|
| | | | | |
|
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM ADMINISTRATION DIVISION OF BUSINESS AND FINANCE SECTION A. CONTRACT AMENDMENT |
1. AMENDMENT NUMBER: 19 | 2. CONTRACT NO.:
YH09-0001 | 3. EFFECTIVE DATE OF CONTRACT: October 1, 2012 | 4. PROGRAM DHCM - ACUTE |
5. CONTRACTOR'S NAME AND ADDRESS: VHS Phoenix Health Plan, LLC 7878 N. 16th Street, Suite 115 Phoenix, AZ 85020
|
6. PURPOSE OF AMENDMENT: To extend the Contract for the term October 1, 2012 through September 30, 2013 and to amend Section B, Capitation Rates, Section C, Definitions, Section D, Program Requirements, Section E, Contract Clauses, and Section J, Attachments . |
7. THE CONTRACT REFERENCED ABOVE IS AMENDED AS FOLLOWS: A. Section B, Capitation Rates have been revised for the period of October 1, 2012 through September 30, 2013. B. Section C, Definitions C. Section D, Program Requirements D. Section E, Contract Terms and Conditions E. Section J, Attachments
Please refer to the individual Contract sections, revised September 26, 2012, for specific changes. Note: Please sign, date and return executed file by E-Mail to: Meggan Harley at meggan.harley@azahcccs.gov Contracts Manager, AHCCCS Contracts & Purchasing and P.J. Schoenstene, Contracts and Policy Administrator, at pj.schoenstene@azahcccs.gov Division of Health Care Management
|
8. EXCEPT AS PROVIDED FOR HEREIN, ALL TERMS AND CONDITIONS OF THE ORIGINAL CONTRACT NOT HERETOFORE CHANGED AND/OR AMENDED REMAIN UNCHANGED AND IN FULL EFFECT. IN WITNESS WHEREOF THE PARTIES HERETO SIGN THEIR NAMES IN AGREEMENT |
9. SIGNATURE OF AUTHORIZED REPRESENTATIVE: /s/ Nancy Novick | 10. SIGNATURE OF AHCCCS CONTRACTING OFFICER: /s/ Michael Veit |
TYPED NAME: NANCY NOVICK | TYPED NAME: MICHAEL VEIT |
TITLE: CHIEF EXECUTIVE OFFICER
| TITLE: CONTRACTS & PURCHASING ADMINISTRATOR |
| DATE: September 28, 2012 | DATE: September 27, 2012 |
1
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
Contract/RFP No. YH09-0001
|
| | | |
| | Tables of Contents | |
| | | |
| SECTION A. | CONTRACT AMENDMENT | 1 |
|
| SECTION B: | CAPITATION RATES AND CONTRACTOR SPECIFIC INFORMATION | 7 |
|
| SECTION C: | DEFINITIONS | 11 |
|
| SECTION D: | PROGRAM REQUIREMENTS | 19 |
|
| INTRODUCTION | | 19 |
|
| 3. | TERM OF CONTRACT AND OPTION TO RENEW | 19 |
|
| 4. | ELIGIBILITY CATEGORIES | 19 |
|
| 5. | ENROLLMENT AND DISENROLLMENT | 20 |
|
| 6. | ANNUAL ENROLLMENT CHOICE | 22 |
|
| 7. | ENROLLMENT AFTER CONTRACT AWARD | 25 |
|
| 8. | AUTO-ASSIGNMENT ALGORITHM | 25 |
|
| 9. | AHCCCS MEMBER IDENTIFICATION CARDS | 26 |
|
| 10. | MAINSTREAMING OF AHCCCS MEMBERS | 26 |
|
| 11. | TRANSITION OF MEMBERS | 26 |
|
| 12. | SCOPE OF SERVICES | 27 |
|
| 13. | SPECIAL HEALTH CARE NEEDS | 36 |
|
| 14. | BEHAVIORAL HEALTH SERVICES | 38 |
|
| 15. | AHCCCS GUIDELINES, POLICIES AND MANUALS | 40 |
|
| 16. | MEDICAID SCHOOL BASED CLAIMING PROGRAM (MSB) | 41 |
|
| 17. | PEDIATRIC IMMUNIZATIONS AND THE VACCINES FOR CHILDREN PROGRAM | 42 |
|
| 18. | STAFF REQUIREMENTS AND SUPPORT SERVICES | 42 |
|
| 19. | WRITTEN POLICIES, PROCEDURES AND JOB DESCRIPTIONS | 47 |
|
| 20. | MEMBER INFORMATION | 48 |
|
| 21. | SURVEYS | 49 |
|
| 22. | CULTURAL COMPETENCY | 50 |
|
| 23. | MEDICAL RECORDS | 50 |
|
| 24. | ADVANCE DIRECTIVES | 51 |
|
| 25. | QUALITY MANAGEMENT (QM) | 52 |
|
| 26. | MEDICAL MANAGEMENT (MM) | 57 |
|
| 27. | ADMINISTRATIVE PERFORMANCE STANDARDS | 59 |
|
| 28. | GRIEVANCE SYSTEM | 60 |
|
| 29. | NETWORK DEVELOPMENT | 61 |
|
| 30. | PROVIDER AFFILIATION TRANSMISSION | 62 |
|
| 31. | NETWORK MANAGEMENT | 62 |
|
| 32. | PRIMARY CARE PROVIDER STANDARDS | 64 |
|
| 33. | MATERNITY CARE PROVIDER STANDARDS | 65 |
|
| 34. | REFERRAL MANAGEMENT PROCEDURES AND STANDARDS | 66 |
|
| 35. | APPOINTMENT STANDARDS | 67 |
|
| 36. | FEDERALLY QUALIFIED HEALTH CENTERS (FQHCS) AND RURAL HEALTH CLINICS (RHCS) | 69 |
|
2
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
Contract/RFP No. YH09-0001
|
| | | |
| 37. | PROVIDER MANUAL | 69 |
|
| 38. | PROVIDER REGISTRATION | 69 |
|
| 39. | SUBCONTRACTS | 69 |
|
| 40. | CLAIMS PAYMENT/HEALTH INFORMATION SYSTEM | 72 |
|
| 41. | SPECIALTY CONTRACTS | 76 |
|
| 42. | HOSPITAL SUBCONTRACTING AND REIMBURSEMENT | 76 |
|
| 43. | RESPONSIBILITY FOR NURSING FACILITY REIMBURSEMENT | 77 |
|
| 44. | PHYSICIAN INCENTIVES/PAY FOR PERFORMANCE | 77 |
|
| 45. | MANAGEMENT SERVICES AGREEMENT AND COST ALLOCATION PLAN | 78 |
|
| 46. | RESERVED | 78 |
|
| 47. | RESERVED | 78 |
|
| 48. | PERFORMANCE BOND OR BOND SUBSTITUTE | 78 |
|
| 49. | AMOUNT OF PERFORMANCE BOND | 79 |
|
| 50. | ACCUMULATED FUND DEFICIT | 79 |
|
| 51. | ADVANCES, DISTRIBUTIONS, LOANS AND INVESTMENTS | 80 |
|
| 52. | FINANCIAL VIABILITY STANDARDS | 80 |
|
| 53. | SEPARATE INCORPORATION | 81 |
|
| 54. | MERGER, REORGANIZATION AND CHANGE OF OWNERSHIP | 81 |
|
| 55. | COMPENSATION | 81 |
|
| 56. | PAYMENTS TO CONTRACTORS | 84 |
|
| 57. | CAPITATION ADJUSTMENTS | 84 |
|
| 58. | MEMBER BILLING AND LIABILITY FOR PAYMENT | 86 |
|
| 59. | REINSURANCE | 86 |
|
| 60. | COORDINATION OF BENEFITS | 90 |
|
| 61. | COPAYMENTS | 95 |
|
| 62. | MEDICARE SERVICES AND COST SHARING | 95 |
|
| 63. | MARKETING | 96 |
|
| 64. | CORPORATE COMPLIANCE | 96 |
|
| 65. | RECORDS RETENTION | 99 |
|
| 66. | DATA EXCHANGE REQUIREMENTS | 100 |
|
| 67. | ENCOUNTER DATA REPORTING | 101 |
|
| 68. | ENROLLMENT AND CAPITATION TRANSACTION UPDATES | 103 |
|
| 69. | PERIODIC REPORT REQUIREMENTS | 103 |
|
| 70. | REQUESTS FOR INFORMATION | 104 |
|
| 71. | DISSEMINATION OF INFORMATION | 104 |
|
| 72. | OPERATIONAL AND FINANCIAL READINESS REVIEWS | 104 |
|
| 73. | OPERATIONAL AND FINANCIAL REVIEWS | 104 |
|
| 74. | SANCTIONS | 105 |
|
| 75. | BUSINESS CONTINUITY AND RECOVERY PLAN | 106 |
|
| 76. | TECHNOLOGICAL ADVANCEMENT | 107 |
|
| 77. | PENDING LEGISLATION / OTHER ISSUES | 108 |
|
3
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
Contract/RFP No. YH09-0001
|
| | | |
| 78. | RESERVED | 109 |
|
| 79. | RESERVED | 109 |
|
| 80. | RESERVED | 109 |
|
| SECTION E: | CONTRACT TERMS AND CONDITIONS | 110 |
|
| 1) | APPLICABLE LAW | 110 |
|
| 2) | AUTHORITY | 110 |
|
| 3) | ORDER OF PRECEDENCE | 110 |
|
| 4) | CONTRACT INTERPRETATION AND AMENDMENT | 110 |
|
| 5) | SEVERABILITY | 110 |
|
| 6) | RELATIONSHIP OF PARTIES | 110 |
|
| 7) | ASSIGNMENT AND DELEGATION | 110 |
|
| 8) | INDEMNIFICATION | 111 |
|
| 9) | INDEMNIFICATION -- PATENT AND COPYRIGHT | 111 |
|
| 10) | COMPLIANCE WITH APPLICABLE LAWS, RULES AND REGULATIONS | 111 |
|
| 11) | ADVERTISING AND PROMOTION OF CONTRACT | 111 |
|
| 12) | THIRD PARTY ANTITRUST VIOLATIONS | 111 |
|
| 13) | RIGHT TO ASSURANCE | 112 |
|
| 14) | TERMINATION FOR CONFLICT OF INTEREST | 112 |
|
| 15) | GRATUITIES | 112 |
|
| 16) | SUSPENSION OR DEBARMENT | 112 |
|
| 17) | TERMINATION FOR CONVENIENCE | 112 |
|
| 18) | TEMPORARY MANAGEMENT/OPERATION OF A CONTRACTOR AND TERMINATION | 113 |
|
| 19) | TERMINATION - AVAILABILITY OF FUNDS | 114 |
|
| 20) | RIGHT OF OFFSET | 114 |
|
| 21) | NON-EXCLUSIVE REMEDIES | 114 |
|
| 22) | NON-DISCRIMINATION | 114 |
|
| 23) | EFFECTIVE DATE | 114 |
|
| 24) | INSURANCE | 114 |
|
| 25) | DISPUTES | 115 |
|
| 26) | RIGHT TO INSPECT PLANT OR PLACE OF BUSINESS | 115 |
|
| 27) | INCORPORATION BY REFERENCE | 115 |
|
| 28) | COVENANT AGAINST CONTINGENT FEES | 115 |
|
| 29) | CHANGES | 116 |
|
| 30) | TYPE OF CONTRACT | 116 |
|
| 31) | AMERICANS WITH DISABILITIES ACT | 116 |
|
| 32) | WARRANTY OF SERVICES | 116 |
|
| 33) | NO GUARANTEED QUANTITIES | 116 |
|
| 34) | CONFLICT OF INTEREST | 116 |
|
| 35) | CONFIDENTIALITY AND DISCLOSURE OF CONFIDENTIAL INFORMATION | 116 |
|
| 36) | COOPERATION WITH OTHER CONTRACTORS | 117 |
|
| 37) | ASSIGNMENT OF CONTRACT AND BANKRUPTCY | 117 |
|
4
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
Contract/RFP No. YH09-0001
|
| | | |
| 38) | OWNERSHIP OF INFORMATION AND DATA | 117 |
|
| 39) | AUDITS AND INSPECTIONS | 118 |
|
| 40) | LOBBYING | 118 |
|
| 41) | CHOICE OF FORUM | 118 |
|
| 42) | DATA CERTIFICATION | 118 |
|
| 43) | OFF-SHORE PERFORMANCE OF WORK PROHIBITED | 118 |
|
| 44) | FEDERAL IMMIGRATION AND NATIONALITY ACT | 118 |
|
| 45) | IRS W-9 FORM | 118 |
|
| 46) | CONTINUATION OF PERFORMANCE THROUGH TERMINATION | 118 |
|
| 47) | E-VERIFY REQUIREMENTS | 118 |
|
| 48) | SCRUTINIZED BUSINESS | 119 |
|
| SECTION F: | RESERVED | 120 |
|
| SECTION G: | RESERVED | 121 |
|
| SECTION H: | RESERVED | 122 |
|
| SECTION I: | RESERVED | 123 |
|
| SECTION J: | LIST OF ATTACHMENTS | 124 |
|
| ATTACHMENT A: | RESERVED | 125 |
|
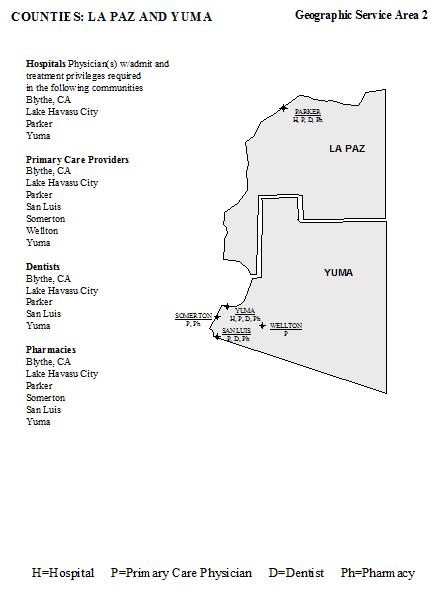
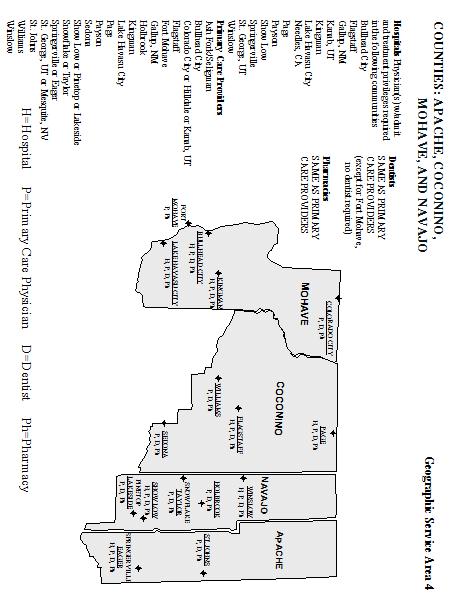
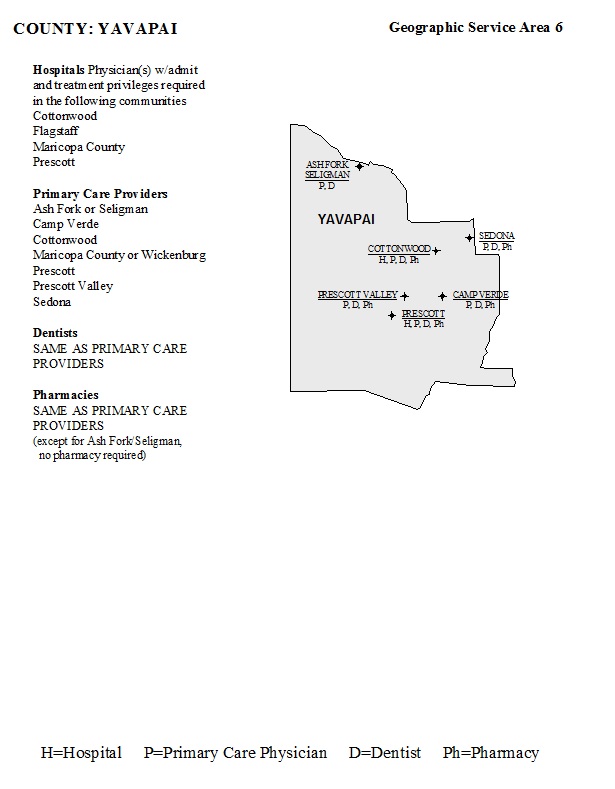
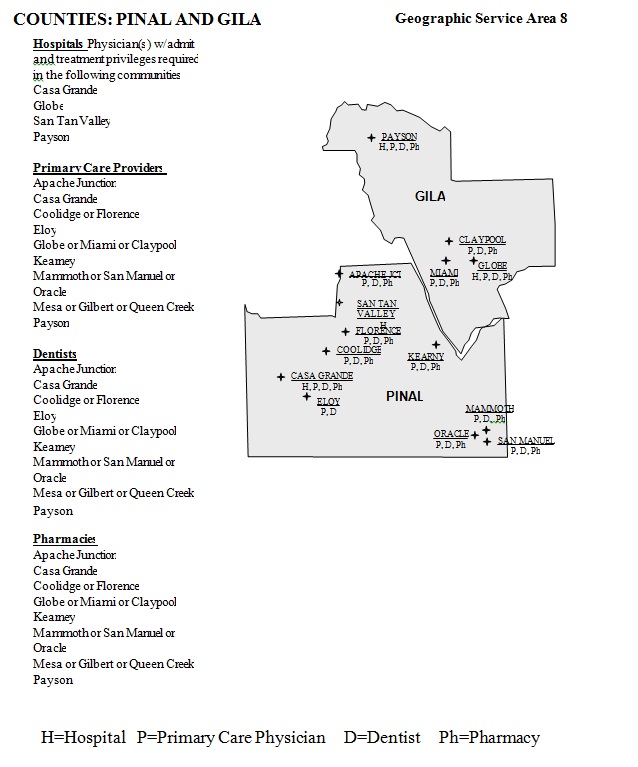
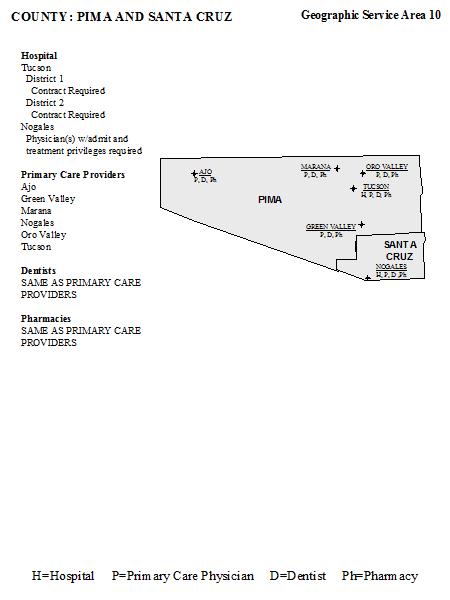
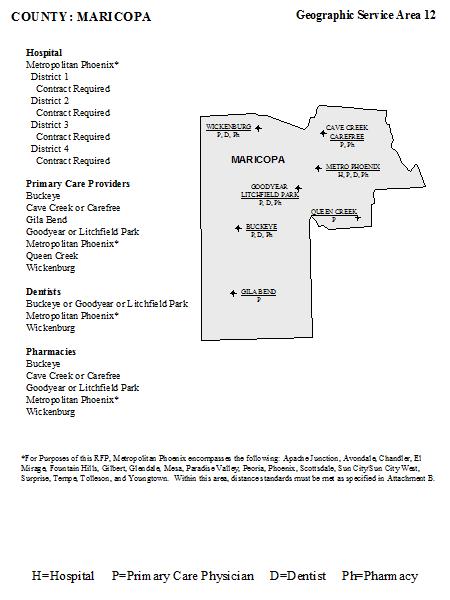
| ATTACHMENT B: | MINIMUM NETWORK STANDARDS (By Geographic Service Area) | 126 |
|
| ATTACHMENT C: | RESERVED | 137 |
|
| ATTACHMENT D: | SAMPLE LETTER OF INTENT | 138 |
|
| ATTACHMENT E: | RESERVED | 143 |
|
| ATTACHMENT F: | CONTRACTORS CHART OF DELIVERABLES | 144 |
|
| ATTACHMENT G: | AUTO-ASSIGNMENT ALGORITHM | 154 |
|
| ATTACHMENT H(1): | ENROLLEE GRIEVANCE SYSTEM STANDARDS AND POLICY | 159 |
|
| ATTACHMENT I: | RESERVED | 165 |
|
| ATTACHMENT J: | RESERVED | 166 |
|
| ATTACHMENT J(2): | RESERVED | 167 |
|
| ATTACHMENT K: | RESERVED | 168 |
|
5
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
Contract/RFP No. YH09-0001
SECTION B: CAPITATION RATES and CONTRACTOR SPECIFIC INFORMATION
The Contractor shall provide services as described in this contract. In consideration for these services, the Contractor will be paid Contractor-specific rates per member per month for the term October 1, 2012 through September 30, 2013.
