
M ay 1 0 , 2 0 2 1 Tr a n s f o r m i n g t h e m a n a g e m e n t o f d e r m a t o l o g i c c a n c e r s a n d o t h e r d e r m a t o l o g i c d i s e a s e s w i t h h i g h u n m e t n e e d

D I S C L A I M E RS F O R W A R D - L O O K I N G S T A T E M E N T S The information in this press release contains forward-looking statements and information within the meaning of Section 27A of the Securities Act of 1933, as amended, and Section 21E of the Securities Exchange Act of 1934, as amended, which are subject to the “safe harbor” created by those sections. These forward-looking statements include, but are not limited to, statements concerning the effects of the COVID-19 pandemic on our business and our efforts to address its impact on our business, statements concerning the estimated size of our total addressable market or our existing and pipeline products, the impact, accuracy and effectiveness of our tests, including DecisionDx-Melanoma, DecisionDx-SCC and DecisionDx DiffDx- Melanoma, on physicians, patients and their treatment plans, our prospects and plans and the objectives of management and statements concerning the expectation that Castle will complete the acquisition of Myriad myPath Laboratory and the expected timing of the consummation of the transaction, Castle's ability to integrate the myPath Melanoma test into its commercial offerings and deliver the most comprehensive molecular testing offering for difficult-to-diagnose melanocytic lesions. The words “anticipates,” “believes,” “estimates,” “expects,” “intends,” “may,” “plans,” “projects,” “will,” “would” and similar expressions are intended to identify forward-looking statements, although not all forward-looking statements contain these identifying words. We may not actually achieve the plans, intentions, or expectations disclosed in our forward-looking statements and you should not place undue reliance on our forward-looking statements. Actual results or events could differ materially from the plans, intentions and expectations disclosed in the forward-looking statements that we make. These forward-looking statements involve risks and uncertainties that could cause our actual results to differ materially from those in the forward-looking statements, including, without limitation, the effects of the COVID-19 pandemic on our business and our efforts to address its impact on our business, subsequent study results and findings that contradict earlier study results and findings, our tests', including DecisionDx-Melanoma, DecisionDx-SCC and DecisionDx DiffDx-Melanoma, ability to provide the aforementioned benefits to patients, the conditions to closing the myPath Melanoma acquisition may not be satisfied and the transaction may be delayed or not close at all, and the risks set forth in our Quarterly Report on Form 10-Q for the quarter ended March 31, 2021, and in our other filings with the SEC. The forward-looking statements are applicable only as of the date on which they are made, and we do not assume any obligation to update any forward-looking statements, except as may be required by law. 2
TRANSFORMING THE MANAGEMENT OF SKIN CANCER AND OTHER DERMATOLOGIC DISEASES WITH HIGH UNMET CLINICAL NEED EXPANSIVE BODY OF EVIDENCE SUITE OF DERMATOLOGIC PROGNOSTIC AND DIAGNOSTIC TESTS STRONG FINANCIAL POSITION ROBUST PIPELINE L E A D I N G D E R M ATO LO G I C D I A G N O S T I C S C O M PA N Y 3 CULTURE OF INNOVATION

F I N A N C I A L S U M M A RY 1 Q 2 0 2 1 1Q21 1Q20 Revenue $22.8M $17.4M Adj. Revenue 1 $17.5M $14.3 Total GEP test reports 2 5,142 4,935 Total Derm test reports 2 4,805 4,574 Operating Cash Flow $(3.6)M $(0.3)M Adj. Operating Cash Flow 1 $(5.5)M $(0.3)M Gross Margin 87% 86% Adj. Gross Margin 1 83% 83% Cash & Cash Equivalents 3 $407M $99M 1See Non-GAAP reconciliations at the end of this presentation. 2Castle had two commercially available GEP tests in 2019. 3 As of 3/31/2021 4

Through this acquisition, which is subject to customary closing conditions and is expected to close in late May 2021, Castle believes more patients will receive actionable results more of the time, enabling a more confident diagnosis and clearer treatment path. myPath Laboratory is a CLIA-certified laboratory in Salt Lake City, where the myPath Melanoma 23-gene expression profile (GEP) test is currently offered Designed to be used as an adjunct to histopathology when the distinction between a benign nevus and a malignant melanoma cannot be made confidently by histopathology alone With the acquisition, Castle strategically expands its suite of genomic tests for skin cancer myPath Melanoma and DIffDx-Melanoma are included in NCCN guidelines myPath Melanoma is currently covered under a MolDX Local Coverage Determination policy through Noridian 5 C a s t l e S i g n s D e f i n i t i v e A g r e e m e n t t o A c q u i re my Pa t h ® M e l a n o m a L a b o ra t o r y C a s t l e e x p e c t s t o m a k e a v a i l a b l e t h e m o s t c o m p r e h e n s i v e m o l e c u l a r t e s t i n g o f f e r i n g f o r d i f f i c u l t - t o - d i a g n o s e m e l a n o c y t i c l e s i o n s

Factors Defining Success Committed to dermatology and informing clinical management decisions Robust development pipeline and proven track record of AI informed GEP algorithms Steering committee with world- class KOLs Large study investment for development and validation E X PA N D I N G C A S T L E ’ S G E N O M I C T E S T S TO N O N - S K I N C A N C E R M E D I C A L D E R M ATO LO GY 6 I n n o v a t i v e p i p e l i n e t e s t f o r p r e d i c t i n g s y s t e m i c t h e r a p y r e s p o n s e Psoriasis Atopic Dermatitis Related Conditions Psoriasis Atopic Dermatitis Gender 49% Female 53% Female Age at Diagnosis (average) Early fifties Mid thirties Severity ~30% moderate to severe >50% moderate to severe

PAT I E N T J O U R N E Y F O R P S O R I A S I S , AT O P I C D E R M AT I T I S A N D R E L AT E D C O N D I T I O N S E x p a n d s o u r r e a c h i n t o n o n - s k i n c a n c e r, m e d i c a l d e r m a t o l o g i c d i s e a s e s 7 Patient presents with skin signs and symptoms to PCP or dermatologist Clinical diagnosis of psoriasis, atopic dermatitis or related condition is made Patient achieves faster treatment response time resulting in improved patient outcomes and QoL Personalized therapy guidance leads to reduced medication switches and health care savings Management plan determined, based on individual biological profile Typically, topical treatment is initiated, while some proceed directly to systemic therapy based on disease severity Depending on initial treatment efficacy or disease severity, systemic treatment is considered Clinician orders innovative test to support decision making
P R O B L E M : T H E U N M E T N E E D I N M O D E R AT E T O S E V E R E P S O R I A S I S A N D AT O P I C D E R M AT I T I S C O M M O N S K I N D I S E A S E S W I T H S I G N I F I C A N T PAT I E N T I M PA C T S A N D C O S T S T O H E A LT H C A R E S Y S T E M Treatments are significantly different for PSO and AD. Previously, treatments for AD were inexpensive (e.g., topical steroids), but are now costly (e.g., Dupixent for ~$38k/year). Costly therapies for moderate/severe psoriasis are common (e.g., Humira for ~$68k/year). Systemic therapy guidance tools have the potential to streamline therapeutic interventions for patients and avoid ineffective, expensive medication courses. Psoriasis (PSO) and Atopic Dermatitis (AD) are among the most frequently seen skin rashes, and their diagnosis is most often made clinically by the treating clinician. 8 Cutaneous T Cell Lymphoma (CTCL) can mimic clinical presentation of AD and PSO. A subset of patients with PSO (approximately 20-30% of affected individuals) will go on to develop psoriatic arthritis, which can produce irreversible joint damage and significant patient morbidity.

Indication/ Test outcome Trade Name Reimbursement Status Peer-Reviewed Publications Primary Customers Initial Launch Targets Initial addressable market, patients2 Estimated U.S. TAM Cutaneous melanoma/ Risk of metastasis MCR, MCRA Commercial – in process 30 Derms (including Mohs), Surgeons __ ~130k patients classified as Stage I, II or III ~$540M Cutaneous squamous cell carcinoma/ Risk of metastasis Expected draft LCD in 2021 4 Derms (including Mohs) ~4,365 current customers3 ~200k w/ high-risk features ~$820M Suspicious pigmented lesions/ Melanoma status Expected draft LCD in 2021 2 Dermpaths, Derms ~1,740 current dermpath customers4 ~300k patients w/indeterminant biopsy ~$600M Pipeline Tests (including psoriasis/AD) Target launches anticipated by the end of 2025 N/A N/A Expected to utilize existing dermatologic sales channels To be announced To be announced ~$3.6B E S T I M AT E D ~ $ 5 . 5 B U. S . TOTA L A D D R E S S A B L E M A R K E T 1 I n m a r ke t a n d p i p e l i n e t e s t s , l e v e r a g i n g e s t a b l i s h e d d e r m a t o l o g i c s a l e s c h a n n e l s 1U.S. TAM = Total addressable market based on estimated patient population assuming average reimbursement rate among all payors. 2 Annual U.S. incidence for Stage I, II o r III melanoma estimated at 130,000; Annual U.S. incidence for squamous cell carcinoma estimated at 1,000,000 with addressable market limited to carcinomas with one or more high risk features; Annual U.S. incidence for suspicious pigmented lesion biopsies estimated at 2,000,000 with addressable market limited to the 15% with an indeterminant biopsy. 3Clinicians who ordered DecisionDx-Melanoma in last twelve months (as of 3/31/2020) 4Pathologists who provided clinical specimens for DecisionDx-Melanoma in last twelve months (as of 3/31/2020) -MCR = Medicare. MCRA = Medicare Advantage; current customer estimates based on last twelve months. 9

