1 1053 Efficacy and Safety of Giroctocogene Fitelparvovec in Adults With Moderately Severe to Severe Hemophilia A: Primary Analysis Results From the Phase 3 AFFINE Gene Therapy Trial Andrew D Leavitt1, Kaan Kavakli2, Laurent Frenzel3, Ali Bülent Antmen4, Margareth Ozelo5, Davide Matino6,7, Hazza Alzahrani8, Barbara A Konkle9, Steven W Pipe10, Jerome M Teitel11, Li-Jung Tseng12, Annie F Fang12, Florence Ganne13, Gregory DiRusso14, Jeremy Rupon14, Pascal Klaus15, Jasmine Healy16, Delphine Agathon13, Francesca Biondo17, Frank Plonski14, on behalf of the AFFINE Investigators 1University of California San Francisco, San Francisco, CA, USA; 2Ege University Faculty of Medicine, Izmir, Turkey; 3Hemophilia Care and Research, Necker Hospital, Institut Imagine, Paris, France; 4Acibadem Adana Hospital, Adana, Turkey; 5Hemocentro UNICAMP, School of Medical Sciences, University of Campinas, Campinas, Brazil; 6Thrombosis and Atherosclerosis Research Institute (TaARI), McMaster University, Hamilton, ON, Canada; 7McMaster University, Hamilton, ON, Canada; 8King Faisal Specialist Hospital and Research Centre, Riyadh, Saudi Arabia; 9Washington Center for Bleeding Disorders and the University of Washington, Seattle, WA, USA; 10University of Michigan, Ann Arbor, MI, USA; 11St. Michael's Hospital, University of Toronto, Toronto, ON, Canada; 12Pfizer Inc, New York, NY, USA; 13Pfizer Inc, Paris, France; 14Pfizer Inc, Collegeville, PA, USA; 15Pfizer Pharma GmbH, Berlin, Germany; 16Pfizer Canada ULC, Kirkland, QC, Canada; 17Pfizer Srl, Rome, Italy 66th Annual Meeting and Exposition of the American Society of Hematology (ASH), December 7–10, 2024, San Diego, CA, USA

22 • Liver-tropic recombinant AAV serotype 6 (rAAV6) vector carrying B-domain–deleted human F8 transgene enabling endogenous FVIII expression in individuals with severe to moderately severe hemophilia A • The completed Alta phase 1/2 dose-ranging study1,2 (up to 5 years) demonstrated a single infusion of giroctocogene