
Use these links to rapidly review the document
TABLE OF CONTENTS
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES INDEX TO FINANCIAL STATEMENTS
UNITED STATES
SECURITIES AND EXCHANGE COMMISSION
Washington, D.C. 20549
FORM 10-K
| ý | ANNUAL REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 | |
For the fiscal year ended December 31, | ||
o | TRANSITION REPORT PURSUANT TO SECTION 13 or 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 | |
For the transition period from to | ||
Commission File No. 1-6639
MAGELLAN HEALTH SERVICES, INC.
(Exact name of registrant as specified in its charter)
| Delaware (State or other jurisdiction of incorporation or organization) | 58-1076937 (I.R.S. Employer Identification No.) | |
55 Nod Road, Avon, Connecticut (Address of principal executive offices) | 06001 (Zip Code) |
Registrant's telephone number, including area code:(860) 507-1900
Securities registered pursuant to Section 12(b) of the Act:None.
| Title of Each Class | Name of Each Exchange on which Registered | |
|---|---|---|
| Ordinary Common Stock, par value $0.01 per share | The NASDAQ Global Market |
Securities registered pursuant to Section 12(g) of the Act:None.
Indicate by check mark if the registrant is a well-known seasoned issuer, as defined in Rule 405 of the Securities Act. Yes ý No o
Indicate by check mark if the registrant is not required to file reports pursuant to Section 13 or 15(d) of the Act. Yes o No ý
Indicate by check mark whether the registrant (1) has filed all reports required to be filed by Section 13 or 15(d) of the Securities Exchange Act of 1934 during the preceding twelve months (or for such shorter period that the registrant was required to file such reports), and (2) has been subject to such filing requirements for the past 90 days. Yes ý No o
Indicate by check mark whether the registrant has submitted electronically and posted on its corporate Web site, if any, every Interactive Data File required to be submitted and posted pursuant to Rule 405 of Regulation S-T (§232.405 of this chapter) during the preceding 12 months (or for such shorter period that the registrant was required to submit and post such files). Yes ý No o
Indicate by check mark if disclosure of delinquent filers pursuant to Item 405 of Regulation S-K is not contained herein, and will not be contained, to the best of registrant's knowledge, in definitive proxy or information statements incorporated by reference in Part III of this Form 10-K or any amendment to this Form 10-K. o
Indicate by check mark whether the registrant is a large accelerated filer, an accelerated filer, or a non-accelerated filer. See definition of "accelerated filer and large accelerated filer" in Rule 12b-2 of the Exchange Act. (Check one):
| Large accelerated filer ý | Accelerated filer o | Non-accelerated filer o (Do not check if a smaller reporting company) | Smaller reporting company o |
Indicate by check mark whether the registrant is a shell company (as defined in Rule 12b-2 of the Exchange Act). Yes o No ý
The aggregate market value of the Ordinary Common Stock ("common stock") held by non-affiliates of the registrant based on the closing price on June 30, 20112012 (the last business day of the registrant's most recently completed second fiscal quarter) was approximately $1.7$1.2 billion.
The number of shares of Magellan Health Services, Inc.'s common stock outstanding as of February 23, 201222, 2013 was 27,192,159.27,007,265.
DOCUMENTS INCORPORATED BY REFERENCE
Portions of the definitive proxy statement for the 20122013 Annual Meeting of Shareholders are incorporated by reference into Part III of this Form 10-K.
MAGELLAN HEALTH SERVICES, INC.
REPORT ON FORM 10-K
For the Fiscal Year Ended December 31, 20112012
Table of Contents
| | | Page | ||
|---|---|---|---|---|
PART I | ||||
Item 1. | Business | 1 | ||
Item 1A. | Risk Factors | |||
Item 1B. | Unresolved Staff Comments | |||
Item 2. | Properties | |||
Item 3. | Legal Proceedings | |||
Item 4. |
| |||
PART II | ||||
Item 5. | Market for Registrant's Common Equity, Related Stockholder Matters and Issuer Purchases of Equity Securities | |||
Item 6. | Selected Financial Data | |||
Item 7. | Management's Discussion and Analysis of Financial Condition and Results of Operations | |||
Item 7A. | Quantitative and Qualitative Disclosures about Market Risk | |||
Item 8. | Financial Statements and Supplementary Data | |||
Item 9. | Changes in and Disagreements with Accountants on Accounting and Financial Disclosure | |||
Item 9A. | Controls and Procedures | |||
Item 9B. | Other Information | |||
PART III | ||||
Item 10. | Directors and Executive Officers of the Registrant | |||
Item 11. | Executive Compensation | |||
Item 12. | Security Ownership of Certain Beneficial Owners and Management and Related Stockholder Matters | |||
Item 13. | Certain Relationships and Related Transactions and Director Independence | |||
Item 14. | Principal Accounting Fees and Services | |||
PART IV | ||||
Item 15. | Exhibits, Financial Statement Schedule and Additional Information |
Cautionary Statement Concerning Forward-Looking Statements
This Form 10-K includes "forward-looking statements" within the meaning of Section 27A of the Securities Act of 1933, as amended (the "Securities Act"), and Section 21E of the Securities Exchange Act of 1934, as amended (the "Exchange Act"). Examples of forward-looking statements include, but are not limited to, statements the Company (as defined below) makes regarding our future operating results and liquidity needs. Although the Company (as defined below) believes that its plans, intentions and expectations reflected in such forward-looking statements are reasonable, it can give no assurance that such plans, intentions or expectations will be achieved. Prospective investors are cautioned that any such forward-looking statements are not guarantees of future performance and involve risks and uncertainties, and that actual results may differ materially from those contemplated by such forward-looking statements. Important factors currently known to management that could cause actual results to differ materially from those in forward-looking statements are set forth under the heading "Risk Factors" in Item 1A and elsewhere in this Form 10-K. When used in this Form 10-K, the words "estimate," "anticipate," "expect," "believe," "should" and similar expressions are intended to be forward-looking statements.
Any forward-looking statement made by the Company in this Form 10-K speaks only as of the date on which it is made. Factors or events that could cause our actual results to differ may emerge from time to time, and it is not possible for the Company to predict all of them. The Company undertakes no obligation to publicly update any forward-looking statement, whether as a result of new information, future developments or otherwise, except as may be required by law.
You should also be aware that while the Company from time to time communicates with securities analysts, the Company does not disclose to them any material non-public information, internal forecasts or other confidential business information. Therefore, to the extent that reports issued by securities analysts contain projections, forecasts or opinions, those reports are not the Company's responsibility and are not endorsed by the Company. You should not assume that the Company agrees with any statement or report issued by any analyst, irrespective of the content of the statement or report.
Magellan Health Services, Inc. ("Magellan") was incorporated in 1969 under the laws of the State of Delaware. Magellan's executive offices are located at 55 Nod Road, Avon, Connecticut 06001, and its telephone number at that location is (860) 507-1900. Reference in this report to the "Company" include the accounts of Magellan and its majority owned subsidiaries.
Business Overview
The Company is engaged in the specialty managed healthcare business. Through 2005, the Company predominantly operated in the managed behavioral healthcare business. As a result of certain acquisitions, the Company expanded into radiology benefits management and specialty pharmaceutical management during 2006, and into Medicaid administration during 2009. The Company provides services to health plans, insurance companies, employers, labor unions and various governmental agencies. The Company's business is divided into the following six segments, based on the services it provides and/or the customers that it serves, as described below.
Managed Behavioral Healthcare
Two of the Company's segments are in the managed behavioral healthcare business. This line of business generally reflects the Company's coordination and management of the delivery of behavioral healthcare treatment services that are provided through its contracted network of third-party treatment providers, which includes psychiatrists, psychologists, other behavioral health professionals, psychiatric
hospitals, general medical facilities with psychiatric beds, residential treatment centers and other treatment facilities. The treatment services provided through the Company's provider network include outpatient programs (such as counseling or therapy), intermediate care programs (such as intensive outpatient programs and partial hospitalization services), inpatient treatment and crisis intervention services. The Company generally does not directly provide or own any provider of treatment services.
The Company provides its management services primarily through: (i) risk-based products, where the Company assumes all or a substantial portion of the responsibility for the cost of providing treatment services in exchange for a fixed per member per month fee, (ii) administrative services only ("ASO") products, where the Company provides services such as utilization review, claims administration and/or provider network management, but does not assume responsibility for the cost of the treatment services, and (iii) employee assistance programs ("EAPs") where the Company provides short-term outpatient behavioral counseling services.
The managed behavioral healthcare business is managed based on the services provided and/or the customers served, through the following two segments:
Commercial. The Managed Behavioral Healthcare Commercial segment ("Commercial") generally reflects managed behavioral healthcare services and EAP services provided under contracts with health plans and insurance companies for some or all of their commercial, Medicaid and Medicare members, as well as with employers, including corporations, governmental agencies, and labor unions. Commercial's contracts encompass risk-based, ASO and EAP arrangements. As of December 31, 2011,2012, Commercial's covered lives were 3.75.4 million, 12.913.4 million and 12.612.0 million for risk-based, ASO and EAP products, respectively. For the year ended December 31, 2011,2012, Commercial's revenue was $370.4$516.6 million, $97.8$118.2 million and $93.6$93.7 million for risk-based, ASO and EAP products, respectively.
Public Sector. The Managed Behavioral Healthcare Public Sector segment ("Public Sector") generally reflects services provided to recipients under Medicaid and other state sponsored programs under contracts with state and local governmental agencies. Public Sector contracts encompass either risk-based or ASO arrangements. As of December 31, 2011,2012, Public Sector's covered lives were 1.61.9 million and 0.31.1 million for risk-based and ASO products, respectively. For the year ended December 31, 2011,2012, Public Sector's revenue was $1.5$1.6 billion and $5.9$27.5 million for risk-based and ASO products, respectively.
Radiology Benefits Management
The Radiology Benefits Management segment ("Radiology Benefits Management") generally reflects the management of the delivery of diagnostic imaging and other therapeutic services to ensure that such services are clinically appropriate and cost effective. The Company's radiology benefits management services currently are provided under contracts with health plans and insurance companies for some or all of their commercial, Medicaid and Medicare members. The Company also contracts with state and local governmental agencies for the provision of such services to Medicaid recipients. The Company offers its radiology benefits management services through risk-based contracts, where the Company assumes all or a substantial portion of the responsibility for the cost of providing diagnostic imaging services, and through ASO contracts, where the Company provides services such as utilization review and claims administration, but does not assume responsibility for the cost of the imaging services. As of December 31, 2011,2012, covered lives for Radiology Benefits Management were 3.64.8 million and 12.012.4 million for risk-based and ASO products, respectively. For the year ended December 31, 2011,2012, revenue for Radiology Benefits Management was $296.0$308.5 million and $48.3$40.6 million for risk-based and ASO products, respectively.
Drug Benefits Management
Two of the Company's segments are in the drug benefits management business. This line of business generally reflects the Company's clinical management of drugs paid under medical and pharmacy benefit programs. The Company's services include the coordination and management of the specialty drug spendspending for health plans, employers, and governmental agencies, and the management of pharmacy programs for Medicaid programs, health plans, and other state-sponsored programs.employers. The two segments in this line of business line are:
Specialty Pharmaceutical Management. The Specialty Pharmaceutical Management segment ("Specialty Pharmaceutical Management") comprises programs that manage specialty drugs used in the treatment of complex conditions such as cancer, multiple sclerosis, hemophilia, infertility, rheumatoid arthritis, chronic forms of hepatitis and other diseases. Specialty pharmaceutical drugs represent high-cost injectible, infused, or oral drugs with sensitive handling or storage needs, many of which may be physician administered. Patients receiving these drugs require greater amounts of clinical support than those taking more traditional agents. Payors require clinical, financial and technological support to maximize the value delivered to their members using these expensive agents. The Company's specialty pharmaceutical management services are provided under contracts with health plans, insurance companies, employers, and governmental agencies for some or all of their commercial, Medicare and Medicaid members. The Company's specialty pharmaceutical services include: (i) contracting and formulary optimization programs; (ii) specialty pharmaceutical dispensing operations; and (iii) medical pharmacy management programs. The Company's Specialty Pharmaceutical Management segment had contracts with 41 health plans and employers, and several pharmaceutical manufacturers and state Medicaid programs as of December 31, 2011.2012.
Medicaid Administration. The Medicaid Administration segment ("Medicaid Administration") generally reflects integrated clinical management services provided to the public sector to manage Medicaid pharmacy, mental health, and long-term care programs.for state benefit programs, and pharmacy benefit management programs for health plans and employers. The primary focus of the Company's Medicaid Administration unit involves providing pharmacy benefits administration ("PBA") and pharmacy benefits management ("PBM") services under contracts with health plans and employers, as well as public sector healthcare clients forsponsoring Medicaid and other state sponsored program recipients.benefit programs. The Company's pharmacy services include pharmacynetwork management, formulary and rebate management, point-of-sale claims processing systems and administration, drug utilization review, clinical prior authorization, and drug utilization review. Magellan's pharmacy strategy combines its Specialty Pharmacy Management and PBM capabilities to provide integrated management of complex drug therapies billed under both the medical and pharmacy benefit. Its mental health and long term care management services include review of service utilization and formulary management services, Preferred Drug List programs, Maximum Allowable Cost programs,compliance with state and drug rebate program services.federal regulations and reimbursement guidelines. Medicaid Administration's contracts encompass both Fee-For-Service ("FFS") and risk-based arrangements. In addition to Medicaid Administration's FFS contracts, effective September 1, 2010, Public Sector has subcontracted with Medicaid Administration to provide pharmacy benefits management services on a risk basis for one of Public Sector's customers.
Corporate
This segment of the Company is comprised primarily of operational support functions such as sales and marketing and information technology, as well as corporate support functions such as executive, finance, human resources and legal.
See Note 11—"Business Segment Information" to the consolidated financial statements for certain segment financial data relating to our business set forth elsewhere herein.
Acquisition of First Health Services
Pursuant to the June 4, 2009 Purchase Agreement (the "Purchase Agreement") with Coventry Health Care ("Coventry"), on July 31, 2009 the Company acquired (the "Acquisition") all of the outstanding equity interests of Coventry's direct and indirect subsidiaries First Health Services
Corporation ("FHS"), FHC, Inc. ("FHC") and Provider Synergies, LLC (together with FHS and FHC,
"First "First Health Services") and certain assets of Coventry which are related to the operation of the business conducted by First Health Services. As consideration for the Acquisition, the Company paid $114.5 million in cash, excluding cash acquired and including net payments of $6.5 million for excess working capital. The Company funded the Acquisition with cash on hand.
Effective July 1, 2010, the Company discontinued the use of the name First Health Services Corporation and officially changed such name to "Magellan Medicaid Administration, Inc." The Company reports the results of operations of Magellan Medicaid Administration, Inc. within the Medicaid Administration segment.
Industry
According to the Centers for Medicare and Medicaid Services ("CMS"), U.S. healthcare spending was projected to have increased 5.24.2 percent to $2.7$2.8 trillion in 2011,2012, representing more than 17nearly 18 percent of the gross domestic product. With the uncertain economic environment, rising healthcare costs, increased fiscal pressures on federal and state governments, and the uncertainty around the implementation of healthcare reform, healthcare spending will continue to be one of the greatest pressing issues for the American public and the government agencies. The rapidly evolving clinical and technological environment demands the expertise of specialized healthcare management services to provide both high-quality and affordable care.
Over the last several years, the Company has transformed itself into a diversified specialty managed healthcare company by entering various healthcare cost and care management areas that represent a meaningful portion of the healthcare dollar and that are growing at a disproportionately higher rate than other areas of healthcare. The Company defines areas of healthcare that can be carved out for specialty healthcare management to be areas where:
Business Strategy
The Company is engaged in the specialty managed healthcare business. It currently provides managed behavioral healthcare services, radiology benefit management services, and drug benefits management services. The Company's strategy is to expand its participation in the healthcare management services market through the expansion of its existing businesses, and diversification into new specialties and services. The Company believes that certain of its clients wouldmay prefer to consolidate outsourced vendors, and that as a vendor offering multiple outsourced products, it will have a competitive advantage in the market. The Company seeks to grow its specialty managed healthcare business through the following initiatives:
Expanding the managed behavioral healthcare business. The Company has operated in both the commercial and public sectors of managed behavioral healthcare by ensuring the delivery of quality outcomes and appropriate care through its unique behavioral healthcare expertise in managing clinical care, provider networks, claims, and customer service. The Company focuses on continually developing and providing innovative and cost effective solutions to its customers, and expanding into new markets. Through its Commercial behavioral segment, the Company seeks to provide a superior outsourced alternative to its health plan, employer, and employergovernment customers. The Company has expanded its product offerings including products dealing with autism. Through its Public Sector segment, the Company seeks to help state and local governments deal with their fiscal pressures resulting from increasing Medicaid enrollment and rising healthcare costs. The Company intends to continue marketing both its risk-based
and ASO products, as well as new products, to its existing customer base and new customers, and to cross-sell its behavioral product portfolio to its other specialty segments' customer base.
Expanding the radiology benefits management services business. In radiology benefits management, the Company's strategy is to deliver innovative and clinically appropriate radiology management
programs that create value for its clients through the reduction in the number of inappropriate radiology services and ensure the delivery of appropriate services through quality providers. The Company seeks to distinguish itself in the marketplace through a focus on clinical excellence, provider partnerships, product and service innovation, and consumerism. The Company continues to expand its product portfolio with customer-focused solutions in new areas of medical management including radiation oncology therapy management, cardiac management, obstetrical ultrasound management, pain management, and other relevant areas. In addition to selling its programs to new customers, the Company's growth strategy is also focused on continuing to develop innovative new products and to expand membership with current customers, upsell additional products to existing customers, and cross-sell to its other specialty segments' customer base.
Expanding the drug benefits management business. The Company has operated in both the Specialty Pharmaceuticalspecialty pharmaceutical management and Medicaid pharmacy administrationbenefits management businesses for several years. In 2011, the Company created a new business unit, Magellan Pharmacy Solutions ("Pharmacy Solutions"), which leverages the strength and assets in these business segments to best position the Company to expand its presence in the pharmaceutical marketplace. This new business unit will offer clinical and financial management solutions that help customers manage their totalthe quality and cost of pharmaceutical care for any drug, spend, regardless of theunder any benefit, at any site of service, methodservice. Pharmacy Solutions provides a comprehensive suite of delivery or claims flow. The Specialty Pharmaceutical Management segment will continue to provide its unique service model, which includes contractingproducts, ranging from pharmacy benefit solutions such as Pharmacy Benefit Manager capabilities; specialty pharmacy solutions including formulary and formulary optimization services,rebate management solutions and specialty pharmaceutical dispensing services,distribution; and its medical pharmacy management product, which manages the cost and quality of therapeutic interventions for complex conditions covered under the medical benefit. In addition, in conditions such as oncology and autoimmune diseases2012, Pharmacy Solutions began offering an integrated drug management solution spanning both the medical and pharmacy benefit plans. The Medicaid Administration business will continue to provide services that help state governments control their pharmacy spending. In 2010, the Company developed additional capabilities to enable it to compete as a risk-bearing pharmacy benefits manager supporting Medicaid managedreduce cost of care, organizations. The Company will continue to utilize its sophisticated clinical tools, operational platform, software development and claims processing expertise to develop pharmacy management products that drive savings and improve quality of care for its customers and members.health outcomes. The company intends to marketCompany is marketing its drug benefits management products to existing and new health plans, employer groups, state governments, exchanges, and Medicaid managed care organizations. The Company implemented its integrated management solution for its first customer on January 1, 2013. The Company continues to cross-sell drug benefits management solutions to its other specialty segments' customer base.
Expanding management services provided to Medicaid and other special populations. The Company seeks to expand its focus on government-sponsored health care plans,the clinically integrated management of special populations including individuals with serious mental illness ("SMI"), those covered under both Medicare and Medicaid (dual-eligibles), and the new solutions that will be developed in response to health care reform and the pressures facing state and local governments. The Company intends to continue to expand its Medicaid business in its existing product lines. The Company believes its significant Medicaid and behavioral health experience will enable it to develop programs to manage specialty populations, such as individuals with Serious Mental Illness, and dual eligibles.other unique high-cost populations. These programs will integrate the management of behavioral and physical health for special populations and utilize the Company's unique expertise to improve health outcomes and lower costs. The Company believes its significant Medicaid, behavioral health and pharmacy experience will enable it to develop programs to manage these specialtyspecial populations. The Company intends to continue to expand its integrated health offerings in its existing product lines. It is developing independent capabilities and may enter into partnerships or joint ventures that facilitate the rate of expansion of special population management in accordance with its Medicaid strategy. The Company believes it is positioned to grow its membership and revenues in the Medicaid marketintegrated care management of special populations over the long term.
Continued selective diversification of business lines. The Company actively evaluates opportunities to enter other significant, high trend specialty healthcare businesses that would leverage its expertise and core competencies and/or that could draw on its existing customer relationships.
Customer Contracts
The Company's contracts with customers typically have terms of one to three years, and in certain cases contain renewal provisions (at the customer's option) for successive terms of between one and two years (unless terminated earlier). Substantially all of these contracts may be immediately
terminated with cause and many of the Company's contracts are terminable without cause by the customer or the Company either upon the giving of requisite notice and the passage of a specified period of time (typically between 60 and 180 days) or upon the occurrence of other specified events. In addition, the Company's contracts with federal, state and local governmental agencies generally are conditioned on legislative appropriations. These contracts generally can be terminated or modified by the customer if such appropriations are not made. The Company's contracts for managed behavioral healthcare and radiology benefits management services generally provide for payment of a per member per month fee to the Company. See "Risk Factors—Risk-Based Products" and "—Reliance on Customer Contracts."
The Company provides behavioral healthcare management and other related services to approximately 683,000 members in Maricopa County, Arizona, (the "Maricopa Contract"). The Maricopa Contract generated net revenues that exceeded, in the aggregate, ten percent of net revenues for the consolidated Company for the years ended December 31, 2009, 2010, 2011 and 2011.2012.
The Company also has a significant concentration of business with various counties in the State of Pennsylvania (the "Pennsylvania Counties") which are part of the Pennsylvania Medicaid program, and with various areas in the State of Florida (the "Florida Areas") which are part of the Florida Medicaid program. See further discussion related to these significant customers in "Risk Factors—Reliance on Customer Contracts." In addition, see "Risk Factors—Dependence on Government Spending" for discussion of risks to the Company related to government contracts.
Provider Network
The Company's managed behavioral healthcare services and EAP treatment services are provided by a contracted network of third-party providers, including psychiatrists, psychologists, other behavioral health professionals, psychiatric hospitals, general medical facilities with psychiatric beds, residential treatment centers and other treatment facilities. The number and type of providers in a particular area depend upon customer preference, site, geographic concentration and demographic composition of the beneficiary population in that area. The Company's managed behavioral healthcare network consists of approximately 79,70070,000 behavioral healthcare providers, including facility locations, providing various levels of care nationwide. The Company's network providers are almost exclusively independent contractors located throughout the local areas in which the Company's customers' beneficiary populations reside. Outpatient network providers work out of their own offices, although the Company's personnel are available to assist them with consultation and other needs.
Non-facility network providers include both individual practitioners, as well as individuals who are members of group practices or other licensed centers or programs. Non-facility network providers typically execute standard contracts with the Company under which they are generally paid on a fee-for-service basis.
Third-party network facilities include inpatient psychiatric and substance abuse hospitals, intensive outpatient facilities, partial hospitalization facilities, community health centers and other community-based facilities, rehabilitative and support facilities and other intermediate care and alternative care facilities or programs. This variety of facilities enables the Company to offer patients a full continuum of care and to refer patients to the most appropriate facility or program within that continuum. Typically, the Company contracts with facilities on a per diem or fee-for-service basis and, in some limited cases, on a "case rate" or capitated basis. The contracts between the Company and inpatient and other facilities typically are for one-year terms and are terminable by the Company or the facility upon 30 to 120 days' notice.
Historically, theThe Company's radiology benefits management services wereare provided by a network of third-party providers that were contracted by the customers of the Company to provide such services to the customers' members or enrollees. To support its offering of risk-based arrangements, the Company has developed and continues to expand a proprietary network of providers directly, through the use of its internal networking resources, and indirectly through a network contracting company. Network providers includeincluding diagnostic imaging centers, radiology departments of hospitals that provide advanced imaging services on an outpatient basis, and individual physicians or physician groups that own advanced imaging equipment and specialize in certain specific areas of care. The Company contracts with theseCertain providers belong to the Company's network, while others are members of networks belonging to the Company's customers. These providers are paid on a fee-for-service basis.
Joint Ventures
Magellan Complete Care of Arizona, Inc. ("MCCAZ"), a joint venture owned 80 percent by the Company and 20 percent by VHS Phoenix Health Plan, LLC (a subsidiary of Vanguard Health Systems, Inc.), was formed to manage integrated behavioral and physical healthcare for recipients with SMI and behavioral healthcare for other Medicaid beneficiaries in Maricopa County. MCCAZ has responded to a Request for Proposal ("RFP") released by the Arizona Department of Health Services ("ADHS") on October 4, 2012. During the year ended December 31, 2012, the Company invested $1.5 million in MCCAZ, which is included within restricted cash on the accompanying consolidated balance sheets. The Company has consolidated the balance sheet and results of operations of MCCAZ in its consolidated financial statements as of December 31, 2012.
The Company currently owns a 49 percent interest in Fallon Total Care, LLC ("Fallon Total Care") which was formed to apply to participate in a demonstration program that will provide integrated healthcare to individuals aged 21 to 64 years who are dually-eligible for Medicare and Medicaid in the State of Massachusetts. The other 51 percent interest in Fallon Total Care is owned by Fallon Community Health Plan. On November 5, 2012, it was announced that Fallon Total Care was selected as a participant in the three-year demonstration program to serve dual-eligible residents in ten counties across Massachusetts. The contract award is subject to completion of readiness review and contract negotiation. During the year ended December 31, 2012 the Company contributed $1.2 million of capital to Fallon Total Care, which is included within other long-term assets on the accompanying consolidated balance sheets. The Company accounts for its investment in Fallon Total Care using the equity method.
Competition
The Company's business is highly competitive. The Company competes with other healthcare organizations as well as with insurance companies, including health maintenance organizations ("HMOs"), preferred provider organizations ("PPOs"), third-party administrators ("TPAs"), independent practitioner associations ("IPAs"), multi-disciplinary medical groups, pharmacy benefit managers ("PBMs"), healthcare information technology solutions, and other specialty healthcare and managed care companies. Many of the Company's competitors, particularly certain insurance companies, HMOs, technology companies, and PBMs are significantly larger and have greater financial, marketing and other resources than the Company, and some of the Company's competitors provide a broader range of services. The Company competes based upon quality and reliability of its services, a focus on clinical excellence, product and service innovation and proven expertise in its business lines. The Company may also encounter competition in the future from new market entrants. In addition, some of the Company's customers that are managed care companies may seek to provide specialty managed healthcare services directly to their subscribers, rather than by contracting with the Company for such services. Because of these factors, the Company does not expect to be able to rely to a significant degree on price increases to achieve revenue growth, and expects to continue experiencing pricing pressures.
Insurance
The Company maintains a program of insurance coverage for a broad range of risks in its business. The Company has renewed its general, professional and managed care liability insurance policies with unaffiliated insurers for a one-year period from June 17, 20112012 to June 17, 2012.2013. The general liability policy is written on an "occurrence" basis, subject to a $0.05 million per claim un-aggregated self-insured retention. The professional liability and managed care errors and omissions liability policies are written on a "claims-made" basis, subject to a $1.0 million per claim ($10.0 million per class action claim) un-aggregated self-insured retention for managed care errors and omissions liability, and a $0.05 million per claim un-aggregated self-insured retention for professional liability.
The Company maintains a separate general and professional liability insurance policy with an unaffiliated insurer for its Specialty Pharmaceutical Management business. The Specialty Pharmaceutical Management insurance policy has a one-year term for the period June 17, 20112012 to June 17, 2012.2013. The general liability policy is written on an "occurrence" basis and the professional liability policy is written on a "claims-made" basis, subject to a $0.05 million per claim and $0.25 million aggregated self-insured retention.
The Company maintains separate professional liability insurance policies with unaffiliated insurers for its Maricopa Contract business for the behavioral health direct care facilities, all of which were divested at various times prior to December 31, 2009. The Maricopa Contract professional liability insurance policies effective dates were from September 1, 2008 to September 1, 2009. The Company purchased a five-year extended reporting period for the professional liability policies effective September 1, 2009 for
the period September 1, 2009 to September 1, 2014.2014, subject to a $0.5 million per claim un-aggregated self-insured retention. The professional liability policies are written on a "claims-made" basis, subject to a $0.5 million per claim un-aggregated self-insured retention.basis.
The Company is responsible for claims within its self-insured retentions, and for portions of claims reported after the expiration date of the policies if they are not renewed, or if policy limits are exceeded. The Company also purchases excess liability coverage in an amount that management believes to be reasonable for the size and profile of the organization.
See "Risk Factors—Professional Liability and Other Insurance," for a discussion of the risks associated with the Company's insurance coverage.
Regulation
General. The specialty managed healthcare industry is subject to extensive and evolving state and federal regulation. The Company is subject to certain state laws and regulations, including those governing the licensing of insurance companies, HMOs, PPOs, TPAs, PBMs, pharmacies and companies engaged in utilization review and specialty pharmaceutical management. In addition, the Company is subject to regulations concerning the licensing of healthcare professionals, including restrictions on business corporations from providing, controlling or exercising excessive influence over healthcare services through the direct employment of physicians, psychiatrists or, in certain states, psychologists and other healthcare professionals. These laws and regulations vary considerably among states and the Company may be subject to different types of laws and regulations depending on the specific regulatory approach adopted by each state to regulate the managed care and specialty pharmacy businesses and the provision of healthcare treatment services. In addition, the Company is subject to certain federal laws as a result of the role it assumes in connection with managing its customers' employee benefit plans. The regulatory scheme generally applicable to the Company's operations is described in this section.
The Company believes its operations are structured to comply in all material respects with applicable laws and regulations and that it has received all licenses and approvals that are material to the operation of its business. However, regulation of the specialty managed healthcare industry is constantly evolving, with new legislative enactments and regulatory initiatives at the state and federal levels being implemented on a regular basis. Consequently, it is possible that a court or regulatory agency may take a position under existing or future laws or regulations, or as a result of a change in the interpretation thereof, that such laws or regulations apply to the Company in a different manner than the Company believes such laws or regulations apply. Moreover, any such position may require significant alterations to the Company's business operations in order to comply with such laws or regulations, or interpretations thereof. Expansion of the Company's business to cover additional geographic areas, to serve different types of customers, to provide new services or to commence new operations could also subject the Company to additional licensure requirements and/or regulation.
Failure to comply with applicable regulatory requirements could have a material adverse affect on the Company.
Licenses. Certain regulatory agencies having jurisdiction over the Company possess discretionary powers when issuing or renewing licenses or granting approval of proposed actions such as mergers, a change in ownership, transfer or assignment of licenses and certain intra-corporate transactions. One or multiple agencies may require as a condition of such license or approval that the Company cease or modify certain of its operations or modify the way it operates in order to comply with applicable regulatory requirements or policies. In addition, the time necessary to obtain a license or approval varies from state to state, and difficulties in obtaining a necessary license or approval may result in delays in the Company's plans to expand operations in a particular state and, in some cases, lost business opportunities.
In recent years, in response to governmental agency inquiries or discussions with regulators, the Company has determined to seek licensing for its managed behavioral healthcare and radiology benefits management business as a single service HMO, TPA or utilization review agent in one or more jurisdictions. The Company maintains network licenses for these lines of business in some states where required by state regulation. The Company has also sought and obtained utilization review licenses in some states for its pharmaceutical management business.business and has also sought pharmacy benefit manager licensure in some states where required to support its expanded pharmacy product offerings.. The Company has obtained HMO licenses to support its Medicaid HMO line of business in some states as well. Compliance activities, mandated changes in the Company's operations, delays in the expansion of the Company's business or lost business opportunities as a result of regulatory requirements or policies could have a material adverse effect on the Company. As discussed below in the section entitled "Regulations Affecting the Company's Pharmacies," the Company is subject to certain state licensure requirements in relation to its specialty pharmaceutical management business.
Insurance, HMO and PPO Activities. To the extent that the Company operates or is deemed to operate in some states as an insurance company, HMO, PPO or similar entity, it may be required to comply with certain laws and regulations that, among other things, may require the Company to maintain certain types of assets and minimum levels of deposits, capital, surplus, reserves or net worth. In many states, entities that assume risk under contracts with licensed insurance companies or HMOs have not been considered by state regulators to be conducting an insurance or HMO business. As a result, the Company has not sought licenses as either an insurer or HMO in certain states.
The National Association of Insurance Commissioners (the "NAIC") has undertaken a comprehensive review of the regulatory status of entities arranging for the provision of healthcare services through a network of providers that, like the Company, may assume risk for the cost and quality of healthcare services, but that are not currently licensed as an HMO or similar entity. As a result of this review, the NAIC developed a "health organizations risk-based capital" formula, designed specifically for managed care organizations, that establishes a minimum amount of capital necessary for a managed care organization to support its overall operations, allowing consideration for the organization's size and risk profile. The NAIC also adopted a model regulation in the area of health plan standards, which could be adopted by individual states in whole or in part, and could result in the Company being required to meet additional or new standards in connection with its existing operations. Certain states, for example, have adopted regulations based on the NAIC initiative, and as a result, the Company has been subject to certain minimum capital requirements in those states. Certain other states, such as Maryland, Texas, New York and New Jersey, have also adopted their own regulatory initiatives that subject entities, such as certain of the Company's subsidiaries, to regulation under state insurance laws. This includes, but is not limited to, requiring adherence to specific financial solvency standards. State insurance laws and regulations may limit the Company's ability to pay dividends, make certain investments and repay certain indebtedness.
Being licensed as an insurance company, HMO or similar entity could also subject the Company to regulations governing reporting and disclosure, mandated benefits, rate setting and other traditional insurance regulatory requirements. PPO regulations to which the Company may be subject may require the Company to register with a state authority and provide information concerning its operations, particularly relating to provider and payor contracting. The imposition of such requirements could increase the Company's cost of doing business and could delay the Company's conduct or expansion of its business in some areas. The licensing process under state insurance laws can be lengthy and, unless the applicable state regulatory agency allows the Company to continue to operate while the licensing process is ongoing, the Company could experience a material adverse effect on its operating results and financial condition while its license application is pending. In addition, failure to obtain and maintain required licenses typically also constitutes an event of default under the Company's contracts with its customers. The loss of business from one or more of the Company's major customers as a result of such an event of default or otherwise could have a material adverse effect on the Company.
Regulators may impose operational restrictions on entities granted licenses to operate as insurance companies or HMOs. For example, the California Department of Managed Health Care has imposed
certain restrictions on the ability of the Company's California subsidiaries to fund the Company's operations in other states, to guarantee or co-sign for the Company's financial obligations, or to pledge or hypothecate the stock of these subsidiaries and on the Company's ability to make certain operational changes with respect to these subsidiaries. In addition, regulators of certain of the Company's subsidiaries may exercise certain discretionary rights under regulations including, without limitation, increasing its supervision of such entities, requiring additional restricted cash or other security.
Utilization Review and Third-Party Administrator Activities. Numerous states in which the Company does business have adopted regulations governing entities engaging in utilization review and TPA activities. Utilization review regulations typically impose requirements with respect to the qualifications of personnel reviewing proposed treatment, timeliness and notice of the review of proposed treatment and other matters. TPA regulations typically impose requirements regarding claims processing and payments and the handling of customer funds. Utilization review and TPA regulations may increase the Company's cost of doing business in the event that compliance requires the Company to retain additional personnel to meet the regulatory requirements and to take other required actions and make necessary filings. Although compliance with utilization review and third party administrator regulations has not had a material adverse effect on the Company, there can be no assurance that specific regulations adopted in the future would not have such a result, particularly since the nature, scope and specific requirements of such provisions vary considerably among states that have adopted regulations of this type.
Numerous states require the licensing or certification of entities performing utilization review or TPA activities; however, certain federal courts have held that such licensing requirements are preempted by the Employment Retirement Income Security Act of 1974, as amended ("ERISA"). ERISA preempts state laws that mandate employee benefit structures or their administration, as well as those that provide alternative enforcement mechanisms. The Company believes that its TPA activities performed for its self-insured employee benefit plan customers are exempt from otherwise applicable state licensing or registration requirements based upon federal preemption under ERISA and have relied on this general principle in determining not to seek licenses for certain of the Company's activities in some states. Existing case law is not uniform on the applicability of ERISA preemption with respect to state regulation of utilization review or TPA activities. There can be no assurance that additional licenses will not be required with respect to utilization review or TPA activities in certain states.
Licensing of Healthcare Professionals. The provision of healthcare treatment services by physicians, psychiatrists, psychologists, pharmacists and other providers is subject to state regulation with respect to the licensing of healthcare professionals. The Company believes that the healthcare professionals, who
provide healthcare treatment on behalf of or under contracts with the Company, and the case managers and other personnel of the health services business, are in compliance with the applicable state licensing requirements and current interpretations thereof. However, there can be no assurance that changes in such state licensing requirements or interpretations thereof will not adversely affect the Company's existing operations or limit expansion. With respect to the Company's employee assistance crisis intervention program, additional licensing of clinicians who provide telephonic assessment or stabilization services to individuals who are calling from out-of-state may be required if such assessment or stabilization services are deemed by regulatory agencies to be treatment provided in the state of such individual's residence. The Company believes that any such additional licenses could be obtained.
Prohibition on Fee Splitting and Corporate Practice of Professions. The laws of some states limit the ability of a business corporation to directly provide, control or exercise excessive influence over healthcare services through the direct employment of physicians, psychiatrists, psychologists, or other healthcare professionals, who are providing direct clinical services. In addition, the laws of some states prohibit physicians, psychiatrists, psychologists, or other healthcare professionals from splitting fees with other persons or entities. These laws and their interpretations vary from state to state and enforcement
by the courts and regulatory authorities may vary from state to state and may change over time. The Company believes that its operations as currently conducted are in material compliance with the applicable laws. However, there can be no assurance that the Company's existing operations and its contractual arrangements with physicians, psychiatrists, psychologists and other healthcare professionals will not be successfully challenged under state laws prohibiting fee splitting or the practice of a profession by an unlicensed entity, or that the enforceability of such contractual arrangements will not be limited. The Company believes that it could, if necessary, restructure its operations to comply with changes in the interpretation or enforcement of such laws and regulations, and that such restructuring would not have a material adverse effect on its operations.
Direct Contracting with Licensed Insurers. Regulators in several states in which the Company does business have adopted policies that require HMOs or, in some instances, insurance companies, to contract directly with licensed healthcare providers, entities or provider groups, such as IPAs, for the provision of treatment services, rather than with unlicensed intermediary companies. In such states, the Company's customary model of contracting directly is modified so that, for example, the IPAs (rather than the Company) contract directly with the HMO or insurance company, as appropriate, for the provision of treatment services.
HIPAA. The Health Insurance Portability and Accountability Act of 1996 ("HIPAA") requires the Secretary of the Department of Health and Human Services ("HHS") to adopt standards relating to the transmission, privacy and security of health information by healthcare providers and healthcare plans. Confidentiality and patient privacy requirements are particularly strict in the Company's behavioral managed care business. Oversight responsibilities for HIPAA compliance is handled by the Company's Corporate Compliance Department. The Company believes it is currently in compliance with the provisions of HIPAA.
The Health Information Technology for Economic and Clinical Health Act ("HITECH Act") passed as part of the American Recovery and Reinvestment Act of 2009 represents a significant expansion of the HIPAA privacy and security laws. The HITECH Act provisions contain multiple effective dates. The Company believes it is currently in compliance with those provisions of the HITECH Act and associated regulations that are currently in effect including the January 2013 "Modifications to the HIPAA Privacy, Security, Enforcement, and Breach Notification Rules under the Health Information Technology for Economic and Clinical Health Act" Rule, and will be in compliance with those portions of the law and regulations that become effective in the future. The Company believes that it can comply with future changes in these laws and regulations, however there can be no
assurance that compliance with such laws and regulations would not have a material adverse effect on its operations.
Other Significant Privacy Regulation. The privacy regulation under HIPAA generally does not preempt state law except under the following limited circumstances: (i) the privacy rights afforded under state law are contrary to those provided by HIPAA so that compliance with both standards is not possible and (ii) HIPAA's privacy protections are more stringent than the state law in question. Because many states have privacy laws that either provide more stringent privacy protections than those imposed by HIPAA or laws that can be followed in addition to HIPAA, the Company must address privacy issues under HIPAA and state law as well. In addition, HIPAA has created an increased awareness of the issues surrounding privacy, which may generate more state regulatory scrutiny in this area.
In addition to HIPAA and the HITECH Act, the Company is also subject to federal laws and regulations governing patient records involving substance abuse, as well as other federal privacy laws and regulations. The Company believes that it is currently in compliance with these applicable laws and regulations.
Federal Anti-Remuneration/Fraud and Abuse Laws. The federal healthcare Anti-Kickback Statute (the "Anti-Kickback Statute") prohibits, among other things, an entity from paying or receiving, subject to certain exceptions and "safe harbors," any remuneration, directly or indirectly, to induce the referral of individuals covered by federally funded healthcare programs, or the purchase, or the arranging for or
recommending of the purchase, of items or services for which payment may be made in whole, or in part, under Medicare, Medicaid, TRICARE or other federally funded healthcare programs. Sanctions for violating the Anti-Kickback Statute may include imprisonment, criminal and civil fines and exclusion from participation in the federally funded healthcare programs. The Anti-Kickback Statute has been interpreted broadly by courts, the Office of Inspector General ("OIG") within the U.S. Department of Health & Human Services ("DHHS"), and other administrative bodies.
It also is a crime under the Public Contractor Anti-Kickback Statute, for any person to knowingly and willfully offer or provide any remuneration to a prime contractor to the United States, including a contractor servicing federally funded health programs, in order to obtain favorable treatment in a subcontract. Violators of this law also may be subject to civil monetary penalties. There have been a series of substantial civil and criminal investigations and settlements, at the state and federal level, by pharmacy benefit managers over the last several years in connection with alleged kickback schemes. The Company believes that it is in compliance with the legal requirements imposed by such anti-remuneration laws and regulations, however, there can be no assurance that the Company will not be subject to scrutiny or challenge under such laws or regulations and that any such challenge would not have a material adverse effect on the Company's business, results of operations, financial condition or cash flows.
Federal Statutes Prohibiting False Claims. The Federal Civil False Claims Act imposes civil penalties for knowingly making or causing to be made false claims with respect to governmental programs, such as Medicare and Medicaid, for services not rendered, or for misrepresenting actual services rendered, in order to obtain higher reimbursement. Private individuals may bringqui tam or whistle blower suits against providers under the Federal Civil False Claims Act, which authorizes the payment of a portion of any recovery to the individual bringing suit. A few federal district courts recently have interpreted the Federal Civil False Claims Act as applying to claims for reimbursement that violate the Anti-Kickback Statute under certain circumstances. The Federal Civil False Claims Act generally provides for the imposition of civil penalties and for treble damages, resulting in the possibility of substantial financial penalties for small billing errors. Criminal provisions that are similar to the Federal Civil False Claims Act provide that a corporation may be fined if it is convicted of presenting to any federal agency a claim or making a statement that it knows to be false, fictitious or fraudulent. Even in situations where the Company does not directly provide services to beneficiaries of
federally funded health programs and, accordingly, does not directly submit claims to the federal government, it is possible that the Company could nevertheless become involved in a situation where false claim issues are raised based on allegations that it caused or assisted a government contractor in making a false claim.
The Company is subject to certain provisions of the Deficit Reduction Act of 2005 (the "Act"). The Act requires entities that receive $5 million or more in annual Medicaid payments to establish written policies that provide detailed information about the Federal Civil False Claims Act and the remedies there under, as well as any state laws pertaining to civil or criminal penalties for false claims and statements, the "whistleblower" protections afforded under such laws, and the role of such laws in preventing and detecting fraud waste and abuse. The written policies are to be disseminated to all employees, contractors and agents which or who, on behalf of the entity, furnishes, or otherwise authorizes the furnishing of, Medicaid healthcare items or services; performs billing or coding functions, or is involved in the monitoring of healthcare provided by the entity. In addition, any such entity that has an employee handbook must include a specific discussion of the federal and state false claims laws, the rights of an employee to be protected as a whistle blower and the entity's policies and procedures for detecting and preventing fraud, waste and abuse. The Company does not believe that it is in violation of the Federal Civil False Claims Act (or its criminal counterparts) and the Company has a corporate compliance and ethics program, policies and procedures and internal controls in place to help maintain an organizational culture of honesty and integrity.
State Anti-Remuneration/False Claims Law. Several states have laws and/or regulations similar to the federal anti-remuneration and Federal Civil False Claims Act described above. Sanctions for violating these state anti-remuneration and false claims laws may include injunction, imprisonment, criminal and civil fines and exclusion from participation in the state Medicaid programs. The Company believes that it is in substantial compliance with the legal requirements imposed by such anti-remuneration laws and regulations. However, there can be no assurance that the Company will not be subject to scrutiny or challenge under such laws or regulations and that any such challenge would not have a material adverse effect on the Company's business, results of operations, financial condition or cash flows.
The Dodd-Frank Wall Street Reform and Consumer Protection Act.Act ("Dodd-Frank"). On July 21, 2010 the President of the United States signed into lawThe Dodd-Frank Wall Street Reform and Consumer Protection Act ("Dodd-Frank"). Dodd-Frank. Under the law, those with independent knowledge of a financial fraud committed by a business required to report to the SECU.S. Securities and Exchange Commission ("SEC") or the USU.S. Commodity Futures Trading Commission ("CFTC") may be entitled to a percentage of the money recovered. Included in Dodd-Frank are provisions which protect employees of publicly traded companies from retaliation for reporting securities fraud, fraud against shareholders and violation of the Securities and Exchange CommissionSEC rules/regulations. Dodd-Frank also amends the Sarbanes-Oxley Act ("SOX") and Federal Civil False Claims Act to expand their whistle-blower protections. On May 25, 2011, the U.S. Securities and Exchange Commission ("SEC")SEC adopted final rules (the "Rules") for the expanded whistleblower program established by the Dodd-Frank Wall Street Reform and Consumer Protection Act ("Dodd-Frank"). MagellanDodd-Frank. The Company believes it is in compliance with these Rules.
ERISA. Certain of the Company's services are subject to the provisions of ERISA. ERISA governs certain aspects of the relationship between employer-sponsored healthcare benefit plans and certain providers of services to such plans through a series of complex laws and regulations that are subject to periodic interpretation by the Internal Revenue Service ("IRS") and the U.S. Department of Labor. In some circumstances, and under certain customer contracts, the Company may be expressly named as a "fiduciary" under ERISA, or be deemed to have assumed duties that make it an ERISA fiduciary, and thus be required to carry out its operations in a manner that complies with ERISA in all material respects. The Company believes that it is in material compliance with ERISA and that such compliance does not currently have a material adverse effect on its operations, however there can be
no assurance that continuing ERISA compliance efforts or any future changes to ERISA will not have a material adverse effect on the Company.
Other Federal Laws and Regulations. The Company is subject to certain federal laws and regulations in connection with its contracts with the federal government. These laws and regulations affect how the Company conducts business with its federal agency customers and may impose added costs on its business. The Company's failure to comply with federal procurement laws and regulations could cause it to lose business, incur additional costs, and subject it to a variety of civil and criminal penalties and administrative sanctions, including termination of contracts, forfeiture of profits, harm to reputation, suspension of payments, fines, and suspension or debarment from doing business with federal government agencies. The Company believes that it is in material compliance with all applicable laws and regulations and that such compliance does not currently have a material adverse effect on its operations.
Regulation of Customers. Regulations imposed upon the Company's customers include, among other things, benefits mandated by statute, exclusions from coverage prohibited by statute, procedures governing the payment and processing of claims, record keeping and reporting requirements, requirements for and payment rates applicable to coverage of Medicaid and Medicare beneficiaries, provider contracting and enrollee rights and confidentiality requirements. Although the Company believes that such regulations do not, at present, materially impair its operations, there can be no assurance that such indirect regulation will not have a material adverse effect on the Company in the future.
In October 2008, the United States Congress passed the Paul Wellstone and Pete Dominici Mental Health Parity Act of 2008 ("MHPAEA") establishing parity in financial requirements (e.g. co-pays, deductibles, etc.) and treatment limitations (e.g., limits on the number of visits) between mental health and substance abuse benefits and medical/surgical benefits for health plan members. This new law does not require coverage for mental health or substance abuse disorders but if coverage is provided it must be provided at parity. No specific disorders are mandated for coverage; health plans are able to define mental health and substance abuse to determine what they are going to cover. State mandated benefits laws are not preempted. The law applies to ERISA plans, Medicaid managed care plans and State Children's Health Insurance Program ("SCHIP") plans. There is an exemption for small employers. On
February 2, 2010, the Department of the Treasury, the Department of Labor and the Department of Health and Human Services issued Interim Final Rules interpreting the MHPAEA ("IFR"). The IFR applies to ERISA plans and insured business;business. A State Medicaid Director Letter was issued in January 2013 discussing applicability of the IFR currently does not apply to Medicaid Managed Caremanaged care plans, or SCHIP plans although itand Alternative Benefit (Benchmark) Plans. It is anticipatedpossible that similar regulatory requirementssome states will change their behavioral health plan benefits or management techniques as a result of this letter. The Health Insurance Exchange regulations provide that plans offered on the exchange must offer behavioral health benefits that are compliant with federal parity law. Further clarification on this requirement is expected to be imposed on that business in the future.issued. The IFR included some concepts not included under the statute including the requirement to conduct the parity review at the category level within the plan, introducing the concept of nonquantitativenon-quantitative treatment limitations, and prohibiting separate but equal deductibles. While some of these regulatory requirements were not anticipated, the Company believes it is in compliance with the requirements of the IFR and that there is no material impact to the companyCompany related to compliance. No assurance can be given that additional interpretive guidance on the legislation and IFR or the release of a final rule will not have a material adverse effect on the Company. However, the Company's risk contracts do allow for repricing to occur effective the same date that any legislation becomes effective if that legislation is projected to have a material effect on cost of care.
Federal and State Medicaid Laws and Regulations. The Company directly contracts with various states to provide Medicaid managed care services to state Medicaid beneficiaries. As such, it is subject to certain federal and state laws and regulations affecting Medicaid as well as state contractual requirements. The Company believes it is in material compliance with these laws, regulations and contractual requirements. The Company also is a sub-contractor to health plans who provide Medicaid managed care services to state Medicaid beneficiaries. In the Company's capacity as a subcontractor with these health plans, the Company is indirectly subject to certain federal and state laws and regulations as well as contractual requirements pertaining to the operation of this business. If a state or a health plan customer determines that the Company has not performed satisfactorily as a subcontractor, a state or the health plan customer may require the Company to cease these activities or responsibilities under the subcontract. While the Company believes that it provides satisfactory levels of service under its respective subcontracts, the Company can give no assurances that a state or health plan will not terminate the Company's business relationships insofar as they pertain to these services.
