UNITED STATES
SECURITIES AND EXCHANGE COMMISSION
Washington, D.C. 20549
Form 10-K
(Mark One)
|
| |
| x | ANNUAL REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 |
FOR THE FISCAL YEAR ENDED DECEMBER 31, 20122014
or
|
| |
| ¨ | TRANSITION REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 |
Commission File Number 1-31719
MOLINA HEALTHCARE, INC.
(Exact name of registrant as specified in its charter)
|
| | |
| Delaware | | 13-4204626 |
| (State or other jurisdiction of | | (I.R.S. Employer |
| incorporation or organization) | | Identification No.) |
200 Oceangate, Suite 100, Long Beach, California 90802
(Address of principal executive offices)
(562) 435-3666
(Registrant’s telephone number, including area code)
Securities registered pursuant to Section 12(b) of the Act:
|
| | |
| Title of Class | | Name of Each Exchange on Which Registered |
| Common Stock, $0.001 Par Value | | New York Stock Exchange |
Securities registered pursuant to Section 12(g) of the Act:
None
Indicate by check mark if the registrant is a well-known seasoned issuer, as defined in Rule 405 of the Securities Act. xý Yes ¨ No
Indicate by check mark if the registrant is not required to file reports pursuant to Section 13 or Section 15(d) of the Act.
¨ Yes xý No
Indicate by check mark whether the registrant (1) has filed all reports required to be filed by Section 13 or 15(d) of the Securities Exchange Act of 1934 during the preceding 12 months (or for such shorter period that the registrant was required to file such reports), and (2) has been subject to such filing requirements for the past 90 days. xý Yes ¨ No
Indicate by check mark whether the registrant has submitted electronically and posted on its corporate Web site, if any, every Interactive Data File required to be submitted and posted pursuant to Rule 405 of Regulation S-T during the preceding 12 months (or for such shorter period that the registrant was required to submit and post such files). xý Yes ¨ No
Indicate by check mark if disclosure of delinquent filers pursuant to Item 405 of Regulation S-K is not contained herein, and will not be contained, to the best of registrant’s knowledge, in definitive proxy or information statements incorporated by reference in Part III of this Form 10-K or any amendment to this Form 10-K. xý
Indicate by check mark whether the registrant is a large accelerated filer, an accelerated filer, a non-accelerated filer, or a smaller reporting company. See the definitions of “large"large accelerated filer,” “accelerated filer”" "accelerated filer" and “smaller"smaller reporting company”company" in Rule 12b-2 of the Exchange Act. (Check one):
|
| | | | |
| Large accelerated filer | xý |
| Accelerated filer | ¨ |
| Non-accelerated filer | ¨ | (Do not check if a smaller reporting company) | Smaller reporting company | ¨ |
Indicate by check mark whether the registrant is a shell company (as defined in Rule 12b-2 of the Exchange Act). ¨ Yes ý No
The aggregate market value of Common Stock held by non-affiliates of the registrant as of June 30, 20122014, the last business day of our most recently completed second fiscal quarter, was approximately $664.3$1,338.4 million (based upon the closing price for shares of the registrant’s Common Stock as reported by the New York Stock Exchange, Inc. on June 30, 20122014).
As of February 22, 2013,20, 2015, approximately 45,154,00049,873,000 shares of the registrant’s Common Stock, $0.001 par value per share, were outstanding.
DOCUMENTS INCORPORATED BY REFERENCE
Portions of the registrant’s Proxy Statement for the 20132015 Annual Meeting of Stockholders to be held on May 1,6, 20132015, are incorporated by reference into Part III of this Form 10-K.
MOLINA HEALTHCARE, INC.
Table of ContentsMolina Healthcare, Inc.
Form 10-K
For the Year Ended December 31, 2014
TABLE OF CONTENTS
This Annual Report on Form 10-K ("Form 10-K") contains forward-looking statements within the meaning of the Private Securities Litigation Reform Act of 1995 that involve risks and uncertainties. Many of the forward-looking statements are located under the headings "Business," and "Management's Discussion and Analysis of Financial Condition and Results of Operations." Forward-looking statements provide current expectations of future events based on certain assumptions and include any statement that does not directly relate to any historical or current fact. Forward-looking statements can also be identified by words such as "future," "anticipates," "believes," "estimates," "expects," "intends," "plans," "predicts," "will," "would," "could," "can," "may," and similar terms. Forward-looking statements are not guarantees of future performance and the Company's actual results may differ significantly from the results discussed in the forward-looking statements. Factors that might cause such differences include, but are not limited to, those discussed in Part I, Item 1A of this Form 10-K under the heading "Risk Factors." Each of the terms "Company," "Molina Healthcare," "we," "our," and "us," as used herein refers collectively to Molina Healthcare, Inc. and its wholly owned subsidiaries, unless otherwise stated. The Company assumes no obligation to revise or update any forward-looking statements for any reason, except as required by law.
PART I
Item 1:Business
OVERVIEW
Molina Healthcare, Inc. provides quality andhealth care to those receiving government assistance. We offer cost-effective Medicaid-related solutions to meet the health care needs of low-income families and individuals, and to assist state agencies in their administration of the Medicaid program.
As of December 31, 2014, our health plans served over 2.6 million members eligible for Medicaid, Medicare, and other government-sponsored health care programs for low-income families and individuals. Dr. C. David Molina founded our company in 1980 as a provider organization serving the Medicaid population in Southern California. Today, we remain a provider-focused company led by his son, Joseph M. Molina, M.D. (Dr.Dr. J. Mario Molina)Molina.
Significant Accomplishments in 2014
Our mission is to provide quality health care to those receiving government assistance. Our goal is to achieve this mission while improving our financial strength. Our significant operational, financial and strategic accomplishments supporting this goal during 2014 included:
Expanding existing markets. Our Health Plans segment enrollment has grown approximately 36% since December 31, 2013, primarily a result of:
| |
| ◦ | Our 2014 growth initiatives associated with the Affordable Care Act (ACA). Since the inception of these programs in January 2014 through the end of fiscal 2014, we have added approximately 385,000 Medicaid expansion members, 18,000 integrated Medicare-Medicaid Plan (MMP) members, and 15,000 Marketplace members; |
| |
| ◦ | The inception and growth of operations at our newer health plans in South Carolina and Illinois, adding over 200,000 members in the aggregate in fiscal 2014; and |
| |
| ◦ | Acquisition of two Medicaid contracts in Florida, which added approximately 73,000 new members in fiscal 2014. |
Entering new strategic markets. In 2014, we were awarded a managed care contract in the Commonwealth of Puerto Rico that is expected to enroll its first members April 1, 2015. Total enrollment is expected to be approximately 350,000 new members, with anticipated annualized revenue of $750 million.
Funding future growth. Debt financing transactions generated net cash of approximately $123 million; such transactions both extended the maturity date and lowered the rate of our convertible senior notes previously due in 2014.
Our Structure
We report our financial performance based on two reportable segments: the Health Plans segment and the Molina Medicaid Solutions.Solutions segment. We derive our revenues primarily from health insurance premiums and service revenues. Refer to Part II, Item 8 of this Form 10-K, Notes to Consolidated Financial Statements, Note 2, "Significant Accounting Policies," and Note 21, "Segment Information," for revenue information by state health plan, and segment revenue, profit and total asset information, respectively.
The Health Plans segment consists of operational health plans in California, Florida, Michigan, New Mexico, Ohio, Texas, Utah, Washington,11 states and Wisconsin, and includes our direct delivery business. As of December 31, 2012, these health plans served approximately 1.8 million members eligible for Medicaid, Medicare, and other government-sponsored health care programs for low-income families and individuals. The health plans are operated by our respective wholly owned subsidiaries in those states, each of which is licensed as a health maintenance organization or HMO.(HMO). Our direct delivery business consists primarily of 24the management of a hospital in southern California under a management services agreement, and the operation of primary care clinics in California, Florida, New Mexico, and Washington, and we manage three county-owned primary care clinics under a contract with Fairfax County, Virginia.
Our Health Plans segment derives its revenue principally in the form of premiums received under Medicaid contracts with theseveral states in which ourwe operate health plans operate. While the health plans receive fixed per-member per-month, or PMPM, premium payments from the states, the health plans are at risk for the medical costs associated with their members' health care.plans. Our Health Plans segment operates in a highly regulated environment, with stringent minimum capitalization requirements whichthat limit the ability of our health plan subsidiaries to pay dividends to us.
Our Molina Medicaid Solutions segment provides design, development, implementation (DDI), and business process outsourcing (BPO) solutions to state governments for their Medicaid Management Information Systems, or MMIS.management information systems (MMIS). MMIS is a core tool used to support the administration of state Medicaid and other health care entitlement programs. Molina Medicaid Solutions currently holds MMIS contracts with the states of Idaho, Louisiana, Maine, New Jersey, and West Virginia, as well asVirginia; the U.S. Virgin Islands; and a contract to provide drugpharmacy rebate administration services for the Florida Medicaid program. We added the Molina Medicaid Solutions segment to our business in May 2010 to expand our product offerings to include support of state Medicaid agency administrative needs, reduce the variability in our earnings resulting from fluctuations in medical care costs, improve our operating profit margin percentages, and improve our cash flow by adding a business for which there are no restrictions on dividend payments.
FromOur reliance on operations in a limited number of states could cause our revenue and profitability to change suddenly and unexpectedly. Additionally, our inability to continue to operate in any of the states in which we currently operate, or a significant change in the nature of our existing operations, could adversely affect our business, financial condition, cash flows, or results of operations.
Health Care Reform
The ACA has made broad-based changes to the U.S. health care system that have significantly affected the U.S. economy and our business. We expect the ACA to continue to significantly impact our business operations and financial results, including our medical care ratios.
Key components of the legislation will continue to be phased in over the next several years, with the most significant changes having occurred at the start of 2014, including the implementation of the Medicaid expansion (in electing states) and Marketplace programs, Medicare and Marketplace minimum medical loss ratios (MLRs), and new industry-wide fees, assessments, and taxes. We have dedicated material resources and have incurred material expenses in implementing and complying with the ACA, and we will continue to do so. As a result of the novelty and extremely broad scale of all of the programmatic changes effected by the ACA, many of the business and market impacts of the ACA will not be known for several years. Further, given the inherent difficulty of foreseeing how individuals will respond to the choices afforded to them by the ACA, we cannot predict the full effect the ACA will have on us.
Our Strategic Growth Initiatives
Our mission is to provide quality health care to those receiving government assistance. This mission drives our strategic perspective, we believe our two business segments allow usgrowth and growth-related initiatives as follows:
Enter New Programs Within Existing Markets
Medicaid Expansion. In the states that have elected to participate, in an expanding sectorthe ACA provides for the expansion of the economyMedicaid program to offer eligibility to nearly all low-income people under age 65 with incomes at or below 138% of the federal poverty line. Medicaid expansion membership phased in beginning January 1, 2014. Since that date, our health plans in California, Illinois, Michigan, New Mexico, Ohio, and continueWashington have begun participating in Medicaid expansion. At December 31, 2014, our missionmembership included approximately 385,000 Medicaid expansion members, or 15% of serving low-incometotal membership.
Health Insurance Marketplace. The ACA authorized the creation of Marketplace insurance exchanges, allowing individuals and small groups to purchase health insurance that is federally subsidized, effective January 1, 2014. We participate in the Marketplace in all of the states in which we operate, except Illinois and South Carolina. At December 31, 2014, we had approximately 15,000 Marketplace members.
Medicare-Medicaid Plans. Policymakers at the federal and state levels are increasingly focused on the design and implementation of programs that improve the coordination of care for those who qualify to receive both Medicare and Medicaid services (the "dual eligible"), and to deliver services to the dual eligible in a more financially efficient manner. As a result of these efforts, 15 states have undertaken demonstration programs to integrate Medicare and Medicaid services for dual-eligible individuals. The health plans participating in such demonstrations are referred to as Medicare-Medicaid Plans (MMPs). Our MMPs in California, Illinois, and Ohio offered coverage beginning in 2014, and we expect to begin offering MMP coverage in South Carolina and Texas in the first quarter of 2015, and in Michigan in the second quarter of 2015.
Direct Delivery. Growth and aging of the U.S. population foreshadows an increasing shortage of physicians over the next 15 years. Health care reform is expected to worsen this shortage. We believe the shortage will be felt most acutely among already under-served populations, such as the financially vulnerable families and individuals eligiblewe serve. While we have no plans to become an organization that fully integrates primary care delivery with our health plans, by leveraging our direct delivery capability on a selective basis we can improve access for government-sponsored healthour plan members in areas that are most under-served by primary care programs. Operationally, our two business segments shareproviders. We operate primary care clinics in the states of California, Florida, New Mexico, Utah, Virginia and Washington. In addition, we perform certain medical and administrative management services for a common systems platform, which allowshospital in Long Beach, California, including the assumption of financial benefit and risk for economiesa number of scale and common experience in meetingacute care beds at the needs of state Medicaid programs.hospital. We also believe that this arrangement improves hospital access for our members in the Long Beach, California area, and enhances our overall direct delivery strategy. We may incur losses while we may have opportunitiesseek to marketmodify various business operations and patient behaviors under the management services agreement.
Enter New Strategic Markets
We plan to continue to enter new markets through both acquisitions and by building our own start-up operations. We intend to focus our expansion in markets with competitive provider communities, supportive regulatory environments, significant size, and, where practicable, mandated Medicaid managed care enrollment. As described above, in December 2014 we entered into a Medicaid contract with the Puerto Rico Health Insurance Administration. The operational start date for the program is expected to be April 1, 2015.
Deliver Administrative Value to Medicaid Agencies
As Medicaid expenditures increase, we believe that an increasing number of states’ and other Medicaid agencies will demand comprehensive solutions that improve both quality and cost-effectiveness. We intend to use our MMIS solution to provide state Medicaid agencies various cost containmentwith a flexible and quality practices used byrobust solution to their administrative needs. We believe that our MMIS platform, together with our extensive experience in health plans, such as care management and care coordination,health plan operations, enables us to offer state and other Medicaid agencies a comprehensive suite of Medicaid-related solutions that meets their needs for incorporation intoquality and for the cost-effective operation of their own fee-for-service Medicaid programs.
Our principal executive offices are locatedLeverage Operational Efficiencies
We intend to leverage the operational efficiencies created by our centralized administrative infrastructure and flexible information systems to earn higher margins on future revenues. We believe our administrative infrastructure has significant expansion capacity, allowing us to integrate new members from expansion within existing markets and enter new markets at 200 Oceangate, Suite 100, Long Beach, California 90802,lower incremental cost. For example, our general and our telephone number is (562) 435-3666. Our website is www.molinahealthcare.com.administrative expenses as a percentage of revenue (the general and administrative expense ratio) declined to 7.9% for the year ended December 31, 2014, compared with 10.1% for the year ended December 31, 2013.
OUR INDUSTRY
Information contained on our website or linked to our website is not incorporated by reference into, or as part of, this annual report. Unless the context otherwise requires, references to “Molina Healthcare,” the “Company,” “we,” “our,” and “us” herein refer to Molina Healthcare, Inc. and its subsidiaries. Our annual reports on Form 10-K, quarterly reports on Form 10-Q, current reports on Form 8-K, and all amendments to these reports, are available free of chargeMedicaid
Medicaid was established in 1965 under the “investors” tab of our website, www.molinahealthcare.com, as soon as reasonably practicable after such reports are electronically filed with or furnishedU.S. Social Security Act to the Securities and Exchange Commission, or SEC. Information regarding our officers and directors, and copies of our Code of Business Conduct and Ethics, Corporate Governance Guidelines, and the charters of our Audit Committee, Compensation Committee, Corporate Governance and Nominating Committee, and Compliance Committee are also available on our website. Such information is also available in print upon the request of any stockholder to our Investor Relations department at the address of our executive offices set forth above. In accordance with New York Stock Exchange, or NYSE, rules, on May 21, 2012, we filed the annual certification by our Chief Executive Officer certifying that he was unaware of any violation by us of the NYSE's corporate governance listing standards at the time of the certification.
Our Industry
The Medicaid and CHIP Programs. The Medicaid program is a federal entitlement program administered by the states. Medicaid providesprovide health care and long-term care services and support to low-income Americans. Although jointly funded by federal and state governments, Medicaid is a state-operated and state-implemented program. Subject to federal laws and regulations, states have significant flexibility to structure their own programs in terms of eligibility, benefits, delivery of services, and provider payments. As a result, there are 56 separate Medicaid is funded jointly by the statesprograms—one for each U.S. state, each U.S. territory, and the federal government. District of Columbia.
The federal government guarantees matching funds to states for qualifying Medicaid expenditures based on each state'sstate’s federal medical assistance percentage or
FMAP.(FMAP). A state'sstate’s FMAP is calculated annually and varies inversely with average personal income in the state. The average FMAP across all states is currently about 57 percent,57%, and ranges from a federally established FMAP floor of 50% to as high as 74%.
The most common state-administered Medicaid program is the Temporary Assistance for Needy Families program (TANF), which covers primarily low-income mothers and children. In states that have elected to participate, Medicaid expansion provides eligibility to nearly all low-income people under age 65 with incomes at or TANF.below 138% of the federal poverty line. Another common state-administered Medicaid program is for aged, blind or disabled (ABD) Medicaid beneficiaries, which covers low-income persons with chronic physical disabilities or behavioral health impairments. ABD beneficiaries represent a growing portion of all Medicaid members. In addition,recipients, and typically use more services because of their critical health issues. Additionally, the Children's Health Insurance Program or CHIP,(CHIP) is a joint federal and state matching program that provides health care coverage to children whose families earn too much to qualify for Medicaid coverage. States have the option of administering CHIP through their Medicaid programs. As of December 31, 2014, approximately 70% of our members were TANF beneficiaries, 15% were Medicaid expansion beneficiaries, 12% were ABD beneficiaries, 2% were Medicare beneficiaries, and 1% were integrated MMP and Marketplace beneficiaries combined. For the year ended December 31, 2014, approximately 54% of our premium revenue was from TANF and Medicaid expansion membership combined; 36% was from ABD membership, 7% was from Medicare membership, 2% was from MMP integrated membership, and 1% was from Marketplace membership.
Each state establishes its own eligibility standards, benefit packages, payment rates, and program administration within broad federal statutory and regulatory guidelines. Every state Medicaid program must balance many potentially competing demands, including the need for quality care, adequate provider access, and cost-effectiveness. In an effort toTo improve quality and provide more uniform and cost-effective care, many states have implemented Medicaid managed care programs. These programs seek to improve access to coordinated health care services, including preventive care, and to control health care costs. Under Medicaid managed care programs, a health plan receives capitation payments from the state. The health plan, in turn, arranges for the provision of health care services by contracting with a network of medical providers. The health plan implements care management and care coordination programs that seek to improve both care access and care quality, while controlling costs more effectively.
While many states have embraced Medicaid managed care programs, others continue to operate traditional fee-for-service programs to serve all or part of their Medicaid populations. Under fee-for-service Medicaid programs, health care services are made available to beneficiaries as they seek that care, without the benefit of a coordinated effort to maintain and improve their health. As a consequence, treatment is often postponed until medical conditions become more severe, leading to higher costs and more unfavorable outcomes. Additionally, providers paid on a fee-for-service basis are compensated based upon services they perform, rather than health outcomes, and therefore lack incentives to coordinate preventive care, monitor utilization, and control costs.
Medicare
Medicare is a federal program that provides eligible persons age 65 and over and some disabled persons a variety of hospital, medical insurance, and prescription drug benefits. Medicare is funded by Congress, and administered by the Centers for Medicare and Medicaid Services (CMS). Medicare beneficiaries may enroll in a Medicare Advantage plan, under which managed care plans contract with CMS to provide benefits that are comparable to original Medicare. Such benefits are provided in exchange for a fixed per-member per-month (PMPM) premium payment that varies based on the county in which a member resides, the demographics of the member, and the member’s health condition.
Since 2006, Medicare beneficiaries have had the option of selecting a new prescription drug benefit from an existing Medicare Advantage plan. The drug benefit, available to beneficiaries for a monthly premium, is subject to certain cost sharing depending upon the specific benefit design of the selected plan.
Medicaid Management Information Systems
Because Medicaid is a state-administered program, every state must have mechanisms, policies, and procedures in place to perform a large number of crucial functions, including the determination of eligibility and the reimbursement of medical providers for services provided. This requirement exists regardless of whether a state has adopted a fee-for-service or a
managed care delivery model. MMIS are used by states to support these administrative activities. The federal government typically reimburses the states for 90% of the costs incurred in the design, development, and implementation of an MMIS and for 75% of the costs incurred in operating an MMIS. Although a small number of states build and operate their own MMIS, a far more typical practice is for states to sub-contract the design, development, implementation, and operation of their MMIS to private parties. Through our Molina Medicaid Solutions segment, we now actively participate in this market.
In certain instances, states have elected to provide medical benefits to individuals and families who are not served by Medicaid. In New Mexico and Washington, our health plan segment participates in programs that are administered in a manner similar to Medicaid and CHIP, but without federal matching funds.
Medicare Advantage Plans. During 2012, all of our health plans, except our Wisconsin health plan, operated Medicare Advantage plans, each of which included a mandatory Part D prescription drug benefit. Our Medicare Advantage special needs plans, or SNPs, operate under the trade name Molina Medicare Options Plus, and serve those beneficiaries who are dually eligible for both Medicare and Medicaid, such as low-income seniors and people with disabilities. Our Medicare Advantage Prescription Drug plans, or MA-PDs, operate under the trade name Molina Medicare Options. Although our MA-PD benefit plans do not exclusively enroll dual eligible beneficiaries, the plans' benefit structure is designed to appeal to lower income beneficiaries. We believe offering these Medicare plans is consistent with our historical mission of serving low-income and medically underserved families and individuals. None of our health plans operates a Medicare Advantage private fee-for-service plan. Total enrollment in our Medicare Advantage plans as of December 31, 2012 was approximately 36,000 members. For the year ended December 31, 2012, premium revenues from Medicare across all health plans represented approximately 8% of our total premium revenues.
As of December 31, 2012, approximately 75% of our members were TANF, 15% were ABD, 8% were CHIP, and 2% were Medicare.
Our Strengths
We focus on serving low-income families and individuals who receive health care benefits through government-sponsored programs within a managed care model. Additionally, we support state Medicaid agencies by providing them with comprehensive solutions to their MMIS development and operating needs. Our approach to our business is based on the following strengths:
Comprehensive Medicaid Services. We offer a complete suite of Medicaid services, ranging from quality care, disease management, cost management, and direct delivery of health care services at our clinics through our Health Plans segment, to state-level MMIS administration through our Molina Medicaid Solutions segment. We have the ability to draw upon our experience and expertise in each of these areas to enhance the quality of the services we offer in the others.
Flexible Service Delivery Systems. Our health plan care delivery systems are diverse and readily adaptable to different markets and changing conditions. We arrange health care services with a variety of providers, including independent physicians and medical groups, hospitals, ancillary providers, and our own clinics. Our systems support multiple types of contract models. Our provider networks are well-suited, based on medical specialty, member proximity, and cultural sensitivity, to provide services to our members. Our Molina Medicaid Solutions platform is based upon commercial off-the-shelf technology. As a result, we believe that our Molina Medicaid Solutions platform has the flexibility to meet a wide variety of state Medicaid administrative needs in a timely and cost-effective manner.
Proven Expansion and Acquisition Capability. We have successfully replicated the business model of our health plan segment through the acquisition of health plans, the start-up development of new operations, and the transition of members from other health plans. The acquisition of our New Mexico and Wisconsin health plans demonstrated our ability to expand into new states. The establishment of our health plans in Utah, Ohio, Texas, and Florida reflects our ability to replicate our business model on a start-up basis in new states, while contract acquisitions in California, Michigan, and Washington have demonstrated our ability to expand our operations within states in which we were already operating.
Administrative Efficiency. We have centralized and standardized various functions and practices to increase administrative efficiency. The steps we have taken include centralizing claims processing and information services onto a single platform. We have standardized medical management programs, pharmacy benefits management contracts, and health education programs. In addition, we have designed our administrative and operational infrastructure to be scalable for cost-effective expansion into new and existing markets.
Recognition for Quality of Care. The National Committee for Quality Assurance, or NCQA, has accredited eight of our nine Medicaid managed care plans. Our Wisconsin plan acquired in September 2010 currently plans to seek NCQA accreditation in early 2014. We believe that these objective measures of the quality of the services that we provide will become increasingly important to state Medicaid agencies.
Experience and Expertise. Since the founding of our Company in 1980 to serve the Medicaid population in Southern California through a small network of primary care clinics, we have increased our membership to 1.8 million members as of December 31, 2012, expanded our Health Plans segment to nine states, and added our Molina Medicaid Solutions segment. Our experience over the last 30 years has allowed us to develop strong relationships with the constituents we serve, establish significant expertise as a government contractor, and develop sophisticated disease management, care coordination and health education programs that address the particular health care needs of our members. We also benefit from a thorough understanding of the cultural and linguistic needs of Medicaid populations.
Our Strategy
Our objective is to provide a comprehensive suite of Medicaid-related services to meet the health care needs of low-income families and individuals and the state Medicaid agencies that serve them. To achieve our objective, we intend to:
Continue to expand within existing markets, including as a result of the Affordable Care Act Medicaid expansion, the duals pilot projects, and the insurance marketplaces. We plan to continue our growth in existing markets. The Patient Protection and Affordable Care Act and the Health Care and Education Affordability Reconciliation Act, commonly referred to together as the Affordable Care Act, or the ACA, provides us with several opportunities for growth, including the expansion of Medicaid eligibility in the states that elect to participate, the implementation of pilot projects for those who are dually eligible for Medicaid and Medicare, and the implementation of insurance marketplaces.
Medicaid expansion. As of February 27, 2013, among the states where we operate our health plans, the states of California, Florida, Michigan, New Mexico, Ohio, and Washington have indicated that they intend to participate in the Medicaid expansion; the states of Texas and Wisconsin have indicated that they do not intend to participate in the expansion; and the state of Utah is undecided. We believe there are significant opportunities to increase our revenues through the Medicaid expansion.
Duals. Nine million low-income elderly and disabled people in the United States are covered under both the Medicare and Medicaid programs. These beneficiaries, often called “dual eligibles” or simply “duals,” are more likely than other Medicare beneficiaries to be frail, live with multiple chronic conditions, and have functional and cognitive impairments. Policymakers at the federal and state level are developing initiatives for dual eligibles both to improve the coordination of their care, and to reduce spending for both Medicare and Medicaid. The Centers for Medicare and Medicaid Services, or CMS, has implemented several demonstrations designed to improve the coordination of care for dual eligibles and reduce spending under Medicare and Medicaid. These demonstrations include issuing contracts to 15 states to design a program to integrate Medicare and Medicaid services for dual eligibles in the state. Our health plans in California, Illinois, Michigan, Ohio, Texas, and Washington intend to take part in the duals demonstrations in those states. Beginning in September 2013, our California plan intends to serve duals in Riverside, San Bernardino and San Diego counties, and may participate with Health Net, Inc. for the duals contract in Los Angeles County. Our new Illinois plan will serve duals
in Central Illinois beginning in 2014. Our Michigan plan will respond to a request for proposals to serve duals also beginning in late 2013. Our Ohio plan will serve duals in three regions in southwestern Ohio (Dayton, Columbus and Cincinnati) beginning in late 2013. The state of Texas announced that it intends to cover duals through its existing Medicaid contracts beginning in 2014. Our Washington plan will respond to a request for proposals to serve duals also beginning in 2014.
Insurance marketplaces. Under the ACA, insurance marketplaces will be online marketplaces organized on a state-by-state basis (although in many instances the insurance marketplace in a state will be operated by the federal government, and there could also be regional marketplaces where states combine their marketplace products). In the insurance marketplace, individuals and groups can purchase health insurance that in many instances will be federally subsidized (up to 400% of the federal poverty level by individual or family). We currently intend to participate in the insurance marketplaces in the states in which we operate our health plans. Our principal focus in participating in the marketplace is to capture the transition in membership that may result from a Medicaid member's income rising above the 138% level of the federal poverty line. By retaining that member in the marketplace, if the member's income subsequently declines, we will continuously serve that same member in all instances and not “lose” the member to another health plan. We endorse the so-called “bridge plan” as the best way to serve low-income persons who may qualify for coverage through the insurance marketplaces, and will be working with legislators and regulators during 2013 to advocate for the merits of the bridge plan.
Continue to enter new strategic markets. We plan to continue to enter new markets through both acquisitions and by building our own start-up operations. We intend to focus our expansion in markets with competitive provider communities, supportive regulatory environments, significant size, and, where practicable, mandated Medicaid managed care enrollment.
Continue to provide quality cost-effective care. We plan to use our strong provider networks and the knowledge gained through the operation of our clinics to further develop and utilize effective medical management and other coordinated programs that address the distinct needs of our members and improve the quality and cost-effectiveness of their care.
Leverage operational efficiencies. We intend to leverage the operational efficiencies created by our centralized administrative infrastructure and flexible information systems to earn higher margins on future revenues. We believe our administrative infrastructure has significant expansion capacity, allowing us to integrate new members from expansion within existing markets and enter new markets at lower incremental cost.
Deliver administrative value to state Medicaid agencies. As Medicaid expenditures increase, we believe that an increasing number of states will demand comprehensive solutions that improve both quality and cost-effectiveness. We intend to use our MMIS solution to provide state Medicaid agencies with a flexible and robust solution to their administrative needs. We believe that our MMIS platform, together with our extensive experience in health care management and health plan operations, enables us to offer state Medicaid agencies a comprehensive suite of Medicaid-related solutions that meets their needs for quality and for the cost-effective operation of their Medicaid programs.
Open additional primary care clinics. The clinic model offers an integrated approach that helps us improve both the quality and cost-effectiveness of the care our members receive. Our Health Plans segment direct delivery business currently consists of primary care clinics in California, Florida, New Mexico, and Washington, and three county-owned clinics in Fairfax County, Virginia that we manage on behalf of the county. The growth and aging of the population of the United States foreshadows an increasing shortage of physicians over the next 15 years. Health care reform is expected to worsen this shortage. We believe the shortage will be felt most acutely among already under-served populations, such as the low income families and individuals we serve. While we have no plans to become an organization that fully integrates primary care delivery with our health plans, by leveraging our direct delivery capability on a selective basis we can improve access for our plan members in areas that are most under-served by primary care providers.
Medicaid Contracts
With the exception of our Wisconsin health plan, which does not serve Medicare members, all of our health plans serve TANF, CHIP, ABD, and Medicare members. For its Medicare members, each health plan enters into a one-year annually renewable contract with CMS. For its other members, each health plan enters into a contract with the state’s Medicaid agency. The contractual relationship with the state is generally for a period of three to four years and renewable on an annual or biannual basis at the discretion of the state. In general, either the state Medicaid agency or the health plan may terminate the state contract with or without cause upon 30 days to nine months prior written notice. Most of these contracts contain renewal options that are exercisable by the state. Our health plan subsidiaries have generally been successful in obtaining the renewal of their contracts in each state prior to the actual expiration of their contracts. Our state contracts are generally at greatest risk of loss when a state issues a new request for proposals, or RFP, subject to competitive bidding by other health plans. If one of our health plans is not a successful responsive bidder to a state RFP, its contract may be subject to non-renewal. For instance, on February 17, 2012, our Missouri
health plan was notified that it was not awarded a new contract under that state’s RFP, and therefore its contract expired on June 30, 2012.
Our contracts with the state determine the type and scope of health care services that we arrange for our members. Generally, our contracts require us to arrange for preventive care, office visits, inpatient and outpatient hospital and medical services, and pharmacy benefits. The contracts also detail the requirements for operating in the Medicaid sector, including provisions relating to: eligibility; enrollment and disenrollment processes; covered benefits; eligible providers; subcontractors; record-keeping and record retention; periodic financial and informational reporting; quality assurance; marketing; financial standards; timeliness of claims payments; health education, wellness and prevention programs; safeguarding of member information; fraud and abuse detection and reporting; grievance procedures; and organization and administrative systems. A health plan’s compliance with these requirements is subject to monitoring by state regulators. A health plan is subject to periodic comprehensive quality assurance evaluation by a third-party reviewing organization and generally by the insurance department of the jurisdiction that licenses the health plan. Most health plans must also submit quarterly and annual statutory financial statements and utilization reports, as well as many other reports in accordance with individual state requirements.
We are usually paid a negotiated PMPM amount, with the PMPM amount varying from contract to contract. Generally, that amount is higher in states where we are required to offer more extensive health benefits. We are also paid an additional amount for each newborn delivery from the Medicaid programs in all of our state health plans, except with respect to our New Mexico health plan.
Provider Networks
We arrange health care services for our members through contracts with providers that include independent physicians and groups, hospitals, ancillary providers, and our own clinics. Our network of providers includes primary care physicians, specialists and hospitals. Our strategy is to contract with providers in those geographic areas and medical specialties necessary to meet the needs of our members. We also strive to ensure that our providers have the appropriate cultural and linguistic experience and skills.
Physicians. We contract with both primary care physicians and specialists, many of whom are organized into medical groups or independent practice associations, or IPAs. Primary care physicians provide office-based primary care services. Primary care physicians may be paid under capitation or fee-for-service contracts and may receive additional compensation by providing certain preventive services. Our specialists care for patients for a specific episode or condition, usually upon referral from a primary care physician, and are usually compensated on a fee-for-service basis. When we contract with groups of physicians on a capitated basis, we monitor their solvency.
Hospitals. We generally contract with hospitals that have significant experience dealing with the medical needs of the Medicaid population. We reimburse hospitals under a variety of payment methods, including fee-for-service, per diems, diagnostic-related groups, or DRGs, capitation, and case rates.
Primary Care Clinics. Our Health Plans segment operates 24 company-owned primary care clinics located in California, Florida, New Mexico and Washington. These clinics are located in neighborhoods where our members live, and provide us a first-hand opportunity to understand the special needs of our members. The clinics assist us in developing and implementing community education, disease management, and other programs. The clinics also give us direct clinic management experience that enables us to better understand the needs of our contracted providers. In addition, we have a subsidiary in Virginia that manages three health care clinics for Fairfax County.
Medical Management
Our experience in medical management extends back to our roots as a provider organization. Primary care physicians are the focal point of the delivery of health care to our members, providing routine and preventive care, coordinating referrals to specialists, and assessing the need for hospital care. This model has proven to be an effective method for coordinating medical care for our members. The underlying challenge we face is to coordinate health care so that our members receive timely and appropriate care from the right provider at the appropriate cost. In support of this goal, and to ensure medical management consistency among our various state health plans, we continuously refine and upgrade our medical management efforts at both the corporate and subsidiary levels.
We seek to ensure quality care for our members on a cost-effective basis through the use of certain key medical management and cost control tools. These tools include utilization management, case and health management, and provider network and contract management.
Utilization Management. We continuously review utilization patterns with the intent to optimize quality of care and ensure that only appropriate services are rendered in the most cost-effective manner. Utilization management, along with our other tools of medical management and cost control, is supported by a centralized corporate medical informatics function which utilizes third-
party software and data warehousing tools to convert data into actionable information. We use predictive modeling that supports a proactive case and health management approach both for us and our affiliated physicians.
Case and Health Management. We seek to encourage quality, cost-effective care through a variety of case and health management programs, including disease management programs, educational programs, and pharmacy management programs.
Disease Management Programs. We develop specialized disease management programs that address the particular health care needs of our members. "motherhood matters!sm" is a comprehensive program designed to improve pregnancy outcomes and enhance member satisfaction. “breathe with ease!” is a multi-disciplinary disease management program that provides health education resources and case management services to assist physicians caring for asthmatic members between the ages of three and 15. “Healthy Living with Diabetes” is a diabetes disease management program. “Heart Health Living” is a cardiovascular disease management program for members who have suffered from congestive heart failure, angina, heart attack, or high blood pressure.
Educational Programs. Educational programs are an important aspect of our approach to health care delivery. These programs are designed to increase awareness of various diseases, conditions, and methods of prevention in a manner that supports our providers while meeting the unique needs of our members. For example, we provide our members with information to guide them through various episodes of care. This information, which is available in several languages, is designed to educate parents on the use of primary care physicians, emergency rooms, and nurse call centers.
Pharmacy Management Programs. Our pharmacy management programs focus on physician education regarding appropriate medication utilization and encouraging the use of generic medications. Our pharmacists and medical directors work with our pharmacy benefits manager to maintain a formulary that promotes both improved patient care and generic drug use. We employ full-time pharmacists and pharmacy technicians who work with physicians to educate them on the uses of specific drugs, the implementation of best practices, and the importance of cost-effective care.
Provider Network and Contract Management. The quality, depth, and scope of our provider network are essential if we are to ensure quality, cost-effective care for our members. In partnering with quality, cost-effective providers, we utilize clinical and financial information derived by our medical informatics function, as well as the experience we have gained in serving Medicaid members to gain insight into the needs of both our members and our providers. As we grow in size, we seek to strengthen our ties with high-quality, cost-effective providers by offering them greater patient volume.
Plan Administration and Operations
Management Information Systems. All of our health plan information technology and systems operate on a single platform. This approach avoids the costs associated with maintaining multiple systems, improves productivity, and enables medical directors to compare costs, identify trends, and exchange best practices among our plans. Our single platform also facilitates our compliance with current and future regulatory requirements.
The software we use is based on client-server technology and is scalable. We believe the software is flexible, easy to use, and allows us to accommodate anticipated enrollment growth and new contracts. The open architecture of the system gives us the ability to transfer data from other systems without the need to write a significant amount of computer code, thereby facilitating the integration of new plans and acquisitions.
We have designed our corporate website with a focus on ease of use and visual appeal. Our website has a secure ePortal which allows providers, members, and trading partners to access individualized data. The ePortal allows the following self-services:
Provider Self Services. Providers have the ability to access information regarding their members and claims. Key functionalities include "Check Member Eligibility," "View Claim," and "View/Submit Authorizations."
Member Self Services. Members can access information regarding their personal data, and can perform the following key functionalities: "View Benefits," "Request New ID Card," "Print Temporary ID Card," and "Request Change of Address/PCP."
File Exchange Services. Various trading partners — such as service partners, providers, vendors, management companies, and individual IPAs — are able to exchange data files (such as those that may be required by the Health Insurance Portability and Accountability Act of 1996, or HIPAA, or any other proprietary format) with us using the file exchange functionality.
Best Practices. We continuously seek to promote best practices. Our approach to quality is broad, encompassing traditional medical management and the improvement of our internal operations. We have staff assigned full-time to the development and implementation of a uniform, efficient, and quality-based medical care delivery model for our health plans. These employees coordinate and implement company-wide programs and strategic initiatives such as preparation of the Healthcare Effectiveness
Data and Information Set, or HEDIS, and accreditation by the NCQA. We use measures established by the NCQA in credentialing the physicians in our network. We routinely use peer review to assess the quality of care rendered by providers. Eight of our health plans are accredited by the NCQA. Our Wisconsin plan acquired in September 2010 currently plans to seek NCQA accreditation in early 2014.
Claims Processing. All of our health plans operate on a single managed care platform for claims processing (the QNXT 4.8 system).
Centralized Management Services. We provide certain centralized medical and administrative services to our health plans pursuant to administrative services agreements, including medical affairs and quality management, health education, credentialing, management, financial, legal, information systems, and human resources services. Fees for such services are based on the fair market value of services rendered and are recorded as operating revenue. Payment is subordinated to the health plan’s ability to comply with minimum capital and other restrictive financial requirements of the states in which they operate.
Compliance. Our health plans have established high standards of ethical conduct. Our compliance programs are modeled after the compliance guidance statements published by the Office of the Inspector General of the U.S. Department of Health and Human Services. Our uniform approach to compliance makes it easier for our health plans to share information and practices and reduces the potential for compliance errors and any associated liability.
Disaster Recovery. We have established a disaster recovery and business resumption plan, with back-up operating sites, to be deployed in the case of a major disruptive event.
Competition
We operate in a highly competitive environment.The Medicaid managed care industry is fragmented, and the competitive landscape is subject to ongoing changes as a result of health care reform, business consolidations and new strategic alliances. We compete with a large number of national, regional, and local Medicaid service providers, principally on the basis of size, location, and quality of provider network, quality of service, and reputation. Our primary competitors in the Medicaid managed care industry include Centene Corporation, WellCare Health Plans, Inc., UnitedHealth Group Incorporated, Anthem, Inc., and Aetna Inc. Competition can vary considerably from state to state. Below is a general description of our principal competitors for state contracts, members, and providers:
Multi-Product Managed Care Organizations — - National and regional managed care organizations that have Medicaid members in addition to numerous commercial health plan and Medicare members.
Medicaid HMOs — - National and regional managed care organizations that focus principally on providing health care services to Medicaid beneficiaries, many of which operate in only one city or state.
Prepaid Health Plans — - Health plans that provide less comprehensive services on an at-risk basis or that provide benefit packages on a non-risk basis.
Primary Care Case Management Programs — - Programs established by the states through contracts with primary care providers to provide primary care services to Medicaid beneficiaries, as well as to provide limited oversight of other services.
We will continue to face varying levels of competition. Health care reform proposals may cause organizations to enter or exit the market for government sponsored health programs. However, the licensing requirements and bidding and contracting procedures in some states may present partial barriers to entry into our industry.
We compete for government contracts, renewals of those government contracts, members, and providers. State agencies consider many factors in awarding contracts to health plans. Among such factors are the health plan’s provider network, medical management, degree of member satisfaction, timeliness of claims payment, and financial resources. Potential members typically choose a health plan based on a specific provider being a part of the network, the quality of care and services available, accessibility of services, and reputation or name recognition of the health plan. We believe factors that providers consider in deciding whether to contract with a health plan include potential member volume, payment methods, timeliness and accuracy of claims payment, and administrative service capabilities.
Molina Medicaid Solutions competes with large MMIS vendors, such as HP Enterprise Services (formerly known as EDS), ACS (owned by Xerox Corporation), Computer Services Corporation, or CSC, and CNSI.
Regulation
Our health plans are highly regulated by both state and federal government agencies. Regulation of managed care products and health care services varies from jurisdiction to jurisdiction, and changes in applicable laws and rules can occur frequently. Regulatory agencies generally have discretion to issue regulations and interpret and enforce laws and rules. Such agencies have
BUSINESS OPERATIONS
Our Strengths
From a strategic perspective, we believe our two business segments allow us to participate in an expanding sector of the economy and continue our mission to provide quality health services to financially vulnerable families and individuals covered by government programs. Our approach to our business is based on the following strengths:
Comprehensive Medicaid Services. We offer a complete suite of Medicaid services, ranging from quality care, disease management, cost management, and direct delivery of health care services, to state-level MMIS administration through our Molina Medicaid Solutions segment. We have the ability to draw upon our experience and expertise in each of these areas to enhance the quality of the services we offer in the others. We also believe that we may have opportunities to market to state Medicaid agencies various cost containment and quality practices used by our health plans, such as care management and care coordination, for incorporation into their own fee-for-service Medicaid programs.
Flexible Service Delivery Systems. Our health plan care delivery systems are diverse and readily adaptable to different markets and changing conditions. We arrange health care services with a variety of providers, including independent physicians and medical groups, hospitals, ancillary providers, and our own clinics. Our systems support multiple types of contract models. Our provider networks are well-suited, based on medical specialty, member proximity, and cultural sensitivity, to provide services to our members. We believe that our Molina Medicaid Solutions platform, which is based on commercial off-the-shelf technology, has the flexibility to meet a wide variety of state Medicaid administrative needs in a timely and cost-effective manner.
Proven Expansion and Acquisition Capability. We have successfully replicated the business model of our Health Plans segment through the acquisition of health plans, the start-up development of new operations, and the transition of members from other health plans. The initial acquisitions of our New Mexico, South Carolina and Wisconsin health plans have demonstrated our ability to expand into new states. The establishment of our health plans in Florida, Illinois, Ohio, Texas and Utah reflects our ability to replicate our business model on a start-up basis in new states, while significant contract acquisitions in California, Michigan, New Mexico and Washington have demonstrated our ability to expand our operations within states in which we were already operating.
Administrative Efficiency. Operationally, our two business segments share a common systems platform, which allows for economies of scale and common experience in meeting the needs of state Medicaid programs. We have centralized and standardized various functions and practices to increase administrative efficiency. The steps we have taken include centralizing claims processing and information services onto a single platform and standardization of medical management programs, pharmacy benefits management contracts, and health education programs. In addition, we have designed our administrative and operational infrastructure to be scalable for cost-effective expansion into new and existing markets.
Recognition for Quality of Care. The National Committee for Quality Assurance (NCQA) has accredited nine of our 11 Medicaid managed care plans. We believe that these objective measures of the quality of the services that we provide will become increasingly activeimportant to state Medicaid agencies.
Experience and Expertise. Since the founding of our company in recent years in their review and scrutiny of health insurers and managed care organization, including those operating in1980 to serve the Medicaid population in southern California through a small network of primary care clinics, we have increased our membership to 2.6 million members as of December 31, 2014, expanded our Health Plans segment to 11 states, and Medicare programs.added our Molina Medicaid Solutions segment. Our experience over more than 30 years has allowed us to develop strong relationships with the constituents we serve, establish significant expertise as a government contractor, and develop sophisticated disease management, care coordination and health education programs that address the particular health care needs of our members. We also benefit from a thorough understanding of the cultural and linguistic needs of Medicaid populations.
To operate aPricing
Medicaid. Under our Medicaid contracts, state government agencies pay our health plan in a givenplans fixed PMPM rates that vary by state, line of business and demographics; and we must applyarrange, pay for and obtain a certificate of authority or license from that state. Our operatingmanage health care services provided to Medicaid beneficiaries. Therefore, our health plans are licensedat risk for the medical costs associated with their members’ health care. The rates we receive are subject to operate aschange by each state and, in some instances, provide for adjustments for health maintenance organizations, or HMOs,risk factors. CMS requires these rates to be actuarially sound. Payments to us under each of our Medicaid contracts are subject to the annual appropriation process in the applicable state.
Medicare. Under Medicare Advantage, managed care plans contract with CMS to provide benefits in exchange for a fixed PMPM premium payment that varies based on the county in which a member resides, and adjusted for demographic and health risk factors. CMS also considers inflation, changes in utilization patterns and average per capita fee-for-service Medicare costs in the calculation of the fixed PMPM premium payment.
Amounts payable to us under the Medicare Advantage contracts are subject to annual revision by CMS, and we elect to participate in each Medicare service area or region on an annual basis. Medicare Advantage premiums paid to us are subject to
federal government reviews and Wisconsin.audits which can result, and have resulted, in retroactive and prospective premium adjustments. Compared with our Medicaid plans, Medicare Advantage contracts generate higher average PMPM revenues and health care costs.
Marketplace. For our Marketplace plans, we develop premium rates during early spring of any given year to take effect on January 1st of the following year. We develop our premium rates based on our estimates of projected member utilization, medical unit costs, and administrative costs, with the intent of realizing a target pretax percentage profit margin. In those statessetting premium rates for our Marketplace plans, we are regulated byalso take into account the agency with responsibilitycompetitive environment on a region–by–region basis. Our actuaries certify the actuarial soundness of Marketplace premiums in the rate filings submitted to the various state and federal authorities for the oversight of HMOs which,approval.
Medical Management
Our experience in most cases, is the state department of insurance. In California, however, the agency with responsibility for the oversight of HMOs is the Department of Managed Health Care. Licensing requirementsmedical management extends back to our roots as a provider organization. Primary care physicians are the samefocal point of the delivery of health care to our members, providing routine and preventive care, coordinating referrals to specialists, and assessing the need for hospital care. This model has proved to be an effective method for coordinating medical care for our members. The underlying challenge we face is to coordinate health care so that our members receive timely and appropriate care from the right provider at the appropriate cost. In support of this goal, and to ensure medical management consistency among our various state health plans, we continuously refine and upgrade our medical management efforts at both the corporate and subsidiary levels.
We seek to ensure quality care for our members on a cost-effective basis through the use of certain key medical management and cost control tools. These tools include utilization management, case and health management, and provider network and contract management.
Utilization Management. We continuously review utilization patterns with the intent to optimize quality of care and ensure that only appropriate services are rendered in the most cost-effective manner. Utilization management, along with our other tools of medical management and cost control, is supported by a centralized corporate medical informatics function which utilizes third-party software and data warehousing tools to convert data into actionable information. We use predictive modeling that supports a proactive case and health management approach both for us and our affiliated physicians.
Case and Health Management. We seek to encourage quality, cost-effective care through a variety of case and health management programs, including disease management programs, educational programs, and pharmacy management programs such as theythe following:
| |
| • | Disease Management Programs. We develop specialized disease management programs that address the particular health care needs of our members. "motherhood matters!sm" is a comprehensive program designed to improve pregnancy outcomes and enhance member satisfaction. "breathe with ease!" is a multi-disciplinary disease management program that provides health education resources and case management services to assist physicians caring for asthmatic members between the ages of three and 15. "Healthy Living with Diabetes" is a diabetes disease management program. "Heart Healthy Living" is a cardiovascular disease management program for members who have suffered from congestive heart failure, angina, heart attack, or high blood pressure. |
Educational Programs. Educational programs are foran important aspect of our approach to health plans serving commercial or Medicarecare delivery. These programs are designed to increase awareness of various diseases, conditions, and methods of prevention in a manner that supports our providers while meeting the unique needs of our members. For example, we provide our members with information to guide them through various episodes of care. This information, which is available in several languages, is designed to educate members on the use of primary care physicians, emergency rooms, and nurse call centers.
Pharmacy Management Programs. Our pharmacy management programs focus on physician education regarding appropriate medication utilization and encouraging the use of generic medications. Our pharmacists and medical directors work with our pharmacy benefits manager to maintain a formulary that promotes both improved patient care and generic drug use. We must demonstrate thatemploy full-time pharmacists and pharmacy technicians who work with physicians to educate them on the uses of specific drugs, the implementation of best practices, and the importance of cost-effective care.
Provider Network and Contract Management. The quality, depth, and scope of our provider network are essential if we are to ensure quality, cost-effective care for our members. In partnering with quality, cost-effective providers, we utilize clinical and financial information derived by our medical informatics function, as well as the experience we have gained in serving Medicaid members, to gain insight into the needs of both our members and our providers. As we grow in size, we seek to strengthen our ties with high-quality, cost-effective providers by offering them greater patient volume.
Provider Networks
We arrange health care services for our members through contracts with providers that include independent physicians and groups, hospitals, ancillary providers, and our own clinics. Our network of providers includes primary care physicians, specialists and hospitals. Our strategy is adequate,to contract with providers in those geographic areas and medical specialties necessary to meet the needs of our members. We also strive to ensure that our quality and utilization management processes comply with state requirements, and that we have adequate procedures in place for responding to member and provider complaints and grievances. We must also demonstrate that we can meet requirements for the timely processing of provider claims, and that we can collect and analyze the information needed to manage our quality improvement activities. In addition, we must prove that weproviders have the financial resources necessaryappropriate cultural and linguistic experience and skills.
Physicians. We contract with both primary care physicians and specialists, many of whom are organized into medical groups or independent practice associations (IPAs). Primary care physicians provide office-based primary care services. Primary care physicians may be paid under capitation or fee-for-service contracts and may receive additional compensation by providing certain preventive services. Our specialists care for patients for a specific episode or condition, usually upon referral from a primary care physician, and are usually compensated on a fee-for-service basis. When we contract with groups of physicians on a capitated basis, we monitor their solvency.
Hospitals. We generally contract with hospitals that have significant experience dealing with the medical needs of the Medicaid population. We reimburse hospitals under a variety of payment methods, including fee-for-service, per diems, diagnostic-related groups (DRGs) capitation, and case rates.
Direct Delivery. The clinics we operate are located in neighborhoods where our members live, and provide us a first-hand opportunity to payunderstand the special needs of our anticipated medical care expensesmembers. The clinics we operate, and the infrastructure neededclinics and hospital services we manage, assist us in developing and implementing community education, disease management, and other programs. Direct clinic management experience also enables us to account forbetter understand the needs of our costs.contracted providers.
Reinsurance
Our health plans are requiredcurrently have reinsurance agreements with an unaffiliated insurer to file quarterlycover certain claims. We enter into these contracts to reduce the risk of catastrophic losses which in turn reduce our capital and annual reportssurplus requirements. We frequently evaluate reinsurance opportunities and review our reinsurance and risk management strategies on a regular basis.
Management Information Systems
All of their operating results with the appropriate state regulatory agencies. These reports are accessible for public viewing. Eachour health plan undergoes periodic examinationsinformation technology systems operate on a single platform. This approach avoids the costs associated with maintaining multiple systems, improves productivity, and reviewsenables medical directors to compare costs, identify trends, and exchange best practices among our plans. Our single platform also facilitates our compliance with current and future regulatory requirements.
The software we use is based on client-server technology and is scalable. We believe the software is flexible, easy to use, and allows us to accommodate anticipated enrollment growth and new contracts. The open architecture of the system gives us the ability to transfer data from other systems without the need to write a significant amount of computer code, thereby facilitating the integration of new plans and acquisitions.
We have designed our corporate website with a focus on ease of use and visual appeal. Our website has a secure ePortal which allows providers, members, and trading partners to access individualized data. The ePortal allows the following self-services:
Provider Self Services - Providers have the ability to access information regarding their members and claims. Key functionalities include "Check Member Eligibility," "View Claim," and "View/Submit Authorizations."
Member Self Services- Members can access information regarding their personal data, and can perform the following key functionalities: "View Benefits," "Request New ID Card," "Print Temporary ID Card," and "Request Change of Address/PCP."
File Exchange Services - Various trading partners, such as service partners, providers, vendors, management companies, and individual IPAs, are able to exchange data files (such as those that may be required by federal health care privacy regulations, or any other proprietary format) with us using the file exchange functionality.
Best Practices. We continuously seek to promote best practices. Our approach to quality is broad, encompassing traditional medical management and the improvement of our internal operations. We have staff assigned full-time to the development and implementation of a uniform, efficient, and quality-based medical care delivery model for our health plans. These employees coordinate and implement company-wide programs and strategic initiatives such as preparation of the Healthcare Effectiveness Data and Information Set (HEDIS), and accreditation by the stateNCQA. We use measures established by the NCQA in which it operates. Thecredentialing the physicians in our network. We routinely use peer review to assess the quality of care rendered by providers.
Claims Processing. All of our health plans generally must obtain approval from the state before declaring dividends in excessoperate on a single managed care platform for claims processing (the QNXT system).
Centralized Management Services. We provide certain thresholds. Eachcentralized medical and administrative services to our health plan must maintain its net worth at an amount determined by statute or regulation. The minimum statutory net worth requirements differ by state,plans pursuant to administrative services agreements, including medical affairs and are generally based on statutory minimum risk-based capital, or RBC, requirements. The RBC requirementsquality management, health education, credentialing, management, financial, legal, information systems, and human resources services. Fees for such services are based on guidelinesthe fair market value of services rendered and are recorded as operating revenue. Payment is subordinated to the health plan’s ability to comply with minimum capital and other restrictive financial requirements of the states in which they operate.
Compliance. Our health plans have established high standards of ethical conduct. Our compliance programs are modeled after the compliance guidance statements published by the National AssociationOffice of Insurance Commissioners, or NAIC,the Inspector General of the U.S. Department of Health and are administered by the states.Human Services (HHS). Our Michigan, New Mexico, Ohio, Texas, Utah, Washington, and Wisconsinuniform approach to compliance makes it easier for our health plans are subject to RBC requirements. Any acquisitionshare information and practices and reduces the potential for compliance errors and any associated liability.
Disaster Recovery. We have established a disaster recovery and business resumption plan, with back-up operating sites, to be deployed in the case of another plan’s members or its state contracts must also be approved by the state, and our ability to invest in certain financial securities may be prescribed by statute.a major disruptive event.
CONTRACTING AND REGULATORY COMPLIANCE
In addition, we are also regulated by each state’s department of health services or the equivalent agency charged with oversight of Medicaid and CHIP. These agencies typically require demonstration of the same capabilities mentioned above and perform periodic audits of performance, usually annually.
Government Contracts
Medicaid. Medicaid was establishedIn all the states in 1965 under the U.S. Social Security Act to provide medical assistance to the poor. Although jointly funded by federal and state governments, Medicaid iswhich we operate health plans, we enter into a state-operated and state-implemented program. Our contractscontract with the statestate’s Medicaid programs impose various requirements on us in additionagency to those imposed by applicable federal and state laws and regulations. Within broad guidelines established by the federal government, each state:
establishes its own member eligibility standards;
determines the type, amount, duration, and scope of services;
sets the rate of payment for healthoffer managed care services; and
administers its own program.
We obtain our Medicaid contracts in different ways.benefits to Medicaid-eligible individuals. Some states award contracts to any applicant demonstrating that it meets the state’s requirements. Otherrequirements, while other states engage in a competitive bidding process. In all cases, we must demonstrate to the satisfaction of the state Medicaid program that we are able to meet the state’s operational and financial requirements. These requirements are in addition to those required for a license and are targeted to the specific needs of the Medicaid population. Forpopulation; for example:
We must measure provider access and availability in terms of the time needed to reach the doctor’s office using public transportation;
Our quality improvement programs must emphasize member education and outreach and include measures designed to promote utilization of preventive services;
We must have linkages with schools, city or county health departments, and other community-based providers of health care, to demonstrate our ability to coordinate all of the sources from which our members may receive care;
We must be able to meet the needs of the disabled and others with special needs;
Our providers and member service representatives must be able to communicate with members who do not speak English or who are deaf; and
Our member handbook, newsletters, and other communications must be written at the prescribed reading level, and must be available in languages other than English.
authority or license from that state. We are regulated by the state agency with responsibility for the oversight of HMOs which, in most cases, is the state department of insurance. In addition,California, however, the agency with responsibility for the oversight of HMOs is the Department of Managed Health Care. Licensing requirements are the same for us as they are for health plans serving commercial or Medicare members. For example, we must demonstrate that wethat:
Our provider network is adequate;
Our quality and utilization management processes comply with state requirements;
We have adequate procedures in place for responding to member and provider complaints and grievances;
We can meet requirements for the timely processing of provider claims;
We can collect and analyze the information needed to manage our quality improvement activities;
We have the financial resources necessary to pay our anticipated medical care expenses and the infrastructure needed to account for our costs;
We have the systems required to process enrollment information, to report on care and services provided, and to process claims for payment in a timely fashion. fashion; and
We must also have the financial resources needed to protect the state, our providers, and our members against the insolvency of one of our health plans.
Our state contracts determine the type and scope of health care services that we arrange for our members. Generally, our contracts require us to arrange for preventive care, office visits, inpatient and outpatient hospital and medical services, and pharmacy benefits. The contracts also detail the requirements for operating in the Medicaid sector, including provisions relating to: eligibility; enrollment and dis-enrollment processes; covered benefits; eligible providers; subcontractors; record-keeping and record retention; periodic financial and informational reporting; quality assurance; marketing; financial standards; timeliness of claims payments; health education, wellness and prevention programs; safeguarding of member information; fraud and abuse detection and reporting; grievance procedures; and organization and administrative systems. A health plan’s compliance with these requirements is subject to monitoring by state regulators. A health plan is subject to periodic comprehensive quality assurance evaluation by a third-party reviewing organization and generally by the insurance department of the jurisdiction that licenses the health plan.
The contractual relationship with the state is generally for a period of three to four years and is renewable on an annual or biennial basis at the discretion of the state. In general, either the state Medicaid agency or the health plan may terminate the state contract with or without cause upon 30 days to nine months’ prior written notice.
Most of these contracts contain renewal options that are exercisable by the state. Our health plan subsidiaries have generally been successful in obtaining the renewal of their contracts in each state prior to the actual expiration of their contracts. Our state contracts are generally at greatest risk of loss when a state issues a new request for proposals (RFP), subject to competitive bidding by other health plans. If one of our health plans is not a successful responsive bidder to a state RFP, its contract may be subject to non-renewal. For instance, in early 2012 our Missouri health plan was notified that it was not awarded a new contract under that state’s RFP, and therefore its contract expired in that year.
Medicare.Under annually renewable contracts with CMS, our state health plans offer Medicare isAdvantage special needs plans which include a federal program that provides eligible persons age 65 and over and some disabled persons a variety of hospital, medical insurance, andmandatory Part D prescription drug benefits.benefit. Molina Medicare Options Plus, our trade name for these plans, serves beneficiaries who are dually eligible for both Medicare and Medicaid, such as low-income seniors and people with disabilities. We believe offering these Medicare plans is funded by Congress,consistent with our historical mission of serving low-income and administered by CMS. Medicare beneficiaries have the optionmedically under-served families and individuals. We employ sales personnel, and engage independent brokers, agents and consultants to enroll innew Molina Medicare Options Plus members. None of our health plans operates a Medicare Advantage private fee-for-service plan. Under
Total enrollment in our Medicare Advantage managed care plans contract with CMS to provide benefits that are comparable to originalas of December 31, 2014 was approximately 49,000 members. For the year ended December 31, 2014, Medicare in exchange for a fixed PMPM premium payment that varies based on the county in which a member resides, the demographics of the member, and the member’s health condition.
The Medicare Prescription Drug, Improvement and Modernization Act of 2003, or MMA, made numerous changes to the Medicare program, including expanding the Medicare program to include a prescription drug benefit. Since 2006, Medicare beneficiaries have had the option of selecting a new prescription drug benefit from an existing Medicare Advantage plan. The drug benefit, available to beneficiaries for a monthly premium, is subject to certain cost sharing depending upon the specific benefit design of the selected plan. Plans are not required to offer the same benefits, but are required to provide coverage that is at least actuarially equivalent to the standard drug coverage delineatedrevenues in the MMA.aggregate represented approximately 7% of our total premium revenues.
On July 15, 2008, the Medicare Improvements for Patients and Providers Act, or MIPPA, became law and, in September 2008, CMS promulgated implementing regulations. MIPPA impacts a broad range of Medicare activities and impacts all types of Medicare managed care plans. MIPPA and subsequent CMS guidanceFederal regulations place prohibitions and limitations on certain sales and marketing activities of Medicare Advantage plans. Among other things, Medicare Advantage plans are not permitted to make unsolicited outbound calls to potential members or engage in other forms of unsolicited contact, establish appointments without documented consent from potential members, or conduct sales events in certain provider-based settings. MIPPA also establishesAdditionally, there are certain restrictions on agent and broker compensation.
HIPAA.Molina Medicaid Solutions. We continually monitor the status of various states’ legacy MMIS capabilities and contracts to determine whether Molina Medicaid Solutions’ value proposition and core strengths will address a state’s MMIS goals. Once an RFP with a Medicaid agency is won, our Molina Medicaid Solutions contracts may extend over a number of years, particularly in circumstances where we deliver extensive and complex DDI services, such as the initial design, development and implementation of a complete MMIS. For example, the initial terms of our most recently implemented Molina Medicaid Solutions contracts (in Idaho and Maine) were each seven years in total, consisting of two years allocated for the delivery of DDI services, followed by five years for the performance of BPO services. The terms of our other Molina Medicaid Solutions contracts - which primarily involve the delivery of BPO services with only minimal DDI activity (consisting of system enhancements) - are shorter in duration than our Idaho and Maine contracts.
The federal government typically reimburses the states for 90% of the costs incurred in the design, development, and implementation of an MMIS and for 75% of the costs incurred in operating a certified MMIS. Federal certification increases the share of the claims processing costs the federal government will pay for monthly operations. With an uncertified system, the federal government contributes approximately 50% of claims processing costs, with the state paying the other half. With a certified system, the federal government pays 75% of costs, reducing the state’s share.
Regulatory Compliance
Our health plans are highly regulated by both state and federal government agencies. Regulation of managed care products and health care services varies from jurisdiction to jurisdiction, and changes in applicable laws and rules occur frequently. Regulatory agencies generally have discretion to issue regulations and interpret and enforce laws and rules. Such agencies have become increasingly active in recent years in their review and scrutiny of health insurers and managed care organizations, including those operating in the Medicaid and Medicare programs.
Health Insurer Fee (HIF). One notable provision of the ACA is an excise tax or annual fee that applies to most health plans, including commercial health plans and Medicaid managed care plans like Molina Healthcare. While characterized as a "fee" in the text of the ACA, the intent of Congress was to impose a broad-based health insurance industry excise tax, with the understanding that the tax could be passed on to consumers, most likely through higher commercial insurance premiums.
However, because Medicaid is a government funded program, Medicaid health plans have no alternative but to look to their respective state partners for payment to offset the impact of this tax. Additionally, when states reimburse us for the amount of the HIF, that reimbursement is itself subject to income tax, the HIF, and applicable state premium taxes. Because the HIF is not deductible for income tax purposes, our net income is reduced by the full amount of the assessment. We expect our 2015 HIF assessment related to our Medicaid business to be approximately $143 million, with an expected tax effect from the reimbursement of the assessment of approximately $88 million. Therefore, the total reimbursement needed as a result of the Medicaid-related HIF is approximately $231 million.
For further discussion of the risks and uncertainties relating to this excise tax, refer to Part II, Item 7 of this Form 10-K, Management’s Discussion and Analysis of Financial Condition and Results of Operations, under the subheading "Liquidity and Capital Resources—Financial Condition."
States’ Risk-Based Capital Requirements. Our health plans are required to file quarterly and annual reports of their operating results with the appropriate state regulatory agencies. These reports are accessible for public viewing. Each health plan undergoes periodic examinations and reviews by the state in which it operates. The health plans generally must obtain approval from the state before declaring dividends in excess of certain thresholds. Each health plan must maintain its net worth at an amount determined by statute or regulation. The minimum statutory net worth requirements differ by state, and are generally based on statutory minimum risk-based capital (RBC) requirements. The RBC requirements are based on guidelines established by the National Association of Insurance Commissioners (NAIC) and are administered by the states. All of our state health plans are subject to RBC requirements, except California and Florida. Any acquisition of another plan’s members or its state contracts must also be approved by the state, and our ability to invest in certain financial securities may be prescribed by statute. For further information regarding RBC requirements, refer to Part II, Item 8 of this Form 10-K, Notes to Consolidated Financial Statements, in Note 20, "Commitments and Contingencies."
In addition, we are also regulated by each state’s department of health services or the equivalent agency charged with oversight of Medicaid and CHIP. These agencies typically require demonstration of the same capabilities mentioned above and perform periodic audits of performance, usually annually.
HIPAA. In 1996, Congress enacted the Health Insurance Portability and Accountability Act or HIPAA.(HIPAA). All health plans are subject to HIPAA, including ours. HIPAA generally requires health plans to:
Establish the capability to receive and transmit electronically certain administrative health care transactions, like claims payments, in a standardized format;
Afford privacy to patient health information; and
Protect the privacy of patient health information through physical and electronic security measures.
The ACAHealth care reform created additional tools for fraud prevention, including increased oversight of providers and suppliers participating or enrolling in Medicaid, CHIP, and Medicare. Those enhancements included mandatory licensure for all providers, and site visits, fingerprinting, and criminal background checks for higher risk providers. On September 23, 2010, CMS issued proposed regulations designed to implement these requirements. It is not clear at this time the degree to which managed care providers would have to comply with these new requirements, many of which resemble procedures that we already have in place.
The Health Information Technology for Economic and Clinical Health Act (“HITECH Act”)(HITECH Act), a part of the American Recovery and Reinvestment Act of 2009, or ARRA, modified certain provisions of HIPAA by, among other things, extending the privacy and security provisions to business associates, mandating new regulations around electronic medical records, expanding enforcement mechanisms, allowing the state Attorneys General to bring enforcement actions, and increasing penalties for violations. The U.S. Department of Health and Human Services, asAs required by ARRA, the Secretary of HHS has promulgated regulations implementing various provisions of the HITECH Act. The Final Omnibus Rule promulgated by HHS in January 2013, included the Final Breach Notification Rule as well as provisions that apply the HIPAA regulatory scheme to business associates. We anticipate that HHS will promulgate additional rules under the HITECH Act has issued interim final rules that set forthto implement provisions of the breach notification obligations applicable to covered entities and their business associates, orstatute which were not addressed in the HHS Breach NotificationFinal Omnibus Rule. The various requirements of the HITECH Act and the HHS Breach NotificationFinal Omnibus Rule have different compliance dates, and in some cases, the applicable compliance date may depend on the publication of which have passed and some of which will occur in the future.additional rules or guidance by HHS. With respect to those requirements whose compliance dates have passed, we believe that we are in compliance with thesesuch provisions. With respect to thoseadditional requirements whose compliance dates arethat may be issued in the future we are reviewing our current practices and identifying those which may be impacted by upcoming regulations. ItHHS, it is our intention to implement theseany such new requirements on or before the applicable compliance dates.
Fraud and Abuse Laws.Our operations are subject to various state and federal health care laws commonly referred to as “fraud"fraud and abuse”abuse" laws. Fraud and abuse prohibitions encompass a wide range of activities, including kickbacks for referral of members, billing for unnecessary medical services, improper marketing, and violations of patient privacy rights. These fraud and abuse laws include the federal False Claims Act which prohibits the knowing filing of a false claim or the knowing use of false statements to obtain payment from the federal government. Many states have false claim act statutes that closely resemble the federal False Claims Act. If an entity is determined to have violated the federal False Claims Act, it must pay three times the actual damages sustained by the government, plus mandatory civil penalties up to fifty thousand dollars for each separate false claim. Suits filed under the Federal False Claims Act, known as "“qui tam”tam" actions, can be brought by any individual on behalf of the government and such individuals (known as “relators”"relators" or, more commonly, as “whistleblowers”"whistleblowers") may share in any amounts paid
by the entity to the government in fines or settlement. Qui tam actions have increased significantly in recent years, causing greater numbers of health care companies to have to defend a false claim action, pay fines or be excluded from the Medicaid, Medicare or other state or Federal health care programs as a result of an investigation arising out of such action. In addition, the Deficit Reduction ActionAct of 2005 or DRA,(DRA) encourages states to enact state-versions of the federal False Claims Act that establish liability to the state for false and fraudulent Medicaid claims and that provide for, among other things, claims to be filed by qui tam relators.
Companies involved in public health care programs such as Medicaid are often the subject of fraud and abuse investigations. The regulations and contractual requirements applicable to participants in these public sector programs are complex and subject to change. Violations of certain fraud and abuse laws applicable to us could result in civil monetary penalties, criminal fines and imprisonment, and/or exclusion from participation in Medicaid, Medicare, other federal health care programs and federally funded state health programs.
Federal and state governments have made investigating and prosecuting health care fraud and abuse a priority. Although we believe that our compliance efforts are adequate, we will continue to devote significant resources to support our compliance efforts.
Executive Officers of the Registrant
J. Mario Molina, M.D., 54, has served as President and Chief Executive Officer since succeeding his father and company founder, Dr. C. David Molina, in 1996. He has also served as Chairman of the Board since 1996. Prior to that, he served as Medical Director from 1991 through 1994 and was Vice President responsible for provider contracting and relations, member services, marketing and quality assurance from 1994 to 1996. He earned an M.D. from the University of Southern California and performed his medical internship and residency at the Johns Hopkins Hospital. Dr. Molina is the brother of John C. Molina.
John C. Molina, J.D., 48, has served in the role of Chief Financial Officer since 1995, and has been employed by the Company for over 30 years in a variety of positions. He also has served as a director since 1994. Mr. Molina is a member of the Los Angeles branch of the Federal Reserve Bank of San Francisco’s board of directors. Mr. Molina holds a Juris Doctorate from the University of Southern California School of Law. Mr. Molina is the brother of Dr. J. Mario Molina.
Terry P. Bayer, 62, has served as our Chief Operating Officer since 2005. She had formerly served as our Executive Vice President, Health Plan Operations. Ms. Bayer has over 30 years of health care management experience, including staff model clinic administration, provider contracting, managed care operations, disease management, and home care. Prior to joining us, her professional experience included regional responsibility at FHP, Inc. and multi-state responsibility as Regional Vice President at Maxicare; Partners National Health Plan, a joint venture of Aetna Life Insurance Company and Voluntary Hospital Association (VHA); and Lincoln National. She has also served as Executive Vice President of Managed Care at Matria Healthcare, President and Chief Operating Officer of Praxis Clinical Services, and as Western Division President of AccentCare. She holds a Juris Doctorate from Stanford University, a Master’s degree in Public Health from the University of California, Berkeley, and a Bachelor’s degree in Communications from Northwestern University.
Joseph W. White, 54, has served as our Chief Accounting Officer since 2007. In his role as Chief Accounting Officer, Mr. White is responsible for oversight of the Company’s accounting, reporting, forecasting, budgeting, actuarial, procurement, treasury and facilities functions. Mr. White has over 30 years of financial management experience in the health care industry. Prior to joining the Company in 2003, Mr. White worked for Maxicare Health Plans, Inc. from 1987 through 2002. Mr. White holds a Master’s degree in Business Administration and a Bachelor’s degree in Commerce from the University of Virginia. Mr. White is a Certified Public Accountant.
Jeff D. Barlow, 50, has served as our Senior Vice President, General Counsel, and Secretary since 2010. As General Counsel, Mr. Barlow is responsible for setting the overall legal strategy of the Company, and for providing legal counsel to senior management, to the board of directors, and to the consolidated organization. Before joining the Company, Mr. Barlow worked for the national law firm of DLA Piper in its corporate securities group. Mr. Barlow holds a Juris Doctorate from the University of Pittsburgh School of Law, a Master's degree in Public Health from the University of California, Berkeley, and a Bachelor's degree in Philosophy from the University of Utah.OTHER INFORMATION
Intellectual Property
We have registered and maintain various service marks, trademarks and trade names that we use in our businesses, including marks and names incorporating the “Molina”"Molina" or “Molina Healthcare”"Molina Healthcare" phrase, and from time to time we apply for additional
registrations of such marks. We utilize these and other marks and names in connection with the marketing and identification of products and services. We believe such marks and names are valuable and material to our marketing efforts.
Employees
As of December 31, 2014, we had approximately 10,500 employees. Our employee base is multicultural and reflects the diverse membership we serve. We believe we have good relations with our employees. None of our employees is represented by a union.
Available Information
We are organized as a C corporation under Delaware law. Our principal executive offices are located at 200 Oceangate, Suite 100, Long Beach, California 90802, and our telephone number is (562) 435-3666.
You can access our website at www.molinahealthcare.com to learn more about our Company. From that site, you can download and print copies of our Annual Reports on Form 10-K, Quarterly Reports on Form 10-Q, and Current Reports on Form 8-K, along with amendments to those reports. You can also download our Corporate Governance Guidelines, Board of Directors committee charters, and Code of Business Conduct and Ethics. We make periodic reports and amendments available, free of charge, as soon as reasonably practicable after we file or furnish these reports to the SEC. We will also provide a copy of any of our corporate governance policies published on our website free of charge, upon request. To request a copy of any of these documents, please submit your request to: Molina Healthcare, Inc., 200 Oceangate, Suite 100, Long Beach, California 90802, Attn: Investor Relations. Information on or linked to our website is neither part of nor incorporated by reference into this Annual Report on Form 10-K or any other SEC filings.
Executive Officers of the Registrant
The following sets forth certain information regarding our executive officers, including the business experience of each executive officer during the past five years:
|
| | |
| Name | Age | Position |
| J. Mario Molina, M.D. | 56 | President and Chief Executive Officer |
| John C. Molina, J.D. | 50 | Chief Financial Officer |
| Terry P. Bayer | 64 | Chief Operating Officer |
| Joseph W. White | 56 | Chief Accounting Officer |
| Jeff D. Barlow | 52 | Chief Legal Officer and Corporate Secretary |
Dr. Molina has served as President and Chief Executive Officer since succeeding his father and company founder, Dr. C. David Molina, in 1996. He has also served as Chairman of the Board of Directors since 1996. Dr. Molina is the brother of John C. Molina.
Mr. Molina has served as Chief Financial Officer since 1995. He also has served as a member of the Board of Directors since 1994. Mr. Molina is the brother of Dr. J. Mario Molina.
Ms. Bayer has served as Chief Operating Officer since 2005.
Mr. White has served as Chief Accounting Officer since 2007.
Mr. Barlow has served as Chief Legal Officer and Corporate Secretary since 2010. From 2004 to 2010, Mr. Barlow served as Vice President, Assistant Secretary, and Assistant General Counsel of Molina Healthcare.
Item 1A:Risk Factors
RISK FACTORS
Safe Harbor Statement under the Private Securities Litigation Reform Act of 1995
This Annual Report on Form 10-K and the documents we incorporate by reference in this report contain forward-looking statements within the meaning of Section 27A of the Securities Act of 1933, as amended (the “Securities Act”"Securities Act"), and Section 21E of the Securities Exchange Act of 1934, as amended (the “Exchange Act”"Exchange Act"). Other than statements of historical fact, all statements that we include in this report and in the documents we incorporate by reference may be deemed to be forward-looking statements for purposes of the Securities Act and the Exchange Act. Such forward-looking statements may be identified by words such as “anticipates,” “believes,” “could,” “estimates,” “expects,” “guidance,” “intends,” “may,” “outlook,” “plans,” “projects,” “seeks,” “will,”"anticipates," "believes," "could," "estimates," "expects," "guidance," "intends," "may," "outlook," "plans," "projects," "seeks," "will," or similar words or expressions.
Investing in our securities involves a high degree of risk. Before making an investment decision, you should carefully read and consider the following risk factors, as well as the other information we include or incorporate by reference in this report and the information in the other reports we file with the U.S. Securities Exchange Commission, or SEC. Such risk factors should be considered not only with regard to the information contained in this annual report, but also with regard to the information and statements in the other periodic or current reports we file with the SEC, as well as our press releases, presentations to securities analysts or investors, or other communications made by or with the approval of one of our executive officers. No assurance can be given that we will actually achieve the results contemplated or disclosed in our forward-looking statements. Such statements may turn out to be wrong due to the inherent uncertainties associated with future events. Accordingly, you should not place undue reliance on our forward-looking statements, which reflect management’s analyses, judgments, beliefs, or expectations only as of the date they are made.
If any of the events described in the following risk factors actually occur, our business, results of operations, financial condition, cash flows, or prospects could be materially adversely affected. The risks and uncertainties described below are those that we currently believe may materially affect us. Additional risks and uncertainties not currently known to us or that we currently deem immaterial may also affect our business and operations. As such, you should not consider this list to be a complete statement of all potential risks or uncertainties. Except to the extent otherwise required by federal securities laws, we do not undertake to address or update forward-looking statements in future filings or communications regarding our business or operating results, and do not undertake to address how any of these factors may have caused results to differ from discussions or information contained in previous filings or communications.
Risks Related to Our Health Plans BusinessSegment
Numerous risks associated with the Affordable Care Act and its implementation could have a material adverse effect on our business, financial condition, cash flows, or results of operations.
In March 2010, President Obama signed both the Patient Protection and Affordable Care Act and the Health Care and Education Affordability Reconciliation Act commonly referred to together as(collectively, the Affordable Care Act, or the ACA.ACA). The ACA enacts comprehensive changes to the United States health care system, elements of which will be phased in at various stages over the next several years. However, the most significant changes effected by the ACA are currently scheduled to bewere implemented as of January 1, 2014. There are a multitude of risks associated with the scope of change in the health care system represented by the ACA, including, but not limited to, the following:
Risks associated with the health care federal excise tax.tax. One notable provision of the ACA is an excise tax or annual fee that applies to most health plans, including both commercial health plans and Medicaid and/or Medicare managed care plans like Molina Healthcare. While characterized as a “fee”"fee" in the text of the ACA, the intent of Congress was to impose a broad-based health insurance industry excise tax, with the understanding that the tax could be passed on to consumers, most likely through slightly higher commercial insurance premiums. However, because Medicaid is jointly paida government funded program, Medicaid health plans have no alternative but to look to their respective state partners for bypayment to offset the federal government and by state governments, so the costimpact of this excise tax, as it may be applied to Medicaid plans, will be passed on intax. Additionally, when states reimburse us for the form of higher Medicaid costs and rates. In Medicaid and Medicare, capitated rates paid to managed care plans are required to be developed using generally accepted principles of actuarial soundness. Actuarial soundness requires that the full costs of doing business, including the costs of both federal and state taxes, be considered and factored into the applicable rate. Thus, for Medicaid and/or Medicare managed care plans like Molina Healthcare, Inc., the excise tax will be included in their capitated rates. Becauseamount of the novelty of this newHIF, that reimbursement is itself subject to income tax, actuaries have never factored the tax intoHIF, and applicable state premium taxes. Because the development of capitated rates, an exercise which must be undertaken during 2013 and well in advance of the 2014 calendar year when the tax is scheduled to go into effect. Moreover, because the tax will be based on a health plan's market share as applied to a total excise tax base of $8 billion in 2014 (and rising thereafter), there is substantial uncertainty regarding the actual size of the tax assessment on Molina. Currently, we project that the excise tax assessment on Molina will be approximately $100 million. Since this amountHIF is not deductible for income tax purposes, under current law, and since our total net income for fiscal year 2011 was $20.8 million, and our net income is reduced by the full amount of the assessment. The state of California has not formally committed to reimburse us for either the HIF itself, or the related tax effects. The states of Michigan and Utah have reimbursed us for the HIF, but have not formally committed to reimbursement for the related tax effect. The total amount of HIF revenue for which agreements were not secured (and revenue was not recognized) amounted to approximately $20 million for fiscal year 2012 was $9.82014. We expect to collect and recognize this revenue related to 2014 in 2015. We further expect to recognize revenue in 2015 sufficient to reimburse us for the full amount of the HIF we will pay (along with related tax effects) in September of 2015. We expect our 2015 HIF assessment related to our Medicaid business to be approximately $143 million, with an expected tax effect from the reimbursement of the assessment of approximately $88 million. Therefore, the total reimbursement needed as a result of the Medicaid-related HIF is approximately $231
our estimated tax rate for 2014 could be driven to 100%, and the excise tax could effectively equal the entire amountmillion. The failure of our projected earnings. Westate partners to reimburse us in full for the HIF and others in the health care industry are working with Congress to carve out the application of the exciseits related tax on Medicaid plans. As an alternative to the repeal of the tax as it applies to Medicaid managed care plans, we and others in the health care industry will also be working with state actuaries to take account of the tax in the calculation of our 2014 rates. However, state budget constraints, inaccurate actuarial calculations, inadequate federal oversight of actuarial soundness, and market competitioneffects could result inhave a failure to reflect in our rates the full amount of the excise tax. If the excise tax is imposed as enactedmaterial adverse effect on Medicaid managed care plans, or we are unable to obtain premium increases to fully offset the impact of the tax or otherwise adjust our business model, our business, financial condition, cash flows andor results of operations could be materially adversely affected.operations.
Risks associated with the duals expansion. expansion. Nine million low-income elderly and disabled people are covered under both the Medicare and Medicaid programs. These beneficiaries often called “dual eligibles,” are more likely than other Medicare beneficiaries to be frail, live with multiple chronic conditions, and have functional and cognitive impairments. Medicare is their primary source of health insurance coverage, as it is for the nearly 50 million elderly and under-65 disabled beneficiaries in 2012. Medicaid supplements Medicare by paying for services not covered by Medicare, such as dental care and long-term care services and supports,support, and by helping to cover Medicare'sMedicare’s premiums and cost-sharing requirements. Together, these two programs help to shield very low-income Medicare beneficiaries from potentially unaffordable out-of-pocket medical and long-term care costs. Policymakers at the federal and state levellevels are increasingly developing initiatives for dual eligibles, both to improvefocused on the coordinationdesign and implementation of their care, and to reduce spending. The Centers for Medicare and Medicaid Services, or CMS, has implemented several demonstration projects designed toprograms that improve the coordination of care for dual eligibles andthose who qualify to reducereceive both Medicare and Medicaid spending. These demonstrations include issuing contractsservices (the "dual eligible"), and to deliver services to the dual eligible in a more financially efficient manner. As a result of these efforts, 15 states to design a programhave undertaken demonstration programs to integrate Medicare and Medicaid services for dual eligiblesdual-eligible individuals. The health plans participating in the relevant state.such demonstrations are referred to as Medicare-Medicaid Plans (MMPs). Our health plansMMPs in California, Illinois, Michigan,and Ohio Texas,offered coverage beginning in 2014, and Washington intendwe expect to take partbegin offering MMP coverage in South Carolina and Texas in the duals demonstrationsfirst quarter of 2015, and in those states. BeginningMichigan in September 2013, our California plan intends to serve duals in Riverside, San Bernardino, and San Diego counties, and may participate with Health Net, Inc. for the duals contract in Los Angeles County. Our new Illinois plan will serve duals in Central Illinois beginning in 2014. Our Michigan plan will respond to a request for proposals to serve duals beginning in late 2013. Our Ohio plan will serve duals in three regions in southwestern Ohio (Dayton, Columbus and Cincinnati) beginning in late 2013. The statesecond quarter of Texas announced that it intends to cover duals through its existing Medicaid contracts beginning in 2014. Our Washington plan will respond to a request for proposals to serve duals also beginning in 2014.2015.