fitelparvovec in the 3e13 vg/kg cohort (n=5) was well tolerated and resulted in: – Sustained FVIII activity levels in the moderate-to-normal range in most participants, no bleeds in the first year post infusion in all participants, and low bleeding rates through follow-up in 4 of 5 participants Giroctocogene fitelparvovec for hemophilia A AAV=adeno-associated virus; BDD=B-domain–deleted; FVIII=factor VIII; hF8=human factor 8; vg=vector genome 1. Harrington TJ, et al. Blood 2023;142(suppl 1):1054. 2. Leavitt AD, et al. Blood 2024;143(9):796–806. AAV6 Capsid Secreted FVIII protein F8 gene (in episomal form) hF8-BDD Transgene Transduction into hepatocytes Infusion of giroctocogene fitelparvovec
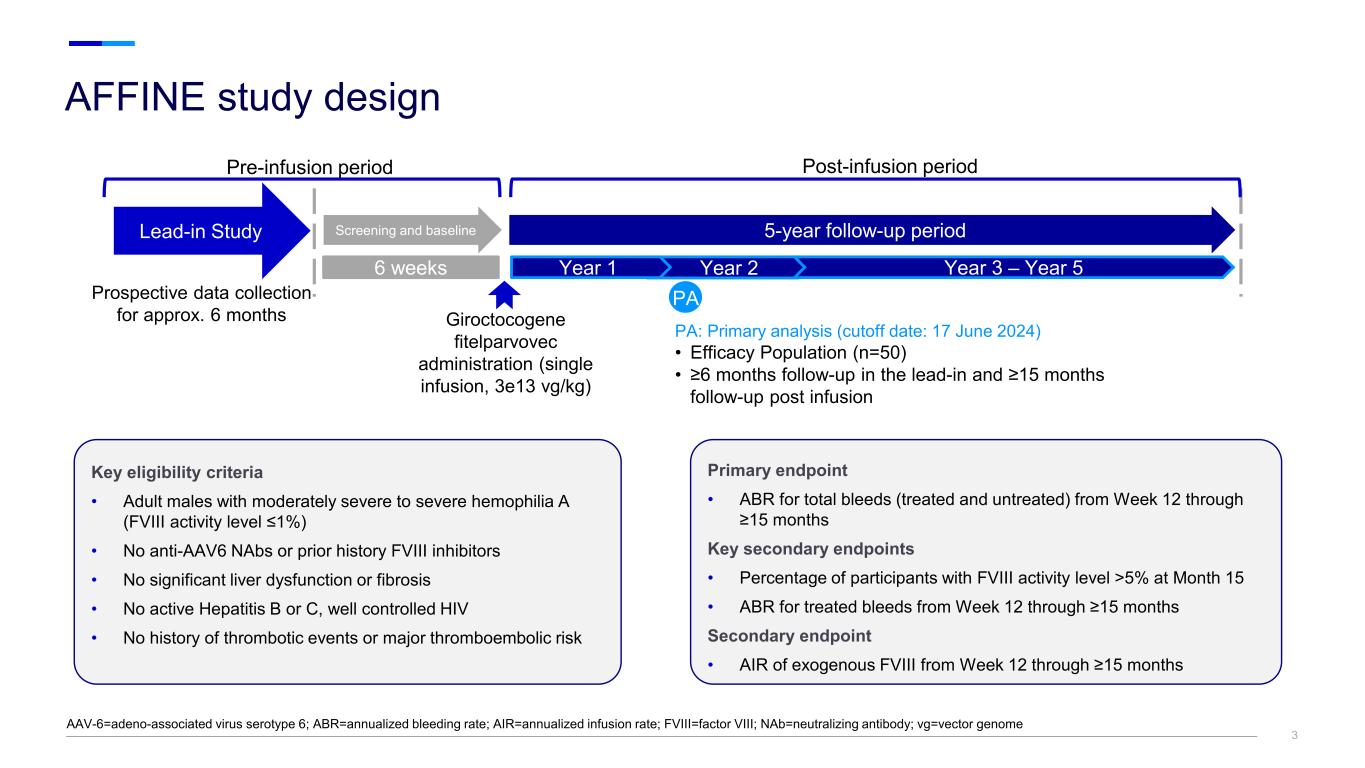
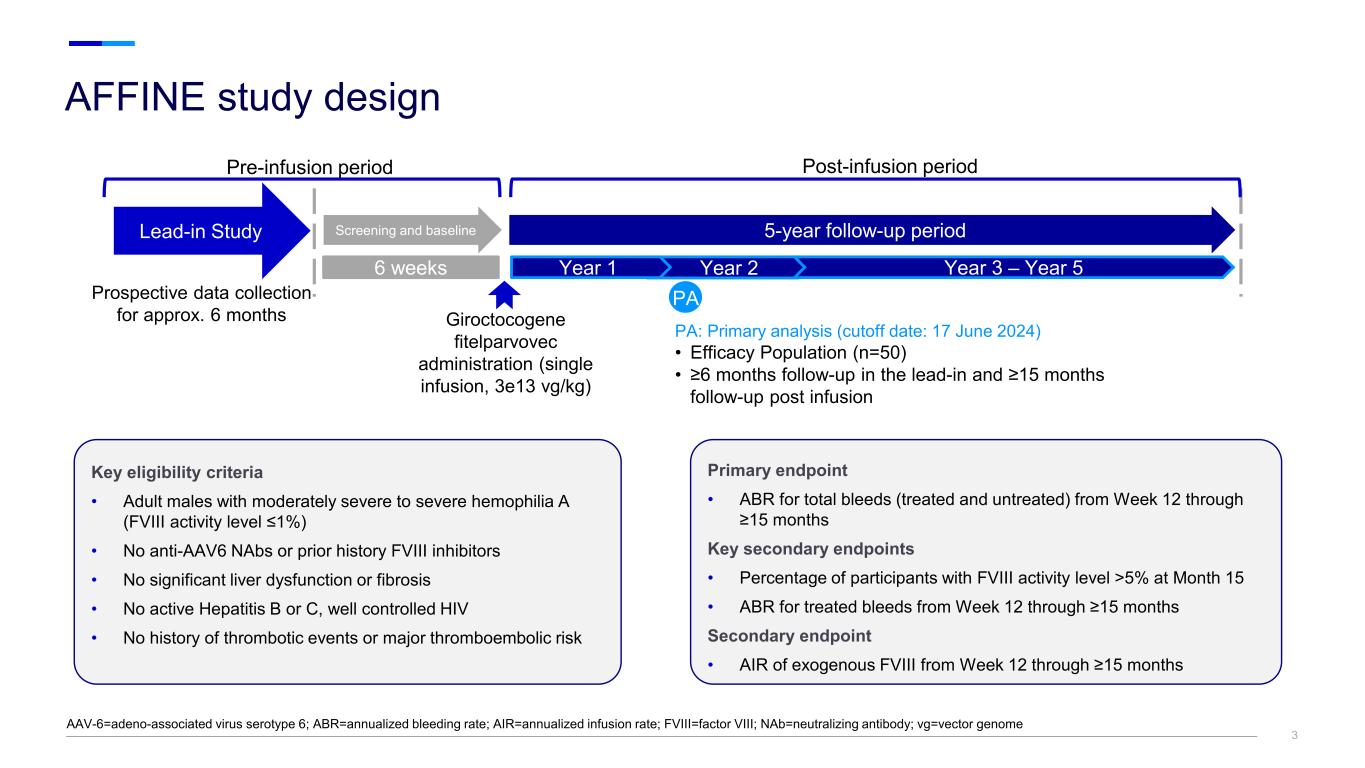
33 AFFINE study design AAV-6=adeno-associated virus serotype 6; ABR=annualized bleeding rate; AIR=annualized infusion rate; FVIII=factor VIII; NAb=neutralizing antibody; vg=vector genome Primary endpoint • ABR for total bleeds (treated and untreated) from Week 12 through ≥15 months Key secondary endpoints • Percentage of participants with FVIII activity level >5% at Month 15 • ABR for treated bleeds from Week 12 through ≥15 months Secondary endpoint • AIR of exogenous FVIII from Week 12 through ≥15 months Key eligibility criteria • Adult males with moderately severe to severe hemophilia A (FVIII activity level ≤1%) • No anti-AAV6 NAbs or prior history FVIII inhibitors • No significant liver dysfunction or fibrosis • No active Hepatitis B or C, well controlled HIV • No history of thrombotic events or major thromboembolic risk Screening and baselineLead-in Study 6 weeks Prospective data collection for approx. 6 months Giroctocogene fitelparvovec administration (single infusion, 3e13 vg/kg) Post-infusion period Year 2Year 1 Pre-infusion period PA PA: Primary analysis (cutoff date: 17 June 2024) • Efficacy Population (n=50) • ≥6 months follow-up in the lead-in and ≥15 months follow-up post infusion Year 3 – Year 5 5-year follow-up period