Phoenix Health Plan special contract language:
HMS Credit Balance Program
I. Purpose:
The purpose of this amendment is to implement a credit balance review program by Health Management Systems, Inc. (HMS) on behalf of Phoenix Health Plan through HMS’s contract with the Arizona Health Care Cost Containment System (AHCCCS). Credit Balance Review is the process used to identify and recover any Medicare or Third Party resource overpayment retained by a provider for an AHCCCS member.
II. Process:
HMS’s credit balance program is comprised of two parts, which when used in conjunction, have proven to be effective recovery tools. The process begins when HMS notifies the selected provider by mail requesting they conduct a self-audit for credit balances. This will be accompanied by the AHCCCS Health Plan third party resource refund worksheet (Attachment A). Instructions allow a provider to return overpayments, which may exclude them from an on-site review. After sufficient time has been allowed for all to respond, the next step is to select providers for on-site reviews of the provider’s credit balance process. Providers are selected for this review based upon their comparative returns of credit balances in the self-audit, AHCCCS and the Health Plan preference, and the likelihood of credit balances existing. AHCCCS will generate a letter to the provider notifying them of the on-site review, explaining the scope, and including a list of accounts that have been targeted for review. This list will be identified through a series of data analysis programs designed to create a profile of a member/patient with a potential credit balance. To perform this function, HMS will use a combination of data files including paid claims history, encounter data, and eligibility files. In addition, provider accounting procedures are verified to ensure the proper posting of contractual allowances, etc. HMS will schedule these reviews approximately thirty (30) days after the provider receives the notification.
Any credit balance accounts under current review or previously identified by the Health Plans shall be reported to AHCCCS prior to HMS’s scheduled review. These accounts should be reported on the AHCCCS Health Plan credit balance accounts under review worksheet (Attachment B) with supporting documentation.
The providers will be directed to send the refund balances to HMS. HMS will receive and identify these refunds. AHCCCS will require HMS to process these refunds in the same manner as currently required by the AHCCCS contract with HMS. AHCCCS will require HMS to research the refunds and to provide a monthly disbursement report of the refund amounts due to the health plans and program contractors. AHCCCS will disburse a payment in the amount due to the health plans and program contractors.
An electronic report of all claims identified as credit balances where reimbursement is received from the provider, will be generated for the Health Plan and for AHCCCS. HMS will research and verify cases needing adjustments as a result of the credit balance. All recoveries are subject to reporting requirements contained in the AHCCCS Recoupment Request Policy. Depending on the program’s initial success, this program may be implemented quarterly, semi-annually or annually.
7
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION C: DEFINITIONS Contract/RFP No. YH09-0001
ATTACHMENT A
Third Party Resource Refund Worksheet
AHCCCS Provider Name: _______________________ Page: ________ of ________
Completed By: ___________________
AHCCCS Provider ID Number: _______________________ Date: ________/_______/_______
|
| | | | | | | | | | | | | | | | | | | | |
| | MEMBER/PATIENT NAME | MEMBER/ PATIENT AHCCCS ID | DATE OF SERVICE PERIOD | CLAIM REFERENCE NUMBER (CRN) | TOTAL BILLED CHARGES | TOTAL AMOUNT PAID BY AHCCCS |
TOTAL AMOUNT PAID BY THIRD PARTY RESOURCE/ INSURANCE |
THIRD PARTY RESOURCE/ INSURANCE NAME | REFUND AMOUNT DUE | REASON FOR REFUND |
| | FROM | TO | | | | |
| | | | | | | | | | | | |
| | | | | | | | | | | | |
| | | | | | | | | | | | |
| | | | | | | | | | | | |
| | | | | | | | | | | | |
| | | | | | | | | | | | |
| | | | | | | | | | | | |
| | | | | | | | | | | | |
This is to certify that the information contained in this report is true, accurate and complete, to the best of my knowledge. I understand that AHCCCS will rely on this certification at the time AHCCCS certifies its expenditures to the Centers for Medicare and Medicaid Services on Form CMS-64.
| |
| 1. | Authorized Signature ___________________________________ Date: _________________________ |
8
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION C: DEFINITIONS Contract/RFP No. YH09-0001
ATTACHMENT B
Credit Balance Accounts Under Review by AHCCCS Program Contractors
Health Plan Name: ________________________ Page: ________ of ________
Completed By: ___________________
Health Plan ID Number: _______________________ Date: ________/_______/_______
|
| | | | | | | | |
AHCCCS PROVIDER NAME |
AHCCCS PROVIDER ID NUMBER |
MEMBER/ PATIENT NAME |
MEMBER/ PATIENT AHCCCS ID |
DATE OF SERVICE PERIOD
|
ENCOUNTER/ CLAIM REFERENCE NUMBER (CRN) |
TOTAL BILLED CHARGES |
THIRD PARTY RESOURCE/INSURANCE NAME |
FROM |
TO |
| | | | | | | | | |
| | | | | | | | | |
| | | | | | | | | |
| | | | | | | | | |
| | | | | | | | | |
| | | | | | | | | |
| | | | | | | | | |
| | | | | | | | | |
| | | | | | | | | |
| | | | | | | | | |
This is to certify that the information contained in this report is true, accurate and complete, to the best of my knowledge. I understand that AHCCCS will rely on this certification at the time AHCCCS certifies its expenditures to the Centers for Medicare and Medicaid Services on Form CMS-64.
| |
| 2. | Authorized Signature ___________________________________ Date:_______________________ |
9
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION C: DEFINITIONS Contract/RFP No. YH09-0001
SECTION C: DEFINITIONS
|
| | |
| 638 TRIBAL FACILITY | A facility that is operated by an Indian tribe and that is authorized to provide services pursuant to Public Law (P.L.) 93-638, as amended. | |
| 1931 (also referred to as TANF related) | Eligible individuals and families under Section 1931 of the Social Security Act, with household income levels at or below 100% of the Federal poverty level (FPL). | |
| | | |
| ACOM | AHCCCS Contractor Operations Manual, available on the AHCCCS website at www.azahcccs.gov. | |
| ADHS | Arizona Department of Health Services, the state agency mandated to serve the public health needs of all Arizona residents.
| |
| ADHS BEHAVIORAL HEALTH RECIPIENT | A Title XIX or Title XXI acute care member who is receiving behavioral health services through ADHS and its subcontractors. | |
| ADJUDICATED CLAIMS | Claims that have been received and processed by the Contractor which resulted in a payment or denial of payment | |
| | | |
| AGENT | Any person who has been delegated the authority to obligate or act on behalf of another person or entity. | |
| AHCCCS | Arizona Health Care Cost Containment System, which is composed of the Administration, Contractors, and other arrangements through which health care services are provided to an eligible person, as defined by A.R.S. § 36-2902, et seq.
| |
| AHCCCS BENEFITS | See “COVERED SERVICES. | |
| AHCCCS CARE | Eligible individuals and childless adults whose income is less than or equal to 100% of the FPL, and who are not categorically linked to another Title XIX program. (Formerly Non-MED) | |
| AHCCCS MEMBER | See “MEMBER”. | |
| ALTCS | The Arizona Long Term Care System, a program under AHCCCS that delivers long-term, acute, behavioral health and case management services to eligible members, as authorized by A.R.S. § 36-2932.
| |
AMBULATORY CARE | Preventive, diagnostic and treatment services provided on an outpatient basis by physicians, nurse practitioners physician assistants and other health care providers.
| |
| AMERICAN INDIAN HEALTH PROGRAM (AIHP) | AIHP is an acute care FFS program administered by AHCCCS for eligible American Indians which reimburses for services provided by and through the Indian Health Service (IHS), tribal health programs operated under PL 93-638 or any other AHCCCS registered provider. AIHP was formerly known as AHCCCS IHS. | |
| AMPM | AHCCCS Medical Policy Manual, available on the AHCCCS website at www.azahcccs.gov. | |
| ANNUAL ENROLLMENT CHOICE (AEC) | The opportunity for a person to change contractors every 12 months, effective on their anniversary date | |
10
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION C: DEFINITIONS Contract/RFP No. YH09-0001
|
| | |
| ANNIVERSARY DATE | The anniversary date is 12 months from the date enrolled with the Contractor and annually thereafter. In some cases, the anniversary date will change based on the last date the member changed Contractors or the last date the member was given an opportunity to change. | |
| APPEAL RESOLUTION | The written determination by the Contractor concerning an appeal. | |
| ARIZONA ADMINISTRATIVE CODE (A.A.C.) | Arizona Administrative Code. State regulations established pursuant to relevant statutes. Referred to in contract as “AHCCCS Rules”. | |
| AT RISK | Refers to the period of time that a member is enrolled with a Contractor during which time the Contractor is responsible to provide AHCCCS covered services under capitation. | |
| A.R.S. | Arizona Revised Statutes. | |
| BIDDER’S LIBRARY | A repository of manuals, statutes, Rules and other reference material located on the AHCCCS website at www.azahcccs.gov. | |
BOARD CERTIFIED
| An individual who has successfully completed all prerequisites of the respective specialty board and successfully passed the required examination for certification.
| |
| BORDER COMMUNITIES | Cities, towns or municipalities located in Arizona and within a designated geographic service area whose residents typically receive primary or emergency care in adjacent Geographic Service Areas (GSA) or neighboring states, excluding neighboring countries, due to service availability or distance. (R9-22-201.F, R9-22-201.G, R9-22-101.B) | |
| BREAST AND CERVICAL CANCER TREATMENT PROGRAM (BCCTP | Eligible individuals under the Title XIX expansion program for women with income up to 250% of the FPL, who are diagnosed with and need treatment for breast and/or cervical cancer or cervical lesions and are not eligible for other Title XIX programs providing full Title XIX services. Qualifying individuals cannot have other creditable health insurance coverage, including Medicare. | |
| CAPITATION | Payment to a Contractor by AHCCCS of a fixed monthly payment per person in advance, for which the Contractor provides a full range of covered services as authorized under A.R.S. § 36-2904 and § 36-2907. | |
| CATEGORICALLY LINKED TITLE XIX MEMBER | Member eligible for Medicaid under Title XIX of the Social Security Act including those eligible under 1931 provisions of the Social Security Act, Sixth Omnibus Budget Reconciliation Act (SOBRA), Supplemental Security Income (SSI), and SSI-related groups. To be categorically linked, the member must be aged 65 or over, blind, disabled, a child under age 19, a parent of a dependent child, or pregnant. | |
| CLAIM DISPUTE | A dispute, filed by a provider or Contractor, whichever is applicable, involving a payment of a claim, denial of a claim, imposition of a sanction or reinsurance. | |
| CLEAN CLAIM | A claim that may be processed without obtaining additional information from the provider of service or from a third party but does not include claims under investigation for fraud or abuse or claims under review for medical necessity, as defined by A.R.S. § 36-2904. | |
| CMS | Centers for Medicare and Medicaid Services, an organization within the U.S. Department of Health and Human Services, which administers the Medicare and Medicaid programs and the State Children’s Health Insurance Program. | |
| COMPETITIVE BID PROCESS | A state procurement system used to select Contractors to provide covered services on a geographic basis. | |
| CONTINUING OFFEROR | An AHCCCS Contractor during the CYE 08 that submits a proposal pursuant to this solicitation. | |
11
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION C: DEFINITIONS Contract/RFP No. YH09-0001
|
| | |
| CONTRACT SERVICES | See “COVERED SERVICES. | |
| CONTRACT YEAR (CY) | Corresponds to the Federal fiscal year (October 1 through September 30).