There are numerous risks associated with the initial implementation of a new program, with a health plan'splan’s expansion into a new service area, orand with the provision of medical services to a new population which has not previously been in managed care. One such risk is the development of actuarially sound rates. Because there is limited historical information on which to develop rates, certain assumptions are required to be made which may subsequently prove to have been inaccurate. Rates of utilization could be significantly higher than had been projected, or the assumptions of policymakers about the amount of savings that could be achieved through the use of utilization management in managed care could be seriously flawed. Moreover, because of our lack of actuarial experience for that program, region, or population, our reserve levels may be set at an inadequate level. For instance, these problems arose at our Texas health plan in the second quarter of 2012, leading to extremely elevated medical care costs and substantial losses at the health plan. All of these risks are presentedpresent in the implementation of the duals demonstration programs. In the event these risks materialize at one or more of our health plans, the negative results of thatthe health plan or plans could adversely affect our business, financial condition, cash flows, andor results of operations.
Risks associated with the Medicaid expansion.expansion Among other things, by January 1, 2014, in. In the states that electhave elected to participate, the ACA provides thatfor the expansion of the Medicaid program will be greatly expanded to provideoffer eligibility to nearly all low-income people under age 65 with incomes at or below 138% of the federal poverty line. As a result, millions of low-income adults without children who currently cannot qualify for coverage, as well as many low-income parents and,Medicaid expansion membership phased in some instances, children now covered through CHIP, will be made eligible for Medicaid. As of February 27, 2013, among the states where we operatebeginning January 1, 2014. Since that date, our health plans the states ofin California, Florida,Illinois, Michigan, New Mexico, Ohio, and Washington have indicated that they intend to participatebegun participating in the Medicaid expansion; the statesexpansion. At December 31, 2014, our membership included approximately 385,000 Medicaid expansion members, or 15% of Texas and Wisconsin have indicated that they do not intend to participate in the expansion; and the state of Utah is undecided. In those states that participate in the expansion, our Medicaid membership is likely to grow appreciably.total membership. The new enrollees in our health plans will represent a population that is different from the population of Medicaid enrollees we have historically managed. In addition, such enrollees may be unfamiliar with managed care, and may have substantial pent-up demand for medical services that could result in greater than anticipated rates of utilization. All of the risk factors described above with regard to the duals demonstration programs apply equally to the Medicaid expansion.
Risks associated with thehealth insurance marketplaces.Under The ACA authorized the ACA,creation of Marketplace insurance marketplaces will be online marketplaces organized on a state-by-state basis (although in many instances the insurance marketplace in a state will be operated by the federal government, and there could also be regional marketplaces where states combine their marketplace products).
In the insurance marketplace,exchanges, allowing individuals and small groups canto purchase health insurance that in many instances will beis federally subsidized, (up to 400% of the federal poverty level by individual or family).effective January 1, 2014. We currently intend to participate in the insurance marketplacesMarketplace in all of the states in which we operate, except Illinois and South Carolina. At December 31, 2014, we had approximately 15,000 Marketplace members, and that enrollment is expected to grow appreciably in 2015, particularly at our Florida health plans. Our principal focus in participating in the marketplace is to capture the transition in membership that may result from a Medicaid member's income rising above the 138% level of the federal poverty line. By retaining that member in the marketplace, if the member's income subsequently declines, we will continuously serve that same member in all instances and not “lose” the member to another health plan. We endorse the so-called “bridge plan” as the best way to serve low-income persons who may qualify for coverage through the insurance marketplaces, and will be working with legislators and regulators during 2013 to advocate for the merits of the bridge plan. All of the risk factors described above with regard to the duals demonstration programs apply equally to our participation in the insurance marketplaces.
Risks associated with the King v. Burwell case. There is a case currently pending before the United States Supreme Court to be argued on March 4, 2015, challenging whether the IRS may permissibly promulgate regulations to extend tax-credit subsidies to coverage purchased through exchanges established by the federal government under Section 1321 of the ACA. In the event the Supreme Court rules against Health and Human Services Secretary Burwell, no federal subsidies would be allowed to be paid to those individuals purchasing health insurance through the federally facilitated exchanges, of which there are currently 36. This would undermine the functioning of those exchanges, and cause major disruption under the entire ACA throughout the nation.
Risk associated with implementing regulations.regulations. There are many parts of the ACA that will require further guidance in the form of regulations. Due to the breadth and complexity of the ACA, the lack of implementing regulations and interpretive guidance, and the phased-inphased nature of the ACA'sACA’s implementation, the overall impact of the ACA on our business and on the health industry in general over the coming years is difficult to predict and not yet fully known.known, and implementing regulations could contain provisions that have a material adverse effect on our business, financial condition, cash flows, or results of operations.
Our profitability depends on our ability to accurately predict and effectively manage our medical care costs.
Our profitability depends to a significant degree on our ability to accurately predict and effectively manage our medical care costs. Historically, our medical care cost ratio, meaning our medical care costs as a percentage of our premium revenue net of premium tax, has fluctuated substantially, and has also varied across our state health plans. Because the premium payments we receive are generally fixed in advance and we operate with a narrow profit margin, relatively small changes in our medical care cost ratio can create significant changes in our overall financial results. For example, if our overall medical care ratio, continuing operations, for the year ended December 31, 20122014 of 89.9%89.5% had been one percentage point higher, or 90.9%90.5%, our resultsnet income from continuing operations for the year ended December 31, 20122014 would have been a net loss of approximately $(0.55)$0.12 per diluted share rather than our actual net income from continuing operations of $0.21$1.30 per diluted share, a decrease of over 300%approximately 91%.
Factors that may affect our medical care costs include the level of utilization of health care services, unexpected patterns in the annual influenza, or flu season, increases in hospital costs, an increased incidence or acuity of high dollar claims related to catastrophic illnesses or medical conditions such as hemophilia for which we do not have adequate reinsurance coverage, increased maternity costs, payment rates that are not actuarially sound, changes in state eligibility certification methodologies, relatively low levels of hospital and specialty provider competition in certain geographic areas, increases in the cost of pharmaceutical products and services, changes in health care regulations and practices, epidemics, new medical technologies, and other various external factors. Many of these factors are beyond our control and could reduce our ability to accurately predict and effectively manage the costs of providing health care services. The inability to forecast and manage our medical care costs or to establish and maintain a satisfactory medical care cost ratio, either with respect to a particular state health plan or across the consolidated entity, could have a material adverse effect on our business, financial condition, cash flows, andor results of operations.
Stateand federal budget deficits may result in Medicaid, CHIP, or Medicare funding cuts which could reduce our revenues and profit margins.
Nearly all of our premium revenues come from the joint federal and state funding of the Medicaid and CHIP programs. Due to high unemployment levels, Medicaid enrollment levels and Medicaid costs remain elevated at the same time that state budgets are suffering from significant fiscal strain. Because Medicaid is one of the largest expenditures in every state budget, and one of the fastest-growing, it is a prime target for cost-containment efforts. All of theThe states in which we currently operate our health plans are currently facingregularly face significant budgetary pressures. These budgetary pressures may result in unexpected Medicaid, CHIP, or Medicare rate cuts which could reduce our revenues and profit margins. Moreover, some federal deficit reduction or entitlement reform proposals would fundamentally change the structure and financing of the Medicaid program. Recently, various proposals have been advanced to reduce annual federal deficits and to slow the increase in the national debt. A number of these proposals include both tax increases and spending reductions in discretionary programs and mandatory programs, such as Social Security, Medicare, and Medicaid.
In addition, potential reductions in Medicare and Medicaid spending have been included in the discussions in Congress regarding deficit reduction measures. The Budget Control Act of 2011 provides that Medicare payments may be reduced by no more than 2% and certain other programs, including Medicaid, would be exempt from the automatic spending cuts associated with sequestration. At this time, weWe are unable to determine how any future Congressional spending cuts will affect Medicare and Medicaid reimbursement in the future. We also cannot predict the initiatives that may be adopted in the future or their full impact.reimbursement. There likely will continue to be legislative and regulatory proposals at the federal and state levels directed at containing or lowering the cost of health care that, if adopted, could potentially have a material adverse effect on our business, financial condition, cash flows, andor results of operations.
A failure to accurately estimate incurred but not reported medical care costs may negatively impact our results of operations.
Because of the time lag between when medical services are actually rendered by our providers and when we receive, process, and pay a claim for those medical services, we must continually estimate our medical claims liability at particular points in time, and establish claims reserves related to such estimates. Our estimated reserves for such “incurred"incurred but not paid,” or IBNP,paid" (IBNP) medical care costs are based on numerous assumptions. We estimate our medical claims liabilities using actuarial methods based on historical data adjusted for claims receipt and payment experience (and variations in that experience), changes in membership, provider billing practices, health care service utilization trends, cost trends, product mix, seasonality, prior authorization of medical services, benefit changes, known outbreaks of disease or increased incidence of illness such as influenza, provider contract changes, changes to Medicaid fee schedules, and the incidence of high dollar or catastrophic claims. Our ability to accurately estimate claims for our newer lines of business or populations, such as with respect to duals, Medicaid expansion members, or aged, blind or disabled Medicaid members, is impacted by the more limited experience we have had with those populations. With regard to the new previously uninsured Medicaid members we expect to enroll in 2014 due to the Medicaid expansion, certain new members may be disproportionately costly due to high utilization in their first several months of Medicaid membership as a result of their previously having been uninsured and therefore not seeking or deferring medical treatment.
The IBNP estimation methods we use and the resulting reserves that we establish are reviewed and updated, and adjustments, if deemed necessary, are reflected in the current period. Given the numerous uncertainties inherent in such estimates, our actual claims liabilities for a particular quarter or other period could differ significantly from the amounts estimated and reserved for that quarter or period. Our actual claims liabilities have varied and will continue to vary from our estimates, particularly in times of significant changes in utilization, medical cost trends, and populations and markets served.
If our actual liability for claims payments is higher than estimated, our earnings per share in any particular quarter or annual period could be negatively affected. Our estimates of IBNP may be inadequate in the future, which would negatively affect our
results of operations for the relevant time period. Furthermore, if we are unable to accurately estimate IBNP, our ability to take timely corrective actions may be limited, further exacerbating the extent of the negative impact on our results.
An increased incidence of flu in 2013 in one or more of the states in which we operate a health plan could significantly increase utilization rates and medical costs.
Our results during 2009 werecan be significantly impacted by the widespread incidence of the H1N1a severe flu season in the states in which we operateoperated our health plans. During December 2012 and January 2013, the CDC reported that the incidence of the flu nationwide had been very high and is expectedWe seek to continue through the 2013 flu season. We have taken steps to appropriately set our IBNP reserves appropriately to account for seasonal spikes in the high incidence of the flu. However, if the actual utilization rates of our members are higher than we had anticipated, our results in the first quarter of 2013relevant periods could be materially and adversely affected.
If the responsive bids of our health plans for new or renewed Medicaid contracts are not successful, or if our government contracts are terminated or are not renewed, our premium revenues could be materially reduced and our operating results could be negatively impacted.
Our government contracts may be subject to periodic competitive bidding. In such process, our health plans may face competition as other plans, many with greater financial resources and greater name recognition, attempt to enter our markets through the competitive bidding process. For instance, the state contract of our Florida health plan will be subject to competitive bidding in 2013 for a new contract commencing January 1, 2014. In the event the responsive bid of our Florida health planone or thosemore of our other health plans areis not successful, we will lose our Medicaid contract in the applicable state or states, and our premium revenues could be materially reduced as a result. Alternatively, even if our responsive bids are successful, the bids may be based upon assumptions regarding enrollment, utilization, medical costs, or other factors which could result in the Medicaid contract being less profitable than we had expected.
In addition, all of our contracts may be terminated for cause if we breach a material provision of the contract or violate relevant laws or regulations. Our contracts with the states are also subject to cancellation by the state in the event of the unavailability of state or federal funding. In some jurisdictions, such cancellation may be immediate and in other jurisdictions a notice period is required. Further, most of our contracts are terminable without cause.
Our government contracts generally run for periods of one yearthree to threefour years, and may be successively extended by amendment for additional periods if the relevant state agency so elects. Our current contracts expire on various dates over the next several years. Although our health plans have generally been successful in obtaining the renewal and/or extension of their state contracts, there can be no guarantee that any of our state government contracts will be renewed or extended, as shown by the loss of our Missouri contract in 2012.2012 in connection with an unsuccessful RFP bid. During 2015, our Michigan Medicaid contract will be subject to a new RFP. We expect the Michigan RFP to be released on May 1, 2015, and for the new contract to become effective on October 1, 2015. If we are unable to renew, successfully re-bid, or compete for any of our government contracts, including our Michigan contract, or if any of our contracts are terminated or renewed on less favorable terms, our business, financial condition, cash flows, andor results of operations could be adversely affected.
In the event the expected reductionIf we sustain a cyberattack or suffer privacy or data security breaches that disrupt our operations or result in the rates paiddissemination of sensitive personal or confidential information, we could suffer increased costs, exposure to significant liability, reputational harm, loss of business, and other serious negative consequences.
As part of our normal operations, we routinely collect, process, store, and transmit large amounts of data in our operations, including sensitive personal information as well as proprietary or confidential information relating to our California health plan isbusiness or third parties. We may be subject to breaches of the information technology systems we use. Experienced computer programmers and hackers may be able to penetrate our layered security controls and misappropriate or compromise sensitive personal information or proprietary or confidential information, create system disruptions, or cause shutdowns. They also may be able to develop and deploy viruses, worms, and other malicious software programs that attack our systems or otherwise exploit any security vulnerabilities. Because the techniques used to circumvent security systems can be highly sophisticated and change frequently, often are not finally implemented, isrecognized until launched against a target, and may originate from less regulated and remote areas around the world, we may be unable to proactively address these techniques or to implement adequate preventive measures. Our facilities may also be vulnerable to security incidents or security attacks; acts of vandalism or theft; misplaced or lost data; human errors; acts of malicious insiders, or other similar events that could negatively affect our systems and our and our members’ data. The cost to eliminate or address the foregoing security threats and vulnerabilities before or after a cyber-incident could be significant. Our remediation efforts may not made effective retroactivelybe successful and could result in interruptions, delays, or cessation of service, and loss of members, vendors, and state contracts. In addition, breaches of our security measures and the unauthorized dissemination of sensitive personal information or proprietary information or confidential information about our members could expose our members to July 1, 2011,the risk of financial or ismedical identity theft, or expose us or other third parties to a risk of loss or misuse of this information, result in litigation and potential liability for us, damage our reputation, or otherwise modified,have a material adverse effect on our business, financial condition, cash flows, or results of operations may be affected.operations.
California Assembly Bill 97,The exorbitant cost of specialty drugs and new generic drugs could have a material adverse effect on the level of our medical costs and our results of operations.
In 2014, Gilead’s pricing of the hepatitis C drug, Sovaldi, at $84,000 per standard course of therapy received major attention as a health care policy and public policy matter. Because of the relatively high incidence of hepatitis C throughout the nation, particularly in the Medicaid population, the pricing of specialty drugs for the treatment of hepatitis C represents a major public health and public financing problem. In the case of Sovaldi, because of its advent on the health care market in early 2014, the cost of the drug was generally not factored into our 2014 capitation rates, thus threatening to undermine the actuarial soundness of those rates. New high priced specialty drugs and generic drugs are expected to enter the health care market in 2015. In addition, evolving regulations and state and federal mandates regarding coverage may impact the ability of our health plans to continue to receive existing price discounts on pharmaceutical products for our members. Other factors affecting our pharmaceutical costs include, but are not limited to, geographic variation in utilization of new and existing pharmaceuticals, and changes in discounts. We will seek to work with state Medicaid agencies to ensure that we receive appropriate and actuarially sound reimbursement for all new drug therapies and pharmaceuticals. In the event we are required to bear the high costs of new specialty drugs or AB 97, is legislation that was signed by Governor Jerry Brown on March 24, 2011. Amonggeneric drugs without an appropriate rate adjustment or other things, AB 97 proposes to effect a 10% reduction in Medi-Cal provider rates. It is currently uncertain whether the rate cut will be implemented, and if it is implemented, whether it will be effective retroactively to July 1, 2011. If the proposed rate cut is not finally implemented, if it is not made effective retroactively to July 1, 2011,reimbursement mechanism, or if it is otherwise modified from its current form, thenew regulations or mandates affect our pharmaceutical costs, our business, financial condition, cash flows, or results of our California health planoperations could be negatively affected depending on the action taken. In addition, recoveries from providers related to any final implemented rate cut could also affect the results of our California health plan.adversely affected.
States may not adequately compensate us for the value of drug rebates that were previously earned by the Companyus but that are now collectible by the states.
The ACA includes certain provisions that change the way drug rebates are handled for drug claims filled by Medicaid managed care plans. Retroactive to March 23, 2010, state Medicaid programs are now required to collect federal rebates on all Medicaid-covered outpatient drugs dispensed or administered to Medicaid managed care enrollees (excluding certain drugs that are already discounted), and pharmaceutical manufacturers are required to pay specified rebates directly to the state Medicaid programs for those claims. This has impacted the level of rebates received by managed care plans from the manufacturers for Medicaid managed care enrollees. Many manufacturers have renegotiated or discontinued their rebate contracts with Medicaid managed care plans and pharmacy benefits managers to offset these new rebates paid directly to state Medicaid programs. As a result, the drug rebate amounts paid to managed care plans like ours continue to remain at levels that are much lower than prior to the ACA implementation. There are provisions in the ACA that require rates paid to Medicaid managed care plans to be actuarially sound in regard to drug rebates. Although we will be pursuing rate increases with state agencies to make us whole for the rebate amounts lost, there can be no assurances that the premium increases we may receive, if any, will be adequate to offset the amount of the lost rebates. If such premium increases prove to be inadequate, our business, financial condition, cash flows, andor results of operations could be adversely affected.
We derive our premium revenues from a relatively small number of state health plans.
We currently derive our premium revenues from nine11 state health plans.plans, with our Puerto Rico health plan expected to commence operations in April 2015. If we are unable to continue to operate in any of those nine11 states, or if our current operations in any portion of the states we are in are significantly curtailed, our revenues could decrease materially. Our reliance on operations in a limited number of states could cause our revenue and profitability to change suddenly and unexpectedly, depending on an abrupt loss of membership, significant rate reductions, a loss of a material contract, legislative actions, changes in Medicaid eligibility methodologies, catastrophic claims, an epidemic, an unexpected increase in utilization, general economic conditions, and similar factors in those states. Our inability to continue to operate in any of the states in which we currently operate, or a significant change in the nature of our existing operations, could adversely affect our business, financial condition, cash flows, andor results of operations.
There are performance risks and other risks associated with certain provisions in the state Medicaid contracts of several of our health plans.
The state contracts of our California, Illinois, New Mexico, Ohio, Texas, Washington, and Wisconsin health plans contain provisions pertaining to at-risk premiums that require us to meet certain quality performance measures to earn all of our contract revenues in those states. In the event we are unsuccessful in achieving the stated performance measure, the health plan will be unable to recognize the revenue associated with that measure. Any failure of our health plans to satisfy one of these performance measure provisions could adversely affecthave a material adverse effect on our business, financial condition, cash flows andor results of operations. In addition, the state contracts of our California, Florida, Illinois, Michigan, New Mexico, Ohio, Texas, and Washington health plans and our contract with CMS, contain provisions pertaining to medical cost floors and corridors, administrative cost and profit ceilings, and profit-sharing arrangements. Our Medicare and Marketplace business is also subject to medical cost floor requirements enacted by the Federal government. These provisions are subject to interpretation and application by our health plans. In the event the applicable state government agency disagrees with our health plan'splan’s interpretation or application of the sometimes complicated contract provisions at issue, the health plan could be required to adjust the amount of its obligations under these provisions and/or make a payment or payments to the state. Any interpretation or application of these provisions at
variance with our health plan'splan’s interpretation or inconsistent with our revenue recognition accounting treatment could adversely affecthave a material adverse effect on our business, financial condition, cash flows, andor results of operations.
Failure to attain profitability in any new start-up operations, including in our new Puerto Rico health plan, could negatively affect our results of operations.
Start-up costs associated with a new business can be substantial. For example, to obtain a certificate of authority to operate as a health maintenance organization in most jurisdictions, we must first establish a provider network, have infrastructure and required systems in place, and demonstrate our ability to obtain a state contract and process claims. Often, we are also required to contribute significant capital to fund mandated net worth requirements, performance bonds or escrows, or contingency guaranties. If we are unsuccessful in obtaining the certificate of authority, winning the bid to provide services, or attracting members in sufficient numbers to cover our costs, any new business of ours would fail. We also could be required by the state to continue to provide services for some period of time without sufficient revenue to cover our ongoing costs or to recover our significant start-up costs.
Even if we are successful in establishing a profitable health plan in a new state, increasing membership, revenues, and medical costs will trigger increased mandated net worth requirements which could substantially exceed the net income generated by the health plan. Rapid growth in an existing state will also result in increased net worth requirements. In such circumstances, we may not be able to fund on a timely basis or at all the increased net worth requirements with our available cash resources. All of these risks will pertain to our new start-up Puerto Rico health plan, which is expected to commence operations in April 2015. The expenses associated with starting up a health plan in a new state or commonwealth, or expanding a health plan in an existing state could have ana material adverse impacteffect on our business, financial condition, cash flows, andor results of operations.
Receipt of inadequate or significantly delayed premiums could negatively affect our business, financial condition, cash flows, andor results of operations.
Our premium revenues consist of fixed monthly payments per member, and supplemental payments for other services such as maternity deliveries. These premiums are fixed by contract, and we are obligated during the contract periods to provide health care services as established by the state governments. We use a large portion of our revenues to pay the costs of health care services delivered to our members. If premiums do not increase when expenses related to medical services rise, our medical margins will be compressed, and our earnings will be negatively affected. A state could increase hospital or other provider rates without making a commensurate increase in the rates paid to us, or could lower our rates without making a commensurate reduction in the rates paid to hospitals or other providers. In addition, if the actuarial assumptions made by a state in implementing a rate or benefit change are incorrect or are at variance with the particular utilization patterns of the members of one of our health plans, our medical margins could be reduced. Any of these rate adjustments in one or more of the states in which we operate could adversely affecthave a material adverse effect our business, financial condition, cash flows, andor results of operations.
Furthermore, a state undergoing a budget crisis may significantly delay the premiums paid to one of our health plans. For instance, due to a prolonged budget impasse during 2010, some of the monthly premium payments made by the state of California to our California health plan were several months late. Any significant delay in the monthly payment of premiums to any of our health plans could have a material adverse affecteffect on our business, financial condition, cash flows, andor results of operations.
Reductions in Medicare payments could reduce our earnings potential for our Medicare Advantage plans and our duals demonstration programs.
The Sequestration Transparency Act of 2012 included a 2% reduction of payments from CMS to our Medicare Advantage plans beginning April 1, 2013. Medicare Advantage plans will continue to be affected until Congress lifts the sequestration mandated under the Sequestration Transparency Act of 2012. The impact of sequestration cuts on our Medicare Advantage revenues is partially mitigated by reductions in provider reimbursements paid to those providers with rates indexed to the Medicare fee-for-service reimbursement rates. Such reduction in our Medicare payments may have an adverse effect on our earnings potential for our Medicare Advantage plans and our duals demonstration programs. In addition, reductions to provider reimbursement rates associated with sequestration may adversely impact our relations with the impacted providers.
Difficulties in executing our acquisition strategy could adversely affect our business.
The acquisitions of other health plans and the assignment and assumption of Medicaid contract rights of other health plans have accounted for a significant amount of our growth over the last several years. Although we cannot predict with certainty our rate of growth as the result of acquisitions, we believe that additional acquisitions of all sizes will be important to our future growth strategy. Many of the other potential purchasers of these assets-particularlyassets—particularly operators of large commercial health plans-haveplans—have significantly greater financial resources than we do. Also, many of the sellers may insist on selling assets that we do not want, such as commercial lines of business, or may insist on transferring their liabilities to us as part of the sale of their companies or assets. Even if we identify suitable targets, we may be unable to complete acquisitions on terms favorable to us, or at all, or obtain the necessary financing for these acquisitions. For these reasons, among others, we cannot provide assurance that we will be able to complete favorable acquisitions, especially in light of the volatility in the capital markets over the past several years.years, or that we will not complete acquisitions that turn out to be unfavorable. Further, to the extent we complete an acquisition, we
may be unable to realize the anticipated benefits from such acquisition because of operational factors or difficulty in integrating the acquisition with our existing business. This may include problems involving the integration of:
additional employees who are not familiar with our operations or our corporate culture,
new provider networks which may operate on terms different from our existing networks,
additional members who may decide to transfer to other health care providers or health plans,
disparate information, claims processing, and record-keeping systems,
internal controls and accounting policies, including those which require the exercise of judgment and complex estimation processes, such as estimates of claims incurred but not paid,reported, accounting for goodwill, intangible assets, stock-based compensation, and income tax matters, and
new regulatory schemes, relationships, practices, and compliance requirements.
Also, we are generally required to obtain regulatory approval from one or more state agencies when making acquisitions of health plans. In the case of an acquisition of a business located in a state in which we do not already operate, we would be required to obtain the necessary licenses to operate in that state. In addition, although we may already operate in a state in which we acquire a new business, we would be required to obtain regulatory approval if, as a result of the acquisition, we will operate in an area of that state in which we did not operate previously. Furthermore, we may be required to renegotiate contracts with the network providers of the acquired business. We may be unable to obtain the necessary governmental approvals, comply with these regulatory requirements or renegotiate the necessary provider contracts in a timely manner, if at all.
In addition, we may be unable to successfully identify, consummate, and integrate future acquisitions, including integrating the acquired businesses on our information technology platform, or to implement our operations strategy in order to operate
acquired businesses profitably. Furthermore, we may incur significant transaction expenses in connection with a potential acquisition which may or may not be consummated. These expenses could impact our selling, general and administrative expense ratio.
For all of the above reasons, we may not be able to consummate our proposed acquisitions as announced from time to time to sustain our pattern of growth or to realize benefits from completed acquisitions.
We face periodic routine and non-routine reviews, audits, and investigations by government agencies, and these reviews and audits could have adverse findings, which could negatively impact our business.
We are subject to various routine and non-routine governmental reviews, audits, and investigations. Violation of the laws, regulations, or contract provisions governing our operations, or changes in interpretations of those laws and regulations, could result in the imposition of civil or criminal penalties, the cancellation of our contracts to provide managed care services, the suspension or revocation of our licenses, the exclusion from participation in government sponsored health programs, or the revision and recoupment of past payments made based on audit findings. If we are unable to correct any noted deficiencies, or become subject to material fines or other sanctions, we mightcould suffer a substantial reduction in profitability, and mightcould also lose one or more of our government contracts and as a result lose significant numbers of members and amounts of revenue. In addition, government receivables are subject to government audit and negotiation, and government contracts are vulnerable to disagreements with the government. The final amounts we ultimately receive under government contracts may be different from the amounts we initially recognize in our financial statements.
We rely on the accuracy of eligibility lists provided by state governments. Inaccuracies in those lists would negatively affect our results of operations.
Premium payments to our health plan segment are based upon eligibility lists produced by state governments. From time to time, states require us to reimburse them for premiums paid to us based on an eligibility list that a state later discovers contains individuals who are not in fact eligible for a government sponsored program or are eligible for a different premium category or a different program. Alternatively, a state could fail to pay us for members for whom we are entitled to payment. Our results of operations would be adversely affected as a result of such reimbursement to the state if we make or have made related payments to providers and are unable to recoup such payments from the providers.
We are subject to extensive fraud and abuse laws which may give rise to lawsuits and claims against us, the outcome of which may have a material adverse effect on our business, financial position,condition, cash flows, or results of operations, and cash flows.operations.
Because we receive payments from federal and state governmental agencies, we are subject to various laws commonly referred to as “fraud"fraud and abuse”abuse" laws, including the federal False Claims Act, which permit agencies and enforcement authorities to institute suit against us for violations and, in some cases, to seek treble damages, penalties, and assessments. Liability under such federal and state statutes and regulations may arise if we know, or it is found that we should have known, that information
we provide to form the basis for a claim for government payment is false or fraudulent, and some courts have permitted False Claims Act suits to proceed if the claimant was out of compliance with program requirements. Qui tam actions under federal and state law can be brought by any individual on behalf of the government. Qui tam actions have increased significantly in recent years, causing greater numbers of health care companies to have to defend a false claim action, pay fines, or be excluded from the Medicare, Medicaid, or other state or federal health care programs as a result of an investigation arising out of such action. Many states, including statesWe are currently defending two qui tam actions where both the federal and state governments declined to intervene: (i) USA and State of Florida ex rel Charles Wilhelm v. Molina Healthcare and Molina Healthcare of Florida; and (ii) USA ex rel Anita Silingo v. Mobile Medical Examination Service, Molina Healthcare of California, et al. We believe we currently operate, have enacted parallel legislation.meritorious defenses to both matters, and intend to defend both matters vigorously. In the event we are subject to liability under athese or other qui tam action,actions, our business, and operatingfinancial condition, cash flows, or results of operations could be adversely affected.
Our business could be adversely impacted by adoption of the new ICD-10 standardized coding set for diagnoses.
The U.S. Department of Health and Human Services, or HHS, has released rules pursuant to the Health Insurance Portability and Accountability Act, or HIPAA, which mandate the use of standard formats in electronic health care transactions. HHS also has published rules requiring the use of standardized code sets and unique identifiers for providers. Originally, the federal government required that health care organizations, including health insurers, upgrade to updated and expanded standardized code sets used for documenting health conditions by October 2013. These new standardized code sets, known as ICD-10, will require substantial investments from health care organizations, including us. However, CMS has now postponedscheduled implementation of ICD-10 toby October 2014. While use1, 2015. Use of the ICD-10 code sets will require significant administrative changes we believe that the cost of compliance with these regulations has not had and is not expected to have a material adverse effect on our cash flows, financial position, or results of operations. However, these changes may result in errors and otherwise negatively impact our service levels, andlevels. In addition, we may experience complications related to supporting customers that are not fully compliant with the revised requirements as of the applicable compliance date. Furthermore, if physicians fail to provide appropriate codes for services provided as a result of the new coding set, we may not be reimbursed, or adequately reimbursed, for such services.
If we are unable to deliver quality care, maintain good relations with the physicians, hospitals, and other providers with whom we contract, or if we are unable to enter into cost-effective contracts with such providers, our profitability could be adversely affected.
We contract with physicians, hospitals, and other providers as a means to ensure access to health care services for our members, to manage health care costs and utilization, and to better monitor the quality of care being delivered. We compete with other health plans to contract with these providers. We believe providers select plans in which they participate based on criteria including reimbursement rates, timeliness and accuracy of claims payment, potential to deliver new patient volume and/or retain existing patients, effectiveness of resolution of calls and complaints, and other factors. We cannot be sure that we will be able to successfully attract and retain providers to maintain a competitive network in the geographic areas we serve. In addition, in any particular market, providers could refuse to contract with us, demand higher payments, or take other actions which could result in higher health care costs, disruption to provider access for current members, a decline in our growth rate, or difficulty in meeting regulatory or accreditation requirements.
The Medicaid program generally pays doctors and hospitals at levels well below those of Medicare and private insurance. Large numbers of doctors, therefore, do not accept Medicaid patients. In the face of fiscal pressures, some states may reduce rates paid to providers, which may further discourage participation in the Medicaid program.
In some markets, certain providers, particularly hospitals, physician/hospital organizations, and some specialists, may have significant market positions or even monopolies. If these providers refuse to contract with us or utilize their market position to negotiate favorable contracts which are disadvantageous to us, our profitability in those areas could be adversely affected.
Some providers that render services to our members are not contracted with our health plans. In those cases, there is no pre-established understanding between the provider and our health plan about the amount of compensation that is due to the provider. In some states, the amount of compensation is defined by law or regulation, but in most instances it is either not defined or it is established by a standard that is not clearly translatable into dollar terms. In such instances, providers may believe they are underpaid for their services and may either litigate or arbitrate their dispute with our health plan. The uncertainty of the amount to pay and the possibility of subsequent adjustment of the payment could adversely affect our business, financial position, cash flows, andcondition, results of operations.operations, and cash flows.
The insolvency of a delegated provider could obligate us to pay its referral claims, which could have an adverse effect on our business, cash flows, andor results of operations.
Circumstances may arise where providers to whom we have delegated risk, due to insolvency or other circumstances, are unable to pay claims they have incurred with third parties in connection with referral services provided to our members. The inability of delegated providers to pay referral claims presents us with both immediate financial risk and potential disruption to member care. Depending on states'states’ laws, we may be held liable for such unpaid referral claims even though the delegated provider has contractually assumed such risk. Additionally, competitive pressures may force us to pay such claims even when we have no legal obligation to do so or we have already paid claims to a delegated provider and payments cannot be recouped when the delegated provider becomes insolvent. To reduce the risk that delegated providers are unable to pay referral claims,
we monitor the operational and financial performance of such providers. We also maintain contingency plans that include transferring members to other providers in response to potential network instability. In certain instances, we have required providers to place funds on deposit with us as protection against their potential insolvency. These funds are frequently in the form of segregated funds received from the provider and held by us or placed in a third-party financial institution. These funds may be used to pay claims that are the financial responsibility of the provider in the event the provider is unable to meet these obligations. However, there can be no assurances that these precautionary steps will fully protect us against the insolvency of a delegated provider. Liabilities incurred or losses suffered as a result of provider insolvency could have an adverse effect on our business, financial condition, cash flows, andor results of operations.
Regulatory actions and negative publicity regarding Medicaid managed care and Medicare Advantage may lead to programmatic changes and intensified regulatory scrutiny and regulatory burdens.
Several of our health care competitors have recently been involved in governmental investigations and regulatory actions which have resulted in significant volatility in the price of their stock. In addition, there has been negative publicity and proposed programmatic changes regarding Medicare Advantage private fee-for-service plans, a part of the Medicare Advantage program in which we do not participate. These actions and the resulting negative publicity could become associated with or imputed to us, regardless of our actual regulatory compliance or programmatic participation. Such an association, as well as any perception of a recurring pattern of abuse among the health plan participants in government programs and the diminished reputation of the managed care sector as a whole, could result in public distrust, political pressure for changes in the programs in which we do not participate, intensified scrutiny by regulators, additional regulatory requirements and burdens, increased stock volatility due to speculative trading, and heightened barriers to new managed care markets and contracts, all of which could have a material adverse effect on our business, financial condition, cash flows, andor results of operations.
If a state fails to renew its federal waiver application for mandated Medicaid enrollment into managed care or such application is denied, our membership in that state will likely decrease.
States may only mandate Medicaid enrollment into managed care under federal waivers or demonstrations. Waivers and programs under demonstrations are approved for two- to five-year periods and can be renewed on an ongoing basis if the state applies and the waiver request is approved or renewed by CMS. We have no control over this renewal process. If a state does not renew its mandated program or the federal government denies the state'sstate’s application for renewal, our business would suffer as a result of a likely decrease in membership.
If state regulators do not approve payments of dividends and distributions by our subsidiaries, it may negatively affect our business strategy.
We are a corporate parent holding company and hold most of our assets at, and conduct most of our operations through, direct subsidiaries. As a holding company, our results of operations depend on the results of operations of our subsidiaries. Moreover, we are dependent on dividends or other inter-companyintercompany transfers of funds from our subsidiaries to meet our debt service and other obligations. The ability of our subsidiaries to pay dividends or make other payments or advances to us will depend on their operating results and will be subject to applicable laws and restrictions contained in agreements governing the debt of such subsidiaries. In addition, our health plan subsidiaries are subject to laws and regulations that limit the amount of dividends and distributions that they can pay to us without prior approval of, or notification to, state regulators. In California, our health plan may dividend, without notice to or approval of the California Department of Managed Health Care, amounts by which its tangible net equity exceeds 130% of the tangible net equity requirement. Our other health plans must give thirty days'days’ advance notice and the opportunity to disapprove “extraordinary”"extraordinary" dividends to the respective state departments of insurance for amounts over the lesser of (a) ten percent of surplus or net worth at the prior year end or (b) the net income for the prior year. The discretion of the state regulators, if any, in approving or disapproving a dividend is not clearly defined. Health plans that declare ordinarynon-extraordinary dividends must usually provide notice to the regulators ten or fifteen days in advance of the intended distribution date of the ordinarynon-extraordinary dividend. For the years ended December 31, 2012, 20112013 and 2010,2012, we received dividends from our health plan subsidiaries amounting to $80.0 million, $76.6$24.4 million and $81.3$101.8 million, respectively. We did not receive any dividends from our health plan subsidiaries during the year ended December 31, 2014. The aggregate additional amounts our health plan subsidiaries could have paid us at December 31, 2012, 20112014, 2013 and 2010,2012, without approval of the regulatory authorities, were approximately $8.1$96 million, $17.5$54 million, and $18.8$24 million, respectively. If the regulators were to deny or significantly restrict our subsidiaries'subsidiaries’ requests to pay dividends to us, the funds available to our company as a whole would be limited, which could harm our ability to implement our business strategy or service our outstanding indebtedness.
Unforeseen changes in pharmaceutical regulations or market conditions may impact our revenues and adversely affect our results of operations.
A significant category of our health care costs relate to pharmaceutical products and services. Evolving regulations and state and federal mandates regarding coverage may impact the ability of our health plans to continue to receive existing price discounts on pharmaceutical products for our members. Other factors affecting our pharmaceutical costs include, but are not limited to, the price of pharmaceuticals, geographic variation in utilization of new and existing pharmaceuticals, and changes in discounts. The unpredictable nature of these factors may have an adverse effect on our business, financial condition, cash flows, and results of operations.
A security breach or unauthorized disclosure of sensitive or confidential member information could have an adverse effect on our business.
As part of our normal operations, we collect, process, and retain confidential member information. We are subject to various federal and state laws and rules regarding the use and disclosure of confidential member information, including HIPAA and the Gramm-Leach-Bliley Act. The Health Information Technology for Economic and Clinical Health Act, or HITECH, provisions of the HITECH American Reinvestment and Recovery Act of 2009 further expand the coverage of HIPAA by, among other things, extending the privacy and security provisions, mandating new regulations around electronic medical records, expanding enforcement mechanisms, allowing the state Attorneys General to bring enforcement actions, increasing penalties for violations, and requiring public disclosure of improper disclosures of the health information of more than 500 individuals.
Under HITECH, civil penalties for HIPAA violations by covered entities and business associates are increased up to an amount of $1.5 million per calendar year for HIPAA violations. In addition, imposition of these penalties is now more likely because HITECH strengthens enforcement.strategy. For example, commencing February 2010, HHS was requiredwe could be hindered in our ability to conduct periodic audits to confirm compliance. Investigations of violations that indicate willful neglect, for which penalties are now mandatory, are statutorily required. In addition, state attorneys general are authorized to bring civil actions seeking either injunctionsmake debt service payments under our convertible senior notes or damages in response to violations of HIPAA privacy and security regulations that threaten the privacy of state residents. Initially monies collected will be transferred to a division of HHS for further enforcement, and within three years, a methodology will be adopted for distributing a percentage of those monies to affected individuals to fund enforcement and provide incentive for individuals to report violations. In addition, HITECH requires us to notify affected individuals, HHS, and in some cases the media when unsecured protected health information is subject to a security breach.
HITECH also contains a number of provisions that provide incentives for providers and states to initiate certain programs related to health care and health care technology, such as electronic health records. While some HITECH provisions may not applyany credit facility.
to us directly, states wishing to apply for grants under HITECH, or otherwise participating in such programs, may impose new health care technology requirements on us through our contracts with state Medicaid agencies. We are unable to predict what such requirements may entail or what their effect on our business may be.
We will continue to assess our compliance obligations as regulations under HITECH are promulgated and more guidance becomes available from HHS and other federal agencies. The new privacy and security requirements, however, may require substantial operational and systems changes, employee education and resources and there is no guarantee that we be able to implement them adequately or prior to their effective date. Given HIPAA's complexity and the anticipated new regulations, which may be subject to changing and perhaps conflicting interpretation, our ongoing ability to comply with all of the HIPAA requirements is uncertain, which may expose us to the criminal and increased civil penalties provided under HITECH and may require us to incur significant costs in order to seek to comply with its requirements.
While we currently expend significant resources and have implemented solutions, processes and procedures to protect against cyber-attacks and security breaches and have no evidence to suggest that such attacks have resulted in a breach of our systems, we may need to expend additional significant resources in the future to continue to protect against potential security breaches or to address problems caused by such attacks or any breach of our systems. Because the techniques used to circumvent security systems can be highly sophisticated and change frequently, often are not recognized until launched against a target, and may originate from less regulated and remote areas around the world, we may be unable to proactively address these techniques or to implement adequate preventive measures.
Despite the security measures we have in place to ensure compliance with applicable laws and rules, our facilities and systems, and those of our third-party service providers, may be vulnerable to security breaches, acts of vandalism, acts of malicious insiders, computer viruses, misplaced or lost data, programming and/or human errors, or other similar events. Any security breach involving the misappropriation, loss or other unauthorized disclosure or use of confidential member information, whether by us or a third party, could subject us to civil and criminal penalties, divert management's time and energy and have a material adverse effect on our business, financial condition, cash flows, or results of operations.
Risks Related to the Operation of Our Molina Medicaid Solutions BusinessSegment
We may be unable to retain or renew the state government contracts of the Molina Medicaid Solutions segment on terms consistent with our expectations or at all.
Molina Medicaid Solutions currently has management contracts in only six states. If we are unable to continue to operate in any of those six states, or if our current operations in any of those six states are significantly curtailed, the revenues and cash flows of Molina Medicaid Solutions could decrease materially, and as a result our profitability would be negatively impacted.
If the responsive bids to RFPs of Molina Medicaid Solutions are not successful, our revenues could be materially reduced and our operating results could be negatively impacted.
The government contracts of Molina Medicaid Solutions may be subject to periodic competitive bidding. In such process, Molina Medicaid Solutions may face competition as other service providers, some with much greater financial resources and greater name recognition, attempt to enter our markets through the competitive bidding process. For instance, in 2012, the government contract of Molina Medicaid Solutions in Louisiana was subject to competitive bidding, and we were unsuccessful in being awarded a new contract. Molina Medicaid Solutions also anticipates bidding in other states which have issued RFPs for procurement of a new MMIS. In the event our responsive bids in other states are not successful, we will be unable to grow in a manner consistent with our projections. Even if our responsive bids are successful, the bids may be based upon assumptions or other factors which could result in the contract being less profitable than we had expected or had been the case prior to competitive re-bidding.
Because of the complexity and duration of the services and systems required to be delivered under the government contracts of Molina Medicaid Solutions, there are substantial risks associated with full performance under the contracts.
The state contracts of Molina Medicaid Solutions typically require significant investment in the early stages that is expected to be recovered through billings over the life of the contracts. These contracts involve the construction of new computer systems and communications networks and the development and deployment of complex technologies. Substantial performance risk exists under each contract. Some or all elements of service delivery under these contracts are dependent upon successful completion of the design, development, construction, and implementation phases. Any increased or unexpected costs or unanticipated delays in connection with the performance of these contracts, including delays caused by factors outside our control, could make these contracts less profitable or unprofitable, which could have an adverse effect on our overall business, financial condition, cash flows, andor results of operations.
If we fail to comply with our state government contracts or government contracting regulations, our business maycould be adversely affected.
Molina Medicaid Solutions'Solutions’ contracts with state government customers may include unique and specialized performance requirements. In particular, contracts with state government customers are subject to various procurement regulations, contract provisions, and other requirements relating to their formation, administration, and performance. Any failure to comply with the specific provisions in our customer contracts or any violation of government contracting regulations could result in the imposition of various civil and criminal penalties, which may include termination of the contracts, forfeiture of profits, suspension of payments, imposition of fines, and suspension from future government contracting. Further, any negative publicity related to our state government contracts or any proceedings surrounding them may damage our business by affecting our ability to compete for new contracts. The termination of a state government contract, our suspension from government work, or any negative impact on our ability to compete for new contracts, could have ana material adverse effect on our business, financial condition, cash flows, andor results of operations.
System security risks and systems integration issues that disrupt our internal operations or information technology services provided to customers could adversely affect our financial results and damage our reputation.
Experienced computerComputer programmers and hackers may be able to penetrate our network security and misappropriate our confidential information or that of third parties, create system disruptions, or cause shutdowns. Computer programmers and hackers also may be able to develop and deploy viruses, worms, and other malicious software programs that attack our products or otherwise exploit any security vulnerabilities of our products. In addition, sophisticated hardware and operating system software and applications that we produce or procure from third parties may contain defects in design or manufacture, including “bugs”"bugs" and other problems that could unexpectedly interfere with the operation of the system. The costs to us to eliminate or alleviate security problems, bugs, viruses, worms, malicious software programs and security vulnerabilities could be significant, and the efforts to address these problems could result in interruptions, delays, cessation of service, and loss of existing or potential government customers.
Molina Medicaid Solutions routinely processes, stores, and transmits large amounts of data for our clients, including sensitive and personally identifiable information. Breaches of our security measures could expose us, our customers, or the individuals affected to a risk of loss or misuse of this information, resulting in litigation and potential liability for us and damage to our
brand and reputation. Accordingly, we could lose existing or potential government customers for outsourcing services or other information technology solutions or incur significant expenses in connection with our customers'customers’ system failures or any actual or perceived security vulnerabilities in our products. In addition, the cost and operational consequences of implementing further data protection measures could be significant.
Portions of our information technology infrastructure also may experience interruptions, delays, or cessations of service or produce errors in connection with systems integration or migration work that takes place from time to time. We may not be successful in implementing new systems and transitioning data, which could cause business disruptions and be more expensive, time consuming, disruptive, and resource-intensive. Such disruptions could adversely impact our ability to fulfill orders and interrupt other processes. Delayed sales, lower margins, or lost government customers resulting from these disruptions could adversely affect our financial results, reputation, and stock price.
In the course of providing services to customers, Molina Medicaid Solutions may inadvertently infringe on the intellectual property rights of others and be exposed to claims for damages.
The solutions we provide to our state government customers may inadvertently infringe on the intellectual property rights of third parties resulting in claims for damages against us. The expense and time of defending against these claims may have a material and adverse impact on our profitability. Additionally, the publicity we may receive as a result of infringing intellectual property rights may damage our reputation and adversely impact our ability to develop new MMIS business or retain existing MMIS business.
Inherent in the government contracting process are various risks which may materially and adversely affect our business and profitability.
We are subject to the risks inherent in the government contracting process. These risks include government audits of billable contract costs and reimbursable expenses and compliance with government reporting requirements. In the event we are found to be out of compliance with government contracting requirements, our reputation may be adversely impacted and our relationship with the government agencies we work with may be damaged, resulting in a material and adverse effect on our profitability.
Our performance on contracts, including those on which we have partnered with third parties, may be adversely affected if we or the third parties fail to deliver on commitments.
In some instances, our contracts require that we partner with other parties, including software and hardware vendors, to provide the complex solutions required by our state government customers. Our ability to deliver the solutions and provide the services required by our customers is dependent on our and our partners'partners’ ability to meet our customers'customers’ delivery schedules. If we or our partners fail to deliver services or products on time, our ability to complete the contract may be adversely affected, which may have a material and adverse impact on our revenuerevenues and profitability.
Risks Related to our General Business Operations
Ineffective management of our growth may negatively affect our business, financial condition, andor results of operations.
Depending on acquisitions and other opportunities, weWe expect to continue to grow our membership and to expand into other markets.markets through acquisitions and other opportunities. Continued rapid growth could place a significant strain on our management and on our other Company resources. Our ability to manage our growth may depend on our ability to strengthen our management team and attract, train, and retain skilled employees, and our ability to implement and improve operational, financial, and management information systems on a timely basis. If we are unable to manage our growth effectively, our business, financial condition, cash flows, andor results of operations could be materially and adversely affected. In addition, due to the initial substantial costs related to acquisitions, rapid growth could adversely affect our short-term profitability and liquidity.
Any changes to the laws and regulations governing our business, or the interpretation and enforcement of those laws or regulations, could cause us to modify our operations and could negatively impact our operating results.
Our business is extensively regulated by the federal government and the states in which we operate. The laws and regulations governing our operations are generally intended to benefit and protect health plan members and providers rather than managed care organizations. The government agencies administering these laws and regulations have broad latitude in interpreting and applying them. These laws and regulations, along with the terms of our government contracts, regulate how we do business, what services we offer, and how we interact with members and the public. For instance, some states mandate minimum medical expense levels as a percentage of premium revenues. These laws and regulations, and their interpretations, are subject to frequent change. The interpretation of certain contract provisions by our governmental regulators may also change. Changes in existing laws or regulations, or their interpretations, or the enactment of new laws or regulations, could reduce our profitability by imposing additional capital requirements, increasing our liability, increasing our administrative and other costs, increasing mandated benefits, forcing us to restructure our relationships with providers, or requiring us to implement additional or
different programs and systems. Changes in the interpretation of our contracts could also reduce our profitability if we have detrimentally relied on a prior interpretation.
Our business depends on our information and medical management systems, and our inability to effectively integrate, manage, and keep secure our information and medical management systems could disrupt our operations.
Our business is dependent on effective and secure information systems that assist us in, among other things, processing provider claims, monitoring utilization and other cost factors, supporting our medical management techniques, and providing data to our regulators. Our providers also depend upon our information systems for membership verifications, claims status, and other information. If we experience a reduction in the performance, reliability, or availability of our information and medical management systems, our operations, ability to pay claims, and ability to produce timely and accurate reports could be adversely affected. In addition, if the licensor or vendor of any software which is integral to our operations were to become insolvent or otherwise fail to support the software sufficiently, our operations could be negatively affected.
Our information systems and applications require continual maintenance, upgrading, and enhancement to meet our operational needs. Moreover, our acquisition activity requires transitions to or from, and the integration of, various information systems. If we experience difficulties with the transition to or from information systems or are unable to properly implement, maintain, upgrade or expand our system, we could suffer from, among other things, operational disruptions, loss of members, difficulty in attracting new members, regulatory problems, and increases in administrative expenses.
Our business requires the secure transmission of confidential information over public networks. Advances in computer capabilities, new discoveries in the field of cryptography, or other events or developments could result in compromises or breaches of our security systems and member data stored in our information systems. Anyone who circumvents our security measures could misappropriate our confidential information or cause interruptions in services or operations. The internet is a public network, and data is sent over this network from many sources. In the past, computer viruses or software programs that disable or impair computers have been distributed and have rapidly spread over the internet. Computer viruses could be introduced into our systems, or those of our providers or regulators, which could disrupt our operations, or make our systems inaccessible to our members, providers, or regulators. We may be required to expend significant capital and other resources to protect against the threat of security breaches or to alleviate problems caused by breaches. Because of the confidential health information we store and transmit, security breaches could expose us to a risk of regulatory action, litigation, possible liability, and loss. Our security measures may be inadequate to prevent security breaches, and our business operations would be negatively impacted by cancellation of contracts and loss of members if security breaches are not prevented.
Because our corporate headquarters are located in Southern California, our business operations may be significantly disrupted as a result of a major earthquake.
Our corporate headquarters is located in Long Beach, California. In addition, the claims of our health plans are also processed in Long Beach. Southern California is exposed to a statistically greater risk of a major earthquake than most other parts of the United States. If a major earthquake were to strike the Los Angeles area, our corporate functions and claims processing could be
significantly impaired for a substantial period of time. Although we have established a disaster recovery and business resumption plan with back-up operating sites to be deployed in the case of such a major disruptive event, there can be no assurances that the disaster recovery plan will be successful or that the business operations of all our health plans, including those that are remote from any such event, would not be substantially impacted by a major Southern California earthquake.
We face claims related to litigation which could result in substantial monetary damages.
We are subject to a variety of legal actions, including medical malpractice actions, provider disputes, employment related disputes, and breach of contract actions. In the event we incur liability materially in excess of the amount for which we have insurance coverage, our profitability would suffer. In addition, our providers involved in medical care decisions are exposed to the risk of medical malpractice claims. As an employer of physicians and ancillary medical personnel and as an operator of primary care clinics, our plans are subject to liability for negligent acts, omissions, or injuries occurring at one of theirour clinics or caused by one of theirour employees. We maintain medical malpractice insurance for our clinics in an amount which we believe to be reasonable in light of our experience to date. However, given the significant amount of some medical malpractice awards and settlements, this insurance may not be sufficient or available at a reasonable cost to protect us from damage awards or other liabilities. Even if any claims brought against us are unsuccessful or without merit, we may have to defend ourselves against such claims. The defense of any such actions may be time-consuming and costly, and may distract our management'smanagement’s attention. As a result, we may incur significant expenses and may be unable to effectively operate our business.
Furthermore, claimants often sue managed care organizations for improper denials of or delays in care, and in some instances improper authorizations of care. Claims of this nature could result in substantial damage awards against us and our providers that could exceed the limits of any applicable medical malpractice insurance coverage. Successful malpractice or tort claims asserted against us, our providers, or our employees could adversely affect our business, financial condition, and profitability.cash flows, or results of operations.
We cannot predict the outcome of any lawsuit with certainty. While we currently have insurance coverage for some of the potential liabilities relating to litigation, other such liabilities may not be covered by insurance, the insurers could dispute coverage, or the amount of insurance could be insufficient to cover the damages awarded. In addition, insurance coverage for all or certain types of liability may become unavailable or prohibitively expensive in the future or the deductible on any such insurance coverage could be set at a level which would result in us effectively self-insuring cases against us.
Although we establish reserves for litigation as we believe appropriate, we cannot provide assuranceassure you that our recorded reserves will be adequate to cover such costs. Therefore, the litigation to which we are subject could have a material adverse effect on our business, financial condition, cash flows, and results of operations, and cash flows, and could prompt us to change our operating procedures.
We are subject to competition which negatively impacts our ability to increase penetration in the markets we serve and could result in the loss of members to other health plans.serve.
We operate in a highly competitive environment and in an industry that is subject to ongoing changes from business consolidations, new strategic alliances, and aggressive marketing practices by other managed care organizations. We compete for members principally on the basis of size, location, and quality of provider network, benefits supplied, quality of service, and reputation. A number of these competitive elements are partially dependent upon and can be positively affected by the financial resources available to a health plan. Many other organizations with which we compete, including large commercial plans, have substantially greater financial and other resources than we do. For these reasons, we may be unable to grow our membership, or may lose members to other health plans.
Failure to maintain effective internal controls over financial reporting could have a material adverse effect on our business, operating results, and stock price.
The Sarbanes-Oxley Act of 2002 requires, among other things, that we maintain effective internal controlscontrol over financial reporting. In particular, we must perform system and process evaluation and testing of our internal controls over financial reporting to allow management to report on, and our independent registered public accounting firm to attest to, our internal controls over financial reporting as required by Section 404 of the Sarbanes-Oxley Act of 2002. Our future testing, or the subsequent testing by our independent registered public accounting firm, may reveal deficiencies in our internal controls over financial reporting that are deemed to be material weaknesses. Our compliance with Section 404 will continue to require that we incur substantial accounting expense and expend significant management time and effort. Moreover, if we are not able to continue to comply with the requirements of Section 404 in a timely manner, or if we or our independent registered public accounting firm identifiesidentify deficiencies in our internal control over financial reporting that are deemed to be material weaknesses, the market price of our stock could decline and we could be subject to sanctions or investigations by the New York Stock Exchange,NYSE, SEC, or other regulatory authorities which would require additional financial and management resources.
Changes in accounting may affect our results of operations.
U.S. generally accepted accounting principles (GAAP) and related implementation guidelines and interpretations can be highly complex and involve subjective judgments. Changes in these rules or their interpretation, or the adoption of new pronouncements could significantly affect our stated results of operations.
The value of our investments is influenced by varying economic and market conditions, and a decrease in value could have an adverse effect on our results of operations, liquidity, and financial condition.
Our investments consist solely of investment-grade debt securities. The unrestricted portion of this portfolio is designated as available-for-sale. Our non-current restricted investments are designated as held-to-maturity. Available-for-sale investments are carried at fair value, and the unrealized gains or losses are included in accumulated other comprehensive income or loss as a separate component of stockholders'stockholders’ equity, unless the decline in value is deemed to be other-than-temporary and we do not have the intent and ability to hold such securities until their full cost can be recovered. For our available-for-sale investments and held-to-maturity investments, if a decline in value is deemed to be other-than-temporary and we do not have the intent and ability to hold such security until its full cost can be recovered, the security is deemed to be other-than-temporarily impaired and it is written down to fair value and the loss is recorded as an expense.
In accordance with applicable accounting standards, we review our investment securities to determine if declines in fair value below cost are other-than-temporary. This review is subjective and requires a high degree of judgment. We conduct this review on a quarterly basis, using both quantitative and qualitative factors, to determine whether a decline in value is other-than-temporary. Such factors considered include the length of time and the extent to which market value has been less than cost, the financial condition and near term prospects of the issuer, recommendations of investment advisors, and forecasts of economic, market or industry trends. This review process also entails an evaluation of our ability and intent to hold individual securities until they mature or full cost can be recovered.
The current economic environment and recent volatility of the securities markets increase the difficulty of assessing investment impairment and the same influences tend to increase the risk of potential impairment of these assets. Over time, the economic and market environment may provide additional insight regarding the fair value of certain securities, which could change our
judgment regarding impairment. This could result in realized losses relating to other-than-temporary declines to be recorded as an expense. Given the current market conditions and the significant judgments involved, there is continuing risk that declines in fair value may occur and material other-than-temporary impairments may result in realized losses in future periods which could have ana material adverse effect on our business, financial condition, cash flows, andor results of operations.
Unanticipated changes in our tax rates or exposure to additional income tax liabilities could affect our profitability.
We are subject to income taxes in the United States. Our effective tax rate could be adversely affected by changes in the mix of earnings in states with different statutory tax rates, changes in the valuation of deferred tax assets and liabilities, changes in U.S. tax laws and regulations, and changes in our interpretations of tax laws, including pending tax law changes, such as the ACAhealth care federal excise tax discussed above. In addition, we are subject to the routine examination of our income tax returns by the Internal Revenue Service and other local and state tax authorities. We regularly assess the likelihood of outcomes resulting from these examinations to determine the adequacy of our estimated income tax liabilities. Adverse outcomes from tax examinations could have ana material adverse effect on our provision for income taxes, estimated income tax liabilities, andor results of operations.
We are dependent on our executive officers and other key employees.
Our operations are highly dependent on the efforts of our executive officers. The loss of their leadership, knowledge, and experience could negatively impact our operations. Replacing many of our executive officers might be difficult or take an extended period of time because a limited number of individuals in the managed care industry have the breadth and depth of skills and experience necessary to operate and expand successfully a business such as ours. Our success is also dependent on our ability to hire and retain qualified management, technical, and medical personnel. It is critical that we recruit, manage, enable, and retain talent to successfully execute our strategic objections which requires aligned policies, a positive work environment, and a robust succession and talent development process. Further, particularly in light of the changing health carehealthcare environment, we must focus on building employee capabilities to help ensure that we can meet upcoming challenges and opportunities. If we are unsuccessful in recruiting, retaining, managing, and enabling such personnel and are unable to meet upcoming challenges and opportunities, our operations could be negatively impacted.
We are subject to risks associated with outsourcing services and functions to third parties.
We contract with independent third party vendors and service providers who provide services to us and our subsidiaries or to whom we delegate selected functions. Our arrangements with third party vendors and service providers may make our operations vulnerable if those third parties fail to satisfy their obligations to us, including their obligations to maintain and protect the security and confidentiality of our information and data. In addition, we may have disagreements with third party vendors and service providers regarding relative responsibilities for any such failures under applicable business associate agreements or other applicable outsourcing agreements. Further, we may not be adequately indemnified against all possible losses through the terms and conditions of our contracts with third party vendors and service providers. Our outsourcing arrangements could be adversely impacted by
changes in vendors'vendors’ or service providers'providers’ operations or financial condition or other matters outside of our control. If we fail to adequately monitor and regulate the performance of our third party vendors and service providers, we could be subject to additional risk. Violations of, or noncompliance with, laws and/or regulations governing our business or noncompliance with contract terms by third party vendors and service providers could increase our exposure to liability to our members, providers, or other third parties, or sanctions and/or fines from the regulators that oversee our business. In turn, this could increase the costs associated with the operation of our business or have an adverse impact on our business and reputation. Moreover, if these vendor and service provider relationships were terminated for any reason, we may not be able to find alternative partners in a timely manner or on acceptable financial terms, and may incur significant costs in connection with any such vendor or service provider transition. As a result, we may not be able to meet the full demands of our customers and, in turn, our business, financial condition, andor results of operations may be harmed. In addition, we may not fully realize the anticipated economic and other benefits from our outsourcing projects or other relationships we enter into with third party vendors and service providers, as a result of regulatory restrictions on outsourcing, unanticipated delays in transitioning our operations to the third party, vendor or service provider noncompliance with contract terms or violations of laws and/or regulations, or otherwise. This could result in substantial costs or other operational or financial problems that could adversely impact our business, financial condition, andcash flows, or results of operations.
An impairment charge with respect to our recorded goodwill, and indefinite-lived intangible assets, or our finite-lived intangible assets, could have a material impact on our financial results.
As of December 31, 2012,2014, the balance of goodwill was $272.0 million, and indefinite-livedthe balance of intangible assets, net, was $151.1$89.3 million. Goodwill and indefinite-lived intangibleIntangible assets are amortized generally on a straight-line basis over their estimated useful lives.
Goodwill represents the amount of the purchase price in excess of the fair values assigned to the underlying identifiable net assets of acquired businesses. Goodwill is not amortized, but areis subject to an annual impairment testing. Testing istest. Tests are performed more frequently if events occur or circumstances change that would more likely than not reduce the fair value of the underlyinga reporting units unit
below theirits carrying amounts. The underlying reporting units generally comprise our health plan subsidiaries and our Molina Medicaid Solutions segment. As of December 31, 2012, the balance of intangible assets, net, was $77.7 million. Intangible assets are amortized generally on a straight-line basis over their estimated useful lives.amount. Our intangible assets are subject to impairment tests when events or circumstances indicate that such an asset'sa finite-lived intangible asset’s (or asset group's)group’s) carrying value may not be recoverable. Consideration is given
The determination of the value of goodwill, and intangible assets, net, requires us to a number of potential impairment indicators, including legal factors, market conditions,make estimates and operational performance.assumptions about estimated asset lives, future business trends, and growth. Such evaluation is significantly impacted by estimates and assumptions of future revenues, costs and expenses, and other factors.
For example, our health plan subsidiaries have generally been successful in obtaining the renewal by amendment of their contracts in each state prior to the actual expiration of their contracts. However, there can be no assurance that these contracts will continue to be renewed. The non-renewal of such a contract would be an indicator of impairment.
If an event or events occur that would cause us to revise our estimates and assumptions used in analyzing the value of our goodwill, and indefinite-lived intangible assets, and intangible assets, net, such revision could result in a non-cash impairment charge that could have a material adverse impact on our financial results.
We are subject to the risks of owning and leasing real property.
We ownare a tenant under numerous leases in multiple states, including a 25-year lease of an approximately 460,000 square foot office building housing our principal executive offices which we purchased in a transaction that closed on December 7, 2011.Long Beach, California. We also own a nearby 32,000186,000 square-foot office building in Long Beach, California,Troy, Michigan, a 160,000 square-foot office building in Columbus, Ohio, a 26,00026,700 square-foot data center in Albuquerque, New Mexico, and a 24,000 square-foot mixed use (office and clinic) facilitycommunity clinic in Pomona, California. Accordingly, we are subject to all of the risks generally associated with leasing and owning real estate, which include, but are not limited to: the possibility of environmental contamination, the costs associated with fixing any environmental problems and the risk of damages resulting from such contamination; risks related to natural disasters, such as earthquakes, flooding or severe weather; adverse changes in the value of the property due to interest rate changes, changes in the neighborhood in which the property is located, or other factors; ongoing maintenance expenses and costs of improvements; the possible need for structural improvements in order to comply with changes in zoning, seismic, disability act, or other requirements; inability to renew or enter into leases for space not utilized by the Companyus on commercially acceptable terms or at all; and possible disputes with neighboring owners or other individuals and entities.
Because we have guaranteed one of our subsidiary's obligations under a loan agreement, if this subsidiary fails to meet its obligations under the loan agreement, we may be required to satisfy such obligations, and such an undertaking could have an adverse affect on our financial condition.
On December 7, 2011, Molina Center LLC, or Molina Center, a wholly owned subsidiary of the Company, entered into a Term Loan Agreement with various lenders and East West Bank, as Administrative Agent, to borrow the aggregate principal amount of $48.6 million to finance a portion of the $81 million purchase price for the acquisition of the office building housing our corporate headquarters. While all amounts due under the Term Loan Agreement and related loan documents are secured by a security interest in the office building in favor of and for the benefit of the Administrative Agent and the other lenders under the Term Loan Agreement, the Company has additionally guaranteed Molina Center's obligations of payment and performance under the Term Loan Agreement, certain promissory notes executed in connection therewith, and other loan documents. The maximum amount of the promissory notes for which the Company is liable under the Guaranty will in no event exceed $20 million, but there
is no cap on the Company's total liability under the Guaranty. Furthermore, Molina Center and the Company also entered into an Environmental Indemnity in favor of the Administrative Agent and the other lenders pursuant to which the Company, jointly and severally with Molina Center, has agreed to indemnify and hold harmless the Administrative Agent and each of the other lenders under the Term Loan Agreement from and against any loss, damage, cost, expense, claim, or liability directly or indirectly arising out of or attributable to the use, generation, storage, release, discharge or disposal, or presence of certain hazardous materials on or about the office building. Neither the Company's nor Molina Center's liability under the Environmental Indemnity is limited by a maximum dollar amount. If Molina Center is unable to comply with the various customary financial covenants of the Term Loan Agreement, if it defaults under the Term Loan Agreement or if there are major environmental liabilities attributed to hazardous materials, such events could have an adverse effect on our business, financial condition, cash flows, and results of operations.
Risks Related to Our Common Stock
Delaware law and our charter documents may impede or discourage a takeover, which could cause the market price of our common stock to decline.
We are subjecta Delaware corporation, and the anti-takeover provisions of Delaware law impose various impediments to the Delaware anti-takeover laws regulating corporate takeovers. These provisions may prohibit stockholders owning 15% or moreability of our outstanding voting stock from merging or combining with us. In addition, any change ina third party to acquire control of our state health plans would require the approval of the applicable insurance regulator in each state in which we operate.
Our certificate of incorporation and bylaws also contain provisions that could have the effect of delaying, deferring, or preventingus, even if a change in control ofwould be beneficial to our company that stockholders may consider favorable or beneficial. These provisions could discourage proxy contests and make it more difficult forexisting stockholders. In addition, our stockholders to elect directors and take other corporate actions. These provisions could also limit the price that investors might be willing to pay in the future for shares of our common stock. These provisions include:
a staggered board of directors so that it would take three successive annual meetings to replace all directors,
prohibition of stockholder action by written consent,
advance notice requirements foror a committee thereof has the submission by stockholders of nominations for election to the board of directors and for proposing matters that can be acted upon by stockholders at a meeting, and
the ability of our board of directors,power, without stockholder approval, to designate the terms of one or more series of preferred stock and issue shares of preferred stock.
In addition, changes of control are often subject to state regulatory notification, and in some cases, prior approval.
Volatility The ability of our board of directors or a committee thereof to create and issue a new series of preferred stock priceand certain provisions of Delaware law and our certificate of incorporation and bylaws could adversely affect stockholders.
Since our initial public offering in July 2003, the sales price ofimpede a merger, takeover or other business combination involving us or discourage a potential acquirer from making a tender offer for our common stock, has ranged from a low of $10.75 to a high of $36.83. A number of factorswhich, under certain circumstances, could continue to influencereduce the market price of our common stock including:
and the implementation of the ACA and duals demonstration programs,
state and federal budget pressures,
changes in expectations as to our future financial performance or changes in financial estimates, if any, by us or by security analysts or investors,
revisions in securities analysts' estimates,
announcements by us or our competitors of significant acquisitions or dispositions, strategic partnerships, joint ventures, or capital commitments,
announcements relating to our business or the businessvalue of our competitors,
changes in government payment levels,
adverse publicity regarding health maintenance organizations and other managed care organizations,
government action regarding member eligibility,
changes in state mandatory programs,
conditions generally affecting the managed care industry or our provider networks,
the success of our operating or acquisition strategy,
the operating and stock price performance of other comparable companies in the health care industry,
the termination of our Medicaid or CHIP contracts with state or county agencies, or subcontracts with other Medicaid managed care organizations that contract with such state or county agencies,
regulatory or legislative change,
general economic conditions, including unemployment rates, inflation, and interest rates, and
the other factors set forth under “Risk factors” in this Annual Report on Form 10-K.
Our common stock may not trade at the same levels as the stock of other health care companies or the market in general. Also, if the trading market for our common stock does not continue to develop, securities analysts may not maintain or initiate research coverage of us and our common stock, and this could depress the market for our common stock.convertible senior notes.
Members of the Molina family own a significant amount of our capital stock, decreasing the influence of other stockholders on stockholder decisions.
Members of the Molina family, either directly or as trustees or beneficiaries of Molina family trusts, in the aggregate ownowned or arewere entitled to receive upon certain events approximately 37%32% of our capital stock as of December 31, 2012.2014. Our president and chief executive officer, as well as our chief financial officer, are members of the Molina family, and they are also on our board of directors. Because of the amount of their shareholdings, Molina family members, if they were to act as a group with the trustees of their family trusts, have the ability to significantly influence all matters submitted to stockholders for approval, including the election of directors, amendments to our charter, and any merger, consolidation, or sale of the Company.our company. A significant concentration of share ownership can also adversely affect the trading price for our common stock because investors often discount the value of stock in companies that have controlling stockholders. Furthermore, the concentration of share ownership in the Molina family could delay or prevent a merger or consolidation, takeover, or other business combination that could be favorable to our stockholders. Finally, the interests and objectives of the Molina family may be different from those of our company or our other stockholders, and they may vote their common stock in a manner that is contrary to the vote of our other stockholders.
Future sales of our common stock or equity-linked securities in the public market could adversely affect the trading price of our common stock and our ability to raise funds in new stock offerings.
We may issue equity securities in the future, or securities that are convertible into or exchangeable for, or that represent the right to receive, shares of our common stock. Sales of a substantial number of shares of our common stock or other equity securities, including sales of shares in connection with any future acquisitions, could be substantially dilutive to our stockholders. These sales may have a harmful effect on prevailing market prices for our common stock and our ability to raise additional capital in the financial markets at a time and price favorable to us. Moreover, to the extent that we issue restricted stock units, stock appreciation rights, options, or warrants to purchase our common stock in the future and those stock appreciation rights, options, or warrants are exercised or as the restricted stock units vest, our stockholders may experience further dilution. Holders of our shares of common stock have no preemptive rights that entitle holders to purchase a pro rata share of any offering of shares of any class or series and, therefore, such sales or offerings could result in increased dilution to our stockholders. Our certificate of incorporation provides that we have authority to issue 80,000,000150,000,000 shares of common stock and 20,000,000 shares of preferred stock. As of December 31, 2012,2014, approximately 46,762,00049,727,000 shares of common stock and no shares of preferred or other capital stock were issued and outstanding.
It may be difficult for a third party to acquire us, which could inhibit stockholders from realizing a premium on their stock price.
We are subject to the Delaware anti-takeover laws regulating corporate takeovers. These provisions may prohibit stockholders owning 15% or more of our outstanding voting stock from merging or combining with us. In addition, any change in control of our state health plans would require the approval of the applicable insurance regulator in each state in which we operate.
Our certificate of incorporation and bylaws also contain provisions that could have the effect of delaying, deferring, or preventing a change in control of our company that stockholders may consider favorable or beneficial. These provisions could discourage proxy contests and make it more difficult for our stockholders to elect directors and take other corporate actions. These provisions could also limit the price that investors might be willing to pay in the future for shares of our common stock. These provisions include:
a staggered board of directors, so that it would take three successive annual meetings to replace all directors,
prohibition of stockholder action by written consent, and
advance notice requirements for the submission by stockholders of nominations for election to the board of directors and for proposing matters that can be acted upon by stockholders at a meeting.
In addition, changes of control are often subject to state regulatory notification, and in some cases, prior approval.
Item 1B:Unresolved Staff Comments
None.
Item 2:Properties
We leaseAs of December 31, 2014, the Health Plans segment leases a total of 7570 facilities and the Molina Medicaid Solutions segment leases a total of 12 facilities. We own a 460,000 square foot office building housing our corporate headquarters in Long Beach, California, and we also own a nearby 32,000186,000 square-foot office building in Long Beach, California,Troy, Michigan, a 160,000 square-foot office building in Columbus, Ohio, a 26,00026,700 square-foot data center in Albuquerque, New Mexico, and a 24,000 square-foot mixed use (office and clinic) facility in Pomona, California. We anticipate leasing additional space in the Long Beach, California area during 2013.under our Health Plans segment. While we believe our current and anticipated facilities will be adequate to meet our operational needs for the foreseeable future, we are continuing to periodically evaluate our employee and operations growth prospects to determine if additional space is required, and where it would be best located.
Item 3:Legal Proceedings
The health care industry isand business process outsourcing industries are subject to numerous laws and regulations of federal, state, and local governments. Compliance with these laws and regulations can be subject to government review and interpretation, as well as regulatory actions unknown and unasserted at this time. Penalties associated with violations of these laws and regulations include significant fines and penalties, exclusion from participating in publicly-fundedpublicly funded programs, and the repayment of previously billed and collected revenues.
We are involved in various legal actions in the normalordinary course of business, some of which seek monetary damages, including claims for punitive damages, which are not covered by insurance. Based uponWe have accrued liabilities for certain matters for which we deem the evaluation of information currently available,loss to be both probable and estimable. Although we believe that our estimates of such losses are reasonable, these estimates could change as a result of further developments of these matters. The outcome of legal actions when finally concludedis inherently uncertain and determined, aresuch pending matters for which accruals have not likelybeen established have not progressed sufficiently through discovery and/or development of important factual information and legal issues to enable us to estimate a range of possible loss, if any. While it is not possible to accurately predict or determine the eventual outcomes of these items, an adverse determination in one or more of these pending matters could have a material adverse effect on our business,consolidated financial condition, cash flows, orposition, results of operations.operations, or cash flows.
State of Louisiana v. Molina Medicaid Solutions et al. On June 26, 2014, the state of Louisiana filed a Petition for Damages against Molina Medicaid Solutions, Molina Healthcare, Inc., Unisys Corporation, and Paramax Systems Corporation, a subsidiary of Unisys, in the Parish of Baton Rouge, 19th Judicial District, versus number 631612. The Petition alleges that between 1989 and 2012, the defendants utilized an incorrect reimbursement formula for the payment of pharmaceutical claims. The petitioner seeks actual damages to be proved at trial, plus interest. We believe we have several meritorious defenses to the claims of the state, and any liability for the alleged claims is not currently probable or reasonably estimable.
USA and State of Florida ex rel. Charles Wilhelm v Molina Healthcare of Florida et al. On July 24, 2014, Molina Healthcare, Inc. and Molina Healthcare of Florida, Inc. were served with a Complaint filed under seal on December 5, 2012 in District Court for the Southern District of Florida by relator, Charles C. Wilhelm, M.D., Case No. 12-24298. The Complaint alleges that, in late 2008 and early 2009, in connection with the acquisition of Florida NetPass by which Molina Healthcare entered into the state of Florida, the defendants failed to adequately staff the plan and provide other services, resulting in a disproportionate number of sicker beneficiaries of Florida NetPass moving back into the Florida fee-for-service Medicaid program. This alleged conduct purportedly resulted in a violation of the federal False Claims Act. The relator seeks treble damages in the alleged amount of $62.3 million, plus interest and penalties. Both the United States of America and the state of Florida have declined to intervene. We believe we have several meritorious defenses to the claims of the relator, and any liability for the alleged claims is not currently probable or reasonably estimable.
United States of America, ex rel., Anita Silingo v. Mobile Medical Examination Services, Inc., et al. On or around October 14, 2014, Molina Healthcare of California, Molina Healthcare of California Partner Plan, Inc., Mobile Medical Examination Services, Inc. (MedXM), and other health plan defendants were served with a Complaint previously filed under seal in the Central District Court of California by relator, Anita Silingo, Case No. SACV13-1348-FMO(SHx). The Complaint alleges that MedXM improperly modified medical records and otherwise took inappropriate steps to increase members’ risk adjustment scores, and that the defendants, including Molina Healthcare of California and Molina Healthcare of California Partner Plan, Inc., purportedly turned a “blind eye” to these unlawful practices. The relator seeks treble damages in the amount of $3 billion, plus interest and penalties. The Department of Justice has declined to intervene. We believe that we have several meritorious defenses to the claims of the relator, and any liability for the alleged claims is not currently probable or reasonably estimable.
Item 4:Mine Safety Disclosures
None.
PART II
Item 5:Market for Registrant’s Common Equity, Related Stockholder Matters and Issuer Purchases of Equity Securities
Our common stock is listed on the New York Stock Exchange under the trading symbol “MOH.”"MOH." As of December 31, 2012,February 20, 2015, there were 130approximately 120 holders of record of our common stock. The high and low intra-day sales prices of our common stock for specified periods are set forth below:
| | | Date Range | High | | Low | High | | Low |
| 2012 | | | | |
| 2014 | | | | |
| First Quarter | $ | 36.83 |
| | $ | 22.25 |
| $ | 39.21 |
| | $ | 32.41 |
|
| Second Quarter | $ | 35.37 |
| | $ | 17.63 |
| $ | 46.17 |
| | $ | 32.86 |
|
| Third Quarter | $ | 27.73 |
| | $ | 21.62 |
| $ | 48.03 |
| | $ | 39.23 |
|
| Fourth Quarter | $ | 29.82 |
| | $ | 21.74 |
| $ | 54.57 |
| | $ | 40.79 |
|
| 2011 | | | | |
| 2013 | | | | |
| First Quarter | $ | 26.86 |
| | $ | 17.77 |
| $ | 33.85 |
| | $ | 25.70 |
|
| Second Quarter | $ | 29.03 |
| | $ | 24.72 |
| $ | 38.74 |
| | $ | 30.26 |
|
| Third Quarter | $ | 28.21 |
| | $ | 14.82 |
| $ | 40.90 |
| | $ | 33.31 |
|
| Fourth Quarter | $ | 26.31 |
| | $ | 13.93 |
| $ | 37.39 |
| | $ | 31.10 |
|
Dividends
To date we have not paid cash dividends on our common stock. We currently intend to retain any future earnings to fund our projected business growth. However, we intend to periodically evaluate our cash position to determine whether to pay a cash dividend in the future.
Our ability to pay dividends is partially dependent on, among other things, our receipt of cash dividends from our regulated subsidiaries. The ability of our regulated subsidiaries to pay dividends to us is limited by the state departments of insurance in the states in which we operate or may operate, as well as requirements of the government-sponsored health programs in which we participate. Any future determination to pay dividends will be at the discretion of our Board and will depend upon, among other factors, our results of operations, financial condition, capital requirements and contractual and regulatory restrictions. For more information regarding restrictions on the ability of our regulated subsidiaries to pay dividends to us, please see Item 7 —of this Form 10-K, Management’s Discussion and Analysis of Financial Condition and Results of Operations, — Liquidityin "Liquidity and Capital Resources, —Regulatory" under the subheading "Regulatory Capital and DividendsDividend Restrictions."
Unregistered Issuances of Equity Securities
None.
Stock Repurchase Programs
Common Stock Repurchase in Connection with Offering of 1.125% Cash Convertible Senior Notes Due 2020. We used a portion of the net proceeds in this offering to repurchase $50 million of our common stock in negotiated transactions with institutional investors in the offering, concurrently with the pricing of the offering. On February 12, 2013, we repurchased a total of 1,624,959 shares at $30.77 per share, which was our closing stock price on that date.
Securities Repurchases and Repurchase Programs. Effective as of February 13, 2013,25, 2015, our board of directors authorized the repurchase of $75up to $50 million in aggregate of either our common stock stock. Stock repurchases under this program may be made through open-market and/or our convertible senior note due 2014.privately negotiated transactions at times and in such amounts as management deems appropriate. The timing and actual number of shares repurchased will depend on a variety of factors including price, corporate and regulatory requirements and market conditions. This newly authorized repurchase program extends through December 31, 2014.
Effective as of October 26, 2011, our board of directors authorized the repurchase of $75 million in aggregate of either our common stock or our convertible senior notes due 2014. The repurchase program expired October 25, 2012. No securities were purchased under this program in 2012.2015.
Purchases of common stock made by or on behalf of the Company during the quarter ended December 31, 2012,2014, including shares withheld by the Company to satisfy our employees’ income tax obligations, are set forth below:
| | | | Total Number of Shares Purchased (a)(b) | | Average Price Paid per Share | | Total Number of Shares Purchased as Part of Publicly Announced Plans or Programs | | Maximum Number (or Approximate Dollar Value) of Shares That May Yet Be Purchased Under the Plans or Programs | Total Number of Shares Purchased (1) | | Average Price Paid per Share (1) | | Total Number of Shares Purchased as Part of Publicly Announced Plans or Programs (2) | | Approximate Dollar Value of Shares That May Yet Be Purchased Under the Plans or Programs (2) |
| October 1 — October 31 | 2,150 |
|
| $ | 25.03 |
| | — |
| | $ | — |
| 1,052 |
| | $ | 41.66 |
| | — |
| | $ | 47,338,505 |
|
| November 1 — November 30 | 1,892 |
|
| $ | 25.31 |
| | — |
| | $ | — |
| 1,781 |
| | $ | 48.64 |
| | — |
| | $ | 47,338,505 |
|
| December 1 — December 31 | 194,974 |
|
| $ | 27.97 |
| | — |
| | $ | — |
| 1,523 |
| | $ | 49.96 |
| | — |
| | $ | 47,338,505 |
|
| Total | 199,016 |
|
| $ | 27.91 |
| | — |
| | | |
| | | 4,356 |
| | $ | 47.42 |
| | — |
| | |
| |
(a) | During the three months ended December 31, 2012, we repurchased shares of our common stock from certain Molina family trusts. Janet M. Watt is the sister, and her husband Lawrence B. Watt is the brother-in-law, of Dr. J. Mario Molina, the Company's Chief Executive Officer, and John Molina, the Company's Chief Financial Officer. Ms. Watt is the sole trustee of the Janet M. Watt Separate Property Trust dated 10/22/2007 (the “Separate Property Trust”) and a co-trustee with Lawrence B. Watt, of the Watt Family Trust dated 10/11/1996 (the “Family Trust” and together with the Separate Property Trust, the “Trusts”). On December 26, 2012, pursuant to a Stock Purchase Agreement between the Company and the Trusts, the Company purchased an aggregate of 110,988 shares of its common stock from the Trusts for an aggregate purchase price of $3,000,005.64, as follows: (i) 43,767 shares from the Family Trust for an aggregate purchase price of $ 1,183,022.01 and (ii) 67,221 shares from the Separate Property Trust for an aggregate purchase price of $1,816,983.63. The shares were purchased at a price per share of $27.03, representing the closing price per share of the Company's common stock on December 26, 2012, as reported by the New York Stock Exchange. The transaction was approved by the Company's board of directors. Other than these repurchases from the Trusts, we did not repurchase any shares of our common stock outside of our publicly announced repurchase program except shares of common stock withheld to settle our employees' income tax obligations described below.
|
| |
(b)(1) | During the quarter we withheld 88,0284,356 shares of common stock under our 2002 Equity Incentive Plan and 2011 Equity Incentive Plan to settle our employees' income tax obligations. |
Securities Authorized for Issuance Under Equity Compensation Plans (as of December 31, 2012)
|
| | | | | | | | | | |
| Plan Category | Number of Securities to be Issued Upon Exercise of Outstanding Options, Warrants and Rights (a) | | Weighted Average Exercise Price of Outstanding Options, Warrants and Rights (b) | | Number of Securities Remaining Available for Future Issuance Under Equity Compensation Plans (Excluding Securities Reflected in Column (a)) (c) | |
| Equity compensation plans approved by security holders | 414,061 |
| (1) | $ | 22.39 |
| | 6,537,592 |
| (2) |
| |
(1) | Options to purchase shares of our common stock issued under the 2002 Equity Incentive Plan. Further grants under the 2002 Equity Incentive Plan have been suspended. |
| |
| (2) | Includes only shares remaining availableEffective as of September 30, 2013, our board of directors authorized the repurchase of up to issue under the 2011 Equity Incentive Plan, and the 2011 Employee Stock Purchase Plan. Further grants under the 2002 Equity Incentive Plan and the 2002 Employee Stock Purchase Plan have been suspended.$50 million in aggregate of our common stock. This repurchase program expired December 31, 2014. |
STOCK PERFORMANCE GRAPH
The following graph and related discussion are being furnished solely to accompany this Annual Report on Form 10-K pursuant to Item 201(e) of Regulation S-K and shall not be deemed to be “soliciting materials”"soliciting materials" or to be “filed”"filed" with the SEC (other than as provided in Item 201) nor shall this information be incorporated by reference into any future filing under the Securities Act or the Exchange Act, whether made before or after the date hereof and irrespective of any general incorporation language contained therein, except to the extent that the Company specifically incorporates it by reference into a filing.