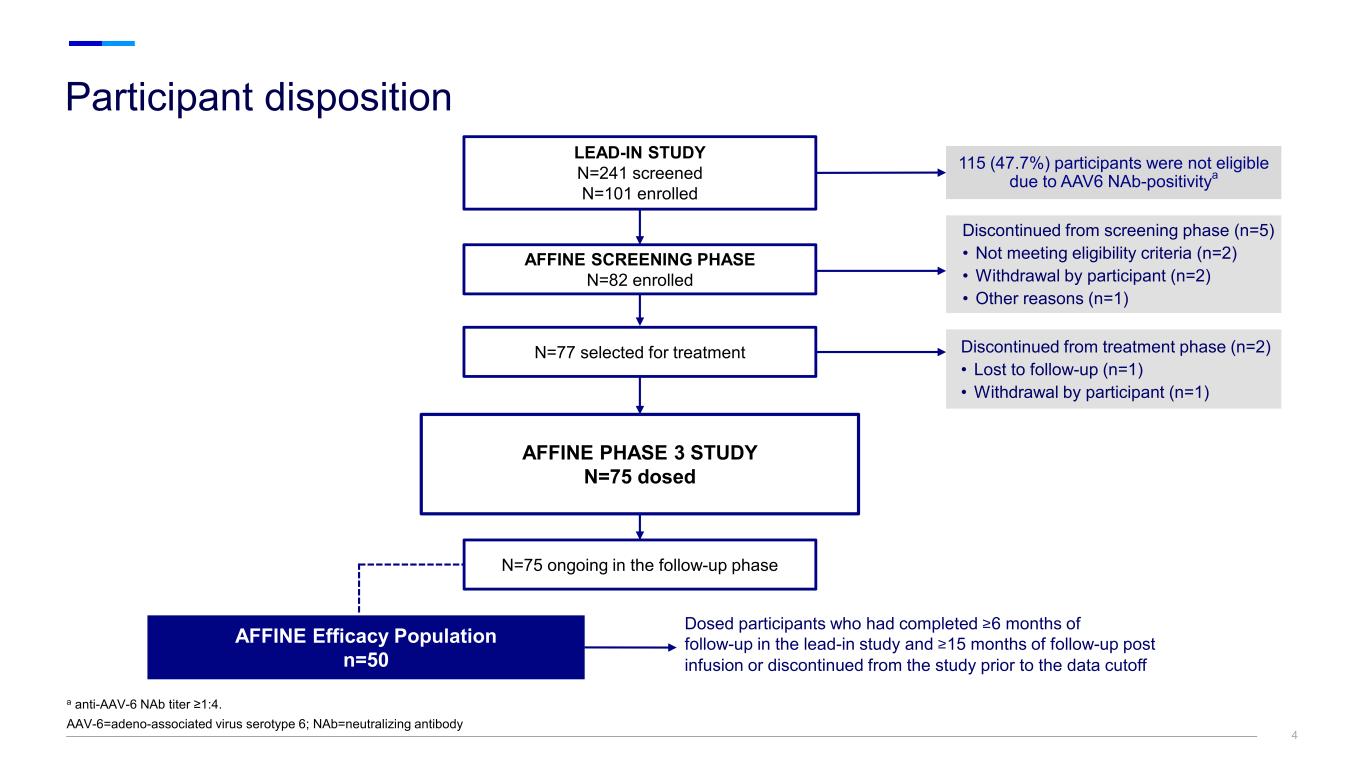
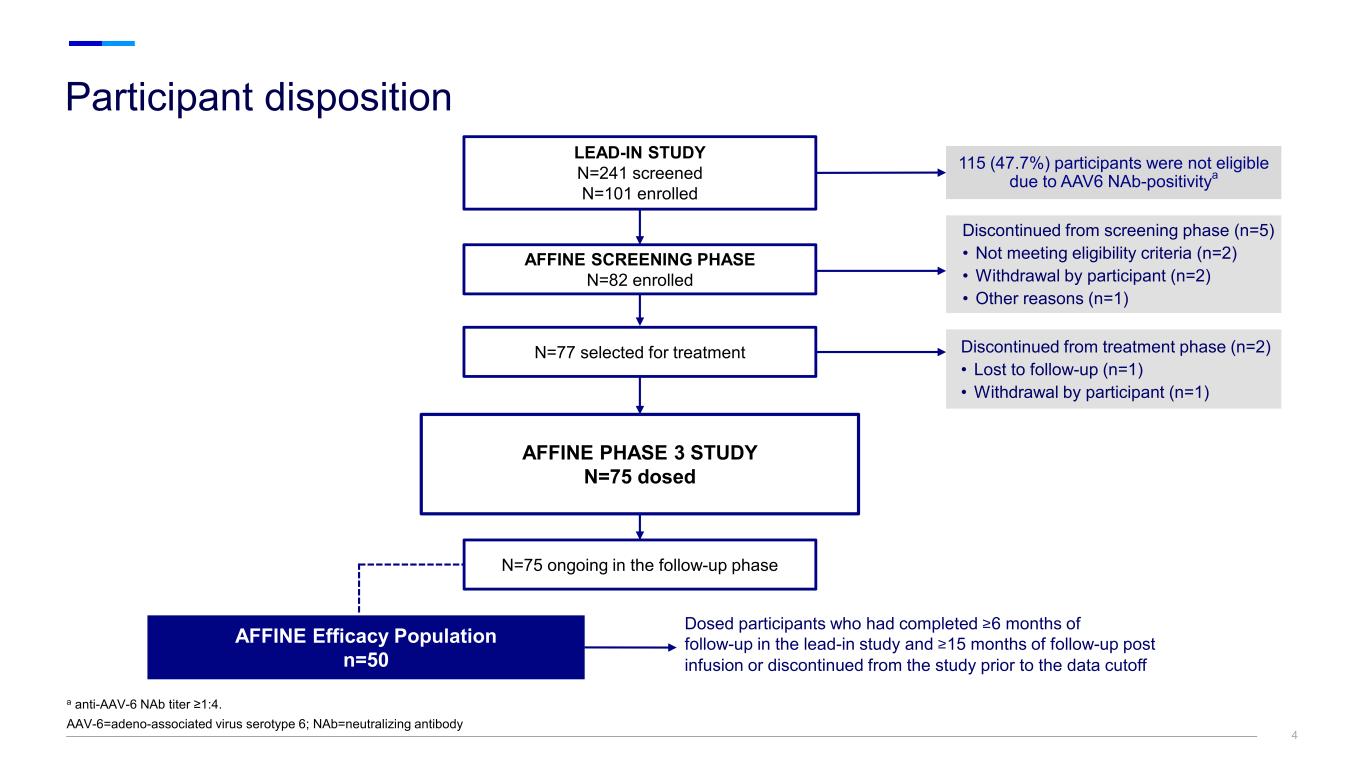
44 Participant disposition a anti-AAV-6 NAb titer ≥1:4. AAV-6=adeno-associated virus serotype 6; NAb=neutralizing antibody AFFINE SCREENING PHASE N=82 enrolled N=77 selected for treatment AFFINE PHASE 3 STUDY N=75 dosed N=75 ongoing in the follow-up phase AFFINE Efficacy Population n=50 LEAD-IN STUDY N=241 screened N=101 enrolled 115 (47.7%) participants were not eligible due to AAV6 NAb-positivitya Dosed participants who had completed ≥6 months of follow-up in the lead-in study and ≥15 months of follow-up post infusion or discontinued from the study prior to the data cutoff Discontinued from screening phase (n=5) • Not meeting eligibility criteria (n=2) • Withdrawal by participant (n=2) • Other reasons (n=1) Discontinued from treatment phase (n=2) • Lost to follow-up (n=1) • Withdrawal by participant (n=1)
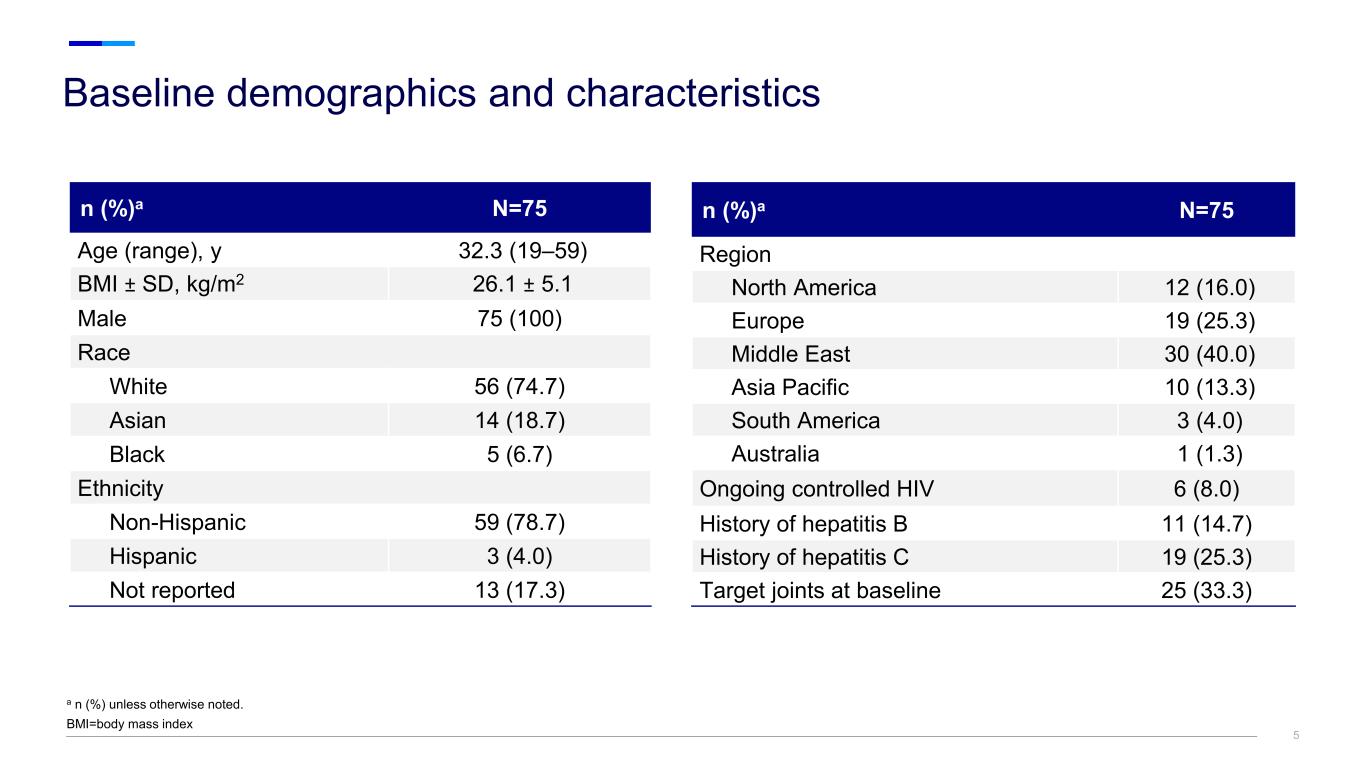
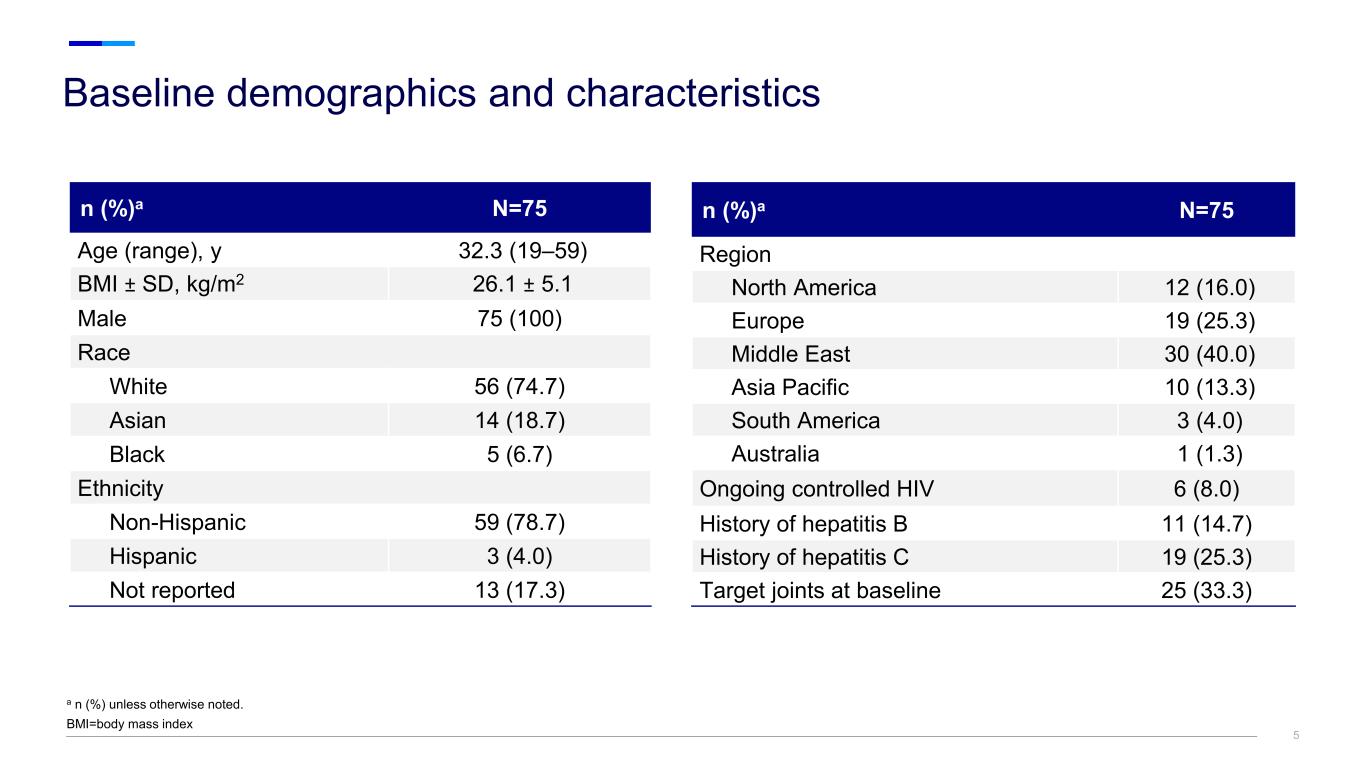
Baseline demographics and characteristics a n (%) unless otherwise noted. BMI=body mass index 5 n (%)a N=75 Region North America 12 (16.0) Europe 19 (25.3) Middle East 30 (40.0) Asia Pacific 10 (13.3) South America 3 (4.0) Australia 1 (1.3) Ongoing controlled HIV 6 (8.0) History of hepatitis B 11 (14.7) History of hepatitis C 19 (25.3) Target joints at baseline 25 (33.3) n (%)a N=75 Age (range), y 32.3 (19–59) BMI ± SD, kg/m2 26.1 ± 5.1 Male 75 (100) Race White 56 (74.7) Asian 14 (18.7) Black 5 (6.7) Ethnicity Non-Hispanic 59 (78.7) Hispanic 3 (4.0) Not reported 13 (17.3)
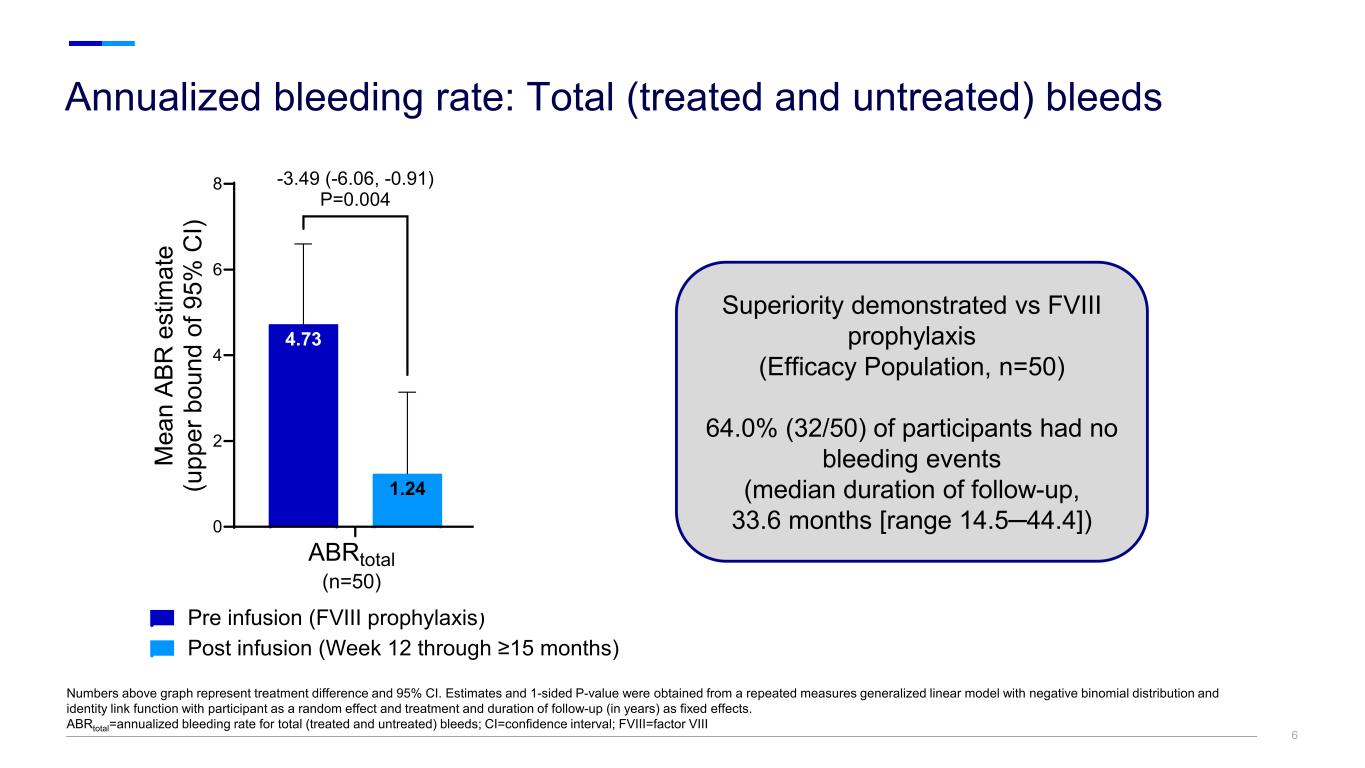
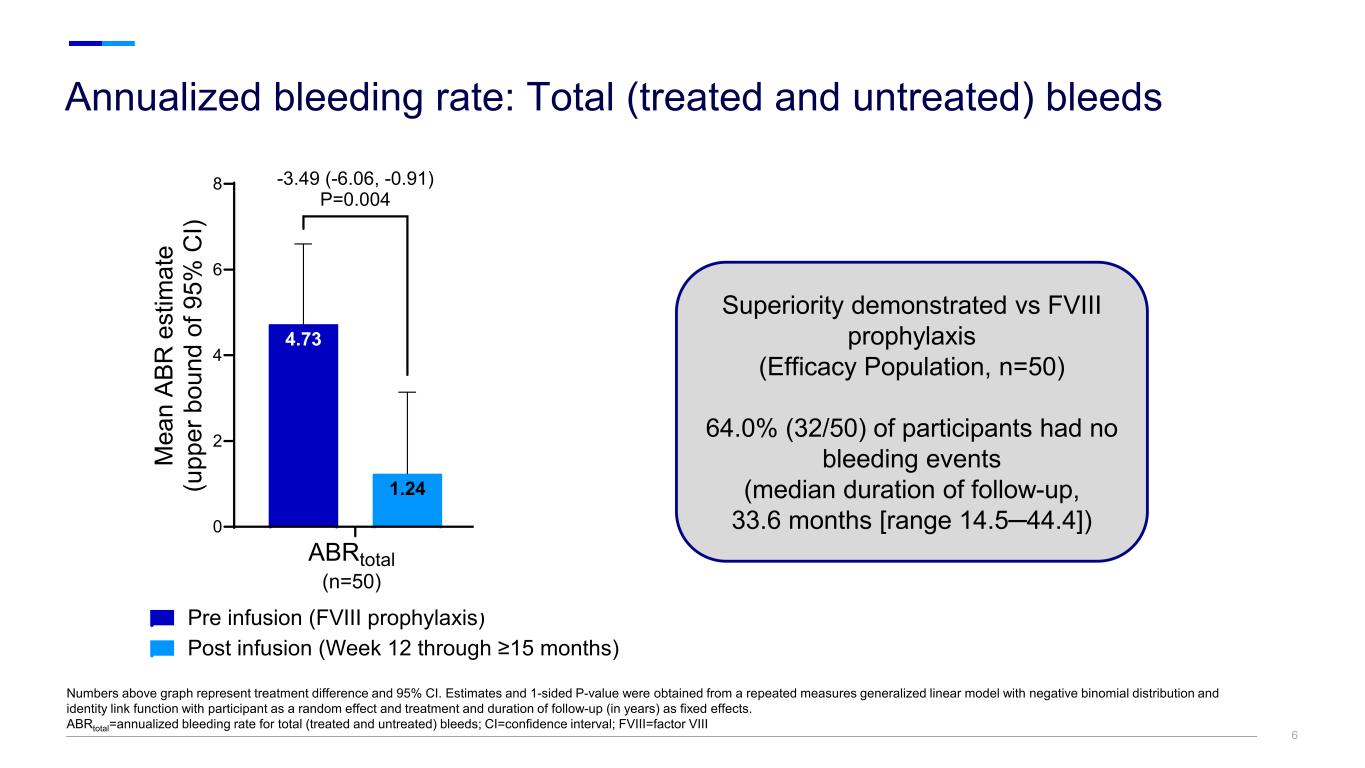
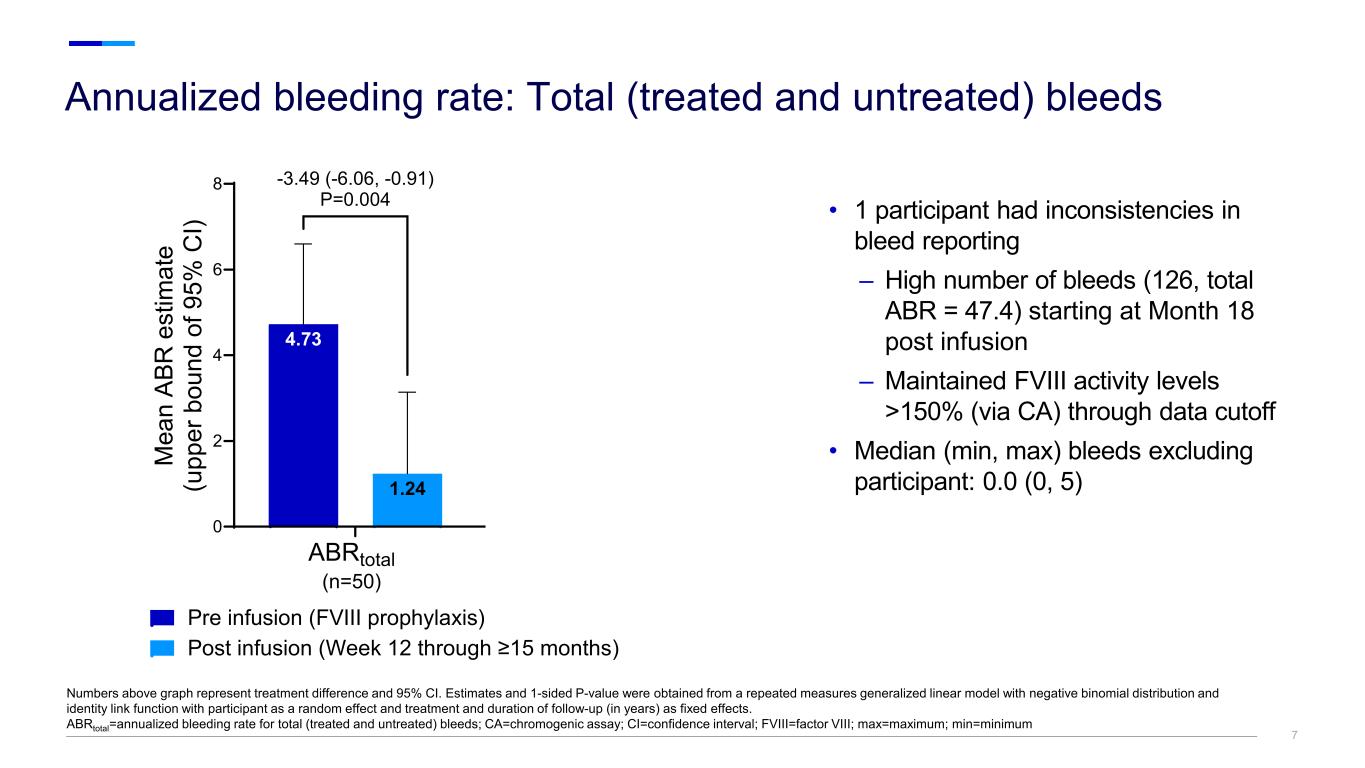