Medicare Laws and Regulations. The Company has been pursuing Medicare Advantage plan licensure in several states. As a Medicare Advantage plan the company is subject to additional regulatory requirements and enhanced scrutiny of this product line. The Company believes that it is in compliance with these requirements.
Medicare Part C and D Laws and Regulations. The Company has submitted an application to become a Medicare Prescription Drug, Improvement, and Modernization Act of 2003 ("MMA") established a voluntary outpatientAdvantage Organization with Medicare prescription drug benefit for Medicare enrollees on an insured basis through Prescription Drug Plans,coverage ("PDPs"MA-PD Plan"), and by Medicare Advantage Plans ("Part D Activities"), in various regions across the United States. The MMA has been amended subsequently by several statutes, most notably the Medicare Improvements for Patients and Providers Act of 2008 (or "MIPPA"), and the federal Centers to serve dual eligible members (eligible for Medicare and Medicaid Services ("CMS") haveMedicaid) in Arizona beginning January 1, 2014. The CMS has issued significant interpretive regulations and guidance regarding MA-PD Plans to which, if approved, the Medicare Part D drug benefit program.Company will be directly subject. Among other things PDPs and Medicare Advantage PlansMA-PD plans are subject to requirements intended to deter fraud, waste and abuse and are monitored strictly by the federal CMSU.S Department of Health and Human Services and its contracted Medicare Drug Integrity Contractors ("MEDICs")vendors to ensure that Part DMedicare program funds are not spent inappropriately. In addition, if approved to provide Part C and D Services, the Company will be ultimately responsible to CMS for any of its subcontractors that may provide services under its agreement. The Company can give no assurance as to whether its MA-PD Plan application will be approved. However, the Company believes that it will be in compliance with these requirements if approval is obtained and business operations commence.
The Company is neither a PDP nor a Medicare Advantage Plan; however,Moreover, in relation to its existing specialty pharmacy business, the Company contracts with PDPs and Medicare Advantage Plans, ("PartMA-PD plans (collectively, "Part D Plans") to provide various services. In the Company's capacity as a subcontractor with certain Part D Plan clients, the Company is indirectly subject to certain federal rules, regulations, and sub-regulatory guidance pertaining to the operation of Medicare Part D. If CMS or a health plan customerPart D Plan determines that the Company has not performed satisfactorily as a subcontractor, CMS or the health plan customerPart D Plan may require the Company to cease its Part D activities or responsibilities under the subcontract. While the Company believes that it provides satisfactory levels of service under its respective subcontracts, the Company can give no assurances that CMS or a Part D Plan will not terminate the Company's business relationships insofar as they pertain to Medicare Part D.
CMS requires PDPs and Medicare AdvantagePart D Plans to report 100% of all price concessions received for PBM services. The applicable CMS guidance suggests that best practices would require
PDPs and Medicare Advantage Part D Plans to contractually require the right to audit their PBMs as well as require 100% transparency as to manufacturer rebates and administrative fees paid for drugs provided under the sponsor's plan, including the portion of such rebates retained by the PBM as part of the price concession for the PBM's services. Additionally, CMS requires Part D Plan sponsorsPlans to ensure through their contractual arrangements with first tier, downstream and related entities (which would include PBMs) that CMS has access to such entities' books and records pertaining to services performed in connection with Part D. The CMS regulations also suggests that Part D Plan sponsorsPlans should contractually require their first tier, downstream and related entities to comply with certain elements of the sponsor'sPart D Plan's compliance program. The Company has not experienced and
does not anticipate that such disclosure and auditing requirements, to the extent required by Medicare planits Part D Plan partners, will have a materially adverse effect on the Company's specialty pharmacy business.
CMS also requires that Part D plan sponsors, beginning in 2010, calculate beneficiary cost sharing based upon the price ultimately received by the pharmacy or other dispensing provider, rather than upon the price paid by the plan. Such calculation could potentially result in lower pharmacy claims reimbursement by Part D plan sponsors. In addition, CMS requires that any profit realized or loss incurred by a PBM through price negotiations with pharmacies or manufacturers be included as administrative costs to the plan rather than being factored into drug costs for reimbursement purposes.
Federal PBM Transparency Laws. On March 23, 2010 the President of the United States signed the Patient Protection and Affordable Care Act and on March 30, 2010 he signed the Health Care and Education Reconciliation Act of 2010 (hereinafter collectively referred to as "ACA"). Beginning in 2014, state and federally run health insurance exchanges authorized by ACA are generally expected to begin operation. The Company has not contracted to provide PBM services to any health insurance exchange products offered by insurers, but may do so in the future. If the Company chooses to directly participate in the exchanges, or offer services to plans that participate in the exchanges, it may be subject to certain financial transparency and disclosure requirements. The ACA mandates that pharmacy benefit managers provide financial transparency and reporting in connection with Medicare Part D plans, as well as plans offered through exchanges. In the event that the Company is determined to be subject to these requirements, the Company does not anticipate that such requirements will have a materially adverse effect on the Company's business.
FDA Regulation. The U.S. Food and Drug Administration ("FDA") generally has authority to regulate drug promotional activities that are performed "by or on behalf of" a drug manufacturer. The Company's business includes the provision of educational seminars for prescribers and other of the Company's customers on behalf of manufacturer clients and thus may be subject to the federal laws applicable to the promotion of prescription drugs. There can be no assurance that the FDA will not attempt to assert jurisdiction over certain aspects of the Company's specialty pharmacy business in the future and, although the Company is not controlled directly or indirectly by any drug manufacturer, the impact of future FDA regulation could materially adversely affect the Company's specialty pharmacy business, results of operations, financial condition or cash flows.
State Comprehensive PBM Regulation. States continue to introduce broad legislation to regulate pharmacy benefits management activities. Some of thisThis legislation could encompass certainencompasses some of the activities ofproducts offered by the specialty pharmacy business of the Company. In particular, some legislation seeks to imposeLegislation in this area is varied and encompasses licensing, audit provision, potential fiduciary duties, orpass through of cost savings and disclosure obligations on entities that provide certain types of pharmacy management services. Both Maineobligations. The regulatory environment is complicated by numerous lawsuits challenging laws and thelegislative repeals and amendments to PBM laws. The District of Columbia havehas enacted statutes designed to impose certain fiduciary obligations on entities providing PBM services. In 2008, Maryland has also implemented comprehensive PBM registration and examination legislation. Other states, including Mississippi, Louisiana, Connecticut, TennesseeGeorgia, Iowa, Kansas, Louisiana, North Dakota, South Dakota and Vermont have recently enacted laws regulating various pharmacy benefit management activities,all require PBMs to register with the state or be licensed. Furthermore, numerous states, including Arkansas, Florida, Indiana, Kentucky, Maryland, Mississippi, Missouri, New Mexico, North Dakota and similar legislation is pending in several more states. Such lawsTennessee subject PBMs to audit provisions and generally require certain financial disclosures. Such state laws do not appear to be having a material adverse effect on the Company's specialty pharmacy business. However, the Company can give no assurance that these and other states will not enact legislation with more adverse consequences in the near future; nor can the Company be certain that future regulations or interpretations of existing laws will not adversely affect its specialty pharmacy business.
State Legislation Affecting Plan or Benefit Design. Some states have enacted legislation that prohibits certain types of managed care plan sponsors from implementing certain restrictive formulary and network design features, and many states have legislation regulating various aspects of managed care plans, including provisions relating to pharmacy benefits. Other states mandate coverage of certain benefits or conditions and require health plan coverage of specific drugs, if deemed medically necessary
by the prescribing physician. Such legislation does not generally apply to the Company directly, but may apply to certain clients of the Company, such as HMOs and health insurers.
Legislation and Regulation Affecting Drug Prices. Specialty pharmaceutical manufacturers generally report various price metrics to the federal government, including "average sales price" ("ASP"), "average manufacturer price" ("AMP") and "best price" ("BP"). The Company does not calculate these price metrics, but the Company notes that the ASP, AMP and BP methodologies may create incentives for some drug manufacturers to reduce the levels of discounts or rebates available to purchasers, including the Company, or their clients with respect to specialty drugs. Any changes in the guidance affecting pharmaceutical manufacturer price metric calculations could materially adversely affect the Company's business.
Additionally, most of the Company's dispensing contracts with its customers use "average wholesale price" ("AWP") as a benchmark for establishing pricing. As partAt least one major third party publisher of settlementsAWP pricing data has ceased to publish such data in the consolidated casespast few years, and there can be no guarantee that AWP will continue to be an available pricing metric in the future. The discontinuance of New England Carpenters Health Benefit Fund, et. al. v. First Data Bank, et. al., Civil Action No. 1:05-CV-11148-PBS (D. Mass.) and District Council 37 Health and Security Plan, et al. v. Medi-Span, a division of Wolters Kluwer Health, Inc., Civil Action No. 07-10988-PBS (D. Mass.), First Data Bank and Medi-Span, two of several companies that reportAWP reporting by one data on prescription drug prices, have agreed to reduce the wholesale average cost ("WAC") to AWP mark up of certain pharmaceutical products. The reduction in WAC to AWP mark up has the effect of reducing the AWP. This settlementsource has not had a material adverse affect on the Company's results of operations.operations and the Company expects that were AWP data to no longer be available, other equitable pricing measures would be available to avoid a material adverse impact on the Company's business. Separately, CMS and several states have taken an interest in attempting to determine the "actual acquisition costs" of pharmacies. In 2012, CMS began conducting surveys and releasing preliminary data on pharmacy acquisition costs. At this time, the Company does not anticipate that actual acquisition cost surveys or pricing should materially adversely impact its operations, but it is too early to speculate what impact, if any such a reimbursement shift might have in pharmacy reimbursement and/or costs in the future..
Regulations Affecting the Company's Pharmacies. The Company owns two pharmacies that provide services to certain of the Company's health plan customers. The activities undertaken by the Company's pharmacies subject the pharmacies to state and federal statutes and regulations governing, among other things, the licensure and operation of mail order and non-resident pharmacies, repackaging of drug products, stocking of prescription drug products and dispensing of prescription drug products, including controlled substances. The Company's pharmacy facilities are located in Florida and New York and are duly licensed to conduct business in those states. Many states, however, require out-of-state mail order pharmacies to register with or be licensed by the state board of pharmacy or similar governing body when pharmaceuticals are delivered by mail into the state, and some states require that an out-of-state pharmacy employ a pharmacist that is licensed in the state into which pharmaceuticals are shipped. The Company holds mail order and non-resident pharmacy licenses where required. The Company also maintains Medicare and Medicaid provider licenses where required for the pharmacies to provide services to these plans.
Regulation of Controlled Substances. The Company's pharmacies must register with the United States Drug Enforcement Administration (the "DEA"), and individual state controlled substance authorities in order to dispense controlled substances. Federal law requires the Company to comply with the DEA's security, recordkeeping, inventory control, and labeling standards in order to dispense controlled substances. State controlled substance law requires registration and compliance with state pharmacy licensure, registration or permit standards promulgated by the state pharmacy licensing authority.
Some of the state regulatory requirements described above may be preempted in whole or in part by ERISA, which provides for comprehensive federal regulation of employee benefit plans. However, the scope of ERISA preemption is uncertain and is subject to conflicting court rulings. As a result, the Company could be subject to overlapping federal and state regulatory requirements in respect of
certain of its operations and may need to implement compliance programs that satisfy multiple regulatory regimes.
Other Regulation of Healthcare Providers. The Company's business is affected indirectly by regulations imposed upon healthcare providers. Regulations imposed upon healthcare providers include but are not limited to, provisions relating to the conduct of, and ethical considerations involved in, the practice of psychiatry, psychology, social work and related behavioral healthcare professions, radiology, pharmacy, accreditation, government healthcare program participation requirements, reimbursements
for patient services, Medicare and Medicaid fraud and abuse and, in certain cases, the common law duty to warn others of danger or to prevent patient self-injury. Changes in these regulatory requirements applicable to healthcare providers could impact the Company's business methods and practices and there can be no assurances that the impact would not be adverse and material.
Federal Regulations affecting Procurement. The Company also provides services to various state Medicaid programs. Services procurement is governed in part by federal regulations because the federal government provides a substantial amount of funding for the services. The Company's state customers risk loss of federal funding if the Company is not in compliance with federal regulations. The Company's non-compliance may also lead to unanticipated, negative financial consequences including corrective action plans or contract default risks. The Company believes the Company is in substantial compliance with various federal regulations and in compliance with contract provisions relating to the services provided by a commercial organization.
Other Proposed Legislation. In the last five years, legislation has periodically been introduced at the state and federal levels providing for new healthcare regulatory programs and materially revising existing healthcare regulatory programs (including, without limitation, legislation to carve out certain classes from generic substitution). Recently some states including Massachusetts, Vermont, Connecticut and California have enacted or considered legislation regarding various forms of mandatory or universal health insurance coverage. Such legislation could include both federal and state bills affecting Medicaid programs which may be pending in, or recently passed by, state legislatures and which are not yet available for review and analysis. In states in which such new state legislation has been enacted, there has been no material adverse impact on the Company. However, the Company at this time is unable to predict whether there may be any effect, positive or negative, on its business as a result of any such future legislation.
Health Care Reform. On March 23, 2010 the President signed the Patient Protection and Affordable Care Act and on March 30, 2010 he signed the Health Care and Education Reconciliation Act of 2010 (hereinafter collectively referred to as "ACA"). The ACA is a broad sweeping piece of legislation creating numerous changes in the healthcare regulatory environment. To date, numerous regulations implementing provisions of the ACA have been released in addition to many requests for information, frequently asked questions and other informational notices. Some of these regulations, most notably the Medical Loss Ratio regulations and the Internal Claims and Appeals and External Review Processes Regulations, have an impact on the Company and its business. Others, such as the regulation on dependent coverage to age 26 and coverage of preventative health services, could impact the nature of the members that we serve and the utilization rates. Recently released regulations on Medicaid expansion and the Health Insurance Exchanges are likely to impact the Company in the future. These regulations take effect in 2014. The Company is also closely monitoring ACA provisions related to taxes and fees to assess their impact to the Company. At this time we do not anticipate any material impact to the Company from these taxes and fees; however this is subject to change as further regulations and interpretive guidance are issued and if the Company contracts for new business that is subject to these fees. The Company believes that it is materially compliant with all applicable provisions of the ACA that are in effect at this time. The Company is closely monitoring legislative and regulatory activity as well as legal actions related to the ACA to identify potential business risks and opportunities. The Company at this time is unable to predict whether there may be any effect, positive or negative, on its business as a result of the ACA.
Employees of the Registrant
At December 31, 2011,2012, the Company had approximately 4,8005,030 full-time and part-time employees. The Company believes it has satisfactory relations with its employees.
History
Magellan was incorporated in 1969 under the laws of the State of Delaware. The Company is engaged in the specialty managed healthcare business. Through 2005, the Company predominantly operated in the managed behavioral healthcare business. As a result of certain acquisitions, the Company expanded into radiology benefits management and specialty pharmaceutical management during 2006, and into Medicaid administration during 2009.
Available Information
The Company makes its annual reports on Form 10-K, quarterly reports on Form 10-Q, current reports on Form 8-K, amendments to those reports filed or furnished pursuant to Section 13(a) or 15(d) of the Securities Exchange Act of 1934, and Section 16 filings available, free of charge, on the Company's website atwww.magellanhealth.com as soon as practicable after the Company has electronically filed such material with, or furnished it to, the Securities and Exchange Commission ("SEC").SEC. The information on the Company's website is not part of or incorporated by reference in this report on Form 10-K.
Reliance on Customer Contracts—The Company's inability to renew, extend or replace expiring or terminated contracts could adversely affect the Company's liquidity, profitability and financial condition.
Substantially all of the Company's net revenue is derived from contracts that may be terminated immediately with cause and many, including some of the Company's most significant contracts, are terminable without cause by the customer upon notice and the passage of a specified period of time (typically between 60 and 180 days), or upon the occurrence of certain other specified events. The Company's ten largest customers accounted for 66.0 percent, 66.6 percent and 66.665.0 percent of the Company's net revenue in the years ended December 31, 2010, 2011 and 2011,2012, respectively. Loss of all of these contracts or customers would, and loss of any one of these contracts or customers could, materially reduce the Company's net revenue and have a material adverse effect on the Company's liquidity, profitability and financial condition.
Significant Customers
Consolidated Company
The Maricopa Contract generated net revenues that exceeded, in the aggregate, ten percent of net revenues for the consolidated Company for the years ended December 31, 2009, 2010, 2011 and 2011. Pursuant to the Maricopa Contract, the Company provides behavioral healthcare management and other related services to approximately 715,000 members in Maricopa County, Arizona.2012. Under the Maricopa Contract, the Company is responsible for providing covered behavioral health services to persons eligible under Title XIX (Medicaid) and Title XXI (State Children's Health Insurance Program) of the Social Security Act, non-Title XIX and non-Title XXI eligible children and adults with a serious mental illness,SMI, and to certain non-Title XIX and non-Title XXI adults with behavioral health or substance abuse disorders. The Maricopa Contract began on September 1, 2007 and extends through September 30, 2013 unless sooner terminated by the parties. The State of Arizona has the right to terminate the Maricopa Contract for cause, as defined, upon ten days' notice with an opportunity to cure, and without cause immediately upon notice from the State. The Maricopa Contract generated net revenues of $807.1 million, $779.5 million and $779.5$758.3 million for the years ended December 31, 2010, 2011 and 2011,2012, respectively.
On October 4, 2012, the ADHS released a RFP for the ADHS Regional Behavioral Health Authority—GSA 6 (Maricopa County). The start date for any contract awarded pursuant to the RFP is expected to be October 1, 2013. This is a single RFP with two components: (i) the RFP maintains the current behavioral health carve-out for the lives the Company currently serves under the Maricopa Contract; (ii) the RFP also introduces a fully integrated program of physical, behavioral, and pharmacy care for approximately 14,000 individuals with SMI, both Medicaid and dual eligible. Under the current Maricopa Contract, these 14,000 individuals are receiving behavioral health and behavioral health pharmacy benefits. MCCAZ has responded to the RFP. There can be no assurance that MCCAZ will be awarded a contract pursuant to the RFP; or that the terms of any contract awarded pursuant to the RFP will be similar to the current Maricopa Contract.
One of the Company's top ten customers during 2010 was WellPoint, Inc. The Company recorded net revenue from contracts with WellPoint, Inc. of $175.7 million for the year ended December 31, 2010. The Company's contracts with WellPoint, Inc. terminated on December 31, 2010.
By Segment
In addition to the Maricopa Contract previously discussed, the following customers generated in excess of ten percent of net revenues for the respective segment for the years ended December 31, 2010, 2011 and 20112012 (in thousands):
Segment | Term Date | 2010 | 2011 | Term Date | 2010 | 2011 | 2012 | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Commercial | Commercial | ||||||||||||||||||||
Customer A | December 31, 2012 | $ | 243,399 | $ | 171,109 | December 31, 2013(2) | $ | 243,399 | $ | 171,109 | $ | 192,415 | |||||||||
Customer B | June 30, 2014 | 71,338 | 67,049 | June 30, 2014 | 71,338 | 67,049 | 67,959 | * | |||||||||||||
Customer C | December 31, 2012 to December 14, 2013(1) | 65,175 | * | 111,607 | December 31, 2012 to December 14, 2013(1)(3) | 65,175 | * | 111,607 | 118,351 | ||||||||||||
Customer D | December 31, 2019 | — | — | 134,885 | |||||||||||||||||
Public Sector | Public Sector | ||||||||||||||||||||
Customer D | June 30, 2012(2) | 153,650 | 191,063 | ||||||||||||||||||
Customer E | June 30, 2013(4) | 153,650 | 191,063 | 240,224 | |||||||||||||||||
Radiology Benefits Management | Radiology Benefits Management | Radiology Benefits Management | |||||||||||||||||||
WellPoint, Inc. | December 31, 2010(3) | 159,644 | — | ||||||||||||||||||
Customer E | November 30, 2012 to April 30, 2013(1) | 121,401 | 134,257 | ||||||||||||||||||
Customer F | June 30, 2011 to November 30, 2011(1)(3) | 66,970 | 38,297 | December 31, 2015 | 121,401 | 134,257 | 117,739 | ||||||||||||||
Customer G | June 30, 2014 | 51,877 | 55,197 | June 30, 2011 to November 30, 2011(1)(5) | 66,970 | 38,297 | — | ||||||||||||||
Customer H | March 31, 2013 | 10,448 | * | 36,293 | June 30, 2014 | 51,877 | 55,197 | 60,094 | |||||||||||||
Specialty Pharmaceutical Management | |||||||||||||||||||||
Customer I | March 31, 2012 to January 1, 2013(1) | 86,850 | 90,563 | July 31, 2015 | 10,448 | * | 36,293 | 57,455 | |||||||||||||
Customer J | April 29, 2012 to September 1, 2012(1) | 57,198 | 56,115 | January 31, 2014 | 935 | * | 32,342 | * | 38,366 | ||||||||||||
Customer E | February 1, 2012 to April 30, 2013(1) | 32,877 | 25,006 | * | |||||||||||||||||
Medicaid Administration | |||||||||||||||||||||
WellPoint, Inc. | December 31, 2010(5) | 159,644 | — | — | |||||||||||||||||
Specialty Pharmaceutical Management | Specialty Pharmaceutical Management | ||||||||||||||||||||
Customer K | December 4, 2011(3) | 31,145 | 28,060 | November 30, 2013 to December 31, 2013(1) | 86,850 | 90,563 | 129,209 | ||||||||||||||
Customer L | September 30, 2013(4) | 26,108 | 82,770 | April 29, 2013 to September 1, 2013(1) | 57,198 | 56,115 | 60,350 | ||||||||||||||
Customer B | September 27, 2013 to December 31, 2013(1) | 11,523 | * | 22,899 | * | 73,785 | |||||||||||||||
Customer F | September 30, 2013 to December 31, 2014(1) | 32,877 | 25,006 | * | 19,787 | * | |||||||||||||||
Medicaid Administration | Medicaid Administration | ||||||||||||||||||||
Customer M | March 16, 2012 to June 30, 2017(1) | 24,432 | 23,683 | December 4, 2011(5) | 31,145 | 28,060 | — | ||||||||||||||
Customer N | June 30, 2012 to June 30, 2013(1) | 22,000 | 18,924 | * | September 30, 2013(6) | 26,108 | 82,770 | 69,090 | |||||||||||||
Customer O | June 30, 2013 to September 30, 2014(1) | 16,249 | * | 22,084 | March 31, 2015 to June 30, 2017(1) | 24,432 | 23,683 | 25,103 | |||||||||||||
Customer P | June 30, 2013 to June 30, 2016(1) | 16,249 | * | 22,084 | 19,518 | ||||||||||||||||
Customer Q | June 30, 2013 to September 30, 2013(1) | 22,000 | 18,924 | * | 13,828 | * | |||||||||||||||
Concentration of Business
The Company also has a significant concentration of business with various counties in the State of Pennsylvania (the "Pennsylvania Counties") which are part of the Pennsylvania Medicaid program, and with various areas in the State of Florida (the "Florida Areas") which are part of the Florida Medicaid program. Net revenues from the Pennsylvania Counties in the aggregate totaled $315.5$334.8 million,
$334.8 $351.6 million and $351.6$354.1 million for the years ended December 31, 2009, 2010, 2011 and 2011,2012, respectively. Net revenues from the Florida Areas in the aggregate totaled $130.9 million, $140.5 million, $131.8 million and $131.8$133.9 million for the years ended December 31, 2009, 2010, 2011 and 2011,2012, respectively.
Integration of Companies Acquired by Magellan—The Company's profitability could be adversely affected if the integration of companies acquired by Magellan is not completed in a timely and effective manner.
One of the Company's growth strategies is to make strategic acquisitions which are complementary to its existing operations. After Magellan closes on an acquisition, it must integrate the acquired company into Magellan's policies, procedures and systems. Failure to effectively integrate an acquired business or the failure of the acquired business to perform as anticipated could result in excessive costs being incurred, a delay in obtaining targeted synergies, decreased customer performance (which could result in contract penalties and/or terminations), increased employee turnover, and lost sales opportunities. Finally, difficulties assimilating acquired operations and services could result in the diversion of capital and management's attention away from other business issues and opportunities.
Changes in the Medical Managed Care Carve-Out Industry—Certain changes in the business practices of this industry could negatively impact the Company's resources, profitability and results of operations.
Substantially all of the Company's Commercial, Radiology Benefits Management and Specialty Pharmaceutical Management segments' net revenues are derived from customers in the medical managed healthcare industry, including managed care companies, health insurers and other health plans. Some types of changes in this industry's business practices could negatively impact the Company. For example, if the Company's managed care customers seek to provide services directly to their subscribers, instead of contracting with the Company for such services, the Company could be adversely affected. In this regard, certain of the Company's major customers in the past have not renewed all or part of their contracts with the Company, and instead provided managed healthcare services directly to their subscribers. Other of the Company's customers that are managed care companies could also seek to provide services directly to their subscribers, rather than by contracting with the Company for such services. In addition, the Company has a significant number of contracts with Blue Cross Blue Shield plans and other regional health plans. Consolidation of the healthcare industry through acquisitions and mergers could potentially result in the loss of contracts for the Company. Any of these changes could reduce the Company's net revenue, and adversely affect the Company's profitability and financial condition.
Changes in the Contracting Model for Medicaid Contracts—Certain changes in the contracting model used by states for managed healthcare services contracts relating to Medicaid lives could negatively impact the Company's resources, profitability and results of operations.
Substantially all of the Company's Public Sector segment net revenue is derived from direct contracts that it has with state or county governments for the provision of services to Medicaid enrollees. Certain states have recently contracted with managed care companies to manage both the behavioral and physical medical care of itstheir Medicaid enrollees. If other governmental entities change the method for contracting for Medicaid business to a fully integrated model, the Company will attempt to subcontract with the managed care organizations to provide behavioral healthcare
management for such Medicaid business; however, there is no assurance that the Company would be able to secure such arrangements. Accordingly, if such a change in the contracting model were to occur, it is possible that the Company could lose current contracted revenues, as well as be unable to bid on potential new business opportunities, thus negatively impacting the Company's profitability and financial condition.
Risk-Based Products—Because the Company provides services at a fixed fee, if the Company is unable to maintain historical margins, or is unable to accurately predict and control healthcare costs, the Company's profitability could decline.
The Company derives its net revenue primarily from arrangements under which the Company assumes responsibility for costs of treatment in exchange for a fixed fee. The Company refers to such arrangements as "risk-based contracts" or "risk-based products," which include EAP services. These arrangements provided 79.8 percent, 79.1 percent and 79.178.3 percent of the Company's net revenue in the years ended December 31, 2010, 2011 and 2011,2012, respectively.
The profitability of the Company's risk contracts could be reduced if the Company is unable to maintain its historical margins. The competitive environment for the Company's risk products could result in pricing pressures which cause the Company to reduce its rates. In addition, customer demands or expectations as to margin levels could cause the Company to reduce its rates. A reduction in risk rates which are not accompanied by a reduction in services covered or expected underlying care trend could result in a decrease in the Company's operating margins.
Profitability of the Company's risk contracts could also be reduced if the Company is unable to accurately estimate the rate of service utilization by members or the cost of such services when the Company prices its services. The Company's assumptions of utilization and costs when the Company prices its services may not ultimately reflect actual utilization rates and costs, many aspects of which are beyond the Company's control. If the cost of services provided to members under a contract together with the administrative costs exceeds the aggregate fees received by the Company under such contract, the Company will incur a loss on the contract.
The Company's profitability could also be reduced if the Company is required to make adjustments to estimates made in reporting historical financial results regarding cost of care, reflected in the Company's financial statements as medical claims payable. Medical claims payable includes reserves for incurred but not reported ("IBNR") claims, which are claims for covered services rendered by the Company's providers which have not yet been submitted to the Company for payment. The Company estimates and reserves for IBNR claims based on past claims payment experience, including the average interval between the date services are rendered and the date the claims are received and between the date services are rendered and the date claims are paid, enrollment data, utilization statistics, adjudication decisions, authorized healthcare services and other factors. This data is incorporated into contract-specific reserve models. The estimates for submitted claims and IBNR claims are made on an accrual basis and adjusted in future periods as required. If such risk-based products are not correctly underwritten, the Company's profitability and financial condition could be adversely affected.
Factors that affect the Company's ability to price the Company's services, or accurately make estimates of IBNR claims and other expenses for which the Company creates reserves may include differences between the Company's assumptions and actual results arising from, among other things:
Some of these factors could impact the ability of the Company to manage and control the medical costs to the extent assumed in the pricing of its services.
If the Company's membership in risk-based business continues to grow (which is a major focus of the Company's strategy), the Company's exposure to potential losses from risk-based products will also increase.
Expansion of Risk-Based Products—Because the Company intends to expand into clinically integrated management of special populations eligible for Medicaid and Medicare including individuals with SMI, and other unique high-cost populations, if the Company is unable to accurately underwrite the healthcare cost risk for this new business and control associated costs, the Company's profitability could decline.
The Company believes that it can leverage its information systems, call center, claims and network infrastructure as well as its financial strength and underwriting expertise to facilitate the development of risk product offerings to states that include behavioral health care and physical medical care for their special Medicaid and dual eligible populations, particularly individuals with SMI. As this represents a new business for the Company, the Company will incur start-up costs to develop and grow this business. The Company's profitability may be negatively impacted until such time that sufficient business is generated to offset these start-up costs.
Furthermore, since this is a new business for the Company, there is an increased risk associated with the underwriting and implementation for this business. Profitability of any such business could be adversely affected if the Company is unable to accurately estimate the rate of service utilization or the cost of such services when the Company prices its services. The Company's assumptions of utilization and costs when the Company prices its services may not ultimately reflect actual utilization rates and costs, many aspects of which are beyond the Company's control. If the cost of services provided to members under a contract together with the administrative costs exceeds the aggregate fees received by the Company under such contract, the Company will incur a loss on the contract.
In addition, the Company has entered into joint ventures in Arizona and Massachusetts to offer integrated healthcare in these states. The Company may also partner with managed care organizations to create joint ventures in other states. Conflicts or disagreements between the Company and any joint venture partner may negatively impact the benefits to be achieved by the relevant joint venture or may ultimately threaten the ability of any such joint venture to continue. The Company is also subject to additional risks and uncertainties because the Company may be dependent upon, and subject to, liability, losses or reputational damage relating to systems, controls and personnel that are not entirely under the Company's control.
Provider Agreements—Failure to maintain or to secure cost-effective health care provider contracts may result in a loss of membership or higher medical costs.
The Company's profitability depends, to an extent, upon the ability to contract favorably with certain healthcare providers. The Company may be unable to enter into agreements with providers in new markets on a timely basis or under favorable terms. If the Company is unable to retain its current provider contracts or enter into new provider contracts timely or on favorable terms, the Company's profitability could be reduced. The Company cannot provide any assurance that it will be able to continue to renew its existing provider contracts or enter into new contracts.
Fluctuation in Operating Results—The Company experiences fluctuations in quarterly operating results and, as a consequence, the Company may fail to meet or exceed market expectations, which could cause the Company's stock price to decline.
The Company's quarterly operating results have varied in the past and may fluctuate significantly in the future due to seasonal and other factors, including:
These factors may affect the Company's quarterly and annual net revenue, expenses and profitability in the future and, accordingly, the Company may fail to meet market expectations, which could cause the Company's stock price to decline.
Dependence on Government Spending—The Company can be adversely affected by changes in federal, state and local healthcare policies, programs, funding and enrollments.
All of the Company's Public Sector and Medicaid Administration segment net revenue, and a portion of the Company's net revenue in the Company's other three operating segments are derived, directly or indirectly, from governmental agencies, including state Medicaid programs. Contract rates vary from state to state, are subject to periodic negotiation and may limit the Company's ability to maintain or increase rates. The Company is unable to predict the impact on the Company's operations of future regulations or legislation affecting Medicaid programs, or the healthcare industry in general, and future regulations or legislation may have a material adverse effect on the Company. Moreover, any reduction in government spending for such programs could also have a material adverse effect on the Company (See "Reliance on Customer Contracts"). In addition, the Company's contracts with federal, state and local governmental agencies, under both direct contract and subcontract arrangements, generally are conditioned upon financial appropriations by one or more governmental agencies, especially in the case of state Medicaid programs. These contracts generally can be terminated or modified by the customer if such appropriations are not made. The Company faces increased risks in this regard as state budgets have come under increasing pressure due to the recent economic downturn. Finally, some of the Company's contracts with federal, state and local governmental agencies, under both direct contract and subcontract arrangements, require the Company to perform additional services if federal, state or local laws or regulations imposed after the contract is
local laws or regulations imposed after the contract is signed so require, in exchange for additional compensation, to be negotiated by the parties in good faith. Government and other third-party payors generally seek to impose lower contract rates and to renegotiate reduced contract rates with service providers in a trend toward cost control.
Restrictive Covenants in the Company's Debt Instruments—Restrictions imposed by the Company's debt agreements limit the Company's operating and financial flexibility. These restrictions may adversely affect the Company's ability to finance the Company's future operations or capital needs or engage in other business activities that may be in the Company's interest.
On December 9, 2011, the Company entered into a Senior Secured Revolving Credit Facility Credit Agreement with Citibank, N.A., Wells Fargo Bank, N.A., Bank of America, N.A., and U.S. Bank, N.A. that provides for up to $230.0 million of revolving loans with a sublimit of up to $70.0 million for the issuance of letters of credit for the account of the Company (the "2011 Credit Facility"), which contains a number of covenants. The 2011 Credit Facility will mature on December 9, 2014.
These covenants limit Company management's discretion in operating the Company's business by restricting or limiting the Company's ability, among other things, to:
These restrictions could adversely affect the Company's ability to finance future operations or capital needs or engage in other business activities that may be in the Company's interest. The 2011 Credit Facility also requires the Company to comply with specified financial ratios and tests. Failure to do so, unless waived by the lenders under the 2011 Credit Facility, pursuant to its terms, would result in an event of default under the 2011 Credit Facility. The 2011 Credit Facility is guaranteed by most of the Company's subsidiaries and is secured by most of the Company's assets and the Company's subsidiaries' assets.
Required Assurances of Financial Resources—The Company's liquidity, financial condition, prospects and profitability can be adversely affected by present or future state regulations and contractual requirements that the Company provide financial assurance of the Company's ability to meet the Company's obligations.
Some of the Company's contracts and certain state regulations require the Company or certain of the Company's subsidiaries to maintain specified cash reserves or letters of credit and/or to maintain certain minimum tangible net equity in certain of the Company's subsidiaries as assurance that the Company has financial resources to meet the Company's contractual obligations. Many of these state regulations also restrict the investment activity of certain of the Company's subsidiaries. Some state regulations also restrict the ability of certain of the Company's subsidiaries to pay dividends to
Magellan. Additional state regulations could be promulgated that would increase the cash or other
security the Company would be required to maintain. In addition, the Company's customers may require additional restricted cash or other security with respect to the Company's obligations under the Company's contracts, including the Company's obligation to pay IBNR claims and other medical claims not yet processed and paid. In addition, certain of the Company's contracts and state regulations limit the profits that the Company may earn on risk-based business. The Company's liquidity, financial condition, prospects and profitability could be adversely affected by the effects of such regulations and contractual provisions. See Note 2—"Summary of Significant Accounting Policies—Restricted Assets" to the consolidated financial statements set forth elsewhere herein for a discussion of the Company's restricted assets.
Competition—The competitive environment in the specialty managed healthcare industry may limit the Company's ability to maintain or increase the Company's rates, which would limit or adversely affect the Company's profitability, and any failure in the Company's ability to respond adequately may adversely affect the Company's ability to maintain contracts or obtain new contracts.
The Company's business is highly competitive. The Company competes with other healthcare organizations as well as with insurance companies, including HMOs, PPOs, TPAs, IPAs, multi-disciplinary medical groups, PBMs, specialty pharmacy companies, radiology benefits management companies and other specialty healthcare and managed care companies. Many of the Company's competitors, particularly certain insurance companies, HMOs and PBMs are significantly larger and have greater financial, marketing and other resources than the Company, which can create downward pressure on prices through economies of scale. The entrance or expansion of these larger companies in the specialty managed healthcare industry (including the Company's customers who have in-sourced or who may choose to in-source healthcare services) could increase the competitive pressures the Company faces and could limit the Company's ability to maintain or increase the Company's rates. If this happens, the Company's profitability could be adversely affected. In addition, if the Company does not adequately respond to these competitive pressures, it could cause the Company to not be able to maintain its current contracts or to not be able to obtain new contracts.
Possible Impact of Federal Healthcare Reform Law—can significantly impact the Company's revenues or profitability.
In March 2010 the Patient Protection and Affordable Care Act and the Health Care Education and Reconciliation Act of 2010 (hereinafter collectively referred to as "ACA") were passed. The ACA is a comprehensive piece of legislation intended to make significant changes to the healthcare system in the United States. The ACA contains various effective dates extending through 2020. Numerous regulations have been promulgated related to the ACA with hundreds more expected in the future.
Significant provisions in the ACA include requiring individuals to purchase health insurance, minimum medical loss ratios for health insurance issuers, significant changes to the Medicare and Medicaid programs and many other changes that affect healthcare insurance and managed care. See "Regulation" above for more information. In addition, dozens of lawsuits have been filed in the courts challenging the constitutionality of the legislation. Therefore, it is uncertain at this time what the financial impact of healthcare reform will be to the Company. The Company cannot predict the effect of this legislation or other legislation that may be adopted by the United States Congress or by the states, and such legislation, if implemented, could have an adverse effect on the Company.
Possible Impact of Federal Mental Health Parity—can significantly impact the Company's revenues or profitability.
In October 2008, the United States Congress passed legislationthe Paul Wellstone and Pete Dominici Mental Health Parity Act of 2008 ("MHPAEA") establishing parity in financial requirements (e.g. co-pays, deductibles, etc.) and treatment limitations (e.g., limits on the number of visits) between mental health and substance abuse benefits and medical/surgical benefits for members.
and substance abuse benefits and medical/surgical benefits for health plan members. This new law does not require coverage for mental health or substance abuse disorders but if coverage is provided it must be provided at parity. No specific disorders are mandated for coverage; health plans are able to define mental health and substance abuse to determine what they are going to cover. State mandated benefits laws are not preempted. The law applies to ERISA plans, Medicaid managed care plans and SCHIPState Children's Health Insurance Program ("SCHIP") plans. There is an exemption for small employers. Interim final regulations ("IFR") were issued onOn February 2, 2010, final regulations have not yet been publishedthe Department of the Treasury, the Department of Labor and interpretive guidance from the regulators has been limited to date.Department of Health and Human Services issued Interim Final Rules interpreting the MHPAEA ("IFR"). The IFR applies to ERISA plans and insured business;business. A State Medicaid Director Letter was issued in January 2013 discussing applicability of the IFR currently does not apply to Medicaid managed care plans, or SCHIP plans although itand Alternative Benefit (Benchmark) Plans. It is anticipatedpossible that similar regulatory requirementssome states will change their behavioral health plan benefits or management techniques as a result of this letter. The Health Insurance Exchange regulations provide that plans offered on the exchange must offer behavioral health benefits that are compliant with federal parity law. Further clarification on this requirement is expected to be imposed on that business in the future.issued. The IFR included some concepts not included under the statute including the requirement to conduct the parity review at the category level within the plan, introducing the concept of nonquantitativenon-quantitative treatment limitations, and prohibiting separate but equal deductibles. While some of these regulatory requirements were not anticipated, the Company believes it is in compliance with the requirements of the IFR and that there is no material impact to the Company related to compliance. No assurance can be given that additional interpretive guidance on the legislation and IFR or the release of a final rule will not have a material adverse effect on the Company. However, the Company's risk behavioral contracts generallydo allow for re-pricingrepricing to occur ineffective the eventsame date that any legislation or regulation results inbecomes effective if that legislation is projected to have a material effect on cost of care.
Government Regulation—The Company is subject to substantial government regulation and scrutiny, which increase the Company's costs of doing business and could adversely affect the Company's profitability.
The specialty managed healthcare industry and the provision of specialty managed healthcare are subject to extensive and evolving federal and state regulation. Such laws and regulations cover, but are not limited to, matters such as licensure, accreditation, government healthcare program participation requirements, information privacy and security, reimbursement for patient services, and Medicare and Medicaid fraud and abuse. The Company's specialty pharmaceutical management business is also the subject of substantial federal and state governmental regulation and scrutiny. Government investigations and allegations have become more frequent concerning possible violations of fraud and abuse and false claims statutes and regulations by healthcare organizations. Violators may be excluded from participating in government healthcare programs, subject to fines or penalties or required to repay amounts received from the government for previously billed services. A violation of such laws and regulations may have a material adverse effect on the Company.
The Company is subject to certain state laws and regulations and federal laws as a result of the Company's role in management of customers' employee benefit plans.
Regulatory issues may also affect the Company's operations including, but not limited to:
The imposition of additional licensing and other regulatory requirements may, among other things, increase the Company's equity requirements, increase the cost of doing business or force significant changes in the Company's operations to comply with these requirements.
The costs associated with compliance with government regulation as discussed above may adversely affect the Company's financial condition and results of operation.
The Company faces risks related to unauthorized disclosure of sensitive or confidential member and other information.
As part of its normal operations, the Company collects, processes and retains confidential member information making the Company subject to various federal and state laws and rules regarding the use and disclosure of confidential member information, including HIPAA. The Company also maintains other confidential information related to its business and operations. Despite appropriate security measures, the Company may be vulnerable to security breaches, acts of vandalism, computer viruses, misplaced or lost data, programming and/or human errors or other similar events. Noncompliance with any privacy or security laws and regulations or any security breach, whether by the Company or by its vendors, could result in enforcement actions, material fines and penalties and could also subject the Company to litigation.
The Company faces additional regulatory risks associated with its Specialty Pharmaceutical Management segment which could subject it to additional regulatory scrutiny and liability and which could adversely affect the profitability of the Specialty Pharmaceutical Management segment in the future.
Various aspects of the Company's Specialty Pharmaceutical Management segment are governed by federal and state laws and regulations. Specialty Pharmaceutical Servicespharmaceutical services are provided by the Company to Medicaid and Medicare plans as well as commercial insurance plans. There has been enhanced scrutiny on federal programs and the Company must remain vigilant in ensuring compliance with the requirements of these programs. In addition there are provisions of the ACA which may impact the Company's pharmaceutical business. Significant sanctions may be imposed for violations of these laws and compliance programs are a significant operational requirement of the Company's business. There are significant uncertainties involving the application of many of these legal requirements to the Company. Accordingly, the Company may be required to incur additional administrative and compliance expenses in determining the applicable requirements and in adapting its compliance practices, or modifying its business practices, in order to satisfy changing interpretations and regulatory policies. In addition, there are numerous proposed healthcare laws and regulations at the federal and state levels, many of which, if adopted, could adversely affect the Company's business. See "Regulation" above.
Risks Related To Realization of Goodwill and Intangible Assets—The Company's profitability could be adversely affected if the value of intangible assets is not fully realized.
The Company's total assets at December 31, 20112012 reflect goodwill of approximately $426.9 million, representing approximately 31.828.2 percent of total assets. The Company completed its annual impairment analysis of goodwill as of October 1, 20112012 noting that no impairment was identified.
At December 31, 2011,2012, identifiable intangible assets (customer lists, contracts and provider networks) totaled approximately $44.6$34.9 million. Intangible assets are amortized over their estimated useful lives, which range from approximately three to eighteen years. The amortization periods used may differ from those used by other entities. In addition, the Company may be required to shorten the amortization period for intangible assets in future periods based on changes in the Company's business. There can be no assurance that such goodwill or intangible assets will be realizable.
The Company evaluates, on a regular basis, whether for any reason the carrying value of the Company's intangible assets and other long-lived assets may no longer be completely recoverable, in which case a charge to earnings for impairment losses could become necessary. When events or changes in circumstances occur that indicate the carrying amount of long-lived assets may not be recoverable, the Company assesses the recoverability of long-lived assets other than goodwill by determining whether the carrying value of such intangible assets will be recovered through the future cash flows expected from the use of the asset and its eventual disposition.
Any event or change in circumstances leading to a future determination requiring write-off of a significant portion of unamortized intangible assets or goodwill would adversely affect the Company's profitability.
Claims for Professional Liability—Pending or future actions or claims for professional liability (including any associated judgments, settlements, legal fees and other costs) could require the Company to make significant cash expenditures and consume significant management time and resources, which could have a material adverse effect on the Company's profitability and financial condition.
Management and administration of the delivery of specialty managed healthcare, and the operation of specialty pharmacies and specialty pharmacy drug dispensing, entail significant risks of liability. In recent years, participants in the healthcare industry generally, as well as the specialty managed healthcare industry, have become subject to an increasing number of lawsuits. From time to time, the Company is subject to various actions and claims of professional liability alleging negligence in performing utilization review and other specialty managed healthcare activities, as well as for the acts or omissions of the Company's employees, including employed physicians and other clinicians, network providers, pharmacists, or others. In the normal course of business, the Company receives reports relating to deaths and other serious incidents involving patients whose care is being managed by the Company. Such incidents occasionally give rise to malpractice, professional negligence and other related actions and claims against the Company, the Company's employees, or the Company's network providers. The Company is also subject to actions and claims for the costs of services for which payment was denied. Many of these actions and claims seek substantial damages and require the Company to incur significant fees and costs related to the Company's defense and consume significant management time and resources. While the Company maintains professional liability insurance, there can be no assurance that future actions or claims for professional liability (including any judgments, settlements or costs associated therewith) will not have a material adverse effect on the Company's profitability and financial condition.
Professional Liability and Other Insurance—Claims brought against the Company that exceed the scope of the Company's liability coverage or denial of coverage could materially and adversely affect the Company's profitability and financial condition.
The Company maintains a program of insurance coverage against a broad range of risks in the Company's business. As part of this program of insurance, the Company carries professional liability insurance, subject to certain deductibles and self-insured retentions. The Company also is sometimes required by customer contracts to post surety bonds with respect to the Company's potential liability on professional responsibility claims that may be asserted in connection with services the Company
provides. As of December 31, 2011,2012, the Company had approximately $103.3$114.6 million of such bonds outstanding. The Company's insurance may not be sufficient to cover any judgments, settlements or costs relating to present or future claims, suits or complaints. Upon expiration of the Company's insurance policies, sufficient insurance may not be available on favorable terms, if at all. To the extent the Company's customers are entitled to indemnification under their contracts with the Company relating to liabilities they incur arising from the operation of the Company's programs, such indemnification may not be covered under the Company's insurance policies. To the extent that certain actions and claims seek punitive and compensatory damages arising from the Company's alleged intentional misconduct, such damages, if awarded, may not be covered, in whole or in part, by the Company's insurance policies. If the Company is unable to secure adequate insurance in the future, or if the insurance the Company carries is not sufficient to cover any judgments, settlements or costs relating to any present or future actions or claims, such judgments, settlements or costs may have a material adverse effect on the Company's profitability and financial condition. If the Company is unable to obtain needed surety bonds in adequate amounts or make alternative arrangements to satisfy
the requirements for such bonds, the Company may no longer be able to operate in those states, which would have a material adverse effect on the Company.
Class Action Suits and Other Legal Proceedings—The Company is subject to class action and other lawsuits that could result in material liabilities to the Company or cause the Company to incur material costs, to change the Company's operating procedures in ways that increase costs or to comply with additional regulatory requirements.
Managed healthcare companies and PBM companies have been targeted as defendants in national class action lawsuits regarding their business practices. The Company has in the past been subject to such national class actions as defendants and is also subject to or a party to other class actions, lawsuits and legal proceedings in conducting the Company's business. In addition, certain of the Company's customers are parties to pending class action lawsuits regarding the customers' business practices for which the customers could seek indemnification from the Company. These lawsuits may take years to resolve and cause the Company to incur substantial litigation expense, and the outcomes could have a material adverse effect on the Company's profitability and financial condition. In addition to potential damage awards, depending upon the outcomes of such cases, these lawsuits may cause or force changes in practices of the Company's industry and may also cause additional regulation of the industry through new federal or state laws or new applications of existing laws or regulations. Such changes could increase the Company's operating costs.
Negative Publicity—The Company may be subject to negative publicity which may adversely affect the Company's business, financial position, results of operations or cash flows.
From time to time, the managed care industry has received negative publicity. This publicity has led to increased legislation, regulation, review of industry practices and private litigation in the commercial sector. These factors may adversely affect the Company's ability to market our services, require the Company to change its services, or increase the overall regulatory burden under which the Company operates. Any of these factors may increase the costs of doing business and adversely affect the Company's business, financial position, results of operations or cash flows.
Government Investigations—The Company may be subjected to additional regulatory requirements and to investigations or regulatory action by governmental agencies, each of which may have a material adverse effect on the Company's business, financial condition and results of operations.
From time to time, the Company receives notifications from and engages in discussions with various government agencies concerning the Company's businesses and operations. As a result of these contacts with regulators, the Company may, as appropriate, be required to implement changes to the
Company's operations, revise the Company's filings with such agencies and/or seek additional licenses to conduct the Company's business. The Company's inability to comply with the various regulatory requirements may have a material adverse effect on the Company's business.
In addition, the Company may become subject to regulatory investigations relating to the Company's business, which may result in litigation or regulatory action. A subsequent legal liability or a significant regulatory action against the Company could have a material adverse effect on the Company's business, financial condition and results of operations. Moreover, even if the Company ultimately prevails in the litigation, regulatory action or investigation, such litigation, regulatory action or investigation could have a material adverse effect on the Company's business, financial condition and results of operations.
Investment Portfolio—The value of the Company's investments is influenced by varying economic and market conditions, and a decrease in value may result in a loss charged to income.
All of the Company's investments are classified as "available-for-sale" and are carried at fair value. The Company's available-for-sale investment securities were $200.9$233.7 million and represented 15.015.5 percent of the Company's total consolidated assets at December 31, 2011.2012.
The current economic environment and recent volatility of securities markets increase the difficulty of assessing investment impairment and the same influences tend to increase the risk of potential impairment of these assets. The Company believes it has adequately reviewed its investment securities for impairment and that its investment securities are carried at fair value. However, over time, the economic and market environment may provide additional insight regarding the fair value of certain securities, which could change the Company's judgment regarding impairment. This could result in
realized losses relating to other-than-temporary declines being charged against future income. Given the current market conditions and the significant judgments involved, there is a risk that declines in fair value may occur and material other-than-temporary impairments may be charged to income in future periods, resulting in realized losses. In addition, if it became necessary for the Company to liquidate its investment portfolio on an accelerated basis, it could have an adverse effect on the Company's results of operations.
Adverse Economic Conditions—The state of the national economy and adverse changes in economic conditions could adversely affect the Company's business and results of operations.