The following line graph compares the percentage change in the cumulative total return on our common stock against the cumulative total return of the Standard & Poor's Corporation Composite 500 Index (the “S(S&P 500”), our old500) and a peer group index (as described below), and a new peer group index (as described below) for the five-year period from December 31, 20072009 to December 31, 2012. We have revised our peer group to match the peer group that is used by our Compensation Committee in benchmarking our executive officers' compensation.2014. The comparison assumes $100 was invested on December 31, 2007,2009, in the Company’s common stock and in each of the foregoing indices and assumes reinvestment of dividends. The stock performance shown on the graph below represents historical stock performance and is not necessarily indicative of future stock price performance.
The old peer group index, used in last year's Annual Report on Form 10-K and also set forth below, consists of Amerigroup Corporation (AGP), Centene Corporation (CNC), Coventry Health Care, Inc. (CVH), Health Net, Inc. (HNT), Humana, Inc. (HUM), UnitedHealth Group Incorporated (UNH), and WellPoint, Inc. (WLP).
The new peer group index consists of Centene Corporation (CNC), Community Health Systems, Inc. (CYH), Coventry Health Care, Inc. (CVH), Health Management Associates, Inc. (HMA), Health Net, Inc. (HNT), Laboratory Corporation of America Holdings (LH), Lifepoint Hospitals, Inc. (LPNT), Magellan Health Services, Inc. (MGLN), Select Medical Holdings Corporation (SEM), Team Health Holdings, Inc. (TMH), Triple-S Management Corporation (GTS), Universal American Corporation (UAM), and WellCare Health Plans, Inc. (WCG).
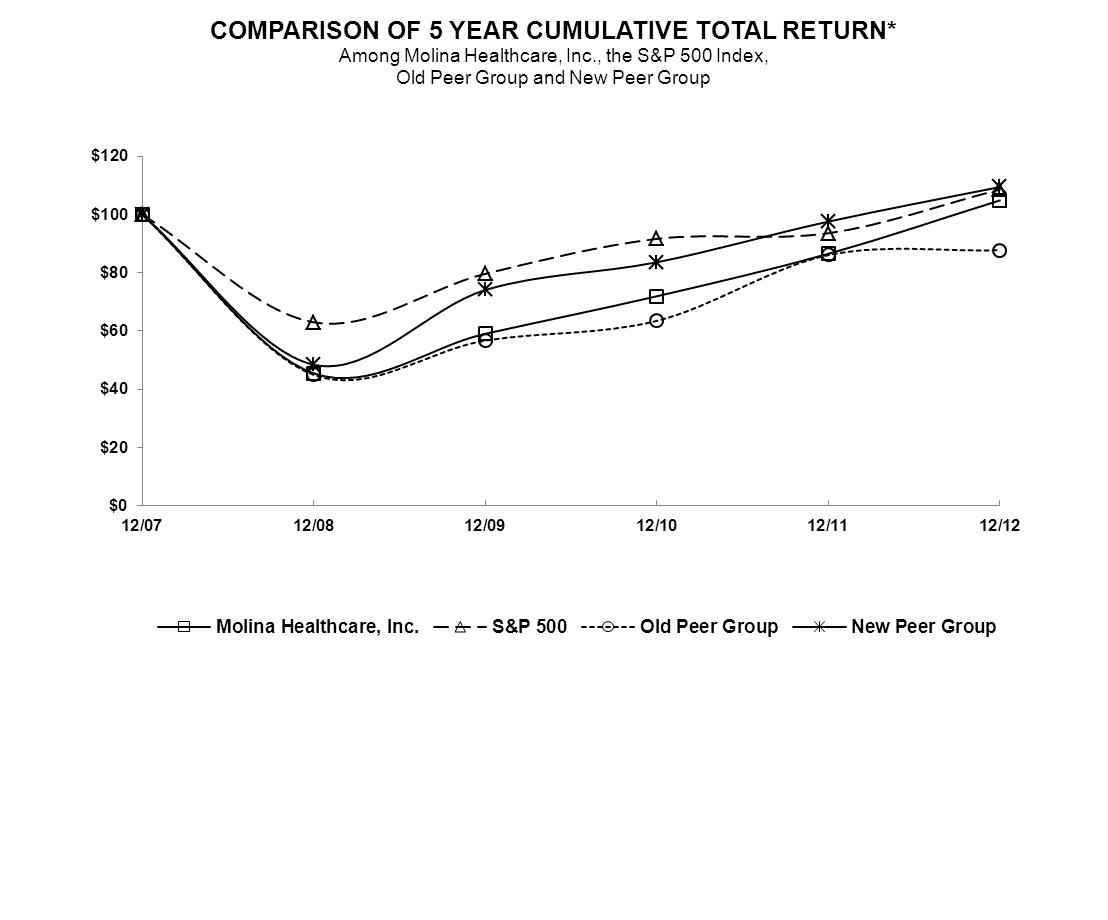
TableThe new peer group index consists of ContentsBrookdale Senior Living, Inc. (BKD), Catamaran Corporation (CTRX), Centene Corporation (CNC), Community Health Systems, Inc. (CYH), DaVita HealthCare Partners, Inc. (DVA), Health Net, Inc. (HNT), Kindred Healthcare, Inc. (KND), Laboratory Corporation of America Holdings (LH), Life Point Hospitals, Inc. (LPNT), Magellan Health, Inc. (MGLN), Omnicare, Inc. (OCR), Quest Diagnostics, Inc. (DGX), Select Medical Holdings Corporation (SEM), Team Health Holdings, Inc. (TMH), Tenet Healthcare Corporation (THC), Universal American Corporation (UAM), Universal Health Services, Inc. (UHS) and WellCare Health Plans, Inc. (WCG).
| | | | | | | | | | | | | | | December 31, |
| Name | 12/07 | 12/08 | 12/09 | 12/10 | 12/11 | 12/12 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 |
| Molina Healthcare, Inc. | $ | 100.00 |
| $ | 45.50 |
| $ | 59.10 |
| $ | 71.96 |
| $ | 86.55 |
| $ | 104.88 |
| $ | 100.00 |
| $ | 121.78 |
| $ | 146.46 |
| $ | 177.48 |
| $ | 227.92 |
| $ | 351.09 |
|
| S&P 500 | 100.00 |
| 63.00 |
| 79.67 |
| 91.67 |
| 93.61 |
| 108.59 |
| 100.00 |
| 115.06 |
| 117.49 |
| 136.30 |
| 180.44 |
| 205.14 |
|
| Old Peer Group | 100.00 |
| 44.97 |
| 56.76 |
| 63.52 |
| 86.09 |
| 87.78 |
| 100.00 |
| 112.08 |
| 135.26 |
| 142.21 |
| 177.30 |
| 236.56 |
|
| New Peer Group | 100.00 |
| 48.44 |
| 74.11 |
| 83.64 |
| 97.61 |
| 109.47 |
| 100.00 |
| 111.51 |
| 124.46 |
| 147.53 |
| 178.64 |
| 225.58 |
|
Item 6.Selected Financial Data
SELECTED FINANCIAL DATA
We derived the following selected consolidated financial data (other than the data under the caption “Operating Statistics”"Operating Statistics, Continuing Operations") for the five years ended December 31, 20122014 from our audited consolidated financial statements. You should read the data in conjunction with our consolidated financial statements, related notes and other financial information included herein. All dollarsdollar amounts are presented in thousands, except per shareper-share data. The data under the caption “Operating Statistics”"Operating Statistics, Continuing Operations" has not been audited.
| | | | Year Ended December 31, | Year Ended December 31, |
| | 2012 | | 2011 | | 2010 | | 2009 | | 2008 | 2014 | | 2013 | | 2012 | | 2011 | | 2010 (1) |
| Statements of Income Data: | | | | | | | | | | | | | | | | | | |
| Revenue: | | | | | | | | | | | | | | | | | | |
| Premium revenue | $ | 5,826,491 |
| | $ | 4,603,407 |
| | $ | 3,989,909 |
| | $ | 3,660,207 |
| | $ | 3,091,240 |
| $ | 9,022,511 |
| | $ | 6,179,170 |
| | $ | 5,544,121 |
| | $ | 4,211,493 |
| | $ | 3,632,142 |
|
| Service revenue (1) | 187,710 |
| | 160,447 |
| | 89,809 |
| | — |
| | — |
| 210,051 |
| | 204,535 |
| | 187,710 |
| | 160,447 |
| | 89,809 |
|
| Premium tax revenue | | 294,388 |
| | 172,017 |
| | 158,991 |
| | 154,589 |
| | 139,775 |
|
| Health insurer fee revenue | | 119,484 |
| | — |
| | — |
| | — |
| | — |
|
| Investment income | 5,188 |
| | 5,539 |
| | 6,259 |
| | 9,149 |
| | 21,126 |
| 8,093 |
| | 6,890 |
| | 5,075 |
| | 5,446 |
| | 6,198 |
|
| Rental income | 9,374 |
| | 547 |
| | — |
| | — |
| | — |
| |
| Other revenue | | 12,074 |
| | 26,322 |
| | 18,312 |
| | 8,288 |
| | 7,140 |
|
| Total revenue | 6,028,763 |
| | 4,769,940 |
| | 4,085,977 |
| | 3,669,356 |
| | 3,112,366 |
| 9,666,601 |
| | 6,588,934 |
| | 5,914,209 |
| | 4,540,263 |
| | 3,875,064 |
|
| Expenses: | | | | | | | | | | |
| Operating expenses: | | | | | | | | | | |
| Medical care costs | 5,096,760 |
| | 3,859,994 |
| | 3,370,857 |
| | 3,176,236 |
| | 2,621,312 |
| 8,076,331 |
| | 5,380,124 |
| | 4,991,188 |
| | 3,664,161 |
| | 3,190,566 |
|
| Cost of service revenue (1) | 141,208 |
| | 143,987 |
| | 78,647 |
| | — |
| | — |
| 156,764 |
| | 161,494 |
| | 141,208 |
| | 143,987 |
| | 78,647 |
|
| General and administrative expenses | 532,627 |
| | 415,932 |
| | 345,993 |
| | 276,027 |
| | 249,646 |
| 764,693 |
| | 665,996 |
| | 518,615 |
| | 393,452 |
| | 326,193 |
|
| Premium tax expenses | 158,991 |
| | 154,589 |
| | 139,775 |
| | 128,581 |
| | 100,165 |
| 294,388 |
| | 172,017 |
| | 158,991 |
| | 154,589 |
| | 139,775 |
|
| Health insurer fee expenses | | 88,591 |
| | — |
| | — |
| | — |
| | — |
|
| Depreciation and amortization | 63,704 |
| | 50,690 |
| | 45,704 |
| | 38,110 |
| | 33,688 |
| 92,917 |
| | 72,743 |
| | 63,114 |
| | 48,253 |
| | 43,246 |
|
| Total operating costs and expenses | 5,993,290 |
| | 4,625,192 |
| | 3,980,976 |
| | 3,618,954 |
| | 3,004,811 |
| |
| Impairment of goodwill and intangible assets (2) | — |
| | (64,575 | ) | | — |
| | — |
| | — |
| |
| Gain on purchase of convertible senior notes | — |
| | — |
| | — |
| | 1,532 |
| | — |
| |
| Total operating expenses | | 9,473,684 |
| | 6,452,374 |
| | 5,873,116 |
| | 4,404,442 |
| | 3,778,427 |
|
| Operating income | 35,473 |
| | 80,173 |
| | 105,001 |
| | 51,934 |
| | 107,555 |
| 192,917 |
| | 136,560 |
| | 41,093 |
| | 135,821 |
| | 96,637 |
|
| Other expenses (income): | | | | | | | | | | |
| Other expenses, net: | | | | | | | | | | |
| Interest expense | 16,769 |
| | 15,519 |
| | 15,509 |
| | 13,777 |
| | 13,231 |
| 56,811 |
| | 52,071 |
| | 16,769 |
| | 15,519 |
| | 15,509 |
|
| Other income | (361 | ) | | — |
| | — |
| | — |
| | — |
| |
| Total other expenses | 16,408 |
| | 15,519 |
| | 15,509 |
| | 13,777 |
| | 13,231 |
| |
| Income before income taxes | 19,065 |
| | 64,654 |
| | 89,492 |
| | 38,157 |
| | 94,324 |
| |
| Provision for income taxes | 9,275 |
| | 43,836 |
| | 34,522 |
| | 7,289 |
| | 34,726 |
| |
| Other expense, net | | 802 |
| | 3,343 |
| | 945 |
| | — |
| | — |
|
| Total other expenses, net | | 57,613 |
| | 55,414 |
| | 17,714 |
| | 15,519 |
| | 15,509 |
|
| Income from continuing operations before income taxes | | 135,304 |
| | 81,146 |
| | 23,379 |
| | 120,302 |
| | 81,128 |
|
| Income tax expense | | 72,726 |
| | 36,316 |
| | 10,513 |
| | 42,914 |
| | 30,511 |
|
| Income from continuing operations | | 62,578 |
| | 44,830 |
| | 12,866 |
| | 77,388 |
| | 50,617 |
|
| (Loss) income from discontinued operations, net of tax (benefit) expense (2) | | (355 | ) | | 8,099 |
| | (3,076 | ) | | (56,570 | ) | | 4,353 |
|
| Net income | $ | 9,790 |
| | $ | 20,818 |
| | $ | 54,970 |
| | $ | 30,868 |
| | $ | 59,598 |
| $ | 62,223 |
| | $ | 52,929 |
| | $ | 9,790 |
| | $ | 20,818 |
| | $ | 54,970 |
|
| Net income per share: | | | | | | | | | | |
| | | | | | | | | | | |
| Basic net income per share: | | | | | | | | | | |
| Income from continuing operations | | $ | 1.34 |
| | $ | 0.98 |
| | $ | 0.28 |
| | $ | 1.69 |
| | $ | 1.23 |
|
| (Loss) income from discontinued operations | | (0.01 | ) | | 0.18 |
| | (0.07 | ) | | (1.24 | ) | | 0.11 |
|
| Basic net income per share | | $ | 1.33 |
| | $ | 1.16 |
| | $ | 0.21 |
| | $ | 0.45 |
| | $ | 1.34 |
|
| Diluted net income per share: | | | | | | | | | | |
| Income from continuing operations | | $ | 1.30 |
| | $ | 0.96 |
| | $ | 0.27 |
| | $ | 1.67 |
| | $ | 1.22 |
|
| (Loss) income from discontinued operations | | (0.01 | ) | | 0.17 |
| | (0.06 | ) | | (1.22 | ) | | 0.10 |
|
| Diluted net income per share | | $ | 1.29 |
| | $ | 1.13 |
| | $ | 0.21 |
| | $ | 0.45 |
| | $ | 1.32 |
|
| | | | | | | | | | | |
| Weighted average shares outstanding: | | | | | | | | | | |
| Basic | $ | 0.21 |
| | $ | 0.45 |
| | $ | 1.34 |
| | $ | 0.80 |
| | $ | 1.44 |
| 46,935,000 |
| | 45,717,000 |
| | 46,380,000 |
| | 45,756,000 |
| | 41,174,000 |
|
| Diluted | $ | 0.21 |
| | $ | 0.45 |
| | $ | 1.32 |
| | $ | 0.79 |
| | $ | 1.43 |
| 48,340,000 |
| | 46,862,000 |
| | 46,999,000 |
| | 46,425,000 |
| | 41,631,000 |
|
| Weighted average number of common shares outstanding | 46,380,000 |
| | 45,756,000 |
| | 41,174,000 |
| | 38,765,000 |
| | 41,514,000 |
| |
| Weighted average number of common shares and potential dilutive common shares outstanding | 46,999,000 |
| | 46,425,000 |
| | 41,631,000 |
| | 38,976,000 |
| | 41,658,000 |
| |
| Operating Statistics: | | | | | | | | | | |
| Operating Statistics, Continuing Operations: | | | | | | | | | | |
| Medical care ratio (3) | 89.9 | % | | 86.8 | % | | 87.6 | % | | 89.9 | % | | 87.6 | % | 89.5 | % | | 87.1 | % | | 90.0 | % | | 87.0 | % | | 87.8 | % |
| General and administrative expense ratio (4) | 8.8 | % | | 8.7 | % | | 8.5 | % | | 7.5 | % | | 8.0 | % | 7.9 | % | | 10.1 | % | | 8.8 | % | | 8.7 | % | | 8.4 | % |
| Premium tax ratio (5) | 2.8 | % | | 3.5 | % | | 3.6 | % | | 3.6 | % | | 3.3 | % | 3.2 | % | | 2.7 | % | | 2.8 | % | | 3.5 | % | | 3.7 | % |
| Members (6) | 1,797,000 |
| | 1,697,000 |
| | 1,613,000 |
| | 1,455,000 |
| | 1,256,000 |
| 2,623,000 |
| | 1,931,000 |
| | 1,797,000 |
| | 1,618,000 |
| | 1,532,000 |
|
| | | | Year Ended December 31, | Year Ended December 31, |
| | 2012 | | 2011 | | 2010 | | 2009 | | 2008 | 2014 | | 2013 | | 2012 | | 2011 | | 2010 |
| Balance Sheet Data: | | | | | | | | | | | | | | | | | | |
| Cash and cash equivalents | $ | 795,770 |
| | $ | 493,827 |
| | $ | 455,886 |
| | $ | 469,501 |
| | $ | 387,162 |
| $ | 1,539,063 |
| | $ | 935,895 |
| | $ | 795,770 |
| | $ | 493,827 |
| | $ | 455,886 |
|
| Total assets | 1,934,822 |
| | 1,652,146 |
| | 1,509,214 |
| | 1,244,035 |
| | 1,148,068 |
| 4,477,215 |
| | 3,002,937 |
| | 1,934,822 |
| | 1,652,146 |
| | 1,509,214 |
|
| Long-term debt (including current maturities) | 262,939 |
| | 218,126 |
| | 164,014 |
| | 158,900 |
| | 164,873 |
| |
| Long-term debt, including current maturities (7) | | 905,389 |
| | 784,862 |
| | 262,939 |
| | 218,126 |
| | 164,014 |
|
| Total liabilities | 1,152,508 |
| | 897,073 |
| | 790,157 |
| | 701,297 |
| | 616,306 |
| 3,466,773 |
| | 2,110,000 |
| | 1,152,508 |
| | 897,073 |
| | 790,157 |
|
| Stockholders’ equity | 782,314 |
| | 755,073 |
| | 719,057 |
| | 542,738 |
| | 531,762 |
| 1,010,442 |
| | 892,937 |
| | 782,314 |
| | 755,073 |
| | 719,057 |
|
_______________________________ | |
| (1) | Service revenue and cost of service revenue represent revenue and costs generated by our Molina Medicaid Solutions segment. Because we acquired this business on May 1, 2010, results for the year ended December 31, 2010 include eight months of results for this segment. |
| |
| (2) | OnAs previously reported, in February 17, 2012 the Division of Purchasing of the Missouri Office of Administration notified us that our Missouri health plan that it was not awarded a contract under the Missouri HealthNet Managed Care Request for Proposal; therefore, ourthe Missouri health plan'splan’s existing contract with the state expired without renewal on June 30, 2012. In connection with this notification, wethe Missouri health plan recorded a non-cash impairment charge of $64.6 million in the fourth quarter of 2011. Results relating to the Missouri health plan have been reported as discontinued operations for all periods presented. (Loss) income from discontinued operations is presented net of income tax (benefit) expense of $(203), $(9,912), $(1,238), $922, and $4,011, respectively. |
| |
| (3) | Medical care ratio represents medical care costs as a percentage of premium revenue, net of premium tax. We now compute the medical care ratio by dividing total medical care costs by premium revenue, net of premium taxes. Previously, we did not adjust premium revenue to remove the impact of premium taxes. We have made this change for all periods presented.revenue. The medical care ratio is a key operating indicator used to measure our performance in delivering efficient and cost effective health care services. Changes in the medical care ratio from period to period result from changes in Medicaid funding by the states, utilization of medical services, our ability to effectively manage costs, contract changes, and changes in accounting estimates related to incurred but not paid claims. See Item 7 — Management’sin this Form 10-K, "Management’s Discussion and Analysis of Financial Condition and Results of Operations," for further discussion. |
| |
| (4) | General and administrative expense ratio represents such expenses as a percentage of total revenue. |
| |
| (5) | Premium tax ratio represents such expenses as a percentage of premium revenue net ofplus premium tax.tax revenue. |
| |
| (6) | Number of members at end of period. |
| |
| (7) | Includes convertible senior notes, lease financing obligations, and other long-term debt. |
Item 7.Management’s Discussion and Analysis of Financial Condition and Results of Operations
The following discussion of our financial condition and results of operations should be read in conjunction with the “SelectedItems 6 and 8 of this Form 10-K, Selected Financial Data”Data, and the accompanying consolidated financial statementsFinancial Statements and the notes to those statements appearing elsewhere in this report.Supplementary Data, respectively. This discussion contains forward-looking statements that involve known and unknown risks and uncertainties, including those set forth underin Part I, Item 1A —of this Form 10-K, Risk Factors, above.Factors.
Overview
Molina Healthcare, Inc. provides quality andhealth care to those receiving government assistance. We offer cost-effective Medicaid-related solutions to meet the health care needs of low-income families and individuals, and to assist state agencies in their administration of the Medicaid program. We report our financial performance based on two reportable segments: the Health Plans segment and the Molina Medicaid Solutions. Solutions segment.
Our Health Plans segment comprisesconsists of health plans in California, Florida, Michigan, New Mexico, Ohio, Texas, Utah, Washington, and Wisconsin,11 states, and includes our direct delivery business. As of December 31, 2012,2014, these health plans served approximately1.8over 2.6 million members eligible for Medicaid, Medicare, and other government-sponsored health care programs for low-income families and individuals. Additionally, we serve a small number of Health Insurance Marketplace members, many of whom are eligible for government premium subsidies. The health plans are operated by our respective wholly owned subsidiaries in those states, each of which is licensed as a health maintenance organization or HMO.(HMO). Our direct delivery business consists primarily of the management of a hospital in southern California under a management services agreement, and the operation of primary care clinics in several states in which we operate.
Our Molina Medicaid Solutions segment provides business processing and information technology development and administrative services to Medicaid agencies in Idaho, Louisiana, Maine, New Jersey, West Virginia, and the U.S. Virgin Islands, and drug rebate administration services in Florida.
We previously reported that our Medicaid managed care contract with the state of Missouri expired without renewal in 2012, and effective June 2013 the transition obligations associated with that contract terminated. Therefore, beginning in the second quarter of 2013, we reported the results relating to the Missouri health plan as discontinued operations for all periods presented. The following discussion and analysis, with the exception of cash flow information, is presented in the context of continuing operations unless otherwise noted.
Fiscal Year 2014 Financial Highlights
Net income from continuing operations increased to $62.6 million in 2014, from $44.8 million in 2013 due to increases in enrollment and revenue, and improved administrative cost efficiency; which offset higher medical costs and higher tax rates.
Strong enrollment growth across all of our programs combined with an 18% increase in premium revenue per member, generated almost $3 billion, or 46%, more premium revenue in 2014 compared with 2013.
General and administrative expenses as a percentage of revenue declined to 7.9% in 2014, versus 10.1% in 2013.
Medical care costs as a percentage of premium revenue increased to 89.5% in 2014, from 87.1% in 2013.
Debt financing transactions generated net cash of $122.6 million; such transactions both extended the maturity date and lowered the rate of our convertible senior notes previously due in 2014.
Health Care Reform
We believe that the government-sponsored initiatives, including the Affordable Care Act (ACA), will continue to provide us with significant opportunities for membership growth in our existing markets and in new programs in the future as follows:
Medicaid Expansion. In the states that have elected to participate, the ACA provides for the expansion of the Medicaid program to offer eligibility to nearly all low-income people under age 65 with incomes at or below 138% of the federal poverty line. Medicaid expansion membership phased in beginning January 1, 2014. Since that date, our health plans in California, Florida,Illinois, Michigan, New Mexico, Ohio, and Washington; additionally,Washington have begun participating in Medicaid expansion. At December 31, 2014 our membership included approximately 385,000 Medicaid expansion members, or 15% of total membership.
Marketplace. The ACA authorized the creation of Marketplace insurance exchanges, allowing individuals and small groups to purchase health insurance that is federally subsidized, effective January 1, 2014. We participate in the Marketplace in all of the states in which we manage three county-owned primaryoperate, except Illinois and South Carolina. At December 31, 2014, we had approximately 15,000 Marketplace members, and that enrollment is expected to grow appreciably in 2015, particularly at our Florida health plan.
Medicare-Medicaid Plans. Policymakers at the federal and state levels are increasingly focused on the design and implementation of programs that improve the coordination of care clinics underfor those who qualify to receive both Medicare and Medicaid services (the "dual eligible"), and to deliver services to the dual eligible in a contract with Fairfax County, Virginia. more financially efficient manner. As a result of these efforts, 15 states have undertaken demonstration programs to integrate Medicare and Medicaid services for dual-eligible individuals. The health plans participating in such demonstrations are referred to as Medicare-Medicaid Plans (MMPs). Our MMPs in California, Illinois, and Ohio offered coverage beginning in 2014, and we expect to begin offering MMP coverage in South Carolina and Texas in the first quarter of 2015, and in Michigan in the second quarter of 2015.
Health Insurer Fee. The ACA imposes an annual fee, or excise tax, on health insurers for each calendar year beginning on or after January 1, 2014. A health insurer’s liability for the payment of the fee (the health insurer fee, or HIF) is established upon first writing business in 2014 or any subsequent year. In other words, an active health insurer becomes liable for the fee on January 1st of any given year. The amount of the HIF for the insurer is based upon the insurer’s share of the industry's net premiums written during the preceding calendar year. The HIF must be paid by the insurer by September 30th of the year in which the insurer becomes liable for the HIF. During the third quarter of 2014 we paid our 2014 HIF assessment, which amounted to $88.6 million. This expense was recognized on a straight-line basis in 2014; and is non-deductible for income tax purposes.
We believe that state Medicaid agencies are required to reimburse us for the HIF imposed on our Medicaid premiums, as well as for the negative financial impact associated with the absence of tax deductibility for the HIF. Although all of our state Medicaid partners have agreed informally to reimbursement of the HIF and the costs of its related tax effects, we have not secured binding commitments to that effect from California, Michigan and Utah. Our 2014 results were adversely affected by our inability to recognize as revenue reimbursement (including reimbursement for tax effects) for the full impact of the HIF from those states. The state of California has not formally committed to reimburse us for either the HIF itself, or the related tax effects. The states of Michigan and Utah have reimbursed us for the HIF, but have not formally committed to reimbursement for the related tax effect. The total amount of HIF revenue for which agreements were not secured (and revenue was not recognized) amounted to approximately $20 million for fiscal 2014. We expect to collect and recognize this revenue related to 2014 in 2015. We further expect to recognize revenue in 2015 sufficient to reimburse us for the full amount of the HIF we will pay (along with related tax effects) in September of 2015. We expect our 2015 HIF assessment related to our Medicaid business to be approximately $143 million, with an expected tax effect from the reimbursement of the assessment of approximately $88 million. Therefore, the total reimbursement needed as a result of the Medicaid-related HIF is approximately $231 million.
For further discussion of the risks and uncertainties relating to the HIF, refer to the subheading below, "Liquidity and Capital Resources—Financial Condition."
Market Updates—Health Plans Segment
Florida. During 2014, our Florida health plan acquired two Medicaid contracts, adding approximately 73,000 members.
Puerto Rico. In 2014, we were awarded a managed care contract in the Commonwealth of Puerto Rico that is expected to enroll its first members April 1, 2015. Total enrollment is expected to be approximately 350,000 new members, with anticipated annualized revenue of $750 million.
South Carolina. Our South Carolina health plan began serving members under the state of South Carolina’s new full-risk Medicaid managed care program effective January 1, 2014.
Market Update—Molina Medicaid Solutions Segment
In 2011, Molina Medicaid Solutions received notice from the state of Louisiana that the state intended to award the contract for a replacement Medicaid management information system (MMIS) to a different vendor, CNSI. However, in March 2013, the state of Louisiana canceled its contract award to CNSI. The state had informed us that we will continue to perform under our current contract until a successor is named. On December 18, 2014, Molina Medicaid Solutions received notice from the state of Louisiana that they have extended our contract through December 31, 2015. We recognized approximately $41 million of service revenue under this contract in 2014.
Composition of Revenue and Membership
Health Plans Segment
Our Health Plans segment derives its revenue, in the form of premiums, chiefly from Medicaid contracts with the states in which our health plans operate; and, to a lesser degree, from Medicare contracts entered into with the Centers for Medicare and Medicaid Services (CMS), a federal government agency.
Our health plans'plans’ state Medicaid contracts generally have terms of three to four years with annual adjustments to premium rates.years. These contracts are renewable at the discretion of the state. In general, eithertypically contain renewal options exercisable by the state Medicaid agency, and allow either the state or the health plan mayto terminate the state contract with or
without cause. Most of these contracts contain renewal options that are exercisable by the state. Our health plan subsidiaries have generally been successful in obtaining the renewal ofretaining their contracts, in each state prior to the actual expiration of their contracts. Our statebut such contracts are generally at greatestsubject to risk of loss when a state issues a new request for proposals or RFP, subject(RFP) open to competitive bidding by other health plans. If one of our health plans is not a successful responsive bidder to a state RFP, its contract may be subject to non-renewal. For instance, on February 17, 2012, the Division of Purchasing of the Missouri Office of Administration notified us that our Missouri health plan was not awarded a contract under the Missouri HealthNet Managed Care Request for Proposal; therefore, our Missouri health plan’s prior contract with theThe state expired without renewal on June 30, 2012 subject to certain transition obligations. As of December 31, 2012, we continued to process claims that were incurred by the Missouri health plan's members through the June 30, 2012 termination date. For the six months ended June 30, 2012, our Missouri health plan contributed premium revenue of $113.8 million, or 4.1% of total premium revenue, and comprised 79,000 members, or 4.3% of total Health Plans segment membership as of June 30, 2012.
With regard to our Ohio health plan, as a result of a lawsuit challenging the selection of several plans including our health plan for the new Medicaid managed care program in Ohio, the Ohio Office of Medical Assistance announced on October 5, 2012, that the operation of the program is being delayed from the previously scheduled January 1, 2013 start date and will now commence on July 1, 2013. Following the trial court's dismissal of the lawsuit, the court of appeals has permitted the state of Ohio to move forward with implementation of the new program and finalizing the provider agreements with our Ohio planprograms and the other selected managed care plans.federal Medicare program periodically adjust premium rates.
OurIn addition to contract renewal, our state Medicaid contracts may be periodically adjustedamended to include or exclude certain health benefits (such as pharmacy services, behavioral health services, or long-term care services); populations (suchsuch as the aged, blind or disabled or ABD)(ABD); and regions or service areas. For example, our Texas health plan added significant membership effective March 1, 2012, in service areas we had not previously served (the Hidalgo and El Paso service areas); and among populations we had not previously served within existing service areas, such as the Temporary Assistance for Needy Families, or TANF, population in the Dallas service area. Additionally, the health benefits provided to our TANF and ABD members in Texas under our contracts with the state were expanded to include inpatient facility and pharmacy services.
During fiscal year 2012, we responded to several RFPs and invitations to negotiate with respect to new business, including proposals to serve dual eligible populations and applications to participate in the Centers for Medicare and Medicaid Services, or CMS', Capitated Financial Alignment Demonstration project. On August 27, 2012, our Ohio health plan was chosen to participate in the Southwest, West Central, and Central markets under the Ohio Integrated Care Delivery System, or ICDS. The Ohio ICDS is intended to improve care coordination for individuals enrolled in both Medicaid and Medicare. The selection of our Ohio health plan was made by the Ohio Department of Jobs and Family Services, or ODJFS, pursuant to the request for applications for qualified health plans to serve in the ICDS issued in April 2012. The commencement of the ICDS is subject to the readiness review of the selected health plans, and the execution of three-way provider agreements between the health plans, ODJFS, and CMS. Enrollment of dual eligible members in the ICDS is expected to begin during the second half of 2013.
On November 15, 2012, we announced that our new Illinois health plan had been chosen to serve members in Central Illinois under the state's Medicare-Medicaid Alignment Initiative (MMAI). The operational start date for the program is currently scheduled for October 2013 with an effective date of January 2014. In addition to the MMAI, we will also serve other seniors and persons with disabilities in the Medicaid Program as the state expands the Integrated Care Program that was implemented in suburban Cook County and the five collar counties in May of 2011.
On February 14, 2013, we announced that the Florida Agency for Health Care Administration awarded our Florida health plan contracts in three regions under the Statewide Medicaid Managed Care Long-Term Care program. As a result of the awards, we will now enter into a comprehensive pre-contracting assessment, with the program currently scheduled to commence on December 1, 2013. Under the program, we will provide long-term care benefits, including institutional and home and community-based services.
On February 11, 2013, we announced that our New Mexico health plan was selected by the New Mexico Human Services Department, or HSD, to participate in the new Centennial Care program. In addition to continuing to provide physical and acute health care services, under the new program our New Mexico health plan will expand its services to provide behavioral health and long-term care services. The selection of our New Mexico health plan was made by HSD pursuant to its request for proposals issued in August 2012. The operational start date for the program is currently scheduled for January 2014.
Our Molina Medicaid Solutions segment provides design, development, implementation, and business process outsourcing solutions to state governments for their Medicaid Management Information Systems, or MMIS. MMIS is a core tool used to support the administration of state Medicaid and other health care entitlement programs. Molina Medicaid Solutions currently holds MMIS contracts with the states of Idaho, Louisiana, Maine, New Jersey, and West Virginia, as well as a contract to provide drug rebate administration services for the Florida Medicaid program.
On October 12, 2012, the Governor of the U.S. Virgin Islands announced a partnership in which we will provide MMIS to the U.S. Virgin Islands through our West Virginia fiscal agent operation. The contract outlining the sharing of our platform went through several rounds of review at the federal level and has been approved by CMS. The partnership will benefit both the Virgin Islands and taxpayers by circumventing the costs associated with establishing an independent system while gaining leverage from operating under a common platform. This partnership can serve as a model for the country by demonstrating that state and territorial governments can reduce local and federal costs by sharing such technologies for their Medicaid populations.
On July 13, 2012, our Molina Medicaid Solutions segment received full federal certification of its Medicaid Management Information System, or MMIS, in the state of Idaho from CMS. As a result of the CMS certification, the state of Idaho is entitled to receive federal reimbursement of 75% of its MMIS operations costs retroactive to June 1, 2010, the date that the system first began processing claims. Our MMIS in Maine received full federal certification from CMS on December 19, 2011.
On June 9, 2011, Molina Medicaid Solutions received notice from the state of Louisiana that the state intends to award the contract for a replacement MMIS to another company. For the year endedDecember 31, 2012, our revenue under the Louisiana MMIS contract was $54.9 million, or 29.2% of total service revenue. We expect that we will continue to perform under this contract through implementation and acceptance of the successor MMIS. Based upon our past experience and our knowledge of the Louisiana MMIS bid process, we believe that implementation and acceptance of the successor MMIS will not occur until 2014 at the earliest. Through implementation and acceptance of the successor MMIS we expect to recognize approximately $40 million in revenue annually under our Louisiana MMIS contract.
Composition of Revenue and Membership
Health Plans Segment
Our Health Plans segment derives its revenue, in the form of premiums, chiefly from Medicaid contracts with the states in which our health plans operate. Premium revenue is fixed in advance of the periods covered and, except as described in “CriticalItem 8 of this Form 10-K, Notes to Consolidated Financial Statements, Note 2 "Significant Accounting Policies” below,Policies," is not generally subject to significant accounting estimates. For the year ended December 31, 2012,2014, we received approximately 96%more than 95% of our premium revenue as a fixed amount per member per month or PMPM,(PMPM), pursuant to our Medicaid, Medicare and Marketplace contracts, with state agencies, our Medicare contracts with CMS, and our contractsincluding agreements with other managed care organizations for which we operate as a subcontractor. These premium revenues are recognized in the month that members are entitled to receive health care services. The state Medicaid programs and the federal Medicare program periodically adjust premium rates.
For the year ended December 31, 2012, we recognized approximately 4% of our premium revenue in the form of “birth income” —Revenue not received on a one-time payment for the delivery of a child — from the Medicaid programs in all of our state health plans except New Mexico. Such payments arefixed PMPM basis is recognized as revenue in the month the birth occurs.earned.
The amount of the premiums paid to us may vary substantially between states and among various government programs. PMPMThe following table sets forth the ranges of premiums paid to our state health plans by program, on a per-member per-month basis for the Children’s Health Insurance Program, or CHIP, members are generally amongyear ended December 31, 2014. The "Consolidated" column represents the weighted-average amounts for our lowest, with rates astotal membership by program.
|
| | | | | | | | | | | | | | |
| | Ending | | PMPM Premiums |
| | Membership | | Low | | High | | Consolidated |
| Temporary Assistance for Needy Families (TANF), CHIP (1) | 1,831,000 |
| | $ | 130.00 |
| | $ | 280.00 |
| | $ | 180.00 |
|
| Medicaid Expansion | 385,000 |
| | 340.00 |
| | 520.00 |
| | 420.00 |
|
| Aged, Blind or Disabled (ABD) | 325,000 |
| | 320.00 |
| | 1,580.00 |
| | 900.00 |
|
| Medicare Special Needs Plans (Medicare) | 49,000 |
| | 970.00 |
| | 1,480.00 |
| | 1,180.00 |
|
| Medicare-Medicaid Plan (MMP) – Integrated (2) | 18,000 |
| | 1,510.00 |
| | 3,240.00 |
| | 1,970.00 |
|
| Marketplace | 15,000 |
| | 190.00 |
| | 560.00 |
| | 320.00 |
|
| |
| (1) | CHIP stands for Children's Health Insurance Program. |
| |
| (2) | MMP members who receive both Medicaid and Medicare coverage from Molina Healthcare. |
low as approximately $75 PMPM in California. Premium revenues for Medicaid members are generally higher. Among the TANF, Medicaid population — the Medicaid group that includes mostly mothers and children — PMPM premiums range between approximately $110 in California to $260 in Ohio. Among our ABD membership, PMPM premiums range from approximately $330 in Utah to $1,400 in Ohio. Contributing to the variability in Medicaid rates among the states is the practice of some states to exclude certain benefits from the managed care contract (most often pharmacy, inpatient, behavioral health and catastrophic case benefits) and retain responsibility for those benefits at the state level. Medicare membership generates the highest PMPM premiums in the aggregate, at approximately $1,200 PMPM.
The following table setstables set forth the approximate total number of members by state health planour Health Plans segment membership as of the dates indicated:
|
| | | | | | | | |
| | As of December 31, |
| | 2014 | | 2013 | | 2012 |
| Ending Membership by Health Plan: | | | | | |
| California | 531,000 |
| | 368,000 |
| | 336,000 |
|
| Florida | 164,000 |
| | 89,000 |
| | 73,000 |
|
| Illinois | 100,000 |
| | 4,000 |
| | — |
|
| Michigan | 242,000 |
| | 213,000 |
| | 220,000 |
|
| New Mexico | 212,000 |
| | 168,000 |
| | 91,000 |
|
| Ohio | 347,000 |
| | 255,000 |
| | 244,000 |
|
| South Carolina (1) | 118,000 |
| | — |
| | — |
|
| Texas | 245,000 |
| | 252,000 |
| | 282,000 |
|
| Utah | 83,000 |
| | 86,000 |
| | 87,000 |
|
| Washington | 497,000 |
| | 403,000 |
| | 418,000 |
|
| Wisconsin | 84,000 |
| | 93,000 |
| | 46,000 |
|
| | 2,623,000 |
| | 1,931,000 |
| | 1,797,000 |
|
| Ending Membership by Program: | | | | | |
| TANF/CHIP | 1,831,000 |
| | 1,624,000 |
| | 1,517,000 |
|
| Medicaid Expansion (2) | 385,000 |
| | — |
| | — |
|
| ABD | 325,000 |
| | 268,000 |
| | 244,000 |
|
| Medicare | 49,000 |
| | 39,000 |
| | 36,000 |
|
| MMP - Integrated | 18,000 |
| | — |
| | — |
|
| Marketplace (2) | 15,000 |
| | — |
| | — |
|
| | 2,623,000 |
| | 1,931,000 |
| | 1,797,000 |
|
|
| | | | | | | | |
| | As of December 31, |
| | 2012 | | 2011 | | 2010 |
| Total Ending Membership by Health Plan: | | | | | |
| California | 336,000 |
| | 355,000 |
| | 344,000 |
|
| Florida | 73,000 |
| | 69,000 |
| | 61,000 |
|
| Michigan | 220,000 |
| | 222,000 |
| | 227,000 |
|
Missouri (1) | — |
| | 79,000 |
| | 81,000 |
|
| New Mexico | 91,000 |
| | 88,000 |
| | 91,000 |
|
| Ohio | 244,000 |
| | 248,000 |
| | 245,000 |
|
| Texas | 282,000 |
| | 155,000 |
| | 94,000 |
|
| Utah | 87,000 |
| | 84,000 |
| | 79,000 |
|
| Washington | 418,000 |
| | 355,000 |
| | 355,000 |
|
| Wisconsin | 46,000 |
| | 42,000 |
| | 36,000 |
|
| Total | 1,797,000 |
| | 1,697,000 |
| | 1,613,000 |
|
| Total Ending Membership by State for our Medicare Advantage Plans: | | | | | |
| California | 7,700 |
| | 6,900 |
| | 4,900 |
|
| Florida | 900 |
| | 800 |
| | 500 |
|
| Michigan | 9,700 |
| | 8,200 |
| | 6,300 |
|
| New Mexico | 900 |
| | 800 |
| | 600 |
|
| Ohio | 300 |
| | 200 |
| | — |
|
| Texas | 1,500 |
| | 700 |
| | 700 |
|
| Utah | 8,200 |
| | 8,400 |
| | 8,900 |
|
| Washington | 6,500 |
| | 5,000 |
| | 2,600 |
|
| Total | 35,700 |
| | 31,000 |
| | 24,500 |
|
| Total Ending Membership by State for our Aged, Blind or Disabled Population: | | | | | |
| California | 44,700 |
| | 31,500 |
| | 13,900 |
|
| Florida | 10,300 |
| | 10,400 |
| | 10,000 |
|
| Michigan | 41,900 |
| | 37,500 |
| | 31,700 |
|
| New Mexico | 5,700 |
| | 5,600 |
| | 5,700 |
|
| Ohio | 28,200 |
| | 29,100 |
| | 28,200 |
|
| Texas | 95,900 |
| | 63,700 |
| | 19,000 |
|
| Utah | 9,000 |
| | 8,500 |
| | 8,000 |
|
| Washington | 30,000 |
| | 4,800 |
| | 4,000 |
|
| Wisconsin | 1,700 |
| | 1,700 |
| | 1,700 |
|
| Total | 267,400 |
| | 192,800 |
| | 122,200 |
|
| |
| (1) | Our contract withSouth Carolina health plan began serving members under the state of Missouri expired without renewal on June 30, 2012South Carolina’s new full-risk Medicaid managed care program effective January 1, 2014. |
| |
| (2) | Medicaid expansion membership phased in, and the Marketplace became available for consumers to access coverage, beginning January 1, 2014. |
Molina Medicaid Solutions Segment
The payments received by our Molina Medicaid Solutions segment under its state contracts are based on the performance of multiple services. The first of these is the design, development and implementation or DDI,(DDI) of an MMIS.a Medicaid management information system (MMIS). An additional service, following completion of DDI, is the operation of the MMIS under a business process outsourcing or BPO(BPO) arrangement. WhileWhen providing BPO services (which include claims payment and eligibility processing) we also provide the state with other services including both hosting and support, and maintenance. Because we have determined the services provided under our Molina Medicaid Solutions contracts represent a single unit of accounting, we recognize revenue associated with such contracts on a straight-line basis over the periodcontract term during which BPO, hosting, and support and maintenance services are delivered.
There may be certain contractual provisions containing contingencies, however that require us to delay recognition of all or part of our service revenue until such contingencies have been removed. For further information regarding revenue recognition for the Molina Medicaid Solutions segment, refer to Item 8 of this Form 10-K, Notes to Consolidated Financial Statements, in Note 2, "Significant Accounting Policies."
Composition of Expenses
Health Plans Segment
Operating expenses for the Health Plans segment include expenses related to the provision of medical care services (including long-term services and supports, or LTSS), general and administrative expenses, and premium tax and health insurer fee expenses. Our results of operations are impacted by our ability to effectively manage expenses related to medical care services and to accurately estimate medical costs incurred. Expenses related to medical care services are captured in the following four categories:
Fee-for-service:Fee-for-service expenses: Physician providers paid on a fee-for-service basis are paid according to a fee schedule set byNearly all hospital services and the state or bymajority of our contracts with these providers. Most hospitalsprimary care and physician specialist services and LTSS costs are paid on a fee-for-service basis in a variety of ways, including per diem amounts, diagnostic-related groups or DRGs, percent of billed charges, and case rates. As discussed below, we also pay a small portion of hospitals on a capitated basis. We also have stop-loss agreements with the hospitals with which we contract. Under all fee-for-service arrangements, we retain the financial responsibility for medical care provided. Expenses related to fee-for-service contractsprovided and incur costs based on actual utilization of services. Such expenses are
recorded in the period in which the related services are dispensed. The costs of drugs administered in a physician or hospital setting that are not billed through our pharmacy benefit manager are included in fee-for-service costs.
Pharmacy expenses: All drug, injectibles, and immunization costs paid through our pharmacy benefit manager are classified as pharmacy expenses. As noted above, drugs and injectibles not paid through our pharmacy benefit manager are included in fee-for-service costs, except in those limited instances where we capitate drug and injectible costs.
Capitation:Capitation expenses: Many of our primary care physicians and a small portion of our specialists and hospitals are paid on a capitated basis. Under capitation contracts,arrangements, we typically pay a fixed amount PMPM payment to the provider without regard to the frequency, extent, or nature of the medical services actually furnished. Under capitated contracts,arrangements, we remain liable for the provision of certain health care services. Certain of our capitated contracts also contain incentive programs based on service delivery, quality of care, utilization management, and other criteria. Capitation payments are fixed in advance of the periods covered and are not subject to significant accounting estimates. These payments are expensed in the period the providers are obligated to provide services. The financial risk for pharmacy services for a small portion of our membership is delegated to capitated providers.
Pharmacy:Direct delivery expenses: PharmacyAll costs include all drug, injectibles, and immunization costs paid throughassociated with our pharmacy benefit manager. As noted above, drugs and injectibles not paid through our pharmacy benefit managerdirect delivery of medical care are included in fee-for-service costs, except in those limited instances where we capitate drug and injectible costs.separately identified.
Other:Other medical care costs includeexpenses: All medically related administrative costs, certain provider incentive costs, reinsurance cost,costs and other health care expense.expenses are classified as other medical expenses. Medically related administrative costs include, for example, expenses relating to health education, quality assurance, case management, care coordination, disease management, and 24-hour on-call nurses. Salary and benefit costs are a substantial portion of these expenses. For the years ended December 31, 2012, 2011,2014, 2013, and 2010,2012, medically related administrative costs were approximately $127.5$262.6 million, $102.3$153.0 million, and $85.5$125.2 million, respectively.
Our medical care costs include amounts that have been paid by us through the reporting date as well as estimated liabilities for medical care costs incurred but not paid by us as of the reporting date. See “Critical"Critical Accounting Policies”Estimates" below, and Item 8 of this Form 10-K, Notes to Consolidated Financial Statements, in Note 11, "Medical Claims and Benefits Payable," for a comprehensive discussion offurther information on how we estimate such liabilities.
Molina Medicaid Solutions Segment
Cost of service revenue consists primarily of the costs incurred to provide business process outsourcingBPO and technology outsourcing services under our MMIS contracts. General and administrative costs consist primarily of indirect administrative costs and business development costs.
In some circumstances we may defer recognition of incremental direct costs (such as direct labor, hardware, and software) associated with a contract if revenue recognition is also deferred. Such deferred contract costs are amortized on a straight-line basis over the remaining original contract term, consistent with the revenue recognition period.
2012 Financial Performance Summary
Financial Performance Summary, Continuing Operations
The following table and narrative briefly summarizessummarize our financial and operating performance from continuing operations for the years ended December 31, 2012, 2011,2014, 2013, and 2010.2012. All ratios, with the exception of the medical care ratio and the premium tax ratio, are showncomputed as a percentage of total revenue. The medical care ratio and the premium tax ratio areis computed as a percentage of premium revenue, netand the premium tax ratio is computed as a percentage of premium revenue plus premium tax revenue, because there are direct relationships exist between premium revenue earned, and the cost of health care and premium taxes.
We have changed our method of calculating the medical care ratio effective December 31, 2012. We now calculate the medical care ratio by dividing total medical care costs by premium revenue, net of premium taxes. Previously, we did not adjust premium revenue to remove the impact of premium taxes when calculating the medical care ratio. We made this change for all periods presented to allow better comparability of the medical care ratio between periods for health plans operating in states where premium taxes are either increased or decreased. Two states where we operate health plans (Michigan and California) either reduced or eliminated their premium tax during 2012.
| | | | Year Ended December 31, | Year Ended December 31, |
| | 2012 | | 2011 | | 2010 | 2014 | | 2013 | | 2012 |
| | (Dollar amounts in thousands, except per-share data) | (Dollar amounts in thousands, except per-share data) |
| Earnings per diluted share | $ | 0.21 |
| | $ | 0.45 |
| | $ | 1.32 |
| |
| Net income per diluted share | | $ | 1.30 |
| | $ | 0.96 |
| | $ | 0.27 |
|
| Adjusted net income per diluted share | | $ | 3.43 |
| | $ | 3.13 |
| | $ | 1.72 |
|
| Premium revenue | $ | 5,826,491 |
| | $ | 4,603,407 |
| | $ | 3,989,909 |
| $ | 9,022,511 |
| | $ | 6,179,170 |
| | $ | 5,544,121 |
|
| Service revenue | $ | 187,710 |
| | $ | 160,447 |
| | $ | 89,809 |
| $ | 210,051 |
| | $ | 204,535 |
| | $ | 187,710 |
|
| Operating income | $ | 35,473 |
| | $ | 80,173 |
| | $ | 105,001 |
| $ | 192,917 |
| | $ | 136,560 |
| | $ | 41,093 |
|
| Net income | $ | 9,790 |
| | $ | 20,818 |
| | $ | 54,970 |
| $ | 62,578 |
| | $ | 44,830 |
| | $ | 12,866 |
|
| | | | | | | |
| Total ending membership | 1,797,000 |
| | 1,697,000 |
| | 1,613,000 |
| 2,623,000 |
| | 1,931,000 |
| | 1,797,000 |
|
| | | | | | | |
| Premium revenue | 96.6 | % | | 96.5 | % | | 97.6 | % | 93.3 | % | | 93.8 | % | | 93.7 | % |
| Service revenue | 3.1 | % | | 3.4 | % | | 2.2 | % | 2.2 |
| | 3.1 |
| | 3.2 |
|
| Premium tax revenue | | 3.1 |
| | 2.6 |
| | 2.7 |
|
| Health insurer fee revenue | | 1.2 |
| | — |
| | — |
|
| Investment income | 0.1 | % | | 0.1 | % | | 0.2 | % | 0.1 |
| | 0.1 |
| | 0.1 |
|
| Rental income | 0.2 | % | | — | % | | — | % | |
| Other revenue | | 0.1 |
| | 0.4 |
| | 0.3 |
|
| Total revenue | 100.0 | % | | 100.0 | % | | 100.0 | % | 100.0 | % | | 100.0 | % | | 100.0 | % |
| | | | | | | | | | | |
| Medical care ratio (1) | 89.9 | % | | 86.8 | % | | 87.6 | % | |
| Medical care ratio | | 89.5 | % | | 87.1 | % | | 90.0 | % |
| General and administrative expense ratio | 8.8 | % | | 8.7 | % | | 8.5 | % | 7.9 | % | | 10.1 | % | | 8.8 | % |
| Premium tax ratio (1) | 2.8 | % | | 3.5 | % | | 3.6 | % | |
| Premium tax ratio | | 3.2 | % | | 2.7 | % | | 2.8 | % |
| Operating income | 0.6 | % | | 1.7 | % | | 2.6 | % | 2.0 | % | | 2.1 | % | | 0.7 | % |
| Net income | 0.2 | % | | 0.4 | % | | 1.3 | % | 0.6 | % | | 0.7 | % | | 0.2 | % |
| Effective tax rate | 48.6 | % | | 67.8 | % | | 38.6 | % | 53.8 | % | | 44.8 | % | | 45.0 | % |
| |
(1) | Medical care ratio represents medical care costs as a percentage of premium revenue, net of premium taxes; premium tax ratio represents premium taxes as a percentage of premium revenue, net of premium taxes. |
Earnings before Interest, Taxes, Depreciation and Amortization, or EBITDANon-GAAP Financial Measures
We calculate ause the following non-GAAP measure, EBITDA, which management usesfinancial measures as a supplemental metricmetrics in evaluating our financial performance, in evaluatingmaking financing and business development decisions, and in forecasting and analyzingplanning for future periods. For these reasons, management believes that EBITDA is asuch measures are useful supplemental measuremeasures to investors in evaluatingcomparing our performance and the performance of other companies in ourthe health care industry. The reconciliation of thisThese non-GAAP financial measures should be considered as supplements to, and not substitutes for or superior to, GAAP financial measure is as followsmeasures (GAAP stands for U.S. generally accepted accounting principles):.
The first of these non-GAAP measures is earnings before interest, taxes, depreciation and amortization, or EBITDA. The following table reconciles net income, which we believe to be the most comparable GAAP measure, to EBITDA.
|
| | | | | | | | | | | |
| | Year Ended December 31, |
| | 2014 | | 2013 | | 2012 |
| | (In thousands) |
| Net income | $ | 62,223 |
| | $ | 52,929 |
| | $ | 9,790 |
|
| Adjustments: | | | | | |
| Depreciation, and amortization of intangible assets and capitalized software | 113,715 |
| | 93,866 |
| | 78,764 |
|
| Interest expense | 56,811 |
| | 52,071 |
| | 16,769 |
|
| Income tax expense | 72,523 |
| | 26,404 |
| | 9,275 |
|
| EBITDA | $ | 305,272 |
| | $ | 225,270 |
| | $ | 114,598 |
|
The second of these non-GAAP measures is adjusted net income and adjusted net income per diluted share, continuing operations. The following tables reconcile net income and net income per diluted share from continuing operations, which we believe to be the most comparable GAAP measures, to adjusted net income and adjusted net income per diluted share, continuing operations.
|
| | | | | | | | | | | |
| | Year Ended December 31, |
| | 2012 | | 2011 | | 2010 |
| | (In thousands) |
| Net income | $ | 9,790 |
| | $ | 20,818 |
| | $ | 54,970 |
|
| Add back: | | | | | |
| Depreciation and amortization reported in the consolidated statements of cash flows | 78,764 |
| | 74,383 |
| | 60,765 |
|
| Interest expense | 16,769 |
| | 15,519 |
| | 15,509 |
|
| Provision for income taxes | 9,275 |
| | 43,836 |
| | 34,522 |
|
EBITDA(1) | $ | 114,598 |
| | $ | 154,556 |
| | $ | 165,766 |
|
|
| | | | | | | | | | | | | | | | | | | | | | | |
| | Year Ended December 31, |
| | 2014 | | 2013 | | 2012 |
| | (In thousands, except diluted per-share amounts) |
| Net income, continuing operations | $ | 62,578 |
| | $ | 1.30 |
| | $ | 44,830 |
| | $ | 0.96 |
| | $ | 12,866 |
| | $ | 0.27 |
|
| Adjustments, net of tax: | | | | | | | | | | | |
| Depreciation, and amortization of capitalized software | 58,770 |
| | 1.21 |
| | 46,018 |
| | 0.98 |
| | 35,267 |
| | 0.75 |
|
| Amortization of convertible senior notes and lease financing obligations | 17,249 |
| | 0.36 |
| | 14,377 |
| | 0.31 |
| | 3,714 |
| | 0.08 |
|
| Share-based compensation | 14,288 |
| | 0.29 |
| | 24,501 |
| | 0.52 |
| | 14,556 |
| | 0.31 |
|
| Amortization of intangible assets | 12,870 |
| | 0.27 |
| | 13,117 |
| | 0.28 |
| | 13,592 |
| | 0.29 |
|
| Change in fair value of derivatives | (10 | ) | | — |
| | 3,580 |
| | 0.08 |
| | 817 |
| | 0.02 |
|
| Adjusted net income per diluted share, continuing operations | $ | 165,745 |
| | $ | 3.43 |
| | $ | 146,423 |
| | $ | 3.13 |
| | $ | 80,812 |
| | $ | 1.72 |
|
________________________
| |
(1) | EBITDA is not prepared in conformity with GAAP because it excludes depreciation and amortization, as well as interest expense, and the provision for income taxes. This non-GAAP financial measure should not be considered as an alternative to the GAAP measures of net income, operating income, operating margin, or cash provided by operating activities; nor should EBITDA be considered in isolation from these GAAP measures of operating performance. |
Results of Operations, Continuing Operations
Year Ended December 31, 20122014 Compared with the Year Ended December 31, 20112013
Fiscal Year 2012 Overview and Highlights
Earnings decreased in2012compared with 2011because lower margins in the Health Plans segment more than offset higher premium revenue.Net income for the year endedDecember 31, 2012, was $9.8 million, or $0.21per diluted share, compared with net income of $20.8 million, or $0.45per diluted share, for the year endedDecember 31, 2011. Results for the quarter and year ended December 31, 2011, were affected by an impairment charge of$64.6 million related to our Missouri health plan.
Lower net income in 2012 was in large part tied to growth in our ABD membership in California and Texas, where margins were considerably lower than our margins in the aggregate. During 2012, both California and Texas transitioned large numbers of ABD members from fee-for-service reimbursement to managed care contracts. It has been our experience that members transitioning from fee-for-service reimbursement to managed care often bring with them pent up demand for medical services; and that the realization of both improved medical outcomes and costs savings from the application of managed care practices takes time as both members and providers acquaint themselves to new ways of accessing and providing care.
The initial reduction to margins associated with the transition of members from fee-for-service reimbursement to managed care was exacerbated by premium rates that assumed unrealistic costs savings from managed care practices. Premium rate increases received later in 2012 at least partially addressed this issue.
Those rate increases, together with the improved health outcomes and the gradual reduction in medical costs resulting from the application of managed care practices, produced improved financial results in the fourth quarter of 2012. Nevertheless, the aggregate impact of the ABD membership transitioned in 2012 was to substantially reduce margins. We believe, however, that in time the higher premium revenue associated with ABD members will allow us to earn acceptable returns on a total dollar basis even if percentage margins remain lower than those earned by serving TANF members, for whom PMPM revenue is much lower.
Health Plans Segment
Premium Revenue
Premium revenue grew27%A 28% increase in the year endedDecember 31, 2012, compared with the year endedDecember 31, 2011, primarily due to a shiftmembership and an 18% increase in member mix to populations generating higher premium revenue PMPM benefit expansions, andin 2014 resulted in an increase in membership.premium revenue of 46%, or over $2.8 billion, when compared with 2013. Medicare premium revenue was $468approximately $627 million in the year ended December 31, 2012,2014, compared with $388approximately $526 million in the year endedDecember 31, 2011.2013.
Growth in our ABDEnrollment growth was primarily due to Medicaid expansion program membership led to higher premium revenue PMPM in 2012. ABD membership, as a percent of total membership, has increased approximately31%year over year. Premium revenue PMPM also increased in the year ended December 31, 2012,added as a result of the inclusion ofAffordable Care Act, and membership added at our South Carolina and Illinois health plans. Higher PMPM premium revenue fromwas primarily the pharmacy benefit for our Ohio health plan effective October 1, 2011, and as a result of the inclusion of revenue for the inpatient facilitylong-term services and pharmacysupports (LTSS) benefits across all of our Texas health plan membership effective March 1, 2012. in various Medicaid managed care programs in California, Florida, Illinois, New Mexico, and Ohio.
Medical Care Costs
Although medical margin (defined as the excess of premium revenue over medical care costs) increased nearly 20% in 2014 over 2013; our consolidated medical care ratio (defined as medical care costs as a percentage of premium revenue) increased to 89.5% in 2014 from 87.1% in 2013.
The medical care ratio increased substantially in 2014 as a result of three developments:
Much of our revenue growth has come from participation in Medicaid programs covering LTSS. Percentage profit margins for LTSS benefits are generally lower than percentage profit margins for acute medical benefits.
Increases to our base premiums in recent years have not kept pace with medical cost trends.
Lack of coordination in the design of profit caps and medical cost floors in some of our state Medicaid contracts is resulting in counterproductive outcomes. In some instances, givebacks due to profitable performance in one product cannot be offset against losses in other products.
Medical care ratios by program for 2014 were as follows: TANF and CHIP - 89.3%; Medicaid expansion - 79.4%;
ABD - 92.3%; Medicare - 95.8%; MMP integrated - 92.1%; and Marketplace - 83.7%.
The following table provides the details of consolidated medical care costs for the periods indicated (dollars in thousands except PMPM amounts):
|
| | | | | | | | | | | | | | | | | | | | | |
| | Year Ended December 31, |
| | 2012 | | 2011 |
| | Amount | | PMPM | | % of Total | | Amount | | PMPM | | % of Total |
| Fee for service | $ | 3,521,960 |
| | $ | 162.60 |
| | 69.1 | % | | $ | 2,764,309 |
| | $ | 139.02 |
| | 71.6 | % |
| Capitation | 557,087 |
| | 25.72 |
| | 10.9 |
| | 518,835 |
| | 26.09 |
| | 13.4 |
|
| Pharmacy | 835,830 |
| | 38.59 |
| | 16.4 |
| | 418,007 |
| | 21.02 |
| | 10.8 |
|
| Other | 181,883 |
| | 8.39 |
| | 3.6 |
| | 158,843 |
| | 8.00 |
| | 4.2 |
|
| Total | $ | 5,096,760 |
| | $ | 235.30 |
| | 100.0 | % | | $ | 3,859,994 |
| | $ | 194.13 |
| | 100.0 | % |
Medical care costs increased in2012primarily due to the same shifts in member mix and the benefit expansions that led to increased premium revenue, particularly in California and Texas. Medical care costs as a percentage of premium revenue, net of premium taxes (the medical care ratio) also increased in 2012 when compared with 2011 because increases in premium rates have not kept pace with increases in medical costs. |
| | | | | | | | | | | | | | | | | | | | | |
| | Year Ended December 31, |
| | 2014 | | 2013 |
| | Amount | | PMPM | | % of Total | | Amount | | PMPM | | % of Total |
| Fee for service | $ | 5,672,483 |
| | $ | 202.87 |
| | 70.2 | % | | $ | 3,611,529 |
| | $ | 160.43 |
| | 67.1 | % |
| Pharmacy | 1,273,329 |
| | 45.54 |
| | 15.8 |
| | 935,204 |
| | 41.54 |
| | 17.4 |
|
| Capitation | 748,388 |
| | 26.77 |
| | 9.3 |
| | 603,938 |
| | 26.83 |
| | 11.2 |
|
| Direct delivery | 96,196 |
| | 3.44 |
| | 1.2 |
| | 48,288 |
| | 2.14 |
| | 0.9 |
|
| Other | 285,935 |
| | 10.22 |
| | 3.5 |
| | 181,165 |
| | 8.05 |
| | 3.4 |
|
| | $ | 8,076,331 |
| | $ | 288.84 |
| | 100.0 | % | | $ | 5,380,124 |
| | $ | 238.99 |
| | 100.0 | % |
Individual Health Plan Analysis
Membership and premium revenue increased significantly at the Texas health plan in 2012 as a result of the transition of large numbers of ABD, TANF and CHIP members from fee-for-service reimbursement into managed care effective March 1, 2012. Also on that date inpatient facility and pharmacy benefits that had previously been reimbursed through fee for service for managed care members were transitioned into managed care contracts; further increasing premium revenue and related medical costs. As noted above, margins on newly transitioned ABD members were considerably less than those experienced by the Company overall.California. The medical care ratio for the TexasCalifornia health plan's ABD membershipplan decreased significantly to 83.3% in total2014, from 88.9% in 2013. Additionally, medical margin improved $171.0 million when compared with 2013. This improvement was the result of higher enrollment, primarily due to the addition of approximately 97.8%107,000 Medicaid expansion members; and premium increases effective October 1, 2013 (2.5%), and July 1, 2014 (5.5%). During 2014, the California health plan benefited from the recognition of approximately $23 million in premium revenue that related to 2013 as a result of certain programmatic changes implemented by the state of California. In 2013, the California health plan recognized approximately $32 million of premium revenue related to 2012 and earlier years as a result of retroactive rate increases from the state of California. The California health plan served its first MMP members in 2014.
Florida. Due to the re-procurement undertaken by the Florida Agency for allHealth Care Administration as part of 2012. Nevertheless,its Managed Medical Assistance program starting in 2014, the Florida health plan transitioned many of its members to other health plans in the second quarter of 2014, and then added approximately 105,000 members in the second half of 2014, both from the addition of new service areas and through acquisitions. Although revenue increased approximately 66% at the Florida health plan for the year ended December 31, 2014, when compared with 2013, profitability fell in 2014. Medical margin declined $14.1 million, and the medical care ratio increased to 95.5% from 87.3% in 2013. The higher medical care costs were the result of 1) the assumption of risk for LTSS benefits for certain members effective December 2013 (as noted above percentage profit margins for LTSS benefits are generally less than those for other benefits); and 2) our inability to recognize revenue related to a rate increase effective September 1, 2014, as a result of those rates not being finalized prior to year end.
Illinois. The medical care ratio for the TexasIllinois health plan overall decreased to 93.7%for all of 2012 compared91.7% in 2014, from 96.9% in 2013. The plan experienced significant growth in 2014; enrollment increased approximately 96,000 members overall, with95.1% for 2011. 78,000 members added in the fourth quarter alone. This growth occurred primarily within the traditional TANF program, and to a lesser degree within the Medicaid expansion program. The Illinois health plan served its first MMP members in 2014.
The medical care ratio at the California health planMichigan. increased significantly in 2012, to 91.1% in 2012 from 86.9% in 2011. As noted above, margins on newly transitioned ABD members were considerably less than those experienced by the Company overall.
The medical care ratio of the Florida health plan decreased to 85.3% in 2012, from 91.9% in 2011 due to a premium rate increase effective September 1, 2011, the re-contracting of portions of the health plan's specialty care network, lower inpatient utilization and lower pharmacy costs.
The medical care ratio of the Michigan health plan was consistent year over year, at 84.6% in 2014, compared with 84.4% in 2013.
increasedNew Mexico. to 88.3% in 2012, from 86.3% in 2011. The primary reasonPremium revenue at the New Mexico health plan increased 141% for the increase in the medical care ratio in 2012 was2014 compared with 2013, primarily as a reduction to premium rates linked to a decrease in premium taxes effective April 1, 2012. The result was a higher medical care ratio in 2012 because premium revenue decreased. There was no impact on profitability because premium tax expense was reduced by the same amount as premium revenue. The remainder of the deterioration inaddition of Medicaid behavioral health and LTSS benefits effective January 1, 2014, and the Michigan plan's medical care ratio was the result of higher pharmacy and fee for service costs. We received a blended rate increase in Michiganaddition of approximately 2%, effective October 1, 2012.
54,000 Medicaid expansion members during the course of 2014. The medical care ratio of the New Mexico health plan increased to 84.7%92.6% in 2012,2014, from 82.4%86.1% in 2011, primarily as a2013. The higher medical care ratio was the result of lower premiums1) the assumption of risk for LTSS benefits effective January 1, 2014; and higher inpatient facility costs.2) premium rates effective January 1, 2014 that did not keep pace with the increase in medical costs in 2014. The New Mexico health plan received a premiumblended rate reductionincrease of approximately 2.5%3% effective JulyJanuary 1, 2011.2015. For the portion of New Mexico health plan’s membership that is eligible for LTSS benefits, the rate increase effective January 1, 2015 was 8%.
Ohio.The medical care ratio of the Ohio health plan increased to 88.6%86.0% in 2012,2014, from 84.1%84.2% in 2011. The2013, primarily due to the increase in the Ohio health plan'sMedicaid expansion enrollment (which is incurring a medical care ratio was partiallyslightly in excess of the resultplan's traditional experience), and the initiation of a 2% rate reductionthe Ohio MMP.
South Carolina. Our South Carolina health plan commenced operations effective January 1, 2012, together2014 and finished the year with a medical care ratio of 84.7%.
Texas. Financial performance at the assumptionTexas health plan declined in 2014, when compared with 2013. The medical care ratio of the lower margin pharmacy benefit effective October 1, 2011.Texas health plan increased to 90.8% in 2014, from 86.4% in 2013. Our inability to recognize a portion of the Texas health
plan's quality revenue reduced income before taxes by approximately $26 million, or $0.33 per diluted share, for the year ended December 31, 2014. Approximately $20 million of this amount is related to measures for which we lack sufficient information to calculate our compliance. Should such information become available in the future, we may be able to recognize all or a portion of such revenue. Removing quality revenue and profit-sharing adjustments would have resulted in a medical care ratio at the Texas health plan of approximately 88% in 2014 and 86% in 2013.
Utah.The medical care ratio of the Utah health plan increased to 92.2% in 2014, from 83.4% in 2013, due to deteriorating margins for both Medicaid and Medicare products.
increasedWashington. Financial performance at the Washington health plan declined in 2014, when compared with 2013. The medical care ratio of the Washington health plan increased to 82.3%93.4% in 2012 from 78.1%2014, compared with 88.0% in 2011.2013, primarily due to the high cost of medical services relative to revenue for members served under the state's program for ABD members; and to the $11.2 million net settlement with the Washington Health Care Authority, as described in Item 8 of this Form 10-K, Notes to Consolidated Financial Statements, in Note 20, "Commitments and Contingencies." The UtahWashington health plan added approximately 102,000 Medicaid expansion members in 2014. The Washington health plan received a premiumblended rate reductionincrease of approximately 2%3% effective JulyJanuary 1, 2012.
The addition of ABD members to2015. For the Washington health plan effective July 1, 2012 increased its medical care ratio to 86.8% in the 2012, compared with 85.4% in 2011. The higher premium revenue PMPM associated with theplan’s ABD membership, however, offset the increased medical care ratio so that income from operationsrate increase effective January 1, 2015 was consistent between 2012 and 2011.11%.
Wisconsin.The medical care ratio of the Wisconsin health plan increased to 96.2%86.8% in 2012,2014, compared with 92.5%79.7% in 2011 primarily due to increases in inpatient costs. The plan has implemented provider contracting initiatives and new utilization management techniques as a part of its efforts to improve profitability.2013.
Health Plans Segment Operating Data
The following table summarizestables summarize member months, premium revenue, medical care costs, medical care ratio, and premium taxesmedical margin by health plan for the periods indicated (PMPM amounts are in whole dollars; member months and other dollar amounts are in thousands):
|
| | | | | | | | | | | | | | | | | | | | | | | | | |
| | Year Ended December 31, 2014 |
| | Member Months (1) | | Premium Revenue | | Medical Care Costs | | MCR (2) | | Medical Margin |
| | | Total | | PMPM | | Total | | PMPM | | |
| California | 5,630 |
| | $ | 1,523,084 |
| | $ | 270.51 |
| | $ | 1,268,937 |
| | $ | 225.37 |
| | 83.3 | % | | $ | 254,147 |
|
| Florida | 1,104 |
| | 439,107 |
| | 397.79 |
| | 419,422 |
| | 379.95 |
| | 95.5 |
| | 19,685 |
|
| Illinois | 307 |
| | 153,271 |
| | 498.48 |
| | 140,480 |
| | 456.88 |
| | 91.7 |
| | 12,791 |
|
| Michigan | 2,802 |
| | 780,896 |
| | 278.68 |
| | 660,790 |
| | 235.81 |
| | 84.6 |
| | 120,106 |
|
| New Mexico | 2,471 |
| | 1,075,330 |
| | 435.17 |
| | 995,626 |
| | 402.92 |
| | 92.6 |
| | 79,704 |
|
| Ohio | 3,650 |
| | 1,552,949 |
| | 425.47 |
| | 1,335,436 |
| | 365.87 |
| | 86.0 |
| | 217,513 |
|
| South Carolina | 1,463 |
| | 381,317 |
| | 260.72 |
| | 323,061 |
| | 220.89 |
| | 84.7 |
| | 58,256 |
|
| Texas | 2,980 |
| | 1,318,192 |
| | 442.32 |
| | 1,197,465 |
| | 401.81 |
| | 90.8 |
| | 120,727 |
|
| Utah | 996 |
| | 309,411 |
| | 310.64 |
| | 285,303 |
| | 286.43 |
| | 92.2 |
| | 24,108 |
|
| Washington | 5,522 |
| | 1,304,605 |
| | 236.27 |
| | 1,218,886 |
| | 220.75 |
| | 93.4 |
| | 85,719 |
|
| Wisconsin | 1,036 |
| | 156,229 |
| | 150.87 |
| | 135,557 |
| | 130.91 |
| | 86.8 |
| | 20,672 |
|
Other (3) | — |
| | 28,120 |
| | — |
| | 95,368 |
| | — |
| | — |
| | (67,248 | ) |
| | 27,961 |
| | $ | 9,022,511 |
| | $ | 322.68 |
| | $ | 8,076,331 |
| | $ | 288.84 |
| | 89.5 | % | | $ | 946,180 |
|
| | | | Year Ended December 31, 2012 | Year Ended December 31, 2013 |
| | Member Months(1) | | Premium Revenue | | Medical Care Costs | | Premium Tax Expense | | MCR Excluding Premium Tax Expense(4) | Member Months (1) | | Premium Revenue | | Medical Care Costs | | MCR (2) | | Medical Margin |
| | | Total | | PMPM | | Total | | PMPM | | | Total | | PMPM | | Total | | PMPM | |
| California | 4,177 |
| | $ | 671,489 |
| | $ | 160.77 |
| | $ | 606,494 |
| | $ | 145.20 |
| | $ | 5,697 |
| | 91.1 | % | 4,233 |
| | $ | 749,755 |
| | $ | 177.10 |
| | $ | 666,592 |
| | $ | 157.46 |
| | 88.9 | % | | $ | 83,163 |
|
| Florida | 850 |
| | 228,828 |
| | 269.36 |
| | 195,226 |
| | 229.80 |
| | (4 | ) | | 85.3 |
| 973 |
| | 264,998 |
| | 272.23 |
| | 231,261 |
| | 237.57 |
| | 87.3 |
| | 33,737 |
|
| Illinois | | 7 |
| | 8,121 |
| | 1,201.34 |
| | 7,869 |
| | 1,164.10 |
| | 96.9 |
| | 252 |
|
| Michigan | 2,639 |
| | 658,741 |
| | 249.59 |
| | 570,636 |
| | 216.20 |
| | 12,190 |
| | 88.3 |
| 2,581 |
| | 676,000 |
| | 261.91 |
| | 570,644 |
| | 221.09 |
| | 84.4 |
| | 105,356 |
|
Missouri(2) | 483 |
| | 113,818 |
| | 236.87 |
| | 113,101 |
| | 234.15 |
| | — |
| | 99.4 |
| |
| New Mexico | 1,069 |
| | 338,770 |
| | 316.90 |
| | 280,108 |
| | 262.03 |
| | 8,208 |
| | 84.7 |
| 1,492 |
| | 446,758 |
| | 299.36 |
| | 384,466 |
| | 257.62 |
| | 86.1 |
| | 62,292 |
|
| Ohio | 3,065 |
| | 1,187,422 |
| | 387.48 |
| | 970,504 |
| | 316.69 |
| | 92,285 |
| | 88.6 |
| 3,007 |
| | 1,098,795 |
| | 365.44 |
| | 924,675 |
| | 307.53 |
| | 84.2 |
| | 174,120 |
|
| South Carolina | | — |
| | — |
| | — |
| | — |
| | — |
| | — |
| | — |
|
| Texas | 3,245 |
| | 1,255,722 |
| | 386.99 |
| | 1,155,433 |
| | 356.08 |
| | 22,101 |
| | 93.7 |
| 3,178 |
| | 1,291,001 |
| | 406.27 |
| | 1,114,852 |
| | 350.84 |
| | 86.4 |
| | 176,149 |
|
| Utah | 1,026 |
| | 298,392 |
| | 290.78 |
| | 245,671 |
| | 239.41 |
| | — |
| | 82.3 |
| 1,040 |
| | 310,895 |
| | 299.05 |
| | 259,397 |
| | 249.51 |
| | 83.4 |
| | 51,498 |
|
| Washington | 4,600 |
| | 992,748 |
| | 215.83 |
| | 845,733 |
| | 183.87 |
| | 18,036 |
| | 86.8 |
| 4,941 |
| | 1,168,405 |
| | 236.47 |
| | 1,028,210 |
| | 208.10 |
| | 88.0 |
| | 140,195 |
|
| Wisconsin | 508 |
| | 70,673 |
| | 139.24 |
| | 67,968 |
| | 133.91 |
| | (5 | ) | | 96.2 |
| 1,060 |
| | 143,465 |
| | 135.40 |
| | 114,340 |
| | 107.91 |
| | 79.7 |
| | 29,125 |
|
Other(3) | — |
| | 9,888 |
| | — |
| | 45,886 |
| | — |
| | 483 |
| | — |
| — |
| | 20,977 |
| | — |
| | 77,818 |
| | — |
| | — |
| | (56,841 | ) |
| | 21,662 |
| | $ | 5,826,491 |
| | $ | 268.99 |
| | $ | 5,096,760 |
| | $ | 235.30 |
| | $ | 158,991 |
| | 89.9 | % | 22,512 |
| | $ | 6,179,170 |
| | $ | 274.48 |
| | $ | 5,380,124 |
| | $ | 238.99 |
| | 87.1 | % | | $ | 799,046 |
|
|
| | | | | | | | | | | | | | | | | | | | | | | | | |
| | Year Ended December 31, 2011 |
| | Member Months(1) | | Premium Revenue | | Medical Care Costs | | Premium Tax Expense | | MCR Excluding Premium Tax Expense(4) |
| | | Total | | PMPM | | Total | | PMPM | | |
| California | 4,190 |
| | $ | 575,176 |
| | $ | 137.27 |
| | $ | 493,419 |
| | $ | 117.75 |
| | $ | 7,499 |
| | 86.9 | % |
| Florida | 788 |
| | 203,945 |
| | 258.70 |
| | 187,358 |
| | 237.66 |
| | 41 |
| | 91.9 |
|
| Michigan | 2,660 |
| | 662,127 |
| | 248.91 |
| | 537,779 |
| | 202.16 |
| | 38,733 |
| | 86.3 |
|
Missouri(2) | 959 |
| | 229,584 |
| | 239.38 |
| | 195,832 |
| | 204.19 |
| | — |
| | 85.3 |
|
| New Mexico | 1,074 |
| | 345,732 |
| | 321.94 |
| | 277,338 |
| | 258.25 |
| | 9,285 |
| | 82.4 |
|
| Ohio | 2,966 |
| | 988,896 |
| | 333.40 |
| | 766,949 |
| | 258.57 |
| | 76,677 |
| | 84.1 |
|
| Texas | 1,616 |
| | 409,295 |
| | 253.40 |
| | 382,390 |
| | 236.74 |
| | 7,117 |
| | 95.1 |
|
| Utah | 972 |
| | 287,290 |
| | 295.51 |
| | 224,513 |
| | 230.94 |
| | — |
| | 78.1 |
|
| Washington | 4,171 |
| | 823,323 |
| | 197.42 |
| | 690,513 |
| | 165.57 |
| | 14,865 |
| | 85.4 |
|
| Wisconsin | 488 |
| | 69,596 |
| | 142.56 |
| | 64,346 |
| | 131.81 |
| | 44 |
| | 92.5 |
|
Other(3) | — |
| | 8,443 |
| | — |
| | 39,557 |
| | — |
| | 328 |
| | — |
|
| | 19,884 |
| | $ | 4,603,407 |
| | $ | 231.51 |
| | $ | 3,859,994 |
| | $ | 194.13 |
| | $ | 154,589 |
| | 86.8 | % |
____________
| |
| (1) | A member month is defined as the aggregate of each month’s ending membership for the period presented. |
| |
| (2) | Our contract with the state of Missouri expired without renewal on June 30, 2012. The Missouri health plan's claims run-out activity subsequent to June 30, 2012, is reported in “Other.” |
| |
(3) | “Other” medical care costs also include medically related administrative costs of the parent company. |
| |
(4) | The “MCR Excluding Premium Tax Expense”"MCR" represents medical costs as a percentage of premium revenues, where premium revenue is reduced by premium tax expense.revenue. |
Days in Medical Claims and Benefits Payable
The days in medical claims and benefits payable were as follows:
|
| | | | | | | | | | | |
| | December 31, |
| | 2012 | | 2011 | | 2010 |
| Days in claims payable: fee-for-service only | 40 days |
| | 40 days |
| | 42 days |
|
| Number of claims in inventory at end of period | 122,700 |
| | 111,100 |
| | 143,600 |
|
| Billed charges of claims in inventory at end of period (in thousands) | $ | 255,200 |
| | $ | 207,600 |
| | $ | 218,900 |
|
| |
| (3) | "Other" medical care costs include primarily medically related administrative costs of the parent company, and direct delivery costs. |
Molina Medicaid Solutions Segment
Performance of the Molina Medicaid Solutions segment was as follows:
| | | | Year Ended December 31, | Year Ended December 31, |
| | 2012 | | 2011 | 2014 | | 2013 |
| | (In thousands) | (In thousands) |
| Service revenue before amortization | $ | 189,281 |
| | $ | 167,269 |
| $ | 212,965 |
| | $ | 207,449 |
|
| Amortization recorded as reduction of service revenue | (1,571 | ) | | (6,822 | ) | (2,914 | ) | | (2,914 | ) |
| Service revenue | 187,710 |
| | 160,447 |
| 210,051 |
| | 204,535 |
|
| Cost of service revenue | 141,208 |
| | 143,987 |
| 156,764 |
| | 161,494 |
|
| General and administrative costs | 17,648 |
| | 9,270 |
| 7,105 |
| | 5,285 |
|
| Amortization of customer relationship intangibles recorded as amortization | 5,127 |
| | 5,127 |
| |
| Amortization of customer relationship intangibles | | 3,355 |
| | 5,127 |
|
| Operating income | $ | 23,727 |
| | $ | 2,063 |
| $ | 42,827 |
| | $ | 32,629 |
|
Operating income for our Molina Medicaid Solutions segment improved$21.7 $10.2 millionfor the year endedDecember 31, 2012, 2014, compared with2011. 2013. This improvement was primarily the result of stabilizationincreased revenues due to higher Medicaid transaction volumes and lower cost of our newest contracts in Idaho and Maine. services overall, as existing contract operations gained efficiencies.
