UNITED STATES
SECURITIES AND EXCHANGE COMMISSION
FORM 10-Q
(Mark One)
|
| |
| ý | QUARTERLY REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 |
For the quarterly period ended September 30, 2017March 31, 2018
OR
|
| |
| ¨ | TRANSITION REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 |
For the transition period from to
Commission file number: 001-31719
MOLINA HEALTHCARE, INC.
(Exact name of registrant as specified in its charter)
|
| | |
| Delaware | | 13-4204626 |
| (State or other jurisdiction of incorporation or organization) | | (I.R.S. Employer Identification No.) |
| | |
200 Oceangate, Suite 100 Long Beach, California | | 90802 |
| (Address of principal executive offices) | | (Zip Code) |
(562) 435-3666
(Registrant’s telephone number, including area code)
Indicate by check mark whether the registrant (1) has filed all reports required to be filed by Section 13 or 15(d) of the Securities Exchange Act of 1934 during the preceding 12 months (or for such shorter period that the registrant was required to file such reports), and (2) has been subject to such filing requirements for the past 90 days. Yes ý No ¨
Indicate by check mark whether the registrant has submitted electronically and posted on its corporate Web site, if any, every Interactive Data File required to be submitted and posted pursuant to Rule 405 of Regulation S-T during the preceding 12 months (or for such shorter period that the registrant was required to submit and post such files). Yes ý No ¨
Indicate by check mark whether the registrant is a large accelerated filer, an accelerated filer, a non-accelerated filer, smaller reporting company, or an emerging growth company. See the definitions of “large accelerated filer,” “accelerated filer,” “smaller reporting company,” and “emerging growth company” in Rule 12b-2 of the Exchange Act.
|
| | | |
| Large accelerated filer | ý | Accelerated filer | ¨ |
| | | | |
| Non-accelerated filer | ¨ (Do not check if a smaller reporting company) | Smaller reporting company | ¨ |
| | | Emerging growth company | ¨ |
|
| |
| If an emerging growth company, indicate by check mark if the registrant has elected not to use the extended transition period for complying with any new or revised financial accounting standards provided pursuant to Section13(a) of the Exchange Act. | |
| ¨ |
Indicate by check mark whether the registrant is a shell company (as defined in Rule 12b-2 of the Exchange Act).
Yes ¨ No ý
The number of shares of the issuer’s Common Stock, $0.001 par value, outstanding as of October 27, 2017,April 25, 2018, was approximately 57,094,000.61,685,000.
MOLINA HEALTHCARE, INC. FORM 10-Q
FOR THE QUARTERLY PERIOD ENDED September 30, 2017March 31, 2018
TABLE OF CONTENTS
CROSS-REFERENCE INDEX
| | | ITEM NUMBER | ITEM NUMBER | Page | ITEM NUMBER | Page |
| | | |
| PART I - Financial Information | PART I - Financial Information | | PART I - Financial Information | |
| | | |
| 1. | | | | |
| | | |
| 2. | | | | |
| | | |
| 3. | |
| |
|
| | | |
| 4. | | | | |
| | | |
| | | | |
| | | |
| 1. | | | | |
| | | |
| 1A. | | | | |
| | | |
| 2. | | | | |
| | | |
| 3. | Defaults Upon Senior Securities | Not Applicable. | Defaults Upon Senior Securities | Not Applicable. |
| | | |
| 4. | Mine Safety Disclosures | Not Applicable. | Mine Safety Disclosures | Not Applicable. |
| | | |
| 5. | Other Information | Not Applicable. | Other Information | Not Applicable. |
| | | |
| 6. | | | | |
| | | |
| | | | | |
| | | |
| | | |
FINANCIAL STATEMENTS
MOLINA HEALTHCARE, INC.
CONSOLIDATED STATEMENTS OF OPERATIONSINCOME | | | | Three Months Ended September 30, | | Nine Months Ended September 30, | Three Months Ended March 31, |
| | 2017 | | 2016 | | 2017 | | 2016 | 2018 | | 2017 |
| | (In millions, except per-share data) (Unaudited) | (In millions, except per-share data) (Unaudited) |
| Revenue: | | | | | | | | | | |
| Premium revenue | $ | 4,777 |
| | $ | 4,191 |
| | $ | 14,165 |
| | $ | 12,215 |
| $ | 4,323 |
| | $ | 4,648 |
|
| Service revenue | 130 |
| | 133 |
| | 390 |
| | 408 |
| 134 |
| | 131 |
|
| Premium tax revenue | 106 |
| | 127 |
| | 331 |
| | 345 |
| 104 |
| | 111 |
|
| Health insurer fee revenue | — |
| | 85 |
| | — |
| | 251 |
| |
| Health insurer fees reimbursed | | 61 |
| | — |
|
| Investment income and other revenue | 18 |
| | 10 |
| | 48 |
| | 29 |
| 24 |
| | 14 |
|
| Total revenue | 5,031 |
| | 4,546 |
| | 14,934 |
| | 13,248 |
| 4,646 |
| | 4,904 |
|
| Operating expenses: | | | | | | | | | | |
| Medical care costs | 4,220 |
| | 3,748 |
| | 12,822 |
| | 10,930 |
| 3,722 |
| | 4,111 |
|
| Cost of service revenue | 123 |
| | 119 |
| | 369 |
| | 362 |
| 120 |
| | 122 |
|
| General and administrative expenses | 383 |
| | 343 |
| | 1,227 |
| | 1,034 |
| 352 |
| | 439 |
|
| Premium tax expenses | 106 |
| | 127 |
| | 331 |
| | 345 |
| 104 |
| | 111 |
|
| Health insurer fee expenses | — |
| | 55 |
| | — |
| | 163 |
| |
| Health insurer fees | | 75 |
| | — |
|
| Depreciation and amortization | 33 |
| | 36 |
| | 109 |
| | 102 |
| 26 |
| | 39 |
|
| Impairment losses | 129 |
| | — |
| | 201 |
| | — |
| |
| Restructuring and separation costs | 118 |
| | — |
| | 161 |
| | — |
| 25 |
| | — |
|
| Total operating expenses | 5,112 |
| | 4,428 |
| | 15,220 |
| | 12,936 |
| 4,424 |
| | 4,822 |
|
| Operating (loss) income | (81 | ) | | 118 |
| | (286 | ) | | 312 |
| |
| Other expenses, net: | | | | | | | | |
| Operating income | | 222 |
| | 82 |
|
| Other expenses (income), net: | | | | |
| Interest expense | 32 |
| | 26 |
| | 85 |
| | 76 |
| 33 |
| | 26 |
|
| Other income, net | — |
| | — |
| | (75 | ) | | — |
| |
| Total other expenses, net | 32 |
| | 26 |
| | 10 |
| | 76 |
| |
| (Loss) income before income tax (benefit) expense | (113 | ) | | 92 |
| | (296 | ) | | 236 |
| |
| Income tax (benefit) expense | (16 | ) | | 50 |
| | (46 | ) | | 137 |
| |
| Net (loss) income | $ | (97 | ) | | $ | 42 |
| | $ | (250 | ) | | $ | 99 |
| |
| Other expense (income), net | | 10 |
| | (75 | ) |
| Total other expenses (income), net | | 43 |
| | (49 | ) |
| Income before income tax expense | | 179 |
| | 131 |
|
| Income tax expense | | 72 |
| | 54 |
|
| Net income | | $ | 107 |
| | $ | 77 |
|
| | | | | | | | | | | |
| Net (loss) income per share: | | | | | | | | |
| Net income per share: | | | | |
| Basic | $ | (1.70 | ) | | $ | 0.77 |
| | $ | (4.44 | ) | | $ | 1.79 |
| $ | 1.79 |
| | $ | 1.38 |
|
| Diluted | $ | (1.70 | ) | | $ | 0.76 |
| | $ | (4.44 | ) | | $ | 1.77 |
| $ | 1.64 |
| | $ | 1.37 |
|
CONSOLIDATED STATEMENTS OF COMPREHENSIVE (LOSS) INCOME
|
| | | | | | | | | | | | | | | |
| | Three Months Ended September 30, | | Nine Months Ended September 30, |
| | 2017 | | 2016 | | 2017 | | 2016 |
| | (Amounts in millions) (Unaudited) |
| Net (loss) income | $ | (97 | ) | | $ | 42 |
| | $ | (250 | ) | | $ | 99 |
|
| Other comprehensive income: | | | | | | | |
| Unrealized investment gain (loss) | 1 |
| | (3 | ) | | 2 |
| | 10 |
|
| Less: effect of income taxes | 1 |
| | (2 | ) | | 1 |
| | 3 |
|
| Other comprehensive (loss) income, net of tax | — |
| | (1 | ) | | 1 |
| | 7 |
|
| Comprehensive (loss) income | $ | (97 | ) | | $ | 41 |
| | $ | (249 | ) | | $ | 106 |
|
|
| | | | | | | |
| | Three Months Ended March 31, |
| | 2018 | | 2017 |
| | (Amounts in millions) (Unaudited) |
| Net income | $ | 107 |
| | $ | 77 |
|
| Other comprehensive (loss) income: | | | |
| Unrealized investment (loss) gain | (7 | ) | | 1 |
|
| Less: effect of income taxes | — |
| | — |
|
| Other comprehensive (loss) income, net of tax | (7 | ) | | 1 |
|
| Comprehensive income | $ | 100 |
| | $ | 78 |
|
See accompanying notes.
MOLINA HEALTHCARE, INC.
CONSOLIDATED BALANCE SHEETS | | | | September 30,
2017 | | December 31,
2016 | March 31,
2018 | | December 31,
2017 |
| | (Amounts in millions, except per-share data) | (Amounts in millions, except per-share data) |
| | (Unaudited) | | | (Unaudited) | | |
ASSETS | | Current assets: | | | | | | |
| Cash and cash equivalents | $ | 3,934 |
| | $ | 2,819 |
| $ | 3,729 |
| | $ | 3,186 |
|
| Investments | 1,787 |
| | 1,758 |
| 2,444 |
| | 2,524 |
|
| Restricted investments | 326 |
| | — |
| 77 |
| | 169 |
|
| Receivables | 1,002 |
| | 974 |
| 950 |
| | 871 |
|
| Income taxes refundable | 60 |
| | 39 |
| |
| Prepaid expenses and other current assets | 174 |
| | 131 |
| 411 |
| | 239 |
|
| Derivative asset | 425 |
| | 267 |
| 585 |
| | 522 |
|
| Total current assets | 7,708 |
| | 5,988 |
| 8,196 |
| | 7,511 |
|
| Property, equipment, and capitalized software, net | 397 |
| | 454 |
| 318 |
| | 342 |
|
| Deferred contract costs | 97 |
| | 86 |
| |
| Intangible assets, net | 101 |
| | 140 |
| |
| Goodwill | 430 |
| | 620 |
| |
| Goodwill and intangible assets, net | | 250 |
| | 255 |
|
| Restricted investments | 117 |
| | 110 |
| 120 |
| | 119 |
|
| Deferred income taxes | 62 |
| | 10 |
| 114 |
| | 103 |
|
| Other assets | 42 |
| | 41 |
| 135 |
| | 141 |
|
| | $ | 8,954 |
| | $ | 7,449 |
| $ | 9,133 |
| | $ | 8,471 |
|
| | | | | | | |
LIABILITIES AND STOCKHOLDERS’ EQUITY | | Current liabilities: | | | | | | |
| Medical claims and benefits payable | $ | 2,478 |
| | $ | 1,929 |
| $ | 2,023 |
| | $ | 2,192 |
|
| Amounts due government agencies | 1,324 |
| | 1,202 |
| 1,714 |
| | 1,542 |
|
| Accounts payable and accrued liabilities | 485 |
| | 385 |
| 713 |
| | 366 |
|
| Deferred revenue | 468 |
| | 315 |
| 404 |
| | 282 |
|
| Current portion of long-term debt | 782 |
| | 472 |
| 566 |
| | 653 |
|
| Derivative liability | 425 |
| | 267 |
| 585 |
| | 522 |
|
| Total current liabilities | 5,962 |
| | 4,570 |
| 6,005 |
| | 5,557 |
|
| Long-term debt | 1,317 |
| | 975 |
| 1,318 |
| | 1,318 |
|
| Lease financing obligations | 198 |
| | 198 |
| 198 |
| | 198 |
|
| Deferred income taxes | — |
| | 15 |
| |
| Other long-term liabilities | 48 |
| | 42 |
| 59 |
| | 61 |
|
| Total liabilities | 7,525 |
| | 5,800 |
| 7,580 |
| | 7,134 |
|
| | | | | | | |
| Stockholders’ equity: | | | | | | |
| Common stock, $0.001 par value; 150 shares authorized; outstanding: 57 shares at September 30, 2017 and at December 31, 2016 | — |
| | — |
| |
| Common stock, $0.001 par value, 150 shares authorized; outstanding: 62 shares at March 31, 2018 and 60 shares at December 31, 2017 | | — |
| | — |
|
| Preferred stock, $0.001 par value; 20 shares authorized, no shares issued and outstanding | — |
| | — |
| — |
| | — |
|
| Additional paid-in capital | 870 |
| | 841 |
| 1,153 |
| | 1,044 |
|
| Accumulated other comprehensive loss | (1 | ) | | (2 | ) | (12 | ) | | (5 | ) |
| Retained earnings | 560 |
| | 810 |
| 412 |
| | 298 |
|
| Total stockholders’ equity | 1,429 |
| | 1,649 |
| 1,553 |
| | 1,337 |
|
| | $ | 8,954 |
| | $ | 7,449 |
| $ | 9,133 |
| | $ | 8,471 |
|
See accompanying notes.
MOLINA HEALTHCARE, INC.CONSOLIDATED STATEMENT OF STOCKHOLDERS’ EQUITY
|
| | | | | | | | | | | | | | | | | | | | | | |
| | Common Stock | | Additional Paid-in Capital | | Accumulated Other Comprehensive Loss | | Retained Earnings | | Total |
| | Outstanding | | Amount | | | | |
| | (In millions) |
| | (Unaudited) |
| Balance at January 1, 2018 | 60 |
| | $ | — |
| | $ | 1,044 |
| | $ | (5 | ) | | $ | 298 |
| | $ | 1,337 |
|
| Net income | — |
| | — |
| | — |
| | — |
| | 107 |
| | 107 |
|
| Adoption of Topic 606 | — |
| | — |
| | — |
| | — |
| | 6 |
| | 6 |
|
| Adoption of ASU 2018-02 | — |
| | — |
| | — |
| | — |
| | 1 |
| | 1 |
|
| 1.625% Convertible Notes exchange transaction | 2 |
| | — |
| | 108 |
| | — |
| | — |
| | 108 |
|
| Other comprehensive loss, net | — |
| | — |
| | — |
| | (7 | ) | | — |
| | (7 | ) |
| Share-based compensation | — |
| | — |
| | 1 |
| | — |
| | — |
| | 1 |
|
| Balance at March 31, 2018 | 62 |
| | $ | — |
| | $ | 1,153 |
| | $ | (12 | ) | | $ | 412 |
| | $ | 1,553 |
|
See accompanying notes.
CONSOLIDATED STATEMENTS OF CASH FLOWS
| | | | Nine Months Ended September 30, | Three Months Ended March 31, |
| | 2017 | | 2016 | 2018 | | 2017 |
| | (Amounts in millions)
(Unaudited) | (Amounts in millions)
(Unaudited) |
| Operating activities: | | | | | | |
| Net (loss) income | $ | (250 | ) | | $ | 99 |
| |
| Adjustments to reconcile net (loss) income to net cash provided by operating activities: | | | | |
| Net income | | $ | 107 |
| | $ | 77 |
|
| Adjustments to reconcile net income to net cash provided by operating activities: | | | | |
| Depreciation and amortization | 139 |
| | 135 |
| 37 |
| | 49 |
|
| Impairment losses | 201 |
| | — |
| |
| Deferred income taxes | (68 | ) | | 20 |
| (6 | ) | | (5 | ) |
| Share-based compensation, including accelerated share-based compensation | 38 |
| | 24 |
| |
| Non-cash restructuring charges | 49 |
| | — |
| |
| Share-based compensation | | 6 |
| | 6 |
|
| Non-cash restructuring costs | | 17 |
| | — |
|
| Amortization of convertible senior notes and lease financing obligations | 24 |
| | 23 |
| 7 |
| | 8 |
|
| Loss on debt extinguishment | | 10 |
| | — |
|
| Other, net | 13 |
| | 14 |
| 2 |
| | 3 |
|
| Changes in operating assets and liabilities: | | | | | | |
| Receivables | (28 | ) | | (427 | ) | (83 | ) | | (32 | ) |
| Prepaid expenses and other assets | (53 | ) | | (116 | ) | |
| Prepaid expenses and other current assets | | (239 | ) | | (12 | ) |
| Medical claims and benefits payable | 549 |
| | 168 |
| (163 | ) | | (3 | ) |
| Amounts due government agencies | 122 |
| | 503 |
| 172 |
| | 373 |
|
| Accounts payable and accrued liabilities | 90 |
| | 1 |
| 319 |
| | 50 |
|
| Deferred revenue | 153 |
| | 157 |
| 130 |
| | 146 |
|
| Income taxes | (22 | ) | | 32 |
| 78 |
| | 59 |
|
| Net cash provided by operating activities | 957 |
| | 633 |
| 394 |
| | 719 |
|
| Investing activities: | | | | | | |
| Purchases of investments | (1,896 | ) | | (1,444 | ) | (389 | ) | | (733 | ) |
| Proceeds from sales and maturities of investments | 1,538 |
| | 1,512 |
| 543 |
| | 433 |
|
| Purchases of property, equipment and capitalized software | (85 | ) | | (143 | ) | (4 | ) | | (26 | ) |
| (Increase) decrease in restricted investments held-to-maturity | (10 | ) | | 4 |
| |
| Net cash paid in business combinations | — |
| | (48 | ) | |
| Increase in restricted investments held-to-maturity | | — |
| | (5 | ) |
| Other, net | (21 | ) | | (12 | ) | (5 | ) | | (6 | ) |
| Net cash used in investing activities | (474 | ) | | (131 | ) | |
| Net cash provided by (used in) investing activities | | 145 |
| | (337 | ) |
| Financing activities: | | | | | | |
| Proceeds from senior notes offering, net of issuance costs | 325 |
| | — |
| |
| Proceeds from borrowings under credit facility | 300 |
| | — |
| |
| Cash paid for financing transaction fees | | (5 | ) | | — |
|
| Proceeds from employee stock plans | 11 |
| | 10 |
| — |
| | 1 |
|
| Other, net | (4 | ) | | 1 |
| — |
| | (2 | ) |
| Net cash provided by financing activities | 632 |
| | 11 |
| |
| Net increase in cash and cash equivalents | 1,115 |
| | 513 |
| |
| Cash and cash equivalents at beginning of period | 2,819 |
| | 2,329 |
| |
| Cash and cash equivalents at end of period | $ | 3,934 |
| | $ | 2,842 |
| |
| Net cash used in financing activities | | (5 | ) | | (1 | ) |
| Net increase in cash, cash equivalents, and restricted cash and cash equivalents | | 534 |
| | 381 |
|
| Cash, cash equivalents, and restricted cash and cash equivalents at beginning of period | | 3,290 |
| | 2,912 |
|
| Cash, cash equivalents, and restricted cash and cash equivalents at end of period | | $ | 3,824 |
| | $ | 3,293 |
|
MOLINA HEALTHCARE, INC.
CONSOLIDATED STATEMENTS OF CASH FLOWS
(continued)
| | | | Nine Months Ended September 30, | Three Months Ended March 31, |
| | 2017 | | 2016 | 2018 | | 2017 |
| | (Amounts in millions)
(Unaudited) | (Amounts in millions)
(Unaudited) |
| Supplemental cash flow information: | | | | | | |
| | | | | | | |
| Schedule of non-cash investing and financing activities: | | | | | | |
| Common stock used for share-based compensation | $ | (21 | ) | | $ | (8 | ) | $ | (5 | ) | | $ | (6 | ) |
| | | | | | | |
| Details of change in fair value of derivatives, net: | | | | | | |
| Gain (loss) on 1.125% Call Option | $ | 158 |
| | $ | (60 | ) | $ | 63 |
| | $ | (86 | ) |
| (Loss) gain on 1.125% Conversion Option | (158 | ) | | 60 |
| (63 | ) | | 86 |
|
| Change in fair value of derivatives, net | $ | — |
| | $ | — |
| $ | — |
| | $ | — |
|
| | | | | | | |
| Details of business combinations: | | | | |
| Fair value of assets acquired | $ | — |
| | $ | (186 | ) | |
| Fair value of liabilities assumed | — |
| | 28 |
| |
| Purchase price amounts accrued/received | — |
| | 8 |
| |
| Reversal of amounts advanced to sellers in prior year | — |
| | 102 |
| |
| Net cash paid in business combinations | $ | — |
| | $ | (48 | ) | |
| 1.625% Convertible Notes exchange transaction: | | | | |
| Common stock issued in exchange for 1.625% Convertible Notes | | $ | 131 |
| | $ | — |
|
| Component of 1.625% Convertible Notes allocated to additional paid-in capital, net of income taxes | | (23 | ) | | — |
|
| Net increase to additional paid-in capital | | $ | 108 |
| | $ | — |
|
See accompanying notes.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (UNAUDITED)
September 30, 2017March 31, 2018
1. Basis of Presentation
Organization and Operations
Molina Healthcare, Inc. provides quality managed health care to people receiving government assistance. We offer cost-effective Medicaid-related solutions to meet the health care needs of low-income families and individuals, and to assist government agencies in their administration of the Medicaid program. We have three reportable segments. These segments consist of our Health Plans segment, which constitutes the vast majority of our operations; our Molina Medicaid Solutions segment; and our Other segment.
The Health Plans segment consists of health plans operating in 1213 states and the Commonwealth of Puerto Rico. As of September 30, 2017,March 31, 2018, these health plans served approximately 4.54.1 million members eligible for Medicaid, Medicare, and other government-sponsored health care programs for low-income families and individuals. This membership includes Affordable Care Act Marketplace (Marketplace) members, most of whom receive government premium subsidies. The health plans are operated by our respective wholly owned subsidiaries in those states, each of which is licensed as a health maintenance organization (HMO).
Our health plans’ state Medicaid contracts generally have terms of three to four years. These contracts typically contain renewal options exercisable by the state Medicaid agency, and allow either the state or the health plan to terminate the contract with or without cause. Our health plan subsidiaries have generally been successful in retaining their contracts, but suchSuch contracts are subject to risk of loss when a state issues a new requestin states that issue requests for proposal (RFP) open to competitive bidding by other health plans. If one of our health plans is not a successful responsive bidder to a state RFP, its contract may not be subject to non-renewal.renewed.
In addition to contract renewal, our state Medicaid contracts may be periodically amended to include or exclude certain health benefits (such as pharmacy services, behavioral health services, or long-term care services); populations such as the aged, blind or disabled (ABD); and regions or service areas.
The Molina Medicaid Solutions segment provides support to state government agencies in theagencies’ administration of their Medicaid programs, including business processing, information technology development and administrative services.
The Other segment includes primarily our Pathways behavioral health and social services provider, and corporate amounts not allocated to other reportable segments.
Recent Developments — Health Plans SegmentPresentation and Reclassification
Illinois Health Plan. We have reclassified certain amounts in the 2017 consolidated statement of cash flows to conform to the 2018 presentation, relating to the presentation of restricted cash and cash equivalents. The reclassification is a result of our adoption of Accounting Standards Update (ASU) 2016-18,In August 2017, Molina Healthcare of Illinois, Inc. was awarded a statewide Medicaid managed care contract by the Illinois Department of Healthcare and Family Services. This Medicaid contract further integrates behavioral health and physical health by combining the State’s three current managed care programs into one program. The contract begins Restricted Cash effective January 1, 2018,2018. See Note 2, “Significant Accounting Policies,” for four years with options to renew annually for up to four additional years.
Mississippi Health Plan. In June 2017, Molina Healthcare of Mississippi, Inc. was awarded a Medicaid Coordinated Care Contract for the statewide administration of the Mississippi Coordinated Access Network (MississippiCAN). The operational start date for the program is currently scheduled for October 1, 2018, pending the completion of a readiness review. The initial term of the contract is through June 2020, with options to renew annually for up to two additional years.
Washington Health Plan. In May 2017, Molina Healthcare of Washington, Inc. was selected by the Washington State Health Care Authority to negotiate and enter into managed care contracts for the North Central region of the state’s Apple Health Integrated Managed Care Program. The start date for the new contract is scheduled for January 1, 2018.
Terminated Medicare Acquisition. In August 2016, we entered into agreements with each of Aetna Inc. and Humana Inc. to acquire certain assets related to their Medicare Advantage business. The transaction was subject to closing
conditionsfurther information, including the completion of the proposed acquisition of Humana by Aetna (the Aetna-Humana Merger). In January 2017, the U.S. District Court for the District of Columbia granted the request for relief made by the U.S. Department of Justice in its civil antitrust lawsuit against Aetna and Humana, to prohibit the Aetna-Humana Merger. In February 2017, our agreements with each of Aetna and Humana were terminated by the parties pursuant to the terms of the agreements. Under the termination agreements, we received an aggregate termination fee of $75 million from Aetna and Humana in the first quarter of 2017, which is reported in “Other income, net”amount reclassified.
We have combined certain line items in the accompanying consolidated statements of operations.balance sheets. For all periods presented, we have combined the presentation of:
New York Health Plan. In August 2016, we closed on our acquisition of the outstanding equity interests of Today’s Options of New York, Inc., which now operates as Molina Healthcare of New York, Inc. The purchase price allocation was completed,Income taxes refundable with “Prepaid expenses and the final purchase price adjustments were recorded, in the first quarter of 2017. Such adjustments were insignificant,other current assets;”
Income taxes payable with “Accounts payable and the final cash purchase price was $38 million.accrued liabilities;”
Impairment Losses
Molina Medicaid Solutions segment. In the third quarter of 2017, we recorded a non-cash goodwill impairment loss of $28 million.See Note 10, “Impairment Losses.”
Other segment. In the third quarter of 2017, we recorded a non-cash goodwill impairment loss of $101 million for our Pathways subsidiary. In the second quarter of 2017, we recorded non-cash goodwillGoodwill, and intangible assets, impairment losses of $72 million, primarily for our Pathways subsidiary. See Note 10, “Impairment Losses.net to a single line; and
Deferred contract costs with “Other assets.”
Consolidation and Interim Financial Information
The consolidated financial statements include the accounts of Molina Healthcare, Inc., its subsidiaries, and variable interest entities (VIEs) in which Molina Healthcare, Inc. is considered to be the primary beneficiary. Such VIEs are insignificant to our consolidated financial position and results of operations. In the opinion of management, all adjustments considered necessary for a fair presentation of the results as of the date and for the interim periods presented have been included; such adjustments consist of normal recurring adjustments. All significant intercompany balances and transactions have been eliminated. The consolidated results of operations for the current interim periodthree
months ended March 31, 2018 are not necessarily indicative of the results for the entire year ending December 31, 2017.2018.
The unaudited consolidated interim financial statements have been prepared under the assumption that users of the interim financial data have either read or have access to our audited consolidated financial statements for the fiscal year ended December 31, 2016.2017. Accordingly, certain disclosures that would substantially duplicate the disclosures contained in theour December 31, 20162017 audited consolidated financial statements have been omitted. These unaudited consolidated interim financial statements should be read in conjunction with our December 31, 20162017 audited consolidated financial statements.
2. Significant Accounting Policies
CertainCash and Cash Equivalents
Cash and cash equivalents consist of cash and short-term, highly liquid investments that are both readily convertible into known amounts of cash and have a maturity of three months or less on the date of purchase. The following table provides a reconciliation of cash, cash equivalents, and restricted cash and cash equivalents reported within the accompanying consolidated balance sheets that sum to the total of the same such amounts presented in the accompanying consolidated statements of cash flows. The restricted cash and cash equivalents presented below are included in non-current “Restricted investments” in the accompanying consolidated balance sheets.
|
| | | | | | | |
| | Three Months Ended March 31, |
| | 2018 | | 2017 |
| | (In millions) |
| Cash and cash equivalents | $ | 3,729 |
| | $ | 3,198 |
|
| Restricted cash and cash equivalents | 95 |
| | 95 |
|
| Total cash, cash equivalents, and restricted cash and cash equivalents presented in the statements of cash flows | $ | 3,824 |
| | $ | 3,293 |
|
Revenue Recognition
We adopted ASU 2014-09, Revenue from Contracts with Customers (Topic 606) effective January 1, 2018, using the modified retrospective approach. The insurance contracts of our significant accounting policies are discussed within the note to which they specifically relate.
Revenue Recognition – Health Plans Segmentsegment, which segment constitutes the vast majority of our operations, are excluded from the scope of Topic 606 because the recognition of revenue under these contracts is dictated by other accounting standards governing insurance contracts. The cumulative effect of initially applying the guidance, relating entirely to our Molina Medicaid Solutions segment contracts, resulted in an immaterial impact to beginning retained earnings, as presented in the accompanying consolidated statement of stockholders’ equity. Topic 606 was only applied to service contracts that were not completed as of December 31, 2017. Refer to “Molina Medicaid Solutions segment” and “Other segment” below for further information.
Health Plans segment
Premium revenue is fixed in advance of the periods covered and, except as described below, is not generally subject to significant accounting estimates. Premium revenues are recognized in the month that members are entitled to receive health care services, and premiums collected in advance are deferred. Certain components of premium revenue are subject to accounting estimates and fall into two broad categories discussed in further detail below: 1) “Contractual Provisions That May Adjust or Limit Revenue or Profit;” and 2) “Quality Incentives.” Liabilities recorded for such provisions are included in “Amounts due government agencies” in the accompanying consolidated balance sheets.
Contractual Provisions That May Adjust or Limit Revenue or Profit
| |
| 1) | Contractual Provisions That May Adjust or Limit Revenue or Profit: |
Medicaid
Medical Cost Floors (Minimums), and Medical Cost Corridors: A portion of our premium revenue may be returned if certain minimum amounts are not spent on defined medical care costs. In the aggregate, we recorded a liability under the terms of such contract provisions of $119$148 million and $272$135 million at September 30, 2017March 31, 2018 and December 31, 2016, respectively, to “Amounts due government agencies.”2017, respectively. Approximately $82$97 million and $244$96 million of the liability
accrued at September 30, 2017March 31, 2018 and December 31, 2016,2017, respectively, relates to our participation in Medicaid Expansion programs.
In certain circumstances, our health plans may receive additional premiums if amounts spent on medical care costs exceed a defined maximum threshold. Receivables relating to such provisions were insignificant at September 30, 2017 and December 31, 2016.
Profit Sharing and Profit Ceiling: Our contracts with certain states contain profit-sharing or profit ceiling provisions under which we refund amounts to the states if our health plans generate profit above a certain specified percentage. In some cases, we are limited in the amount of administrative costs that we may deduct in calculating the refund, if any. Liabilities for profits in excess of the amount we are allowed to retain under these provisions were insignificant at September 30, 2017 and December 31, 2016.
Retroactive Premium Adjustments: State Medicaid programs periodically adjust premium rates on a retroactive basis. In these cases, we must adjust our premium revenue in the period in which we learn of the adjustment, rather than in the months of service to which the retroactive adjustment applies.
Medicare
Risk Adjustment: Our Medicare premiums are subject to retroactive increase or decrease based on the health status of our Medicare members (measured as a member risk score). We estimate our members’ risk scores and the related amount of Medicare revenue that will ultimately be realized for the periods presented based on our knowledge of our members’ health status, risk scores and the Centers for Medicare & Medicaid Services (CMS) practices. Consolidated balance sheet amounts related to anticipated Medicare risk adjustment premiums and Medicare Part D settlements were insignificant at September 30, 2017 and December 31, 2016.
Minimum MLR: Additionally, federalFederal regulations have established a minimum annual medical loss ratio (Minimum MLR) of 85% for Medicare. The medical loss ratio represents medical costs as a percentage of premium revenue. Federal regulations define what constitutes medical costs and premium revenue. If the Minimum MLR is not met, we may be required to pay rebates to the federal government. We recognize estimated rebates under the Minimum MLR as an adjustment to premium revenue in our consolidated statements of operations.income.
Marketplace
Premium Stabilization Programs: The Affordable Care Act (ACA) established Marketplace premium stabilization programs effective January 1, 2014. These programs, commonly referred to as the “3R’s,” include a permanent risk adjustment program, a transitional reinsurance program, and a temporary risk corridor program. We record receivables or payables related to the 3R programs and the Minimum MLR when the amounts are reasonably estimable as described below, and, for receivables, when collection is reasonably assured. Our receivables (payables) for each of these programs, as of the dates indicated, were as follows:
|
| | | | | | | | | | | | | | | |
| | September 30, 2017 | | December 31,
2016 |
| | Current Benefit Year | | Prior Benefit Years | | Total | |
| | | | | | | | |
| | (In millions) |
| Risk adjustment | $ | (655 | ) | | $ | — |
| | $ | (655 | ) | | $ | (522 | ) |
| Reinsurance | — |
| | 10 |
| | 10 |
| | 55 |
|
| Risk corridor | — |
| | — |
| | — |
| | (1 | ) |
| Minimum MLR | (27 | ) | | — |
| | (27 | ) | | (1 | ) |
Risk adjustment: Under this permanent program, our health plans’ composite risk scores are compared with the overall average risk score for the relevant state and market pool. Generally, our health plans will make a risk transfer payment into the pool if their composite risk scores are below the average risk score, and will receive a risk transfer payment from the pool if their composite risk scores are above the average risk score. We estimate our ultimate premium based on insurance policy year-to-date experience, and recognize estimated premiums relating to the risk adjustment program as an adjustment to premium revenue in our consolidated statements of operations.
Reinsurance: This program was designed to provide reimbursement to insurers for high cost membersincome. As of March 31, 2018, and ended December 31, 2016; we expect2017 the Marketplace risk adjustment payable amounted to settle the outstanding receivable balance in 2017.$1,129 million and $912 million, respectively.
Risk corridor: This program was intended to limit gains and losses of insurers by comparing allowable costs to a target amount as defined by CMS, and ended December 31, 2016; all outstanding balances were settled as of September 30, 2017.
Additionally, theMinimum MLR: The ACA has established a Minimum MLR of 80% for the Marketplace. The medical loss ratio represents medical costs as a percentage of premium revenue. Federal regulations define what constitutes medical costs and premium revenue. If the Minimum MLR is not met, we may be required to pay rebates to our Marketplace policyholders. Each of the 3R programsThe Marketplace risk adjustment program is taken into consideration when computing the Minimum MLR. We recognize estimated rebates under the Minimum MLR as an adjustment to premium revenue in our consolidated statements of operations.income.
Quality Incentives
At severalmany of our health plans, revenue ranging from approximately 1% to 3% of certain health plan premiums is earned only if certain performance measures are met.
The following table quantifies the quality incentive premium revenue recognized for the periods presented, including the amounts earned in the periods presented and prior periods. Although the reasonably possible effects of a change in estimate related to quality incentive premium revenue as of September 30, 2017March 31, 2018 are not known, we have no reason to believe that the adjustments to prior years noted below are not indicative of the potential future changes in our estimates as of September 30, 2017.March 31, 2018.
| | | | Three Months Ended September 30, | | Nine Months Ended September 30, | Three Months Ended March 31, |
| | 2017 | | 2016 | | 2017 | | 2016 | 2018 | | 2017 |
| | (Dollars in millions) | (Dollars in millions) |
| Maximum available quality incentive premium - current period | $ | 36 |
| | $ | 33 |
| | $ | 113 |
| | $ | 114 |
| $ | 40 |
| | $ | 38 |
|
| Quality incentive premium revenue recognized in current period: | | | | | | | | | | |
| Earned current period | $ | 24 |
| | $ | 26 |
| | $ | 72 |
| | $ | 80 |
| $ | 24 |
| | $ | 19 |
|
| Earned prior periods | 3 |
| | — |
| | 9 |
| | 54 |
| 11 |
| | 5 |
|
| Total | $ | 27 |
| | $ | 26 |
| | $ | 81 |
| | 134 |
| $ | 35 |
| | $ | 24 |
|
| | | | | | | | | | | |
| Quality incentive premium revenue recognized as a percentage of total premium revenue | 0.6 | % | | 0.6 | % | | 0.6 | % | | 1.1 | % | 0.8 | % | | 0.5 | % |
Molina Medicaid Solutions segment
Molina Medicaid Solutions is under contract with Medicaid agencies in six states and the U.S. Virgin Islands. Our existing contracts have terms that currently extend to 2018 through 2025, before renewal options. As of March 31, 2018, the aggregate amount of service revenue relating to unsatisfied performance obligations amounted to $571 million.
Business process outsourcing services are billed immediately following the end of the month in which such services are performed, with payment received soon thereafter. Payments for the design, development and implementation (DDI) of Medicaid management information systems milestones are received following our performance, and the
customer’s acceptance, of the milestone deliverable. However, DDI revenue is deferred until the system ‘go-live’ date, and is amortized over the initial contract hosting period.
Other segment
Our Pathways behavioral health subsidiary’s revenue is variable, and generally invoiced after services are rendered; customer payment follows invoicing. We have concluded that there is no change to revenue recognition under Topic 606 for our Pathways behavioral health subsidiary, and therefore no impact to retained earnings effective January 1, 2018.
The following table presents the opening and closing balances of receivables, deferred contract costs (contract assets), and deferred revenue (contract liabilities) from contracts with customers, by segment.
|
| | | | | | | |
| | March 31,
2018 | | December 31,
2017 |
| | (In millions) |
| Receivables: | | | |
| Molina Medicaid Solutions | $ | 41 |
| | $ | 30 |
|
| Other | 46 |
| | 44 |
|
| Deferred contract costs (contract assets) – Molina Medicaid Solutions | 103 |
| | 101 |
|
| Deferred revenue (contract liabilities) – Molina Medicaid Solutions | 41 |
| | 49 |
|
Medical Care Costs - Marketplace Cost Share Reduction (CSR) Update
During the first quarter of 2018, we recognized a benefit of approximately $70 million in reduced medical expense related to 2017 dates of service as a result of the federal government’s confirmation that the reconciliation of 2017 Marketplace CSR subsidies would be performed on an annual basis. In the fourth quarter of 2017, we had assumed a nine-month reconciliation of this item pending confirmation of the time period to which the 2017 reconciliation would be applied.
Income Taxes
The provision for income taxes is determined using an estimated annual effective tax rate, which generally differs from the U.S. federal statutory rate primarily because of state taxes, nondeductible expenses such as the Health Insurer Fee (HIF), goodwill impairment, certain compensation, and other general and administrative expenses. The effective tax rate was not impacted by HIF in 2017 given the 2017 HIF moratorium.
The effective tax rate may be subject to fluctuations during the year, particularly as a result of the level of pretax earnings, and also as new information is obtained. Such information may affect the assumptions used to estimate the annual effective tax rate, including factors such as the mix of pretax earnings in the various tax jurisdictions in which we operate, valuation allowances against deferred tax assets, the recognition or the reversal of the recognition of tax benefits related to uncertain tax positions, and changes in or the interpretation of tax laws in jurisdictions where we conduct business. We recognize deferred tax assets and liabilities for temporary differences between the financial reporting basis and the tax basis of our assets and liabilities, along with net operating loss and tax credit carryovers.