The state of the economy has negatively affected state budgets and could adversely affect the Company's reimbursement from state Medicaid programs in its Medicaid Administration and Public Sector segments. The state of the economy and adverse economic conditions could also adversely affect the Company's customers in the Commercial, Radiology Benefits Management and Specialty Pharmaceutical Management segments resulting in increased pressures on the Company's operating margins. In addition, the economic conditions may result in decreased membership in the Commercial, Radiology Benefits Management, and Specialty Pharmaceutical Management segments, thereby adversely affecting the revenues to the Company from such customers as well as the Company's operating profitability.
Adverse economic conditions in the debt markets may affect the Company's ability to refinance the Company's existing 2011 Credit Facility on December 9, 2014 upon maturity on acceptable terms, or at all.
Item 1B. Unresolved Staff Comments
None.
The Company currently leases approximately 1.1one million square feet of office space comprising 6255 offices in 2625 states and the District of Columbia with terms expiring between January 20122013 and October 2016.January 2023. The Company's principal executive offices are located in Avon, Connecticut, which lease expires in September 2012.2019. The Company believes that its current facilities are suitable for and adequate to support the level of its present operations.
The management and administration of the delivery of specialty managed healthcare entails significant risks of liability. From time to time, the Company is subject to various actions and claims arising from the acts or omissions of its employees, network providers or other parties. In the normal course of business, the Company receives reports relating to deaths and other serious incidents involving patients whose care is being managed by the Company. Such incidents occasionally give rise to malpractice, professional negligence and other related actions and claims against the Company or its network providers. Many of these actions and claims received by the Company seek substantial damages and therefore require the Company to incur significant fees and costs related to their defense. The Company is also subject to or party to certain class actions, litigation and claims relating to its operations andor business practices. In the opinion of management, the Company has recorded reserves that are adequate to cover litigation, claims or assessments that have been or may be asserted against the Company, and for which the outcome is probable and reasonably estimable. Management believes that the resolution of such litigation and claims will not have a material adverse effect on the Company's financial condition or results of operations; however, there can be no assurance in this regard.
Item 4. (Removed and Reserved)Mine Safety Disclosures
Not applicable.
Item 5. Market for Registrant's Common Equity, Related Stockholder Matters and Issuer Purchases of Equity Securities
Since January 6, 2004, shares of the Company's Ordinary Common Stock, $0.01 par value per share ("common stock") have traded on the NASDAQ Stock Market under the symbol "MGLN." For further information regarding the Company's common stock, see Note 6—"Stockholders' Equity" to the consolidated financial statements set forth elsewhere herein. The following tables set forth the high and low closing bid prices of the Company's common stock as reported by the NASDAQ Stock Market for the years ended December 31, 20102011 and 2011,2012, as follows:
| | Common Stock Sales Prices | Common Stock Sales Prices | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| | High | Low | High | Low | ||||||||||
2010 | ||||||||||||||
First Quarter | $ | 44.63 | $ | 37.97 | ||||||||||
Second Quarter | 43.25 | 36.32 | ||||||||||||
Third Quarter | 47.51 | 34.96 | ||||||||||||
Fourth Quarter | 49.80 | 45.56 | ||||||||||||
2011 | ||||||||||||||
First Quarter | 51.42 | 46.05 | 51.42 | 46.05 | ||||||||||
Second Quarter | 54.74 | 46.83 | 54.74 | 46.83 | ||||||||||
Third Quarter | 56.13 | 41.85 | 56.13 | 41.85 | ||||||||||
Fourth Quarter | 54.37 | 45.88 | 54.37 | 45.88 | ||||||||||
2012 | ||||||||||||||
First Quarter | 50.15 | 46.30 | ||||||||||||
Second Quarter | 49.38 | 40.81 | ||||||||||||
Third Quarter | 55.89 | 44.83 | ||||||||||||
Fourth Quarter | 53.52 | 47.48 | ||||||||||||
As of December 31, 2011,2012, there were approximately 331305 stockholders of record of the Company's common stock. The stockholders of record data for common stock does not reflect persons whose stock was held on that date by the Depository Trust Company or other intermediaries.
Comparison of Cumulative Total Returns
The following graph compares the change in the cumulative total return on the Company's common stock to (a) the change in the cumulative total return on the stocks included in the Standard & Poor's 500 Stock Index and (b) the change in the cumulative total return on the stocks included in the S&P Managed Health Care Index, assuming an investment of $100 made at the close of trading on December 31, 2006,2007, and comparing relative values on December 31, 2007, 2008, 2009, 2010, 2011 and 2011.2012. The Company did not pay any dividends during the period reflected in the graph. The common stock price performance shown below should not be viewed as being indicative of future performance.
Comparison of Cumulative Total Return

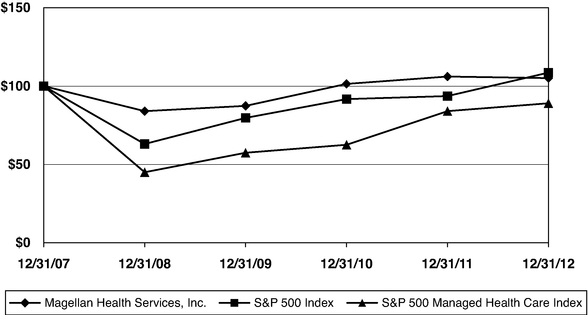
| | December 31, | December 31, | ||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | ||||||||||||||||||||||||||
Magellan Health Services, Inc. | $ | 100.00 | $ | 107.89 | $ | 90.61 | $ | 94.24 | $ | 109.39 | $ | 114.46 | $ | 100.00 | $ | 83.98 | $ | 87.35 | $ | 101.39 | $ | 106.09 | $ | 105.08 | ||||||||||||||
S&P 500 Index | 100.00 | 105.49 | 66.46 | 84.05 | 96.71 | 98.76 | 100.00 | 63.00 | 79.67 | 91.68 | 93.61 | 108.59 | ||||||||||||||||||||||||||
S&P 500 Managed Health Care Index(1) | 100.00 | 115.56 | 51.96 | 66.34 | 72.23 | 97.07 | 100.00 | 44.96 | 57.41 | 62.50 | 84.00 | 89.01 | ||||||||||||||||||||||||||
The information set forth above under the "Comparison of Cumulative Total Returns" does not constitute soliciting material and should not be deemed filed or incorporated by reference into any other of the Company's filings under the Securities Act or the Exchange Act, except to the extent the filing specifically incorporates such information by reference therein.
Stock Repurchases
On July 30, 2008 theThe Company's board of directors approvedhas previously authorized a series of stock repurchase plan which authorized the Company to purchase up to $200 million of its outstanding common stock through January 31, 2010.plans. Stock repurchases under the programfor each such plan could be executed through open market repurchases, privately negotiated transactions, accelerated share repurchases or other means. The board of directors authorized management to execute stock repurchase transactions under the program from time to time and in such
time to time and in such amounts and via such methods as management deemed appropriate. TheEach stock repurchase program could be limited or terminated at any time without prior notice. Pursuant to this program, the Company made open market purchases of 3,866,505 shares of the Company's common stock at an aggregate cost of $136.0 million (excluding broker commissions) during the year ended December 31, 2008 and made open market purchases of 1,859,959 shares of the Company's common stock at an average share price of $34.39 per share for an aggregate cost of $64.0 million (excluding broker commissions) during the period January 1, 2009 through April 7, 2009, which was the date that the repurchase program was completed.
On July 28, 2009 the Company's board of directors approved a stock repurchase plan which authorized the Company to purchase up to $100 million of its outstanding common stock through July 28, 2011. Stock repurchases under the program could be executed through open market repurchases, privately negotiated transactions, accelerated share repurchases or other means. The board of directors authorized management to execute stock repurchase transactions under the program from time to time and in such amounts and via such methods as management deemed appropriate. The stock repurchase program could be limited or terminated at any time without prior notice. Pursuant to this program, the Company made open market purchases of 782,400 shares of the Company's common stock at an average price of $32.75 per share for an aggregate cost of $25.6 million (excluding broker commissions) during the period from August 17, 2009 through December 31, 2009. Pursuant to this program, the Company made open market purchases of 1,711,881 shares of the Company's common stock at an average price of $43.46 per share for an aggregate cost of $74.4 million (excluding broker commissions) during the period January 1, 2010 through April 1, 2010, which was the date that the repurchase program was completed.
On July 27, 2010 the Company's board of directors approved a stock repurchase plan which authorized the Company to purchase up to $350 million of its outstanding common stock through July 28, 2012. On February 18, 2011, the Company's board of directors increased the stock repurchase program by an additional $100 million. Stock repurchases under the program could be executed through open market repurchases, privately negotiated transactions, accelerated share repurchases or other means. The boardmillion, to a total of directors authorized management to execute stock repurchase transactions from time to time and in such amounts and via such methods as management deemed appropriate. The stock repurchase program could be limited or terminated at any time without prior notice.$450 million. Pursuant to this program, the Company made open market purchases of 1,684,510 shares of the Company's common stock at an average price of $48.36 per share for an aggregate cost of $81.5 million (excluding broker commissions) during the period from November 3, 2010 through December 31, 2010. Pursuant to this program, the Company made open market purchases of 7,534,766 shares of the Company's common stock at an average price of $48.91 per share for an aggregate cost of $368.5 million (excluding broker commissions) during the period January 1, 2011 through November 10, 2011, which was the date the repurchase program was completed.
On October 25, 2011 the Company's board of directors approved a stock repurchase plan which authorizesauthorized the Company to purchase up to $200 million of its outstanding common stock through October 25, 2013. Stock repurchases under the program may be executed through open market repurchases, privately negotiated transactions, accelerated share repurchases or other means. The board of directors authorized management to execute stock repurchase transactions from time to time and in such amounts and via such methods as management deems appropriate. The stock repurchase program may be limited or terminated at any time without prior notice. Pursuant to this program, the Company made open market purchases of 671,776 shares of the Company's common stock at an average price of $48.72 per share for an aggregate cost of $32.7 million (excluding broker commissions) during the period from November 11, 2011 through December 31, 2011.
Table Pursuant to this program, the Company made open market purchases of Contents459,252 shares of the Company's common stock at an average price of $50.27 per share for an aggregate cost of $23.1 million (excluding broker commissions) during 2012.
Following is a summary of stock repurchases made during the three months ended December 31, 2011:2012:
Period | Total number of Shares Purchased | Average Price Paid per Share(2) | Total Number of Shares Purchased as Part of Publicly Announced Plans or Programs | Approximate Dollar Value of Shares that May Yet Be Purchased Under the Plans(1)(2) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
October 1–31, 2011 | 620,665 | $ | 50.04 | 620,665 | $ | 209,533 | |||||||
November 1–30, 2011 | 267,684 | $ | 50.90 | 267,684 | 195,907 | ||||||||
December 1–31, 2011 | 589,971 | $ | 48.53 | 589,971 | 167,274 | ||||||||
| 1,478,320 | 1,478,320 | $ | 167,274 | ||||||||||
Period | Total number of Shares Purchased | Average Price Paid per Share(2) | Total Number of Shares Purchased as Part of Publicly Announced Plans or Programs | Approximate Dollar Value of Shares that May Yet Be Purchased Under the Plans(1)(2) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
October 1–31, 2012 | 11,773 | $ | 50.14 | 11,773 | $ | 166,684 | |||||||
November 1–30, 2012 | 284,144 | $ | 49.50 | 284,144 | 152,618 | ||||||||
December 1–31, 2012 | 163,335 | $ | 51.62 | 163,335 | 144,186 | ||||||||
| 459,252 | 459,252 | $ | 144,186 | ||||||||||
The Company made no share repurchasesDuring the period from January 1, 20122013 through February 23, 2012.22, 2013, the Company made additional open market purchases of 366,650 shares of the Company's common stock at an aggregate cost of $18.6 million (excluding broker commissions).
Dividends
The Company did not declare any dividends during either of the years ended December 31, 20102011 or 20112012 and does not expect to pay a dividend in 2012.2013. The Company is prohibited from paying dividends on its common stock under the terms of the 2011 Credit Facility, except in limited circumstances. The declaration and payment of any dividends in the future by the Company will be subject to the sole discretion of the Company's board of directors and will depend upon many factors, including the Company's financial condition, earnings, covenants associated with the Company's 2011 Credit Facility and any similar future agreement, legal requirements, regulatory constraints and other factors deemed relevant by the Company's board of directors. Moreover, should the Company pay any dividends in the future, there can be no assurance that the Company will continue to pay such dividends.
Recent Sales of Unregistered Securities
On January 28, 2011, the Company and Blue Shield of California ("Blue Shield") entered into a Share Purchase Agreement (the "Share Purchase Agreement") pursuant to which on January 31, 2011 Blue Shield purchased 416,840 shares of the Company's common stock (the "Shares") for a total purchase price of $20 million. The Shares were issued to Blue Shield, an accredited investor, in a private placement pursuant to Regulation D of the Securities Act. Blue Shield has agreed not to transfer such Shares for a two year period, except in the event of any change in control of the Company as defined in the Share Purchase Agreement. The purchase price for the Shares issued was determined taking into account the recent trading price of the Company's common stock on NASDAQ and the restrictions on transfer of the Shares agreed to by Blue Shield.
Item 6. Selected Financial Data
The following table sets forth selected historical consolidated financial information of the Company as of and for the years ended December 31, 2007, 2008, 2009, 2010, 2011 and 2011.2012.
Selected consolidated financial information for the years ended December 31, 2009, 2010, 2011 and 20112012 and as of December 31, 20102011 and 20112012 presented below, have been derived from, and should be read in conjunction with, the consolidated financial statements and the notes thereto included elsewhere herein. Selected consolidated financial information for the years ended December 31, 20072008 and 20082009 has been derived from the Company's audited consolidated financial statements not included in this Form 10-K. The selected financial data set forth below also should be read in conjunction with the Company's financial statements and accompanying notes and "Management's Discussion and Analysis of Financial Condition and Results of Operations" appearing elsewhere herein.
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
(In thousands, except per share amounts)
| | Year Ended December 31, | Year Ended December 31, | ||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| | 2007 | 2008 | 2009 | 2010 | 2011 | 2008 | 2009 | 2010 | 2011 | 2012 | ||||||||||||||||||||||
Statement of Operations Data: | ||||||||||||||||||||||||||||||||
Net revenue | $ | 2,155,953 | $ | 2,625,394 | $ | 2,641,814 | $ | 2,969,240 | $ | 2,799,400 | $ | 2,625,394 | $ | 2,641,814 | $ | 2,969,240 | $ | 2,799,400 | $ | 3,207,397 | ||||||||||||
Cost of care | 1,409,103 | 1,830,542 | 1,765,313 | 1,907,985 | 1,784,724 | 1,830,542 | 1,765,313 | 1,907,985 | 1,784,724 | 2,071,890 | ||||||||||||||||||||||
Cost of goods sold | 149,585 | 181,356 | 203,336 | 218,630 | 232,038 | 181,356 | 203,336 | 218,630 | 232,038 | 328,414 | ||||||||||||||||||||||
Direct service costs and other operating expenses(1) | 404,003 | 426,627 | 465,710 | 566,582 | 529,634 | 426,627 | 465,710 | 566,582 | 529,634 | 557,512 | ||||||||||||||||||||||
Depreciation and amortization | 57,524 | 60,810 | 47,268 | 54,682 | 58,623 | 60,810 | 47,268 | 54,682 | 58,623 | 60,488 | ||||||||||||||||||||||
Interest expense | 6,386 | 2,846 | 2,424 | 2,233 | 2,502 | 2,846 | 2,424 | 2,233 | 2,502 | 2,247 | ||||||||||||||||||||||
Interest income | (23,836 | ) | (17,030 | ) | (6,245 | ) | (3,275 | ) | (2,781 | ) | (17,030 | ) | (6,245 | ) | (3,275 | ) | (2,781 | ) | (2,019 | ) | ||||||||||||
Income before income taxes | 153,188 | 140,243 | 164,008 | 222,403 | 194,660 | 140,243 | 164,008 | 222,403 | 194,660 | 188,865 | ||||||||||||||||||||||
Provision for income taxes | 59,030 | 54,038 | 57,337 | 83,744 | 65,037 | 54,038 | 57,337 | 83,744 | 65,037 | 37,838 | ||||||||||||||||||||||
Net income | $ | 94,158 | $ | 86,205 | $ | 106,671 | $ | 138,659 | $ | 129,623 | $ | 86,205 | $ | 106,671 | $ | 138,659 | $ | 129,623 | $ | 151,027 | ||||||||||||
Income per common share—basic: | $ | 2.42 | $ | 2.18 | $ | 3.03 | $ | 4.10 | $ | 4.25 | $ | 2.18 | $ | 3.03 | $ | 4.10 | $ | 4.25 | $ | 5.51 | ||||||||||||
Income per common share—diluted: | $ | 2.36 | $ | 2.16 | $ | 3.01 | $ | 4.03 | $ | 4.17 | $ | 2.16 | $ | 3.01 | $ | 4.03 | $ | 4.17 | $ | 5.42 | ||||||||||||
| | December 31, | December 31, | ||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| | 2007 | 2008 | 2009 | 2010 | 2011 | 2008 | 2009 | 2010 | 2011 | 2012 | ||||||||||||||||||||||
Balance Sheet Data: | ||||||||||||||||||||||||||||||||
Current assets | $ | 803,092 | $ | 822,420 | $ | 753,588 | $ | 858,487 | $ | 732,709 | $ | 822,420 | $ | 753,588 | $ | 858,487 | $ | 732,709 | $ | 871,418 | ||||||||||||
Current liabilities | 375,859 | 373,881 | 369,164 | 390,169 | 369,550 | 373,881 | 369,164 | 390,169 | 369,550 | 393,202 | ||||||||||||||||||||||
Property and equipment, net | 105,735 | 88,436 | 108,219 | 111,814 | 118,022 | 88,436 | 108,219 | 111,814 | 118,022 | 136,548 | ||||||||||||||||||||||
Total assets | 1,435,123 | 1,417,564 | 1,441,041 | 1,549,432 | 1,341,167 | 1,417,564 | 1,441,041 | 1,549,432 | 1,341,167 | 1,512,133 | ||||||||||||||||||||||
Total debt and capital lease obligations | 13,969 | 28 | — | 559 | — | 28 | — | 559 | — | — | ||||||||||||||||||||||
Stockholders' equity | $ | 908,232 | $ | 908,073 | $ | 950,492 | $ | 1,039,015 | $ | 845,274 | $ | 908,073 | $ | 950,492 | $ | 1,039,015 | $ | 845,274 | $ | 1,017,333 | ||||||||||||
Item 7. Management's Discussion and Analysis of Financial Condition and Results of Operations
The following discussion and analysis of the Company's financial condition and results of operations should be read in conjunction with the Company's selected financial data and the Company's financial statements and the accompanying notes included herein. The following discussion may contain "forward-looking statements" within the meaning of the Securities Act and the Exchange
Act. When used in this Form 10-K, the words "estimate," "anticipate," "expect," "believe," "should" and similar expressions are intended to be forward-looking statements. Although the Company believes that its plans, intentions and expectations reflected in such forward-looking statements are reasonable, it can give no assurance that such plans, intentions or expectations will be achieved. Prospective investors are cautioned that any such forward-lookingforward- looking statements are not guarantees of future performance and involve risks and uncertainties, and that actual results may differ materially from those contemplated by such forward-looking statements. Important factors currently known to management that could cause actual results to differ materially from those in forward-looking statements are set forth under the heading "Risk Factors" in Item 1A and elsewhere in this Form 10-K. Capitalized or defined terms included in this Item 7 have the meanings set forth in Item 1 of this Form 10-K.
Business Overview
The Company is engaged in the specialty managed healthcare business. Through 2005, the Company predominantly operated in the managed behavioral healthcare business. As a result of certain acquisitions, the Company expanded into radiology benefits management and specialty pharmaceutical management during 2006, and into Medicaid administration during 2009. The Company provides services to health plans, insurance companies, employers, labor unions and various governmental agencies. The Company's business is divided into the following six segments, based on the services it provides and/or the customers that it serves, as described below.
Managed Behavioral Healthcare
Two of the Company's segments are in the managed behavioral healthcare business. This line of business generally reflects the Company's coordination and management of the delivery of behavioral healthcare treatment services that are provided through its contracted network of third-party treatment providers, which includes psychiatrists, psychologists, other behavioral health professionals, psychiatric hospitals, general medical facilities with psychiatric beds, residential treatment centers and other treatment facilities. The treatment services provided through the Company's provider network include outpatient programs (such as counseling or therapy), intermediate care programs (such as intensive outpatient programs and partial hospitalization services), inpatient treatment and crisis intervention services. The Company generally does not directly provide or own any provider of treatment services.
The Company provides its management services primarily through: (i) risk-based products, where the Company assumes all or a substantial portion of the responsibility for the cost of providing treatment services in exchange for a fixed per member per month fee, (ii) administrative services only ("ASO")ASO products, where the Company provides services such as utilization review, claims administration and/or provider network management, but does not assume responsibility for the cost of the treatment services, and (iii) employee assistance programs ("EAPs")EAPs where the Company provides short-term outpatient behavioral counseling services.
The managed behavioral healthcare business is managed based on the services provided and/or the customers served, through the following two segments:
Commercial. The Managed Behavioral Healthcare Commercial segment ("Commercial") generally reflects managed behavioral healthcare services and EAP services provided under contracts with health plans and insurance companies for some or all of their commercial, Medicaid and Medicare members, as well as with employers, including corporations, governmental agencies, and labor unions. Commercial's contracts encompass risk-based, ASO and EAP
arrangements. As of December 31, 2011,2012, Commercial's covered lives were 3.75.4 million, 12.913.4 million and 12.612.0 million for risk-based, ASO and EAP products, respectively. For the year ended December 31, 2011,2012, Commercial's revenue was $370.4$516.6 million, $97.8$118.2 million and $93.6$93.7 million for risk-based, ASO and EAP products, respectively.
Public Sector. The Managed Behavioral Healthcare Public Sector segment ("Public Sector") generally reflects services provided to recipients under Medicaid and other state sponsored programs under contracts with state and local governmental agencies. Public Sector contracts encompass either risk-based or ASO arrangements. As of December 31, 2011,2012, Public Sector's covered lives were 1.61.9 million and 0.31.1 million for risk-based and ASO products, respectively. For the year ended December 31, 2011,2012, Public Sector's revenue was $1.5$1.6 billion and $5.9$27.5 million for risk-based and ASO products, respectively.
The Maricopa Contract began on September 1, 2007 and extends through September 30, 2013 unless sooner terminated by the parties. The ADHS released an RFP for the ADHS Regional Behavioral Health Authority-GSA 6 (Marciopa County), which includes the current behavioral carve-out for the lives the Company currently serves under the Maricopa Contract. MCCAZ, a joint venture in which the Company has an 80% ownership interest, has responded to this RFP. There can be no assurance that MCCAZ will be awarded a contract pursuant to the RFP, or that the terms of any contract awarded pursuant to the RFP will be similar to the Maricopa Contract. The Maricopa Contract generated net revenues of $807.1 million, $779.5 million, and $758.3 million for the years ended December 31, 2010, 2011, and 2012, respectively.
Radiology Benefits Management
The Radiology Benefits Management segment ("Radiology Benefits Management") generally reflects the management of the delivery of diagnostic imaging and other therapeutic services to ensure that such services are clinically appropriate and cost effective. The Company's radiology benefits management services currently are provided under contracts with health plans and insurance companies for some or all of their commercial, Medicaid and Medicare members. The Company also contracts with state and local governmental agencies for the provision of such services to Medicaid recipients. The Company offers its radiology benefits management services through risk-based contracts, where the Company assumes all or a substantial portion of the responsibility for the cost of providing diagnostic imaging services, and through ASO contracts, where the Company provides services such as utilization review and claims administration, but does not assume responsibility for the cost of the imaging services. As of December 31, 2011,2012, covered lives for Radiology Benefits Management were 3.64.8 million and 12.012.4 million for risk-based and ASO products, respectively. For the year ended December 31, 2011,2012, revenue for Radiology Benefits Management was $296.0$308.5 million and $48.3$40.6 million for risk-based and ASO products, respectively.
Drug Benefits Management
Two of the Company's segments are in the drug benefits management business. This line of business generally reflects the Company's clinical management of drugs paid under medical and pharmacy benefit programs. The Company's services include the coordination and management of the specialty drug spendspending for health plans, employers, and governmental agencies, and the management of pharmacy programs for Medicaid programs, health plans, and other state-sponsored programs.employers. The two segments in this line of business line are:
Specialty Pharmaceutical Management. The Specialty Pharmaceutical Management segment ("Specialty Pharmaceutical Management") comprises programs that manage specialty drugs used in the treatment of complex conditions such as cancer, multiple sclerosis, hemophilia, infertility, rheumatoid arthritis, chronic forms of hepatitis and other diseases. Specialty pharmaceutical drugs represent high-cost injectible, infused, or oral drugs with sensitive handling or storage needs, many of which may be physician administered. Patients receiving these drugs require greater amounts of clinical support than those taking more traditional agents. Payors require
clinical, financial and technological support to maximize the value delivered to their members using these expensive agents. The Company's specialty pharmaceutical management services are provided under contracts with health plans, insurance companies, employers, and governmental agencies for some or all of their commercial, Medicare and Medicaid members. The Company's specialty pharmaceutical services include: (i) contracting and formulary optimization programs; (ii) specialty pharmaceutical dispensing operations; and (iii) medical pharmacy management programs. The Company's Specialty Pharmaceutical Management segment had contracts with 41 health plans and employers, and several pharmaceutical manufacturers and state Medicaid programs as of December 31, 2011.2012.
Medicaid Administration. The Medicaid Administration segment ("Medicaid Administration") generally reflects integrated clinical management services provided to the public sector to manage Medicaid pharmacy, mental health, and long-term care programs.for state benefit programs, and pharmacy benefit management programs for health plans and employers. The primary focus of the Company's
Medicaid Administration unit involves providing pharmacy benefits administration ("PBA")PBA and pharmacy benefits management ("PBM")PBM services under contracts with health plans and employers, as well as public sector healthcare clients forsponsoring Medicaid and other state sponsored program recipients.benefit programs. The Company's pharmacy services include pharmacynetwork management, formulary and rebate management, point-of-sale claims processing systems and administration, drug utilization review, clinical prior authorization, and drug utilization review. Magellan's pharmacy strategy combines its Specialty Pharmacy Management and PBM capabilities to provide integrated management of complex drug therapies billed under both the medical and pharmacy benefit. Its mental health and long term care management services include review of service utilization and formulary management services, Preferred Drug List programs, Maximum Allowable Cost programs,compliance with state and drug rebate program services.federal regulations and reimbursement guidelines. Medicaid Administration's contracts encompass Fee-For-Service ("FFS")both FFS and risk-based arrangements. In addition to Medicaid Administration's FFS contracts, effective September 1, 2010, Public Sector has subcontracted with Medicaid Administration to provide pharmacy benefits management services on a risk basis for one of Public Sector's customers.
Corporate
This segment of the Company is comprised primarily of operational support functions such as sales and marketing and information technology, as well as corporate support functions such as executive, finance, human resources and legal.
Acquisition of First Health Services
Pursuant to the June 4, 2009 Purchase Agreement (the "Purchase Agreement") with Coventry Health Care ("Coventry"), on July 31, 2009 the Company acquired (the "Acquisition") all of the outstanding equity interests of Coventry's direct and indirect subsidiaries First Health Services Corporation ("FHS"), FHC, Inc. ("FHC") and Provider Synergies, LLC (together with FHS and FHC, "First Health Services") and certain assets of Coventry which are related to the operation of the business conducted by First Health Services. As consideration for the Acquisition, the Company paid $114.5 million in cash, excluding cash acquired and including net payments of $6.5 million for excess working capital. The Company funded the Acquisition with cash on hand.
Effective July 1, 2010 the Company discontinued the use of the name First Health Services Corporation and officially changed such name to "Magellan Medicaid Administration, Inc." The Company reports the results of operations of Magellan Medicaid Administration, Inc. within the Medicaid Administration segment.
Managed Care Revenue
Managed care revenue, inclusive of revenue from the Company's risk, EAP and ASO contracts, is recognized over the applicable coverage period on a per member basis for covered members. The Company is paid a per member fee for all enrolled members, and this fee is recorded as revenue in the month in which members are entitled to service. The Company adjusts its revenue for retroactive membership terminations, additions and other changes, when such adjustments are identified, with the
exception of retroactivity that can be reasonably estimated. The impact of retroactive rate amendments is generally recorded in the accounting period that terms to the amendment are finalized, and that the amendment is executed. Any fees paid prior to the month of service are recorded as deferred revenue. Managed care revenues approximated $2.4 billion, $2.2 billion $2.4 billion and $2.2$2.5 billion for the years ended December 31, 2009, 2010, 2011 and 2011,2012, respectively.
Fee-For-Service and Cost-Plus Contracts
The Company has certain FFS contracts, including cost-plus contracts, with customers under which the Company recognizes revenue as services are performed and as costs are incurred. Revenues from these contracts approximated $104.4 million, $192.9 million, $174.5 million and $174.5$151.4 million for the years ended December 31, 2009, 2010, 2011 and 2011,2012, respectively.
Block Grant Revenues
The Maricopa ContractPublic Sector has a contract that is partially funded by federal, state and county block grant money, which represents annual appropriations. The Company recognizes revenue from block grant activity ratably over the period to which the block grant funding applies. Block grant revenues were approximately $106.6 million, $109.1 million, $114.4 million and $114.4$124.8 million for the years ended December 31, 2009, 2010, 2011 and 2011,2012, respectively.
Dispensing Revenue
The Company recognizes dispensing revenue, which includes the co-payments received from members of the health plans the Company serves, when the specialty pharmaceutical drugs are shipped. At the time of shipment, the earnings process is complete; the obligation of the Company's customer to pay for the specialty pharmaceutical drugs is fixed, and, due to the nature of the product, the member may neither return the specialty pharmaceutical drugs nor receive a refund. Revenues from the dispensing of specialty pharmaceutical drugs on behalf of health plans were $221.6 million, $234.8 million, $247.4 million and $247.4$350.3 million for the years ended December 31, 2009, 2010, 2011 and 2011,2012, respectively.
Performance-Based Revenue
The Company has the ability to earn performance-based revenue under certain risk and non-risk contracts. Performance-based revenue generally is based on either the ability of the Company to manage care for its clients below specified targets, or on other operating metrics. For each such contract, the Company estimates and records performance-based revenue after considering the relevant contractual terms and the data available for the performance-based revenue calculation. Pro-rata performance-based revenue ismay be recognized on an interim basis pursuant to the rights and obligations of each party upon termination of the contracts.contracts, among other factors. Performance-based revenues were $7.6 million, $13.1 million, $26.5 million and $26.5$25.4 million for the years ended December 31, 2009, 2010, 2011 and 2011,2012, respectively.
Rebate Revenue
The Company administers a rebate program for certain clients through which the Company coordinates the achievement, calculation and collection of rebates and administrative fees from pharmaceutical manufacturers on behalf of clients. Each period, the Company estimates the total rebates earned based on actual volumes of pharmaceutical purchases by the Company's clients, as well as historical and/or anticipated sharing percentages. The Company earns fees based upon the volume of rebates generated for its clients. The Company does not record as rebate revenue any rebates that are passed through to its clients. Total rebate revenues for the years ended December 31, 2009, 2010, 2011 and 20112012 were $29.4 million, $25.5 million, and $32.8 million and $40.2 million, respectively.
Cost of Care, Medical Claims Payable and Other Medical Liabilities
Cost of care is recognized in the period in which members receive managed healthcare services. In addition to actual benefits paid, cost of care in a period also includes the impact of accruals for estimates of medical claims payable. Medical claims payable represents the liability for healthcare claims reported but not yet paid and claims incurred but not yet reported ("IBNR")IBNR related to the Company's managed healthcare businesses.
Such liabilities are determined by employing actuarial methods that are commonly used by health insurance actuaries and that meet actuarial standards of practice.
The IBNR portion of medical claims payable is estimated based on past claims payment experience for member groups, enrollment data, utilization statistics, authorized healthcare services and other factors. This data is incorporated into contract-specific actuarial reserve models and is further
analyzed to create "completion factors" that represent the average percentage of total incurred claims that have been paid through a given date after being incurred. Factors that affect estimated completion factors include benefit changes, enrollment changes, shifts in product mix, seasonality influences, provider reimbursement changes, changes in claims inventory levels, the speed of claims processing and changes in paid claim levels. Completion factors are applied to claims paid through the financial statement date to estimate the ultimate claim expense incurred for the current period. Actuarial estimates of claim liabilities are then determined by subtracting the actual paid claims from the estimate of the ultimate incurred claims. For the most recent incurred months (generally the most recent two months), the percentage of claims paid for claims incurred in those months is generally low. This makes the completion factor methodology less reliable for such months. Therefore, incurred claims for any month with a completion factor that is less than 70 percent are generally not projected from historical completion and payment patterns; rather they are projected by estimating claims expense based on recent monthly estimated cost incurred per member per month times membership, taking into account seasonality influences, benefit changes and healthcare trend levels, collectively considered to be "trend factors."
Medical claims payable balances are continually monitored and reviewed. If it is determined that the Company's assumptions in estimating such liabilities are significantly different than actual results, the Company's results of operations and financial position could be impacted in future periods. Adjustments of prior period estimates may result in additional cost of care or a reduction of cost of care in the period an adjustment is made. Further, due to the considerable variability of healthcare costs, adjustments to claim liabilities occur each period and are sometimes significant as compared to the net income recorded in that period. Prior period development is recognized immediately upon the actuary's judgment that a portion of the prior period liability is no longer needed or that additional
liability should have been accrued. The following table presents the components of the change in medical claims payable for the years ended December 31, 2009, 2010, 2011 and 20112012 (in thousands):
| | 2009 | 2010 | 2011 | 2010 | 2011 | 2012 | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Claims payable and IBNR, beginning of period | $ | 184,422 | $ | 168,851 | $ | 166,095 | $ | 168,851 | $ | 166,095 | $ | 157,099 | ||||||||
Cost of care: | ||||||||||||||||||||
Current year | 1,771,213 | 1,919,785 | 1,790,124 | 1,919,785 | 1,790,124 | 2,076,190 | ||||||||||||||
Prior years | (5,900 | ) | (11,800 | ) | (5,400 | ) | (11,800 | ) | (5,400 | ) | (4,300 | ) | ||||||||
Total cost of care | 1,765,313 | 1,907,985 | 1,784,724 | 1,907,985 | 1,784,724 | 2,071,890 | ||||||||||||||
Claim payments and transfers to other medical liabilities(1): | ||||||||||||||||||||
Current year | 1,624,626 | 1,777,356 | 1,657,291 | 1,777,356 | 1,657,291 | 1,877,459 | ||||||||||||||
Prior years | 156,258 | 133,385 | 136,429 | 133,385 | 136,429 | 128,601 | ||||||||||||||
Total claim payments and transfers to other medical liabilities | 1,780,884 | 1,910,741 | 1,793,720 | 1,910,741 | 1,793,720 | 2,006,060 | ||||||||||||||
Claims payable and IBNR, end of period | 168,851 | 166,095 | 157,099 | 166,095 | 157,099 | 222,929 | ||||||||||||||
Withhold receivables, end of period(2) | (25,182 | ) | (23,424 | ) | (19,126 | ) | (23,424 | ) | (19,126 | ) | (24,500 | ) | ||||||||
Medical claims payable, end of period | $ | 143,669 | $ | 142,671 | $ | 137,973 | $ | 142,671 | $ | 137,973 | $ | 198,429 | ||||||||
Actuarial standards of practice require that the claim liabilities be adequate under moderately adverse circumstances. Adverse circumstances are situations in which the actual claims experience could be higher than the otherwise estimated value of such claims. In many situations, the claims paid amount experienced will be less than the estimate that satisfies the actuarial standards of practice.
Care trend factors and completion factors can have a significant impact on the medical claims payable liability. The following example provides the estimated impact to the Company's December 31, 20112012 unpaid medical claims payable liability assuming hypothetical changes in care trend factors and completion factors:
| Care Trend Factor(1) | Care Trend Factor(1) | Completion Factor(2) | Care Trend Factor(1) | Completion Factor(2) | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (Decrease) Increase | (Decrease) Increase | (Decrease) Increase | (Decrease) Increase | (Decrease) Increase | ||||||||||||||||||
Trend Factor | Trend Factor | Medical Claims Payable | Completion Factor | Medical Claims Payable | Trend Factor | Medical Claims Payable | Completion Factor | Medical Claims Payable | ||||||||||||||
| | | (in thousands) | | (in thousands) | | (in thousands) | | (in thousands) | ||||||||||||||
| -3 | % | $ | (18,000 | ) | -3 | % | $ | (32,000 | ) | -3 | % | $ | (25,500 | ) | -3 | % | $ | (39,500 | ) | |||
| -2 | % | (11,500 | ) | -2 | % | (21,000 | ) | -2 | % | (16,000 | ) | -2 | % | (26,000 | ) | |||||||
| -1 | % | (5,500 | ) | -1 | % | (10,500 | ) | -1 | % | (7,500 | ) | -1 | % | (13,000 | ) | |||||||
| 1 | % | 5,500 | 1 | % | 10,500 | 1 | % | 7,500 | 1 | % | 13,000 | |||||||||||
| 2 | % | 11,500 | 2 | % | 21,000 | 2 | % | 16,000 | 2 | % | 26,000 | |||||||||||
| 3 | % | 18,000 | 3 | % | 32,000 | 3 | % | 25,500 | 3 | % | 39,500 | |||||||||||
Approximately 70 percent of IBNR dollars is based on care trend factors. | ||||||||||||||||||||||
Approximately 70 percent of IBNR dollars is based on care trend factors.
Due to the existence of risk sharing and reinvestment provisions in certain customer contracts, a change in the estimate for medical claims payable does not necessarily result in an equivalent impact on cost of care.
The Company believes that the amount of medical claims payable is adequate to cover its ultimate liability for unpaid claims as of December 31, 2011;2012; however, actual claims payments may differ from established estimates.
Other medical liabilities consist primarily of "reinvestment" payables under certain managed behavioral healthcare contracts with Medicaid customers and "profit share" payables under certain risk-based contracts. Under a contract with reinvestment features, if the cost of care is less than certain minimum amounts specified in the contract (usually as a percentage of revenue), the Company is required to "reinvest" such difference in behavioral healthcare programs when and as specified by the customer or to pay the difference to the customer for their use in funding such programs. Under a contract with profit share provisions, if the cost of care is below certain specified levels, the Company will "share" the cost savings with the customer at the percentages set forth in the contract.
Long-lived Assets
Long-lived assets, including property and equipment and intangible assets to be held and used, are currently reviewed for impairment whenever events or changes in circumstances indicate that the carrying amount should be addressed. Impairment is determined by comparing the carrying value of these long-lived assets to management's best estimate of the future undiscounted cash flows expected to result from the use of the assets and their eventual disposition. The cash flow projections used to make this assessment are consistent with the cash flow projections that management uses internally in making key decisions. In the event an impairment exists, a loss is recognized based on the amount by which the carrying value exceeds the fair value of the asset, which is generally determined by using quoted market prices or the discounted present value of expected future cash flows.
Goodwill
The Company is required to test its goodwill for impairment on at least an annual basis. The Company has selected October 1 as the date of its annual impairment test. The goodwill impairment test is a two-step process that requires management to make judgments in determining what assumptions to use in the calculation. The first step of the process consists of estimating the fair value of each reporting unit with goodwill based on various valuation techniques, with the primary technique being a discounted cash flow analysis, which requires the input of various assumptions with respect to revenues, operating margins, growth rates and discount rates. The estimated fair value for each reporting unit is compared to the carrying value of the reporting unit, which includes goodwill. If the estimated fair value is less than the carrying value, a second step is performed to compute the amount of the impairment by determining an "implied fair value" of goodwill. The determination of a reporting unit's "implied fair value" of goodwill requires the Company to allocate the estimated fair value of the reporting unit to the assets and liabilities of the reporting unit. Any unallocated fair value represents the "implied fair value" of goodwill, which is compared to its corresponding carrying value.
The fair value of the Health Plan (a component of the Commercial segment), Radiology Benefits Management and the Radiology BenefitsSpecialty Pharmaceutical Management reporting units were determined using a discounted cash flow method. This method involves estimating the present value of estimated future cash flows utilizing a risk adjusted discount rate. Key assumptions for this method include cash flow projections, terminal growth rates and discount rates.
The fair value of the Specialty Pharmaceutical ManagementMedicaid Administration reporting unit was determined using the discounted cash flow, guideline company and similar transaction methods. Key assumptions for the discounted cash flow method are consistent with those described above. For the guideline company method, revenue and earnings before interest, taxes, depreciation, and amortization ("EBITDA") multiples for guideline companies were applied to the reporting unit's actual revenue and EBTIDAEDITDA for the twelve-month period ended September 30, 20112012 and to the reporting unit's projected revenue and EBITDA for 2012. For the similar transaction method, an EBITDA multiple based on merger and acquisition transactions for similar companies was applied to the reporting unit's actual EBITDA for the twelve-month period ended September 30, 2011. The weighting applied to the fair values determined using the discounted cash flow, guideline company and similar transaction methods to determine an overall fair value for the Specialty Pharmaceutical Management reporting unit was 60 percent, 24 percent and 16 percent, respectively. The weighting of each of the methods described above was based on the relevance of the approach. A change in the weighting would not change the outcome of the first step of the impairment test.
The fair value of the Medicaid Administration reporting unit was determined using discounted cash flow, guideline company and similar transaction methods. Key assumptions for the discounted cash flow method are consistent with those described above. For the guideline company method, an EBITDA multiple for guideline companies was applied to the reporting unit's projected EBITDA for 2012.2013. For the similar transaction method, revenue and EBITDA multiples based on merger and acquisition transactions for similar companies were applied to the reporting unit's actual revenue and EBITDA for the twelve-month period ended September 30, 2011.2012. The weighting applied to the fair values determined using the discounted cash flow, guideline company and similar transaction methods to determine an overall fair value for the Medicaid Administration reporting unit was 75 percent, 22.5 percent and 2.5 percent, respectively. The weighting of each of the methods described above was based on the relevance of the approach. A change in the weighting would not change the outcome of the first step of the impairment test.
As a result of the first step of the 20112012 annual goodwill impairment analysis, the fair value of each reporting unit with goodwill exceeded its carrying value. Therefore, the second step was not necessary. However, a 20 percent decline in the fair value of Health Plan, a 56 percent decline in fair value of the Health Plan reporting unit, a 54 percent decline in
fair value of Radiology Benefits Management, or a 2035 percent decline in fair value of Specialty Pharmaceutical Management and a 30 percent decline in fair value of Medicaid Administration reporting units would have caused the carrying values for these reporting units to be in excess of fair values, which would require the second step to be performed. The second step could have resulted in an impairment loss for goodwill.
While there are numerous assumptions that impact the calculation of the fair value of the reporting units, the most sensitive assumptions relate to the discount rate and estimated future cash flows when determining fair value using the discounted cash flow method. For Medicaid Administration, an 8those reporting units with a projected fair value within 30 percent of the carrying value, the impact of changes in the discount rate and estimated future cash flows was reviewed for sensitivity.
For Health Plan, a 20 percent decline in fair value, or approximately $10$40 million, would have caused the carrying value to be in excess of its fair value as of October 1, 2011. While there are numerous assumptions that impact the calculation of the fair value of this reporting unit, the most sensitive assumptions relate to the discount rate and the estimated future cash flows.2012. A decline in fair value of approximately $10$40 million would occur upon either: (1) an increase of 0.85338 basis points in the discount rate utilized to determine the present value of the projected net cash flows; or (2) a decline between 20 and 40 percent in estimated future cash flows, with the percentage decrease varying depending upon whether the cash flow decrease were to occur in the near term or long term. For Medicaid Administration, a 30 percent decline in fair value, or approximately $50 million, would have caused the carrying value to be in excess of its fair value as of October 1, 2012. A decline in fair value of approximately $50 million would occur upon either: (1) an increase of 350 basis points in the discount rate utilized to determine the present value of the projected net cash flows; or (2) a decline of between 1230 and 2540 percent in estimated future cash flows, with the percentage decrease varying depending upon whether the cash flow decrease were to occur in the near term or the long term. Such declinedeclines in the future cash flows could be the result of a loss of one or more significant customers without the generation of new business to offset such losses.losses or an inability to meet the respective reporting unit's growth targets, which could include expansion into new product offerings. A decline in the fair valuevalues for Health Plan and Medicaid Administration could result in a carrying value for Medicaid Administrationvalues in excess of fair value,values, which would require the second step of goodwill testing to be performed. The second step could result in an impairment loss for goodwill.
Goodwill for each of the Company's reporting units isare as follows (in thousands):
| | December 31, | ||||||
|---|---|---|---|---|---|---|---|
| | 2010 | 2011 | |||||
Commercial | $ | 120,485 | $ | 120,485 | |||
Radiology Benefits Management | 104,549 | 104,549 | |||||
Specialty Pharmaceutical Management | 142,291 | 142,291 | |||||
Medicaid Administration | 59,614 | 59,614 | |||||
Total | $ | 426,939 | $ | 426,939 | |||
The changes in the carrying amount of goodwill for the years ended December 31, 2010 and 2011 are reflected in the table below (in thousands):
| | 2010 | 2011 | |||||
|---|---|---|---|---|---|---|---|
Balance as of beginning of period | $ | 426,471 | $ | 426,939 | |||
Adjustment related to acquisition of Medicaid Administration | 468 | — | |||||
Balance as of end of period | $ | 426,939 | $ | 426,939 | |||
| | December 31, | ||||||
|---|---|---|---|---|---|---|---|
| | 2011 | 2012 | |||||
Health Plan | $ | 120,485 | $ | 120,485 | |||
Radiology Benefits Management | 104,549 | 104,549 | |||||
Specialty Pharmaceutical Management | 142,291 | 142,291 | |||||
Medicaid Administration | 59,614 | 59,614 | |||||
Total | $ | 426,939 | $ | 426,939 | |||
Stock Compensation
At December 31, 20102011 and 2011,2012, the Company had equity-based employee incentive plans, which are described more fully in Note 6—"Stockholders' Equity" to the consolidated financial statements set forth elsewhere herein. The Company recorded stock compensation expense of $15.1$17.4 million and $17.4$17.8 million for the years ended December 31, 20102011 and 2011,2012, respectively. The Company recognizes substantially all of these compensation costs for awards that do not contain performance conditions on a straight-line basis over the requisite service period, which is generally the vesting term of three years. For restricted stock units that include performance conditions, stock compensation is recognized using an accelerated method over the vesting period.
The Company estimates the fair value of substantially all stock options using the Black-Scholes-Merton option pricing model that employs certain factors including expected volatility of stock price, expected life of the option, risk-free interest rate and expected dividend yield. For the years ended December 31, 2009, 20102011 and 2011,2012, such volatility was based on the historical volatility of the Company's stock price.
The expected term of the option is based on historical employee stock option exercise behavior and the vesting terms of the respective option. Risk-free interest rates are based on the U.S. Treasury yield in effect at the time of grant.
The Company recognizes compensation expense for only the portion of options, restricted stock or restricted stock units that are ultimately expected to vest. Therefore, estimated forfeiture rates are derived from historical employee termination behavior. The Company's estimated forfeiture ratesrate for the years ended December 31, 2009, 20102011 and 2011 were five percent, five percent, and2012 was four percent respectively.percent. If the actual number of forfeitures differs from those estimated, additional adjustments to compensation expense may be required in future periods. If vesting of an award is conditioned upon the achievement of performance goals, compensation expense during the performance period is estimated using the most probable outcome of the performance goals, and adjusted as the expected outcome changes.
Income Taxes
The Company files a consolidated federal income tax return for the Company and its eighty-percent or more owned subsidiaries, and the Company and its subsidiaries file income tax returns in various statesstate and local jurisdictions.
The Company estimates income taxes for each of the jurisdictions in which it operates. This process involves estimating current tax exposures together with assessingdetermining both permanent and temporary differences resulting from differing treatment of items for tax and book purposes. Deferred tax assets and/or liabilities are determined by multiplying the temporary differences between the financial reporting and tax reporting bases for assets and liabilities by the enacted tax rates expected to be in effect when such differences are recovered or settled. The Company then assesses the likelihood that the deferred tax assets will be recovered from the reversal of temporary timing differences, the implementation of feasible and prudent tax planning
strategies, and future taxable income. To the extent the Company cannot conclude that recovery is more likely than not, it establishes a valuation allowance. The effect of a change in tax rates on deferred taxes is recognized in income in the period that includes the enactment date.
The Company has federal net operating loss carryforwards ("NOLs") as of December 31, 20112012 of $4.8$4.2 million available to reduce future federal taxable income. These NOLs, if not used, will expire in 2017 through 2019 and are subject to examination and adjustment by the Internal Revenue Service ("IRS"). In addition, the Company's utilizationIRS. Utilization of suchthese NOLs is also subject to limitation under Internal Revenue Code Section 382 ("Section 382") which affects thecertain timing of the use of these NOLs. At this time,limitations, although the Company does not believe these limitations will limit the Company'srestrict its ability to use any federal NOLs before they expire.
The Company's valuation allowances against deferred tax assets were $5.3$3.4 million and $3.4$3.1 million as of December 31, 20102011 and 2011,2012, respectively, mostly relating to uncertainties regarding the eventual realization of certain state NOLs. Determination of the amount of deferred tax assets considered realizable requires significant judgment and estimation regarding the forecasts of future taxable income which are consistent with the plans and estimates the Company uses to manage the underlying businesses. Changes in these estimatesFuture changes in the futureestimated realizable portion of deferred tax assets could materially affect the Company's financial condition and results of operations.
Reversals of both valuation allowances and unrecognized tax benefits are recorded in the period they occur, typically as reductions to income tax expense. However, reversals of unrecognized tax benefits related to deductions for stock compensation in excess of the related book expense are recorded as increases in additional paid-in capital. To the extent reversals of unrecognized tax benefits cannot be specifically traced to these excess deductions due to complexities in the tax law, the Company records the tax benefit for such reversals to additional paid-in-capital on a pro-rata basis.
The tax benefit from an uncertain tax position is recognized when it is more likely than not that, based on technical merit, the position will be sustained upon examination, including resolution of any related appeals or litigation processes. As of December 31, 2010 and 2011, $111.62012, $56.6 million and $99.2 million, respectively, of unrecognized tax benefits were included in tax contingencies. If these unrecognized tax benefits had been realized as of December 31, 2010 and 2011, $88.22012, $45.1 million and $80.3 million, respectively, would have impacted the effectivereduced income tax rate.expense.
The statutes of limitationlimitations regarding the assessment of federal and certain state and local income taxes for the year ended December 31, 20072008 expired during 2011. With few exceptions, the Company is no longer subject to income tax assessments by tax authorities for years ended prior to December 31, 2008.2012. As a result, $15.0$43.3 million of unrecognized tax benefits (excluding interest costs) recorded as of December 31, 20102011 were reversed in the current year as a result of statute expirations, of which $35.7 million is reflected as a reduction to income tax expense, $6.2 million as an increase to additional paid-in capital, and the remainder as a decrease to deferred tax assets. Additionally, $1.4 million of accrued interest and $0.8 million of unrecognized state tax benefits were reversed in 2012 and reflected as reductions to income tax expense due to the closing of statutes of limitations on tax assessments and changes in tax return elections, respectively.