Consolidated Expenses
General and Administrative Expenses
General and administrative expenses increaseddecreased to 8.8%7.9% of revenue in 2014, from 10.1% in 2013. The significant decline in the ratio of general and administrative expenses relative to total revenue forwas primarily the year ended December 31, 2012, compared with 8.7%result of improved leverage of fixed administrative expenses over higher total revenue for the year ended December 31, 2011.revenue.
Premium Tax Expense
Premium tax expense decreasedwas 3.2% in 2014, compared with 2.7% in 2013. In June 2014, the state of Michigan instituted a 6% use tax on medical premiums. That state has agreed to 2.8% offund this tax through rate increases; as a result, we recorded approximately $30 million in additional premium revenue net ofin 2014, as well as corresponding premium tax expense.
Health Insurer Fee Revenue and Expenses
Refer to "Liquidity and Capital Resources—Financial Condition" below for a comprehensive discussion of the year ended December 31, 2012, compared with 3.5% of total premium revenue for the year ended December 31, 2011. The decrease in 2012 was primarily due to the reduction of premium taxes at the Michigan and California health plans effective in 2012, and the growth in revenue at our Texas health plan, which is subject to a lower premium tax rate (measured as a percentage of premium revenue) than our consolidated average.HIF.
Depreciation and Amortization
Depreciation and amortization related to our Health Plans segment is all recorded in “Depreciation and Amortization” in the consolidated statements of income. Depreciation and amortization related to our Molina Medicaid Solutions segment is recorded within three different headings in the consolidated statements of income as follows:
Amortization of purchased intangibles relating to customer relationships is reported as amortization within the heading “Depreciation and amortization;”
Amortization of purchased intangibles relating to contract backlog is recorded as a reduction of “Service revenue;” and
Depreciation is recorded within the heading “Cost of service revenue.”
The following table presents all depreciation and amortization recorded in our consolidated statements of income, regardless of whether the item appears as depreciation and amortization, a reduction of revenue, or as cost of service revenue.
|
| | | | | | | | | | | | | |
| | Year Ended December 31, |
| | 2014 | | 2013 |
| | Amount | | % of Total Revenue | | Amount | | % of Total Revenue |
| | (Dollar amounts in thousands) |
| Depreciation, and amortization of capitalized software, continuing operations | $ | 75,402 |
| | 0.8 | % | | $ | 54,837 |
| | 0.8 | % |
| Amortization of intangible assets, continuing operations | 17,515 |
| | 0.2 |
| | 17,906 |
| | 0.3 |
|
| Depreciation and amortization, continuing operations | 92,917 |
| | 1.0 |
| | 72,743 |
| | 1.1 |
|
| Depreciation and amortization, discontinued operations | — |
| | — |
| | 2 |
| | — |
|
| Amortization recorded as reduction of service revenue | 2,914 |
| | — |
| | 2,914 |
| | — |
|
| Amortization of capitalized software recorded as cost of service revenue | 38,573 |
| | 0.4 |
| | 18,207 |
| | 0.3 |
|
| Depreciation and amortization reported in statement of cash flows | $ | 134,404 |
| | 1.4 | % | | $ | 93,866 |
| | 1.4 | % |
Interest Expense
Interest expense increased to $56.8 million for the year ended December 31, 2014, compared with $52.1 million for the year ended December 31, 2013. The increase was due primarily to our 3.75% Notes exchange transaction and related issuance of 1.625% Notes in the third quarter of 2014, and lease financing transactions executed in 2013. For further details regarding these transactions, please refer to Item 8 of this Form 10-K, Notes to Consolidated Financial Statements, in Note 12, "Long-Term Debt."
Interest expense includes non-cash interest expense relating to the amortization of the discount on our long-term debt obligations, which amounted to $27.4 million and $22.8 million for the years ended December 31, 2014 and 2013, respectively.
Other Expenses, Net
Other expenses, net decreased to $0.8 million for the year endedDecember 31, 2014, from $3.3 million for the year ended December 31, 2013. Other expenses, net include primarily gains or losses associated with changes in the fair value of our derivative financial instruments. In the second quarter of 2013 we recorded a one-time non-cash charge of $3.9 million related to the change in fair value of warrants issued in connection with the 1.125% Notes, with no comparable activity in 2014.
Income Taxes
The provision for income taxes in continuing operations is recorded at an effective rate of 53.8% for the year ended December 31, 2014, compared with 44.8% for the year ended December 31, 2013. The increase is primarily due to the nondeductible health insurer fee in 2014 that did not exist in 2013.
|
| | | | | | | | | | | | | |
| | Year Ended December 31, |
| | 2012 | | 2011 |
| | Amount | | % of Total Revenue | | Amount | | % of Total Revenue |
| | (Dollar amounts in thousands) |
| Depreciation, and amortization of capitalized software | $ | 43,201 |
| | 0.7 | % | | $ | 30,864 |
| | 0.7 | % |
| Amortization of intangible assets | 20,503 |
| | 0.3 |
| | 19,826 |
| | 0.4 |
|
| Depreciation and amortization reported as such in the consolidated statements of income | 63,704 |
| | 1.0 |
| | 50,690 |
| | 1.1 |
|
| Amortization recorded as reduction of service revenue | 1,571 |
| | — |
| | 6,822 |
| | 0.1 |
|
| Amortization of capitalized software recorded as cost of service revenue | 13,489 |
| | 0.2 |
| | 16,871 |
| | 0.4 |
|
| Total | $ | 78,764 |
| | 1.2 | % | | $ | 74,383 |
| | 1.6 | % |
ImpairmentResults of Goodwill and Intangible AssetsOperations, Continuing Operations
We did not record an impairment charge in 2012. On February 17, 2012, our Missouri health plan was notified that it was not awarded a new contract underYear Ended December 31, 2013 Compared with the state’s RFP, and therefore its contract expired on June 30, 2012. As a result, we recorded a non-cash impairment charge of approximately $64.6 million, or $1.34 per diluted share, in the fourth quarter of 2011. Of the total charge, $58.5 million was not tax deductible, resulting in a disproportionate impact to net income and to the effective tax rate.
Interest Expense
Interest expense was $16.8 million for the year ended Year Ended December 31, 2012, compared with $15.5
Premium Revenue
Premium revenue in 2013 increased 11% over 2012, due to a 6% increase in member months, and a 5% increase in revenue PMPM. Medicare premium revenue was $526 million for the year ended December 31, 2011. Interest expense includes non-cash interest expense relating to our convertible senior notes, which amounted to $5.9 million and $5.5 million for the years ended December 31, 2012 and 2011, respectively.
Income Taxes
Income tax expense is recorded at an effective rate of 48.6% for the year ended December 31, 2012, compared with 67.8% for the year ended December 31, 2011. The effective rate for the year ended December 31, 2012 is higher than our statutory rate primarily due to nondeductible expenses primarily relating to compensation and changes in the fair value of contingent consideration. The effective rate2013, compared with $468 million for the year ended December 31, 2011 reflects the nondeductible nature of the majority of the Missouri impairment charge and certain discrete tax benefits.
Year Ended December 31, 2011 Compared with the Year Ended December 31, 2010
Fiscal Year 2011 Overview and Highlights
For the year, our net income was $20.8 million, or $0.45 per diluted share, a decrease of 66% over 2010. We recorded a non-cash impairment charge of approximately $64.6 million, or $1.34 per diluted share, in connection with the expiration of our Missouri health plan's contract with the state of Missouri effective June 30, 2012. Absent this impairment charge, improved performance of the Health Plans segment drove our improved performance overall for the year ended December 31, 2011.
We earned premium revenues of $4.6 billion, up 15.4% over the previous year. Meanwhile, we achieved a medical care ratio of 86.8%, compared with a medical care ratio of 87.6% for fiscal year 2010.
Health Plans Segment
Premium Revenue
Premium revenue increased 15.4% in the year ended December 31, 2011, compared with the year ended December 31, 2010, due to a membership increase of approximately 8.4% (on a member-month basis), and PMPM revenue increase of approximately 6.4%. Premium revenues were impacted by the following in 2011:
In the fourth quarter of 2011, our New Mexico health plan entered into a contract amendment that more closely aligns the calculation of revenue with the methodology adopted under the Affordable Care Act. The contract amendment changed the calculation of the amount of revenue that may be recognized relative to medical costs, and resulted in the recognition of approximately $5.6 million of premium revenue which all related to periods prior to 2011.
Also in the fourth quarter of 2011, the addition of pharmacy benefits at our Ohio health plan effective October 1, 2011, increased premium revenue.
Absent the adjustment to New Mexico premium revenue and the addition of the pharmacy benefit in Ohio, premium revenue PMPM increased approximately 4.4%, from $218 in 2010 to $227 in 2011. Increased enrollment among the ABD and Medicare populations contributed to the higher premium revenue PMPM. Medicare premium revenue was $388 million for the year ended December 31, 2011, compared with $265 million for the year ended December 31, 2010.
Medical Care Costs
The following table provides the details of consolidated medical care costs for the periods indicated (dollars in thousands except PMPM amounts):
| | | | Year Ended December 31, | Year Ended December 31, |
| | 2011 | | 2010 | 2013 | | 2012 |
| | Amount | | PMPM | | % of Total | | Amount | | PMPM | | % of Total | Amount | | PMPM | | % of
Total | | Amount | | PMPM | | % of Total |
| Fee for service | $ | 2,764,309 |
| | $ | 139.02 |
| | 71.6 | % | | $ | 2,360,858 |
| | $ | 128.73 |
| | 70.0 | % | $ | 3,611,529 |
| | $ | 160.43 |
| | 67.1 | % | | $ | 3,423,751 |
| | $ | 161.67 |
| | 68.6 | % |
| Pharmacy | | 935,204 |
| | 41.54 |
| | 17.4 |
| | 835,830 |
| | 39.47 |
| | 16.7 |
|
| Capitation | 518,835 |
| | 26.09 |
| | 13.4 |
| | 555,487 |
| | 30.29 |
| | 16.5 |
| 603,938 |
| | 26.83 |
| | 11.2 |
| | 552,136 |
| | 26.07 |
| | 11.1 |
|
| Pharmacy | 418,007 |
| | 21.02 |
| | 10.8 |
| | 325,935 |
| | 17.77 |
| | 9.7 |
| |
| Direct delivery | | 48,288 |
| | 2.14 |
| | 0.9 |
| | 33,920 |
| | 1.60 |
| | 0.7 |
|
| Other | 158,843 |
| | 8.00 |
| | 4.2 |
| | 128,577 |
| | 7.01 |
| | 3.8 |
| 181,165 |
| | 8.05 |
| | 3.4 |
| | 145,551 |
| | 6.87 |
| | 2.9 |
|
| Total | $ | 3,859,994 |
| | $ | 194.13 |
| | 100.0 | % | | $ | 3,370,857 |
| | $ | 183.80 |
| | 100.0 | % | |
| | | $ | 5,380,124 |
| | $ | 238.99 |
| | 100.0 | % | | $ | 4,991,188 |
| | $ | 235.68 |
| | 100.0 | % |
Excluding our Illinois health plan, which was not operational until 2013, eight of our nine health plans reported higher medical margins in 2013 than in 2012. The consolidated medical margin increased by approximately 45% year over year. Our consolidated medical care ratio decreased to 87.1% for the year ended December 31, 2013, compared with 90.0% for the year ended December 31, 2012.
Individual Health Plan Analysis
California. Financial performance improved at the California health plan in 2013, when compared with 2012, primarily due to the receipt of premium rate increases for both TANF and ABD membership; and lower inpatient facility costs for the TANF membership. Approximately $32 million of premium revenue received and recognized in 2013 related to 2012 and earlier years. The medical care ratio decreased to 86.8% for the year ended December 31, 2011, compared with 87.6% for the year ended December 31, 2010.
The medical care ratio ofat the California health plan increaseddecreased to 86.9% for the year ended December 31, 2011,88.9% in 2013 from 84.6% for the year ended December 31, 2010. The California health plan received premium reductions of approximately 3% and 1% effective July 1, 2011, and October 1, 2011, respectively. In the second half of 2011, the California health plan added approximately 14,500 new ABD members with average premium revenue of approximately $385 PMPM.91.1% in 2012.
Florida. The medical care ratio of the Florida health plan increased to 87.3% in 2013, from 85.3% in 2012, due to higher fee-for-service costs that more than offset lower pharmacy costs.
decreasedIllinois. to 91.9%The medical care ratio for the year ended December 31, 2011, from 95.4% for the year ended December 31, 2010, primarily due to initiatives that have reduced pharmacy and behavioralIllinois health costs, and a premium rate increase of approximately 7.5%plan was 96.9% in 2013. The Illinois health plan served its first member effective September 1, 2011.2013.
Michigan. Financial performance improved at the Michigan health plan in 2013, when compared with 2012. The medical care ratio of the Michigan health plan decreased to 86.3% for the year ended December 31, 2011,84.4% in 2013, from 89.3% for the year ended December 31, 2010,88.3% in 2012, primarily due to lower fee-for-service and pharmacy costs for both the ABD and the TANF membership.
New Mexico. Financial performance improved Medicare performance and lower inpatient facility costs. The Michiganat the New Mexico health plan received a premium rate increase of approximately 1% effective October 1, 2011.
The medical care ratio of the Missouri health plan decreased to 85.3% for the year ended December 31, 2011, from 85.5% for the year ended December 31, 2010. The health plan received a premium rate increase of approximately 5% effective July 1, 2011.
in 2013, when compared with 2012. The medical care ratio of the New Mexico health plan decreased to 82.4% for the year ended December 31, 2011,86.1% in 2013, from 82.7% for the year ended December 31, 2010.87.0% in 2012, primarily as a result of higher Medicaid premium rates PMPM effective January 1, 2013, and stable medical costs PMPM. The New Mexico health plan receivedadded approximately 80,000 new members in 2013, as a premium rate reductionresult of approximately 2.5% effective July 1, 2011. As discussed above,its acquisition of Lovelace Community Health Plan's contract for the New Mexico Medicaid Salud! Program effective August 1, 2013.
Ohio. Financial performance improved at the Ohio health plan entered into a contract amendment that changed the calculation of the amount of revenue that may be recognized relative to medical costs in the fourth quarter of 2011. Consequently, premium revenue recognized in the year ended December 31, 2011, includes $5.6 million related to periods prior to 2011.
2013, when compared with 2012. The medical care ratio of the Ohio health plan decreased to 84.1%84.2% in 2013, from 88.6% in 2012, primarily due to lower fee-for-service and pharmacy costs for both the ABD and the TANF membership. Financial performance deteriorated in the second half of 2013 due to both premium decreases, and increases to fee schedules effective July 1, 2013, that combined to reduce medical margin approximately 3% for the year ended December 31, 2011, from 85.9% for the year ended December 31, 2010, due tosecond half of 2013. We also experienced an increaseadditional 1.5% decrease in Medicaid premium PMPM of approximately 4.5% effective January 1, 2011, and relatively flat fee-for-service costs. The pharmacy benefit was restored to all managed care plansrates in Ohio effective OctoberJuly 1, 2011.2013, due to a re-basing of revenue risk adjusters.
Texas. Financial performance improved at the Texas health plan in 2013, when compared with 2012. The medical care ratio of the Texas health plan increaseddecreased to 95.1% for the year ended December 31, 2011,86.4% in 2013, from 87.7% for the year ended December 31, 2010. Effective February 1, 2011, we added approximately 30,000 ABD members93.7% in the Dallas-Fort Worth area and effective2012, primarily due to rate increases received on September 1, 2011, we added approximately 8,000 ABD members2013 and 3,000 TANF members2012, respectively.
Utah. Financial performance deteriorated at the Utah health plan in the Jefferson Service area. Medical costs in the Dallas-Fort Worth area were well in excess of premium revenue. Excluding the ABD population in the Dallas-Fort Worth region,2013, when compared with 2012. Reductions to the medical care ratioportion of the Texas health plan was 87.2% forMedicaid premium, and the year ended December 31, 2011.
addition of the pharmacy benefit to our Medicaid premium, both effective January 1, 2013, more than offset stable medical costs. The medical care ratio of the Utah health plan increased to 83.4% in 2013, from 82.3% in 2012.
decreasedWashington. to 78.1% for the year ended December 31, 2011, from 91.3% for the year ended December 31, 2010, primarily due to reduced fee-for-service inpatient and physician costs and an increase in
Medicaid premiums PMPM. Effective July 1, 2010, the Utah health plan received a premium rate increase of approximately 7%. Lower fee-for-service costs were the result of both lower unit costs and lower utilization. During the second quarter of 2011 we settled certain claims with the state regarding the savings share provision of our contract in effect from 2003 through June of 2009. We settled for the contract years 2006 through 2009 and recognized $6.9 million in premium revenue without any corresponding charge to expense. The Utah health plan received a premium rate reduction of approximately 2% effective July 1, 2011.
The medical care ratio of the Washington health plan remained flat at 85.4% for the year ended December 31, 2011increased to 88.0% in 2013, compared with 86.8% in 2012, due to the year ended December 31, 2010. Higher fee-for-serviceaddition of ABD members effective July 1, 2012 and pharmacy costs werelower TANF premium rates. The higher premium revenue PMPM associated with the ABD membership, however, offset by lower capitation costs.the increased medical care ratio, so that medical margin increased to $140.2 million in 2013, from $129.0 million in 2012.
Wisconsin. Financial performance improved at the Wisconsin health plan in 2013, when compared with 2012. The medical care ratio of the Wisconsin health plan (acquired September 1, 2010) was 92.5% fordecreased to 79.7% in 2013, compared with 96.2% in 2012, due to both higher revenue PMPM and lower fee-for-service physician, specialty and outpatient costs PMPM. Additionally, the year ended December 31, 2011. The statehealth plan gained approximately 50,000 members in the first half of Wisconsin reduced capitation rates by 11% on January 1, 2011.2013 due to another health plan's exit from the market.
Health Plans Segment Operating Data
The following table summarizes member months, premium revenue, medical care costs, medical care ratio, and premium taxesmedical margin by health plan for the periods indicated (PMPM amounts are in whole dollars; member months and other dollar amounts are in thousands):
|
| | | | | | | | | | | | | | | | | | | | | | | | | |
| | Year Ended December 31, 2013 |
| | Member Months (2) | | Premium Revenue (1) | | Medical Care Costs (1) | | MCR (3) | | Medical Margin |
| | | Total | | PMPM | | Total | | PMPM | | |
| California | 4,233 |
| | $ | 749,755 |
| | $ | 177.10 |
| | $ | 666,592 |
| | $ | 157.46 |
| | 88.9 | % | | $ | 83,163 |
|
| Florida | 973 |
| | 264,998 |
| | 272.23 |
| | 231,261 |
| | 237.57 |
| | 87.3 |
| | 33,737 |
|
| Illinois | 7 |
| | 8,121 |
| | 1,201.34 |
| | 7,869 |
| | 1,164.10 |
| | 96.9 |
| | 252 |
|
| Michigan | 2,581 |
| | 676,000 |
| | 261.91 |
| | 570,644 |
| | 221.09 |
| | 84.4 |
| | 105,356 |
|
| New Mexico | 1,492 |
| | 446,758 |
| | 299.36 |
| | 384,466 |
| | 257.62 |
| | 86.1 |
| | 62,292 |
|
| Ohio | 3,007 |
| | 1,098,795 |
| | 365.44 |
| | 924,675 |
| | 307.53 |
| | 84.2 |
| | 174,120 |
|
| Texas | 3,178 |
| | 1,291,001 |
| | 406.27 |
| | 1,114,852 |
| | 350.84 |
| | 86.4 |
| | 176,149 |
|
| Utah | 1,040 |
| | 310,895 |
| | 299.05 |
| | 259,397 |
| | 249.51 |
| | 83.4 |
| | 51,498 |
|
| Washington | 4,941 |
| | 1,168,405 |
| | 236.47 |
| | 1,028,210 |
| | 208.10 |
| | 88.0 |
| | 140,195 |
|
| Wisconsin | 1,060 |
| | 143,465 |
| | 135.40 |
| | 114,340 |
| | 107.91 |
| | 79.7 |
| | 29,125 |
|
Other(4) | — |
| | 20,977 |
| | — |
| | 77,818 |
| | — |
| | — |
| | (56,841 | ) |
| | 22,512 |
| | $ | 6,179,170 |
| | $ | 274.48 |
| | $ | 5,380,124 |
| | $ | 238.99 |
| | 87.1 | % | | $ | 799,046 |
|
| | | | Year Ended December 31, 2011 | Year Ended December 31, 2012 |
| | Member Months(1) | | Premium Revenue | | Medical Care Costs | | Premium Tax Expense | | MCR Excluding Premium Tax Expense(4) | Member Months (2) | | Premium Revenue (1) | | Medical Care Costs (1) | | MCR (3) | | Medical Margin |
| | | Total | | PMPM | | Total | | PMPM | | | | Total | | PMPM | | Total | | PMPM | |
| California | 4,190 |
| | $ | 575,176 |
| | $ | 137.27 |
| | $ | 493,419 |
| | $ | 117.75 |
| | $ | 7,499 |
| | 86.9 | % | 4,177 |
| | $ | 665,600 |
| | $ | 159.36 |
| | $ | 606,494 |
| | $ | 145.20 |
| | 91.1 | % | | $ | 59,106 |
|
| Florida | 788 |
| | 203,945 |
| | 258.70 |
| | 187,358 |
| | 237.66 |
| | 41 |
| | 91.9 |
| 850 |
| | 228,832 |
| | 269.36 |
| | 195,226 |
| | 229.80 |
| | 85.3 |
| | 33,606 |
|
| Illinois | | — |
| | — |
| | — |
| | — |
| | — |
| | — |
| | — |
|
| Michigan | 2,660 |
| | 662,127 |
| | 248.91 |
| | 537,779 |
| | 202.16 |
| | 38,733 |
| | 86.3 |
| 2,639 |
| | 646,551 |
| | 244.97 |
| | 570,636 |
| | 216.20 |
| | 88.3 |
| | 75,915 |
|
Missouri(2) | 959 |
| | 229,584 |
| | 239.38 |
| | 195,832 |
| | 204.19 |
| | — |
| | 85.3 |
| |
| New Mexico | 1,074 |
| | 345,732 |
| | 321.94 |
| | 277,338 |
| | 258.25 |
| | 9,285 |
| | 82.4 |
| 1,069 |
| | 321,853 |
| | 301.08 |
| | 280,108 |
| | 262.03 |
| | 87.0 |
| | 41,745 |
|
| Ohio | 2,966 |
| | 988,896 |
| | 333.40 |
| | 766,949 |
| | 258.57 |
| | 76,677 |
| | 84.1 |
| 3,065 |
| | 1,095,137 |
| | 357.36 |
| | 970,504 |
| | 316.69 |
| | 88.6 |
| | 124,633 |
|
| Texas | 1,616 |
| | 409,295 |
| | 253.40 |
| | 382,390 |
| | 236.74 |
| | 7,117 |
| | 95.1 |
| 3,245 |
| | 1,233,621 |
| | 380.18 |
| | 1,155,433 |
| | 356.08 |
| | 93.7 |
| | 78,188 |
|
| Utah | 972 |
| | 287,290 |
| | 295.51 |
| | 224,513 |
| | 230.94 |
| | — |
| | 78.1 |
| 1,026 |
| | 298,392 |
| | 290.78 |
| | 245,671 |
| | 239.41 |
| | 82.3 |
| | 52,721 |
|
| Washington | 4,171 |
| | 823,323 |
| | 197.42 |
| | 690,513 |
| | 165.57 |
| | 14,865 |
| | 85.4 |
| 4,600 |
| | 974,712 |
| | 211.91 |
| | 845,733 |
| | 183.87 |
| | 86.8 |
| | 128,979 |
|
| Wisconsin | 488 |
| | 69,596 |
| | 142.56 |
| | 64,346 |
| | 131.81 |
| | 44 |
| | 92.5 |
| 508 |
| | 70,678 |
| | 139.25 |
| | 67,968 |
| | 133.91 |
| | 96.2 |
| | 2,710 |
|
Other(3)(4) | — |
| | 8,443 |
| | — |
| | 39,557 |
| | — |
| | 328 |
| | — |
| — |
| | 8,745 |
| | — |
| | 53,415 |
| | — |
| | — |
| | (44,670 | ) |
| | 19,884 |
| | $ | 4,603,407 |
| | $ | 231.51 |
| | $ | 3,859,994 |
| | $ | 194.13 |
| | $ | 154,589 |
| | 86.8 | % | 21,179 |
| | $ | 5,544,121 |
| | $ | 261.79 |
| | $ | 4,991,188 |
| | $ | 235.68 |
| | 90.0 | % | | $ | 552,933 |
|
|
| | | | | | | | | | | | | | | | | | | | | | | | | |
| | Year Ended December 31, 2010 |
| | Member Months(1) | | Premium Revenue | | Medical Care Costs | | Premium Tax Expense | | MCR Excluding Premium Tax Expenses(4) |
| | | Total | | PMPM | | Total | | PMPM | | |
| California | 4,197 |
| | $ | 506,871 |
| | $ | 120.77 |
| | $ | 423,021 |
| | $ | 100.79 |
| | $ | 6,912 |
| | 84.6 | % |
| Florida | 664 |
| | 170,683 |
| | 256.87 |
| | 162,839 |
| | 245.07 |
| | 1 |
| | 95.4 |
|
| Michigan | 2,708 |
| | 630,134 |
| | 232.66 |
| | 527,596 |
| | 194.80 |
| | 39,187 |
| | 89.3 |
|
Missouri(2) | 946 |
| | 210,852 |
| | 222.98 |
| | 180,291 |
| | 190.66 |
| | — |
| | 85.5 |
|
| New Mexico | 1,104 |
| | 366,784 |
| | 332.02 |
| | 295,633 |
| | 267.61 |
| | 9,300 |
| | 82.7 |
|
| Ohio | 2,817 |
| | 860,324 |
| | 305.42 |
| | 680,802 |
| | 241.69 |
| | 67,358 |
| | 85.9 |
|
| Texas | 708 |
| | 188,716 |
| | 266.72 |
| | 162,714 |
| | 229.97 |
| | 3,251 |
| | 87.7 |
|
| Utah | 921 |
| | 258,076 |
| | 280.27 |
| | 235,576 |
| | 255.84 |
| | — |
| | 91.3 |
|
| Washington | 4,141 |
| | 758,849 |
| | 183.27 |
| | 636,617 |
| | 153.75 |
| | 13,513 |
| | 85.4 |
|
| Wisconsin | 134 |
| | 30,033 |
| | 224.75 |
| | 27,574 |
| | 206.35 |
| | — |
| | 91.8 |
|
Other(3) | — |
| | 8,587 |
| | — |
| | 38,194 |
| | — |
| | 253 |
| | — |
|
| | 18,340 |
| | $ | 3,989,909 |
| | $ | 217.56 |
| | $ | 3,370,857 |
| | $ | 183.80 |
| | $ | 139,775 |
| | 87.6 | % |
| |
| (1) | Premium revenue for our former Missouri health plan was $0.2 million and $114.4 million for the years ended December 31, 2013 and 2012, respectively. Medical care costs for the plan were $1.5 million and $105.6 million for the years ended December 31, 2013 and 2012, respectively. These amounts are excluded from the tables above because the results of this health plan are classified as discontinued operations. |
| |
| (2) | A member month is defined as the aggregate of each month’s ending membership for the period presented. |
| |
(2) | Our contract with the state of Missouri expired without renewal on June 30, 2012. |
| |
| (3) | “Other” medical care costs also include medically related administrative costs at the parent company. |
| |
(4) | The “MCR Excluding Premium Tax Expense”"MCR" represents medical costs as a percentage of premium revenues, where premium revenue is reduced by premium tax expense.revenue. |
| |
| (4) | "Other" medical care costs include primarily medically related administrative costs of the parent company, and direct delivery costs. |
Molina Medicaid Solutions Segment
We acquired Molina Medicaid Solutions on May 1, 2010; therefore, the year ended December 31, 2010, includes only eight months of operating results for this segment. Performance of the Molina Medicaid Solutions segment was as follows:
| | | | | | | | Year Ended December 31, |
| | Year Ended December 31, 2011 | Eight Months Ended December 31, 2010 | 2013 | | 2012 |
| | (In thousands) | (In thousands) |
| Service revenue before amortization | $ | 167,269 |
| $ | 98,125 |
| $ | 207,449 |
| | $ | 189,281 |
|
| Amortization recorded as reduction of service revenue | (6,822 | ) | (8,316 | ) | (2,914 | ) | | (1,571 | ) |
| Service revenue | 160,447 |
| 89,809 |
| 204,535 |
| | 187,710 |
|
| Cost of service revenue | 143,987 |
| 78,647 |
| 161,494 |
| | 141,208 |
|
| General and administrative costs | 9,270 |
| 5,135 |
| 5,285 |
| | 17,648 |
|
| Amortization of customer relationship intangibles recorded as amortization | 5,127 |
| 3,418 |
| |
| Amortization of customer relationship intangibles | | 5,127 |
| | 5,127 |
|
| Operating income | $ | 2,063 |
| $ | 2,609 |
| $ | 32,629 |
| | $ | 23,727 |
|
ForOperating income for our Molina Medicaid Solutions segment increased $8.9 million for the year ended December 31, 2011, cost2013, compared with 2012. The increase in operating income was primarily the result of service revenue included $11.5 millionadditional sales in existing markets, and the favorable resolution of direct costs associated withcertain contingencies related to the Idaho contract that would otherwise have been recorded as deferred contract costs. In assessing the recoverability of the deferred contract costs associated with the Idaho contract during 2011, we determined that these costs should be expensed as a period cost. In December 2011, our MMIS in Maine received full certification from CMS.contract.
Consolidated Expenses and Other
General and Administrative Expenses
General and administrative expenses were $415.9increased to 10.1% of revenue in 2013, from 8.8% in 2012, primarily due to higher costs incurred as we prepared for significant membership growth anticipated in 2014. Increased administrative expenses related to anticipated membership growth represented approximately 2% of premium revenue, or $135 million or 8.7% of total revenue, for the year ended December 31, 2011, compared with $346.0 million, or 8.5% of total revenue, for the year ended December 31, 2010.during 2013.
Premium Tax Expense
Premium tax expense decreased to 3.5% of premium revenue net of premium tax for thewas consistent year ended December 31, 2011, compared with 3.6% for December 31, 2010.over year.
Depreciation and Amortization
The following table presents all depreciation and amortization recorded in our consolidated statements of income, regardless of whether the item appears as depreciation and amortization, a reduction of service revenue, or as cost of service revenue.
|
| | | | | | | | | | | | | |
| | Year Ended December 31, |
| | 2013 | | 2012 |
| | Amount | | % of Total Revenue | | Amount | | % of Total Revenue |
| | (Dollar amounts in thousands) |
| Depreciation, and amortization of capitalized software, continuing operations | $ | 54,837 |
| | 0.8 | % | | $ | 42,938 |
| | 0.7 | % |
| Amortization of intangible assets, continuing operations | 17,906 |
| | 0.3 |
| | 20,176 |
| | 0.3 |
|
| Depreciation and amortization, continuing operations | 72,743 |
| | 1.1 |
| | 63,114 |
| | 1.0 |
|
| Depreciation and amortization, discontinued operations | 2 |
| | — |
| | 590 |
| | — |
|
| Amortization recorded as reduction of service revenue | 2,914 |
| | — |
| | 1,571 |
| | — |
|
| Amortization of capitalized software recorded as cost of service revenue | 18,207 |
| | 0.3 |
| | 13,489 |
| | 0.2 |
|
| | $ | 93,866 |
| | 1.4 | % | | $ | 78,764 |
| | 1.2 | % |
|
| | | | | | | | | | | | | |
| | Year Ended December 31, |
| | 2011 | | 2010 |
| | Amount | | % of Total Revenue | | Amount | | % of Total Revenue |
| | (Dollar amounts in thousands) |
| Depreciation, and amortization of capitalized software | $ | 30,864 |
| | 0.7 | % | | $ | 27,230 |
| | 0.7 | % |
| Amortization of intangible assets | 19,826 |
| | 0.4 |
| | 18,474 |
| | 0.4 |
|
| Depreciation and amortization reported as such in the consolidated statements of income | 50,690 |
| | 1.1 |
| | 45,704 |
| | 1.1 |
|
| Amortization recorded as reduction of service revenue | 6,822 |
| | 0.1 |
| | 8,316 |
| | 0.2 |
|
| Amortization of capitalized software recorded as cost of service revenue | 16,871 |
| | 0.4 |
| | 6,745 |
| | 0.2 |
|
| Total | $ | 74,383 |
| | 1.6 | % | | $ | 60,765 |
| | 1.5 | % |
Impairment of Goodwill and Intangible Assets
On February 17, 2012, our Missouri health plan was notified that it was not awarded a new contract under the state’s RFP, and therefore its contract expired on June 30, 2012. As a result, we recorded a non-cash impairment charge of approximately $64.6 million, or $1.34 per diluted share, in the fourth quarter of 2011. Of the total charge, $58.5 million is not tax deductible, resulting in a disproportionate impact to net income and the effective tax rate. We did not record an impairment charge in 2010.
Interest Expense
Interest expense was $15.5$52.1 million for each of the yearsyear ended December 31, 2011 and 2010.2013, compared with $16.8 million for the year ended December 31, 2012. Interest expense includes non-cash interest expense relating to the amortization of the discount on our convertible senior notes,long-term debt obligations, which amounted to $5.5$22.8 million and $5.1$5.9 million for the years ended December 31, 2013 and 2012, respectively. The increase in interest expense for the year ended December 31, 2013, was primarily due to our issuance of $550.0 million aggregate principal amount 1.125% cash convertible senior notes due 2020 (the 1.125% Notes) in the first quarter of 2013. Interest expense in 2013 also included the immediate recognition of approximately $6 million in debt issuance costs associated with this transaction. The remaining fees associated with that issuance, amounting to approximately $12 million, are being amortized over the life of the 1.125% Notes. For the year ended December 31, 2013, interest expense also includes amounts relating to lease financing transactions executed in the second quarter of 2013.
Other Expenses, Net
Other expenses, net increased to $3.3 million for the year endedDecember 31, 2011 and 2010, respectively.2013, from $0.9 million for the year ended December 31, 2012. Other expenses, net include primarily gains or losses associated with changes in the fair value of our derivative financial instruments. In the second quarter of 2013 we recorded a one-time non-cash charge of $3.9 million related to the change in fair value of warrants issued in connection with the 1.125% Notes. We settled the interest rate swap in the second quarter of 2013, which resulted in a gain of $0.4 million, partially offsetting the $3.9 million charge described above. Other expenses, net was $0.9 million for the year ended December 31, 2012, primarily due to the change in fair value of the interest rate swap.
Income Taxes
Income tax expense wasThe provision for income taxes in continuing operations is recorded at an effective rate of 67.8% for the year ended December 31, 2011, compared with 38.6% for the year ended December 31, 2010. The effective rate44.8% for the year ended December 31, 2011 reflects the non-deductible nature of the majority of the Missouri impairment charge, discrete tax benefits of $1.7 million recognized for statute closures, prior year tax return to provision reconciliations, and certain non-recurring income that is not subject to income tax. Excluding the impact from the Missouri impairment charge and discrete tax benefits, the effective tax rate2013, compared with 45.0% for the year ended December 31, 2011 was 37.9%.
Acquisitions
Molina Center. On December 7, 2011, our wholly owned subsidiary Molina Center LLC closed on its acquisition of the 460,000 square foot office building located in Long Beach, California. The building, or Molina Center, consists of two conjoined fourteen-story office towers on approximately five acres of land. For the last several years we have leased approximately 155,000 square feet of the Molina Center for use as our corporate headquarters and also for use by our California health plan subsidiary. The final purchase price was $81 million, which amount was paid with a combination of cash on hand and bank financing under a term loan agreement. We acquired this business primarily to facilitate space needs for the projected future growth of the Company.
Molina Medicaid Solutions. On May 1, 2010, we acquired a health information management business which we operate under the name, Molina Medicaid SolutionsSM.
Other Transactions
As described above, our Missouri health plan, Alliance for Community Health, LLC, or ACH, was not awarded a contract under the Missouri HealthNet Managed Care Request for Proposal; therefore, our Missouri health plan's prior contract with the state (the “MC+ Contract”) expired without renewal on June 30, 2012, subject to certain transition obligations which terminate 365 days after June 30, 2012. ACH intends to enter into an assignment and assumption agreement with another one of our wholly owned subsidiaries, Molina Healthcare of Illinois, Inc., or Molina Illinois, pursuant to which ACH intends to assign to Molina Illinois substantially all of its assets and liabilities, including its surviving rights, duties and obligations, including all of the post-expiration duties and services under the MC+ Contract. Such assignment is subject to prior approval by the Missouri Department of Insurance, Financial Institutions and Professional Registration, the Illinois Department of Insurance, and the written consent of Mo HealthNet. Subsequent to the effectiveness of the assignment and assumption agreement between ACH and Molina Illinois and ACH's surrender of its Missouri certificate of authority, we intend to abandon our equity interests in ACH to an unrelated
entity. Subject to appropriate regulatory approvals discussed above, ACH will retain certain assets and investments, to which we will no longer have access after the abandonment transaction is effected and which amounts we intend to write off.
Liquidity and Capital Resources
Introduction
We manage our cash, investments, and capital structure to meet the short- and long-term obligations of our business while maintaining liquidity and financial flexibility. We forecast, analyze, and monitor our cash flows to enable prudent investment management and financing within the confines of our financial strategy.
Our regulated subsidiaries generate significant cash flows from premium revenue. Such cash flows are our primary source of liquidity. Thus, any future decline in our profitability may have a negative impact on our liquidity. We generally receive premium revenue in advance of the payment of claimsa short time before we pay for the related health care services. A majority of the assets held by our regulated subsidiaries are in the form of cash, cash equivalents, and investments. After considering expected cash flows from operating activities, we generally invest cash of regulated subsidiaries that exceeds our expected short-term obligations in longer term, investment-grade, and marketable debt securities to improve our overall investment return. These investments are made pursuant to board approved investment policies which conform to applicable state laws and regulations. Our investment policies are designed to provide liquidity, preserve capital, and maximize total return on invested assets, all in a manner consistent with state requirements that prescribe the types of instruments in which our subsidiaries may invest. These investment policies require that our investments have final maturities of five10 years or less (excluding auction rate securities and variable rate securities, for which interest rates are periodically reset) and that the average maturity be twothree years or less. Professional portfolio managers operating under documented guidelines manage our investments. As of December 31, 2012,2014, a substantial portion of our cash was invested in a portfolio of highly liquid money market securities, and our investments consisted solely of investment-grade debt securities. All of our investments are classified as current assets, except for our restricted investments, and our investments in auction rate securities, which are classified as non-current assets. Our restricted investments are invested principally in certificates of deposit and U.S. treasury securities.
Investment income decreasedincreased to $5.2$8.1 million for the year ended December 31, 2012,2014, compared with $5.5$6.9 million for the year ended December 31, 2011.2013, primarily due to the increase in invested assets. Our annualized portfolio yields for the years ended December 31, 2012, 2011,2014 and 20102013 were 0.5%, 0.6%,0.4% and 0.7%, respectively.for 2012 was 0.5%.
Investments and restricted investments are subject to interest rate risk and will decrease in value if market rates increase. We have the ability to hold our restricted investments until maturity. Declines in interest rates over time will reduce our investment income.
Cash in excess of the capital needs of our regulated health plans is generally paid to our non-regulated parent company in the form of dividends, when and as permitted by applicable regulations, for general corporate use. We did not receive any dividends from our health plan subsidiaries during the year ended December 31, 2014, because significant growth across all of our health plans necessitated that the plans retain their capital for operations. See further discussion below,in Item 8 of this Form 10-K, Notes to Consolidated Financial Statements, Note 20, "Commitments and Contingencies," under the subheading
"Regulatory Capital and Dividend Restrictions.
Restrictions," and Note 23, "Condensed Financial Information of Registrant," under "Note C - Dividends and Capital Contributions."
Liquidity
A condensed schedule of cash flows to facilitate our discussion of liquidity follows:
|
| | | | | | | | | | | |
| | Year Ended December 31, |
| | 2014 | | 2013 | | Change |
| | (In thousands) |
| Net cash provided by operating activities | $ | 1,060,257 |
| | $ | 190,083 |
| | $ | 870,174 |
|
| Net cash used in investing activities | (535,729 | ) | | (543,311 | ) | | 7,582 |
|
| Net cash provided by financing activities | 78,640 |
| | 493,353 |
| | (414,713 | ) |
| Net increase in cash and cash equivalents | $ | 603,168 |
| | $ | 140,125 |
| | $ | 463,043 |
|
|
| | | | | | | | | | | |
| | Year Ended December 31, |
| | 2013 | | 2012 | | Change |
| | (In thousands) |
| Net cash provided by operating activities | $ | 190,083 |
| | $ | 347,784 |
| | $ | (157,701 | ) |
| Net cash used in investing activities | (543,311 | ) | | (93,584 | ) | | (449,727 | ) |
| Net cash provided by financing activities | 493,353 |
| | 47,743 |
| | 445,610 |
|
| Net increase in cash and cash equivalents | $ | 140,125 |
| | $ | 301,943 |
| | $ | (161,818 | ) |
Operating Activities.Cash provided by operating activities was $347.8$1,060.3 million in 20122014 compared with$225.4 $190.1 million in 2011,2013, an increase of $870.2 million. This increase was due primarily to the following:
$122.4441.8 million. increase in amounts due to government agencies, due to a significant increase in amounts accrued for medical cost floor contract provisions primarily associated with our Medicaid expansion membership; and
$355.5 million increase in medical claims and benefits payable due to significant membership growth in 2014.
In 2013, cash provided by operating activities was $190.1 million compared with $347.8 million for 2012,, a decrease of $157.7 million. In 2013, deferred revenue was a sourceuse of cash from operations amounting to $90.9$19.6 million,, compared with a usesource of cash amounting to $8.2$90.9 million in 2011.2012. This increase was primarily due to an increase in deferred revenue relating to an advance premium payment received by our Washington health plan in December 2012. 2012, with no comparable advance premium receipts in December 2013.
Investing Activities. Cash used in investing activities decreased to $535.7 million in 2014, compared with $543.3 million in 2013. This $7.6 million decline in cash used was primarily due to lower purchases of investments, net of sales and maturities, compared with 2013. As described below, there was greater investment activity in 2013 associated with significant debt financing transactions.
In 2011,2013, cash provided by operatingused in investing activities was $225.4$543.3 million compared with $161.4$93.6 million for 2010, an increase of $64.0 in 2012. This $449.7 million. This increase was primarily due to higher operating income before giving effectgreater purchases of investments in 2013, as a result of the cash generated in financing activities, described below. In addition to the $64.6increased purchases of investments, we paid $61.5 million non-cash impairment of goodwill and intangible assets relating to our Missouri health plan's state contract termination recorded in the fourth quarter of 2011.
Cash used in investing activities was $93.6 million in 2012 comparedconnection with$236.9 million in 2011, a decrease of $143.3 million. This decrease was primarily due to the change in cash paid in business combinations resulting from our fourth quarter 2011 acquisition of the Molina Center amounting to $81.0 million,in 2013, with no comparable activity in 2012.
Financing Activities. Cash provided by financing activities was $78.6 million in 2014 compared with $493.4 million in 2013, a decrease of $414.7 million. Cash provided by financing activities in 2014 included primarily $122.6 million net proceeds from our fiscal 2014 offering of 1.625% Notes, partially offset by $50.3 million paid in the settlement of contingent consideration liabilities associated with our 2013 business combinations. Cash provided by financing activities in 2014 was significantly outpaced by debt financing activities in 2013, as described below.
In 2011,2013, cash provided by financing activities was $236.9 million compared with $288.8 million in 2010, a decrease of $51.9 million. This decrease was primarily due to $46.5 million less cash paid for business combinations in 2011. We acquired Molina Medicaid Solutions in the second quarter of 2010 for $131.1$493.4 million compared with $81.0$47.7 million spent to acquire the Molina Center in 2011.
Cash2012, an increase of $445.6 million. The increase in cash provided by financing activities was $47.7 million in 2012 compared with $49.5 million in 2011, a decrease of $1.8 million. Cash provided from borrowings under our credit facility in 2012 amounting to $40.0 million was consistent with cash provided from the $48.6 million term loan in 2011 used to finance the acquisition of the Molina Center. In 2011, cash provided
by financing activities was $49.5 million compared with $113.8 million in 2010, a decrease of $64.3 million. This decrease was due to $111.1 million of net proceeds from our common stock offering in the third quarter of 2010, compared with the $48.6 million term loan to acquire the Molina Center in 2011.
Financial Condition
On a consolidated basis, at December 31, 2012, we had working capital of $521.1 million compared with $446.2 million at December 31, 2011. At December 31, 2012 we had cash and investments of $1,196.1 million, compared with $893.0 million of cash and investments at December 31, 2011. We believe that our cash resources and internally generated funds will be sufficient to support our operations, regulatory requirements, and capital expenditures for at least the next 12 months.
Regulatory Capital and Dividend Restrictions
Our health plans, which are operated by our respective wholly owned subsidiaries in those states, are subject to state laws and regulations that, among other things, require the maintenance of minimum levels of statutory capital, as defined by each state. Such state laws and regulations also restrict the timing, payment, and amount of dividends and other distributions that may be paid to us as the sole stockholder. To the extent the subsidiaries must comply with these regulations, they may not have the financial flexibility to transfer funds to us. The net assets in these subsidiaries (after inter-company eliminations) which may not be transferable to us in the form of loans, advances, or cash dividends was $549.7 million atDecember 31, 2012, and $492.4 million at December 31, 2011. Because of the statutory restrictions that inhibit the ability of our health plans to transfer net assets to us, the amount of retained earnings readily available to pay dividends to our stockholders are generally limited to cash, cash equivalents and investments held by the parent company – Molina Healthcare, Inc. Such cash, cash equivalents and investments amounted to $46.9 million and $23.6 million as of December 31, 2012, and 2011, respectively. This increase was primarily due to increased dividends2013 activity including $538.0 million in proceeds received from our subsidiaries during 2012.
The National Associationoffering of Insurance Commissioners, or NAIC, adopted rules effective December 31, 1998, which, if implemented by the states, set minimum capitalization requirements for insurance companies, HMOs, and other entities bearing risk for health care coverage. The requirements take the form of risk-based capital, or RBC, rules. Michigan, New Mexico, Ohio, Texas, Utah, Washington, and Wisconsin have adopted these rules, which may vary1.125% Notes, $158.7 million received from state to state. California and Florida have not yet adopted NAIC risk-based capital requirements for HMOs and have not formally given notice of their intention to do so. Such requirements, if adopted by California and Florida, may increase the minimum capital required for those states.
As ofDecember 31, 2012, our health plans had aggregate statutory capital and surplus of approximately $557.9 million compared with the required minimum aggregate statutory capital and surplus of approximately $345.7 million. All of our health plans were in compliance with the minimum capital requirements at December 31, 2012. We have the ability and commitment to provide additional capital to each of our health plans when necessary to ensure that statutory capital and surplus continue to meet regulatory requirements.
Future Sources and Uses of Liquidity
1.125% Cash Convertible Senior Notes due 2020
On February 15, 2013, we issued $550 million aggregate principal amount of 1.125% Cash Convertible Senior Notes due 2020, or the Notes. The Notes bear interest at a rate of 1.125% per year, payable semiannually in arrears on January 15 and July 15 of each year, beginning on July 15, 2013. The Notes will mature on January 15, 2020.
The Notes are not convertible into our common stock or any other securities under any circumstances. Holders may convert their Notes solely into cash at their option at any time prior to the close of business on the business day immediately preceding July 15, 2019 only under the following circumstances: (1) during any calendar quarter commencing after the calendar quarter ending on June 30, 2013 (and only during such calendar quarter), if the last reported sale price of the common stock for at least 20 trading days (whether or not consecutive) during a period of 30 consecutive trading days ending on the last trading day of the immediately preceding calendar quarter is greater than or equal to 130% of the conversion price on each applicable trading day; (2) during the five business day period immediately after any five consecutive trading day period in which the trading price per $1,000 principal amount of Notes for each trading day of the measurement period was less than 98% of the product of the last reported sale price of our common stock and the conversion rate on each such trading day; or (3) upon the occurrence of specified corporate events. On or after July 15, 2019 until the close of business on the second scheduled trading day immediately preceding the maturity date, holders may convert their Notes solely into cash at any time, regardless of the foregoing circumstances. Upon conversion, in lieu of receiving shares of our common stock, a holder will receive an amount in cash, per $1,000 principal amount of Notes, equal to the settlement amount, determined in the manner set forth in the Indenture.
The initial conversion rate will be 24.5277 shares of our common stock per $1,000 principal amount of Notes (equivalent to an initial conversion price of approximately $40.77 per share of common stock). The conversion rate will be subject to adjustment
in some events but will not be adjusted for any accrued and unpaid interest. In addition, following certain corporate events that occur prior to the maturity date, we will pay a cash make-whole premium by increasing the conversion rate for a holder who elects to convert its Notes in connection with such a corporate event in certain circumstances. We may not redeem the Notes prior to the maturity date, and no sinking fund is provided for the Notes.
If we undergo a fundamental change (as defined in the indenture to the Notes), holders may require us to repurchase for cash all or part of their Notes at a repurchase price equal to 100% of the principal amount of the Notes to be repurchased, plus accrued and unpaid interest to, but excluding, the fundamental change repurchase date. The indenture provides for customary events of default, including cross acceleration to certain other indebtedness of ours, and our significant subsidiaries.
The Notes will be senior unsecured obligations of the Company and will rank senior in right of payment to any of our indebtedness that is expressly subordinated in right of payment to the Notes; equal in right of payment to any of our unsecured indebtedness that is not so subordinated; effectively junior in right of payment to any of our secured indebtedness to the extent of the value of the assets securing such indebtedness; and structurally junior to all indebtedness and other liabilities (including trade payables) of our subsidiaries.
Cash Convertible Note Hedge and Warrant Transactions
In connection with the pricing of the Notes, on February 11, 2013, we entered into cash convertible note hedgesale-leaseback transactions, and warrant transactions relating to a notional number of shares of our common stock underlying the Notes to be issued by us (without regard to the initial purchasers' $100$75.1 million over-allotment option) with two counterparties, JPMorgan Chase Bank, National Association, London Branch and Bank of America, N.A. (the “Option Counterparties”). The cash convertible note hedge transactions are intended to offset cash payments due upon any conversion of the Notes. However, the warrant transactions could separately have a dilutive effect to the extent that the market value per share of our common stock (as measured under the terms of the warrant transactions) exceeds the applicable strike price of the warrants. The strike price of the warrants will initially be $53.8475 per share, which is 75% above the last reported sale price of our common stock on February 11, 2013.
In connection with the exercise in full by the initial purchasers of their over-allotment option in respect of the Notes, on February 13, 2013, we and the Option Counterparties amended the cash convertible note hedge transactions entered into on February 11, 2013 to upsize such transactions by a notional number of shares of our common stock corresponding to the number of shares underlying the Notes purchased pursuant to the exercise of such over-allotment option. On February 13, 2013, we also entered into additional warrant transactions with the Option Counterparties relating to a number of shares of our common stock corresponding to the number of shares underlying the Notes purchased pursuant to the exercise of such over-allotment option. Each of the amendments to the cash convertible note hedge transactions and the additional warrant transactions were on substantially similar terms to the corresponding transactions entered into on February 11, 2013. Pursuant to these warrant transactions, we issued 13,490,236 warrants with a strike price of $53.8475 per share. The number of warrants and the strike price are subject to adjustment under certain circumstances.
We used approximately $74.3 million of the net proceeds from the offering to pay the cost of the cash convertible note hedge transactions (after such cost was partially offset by the proceeds to us from the sale of warrants, inpartially offset by $149.3 million paid for the warrant transactions and the additional warrant transactions).
Aside from the initial payment of a premiumpurchased call option relating to the Option Counterparties of approximately $149.31.125% Notes, $52.7 million, we will not be required to make any cash payments to the Option Counterparties under the cash convertible note hedge transactions and will be entitled to receive from the Option Counterparties an amount of cash, generally equal to the amount by which the market price per share of common stock exceeds the strike price of the cash convertible note hedge transactions during the relevant valuation period. The strike price under the cash convertible note hedge transactions is initially equal to the conversion price of the Notes. Additionally, if the market value per share paid for repurchases of our common stock, exceeds$47.5 million used to repay our term loan, and $40.0 million used to repay our credit facility. Our credit facility was terminated in early 2013 when the strike price of the warrants on any trading day during the 160 trading day measurement period under the warrant transactions and the additional warrant transactions, we will be obligated to issue to the Option Counterparties a number of shares equal in value to the product of the amount by which such market value exceeds such strike price and 1/160th of the aggregate number of shares of our common stock underlying the warrant transactions and the additional warrant transactions, subject to a share delivery cap. The Company will not receive any additional proceeds if warrants are exercised.
Repurchase in Connection with Offering of 1.125% Cash Convertible Senior Notes Due 2020
We used a portion of the net proceeds in this offering to repurchase $50 million of our common stock in negotiated transactions with institutional investors in the offering, concurrently with the pricing of the offering. On February 12, 2013, we repurchased a total of 1,624,959 shares at $30.77 per share, whichbalance was our closing stock price on that date.
repaid.
Credit FacilityFinancial Condition
On a consolidated basis, at December 31, 2014, our working capital was $1,070.6 million compared with $745.7 million at December 31, 2013. At December 31, 2014, our cash and investments amounted to $2,665.9 million, compared with $1,712.9 million of cash and investments at December 31, 2013.
On February 15, 2013, we used approximatelyHealth Insurer Fee $40.0 million . One notable provision of the net proceeds fromACA is an excise tax or annual fee that applies to most health plans, including commercial health plans and Medicaid managed care plans like Molina Healthcare. While characterized as a "fee" in the offeringtext of the NotesACA, the intent of Congress was to repay all ofimpose a broad-based health insurance industry excise tax, with the outstanding indebtedness under our $170 million revolving credit facility, orunderstanding that the Credit Facility, with various lenders and U.S. Bank National Association, as Line of Credit Issuer, Swing Line Lender, and Administrative Agent. As of December 31, 2012, there was $40.0 million outstanding under the Credit Facility. tax could be passed on to consumers, most likely through higher commercial insurance premiums.
We terminated the Credit Facility in connection with the closing of the offering and sale of the Notes. Two letters of credit in the aggregate principal amount of $10.3 million that reduced the amount available for borrowing under the Credit Facilityas of December 31, 2012, were transferred to direct issue letters of credit with another financial institution. The Credit Facility had a term of five years under which all amounts outstanding would have been due and payable on September 9, 2016.
Borrowings under the Credit Facility accrued interest based, at our election, on the base rate plus an applicable margin or the Eurodollar rate. The base rate is, for any day, a rate of interest per annum equal to the highest of (i) the prime rate of interest announced from time to time by U.S. Bank or its parent, (ii) the sum of the federal funds rate for such day plus 0.50% per annum and (iii) the Eurodollar rate (without giving effect to the applicable margin) for a one month interest period on such day (or if such day is not a business day, the immediately preceding business day) plus 1.00%. The Eurodollar rateHowever, because Medicaid is a reserve adjusted rate at which Eurodollar deposits are offered ingovernment funded program, Medicaid health plans have no alternative but to look to their respective state partners for payment to offset the interbank Eurodollar market plus an applicable margin. In addition to interest payable onimpact of this tax. Additionally, when states reimburse us for the principal amount of indebtedness outstanding from time to time under the Credit Facility, we were required to pay a quarterly commitment fee of 0.25% to 0.50% (based upon our leverage ratio) of the unused amount of the lenders' commitments underHIF, that reimbursement is itself subject to income tax, the Credit Facility. TheHIF, and applicable margins ranged between 0.75% to 1.75% state premium taxes. Because the HIF is not deductible for base rate loans and 1.75% to 2.75% for Eurodollar loans, in each case, based uponincome tax purposes, our leverage ratio.
Our obligations undernet income is reduced by the Credit Facility were secured by a lien on substantially all of our assets, with the exception of certain of our real estate assets, and by a pledge of the capital stock or membership interests of our operating subsidiaries and health plans (with the exception of the California health plan). The Credit Facility included usual and customary covenants for credit facilities of this type, including covenants limiting liens, mergers, asset sales, other fundamental changes, debt, acquisitions, dividends and other distributions, capital expenditures, and investments. The Credit Facility also required us to maintain as of the end of any fiscal quarter (calculated for each four consecutive fiscal quarter period) a ratio of total consolidated debt to total consolidated EBITDA, as defined in the Credit Facility, of not more than 2.75 to 1.00, and a fixed charge coverage ratio of not less than 1.75 to 1.00. AtDecember 31, 2012, we were in compliance with all financial covenants under the Credit Facility.
3.75% Convertible Senior Notes due 2014
As of December 31, 2012, $187.0 million in aggregate principal amount of our 3.75% Convertible Senior Notes due 2014, or the 3.75% Notes, remain outstanding. The 3.75% Notes rank equally in right of payment with our existing and future senior indebtedness. The 3.75% Notes are convertible into cash and, under certain circumstances, shares of our common stock. The initial conversion rate is 31.9601 shares of our common stock per one thousand dollar principalfull amount of the 3.75% Notes. This representsassessment. We expect our 2015 HIF assessment related to our Medicaid business to be approximately $143 million, with an initial conversion priceexpected tax effect from the reimbursement of the assessment of approximately $88 million. Therefore, the total reimbursement needed as a result of the Medicaid-related HIF is approximately $231 million.
Our 2014 HIF assessment amounted to $88.6 million, which was paid in September 2014. As indicated in the table below, it was necessary for the states to pay us an incremental amount of approximately $131 million during 2014 to account for the HIF and the absence of its deductibility.
The state of California has not formally committed to reimburse us for either the HIF itself, or the related tax effects. The states of Michigan and Utah have reimbursed us for the HIF, but have not formally committed to reimbursement for the related tax effect. The total amount of HIF revenue for which agreements were not secured (and revenue was not recognized) amounted to approximately $20 million for fiscal 2014. We expect to collect and recognize this revenue related to 2014 in 2015. We further expect to recognize revenue in 2015 sufficient to reimburse us for the full amount of the HIF we will pay (along with related tax effects) in September of 2015.
$31.29 per shareWe continue to work with our state partners to obtain reimbursement for the full economic impact of the excise tax. The failure of our common stock. In addition, if certain corporate transactions that constitute a change of control occur priorstate partners to maturity, we will increase the conversion ratereimburse us in certain circumstances.
Term Loan
On December 7, 2011, our wholly owned subsidiary Molina Center LLC entered into a Term Loan Agreement, dated as of December 1, 2011, with various lenders and East West Bank, as Administrative Agent (the “Administrative Agent”). Pursuant to the terms of the Term Loan Agreement, Molina Center LLC borrowed the aggregate principal amount of $48.6 million to finance a portion of the $81 million purchase pricefull for the acquisitionHIF and its related tax effects could have a material adverse effect on our business, financial condition, cash flows or results of the Molina Center, located in Long Beach, California.operations.
The outstanding principal amount underfollowing table provides the Term Loan Agreement bears interest at the Eurodollar rate for each Interest Period (as defined below) commencing January 1, 2012. The Eurodollar rate is a per annum ratedetails of interest equalour HIF revenue reimbursement by health plan to the greater of (a) the rate that is publisheddate in the Wall Street Journal as the London interbank offered rate for deposits in United States dollars, for a period of one month, two business days prior to the commencement of an Interest Period, multiplied by a statutory reserve rate established by the Board of Governors of the Federal Reserve System, or (b)2014 (in thousands): 4.25%. "Interest Period" means the period commencing on the first day of each calendar month and ending on the last day of each calendar month. The loan matures on November 30, 2018, and is subject to a 25-year amortization schedule that commenced on January 1, 2012. The Term Loan Agreement contains customary representations, warranties, and financial covenants. In the event of a default as described in the Term Loan Agreement, the outstanding principal amount under the Term Loan Agreement will bear interest at a rate 5.00% per annum higher than the otherwise applicable rate. All amounts due under the Term Loan Agreement and related loan documents are secured by a security interest in the Molina Center in favor of and for the benefit of the Administrative Agent and the other lenders under the Term Loan Agreement. |
| | | | | | | | | | | | | | | | | | | | | | | |
| | HIF Reimbursement Recognized | | Required HIF Reimbursement through Dec. 31, 2014 |
| | Three Months Ended | | Year Ended Dec. 31, 2014 | |
| | March 31, 2014 | | June 30, 2014 | | Sept. 30, 2014 | | Dec. 31, 2014 | | |
| | Gross (1) |
| California | $ | — |
| | $ | — |
| | $ | — |
| | $ | — |
| | $ | — |
| | $ | 11,616 |
|
| Florida | 1,416 |
| | 1,473 |
| | 1,487 |
| | 1,459 |
| | 5,835 |
| | 5,835 |
|
| Illinois | 40 |
| | 42 |
| | 40 |
| | 40 |
| | 162 |
| | 162 |
|
| Michigan | — |
| | — |
| | 8,011 |
| | 2,663 |
| | 10,674 |
| | 17,471 |
|
| New Mexico | — |
| | — |
| | — |
| | 11,322 |
| | 11,322 |
| | 11,322 |
|
| Ohio | 7,791 |
| | 8,117 |
| | 6,912 |
| | 7,606 |
| | 30,426 |
| | 30,426 |
|
| Texas | — |
| | — |
| | — |
| | 18,518 |
| | 18,518 |
| | 18,518 |
|
| Utah | — |
| | — |
| | 3,000 |
| | 1,049 |
| | 4,049 |
| | 5,332 |
|
| Washington | 6,229 |
| | 6,489 |
| | 6,217 |
| | 6,311 |
| | 25,246 |
| | 25,246 |
|
| Wisconsin | 1,080 |
| | 1,126 |
| | 1,372 |
| | 1,193 |
| | 4,771 |
| | 4,771 |
|
| Medicaid | 16,556 |
| | 17,247 |
| | 27,039 |
| | 50,161 |
| | 111,003 |
| | 130,699 |
|
| Medicare | 2,892 |
| | 3,199 |
| | 3,068 |
| | 3,053 |
| | 12,212 |
| | 12,212 |
|
| | $ | 19,448 |
| | $ | 20,446 |
| | $ | 30,107 |
| | $ | 53,214 |
| | $ | 123,215 |
| | $ | 142,911 |
|
| Recognized in: | | | | | | | | | | | |
| Health insurer fee revenue | $ | 18,696 |
| | $ | 19,662 |
| | $ | 29,427 |
| | $ | 51,699 |
| | $ | 119,484 |
| | |
| Premium tax revenue | 752 |
| | 784 |
| | 680 |
| | 1,515 |
| | 3,731 |
| | |
| | $ | 19,448 |
| | $ | 20,446 |
| | $ | 30,107 |
| | $ | 53,214 |
| | $ | 123,215 |
| | |
Interest Rate Swap_____________
| |
| (1) | Amounts in the table include the full economic impact of the excise tax including premium tax and the income tax effect. |
Regulatory Capital and Dividend Restrictions
In May 2012, we entered intoFor a $42.5 million notional amount interest rate swap agreement, or Swap Agreement, with an effective datecomprehensive discussion of March 1,our regulatory capital requirements and dividend restrictions, refer to Item 8 of this Form 10-K, Notes to Consolidated Financial Statements, in Note 20 "Commitments and Contingencies."
Future Sources and Uses of Liquidity
For a comprehensive discussion of our debt instruments, including our convertible senior notes transactions in 2014 and 2013,. While not designated as refer to Item 8 of this Form 10-K, Notes to Consolidated Financial Statements, in Note 12 "Long-Term Debt."
For a hedge during the year ended December 31, 2012, the Swap Agreement is intended to reducediscussion of our exposure to fluctuations in the contractual variable interest rates under our Term Loan Agreement, and expires on the maturity date of the Term Loan Agreement, which is November 30, 2018. Under the Swap Agreement, we will receive a variable rate of the one-month LIBOR plus 3.25%, and pay a fixed rate of 5.34%. The Swap Agreement is measured and reported at fair value on a recurring basis, within Level 2 of the fair value hierarchy. Gains and losses relating to changes in fair value are reported in earnings in the current period. For the year endedDecember 31, 2012, we have recorded losses of $1.3 million to general and administrative expense. As ofDecember 31, 2012the fair value of the Swap Agreement is a liability of $1.3 million, recorded to other noncurrent liabilities. We do not use derivatives for trading or speculative purposes. We believe that we are not exposed to more than a nominal amount of credit risk relating to the Swap Agreement because the counterparty is an established and well-capitalized financial institution.
Shelf Registration Statement
In May 2012, we filed an automatic shelf registration statement, on Form S-3 with the Securities and Exchange Commission covering the issuance of an indeterminate number of our securities including common stock, warrants, or debt securities. We may publicly offer securities from timerepurchase programs through December 31, 2014, refer to time at prices and termsItem 8 of this Form 10-K, Notes to be determined at the time of the offering.
Securities Repurchase ProgramConsolidated Financial Statements, in Note 15, "Stockholders' Equity."
Effective as of February 13, 2013,25, 2015, our board of directors authorized the repurchase of $75up to $50 million in aggregate of either our common stock stock. Stock repurchases under this program may be made through open-market and/or our convertible senior note due 2014.privately negotiated transactions at times and in such amounts as management deems appropriate. The timing and actual number of shares repurchased will depend on a variety of factors including price, corporate and regulatory requirements and market conditions. This newly authorized repurchase program extends through December 31, 2014.
2015.
Critical Accounting PoliciesEstimates
When we prepare our consolidated financial statements, we use estimates and assumptions that may affect reported amounts and disclosures. Actual results could differ from these estimates. Our most significant accounting policiesestimates relate to:
Health Plans segment medical claims and benefits payable (see discussion below).
Health planPlans segment contractual provisions that may adjust or limit revenue based upon the costs incurred or the profits realized underprofit. For a specific contract;
Health plan quality incentives that allow us to recognize incremental revenue if certain quality standards are met;
The recognitioncomprehensive discussion of revenue and costs associated with contracts held by our Molina Medicaid Solutions segment; and;
The determination of medical claims and benefits payable.
Revenue Recognition — Health Plans Segment
Premium revenue is fixed in advance of the periods covered and, except as described below, is not generally subject to significant accounting estimates. Premium revenues are recognized in the month that members are entitled to receive health care services.
Certain components of premium revenue are subject to accounting estimates. The components of premium revenue subject to estimation fall into two categories:
Contractual provisions that may limit revenue based upon the costs incurred or the profits realized under a specific contract. These are contractual provisions that require the health plan to return premiums to the extent that certain thresholds are not met. In some instances premiums are returned when medical costs fall below a certain percentage of gross premiums; or when administrative costs or profits exceed a certain percentage of gross premiums. In other instances, premiums are partially determined by the acuity of care provided to members (risk adjustment). To the extent that our expenses and profits change from thethis topic, including amounts previously reported (due to changes in estimates) our revenue earned for those periods will also change. In all of these instances our revenue is only subject to estimate due to the fact that the thresholds themselves contain elements (expense or profit) that are subject to estimate. While we have adequate experience and data to make sound estimates of our expenses or profits, changes to those estimates may be necessary, which in turn will lead to changesrecorded in our estimates of revenue. In general, a change in estimate relatingconsolidated financial statements, refer to expense or profit would offset any related change in estimate to premium, resulting in no or small impact to net income. The following contractual provisions fall into this category:
California Health Plan Medical Cost Floors (Minimums):A portion of certain premiums received by our California health plan may be returned to the state if certain minimum amounts are not spent on defined medical care costs. We
recorded a liability under the terms of these contract provisions of $0.3 million and $1.0 million at December 31, 2012, and December 31, 2011, respectively.
Florida Health Plan Medical Cost Floor (Minimum) for Behavioral Health:A portion of premiums received by our Florida health plan may be returned to the state if certain minimum amounts are not spent on defined behavioral health care costs. At bothDecember 31, 2012 and December 31, 2011, we had not recorded any liability under the termsItem 8 of this contract provision since behavioral health expenses are not less than the contractual floor. Form 10-K, Notes to Consolidated Financial Statements, in Note 2, "Significant Accounting Policies."
New Mexico Health Plan Medical Cost Floors (Minimums) and Administrative Cost and Profit Ceilings (Maximums): Plans segment quality incentives.Our contract with the state For a comprehensive discussion of New Mexico directs that a portionthis topic, including amounts recorded in our consolidated financial statements, refer to Item 8 of premiums received may be returnedthis Form 10-K, Notes to the state if certain minimum amounts are not spent on defined medical care costs, or if administrative costs or profit (as defined) exceed certain amounts. At both December 31, 2012, and December 31, 2011, we had not recorded any liability under the terms of these contract provisions. Consolidated Financial Statements, in Note 2, "Significant Accounting Policies."
Texas Health Plan Profit Sharing: Under our contract with the state of Texas, there is a profit-sharing agreement under which we pay a rebate to the state of Texas if our Texas health plan generates pretax income, as defined in the contract, above a certain specified percentage, as determined in accordance with a tiered rebate schedule. We are limited in the amount of administrative costs that we may deduct in calculating the rebate, if any. As a result of profits in excess of the amount we are allowed to fully retain, we accrued an aggregate liability of approximately $3.2 million and $0.7 million pursuant to our profit-sharing agreement with the state of Texas at December 31, 2012 and December 31, 2011, respectively.
Washington Health Plan Medical Cost Floors (Minimums): A portion of certain premiums received by our Washington health plan may be returned to the state if certain minimum amounts are not spent on defined medical care costs. At both December 31, 2012, andDecember 31, 2011, we had not recorded any liability under the terms of this contract provision because medical expenses are not less than the contractual floor.
Medicare Revenue Risk Adjustment:Based on member encounter data that we submit to CMS, our Medicare premiums are subject to retroactive adjustment for both member risk scores and member pharmacy cost experience for up to two years after the original year of service. This adjustment takes into account the acuity of each member’s medical needs relative to what was anticipated when premiums were originally set for that member. In the event that a member requires less acute medical care than was anticipated by the original premium amount, CMS may recover premium from us. In the event that a member requires more acute medical care than was anticipated by the original premium amount, CMS may pay us additional retroactive premium. A similar retroactive reconciliation is undertaken by CMS for our Medicare members’ pharmacy utilization. We estimate the amount of Medicare revenue that will ultimately be realized for the periods presented based on our knowledge of our members’ heath care utilization patterns and CMS practices. Based on our knowledge of member health care utilization patterns and expenses we have recorded a net receivable of approximately $0.3 million and $5.0 million for anticipated Medicare risk adjustment premiums at December 31, 2012, and December 31, 2011, respectively.
Quality incentives that allow us to recognize incremental revenue if certain quality standards are met.These are contract provisions that allow us to earn additional premium revenue in certain states if we achieve certain quality-of-care or administrative measures. We estimate the amount of revenue that will ultimately be realized for the periods presented based on our experience and expertise in meeting the quality and administrative measures as well as our ongoing and current monitoring of our progress in meeting those measures. The amount of the revenue that we will realize under these contractual provisions is determinable based upon that experience. The following contractual provisions fall into this category:
New Mexico Health Plan Quality Incentive Premiums:Under our contract with the state of New Mexico, incremental revenue of up to 0.75% of our total premium is earned if certain performance measures are met. These performance measures are generally linked to various quality-of-care and administrative measures dictated by the state.
Ohio Health Plan Quality Incentive Premiums:Under our contract with the state of Ohio, incremental revenue of up to 1% of our total premium is earned if certain performance measures are met. These performance measures are generally linked to various quality-of-care measures dictated by the state.
Texas Health Plan Quality Incentive Premiums:Effective March 1, 2012, under our contract with the state of Texas, incremental revenue of up to 5% of our total premium may be earned if certain performance measures are met. These performance measures are generally linked to various quality-of-care measures established by the state.
Wisconsin Health Plan Quality Incentive Premiums:Under our contract with the state of Wisconsin, effective beginning in 2011, up to 3.25% of premium revenue is withheld by the state. The withheld premiums can be earned by the health plan by meeting certain performance measures. These performance measures are generally linked to various quality-of-care measures dictated by the state.
The following table quantifies the quality incentive premium revenue recognized for the periods presented, including the amounts earned in the period presented and prior periods. Although the reasonably possible effects of a change in estimate related to quality incentive premium revenue as of December 31, 2012are not known, we have no reason to believe that the adjustments to prior years noted below are not indicative of the potential future changes in our estimates as of December 31, 2012.
|
| | | | | | | | | | | | | | | | | | | |
| | Year Ended December 31, 2012 |
| | Maximum Available Quality Incentive Premium – Current Year | | Amount of Current Year Quality Incentive Premium Revenue Recognized | | Amount of Quality Incentive Premium Revenue Recognized from Prior Year | | Total Quality Incentive Premium Revenue Recognized | | Total Revenue Recognized |
| | (In thousands) |
| New Mexico | $ | 2,244 |
| | $ | 1,889 |
| | $ | 643 |
| | $ | 2,532 |
| | $ | 338,770 |
|
| Ohio | 12,033 |
| | 8,079 |
| | 966 |
| | 9,045 |
| | 1,187,422 |
|
| Texas | 58,516 |
| | 52,521 |
| | — |
| | 52,521 |
| | 1,255,722 |
|
| Wisconsin | 1,771 |
| | — |
| | 593 |
| | 593 |
| | 70,673 |
|
| | $ | 74,564 |
| | $ | 62,489 |
| | $ | 2,202 |
| | $ | 64,691 |
| | $ | 2,852,587 |
|
|
| | | | | | | | | | | | | | | | | | | |
| | Year Ended December 31, 2011 |
| | Maximum Available Quality Incentive Premium – Current Year | | Amount of Current Year Quality Incentive Premium Revenue Recognized | | Amount of Quality Incentive Premium Revenue Recognized from Prior Year | | Total Quality Incentive Premium Revenue Recognized | | Total Revenue Recognized |
| | (In thousands) |
| New Mexico | $ | 2,271 |
| | $ | 1,558 |
| | $ | 378 |
| | $ | 1,936 |
| | $ | 345,732 |
|
| Ohio | 10,212 |
| | 8,363 |
| | 3,501 |
| | 11,864 |
| | 988,896 |
|
| Texas | — |
| | — |
| | — |
| | — |
| | 409,295 |
|
| Wisconsin | 1,705 |
| | 542 |
| | — |
| | 542 |
| | 69,596 |
|
| | $ | 14,188 |
| | $ | 10,463 |
| | $ | 3,879 |
| | $ | 14,342 |
| | $ | 1,813,519 |
|
|
| | | | | | | | | | | | | | | | | | | |
| | Year Ended December 31, 2010 |
| | Maximum Available Quality Incentive Premium – Current Year | | Amount of Current Year Quality Incentive Premium Revenue Recognized | | Amount of Quality Incentive Premium Revenue Recognized from Prior Year | | Total Quality Incentive Premium Revenue Recognized | | Total Revenue Recognized |
| | (In thousands) |
| New Mexico | $ | 2,581 |
| | $ | 1,311 |
| | $ | 579 |
| | $ | 1,890 |
| | $ | 366,784 |
|
| Ohio | 9,881 |
| | 3,114 |
| | (1,248 | ) | | 1,866 |
| | 860,324 |
|
| Texas | 1,771 |
| | 1,771 |
| | — |
| | 1,771 |
| | 188,716 |
|
| | $ | 14,233 |
| | $ | 6,196 |
| | $ | (669 | ) | | $ | 5,527 |
| | $ | 1,415,824 |
|
Service Revenue and Cost of Service Revenue — Molina Medicaid Solutions Segment
The payments received by our Molina Medicaid Solutions segment under its state contracts are based on the performance of multiple services. The first of these is the design, developmentrevenue and implementation, or DDI, ofcost recognition. For a Medicaid Management Information System, or MMIS. An additional service, following completion of DDI, is the operation of the MMIS under a business process outsourcing, or BPO arrangement. While providing BPO services (which include claims payment and eligibility processing) we also provide the state with other services including both hosting and support and maintenance. Our Molina Medicaid Solutions contracts may extend over a number of years, particularly in circumstances where we are delivering extensive and complex DDI services, such as the initial design, development and implementation of a complete MMIS. For example, the terms of our most recently implemented Molina Medicaid Solutions contracts (in Idaho and Maine) were each seven years in total, consisting of two years allocated for the delivery of DDI services, followed by five years for the performance of BPO services. We receive progress payments from the state during the performance of DDI services based upon the attainment of predetermined milestones. We receive a flat monthly payment for BPO services under our Idaho and Maine contracts. The terms of our other Molina Medicaid
Solutions contracts - which primarily involve the delivery of BPO services with only minimal DDI activity (consisting of system enhancements) - are shorter in duration than our Idaho and Maine contracts.
We have evaluated our Molina Medicaid Solutions contracts to determine if such arrangements include a software element. Based on this evaluation, we have concluded that these arrangements do not include a software element. As such, we have concluded that our Molina Medicaid Solutions contracts are multiple-element service arrangements under the scope of FASB Accounting Standards Codification Subtopic 605-25, Revenue Recognition –– Multiple–Element Arrangements, and SEC Staff Accounting Bulletin Topic 13, Revenue Recognition.
Effective January 1, 2011, we adopted a new accounting standard that amends the guidance on the accounting for multiple-element arrangements. Pursuant to the new standard, each required deliverable is evaluated to determine whether it qualifies as a separate unit of accounting which is generally based on whether the deliverable has standalone value to the customer. In addition to standalone value, previous guidance also required objective and reliable evidence of fair value of a deliverable in order to treat the deliverable as a separate unit of accounting. The arrangement’s consideration that is fixed or determinable is then allocated to each separate unit of accounting based on the relative selling price of each deliverable. In general, the consideration allocated to each unit of accounting is recognized as the related goods or services are delivered, limited to the consideration that is not contingent. We have adopted this guidance on a prospective basis for all new or materially modified revenue arrangements with multiple deliverables entered into on or after January 1, 2011. Our adoptioncomprehensive discussion of this guidance has not impacted the timing or patterntopic, refer to Item 8 of our revenue recognitionthis Form 10-K, Notes to Consolidated Financial Statements, in 2011 or 2012. Also, there would have been no change in revenue recognized relating to multiple-element arrangements if we had adopted this guidance retrospectively for contracts entered into prior to January 1, 2011. Note 2, "Significant Accounting Policies."
We have concluded that the various service elements in our Molina Medicaid Solutions contracts represent a single unit of accounting due to the fact that DDI, which is the only service performed in advance of the other services (all other services are performed over an identical period), does not have standalone value because our DDI services are not sold separately by any vendor and the customer could not resell our DDI services. Further, we have no objective and reliable evidence of fair value for any of the individual elements in these contracts, and at no point in the contract will we have objective and reliable evidence of fair value for the undelivered elements in the contracts. For contracts entered into prior to January 1, 2011, objective and reliable evidence of fair value would be required, in addition to DDI standalone value which we do not have, in order to treat DDI as a separate unit of accounting. We lack objective and reliable evidence of the fair value of the individual elements of our Molina Medicaid Solutions contracts for the following reasons:
Each contract calls for the provision of its own specific set of services. While all contracts support the system of record for state MMIS, the actual services we provide vary significantly between contracts; and
The nature of the MMIS installed varies significantly between our older contracts (proprietary mainframe systems) and our new contracts (commercial off-the-shelf technology solutions)
Because we have determined the services provided under our Molina Medicaid Solutions contracts represent a single unit of accounting, and because we are unable to determine a pattern of performance of services during the contract period, we recognize all revenue (both the DDI and BPO elements) associated with such contracts on a straight-line basis over the period during which BPO, hosting, and support and maintenance services are delivered. As noted above, the period of performance of BPO services under our Idaho and Maine contracts is five years. Therefore, absent any contingencies as discussed in the following paragraph, we would recognize all revenue associated with those contracts over a period of five years. In cases where there is no DDI element associated with our contracts, BPO revenue is recognized on a monthly basis as specified in the applicable contract or contract extension.
Provisions specific to each contract may, however, lead us to modify this general principle. In those circumstances, the right of the state to refuse acceptance of services, as well as the related obligation to compensate us, may require us to delay recognition of all or part of our revenue until that contingency (the right of the state to refuse acceptance) has been removed. In those circumstances we defer recognition of any contingent revenue (whether DDI, BPO services, hosting, and support and maintenance services) until the contingency has been removed. These types of contingency features are present in our Maine and Idaho contracts. In those states, we deferred recognition of revenue until the contingencies were removed.
Costs associated with our Molina Medicaid Solutions contracts include software related costs and other costs. With respect to software related costs, we apply the guidance for internal-use software and capitalize external direct costs of materials and services consumed in developing or obtaining the software, and payroll and payroll-related costs associated with employees who are directly associated with and who devote time to the computer software project. With respect to all other direct costs, such costs are expensed as incurred, unless corresponding revenue is being deferred. If revenue is being deferred, direct costs relating to delivered service elements are deferred as well and are recognized on a straight-line basis over the period of revenue recognition, in a manner consistent with our recognition of revenue that has been deferred. Such direct costs can include:
Transaction processing costs.
Employee costs incurred in performing transaction services.
Vendor costs incurred in performing transaction services.
Costs incurred in performing required monitoring of and reporting on contract performance.
Costs incurred in maintaining and processing member and provider eligibility.
Costs incurred in communicating with members and providers.
The recoverability of deferred contract costs associated with a particular contract is analyzed on a periodic basis using the undiscounted estimated cash flows of the whole contract over its remaining contract term. If such undiscounted cash flows are insufficient to recover the long-lived assets and deferred contract costs, the deferred contract costs are written down by the amount of the cash flow deficiency. If a cash flow deficiency remains after reducing the balance of the deferred contract costs to zero, any remaining long-lived assets are evaluated for impairment. Any such impairment recognized would equal the amount by which the carrying value of the long-lived assets exceeds the fair value of those assets.
Medical Claims and Benefits Payable — Health Plans Segment
The following table provides the details of our medical claims and benefits payable as of the dates indicated:
|
| | | | | | | | | | | |
| | December 31, |
| | 2014 | | 2013 | | 2012 |
| | (In thousands) |
| Fee-for-service claims incurred but not paid (IBNP) | $ | 870,429 |
| | $ | 424,173 |
| | $ | 377,614 |
|
| Pharmacy payable | 71,412 |
| | 45,037 |
| | 38,992 |
|
| Capitation payable | 28,150 |
| | 20,267 |
| | 49,066 |
|
| Other (1) | 230,531 |
| | 180,310 |
| | 28,858 |
|
| | $ | 1,200,522 |
| | $ | 669,787 |
| | $ | 494,530 |
|
|
| | | | | | | | | | | |
| | December 31, |
| | 2012 | | 2011 | | 2010 |
| | (In thousands) |
| Fee-for-service claims incurred but not paid (IBNP) | $ | 377,614 |
| | $ | 301,020 |
| | $ | 275,259 |
|
| Capitation payable | 49,066 |
| | 53,532 |
| | 49,598 |
|
| Pharmacy | 38,992 |
| | 26,178 |
| | 14,649 |
|
| Other | 28,858 |
| | 21,746 |
| | 14,850 |
|
| | $ | 494,530 |
| | $ | 402,476 |
| | $ | 354,356 |
|
| |
| (1) | "Other" medical claims and benefits payable include amounts payable to certain providers for which we act as an intermediary on behalf of various state agencies without assuming financial risk. Such receipts and payments do not impact our consolidated statements of income. As of December 31, 2014 and 2013, we recorded non-risk provider payables relating to such intermediary arrangements of approximately $119.3 million and $151.3 million, respectively. |
The determination of our liability for claims and medical benefits payable is particularly important to the determination of our financial position and results of operations in any given period. Such determination of our liability requires the application of a significant degree of judgment by our management.