Premium Deficiency ReservesThe Tax Cuts and Jobs Act (TCJA) was enacted on Loss Contracts
We assessDecember 22, 2017. The TCJA, in part, reduced the profitabilityU.S. federal statutory corporate income tax rate from 35% to 21% effective January 1, 2018. Accounting guidance allows filers one year subsequent to the end of the tax year to finalize the valuation of deferred tax assets and liabilities. At March 31, 2018, we had not completed our accounting for the tax effects resulting from enactment of TCJA with respect to valuation of our medical care policiesdeferred tax assets and liabilities. We will continue to identify groupsmake and refine our calculations as additional analysis is completed. In addition, our estimates may also be affected as we gain a more thorough understanding of contracts where current operating results or forecasts indicate probablethe tax law based on expected future losses. If anticipated future variable costs exceed anticipated future premiums and investment income, a premium deficiency reserve is recognized. We assume a full-year CSR reconciliation (see further information below) in the premium deficiency reserve calculation for the Marketplace program. We recorded a premium deficiency reserve to “Medical claims and benefits payable” on our accompanying consolidated balance sheets relating to our Marketplace program of $30 million as of December 31, 2016, which increased to $100 million as of June 30, 2017, and then decreased to $70 million as of September 30, 2017. If a nine-month CSR reconciliation had been included in the computation rather than a full year, the premium deficiency reserve would have increased by $55 million, to $125 million as of September 30, 2017. The theoretical $55 million increase to the premium deficiency reserve is less than the potential fourth quarter 2017 impact described below, or $85 million, because such adjustment only recognizes the potential CSR impact to the extent it would have created a deficiency in premiums at September 30, 2017.
Marketplace Cost Share Reduction (CSR) Update
Our third quarter results do not include any potential impactguidance from the October 12, 2017, direction to Centers for MedicareInternal Revenue Service and Medicaid Services (CMS) from Acting Department of Health and Human Services Secretary Hargan to cease payment of Marketplace CSR subsidies. At September 30, 2017, we had a total of approximately $220 million in excess CSR subsidies, recorded as a payable to CMS. This payable represents the extent to which payments received by us from CMS exceeded our estimate of the actual cost of member subsidies incurred by us through September 30, 2017.
We expect to incur approximately $85 million in unreimbursed expense associated with the cessation of CSR subsidies in the fourth quarter of 2017. It has been the practice of CMS to perform a reconciliation on an annual basis of CSR subsidies paid to all health plans against the actual costs incurred by the health plans. Were such a reconciliation to be performed for the full calendar year of 2017—consistent with past practice—we would be able to offset nearly all of the $85 million expense incurred in the fourth quarter against the excess amounts received prior to September 30, 2017. However, should CMS transition to a nine month reconciliation period ending September 30, 2017—the last month for which CSR subsidies have been paid—the absence of CSR subsidy reimbursement would reduce income before income tax expense by approximately $85 million in the fourth quarter of 2017.U.S. Treasury.
Recent Accounting Pronouncements Adopted
Goodwill Impairment.Revenue Recognition (Topic 606). See discussion above, in “Revenue Recognition.”
Comprehensive Income. In January 2017,February 2018, the Financial Accounting Standards Board (FASB) issued Accounting Standards Update (ASU) 2017-04,ASU 2018-02, Simplifying the Test for Goodwill ImpairmentReclassification of Certain Tax Effects from Accumulated Other Comprehensive Income, which eliminatesallows a reclassification from accumulated other comprehensive income to retained earnings for stranded tax effects resulting from the requirement to calculate the implied fair value of goodwill to measure a goodwill impairment loss. Instead, an impairment loss is measured as the excess of the carrying amount of the reporting unit, including goodwill, over the fair value of the reporting unit.TCJA. ASU 2017-042018-02 is effective beginning January 1, 2020;2019; we early adopted this ASU 2017-04effective
January 1, 2018. The effect of applying the guidance resulted in an immaterial impact to beginning retained earnings, as presented in the accompanying consolidated statement of June 30, 2017, in connection with the interim assessment of our Pathways subsidiary. See further discussion at Note 10, “Impairment Losses.”stockholders’ equity.
Restricted Cash. In November 2016, the FASB issued ASU 2016-18, Restricted Cash, which will requirerequires us to include in our consolidated statements of cash flows the balances of cash, cash equivalents, restricted cash and restricted cash equivalents. When these items are presented in more than one line item on the balance sheet, the new guidance requires a reconciliation of the totals in the statement of cash flows to the related captions in the balance sheet. Transfers between cash and cash equivalents and restricted cash and restricted cash equivalents willare no longer be presented in the statement of cash flows. ASU 2016-18 is effective beginning January 1, 2018; early adoption is permitted. We are currently evaluating the changes that will be required in our consolidated statements of cash flows.
Stock Compensation. In March 2016, the FASB issued ASU 2016-09, Improvements to Employee Share-Based Payment Accounting, which amends ASC Topic 718, Compensation – Stock Compensation. ASU 2016-09 simplifies several aspects of accounting for employee share-based payment transactions, including the accounting for income taxes, forfeitures, statutory tax and classification in the statement of cash flows. We adopted ASU 2016-092016-18 on January 1, 2018. We have applied the guidance retrospectively to all periods presented. Such retrospective adoption resulted in a $95 million reclassification of restricted cash and cash equivalents from “Investing activities” to the first quarterbeginning and ending balances of 2017; such adoption did not significantly impactcash and cash equivalents in our consolidated financial statements. In addition, the prior period presentation in the statementstatements of cash flows for the quarter ended March 31, 2017. There was not adjusted because such adjustments were insignificant.no impact to our consolidated statements of income, balance sheets, or stockholders’ equity. The reconciliation of cash and cash equivalents to cash, cash equivalents and restricted cash and cash equivalents is presented at the beginning of this note.
Recent Accounting Pronouncements Not Yet Adopted
Credit Losses. In June 2016, the FASB issued ASU 2016-13, Measurement of Credit Losses on Financial Instruments. Rather than generally recognizing credit losses when it is probable that the loss has been incurred, the revised guidance requires companies to recognize an allowance for credit losses for the difference between the amortized cost basis of a financial instrument and the amount of amortized cost that the company expects to collect over the instrument’s contractual life. ASU 2016-13 is effective for us beginning January 1, 2020, and must be adopted as a cumulative effect adjustment to retained earnings; early adoption is permitted. We are evaluating the effect of this guidance.
Leases. In February 2016, the FASB issued ASU 2016-02, Leases (Topic 842), as modified by ASU 2017-03, Transition and Open Effective Date Information. Under ASU 2016-02, an entity will be required to recognize assets and liabilities for the rights and obligations created by leases on the entity’s balance sheet for both financefinancing and operating leases. For leases with a term of 12 months or less, an entity canmay elect to not recognize lease assets and lease liabilities and expense the lease over a straight-line basis for the term of the lease. ASU 2016-02 will require new disclosures that depict the amount, timing, and uncertainty of cash flows pertaining to an entity’s leases. ASU 2016-02 is effective for us beginning January 1, 2019, and must be adopted using a modified retrospective approach for annual and interim periods beginning after December 15, 2018. Early adoption is permitted. Under this guidance, we will record assets and liabilities relating primarily to our long-term office leases. We are evaluatingcurrently updating the effect toconfiguration of our lease database management system for the adoption of Topic 842, and we are in the early stages of computing the impact of Topic 842 on our consolidated financial statements.
Revenue Recognition. In May 2014, the FASB issued ASU 2014-09, Revenue from Contracts with Customers (Topic 606). We intend to adopt this standard and the related modifications on January 1, 2018, using the modified retrospective approach. Under this approach, the cumulative effect of initially applying the guidance will be reflected as an adjustment to beginning retained earnings.
We have determined that the insurance contracts of our Health Plans segment, which segment constitutes the vast majority of our operations, are excluded from the scope of Topic 606 because the recognition of revenue under these contracts is dictated by other accounting standards governing insurance contracts.
For our Molina Medicaid Solutions segment, we have reevaluated our earlier assessment and determined that revenue for contracts that include design, development and implementation of Medicaid managed care systems shall be deferred until the system ‘go-live’ date, and then generally recognized on a straight-line basis over the hosting period. This approach is consistent with the FASB/IASB Joint Transition Resource Group for Revenue Recognition view for entities that provide software as a service solution, and similar to our historical revenue recognition methodology. We are continuing to evaluate the existence of customers’ rights with regard to renewal options and whether such rights may constitute separate performance obligations. We expect that cost of service revenue will generally be recognized in a manner consistent with the corresponding revenue recognition.
We believe the cumulative adjustment to retained earnings associated with the adoption of Topic 606 effective January 1, 2018, will be insignificant for both our Molina Medicaid Solutions and Other segments.
Other recent accounting pronouncements issued by the FASB (including its Emerging Issues Task Force), the American Institute of Certified Public Accountants, and the Securities and Exchange Commission (SEC) did not have, or are not believed by management to have, a significant impact on our present or future consolidated financial statements.
3. Net (Loss) Income per Share
The following table sets forth the calculation of basic and diluted net (loss) income per share: | | | | Three Months Ended September 30, | | Nine Months Ended September 30, | Three Months Ended March 31, |
| | 2017 | | 2016 | | 2017 | | 2016 | 2018 | | 2017 |
| | (In millions, except net income per share) | (In millions, except net income per share) |
| Numerator: | | | | | | | | | | |
| Net (loss) income | $ | (97 | ) | | $ | 42 |
| | $ | (250 | ) | | $ | 99 |
| |
| Net income | | $ | 107 |
| | $ | 77 |
|
| Denominator: | | | | | | | | | | |
| Denominator for basic net (loss) income per share | 57 |
| | 56 |
| | 56 |
| | 55 |
| |
| Shares outstanding at the beginning of the period | | 59 |
| | 56 |
|
| Weighted-average number of shares issued: | | | | |
1.625% Exchange (1) | | 1 |
| | — |
|
| Denominator for basic net income per share | | 60 |
| | 56 |
|
| Effect of dilutive securities: | | | | | | | | | | |
Convertible senior notes (1) | | 1 |
| | — |
|
1.125% Warrants (1) | — |
| | — |
| | — |
| | 1 |
| 4 |
| | — |
|
| Denominator for diluted net (loss) income per share | 57 |
| | 56 |
| | 56 |
| | 56 |
| |
| Denominator for diluted net income per share | | 65 |
| | 56 |
|
| | | | | | | | | | | |
Net (loss) income per share: (2) | | | | | | | | |
Net income per share: (2) | | | | |
| Basic | $ | (1.70 | ) | | $ | 0.77 |
| | $ | (4.44 | ) | | $ | 1.79 |
| $ | 1.79 |
| | $ | 1.38 |
|
| Diluted | $ | (1.70 | ) | | $ | 0.76 |
| | $ | (4.44 | ) | | $ | 1.77 |
| $ | 1.64 |
| | $ | 1.37 |
|
| | | | | | | | | |
| Potentially dilutive common shares excluded from calculations: | | | | | | | | |
1.125% Warrants (1) | 2 |
| | — |
| | 2 |
| | — |
| |
1.625% Notes (1) | 1 |
| | — |
| | — |
| | — |
| |
| |
| (1) | For more information regarding the 1.625% Exchange and the convertible senior notes, refer to Note 7, “Debt.” For more information regarding the 1.125% Warrants, refer to Note 9, “Stockholders' Equity.” For more information regarding the 1.625% Notes, refer to Note 7, “Debt.” The dilutive effect of all potentially dilutive common shares is calculated using the treasury stock method. Potentially dilutive common shares were not included in the computation of diluted net loss per share in the three and nine months ended September 30, 2017, because to do so would have been anti-dilutive. |
| |
| (2) | Source data for calculations in thousands. |
4. Fair Value Measurements
We consider the carrying amounts of cash, cash equivalents and other current assets and current liabilities (not including derivatives and the current portion of long-term debt) to approximate their fair values because of the
relatively short period of time between the origination of these instruments and their expected realization or payment. For our financial instruments measured at fair value on a recurring basis, we prioritize the inputs used in measuring fair value according to the three-tier fair value hierarchy. For a description of the methods and assumptions that we use to a) estimate the fair value; and b) determine the classification according to the fair value hierarchy for each financial instrument, see Note 5,4, “Fair Value Measurements,” in our 20162017 Annual Report on Form 10-K.
Derivative financial instruments include the 1.125% Call Option derivative asset and the 1.125% Conversion Option derivative liability. These derivatives are not actively traded and are valued based on an option pricing model that uses observable and unobservable market data for inputs. Significant market data inputs used to determine fair value as of September 30, 2017,March 31, 2018, included the price of our common stock, the time to maturity of the derivative instruments, the risk-free interest rate, and the implied volatility of our common stock. As described further in Note 8, “Derivatives,” the 1.125% Call Option derivative asset and the 1.125% Conversion Option derivative liability were designed such that changes in their fair values would offset, with minimal impact to the consolidated statements of operations.income. Therefore, the sensitivity of changes in the unobservable inputs to the option pricing model for such derivative instruments is mitigated.
The net changes in fair value of Level 3 financial instruments were insignificant to our results of operations for the ninethree months ended September 30, 2017.March 31, 2018.
Our financial instruments measured at fair value on a recurring basis at September 30, 2017,March 31, 2018, were as follows: | | | | Total | | Quoted Market Prices (Level 1) | | Significant Other Observable Inputs (Level 2) | | Significant Unobservable Inputs (Level 3) | Total | | Quoted Market Prices (Level 1) | | Significant Other Observable Inputs (Level 2) | | Significant Unobservable Inputs (Level 3) |
| | (In millions) | (In millions) |
| Corporate debt securities | $ | 1,162 |
| | $ | — |
| | $ | 1,162 |
| | $ | — |
| $ | 1,618 |
| | $ | — |
| | $ | 1,618 |
| | $ | — |
|
| U.S. treasury notes | | 329 |
| | 329 |
| | — |
| | — |
|
| Government-sponsored enterprise securities (GSEs) | 220 |
| | 220 |
| | — |
| | — |
| 227 |
| | 227 |
| | — |
| | — |
|
| Municipal securities | 131 |
| | — |
| | 131 |
| | — |
| 131 |
| | — |
| | 131 |
| | — |
|
| Asset-backed securities | 125 |
| | — |
| | 125 |
| | — |
| 110 |
| | — |
| | 110 |
| | — |
|
| U.S. treasury notes | 121 |
| | 121 |
| | — |
| | — |
| |
| Certificates of deposit | 28 |
| | — |
| | 28 |
| | — |
| |
| Certificate of deposit | | 27 |
| | — |
| | 27 |
| | — |
|
| Other | | 2 |
| | — |
| | 2 |
| | — |
|
| Subtotal - current investments | 1,787 |
| | 341 |
| | 1,446 |
| | — |
| 2,444 |
| | 556 |
| | 1,888 |
| | — |
|
| Corporate debt securities | 229 |
| | — |
| | 229 |
| | — |
| 66 |
| | — |
| | 66 |
| | — |
|
| U.S. treasury notes | 97 |
| | 97 |
| | — |
| | — |
| 11 |
| | 11 |
| | — |
| | — |
|
| Subtotal - current restricted investments | 326 |
| | 97 |
| | 229 |
| | — |
| 77 |
| | 11 |
| | 66 |
| | — |
|
| 1.125% Call Option derivative asset | 425 |
| | — |
| | — |
| | 425 |
| 585 |
| | — |
| | — |
| | 585 |
|
| Total assets | $ | 2,538 |
| | $ | 438 |
| | $ | 1,675 |
| | $ | 425 |
| $ | 3,106 |
| | $ | 567 |
| | $ | 1,954 |
| | $ | 585 |
|
| | | | | | | | | | | | | | | |
| 1.125% Conversion Option derivative liability | $ | 425 |
| | $ | — |
| | $ | — |
| | $ | 425 |
| $ | 585 |
| | $ | — |
| | $ | — |
| | $ | 585 |
|
| Total liabilities | $ | 425 |
| | $ | — |
| | $ | — |
| | $ | 425 |
| $ | 585 |
| | $ | — |
| | $ | — |
| | $ | 585 |
|
Our financial instruments measured at fair value on a recurring basis at December 31, 2016,2017, were as follows: | | | | Total | | Quoted Market Prices (Level 1) | | Significant Other Observable Inputs (Level 2) | | Significant Unobservable Inputs (Level 3) | Total | | Quoted Market Prices (Level 1) | | Significant Other Observable Inputs (Level 2) | | Significant Unobservable Inputs (Level 3) |
| | (In millions) | (In millions) |
| Corporate debt securities | $ | 1,179 |
| | $ | — |
| | $ | 1,179 |
| | $ | — |
| $ | 1,588 |
| | $ | — |
| | $ | 1,588 |
| | $ | — |
|
| U.S. treasury notes | | 388 |
| | 388 |
| | — |
| | — |
|
| GSEs | 231 |
| | 231 |
| | — |
| | — |
| 253 |
| | 253 |
| | — |
| | — |
|
| Municipal securities | 142 |
| | — |
| | 142 |
| | — |
| 141 |
| | — |
| | 141 |
| | — |
|
| Asset-backed securities | 69 |
| | — |
| | 69 |
| | — |
| 117 |
| | — |
| | 117 |
| | — |
|
| U.S. treasury notes | 84 |
| | 84 |
| | — |
| | — |
| |
| Certificates of deposit | 53 |
| | — |
| | 53 |
| | — |
| 37 |
| | — |
| | 37 |
| | — |
|
| Subtotal - current investments | 1,758 |
| | 315 |
| | 1,443 |
| | — |
| 2,524 |
| | 641 |
| | 1,883 |
| | — |
|
| Corporate debt securities | | 101 |
| | — |
| | 101 |
| | — |
|
| U.S. treasury notes | | 68 |
| | 68 |
| | — |
| | — |
|
| Subtotal - current restricted investments | | 169 |
| | 68 |
| | 101 |
| | — |
|
| 1.125% Call Option derivative asset | 267 |
| | — |
| | — |
| | 267 |
| 522 |
| | — |
| | — |
| | 522 |
|
| Total assets | $ | 2,025 |
| | $ | 315 |
| | $ | 1,443 |
| | $ | 267 |
| $ | 3,215 |
| | $ | 709 |
| | $ | 1,984 |
| | $ | 522 |
|
| | | | | | | | | | | | | | | |
| 1.125% Conversion Option derivative liability | $ | 267 |
| | $ | — |
| | $ | — |
| | $ | 267 |
| $ | 522 |
| | $ | — |
| | $ | — |
| | $ | 522 |
|
| Total liabilities | $ | 267 |
| | $ | — |
| | $ | — |
| | $ | 267 |
| $ | 522 |
| | $ | — |
| | $ | — |
| | $ | 522 |
|
There were no current restricted investments as of December 31, 2016.
Fair Value Measurements – Disclosure Only
The carrying amounts and estimated fair values of our senior notes are classified as Level 2 financial instruments. Fair value for these securities is determined using a market approach based on quoted market prices for similar securities in active markets or quoted prices for identical securities in inactive markets. The carrying amount and estimated fair value of the amount due under our Credit Facility is classified as a Level 3 financial instrument, because certain inputs used to determine its fair value are not observable. As of September 30, 2017, theThe carrying valueamount of the amount due under the Credit Facility approximates itits fair value because of the recency of this borrowing during the third quarter of 2017.Credit Facility’s interest rate is a variable rate that approximates rates currently available to us.
| | | | September 30, 2017 | | December 31, 2016 | March 31, 2018 | | December 31, 2017 |
| | Carrying Value | |
Fair Value | | Carrying Value | |
Fair Value | Carrying Value | |
Fair Value | | Carrying Value | |
Fair Value |
| | (In millions) | (In millions) |
| 5.375% Notes | $ | 692 |
| | $ | 726 |
| | $ | 691 |
| | $ | 714 |
| $ | 693 |
| | $ | 694 |
| | $ | 692 |
| | $ | 730 |
|
| 1.125% Convertible Notes | 489 |
| | 927 |
| | 471 |
| | 792 |
| 502 |
| | 1,111 |
| | 496 |
| | 1,052 |
|
| 4.875% Notes | 325 |
| | 324 |
| | — |
| | — |
| 326 |
| | 307 |
| | 325 |
| | 329 |
|
| Credit Facility | 300 |
| | 300 |
| | — |
| | — |
| 300 |
| | 300 |
| | 300 |
| | 300 |
|
| 1.625% Convertible Notes | 292 |
| | 373 |
| | 284 |
| | 344 |
| 63 |
| | 90 |
| | 157 |
| | 220 |
|
| | $ | 2,098 |
| | $ | 2,650 |
| | $ | 1,446 |
| | $ | 1,850 |
| $ | 1,884 |
| | $ | 2,502 |
| | $ | 1,970 |
| | $ | 2,631 |
|
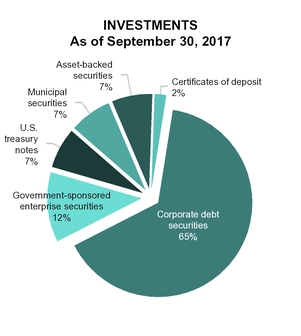
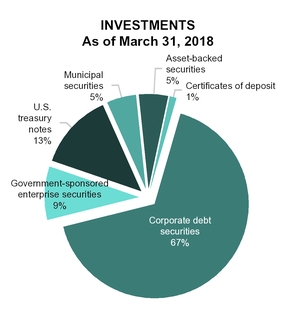
5. Investments
Available-for-Sale Investments
We consider all of our investments classified as current assets (including restricted investments) to be available-for-sale. Certain of our senior notes, as further discussed in Note 7, “Debt,” contain a limitation on the use of proceeds which required us to deposit the net proceeds from their issuance into a segregated deposit account, a current asset reported as “Restricted investments” in the accompanying consolidated balance sheets. Such proceeds, while restricted as to their use and held in a segregated deposit account, are available-for-sale based upon our contractual liquidity requirements.
The following tables summarize our investments as of the dates indicated: | | | | September 30, 2017 | March 31, 2018 |
| | Amortized | | Gross Unrealized | | Estimated Fair | Amortized | | Gross Unrealized | | Estimated Fair |
| | Cost | | Gains | | Losses | | Value | Cost | | Gains | | Losses | | Value |
| | (In millions) | (In millions) |
| Corporate debt securities | $ | 1,162 |
| | $ | 1 |
| | $ | 1 |
| | $ | 1,162 |
| $ | 1,627 |
| | $ | — |
| | $ | 9 |
| | $ | 1,618 |
|
| U.S. treasury notes | | 330 |
| | — |
| | 1 |
| | 329 |
|
| GSEs | 221 |
| | — |
| | 1 |
| | 220 |
| 229 |
| | — |
| | 2 |
| | 227 |
|
| Municipal securities | 132 |
| | — |
| | 1 |
| | 131 |
| 133 |
| | — |
| | 2 |
| | 131 |
|
| Asset-backed securities | 125 |
| | — |
| | — |
| | 125 |
| |
| U.S. treasury notes | 121 |
| | — |
| | — |
| | 121 |
| |
| Asset backed securities | | 111 |
| | — |
| | 1 |
| | 110 |
|
| Certificates of deposit | 28 |
| | — |
| | — |
| | 28 |
| 27 |
| | — |
| | — |
| | 27 |
|
| Other | | 2 |
| | — |
| | — |
| | 2 |
|
| Subtotal - current investments | 1,789 |
| | 1 |
| | 3 |
| | 1,787 |
| 2,459 |
| | — |
| | 15 |
| | 2,444 |
|
| Corporate debt securities | 229 |
| | — |
| | — |
| | 229 |
| 66 |
| | — |
| | — |
| | 66 |
|
| U.S. treasury notes | 97 |
| | — |
| | — |
| | 97 |
| 11 |
| | — |
| | — |
| | 11 |
|
| Subtotal - current restricted investments | 326 |
| | — |
| | — |
| | 326 |
| 77 |
| | — |
| | — |
| | 77 |
|
| | $ | 2,115 |
| | $ | 1 |
| | $ | 3 |
| | $ | 2,113 |
| $ | 2,536 |
| | $ | — |
| | $ | 15 |
| | $ | 2,521 |
|
| | | | December 31, 2016 | December 31, 2017 |
| | Amortized | | Gross Unrealized | | Estimated Fair | Amortized | | Gross Unrealized | | Estimated Fair |
| | Cost | | Gains | | Losses | | Value | Cost | | Gains | | Losses | | Value |
| | (In millions) | (In millions) |
| Corporate debt securities | $ | 1,180 |
| | $ | 1 |
| | $ | 2 |
| | $ | 1,179 |
| $ | 1,591 |
| | $ | 1 |
| | $ | 4 |
| | $ | 1,588 |
|
| U.S. treasury notes | | 389 |
| | — |
| | 1 |
| | 388 |
|
| GSEs | 232 |
| | — |
| | 1 |
| | 231 |
| 255 |
| | — |
| | 2 |
| | 253 |
|
| Municipal securities | 143 |
| | — |
| | 1 |
| | 142 |
| 142 |
| | — |
| | 1 |
| | 141 |
|
| Asset-backed securities | 69 |
| | — |
| | — |
| | 69 |
| 117 |
| | — |
| | — |
| | 117 |
|
| Certificates of deposit | | 37 |
| | — |
| | — |
| | 37 |
|
| Subtotal - current investments | | 2,531 |
| | 1 |
| | 8 |
| | 2,524 |
|
| Corporate debt securities | | 101 |
| | — |
| | — |
| | 101 |
|
| U.S. treasury notes | 84 |
| | — |
| | — |
| | 84 |
| 68 |
| | — |
| | — |
| | 68 |
|
| Certificates of deposit | 53 |
| | — |
| | — |
| | 53 |
| |
| Subtotal - current restricted investments | | 169 |
| | — |
| | — |
| | 169 |
|
| | $ | 1,761 |
| | $ | 1 |
| | $ | 4 |
| | $ | 1,758 |
| $ | 2,700 |
| | $ | 1 |
| | $ | 8 |
| | $ | 2,693 |
|
There were no current restricted investments as of December 31, 2016.
The contractual maturities of our available-for-sale investments as of September 30, 2017March 31, 2018 are summarized below: | | | | Amortized Cost | | Estimated Fair Value | Amortized Cost | | Estimated Fair Value |
| | (In millions) | (In millions) |
| Due in one year or less | $ | 1,154 |
| | $ | 1,153 |
| $ | 1,576 |
| | $ | 1,573 |
|
| Due after one year through five years | 944 |
| | 943 |
| 959 |
| | 947 |
|
| Due after five years through ten years | 17 |
| | 17 |
| 1 |
| | 1 |
|
| | $ | 2,115 |
| | $ | 2,113 |
| $ | 2,536 |
| | $ | 2,521 |
|
Gross realized gains and losses from sales of available-for-sale securities are calculated under the specific identification method and are included in investment income. Gross realized investment gains and losses for the three and nine months ended September 30,March 31, 2018 and 2017 and 2016 were insignificant.
We have determined that unrealized losses at September 30, 2017March 31, 2018 and December 31, 2016,2017, are temporary in nature, because the change in market value for these securities has resulted from fluctuating interest rates, rather than a deterioration of the creditworthiness of the issuers. So long as we maintain the intent and ability to hold these securities to maturity, we are unlikely to experience losses. In the event that we dispose of these securities before maturity, we expect that realized losses, if any, will be insignificant.
The following table segregates those available-for-sale investments that have been in a continuous loss position for less than 12 months, and those that have been in a continuous loss position for 12 months or more as of September 30, 2017:March 31, 2018:
| | | | In a Continuous Loss Position for Less than 12 Months | | In a Continuous Loss Position for 12 Months or More | In a Continuous Loss Position for Less than 12 Months | | In a Continuous Loss Position for 12 Months or More |
| | Estimated Fair Value | | Unrealized Losses | | Total Number of Positions | | Estimated Fair Value | | Unrealized Losses | | Total Number of Positions | Estimated Fair Value | | Unrealized Losses | | Total Number of Positions | | Estimated Fair Value | | Unrealized Losses | | Total Number of Positions |
| | (Dollars in millions) | (Dollars in millions) |
| Corporate debt securities | $ | 783 |
| | $ | 1 |
| | 314 |
| | $ | — |
| | $ | — |
| | — |
| $ | 1,276 |
| | $ | 7 |
| | 610 |
| | $ | 93 |
| | $ | 2 |
| | 71 |
|
| U.S. Treasury notes | | 364 |
| | 1 |
| | 81 |
| | — |
| | — |
| | — |
|
| GSEs | — |
| | — |
| | — |
| | 58 |
| | 1 |
| | 20 |
| 179 |
| | 1 |
| | 67 |
| | 95 |
| | 1 |
| | 47 |
|
| Municipal securities | 97 |
| | 1 |
| | 116 |
| | — |
| | — |
| | — |
| 85 |
| | 1 |
| | 97 |
| | 38 |
| | 1 |
| | 46 |
|
| Asset backed securities | | 97 |
| | 1 |
| | 60 |
| | — |
| | — |
| | — |
|
| | $ | 880 |
| | $ | 2 |
| | 430 |
| | $ | 58 |
| | $ | 1 |
| | 20 |
| $ | 2,001 |
| | $ | 11 |
| | 915 |
| | $ | 226 |
| | $ | 4 |
| | 164 |
|
The following table segregates those available-for-sale investments that have been in a continuous loss position for less than 12 months, and those that have been in a continuous loss position for 12 months or more as of December 31, 2016:2017:
| | | | In a Continuous Loss Position for Less than 12 Months | | In a Continuous Loss Position for 12 Months or More | In a Continuous Loss Position for Less than 12 Months | | In a Continuous Loss Position for 12 Months or More |
| | Estimated Fair Value | | Unrealized Losses | | Total Number of Positions | | Estimated Fair Value | | Unrealized Losses | | Total Number of Positions | Estimated Fair Value | | Unrealized Losses | | Total Number of Positions | | Estimated Fair Value | | Unrealized Losses | | Total Number of Positions |
| | (Dollars in millions) | (Dollars in millions) |
| Corporate debt securities | $ | 542 |
| | $ | 2 |
| | 378 |
| | $ | — |
| | $ | — |
| | — |
| $ | 1,297 |
| | $ | 3 |
| | 561 |
| | $ | 94 |
| | $ | 1 |
| | 69 |
|
| U.S. Treasury Notes | | 470 |
| | 1 |
| | 89 |
| | — |
| | — |
| | — |
|
| GSEs | 198 |
| | 1 |
| | 73 |
| | — |
| | — |
| | — |
| 173 |
| | 1 |
| | 69 |
| | 95 |
| | 1 |
| | 47 |
|
| Municipal securities | 101 |
| | 1 |
| | 129 |
| | — |
| | — |
| | — |
| — |
| | — |
| | — |
| | 38 |
| | 1 |
| | 48 |
|
| | $ | 841 |
| | $ | 4 |
| | 580 |
| | $ | — |
| | $ | — |
| | — |
| $ | 1,940 |
| | $ | 5 |
| | 719 |
| | $ | 227 |
| | $ | 3 |
| | 164 |
|
Held-to-Maturity Investments
Pursuant to the regulations governing our Health Plans segment subsidiaries, we maintain statutory deposits and deposits required by government authorities primarily in certificates of deposit and U.S. treasury securities. We also maintain restricted investments as protection against the insolvency of certain capitated providers. The use of these funds is limited as required by regulationregulations in the various states in which we operate, or as needed in the event of insolvency of capitated providers. Therefore, such investments are reported as non-current “Restricted investments” in the accompanying consolidated balance sheets. We have the ability to hold these restricted investments until maturity, and as a result, we would not expect the value of these investments to decline significantly due to a sudden change in market interest rates.
The contractual maturities of our held-to-maturity restricted investments, which are carried at amortized cost, which approximates fair value, as of September 30, 2017March 31, 2018, are summarized below: | | | | Amortized Cost | | Estimated Fair Value | Amortized Cost | | Estimated Fair Value |
| | (In millions) | (In millions) |
| Due in one year or less | $ | 100 |
| | $ | 100 |
| $ | 117 |
| | $ | 117 |
|
| Due after one year through five years | 17 |
| | 17 |
| 3 |
| | 3 |
|
| | $ | 117 |
| | $ | 117 |
| $ | 120 |
| | $ | 120 |
|
6. Medical Claims and Benefits Payable
The following table provides the details of our medical claims and benefits payable (including amounts payable for the provision of long-term services and supports, or LTSS) as of the dates indicated:
| | | | September 30,
2017 | | December 31,
2016 | March 31,
2018 | | December 31,
2017 |
| | (In millions) | (In millions) |
| Fee-for-service claims incurred but not paid (IBNP) | $ | 1,681 |
| | $ | 1,352 |
| $ | 1,586 |
| | $ | 1,717 |
|
| Pharmacy payable | 125 |
| | 112 |
| 127 |
| | 112 |
|
| Capitation payable | 57 |
| | 37 |
| 62 |
| | 67 |
|
| Other | 615 |
| | 428 |
| 248 |
| | 296 |
|
| | $ | 2,478 |
| | $ | 1,929 |
| $ | 2,023 |
| | $ | 2,192 |
|
“Other” medical claims and benefits payable includeincludes amounts payable to certain providers for which we act as an intermediary on behalf of various government agencies without assuming financial risk. Such receipts and payments do not impact our consolidated statements of operations.income. Non-risk provider payables amounted to $403$146 million and $225$122 million as of September 30, 2017March 31, 2018 and December 31, 2016,2017, respectively.
Reinsurance recoverables of $16 million and $72 million as of September 30, 2017 and 2016, respectively, are included in “Receivables” in the accompanying consolidated balance sheets.
The following table presents the components of the change in our medical claims and benefits payable for the periods indicated. The amounts presented for “Components of medical care costs related to: Prior periods” represent the amounts by which our original estimate of medical claims and benefits payable at the beginning of the
period were less (more)more than the actual amount of the liability based on information (principally the payment of claims) developed since that liability was first reported.
| | | | Nine Months Ended September 30, | Three Months Ended March 31, |
| | 2017 | | 2016 | 2018 | | 2017 |
| | (Dollars in millions) | (Dollars in millions) |
| Medical claims and benefits payable, beginning balance | $ | 1,929 |
| | $ | 1,685 |
| $ | 2,192 |
| | $ | 1,929 |
|
| Components of medical care costs related to: | | | | | | |
| Current period | 12,813 |
| | 11,120 |
| 3,963 |
| | 4,253 |
|
| Prior periods | 9 |
| | (190 | ) | (241 | ) | | (142 | ) |
| Total medical care costs | 12,822 |
| | 10,930 |
| 3,722 |
| | 4,111 |
|
| | | | | | | |
| Change in non-risk provider payables | 172 |
| | 70 |
| 45 |
| | (96 | ) |
| | | | | | | |
| Payments for medical care costs related to: | | | | | | |
| Current period | 10,944 |
| | 9,536 |
| 2,498 |
| | 2,683 |
|
| Prior periods | 1,501 |
| | 1,278 |
| 1,438 |
| | 1,335 |
|
| Total paid | 12,445 |
| | 10,814 |
| 3,936 |
| | 4,018 |
|
| Medical claims and benefits payable, ending balance | $ | 2,478 |
| | $ | 1,871 |
| $ | 2,023 |
| | $ | 1,926 |
|
| Benefit from prior period as a percentage of: | | | | | | |
| Balance at beginning of period | (0.5 | )% | | 11.3 | % | 11.0 | % | | 7.4 | % |
| Premium revenue, trailing twelve months | — | % | | 1.2 | % | 1.3 | % | | 0.8 | % |
| Medical care costs, trailing twelve months | (0.1 | )% | | 1.3 | % | 1.4 | % | | 0.9 | % |
Assuming that our initial estimate of IBNP is accurate, we believe that amounts ultimately paid would generally be between 8% and 10% less than the IBNP liability recorded at the end of the period as a result of the inclusion in that liability of the provision for adverse claims deviation and the accrued cost of settling those claims. Because we establish the provision for adverse claims deviation and the accrued cost of settling claims on a consistent basis every quarter, the lower cost recognized in a subsequent period if such a provision proved unnecessary would be offset by the establishment of a similar provision during that subsequent period.
Because the amount of our initial liability is merely an estimate (and therefore not perfectly accurate), we will always experience variability in that estimate as new information becomes available with the passage of time. Therefore, there can be no assurance that amounts ultimately paid out will fall within the range of 8% to 10% lower than the liability that was initially recorded. Furthermore, because our initial estimate of IBNP is derived from many factors, some of which are qualitative in nature rather than quantitative, we are seldom able to assign specific values to the reasons for a change in estimate—we only know when the circumstances for any one or more factors are out of the ordinary.
The differences between our original estimates and the amounts ultimately paid out (or now expected to be ultimately paid out) for the most part relatedrelate to IBNP. While many related factors working in conjunction with one another serve to determine the accuracy of our estimates, we are seldom able to quantify the impact that any single
factor has on a change in estimate. In addition, given the variability inherent in the reserving process, we will only be able to identify specific factors if they represent a significant departure from expectations. As a result, we do not expect to be able to fully quantify the impact of individual factors on changes in estimates.
Prior period development of our estimate as of December 31, 2016, through September 30, 2017, was unfavorable by $9 million, which is substantially less than the favorable prior period development of $190 million we recognized for the same period in the prior year. Further, the unfavorable development through September 30, 2017, was less than the 8% to 10% favorable development we typically expect.
We believe that the most significant uncertainties surrounding our IBNP estimates at September 30, 2017March 31, 2018 are as follows:
AtAcross all of our Florida health plan,plans, the inventory of unpaid claims increased significantly during the first two quartershalf of 2017, then decreased in the last half of 2017 and then droppedinto 2018. Changes in the third quarter. For this reason,claims inventories impact the timing between the datesdate of service and the dates claims are paid will be impacted, makingdate of claim payment, increasing the volatility of our liability estimates subjectestimates.
According to The Centers for Disease Control and Prevention, and confirmed by our own claims experience, the influenza season was much more severe this year than the usual amount of uncertainty.
At our Illinoislast year in several states in which we operate health plan, in 2017plans. Although we paid a large number of claims that had previously been denied and were subsequently disputed by providers. We have also established a liabilityliabilities for additional expected claims resulting from provider disputes. This has created some distortion in the claims payment patterns, making our liability estimates subjectrelated to more than the usual amount of uncertainty.
At our California health plan, we adjusted our inpatient authorization process. As a result, due to the expected increase in authorized inpatient stays,influenza, our liability estimates are subject to more than the usual amount of uncertainty.
At our Illinois and New YorkFlorida health plans, weplan a new clinical service system was implemented in the first quarter of 2018. This system impacted the reporting of inpatient authorizations used in our development of claims liabilities, which makes our liability estimates subject to more than the usual amount of uncertainty.
We recently implemented a new process for increased quality review of claims payments.payments in nine of our health plans. While we do not anticipate this new process will impact the percentage of claims paid within the timely turnaround requirements, we believe it will have a minor impact on the timing of some paid claims. For this reason, our liability estimates in these twothe nine health plans are subject to more than the usual amount of uncertainty.
AtWe recognized favorable prior period claims development in the amount of $241 million for the three months ended March 31, 2018. This amount represents our Puerto Rico health plan, Hurricane Maria had a significant impact on both utilizationestimate as of servicesMarch 31, 2018, of the extent to which our initial estimate of medical claims and our ability to process claims payments in Puerto Rico. For these reasons, we believe our liability estimates are subject tobenefits payable at December 31, 2017, was more than the usual amount that will ultimately be paid out in satisfaction of uncertainty.that liability. We believe the overestimation was due primarily to the following factors:
The impact of the provision for adverse claims deviation and the accrued cost of settling claims as discussed above. Because we re-establish the provision for adverse claims deviation and the accrued cost of settling claims on a consistent basis every quarter, the impact of this item on first quarter 2018 results was minimal.
Across all of our health plans, the inventory of unpaid claims increased significantly during the first half of 2017, then decreased in the last half of 2017. In hindsight, the impact of the changes in claims processing timing reduced our liabilities more than we had anticipated.
December 2017 data from The Centers for Disease Control and Prevention indicated widespread influenza activity in several states in which we operate health plans. The additional liabilities established in consideration of increased claims related to a more severe influenza season turned out to be conservative.
In establishing our liability at December 31, 2017, we anticipated an increase in the utilization of medical services by Marketplace members concerned about the future of their healthcare coverage as a result of uncertainties related to high premium increases and issuer exits. This induced demand did not materialize to the degree we expected.