66 Annualized bleeding rate: Total (treated and untreated) bleeds Numbers above graph represent treatment difference and 95% CI. Estimates and 1-sided P-value were obtained from a repeated measures generalized linear model with negative binomial distribution and identity link function with participant as a random effect and treatment and duration of follow-up (in years) as fixed effects. ABRtotal=annualized bleeding rate for total (treated and untreated) bleeds; CI=confidence interval; FVIII=factor VIII 0 2 4 6 8 1.24 4.73 4.65 M ea n AB R e st im at e (u pp er b ou nd o f 9 5% C I) Pre infusion (FVIII prophylaxis) Post infusion (Week 12 through ≥15 months) ABRtotal (n=50) ABRtotal (n=49) -3.49 (-6.06, -0.91) P=0.004 -4.40 (-6.31, -2.48) P<0.0001 Superiority demonstrated vs FVIII prophylaxis (Efficacy Population, n=50) 64.0% (32/50) of participants had no bleeding events (median duration of follow-up, 33.6 months [range 14.5─44.4])
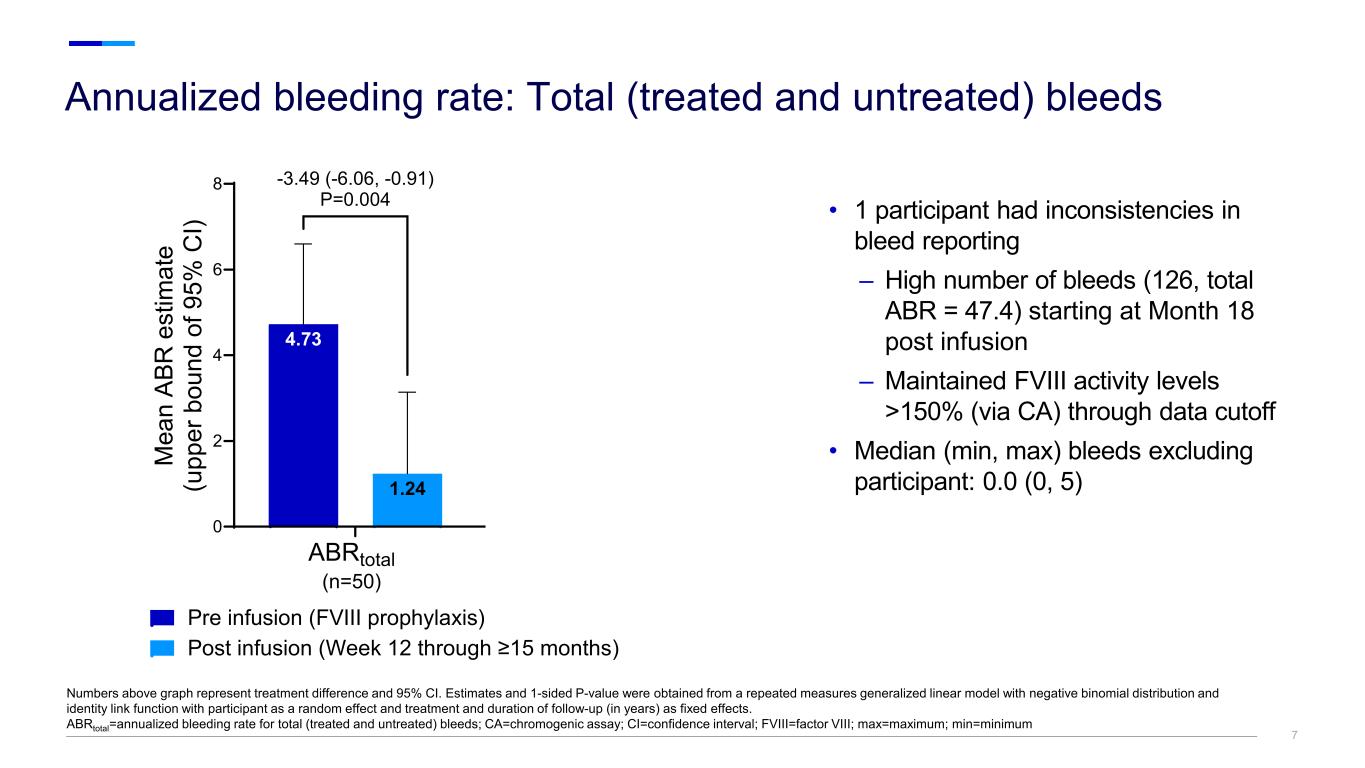
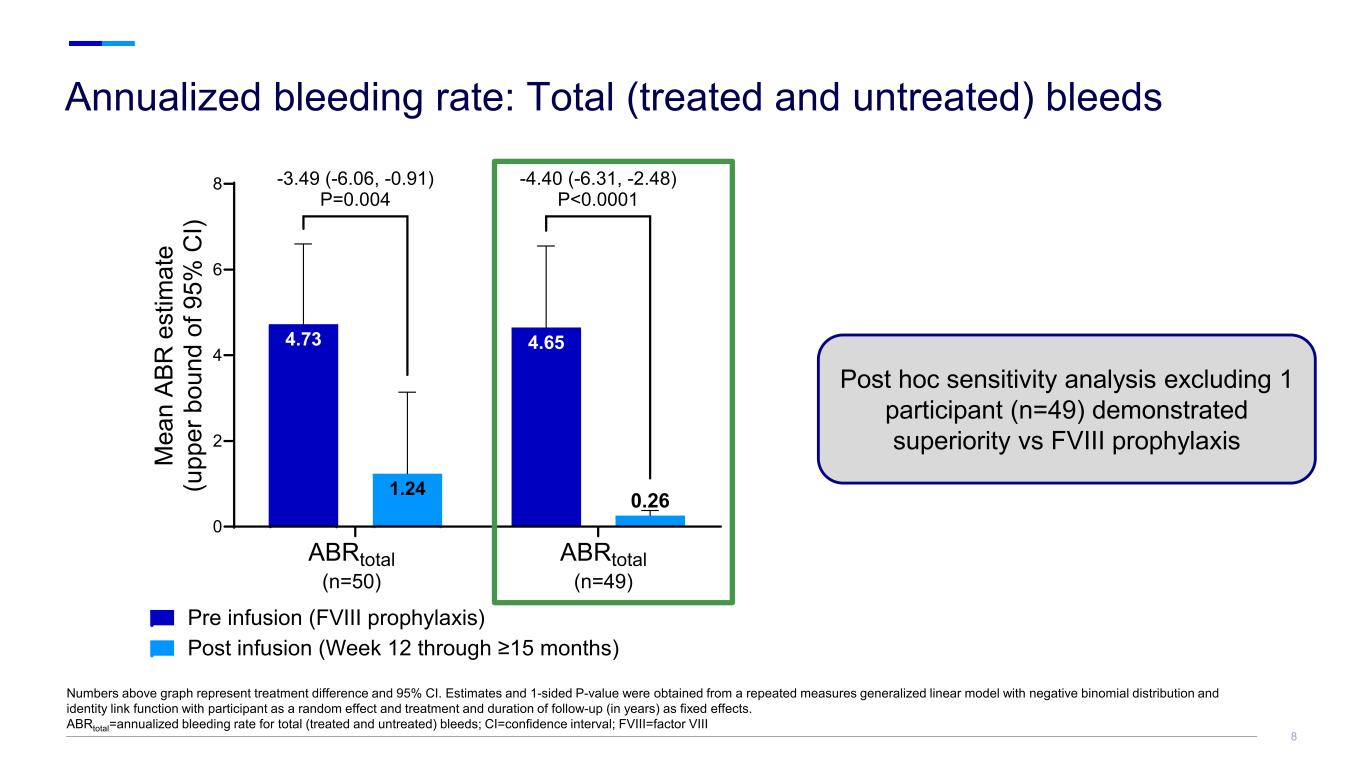
7 0 2 4 6 8 1.24 4.73 4.65 M ea n AB R e st im at e (u pp er b ou nd o f 9 5% C I) Pre infusion (FVIII prophylaxis) Post infusion (Week 12 through ≥15 months) ABRtotal (n=50) ABRtotal (n=49) -3.49 (-6.06, -0.91) P=0.004 -4.40 (-6.31, -2.48) P<0.0001 0.26 7 Annualized bleeding rate: Total (treated and untreated) bleeds Numbers above graph represent treatment difference and 95% CI. Estimates and 1-sided P-value were obtained from a repeated measures generalized linear model with negative binomial distribution and identity link function with participant as a random effect and treatment and duration of follow-up (in years) as fixed effects. ABRtotal=annualized bleeding rate for total (treated and untreated) bleeds; CA=chromogenic assay; CI=confidence interval; FVIII=factor VIII; max=maximum; min=minimum • 1 participant had inconsistencies in bleed reporting – High number of bleeds (126, total ABR = 47.4) starting at Month 18 post infusion – Maintained FVIII activity levels >150% (via CA) through data cutoff • Median (min, max) bleeds excluding participant: 0.0 (0, 5)
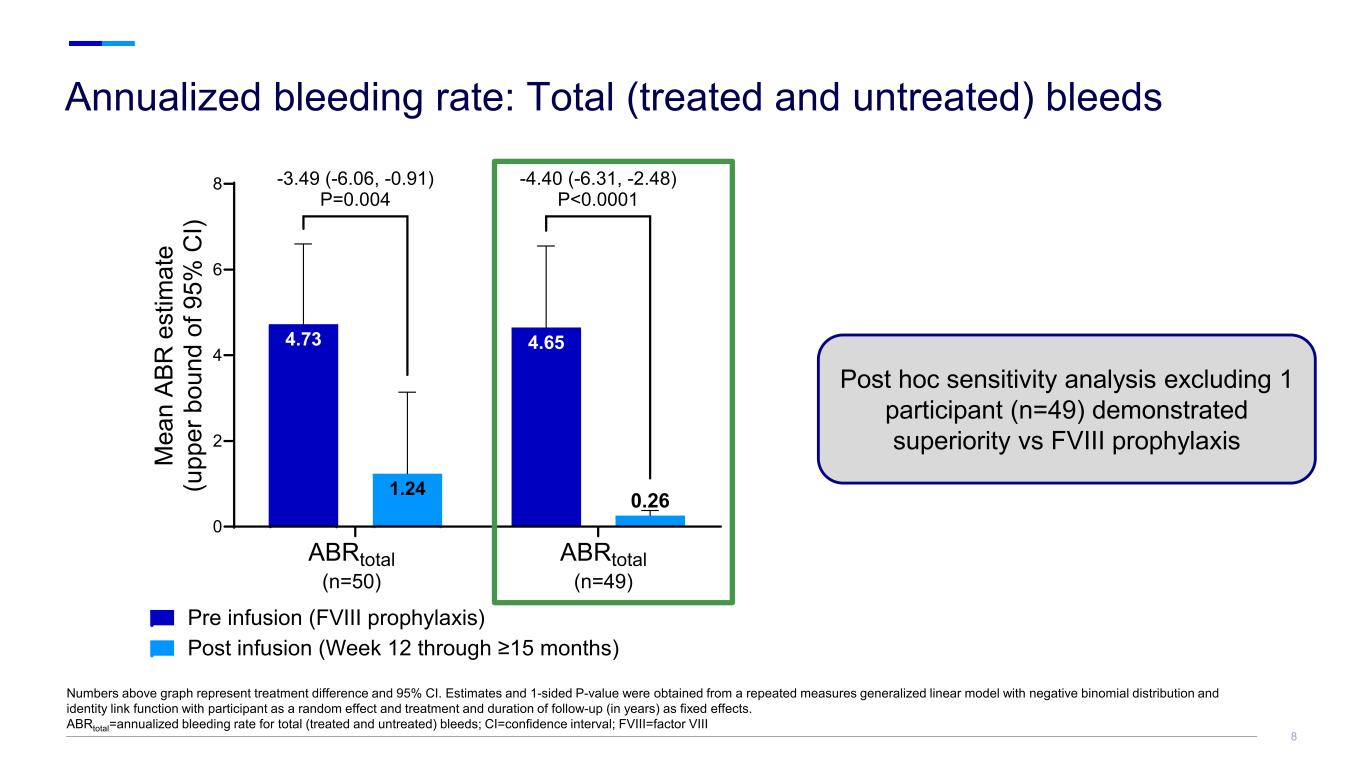