The statutes of limitations regarding the assessment of federal and certain state and local income taxes for 2007 closed during 2011. As a result, $15.0 million of unrecognized tax benefits recorded as of December 31, 2010 were reversed in 2011, of which $10.4 million iswas reflected as a reduction to income tax expense, $2.5 million as an increase to additional paid-in capital, and the remainder as a decrease to deferred tax assets. Additionally, $2.2 million of accrued interest was reversed in 2011 and reflected as a reduction to income tax expense due to these statute closings.
With few exceptions, the Company is no longer subject to income tax assessments by tax authorities for years ended prior to 2009. Further, it is reasonably possible the statutestatutes of limitations regarding the assessment of federal and most state and local income taxes for the year ended December 31, 2008 will2009 could expire during 2012.2013. The Company anticipates that up to $43.2$28.6 million of unrecognized tax benefits (excluding interest costs) recorded as of December 31, 20112012 could be reversed during 20122013 as a result of statute expirations, of which $35.6$23.2 million would be reflected as a reduction to income tax expense, $6.2$3.9 million as an increase to additional paid-in capital, and the remainder as a decrease to deferred tax assets. All such reversals (net
Table of the related indirect tax benefits) Contents
would be reflected as discrete adjustments during the quarter in which the respective statute expiration occurs, primarily in the 3rd quarter.
TheIn addition to reversals for statute closings, the Company also adjusts these liabilities for unrecognized tax benefits when its judgment changes as a result of the evaluation of new information not previously available. Due to the complexity of some of these uncertainties,However, the ultimate resolution mayof a disputed tax position following an examination by a taxing authority could result in a payment that is materially different from that accrued by the Company's current estimate of the tax liabilities.Company. These differences will beare reflected as increases or decreases to income tax expense in the period in which they are determined.
Results of Operations
The accounting policies of the Company's segments are the same as those described in Note 1—"General." The Company evaluates performance of its segments based on profit or loss from continuing operations before stock compensation expense, depreciation and amortization, interest expense, interest income, gain on sale of assets, special charges or benefits, and income taxes ("Segment Profit"). Management uses Segment Profit information for internal reporting and control purposes and considers it important in making decisions regarding the allocation of capital and other resources, risk assessment and employee compensation, among other matters. Effective September 1, 2010, Public Sector has subcontracted with Medicaid Administration to provide pharmacy benefits management services on a risk basis for one of Public Sector's customers. As such, revenue and cost of care related to this intersegment arrangement are eliminated. The Company's segments are defined above.
The table below summarizes,following tables summarize, for the periods indicated, operating results by business segment (in thousands):
| | Commercial | Public Sector | Radiology Benefits Management | Specialty Pharmaceutical Management | Medicaid Administration | Corporate and Elimination | Consolidated | Commercial | Public Sector | Radiology Benefits Management | Specialty Pharmaceutical Management | Medicaid Administration | Corporate and Elimination | Consolidated | ||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Year Ended December 31, 2009 | ||||||||||||||||||||||||||||||||||||||||||||
Net revenue | $ | 650,139 | $ | 1,362,420 | $ | 305,251 | $ | 259,745 | $ | 64,259 | $ | — | $ | 2,641,814 | ||||||||||||||||||||||||||||||
Year Ended December 31, 2010 | ||||||||||||||||||||||||||||||||||||||||||||
Managed care and other revenue | $ | 652,221 | $ | 1,442,093 | $ | 454,105 | $ | 35,812 | $ | 176,283 | $ | (26,108 | ) | $ | 2,734,406 | |||||||||||||||||||||||||||||
Dispensing revenue | — | — | — | 234,834 | — | — | 234,834 | |||||||||||||||||||||||||||||||||||||
Cost of care | (351,270 | ) | (1,208,451 | ) | (205,592 | ) | — | — | — | (1,765,313 | ) | (365,115 | ) | (1,246,779 | ) | (298,516 | ) | — | (23,683 | ) | 26,108 | (1,907,985 | ) | |||||||||||||||||||||
Cost of goods sold | — | — | — | (203,336 | ) | — | — | (203,336 | ) | — | — | — | (218,630 | ) | — | — | (218,630 | ) | ||||||||||||||||||||||||||
Direct service costs | (152,280 | ) | (67,835 | ) | (51,732 | ) | (24,901 | ) | (54,874 | ) | — | (351,622 | ) | |||||||||||||||||||||||||||||||
Other operating expenses | — | — | — | — | — | (114,088 | ) | (114,088 | ) | |||||||||||||||||||||||||||||||||||
Direct service costs and other | (156,278 | ) | (67,577 | ) | (67,672 | ) | (26,368 | ) | (124,312 | ) | (124,375 | ) | (566,582 | ) | ||||||||||||||||||||||||||||||
Stock compensation expense(1) | 953 | 690 | 1,260 | 5,383 | 27 | 11,469 | 19,782 | 714 | 714 | 1,485 | 424 | 74 | 11,691 | 15,102 | ||||||||||||||||||||||||||||||
Segment profit (loss) | $ | 147,542 | $ | 86,824 | $ | 49,187 | $ | 36,891 | $ | 9,412 | $ | (102,619 | ) | $ | 227,237 | $ | 131,542 | $ | 128,451 | $ | 89,402 | $ | 26,072 | $ | 28,362 | $ | (112,684 | ) | $ | 291,145 | ||||||||||||||
| | Commercial | Public Sector | Radiology Benefits Management | Specialty Pharmaceutical Management | Medicaid Administration | Corporate and Elimination | Consolidated | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Year Ended December 31, 2011 | ||||||||||||||||||||||
Managed care and other revenue | $ | 561,780 | $ | 1,459,659 | $ | 344,335 | $ | 48,534 | $ | 220,453 | $ | (82,770 | ) | $ | 2,551,991 | |||||||
Dispensing revenue | — | — | — | 247,409 | — | — | 247,409 | |||||||||||||||
Cost of care | (314,178 | ) | (1,271,532 | ) | (205,240 | ) | — | (76,544 | ) | 82,770 | (1,784,724 | ) | ||||||||||
Cost of goods sold | — | — | — | (232,038 | ) | — | — | (232,038 | ) | |||||||||||||
Direct service costs and other | (152,760 | ) | (67,227 | ) | (61,681 | ) | (24,344 | ) | (103,254 | ) | (120,368 | ) | (529,634 | ) | ||||||||
Stock compensation expense(1) | 839 | 872 | 1,563 | 693 | 124 | 13,327 | 17,418 | |||||||||||||||
Segment profit (loss) | $ | 95,681 | $ | 121,772 | $ | 78,977 | $ | 40,254 | $ | 40,779 | $ | (107,041 | ) | $ | 270,422 | |||||||
| | Commercial | Public Sector | Radiology Benefits Management | Specialty Pharmaceutical Management | Medicaid Administration | Corporate and Elimination | Consolidated | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Year Ended December 31, 2010 | ||||||||||||||||||||||
Net revenue | $ | 652,221 | $ | 1,442,093 | $ | 454,105 | $ | 270,646 | $ | 176,283 | $ | (26,108 | ) | $ | 2,969,240 | |||||||
Cost of care | (365,115 | ) | (1,246,779 | ) | (298,516 | ) | — | (23,683 | ) | 26,108 | (1,907,985 | ) | ||||||||||
Cost of goods sold | — | — | — | (218,630 | ) | — | — | (218,630 | ) | |||||||||||||
Direct service costs | (156,278 | ) | (67,577 | ) | (67,672 | ) | (26,368 | ) | (124,312 | ) | — | (442,207 | ) | |||||||||
Other operating expenses | — | — | — | — | — | (124,375 | ) | (124,375 | ) | |||||||||||||
Stock compensation expense(1) | 714 | 714 | 1,485 | 424 | 74 | 11,691 | 15,102 | |||||||||||||||
Segment profit (loss) | $ | 131,542 | $ | 128,451 | $ | 89,402 | $ | 26,072 | $ | 28,362 | $ | (112,684 | ) | $ | 291,145 | |||||||
| | Commercial | Public Sector | Radiology Benefits Management | Specialty Pharmaceutical Management | Medicaid Administration | Corporate and Elimination | Consolidated | Commercial | Public Sector | Radiology Benefits Management | Specialty Pharmaceutical Management | Medicaid Administration | Corporate and Elimination | Consolidated | ||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Year Ended December 31, 2011 | ||||||||||||||||||||||||||||||||||||||||||||
Net revenue | $ | 561,780 | $ | 1,459,659 | $ | 344,335 | $ | 295,943 | $ | 220,453 | $ | (82,770 | ) | $ | 2,799,400 | |||||||||||||||||||||||||||||
Year Ended December 31, 2012 | ||||||||||||||||||||||||||||||||||||||||||||
Managed care and other revenue | $ | 728,512 | $ | 1,620,875 | $ | 349,133 | $ | 55,178 | $ | 172,491 | $ | (69,090 | ) | $ | 2,857,099 | |||||||||||||||||||||||||||||
Dispensing revenue | — | — | — | 350,298 | — | — | 350,298 | |||||||||||||||||||||||||||||||||||||
Cost of care | (314,178 | ) | (1,271,532 | ) | (205,240 | ) | — | (76,544 | ) | 82,770 | (1,784,724 | ) | (437,518 | ) | (1,413,320 | ) | (228,383 | ) | — | (61,759 | ) | 69,090 | (2,071,890 | ) | ||||||||||||||||||||
Cost of goods sold | — | — | — | (232,038 | ) | — | — | (232,038 | ) | — | — | — | (328,414 | ) | — | — | (328,414 | ) | ||||||||||||||||||||||||||
Direct service costs | (152,760 | ) | (67,227 | ) | (61,681 | ) | (24,344 | ) | (103,254 | ) | — | (409,266 | ) | |||||||||||||||||||||||||||||||
Other operating expenses | — | — | — | — | — | (120,368 | ) | (120,368 | ) | |||||||||||||||||||||||||||||||||||
Direct service costs and other | (172,035 | ) | (89,129 | ) | (55,418 | ) | (26,709 | ) | (84,884 | ) | (129,337 | ) | (557,512 | ) | ||||||||||||||||||||||||||||||
Stock compensation expense(1) | 839 | 872 | 1,563 | 693 | 124 | 13,327 | 17,418 | 532 | 1,111 | 1,567 | 672 | 335 | 13,566 | 17,783 | ||||||||||||||||||||||||||||||
Segment profit (loss) | $ | 95,681 | $ | 121,772 | $ | 78,977 | $ | 40,254 | $ | 40,779 | $ | (107,041 | ) | $ | 270,422 | $ | 119,491 | $ | 119,537 | $ | 66,899 | $ | 51,025 | $ | 26,183 | $ | (115,771 | ) | $ | 267,364 | ||||||||||||||
�� The following table reconciles Segment Profit to consolidated income before income taxes for the years ended December 31, 2009, 2010, 2011 and 20112012 (in thousands):
| | 2009 | 2010 | 2011 | 2010 | 2011 | 2012 | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Segment Profit | $ | 227,237 | $ | 291,145 | $ | 270,422 | $ | 291,145 | $ | 270,422 | $ | 267,364 | ||||||||
Stock compensation expense | (19,782 | ) | (15,102 | ) | (17,418 | ) | (15,102 | ) | (17,418 | ) | (17,783 | ) | ||||||||
Depreciation and amortization | (47,268 | ) | (54,682 | ) | (58,623 | ) | (54,682 | ) | (58,623 | ) | (60,488 | ) | ||||||||
Interest expense | (2,424 | ) | (2,233 | ) | (2,502 | ) | (2,233 | ) | (2,502 | ) | (2,247 | ) | ||||||||
Interest income | 6,245 | 3,275 | 2,781 | 3,275 | 2,781 | 2,019 | ||||||||||||||
Income before income taxes | $ | 164,008 | $ | 222,403 | $ | 194,660 | $ | 222,403 | $ | 194,660 | $ | 188,865 | ||||||||
Year ended December 31, 2012 ("2012") compared to the year ended December 31, 2011 ("2011")
Commercial
Revenue
Revenue related to Commercial increased by 29.7 percent or $166.7 million from 2011 to 2012. The increase in revenue is mainly due to new contracts implemented after 2011 of $149.8 million, favorable rate changes of $29.7 million, and higher performance-based revenue recorded in 2012 of $10.5 million ($5.9 million relating to the prior year), which increases were partially offset by favorable retroactive membership and rate adjustments recorded in 2011 of $8.6 million, program changes of $6.4 million, terminated contracts of $3.3 million, retroactive risk share adjustments recorded in 2012 of $1.6 million, net decreased membership from existing customers of $1.4 million, and other net decreases of $2.0 million.
Cost of Care
Cost of care increased by 39.3 percent or $123.3 million from 2011 to 2012. The increase in cost of care is primarily due to new contracts implemented after 2011 of $115.5 million and unfavorable care trends and other net variances of $24.2 million, which increases were partially offset by program changes of $6.2 million, favorable medical claims development for 2011 which was recorded after 2011 of $3.7 million, favorable prior period medical claims development recorded in 2012 of $3.8 million, and net decreased membership from existing customers of $2.7 million. Cost of care increased as a percentage of risk revenue (excluding EAP business) from 77.0 in 2011 to 78.0 percent in 2012, mainly due to unfavorable care trends in excess of rate increases and changes in business mix.
Direct Service Costs
Direct service costs increased by 12.6 percent or $19.3 million from 2011 to 2012. The increase in direct service costs is mainly due to costs to support new contracts. Direct service costs decreased as a percentage of revenue from 27.2 percent in 2011 to 23.6 percent in 2012, mainly due to changes in business mix.
Public Sector
Revenue
Revenue related to Public Sector increased by 11.0 percent or $161.2 million from 2011 to 2012. This increase is primarily due to new contracts implemented after 2011 of $177.4 million, unfavorable retroactive contract funding adjustments in 2011 of $12.6 million, timing of incentive revenue for 2012 of $5.8 million, and the revenue impact for favorable prior period medical claims development recorded in 2011 of $2.0 million. The revenue increases were partially offset by unfavorable rate changes and program funding of $23.0 million, retroactive incentive revenue recorded in 2011 of $6.8 million, 2011 incentive revenue recorded in 2011 of $5.2 million, and net decreased membership from existing customers of $1.6 million.
Cost of Care
Cost of care increased by 11.2 percent or $141.8 million from 2011 to 2012. This increase is primarily due to new contracts implemented after 2011 of $132.4 million, care associated with retroactive contract funding changes in 2011 of $14.4 million, favorable prior period medical claims development recorded in 2011 of $2.3 million, and unfavorable care trends and other net variances of $20.8 million, which increases were partially offset by care associated with rate changes for contracts with minimum care requirements of $25.9 million, and favorable contractual settlements of $2.2 million in 2012. Cost of care increased as a percentage of risk revenue from 87.5 percent in 2011 to
88.7 percent in 2012, mainly due to unfavorable rate changes, unfavorable care trends, and changes in business mix.
Direct Service Costs
Direct service costs increased by 32.6 percent or $21.9 million from 2011 to 2012, mainly due to costs to support new contracts. Direct service costs increased as a percentage of revenue from 4.6 percent for 2011 to 5.5 percent in 2012 mainly due to rate decreases and changes in business mix.
Radiology Benefits Management
Revenue
Revenue related to Radiology Benefits Management increased by 1.4 percent or $4.8 million from 2011 to 2012. This increase is primarily due to the net impact of new contracts implemented after (or during) 2011 of $54.3 million, favorable contractual settlements of $4.4 million in 2012, and program changes of $2.9 million which increases were partially offset by decreased membership from terminated contracts and existing customers of $39.7 million, unfavorable rate changes of $14.5 million, and other net unfavorable variances of $2.6 million.
Cost of Care
Cost of care increased by 11.3 percent or $23.1 million from 2011 to 2012. This increase is primarily attributed to new contracts implemented after (or during) 2011 of $38.4 million, program changes of $2.9 million, and favorable prior period medical claims development recorded in 2011 of $3.1 million, which increases were partially offset by decreased membership from terminated contracts and existing customers of $18.3 million, favorable prior period medical claims development recorded in 2012 of $0.4 million, and care trends and other net favorable variances of $2.6 million. Cost of care increased as a percentage of risk revenue from 69.3 percent in 2011 to 74.0 percent in 2012 mainly due to unfavorable rate changes in excess of care trends and changes in business mix.
Direct Service Costs
Direct service costs decreased by 10.2 percent or $6.3 million from 2011 to 2012. The decrease in direct service costs is mainly attributable to terminated contracts. As a percentage of revenue, direct service costs decreased from 17.9 percent in 2011 to 15.9 percent in 2012, mainly due to changes in business mix.
Specialty Pharmaceutical Management
Revenue
Revenue related to Specialty Pharmaceutical Management increased by 37.0 percent or $109.5 million from 2011 to 2012. This increase is primarily due to net increased dispensing activity of $102.9 million (mainly due to increased business from new and existing customers), formulary optimization revenue of $6.0 million, retroactive revenue adjustments recorded in 2012 of $0.9 million, and medical pharmacy management revenue of $0.3 million. These increases were partially offset by other net decreases of $0.6 million.
Cost of Goods Sold
Cost of goods sold increased by 41.5 percent or $96.4 million from 2011 to 2012. This increase is primarily due to net increased dispensing activity. As a percentage of the portion of net revenue that relates to dispensing activity, cost of goods sold was 93.8 percent in 2012, which is consistent with 2011.
Direct Service Costs
Direct service costs increased by 9.7 percent or $2.4 million from 2011 to 2012. This increase is primarily due to costs to support increased business. As a percentage of revenue, direct service costs decreased from 8.2 percent in 2011 to 6.6 percent in 2012, mainly due to changes in business mix.
Medicaid Administration
Revenue
Revenue related to Medicaid Administration decreased by 21.8 percent or $48.0 million from 2011 to 2012. This decrease is primarily due to terminated contracts of $28.8 million, decreased pharmacy revenue of $5.1 million, decreased revenue due to lower cost of care associated with the subcontract with Public Sector of $13.7 million, and other net decreases of $0.4 million. The terminated contracts are associated with the Company's decision to exit the fiscal agent services ("FAS") market, with the Company's last FAS contract terminating in late 2011.
Cost of Care
Cost of care decreased by 19.3 percent or $14.8 million from 2011 to 2012. This decrease is primarily due to favorable care trends. Cost of care decreased as a percentage of risk revenue from 92.5 percent in 2011 to 89.4 percent in 2012, mainly due to favorable care trends.
Direct Service Costs
Direct service costs decreased by 17.8 percent or $18.4 million. This decrease was primarily due to terminated contracts. As a percentage of revenue, direct service costs increased from 46.8 percent in 2011 to 49.2 percent in 2012, mainly due to changes in business mix.
Corporate and Other
Other Operating Expenses
Other operating expenses related to the Corporate and Other Segment increased by 7.5 percent or $9.0 million from 2011 to 2012. The increase results primarily from an increase in costs of $10.6 million related to our growth initiatives, partially offset by other net unfavorable variances of $1.6 million. As a percentage of total net revenue, other operating expenses were 4.0 percent for 2012, which decreased slightly from 2011.
Depreciation and Amortization
Depreciation and amortization expense increased by 3.2 percent or $1.9 million from 2011 to 2012, primarily due to asset additions after 2011.
Interest Expense
Interest expense decreased by $0.3 million from 2011 to 2012.
Interest Income
Interest income decreased by $0.8 million from 2011 to 2012, mainly due to lower yields.
Income Taxes
The Company's effective income tax rate was 33.4 percent in 2011 and 20.0 percent in 2012. These rates differ from the federal statutory income tax rate primarily due to state income taxes, permanent
differences between book and tax income, and changes to recorded tax contingencies. The Company also accrues interest and penalties related to unrecognized tax benefits in its provision for income taxes. The effective income tax rate for 2012 is lower than 2011 mainly due to more significant reversals of tax contingencies in 2012 as a result of closure of federal and state statutes of limitations.
The statutes of limitations regarding the assessment of federal and certain state and local income taxes for 2008 expired during 2012. As a result, $43.3 million of unrecognized tax benefits recorded as of December 31, 2011 were reversed in 2012 as a result of statute expirations, of which $35.7 million is reflected as an adjustment to income tax expense, $6.2 million as an increase to additional paid-in capital, and the remainder as a decrease to deferred tax assets. Additionally, $1.4 million of accrued interest and $0.8 million of unrecognized state tax benefits were reversed in 2012 and reflected as reductions to income tax expense due to the closing of statutes of limitations on tax assessments and changes in tax return elections, respectively.
The statutes of limitations regarding the assessment of federal and certain state and local income taxes for 2007 closed during 2011. As a result, $15.0 million of unrecognized tax benefits recorded as of December 31, 2010 were reversed in 2011, of which $10.4 million was reflected as a reduction to income tax expense, $2.5 million as an increase to additional paid-in capital, and the remainder as a decrease to deferred tax assets. Additionally, $2.2 million of accrued interest was reversed in 2011 and reflected as a reduction to income tax expense due to these statute closings.
2011 compared to the year ended December 31, 2010 ("2010")
Commercial
Net Revenue
Net revenueRevenue related to Commercial decreased by 13.9 percent or $90.4 million from 2010 to 2011. The decrease in revenue is mainly due to program changes of $94.6 million, terminated contracts of $57.8 million, net decreased membership from existing customers of $12.9 million, and other net unfavorable variances of $0.4 million, which decreases were partially offset by new contracts implemented after (or during) 2010 of $42.5 million, favorable rate changes of $22.9 million, favorable retroactive membership and rate adjustments recorded in 2011 of $8.6 million, and unfavorable retroactive rate adjustments recorded in 2010 of $1.3 million.
Cost of Care
Cost of care decreased by 14.0 percent or $50.9 million from 2010 to 2011. The decrease in cost of care is primarily due to program changes of $92.8 million, terminated contracts of $11.2 million, and decreased membership from existing customers of $7.0 million, which decreases were partially offset by new business of $36.5 million, favorable prior period medical claims development recorded in 2010 of $2.7 million, and care trends and other net variances of $20.9 million. Cost of care decreased as a percentage of risk revenue (excluding EAP business) from 77.6 percent in 2010 to 77.0 percent in 2011, mainly due to changes in business mix.
Direct Service Costs
Direct service costs decreased by 2.3 percent or $3.5 million from 2010 to 2011. The decrease in direct service costs is mainly attributable to one-time severance charges in 2010 of $2.0 million associated with terminated contracts. Direct service costs increased as a percentage of revenue from 24.0 percent in 2010 to 27.2 percent in 2011, mainly due to changes in business mix.
Public Sector
Net Revenue
Net revenueRevenue related to Public Sector increased by 1.2 percent or $17.6 million from 2010 to 2011. This increase is primarily due to increased membership from existing customers of $68.6 million, retroactive incentive revenue recorded in 2011 of $6.8 million, timing of incentive revenue for 2011 of $5.2 million, and other net increases of $2.5 million, which increases were partially offset by unfavorable rate and funding changes of $34.1 million, the recognition in 2010 of $12.5 million of previously deferred revenue on the Maricopa Contract, unfavorable retroactive contract funding adjustments recorded in 2011 of $12.6 million, the revenue impact for favorable prior period medical claims development for 2010 which was recorded after 2010 of $4.3 million, and the revenue impact for favorable prior period medical claims development recorded in 2011 of $2.0 million.
Cost of Care
Cost of care increased by 2.0 percent or $24.8 million from 2010 to the 2011. This increase is primarily due to increased membership from existing customers of $61.8 million, favorable prior period medical claims development recorded in 2010 of $7.1 million, and care trends and other net unfavorable variances of $1.5 million, which increases were partially offset by care associated with rate changes for contracts with minimum care requirements of $24.9 million, care associated with retroactive contract funding adjustments of $14.4 million, favorable prior period medical claims development for 2010 which was recorded after 2010 of $4.0 million, and favorable prior period medical claims development recorded in 2011 of $2.3 million. Cost of care increased as a percentage of risk revenue
from 86.8 percent in 2010 to 87.5 percent in 2011, mainly due to the net impact of care development between years.
Direct Service Costs
Direct service costs decreased by 0.5 percent or $0.4 million from 2010 to 2011. Direct service costs as a percentage of revenue was 4.6 percent in 2011, which is consistent with 2010.
Radiology Benefits Management
Net Revenue
Net revenueRevenue related to Radiology Benefits Management decreased by 24.2 percent or $109.8 million from 2010 to 2011. This decrease is primarily due to terminated contracts of $188.4 million and decreased membership from existing customers of $5.1 million. These decreases were partially offset by new contracts implemented after (or during) 2010 of $34.9 million, program changes of $31.3 million, favorable rate changes of $10.4 million, and other net increases of $7.1 million.
Cost of Care
Cost of care decreased by 31.2 percent or $93.3 million from 2010 to 2011. This decrease is primarily attributed to terminated contracts of $135.4 million, favorable prior period medical claims development recorded in 2011 of $3.1 million, favorable medical claims development for 2010 which was recorded after 2010 of $2.8 million, decreased membership from existing customers of $2.4 million, and care trends and other net variances of $13.1 million. These decreases were partially offset by new contracts implemented after (or during) 2010 of $31.0 million, program changes of $30.5 million, and favorable prior period medical claims development recorded in 2010 of $2.0 million. Cost of care decreased as a percentage of risk revenue from 74.0 percent in 2010 to 69.3 percent in 2011 mainly due to net favorable care trends and development, and changes in business mix.
Direct Service Costs
Direct service costs decreased by 8.9 percent or $6.0 million from 2010 to 2011. The decrease in direct service costs is mainly attributable to terminated contracts. As a percentage of revenue, direct service costs increased from 14.9 percent in 2010 to 17.9 percent in 2011, mainly due to changes in business mix.
Specialty Pharmaceutical Management
Net Revenue
Net revenueRevenue related to Specialty Pharmaceutical Management increased by 9.3 percent or $25.3 million from 2010 to 2011. This increase is primarily due to net increased dispensing activity of $13.2$12.6 million, formulary optimization revenue of $7.6 million, and medical pharmacy management revenue of $5.7 million, which increases were partially offset by other net decreases of $1.2$0.6 million.
Cost of Goods Sold
Cost of goods sold increased by 6.1 percent or $13.4 million from 2010 to 2011. This increase is primarily due to net increased dispensing activity. As a percentage of the portion of net revenue that relates to dispensing activity, cost of goods sold increased from 93.1 percent in 2010 to 93.8 percent in 2011, mainly due to changes in business mix.
Direct Service Costs
Direct service costs decreased by 7.7 percent or $2.0 million from 2010 to 2011. This decrease is primarily due to decreased employee compensation and benefits. As a percentage of revenue, direct service costs decreased from 9.7 percent in 2010 to 8.2 percent in 2011, mainly due to decreased employee compensation and benefits, and changes in business mix.
Medicaid Administration
Net Revenue
Net revenueRevenue related to Medicaid Administration increased by 25.1 percent or $44.2 million from 2010 to 2011. This increase is primarily due to a subcontract with Public Sector for Medicaid Administration to provide pharmacy benefits management services on a risk basis for one of Public Sector's customers which started September 1, 2010, partially offset by terminated contracts.
Cost of Care
Cost of care increased by 223.2 percent or $52.9 million from 2010 to 2011. This increase is attributed to the subcontract with Public Sector. Cost of care increased as a percentage of risk revenue from 90.7 percent in 2010 to 92.5 percent in 2011, mainly due to unfavorable care trends.
Direct Service Costs
Direct service costs decreased by 16.9 percent or $21.1 million. This decrease was primarily due to terminated contracts and operating efficiencies. As a percentage of revenue, direct service costs decreased from 70.5 percent in 2010 to 46.8 percent in 2011, mainly due to changes in business mix, including the new risk-based subcontract discussed above.
Corporate and Other
Other Operating Expenses
Other operating expenses related to the Corporate and Other Segment decreased by 3.2 percent or $4.0 million from 2010 to 2011. The decrease results primarily from net one-time unfavorable adjustments recorded in 2010 of $4.8 million, partially offset by other net unfavorable variances of $0.8 million. As a percentage of total net revenue, other operating expenses were 4.3 percent for 2011, which is consistent with 2010.
Depreciation and Amortization
Depreciation and amortization expense increased by 7.2 percent or $3.9 million from 2010 to 2011, primarily due to asset additions after 2010.
Interest Expense
Interest expense increased by $0.3 million from 2010 to 2011, mainly due to the acceleration of deferred loan costs associated with the 2010 Credit Facility.
Interest Income
Interest income decreased by $0.5 million from 2010 to 2011, mainly due to lower yields.
Income Taxes
The Company's effective income tax rate was 37.7 percent in 2010 and 33.4 percent in 2011. These rates differ from the federal statutory income tax rate primarily due to state income taxes, permanent differences between book and tax income, and changes to recorded tax contingencies. The Company also accrues interest and penalties related to unrecognized tax benefits in its provision for income taxes. The effective income tax rate for 2011 iswas lower than 2010 mainly due to more significant reversals of tax contingencies in 2011 as a result of closure of federal and state statutes of limitations.
The statutes of limitation regarding the assessment of federal and certain state and local income taxes for the year ended December 31, 2007 expired during 2011. With few exceptions, the Company is no longer subject to state or local income tax assessments by tax authorities for years ended prior to December 31, 2008. As a result, $15.0 million of unrecognized tax benefits (excluding interest costs) recorded as of December 31, 2010 were reversed in the current year as a result of statute expirations,2011, of which $10.4 million iswas reflected as an adjustment to income tax expense, $2.5 million as an increase to additional paid-in capital, and the remainder as a decrease to deferred tax assets.
2010 compared to the year ended December 31, 2009 ("2009")
Commercial
Net Revenue
Net revenue related to the Commercial segment increased by 0.3 percent or $2.1 million from 2009 to 2010. The increase in revenue is mainly due to revenue from new contracts implemented after 2009 of $22.2 million and favorable rate changes of $17.9 million, which increases were partially offset by terminated contracts of $28.5 million, the favorable impact of contractual settlements in 2009 of $5.7 million, unfavorable retroactive rate adjustments of $1.3 million recorded in 2010, and other net unfavorable variances of $2.5 million.
Cost of Care
Cost of care increased by 3.9 percent or $13.8 million from 2009 to 2010. The increase in cost of care is primarily due to new contracts implemented after 2009 of $14.1 million, the impact of favorable contractual settlements recorded in 2009 of $2.7 million, favorable prior period medical claims development recorded in 2009 of $2.5 million, and care trends and other net unfavorable variances of $12.8 million, which increases were partially offset by terminated contracts of $12.9 million, favorable prior period medical claims development recorded in 2010 of $2.7 million, and favorable medical claims development for 2009 which was recorded in 2010 of $2.7 million. Cost of care as a percentage of risk revenue (excluding EAP revenue) increased from 76.4 percent in 2009 to 77.6 percent in 2010, mainly due to unfavorable care trends and business mix.
Direct Service Costs
Direct service costs increased by 2.6 percent or $4.0 million from 2009 to 2010. The increase in direct service costs is mainly attributable to one-time severance charges in 2010 of $2.0 million associated with terminated contracts and increased employee compensation and benefits. Direct service costs increased as a percentage of revenue from 23.4 percent in 2009 to 24.0 percent in 2010, mainly due to one-time severance charges in 2010 and changes in business mix.
Public Sector
Net Revenue
Net revenue related to Public Sector increased by 5.8 percent or $79.7 million from 2009 to 2010. This increase is primarily due to increased membership from existing customers of $125.3 million, $19.3 million related to the recognition in 2010 of previously deferred revenue on the Maricopa Contract as well as the lack of deferral of revenue for the current contract year due to a change in contractual provisions, the revenue impact for out of period care development pertaining to 2009 of $3.2 million, and other net favorable variances of $24.0 million, which increases were partially offset by terminated contracts of $38.6 million, net unfavorable rate changes of $37.2 million, and the recognition in 2009 of $16.3 million of deferred revenue on the Maricopa Contract.
Cost of Care
Cost of care increased by 3.2 percent or $38.3 million from 2009 to 2010. This increase is primarily due to increased membership from existing customers of $107.5 million, favorable prior period medical claims development recorded in 2009 of $2.6 million, and care trends and other net unfavorable variances of $5.9 million, which increases were partially offset by terminated contracts of $35.0 million, lower care associated with rate changes for contracts with minimum care requirements recorded in 2010 of $27.6 million, favorable medical claims development for 2009 which was recorded in 2010 of $8.0 million, and favorable prior period medical claims development recorded in 2010 of $7.1 million. Cost of care decreased as a percentage of risk revenue from 89.1 percent in 2009 to 86.8 percent in 2010 mainly due to business mix and net favorable care development.
Direct Service Costs
Direct service costs decreased by 0.4 percent or $0.3 million from 2009 to 2010. The decrease in direct service costs is primarily due to terminated contracts, partially offset by staffing required to support certain contracts. As a percentage of revenue, direct service costs decreased from 5.0 percent in 2009 to 4.7 percent in 2010 mainly due to changes in business mix.
Radiology Benefits Management
Net Revenue
Net revenue related to the Radiology Benefits Management segment increased by 48.8 percent or $148.9 million from 2009 to 2010. This increase is primarily due to revenue from new contracts implemented after 2009 (or during) of $155.9 million and favorable rate changes of $21.8 million, which increases were partially offset by decreased membership from existing customers of $18.3 million, favorable retroactive membership, rate, and contractual settlements recorded in 2009 of $2.4 million, terminated contracts of $1.7 million, and other net decreases of $6.4 million.
Cost of Care
Cost of care increased by 45.2 percent or $92.9 million from 2009 to 2010. This increase is primarily attributed to new contracts implemented after 2009 (or during) of $113.8 million, favorable contractual settlements recorded in 2009 of $4.7 million, and favorable prior period medical claims development recorded in 2009 of $0.8 million, which increases were partially offset by decreased membership from existing customers of $19.1 million, favorable medical claims development for 2009 which was recorded in 2010 of $2.1 million, favorable prior period medical claims development recorded in 2010 of $2.0 million, and care trends and other net favorable variances of $3.2 million. Cost of care decreased as a percentage of risk revenue from 80.8 percent in 2009 to 74.0 percent in 2010 mainly due to rate increases and business mix.
Direct Service Costs
Direct service costs increased 30.8 percent or $15.9 million from 2009 to 2010. The increase in direct service costs is mainly attributable to increased employee compensation and benefits, and costs associated with new business. As a percentage of revenue, direct service costs decreased from 16.9 percent in 2009 to 14.9 percent in 2010, mainly due to business mix.
Specialty Pharmaceutical Management
Net Revenue
Net revenue related to the Specialty Pharmaceutical Management segment increased 4.2 percent or $10.9 million from 2009 to 2010. This increase is primarily due to net increased dispensing activity from new and existing customers of $13.7 million, which increase was partially offset by other net decreases of $2.8 million.
Cost of Cost of Goods Sold
Cost of goods sold increased 7.5 percent or $15.3 million from 2009 to 2010, primarily due to net increased dispensing activity from new and existing customers. As a percentage of the portion of net revenue that relates to dispensing revenue, cost of goods sold increased from 91.8 percent in 2009 to 93.1 percent in 2010, mainly due to business mix.
Direct Service Costs
Direct service costs increased by 5.9 percent or $1.5 million from 2009 to 2010. This increase is primarily due to increased employee compensation and benefits, and expenses to support the development of new products, partially offset by a reduction in stock compensation expense. As a percentage of revenue, direct service costs increased slightly from 9.6 percent in 2009 to 9.7 percent in 2010.
Medicaid Administration
Net Revenue
Net revenue related to Medicaid Administration increased 174.3 percent or $112.0 million from 2009 to the 2010. This increase is primarily the result of the inclusion of only five months of operating results in 2009 due to the closing of the acquisition of First Health Services on July 31, 2009.
Cost of Care
Cost of care in 2010 of $23.7 million is attributed to a subcontract with Public Sector for Medicaid Administration to provide pharmacy benefits management services on a risk basis for one of Public Sector's customers starting September 1, 2010.
Direct Service Costs
Direct service costs increased 126.5 percent or $69.4 million from 2009 to 2010. This increase is primarily the result of the inclusion of only five months of operating results in 2009 due to the closing of the acquisition of First Health Services on July 31, 2009. As a percentage of revenue, direct service costs decreased from 85.4 percent in 2009 to 70.5 percent in 2010, mainly due to changes in business mix, including the new risk based subcontract discussed above.
Corporate
Other Operating Expenses
Other operating expenses related to the Corporate and Other segment increased by 9.0 percent or $10.3 million from 2009 to 2010. The increase results primarily from net one-time unfavorable adjustments recorded in 2010 of $4.8 million, unfavorable employee benefit and termination costs of $4.2 million, and other net increases of $2.7 million, which increases were partially offset by one-time acquisition-related expenses incurred in 2009 of $1.4 million. As a percentage of total net revenue, other operating expenses decreased slightly from 4.3 percent for 2009 to 4.2 percent for 2010, mainly due to business mix.
Depreciation and Amortization
Depreciation and amortization expense increased by 15.7 percent or $7.4 million from 2009 to 2010, primarily due to asset additions after (or during) 2009 (inclusive of assets related to the acquisition of First Health Services).
Interest Expense
Interest expense decreased by 7.9 percent or $0.2 million from 2009 to 2010, mainly due to lower costs associated with the 2010 Credit Facility.
Interest Income
Interest income decreased by 47.6 percent or $3.0 million from 2009 to 2010, mainly due to lower yields.
Income Taxes
The Company's effective income tax rate was 35.0 percent in 2009 and 37.7 percent in 2010. The 2009 and 2010 effective income tax rates differ from the federal statutory income tax rate primarily due to state income taxes and permanent differences between book and tax income. The Company also accrues interest related to unrecognized tax benefits in its provision for income taxes. The effective income tax rate in 2010 is higher than 2009 mainly due to more significant reversals in 2009 of valuation allowances on deferred state taxes and tax contingencies due to closure of statutes of limitation.
Outlook—Results of Operations
The Company's Segment Profit and net income are subject to significant fluctuations from period to period. These fluctuations may result from a variety of factors such as those set forth under Item 1A—"Risk Factors" as well as a variety of other factors including: (i) changes in utilization levels by enrolled members of the Company's risk-based contracts, including seasonal utilization patterns; (ii) contractual adjustments and settlements; (iii) retrospective membership adjustments; (iv) timing of implementation of new contracts, enrollment changes and contract terminations; (v) pricing adjustments upon contract renewals (and price competition in general); and (vi) changes in estimates regarding medical costs and IBNR.
A portion of the Company's business is subject to rising care costs due to an increase in the number and frequency of covered members seeking behavioral healthcare or radiology services, and higher costs per inpatient day or outpatient visit for behavioral services, and higher costs per scan for radiology services. Many of these factors are beyond the Company's control. Future results of
operations will be heavily dependent on management's ability to obtain customer rate increases that are consistent with care cost increases and/or to reduce operating expenses.
In relation to the managed behavioral healthcare business, the Company is a market leader in a mature market with many viable competitors. The Company is continuing its attempts to grow its business in the managed behavioral healthcare industry through aggressive marketing and development of new products; however, due to the maturity of the market, the Company believes that the ability to grow its current business lines may be limited. In addition, as previously discussed, substantially all of the Company's Commercial segment revenues are derived from Blue Cross Blue Shield health plans and other managed care companies, health insurers and health plans. In the past, certain of the managed care customers of the Company have decided not to renew all or part of their contracts with the Company, and to instead manage the behavioral healthcare services directly for their subscribers.
Care Trends. The Company expects that same-store normalized cost of care trend for the 12 month forward outlook to be 7 to 9 percent for Commercial, 1 to 3 percent for Public Sector and 4 to 6 percent for Radiology Benefits Management.
Interest Rate Risk. Changes in interest rates affect interest income earned on the Company's cash equivalents and investments, as well as interest expense on variable interest rate borrowings under the Company's 2011 Credit Facility. Based on the amount of cash equivalents and investments and the borrowing levels under the 2011 Credit Facility as of December 31, 2011,2012, a hypothetical 10 percent increase or decrease in the interest rate associated with these instruments, with all other variables held constant, would not materially affect the Company's future earnings and cash outflows.
Historical—Liquidity and Capital Resources
2012 compared to 2011
Operating Activities. The Company reported net cash provided by operating activities of $112.0 million and $181.3 million for 2011 and 2012, respectively. The $69.3 million increase in operating cash flows from 2011 to 2012 is primarily attributable to the net shift of restricted funds between cash and investments, which results in an operating cash flow change that is directly offset by an investing cash flow change, as well as the net favorable impact of working capital changes between periods. Partially offsetting these items is a reduction in Segment Profit and increase in tax payments between years.
During 2011 and 2012, restricted investments of $62.3 million and $16.7 million, respectively, were shifted to restricted cash that reduced operating cash flows for both years, resulting in a net increase of operating cash flows between years of $45.6 million. The net favorable impact of working capital changes between years totaled $34.1 million, with $12.5 million of the change related to restricted cash requirements for the Company's regulated entities and $11.2 million of the change related to pharmaceutical inventory levels and the timing of the settlement of the associated inventory payables. In 2011 and 2012, the Company was required to restrict additional funds of $17.9 million and $5.4 million, respectively. Segment Profit for 2012 decreased $3.1 million from 2011. Tax payments for 2012 totaled $57.7 million, which is an increase of $7.3 million from 2011.
During 2012, the Company's restricted cash increased $40.8 million. The change is attributable to the shift of restricted investments of $16.7 million to restricted cash, net increases in restricted cash of $24.3 million related to the Company's regulated entities, partially offset by other net decreases of $0.2 million. The net change in restricted cash for the Company's regulated entities is attributable to an increase in restricted cash of $18.9 million that is offset by changes in other assets and liabilities, primarily accounts receivable, accrued liabilities, medical claims payable and other medical liabilities, thus having no impact on operating cash flows, and a net increase of $5.4 million in restricted cash requirements that resulted in an operating cash flow use.
Investing Activities. The Company utilized $54.4 million and $69.5 million during 2011 and 2012, respectively, for capital expenditures. The additions related to hard assets (equipment, furniture, leaseholds) and capitalized software for 2011 were $25.4 million and $29.0 million, respectively, as compared to additions for 2012 related to hard assets and capitalized software of $31.7 million and $37.9 million, respectively. In addition, during 2011 the Company received net cash of $71.0 million from the net maturity of "available for sale" securities, with the Company using net cash during 2012 of $39.8 million for the net purchase of "available for sale" securities. During 2011, the Company purchased provider network contracts for $1.3 million that resulted in the establishment of an intangible asset. In addition, during 2011, the Company received the final working capital settlement of $0.9 million from Coventry in regards to the Company's acquisition of First Health. In 2012, the Company contributed $1.2 million of capital to Fallon Total Care, LLC, with the Company owning a 49.0 percent interest in the entity.
Financing Activities. During 2011, the Company paid $407.6 million for the repurchase of treasury stock under the Company's share repurchase program and paid $0.6 million for capital lease obligations. In addition, the Company received $20.0 million under a share purchase agreement pursuant to which Blue Shield of California purchased shares of the Company's common stock, received $41.8 million from the exercise of stock options and warrants, and had other net favorable items of $0.8 million.
During 2012, the Company paid $21.9 million for the repurchase of treasury stock under the Company's share repurchase program. In addition, the Company received $20.5 million from the exercise of stock options and had other net favorable items of $0.3 million.
2011 compared to 2010
Operating Activities. The Company reported net cash provided by operating activities of $308.9 million and $112.0 million for 2010 and 2011, respectively. The $196.9 million decrease in operating cash flows from 2010 to 2011 is primarily attributable to the decrease in Segment Profit, the net shift of restricted funds between cash and investments that results in an operating cash flow change that is directly offset by an investing cash flow change, and other net unfavorable items primarily associated with working capital changes, partially offset by a reduction in tax payments.
Segment Profit for 2011 decreased $20.7 million from 2010. During 2010, $36.7 million of restricted cash was shifted to restricted investments as compared to 2011, in which $62.3 million of restricted investments were shifted to restricted cash, resulting in a net decrease in operating cash flows between periods of $99.0 million. Operating cash flows for 2010 were impacted by net favorable working capital changes of $42.9 million as compared to net unfavorable working capital changes of $45.8 million 2011. The favorable working capital changes for 2010 were largely attributable to the build-up of medical claims payable for Radiology Benefits Management associated with new risk business and other items due to timing. The unfavorable working capital changes for 2011 were largely attributable to the increase in inventory associated with Specialty Pharmaceutical Management and the increase in restricted cash related to the Company's regulated entities to comply with capital requirements. Tax payments for 2011 totaled $50.3 million, which is a reduction of $11.5 million from 2010.
During 2011, the Company's restricted cash increased $69.1 million. The change is attributable to the shift of restricted investments of $62.3 million to restricted cash, net increases in restricted cash of $19.1 million related to the Company's regulated entities and other net increases of $0.6 million, partially offset by the release of restricted cash of $12.9 million associated with a previously terminated customer contract. The increase in restricted cash for the Company's regulated entities is primarily due to increased capital requirements associated with the award of a new contract.
Investing Activities. The Company utilized $46.2 million and $54.4 million during 2010 and 2011, respectively, for capital expenditures. The additions related to hard assets (equipment, furniture, leaseholds) and capitalized software for 2010 were $23.2 million and $23.0 million, respectively, as compared to additions for 2011 related to hard assets and capitalized software of $25.4 million and $29.0 million, respectively. During 2010, the Company used net cash of $64.3 million for the net purchase of "available for sale" securities, with the Company receiving net cash of $71.0 million during 2011 from the net maturity of "available for sale" investments. During 2011, the Company purchased provider network contracts for $1.3 million that resulted in the establishment of an intangible asset. In addition, during 2011 the Company received the final working capital settlement of $0.9 million from Coventry in relationship to the Company's acquisition of First Health.
Financing Activities. During 2010, the Company paid $149.8 million for the repurchase of treasury stock under the Company's share repurchase program, and paid $1.1 million related to capital lease obligations. In addition, the Company received $92.9 million from the exercise of stock options and warrants and had other net favorable items of $0.2 million.
During 2011, the Company paid $407.6 million for the repurchase of treasury stock under the Company's share repurchase program and paid $0.6 million related to capital lease obligations. In addition, the Company received $20.0 million under a share purchase agreement pursuant to which Blue Shield of California purchased shares of the Company's common stock, received $41.8 million from the exercise of stock options and warrants, and had other net favorable items of $0.8 million.
2010 compared to 2009
Operating Activities. The Company reported net cash provided by operating activities of $218.6 million and $308.9 million for 2009 and 2010, respectively. Both years were positively impacted by the shift of restricted funds between cash and investments that resulted in operating cash flow sources directly offset by investing cash flow uses, with $38.5 million and $36.7 million of restricted cash shifted to restricted investments in 2009 and 2010, respectively. The $90.3 million increase in operating cash flows from 2009 to 2010 is primarily attributable to the increase in Segment Profit and net favorable working capital changes between years largely related to growth in the Company's business segments (including the build of medical claims payable balances and other contract liabilities associated with new contracts), partially offset by higher tax payments. Segment Profit for 2010 increased $63.9 million compared to 2009. Net favorable year over year working capital changes were primarily attributable to the build of medical claims payable balances and other contract liabilities associated with new contracts. Tax payments in 2010 were $45.3 million higher than 2009, mostly due to the Company's utilization of the majority of its NOLs prior to 2010.
During 2010, the Company's restricted cash decreased $42.9 million. The decrease is attributable to a reduction in restricted cash of $4.1 million associated with the Company's regulated entities, the shift of restricted cash to restricted investments of $36.7 million and other net decreases of $2.1 million. In regards to the decrease in restricted cash for the Company's regulated entities, $11.8 million is offset by changes in other assets and liabilities, primarily accounts receivable, accrued liabilities, medical claims payable and other medical liabilities, thus having no impact on operating cash flows. Partially offsetting these net reductions is the net funding of $7.7 million in additional restricted cash associated with the Company's regulated entities.
Investing Activities. The Company utilized $33.2 million and $46.2 million during 2009 and 2010, respectively, for capital expenditures. The majority of the increase in capital expenditures of $13.0 million is attributable to management information systems and related equipment, with significant current year expenditures related to the Medicaid Administration segment. The Company also used cash of $0.8 million and $64.3 million for the net purchase of "available-for-sale" investments during 2009 and 2010, respectively. During 2009, the Company paid $115.4 million for the acquisition of First
Health Services, excluding cash acquired of $2.0 million but including payment of $7.4 million for excess working capital.
Financing Activities. During 2009, the Company paid $89.7 million for the repurchase of treasury stock under the Company's share repurchase program. In addition, the Company received $2.6 million from the exercise of stock options and warrants and had other net favorable items of $2.7 million.
During 2010, the Company paid $149.8 million for the repurchase of treasury stock under the Company's share repurchase program, and paid $1.1 million related to capital lease obligations. In addition, the Company received $92.9 million from the exercise of stock options and warrants and had other net favorable items of $0.8 million.
Outlook—Liquidity and Capital Resources
Liquidity. During 2012,2013, the Company expects to fund its estimated capital expenditures of $61$52 to $71$62 million with cash from operations. The Company does not anticipate that it will need to draw on amounts available under the 2011 Credit Facility for cash flow needs related to its operations, capital needs or debt service in 2012.2013. The Company also currently expects to have adequate liquidity to satisfy its existing financial commitments over the periods in which they will become due. The Company plans to maintain its current investment strategy of investing in a diversified, high quality, liquid portfolio of investments and continues to closely monitor the situation in the financial markets. The Company estimates that it has no risk of any material permanent loss on its investment portfolio; however, there can be no assurance that the Company will not experience any such losses in the future.
Contractual Obligations and Commitments
The following table sets forth the future financial commitments of the Company as of the December 31, 20112012 (in thousands):
| | Payments due by period | Payments due by period | ||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Contractual Obligations | Total | Less than 1 year | 1-3 years | 3-5 years | More than 5 years | Total | Less than 1 year | 1 - 3 years | 3 - 5 years | More than 5 years | ||||||||||||||||||||||
Operating leases(1) | $ | 59,770 | $ | 17,878 | $ | 25,445 | $ | 16,447 | $ | — | $ | 71,223 | $ | 14,266 | $ | 31,623 | $ | 13,906 | $ | 11,428 | ||||||||||||
Letters of credit(2) | 68,109 | — | — | — | — | 31,952 | — | — | — | — | ||||||||||||||||||||||
Purchase commitments(3) | 621 | 621 | — | — | — | 1,501 | 1,501 | — | — | — | ||||||||||||||||||||||
Tax contingency reserves(4) | 99,230 | 1,482 | — | — | — | 56,601 | 384 | — | — | — | ||||||||||||||||||||||
| $ | 227,730 | $ | 19,981 | $ | 25,445 | $ | 16,447 | $ | — | $ | 161,277 | $ | 16,151 | $ | 31,623 | $ | 13,906 | $ | 11,428 | |||||||||||||
In addition to the contractual obligations and commitments discussed above, the Company has a variety of other contractual agreements related to acquiring materials and services used in the Company's operations. However, the Company does not believe these other agreements contain material noncancelable commitments.