7. Debt
Substantially all of our debt is held at the parent, which is reported in the Other segment. The following table summarizes our outstanding debt obligations and their classification in the accompanying consolidated balance sheets (in millions):sheets:
| | | | | | | March 31,
2018 | | December 31,
2017 |
| | September 30,
2017 | | December 31,
2016 | (In millions) |
| Current portion of long-term debt: | | | | | | |
| 1.125% Convertible Notes, net of unamortized discount | $ | 494 |
| | $ | 477 |
| $ | 505 |
| | $ | 499 |
|
| 1.625% Convertible Notes, net of unamortized premium and discount | 293 |
| | — |
| |
| 1.625% Convertible Notes, net of unamortized discount | | 63 |
| | 157 |
|
| Lease financing obligations | 1 |
| | 1 |
| 1 |
| | 1 |
|
| Debt issuance costs | (6 | ) | | (6 | ) | (3 | ) | | (4 | ) |
| | 782 |
| | 472 |
| 566 |
| | 653 |
|
| Non-current portion of long-term debt: | | | | | | |
| 5.375% Notes | 700 |
| | 700 |
| 700 |
| | 700 |
|
| 4.875% Notes | 330 |
| | — |
| 330 |
| | 330 |
|
| Credit Facility | 300 |
| | — |
| 300 |
| | 300 |
|
| 1.625% Convertible Notes, net of unamortized premium and discount | — |
| | 286 |
| |
| Debt issuance costs | (13 | ) | | (11 | ) | (12 | ) | | (12 | ) |
| | 1,317 |
| | 975 |
| 1,318 |
| | 1,318 |
|
| Lease financing obligations | 198 |
| | 198 |
| 198 |
| | 198 |
|
| | $ | 2,297 |
| | $ | 1,645 |
| $ | 2,082 |
| | $ | 2,169 |
|
Interest cost recognized relating to our convertible senior notes for the periods presented was as follows:
|
| | | | | | | |
| | Three Months Ended March 31, |
| | 2018 | | 2017 |
| | (In millions) |
| Contractual interest at coupon rate | $ | 2 |
| | $ | 3 |
|
| Amortization of the discount | 7 |
| | 8 |
|
| | $ | 9 |
| | $ | 11 |
|
Credit Facility
In January 2017, weentered into an amended unsecured $500 million revolving credit facility (Credit Facility). The Credit Facility has a term of five years and all amounts outstanding will be due and payable on January 31, 2022. As of March 31, 2018, $300 million was outstanding under the Credit Facility, and outstanding letters of credit amounting to $6 million reduced our remaining borrowing capacity under the Credit Facility to $194 million.
Borrowings under our Credit Facility bear interest based, at our election, on a base rate or an adjusted London Interbank Offered Rate (LIBOR), plus in each case the applicable margin. In addition to interest payable on the principal amount of indebtedness outstanding from time to time under the Credit Facility, we are required to pay a quarterly commitment fee. The Credit Facility contains customary non-financial and financial covenants, including a net leverage ratio and an interest coverage ratio. As of March 31, 2018, we were in compliance with all financial and non-financial covenants under the Credit Facility and other long-term debt.
Bridge Credit Agreement
In January 2018, we entered into a bridge credit agreement (Bridge Credit Agreement) with several banks. Under the Bridge Credit Agreement, we may borrow up to $550 million to: (i) satisfy conversions of our 1.125% Convertible Notes; (ii) satisfy and/or refinance indebtedness incurred to satisfy conversion of the 1.125% Convertible Notes; (iii) repay or refinance our Credit Facility; and (iv) pay fees and expenses in connection with the foregoing. Subject to the satisfaction of certain conditions, the remaining amount of any borrowing may be used for general corporate purposes.
Borrowings under the Bridge Credit Agreement are reduced by the following:
Any future debt and/or equity transactions including term loans, but excluding any Credit Facility drawing (excluding transactions with proceeds used for working capital purposes and acquisition financings up to $300 million); and
On August 20, 2018 (the first put date for the 1.625% Convertible Notes), the Bridge Credit Agreement shall permanently be reduced by the greater of $150 million; and the principal amount of the 1.625% Convertible Notes that are exchanged into equity or otherwise defeased on or prior to that date.
The Bridge Credit Agreement matures on January 1, 2019 and, subject to the satisfaction of certain conditions, we may elect to extend twice the initial maturity date by a period of six months each. The amount available for borrowing under the Bridge Credit Agreement at March 31, 2018, was $550 million.
Borrowings under the Bridge Credit Agreement will bear interest based, at our election, at a base rate or an adjusted LIBOR rate, plus in each case the applicable margin. Our wholly owned subsidiaries that guarantee our obligations under the indenture governing the 4.875% Notes, the 5.375% Notes, and the Credit Facility have jointly and severally guaranteed our obligations under the Bridge Credit Agreement.
The Bridge Credit Agreement contains usual and customary (a) affirmative covenants for credit facilities of this type and substantially similar to those contained in the Credit Facility, (b) negative covenants consistent with those contained in the 4.875% Notes and (c) events of default for credit facilities of this type and substantially similar to those contained in the 4.875% Notes.
4.875% Notes due 2025
On June 6, 2017, we completed the private offering ofWe have outstanding $330 million aggregate principal amount of senior notes (4.875% Notes) due June 15, 2025, unless earlier redeemed. Interest on the 4.875% Notes is payable semiannually in arrears on June 15 and December 15. According to their terms, the guaranteesGuarantees under the 4.875% Notes mirror those of the Credit Facility, defined and described below.Facility. See Note 16,13, “Supplemental Condensed Consolidating Financial Information,” for more information on the guarantors. The 4.875% Notes contain customary non-financial covenants and change of control provisions.
The 4.875% Notes contain a limitation on the use of proceeds which required us to deposit the net proceeds from their issuance into a segregated deposit account, a current asset reported as “Restricted investments” in our consolidated balance sheets. These funds may be used by us as follows:
On or prior to August 20, 2018, to:
| |
| ◦ | Redeem, repurchase, repay, tender for, or acquire for value all or any portion of our 1.625% Convertible Notes, defined and discussed further below, or to satisfy the cash portion of any consideration due upon any conversion of the 1.625% Convertible Notes; and/or |
| |
| ◦ | Pay any interest due on all or any portion of the 4.875% Notes. |
On or after August 20, 2018, to repurchase all or any portion of the 1.625% Convertible Notes that we are obligated to repurchase; and
Subsequent to August 20, 2018 (or such earlier date in the event that there are no longer any 1.625% Convertible Notes outstanding), in any other manner not otherwise prohibited in the indenture governing the 4.875% Notes.
The investments that constitute the segregated funds are current assets reported as “Restricted investments” in the accompanying consolidated balance sheets. As a result of the 1.625% Exchange described below, approximately $94 million of such investments were transferred to unrestricted current investments in the first quarter of 2018. As of March 31, 2018, the balance of current restricted investments was
$77 million.5.375% Notes due 2022
We have outstanding $700 million aggregate principal amount of senior notes (5.375% Notes) due November 15, 2022, unless earlier redeemed. According to their terms,Interest on the guarantees5.375% Notes is payable semiannually in arrears on May 15 and November 15. Certain of our wholly owned subsidiaries guarantee our obligations under the 5.375% NotesNotes. Such guarantees mirror those of the Credit Facility, defined and described below.Facility. See Note 16,13, “Supplemental Condensed Consolidating Financial Information,” for more information on the guarantors.
Credit Facility
In January 2017, weentered into an amended unsecured $500 million revolving credit facility (Credit Facility), referred to as the First Amendment. The Credit Facility has a term of five years and all amounts outstanding will be due and payable on January 31, 2022. As of September 30, 2017, $300 million was outstanding under the Credit Facility, and we were in compliance with all financial and5.375% Notes contain customary non-financial covenants under the Credit Facility. Also as of September 30, 2017, outstanding letters of credit amounting to $6 million reduced our remaining borrowing capacity under the Credit Facility to $194 million.and change in control provisions.
In addition to increasing amounts available to borrow under the Credit Facility and extending its term, the First Amendment provided that all guarantors immediately prior to January 3, 2017, other than Molina Information Systems, LLC, d/b/a Molina Medicaid Solutions, Molina Pathways, LLC, and Pathways Health and Community Support LLC, were automatically and unconditionally released from their obligations as guarantors of the Credit Facility and the 5.375% Notes.
The Credit Facility contains customary non-financial and financial covenants, including a net leverage ratio and an interest coverage ratio. In February 2017, we entered into a second amendment to the Credit Facility (the Second Amendment) which modified the Credit Facility’s definition of the earnings measure used in the financial covenant computations to a) allow us to receive credit for risk corridor payments owed to, but not received or accrued by us during 2016; and b) account for the difference between the amount of actual risk transfer payments made or accrued by us during 2016, and the amount of risk transfer payments that would have been due under the federal government’s proposed 2018 risk adjustment payment transfer formula.
In May 2017, we entered into a third amendment to the Credit Facility (the Third Amendment) which modified the Credit Facility’s definition of specified cash, to permit cash that is either subject to customary escrow arrangements or held in a segregated account to be netted from the Credit Facility’s consolidated net leverage ratio if the use of the cash is limited to the repayment of other indebtedness. The Third Amendment also adds a carve-out to the Credit Facility’s negative pledge covenant to allow for the escrow arrangements and segregated accounts.
In August 2017, we entered into a fourth amendment to the Credit Facility (the Fourth Amendment). The Fourth Amendment modified the definition of consolidated adjusted EBITDA to permit the add-back of certain restructuring charges and cost savings subject to certain limitations, and modified the definition of the consolidated interest coverage ratio to include, when calculating such ratio, consolidated interest expense “paid in cash” only.
1.125% Cash Convertible Senior Notes due 2020
We have outstanding $550 million aggregate principal amount of 1.125% cash convertible senior notes due January 15, 2020 (1.125% Convertible Notes), unless earlier repurchased or converted. We also have outstanding $302 million aggregate principal amount of 1.625% convertible senior notes due August 14, 2044 (1.625% Convertible Notes), unless earlier repurchased, redeemed, or converted. Interest is payable semiannually in arrears on January 15 and July 15.
The 1.125% Convertible Notes are convertible entirelyonly into cash, and the 1.625% Convertible Notes are convertible partiallynot into cash, each prior to their respective maturity dates under certain circumstances, one of which relates to the closing priceshares of our common stock overor any other securities. The initial conversion rate for the 1.125% Convertible Notes is 24.5277 shares of our common stock per $1,000 principal amount, or approximately $40.77 per share of our common stock. Upon conversion, in lieu of receiving shares of our common stock, a specified period.holder will receive an amount in cash, per $1,000 principal amount of 1.125% Convertible Notes, equal to the settlement amount, determined in the manner set forth in the indenture. We refermay not redeem the 1.125% Convertible Notes prior to this conversion trigger as the stock price trigger.maturity date.
The stock price trigger for the 1.125% Convertible Notes is $53.00 per share. The 1.125% Convertible Notes met this trigger in the quarter ended September 30, 2017;March 31, 2018; therefore, they are convertible into cash and are reported in current portion of long-term debt as of September 30, 2017.March 31, 2018.
The 1.125% Convertible Notes contain an embedded cash conversion option (the 1.125% Conversion Option), which was separated from the 1.125% Convertible Notes and accounted for separately as a derivative liability, with changes in fair value reported in our consolidated statements of income until the 1.125% Conversion Option settles or expires. The effective interest rate approximating what we would have incurred had nonconvertible debt with otherwise similar terms been issued is approximately 6%. As of March 31, 2018, the 1.125% Convertible Notes had a remaining amortization period of 1.8 years. The 1.125% Convertible Notes’ if-converted value exceeded their principal amount by approximately $527 million and $406 million as of March 31, 2018 and December 31, 2017, respectively.
1.625% Convertible Senior Notes due 2044
In March 2018, we entered into separate, privately negotiated, synthetic exchange agreements (1.625% Exchange) with certain holders of our outstanding 1.625% convertible senior notes due 2044 (1.625% Convertible Notes). In this transaction, we exchanged $97 million aggregate principal amount and accrued interest for 1.8 million shares of our common stock. We recorded a loss on debt extinguishment, including transaction fees, of $10 million, for the transaction, primarily relating to the inducement premium paid to the bondholders, which is recorded in “Other
expenses (income), net” in the accompanying consolidated statements of income. We did not receive any proceeds from the 1.625% Exchange.
Following the 1.625% Exchange, we have outstanding $64 million aggregate principal amount of the 1.625% Convertible Notes. The initial conversion rate for the 1.625% Convertible Notes is 17.2157 shares of our common stock per $1,000 principal amount, or approximately $58.09 per share of our common stock. Upon conversion, we will pay cash and, if applicable, deliver shares of our common stock to the converting holder in an amount per $1,000 principal amount of 1.625% Notes equal to the settlement amount (as defined in the related indenture).
The stock price trigger for the 1.625% Convertible Notes is $75.51 per share. The 1.625% Convertible Notes did not meet this stock price trigger in the quarter ended September 30, 2017.March 31, 2018. However, on contractually specified dates beginning in August 2018, holders of the 1.625% Convertible Notes may require us to repurchase some or all of such notes. In addition, beginning May 15, 2018 until August 19, 2018, holders may convert some or all of the 1.625% Convertible Notes. Because of these put and conversion features, the 1.625% Convertible Notes are reported in current portion of long-term debt as of September 30, 2017.March 31, 2018. As noted above, because the proceeds from the 4.875% Notes are initially restricted to payments upon conversion or redemption of the 1.625% Convertible Notes, such restricted investments are also classified as current in the accompanying consolidated balance sheets.
The expected life of the 1.625% Convertible Notes is approximately four years, beginning on the issuance date and ending on the first date we may redeem the 1.625% Convertible Notes in August 2018. As of March 31, 2018, the 1.625% Convertible Notes had a remaining amortization period of 0.4 years. The effective interest rate approximating what we would have incurred had nonconvertible debt with otherwise similar terms been issued is approximately 5%. The outstanding 1.625% Convertible Notes’ if-converted value exceeded their principal amount at March 31, 2018 and December 31, 2017 by approximately $19 million and $50 million, respectively. At March 31, 2018 and December 31, 2017, the equity component of the 1.625% Convertible Notes, including the impact of deferred taxes, was $5 million and $12 million, respectively.
Cross-Default Provisions
The terms of ourindentures governing the 4.875% Notes, the 5.375% Notes, and each of the 1.125% Convertible Notes and the 1.625% Convertible Notes contain cross-default provisions with the Credit Facility that are triggered upon an eventdefault by us or any of default underour subsidiaries on any indebtedness in excess of the Credit Facility, and when borrowings under the Credit Facility equal or exceed certain amounts as definedamount specified in the related indentures.
Debt Commitment Letter
In connection with the terminated Medicare Acquisition, we entered into a debt commitment letter with Barclays Bank PLC (Barclays) in August 2016. Under this debt commitment letter, Barclays agreed to lend us up to $400 million, subject to satisfaction of certain conditions, including consummation of the terminated Medicare Acquisition. The debt commitment letter automatically terminated in February 2017 as a result of the termination of this transaction. The costs associated with the debt commitment letter and its termination were reimbursed as described in Note 1, “Basis of Presentation–Health Plans Segment Recent Developments.”applicable indenture.
8. Derivatives
The following table summarizes the fair values and the presentation of our derivative financial instruments (defined and discussed individually below) in the accompanying consolidated balance sheets:
| | | | Balance Sheet Location | | September 30,
2017 | | December 31,
2016 | Balance Sheet Location | | March 31,
2018 | | December 31,
2017 |
| | | (In millions) | | (In millions) |
| Derivative asset: | | | | | | | | |
| 1.125% Call Option | Current assets: Derivative asset | | $ | 425 |
| | $ | 267 |
| Current assets: Derivative asset | | $ | 585 |
| | $ | 522 |
|
| Derivative liability: | | | | | | | | |
| 1.125% Conversion Option | Current liabilities: Derivative liability | | $ | 425 |
| | $ | 267 |
| Current liabilities: Derivative liability | | $ | 585 |
| | $ | 522 |
|
Our derivative financial instruments do not qualify for hedge treatment; therefore, the change in fair value of these instruments is recognized immediately in our consolidated statements of operations,income, and reported in “Other income,expenses (income), net.” Gains and losses for our derivative financial instruments are presented individually in the accompanying consolidated statements of cash flows, “Supplemental cash flow information.”
1.125% Notes Call Spread Overlay. Concurrent with the issuance of the 1.125% Convertible Notes in 2013, we entered into privately negotiated hedge transactions (collectively, the 1.125% Call Option) and warrant transactions (collectively, the 1.125% Warrants), with certain of the initial purchasers of the 1.125% Convertible Notes (the Counterparties). We refer to these transactions collectively as the Call Spread Overlay. Under the Call Spread Overlay, the cost of the 1.125% Call Option we purchased to cover the cash outlay upon conversion of the 1.125% Convertible Notes was reduced by proceeds from the sale of the 1.125% Warrants. Assuming full performance by the Counterparties (and 1.125% Warrants strike prices in excess of the conversion price of the 1.125% Convertible Notes), these transactions are intended to offset cash payments in excess of the principal amount of the 1.125% Convertible Notes due upon any conversion of such notes.
1.125% Call Option. The 1.125% Call Option, which is indexed to our common stock, is a derivative asset that requires mark-to-market accounting treatment due to cash settlement features until the 1.125% Call Option settles or expires. For further discussion of the inputs used to determine the fair value of the 1.125% Call Option, refer to Note 4, “Fair Value Measurements.”
1.125% Conversion Option. The embedded cash conversion option within the 1.125% Convertible Notes is accounted for separately as a derivative liability, with changes in fair value reported in our consolidated statements of operationsincome until the cash conversion option settles or expires. For further discussion of the inputs used to determine the fair value of the 1.125% Conversion Option, refer to Note 4, “Fair Value Measurements.”
As of September 30, 2017,March 31, 2018, the 1.125% Call Option and the 1.125% Conversion Option were classified as a current asset and current liability, respectively, because the 1.125% Convertible Notes may be converted within twelve months of September 30, 2017,March 31, 2018, as described in Note 7, “Debt.”
9. Stockholders' Equity
Stockholders’ equity decreased $2201.625% Exchange
As described in Note 7, “Debt,” we issued 1.8 million during shares of our common stock in connection with the nine months ended September 30, 2017 compared with stockholders’ equity at December 31, 2016. The decrease was due primarily to the net loss of $250 million, partially offset by $29 million related to employee stock transactions1.625% Exchange in the nine months ended September 30, 2017.
March 2018.
1.125% Warrants
In connection with the Call Spread Overlay transaction described in Note 8, “Derivatives,” in 2013, we issued 13,490,236 warrants with a strike price of $53.8475 per share. Under certain circumstances, beginning in April 2020, when the price of our common stock exceeds the strike price of the 1.125% Warrants, we will be obligated to issue shares of our common stock subject to a share delivery cap. The 1.125% Warrants could separately have a dilutive effect to the extent that the market value per share of our common stock exceeds the applicable strike price of the 1.125% Warrants. Refer to Note 3, “Net (Loss) Income per Share,” for dilution information for the periods presented. We will not receive any additional proceeds if the 1.125% Warrants are exercised.
Stock Incentive PlansShare-Based Compensation
In connection with our equity incentive plans and employee stock purchase plan, approximately 702,000127,000 shares of common stock vested or were purchased, net of shares used to settle employees’ income tax obligations, during the ninethree months ended September 30, 2017.March 31, 2018.
Except as noted below, weWe record share-based compensation as “General and administrative expenses” in the accompanying consolidated statements of operations. Restricted stock awards (RSAs), performance stock awards (PSAs) and performance stock units (PSUs) activity for the nine months ended September 30, 2017 is summarized below: |
| | | | | | | | | | | | | | | |
| | Restricted Stock Awards | | Performance Stock Awards | | Performance Stock Units | | Total | | Weighted Average Grant Date Fair Value |
| Unvested balance, December 31, 2016 | 577,244 |
| | 345,656 |
| | — |
| | 922,900 |
| | $ | 58.15 |
|
| Granted | 386,273 |
| | — |
| | 231,100 |
| | 617,373 |
| | 57.16 |
|
| Vested | (391,680 | ) | | (260,894 | ) | | (139,272 | ) | | (791,846 | ) | | 57.78 |
|
| Forfeited | (69,346 | ) | | — |
| | — |
| | (69,346 | ) | | 54.37 |
|
| Unvested balance, September 30, 2017 | 502,491 |
| | 84,762 |
| | 91,828 |
| | 679,081 |
| | 57.61 |
|
The total fair value of RSAs granted during the nine months ended September 30, 2017 and 2016 was $19 million and $18 million, respectively. The total fair value of RSAs which vested during the nine months ended September 30, 2017 and 2016 was $21 million and $22 million, respectively.
No PSAs were granted during the nine months ended September 30, 2017. The total fair value of PSAs granted during the nine months ended September 30, 2016 was $15 million. The total fair value of PSAs which vested during the nine months ended September 30, 2017 was $15 million. No PSAs vested during the nine months ended September 30, 2016.
The total fair value of PSUs granted during the nine months ended September 30, 2017 was $16 million. The total fair value of PSUs which vested during the nine months ended September 30, 2017 was $9 million. There were no PSUs granted or vested in 2016.
During the nine months ended September 30, 2017, the vesting of 133,957 RSAs, 153,574 PSAs and 139,272 PSUs was accelerated in connection with the termination of our former Chief Executive Officer (CEO) and former Chief Financial Officer (CFO) in May 2017. Share-based compensation expense of $38 million was recorded during the nine months ended September 30, 2017, of which $23 million was recorded to “Restructuring and separation costs” in the accompanying consolidated statements of operations. See Note 11, “Restructuring and Separation Costs” for further discussion. We recorded share-based compensation expense of $24 million in the nine months ended September 30, 2016.
income. As of September 30, 2017,March 31, 2018, there was $27$53 million of total unrecognized compensation expense related to unvested RSAs, PSAs,restricted stock awards (RSAs), performance stock awards (PSAs), and PSUs,performance stock units (PSUs), which we expect to recognize over a remaining weighted-average period of 2.23.2 years, 0.9 years and 1.92.7 years, respectively. This unrecognized compensation cost assumes an estimated forfeiture rate of 4.5%9.7% for non-executive employees as of September 30, 2017.March 31, 2018.
10. Impairment Losses
Goodwill represents the excessAlso as of the purchase price over the fair valueMarch 31, 2018, there was $13 million of net assets acquired in business combinations. Goodwill is not amortized, but is subject to an annual impairment test.We are required to test at least annually for impairment, or more frequently if adverse events or changes in circumstances indicate that the asset may be impaired. When testing goodwill for impairment, we may first assess qualitative factors, such as industry and market factors, cost factors, and changes in overall performance, to determine if it is more likely than not that the carrying value of a reporting unit exceeds its estimated fair value. If our qualitative assessment indicates that goodwill impairment is more likely than not, we perform additional quantitative analysis. We may also elect to skip the qualitative testing and proceed directly to the quantitative testing.
An impairment loss is measured as the excess of the carrying amount of the reporting unit, including goodwill, over the fair value of the reporting unit. We estimate the fair values of our reporting units using discounted cash flows. We apply our weighted average cost of capital (WACC) as the best estimate to discount future estimated cash flows to present value. The WACC is based on externally available data considering market participants’ cost of equity and debt, and capital structure. In addition, we apply a terminal growth rate that corresponds to the reporting unit’s long-term growth prospects.
In the discounted cash flow analyses, we must make assumptions about a wide variety of internal and external factors, and consider the price that would be received to sell the reporting unit as a whole in an orderly transaction between market participants at the measurement date. Significant assumptions include financial projections of free cash flow (including significant assumptions about operations, capital requirements and income taxes), long-term growth rates for determining terminal value beyond the discretely forecasted periods, and discount rates.
Molina Medicaid Solutions Segment
As described in Note 11, “Restructuring and Separation Costs,” in the third quarter of 2017 we wrote off certain costs capitalized at our Molina Medicaid Solutions segment that supported our Health Plans segment provider information management processes to be re-designed. Although the intercompany revenues recorded by Molina Medicaid Solutions under this arrangement were insignificant on a consolidated basis, the termination of such revenue resulted in a triggering event for an interim goodwill impairment analysis of this segment in the third quarter of 2017. In the Molina Medicaid Solutions’ discounted cash flow model, we incorporated significant estimates and assumptionstotal unrecognized compensation expense related to future periods, such as intercompany business support opportunities and prospects for new Medicaid management information systems contracts. Because management has determined that Molina Medicaid Solutions will provide fewer future benefits for its supportunvested stock options, which we expect to recognize over a weighted-average period of the Health Plans segment, the test resulted2.5 years. No stock options were granted or exercised in a fair value less than Molina Medicaid Solutions’ carrying amount; therefore, we recorded a goodwill impairment loss for the difference, or $28 million, in the third quarter of 2017.
Other Segment
In the course of developing the Restructuring Plan in the second quarter of 2017, we determined that future benefits to be derived from our Pathways subsidiary, including the integration of its operations with our Health Plans segment, would be less than previously anticipated. In addition, poorer than expected year-to-date operating results, as well as lower projections of operating results for periods in the near term at our Pathways subsidiary, led us to conclude that a triggering event for an interim impairment analysis had occurred in the second quarter of 2017.
In the third quarter of 2017, management determined that Pathways will not provide future benefits relating to the integration of its operations with the Health Plans segment to the extent previously expected. Therefore, we conducted an additional interim impairment analysis.
Intangible assets. In the second quarter of 2017, we evaluated Pathways’ finite-lived intangible assets (customer relationships and contract licenses) for impairment, using undiscounted cash flows expected over the longest remaining useful life of the assets tested. Because the undiscounted cash flows over the remaining useful life were less than Pathways’ carrying amount, the intangible assets were impaired. We recorded an impairment loss for the carrying amount of the intangible assets, or $11 million, in the second quarter of 2017.
Goodwill. As noted above, we estimated Pathways’ fair value using discounted cash flows, incorporating significant estimates and assumptions related to future periods. Such estimates included anticipated client census which drives service revenue; the likelihood of future benefits to be derived from Pathways (including integration with our health plans); current prospects relating to the behavioral services labor market which drives cost of service revenue; and anticipated capital expenditures. The tests in each of the three months ended June 30, 2017,March 31, 2018.
Activity for RSAs, PSAs and September 30, 2017, resulted in a fair value less than Pathways’ carrying amount; therefore, we recorded an
impairment lossPSUs, for the difference. The Pathways goodwill impairment losses amounted to $101 million in the third quarter of 2017, and $59 million in the second quarter of 2017. In the second quarter of 2017, we also recorded a goodwill impairment loss of $2 million for a separate subsidiary in the Other segment that did not pass its impairment test.
There were no impairments of intangible assets or goodwill during 2016.
The goodwill impairment losses are recorded to the segments as indicated in following table, and reported as “Impairment losses” in the accompanying consolidated statements of operations.three months ended March 31, 2018, is summarized below:
|
| | | | | | | | | | | | | | | |
| | Health Plans | | Molina Medicaid Solutions | | Other | | Total |
| | (In millions) |
| Historical goodwill | $ | 445 |
| | $ | 71 |
| | $ | 162 |
| | $ | 678 |
|
| Accumulated impairment losses at December 31, 2016 | (58 | ) | | — |
| | — |
| | (58 | ) |
| Balance, December 31, 2016 | 387 |
| | 71 |
| | 162 |
| | 620 |
|
| Impairment losses, three months ended June 30, 2017 | — |
| | — |
| | (61 | ) | | (61 | ) |
| Impairment losses, three months ended September 30, 2017 | — |
| | (28 | ) | | (101 | ) | | (129 | ) |
| Balance, September 30, 2017 | $ | 387 |
| | $ | 43 |
| | $ | — |
| | $ | 430 |
|
| Accumulated impairment losses at September 30, 2017 | $ | 58 |
| | $ | 28 |
| | $ | 162 |
| | $ | 248 |
|
|
| | | | | | | | | | | | | | | |
| | Restricted Stock Awards | | Performance Stock Awards | | Performance Stock Units | | Total | | Weighted Average Grant Date Fair Value |
| Unvested balance, December 31, 2017 | 401,804 |
| | 84,762 |
| | 91,828 |
| | 578,394 |
| | $ | 58.35 |
|
| Granted | 321,798 |
| | — |
| | 188,455 |
| | 510,253 |
| | 72.46 |
|
| Vested | (163,043 | ) | | (32,929 | ) | | — |
| | (195,972 | ) | | 55.16 |
|
| Forfeited | (59,931 | ) | | (44,384 | ) | | (47,650 | ) | | (151,965 | ) | | 62.99 |
|
| Unvested balance, March 31, 2018 | 500,628 |
| | 7,449 |
| | 232,633 |
| | 740,710 |
| | 67.96 |
|
The total fair value of awards granted and vested is presented in the following table:
|
| | | | | | | |
| | Three Months Ended March 31, |
| | 2018 | | 2017 |
| | (In millions) |
| Granted: | | | |
| Restricted stock awards | $ | 23 |
| | $ | 17 |
|
| Performance stock units | 14 |
| | — |
|
| | $ | 37 |
| | $ | 17 |
|
| Vested: | | | |
| Restricted stock awards | $ | 12 |
| | $ | 10 |
|
| Performance stock awards | 3 |
| | 6 |
|
| | $ | 15 |
| | $ | 16 |
|
11.10. Restructuring and Separation Costs
Following a management-initiated, broad operational assessment in early 2017, designedour board of directors approved, and we committed to, improve our profitability and expand our core Medicaid business, in June 2017, we accelerated the implementation of a comprehensive restructuring and profitability improvement plan in June 2017 (the 2017 Restructuring Plan). UnderKey activities under this plan to date have included:
Streamlining of our organizational structure to eliminate redundant layers of management, consolidate regional support services, and other staff reductions to improve efficiency and the speed and quality of decision making;
Re-design of core operating processes such as provider payment, utilization management, quality monitoring and improvement, and information technology, to achieve more effective and cost-efficient outcomes;
Remediation of high-cost provider contracts and enhancement of high quality, cost-effective networks;
Restructuring, Plan, we are takingincluding selective exits, of direct delivery operations; and
Partnering with the following actions:lowest-cost, most effective vendors.
| |
1. | We have streamlined our organizational structure, including the elimination of redundant layers of management, the consolidation of regional support services, and other reductions to our workforce, to improve efficiency as well as the speed and quality of our decision-making. |
| |
2. | We are re-designing core operating processes such as provider payment, utilization management, quality monitoring and improvement, and information technology to achieve more effective and cost efficient outcomes. |
| |
3. | We are remediating high cost provider contracts and building around high quality, cost-effective networks. |
| |
4. | We are restructuring our existing direct delivery operations. |
| |
5. | We are reviewing our vendor base to ensure that we are partnering with the lowest-cost, most-effective vendors. |
| |
6. | Throughout this process, we are taking precautions to ensure that our actions do not impede our ability to continue to deliver quality health care, retain existing managed care contracts, and to secure new managed care contracts. |
Costs Incurred
In addition to costsour 2017 Annual Report on Form 10-K, we reported that we had incurred undersubstantially all of the Restructuring Plan, we have recorded costs associated with the separation of our former CEO and former CFO, described in further detail below.
Expected Costs
We estimate that total pre-tax costs associated with the restructuring plan will be approximately $70 million to $90 million in the fourth quarter of 2017 with an additional $20 million to $40 million to be incurred in 2018. Since the initiation of our Restructuring Plan in 2017, amounting to $234 million. In the secondfirst quarter of 2017, the range2018, we incurred an additional $25 million in such costs, primarily as a result of total estimated costs have increased by approximately $50 million due primarily to non-cash write-offsour further evaluation of certain capitalized software in connectiona utilization and care management project terminated because of its inconsistency with the re-designgoals of core processes. Such write-offsthe 2017 Restructuring Plan. As a result, assets relating to this project were not included in our initial total cost estimates, but as our evaluation of core operating processes proceeded in the third quarter, we determined that certain projects were inconsistent with our future operating goals and were therefore written off.
In addition, in the second quarter of 2017, we reported that we expected restructuring costs to relate only to the Health Plans and Other segments. In the third quarter of 2017, however, we wrote off certain costs capitalized at our Molina Medicaid Solutions segment that supported our Health Plans segment provider information management
processes to be re-designed. In addition, we now expect to incurrecorded nominal amounts for one-time termination benefits, and true-ups of consulting fees in connection with the review of Molina Medicaid Solutions’ core operating processes.
The following table illustrates our estimates of the totaland contract termination costs by segment and major type of cost, that we expect to incur under the Restructuring Plan, and includes costs incurred through September 30,recorded in 2017. We expect to complete all activities under the 2017 Restructuring Plan in 2018, with the exception of the settlement of lease termination liabilities. We expect to be completed bycontinue to settle those liabilities through 2025, unless the end of 2018. |
| | | | | | | | | |
Estimated Costs Expected to be Incurred by Reportable Segment | | Health Plans | | Molina Medicaid Solutions | | Other | | Total |
| | (In millions) |
Termination benefits | | $30 to $35 | | — |
| | $30 to $35 | | $60 to $70 |
Other restructuring costs | | $40 to $45 | | $10 | | $110 to $115 | | $160 to $170 |
| | $70 to $80 | | $10 | | $140 to $150 | | $220 to $240 |
Costs Incurred
Restructuring Plan
Restructuring costs incurred to date consist primarily of termination benefits, write-offs of capitalized software due to the re-design of our core operating processes, restructuring of our direct delivery operations, and consulting fees.
Separation Costs
On May 2, 2017, weleases are terminated the employment of our former CEO and CFO without cause. Under their amended and restated employment agreements, they were each entitled to receive 400% of their base salary, a prorated termination bonus (150% of base salary for the former CEO and 125% of base salary for the former CFO), full vesting of equity compensation, and a cash payment for health and welfare benefits. We recorded separation costs of $35 million primarily related to these former executives under FASB ASC Topic 712, Nonretirement and Postemployment Benefits. Of this total, $23 million related to the acceleration of their share-based compensation, as further discussed in Note 9, “Stockholders' Equity.” Employee separation costs were insignificant in 2016.sooner.
Restructuring and separation costs are reported in “Restructuring and separation costs”by the same name in the accompanying consolidated statements of operations.income. The following tables present the major types of such costs by segment. Long-livedCurrent and long-lived assets include current and non-current capitalized project costs, and capitalized software intangible assets and furniture, fixtures and equipment.determined to be unrecoverable.
| | | | Three Months Ended September 30, 2017 | Three Months Ended March 31, 2018 |
| | Separation Costs - Former Executives | | One-Time Termination Benefits | | Other Restructuring Costs | | Total | One-Time Termination Benefits | | Other Restructuring Costs | | Total |
| | | Write-offs of Long-lived Assets | | Consulting Fees | | Contract Termination Costs | | | Write-offs of Current and Long-lived Assets | | Consulting Fees | | Contract Termination Costs | |
| | (In millions) | (In millions) |
| Health Plans | $ | — |
| | $ | 27 |
| | $ | 6 |
| | $ | — |
| | $ | — |
| | $ | 33 |
| $ | 1 |
| | $ | (1 | ) | | $ | — |
| | $ | (1 | ) | | $ | (1 | ) |
| Molina Medicaid Solutions | — |
| | — |
| | 8 |
| | — |
| | — |
| | 8 |
| |
| Other | — |
| | 23 |
| | 35 |
| | 16 |
| | 3 |
| | 77 |
| 5 |
| | 20 |
| | 1 |
| | — |
| | 26 |
|
| | $ | — |
| | $ | 50 |
| | $ | 49 |
| | $ | 16 |
| | $ | 3 |
| | $ | 118 |
| $ | 6 |
| | $ | 19 |
| | $ | 1 |
| | $ | (1 | ) | | $ | 25 |
|
No restructuring costs were reported in the first quarter of 2017.
As of March 31, 2018, we had incurred cumulative restructuring costs under the 2017 Restructuring Plan as follows: | | | | Nine Months Ended September 30, 2017 | | | | | | | | | | | | | |
| | Separation Costs - Former Executives | | One-Time Termination Benefits | | Other Restructuring Costs | | Total | Separation Costs - Former Executives | | One-Time Termination Benefits | | Other Restructuring Costs | | Total |
| | | Write-offs of Long-lived Assets | | Consulting Fees | | Contract Termination Costs | | | Write-offs of Current and Long-lived Assets | | Consulting Fees | | Contract Termination Costs | |
| | (In millions) | (In millions) |
| Health Plans | $ | — |
| | $ | 27 |
| | $ | 6 |
| | $ | — |
| | $ | — |
| | $ | 33 |
| $ | — |
| | $ | 34 |
| | $ | 15 |
| | $ | — |
| | $ | 23 |
| | $ | 72 |
|
| Molina Medicaid Solutions | — |
| | — |
| | 8 |
| | — |
| | — |
| | 8 |
| — |
| | — |
| | 8 |
| | — |
| | — |
| | 8 |
|
| Other | 35 |
| | 23 |
| | 35 |
| | 24 |
| | 3 |
| | 120 |
| 36 |
| | 39 |
| | 57 |
| | 45 |
| | 2 |
| | 179 |
|
| | $ | 35 |
| | $ | 50 |
| | $ | 49 |
| | $ | 24 |
| | $ | 3 |
| | $ | 161 |
| $ | 36 |
| | $ | 73 |
| | $ | 80 |
| | $ | 45 |
| | $ | 25 |
| | $ | 259 |
|
Reconciliation of Liability
For those restructuring and separation costs that require cash settlement (primarily separation costs, one-time termination benefits, consulting fees and consulting fees)contract termination costs), the following table presents a roll-forward of the accrued liability, which is reported in “Accounts payable and accrued liabilities” in the accompanying consolidated balance sheets:sheets. The adjustments are due to true-ups of consulting fees and contract termination costs recorded in 2017. | | | | Separation Costs - Former Executives | | One-Time Termination Benefits | | Other Restructuring Costs | | Total | Separation Costs - Former Executives | | One-Time Termination Benefits | | Other Restructuring Costs | | Total |
| | (In millions) | (In millions) |
| Accrued as of December 31, 2016 | $ | — |
| | $ | — |
| | $ | — |
| | $ | — |
| |
| Accrued as of December 31, 2017 | | $ | 2 |
| | $ | 11 |
| | $ | 35 |
| | $ | 48 |
|
| Adjustments | | — |
| | — |
| | (1 | ) | | (1 | ) |
| Charges | 12 |
| | 50 |
| | 27 |
| | 89 |
| — |
| | 6 |
| | 2 |
| | 8 |
|
| Cash payments | (1 | ) | | (9 | ) | | (14 | ) | | (24 | ) | (2 | ) | | (12 | ) | | (9 | ) | | (23 | ) |
| Accrued as of September 30, 2017 | $ | 11 |
| | $ | 41 |
| | $ | 13 |
| | $ | 65 |
| |
| Accrued as of March 31, 2018 | | $ | — |
| | $ | 5 |
| | $ | 27 |
| | $ | 32 |
|
12. Segment Information11. Segments
We have three reportable segments. These segments consist of our Health Plans segment, which constitutes the vast majority of our operations; our Molina Medicaid Solutions segment; and our Other segment. Our reportable segments are consistent with how we currently manage the business and view the markets we serve.
Gross margin is the appropriate earnings measure for our reportable segments, based on how our chief operating decision maker currently reviews results, assesses performance, and allocates resources.
Gross margin for our Health Plans segment is referred to as “Medical margin,” and for our Molina Medicaid Solutions and Other segments, as “Service margin.” Medical margin represents the amount earned by the Health Plans segment after medical care costs are deducted from premium revenue. The medical care ratio represents medical care costs as a percentage of premium revenue, and is one of the key metrics used to assess the performance of the Health Plans segment. Therefore, the underlying medical margin is the most important measure
of earnings reviewed by the chief operating decision maker. The service margin is equal to service revenue minus cost of service revenue.