As a result, the determination of our liability for claims and medical benefits payable is subject to an inherent degree of uncertainty. Our medical care costs include amounts that have been paid by us through the reporting date, as well as estimated
liabilities for medical care costs incurred but not paid by us as of the reporting date. Such medical care cost liabilities include, among other items, unpaid fee-for-service claims, capitation payments owed providers, unpaid pharmacy invoices, and various medically related administrative costs that have been incurred but not paid. We use judgment to determine the appropriate assumptions for determining the required estimates.
The most important element in estimating our medical care costs is our estimate for fee-for-service claims which have been incurred but not paid by us. These fee-for-service costs that have been incurred but have not been paid at the reporting date are collectively referred to as medical costs that are “Incurred But Not Paid,” or IBNP.incurred but not paid (IBNP). Our IBNP, as reported on our balance sheet, represents our best estimate of the total amount of claims we will ultimately pay with respect to claims that we have incurred as of the balance sheet date. We estimate our IBNP monthly using actuarial methods based on a number of factors. As indicated in the table above, our estimated IBNP liability represented $377.6$870.4 million of our total medical claims and benefits payable of $494.5$1,200.5 million as of December 31, 2012.2014. Excluding amounts that we anticipate paying on behalf of acertain capitated providerproviders in Ohio (which we will subsequently withhold from that provider’sthose providers' monthly capitation payment)payments), our IBNP liability at December 31, 2012,2014, was $371.4 million.$861.8 million.
The factors we consider when estimating our IBNP include, without limitation, claims receipt and payment experience (and variations in that experience), changes in membership, provider billing practices, health care service utilization trends, cost trends, product mix, seasonality, prior authorization of medical services, benefit changes, known outbreaks of disease or increased incidence of illness such as influenza, provider contract changes, changes to Medicaid fee schedules, and the incidence of high dollar or catastrophic claims. Our assessment of these factors is then translated into an estimate of our IBNP liability at the relevant measuring point through the calculation of a base estimate of IBNP, a further reserveprovision for adverse claims development,deviation, and an estimate of the
administrative costs of settling all claims incurred through the reporting date. The base estimate of IBNP is derived through application of claims payment completion factors and trended PMPM cost estimates.
For the fifth month of service prior to the reporting date and earlier, we estimate our outstanding claims liability based on actual claims paid, adjusted for estimated completion factors. Completion factors seek to measure the cumulative percentage of claims expense that will have been paid for a given month of service as of the reporting date, based on historical payment patterns.
The following table reflects the change in our estimate of claims liability as of December 31, 20122014 that would have resulted had we changed our completion factors for the fifth through the twelfth months preceding December 31, 2012,2014, by the percentages indicated. A reduction in the completion factor results in an increase in medical claims liabilities. Dollar amounts are in thousands.
| | | (Decrease) Increase in Estimated Completion Factors | Increase (Decrease) in Medical Claims and Benefits Payable | |
| Increase (Decrease) in Estimated Completion Factors | | Increase (Decrease) in Medical Claims and Benefits Payable |
| (6)% | $ | 152,598 |
| $ | 223,129 |
|
| (4)% | 101,732 |
| 148,753 |
|
| (2)% | 50,866 |
| 74,376 |
|
| 2% | (50,866 | ) | (74,376 | ) |
| 4% | (101,732 | ) | (148,753 | ) |
| 6% | (152,598 | ) | (223,129 | ) |
For the four months of service immediately prior to the reporting date, actual claims paid are not a reliable measure of our ultimate liability, given the inherent delay between the patient/physician encounter and the actual submission of a claim for payment. For these months of service, we estimate our claims liability based on trended PMPM cost estimates. These estimates are designed to reflect recent trends in payments and expense, utilization patterns, authorized services, and other relevant factors. The following table reflects the change in our estimate of claims liability as of December 31, 20122014 that would have resulted had we altered our trend factors by the percentages indicated. An increase in the PMPM costs results in an increase in medical claims liabilities. Dollar amounts are in thousands.
| | | (Decrease) Increase in Trended Per member Per Month Cost Estimates | Increase (Decrease) in Medical Claims and Benefits Payable | (Decrease) Increase in Medical Claims and Benefits Payable |
| (6)% | $ | (75,312 | ) | $ | (135,631 | ) |
| (4)% | (50,208 | ) | (90,421 | ) |
| (2)% | (25,104 | ) | (45,210 | ) |
| 2% | 25,104 |
| 45,210 |
|
| 4% | 50,208 |
| 90,421 |
|
| 6% | 75,312 |
| 135,631 |
|
The following per-share amounts are based on a combined federal and state statutory tax rate of 37.5%37%, and $47.048.3 million diluted shares outstanding for the year ended December 31, 2012.2014. Assuming a hypothetical 1% change in completion factors from those used in our calculation of IBNP at December 31, 2012,2014, net income for the year ended December 31, 20122014 would increase or decrease by approximately $15.9$23 million, or $0.34$0.48 per diluted share. Assuming a hypothetical 1% change in PMPM cost estimates from those used in our calculation of IBNP at December 31, 2012,2014, net income for the year ended December 31, 20122014 would increase or decrease by approximately $7.8$14 million, or $0.17$0.29 per diluted share. The corresponding figures for a 5% change in completion factors and PMPM cost estimates would be $79.5$117 million, or $1.69$2.42 per diluted share, and $39.2$71 million, or $0.83$1.47 per diluted share, respectively.
It is important to note that any change in the estimate of either completion factors or trended PMPM costs would usually be accompanied by a change in the estimate of the other component, and that a change in one component would almost always compound rather than offset the resulting distortion to net income. When completion factors are overestimated, trended PMPM costs tend to be underestimated. Both circumstances will create an overstatement of net income. Likewise, when completion factors are underestimated, trended PMPM costs tend to be overestimated, creating an understatement of net income. In other words, errors in estimates involving both completion factors and trended PMPM costs will usually act to drive estimates of claims liabilities and medical care costs in the same direction. If completion factors were overestimated by 1%, resulting in an overstatement of
net income by approximately $15.9$23 million, it is likely that trended PMPM costs would be underestimated, resulting in an additional overstatement of net income.
After we have established our base IBNP reserve through the application of completion factors and trended PMPM cost estimates, we then compute an additional liability, once again using actuarial techniques, to account for adverse developmentsdeviation in our claims payments which the base actuarial model is not intended to and does not account for. We refer to this additional liability as the provision for adverse claims development.deviation. The provision for adverse claims developmentdeviation is a component of our overall determination of the adequacy of our IBNP. It is intended to capture the potential inadequacy of our IBNP estimate as a result of our inability to adequately assess the impact of factors such as changes in the speed of claims receipt and payment, the relative magnitude or severity of claims, known outbreaks of disease such as influenza, our entry into new geographical markets, our provision of services to new populations such as the aged, blind or disabled (ABD), changes to state-controlled fee schedules upon which a large proportion of our provider payments are based, modifications and upgrades to our claims processing systems and practices, and increasing medical costs. Because of the complexity of our business, the number of states in which we operate, and the need to account for different health care benefit packages among those states, we make an overall assessment of IBNP after considering the base actuarial model reserves and the provision for adverse claims development. deviation.
We also include in our IBNP liability an estimate of the administrative costs of settling all claims incurred through the reporting date.
The development of IBNP is a continuous process that we monitor and refine on a monthly basis as additional claims payment information becomes available. As additional information becomes known to us, we adjust our actuarial model accordingly to establish IBNP.accordingly.
On a monthly basis, we review and update our estimated IBNP and the methods used to determine that liability. Any adjustments, if appropriate, are reflected in the period known. While we believe our current estimates are adequate, we have in the past been required to increase significantly our claims reserves for periods previously reported, and may be required to do so again in the future. Any significant increases to prior period claims reserves would materially decrease reported earnings for the period in which the adjustment is made.
In our judgment, the estimates for completion factors will likely prove to be more accurate than trended PMPM cost estimates because estimated completion factors are subject to fewer variables in their determination. Specifically, completion factors are developed over long periods of time, and are most likely to be affected by changes in claims receipt and payment experience and by provider billing practices. Trended PMPM cost estimates, while affected by the same factors, will also be influenced by health care service utilization trends, cost trends, product mix, seasonality, prior authorization of medical services, benefit changes, outbreaks of disease or increased incidence of illness, provider contract changes, changes to Medicaid fee schedules, and the incidence of high dollar or catastrophic claims. As discussed above, however, errors in estimates involving trended
PMPM costs will almost always be accompanied by errors in estimates involving completion factors, and vice versa. In such circumstances, errors in estimation involving both completion factors and trended PMPM costs will act to drive estimates of claims liabilities (and therefore medical care costs) in the same direction.
Assuming thatRefer to Item 8 of this Form 10-K, Notes to Consolidated Financial Statements, in Note 11, "Medical Claims and Benefits Payable," for additional information regarding the specific factors used to determine our initial estimatechanges in estimates of IBNP is accurate, we believe that amounts ultimately paid out would generally be between 8% and 10% less than the liability recorded at the end of the period as a result of the inclusion in that liability of the allowance for adverse claims development and the accrued cost of settling those claims. Because the amount of our initial liability is merely an estimate (and therefore never perfectly accurate), we will always experience variability in that estimate as new information becomes available with the passage of time. Therefore, there can be no assurance that amounts ultimately paid out will not be higher or lower than this 8% to 10% range. For example, for the years ended December 31, 2011 and 2010, the amounts ultimately paid out were less than the amount of the reserves we had established as of December 31, 2010 and 2009, by 14.6% and 15.7%, respectively. Furthermore, because the initial estimate of IBNP is derived from many factors, some of which are qualitative in nature rather than quantitative, we are seldom able to assign specific values to the reasons for a change in estimate - we only know when the circumstances for any one or more of those factors are out of the ordinary.
As shown in greater detailall periods presented in the table below, the amounts ultimately paid out on our liabilities in fiscal yearsaccompanying consolidated financial statements. 2012, 2011, and 2010were less than what we had expected when we established our reserves. While many related factors working in conjunction with one another determine the accuracy of our estimates, we are seldom able to quantify the impact that any single factor has on a change in estimate. In addition, given the variability inherent in the reserving process, we will only be able to identify specific factors if they represent a significant departure from expectations. As a result, we do not expect to be able to fully quantify the impact of individual factors on changes in estimate.
We recognized a benefit from prior period claims development in the amount of $39.3 millionfor the year endedDecember 31, 2012. This amount represents our estimate as of December 31, 2012, of the extent to which our initial estimate of medical claims and benefits payable at December 31, 2011was more than the amount that will ultimately be paid out in satisfaction of that liability. We believe that the overestimation of our claims liability atDecember 31, 2011was due primarily to the following factors:
At our Washington health plan, we underestimated the amount of recoveries we would collect for certain high-cost newborn claims, resulting in an overestimation of reserves at year end.
At our Texas health plan, we overestimated the cost of new members in STAR+PLUS (the name of our ABD program in Texas), in the Dallas region.
In early 2011, the state of Michigan was delayed in the enrollment of newborns in managed care plans; the delay was resolved by mid-2011. This caused a large number of claims with older dates of service to be paid during late 2011, resulting in an artificial increase in the lag time for claims payment at our Michigan health plan. We adjusted reserves downward for this issue at December 31, 2011, but the adjustment did not capture all of the claims overestimation.
The overestimation of our liability for medical claims and benefits payable was partially offset by an underestimation of that liability at our Missouri health plan, as a result of the costs associated with an unusually large number of premature infants during the fourth quarter of 2011.
We recognized a benefit from prior period claims development in the amount of$51.8 millionfor the year endedDecember 31, 2011. This amount represents our estimate as of December 31, 2011, of the extent to which our initial estimate of medical claims and benefits payable at December 31, 2010was more than the amount that will ultimately be paid out in satisfaction of that liability. We believe that the overestimation of our claims liability atDecember 31, 2010 was due primarily to the following factors:
At our Ohio health plan, we overestimated the impact of a buildup in claims inventory.
At our California health plan, we overestimated the impact of the settlement of disputed provider claims.
At our New Mexico health plan, we underestimated the impact of a reduction in the outpatient facility fee schedule.
We recognized a benefit from prior period claims development in the amount of$49.4 millionfor the year ended December 31, 2010. This amount represents our estimate as ofDecember 31, 2010, of the extent to which our initial estimate of medical claims and benefits payable at December 31, 2009was more than the amount that will ultimately be paid out in satisfaction of that liability. We believe that the overestimation of our claims liability atDecember 31, 2009was due primarily to the following factors:
At our New Mexico health plan, we underestimated the degree to which cuts to the Medicaid fees schedule would reduce our liability as of December 31, 2009.
At our California health plan, we underestimated the extent to which various network restructuring, provider contracting, and medical management initiatives had reduced our medical care costs during the second half of 2009, thereby resulting in a lower liability at December 31, 2009.
In estimating our claims liability atDecember 31, 2012, we adjusted our base calculation to take account of the numerous factors that we believe will likely change our final claims liability amount. We believe that the most significant among those factors are:
Our Texas health plan membership nearly doubled effective March 1, 2012. In addition, effective March 1, 2012, we assumed inpatient medical liability for ABD members for which we were not previously responsible. Reserves for new coverage and new regions are now based on the newly developing claims lag patterns. While the lag patterns are now beginning to stabilize for the new membership and coverage, the true reserve liability continues to be more uncertain than usual.
Data published by the Centers for Disease Control, or CDC, indicated a significant increase in the percentage of office visits for influenza-like illnesses, or ILI, during December 2012. This indicated that the annual flu season was starting earlier than it had in most recent years. This was most noticeable in the southeast region of the country, but impacted other areas as well. Our leading indicators, including inpatient authorizations and overall pharmacy utilization, did not show as great an increase as we had expected based on the severity of the CDC's flu-related indices. However, we did see a significant increase in the use of prescription flu medication, especially in our Texas health plan. Therefore, we increased our reserves to account for expected additional utilization due to the early onset of the flu season.
Our California health plan has enrolled approximately 20,000 new ABD members since September 30, 2011, as a result of the mandatory assignment of ABD members to managed care plans effective July 1, 2011. These new members converted from a fee-for-service environment. Due to the relatively recent transition of these members to managed care, their utilization of medical services is less predictable than it is for many of our other members.
Prior to July 2012, it was the state of Washington's practice to disenroll certain sick newborns from the Healthy Options Medicaid managed care program and cover them under the Supplemental Security Income program, or SSI, instead. When this occurred, the health plan would reimburse the premiums received for that member back to the state and the state in turn reimbursed the health plan for the cost of care, usually retroactively to the date of birth. Effective July 1, 2012, the health plans now retain these members and cover them under a new ABD program entitled Healthy Options Blind and Disabled, or HOBD. The premium we receive from the state for the HOBD members is very high to cover
the substantial cost of care. By December, we had enrolled approximately 26,000 members under HOBD. Because the program is relatively new, there is still some uncertainty as to the level of claims to be expected from these high-cost members.
The use of a consistent methodology in estimating our liability for claims and medical benefits payable minimizes the degree to which the under- or overestimation of that liability at the close of one period may affect consolidated results of operations in subsequent periods. Facts and circumstances unique to the estimation process at any single date, however, may still lead to a material impact on consolidated results of operations in subsequent periods. Any absence of adverse claims development (as well as the expensing through general and administrative expense of the costs to settle claims held at the start of the period) will lead to the recognition of a benefit from prior period claims development in the period subsequent to the date of the original estimate. In 2012, 2011and2010, the absence of adverse development of the liability for claims and medical benefits payable at the close of the previous period resulted in the recognition of substantial favorable prior period development. In these years, however, the recognition of a benefit from prior period claims development did not have a material impact on our consolidated results of operations because the amount of benefit recognized in each year was roughly consistent with that recognized in the previous year.
The following table presents the components of the change in our medical claims and benefits payable from continuing and discontinued operations combined for the periods presented.indicated. The negative amounts displayedpresented for “Components"Components of medical care costs related to: Prior year”periods" represent the amount by which our original estimate of medical claims and benefits payable at the beginning of the period waswere more than the actual amount of the liability based on information (principally the payment of claims) developed since that liability was first reported.
| | | | Year ended December 31, | Year ended December 31, |
| | 2012 | | 2011 | | 2010 | 2014 | | 2013 | | 2012 |
| | (Dollars in thousands, except per-member amounts) | (Dollars in thousands, except per-member amounts) |
| Balances at beginning of period | $ | 402,476 |
| | $ | 354,356 |
| | $ | 315,316 |
| $ | 669,787 |
| | $ | 494,530 |
| | $ | 402,476 |
|
| Balance of acquired subsidiary | — |
| | — |
| | 3,228 |
| |
| Components of medical care costs related to: | | | | | | | | | | |
| Current year | 5,136,055 |
| | 3,911,803 |
| | 3,420,235 |
| |
| Prior year | (39,295 | ) | | (51,809 | ) | | (49,378 | ) | |
| Current period | | 8,122,885 |
| | 5,434,443 |
| | 5,136,055 |
|
| Prior periods | | (45,979 | ) | | (52,779 | ) | | (39,295 | ) |
| Total medical care costs | 5,096,760 |
| | 3,859,994 |
| | 3,370,857 |
| 8,076,906 |
| | 5,381,664 |
| | 5,096,760 |
|
| | | | | | | |
| Change in non-risk provider payables | | (31,973 | ) | | 111,267 |
| | (7,004 | ) |
| | | | | | | |
| Payments for medical care costs related to: | | | | | | | | | | |
| Current year | 4,649,363 |
| | 3,516,994 |
| | 3,085,388 |
| |
| Prior year | 355,343 |
| | 294,880 |
| | 249,657 |
| |
| Current period | | 7,064,427 |
| | 4,932,195 |
| | 4,689,395 |
|
| Prior periods | | 449,771 |
| | 385,479 |
| | 308,307 |
|
| Total paid | 5,004,706 |
| | 3,811,874 |
| | 3,335,045 |
| 7,514,198 |
| | 5,317,674 |
| | 4,997,702 |
|
| Balances at end of year | $ | 494,530 |
| | $ | 402,476 |
| | $ | 354,356 |
| |
| Benefit from prior years as a percentage of: | | | | | | |
| Balance at beginning of year | 9.8 | % | | 14.6 | % | | 15.7 | % | |
| Balances at end of period | | $ | 1,200,522 |
| | $ | 669,787 |
| | $ | 494,530 |
|
| | | | | | | |
| Benefit from prior periods as a percentage of: | | | | | | |
| Balance at beginning of period | | 6.9 | % | | 10.7 | % | | 9.8 | % |
| Premium revenue | 0.7 | % | | 1.1 | % | | 1.2 | % | 0.5 | % | | 0.9 | % | | 0.7 | % |
| Total medical care costs | 0.8 | % | | 1.3 | % | | 1.5 | % | |
| Claims Data | | | | | | |
| Medical care costs | | 0.6 | % | | 1.0 | % | | 0.8 | % |
| | | | | | | |
| Claims Data: | | | | | | |
| Days in claims payable, fee for service | 40 |
| | 40 |
| | 42 |
| 49 |
| | 43 |
| | 40 |
|
| Number of members at end of period | 1,797,000 |
| | 1,697,000 |
| | 1,613,000 |
| 2,623,000 |
| | 1,931,000 |
| | 1,797,000 |
|
| Number of claims in inventory at end of period | 122,700 |
| | 111,100 |
| | 143,600 |
| 307,700 |
| | 145,800 |
| | 122,700 |
|
| Billed charges of claims in inventory at end of period | $ | 255,200 |
| | $ | 207,600 |
| | $ | 218,900 |
| $ | 718,500 |
| | $ | 276,500 |
| | $ | 255,200 |
|
| Claims in inventory per member at end of period | 0.07 |
| | 0.07 |
| | 0.09 |
| 0.12 |
| | 0.08 |
| | 0.07 |
|
| Billed charges of claims in inventory per member end of period | $ | 142.01 |
| | $ | 122.33 |
| | $ | 135.71 |
| $ | 273.92 |
| | $ | 143.19 |
| | $ | 142.01 |
|
| Number of claims received during the period | 20,842,400 |
| | 17,207,500 |
| | 14,554,800 |
| 27,597,000 |
| | 21,317,500 |
| | 20,842,400 |
|
| Billed charges of claims received during the period | $ | 19,429,300 |
| | $ | 14,306,500 |
| | $ | 11,686,100 |
| $ | 30,315,600 |
| | $ | 21,414,600 |
| | $ | 19,429,300 |
|
Commitments and Contingencies
We are not an obligor to or guarantor of any indebtedness of any other party, except for our obligation to pay benefits under policies in-force relating to an insurance subsidiary we sold in the first quarter of 2012, in the event such benefits are not paid by the reinsurer or current owner. This transaction is more fully described in Note 19 to the accompanying audited consolidated financial statements for the year ended December 31, 2012.
We are not a party to off-balance sheet financing arrangements, except for operating leases which are disclosed in Item 8 of this Form 10-K, Notes to Consolidated Financial Statements, in Note 19 to the accompanying audited consolidated financial statements for the year ended December 31, 2012.20 ,"Commitments and Contingencies."
Contractual Obligations
In the table below, we present our contractual obligations as of December 31, 20122014..(1) Some of the amounts we have included in this table are based on management’s estimates and assumptions about these obligations, including their duration, the possibility of renewal, anticipated actions by third parties, and other factors. Because these estimates and assumptions are necessarily subjective, the contractual obligations we will actually pay in future periods may vary from those reflected in the table. Amounts are in thousands.
| | | | Total | | 2013 | | 2014-2015 | | 2016-2017 | | 2018 and Beyond | Total | | 2015 | | 2016-2017 | | 2018-2019 | | 2020 and Beyond |
| Medical claims and benefits payable | $ | 494,530 |
| | $ | 494,530 |
| | $ | — |
| | $ | — |
| | $ | — |
| $ | 1,200,522 |
| | $ | 1,200,522 |
| | $ | — |
| | $ | — |
| | $ | — |
|
| Principal amount of long-term debt(1) | 274,471 |
| | 1,155 |
| | 189,465 |
| | 42,681 |
| | 41,170 |
| |
| Principal amount of convertible senior notes (2) | | 851,551 |
| | — |
| | — |
| | — |
| | 851,551 |
|
| Amounts due government agencies | | 527,193 |
| | 527,193 |
| | — |
| | — |
| | — |
|
| Lease financing obligations | | 380,956 |
| | 11,397 |
| | 23,830 |
| | 25,282 |
| | 320,447 |
|
| Interest on long-term debt | | 176,405 |
| | 11,088 |
| | 22,176 |
| | 22,175 |
| | 120,966 |
|
| Operating leases | 86,276 |
| | 26,866 |
| | 36,228 |
| | 15,411 |
| | 7,771 |
| 122,035 |
| | 29,142 |
| | 44,591 |
| | 33,073 |
| | 15,229 |
|
| Interest on long-term debt | 23,465 |
| | 9,035 |
| | 9,150 |
| | 3,675 |
| | 1,605 |
| |
| Lease financing obligations - related party | | 102,394 |
| | 5,346 |
| | 11,243 |
| | 12,021 |
| | 73,784 |
|
| Purchase commitments | 37,537 |
| | 19,367 |
| | 17,645 |
| | 525 |
| | — |
| 26,029 |
| | 14,232 |
| | 11,797 |
| | — |
| | — |
|
| Total contractual obligations | $ | 916,279 |
| | $ | 550,953 |
| | $ | 252,488 |
| | $ | 62,292 |
| | $ | 50,546 |
| |
| | | $ | 3,387,085 |
| | $ | 1,798,920 |
| | $ | 113,637 |
| | $ | 92,551 |
| | $ | 1,381,977 |
|
| |
| (1) | As of December 31, 2014, we have recorded approximately $2.6 million of unrecognized tax benefits. The table does not contain this amount because we cannot reasonably estimate when or if such amount may be settled. For further information, refer to Item 8 of this Form 10-K, Notes to Consolidated Financial Statements, in Note 14, "Income Taxes." |
| |
| (2) | Represents the principal amountamounts due on our 3.75%1.125% Cash Convertible Senior Notes due 2014,2020, and our term loan1.625% Convertible Senior Notes due 2044 (1.625% Notes). The 1.625% Notes have a contractual maturity date in 2044; however, on specified dates beginning in 2018 andholders of the Credit Facility due 2016.1.625% Notes may require us to repurchase some or all of the 1.625% Notes, as described in Item 8 of this Form 10-K, Notes to Consolidated Financial Statements, in Note 12, "Long-Term Debt." |
As of December 31, 2012, we have recorded approximately $10.6 million of unrecognized tax benefits. The above table does not contain this amount because we cannot reasonably estimate when or if such amount may be settled. See Note 13 to the accompanying audited consolidated financial statements for the year ended December 31, 2012 for further information.
Item 7A.Quantitative and Qualitative Disclosures About Market Risk
Quantitative and Qualitative Disclosures About Market Risk
Refer to Item 8 of this Form 10-K, Notes to Consolidated Financial instruments that potentially subject us to concentrations of credit risk consist primarily of cashStatements, in Note 2, "Significant Accounting Policies," Note 5, "Fair Value Measurements," and cash equivalents, investments, receivables, and restricted investments. We invest a substantial portion of our cash in the PFM Fund Prime Series — Institutional Class, and the PFM Fund Government Series. These funds represent a portfolio of highly liquid money market securities that are managed by PFM Asset Management LLC (PFM), a Virginia business trust registered as an open-end management investment fund. Our investments and a portion of our cash equivalents are managed by professional portfolio managers operating under documented investment guidelines. No investment that is in a loss position can be sold by our managers without our prior approval. Our investments consist solely of investment grade debt securities with a maximum maturity of five years and an average duration of two years or less. Restricted investments are invested principally in certificates of deposit and U.S. treasury securities. Concentration of credit risk with respect to accounts receivable is limited due to payors consisting principally of the governments of each state in which our Health Plans segment and our Molina Medicaid Solutions segment operate.
We are also exposed to interest rate risk relating to contractual variable interest rates under our Term Loan Agreement which matures on November 30, 2018. The outstanding principal amount under the Term Loan Agreement bears interest at the Eurodollar rate for each Interest Period commencing January 1, 2012. We manage this floating rate debt using an Interest Rate Swap Agreement that is intended to reduce our exposure to the impact of changing interest rates to our consolidated results of operations and future outflows for interest expense. Under the Swap Agreement, we will receive a variable rate of one-month LIBOR plus 3.25%, and pay a fixed rate of 5.34%. At December 31, 2012, a hypothetical 1% increase in the Eurodollar rate would result in a $1.6 million favorable change in the fair value of our Interest Rate Swap Agreement. This favorable change would reduce our exposure to a hypothetical 1% increase in the Eurodollar rate on the outstanding borrowings of our Term Loan, that would result in additional interest expense of only $0.5 million. See Note 12 of the accompanying audited consolidated financial statements for the year ended December 31, 2012 for more information on the Term Loan Agreement and Interest Rate Swap Agreement.6, "Investments."
Inflation
We use various strategies to mitigate the negative effects of health care cost inflation. Specifically, our health plans try to control medical and hospital costs through contracts with independent providers of health care services. Through these contracted providers, our health plans emphasize preventive health care and appropriate use of specialty and hospital services. There can be no assurance, however, that our strategies to mitigate health care cost inflation will be successful. Competitive pressures, new health care and pharmaceutical product introductions, demands from health care providers and customers, applicable regulations, or other factors may affect our ability to control health care costs.
Compliance Costs
Our health plans are regulated by both state and federal government agencies. Regulation of managed care products and health care services is an evolving area of law that varies from jurisdiction to jurisdiction. Regulatory agencies generally have discretion to issue regulations and interpret and enforce laws and rules. Changes in applicable laws and rules occur frequently. Compliance with such laws and rules may lead to additional costs related to the implementation of additional systems, procedures and programs that we have not yet identified.
Item 8.Financial Statements and Supplementary Data
INDEX TO FINANCIAL STATEMENTS
|
| |
| | Page |
| MOLINA HEALTHCARE INC. | |
| |
| |
| |
| |
| |
| |
REPORT OF INDEPENDENT REGISTERED PUBLIC ACCOUNTING FIRM
The Board of Directors and Stockholders
of Molina Healthcare, Inc.
We have audited the accompanying consolidated balance sheets of Molina Healthcare, Inc. (the Company) as of December 31, 20122014 and 20112013, and the related consolidated statements of income, and comprehensive income, stockholders’ equity and cash flows for each of the three years in the period ended December 31, 20122014. These financial statements are the responsibility of the Company’s management. Our responsibility is to express an opinion on these financial statements based on our audits.
We conducted our audits in accordance with the standards of the Public Company Accounting Oversight Board (United States). Those standards require that we plan and perform the audit to obtain reasonable assurance about whether the financial statements are free of material misstatement. An audit includes examining, on a test basis, evidence supporting the amounts and disclosures in the financial statements. An audit also includes assessing the accounting principles used and significant estimates made by management, as well as evaluating the overall financial statement presentation. We believe that our audits provide a reasonable basis for our opinion.
In our opinion, the financial statements referred to above present fairly, in all material respects, the consolidated financial position of Molina Healthcare, Inc. at December 31, 20122014 and 20112013, and the consolidated results of its operations and its cash flows for each of the three years in the period ended December 31, 20122014, in conformity with U.S. generally accepted accounting principles.
We also have audited, in accordance with the standards of the Public Company Accounting Oversight Board (United States), Molina Healthcare, Inc.’s internal control over financial reporting as of December 31, 20122014, based on criteria established in Internal Control — Integrated Framework issued by the Committee of Sponsoring Organizations of the Treadway Commission (2013 framework) and our report dated February 28, 201326, 2015 expressed an unqualified opinion thereon.
/s/ ERNST & YOUNG LLP
Los Angeles, California
February 28, 201326, 2015
MOLINA HEALTHCARE, INC.
CONSOLIDATED BALANCE SHEETS
| | | | December 31, | December 31, |
| | 2012 | | 2011 | 2014 | | 2013 |
| | (Amounts in thousands, except per-share data) | (Amounts in thousands, except per-share data) |
| ASSETS | | | | ASSETS |
| Current assets: | | | | | | |
| Cash and cash equivalents | $ | 795,770 |
| | $ | 493,827 |
| $ | 1,539,063 |
| | $ | 935,895 |
|
| Investments | 342,845 |
| | 336,916 |
| 1,019,462 |
| | 703,052 |
|
| Receivables | 149,682 |
| | 167,898 |
| 596,456 |
| | 298,935 |
|
| Income tax refundable | — |
| | 11,679 |
| — |
| | 32,742 |
|
| Deferred income taxes | 32,443 |
| | 18,327 |
| 39,532 |
| | 26,556 |
|
| Prepaid expenses and other current assets | 28,386 |
| | 19,435 |
| 50,884 |
| | 42,484 |
|
| Total current assets | 1,349,126 |
| | 1,048,082 |
| 3,245,397 |
| | 2,039,664 |
|
| Property, equipment, and capitalized software, net | 221,443 |
| | 190,934 |
| 340,778 |
| | 292,083 |
|
| Deferred contract costs | 58,313 |
| | 54,582 |
| 53,675 |
| | 45,675 |
|
| Intangible assets, net | 77,711 |
| | 101,796 |
| 89,273 |
| | 98,871 |
|
| Goodwill and indefinite-lived intangible assets | 151,088 |
| | 153,954 |
| |
| Auction rate securities | 13,419 |
| | 16,134 |
| |
| Goodwill | | 271,964 |
| | 230,738 |
|
| Restricted investments | 44,101 |
| | 46,164 |
| 102,479 |
| | 63,093 |
|
| Receivable for ceded life and annuity contracts | — |
| | 23,401 |
| |
| Derivative asset | | 329,323 |
| | 186,351 |
|
| Other assets | 19,621 |
| | 17,099 |
| 44,326 |
| | 46,462 |
|
| | | $ | 4,477,215 |
| | $ | 3,002,937 |
|
| | $ | 1,934,822 |
| | $ | 1,652,146 |
| | | |
| LIABILITIES AND STOCKHOLDERS’ EQUITY | | | | LIABILITIES AND STOCKHOLDERS’ EQUITY |
| Current liabilities: | | | | | | |
| Medical claims and benefits payable | $ | 494,530 |
| | $ | 402,476 |
| $ | 1,200,522 |
| | $ | 669,787 |
|
| Accounts payable and accrued liabilities | 184,034 |
| | 147,214 |
| 241,654 |
| | 263,043 |
|
| Amounts due government agencies | | 527,193 |
| | 56,922 |
|
| Deferred revenue | 141,798 |
| | 50,947 |
| 196,076 |
| | 122,216 |
|
| Income taxes payable | 6,520 |
| | — |
| 8,987 |
| | — |
|
| Current maturities of long-term debt | 1,155 |
| | 1,197 |
| 341 |
| | 182,008 |
|
| Total current liabilities | 828,037 |
| | 601,834 |
| 2,174,773 |
| | 1,293,976 |
|
| Long-term debt | 261,784 |
| | 216,929 |
| |
| Convertible senior notes | | 704,097 |
| | 416,368 |
|
| Lease financing obligations | | 160,710 |
| | 159,394 |
|
| Lease financing obligations - related party | | 40,241 |
| | 27,092 |
|
| Deferred income taxes | 37,900 |
| | 33,127 |
| 24,271 |
| | 580 |
|
| Liability for ceded life and annuity contracts | — |
| | 23,401 |
| |
| Derivative liability | | 329,194 |
| | 186,239 |
|
| Other long-term liabilities | 24,787 |
| | 21,782 |
| 33,487 |
| | 26,351 |
|
| Total liabilities | 1,152,508 |
| | 897,073 |
| 3,466,773 |
| | 2,110,000 |
|
| Stockholders’ equity: | | | | | | |
| Common stock, $0.001 par value; 80,000 shares authorized; outstanding: | 47 |
| | 46 |
| |
| 46,762 shares at December 31, 2012 and 45,815 shares at December 31, 2011 | | | | |
| Common stock, $0.001 par value; 150,000 shares authorized; outstanding: 49,727 shares at December 31, 2014 and 45,871 shares at December 31, 2013 | | 50 |
| | 46 |
|
| Preferred stock, $0.001 par value; 20,000 shares authorized, no shares issued and outstanding | — |
| | — |
| — |
| | — |
|
| Additional paid-in capital | 285,524 |
| | 266,022 |
| 396,059 |
| | 340,848 |
|
| Accumulated other comprehensive loss | (457 | ) | | (1,405 | ) | (1,019 | ) | | (1,086 | ) |
| Treasury stock, at cost; 111 shares at December 31, 2012 | (3,000 | ) | | — |
| |
| Retained earnings | 500,200 |
| | 490,410 |
| 615,352 |
| | 553,129 |
|
| Total stockholders’ equity | 782,314 |
| | 755,073 |
| 1,010,442 |
| | 892,937 |
|
| | $ | 1,934,822 |
| | $ | 1,652,146 |
| $ | 4,477,215 |
| | $ | 3,002,937 |
|
See accompanying notes.
MOLINA HEALTHCARE, INC.
CONSOLIDATED STATEMENTS OF INCOME
| | | | Year Ended December 31, | Year Ended December 31, |
| | 2012 | | 2011 | | 2010 | 2014 | | 2013 | | 2012 |
| | (In thousands, except per-share data) | (In thousands, except per-share data) |
| Revenue: | | | | | | | | | | |
| Premium revenue | $ | 5,826,491 |
| | $ | 4,603,407 |
| | $ | 3,989,909 |
| $ | 9,022,511 |
| | $ | 6,179,170 |
| | $ | 5,544,121 |
|
| Service revenue | 187,710 |
| | 160,447 |
| | 89,809 |
| 210,051 |
| | 204,535 |
| | 187,710 |
|
| Premium tax revenue | | 294,388 |
| | 172,017 |
| | 158,991 |
|
| Health insurer fee revenue | | 119,484 |
| | — |
| | — |
|
| Investment income | 5,188 |
| | 5,539 |
| | 6,259 |
| 8,093 |
| | 6,890 |
| | 5,075 |
|
| Rental income | 9,374 |
| | 547 |
| | — |
| |
| Other revenue | | 12,074 |
| | 26,322 |
| | 18,312 |
|
| Total revenue | 6,028,763 |
| | 4,769,940 |
| | 4,085,977 |
| 9,666,601 |
| | 6,588,934 |
| | 5,914,209 |
|
| Expenses: | | | | | | |
| Operating expenses: | | | | | | |
| Medical care costs | 5,096,760 |
| | 3,859,994 |
| | 3,370,857 |
| 8,076,331 |
| | 5,380,124 |
| | 4,991,188 |
|
| Cost of service revenue | 141,208 |
| | 143,987 |
| | 78,647 |
| 156,764 |
| | 161,494 |
| | 141,208 |
|
| General and administrative expenses | 532,627 |
| | 415,932 |
| | 345,993 |
| 764,693 |
| | 665,996 |
| | 518,615 |
|
| Premium tax expenses | 158,991 |
| | 154,589 |
| | 139,775 |
| 294,388 |
| | 172,017 |
| | 158,991 |
|
| Health insurer fee expenses | | 88,591 |
| | — |
| | — |
|
| Depreciation and amortization | 63,704 |
| | 50,690 |
| | 45,704 |
| 92,917 |
| | 72,743 |
| | 63,114 |
|
| Total expenses | 5,993,290 |
| | 4,625,192 |
| | 3,980,976 |
| |
| Impairment of goodwill and intangible assets | — |
| | (64,575 | ) | | — |
| |
| Total operating expenses | | 9,473,684 |
| | 6,452,374 |
| | 5,873,116 |
|
| Operating income | 35,473 |
| | 80,173 |
| | 105,001 |
| 192,917 |
| | 136,560 |
| | 41,093 |
|
| Other expenses (income): | | | | | | |
| Other expenses, net: | | | | | | |
| Interest expense | 16,769 |
| | 15,519 |
| | 15,509 |
| 56,811 |
| | 52,071 |
| | 16,769 |
|
| Other income | (361 | ) | | — |
| | — |
| |
| Total other expenses (income) | 16,408 |
| | 15,519 |
| | 15,509 |
| |
| Income before income taxes | 19,065 |
| | 64,654 |
| | 89,492 |
| |
| Provision for income taxes | 9,275 |
| | 43,836 |
| | 34,522 |
| |
| Other expense, net | | 802 |
| | 3,343 |
| | 945 |
|
| Total other expenses, net | | 57,613 |
| | 55,414 |
| | 17,714 |
|
| Income from continuing operations before income tax expense | | 135,304 |
| | 81,146 |
| | 23,379 |
|
| Income tax expense | | 72,726 |
| | 36,316 |
| | 10,513 |
|
| Income from continuing operations | | 62,578 |
| | 44,830 |
| | 12,866 |
|
| (Loss) income from discontinued operations, net of tax (benefit) expense of $(203), $(9,912), and $(1,238), respectively | | (355 | ) | | 8,099 |
| | (3,076 | ) |
| Net income | $ | 9,790 |
| | $ | 20,818 |
| | $ | 54,970 |
| $ | 62,223 |
| | $ | 52,929 |
| | $ | 9,790 |
|
| Net income per share: | | | | | | |
| Basic | $ | 0.21 |
| | $ | 0.45 |
| | $ | 1.34 |
| |
| Diluted | 0.21 |
| | 0.45 |
| | 1.32 |
| |
| | | | | | | |
| | | | | | | |
| Basic net income per share: | | | | | | |
| Income from continuing operations | | $ | 1.34 |
| | $ | 0.98 |
| | $ | 0.28 |
|
| (Loss) income from discontinued operations | | (0.01 | ) | | 0.18 |
| | (0.07 | ) |
| Basic net income per share | | $ | 1.33 |
| | $ | 1.16 |
| | $ | 0.21 |
|
| Diluted net income per share: | | | | | | |
| Income from continuing operations | | $ | 1.30 |
| | $ | 0.96 |
| | $ | 0.27 |
|
| (Loss) income from discontinued operations | | (0.01 | ) | | 0.17 |
| | (0.06 | ) |
| Diluted net income per share | | $ | 1.29 |
| | $ | 1.13 |
| | $ | 0.21 |
|
| Weighted average shares outstanding: | | | | | | | | | | |
| Basic | 46,380 |
| | 45,756 |
| | 41,174 |
| 46,935 |
| | 45,717 |
| | 46,380 |
|
| Diluted | 46,999 |
| | 46,425 |
| | 41,631 |
| 48,340 |
| | 46,862 |
| | 46,999 |
|
See accompanying notes.
MOLINA HEALTHCARE, INC.
CONSOLIDATED STATEMENTS OF COMPREHENSIVE INCOME
|
| | | | | | | | | | | |
| | Year Ended December 31, |
| | 2012 | | 2011 | | 2010 |
| | (In thousands) |
| Net income | $ | 9,790 |
| | $ | 20,818 |
| | $ | 54,970 |
|
| Other comprehensive income (loss), before tax: | | | | | |
| Unrealized gain (loss) on investments | 1,529 |
| | 1,167 |
| | (613 | ) |
| Total other comprehensive income (loss), before tax | 1,529 |
| | 1,167 |
| | (613 | ) |
| Income tax expense (benefit) related to items of other comprehensive income | 581 |
| | 380 |
| | (233 | ) |
| Total other comprehensive income (loss), net of tax | 948 |
| | 787 |
| | (380 | ) |
| Comprehensive income | $ | 10,738 |
| | $ | 21,605 |
| | $ | 54,590 |
|
|
| | | | | | | | | | | |
| | Year Ended December 31, |
| | 2014 | | 2013 | | 2012 |
| | (In thousands) |
| Net income | $ | 62,223 |
| | $ | 52,929 |
| | $ | 9,790 |
|
| Other comprehensive income (loss): | | | | | |
| Unrealized investment gain (loss) | 108 |
| | (1,015 | ) | | 1,529 |
|
| Effect of income tax expense (benefit) | 41 |
| | (386 | ) | | 581 |
|
| Other comprehensive income (loss), net of tax | 67 |
| | (629 | ) | | 948 |
|
| Comprehensive income | $ | 62,290 |
| | $ | 52,300 |
| | $ | 10,738 |
|
See accompanying notes.
MOLINA HEALTHCARE, INC.
CONSOLIDATED STATEMENTS OF CASH FLOWS
|
| | | | | | | | | | | |
| | Year Ended December 31, |
| | 2012 | | 2011 | | 2010 |
| | | | (In thousands) | | |
| Operating activities: | | | | | |
| Net income | $ | 9,790 |
| | $ | 20,818 |
| | $ | 54,970 |
|
| Adjustments to reconcile net income to net cash provided by operating activities: | | | | | |
| Depreciation and amortization | 78,764 |
| | 74,383 |
| | 60,765 |
|
| Deferred income taxes | (9,887 | ) | | 13,836 |
| | (4,092 | ) |
| Stock-based compensation | 20,018 |
| | 17,052 |
| | 9,531 |
|
| Non-cash interest on convertible senior notes | 5,942 |
| | 5,512 |
| | 5,114 |
|
| Impairment of goodwill and intangible assets | — |
| | 64,575 |
| | — |
|
| Change in fair value of interest rate swap | 1,307 |
| | — |
| | — |
|
| Amortization of premium/discount on investments | 6,746 |
| | 7,242 |
| | 2,029 |
|
| Amortization of deferred financing costs | 1,089 |
| | 2,818 |
| | 1,780 |
|
| Gain on sale of subsidiary | (1,747 | ) | | — |
| | — |
|
| Loss on disposal of property and equipment | 2,608 |
| | — |
| | — |
|
| Gain on acquisition | — |
| | (1,676 | ) | | — |
|
| Unrealized gain on trading securities | — |
| | — |
| | (4,170 | ) |
| Loss on rights agreement | — |
| | — |
| | 3,807 |
|
| Tax deficiency from employee stock compensation | (526 | ) | | (714 | ) | | (968 | ) |
| Changes in operating assets and liabilities: | | | | | |
| Receivables | 18,216 |
| | 352 |
| | (7,539 | ) |
| Prepaid expenses and other current assets | (8,958 | ) | | 3,308 |
| | (12,034 | ) |
| Medical claims and benefits payable | 92,054 |
| | 48,120 |
| | 34,363 |
|
| Accounts payable and accrued liabilities | 23,345 |
| | 2,778 |
| | 40,482 |
|
| Deferred revenue | 90,851 |
| | (8,154 | ) | | (41,899 | ) |
| Income taxes | 18,172 |
| | (24,855 | ) | | 19,258 |
|
| Net cash provided by operating activities | 347,784 |
| | 225,395 |
| | 161,397 |
|
| Investing activities: | | | | | |
| Purchases of equipment | (78,145 | ) | | (60,581 | ) | | (48,538 | ) |
| Purchases of investments | (306,437 | ) | | (345,968 | ) | | (302,842 | ) |
| Sales and maturities of investments | 298,006 |
| | 302,667 |
| | 223,077 |
|
| Net cash paid in business combinations | — |
| | (84,253 | ) | | (130,743 | ) |
| Proceeds from sale of subsidiary, net of cash surrendered | 9,162 |
| | — |
| | — |
|
| Increase in deferred contract costs | (11,610 | ) | | (42,830 | ) | | (29,319 | ) |
| Increase in restricted investments | (2,647 | ) | | (4,064 | ) | | (5,566 | ) |
| Change in other noncurrent assets and liabilities | (1,913 | ) | | (1,898 | ) | | 5,108 |
|
| Net cash used in investing activities | (93,584 | ) | | (236,927 | ) | | (288,823 | ) |
| Financing activities: | | | | | |
| Amount borrowed under term loan | — |
| | 48,600 |
| | — |
|
| Amount borrowed under credit facility | 60,000 |
| | — |
| | 105,000 |
|
| Proceeds from common stock offering, net of issuance costs | — |
| | — |
| | 111,131 |
|
| Repayment of amount borrowed under credit facility | (20,000 | ) | | — |
| | (105,000 | ) |
| Treasury stock purchases | (3,000 | ) | | (7,000 | ) | | — |
|
| Credit facility fees paid | — |
| | (1,125 | ) | | (1,671 | ) |
| Principal payments on term loan | (1,129 | ) | | — |
| | — |
|
| Proceeds from employee stock plans | 8,205 |
| | 7,347 |
| | 4,056 |
|
| Excess tax benefits from employee stock compensation | 3,667 |
| | 1,651 |
| | 295 |
|
| Net cash provided by financing activities | 47,743 |
| | 49,473 |
| | 113,811 |
|
| Net increase (decrease) in cash and cash equivalents | 301,943 |
| | 37,941 |
| | (13,615 | ) |
| Cash and cash equivalents at beginning of period | 493,827 |
| | 455,886 |
| | 469,501 |
|
| Cash and cash equivalents at end of period | $ | 795,770 |
| | $ | 493,827 |
| | $ | 455,886 |
|
See accompanying notes.
MOLINA HEALTHCARE, INC.
CONSOLIDATED STATEMENTS OF CASH FLOWS — (continued)
|
| | | | | | | | | | | |
| | Year Ended December 31, |
| | 2012 | | 2011 | | 2010 |
| | (In thousands) |
| Supplemental cash flow information: | | | | | |
| Cash (received) paid during the period for: | | | | | |
| Income taxes | $ | (4,634 | ) | | $ | 54,663 |
| | $ | 18,299 |
|
| Interest | $ | 10,099 |
| | $ | 11,399 |
| | $ | 10,951 |
|
| Schedule of non-cash investing and financing activities: | | | | | |
| Retirement of treasury stock | $ | — |
| | $ | 7,000 |
| | $ | — |
|
| Retirement of common stock used for stock-based compensation | $ | (11,862 | ) | | $ | (3,926 | ) | | $ | (2,316 | ) |
| Details of sale of subsidiary | | | | | |
| Decrease in carrying value of assets | 30,942 |
| | — |
| | — |
|
| Decrease in carrying value of liabilities | (23,527 | ) | | — |
| | — |
|
| Gain on sale | 1,747 |
| | — |
| | — |
|
| Proceeds from sale of subsidiary, net of cash surrendered | 9,162 |
| | — |
| | — |
|
| Details of business combinations: | | | | | |
| Increase in fair value of assets acquired | $ | — |
| | $ | (81,256 | ) | | $ | (159,916 | ) |
| (Decrease) increase in fair value of liabilities assumed | — |
| | (1,045 | ) | | 24,450 |
|
| (Decrease) increase in payable to seller | — |
| | (1,952 | ) | | 4,723 |
|
| Net cash paid in business combinations | $ | — |
| | $ | (84,253 | ) | | $ | (130,743 | ) |
See accompanying notes.
MOLINA HEALTHCARE, INC.
CONSOLIDATED STATEMENTS OF STOCKHOLDERS’ EQUITY
|
| | | | | | | | | | | | | | | | | | | | | | | | | | |
| | Common Stock | | Additional Paid-in Capital | | Accumulated Other Comprehensive Loss | | Retained Earnings | | Treasury Stock | | |
| | Outstanding | | Amount | | | | | | Total |
| | (In thousands) |
| Balance at January 1, 2010 | 38,410 |
| | $ | 38 |
| | $ | 129,890 |
| | $ | (1,812 | ) | | $ | 414,622 |
| | $ | — |
| | $ | 542,738 |
|
| Net income | — |
| | — |
| | — |
| | — |
| | 54,970 |
| | — |
| | 54,970 |
|
| Other comprehensive loss, net of tax | — |
| | — |
| | — |
| | (380 | ) | | — |
| | — |
| | (380 | ) |
| Common stock issued, net of issuance costs | 6,525 |
| | 7 |
| | 111,124 |
| | — |
| | — |
| | — |
| | 111,131 |
|
| Employee stock grants and employee stock purchase plans | 528 |
| | — |
| | 11,271 |
| | — |
| | — |
| | — |
| | 11,271 |
|
| Tax deficiency from employee stock compensation | — |
| | — |
| | (673 | ) | | — |
| | — |
| | — |
| | (673 | ) |
| Balance at December 31, 2010 | 45,463 |
| | 45 |
| | 251,612 |
| | (2,192 | ) | | 469,592 |
| | — |
| | 719,057 |
|
| Net income | — |
| | — |
| | — |
| | — |
| | 20,818 |
| | — |
| | 20,818 |
|
| Other comprehensive income, net of tax | — |
| | — |
| | — |
| | 787 |
| | — |
| | — |
| | 787 |
|
| Purchase of treasury stock | — |
| | — |
| | — |
| | — |
| | — |
| | (7,000 | ) | | (7,000 | ) |
| Retirement of treasury stock | (400 | ) | | — |
| | (7,000 | ) | | — |
| | — |
| | 7,000 |
| | — |
|
| Employee stock grants and employee stock plan purchases | 752 |
| | 1 |
| | 20,473 |
| | — |
| | — |
| | — |
| | 20,474 |
|
| Tax benefit from employee stock compensation | — |
| | — |
| | 937 |
| | — |
| | — |
| | — |
| | 937 |
|
| Balance at December 31, 2011 | 45,815 |
| | 46 |
| | 266,022 |
| | (1,405 | ) | | 490,410 |
| | — |
| | 755,073 |
|
| Net income | — |
| | — |
| | — |
| | — |
| | 9,790 |
| | — |
| | 9,790 |
|
| Other comprehensive income, net of tax | — |
| | — |
| | — |
| | 948 |
| | — |
| | — |
| | 948 |
|
| Purchase of treasury stock | (111 | ) | | — |
| | — |
| | — |
| | — |
| | (3,000 | ) | | (3,000 | ) |
| Employee stock grants and employee stock plan purchases | 1,058 |
| | 1 |
| | 16,361 |
| | — |
| | — |
| | — |
| | 16,362 |
|
| Tax benefit from employee stock compensation | — |
| | — |
| | 3,141 |
| | — |
| | — |
| | — |
| | 3,141 |
|
| Balance at December 31, 2012 | 46,762 |
| | $ | 47 |
| | $ | 285,524 |
| | $ | (457 | ) | | $ | 500,200 |
| | $ | (3,000 | ) | | $ | 782,314 |
|
|
| | | | | | | | | | | | | | | | | | | | | | | | | | |
| | Common Stock | | Additional Paid-in Capital | | Accumulated Other Comprehensive Loss | | Retained Earnings | | Treasury Stock | | |
| | Outstanding | | Amount | | | | | | Total |
| | (In thousands) |
| Balance at January 1, 2012 | 45,815 |
| | $ | 46 |
| | $ | 266,022 |
| | $ | (1,405 | ) | | $ | 490,410 |
| | $ | — |
| | $ | 755,073 |
|
| Net income | — |
| | — |
| | — |
| | — |
| | 9,790 |
| | — |
| | 9,790 |
|
| Other comprehensive income, net | — |
| | — |
| | — |
| | 948 |
| | — |
| | — |
| | 948 |
|
| Purchase of treasury stock | (111 | ) | | — |
| | — |
| | — |
| | — |
| | (3,000 | ) | | (3,000 | ) |
| Share-based compensation | 1,058 |
| | 1 |
| | 16,361 |
| | — |
| | — |
| | — |
| | 16,362 |
|
| Tax benefit from share-based compensation | — |
| | — |
| | 3,141 |
| | — |
| | — |
| | — |
| | 3,141 |
|
| Balance at December 31, 2012 | 46,762 |
| | 47 |
| | 285,524 |
| | (457 | ) | | 500,200 |
| | (3,000 | ) | | 782,314 |
|
| Net income | — |
| | — |
| | — |
| | — |
| | 52,929 |
| | — |
| | 52,929 |
|
| Other comprehensive loss, net | — |
| | — |
| | — |
| | (629 | ) | | — |
| | — |
| | (629 | ) |
| Purchase of treasury stock | (1,710 | ) | | (2 | ) | | — |
| | — |
| | — |
| | (52,660 | ) | | (52,662 | ) |
| Retirement of treasury stock | — |
| | — |
| | (55,660 | ) | | — |
| | — |
| | 55,660 |
| | — |
|
| Issuance of warrants | — |
| | — |
| | 78,997 |
| | — |
| | — |
| | — |
| | 78,997 |
|
| Share-based compensation | 819 |
| | 1 |
| | 30,385 |
| | — |
| | — |
| | — |
| | 30,386 |
|
| Tax benefit from share-based compensation | — |
| | — |
| | 1,602 |
| | — |
| | — |
| | — |
| | 1,602 |
|
| Balance at December 31, 2013 | 45,871 |
| | 46 |
| | 340,848 |
| | (1,086 | ) | | 553,129 |
| | — |
| | 892,937 |
|
| Net income | — |
| | — |
| | — |
| | — |
| | 62,223 |
| | — |
| | 62,223 |
|
| Other comprehensive income, net | — |
| | — |
| | — |
| | 67 |
| | — |
| | — |
| | 67 |
|
| Convertible senior notes transactions, including issuance costs | 1,787 |
| | 2 |
| | 21,961 |
| | — |
| | — |
| | — |
| | 21,963 |
|
| Share-based compensation | 2,069 |
| | 2 |
| | 30,261 |
| | — |
| | — |
| | — |
| | 30,263 |
|
| Tax benefit from share-based compensation | — |
| | — |
| | 2,989 |
| | — |
| | — |
| | — |
| | 2,989 |
|
| Balance at December 31, 2014 | 49,727 |
| | $ | 50 |
| | $ | 396,059 |
| | $ | (1,019 | ) | | $ | 615,352 |
| | $ | — |
| | $ | 1,010,442 |
|
See accompanying notes.
MOLINA HEALTHCARE, INC.
CONSOLIDATED STATEMENTS OF CASH FLOWS
|
| | | | | | | | | | | |
| | Year Ended December 31, |
| | 2014 | | 2013 | | 2012 |
| | (In thousands) |
| Operating activities: | | | | | |
| Net income | $ | 62,223 |
| | $ | 52,929 |
| | $ | 9,790 |
|
| Adjustments to reconcile net income to net cash provided by operating activities: | | | | | |
| Depreciation and amortization | 134,404 |
| | 93,866 |
| | 78,764 |
|
| Deferred income taxes | (2,352 | ) | | (31,047 | ) | | (9,887 | ) |
| Share-based compensation | 21,727 |
| | 28,694 |
| | 20,018 |
|
| Amortization of convertible senior notes and lease financing obligations | 27,379 |
| | 22,820 |
| | 5,942 |
|
| Gain on sale of subsidiary | — |
| | — |
| | (1,747 | ) |
| Other, net | 6,222 |
| | 17,729 |
| | 11,224 |
|
| Changes in operating assets and liabilities: | | | | | |
| Receivables | (297,521 | ) | | (149,253 | ) | | 18,216 |
|
| Prepaid expenses and other current assets | (19,517 | ) | | (23,064 | ) | | (8,958 | ) |
| Medical claims and benefits payable | 530,735 |
| | 175,257 |
| | 92,054 |
|
| Accounts payable and accrued liabilities | 11,097 |
| | 32,550 |
| | 8,078 |
|
| Amounts due government agencies | 470,271 |
| | 28,446 |
| | 15,267 |
|
| Deferred revenue | 73,860 |
| | (19,582 | ) | | 90,851 |
|
| Income taxes | 41,729 |
| | (39,262 | ) | | 18,172 |
|
| Net cash provided by operating activities | 1,060,257 |
| | 190,083 |
| | 347,784 |
|
| Investing activities: | | | | | |
| Purchases of investments | (953,355 | ) | | (770,083 | ) | | (306,437 | ) |
| Proceeds from sales and maturities of investments | 632,800 |
| | 399,595 |
| | 298,006 |
|
| Purchases of equipment | (114,934 | ) | | (98,049 | ) | | (78,145 | ) |
| Net cash paid in business combinations | (44,133 | ) | | (61,521 | ) | | — |
|
| Increase in restricted investments | (33,661 | ) | | (18,992 | ) | | (2,647 | ) |
| Proceeds from sale of subsidiary, net of cash surrendered | — |
| | — |
| | 9,162 |
|
| Other, net | (22,446 | ) | | 5,739 |
| | (13,523 | ) |
| Net cash used in investing activities | (535,729 | ) | | (543,311 | ) | | (93,584 | ) |
| Financing activities: | | | | | |
| Proceeds from issuance of convertible senior notes, net of financing costs paid | 122,625 |
| | 537,973 |
| | — |
|
| Proceeds from sale-leaseback transactions | — |
| | 158,694 |
| | — |
|
| Purchase of call option | — |
| | (149,331 | ) | | — |
|
| Proceeds from issuance of warrants | — |
| | 75,074 |
| | — |
|
| Contingent consideration liabilities settled | (50,349 | ) | | — |
| | — |
|
| Treasury stock purchases | — |
| | (52,662 | ) | | (3,000 | ) |
| Principal payments on term loan | — |
| | (47,471 | ) | | (1,129 | ) |
| Repayment of amount borrowed under credit facility | — |
| | (40,000 | ) | | (20,000 | ) |
| Proceeds from employee stock plans | 14,040 |
| | 9,402 |
| | 8,205 |
|
| Principal payments on convertible senior notes | (10,449 | ) | | — |
| | — |
|
| Amount borrowed under credit facility | — |
| | — |
| | 60,000 |
|
| Other, net | 2,773 |
| | 1,674 |
| | 3,667 |
|
| Net cash provided by financing activities | 78,640 |
| | 493,353 |
| | 47,743 |
|
| Net increase in cash and cash equivalents | 603,168 |
| | 140,125 |
| | 301,943 |
|
| Cash and cash equivalents at beginning of period | 935,895 |
| | 795,770 |
| | 493,827 |
|
| Cash and cash equivalents at end of period | $ | 1,539,063 |
| | $ | 935,895 |
| | $ | 795,770 |
|
See accompanying notes.
MOLINA HEALTHCARE, INC.
CONSOLIDATED STATEMENTS OF CASH FLOWS
(continued)
|
| | | | | | | | | | | |
| | Year Ended December 31, |
| | 2014 | | 2013 | | 2012 |
| | (Amounts in thousands) |
| | (Unaudited) |
| Supplemental cash flow information: | | | | | |
| | | | | | |
| Cash paid (received) during the period for: | | | | | |
| Income taxes | $ | 30,413 |
| | $ | 95,240 |
| | $ | (4,634 | ) |
| Interest | $ | 29,178 |
| | $ | 34,881 |
| | $ | 10,099 |
|
| | | | | | |
| Schedule of non-cash investing and financing activities: | | | | | |
| 3.75% Notes exchanged for 1.625% Notes | $ | 176,551 |
| | $ | — |
| | $ | — |
|
| Retirement of treasury stock | $ | — |
| | $ | 55,660 |
| | $ | — |
|
| Increase in non-cash lease financing obligation - related party | $ | 13,841 |
| | $ | 27,211 |
| | $ | — |
|
| Common stock used for stock-based compensation | $ | (8,802 | ) | | $ | (7,711 | ) | | $ | (11,862 | ) |
| | | | | | |
| Details of business combinations: | | | | | |
| Fair value of assets acquired | $ | (52,057 | ) | | $ | (121,801 | ) | | $ | — |
|
| Fair value of contingent consideration liabilities incurred | — |
| | 59,948 |
| | — |
|
| Payable to seller | 7,924 |
| | — |
| | — |
|
| Escrow deposit | — |
| | 332 |
| | — |
|
| Net cash paid in business combinations | $ | (44,133 | ) | | $ | (61,521 | ) | | $ | — |
|
| | | | | | |
| Details of change in fair value of derivatives, net: | | | | | |
| Gain on 1.125% Call Option | $ | 142,972 |
| | $ | 37,020 |
| | $ | — |
|
| Loss on 1.125% Notes Conversion Option | (142,955 | ) | | (36,908 | ) | | — |
|
| Loss on 1.125% Warrants | — |
| | (3,923 | ) | | — |
|
| Gain (loss) on interest rate swap | — |
| | 433 |
| | (1,307 | ) |
| Change in fair value of derivatives, net | $ | 17 |
| | $ | (3,378 | ) | | $ | (1,307 | ) |
| | | | | | |
| Details of sale of subsidiary: | | | | | |
| Decrease in carrying value of assets | $ | — |
| | $ | — |
| | $ | 30,942 |
|
| Decrease in carrying value of liabilities | — |
| | — |
| | (23,527 | ) |
| Gain on sale | — |
| | — |
| | 1,747 |
|
| Proceeds from sale of subsidiary, net of cash surrendered | $ | — |
| | $ | — |
| | $ | 9,162 |
|
See accompanying notes.
MOLINA HEALTHCARE, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS
1. Basis of Presentation
Organization and Operations
Molina Healthcare, Inc. provides quality andhealth care to those receiving government assistance. We offer cost-effective Medicaid-related solutions to meet the health care needs of low-income families and individuals, and to assist state agencies in their administration of the Medicaid program. We report our financial performance based on two reportable segments: the Health Plans segment and the Molina Medicaid Solutions. Solutions segment.
Our Health Plans segment comprisesconsists of health plans in California, Florida, Michigan, New Mexico, Ohio, Texas, Utah, Washington, and Wisconsin,11 states, and includes our direct delivery business. As of December 31, 2012,2014, these health plans served approximately1.8over 2.6 million members eligible for Medicaid, Medicare, and other government-sponsored health care programs for low-income families and individuals. Additionally, we serve a small number of Health Insurance Marketplace members, many of whom are eligible for government premium subsidies. The health plans are operated by our respective wholly owned subsidiaries in those states, each of which is licensed as a health maintenance organization or HMO.(HMO). Our direct delivery business consists primarily of the management of a hospital in southern California under a management services agreement, and the operation of primary care clinics in California, Florida, New Mexico and Washington; additionally,several states in which we manage three county-owned primary care clinics under a contract with Fairfax County, Virginia.operate.
Our health plans'plans’ state Medicaid contracts generally have terms of three to four years with annual adjustments to premium rates.years. These contracts are renewable at the discretion of the state. In general, eithertypically contain renewal options exercisable by the state Medicaid agency, and allow either the state or the health plan mayto terminate the state contract with or without cause. Most of these contracts contain renewal options that are exercisable by the state. Our health plan subsidiaries have generally been successful in obtaining the renewal ofretaining their contracts, in each state prior to the actual expiration of their contracts. Our statebut such contracts are generally at greatestsubject to risk of loss when a state issues a new request for proposals or RFP, subject(RFP) open to competitive bidding by other health plans. If one of our health plans is not a successful responsive bidder to a state RFP, its contract may be subject to non-renewal. For instance, on February 17, 2012, the Division of Purchasing of the Missouri Office of Administration notified us that our Missouri health plan was not awarded a contract under the Missouri HealthNet Managed Care Request for Proposal; therefore, our Missouri health plan’s prior contract with the state expired without renewal on June 30, 2012 subject to certain transition obligations. As of December 31, 2012, we continued to process claims that were incurred by the Missouri health plan's members through the June 30, 2012 termination date. For the six months ended June 30, 2012, our Missouri health plan contributed premium revenue of$113.8 million, or 4.1%of total premium revenue, and comprised79,000 members, or 4.3%of total Health Plans segment membership as of June 30, 2012.
Our state Medicaid contracts may be periodically adjusted to include or exclude certain health benefits (such as pharmacy services, behavioral health services, or long-term care services); populations (such as the aged, blind or disabled, or ABD); and regions or service areas. For example, our Texas health plan added significant membership effective March 1, 2012, in service areas we had not previously served (the Hidalgo and El Paso service areas); and among populations we had not previously served within existing service areas, such as the Temporary Assistance for Needy Families, or TANF, population in the Dallas service area. Additionally, the health benefits provided to our TANF and ABD members in Texas under our contracts with the state were expanded to include inpatient facility and pharmacy services.
Our Molina Medicaid Solutions segment provides business processing and information technology development and administrative services to Medicaid agencies in Idaho, Louisiana, Maine, New Jersey, and West Virginia, and the U.S. Virgin Islands, and drug rebate administration services in Florida.
Market Updates—Health Plans Segment
On July 13, 2012,Florida. During 2014, our Florida health plan acquired two Medicaid contracts, adding approximately 73,000 members. See Note 4, "Business Combinations," for further information.
Puerto Rico. In 2014, we were awarded a managed care contract in the Commonwealth of Puerto Rico that is expected to enroll its first members April 1, 2015.
South Carolina. Our South Carolina health plan began serving members under the state of South Carolina’s new full-risk Medicaid managed care program effective January 1, 2014.
Market Update—Molina Medicaid Solutions segment received full federal certification of its Medicaid Management Information System, or MMIS, in the state of Idaho from CMS. As a result of the CMS certification, the state of Idaho is entitled to receive federal reimbursement of 75% of its MMIS operations costs retroactive to June 1, 2010, the date that the system first began processing claims. Our MMIS in Maine received full federal certification from CMS on December 19, 2011.Segment
On June 9,In 2011, Molina Medicaid Solutions received notice from the state of Louisiana that the state intendsintended to award the contract for a replacement MMISMedicaid management information system (MMIS) to another company. Fora different vendor, CNSI. However, in March 2013, the year endedDecember 31, 2012, our revenue under thestate of Louisiana MMIScanceled its contract was$54.9 million, or 29.2%of total service revenue. We expectaward to CNSI. The state had informed us that we will continue to perform under our current contract until a successor is named. On December 18, 2014, Molina Medicaid Solutions received notice from the state of Louisiana that they have extended our contract through December 31, 2015. We recognized approximately $41 million of service revenue under this contract through implementation and acceptance of the successor MMIS. Based upon our past experience and our knowledge of the Louisiana MMIS bid process, we believe that implementation and acceptance of the successor MMIS will not occur until 2014 at the earliest. Through implementation and acceptance of the successor MMIS we expect to recognize approximately$40 millionin revenue annually under our Louisiana MMIS contract.2014.
Consolidation and Presentation
The consolidated financial statements include the accounts of Molina Healthcare, Inc., its wholly owned subsidiaries, and two variable interest entities in which Molina Healthcare, Inc. is considered to be the primary beneficiary. See Note 18,
“Variable19, "Variable Interest Entities,”" for more information regarding these variable interest entities. In the opinion of management, all adjustments considered necessary for a fair presentation of the results as of the date and for the interim periods presented have been included; such adjustments consist of normal recurring adjustments. All significant inter-company balances and transactions have been eliminated in consolidation. Financial information related to subsidiaries acquired during any year is included only for periods subsequent to their acquisition.
Presentation and Reclassifications
We previously reported that our Medicaid managed care contract with the state of Missouri expired without renewal in 2012, and effective June 2013 the transition obligations associated with that contract terminated. Therefore, beginning in the second quarter of 2013, we reported the results relating to the Missouri health plan as discontinued operations for all periods presented. Additionally, we abandoned our equity interests in the Missouri health plan during the second quarter of 2013, resulting in the
recognition of a tax benefit of $9.5 million, which is also included in discontinued operations in the consolidated statements of income. The Missouri health plan's premium revenues were insignificant in 2014 and 2013, and amounted to $114.4 million for the year ended December 31, 2012.
We have reclassified certain amounts in the 2013 consolidated balance sheet, and 2013 and 2012 statements of cash flows to conform to the 2014 presentation, including the presentation of amounts due government agencies as a separate line item in the consolidated balance sheets and statements of cash flows.
Use of Estimates
The preparation of consolidated financial statements in conformity with U.S. generally accepted accounting principles requires management to make estimates and assumptions that affect the reported amounts of assets and liabilities and the disclosure of contingent assets and liabilities at the date of the financial statements. Estimates also affect the reported amounts of revenues and expenses during the reporting period. Actual results could differ from these estimates. Principal areas requiring the use of estimates include:
Health plan contractual provisions that may limit revenue recognition based upon the costs incurred or the profits realized under a specific contract;
Health plan quality incentives that allow us to recognize incremental revenue if certain quality standards are met;
The determination of medical claims and benefits payable of our Health Plans segment;
The valuation of certain investments;
Settlements under risk or savings sharing programs;
The assessment of deferred contract costs, deferred revenue, long-lived and intangible assets, and goodwill for impairment;
The determination of professional and general liability claims, and reserves for potential absorption of claims unpaid by insolvent providers;
The determination of reserves for the outcome of litigation;
The determination of valuation allowances for deferred tax assets; and
The determination of unrecognized tax benefits.
2. Significant Accounting Policies
Cash and Cash Equivalents
Cash and cash equivalents consist of cash and short-term, highly liquid investments that are both readily convertible into known amounts of cash and have a maturity of three months or less on the date of purchase.
Investments
Our investments are principally held in debt securities, which are grouped into two separate categories for accounting and reporting purposes: available-for-sale securities, and held-to-maturity securities. Available-for-sale securities are recorded at fair value and unrealized gains and losses, if any, are recorded in stockholders’ equity as other comprehensive income, net of applicable income taxes. Held-to-maturity securities are recorded at amortized cost, which approximates fair value, and unrealized holding gains or losses are not generally recognized. Realized gains and losses and unrealized losses judged to be other than temporary with respect to available-for-sale and held-to-maturity securities are included in the determination of net income. The cost of securities sold is determined using the specific-identification method, on an amortized cost basis.
Our investment policy requires that all of our investments have final maturities of five10 years or less (excluding auction rate and variable rate securities where interest rates may be periodically reset), and that the average maturity be twothree years or less.less. Investments and restricted investments are subject to interest rate risk and will decrease in value if market rates increase. Declines in interest rates over time will reduce our investment income.
In general, our available-for-sale securities are classified as current assets without regard to the securities’ contractual maturity dates because they may be readily liquidated. Our auction rate securities are classified as non-current assets and reported in other assets. We monitor our investments for other-than-temporary impairment. For comprehensive discussions of the fair value and classification of our current and non-current investments, including auction rate securities, see Note 5,, “Fair "Fair Value Measurements,”" Note 6,, “Investments” "Investments," and Note 10,, “Restricted "Restricted Investments.”
"
Receivables
Receivables are readily determinable and because our creditors are primarily state governments, and our allowance for doubtful accounts is immaterial. Any amounts determined to be uncollectible are charged to expense when such determination is made. See Note 7, "Receivables."
Property, Equipment, and Capitalized Software
Property and equipment are stated at historical cost. Replacements and major improvements are capitalized, and repairs and maintenance are charged to expense as incurred. Furniture and equipment are generally depreciated using the straight-line method over estimated useful lives ranging from three to seven years. Software developed for internal use is capitalized. Software is generally amortized over its estimated useful life of three years. Leasehold improvements are amortized over the term of the lease, or over their useful lives from five to 10 years, whichever is shorter. Buildings are depreciated over their estimated useful lives of 31.5 to 40 years. See Note 8,, “Property, "Property, Equipment, and Capitalized Software.”"
As discussed below, the costs associated with certain of our Molina Medicaid Solutions segment equipment and software are capitalized and recorded as deferred contract costs. Such costs are amortized on a straight-line basis over the shorter of the useful life or the contract period.
Depreciation and Amortization
Depreciation and amortization related to our Health Plans segment is all recorded in “Depreciation"Depreciation and Amortization”Amortization" in the consolidated statements of income. Depreciation and amortization related to our Molina Medicaid Solutions segment is recorded within three different headings in the consolidated statements of income as follows:
Amortization of purchased intangibles relating to customer relationships is reported as amortization within the heading “Depreciation"Depreciation and amortization;”
"
Amortization of purchased intangibles relating to contract backlog is recorded as a reduction of “Service"Service revenue;”" and
DepreciationAmortization of capitalized software is recorded within the heading “Cost"Cost of service revenue.”
"
The following table presents all depreciation and amortization recorded in our consolidated statements of income, regardless of whether the item appears as depreciation and amortization, a reduction of revenue, or as cost of service revenue.
|
| | | | | | | | | | | |
| | Year Ended December 31, |
| | 2012 | | 2011 | | 2010 |
| | (Dollar amounts in thousands) |
| Depreciation, and amortization of capitalized software | $ | 43,201 |
| | $ | 30,864 |
| | $ | 27,230 |
|
| Amortization of intangible assets | 20,503 |
| | 19,826 |
| | 18,474 |
|
| Depreciation and amortization reported as such in the consolidated statements of income | 63,704 |
| | 50,690 |
| | 45,704 |
|
| Amortization recorded as reduction of service revenue | 1,571 |
| | 6,822 |
| | 8,316 |
|
| Amortization of capitalized software recorded as cost of service revenue | 13,489 |
| | 16,871 |
| | 6,745 |
|
| Total | $ | 78,764 |
| | $ | 74,383 |
| | $ | 60,765 |
|
|
| | | | | | | | | | | |
| | Year Ended December 31, |
| | 2014 | | 2013 | | 2012 |
| | (In thousands) |
| Depreciation, and amortization of capitalized software, continuing operations | $ | 75,402 |
| | $ | 54,837 |
| | $ | 42,938 |
|
| Amortization of intangible assets, continuing operations | 17,515 |
| | 17,906 |
| | 20,176 |
|
| Depreciation and amortization, continuing operations | 92,917 |
| | 72,743 |
| | 63,114 |
|
| Depreciation and amortization, discontinued operations | — |
| | 2 |
| | 590 |
|
| Amortization recorded as reduction of service revenue | 2,914 |
| | 2,914 |
| | 1,571 |
|
| Amortization of capitalized software recorded as cost of service revenue | 38,573 |
| | 18,207 |
| | 13,489 |
|
| Depreciation and amortization reported in the statement of cash flows | $ | 134,404 |
| | $ | 93,866 |
| | $ | 78,764 |
|
Long-Lived Assets, including Intangible Assets
Long-lived assets comprise primarily property, equipment, capitalized software and intangible assets. Finite-lived, separately-identifiable intangible assets are acquired in business combinations and are assets that represent future expected benefits but lack physical substance (such as purchased contract rights and provider contracts). Intangible assets are initially recorded at their fair values and are then amortized on a straight-line basis over their expected useful lives, generally between onethree and 15 years.
Identifiable intangible assets associated with Molina Medicaid Solutions are classified as either contract backlog or customer relationships as follows:
The contract backlog intangible asset comprises all contractual cash flows anticipated to be received during the remaining contracted period for each specific contract relating to work that was performed prior to the acquisition. Because each
acquired contract constitutes a single revenue stream, amortization of the contract backlog intangible is recorded to contra-service revenue so that amortization is matched to any revenues associated with contract performance that occurred prior to the acquisition date. The contract backlog intangible asset is amortized on a
straight-line basis for each specific contract over periods generally ranging from one to six years. The contract backlog intangible assets will be fully amortized in 2015.
The customer relationship intangible asset comprises all contractual cash flows that are anticipated to be received during the option periods of each specific contract as well as anticipated renewals of those contracts. The customer relationship intangible is amortized on a straight-line basis for each specific contract over periods generally ranging from four to nine years.
Our intangible assets are subject to impairment tests when events or circumstances indicate that a finite-lived intangible asset’s (or asset group’s) carrying value may not be recoverable. Consideration is given to a number of potential impairment indicators. For example, our health plan subsidiaries have generally been successful in obtaining the renewal by amendment of their contracts in each state prior to the actual expiration of their contracts. However, there can be no assurance that these contracts will continue to be renewed as in the case of our Missouri health plan, described below.renewed.
Following the identification of any potential impairment indicators, to determine whether an impairment exists, we would compare the carrying amount of a finite-lived intangible asset with the undiscounted cash flows that are expected to result from the use of the asset or related group of assets. If it is determined that the carrying amount of the asset is not recoverable, the amount by which the carrying value exceeds the estimated fair value is recorded as an impairment.
On February 17, 2012, we received notification that our Missouri Health plan's contract with the state of Missouri would expire without renewal on June 30, 2012. As a result, we recorded a total non-cash impairment charge of $64.6 million in 2011, of which $6.1 million related to finite-lived intangible assets, and $58.5 million related to goodwill, discussed below. The impairment charge comprised substantially all intangible assets relating to contract rights and licenses, and provider networks recorded at the time of our acquisition of the Missouri health plan in 2007. No significant impairment charges relating to long-lived assets, including intangible assets, were recorded in the years ended December 31, 2012,2014, 2013, and 2010.2012.
Goodwill
Goodwill represents the amount of the purchase price in excess of the fair values assigned to the underlying identifiable net assets of acquired businesses. Goodwill is not amortized, but is subject to an annual impairment test. Tests are performed more frequently if events occur or circumstances change that would more likely than not reduce the fair value of thea reporting unit below its carrying amount.
To determine whether goodwill is impaired, we measure the fair values of our reporting units and compare them to their aggregatethe carrying values of the respective units, including goodwill. If the fair value is less than the carrying value of the reporting unit, then the implied value of goodwill would be calculated and compared to the carrying amount of goodwill to determine whether goodwill is impaired.
We estimate the fair values of our reporting units using discounted cash flows. To determine fair values, we must make assumptions about a wide variety of internal and external factors. Significant assumptions used in the impairment analysis include financial projections of free cash flow (including significant assumptions about operations, capital requirements and income taxes), long-term growth rates for determining terminal value, and discount rates.
In connection with our Missouri health plan as described above, we recorded a non-cash impairment charge of $58.5 million in the fourth quarter of 2011. The impairment charge comprised all of the goodwill recorded at the time of our acquisition of the Missouri health plan in 2007, and was not tax deductible. No impairment charges relating to goodwill were recorded in the years ended December 31, 2012,2014, 2013, and 2010.2012.
Restricted Investments
Restricted investments, which consist of certificates of deposit and U.S. treasury securities, are designated as held-to-maturity and are carried at amortized cost, which approximates market value. The use of these funds is limited to specific purposes as required by each state, or as protection against the insolvency of capitated providers. We have the ability to hold our restricted investments until maturity and, as a result, we would not expect the value of these investments to decline significantly due to a sudden change in market interest rates. See Note 10,, “Restricted "Restricted Investments.”"
Other Assets
Significant items included in otherOther assets includeprimarily includes deferred financing costs associated with our convertible senior notes and with our credit facility,lease financing obligations, and certain investments held in connection with our employee deferred compensation program, and an
investment in a vision services provider (see Note 17, “Related Party Transactions”).program. The deferred financing costs are being amortized on a straight-line basis over the seven-year termterms of the convertible senior notes and the five-year termlease financing obligations.
Delegated Provider Insolvency
Circumstances may arise where providers to whom we have delegated risk due to insolvency or other circumstances, are unable to pay claims they have incurred with third parties in connection with referral services (including hospital inpatient services) provided to our members. The inability of delegated providers to pay referral claims presents us with both immediate financial risk and potential disruption to member care. Depending on states’ laws, we may be held liable for such unpaid referral claims even though the delegated provider has contractually assumed such risk. Additionally, competitive pressures may force us to pay such claims even when we have no legal obligation to do so. To reduce the risk that delegated providers are unable to pay referral claims, we monitor the operational and financial performance of such providers. We also maintain contingency plans that include transferring members to other providers in response to potential network instability.
In certain instances, we have required providers to place funds on deposit with us as protection against their potential insolvency. These reserves are frequently in the form of segregated funds received from the provider and held by us or placed in a third-party financial institution. These funds may be used to pay claims that are the financial responsibility of the provider in the event the provider is unable to meet these obligations. Additionally, we have recorded liabilities for estimated losses arising from provider instability or insolvency in excess of provider funds on deposit with us. Such liabilities were not material at December 31, 2012, or December 31, 2011.2014 and 2013.
Premium Revenue
Premium revenue is fixed in advance of the periods covered and, except as described below, is not generally subject to significant accounting estimates. For the year ended December 31, 20122014, we received approximately 96%more than 95% of our premium revenue as a fixed amount per member per month or PMPM,(PMPM), pursuant to our contracts with state Medicaid, agencies, Medicare and Marketplace contracts, including agreements with other managed care organizations for which we operate as a subcontractor. These premium revenues are recognized in the month that members are entitled to receive health care services. Revenue not received on a fixed PMPM basis is recognized as earned. The state Medicaid programs and the federal Medicare program periodically adjust premium rates.