Pipeline Expansion 2022 C A S T L E ’ S L O N G - T E R M R E V E N U E G R O W T H P OT E N T I A L 10 CUTANEOUS MELANOMA 2021 SQUAMOUS CELL CARCINOMA CUTANEOUS MELANOMA ADDITIONAL TESTS FOR DERMATOLOGIC DISEASES 2025 (Expanded LCD effective Dec 2020) (Potential LCDs effective in 2022) (Expected launches ~2025)
T H E C A S T L E A P P R O A C H CAP-accredited, CLIA- certified commercial labs Identify dermatologic diseases with high unmet medical need, where genomic information has the potential to improve management decisions Suite of skin cancer tests designed to provide clinicians with precise, personalized information, enabling more accurate treatment plan decisions Leveraging artificial intelligence, tests are designed to provide actionable information based on tumor gene expression patterns Test results inform management decisions within nationally accepted treatment guidelines 11

Informing clinical decision making for patients with invasive melanoma

If melanoma, clinician orders to answer SLNB and/or management questions: • Is the risk of SLN-positivity high enough to warrant referral for the SLNB surgery? • What is the individual risk of recurrence? D E C I S I O N D X - M E L A N O M A : A F T E R D I A G N O S I S O F C A N C E R 13 Patient presents with mole to PCP or dermatologist Physician may order biopsy Biopsy results received: • Positive for melanoma • Negative • Uncertain malignant potential Physician may order SLNB, if warranted per clinicopathological features and Management plan determined, based on personalized risk
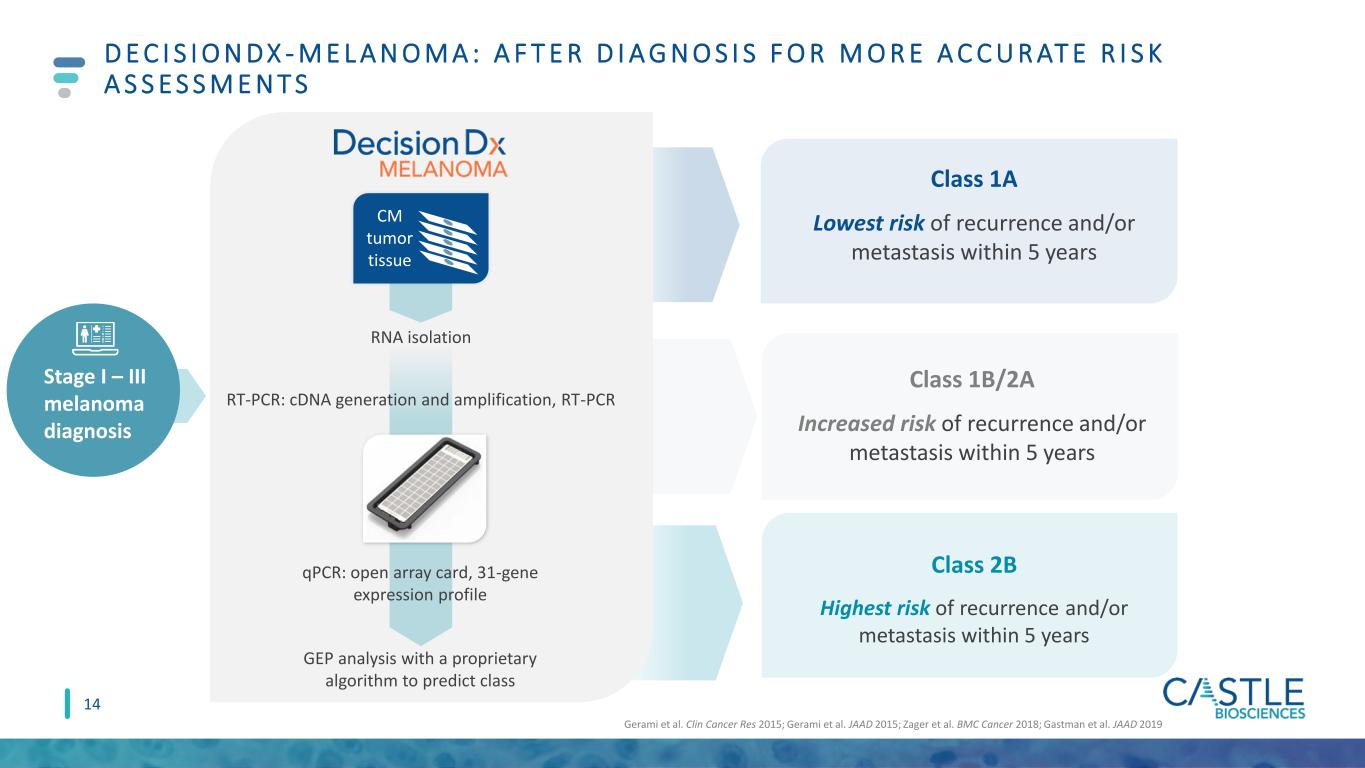
Gerami et al. Clin Cancer Res 2015; Gerami et al. JAAD 2015; Zager et al. BMC Cancer 2018; Gastman et al. JAAD 2019 D E C I S I O N D X - M E L A N O M A : A F T E R D I A G N O S I S F O R M O R E A C C U R AT E R I S K A S S E S S M E N T S qPCR: open array card, 31-gene expression profile CM tumor tissue RNA isolation RT-PCR: cDNA generation and amplification, RT-PCR GEP analysis with a proprietary algorithm to predict class Stage I – III melanoma diagnosis Class 1A Lowest risk of recurrence and/or metastasis within 5 years Class 2B Highest risk of recurrence and/or metastasis within 5 years 14 Class 1B/2A Increased risk of recurrence and/or metastasis within 5 years

I N T E G R AT E D T E S T R E S U LT i 3 1 - G E P u t i l i z e s a r t i f i c i a l i n t e l l i g e n c e d e s i g n e d t o p r o v i d e a m o r e p r e c i s e p r e d i c t i o n o f S L N p o s i t i v i t y r i s k 15 The new Integrated Test Result incorporates traditional clinicopathologic factors with the DecisionDx-Melanoma continuous score designed to provide a precise, personalized likelihood of sentinel lymph node positivity
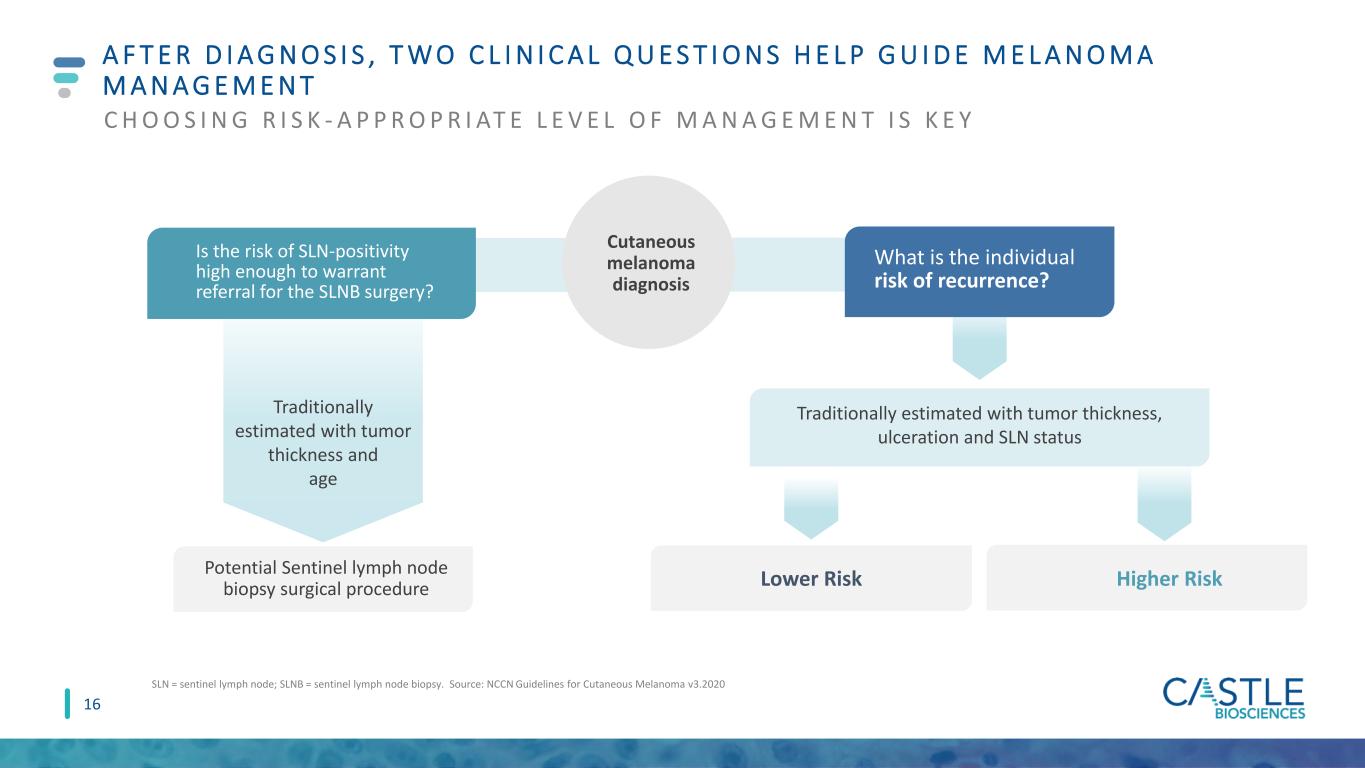
Cutaneous melanoma diagnosis A F T E R D I A G N O S I S , T W O C L I N I C A L Q U E S T I O N S H E L P G U I D E M E L A N O M A M A N A G E M E N T C H O O S I N G R I S K - A P P R O P R I AT E L E V E L O F M A N A G E M E N T I S K E Y SLN = sentinel lymph node; SLNB = sentinel lymph node biopsy. Source: NCCN Guidelines for Cutaneous Melanoma v3.2020 What is the individual risk of recurrence? Higher RiskLower Risk 16 Traditionally estimated with tumor thickness, ulceration and SLN status Traditionally estimated with tumor thickness and age Is the risk of SLN-positivity high enough to warrant referral for the SLNB surgery? Potential Sentinel lymph node biopsy surgical procedure