0 2 4 6 8 1.24 4.73 4.65 M ea n AB R e st im at e (u pp er b ou nd o f 9 5% C I) Pre infusion (FVIII prophylaxis) Post infusion (Week 12 through ≥15 months) ABRtotal (n=50) ABRtotal (n=49) -3.49 (-6.06, -0.91) P=0.004 -4.40 (-6.31, -2.48) P<0.0001 0.26 8 Annualized bleeding rate: Total (treated and untreated) bleeds Numbers above graph represent treatment difference and 95% CI. Estimates and 1-sided P-value were obtained from a repeated measures generalized linear model with negative binomial distribution and identity link function with participant as a random effect and treatment and duration of follow-up (in years) as fixed effects. ABRtotal=annualized bleeding rate for total (treated and untreated) bleeds; CI=confidence interval; FVIII=factor VIII Post hoc sensitivity analysis excluding 1 participant (n=49) demonstrated superiority vs FVIII prophylaxis
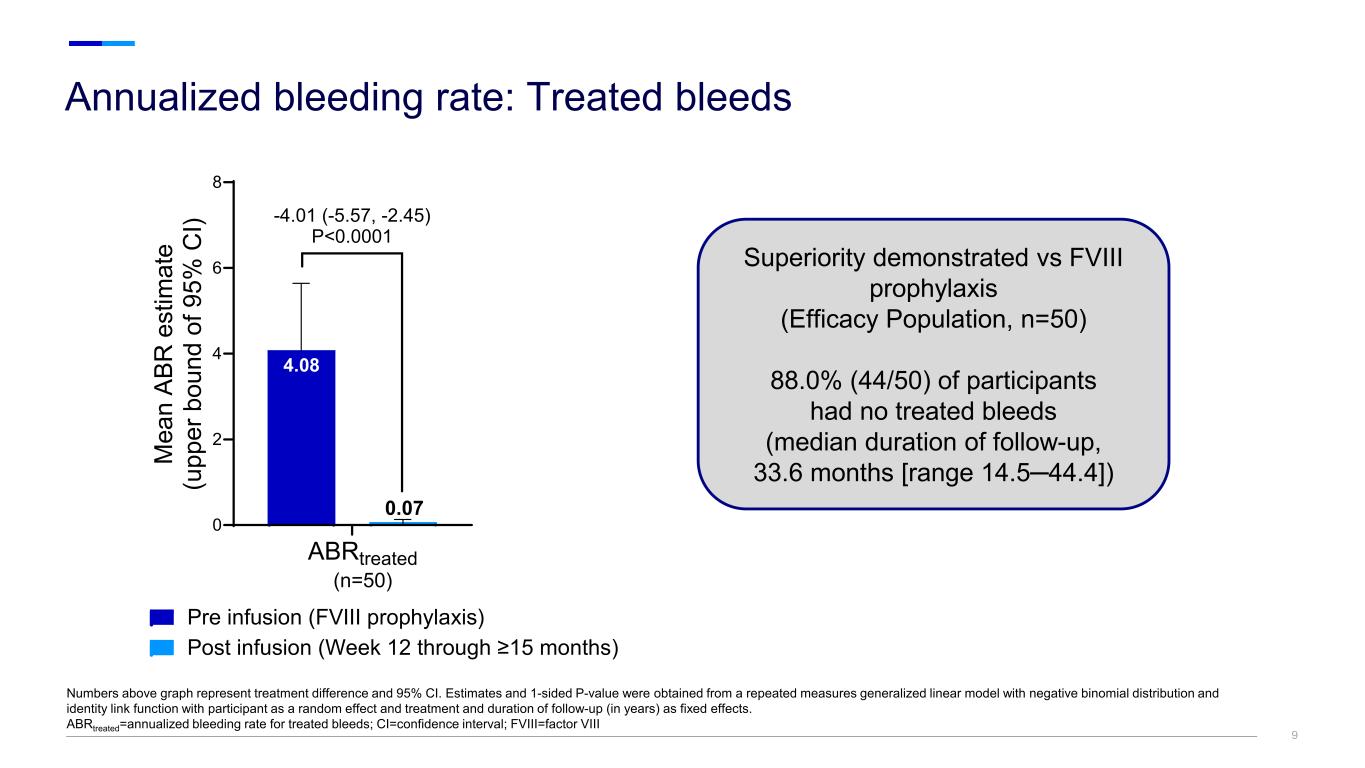
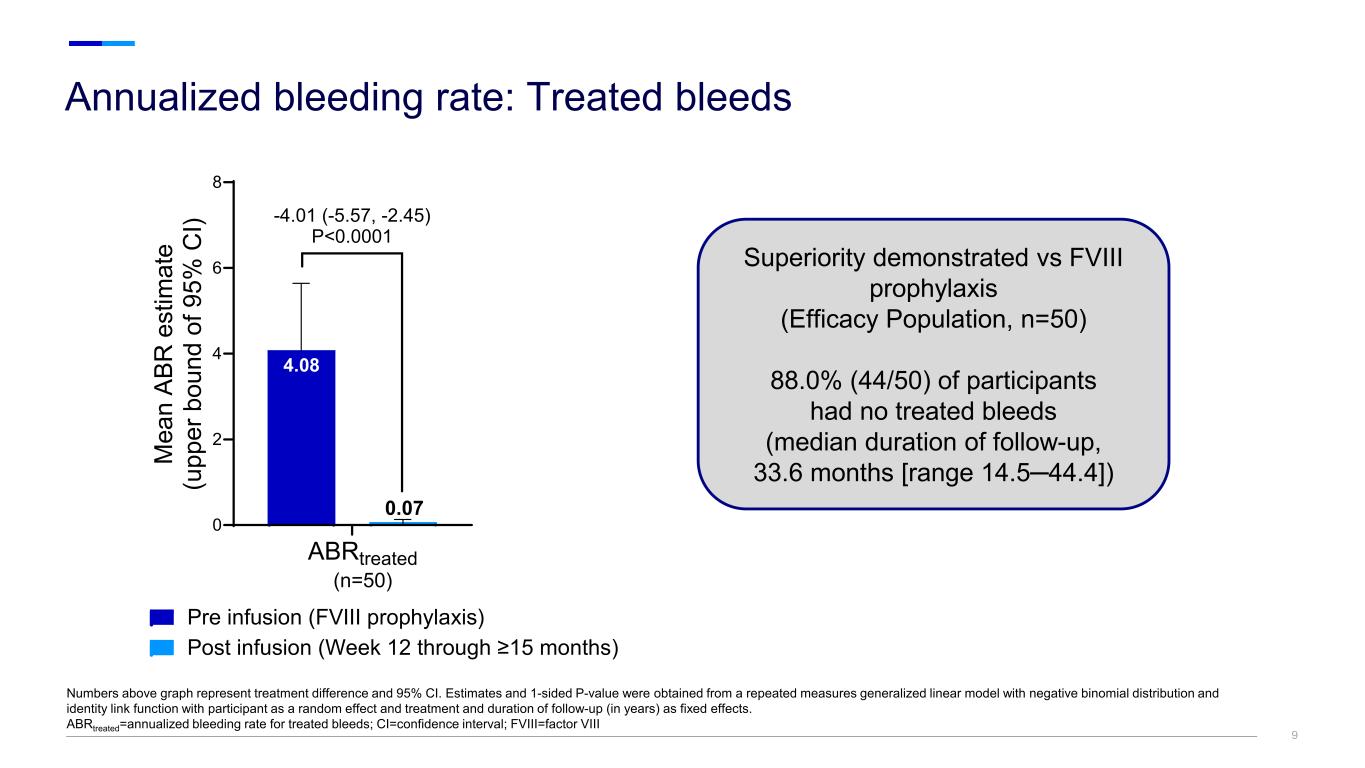
99 Annualized bleeding rate: Treated bleeds Numbers above graph represent treatment difference and 95% CI. Estimates and 1-sided P-value were obtained from a repeated measures generalized linear model with negative binomial distribution and identity link function with participant as a random effect and treatment and duration of follow-up (in years) as fixed effects. ABRtreated=annualized bleeding rate for treated bleeds; CI=confidence interval; FVIII=factor VIII Superiority demonstrated vs FVIII prophylaxis (Efficacy Population, n=50) 88.0% (44/50) of participants had no treated bleeds (median duration of follow-up, 33.6 months [range 14.5─44.4]) 0 2 4 6 8 4.08 M ea n AB R e st im at e (u pp er b ou nd o f 9 5% C I) Pre infusion (FVIII prophylaxis) Post infusion (Week 12 through ≥15 months) ABRtreated (n=50) -4.01 (-5.57, -2.45) P<0.0001 0.07
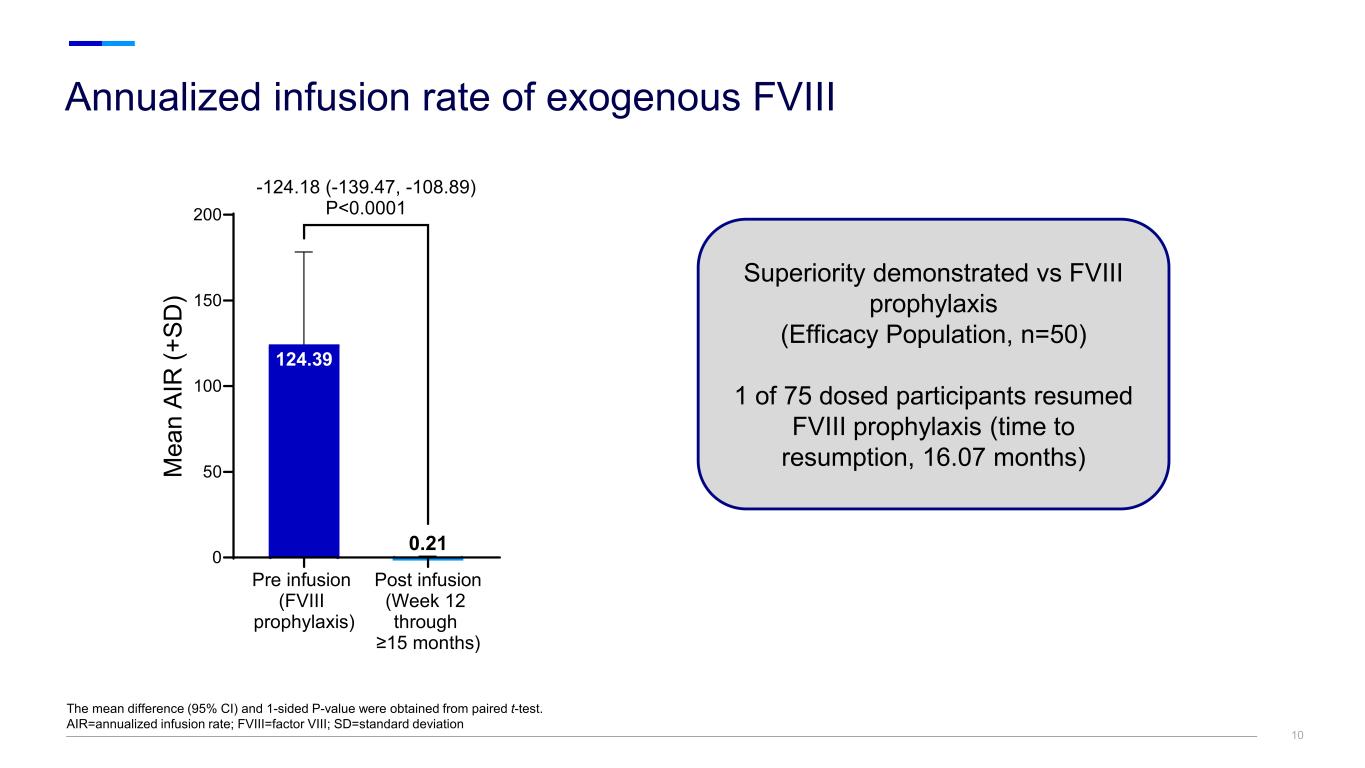
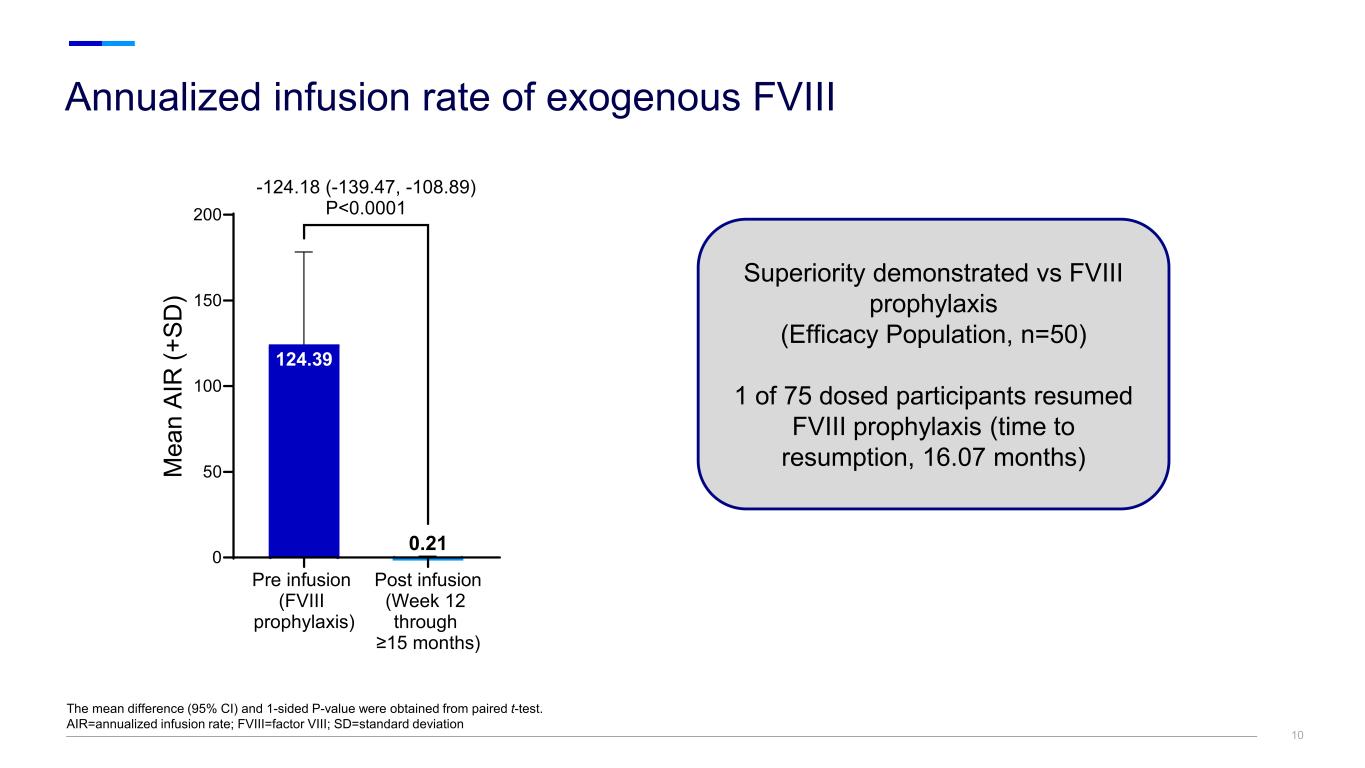