The following table summarizes premium revenue by health planfrom continuing operations for the periods indicated:
|
| | | | | | | | | | | |
| | Year Ended December 31, |
| | 2012 | | 2011 | | 2010 |
| | (In thousands) |
| California | $ | 671,489 |
| | $ | 575,176 |
| | $ | 506,871 |
|
| Florida | 228,828 |
| | 203,945 |
| | 170,683 |
|
| Michigan | 658,741 |
| | 662,127 |
| | 630,134 |
|
| Missouri(1) | 113,818 |
| | 229,584 |
| | 210,852 |
|
| New Mexico | 338,770 |
| | 345,732 |
| | 366,784 |
|
| Ohio | 1,187,422 |
| | 988,896 |
| | 860,324 |
|
| Texas | 1,255,722 |
| | 409,295 |
| | 188,716 |
|
| Utah | 298,392 |
| | 287,290 |
| | 258,076 |
|
| Washington | 992,748 |
| | 823,323 |
| | 758,849 |
|
| Wisconsin | 70,673 |
| | 69,596 |
| | 30,033 |
|
| Other | 9,888 |
| | 8,443 |
| | 8,587 |
|
| | $ | 5,826,491 |
| | $ | 4,603,407 |
| | $ | 3,989,909 |
|
| |
(1) | Our contract with the state of Missouri expired without renewal on June 30, 2012. |
For the year ended December 31, 2012, we received approximately 4% of our premium revenue in the form of “birth income” — a one-time payment for the delivery of a child — from the Medicaid programs in all of our state health plans except New Mexico. Such payments are recognized as revenue in the month the birth occurs. |
| | | | | | | | | | | | | | | | | | | | |
| | Year Ended December 31, |
| | 2014 | | 2013 | | 2012 |
| | Amount | | % of Total | | Amount | | % of Total | | Amount | | % of Total |
| | (Dollars in thousands) |
| California | $ | 1,523,084 |
| | 16.9 | % | | $ | 749,755 |
| | 12.1 | % | | $ | 665,600 |
| | 12.0 | % |
| Florida | 439,107 |
| | 4.9 |
| | 264,998 |
| | 4.3 |
| | 228,832 |
| | 4.1 |
|
| Illinois | 153,271 |
| | 1.7 |
| | 8,121 |
| | 0.1 |
| | — |
| | — |
|
| Michigan | 780,896 |
| | 8.7 |
| | 676,000 |
| | 11.0 |
| | 646,551 |
| | 11.7 |
|
| New Mexico | 1,075,330 |
| | 11.9 |
| | 446,758 |
| | 7.2 |
| | 321,853 |
| | 5.8 |
|
| Ohio | 1,552,949 |
| | 17.2 |
| | 1,098,795 |
| | 17.8 |
| | 1,095,137 |
| | 19.7 |
|
| South Carolina | 381,317 |
| | 4.2 |
| | — |
| | — |
| | — |
| | — |
|
| Texas | 1,318,192 |
| | 14.6 |
| | 1,291,001 |
| | 20.9 |
| | 1,233,621 |
| | 22.2 |
|
| Utah | 309,411 |
| | 3.4 |
| | 310,895 |
| | 5.0 |
| | 298,392 |
| | 5.4 |
|
| Washington | 1,304,605 |
| | 14.5 |
| | 1,168,405 |
| | 18.9 |
| | 974,712 |
| | 17.6 |
|
| Wisconsin | 156,229 |
| | 1.7 |
| | 143,465 |
| | 2.3 |
| | 70,678 |
| | 1.3 |
|
| Direct delivery | 28,120 |
| | 0.3 |
| | 20,977 |
| | 0.4 |
| | 8,745 |
| | 0.2 |
|
| | $ | 9,022,511 |
| | 100.0 | % | | $ | 6,179,170 |
| | 100.0 | % | | $ | 5,544,121 |
| | 100.0 | % |
Certain components of premium revenue are subject to accounting estimates. The components of premium revenue subject to estimationestimates and fall into twothe following categories:
77Contractual Provisions That May Adjust or Limit Revenue or Profit
Contractual provisions that may limit revenue based upon the costs incurred or the profits realized under a specific contract.These are contractual provisions that require the health plan to return premiums to the extent that certain thresholds are not met. In some instances premiums are returned when medical costs fall below a certain percentage of gross premiums; or when administrative costs or profits exceed a certain percentage of gross premiums. In other instances, premiums are partially determined by the acuity of care provided to members (risk adjustment). To the extent that our expenses and profits change from the amounts previously reported (due to changes in estimates) our revenue earned for those periods will also change. In all of these instances our revenue is only subject to estimate due to the fact that the thresholds themselves contain elements (expense or profit) that are subject to estimate. While we have adequate experience and data to make sound estimates of our expenses or profits, changes to those estimates may be necessary, which in turn will lead to changes in our estimates of revenue. In general, a change in estimate relating to expense or profit would offset any related change in estimate to premium, resulting in no or small impact to net income. The following contractual provisions fall into this category:
California Health Plan Medical Cost Floors (Minimums), Medical Cost Corridors, and Administrative Cost Ceilings (Maximums): A portion of certain Medicaid, Medicare, and Marketplace premiums received by our California health planplans may be returned to the state if certain minimum amounts are not spent on defined medical care costs. WeIn the aggregate, we recorded a liability under the terms of thesesuch contract provisions of $0.3$392.4 million and $1.0$1.4 million at December 31, 2012,2014, and December 31, 2011, respectively.2013, respectively, to amounts due government agencies. Such liability amounts could be subject to future changes in estimate. The increase is primarily driven by contractual provisions relating to the Medicaid expansion program, which began to phase in during January 2014. Beginning in 2014, the health plans may receive additional premiums if amounts spent on medical care costs exceed a defined
Florida Health Plan Medical Cost Floor (Minimum) for Behavioral Health:A portion71
maximum threshold. Separately, in certain states we may be returned to the state if certain minimum amounts are not spent on defined behavioral health care costs. At bothDecember 31, 2012, and December 31, 2011, we had not recorded any liability under the terms of this contract provision since behavioral health expenses are not less than the contractual floor.
New Mexico Health Plan Medical Cost Floors (Minimums) and Administrative Cost and Profit Ceilings (Maximums):Our contractlevied with the state of New Mexico directs that a portion of premiums received may be returned to the statenon-monetary sanctions if certain minimum amounts are not spent on defined medical care costs, or if administrative costs or profit (as defined) exceed certain amounts. At both December 31, 2012, and December 31, 2011we had not recorded any liability under the terms of these contract provisions.
Texas Health Plan Profit Sharing:Sharing and Profit Ceiling:Under our contract Our contracts with the state of Texas, there is acertain states contain profit-sharing agreementor profit ceiling provisions under which we pay a rebaterefund amounts to the state of Texasstates if our Texas health plan generates pretax income, as defined in the contract,plans generate profit above a certain specified percentage, as determinedin some cases in accordance with a tiered rebate schedule. WeIn some cases, we are limited in the amount of administrative costs that we may deduct in calculating the rebate,refund, if any. As a result of profits in excess of the amount we are allowed to fully retain, we accrued an aggregaterecorded a liability of approximately$3.2$0.5 million and $0.7$2.5 millionpursuant to our profit-sharing agreement with the state of Texas at December 31, 20122014 and December 31, 2011,2013, respectively.
Washington Health Plan Medical Cost Floors (Minimums): A portion of certain premiums received by our Washington health plan may be returned to the state if certain minimum amounts are not spent on defined medical care costs. At both December 31, 2012, andDecember 31, 2011, we had not recorded any liability under the terms of this contract provision because medical expenses are not less than the contractual floor.
Medicare Revenue Risk Adjustment:Based on member encounter data that we submit to CMS,the Centers for Medicare and Medicaid Services (CMS), our Medicare premiums are subject to retroactive adjustment for both member risk scores and member pharmacy cost experience for up to2 two years after the original year of service. This adjustment takes into account the acuity of each member’s medical needs relative to what was anticipated when premiums were originally set for that member. In the event that a member requires less acute medical care than was anticipated by the original premium amount, CMS may recover premium from us. In the event that a member requires more acute medical care than was anticipated by the original premium amount, CMS may pay us additional retroactive premium. A similar retroactive reconciliation is undertaken by CMS for our Medicare members’ pharmacy utilization. We estimate the amount of Medicare revenue that will ultimately be realized for the periods presented based on our knowledge of our members’ heathhealth care utilization patterns and CMS practices. Based on our knowledge of member health care utilization patterns and expenses we have recorded a net receivable of approximately$0.3$7.6 million and $5.0$20.8 millionfor anticipated Medicare risk adjustment premiums at December 31, 20122014 and December 31, 2011,2013, respectively.
Quality Incentives
Quality incentives that allow us to recognize incremental revenue if certain quality standards are met.These are contract provisions that allow us to earn additional premium revenue in certain states if we achieve certain quality-of-care or administrative measures. We estimate the amount of revenue that will ultimately be realized for the periods presented based onAt our experience and expertise in meeting the quality and administrative measures as well as our ongoing and current monitoring of our progress
in meeting those measures. The amount of the revenue that we will realize under these contractual provisions is determinable based upon that experience. The following contractual provisions fall into this category:
California, Illinois, New Mexico, Health Plan Quality Incentive Premiums:Under our contract with the stateOhio, Texas, Washington and Wisconsin health plans, revenue ranging from approximately 1% to 4% of New Mexico, incremental revenue of up to 0.75%of our total premiumcertain health plan premiums is earned if certain performance measures are met. These performance measures are generally linked to various quality-of-care and administrative measures dictated by the state.
Ohio Health Plan Quality Incentive Premiums:Under our contract with the state of Ohio, incremental revenue of up to1%of our total premium is earned if certain performance measures are met. These performance measures are generally linked to various quality-of-care measures dictated by the state.
Texas Health Plan Quality Incentive Premiums:Effective March 1, 2012, under our contract with the state of Texas, incremental revenue of up to5%of our total premium may be earned if certain performance measures are met. These performance measures are generally linked to various quality-of-care measures established by the state.
Wisconsin Health Plan Quality Incentive Premiums:Under our contract with the state of Wisconsin, effective beginning in 2011, up to3.25%of premium revenue is withheld by the state. The withheld premiums can be earned by the health plan by meeting certain performance measures. These performance measures are generally linked to various quality-of-care measures dictated by the state.
The following table quantifies the quality incentive premium revenue recognized for the periods presented, including the amounts earned in the period presented and prior periods. Although the reasonably possible effects of a change in estimate related to quality incentive premium revenue as of December 31, 20122014 are not known, we have no reason to believe that the adjustments to prior years noted below are not indicative of the potential future changes in our estimates as of December 31, 2012.
2014.
|
| | | | | | | | | | | | | | | | | | | |
| | Year Ended December 31, 2012 |
| | Maximum Available Quality Incentive Premium – Current Year | | Amount of Current Year Quality Incentive Premium Revenue Recognized | | Amount of Quality Incentive Premium Revenue Recognized from Prior Year | | Total Quality Incentive Premium Revenue Recognized | | Total Revenue Recognized |
| | (In thousands) |
| New Mexico | $ | 2,244 |
| | $ | 1,889 |
| | $ | 643 |
| | $ | 2,532 |
| | $ | 338,770 |
|
| Ohio | 12,033 |
| | 8,079 |
| | 966 |
| | 9,045 |
| | 1,187,422 |
|
| Texas | 58,516 |
| | 52,521 |
| | — |
| | 52,521 |
| | 1,255,722 |
|
| Wisconsin | 1,771 |
| | — |
| | 593 |
| | 593 |
| | 70,673 |
|
| | $ | 74,564 |
| | $ | 62,489 |
| | $ | 2,202 |
| | $ | 64,691 |
| | $ | 2,852,587 |
|
|
| | | | | | | | | | | |
| | Year Ended December 31, |
| | 2014 | | 2013 | | 2012 |
| | (In thousands) |
| Maximum available quality incentive premium - current period | $ | 90,327 |
| | $ | 63,311 |
| | $ | 74,564 |
|
| | | | | | |
| Amount of quality incentive premium revenue recognized in current period: | | | | | |
| Earned current period | $ | 40,396 |
| | $ | 45,803 |
| | $ | 62,489 |
|
| Earned prior periods | 3,950 |
| | 9,056 |
| | 2,202 |
|
| Total | $ | 44,346 |
| | $ | 54,859 |
| | $ | 64,691 |
|
| | | | | | |
| Total premium revenue recognized for state health plans with quality incentive premiums | $ | 7,083,660 |
| | $ | 2,980,019 |
| | $ | 2,721,289 |
|
California Health Plan Rate Settlement Agreement
In the fourth quarter of 2013, our California health plan entered into a settlement agreement with the California Department of Health Care Services (DHCS). The agreement settled rate disputes initiated by our California health plan dating back to 2003 with respect to its participation in Medi-Cal (California’s Medicaid program). Under the terms of the agreement, a settlement account (the Account) applicable to the California health plan’s managed care contracts has been established. |
| | | | | | | | | | | | | | | | | | | |
| | Year Ended December 31, 2011 |
| | Maximum Available Quality Incentive Premium – Current Year | | Amount of Current Year Quality Incentive Premium Revenue Recognized | | Amount of Quality Incentive Premium Revenue Recognized from Prior Year | | Total Quality Incentive Premium Revenue Recognized | | Total Revenue Recognized |
| | (In thousands) |
| New Mexico | $ | 2,271 |
| | $ | 1,558 |
| | $ | 378 |
| | $ | 1,936 |
| | $ | 345,732 |
|
| Ohio | 10,212 |
| | 8,363 |
| | 3,501 |
| | 11,864 |
| | 988,896 |
|
| Texas | — |
| | — |
| | — |
| | — |
| | 409,295 |
|
| Wisconsin | 1,705 |
| | 542 |
| | — |
| | 542 |
| | 69,596 |
|
| | $ | 14,188 |
| | $ | 10,463 |
| | $ | 3,879 |
| | $ | 14,342 |
| | $ | 1,813,519 |
|
Effective January 1, 2014, the Account was established with an initial balance of zero, and will be settled after December 31, 2017. DHCS will make an interim partial settlement payment to us if it terminates early, without replacement, any of our managed care contracts. The Account will be adjusted annually to reflect a calendar year deficit or surplus, which is determined by comparing the California health plan’s pre-tax margin and a target margin established in the settlement agreement. Upon expiration of the settlement agreement, if the Account is in a deficit position, then DHCS will pay the amount of the deficit to us, subject to an alternative minimum payment amount. If the Account is in a surplus position, then no amount is owed to either party. The maximum amount that DHCS would pay to us under the terms of the settlement agreement is $40.0 million.
|
| | | | | | | | | | | | | | | | | | | |
| | Year Ended December 31, 2010 |
| | Maximum Available Quality Incentive Premium – Current Year | | Amount of Current Year Quality Incentive Premium Revenue Recognized | | Amount of Quality Incentive Premium Revenue Recognized from Prior Year | | Total Quality Incentive Premium Revenue Recognized | | Total Revenue Recognized |
| | (In thousands) |
| New Mexico | $ | 2,581 |
| | $ | 1,311 |
| | $ | 579 |
| | $ | 1,890 |
| | $ | 366,784 |
|
| Ohio | 9,881 |
| | 3,114 |
| | (1,248 | ) | | 1,866 |
| | 860,324 |
|
| Texas | 1,771 |
| | 1,771 |
| | — |
| | 1,771 |
| | 188,716 |
|
| | $ | 14,233 |
| | $ | 6,196 |
| | $ | (669 | ) | | $ | 5,527 |
| | $ | 1,415,824 |
|
Medical Care Costs
Expenses related to medical care services are captured in the following four categories:
Fee-for-service:Fee-for-service expenses: Physician providers paid on a fee-for-service basis are paid according to a fee schedule set byNearly all hospital services and the state or bymajority of our contracts with these providers. Most hospitalsprimary care and physician specialist services and LTSS costs are paid on a fee-for-service basis in a variety of ways, including per diem amounts, diagnostic-related groups, or DRGs, percent of billed charges, and case rates. As discussed below, we also pay a small portion of hospitals on a capitated basis. We also have stop-loss agreements with the hospitals with which we contract. Under all fee-for-service arrangements, we retain the financial responsibility for medical care provided. Expenses related to fee-for-service contractsprovided and incur costs based on actual utilization of services. Such expenses are recorded in the period in which the related services are dispensed. The costs of drugs administered in a physician or hospital setting that are not billed through our pharmacy benefit manager are included in fee-for-service costs.
Capitation:Pharmacy expenses: All drug, injectibles, and immunization costs paid through our pharmacy benefit manager are classified as pharmacy expenses. As noted above, drugs and injectibles not paid through our pharmacy benefit manager are included in fee-for-service costs, except in those limited instances where we capitate drug and injectible costs.
Capitation expenses: Many of our primary care physicians and a small portion of our specialists and hospitals are paid on a capitated basis. Under capitation contracts,arrangements, we typically pay a fixed per-member per-month, oramount PMPM payment to the provider without regard to the frequency, extent, or nature of the medical services actually furnished. Under capitated contracts,arrangements, we remain liable for the provision of certain health care services. Certain of our capitated contracts also contain incentive programs based on service delivery, quality of care, utilization management, and other criteria. Capitation payments are fixed in advance of the periods covered and are not subject to significant accounting estimates. These payments are expensed in the period the providers are obligated to provide services. The financial risk for pharmacy services for a small portion of our membership is delegated to capitated providers.
Pharmacy:Direct delivery expenses: PharmacyAll costs include all drug, injectibles, and immunization costs paid throughassociated with our pharmacy benefit manager. As noted above, drugs and injectibles not paid through our pharmacy benefit managerdirect delivery of medical care are included in fee-for-service costs, except in those limited instances where we capitate drug and injectible costs.separately identified.
Other:Other medical care costs includeexpenses: All medically related administrative costs, certain provider incentive costs, reinsurance cost,costs and other health care expense.expenses are classified as other medical expenses. Medically related administrative costs include, for example, expenses relating to health education, quality assurance, case management, care coordination, disease management, and 24-hour on-call nurses. Salary and benefit costs are a substantial portion of these expenses. For the years ended December 31, 2012, 2011,2014, 2013, and 2010,2012, medically related administrative costs were approximately $127.5$262.6 million,, $102.3 $153.0 million,, and $85.5$125.2 million,, respectively.
The following table provides the details of our consolidated medical care costs from continuing operations for the periods indicated (dollars in thousands, except PMPM amounts):
| | | | Year Ended December 31, | Year Ended December 31, |
| | 2012 | | 2011 | | 2010 | 2014 | | 2013 | | 2012 |
| | Amount | | PMPM | | % of Total | | Amount | | PMPM | | % of Total | | Amount | | PMPM | | % of Total | Amount | | PMPM | | % of Total | | Amount | | PMPM | | % of Total | | Amount | | PMPM | | % of Total |
| Fee-for-service | $ | 3,521,960 |
| | $ | 162.60 |
| | 69.1 | % | | $ | 2,764,309 |
| | $ | 139.02 |
| | 71.6 | % | | $ | 2,360,858 |
| | $ | 128.73 |
| | 70.0 | % | $ | 5,672,483 |
| | $ | 202.87 |
| | 70.2 | % | | $ | 3,611,529 |
| | $ | 160.43 |
| | 67.1 | % | | $ | 3,423,751 |
| | $ | 161.67 |
| | 68.6 | % |
| Pharmacy | | 1,273,329 |
| | 45.54 |
| | 15.8 |
| | 935,204 |
| | 41.54 |
| | 17.4 |
| | 835,830 |
| | 39.47 |
| | 16.7 |
|
| Capitation | 557,087 |
| | 25.72 |
| | 10.9 |
| | 518,835 |
| | 26.09 |
| | 13.4 |
| | 555,487 |
| | 30.29 |
| | 16.5 |
| 748,388 |
| | 26.77 |
| | 9.3 |
| | 603,938 |
| | 26.83 |
| | 11.2 |
| | 552,136 |
| | 26.07 |
| | 11.1 |
|
| Pharmacy | 835,830 |
| | 38.59 |
| | 16.4 |
| | 418,007 |
| | 21.02 |
| | 10.8 |
| | 325,935 |
| | 17.77 |
| | 9.7 |
| |
| Direct delivery | | 96,196 |
| | 3.44 |
| | 1.2 |
| | 48,288 |
| | 2.14 |
| | 0.9 |
| | 33,920 |
| | 1.60 |
| | 0.7 |
|
| Other | 181,883 |
| | 8.39 |
| | 3.6 |
| | 158,843 |
| | 8.00 |
| | 4.2 |
| | 128,577 |
| | 7.01 |
| | 3.8 |
| 285,935 |
| | 10.22 |
| | 3.5 |
| | 181,165 |
| | 8.05 |
| | 3.4 |
| | 145,551 |
| | 6.87 |
| | 2.9 |
|
| Total | $ | 5,096,760 |
| | $ | 235.30 |
| | 100.0 | % | | $ | 3,859,994 |
| | $ | 194.13 |
| | 100.0 | % | | $ | 3,370,857 |
| | $ | 183.80 |
| | 100.0 | % | $ | 8,076,331 |
| | $ | 288.84 |
| | 100.0 | % | | $ | 5,380,124 |
| | $ | 238.99 |
| | 100.0 | % | | $ | 4,991,188 |
| | $ | 235.68 |
| | 100.0 | % |
The Missouri health plan's medical care costs, which are not included in the table above, amounted to $0.6 million, $1.5 million, and $105.6 million for the years ended December 31, 2014, 2013, and 2012, respectively.
Our medical care costs include amounts that have been paid by us through the reporting date, as well as estimated liabilities for medical care costs incurred but not paid by us as of the reporting date. Such medical care cost liabilities include, among other items, unpaid fee-for-service claims, capitation payments owed providers, unpaid pharmacy invoices, and various medically related
administrative costs that have been incurred but not paid. We use judgment to determine the appropriate assumptions for determining the required estimates.
The most important element in estimating our medical care costs is our estimate for fee-for-service claims which have been incurred but not paid by us. These fee-for-service costs that have been incurred but have not been paid at the reporting date are collectively referred to as medical costs that are “Incurred But Not Paid,” or IBNP.incurred but not paid (IBNP). Our IBNP claims reserve, as reported in our
balance sheet, represents our best estimate of the total amount of claims we will ultimately pay with respect to claims that we have incurred as of the balance sheet date. We estimate our IBNP monthly using actuarial methods based on a number of factors.
The factors we consider when estimating our IBNP include, without limitation, claims receipt and payment experience (and variations in that experience), changes in membership, provider billing practices, health care service utilization trends, cost trends, product mix, seasonality, prior authorization of medical services, benefit changes, known outbreaks of disease or increased incidence of illness such as influenza, provider contract changes, changes to Medicaid fee schedules, and the incidence of high dollar or catastrophic claims. Our assessment of these factors is then translated into an estimate of our IBNP liability at the relevant measuring point through the calculation of a base estimate of IBNP, a For further reserve for adverse claims development, and an estimate of the administrative costs of settling all claims incurred through the reporting date. The base estimate of IBNP is derived through application of claims payment completion factors and trended PMPM cost estimates. Seeinformation, see Note 11,, “Medical "Medical Claims and Benefits Payable.”"
We report reinsurance premiums as medical care costs, while related reinsurance recoveries are reported as deductions from medical care costs. We limit our risk of catastrophic losses by maintaining high deductible reinsurance coverage. We do not consider this coverage to be material because the cost is not significant and the likelihood that coverage will apply is low.
Taxes Based on Premiums
Our California (through June 30, 2012), Florida, Michigan, New Mexico, Ohio, TexasHealth Insurer Fee. The federal government under the Patient Protection and WashingtonAffordable Care Act and the Health Care and Education Reconciliation Act of 2010 (collectively, the Affordable Care Act, or ACA) imposes an annual fee, or excise tax, on health insurers for each calendar year. The health insurer fee (HIF) is based on a company's share of the industry's net premiums written during the preceding calendar year, and is non-deductible for income tax purposes. We recognize expense for the HIF over the year on a straight-line basis. Because we primarily serve individuals in government-sponsored programs, we must secure additional reimbursement from our state partners for this added cost. We recognize the related revenue when we have obtained a contractual commitment from a state to reimburse us for the HIF; such HIF revenue is recognized ratably throughout the year.
Premium and Use Tax. Certain of our health plans are assessed a tax based on premium revenue collected. The premium revenues we receive from these states include the premium tax assessment. We reporthave reported these taxes on a gross basis, included inas premium tax expense.revenue and as premium tax expense in the consolidated statements of income.
Premium Deficiency Reserves on Loss Contracts
We assess the profitability of our contracts for providing medical care services to our members and identify those contracts where current operating results or forecasts indicate probable future losses. Anticipated future premiums are compared to anticipated medical care costs, including the cost of processing claims. If the anticipated future costs exceed the premiums, a loss contract accrual is recognized. No such accrual was recorded as of December 31, 2012,2014, or 2011.2013.
Service Revenue and Cost of Service Revenue — Molina Medicaid Solutions Segment
The payments received by our Molina Medicaid Solutions segment under its state contracts are based on the performance of multiple services. The first of these is the design, development and implementation or DDI,(DDI) of a Medicaid Management Information System, or MMIS.management information system (MMIS). An additional service, following completion of DDI, is the operation of the MMIS under a business process outsourcing or BPO(BPO) arrangement. WhileWhen providing BPO services (which include claims payment and eligibility processing) we also provide the state with other services including both hosting and support, and maintenance. OurBecause we have determined the services provided under our Molina Medicaid Solutions contracts represent a single unit of accounting, we recognize revenue associated with such contracts on a straight-line basis over the contract term during which BPO, hosting, and support and maintenance services are delivered. There may extend over a numberbe certain contractual provisions containing contingencies, however that require us to delay recognition of years, particularly in circumstances where we are delivering extensive and complex DDI services, such as the initial design, development and implementation of a complete MMIS. For example, the termsall or part of our most recently implemented Molina Medicaid Solutions contracts (in Idaho and Maine) were each seven years in total, consisting of two years allocated for the delivery of DDI services, followed by five years for the performance of BPO services. We receive progress payments from the state during the performance of DDI services based upon the attainment of predetermined milestones. We receive a flat monthly payment for BPO services under our Idaho and Maine contracts. The terms of our other Molina Medicaid Solutions contracts - which primarily involve the delivery of BPO services with only minimal DDI activity (consisting of system enhancements) - are shorter in duration than our Idaho and Maine contracts.service revenue until such contingencies have been removed.
We have evaluated our Molina Medicaid Solutions contracts to determine if such arrangements include a software element. Based on this evaluation, we have concluded that these arrangements do not include a software element. As such, we have concluded that our Molina Medicaid Solutions contractselement, and are therefore multiple-element service arrangements under the scope of FASB Accounting Standards Codification Subtopic 605-25, Revenue Recognition –– Multiple–Element Arrangements, and SEC Staff Accounting Bulletin Topic 13, Revenue Recognition. arrangements.
Effective January 1, 2011,Additionally, we adopted a new accounting standard that amends the guidance on the accounting for multiple-element arrangements. Pursuant to the new standard,evaluate each required deliverable is evaluatedunder our multiple-element service arrangements to determine whether it qualifies as a separate unit of accounting whichaccounting. Such evaluation is generally based on whether the deliverable has standalone value to the customer. In addition toIf the deliverable has standalone value, previous guidance also required objective and reliable evidence of fair value of a deliverable in order to treat the deliverable as a separate unit of accounting. The arrangement’s consideration that is fixed or determinable is then allocated to
each separate unit of accounting based on the relative selling price of each deliverable. In general, the consideration allocated to each unit of accounting is recognized as the related goods or services are delivered, limited to the consideration that is not contingent. We have adopted this guidance on a prospective basis for all new or materially modified revenue arrangements with multiple deliverables entered into on or after January 1, 2011. Our adoption of this guidance has not impacted the timing or pattern of our revenue recognition in 2011 or 2012. Also, there would have been no change in revenue recognized relating to multiple-element arrangements if we had adopted this guidance retrospectively for contracts entered into prior to January 1, 2011.
We have concluded that the various service elements in our Molina Medicaid Solutions contracts represent a single unit of accounting due to the fact that DDI, which is the only service performed in advance of the other services (all other services are performed over an identical period), does not have standalone value because our DDI services are not sold separately by any vendor and the customer could not resell our DDI services. Further, we have no objective and reliable evidence of fair value for any of the individual elements in these contracts, and at no point in the contract will we have objective and reliable evidence of fair value for the undelivered elements in the contracts. For contracts entered into prior to January 1, 2011, objective and reliable evidence of fair value would be required, in addition to DDI standalone value which we do not have, in order to treat DDI as a separate unit of accounting. We lack objective and reliable evidence of the fair value of the individual elements of our Molina Medicaid Solutions contracts for the following reasons:
Each contract calls for the provision of its own specific set of services. While all contracts support the system of record for state MMIS, the actual services we provide vary significantly between contracts; and
The nature of the MMIS installed varies significantly between our older contracts (proprietary mainframe systems) and our new contracts (commercial off-the-shelf technology solutions).
Because we have determined the services provided under our Molina Medicaid Solutions contracts represent a single unit of accounting, and because we are unable to determine a pattern of performance of services during the contract period, we recognize all revenue (both the DDI and BPO elements) associated with such contracts on a straight-line basis over the period during which BPO, hosting, and support and maintenance services are delivered. As noted above, the period of performance of BPO services under our Idaho and Maine contracts is five years. Therefore, absent any contingencies as discussed in the following paragraph, or contract extensions, we would recognize all revenue associated with those contracts over the initial contract period. When a periodcontract is extended, we generally consider the extension to be a continuation of five years.the single unit of accounting; therefore, the deferred revenue as of the extension date is recognized prospectively over the new remaining term of the contract. In cases where there is no DDI element associated with our contracts, BPO revenue is recognized on a monthly basis as specified in the applicable contract or contract extension.
Provisions specific to each contract may, however, lead us to modify this general principle. In those circumstances, the right of the state to refuse acceptance of services, as well as the related obligation to compensate us, may require us to delay recognition of all or part of our revenue until that contingency (the right of the state to refuse acceptance) has been removed. In those circumstances, we defer recognition of any contingent revenue (whether DDI, BPO services, hosting, and support and maintenance services) until the contingency has been removed. These types of contingency features are present in our Maine and Idaho contracts.contracts, for example. In those states, we deferred recognition of revenue until the contingencies were removed.
Costs associated with our Molina Medicaid Solutions contracts include software related costs and other costs. With respect to software related costs, we apply the guidance for internal-use software and capitalize external direct costs of materials and services consumed in developing or obtaining the software, and payroll and payroll-related costs associated with employees who are directly associated with and who devote time to the computer software project. With respect to all other direct costs, such costs are expensed as incurred, unless corresponding revenue is being deferred. If revenue is being deferred, direct costs relating to delivered service elements are deferred as well and are recognized on a straight-line basis over the period of revenue recognition, in a manner consistent with our recognition of revenue that has been deferred. Such direct costs can include:
Transaction processing costs.
costs;Employee costs incurred in performing transaction services.
services;Vendor costs incurred in performing transaction services.
services;Costs incurred in performing required monitoring of and reporting on contract performance.
performance;Costs incurred in maintaining and processing member and provider eligibility.
eligibility; andCosts incurred in communicating with members and providers.
The recoverability of deferred contract costs associated with a particular contract is analyzed on a periodic basis using the undiscounted estimated cash flows of the whole contract over its remaining contract term. If such undiscounted cash flows are insufficient to recover the long-lived assets and deferred contract costs, the deferred contract costs are written down by the amount of the cash flow deficiency. If a cash flow deficiency remains after reducing the balance of the deferred contract costs to zero, any
remaining long-lived assets are evaluated for impairment. Any such impairment recognized would equal the amount by which the carrying value of the long-lived assets exceeds the fair value of those assets.
Income Taxes
The provision for income taxes is determined using an estimated annual effective tax rate, which is generally greater than the U.S. federal statutory rate primarily because of state taxes, andnondeductible HIF expenses, nondeductible compensation and other general and administrative expenses. The effective tax rate may be subject to fluctuations during the year, particularly as a result of the mathematical impact of the level of pretax earnings, and also as new information is obtained. Such information may affect the assumptions used to estimate the annual effective tax rate, including factors such as the mix of pretax earnings in the various tax jurisdictions in which we operate, valuation allowances against deferred tax assets, the recognition or derecognitionthe reversal of the recognition of tax benefits related to uncertain tax positions, and changes in or the interpretation of tax laws in jurisdictions where we conduct business. We recognize deferred tax assets and liabilities for temporary differences between the financial reporting basis and the tax basis of our assets and liabilities, along with net operating loss and tax credit carryovers. For further discussion and disclosure, see Note 13, “Income14, "Income Taxes.”
"
Concentrations of Credit Risk
Financial instruments that potentially subject us to concentrations of credit risk consist primarily of cash and cash equivalents, investments, receivables, and restricted investments. We invest a substantial portion of our cash in the PFM Funds Prime Series — Institutional Class, and the PFM Funds Government Series. These funds represent a portfolio of highly liquid money market securities that are managed by PFM Asset Management LLC (PFM), a Virginia business trust registered as an open-end
management investment fund. As of December 31, 2012,2014, and 2011,2013, our investments with PFM totaled $428amounted to approximately $321 million and $209$374 million,, respectively. Our investments and a portion of our cash equivalents are managed by professional portfolio managers operating under documented investment guidelines. No investment that is in a loss position can be sold by our managers without our prior approval. Our investments consist solely of investment grade debt securities with a maximum maturity of 10 years and an average duration of three years or less. Restricted investments are invested principally in certificates of deposit and U.S. treasury securities. Concentration of credit risk with respect to accounts receivable is limited due to payors consisting principally of the governments of each state in which our health plan subsidiaries operate.
Risks and Uncertainties
Our profitability depends in large part on our ability to accurately predict and effectively manage medical care costs. We continually review our medical costs in light of our underlying claims experience and revised actuarial data. However, several factors could adversely affect medical care costs. These factors, which include changes in health care practices, inflation, new technologies, major epidemics, natural disasters, and malpractice litigation, are beyond our control and may have an adverse effect on our ability to accurately predict and effectively control medical care costs. Costs in excess of those anticipated could have a material adverse effect on our financial condition, results of operations, or cash flows.
At December 31, 2012, we operatedWe operate health plans in nine11 states, primarily as a direct contractor with the states, and in Los Angeles County, California, as a subcontractor to another health plan holding a direct contract with the state. We are therefore dependent upon a small number of contracts to support our revenue. The loss of any one of those contracts could have a material adverse effect on our financial position, results of operations, or cash flows. Our ability to arrange for the provision of medical services to our members is dependent upon our ability to develop and maintain adequate provider networks. Our inability to develop or maintain such networks might, in certain circumstances, have a material adverse effect on our financial position, results of operations, or cash flows.
Recent Accounting Pronouncements
Technical Corrections and Improvements. Health Insurer Fee.In October 2012,the first quarter of 2014, we adopted the guidance of the Financial Accounting Standards Board or FASB, issued guidance related to amendments that cover a wide range of Topics in the Accounting Standards Codification. These amendments include technical corrections and improvements to the Accounting Standards Codification and conforming amendments related to fair value measurements. The amendments that do not have transition guidance became effective upon issuance. The amendments that are subject to transition guidance become effective for fiscal periods beginning after December 15, 2012. The adoption of this new guidance in 2012 did not impact our financial position, results of operations or cash flows.
Balance Sheet Offsetting. In January 2013, the FASB issued guidance for new disclosure requirements related to the nature of an entity's rights of setoff and related arrangements associated with certain financial instruments and derivative instruments. The new guidance is effective for annual reporting periods, and interim periods within those years, beginning on or after January 1, 2013. While we do not expect the adoption of this guidance in 2013 to impact our financial position, results of operations or cash flows, it may change our disclosure policies relative to certain arrangements with rights of setoff.
Goodwill. In September 2011, the FASB issued guidance related to evaluating goodwill for impairment. The new guidance provides entities with the option to perform a qualitative assessment of whether it is more likely than not that the fair value of a reporting unit is less than its carrying amount before applying the quantitative two-step goodwill impairment test. If an entity
concludes that it is not more likely than not that the fair value of a reporting unit is less than its carrying amount, it would not be required to perform the quantitative two-step goodwill impairment test. Entities also have the option to bypass the assessment of qualitative factors for any reporting unit in any period and proceed directly to performing the first step of the quantitative two-step goodwill impairment test, as was required prior to the issuance of this new guidance. An entity may begin or resume performing the qualitative assessment in any subsequent period. The new guidance became effective for annual reporting periods, and interim periods within those years, beginning after December 15, 2011, with early adoption permitted. The adoption of this new guidance in 2012 did not impact our financial position, results of operations or cash flows.
Federal Premium-Based Assessment. In July 2011, the FASB issued guidance(FASB) related to accounting for the fees to be paid by health insurers to the federal government under the Patient Protection and Affordable Care Act, as amended byACA, specifically the Health Care and Education Reconciliation Act (the “Affordable Care Act”).HIF. The Affordable Care Act imposes an annual fee on health insurers for each calendar yearHIF is imposed beginning on or after January 1,in 2014, that is allocated to health insurers based on the ratioa company's share of the amount of an entity'sindustry's net premium revenuespremiums written during the preceding calendar year, to the amount of health insurance for any U.S. health risk that is written during the preceding calendar year. The new guidance specifies that the liability for the fee should be estimated and recorded in full once the entity provides qualifying health insurance in the applicable calendar year in which the fee is payable with a corresponding deferred cost that is amortizedon September 30 of each year. Effective January 1, 2014, we recorded our estimate of the 2014 liability to expense using a straight-line methodaccounts payable and accrued liabilities. During the third quarter of allocation unless another method better allocates the fee over the calendar year that it is payable. The new guidance is effective for annual reporting periods beginning after December 31, 2013, when the fee initially becomes effective. As enacted, this federal premium-based2014 we paid our 2014 HIF assessment, is non-deductible for income tax purposes, and is anticipatedwhich amounted to be significant. It is yet undetermined how this premium-based assessment will be factored into the calculation of our premium rates, if at all. Accordingly, adoption of this guidance and the enactment of this assessment as currently written will have a material impact on our financial position, results of operations, or cash flows in future periods.$88.6 million.
Comprehensive Income.Revenue Recognition. In June 2011,May 2014, the FASB issued guidance, as amended in December 2011, related to the presentation of other comprehensive income. The new guidance provides entities with an option to either replace the statement of income with a statement of comprehensive income which would display both the components of net income and comprehensive income in a combined statement, or to present a separate statement of comprehensive income immediately following the statement of income. The new guidance does not affect the components of other comprehensive income or the calculation of earnings per share. To be applied retrospectively with early adoption permitted, the new guidance became effective for annual reporting periods, and interim periods within those years, beginning after December 15, 2011. We have elected to present a separate statement of comprehensive income immediately following the statement of income. The adoption of this new guidance in 2012 did not impact our financial position, results of operations or cash flows.
Fair Value.In May 2011, the FASB issued guidance related to fair value measurement and disclosure. The new guidance is a result of joint efforts by the FASB and the International Accounting Standards Board to develop a single converged fair value framework. The newUpdate (ASU) 2014-09 - Revenue from Contracts with Customers, which will supersede nearly all existing revenue recognition guidance expands existing disclosure requirements for fair value measurements and makes other amendments; mostly to eliminate wording differences betweenunder U.S. generally accepted accounting principles (GAAP). The core principal of this ASU is that an entity should recognize revenue when it transfers promised goods or GAAP,services to customers in an amount that reflects the consideration to which the entity expects to be entitled in exchange for those goods or services. This ASU also requires additional disclosure about the nature, amount, timing and international financial reporting standards. Touncertainty of revenue and cash flows arising from customer contracts, including significant judgments and changes in judgments and assets recognized from costs incurred to obtain or fulfill a contract. This ASU will be applied prospectively, the new guidance became effective for annual reporting periods,us in the first quarter of 2017; early adoption is not permitted. The ASU allows for either full retrospective or modified retrospective adoption. We are evaluating the transition method that will be elected and interim periods within those years, beginning after December 15, 2011. Althoughthe potential effects of the adoption of this new guidance in 2012 did not impactASU on our financial position, resultsstatements.
Discontinued Operations. In April 2014, the FASB issued ASU 2014-08 - Reporting Discontinued Operations and Disclosures of Disposal of Components of an Entity, which raises the threshold for disposals to qualify as discontinued operations by focusing on strategic shifts that have or cash flows, it did changewill have a major effect on an entity’s operations and financial results. This ASU will be effective for us in the first quarter of 2015, and is applied prospectively. Early adoption is permitted but only for disposals (or classifications as held for sale) that have not been reported in financial statements previously issued or available for issue. We are evaluating the potential effects of the adoption of the ASU on our disclosure policies relative to fair value measurements.financial statements.
Other recent accounting pronouncements issued by the FASB (including its Emerging Issues Task Force), the American Institute of Certified Public Accountants or AICPA,(AICPA), and the Securities and Exchange Commission or SEC,(SEC), did not have, or are not believed by management to have, a material impact on our present or future consolidated financial statements.
3. Earnings per Share
The denominators for the computation of basic and diluted earnings per share were calculated as follows:
3. Net Income per Share
The following table sets forth the calculation of the denominators used to compute basic and diluted net income per share:
|
| | | | | | | | |
| | December 31, |
| | 2012 | | 2011 | | 2010 |
| | (In thousands) |
| Shares outstanding at the beginning of the period | 45,815 |
| | 45,463 |
| | 38,410 |
|
| Weighted-average number of shares issued under equity offering | — |
| | — |
| | 2,506 |
|
| Weighted-average number of shares purchased | (2 | ) | | (160 | ) | | — |
|
| Weighted-average number of shares issued under employee stock plans | 567 |
| | 453 |
| | 258 |
|
| Denominator for basic earnings per share | 46,380 |
| | 45,756 |
| | 41,174 |
|
| Dilutive effect of employee stock options and stock grants(1) | 619 |
| | 669 |
| | 457 |
|
| Denominator for diluted earnings per share(2) | 46,999 |
| | 46,425 |
| | 41,631 |
|
|
| | | | | | | | |
| | December 31, |
| | 2014 | | 2013 | | 2012 |
| | (In thousands) |
| Shares outstanding at the beginning of the period | 45,871 |
| | 46,762 |
| | 45,815 |
|
| Weighted-average number of shares: | | | | | |
| Repurchased | — |
| | (1,445 | ) | | (2 | ) |
| Issued, 3.75% Notes and 3.75% Exchange (1) | 566 |
| | — |
| | — |
|
| Issued, share-based compensation | 498 |
| | 400 |
| | 567 |
|
| Denominator for basic net income per share | 46,935 |
| | 45,717 |
| | 46,380 |
|
| Effect of dilutive securities: | | | | | |
| Share-based compensation | 498 |
| | 643 |
| | 619 |
|
| 3.75% Notes and 3.75% Exchange (1) | 907 |
| | 502 |
| | — |
|
| Denominator for diluted net income per share | 48,340 |
| | 46,862 |
| | 46,999 |
|
| | | | | | |
| Potentially dilutive common shares excluded from calculations (2): | | | | | |
| Stock options | — |
| | 51 |
| | 87 |
|
| 1.125% Warrants | 13,490 |
| | 11,975 |
| | — |
|
| Restricted shares | — |
| | — |
| | 304 |
|
_______________________________
| |
| (1) | OptionsFor more information regarding the 3.75% Exchange and 3.75% Notes, refer to purchase common shares are included in the calculation of diluted earnings per share when their exercise prices are below the average fair value of the common shares for each of the periods presented. For the years ended December 31, 2012, 2011, and 2010 there were approximately 87,000, 137,000 and 478,000 anti-dilutive weighted options, respectively. Restricted shares are included in the calculation of diluted earnings per share when their grant date fair values are below the average fair value of the common shares for each of the periods presented. For the year ended December 31, 2012, there were approximately 304,000 anti-dilutive restricted shares. For the years ended December 31, 2011 and 2010, anti-dilutive restricted shares were insignificant.
Note 12, "Long-Term Debt." |
| |
| (2) | Potentially dilutive shares issuable pursuant to certain of our convertible senior notesemployee stock options, 1.125% Warrants (defined in Note 13, "Derivative Financial Instruments"), and 1.625% Notes (defined in Note 12, "Long-Term Debt") were not included in the computation of diluted earningsnet income per share because to do so would have been anti-dilutive for the years ended December 31, 2012, 2011, and 2010. anti-dilutive. |
4. Business Combinations
Molina Center
OnHealth Plans Segment
Florida.In December 7, 2011,2014, our wholly owned subsidiary Molina CenterFlorida health plan acquired certain assets relating to the Medicaid business of First Coast Advantage, LLC acquired a 460,000 square foot office building located in Long Beach, California. The building, or Molina Center, consists of two conjoined fourteen-story office towers on approximately five acres of land. For the last several years we have leased approximately 155,000 square feet(FCA). As part of the Molina Centertransaction, we assumed FCA's Medicaid contract and certain provider agreements for useRegion 4 of the Statewide Medicaid Managed Care Managed Medical Assistance Program in the state of Florida. The Florida health plan's membership increased by approximately 62,000 members as a result of this transaction. We estimate that the final purchase price for this acquisition, to be settled in the first quarter of 2015, will be approximately $44.6 million.
In August 2014, our corporate headquarters and also for use by our CaliforniaFlorida health plan subsidiary.acquired certain assets relating to the Medicaid business of Healthy Palm Beaches, Inc. The final purchase price for this acquisition was $81$7.5 million. The Florida health plan's membership increased by approximately 11,000 members as a result of this transaction.
In connection with these transactions, we recorded goodwill amounting to $41.2 million,, which relates to future economic benefits arising from expected synergies to be achieved. Such synergies include use of our existing infrastructure to support the added membership. The amount recorded as goodwill represents intangible assets that do not qualify for separate recognition as identifiable intangible assets. Goodwill is not amortized, but is subject to an annual impairment test. The entire amount recorded as goodwill is deductible for income tax purposes. We also recorded intangible assets in the following major classes: contract rights and licenses amounting to $5.8 million, and provider networks amounting to $5.0 million. Contract rights and licenses are amortized over a period of five years, and provider networks are amortized over a period of 10 years. The weighted-average amortization period, in the aggregate, is 7.3 years.
South Carolina.In July 2013, we entered into an agreement with Community Health Solutions of America, Inc. (CHS) to acquire certain assets, including rights to convert certain of CHS' Medicaid members covered by South Carolina's full-risk Medicaid managed care program. The conversion conditions under the agreement were satisfied by January 1, 2014, and on that date such Medicaid members were converted to the managed care program and enrolled with our South Carolina health plan. The total purchase price for the converted Medicaid membership amounted to $57.2 million, of which $49.7 million was
paid in the first half of 2014, and $7.5 million was paid when the agreement was executed in 2013. The total amount paid included indemnification withhold funds transferred to restricted investments amounting to $5.7 million, which were released to CHS in January 2015.
Because the number of Medicaid members we would ultimately convert was unknown as of the acquisition date in 2013, we recorded a contingent consideration liability for such members to be settled when the final purchase price was known in the second quarter of 2014. In addition, we recorded a contingent consideration liability for dual-eligible members we expect to enroll in our Medicare-Medicaid Plan (MMP) implementation in South Carolina in 2015. The contingent consideration liability is remeasured to fair value at each quarter until the contingency is resolved with a combinationfair value adjustments, if any, recorded to operations. As of cash on hand and bank financing under a term loan agreement. We acquired this business primarily to facilitate space needsDecember 31, 2014, the fair value of the remaining contingent consideration liability for the projected future growthMMP implementation amounted to $0.5 million. The aggregate contingent consideration liability fair value adjustments for the South Carolina transaction resulted in a gain of $5.2 million in the year ended December 31, 2014.
New Mexico. In August 2013, our New Mexico health plan acquired Lovelace Community Health Plan's contract for the state of New Mexico's Medicaid program. In addition to Lovelace's Medicaid members, we also added membership previously covered under New Mexico's State Coverage Insurance (SCI) program with Lovelace. Effective January 1, 2014, these SCI members were either enrolled in New Mexico's Medicaid program, or eligible to enroll in New Mexico's Marketplace. Because the number of SCI members we would ultimately retain was unknown as of the Company.acquisition date in 2013, we recorded a contingent consideration liability for such members to be settled when the final purchase price was known in the second quarter of 2014. The aggregate contingent consideration liability fair value adjustments for the New Mexico transaction resulted in a gain of $1.5 million in the year ended December 31, 2014.
5. Fair Value Measurements
Our consolidated balance sheets include the following financial instruments: cash and cash equivalents, investments, receivables, other assets, trade accounts payable, medical claims and benefits payable, amounts due government agencies, long-term debt, and other liabilities. We consider the carrying amounts of cash and cash equivalents, receivables, other current assets and current liabilities (excluding contingent consideration) to approximate their fair valuevalues because of the relatively short period of time between the origination of these instruments and their expected realization or payment. For our financial instruments measured at fair value on a recurring basis, we prioritize the inputs used in measuring fair value according to a three-tier fair value hierarchy as follows:
Level 1 — Observable inputs such as quoted prices in active markets: Our Inputs
Level 1 financial instruments recorded at fair value consist of investments including government-sponsored enterprise securities (GSEs) and U.S. treasury notes that are classified as current investments in the accompanying consolidated balance sheets. These financial instruments are actively traded and therefore the fair value for these securities is based on quoted market prices on one or more securities exchanges.
Level 2 — Inputs other than quoted prices in active markets that are either directlyDirectly or indirectly observable: Our Indirectly Observable Inputs
Level 2 financial instruments recorded at fair value consist of investments including corporate debt securities, municipal securities, and certificates of deposit that are classified as current investments in the accompanying consolidated balance sheets, and an interest rate swap derivative recorded as a noncurrent liability. Oursheets. Such investments classified as Level 2 are traded frequently though not necessarily daily. Fair value for these investments is determined using a market approach based on quoted prices for similar securities in active markets or quoted prices for identical securities in inactive markets. Fair value for the interest rate swap derivative is based on forward LIBOR rates that are and will be observable at commonly
quoted intervals for the full term of the interest rate swap agreement. See Note 12, “Long-Term Debt,” for further information regarding the interest rate swap agreement.
Level 3 — Unobservable inputs in which little or noInputs
Derivative financial instruments. Derivative financial instruments include the 1.125% Call Option derivative asset and the 1.125% Notes Conversion Option derivative liability. These derivatives are not actively traded and are valued based on an option pricing model that uses observable and unobservable market data exists, therefore requiring an entityfor inputs. Significant market data inputs used to develop its own assumptions: Our Level 3 financial instruments recorded atdetermine fair value consistas of non-current auctionDecember 31, 2014 included our common stock price, time to maturity of the derivative instruments, the risk-free interest rate, and the implied volatility of our common stock. As described further in Note 13, "Derivative Financial Instruments," the 1.125% Call Option asset and the 1.125% Notes Conversion Option liability were designed such that changes in their fair values would offset, with minimal impact to the consolidated statements of income. Therefore, the sensitivity of changes in the unobservable inputs to the option pricing model for such instruments is mitigated.
Contingent consideration liability. Such liability relates to our South Carolina health plan acquisition described in Note 4, "Business Combinations," and is recorded in accounts payable and accrued liabilities. We applied a cash flow analysis to determine the fair value of this liability. Significant unobservable inputs primarily related to the purchase price estimate for the projected membership.
Auction rate securities that. Auction rate securities are designated as available-for-sale and are reported at fair value of $13.4 million (par value of $14.7 million) as of December 31, 2012.in other assets. To estimate the fair value of these securities we use valuation data from our primary pricing source, a third party who provides
a marketplace for illiquid assets with over 10,000 participants including global financial institutions, hedge funds, private equity funds, mutual funds, corporations and other institutional investors.participants. This valuation data is based on a range of prices that represent indicative bids from potential buyers. To validate the reasonableness of the data, we compare these valuations to data from two other third-party pricing sources, which also provide a range of prices representing indicative bids from potential buyers. We have concluded that these estimates, given the lack of market available pricing, provide a reasonable basis for determining the fair value of the auction rate securities as of December 31, 2012.
2014.Our financial instruments measured at fair value on a recurring basis at December 31, 2012,2014, were as follows:
| | | | Total | | Level 1 | | Level 2 | | Level 3 | Total | | Level 1 | | Level 2 | | Level 3 |
| | (In thousands) | (In thousands) |
| Corporate debt securities | $ | 191,008 |
| | $ | — |
| | $ | 191,008 |
| | $ | — |
| $ | 641,729 |
| | $ | — |
| | $ | 641,729 |
| | $ | — |
|
| Municipal securities | | 127,045 |
| | — |
| | 127,045 |
| | — |
|
| GSEs | 29,525 |
| | 29,525 |
| | — |
| | — |
| 122,269 |
| | 122,269 |
| | — |
| | — |
|
| Municipal securities | 75,848 |
| | — |
| | 75,848 |
| | — |
| |
| U.S. treasury notes | 35,740 |
| | 35,740 |
| | — |
| | — |
| 59,543 |
| | 59,543 |
| | — |
| | — |
|
| Certificates of deposit | | 68,876 |
| | — |
| | 68,876 |
| | — |
|
| Auction rate securities | 13,419 |
| | — |
| | — |
| | 13,419 |
| 4,847 |
| | — |
| | — |
| | 4,847 |
|
| Certificates of deposit | 10,724 |
| | — |
| | 10,724 |
| | — |
| |
| Total assets at fair value | $ | 356,264 |
| | $ | 65,265 |
| | $ | 277,580 |
| | $ | 13,419 |
| |
| 1.125% Call Option derivative asset | | 329,323 |
| | — |
| | — |
| | 329,323 |
|
| Total assets measured at fair value on a recurring basis | | $ | 1,353,632 |
| | $ | 181,812 |
| | $ | 837,650 |
| | $ | 334,170 |
|
| | | | | | | | | | | | | | | |
| Interest rate swap liability | $ | 1,307 |
| | $ | — |
| | $ | 1,307 |
| | $ | — |
| |
| 1.125% Notes Conversion Option derivative liability | | $ | 329,194 |
| | $ | — |
| | $ | — |
| | $ | 329,194 |
|
| Contingent consideration liability | | 500 |
| | — |
| | — |
| | 500 |
|
| Total liabilities measured at fair value on a recurring basis | | $ | 329,694 |
| | $ | — |
| | $ | — |
| | $ | 329,694 |
|
Our financial instruments measured at fair value on a recurring basis at December 31, 2011,2013, were as follows:
| | | | Total | | Level 1 | | Level 2 | | Level 3 | Total | | Level 1 | | Level 2 | | Level 3 |
| | (In thousands) | (In thousands) |
| Corporate debt securities | $ | 231,634 |
| | $ | — |
| | $ | 231,634 |
| | $ | — |
| $ | 449,772 |
| | $ | — |
| | $ | 449,772 |
| | $ | — |
|
| Municipal securities | | 113,330 |
| | — |
| | 113,330 |
| | — |
|
| GSEs | 33,949 |
| | 33,949 |
| | — |
| | — |
| 68,817 |
| | 68,817 |
| | — |
| | — |
|
| Municipal securities | 47,313 |
| | — |
| | 47,313 |
| | — |
| |
| U.S. treasury notes | 21,748 |
| | 21,748 |
| | — |
| | — |
| 37,376 |
| | 37,376 |
| | — |
| | — |
|
| Certificates of deposit | | 33,757 |
| | — |
| | 33,757 |
| | — |
|
| Auction rate securities | 16,134 |
| | — |
| | — |
| | 16,134 |
| 10,898 |
| | — |
| | — |
| | 10,898 |
|
| Certificates of deposit | 2,272 |
| | — |
| | 2,272 |
| | — |
| |
| Total assets at fair value | $ | 353,050 |
| | $ | 55,697 |
| | $ | 281,219 |
| | $ | 16,134 |
| |
| 1.125% Call Option derivative asset | | 186,351 |
| | — |
| | — |
| | 186,351 |
|
| Total assets measured at fair value on a recurring basis | | $ | 900,301 |
| | $ | 106,193 |
| | $ | 596,859 |
| | $ | 197,249 |
|
| | | | | | | | | | | | | | | |
| Interest rate swap liability | $ | — |
| | $ | — |
| | $ | — |
| | $ | — |
| |
| 1.125% Notes Conversion Option derivative liability | | $ | 186,239 |
| | $ | — |
| | $ | — |
| | $ | 186,239 |
|
| Contingent consideration liabilities | | 57,548 |
| | — |
| | — |
| | 57,548 |
|
| Total liabilities measured at fair value on a recurring basis | | $ | 243,787 |
| | $ | — |
| | $ | — |
| | $ | 243,787 |
|
The following table presents activity for the year ended December 31, 2012, relating to our assets (liabilities) measured at fair value on a recurring basis using significant unobservable inputs (Level 3):
|
| | | |
| | (Level 3) |
| | (In thousands) |
| Balance at December 31, 2011 | $ | 16,134 |
|
| Total gains (unrealized only): | |
| Included in other comprehensive income | 1,635 |
|
| Settlements | (4,350 | ) |
| Balance at December 31, 2012 | $ | 13,419 |
|
| The amount of total unrealized gains for the period included in other comprehensive income attributable to the change in accumulated other comprehensive losses relating to assets still held at December 31, 2012 | $ | 1,059 |
|
|
| | | | | | | | | | | |
| | Changes in Level 3 Instruments |
| | Auction Rate Securities | | Derivatives, Net | | Contingent Consideration Liabilities |
| | (In thousands) |
| Balance at December 31, 2013 | $ | 10,898 |
| | $ | 112 |
| | $ | (57,548 | ) |
| Total gains for the period recognized in: | | | | | |
| General and administrative expenses | — |
| | — |
| | 6,699 |
|
| Other expense, net | — |
| | 17 |
| | — |
|
| Other comprehensive income | 249 |
| | — |
| | — |
|
| Settlements | (6,300 | ) | | — |
| | 50,349 |
|
| Balance at December 31, 2014 | $ | 4,847 |
| | $ | 129 |
| | $ | (500 | ) |
Fair Value Measurements - Disclosure Only
The carrying amounts and estimated fair values of our long-term debt as well as the applicable fair value hierarchy tier, at December 31, 2012, are contained in the table below. Our convertible senior notes, which are classified as Level 2 financial instruments.instruments, are indicated in the following table. Fair value for these securities is determined using a market approach based on quoted prices for similar securities in active markets or quoted prices for identical securities in inactive markets. Borrowings under our credit facility and our term loan are classified as Level 3 financial instruments, because certain inputs used to determine the fair value of these agreements are unobservable. The carrying value of the credit facility at December 31, 2012 is equal to fair value because we repaid the $40 million outstanding under the Credit Facility in February 2013. The carrying value of the term loan at December 31, 2012, approximates its fair value because there has been no significant change to our credit risk relating to this instrument from the term loan's origination date in December 2011, to December 31, 2012.
|
| | | | | | | | | | | | | | | |
| | December 31, 2012 |
| | Carrying | Total | | | |
| | Value | Fair Value | Level 1 | Level 2 | Level 3 |
| | (In thousands) |
| Convertible senior notes | $ | 175,468 |
| $ | 208,460 |
| $ | — |
| $ | 208,460 |
| $ | — |
|
| Credit facility | 40,000 |
| 40,000 |
| — |
| — |
| 40,000 |
|
| Term loan | 47,471 |
| 47,471 |
| — |
| — |
| 47,471 |
|
| | $ | 262,939 |
| $ | 295,931 |
| $ | — |
| $ | 208,460 |
| $ | 87,471 |
|
| | |
| | December 31, 2011 |
| | Carrying | Total | | | |
| | Value | Fair Value | Level 1 | Level 2 | Level 3 |
| | (In thousands) |
| Convertible senior notes | $ | 169,526 |
| $ | 192,049 |
| $ | — |
| $ | 192,049 |
| $ | — |
|
| Credit facility | — |
| — |
| — |
| — |
| — |
|
| Term loan | 48,600 |
| 48,600 |
| — |
| — |
| 48,600 |
|
| | $ | 218,126 |
| $ | 240,649 |
| $ | — |
| $ | 192,049 |
| $ | 48,600 |
|
|
| | | | | | | | | | | | | | | | | | | |
| | December 31, 2014 |
| | Carrying | | Total | | | | | | |
| | Amount | | Fair Value | | Level 1 | | Level 2 | | Level 3 |
| | (In thousands) |
| 1.125% Notes | $ | 435,330 |
| | $ | 767,377 |
| | $ | — |
| | $ | 767,377 |
| | $ | — |
|
| 1.625% Notes | 268,767 |
| | 337,292 |
| | — |
| | 337,292 |
| | — |
|
| | $ | 704,097 |
| | $ | 1,104,669 |
| | $ | — |
| | $ | 1,104,669 |
| | $ | — |
|
| | |
| | December 31, 2013 |
| | Carrying | | Total | | | | | | |
| | Amount | | Fair Value | | Level 1 | | Level 2 | | Level 3 |
| | (In thousands) |
| 1.125% Notes | $ | 416,368 |
| | $ | 572,627 |
| | $ | — |
| | $ | 572,627 |
| | $ | — |
|
| 3.75% Notes | 181,872 |
| | 219,491 |
| | — |
| | 219,491 |
| | — |
|
| | $ | 598,240 |
| | $ | 792,118 |
| | $ | — |
| | $ | 792,118 |
| | $ | — |
|
6. Investments
The following tables summarize our investments as of the dates indicated:
|
| | | | | | | | | | | | | | | |
| | December 31, 2014 |
| | Amortized | | Gross Unrealized | | Estimated |
| | Cost | | Gains | | Losses | | Fair Value |
| | (In thousands) |
| Corporate debt securities | $ | 642,910 |
| | $ | 201 |
| | $ | 1,382 |
| | $ | 641,729 |
|
| Municipal securities | 127,185 |
| | 129 |
| | 269 |
| | 127,045 |
|
| GSEs | 122,317 |
| | 34 |
| | 82 |
| | 122,269 |
|
| U.S. treasury notes | 59,546 |
| | 30 |
| | 33 |
| | 59,543 |
|
| Certificates of deposit | 68,893 |
| | 1 |
| | 18 |
| | 68,876 |
|
| Subtotal - current investments | 1,020,851 |
| | 395 |
| | 1,784 |
| | 1,019,462 |
|
| Auction rate securities | 5,100 |
| | — |
| | 253 |
| | 4,847 |
|
| | $ | 1,025,951 |
| | $ | 395 |
| | $ | 2,037 |
| | $ | 1,024,309 |
|
| | | | December 31, 2012 | December 31, 2013 |
| | Amortized | | Gross Unrealized | | Estimated | Amortized | | Gross Unrealized | | Estimated |
| | Cost | | Gains | | Losses | | Fair Value | Cost | | Gains | | Losses | | Fair Value |
| | (In thousands) | (In thousands) |
| Corporate debt securities | $ | 190,545 |
| | $ | 528 |
| | $ | 65 |
| | $ | 191,008 |
| $ | 450,162 |
| | $ | 442 |
| | $ | 832 |
| | $ | 449,772 |
|
| Municipal securities | | 114,126 |
| | 119 |
| | 915 |
| | 113,330 |
|
| GSEs | 29,481 |
| | 45 |
| | 1 |
| | 29,525 |
| 68,898 |
| | 6 |
| | 87 |
| | 68,817 |
|
| Municipal securities | 75,909 |
| | 185 |
| | 246 |
| | 75,848 |
| |
| U.S. treasury notes | 35,700 |
| | 42 |
| | 2 |
| | 35,740 |
| 37,360 |
| | 44 |
| | 28 |
| | 37,376 |
|
| Certificates of deposit | | 33,756 |
| | 2 |
| | 1 |
| | 33,757 |
|
| Subtotal - current investments | | 704,302 |
| | 613 |
| | 1,863 |
| | 703,052 |
|
| Auction rate securities | 14,650 |
| | — |
| | 1,231 |
| | 13,419 |
| 11,400 |
| | — |
| | 502 |
| | 10,898 |
|
| Certificates of deposit | 10,715 |
| | 9 |
| | — |
| | 10,724 |
| |
| | $ | 357,000 |
| | $ | 809 |
| | $ | 1,545 |
| | $ | 356,264 |
| $ | 715,702 |
| | $ | 613 |
| | $ | 2,365 |
| | $ | 713,950 |
|
|
| | | | | | | | | | | | | | | |
| | December 31, 2011 |
| | Amortized | | Gross Unrealized | | Estimated |
| | Cost | | Gains | | Losses | | Fair Value |
| | (In thousands) |
| Corporate debt securities | $ | 231,407 |
| | $ | 442 |
| | $ | 215 |
| | $ | 231,634 |
|
| GSEs | 33,912 |
| | 46 |
| | 9 |
| | 33,949 |
|
| Municipal securities | 47,099 |
| | 232 |
| | 18 |
| | 47,313 |
|
| U.S. treasury notes | 21,627 |
| | 121 |
| | — |
| | 21,748 |
|
| Auction rate securities | 19,000 |
| | — |
| | 2,866 |
| | 16,134 |
|
| Certificates of deposit | 2,272 |
| | — |
| | — |
| | 2,272 |
|
| | $ | 355,317 |
| | $ | 841 |
| | $ | 3,108 |
| | $ | 353,050 |
|
The contractual maturities of our investments as of December 31, 20122014 are summarized below:
| | | | Amortized Cost | | Estimated Fair Value | Amortized Cost | | Estimated Fair Value |
| | (In thousands) | (In thousands) |
| Due in one year or less | $ | 195,986 |
| | $ | 196,201 |
| $ | 448,880 |
| | $ | 448,732 |
|
| Due one year through five years | 146,364 |
| | 146,644 |
| 571,971 |
| | 570,730 |
|
| Due after ten years | 14,650 |
| | 13,419 |
| 5,100 |
| | 4,847 |
|
| | $ | 357,000 |
| | $ | 356,264 |
| $ | 1,025,951 |
| | $ | 1,024,309 |
|
Gross realized gains and losses from sales of available-for-sale securities are calculated under the specific identification method and are included in investment income. Total proceeds from salesGross realized investment gains and maturities of available-for-sale securities were $298.0 million, $302.7 million, and $182.3 millionlosses for the year ended December 31, 2012, 2011,2014, 2013, and 2010, respectively. Net realized investment gains for the year ended December 31, 2012, 2011, and 2010 were $293,000, $367,000, and $110,000, respectively.insignificant.
We monitor our investments for other-than-temporary impairment. For investments other than our auction rate securities, as describeddiscussed below, we have determined that unrealized gains and losses at December 31, 2012,2014, and 2011,2013, are temporary in nature, because the change in market value for these securities has resulted from fluctuating interest rates, rather than a deterioration of the credit worthiness of the issuers. So long as we hold these securities to maturity, we are unlikely to experience gains or losses. In the event that we dispose of these securities before maturity, we expect that realized gains or losses, if any, will be immaterial.
The following table segregates those available-for-sale investments that have been in a continuous loss position for less than 12 months, and those that have been in a loss position for 12 months or more as of December 31, 2014.
|
| | | | | | | | | | | | | | | | | | | | | |
| | In a Continuous Loss Position for Less than 12 Months | | In a Continuous Loss Position for 12 Months or More |
| | Estimated Fair Value | | Unrealized Losses | | Total Number of Positions | | Estimated Fair Value | | Unrealized Losses | | Total Number of Positions |
| | (Dollars in thousands) |
| Corporate debt securities | $ | 379,034 |
| | $ | 1,151 |
| | 265 |
| | $ | 28,668 |
| | $ | 231 |
| | 10 |
|
| Municipal securities | 53,626 |
| | 168 |
| | 64 |
| | 11,075 |
| | 101 |
| | 13 |
|
| GSEs | 75,025 |
| | 69 |
| | 22 |
| | 2,986 |
| | 13 |
| | 3 |
|
| U.S. treasury notes | 19,199 |
| | 33 |
| | 13 |
| | — |
| | — |
| | — |
|
| Certificates of deposit | 12,591 |
| | 18 |
| | 52 |
| | — |
| | — |
| | — |
|
| Auction rate securities | — |
| | — |
| | — |
| | 4,847 |
| | 253 |
| | 6 |
|
| | $ | 539,475 |
| | $ | 1,439 |
| | 416 |
| | $ | 47,576 |
| | $ | 598 |
| | 32 |
|
The following table segregates those available-for-sale investments that have been in a continuous loss position for less than 12 months, and those that have been in a loss position for 12 months or more as of December 31, 2013.
|
| | | | | | | | | | | | | | | | | | | | | |
| | In a Continuous Loss Position for Less than 12 Months | | In a Continuous Loss Position for 12 Months or More |
| | Estimated Fair Value | | Unrealized Losses | | Total Number of Positions | | Estimated Fair Value | | Unrealized Losses | | Total Number of Positions |
| | (Dollars in thousands) |
| Corporate debt securities | $ | 210,057 |
| | $ | 802 |
| | 91 |
| | $ | 2,540 |
| | $ | 30 |
| | 3 |
|
| Municipal securities | 30,715 |
| | 398 |
| | 49 |
| | 31,091 |
| | 517 |
| | 39 |
|
| GSEs | 53,308 |
| | 87 |
| | 21 |
| | — |
| | — |
| | — |
|
| U.S. treasury notes | 12,037 |
| | 28 |
| | 11 |
| | — |
| | — |
| | — |
|
| Certificates of deposit | 414 |
| | 1 |
| | 2 |
| | — |
| | — |
| | — |
|
| Auction rate securities | — |
| | — |
| | — |
| | 10,898 |
| | 502 |
| | 15 |
|
| | $ | 306,531 |
| | $ | 1,316 |
| | 174 |
| | $ | 44,529 |
| | $ | 1,049 |
| | 57 |
|
Auction Rate Securities
Securities. Due to events in the credit markets, the auction rate securities held by us experienced failed auctions beginning in the first quarter of 2008, and such auctions have not resumed. Therefore, quoted prices in active markets have not been available since early 2008. Our investments in auction rate securities are collateralized by student loan portfolios guaranteed by the U.S.
government, and the range of maturities for such securities is from 1816 years to 3432 years. Considering the relative insignificance of these securities when compared with our liquid assets and other sources of liquidity, we have no current intention of selling these securities nor do we expect to be required to sell these securities before a recovery in their cost basis. For this reason, and because the decline in the fair value of the auction rate securities was not due to the credit quality of the issuers, we do not consider the auction rate securities to be other-than-temporarily impaired at December 31, 2012.2014. At the time of the first failed auctions during first quarter 2008, we held a total of $82.1$82.1 million in auction rate securities at par value; since that time, we have settled $67.4$77.0 million of these instruments at par value.
For the years ended December 31, 2012,2014, 2013 and 2011,2012, we recorded pretax unrealized gains of $1.6$0.2 million, $0.7 million and $1.2$1.6 million,, respectively, to accumulated other comprehensive income for the changes in their fair value. Any future fluctuationsfluctuation in fair value related to these instruments that we deem to be temporary, including any recoveries of previous write-downs, would be recorded to accumulated other comprehensive income. If we determine that any future valuation adjustment wasimpairment is other-than-temporary, we wouldwill record a charge to earnings as appropriate.
7. Receivables
The following tables segregate those available-for-sale investments that have been in a continuous loss position for less than 12 months, and those that have been in a loss position for 12 months or more as of December 31, 2012.
|
| | | | | | | | | | | | | | | | | | | | | |
| | In a Continuous Loss Position for Less than 12 Months | | In a Continuous Loss Position for 12 Months or More |
| | Estimated Fair Value | | Unrealized Losses | | Total Number of Securities | | Estimated Fair Value | | Unrealized Losses | | Total Number of Securities |
| | (In thousands, except number of securities) |
| Corporate debt securities | $ | 44,457 |
| | $ | 65 |
| | 23 |
| | $ | — |
| | $ | — |
| | — |
|
| GSEs | 5,004 |
| | 1 |
| | 1 |
| | — |
| | — |
| | — |
|
| Municipal securities | 35,223 |
| | 246 |
| | 43 |
| | — |
| | — |
| | — |
|
| U.S. treasury notes | 4,511 |
| | 2 |
| | 5 |
| | — |
| | — |
| | — |
|
| Auction rate securities | — |
| | — |
| | — |
| | 13,419 |
| | 1,231 |
| | 21 |
|
| Total temporarily impaired securities | $ | 89,195 |
| | $ | 314 |
| | 72 |
| | $ | 13,419 |
| | $ | 1,231 |
| | 21 |
|
The following table segregates those available-for-sale investments that have been in a continuous loss position for less than 12 months, and those that have been in a loss position for 12 months or more as of December 31, 2011.
|
| | | | | | | | | | | | | | | | | | | | | |
| | In a Continuous Loss Position for Less than 12 Months | | In a Continuous Loss Position for 12 Months or More |
| | Estimated Fair Value | | Unrealized Losses | | Total Number of Securities | | Estimated Fair Value | | Unrealized Losses | | Total Number of Securities |
| | (In thousands, except number of securities) |
| Corporate debt securities | $ | 72,766 |
| | $ | 215 |
| | 47 |
| | $ | — |
| | $ | — |
| | — |
|
| GSEs | 11,493 |
| | 9 |
| | 9 |
| | — |
| | — |
| | — |
|
| Municipal securities | 12,033 |
| | 18 |
| | 8 |
| | — |
| | — |
| | — |
|
| Auction rate securities | — |
| | — |
| | — |
| | 16,134 |
| | 2,866 |
| | 27 |
|
| Total temporarily impaired securities | $ | 96,292 |
| | $ | 242 |
| | 64 |
| | $ | 16,134 |
| | $ | 2,866 |
| | 27 |
|
7. Receivables
Health Plans segment receivables consist primarily of amounts due from the various states in which we operate.operate, which may be subject to potential retroactive adjustments. Because all of our receivable amounts are readily determinable and substantially all of our creditors are state governments, our allowance for doubtful accounts is immaterial. Accounts receivable wereincreased as follows:
Table of ContentsDecember 31, 2014, primarily due to significant enrollment growth in 2014.
| | | | December 31, | December 31, |
| | 2012 | | 2011 | 2014 | | 2013 |
| | (In thousands) | (In thousands) |
| Health Plans segment: | | | | |
| California | $ | 28,553 |
| | $ | 22,175 |
| $ | 310,938 |
| | $ | 148,654 |
|
| Florida | | 2,141 |
| | 2,901 |
|
| Illinois | | 31,594 |
| | 5,773 |
|
| Michigan | 12,873 |
| | 8,864 |
| 19,880 |
| | 15,253 |
|
| Missouri | 1,053 |
| | 27,092 |
| |
| New Mexico | 9,059 |
| | 9,350 |
| 49,609 |
| | 17,056 |
|
| Ohio | 40,980 |
| | 27,458 |
| 45,187 |
| | 43,969 |
|
| South Carolina | | 4,134 |
| | — |
|
| Texas | 7,459 |
| | 1,608 |
| 29,348 |
| | 9,736 |
|
| Utah | 3,359 |
| | 2,825 |
| 6,389 |
| | 10,953 |
|
| Washington | 17,587 |
| | 15,006 |
| 42,848 |
| | 13,455 |
|
| Wisconsin | 4,098 |
| | 4,909 |
| 8,102 |
| | 8,087 |
|
| Others | 2,077 |
| | 2,489 |
| |
| Direct delivery and other | | 11,295 |
| | 2,463 |
|
| Total Health Plans segment | 127,098 |
| | 121,776 |
| 561,465 |
| | 278,300 |
|
| Molina Medicaid Solutions segment | 22,584 |
| | 46,122 |
| 34,991 |
| | 20,635 |
|
| | $ | 149,682 |
| | $ | 167,898 |
| $ | 596,456 |
| | $ | 298,935 |
|
8. Property, Equipment, and Capitalized Software
A summary of property, equipment, and capitalized software is as follows:
| | | | December 31, | December 31, |
| | 2012 | | 2011 | 2014 | | 2013 |
| | (In thousands) | (In thousands) |
| Land | $ | 15,764 |
| | $ | 14,094 |
| $ | 15,514 |
| | $ | 15,764 |
|
| Building and improvements | 124,163 |
| | 109,789 |
| 195,405 |
| | 165,670 |
|
| Furniture and equipment | 97,865 |
| | 79,112 |
| 140,691 |
| | 131,478 |
|
| Capitalized software | 154,708 |
| | 116,389 |
| 266,782 |
| | 187,105 |
|
| | 392,500 |
| | 319,384 |
| 618,392 |
| | 500,017 |
|
| Less: accumulated depreciation and amortization on building and improvements, furniture and equipment | (84,156 | ) | | (65,518 | ) | (129,161 | ) | | (103,918 | ) |
| Less: accumulated amortization for capitalized software | (86,901 | ) | | (62,932 | ) | (148,453 | ) | | (104,016 | ) |
| | (171,057 | ) | | (128,450 | ) | (277,614 | ) | | (207,934 | ) |
| Property, equipment, and capitalized software, net | $ | 221,443 |
| | $ | 190,934 |
| $ | 340,778 |
| | $ | 292,083 |
|
Depreciation recognized for building and improvements, and furniture and equipment was $20.5$34.6 million,, $17.5 $26.6 million,, and $13.9$20.5 million for the years ended December 31, 2012, 20112014, 2013 and 2010,2012, respectively. Amortization of capitalized software was $36.2$58.7 million,, $30.2 $46.4 million,, and $20.1$36.2 million for the years ended December 31, 2012, 20112014, 2013 and 2010,2012, respectively.
Molina Center
As described in NoteMolina Center. 4, “Business Combinations,” weWe acquired the Molina Center in December 2011. At December 31, 2012,Subsequently, in June 2013 we entered into a sale-leaseback transaction for the carrying amountsale and contemporaneous leaseback of the Molina Center buildingCenter. Due to our continuing involvement with the leased property, the sale did not qualify for sale-leaseback accounting treatment and leasehold improvements was $44.4 million andwe remain the accumulated depreciation was "accounting owner" of the property. See Note 12, "Long-Term Debt."$1.8 million. Future minimum rentals on noncancelable leases are as follows:
Future minimum rental income on noncancelable leases from third party tenants of the Molina Center is sublease rental income, and is reported in other revenue in our consolidated statements of income. The future minimum rental income is as follows:
| | | | (In thousands) | (In thousands) |
| 2013 | $ | 9,784 |
| |
| 2014 | 9,954 |
| |
| 2015 | 9,878 |
| $ | 4,313 |
|
| 2016 | 8,054 |
| 4,035 |
|
| 2017 | 7,419 |
| 4,256 |
|
| 2018 | | 4,116 |
|
| 2019 | | 1,557 |
|
| Thereafter | 10,295 |
| 2,164 |
|
| Total minimum future rentals | $ | 55,384 |
| $ | 20,441 |
|
9. Goodwill and Intangible Assets
Other intangible assets are amortized over their useful lives ranging from one to 15 years. The weighted average amortization period for contract rights and licenses is approximately 11 years, for customer relationships is approximately five years, for backlog is approximately two years, and for provider networks is approximately 10 years. Based on the balances of our identifiable intangible assets as of December 31, 2012, we estimate that our intangible asset amortization will be $17.9 million in 2013, $17.0 million in 2014, $12.1 million in 2015, $9.4 million in 2016, and $9.3 million in 2017. The following table provides the details of identified intangible assets, by major class, for the periods indicated. As described in Note 2, “Significant Accounting Policies,” no impairment charges relating to long-lived assets, includingindicated:
|
| | | | | | | | | | | |
| | Cost | | Accumulated Amortization | | Net Balance |
| | (In thousands) |
| Intangible assets: | | | | | |
| Contract rights and licenses | $ | 182,228 |
| | $ | 105,613 |
| | $ | 76,615 |
|
| Customer relationships | 24,550 |
| | 22,154 |
| | 2,396 |
|
| Contract backlog | 23,600 |
| | 22,540 |
| | 1,060 |
|
| Provider networks | 18,401 |
| | 9,199 |
| | 9,202 |
|
| Balance at December 31, 2014 | $ | 248,779 |
| | $ | 159,506 |
| | $ | 89,273 |
|
| Intangible assets: | | | | | |
| Contract rights and licenses | $ | 176,428 |
| | $ | 92,789 |
| | $ | 83,639 |
|
| Customer relationships | 24,550 |
| | 18,801 |
| | 5,749 |
|
| Contract backlog | 23,600 |
| | 19,624 |
| | 3,976 |
|
| Provider networks | 13,370 |
| | 7,863 |
| | 5,507 |
|
| Balance at December 31, 2013 | $ | 237,948 |
| | $ | 139,077 |
| | $ | 98,871 |
|
Based on the balances of our identifiable intangible assets were recorded in the year ended as of December 31, 2012.2014, we estimate that our intangible asset amortization will be $16.3 million in 2015, $14.4 million in 2016, $14.1 million in 2017, $13.8 million in 2018, and $9.2 million in 2019. For a descriptionpresentation of our goodwill and intangible assets by reportable segment, refer to Note 20, “Segment Reporting.”21, "Segment Information."
|
| | | | | | | | | | | |
| | Cost | | Accumulated Amortization | | Net Balance |
| | (In thousands) |
| Intangible assets: | | | | | |
| Contract rights and licenses | $ | 135,932 |
| | $ | 81,376 |
| | $ | 54,556 |
|
| Customer relationships | 24,550 |
| | 12,513 |
| | 12,037 |
|
| Contract backlog | 23,600 |
| | 17,870 |
| | 5,730 |
|
| Provider networks | 11,990 |
| | 6,602 |
| | 5,388 |
|
| Balance at December 31, 2012 | $ | 196,072 |
| | $ | 118,361 |
| | $ | 77,711 |
|
| Intangible assets: | | | | | |
| Contract rights and licenses | $ | 140,242 |
| | $ | 69,515 |
| | $ | 70,727 |
|
| Customer relationships | 24,550 |
| | 8,546 |
| | 16,004 |
|
| Contract backlog | 23,600 |
| | 15,139 |
| | 8,461 |
|
| Provider networks | 11,990 |
| | 5,386 |
| | 6,604 |
|
| Balance at December 31, 2011 | $ | 200,382 |
| | $ | 98,586 |
| | $ | 101,796 |
|
The following table presents the balances of goodwill and indefinite-lived intangible assets as of December 31, 20122014 and 2011:
2013:
|
| | | | | | | | | | | |
| | December 31, 2011 | | Reductions | | December 31, 2012 |
| | (In thousands) |
| Goodwill and indefinite-lived intangible assets, gross | $ | 212,484 |
| | $ | (2,866 | ) | | $ | 209,618 |
|
| Accumulated impairment losses | (58,530 | ) | | — |
| | (58,530 | ) |
| Goodwill and indefinite-lived intangible assets, net | $ | 153,954 |
| | $ | (2,866 | ) | | $ | 151,088 |
|
|
| | | | | | | | | | | |
| | December 31, 2013 | | Acquisitions | | December 31, 2014 |
| | (In thousands) |
| Goodwill, gross | $ | 289,268 |
| | $ | 41,226 |
| | $ | 330,494 |
|
| Accumulated impairment losses | (58,530 | ) | | — |
| | (58,530 | ) |
| Goodwill, net | $ | 230,738 |
| | $ | 41,226 |
| | $ | 271,964 |
|
The change in the carrying amount of goodwill in 20122014 was due to the sale of the Molina Healthcare Insurance Company.
acquisitions described in Note 4, "Business Combinations."
10. Restricted Investments
Pursuant to the regulations governing our Health PlanPlans segment subsidiaries, we maintain statutory deposits and deposits required by state Medicaid authorities in certificates of deposit and U.S. treasury securities. Additionally, weWe also maintain restricted investments as protection against the insolvency of certain capitated providers. Additionally, in connection with a Molina Medicaid Solutions segment state contract, we maintain restricted investments as collateral for a letter of credit. The following table presents the balances of restricted investments:
| | | | December 31, | December 31, |
| | 2012 | | 2011 | 2014 | | 2013 |
| | (In thousands) | (In thousands) |
| California | $ | 373 |
| | $ | 372 |
| $ | 373 |
| | $ | 373 |
|
| Florida | 5,738 |
| | 5,198 |
| 28,649 |
| | 9,242 |
|
| Insurance Company | — |
| | 4,711 |
| |
| Illinois | | 311 |
| | 310 |
|
| Michigan | 1,014 |
| | 1,000 |
| 1,014 |
| | 1,014 |
|
| Missouri | 500 |
| | 504 |
| |
| New Mexico | 15,915 |
| | 15,905 |
| 35,135 |
| | 24,622 |
|
| Ohio | 9,082 |
| | 9,078 |
| 12,719 |
| | 9,080 |
|
| South Carolina | | 6,040 |
| | 310 |
|
| Texas | 3,503 |
| | 3,518 |
| 3,500 |
| | 3,500 |
|
| Utah | 3,126 |
| | 2,895 |
| 3,601 |
| | 3,301 |
|
| Washington | 151 |
| | 151 |
| 151 |
| | 151 |
|
| Other | 4,699 |
| | 2,832 |
| 5,985 |
| | 886 |
|
| Total Health Plans segment | | 97,478 |
| | 52,789 |
|
| Molina Medicaid Solutions segment | | 5,001 |
| | 10,304 |
|
| | $ | 44,101 |
| | $ | 46,164 |
| $ | 102,479 |
| | $ | 63,093 |
|
The contractual maturities of our held-to-maturity restricted investments as of December 31, 20122014 are summarized below.
| | | | Amortized Cost | | Estimated Fair Value | Amortized Cost | | Estimated Fair Value |
| | (In thousands) | (In thousands) |
| Due in one year or less | $ | 39,733 |
| | $ | 39,738 |
| $ | 101,017 |
| | $ | 101,022 |
|
| Due one year through five years | 4,368 |
| | 4,368 |
| 1,462 |
| | 1,462 |
|
| | $ | 44,101 |
| | $ | 44,106 |
| $ | 102,479 |
| | $ | 102,484 |
|
11. Medical Claims and Benefits Payable
The following table provides the details of our medical claims and benefits payable (including amounts payable for the provision of long-term services and supports, or LTSS) as of the dates indicated.
|
| | | | | | | | | | | |
| | December 31, |
| | 2014 | | 2013 | | 2012 |
| | (In thousands) |
| Fee-for-service claims incurred but not paid (IBNP) | $ | 870,429 |
| | $ | 424,173 |
| | $ | 377,614 |
|
| Pharmacy payable | 71,412 |
| | 45,037 |
| | 38,992 |
|
| Capitation payable | 28,150 |
| | 20,267 |
| | 49,066 |
|
| Other | 230,531 |
| | 180,310 |
| | 28,858 |
|
| | $ | 1,200,522 |
| | $ | 669,787 |
| | $ | 494,530 |
|
"Other" medical claims and benefits payable include amounts payable to certain providers for which we act as an intermediary on behalf of various state agencies without assuming financial risk. Such receipts and payments do not impact our consolidated statements of income. Such non-risk provider payables amounted to $119.3 million and $151.3 million as of December 31, 2014 and 2013, respectively.