D E C I S I O N D X - M E L A N O M A I N F O R M S B OT H R I S K A S S E S S M E N T S , N O W W I T H i 3 1 - G E P TO P R E D I C T S L N P O S I T I V I T Y R I S K Vetto et al. Future Oncol 2019; Marks et al SKIN J Cutaneous Med 2019 NEW i31-GEP algorithm Risk of existing metastasis to SLN For SLNB eligible patients with: DecisionDx-Melanoma informs management (clinical follow- up, referrals, imaging, adjuvant therapy) Risk of recurrence • T ≥0.3 mm • T1a with adverse features • T1b-T4 DecisionDx-Melanoma informs use of SLNB 17 For patients with: 31-GEP continuous score + Breslow Thickness Ulceration Mitotic rate Age i31-GEP algorithm integrates test score with clinicopathologic factors for precise and personalized risk Class 1A: lowest risk Class 1B/2A: increased risk Class 2B: highest risk

D E C I S I O N D X - M E L A N O M A S T R AT I F I ES R I S K O F P O S I T I V E S L N TO I N F O R M D I S C U S S I O N S Objective: right treatment, right patient, right time Text sources: 1Systematic review of 21 articles representing 9,047 patients (Moody Eur J Sur Onc 2016); 2Morton NEJM 2014; 3False negative rate definition limited to metastasis to the regional lymphatics, not to distant metastasis or death. Median false negative rate = 17.6%; 3Sondak & Zager Ann Surg Oncol 2010 Graph sources: • SLN = sentinel lymph node; SLNB = sentinel lymph node biopsy. MCR=Medicare Cost Report. • Source: AJCC v7 J Clin Oncol 2009; SEER data release 2017; Morton et al. N Engl J Med 2014; Whiteman et al. J Invest Dermatol 2015; Shaikh et al. J Natl Cancer Inst 2016; Poklepovic and Carvajal. Oncology 2018; Sondak and Zager. Ann Surg Oncol 2010. Moody et al. Euro Jrnl Surg Onc 2017. LIMITATIONS OF CURRENT STAGING TO INFORM SLNB SURGERY 12% 11% 18% $20-24k SLNB Positivity Average Complication Rate Median Regional False Negative Rate Average Reimbursed Cost SLNB: risky, poor prognostic tool • 88% SLNB recipients negative • Anesthesia risks, surgical complications: 11% 1 • False negative: 5% - 21%3 • No survival benefit, low sensitivity: • 2/3 of melanoma deaths were SLN-negative 2 18

S O LU T I O N 1 : D E C I S I O N D X - M E L A N O M A I N F O R M S S L N B S U R G E RY D I S C U S S I O N S I N T 1 a – T 4 M E L A N O M A S I31-GEP is designed to take patients from population-based risk to more precise, personalized risk to guide SLNB discussions DecisionDx-Melanoma could result in 74% fewer SLNB surgeries, potentially saving U.S. healthcare system $250M1,3 1Vetto et al. Future Oncol 2019. 2Hsueh et al. Poster discussion abstract, ASCO 2019. 3Clearview health economic model, data on file. T1-T2 tumors are ≤2.0mm thick (“Breslow’s” thickness or depth). MSS = melanoma specific survival. OS = overall survival. DMFS = distant metastasis free survival. RFS = recurrence free survival. n/r = not reported. Outcomes confirmed in prospective, multi-center study2 19

Text sources:1Poklepovic and Carvajal. ONCOLOGY 2018; 2Ribas et al. JAMA 2016; 3Schadendorf et al. Eur J Can 2017; 4Robert et al. J Clin Oncol 2017; 5Joseph et al. Clin Cancer Res 2018; 6SEER data release 2017; 7Whiteman et al. J Invest Dermatol 2015; 8Shaikh et al. J Natl Cancer Inst 2016 Graph sources: AJCC v7 J Clin Oncol 2009; SEER data release 2017; Morton et al. N Engl J Med 2014; Whiteman et al. J Invest Dermatol 2015; Shaikh et al. J Natl Cancer Inst 2016; Poklepovic and Carvajal. Oncology 2018; Sondak and Zager. Ann Surg Oncol 2010. Moody et al. Euro Jrnl Surg Onc 2017. P R O B L E M 2 : U N D E R - M A N A G E M E N T E V I D E N T I N M E L A N O M A C U R R E N T R I S K A S S E S S M E N T S M I S S PAT I E N T S W I T H A G G R E S S I V E T U M O R B I O L O G Y 34% 66% “High-risk” patients “Low-risk” patients DEATHS FROM MELANOMAEarly detection, lower tumor burden associated with better therapy responses, survival outcomes1-5 Appropriate surveillance, including imaging of high-risk patients, is critical1-5 AJCC clinicopathologic factors are helpful clinically, but majority of deaths occur in patients diagnosed with early-stage disease6-8 Prognostic accuracy must improve to determine the most appropriate melanoma management strategy for each patient 20
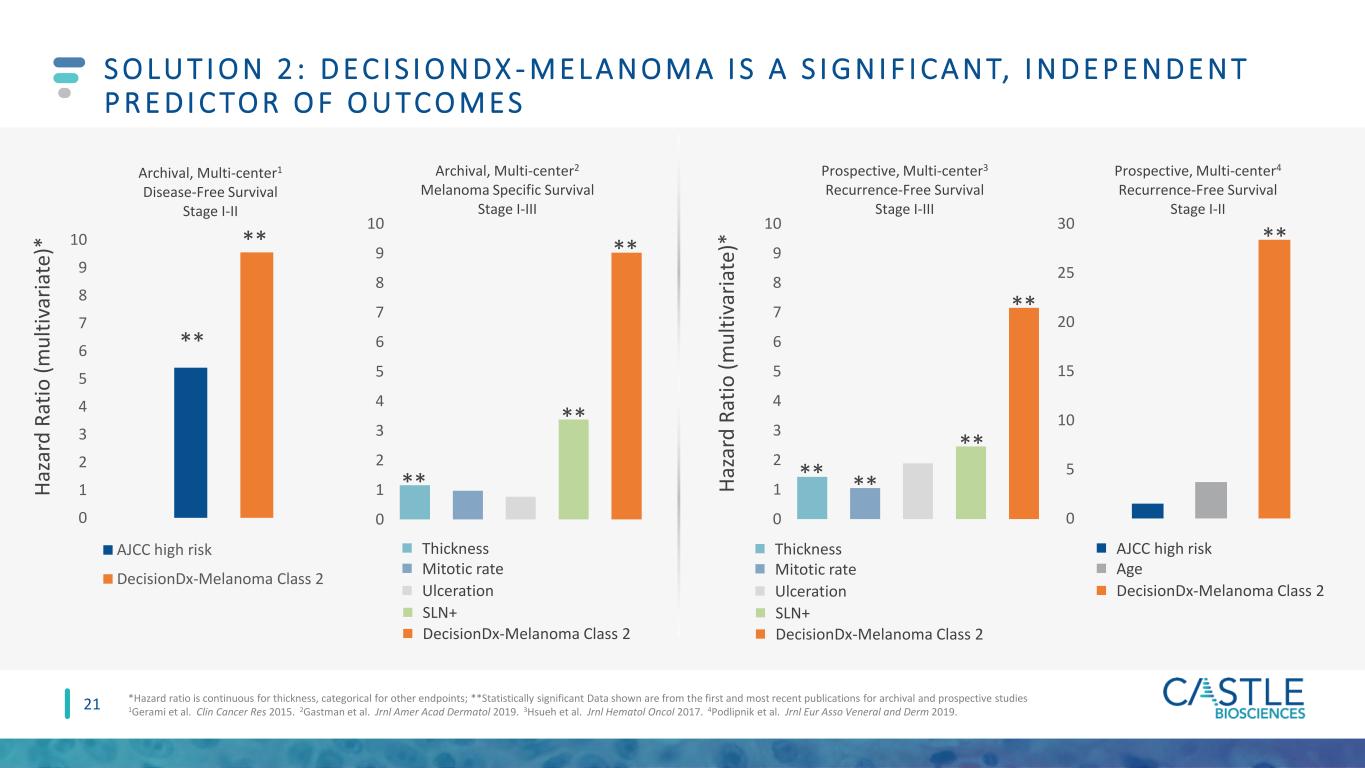
0 1 2 3 4 5 6 7 8 9 10 Archival, Multi-center1 Disease-Free Survival Stage I-II AJCC high risk DecisionDx-Melanoma Class 2 0 5 10 15 20 25 30 Prospective, Multi-center4 Recurrence-Free Survival Stage I-II 0 1 2 3 4 5 6 7 8 9 10 Archival, Multi-center2 Melanoma Specific Survival Stage I-III 0 1 2 3 4 5 6 7 8 9 10 Prospective, Multi-center3 Recurrence-Free Survival Stage I-III H a za rd R a ti o ( m u lt iv a ri a te )* H a za rd R a ti o ( m u lt iv a ri a te )* ** ** ** ** ** ** ** ** ** ** S O LU T I O N 2 : D E C I S I O N D X - M E L A N O M A I S A S I G N I F I C A N T, I N D E P E N D E N T P R E D I C TO R O F O U TC O M E S *Hazard ratio is continuous for thickness, categorical for other endpoints; **Statistically significant Data shown are from the first and most recent publications for archival and prospective studies 1Gerami et al. Clin Cancer Res 2015. 2Gastman et al. Jrnl Amer Acad Dermatol 2019. 3Hsueh et al. Jrnl Hematol Oncol 2017. 4Podlipnik et al. Jrnl Eur Asso Veneral and Derm 2019. AJCC high risk Age DecisionDx-Melanoma Class 2 Thickness Mitotic rate Ulceration SLN+ DecisionDx-Melanoma Class 2 Thickness Mitotic rate Ulceration SLN+ DecisionDx-Melanoma Class 2 21