| |
| CONTRACTOR | A person, organization or entity agreeing through a direct contracting relationship with AHCCCS to provide the goods and services specified by this contract in conformance with the stated contract requirements, AHCCCS statute and Rules, and Federal law and regulations as defined in A.R.S. § 36-2901. | |
| CONVICTED | A judgment of conviction has been entered by a Federal, State or local court, regardless of whether an appeal from that judgment is pending. | |
| COPAYMENT | A monetary amount specified by the Director that the member pays directly to a Contractor or provider at the time covered services are rendered, as defined in 9 A.A.C. 22, Article 7. | |
| COST AVOIDANCE | The process of identifying and utilizing all sources of first or third-party benefits before services are rendered by the Contractor or before payment is made by the Contractor. (This assumes the Contractor can avoid costs by not paying until the first or third party has paid what it covers first, or having the first or third party render the service so that the Contractor is only liable for coinsurance and/or deductibles.) | |
| COVERED SERVICES | The health and medical services to be delivered by the Contractor as defined in 9 A.A.C. 22, Article 2 and 9 A.A.C. 31, Article 2, the AMPM and Section D of this contract. [42 CFR 438.210(a)(4)] | |
| CRS – Children’s Rehabilitation Services | A program administered by the AHCCCS CRS Contractor. The CRS Contractor provides services to Title XIX and Title XXI members who have completed the CRS application and have met the eligibility criteria to receive CRS covered services as specified in 9 A.A.C.7. | |
| CRS-ELIGIBLE | An individual who has completed the CRS application process, as delineated in the CRS Policy and Procedure Manual, and has met all applicable criteria to be eligible to receive CRS covered - services. | |
| CRS RECIPIENT | An individual who has completed the CRS application process, and has met all applicable criteria to be eligible to receive CRS covered Services. | |
| DAYS | Calendar days, unless otherwise specified as defined in the text, as defined in9 A.A.C. 22, Article 1. | |
| DELEGATED AGREEMENT | A type of subcontract agreement with a qualified organization or person to perform one or more functions required to be performed by the Contractor pursuant to this contract. | |
| DIRECTOR | The Director of AHCCCS. | |
| DISENROLLMENT | The discontinuance of a member’s ability to receive covered services through a Contractor. | |
| DME | Durable medical equipment is an item or appliance that can withstand repeated use, is designated to serve a medical purpose, and are not generally useful to a person in the absence of a medical condition, illness or injury as defined in9 A.A.C. 22, Article 1. | |
| DUAL ELIGIBLE | A member who is eligible for both Medicare and Medicaid. | |
| ELIGIBILITY DETERMINATION | A process of determining, through a written application and required documentation, whether an applicant meets the qualifications for Title XIX or Title XXI | |
12
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION C: DEFINITIONS Contract/RFP No. YH09-0001
|
| | |
| EMERGENCY MEDICAL CONDITION | A medical condition manifesting itself by acute symptoms of sufficient severity (including severe pain) such that a prudent layperson who possesses an average knowledge of health and medicine could reasonably expect the absence of immediate medical attention to result in: a) placing the patient’s health (or, with respect to a pregnant woman, the health of the woman or her unborn child) in serious jeopardy, b) serious impairment to bodily functions, or c) serious dysfunction of any bodily organ or part [42 CFR 438.114(a)]. | |
| EMERGENCY MEDICAL SERVICE | Covered inpatient and outpatient services provided after the sudden onset of an emergency medical condition as defined above. These services must be furnished by a qualified provider, and must be necessary to evaluate or stabilize the emergency medical condition [42 CFR 438.114(a)]. | |
| ENCOUNTER | A record of a health care-related service rendered by a provider or providers registered with AHCCCS to a member who is enrolled with a Contractor on the date of service. | |
| ENROLLEE | A Medicaid recipient who is currently enrolled with a Contractor. [42 CFR 438.10(a)] | |
| ENROLLMENT | The process by which an eligible person becomes a member of a Contractor’s plan. | |
| EPSDT | Early and Periodic Screening, Diagnostic and Treatment services for eligible persons or members less than 21 years of age as, defined in 9 A.A.C. 22, Article 2. | |
| FAMILY PLANNING SERVICES EXTENSION PROGRAM | A program that provides only family planning services for a maximum of two consecutive 12-month periods to a SOBRA woman whose pregnancy has ended and who is not otherwise eligible for full Title XIX services | |
FEDERALLY QUALIFIED HEALTH CENTER (FQHC)
| An entity that meets the requirements and receives a grant and funding pursuant to Section 330 of the Public Health Service Act. An FQHC includes an outpatient health program or facility operated by a tribe or tribal organization under the Indian Self-Determination and Education Assistance Act (P.L. 93-638) or an urban Indian organization receiving funds under Title V of the Indian Health Care Improvement Act (P.L. 94-437). | |
FEDERALLY QUALIFIED HEALTH CENTER Look-Alike
| An organization that meets all of the eligibility requirements of an organization that receives a Public Health Service Section 330 Grant (FQHC), but does not receive grant funding. AHCCCS requires Contractors to credential providers employed by an FQHC Look-Alike through the temporary or provisional credentialing process. | |
| FEE‑FOR‑SERVICE (FFS) | Fee‑For‑Service, a method of payment to registered providers on an amount-per-service basis. | |
| FES | Federal Eemergency Services program covered under R9-22-217, to treat an emergency medical condition for a member who is determined eligible under A.R.S. § 36-2903.03 (D). | |
| FFP | Federal financial participation (FFP) refers to the contribution that the Federal government makes to the Title XIX and Title XXI program portions of AHCCCS, as defined in 42 CFR 400.203. | |
| FIRST PARTY LIABILITY | The resources available from any insurance or other coverage obtained directly or indirectly by a member or eligible person that provides benefits directly to the member or eligible person and is liable to pay all or part of the expenses for medical services incurred by an AHCCCS, Contractor, or member. | |
| FISCAL YEAR (FY) | Federal Fiscal Year, October 1 through September 30. | |
| FREEDOM OF CHOICE (FC) | The opportunity given to each member who does not specify a Contractor preference at the time of enrollment to choose between the Contractors available within the Geographic Service Area in which the member is enrolled. | |
13
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION C: DEFINITIONS Contract/RFP No. YH09-0001
|
| | |
| FRAUD | An intentional deception or misrepresentation made by a person with the knowledge that the deception could result in some unauthorized benefit to himself or some other person. It includes any act that constitutes fraud under applicable State or Federal law, as defined in 42 CFR 455.2. | |
| FREEDOM TO WORK (TICKET TO WORK | Eligible individuals under the Title XIX expansion program that extends eligibility to individuals 16 through 64 years old who meet SSI disability criteria; whose earned income, after allowable deduction, is at or below 250% of the FPL and who are not eligible for any other Medicaid program. | |
| GEOGRAPHIC SERVICE AREA (GSA) | An area designated by AHCCCS within which a Contractor of record provides, directly or through subcontract, covered health care service to a member enrolled with that Contractor of record, as defined in 9 A.A.C. 22, Article 1. | |
| GRIEVANCE SYSTEM | A system that includes a process for enrollee grievances, enrollee appeals, provider claim disputes, and access to the state fair hearing system. | |
| HEALTHCARE GROUP OF ARIZONA (HCG) | A prepaid medical coverage plan marketed to small, uninsured businesses and political subdivisions within the state. | |
| HEALTH PLAN | See “CONTRACTOR”. | |
| HIPAA | The Health Insurance Portability and Accountability Act (P.L. 104-191); also known as the Kennedy-Kassebaum Act, signed August 21, 1996. | |
| IBNR | Incurred but not reported liability for services rendered for which claims have not been received. | |
| IHS | Indian Health Service authorized as a Federal agency pursuant to 25 U.S.C. 1661. | |
| KIDSCARE | Federal and State Children’s Health Insurance Program (Title XXI – SCHIP) administered by AHCCCS. The KidsCare program offers comprehensive medical, preventive and treatment services and a full array of behavioral health care services statewide to eligible children under the age of 19, in households with income at or below 200% Federal Poverty Level (FPL). All members, except American Indian members, are required to pay a premium amount based on the number of children in the family and the gross family income. Also referred to as “Title XXI”. | |
| KIDSCARE II | A children’s coverage program that has the same benefits and premium requirements as KidsCare but income limits for KidsCare II cannot be greater than 175% FPL. KidsCare II is available August 1, 2012 through December 31, 2013. | |
| LIABLE PARTY | A person or entity that is or may be, by agreement, circumstance or otherwise, liable to pay all or part of the medical expenses incurred by an AHCCCS applicant or member. | |
| LIEN | A legal claim, filed with the County Recorder’s office in which a member resides and in the county an injury was sustained for the purpose of ensuring that AHCCCS receives reimbursement for medical services paid. The lien is attached to any settlement the member may receive as a result of an injury. | |
| MANAGED CARE | Systems that integrate the financing and delivery of health care services to covered individuals by means of arrangements with selected providers to furnish comprehensive services to members; establish explicit criteria for the selection of health care providers; have financial incentives for members to use providers and procedures associated with the plan; and have formal programs for quality, medical management and the coordination of care. | |
| MANAGEMENT SERVICES AGREEMENT | A type of subcontract with an entity in which the owner of the Contractor delegates some or all of the comprehensive management and administrative services necessary for the operation of the Contractor.
| |
14
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION C: DEFINITIONS Contract/RFP No. YH09-0001
|
| | |
| MANAGEMENT SERVICES SUBCONTRACTOR | An entity to which the Contractor delegates the comprehensive management and administrative services necessary for the operation of the Contractor. | |
| MANAGING EMPLOYEE | A general manager, business manager, administrator, director, or other individual who exercises operational or managerial control over or who directly or indirectly conducts the day-to-day operation of an institution, organization or agency. | |
| MATERIAL OMISSION | A fact, data or other information excluded from a report, contract, etc., the absence of which could lead to erroneous conclusions following reasonable review of such report, contract, etc. | |
| MAJOR UPGRADE | Any upgrade or changes that may result in a disruption to the following: loading of contracts, providers or members, issuing prior authorizations or the adjudication of claims. | |
| MEDICAID | A Federal/State program authorized by Title XIX of the Social Security Act, as amended. | |
| MEDICAL EXPENSE DEDUCTION (MED) | Title XIX waiver member whose family income exceeds the limits of all other Title XIX categories (except ALTCS) and has family medical expenses that reduce income to or below 40% of the FPL. MED members may or may not have a categorical link to Title XIX.
| |
| MEDICAL MANAGEMENT | Is an integrated process or system that is designed to assure appropriate utilization of health care resources, in the amount and duration necessary to achieve desired health outcomes, across the continuum of care (from prevention to end of life care). | |
| MEDICARE | A Federal program authorized by Title XVIII of the Social Security Act, as amended. | |
| MEDICARE MANAGED CARE PLAN | A managed care entity that has a Medicare contract with CMS to provide services to Medicare beneficiaries, including Medicare Advantage Plan (MAP), Medicare Advantage Prescription Drug Plan (MAPDP), MAPDP Special Needs Plan, or Medicare Prescription Drug Plan. | |
| MEDICARE PART D EXCLUDED DRUGS | Medicare Part D is the Prescription Drug Coverage option available to Medicare beneficiaries, including those also eligible for Medicaid. Medications that are available under this benefit will not be covered by AHCCCS for dual eligible members. There are certain drugs that are excluded from coverage by Medicare, and will continue to be covered by AHCCCS. Those medications are barbiturates, benzodiazepines, and over-the-counter medication as defined in the AMPM. Prescription medications that are covered under Medicare, but are not on a Part D Health Plan’s formulary are not considered excluded drugs, and are not covered by AHCCCS. | |
| MEMBER | An eligible person who is enrolled in AHCCCS, as defined in A.R.S. §§ 36-2931, 36-2901, 36-2901.01 and A.R.S. §36-2981. | |
| NON-CONTRACTING PROVIDER | A person or entity that provides services as prescribed in A.R.S. § 36-2901 who does not have a subcontract with an AHCCCS Contractor. | |
| NON-MEDICAL EXPENSE DEDUCTION (Formerly NON MED) MEMBER | See “AHCCCS CARE”. | |
| NPI | National Provider Identifier assigned by the CMS contracted national enumerator. | |
| OFFEROR | An organization or other entity that submits a proposal to AHCCCS in response to a Request For Proposal as defined in9 A.A.C. 22, Article 1. | |
15
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION C: DEFINITIONS Contract/RFP No. YH09-0001
|
| | |
| PAY AND CHASE | Recovery method used by the Contractor to collect from legally liable first or third parties after the Contractor pays the member’s medical bills. The service may be provided by a contracted or non-contracted provider. Regardless of who provides the service, pay and chase assumes that the Contractor will pay the provider, then seek reimbursement from the first or third party. | |
| PERFORMANCE STANDARDS | A set of standardized measures designed to assist AHCCCS in evaluating, comparing and improving the performance of its Contractors | |
| PIP | Performance Improvement Project (PIP), formerly referred to as Quality Improvement Project (QIP). | |
| PMMIS | AHCCCS’ Prepaid Medical Management Information System. | |
| POST STABILIZATION SERVICES | Medically necessary services, related to an emergency medical condition provided after the member’s condition is sufficiently stabilized in order to maintain, improve or resolve the member’s condition so that the member could alternatively be safely discharged or transferred to another location [42 CFR 438-114(a)]. | |
| POTENTIAL ENROLLEE | A Medicaid-eligible recipient who is not yet enrolled with a Contractor [42 CFR 438.10(a)]. | |
| PRIMARY CARE PROVIDER (PCP | Primary Care Provider/Practitioner, an individual who meets the requirements of A.R.S. § 36-2901, and who is responsible for the management of the member’s or eligible person’s health care. A PCP may be a physician defined as a person licensed as an allopathic or osteopathic physician according to A.R.S. Title 32, Chapter 13 or Chapter 17 or a practitioner defined as a physician assistant licensed under A.R.S. Title 32, Chapter 25, or a certified nurse practitioner licensed under A.R.S. Title 32, Chapter 15. | |
| PRIOR PERIOD COVERAGE (PPC | The period prior to a member’s enrollment, during which a member is eligible for covered services. The time frame is from the effective date of eligibility to the day a member is enrolled with a Contractor. | |
| PROVIDER | Any person or entity that contracts with AHCCCS or a Contractor for the provision of covered services to members according to the provisions A.R.S. § 36-2901 or any subcontractor of a provider delivering services pursuant to A.R.S. § 36-2901. | |
| QUALIFIED MEDICARE BENEFICIARY DUAL ELIGIBLE (QMB DUAL) | A person, eligible under A.R.S. § 36-2971(6), who is entitled to Medicare Part A insurance and meets certain income and residency requirements of the Qualified Medicare Beneficiary program. A QMB, who is also eligible for Medicaid, is commonly referred to as a QMB dual eligible. | |
| RATE CODE | Eligibility classification for capitation payment purposes. | |
| REGIONAL BEHAVIORAL HEALTH AUTHORITY (RBHA) | An organization under contract with ADHS to administer covered behavioral health services in a geographically specific area of the state. Tribal governments, through an agreement with ADHS, may operate a tribal regional behavioral health authority (TRBHA) for the provision of behavioral health services to American Indians. | |
| REINSURANCE | A risk-sharing program provided by AHCCCS to Contractors for the reimbursement of certain contract service costs incurred for a member beyond a predetermined monetary threshold. | |
| RELATED PARTY | A party that has, or may have, the ability to control or significantly influence a Contractor, or a party that is, or may be, controlled or significantly influenced by a Contractor. "Related parties" include, but are not limited to, agents, managing employees, persons with an ownership or controlling interest in the Offeror and their immediate families, subcontractors, wholly-owned subsidiaries or suppliers, parent companies, sister companies, holding companies, and other entities controlled or managed by any such entities or persons. | |
| RISK GROUP | Grouping of rate codes that are paid at the same capitation rate. | |
16
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION C: DEFINITIONS Contract/RFP No. YH09-0001
|
| | |
| RFP | Request For Proposal, a document prepared by AHCCCS that describes the services required and instructs prospective Offerors about how to prepare a response (proposal), as defined in 9 A.A.C. 22, Article 1. | |
| RURAL HEALTH CLINIC (RHC) | A clinic located in an area designated by the Bureau of Census as rural, and by the Secretary of the DHHS as medically underserved or having an insufficient number of physicians, which meets the requirements under 42 CFR 491. | |
| SCHIP | State Children’s Health Insurance Program under Title XXI of the Social Security Act (Also known as CHIP). The Arizona version of CHIP is referred to as “KidsCare”. See “KIDSCARE”. | |
| SCOPE OF SERVICES | See “COVERED SERVICES. | |
| SERVICE LEVEL AGREEMENT | A type of subcontract with a corporate owner or any of its Divisions or Subsidiaries that requires specific levels of service for administrative functions or services for the Contractor specifically related to fulfilling the Contractor’s obligations to AHCCCS under the terms of this contract. | |