Stock Repurchases
On July 30, 2008 theThe Company's board of directors approvedhas previously authorized a series of stock repurchase plan which authorized the Company to purchase up to $200 million of its outstanding common stock through January 31, 2010.plans. Stock repurchases under the programfor each such plan could be executed through open market repurchases, privately negotiated transactions, accelerated share repurchases or other means. The board of directors authorized management to execute stock repurchase transactions under the program from time to time and in such amounts and via such methods as management deemed appropriate. TheEach stock repurchase program could be limited or terminated at any time without prior notice. Pursuant to this program, the Company made open market purchases of 3,866,505 shares of the Company's common stock at an aggregate cost of $136.0 million (excluding broker commissions) during the year ended December 31, 2008 and made open market purchases of 1,859,959 shares of the Company's common stock at an average share price of $34.39 per share for an aggregate cost of $64.0 million (excluding broker commissions) during the period January 1, 2009 through April 7, 2009, which was the date that the repurchase program was completed.
On July 28, 2009 the Company's board of directors approved a stock repurchase plan which authorized the Company to purchase up to $100 million of its outstanding common stock through July 28, 2011. Stock repurchases under the program could be executed through open market repurchases, privately negotiated transactions, accelerated share repurchases or other means. The board of directors authorized management to execute stock repurchase transactions under the program from time to time and in such amounts and via such methods as management deemed appropriate. The stock repurchase program could be limited or terminated at any time without prior notice. Pursuant to this program, the Company made open market purchases of 782,400 shares of the Company's common stock at an average price of $32.75 per share for an aggregate cost of $25.6 million (excluding broker commissions) during the period from August 17, 2009 through December 31, 2009. Pursuant to this program, the Company made open market purchases of 1,711,881 shares of the Company's common stock at an average price of $43.46 per share for an aggregate cost of $74.4 million (excluding broker commissions) during the period January 1, 2010 through April 1, 2010, which was the date that the repurchase program was completed.
On July 27, 2010 the Company's board of directors approved a stock repurchase plan which authorized the Company to purchase up to $350 million of its outstanding common stock through July 28, 2012. On February 18, 2011, the Company's board of directors increased the stock repurchase program by an additional $100 million. Stock repurchases under the program could be executed through open market repurchases, privately negotiated transactions, accelerated share repurchases or other means. The boardmillion, to a total of directors authorized management to execute stock repurchase transactions from time to time and in such amounts and via such methods as management deemed appropriate. The stock repurchase program could be limited or terminated at any time without prior notice.$450 million. Pursuant to this program, the Company made open market purchases of 1,684,510 shares of the Company's common stock at an average price of $48.36 per share for an aggregate cost of $81.5 million (excluding broker commissions) during the period from November 3, 2010 through December 31, 2010. Pursuant to this program, the Company made open market purchases of 7,534,766 shares of the Company's common stock at an average price of $48.91 per share for an aggregate cost of $368.5 million (excluding broker commissions) during the period January 1, 2011 through November 10, 2011, which was the date the repurchase program was completed.
On October 25, 2011 the Company's board of directors approved a stock repurchase plan which authorizesauthorized the Company to purchase up to $200 million of its outstanding common stock through October 25, 2013. Stock repurchases under the program may be executed through open market repurchases, privately negotiated transactions, accelerated share repurchases or other means. The board of directors authorized management to execute stock repurchase transactions from time to time and in such amounts and via such methods as management deems appropriate. The stock repurchase program may be limited or terminated at any time without prior notice. Pursuant to this program, the Company made open market purchases of 671,776 shares of the Company's common stock at an average price of $48.72 per share for an aggregate cost of $32.7 million (excluding broker commissions) during the period from November 11, 2011 through December 31, 2011.
The Pursuant to this program, the Company made noopen market purchases of 459,252 shares of the Company's common stock at an average price of $50.27 per share repurchasesfor an aggregate cost of $23.1 million (excluding broker commissions) during 2012.
During the period from January 1, 20122013 through February 23, 2012.22, 2013, the Company made additional open market purchases of 366,650 shares of the Company's common stock at an aggregate cost of $18.6 million (excluding broker commissions).
Recent Sales of Unregistered Securities
On January 28, 2011, the Company and Blue Shield of California ("Blue Shield") entered into a Share Purchase Agreement (the "Share Purchase Agreement") pursuant to which on January 31, 2011 Blue Shield purchased 416,840 shares of the Company's common stock (the "Shares") for a total purchase price of $20 million. The Shares were issued to Blue Shield, an accredited investor, in a private placement pursuant to Regulation D of the Securities Act. Blue Shield has agreed not to transfer such Shares for a two year period, except in the event of any change in control of the Company as defined in the Share Purchase Agreement. The purchase price for the Shares issued was determined taking into account the recent trading price of the Company's common stock on NASDAQ and the restrictions on transfer of the Shares agreed to by Blue Shield.
Off-Balance Sheet Arrangements. As of December 31, 2011,2012, the Company has no material off-balance sheet arrangements.
2011 Credit Facility. On December 9, 2011, the Company entered into a Senior Secured Revolving Credit Facility Credit Agreement with Citibank, N.A., Wells Fargo Bank, N.A., Bank of America, N.A., and U.S. Bank, N.A. that provides for up to $230.0 million of revolving loans with a sublimit of up to $70.0 million for the issuance of letters of credit for the account of the Company (the "2011 Credit Facility"). The 2011 Credit Facility is guaranteed by substantially all of the subsidiaries of the Company and is secured by substantially all of the assets of the Company and the subsidiary guarantors. The 2011 Credit Facility will mature on December 9, 2014.
Under the 2011 Credit Facility, the annual interest rate on Revolving Loan borrowings is equal to (i) in the case of U.S. dollar denominated loans, the sum of a borrowing margin of 1.000.75 percent plus the higher of the prime rate, one-half of one percent in excess of the overnight "federal funds" rate, or the Eurodollar rate for one month plus 1.00%,1.00 percent, or (ii) in the case of Eurodollar denominated loans, the sum of a borrowing margin of 2.001.75 percent plus the Eurodollar rate for the selected interest period. The Company has the option to borrow in U.S. dollar denominated loans or Eurodollar denominated loans at its discretion. Letters of Credit issued under the Revolving Loan Commitment bear interest at the rate of 2.1251.875 percent. The commitment commission on the 2011 Credit Facility is 0.375 percent of the unused Revolving Loan Commitment.
Restrictive Covenants in Debt Agreements. The 2011 Credit Facility contains covenants that limit management's discretion in operating the Company's business by restricting or limiting the Company's ability, among other things, to:
These restrictions could adversely affect the Company's ability to finance future operations or capital needs or engage in other business activities that may be in the Company's interest.
The 2011 Credit Facility also requires the Company to comply with specified financial ratios and tests. Failure to do so, unless waived by the lenders under the 2011 Credit Facility, pursuant to its terms, would result in an event of default under the 2011 Credit Facility. As of December 31, 2011,2012, the Company was in compliance with all covenants, including financial covenants, under the 2011 Credit Facility.
Although the 2011 Credit Facility expires on December 9, 2014, the Company believes it will be able to obtain a new facility or, if not, to use cash on hand to fund letters of credit and other liquidity needs.
Net Operating Loss Carryforwards. The Company has federal NOLs as of December 31, 20112012 of approximately $4.8$4.2 million available to reduce future federal taxable income. These NOLs, if not used, expire in 2017 through 2019 and are subject to examination and adjustment by the IRS. In addition, the Company's utilizationUtilization of suchthese NOLs is also subject to limitation under Section 382, which affects thecertain timing of the use of these NOLs. At this time,limitations, although the Company does not believe these limitations will limit the Company'srestrict its ability to use any federal NOLs before they expire.
As of December 31, 2011,2012, the Company's valuation allowances against deferred tax assets were $3.4$3.1 million, mostly relating to uncertainties regarding the eventual realization of certain state NOLs. Determination of the amount of deferred tax assets considered realizable requires significant judgment and estimation regarding the forecasts of future taxable income which are consistent with the plans and estimates the Company uses to manage the underlying businesses. Changes in these estimatesFuture changes in the futureestimated realizable portion of deferred taxes could materially affect the Company's financial condition and results of operations.
Recent Accounting Pronouncements
In January 2010,May 2011, the Financial Accounting Standards Board ("FASB") issued Accounting Standards Update ("ASU"), No. 2010-24, "Health Care Entities—Presentation of Insurance Claims2011-04, "Fair Value Measurement (Topic 820): Amendments to Achieve Common Fair Value Measurement and Related Insurance Recoveries"Disclosure Requirements in U.S. GAAP and IFRSs", ("ASU 2010-24"2011-04"). ASU 2010-24 clarifies that a health care entity should not net insurance recoveries against a related claim liability. Additionally, the amount of the claim liability2011-04 amends ASC Topic 820, "Fair Value Measurements and Disclosures", to provide guidance on how fair value measurement should be determined without consideration of insurance recoveries. This guidance isapplied where existing GAAP already requires or permits fair value measurements. In addition, ASU 2011-04 requires expanded disclosures regarding fair value measurements. ASU 2011-04 became effective for fiscal years beginning after December 15, 2010. Accordingly, the Company adopted ASU 2010-24 on January 1, 2011.2012. The adoption of this standardASU 2011-04 did not have a material impact on the Company's consolidated results of operations, financial statements.position or cash flows.
In June 2011, the FASB issued ASU No. 2011-05, "Comprehensive Income (Topic 220): Presentation of Comprehensive Income" ("ASU 2011-05"). ASU 2011-05 requires an entity to present the total of comprehensive income, the components of net income, and the components of other comprehensive income either in a single continuous statement of comprehensive income or in two separate but consecutive statements and eliminates the option to present the components of other comprehensive income as part of the statement of equity. ASU 2011-05 is effective for fiscal years, and interim periods within those fiscal years, beginning on or after December 15, 2011, with early adoption
permitted. While the adoption of this guidance is expected to impactimpacts the Company's disclosures for annual and interim filings for the year ending December 31, 2012, it willdid not have an impact on the Company's consolidated results of operations, financial position, or cash flows.
In July 2011, the FASB issued ASU No. 2011-06, "Other Expenses (Topic 720): Fees Paid to the Federal Government by Health Insurers (a consensus of the FASB Emerging Issues Task Force)" ("ASU 2011-06"), which addresses how fees mandated by the Patient Protection and Affordable Care Act, as amended by the Health Care and Education Reconciliation Act of 2010 (collectively, the
"Health Reform Law"), should be recognized and classified in the income statements of health insurers. The Health Reform Law imposes a mandatory annual fee on health insurers for each calendar year beginning on or after January 1, 2014. ASU 2011-06 stipulates that the liability incurred for that fee be amortized to expense over the calendar year in which it is payable. This ASU is effective for calendar years beginning after December 31, 2013, when the fee initially becomes effective. The adoption of ASU 2011-06 is not expected to significantly impact the Company's consolidated results of operations, financial condition.position, or cash flows.
In September 2011, the FASB issued ASU 2011-08, "Testing Goodwill for Impairment" ("ASU 2011-8"), which provides authoritative guidance to simplify how entities, both public and nonpublic, test goodwill for impairment. This accounting update permits an entity to first assess qualitative factors to determine whether it is more likely than not that the fair value of a reporting unit is less than its carrying amount as a basis for determining whether it is necessary to perform the two-step goodwill impairment test. This guidance will bewas effective for the Company beginning on January 1, 2012, with early adoption permitted.2012; however the Company did not elect to use the qualitative screen for any reporting units in 2012. The Company doesguidance did not expect the guidance to impact the Company's financial position,consolidated results of operations, financial position, or cash flows.
In December 2011, the FASB issued ASU 2011-12, "Deferral of the Effective Date for Amendments to the Presentation of Reclassifications of Items Out of Accumulated Other Comprehensive Income in ASU 2011-05" ("ASU 2011-12"), which defers the requirement that companies present reclassification adjustments for each component of accumulated other comprehensive income in both net income and other comprehensive income on the face of the financial statements. The effective dates for ASU 2011-12 are consistent with the effective dates for ASU 2011-05 and, similar to our expectations for the adoption of ASU 2011-05, while the adoption of this guidance is expected to impactimpacts the Company's disclosures for annual and interim filings for the year ending December 31, 2012, it willdid not have an impact on the Company's consolidated results of operations, financial position or cash flows.
In October 2012, the FASB issued ASU 2012-04, "Technical Corrections and Improvements" ("ASC 2012-04"). The amendments in this update cover a wide range of Topics in the Accounting Standards Codification. These amendments include technical corrections and improvements to the Accounting Standards Codification and conforming amendments related to fair value measurements. The amendments in this guidance that will not have transition guidance are effective upon issuance. The amendments that are subject to transition guidance are effective for fiscal periods beginning after December 15, 2012. The guidance did not impact the Company's consolidated results of operations, financial condition.position, or cash flows.
Item 7A. Quantitative and Qualitative Disclosures about Market Risk
Changes in interest rates affect interest income earned on the Company's cash equivalents and restricted cash and investments, as well as interest expense on variable interest rate borrowings under the 2011 Credit Facility. Based on the Company's investment balances, and the borrowing levels under the 2011 Credit Facility as of December 31, 2011,2012, a hypothetical 10 percent increase or decrease in the interest rate associated with these instruments, with all other variables held constant, would not materially affect the Company's future earnings and cash outflows.
Item 8. Financial Statements and Supplementary Data
Information with respect to this item is contained in the Company's consolidated financial statements, including the reports of independent accountants, set forth elsewhere herein and financial statement schedule indicated in the Index on Page F-1 of this Report on Form 10-K, and is included herein.
Item 9. Changes in and Disagreements with Accountants on Accounting and Financial Disclosure
None.
Item 9A. Controls and Procedures
EVALUATION OF DISCLOSURE CONTROLS AND PROCEDURES
The Company's management evaluated, with the participation of the Company's principal executive and principal financial officers, the effectiveness of the Company's disclosure controls and procedures (as defined in Rules 13a-15(e) and 15d-15(e) under the Securities Exchange Act of 1934, as amended (the "Exchange Act")), as of December 31, 2011.2012. Based on their evaluation, management has concluded that the Company's disclosure controls and procedures were effective as of December 31, 2011.
Table of Contents2012.
CHANGES IN INTERNAL CONTROL OVER FINANCIAL REPORTING
In the fourth quarter ended December 31, 2011,2012, there have been no changes in the Company's internal controls over financial reporting that have materially affected, or are reasonably likely to materially affect, the Company's internal controls over financial reporting.
MANAGEMENT'S REPORT ON INTERNAL CONTROL OVER FINANCIAL REPORTING
The Company's management is responsible for establishing and maintaining adequate internal control over financial reporting (as defined in Rule 13a-15(f) under the Securities Exchange Act of 1934, as amended). The Company's internal control system was designed to provide reasonable assurance regarding the preparation and fair presentation of published financial statements. Because of its inherent limitations, internal control over financial reporting may not prevent or detect misstatements. Also, projections of any evaluation of effectiveness to future periods are subject to the risk that controls may become inadequate because of changes in conditions, or that the degree of compliance with the policies or procedures may deteriorate. Under the supervision and with the participation of management, including the Company's Chief Executive Officer and Chief Financial Officer, the Company assessed the effectiveness of internal control over financial reporting as of December 31, 2011.2012. In making this assessment, management used the criteria set forth by the Committee of Sponsoring Organizations of the Treadway Commission ("COSO") in its statement "Internal Control-Integrated Framework."
Based on this assessment, management has concluded that, as of December 31, 2011,2012, internal control over financial reporting is effective based on these criteria.
The Company's independent registered public accounting firm has issued an audit report on the Company's internal control over financial reporting. This report dated February 28, 20122013 appears on page 6266 of this Form 10-K.
Report of Independent Registered Public Accounting Firm
The Board of Directors and Stockholders of Magellan Health Services, Inc.
We have audited Magellan Health Services, Inc.'s (the "Company") internal control over financial reporting as of December 31, 2011,2012, based on criteria established in Internal Control—Integrated Framework issued by the Committee of Sponsoring Organizations of the Treadway Commission (the "COSO criteria"). The Company's management is responsible for maintaining effective internal control over financial reporting, and for its assessment of the effectiveness of internal control over financial reporting included in the accompanying Management's Report on Internal Control over Financial Reporting. Our responsibility is to express an opinion on the Company's internal control over financial reporting based on our audit.
We conducted our audit in accordance with the standards of the Public Company Accounting Oversight Board (United States). Those standards require that we plan and perform the audit to obtain reasonable assurance about whether effective internal control over financial reporting was maintained in all material respects. Our audit included obtaining an understanding of internal control over financial reporting, assessing the risk that a material weakness exists, testing and evaluating the design and operating effectiveness of internal control based on the assessed risk, and performing such other procedures as we considered necessary in the circumstances. We believe that our audit provides a reasonable basis for our opinion.
A company's internal control over financial reporting is a process designed to provide reasonable assurance regarding the reliability of financial reporting and the preparation of financial statements for external purposes in accordance with generally accepted accounting principles. A company's internal control over financial reporting includes those policies and procedures that (1) pertain to the maintenance of records that, in reasonable detail, accurately and fairly reflect the transactions and dispositions of the assets of the company; (2) provide reasonable assurance that transactions are recorded as necessary to permit preparation of financial statements in accordance with generally accepted accounting principles, and that receipts and expenditures of the company are being made only in accordance with authorizations of management and directors of the company; and (3) provide reasonable assurance regarding prevention or timely detection of unauthorized acquisition, use, or disposition of the company's assets that could have a material effect on the financial statements.
Because of its inherent limitations, internal control over financial reporting may not prevent or detect misstatements. Also, projections of any evaluation of effectiveness to future periods are subject to the risk that controls may become inadequate because of changes in conditions, or that the degree of compliance with the policies or procedures may deteriorate.
In our opinion, the Company maintained, in all material respects, effective internal control over financial reporting as of December 31, 2011,2012, based on the COSO criteria.
We also have audited, in accordance with the standards of the Public Company Accounting Oversight Board (United States), the consolidated balance sheets of Magellan Health Services, Inc. as of December 31, 20102011 and 2011,2012, and the related consolidated statements of comprehensive income, changes in stockholders' equity, and cash flows for each of the three years in the period ended December 31, 20112012 of Magellan Health Services, Inc. and our report dated February 28, 20122013 expressed an unqualified opinion thereon.
/s/ERNST & YOUNG LLP
Baltimore, Maryland
February 28, 20122013
The information required by Items 10 through 14 is incorporated by reference to the Registrant's definitive proxy statement to be filed pursuant to Regulation 14A under the Securities Exchange Act of 1934, as amended, within 120 days after December 31, 2011,2012, except for the following information required by Item 12 of this Part III.
Securities Authorized for Issuance under Equity Compensation Plans
The following table sets forth certain information as of December 31, 20112012 with respect to the Company's compensation plans under which equity securities are authorized for issuance:
Plan category | Number of securities to be issued upon exercise of outstanding options, warrants and rights | Weighted average exercise price of outstanding options, warrants and rights | Number of securitie remaining available for future issuance under equity compensation plans (excluding securities reflected in column(a)) | Number of securities to be issued upon exercise of outstanding options, warrants and rights | Weighted average exercise price of outstanding options, warrants and rights | Number of securities remaining available for future issuance under equity compensation plans (excluding securities reflected in column(a)) | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| | (a) | | | (a) | | | ||||||||||||||
Equity compensation plans approved by security holders | 3,841,233 | $ | 42.65 | 4,886,385 | (1) | 4,268,240 | $ | 44.35 | 3,734,703 | (1) | ||||||||||
Equity compensation plans not approved by security holders | — | — | — | — | — | — | ||||||||||||||
Total | 3,841,233 | $ | 42.65 | 4,886,385 | (1) | 4,268,240 | $ | 44.35 | 3,734,703 | (1) | ||||||||||
For further discussion, see Note 6—"Stockholders' Equity" to the consolidated financial statements set forth elsewhere herein.
Item 15. Exhibits, Financial Statement Schedule and Additional Information
(a) Documents furnished as part of the Report:
1. Financial Statements
Information with respect to this item is contained on Pages F-1 to F-44 of this Report on Form 10-K.
2. Financial Statement Schedule
Information with respect to this item is contained on page S-1 of this Report on Form 10-K.
3. Exhibits
| Exhibit No. | Description of Exhibit | ||
|---|---|---|---|
| 2.1 | |||
Share Purchase Agreement between Magellan Health Services, Inc. and California Physicians' Service D/B/A Blue Shield of California, dated January 28, 2011, which was filed as Exhibit 2.3 to the Company's Annual Report on Form 10-K for the year ended December 31, 2010, which was | |||
3.1 | Bylaws of the company, which were filed as Exhibit 3.1 to the Company's Quarterly Report on Form 10-Q for the quarterly period ended March 31, 2008, which was filed on May 2, 2008, and is incorporated herein by reference. | ||
3.2 | Amended and Restated Certificate of Incorporation of the Company, which was filed as Exhibit 3.2 to the Company's Annual Report on Form 10-K for the period ended December 31, 2004, which was filed on March 30, 2004, and is incorporated herein by reference. | ||
4.1 | Credit Agreement, dated | ||
*10.1 | Magellan Health Services, Inc.—2003 Management Incentive Plan, effective as of January 5, 2004, which was filed as Exhibit 2.14 to the Company's current report on Form 8-K, which was filed on January 6, 2004, and is incorporated herein by reference. | ||
*10.2 | Magellan Health Services, Inc.—2005 Director Stock Compensation Plan, effective as of March 3, 2005, which was filed as Appendix B to the Company's definitive proxy statement, filed on April 18, 2005, and is incorporated herein by reference. | ||
*10.3 | Form of Stock Option Agreement, relating to options granted under the Company's 2003 Management Incentive Plan, which was filed as Exhibit 10.1 to the Company's current report on Form 8-K, which was filed on March 17, 2005, and is incorporated herein by reference. | ||
*10.4 | |||
| Form of First Amendment to Stock Option Agreement, relating to options granted under the Company's 2003 Management Incentive Plan, which was filed as Exhibit 10.1 to the Company's current report on Form 8-K, which was filed on January 9, 2006, and is incorporated herein by reference. | |||
*10.5 | Form of Notice of March 2005 Stock Option Grant, relating to options granted under the Company's 2003 Management Incentive Plan, which was filed as Exhibit 10.2 to the Company's current report on Form 8-K, which was filed on March 17, 2005, and is incorporated herein by reference. | ||
*10.6 | Form of Restricted Stock Agreement, relating to restricted shares granted under the Company's 2003 Management Incentive Plan, which was filed as Exhibit 10.3 to the Company's current report on Form 8-K, which was filed on March 17, 2005, and is incorporated herein by reference. | ||
*10.7 | Form of Notice of March 2005 Restricted Stock Award, relating to restricted shares granted under the Company's 2003 Management Incentive Plan, which was filed as Exhibit 10.4 to the Company's current report on Form 8-K, which was filed on March 17, 2005, and is incorporated herein by reference. | ||
| Exhibit No. | Description of Exhibit | ||
|---|---|---|---|
* | First form of Notice of Amendment of Stock Option Grant, relating to options granted under the Company's 2003 Management Incentive Plan and dated as of January 3, 2006, between the Company and Steven J. Shulman, Chief Executive Officer of the Company, Rene Lerer, Chief Operating Officer of the Company, and Mark S. Demilio, Chief Financial Officer of the Company, which was filed as Exhibit 10.2 to the Company's current report on Form 8-K, which was filed on January 9, 2006, and is incorporated herein by reference. | ||
* | Second form of Notice of Stock Option Grant, relating to options granted under the Company's 2003 Management Incentive Plan and dated as of January 5, 2004, between the Company and Steven J. Shulman, Chief Executive Officer of the Company, Rene Lerer, Chief Operating Officer of the Company, and Mark S. Demilio, Chief Financial Officer of the Company, which was filed as Exhibit 10.6 to the Company's current report on Form 8-K, which was filed on March 17, 2005, and is incorporated herein by reference. | ||
* | Second form of Notice of Amendment of Stock Option Grant, relating to options granted under the Company's 2003 Management Incentive Plan and dated as of January 3, 2006, between the Company and Steven J. Shulman, Chief Executive Officer of the Company, Rene Lerer, Chief Operating Officer of the Company, and Mark S. Demilio, Chief Financial Officer of the Company, which was filed as Exhibit 10.3 to the Company's current report on Form 8-K, which was filed on January 9, 2006, and is incorporated herein by reference. | ||
*10.11 | |||
| Third form of Notice of Stock Option Grant, relating to options granted under the Company's 2003 Management Incentive Plan and dated as of January 5, 2004, between the Company and Steven J. Shulman, Chief Executive Officer of the Company, Rene Lerer, Chief Operating Officer of the Company, and Mark S. Demilio, Chief Financial Officer of the Company, which was filed as Exhibit 10.7 to the Company's current report on Form 8-K, which was filed on March 17, 2005, and is incorporated herein by reference. | |||
* | Third form of Notice of Amendment of Stock Option Grant, relating to options granted under the Company's 2003 Management Incentive Plan and dated as of January 3, 2006, between the Company and Steven J. Shulman, Chief Executive Officer of the Company, Rene Lerer, Chief Operating Officer of the Company, and Mark S. Demilio, Chief Financial Officer of the Company, which was filed as Exhibit 10.4 to the Company's current report on Form 8-K, which was filed on January 9, 2006, and is incorporated herein by reference. | ||
* | Form of Notice of Restricted Stock Award, relating to restricted shares granted under the Company's 2003 Management Incentive Plan and dated as of January 5, 2004, between the Company and Steven J. Shulman, Chief Executive Officer of the Company, Rene Lerer, Chief Operating Officer of the Company and Mark S. Demilio, Chief Financial Officer of the Company, which was filed as Exhibit 10.8 to the Company's current report on Form 8-K, which was filed on March 17, 2005, and is incorporated herein by reference. | ||
* | Notice of Restricted Stock Award, relating to restricted shares granted under the Company's 2003 Management Incentive Plan and dated as of January 5, 2004, between the Company and Steven J. Shulman, Chief Executive Officer of the Company, which was filed as Exhibit 10.9 to the Company's current report on Form 8-K, which was filed on March 17, 2005, and is incorporated herein by reference. | ||
| Exhibit No. | Description of Exhibit | ||
|---|---|---|---|
| *10.15 | Supplemental Accumulation Plan, adopted in 2002, which was filed as Exhibit 10.10 to the Company's current report on Form 8-K, which was filed on March 17, 2005, and is incorporated herein by reference. | ||
* | Form of Stock Option Agreement, relating to the 2006 Management Incentive Plan, which was filed as Exhibit 10.1 to the Company's current report on Form 8-K, which was filed on May 22, 2006, and is incorporated herein by reference. | ||
* | Form of Notice of Stock Option Grant, pursuant to the 2006 Management Incentive Plan, which was filed as Exhibit 10.2 to the Company's current report on Form 8-K, which was filed on May 22, 2006, and is incorporated herein by reference. | ||
* | Form of Restricted Stock Unit Agreement, pursuant to the 2006 Management Incentive Plan, which was filed as Exhibit 10.3 to the Company's current report on Form 8-K, which was filed on May 22, 2006, and is incorporated herein by reference. | ||
* | Form of Notice of Restricted Stock Unit Award, pursuant to the 2006 Management Incentive Plan, which was filed as Exhibit 10.4 to the Company's current report on Form 8-K, which was filed on May 22, 2006, and is incorporated herein by reference. | ||
* | Form of Restricted Stock and Stock Option Award Agreement, pursuant to the 2006 Director Equity Compensation Plan, which was filed as Exhibit 10.5 to the Company's current report on Form 8-K, which was filed on May 22, 2006, and is incorporated herein by reference. | ||
*10.21 | |||
| Magellan Health Services, Inc.—2006 Management Incentive Plan, effective as of May 16, 2006, which was filed as Exhibit 10.1 to the Company's Quarterly report on Form 10-Q for the quarterly period ended June 30, 2006, which was filed on July 28, 2006, and is incorporated herein by reference. | |||
* | Magellan Health Services, Inc.—2006 Director Equity Compensation Plan, effective as of May 16, 2006, which was filed as Exhibit 10.2 to the Company's Quarterly report on Form 10-Q for the quarterly period ended June 30, 2006, which was filed on July 28, 2006, and is incorporated herein by reference. | ||
* | Magellan Health Services, Inc.—2006 Employee Stock Purchase Plan, effective as of May 16, 2006 which was filed as Exhibit 10.3 to the Company's Quarterly report on Form 10-Q for the quarterly period ended June 30, 2006, which was filed on July 28, 2006, and is incorporated herein by reference. | ||
* | Amended and Restated Supplemental Accumulation Plan, effective as of January 1, 2005, which was filed as Exhibit 10.1 to the Company's Quarterly report on Form 10-Q for the quarter ended September 30, 2006, which was filed on October 26, 2006, and is incorporated herein by reference. | ||
* | Amendment to Employment Agreement, dated July 28, 2006, between the Company and Jeffrey N. West, Senior Vice President and Controller of the Company, which was filed as Exhibit 10.2 to the Company's Quarterly report on Form 10-Q for the quarter ended September 30, 2006, which was filed on October 26, 2006, and is incorporated herein by reference. | ||
* | Amendment to Agreements and Documents Governing Restricted Stock Units, dated December 1, 2008, between the Company and Rene Lerer, Chief Executive Officer which was filed as Exhibit 10.66 to the Company's Annual Report on Form 10-K, which was filed on February 29, 2008 and is incorporated herein by reference. | ||
| Exhibit No. | Description of Exhibit | ||
|---|---|---|---|
| *10.27 | Employment Agreement dated February 19, 2008 between the Company and Rene Lerer, M.D., which was filed as Exhibit 10.1 to the Company's current report on Form 8-K, which was filed on February 25, 2008 and is incorporated herein by reference. | ||
* | Employment Agreement, dated February 25, 2008, between the Company and Tina Blasi, which was filed as Exhibit 10.46 to the Company's Annual Report on Form 10-K, which was filed on February 29, 2008 and is incorporated herein by reference. | ||
* | Amendment to Employment Agreement, dated February 25, 2008, between the Company and Tina Blasi, which was filed as Exhibit 10.47 to the Company's Annual Report on Form 10-K, which was filed on February 29, 2008 and is incorporated herein by reference. | ||
* | Form of Stock Option Agreement, relating to options granted under the Company's 2008 Management Incentive Plan, which was filed as Exhibit 10.1 to the Company's current report on Form 8-K, which was filed on May 27, 2008 and is incorporated herein by reference. | ||
* | Form of Notice of March 2008 Stock Option Grant, relating to options granted under the Company's 2008 Management Incentive Plan, which was filed as Exhibit 10.2 to the Company's current report on Form 8-K, which was filed on May 27, 2008 and is incorporated herein by reference. | ||
*10.32 | |||
| Form of Restricted Stock Unit Agreement, relating to restricted stock units granted under the Company's 2008 Management Incentive Plan, which was filed as Exhibit 10.3 to the Company's current report on Form 8-K, which was filed on May 27, 2008 and is incorporated herein by reference. | |||
* | Form of Notice of Restricted Stock Unit Award, relating to restricted stock units granted under the Company's 2008 Management Incentive Plan, which was filed as Exhibit 10.4 to the Company's current report on Form 8-K, which was filed on May 27, 2008 and is incorporated herein by reference. | ||
* | Employment Agreement, dated August 11, 2008 between the Company and Jonathan Rubin, Chief Financial Officer, which was filed as Exhibit 10.1 to the Company's current report on Form 8-K, which was filed on August 13, 2008, and is incorporated herein by reference. | ||
* | Magellan Health Services, Inc.—2008 Management Incentive Plan, effective as of February 27, 2008, which was filed as Appendix A to the Company's Definitive Proxy Statement, which was filed on April 11, 2008, and is incorporated herein by reference. | ||
* | Amendment to Employment Agreement, dated December 1, 2008, between the Company and Jeffrey West, Senior Vice President and Controller which was filed as Exhibit 10.56 to the Company's Annual Report on Form 10-K, which was filed on February 29, 2008 and is incorporated herein by reference. | ||
* | Amendment to Employment Agreement, dated December 1, 2008, between the Company and Tina Blasi, Chief Executive Officer of National Imaging Associates, Inc. which was filed as Exhibit 10.57 to the Company's Annual Report on Form 10-K, which was filed on February 29, 2008 and is incorporated herein by reference. | ||
* | Amendment to Employment Agreement, dated December 1, 2008, between the Company and Daniel N. Gregoire, Executive Vice President, General Counsel and Secretary which was filed as Exhibit 10.58 to the Company's Annual Report on Form 10-K, which was filed on February 29, 2008 and is incorporated herein by reference. | ||
| Exhibit No. | Description of Exhibit | ||
|---|---|---|---|
| *10.39 | Amendment to Agreements and Documents Governing Restricted Stock Units, dated December 1, 2008, between the Company and Caskie Lewis-Clapper, Chief Human Resources Officer which was filed as Exhibit 10.61 to the Company's Annual Report on Form 10-K, which was filed on February 29, 2008 and is incorporated herein by reference. | ||
* | Amendment to Agreements and Documents Governing Restricted Stock Units, dated December 1, 2008, between the Company and Tina Blasi, Chief Executive Officer of National Imaging Associates, Inc. which was filed as Exhibit 10.62 to the Company's Annual Report on Form 10-K, which was filed on February 29, 2008 and is incorporated herein by reference. | ||
* | Amendment to Agreements and Documents Governing Restricted Stock Units, dated December 1, 2008, between the Company and Jeffrey West, Senior Vice President and Controller which was filed as Exhibit 10.63 to the Company's Annual Report on Form 10-K, which was filed on February 29, 2008 and is incorporated herein by reference. | ||
* | Amendment to Agreements and Documents Governing Restricted Stock Units, dated December 1, 2008, between the Company and Daniel N. Gregoire, Executive Vice President, General Counsel and Secretary which was filed as Exhibit 10.64 to the Company's Annual Report on Form 10-K, which was filed on February 29, 2008 and is incorporated herein by reference. | ||
*10.43 | |||
| Amendment to Employment Agreement, as amended and restated December 16, 2008, between the Company and Rene Lerer, M.D, Chief Executive Officer which was filed as Exhibit 10.65 to the Company's Annual Report on Form 10-K, which was filed on February 29, 2008 and is incorporated herein by reference. | |||
* | Amendment to Agreements and Documents Governing Restricted Stock Units, dated December 1, 2008, between the Company and Rene Lerer, Chief Executive Officer which was filed as Exhibit 10.66 to the Company's Annual Report on Form 10-K, which was filed on February 29, 2008 and is incorporated herein by reference. | ||
* | Form of Stock Option Agreement, relating to options granted under the Company's 2008 Management Incentive Plan, which was filed as Exhibit 10.1 to the Company's current report on Form 8-K, which was filed on May 4, 2009 and is incorporated herein by reference. | ||
* | Form of Notice of March 2008 Stock Option Grant, relating to options granted under the Company's 2008 Management Incentive Plan, which was filed as Exhibit 10.2 to the Company's current report on Form 8-K, which was filed on May 4, 2009 and is incorporated herein by reference. | ||
* | Form of Restricted Stock Unit Agreement, relating to restricted stock units granted under the Company's 2008 Management Incentive Plan, which was filed as Exhibit 10.3 to the Company's current report on Form 8-K, which was filed on May 4, 2009 and is incorporated herein by reference. | ||
* | Form of Notice of Restricted Stock Unit Award, relating to restricted stock units granted under the Company's 2008 Management Incentive Plan, which was filed as Exhibit 10.4 to the Company's current report on Form 8-K, which was filed on May 4, 2009 and is incorporated herein by reference. | ||
| Exhibit No. | Description of Exhibit | ||
|---|---|---|---|
| *10.49 | Employment Agreement, dated July 28, 2009 between Karen S. Rohan and Magellan Health Services, Inc., which was filed as Exhibit 10.1 to the Company's Quarterly Report on Form 10-Q for the quarterly period ended June 30, 2009, which was filed on July 31, 2009 and is incorporated herein by reference. | ||
* | Amendment to Employment Agreement, dated July 28, 2009 between Magellan Health Services, Inc. and Karen S. Rohan, which was filed as Exhibit 10.2 to the Company's Quarterly Report on Form 10-Q for the quarterly period ended June 30, 2009, which was filed on July 31, 2009 and is incorporated herein by reference. | ||
* | Form of Stock Option Agreement, relating to options granted under the Company's 2008 Management Incentive Plan, which was filed as Exhibit 10.1 to the Company's current report on Form 8-K, which was filed on March 5, 2010 and is incorporated herein by reference. | ||
* | Form of Notice of March 2008 Stock Option Grant, relating to options granted under the Company's 2008 Management Incentive Plan, which was filed as Exhibit 10.2 to the Company's current report on Form 8-K, which was filed on March 5, 2010 and is incorporated herein by reference. | ||
* | Form of Restricted Stock Unit Agreement, relating to restricted stock units granted under the Company's 2008 Management Incentive Plan, which was filed as Exhibit 10.3 to the Company's current report on Form 8-K, which was filed on March 5, 2010 and is incorporated herein by reference. | ||
*10.54 | Form of Notice of Restricted Stock Unit Award, relating to restricted stock units granted under the Company's 2008 Management Incentive Plan, which was filed as Exhibit 10.4 to the Company's current report on Form 8-K, which was filed on March 5, 2010 and is incorporated herein by reference. | ||||||
*10.55 | Form of Stock Option Agreement, relating to options granted under the Company's 2008 Management Incentive Plan, which was filed as Exhibit | ||||||
* | Form of Notice of Stock Option Grant, relating to options granted under the Company's 2008 Management Incentive Plan, which was filed as Exhibit 10.2 to the Company's current report on Form 8-K, which was filed on March 8, 2011 and is incorporated herein by reference. | ||||||
*10.57 | Form of Restricted Stock Unit Agreement, relating to restricted stock units granted under the Company's 2008 Management Incentive Plan, which was filed as Exhibit 10.3 to the Company's current report on Form 8-K, which was filed on March 8, 2011 and is incorporated herein by reference. | ||||||
*10.58 | Form of Notice of Restricted Stock Unit Award, relating to restricted stock units granted under the Company's 2008 Management Incentive Plan, which was filed as Exhibit 10.4 to the Company's current report on Form 8-K, which was filed on March 8, 2011 and is incorporated herein by reference. | ||||||
*10.59 | Magellan Health Services, Inc. 2011 Management Incentive Plan, effective as of May 18, 2011, which was filed as Appendix A to the Company's Definitive Proxy Statement, which was filed on April 8, 2011, and is incorporated herein by reference. | ||||||
| Exhibit No. | Description of Exhibit | ||
|---|---|---|---|
* | Magellan Health Services, Inc. 2011 Employee Stock Purchase Plan, effective as of May 18, 2011, which was filed as Appendix B to the Company's Definitive Proxy Statement, which was filed on April 8, 2011, and is incorporated herein by reference. | ||
*10.61 | Form of Stock Option Agreement, relating to options granted under the Company's 2011 Management Incentive Plan, which was filed as Exhibit 10.1 to the Company's current report on Form 8-K, which was filed on March 7, 2012 and is incorporated herein by reference. | ||
*10.62 | Form of Notice of Stock Option Grant, relating to options granted under the Company's 2011 Management Incentive Plan, which was filed as Exhibit 10.2 to the Company's current report on Form 8-K, which was filed on March 7, 2012 and is incorporated herein by reference. | ||
*10.63 | Form of Restricted Stock Unit Agreement, relating to restricted stock units granted under the Company's 2011 Management Incentive Plan, which was filed as Exhibit 10.3 to the Company's current report on Form 8-K, which was filed on March 7, 2012 and is incorporated herein by reference. | ||
*10.64 | Form of Notice of Restricted Stock Unit Award, relating to restricted stock units granted under the Company's 2011 Management Incentive Plan, which was filed as Exhibit 10.4 to the Company's current report on Form 8-K, which was filed on March 7, 2012 and is incorporated herein by reference. | ||
*10.65 | Amendment to Employment Agreement, dated December 10, 2012 between Magellan Health Services, Inc. and Rene Lerer, M.D., which was filed as Exhibit 10.1 to the Company's current report on Form 8-K, which was filed on December 12, 2012, and is incorporated herein by reference. | ||
*10.66 | Employment Agreement dated December 10, 2012 between the Company and Barry M. Smith, which was filed as Exhibit 10.2 to the Company's current report on Form 8-K, which was filed on December 12, 2012, and is incorporated herein by reference. | ||
*10.67 | Form of Stock Option Agreement, relating to options granted under the Company's 2011 Management Incentive Plan, which was filed as Exhibit 10.1 to the Company's current report on Form 8-K, which was filed on February 7, 2013 and is incorporated herein by reference. | ||
*10.68 | Form of Notice of Stock Option Grant, relating to options granted under the Company's 2011 Management Incentive Plan, which was filed as Exhibit 10.2 to the Company's current report on Form 8-K, which was filed on February 7, 2013 and is incorporated herein by reference. | ||
*10.69 | Form of Restricted Stock Unit Agreement, relating to restricted stock units granted under the Company's 2011 Management Incentive Plan, which was filed as Exhibit 10.3 to the Company's current report on Form 8-K, which was filed on February 7, 2013 and is incorporated herein by reference. | ||
*10.70 | Form of Notice of Restricted Stock Unit Award, relating to restricted stock units granted under the Company's 2011 Management Incentive Plan, which was filed as Exhibit 10.4 to the Company's current report on Form 8-K, which was filed on February 7, 2013 and is incorporated herein by reference. | ||
#21 | List of subsidiaries of the Company. | ||
#23 | Consent of Independent Registered Public Accounting Firm. | ||
| Exhibit No. | Description of Exhibit | ||
|---|---|---|---|
| #31.1 | Certification of Chief Executive Officer pursuant to Section 302 of the Sarbanes-Oxley Act of 2002. | ||
#31.2 | Certification of Chief Financial Officer pursuant to Section 302 of the Sarbanes-Oxley Act of 2002. | ||
†32.1 | Certification of Chief Executive Officer pursuant to Section 906 of the Sarbanes-Oxley Act of 2002. | ||
†32.2 | Certification of Chief Financial Officer pursuant to Section 906 of the Sarbanes-Oxley Act of 2002. | ||
†101 | The following materials from the Company's Annual Report on Form 10-K for the fiscal year ended December 31, 2011 formatted in Extensible Business Reporting Language (XBRL): (i) the Consolidated Statements of Income, (ii) the Consolidated Balance Sheets, (iii) the Consolidated Statements of Changes in Shareholders' Equity (iv) the Consolidated Statements of Cash Flows and (v) related notes. | ||
(b) Exhibits Required by Item 601 of Regulation S-K:
Exhibits required to be filed by the Company pursuant to Item 601 of Regulation S-K are contained in a separate volume.
(c) Financial statements and schedules required by Regulation S-X Item 14(d):
(1) Not applicable.
(2) Not applicable.
(3) Information with respect to this item is contained on page S-1 of this Report on Form 10-K.
4. Additional Information
The Company will provide to any person without charge, upon request, a copy of its annual Report on Form 10-K (without exhibits) for the year ended December 31, 2011,2012, as filed with the Securities and Exchange Commission. The Company will also provide to any person without charge, upon request, copies of its Code of Ethics for Directors, Code of Ethics for Covered Officers, and Corporate Compliance Handbook for all employees (hereinafter referred to as the "Codes of Ethics"). Any such requests should be made in writing to the Investor Relations Department, Magellan Health
Services, Inc., 55 Nod Road, Avon, Connecticut 06001. The documents referred to above and other Securities and Exchange Commission filings of the Company are available on the Company's website atwww.magellanhealth.com. The Company intends to disclose any future amendments to the provisions of the Codes of Ethics and waivers from such Codes of Ethics, if any, made with respect to any of its directors and executive officers, on its internet site.
Pursuant to the requirements of Section 13 or 15(d) of the Securities Exchange Act of 1934, the Registrant has duly caused this Report to be signed on its behalf by the undersigned thereunto duly authorized.
| MAGELLAN HEALTH SERVICES, INC. (Registrant) | ||
Date: February 28, | /s/ JONATHAN N. RUBIN Jonathan N. Rubin Executive Vice President and Chief Financial Officer (Principal Financial Officer) | |
Date: February 28, | /s/ JEFFREY N. WEST Jeffrey N. West Senior Vice President and Controller (Principal Accounting Officer) |
Pursuant to the requirements of the Securities Exchange Act of 1934, the following persons on behalf of the Registrant and in the capacities and on the dates indicated have signed this Report below.
Signature | Title | Date | ||
|---|---|---|---|---|
| /s/ | Chief Executive Officer and | February 28, | ||
/s/ RENE LERER Rene Lerer | Executive Chairman of the Board of Directors | February 28, 2013 | ||
/s/ ERAN BROSHY Eran Broshy | Director | February 28, | ||
/s/ MICHAEL DIAMENT Michael Diament | Director | February 28, | ||
/s/ WILLIAM D. FORREST William D. Forrest | Director | February 28, | ||
/s/ ROBERT M. LE BLANC Robert M. Le Blanc | Director | February 28, | ||
Signature | Title | Date | ||
|---|---|---|---|---|
| /s/ WILLIAM J. MCBRIDE William J. McBride | Director | February 28, 2013 | ||
/s/ MICHAEL P. RESSNER Michael P. Ressner | Director | February 28, | ||
/s/ MARY SAMMONS Mary Sammons | Director | February 28, | ||
/s/ JONATHAN N. RUBIN Jonathan N. Rubin | Executive Vice President and Chief Financial Officer (Principal Financial Officer) | February 28, | ||
/s/ JEFFREY N. WEST Jeffrey N. West | Senior Vice President and Controller | February 28, |
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
INDEX TO FINANCIAL STATEMENTS
The following consolidated financial statements of the registrant and its subsidiaries are submitted herewith in response to Item 8 and Item 15(a)1:
| | Page(s) | ||
|---|---|---|---|
Magellan Health Services, | |||
Audited Consolidated Financial Statements | |||
Report of independent registered public accounting firm | F-2 | ||
Consolidated balance sheets as of December 31, | F-3 | ||
Consolidated statements of comprehensive income for the years ended December 31, | F-4 | ||
Consolidated statements of changes in stockholders' equity for the years ended December 31, | F-5 | ||
Consolidated statements of cash flows for the years ended December 31, | F-6 | ||
Notes to consolidated financial statements | F-7 | ||
The following financial statement schedule of the registrant and its subsidiaries is submitted herewith in response to Item 15(a)2: | |||
Schedule II—Valuation and qualifying accounts | S-1 | ||
All other schedules for which provision is made in the applicable accounting regulation of the Securities and Exchange Commission are not required under the related instructions or are inapplicable and therefore have been omitted.
Report of Independent Registered Public Accounting Firm
The Board of Directors and Stockholders of Magellan Health Services, Inc.
We have audited the accompanying consolidated balance sheets of Magellan Health Services, Inc. and subsidiaries (the "Company") as of December 31, 20102011 and 2011,2012, and the related consolidated statements of comprehensive income, changes in stockholders' equity, and cash flows for each of the three years in the period ended December 31, 2011.2012. Our audits also included the financial statement schedule of the Company for the years ended December 31, 2009, 2010, and 2011 as listed in the Index at Item 15(a)2. These financial statements and schedule are the responsibility of the Company's management. Our responsibility is to express an opinion on these financial statements and schedule based on our audits.
We conducted our audits in accordance with the standards of the Public Company Accounting Oversight Board (United States). Those standards require that we plan and perform the audit to obtain reasonable assurance about whether the financial statements are free of material misstatement. An audit includes examining, on a test basis, evidence supporting the amounts and disclosures in the financial statements. An audit also includes assessing the accounting principles used and significant estimates made by management, as well as evaluating the overall financial statement presentation. We believe that our audits provide a reasonable basis for our opinion.
In our opinion, the financial statements referred to above present fairly, in all material respects, the consolidated financial position of the Company at December 31, 20102011 and 2011,2012, and the consolidated results of its operations and its cash flows for each of the three years in the period ended December 31, 2011,2012, in conformity with U.S. generally accepted accounting principles. Also in our opinion, the related financial statement schedule, when considered in relation to the basic financial statements taken as a whole, presents fairly in all material respects the information set forth therein.
We also have audited, in accordance with the standards of the Public Company Accounting Oversight Board (United States), the Company's internal control over financial reporting as of December 31, 2011,2012, based on criteria established in Internal Control—Integrated Framework issued by the Committee of Sponsoring Organizations of the Treadway Commission and our report dated February 28, 20122013 expressed an unqualified opinion thereon.