The following table presents total revenue by segment. Inter-segment revenue is insignificant for all periods presented.
|
| | | | | | | | | | | | | | | | |
| | | Health Plans | | Molina Medicaid Solutions | | Other | | Consolidated |
| | | | | |
| | | (In millions) |
| Three Months Ended September 30, 2017 | | | | | | | | |
Total revenue (1) | | $ | 4,899 |
| | $ | 47 |
| | $ | 85 |
| | $ | 5,031 |
|
| Gross margin | | 557 |
| | 5 |
| | 2 |
| | 564 |
|
| Impairment losses | | — |
| | (28 | ) | | (101 | ) | | (129 | ) |
| Restructuring and separation costs | | (33 | ) | | (8 | ) | | (77 | ) | | (118 | ) |
| | | | | | | | | |
| Nine Months Ended September 30, 2017 | | | | | | | | |
Total revenue (1) | | $ | 14,538 |
| | $ | 140 |
| | $ | 256 |
| | $ | 14,934 |
|
| Gross margin | | 1,343 |
| | 13 |
| | 8 |
| | 1,364 |
|
| Impairment losses | | — |
| | (28 | ) | | (173 | ) | | (201 | ) |
| Restructuring and separation costs | | (33 | ) | | (8 | ) | | (120 | ) | | (161 | ) |
| | | | | | | | | |
| Three Months Ended September 30, 2016 | | | | | | | | |
Total revenue (1) | | $ | 4,412 |
| | $ | 48 |
| | $ | 86 |
| | $ | 4,546 |
|
| Gross margin | | 443 |
| | 6 |
| | 8 |
| | 457 |
|
| Impairment losses | | — |
| | — |
| | — |
| | — |
|
| Restructuring and separation costs | | — |
| | — |
| | — |
| | — |
|
| | | | | | | | | |
| Nine Months Ended September 30, 2016 | | | | | | | | |
Total revenue (1) | | $ | 12,835 |
| | $ | 146 |
| | $ | 267 |
| | $ | 13,248 |
|
| Gross margin | | 1,285 |
| | 17 |
| | 29 |
| | 1,331 |
|
| Impairment losses | | — |
| | — |
| | — |
| | — |
|
| Restructuring and separation costs | | — |
| | — |
| | — |
| | — |
|
| | | | | | | | | |
| Total assets | | | | | | | | |
| September 30, 2017 | | $ | 7,031 |
| | $ | 233 |
| | $ | 1,690 |
| | $ | 8,954 |
|
| December 31, 2016 | | 5,897 |
| | 267 |
| | 1,285 |
| | 7,449 |
|
| | | | | | | | | |
| Goodwill and intangible assets, net | | | | | | | | |
| September 30, 2017 | | $ | 488 |
| | $ | 43 |
| | $ | — |
| | $ | 531 |
|
| December 31, 2016 | | 513 |
| | 72 |
| | 175 |
| | 760 |
|
______________________
| |
(1) | Total revenue consists primarily of premium revenue, premium tax revenue and health insurer fee revenue for the Health Plans segment, and service revenue for the Molina Medicaid Solutions and Other segments. Inter-segment revenue is insignificant for all periods presented. |
|
| | | | | | | |
| | Three Months Ended March 31, |
| | 2018 | | 2017 |
| | (In millions) |
| Total revenue: | | | |
| Health Plans | $ | 4,509 |
| | $ | 4,771 |
|
| Molina Medicaid Solutions | 51 |
| | 46 |
|
| Other | 86 |
| | 87 |
|
| Consolidated | $ | 4,646 |
| | $ | 4,904 |
|
The following table reconciles gross margin by segment to consolidated income before income tax expense: | | | | Three Months Ended September 30, | | Nine Months Ended September 30, | Three Months Ended March 31, |
| | 2017 | | 2016 | | 2017 | | 2016 | 2018 | | 2017 |
| | (In millions) | (In millions) |
| Gross margin: | | | | | | | | | | |
| Health Plans | $ | 557 |
| | $ | 443 |
| | $ | 1,343 |
| | $ | 1,285 |
| $ | 601 |
| | $ | 537 |
|
| Molina Medicaid Solutions | 5 |
| | 6 |
| | 13 |
| | 17 |
| 8 |
| | 4 |
|
| Other | 2 |
| | 8 |
| | 8 |
| | 29 |
| 6 |
| | 5 |
|
| Total gross margin | 564 |
| | 457 |
| | 1,364 |
| | 1,331 |
| 615 |
| | 546 |
|
Add: other operating revenues (1) | 124 |
| | 222 |
| | 379 |
| | 625 |
| 189 |
| | 125 |
|
Less: other operating expenses (2) | (769 | ) | | (561 | ) | | (2,029 | ) | | (1,644 | ) | (582 | ) | | (589 | ) |
| Operating (loss) income | (81 | ) | | 118 |
| | (286 | ) | | 312 |
| |
| Other expenses, net | 32 |
| | 26 |
| | 10 |
| | 76 |
| |
| (Loss) income before income taxes | $ | (113 | ) | | $ | 92 |
| | $ | (296 | ) | | $ | 236 |
| |
| Operating income | | 222 |
| | 82 |
|
| Other expenses (income), net | | 43 |
| | (49 | ) |
| Income before income taxes | | $ | 179 |
| | $ | 131 |
|
______________________
| |
| (1) | Other operating revenues include premium tax revenue, health insurer fee revenue,fees reimbursed, and investment income and other revenue. |
| |
| (2) | Other operating expenses include general and administrative expenses, premium tax expenses, health insurer fee expenses,fees, depreciation and amortization, impairment losses, and restructuring and separation costs. |
13.12. Commitments and Contingencies
Regulatory Capital Requirements and Dividend Restrictions
Our health plans, which are operated by our wholly owned subsidiaries in the states in which our health plans operate, are subject to state laws and regulations that, among other things, require the maintenance of minimum levels of statutory capital, as defined by each state. Regulators in some states may also attempt to enforce capital requirements that require the retention of net worth in excess of amounts formally required by statute or regulation. Such statutes, regulations and informal capital requirements also restrict the timing, payment, and amount of dividends and other distributions that may be paid to us as the sole stockholder. To the extent our subsidiaries must comply with these regulations, they may not have the financial flexibility to transfer funds to us. Based on current statutes and regulations, the net assets in these subsidiaries (after intercompany eliminations) which may not be transferable to us in the form of loans, advances, or cash dividends was approximately $1,696$1,777 million at September 30, 2017,March 31, 2018, and $1,492$1,691 million at December 31, 2016.2017. Because of the statutory restrictions that inhibit the ability of our health plans to transfer net assets to us, the amount of retained earnings readily available to pay dividends to our stockholders is generally limited to cash, cash equivalents and investments (excluding restricted investments) held by the parent company – company—Molina Healthcare, Inc. Such cash, cash equivalents and investments (excluding restricted investments) amounted to $391$706 million and $264$696 million as of September 30, 2017March 31, 2018 and December 31, 2016,2017, respectively.
The National Association of Insurance Commissioners (NAIC) adopted rules effective December 31, 1998, which, if implemented by the states, set minimum capitalization requirements for insurance companies, HMOs, and other entities bearing risk for health care coverage. The requirements take the form of risk-based capital (RBC) rules which may vary from state to state. All of the states and Commonwealth in which our health plans operate, except California, Florida and New York, have adopted these rules. Such requirements, if adopted by California, Florida and New York, may increase the minimum capital required for those states.
As of September 30, 2017,March 31, 2018, our health plans had aggregate statutory capital and surplus of approximately $1,828$1,904 million compared with the required minimum aggregate statutory capital and surplus of approximately $1,113$1,181 million. All of our health plans were in compliance with the minimum capital requirements at September 30, 2017.March 31, 2018. We have the ability, and have committed to provide, additional capital to each of our health plans as necessary to ensure compliance with statutory capital and surplus requirements.
Legal Proceedings
The health care and Medicaid-related business process outsourcing industries are subject to numerous laws and regulations of federal, state, and local governments. Compliance with these laws and regulations can be subject to government review and interpretation, as well as regulatory actions unknown and unasserted at this time. Penalties
associated with violations of these laws and regulations include significant fines, exclusion from participating in publicly funded programs, and the repayment of previously billed and collected revenues.
We are involved in legal actions in the ordinary course of business, some of which seek monetary damages, including claims for punitive damages, which are not covered by insurance. We have accrued liabilities for certain matters for which we deem the loss to be both probable and reasonably estimable, but the outcome of legal actions is inherently uncertain and our estimates of such losses could change as a result of further developments of these matters. For certain pending matters, accruals have not been established because such matters have not progressed sufficiently through discovery, and/or development of important factual information and legal issues is insufficient to enable us to estimate a range of possible loss, if any. An adverse determination in one or more of these pending matters could have a material adverse effect on our consolidated financial position, results of operations, or cash flows.
Marketplace Risk Corridor Program. On January 19, 2017, we filed suit against the United States of America in the United States Court of Federal Claims, Case Number 1:55-cv-01000-UNJ, on behalf of our health plans seeking recovery from the federal government of approximately $52 million in Marketplace risk corridor payments for calendar year 2015. Based upon current estimates, we believe our health plans are also owed approximately $76 million in Marketplace risk corridor payments from the federal government for calendar year 2016. We have not recognized revenue, nor have we recorded a receivable, for any amount due from the federal government for unpaid Marketplace risk corridor payments as of September 30, 2017. We have fully recognized all liabilities due to the federal government that we have incurred under the Marketplace risk corridor program, and have paid all amounts due to the federal government as required.
RodriguezSteamfitters Local 449 Pension Plan v. Providence Community Corrections.Molina Healthcare, Inc, et al. On October 1, 2015, seven individuals, on behalf of themselves and all others similarly situated,April 27, 2018, the Steamfitters Local 449 Pension Plan filed a class action securities complaint in the District Court for the Middle District of Tennessee, Nashville Division, Case No. 3:15-cv-01048 (the Rodriquez Litigation), against Providence Community Corrections, Inc. (now known as Pathways Community Corrections, Inc., or PCC). Rutherford County, Tennessee formerly contracted with PCC for the administration of misdemeanor probation, which involved the collection of court costs and fees from probationers. The complaint alleges, among other things, that PCC illegally assessed fees and surcharges against probationers and made improper threats of arrest and probation revocation if the probationers did not pay such amounts. The plaintiffs in the Rodriguez Litigation seek alleged compensatory, treble, and punitive damages, plus attorneys’ fees, for alleged federal and state constitutional violations, as well as alleged violations of the Racketeer Influenced and Corrupt Organization Act. PCC’s agreement with Rutherford County terminated effective March 31, 2016. On November 1, 2015, one month after the Rodriguez Litigation commenced, we acquired PCC from The Providence Service Corporation (Providence) pursuant to a membership interest purchase agreement. In September 2016, the parties to the Rodriguez Litigation accepted a mediation proposal for settlement pursuant to which PCC and Rutherford County would pay the plaintiffs $14 million and $3 million, respectively. The parties are in the process of finalizing the settlement agreement. We expect to recover the full amount of the settlement under the indemnification provisions of the membership interest purchase agreement with Providence.
United States of America, ex rel., Anita Silingo v. Mobile Medical Examination Services, Inc., et al. On or around October 14, 2014, Molina Healthcare of California, Molina Healthcare of California Partner Plan, Inc., Mobile Medical Examination Services, Inc. (MedXM), and other health plan defendants were served with a complaint previously filed under seal in the Central District Court of California by Relator, Anita Silingo,against the Company and its former executive officers, J. Mario Molina, John C. Molina, Terry P. Bayer, and Rick Hopfer, Case No. SACV13-1348-FMO(SHx).2:18-cv-03579. The complaint alleges that MedXM improperly modified medical recordspurports to seek recovery on behalf of all persons or entities who purchased Molina common stock between October 31, 2014 and otherwise took inappropriate steps to increase members’ risk adjustment scores,August 2, 2017 for alleged violations under Sections 10(b) and that20(a) of the Securities Exchange Act and Rule 10b-5 promulgated thereunder. The plaintiff alleges the defendants including Molina Healthcaremisled investors regarding the scalability of Californiathe Company’s administrative infrastructure during the identified class period. The Company believes it has meritorious defenses to the alleged claims and Molina Healthcare of California Partner Plan, Inc., purportedly turned a “blind eye”intends to these unlawful practices. On October 22, 2015,defend the Relator filed a third amended complaint, seeking general and compensatory damages, treble damages, civil penalties, plus interest and attorneys’ fees. On July 11, 2016, the District Court dismissed with prejudice the third amended complaint, without leave to amend. On September 23, 2016, the plaintiff filed an appeal with the Ninth Circuit Court of Appeals. The appeal has been fully briefed by the parties and we are awaiting the Court’s decision.matter vigorously.
States’ Budgets
From time to time,Nearly all of our premium revenues come from the joint federal and state funding of the Medicaid and CHIP programs. The states and Commonwealth in which we operate our health plans operate may experience financial difficulties, which could lead to delays in premium payments. Until July 4, 2017, the state of Illinois operated without a budget for its current fiscal year. As of September 30, 2017, our Illinois health plan served approximately 163,000 members, and recognized premium revenue of approximately $447 million in the nine months ended September 30, 2017. As of September 30, 2017, the state of Illinois owed us approximately $220 million for certain March through September 2017 premiums.
On May 3, 2017, Puerto Rico’s financial oversight board filed for a form of bankruptcy in the U.S. District Court in Puerto Rico under Title III of PROMESA. The Title III provision allows for a court debt restructuring process similar to U.S. bankruptcy protection. To the extent such bankruptcy results in our failure to receive payment of amounts due under our Medicaid contract with the Commonwealth or the inability of the Commonwealth to extend our Medicaid contract at the end of its current term, such bankruptcy could have a material adverse effect on our business, financial condition, cash flows, or results of operations. As of September 30, 2017, the plan served approximately 306,000 members and recorded premium revenue of approximately $553 million in the nine months ended September 30, 2017. As of October 27, 2017, the Commonwealth was current with its premium payments.regularly face significant budgetary pressures.
14. Related Party Transactions
Our California health plan has entered into a provider agreement with Pacific Healthcare IPA (Pacific), which is 50% owned by the brother-in-law of Dr. J. Mario Molina and John C. Molina, who are members of our board of directors. Under the terms of this provider agreement, the California health plan pays Pacific for medical care Pacific provides to health plan members. For the three and nine months ended September 30, 2017 and 2016, the amounts paid to Pacific were insignificant.
Refer to Note 15, “Variable Interest Entities (VIEs),” for a discussion of theJoseph M. Molina, M.D. Professional Corporations.
15. Variable Interest Entities (VIEs)
TheJoseph M. Molina, M.D. Professional Corporations (JMMPC) were created to further advance our direct delivery business. Effective September 30, 2017, we terminated our relationship with JMMPC in Florida, Michigan, Washington, and Utah. Therefore, the agreements described below, for all of our health plans other than those in California and New Mexico, were terminated effective September 30, 2017.
JMMPC’s primary shareholder is Dr. J. Mario Molina, who is a member of our board of directors. Dr. Molina is paid no salary and receives no dividends in connection with his work for, or ownership of, JMMPC. JMMPC provides primary care medical services through its employed physicians and other medical professionals. JMMPC also provides certain specialty referral services to our California health plan members through a contracted provider network. The health plans had entered into primary care services agreements with JMMPC, under which the health plans paid $29 million and $31 million to JMMPC for health care services provided in the three months ended September 30, 2017 and 2016, respectively, and $89 million and $92 million for the nine months ended September 30, 2017 and 2016, respectively. JMMPC does not have agreements to provide professional medical services with any other entities.
Our wholly owned subsidiary, Molina Medical Management, Inc. (MMM), had also entered into services agreements with JMMPC to provide clinic facilities, clinic administrative support staff, patient scheduling services and medical supplies to JMMPC. For the three months ended September 30, 2017 and 2016, JMMPC paid $12 million and $13 million to MMM for clinic administrative services, respectively. For the nine months ended September 30, 2017 and 2016, JMMPC paid $38 million and $40 million, respectively, to MMM for clinic administrative services.
As of September 30, 2017, we determined that JMMPC is a VIE, and that we are its primary beneficiary. We reached this conclusion under the power and benefits criterion model according to GAAP. Specifically, we had the power to direct the activities (excluding clinical decisions) that most significantly affected JMMPC’s economic performance, and the obligation to absorb losses or right to receive benefits that were potentially significant to the VIE, under the agreements described above. Because we were its primary beneficiary, we consolidated JMMPC. JMMPC’s assets may be used to settle only JMMPC’s obligations, and JMMPC’s creditors have no recourse to the general credit of Molina Healthcare, Inc. As of September 30, 2017, JMMPC had total assets of $20 million, and total liabilities of $24 million. As of December 31, 2016, JMMPC had total assets of $18 million, and total liabilities of $18 million.
Our maximum exposure to loss as a result of our involvement with JMMPC is generally limited to the amounts needed to fund JMMPC’s ongoing payroll, employee benefits and medical care costs associated with JMMPC’s specialty referral activities.
16.13. Supplemental Condensed Consolidating Financial Information
The 5.375% Notes describedAs discussed in Note 7, “Debt,” we have outstanding $700 million aggregate principal amount of 5.375% Notes due November 15, 2022, unless earlier redeemed. The 5.375% Notes were registered in September 2016, and are fully and unconditionally guaranteed by certain of our 100%wholly owned subsidiaries on a joint and several basis, with certain exceptions considered customary for such guarantees. The 5.375% Notes and
For all periods presented, the guarantees are effectively subordinated to all of our and our guarantors’ existing and future secured debt to the extent of the assets securing such debt. In addition, the 5.375% Notes and the guarantees are structurally subordinated to all indebtedness and other liabilities and preferred stock, if any, of our subsidiaries that do not guarantee the 5.375% Notes.
As discussed in Note 7, “Debt,” the First Amendment to the Credit Facility provided that all guarantors immediately prior to January 3, 2017, other than Molina Information Systems, LLC, d/b/a Molina Medicaid Solutions, Molina Pathways, LLC, and Pathways Health and Community Support LLC, were automatically and unconditionally released from their obligations as guarantors under the Credit Facility and the 5.375% Notes.
The following condensed consolidating financial statements present Molina Healthcare, Inc. (as parent guarantor)“Parent Guarantor”), the subsidiary guarantors (as “Other Guarantors”), the subsidiary non-guarantors (as “Non-Guarantors”) and eliminations,“Eliminations”, according to the guarantor structure as assessed atas of and for the most recent balance sheet date, September 30, 2017.three months ended March 31, 2018.
CONDENSED CONSOLIDATING STATEMENTS OF OPERATIONS
|
| | | | | | | | | | | | | | | | | | | |
| | Three Months Ended September 30, 2017 |
| | Parent Guarantor | | Other Guarantors | | Non-Guarantors | | Eliminations | | Consolidated |
| | (In millions) |
| Revenue: | | | | | | | | | |
| Total revenue | $ | 380 |
| | $ | 47 |
| | $ | 4,983 |
| | $ | (379 | ) | | $ | 5,031 |
|
| Expenses: | | | | | | | | | |
| Medical care costs | 3 |
| | — |
| | 4,217 |
| | — |
| | 4,220 |
|
| Cost of service revenue | — |
| | 42 |
| | 81 |
| | — |
| | 123 |
|
| General and administrative expenses | 244 |
| | (1 | ) | | 519 |
| | (379 | ) | | 383 |
|
| Premium tax expenses | — |
| | — |
| | 106 |
| | — |
| | 106 |
|
| Depreciation and amortization | 23 |
| | 1 |
| | 9 |
| | — |
| | 33 |
|
| Impairment losses | — |
| | 28 |
| | 101 |
| | — |
| | 129 |
|
| Restructuring and separation costs | 77 |
| | 8 |
| | 33 |
| | — |
| | 118 |
|
| Total operating expenses | 347 |
| | 78 |
| | 5,066 |
| | (379 | ) | | 5,112 |
|
| Operating income (loss) | 33 |
| | (31 | ) | | (83 | ) | | — |
| | (81 | ) |
| Interest expense | 32 |
| | — |
| | — |
| | — |
| | 32 |
|
| Income (loss) before income taxes | 1 |
| | (31 | ) | | (83 | ) | | — |
| | (113 | ) |
| Income tax expense (benefit) | 9 |
| | (10 | ) | | (15 | ) | | — |
| | (16 | ) |
| Net loss before equity in net losses of subsidiaries | (8 | ) | | (21 | ) | | (68 | ) | | — |
| | (97 | ) |
| Equity in net losses of subsidiaries | (89 | ) | | (77 | ) | | — |
| | 166 |
| | — |
|
| Net loss | $ | (97 | ) | | $ | (98 | ) | | $ | (68 | ) | | $ | 166 |
| | $ | (97 | ) |
CONDENSED CONSOLIDATING STATEMENTS OF COMPREHENSIVE LOSS
|
| | | | | | | | | | | | | | | | | | | |
| | Three Months Ended September 30, 2017 |
| | Parent Guarantor | | Other Guarantors | | Non-Guarantors | | Eliminations | | Consolidated |
| | (In millions) |
| Net loss | $ | (97 | ) | | $ | (98 | ) | | $ | (68 | ) | | $ | 166 |
| | $ | (97 | ) |
| Other comprehensive loss, net of tax | — |
| | — |
| | — |
| | — |
| | — |
|
| Comprehensive loss | $ | (97 | ) | | $ | (98 | ) | | $ | (68 | ) | | $ | 166 |
| | $ | (97 | ) |
CONDENSED CONSOLIDATING STATEMENTS OF INCOME
| | | | Three Months Ended September 30, 2016 | Three Months Ended March 31, 2018 |
| | Parent Guarantor | | Other Guarantors | | Non-Guarantors | | Eliminations | | Consolidated | Parent Guarantor | | Other Guarantors | | Non-Guarantors | | Eliminations | | Consolidated |
| | (In millions) | (In millions) |
| Revenue: | | | | | | | | | | | | | | | | | | |
| Total revenue | $ | 274 |
| | $ | 48 |
| | $ | 4,498 |
| | $ | (274 | ) | | $ | 4,546 |
| $ | 333 |
| | $ | 52 |
| | $ | 4,592 |
| | $ | (331 | ) | | $ | 4,646 |
|
| Expenses: | | | | | | | | | | | | | | | | | | |
| Medical care costs | 19 |
| | — |
| | 3,730 |
| | (1 | ) | | 3,748 |
| 4 |
| | — |
| | 3,718 |
| | — |
| | 3,722 |
|
| Cost of service revenue | — |
| | 42 |
| | 77 |
| | — |
| | 119 |
| — |
| | 43 |
| | 77 |
| | — |
| | 120 |
|
| General and administrative expenses | 223 |
| | (4 | ) | | 397 |
| | (273 | ) | | 343 |
| 267 |
| | 4 |
| | 412 |
| | (331 | ) | | 352 |
|
| Premium tax expenses | — |
| | — |
| | 127 |
| | — |
| | 127 |
| — |
| | — |
| | 104 |
| | — |
| | 104 |
|
| Health insurer fee expenses | — |
| | — |
| | 55 |
| | — |
| | 55 |
| |
| Health insurer fees | | — |
| | — |
| | 75 |
| | — |
| | 75 |
|
| Depreciation and amortization | 25 |
| | 2 |
| | 9 |
| | — |
| | 36 |
| 18 |
| | — |
| | 8 |
| | — |
| | 26 |
|
| Restructuring and separation costs | | 26 |
| | — |
| | (1 | ) | | — |
| | 25 |
|
| Total operating expenses | 267 |
| | 40 |
| | 4,395 |
| | (274 | ) | | 4,428 |
| 315 |
| | 47 |
| | 4,393 |
| | (331 | ) | | 4,424 |
|
| Operating income | 7 |
| | 8 |
| | 103 |
| | — |
| | 118 |
| 18 |
| | 5 |
| | 199 |
| | — |
| | 222 |
|
| Interest expense | 26 |
| | — |
| | — |
| | — |
| | 26 |
| 33 |
| | — |
| | — |
| | — |
| | 33 |
|
| Other expenses, net | | 10 |
| | — |
| | — |
| | — |
| | 10 |
|
| (Loss) income before income taxes | (19 | ) | | 8 |
| | 103 |
| | — |
| | 92 |
| (25 | ) | | 5 |
| | 199 |
| | — |
| | 179 |
|
| Income tax expense | 4 |
| | — |
| | 46 |
| | — |
| | 50 |
| 9 |
| | 1 |
| | 62 |
| | — |
| | 72 |
|
| Net (loss) income before equity in net earnings of subsidiaries | (23 | ) | | 8 |
| | 57 |
| | — |
| | 42 |
| |
| Equity in net earnings of subsidiaries | 65 |
| | — |
| | — |
| | (65 | ) | | — |
| |
| Net (loss) income before equity in net losses of subsidiaries | | (34 | ) | | 4 |
| | 137 |
| | — |
| | 107 |
|
| Equity in net earnings (losses) of subsidiaries | | 141 |
| | (3 | ) | | — |
| | (138 | ) | | — |
|
| Net income | $ | 42 |
| | $ | 8 |
| | $ | 57 |
| | $ | (65 | ) | | $ | 42 |
| $ | 107 |
| | $ | 1 |
| | $ | 137 |
| | $ | (138 | ) | | $ | 107 |
|
CONDENSED CONSOLIDATING STATEMENTS OF COMPREHENSIVE INCOME
|
| | | | | | | | | | | | | | | | | | | |
| | Three Months Ended September 30, 2016 |
| | Parent Guarantor | | Other Guarantors | | Non-Guarantors | | Eliminations | | Consolidated |
| | | | | | | | | | |
| | (In millions) |
| Net income | $ | 42 |
| | $ | 8 |
| | $ | 57 |
| | $ | (65 | ) | | $ | 42 |
|
| Other comprehensive loss, net of tax | (1 | ) | | — |
| | (1 | ) | | 1 |
| | (1 | ) |
| Comprehensive income | $ | 41 |
| | $ | 8 |
| | $ | 56 |
| | $ | (64 | ) | | $ | 41 |
|
CONDENSED CONSOLIDATING STATEMENTS OF OPERATIONS
|
| | | | | | | | | | | | | | | | | | | |
| | Nine Months Ended September 30, 2017 |
| | Parent Guarantor | | Other Guarantors | | Non-Guarantors | | Eliminations | | Consolidated |
| | (In millions) |
| Revenue: | | | | | | | | | |
| Total revenue | $ | 1,010 |
| | $ | 146 |
| | $ | 14,792 |
| | $ | (1,014 | ) | | $ | 14,934 |
|
| Expenses: | | | | | | | | | |
| Medical care costs | 10 |
| | — |
| | 12,812 |
| | — |
| | 12,822 |
|
| Cost of service revenue | — |
| | 127 |
| | 242 |
| | — |
| | 369 |
|
| General and administrative expenses | 799 |
| | 13 |
| | 1,429 |
| | (1,014 | ) | | 1,227 |
|
| Premium tax expenses | — |
| | — |
| | 331 |
| | — |
| | 331 |
|
| Depreciation and amortization | 75 |
| | 1 |
| | 33 |
| | — |
| | 109 |
|
| Impairment losses | — |
| | 28 |
| | 173 |
| | — |
| | 201 |
|
| Restructuring and separation costs | 120 |
| | 8 |
| | 33 |
| | — |
| | 161 |
|
| Total operating expenses | 1,004 |
| | 177 |
| | 15,053 |
| | (1,014 | ) | | 15,220 |
|
| Operating income (loss) | 6 |
| | (31 | ) | | (261 | ) | | — |
| | (286 | ) |
| Interest expense | 85 |
| | — |
| | — |
| | — |
| | 85 |
|
| Other income, net | (75 | ) | | — |
| | — |
| | — |
| | (75 | ) |
| Loss before income taxes | (4 | ) | | (31 | ) | | (261 | ) | | — |
| | (296 | ) |
| Income tax expense (benefit) | 26 |
| | (10 | ) | | (62 | ) | | — |
| | (46 | ) |
| Net loss before equity in net losses of subsidiaries | (30 | ) | | (21 | ) | | (199 | ) | | — |
| | (250 | ) |
| Equity in net losses of subsidiaries | (220 | ) | | (143 | ) | | — |
| | 363 |
| | — |
|
| Net loss | $ | (250 | ) | | $ | (164 | ) | | $ | (199 | ) | | $ | 363 |
| | $ | (250 | ) |
CONDENSED CONSOLIDATING STATEMENTS OF COMPREHENSIVE LOSS
|
| | | | | | | | | | | | | | | | | | | |
| | Nine Months Ended September 30, 2017 |
| | Parent Guarantor | | Other Guarantors | | Non-Guarantors | | Eliminations | | Consolidated |
| | (In millions) |
| Net loss | $ | (250 | ) | | $ | (164 | ) | | $ | (199 | ) | | $ | 363 |
| | $ | (250 | ) |
| Other comprehensive income, net of tax | 1 |
| | — |
| | 1 |
| | (1 | ) | | 1 |
|
| Comprehensive loss | $ | (249 | ) | | $ | (164 | ) | | $ | (198 | ) | | $ | 362 |
| | $ | (249 | ) |
|
| | | | | | | | | | | | | | | | | | | |
| | Three Months Ended March 31, 2018 |
| | Parent Guarantor | | Other Guarantors | | Non-Guarantors | | Eliminations | | Consolidated |
| | (In millions) |
| Net income | $ | 107 |
| | $ | 1 |
| | $ | 137 |
| | $ | (138 | ) | | $ | 107 |
|
| Other comprehensive loss, net of tax | (7 | ) | | — |
| | (7 | ) | | 7 |
| | (7 | ) |
| Comprehensive income | $ | 100 |
| | $ | 1 |
| | $ | 130 |
| | $ | (131 | ) | | $ | 100 |
|
CONDENSED CONSOLIDATING STATEMENTS OF INCOME
| | | | Nine Months Ended September 30, 2016 | Three Months Ended March 31, 2017 |
| | Parent Guarantor | | Other Guarantors | | Non-Guarantors | | Eliminations | | Consolidated | Parent Guarantor | | Other Guarantors | | Non-Guarantors | | Eliminations | | Consolidated |
| | (In millions) | (In millions) |
| Revenue: | | | | | | | | | | | | | | | | | | |
| Total revenue | $ | 786 |
| | $ | 147 |
| | $ | 13,099 |
| | $ | (784 | ) | | $ | 13,248 |
| $ | 341 |
| | $ | 48 |
| | $ | 4,857 |
| | $ | (342 | ) | | $ | 4,904 |
|
| Expenses: | | | | | | | | | | | | | | | | | | |
| Medical care costs | 50 |
| | — |
| | 10,881 |
| | (1 | ) | | 10,930 |
| 4 |
| | — |
| | 4,107 |
| | — |
| | 4,111 |
|
| Cost of service revenue | — |
| | 130 |
| | 232 |
| | — |
| | 362 |
| — |
| | 42 |
| | 80 |
| | — |
| | 122 |
|
| General and administrative expenses | 659 |
| | 5 |
| | 1,153 |
| | (783 | ) | | 1,034 |
| 297 |
| | 7 |
| | 477 |
| | (342 | ) | | 439 |
|
| Premium tax expenses | — |
| | — |
| | 345 |
| | — |
| | 345 |
| — |
| | — |
| | 111 |
| | — |
| | 111 |
|
| Health insurer fee expenses | — |
| | — |
| | 163 |
| | — |
| | 163 |
| |
| Depreciation and amortization | 70 |
| | 5 |
| | 27 |
| | — |
| | 102 |
| 27 |
| | — |
| | 12 |
| | — |
| | 39 |
|
| Total operating expenses | 779 |
| | 140 |
| | 12,801 |
| | (784 | ) | | 12,936 |
| 328 |
| | 49 |
| | 4,787 |
| | (342 | ) | | 4,822 |
|
| Operating income | 7 |
| | 7 |
| | 298 |
| | — |
| | 312 |
| |
| Operating income (loss) | | 13 |
| | (1 | ) | | 70 |
| | — |
| | 82 |
|
| Interest expense | 76 |
| | — |
| | — |
| | — |
| | 76 |
| 26 |
| | — |
| | — |
| | — |
| | 26 |
|
| (Loss) income before income taxes | (69 | ) | | 7 |
| | 298 |
| | — |
| | 236 |
| |
| Income tax (benefit) expense | (24 | ) | | (1 | ) | | 162 |
| | — |
| | 137 |
| |
| Net (loss) income before equity in earnings of subsidiaries | (45 | ) | | 8 |
| | 136 |
| | — |
| | 99 |
| |
| Equity in net earnings of subsidiaries | 144 |
| | 3 |
| | — |
| | (147 | ) | | — |
| |
| Net income | $ | 99 |
| | $ | 11 |
| | $ | 136 |
| | $ | (147 | ) | | $ | 99 |
| |
| Other income, net | | (75 | ) | | — |
| | — |
| | — |
| | (75 | ) |
| Income (loss) before income taxes | | 62 |
| | (1 | ) | | 70 |
| | — |
| | 131 |
|
| Income tax expense | | 31 |
| | — |
| | 23 |
| | — |
| | 54 |
|
| Net income (losses) before equity in earnings (losses) of subsidiaries | | 31 |
| | (1 | ) | | 47 |
| | — |
| | 77 |
|
| Equity in net earnings (losses) of subsidiaries | | 46 |
| | (2 | ) | | — |
| | (44 | ) | | — |
|
| Net income (loss) | | $ | 77 |
| | $ | (3 | ) | | $ | 47 |
| | $ | (44 | ) | | $ | 77 |
|
CONDENSED CONSOLIDATING STATEMENTS OF COMPREHENSIVE INCOME
|
| | | | | | | | | | | | | | | | | | | |
| | Nine Months Ended September 30, 2016 |
| | Parent Guarantor | | Other Guarantors | | Non-Guarantors | | Eliminations | | Consolidated |
| | (In millions) |
| Net income | $ | 99 |
| | $ | 11 |
| | $ | 136 |
| | $ | (147 | ) | | $ | 99 |
|
| Other comprehensive income, net of tax | 7 |
| | — |
| | 6 |
| | (6 | ) | | 7 |
|
| Comprehensive income | $ | 106 |
| | $ | 11 |
| | $ | 142 |
| | $ | (153 | ) | | $ | 106 |
|
|
| | | | | | | | | | | | | | | | | | | |
| | Three Months Ended March 31, 2017 |
| | Parent Guarantor | | Other Guarantors | | Non-Guarantors | | Eliminations | | Consolidated |
| | (In millions) |
| Net income (loss) | $ | 77 |
| | $ | (3 | ) | | $ | 47 |
| | $ | (44 | ) | | $ | 77 |
|
| Other comprehensive income, net of tax | 1 |
| | — |
| | 1 |
| | (1 | ) | | 1 |
|
| Comprehensive income (loss) | $ | 78 |
| | $ | (3 | ) | | $ | 48 |
| | $ | (45 | ) | | $ | 78 |
|
CONDENSED CONSOLIDATING BALANCE SHEETS
| | | | September 30, 2017 | March 31, 2018 |
| | Parent Guarantor | | Other Guarantors | | Non-Guarantors | | Eliminations | | Consolidated | Parent Guarantor | | Other Guarantors | | Non-Guarantors | | Eliminations | | Consolidated |
| | (In millions) | (In millions) |
ASSETS | | Current assets: | | | | | | | | | | | | | | | | | | |
| Cash and cash equivalents | $ | 356 |
| | $ | 58 |
| | $ | 3,520 |
| | $ | — |
| | $ | 3,934 |
| $ | 307 |
| | $ | 27 |
| | $ | 3,395 |
| | $ | — |
| | $ | 3,729 |
|
| Investments | 35 |
| | — |
| | 1,752 |
| | — |
| | 1,787 |
| 399 |
| | — |
| | 2,045 |
| | — |
| | 2,444 |
|
| Restricted investments | 326 |
| | — |
| | — |
| | — |
| | 326 |
| 77 |
| | — |
| | — |
| | — |
| | 77 |
|
| Receivables | 2 |
| | 25 |
| | 975 |
| | — |
| | 1,002 |
| 2 |
| | 41 |
| | 907 |
| | — |
| | 950 |
|
| Income taxes refundable | 2 |
| | — |
| | 58 |
| | — |
| | 60 |
| |
| Due from (to) affiliates | 203 |
| | (5 | ) | | (198 | ) | | — |
| | — |
| 147 |
| | (5 | ) | | (142 | ) | | — |
| | — |
|
| Prepaid expenses and other current assets | 65 |
| | 20 |
| | 89 |
| | — |
| | 174 |
| 60 |
| | 8 |
| | 343 |
| | — |
| | 411 |
|
| Derivative asset | 425 |
| | — |
| | — |
| | — |
| | 425 |
| 585 |
| | — |
| | — |
| | — |
| | 585 |
|
| Total current assets | 1,414 |
| | 98 |
| | 6,196 |
| | — |
| | 7,708 |
| 1,577 |
| | 71 |
| | 6,548 |
| | — |
| | 8,196 |
|
| Property, equipment, and capitalized software, net | 261 |
| | 37 |
| | 99 |
| | — |
| | 397 |
| 206 |
| | 30 |
| | 82 |
| | — |
| | 318 |
|
| Deferred contract costs | — |
| | 97 |
| | — |
| | — |
| | 97 |
| |
| Goodwill and intangible assets, net | 55 |
| | 43 |
| | 433 |
| | — |
| | 531 |
| 15 |
| | 43 |
| | 192 |
| | — |
| | 250 |
|
| Restricted investments | — |
| | — |
| | 117 |
| | — |
| | 117 |
| — |
| | — |
| | 120 |
| | — |
| | 120 |
|
| Investment in subsidiaries, net | 2,625 |
| | 95 |
| | — |
| | (2,720 | ) | | — |
| 2,531 |
| | 79 |
| | — |
| | (2,610 | ) | | — |
|
| Deferred income taxes | 10 |
| | — |
| | 96 |
| | (44 | ) | | 62 |
| 28 |
| | — |
| | 104 |
| | (18 | ) | | 114 |
|
| Other assets | 50 |
| | 2 |
| | 6 |
| | (16 | ) | | 42 |
| 41 |
| | 105 |
| | 5 |
| | (16 | ) | | 135 |
|
| | $ | 4,415 |
| | $ | 372 |
| | $ | 6,947 |
| | $ | (2,780 | ) | | $ | 8,954 |
| $ | 4,398 |
| | $ | 328 |
| | $ | 7,051 |
| | $ | (2,644 | ) | | $ | 9,133 |
|
| | | | | | | | | | | | | | | | | | | |
LIABILITIES AND STOCKHOLDERS’ EQUITY | | Current liabilities: | | | | | | | | | | | | | | | | | | |
| Medical claims and benefits payable | $ | — |
| | $ | — |
| | $ | 2,478 |
| | $ | — |
| | $ | 2,478 |
| $ | 3 |
| | $ | — |
| | $ | 2,020 |
| | $ | — |
| | $ | 2,023 |
|
| Amounts due government agencies | — |
| | — |
| | 1,324 |
| | — |
| | 1,324 |
| — |
| | 1 |
| | 1,713 |
| | — |
| | 1,714 |
|
| Accounts payable and accrued liabilities | 227 |
| | 40 |
| | 218 |
| | — |
| | 485 |
| 151 |
| | 40 |
| | 522 |
| | — |
| | 713 |
|
| Deferred revenue | — |
| | 52 |
| | 416 |
| | — |
| | 468 |
| — |
| | 41 |
| | 363 |
| | — |
| | 404 |
|
| Current portion of long-term debt | 782 |
| | — |
| | — |
| | — |
| | 782 |
| 566 |
| | — |
| | — |
| | — |
| | 566 |
|
| Derivative liability | 425 |
| | — |
| | — |
| | — |
| | 425 |
| 585 |
| | — |
| | — |
| | — |
| | 585 |
|
| Total current liabilities | 1,434 |
| | 92 |
| | 4,436 |
| | — |
| | 5,962 |
| 1,305 |
| | 82 |
| | 4,618 |
| | — |
| | 6,005 |
|
| Long-term debt | 1,515 |
| | — |
| | 16 |
| | (16 | ) | | 1,515 |
| 1,516 |
| | — |
| | 16 |
| | (16 | ) | | 1,516 |
|
| Deferred income taxes | 12 |
| | 32 |
| | — |
| | (44 | ) | | — |
| — |
| | 18 |
| | — |
| | (18 | ) | | — |
|
| Other long-term liabilities | 25 |
| | 1 |
| | 22 |
| | — |
| | 48 |
| 24 |
| | 1 |
| | 34 |
| | — |
| | 59 |
|
| Total liabilities | 2,986 |
| | 125 |
| | 4,474 |
| | (60 | ) | | 7,525 |
| 2,845 |
| | 101 |
| | 4,668 |
| | (34 | ) | | 7,580 |
|
| Total stockholders’ equity | 1,429 |
| | 247 |
| | 2,473 |
| | (2,720 | ) | | 1,429 |
| 1,553 |
| | 227 |
| | 2,383 |
| | (2,610 | ) | | 1,553 |
|
| | $ | 4,415 |
| | $ | 372 |
| | $ | 6,947 |
| | $ | (2,780 | ) | | $ | 8,954 |
| $ | 4,398 |