Low Risk Stage I-IIA High Risk Stage IIB-III NCCN Risk Category Prado et al. SKIN J Cutan Med 2018:suppl 2. n=690 D E C I S I O N D X - M E L A N O M A F U R T H E R S T R AT I F I ES R I S K O F R E C U R R E N C E B E YO N D A J C C ( 8 T H E d . ) S TA G I N G 22 STAGE M e la n o m a -S p e ci fi c S u rv iv a l (M S S ) (% ) 100% 90% 80% 70% 60% I 99.6% ≈AJCC IA 89.5% ≈AJCC IIIA 98% II >99% ≈AJCC IA 84.7% ≈AJCC IIIB 90% III 94.8% ≈AJCC IIA 61.2% ≈AJCC IIIC+ 77% Castle Class 1A MSS Castle Class 2B MSS AJCC MSS

S O LU T I O N 2 : D E C I S I O N D X - M E L A N O M A C H A N G E D M A N A G E M E N T F O R 5 0 % O F PAT I E N T S 1Berger, et al. 2016 Curr Med Res Opin; 2Dillon et al. 2018 Skin; 3Farberg et al. 2017 Jrnl Drugs Derm; 4Schuitevoerder, et al. 2018 Jrnl Drugs Derm. Changes in patient management include: Imaging and labs Sentinel lymph node biopsy guidance Clinical visit frequency Referrals Study Design # of Patients % Change in Management Berger1 Prospectively tested cohort, multi-center. Retrospective pre-test / post-test management. 156 53% Dillon2 Prospective, multi-center: pre-test / post-test management 247 49% Farberg3 169 physician impact study: patient vignettes with pre-test / post-test management n/a 47-50% Schuitevoerder4 Prospectively tested cohort, single center. Retrospective pre-test / post-test management; modeling of prospective cohort 91 52% 4 consecutive clinical impact studies: 47-53% change in risk-of-recurrence-based management 23

D E C I S I O N D X - M E L A N O M A : W E L L - S T U D I E D, I N F O R M S C A N C E R M A N A G E M E N T D E C I S I O N S * A C C O R D I N G T O S O R T S Y S T E M , U S E D B Y A A D Patients included in studies including independent validation >5,700 Peer-reviewed, published studies including 2 meta-analyses 30 Demonstrated change in management for 1 of 2 patients tested 50% Level 1A evidence* 1A Patients with a DecisionDx-Melanoma order from more than 7,700 clinicians ~74,000 Covered by Medicare and multiple private insurers with an industry- leading patient assistance program Medicare+ 24

Identifying the risk of metastasis in patients with cutaneous squamous cell carcinoma with one or more risk factors

PAT I E N T J O U R N E Y: W H E R E D E C I S I O N DX - S C C F I T S 26 Patient referred to a dermatologist who performs a skin exam History and physical • Complete skin exam • Regional lymph node exam Skin biopsy Lesion suspicious for skin cancer discovered by patient or PCP Diagnosis of SCC with≥1 risk factor Order placed for Test results received for Treatment plan defined • Curettage and electrodesiccation • Standard excision • Excision with wide margins • Mohs

P R O B L E M : T H E U N M E T N E E D I N H I G H - R I S K S C C PAT I E N T S : W H O I S R E A L LY AT L O W R I S K O R H I G H R I S K F O R M E TA S TA S I S ? NCCN=National Comprehensive Cancer Network; BWH = Brigham and Women’s Hospital; AJCC = American Joint Committee on Cancer ~20% of SCC patients (200,000 annually) have one or more clinical or pathological risk factors, and a subset will develop metastasis. They suffer the majority of SCC mortality. These factors alone are often not specific enough to determine risk-appropriate treatment and further management. SCC treatment plans are guided by risk of metastasis. Risk-appropriate SCC management is currently limited by classification systems (NCCN, BWH, AJCC) with low positive predictive value (PPV). Deaths from SCC are now estimated to exceed those from melanoma. 27
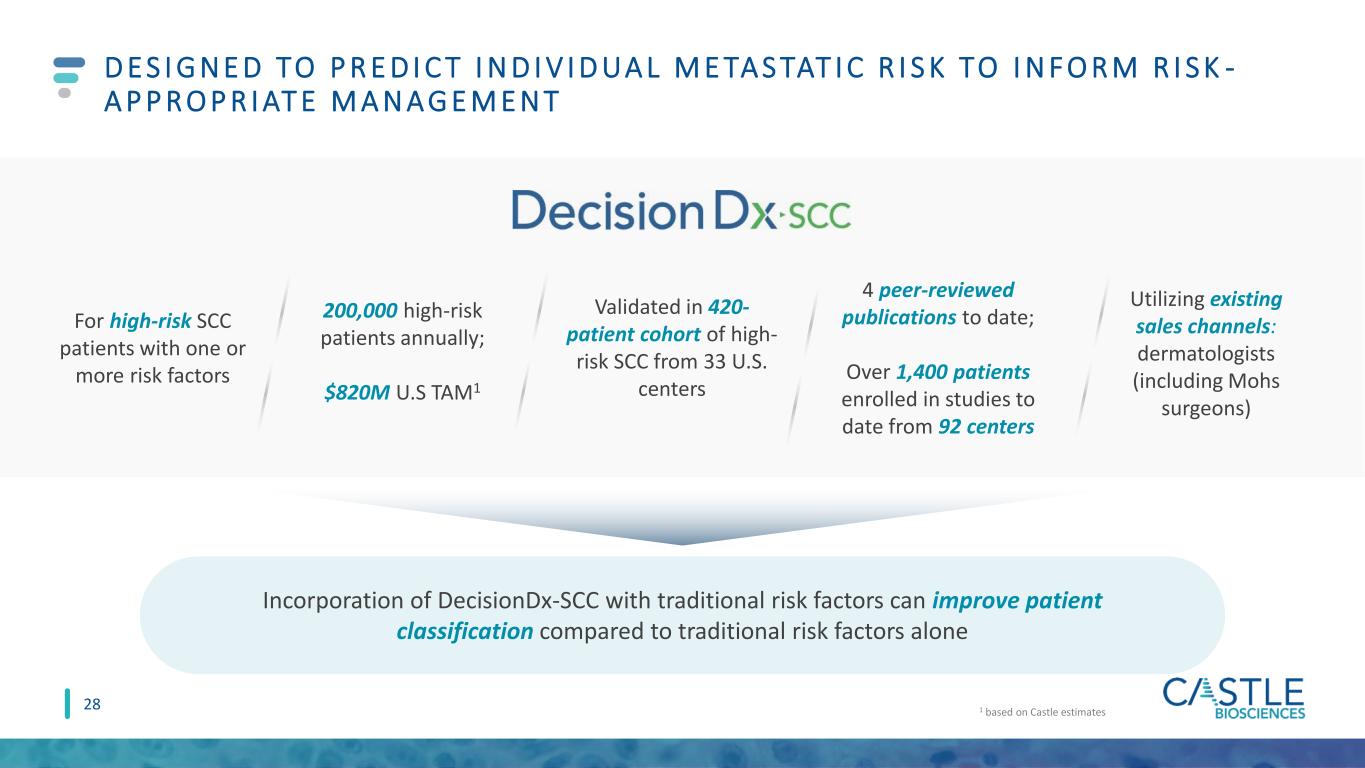
200,000 high-risk patients annually; $820M U.S TAM1 Validated in 420- patient cohort of high- risk SCC from 33 U.S. centers 4 peer-reviewed publications to date; Over 1,400 patients enrolled in studies to date from 92 centers D E S I G N E D TO P R E D I C T I N D I V I D UA L M E TA S TAT I C R I S K TO I N F O R M R I S K - A P P R O P R I AT E M A N A G E M E N T 1 based on Castle estimates Incorporation of DecisionDx-SCC with traditional risk factors can improve patient classification compared to traditional risk factors alone For high-risk SCC patients with one or more risk factors Utilizing existing sales channels: dermatologists (including Mohs surgeons) 28