/s/ERNST & YOUNG LLP
Baltimore, Maryland
February 28, 20122013
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
CONSOLIDATED BALANCE SHEETS AS OF DECEMBER 31,
(In thousands, except per share amounts)
| | 2010 | 2011 | 2011 | 2012 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
ASSETS | ||||||||||||||
Current Assets: | ||||||||||||||
Cash and cash equivalents | $ | 337,179 | $ | 119,862 | $ | 119,862 | $ | 189,464 | ||||||
Restricted cash | 116,734 | 185,794 | 185,794 | 226,554 | ||||||||||
Accounts receivable, less allowance for doubtful accounts of $1,985 and $3,336 at December 31, 2010 and 2011, respectively | 106,934 | 121,606 | ||||||||||||
Short-term investments (restricted investments of $114,903 and $129,599 at December 31, 2010 and 2011, respectively) | 189,530 | 192,947 | ||||||||||||
Accounts receivable, less allowance for doubtful accounts of $3,336 and $4,612 at December 31, 2011 and 2012, respectively | 121,606 | 138,253 | ||||||||||||
Short-term investments (restricted investments of $129,599 and $88,332 at December 31, 2011 and 2012, respectively) | 192,947 | 201,127 | ||||||||||||
Deferred income taxes | 28,439 | 35,138 | 35,138 | 31,698 | ||||||||||
Pharmaceutical inventory | 27,910 | 39,567 | 39,567 | 45,727 | ||||||||||
Other current assets (restricted deposits of $21,302 and $20,453 at December 31, 2010 and 2011, respectively) | 51,761 | 37,795 | ||||||||||||
Other current assets (restricted deposits of $20,453 and $20,846 at December 31, 2011 and 2012, respectively) | 37,795 | 38,595 | ||||||||||||
Total Current Assets | 858,487 | 732,709 | 732,709 | 871,418 | ||||||||||
Property and equipment, net | 111,814 | 118,022 | 118,022 | 136,548 | ||||||||||
Long-term investments (restricted investments of $84,950 and $7,956 at December 31, 2010 and 2011, respectively) | 94,974 | 7,956 | ||||||||||||
Deferred income taxes | 825 | — | ||||||||||||
Restricted long-term investments | 7,956 | 32,563 | ||||||||||||
Other long-term assets | 2,396 | 10,952 | 10,952 | 9,730 | ||||||||||
Goodwill | 426,939 | 426,939 | 426,939 | 426,939 | ||||||||||
Other intangible assets, net | 53,997 | 44,589 | 44,589 | 34,935 | ||||||||||
Total Assets | $ | 1,549,432 | $ | 1,341,167 | $ | 1,341,167 | $ | 1,512,133 | ||||||
LIABILITIES AND STOCKHOLDERS' EQUITY | ||||||||||||||
Current Liabilities: | ||||||||||||||
Accounts payable | $ | 31,878 | $ | 18,690 | $ | 18,690 | $ | 17,081 | ||||||
Accrued liabilities | 105,776 | 106,809 | 106,809 | 100,778 | ||||||||||
Medical claims payable | 142,671 | 137,973 | 137,973 | 198,429 | ||||||||||
Other medical liabilities | 109,285 | 106,078 | 106,078 | 76,914 | ||||||||||
Current maturities of long-term capital lease obligation | 559 | — | ||||||||||||
Total Current Liabilities | 390,169 | 369,550 | 369,550 | 393,202 | ||||||||||
Deferred income taxes | — | 18,509 | 18,509 | 34,086 | ||||||||||
Tax Contingencies | 117,599 | 102,919 | ||||||||||||
Tax contingencies | 102,919 | 60,697 | ||||||||||||
Deferred credits and other long-term liabilities | 2,649 | 4,915 | 4,915 | 6,815 | ||||||||||
Total Liabilities | 510,417 | 495,893 | 495,893 | 494,800 | ||||||||||
Preferred stock, par value $.01 per share | ||||||||||||||
Authorized—10,000 shares—Issued and outstanding—none | — | — | ||||||||||||
Authorized—10,000 shares at December 31, 2011 and December 31, 2012—Issued and outstanding—none | — | — | ||||||||||||
Ordinary common stock, par value $.01 per share | ||||||||||||||
Authorized—100,000 shares at December 31, 2010 and 2011—Issued and outstanding—43,687 shares and 33,782 shares at December 31, 2010, respectively, and 45,285 and 27,173 shares at December 31, 2011, respectively | 437 | 453 | ||||||||||||
Authorized—100,000 shares at December 31, 2011 and December 31, 2012—Issued and outstanding—45,285 shares and 27,173 shares at December 31, 2011, respectively, and 45,928 and 27,353 shares at December 31, 2012, respectively | 453 | 459 | ||||||||||||
Multi-Vote common stock, par value $.01 per share | ||||||||||||||
Authorized—40,000 shares—Issued and outstanding—none | — | — | ||||||||||||
Authorized—40,000 shares at December 31, 2011 and December 31, 2012—Issued and outstanding—none | — | — | ||||||||||||
Other Stockholders' Equity: | ||||||||||||||
Additional paid-in capital | 725,322 | 804,035 | 804,035 | 848,238 | ||||||||||
Retained earnings | 694,582 | 824,205 | 824,205 | 975,232 | ||||||||||
Warrants outstanding | 420 | — | ||||||||||||
Accumulated other comprehensive income (loss) | 9 | (150 | ) | |||||||||||
Ordinary common stock in treasury, at cost, 9,905 shares and 18,112 shares at December 31, 2010 and 2011, respectively | (381,755 | ) | (783,269 | ) | ||||||||||
Accumulated other comprehensive loss | (150 | ) | (35 | ) | ||||||||||
Ordinary common stock in treasury, at cost, 18,112 shares and 18,575 shares at | ||||||||||||||
December 31, 2011 and December 31, 2012, respectively | (783,269 | ) | (806,561 | ) | ||||||||||
Total Stockholders' Equity | 1,039,015 | 845,274 | 845,274 | 1,017,333 | ||||||||||
Total Liabilities and Stockholders' Equity | $ | 1,549,432 | $ | 1,341,167 | $ | 1,341,167 | $ | 1,512,133 | ||||||
See accompanying notes to consolidated financial statements.
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
CONSOLIDATED STATEMENTS OF COMPREHENSIVE INCOME
FOR THE YEARS ENDED DECEMBER 31,
(In thousands, except per share amounts)
| | 2009 | 2010 | 2011 | 2010 | 2011 | 2012 | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Net revenue | $ | 2,641,814 | $ | 2,969,240 | $ | 2,799,400 | ||||||||||||||
Net revenue: | ||||||||||||||||||||
Managed care and other | $ | 2,734,406 | $ | 2,551,991 | $ | 2,857,099 | ||||||||||||||
Dispensing | 234,834 | 247,409 | 350,298 | |||||||||||||||||
Cost and expenses: | ||||||||||||||||||||
Total net revenue | 2,969,240 | 2,799,400 | 3,207,397 | |||||||||||||||||
Costs and expenses: | ||||||||||||||||||||
Cost of care | 1,765,313 | 1,907,985 | 1,784,724 | 1,907,985 | 1,784,724 | 2,071,890 | ||||||||||||||
Cost of goods sold | 203,336 | 218,630 | 232,038 | 218,630 | 232,038 | 328,414 | ||||||||||||||
Direct service costs and other operating expenses(1) | 465,710 | 566,582 | 529,634 | 566,582 | 529,634 | 557,512 | ||||||||||||||
Depreciation and amortization | 47,268 | 54,682 | 58,623 | 54,682 | 58,623 | 60,488 | ||||||||||||||
Interest expense | 2,424 | 2,233 | 2,502 | 2,233 | 2,502 | 2,247 | ||||||||||||||
Interest income | (6,245 | ) | (3,275 | ) | (2,781 | ) | (3,275 | ) | (2,781 | ) | (2,019 | ) | ||||||||
| 2,477,806 | 2,746,837 | 2,604,740 | ||||||||||||||||||
Total costs and expenses | 2,746,837 | 2,604,740 | 3,018,532 | |||||||||||||||||
Income before income taxes | 164,008 | 222,403 | 194,660 | 222,403 | 194,660 | 188,865 | ||||||||||||||
Provision for income taxes | 57,337 | 83,744 | 65,037 | 83,744 | 65,037 | 37,838 | ||||||||||||||
Net income | 106,671 | 138,659 | 129,623 | 138,659 | 129,623 | 151,027 | ||||||||||||||
Other comprehensive loss(2) | (58 | ) | (105 | ) | (159 | ) | ||||||||||||||
Net income per common share—basic: | $ | 4.10 | $ | 4.25 | $ | 5.51 | ||||||||||||||
Net income per common share—diluted: | $ | 4.03 | $ | 4.17 | $ | 5.42 | ||||||||||||||
Other comprehensive (loss) income: | ||||||||||||||||||||
Unrealized (losses) gains on available-for-sale securities(2) | (105 | ) | (159 | ) | 115 | |||||||||||||||
Comprehensive income | $ | 106,613 | $ | 138,554 | $ | 129,464 | $ | 138,554 | $ | 129,464 | $ | 151,142 | ||||||||
Weighted average number of common shares outstanding—basic (See Note 6) | 35,248 | 33,779 | 30,478 | |||||||||||||||||
Weighted average number of common shares outstanding—diluted (See Note 6) | 35,416 | 34,441 | 31,058 | |||||||||||||||||
Net income per common share—basic: | $ | 3.03 | $ | 4.10 | $ | 4.25 | ||||||||||||||
Net income per common share—diluted: | $ | 3.01 | $ | 4.03 | $ | 4.17 | ||||||||||||||
See accompanying notes to consolidated financial statements.
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
CONSOLIDATED STATEMENTS OF CHANGES IN STOCKHOLDERS' EQUITY
(In thousands)
| | | | Common Stock In Treasury | | | | | | | | Common Stock In Treasury | | | | | | ||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| | Common Stock | | | | Accumulated Other Comprehensive Income (Loss) | | Common Stock | | | | Accumulated Other Comprehensive Income (Loss) | | ||||||||||||||||||||||||||||||||||||||||||||
| | Common Stock In Treasury | Warrants Outstanding | Total Stockholders' Equity | Common Stock In Treasury | Warrants Outstanding | Total Stockholders' Equity | ||||||||||||||||||||||||||||||||||||||||||||||||||
| | Shares | Amount | Additional Paid in Capital | Retained Earnings | Accumulated Other Comprehensive Income (Loss) | |||||||||||||||||||||||||||||||||||||||||||||||||||
Balance at December 31, 2008 | 40,873 | $ | 409 | $ | 5,382 | $ | 172 | $ | 908,073 | |||||||||||||||||||||||||||||||||||||||||||||||
Stock compensation expense | — | — | — | — | 19,782 | — | — | — | 19,782 | |||||||||||||||||||||||||||||||||||||||||||||||
Exercise of stock options | 77 | 1 | — | — | 2,578 | — | — | — | 2,579 | |||||||||||||||||||||||||||||||||||||||||||||||
Tax benefit from exercise of stock options and vesting of stock awards | — | — | — | — | 2,917 | — | — | — | 2,917 | |||||||||||||||||||||||||||||||||||||||||||||||
Exercise of stock warrants | — | — | — | — | 1 | — | — | — | 1 | |||||||||||||||||||||||||||||||||||||||||||||||
Issuance of equity | 94 | — | — | — | 194 | — | — | — | 194 | |||||||||||||||||||||||||||||||||||||||||||||||
Repurchase of stock | — | — | (2,642 | ) | (89,667 | ) | — | — | — | — | (89,667 | ) | ||||||||||||||||||||||||||||||||||||||||||||
Net income | — | — | — | — | — | 106,671 | — | — | 106,671 | |||||||||||||||||||||||||||||||||||||||||||||||
Other comprehensive loss—other | — | — | — | — | — | — | — | (58 | ) | (58 | ) | |||||||||||||||||||||||||||||||||||||||||||||
| Shares | Amount | Additional Paid in Capital | Retained Earnings | Shares | Amount | Warrants Outstanding | Accumulated Other Comprehensive Income (Loss) | Total Stockholders' Equity | Accumulated Other Comprehensive Income (Loss) | |||||||||||||||||||||||||||||||||||||||||||||||
Balance at December 31, 2009 | 41,044 | 410 | (6,509 | ) | (225,820 | ) | 614,483 | 555,923 | 5,382 | 114 | 950,492 | 41,044 | $ | 410 | ) | $ | 614,483 | $ | 555,923 | |||||||||||||||||||||||||||||||||||||
Stock compensation expense | — | — | — | — | 15,102 | — | — | — | 15,102 | — | — | — | — | 15,102 | — | — | 15,102 | |||||||||||||||||||||||||||||||||||||||
Exercise of stock options | 2,027 | 21 | — | — | 76,845 | — | — | — | 76,866 | 2,027 | 21 | — | — | 76,845 | — | — | — | 76,866 | ||||||||||||||||||||||||||||||||||||||
Tax benefit (cost) from exercise of stock options and vesting of stock awards | — | — | — | — | (1,384 | ) | — | — | — | (1,384 | ) | — | — | — | — | (1,384 | ) | — | — | — | (1,384 | ) | ||||||||||||||||||||||||||||||||||
Exercise of stock warrants | 526 | 6 | — | — | 20,966 | — | (4,962 | ) | — | 16,010 | 526 | 6 | — | — | 20,966 | — | (4,962 | ) | — | 16,010 | ||||||||||||||||||||||||||||||||||||
Issuance of equity | 90 | — | — | — | (690 | ) | — | — | — | (690 | ) | 90 | — | — | — | (690 | ) | — | — | — | (690 | ) | ||||||||||||||||||||||||||||||||||
Repurchase of stock | — | — | (3,396 | ) | (155,935 | ) | — | — | — | — | (155,935 | ) | — | — | (3,396 | ) | (155,935 | ) | — | — | — | — | (155,935 | ) | ||||||||||||||||||||||||||||||||
Net income | — | — | — | — | — | 138,659 | — | — | 138,659 | — | — | — | — | — | 138,659 | — | — | 138,659 | ||||||||||||||||||||||||||||||||||||||
Other comprehensive loss—other | — | — | — | — | — | — | — | (105 | ) | (105 | ) | — | — | — | — | — | — | — | (105 | ) | (105 | ) | ||||||||||||||||||||||||||||||||||
Balance at December 31, 2010 | 43,687 | 437 | (9,905 | ) | (381,755 | ) | 725,322 | 694,582 | 420 | 9 | 1,039,015 | 43,687 | 437 | (9,905 | ) | (381,755 | ) | 725,322 | 694,582 | 420 | 9 | 1,039,015 | ||||||||||||||||||||||||||||||||||
Stock compensation expense | — | — | — | — | 17,256 | — | — | — | 17,256 | — | — | — | — | 17,256 | — | — | — | 17,256 | ||||||||||||||||||||||||||||||||||||||
Exercise of stock options | 1,065 | 11 | — | — | 40,830 | — | — | — | 40,841 | 1,065 | 11 | — | — | 40,830 | — | — | — | 40,841 | ||||||||||||||||||||||||||||||||||||||
Tax benefit (cost) from exercise of stock options and vesting of stock awards | — | — | — | — | (1,213 | ) | — | — | — | (1,213 | ) | — | — | — | — | (1,213 | ) | — | — | — | (1,213 | ) | ||||||||||||||||||||||||||||||||||
Exercise of stock warrants | 31 | — | — | — | 1,251 | — | (296 | ) | — | 955 | 31 | — | — | — | 1,251 | — | (296 | ) | — | 955 | ||||||||||||||||||||||||||||||||||||
Issuance of equity | 502 | 5 | — | — | 17,975 | — | — | — | 17,980 | 502 | 5 | — | — | 17,975 | — | — | — | 17,980 | ||||||||||||||||||||||||||||||||||||||
Repurchase of stock | — | — | (8,207 | ) | (401,514 | ) | — | — | — | — | (401,514 | ) | — | — | (8,207 | ) | (401,514 | ) | — | — | — | — | (401,514 | ) | ||||||||||||||||||||||||||||||||
Adjustment to additional paid in capital due to reversal of tax contingency | — | — | — | — | 2,490 | — | — | — | 2,490 | — | — | — | — | 2,490 | — | — | — | 2,490 | ||||||||||||||||||||||||||||||||||||||
Forfeiture of stock warrants | — | — | — | — | 124 | — | (124 | ) | — | — | — | — | — | — | 124 | — | (124 | ) | — | — | ||||||||||||||||||||||||||||||||||||
Net income | — | — | — | — | — | 129,623 | — | — | 129,623 | — | — | — | — | — | 129,623 | — | — | 129,623 | ||||||||||||||||||||||||||||||||||||||
Other comprehensive loss—other | — | — | — | — | — | — | — | (159 | ) | (159 | ) | — | — | — | — | — | — | — | (159 | ) | (159 | ) | ||||||||||||||||||||||||||||||||||
Balance at December 31, 2011 | 45,285 | $ | 453 | (18,112 | ) | $ | (783,269 | ) | $ | 804,035 | $ | 824,205 | $ | — | $ | (150 | ) | $ | 845,274 | 45,285 | 453 | (18,112 | ) | (783,269 | ) | 804,035 | 824,205 | — | (150 | ) | 845,274 | |||||||||||||||||||||||||
Stock compensation expense | — | — | — | — | 17,945 | — | — | — | 17,945 | |||||||||||||||||||||||||||||||||||||||||||||||
Exercise of stock options | 531 | 5 | — | — | 20,717 | — | — | — | 20,722 | |||||||||||||||||||||||||||||||||||||||||||||||
Tax benefit (cost) from exercise of stock options and vesting of stock awards | — | — | — | — | 112 | — | — | — | 112 | |||||||||||||||||||||||||||||||||||||||||||||||
Issuance of equity | 112 | 1 | — | — | (733 | ) | — | — | — | (732 | ) | |||||||||||||||||||||||||||||||||||||||||||||
Repurchase of stock | — | — | (463 | ) | (23,292 | ) | — | — | — | — | (23,292 | ) | ||||||||||||||||||||||||||||||||||||||||||||
Adjustment to additional paid in capital due to reversal of tax contingency | — | — | — | — | 6,162 | — | — | — | 6,162 | |||||||||||||||||||||||||||||||||||||||||||||||
Net income | — | — | — | — | — | 151,027 | — | — | 151,027 | |||||||||||||||||||||||||||||||||||||||||||||||
Other comprehensive income—other | — | — | — | — | — | — | — | 115 | 115 | |||||||||||||||||||||||||||||||||||||||||||||||
Balance at December 31, 2012 | 45,928 | $ | 459 | (18,575 | ) | $ | (806,561 | ) | $ | 848,238 | $ | 975,232 | $ | — | $ | (35 | ) | $ | 1,017,333 | |||||||||||||||||||||||||||||||||||||
See accompanying notes to consolidated financial statements.
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
CONSOLIDATED STATEMENTS OF CASH FLOWS FOR THE YEARS ENDED DECEMBER 31,
(In thousands)
| | 2009 | 2010 | 2011 | 2010 | 2011 | 2012 | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Cash flows from operating activities: | ||||||||||||||||||||
Net income | $ | 106,671 | $ | 138,659 | $ | 129,623 | $ | 138,659 | $ | 129,623 | $ | 151,027 | ||||||||
Adjustments to reconcile net income to net cash provided by operating activities: | ||||||||||||||||||||
Depreciation and amortization | 47,268 | 54,682 | 58,623 | 54,682 | 58,623 | 60,488 | ||||||||||||||
Non-cash interest expense | 899 | 569 | 1,033 | 569 | 1,033 | 728 | ||||||||||||||
Non-cash stock compensation expense | 19,782 | 15,102 | 17,418 | 15,102 | 17,418 | 17,783 | ||||||||||||||
Non-cash income tax expense | 30,033 | 42,251 | 8,308 | 42,251 | 8,285 | 17,306 | ||||||||||||||
Non-cash amortization on investments | 4,161 | 10,155 | 12,309 | 10,155 | 12,309 | 7,193 | ||||||||||||||
Cash flows from changes in assets and liabilities, net of effects from acquisitions of businesses: | ||||||||||||||||||||
Restricted cash | 32,736 | 42,925 | (69,060 | ) | 42,925 | (69,060 | ) | (40,760 | ) | |||||||||||
Accounts receivable, net | (3,328 | ) | 3,262 | (15,609 | ) | 3,262 | (15,609 | ) | (16,411 | ) | ||||||||||
Inventory | (7,577 | ) | (2,347 | ) | (11,657 | ) | ||||||||||||||
Pharmaceutical inventory | (2,347 | ) | (11,657 | ) | (6,160 | ) | ||||||||||||||
Other assets | (1,359 | ) | (14,847 | ) | (5,672 | ) | (14,847 | ) | 3,804 | 414 | ||||||||||
Accounts payable and accrued liabilities | (2,908 | ) | 14,447 | (7,251 | ) | 14,447 | (7,251 | ) | (8,321 | ) | ||||||||||
Medical claims payable and other medical liabilities | (7,495 | ) | 3,638 | (7,905 | ) | 3,638 | (7,905 | ) | 31,292 | |||||||||||
Tax contingencies | — | (9,453 | ) | (35,376 | ) | |||||||||||||||
Other | (310 | ) | 445 | 1,843 | 445 | 1,843 | 2,090 | |||||||||||||
Net cash provided by operating activities | 218,573 | 308,941 | 112,003 | 308,941 | 112,003 | 181,293 | ||||||||||||||
Cash flows from investing activities: | ||||||||||||||||||||
Capital expenditures | (33,220 | ) | (46,162 | ) | (54,394 | ) | (46,162 | ) | (54,394 | ) | (69,549 | ) | ||||||||
Acquisitions and investments in businesses, net of cash acquired | (115,438 | ) | — | (376 | ) | — | (376 | ) | — | |||||||||||
Purchase of investments | (299,357 | ) | (291,289 | ) | (259,552 | ) | (291,289 | ) | (259,552 | ) | (321,541 | ) | ||||||||
Maturity of investments | 298,556 | 226,957 | 330,583 | 226,957 | 330,583 | 281,748 | ||||||||||||||
Investment in equity method joint ventures | — | — | (1,225 | ) | ||||||||||||||||
Net cash (used in) provided by investing activities | (149,459 | ) | (110,494 | ) | 16,261 | (110,494 | ) | 16,261 | (110,567 | ) | ||||||||||
Cash flows from financing activities: | ||||||||||||||||||||
Payments on long-term debt and capital lease obligations | (3 | ) | (1,120 | ) | (559 | ) | (1,120 | ) | (559 | ) | — | |||||||||
Payments to acquire treasury stock | (149,805 | ) | (407,645 | ) | (21,868 | ) | ||||||||||||||
Proceeds from issuance of equity | — | — | 20,000 | — | 20,000 | — | ||||||||||||||
Payments to acquire treasury stock | (89,667 | ) | (149,805 | ) | (407,645 | ) | ||||||||||||||
Proceeds from exercise of stock options and warrants | 2,580 | 92,876 | 41,796 | 92,876 | 41,796 | 20,486 | ||||||||||||||
Tax benefit from exercise of stock options and vesting of stock awards | 2,917 | 1,121 | 2,038 | 1,121 | 2,038 | 990 | ||||||||||||||
Other | (259 | ) | (847 | ) | (1,211 | ) | (847 | ) | (1,211 | ) | (732 | ) | ||||||||
Net cash used in financing activities | (84,432 | ) | (57,775 | ) | (345,581 | ) | (57,775 | ) | (345,581 | ) | (1,124 | ) | ||||||||
Net (decrease) increase in cash and cash equivalents | (15,318 | ) | 140,672 | (217,317 | ) | |||||||||||||||
Net increase (decrease) in cash and cash equivalents | 140,672 | (217,317 | ) | 69,602 | ||||||||||||||||
Cash and cash equivalents at beginning of period | 211,825 | 196,507 | 337,179 | 196,507 | 337,179 | 119,862 | ||||||||||||||
Cash and cash equivalents at end of period | $ | 196,507 | $ | 337,179 | $ | 119,862 | $ | 337,179 | $ | 119,862 | $ | 189,464 | ||||||||
See accompanying notes to consolidated financial statements.
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS
December 31, 20112012
1. General
Basis of Presentation
The consolidated financial statements of Magellan Health Services, Inc., a Delaware corporation ("Magellan"), include the accounts of Magellan, its majority owned subsidiaries, and all variable interest entities ("VIEs") for which Magellan is the primary beneficiary (together with Magellan, the "Company"). All significant intercompany accounts and transactions have been eliminated in consolidation.
Business Overview
The Company is engaged in the specialty managed healthcare business. Through 2005, the Company predominantly operated in the managed behavioral healthcare business. As a result of certain acquisitions, the Company expanded into radiology benefits management and specialty pharmaceutical management during 2006, and into Medicaid administration during 2009. The Company provides services to health plans, insurance companies, employers, labor unions and various governmental agencies. The Company's business is divided into the following six segments, based on the services it provides and/or the customers that it serves, as described below.
Managed Behavioral Healthcare
Two of the Company's segments are in the managed behavioral healthcare business. This line of business generally reflects the Company's coordination and management of the delivery of behavioral healthcare treatment services that are provided through its contracted network of third-party treatment providers, which includes psychiatrists, psychologists, other behavioral health professionals, psychiatric hospitals, general medical facilities with psychiatric beds, residential treatment centers and other treatment facilities. The treatment services provided through the Company's provider network include outpatient programs (such as counseling or therapy), intermediate care programs (such as intensive outpatient programs and partial hospitalization services), inpatient treatment and crisis intervention services. The Company generally does not directly provide or own any provider of treatment services.
The Company provides its management services primarily through: (i) risk-based products, where the Company assumes all or a substantial portion of the responsibility for the cost of providing treatment services in exchange for a fixed per member per month fee, (ii) administrative services only ("ASO") products, where the Company provides services such as utilization review, claims administration and/or provider network management, but does not assume responsibility for the cost of the treatment services, and (iii) employee assistance programs ("EAPs") where the Company provides short-term outpatient behavioral counseling services.
The managed behavioral healthcare business is managed based on the services provided and/or the customers served, through the following two segments:
Commercial. The Managed Behavioral Healthcare Commercial segment ("Commercial") generally reflects managed behavioral healthcare services and EAP services provided under contracts with health plans and insurance companies for some or all of their commercial, Medicaid and Medicare members, as well as with employers, including corporations, governmental agencies, and labor unions. Commercial's contracts encompass risk-based, ASO and EAP arrangements.
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
December 31, 20112012
1. General (Continued)
Public Sector. The Managed Behavioral Healthcare Public Sector segment ("Public Sector") generally reflects services provided to recipients under Medicaid and other state sponsored programs under contracts with state and local governmental agencies. Public Sector contracts encompass either risk-based or ASO arrangements.
Radiology Benefits Management
The Radiology Benefits Management segment ("Radiology Benefits Management") generally reflects the management of the delivery of diagnostic imaging and other therapeutic services to ensure that such services are clinically appropriate and cost effective. The Company's radiology benefits management services currently are provided under contracts with health plans and insurance companies for some or all of their commercial, Medicaid and Medicare members. The Company also contracts with state and local governmental agencies for the provision of such services to Medicaid recipients. The Company offers its radiology benefits management services through risk-based contracts, where the Company assumes all or a substantial portion of the responsibility for the cost of providing diagnostic imaging services, and through ASO contracts, where the Company provides services such as utilization review and claims administration, but does not assume responsibility for the cost of the imaging services.
Drug Benefits Management
Two of the Company's segments are in the drug benefits management business. This line of business generally reflects the Company's clinical management of drugs paid under medical and pharmacy benefit programs. The Company's services include the coordination and management of the specialty drug spendspending for health plans, employers, and governmental agencies, and the management of pharmacy programs for Medicaid programs, health plans, and other state-sponsored programs.employers. The two segments in this line of business are:
Specialty Pharmaceutical Management. The Specialty Pharmaceutical Management segment ("Specialty Pharmaceutical Management") comprises programs that manage specialty drugs used in the treatment of complex conditions such as cancer, multiple sclerosis, hemophilia, infertility, rheumatoid arthritis, chronic forms of hepatitis and other diseases. Specialty pharmaceutical drugs represent high-cost injectible, infused, or oral drugs with sensitive handling or storage needs, many of which may be physician administered. Patients receiving these drugs require greater amounts of clinical support than those taking more traditional agents. Payors require clinical, financial and technological support to maximize the value delivered to their members using these expensive agents. The Company's specialty pharmaceutical management services are provided under contracts with health plans, insurance companies, employers, and governmental agencies for some or all of their commercial, Medicare and Medicaid members. The Company's specialty pharmaceutical services include: (i) contracting and formulary optimization programs; (ii) specialty pharmaceutical dispensing operations; and (iii) medical pharmacy management programs.
The Company's Specialty Pharmaceutical Management segment had contracts with 41 health plans and employers, and several pharmaceutical manufacturers and state Medicaid Administration. The Medicaid Administration segment ("Medicaid Administration") generally reflects integrated clinical management services provided to the public sector to manage Medicaid pharmacy, mental health, and long-term care programs. The primary focusprograms as of the Company'sDecember 31, 2012.
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
December 31, 20112012
1. General (Continued)
Medicaid Administration. The Medicaid Administration segment ("Medicaid Administration") generally reflects integrated clinical management services provided to manage pharmacy, mental health, and long-term care for state benefit programs, and pharmacy benefit management programs for health plans and employers. The primary focus of the Company's Medicaid Administration unit involves providing pharmacy benefits administration ("PBA") and pharmacy benefits management ("PBM") services under contracts with health plans and employers, as well as public sector healthcare clients forsponsoring Medicaid and other state sponsored program recipients.benefit programs. The Company's pharmacy services include pharmacynetwork management, formulary and rebate management, point-of-sale claims processing systems and administration, drug utilization review, clinical prior authorization, and drug utilization review. Magellan's pharmacy strategy combines its Specialty Pharmacy Management and PBM capabilities to provide integrated management of complex drug therapies billed under both the medical and pharmacy benefit. Its mental health and long term care management services include review of service utilization and formulary management services, Preferred Drug List programs, Maximum Allowable Cost programs,compliance with state and drug rebate program services.federal regulations and reimbursement guidelines. Medicaid Administration's contracts encompass both Fee-For-Service ("FFS") and risk-based arrangements. In addition to Medicaid Administration's FFS contracts, effective September 1, 2010, Public Sector has subcontracted with Medicaid Administration to provide pharmacy benefits management services on a risk basis for one of Public Sector's customers.
Corporate
This segment of the Company is comprised primarily of operational support functions such as sales and marketing and information technology, as well as corporate support functions such as executive, finance, human resources and legal.
2. Summary of Significant Accounting Policies
Recent Accounting Pronouncements
In January 2010,May 2011, the Financial Accounting Standards Board ("FASB") issued Accounting Standards Update ("ASU"), No. 2010-24, "Health Care Entities—Presentation of Insurance Claims2011-04, "Fair Value Measurement (Topic 820): Amendments to Achieve Common Fair Value Measurement and Related Insurance Recoveries"Disclosure Requirements in U.S. GAAP and IFRSs", ("ASU 2010-24"2011-04"). ASU 2010-24 clarifies that a health care entity should not net insurance recoveries against a related claim liability. Additionally, the amount of the claim liability2011-04 amends ASC Topic 820, "Fair Value Measurements and Disclosures", to provide guidance on how fair value measurement should be determined without consideration of insurance recoveries. This guidance isapplied where existing GAAP already requires or permits fair value measurements. In addition, ASU 2011-04 requires expanded disclosures regarding fair value measurements. ASU 2011-04 became effective for fiscal years beginning after December 15, 2010. Accordingly, the Company adopted ASU 2010-24 on January 1, 2011.2012. The adoption of this standardASU 2011-04 did not have a material impact on the Company's consolidated results of operations, financial statements.position or cash flows.
In June 2011, the FASB issued ASU No. 2011-05, "Comprehensive Income (Topic 220): Presentation of Comprehensive Income" ("ASU 2011-05"). ASU 2011-05 requires an entity to present the total of comprehensive income, the components of net income, and the components of other comprehensive income either in a single continuous statement of comprehensive income or in two separate but consecutive statements and eliminates the option to present the components of other comprehensive income as part of the statement of equity. ASU 2011-05 is effective for fiscal years, and interim periods within those fiscal years, beginning on or after December 15, 2011, with early adoption permitted. While the adoption of this guidance is expected to impactimpacts the Company's disclosures for annual and interim filings for the year endingended December 31, 2012, it willdid not have an impact on the Company's consolidated results of operations, financial position, or cash flows.
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
December 31, 2012
2. Summary of Significant Accounting Policies (Continued)
In July 2011, the FASB issued ASU No. 2011-06, "Other Expenses (Topic 720): Fees Paid to the Federal Government by Health Insurers (a consensus of the FASB Emerging Issues Task Force)" ("ASU 2011-06"), which addresses how fees mandated by the Patient Protection and Affordable Care Act, as amended by the Health Care and Education Reconciliation Act of 2010 (collectively, the "Health Reform Law"), should be recognized and classified in the income statements of health insurers. The Health Reform Law imposes a mandatory annual fee on health insurers for each calendar year beginning on or after January 1, 2014. ASU 2011-06 stipulates that the liability incurred for that fee be amortized to expense over the calendar year in which it is payable. This ASU is effective for calendar years beginning after December 31, 2013, when the fee initially becomes effective. The adoption of ASU 2011-06 is not expected to significantly impact the Company's consolidated results of operations, financial condition.position, or cash flows.
In September 2011, the FASB issued ASU 2011-08, "Testing Goodwill for Impairment" ("ASU 2011-8"2011-08"), which provides authoritative guidance to simplify how entities, both public and nonpublic, test goodwill for impairment. This accounting update permits an entity to first assess qualitative factors to determine whether it is more likely than not that the fair value of a reporting unit is less than its carrying amount as a basis for determining whether it is necessary to perform the two-step goodwill
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
December 31, 2011
2. Summary of Significant Accounting Policies (Continued)
impairment test. This guidance will bewas effective for the Company beginning on January 1, 2012, with early adoption permitted.however the Company did not elect to use the qualitative screen for any reporting units in 2012. The Company doesguidance did not expect the guidance to impact the Company's financial position,consolidated results of operations, financial position, or cash flows.
In December 2011, the FASB issued ASU 2011-12, "Deferral of the Effective Date for Amendments to the Presentation of Reclassifications of Items Out of Accumulated Other Comprehensive Income in ASU 2011-05" ("ASU 2011-12"), which defers the requirement that companies present reclassification adjustments for each component of accumulated other comprehensive income in both net income and other comprehensive income on the face of the financial statements. The effective dates for ASU 2011-12 are consistent with the effective dates for ASU 2011-05 and, similar to our expectations for the adoption of ASU 2011-05, while the adoption of this guidance is expected to impactimpacts the Company's disclosures for annual and interim filings for the year endingended December 31, 2012, it willdid not have an impact on the Company's consolidated results of operations, financial position or cash flows.
In October 2012, the FASB issued ASU 2012-04, "Technical Corrections and Improvements" ("ASC 2012-04"). The amendments in this update cover a wide range of Topics in the Accounting Standards Codification. These amendments include technical corrections and improvements to the Accounting Standards Codification and conforming amendments related to fair value measurements. The amendments in this guidance that will not have transition guidance are effective upon issuance. The amendments that are subject to transition guidance are effective for fiscal periods beginning after December 15, 2012. The guidance did not impact the Company's consolidated results of operations, financial condition.position, or cash flows.
Use of Estimates
The preparation of financial statements in conformity with accounting principles generally accepted in the United States requires management to make estimates and assumptions that affect the reported
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
December 31, 2012
2. Summary of Significant Accounting Policies (Continued)
amounts of assets and liabilities and the disclosure of contingent assets and liabilities at the date of the financial statements and the reported amounts of revenue and expenses during the reporting period. Significant estimates of the Company include, among other things, accounts receivable realization, valuation allowances for deferred tax assets, valuation of goodwill and intangible assets, medical claims payable, other medical liabilities, stock compensation assumptions, tax contingencies and legal liabilities. Actual results could differ from those estimates.
Managed Care Revenue
Managed care revenue, inclusive of revenue from the Company's risk, EAP and ASO contracts, is recognized over the applicable coverage period on a per member basis for covered members. The Company is paid a per member fee for all enrolled members, and this fee is recorded as revenue in the month in which members are entitled to service. The Company adjusts its revenue for retroactive membership terminations, additions and other changes, when such adjustments are identified, with the exception of retroactivity that can be reasonably estimated. The impact of retroactive rate amendments is generally recorded in the accounting period that terms to the amendment are finalized, and that the amendment is executed. Any fees paid prior to the month of service are recorded as deferred revenue. Managed care revenues approximated $2.4 billion, $2.2 billion $2.4 billion and $2.2$2.5 billion for the years ended December 31, 2009, 2010, 2011 and 2011,2012, respectively.
Fee-For-Service and Cost-Plus Contracts
The Company has certain FFS contracts, including cost-plus contracts, with customers under which the Company recognizes revenue as services are performed and as costs are incurred. Revenues from these contracts approximated $104.4 million, $192.9 million, $174.5 million and $174.5$151.4 million for the years ended December 31, 2009, 2010, 2011 and 2011,2012, respectively.
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
December 31, 2011
2. Summary of Significant Accounting Policies (Continued)
Block Grant Revenues
The Maricopa ContractPublic Sector has a contract that is partially funded by federal, state and county block grant money, which represents annual appropriations. The Company recognizes revenue from block grant activity ratably over the period to which the block grant funding applies. Block grant revenues were approximately $106.6 million, $109.1 million, $114.4 million and $114.4$124.8 million for the years ended December 31, 2009, 2010, 2011 and 2011,2012, respectively.
Dispensing Revenue
The Company recognizes dispensing revenue, which includes the co-payments received from members of the health plans the Company serves, when the specialty pharmaceutical drugs are shipped. At the time of shipment, the earnings process is complete; the obligation of the Company's customer to pay for the specialty pharmaceutical drugs is fixed, and, due to the nature of the product, the member may neither return the specialty pharmaceutical drugs nor receive a refund. Revenues from the dispensing of specialty pharmaceutical drugs on behalf of health plans were $221.6 million, $234.8 million, $247.4 million and $247.4$350.3 million for the years ended December 31, 2009, 2010, 2011 and 2011,2012, respectively.
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
December 31, 2012
2. Summary of Significant Accounting Policies (Continued)
Performance-Based Revenue
The Company has the ability to earn performance-based revenue under certain risk and non-risk contracts. Performance-based revenue generally is based on either the ability of the Company to manage care for its clients below specified targets, or on other operating metrics. For each such contract, the Company estimates and records performance-based revenue after considering the relevant contractual terms and the data available for the performance-based revenue calculation. Pro-rata performance-based revenue ismay be recognized on an interim basis pursuant to the rights and obligations of each party upon termination of the contracts.contracts, among other factors. Performance-based revenues were $7.6 million, $13.1 million, $26.5 million and $26.5$25.4 million for the years ended December 31, 2009, 2010, 2011 and 2011,2012, respectively.
Rebate Revenue
The Company administers a rebate program for certain clients through which the Company coordinates the achievement, calculation and collection of rebates and administrative fees from pharmaceutical manufacturers on behalf of clients. Each period, the Company estimates the total rebates earned based on actual volumes of pharmaceutical purchases by the Company's clients, as well as historical and/or anticipated sharing percentages. The Company earns fees based upon the volume of rebates generated for its clients. The Company does not record as rebate revenue any rebates that are passed through to its clients. Total rebate revenues were $25.5 million, $32.8 million and $40.2 million for the years ended December 31, 2009, 2010, 2011 and 2011 were $29.4 million, $25.5 million, and $32.8 million,2012, respectively.
Significant Customers
Consolidated Company
The Company provides behavioral healthcare management and other related services to approximately 683,000 members in Maricopa County, Arizona, (the "Maricopa Contract").
The Maricopa Contract generated net revenues that exceeded, in the aggregate, ten percent of net revenues for the consolidated Company for the years ended December 31, 2009, 2010, 2011 and 2011. Pursuant to the Maricopa Contract, the Company provides behavioral healthcare management and
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
December 31, 2011
2. Summary of Significant Accounting Policies (Continued)
other related services to approximately 715,000 members in Maricopa County, Arizona.2012. Under the Maricopa Contract, the Company is responsible for providing covered behavioral health services to persons eligible under Title XIX (Medicaid) and Title XXI (State Children's Health Insurance Program) of the Social Security Act, non-Title XIX and non-Title XXI eligible children and adults with a serious mental illness ("SMI"), and to certain non-Title XIX and non-Title XXI adults with behavioral health or substance abuse disorders. The Maricopa Contract began on September 1, 2007 and extends through September 30, 2013 unless sooner terminated by the parties. The State of Arizona has the right to terminate the Maricopa Contract for cause, as defined, upon ten days' notice with an opportunity to cure, and without cause immediately upon notice from the State. The Maricopa Contract generated net revenues of $725.0 million, $807.1 million, $779.5 million and $779.5$758.3 million for the years ended December 31, 2009, 2010, 2011 and 2011,2012, respectively.
On October 4, 2012, the Arizona Department of Health Services ("ADHS") released a Request for Proposal ("RFP") for the ADHS Regional Behavioral Health Authority—GSA 6 (Maricopa County). The start date for any contract awarded pursuant to the RFP is expected to be October 1, 2013. This is a single RFP with two components: (i) the RFP maintains the current behavioral health carve-out for
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
December 31, 2012
2. Summary of Significant Accounting Policies (Continued)
the lives the Company currently serves under the Maricopa Contract; (ii) the RFP also introduces a fully integrated program of physical, behavioral, and pharmacy care for approximately 14,000 individuals with SMI, both Medicaid and dual eligible. Under the current Maricopa Contract, these 14,000 individuals are receiving behavioral health and behavioral health pharmacy benefits. Magellan Complete Care of Arizona, Inc. ("MCCAZ"), a joint venture owned 80 percent by the Company and 20 percent by VHS Phoenix Health Plan, LLC (a subsidiary of Vanguard Health Systems, Inc.), has responded to the RFP. There can be no assurance that MCCAZ will be awarded a contract pursuant to the RFP; or that the terms of any contract awarded pursuant to the RFP will be similar to the current Maricopa Contract.
One of the Company's top ten customers during 2009 and 2010 was WellPoint, Inc. The Company recorded net revenue from contracts with WellPoint, Inc. of $170.4 million and $175.7 million for the yearsyear ended December 31, 2009 and 2010, respectively.2010. The Company's contracts with WellPoint, Inc. terminated on December 31, 2010.
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
December 31, 20112012
2. Summary of Significant Accounting Policies (Continued)
By Segment
In addition to the Maricopa Contract previously discussed, the following customers generated in excess of ten percent of net revenues for the respective segment for the years ended December 31, 2009, 2010, 2011 and 20112012 (in thousands):
Segment | Term Date | 2009 | 2010 | 2011 | Term Date | 2010 | 2011 | 2012 | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Commercial | ||||||||||||||||||||||||
Customer A | December 31, 2012 | $ | 235,002 | $ | 243,399 | $ | 171,109 | December 31, 2013(2) | $ | 243,399 | $ | 171,109 | $ | 192,415 | ||||||||||
Customer B | June 30, 2014 | 85,842 | 71,338 | 67,049 | June 30, 2014 | 71,338 | 67,049 | 67,959 | * | |||||||||||||||
Customer C | December 31, 2012 to December 14, 2013(1) | 40,697 | * | 65,175 | * | 111,607 | December 31, 2012 to December 14, 2013(1)(3) | 65,175 | * | 111,607 | 118,351 | |||||||||||||
Customer D | December 31, 2019 | — | — | 134,885 | ||||||||||||||||||||
Public Sector | ||||||||||||||||||||||||
Customer D | June 30, 2012(2) | 147,734 | 153,650 | 191,063 | ||||||||||||||||||||
Customer E | June 30, 2013(4) | 153,650 | 191,063 | 240,224 | ||||||||||||||||||||
Radiology Benefits Management | Radiology Benefits Management | Radiology Benefits Management | ||||||||||||||||||||||
WellPoint, Inc. | December 31, 2010(3) | 155,933 | 159,644 | — | ||||||||||||||||||||
Customer E | November 30, 2012 to April 30, 2013(1) | — | 121,401 | 134,257 | ||||||||||||||||||||
Customer F | June 30, 2011 to November 30, 2011(1)(3) | 80,368 | 66,970 | 38,297 | December 31, 2015 | 121,401 | 134,257 | 117,739 | ||||||||||||||||
Customer G | June 30, 2014 | 23,331 | * | 51,877 | 55,197 | June 30, 2011 to November 30, 2011(1)(5) | 66,970 | 38,297 | — | |||||||||||||||
Customer H | March 31, 2013 | — | 10,448 | * | 36,293 | June 30, 2014 | 51,877 | 55,197 | 60,094 | |||||||||||||||
Specialty Pharmaceutical Management | ||||||||||||||||||||||||
Customer I | March 31, 2012 to January 1, 2013(1) | 85,725 | 86,850 | 90,563 | July 31, 2015 | 10,448 | * | 36,293 | 57,455 | |||||||||||||||
Customer J | April 29, 2012 to September 1, 2012(1) | 43,937 | 57,198 | 56,115 | January 31, 2014 | 935 | * | 32,342 | * | 38,366 | ||||||||||||||
Customer E | February 1, 2012 to April 30, 2013(1) | 30,856 | 32,877 | 25,006 | * | |||||||||||||||||||
Customer Q | December 31, 2012 | 42,465 | 24,897 | * | 18,943 | * | ||||||||||||||||||
Medicaid Administration | ||||||||||||||||||||||||
WellPoint, Inc. | December 31, 2010(5) | 159,644 | — | — | ||||||||||||||||||||
Specialty Pharmaceutical Management | Specialty Pharmaceutical Management | |||||||||||||||||||||||
Customer K | December 4, 2011(3) | 11,353 | 31,145 | 28,060 | November 30, 2013 to December 31, 2013(1) | 86,850 | 90,563 | 129,209 | ||||||||||||||||
Customer L | September 30, 2013(4) | — | 26,108 | 82,770 | April 29, 2013 to September 1, 2013(1) | 57,198 | 56,115 | 60,350 | ||||||||||||||||
Customer B | September 27, 2013 to December 31, 2013(1) | 11,523 | * | 22,899 | * | 73,785 | ||||||||||||||||||
Customer F | September 30, 2013 to December 31, 2014(1) | 32,877 | 25,006 | * | 19,787 | * | ||||||||||||||||||
Medicaid Administration | Medicaid Administration | |||||||||||||||||||||||
Customer M | March 16, 2012 to June 30, 2017(1) | 10,528 | 24,432 | 23,683 | December 4, 2011(5) | 31,145 | 28,060 | — | ||||||||||||||||
Customer N | June 30, 2012 to June 30, 2013(1) | 8,995 | 22,000 | 18,924 | * | September 30, 2013(6) | 26,108 | 82,770 | 69,090 | |||||||||||||||
Customer O | June 30, 2010(3) | 8,815 | 10,319 | * | — | March 31, 2015 to June 30, 2017(1) | 24,432 | 23,683 | 25,103 | |||||||||||||||
Customer P | June 30, 2013 to September 30, 2014(1) | 6,036 | * | 16,249 | * | 22,084 | June 30, 2013 to June 30, 2016(1) | 16,249 | * | 22,084 | 19,518 | |||||||||||||
Customer Q | June 30, 2013 to September 30, 2013(1) | 22,000 | 18,924 | * | 13,828 | * | ||||||||||||||||||
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
December 31, 20112012
2. Summary of Significant Accounting Policies (Continued)
Concentration of Business
The Company also has a significant concentration of business with various counties in the State of Pennsylvania (the "Pennsylvania Counties") which are part of the Pennsylvania Medicaid program, and with various areas in the State of Florida (the "Florida Areas") which are part of the Florida Medicaid program. Net revenues from the Pennsylvania Counties in the aggregate totaled $315.5 million, $334.8 million, $351.6 million and $351.6$354.1 million for the years ended December 31, 2009, 2010, 2011 and 2011,2012, respectively. Net revenues from the Florida Areas in the aggregate totaled $130.9 million, $140.5 million, $131.8 million and $131.8$133.9 million for the years ended December 31, 2009, 2010, 2011 and 2011,2012, respectively.
The Company's contracts with customers typically have terms of one to three years, and in certain cases contain renewal provisions (at the customer's option) for successive terms of between one and two years (unless terminated earlier). Substantially all of these contracts may be immediately terminated with cause and many of the Company's contracts are terminable without cause by the customer or the Company either upon the giving of requisite notice and the passage of a specified period of time (typically between 60 and 180 days) or upon the occurrence of other specified events. In addition, the Company's contracts with federal, state and local governmental agencies generally are conditioned on legislative appropriations. These contracts generally can be terminated or modified by the customer if such appropriations are not made.
Income Taxes
The Company files a consolidated federal income tax return for the Company and its eighty-percent or more owned subsidiaries, and the Company and its subsidiaries file income tax returns in various statesstate and local jurisdictions.
The Company estimates income taxes for each of the jurisdictions in which it operates. This process involves estimating current tax exposures together with assessingdetermining both permanent and temporary differences resulting from differing treatment of items for tax and book purposes. Deferred tax assets and/or liabilities are determined by multiplying the temporary differences between the financial reporting and tax reporting bases for assets and liabilities by the enacted tax rates expected to be in effect when such differences are recovered or settled. The Company establishes valuation allowances against deferred tax assets if it is more likely than not that the deferred tax asset will not be realized. The need for a valuation allowance is determined based on the evaluation of various factors, including expectations of future earnings and management's judgment. The effect of a change in tax rates on deferred taxes is recognized in income in the period that includes the enactment date.
The Company periodically performs a comprehensive review of its tax positions and accrues amounts for tax contingencies related to uncertain tax positions. Based upon these reviews, the status of ongoing tax audits, and the expiration of applicable statutes of limitations, accruals are adjusted as necessary. The tax benefit from an uncertain tax position is recognized when it is more likely than not that, based on technical merit, the position will be sustained upon examination, including resolution of any related appeals or litigation processes. Total accruals for unrecognized tax benefits as of December 31, 2010 and 2011 were $111.6 million and $99.2 million, respectively, and were included within the accompanying consolidated balance sheets in tax contingencies.
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
December 31, 2011
2. Summary of Significant Accounting Policies (Continued)
The Company adjusts these liabilities for unrecognized tax benefits when its judgment changes as a result of the evaluation of new information not previously available. The resolution of tax audits is unpredictable and could result in tax liabilities that are significantly different than those which have been estimated and accrued by the Company. Due to the complexity of some of these uncertainties, the ultimate resolution may result in a payment that is materially different from the Company's current estimate of the tax liabilities. These differences will be reflected as increases or decreases to income tax expense in the period in which they are determined. If the Company's unrecognized tax benefits had been fully realized as of December 31, 2010 and 2011, $88.2 million and $80.3 million, respectively, would have impacted the effective tax rate.
Reversals of both valuation allowances and unrecognized tax benefits are recorded in the period they occur, typically as reductions to income tax expense. However, reversals of unrecognized tax benefits related to deductions for stock compensation in excess of the related book expense are recorded as increases in additional paid-in capital. To the extent reversals of unrecognized tax benefits cannot be specifically traced to these excess deductions due to complexities in the tax law, the Company records the tax benefit for such reversals to additional paid-in capitalpaid-in-capital on a pro-rata basis.
The Company recognizes interim period income taxes by estimating an annual effective tax rate and applying it to year-to-date results. The estimated annual effective tax rate is periodically updated throughout the year based on actual results to date and an updated projection of full year income.
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
December 31, 2012
2. Summary of Significant Accounting Policies (Continued)
Although the effective tax rate approach is generally used for interim periods, taxes on significant, unusual and infrequent items are recognized at the statutory tax rate entirely in the period the amounts are realized.
Cash and Cash Equivalents
Cash equivalents are short-term, highly liquid interest-bearing investments with maturity dates of three months or less when purchased, consisting primarily of money market instruments. At December 31, 2011,2012, the Company's excess capital and undistributed earnings for the Company's regulated subsidiaries of $56.3$47.3 million are included in cash and cash equivalents.
Restricted Assets
The Company has certain assets which are considered restricted for: (i) the payment of claims under the terms of certain managed care contracts; (ii) regulatory purposes related to the payment of claims in certain jurisdictions; and (iii) the maintenance of minimum required tangible net equity levels for certain of the Company's subsidiaries. Significant restricted assets of the Company as of December 31, 20102011 and 20112012 were as follows (in thousands):
| | 2010 | 2011 | 2011 | 2012 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Restricted cash | $ | 116,734 | $ | 185,794 | $ | 185,794 | $ | 226,554 | ||||||
Restricted short-term investments | 114,903 | 129,599 | 129,599 | 88,332 | ||||||||||
Restricted deposits (included in other current assets) | 21,302 | 20,453 | 20,453 | 20,846 | ||||||||||
Restricted long-term investments | 84,950 | 7,956 | 7,956 | 32,563 | ||||||||||
Total | $ | 337,889 | $ | 343,802 | $ | 343,802 | $ | 368,295 | ||||||
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
December 31, 2011
2. Summary of Significant Accounting Policies (Continued)
Investments
All of the Company's investments are classified as "available-for-sale" and are carried at fair value. Securities which have been classified as Level 1 are measured using quoted market prices while those which have been classified as Level 2 are measured using quoted prices for identical assets and liabilities in markets that are not active. The Company's policy is to classify all investments with contractual maturities within one year as current. Investment income is recognized when earned and reported net of investment expenses. Net unrealized holding gains or losses are excluded from earnings and are reported, net of tax, as "accumulated other comprehensive income (loss)" in the accompanying consolidated balance sheets and consolidated statements of comprehensive income until realized, unless the losses are deemed to be other-than-temporary. Realized gains or losses, including any provision for other-than-temporary declines in value, are included in the consolidated statements of comprehensive income.