| SOBRA | Eligible pregnant women under Section 9401 of the Sixth Omnibus Budget and Reconciliation Act of 1986, amended by the Medicare Catastrophic Coverage Act of 1988, 42 U.S.C. 1396 a(a)(10)(A)(ii)(IX), November 5, 1990, with individually budgeted incomes at or below 150% of the FPL, and children in families with individually budgeted incomes ranging from below 100% to 140% of the FPL, depending on the age of the child. | |
| SOBRA FAMILY PLANNING | Female members eligible for family planning services only, for a maximum of two consecutive 12-month periods following the loss of SOBRA eligibility. | |
| SPECIAL HEALTH CARE NEEDS | Members with special health care needs are those members who have serious and chronic physical, developmental or behavioral conditions, and who also require medically necessary health and related services of a type or amount beyond that generally required by members. | |
| STATE | The State of Arizona. | |
| STATE ONLY TRANSPLANT MEMBERS | Individuals who are eligible under one of the Title XIX eligibility categories and found eligible for a transplant, but subsequently lose Title XIX eligibility due to excess income become eligible for one of two extended eligibility options as specified in A.R.S. 36-2907.10 and A.R.S. 36-2907.11. | |
| STATE PLAN | The written agreements between the State and CMS, which describes how the AHCCCS program meets CMS requirements for participation in the Medicaid program and the State Children’s Health Insurance Program. | |
| SUBCONTRACT | An agreement entered into by the Contractor with any of the following: a provider of health care services who agrees to furnish covered services to member or with any other organization or person who agrees to perform any administrative function or service for the Contractor specifically related to fulfilling the Contractor's obligations to AHCCCS under the terms of this contract, as defined in9 A.A.C. 22, Article 1. | |
| SUBCONTRACTOR | (1) A provider of health care who agrees to furnish covered services to members. (2) A person, agency or organization with which the Contractor has contracted or delegated some of its management/administrative functions or responsibilities. (3) A person, agency or organization with which a fiscal agent has entered into a contract, agreement, purchase order or lease (or leases of real property) to obtain space, supplies equipment or services provided under the AHCCCS agreement. | |
| SUPPLEMENTAL SECURITY INCOME (SSI) AND SSI RELATED GROUPS | Eligible individuals receiving income through Federal cash assistance programs under Title XVI of the Social Security Act who are aged, blind or disabled and have household income levels at or below 100% of the FPL. | |
17
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION C: DEFINITIONS Contract/RFP No. YH09-0001
|
| | |
| TEMPORARY ASSISTANCE TO NEEDY FAMILIES (TANF) | A Federal cash assistance program under Title IV of the Social Security Act established by the Personal Responsibility and Work Opportunity Reconciliation Act of 1996 (P.L. 104-193). It replaced Aid To Families With Dependent Children (AFDC). | |
| THIRD PARTY LIABILITY (TPL) | See “LIABLE PARTY”. | |
| TITLE XIX MEMBER | Member eligible for Medicaid under Title XIX of the Social Security Act including those eligible under 1931 provisions of the Social Security Act (previously AFDC), Sixth Omnibus Budget Reconciliation Act (SOBRA), Supplemental Security Income (SSI) or SSI-related groups, Medicare Cost Sharing groups, Title XIX Waiver groups, Breast and Cervical Cancer Treatment program and Freedom to Work | |
| TITLE XXI MEMBER | A member eligible for acute care services under Title XXI of the Social Security Act, referred to in Federal legislation as the “State Children’s Health Insurance Program” (SCHIP or CHIP). The Arizona version of CHIP is referred to as “KidsCare” | |
| TRIBAL/REGIONAL BEHAVIORAL HEALTH AUTHORITY (T/RBHA) | An organization under contract with ADHS/DBHS that administers covered behavioral health services in a geographically specific area of the state. Tribal governments, through an agreement with ADHS, may operate a Tribal Regional Behavioral Health Authority for the provision of behavioral health services to American Indian members. | |
| WWHP | Well Woman Health-Check Program, administered by the Arizona Department of Health Services and funded by the Centers for Disease Control and Prevention. (See AMPM Chapter 300, Section 320) | |
| YOUNG ADULT TRANSITIONAL INSURANCE (YATI) | Eligible individuals, between 18 and 21 years of age who were formerly enrolled through the foster care program. | |
[END OF DEFINITIONS]
SECTION D: PROGRAM REQUIREMENTS
INTRODUCTION
The Arizona Health Care Cost Containment System (AHCCCS) is the single state agency for the Medicaid and CHIP programs. AHCCCS has operated under an 1115 Research and Demonstration Waiver since 1982 when it became the first statewide Medicaid managed care system in the nation. The program is a model public-private collaboration that includes the state and its counties, the Federal government, and managed care Contractors and providers from both the public and private sectors. AHCCCS has remained a leader in Medicaid Managed Care through the diligent pursuit of excellence and cost effectiveness by Managed Care Contractors (MCOs) in collaboration with AHCCCS.
In order to continue this collaboration, Contractors must continue to add value to the program. A Contractor adds value when it:
| |
| • | Recognizes that Medicaid members are entitled to care and assistance navigating the service delivery system and demonstrates special effort to assure members receive necessary services, including prevention and screening services. |
| |
| • | Recognizes that Medicaid members with special health care needs or chronic health conditions require care coordination, and provides that coordination. This is particularly true if a member must receive services from other AHCCCS Contractors in addition to the Contractor. |
| |
| • | Recognizes that Medicaid members have the right to contact their elected officials in an effort to secure necessary services and assist members in order to reduce their need to contact elected officials. The Contractor provides information to elected officials to help them respond to the member. |
18
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
| |
| • | Recognizes that health care providers are an essential partner in the delivery of health care services, and operates in a manner that is efficient and effective for health care providers as well as the Contractor. |
| |
| • | Avoids administrative practices that place unnecessary burdens on providers with little or no impact on quality of care or cost containment. |
| |
| • | Recognizes that performance improvement is both clinical and operational in nature and self-monitors and self corrects as necessary to improve contract compliance or operational excellence. |
| |
| • | Recognizes that the program is publicly funded, and as such is subject to public scrutiny and behaves in a manner that is supported by the general public. |
| |
| • | Recognizes that the program is subject to significant regulation and operates in compliance with those regulations. |
AHCCCS encourages Contractor innovation and application of best practices. AHCCCS is always looking for ways to reduce administrative costs and improve program efficiency. Over the term of the contract, AHCCCS will work collaboratively with Contractors to evaluate ways to reduce program complexity, improve chronic disease management, reduce administrative burdens, leverage joint purchasing power, and reduce unnecessary Medicaid/CHIP administrative and medical costs.
| |
| 3. | TERM OF CONTRACT AND OPTION TO RENEW |
The initial term of this contract shall be 10/1/12 through 9/30/13, with two additional one-year options to renew. All contract renewals shall be through contract amendment. AHCCCS shall issue amendments prior to the end date of the contract when there is an adjustment to capitation rates and/or changes to the scope of services contained herein. Changes to the scope of services include, but are not limited, to changes in the enrolled population, changes in covered services and changes in GSAs.
If the Contractor has been awarded a contract in more than one GSA, each such contract will be considered separately renewable. AHCCCS may renew the Contractor’s contract in one GSA, but not in another. In addition, if the Contractor has had significant problems of non-compliance in one GSA, it may result in the capping of the Contractor’s enrollment in all GSAs. Further, AHCCCS may require the Contractor to renew all currently awarded GSAs, or may terminate the contract if the Contractor does not agree to renew all currently awarded GSAs.
When the Contracting Officer issues an amendment to extend the contract, the provisions of such extension will be deemed to have been accepted 60 days after the date of mailing by the Contracting Officer, even if the extension amendment has not been signed by the Contractor, unless within that time the Contractor notifies the Contracting Officer in writing that it refuses to sign the extension amendment. If the Contractor provides such notification, the Contracting Officer will initiate contract termination proceedings.
Contractor’s Notice of Intent Not To Renew: If the Contractor chooses not to renew this contract, the Contractor may be liable for certain costs associated with the transition of its members to a different Contractor. The Contractor is required to provide 180 days advance written notice to the Contracts and Purchasing Administrator of its intent not to renew the contract. If the Contractor provides the Contracts and Purchasing Administrator written notice of its intent not to renew this contract at least 180 days before its expiration, this liability for transition costs may be waived by the Contracting Officer.
Contract Termination: In the event that the contract or any portion thereof, is terminated for any reason, or expires, the Contractor shall assist AHCCCS in the transition of its members to other Contractors, and shall abide by standards and protocols set forth in Paragraph 9, Transition of Members. In addition, AHCCCS reserves the right to extend the term of the contract on a month-to-month basis to assist in any transition of members. AHCCCS may discontinue enrollment of members with the Contractor three months prior to the contract termination date. The Contractor shall make provision for continuing all management and administrative services until the transition of all members is completed and all other requirements of this contract are satisfied. The Contractor shall submit,
19
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
upon request, to AHCCCS for approval a detailed plan for the transition of its members in the event of contract expiration or termination. The name and title of the Contractor’s transition coordinator shall be included in the transition plan. The Contractor shall be responsible for providing all reports set forth in this contract and necessary for the transition process, and shall be responsible for the following:
| |
| a. | Notification of subcontractors and members. |
| |
| b. | Payment of all outstanding obligations for medical care rendered to members until AHCCCS is satisfied that the Contractor has paid all such obligations The Contractor shall provide a monthly claims aging report including IBNR amounts due the 15th day of the month, for the prior month. |
| |
| c. | Providing Quarterly and Audited Financial Statements up to the date of contract termination. The financial statement requirement will not be absolved without an official release from AHCCCS. |
| |
| d. | Continuing encounter reporting until all services rendered prior to contract termination have reached adjudicated status and data validation of the information has been completed, as communicated by a letter of release from AHCCCS. |
| |
| e. | Cooperation with reinsurance audit activities on prior contract years until release has been granted by AHCCCS. |
| |
| f. | Cooperating with AHCCCS to complete and finalize any open reconciliations until release has been granted by AHCCCS. AHCCCS will work to complete any pending reconciliations as timely as possible, allowing for appropriate lag time for claims run-out and/or changes to be entered into the system. |
| |
| g. | Supplying quarterly Quality Management and Medical Management reports will be submitted as required by Section D, Paragraphs 23, Quality Management, and 24, Medical Management, as appropriate to provide AHCCCS with information on services rendered up to the date of contract termination. This will include quality of care (QOC) concern reporting based on the date of service |
| |
| h. | Participating in and closing out Performance Measures and Performance Improvement Projects as requested by AHCCCS. |
| |
| i. | Maintaining a Performance Bond as long as the Contractor has AHCCCS-related liabilities of $50,000 or more outstanding or 15 months following the termination date of this contract, whichever is later. At that time, a formal request to release the performance bond, as well as a balance sheet, must be submitted. |
| |
| j. | Indemnify AHCCCS for any claim by any third party against the State or AHCCCS arising from the Contractor's performance of this contract and for which the Contractor would otherwise be liable under this contract. |
| |
| k. | Returning to AHCCCS, any funds advanced to the Contractor for coverage of members for periods after the date of termination. Funds must be returned to AHCCCS within 30 days of termination of the contract. |
| |
| l. | Providing a monthly accounting of Member Grievances and Claim Disputes and their disposition. |
| |
| m. | Preserving and making available all records for a period of five years from the date of final payment under contract. Records covered under HIPAA must be preserved and made available for six years per 45 CFR 164.530(j)(2). |
The above list is not exhaustive and additional information may be requested to ensure that all operational and reporting requirements have been met. Any dispute by the Contractor, with respect to termination or suspension of this contract by AHCCCS, shall be exclusively governed by the provisions of Section E, Contract Terms and Conditions, Paragraph 26, Disputes.
AHCCCS is Arizona’s Title XIX Medicaid program operating under an 1115 Waiver and Title XXI program operating under Title XXI State Plan authority. Arizona has the authority to require mandatory enrollment in managed care. All Acute Care Program members eligible for AHCCCS benefits, with exceptions as identified below, are enrolled with Acute Care Contractors that are paid on a capitated basis. AHCCCS pays for health care expenses on a fee-for-service (FFS) basis for Title XIX- and Title XXI- eligible members who receive services
20
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
through the Indian Health Service; for Title XIX eligible members who are entitled to emergency services under the Federal Emergency Services (FES) program; and for Medicare cost sharing beneficiaries under QMB program.
The following describes the eligibility groups enrolled in the managed care program and covered under this contract [42 CFR 434.6(a)(2)].
Title XIX
1931 (Also referred to as TANF-related): Eligible individuals and families under the 1931 provision of the Social Security Act, with household income levels at or below 100% of the FPL.
SSI Cash: Eligible individuals receiving Supplemental Security Income through Federal cash assistance programs under Title XVI of the Social Security Act who are aged, blind or disabled and have household income levels at or below 100% of the Federal Benefit Rate (FBR).
SSI Medical Assistance Only (SSI MAO) and Related Groups: Eligible individuals are individuals who are aged, blind or disabled and have household income levels at or below 100% of the FPL.
Freedom to Work (Ticket to Work): Eligible individuals under the Title XIX expansion program that extends eligibility to individuals 16 through 64 years old who meet SSI disability criteria, and whose earned income after allowable deductions is at or below 250% of the FPL, and who are not eligible for any other Medicaid program. These members must pay a premium to AHCCCS, depending on income.
SOBRA: Under the Sixth Omnibus Budget Reconciliation Act of 1986, eligible pregnant women, with individually budgeted income at or below 150% of the FPL, and children in families with individually budgeted incomes ranging from below 100% to 140% of the FPL, depending on the age of the child.
SOBRA Family Planning: Family planning extension program that covers the costs for family planning services only, for a maximum of two consecutive 12-month periods following the loss of SOBRA eligibility.
Breast and Cervical Cancer Treatment Program (BCCTP): Eligible individuals under the Title XIX expansion program for women with incomes up to 250% of the FPL, who are diagnosed with and need treatment for breast and/or cervical cancer or cervical lesions and are not eligible for other Title XIX programs. Eligible members cannot have other creditable health insurance coverage, including Medicare.
Title IV-E Foster Care and Adoption Subsidy: Children with special medical needs who have been placed in foster homes or have been adopted.
Young Adult Transitional Insurance (YATI): Former foster care children between 18 and 21 years of age.
Title XIX Waiver Group
AHCCCS Care: Eligible individuals and couples whose income is at or below 100% of the FPL, and who are not categorically linked to another Title XIX program. Formerly known as Non-MED members.
Title XXI
KidsCare: Individuals under the age of 19 years, eligible under the Federal State Children’s Health Insurance Program (CHIP), who are in households with incomes at or below 200% FPL. All members except American
21
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
Indian members are required to pay a premium amount based on the number of children in the family and the gross family income. Also referred to as Title XXI.
State-Only
State-Only Transplants: Title XIX individuals, for whom medical necessity for a transplant has been established and who subsequently lose Title XIX eligibility may become eligible for and select one of two extended eligibility options as specified in A.R.S. 36-2907.10 and A.R.S. 36-2907.11. The extended eligibility is authorized only for those individuals who have met all of the following conditions:
| |
| 1. | The individual has been determined ineligible for Title XIX due to excess income; |
| |
| 2. | The individual had been placed on a donor waiting list before eligibility expired; |
| |
| 3. | The individual has entered into a contractual arrangement with the transplant facility to pay the amount of income which is in excess of the eligibility income standards (referred to as transplant share of cost). |
The following options for extended eligibility are available to these members:
Option 1: Extended eligibility is for one 12-month period immediately following the loss of AHCCCS eligibility. The member is eligible for all AHCCCS covered services as long as they continue to be medically eligible for a transplant. If determined medically ineligible for a transplant at any time during the period, eligibility will terminate at the end of the calendar month in which the determination is made.