W O R K F LOW F O R D E C I S I O N D X - S C C : P R O C E S S I D E N T I C A L TO D E C I S I O N D X - M E L A N O M A qPCR: open array card 34 discriminant gene targets and 6 control genes Class 1 low metastatic risk (~50% of results)a Class 2A moderate metastatic risk (~40% of results) Class 2B high metastatic risk (<10% of results) SCC tumor tissue RNA isolation RT-PCR: cDNA generation and amplification Analysis of GEP with a proprietary algorithm to determine Class and metastatic risk Wysong et al. JAAD 2020; Data on file, Castle Biosciences NCCN Guidelines for Squamous Cell Skin Cancer v1.2020, Likhacheva et al. Pract Radiat Oncol 2020, Farberg et al. CMRO 2020, Litchman et al. CMRO 2020, Teplitz et al. JDD 2019, Alam et al. JAAD 2018 . DecisionDx-SCC results can inform management decisions within established guidelines • Surgery, if feasible • Consider nodal imaging / staging • Consider oncology referral • Surgery, if feasible • Nodal imaging / staging • Consultation: radiation oncology • Consultation: medical oncology Treatment plans may include • Surgery, if feasible • Clinical nodal exam Follow-up plans may include • Clinical follow-up: 1-2x per year • Clinical nodal exam • Clinical follow-up: 2-4x per year for 3 years • Baseline and annual nodal US/CT for 2 years • Clinical follow-up: 4-12x per year for 3 years • Baseline and 4x per year nodal US/CT for 2 years Patient diagnosed with SCC and one or more risk factors 29

M e ta st a si s- fr e e s u rv iv a l (M FS ) Years Kaplan-Meier Estimated MFS n = 420 p < 0.0001 D E C I S I O N D X - S C C I S VA L I D AT E D TO P R E D I C T M E TA S TAT I C R I S K F O R I N D I V I D UA L S C C PAT I E N T S W I T H O N E O R M O R E R I S K FA C TO R S Wysong et al. JAAD 2020; Ibrahim et al. submitted; Data on file, Castle Biosciences. Class 1 – Low Biological Risk Less than half the general study population risk Class 2A – Moderate Biological Risk Similar to the strongest traditional factors Class 2B – High Biological Risk ≥50% risk of metastasis 30

C L A S S 2 A A N D C L A S S 2 B A R E I N D E P E N D E N T P R E D I C TO RS O F M E TA S TA S I S Deep invasion: beyond subcutaneous fat, depth >6mm, or Clark level V. Wysong et al. JAAD 2020; Ibrahim et al. submitted; Data on file, Castle Biosciences. W h a t i s t h e i m p a c t o f D e c i s i o n D x - S C C ? Immunosuppression Tumor diameter (per cm) Perineural invasion Deep invasion Poor differentiation Class 2A Class 2B Univariate Analysis Multivariate Analysis NA 1.1 (ns) 1.2 (ns) 2.1 (p<0.001) 2.3 (p<0.001) 2.3 (p<0.001) 6.9 (p<0.001) 1.5 (ns) 1.2 (p<0.001) 3.3 (p<0.001) 3.1 (p<0.001) 3.9 (p<0.001) 3.2 (p<0.001) 11.6 (p<0.001) Hazard Ratio (HR) Hazard Ratio (HR) 0 5 10 Hazard Ratio 0 5 10 azard Ratio An SCC with deep invasion is 2.1x more likely to metastasize than without. Adding a Class 2A results shifts that to 4.8x more likely to metastasize. Adding a Class 2B result shifts that to 14.5x more likely to metastasize. 31

A highly accurate and objective test for melanocytic lesions of unknown malignant potential
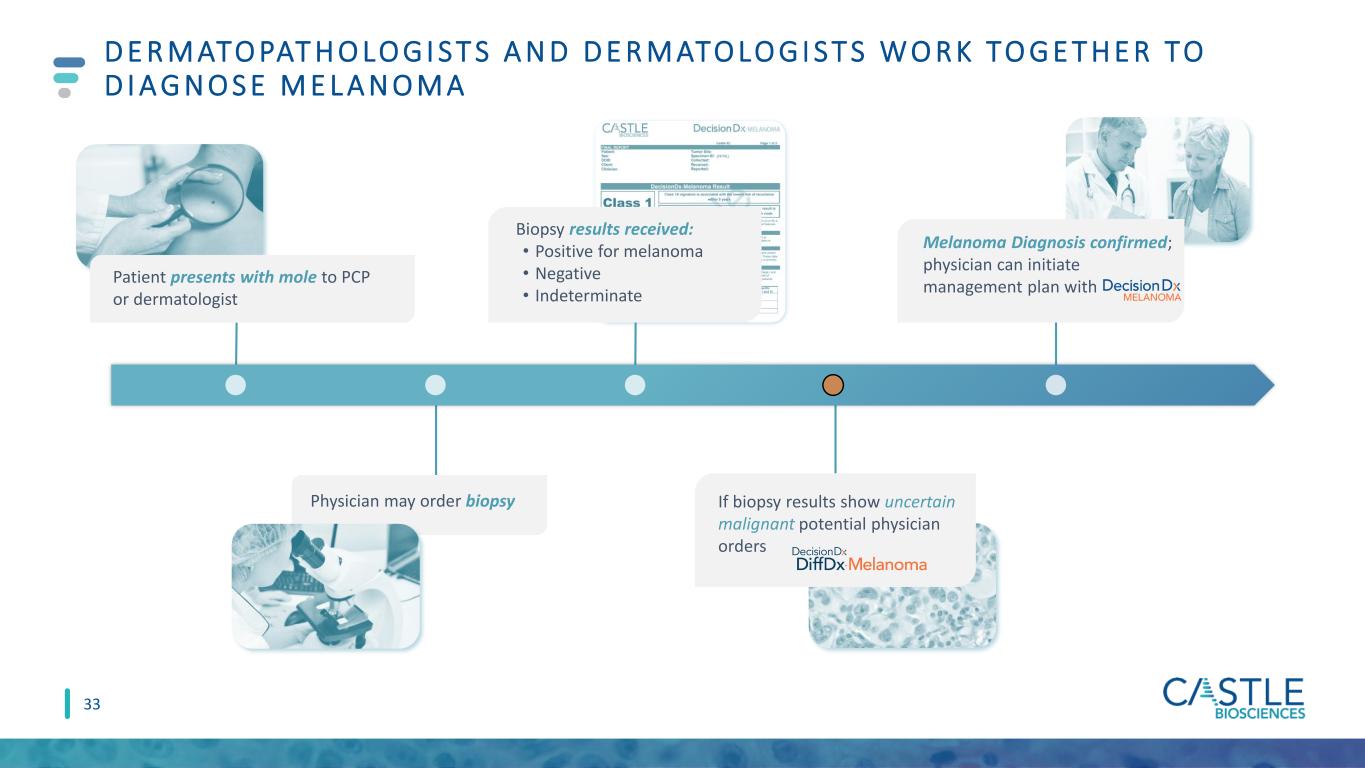
D E R M ATO PAT H O LO G I S T S A N D D E R M ATO LO G I S T S W O R K TO G E T H E R TO D I A G N O S E M E L A N O M A 33 Patient presents with mole to PCP or dermatologist Biopsy results received: • Positive for melanoma • Negative • Indeterminate If biopsy results show uncertain malignant potential physician orders Melanoma Diagnosis confirmed; physician can initiate management plan with Physician may order biopsy