The following table presents the components of the change in our medical claims and benefits payable from continuing and discontinued operations combined for the years ended December 31, 2012, 2011, and 2010.periods indicated. The amounts displayedpresented for “Components"Components of medical care costs related to: Prior period”periods" represent the amount by which our original estimate of medical claims and benefits payable at the beginning of the period were (more) or lessmore than the actual amount of the liability based on information (principally the payment of claims) developed since that liability was first reported.
| | | | Year Ended December 31, | Year Ended December 31, |
| | 2012 | | 2011 | | 2010 | 2014 | | 2013 | | 2012 |
| | (Dollars in thousands, except per-member amounts) | (Dollars in thousands) |
| Balances at beginning of period | $ | 402,476 |
| | $ | 354,356 |
| | $ | 315,316 |
| $ | 669,787 |
| | $ | 494,530 |
| | $ | 402,476 |
|
| Balance of acquired subsidiary | — |
| | — |
| | 3,228 |
| |
| Components of medical care costs related to: | | | | | | | | | | |
| Current period | 5,136,055 |
| | 3,911,803 |
| | 3,420,235 |
| 8,122,885 |
| | 5,434,443 |
| | 5,136,055 |
|
| Prior period | (39,295 | ) | | (51,809 | ) | | (49,378 | ) | |
| Prior periods | | (45,979 | ) | | (52,779 | ) | | (39,295 | ) |
| Total medical care costs | 5,096,760 |
| | 3,859,994 |
| | 3,370,857 |
| 8,076,906 |
| | 5,381,664 |
| | 5,096,760 |
|
| | | | | | | |
| Change in non-risk provider payables | | (31,973 | ) | | 111,267 |
| | (7,004 | ) |
| | | | | | | |
| Payments for medical care costs related to: | | | | | | | | | | |
| Current period | 4,649,363 |
| | 3,516,994 |
| | 3,085,388 |
| 7,064,427 |
| | 4,932,195 |
| | 4,689,395 |
|
| Prior period | 355,343 |
| | 294,880 |
| | 249,657 |
| |
| Prior periods | | 449,771 |
| | 385,479 |
| | 308,307 |
|
| Total paid | 5,004,706 |
| | 3,811,874 |
| | 3,335,045 |
| 7,514,198 |
| | 5,317,674 |
| | 4,997,702 |
|
| Balances at end of period | $ | 494,530 |
| | $ | 402,476 |
| | $ | 354,356 |
| $ | 1,200,522 |
| | $ | 669,787 |
| | $ | 494,530 |
|
| Benefit from prior period as a percentage of: | | | | | | |
| Balance at beginning of period | 9.8 | % | | 14.6 | % | | 15.7 | % | |
| Premium revenue | 0.7 | % | | 1.1 | % | | 1.2 | % | |
| Total medical care costs | 0.8 | % | | 1.3 | % | | 1.5 | % | |
That portion of our total medical claims and benefits payable liability that is most subject to variability in the estimate is fee-for-service claims incurred but not paid (IBNP). Our IBNP, as included in medical claims and benefits payable, represents our best estimate of the total amount of claims we will ultimately pay with respect to claims that we have incurred as of the balance sheet date. We estimate our IBNP monthly using actuarial methods based on a number of factors.
Assuming that our initial estimate of IBNP is accurate, we believe that amounts ultimately paid out would generally be between 8% and 10% less than the IBNP liability recorded at the end of the period as a result of the inclusion in that liability of the allowanceprovision for adverse claims developmentdeviation and the accrued cost of settling those claims. Because the amount of our initial liability is merely an estimate (and therefore nevernot perfectly accurate), we will always experience variability in that estimate as new information becomes available with the passage of time. Therefore, there can be no assurance that amounts ultimately paid out will not be higher or lower than thisfall within the range of 8% to 10% range. For example, for the years ended December 31, 2011 and 2010, the amounts ultimately paid out were lesslower than the amount of the reserves we had established as of December 31, 2010 and 2009, by 14.6% and 15.7%, respectively.liability that was initially recorded. Furthermore, because theour initial estimate of IBNP is derived from many factors, some of which are qualitative in nature rather than quantitative, we are seldom able to assign specific values to the reasons for a change in estimate - estimate—we only know when the circumstances for any one or more of those factors are out of the ordinary.
The use of a consistent methodology in estimating our liability for claims and medical benefits payable minimizes the degree to which the under– or overestimation of that liability at the close of one period may affect consolidated results of operations in subsequent periods. In particular, the use of a consistent methodology should result in the replenishment of reserves during any given period in a manner that generally offsets the benefit of favorable prior period development in that period. Facts and circumstances unique to the estimation process at any single date, however, may still lead to a material impact on consolidated results of operations in subsequent periods. Any absence of adverse claims development (as well as the expensing through general and administrative expense of the costs to settle claims held at the start of the period) will lead to the recognition of a benefit from prior period claims development in the period subsequent to the date of the original estimate.
As indicated above, the amounts ultimately paid out on our medical claims and benefits payable liabilities in fiscal years 2012, 2011,2014, 2013, and 20102012 were less than what we had expected when we had established those liabilities. The differences between our reserves.original estimates and the amounts ultimately paid out (or now expected to be ultimately paid out) for the most part related to IBNP. While many related factors working in conjunction with one another determine the accuracy of our estimates, we are seldom able to quantify the impact that any single factor has on a change in estimate. In addition, given the variability inherent in the reserving process, we will only be able to identify specific factors if they represent a significant departure from expectations. As a result, we do not expect to be able to fully quantify the impact of individual factors on changes in estimate.estimates.
2014
We believe that the most significant factors that will determine the accuracy of our IBNP estimates at December 31, 2014 are:
The addition since January 1, 2014, of 385,000 members under Medicaid expansion in six of our health plans. Because these members are transitioning into managed care, and have different demographics than those of our legacy membership, we have little insight into their utilization of medical services. Additionally, as of December 31, 2014, we have relatively little medical claims payment history related to Medicaid expansion membership in Illinois, Michigan and Ohio because such members were enrolled in these states later in the year. Accordingly, our estimates of the claims liability for this population are subject to a higher degree of uncertainty.
The addition of approximately 6,000 to 8,000 members per month on a retroactive basis during the last several months of 2014 at our New Mexico health plan. Because we have no claims payment history for these members, our estimates of the claims liability for this population are subject to a higher degree of uncertainty. However, for these members, the state will reimburse the health plan for claims with dates of services during the retroactive period on a cost-plus basis (claims paid plus an administration fee).
The addition of new membership to our MMP and aged, blind or disabled (ABD) programs at several of our health plans whose benefits include a substantial amount of managed LTSS benefits. Because these are newer members with substantially different benefits than our legacy members, our estimates of the claims liability for this population are subject to a higher degree of uncertainty.
We recognized a benefit fromfavorable prior period claims development in the amount of $39.3$46.0 millionfor the year endedDecember 31, 2012.2014. This amount represents our estimate as of December 31, 2012,2014, of the extent to which our initial estimate of medical claims and benefits payable at December 31, 20112013 was more than the amount that will ultimately be paid out in satisfaction of that liability. We believe that the overestimation of our claims liability atDecember 31, 2011was due primarily to the following factors:
At our WashingtonOhio health plan, we underestimatedentered new regions in the amountstate, and a new product, ABD Kids, in July 2013. Since we did not have enough historical claims data to use the pattern of recoveriespaid and incurred claims, we would collectinitially estimated the reserves for certain high-cost newborn claims, resultingthese new members by applying an estimated medical care ratio (MCR). This resulted in an overestimationoverstatement of reserves at year end.
our reserve liability as of December 31, 2013.
At our TexasMichigan health plan, we overestimated the costimpact of new memberscertain unpaid potentially high-dollar claims. In addition, we overestimated the impact of the flu season on the outpatient claims for November and December 2013, which caused an overestimation in STAR+PLUS (the nameour outpatient reserve liability as of our ABD program in Texas), in the Dallas region.
In early 2011, the state of Michigan was delayed in the enrollment of newborns in managed care plans; the delay was resolved by mid-2011. This caused a large number of claims with older dates of service to be paid during late 2011, resulting in an artificial increase in the lag time for claims payment at our Michigan health plan. We adjusted reserves downward for this issue at December 31, 2011, but the adjustment did not capture all of the claims overestimation.
2013.
The overestimation of our liability for medical claims and benefits payable was partially offset by an underestimation of that liability at our Missouri health plan, as a result of the costs associated with an unusually large number of premature infants during the fourth quarter of 2011.
2013We recognized a benefit fromfavorable prior period claims development in the amount of$51.8 $52.8 millionfor the year endedDecember 31, 2011.2013. This amount represents our estimate as of December 31, 2011,2013, of the extent to which our initial estimate of medical claims and benefits payable at December 31, 20102012 was more than the amount that willwas ultimately be paid out in satisfaction of that liability. We believe that the overestimation of our claims liability atDecember 31, 2010was due primarily to the following factors:
At our Washington health plan certain high-cost newborns, as well as other high-cost disabled members, were covered by the health plan effective July 1, 2012. At the end of 2012, we had limited claims history with which to estimate the claims liability of these members, and overstated the liability for such members.
At our New Mexico health plan, we overestimated the impact of certain high-dollar outstanding claim payments as of December 31, 2012.
At our Ohio health plan, we overestimated the impact of a buildup inseveral potential high-dollar claims inventory.
relating to our ABD members.At our California health plan, we overestimated the impact of the settlement of disputed provider claims.
2012At our New Mexico health plan, we underestimated the impact of a reduction in the outpatient facility fee schedule.
We recognized a benefit from priorPrior period claims development in the amount of$49.4 millionfor the year ended December 31, 2010. This amount represents our estimate as ofDecember 31, 2010, of the extent to which our initial estimate of medical claims and benefits payable at December 31, 2009was more than the amount that will ultimately be paid out in satisfaction of that liability. We believe that the overestimation of our claims liability atDecember 31, 2009was due primarily to the following factors:
At our New Mexico health plan, we underestimated the degree to which cuts to the Medicaid fees schedule would reduce our liability as of December 31, 2009.
At our California health plan, we underestimated the extent to which various network restructuring, provider contracting, and medical management initiatives had reduced our medical care costs during the second half of 2009, thereby resulting in a lower liability at December 31, 2009.
In estimating our claims liability at2011 through December 31, 2012 we adjusted our base calculation to take account of the numerous factors that we believe will likely change our final claims liability amount. We believe that the most significant among those factors are:
Our Texas health plan membership nearly doubled effective March 1, 2012. In addition, effective March 1, 2012, we assumed inpatient medical liability for ABD members for which we were not previously responsible. Reserves for new coverage and new regions are now based on the newly developing claims lag patterns. While the lag patterns are now beginning to stabilize for the new membership and coverage, the true reserve liability continues to be more uncertain than usual.
Data publishedwas favorable by the Centers for Disease Control, or CDC, indicated a significant increase in the percentage of office visits for influenza-like illnesses, or ILI, during December 2012. This indicated that the annual flu season was starting earlier than it had in most recent years. This was most noticeable in the southeast region of the country, but impacted other areas as well. Our leading indicators, including inpatient authorizations and overall pharmacy utilization, did not show as great an increase as we had expected based on the severity of the CDC's flu-related indices. However, we did see a significant increase in the use of prescription flu medication, especially in our Texas health plan. Therefore, we increased our reserves to account for expected additional utilization due to the early onset of the flu season.
Our California health plan has enrolled approximately 20,000 new ABD members since September 30, 2011, as a result of the mandatory assignment of ABD members to managed care plans effective July 1, 2011. These new members converted from a fee-for-service environment. Due to the relatively recent transition of these members to managed care, their utilization of medical services is less predictable than it is for many of our other members.
Prior to July 2012, it was the state of Washington's practice to disenroll certain sick newborns from the Healthy Options Medicaid managed care program and cover them under the Supplemental Security Income program, or SSI, instead. When this occurred, the health plan would reimburse the premiums received for that member back to the state and the state in turn reimbursed the health plan for the cost of care, usually retroactively to the date of birth. Effective July 1, 2012, the health plans now retain these members and cover them under a new ABD program entitled Healthy Options Blind and Disabled, or HOBD. The premium we receive from the state for the HOBD members is very high to cover the substantial cost of care. By December, we had enrolled approximately 26,000 members under HOBD. Because the program is relatively new, there is still some uncertainty as to the level of claims to be expected from these high-cost members.
The use of a consistent methodology in estimating our liability for claims and medical benefits payable minimizes the degree to which the under- or overestimation of that liability at the close of one period may affect consolidated results of operations in subsequent periods. Facts and circumstances unique to the estimation process at any single date, however, may still lead to a$39.3 million.
material impact on consolidated results of operations in subsequent periods. Any absence of adverse claims development (as well as the expensing through general and administrative expense of the costs to settle claims held at the start of the period) will lead to the recognition of a benefit from prior period claims development in the period subsequent to the date of the original estimate. In 2012, 2011and2010, the absence of adverse development of the liability for claims and medical benefits payable at the close of the previous period resulted in the recognition of substantial favorable prior period development. In these years, however, the recognition of a benefit from prior period claims development did not have a material impact on our consolidated results of operations because the amount of benefit recognized in each year was roughly consistent with that recognized in the previous year.
12. Long-Term Debt
As of December 31, 2014, maturities of long-term debt for the years ending December 31 are as follows (in thousands):
|
| | | | | | | | | | | | | | | | | | | | | | | | | | | |
| | Total | | 2015 | | 2016 | | 2017 | | 2018 | | 2019 | | Thereafter |
| 1.125% Notes | $ | 550,000 |
| | $ | — |
| | $ | — |
| | $ | — |
| | $ | — |
| | $ | — |
| | $ | 550,000 |
|
| 1.625% Notes (1) | 301,551 |
| | — |
| | — |
| | — |
| | — |
| | — |
| | 301,551 |
|
| | $ | 851,551 |
| | $ | — |
| | $ | — |
| | $ | — |
| | $ | — |
| | $ | — |
| | $ | 851,551 |
|
| |
| (1) | The 1.625% Notes have a contractual maturity date in 2044; however, on specified dates beginning in 2018 as described below, holders of the 1.625% Notes may require us to repurchase some or all of the 1.625% Notes, or we may redeem any or all of the 1.625% Notes. |
1.125% Cash Convertible Senior Notes due 2020
2020.OnIn February 15, 2013, we issued$550 $550.0 millionaggregate principal amount of1.125%Cash Convertible Senior cash convertible senior notes (the 1.125% Notes) due January 15, 2020, unless earlier repurchased or converted. Interest on the 1.125% Notes due 2020, or the Notes. The Notes bear interest at a rate of1.125% per year,is payable semiannually in arrears on January 15 and July 15 at a rate of each year, beginning on July 15, 2013. The Notes will mature on January 15, 2020. 1.125% per annum.
The 1.125% Notes are senior unsecured obligations and rank senior in right of payment to any of our indebtedness that is expressly subordinated in right of payment to the 1.125% Notes; equal in right of payment to any of our unsecured indebtedness that is not subordinated; effectively junior in right of payment to any of our secured indebtedness to the extent of the value of the assets securing such indebtedness; and structurally junior to all indebtedness and other liabilities of our subsidiaries.
The 1.125% Notes are convertible only into cash, and not into shares of our common stock or any other securities undersecurities. The initial conversion rate for the 1.125% Notes is 24.5277 shares of our common stock per $1,000 principal amount of the 1.125% Notes. This represents an initial conversion price of approximately $40.77 per share of our common stock. The conversion rate is subject to adjustment in some events but will not be adjusted for any circumstances.accrued and unpaid interest. Holders may convert their 1.125% Notes solely into cash at their option at any time prior to the close of business on the business day immediately preceding July 15, 2019 only under the following circumstances: (1)
during any calendar quarter commencing after the calendar quarter ending on June 30, 2013 (and only during such calendar quarter), if the last reported sale price of the common stock for at least 20 trading days (whether or not consecutive) during a period of30consecutive trading days ending on the last trading day of the immediately preceding calendar quarter is greater than or equal to130%of the conversion price on each applicable trading day; (2)
during the five business day period immediately after any five consecutive trading day period (the measurement period) in which the trading price per$1,000 $1,000 principal amount of 1.125% Notes for each trading day of the measurement period was less than98%of the product of the last reported sale price of our common stock and the conversion rate on each such trading day; or (3)
upon the occurrence of specified corporate events. Onevents; or
at any time on or after July 15, 2019 until the close of business on the second scheduled trading day immediately preceding the maturity date, holders may convert their Notes solely into cash at any time, regardless of the foregoing circumstances.date. Upon conversion, in lieu of receiving shares of our common stock, a holder will receive an amount in cash, per$1,000 $1,000 principal amount of 1.125% Notes, equal to the settlement amount, determined in the manner set forth in the Indenture. indenture. We may not redeem the 1.125% Notes prior to the maturity date.
As of December 31, 2014, the 1.125% Notes were not convertible.
The 1.125% Notes contain an embedded cash conversion option (the 1.125% Notes Conversion Option), which was separated from the 1.125% Notes and accounted for separately as a derivative liability, with changes in fair value reported in our consolidated statements of income until the 1.125% Notes Conversion Option transaction settles or expires. The initial conversionfair value liability of the 1.125% Notes Conversion Option simultaneously reduced the carrying value of the 1.125% Notes (effectively an original issuance discount). This discount is amortized to the 1.125% Notes' principal amount through the recognition of non-cash interest expense over the expected life of the debt. This has resulted in our recognition of interest expense on the 1.125% Notes at an effective rate willapproximating what we would have incurred had nonconvertible debt with otherwise similar terms been issued, or approximately 6%. As of December 31, 2014, we expect the 1.125% Notes to be outstanding until their maturity date, for a remaining amortization period of 5.0 years. The 1.125% Notes' if-converted value exceeded their principal amount by approximately $93 million as of December 31, 2014, and did not exceed their principal amount as of December 31, 2013.
3.75% Exchange.24.5277 In August 2014, we entered into separate, privately negotiated, exchange agreements (the 3.75% Exchange) with certain holders of our outstanding 3.75% convertible senior notes due 2014 (the 3.75% Notes). In this transaction, we
exchanged $176.6 million aggregate principal amount of the 3.75% Notes for $176.6 million principal amount of 1.625% convertible senior notes due 2044 (see further discussion below), approximately 1.7 million shares of our common stock, perand payment of accrued interest on the exchanged 3.75% Notes. We did not receive any proceeds related to the 3.75% Exchange.
1.625% Convertible Senior Notes due 2044. $1,000In September 2014, we issued $125.0 million principal amount of 1.625% convertible senior notes (the 1.625% Notes) due August 15, 2044, unless earlier repurchased, redeemed or converted. Combined with the 1.625% Notes (equivalent to an initial conversion price of approximately$40.77per share of common stock). The conversion rate will be subject to adjustment in some events but will not be adjusted for any accrued and unpaid interest. In addition, following certain corporate events that occur prior to the maturity date, we will pay a cash make-whole premium by increasing the conversion rate for a holder who elects to convert its Notesissued in connection with such a corporate eventthe 3.75% Exchange described above, the aggregate principal amount issued under the 1.625% Notes was $301.6 million.
Interest on the 1.625% Notes is payable semiannually in certain circumstances. We may not redeem the Notes prior to the maturity date,arrears on February 15 and no sinking fund is provided for the Notes.
If we undergo a fundamental change (as defined in the indenture to the Notes), holders may require us to repurchase for cash all or part of their NotesAugust 15, at a repurchase price equal to100%rate of 1.625% per annum, beginning on February 15, 2015. In addition, beginning with the semiannual interest period commencing immediately following the interest payment date on August 15, 2018, contingent interest will accrue on the 1.625% Notes during any semiannual interest period in which certain conditions or events occur, or under certain events of default. For example, additional interest of 0.25% per year will be payable on the 1.625% Notes for any semiannual interest period for which the principal amount of 1.625% Notes outstanding is less than $100 million.
The proceeds from the issuance of the 1.625% Notes amounted to be repurchased, plus accrued$122.6 million, including a premium of $0.6 million, and unpaid interest to, but excluding,net of deferred issuance costs paid for both the fundamental change repurchase date. The indenture provides for customary events3.75% Exchange and the additional $125.0 million principal amount issued. In connection with aggregate principal amount of default, including cross acceleration to certain other indebtednessthe 1.625% Notes, we have recorded total deferred issuance costs of ours, and our significant subsidiaries.
The Notesapproximately $6 million, which will be amortized over the expected term of the debt, as discussed further below.
The 1.625% Notes are senior unsecured obligations of the Company and will rank senior in right of payment to any of our indebtedness that is expressly subordinated in right of payment to the 1.625% Notes; equal in right of payment to any of our unsecured indebtedness that is not so subordinated; effectively junior in right of payment to any of our secured indebtedness to the extent of the value of the assets securing such indebtedness; and structurally junior to all indebtedness and other liabilities (including trade payables) of our subsidiaries.
Cash Convertible Note Hedge and Warrant Transactions
In connection withThe initial conversion rate for the pricing of the1.625% Notes on February 11, 2013, we entered into cash convertible note hedge transactions and warrant transactions relating to a notional number ofis 17.2157 shares of our common stock underlyingper $1,000 principal amount of the 1.625% Notes. This represents an initial conversion price of approximately $58.09 per share of our common stock. Upon conversion, we will pay cash and, if applicable, deliver shares of our common stock to the converting holder in an amount per $1,000 principal amount of 1.625% Notes equal to the settlement amount (as defined in the related indenture). Holders may convert their 1.625% Notes only under the following circumstances:
during any calendar quarter commencing after the calendar quarter ending on September 30, 2014 (and only during such calendar quarter), if the last reported sale price of the common stock for at least 20 trading days (whether or not consecutive) during a period of 30 consecutive trading days ending on the last trading day of the immediately preceding calendar quarter is greater than or equal to 130% of the conversion price on each applicable trading day;
during the five business day period after any five consecutive trading day period (the measurement period) in which the trading price per $1,000 principal amount of 1.625% Notes for each trading day of the measurement period was less than 98% of the product of the last reported sale price of our common stock and the conversion rate on each such trading day;
upon the occurrence of specified corporate events;
if we call any 1.625% Notes for redemption, at any time until the close of business on the business day immediately preceding the redemption date;
during the period from, and including, May 15, 2018 to the close of business on the business day immediately preceding August 19, 2018; or
at any time on or after February 15, 2044 until the close of business on the second scheduled trading day immediately preceding the maturity date, holders may convert their 1.625% Notes, in integral multiples of $1,000 principal amount, at the option of the holder regardless of the foregoing circumstances.
As of December 31, 2014, the 1.625% Notes were not convertible.
We may not redeem the 1.625% Notes prior to August 19, 2018. On or after August 19, 2018, we may redeem for cash all or part of the 1.625% Notes, except for the 1.625% Notes we are required to repurchase in connection with a fundamental change or on any specified repurchase date. The redemption price for the 1.625% Notes will equal 100% of the principal amount of the 1.625% Notes being redeemed, plus accrued and unpaid interest. In addition, holders of the 1.625% Notes may require us to repurchase some or all of the 1.625% Notes for cash on August 19, 2018, August 19, 2024, August 19, 2029, August 19, 2034 and August 19, 2039, in each case, at a specified price equal to 100% of the principal amount of the 1.625% Notes to be issued by us (without regardrepurchased, plus accrued and unpaid interest.
Because the 1.625% Notes have cash settlement features, we have allocated the principal amount between a liability component and an equity component. The reduced carrying value on the 1.625% Notes resulted in a debt discount that is amortized back to the initial purchasers'$100 million over-allotment option)1.625% Notes' principal amount through the recognition of non-cash interest expense over the expected life of the debt. The expected life of the debt is approximately four years, beginning on the issuance date and ending on the first date we may redeem the notes in August 2018. As of December 31, 2014, we expect the 1.625% Notes to be outstanding until August 2018, for a remaining amortization period of 3.6 years. This has resulted in our recognition of interest expense on the 1.625% Notes at an effective rate approximating what we would have incurred had nonconvertible debt with twocounterparties, JPMorgan Chase Bank, National Association, London Branch and Bank of America, N.A. (the “Option Counterparties”)otherwise similar terms been issued, or approximately 5%. The outstanding 1.625% Notes’ if-converted value did not exceed their principal amount as of December 31, 2014. At December 31, 2014, the equity component of the 1.625% Notes, including the impact of deferred taxes, was $22.9 million.
3.75% Convertible Senior Notes due 2014. As described above, we entered into the 3.75% Exchange transaction in August 2014, under which we exchanged $176.6 million of the outstanding principal amount of the 3.75% Notes for the 1.625% Notes. The remaining $10.4 million principle amount was repaid in full in October 2014. In addition to the repayment of the outstanding principle balance, in early October 2014 we issued approximately 0.1 million shares to settle the 3.75% Notes' conversion feature.
The principal amounts, unamortized discount (net of premium related to 1.625% Notes), and net carrying amounts of the convertible senior notes were as follows:
|
| | | | | | | | | | | |
| | Principal Balance | | Unamortized Discount | | Net Carrying Amount |
| | (In thousands) |
| December 31, 2014: | | | | | |
| 1.125% Notes | $ | 550,000 |
| | $ | 114,670 |
| | $ | 435,330 |
|
| 1.625% Notes | 301,551 |
| | 32,784 |
| | 268,767 |
|
| | $ | 851,551 |
| | $ | 147,454 |
| | $ | 704,097 |
|
| December 31, 2013: | | | | | |
| 1.125% Notes | $ | 550,000 |
| | $ | 133,632 |
| | $ | 416,368 |
|
| 3.75% Notes | 187,000 |
| | 5,128 |
| | 181,872 |
|
| | $ | 737,000 |
| | $ | 138,760 |
| | $ | 598,240 |
|
|
| | | | | | | | | | | |
| | Years Ended December 31, |
| | 2014 | | 2013 | | 2012 |
| | (In thousands) |
| Interest cost recognized for the period relating to the: | | | | | |
| Contractual interest coupon rate | $ | 12,504 |
| | $ | 12,427 |
| | $ | 7,012 |
|
| Amortization of the discount | 26,064 |
| | 22,103 |
| | 5,942 |
|
| | $ | 38,568 |
| | $ | 34,530 |
| | $ | 12,954 |
|
Lease Financing Obligations.In 2013 we entered into a sale-leaseback transaction for the sale and contemporaneous leaseback of the Molina Center located in Long Beach, California, and our Ohio health plan office building located in Columbus, Ohio. Due to our continuing involvement with these leased properties, the sale did not qualify for sale-leaseback accounting treatment and we remain the "accounting owner" of the properties. These assets continue to be included in our consolidated balance sheets, and also continue to be depreciated and amortized over their remaining useful lives. The lease financing obligation is amortized over the 25-year lease term such that there will be no gain or loss recorded if the lease is not extended at the end of its term. Rent will increase 3% per year through the initial term. Payments under the lease adjust the lease financing obligation, and the imputed interest is recorded to interest expense in our consolidated statements of income. Such interest amounted to $12.5 million and $6.8 million for the year ended December 31, 2014 and 2013, respectively.
As described and defined in further detail in Note 18, "Related Party Transactions," we entered into a lease for office space in February 2013 consisting of two office buildings. We have concluded that we are the accounting owner of the buildings due to our continuing involvement with the properties. We have recorded $38.4 million to property, equipment and capitalized software, net, in the accompanying consolidated balance sheet as of December 31, 2014, which represents the total cost incurred by the Landlord for the construction of the buildings, net of accumulated depreciation. As of December 31, 2014, the aggregate amount recorded to lease financing obligations, including the current portion, amounted to $40.6 million. Payments under the lease adjust the lease financing obligation, and the imputed interest is recorded to interest expense in our consolidated statements of income. Such interest expense for the years ended December 31, 2014, and 2013, was $3.2 million and $1.3
million, respectively. In addition to the capitalization of the costs incurred by the Landlord, we impute and record rent expense relating to the ground leases for the property sites. Such rent expense is computed based on the fair value of the land and our incremental borrowing rate, amounting to $1.1 million for the year ended December 31, 2014, and insignificant for the year ended December 31, 2013. For information regarding the future minimum lease obligation, refer to Note 20, "Commitments and Contingencies."
13. Derivative Financial Instruments
The following table summarizes the fair values and the presentation of our derivative financial instruments (defined and discussed individually below) in the consolidated balance sheets:
|
| | | | | | | | | |
| | | | December 31, |
| | Balance Sheet Location | | 2014 | | 2013 |
| | | | (In thousands) |
| Derivative asset: | | | | | |
| 1.125% Call Option | Non-current assets: Derivative asset | | $ | 329,323 |
| | $ | 186,351 |
|
| | | | | | |
| Derivative liability: | | | | | |
| 1.125% Notes Conversion Option | Non-current liabilities: Derivative liability | | $ | 329,194 |
| | $ | 186,239 |
|
Our derivative financial instruments do not qualify for hedge treatment, therefore the change in fair value of these instruments is recognized immediately in our consolidated statements of income, and reported in other expense, net. Gains and losses for our derivative financial instruments are presented individually in the consolidated statements of cash convertible noteflows, supplemental cash flow information.
1.125% Notes Call Spread Overlay.Concurrent with the issuance of the 1.125% Notes in 2013 as described in Note 12, "Long-Term Debt," we entered into privately negotiated hedge transactions (collectively, the 1.125% Call Option) and warrant transactions (collectively, the 1.125% Warrants), with certain of the initial purchasers of the 1.125% Notes (the Counterparties). We refer to these transactions collectively as the Call Spread Overlay. Under the Call Spread Overlay, the cost of the 1.125% Call Option we purchased to cover the cash outlay upon conversion of the 1.125% Notes was reduced by proceeds from the sale of the 1.125% Warrants. Assuming full performance by the Counterparties (and 1.125% Warrants strike prices in excess of the conversion price of the 1.125% Notes), these transactions are intended to offset cash payments due upon any conversion of the 1.125% Notes. However, the warrant transactions could separately have a dilutive effect
1.125% Call Option.The 1.125% Call Option, which is indexed to the extent that the market value per share of our common stock, (as measured underis a derivative asset that requires mark-to-market accounting treatment due to cash settlement features until the terms1.125% Call Option settles or expires. For further discussion of the warrant transactions) exceedsinputs used to determine the applicable strike pricefair value of the warrants. 1.125% Call Option, refer to Note 5, "Fair Value Measurements."
1.125% Notes Conversion Option. The strike priceembedded cash conversion option within the 1.125% Notes is accounted for separately as a derivative liability, with changes in fair value reported in our consolidated statements of income until the cash conversion option settles or expires. For further discussion of the warrants will initially be$53.8475per share, which is75%aboveinputs used to determine the last reported sale price of our common stock on February 11, 2013.
In connection with the exercise in full by the initial purchasers of their over-allotment option in respectfair value of the 1.125% Notes on February 13, 2013, we and theConversion Option, Counterparties amended the cash convertible note hedge transactions entered into on February 11, 2013refer to upsize such transactions by a notional number of shares of our common stock corresponding to the number of shares underlying the Notes purchased pursuant to the exercise of such over-allotment option. On February 13, 2013, we also entered into additional warrant transactions with the Option Counterparties relating to a number of shares of our common stock corresponding to the number of shares underlying the Notes purchased pursuant to the exercise of such over-allotment option. Each of the amendments to the cash convertible note hedge transactions and the additional warrant transactions were on substantially similar terms to the corresponding transactions entered into on February 11, 2013. Pursuant to these warrant transactions, we issued13,490,236warrants with a strike price of$53.8475per share. The number of warrants and the strike price are subject to adjustment under certain circumstances.Note 5, "Fair Value Measurements."
We used approximately$74.3 millionof the net proceeds from the offering to pay the cost of the cash convertible note hedge transactions (after such cost was partially offset by the proceeds to us from the sale of warrants in the warrant transactions and the additional warrant transactions).
Aside from the initial payment of a premium to the Option Counterparties of approximately$149.3 million, we will not be required to make any cash payments to the Option Counterparties under the cash convertible note hedge transactions and will be entitled to receive from the Option Counterparties an amount of cash, generally equal to the amount by which the market price per share of common stock exceeds the strike price of the cash convertible note hedge transactions during the relevant valuation period. The strike price under the cash convertible note hedge transactions is initially equal to the conversion price of the Notes. Additionally, if the market value per share of our common stock exceeds the strike price of the warrants on any trading day during the160trading day measurement period under the warrant transactions and the additional warrant transactions, we will be obligated to issue to the Option Counterparties a number of shares equal in value to the product of the amount by which such market value exceeds such strike price and1/160thof the aggregate number of shares of our common stock underlying the warrant transactions and the additional warrant transactions, subject to a share delivery cap. The Company will not receive any additional proceeds if warrants are exercised.
As of December 31, 2012, maturities of long-term debt for the years ending December 31 are as follows (in thousands):
|
| | | | | | | | | | | | | | | | | | | | | | | | | | | |
| | Total | | 2013 | | 2014 | | 2015 | | 2016 | | 2017 | | Thereafter |
| Credit Facility | $ | 40,000 |
| | $ | — |
| | $ | — |
| | $ | — |
| | $ | 40,000 |
| | $ | — |
| | $ | — |
|
| Convertible senior notes | 187,000 |
| | — |
| | 187,000 |
| | — |
| | — |
| | — |
| | — |
|
| Term loan | 47,471 |
| | 1,155 |
| | 1,206 |
| | 1,259 |
| | 1,309 |
| | 1,372 |
| | 41,170 |
|
| | $ | 274,471 |
| | $ | 1,155 |
| | $ | 188,206 |
| | $ | 1,259 |
| | $ | 41,309 |
| | $ | 1,372 |
| | $ | 41,170 |
|
Credit Facility
On February 15, 2013, we used approximately$40.0 millionof the net proceeds from the offering of the Notes to repay all of the outstanding indebtedness under our$170 millionrevolving credit facility, or the Credit Facility, with various lenders and U.S. Bank National Association, as Line of Credit Issuer, Swing Line Lender, and Administrative Agent. As of December 31, 2012, there was$40.0 millionoutstanding under the Credit Facility.
We terminated the Credit Facility in connection with the closing of the offering and sale of the Notes.twoletters of credit in the aggregate principal amount of$10.3 millionthat reduced the amount available for borrowing under the Credit Facilityas of December 31, 2012, were transferred to direct issue letters of credit with another financial institution. The Credit Facility had a term offive yearsunder which all amounts outstanding would have been due and payable on September 9, 2016.
Borrowings under the Credit Facility accrued interest based, at our election, on the base rate plus an applicable margin or the Eurodollar rate. The base rate is, for any day, a rate of interest per annum equal to the highest of (i) the prime rate of interest announced from time to time by U.S. Bank or its parent, (ii) the sum of the federal funds rate for such day plus0.50%per annum and (iii) the Eurodollar rate (without giving effect to the applicable margin) for a one month interest period on such day (or if such day is not a business day, the immediately preceding business day) plus1.00%. The Eurodollar rate is a reserve adjusted rate at which Eurodollar deposits are offered in the interbank Eurodollar market plus an applicable margin. In addition to interest payable on the principal amount of indebtedness outstanding from time to time under the Credit Facility, we were required to pay a quarterly commitment fee of0.25% to 0.50%(based upon our leverage ratio) of the unused amount of the lenders' commitments under the Credit Facility. The applicable margins ranged between0.75% to 1.75%for base rate loans and1.75% to 2.75%for Eurodollar loans, in each case, based upon our leverage ratio.
Our obligations under the Credit Facility were secured by a lien on substantially all of our assets, with the exception of certain of our real estate assets, and by a pledge of the capital stock or membership interests of our operating subsidiaries and health plans (with the exception of the California health plan). The Credit Facility included usual and customary covenants for credit facilities of this type, including covenants limiting liens, mergers, asset sales, other fundamental changes, debt, acquisitions, dividends and other distributions, capital expenditures, and investments. The Credit Facility also required us to maintain as of the end of any fiscal quarter (calculated for each four consecutive fiscal quarter period) a ratio of total consolidated debt to total consolidated EBITDA, as defined in the Credit Facility, of not more than2.75 to 1.00, and a fixed charge coverage ratio of not less than1.75 to 1.00.. AtDecember 31, 2012, we were in compliance with all financial covenants under the Credit Facility.
3.75% Convertible Senior Notes due 2014
As of December 31, 2012, $187.0 millionin aggregate principal amount of our 3.75%Convertible Senior Notes due 2014, or the 3.75% Notes, remain outstanding. The 3.75% Notes rank equally in right of payment with our existing and future senior indebtedness. The 3.75% Notes are convertible into cash and, under certain circumstances, shares of our common stock. The initial conversion rate is31.9601shares of our common stock per one thousand dollar principal amount of the 3.75% Notes. This represents an initial conversion price of approximately$31.29per share of our common stock. In addition, if certain corporate transactions that constitute a change of control occur prior to maturity, we will increase the conversion rate in certain circumstances. Prior to July 2014, holders may convert their 3.75% Notes only under the following circumstances:
During any fiscal quarter after our fiscal quarter ending December 31, 2007, if the closing sale price per share of our common stock, for each of at least 20 trading days during the period of 30 consecutive trading days ending on the last trading day of the previous fiscal quarter, is greater than or equal to 120% of the conversion price per share of our common stock;
During the five business day period immediately following any five consecutive trading day period in which the trading price per one thousand dollar principal amount of the 3.75% Notes for each trading day of such period was less than 98% of the product of the closing price per share of our common stock on such day and the conversion rate in effect on such day; or
Upon the occurrence of specified corporate transactions or other specified events.
On or after July 1, 2014, holders may convert their 3.75% Notes at any time prior to the close of business on the scheduled trading day immediately preceding the stated maturity date regardless of whether any of the foregoing conditions is satisfied.
We will deliver cash and shares of our common stock, if any, upon conversion of each $1,000 principal amount of 3.75% Notes, as follows:
An amount in cash (the “principal return”) equal to the sum of, for each of the 20 Volume-Weighted Average Price ("VWAP") trading days during the conversion period, the lesser of the daily conversion value for such VWAP trading day and fifty dollars (representing 1/20th of one thousand dollars); and
A number of shares based upon, for each of the 20 VWAP trading days during the conversion period, any excess of the daily conversion value above fifty dollars.
The proceeds from the issuance of the 3.75% Notes have been allocated between a liability component and an equity component. We have determined that the effective interest rate of the 3.75% Notes is 7.5%, principally based on the seven-year U.S. Treasury note rate as of the October 2007 issuance date, plus an appropriate credit spread. The resulting debt discount is being amortized over the period the 3.75% Notes are expected to be outstanding, as additional non-cash interest expense. As of December 31, 2012, we expect the 3.75% Notes to be outstanding until their October 1, 2014 maturity date, for a remaining amortization period of 21 months. The 3.75% Notes’ if-converted value did not exceed their principal amount as of December 31, 2012. At December 31, 2012, the equity component of the 3.75% Notes, net of the impact of deferred taxes, was $24.0 million. The following table provides the details of the liability amounts recorded:
|
| | | | | | | |
| | December 31, |
| | 2012 | | 2011 |
| | (In thousands) |
| Details of the liability component: | | | |
| Principal amount | $ | 187,000 |
| | $ | 187,000 |
|
| Unamortized discount | (11,532 | ) | | (17,474 | ) |
| Net carrying amount | $ | 175,468 |
| | $ | 169,526 |
|
|
| | | | | | | | | | | |
| | Years Ended December 31, |
| | 2012 | | 2011 | | 2010 |
| | (In thousands) |
| Interest cost recognized for the period relating to the: | | | | | |
| Contractual interest coupon rate of 3.75% | $ | 7,012 |
| | $ | 7,012 |
| | $ | 7,012 |
|
| Amortization of the discount on the liability component | 5,942 |
| | 5,512 |
| | 5,114 |
|
| Total interest cost recognized | $ | 12,954 |
| | $ | 12,524 |
| | $ | 12,126 |
|
Term Loan
On December 7, 2011, our wholly owned subsidiary Molina Center LLC entered into a Term Loan Agreement, dated as of December 1, 2011, with various lenders and East West Bank, as Administrative Agent (the “Administrative Agent”). Pursuant to the terms of the Term Loan Agreement, Molina Center LLC borrowed the aggregate principal amount of$48.6 millionto finance a portion of the$81 millionpurchase price for the acquisition of the Molina Center, located in Long Beach, California.
The outstanding principal amount under the Term Loan Agreement bears interest at the Eurodollar rate for each Interest Period (as defined below) commencing January 1, 2012. The Eurodollar rate is a per annum rate of interest equal to the greater of (a) the rate that is published in the Wall Street Journal as the London interbank offered rate for deposits in United States dollars, for a period of one month, two business days prior to the commencement of an Interest Period, multiplied by a statutory reserve rate established by the Board of Governors of the Federal Reserve System, or (b)4.25%. "Interest Period" means the period commencing on the first day of each calendar month and ending on the last day of each calendar month. The loan matures on November 30, 2018, and is subject to a 25-yearamortization schedule that commenced on January 1, 2012.
The Term Loan Agreement contains customary representations, warranties, and financial covenants. In the event of a default as described in the Term Loan Agreement, the outstanding principal amount under the Term Loan Agreement will bear interest at a rate 5.00% per annum higher than the otherwise applicable rate. All amounts due under the Term Loan Agreement and related loan documents are secured by a security interest in the Molina Center in favor of and for the benefit of the Administrative Agent and the other lenders under the Term Loan Agreement.
Interest Rate Swap
Swap.In May 2012, we entered into a $42.5$42.5 millionnotional amount interest rate swap, agreement, or Swap Agreement, with an effective date of March 1, 2013. While not designated as a hedge during the year ended December 31, 2012, the Swap Agreement iswhich was intended to reduce our exposure to fluctuations in the contractual variable interest rates under our Term Loan Agreement, and expires onterm loan agreement that was repaid in June 2013. In June 2013, we settled the maturity date of the Term Loan Agreement, which is November 30, 2018. Under the Swap Agreement, we will receive a variableinterest rate of the one-month LIBOR plus3.25%, and pay a fixed rate of5.34%. The Swap Agreement is measured and reported at fair value on a recurring basis, within Level 2 of the fair value hierarchy. Gains and losses relating to changes in fair value are reported in earnings in the current period. For the year endedDecember 31, 2012, we have recorded losses of$1.3 millionto general and administrative expense. As ofDecember 31, 2012the fair value of the Swap Agreement is a liability of $1.3 million, recorded to other noncurrent liabilities. We do not use derivativesswap for trading or speculative purposes. We believe that we are not exposed to more than a nominal amount of credit risk relating to the Swap Agreement because the counterparty is an established and well-capitalized financial institution.$0.9 million.
13. Income Taxes
The provision for income taxes consisted of the following:
14. Income Taxes
The provision for income taxes for continuing operations consisted of the following:
| | | | Years Ended December 31, | Year Ended December 31, |
| | 2012 | | 2011 | | 2010 | 2014 | | 2013 | | 2012 |
| | (In thousands) | (In thousands) |
| Current: | | | | | | | | | | |
| Federal | $ | 17,853 |
| | $ | 28,336 |
| | $ | 36,395 |
| $ | 72,040 |
| | $ | 66,883 |
| | $ | 23,019 |
|
| State | 1,308 |
| | 1,639 |
| | 2,144 |
| 3,038 |
| | 581 |
| | 1,254 |
|
| Total current | 19,161 |
| | 29,975 |
| | 38,539 |
| 75,078 |
| | 67,464 |
| | 24,273 |
|
| Deferred: | | | | | | | | | | |
| Federal | (6,300 | ) | | 14,028 |
| | (4,717 | ) | (72 | ) | | (25,498 | ) | | (9,205 | ) |
| State | (3,586 | ) | | (167 | ) | | 700 |
| (2,280 | ) | | (5,650 | ) | | (4,555 | ) |
| Total deferred | (9,886 | ) | | 13,861 |
| | (4,017 | ) | (2,352 | ) | | (31,148 | ) | | (13,760 | ) |
| Total provision for income taxes | $ | 9,275 |
| | $ | 43,836 |
| | $ | 34,522 |
| |
| | | $ | 72,726 |
| | $ | 36,316 |
| | $ | 10,513 |
|
A reconciliation of the U.S. federal statutory income tax rate to the combined effective income tax rate for continuing operations is as follows:
| | | | Years Ended December 31, | Year Ended December 31, |
| | 2012 | | 2011 | | 2010 | 2014 | | 2013 | | 2012 |
| Statutory federal tax rate | 35.0 | % | | 35.0 | % | | 35.0 | % | 35.0 | % | | 35.0 | % | | 35.0 | % |
| State income taxes, net of federal benefit | (7.8 | ) | | 1.5 |
| | 2.1 |
| 0.4 |
| | (0.5 | ) | | (9.2 | ) |
| Benefit for unrecognized tax benefits | (1.2 | ) | | (0.6 | ) | | (0.1 | ) | |
| Change in unrecognized tax benefits | | (0.1 | ) | | (3.7 | ) | | 0.7 |
|
| Nondeductible health insurer fee (HIF) | | 22.9 |
| | — |
| | — |
|
| Nondeductible compensation | 7.6 |
| | — |
| | 1.0 |
| (4.1 | ) | | 9.6 |
| | 6.2 |
|
| Nondeductible goodwill | — |
| | 31.7 |
| | — |
| |
| Nondeductible lobbying | 5.2 |
| | 1.1 |
| | 0.7 |
| (0.3 | ) | | 1.6 |
| | 4.2 |
|
| Purchase accounting adjustment | — |
| | (1.5 | ) | | — |
| |
| Change in fair value of contingent consideration | 5.9 |
| | — |
| | — |
| |
| Nondeductible fair value of 1.125% Warrants | | — |
| | 2.4 |
| | — |
|
| Change in fair value of contingent consideration liabilities | | — |
| | (0.3 | ) | | 4.8 |
|
| Other | 3.9 |
| | 0.6 |
| | (0.1 | ) | — |
| | 0.7 |
| | 3.3 |
|
| Effective tax rate | 48.6 | % | | 67.8 | % | | 38.6 | % | 53.8 | % | | 44.8 | % | | 45.0 | % |
Our effective tax rate is based on expected income, statutory tax rates, and tax planning opportunities available to us in the various jurisdictions in which we operate. Significant management estimates and judgments are required in determining our effective tax rate. We are routinely under audit by federal, state, or local authorities regarding the timing and amount of deductions, nexus of income among various tax jurisdictions, and compliance with federal, state, and local tax laws. We have pursued various strategies
During 2014, the Internal Revenue Service (IRS) issued final regulations related to reduce our federal, statecompensation deduction limitations applicable to certain health insurance issuers. Pursuant to these final regulations, we reversed amounts treated as nondeductible in 2013 and local taxes. Asrecognized a result, we have reduced our state income tax expense due to California enterprise zone credits.benefit during 2014.
During 20122014, 2013, and 2011,2012, excess tax benefits from shared-basedshare-based compensation were $3.1amounted to $3.0 million, $1.6 million, and $937,000,$3.1 million, respectively. These amounts were recorded as a decrease to income taxes payable and an increase to additional paid-in capital. During 2010, tax-related deficiencies on share-based compensation were $673,000. This amount was recorded as an adjustment to income taxes payable with a corresponding decrease to additional paid-in capital.
Deferred tax assets and liabilities are classified as current or non-current according to the classification of the related asset or liability. Significant components of our deferred tax assets and liabilities as of December 31, 20122014 and 20112013 were as follows:
| | | | December 31, | December 31, |
| | 2012 | | 2011 | 2014 | | 2013 |
| | (In thousands) | (In thousands) |
| Accrued expenses | $ | 15,381 |
| | $ | 14,541 |
| $ | 13,323 |
| | $ | 19,545 |
|
| Reserve liabilities | 2,936 |
| | 1,292 |
| 2,487 |
| | 1,712 |
|
| State taxes | (606 | ) | | (396 | ) | (134 | ) | | (1,323 | ) |
| Other accrued medical costs | 2,518 |
| | 2,051 |
| 3,800 |
| | 2,540 |
|
| Net operating losses | 27 |
| | 27 |
| 27 |
| | 27 |
|
| Unrealized gains | (283 | ) | | (316 | ) | |
| Unrealized losses | | 444 |
| | 380 |
|
| Unearned premiums | 15,675 |
| | 4,139 |
| 21,749 |
| | 10,543 |
|
| Prepaid expenses | (4,390 | ) | | (3,032 | ) | (5,920 | ) | | (5,354 | ) |
| Basis in debt | | (210 | ) | | (2,162 | ) |
| Deferred compensation | 1,611 |
| | — |
| 5,252 |
| | 2,087 |
|
| Other, net | (426 | ) | | 21 |
| (244 | ) | | (928 | ) |
| Valuation allowance | | (1,042 | ) | | (511 | ) |
| Deferred tax asset, net of valuation allowance — current | 32,443 |
| | 18,327 |
| 39,532 |
| | 26,556 |
|
| Accrued expenses | — |
| | 223 |
| |
| Reserve liabilities | 2,013 |
| | 3,015 |
| 2,017 |
| | 1,909 |
|
| State tax credit carryover | 4,149 |
| | 2,609 |
| 8,157 |
| | 7,027 |
|
| Net operating losses | 3,341 |
| | 2,694 |
| 3,138 |
| | 2,326 |
|
| Unrealized losses | 563 |
| | 1,176 |
| 181 |
| | 286 |
|
| Depreciation and amortization | (44,198 | ) | | (39,939 | ) | (57,068 | ) | | (40,433 | ) |
| Deferred compensation | 3,323 |
| | 7,904 |
| 4,405 |
| | 3,404 |
|
| Debt basis | (5,410 | ) | | (7,604 | ) | |
| Lease financing obligation | | 34,084 |
| | 27,543 |
|
| Basis in debt | | (14,724 | ) | | 466 |
|
| Other, net | 702 |
| | (278 | ) | (96 | ) | | (24 | ) |
| Valuation allowance | (2,383 | ) | | (2,927 | ) | (4,365 | ) | | (3,084 | ) |
| Deferred tax liability, net of valuation allowance — long term | (37,900 | ) | | (33,127 | ) | (24,271 | ) | | (580 | ) |
| Net deferred income tax liability | $ | (5,457 | ) | | $ | (14,800 | ) | |
| Net deferred income tax asset | | $ | 15,261 |
| | $ | 25,976 |
|
At December 31, 2012,2014, we had federal and state net operating loss carryforwards of $319,000$0.2 million and $73.0$84.0 million,, respectively. The federal net operating loss begins expiring in 2018, and state net operating losses begin expiring in 2013.2015. The utilization of the net operating losses is subject to certain limitations under federal law.
At December 31, 2012,2014, we had California enterprise zone tax credit carryovers of $6.3$12.5 million which do not expire.expire in 2024.
We evaluate the need for a valuation allowance taking into consideration the ability to carry back and carry forward tax credits and losses, available tax planning strategies and future income, including reversal of temporary differences. We have determined that as of December 31, 2012, $3.02014, $5.4 million of deferred tax assets did not satisfy the recognition criteria due to uncertainty regarding the realization of some of our state tax operating loss carryforwards. WeTherefore, we increased our valuation allowance $100,000by $1.8 million, from $2.9$3.6 million at December 31, 20112013, to $3.0$5.4 million as of December 31, 2012.2014.
We recognize tax benefits only if the tax position is more likely than not to be sustained. We are subject to income taxes in the U.S. and numerous state jurisdictions. Significant judgment is required in evaluating our tax positions and determining our provision for income taxes. During the ordinary course of business, there are many transactions and calculations for which the ultimate tax determination is uncertain. We establish reserves for tax-related uncertainties based on estimates of whether, and the extent to which, additional taxes will be due. These reserves are established when we believe that certain positions might be challenged despite our belief that our tax return positions are fully supportable. We adjust these reserves in light of changing facts and circumstances, such as the outcome of tax audits. The provision for income taxes includes the impact of reserve provisions and changes to reserves that are considered appropriate.
The roll-forwardroll forward of our unrecognized tax benefits is as follows:
| | | | Years Ended December 31, | Year Ended December 31, |
| | 2012 | | 2011 | | 2010 | 2014 | | 2013 | | 2012 |
| | (In thousands) | (In thousands) |
| Gross unrecognized tax benefits at beginning of period | $ | (10,712 | ) | | $ | (10,962 | ) | | $ | (4,128 | ) | $ | (8,030 | ) | | $ | (10,622 | ) | | $ | (10,712 | ) |
| Increases in tax positions for prior years | (441 | ) | | (137 | ) | | (6,891 | ) | — |
| | — |
| | (441 | ) |
| Decreases in tax positions for prior years | 320 |
| | — |
| | — |
| — |
| | 3,615 |
| | 320 |
|
| Increases in tax positions for current year | | (777 | ) | | (2,084 | ) | | — |
|
| Decreases in tax positions for current year | | — |
| | 886 |
| | — |
|
| Settlements | — |
| | — |
| | — |
| 5,960 |
| | — |
| | — |
|
| Lapse in statute of limitations | 211 |
| | 387 |
| | 57 |
| 253 |
| | 175 |
| | 211 |
|
| Gross unrecognized tax benefits at end of period | $ | (10,622 | ) | | $ | (10,712 | ) | | $ | (10,962 | ) | $ | (2,594 | ) | | $ | (8,030 | ) | | $ | (10,622 | ) |
As of December 31, 2012, we had $10.6 millionThe total amount of unrecognized tax benefits of which $7.4 million,at December 31, 2014, 2013 and 2012 that, if fully recognized, would affect ourthe effective tax rate. Approximately $8.4rates is $1.6 million, of the unrecognized tax benefits recorded at December 31, 2012 relates to a tax position claimed on a state refund claim that will not result in a cash payment for income taxes if our claim is denied. $5.7 million and $7.4 million, respectively. We expect that during the next 12 months it is reasonably possible that unrecognized tax benefit liabilities may decrease by as much as $8.6$0.1 million due the resolution to the state refund claim as well as the normal expiration of statutestatutes of limitations.limitation.
Our continuing practice is to recognize interest and/or penalties related to unrecognized tax benefits in income tax expense. As of December 31, 2012, December 31, 2011, and December 31, 2010, we hadAmounts accrued$56,000, $65,000, and $82,000, respectively, for the payment of interest and penalties.penalties as of December 31, 2014, and 2013 were insignificant.
We are under examination by the IRS for calendar year 2011 and may be subject to examination by the Internal Revenue Service, or IRS, for calendar years 20092012 through 2012.2014. We are under examination, or may be subject to examination, in certain state and local jurisdictions, with the major jurisdictions being California, Missouri,Utah, and Michigan, for the years 20042010 through 2012.
2014.
14. Stockholders’15. Stockholders' Equity
Repurchase in Connection with Offering of 1.125% Cash Convertible Senior Notes Due 2020. Subsequent toStockholders' equity increased $117.5 million during the year ended December 31, 2012,2014. The increase was due to net income of $62.2 million, $22.0 million related to 1.625% Notes and 3.75% Exchange, $33.2 million related to share-based compensation transactions, and $0.1 million related to other comprehensive income.
3.75% Exchange and 3.75% Notes. As described in Note 12, "Long-Term Debt," we issued approximately 1.8 million shares in connection with the 3.75% Exchange, and the 3.75% Notes settlement in 2014; additionally, we issued approximately 81,000 shares of common stock for services rendered in connection with the 3.75% Exchange.
1.125% Warrants. In connection with the 1.125% Notes Call Spread Overlay transaction described in Note 13, "Derivative Financial Instruments," we issued 13,490,236 warrants with a strike price of $53.8475 per share. The number of warrants and the strike price are subject to adjustment under certain circumstances. If the market value per share of our common stock exceeds the strike price of the 1.125% Warrants on any trading day during the 160 trading day measurement period under the 1.125% Warrants, we will be obligated to issue to the Counterparties a number of shares equal in value to the product of the amount by which such market value exceeds such strike price and 1/160th of the aggregate number of shares of our common stock underlying the 1.125% Warrants, subject to a share delivery cap. The 1.125% Warrants could separately have a dilutive effect to the extent that the market value per share of our common stock (as measured under the terms of the warrant transactions) exceeds the applicable strike price of the 1.125% Warrants. We will not receive any additional proceeds if the 1.125% Warrants are exercised.
Securities Repurchases. In connection with the issuance and settlement of the 1.125% Notes, we used a portion of the net proceeds from the offering to repurchase $50$50 million of our common stock in negotiated transactions with institutional investors in the offering, concurrently with the pricing of the offering. OnIn February 12, 2013, we repurchased a total of 1,624,959 shares at $30.77$30.77 per share, which was our closing stock price on that date.
Securities Repurchases and Repurchase Programs. Effective as of February 13,25, 2015, our board of directors authorized the repurchase of up to $50 million in aggregate of our common stock. Stock repurchases under this program may be made through open-market and/or privately negotiated transactions at times and in such amounts as management deems appropriate. The timing and actual number of shares repurchased will depend on a variety of factors including price, corporate and regulatory requirements and market conditions. This newly authorized repurchase program extends through December 31, 2015.
Effective as of September 30, 2013, our board of directors authorized the repurchase of $75up to $50 million in aggregate of either our common stock or our convertible senior note due 2014. The repurchase program extends through December 31, 2014.
On December 26, 2012, we purchased 110,988 shares of our common stock from certain Molina family trusts for an aggregate purchase price of $3.0 million. This purchase transaction was approved by our board of directors. The shares were purchased at a price of $27.03, representing the closing price per share of our common stock on December 26, 2012. See Note 17, "Related Party Transactions."
Effective as of October 26, 2011, our board of directors authorized the repurchase of $75 million in aggregate of either our common stock or our convertible senior notes due 2014 (see Note 12, “Long-Term Debt”). The repurchase program expired October 25, 2012. No securities were purchased under this program in 2012.
In July 2011, our board of directors approved a stock repurchase program of up to $7.0 million, to be used to purchase shares of our common stock under a Rule 10b5-1 trading plan.stock. Under this program, we purchased approximately 400,00085,000 shares of our common stock for $7.0$2.7 million (average cost of approximately $17.47$31.28 per share) during August 2011. These purchases did not materially impact diluted earnings per share for the year endedNovember 2013. This repurchase program expired December 31, 2011. Subsequently, we retired the $7.0 million2014.
Shelf Registration Statement. In May 2012, we filed an automatic shelf registration statement on Form S-3 with the Securities and Exchange CommissionSEC covering the issuance of an indeterminate number of our securities, including common stock, warrants, or debt securities. We may publicly offer securities from time to time at prices and terms to be determined at the time of the offering.
Stock Split. On April 27, 2011, we announced that our board of directors authorized a 3-for-2 stock split of our common stock to be effected in the form of a stock dividend of one share of our stock for every two shares outstanding. The dividend was distributed on May 20, 2011.
Stock Plans. In connection with the stock plans described in Note 16, “Share-Based17, "Share-Based Compensation,”" we issued approximately 1,057,000840,000, and 820,000 shares of common stock, net of shares used to settle employees’ income tax obligations, for the yearyears ended December 31, 20122014 and 2013, respectively.. Stock plan activity resulted in a $19.5 million increase to additional paid-in capital for the same period.
15.16. Employee Benefits
We sponsor a defined contribution 401(k) plan that covers substantially all full-time salaried and hourly employees of our company and its subsidiaries. Eligible employees are permitted to contribute up to the maximum amount allowed by law. We match up to the first 4% of compensation contributed by employees. Expense recognized in connection with our contributions to the 401(k) plan totaled $10.7$21.2 million,, $8.5 $12.8 million and $5.9$10.7 million in the years ended December 31, 2012, 2011,2014, 2013, and 2010,2012, respectively.
We also have a nonqualified deferred compensation plan for certain key employees. Under this plan, eligible participants may defer up to 100% of their base salary and 100% of their bonus to provide tax-deferred growth for retirement. The funds deferred are invested in corporate-owned life insurance, under a rabbi trust.
16.17. Share-Based Compensation
In 2011,At December 31, 2014, we adoptedhad employee equity incentives outstanding under two plans: (1) the 2011 Equity Incentive Plan (the “2011 Plan”) ,(2011 Plan); and (2) the 2002 Equity Incentive Plan (from which equity incentives are no longer awarded).
The 2011 Plan provides for the award of stock options, restricted shares and units, performance shares and units, and stock bonuses to the company’s officers, employees, directors, consultants, advisors,advisers, and other service providers. The 2011 Plan allows for the issuance of 4.5 million shares of common stock.
At In March 2014, our named executive officers were granted a total of 356,292 restricted shares with service, market, and performance conditions. In the event the vesting conditions are not achieved, the awards shall lapse. As of December 31, 2012,2014, we had equity incentives outstanding under two plans: (1)expect the 2011 Plan; and (2) the 2002 Equity Incentive Plan (from which equity incentives are no longer awarded). In March 2012, our chief executive officer, chief financial officer, and chief operating officer were awarded 94,050performance units, 53,236 performance units, and 30,167 performance units, respectively, that would vest and be settled in shares of the Company's common stock equal in number to the units awarded upon the achievement of certain performance and service conditions as follows: (i) the Company’s total operating revenue for 2012 is equal to or greater than $5.5 billion, and (ii) the respective officer continues to be employed by the Company if and when the operating revenue target is met. Such awards vested when the performance and service conditions were met in December 2012. Also in March 2012, our chief executive officer, chief financial officer, chief operating officer, and chief accounting officer were awarded 8,000 performance units, 8,000 performance units, 8,000 performance units, and 3,000 performance units respectively, that would vest and be settled in shares of the Company's common stock equal in number to the units granted upon the certification of our Idaho MMIS by CMS. Such awards vested when the Idaho MMIS was certified in July 2012.full.
Restricted share awards are granted with a fair value equal to the market price of our common stock on the date of grant, and generally vest in equal annual installments over periods up to four years from the date of grant. Stock option awards have an exercise price equal to the fair market value of our common stock on the date of grant, generally vest in equal annual installments over periods up to four years from the date of grant, and have a maximum term of ten years from the date of grant.
Under our employee stock purchase plan (the “ESPP”)(ESPP), eligible employees may purchase common shares at 85% of the lower of the fair market value of our common stock on either the first or last trading day of each six-month offering period. Each participant is limited to a maximum purchase of $25,000$25,000 (as measured by the fair value of the stock acquired) per year through payroll deductions. We estimate the fair value of the stock issued 277,400using the Black-Scholes option pricing model. For the years ended December 31, 2014, 2013, 2012, the inputs to this model were as follows: risk-free interest rates ranging from approximately 0.1% to 0.2%; expected volatilities ranging from approximately 30% to 50%, dividend yields of 0%, and 201,700an average expected life of 0.5 years. We issued approximately 327,200, 299,600 and 277,400 shares of our common stock under the ESPP during the years ended December 31, 20122014, 2013, and 2011,2012, respectively. In 2011, stockholders approved our 2011 ESPP, which superseded the 2002 Employee Stock Purchase Plan. The 2011 ESPP allows for the issuance of three million shares of common stock.
The following table illustrates the components of our share-based compensation expense that are reported in general and administrative expenses in the consolidated statements of income:
|
| | | | | | | | | | | | | | | | | | | | | | | |
| | Year Ended December 31, |
| | 2012 | | 2011 | | 2010 |
| | (In thousands) |
| | Pretax Charges | | Net-of-Tax Amount | | Pretax Charges | | Net-of-Tax Amount | | Pretax Charges | | Net-of-Tax Amount |
| Restricted share and performance unit awards | $ | 18,106 |
| | $ | 12,943 |
| | $ | 15,914 |
| | $ | 9,946 |
| | $ | 8,007 |
| | $ | 5,044 |
|
| Stock options (including expense relating to our ESPP) | 1,912 |
| | 1,613 |
| | 1,138 |
| | 712 |
| | 1,524 |
| | 960 |
|
| $ | 20,018 |
| | $ | 14,556 |
| | $ | 17,052 |
| | $ | 10,658 |
| | $ | 9,531 |
| | $ | 6,004 |
|
|
| | | | | | | | | | | | | | | | | | | | | | | |
| | Year Ended December 31, |
| | 2014 | | 2013 | | 2012 |
| | (In thousands) |
| | Pretax Charges | | Net-of-Tax Amount | | Pretax Charges | | Net-of-Tax Amount | | Pretax Charges | | Net-of-Tax Amount |
| Restricted stock and performance awards | $ | 18,535 |
| | $ | 11,936 |
| | $ | 26,116 |
| | $ | 22,489 |
| | $ | 18,106 |
| | $ | 12,943 |
|
| Employee stock purchase plan and stock options | 3,192 |
| | 2,352 |
| | 2,578 |
| | 2,012 |
| | 1,912 |
| | 1,613 |
|
| | $ | 21,727 |
| | $ | 14,288 |
| | $ | 28,694 |
| | $ | 24,501 |
| | $ | 20,018 |
| | $ | 14,556 |
|
As of December 31, 2012,2014, there was $15.1$24.5 million of total unrecognized compensation expense related to unvested restricted share awards, including those with performance conditions, which we expect to recognize over a remaining weighted-average period of 2.1 years.1.7 years. This unrecognized compensation cost assumes an estimated forfeiture rate of 7.5%4.0% as of December 31, 2012.
2014. Also as of December 31, 2012,2014, there was $0.1$0.3 million of unrecognized compensation expense related to unvested stock options, which we expect to recognize over a weighted-average period of 2.1 years.1.0 year.
Restricted shareand performance stock activity for the year ended December 31, 20122014 is summarized below:
|
| | | | | | |
| | Shares | | Weighted Average Grant Date Fair Value |
| Unvested balance as of December 31, 2011 | 1,435,882 |
| | $ | 18.97 |
|
| Granted | 511,557 |
| | 31.71 |
|
| Vested | (786,135 | ) | | 20.49 |
|
| Forfeited | (174,727 | ) | | 22.53 |
|
| Unvested balance as of December 31, 2012 | 986,577 |
| | 23.74 |
|
|
| | | | | | |
| | Shares | | Weighted Average Grant Date Fair Value |
| Unvested balance as of December 31, 2013 | 1,299,852 |
| | $ | 29.03 |
|
| Granted - restricted stock | 420,352 |
| | 38.06 |
|
| Granted - performance stock | 249,402 |
| | 34.61 |
|
| Vested - restricted stock | (423,970 | ) | | 26.70 |
|
| Vested - performance stock | (199,948 | ) | | 30.18 |
|
| Forfeited | (63,616 | ) | | 31.31 |
|
| Unvested balance as of December 31, 2014 | 1,282,072 |
| | 33.55 |
|
The total fair value of restricted shares and performance sharesawards granted during the year ended December 31, 2012, 2011,2014, 2013, and 20102012 was $16.2$25.4 million,, $18.4 $33.3 million,, and $12.7$16.2 million,, respectively. The total fair value of restricted sharesawards, including those with performance and market conditions which vested during the year ended December 31, 2012, 2011,2014, 2013, and 20102012 was $25.4$23.7 million,, $12.2 $22.3 million,, and $6.4$25.4 million,, respectively.
Performance and restricted unit activity for the year ended December 31, 2012 is summarized below:
|
| | | | | | | | | | | | |
| | Shares | | Weighted Average Grant Date Fair Value | | Aggregate Intrinsic Value | | Weighted Average Remaining Contractual term |
| | | | | | (In thousands) | | (Years) |
| Outstanding as of December 31, 2011 | — |
| | $ | — |
| | | | |
| Granted | 213,022 |
| | 33.59 |
| | | | |
| Vested | (210,880 | ) | | 33.58 |
| | $ | 6,066 |
| | |
| Outstanding as of December 31, 2012 | 2,142 |
| | 35.01 |
| | $ | 58 |
| | 0.2 |
| Performance and restricted units expected to vest as of December 31, 2012 | 2,142 |
| | 35.01 |
| | $ | 58 |
| | 0.2 |
The total fair value of performance and restricted units granted during the year ended December 31, 2012 was $7.2 million No performance or restricted units were granted or vested in 2011 and 2010.
Stock option activity for the year ended December 31, 2012 is summarized below:
|
| | | | | | | | | | | | |
| | Shares | | Weighted Average Exercise Price | | Aggregate Intrinsic Value | | Weighted Average Remaining Contractual term |
| | | | | | (In thousands) | | (Years) |
| Stock options outstanding as of December 31, 2011 | 553,049 |
| | $ | 20.91 |
| | | | |
| Granted | 15,000 |
| | 34.82 |
| | | | |
| Exercised | (153,238 | ) | | 18.27 |
| | | | |
| Forfeited | (750 | ) | | 22.37 |
| | | | |
| Stock options outstanding as of December 31, 2012 | 414,061 |
| | 22.39 |
| | $ | 2,204 |
| | 3.3 |
| Stock options exercisable and expected to vest as of December 31, 2012 | 414,061 |
| | 22.39 |
| | $ | 2,204 |
| | 3.3 |
| Exercisable as of December 31, 2012 | 399,061 |
| | 21.93 |
| | $ | 2,204 |
| | 3.1 |
The weighted-average grant date fair value per share of the sole stock option awarded during 2012performance awards with vesting conditions based on one-year Total Stockholder Return (TSR) was $13.97. To determine this$27.25. We estimated the fair value we appliedon the grant date using a Monte Carlo Simulation to project TSR over the performance period using correlations and volatilities of the ISS peer group. Additional inputs included a risk-free interest rate of 1.1%0.1%, expected volatility of 43.0%, an expected option life of 6 years, and expected dividend yield of 0%., and an expected life of 0.8 years. The weighted-average grant date fair value per share of the performance awards with vesting conditions based on three-year TSR, as described above, was $26.60. Additional inputs included a risk-free interest rate of 0.5%, dividend yield of 0%, and an expected life of 2.8 years.
The total fair value of restricted stock units granted during the year ended December 31, 2012 was $0.3 million with a weighted average grant date fair value of $35.01. These restricted stock units vested during 2013. No restricted stock units were granted in 2014 and 2013 and there were no outstanding restricted stock units as of December 31, 2014.
Stock option activity for the year ended December 31, 2014 is summarized below:
|
| | | | | | | | | | | | |
| | Shares | | Weighted Average Exercise Price | | Aggregate Intrinsic Value | | Weighted Average Remaining Contractual term |
| | | | | | (In thousands) | | (Years) |
| Stock options outstanding as of December 31, 2013 | 379,221 |
| | $ | 24.14 |
| | | | |
| Exercised | (122,523 | ) | | 24.93 |
| | | | |
| Stock options outstanding as of December 31, 2014 | 256,698 |
| | 23.77 |
| | $ | 7,640 |
| | 3.3 |
| Stock options exercisable and expected to vest as of December 31, 2014 | 256,698 |
| | 23.77 |
| | $ | 7,640 |
| | 3.3 |
| Exercisable as of December 31, 2014 | 221,698 |
| | 22.26 |
| | $ | 6,932 |
| | 2.5 |
The weighted-average grant date fair value per share of the stock options awarded to the new members of our board of directors during 2013 was $14.67. The weighted-average grant date fair value per share of the stock option awarded to the director appointed during 2012 was $13.97. We estimate the fair value of each stock option award on the grant date using the Black-Scholes option pricing model. To determine the fair value of these stock options we applied risk-free interest rates of 1.1% to 1.4%, expected volatilities of 41.3% to 43.0%, dividend yields of 0%, and expected lives of 6 years to 7 years. No stock options were granted in 2011 or 2010.2014.
The total intrinsic value of options exercised during the year ended December 31, 2014, 2013, and 2012 was $2.1 million, $1.2 million, and $2.0 million, respectively. The following is a summary of information about stock options outstanding and exercisable at December 31, 2012:
2014:
| | | | Options Outstanding | | Options Exercisable | Options Outstanding | | Options Exercisable |
| Range of Exercise Prices | Number Outstanding | | Weighted- Average Remaining Contractual Life (Years) | | Weighted- Average Exercise Price | | Number Exercisable | | Weighted- Average Exercise Price | Number Outstanding | | Weighted- Average Remaining Contractual Life (Years) | | Weighted- Average Exercise Price | | Number Exercisable | | Weighted- Average Exercise Price |
| $16.89 – $19.11 | 137,161 |
| | 2.5 | | $ | 18.46 |
| | 137,161 |
| | $ | 18.46 |
| |
| $19.11 | | 46,148 |
| | 1.1 | | $ | 19.11 |
| | 46,148 |
| | $ | 19.11 |
|
| $20.88 | 148,500 |
| | 4.1 | | 20.88 |
| | 148,500 |
| | 20.88 |
| 139,500 |
| | 2.2 | | 20.88 |
| | 139,500 |
| | 20.88 |
|
| $22.86 – $34.82 | 128,400 |
| | 3.3 | | 28.35 |
| | 113,400 |
| | 27.49 |
| 71,050 |
| | 6.9 | | 32.46 |
| | 36,050 |
| | 31.66 |
|
| | 414,061 |
| | | | 399,061 |
| | | 256,698 |
| | | | 221,698 |
| | |
17.18. Related Party Transactions
OnIn February 27, 2013, wethe Parent (as defined in Note 23, "Condensed Financial Information of Registrant,") entered into a lease (the “Lease”) with 6th6th & Pine Development, LLC (the “Landlord”)Landlord) for two office space locatedbuildings, referred to as Building A and Building B, in Long Beach, California. The lease consists of two office buildings as follows:
an existing building, which comprises approximately 70,000 square feet of office space, and
a new building, which is expected to comprise approximately 120,000 square feet of office space.
The term of the Lease with respect to the existing building is expected to commence onfor Building A commenced in June 1, 2013, and the term of the Lease with respect to the new building is expected to commence on November 1, 2014. The initial term of the Lease with respect to both buildings expires on December 31, 2024, subject to two options to extend thelease term for a period of five years each. Initial annual rent for the existing building is expected to be approximately $2.5 million and initial annual rent for the new building is expected to be approximately $4.0 million. Rent will increase 3.75% per year through the initial term. Rent during the extension terms will be the greater of then-current rent or fair market rent.Building B commenced in July 2014.
The principal members of the Landlord are John C. Molina, the Chief Financial Officerour chief financial officer and a director of the Company, and his wife. In addition, in connection with the development of the buildings being leased, the LandlordJohn C. Molina has pledged shares of common stock in the Company that he holds as trustee.holds. Dr. J. Mario Molina, the Company's Chief Executive Officerour chief executive officer, president and Chairmanchairman of the Boardboard of Directors,directors, holds a partial interest in such shares as trust beneficiary.
We have an equity investment in a medical service provider that provides certain vision servicesEffective October 31, 2014, the Parent entered into the First Amendment to our members. We account for this investmentOffice Building Lease (the Amended Lease) with the Landlord. The Amended Lease reduced the annual rent escalator under the equity method of accounting because we have an ownership interest inoriginal lease from 3.75% per year to 3.4% per year. The Amended Lease also extended the investee that confers significant influence over operating and financial policiesinitial base term of the investee. For bothoriginal lease by five years ended such that the Amended Lease will now expire on December 31, 2012, and 2011 our carrying amount for this investment amounted to $3.9 million. For2029, unless extended or earlier terminated. The Amended Lease also converted the years ended December 31, 2012, 2011, and 2010, we paid $28.4 million, $24.3 million, and $22.0 million, respectively, for medicaloriginal lease from a full service fees to this provider.
We are a partygross lease to a fee-for-service agreement with Pacific Hospitaltriple-net lease. For information regarding the future minimum lease payments, refer to Note 20, "Commitments and Contingencies." For information regarding the lease financing obligation, refer to Note 12, "Long-Term Debt."
Refer to Note 19, "Variable Interest Entities," for a discussion of Long Beach, or Pacific Hospital. Pacific Hospital is owned by Abrazos Healthcare, Inc. Until October 12, 2010, the majority of the shares of Abrazos Healthcare, Inc. were held as community property by Dr. Martha Bernadett and her husband. Dr. Martha Bernadett is the sister of Joseph M. Molina, M.D. (Dr. J. Mario Molina), our Chief Executive Officer, and John Molina, our Chief Financial Officer. On October 12, 2010, Dr. Bernadett and her husband sold their shares in Abrazos Healthcare, Inc., terminating our related party relationship with Pacific Hospital. Under the terms of this fee-for-service agreement we paid Pacific Hospital$0.8 millionfor the period from January 1, 2010 to October 12, 2010. Professional Corporations.
On December 26, 2012, we purchased 110,988 shares of our common stock from certain Molina family trusts for an aggregate purchase price of $3.0 million. This purchase transaction was approved by our board of directors. The shares were purchased at a price of $27.03, representing the closing price per share of our common stock on December 26, 2012. The shares were purchased from the Janet M. Watt Separate Property Trust dated 10/22/2007, or the Separate Property Trust, and the Watt Family Trust dated 10/11/1996, or the Family Trust. Janet M. Watt is the sister, and her husband Lawrence B. Watt is the brother-in-law, of Dr. J. Mario Molina and John Molina. Ms. Watt is the sole trustee of the Separate Property Trust, and a co-trustee with Lawrence B. Watt of the Family Trust.
18.19. Variable Interest Entities
Joseph M. Molina M.D., Professional Corporations
Our wholly owned subsidiary, American Family Care, Inc., or AFC, operates our primary care clinics. In 2012, AFC entered into services agreements with theThe Joseph M. Molina, M.D. Professional Corporations or JMMPC. JMMPC was(JMMPC) were created in 2012 to further advance our direct delivery line of business. ItsJMMPC's sole shareholder is Dr. J. Mario Molina, our Chairmanchief executive officer, president, and chairman of the Board, President and Chief Executive Officer.board of directors. Dr. Molina is paid no salary and receives no dividends in connection with his work for, or ownership of, JMMPC. Under the services agreements, AFC provides the clinic facilities, clinic administrative support staff, patient scheduling services and medical supplies to JMMPC, and JMMPC provides outpatient professionalprimary care medical services tothrough its employed physicians and other medical professionals. Beginning in the general public for routine non-life threatening, outpatient health care needs. Whilefourth quarter of 2014, JMMPC may providealso provided certain specialty referral services to the general public, substantiallyour California health plan members through a contracted provider network. Substantially all of the individuals served by JMMPC are members of our health plans. JMMPC does not have agreements to provide professional medical services with any other entities. In addition to the
Our wholly owned subsidiary, Molina Medical Management, Inc. (MMM), has entered into services agreements with AFC, JMMPC hasto provide clinic facilities, clinic administrative support staff, patient scheduling services and medical supplies to JMMPC. The services agreements were designed such that JMMPC will operate at break even, ensuring the availability of quality care and access for our health plan members. The services agreements provide that the administrative fees charged to JMMPC by MMM are reviewed annually to assure the achievement of this goal.
Separately, our California, Florida, New Mexico, Utah and Washington health plans have entered into affiliationprimary care services agreements with us. Under theseJMMPC. These agreements we have agreeddirect our health plans to perform a monthly reconciliation, to either fund JMMPC's operating deficits, or receive JMMPC's operating surpluses, based on a monthly reconciliation such that JMMPC will operate at break even and derive no profit.profit or loss. Because the MMM services agreements described above mitigate the likelihood of significant operating deficits or surpluses, such monthly reconciliation amounts are generally insignificant.
We have determined that JMMPC is a variable interest entity or VIE,(VIE), and that we are its primary beneficiary. We have reached this conclusion under the power and benefits criterion model according to U.S. generally accepted accounting principles.GAAP. Specifically, we have the power to direct the activities that most significantly affect JMMPC's economic performance, and the obligation to absorb losses or right to receive
benefits that are potentially significant to the VIE, under the services and affiliation agreements described above. Because we are its primary beneficiary, we have consolidated JMMPC. JMMPC's assets may be used to settle only JMMPC's obligations, and JMMPC's creditors have no recourse to the general credit of Molina Healthcare, Inc. As of December 31, 2012,2014, JMMPC had total assets of $1.4$31.1 million,, comprising primarily cash and equivalents, and total liabilities of $1.1$30.8 million. As of December 31, 2013, JMMPC had total assets of $6.9 million,, comprising primarily accrued payroll and employee benefits.total liabilities of $6.6 million.
Our maximum exposure to loss as a result of our involvement with this entityJMMPC is equalgenerally limited to the amounts needed to fund JMMPC's ongoing payroll and employee benefits. Additionally, in connection with specialty referral services provided beginning in 2014, our exposure to loss includes medical care costs associated with such services. We believe that such loss exposureexposures will be immaterial to our consolidated operating results and cash flows for the foreseeable future. For the year ended December 31, 2012, we provided an initial cash infusion of $0.3 million to JMMPC in the first quarter of 2012 to fund its start-up operations. During 2012 our health plans received $0.2 million from JMMPC under the terms of the affiliation agreement.
New Markets Tax Credit
During the fourth quarter ofIn 2011, our New Mexico data center subsidiary entered into a financing transaction with Wells Fargo Community Investment Holdings, LLC or Wells Fargo,(Wells Fargo), its wholly owned subsidiary New Mexico Healthcare Data Center Investment Fund, LLC or Investment Fund,(Investment Fund), and certain of Wells Fargo's affiliated Community Development Entities or CDEs,(CDEs), in connection with our participation in the federal government's New Markets Tax Credit Program or NMTC.(NMTC). The NMTC was established by Congress in 2000 to facilitate new or increased investments in businesses and real estate projects in low-income communities. The NMTC attracts investment capital to low-income communities by permitting investors to receive a tax credit against their federal income tax return in exchange for equity investments in specialized financial institutions, called CDEs, which provide financing to qualified active businesses operating in low-income communities. The credit amounts to 39% of the original investment amount and is claimed over a period of seven years (five(five percent for each of the first three years, and six percent for each of the remaining four years)years). The investment in the CDE cannot be redeemed before the end of the seven-year period.
In the fourth quarter of 2011, as a result of a series of simultaneous financing transactions, Wells Fargo contributed capital of $5.9$5.9 million to the Investment Fund, and Molina Healthcare, Inc. loaned the principal amount of $15.5$15.5 million to the Investment Fund. The Investment Fund then contributed the proceeds to certain CDEs, which, in turn, loaned the proceeds of $20.9$20.9 million to our New Mexico data center subsidiary. Wells Fargo will be entitled to claim the NMTC while we effectively received net loan proceeds equal to Wells Fargo's contribution to the Investment Fund, or approximately $5.9 million.$5.9 million. Additionally, financing costs incurred in structuring the arrangement amounting to $1.2$1.2 million were deferred and will be recognized as expense over the term of the loans. This transaction also includes a put/call feature that becomes enforceable at the end of the seven-year compliance period. Wells Fargo may exercise its put option or we can exercise the call, both of which will serve to transfer the debt obligation to us. Incremental costs to maintain the structure during the compliance period will be recognized as incurred.
We have determined that the financing arrangement with Investment Fund and CDEs is a VIE, and that we are the primary beneficiary of the VIE. We reached this conclusion based on the following:
The ongoing activities of the VIE-collectingVIE—collecting and remitting interest and fees and NMTC compliance-werecompliance—were all considered in the initial design and are not expected to significantly affect economic performance throughout the life of the VIE;
Contractual arrangements obligate us to comply with NMTC rules and regulations and provide various other guarantees to Investment Fund and CDEs;
Wells Fargo lacks a material interest in the underling economics of the project; and
We are obligated to absorb losses of the VIE.
Because we are the primary beneficiary of the VIE, we have included it in our consolidated financial statements. Wells Fargo's contribution of $5.9$5.9 million is included in cash at December 31, 20122014 and December 31, 2013 and the offsetting Wells Fargo's interest in the financing arrangement is included in other liabilities in the accompanying consolidated balance sheets.
As described above, this transaction also includes a put/call provision whereby we may be obligated or entitled to repurchase Wells Fargo's interest in the Investment Fund. The value attributed to the put/call is nominal. The NMTC is subject to 100% recapture for a period of seven years as provided in the Internal Revenue Code and applicable U.S. Treasury regulations. We are required to be in compliance with various regulations and contractual provisions that apply to the NMTC arrangement. Non-compliance with applicable requirements could result in Wells Fargo's projected tax benefits not being realized and, therefore, require us to indemnify Wells Fargo for any loss or recapture of NMTCs related to the financing until such time as the recapture provisions have expired under the applicable statute of limitations. We do not anticipate any credit recaptures will be required in connection with this arrangement.
98
20. Commitments and Contingencies
LeasesCertain Leasing Transactions.As described in Note 12, "Long-Term Debt," we entered into certain leasing transactions that have been classified as lease financing obligations. Such leases have initial terms that range from 16.5 years to 25 years. Additionally, the leases provide for renewal options ranging from 10 years to 25 years in aggregate.
Operating Leases.We lease administrative and clinic facilities and certain equipment under non-cancelable operating leases expiring at various dates through 2021.2023. Facility lease terms generally range from five to ten10 years with one to two renewal options for extended terms. In most cases, we are required to make additional payments under facility operating leases for taxes, insurance and other operating expenses incurred during the lease period. Certain of our leases contain rent escalation clauses or lease incentives, including rent abatements and tenant improvement allowances. Rent escalation clauses and lease incentives are taken into account in determining total rent expense to be recognized during the lease term.