Annualized infusion rate of exogenous FVIII The mean difference (95% CI) and 1-sided P-value were obtained from paired t-test. AIR=annualized infusion rate; FVIII=factor VIII; SD=standard deviation 10 Pre infusion (FVIII prophylaxis) Post infusion (Week 12 through ≥15 months) 0 50 100 150 200 124.39 M ea n AI R (+ SD ) -124.18 (-139.47, -108.89) P<0.0001 0.21 Superiority demonstrated vs FVIII prophylaxis (Efficacy Population, n=50) 1 of 75 dosed participants resumed FVIII prophylaxis (time to resumption, 16.07 months)
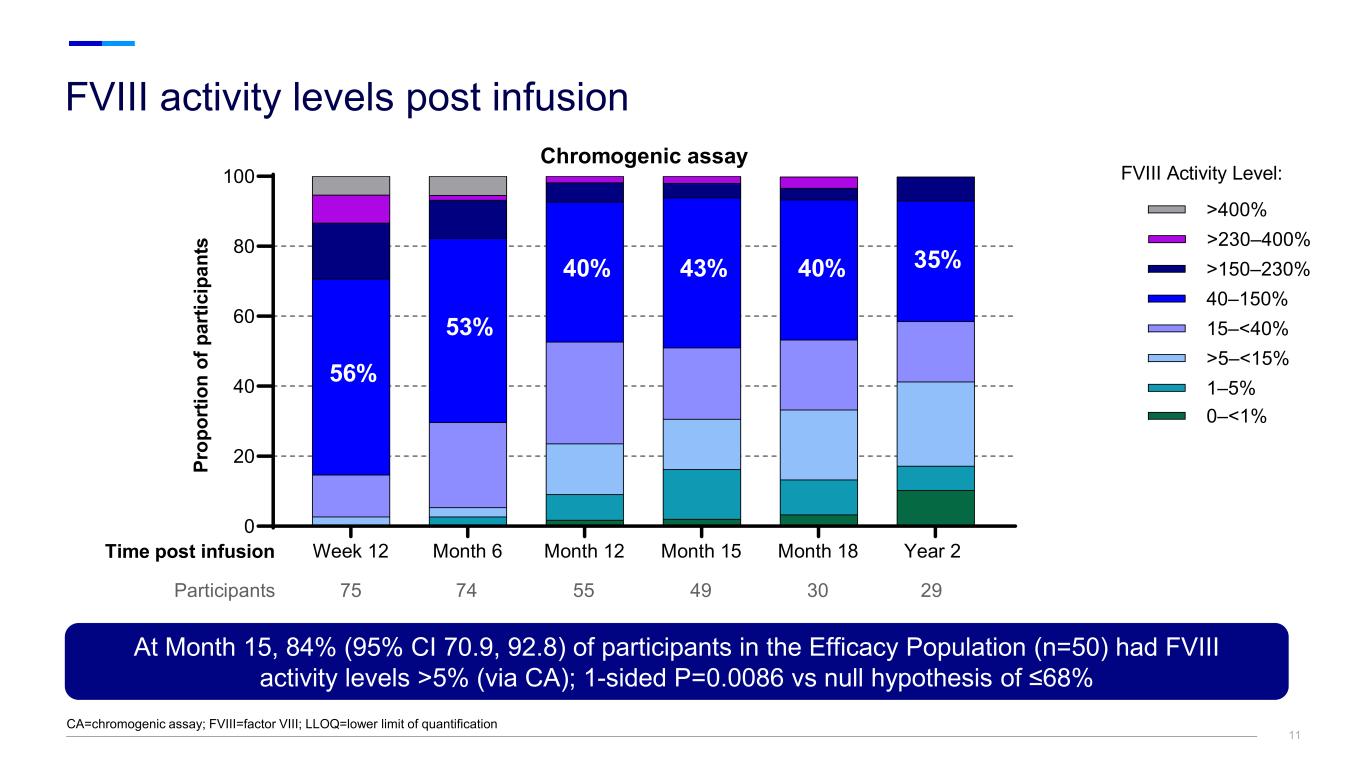
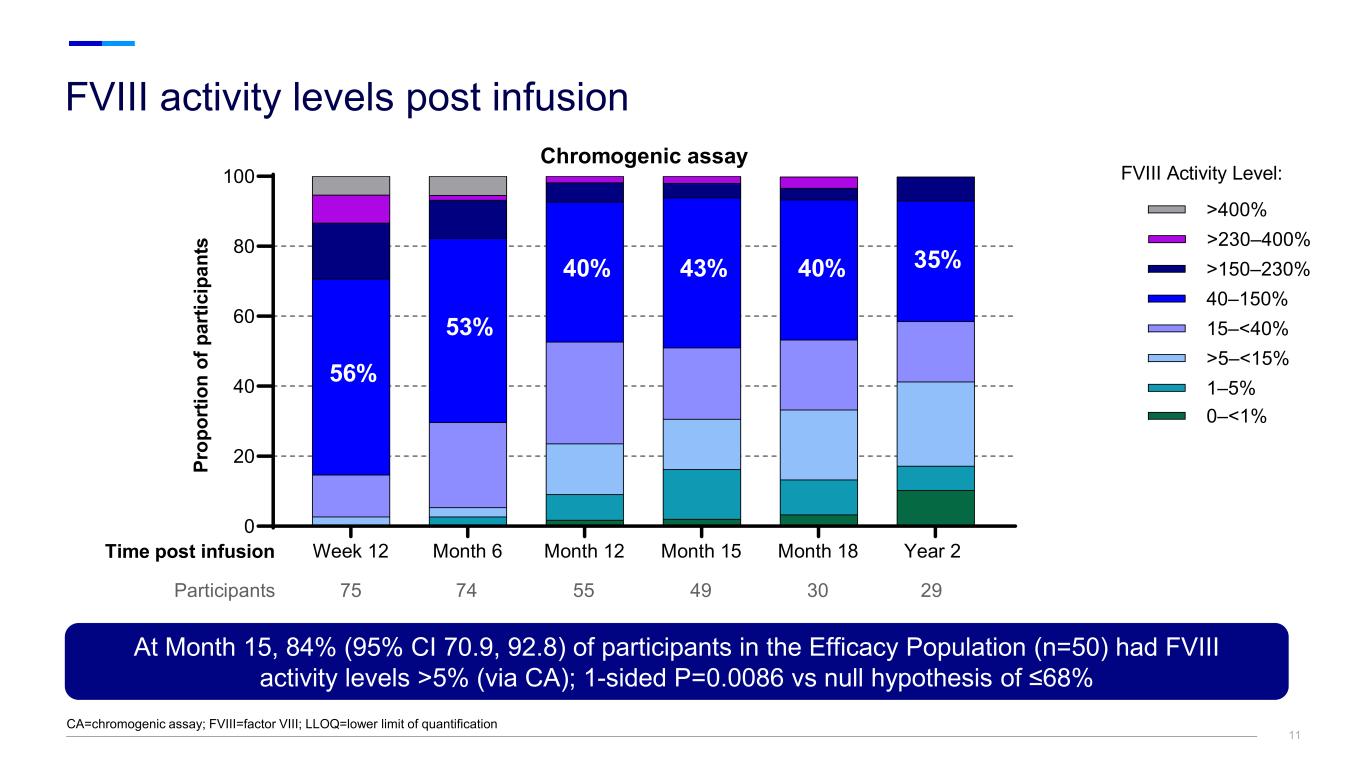
FVIII activity levels post infusion CA=chromogenic assay; FVIII=factor VIII; LLOQ=lower limit of quantification 11 At Month 15, 84% (95% CI 70.9, 92.8) of participants in the Efficacy Population (n=50) had FVIII activity levels >5% (via CA); 1-sided P=0.0086 vs null hypothesis of ≤68% Week 12 Month 6 Month 12 Month 15 Month 18 Year 2 0 20 40 60 80 100 Chromogenic assay Pr op or tio n of p ar tic ip an ts Participants 75 74 55 49 30 29 FVIII Activity Level: 15–<40% >400% >230–400% >150–230% 40–150% >5–<15% 1–5% 0–<1% 56% 53% 40% 43% 40% 35% Time post infusion

12 FVIII activity levels through Year 3 Values >300% not shown. CA=chromogenic assay; BLOQ=below lower limit of quantification; FVIII=factor VIII; IQR=interquartile range; max=maximum; min=minimum; Q=quartile Fa ct or V III A ct iv ity (c hr om og en ic , % ) Post infusion (Weeks) 50% 5% Year 2 51.9 (54.43) 36.5 (BLOQ–209.2) Year 3 40.7 (39.20) 38.0 (BLOQ–105.1) 12 Week 12 mean (SD):139.7 (143.81) median (range): 88.9 (8.8–843.1) Year 1 53.3 (53.89) 38.6 (BLOQ–234.7) Box length=Q1–Q3 (IQR) Whiskers=Q1/Q3-/+1.5*IQR =mean =median =outliers

13 • No infusion interruptions or rate slowing • Infusion-related reactions (events occurring within 2 days post infusion) in 58 (77.3%) participants – Mostly mild (n=39/58; 67.2%) with resolution within 2 days • At data cutoff (mean [range] follow-up, 21.88 [7.8-44.4] months): – No FVIII inhibitors – No malignancies related to study drug – One thrombotic event in a participant with major protocol deviation (prior history of DVT and PE) and multiple thrombotic risk