T H E C L I N I C A L I S S U E : U N C E R TA I N T Y C R E AT E S A N O V E R - O R U N D E R - T R E AT M E N T D I L E M M A Definitive melanoma diagnoses (invasive or in situ) Definitive benign diagnoses SLNB Imaging Increased Follow-up No additional treatment Routine follow-up Clinically evaluated suspicious pigmented lesions Wide Local Excision ~2 million melanocytic skin biopsies Uncertain malignant potential Primary treatment Staging, surveillance, and follow-up options Histopathologic evaluation 34

D E C I S I O N D X D I F F DX - M E L A N O M A I S D E S I G N E D F O R U S E F O L LO W I N G I M M U N O H I S TO C H E M I S T R Y ( I H C ) A N D / O R LO C A L C O N S E N S U S Uncertain malignant potential IHC stains/recuts or local consensus conference/colleagues Uncertain malignant potential Benign Malignant Additional ancillary testing 35

RNA isolation cDNA generation and amplification • Open array card 32 discriminant gene targets and 3 control genes Analysis of GEP with a proprietary AI algorithm to determine risk Benign Suggestive of benign neoplasm Intermediate-Risk Cannot exclude malignancy Malignant Suggestive of melanoma FFPE tissue RT qPCR Dermatopathologist OR Dermatology clinician orders W O R K F LOW F O R D E C I S I O N D X D I F F D X - M E L A N O M A : P R O C E S S I D E N T I C A L T O D E C I S I O N D X - M E L A N O M A Diagnostically challenging pigmented (melanocytic) lesion 36

D E C I S I O N D X D I F F DX - M E L A N O M A : D E S I G N E D A N D VA L I DAT E D TO I M P R O V E D I A G N O S T I C R E S O LU T I O N F O R T H E B E N E F I T O F PAT I E N T C A R E All ages N=503 Age > 65 years N=178 DecisionDx DiffDx-Melanoma 95% CI DecisionDx DiffDx-Melanoma 95% CI Sensitivity 99.1% 97.9-100 99.2% 97.6-100 Specificity 94.3% 91.5-97.1 100% 100-100 PPV 93.6% 90.5-96.7 100% 100-100 NPV 99.2% 98.1-100 98.1% 94.3-100 Intermediate-risk result 3.6% 3.4% Technical success rate 96% Samples that fall in intermediate-risk zone were excluded from the calculation. PPV – positive predictive value; NPV – negative predictive value; CI – confidence interval. Estrada et al. (2020) SKIN J Cutan Med 37
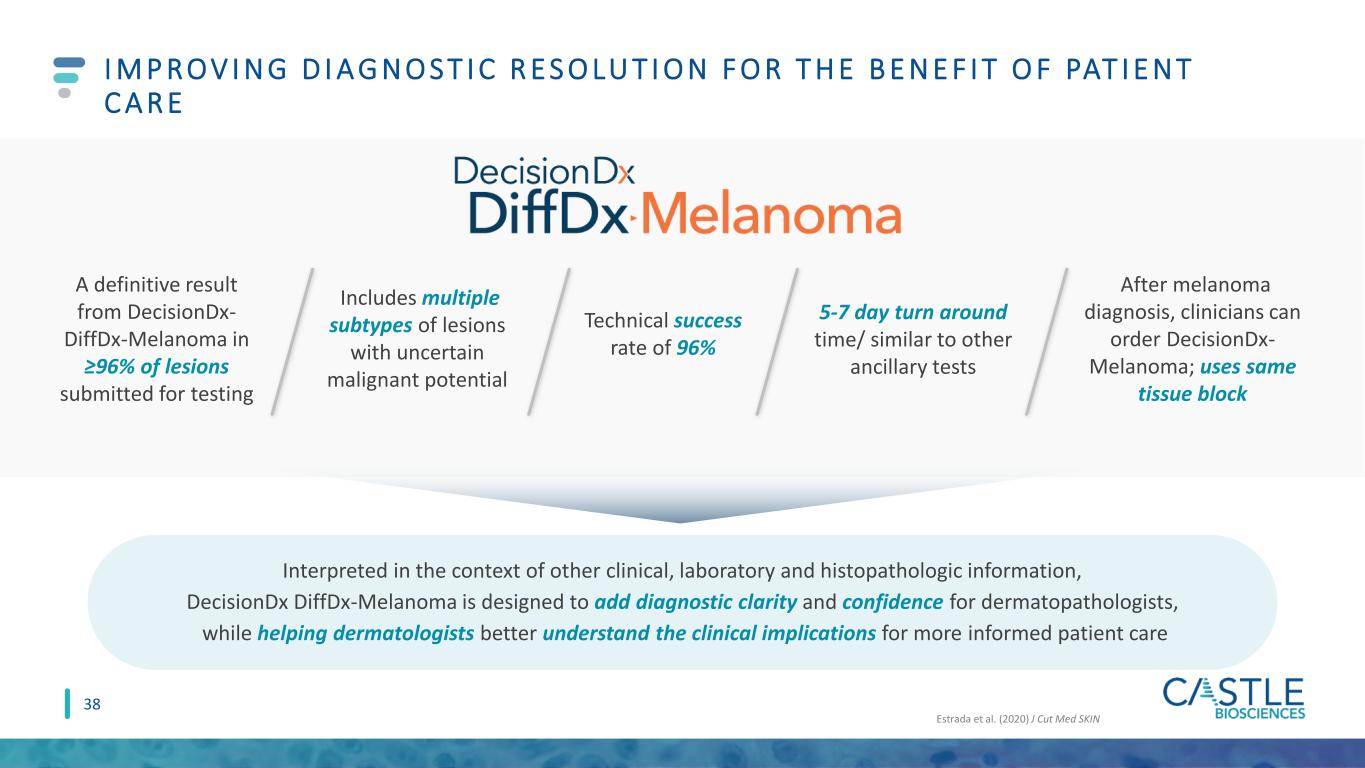
I M P R O V I N G D I A G N O S T I C R E S O LU T I O N F O R T H E B E N E F I T O F PAT I E N T C A R E Interpreted in the context of other clinical, laboratory and histopathologic information, DecisionDx DiffDx-Melanoma is designed to add diagnostic clarity and confidence for dermatopathologists, while helping dermatologists better understand the clinical implications for more informed patient care Estrada et al. (2020) J Cut Med SKIN A definitive result from DecisionDx- DiffDx-Melanoma in ≥96% of lesions submitted for testing Includes multiple subtypes of lesions with uncertain malignant potential Technical success rate of 96% 5-7 day turn around time/ similar to other ancillary tests After melanoma diagnosis, clinicians can order DecisionDx- Melanoma; uses same tissue block 38