Future minimum lease payments by year and in the aggregate under all operating leases and lease financing obligations consist of the following approximate amounts:
| | | | (In thousands) | Lease Financing Obligations | | Lease Financing Obligations - Related Party | | Operating Leases | | Total |
| 2013 | $ | 26,866 |
| |
| 2014 | 21,420 |
| |
| | | (In thousands) |
| 2015 | 14,808 |
| $ | 11,397 |
| | $ | 5,346 |
| | $ | 29,142 |
| | $ | 45,885 |
|
| 2016 | 8,472 |
| 11,739 |
| | 5,528 |
| | 22,989 |
| | 40,256 |
|
| 2017 | 6,939 |
| 12,091 |
| | 5,715 |
| | 21,602 |
| | 39,408 |
|
| 2018 | | 12,454 |
| | 5,910 |
| | 20,296 |
| | 38,660 |
|
| 2019 | | 12,828 |
| | 6,111 |
| | 12,777 |
| | 31,716 |
|
| Thereafter | 7,771 |
| 320,447 |
| | 73,784 |
| | 15,229 |
| | 409,460 |
|
| Total minimum lease payments | $ | 86,276 |
| |
| | | $ | 380,956 |
| | $ | 102,394 |
| | $ | 122,035 |
| | $ | 605,385 |
|
Rental expense related to theseoperating leases amounted to $20.5$32.4 million,, $23.1 $24.5 million,, and $25.1$20.5 million for the years ended December 31, 2012, 2011,2014, 2013, and 2010,2012, respectively.
Employment Agreements The amounts reported in "Lease Financing Obligations," and "Lease Financing Obligations - Related Party," above represent our contractual lease commitments for the properties described in Note 12, "Long-Term Debt" under the subheading "Lease Financing Obligations." Payments under these leases adjust the lease financing obligation, and the imputed interest is recorded to interest expense in our consolidated statements of income.
InEmployment Agreements.In 2002 we entered into employment agreements with our Chief Executive Officer and Chief Financial Officer, which have beenwere amended and restated as of December 31,in 2009. These employment agreements had initial terms of one to three years and are subject to automatic one-year extensions thereafter. Should the executives be terminated without cause or resign for good reason before a change of control, as defined, we will pay one year’s base salary and termination bonus, as defined, in addition to full vesting of 401(k) employer contributions and stock-based awards, and a cash sum equal in value topayment for health and welfare benefits.
In 2013 we entered into employment agreements with our Chief Operating Officer, Chief Accounting Officer, and Chief Legal Officer. These agreements continue until terminated by us, or the executive resigns. If the executive’s employment is terminated by us without cause or the executive resigns for good reason, the executive will be entitled to receive one year’s base salary and termination bonus, as defined, full vesting of all time-based equity compensation, and a cash payment for health and welfare benefits.
Payment of the executives’ severance benefits provided for 18 months.is contingent upon the executive’s signing a release agreement waiving claims against us. If the executives are terminated for cause, no further payments are due under the contracts.
If termination occurs within two years following a change of control, the executives will receive two times their base salary and termination bonus, in addition to full vesting of 401(k) employer contributions and stock-based awards, and a cash sum equal in value to health and welfare benefits provided for three years.
Legal Proceedings
Proceedings.The health care and business process outsourcing industries are subject to numerous laws and regulations of federal, state, and local governments. Compliance with these laws and regulations can be subject to government review and interpretation, as well as regulatory actions unknown and unasserted at this time. Penalties associated with violations of these laws and regulations include significant fines and penalties, exclusion from participating in publicly funded programs, and the repayment of previously billed and collected revenues.
We are involved in legal actions in the ordinary course of business, some of which seek monetary damages, including claims for punitive damages, which are not covered by insurance. We have accrued liabilities for certain matters for which we deem the loss to be both probable and estimable. Although we believe that our estimates of such losses are reasonable, these estimates could change as a result of further developments of these matters. The outcome of legal actions is inherently uncertain and such pending matters for which accruals have not been established have not progressed sufficiently through
discovery and/or development of important factual information and legal issues to enable us to estimate a range of possible loss, if any. While it is not possible to accurately predict or determine the eventual outcomes of these items, an adverse determination in one or more of these pending matters could have a material adverse effect on our consolidated financial position, results of operations, or cash flows.
Washington Health Plan. In September 2014, our Washington health plan paid $19.2 million to the Washington Health Care Authority (HCA) to settle two outstanding overpayment matters. The matters related to demands for recoupment of claims for psychotropic drugs and claims for health plan members under the Washington Community Options Program Entry System (COPES). Additionally, in September 2014 HCA paid our Washington health plan $8.0 million to settle certain matters brought by the Washington health plan related to auto-assignment provisions in the parties' contract. The net effect of these settlements resulted in a premium revenue reduction of $11.2 million in the third quarter of 2014, and resolved all pending disputes between the parties.
State of Louisiana. On June 26, 2014, the state of Louisiana filed a Petition for Damages against Molina Medicaid Solutions, Molina Healthcare, Inc., Unisys Corporation, and Paramax Systems Corporation, a subsidiary of Unisys, in the Parish of Baton Rouge, 19th Judicial District, versus number 631612. The Petition alleges that between 1989 and 2012, the defendants utilized an incorrect reimbursement formula for the payment of pharmaceutical claims. We believe we have several meritorious defenses to the claims of the state, and any liability for the alleged claims is not currently probable or reasonably estimable.
USA and State of Florida ex rel. Charles Wilhelm. On July 24, 2014, Molina Healthcare, Inc. and Molina Healthcare of Florida, Inc. were served with a Complaint filed under seal on December 5, 2012 in District Court for the Southern District of Florida by relator, Charles C. Wilhelm, M.D., Case No. 12-24298. The Complaint alleges that, in late 2008 and early 2009, in connection with the acquisition of Florida NetPass by which Molina Healthcare entered into the state of Florida, the defendants failed to adequately staff the plan and provide other services, resulting in a disproportionate number of sicker beneficiaries of Florida NetPass moving back into the Florida fee-for-service Medicaid program. This alleged conduct purportedly resulted in a violation of the federal False Claims Act. Both the United States of America and the state of Florida have declined to intervene. We believe we have several meritorious defenses to the claims of the relator, and any liability for the alleged claims is not currently probable or reasonably estimable.
United States of America, ex rel., Anita Silingo v. Mobile Medical Examination Services, Inc., et al. On or around October 14, 2014, Molina Healthcare of California, Molina Healthcare of California Partner Plan, Inc., Mobile Medical Examination Services, Inc. (MedXM), and other health plan defendants were served with a Complaint previously filed under seal in the Central District Court of California by relator, Anita Silingo, Case No. SACV13-1348-FMO(SHx). The Complaint alleges that MedXM improperly modified medical records and otherwise took inappropriate steps to increase members’ risk adjustment scores, and that the defendants, including Molina Healthcare of California and Molina Healthcare of California Partner Plan, Inc., purportedly turned a “blind eye” to these unlawful practices. The Department of Justice has declined to intervene. We believe that we have several meritorious defenses to the claims of the relator, and any liability for the alleged claims is not currently probable or reasonably estimable.
Professional Liability Insurance
Insurance.We carry medical professional liability insurance for health care services rendered through our clinics in California, Florida, New Mexico, Virginia,the primary care and Washington. Wehospital institutions that we manage. In addition, we also carry claims-made managed care errors and omissions professional liability insurance for our health plan operations.all Molina entities.
Provider Claims
Claims.Many of our medical contracts are complex in nature and may be subject to differing interpretations regarding amounts due for the provision of various services. Such differing interpretations have led certain medical providers to pursue us for additional compensation. The claims made by providers in such circumstances often involve issues of contract compliance, interpretation, payment methodology, and intent. These claims often extend to services provided by the providers over a number of years.
Various providers have contacted us seeking additional compensation for claims that we believe to have been settled. These matters, when finally concluded and determined, will not, in our opinion, have a material adverse effect on our business, consolidated financial position, results of operations, or cash flows.
Regulatory Capital and Dividend Restrictions
Restrictions.Our health plans, which are operated by our respective wholly owned subsidiaries in those states, are subject to state laws and regulations that, among other things, require the maintenance of minimum levels of statutory capital, as defined by each state. Regulators in some states may also attempt to enforce capital requirements upon us that require the retention of net worth in excess of amounts formally required by statute or regulation. Such state lawsstatutes, regulations and regulationsinformal capital requirements also restrict the timing, payment, and amount of dividends and other distributions that may be paid to us as the sole stockholder. To the extent theour subsidiaries must comply with these regulations, they may not have the financial flexibility to transfer funds to us. TheBased upon current statutes and regulations, the net assets in these subsidiaries (after inter-companyintercompany eliminations) which may not be transferable to us in the form of loans, advances, or cash dividends was $549.7approximately $859 million atDecember 31, 2012,2014, and$492.4 $608 million at December 31, 2011.2013. Because of the statutory restrictions that inhibit the ability of our health plans to transfer net assets to us, the amount of retained
earnings readily available to pay dividends to our stockholders areis generally limited to cash, cash equivalents and investments held by the parent company – Molina Healthcare, Inc. Such cash, cash equivalents and investments amounted to $46.9$202.6 million and $23.6$365.2 million as of December 31, 2012,2014, and 2011,2013, respectively.
The National Association of Insurance Commissioners or NAIC,(NAIC), adopted rules effective December 31, 1998, which, if implemented by the states, set minimum capitalization requirements for insurance companies, HMOs, and other entities bearing risk for health care coverage. The requirements take the form of risk-based capital or RBC,(RBC), rules. Illinois, Michigan, New Mexico, Ohio, South Carolina, Texas, Utah, Washington, and Wisconsin have adopted these rules, which may vary from state to state. California and Florida have not yet adopted NAIC risk-based capital requirements for HMOs, and have not formally given notice of their intention to do so. Such requirements, if adopted by California and Florida, may increase the minimum capital required for those states.
As ofDecember 31, 2012,2014, our health plans had aggregate statutory capital and surplus of approximately$557.9 $955 millioncompared with the required minimum aggregate statutory capital and surplus of approximately$345.7 $541 million. All of our health plans were in compliance with the minimum capital requirements at December 31, 2012.2014, with the exception of our Florida health plan, which was funded in February 2015 to meet the minimum capital requirement. We have the ability and commitment to provide additional capital to each of our health plans when necessary to ensure that statutory capital and surplus continue to meet regulatory requirements.
Receivable/Liability for Ceded Life and Annuity Contracts
Prior to February 17, 2012, we reported a 100% ceded reinsurance arrangement for life insurance policies written and held by our then wholly owned insurance subsidiary, Molina Healthcare Insurance Company, by recording a non-current receivable
from the reinsurer with a corresponding non-current liability for ceded life and annuity contracts. Effective February 17, 2012, we sold Molina Healthcare Insurance Company. The transaction resulted in the elimination of both the noncurrent receivable and liability for ceded life and annuity contracts, each amounting to $23.4 million as of December 31, 2011. Additionally, we recorded a gain of approximately $1.7 million to general and administrative expenses in the first quarter of 2012 upon closing of the transaction.
Molina Healthcare Insurance Company is now named Catamaran Insurance of Ohio, or Catamaran. In the event that both the reinsurer and Catamaran are unable to pay benefit on policies that were in-force as of the sale date, we remain ultimately liable for payment of such benefits. Because we no longer own Catamaran, we no longer have access to its financial records; therefore, the maximum amount of potential future payments is not determinable. We believe the possibility of our having to pay such benefits is remote, and no provision for the payment of such benefits is included in our consolidated financial statements.
20.21. Segment ReportingInformation
We report our financial performance based on two reportable segments: the Health Plans segment and the Molina Medicaid Solutions.Solutions segment. Our reportable segments are consistent with how we manage the business and view the markets we serve. Our Health Plans segment consists of our state health plans which serve Medicaid populations in nine states, subsequent to the termination ofand our Medicaid contract in Missouri effective June 30, 2012, and also includes our smaller direct delivery line of business. Our state health plans represent operating segments that have been aggregated for reporting purposes because they share similar economic characteristics.
Our Molina Medicaid Solutions segment provides MMIS design, development, implementation; business process outsourcing solutions; hosting services; and information technology support services to state Medicaid agencies in an additional five states. The Molina Medicaid Solutions segment was added to our internal financial reporting structure when we acquired this business in the second quarteragencies.
We rely on an internal management reporting process that provides segment information to the operating income level for purposes of making financial decisions and allocating resources. The accounting policies of the segments are the same as those described in Note 2,, “Significant "Significant Accounting Policies.” The" For presentation purposes, the cost of centralized services shared betweenis reported within the Health Plans segment.
|
| | | | | | | | | | | |
| | Year Ended December 31, |
| | 2014 | | 2013 | | 2012 |
| | (In thousands) |
| Revenue, continuing operations: | | | | | |
| Health Plans segment: | | | | | |
| Premium revenue | $ | 9,022,511 |
| | $ | 6,179,170 |
| | $ | 5,544,121 |
|
| Premium tax revenue | 294,388 |
| | 172,017 |
| | 158,991 |
|
| Health insurer fee revenue | 119,484 |
| | — |
| | — |
|
| Investment income | 8,093 |
| | 6,890 |
| | 5,075 |
|
| Other revenue | 12,074 |
| | 26,322 |
| | 18,312 |
|
| Molina Medicaid Solutions segment: | | | | | |
| Service revenue | 210,051 |
| | 204,535 |
| | 187,710 |
|
| | $ | 9,666,601 |
| | $ | 6,588,934 |
| | $ | 5,914,209 |
|
| | | | | | |
| Depreciation and amortization reported in the consolidated statements of cash flows: | | | | | |
| Health Plans segment | $ | 89,438 |
| | $ | 67,446 |
| | $ | 58,577 |
|
| Molina Medicaid Solutions segment | 44,966 |
| | 26,420 |
| | 20,187 |
|
| | $ | 134,404 |
| | $ | 93,866 |
| | $ | 78,764 |
|
| Income from continuing operations before income tax expense: | | | | | |
| Health Plans segment | $ | 150,090 |
| | $ | 103,931 |
| | $ | 17,366 |
|
| Molina Medicaid Solutions segment | 42,827 |
| | 32,629 |
| | 23,727 |
|
| Operating income, continuing operations | 192,917 |
| | 136,560 |
| | 41,093 |
|
| Other expenses, net | 57,613 |
| | 55,414 |
| | 17,714 |
|
| | $ | 135,304 |
| | $ | 81,146 |
| | $ | 23,379 |
|
|
| | | | | | | | | | | |
| | As of December 31, |
| | 2014 | | 2013 | | 2012 |
| | (In thousands) |
| Goodwill and intangible assets, net: | | | | | |
| Health Plans segment | $ | 286,459 |
| | $ | 248,562 |
| | $ | 139,710 |
|
| Molina Medicaid Solutions segment | 74,778 |
| | 81,047 |
| | 89,089 |
|
| | $ | 361,237 |
| | $ | 329,609 |
| | $ | 228,799 |
|
| Total assets: | | | | | |
| Health Plans segment | $ | 4,270,870 |
| | $ | 2,809,439 |
| | $ | 1,702,212 |
|
| Molina Medicaid Solutions segment | 206,345 |
| | 193,498 |
| | 232,610 |
|
| | $ | 4,477,215 |
| | $ | 3,002,937 |
| | $ | 1,934,822 |
|
Goodwill and Molina Medicaid Solutions segments is charged tointangible assets increased in the Health Plans segment.
Molina Medicaid Solutions was acquired on May 1, 2010; therefore,segment due to the year ended December 31, 2010 includes only eight months of operating results for this segment. Operating segment information is as follows:
acquisitions described in Note 4, "Business Combinations."
|
| | | | | | | | | | | |
| | Year Ended December 31, |
| | 2012 | | 2011 | | 2010 |
| | (In thousands) |
| Segment Information: | | | | | |
| Revenue: | | | | | |
| Health Plans: | | | | | |
| Premium revenue | $ | 5,826,491 |
| | $ | 4,603,407 |
| | $ | 3,989,909 |
|
| Investment income | 5,188 |
| | 5,539 |
| | 6,259 |
|
| Rental income | 9,374 |
| | 547 |
| | — |
|
| Molina Medicaid Solutions: | | | | | |
| Service revenue | 187,710 |
| | 160,447 |
| | 89,809 |
|
| | $ | 6,028,763 |
| | $ | 4,769,940 |
| | $ | 4,085,977 |
|
| Depreciation and amortization: | | | | | |
| Health Plans | $ | 58,577 |
| | $ | 45,734 |
| | $ | 42,282 |
|
| Molina Medicaid Solutions | 20,187 |
| | 28,649 |
| | 18,483 |
|
| | $ | 78,764 |
| | $ | 74,383 |
| | $ | 60,765 |
|
| Operating Income: | | | | | |
| Health Plans | $ | 11,746 |
| | $ | 78,110 |
| | $ | 102,392 |
|
| Molina Medicaid Solutions | 23,727 |
| | 2,063 |
| | 2,609 |
|
| Total operating income | 35,473 |
| | 80,173 |
| | 105,001 |
|
| Interest expense | (16,769 | ) | | (15,519 | ) | | (15,509 | ) |
| Other income | 361 |
| | — |
| | — |
|
| Income before income taxes | $ | 19,065 |
| | $ | 64,654 |
| | $ | 89,492 |
|
|
| | | | | | | |
| | As of December 31, |
| | 2012 | | 2011 |
| | (In thousands) |
| Goodwill and intangible assets, net: | | | |
| Health Plans | $ | 139,710 |
| | $ | 159,963 |
|
| Molina Medicaid Solutions | 89,089 |
| | 95,787 |
|
| | $ | 228,799 |
| | $ | 255,750 |
|
| Total assets: | | | |
| Health Plans | $ | 1,702,212 |
| | $ | 1,429,283 |
|
| Molina Medicaid Solutions | 232,610 |
| | 222,863 |
|
| | $ | 1,934,822 |
| | $ | 1,652,146 |
|
21.22. Quarterly Results of Operations (Unaudited)
The following is a summary of thetable summarizes quarterly unaudited results of operations for the years ended December 31, 20122014 and 2011.
|
| | | | | | | | | | | | | | | |
| | For The Quarter Ended, |
| | March 31, 2012 | | June 30, 2012 | | September 30, 2012 | | December 31,
2012 |
| | (In thousands, except per-share data) |
| Premium revenue | $ | 1,327,449 |
| | $ | 1,492,272 |
| | $ | 1,488,718 |
| | $ | 1,518,052 |
|
| Service revenue | 42,205 |
| | 41,724 |
| | 48,422 |
| | 55,359 |
|
| Operating income (loss) | 33,420 |
| | (59,267 | ) | | 7,187 |
| | 54,133 |
|
| Income (loss) before income taxes | 29,122 |
| | (63,075 | ) | | 2,872 |
| | 50,146 |
|
| Net income (loss) | 18,089 |
| | (37,306 | ) | | 3,364 |
| | 25,643 |
|
| Net income (loss) per share (2): | | | | | | | |
| Basic | $ | 0.39 |
| | $ | (0.80 | ) | | $ | 0.07 |
| | $ | 0.55 |
|
| Diluted | $ | 0.39 |
| | $ | (0.80 | ) | | $ | 0.07 |
| | $ | 0.54 |
|
Presentation," the results of the Missouri health plan are reported as discontinued operations for all periods presented. For further information relating to our segment reporting, refer to Note 21, "Segment Information."
| | | | For The Quarter Ended, | For The Quarter Ended |
| | March 31, 2011 | | June 30, 2011 | | September 30, 2011 | | December 31,
2011(1) | March 31,
2014 | | June 30,
2014 | | September 30, 2014 | | December 31,
2014 |
| | (In thousands, except per-share data) | (In thousands, except per-share data) |
| Premium revenue | $ | 1,081,438 |
| | $ | 1,128,770 |
| | $ | 1,138,230 |
| | $ | 1,254,969 |
| $ | 1,940,337 |
| | $ | 2,167,142 |
| | $ | 2,316,759 |
| | $ | 2,598,273 |
|
| Service revenue | 36,674 |
| | 36,888 |
| | 37,728 |
| | 49,157 |
| 53,630 |
| | 50,232 |
| | 52,557 |
| | 53,632 |
|
| Operating income (loss) | 31,300 |
| | 31,410 |
| | 33,566 |
| | (16,103 | ) | |
| Income (loss) before income taxes | 27,697 |
| | 27,727 |
| | 29,186 |
| | (19,956 | ) | |
| Net income (loss) | 17,388 |
| | 17,440 |
| | 18,950 |
| | (32,960 | ) | |
| Net income (loss) per share (2): | | | | | | | | |
| Operating income, Health Plans segment | | 14,019 |
| | 21,986 |
| | 29,874 |
| | 84,211 |
|
| Operating income, Molina Medicaid Solutions segment | | 10,248 |
| | 10,441 |
| | 9,905 |
| | 12,233 |
|
| | | | | | | | | |
| Income from continuing operations | | $ | 4,834 |
| | $ | 7,741 |
| | $ | 16,070 |
| | $ | 33,933 |
|
| (Loss) income from discontinued operations | | (336 | ) | | 70 |
| | 52 |
| | (141 | ) |
| Net income | | $ | 4,498 |
| | $ | 7,811 |
| | $ | 16,122 |
| | $ | 33,792 |
|
| | | | | | | | | |
| Net income per share (1): | | | | | | | | |
| Basic | $ | 0.38 |
| | $ | 0.38 |
| | $ | 0.41 |
| | $ | (0.72 | ) | $ | 0.10 |
| | $ | 0.17 |
| | $ | 0.34 |
| | $ | 0.70 |
|
| Diluted | $ | 0.38 |
| | $ | 0.38 |
| | $ | 0.41 |
| | $ | (0.72 | ) | $ | 0.09 |
| | $ | 0.16 |
| | $ | 0.33 |
| | $ | 0.69 |
|
|
| | | | | | | | | | | | | | | |
| | For The Quarter Ended |
| | March 31,
2013 | | June 30,
2013 (2) | | September 30, 2013 | | December 31,
2013 |
| | (In thousands, except per-share data) |
| Premium revenue | $ | 1,497,433 |
| | $ | 1,501,729 |
| | $ | 1,584,656 |
| | $ | 1,595,352 |
|
| Service revenue | 49,756 |
| | 49,672 |
| | 51,100 |
| | 54,007 |
|
| Operating income (loss), Health Plans segment | 61,520 |
| | 40,151 |
| | 16,929 |
| | (14,669 | ) |
| Operating income, Molina Medicaid Solutions segment | 6,353 |
| | 6,295 |
| | 7,997 |
| | 11,984 |
|
| | | | | | | | |
| Income (loss) from continuing operations | $ | 30,522 |
| | $ | 15,796 |
| | $ | 7,553 |
| | $ | (9,041 | ) |
| (Loss) income from discontinued operations | (607 | ) | | 8,775 |
| | 16 |
| | (85 | ) |
| Net income (loss) | $ | 29,915 |
| | $ | 24,571 |
| | $ | 7,569 |
| | $ | (9,126 | ) |
| | | | | | | | |
| Net income (loss) per share (1): | | | | | | | |
| Basic | $ | 0.65 |
| | $ | 0.54 |
| | $ | 0.17 |
| | $ | (0.20 | ) |
| Diluted | $ | 0.64 |
| | $ | 0.53 |
| | $ | 0.16 |
| | $ | (0.20 | ) |
| |
| (1) | On February 17, 2012, the Division of Purchasing of the Missouri Office of Administration notified us that our Missouri health plan was not awarded a contract under the Missouri HealthNet Managed Care Request for Proposal; therefore, our Missouri health plan's existing contract with the state expired without renewal on June 30, 2012. In connection with this notification, we recorded a total non-cash impairment charge of $64.6 million in the fourth quarter of 2011, of which $6.1 million related to finite-lived intangible assets, and $58.5 million related to goodwill. The impairment charge comprised substantially all intangible assets relating to contract rights and licenses, and provider networks recorded at the time of our acquisition of the Missouri health plan in 2007. For the quarter ended December 31, 2011, the impairment charge reduced diluted earnings per share by $1.34.
|
| |
(2) | Potentially dilutive shares issuable pursuant to our 2007 offering of convertible senior notes1.125% Warrants and 1.625% Notes were not included in the computation of diluted net income per share, because to do so would have been anti-dilutiveanti-dilutive. Potentially dilutive shares issuable pursuant to our 3.75% Notes were not included in the computation of diluted net income per share for the yearsquarter ended DecemberMarch 31, 2012, and 2011. 2013, because to do so would have been anti-dilutive. |
| |
| (2) | We abandoned our equity interests in the Missouri health plan during the second quarter of 2013, resulting in the recognition of a tax benefit of $9.5 million, which is reported in (loss) income from discontinued operations. |
22.23. Condensed Financial Information of Registrant
Following are our parent company only condensed balance sheets as of December 31, 20122014 and 2011,2013, and our condensed statements of income, condensed statements of comprehensive income and condensed statements of cash flows for each of the three years in the period ended December 31, 2012.2014.
Condensed Balance Sheets
|
| | | | | | | |
| | December 31, |
| | 2012 | | 2011 |
| | (Amounts in thousands, except per-share data) |
| ASSETS | | | |
| Current assets: | |
| | |
| Cash and cash equivalents | $ | 39,068 |
| | $ | 14,650 |
|
| Investments | 2,015 |
| | 2,010 |
|
| Income tax refundable | 8,868 |
| | 14,126 |
|
| Deferred income taxes | 9,706 |
| | 9,133 |
|
| Due from affiliates | 55,382 |
| | 60,569 |
|
| Prepaid and other current assets | 19,164 |
| | 10,467 |
|
| Total current assets | 134,203 |
| | 110,955 |
|
| Property and equipment, net | 108,808 |
| | 82,437 |
|
| Goodwill | 52,302 |
| | 53,769 |
|
| Auction rate securities | 3,615 |
| | 4,694 |
|
| Investments in subsidiaries | 768,765 |
| | 740,345 |
|
| Advances to related parties and other assets | 34,600 |
| | 32,473 |
|
| | $ | 1,102,293 |
| | $ | 1,024,673 |
|
| LIABILITIES AND STOCKHOLDERS' EQUITY | | | |
| Liabilities: | | | |
| Accounts payable and accrued liabilities | $ | 73,883 |
| | $ | 71,392 |
|
| Long-term debt | 215,468 |
| | 169,526 |
|
| Deferred income taxes | 17,122 |
| | 16,909 |
|
| Other long-term liabilities | 13,506 |
| | 11,773 |
|
| Total liabilities | 319,979 |
| | 269,600 |
|
| Stockholders' equity: | | | |
|
| Common stock, $0.001 par value; 80,000 shares authorized; outstanding: | | | |
|
| 46,762 shares at December 31, 2012 and 45,815 shares at December 31, 2011 | 47 |
| | 46 |
|
| Preferred stock, $0.001 par value; 20,000 shares authorized, no shares issued and outstanding | — |
| | — |
|
| Paid-in capital | 285,524 |
| | 266,022 |
|
| Accumulated other comprehensive loss | (457 | ) | | (1,405 | ) |
| Treasury stock, at cost; 111 shares at December 31, 2012 | (3,000 | ) | | — |
|
| Retained earnings | 500,200 |
| | 490,410 |
|
| Total stockholders' equity | 782,314 |
| | 755,073 |
|
| | $ | 1,102,293 |
| | $ | 1,024,673 |
|
|
| | | | | | | |
| | December 31, |
| | 2014 | | 2013 |
| | (Amounts in thousands, except per-share data) |
| ASSETS |
| Current assets: | |
| | |
| Cash and cash equivalents | $ | 74,696 |
| | $ | 99,698 |
|
| Investments | 126,439 |
| | 262,665 |
|
| Income tax refundable | 13,413 |
| | 8,403 |
|
| Deferred income taxes | 8,546 |
| | 10,073 |
|
| Due from affiliates | 17,567 |
| | 35,928 |
|
| Prepaid expenses and other current assets | 36,143 |
| | 28,387 |
|
| Total current assets | 276,804 |
| | 445,154 |
|
| Property, equipment, and capitalized software, net | 265,110 |
| | 225,522 |
|
| Goodwill and intangible assets, net | 64,972 |
| | 68,902 |
|
| Investments in subsidiaries | 1,376,613 |
| | 992,998 |
|
| Deferred income taxes | 2,824 |
| | 17,245 |
|
| Derivative asset | 329,323 |
| | 186,351 |
|
| Advances to related parties and other assets | 57,263 |
| | 52,615 |
|
| | $ | 2,372,909 |
| | $ | 1,988,787 |
|
| | | | |
| LIABILITIES AND STOCKHOLDERS' EQUITY |
| Liabilities: | | | |
| Accounts payable and accrued liabilities | $ | 106,212 |
| | $ | 109,388 |
|
| Long-term debt | 865,148 |
| | 757,770 |
|
| Lease financing obligations - related party | 40,241 |
| | 27,092 |
|
| Derivative liability | 329,194 |
| | 186,239 |
|
| Other long-term liabilities | 21,672 |
| | 15,361 |
|
| Total liabilities | 1,362,467 |
| | 1,095,850 |
|
| Stockholders' equity: | | | |
| Common stock, $0.001 par value; 150,000 shares authorized; outstanding: | | |
|
|
| 49,727 shares at December 31, 2014 and 45,871 shares at December 31, 2013 | 50 |
| | 46 |
|
| Preferred stock, $0.001 par value; 20,000 shares authorized, no shares issued and outstanding | — |
| | — |
|
| Additional paid-in capital | 396,059 |
| | 340,848 |
|
| Accumulated other comprehensive loss | (1,019 | ) | | (1,086 | ) |
| Retained earnings | 615,352 |
| | 553,129 |
|
| Total stockholders' equity | 1,010,442 |
| | 892,937 |
|
| | $ | 2,372,909 |
| | $ | 1,988,787 |
|
Condensed Statements of Income
|
| | | | | | | | | | | |
| | Year Ended December 31, |
| | 2014 | | 2013 | | 2012 |
| | (In thousands) |
| Revenue: | | | | | |
| Management fees and other operating revenue | $ | 703,710 |
| | $ | 599,049 |
| | $ | 406,981 |
|
| Investment income | 2,218 |
| | 2,768 |
| | 550 |
|
| Total revenue | 705,928 |
| | 601,817 |
| | 407,531 |
|
| Expenses: | | | | | |
|
| Medical care costs | 46,437 |
| | 37,862 |
| | 33,102 |
|
| General and administrative expenses | 582,587 |
| | 503,781 |
| | 367,606 |
|
| Depreciation and amortization | 72,995 |
| | 51,562 |
| | 38,794 |
|
| Total operating expenses | 702,019 |
| | 593,205 |
| | 439,502 |
|
| Operating income (loss) | 3,909 |
| | 8,612 |
| | (31,971 | ) |
| Interest expense | 56,728 |
| | 50,508 |
| | 14,469 |
|
| Other expense | 844 |
| | 3,811 |
| | — |
|
| Loss before income taxes and equity in net income of subsidiaries | (53,663 | ) | | (45,707 | ) | | (46,440 | ) |
| Income tax benefit | (26,776 | ) | | (15,455 | ) | | (15,779 | ) |
| Net loss before equity in net income of subsidiaries | (26,887 | ) | | (30,252 | ) | | (30,661 | ) |
| Equity in net income of subsidiaries | 89,110 |
| | 83,181 |
| | 40,451 |
|
| Net income | $ | 62,223 |
| | $ | 52,929 |
| | $ | 9,790 |
|
Condensed Statements of Comprehensive Income
|
| | | | | | | | | | | |
| | Year Ended December 31, |
| | 2012 | | 2011 | | 2010 |
| | (In thousands) |
| Revenue: | | | | | |
| Management fees and other operating revenue | $ | 406,981 |
| | $ | 308,287 |
| | $ | 238,883 |
|
| Investment income | 550 |
| | 81 |
| | 1,153 |
|
| Total revenue | 407,531 |
| | 308,368 |
| | 240,036 |
|
| Expenses: | | | |
| | |
|
| Medical care costs | 33,102 |
| | 31,672 |
| | 30,582 |
|
| General and administrative expenses | 367,606 |
| | 272,302 |
| | 218,834 |
|
| Depreciation and amortization | 38,794 |
| | 31,355 |
| | 27,166 |
|
| Total expenses | 439,502 |
| | 335,329 |
| | 276,582 |
|
| Operating loss | (31,971 | ) | | (26,961 | ) | | (36,546 | ) |
| Interest expense | 14,469 |
| | 14,958 |
| | 15,500 |
|
| Loss before income taxes and equity in net income of subsidiaries | (46,440 | ) | | (41,919 | ) | | (52,046 | ) |
| Income tax benefit | (15,779 | ) | | (14,826 | ) | | (16,936 | ) |
| Net loss before equity in net income of subsidiaries | (30,661 | ) | | (27,093 | ) | | (35,110 | ) |
| Equity in net income of subsidiaries | 40,451 |
| | 47,911 |
| | 90,080 |
|
| Net income | $ | 9,790 |
| | $ | 20,818 |
| | $ | 54,970 |
|
|
| | | | | | | | | | | |
| | Year Ended December 31, |
| | 2014 | | 2013 | | 2012 |
| | (In thousands) |
| Net income | $ | 62,223 |
| | $ | 52,929 |
| | $ | 9,790 |
|
| Other comprehensive income (loss): | | | | | |
| Unrealized investment gain (loss) | 108 |
| | (1,015 | ) | | 1,529 |
|
| Effect of income tax expense (benefit) | 41 |
| | (386 | ) | | 581 |
|
| Other comprehensive income (loss), net of tax | 67 |
| | (629 | ) | | 948 |
|
| Comprehensive income | $ | 62,290 |
| | $ | 52,300 |
| | $ | 10,738 |
|
Condensed Statements of Cash Flows
| | | | Year Ended December 31, | Year Ended December 31, |
| | 2012 | | 2011 | | 2010 | 2014 | | 2013 | | 2012 |
| | (In thousands) | (In thousands) |
| Operating activities: | | | | | | | | | | |
| Cash provided by operating activities | $ | 20,611 |
| | $ | 28,606 |
| | $ | 19,380 |
| |
| Net cash provided by operating activities | | $ | 73,674 |
| | $ | 62,602 |
| | $ | 20,611 |
|
| Investing activities: | | | |
| | |
| | | | | |
|
| Net dividends from and capital contributions to subsidiaries | 1,579 |
| | 27,872 |
| | 70,800 |
| |
| Capital contributions to subsidiaries | | (292,232 | ) | | (166,112 | ) | | (100,221 | ) |
| Dividends received from subsidiaries | | — |
| | 24,429 |
| | 101,800 |
|
| Purchases of investments | (1,905 | ) | | (2,020 | ) | | (2,019 | ) | (128,996 | ) | | (362,927 | ) | | (1,905 | ) |
| Sales and maturities of investments | 4,067 |
| | 3,760 |
| | 14,083 |
| |
| Cash paid in business combinations | — |
| | — |
| | (139,762 | ) | |
| Proceeds from sales and maturities of investments | | 263,479 |
| | 97,713 |
| | 4,067 |
|
| Proceeds from sale of subsidiary, net of cash surrendered | 9,162 |
| | — |
| | — |
| — |
| | — |
| | 9,162 |
|
| Purchases of equipment | (61,813 | ) | | (30,930 | ) | | (40,419 | ) | (93,610 | ) | | (76,873 | ) | | (61,813 | ) |
| Changes in amounts due to and due from affiliates | 5,187 |
| | (50,090 | ) | | (5,723 | ) | |
| Change in other assets and liabilities | (1,342 | ) | | (20,441 | ) | | 829 |
| |
| Change in amounts due to/from affiliates | | 16,054 |
| | (5,888 | ) | | 5,187 |
|
| Other, net | | 7,640 |
| | (6,175 | ) | | (1,342 | ) |
| Net cash used in investing activities | (45,065 | ) | | (71,849 | ) | | (102,211 | ) | (227,665 | ) | | (495,833 | ) | | (45,065 | ) |
| Financing activities: | | | |
| | |
| | | | | |
|
| Proceeds from common stock offering, net of issuance costs | — |
| | — |
| | 111,131 |
| |
| Proceeds from issuance of convertible senior notes, net of financing costs paid | | 122,625 |
| | 537,973 |
| | — |
|
| Proceeds from sale-leaseback transactions | | — |
| | 158,694 |
| | — |
|
| Purchase of call option | | — |
| | (149,331 | ) | | — |
|
| Proceeds from issuance of warrants | | — |
| | 75,074 |
| | — |
|
| Treasury stock repurchases | | — |
| | (52,662 | ) | | (3,000 | ) |
| Principal payment on term loan of subsidiary | | — |
| | (46,963 | ) | | — |
|
| Repayment of amount borrowed under credit facility | | — |
| | (40,000 | ) | | (20,000 | ) |
| Proceeds from employee stock plans | | 14,040 |
| | 9,402 |
| | 8,205 |
|
| Principal payments on convertible senior notes | | (10,449 | ) | | — |
| | — |
|
| Amount borrowed under credit facility | 60,000 |
| | — |
| | 105,000 |
| — |
| | — |
| | 60,000 |
|
| Repayment of amount borrowed under credit facility | (20,000 | ) | | — |
| | (105,000 | ) | |
| Treasury stock repurchases | (3,000 | ) | | (7,000 | ) | | — |
| |
| Payment of credit facility fees | — |
| | (1,125 | ) | | (1,671 | ) | |
| Excess tax benefits from employee stock compensation | 3,667 |
| | 1,651 |
| | 295 |
| |
| Proceeds from exercise of stock options and employee stock plan purchases | 8,205 |
| | 7,347 |
| | 4,056 |
| |
| Other, net | | 2,773 |
| | 1,674 |
| | 3,667 |
|
| Net cash provided by financing activities | 48,872 |
| | 873 |
| | 113,811 |
| 128,989 |
| | 493,861 |
| | 48,872 |
|
| Net increase (decrease) in cash and cash equivalents | 24,418 |
| | (42,370 | ) | | 30,980 |
| |
| Net (decrease) increase in cash and cash equivalents | | (25,002 | ) | | 60,630 |
| | 24,418 |
|
| Cash and cash equivalents at beginning of year | 14,650 |
| | 57,020 |
| | 26,040 |
| 99,698 |
| | 39,068 |
| | 14,650 |
|
| Cash and cash equivalents at end of year | $ | 39,068 |
| | $ | 14,650 |
| | $ | 57,020 |
| $ | 74,696 |
| | $ | 99,698 |
| | $ | 39,068 |
|
Notes to Condensed Financial Information of Registrant
Note A - Basis of Presentation
Molina Healthcare, Inc., (the Registrant, or the Registrant,Parent), was incorporated on July 24, 2002. Prior to that date, Molina Healthcare of California (formerly known as Molina Medical Centers) operated as a California health plan and as the parent company for Molina Healthcare of Utah, Inc., Molina Healthcare of Michigan, Inc., and Molina Healthcare of Washington, Inc. In June 2003, the employees and operations of the corporate entity were transferred from Molina Healthcare of California to the Registrant.
The Registrant's investment in subsidiaries is stated at cost plus equity in undistributed earnings of subsidiaries since the date of acquisition. The accompanying condensed financial information of the Registrant should be read in conjunction with the consolidated financial statements and accompanying notes.
Note B - Transactions with Subsidiaries
The Registrant provides certain centralized medical and administrative services to its subsidiaries pursuant to administrative services agreements, including medical affairs and quality management, health education, credentialing, management,
financial, legal, information systems and human resources services. Fees are based on the fair market value of services rendered and are recorded as operating revenue. Payment is subordinated to the subsidiaries' ability to comply with minimum capital and other restrictive financial requirements of the states in which they operate. Charges in 2012, 2011,2014, 2013, and 20102012 for these services totaled $406.4amounted to $691.6 million,, $307.9 $592.1 million,, and $238.5$406.4 million,, respectively, whichand are included in operating revenue.
During 2013, the Registrant used a portion of the proceeds from the sale of the Molina Center, described in Note 12, "Long-Term Debt," to repay the remaining principal balance of the related term loan, on behalf of a subsidiary of the Registrant.
The Registrant and its subsidiaries are included in the consolidated federal and state income tax returns filed by the Registrant. Income taxes are allocated to each subsidiary in accordance with an intercompany tax allocation agreement. The agreement allocates income taxes in an amount generally equivalent to the amount which would be expensed by the subsidiary if it filed a separate
tax return. Net operating loss benefits are paid to the subsidiary by the Registrant to the extent such losses are utilized in the consolidated tax returns.
Note C - Capital Contribution, Dividends and Surplus NoteCapital Contributions
During 2012, 2011,2013 and 2010,2012, the Registrant received dividends from its subsidiaries amounting to $101.8 million, $76.6 million, and $81.3 million, respectively.subsidiaries. Such amounts have been recorded as a reduction to the investments in the respective subsidiaries. In addition, in 2011 a subsidiary of the Registrant repaid a surplus note in favor of the Registrant amounting to $9.7 million, including accrued interest. Such amount was a reduction of due from affiliates
During 2014, 2013, and prepaid and other current assets.
During 2012,, 2011, and 2010, the Registrant made capital contributions to certain subsidiaries amounting to $100.2 million, $58.4 million, and $10.5 million, respectively, primarily to comply with minimum net worth requirements and to fund contract acquisitions. Such amounts have been recorded as an increase in investment in the respective subsidiaries.subsidiaries, net of insignificant returns of capital.
Note D - Related Party Transactions
On February 27, 2013, the Registrant entered into a lease (the “Lease”) with 6th & Pine Development, LLC (the “Landlord”) for office space located in Long Beach, California. The lease consists of two office buildings as follows:
an existing building, which comprises approximately 70,000 square feet of office space, and
a new building, which is expected to comprise approximately 120,000 square feet of office space.
The term of the Lease with respect to the existing building is expected to commence on June 1, 2013, and the term of the Lease with respect to the new building is expected to commence on November 1, 2014. The initial term of the Lease with respect to both buildings expires on December 31, 2024, subject to two options to extend the term for a period of five years each. Initial annual rent for the existing building is expected to be approximately $2.5 million and initial annual rent for the new building is expected to be approximately $4.0 million. Rent will increase 3.75% per year through the initial term. Rent during the extension terms will be the greater of then-current rent or fair market rent.
The principal members of the Landlord are John C. Molina, the Chief Financial Officer and a director of the Registrant, and his wife. In addition, in connection with the development of the buildings being leased, the Landlord has pledged shares of common stock in the Registrant he holds as trustee. Dr. J. Mario Molina, the Registrant's Chief Executive Officer and Chairman of the Board of Directors, holds a partial interest in such shares as trust beneficiary.
The Registrant has an equity investment in a medical service provider that provides certain vision services to its members. The Registrant accounts for this investment under the equity method of accounting because the Registrant has an ownership interest in the investee that confers significant influence over operating and financial policies of the investee. For both years ended December 31, 2012 and 2011, the Registrant's carrying amount for this investment amounted to $3.9 million. For the years ended December 31, 2012, 2011, and 2010, the Registrant paid $28.4 million, $24.3 million, and $22.0 million, respectively, for medical service fees to this provider.
The Registrant is party to a fee-for-service agreement with Pacific Hospital of Long Beach, or Pacific Hospital. Pacific Hospital is owned by Abrazos Healthcare, Inc. Until October 12, 2010, the majority of the shares of Abrazos Healthcare, Inc. were held as community property by Dr. Martha Bernadett and her husband. Dr. Martha Bernadett is the sister of Joseph M. Molina, M.D. (Dr. J. Mario Molina), our Chief Executive Officer, and John Molina, our Chief Financial Officer. On October 12, 2010, Dr. Bernadett and her husband sold their shares in Abrazos Healthcare, Inc., terminating our related party relationship with Pacific Hospital. Under the terms of this fee-for-service agreement we paid Pacific Hospital$0.8 millionfor the period from January 1, 2010 to October 12, 2010.
On December 26, 2012, the Registrant purchased 110,988 shares of its common stock from certain Molina family trusts for an aggregate purchase price of $3.0 million. This purchase transaction was approved by the Registrant's board of directors. The shares were purchased at a price of $27.03, representing the closing price per share of the Registrant's common stock on December 26, 2012. The shares were purchased from the Janet M. Watt Separate Property Trust dated 10/22/2007, or the Separate Property Trust, and the Watt Family Trust dated 10/11/1996, or the Family Trust. Janet M. Watt is the sister, and her husband Lawrence B. Watt is the brother-in-law, of Dr. J. Mario Molina and John Molina. Ms. Watt is the sole trustee of the Separate Property Trust, and a co-trustee with Lawrence B. Watt of the Family Trust.
23. Subsequent Event
New Mexico Health Plan
On February 11, 2013, we announced that our New Mexico health plan was selected by the New Mexico Human Services Department (HSD) to participatetransactions are described in the new Centennial Care program. In addition to continuing to provide physical and acute health care services, under the new program Molina Healthcare of New Mexico will expand its services to provide behavioralNote 18, "Related Party Transactions."
health and long-term care services. The selection of Molina Healthcare of New Mexico was made by HSD pursuant to its request for proposals issued in August 2012. The operational start date for the program is currently scheduled for January 2014.
Item 9.Changes in and Disagreements with Accountants on Accounting and Financial Disclosures
None.
Item 9A.Controls and Procedures
Disclosure Controls and Procedures: Our management is responsible for establishing and maintaining effective internal control over financial reporting as defined in Rules 13a-15(f) and 15d-15(f) under the Securities Exchange Act of 1934 (the “Exchange Act”"Exchange Act"). Our internal control over financial reporting is designed to provide reasonable assurance to our management and board of directors regarding the preparation and fair presentation of published financial statements. We maintain controls and procedures designed to ensure that we are able to collect the information we are required to disclose in the reports we file with the Securities and Exchange Commission, and to process, summarize and disclose this information within the time periods specified in the rules of the Securities and Exchange Commission.
Evaluation of Disclosure Controls and Procedures: Our management, with the participation of our Chief Executive Officer and our Chief Financial Officer, has conducted an evaluation of the design and operation of our “disclosure"disclosure controls and procedures”procedures" (as defined in Rules 13a-15(e) and 15d-15(e)) under the Exchange Act. Based on this evaluation, our Chief Executive Officer and our Chief Financial Officer have concluded that our disclosure controls and procedures are effective as of the end of the period covered by this report to ensure that information required to be disclosed in the reports that we file or submit under the Exchange Act is recorded, processed, summarized and reported within the time periods specified in the Securities and Exchange Commission’s rules and forms.
Because of its inherent limitations, internal control over financial reporting may not prevent or detect misstatements. Therefore, even those systems determined to be effective can provide only reasonable assurance with respect to financial statement preparation and presentation.
Changes in Internal Controls: There were no changes in our internal control over financial reporting that occurred during the quarter ended December 31, 2012, that have materially affected, or are reasonably likely to materially affect, our internal control over financial reporting.
Management’s Report on Internal Control over Financial Reporting: Management of the Company is responsible for establishing and maintaining adequate internal control over financial reporting, as such term is defined in Rule 13a-15(f) under the Exchange Act. The Company’s internal control over financial reporting is designed to provide reasonable assurance regarding the reliability of financial reporting and the preparation of financial statements for external purposes in accordance with generally accepted accounting principles in the United States. However, all internal control systems, no matter how well designed, have inherent limitations. Therefore, even those systems determined to be effective can provide only reasonable assurance with respect to financial statement preparation and reporting.
Management assessed the effectiveness of the Company’s internal control over financial reporting as of December 31, 20122014. In making this assessment, management used the criteria set forth by the Committee of Sponsoring Organizations of the Treadway Commission (“COSO”)(COSO) in Internal Control-Integrated Framework.Framework (2013 framework).
Based on our assessment, management believes that the Company maintained effective internal control over financial reporting as of December 31, 20122014, based on those criteria.
The effectiveness ofErnst & Young, LLP, the independent registered public accounting firm who audited the Company’s Consolidated Financial Statements included in this Form 10-K, has issued a report on the Company’s internal control over financial reporting, has been audited by Ernst & Young LLP, an independent registered public accounting firm, as statedwhich is included herein.
Changes in their report appearing on page 117 of this Annual Report on Form 10-K, which expresses an unqualified opinion on the effectiveness ofInternal Control over Financial Reporting. There were no changes in the Company’s internal control over financial reporting as(as defined in Rule 13a-15(f) of the Exchange Act) during the quarter ended December 31, 20122014., that have materially affected, or are reasonably likely to materially affect, the Company’s internal control over financial reporting.
Item 9B.Other Information
6th and Pine Lease
On February 27, 2013, Molina Healthcare, Inc. (the “Company”) entered into a build-to-suit office building lease (the “Lease”) with 6th & Pine Development, LLC (the “Landlord”) for approximately 190,000 rentable square feet of office space and 15,000 square feet of storage space located at 604 Pine Avenue, Long Beach, California (the “Project”). The Landlord is expected to construct the Project on a “turnkey” basis, which will consist of two office buildings, on-site parking, common areas and certain amenities, and the right to use up to 500 off-site parking spaces to be secured by the Landlord. The two office buildings will be comprised of:
an existing building located on the site and commonly known as the Independent Press Telegram building (the “Existing Building”), which the Landlord is required to substantially refurbish as part of Phase I of the Project. Upon completion of the refurbishment, the Existing Building is expected to contain approximately 70,000 square feet of office space and 15,000 square feet of storage space, and
a new building (the “New Building”), which the Landlord is required to construct as part of Phase II of the Project following the demolition of a building currently located on the site commonly known as the Meeker-Baker building. Upon completion of the construction, the New Building is expected to contain approximately 120,000 square feet of office space.
The term of the Lease with respect to the Existing Building is expected to commence on June 1, 2013, and the term of the Lease with respect to the New Building is expected to commence on November 1, 2014. The initial term of the Lease with respect to both buildings expires on December 31, 2024, subject to two options to extend the term for a period of five years each.
Commencing on the commencement date of the lease for the Existing Building, the monthly base rent due under the Lease is (i) for the office space, initially $2.70 per rentable square foot, increasing by 3.75% per year through the initial term, and (ii) for the storage space, $1.40 per rentable square foot, increasing by 3.75% per year through the initial term. Base rent during the extension terms will be the greater of then-current base rent or fair market rent. The Lease is a full service, base year, gross lease. Accordingly, the rent payable by the Company includes the cost of all utilities, taxes, insurance and maintenance with respect to the Project for the base year, 2015. The Company will be responsible for any increases in the cost of utilities, taxes, insurance and/or maintenance in excess of the cost therefor during the base year, 2015 (subject to certain customary limitations). The Company will also pay $600 per year for each on-site parking space (213) and for each off-site parking space that the Company elects to use (up to 500). The per year, per space parking rate will increase by 3% each year for each on-site parking space and by CPI, with a cap of 3%, for each off-site space.
During the first five years of the term of the Lease, the Company has a right of first offer to purchase the Project (including any transferable off-site parking rights held by the Landlord), and from and after year five of the Lease, the Company has an option to purchase the Project (including any transferable off-site parking rights held by the Landlord) for a purchase price equal to the fair market value for the Project.
The principal members of the Landlord are John C. Molina, the Chief Financial Officer and a director of the Company, and his wife. In addition, in connection with the Project the Landlord has pledged shares of common stock in the Company he holds as trustee. Dr. J. Mario Molina, the Company's Chief Executive Officer and Chairman of the Board of Directors, holds a partial interest in such shares as trust beneficiary.
In November 2011, the Company's Board of Directors organized a special committee of five independent directors (the “Special Committee”) consisting of Steve Orlando, Ronna Romney, John Szabo, Charles Fedak, and Dr. Frank Murray, and delegated to the Special Committee full power and authority to consider and enter into any real property transaction to meet the Company's space needs. Following its formation, the Special Committee undertook a review of, among other things, the Company's projected space needs and available space options. In connection with its work, the Special Committee retained Latham & Watkins LLP, as its independent legal counsel, and Duff & Phelps LLC, as its independent real estate advisor. Following the completion of its work, the Committee determined that it was appropriate to enter into the Lease with the Landlord under its terms and conditions, and accordingly approved the Company's entry into the Lease.
The foregoing description of the Lease is not complete and is qualified in its entirety by reference to the full text of such agreement, a copy of which is filed as Exhibit 10.32 herewith and which is incorporated herein by reference.None.
REPORT OF INDEPENDENT REGISTERED PUBLIC ACCOUNTING FIRM
The Board of Directors and Stockholders
of Molina Healthcare, Inc.
We have audited Molina Healthcare, Inc.’s (the “Company’s”"Company’s") internal control over financial reporting as of December 31, 20122014, based on criteria established in Internal Control — Integrated Framework issued by the Committee of Sponsoring Organizations of the Treadway Commission (2013 framework) (the COSO criteria). The Company’s management is responsible for maintaining effective internal control over financial reporting, and for its assessment of the effectiveness of internal control over financial reporting included in the accompanying Management’s Report on Internal Control over Financial Reporting. Our responsibility is to express an opinion on the Company’s internal control over financial reporting based on our audit.
We conducted our audit in accordance with the standards of the Public Company Accounting Oversight Board (United States). Those standards require that we plan and perform the audit to obtain reasonable assurance about whether effective internal control over financial reporting was maintained in all material respects. Our audit included obtaining an understanding of internal control over financial reporting, assessing the risk that a material weakness exists, testing and evaluating the design and operating effectiveness of internal control based on the assessed risk, and performing such other procedures as we considered necessary in the circumstances. We believe that our audit provides a reasonable basis for our opinion.
A company’s internal control over financial reporting is a process designed to provide reasonable assurance regarding the reliability of financial reporting and the preparation of financial statements for external purposes in accordance with generally accepted accounting principles. A company’s internal control over financial reporting includes those policies and procedures that (1) pertain to the maintenance of records that, in reasonable detail, accurately and fairly reflect the transactions and dispositions of the assets of the company; (2) provide reasonable assurance that transactions are recorded as necessary to permit preparation of financial statements in accordance with generally accepted accounting principles, and that receipts and expenditures of the company are being made only in accordance with authorizations of management and directors of the company; and (3) provide reasonable assurance regarding prevention or timely detection of unauthorized acquisition, use, or disposition of the company’s assets that could have a material effect on the financial statements.
Because of its inherent limitations, internal control over financial reporting may not prevent or detect misstatements. Also, projections of any evaluation of effectiveness to future periods are subject to the risk that controls may become inadequate because of changes in conditions, or that the degree of compliance with the policies or procedures may deteriorate.
In our opinion, Molina Healthcare, Inc. maintained, in all material respects, effective internal control over financial reporting as of December 31, 20122014, based on the COSO criteria.
We also have audited, in accordance with the standards of the Public Company Accounting Oversight Board (United States), the consolidated balance sheets of Molina Healthcare, Inc. as of December 31, 20122014 and 20112013, and the related consolidated statements of income, and comprehensive income, stockholders’ equity, and cash flows for each of the three years in the period ended December 31, 20122014 and our report dated February 28, 201326, 2015 expressed an unqualified opinion thereon.
Los Angeles, California
February 28, 201326, 2015
PART III
Item 10.Directors, Executive Officers, and Corporate Governance
Pursuant to General Instruction G(3) to Form 10-K and Instruction 3 to Item 401(b) of Regulation S-K, information regarding our executive officers is provided in Item 1 of Part I of this Annual Report on Form 10-K under the caption “Executive"Executive Officers of the Registrant,”" and will also appear in our definitive proxy statement for our 20132015 Annual Meeting of Stockholders. The remaining information required by Items 401, 405, 406 and 407(c)(3), (d)(4) and (d)(5) of Regulation S-K will be included under the headings “Election"Election of Directors,” “Corporate" "Corporate Governance,”" and “Section"Section 16(a) Beneficial Ownership Reporting Compliance”Compliance" in our definitive proxy statement for our 20132015 Annual Meeting of Shareholders,Stockholders, and such required information is incorporated herein by reference.
Item 11.Executive Compensation
The information required by Items 402, 407(e)(4), and (e)(5) of Regulation S-K will be included under the headings “Executive Compensation”"Executive Compensation" and “Compensation"Compensation Committee Interlocks and Insider Participation”Participation" in our definitive proxy statement for our 20132015 Annual Meeting of Shareholders,Stockholders, and such required information is incorporated herein by reference.
Item 12.Security Ownership of Certain Beneficial Owners and Management and Related Stockholder Matters
The information required by this item regarding our equity compensation plans is set forth in Part II, Item 5Securities Authorized for Issuance Under Equity Compensation Plans (as of this report and incorporated herein by reference. December 31, 2014)
|
| | | | | | | | | | |
| Plan Category | Number of Securities to be Issued Upon Exercise of Outstanding Options, Warrants and Rights (a) | | Weighted Average Exercise Price of Outstanding Options, Warrants and Rights (b) | | Number of Securities Remaining Available for Future Issuance Under Equity Compensation Plans (Excluding Securities Reflected in Column (a)) (c) | |
| Equity compensation plans approved by security holders | 256,698 |
| (1) | $ | 23.77 |
| | 4,529,223 |
| (2) |
| |
| (1) | Options to purchase shares of our common stock issued under the 2002 Equity Incentive Plan and 2011 Equity Incentive Plan. Further grants under the 2002 Equity Incentive Plan have been suspended. |
| |
| (2) | Includes shares remaining available to issue under the 2011 Equity Incentive Plan, and the 2011 Employee Stock Purchase Plan. |
The remaining information required by Item 403 of Regulation S-K will be included under the heading “Security"Security Ownership of Certain Beneficial Owners and Management”Management" in our definitive proxy statement for our 20132015 Annual Meeting of Shareholders,Stockholders, and such required information is incorporated herein by reference.
Item 13.Certain Relationships and Related Transactions, and Director Independence
The information required by Items 404 and 407(a) of Regulation S-K will be included under the headings “Certain Relationships"Related Party Transactions," "Corporate Governance," and Transactions” and “Corporate Governance”"Director Independence" in our definitive proxy statement for our 20132015 Annual Meeting of Shareholders,Stockholders, and such required information is incorporated herein by reference.
JosephAdditionally, refer to Part II, Item 8 of this Form 10-K, Notes to Consolidated Financial Statements, in Note 18, "Related Party Transactions," and Note 19, "Variable Interest Entities," under the subheading "Joseph M. Molina M.D., Professional Corporations
Our wholly owned subsidiary, American Family Care, Inc., or AFC, operates our primary care clinics. In 2012, AFC entered into services agreements with theCorporations."Joseph M. Molina, M.D. Professional Corporations, or JMMPC. JMMPC was created to further advance our direct delivery line of business. Its sole shareholder is Joseph M. Molina, M.D. (Dr. J. Mario Molina), our Chairman of the Board, President and Chief Executive Officer. Dr. Molina is paid no salary and receives no dividends in connection with his work for, or ownership of, JMMPC. Under the services agreements, AFC provides the clinic facilities, clinic administrative support staff, patient scheduling services and medical supplies to JMMPC, and JMMPC provides outpatient professional medical services to the general public for routine non-life threatening, outpatient health care needs. While JMMPC may provide services to the general public, substantially all of the individuals served by JMMPC are members of our health plans. JMMPC does not have agreements to provide professional medical services with any other entities. In addition to the services agreements with AFC, JMMPC has entered into affiliation agreements with us. Under these agreements, we have agreed to fund JMMPC's operating deficits, or receive JMMPC's operating surpluses, based on a monthly reconciliation such that JMMPC will operate at break even and derive no profit.
We have determined that JMMPC is a variable interest entity, or VIE, and that we are its primary beneficiary. We have reached this conclusion under the power and benefits criterion model according to U.S. generally accepted accounting principles. Specifically, we have the power to direct the activities that most significantly affect JMMPC's economic performance, and the obligation to absorb losses or right to receive benefits that are potentially significant to the VIE, under the services and affiliation agreements described above. Because we are its primary beneficiary, we have consolidated JMMPC. JMMPC's assets may be used to settle only JMMPC's obligations, and JMMPC's creditors have no recourse to the general credit of Molina Healthcare, Inc. As of December 31, 2012, JMMPC had total assets of $1.4 million, comprising primarily cash and equivalents, and total liabilities of $1.1 million, comprising primarily accrued payroll and employee benefits.
Our maximum exposure to loss as a result of our involvement with this entity is equal to the amounts needed to fund JMMPC's ongoing payroll and employee benefits. We believe that such loss exposure will be immaterial to our consolidated
operating results and cash flows for the foreseeable future. For the year ended December 31, 2012, we provided an initial cash infusion of $0.3 million to JMMPC in the first quarter of 2012 to fund its start-up operations. During 2012 our health plans received $0.2 million from JMMPC under the terms of the affiliation agreement.
Stock Repurchase
Janet M. Watt is the sister, and her husband Lawrence B. Watt is the brother-in-law, of Dr. J. Mario Molina, the Company's Chief Executive Officer, and John Molina, the Company's Chief Financial Officer. Ms. Watt is the sole trustee of the Janet M. Watt Separate Property Trust dated 10/22/2007 (the “Separate Property Trust”) and a co-trustee with Lawrence B. Watt, of the Watt Family Trust dated 10/11/1996 (the “Family Trust” and together with the Separate Property Trust, the “Trusts”). On December 26, 2012, pursuant to a Stock Purchase Agreement between the Company and the Trusts, the Company purchased an aggregate of 110,988 shares of its common stock from the Trusts for an aggregate purchase price of $3,000,005.64, as follows: (i) 43,767 shares from the Family Trust for an aggregate purchase price of $ 1,183,022.01 and (ii) 67,221 shares from the Separate Property Trust for an aggregate purchase price of $1,816,983.63. The shares were purchased at a price per share of $27.03, representing the closing price per share of the Company's common stock on December 26, 2012, as reported by the New York Stock Exchange. The transaction was approved by the Company's Board of Directors.
6th and Pine Lease
Please see the information disclosed under Part II, Item 9B. Other Information, in this Annual Report, which disclosure is incorporated herein by reference.
Item 14.Principal Accountant Fees and Services
The information required by Item 9(e) of Schedule 14A will be included under the heading “Independent Registered Public Accounting Firm”"Disclosure of Auditor Fees" in our definitive proxy statement for our 20132015 Annual Meeting of Shareholders,Stockholders, and such required information is incorporated herein by reference.
PART IV
Item 15. Exhibits and Financial Statement Schedules
| |
| (a) | The consolidated financial statements and exhibits listed below are filed as part of this report. |
| |
| (1) | The Company's consolidated financial statements the notes thereto and the report of the Independent Registered Public Accounting Firm are on pages 64 through 108included in Item 8 of this Annual Report on Form 10-K, Financial Statements and Supplementary Data, above are incorporated by reference.filed as part of this annual report. |
Report of Independent Registered Public Accounting Firm
Consolidated Balance Sheets - At December 31, 2012 and 2011
Consolidated Statements of Income - Years ended December 31, 2012, 2011, and 2010
Consolidated Statements of Stockholders' Equity - Years ended December 31, 2012, 2011, and 2010
Consolidated Statements of Cash Flows - Years ended December 31, 2012, 2011, and 2010
Notes to Consolidated Financial Statements
| |
| (2) | Financial Statement Schedules |
None of the schedules apply, or the information required is included in the Notes to the Consolidated Financial Statements.
Reference is made to the accompanying Index to Exhibits.
SIGNATURES
Pursuant to the requirements of Section 13 or 15(d) of the Securities Exchange Act of 1934, as amended, the undersigned registrant has duly caused this report to be signed on its behalf by the undersigned, thereunto duly authorized, on the 26th day of February, 2015.
|
| | | |
| MOLINA HEALTHCARE, INC. |
| | | |
| By: | | /s/ Joseph M. Molina |
| | | Joseph M. Molina, M.D. (Dr. J. Mario Molina) |
| | | Chief Executive Officer (Principal Executive Officer) |
Pursuant to the requirements of the Securities Exchange Act of 1934, as amended, this report has been signed below by the following persons on behalf of the registrant and in the capacities and on the dates indicated.
|
| | | | |
| Signature | | Title | | Date |
| | | | |
| /s/ Joseph M. Molina | | Chairman of the Board, Chief Executive Officer, and President | | February 26, 2015 |
| Joseph M. Molina, M.D. | | (Principal Executive Officer) | | |
| | | | |
| /s/ John C. Molina | | Director, Chief Financial Officer, and Treasurer | | February 26, 2015 |
| John C. Molina, J.D. | | (Principal Financial Officer) | | |
| | | | |
| /s/ Joseph W. White | | Chief Accounting Officer | | February 26, 2015 |
| Joseph W. White | | (Principal Accounting Officer) | | |
| | | | |
| /s/ Garrey E. Carruthers | | Director | | February 26, 2015 |
| Garrey E. Carruthers, Ph.D. | | | | |
| | | | |
| /s/ Daniel Cooperman | | Director | | February 26, 2015 |
| Daniel Cooperman | | | | |
| | | | |
| /s/ Charles Z. Fedak | | Director | | February 26, 2015 |
| Charles Z. Fedak | | | | |
| | | | |
| /s/ Steven G. James | | Director | | February 26, 2015 |
| Steven G. James | | | | |
| | | | |
| /s/ Frank E. Murray | | Director | | February 26, 2015 |
| Frank E. Murray, M.D. | | | | |
| | | | |
| /s/ Steven J. Orlando | | Director | | February 26, 2015 |
| Steven J. Orlando | | | | |
| | | | |
| /s/ Ronna E. Romney | | Director | | February 26, 2015 |
| Ronna E. Romney | | | | |
| | | | |
| /s/ John P. Szabo, Jr. | | Director | | February 26, 2015 |
| John P. Szabo, Jr. | | | | |
| | | | |
| /s/ Dale B. Wolf | | Director | | February 26, 2015 |
| Dale B. Wolf | | | | |
| | | | |
INDEX TO EXHIBITS
The following exhibits, which are furnished with this annual report or incorporated herein by reference, are filed as part of this annual report.
The agreements included or incorporated by reference as exhibits to this Annual Report on Form 10-K may contain representations and warranties by each of the parties to the applicable agreement. These representations and warranties were made solely for the benefit of the other parties to the applicable agreement and (i) were not intended to be treated as categorical statements of fact, but rather as a way of allocating the risk to one of the parties if those statements prove to be inaccurate; (ii) may have been qualified in such agreement by disclosures that were made to the other party in connection with the negotiation of the applicable agreement; (iii) may apply contract standards of “materiality”"materiality" that are different from “materiality”"materiality" under the applicable securities laws; and (iv) were made only as of the date of the applicable agreement or such other date or dates as may be specified in the agreement. The Company acknowledges that, notwithstanding the inclusion of the foregoing cautionary statements, it is responsible for considering whether additional specific disclosures of material information regarding material contractual provisions are required to make the statements in this Annual Report on Form 10-K not misleading.
|
| | | | |
| Number | | Description | | Method of Filing |
| 1.1 | | Purchase Agreement, dated as of February 11, 2013, among Molina Healthcare, Inc. and J.P. Morgan Securities LLC and Merrill Lynch, Pierce, Fenner & Smith Incorporated, as Representatives of the Initial Purchasers.Purchasers | | Filed as Exhibit 1.1 to registrant's Form 8-K filed February 15, 2013. |
| 2.1 | | Asset Purchase Agreement between Molina Healthcare, Inc. and Unisys Corporation dated as of January 18, 2010 | | Filed as Exhibit 2.1 to registrant's Form 8-K filed January 19, 2010. |
| 3.1 | | Certificate of Incorporation | | Filed as Exhibit 3.2 to registrant's Registration Statement on Form S-1 filed December 30, 2002. |
| 3.2 | | Amended and Restated BylawsCertificate of Amendment to Certificate of Incorporation | | Filed as Exhibit 3.23.1 to registrant'sregistrant’s Form 8-K filed February 17, 2009.July 24, 2013. |
4.13.3 | | Indenture dated asThird Amended and Restated Bylaws of October 11, 2008Molina Healthcare, Inc. | | Filed as Exhibit 4.13.1 to registrant's Form 8-K10-Q filed October 5, 2007.July 30, 2014. |
4.2 | | First Supplemental Indenture dated as of October 11, 2008 | | Filed as Exhibit 4.2 to registrant's Form 8-K filed October 5, 2007. |
4.3 | | Global Form of 3.75% Convertible Senior Note due 2014 | | Filed as Exhibit 4.3 to registrant's Form 8-K filed October 5, 2007. |
4.44.1 | | Indenture, dated as of February 15, 2013, by and between Molina Healthcare, Inc. and U.S. Bank, National Association.Association | | Filed as Exhibit 4.1 to registrant's Form 8-K filed February 15, 2013. |
4.54.2 | | Form of 1.125% Cash Convertible Senior Note due 2020 | | Included in Exhibit 4.1 to registrant's Form 8-K filed February 15, 2013. |
10.14.3 | | 2000 Omnibus StockIndenture, dated as of September 5, 2014, by and Incentive Planbetween Molina Healthcare, Inc. and U.S. Bank National Association | | Filed as Exhibit 10.124.1 to registrant'sregistrant’s Form S-18-K filed December 30, 2002.September 8, 2014. |
10.24.4 | | Form of 1.625% Convertible Senior Note due 2044 | | Included in Exhibit 4.1 to registrant’s Form 8-K filed September 8, 2014. |
| 4.5 | | Form of 1.625% Convertible Senior Notes Due 2044 Note Purchase Agreement, dated as of September 11, 2014, by and between Molina Healthcare, Inc. and certain institutional investors | | Filed as Exhibit 10.1 to registrant’s Form 8-K filed September 12, 2014. |
| 4.6 | | First Supplemental Indenture, dated as of September 16, 2014, by and between Molina Healthcare, Inc. and the U.S. Bank National Association | | Filed as Exhibit 4.1 to registrant’s Form 8-K filed September 17, 2014. |
| 4.7 | | Form of 1.625% Convertible Senior Note due 2044 | | Included in Exhibit 4.1 to registrant’s Form 8-K filed September 17, 2014. |
| *10.1 | | 2002 Equity Incentive Plan | | Filed as Exhibit 10.13 to registrant's Form S-1 filed December 30, 2002. |
10.3*10.2 | | 2002 Employee Stock PurchaseMolina Healthcare, Inc. Amended and Restated Deferred Compensation Plan (2013) | | Filed as Exhibit 10.1410.5 to registrant'sregistrant’s Form S-110-K filed December 30, 2002.February 26, 2014. |
10.4*10.3 | | 2005Amendment No. 1 to the Molina Healthcare, Inc. Amended and Restated Deferred Compensation Plan adopted November 6, 2006(2013) | | Filed as Exhibit 10.410.6 to registrant'sregistrant’s Form 10-Q10-K filed November 9, 2006.February 26, 2014. |
10.5*10.4 | | 2005 IncentiveAmendment No. 2 to the Molina Healthcare, Inc. Amended and Restated Deferred Compensation Plan (2013) | | Filed as Appendix A to registrant's Proxy Statement filed March 28, 2005.herewith. |
10.6*10.5 | | 2011 Equity Incentive Plan | | Filed as Exhibit 10.210.8 to registrant'sregistrant’s Form 8-K10-K filed May 2, 2011.February 26, 2014. |
|
10.7 | | | | |
| Number | | Description | | Method of Filing |
| *10.6 | | 2011 Employee Stock Purchase Plan | | Filed as Exhibit 10.1 to registrant's Form 8-K filed May 2, 2011.herewith. |
10.8*10.7 | | Form of Restricted Stock Award Agreement (Executive Officer) under Molina Healthcare, Inc. Equity Incentive Plan | | Filed as Exhibit 10.1 to registrant's Form 10-Q filed August 9, 2005. |
10.9*10.8 | | Form of Restricted Stock Award Agreement (Outside Director) under Molina Healthcare, Inc. Equity Incentive Plan | | Filed as Exhibit 10.1 to registrant's Form 10-Q filed August 9, 2005. |
|
| | | | |
Number | | Description | | Method of Filing |
10.10*10.9 | | Form of Restricted Stock Award Agreement (Employee) under Molina Healthcare, Inc. Equity Incentive Plan | | Filed as Exhibit 10.1 to registrant's Form 10-Q filed August 9, 2005. |
10.11*10.10 | | Form of Stock Option Agreement under Equity Incentive Plan | | Filed as Exhibit 10.3 to registrant's Form 10-K filed March 14, 2007. |
10.12*10.11 | | Amended and Restated Employment Agreement with J. Mario Molina, M.D. dated as of December 31, 2009 | | Filed as Exhibit 10.1 to registrant's Form 8-K filed January 7, 2010. |
10.13*10.12 | | Amended and Restated Employment Agreement with John C. Molina dated as of December 31, 2009 | | Filed as Exhibit 10.2 to registrant's Form 8-K filed January 7, 2010. |
| *10.13 | | Employment Agreement with Terry Bayer dated June 14, 2013 | | Filed as Exhibit 10.1 to registrant’s Form 8-K filed June 14, 2013. |
| *10.14 | | Employment Agreement with Joseph White dated June 14, 2013 | | Filed as Exhibit 10.2 to registrant’s Form 8-K filed June 14, 2013. |
| *10.15 | | Employment Agreement with Jeff Barlow, dated June 14, 2013 | | Filed as Exhibit 10.3 to registrant’s Form 8-K filed June 14, 2013. |
| *10.16 | | Amended and Restated Change in Control Agreement with Terry Bayer, dated as of December 31, 2009 | | Filed as Exhibit 10.4 to registrant's Form 8-K filed January 7, 2010. |
10.15*10.17 | | Amended and Restated Change in Control Agreement with Joseph W. White, dated as of December 31, 2009 | | Filed as Exhibit 10.6 to registrant's Form 8-K filed January 7, 2010. |
10.16*10.18 | | Change in Control Agreement with Jeff D. Barlow, dated as of September 18, 2012 | | Filed herewith.as Exhibit 10.16 to registrant’s Form 10-K filed February 28, 2013. |
10.1710.19 | | Form of Indemnification Agreement | | Filed as Exhibit 10.14 to registrant's Form 10-K filed March 14, 2007. |
10.1810.20 | | Base Call Option Transaction Confirmation, dated as of February 11, 2013, between Molina Healthcare, Inc. and JPMorgan Chase Bank, National Association, London Branch.Branch | | Filed as Exhibit 10.1 to registrant's Form 8-K filed February 15, 2013. |
10.1910.21 | | Base Call Option Transaction Confirmation, dated as of February 11, 2013, between Molina Healthcare, Inc. and Bank of America, N.A. | | Filed as Exhibit 10.2 to registrant's Form 8-K filed February 15, 2013. |
10.2010.22 | | Base Warrants Confirmation, dated as of February 11, 2013, between Molina Healthcare, Inc. and JPMorgan Chase Bank, National Association, London Branch.Branch | | Filed as Exhibit 10.3 to registrant's Form 8-K filed February 15, 2013. |
10.2110.23 | | Base Warrants Confirmation, dated as of February 11, 2013, between Molina Healthcare, Inc. and Bank of America, N.A. | | Filed as Exhibit 10.4 to registrant's Form 8-K filed February 15, 2013. |
10.2210.24 | | Amendment to Base Call Option Transaction Confirmation, dated as of February 13, 2013, between Molina Healthcare, Inc. and JPMorgan Chase Bank, National Association, London Branch.Branch | | Filed as Exhibit 10.5 to registrant's Form 8-K filed February 15, 2013. |
10.2310.25 | | Amendment to Base Call Option Transaction Confirmation, dated as of February 13, 2013, between Molina Healthcare, Inc. and Bank of America, N.A. | | Filed as Exhibit 10.6 to registrant's Form 8-K filed February 15, 2013. |
10.2410.26 | | Additional Base Warrants Confirmation, dated as of February 13, 2013, between Molina Healthcare, Inc. and JPMorgan Chase Bank, National Association, London Branch.Branch | | Filed as Exhibit 10.7 to registrant's Form 8-K filed February 15, 2013. |
10.2510.27 | | Additional Base Warrants Confirmation, dated as of February 13, 2013, between Molina Healthcare, Inc. and Bank of America, N.A. | | Filed as Exhibit 10.8 to registrant's Form 8-K filed February 15, 2013. |
10.26 | | Term Loan Agreement, dated as of December 1, 2011, among Molina Center LLC, various lenders and East West Bank, as Administrative Agent | | Filed as Exhibit 10.18 to registrant's From 10-K filed February 29, 2012. |
10.27 | | Guaranty, dated as of December 1, 2011, by Molina Healthcare, Inc. in favor of East West Bank, as Administrative Agent | | Filed as Exhibit 10.9 to registrant's Form 10-K filed February 29, 2012. |
10.28 | | Environmental Indemnity, dated as of December 1, 2011, by Molina Center LLC and Molina Healthcare, Inc. for the benefit of certain lenders and East West Bank, as Administrative Agent | | Filed as Exhibit 10.20 to registrant's Form 10-K filed February 29, 2012. |
10.29 | | Purchase Agreement, dated as of October 11, 2011, between Molina Center LLC and 200 Oceangate, LLC | | Filed as Exhibit 10.21 to registrant's Form 10-K filed February 29, 2012. |
| | | | |
|
| | | | |
| Number | | Description | | Method of Filing |
10.3010.28 | | First Amendment to Purchase Agreement,Amended and Restated Base Warrants Confirmation, dated as of November 10, 2011,April 22, 2013, between Molina Center LLCHealthcare, Inc. and 200 Oceangate, LLCJPMorgan Chase Bank, National Association, London Branch | | Filed as Exhibit 10.2210.1 to registrant's Form 10-K10-Q filed February 29, 2012.May 3, 2013. |
10.3110.29 | | Second Amendment to Purchase Agreement,Amended and Restated Base Warrants Confirmation, dated as of November 30, 2011,April 22, 2013, between Molina Center LLCHealthcare, Inc. and 200 Oceangate, LLCBank of America, N.A. | | Filed as Exhibit 10.2310.2 to registrant's Form 10-K10-Q filed February 29, 2012.May 3, 2013. |
| 10.30 | | Additional Amended and Restated Base Warrants Confirmation, dated as of April 22, 2013, between Molina Healthcare, Inc. and JPMorgan Chase Bank, National Association, London Branch | | Filed as Exhibit 10.3 to registrant's Form 10-Q filed May 3, 2013. |
| 10.31 | | Additional Amended and Restated Base Warrants Confirmation, dated as of April 22, 2013, between Molina Healthcare, Inc. and Bank of America, N.A. | | Filed as Exhibit 10.4 to registrant's Form 10-Q filed May 3, 2013. |
| 10.32 | | Lease Agreement, dated as of February 27, 2013, by and between 6th & Pine Development, LLC and Molina Healthcare, Inc. | | Filed herewith.as Exhibit 10.32 to registrant’s Form 10-K filed February 28, 2013. |
| 10.33 | | First Amendment to Office Building Lease, effective as of October 31, 2014, by and between 6th & Pine Development, LLC and Molina Healthcare, Inc. | | Filed as Exhibit 10.1 to registrant’s Form 8-K filed November 5, 2014. |
| 10.34 | | Settlement Agreement entered into on October 30, 2013, by and between the Department of Health Care Services and Molina Healthcare of California and Molina Healthcare of California Partner Plan, Inc. | | Filed as Exhibit 10.1 to registrant's Form 10-Q filed October 30, 2013. |
| 10.35 | | Agreement of Purchase and Sale, dated as of June 12, 2013, by and between Molina Healthcare, Inc. and Molina Center, LLC, and AG Net Lease Acquisition Corp. | | Filed as Exhibit 10.1 to registrant's Form 10-Q filed July 25, 2013. |
| 10.36 | | Lease Agreement, dated as of June 13, 2013, by and between AGNL Clinic, L.P., and Molina Healthcare, Inc. | | Filed as Exhibit 10.2 to registrant's Form 10-Q filed July 25, 2013. |
| 10.37 | | Form of Exchange Agreement, dated August 11, 2014, by and between Molina Healthcare, Inc. and certain beneficial owners of Molina Healthcare, Inc.’s 3.75% Convertible Senior Notes due 2014 | | Filed as Exhibit 10.1 to registrant’s Form 8-K filed August 12, 2014. |
| 12.1 | | Computation of Ratio of Earnings to Fixed Charges | | Filed herewith. |
| 21.1 | | List of subsidiaries | | Filed herewith. |
| 23.1 | | Consent of Independent Registered Public Accounting Firm | | Filed herewith. |
| 31.1 | | Section 302 Certification of Chief Executive Officer | | Filed herewith. |
| 31.2 | | Section 302 Certification of Chief Financial Officer | | Filed herewith. |
| 32.1 | | Certificate of Chief Executive Officer pursuant to 18 U.S.C. Section 1350, as adopted pursuant to Section 906 of the Sarbanes-Oxley Act of 2002 | | Filed herewith. |
| 32.2 | | Certificate of Chief Financial Officer pursuant to 18 U.S.C. Section 1350, as adopted pursuant to Section 906 of the Sarbanes-Oxley Act of 2002 | | Filed herewith. |
101.INS(1)101.INS | | XBRL Taxonomy Instance Document | | Filed herewith. |
101.SCH(1)101.SCH | | XBRL Taxonomy Extension Schema Document | | Filed herewith. |
101.CAL(1)101.CAL | | XBRL Taxonomy Extension Calculation Linkbase Document | | Filed herewith. |
101.DEF(1)101.DEF | | XBRL Taxonomy Extension Definition Linkbase Document | | Filed herewith. |
101.LAB(1)101.LAB | | XBRL Taxonomy Extension Label Linkbase Document | | Filed herewith. |
101.PRE(1)101.PRE | | XBRL Taxonomy Extension Presentation Linkbase Document | | Filed herewith. |
(1) Pursuant to Rule 406T of Regulation S-T, XBRL (eXtensible Business Reporting Language) information is furnished and not filed or a part of a registration statement or prospectus for purposes of Sections 11 or 12 of the Securities Act of 1933, as amended, is deemed not filed for purposes of Section 18 of the Securities Exchange Act of 1934, as amended, and otherwise is not subject to liability under these sections.
SIGNATURES
Pursuant to the requirements of Section 13 or 15(d) of the Securities Exchange Act of 1934, as amended, the undersigned registrant has duly caused this report to be signed on its behalf by the undersigned, thereunto duly authorized, on the 28th day of February, 2013.
|
| | | |
| * | MOLINA HEALTHCARE, INC. |
| | | |
| By: | | /s/ Joseph M. Molina |
| | | Joseph M. Molina, M.D. (Dr. J. Mario Molina) |
| | | Chief Executive Officer
(Principal Executive Officer)
|
Pursuant to the requirements of the Securities Exchange Act of 1934, as amended, this report has been signed below by the following persons on behalf of the registrant and in the capacities and on the dates indicated.
|
| | | | |
Signature | | Title | | Date |
| | | | |
/s/ Joseph M. Molina | | ChairmanManagement contract or compensatory plan or arrangement required to be filed (and/or incorporated by reference) as an exhibit to this Annual Report on Form 10-K pursuant to Item 15(b) of the Board, Chief Executive Officer, and President | | February 28, 2013 |
Joseph M. Molina, M.D. | | (Principal Executive Officer) | | |
| | | | |
/s/ John C. Molina | | Director, Chief Financial Officer, and Treasurer | | February 28, 2013 |
John C. Molina, J.D. | | (Principal Financial Officer) | | |
| | | | |
/s/ Joseph W. White | | Chief Accounting Officer | | February 28, 2013 |
Joseph W. White, CPA, MBA | | (Principal Accounting Officer) | | |
| | | | |
/s/ Garrey E. Carruthers | | Director | | February 28, 2013 |
Garrey E. Carruthers, Ph.D. | | | | |
| | | | |
/s/ Charles Z. Fedak | | Director | | February 28, 2013 |
Charles Z. Fedak, CPA, MBA | | | | |
| | | | |
/s/ Frank E. Murray | | Director | | February 28, 2013 |
Frank E. Murray, M.D. | | | | |
| | | | |
/s/ Steven Orlando | | Director | | February 28, 2013 |
Steven Orlando, CPA (inactive) | | | | |
| | | | |
/s/ Ronna Romney | | Director | | February 28, 2013 |
Ronna Romney | | | | |
| | | | |
/s/ John P. Szabo, Jr. | | Director | | February 28, 2013 |
John P. Szabo, Jr. | | | | Form 10-K. |