If a debt security is in an unrealized loss position and the Company has the intent to sell the debt security, or it is more likely than not that the Company will have to sell the debt security before recovery of its amortized cost basis, the decline in value is deemed to be other-than-temporary and is recorded to other-than-temporary impairment losses recognized in income in the consolidated statements of comprehensive income. For impaired debt securities that the Company does not intend to
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
December 31, 2012
2. Summary of Significant Accounting Policies (Continued)
sell or it is more likely than not that the Company will not have to sell such securities, but the Company expects that it will not fully recover the amortized cost basis, the credit component of the other-than-temporary impairment is recognized in other-than-temporary impairment losses recognized in income in the consolidated statements of comprehensive income and the non-credit component of the other-than-temporary impairment is recognized in other comprehensive income.
The credit component of an other-than-temporary impairment is determined by comparing the net present value of projected future cash flows with the amortized cost basis of the debt security. The net present value is calculated by discounting the best estimate of projected future cash flows at the effective interest rate implicit in the debt security at the date of acquisition. Cash flow estimates are driven by assumptions regarding probability of default, including changes in credit ratings, and estimates regarding timing and amount of recoveries associated with a default. Furthermore, unrealized losses entirely caused by non-credit related factors related to debt securities for which the Company expects to fully recover the amortized cost basis continue to be recognized in accumulated other comprehensive income.
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
December 31, 2011
2. Summary of Significant Accounting Policies (Continued)
As of December 31, 20102011 and 2011,2012, there were no unrealized losses that the Company believed to be other-than-temporary. No realized gains or losses were recorded for the years ended December 31, 2009, 2010, 2011 or 2011.2012. The following is a summary of short-term and long-term investments at December 31, 20102011 and 20112012 (in thousands):
| | December 31, 2010 | December 31, 2011 | ||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| | Amortized Cost | Gross Unrealized Gains | Gross Unrealized Losses | Estimated Fair Value | Amortized Cost | Gross Unrealized Gains | Gross Unrealized Losses | Estimated Fair Value | ||||||||||||||||||
U.S. Government and agency securities | $ | 2,178 | $ | 1 | $ | — | $ | 2,179 | $ | 697 | $ | — | $ | — | $ | 697 | ||||||||||
Obligations of government-sponsored enterprises(1) | 10,142 | 7 | (11 | ) | 10,138 | 8,293 | 3 | (3 | ) | 8,293 | ||||||||||||||||
Corporate debt securities | 268,739 | 245 | (215 | ) | 268,769 | 192,059 | 31 | (277 | ) | 191,813 | ||||||||||||||||
Certificates of deposit | 750 | — | — | 750 | 100 | — | — | 100 | ||||||||||||||||||
Taxable municipal bonds | 2,680 | (12 | ) | 2,668 | ||||||||||||||||||||||
Total investments at December 31, 2010 | $ | 284,489 | $ | 253 | $ | (238 | ) | $ | 284,504 | |||||||||||||||||
Total investments at December 31, 2011 | $ | 201,149 | $ | 34 | $ | (280 | ) | $ | 200,903 | |||||||||||||||||
| | December 31, 2011 | December 31, 2012 | ||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| | Amortized Cost | Gross Unrealized Gains | Gross Unrealized Losses | Estimated Fair Value | Amortized Cost | Gross Unrealized Gains | Gross Unrealized Losses | Estimated Fair Value | ||||||||||||||||||
U.S. Government and agency securities | $ | 697 | $ | — | $ | — | $ | 697 | $ | 1,065 | $ | — | $ | — | $ | 1,065 | ||||||||||
Obligations of government-sponsored enterprises | 8,293 | 3 | (3 | ) | 8,293 | 6,126 | 4 | (2 | ) | 6,128 | ||||||||||||||||
Corporate debt securities | 192,059 | 31 | (277 | ) | 191,813 | 214,603 | 66 | (122 | ) | 214,547 | ||||||||||||||||
Certificates of deposit | 100 | — | — | 100 | 150 | — | — | 150 | ||||||||||||||||||
Taxable municipal bonds | 11,805 | (5 | ) | 11,800 | ||||||||||||||||||||||
Total investments at December 31, 2011 | $ | 201,149 | $ | 34 | $ | (280 | ) | $ | 200,903 | |||||||||||||||||
Total investments at December 31, 2012 | $ | 233,749 | $ | 70 | $ | (129 | ) | $ | 233,690 | |||||||||||||||||
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
December 31, 2012
2. Summary of Significant Accounting Policies (Continued)
The maturity dates of the Company's investments as of December 31, 20112012 are summarized below (in thousands):
| | Amortized Cost | Estimated Fair Value | |||||
|---|---|---|---|---|---|---|---|
2012 | $ | 193,147 | $ | 192,947 | |||
2013 | 8,002 | 7,956 | |||||
Total investments at December 31, 2011 | $ | 201,149 | $ | 200,903 | |||
| | Amortized Cost | Estimated Fair Value | |||||
|---|---|---|---|---|---|---|---|
2013 | $ | 201,198 | $ | 201,127 | |||
2014 | 32,551 | 32,563 | |||||
Total investments at December 31, 2012 | $ | 233,749 | $ | 233,690 | |||
Accounts Receivable
The Company's accounts receivable consists of amounts due from customers throughout the United States. Collateral is generally not required. The Company establishes an allowance for doubtful
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
December 31, 2011
2. Summary of Significant Accounting Policies (Continued)
accounts based upon factors surrounding the credit risk of specific customers, historical trends and other information. Management believes the allowance for doubtful accounts is adequate to provide for normal credit losses.
Concentration of Credit Risk
Accounts receivable subjects the Company to a concentration of credit risk with third party payors that include health insurance companies, managed healthcare organizations, healthcare providers and governmental entities.
The Company maintains cash and cash equivalents balances at financial institutions and are insured by the Federal Deposit Insurance Corporation ("FDIC"). At times, balances in certain bank accounts may exceed the FDIC insured limits.
Pharmaceutical Inventory
Pharmaceutical inventory consists solely of finished productsgoods (primarily prescription drugs) and are stated at the lower of first-in first-out cost or market.
Long-lived Assets
Long-lived assets, including property and equipment and intangible assets to be held and used, are currently reviewed for impairment whenever events or changes in circumstances indicate that the carrying amount should be addressed. Impairment is determined by comparing the carrying value of these long-lived assets to management's best estimate of the future undiscounted cash flows expected to result from the use of the assets and their eventual disposition. The cash flow projections used to make this assessment are consistent with the cash flow projections that management uses internally in making key decisions. In the event an impairment exists, a loss is recognized based on the amount by which the carrying value exceeds the fair value of the asset, which is generally determined by using quoted market prices or the discounted present value of expected future cash flows.
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
December 31, 2012
2. Summary of Significant Accounting Policies (Continued)
Property and Equipment
Property and equipment is stated at cost, except for assets that have been impaired, for which the carrying amount has been reduced to estimated fair value. Expenditures for renewals and improvements are capitalized to the property accounts. Replacements and maintenance and repairs that do not improve or extend the life of the respective assets are expensed as incurred. The Company capitalizes costs incurred to develop internal-use software during the application development stage. Capitalization of software development costs occurs after the preliminary project stage is complete, management authorizes the project, and it is probable that the project will be completed and the software will be used for the function intended. Amortization of capital lease assets is included in depreciation expense and is included in accumulated depreciation as reflected in the table below. Depreciation is provided on a straight-line basis over the estimated useful lives of the assets, which is generally two to ten years for buildings andbuilding improvements (or the lease term, if shorter), three to fifteen years for equipment and three to five years for capitalized internal-use software. The net capitalized internal use software as of December 31, 20102011 and 20112012 was $61.9$62.0 million and $62.0$71.1 million, respectively. Depreciation expense was $37.8 million, $43.9 million, $47.9 million and $47.9$50.8 million for the years ended December 31, 2009, 2010, 2011 and 2011,2012, respectively. Included in the depreciation expense for the years ended December 31, 2009, 2010, 2011 and 20112012 was $20.2 million, $26.6 million, $28.9 million and $28.9$28.8 million, respectively, related to capitalized internal use software.
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
December 31, 2011
2. Summary of Significant Accounting Policies (Continued)
Property and equipment, net, consisted of the following at December 31, 20102011 and 20112012 (in thousands):
| | 2010 | 2011 | 2011 | 2012 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Buildings and improvements | $ | 5,321 | $ | 5,037 | ||||||||||
Building improvements | $ | 5,037 | $ | 7,285 | ||||||||||
Equipment | 141,427 | 150,874 | 150,874 | 168,400 | ||||||||||
Capitalized internal-use software | 195,223 | 224,190 | 224,190 | 261,833 | ||||||||||
| 341,971 | 380,101 | 380,101 | 437,518 | |||||||||||
Accumulated depreciation | (230,157 | ) | (262,079 | ) | (262,079 | ) | (300,970 | ) | ||||||
Property and equipment, net | $ | 111,814 | $ | 118,022 | $ | 118,022 | $ | 136,548 | ||||||
Goodwill
The Company is required to test its goodwill for impairment on at least an annual basis. The Company has selected October 1 as the date of its annual impairment test. The goodwill impairment test is a two-step process that requires management to make judgments in determining what assumptions to use in the calculation. The first step of the process consists of estimating the fair value of each reporting unit with goodwill based on various valuation techniques, with the primary technique being a discounted cash flow analysis, which requires the input of various assumptions with respect to revenues, operating margins, growth rates and discount rates. The estimated fair value for each reporting unit is compared to the carrying value of the reporting unit, which includes goodwill. If the estimated fair value is less than the carrying value, a second step is performed to compute the amount of the impairment by determining an "implied fair value" of goodwill. The determination of a reporting unit's "implied fair value" of goodwill requires the Company to allocate the estimated fair value of the
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
December 31, 2012
2. Summary of Significant Accounting Policies (Continued)
reporting unit to the assets and liabilities of the reporting unit. Any unallocated fair value represents the "implied fair value" of goodwill, which is compared to its corresponding carrying value.
The fair value of the Health Plan (a component of the Commercial segment), Radiology Benefits Management and the Radiology BenefitsSpecialty Pharmaceutical Management reporting units were determined using a discounted cash flow method. This method involves estimating the present value of estimated future cash flows utilizing a risk adjusted discount rate. Key assumptions for this method include cash flow projections, terminal growth rates and discount rates.
The fair value of the Specialty Pharmaceutical ManagementMedicaid Administration reporting unit was determined using the discounted cash flow, guideline company and similar transaction methods. Key assumptions for the discounted cash flow method are consistent with those described above. For the guideline company method, revenue and earnings before interest, taxes, depreciation, and amortization ("EBITDA") multiples for guideline companies were applied to the reporting unit's actual revenue and EBTIDAEDITDA for the twelve-month period ended September 30, 20112012 and to the reporting unit's projected revenue and EBITDA for 2012. For the similar transaction method, an EBITDA multiple based on merger and acquisition transactions for similar companies was applied to the reporting unit's actual EBITDA for the twelve-month period ended September 30, 2011. The weighting applied to the fair values determined using the discounted cash flow, guideline company and similar transaction methods to determine an overall fair value for the Specialty Pharmaceutical Management reporting unit was 60 percent, 24 percent and 16 percent,
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
December 31, 2011
2. Summary of Significant Accounting Policies (Continued)
respectively. The weighting of each of the methods described above was based on the relevance of the approach. A change in the weighting would not change the outcome of the first step of the impairment test.
The fair value of the Medicaid Administration reporting unit was determined using discounted cash flow, guideline company and similar transaction methods. Key assumptions for the discounted cash flow method are consistent with those described above. For the guideline company method, an EBITDA multiple for guideline companies was applied to the reporting unit's projected EBITDA for 2012.2013. For the similar transaction method, revenue and EBITDA multiples based on merger and acquisition transactions for similar companies were applied to the reporting unit's actual revenue and EBITDA for the twelve-month period ended September 30, 2011.2012. The weighting applied to the fair values determined using the discounted cash flow, guideline company and similar transaction methods to determine an overall fair value for the Medicaid Administration reporting unit was 75 percent, 22.5 percent and 2.5 percent, respectively. The weighting of each of the methods described above was based on the relevance of the approach. A change in the weighting would not change the outcome of the first step of the impairment test.
As a result of the first step of the 20112012 annual goodwill impairment analysis, the fair value of each reporting unit with goodwill exceeded its carrying value. Therefore, the second step was not necessary. However, a 5620 percent decline in the fair value of the Health Plan, reporting unit, a 5456 percent decline in fair value of Radiology Benefits Management, or a 2035 percent decline in fair value of Specialty Pharmaceutical Management and a 30 percent decline in fair value of Medicaid Administration reporting units would have caused the carrying values for these reporting units to be in excess of fair values, which would require the second step to be performed. The second step could have resulted in an impairment loss for goodwill.
While there are numerous assumptions that impact the calculation of the fair value of the reporting units, the most sensitive assumptions relate to the discount rate and estimated future cash flows when determining fair value using the discounted cash flow method. For Medicaid Administration, an 8those reporting units with a projected fair value within 30 percent of the carrying value, the impact of changes in the discount rate and estimated future cash flows was reviewed for sensitivity.
For Health Plan, a 20 percent decline in fair value, or approximately $10$40 million, would have caused the carrying value to be in excess of its fair value as of October 1, 2011. While there are numerous assumptions that impact the calculation of the fair value of this reporting unit, the most sensitive assumptions relate to the discount rate and the estimated future cash flows.2012. A decline in fair value of approximately $10$40 million would occur upon either: (1) an increase of 0.85338 basis points in the discount rate utilized to determine the present value of the projected net cash flows; or (2) a decline between 20 and 40 percent in estimated future cash flows, with the percentage decrease varying depending upon whether the cash flow decrease were to occur in the near term or long term. For Medicaid Administration, a 30 percent decline in fair value, or approximately $50 million, would have
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
December 31, 2012
2. Summary of Significant Accounting Policies (Continued)
caused the carrying value to be in excess of its fair value as of October 1, 2012. A decline in fair value of approximately $50 million would occur upon either: (1) an increase of 350 basis points in the discount rate utilized to determine the present value of the projected net cash flows; or (2) a decline of between 1230 and 2540 percent in estimated future cash flows, with the percentage decrease varying depending upon whether the cash flow decrease were to occur in the near term or the long term. Such declinedeclines in the future cash flows could be the result of a loss of one or more significant customers without the generation of new business to offset such losses.losses or an inability to meet the respective reporting unit's growth targets, which could include expansion into new product offerings. A decline in the fair valuevalues for Health Plan and Medicaid Administration could result in a carrying value for Medicaid Administrationvalues in excess of fair value,values, which would require the second step of goodwill testing to be performed. The second step could result in an impairment loss for goodwill.
Goodwill for each of the Company's reporting units are as follows (in thousands):
| | December 31, | ||||||
|---|---|---|---|---|---|---|---|
| | 2011 | 2012 | |||||
Health Plan | $ | 120,485 | $ | 120,485 | |||
Radiology Benefits Management | 104,549 | 104,549 | |||||
Specialty Pharmaceutical Management | 142,291 | 142,291 | |||||
Medicaid Administration | 59,614 | 59,614 | |||||
Total | $ | 426,939 | $ | 426,939 | |||
Intangible Assets
The following is a summary of intangible assets at December 31, 2011 and 2012, and the estimated useful lives for such assets (in thousands):
| | December 31, 2011 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
Asset | Estimated Useful Life | Gross Carrying Amount | Accumulated Amortization | Net Carrying Amount | ||||||||
Customer agreements and lists | 3 to 18 years | $ | 121,490 | $ | (81,388 | ) | $ | 40,102 | ||||
Provider networks and other | 5 to 16 years | 8,743 | (4,256 | ) | 4,487 | |||||||
| $ | 130,233 | $ | (85,644 | ) | $ | 44,589 | ||||||
| | December 31, 2012 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
Asset | Estimated Useful Life | Gross Carrying Amount | Accumulated Amortization | Net Carrying Amount | ||||||||
Customer agreements and lists | 3 to 18 years | $ | 121,490 | $ | (90,548 | ) | $ | 30,942 | ||||
Provider networks and other | 5 to 16 years | 8,743 | (4,750 | ) | 3,993 | |||||||
| $ | 130,233 | $ | (95,298 | ) | $ | 34,935 | ||||||
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
December 31, 20112012
2. Summary of Significant Accounting Policies (Continued)
Goodwill for each of the Company's reporting units is as follows (in thousands):
| | December 31, | ||||||
|---|---|---|---|---|---|---|---|
| | 2010 | 2011 | |||||
Commercial | $ | 120,485 | $ | 120,485 | |||
Radiology Benefits Management | 104,549 | 104,549 | |||||
Specialty Pharmaceutical Management | 142,291 | 142,291 | |||||
Medicaid Administration | 59,614 | 59,614 | |||||
Total | $ | 426,939 | $ | 426,939 | |||
The changes in the carrying amount of goodwillAmortization expense was $10.8 million, $10.7 million and $9.7 million for the years ended December 31, 2010, and 2011 are reflected in the table below (in thousands):
| | 2010 | 2011 | |||||
|---|---|---|---|---|---|---|---|
Balance as of beginning of period | $ | 426,471 | $ | 426,939 | |||
Adjustment related to acquisition of Medicaid Administration | 468 | — | |||||
Balance as of end of period | $ | 426,939 | $ | 426,939 | |||
Intangible Assets
The following is a summary of intangible assets at December 31, 2010 and 2011 and the estimated useful lives for such assets (in thousands):
| | December 31, 2010 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
Asset | Estimated Useful Life | Gross Carrying Amount | Accumulated Amortization | Net Carrying Amount | ||||||||
Customer agreements and lists | 3 to 18 years | $ | 121,490 | $ | (71,165 | ) | $ | 50,325 | ||||
Provider networks and other | 5 to 16 years | 7,430 | (3,758 | ) | 3,672 | |||||||
| $ | 128,920 | $ | (74,923 | ) | $ | 53,997 | ||||||
| | December 31, 2011 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
Asset | Estimated Useful Life | Gross Carrying Amount | Accumulated Amortization | Net Carrying Amount | ||||||||
Customer agreements and lists | 3 to 18 years | $ | 121,490 | $ | (81,388 | ) | $ | 40,102 | ||||
Provider networks and other | 5 to 16 years | 8,743 | (4,256 | ) | 4,487 | |||||||
| $ | 130,233 | $ | (85,644 | ) | $ | 44,589 | ||||||
Amortization expense was $9.5 million, $10.8 million and $10.7 million for the years ended December 31, 2009, 2010 and 2011,2012, respectively. The Company estimates amortization expense will be
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
December 31, 2011
2. Summary of Significant Accounting Policies (Continued)
$9.7 million, $9.1 million, $9.1 million, $8.0 million, $5.3 million and $5.3$1.9 million for the years ending December 31, 2012, 2013, 2014, 2015, 2016, and 20162017 respectively.
Cost of Care, Medical Claims Payable and Other Medical Liabilities
Cost of care is recognized in the period in which members receive managed healthcare services. In addition to actual benefits paid, cost of care in a period also includes the impact of accruals for estimates of medical claims payable. Medical claims payable represents the liability for healthcare claims reported but not yet paid and claims incurred but not yet reported ("IBNR") related to the Company's managed healthcare businesses.
Such liabilities are determined by employing actuarial methods that are commonly used by health insurance actuaries and that meet actuarial standards of practice.
The IBNR portion of medical claims payable is estimated based on past claims payment experience for member groups, enrollment data, utilization statistics, authorized healthcare services and other factors. This data is incorporated into contract-specific actuarial reserve models and is further analyzed to create "completion factors" that represent the average percentage of total incurred claims that have been paid through a given date after being incurred. Factors that affect estimated completion factors include benefit changes, enrollment changes, shifts in product mix, seasonality influences, provider reimbursement changes, changes in claims inventory levels, the speed of claims processing and changes in paid claim levels. Completion factors are applied to claims paid through the financial statement date to estimate the ultimate claim expense incurred for the current period. Actuarial estimates of claim liabilities are then determined by subtracting the actual paid claims from the estimate of the ultimate incurred claims. For the most recent incurred months (generally the most recent two months), the percentage of claims paid for claims incurred in those months is generally low. This makes the completion factor methodology less reliable for such months. Therefore, incurred claims for any month with a completion factor that is less than 70 percent are generally not projected from historical completion and payment patterns; rather they are projected by estimating claims expense based on recent monthly estimated cost incurred per member per month times membership, taking into account seasonality influences, benefit changes and healthcare trend levels, collectively considered to be "trend factors."
Medical claims payable balances are continually monitored and reviewed. If it is determined that the Company's assumptions in estimating such liabilities are significantly different than actual results, the Company's results of operations and financial position could be impacted in future periods. Adjustments of prior period estimates may result in additional cost of care or a reduction of cost of care in the period an adjustment is made. Further, due to the considerable variability of healthcare costs, adjustments to claim liabilities occur each period and are sometimes significant as compared to the net income recorded in that period. Prior period development is recognized immediately upon the actuary's judgment that a portion of the prior period liability is no longer needed or that additional
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
December 31, 20112012
2. Summary of Significant Accounting Policies (Continued)
liability should have been accrued. The following table presents the components of the change in medical claims payable for the years ended December 31, 2009, 2010, 2011 and 20112012 (in thousands):
| | 2009 | 2010 | 2011 | 2010 | 2011 | 2012 | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Claims payable and IBNR, beginning of period | $ | 184,422 | $ | 168,851 | $ | 166,095 | $ | 168,851 | $ | 166,095 | $ | 157,099 | ||||||||
Cost of care: | ||||||||||||||||||||
Current year | 1,771,213 | 1,919,785 | 1,790,124 | 1,919,785 | 1,790,124 | 2,076,190 | ||||||||||||||
Prior years | (5,900 | ) | (11,800 | ) | (5,400 | ) | (11,800 | ) | (5,400 | ) | (4,300 | ) | ||||||||
Total cost of care | 1,765,313 | 1,907,985 | 1,784,724 | 1,907,985 | 1,784,724 | 2,071,890 | ||||||||||||||
Claim payments and transfers to other medical liabilities(1): | ||||||||||||||||||||
Current year | 1,624,626 | 1,777,356 | 1,657,291 | 1,777,356 | 1,657,291 | 1,877,459 | ||||||||||||||
Prior years | 156,258 | 133,385 | 136,429 | 133,385 | 136,429 | 128,601 | ||||||||||||||
Total claim payments and transfers to other medical liabilities | 1,780,884 | 1,910,741 | 1,793,720 | 1,910,741 | 1,793,720 | 2,006,060 | ||||||||||||||
Claims payable and IBNR, end of period | 168,851 | 166,095 | 157,099 | 166,095 | 157,099 | 222,929 | ||||||||||||||
Withhold receivables, end of period(2) | (25,182 | ) | (23,424 | ) | (19,126 | ) | (23,424 | ) | (19,126 | ) | (24,500 | ) | ||||||||
Medical claims payable, end of period | $ | 143,669 | $ | 142,671 | $ | 137,973 | $ | 142,671 | $ | 137,973 | $ | 198,429 | ||||||||
Actuarial standards of practice require that the claim liabilities be adequate under moderately adverse circumstances. Adverse circumstances are situations in which the actual claims experience could be higher than the otherwise estimated value of such claims. In many situations, the claims paid amount experienced will be less than the estimate that satisfies the actuarial standards of practice.
Due to the existence of risk sharing and reinvestment provisions in certain customer contracts, principally in the Public Sector segment, a change in the estimate for medical claims payable does not necessarily result in an equivalent impact on cost of care.
The Company believes that the amount of medical claims payable is adequate to cover its ultimate liability for unpaid claims as of December 31, 2011;2012; however, actual claims payments may differ from established estimates.
Other medical liabilities consist primarily of "reinvestment" payables under certain managed behavioral healthcare contracts with Medicaid customers and "profit share" payables under certain risk-based contracts. Under a contract with reinvestment features, if the cost of care is less than certain
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
December 31, 2011
2. Summary of Significant Accounting Policies (Continued)
minimum amounts specified in the contract (usually as a percentage of revenue), the Company is required to "reinvest" such difference in behavioral healthcare programs when and as specified by the customer or to pay the difference to the customer for their use in funding such programs. Under a
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
December 31, 2012
2. Summary of Significant Accounting Policies (Continued)
contract with profit share provisions, if the cost of care is below certain specified levels, the Company will "share" the cost savings with the customer at the percentages set forth in the contract.
Accrued Liabilities
As of December 31, 20102011 and 2011,2012, the only individual current liability that exceeded five percent of total current liabilities related to accrued employee compensation liabilities of $34.5$32.7 million and $32.7$36.5 million, respectively.
Net Income per Common Share
Net income per common share is computed based on the weighted average number of shares of common stock and common stock equivalents outstanding during the period (see Note 6—"Stockholders' Equity").
Stock Compensation
The Company uses the Black-Scholes-Merton formula to estimate the fair value of substantially all stock options granted to employees, and recorded stock compensation expense of $19.8 million, $15.1 million, $17.4 million and $17.4$17.8 million for the years ended December 31, 2009, 2010, 2011 and 2011,2012, respectively. As stock compensation expense recognized in the consolidated statements of comprehensive income for the years ended December 31, 2009, 2010, 2011 and 20112012 is based on awards ultimately expected to vest, it has been reduced for annual estimated forfeitures of five percent, fivefour percent and four percent, respectively. If the actual number of forfeitures differs from those estimated, additional adjustments to compensation expense may be required in future periods. If vesting of an award is conditioned upon the achievement of performance goals, compensation expense during the performance period is estimated using the most probable outcome of the performance goals, and adjusted as the expected outcome changes. The Company recognizes substantially all of these compensation costs for awards that do not contain performance conditions on a straight-line basis over the requisite service period, which is generally the vesting term of three years. For restricted stock units that include performance conditions, stock compensation is recognized using an accelerated method over the vesting period.
Fair Value Measurements
The Company currently does not have non-financial assets and non-financial liabilities that are required to be measured at fair value on a recurring basis. Financial assets and liabilities are to be measured using inputs from the three levels of the fair value hierarchy, which are as follows:
Level 1—Inputs are unadjusted quoted prices in active markets for identical assets or liabilities that the Company has the ability to access at the measurement date.
Level 2—Inputs include quoted prices for similar assets and liabilities in active markets, quoted prices for identical or similar assets or liabilities in markets that are not active, inputs other than quoted prices that are observable for the asset or liability (i.e., interest rates, yield curves, etc.), and inputs that are derived principally from or corroborated by observable market data by correlation or other means (market corroborated inputs).
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
December 31, 20112012
2. Summary of Significant Accounting Policies (Continued)
Level 3—Unobservable inputs that reflect the Company's assumptions about the assumptions that market participants would use in pricing the asset or liability. The Company develops these inputs based on the best information available, including the Company's data.
In accordance with the fair value hierarchy described above, the following table shows the fair value of the Company's financial assets and liabilities that are required to be measured at fair value as of December 31, 20102011 and 20112012 (in thousands):
| Fair Value Measurements at December 31, 2011 | ||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| | Level 1 | Level 2 | Level 3 | Total | Level 1 | Level 2 | Level 3 | Total | ||||||||||||||||||
Cash and Cash Equivalents(1) | $ | — | $ | 68,726 | $ | — | $ | 68,726 | $ | — | $ | 1,296 | $ | — | $ | 1,296 | ||||||||||
Restricted Cash(2) | — | 72,698 | — | 72,698 | — | 47,972 | — | 47,972 | ||||||||||||||||||
Investments: | ||||||||||||||||||||||||||
U.S. Government and agency securities | 2,179 | — | — | 2,179 | 697 | — | — | 697 | ||||||||||||||||||
Obligations of government-sponsored enterprises(3) | — | 10,138 | — | 10,138 | — | 8,293 | — | 8,293 | ||||||||||||||||||
Corporate debt securities | — | 268,769 | — | 268,769 | — | 191,813 | — | 191,813 | ||||||||||||||||||
Taxable municipal bonds | — | 2,668 | — | 2,668 | ||||||||||||||||||||||
Certificates of deposit | — | 750 | — | 750 | — | 100 | — | 100 | ||||||||||||||||||
December 31, 2010 | $ | 2,179 | $ | 423,749 | $ | — | $ | 425,928 | ||||||||||||||||||
December 31, 2011 | $ | 697 | $ | 249,474 | $ | — | $ | 250,171 | ||||||||||||||||||
| Fair Value Measurements at December 31, 2012 | ||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| | Level 1 | Level 2 | Level 3 | Total | Level 1 | Level 2 | Level 3 | Total | ||||||||||||||||||
Cash and Cash Equivalents(4) | $ | — | $ | 1,296 | $ | — | $ | 1,296 | $ | — | $ | 102,137 | $ | — | $ | 102,137 | ||||||||||
Restricted Cash(5) | — | 47,972 | — | 47,972 | — | 82,839 | — | 82,839 | ||||||||||||||||||
Investments: | ||||||||||||||||||||||||||
U.S. Government and agency securities | 697 | — | — | 697 | 1,065 | — | — | 1,065 | ||||||||||||||||||
Obligations of government-sponsored enterprises(6) | — | 8,293 | — | 8,293 | ||||||||||||||||||||||
Obligations of government-sponsored enterprises(3) | — | 6,128 | — | 6,128 | ||||||||||||||||||||||
Corporate debt securities | — | 191,813 | — | 191,813 | — | 214,547 | — | 214,547 | ||||||||||||||||||
Taxable municipal bonds | — | — | — | — | — | 11,800 | — | 11,800 | ||||||||||||||||||
Certificates of deposit | — | 100 | — | 100 | — | 150 | — | 150 | ||||||||||||||||||
December 31, 2011 | $ | 697 | $ | 249,474 | $ | — | $ | 250,171 | ||||||||||||||||||
December 31, 2012 | $ | 1,065 | $ | 417,601 | $ | — | $ | 418,666 | ||||||||||||||||||
Reclassifications
Certain prior year amounts have been reclassified to conform with the Federal Home Loan Bank.current year presentation.
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
December 31, 20112012
2. Summary of Significant Accounting Policies (Continued)
Reclassifications
Certain prior year amounts have been reclassified to conform with the current year presentation.
3. Acquisitions
Acquisition of First Health ServicesJoint Ventures
PursuantThe Company currently owns an 80 percent interest in MCCAZ, which was formed to manage integrated behavioral and physical healthcare for recipients with SMI and behavioral healthcare for other Medicaid beneficiaries in Maricopa County. MCCAZ has responded to a RFP released by the JuneADHS on October 4, 2009 Purchase Agreement (the "Purchase Agreement") with Coventry Health Care ("Coventry"), on July2012. During the year ended December 31, 20092012, the Company acquired (the "Acquisition") all of the outstanding equity interests of Coventry's direct and indirect subsidiaries First Health Services Corporation ("FHS"), FHC, Inc. ("FHC") and Provider Synergies, LLC (together with FHS and FHC, "First Health Services") and certain assets of Coventry which are related to the operation of the business conducted by First Health Services. As consideration for the Acquisition, the Company paid $114.5invested $1.5 million in MCCAZ, which is included within restricted cash excluding cash acquired and including net payments of $6.5 million for excess working capital.on the accompanying consolidated balance sheets. The Company fundedhas consolidated the Acquisition with cash on hand.
Effective July 1, 2010 the Company discontinued the use of the name First Health Services Corporationbalance sheet and officially changed such name to "Magellan Medicaid Administration, Inc." The Company reports the results of operations of MagellanMCCAZ in its consolidated financial statements as of December 31, 2012.
The Company currently owns a 49 percent interest in Fallon Total Care, LLC ("Fallon Total Care"), which was formed to apply to participate in a demonstration program that will provide integrated healthcare to individuals aged 21 to 64 years who are dually-eligible for Medicare and Medicaid Administration, Inc.in the State of Massachusetts. The other 51 percent interest in Fallon Total Care is owned by Fallon Community Health Plan. On November 5, 2012, it was announced that Fallon Total Care was selected as a participant in the three-year demonstration program to serve dual-eligible residents in ten counties across Massachusetts. The contract award is subject to completion of readiness review and contract negotiation. During the year ended December 31, 2012, the Company contributed $1.2 million of capital to Fallon Total Care, which is included within other long-term assets on the Medicaid Administration segment.accompanying consolidated balance sheets. The Company accounts for its investment in Fallon Total Care using the equity method.
4. Benefit Plans
The Company has a defined contribution retirement plan (the "401(k) Plan"). Employee participants can elect to contribute up to 75 percent of their compensation, subject to Internal Revenue Service ("IRS") deferral limitations. The Company makes contributions to the 401(k) Plan based on employee compensation and contributions. The Company matches 50 percent of each employee's contribution up to 6 percent of their annual compensation. The Company recognized $5.1 million, $5.6 million, $5.8 million and $5.8$6.3 million of expense for the years ended December 31, 2009, 2010, 2011 and 2011,2012, respectively, for matching contributions to the 401(k) Plan.
5. Long-Term Debt and Capital Lease Obligations
On April 30, 2008,29, 2009, the Company entered into a credit facility with Deutsche Bank AG and Citigroup Global Markets Inc. that provided for a $100.0 million Revolving Loan Commitment for the issuance of letters of credit for the account of the Company with a sublimit of up to $30.0 million for revolving loans (the "2008 Credit Facility").
On April 29, 2009, the Company entered into an amendment to the 2008 Credit Facility with Deutsche Bank AG, Citibank, N.A., and Bank of America, N.A. that provided for an $80.0 million Revolving Loan Commitment for the issuance of letters of credit for the account of the Company with a sublimit of up to $30.0 million for revolving loans (the "2009 Credit Facility"). Borrowings under the 2009 Credit Facility matured on April 28, 2010. The 2009 Credit Facility was guaranteed by substantially all of the subsidiaries of the Company and was secured by substantially all of the assets of the Company and the subsidiary guarantors.
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
December 31, 2011
5. Long-Term Debt and Capital Lease Obligations (Continued)
Under the 2009 Credit Facility, the annual interest rate on Revolving Loan borrowings was equal to (i) in the case of U.S. dollar denominated loans, the sum of a borrowing margin of 2.25 percent plus the higher of the prime rate or one-half of one percent in excess of the overnight "federal funds" rate, or (ii) in the case of Eurodollar denominated loans, the sum of a borrowing margin of 3.25 percent plus the Eurodollar rate for the selected interest period. The Company had the option to borrow in U.S. dollar denominated loans or Eurodollar denominated loans at its discretion. Letters of Credit issued under the Revolving Loan Commitment bore interest at the rate of 3.375 percent. The commitment commission on the 2009 Credit Facility was 0.625 percent of the unused Revolving Loan Commitment.
On April 28, 2010, the Company entered into an amendment to the 2009 Credit Facility with Deutsche Bank AG, Citibank, N.A., and Bank of America, N.A. that provided for an $80.0 million Revolving Loan Commitment for the issuance of letters of credit for the account of the Company with a sublimit of up to $30.0 million for revolving loans (the "2010 Credit Facility"). Borrowings under the 2010 Credit Facility mature on April 28, 2013. The 2010 Credit Facility is guaranteed by substantially all
Table of the subsidiaries of the CompanyContents
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
December 31, 2012
5. Long-Term Debt and is secured by substantially all of the assets of the Company and the subsidiary guarantors.Capital Lease Obligations (Continued)
Under the 2010 Credit Facility, the annual interest rate on Revolving Loan borrowings iswas equal to (i) in the case of U.S. dollar denominated loans, the sum of a borrowing margin of 1.75 percent plus the higher of the prime rate or one-half of one percent in excess of the overnight "federal funds" rate, or (ii) in the case of Eurodollar denominated loans, the sum of a borrowing margin of 2.75 percent plus the Eurodollar rate for the selected interest period. The Company hashad the option to borrow in U.S. dollar denominated loans or Eurodollar denominated loans at its discretion. Letters of Credit issued under the Revolving Loan Commitment bearbore interest at the rate of 2.875 percent. The commitment commission on the 2010 Credit Facility iswas 0.50 percent of the unused Revolving Loan Commitment.
On December 9, 2011, the Company entered into a Senior Secured Revolving Credit Facility Credit Agreement with Citibank, N.A., Wells Fargo Bank, N.A., Bank of America, N.A., and U.S. Bank, N.A. that provides for up to $230.0 million of revolving loans with a sublimit of up to $70.0 million for the issuance of letters of credit for the account of the Company (the "2011 Credit Facility"). At such point, the 2010 Credit Facility was terminated. The 2011 Credit Facility is guaranteed by substantially all of the subsidiaries of the Company and is secured by substantially all of the assets of the Company and the subsidiary guarantors. The 2011 Credit Facility will mature on December 9, 2014.
Under the 2011 Credit Facility, the annual interest rate on Revolving Loan borrowings is equal to (i) in the case of U.S. dollar denominated loans, the sum of a borrowing margin of 1.000.75 percent plus the higher of the prime rate, one-half of one percent in excess of the overnight "federal funds" rate, or the Eurodollar rate for one month plus 1.00%,1.00 percent, or (ii) in the case of Eurodollar denominated loans, the sum of a borrowing margin of 2.001.75 percent plus the Eurodollar rate for the selected interest period. The Company has the option to borrow in U.S. dollar denominated loans or Eurodollar denominated loans at its discretion. Letters of Credit issued under the Revolving Loan Commitment bear interest at the rate of 2.1251.875 percent. The commitment commission on the 2011 Credit Facility is 0.375 percent of the unused Revolving Loan Commitment.
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
December 31, 2011
5. Long-Term Debt and Capital Lease Obligations (Continued)
The 2011 Credit Facility contains covenants that limit management's discretion in operating the Company's business by restricting or limiting the Company's ability, among other things, to:
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
December 31, 2012
5. Long-Term Debt and Capital Lease Obligations (Continued)
There were $0.6$68.1 million and $0 million of capital lease obligations at December 31, 2010 and 2011, respectively, $44.9 million and $68.1$32.0 million of letters of credit outstanding at December 31, 20102011 and 2011,2012, respectively, and no Revolving Loan borrowings or capital lease obligations at December 31, 20102011 or December 31, 2011.2012.
6. Stockholders' Equity
Stock Compensation
At December 31, 20102011 and 2011,2012, the Company had equity-based employee incentive plans. Prior to May 18, 2011, the Company utilized the 2008 Management Incentive Plan (the "2008 MIP"), 2006 Management Incentive Plan (the "2006 MIP"), 2003 Management Incentive Plan (the "2003 MIP") and 2006 Directors' Equity Compensation Plan (collectively the "Preexisting Plans") for grants of stock options, restricted stock, restricted stock units, and stock appreciation rights, to provide incentives to officers, employees and non-employee directors.
On February 18, 2011 the board of directors of the Company approved the 2011 Management Incentive Plan ("2011 MIP"), and the 2011 MIP was approved by the Company's shareholders at the 2011 Annual Meeting of Shareholders on May 18, 2011. The 2011 MIP provides for the delivery of up to a number of shares equal to (i) 5,000,000 shares of common stock, plus (ii) the number of shares subject to outstanding awards under the Preexisting Plans which become available after shareholder approval of the 2011 MIP as a result of forfeitures, expirations, and in other permitted ways under the share recapture provisions of the 2011 MIP. Delivery of shares under "full-value" awards (awards other than options or stock appreciation rights) will be counted for each share delivered as 2.29 shares against the total number of shares reserved under the 2011 MIP. Upon shareholder approval of the 2011 MIP, no further awards were made under the Preexisting Plans, and any shares that remained available for new awards (i.e.,were not committed for outstanding awards) under the Preexisting Plans were not carried forward to the 2011 MIP.
The 2011 MIP provides for awards of stock options, restictedrestricted stock awards ("RSAs"), restricted stock units ("RSUs"), stock appreciation rights, cash-denominated awards and any combination of the
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
December 31, 2011
6. Stockholders' Equity (Continued)
foregoing. A restricted stock unit is a notional account representing the right to receive a share of the Company's Common Stock (or, at the Company's option, cash in lieu thereof) at some future date. In general, stock options vest ratably on each anniversary over the three years subsequent to grant, and have a ten year life. RSAs generally vest on the anniversary of the grant, whilegrant. The RSUs vest ratably on each anniversary over the three years subsequent to grant.grant, assuming that the associated performance hurdle(s) for that vesting year are met. Stock compensation expense is recognized using an accelerated method over the vesting period based upon the continued employment of the RSU holder and the probability of achievement of the performance hurdle(s). RSUs granted in 2010 and 2011 have performance thresholds based on EPS, while RSUs granted in 2012 have performance thresholds based on EPS and return on equity ("ROE").
The 2011 MIP additionally provides for the ability of employees to purchase common stock at a discount under the employee stock purchase plan ("ESPP"). At December 31, 2011, 4,886,3852012, 3,734,703 shares of the Company's common stock remain available for future grant under the Company's 2011 MIP.
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
December 31, 2012
6. Stockholders' Equity (Continued)
Stock Options
Summarized information related to the Company's stock options for the years ended December 31, 2009, 2010, 2011 and 20112012 is as follows:
| | 2009 | 2010 | 2010 | 2011 | ||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| | Options | Weighted Average Exercise Price | Options | Weighted Average Exercise Price | Options | Weighted Average Exercise Price | Options | Weighted Average Exercise Price | ||||||||||||||||||
Outstanding, beginning of period | 4,668,490 | $ | 39.82 | 5,185,091 | $ | 38.19 | 5,185,091 | $ | 38.19 | 3,775,586 | $ | 39.27 | ||||||||||||||
Granted | 1,326,694 | 33.00 | 951,072 | 42.70 | 951,072 | 42.70 | 1,217,958 | 49.30 | ||||||||||||||||||
Forfeited | (732,846 | ) | 39.68 | (332,105 | ) | 40.66 | (332,105 | ) | 40.66 | (86,986 | ) | 42.13 | ||||||||||||||
Exercised | (77,247 | ) | 33.38 | (2,028,472 | ) | 37.89 | (2,028,472 | ) | 37.89 | (1,065,325 | ) | 38.34 | ||||||||||||||
Outstanding, end of period | 5,185,091 | $ | 38.19 | 3,775,586 | $ | 39.27 | 3,775,586 | $ | 39.27 | 3,841,233 | $ | 42.65 | ||||||||||||||
| | 2011 | 2012 | ||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| | Options | Weighted Average Exercise Price | Weighted Average Remaining Contractual Term (in years) | Aggregate Intrinsic Value (in thousands) | Options | Weighted Average Exercise Price | Weighted Average Remaining Contractual Term (in years) | Aggregate Intrinsic Value (in thousands) | ||||||||||||||||||
Outstanding, beginning of period | 3,775,586 | $ | 39.27 | 3,841,233 | $ | 42.65 | ||||||||||||||||||||
Granted | 1,217,958 | 49.30 | 1,402,800 | 47.54 | ||||||||||||||||||||||
Forfeited | (86,986 | ) | 42.13 | (444,939 | ) | 46.08 | ||||||||||||||||||||
Exercised | (1,065,325 | ) | 38.34 | (530,854 | ) | 39.03 | ||||||||||||||||||||
Outstanding, end of period | 3,841,233 | $ | 42.65 | 7.47 | $ | 26,446 | 4,268,240 | $ | 44.35 | 7.17 | $ | 20,339 | ||||||||||||||
Vested and expected to vest at end of period | 3,763,158 | $ | 42.55 | 7.44 | $ | 26,251 | 4,229,455 | $ | 44.31 | 7.16 | $ | 20,288 | ||||||||||||||
Exercisable, end of period | 1,720,871 | $ | 40.02 | 6.03 | $ | 16,268 | 2,162,893 | $ | 41.26 | 5.71 | $ | 16,884 | ||||||||||||||
The aggregate intrinsic value in the table above represents the total pre-tax intrinsic value (based upon the difference between the Company's closing stock price on the last trading day of 20112012 of $49.47$49.00 and the exercise price) for all in-the-money options as of December 31, 2011.2012. This amount changes based on the fair market value of the Company's common stock.
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
December 31, 2011
6. Stockholders' Equity (Continued)
The total pre-tax intrinsic value of options exercised (based on the difference between the Company's closing stock price on the day the option was exercised and the exercise price) during the years ended December 31, 2009, 2010, 2011 and 20112012 was $0.4 million, $18.2 million, $13.1 million, and $13.1$6.4 million, respectively.
The weighted average grant date fair value of substantially all stock options granted during the years ended December 31, 2009, 2010, 2011 and 20112012 was $8.69, $11.74, $12.72 and $12.72,$11.65, respectively, as
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
December 31, 2012
6. Stockholders' Equity (Continued)
estimated using the Black- Scholes-Merton option pricing model based on the following weighted average assumptions:
| | 2009 | 2010 | 2011 | 2010 | 2011 | 2012 | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Risk-free interest rate | 1.67 | % | 1.74 | % | 1.63 | % | 1.74 | % | 1.63 | % | 0.66 | % | ||||||||
Expected life | 4 years | 4 years | 4 years | 4 years | 4 years | 4 years | ||||||||||||||
Expected volatility | 30.20 | % | 31.70 | % | 29.88 | % | 31.70 | % | 29.88 | % | 30.30 | % | ||||||||
Expected dividend yield | 0.00 | % | 0.00 | % | 0.00 | % | 0.00 | % | 0.00 | % | 0.00 | % | ||||||||
For the years ended December 31, 2009, 2010, 2011 and 2011,2012, expected volatility was based on the historical volatility of the Company's stock price.
As of December 31, 2011,2012, there was $16.9$16.4 million of total unrecognized compensation expense related to nonvested stock options that is expected to be recognized over a weighted average remaining recognition period of 1.891.81 years. The total fair value of options vested during the year ended December 31, 20112012 was $10.3$11.0 million.
The benefits of tax deductions from exercises of stock options and vesting of stock awards are reported as a financing cash flow, rather than as an operating cash flow. In the years ended December 31, 2009, 2010, 2011 and 2011,2012, approximately $2.9 million, $1.1 million, $2.0 million and $2.0$1.0 million, respectively, of benefits of such tax deductions related to stock compensation expense were realized and as such were reported as financing cash flows. For the yearsyear ended December 31, 2009 and 2011, $2.9 million and $2.0 million, respectively, were reflected as increases2012, the change to additional paid-in capital.capital related to tax benefits (deficiencies) was $0.1 million which includes the $1.0 million of excess tax benefits offset by $0.9 million of tax deficiencies and adjustments to prior years' tax benefit from exercise of stock options and vesting of stock awards. For the year ended December 31, 2011, the change to additional paid-in capital related to tax benefits (deficiencies) was $(1.2) million which includes the $2.0 million of excess tax benefits offset by $3.2 million of tax deficiencies and adjustments to prior years' tax benefit from exercise of stock options and vesting of stock awards. For the year ended December 31, 2010, the change to additional paid-in capital related to tax benefits (deficiencies) was $(1.4) million which includes the $1.1 million of excess tax benefits offset by $2.5 million of tax deficiencies.
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
December 31, 20112012
6. Stockholders' Equity (Continued)
Restricted Stock Awards
Summarized information related to the Company's nonvested RSAs for the years ended December 31, 2009, 2010, 2011 and 20112012 is as follows:
| | 2009 | 2010 | 2011 | 2010 | 2011 | 2012 | ||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| | Shares | Weighted Average Grant Date Fair Value | Shares | Weighted Average Grant Date Fair Value | Shares | Weighted Average Grant Date Fair Value | Shares | Weighted Average Grant Date Fair Value | Shares | Weighted Average Grant Date Fair Value | Shares | Weighted Average Grant Date Fair Value | ||||||||||||||||||||||||||
Outstanding, beginning of period | 321,935 | $ | 42.92 | 28,910 | $ | 30.27 | 22,309 | $ | 39.23 | 28,910 | $ | 30.27 | 22,309 | $ | 39.23 | 18,748 | $ | 52.11 | ||||||||||||||||||||
Awarded | 30,385 | 30.36 | 22,309 | 39.23 | 18,748 | 52.11 | 22,309 | 39.23 | 18,748 | 52.11 | 23,672 | 42.25 | ||||||||||||||||||||||||||
Vested | (319,547 | ) | 42.97 | (28,910 | ) | 30.27 | (22,309 | ) | 39.23 | (28,910 | ) | 30.27 | (22,309 | ) | 39.23 | (18,748 | ) | 52.11 | ||||||||||||||||||||
Forfeited | (3,863 | ) | 36.66 | — | — | — | — | — | — | — | — | — | — | |||||||||||||||||||||||||
Outstanding, ending of period | 28,910 | $ | 30.27 | 22,309 | $ | 39.23 | 18,748 | $ | 52.11 | 22,309 | $ | 39.23 | 18,748 | $ | 52.11 | 23,672 | $ | 42.25 | ||||||||||||||||||||
As of December 31, 2011,2012, there was $0.4 million of unrecognized stock compensation expense related to nonvested restricted stock awards. This cost is expected to be recognized over a weighted-average period of 0.380.37 years.
Restricted Stock Units
Summarized information related to the Company's nonvested RSUs for the years ended December 31, 2009, 2010, 2011 and 20112012 is as follows:
| | 2009 | 2010 | 2011 | 2010 | 2011 | 2012 | ||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| | Shares | Weighted Grant Date Fair Value | Shares | Weighted Grant Date Fair Value | Shares | Weighted Grant Date Fair Value | Shares | Weighted Average Grant Date Fair Value | Shares | Weighted Average Grant Date Fair Value | Shares | Weighted Average Grant Date Fair Value | ||||||||||||||||||||||||||
Outstanding, beginning of period | 176,112 | $ | 38.72 | 184,454 | $ | 34.99 | 190,488 | $ | 38.43 | 184,454 | $ | 34.99 | 190,488 | $ | 38.43 | 206,338 | $ | 44.63 | ||||||||||||||||||||
Awarded | 121,065 | 32.91 | 101,812 | 42.75 | 115,003 | 49.14 | 101,812 | 42.75 | 115,003 | 49.14 | 131,913 | 47.48 | ||||||||||||||||||||||||||
Vested | (73,465 | ) | 39.16 | (84,615 | ) | 36.20 | (90,853 | ) | 37.50 | (84,615 | ) | 36.20 | (90,853 | ) | 37.50 | (99,976 | ) | 41.81 | ||||||||||||||||||||
Forfeited | (39,258 | ) | 37.60 | (11,163 | ) | 37.97 | (8,300 | ) | 42.94 | (11,163 | ) | 37.97 | (8,300 | ) | 42.94 | (35,585 | ) | 47.43 | ||||||||||||||||||||
Outstanding, ending of period | 184,454 | $ | 34.99 | 190,488 | $ | 38.43 | 206,338 | $ | 44.63 | 190,488 | $ | 38.43 | 206,338 | $ | 44.63 | 202,690 | $ | 47.38 | ||||||||||||||||||||
As of December 31, 2011,2012, there was $3.8$3.7 million of unrecognized stock compensation expense related to nonvested restricted stock units. This cost is expected to be recognized over a weighted-average period of 1.891.90 years.