The Standard of Care for Evaluating Metastatic Risk in Uveal Melanoma
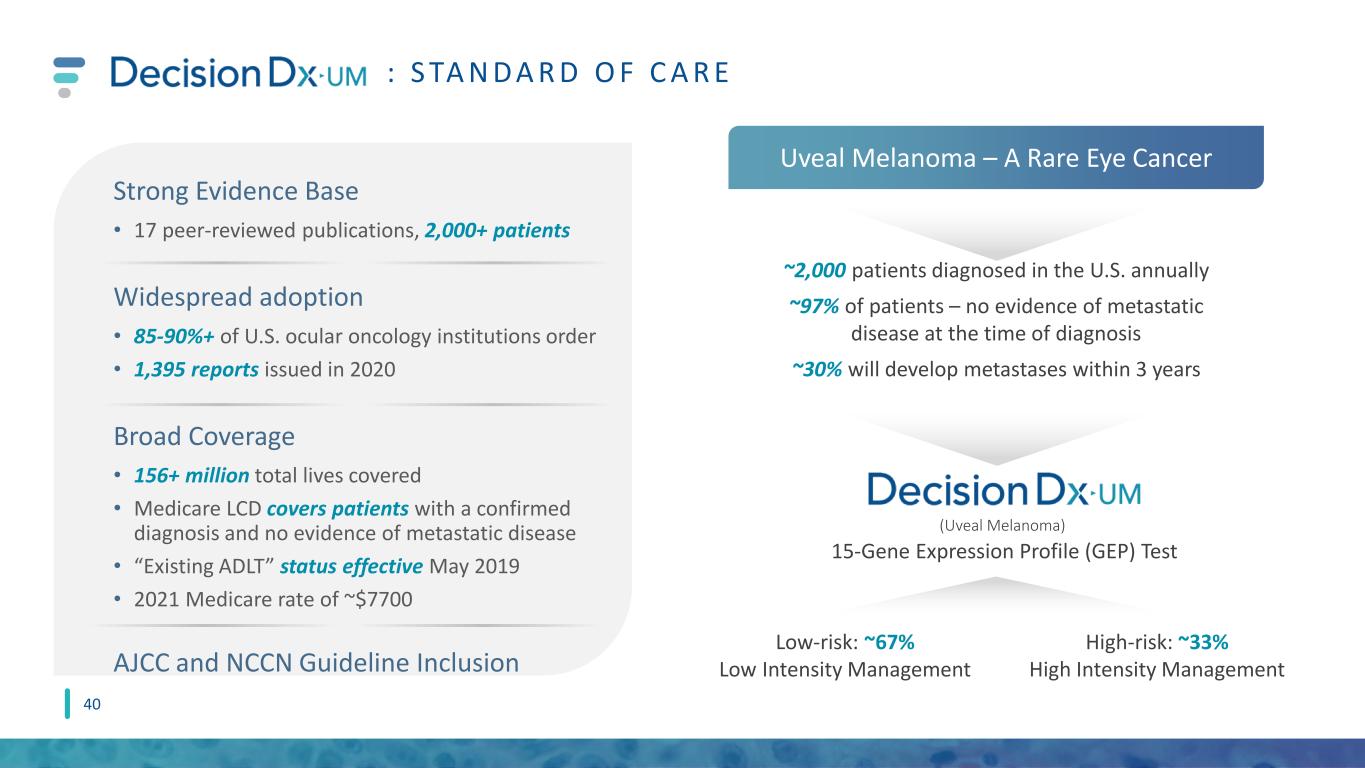
z : S TA N D A R D O F C A R E ~2,000 patients diagnosed in the U.S. annually ~97% of patients – no evidence of metastatic disease at the time of diagnosis ~30% will develop metastases within 3 years Low-risk: ~67% Low Intensity Management High-risk: ~33% High Intensity Management (Uveal Melanoma) Strong Evidence Base • 17 peer-reviewed publications, 2,000+ patients Widespread adoption • 85-90%+ of U.S. ocular oncology institutions order • 1,395 reports issued in 2020 Broad Coverage • 156+ million total lives covered • Medicare LCD covers patients with a confirmed diagnosis and no evidence of metastatic disease • “Existing ADLT” status effective May 2019 • 2021 Medicare rate of ~$7700 AJCC and NCCN Guideline Inclusion Uveal Melanoma – A Rare Eye Cancer 15-Gene Expression Profile (GEP) Test 40

MARKET AND FINANCIAL OVERVIEW

Indication/ Test outcome Trade Name Reimbursement Status Peer-Reviewed Publications Primary Customers Initial Launch Targets Initial addressable market, patients2 Estimated U.S. TAM Cutaneous melanoma/ Risk of metastasis MCR, MCRA Commercial – in process 30 Derms (including Mohs), Surgeons __ ~130k patients classified as Stage I, II or III ~$540M Cutaneous squamous cell carcinoma/ Risk of metastasis Expected draft LCD in 2021 4 Derms (including Mohs) ~4,365 current customers3 ~200k w/ high-risk features ~$820M Suspicious pigmented lesions/ Melanoma status Expected draft LCD in 2021 2 Dermpaths, Derms ~1,740 current dermpath customers4 ~300k patients w/indeterminant biopsy ~$600M Pipeline Tests (including psoriasis/AD) Target launches anticipated by the end of 2025 N/A N/A Expected to utilize existing dermatologic sales channels To be announced To be announced ~$3.6B E S T I M AT E D ~ $ 5 . 5 B U. S . TOTA L A D D R E S S A B L E M A R K E T 1 I n m a r ke t a n d p i p e l i n e t e s t s , l e v e r a g i n g e s t a b l i s h e d d e r m a t o l o g i c s a l e s c h a n n e l s 1U.S. TAM = Total addressable market based on estimated patient population assuming average reimbursement rate among all payors. 2 Annual U.S. incidence for Stage I, II o r III melanoma estimated at 130,000; Annual U.S. incidence for squamous cell carcinoma estimated at 1,000,000 with addressable market limited to carcinomas with one or more high risk features; Annual U.S. incidence for suspicious pigmented lesion biopsies estimated at 2,000,000 with addressable market limited to the 15% with an indeterminant biopsy. 3Clinicians who ordered DecisionDx-Melanoma in last twelve months (as of 3/31/2020) 4Pathologists who provided clinical specimens for DecisionDx-Melanoma in last twelve months (as of 3/31/2020) -MCR = Medicare. MCRA = Medicare Advantage; current customer estimates based on last twelve months. 42

R E C E N T A C H I E V E M E N T S A N D E X P E C T E D F U T U R E M I L E S TO N ES 2 0 2 1 M I L E S T O N E S O N T R A C K Oct 2020: LCD expansion finalized for DecisionDx-Melanoma, effective date 12/6/20 2021: Potential draft LCD for DecisionDx-SCC and DecisionDx DiffDx-Melanoma 2020 2021 2019 2022 2H2020: Initiation of work on additional dermatology pipeline products 4Q2020: Launch of DecisionDx DiffDx-Melanoma 2022: Potential effective LCD for DecisionDx-SCC and DecisionDx DiffDx- Melanoma 3Q2020: Commercial team expansion Sept 2020: Launch of DecisionDx-SCC July 2019: IPO Dec 2019: Expanded outside sales territories to 32 = Achieved Feb 2019: Expanded outside sales territories to 23 Aug 2019: Expanded draft LCD for DecisionDx- Melanoma posted 43 1H2021: Planned commercial team expansion to ~60 2018 Dec 2018: Initial LCD effective for DecisionDx-Melanoma 2021+: Continued evidence development for all commercialized products 2021+: Continued development of dermatologic pipeline products; potential launches in 2025 2021: Signed definitive agreement to acquire myPath® Melanoma 2021: Planned announcement of pipeline indications

FA C TO RS D R I V I N G N E A R - A N D LO N G - T E R M G R O W T H REVENUE PROFITABILITY PIPELINE Gross Margins • 87% in Q1 2021 • Continued margin expansion of existing products (increasing ASPs and efficiencies of scale) could be offset by uptake of pipeline products ahead of reimbursement New Product Development • Launched two skin cancer tests in 2020 with estimated $1.4B+ U.S. TAM • Leverage of our existing skin cancer sales channels to support new products • Initiated new pipeline products in dermatologic diseases with high unmet need; potential to launch 3-5 new tests by the end of 2025 Test Report Volume • Commercial sales team expansion in 1H21 to ~60-65 Reimbursement • Strong ASP growth • DecisionDx-Melanoma $7,193 PAMA rate through 2021 • DecisionDx-UM $7,776 PAMA rate through 2021 44
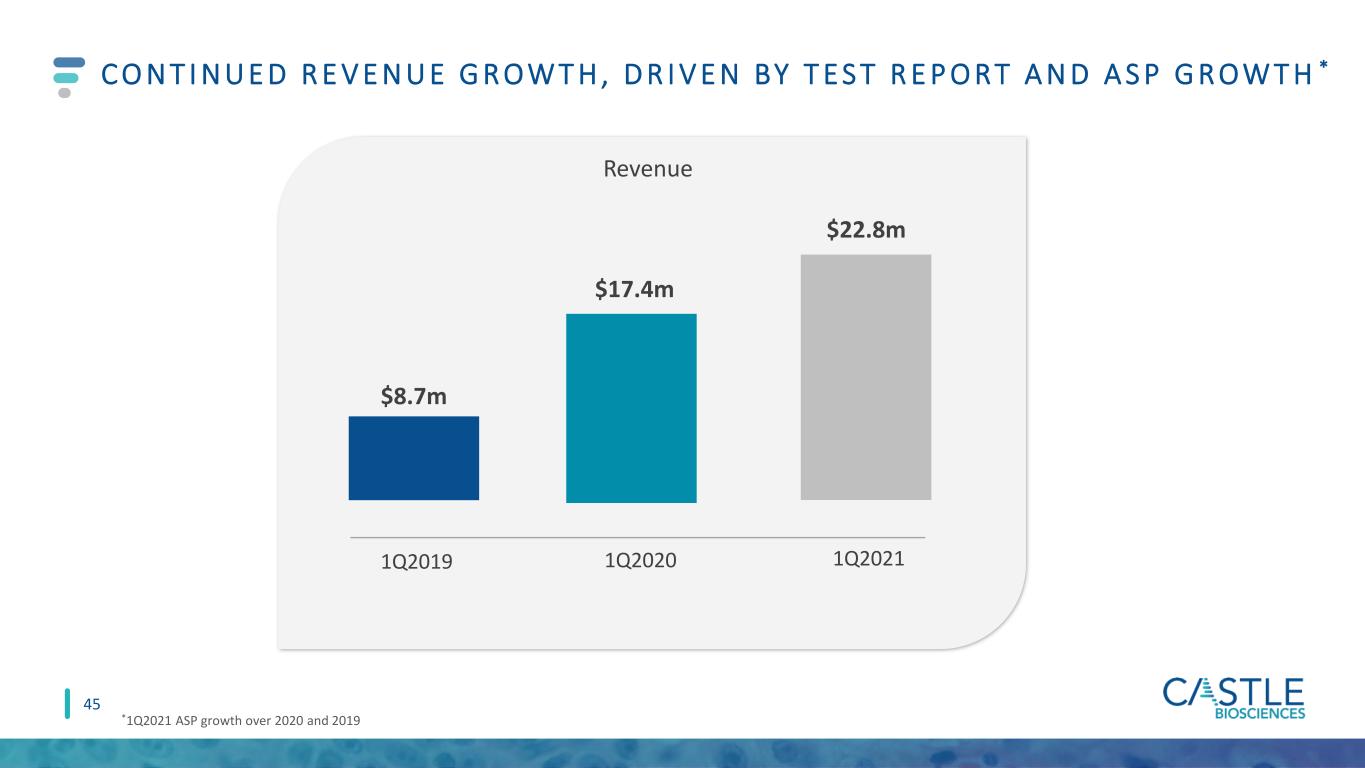
C O N T I N U E D R E V E N U E G R O W T H , D R I V E N BY T E S T R E P O R T A N D A S P G R O W T H * 1Q2019 1Q2020 1Q2021 Revenue *1Q2021 ASP growth over 2020 and 2019 $22.8m $17.4m $8.7m 45