| | $ | 328 |
| | $ | 7,051 |
| | $ | (2,644 | ) | | $ | 9,133 |
|
CONDENSED CONSOLIDATING BALANCE SHEETS
| | | | December 31, 2016 | December 31, 2017 |
| | Parent Guarantor | | Other Guarantors | | Non-Guarantors | | Eliminations | | Consolidated | Parent Guarantor | | Other Guarantors | | Non-Guarantors | | Eliminations | | Consolidated |
| | (In millions) | (In millions) |
ASSETS | | Current assets: | | | | | | | | | | | | | | | | | | |
| Cash and cash equivalents | $ | 86 |
| | $ | 6 |
| | $ | 2,727 |
| | $ | — |
| | $ | 2,819 |
| $ | 504 |
| | $ | 28 |
| | $ | 2,654 |
| | $ | — |
| | $ | 3,186 |
|
| Investments | 178 |
| | — |
| | 1,580 |
| | — |
| | 1,758 |
| 192 |
| | — |
| | 2,332 |
| | — |
| | 2,524 |
|
| Restricted investments | | 169 |
| | — |
| | — |
| | — |
| | 169 |
|
| Receivables | 2 |
| | 34 |
| | 938 |
| | — |
| | 974 |
| 2 |
| | 30 |
| | 839 |
| | — |
| | 871 |
|
| Income tax refundable | 17 |
| | 4 |
| | 18 |
| | — |
| | 39 |
| |
| Due from (to) affiliates | 104 |
| | (5 | ) | | (99 | ) | | — |
| | — |
| 148 |
| | (6 | ) | | (142 | ) | | — |
| | — |
|
| Prepaid expenses and other current assets | 58 |
| | 30 |
| | 43 |
| | — |
| | 131 |
| 103 |
| | 14 |
| | 138 |
| | (16 | ) | | 239 |
|
| Derivative asset | 267 |
| | — |
| | — |
| | — |
| | 267 |
| 522 |
| | — |
| | — |
| | — |
| | 522 |
|
| Total current assets | 712 |
| | 69 |
| | 5,207 |
| | — |
| | 5,988 |
| 1,640 |
| | 66 |
| | 5,821 |
| | (16 | ) | | 7,511 |
|
| Property, equipment, and capitalized software, net | 301 |
| | 46 |
| | 107 |
| | — |
| | 454 |
| 223 |
| | 33 |
| | 86 |
| | — |
| | 342 |
|
| Deferred contract costs | — |
| | 86 |
| | — |
| | — |
| | 86 |
| |
| Goodwill and intangible assets, net | 58 |
| | 73 |
| | 629 |
| | — |
| | 760 |
| 15 |
| | 43 |
| | 197 |
| | — |
| | 255 |
|
| Restricted investments | — |
| | — |
| | 110 |
| | — |
| | 110 |
| — |
| | — |
| | 119 |
| | — |
| | 119 |
|
| Investment in subsidiaries, net | 2,609 |
| | 246 |
| | — |
| | (2,855 | ) | | — |
| 2,306 |
| | 82 |
| | — |
| | (2,388 | ) | | — |
|
| Deferred income taxes | 10 |
| | — |
| | — |
| | — |
| | 10 |
| 17 |
| | — |
| | 101 |
| | (15 | ) | | 103 |
|
| Other assets | 48 |
| | 3 |
| | 6 |
| | (16 | ) | | 41 |
| 32 |
| | 103 |
| | 7 |
| | (1 | ) | | 141 |
|
| | $ | 3,738 |
| | $ | 523 |
| | $ | 6,059 |
| | $ | (2,871 | ) | | $ | 7,449 |
| $ | 4,233 |
| | $ | 327 |
| | $ | 6,331 |
| | $ | (2,420 | ) | | $ | 8,471 |
|
| | | | | | | | | | | | | | | | | | | |
LIABILITIES AND STOCKHOLDERS’ EQUITY | | Current liabilities: | | | | | | | | | | | | | | | | | | |
| Medical claims and benefits payable | $ | 1 |
| | $ | — |
| | $ | 1,928 |
| | $ | — |
| | $ | 1,929 |
| $ | 3 |
| | $ | — |
| | $ | 2,189 |
| | $ | — |
| | $ | 2,192 |
|
| Amounts due government agencies | — |
| | — |
| | 1,202 |
| | — |
| | 1,202 |
| — |
| | 1 |
| | 1,541 |
| | — |
| | 1,542 |
|
| Accounts payable and accrued liabilities | 146 |
| | 34 |
| | 205 |
| | — |
| | 385 |
| 178 |
| | 40 |
| | 148 |
| | — |
| | 366 |
|
| Deferred revenue | — |
| | 40 |
| | 275 |
| | — |
| | 315 |
| — |
| | 49 |
| | 233 |
| | — |
| | 282 |
|
| Current portion of long-term debt | 472 |
| | — |
| | — |
| | — |
| | 472 |
| 653 |
| | — |
| | 16 |
| | (16 | ) | | 653 |
|
| Derivative liability | 267 |
| | — |
| | — |
| | — |
| | 267 |
| 522 |
| | — |
| | — |
| | — |
| | 522 |
|
| Total current liabilities | 886 |
| | 74 |
| | 3,610 |
| | — |
| | 4,570 |
| 1,356 |
| | 90 |
| | 4,127 |
| | (16 | ) | | 5,557 |
|
| Long-term debt | 1,173 |
| | — |
| | 16 |
| | (16 | ) | | 1,173 |
| 1,516 |
| | — |
| | — |
| | — |
| | 1,516 |
|
| Deferred income taxes | 11 |
| | 39 |
| | (35 | ) | | — |
| | 15 |
| — |
| | 15 |
| | — |
| | (15 | ) | | — |
|
| Other long-term liabilities | 19 |
| | 1 |
| | 22 |
| | — |
| | 42 |
| 24 |
| | 2 |
| | 36 |
| | (1 | ) | | 61 |
|
| Total liabilities | 2,089 |
| | 114 |
| | 3,613 |
| | (16 | ) | | 5,800 |
| 2,896 |
| | 107 |
| | 4,163 |
| | (32 | ) | | 7,134 |
|
| Total stockholders’ equity | 1,649 |
| | 409 |
| | 2,446 |
| | (2,855 | ) | | 1,649 |
| 1,337 |
| | 220 |
| | 2,168 |
| | (2,388 | ) | | 1,337 |
|
| | $ | 3,738 |
| | $ | 523 |
| | $ | 6,059 |
| | $ | (2,871 | ) | | $ | 7,449 |
| $ | 4,233 |
| | $ | 327 |
| | $ | 6,331 |
| | $ | (2,420 | ) | | $ | 8,471 |
|
CONDENSED CONSOLIDATING STATEMENTS OF CASH FLOWS
|
| | | | | | | | | | | | | | | | | | | |
| | Nine Months Ended September 30, 2017 |
| | Parent Guarantor | | Other Guarantors | | Non-Guarantors | | Eliminations | | Consolidated |
| | (In millions) |
| Operating activities: | | | | | | | | | |
| Net cash provided by operating activities | $ | 215 |
| | $ | 81 |
| | $ | 661 |
| | $ | — |
| | $ | 957 |
|
| Investing activities: | | | | | | | | | |
| Purchases of investments | (333 | ) | | — |
| | (1,563 | ) | | — |
| | (1,896 | ) |
| Proceeds from sales and maturities of investments | 150 |
| | — |
| | 1,388 |
| | — |
| | 1,538 |
|
| Purchases of property, equipment and capitalized software | (67 | ) | | (10 | ) | | (8 | ) | | — |
| | (85 | ) |
| Increase in restricted investments held-to-maturity | — |
| | — |
| | (10 | ) | | — |
| | (10 | ) |
| Capital contributions to/from subsidiaries | (363 | ) | | 2 |
| | 361 |
| | — |
| | — |
|
| Dividends to/from subsidiaries | 136 |
| | — |
| | (136 | ) | | — |
| | — |
|
| Change in amounts due to/from affiliates | (100 | ) | | — |
| | 100 |
| | — |
| | — |
|
| Other, net | — |
| | (21 | ) | | — |
| | — |
| | (21 | ) |
| Net cash (used in) provided by investing activities | (577 | ) | | (29 | ) | | 132 |
| | — |
| | (474 | ) |
| Financing activities: | | | | | | | | | |
| Proceeds from senior notes offering, net of issuance costs | 325 |
| | — |
| | — |
| | — |
| | 325 |
|
| Proceeds from borrowings under credit facility | 300 |
| | — |
| | — |
| | — |
| | 300 |
|
| Proceeds from employee stock plans | 11 |
| | — |
| | — |
| | — |
| | 11 |
|
| Other, net | (4 | ) | | — |
| | — |
| | — |
| | (4 | ) |
| Net cash provided by financing activities | 632 |
| | — |
| | — |
| | — |
| | 632 |
|
| Net increase in cash and cash equivalents | 270 |
| | 52 |
| | 793 |
| | — |
| | 1,115 |
|
| Cash and cash equivalents at beginning of period | 86 |
| | 6 |
| | 2,727 |
| | — |
| | 2,819 |
|
| Cash and cash equivalents at end of period | $ | 356 |
| | $ | 58 |
| | $ | 3,520 |
| | $ | — |
| | $ | 3,934 |
|
CONDENSED CONSOLIDATING STATEMENTS OF CASH FLOWS
|
| | | | | | | | | | | | | | | | | | | |
| | Three Months Ended March 31, 2018 |
| | Parent Guarantor | | Other Guarantors | | Non-Guarantors | | Eliminations | | Consolidated |
| | (In millions) |
| Operating activities: | | | | | | | | | |
| Net cash provided by operating activities | $ | 6 |
| | $ | 9 |
| | $ | 379 |
| | $ | — |
| | $ | 394 |
|
| Investing activities: | | | | | | | | | |
| Purchases of investments | (130 | ) | | — |
| | (259 | ) | | — |
| | (389 | ) |
| Proceeds from sales and maturities of investments | 5 |
| | — |
| | 538 |
| | — |
| | 543 |
|
| Purchases of property, equipment and capitalized software | (1 | ) | | (2 | ) | | (1 | ) | | — |
| | (4 | ) |
| Capital contributions to subsidiaries | (80 | ) | | — |
| | 80 |
| | — |
| | — |
|
| Change in amounts due to/from affiliates | (3 | ) | | (2 | ) | | 5 |
| | — |
| | — |
|
| Other, net | 2 |
| | (6 | ) | | (1 | ) | | — |
| | (5 | ) |
| Net cash (used in) provided by investing activities | (207 | ) | | (10 | ) | | 362 |
| | — |
| | 145 |
|
| Financing activities: | | | | | | | | | |
| Cash paid for financing transaction fees | (5 | ) | | — |
| | — |
| | — |
| | (5 | ) |
| Net cash used in financing activities | (5 | ) | | — |
| | — |
| | — |
| | (5 | ) |
| Net (decrease) increase in cash, cash equivalents, and restricted cash and cash equivalents | (206 | ) | | (1 | ) | | 741 |
| | — |
| | 534 |
|
| Cash, cash equivalents, and restricted cash and cash equivalents at beginning of period | 513 |
| | 28 |
| | 2,749 |
| | — |
| | 3,290 |
|
| Cash, cash equivalents, and restricted cash and cash equivalents at end of period | $ | 307 |
| | $ | 27 |
| | $ | 3,490 |
| | $ | — |
| | $ | 3,824 |
|
| | | | Nine Months Ended September 30, 2016 | Three Months Ended March 31, 2017 |
| | Parent Guarantor | | Other Guarantors | | Non-Guarantors | | Eliminations | | Consolidated | Parent Guarantor | | Other Guarantors | | Non-Guarantors | | Eliminations | | Consolidated |
| | (In millions) | (In millions) |
| Operating activities: | | | | | | | | | | | | | | | | | | |
| Net cash provided by operating activities | $ | 43 |
| | $ | 34 |
| | $ | 556 |
| | $ | — |
| | $ | 633 |
| $ | 144 |
| | $ | 21 |
| | $ | 554 |
| | $ | — |
| | $ | 719 |
|
| Investing activities: | | | | | | | | | | | | | | | | | | |
| Purchases of investments | (114 | ) | | — |
| | (1,330 | ) | | — |
| | (1,444 | ) | — |
| | — |
| | (733 | ) | | — |
| | (733 | ) |
| Proceeds from sales and maturities of investments | 103 |
| | — |
| | 1,409 |
| | — |
| | 1,512 |
| 92 |
| | — |
| | 341 |
| | — |
| | 433 |
|
| Purchases of property, equipment and capitalized software | (102 | ) | | (23 | ) | | (18 | ) | | — |
| | (143 | ) | (18 | ) | | (5 | ) | | (3 | ) | | — |
| | (26 | ) |
| Decrease in restricted investments held-to-maturity | — |
| | — |
| | 4 |
| | — |
| | 4 |
| — |
| | — |
| | (5 | ) | | — |
| | (5 | ) |
| Net cash paid in business combinations | — |
| | (5 | ) | | (43 | ) | | — |
| | (48 | ) | |
| Capital contributions to/from subsidiaries | (221 | ) | | 7 |
| | 214 |
| | — |
| | — |
| |
| Dividends to/from subsidiaries | 50 |
| | — |
| | (50 | ) | | — |
| | — |
| |
| Capital contributions to subsidiaries | | (106 | ) | | 1 |
| | 105 |
| | — |
| | — |
|
| Dividends from subsidiaries | | 50 |
| | — |
| | (50 | ) | | — |
| | — |
|
| Change in amounts due to/from affiliates | (12 | ) | | 4 |
| | 8 |
| | — |
| | — |
| (60 | ) | | 2 |
| | 58 |
| | — |
| | — |
|
| Other, net | 6 |
| | (19 | ) | | 1 |
| | — |
| | (12 | ) | — |
| | (6 | ) | | — |
| | — |
| | (6 | ) |
| Net cash (used in) provided by investing activities | (290 | ) | | (36 | ) | | 195 |
| | — |
| | (131 | ) | |
| Net cash used in investing activities | | (42 | ) | | (8 | ) | | (287 | ) | | — |
| | (337 | ) |
| Financing activities: | | | | �� | | | | | | | | | | | | | | |
Proceeds from employee stock plans
| 10 |
| | — |
| | — |
| | — |
| | 10 |
| 1 |
| | — |
| | — |
| | — |
| | 1 |
|
| Other, net | 2 |
| | — |
| | (1 | ) | | — |
| | 1 |
| (2 | ) | | — |
| | — |
| | — |
| | (2 | ) |
| Net cash provided by (used in) financing activities | 12 |
| | — |
| | (1 | ) | | — |
| | 11 |
| |
| Net (decrease) increase in cash and cash equivalents | (235 | ) | | (2 | ) | | 750 |
| | — |
| | 513 |
| |
| Cash and cash equivalents at beginning of period | 360 |
| | 13 |
| | 1,956 |
| | — |
| | 2,329 |
| |
| Cash and cash equivalents at end of period | $ | 125 |
| | $ | 11 |
| | $ | 2,706 |
| | $ | — |
| | $ | 2,842 |
| |
| Net cash used in financing activities | | (1 | ) | | — |
| | — |
| | — |
| | (1 | ) |
| Net increase in cash, cash equivalents, and restricted cash and cash equivalents | | 101 |
| | 13 |
| | 267 |
| | — |
| | 381 |
|
| Cash, cash equivalents, and restricted cash and cash equivalents at beginning of period | | 86 |
| | 6 |
| | 2,820 |
| | — |
| | 2,912 |
|
| Cash, cash equivalents, and restricted cash and cash equivalents at end of period | | $ | 187 |
| | $ | 19 |
| | $ | 3,087 |
| | $ | — |
| | $ | 3,293 |
|
MANAGEMENT’S DISCUSSION AND ANALYSIS OF FINANCIAL CONDITION AND RESULTS OF OPERATIONS (MD&A)
FORWARD-LOOKING STATEMENTS
This quarterly report on Form 10-Q contains forward-looking statements regarding our business, financial condition, and results of operations within the meaning of Section 27A of the Securities Act of 1933, or Securities Act, and Section 21E of the Securities Exchange Act of 1934, or Securities Exchange Act. We intend such forward-looking statements to be covered by the safe harbor provisions for forward-looking statements contained in the Private Securities Litigation Reform Act of 1995, and we are including this statement for purposes of complying with these safe harbor provisions. All statements, other than statements of historical facts, included in this quarterly report may be deemed to be forward-looking statements for purposes of the Securities Act and the Securities Exchange Act. Without limiting the foregoing, we use the words “anticipate(s),” “believe(s),” “estimate(s),” “expect(s),” “intend(s),” “may,” “plan(s),” “project(s),” “will,” “would,” “could,” “should” and similar expressions to identify forward-looking statements, although not all forward-looking statements contain these identifying words. We cannot guarantee that we will actually achieve the plans, intentions, or expectations disclosed in our forward-looking statements and, accordingly, you should not place undue reliance on our forward-looking statements. We caution you that we do not undertake any obligation to update forward-looking statements made by us. Forward-looking statements involve known and unknown risks and uncertainties that may cause our actual results in future periods to differ materially from those projected, estimated, expected, or contemplated. Those known risks and uncertainties include, but are not limited to, the following:
the success of our previously announced restructuring plan,the Company’s profit improvement and maintenance initiatives, including the timing and amounts of the benefits realized;realized, and administrative savings achieved;
the numerous political and market-based uncertainties associated with the Affordable Care Act (the “ACA”) or “Obamacare,“Obamacare;” including any potential repeal and replacement of the law, amendment of the law, or move to state block grants for Medicaid;
the market dynamics surrounding the ACA Marketplaces, including but not limited to uncertainties associated with risk transfer requirements, the potential for disproportionate enrollment of higher acuity members, the discontinuation of premium tax credits, and the adequacy of agreed rates, and potential disruption associated with market withdrawal from Utah, Wisconsin, or other states;rates;
subsequent adjustments to reported premium revenue based upon subsequent developments or new information, including changes to estimated amounts payable or receivable related to Marketplace risk adjustment/risk transfer, risk corridors, and reinsurance;transfer;
effective management of ourthe Company’s medical costs;
ourthe Company’s ability to predict with a reasonable degree of accuracy utilization rates, including utilization rates associated with seasonal flu patterns or other newly emergent diseases;
significant budget pressures on state governments and their potential inability to maintain current rates, to implement expected rate increases, or to maintain existing benefit packages or membership eligibility thresholds or criteria, including the payment of all amounts due to our Illinois health plan following the resolution of the Illinois budget impasse;criteria;
the success of our efforts to retain existing managed care contracts, including those in Florida, New Mexico, Puerto Rico, and Texas, and to obtain new government contracts in connection with state requests for proposals (RFPs) in both existing and new states;
any adverse impact resulting from the significant changes to our executive leadership team and the rightsizing of our workforce;
the impact of our decision to exit the Utah and Wisconsin ACA Marketplace markets effective December 31, 2017;
ourCompany’s ability to manage ourits operations, including maintaining and creating adequate internal systems and controls relating to authorizations, approvals, provider payments, and the overall success of ourits care management initiatives;
ourthe Company’s ability to consummate and realize benefits from acquisitions or divestitures;
ourthe Company’s receipt of adequate premium rates to support increasing pharmacy costs, including costs associated with specialty drugs and costs resulting from formulary changes that allow the option of higher-priced non-generic drugs;
ourthe Company’s ability to operate profitably in an environment where the trend in premium rate increases lags behind the trend in increasing medical costs;
the interpretation and implementation of federal or state medical cost expenditure floors, administrative cost and profit ceilings, premium stabilization programs, profit sharing arrangements, and risk adjustment provisions;provisions and requirements;
ourthe Company’s estimates of amounts owed for such cost expenditure floors, administrative cost and profit ceilings, premium stabilization programs, profit-sharing arrangements, and risk adjustment provisions;
the Medicaid expansion cost corridors in California, New Mexico, and Washington, and any other retroactive adjustment to revenue where methodologies and procedures are subject to interpretation or dependent upon information about the health status of participants other than Molina members;
the interpretation and implementation of at-risk premium rules and state contract performance requirements regarding the achievement of certain quality measures, and ourthe Company’s ability to recognize revenue amounts associated therewith;
cyber-attacks or other privacy or data security incidents resulting in an inadvertent unauthorized disclosure of protected health information;
the success of ourthe Company’s health plan in Puerto Rico, including the resolution of the Puerto Rico debt crisis, payment of all amounts due under ourthe Company’s Medicaid contract, the effect of the PROMESA law, the impact of Hurricane Maria and ourthe Company’s efforts to better manage the health care costs of ourits Puerto Rico health plan;
the success and renewal of ourthe Company’s duals demonstration programs in California, Illinois, Michigan, Ohio, South Carolina, and Texas;
the accurate estimation of incurred but not reported or paid medical costs across ourthe Company’s health plans;
efforts by states to recoup previously paid and recognized premium amounts;
complications, member confusion, or enrollment backlogs related to the annual renewal of Medicaid coverage;
government audits and reviews, or potential investigations, and any fine, sanction, enrollment freeze, monitoring program, or premium recovery that may result therefrom, including any potential demand by the state of New Mexico to recover purportedly underpaid premium taxes;therefrom;
changes with respect to ourthe Company’s provider contracts and the loss of providers;
approval by state regulators of dividends and distributions by ourthe Company’s health plan subsidiaries;
changes in funding under ourthe Company’s contracts as a result of regulatory changes, programmatic adjustments, or other reforms;
high dollar claims related to catastrophic illness;
the favorable resolution of litigation, arbitration, or administrative proceedings;
the relatively small number of states in which we operate health plans, including the greater scale and revenues of the Company’s California, Ohio, Texas, and Washington health plans;
the availability of adequate financing on acceptable terms to fund and capitalize ourthe Company’s expansion and growth, repay ourthe Company’s outstanding indebtedness at maturity and meet ourits liquidity needs, including the interest expense and other costs associated with such financing;
ourthe Company’s failure to comply with the financial or other covenants in ourits credit agreementagreements or the indentures governing ourits outstanding notes;
the sufficiency of ourthe Company’s funds on hand to pay the amounts due upon conversion or maturity of ourits outstanding notes;
the failure of a state in which we operate to renew its federal Medicaid waiver;
changes generally affecting the managed care or Medicaid management information systems industries;
increases in government surcharges, taxes, and assessments, including but not limited to the deductibility of certain compensation costs;
newly emergent viruses or widespread epidemics, public catastrophes or terrorist attacks, and associated public alarm; and
increasing competition and consolidation in the Medicaid industry;
Readers should refer to the section entitled “Risk Factors” in each of our Annual Report on Form 10-K for the year ended December 31, 2016, our Quarterly Reports on Form 10-Q for the quarters ended March 31, 2017 and June 30, 2017, and this Quarterly Report on Form 10-Q, for a discussion of certain risk factors that could materially affect our business, financial condition, cash flows, or results of operations. Given these risks and uncertainties, we can give no assurance that any results or events projected or contemplated by our forward-looking statements will in fact occur.
This quarterly reportQuarterly Report on Form 10-Q and the following discussion of our financial condition and results of operations should be read in conjunction with the accompanying consolidated financial statements and the notes to those statements appearing elsewhere in this report, and the audited financial statements and Management’s Discussion and Analysis appearing in our Annual Report on Form 10-K for the year ended December 31, 2016.2017.
ABOUT MOLINA HEALTHCARE
OUR MISSION IS TO PROVIDE QUALITY HEALTHCARE TO PEOPLE RECEIVING GOVERNMENT ASSISTANCE.
Molina Healthcare, Inc. provides quality managed health care to people receiving government assistance. We offer cost-effective Medicaid-related solutions to meet the health care needs of low-income families and individuals, and to assist government agencies in their administration of the Medicaid program. We have three reportable segments. These segments consist of our Health Plans segment, which constitutes the vast majority of our operations; our Molina Medicaid Solutions segment; and our Other segment.
KEY PERFORMANCE INDICATORS |
| | | | | | | |
| | Three Months Ended March 31, |
| | 2018 | | 2017 |
| | (Dollar amounts in millions, except per-share amounts) |
| Ending total membership | 4.1 |
| | 4.8 |
|
| | | | |
| Premium revenue | $ | 4,323 |
| | $ | 4,648 |
|
Health Plans segment medical margin (1) | $ | 601 |
| | $ | 537 |
|
| Operating income | $ | 222 |
| | $ | 82 |
|
| | | | |
| Net income | $ | 107 |
| | $ | 77 |
|
| Net income per diluted share | $ | 1.64 |
| | $ | 1.37 |
|
| Diluted weighted average shares outstanding | 65.2 |
| | 56.2 |
|
| | | | |
| Adjusted net income per diluted share* | $ | 1.71 |
| | $ | 1.47 |
|
| EBITDA* | $ | 246 |
| | $ | 203 |
|
| | | | |
| Operating Statistics: | | | |
MCR (2) | 86.1 | % | | 88.4 | % |
G&A ratio (3) | 7.6 | % | | 8.9 | % |
Premium tax ratio (2) | 2.3 | % | | 2.3 | % |
| Effective income tax expense rate | 40.3 | % | | 41.6 | % |
Net profit margin (3) | 2.3 | % | | 1.6 | % |
________________________
| |
| (1) | Medical margin is equal to premium revenue minus medical care costs. |
| |
| (2) | MCR represents medical care costs as a percentage of premium revenue; premium tax ratio represents premium tax expenses as a percentage of premium revenue plus premium tax revenue. |
| |
| (3) | G&A ratio represents general and administrative expenses as a percentage of total revenue. Net profit margin represents net income as a percentage of total revenue. |
*Non-GAAP Financial Measures
We use non-GAAP financial measures as supplemental metrics in evaluating our financial performance, making financing and business decisions, and forecasting and planning for future periods. For these reasons, management believes such measures are useful supplemental measures to investors in comparing our performance to the performance of other public companies in the health care industry. These non-GAAP financial measures should be considered as supplements to, and not as substitutes for or superior to, GAAP measures.
See further information regarding non-GAAP measures in the “Supplemental Information” section of this MD&A, including the reconciliations to U.S. GAAP. Non-GAAP financial measures referred to in this report are designated with an asterisk (*).
|
| | | | | | | | | | | | | | | |
| | Three Months Ended September 30, | | Nine Months Ended September 30, |
| | 2017 | | 2016 | | 2017 | | 2016 |
| | (Dollar amounts in millions, except per-share amounts) |
| Net (loss) income | $ | (97 | ) | | $ | 42 |
| | $ | (250 | ) | | $ | 99 |
|
| Net (loss) income per diluted share | $ | (1.70 | ) | | $ | 0.76 |
| | $ | (4.44 | ) | | $ | 1.77 |
|
MCR (1) | 88.3 | % | | 89.4 | % | | 90.5 | % | | 89.5 | % |
G&A ratio (2) | 7.6 | % | | 7.6 | % | | 8.2 | % | | 7.8 | % |
Premium tax ratio (1) | 2.2 | % | | 2.9 | % | | 2.3 | % | | 2.7 | % |
| Effective tax rate | 14.6 | % | | 54.0 | % | | 15.5 | % | | 58.0 | % |
Net profit margin (2) | (1.9 | )% | | 0.9 | % | | (1.7 | )% | | 0.7 | % |
| EBITDA* | $ | (42 | ) | | $ | 160 |
| | $ | (82 | ) | | $ | 430 |
|
| Adjusted net (loss) income* | $ | (93 | ) | | $ | 47 |
| | $ | (235 | ) | | $ | 114 |
|
| Adjusted net (loss) income per diluted share* | $ | (1.62 | ) | | $ | 0.85 |
| | $ | (4.17 | ) | | $ | 2.03 |
|
________________________
| |
(1) | MCR represents medical care costs as a percentage of premium revenue; premium tax ratio represents premium tax expenses as a percentage of premium revenue plus premium tax revenue. |
| |
(2) | G&A ratio represents general and administrative expenses as a percentage of total revenue. Net profit margin represents net income as a percentage of total revenue. |
CONSOLIDATED RESULTS
Three Months Ended September 30, 2017March 31, 2018 Compared with Three Months Ended September 30, 2016March 31, 2017
Net lossincome for the first quarter of 2018 was $107 million, compared with net income of $77 million for the first quarter of 2017. Net income per diluted share was $1.70$1.64 for the thirdfirst quarter of 20172018 compared with net income per diluted share of $0.76$1.37 reported for the third quarter of 2016. Adjusted net loss per diluted share* was $1.62 in the third quarter of 2017, compared with adjusted net income per diluted share* of $0.85 in the third quarter of 2016. Loss before income tax benefit for the third quarter of 2017 was $113 million.
Medical care costs measured as a percentage of premium revenue (the “medical care ratio”) declined to 88.3% in the third quarter of 2017 from 89.4% in the third quarter of 2016 and from 94.8% in the secondfirst quarter of 2017. Improved medical cost performance in the thirdfirst quarter of 2018 resulted from improved medical and administrative cost efficiency.
Net income for the first quarter of 2018 included a net benefit of $35 million ($0.38 per diluted share) for certain items significant to our financial performance described below. Net income for the first quarter of 2017 included a benefit of $75 million ($0.84 per diluted share) for the receipt of an acquisition termination fee.
Premium revenue decreased approximately 7% when compared with the first quarter of 2017. Lower premium revenue was driven by a decrease in Marketplace membership of over 50%, partially offset by Marketplace premium rate increases. As previously disclosed, we have increased premium rates and reduced our Marketplace presence effective January 1, 2018, as part of our overall program to improve profitability.
Overall, the result of:
| |
◦ | Improved sequential performance at our Illinois, New Mexico, Ohio, Puerto Rico, Texas, and Washington health plans, exclusive of the Marketplace program.
|
| |
◦ | Improved performance of our Marketplace program, including a reduction to the premium deficiency reserve of $30 million ($0.33 per diluted share, net of tax). The reserve, which was $100 million at June 30, 2017, decreased to $70 million as of September 30, 2017. |
General and administrative costs, measured as a percentage of total revenue (the “administrative cost ratio”)medical care ratio decreased to 86.1%, were 7.6%from 88.4% in the third quarter of 2017, consistent with the third quarter of 2016, and 50 basis points lower than the secondfirst quarter of 2017. Excluding the benefit of the 2017 CSR reimbursement, the consolidated medical care ratio was 87.7% in the first quarter of 2018.
The medical care ratio for the Medicaid and Medicare programs combined decreased to 90.0%, from 91.0% in the first quarter of 2017. Improved performance at the Florida, Illinois, Ohio and South Carolina health plans, partially offset by a decline in performance at the Washington health plan, drove the decrease in the consolidated medical care ratio for Medicaid and Medicare combined. The 2017 CSR reimbursement had no impact on the medical care ratio for the Company’s Medicaid and Medicare programs.
The medical care ratio for the Marketplace operations was 50.6% for the first quarter of 2018. Excluding the impact of the 2017 Marketplace CSR adjustment noted below, the medical care ratio for Marketplace operations decreased to approximately 67%, from 75% in the first quarter of 2017. Improved profitability in Marketplace operations is primarily the result of premium increases implemented effective January 1, 2018.
The general and administrative (G&A) expense ratio decreased to 7.6%, from 8.9% in the first quarter of 2017. Excluding the impact of Marketplace broker commissioncommissions and exchange fees in both periods, the administrative costG&A ratio decreased 30 basis pointsto 6.8%, from 7.5% in the thirdfirst quarter of 2016.2017.This improvement is primarily the result of our efforts to reduce G&A costs under the 2017 Restructuring Plan.
Restructuring costs andWe recognized a benefit of approximately $70 million ($0.83 per diluted share) in reduced medical expense related to 2017 dates of service as a result of the impairmentfederal government’s confirmation that the reconciliation of certain purchased intangible assets increased loss before income tax benefit in2017 Marketplace CSR subsidies would be performed on an annual basis. In the thirdfourth quarter of 2017, by approximately $247 million. Specifically:we had assumed a nine-month reconciliation of this item pending confirmation of the time period to which the 2017 reconciliation would be applied.
We recorded $118Approximately $25 million ($1.390.30 per diluted share, net of tax)share) of restructuring costs were recognized in the thirdfirst quarter, of 2017. Restructuring costs incurred to date consist primarily of termination benefits, write-offs of capitalized software due to the re-design of our core operating processes, restructuring of our direct delivery operations, and consulting fees.
We recorded $129 million ($1.77 per diluted share, net of tax) in non-cash goodwill impairment losses for our Pathways behavioral health subsidiary and our Molina Medicaid Solutions (MMS) segment. In the third quarter of 2017, management determined that neither business will provide future benefits relating to the integrationwrite-off of their operationsprepaid and other assets in connection with the Health Plans segment tocontinuing re-design of core processes.
Approximately $10 million ($0.15 per diluted share) loss on debt extinguishment was recognized in the extent previously expected.
first quarter in connection with the issuance of 1.8 million common shares in exchange for $97 million principal amount of our 1.625% Convertible Notes.The table below summarizes the impact of certain items significant to our financial performance in the periods presented. The individual items presented below increase (decrease) income before income tax expense.
|
| | | | | | | | | | | | | | | |
| | Three Months Ended March 31, |
| | 2018 | | 2017 |
| | Amount | | Per Diluted Share (1) | | Amount | | Per Diluted Share (1) |
| | (In millions, except per diluted share amounts) |
| Reimbursement of Marketplace CSR subsidies, for 2017 dates of service | $ | 70 |
| | $ | 0.83 |
| | $ | — |
| | $ | — |
|
| Restructuring costs | (25 | ) | | (0.30 | ) | | — |
| | — |
|
| Loss on debt extinguishment | (10 | ) | | (0.15 | ) | | — |
| | — |
|
| Fee received for terminated acquisition | — |
| | — |
| | 75 |
| | 0.84 |
|
| | $ | 35 |
| | $ | 0.38 |
| | $ | 75 |
| | $ | 0.84 |
|
|
| | | | | | | | | | | | | | | |
| Summary of Significant Items Affecting 2017 Financial Results |
| | Three Months Ended | | Nine Months Ended |
| | September 30, 2017 | | September 30, 2017 |
| | (In millions, except per diluted share amounts) |
| | Amount | | Per Diluted Share (1) | | Amount | | Per Diluted Share (1) |
| Restructuring and separation costs | $ | 118 |
| | $ | 1.39 |
| | $ | 161 |
| | $ | 1.92 |
|
| Impairment losses | 129 |
| | 1.77 |
| | 201 |
| | 2.77 |
|
| Change in Marketplace premium deficiency reserve for 2017 service dates | (30 | ) | | (0.33 | ) | | 40 |
| | 0.45 |
|
| Termination fee received for terminated Medicare acquisition | — |
| | — |
| | (75 | ) | | (0.84 | ) |
| | $ | 217 |
| | $ | 2.83 |
| | $ | 327 |
| | $ | 4.30 |
|
__________________________________________
| |
| (1) | Except for certain items that are not deductible for tax purposes, per diluted share amounts are generally calculated at our statutory income tax raterates of 22% and 37%, which is in excess for the first quarters of the effective tax rate recorded in our consolidated statements of operations. 2018 and 2017, respectively. |
Marketplace Cost Share Reduction (CSR) Update
Our third quarter results do not include any potential impact from the October 12, 2017, direction to Centers for Medicare and Medicaid Services (CMS) from Acting Department of Health and Human Services Secretary Hargan to cease payment of Marketplace CSR subsidies. At September 30, 2017, we had a total of approximately $220 million in excess CSR subsidies, recorded as a payable to CMS. This payable represents the extent to which payments received by us from CMS exceeded our estimate of the actual cost of member subsidies incurred by us through September 30, 2017.
We expect to incur approximately $85 million in unreimbursed expense associated with the cessation of CSR subsidies in the fourth quarter of 2017. It has been the practice of CMS to perform a reconciliation on an annual
basis of CSR subsidies paid to all health plans against the actual costs incurred by the health plans. Were such a reconciliation to be performed for the full calendar year of 2017—consistent with past practice—we would be able to offset nearly all of the $85 million expense incurred in the fourth quarter against the excess amounts received prior to September 30, 2017. However, should CMS transition to a nine month reconciliation period ending September 30, 2017—the last month for which CSR subsidies have been paid—the absence of CSR subsidy reimbursement would reduce income before income tax expense by approximately $85 million in the fourth quarter of 2017.
Nine Months ended September 30, 2017 Compared with Nine Months Ended September 30, 2016
Net loss per diluted share was $4.44 in the nine months ended September 30, 2017 compared with net income per diluted share of $1.77 reported for the nine months ended September 30, 2016. Adjusted net loss per diluted share* was $4.17 in the nine months ended September 30, 2017, compared with adjusted net income per diluted share* of $2.03 in the nine months ended September 30, 2016. Loss before income tax benefit for the nine months ended September 30, 2017 was $296 million. Results for the nine months ended September 30, 2017, were affected by the significant items presented in the table, and as further described, above. In total, these adjustments increased pretax loss in the nine months ended September 30, 2017 by $327 million.
RESTRUCTURING AND PROFIT IMPROVEMENT PLAN UPDATE
As previously disclosed, we estimate that our restructuring plan will reduce annualized run-rate expenses by approximately $300 million to $400 million when completed by the end of 2018. We have already achieved $200 million of these run-rate reductions on an annualized basis, which will take full effect no later than January 1, 2018. Our third quarter results include approximately $10 million of these reductions. All savings targets discussed in regards to the restructuring plan represent annualized run-rate savings that we expect to achieve during the year following the indicated implementation date. We expect one-time costs associated with the restructuring plan to exceed the benefits realized in 2017 due to the upfront payment of implementation costs and the delayed benefit of full savings until the beginning of 2018.