Option 2: As long as medical eligibility for a transplant (status on a transplant waiting list) is maintained, at the time that the transplant is scheduled to be performed the transplant candidate will reapply and will be re-enrolled with their previous Contractor to receive all covered transplant services. Option 2-eligible individuals are not eligible for any non-transplant related health care services from AHCCCS.
| |
| 5. | ENROLLMENT AND DISENROLLMENT |
AHCCCS has the exclusive authority to enroll and disenroll members. The Contractor shall not disenroll any member for any reason unless directed to do so by AHCCCS. The Contractor may request AHCCCS to change the member’s enrollment in accordance with the ACOM Policy 401. The Contractor may not request disenrollment because of an adverse change in the enrollee’s health status, or because of the enrollee’s utilization of medical services, diminished mental capacity, or uncooperative or disruptive behavior resulting from his or her special needs. An AHCCCS member may request disenrollment from the Contractor for cause at any time. Please refer those requests due to situations defined in Section A (1) of the ACOM Policy 401 to the AHCCCS Division of Member Services via mail or at (602) 417-4000 or (800) 962-6690. For medical continuity requests, the Contractor shall follow the procedures outlined in the ACOM Policy 401, before notifying AHCCCS.
AHCCCS will disenroll the member from the Contractor when:
| |
| • | The member becomes ineligible for the AHCCCS program ; |
| |
| • | In certain situations when they move out of the Contractor’s service areas; |
| |
| • | The member changes Contractors during the member’s open enrollment/annual enrollment choice period; |
| |
| • | The Contractor does not, because of moral or religious objections, cover the service the member seeks; or |
| |
| • | The member is approved for a Contractor change through the ACOM Policy 401. [42 CFR 438.56]. |
Members may submit plan change requests to the Contractor or AHCCCS. A denial of any plan change request must include a description of the member’s right to appeal the denial.
22
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
Eligibility for the various AHCCCS coverage groups is determined by one of the following agencies:
|
| |
Social Security Administration (SSA)
| SSA determines eligibility for the Supplemental Security Income (SSI) cash program. SSI cash recipients are automatically eligible for AHCCCS coverage.
|
Department of Economic Security (DES)
| DES determines eligibility for families with children under section 1931 of the Social Security Act, pregnant women and children under SOBRA, the Adoption Subsidy Program, Title IV-E foster care children, Young Adult Transitional Insurance Program, the Federal Emergency Services program (FES) and Title XIX Waiver Members. (AHCCCS Care)
|
AHCCCS
| AHCCCS determines eligibility for the SSI/Medical Assistance Only groups, including the FES program for this population (aged, disabled, blind), the Arizona Long Term Care System (ALTCS), the Qualified Medicare Beneficiary program and other Medicare cost sharing programs, BCCTP, the Freedom to Work program, the Title XXI KidsCare program and the State-Only Transplant program.
|
| |
AHCCCS Acute Care members are enrolled with Contractors in accordance with the Rules set forth in A.A.C R9-22, Article 17, A.A.C. R9-31, Articles 3 and 17.
Member Choice of Contractor
All AHCCCS members eligible for services covered under this contract have a choice of available Contractors. Contact information for the Contractors is provided during the application process for AHCCCS benefits. If there is only one Contractor available for the applicant’s Geographic Service Area, no choice is offered as long as the Contractor offers the member a choice of PCPs. Members who do not choose a Contractor prior to AHCCCS being notified of their eligibility are automatically assigned to a Contractor based on family continuity or the auto-assignment algorithm. Once assigned, AHCCCS sends a Freedom of Choice notice to the member and gives them 30 days to choose a different Contractor from the auto-assigned Contractor. See Section D, Paragraph 6, Auto-Assignment Algorithm, for further explanation.
The Contractor will share with AHCCCS the cost of providing information about the Acute Care Contractors to potential members and to those eligible for annual enrollment choice.
Exceptions to the above enrollment policies for Title XIX members include previously enrolled members who have been disenrolled for less than 90 days. These members will be automatically enrolled with the same Contractor, if still available. Women who become eligible for the Family Planning Services Extension Program, will remain assigned to their current Contractor.
The effective date of enrollment for a new Title XIX member with the Contractor is the day AHCCCS takes the enrollment action. The Contractor is responsible for payment of medically necessary covered services retroactive to the member’s beginning date of eligibility, as reflected in PMMIS.
The effective date of enrollment for a Title XXI member will be the first day of the month following notification to the Contractor. In the event that eligibility is determined on or after the 25th day of the month, eligibility will begin on the 1st day of the second month following the determination.
23
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
When a member is transferred from Title XIX to Title XXI and has not made a Contractor choice for Title XXI, the member will remain with their current Contractor and a Freedom of Choice notice will be sent to the member. The member may then change plans no later than 30 days from the date the Freedom of Choice notice is sent.
Prior Period Coverage: AHCCCS provides prior period coverage for the period of time prior to the Title XIX member’s enrollment during which the member is eligible for covered services. Prior Period Coverage means the time frame from the effective date of eligibility to the day the member is enrolled with the Contractor. The Contractor receives notification from AHCCCS of the member’s enrollment. The Contractor is responsible for payment of all claims for medically necessary covered services, excluding most behavioral health services, provided to members during prior period coverage. This may include services provided prior to the contract year (See Section D, Paragraph 53, Compensation, for a description of the Contractor’s reimbursement from AHCCCS for this eligibility time period).
For behavioral health services, the Contractor is responsible for the same services as outlined in Section D, Paragraph 12, Behavioral Health Services, for the prospective period.
Newborns: Newborns born to AHCCCS eligible mothers enrolled at the time of the child's birth will be enrolled with the mother's Contractor, when newborn notification is received by AHCCCS. The Contractor is responsible for notifying AHCCCS of a child’s birth to an enrolled member. Capitation for the newborn will begin on the date notification is received by AHCCCS. The effective date of AHCCCS eligibility will be the newborn’s date of birth, and the Contractor is responsible for all covered services to the newborn, whether or not AHCCCS has received notification of the child’s birth. AHCCCS is currently available to receive notification 24 hours a day, seven days a week via phone or the AHCCCS website. Each eligible mother of a newborn is sent a letter advising her of her right to choose a different Contractor for her child; the date of the change will be the date of processing the request from the mother. If the mother does not request a change, the child will remain with the mother's Contractor.
Newborns of FES mothers are auto-assigned to a Contractor and mothers of these newborns sent letters advising them of their right to choose a different Contractor for their children. In the event the FES mother chooses a different Contractor, AHCCCS will recoup all capitation paid to the originally assigned Contractor and the baby will be enrolled retroactive to the date of birth with the second Contractor. The second Contractor will receive prior period capitation from the date of birth to the day before assignment and prospective capitation from the date of assignment forward. The second Contractor will be responsible for all covered services to the newborn from date of birth.
Enrollment Guarantees: Upon initial capitated enrollment as a Title XIX-eligible member, the member is guaranteed a minimum of five full months of continuous enrollment. Upon initial capitated enrollment as a Title XXI-eligible member, the member is guaranteed a minimum of 12 full months of continuous enrollment. The enrollment guarantee is a one-time benefit. If a member changes from one Contractor to another within the enrollment guarantee period, the remainder of the guarantee period applies to the new Contractor. AHCCCS Rules R9-22, Article 17, and R9-31, Article 3, describes other reasons for which the enrollment guarantee may not apply.
American Indians: American Indians, on- or off-reservation, may choose to receive services from Indian Health Service (IHS), a 638 tribal facility or any available Contractor. If a choice is not made within the specified time limit, American Indian Title XIX members living on-reservation will be assigned to the AHCCCS American Indian Health Program (AIHP) as FFS members. The designation of a zip code as a ‘reservation zip code’, not the physical location of the residence, is the factor that determines whether a member is considered on or off-reservation for these purposes. Further, if the member resides in a zip code that contains land on both sides of a reservation boundary and the zip code is assigned as off-reservation, the physical location of the residence does not change the off-reservation designation for the member. American Indian Title XIX members living off-
24
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
reservation who do not make a Contractor choice will be assigned to an available Contractor using the AHCCCS protocol for family continuity and the auto-assignment algorithm. American Indian Title XXI members may change from AHCCCS AIHP FFS to a Contractor or from a Contractor to AHCCCS AIHP FFS at any time.
| |
| 6. | ANNUAL ENROLLMENT CHOICE |
AHCCCS conducts an Annual Enrollment Choice (AEC) for members on their annual anniversary date [42 CFR 438.56(c)(2)(ii)]. AHCCCS may hold an open enrollment in any GSA or combination of GSAs as deemed necessary. During AEC, members may change Contractors subject to the availability of other Contractors within their Geographic Service Area. A member is mailed a printed enrollment form and other information required by the Medicaid Managed Care Regulations 60 days prior to their AEC date and may choose a new Contractor by contacting AHCCCS to complete the enrollment process. If the member does not participate in the AEC, no change of Contractor will be made (except for approved changes under the ACOM Policy 401) during the new anniversary year. This holds true if a Contractor’s contract is renewed and the member continues to live in a Contractor’s service area. The Contractor shall comply with the ACOM Policy 402, , and the AMPM.
| |
| 7. | ENROLLMENT AFTER CONTRACT AWARD |
In the event that AHCCCS does not award a CYE ’09 contract to an incumbent Contractor, AHCCCS will direct enrollment effective October 1, 2008, for those members enrolled with an exiting Contractor. Members will be auto assigned to all or select Contractors utilizing the auto assignment algorithm found in the Conversion Group Assignment section of Attachment G, Auto-Assignment Algorithm. The members in the Conversion Group will have the opportunity to choose an alternate Contractor, according to the details in Attachment G, Auto-Assignment Algorithm.
AHCCCS will also use an enhanced auto-assignment algorithm in certain GSAs for new Contractors or those incumbent Contractors defined as small Contractors. This enhanced algorithm may be in effect beginning October 1, 2008, for a period of no less than three months and no more than six months. Those Contractors not defined as new or small Contractors in a GSA may not receive auto-assigned members during the enhanced algorithm period. See Attachment G, Auto-Assignment Algorithm, for details.
In addition to auto-assignment, AHCCCS will make changes to both annual enrollment choice materials and new enrollee materials prior to October 1, 2008, to reflect the change in available Contractors. The auto assignment algorithm will be adjusted to exclude auto assignment of new enrollees to exiting Contractor(s) effective August 1, 2008.
| |
| 8. | AUTO-ASSIGNMENT ALGORITHM |
Members who do not exercise their right to choose and do not have family continuity are assigned to a Contractor through an auto-assignment algorithm. Once auto-assigned, AHCCCS sends a Freedom of Choice notice to the member and gives him/her 30 days to choose a different Contractor from the auto-assigned Contractor. The algorithm is a mathematical formula used to distribute members to the various Contractors in a manner that is predictable and consistent with AHCCCS goals. For CYE 09 through CYE 12, the algorithm favors those Contractors with lower capitation rates and higher Program scores in this procurement and as described below. AHCCCS may change the algorithm at any time during the term of the contract in response to Contractor-specific issues (e.g. imposition of an enrollment cap).
AHCCCS may adjust the auto-assignment algorithm in consideration of Contractors’ clinical performance measure results when calculating target percentages. Ranking in the algorithm may be weighted, based on the number of Performance Measures for which a Contractor is meeting the current AHCCCS Minimum Performance Standard
25
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
(MPS) as a percentage of the total number of measures utilized in the calculation. AHCCCS will determine and communicate the adjusted auto-assignment algorithm to be used prior to the beginning of the contract year to be measured. For further details on the AHCCCS Auto-Assignment Algorithm for CYE 13, refer to Attachment G.
| |
| 9. | AHCCCS MEMBER IDENTIFICATION CARDS |
The Contractor is responsible for paying the costs of producing AHCCCS member identification cards. The Contractor will receive an invoice the month following the issue date of the identification card.
| |
| 10. | MAINSTREAMING OF AHCCCS MEMBERS |
To ensure mainstreaming of AHCCCS members, the Contractor shall take affirmative action so that members are provided covered services without regard to payer source, race, color, creed, gender, religion, age, national origin (to include those with limited English proficiency), ancestry, marital status, sexual preference, genetic information, or physical or intellectual disability, except where medically indicated. The Contractor must take into account a member’s literacy and culture when addressing members and their concerns, and must take reasonable steps to ensure subcontractors to do the same. The Contractor must make interpreters, including assistance for the visual- or hearing- impaired, available at no cost for all members to ensure appropriate delivery of covered services. The Contractor must provide to members with information instructing them how to access these services.
Prohibited practices include, but are not limited to, the following, in accordance with 42 CFR 438.6(f) :
| |
| a. | Denying or not providing a member any covered service or access to an available facility. |
| |
| b. | Providing to a member any medically necessary covered service which is different, or is provided in a different manner or at a different time from that provided to other members, other public or private patients or the public at large, except where medically necessary. |
| |
| c. | Subjecting a member to segregation or separate treatment in any manner related to the receipt of any covered service; restricting a member in any way in his or her enjoyment of any advantage or privilege enjoyed by others receiving any covered service. |
| |
| d. | The assignment of times or places for the provision of services on the basis of the race, color, creed, religion, age, sex, national origin, ancestry, marital status, sexual preference, income status, AHCCCS membership, or physical or intellectual disability of the participants to be served. |
If the Contractor knowingly executes a subcontract with a provider with the intent of allowing or permitting the subcontractor to implement barriers to care (i.e., the terms of the subcontract act to discourage the full utilization of services by some members); the Contractor will be in default of its contract.
If the Contractor identifies a problem involving discrimination by one of its providers, it shall promptly intervene and require a corrective action plan from the provider. Failure to take prompt corrective measures may place the Contractor in default of its contract.
The Contractor shall comply with the AMPM and the ACOM Policy 402 standards for member transitions between Contractors or GSAs, participation in or discharge from CRS or CMDP, to or from an ALTCS Contractor and upon termination or expiration of a contract. The exiting Contractor shall be responsible for performing all transition activities at no cost. AHCCCS may discontinue enrollment of members with the Contractor three months prior to the contract termination date. The Contractor shall develop and implement policies and procedures which comply with these policies to address transition of:
26
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
| |
| a. | Members with significant medical conditions such as a high-risk pregnancy or pregnancy within the last 30 days, the need for organ or tissue transplantation, chronic illness resulting in hospitalization or nursing facility placement, etc.; |
| |
| b. | Members who are receiving ongoing services such as dialysis, home health, chemotherapy and/or radiation therapy, or who are hospitalized at the time of transition; |
| |
| c. | Members who have conditions requiring ongoing monitoring or screening such as elevated blood lead levels and members who were in the NICU after birth; |
| |
| d. | Members who frequently contact AHCCCS, state and local officials, the Governor’s Office and/or the media; |
| |
| e. | Members who have received prior authorization for services such as scheduled surgeries, post surgical follow-up visits, out-of-area specialty services, or nursing home admission; |
| |
| f. | Prescriptions, DME and medically necessary transportation ordered for the transitioning member by the relinquishing Contractor; and |
| |
| g. | Medical records of the transitioning member (the cost, if any, of reproducing and forwarding medical records shall be the responsibility of the relinquishing AHCCCS Contractor). |
| |
| h. | Any members transitioning to CMDP. |
When relinquishing members, the Contractor is responsible for timely notification to the receiving Contractor regarding pertinent information related to any special needs of transitioning members. The Contractor, when receiving a transitioning member with special needs, is responsible for coordinating care with the relinquishing Contractor in order that services are not interrupted, and for providing the new member with Contractor and service information, emergency numbers and instructions about how to obtain services.
The Contractor shall provide covered services to AHCCCS members in accordance with all applicable Federal and State laws regulations and policies, including those listed by reference in attachments and this contract. The services are described in detail in AHCCCS Rules R9-22, Article 2, the AHCCCS Medical Policy Manual (AMPM) and the AHCCCS Contractor Operations Manual (ACOM), all of which are incorporated herein by reference, except for provisions specific to the Fee-for-Service program, and may be found on the AHCCCS website (http://www.azahcccs.gov/) [42 CFR 438.210(a)(1)]. To be covered, services must be medically necessary and cost effective. The covered services are briefly described below. Except for annual well woman exams, behavioral health and children’s dental services and consistent with the terms of the demonstration, covered services must be provided by or coordinated with a primary care provider.