factors AE=adverse event; AESI=adverse event of special interest; DVT=deep vein thrombosis; FVIII=factor VIII; PE=pulmonary embolism; SAE=serious adverse event Participants with AEs, n (%) and number of events (when specified) Dosed Population N=75 AEs 74 (98.7) Number of events 740 Discontinued due to AEs 0 (0) SAEs 15 (20.0) Number of events 26 Treatment-related AEs 68 (90.7) Selected treatment-related AESIs Hepatotoxicity (transaminase increased) 47 (62.7) Infusion-related reactions 55 (73.3) Pyrexia 38 (50.7) Headache 23 (30.7) Chills 14 (18.7) Deep vein thrombosis 1 (1.3) Safety overview

14 • ALT elevations were mild and manageable – ALT elevations resolved within a median of 28.0 days • Overall, corticosteroids were well tolerated, with corticosteroid-related AEs reported in 19 (25.3%) participants • At the time of the data cutoff, no participants in the Efficacy Population remained on corticosteroids • 5 (6.7%) participants received alternative immunosuppressive therapies following corticosteroid treatment, including MMF in 4 participants, and azathioprine in 1 participant a The highest CTCAE grade among all post baseline assessments from each participant are reported. AE=adverse event; ALT=alanine aminotransferase; CTCAE=common terminology criteria for adverse events; MMF=mycophenolate mofetil; pts=participants; SAE=serious adverse event; ULN=upper limit of normal ALT and corticosteroid use N=75 Treatment-related AEs related to hepatotoxicity (transaminase increased), n (%) 47 (62.7) SAEs related to transaminase increased, n (%) 2 (2.7) Participants with ALT increase >ULN, n (%) 46 (61.3) ALT grades (CTCAE grading)a among all dosed participants, n (%) Normal 30 (40.0) Grade 1 40 (53.3) Grade 2 4 (5.3) Grade 3 1 (1.3) Grade 4 0 (0) Pts with corticosteroid use, n (%) 47 (62.7) Time to corticosteroid initiation, median (range), days 84 (7–193) Corticosteroid courses per participant, mean (range), days 2.0 (1–5) Duration of corticosteroid use, mean (range), days 114.6 (11–296) ALT elevations and corticosteroid use