TRENDS AND UNCERTAINTIES
ACA and the Marketplace
The future of the Affordable Care Act (ACA) and its underlying programs, including the Marketplace, are subject to substantial uncertainty. We have taken the following steps in regards to our participation in the ACA Marketplace in 2018:
| |
1. | As previously announced, we will exit the Utah and Wisconsin ACA Marketplaces effective December 31, 2017. |
| |
2. | In our remaining Marketplace plans, we are increasing 2018 premiums by 55% to take into account the absence of cost sharing reduction (CSR) subsidies and other risks related to ACA Marketplace uncertainties. |
| |
3. | We have reduced the scope of our 2018 participation in the state of Washington Marketplace. |
| |
4. | We continue to monitor the current political and programmatic developments pertaining to the ACA Marketplace.
|
Medicaid Contract Re-ProcurementMEDICAID CONTRACT RE-PROCUREMENT
The following table illustrates Health Plans segment Medicaid contracts scheduled for re-procurement in the near term. While we have been notified of the Medicaid regulators’ intention to re-procure the contracts, the anticipated award dates and effective dates are management’s current best estimates; such dates are subject to change. Premium revenue is stated in millions.
| | | | | | | Premium Revenue | | | | | Premium Revenue | |
| | | Membership as of | | Nine Months Ended | | Anticipated | | Membership as of | | Three Months Ended | | Anticipated |
| State Health Plan | | Medicaid Program(s) | | September 30, 2017 | | September 30, 2017 | | Award Date | | Effective Date | | Medicaid Program(s) | | March 31, 2018 | | March 31, 2018 | | Award Date | | Effective Date |
| Florida | | All | | 355,000 |
| | $ | 1,105 |
| | Q2 2018 | | 1/1/2019 | |
| New Mexico | | All | | 225,000 |
| | 893 |
| | Q1 2018 | | 1/1/2019 | |
| Puerto Rico | | | All | | 316,000 |
| | $ | 186 |
| | Q2 2018 | | 10/1/2018 |
| Texas | | ABD | | 87,000 |
| | 1,065 |
| | Q3 2018 | | 9/1/2019 | | ABD, MMP | | 99,000 |
| | 479 |
| | Q3 2018 | | 1/1/2020 |
| Texas | | CHIP | | 24,000 |
| | 31 |
| | Q4 2017 | | 9/1/2018 | | TANF, CHIP | | 129,000 |
| | 77 |
| | Q1 2019 | | 1/1/2020 |
Washington (1) | | | All in 7 of 9 regions | | 606,000 |
| | 444 |
| | Q2 2018 | | 1/1/2019 |
__________________
| |
| (1) | The re-procurement information presented for the Washington health plan includes all Medicaid membership in the following regions: Northeast, Northwest, Central and Southeast, Pierce County, King County, Olympic Peninsula, and West-Central. Five of the seven largest regions’ contracts that are awarded will be effective January 1, 2019. The remaining two will be effective on January 1, 2020. |
Illinois Health Plan.Florida and New Mexico RFP Update. In Augustour Form 10-K Annual Report for 2017, Molina Healthcarewe reported that we were selected by Florida’s Medicaid agency to negotiate for a tentative award of Illinois, Inc. wasa 2019 Medicaid contract in Region 11 of the state. We were selected for no other regions besides Region 11. On April 24, 2018, the state notified us that we were not awarded a statewide Medicaid managed care contract for Region 11. While we protest the Florida RFP awards, we continue to evaluate our options for 2019 participation in the Florida Marketplace, which business has shown signs of improvement. Also in our Form 10-K for 2017, we reported that we were notified by the Illinois DepartmentNew Mexico Medicaid agency that we had not been selected for a tentative award of Healthcarea 2019 Medicaid contract. We are pursuing a protest of the New Mexico RFP awards. Without a reversal of the RFP awards, our New Mexico health plan will be in run-off. Subject to future developments, we will continue to evaluate our business profile in New Mexico for 2019.
PRESSURES ON MEDICAID FUNDING
Currently, there are a number of different legislative proposals being considered, some of which would involve significantly reduced federal spending on the Medicaid program, and Family Services. Thisconstitute a fundamental change in the federal role in health care. These proposals include elements such as the following:
Ending the entitlement nature of Medicaid contract further integrates behavioralby capping future increases in federal health spending for these programs, and physicalshifting more of the risk for health by combiningcosts in the State’s three current managed carefuture to states and consumers;
Reversing the ACA’s expansion of Medicaid that enables states to cover low-income childless adults;
Changing Medicaid to a state block grant program, including potentially capping spending on a per-enrollee basis (a “per capita cap”);
Requiring Medicaid beneficiaries to work;
Limiting the amount of lifetime benefits for Medicaid beneficiaries; and
Numerous other potential changes and reforms.
ACA AND THE MARKETPLACE
The future of the Affordable Care Act (ACA) and its underlying programs, into one program. The contract beginsincluding the Marketplace, are subject to substantial uncertainty. Effective January 1, 2018, for four years with options to renew annually for up to four additional years. we have:
Exited the Utah and Wisconsin Marketplaces;
Reduced the scope of our Washington Health Plan. In May 2017, Molina Healthcare of Washington, Inc. was selected by the Washington State Health Care Authority to negotiate and enter into managed care contracts for the North Central region of the state’s Apple Health Integrated Managed Care Program. The start date for the new contract is scheduled for January 1, 2018.state participation;
Increased premiums averaging 58%
Mitigated our exposure to uncertainties relating to cost share reduction (CSR) funding and reconciliation; and
Adjusted broker commissions to market rates.
REPORTABLE SEGMENTS
How We Assess PerformanceHOW WE ASSESS PERFORMANCE
We derive our revenues primarily from health insurance premiums, and our primary customers are state Medicaid agencies and the federal government.
One of the key metrics used to assess the performance of our most significant segment, the Health Plans segment, is the medical care ratio, or MCR.(“MCR”). The medical care ratio represents medical care costs as a percentage of premium revenue. Therefore, the underlying gross margin, or the amount earned by the Health Plans segment after medical costs are deducted from premium revenue, is the most important measure of earnings reviewed by management.
Gross margin for our Health Plans segment is referred to as “Medical margin,” and for our Molina Medicaid Solutions and Other segments, as “Service margin.” The service margin is equal to service revenue minus cost of service revenue. Management’s discussion and analysis of the changes in the individual components of grossmedical margin by reportable segment, is presented in the “Health Plans—Financial Overview,” “Molina Medicaid Solutions—Financial Overview,” and “Other—Financial Overview” sections of this MD&A.
service margin follows.
SEGMENT SUMMARY
|
| | | | | | | | | | | | | | | |
| | Three Months Ended September 30, | | Nine Months Ended September 30, |
| | 2017 | | 2016 | | 2017 | | 2016 |
| | (In millions) |
| Segment gross margin: | | | | | | | |
Health Plans medical margin (1) | $ | 557 |
| | $ | 443 |
| | $ | 1,343 |
| | $ | 1,285 |
|
Molina Medicaid Solutions service margin (2) | 5 |
| | 6 |
| | 13 |
| | 17 |
|
Other (2) | 2 |
| | 8 |
| | 8 |
| | 29 |
|
| Total segment gross margin | 564 |
| | 457 |
| | 1,364 |
| | 1,331 |
|
Other operating revenues (3) | 124 |
| | 222 |
| | 379 |
| | 625 |
|
Other operating expenses (4) | (769 | ) | | (561 | ) | | (2,029 | ) | | (1,644 | ) |
| Operating (loss) income | (81 | ) | | 118 |
| | (286 | ) | | 312 |
|
| Other expenses, net | 32 |
| | 26 |
| | 10 |
| | 76 |
|
| (Loss) income before income tax expense | (113 | ) | | 92 |
| | (296 | ) | | 236 |
|
| Income tax (benefit) expense | (16 | ) | | 50 |
| | (46 | ) | | 137 |
|
| Net (loss) income | $ | (97 | ) | | $ | 42 |
| | $ | (250 | ) | | 99 |
|
| | | | | | | |
| | Three Months Ended March 31, |
| | 2018 | | 2017 |
| | (In millions) |
Health Plans segment medical margin (1) | $ | 601 |
| | $ | 537 |
|
Molina Medicaid Solutions segment service margin (2) | 8 |
| | 4 |
|
Other segment service margin (2) | 6 |
| | 5 |
|
| | $ | 615 |
| | $ | 546 |
|
| | | | |
| Health Plans segment medical care ratio | 86.1 | % | | 88.4 | % |
_______________________
| |
| (1) | Represents premium revenue minus medical care costs. |
| |
| (2) | Represents service revenue minus cost of service revenue. |
| |
(3) | Other operating revenues include premium tax revenue, health insurer fee revenue, investment income and other revenue. |
| |
(4) | Other operating expenses include general and administrative expenses, premium tax expenses, health insurer fee expenses, depreciation and amortization, impairment losses, and restructuring and separation costs. |
HEALTH PLANS
The Health Plans segment consists of health plans operating in 1213 states and the Commonwealth of Puerto Rico. As of September 30, 2017,March 31, 2018, these health plans served approximately 4.54.1 million members eligible for Medicaid, Medicare, and other government-sponsored health care programs for low-income families and individuals. This membership includes Affordable Care Act Marketplace (Marketplace) members, most of whom receive government premium subsidies.
BUSINESS OVERVIEW
Recent Developments — Health Plans Segment
Refer to Notes to Consolidated Financial Statements, Note 1, “Basis of Presentation.”
Health Plans Membership
The following tables set forth our Health Plans membership as of the dates indicated: | | | | September 30,
2017 | | December 31,
2016 | | September 30,
2016 | March 31,
2018 | | December 31,
2017 | | March 31,
2017 |
| Ending Membership by Program: | | | | | | | | | | |
| Temporary Assistance for Needy Families (TANF) and Children’s Health Insurance Program (CHIP) | 2,451,000 |
| | 2,536,000 |
| | 2,529,000 |
| 2,435,000 |
| | 2,457,000 |
| | 2,548,000 |
|
| Marketplace | 877,000 |
| | 526,000 |
| | 568,000 |
| |
| Medicaid Expansion | 662,000 |
| | 673,000 |
| | 658,000 |
| 662,000 |
| | 668,000 |
| | 684,000 |
|
| Aged, Blind or Disabled (ABD) | 411,000 |
| | 396,000 |
| | 395,000 |
| 411,000 |
| | 412,000 |
| | 401,000 |
|
| Total Medicaid | | 3,508,000 |
| | 3,537,000 |
| | 3,633,000 |
|
Medicare-Medicaid Plan (MMP) – Integrated (1) | 58,000 |
| | 51,000 |
| | 51,000 |
| 56,000 |
| | 57,000 |
| | 55,000 |
|
| Medicare Special Needs Plans (Medicare) | 44,000 |
| | 45,000 |
| | 45,000 |
| 44,000 |
| | 44,000 |
| | 43,000 |
|
| Total Medicare | | 100,000 |
| | 101,000 |
| | 98,000 |
|
| Non-Marketplace | | 3,608,000 |
| | 3,638,000 |
| | 3,731,000 |
|
| Marketplace | | 453,000 |
| | 815,000 |
| | 1,035,000 |
|
| | | 4,061,000 |
| | 4,453,000 |
| | 4,766,000 |
|
| | 4,503,000 |
| | 4,227,000 |
| | 4,246,000 |
| | | | | |
| Ending Membership by Health Plan: | | | | | | | | | | |
| California | 751,000 |
| | 683,000 |
| | 683,000 |
| 656,000 |
| | 746,000 |
| | 765,000 |
|
| Florida | 641,000 |
| | 553,000 |
| | 563,000 |
| 414,000 |
| | 625,000 |
| | 711,000 |
|
Idaho (2) | | 2,000 |
| | — |
| | — |
|
| Illinois | 163,000 |
| | 195,000 |
| | 195,000 |
| 151,000 |
| | 165,000 |
| | 194,000 |
|
| Michigan | 399,000 |
| | 391,000 |
| | 387,000 |
| 388,000 |
| | 398,000 |
| | 417,000 |
|
| New Mexico | 256,000 |
| | 254,000 |
| | 253,000 |
| 250,000 |
| | 253,000 |
| | 270,000 |
|
| New York | 33,000 |
| | 35,000 |
| | 37,000 |
| 32,000 |
| | 32,000 |
| | 34,000 |
|
| Ohio | 343,000 |
| | 332,000 |
| | 339,000 |
| 328,000 |
| | 327,000 |
| | 351,000 |
|
| Puerto Rico | 306,000 |
| | 330,000 |
| | 331,000 |
| 316,000 |
| | 314,000 |
| | 326,000 |
|
| South Carolina | 113,000 |
| | 109,000 |
| | 109,000 |
| 117,000 |
| | 116,000 |
| | 111,000 |
|
| Texas | 444,000 |
| | 337,000 |
| | 352,000 |
| 476,000 |
| | 430,000 |
| | 493,000 |
|
| Utah | 160,000 |
| | 146,000 |
| | 150,000 |
| 90,000 |
| | 152,000 |
| | 172,000 |
|
| Washington | 770,000 |
| | 736,000 |
| | 716,000 |
| 779,000 |
| | 777,000 |
| | 785,000 |
|
| Wisconsin | 124,000 |
| | 126,000 |
| | 131,000 |
| 62,000 |
| | 118,000 |
| | 137,000 |
|
| | 4,503,000 |
| | 4,227,000 |
| | 4,246,000 |
| 4,061,000 |
| | 4,453,000 |
| | 4,766,000 |
|
_________________________ | |
| (1) | MMP members receive both Medicaid and Medicare coverage from Molina Healthcare. |
| |
| (2) | Idaho operations commenced January 1, 2018. |
Premiums by Program
The amount of the premiums paid to our health plans may vary substantially between states and among various government programs. The following table sets forth the ranges of premiums paid to our state health plans by program on a per member per month (PMPM) basis, for the ninethree months ended September 30, 2017.March 31, 2018. The “Consolidated” column represents the weighted-average amounts for our total membership by program.
| | | | PMPM Premiums | PMPM Premiums |
| | Low | | High | | Consolidated | Low | | High | | Consolidated |
| TANF and CHIP | $ | 120.00 |
| | $ | 310.00 |
| | $ | 180.00 |
| $ | 130.00 |
| | $ | 330.00 |
| | $ | 190.00 |
|
| Marketplace | 190.00 |
| | 470.00 |
| | 280.00 |
| |
| Medicaid Expansion | 320.00 |
| | 510.00 |
| | 390.00 |
| 330.00 |
| | 500.00 |
| | 370.00 |
|
| ABD | 380.00 |
| | 1,480.00 |
| | 1,030.00 |
| 440.00 |
| | 1,530.00 |
| | 1,010.00 |
|
| MMP – Integrated | 1,250.00 |
| | 3,280.00 |
| | 2,190.00 |
| 1,320.00 |
| | 3,200.00 |
| | 2,140.00 |
|
| Medicare | 960.00 |
| | 1,260.00 |
| | 1,140.00 |
| 600.00 |
| | 1,380.00 |
| | 1,190.00 |
|
| Marketplace | | 220.00 |
| | 530.00 |
| | 310.00 |
|
FINANCIAL OVERVIEW
In the thirdfirst quarter of 2017,2018, premium revenue increaseddecreased approximately 14%7%, or $586$325 million, when compared with the thirdfirst quarter of 2016.2017. Member months grew 8% whiledeclined 13%, partially offset by a revenue PMPM increasedincrease of 6%. Medical margin increased 12% in the first quarter of 2018 compared with the first quarter of 2017.
Medical care costs as a percent of premium revenue decreased to 88.3%86.1% in the thirdfirst quarter of 20172018 from 89.4%88.4% in the thirdfirst quarter of 2016. Medical margin increased 26%2017. This improvement reflects improved performance and favorable medical cost trends that were partially offset by a lower mix of Marketplace revenue. On balance, inpatient and physician utilization as well as unit costs improved in the third quarter, while pharmacy costs ran higher than expected. This netted to an overall favorable medical cost trend despite the higher pharmacy costs and approximately $18 million of 2017above normal influenza-related expenses.
We have also started to see some of the early benefits from the third quarter of 2016.
In the nine months ended September 30, 2017, premium revenue increased approximately 16%,contracting efforts that we undertook last year in Florida, South Carolina and Texas, where we eliminated or $1,950 million, when compared with the nine months ended September 30, 2016. Member months grew 11% while revenue PMPM increased 5%. Medical care costs as a percent of premium revenue increased to 90.5% in the nine months ended September 30, 2017 from 89.5% in the nine months ended September 30, 2016. Medical margin increased 5% in the nine months ended September 30, 2017 from the nine months ended September 30, 2016.renegotiated high cost provider contracts for in-patient, and ancillary services.
FINANCIAL PERFORMANCE BY PROGRAM
The following tables summarize member months, premium revenue, medical care costs, medical care ratio and medical margin by program for the periods indicated (PMPM amounts are in whole dollars; member months and other dollar amounts are in millions):
| | | | Three Months Ended September 30, 2017 | Three Months Ended March 31, 2018 |
| | Member Months (1) | | Premium Revenue | | Medical Care Costs | | MCR (2) | | Medical Margin | Member Months (1) | | Premium Revenue | | Medical Care Costs | | MCR (2) | | Medical Margin |
| | | Total | | PMPM | | Total | | PMPM | | | Total | | PMPM | | Total | | PMPM | |
| TANF and CHIP | 7.5 |
| | $ | 1,392 |
| | $ | 185.95 |
| | $ | 1,242 |
| | $ | 165.76 |
| | 89.1 | % | | $ | 150 |
| 7.4 |
| | $ | 1,373 |
| | $ | 185.14 |
| | $ | 1,272 |
| | $ | 171.56 |
| | 92.7 | % | | $ | 101 |
|
| Medicaid Expansion | 2.0 |
| | 773 |
| | 385.58 |
| | 667 |
| | 332.99 |
| | 86.4 |
| | 106 |
| 2.0 |
| | 752 |
| | 372.75 |
| | 641 |
| | 317.46 |
| | 85.2 |
| | 111 |
|
| ABD | 1.2 |
| | 1,288 |
| | 1,038.85 |
| | 1,259 |
| | 1,016.06 |
| | 97.8 |
| | 29 |
| 1.2 |
| | 1,254 |
| | 1,014.23 |
| | 1,155 |
| | 934.55 |
| | 92.1 |
| | 99 |
|
| Total Medicaid | 10.7 |
| | 3,453 |
| | 321.77 |
| | 3,168 |
| | 295.23 |
| | 91.8 |
| | 285 |
| 10.6 |
| | 3,379 |
| | 316.69 |
| | 3,068 |
| | 287.56 |
| | 90.8 |
| | 311 |
|
| MMP | 0.2 |
| | 378 |
| | 2,263.07 |
| | 336 |
| | 2,013.67 |
| | 89.0 |
| | 42 |
| 0.2 |
| | 357 |
| | 2,137.88 |
| | 305 |
| | 1,824.21 |
| | 85.3 |
| | 52 |
|
| Medicare | 0.1 |
| | 163 |
| | 1,231.61 |
| | 126 |
| | 951.01 |
| | 77.2 |
| | 37 |
| 0.1 |
| | 157 |
| | 1,188.97 |
| | 131 |
| | 994.81 |
| | 83.7 |
| | 26 |
|
| Total Medicare | 0.3 |
| | 541 |
| | 1,806.26 |
| | 462 |
| | 1,543.05 |
| | 85.4 |
| | 79 |
| 0.3 |
| | 514 |
| | 1,718.61 |
| | 436 |
| | 1,457.75 |
| | 84.8 |
| | 78 |
|
| Excluding Marketplace | 11.0 |
| | 3,994 |
| | 362.04 |
| | 3,630 |
| | 329.08 |
| | 90.9 |
| | 364 |
| |
| Non-Marketplace | | 10.9 |
| | 3,893 |
| | 354.94 |
| | 3,504 |
| | 319.48 |
| | 90.0 |
| | 389 |
|
| Marketplace | 2.7 |
| | 783 |
| | 301.72 |
| | 590 |
| | 227.22 |
| | 75.3 |
| | 193 |
| 1.4 |
| | 430 |
| | 312.87 |
| | 218 |
| | 158.40 |
| | 50.6 |
| | 212 |
|
| | 13.7 |
| | $ | 4,777 |
| | $ | 350.55 |
| | $ | 4,220 |
| | $ | 309.68 |
| | 88.3 | % | | $ | 557 |
| 12.3 |
| | $ | 4,323 |
| | $ | 350.25 |
| | $ | 3,722 |
| | $ | 301.55 |
| | 86.1 | % | | $ | 601 |
|
|
| | | | | | | | | | | | | | | | | | | | | | | | | |
| | Three Months Ended September 30, 2016 |
| | Member Months (1) | | Premium Revenue | | Medical Care Costs | | MCR (2) | | Medical Margin |
| | | Total | | PMPM | | Total | | PMPM | | |
| TANF and CHIP | 7.6 |
| | $ | 1,373 |
| | $ | 180.74 |
| | $ | 1,246 |
| | $ | 164.04 |
| | 90.8 | % | | $ | 127 |
|
| Medicaid Expansion | 2.0 |
| | 763 |
| | 386.98 |
| | 642 |
| | 325.68 |
| | 84.2 |
| | 121 |
|
| ABD | 1.1 |
| | 1,186 |
| | 1,008.28 |
| | 1,094 |
| | 929.93 |
| | 92.2 |
| | 92 |
|
| Total Medicaid | 10.7 |
| | 3,322 |
| | 309.19 |
| | 2,982 |
| | 277.55 |
| | 89.8 |
| | 340 |
|
| MMP | 0.2 |
| | 334 |
| | 2,165.26 |
| | 280 |
| | 1,818.75 |
| | 84.0 |
| | 54 |
|
| Medicare | 0.1 |
| | 136 |
| | 1,019.19 |
| | 134 |
| | 1,003.85 |
| | 98.5 |
| | 2 |
|
| Total Medicare | 0.3 |
| | 470 |
| | 1,633.62 |
| | 414 |
| | 1,440.73 |
| | 88.2 |
| | 56 |
|
| Excluding Marketplace | 11.0 |
| | 3,792 |
| | 343.68 |
| | 3,396 |
| | 307.84 |
| | 89.6 |
| | 396 |
|
| Marketplace | 1.7 |
| | 399 |
| | 238.86 |
| | 352 |
| | 210.38 |
| | 88.1 |
| | 47 |
|
| | 12.7 |
| | $ | 4,191 |
| | $ | 329.88 |
| | $ | 3,748 |
| | $ | 295.01 |
| | 89.4 | % | | $ | 443 |
|
|
| | | | | | | | | | | | | | | | | | | | | | | | | |
| | Nine Months Ended September 30, 2017 |
| | Member Months (1) | | Premium Revenue | | Medical Care Costs | | MCR (2) | | Medical Margin |
| | | Total | | PMPM | | Total | | PMPM | | |
| TANF and CHIP | 22.8 |
| | $ | 4,185 |
| | $ | 183.69 |
| | $ | 3,861 |
| | $ | 169.44 |
| | 92.2 | % | | $ | 324 |
|
| Medicaid Expansion | 6.1 |
| | 2,376 |
| | 389.14 |
| | 2,045 |
| | 334.93 |
| | 86.1 |
| | 331 |
|
| ABD | 3.6 |
| | 3,769 |
| | 1,033.45 |
| | 3,634 |
| | 996.58 |
| | 96.4 |
| | 135 |
|
| Total Medicaid | 32.5 |
| | 10,330 |
| | 317.49 |
| | 9,540 |
| | 293.21 |
| | 92.4 |
| | 790 |
|
| MMP | 0.5 |
| | 1,083 |
| | 2,189.96 |
| | 976 |
| | 1,974.22 |
| | 90.1 |
| | 107 |
|
| Medicare | 0.4 |
| | 449 |
| | 1,142.68 |
| | 369 |
| | 939.21 |
| | 82.2 |
| | 80 |
|
| Total Medicare | 0.9 |
| | 1,532 |
| | 1,726.39 |
| | 1,345 |
| | 1,516.09 |
| | 87.8 |
| | 187 |
|
| Excluding Marketplace | 33.4 |
| | 11,862 |
| | 354.88 |
| | 10,885 |
| | 325.66 |
| | 91.8 |
| | 977 |
|
| Marketplace | 8.4 |
| | 2,303 |
| | 276.27 |
| | 1,937 |
| | 232.31 |
| | 84.1 |
| | 366 |
|
| | 41.8 |
| | $ | 14,165 |
| | $ | 339.19 |
| | $ | 12,822 |
| | $ | 307.03 |
| | 90.5 | % | | $ | 1,343 |
|
| | | | Nine Months Ended September 30, 2016 | Three Months Ended March 31, 2017 |
| | Member Months (1) | | Premium Revenue | | Medical Care Costs | | MCR (2) | | Medical Margin | Member Months (1) | | Premium Revenue | | Medical Care Costs | | MCR (2) | | Medical Margin |
| | | Total | | PMPM | | Total | | PMPM | | | Total | | PMPM | | Total | | PMPM | |
| TANF and CHIP | 22.5 |
| | $ | 3,999 |
| | $ | 177.60 |
| | $ | 3,646 |
| | $ | 161.93 |
| | 91.2 | % | | $ | 353 |
| 7.7 |
| | $ | 1,402 |
| | $ | 182.69 |
| | $ | 1,304 |
| | $ | 170.02 |
| | 93.1 | % | | $ | 98 |
|
| Medicaid Expansion | 5.8 |
| | 2,184 |
| | 376.98 |
| | 1,850 |
| | 319.38 |
| | 84.7 |
| | 334 |
| 2.0 |
| | 817 |
| | 398.70 |
| | 689 |
| | 336.51 |
| | 84.4 |
| | 128 |
|
| ABD | 3.5 |
| | 3,466 |
| | 987.20 |
| | 3,173 |
| | 903.85 |
| | 91.6 |
| | 293 |
| 1.2 |
| | 1,196 |
| | 1,006.84 |
| | 1,130 |
| | 951.32 |
| | 94.5 |
| | 66 |
|
| Total Medicaid | 31.8 |
| | 9,649 |
| | 303.23 |
| | 8,669 |
| | 272.46 |
| | 89.9 |
| | 980 |
| 10.9 |
| | 3,415 |
| | 312.98 |
| | 3,123 |
| | 286.35 |
| | 91.5 |
| | 292 |
|
| MMP | 0.5 |
| | 989 |
| | 2,160.14 |
| | 867 |
| | 1,894.38 |
| | 87.7 |
| | 122 |
| 0.2 |
| | 344 |
| | 2,088.96 |
| | 307 |
| | 1,859.41 |
| | 89.0 |
| | 37 |
|
| Medicare | 0.4 |
| | 396 |
| | 1,015.14 |
| | 385 |
| | 986.40 |
| | 97.2 |
| | 11 |
| 0.1 |
| | 138 |
| | 1,068.20 |
| | 117 |
| | 902.67 |
| | 84.5 |
| | 21 |
|
| Total Medicare | 0.9 |
| | 1,385 |
| | 1,633.26 |
| | 1,252 |
| | 1,476.57 |
| | 90.4 |
| | 133 |
| 0.3 |
| | 482 |
| | 1,640.63 |
| | 424 |
| | 1,439.20 |
| | 87.7 |
| | 58 |
|
| Excluding Marketplace | 32.7 |
| | 11,034 |
| | 337.76 |
| | 9,921 |
| | 303.72 |
| | 89.9 |
| | 1,113 |
| |
| Non-Marketplace | | 11.2 |
| | 3,897 |
| | 347.84 |
| | 3,547 |
| | 316.62 |
| | 91.0 |
| | 350 |
|
| Marketplace | 5.1 |
| | 1,181 |
| | 231.69 |
| | 1,009 |
| | 197.77 |
| | 85.4 |
| | 172 |
| 2.9 |
| | 751 |
| | 262.16 |
| | 564 |
| | 196.72 |
| | 75.0 |
| | 187 |
|
| | 37.8 |
| | $ | 12,215 |
| | $ | 323.44 |
| | $ | 10,930 |
| | $ | 289.41 |
| | 89.5 | % | | $ | 1,285 |
| 14.1 |
| | $ | 4,648 |
| | $ | 330.39 |
| | $ | 4,111 |
| | $ | 292.20 |
| | 88.4 | % | | $ | 537 |
|
_______________________
| |
| (1) | A member month is defined as the aggregate of each month’s ending membership for the period presented. |
| |
| (2) | “MCR” represents medical costs as a percentage of premium revenue. |
Medicaid: TANF/CHIP, Medicaid Expansion
TANF and ABD
CHIP. The medical care ratios of the combined TANF/ratio for TANF and CHIP Medicaid Expansion and ABD programs increased to 91.8%was 92.7% in the thirdfirst quarter of 2017,2018, a slight improvement from 89.8%93.1% in the thirdfirst quarter of 2016. Margin pressures at2017. However, the California health plan (primarilycurrent quarter results modestly underperformed our expectations due to reduced high acuity inpatient cases in Washington, and higher behavioral health costs in New Mexico.
Medicaid Expansion premium rates effective July 1, 2017), the Florida health plan; and the Illinois health plan more than offset improved performance at the Washington health plan.
Expansion.The medical care ratios of the combined TANF/CHIP,ratio for Medicaid Expansion and ABD programs increased to 92.4%was 85.2% in the nine months ended September 30, 2017, from 89.9%first quarter of 2018, compared with 84.4% in the nine months ended September 30, 2016. Forfirst quarter of 2017. This increase was primarily due to the nine months ended September 30, 2017, margin pressures at the Florida, Illinois, New Mexicopremium reduction we received in California last July. Medicaid Expansion has performed well because rate adequacy has trended favorably, and Texasmembership is concentrated in our higher performing health plans, more than offset improved performance atparticularly, California, Michigan and Ohio.
ABD. The medical care ratio for ABD was 92.1% in the Washington health plan. Financial results forfirst quarter of 2018, compared with 94.5% in the Texas health plan in 2016 benefited from the recognitionfirst quarter of $44 million of quality revenue related2017. The year over year improvement can be attributed to 2015our continued advancement on key, high acuity management fundamentals.
Medicare and 2014.
MMP and Medicare
The medical care ratio for thesethe combined Medicare programs decreased to 84.8% in the aggregate, decreasedfirst quarter of 2018, from 87.7% in the thirdfirst quarter of 2017. Much of this improvement relates to the recognition of additional MMP at‑risk revenue for dates of service in 2016 and 2017, when compared withbecause at‑risk revenue is often recognized long after medical services have been provided. The Medicare business also benefited from favorable medical care trends and improved medical management of inpatient utilization for this population. Our Michigan health plan, which serves about 25% of our Medicare membership, has shown particular improvement in the thirdfirst quarter of 2016,2018. Accurate and also incomplete risk score documentation and effective management of chronic and high acuity conditions are critical to the nine months ended September 30, 2017, compared with the nine months ended September 30, 2016. Utilizationsuccessful management of inpatient and pharmacy services among our Medicare members has been subduedthis program for the first nine monthsrest of 2017.the year.
Marketplace
Lower Marketplace member monthspremium revenue was driven by a decrease in membership of over 50%, partially offset by premium rate increases. As previously disclosed, we have increased 64% in the nine months ended September 30, 2017, when compared with the nine months ended September 30, 2016,premium rates and reduced our Marketplace presence effective January 1, 2018, as a resultpart of membership growth primarily in California, Florida and Texas.
our overall program to improve profitability.
The medical care ratio for the Marketplace program decreased to 75.3%50.6% in the thirdfirst quarter of 2017,2018, from 88.1%75.0% in the thirdfirst quarter of 2016.2017. The lower medical care ratio in 2018 was the result of the premium increases implemented effective January 2018 and the 2017 Marketplace CSR adjustment described in “Consolidated Results” above. Absent a $30 million reduction to a previously established premium deficiency reserve,the 2017 Marketplace CSR adjustment, the medical care ratio for our Marketplace program would have been approximately 79%67% in the thirdfirst quarter of 2017. The medical care ratio of the Marketplace program for the nine months ended September 30, 2017 was 84.1%, and generally consistent with the medical care ratio reported for the same period in 2016.2018.