The Contractor must ensure the coordination of services it provides with services the member receives from other entities, including behavioral health services the member receives through an ADHS/RBHA provider and Children’s Rehabilitative Services (CRS). The Contractor shall ensure that, in the process of coordinating care, each member’s privacy is protected in accordance with the privacy requirements in 45 CFR Parts 160 and 164, Subparts A and E, to the extent that they are applicable [42 CFR 438.208 (b)(2) and (b)(4) and 438.224].
Services must be rendered by providers that are appropriately licensed or certified, operating within their scope of practice, and registered as an AHCCCS provider. The Contractor shall provide the same standard of care for all members, regardless of the member's eligibility category. The Contractor shall ensure that the services are sufficient in amount, duration and scope to reasonably be expected to achieve the purpose for which the services are furnished. The Contractor shall not arbitrarily deny or reduce the amount, duration, or scope of a required service solely because of diagnosis, type of illness, or condition of the member. The Contractor may place appropriate limits on a service on the basis of criteria such as medical necessity; or for utilization control, provided the services furnished can reasonably be expected to achieve their purpose [42 CFR 438.210(a)(3)].
The Contractor must notify AHCCCS if, on the basis of moral or religious grounds, it elects to not provide or reimburse for a covered service. Notification must be submitted prior to entering into a contract with AHCCCS
27
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
or prior to adopting the policy during the term of the contract [42 CFR 438.102(a)(2) and (b)(1)]. Members must be notified on how to access the services. The notification and policy must be consistent with the provisions of 42 CFR 438.10, must be provided to members during their initial appointment, and must be provided to members at least 30 days prior to the effective date of the policy. AHCCCS will disenroll from the Contractor members who are seeking these services and assign the members to another Contractor [42 CFR 438.56].
Authorization of Services: For the processing of requests for initial and continuing authorizations of services, the Contractor shall have in place, and follow, written policies and procedures. The Contractor must have mechanisms in place to ensure consistent application of review criteria for authorization decisions. Any decision to deny a service authorization request or to authorize a service in an amount, duration or scope that is less than requested, must be made by a health care professional who has appropriate clinical expertise in treating the member’s condition or disease [42 CFR 438.210(b)].
Notice of Action: The Contractor must notify the requesting provider and give the member written notice of any decision by the Contractor to deny, reduce, suspend or terminate a service authorization request, or to authorize a service in an amount, duration, or scope that is less than requested, or for any action as defined in Attachment H(1).[42 CFR 438.400(b)] The notice shall meet the requirements of 42 CFR 438.404, AHCCCS Rules and ACOM Policy 414. The notice to the provider must also be in writing as specified in Attachment H(1) of this contract [42 CFR 438.210 (c)]. The Contractor must comply with all decision timelines outlined in ACOM Policy 414.
The Contractor shall ensure that its providers, within the lawful scope of their practice, are not prohibited or otherwise restricted from communicating freely with members regarding their health care, medical needs and treatment options, even if needed services are not covered by the Contractor.
Ambulatory Surgery: The Contractor shall provide surgical services for either emergency or scheduled surgeries when provided in an ambulatory or outpatient setting, such as a freestanding surgical center or a hospital-based outpatient surgical setting.
American Indian Health Program (AIHP): AHCCCS Division of Fee For Service Management (DFSM) will reimburse claims for acute care services that are medically necessary, eligible for 100% Federal reimbursement, and are provided to Title XIX members enrolled with the Contractor by an IHS or a 638 tribal facility and when the member is eligible to receive services at the IHS or a tribally operated 638 program. Encounters for Title XIX services billed by an IHS or tribal facilities will not be accepted by AHCCCS or considered in capitation rate development.
The Contractor is responsible for reimbursement to IHS or tribal facilities for services provided to Title XXI American Indian members enrolled with the Contractor. The Contractor may choose to subcontract with an IHS or 638 tribal facility as part of its provider network for the delivery of Title XXI covered services. Expenses incurred by the Contractor for Title XXI services billed by an IHS or 638 tribal facility shall be encountered and considered in capitation rate development.
Anti-hemophilic Agents and Related Services: The Contractor shall provide services for the treatment of hemophilia and Von Willebrand’s disease (See Section D, Paragraph 57, Reinsurance, Catastrophic Reinsurance).
Audiology: The Contractor shall provide medically necessary audiology services to evaluate hearing loss for all members, on both an inpatient and outpatient basis. Hearing aids are covered only for members under the age of 21 receiving EPSDT services.
28
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
Behavioral Health: The Contractor shall provide behavioral health services as described in Section D, Paragraph 12, Behavioral Health Services. Also refer to Prior Period Coverage in Section D, Paragraph 3, Enrollment and Disenrollment.
Children's Rehabilitative Services (CRS): Is a program for children with special health care needs. The CRS program is administered by AHCCCS utilizing a CRS Contractor for children who meet CRS eligibility criteria. The Contractor shall refer children to CRS who are potentially eligible for services related to CRS-covered conditions, as specified in R9-22, Article 2, and A.R.S. Title 36, Chapter 2, Article 3. In addition, the Contractor shall notify the member when a referral to CRS has been made. The Contractor is responsible for care of members until those members are determined eligible by the CRS Contractor. In addition, the Contractor is responsible for covered services for CRS-eligible members unless and until the Contractor has received written confirmation from the CRS Contractor that the CRS Contractor will provide the medically necessary, CRS covered service. The Contractor shall require the member’s Primary Care Provider (PCP) to coordinate the member’s care with the CRS Contractor. For more detailed information regarding eligibility criteria, referral practices, and Contractor-CRS coordination issues, refer to the AHCCCS Medical Policy Manual (AMPM) and the AHCCCS Contractor’s Operation Manual (ACOM) located on the AHCCCS website at www.azahcccs.gov.
The Contractor shall respond to requests for services potentially covered by CRSA in accordance with the related ACOM and AMPM policies. The Contractor is responsible for addressing prior authorization requests if CRSA fails to comply with the timeframes specified in the related ACOM policy. The Contractor is responsible for the payment of emergency department facility and professional claims (in or out of network), regardless of whether the service is related to the CRS condition. In addition, the Contractor remains ultimately responsible for the provision of all AHCCCS-covered services to its members including services denied by the CRS Contractor for the reason that it is not a service related to a CRS condition.
Referral to the CRS Contractor does not relieve the Contractor of the responsibility for providing timely medically necessary AHCCCS services not covered by the CRS Contractor. In the event that the CRS Contractor denies a medically necessary AHCCCS service for the reason that it is not related to a CRS covered condition, the Contractor must promptly respond to the service authorization request and authorize the provision of medically necessary services. The CRS Contractor cannot contest the Contractor prior authorization determination if the CRS Contractor fails to timely respond to a service authorization request. Contractors, through their Medical Directors, may request review from the CRS Contractor Medical Director when it denies a service for the reason that it is not covered by the CRS Program. The Contractor may also request a review of the decision with AHCCCS if it is dissatisfied with the CRS Contractor’s determination. If the AHCCCS review determines that the service should have been provided by the CRS Contractor, the CRS Contractor shall be financially responsible for the costs incurred by the Contractor in providing the service.
A member with private insurance is not required to utilize CRS. This includes members with Medicare whether they are enrolled in Medicare FFS or a Medicare Managed Care Plan. If the member uses a private insurance network for a CRS covered condition, the Contractor is responsible for all applicable deductibles and copayments. If the member is on Medicare, ACOM Policy 201 and Policy 202 shall apply. When private insurance or Medicare is exhausted, or certain annual or lifetime limits are reached with respect to the CRS covered conditions, the Contractor shall refer the member to CRS for determination of eligibility. If the member with private insurance or Medicare chooses to enroll with CRS, CRS becomes the secondary payer responsible for all applicable deductibles and copayments. The Contractor is not responsible to provide services in instances when a member with a CRS covered condition who has no primary insurance or Medicare, refuses to participate in the CRS application process, or refuses to receive CRS covered services through the CRS program. The member may be billed by the provider in accordance with AHCCCS regulations regarding billing for unauthorized services.
Chiropractic Services: The Contractor shall provide chiropractic services to members under age 21 when prescribed by the member’s PCP and approved by the Contractor in order to ameliorate the member’s medical
29
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
condition. Medicare approved chiropractic services for any member shall be covered, subject to limitations specified in 42 CFR 410.22, for Qualified Medicare Beneficiaries, regardless of age, if prescribed by the member’s PCP and approved by the Contractor.
Dialysis: The Contractor shall provide medically necessary dialysis, supplies, diagnostic testing and medication for all members when provided by Medicare-certified hospitals or Medicare-certified end stage renal disease (ESRD) providers. Services may be provided on an outpatient basis or on an inpatient basis if the hospital admission is not solely to provide chronic dialysis services.
Early and Periodic Screening, Diagnostic and Treatment (EPSDT): The Contractor shall provide comprehensive health care services through primary prevention, early intervention, diagnosis and medically necessary treatment to correct or ameliorate defects and physical or intellectual disabilities discovered by the screenings for members under age 21. The Contractor shall ensure that these members receive required health screenings, including developmental and behavioral health screenings, in compliance with the AHCCCS EPSDT Periodicity Schedule, and the AHCCCS Dental Periodicity Schedule (Exhibit 430-1 in the AMPM).
The Contractor shall ensure the initiation and coordination of a referral to the T/RBHA system for members in need of behavioral health services. The Contractor shall follow up with the T/RBHA to monitor whether members have received these health services. The Contractor will ensure the Health Plan coordinates referrals and follow-up collaboration, as necessary, for members identified by the ADHS as needing acute care services.
Early Detection Health Risk Assessment, Screening, Treatment and Primary Prevention: The Contractor shall provide health care services through screening, diagnostic and medically necessary treatment for members 21 years of age and older. These services include, but are not limited to, screening and treatment for hypertension; elevated cholesterol; colon cancer; sexually transmitted diseases; tuberculosis; HIV/AIDS; breast cancer, cervical cancer; and prostate cancer. Nutritional assessment and treatment are covered when medically necessary to meet the over and under nutritional needs of members who may have a chronic debilitating disease. Physical examinations, diagnostic work-ups and medically necessary immunizations are also covered as specified in Arizona Administrative Code Section R9-22-205. AHCCCS does not cover well exams (i.e., physical examinations in the absence of any known disease or symptom or any specific medical complaint by the patient precipitating the examination) for adult members.
Emergency Services: The Contractor shall provide emergency services per the AHCCCS AMPM Policy and the following:
| |
| a. | Emergency services facilities adequately staffed by qualified medical professionals to provide pre-hospital, emergency care on a 24-hour-a-day, 7-day-a-week basis, for an emergency medical condition as defined by AHCCCS Rule 9 A.A.C. 22, Article 1. Emergency medical services are covered without prior authorization. The Contractor is encouraged to contract with emergency service facilities for the provision of emergency services. The Contractor shall be responsible for educating members and providers regarding appropriate utilization of emergency room services including behavioral health emergencies. [42 CFR 438.206(c)(1)(i)]The Contractor shall monitor emergency service utilization (by both provider and member) and shall have guidelines for implementing corrective action for inappropriate utilization. For utilization review, the test for appropriateness of the request for emergency services shall be whether a prudent layperson, similarly situated, would have requested such services. For the purposes of this contract, a prudent layperson is a person who possesses an average knowledge of health and medicine. |
| |
| b. | All medical services necessary to rule out an emergency condition; and |
| |
| c. | Emergency transportation. |
Per the Medicaid Managed Care regulations, 42 CFR 438.114, 422.113, 422.133 the following conditions apply with respect to coverage and payment of emergency services:
30
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
The Contractor must cover and pay for emergency services regardless of whether the provider that furnishes the service has a contract with the Contractor.
The Contractor may not deny payment for treatment obtained under either of the following circumstances:
| |
| 1. | A member had an emergency medical condition, including cases in which the absence of medical attention would not have resulted in the outcomes identified in the definition of emergency medical condition under 42 CFR 438.114. |
| |
| 2. | A representative of the Contractor (an employee or subcontracting provider) instructs the member to seek emergency medical services. |
Additionally, the Contractor may not:
| |
| 1. | Limit what constitutes an emergency medical condition as defined in 42 CFR 438.114, on the basis of lists of diagnoses or symptoms. |
| |
| 2. | Refuse to cover emergency services based on the failure of the emergency room provider, hospital, or fiscal agent to notify the Contractor of the member’s screening and treatment within 10 calendar days of presentation for emergency services. Claims submission by the hospital within 10 calendar days of the member’s presentation for the emergency services constitutes notice to the Contractor. This notification stipulation is only related to the provision of emergency services. |
| |
| 3. | Require notification of Emergency Department treat and release visits as a condition of payment unless the plan has prior approval from AHCCCS. |
A member who has an emergency medical condition may not be held liable for payment of subsequent screening and treatment needed to diagnose the specific condition or stabilize the patient.
The attending emergency physician, or the provider actually treating the member, is responsible for determining when the member is sufficiently stabilized for transfer or discharge, and such determination is binding on the Contractor responsible for coverage and payment. The Contractor shall comply with Medicaid Managed Care guidelines regarding the coordination of post-stabilization care.
For additional information and requirements regarding emergency services, refer to AHCCCS Rules R9-22-201 et seq. and 42 CFR 438.114.
Family Planning: The Contractor shall provide family planning services in accordance with the AMPM and consistent with the terms of the demonstration, for all members who choose to delay or prevent pregnancy. These include medical, surgical, pharmacological and laboratory services, as well as contraceptive devices. Information and counseling, which allow members to make informed decisions regarding family planning methods, are also included. If the Contractor does not provide family planning services, it must contract for these services through another health care delivery system or AHCCCS will disenroll from the Contractor members who are seeking these services and assign the members to another Contractor.
The Contractor shall provide services to members enrolled in the Family Planning Services Extension Program, a program that provides family planning services only, for a maximum of two consecutive 12-month periods, to women whose SOBRA eligibility has terminated. The Contractor is also responsible for notifying AHCCCS when a SOBRA woman is sterilized to prevent inappropriate enrollment in the SOBRA Family Planning Services Extension Program. Notification should be made at the time the newborn is reported or after the sterilization procedure is completed.
31
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
Foot and Ankle Services Children: The Contractor shall provide foot and ankle services for members under the age of 21 to include bunionectomies, casting for the purpose of constructing or accommodating orthotics, medically necessary orthopedic shoes that are an integral part of a brace, and medically necessary routine foot care for patients with a severe systemic disease that prohibits care by a nonprofessional person.
Foot and Ankle Services Adults: The Contractor shall provide foot and ankle care services to include wound care, treatment of pressure ulcers, fracture care, reconstructive surgeries, and limited bunionectomy services. Medically necessary routine foot care services are only available for members with a severe systemic disease that prohibits care by a nonprofessional person as described in the AMPM. Services are not covered for members 21 years of age and older, when provided by a podiatrist or podiatric surgeon.
Home and Community Based Services (HCBS): Assisted living facility, alternative residential setting, or home and community based services (HCBS) as defined in R9-22, Article 2, and R9-28, Article 2 that meet the provider standards described in R9-28, Article 5, and subject to the limitations set forth in the AMPM. These services are covered in lieu of a nursing facility.
Home Health: This service shall be provided under the direction of a physician to prevent hospitalization or institutionalization and may include nursing, therapies, supplies and home health aide services. It shall be provided on a part-time or intermittent basis.
Hospice: These services are covered for members who are certified by a physician as being terminally ill and having six months or less to live. See the AMPM for details on covered hospice services.
Hospital: Inpatient services include semi-private accommodations for routine care, intensive and coronary care, surgical care, obstetrics and newborn nurseries, and behavioral health emergency/crisis services. If the member’s medical condition requires isolation, private inpatient accommodations are covered. Nursing services, dietary services and ancillary services such as laboratory, radiology, pharmaceuticals, medical supplies, blood and blood derivatives, etc. are also covered. Outpatient hospital services include any of the above services which may be appropriately provided on an outpatient or ambulatory basis (i.e., laboratory, radiology, therapies, ambulatory surgery, etc.). Observation services may be provided on an outpatient basis, if determined reasonable and necessary to decide whether the member should be admitted for inpatient care. Observation services include the use of a bed and periodic monitoring by hospital nursing staff and/or other staff to evaluate, stabilize or treat medical conditions of a significant degree of instability and/or disability. Refer to the AHCCCS Medical Policy Manual for limitations on hospital stays.