Common Stock Warrants
On January 5, 2004, the Company issued 570,825 warrants to purchase common stock of the Company at a purchase price of $30.46 per share at anytime until January 5, 2011 and at an approximate fair value per warrant of $9.44 ("2004 Warrants"). As of December 31, 2010, 44,561 of these 2004 Warrants remained outstanding. In January 2011, 31,362 warrants were exercised and the remaining 13,199 warrants were forfeited. There were no warrants outstanding as of December 31, 2011.2012.
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
December 31, 20112012
6. Stockholders' Equity (Continued)
Income per Common Share
The following table reconciles income (numerator) and shares (denominator) used in the Company's computations of net income per share for the years ended December 31, 2009, 2010, 2011 and 20112012 (in thousands, except per share amounts)data):
| | 2009 | 2010 | 2011 | 2010 | 2011 | 2012 | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Numerator: | ||||||||||||||||||||
Net income | $ | 106,671 | $ | 138,659 | $ | 129,623 | $ | 138,659 | $ | 129,623 | $ | 151,027 | ||||||||
Denominator: | ||||||||||||||||||||
Weighted average number of common shares outstanding—basic | 35,248 | 33,779 | 30,478 | 33,779 | 30,478 | 27,386 | ||||||||||||||
Common stock equivalents—stock options | 46 | 448 | 480 | 448 | 480 | 406 | ||||||||||||||
Common stock equivalents—warrants | 52 | 116 | — | 116 | — | — | ||||||||||||||
Common stock equivalents—restricted stock awards | 29 | 12 | 9 | 12 | 9 | 11 | ||||||||||||||
Common stock equivalents—restricted stock units | 41 | 86 | 91 | 86 | 91 | 77 | ||||||||||||||
Common stock equivalents—employee stock purchase plan | — | — | 2 | |||||||||||||||||
Weighted average number of common shares outstanding—diluted | 35,416 | 34,441 | 31,058 | 34,441 | 31,058 | 27,882 | ||||||||||||||
Net income per common share—basic | $ | 3.03 | $ | 4.10 | $ | 4.25 | $ | 4.10 | $ | 4.25 | $ | 5.51 | ||||||||
Net income per common share—diluted | $ | 3.01 | $ | 4.03 | $ | 4.17 | $ | 4.03 | $ | 4.17 | $ | 5.42 | ||||||||
The weighted average number of common shares outstanding for the years ended December 31, 2009, 2010, 2011 and 20112012 was calculated using outstanding shares of the Company's common stock. Common stock equivalents included in the calculation of diluted weighted average common shares outstanding for the years ended December 31, 2009, 2010, 2011 and 20112012 represent stock options to purchase shares of the Company's common stock, restricted stock awards and restricted stock units, stock purchased under the ESPP and shares of common stock related to certain warrants issued on January 5, 2004.
For the years ended December 31, 2009, 2010, 2011 and 2011,2012, the Company had additional potential dilutive securities outstanding representing 5.2 million, 2.0 million, 1.0 million and 1.02.2 million options, respectively, that were not included in the computation of dilutive securities because they were anti-dilutive for such periods. Had these shares not been anti-dilutive, all of these shares would not have been included in the net income per common share calculation as the Company uses the treasury stock method of calculating diluted shares.
Stock Repurchases
On July 30, 2008 theThe Company's board of directors approvedhas previously authorized a series of stock repurchase plan which authorized the Company to purchase up to $200 million of its outstanding common stock through January 31, 2010.plans. Stock repurchases under the programfor each such plan could be executed through open market repurchases, privately negotiated transactions, accelerated share repurchases or other means. The board of directors authorized management to execute stock repurchase transactions under the program from time to time and in such amounts and via such methods as management deemed appropriate. TheEach stock repurchase program could be limited or terminated at any time without prior notice. Pursuant to
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
December 31, 20112012
6. Stockholders' Equity (Continued)
this program, the Company made open market purchases of 3,866,505 shares of the Company's common stock at an aggregate cost of $136.0 million (excluding broker commissions) during the year ended December 31, 2008 and made open market purchases of 1,859,959 shares of the Company's common stock at an average share price of $34.39 per share for an aggregate cost of $64.0 million (excluding broker commissions) during the period January 1, 2009 through April 7, 2009, which was the date that the repurchase program was completed.
On July 28, 2009 the Company's board of directors approved a stock repurchase plan which authorized the Company to purchase up to $100 million of its outstanding common stock through July 28, 2011. Stock repurchases under the program could be executed through open market repurchases, privately negotiated transactions, accelerated share repurchases or other means. The board of directors authorized management to execute stock repurchase transactions under the program from time to time and in such amounts and via such methods as management deemed appropriate. The stock repurchase program could be limited or terminated at any time without prior notice. Pursuant to this program, the Company made open market purchases of 782,400 shares of the Company's common stock at an average price of $32.75 per share for an aggregate cost of $25.6 million (excluding broker commissions) during the period from August 17, 2009 through December 31, 2009. Pursuant to this program, the Company made open market purchases of 1,711,881 shares of the Company's common stock at an average price of $43.46 per share for an aggregate cost of $74.4 million (excluding broker commissions) during the period January 1, 2010 through April 1, 2010, which was the date that the repurchase program was completed.
On July 27, 2010 the Company's board of directors approved a stock repurchase plan which authorized the Company to purchase up to $350 million of its outstanding common stock through July 28, 2012. On February 18, 2011, the Company's board of directors increased the stock repurchase program by an additional $100 million. Stock repurchases under the program could be executed through open market repurchases, privately negotiated transactions, accelerated share repurchases or other means. The boardmillion, to a total of directors authorized management to execute stock repurchase transactions from time to time and in such amounts and via such methods as management deemed appropriate. The stock repurchase program could be limited or terminated at any time without prior notice.$450 million. Pursuant to this program, the Company made open market purchases of 1,684,510 shares of the Company's common stock at an average price of $48.36 per share for an aggregate cost of $81.5 million (excluding broker commissions) during the period from November 3, 2010 through December 31, 2010. Pursuant to this program, the Company made open market purchases of 7,534,766 shares of the Company's common stock at an average price of $48.91 per share for an aggregate cost of $368.5 million (excluding broker commissions) during the period January 1, 2011 through November 10, 2011, which was the date the repurchase program was completed.
On October 25, 2011 the Company's board of directors approved a stock repurchase plan which authorizesauthorized the Company to purchase up to $200 million of its outstanding common stock through October 25, 2013. Stock repurchases under the program may be executed through open market repurchases, privately negotiated transactions, accelerated share repurchases or other means. The board of directors authorized management to execute stock repurchase transactions from time to time and in such amounts and via such methods as management deems appropriate. The stock repurchase program may be limited or terminated at any time without prior notice. Pursuant to this program, the Company
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
December 31, 2011
6. Stockholders' Equity (Continued)
made open market purchases of 671,776 shares of the Company's common stock at an average price of $48.72 per share for an aggregate cost of $32.7 million (excluding broker commissions) during the period from November 11, 2011 through December 31, 2011.
The Pursuant to this program, the Company made noopen market purchases of 459,252 shares of the Company's common stock at an average price of $50.27 per share repurchasesfor an aggregate cost of $23.1 million (excluding broker commissions) during 2012.
During the period from January 1, 20122013 through February 23, 2012.22, 2013, the Company made additional open market purchases of 366,650 shares of the Company's common stock at an aggregate cost of $18.6 million (excluding broker commissions).
Recent Sales of Unregistered Securities
On January 28, 2011, the Company and Blue Shield of California ("Blue Shield") entered into a Share Purchase Agreement (the "Share Purchase Agreement") pursuant to which on January 31, 2011 Blue Shield purchased 416,840 shares of the Company's Common Stock (the "Shares") for a total purchase price of $20 million. The Shares were issued to Blue Shield, an accredited investor, in a private placement pursuant to Regulation D of the Securities Act. Blue Shield has agreed not to transfer such Shares for a two year period, except in the event of any change in control of the Company as defined in the Share Purchase Agreement. The purchase price for the Shares issued was determined taking into account the recent trading price of the Company's Common Stock on NASDAQ and the restrictions on transfer of the Shares agreed to by Blue Shield.
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
December 31, 2012
7. Income Taxes
Income Tax Expense
The components of income tax expense (benefit) expense for the following years ended December 31 were as follows (in thousands):
| | 2009 | 2010 | 2011 | 2010 | 2011 | 2012 | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Income taxes currently payable: | ||||||||||||||||||||
Federal | $ | 17,003 | $ | 34,235 | $ | 51,195 | $ | 34,235 | $ | 51,195 | $ | 18,345 | ||||||||
State | 4,443 | 6,722 | 5,534 | 6,722 | 5,534 | 2,187 | ||||||||||||||
| 21,446 | 40,957 | 56,729 | 40,957 | 56,729 | 20,532 | |||||||||||||||
Deferred income taxes: | ||||||||||||||||||||
Federal | 40,348 | 44,310 | 8,644 | 44,310 | 8,644 | 14,922 | ||||||||||||||
State | (4,457 | ) | (1,523 | ) | (336 | ) | (1,523 | ) | (336 | ) | 2,384 | |||||||||
| 35,891 | 42,787 | 8,308 | 42,787 | 8,308 | 17,306 | |||||||||||||||
Total income tax expense | $ | 57,337 | $ | 83,744 | $ | 65,037 | ||||||||||||||
Total provision for income taxes | $ | 83,744 | $ | 65,037 | $ | 37,838 | ||||||||||||||
Total income tax expense for the years ended December 31 was different from the amount computed using the statutory federal income tax rate of 35 percent for the following reasons (in thousands):
| | 2010 | 2011 | 2012 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
Income tax expense at federal statutory rate | $ | 77,841 | $ | 68,458 | $ | 67,107 | ||||
State income taxes, net of federal income tax benefit | 7,491 | 7,013 | 6,812 | |||||||
Tax contingencies reversed due to statute closings | (3,002 | ) | (12,521 | ) | (37,093 | ) | ||||
Net change in valuation allowances | (2,554 | ) | (1,163 | ) | (288 | ) | ||||
Other-net | 3,968 | 3,250 | 1,300 | |||||||
Total provision for income taxes | $ | 83,744 | $ | 65,037 | $ | 37,838 | ||||
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
December 31, 20112012
7. Income Taxes (Continued)
Total income tax expense for the years ended December 31 was different from the amount computed using the statutory federal income tax rate of 35% for the following reasons (in thousands):
| | 2009 | 2010 | 2011 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
Income tax expense at federal statutory rate | $ | 57,403 | $ | 77,841 | $ | 68,458 | ||||
State income taxes, net of federal income tax benefit | 6,805 | 7,491 | 7,013 | |||||||
Tax contingencies reversed due to statute closings | (5,763 | ) | (3,002 | ) | (12,521 | ) | ||||
Net change in valuation allowances | (4,342 | ) | (2,554 | ) | (1,163 | ) | ||||
Other—net | 3,234 | 3,968 | 3,250 | |||||||
Total income tax expense | $ | 57,337 | $ | 83,744 | $ | 65,037 | ||||
Deferred Income Taxes
The significant components of deferred tax assets and liabilities at December 31 were as follows (in thousands):
| | 2010 | 2011 | 2011 | 2012 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Deferred tax assets: | ||||||||||||||
Intangible assets | $ | 2,966 | $ | — | ||||||||||
Accrued compensation | 3,404 | 3,258 | $ | 3,258 | $ | 3,891 | ||||||||
Operating loss carryforwards | 12,936 | 10,969 | 10,969 | 10,116 | ||||||||||
Stock compensation | 15,094 | 13,431 | 13,431 | 16,225 | ||||||||||
Community reinvestment reserves | 5,420 | 8,065 | 8,065 | 6,276 | ||||||||||
Other non-deductible book accruals | 4,480 | 5,543 | 6,988 | 5,678 | ||||||||||
Claims reserves | 5,703 | 5,438 | 5,438 | 7,244 | ||||||||||
Self-insured medical reserves | 2,448 | 4,167 | 4,167 | 2,403 | ||||||||||
Refundable tax credits | 4,855 | — | ||||||||||||
Indirect tax benefits | 8,506 | 6,947 | 6,947 | 5,897 | ||||||||||
Other | 5,287 | 7,344 | ||||||||||||
Other assets | 5,899 | 3,691 | ||||||||||||
Total deferred tax assets | 71,099 | 65,162 | 65,162 | 61,421 | ||||||||||
Valuation allowance | (5,319 | ) | (3,424 | ) | (3,424 | ) | (3,130 | ) | ||||||
Deferred tax assets after valuation allowance | 65,780 | 61,738 | 61,738 | 58,291 | ||||||||||
Deferred tax liabilities: | ||||||||||||||
Property and depreciation | (33,356 | ) | (37,712 | ) | (37,712 | ) | (44,728 | ) | ||||||
Intangible assets | — | (7,358 | ) | |||||||||||
Goodwill and intangible assets | (7,358 | ) | (15,782 | ) | ||||||||||
Other liabilities | (3,160 | ) | (39 | ) | (39 | ) | (169 | ) | ||||||
Total deferred tax liabilities | (36,516 | ) | (45,109 | ) | (45,109 | ) | (60,679 | ) | ||||||
Net deferred tax assets | $ | 29,264 | $ | 16,629 | ||||||||||
Net deferred tax assets (liabilities) | $ | 16,629 | $ | (2,388 | ) | |||||||||
The Company's valuation allowances against deferred tax assets were $5.3$3.4 million and $3.4$3.1 million as of December 31, 20102011 and 2011,2012, respectively, mostly relating to uncertainties regarding the eventual
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
December 31, 2011
7. Income Taxes (Continued)
realization of certain state net operating loss carryforwards ("NOLs"). Determination of the amount of deferred tax assets considered realizable requires significant judgment and estimation regarding the forecasts of future taxable income which are consistent with the plans and estimates the Company uses to manage the underlying businesses. The Company believes taxable income expected to be generated in the future will be sufficient to support realization of the Company's deferred tax assets, as reduced by valuation allowances. This determination is based upon its consistent overall earnings history and future earnings expectations. Other than deferred tax benefits attributable to operating loss carryforwards, there are no time constraints within which the Company's deferred tax assets must be realized. Changes in these estimates in the future could materially affect the Company's financial condition and results of operations. Reversals of valuation allowances are recorded as reductions to income tax expense in the period they occur.
The Company has federal NOLs as of December 31, 20112012 of $4.8$4.2 million available to reduce future federal taxable income. These NOLs, if not used, will expire in 2017 through 2019 and are subject to examination and adjustment by the Internal Revenue Service ("IRS"). In addition, the Company's utilizationIRS. Utilization of suchthese NOLs is also subject to limitation under Internal Revenue Code Section 382 ("Section 382") which affects the certain
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
December 31, 2012
7. Income Taxes (Continued)
timing of the use of these NOLs. At this time,limitations, although the Company does not believe these limitations will limit the Company'srestrict its ability to use any federal NOLs before they expire.
Uncertain Tax Positions
A reconciliation of the beginning and ending amount of gross unrecognized tax benefits is as follows (in thousands):
| | 2009 | 2010 | 2011 | 2010 | 2011 | 2012 | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Balance as of beginning of period | $ | 129,157 | $ | 113,100 | $ | 111,594 | $ | 113,100 | $ | 111,594 | $ | 99,230 | ||||||||
Additions based on tax positions related to the current year | 4,023 | 3,317 | 3,240 | |||||||||||||||||
Additions for current year tax positions | 3,317 | 3,240 | 1,904 | |||||||||||||||||
Additions for tax positions of prior years | 4,759 | 422 | 948 | 422 | 948 | 403 | ||||||||||||||
Reductions for tax positions of prior years | (17,866 | ) | (1,916 | ) | (1,492 | ) | (1,916 | ) | (1,492 | ) | (1,618 | ) | ||||||||
Reductions due to lapses of applicable statutes of limitations | (6,822 | ) | (3,329 | ) | (15,011 | ) | (3,329 | ) | (15,011 | ) | (43,297 | ) | ||||||||
Settlements | (151 | ) | — | (49 | ) | |||||||||||||||
Reductions due to settlements with taxing authorities | — | (49 | ) | (21 | ) | |||||||||||||||
Balance as of end of period | $ | 113,100 | $ | 111,594 | $ | 99,230 | $ | 111,594 | $ | 99,230 | $ | 56,601 | ||||||||
If these unrecognized tax benefits had been realized as of December 31, 20102011 and 2011, $88.22012, $80.3 million and $80.3$45.1 million, respectively, would have impacted the effectivereduced income tax rate.expense.
The Company periodicallycontinually performs a comprehensive review of its tax positions and accrues amounts for tax contingencies related to uncertain tax positions. Based upon these reviews, the status of ongoing tax audits, and the expiration of applicable statutes of limitations, accruals are adjusted as necessary. The tax benefit from an uncertain tax position is recognized when it is more likely than not that, based on technical merit, the position will be sustained upon examination, including resolution of any related appeals or litigation processes. The resolution of tax audits is unpredictable and could result in tax liabilities that are significantly different than those which have been estimated and accrued
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
December 31, 2011
7. Income Taxes (Continued)
by the Company. Such amounts are included within the accompanying consolidated balance sheets in tax contingencies, and the remainder reducing deferred tax assets.
The Company also adjusts these liabilities for unrecognized tax benefits when its judgment changes as a result of the evaluation of new information not previously available. Due to the complexity of some of these uncertainties,However, the ultimate resolution mayof a disputed tax position following an examination by a taxing authority could result in a payment that is materially different from that accrued by the Company's current estimate of theCompany. These differences are reflected as increases or decreases to income tax liabilities. Reversals of unrecognized tax benefits are recordedexpense in the period in which they occur, typically as reductions to income tax expense.are determined. However, reversals of unrecognized tax benefits related to deductions for stock compensation in excess of the related book expense are recorded as increases in additional paid-in capital. To the extent reversals of unrecognized tax benefits cannot be specifically traced to these excess deductions due to complexities in the tax law, the Company records the tax benefit for such reversals to additional paid-in capital on a pro-rata basis.
The statutes of limitationlimitations regarding the assessment of federal and certain state and local income taxes for the year ended December 31, 20072008 expired during 2011. With few exceptions, the Company is no longer subject to income tax assessments by tax authorities for years ended prior to December 31, 2008.2012. As a result, $15.0$43.3 million of unrecognized tax benefits (excluding interest costs) recorded as of December 31, 20102011 were reversed in the current year as a result of statute expirations, of which $35.7 million is reflected as a reduction to income tax expense, $6.2 million as an increase to additional paid-in capital, and the remainder as a decrease to deferred tax assets. Additionally, $1.4 million of accrued interest and $0.8 million of unrecognized state tax benefits were reversed in 2012 and reflected
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
December 31, 2012
7. Income Taxes (Continued)
as reductions to income tax expense due to the closing of statutes of limitations on tax assessments and changes in tax return elections, respectively.
The statutes of limitations regarding the assessment of federal and certain state and local income taxes for 2007 closed during 2011. As a result, $15.0 million of unrecognized tax benefits recorded as of December 31, 2010 were reversed in the prior year, of which $10.4 million iswas reflected as a reduction to income tax expense, $2.5 million as an increase to additional paid-in capital, and the remainder as a decrease to deferred tax assets. Additionally, $2.2 million of accrued interest was reversed in 2011 and reflected as a reduction to income tax expense due to these statute closings.
With few exceptions, the Company is no longer subject to income tax assessments by tax authorities for years ended prior to 2009. Further, it is reasonably possible the statutestatutes of limitations regarding the assessment of federal and most state and local income taxes for the year ended December 31, 2008 will2009 could expire during 2012.2013. The Company anticipates that up to $43.2$28.6 million of unrecognized tax benefits (excluding interest costs) recorded as of December 31, 20112012 could be reversed during 20122013 as a result of statute expirations, of which $35.6$23.2 million would be reflected as a reduction to income tax expense, $6.2$3.9 million as an increase to additional paid-in capital, and the remainder as a decrease to deferred tax assets. All such reversals (net of the related indirect tax benefits) would be reflected as discrete adjustments during the quarter in which the respective statute expiration occurs, primarily in the 3rd quarter.
As of December 31, 20102011 and 2011,2012, the Company had accrued approximately $3.7$2.8 million and $2.8$2.7 million, respectively, for the potential payment of interest and penalties (net of indirect benefits). The Company accrues interest and penalties related to unrecognized tax benefits in its provision for income taxes. During the years ended December 31, 2009, 2010, 2011 and 2011,2012, the Company recorded approximately $(0.7) million, $0.2 million, $(0.9) million and $(0.9)$(0.1) million in interest and penalties.
8. Supplemental Cash Flow Information
Supplemental cash flow information for the years ended December 31, 2009, 2010, 2011 and 20112012 is as follows (in thousands):
| | 2009 | 2010 | 2011 | 2010 | 2011 | 2012 | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Income taxes paid, net of refunds | $ | 16,599 | $ | 61,861 | $ | 50,324 | $ | 61,861 | $ | 50,324 | $ | 57,663 | ||||||||
Interest paid | $ | 1,470 | $ | 1,685 | $ | 1,521 | $ | 1,685 | $ | 1,521 | $ | 1,594 | ||||||||
Assets acquired through capital leases | $ | — | $ | 1,680 | $ | — | $ | 1,680 | $ | — | $ | — | ||||||||
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
December 31, 20112012
9. Commitments and Contingencies
Insurance
The Company maintains a program of insurance coverage for a broad range of risks in its business. The Company has renewed its general, professional and managed care liability insurance policies with unaffiliated insurers for a one-year period from June 17, 20112012 to June 17, 2012.2013. The general liability policy is written on an "occurrence" basis, subject to a $0.05 million per claim un-aggregated self-insured retention. The professional liability and managed care errors and omissions liability policies are written on a "claims-made" basis, subject to a $1.0 million per claim ($10.0 million per class action claim) un-aggregated self-insured retention for managed care errors and omissions liability, and a $0.05 million per claim un-aggregated self-insured retention for professional liability.
The Company maintains a separate general and professional liability insurance policy with an unaffiliated insurer for its Specialty Pharmaceutical Management business. The Specialty Pharmaceutical Management insurance policy has a one-year term for the period June 17, 20112012 to June 17, 2012.2013. The general liability policy is written on an "occurrence" basis and the professional liability policy is written on a "claims-made" basis, subject to a $0.05 million per claim and $0.25 million aggregated self-insured retention.
The Company maintains separate professional liability insurance policies with unaffiliated insurers for its Maricopa Contract business for the behavioral health direct care facilities.facilities, all of which were divested at various times prior to December 31, 2009. The Maricopa Contract professional liability insurance policies effective dates were from September 1, 2008 to September 1, 2009. The Company purchased a five-year extended reporting period for the professional liability policies effective September 1, 2009 for the period September 1, 2009 to September 1, 2014, subject to a $0.5 million per claim un-aggregated self-insured retention. The professional liability policies are written on a "claims-made" basis.
The Company is responsible for claims within its self-insured retentions, and for portions of claims reported after the expiration date of the policies if they are not renewed, or if policy limits are exceeded. The Company also purchases excess liability coverage in an amount that management believes to be reasonable for the size and profile of the organization.
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
December 31, 2011
9. Commitments and Contingencies (Continued)
Regulatory Issues
The specialty managed healthcare industry is subject to numerous laws and regulations. The subjects of such laws and regulations cover, but are not limited to, matters such as licensure, accreditation, government healthcare program participation requirements, information privacy and security, reimbursement for patient services, and Medicare and Medicaid fraud and abuse. Over the past several years, government activity has increased with respect to investigations and/or allegations concerning possible violations of fraud and abuse and false claims statutes and/or regulations by healthcare organizations and insurers. Entities that are found to have violated these laws and regulations may be excluded from participating in government healthcare programs, subjected to fines or penalties or required to repay amounts received from the government for previously billed patient services. Compliance with such laws and regulations can be subject to future government review and interpretation, as well as regulatory actions unknown or unasserted at this time.
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
December 31, 2012
9. Commitments and Contingencies (Continued)
In addition, regulators of certain of the Company's subsidiaries may exercise certain discretionary rights under regulations including increasing their supervision of such entities, requiring additional restricted cash or other security or seizing or otherwise taking control of the assets and operations of such subsidiaries.
Legal
The management and administration of the delivery of specialty managed healthcare entails significant risks of liability. From time to time, the Company is subject to various actions and claims arising from the acts or omissions of its employees, network providers or other parties. In the normal course of business, the Company receives reports relating to deaths and other serious incidents involving patients whose care is being managed by the Company. Such incidents occasionally give rise to malpractice, professional negligence and other related actions and claims against the Company or its network providers. Many of these actions and claims received by the Company seek substantial damages and therefore require the Company to incur significant fees and costs related to their defense. The Company is also subject to or party to certain class actions, litigation and claims relating to its operations andor business practices. In the opinion of management, the Company has recorded reserves that are adequate to cover litigation, claims or assessments that have been or may be asserted against the Company, and for which the outcome is probable and reasonably estimable. Management believes that the resolution of such litigation and claims will not have a material adverse effect on the Company's financial condition or results of operations; however, there can be no assurance in this regard.
Operating Leases
The Company leases certain of its operating facilities and equipment. The leases, which expire at various dates through November 2019,January 2023, generally require the Company to pay all maintenance, property tax and insurance costs.
At December 31, 2011,2012, aggregate amounts of future minimum payments under operating leases were as follows: 2012—$17.9 million; 2013—$10.314.3 million; 2014—$8.311.7 million; 2015—$6.910.5 million;
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
December 31, 2011
9. Commitments and Contingencies (Continued)
2016—$5.49.4 million; 20172017—$7.2 million; 2018—$6.7 million; 2019 and beyond—$11.011.4 million. Operating lease obligations include estimated future lease payments for both open and closed offices.
At December 31, 2011,2012, aggregate amounts of future minimum rentals to be received under operating subleases were as follows: 2012—$0.7 million; 2013—$0.6 million; 2014—$0.5 million; 2015—$0.3 million; 2016 and beyond—$0.0 million. Operating sublease rentals to be received relate primarily to behavioral health direct care facilities transitioned to third parties pursuant to the Maricopa Contract.
Rent expense is recognized on a straight-line basis over the terms of the leases. Rent expense was $20.3 million, $19.8 million, $19.3 million and $19.3$19.5 million for the years ended December 31, 2009, 2010, 2011 and 2011,2012, respectively.
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
December 31, 2012
10. Certain Relationships and Related Party Transactions
On February 25, 2009, Allen Wise resigned from the board of directors of the Company as a result of his appointment as Chief Executive Officer of Coventry. On July 31, 2009, the Company completed the acquisition of First Health Services as described in Note 3—"Acquisitions". Mr. Wise was no longer a Director of the Company at the time that the Company negotiated and closed on the acquisition of First Health Services from Coventry. At the same time that the Company acquired First Health Services, the Company also executed agreements to provide radiology and oncology services for certain Coventry markets. The Company derived revenues from Coventry of approximately $124.1 million and $135.8 million during the years ended December 31, 2010 and 2011, respectively.
William McBride, a Director of the Company, servesserved as a member of the board of directors of AmeriGroup Corporation.Corporation ("AmeriGroup"). The Company has a radiology benefits management agreement with a subsidiary of AmeriGroup under which the Company derived revenues of approximately $1.7 million, $1.8 million and $1.8$2.2 million in 2010, 2011 and 2011,2012, respectively. In December 2012, Amerigroup was acquired by WellPoint, Inc. ("WellPoint"), with AmeriGroup operating as a wholly owned subsidiary within WellPoint. As a result, William McBride no longer serves as a member of the board of directors of AmeriGroup.
11. Business Segment Information
The accounting policies of the Company's segments are the same as those described in Note 1—"General." The Company evaluates performance of its segments based on profit or loss from operationsincome before income taxes, before stock compensation expense, depreciation and amortization, interest expense, interest income, gain on sale of assets, and special charges or benefits and income taxes ("Segment Profit"). Management uses Segment Profit information for internal reporting and control purposes and considers it important in making decisions regarding the allocation of capital and other resources, risk assessment and employee compensation, among other matters. Effective September 1, 2010, Public Sector has subcontracted with Medicaid AdministrationPharmacy to provide pharmacy benefits management services on a risk basis for one of Public Sector's customers. As such, revenue and cost of care related to this intersegment arrangement are eliminated.
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
December 31, 20112012
11. Business Segment Information (Continued)
intersegment arrangement are eliminated. The Company's segments are defined above.previously. The following tables summarize, for the periods indicated, operating results by business segment (in thousands):
| | Commercial | Public Sector | Radiology Benefits Management | Specialty Pharmaceutical Management | Medicaid Administration | Corporate and Elimination | Consolidated | Commercial | Public Sector | Radiology Benefits Management | Specialty Pharmaceutical Management | Medicaid Administration | Corporate and Elimination | Consolidated | ||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Year Ended December 31, 2009 | ||||||||||||||||||||||||||||||||||||||||||||
Net revenue | $ | 650,139 | $ | 1,362,420 | $ | 305,251 | $ | 259,745 | $ | 64,259 | $ | — | $ | 2,641,814 | ||||||||||||||||||||||||||||||
Year Ended December 31, 2010 | ||||||||||||||||||||||||||||||||||||||||||||
Managed care and other revenue | $ | 652,221 | $ | 1,442,093 | $ | 454,105 | $ | 35,812 | $ | 176,283 | $ | (26,108 | ) | $ | 2,734,406 | |||||||||||||||||||||||||||||
Dispensing revenue | — | — | — | 234,834 | — | — | 234,834 | |||||||||||||||||||||||||||||||||||||
Cost of care | (351,270 | ) | (1,208,451 | ) | (205,592 | ) | — | — | — | (1,765,313 | ) | (365,115 | ) | (1,246,779 | ) | (298,516 | ) | — | (23,683 | ) | 26,108 | (1,907,985 | ) | |||||||||||||||||||||
Cost of goods sold | — | — | — | (203,336 | ) | — | — | (203,336 | ) | — | — | — | (218,630 | ) | — | — | (218,630 | ) | ||||||||||||||||||||||||||
Direct service costs | (152,280 | ) | (67,835 | ) | (51,732 | ) | (24,901 | ) | (54,874 | ) | — | (351,622 | ) | |||||||||||||||||||||||||||||||
Other operating expenses | — | — | — | — | — | (114,088 | ) | (114,088 | ) | |||||||||||||||||||||||||||||||||||
Direct service costs and other | (156,278 | ) | (67,577 | ) | (67,672 | ) | (26,368 | ) | (124,312 | ) | (124,375 | ) | (566,582 | ) | ||||||||||||||||||||||||||||||
Stock compensation expense(1) | 953 | 690 | 1,260 | 5,383 | 27 | 11,469 | 19,782 | 714 | 714 | 1,485 | 424 | 74 | 11,691 | 15,102 | ||||||||||||||||||||||||||||||
Segment profit (loss) | $ | 147,542 | $ | 86,824 | $ | 49,187 | $ | 36,891 | $ | 9,412 | $ | (102,619 | ) | $ | 227,237 | $ | 131,542 | $ | 128,451 | $ | 89,402 | $ | 26,072 | $ | 28,362 | $ | (112,684 | ) | $ | 291,145 | ||||||||||||||
Identifiable assets by business segment(2) | ||||||||||||||||||||||||||||||||||||||||||||
Restricted cash | $ | 20,398 | $ | 133,123 | $ | 2,272 | $ | — | $ | — | $ | 3,866 | $ | 159,659 | $ | 22,501 | $ | 82,813 | $ | 7,890 | $ | — | $ | — | $ | 3,530 | $ | 116,734 | ||||||||||||||||
Net accounts receivable | 23,025 | 16,450 | 6,085 | 30,371 | 31,021 | 7,482 | 114,434 | 26,564 | 15,086 | 2,496 | 28,309 | 29,632 | 4,847 | 106,934 | ||||||||||||||||||||||||||||||
Investments | 14,337 | 133,392 | 12,676 | — | — | 70,040 | 230,445 | 8,507 | 183,632 | 5,005 | — | — | 87,360 | 284,504 | ||||||||||||||||||||||||||||||
Goodwill | 120,485 | — | 104,549 | 142,291 | 59,146 | — | 426,471 | 120,485 | — | 104,549 | 142,291 | 59,614 | — | 426,939 | ||||||||||||||||||||||||||||||
| | Commercial | Public Sector | Radiology Benefits Management | Specialty Pharmaceutical Management | Medicaid Administration | Corporate and Elimination | Consolidated | Commercial | Public Sector | Radiology Benefits Management | Specialty Pharmaceutical Management | Medicaid Administration | Corporate and Elimination | Consolidated | ||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Year Ended December 31, 2010 | ||||||||||||||||||||||||||||||||||||||||||||
Net revenue | $ | 652,221 | $ | 1,442,093 | $ | 454,105 | $ | 270,646 | $ | 176,283 | $ | (26,108 | ) | $ | 2,969,240 | |||||||||||||||||||||||||||||
Year Ended December 31, 2011 | ||||||||||||||||||||||||||||||||||||||||||||
Managed care and other revenue | $ | 561,780 | $ | 1,459,659 | $ | 344,335 | $ | 48,534 | $ | 220,453 | $ | (82,770 | ) | $ | 2,551,991 | |||||||||||||||||||||||||||||
Dispensing revenue | — | — | — | 247,409 | — | — | 247,409 | |||||||||||||||||||||||||||||||||||||
Cost of care | (365,115 | ) | (1,246,779 | ) | (298,516 | ) | — | (23,683 | ) | 26,108 | (1,907,985 | ) | (314,178 | ) | (1,271,532 | ) | (205,240 | ) | — | (76,544 | ) | 82,770 | (1,784,724 | ) | ||||||||||||||||||||
Cost of goods sold | — | — | — | (218,630 | ) | — | — | (218,630 | ) | — | — | — | (232,038 | ) | — | — | (232,038 | ) | ||||||||||||||||||||||||||
Direct service costs | (156,278 | ) | (67,577 | ) | (67,672 | ) | (26,368 | ) | (124,312 | ) | — | (442,207 | ) | |||||||||||||||||||||||||||||||
Other operating expenses | — | — | — | — | — | (124,375 | ) | (124,375 | ) | |||||||||||||||||||||||||||||||||||
Direct service costs and other | (152,760 | ) | (67,227 | ) | (61,681 | ) | (24,344 | ) | (103,254 | ) | (120,368 | ) | (529,634 | ) | ||||||||||||||||||||||||||||||
Stock compensation expense(1) | 714 | 714 | 1,485 | 424 | 74 | 11,691 | 15,102 | 839 | 872 | 1,563 | 693 | 124 | 13,327 | 17,418 | ||||||||||||||||||||||||||||||
Segment profit (loss) | $ | 131,542 | $ | 128,451 | $ | 89,402 | $ | 26,072 | $ | 28,362 | $ | (112,684 | ) | $ | 291,145 | $ | 95,681 | $ | 121,772 | $ | 78,977 | $ | 40,254 | $ | 40,779 | $ | (107,041 | ) | $ | 270,422 | ||||||||||||||
Identifiable assets by business segment(2) | ||||||||||||||||||||||||||||||||||||||||||||
Restricted cash | $ | 22,501 | $ | 82,813 | $ | 7,890 | $ | — | $ | — | $ | 3,530 | $ | 116,734 | $ | 18,319 | $ | 164,479 | $ | — | $ | — | $ | — | $ | 2,996 | $ | 185,794 | ||||||||||||||||
Net accounts receivable | 26,564 | 15,086 | 2,496 | 28,309 | 29,632 | 4,847 | 106,934 | 26,822 | 28,331 | 1,398 | 21,370 | 30,654 | 13,031 | 121,606 | ||||||||||||||||||||||||||||||
Investments | 8,507 | 183,632 | 5,005 | — | — | 87,360 | 284,504 | 5,320 | 131,261 | — | — | — | 64,322 | 200,903 | ||||||||||||||||||||||||||||||
Goodwill | 120,485 | — | 104,549 | 142,291 | 59,614 | — | 426,939 | 120,485 | — | 104,549 | 142,291 | 59,614 | — | 426,939 | ||||||||||||||||||||||||||||||
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
December 31, 20112012
11. Business Segment Information (Continued)
| | Commercial | Public Sector | Radiology Benefits Management | Specialty Pharmaceutical Management | Medicaid Administration | Corporate and Elimination | Consolidated | Commercial | Public Sector | Radiology Benefits Management | Specialty Pharmaceutical Management | Medicaid Administration | Corporate and Elimination | Consolidated | ||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Year Ended December 31, 2011 | ||||||||||||||||||||||||||||||||||||||||||||
Net revenue | $ | 561,780 | $ | 1,459,659 | $ | 344,335 | $ | 295,943 | $ | 220,453 | $ | (82,770 | ) | $ | 2,799,400 | |||||||||||||||||||||||||||||
Year Ended December 31, 2012 | ||||||||||||||||||||||||||||||||||||||||||||
Managed care and other revenue | $ | 728,512 | $ | 1,620,875 | $ | 349,133 | $ | 55,178 | $ | 172,491 | $ | (69,090 | ) | $ | 2,857,099 | |||||||||||||||||||||||||||||
Dispensing revenue | — | — | — | 350,298 | — | — | 350,298 | |||||||||||||||||||||||||||||||||||||
Cost of care | (314,178 | ) | (1,271,532 | ) | (205,240 | ) | — | (76,544 | ) | 82,770 | (1,784,724 | ) | (437,518 | ) | (1,413,320 | ) | (228,383 | ) | — | (61,759 | ) | 69,090 | (2,071,890 | ) | ||||||||||||||||||||
Cost of goods sold | — | — | — | (232,038 | ) | — | — | (232,038 | ) | — | — | — | (328,414 | ) | — | — | (328,414 | ) | ||||||||||||||||||||||||||
Direct service costs | (152,760 | ) | (67,227 | ) | (61,681 | ) | (24,344 | ) | (103,254 | ) | — | (409,266 | ) | |||||||||||||||||||||||||||||||
Other operating expenses | — | — | — | — | — | (120,368 | ) | (120,368 | ) | |||||||||||||||||||||||||||||||||||
Direct service costs and other | (172,035 | ) | (89,129 | ) | (55,418 | ) | (26,709 | ) | (84,884 | ) | (129,337 | ) | (557,512 | ) | ||||||||||||||||||||||||||||||
Stock compensation expense(1) | 839 | 872 | 1,563 | 693 | 124 | 13,327 | 17,418 | 532 | 1,111 | 1,567 | 672 | 335 | 13,566 | 17,783 | ||||||||||||||||||||||||||||||
Segment profit (loss) | $ | 95,681 | $ | 121,772 | $ | 78,977 | $ | 40,254 | $ | 40,779 | $ | (107,041 | ) | $ | 270,422 | $ | 119,491 | $ | 119,537 | $ | 66,899 | $ | 51,025 | $ | 26,183 | $ | (115,771 | ) | $ | 267,364 | ||||||||||||||
Identifiable assets by business segment(2) | ||||||||||||||||||||||||||||||||||||||||||||
Restricted cash | $ | 18,319 | $ | 164,479 | $ | — | $ | — | $ | — | $ | 2,996 | $ | 185,794 | $ | 18,254 | $ | 147,766 | $ | — | $ | — | $ | — | $ | 60,534 | $ | 226,554 | ||||||||||||||||
Net accounts receivable | 26,822 | 28,331 | 1,398 | 21,370 | 30,654 | 13,031 | 121,606 | 39,678 | 27,415 | 7,580 | 44,975 | 20,780 | (2,175 | ) | 138,253 | |||||||||||||||||||||||||||||
Investments | 5,320 | 131,261 | — | — | — | 64,322 | 200,903 | 21,273 | 101,093 | — | — | — | 111,324 | 233,690 | ||||||||||||||||||||||||||||||
Goodwill | 120,485 | — | 104,549 | 142,291 | 59,614 | — | 426,939 | 120,485 | — | 104,549 | 142,291 | 59,614 | — | 426,939 | ||||||||||||||||||||||||||||||
The following table reconciles Segment Profit to consolidated income before income taxes for the years ended December 31, 2009, 2010, 2011 and 20112012 (in thousands):
| | 2009 | 2010 | 2011 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
Segment Profit | $ | 227,237 | $ | 291,145 | $ | 270,422 | ||||
Stock compensation expense | (19,782 | ) | (15,102 | ) | (17,418 | ) | ||||
Depreciation and amortization | (47,268 | ) | (54,682 | ) | (58,623 | ) | ||||
Interest expense | (2,424 | ) | (2,233 | ) | (2,502 | ) | ||||
Interest income | 6,245 | 3,275 | 2,781 | |||||||
Income before income taxes | $ | 164,008 | $ | 222,403 | $ | 194,660 | ||||
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
December 31, 2011
12. Selected Quarterly Financial Data (Unaudited)
The following is a summary of the unaudited quarterly results of operations for the years ended December 31, 2010 and 2011 (in thousands, except per share amounts):
| | For the Quarter Ended | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| | March 31, 2010 | June 30, 2010 | September 30, 2010 | December 31, 2010 | |||||||||
Fiscal Year Ended December 31, 2010 | |||||||||||||
Net revenue | $ | 728,053 | $ | 741,658 | $ | 750,319 | $ | 749,210 | |||||
Cost and expenses: | |||||||||||||
Cost of care | 476,679 | 472,478 | 467,160 | 491,668 | |||||||||
Cost of goods sold | 56,296 | 54,771 | 55,071 | 52,492 | |||||||||
Direct service costs and other operating expenses(1) | 138,254 | 139,617 | 141,581 | 147,130 | |||||||||
Depreciation and amortization | 13,422 | 14,235 | 13,950 | 13,075 | |||||||||
Interest expense | 685 | 584 | 482 | 482 | |||||||||
Interest income | (817 | ) | (803 | ) | (846 | ) | (809 | ) | |||||
| 684,519 | 680,882 | 677,398 | 704,038 | ||||||||||
Income before income taxes | 43,534 | 60,776 | 72,921 | 45,172 | |||||||||
Provision for income taxes | 18,015 | 25,348 | 28,137 | 12,244 | |||||||||
Net income | $ | 25,519 | $ | 35,428 | $ | 44,784 | $ | 32,928 | |||||
Weighted average number of common shares outstanding—basic | 34,382 | 33,323 | 33,450 | 33,971 | |||||||||
Weighted average number of common shares outstanding—diluted | 35,074 | 33,800 | 34,171 | 34,730 | |||||||||
Net income per common share—basic: | $ | 0.74 | $ | 1.06 | $ | 1.34 | $ | 0.97 | |||||
Net income per common share—diluted: | $ | 0.73 | $ | 1.05 | $ | 1.31 | $ | 0.95 | |||||
| | 2010 | 2011 | 2012 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
Segment Profit | $ | 291,145 | $ | 270,422 | $ | 267,364 | ||||
Stock compensation expense | (15,102 | ) | (17,418 | ) | (17,783 | ) | ||||
Depreciation and amortization | (54,682 | ) | (58,623 | ) | (60,488 | ) | ||||
Interest expense | (2,233 | ) | (2,502 | ) | (2,247 | ) | ||||
Interest income | 3,275 | 2,781 | 2,019 | |||||||
Income before income taxes | $ | 222,403 | $ | 194,660 | $ | 188,865 | ||||
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
December 31, 2012
12. Selected Quarterly Financial Data (Unaudited)
The following is a summary of the unaudited quarterly results of operations for the years ended December 31, 2011 and 2012 (in thousands, except per share amounts):
| | For the Quarter Ended | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| | March 31, 2011 | June 30, 2011 | September 30, 2011 | December 31, 2011 | |||||||||
Fiscal Year Ended December 31, 2011 | |||||||||||||
Net revenue: | |||||||||||||
Managed care and other | $ | 632,366 | $ | 641,742 | $ | 625,079 | $ | 652,804 | |||||
Dispensing | 60,389 | 56,596 | 61,764 | 68,660 | |||||||||
Total net revenue | 692,755 | 698,338 | 686,843 | 721,464 | |||||||||
Costs and expenses: | |||||||||||||
Cost of care | 433,700 | 441,446 | 448,051 | 461,527 | |||||||||
Cost of goods sold | 56,519 | 53,404 | 57,636 | 64,479 | |||||||||
Direct service costs and other operating expenses(1) | 131,567 | 131,779 | 130,038 | 136,250 | |||||||||
Depreciation and amortization | 13,952 | 14,267 | 15,069 | 15,335 | |||||||||
Interest expense | 471 | 494 | 457 | 1,080 | |||||||||
Interest income | (815 | ) | (858 | ) | (592 | ) | (516 | ) | |||||
Total costs and expenses | 635,394 | 640,532 | 650,659 | 678,155 | |||||||||
Income before income taxes | 57,361 | 57,806 | 36,184 | 43,309 | |||||||||
Provision for income taxes | 23,063 | 23,575 | 4,829 | 13,570 | |||||||||
Net income | $ | 34,298 | $ | 34,231 | $ | 31,355 | $ | 29,739 | |||||
Weighted average number of common shares outstanding—basic | 33,051 | 31,301 | 29,900 | 27,724 | |||||||||
Weighted average number of common shares outstanding—diluted | 33,656 | 31,903 | 30,438 | 28,300 | |||||||||
Net income per common share—basic: | $ | 1.04 | $ | 1.09 | $ | 1.05 | $ | 1.07 | |||||
Net income per common share—diluted: | $ | 1.02 | $ | 1.07 | $ | 1.03 | $ | 1.05 | |||||
MAGELLAN HEALTH SERVICES, INC. AND SUBSIDIARIES
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (Continued)
December 31, 2012
12. Selected Quarterly Financial Data (Unaudited) (Continued)
| | For the Quarter Ended | For the Quarter Ended | ||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| | March 31, 2011 | June 30, 2011 | September 30, 2011 | December 31, 2011 | March 31, 2012 | June 30, 2012 | September 30, 2012 | December 31, 2012 | ||||||||||||||||||
Fiscal Year Ended December 31, 2011 | ||||||||||||||||||||||||||
Net revenue | $ | 692,755 | $ | 698,338 | $ | 686,843 | $ | 721,464 | ||||||||||||||||||
Fiscal Year Ended December 31, 2012 | ||||||||||||||||||||||||||
Net revenue: | ||||||||||||||||||||||||||
Managed care and other | $ | 686,059 | $ | 716,998 | $ | 711,092 | $ | 742,950 | ||||||||||||||||||
Dispensing | 87,154 | 88,475 | 87,345 | 87,324 | ||||||||||||||||||||||
Cost and expenses: | ||||||||||||||||||||||||||
Total net revenue | 773,213 | 805,473 | 798,437 | 830,274 | ||||||||||||||||||||||
Costs and expenses: | ||||||||||||||||||||||||||
Cost of care | 433,700 | 441,446 | 448,051 | 461,527 | 505,293 | 521,830 | 516,238 | 528,529 | ||||||||||||||||||
Cost of goods sold | 56,519 | 53,404 | 57,636 | 64,479 | 81,038 | 82,855 | 81,662 | 82,859 | ||||||||||||||||||
Direct service costs and other operating expenses(2) | 131,567 | 131,779 | 130,038 | 136,250 | 136,589 | 140,333 | 135,574 | 145,016 | ||||||||||||||||||
Depreciation and amortization | 13,952 | 14,267 | 15,069 | 15,335 | 14,781 | 15,152 | 15,239 | 15,316 | ||||||||||||||||||
Interest expense | 471 | 494 | 457 | 1,080 | 600 | 576 | 537 | 534 | ||||||||||||||||||
Interest income | (815 | ) | (858 | ) | (592 | ) | (516 | ) | (412 | ) | (857 | ) | (350 | ) | (400 | ) | ||||||||||
| 635,394 | 640,532 | 650,659 | 678,155 | |||||||||||||||||||||||
Total costs and expenses | 737,889 | 759,889 | 748,900 | 771,854 | ||||||||||||||||||||||
Income before income taxes | 57,361 | 57,806 | 36,184 | 43,309 | 35,324 | 45,584 | 49,537 | 58,420 | ||||||||||||||||||
Provision for income taxes | 23,063 | 23,575 | 4,829 | 13,570 | ||||||||||||||||||||||
Provision (benefit) for income taxes | 14,534 | 18,611 | (16,725 | ) | 21,418 | |||||||||||||||||||||
Net income | $ | 34,298 | $ | 34,231 | $ | 31,355 | $ | 29,739 | $ | 20,790 | $ | 26,973 | $ | 66,262 | $ | 37,002 | ||||||||||
Weighted average number of common shares outstanding—basic | 33,051 | 31,301 | 29,900 | 27,724 | 27,199 | 27,317 | 27,521 | 27,505 | ||||||||||||||||||
Weighted average number of common shares outstanding—diluted | 33,656 | 31,903 | 30,438 | 28,300 | 27,747 | 27,717 | 28,042 | 28,020 | ||||||||||||||||||
Net income per common share—basic: | $ | 1.04 | $ | 1.09 | $ | 1.05 | $ | 1.07 | $ | 0.76 | $ | 0.99 | $ | 2.41 | $ | 1.35 | ||||||||||
Net income per common share—diluted: | $ | 1.02 | $ | 1.07 | $ | 1.03 | $ | 1.05 | $ | 0.75 | $ | 0.97 | $ | 2.36 | $ | 1.32 | ||||||||||
MAGELLAN HEALTH SERVICES, INC.
SCHEDULE II—VALUATION AND QUALIFYING ACCOUNTS
(In thousands)
Classification | Balance at Beginning of Period | Charged to Costs and Expenses | Charged to Other Accounts | Addition | Deduction | Balance at End of Period | Balance at Beginning of Period | Charged to Costs and Expenses | Charged to Other Accounts | Addition | Deduction | Balance at End of Period | ||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Year Ended December 31, 2009 | ||||||||||||||||||||||||||||||||||||||
Allowance for doubtful accounts | $ | 1,915 | $ | 112 | (3) | $ | (650) | (1) | $ | 116 | (4) | $ | (135) | (2) | $ | 1,358 | ||||||||||||||||||||||
Year Ended December 31, 2010 | ||||||||||||||||||||||||||||||||||||||
Allowance for doubtful accounts | 1,358 | 925 | (3) | (130) | (1) | — | (168) | (2) | 1,985 | $ | 1,358 | $ | 925 | (3) | $ | (130 | )(1) | — | $ | (168 | )(2) | $ | 1,985 | |||||||||||||||
Year Ended December 31, 2011 | ||||||||||||||||||||||||||||||||||||||
Allowance for doubtful accounts | 1,985 | 1,528 | (3) | (150) | (1) | — | (27) | (2) | 3,336 | 1,985 | 1,528 | (3) | (150 | )(1) | — | (27 | )(2) | 3,336 | ||||||||||||||||||||
Year Ended December 31, 2012 | ||||||||||||||||||||||||||||||||||||||
Allowance for doubtful accounts | 3,336 | 1,947 | (3) | (346 | )(1) | — | (325 | )(2) | 4,612 | |||||||||||||||||||||||||||||