FINANCIAL PERFORMANCE BY STATE
The following tables summarize member months, premium revenue, medical care costs, medical care ratio, and medical margin by state health plan for the periods indicated (PMPM amounts are in whole dollars; member months and other dollar amounts are in millions):
Health Plans Segment Financial Data — Non-Marketplace
| | | | Three Months Ended September 30, 2017 | Three Months Ended March 31, 2018 |
| | Member
Months | | Premium Revenue | | Medical Care Costs | | MCR | | Medical Margin | Member
Months | | Premium Revenue | | Medical Care Costs | | MCR | | Medical Margin |
| | | Total | | PMPM | | Total | | PMPM | | | Total | | PMPM | | Total | | PMPM | |
| California | 1.9 |
| | $ | 601 |
| | $ | 322.97 |
| | $ | 563 |
| | $ | 302.67 |
| | 93.7 | % | | $ | 38 |
| 1.8 |
| | $ | 494 |
| | $ | 272.61 |
| | $ | 412 |
| | $ | 227.31 |
| | 83.4 | % | | $ | 82 |
|
| Florida | 1.0 |
| | 388 |
| | 355.59 |
| | 390 |
| | 356.83 |
| | 100.3 |
| | (2 | ) | 1.0 |
| | 382 |
| | 351.58 |
| | 345 |
| | 317.41 |
| | 90.3 |
| | 37 |
|
Idaho (1) | | — |
| | 4 |
| | 960.33 |
| | 4 |
| | 977.00 |
| | 101.8 |
| | — |
|
| Illinois | 0.5 |
| | 137 |
| | 287.69 |
| | 138 |
| | 289.36 |
| | 100.6 |
| | (1 | ) | 0.5 |
| | 141 |
| | 298.17 |
| | 122 |
| | 257.50 |
| | 86.4 |
| | 19 |
|
| Michigan | 1.2 |
| | 390 |
| | 337.17 |
| | 345 |
| | 298.83 |
| | 88.6 |
| | 45 |
| 1.1 |
| | 376 |
| | 336.64 |
| | 331 |
| | 296.19 |
| | 88.0 |
| | 45 |
|
| New Mexico | 0.7 |
| | 304 |
| | 429.07 |
| | 277 |
| | 390.91 |
| | 91.1 |
| | 27 |
| 0.7 |
| | 319 |
| | 466.17 |
| | 310 |
| | 453.30 |
| | 97.2 |
| | 9 |
|
| New York (3) | 0.1 |
| | 43 |
| | 435.00 |
| | 41 |
| | 413.02 |
| | 94.9 |
| | 2 |
| |
| New York | | 0.1 |
| | 46 |
| | 468.91 |
| | 39 |
| | 396.76 |
| | 84.6 |
| | 7 |
|
| Ohio | 0.9 |
| | 549 |
| | 560.06 |
| | 483 |
| | 492.61 |
| | 88.0 |
| | 66 |
| 0.9 |
| | 551 |
| | 576.60 |
| | 460 |
| | 481.26 |
| | 83.5 |
| | 91 |
|
| Puerto Rico | 1.0 |
| | 191 |
| | 202.59 |
| | 159 |
| | 168.25 |
| | 83.1 |
| | 32 |
| 1.0 |
| | 186 |
| | 193.13 |
| | 174 |
| | 181.39 |
| | 93.9 |
| | 12 |
|
| South Carolina | 0.3 |
| | 113 |
| | 332.48 |
| | 101 |
| | 297.74 |
| | 89.6 |
| | 12 |
| 0.3 |
| | 122 |
| | 348.08 |
| | 104 |
| | 297.52 |
| | 85.5 |
| | 18 |
|
| Texas | 0.7 |
| | 541 |
| | 778.50 |
| | 506 |
| | 728.19 |
| | 93.5 |
| | 35 |
| 0.7 |
| | 562 |
| | 809.90 |
| | 519 |
| | 747.53 |
| | 92.3 |
| | 43 |
|
| Utah | 0.2 |
| | 89 |
| | 318.98 |
| | 71 |
| | 254.99 |
| | 79.9 |
| | 18 |
| 0.3 |
| | 92 |
| | 339.71 |
| | 77 |
| | 284.61 |
| | 83.8 |
| | 15 |
|
| Washington | 2.3 |
| | 612 |
| | 276.73 |
| | 522 |
| | 236.11 |
| | 85.3 |
| | 90 |
| 2.3 |
| | 584 |
| | 256.66 |
| | 574 |
| | 252.41 |
| | 98.3 |
| | 10 |
|
| Wisconsin | 0.2 |
| | 34 |
| | 175.77 |
| | 27 |
| | 141.78 |
| | 80.7 |
| | 7 |
| 0.2 |
| | 34 |
| | 183.97 |
| | 29 |
| | 154.53 |
| | 84.0 |
| | 5 |
|
| Other (4) | — |
| | 2 |
| | — |
| | 7 |
| | — |
| | — |
| | (5 | ) | |
Other (2) | | — |
| | — |
| | — |
| | 4 |
| | — |
| | — |
| | (4 | ) |
| | 11.0 |
| | $ | 3,994 |
| | $ | 362.04 |
| | $ | 3,630 |
| | $ | 329.08 |
| | 90.9 | % | | $ | 364 |
| 10.9 |
| | $ | 3,893 |
| | $ | 354.94 |
| | $ | 3,504 |
| | $ | 319.48 |
| | 90.0 | % | | $ | 389 |
|
| | | | Three Months Ended September 30, 2016 | Three Months Ended March 31, 2017 |
| | Member
Months | | Premium Revenue | | Medical Care Costs | | MCR | | Medical Margin | Member
Months | | Premium Revenue | | Medical Care Costs | | MCR | | Medical Margin |
| | | Total | | PMPM | | Total | | PMPM | | | Total | | PMPM | | Total | | PMPM | |
| California | 1.8 |
| | $ | 575 |
| | $ | 310.64 |
| | $ | 493 |
| | $ | 266.81 |
| | 85.9 | % | | $ | 82 |
| 1.8 |
| | $ | 572 |
| | $ | 308.57 |
| | $ | 484 |
| | $ | 261.31 |
| | 84.7 | % | | $ | 88 |
|
| Florida | 1.0 |
| | 335 |
| | 323.98 |
| | 317 |
| | 305.71 |
| | 94.4 |
| | 18 |
| 1.1 |
| | 364 |
| | 339.30 |
| | 352 |
| | 328.45 |
| | 96.8 |
| | 12 |
|
Idaho (1) | | — |
| | — |
| | — |
| | — |
| | — |
| | — |
| | — |
|
| Illinois | 0.6 |
| | 163 |
| | 275.26 |
| | 145 |
| | 244.86 |
| | 89.0 |
| | 18 |
| 0.6 |
| | 161 |
| | 276.58 |
| | 180 |
| | 310.08 |
| | 112.1 |
| | (19 | ) |
| Michigan | 1.2 |
| | 385 |
| | 335.34 |
| | 335 |
| | 291.69 |
| | 87.0 |
| | 50 |
| 1.2 |
| | 382 |
| | 327.41 |
| | 333 |
| | 284.58 |
| | 86.9 |
| | 49 |
|
| New Mexico | 0.7 |
| | 323 |
| | 451.06 |
| | 293 |
| | 409.24 |
| | 90.7 |
| | 30 |
| 0.7 |
| | 308 |
| | 422.87 |
| | 299 |
| | 410.75 |
| | 97.1 |
| | 9 |
|
| New York (3) | 0.1 |
| | 32 |
| | 427.40 |
| | 30 |
| | 403.71 |
| | 94.5 |
| | 2 |
| |
| New York | | 0.1 |
| | 46 |
| | 441.19 |
| | 42 |
| | 409.63 |
| | 92.8 |
| | 4 |
|
| Ohio | 1.0 |
| | 492 |
| | 497.08 |
| | 417 |
| | 421.95 |
| | 84.9 |
| | 75 |
| 1.0 |
| | 520 |
| | 527.79 |
| | 462 |
| | 469.04 |
| | 88.9 |
| | 58 |
|
| Puerto Rico | 1.0 |
| | 184 |
| | 183.46 |
| | 167 |
| | 167.44 |
| | 91.3 |
| | 17 |
| 1.0 |
| | 183 |
| | 186.51 |
| | 165 |
| | 168.18 |
| | 90.2 |
| | 18 |
|
| South Carolina | 0.3 |
| | 102 |
| | 312.28 |
| | 94 |
| | 285.97 |
| | 91.6 |
| | 8 |
| 0.3 |
| | 105 |
| | 317.07 |
| | 98 |
| | 293.34 |
| | 92.5 |
| | 7 |
|
| Texas | 0.7 |
| | 534 |
| | 728.84 |
| | 484 |
| | 662.79 |
| | 90.9 |
| | 50 |
| 0.7 |
| | 527 |
| | 751.86 |
| | 489 |
| | 696.43 |
| | 92.6 |
| | 38 |
|
| Utah | 0.3 |
| | 83 |
| | 288.59 |
| | 71 |
| | 242.77 |
| | 84.1 |
| | 12 |
| 0.3 |
| | 89 |
| | 313.20 |
| | 72 |
| | 253.75 |
| | 81.0 |
| | 17 |
|
| Washington | 2.0 |
| | 546 |
| | 264.01 |
| | 500 |
| | 241.49 |
| | 91.5 |
| | 46 |
| 2.2 |
| | 605 |
| | 273.18 |
| | 535 |
| | 241.77 |
| | 88.5 |
| | 70 |
|
| Wisconsin | 0.3 |
| | 35 |
| | 166.82 |
| | 26 |
| | 125.86 |
| | 75.4 |
| | 9 |
| 0.2 |
| | 33 |
| | 165.40 |
| | 27 |
| | 135.91 |
| | 82.2 |
| | 6 |
|
| Other (4) | — |
| | 3 |
| | — |
| | 24 |
| | — |
| | — |
| | (21 | ) | |
Other (2) | | — |
| | 2 |
| | — |
| | 9 |
| | — |
| | — |
| | (7 | ) |
| | 11.0 |
| | $ | 3,792 |
| | $ | 343.68 |
| | $ | 3,396 |
| | $ | 307.84 |
| | 89.6 | % | | $ | 396 |
| 11.2 |
| | $ | 3,897 |
| | $ | 347.84 |
| | $ | 3,547 |
| | $ | 316.62 |
| | 91.0 | % | | $ | 350 |
|
|
| | | | | | | | | | | | | | | | | | | | | | | | | |
| | Nine Months Ended September 30, 2017 |
| | Member
Months | | Premium Revenue | | Medical Care Costs | | MCR | | Medical Margin |
| | | Total | | PMPM | | Total | | PMPM | | |
| California | 5.6 |
| | $ | 1,771 |
| | $ | 316.83 |
| | $ | 1,586 |
| | $ | 283.82 |
| | 89.6 | % | | $ | 185 |
|
| Florida | 3.2 |
| | 1,132 |
| | 347.41 |
| | 1,112 |
| | 341.15 |
| | 98.2 |
| | 20 |
|
| Illinois | 1.6 |
| | 447 |
| | 284.18 |
| | 492 |
| | 312.54 |
| | 110.0 |
| | (45 | ) |
| Michigan | 3.5 |
| | 1,162 |
| | 332.60 |
| | 1,035 |
| | 296.28 |
| | 89.1 |
| | 127 |
|
| New Mexico | 2.2 |
| | 933 |
| | 431.70 |
| | 887 |
| | 410.24 |
| | 95.0 |
| | 46 |
|
| New York (3) | 0.3 |
| | 135 |
| | 444.77 |
| | 128 |
| | 421.58 |
| | 94.8 |
| | 7 |
|
| Ohio | 2.9 |
| | 1,598 |
| | 541.56 |
| | 1,434 |
| | 486.02 |
| | 89.7 |
| | 164 |
|
| Puerto Rico | 2.9 |
| | 553 |
| | 190.99 |
| | 513 |
| | 177.01 |
| | 92.7 |
| | 40 |
|
| South Carolina | 1.0 |
| | 329 |
| | 325.43 |
| | 301 |
| | 298.43 |
| | 91.7 |
| | 28 |
|
| Texas | 2.1 |
| | 1,592 |
| | 760.76 |
| | 1,468 |
| | 701.32 |
| | 92.2 |
| | 124 |
|
| Utah | 0.8 |
| | 267 |
| | 315.35 |
| | 219 |
| | 258.64 |
| | 82.0 |
| | 48 |
|
| Washington | 6.7 |
| | 1,835 |
| | 275.60 |
| | 1,603 |
| | 240.83 |
| | 87.4 |
| | 232 |
|
| Wisconsin | 0.6 |
| | 101 |
| | 170.64 |
| | 80 |
| | 136.04 |
| | 79.7 |
| | 21 |
|
| Other (4) | — |
| | 7 |
| | — |
| | 27 |
| | — |
| | — |
| | (20 | ) |
| | 33.4 |
| | $ | 11,862 |
| | $ | 354.88 |
| | $ | 10,885 |
| | $ | 325.66 |
| | 91.8 | % | | $ | 977 |
|
|
| | | | | | | | | | | | | | | | | | | | | | | | | |
| | Nine Months Ended September 30, 2016 |
| | Member
Months | | Premium Revenue | | Medical Care Costs | | MCR | | Medical Margin |
| | | Total | | PMPM | | Total | | PMPM | | |
| California | 5.5 |
| | $ | 1,603 |
| | $ | 291.20 |
| | $ | 1,411 |
| | $ | 256.41 |
| | 88.1 | % | | $ | 192 |
|
| Florida | 3.0 |
| | 974 |
| | 322.69 |
| | 892 |
| | 295.43 |
| | 91.6 |
| | 82 |
|
| Illinois | 1.8 |
| | 466 |
| | 266.11 |
| | 414 |
| | 236.39 |
| | 88.8 |
| | 52 |
|
| Michigan | 3.6 |
| | 1,136 |
| | 323.08 |
| | 1,013 |
| | 288.13 |
| | 89.2 |
| | 123 |
|
| New Mexico | 2.1 |
| | 974 |
| | 460.71 |
| | 873 |
| | 412.92 |
| | 89.6 |
| | 101 |
|
| New York (3) | 0.1 |
| | 32 |
| | 427.40 |
| | 30 |
| | 403.71 |
| | 94.5 |
| | 2 |
|
| Ohio | 2.9 |
| | 1,444 |
| | 489.63 |
| | 1,286 |
| | 435.99 |
| | 89.0 |
| | 158 |
|
| Puerto Rico | 3.0 |
| | 535 |
| | 176.44 |
| | 516 |
| | 170.46 |
| | 96.6 |
| | 19 |
|
| South Carolina | 0.9 |
| | 273 |
| | 288.93 |
| | 232 |
| | 245.13 |
| | 84.8 |
| | 41 |
|
| Texas | 2.2 |
| | 1,650 |
| | 744.71 |
| | 1,466 |
| | 662.01 |
| | 88.9 |
| | 184 |
|
| Utah | 0.9 |
| | 255 |
| | 293.33 |
| | 221 |
| | 253.79 |
| | 86.5 |
| | 34 |
|
| Washington | 6.0 |
| | 1,576 |
| | 261.23 |
| | 1,431 |
| | 237.20 |
| | 90.8 |
| | 145 |
|
| Wisconsin | 0.7 |
| | 107 |
| | 165.53 |
| | 78 |
| | 120.82 |
| | 73.0 |
| | 29 |
|
| Other (4) | — |
| | 9 |
| | — |
| | 58 |
| | — |
| | — |
| | (49 | ) |
| | 32.7 |
| | $ | 11,034 |
| | $ | 337.76 |
| | $ | 9,921 |
| | $ | 303.72 |
| | 89.9 | % | | $ | 1,113 |
|
Health Plans Segment Financial Data — Marketplace
|
| | | | | | | | | | | | | | | | | | | | | | | | | |
| | Three Months Ended September 30, 2017 |
| | Member
Months | | Premium Revenue | | Medical Care Costs | | MCR | | Medical Margin |
| | | Total | | PMPM | | Total | | PMPM | | |
| California | 0.3 |
| | $ | 88 |
| | $ | 208.19 |
| | $ | 63 |
| | $ | 147.87 |
| | 71.0 | % | | $ | 25 |
|
| Florida | 0.9 |
| | 260 |
| | 313.36 |
| | 235 |
| | 283.13 |
| | 90.4 |
| | 25 |
|
| Michigan | — |
| | 14 |
| | 212.08 |
| | 10 |
| | 150.24 |
| | 70.8 |
| | 4 |
|
| New Mexico | 0.1 |
| | 29 |
| | 383.58 |
| | 20 |
| | 269.28 |
| | 70.2 |
| | 9 |
|
| Ohio | 0.1 |
| | 23 |
| | 386.09 |
| | 20 |
| | 364.31 |
| | 94.4 |
| | 3 |
|
| Texas | 0.7 |
| | 183 |
| | 291.14 |
| | 109 |
| | 172.70 |
| | 59.3 |
| | 74 |
|
| Utah | 0.3 |
| | 49 |
| | 241.65 |
| | 31 |
| | 155.13 |
| | 64.2 |
| | 18 |
|
| Washington | 0.1 |
| | 42 |
| | 327.40 |
| | 33 |
| | 256.52 |
| | 78.3 |
| | 9 |
|
| Wisconsin | 0.2 |
| | 95 |
| | 527.17 |
| | 70 |
| | 385.65 |
| | 73.2 |
| | 25 |
|
Other (3) | — |
| | — |
| | — |
| | (1 | ) | | — |
| | — |
| | 1 |
|
| | 2.7 |
| | $ | 783 |
| | $ | 301.72 |
| | $ | 590 |
| | $ | 227.22 |
| | 75.3 | % | | $ | 193 |
|
|
| | | | | | | | | | | | | | | | | | | | | | | | | |
| | Three Months Ended September 30, 2016 |
| | Member
Months | | Premium Revenue | | Medical Care Costs | | MCR | | Medical Margin |
| | | Total | | PMPM | | Total | | PMPM | | |
| California | 0.3 |
| | $ | 37 |
| | $ | 185.04 |
| | $ | 30 |
| | $ | 140.10 |
| | 75.7 | % | | $ | 7 |
|
| Florida | 0.6 |
| | 159 |
| | 253.16 |
| | 145 |
| | 231.78 |
| | 91.6 |
| | 14 |
|
| Michigan | — |
| | 2 |
| | 221.84 |
| | 2 |
| | 132.62 |
| | 59.8 |
| | — |
|
| New Mexico | 0.1 |
| | 15 |
| | 290.63 |
| | 11 |
| | 220.32 |
| | 75.8 |
| | 4 |
|
| Ohio | — |
| | 9 |
| | 307.24 |
| | 7 |
| | 215.01 |
| | 70.0 |
| | 2 |
|
| Texas | 0.4 |
| | 63 |
| | 189.85 |
| | 41 |
| | 121.06 |
| | 63.8 |
| | 22 |
|
| Utah | 0.1 |
| | 23 |
| | 142.10 |
| | 33 |
| | 208.48 |
| | 146.7 |
| | (10 | ) |
| Washington | 0.1 |
| | 23 |
| | 307.55 |
| | 21 |
| | 300.71 |
| | 97.8 |
| | 2 |
|
| Wisconsin | 0.1 |
| | 68 |
| | 375.60 |
| | 64 |
| | 357.60 |
| | 95.2 |
| | 4 |
|
| Other (3) | — |
| | — |
| | — |
| | (2 | ) | | — |
| | — |
| | 2 |
|
| | 1.7 |
| | $ | 399 |
| | $ | 238.86 |
| | $ | 352 |
| | $ | 210.38 |
| | 88.1 | % | | $ | 47 |
|
|
| | | | | | | | | | | | | | | | | | | | | | | | | |
| | Nine Months Ended September 30, 2017 |
| | Member
Months | | Premium Revenue | | Medical Care Costs | | MCR | | Medical Margin |
| | | Total | | PMPM | | Total | | PMPM | | |
| California | 1.2 |
| | $ | 241 |
| | $ | 193.33 |
| | $ | 156 |
| | $ | 124.32 |
| | 64.3 | % | | $ | 85 |
|
| Florida | 2.8 |
| | 821 |
| | 296.14 |
| | 758 |
| | 273.55 |
| | 92.4 |
| | 63 |
|
| Michigan | 0.2 |
| | 41 |
| | 187.96 |
| | 27 |
| | 126.76 |
| | 67.4 |
| | 14 |
|
| New Mexico | 0.2 |
| | 82 |
| | 338.18 |
| | 62 |
| | 256.05 |
| | 75.7 |
| | 20 |
|
| Ohio | 0.2 |
| | 68 |
| | 365.35 |
| | 64 |
| | 346.93 |
| | 95.0 |
| | 4 |
|
| Texas | 2.1 |
| | 517 |
| | 252.32 |
| | 351 |
| | 171.57 |
| | 68.0 |
| | 166 |
|
| Utah | 0.7 |
| | 135 |
| | 209.43 |
| | 135 |
| | 209.13 |
| | 99.9 |
| | — |
|
| Washington | 0.4 |
| | 123 |
| | 315.95 |
| | 128 |
| | 327.51 |
| | 103.7 |
| | (5 | ) |
| Wisconsin | 0.6 |
| | 275 |
| | 469.44 |
| | 260 |
| | 443.41 |
| | 94.5 |
| | 15 |
|
| Other (3) | — |
| | — |
| | — |
| | (4 | ) | | — |
| | — |
| | 4 |
|
| | 8.4 |
| | $ | 2,303 |
| | $ | 276.27 |
| | $ | 1,937 |
| | $ | 232.31 |
| | 84.1 | % | | $ | 366 |
|
|
| | | | | | | | | | | | | | | | | | | | | | | | | |
| | Nine Months Ended September 30, 2016 |
| | Member
Months | | Premium Revenue | | Medical Care Costs | | MCR | | Medical Margin |
| | | Total | | PMPM | | Total | | PMPM | | |
| California | 0.6 |
| | $ | 104 |
| | $ | 177.57 |
| | $ | 74 |
| | $ | 124.29 |
| | 70.0 | % | | $ | 30 |
|
| Florida | 2.0 |
| | 473 |
| | 237.37 |
| | 409 |
| | 205.37 |
| | 86.5 |
| | 64 |
|
| Michigan | — |
| | 7 |
| | 213.35 |
| | 5 |
| | 138.37 |
| | 64.9 |
| | 2 |
|
| New Mexico | 0.2 |
| | 42 |
| | 264.76 |
| | 32 |
| | 201.73 |
| | 76.2 |
| | 10 |
|
| Ohio | 0.1 |
| | 28 |
| | 322.36 |
| | 20 |
| | 232.44 |
| | 72.1 |
| | 8 |
|
| Texas | 1.1 |
| | 202 |
| | 196.45 |
| | 133 |
| | 128.97 |
| | 65.7 |
| | 69 |
|
| Utah | 0.4 |
| | 75 |
| | 160.33 |
| | 91 |
| | 194.78 |
| | 121.5 |
| | (16 | ) |
| Washington | 0.2 |
| | 58 |
| | 281.80 |
| | 48 |
| | 235.78 |
| | 83.7 |
| | 10 |
|
| Wisconsin | 0.5 |
| | 192 |
| | 357.80 |
| | 200 |
| | 373.94 |
| | 104.5 |
| | (8 | ) |
| Other (3) | — |
| | — |
| | — |
| | (3 | ) | | — |
| | — |
| | 3 |
|
| | 5.1 |
| | $ | 1,181 |
| | $ | 231.69 |
| | $ | 1,009 |
| | $ | 197.77 |
| | 85.4 | % | | $ | 172 |
|
Health Plans Segment Financial Data — Total
|
| | | | | | | | | | | | | | | | | | | | | | | | | |
| | Three Months Ended September 30, 2017 |
| | Member Months | | Premium Revenue | | Medical Care Costs | | MCR | | Medical Margin |
| | | Total | | PMPM | | Total | | PMPM | | |
| California | 2.2 |
| | $ | 689 |
| | $ | 301.64 |
| | $ | 626 |
| | $ | 273.90 |
| | 90.8 | % | | $ | 63 |
|
| Florida | 1.9 |
| | 648 |
| | 337.40 |
| | 625 |
| | 325.09 |
| | 96.4 |
| | 23 |
|
| Illinois | 0.5 |
| | 137 |
| | 287.69 |
| | 138 |
| | 289.36 |
| | 100.6 |
| | (1 | ) |
| Michigan | 1.2 |
| | 404 |
| | 330.27 |
| | 355 |
| | 290.63 |
| | 88.0 |
| | 49 |
|
| New Mexico | 0.8 |
| | 333 |
| | 424.61 |
| | 297 |
| | 378.98 |
| | 89.3 |
| | 36 |
|
New York (1) | 0.1 |
| | 43 |
| | 435.00 |
| | 41 |
| | 413.02 |
| | 94.9 |
| | 2 |
|
| Ohio | 1.0 |
| | 572 |
| | 550.75 |
| | 503 |
| | 485.61 |
| | 88.2 |
| | 69 |
|
| Puerto Rico | 1.0 |
| | 191 |
| | 202.59 |
| | 159 |
| | 168.25 |
| | 83.1 |
| | 32 |
|
| South Carolina | 0.3 |
| | 113 |
| | 332.48 |
| | 101 |
| | 297.74 |
| | 89.6 |
| | 12 |
|
| Texas | 1.4 |
| | 724 |
| | 546.57 |
| | 615 |
| | 463.83 |
| | 84.9 |
| | 109 |
|
| Utah | 0.5 |
| | 138 |
| | 286.39 |
| | 102 |
| | 212.91 |
| | 74.3 |
| | 36 |
|
| Washington | 2.4 |
| | 654 |
| | 279.52 |
| | 555 |
| | 237.23 |
| | 84.9 |
| | 99 |
|
| Wisconsin | 0.4 |
| | 129 |
| | 345.63 |
| | 97 |
| | 259.66 |
| | 75.1 |
| | 32 |
|
Other (2) | — |
| | 2 |
| | — |
| | 6 |
| | — |
| | — |
| | (4 | ) |
| | 13.7 |
| | $ | 4,777 |
| | $ | 350.55 |
| | $ | 4,220 |
| | $ | 309.68 |
| | 88.3 | % | | $ | 557 |
|
|
| | | | | | | | | | | | | | | | | | | | | | | | | |
| | Three Months Ended September 30, 2016 |
| | Member Months | | Premium Revenue | | Medical Care Costs | | MCR | | Medical Margin |
| | | Total | | PMPM | | Total | | PMPM | | |
| California | 2.1 |
| | $ | 612 |
| | $ | 298.05 |
| | $ | 523 |
| | $ | 254.11 |
| | 85.3 | % | | $ | 89 |
|
| Florida | 1.6 |
| | 494 |
| | 297.24 |
| | 462 |
| | 277.79 |
| | 93.5 |
| | 32 |
|
| Illinois | 0.6 |
| | 163 |
| | 275.26 |
| | 145 |
| | 244.86 |
| | 89.0 |
| | 18 |
|
| Michigan | 1.2 |
| | 387 |
| | 334.25 |
| | 337 |
| | 290.16 |
| | 86.8 |
| | 50 |
|
| New Mexico | 0.8 |
| | 338 |
| | 440.12 |
| | 304 |
| | 396.35 |
| | 90.1 |
| | 34 |
|
New York (1) | 0.1 |
| | 32 |
| | 427.40 |
| | 30 |
| | 403.71 |
| | 94.5 |
| | 2 |
|
| Ohio | 1.0 |
| | 501 |
| | 491.51 |
| | 424 |
| | 415.87 |
| | 84.6 |
| | 77 |
|
| Puerto Rico | 1.0 |
| | 184 |
| | 183.46 |
| | 167 |
| | 167.44 |
| | 91.3 |
| | 17 |
|
| South Carolina | 0.3 |
| | 102 |
| | 312.28 |
| | 94 |
| | 285.97 |
| | 91.6 |
| | 8 |
|
| Texas | 1.1 |
| | 597 |
| | 559.98 |
| | 525 |
| | 493.07 |
| | 88.1 |
| | 72 |
|
| Utah | 0.4 |
| | 106 |
| | 236.31 |
| | 104 |
| | 230.53 |
| | 97.6 |
| | 2 |
|
| Washington | 2.1 |
| | 569 |
| | 265.48 |
| | 521 |
| | 243.49 |
| | 91.7 |
| | 48 |
|
| Wisconsin | 0.4 |
| | 103 |
| | 262.32 |
| | 90 |
| | 231.86 |
| | 88.4 |
| | 13 |
|
Other (2) | — |
| | 3 |
| | — |
| | 22 |
| | — |
| | — |
| | (19 | ) |
| | 12.7 |
| | $ | 4,191 |
| | $ | 329.88 |
| | $ | 3,748 |
| | $ | 295.01 |
| | 89.4 | % | | $ | 443 |
|
|
| | | | | | | | | | | | | | | | | | | | | | | | | |
| | Nine Months Ended September 30, 2017 |
| | Member Months | | Premium Revenue | | Medical Care Costs | | MCR | | Medical Margin |
| | | Total | | PMPM | | Total | | PMPM | | |
| California | 6.8 |
| | $ | 2,012 |
| | $ | 294.26 |
| | $ | 1,742 |
| | $ | 254.67 |
| | 86.5 | % | | $ | 270 |
|
| Florida | 6.0 |
| | 1,953 |
| | 323.86 |
| | 1,870 |
| | 310.09 |
| | 95.7 |
| | 83 |
|
| Illinois | 1.6 |
| | 447 |
| | 284.18 |
| | 492 |
| | 312.54 |
| | 110.0 |
| | (45 | ) |
| Michigan | 3.7 |
| | 1,203 |
| | 324.12 |
| | 1,062 |
| | 286.35 |
| | 88.3 |
| | 141 |
|
| New Mexico | 2.4 |
| | 1,015 |
| | 422.25 |
| | 949 |
| | 394.66 |
| | 93.5 |
| | 66 |
|
New York (1) | 0.3 |
| | 135 |
| | 444.77 |
| | 128 |
| | 421.58 |
| | 94.8 |
| | 7 |
|
| Ohio | 3.1 |
| | 1,666 |
| | 531.17 |
| | 1,498 |
| | 477.81 |
| | 90.0 |
| | 168 |
|
| Puerto Rico | 2.9 |
| | 553 |
| | 190.99 |
| | 513 |
| | 177.01 |
| | 92.7 |
| | 40 |
|
| South Carolina | 1.0 |
| | 329 |
| | 325.43 |
| | 301 |
| | 298.43 |
| | 91.7 |
| | 28 |
|
| Texas | 4.2 |
| | 2,109 |
| | 509.09 |
| | 1,819 |
| | 439.11 |
| | 86.3 |
| | 290 |
|
| Utah | 1.5 |
| | 402 |
| | 269.48 |
| | 354 |
| | 237.20 |
| | 88.0 |
| | 48 |
|
| Washington | 7.1 |
| | 1,958 |
| | 277.83 |
| | 1,731 |
| | 245.62 |
| | 88.4 |
| | 227 |
|
| Wisconsin | 1.2 |
| | 376 |
| | 319.57 |
| | 340 |
| | 289.24 |
| | 90.5 |
| | 36 |
|
Other (2) | — |
| | 7 |
| | — |
| | 23 |
| | — |
| | — |
| | (16 | ) |
| | 41.8 |
| | $ | 14,165 |
| | $ | 339.19 |
| | $ | 12,822 |
| | $ | 307.03 |
| | 90.5 | % | | $ | 1,343 |
|
|
| | | | | | | | | | | | | | | | | | | | | | | | | |
| | Nine Months Ended September 30, 2016 |
| | Member Months | | Premium Revenue | | Medical Care Costs | | MCR | | Medical Margin |
| | | Total | | PMPM | | Total | | PMPM | | |
| California | 6.1 |
| | $ | 1,707 |
| | $ | 280.21 |
| | $ | 1,485 |
| | $ | 243.64 |
| | 86.9 | % | | $ | 222 |
|
| Florida | 5.0 |
| | 1,447 |
| | 288.74 |
| | 1,301 |
| | 259.60 |
| | 89.9 |
| | 146 |
|
| Illinois | 1.8 |
| | 466 |
| | 266.11 |
| | 414 |
| | 236.39 |
| | 88.8 |
| | 52 |
|
| Michigan | 3.6 |
| | 1,143 |
| | 322.08 |
| | 1,018 |
| | 286.77 |
| | 89.0 |
| | 125 |
|
| New Mexico | 2.3 |
| | 1,016 |
| | 447.07 |
| | 905 |
| | 398.22 |
| | 89.1 |
| | 111 |
|
New York (1) | 0.1 |
| | 32 |
| | 427.40 |
| | 30 |
| | 403.71 |
| | 94.5 |
| | 2 |
|
| Ohio | 3.0 |
| | 1,472 |
| | 484.82 |
| | 1,306 |
| | 430.14 |
| | 88.7 |
| | 166 |
|
| Puerto Rico | 3.0 |
| | 535 |
| | 176.44 |
| | 516 |
| | 170.46 |
| | 96.6 |
| | 19 |
|
| South Carolina | 0.9 |
| | 273 |
| | 288.93 |
| | 232 |
| | 245.13 |
| | 84.8 |
| | 41 |
|
| Texas | 3.3 |
| | 1,852 |
| | 570.65 |
| | 1,599 |
| | 492.79 |
| | 86.4 |
| | 253 |
|
| Utah | 1.3 |
| | 330 |
| | 246.78 |
| | 312 |
| | 233.14 |
| | 94.5 |
| | 18 |
|
| Washington | 6.2 |
| | 1,634 |
| | 261.91 |
| | 1,479 |
| | 237.15 |
| | 90.5 |
| | 155 |
|
| Wisconsin | 1.2 |
| | 299 |
| | 252.45 |
| | 278 |
| | 235.25 |
| | 93.2 |
| | 21 |
|
Other (2) | — |
| | 9 |
| | — |
| | 55 |
| | — |
| | — |
| | (46 | ) |
| | 37.8 |
| | $ | 12,215 |
| | $ | 323.44 |
| | $ | 10,930 |
| | $ | 289.41 |
| | 89.5 | % | | $ | 1,285 |
|
| |
| (1) | The New York health plan was acquired on AugustIdaho operations commenced January 1, 2016.2018. |
| |
| (2) | “Other” medical care costs include primarily medically related administrative costs ofat the parent company,company. |
Health Plans Segment Financial Data — Marketplace
|
| | | | | | | | | | | | | | | | | | | | | | | | | |
| | Three Months Ended March 31, 2018 |
| | Member
Months | | Premium Revenue | | Medical Care Costs | | MCR | | Medical Margin |
| | | Total | | PMPM | | Total | | PMPM | | |
| California | 0.2 |
| | $ | 49 |
| | $ | 253.93 |
| | $ | 31 |
| | $ | 162.64 |
| | 64.0 | % | | $ | 18 |
|
| Florida | 0.2 |
| | 45 |
| | 271.12 |
| | (16 | ) | | (95.60 | ) | | (35.3 | ) | | 61 |
|
| Michigan | 0.1 |
| | 13 |
| | 224.11 |
| | 9 |
| | 144.16 |
| | 64.3 |
| | 4 |
|
| New Mexico | 0.1 |
| | 34 |
| | 438.67 |
| | 19 |
| | 246.50 |
| | 56.2 |
| | 15 |
|
| Ohio | 0.1 |
| | 26 |
| | 403.44 |
| | 17 |
| | 262.87 |
| | 65.2 |
| | 9 |
|
| Texas | 0.7 |
| | 229 |
| | 308.74 |
| | 146 |
| | 196.89 |
| | 63.8 |
| | 83 |
|
Utah (1) | — |
| | (3 | ) | | NM |
| | (10 | ) | | NM |
| | NM |
| | 7 |
|
| Washington | — |
| | 39 |
| | 526.36 |
| | 30 |
| | 405.40 |
| | 77.0 |
| | 9 |
|
Wisconsin (1) | — |
| | (2 | ) | | NM |
| | (8 | ) | | NM |
| | NM |
| | 6 |
|
| Other | — |
| | — |
| | — |
| | — |
| | — |
| | — |
| | — |
|
| | 1.4 |
| | $ | 430 |
| | $ | 312.87 |
| | $ | 218 |
| | $ | 158.40 |
| | 50.6 | % | | $ | 212 |
|
|
| | | | | | | | | | | | | | | | | | | | | | | | | |
| | Three Months Ended March 31, 2017 |
| | Member
Months | | Premium Revenue | | Medical Care Costs | | MCR | | Medical Margin |
| | | Total | | PMPM | | Total | | PMPM | | |
| California | 0.4 |
| | $ | 72 |
| | $ | 184.34 |
| | $ | 26 |
| | $ | 65.53 |
| | 35.5 | % | | $ | 46 |
|
| Florida | 1.0 |
| | 292 |
| | 292.80 |
| | 206 |
| | 205.91 |
| | 70.3 |
| | 86 |
|
| Michigan | 0.1 |
| | 11 |
| | 149.23 |
| | 6 |
| | 95.92 |
| | 64.3 |
| | 5 |
|
| New Mexico | 0.1 |
| | 22 |
| | 265.06 |
| | 19 |
| | 232.50 |
| | 87.7 |
| | 3 |
|
| Ohio | 0.1 |
| | 21 |
| | 334.26 |
| | 17 |
| | 273.72 |
| | 81.9 |
| | 4 |
|
| Texas | 0.7 |
| | 157 |
| | 222.40 |
| | 113 |
| | 161.02 |
| | 72.4 |
| | 44 |
|
| Utah | 0.2 |
| | 45 |
| | 202.48 |
| | 51 |
| | 228.20 |
| | 112.7 |
| | (6 | ) |
| Washington | 0.1 |
| | 37 |
| | 302.51 |
| | 46 |
| | 365.94 |
| | 121.0 |
| | (9 | ) |
| Wisconsin | 0.2 |
| | 94 |
| | 453.39 |
| | 81 |
| | 389.80 |
| | 86.0 |
| | 13 |
|
| Other | — |
| | — |
| | — |
| | (1 | ) | | — |
| | — |
| | 1 |
|
| | 2.9 |
| | $ | 751 |
| | $ | 262.16 |
| | $ | 564 |
| | $ | 196.72 |
| | 75.0 | % | | $ | 187 |
|
_________________________
| |
| (1) | We terminated Marketplace operations at our Utah and direct delivery costs.Wisconsin health plans effective January 1, 2018, so the ratios for 2018 periods are not meaningful for those health plans. |
Health Plans Segment Financial Data — Total
|
| | | | | | | | | | | | | | | | | | | | | | | | | |
| | Three Months Ended March 31, 2018 |
| | Member Months | | Premium Revenue | | Medical Care Costs | | MCR | | Medical Margin |
| | | Total | | PMPM | | Total | | PMPM | | |
| California | 2.0 |
| | $ | 543 |
| | $ | 270.80 |
| | $ | 443 |
| | $ | 221.03 |
| | 81.6 | % | | $ | 100 |
|
| Florida | 1.2 |
| | 427 |
| | 340.91 |
| | 329 |
| | 262.65 |
| | 77.0 |
| | 98 |
|
| Idaho | — |
| | 4 |
| | 960.33 |
| | 4 |
| | 977.00 |
| | 101.8 |
| | — |
|
| Illinois | 0.5 |
| | 141 |
| | 298.17 |
| | 122 |
| | 257.50 |
| | 86.4 |
| | 19 |
|
| Michigan | 1.2 |
| | 389 |
| | 331.08 |
| | 340 |
| | 288.68 |
| | 87.2 |
| | 49 |
|
| New Mexico | 0.8 |
| | 353 |
| | 463.33 |
| | 329 |
| | 431.94 |
| | 93.2 |
| | 24 |
|
| New York | 0.1 |
| | 46 |
| | 468.91 |
| | 39 |
| | 396.76 |
| | 84.6 |
| | 7 |
|
| Ohio | 1.0 |
| | 577 |
| | 565.62 |
| | 477 |
| | 467.41 |
| | 82.6 |
| | 100 |
|
| Puerto Rico | 1.0 |
| | 186 |
| | 193.13 |
| | 174 |
| | 181.39 |
| | 93.9 |
| | 12 |
|
| South Carolina | 0.3 |
| | 122 |
| | 348.08 |
| | 104 |
| | 297.52 |
| | 85.5 |
| | 18 |
|
| Texas | 1.4 |
| | 791 |
| | 551.28 |
| | 665 |
| | 463.37 |
| | 84.1 |
| | 126 |
|
| Utah | 0.3 |
| | 89 |
| | 328.83 |
| | 67 |
| | 246.78 |
| | 75.0 |
| | 22 |
|
| Washington | 2.3 |
| | 623 |
| | 265.20 |
| | 604 |
| | 257.25 |
| | 97.0 |
| | 19 |
|
| Wisconsin | 0.2 |
| | 32 |
| | 172.09 |
| | 21 |
| | 110.91 |
| | 64.4 |
| | 11 |
|
| Other | — |
| | — |
| | — |
| | 4 |
| | — |
| | — |
| | (4 | ) |
| | 12.3 |
| | $ | 4,323 |
| | $ | 350.25 |
| | $ | 3,722 |
| | $ | 301.55 |
| | 86.1 | % | | $ | 601 |
|
|
| | | | | | | | | | | | | | | | | | | | | | | | | |
| | Three Months Ended March 31, 2017 |
| | Member Months | | Premium Revenue | | Medical Care Costs | | MCR | | Medical Margin |
| | | Total | | PMPM | | Total | | PMPM | | |
| California | 2.2 |
| | $ | 644 |
| | $ | 286.92 |
| | $ | 510 |
| | $ | 227.19 |
| | 79.2 | % | | $ | 134 |
|
| Florida | 2.1 |
| | 656 |
| | 316.86 |
| | 558 |
| | 269.33 |
| | 85.0 |
| | 98 |
|
| Idaho | — |
| | — |
| | — |
| | — |
| | — |
| | — |
| | — |
|
| Illinois | 0.6 |
| | 161 |
| | 276.58 |
| | 180 |
| | 310.08 |
| | 112.1 |
| | (19 | ) |
| Michigan | 1.3 |
| | 393 |
| | 316.80 |
| | 339 |
| | 273.36 |
| | 86.3 |
| | 54 |
|
| New Mexico | 0.8 |
| | 330 |
| | 406.90 |
| | 318 |
| | 392.72 |
| | 96.5 |
| | 12 |
|
| New York | 0.1 |
| | 46 |
| | 441.19 |
| | 42 |
| | 409.63 |
| | 92.8 |
| | 4 |
|
| Ohio | 1.1 |
| | 541 |
| | 516.00 |
| | 479 |
| | 457.14 |
| | 88.6 |
| | 62 |
|
| Puerto Rico | 1.0 |
| | 183 |
| | 186.51 |
| | 165 |
| | 168.18 |
| | 90.2 |
| | 18 |
|
| South Carolina | 0.3 |
| | 105 |
| | 317.07 |
| | 98 |
| | 293.34 |
| | 92.5 |
| | 7 |
|
| Texas | 1.4 |
| | 684 |
| | 486.96 |
| | 602 |
| | 428.55 |
| | 88.0 |
| | 82 |
|
| Utah | 0.5 |
| | 134 |
| | 264.73 |
| | 123 |
| | 242.57 |
| | 91.6 |
| | 11 |
|
| Washington | 2.3 |
| | 642 |
| | 274.74 |
| | 581 |
| | 248.40 |
| | 90.4 |
| | 61 |
|
| Wisconsin | 0.4 |
| | 127 |
| | 311.30 |
| | 108 |
| | 264.53 |
| | 85.0 |
| | 19 |
|
| Other | — |
| | 2 |
| | — |
| | 8 |
| | — |
| | — |
| | (6 | ) |
| | 14.1 |
| | $ | 4,648 |
| | $ | 330.39 |
| | $ | 4,111 |
| | $ | 292.20 |
| | 88.4 | % | | $ | 537 |
|
MEDICAL CARE COSTS BY TYPE
The following table provides the details of consolidated medical care costs by category for the periods indicated (dollars in millions except PMPM amounts):
|
| | | | | | | | | | | | | | | | | | | | | |
| | Three Months Ended September 30, |
| | 2017 | | 2016 |
| | Amount | | PMPM | | % of Total | | Amount | | PMPM | | % of Total |
| Fee for service | $ | 3,196 |
| | $ | 234.51 |
| | 75.8 | % | | $ | 2,799 |
| | $ | 220.29 |
| | 74.7 | % |
| Pharmacy | 638 |
| | 46.85 |
| | 15.1 |
| | 567 |
| | 44.65 |
| | 15.1 |
|
| Capitation | 342 |
| | 25.07 |
| | 8.1 |
| | 302 |
| | 23.83 |
| | 8.1 |
|
| Direct delivery | 18 |
| | 1.37 |
| | 0.4 |
| | 21 |
| | 1.66 |
| | 0.5 |
|
| Other | 26 |
| | 1.88 |
| | 0.6 |
| | 59 |
| | 4.58 |
| | 1.6 |
|
| | $ | 4,220 |
| | $ | 309.68 |
| | 100.0 | % | | $ | 3,748 |
| | $ | 295.01 |
| | 100.0 | % |
| | | | Nine Months Ended September 30, | Three Months Ended March 31, |
| | 2017 | | 2016 | 2018 | | 2017 |
| | Amount | | PMPM | | % of Total | | Amount | | PMPM | | % of Total | Amount | | PMPM | | % of Total | | Amount | | PMPM | | % of Total |
| Fee for service | $ | 9,630 |
| | $ | 230.58 |
| | 75.1 | % | | $ | 8,156 |
| | $ | 215.96 |
| | 74.6 | % | $ | 2,745 |
| | $ | 222.38 |
| | 73.8 | % | | $ | 3,086 |
| | $ | 219.32 |
| | 75.1 | % |
| Pharmacy | 1,904 |
| | 45.60 |
| | 14.8 |
| | 1,621 |
| | 42.93 |
| | 14.8 |
| 583 |
| | 47.25 |
| | 15.6 |
| | 616 |
| | 43.76 |
| | 15.0 |
|
| Capitation | 1,022 |
| | 24.47 |
| | 8.0 |
| | 901 |
| | 23.86 |
| | 8.3 |
| 312 |
| | 25.28 |
| | 8.4 |
| | 324 |
| | 23.06 |
| | 7.9 |
|
| Direct delivery | 62 |
| | 1.50 |
| | 0.5 |
| | 55 |
| | 1.46 |
| | 0.5 |
| |
| Other | 204 |
| | 4.88 |
| | 1.6 |
| | 197 |
| | 5.20 |
| | 1.8 |
| 82 |
| | 6.64 |
| | 2.2 |
| | 85 |
| | 6.06 |
| | 2.0 |
|
| | $ | 12,822 |
| | $ | 307.03 |
| | 100.0 | % | | $ | 10,930 |
| | $ | 289.41 |
| | 100.0 | % | $ | 3,722 |
| | $ | 301.55 |
| | 100.0 | % | | $ | 4,111 |
| | $ | 292.20 |
| | 100.0 | % |
PREMIUM TAXES
The premium tax ratio (premium tax expense as a percentage of premium revenue plus premium tax revenue) was 2.2%2.3% in both the first quarter of 2018 and 2017.
HEALTH INSURER FEES (HIF)
Health insurer fees reimbursed amounted to $61 million, and health insurer fees amounted to $75 million, in the thirdfirst quarter of 2017 compared with 2.9%2018. Approximately $10 million of revenue related to the reimbursement of Medicaid health insurer fees from New Mexico, New York and Puerto Rico was not recognized in the thirdfirst quarter of 2016 and 2.3%2018 because as of March 31, 2018 we had not received adequate documentation of the intent to reimburse such fees.
There were no HIF reimbursed or expensed in the nine months
ended September 30, 2017 compared with 2.7% in the nine months ended September 30, 2016. This decline was primarily due to the temporary suspension of a Michigan HMO use tax effective January 1, 2017, which was partially offset by a higher California premium tax rate effective July 1, 2016, and significant revenue growth at our Florida health plan, which operates in a state with no premium tax.
HEALTH INSURER FEE (HIF) REVENUE AND EXPENSES
TheHIF moratorium under the Consolidated Appropriations Act of 2016 provided for a HIF moratorium in 2017. Therefore, there are no HIF revenues or expenses in 2017.2016.
MOLINA MEDICAID SOLUTIONS
The Molina Medicaid Solutions segment provides support to state government agencies in theagencies’ administration of their Medicaid programs, including business processing, information technology development and administrative services.
FINANCIAL OVERVIEW
The Molina Medicaid Solutions segment service margin for the third quarter of 2017 and 2016, and for the ninethree months ended September 30,March 31, 2018 and 2017, and 2016, was insignificant.
As discussed further in Notes to Consolidated Financial Statements, Note 10, “Impairment Losses,” we recorded a goodwill impairment charge of $28 million, reported in our consolidated statements of operations as “Impairment losses.”
OTHER
The Other segment includes primarily our Pathways behavioral health and social services provider, and corporate amounts not allocated to other reportable segments.
FINANCIAL OVERVIEW
The Other segment service margin for the third quarter of 2017 and 2016, and for the ninethree months ended September 30,March 31, 2018 and 2017, and 2016, was insignificant.
As discussed further in Notes to Consolidated Financial Statements, Note 10, “Impairment Losses,” in the second quarter of 2017 we recorded impairment losses, primarily relating to our Pathways subsidiary, of $61 million for goodwill and $11 million for intangible assets, or $72 million in the aggregate. In the third quarter of 2017, we recorded a further goodwill impairment loss relating to the Pathways subsidiary, of $101 million.