Immunizations: The Contractor shall provide medically necessary immunizations for adults 21 years of age and older. Human Pappiloma virus (HPV) is covered only for EPSDT aged male and female members (through age 20). (Please refer to the AMPM for current immunization requirements.)The Contractor is required to meet specific immunization rates for members under the age of 21, which are described in Section D, Paragraph 23, Quality Management.
Incontinence Supplies: The Contractor shall cover incontinence supplies as specified in AHCCCS Rule A.A.C. R9-22-212 and the AMPM.
Laboratory: Laboratory services for diagnostic, screening and monitoring purposes are covered when ordered by the member’s PCP, other attending physician or dentist, and provided by a CLIA (Clinical Laboratory Improvement Act) approved free-standing laboratory or hospital laboratory, clinic, physician office or other health care facility laboratory.
Upon written request, the Contractor may obtain laboratory test data on members from a laboratory or hospital- based laboratory subject to the requirements specified in A.R.S. § 36-2903(Q) and (R). The data shall be used
32
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
exclusively for quality improvement activities and health care outcome studies required and/or approved by AHCCCS.
Maternity: The Contractor shall provide pregnancy identification, prenatal care, treatment of pregnancy related conditions, labor and delivery services, and postpartum care for members. Services may be provided by physicians, physician assistants, nurse practitioners, certified nurse midwives, or licensed midwives. Members may select or be assigned to a PCP specializing in obstetrics while they are pregnant. Members anticipated to have a low-risk delivery, may elect to receive labor and delivery services in their home from their maternity provider if this setting is included in the allowable settings for the Contractor, and the Contractor has providers in its network that offer home labor and delivery services. Members anticipated to have a low-risk prenatal course and delivery may elect to receive maternity services of prenatal care, labor and delivery and postpartum care provided by certified nurse midwives or licensed midwives, if they are in the Contractor’s provider network. Members receiving maternity services from a certified nurse midwife or a licensed midwife must also be assigned to a PCP for other health care and medical services. A certified nurse midwife may provide those primary care services that s/he is willing to provide and that the member elects to receive from the certified nurse midwife. Members receiving care from a certified nurse midwife may also elect to receive some or all her primary care from the assigned PCP. Licensed midwives may not provide any additional medical services as primary care is not within their scope of practice.
The Contractor shall allow women and their newborns to receive up to 48 hours of inpatient hospital care after a routine vaginal delivery and up to 96 hours of inpatient care after a cesarean delivery. The attending health care provider, in consultation with the mother, may discharge the mother or newborn prior to the minimum length of stay. A normal newborn may be granted an extended stay in the hospital of birth when the mother’s continued stay in the hospital is beyond the 48 or 96 hour stay. However, for payment purposes, inpatient limits will apply to the extent consistent with EPSDT.
The Contractor shall inform all assigned AHCCCS pregnant women of voluntary prenatal testing and the availability of medical counseling if the test is positive. The Contractor shall provide information in the Member Handbook and annually in the member newsletter, to encourage pregnant women to be tested and instructions about where to be tested. Semi-annually, the Contractor shall report to AHCCCS, Division of Health Care Management (DHCM) the number of pregnant women who have been identified as HIV/AIDS-positive for each quarter during the contract year. This report is due no later than 30 days after the end of the second and fourth quarters of the contract year.
Medical Foods: Medical foods are covered within limitations defined in the AMPM for members diagnosed with a metabolic condition included under the ADHS Newborn Screening Program and specified in the AMPM. The medical foods, including metabolic formula and modified low protein foods, must be prescribed or ordered under the supervision of a physician.
Medical Supplies, Durable Medical Equipment (DME), and Prosthetic Devices: These services are covered when prescribed by the member’s PCP, attending physician or practitioner, or by a dentist as described in the AMPM. Prosthetic devices must be medically necessary and meet criteria as described in the AMPM. For persons age 21 or older, AHCCCS will not pay for microprocessor controlled lower limbs and microprocessor controlled joints for lower limbs. Medical equipment may be rented or purchased only if other sources are not available which provide the items at no cost. The total cost of the rental must not exceed the purchase price of the item. Reasonable repairs or adjustments of purchased equipment are covered to make the equipment serviceable and/or when the repair cost is less than renting or purchasing another unit.
Nursing Facility: The Contractor shall provide services in nursing facilities, including religious non-medical health care institutions, for members who require short-term convalescent care not to exceed 90 days per contract year. In lieu of a nursing facility, the member may be placed in an assisted living facility, an alternative residential
33
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
setting, or receive home and community based services (HCBS) as defined in R9-22, Article 2 and R9-28, Article 2 that meet the provider standards described in R9-28, Article 5, and subject to the limitations set forth in the AMPM.
Nursing facility services must be provided in a dually-certified Medicare/Medicaid nursing facility, which includes in the per-diem rate: nursing services; basic patient care equipment and sickroom supplies; dietary services; administrative physician visits; non-customized DME; necessary maintenance and rehabilitation therapies; over-the-counter medications; social, recreational and spiritual activities; and administrative, operational medical direction services. See Section D, Paragraph 41, Responsibility for Nursing Facility Reimbursement, for further details.
The Contractor shall notify the Assistant Director of the Division of Member Services, by Email, when a member has been residing in a nursing facility, alternative residential facility or receiving home and community based services for 45 days. This will allow AHCCCS time to follow-up on the status of the ALTCS application and to consider potential fee-for-service coverage, if the stay goes beyond the 90-day per contract year maximum. The notice should be sent via e-mail to HealthPlan45DayNotice@azahcccs.gov.
Notifications must include:
| |
| 5. | Admission Date to the Facility |
| |
| 6. | Date they reach the 45 days |
| |
| 7. | Name of Contractor of enrollment |
Nutrition: Nutritional assessments are conducted as a part of the EPSDT screenings for members under age 21, and to assist members 21 years of age and older whose health status may improve with over and under-nutritional intervention. Assessment of nutritional status on a periodic basis may be provided as determined necessary, and as a part of the health risk assessment and screening services provided by the member’s PCP. Assessments may also be provided by a registered dietitian when ordered by the member’s PCP. AHCCCS covers nutritional therapy on an enteral, parenteral or oral basis, when determined medically necessary, according to the criteria specified in the AMPM, to provide either complete daily dietary requirements or to supplement a member’s daily nutritional and caloric intake.
Oral Health: The Contractor shall provide all members under the age of 21 years with all medically necessary dental services including emergency dental services, dental screening, preventive services, therapeutic services and dental appliances in accordance with the AHCCCS Dental Periodicity Schedule and pre-transplantation dental services. The Contractor shall monitor compliance with the AHCCCS Dental Periodicity Schedule for dental screening services. The Contractor is required to meet specific utilization rates for members as described in Section D, Paragraph 23, Quality Management The Contractor shall ensure that members are notified when dental screenings are due if the member has not been scheduled for a visit. If a dental screening is not received by the member, a second notice must be sent. Members under the age of 21 may request dental services without referral and may choose a dental provider from the Contractor’s provider network.
Pursuant to A.A.C. R9-22-207, for members who are 21 years of age and older, the Contractor shall cover medical and surgical services furnished by a dentist only to the extent such services may be performed under state law either by a physician or by a dentist. These services would be considered physician services if furnished by a physician. Limited dental services are covered for pre-transplant candidates and for members with cancer of the jaw, neck or head. Refer to the AMPM for specific details.
34
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
Orthotics: These services are covered for members under the age of 21 when prescribed by the member’s PCP, attending physician, practitioner, or by a dentist as described in the AMPM. Medical equipment may be rented or purchased only if other sources, which provide the items at no cost, are not available. The total cost of the rental must not exceed the purchase price of the item.
Reasonable repairs or adjustments of purchased equipment are covered for all members over and under the age of 21 to make the equipment serviceable and/or when the repair cost is less than renting or purchasing another unit. The component will be replaced if at the time authorization is sought documentation is provided to establish that the component is not operating effectively.
Physician: The Contractor shall provide physician services to include medical assessment, treatments and surgical services provided by licensed allopathic or osteopathic physicians.
Post-stabilization Care Services Coverage and Payment: Pursuant to AHCCCS Rule A.A.C. R9-22-210 and 42 CFR 438.114, 422.113(c) and 422.133, the following conditions apply with respect to coverage and payment of emergency and of post-stabilization care services, except where otherwise noted in the contract:
The Contractor must cover and pay for post-stabilization care services without authorization, regardless of whether the provider that furnishes the service has a contract with the Contractor, for the following situations:
| |
| 1. | Post-stabilization care services that were pre-approved by the Contractor; or |
| |
| 2. | Post-stabilization care services were not pre-approved by the Contractor because the Contractor did not respond to the treating provider’s request for pre-approval within one hour after being requested to approve such care or could not be contacted for pre-approval. |
| |
| 3. | The Contractor representative and the treating physician cannot reach agreement concerning the member’s care and a Contractor physician is not available for consultation. In this situation, the Contractor must give the treating physician the opportunity to consult with a Contractor physician and the treating physician may continue with care of the patient until a Contractor physician is reached or one of the criteria in 42 CFR 422.113(c)(3) is met. |
Pursuant to 42 CFR 422.113(c)(3), the Contractor’s financial responsibility for post-stabilization care services that have not been pre-approved ends when:
| |
| 1. | A Contractor physician with privileges at the treating hospital assumes responsibility for the member’s care; |
| |
| 2. | A Contractor physician assumes responsibility for the member’s care through transfer; |
| |
| 3. | A Contractor representative and the treating physician reach an agreement concerning the member’s care; or |
| |
| 4. | The member is discharged. |
Pregnancy Terminations: AHCCCS covers pregnancy termination if the pregnant member suffers from a physical disorder, physical injury, or physical illness, including a life endangering physical condition caused by or arising from the pregnancy itself, that would, as certified by a physician, place the member in danger of death unless the pregnancy is terminated, or the pregnancy is a result of rape or incest.
The attending physician must acknowledge that a pregnancy termination has been determined medically necessary by submitting the Certificate of Necessity for Pregnancy Termination. This certificate must be submitted to the Contractor’s Medical Director and meet the requirements specified in the AMPM. The Certificate must certify that, in the physician's professional judgment, one or more of the previously mentioned criteria have been met.
Prescription Medications: Medications ordered by a PCP, attending physician, dentist or other authorized prescriber and dispensed under the direction of a licensed pharmacist are covered subject to limitations related to prescription supply amounts, Contractor formularies and prior authorization requirements. An appropriate
35
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
over-the-counter medication may be prescribed as defined in the AMPM when it is determined to be a lower-cost alternative to a prescription medication.
Medicare Part D: AHCCCS covers those drugs ordered by a PCP, attending physician, dentist or other authorized prescriber and dispensed under the direction of a licensed pharmacist subject to limitations related to prescription supply amounts, and the Contractor’s prior authorization requirements if they are excluded from Medicare Part D coverage. Medications that are covered by Part D, but are not on a specific Part D Health Plan’s formulary are not considered excluded drugs and will not be covered by AHCCCS. This applies to members that are enrolled in Medicare Part D or are eligible for Medicare Part D.
Primary Care Provider (PCP): PCP services are covered when provided by a physician, physician assistant or nurse practitioner selected by, or assigned to, the member. The PCP provides primary health care and serves as a coordinator in referring the member for specialty medical services [42 CFR 438.208(b)]. The PCP is responsible for maintaining the member’s primary medical record, which contains documentation of all health risk assessments and health care services of which they are aware whether or not they were provided by the PCP.
Radiology and Medical Imaging: These services are covered when ordered by the member’s PCP, attending physician or dentist and are provided for diagnosis, prevention, treatment or assessment of a medical condition.
Rehabilitation Therapy: The Contractor shall provide occupational, physical and speech therapies. Therapies must be prescribed by the member’s PCP or attending physician for an acute condition and the member must have the potential for improvement due to the rehabilitation.
Occupational and Speech therapy is covered for all members receiving inpatient hospital (or nursing facility services). Occupational Therapy and Speech therapy services provided on an outpatient basis are only covered for members under the age of 21. Physical Therapy is covered for all members in both inpatient and outpatient settings. Outpatient physical therapy for members 21 years of age or older are subject to a 15 visit limit per contract year as described in the AMPM.
Respiratory Therapy: Respiratory therapy is covered when prescribed by the member’s PCP or attending physician, and is necessary to restore, maintain or improve respiratory functioning.
Transplantation of Organs and Tissue, and Related Immunosuppressant Drugs: These services are covered within limitations defined in the AMPM for members diagnosed with specified medical conditions. Services include: pre-transplant inpatient or outpatient evaluation; donor search; organ/tissue harvesting or procurement; preparation and transplantation services; and convalescent care. In addition, if a member receives a transplant covered by a source other than AHCCCS, medically necessary non-experimental services are provided, within limitations, after the discharge from the acute care hospitalization for the transplantation. AHCCCS maintains specialty contracts with transplantation facility providers for the Contractor’s use or the Contractor may select its own transplantation provider.
Transportation: These services include emergency and non-emergency medically necessary transportation. Emergency transportation, including transportation initiated by an emergency response system such as 911, may be provided by ground, air or water ambulance to manage an AHCCCS member’s emergency medical condition at an emergency scene and transport the member to the nearest appropriate medical facility. Non-emergency transportation shall be provided for members who are unable to provide their own transportation for medically necessary services using the appropriate mode based on the needs of the member. The Contractor shall ensure that members have coordinated, reliable, medically necessary transportation to ensure members arrive on-time for regularly scheduled appointments and are picked up upon completion of the entire scheduled treatment.
36
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
Triage/Screening and Evaluation: These are covered services when provided by acute care hospitals, IHS facilities, a 638 tribal facility and after-hours settings to determine whether or not an emergency exists, assess the severity of the member’s medical condition and determine services necessary to alleviate or stabilize the emergent condition. Triage/screening services must be reasonable, cost effective and meet the criteria for severity of illness and intensity of service.
Vision Services/Ophthalmology/Optometry: The Contractor shall provide all medically necessary emergency eye care, vision examinations, prescriptive lenses, frames, and treatments for conditions of the eye for all members under the age of 21. For members who are 21 years of age and older, the Contractor shall provide emergency care for eye conditions which meet the definition of an emergency medical condition, cataract removal, and/or medically necessary vision examinations and prescriptive lenses and frames, if required following cataract removal and other eye conditions as specified in the AMPM.
Members shall have full freedom to choose, within the Contractor’s network, a practitioner in the field of eye care, acting within the scope of their practice, to provide the examination, care or treatment for which the member is eligible. A “practitioner in the field of eye care” is defined to be either an ophthalmologist or an optometrist.
| |
| 13. | SPECIAL HEALTH CARE NEEDS |
AHCCCS has specified in its Quality Strategy certain populations with special health care needs including members enrolled in DDD, CRS and those receiving behavioral health services. The Contractor shall have in place a mechanism to identify all members with special health care needs [42 CFR 438.240(b)(4)]. The Contractor shall implement mechanisms to assess each member identified as having special health care needs, in order to identify any ongoing special conditions of the member which require a course of treatment or regular care monitoring. The assessment mechanisms shall use appropriate health care professionals [42 CFR 438.208(c)(2)]. The Contractor shall share with other entities providing services to that member the results of its identification and assessment of that member’s needs so that those activities need not be duplicated [42 CFR 438.208(b)(3)].
For members with special health care needs determined to need a specialized course of treatment or regular care monitoring, the Contractor must have procedures in place to allow members to directly access a specialist (for example through a standing referral or an approved number of visits) as appropriate for the member’s condition and identified needs [42 CFR 438.208(c)(4)].
The Contractor shall have a methodology to identify providers willing to provide medical home services and make reasonable efforts to offer access to these providers.
The American Academy of Pediatrics (AAP) describes care from a medical home as:
The Contractor shall ensure that populations with ongoing medical needs, including but not limited to dialysis, radiation and chemotherapy, have coordinated, reliable, medically necessary transportation to ensure members arrive on-time for regularly scheduled appointments and are picked up upon completion of the entire scheduled treatment.