Asian Black or African American Hispanic or Latino Two or more races (not Hispanic or Latino) White Othe (n t Hispanic r Latino) Female Male Female Male C O M M I T M E N T TO D I V E RS I T Y 46 37.3% 62.7% 68.2% 31.8% 79.1% 5% 9.5 4.9% 1.5% A ll E m p lo y e e s E xe cu ti v e s E T H N I C I T Y/ R A C E G E N D E R Data as of 12/31/20, Executive= Executive Director or Regional Business Director level and above American Indian or Alaska Native Two or more races (not Hispanic or Latino) White Hispanic or Latino 86.36% 4.55% 4.55% 4.55%

TRANSFORMING THE MANAGEMENT OF SKIN CANCER AND OTHER DERMATOLOGIC DISEASES WITH HIGH UNMET CLINICAL NEED EXPANSIVE BODY OF EVIDENCE SUITE OF SKIN CANCER PROGNOSTIC AND DIAGNOSTIC TESTS STRONG FINANCIAL POSITION ROBUST PIPELINE L E A D I N G D E R M ATO LO G I C D I A G N O S T I C S C O M PA N Y 47 CULTURE OF INNOVATION

THANK YOU

U S E O F N O N - G A A P F I N A N C I A L M E A S U R ES ( U N A U D I T E D ) 49 • In this presentation, we use the metrics of Adjusted Revenue, Adjusted Gross Margin and Adjusted Operating Cash Flow, which are non-GAAP financial measures and are not calculated in accordance with generally accepted accounting principles in the United States (GAAP). Adjusted Revenue and Adjusted Gross Margin reflect adjustments to net revenues to exclude changes in variable consideration related to test reports delivered in previous periods. Adjusted Operating Cash Flow excludes the effects of cash activity associated with COVID-19 government relief payments to healthcare providers. • We use Adjusted Revenue, Adjusted Gross Margin and Adjusted Operating Cash Flow internally because we believe these metrics provide useful supplemental information in assessing our revenue and cash flow performance, respectively. We believe Adjusted Revenue and Adjusted Gross Margin are also useful to investors because they provide additional information on current-period performance by removing the effects of revenue adjustments related to tests delivered in previous periods, which we believe may facilitate revenue and gross margin comparisons to historical periods. We believe Adjusted Operating Cash Flow is also useful to investors as a supplement to GAAP measures in the assessment of our cash flow performance by removing the effects of COVID-19 government relief payments, which we believe are not indicative of our ongoing operations. However, these non-GAAP financial measures may be different from non-GAAP financial measures used by other companies, even when the same or similarly titled terms are used to identify such measures, limiting their usefulness for comparative purposes. These non-GAAP financial measures are not meant to be substitutes for net revenues or net cash (used in) provided by operating activities reported in accordance with GAAP and should be considered in conjunction with our financial information presented on GAAP basis. Accordingly, investors should not place undue reliance on non-GAAP financial measures. Reconciliations of these non-GAAP financial measures to the most directly comparable GAAP financial measures are presented in the next slide.
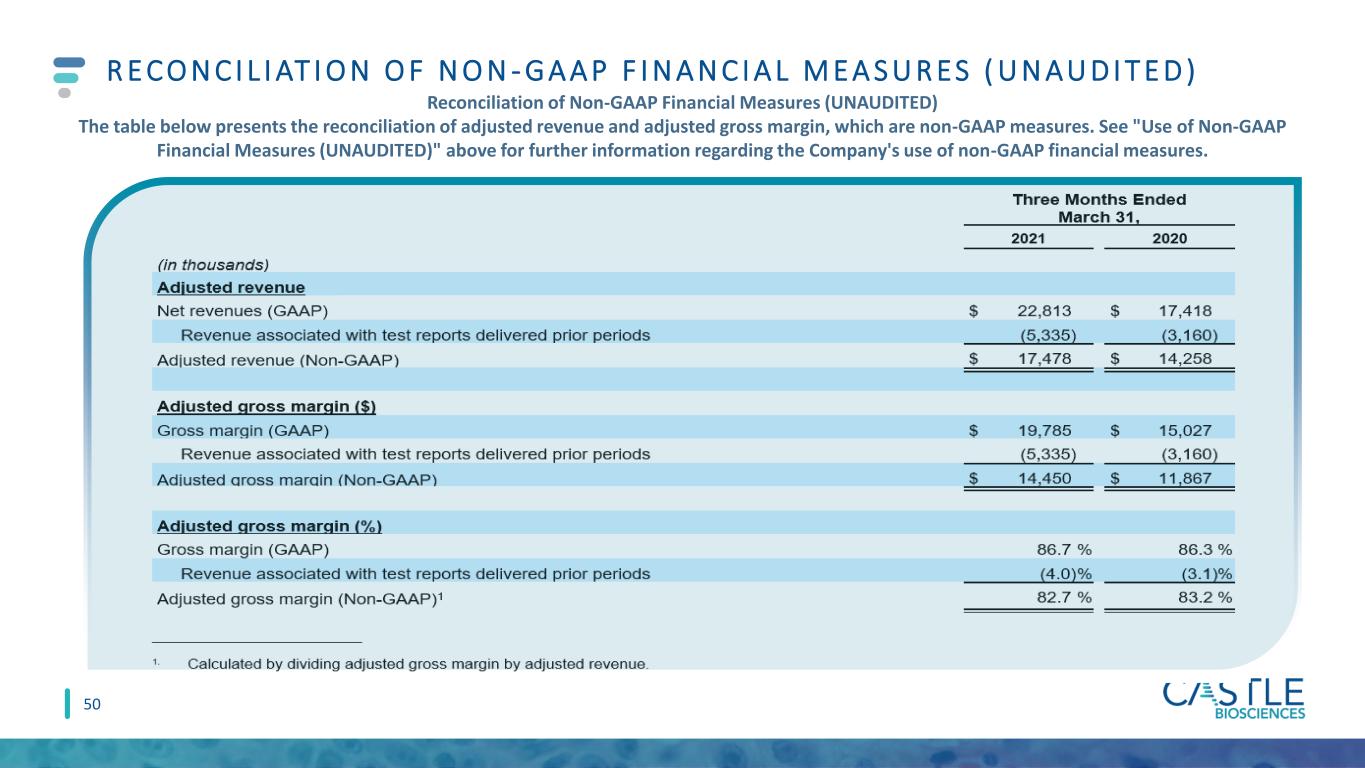
R E C O N C I L I AT I O N O F N O N - G A A P F I N A N C I A L M E A S U R ES ( U N A U D I T E D ) Reconciliation of Non-GAAP Financial Measures (UNAUDITED) The table below presents the reconciliation of adjusted revenue and adjusted gross margin, which are non-GAAP measures. See "Use of Non-GAAP Financial Measures (UNAUDITED)" above for further information regarding the Company's use of non-GAAP financial measures. 50

R E C O N C I L I AT I O N O F N O N - G A A P F I N A N C I A L M E A S U R ES ( U N A U D I T E D ) The table below presents the reconciliation of adjusted operating cash flow, which is a non-GAAP measure. See "Use of Non-GAAP Financial Measures (UNAUDITED)" above for further information regarding the Company's use of non- GAAP financial measures 51

APPENDIX

Stuart Pharmaceuticals Robert Cook, PhD Senior Vice President, Research & Development L E A D E RS H I P T E A M O V E RV I E W B O A R D O F D I R E C T O R S M A N A G E M E N T T E A M Derek Maetzold Founder, Director, President and CEO Frank Stokes Chief Financial Officer Bernhard Spiess Chief Business Officer Toby Juvenal Chief Commercial Officer Kristen Oelschlager, RN, CHC Chief Operating Officer Dan Bradbury Derek Maetzold Mara Aspinall Brad Cole Miles D. Harrison David Kabakoff 53 Matthew Goldberg, MD Medical Director Tiffany Olson