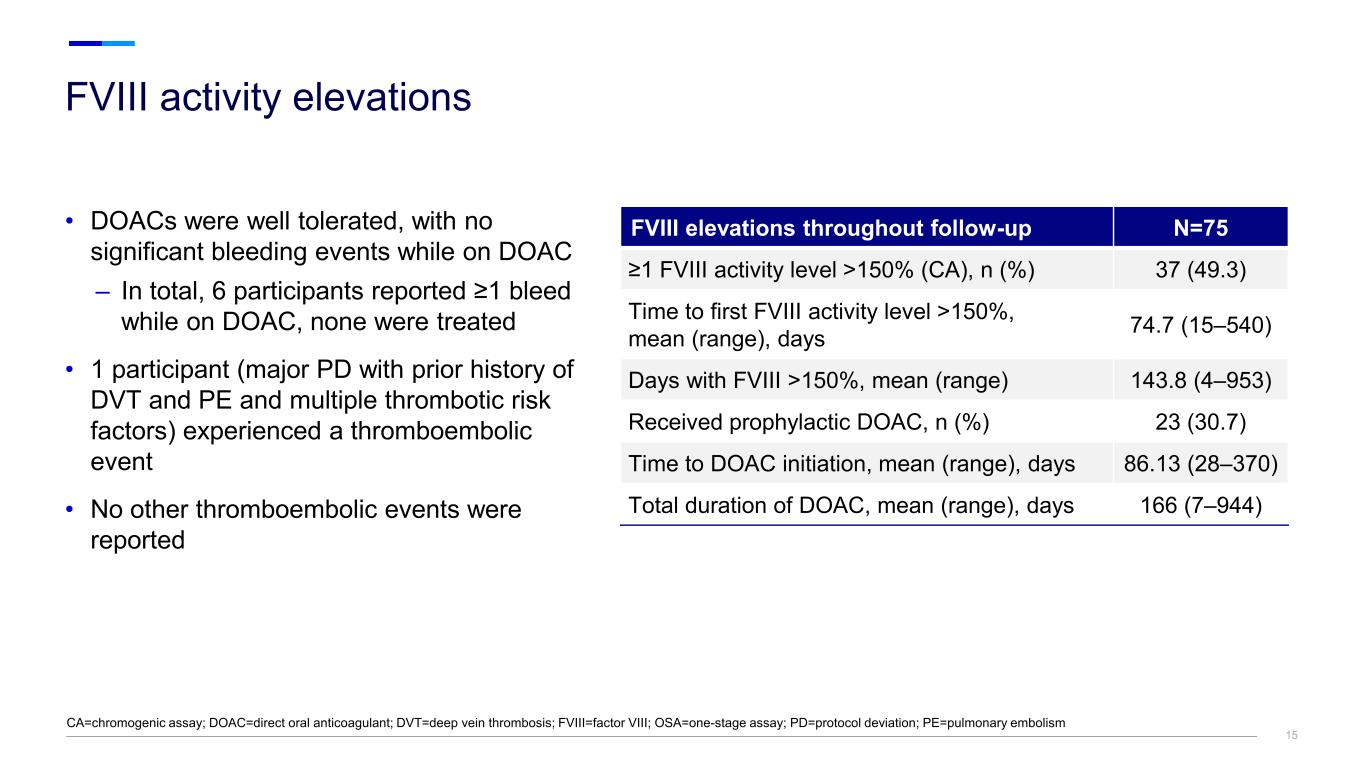
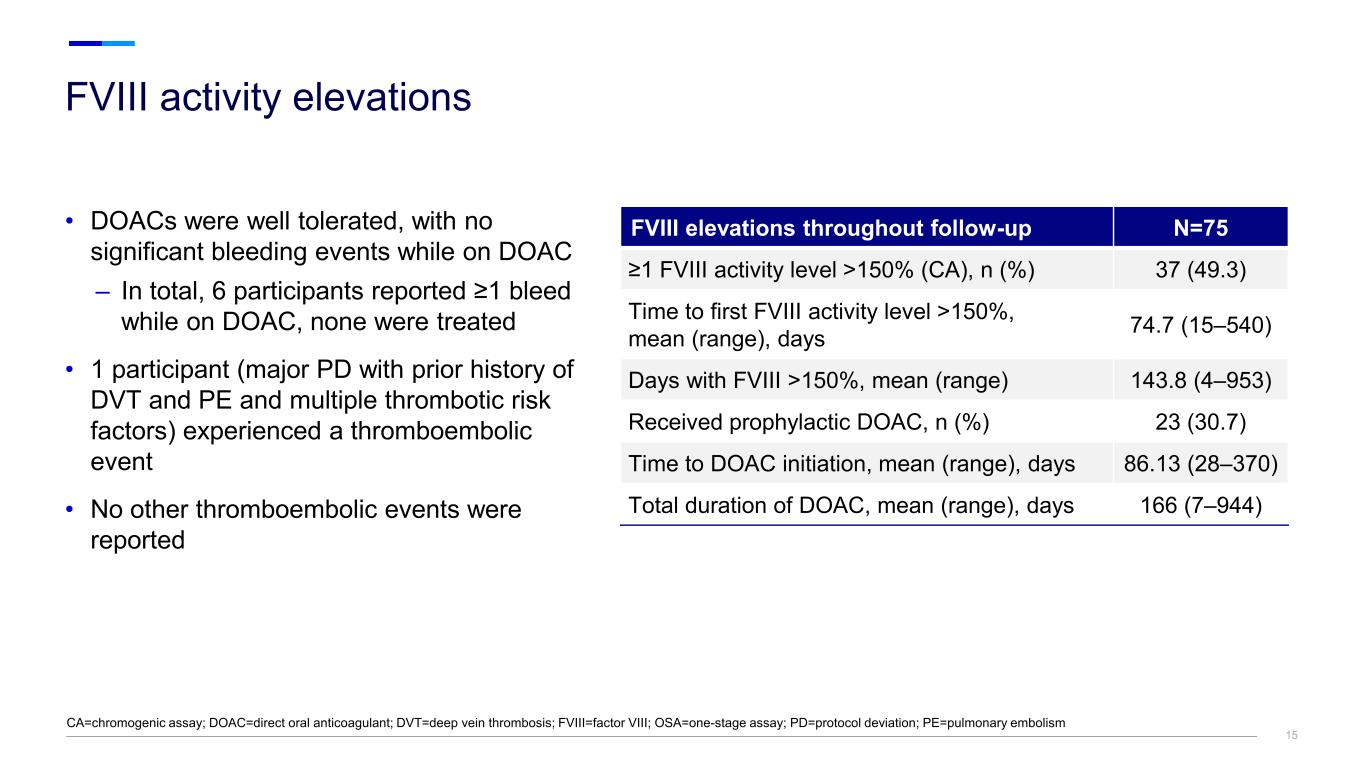
15 • DOACs were well tolerated, with no significant bleeding events while on DOAC – In total, 6 participants reported ≥1 bleed while on DOAC, none were treated • 1 participant (major PD with prior history of DVT and PE and multiple thrombotic risk factors) experienced a thromboembolic event • No other thromboembolic events were reported CA=chromogenic assay; DOAC=direct oral anticoagulant; DVT=deep vein thrombosis; FVIII=factor VIII; OSA=one-stage assay; PD=protocol deviation; PE=pulmonary embolism FVIII elevations throughout follow-up N=75 ≥1 FVIII activity level >150% (CA), n (%) 37 (49.3) Time to first FVIII activity level >150%, mean (range), days 74.7 (15–540) Days with FVIII >150%, mean (range) 143.8 (4–953) Received prophylactic DOAC, n (%) 23 (30.7) Time to DOAC initiation, mean (range), days 86.13 (28–370) Total duration of DOAC, mean (range), days 166 (7–944) FVIII activity elevations
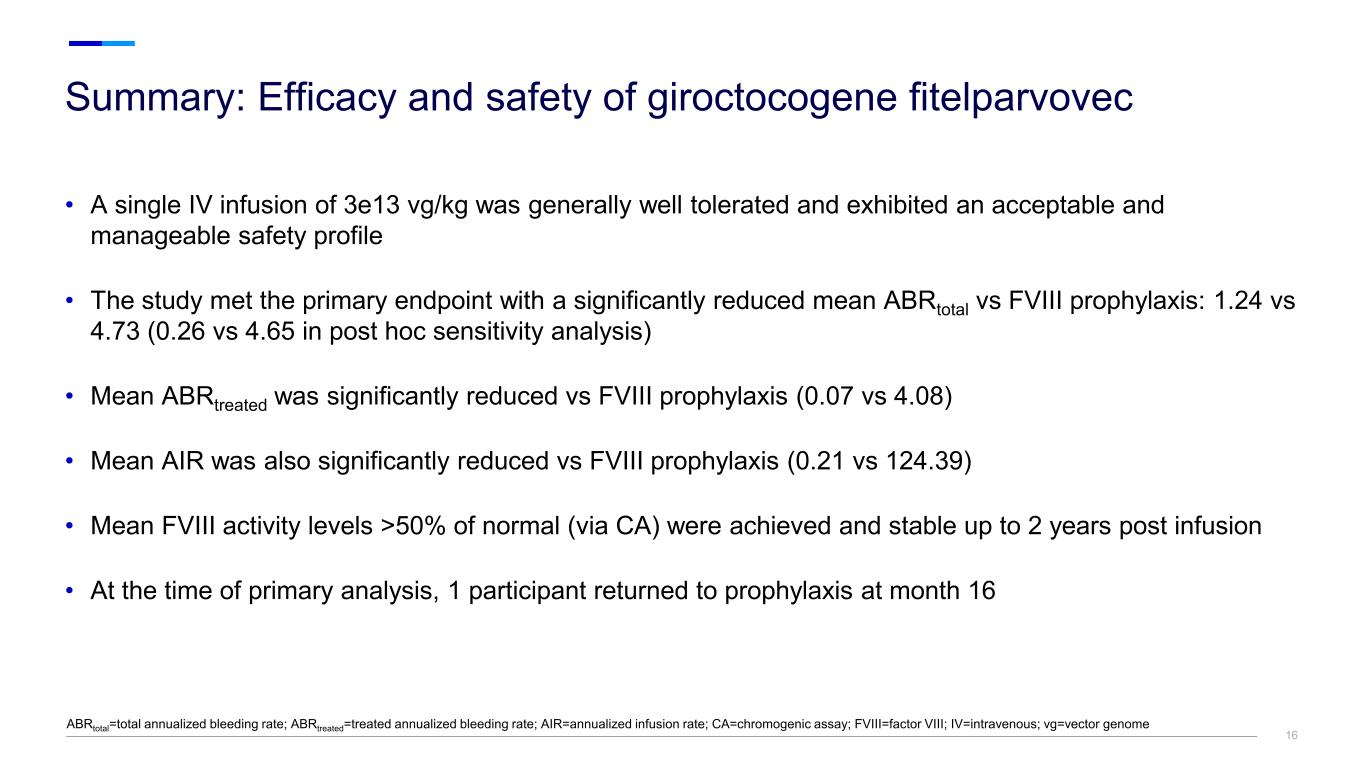
16 • A single IV infusion of 3e13 vg/kg was generally well tolerated and exhibited an acceptable and manageable safety profile • The study met the primary endpoint with a significantly reduced mean ABRtotal vs FVIII prophylaxis: 1.24 vs 4.73 (0.26 vs 4.65 in post hoc sensitivity analysis) • Mean ABRtreated was significantly reduced vs FVIII prophylaxis (0.07 vs 4.08) • Mean AIR was also significantly reduced vs FVIII prophylaxis (0.21 vs 124.39) • Mean FVIII activity levels >50% of normal (via CA) were achieved and stable up to 2 years post infusion • At the time of primary analysis, 1 participant returned to prophylaxis at month 16 Summary: Efficacy and safety of giroctocogene fitelparvovec ABRtotal=total annualized bleeding rate; ABRtreated=treated annualized bleeding rate; AIR=annualized infusion rate; CA=chromogenic assay; FVIII=factor VIII; IV=intravenous; vg=vector genome