OTHER CONSOLIDATED INFORMATION
GENERAL AND ADMINISTRATIVE EXPENSES
The G&A ratio wasdecreased to 7.6% for both the thirdfirst quarter of 2017 and 2016. The G&A ratio increased to 8.2%2018, compared with 8.9% for the nine months ended September 30, 2017, compared with 7.8% for the nine months ended September 30, 2016.first quarter of 2017. Refer to discussion above, in “Consolidated Results.”
DEPRECIATION AND AMORTIZATION
Depreciation and amortization, as a percentage of total revenue, was 0.7%0.6% and 0.8% in the nine months ended September 30,first quarter of 2018 and 2017, and 2016, respectively.
IMPAIRMENT LOSSES
See Notes to Consolidated Financial Statements, Note 10, “Impairment Losses.”
RESTRUCTURING AND SEPARATION COSTS
See Notes to Consolidated Financial Statements, Note 11,10, “Restructuring and Separation Costs.”
INTEREST EXPENSE
Interest expense was $32$33 million for the thirdfirst quarter of 2017,2018, compared with $26 million for the thirdfirst quarter of 2016. Interest expense was $85 million for the nine months ended September 30, 2017, compared with $76 million for the nine months ended September 30, 2016.2017. Interest expense includes non-cash interest expense relating primarily to the amortization of the discount on convertible senior notes, which amounted to $8 million for both the third quarter of 2017 and 2016, and $24$7 million and $23$8 million in the nine months ended September 30,first quarter of 2018 and 2017, and 2016, respectively. We expect interest expense to continue to increase in future periods as a result of our recent $330 million offering of 4.875% Notes, and borrowings under the Credit Facility. See further discussion in Notes to Consolidated Financial Statements, Note 7, “Debt.”
OTHER INCOME,EXPENSES (INCOME), NET
AsIn the first quarter of 2018, we recorded other expenses of $10 million due to the loss on debt extinguishment resulting from our 1.625% Exchange. The 1.625% Exchange is described further in Notes to Consolidated Financial Statements, Note 1, “Basis7, “Debt.” In the first quarter of Presentation,” in February 2017, we received an aggregate termination fee ofa $75 million for thefee in connection with a terminated Medicare Acquisition. This amount is reported in “Other income, net” in our consolidated statements of operations.acquisition transaction.
INCOME TAXES
The (benefit) provision for income taxes was recorded at an effective rate of 14.6%40.3% for the thirdfirst quarter of 2017,2018, compared with 54.0%41.6% for the thirdfirst quarter of 2016, and an effective rate of 15.5% for the nine months ended September 30, 2017 compared with 58.0% for the nine months ended September 30, 2016.2017. The significant change in the effective tax rate was primarilyfor 2018 is lower than 2017 as a result of pretax lossesthe reduction in the federal statutory rate from 35% to 21% under the TCJA, combined with higher non-deductible expenses in 2018 primarily related to the non-deductible HIF. The HIF was not applicable in 2017 combined with significant nondeductible expenses (primarily, separation costs and goodwill impairment) anddue to the 2017 HIF moratorium as described above in “Health Plans—Health Insurer Fee (HIF) Revenue and Expenses.”moratorium.
LIQUIDITY AND FINANCIAL CONDITION
INTRODUCTION
We manage our cash, investments, and capital structure to meet the short- and long-term obligations of our business while maintaining liquidity and financial flexibility. We forecast, analyze, and monitor our cash flows to enable prudent investment management and financing within the confines of our financial strategy.
A majority of the assets held by our Health Plans segment regulated subsidiaries is in the form of cash, cash equivalents, and investments. After considering expected cash flows from operating activities, we generally invest cash of regulated subsidiaries that exceeds our expected short-term obligations in longer term, investment-grade, and marketable debt securities to improve our overall investment return. These investments are made pursuant to board-approved investment policies that conform to applicable state laws and regulations.
Our investments are classified as current assets, except for our held-to-maturity restricted investments, which are classified as non-current assets, and which are not included in the totals below. Our held-to-maturity restricted investments are invested principally in certificates of deposit and U.S. treasury securities.
Investment income increased to $37$19 million for the ninethree months ended September 30, 2017,March 31, 2018, compared with $25$10 million for the ninethree months ended September 30, 2016,March 31, 2017, primarily due to the increase in invested assets.
MARKET RISK
Our earnings and financial position are exposed to financial market risk relating to changes in interest rates, and the resulting impact on investment income and interest expense.
Substantially all of our investments and restricted investments are subject to interest rate risk and will decrease in value if market interest rates increase. Assuming a hypothetical and immediate 1% increase in market interest rates at September 30, 2017,March 31, 2018, the fair value of our fixed income investments would decrease by approximately $25$21 million. Declines in interest rates over time will reduce our investment income.
For further information on fair value measurements and our investment portfolio, please refer to Notes to Consolidated Financial Statements, Note 4, “Fair Value Measurements,” and Note 5, “Investments.”
Borrowings under our Credit Facility bear interest based, at our election, on a base rate or an adjusted London Interbank Offered Rate (LIBOR), plus in each case the applicable margin. As of September 30, 2017,March 31, 2018, $300 million was outstanding under the Credit Facility.
LIQUIDITY
A condensed schedule of cash flows to facilitate our discussion of liquidity follows:
|
| | | | | | | | | | | |
| | Nine Months Ended September 30, |
| | 2017 | | 2016 | | Change |
| | (In millions) |
| Net cash provided by operating activities | $ | 957 |
| | $ | 633 |
| | $ | 324 |
|
| Net cash used in investing activities | (474 | ) | | (131 | ) | | (343 | ) |
| Net cash provided by financing activities | 632 |
| | 11 |
| | 621 |
|
| Net increase in cash and cash equivalents | $ | 1,115 |
| | $ | 513 |
| | $ | 602 |
|
|
| | | | | | | | | | | |
| | Three Months Ended March 31, |
| | 2018 | | 2017 | | Change |
| | (In millions) |
| Net cash provided by operating activities | $ | 394 |
| | $ | 719 |
| | $ | (325 | ) |
| Net cash provided by (used in) investing activities | 145 |
| | (337 | ) | | 482 |
|
| Net cash used in financing activities | (5 | ) | | (1 | ) | | (4 | ) |
| Net increase in cash, cash equivalents, and restricted cash and cash equivalents | $ | 534 |
| | $ | 381 |
| | $ | 153 |
|
Operating Activities
Cash provided by operating activities increased $324 million in the nine months ended September 30, 2017 compared with the nine months ended September 30, 2016. The change in net (loss) income, partially offset by the effect of adjustments to reconcile net loss to netNet cash provided by operating activities reduced cash provided by operating activities by $169 million. This changedecreased $325 million in the first quarter of 2018, compared with the first quarter of 2017, primarily due to the following:
Prepaid expenses and other current assets, and accounts payable and accrued liabilities. Each of these accounts increased significantly in the first quarter of 2018, primarily due to amounts recorded in connection with the reinstatement of the HIF in 2018; such increase in accounts payable and accrued liabilities was more thanlargely offset by the aggregate of the following changes:increase in prepaid expenses and other current assets.
Medical claims and benefits payable. In 2017,the first quarter of 2018, the change in medical claims and benefits payable increaseddecreased cash flows from operations by $381$160 million, primarily due to additional accruals relating to increaseda decline in reserves as a result of reduced Marketplace membership in 2017.
ReceivablesFlorida, Utah and deferred revenue. In 2017, the aggregate change in receivables and deferred revenue increased cash flows from operations by $395 million. Cash flows from operations in each period were impacted by the timing of premium revenues receipts. In general, state or federal payors may delay our premium payments, which we record as a receivable, or they may prepay the following month’s premium payment, which we record as deferred revenue. We typically receive capitation payments monthly; however, state or federal payors may decide to adjust their payment schedules which could positively or negatively impact our reported cash flows from operating activities in any given period.Wisconsin.
Amounts due government agencies. In 2017, the change inWhile amounts due government agencies decreasedincreased $172 million in the first quarter of 2018, this increase was less than the increase experienced in the first quarter of 2017, resulting in a year over year decrease of cash flows from operations by $381 million,of $201 million. This decrease was primarily due to paymentsa decline in the thirdamounts accrued for Marketplace CSR subsidies year over year.
Investing Activities
Investing activities were a source of cash of $145 million in the first quarter of 2017.2018, and a use of cash of $337 million in the first quarter of 2017, primarily due to reduced purchases of investments and higher proceeds from sales and maturities of investments, in the first quarter of 2018.
InvestingFinancing Activities
Net cash used in investingfinancing activities increased $343$4 million in the nine months ended September 30, 2017first quarter of 2018 compared with the nine months ended September 30, 2016, primarilyfirst quarter of 2017, due to higher purchases of investments, net of salescash paid for financing transaction fees, including the 1.625% Exchange and maturities,our Bridge Credit Agreement, in the current year.
Financing Activities
Net cash provided by financing activities increased $621 million in the nine months ended September 30, 2017 compared with the nine months ended September 30, 2016, due to proceeds received from the 4.875% Notes offering and borrowings under the Credit Facility.first quarter of 2018.
FINANCIAL CONDITION
We believe that our cash resources, combined withour borrowing capacity available under our Bridge Credit Agreement and Credit Facility as discussed further below in “Future Sources and Uses of Liquidity—Sources”,Sources,” and internally generated funds will be sufficient to support costs under the Restructuring Plan, operations, regulatory requirements, debt repayment obligations and capital expenditures for at least the next 12 months.
On a consolidated basis, at September 30, 2017,March 31, 2018, our working capital was $1,746$2,191 million, compared with $1,418$1,954 million at December 31, 2016.2017. At September 30, 2017,March 31, 2018, our cash and investments amounted to $6,166$6,372 million, compared with $4,689$6,000 million at December 31, 2016.2017.
Because of the statutory restrictions that inhibit the ability of our health plans to transfer net assets to us, the amount of retained earnings readily available to pay dividends to our stockholders is generally limited to cash, cash equivalents and investments (excluding restricted investments) held by the parent company—Molina Healthcare, Inc. Such cash, cash equivalents and investments (excluding restricted investments) amounted to $706 million and $696 million as of March 31, 2018 and December 31, 2017, respectively.
Debt Ratings. Our 5.375% Notes are rated “BB”“BB-” by Standard & Poor’s, and “B2”“B3” by Moody’s Investor Service, Inc. A significant downgrade in our ratings could adversely affect our borrowing capacity and increase our borrowing costs.
Financial Covenants. Our Credit Facility contains customary non-financial and financial covenants, including a net leverage ratio and an interest coverage ratio. Such ratios, presented below, are computed as defined by the terms of the Credit Facility.
|
| | | |
| Credit Facility Financial Covenants | Required Per Agreement | | As of September 30, 2017March 31, 2018 |
| | | | |
| Net leverage ratio | <4.0x | | 2.5x2.7x |
| Interest coverage ratio | >3.5x | | 8.8x6.9x |
In addition, the terms of ourindentures governing the 4.875% Notes, the 5.375% Notes, and each of the 1.125% Convertible Notes and the 1.625% Convertible Notes contain cross-default provisions with the Credit Facility that are triggered upon an eventdefault by us or any of default underour subsidiaries on any indebtedness in excess of the Credit Facility, and when borrowings under the Credit Facility equal or exceed certain amounts as definedamount specified in the related indentures.applicable indenture. As of September 30, 2017,March 31, 2018, we were in compliance with all covenants under the Credit Facility.Facility and the indentures governing our outstanding notes.
FUTURE SOURCES AND USES OF LIQUIDITY
Sources
Our Health Plans segment regulated subsidiaries generate significant cash flows from premium revenue, which we generally receive a short time before we pay for the related health care services. Such cash flows are our primary source of liquidity. Thus, any future decline in our profitability may have a negative impact on our liquidity.
Dividends from Subsidiaries. When available and as permitted by applicable regulations, cash in excess of the capital needs of our regulated health plans is generally paid in the form of dividends to our unregulated parent company to be used for general corporate purposes. In the nine months ended September 30,first quarter of 2018, we did not receive dividends from our subsidiaries. In the first quarter of 2017, and 2016, we received $100 million and $50 million respectively, in dividends from our regulated health plan subsidiaries. We received $36 million in dividends from our unregulated subsidiaries in the nine months ended September 30, 2017. See further discussion in Notes to Consolidated Financial Statements, Note 13,12, “Commitments and Contingencies—Regulatory Capital Requirements and Dividend Restrictions.”
Borrowing Capacity and Debt Financing. We have available borrowing capacity of $550 million under our Bridge Credit Agreement (which amount is subject to the use of proceeds restrictions set forth in the Bridge Credit Agreement), and $194 million under our Credit Facility. We have adequate cash held in a restricted account available to repay the $64 million principal balance outstanding under our 1.625% Convertible Notes, if noteholders exercise their conversion or put rights in 2018. See further discussion in the Notes to Consolidated Financial Statements, Note 7, “Debt.”
2017 Restructuring Plan. As previously disclosed, we estimate that our restructuring planthe 2017 Restructuring Plan will reduce annualized run-rate expenses by approximately $300 million to $400 million when completed by the end of 2018. We have already achieved $200 million of these run-rate reductions on an annualized basis, which will take full effect no later than January 1, 2018. All savings targets discussed in regards to the restructuring plan represent annualizedThis estimate includes run-rate savings that we expectof approximately $10 million relating to achieve duringactions taken in the year following the indicated implementation date. We expect one-time costs associated with the restructuring plan to exceed the benefits realized in 2017 due to the upfront payment of implementation costs and the delayed benefit of full savings until the beginningfirst quarter of 2018. We expect the cost savings to reduce both “General and administrative expenses” and “Medical care costs” reported onin our consolidated statements of operations.
income. The following table illustrates our estimates of run-rate savings associated with the restructuring plan.2017 Restructuring Plan, which have not changed significantly since our estimate at December 31, 2017. Such savings will be offset, through the end of 2018, by the costs notedreferred to below in “Uses.” Following 2018, the savings will be offset by approximately $20 million in run-rate expenses resulting from the implementation of restructuring plan initiatives. |
| | | | | | |
| Estimated Savings Expected to be Realized by Reportable Segment | | Health Plans | | Other | | Total |
| | | (In millions) |
| General and administrative expenses | | $5065 | | $12092 to $140$152 | | $170157 to $190$217 |
| Medical care costs | | $110126 to $190$166 | | $2017 | | $130143 to $210$183 |
| | | $160191 to $240$231 | | $140109 to $160$169 | �� | $300 to $400 |
Credit Facility. Refer to Notes to Consolidated Financial Statements, Note 7, “Debt,” for a detailed discussion of our Credit Facility. In August 2017, we drew against the Credit Facility in the amount of $300 million.
4.875% Notes. The 4.875% Notes contain a limitation on the use of proceeds which required us to deposit the net proceeds from their issuance into a segregated deposit account, a current asset reported as “Restricted investments” in our consolidated balance sheets. See further discussion in Notes to Consolidated Financial Statements, Note 7, “Debt.”
Shelf Registration Statement. We have a shelf registration statement on file with the Securities and Exchange Commission to register an unlimited amount of any combination of debt or equity securities in one or more offerings. Specific information regarding the terms and securities being offered will be provided at the time of an offering. Proceeds from future offerings are expected to be used for general corporate purposes, including, but not limited to, the repayment of debt, investments in or extensions of credit to our subsidiaries and the financing of possible acquisitions or business expansion.
Uses
Restructuring. We recorded $118 million of restructuring costs in the third quarter of 2017. Restructuring costs incurred to date consist primarily of termination benefits, write-offs of capitalized software due to the re-design of our core operating processes, restructuring of our direct delivery operations, and consulting fees. Under the restructuring plan, and also including separation costs to former executives, we have made cash payments of $24 million in the nine months ended September 30, 2017, and have accrued a liability of $65 million for future payments as of September 30, 2017.
We estimate that total pre-tax costs associated with the restructuring plan will be approximately $70 million to $90 million in the fourth quarter of 2017, with an additional $20 million to $40 million to be incurred in 2018. We currently estimate that a majority of the costs we expect to incur in the fourth quarter of 2017 will be settled in cash. The costs we incur associated with the restructuring plan are reported in “Restructuring and separation costs” in our consolidated statements of operations.
|
| | | | | | | | | |
Estimated Costs Expected to be Incurred by Reportable Segment | | Health Plans | | Molina Medicaid Solutions | | Other | | Total |
| | (In millions) |
Termination benefits | | $30 to $35 | | — |
| | $30 to $35 | | $60 to $70 |
Other restructuring costs | | $40 to $45 | | $10 | | $110 to $115 | | $160 to $170 |
| | $70 to $80 | | $10 | | $140 to $150 | | $220 to $240 |
Regulatory Capital Requirements and Dividend Restrictions. In the first quarter of 2018 and 2017, the parent company contributed capital of $80 million and $106 million, respectively, to our health plans subsidiaries to satisfy statutory net worth requirements. For more information on our regulatory capital requirements and dividend restrictions, refer to Notes to Consolidated Financial Statements, Note 13,12, “Commitments and Contingencies.”
States’ Budgets. 2017 Restructuring PlanFrom time. Refer to time,Notes to Consolidated Financial Statements, Note 10, “Restructuring and Separation Costs,” for a detailed discussion and update of the states in which our health plans operate may experience financial difficulties, which could lead to delays in premium payments. Until July 4, 2017 the state of Illinois operated without a budget for its current fiscal year. As of September 30, 2017, our Illinois health plan served approximately 163,000 members, and recognized premium revenue of approximately $447 millionRestructuring Plan, including costs incurred in the nine months ended September 30, 2017. Asfirst quarter of October 27, 2017,2018.
Convertible Senior Notes. Refer to the state of Illinois owed us approximately $220 million for certain March through September 2017 premiums.
On May 3, 2017, Puerto Rico’s financial oversight board filedNotes to Consolidated Financial Statements, Note 7, “Debt,” for a formdetailed discussion of bankruptcy in the U.S. District Court in Puerto Rico under Title IIIour Convertible Senior Notes. The principal amounts of PROMESA. The Title III provision allows for a court debt restructuring process similar to U.S. bankruptcy protection. To the extent such bankruptcy results in our failure to receive payment of amounts due under our Medicaid contract with the Commonwealth or the inability of the Commonwealth to extend our Medicaid contract at the end of its current term, such bankruptcy could have a material adverse effect on our business, financial condition, cash flows, or results of operations. As of September 30, 2017, the plan served approximately 306,000 members and recorded premium revenue of approximately $553 million in the nine months ended September 30, 2017. As of October 27, 2017, the Commonwealth was current with its premium payments.
Convertible Notes. We have outstanding $550 million aggregate principal amount of 1.125% cash convertible senior notes due January 15, 2020, unless earlier repurchased or converted. We refer to these notes as our 1.125% Convertible Notes. We also have outstanding $302 million aggregate principal amount of 1.625% convertible senior notes due August 14, 2044, unless earlier repurchased, redeemed, or converted. We refer to these notes asboth our 1.625% Convertible Notes. We refer to the 1.125% Convertible Notes and 1.625% Convertible Notes collectively as the Convertible Notes. Theour 1.125% Convertible Notes are convertible entirely into cash and the 1.625% Convertible Notes are convertible partially into cash, each prior to their respective maturity dates under certain circumstances, one of which relates to the closing price of our common stock over a specified period. We refer to this conversion trigger as the stock price trigger.
The stock price trigger for the 1.125% Convertible Notes is $53.00 per share. The 1.125% Convertible Notes met this trigger in the quarter ended September 30, 2017; therefore, they are convertible into cash and are reported in current portion of long-term debt as of September 30, 2017.
The stock price trigger for the 1.625% Convertible Notes is $75.51 per share. The 1.625% Convertible Notes did not meet this stock price trigger in the quarter ended September 30, 2017.March 31, 2018. However, on contractually specified dates beginning in August 2018, holders of the 1.625% Convertible Notes may require us to repurchase some or all of such notes. In addition, beginning May 15, 2018 until August 19, 2018, holders may convert some or all of the 1.625% Convertible Notes. Because of these put and conversion features, the 1.625% Convertible Notes are reported in current portion of long-term debt as of September 30, 2017.March 31, 2018. As noteddescribed above, because the proceeds from the 4.875% Notes are initiallywe have adequate cash held in a restricted account available to payments upon conversion or redemption ofrepay the 1.625% Convertible Notes, such restricted investments are also classified as currentif noteholders exercise their conversion or put rights in 2018.
The stock price trigger for the 1.125% Notes is $53.00 per share. The 1.125% Convertible Notes met this trigger in the accompanying consolidated balance sheets.
quarter ended March 31, 2018, and are convertible to cash through at least June 30, 2018. Because the 1.125% Convertible Notes may be converted into cash within 12 months, the $550 million carrying amount is reported in current portion of long-term debt as of March 31, 2018. For economic reasons related to the trading market for our 1.125% Convertible Notes, we believe that the amount of the notes that may be converted over the next twelve months, if any, will not be significant. However, if the trading market for our 1.125% Convertible Notes becomes closed or restricted due to market turmoil or other reasons such that the notes cannot be traded, or if the trading price of our Convertible1.125% Notes, which normally trade at a marginal premium to the underlying composite stock-and-interest economic value, no longer includes that marginal premium, holders of our 1.125% Convertible Notes may elect to convert the notes to cash.
If conversion requests are received, the settlement of the notes must be paid in cash pursuant to the terms of the relevant indentures. We currently have sufficient available cash, combined with borrowing capacity available under our Credit Facility and Bridge Credit Agreement, to fund such conversions.conversions should they occur.
CONTRACTUAL OBLIGATIONS
A summary of future obligations under our various contractual obligations and commitments as of December 31, 2016,2017, was disclosed in our 20162017 Annual Report on Form 10-K.
As described further in the Notes to Consolidated Financial Statements, Note 7 “Debt,” on June 6, 2017, we completed the private offering of $330 million aggregate principal amount of senior notes (4.875% Notes) due June 15, 2025. In addition, in the third quarter of 2017, we borrowed $300 million under our Credit Facility.
Other than the transactions described above,Bridge Credit Agreement we executed in January 2018, and the 1.625% Exchange in March 2018, there were no material changes to this previously filed information outside the ordinary course of business during the ninethree months ended September 30, 2017.March 31, 2018. Refer to Notes to Consolidated Financial Statements, Note 7, “Debt,” for further information on the transactions noted above.
CRITICAL ACCOUNTING ESTIMATES
When we prepare our consolidated financial statements, we use estimates and assumptions that may affect reported amounts and disclosures; actual results could differ from these estimates. Our critical accounting estimates relate to:
Health Plans segment medical claims and benefits payable. Refer to Notes to Consolidated Financial Statements, Note 6, “Medical Claims and Benefits Payable,” for a table that presents the components of the change in medical claims and benefits payable, and for additional information regarding the factors used to determine our changes in estimates for all periods presented in the accompanying consolidated financial statements. Other than the discussion as noted above, there have been no significant changes during the ninethree months ended September 30, 2017,March 31, 2018, to our disclosure reported in “Critical Accounting Estimates” in our Annual Report on Form 10-K for the year ended December 31, 2016.2017.
Health Plans segment contractual provisions that may adjust or limit revenue or profit. For a discussion of this topic, including amounts recorded in our consolidated financial statements, refer to Notes to Consolidated Financial Statements, Note 2, “Significant Accounting Policies.”
Health Plans segment quality incentives. For a discussion of this topic, including amounts recorded in our consolidated financial statements, refer to Notes to Consolidated Financial Statements, Note 2, “Significant Accounting Policies.”
Molina Medicaid Solutions segment revenueGoodwill and cost recognitionintangible assets, net.. There have been no significant changes during the ninethree months ended September 30, 2017,March 31, 2018, to our disclosure reported in “Critical Accounting Estimates” in our Annual Report on Form 10-K for the year ended December 31, 2016.
Goodwill and intangible assets, net. Please refer to Notes to Consolidated Financial Statements, Note 2, “Significant Accounting Policies,” regarding our adoption of Accounting Standards Update No. 2017-04 as of June 30, 2017, which has simplified the test for goodwill impairment. In the third quarter of 2017, we2017.
recorded impairment charges of $129 million for goodwill, and in the second quarter of 2017, we recorded impairment charges of $61 million for goodwill and $11 million for intangible assets, or $72 million in the aggregate. Such charges are reported in the accompanying consolidated statements of operations as “Impairment losses.” At September 30, 2017, goodwill and intangible assets, net, represented approximately 6% of total assets and 37% of total stockholders’ equity, compared with 10% and 46%, respectively, at December 31, 2016. Refer to Notes to Consolidated Financial Statements, Note 10, “Impairment Losses.”
SUPPLEMENTAL INFORMATION
FINANCIAL MEASURES THAT SUPPLEMENT U.S. GAAP (NON-GAAP FINANCIAL MEASURES)
We use these non-GAAP financial measures as supplemental metrics in evaluating our financial performance, making financing and business decisions, and forecasting and planning for future periods. For these reasons, management believes such measures are useful supplemental measures to investors in comparing our performance to the performance of other public companies in the health care industry.
EBITDA*
We believe that earnings before interest, taxes, depreciation and amortization (EBITDA*) is helpful in assessing our ability to meet the cash demands of our operating units.
| | | | Three Months Ended September 30, | | Nine Months Ended September 30, | Three Months Ended March 31, |
| 2017 | | 2016 | | 2017 | | 2016 | 2018 | | 2017 |
| | (In millions) | (In millions) |
| Net (loss) income | $ | (97 | ) | | $ | 42 |
| | $ | (250 | ) | | $ | 99 |
| |
| Net income | | $ | 107 |
| | $ | 77 |
|
| Adjustments: | | | | | | | | | | |
| Depreciation, and amortization of intangible assets and capitalized software | 39 |
| | 42 |
| | 129 |
| | 118 |
| 34 |
| | 46 |
|
| Interest expense | 32 |
| | 26 |
| | 85 |
| | 76 |
| 33 |
| | 26 |
|
| Income tax (benefit) expense | (16 | ) | | 50 |
| | (46 | ) | | 137 |
| |
| Income tax expense | | 72 |
| | 54 |
|
| EBITDA* | $ | (42 | ) | | $ | 160 |
| | $ | (82 | ) | | $ | 430 |
| $ | 246 |
| | $ | 203 |
|
ADJUSTED NET (LOSS) INCOME* AND ADJUSTED NET (LOSS) INCOME PER SHARE*
We believe that adjusted net (loss) income* and adjusted net (loss) income per diluted share* are helpful in assessing our financial performance exclusive of the non-cash impact of the amortization of purchased intangibles. The following table reconciles net income, which we believe to be the most comparable GAAP measure, to adjusted net (loss) income*.
| | | | Three Months Ended September 30, | | Nine Months Ended September 30, | Three Months Ended March 31, |
| 2017 | | 2016 | | 2017 | | 2016 | 2018 | | 2017 |
| | (In millions, except diluted per-share amounts) | (In millions, except diluted per-share amounts) |
| Net (loss) income | $ | (97 | ) | | $ | (1.70 | ) | | $ | 42 |
| | $ | 0.76 |
| | $ | (250 | ) | | $ | (4.44 | ) | | $ | 99 |
| | $ | 1.77 |
| |
| Net income | | $ | 107 |
| | $ | 1.64 |
| | $ | 77 |
| | $ | 1.37 |
|
| Adjustment: | | | | | | | | | | | | | | | | | | | | | | |
| Amortization of intangible assets | 7 |
| | 0.13 |
| | 9 |
| | 0.15 |
| | 24 |
| | 0.43 |
| | 24 |
| | 0.42 |
| 5 |
| | 0.08 |
| | 9 |
| | 0.16 |
|
Income tax effect (1) | (3 | ) | | (0.05 | ) | | (4 | ) | | (0.06 | ) | | (9 | ) | | (0.16 | ) | | (9 | ) | | (0.16 | ) | (1 | ) | | (0.01 | ) | | (3 | ) | | (0.06 | ) |
| Amortization of intangible assets, net of tax effect | 4 |
| | 0.08 |
| | 5 |
| | 0.09 |
| | 15 |
| | 0.27 |
| | 15 |
| | 0.26 |
| 4 |
| | 0.07 |
| | 6 |
| | 0.10 |
|
| Adjusted net (loss) income* | $ | (93 | ) | | $ | (1.62 | ) | | $ | 47 |
| | $ | 0.85 |
| | $ | (235 | ) | | $ | (4.17 | ) | | $ | 114 |
| | $ | 2.03 |
| |
| Adjusted net income* | | $ | 111 |
| | $ | 1.71 |
| | $ | 83 |
| | $ | 1.47 |
|
__________________________
| |
| (1) | Income tax effect of adjustments calculated at the blended federal and state statutory tax raterates of 22% and 37%. for the first quarters of 2018 and 2017, respectively. |
CONTROLS AND PROCEDURES
Evaluation of Disclosure Controls and Procedures: Our management, with the participation of our interim chief executive officer and our chief financial officer, has concluded, based upon its evaluation as of the end of the period covered by this report, that the Company’s “disclosure controls and procedures” (as defined in Rules 13a-15(e) and 15d-15(e) under the Securities Exchange Act of 1934, as amended (the “Exchange Act”)), were notare effective at the reasonable assurance level because of the material weakness in our internal control over financial reporting described below. Notwithstanding the material weakness described below, management has concludedto ensure that our consolidated financial statements included in this interim report on Form 10-Q are fairly stated in all material respects in accordance with U.S. generally accepted accounting principles (GAAP) for each of the periods presented herein.
Existence of a Material Weakness in Internal Control as of September 30, 2017
During the quarter ended September 30, 2017, we determined that a material weakness existed in our internal control over financial reporting relatinginformation required to the design and operating effectiveness of our internal control for our interim goodwill impairment tests for our Pathways subsidiary and Molina Medicaid Solutions segment. Specifically, spreadsheet formula errors in our valuation model, and errors madebe disclosed in the calculation of impairment lossesreports that we file or submit under the Exchange Act is recorded, were not detected in our review procedures. As a result, we initially miscalculatedprocessed, summarized, and reported within the goodwill impairmenttime periods specified in the threeSEC’s rules and nine months ended September 30, 2017. The impairment calculation was corrected prior to the filing of our unaudited consolidated financial statements as of and for the three and nine months ended September 30, 2017.
Remediation Plan for Material Weakness
We will implement a remediation plan developed to address this material weakness as of September 30, 2017. The remediation efforts we intend to implement include the enhancement of the design of the controls relating to the computation and rigor of review of the goodwill impairment tests. The enhancement of the controls will include the engagement of additional subject matter experts to support the valuation calculations, key assumptions and review process. In addition, we intend to develop new review controls that operate at an appropriate level of precision to prevent or detect potential material errors within the valuation calculations. We believe these measures will remediate the material weakness identified above and will strengthen our internal control over financial reporting for the computation of reporting unit fair value and potential consequent goodwill impairment. We are currently targeting to complete the implementation of the control enhancements during the fourth quarter of 2017. We will test the operating effectiveness of the control enhancements subsequent to implementation. If the remedial measures described above are insufficient to address the material weakness described above, or are not implemented timely, or additional deficiencies arise in the future, material misstatements in our interim or annual financial statements may occur in the future and could have the effects described in “Risk Factors,” in our Annual Report on Form 10-K for the year ended December 31, 2016.forms.
Changes in Internal Control Over Financial Reporting:Reporting. Except as described above, management did not identify anyThere has been no change in our internal control over financial reporting during the fiscal quarter ended September 30, 2017March 31, 2018 that has materially affected, or is reasonably likely to materially affect, our internal controls over financial reporting.
Existence of a Material Weakness in Internal Control as of December 31, 2016
As disclosed in our Annual Report on Form 10-K for the year ended December 31, 2016, our management assessed the effectiveness of our internal control over financial reporting as of December 31, 2016, based on the framework set forth in Internal Control-Integrated Framework (2013)issued by the Committee of Sponsoring Organizations of the Treadway Commission (COSO). A material weakness is a deficiency, or a combination of deficiencies, in internal control over financial reporting, such that there is a reasonable possibility that a material misstatement of the annual or interim financial statements will not be prevented or detected on a timely basis.
We determined that a material weakness existed in our internal control over financial reporting relating to the operation of an element of our process for calculating the amount owed to California by our California health plan. More specifically, a Medicaid Expansion contract amendment executed in the fourth quarter of 2016 changed the medical loss ratio corridor formula and such amendment was not initially considered in determining the liability. As a result, we understated net income by $44 million for the year ended December 31, 2016, which was material to our consolidated results for the year ended December 31, 2016. This amount was corrected prior to the issuance of our consolidated financial statements as of and for the year ended December 31, 2016.
Because of this material weakness, management concluded that we did not maintain effective internal control over financial reporting as of December 31, 2016, based on criteria described in Internal Control - Integrated Framework (2013) issued by COSO.
Remediation Plan for Material Weakness
We are executing the remediation plan developed to address the material weakness reported as of December 31, 2016. The remediation efforts we have implemented include the development of robust protocols to ensure that the control, relating to the review of a contractual amendment affecting the computation of the Medicaid Expansion medical loss ratio corridor for our California health plan, is operating as designed. We believe these measures will remediate the material weakness identified above and will strengthen our internal control over financial reporting for the computation of our California Medicaid Expansion medical loss ratio corridor. We currently are targeting to complete the implementation of the control enhancements during 2017. We will test the ongoing operating effectiveness of the control enhancements subsequent to implementation, and consider the material weakness remediated after the applicable remedial control enhancements operate effectively for a sufficient period of time. If the remedial measures described above are insufficient to address the material weakness described above, or are not implemented timely, or additional deficiencies arise in the future, material misstatements in our interim or annual financial statements may occur in the future and could have the effects described in “Risk Factors” in our Annual Report on Form 10-K for the year ended December 31, 2016.
LEGAL PROCEEDINGS
For information regarding legal proceedings, see Notes to Consolidated Financial Statements, Note 13,12, “Commitments and Contingencies.”
RISK FACTORS
Certain risks may have a material adverse effect on our business, financial condition, cash flows, results of operations, or stock price, and you should carefully consider them before making an investment decision. In addition to the other information set forth in this report, you should carefully consider the risk factors discussed in “Risk Factors,” in our Annual Report on Form 10-K for the year ended December 31, 2016 and our Quarterly Reports on Form 10-Q for the quarters ended March 31, 2017 and June 30, 2017. The risk factors described in our 20162017 Annual Report on Form 10-K and our Quarterly Reports on Form 10-Q for the quarters ended March 31, 2017 and June 30, 2017, are not the only risks that we face. Additional risks and uncertainties not currently known to us or that we currently deem to be immaterial may also materially adversely affect our business, financial condition, cash flows, results of operations, or stock price.
UNREGISTERED SALES OF EQUITY SECURITIES AND USE OF PROCEEDS
ISSUER PURCHASES OF EQUITY SECURITIES
Purchases of common stock made by us, or on our behalf during the quarter ended September 30, 2017,March 31, 2018, including shares withheld by us to satisfy our employees’ income tax obligations, are set forth below: |
| | | | | | | | | | | | | |
| | Total Number of Shares Purchased (1) | | Average Price Paid per Share | | Total Number of Shares Purchased as Part of Publicly Announced Plans or Programs | | Approximate Dollar Value of Shares Authorized to Be Purchased Under the Plans or Programs |
| July 1 - July 31 | 665 |
| | $ | 69.18 |
| | — |
| | $ | — |
|
| August 1 - August 31 | 285 |
| | $ | 57.03 |
| | — |
| | $ | — |
|
| September 1 - September 30 | — |
| | $ | — |
| | — |
| | $ | — |
|
| Total | 950 |
| | $ | 65.54 |
| | — |
| | |
|
| | | | | | | | | | | | | |
| | Total Number of Shares Purchased (1) | | Average Price Paid per Share | | Total Number of Shares Purchased as Part of Publicly Announced Plans or Programs | | Approximate Dollar Value of Shares Authorized to Be Purchased Under the Plans or Programs |
| January 1 - January 31 | 2,705 |
| | $ | 91.83 |
| | — |
| | $ | — |
|
| February 1 - February 28 | 17,365 |
| | $ | 90.63 |
| | — |
| | $ | — |
|
| March 1 - March 31 | 48,853 |
| | $ | 72.36 |
| | — |
| | $ | — |
|
| Total | 68,923 |
| | $ | 77.73 |
| | — |
| | |
_______________________
| |
| (1) | During the three months ended September 30, 2017,March 31, 2018, we withheld 95068,923 shares of common stock under our 2011 Equity Incentive Plan to settle employee income tax obligations. |
INDEX TO EXHIBITS
|
| | | | |
| Exhibit No. | | Title | | Method of Filing |
| | | |
| | Fourth Amended and Restated Bylaws of Molina Healthcare, Inc. | | Filed as Exhibit 3.1 to registrant’s Form 8-K filed March 2, 2018. |
| | | | |
| | Employment Agreement,Amended and Restated Commitment Letter, dated October 9, 2017,as of January 2, 2018, by and betweenamong Molina Healthcare, Inc., SunTrust Bank, SunTrust Robinson Humphrey, Inc., Barclays Bank PLC, MUFG, Bank of America, N.A., Merrill Lynch, Pierce, Fenner & Smith Incorporated, and Joseph M. Zubretsky. Morgan Stanley Senior Funding, Inc. | | Filed as Exhibit 10.1 to registrant’s Form 8-K filed October 10, 2017.January 2, 2018. |
| | | | |
| | Bridge Credit Agreement, dated as of January 2, 2018, by and among Molina Healthcare, Inc., as the Borrower, Molina Information Systems, LLC, Molina Pathways LLC and Pathways Health and Community Support LLC, as the Guarantors, SunTrust Bank, Barclays Bank PLC, The Bank of Tokyo-Mitsubishi UFJ, Ltd., Bank of America, N.A., and Morgan Stanley Senior Funding, Inc., as Lenders, and SunTrust Bank, as Administrative Agent. | | Filed as Exhibit 10.2 to registrant’s Form 8-K filed January 2, 2018. |
| | | | |
| | | | Filed herewith. |
| | | |
| | Section 302 Certification of Chief Financial Officer pursuant to Rules 13a-14(a)/15d-14(a) under the Securities Exchange Act of 1934, as amended. | | Filed herewith. |
| | | | |
| | | | Filed herewith. |
| | | |
| | Certification of Chief Financial Officer pursuant to 18 U.S.C. Section 1350, as adopted pursuant to Section 906 of the Sarbanes-Oxley Act of 2002. | | Filed herewith. |
| | | | |
| 101.INS | | XBRL Taxonomy Instance Document. | | Filed herewith. |
| | | |
| 101.SCH | | XBRL Taxonomy Extension Schema Document. | | Filed herewith. |
| | | |
| 101.CAL | | XBRL Taxonomy Extension Calculation Linkbase Document. | | Filed herewith. |
| | | |
| 101.DEF | | XBRL Taxonomy Extension Definition Linkbase Document. | | Filed herewith. |
| | | |
| 101.LAB | | XBRL Taxonomy Extension Label Linkbase Document. | | Filed herewith. |
| | | |
| 101.PRE | | XBRL Taxonomy Extension Presentation Linkbase Document | | Filed herewith. |
SIGNATURES
Pursuant to the requirements of the Securities Exchange Act of 1934, the registrant has duly caused this report to be signed on its behalf by the undersigned thereunto duly authorized.
|
| | | |
| | | | MOLINA HEALTHCARE, INC. |
| | | | (Registrant) |
| | | |
| Dated: | November 5, 2017April 30, 2018 | | /s/ JOSEPH W. WHITEM. ZUBRETSKY |
| | | | Joseph W. WhiteM. Zubretsky |
| | | | Interim Chief Executive Officer
|
| | | | (Principal Executive Officer) |
| | | |
| Dated: | November 5, 2017April 30, 2018 | | /s/ JOSEPH W. WHITE |
| | | | Joseph W. White |
| | | | Chief Financial Officer and Treasurer |
| | | | (Principal Financial Officer) |
Molina Healthcare, Inc. 2017March 31, 2018 Form 10-Q | 6755