37
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
| |
| 14. | BEHAVIORAL HEALTH SERVICES |
AHCCCS members, except for SOBRA Family Planning members, are eligible for comprehensive behavioral health services. For SOBRA Family Planning members, there is no behavioral health coverage. With the exception of the Contractor’s providers’ medical management of certain behavioral health conditions as described under “Medication Management Services”, the behavioral health benefit for these members is provided through the ADHS - Regional Behavioral Health Authority (RBHA) system. The Contractor shall be responsible for member education regarding these benefits; provision of limited emergency inpatient services; and screening and referral to the RBHA system of members identified as requiring behavioral health services.
Member Education: The Contractor shall be responsible for educating members in the Member Handbook and other printed documents about covered behavioral health services and where and how to access services. Covered services include:
| |
| a. | Behavior Management (personal care, family support/home care training, peer support) |
| |
| b. | Behavioral Health Case Management Services |
| |
| c. | Behavioral Health Nursing Services |
| |
| d. | Emergency Behavioral Health Care |
| |
| e. | Emergency and Non-Emergency Transportation |
| |
| f. | Evaluation and Assessment |
| |
| g. | Individual, Group and Family Therapy and Counseling |
| |
| h. | Inpatient Hospital Services (the Contractor may provide services in alternative inpatient settings that are licensed by the Arizona Department of Health Services, Division of Assurance and Licensure, the Office of Behavioral Health Licensure, in lieu of services in an inpatient hospital. These alternative settings must be lower cost than traditional inpatient settings. ) |
| |
| i. | Non-Hospital Inpatient Psychiatric Facilities Services (Level I residential treatment centers and sub-acute facilities) |
| |
| j. | Laboratory and Radiology Services for Psychotropic Medication Regulation and Diagnosis |
| |
| k. | Opioid Agonist Treatment |
| |
| l. | Partial Care (Supervised day program, therapeutic day program and medical day program) |
| |
| m. | Psychosocial Rehabilitation (living skills training; health promotion; supportive employment services) |
| |
| n. | Psychotropic Medication |
| |
| o. | Psychotropic Medication Adjustment and Monitoring |
| |
| p. | Respite Care (with limitations) |
| |
| q. | Rural Substance Abuse Transitional Agency Services |
| |
| s. | Home Care Training to Home Care Client |
Referrals: As specified in Section D, Paragraph 10, Scope of Services, EPSDT, the Contractor must provide developmental/behavioral health screenings for members up to 21 years of age in compliance with the AHCCCS periodicity schedule. The Contractor shall ensure the initiation and coordination of behavioral health referrals of these members to the RBHA when determined necessary through the screening process.
The Contractor is responsible for collaborating with RBHAs regarding referrals and follow up activities, as necessary, for other members identified by the AHCCCS Contractor as needing behavioral health evaluation and treatment. Members may also access the RBHA system for evaluation by self-referral or be referred by schools, State agencies or other service providers. The Contractor is responsible for providing transportation to a member’s first RBHA evaluation appointment if a member is unable to provide his/her own transportation. The Contractor will ensure coordination of referrals and follow-up collaboration, as necessary, for members identified by ADHS as needing acute care services.
38
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
Emergency Services: When members present in an emergency room setting, the Contractor is responsible for all emergency medical services including triage, physician assessment and diagnostic tests. The Contractor is responsible for reimbursement of ambulance transportation and/or other medically necessary transportation provided to a member. Refer to ACOM Policy 432. ADHS is responsible for medically necessary professional psychiatric consultations in either emergency room or inpatient settings. ADHS is responsible for reimbursement of ambulance transportation and/or other medically necessary transportation provided to a member who requires behavioral services after medical stabilization.
Reimbursement for court ordered screening and evaluation services is not the responsibility of the Contractor and instead falls to the county pursuant to A.R.S. 36-545. For additional information regarding behavioral health services refer to Title 9 Chapter 22 Articles 2 and 12. It is expected that the Contractor initiate a referral to the T/RBHA for evaluation and behavioral health recipient eligibility as soon as possible after admission.
Co-Morbidities: The Contractor must ensure that members with diabetes who are being discharged from the Arizona State Hospital (AzSH) are issued the same brand and model of both glucometer and supplies they were trained to use while in the facility. Care must be coordinated with the AzSH prior to discharge to ensure that all supplies are authorized and available to the member upon discharge.
In the event that a member’s mental health status renders them incapable or unwilling to manage their medical condition and the member has a skilled medical need, the Contractor must arrange ongoing medically necessary nursing services. The Contractor shall also have a mechanism in place for tracking members for whom ongoing medically necessary services are required.
For enrolled members who are inpatient at the Arizona State Hospital, the Contractor is required to follow ACOM Policy 422 regarding medical care coordination for these members.
Coordination of Care: The Contractor is responsible for ensuring that a medical record is established by the PCP when behavioral health information is received from the RBHA or provider about an assigned member even if the PCP has not yet seen the assigned member. In lieu of actually establishing a medical record, such information may be kept in an appropriately labeled file but must be associated with the member’s medical record as soon as one is established. The Contractor shall require the PCP to respond to RBHA/provider information requests pertaining to ADHS behavioral health recipient members within 10 business days of receiving the request. The response should include all pertinent information, including, but not limited to, current diagnoses, medications, laboratory results, last PCP visit, and recent hospitalizations. The Contractor shall require the PCP to document or initial signifying review of member behavioral health information received from a RBHA behavioral health provider who is also treating the member. For guidance in addressing the needs of members with multi system involvement and complex behavior health and co-occurring conditions, refer to the AHCCCS AMPM Policy, Community Collaborative Care Teams, effective March 2012.
Medication Management Services: The Contractor shall allow PCPs to provide medication management services (prescriptions, medication monitoring visits, laboratory and other diagnostic tests necessary for diagnosis and treatment of behavioral disorders) to members with diagnoses of depression, anxiety and attention deficit hyperactivity disorder. The Contractor shall make available, on the Contractor’s formulary, medications for the treatment of these disorders. AHCCCS has facilitated the development of Clinical tool kits for the treatment of anxiety, depression, and ADHD. These tool kits are a resource only and may not apply to all patients and all clinical situations. They are not intended to replace clinical judgment. The Contractor shall ensure that PCPs and Pediatricians who have an interest or are actively treating members with these disorders are aware of these resources and/or are utilizing other recognized tools/evidence-based guidelines. The Contractor shall develop a monitoring process to ensure that PCPs utilize evidence-based guidelines/recognized clinical tools when prescribing medications to treat depression, anxiety, and ADHD.
39
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
The Contractor may implement step therapy for behavioral health medications used for treating anxiety, depression and ADHD disorders. The Contractor shall provide education and training for providers regarding the concept of step therapy. If the RBHA/behavioral health provider provides documentation to the Contractor that step therapy has already been completed, or is medically contraindicated, the Contractor shall continue to provide the medication at the dosage at which the member has been stabilized, unless there is subsequently a change in medical condition of the member. The Contractor shall monitor PCPs to ensure that they prescribe medication at the dosage at which the member has been stabilized.
The Contractor shall ensure that training and education are available to PCPs regarding behavioral health referral and consultation procedures. The Contractor shall establish policies and procedures for referral and consultation and shall describe them in its provider manual. Policies for referral must include, at a minimum, criteria, processes, responsible parties and minimum requirements no less stringent than those specified in this contract for the forwarding of member medical information.
Transfer of Care: When a PCP has initiated medication management services for a member to treat a behavioral health disorder, and it is subsequently determined by the PCP or Contractor that the member should be transferred to a RBHA prescriber for evaluation and/or continued medication management services, the Contractor will require and ensure that the PCP or Contractor coordinates the transfer of care. All affected subcontracts shall include this provision. The Contractor shall establish policies and procedures for the transition of members who are referred to the RBHA for ongoing treatment. The Contractor shall ensure that PCPs maintain continuity of care for these members. The policies and procedures must address, at a minimum, the following:
| |
| 1. | Guidelines for when a transition of the member to the RBHA for ongoing treatment is indicated. |
| |
| 2. | Protocols for notifying the RBHA of the member’s transfer, including reason for transfer, diagnostic information, and medication history. |
| |
| 3. | Protocols and guidelines for the transfer of medical records, including but not limited to which parts of the medical record are to be copied, timeline for making the medical record available to the RBHA, observance of confidentiality of the member’s medical record, and protocols for responding to RBHA requests for additional medical record information. |
| |
| 4. | Protocols for transition of prescription services, including but not limited to notification to the RBHA of the member’s current medications and timeframes for dispensing and refilling medications during the transition period. This coordination must ensure at a minimum, that the member does not run out of prescribed medications prior to the first appointment with a RBHA prescriber and that all relevant member pertinent medical information as outlined above and including the reason for transfer is forwarded to the receiving RBHA prescriber prior to the member’s first scheduled appointment with the RBHA prescriber. |
| |
| 5. | Contractor activities to monitor to ensure that members are appropriately transitioned to the RBHA for care. |
The Contractor shall ensure that its quality management program incorporates monitoring of the PCP’s management of behavioral health disorders and referral to, coordination of care with and transfer of care to RBHA providers as required under this contract.
| |
| 15. | AHCCCS GUIDELINES, POLICIES AND MANUALS |
All AHCCCS guidelines, policies and manuals are hereby incorporated by reference into this contract. All guidelines, policies and manuals are available on the AHCCCS website, located at www,azahcccs.gov. The Contractor is responsible for complying with the requirements set forth within. In addition, linkages to AHCCCS Rules (Arizona Administrative Code), Statutes and other resources are also available to all interested parties through the AHCCCS website. Upon adoption by AHCCCS, updates will be made available to the Contractor. The Contractor shall be responsible for implementing these requirements and maintaining current copies of updates.
40
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
| |
| 16. | MEDICAID SCHOOL BASED CLAIMING PROGRAM (MSB) |
Pursuant to an Intergovernmental Agreement with the Department of Education, and a contract with a Third Party Administrator, AHCCCS pays participating school districts for specifically identified Medicaid services when provided to Medicaid eligible children who are included under the Individuals with Disabilities Education Act (IDEA). The Medicaid services must be identified in the member’s Individual Education Plan (IEP) as medically necessary for the child to obtain a public school education.
MSB services are provided in a school setting or other approved setting specifically to allow children to receive a public school education. They do not replace medically necessary services provided outside the school setting or other MSB approved alternative setting. Currently, services include audiology, therapies (OT, PT and speech/language); behavioral health evaluation and counseling; nursing and attendant care (health aid services provided in the classroom); and specialized transportation to and from school on days when the child receives an AHCCCS-covered MSB service.
The Contractor’s evaluations and determinations of medical necessity shall be made independent of the fact that the child is receiving MSB services. If a request is made for services that also are covered under the MSB program for a child enrolled with the Contractor, the request shall be evaluated on the same basis as any request for a covered service.
The Contractor and its providers should coordinate with schools and school districts that provide MSB services to the Contractor’s enrolled members. Services should not be duplicative. Contractor case managers, working with special needs children, should coordinate with the appropriate school staff working with these members. Transfer of member medical information and progress toward treatment goals between the Contractor and the member’s school or school district is required as appropriate and should be used to enhance the services provided to members.
41
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
| |
| 17. | PEDIATRIC IMMUNIZATIONS AND THE VACCINES FOR CHILDREN PROGRAM |
Through the Vaccines for Children Program, the Federal and State governments purchase, and make available to providers free of charge, vaccines for AHCCCS children under age 19. The Contractor shall not utilize AHCCCS funding to purchase vaccines for members under the age of 19. If vaccines are not available through the VFC Program, the Contractor shall contact the AHCCCS Division of Health Care Management, Clinical Quality Management Unit for guidance. Any provider, licensed by the State to administer immunizations, may register with ADHS as a "VFC provider" and receive free vaccines. The Contractor shall not reimburse providers for the administration of the vaccines in excess of the maximum allowable as set by CMS, found in the AHCCCS fee schedule. The Contractor shall comply with all VFC requirements and monitor its providers to ensure that, a physician when acting as primary care physician (PCP) to members under the age of 19 is registered with ADHS/VFC.
In some GSAs, providers may choose not to provide vaccinations due to low numbers of children in their panels, etc. The Contractor must develop processes to ensure that vaccinations are available through a VFC enrolled provider or through the county Health Department. In all instances, the antigens are to be provided through the VFC program. The Contractor must develop processes to pay the administration fee to whoever administers the vaccine regardless of their contract status with the Contractor.
Arizona State law requires the reporting of all immunizations given to children under the age of 19. Immunizations must be reported at least monthly to the ADHS. Reported immunizations are held in a central database known as ASIIS (Arizona State Immunization Information System), which can be accessed by providers to obtain complete, accurate immunization records. Software is available from ADHS to assist providers in meeting this reporting requirement. The Contractor must educate its provider network about these reporting requirements and the use of this resource and monitor to ensure compliance.
| |
| 18. | STAFF REQUIREMENTS AND SUPPORT SERVICES |
The Contractor shall have in place the organizational, operational, managerial and administrative systems capable of fulfilling all contract requirements. For the purposes of this contract, the Contractor shall not employ or contract with any individual who has been debarred, suspended or otherwise lawfully prohibited from participating in any public procurement activity or from participating in non-procurement activities under regulations issued under Executive Order No. 12549 or under guidelines implementing Executive Order 12549 [42 CFR 438.610 (a) & (b), 42 CFR §1001.1901(b), 42 CFR §1003.102(a)(2)]. The Contractor is obligated to screen all employees and Contractors to determine whether any of them have been excluded from participation in Federal health care programs. You can search the HHS-OIG website by the names of any individuals. The database can be accessed at http://www.oig.hhs.gov/fraud/exclusions.asp.
The Contractor is responsible for maintaining a significant local (within the State of Arizona) presence. This presence includes staff designated below with an asterisk (*). All staff or functions designated with an asterisk must be located within the State of Arizona at all times throughout the term of the contract. The Contractor must obtain approval from AHCCCS prior to moving any functions not designated with an asterisk outside the State of Arizona after contract initiation. Such a request for approval must be submitted to the Division of Health Care Management at least 60 days prior to the proposed change in operations and must include a description of the processes in place that assure rapid responsiveness to effect changes for contract compliance. The Contractor shall be responsible for any additional costs associated with on-site audits or other oversight activities of required functions located outside of the State of Arizona. At the beginning of each contract year the Contractor must provide, to the Division of Health Care Management, a listing of all functions and their locations.
42
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
The Contractor must employ sufficient staffing and utilize appropriate resources to achieve contractual compliance. The Contractor’s resource allocation must be adequate to achieve outcomes in all functional areas within the organization. Adequacy will be evaluated based on outcomes and compliance with contractual and AHCCCS policy requirements, including the requirement for providing culturally competent services. If the Contractor does not achieve the desired outcomes or maintain compliance with contractual obligations, additional monitoring and regulatory action may be employed by AHCCCS, including but not limited to, requiring the Contractor to hire additional staff and actions specified in Section D, Paragraph 72, Sanctions, of the contract.
The Contractor shall have local staff available 24 hours a day, seven days a week to work with AHCCCS and/or other State agencies (for example ADHS Licensure) on urgent issue resolutions, such as in the case of an Immediate Jeopardy (IJ), fires, or other public emergency situations. These staff person(s) shall have access to information necessary to identify members who may be at risk, their current health/service status, ability to initiate new placements/services, and to be available to perform status checks at affected facilities and potentially ongoing monitoring, if necessary. The Contractor shall supply AHCCCS CQM with the contact information for these staff persons, such as a telephone number, to call in these urgent situations.
An individual staff member shall be limited to occupying a maximum of two of the Key Staff positions listed below. The Contractor shall inform AHCCCS, Division of Health Care Management, in writing within seven days, when an employee leaves one of the Key Staff positions listed below (this requirement does not apply to Additional Required Staff, also listed below). The name of the interim contact person should be included with the notification. The name and resume of the permanent employee should be submitted as soon as the new hire has taken place. Each year on October 15th, the Contractor must provide the name, Social Security Number and date of birth of the staff members performing the duties of the Key Staff listed as a, b and c below, to the Office of the Inspector General (OIG). AHCCCS will compare this information against Federal databases to confirm that those individuals have not been banned or debarred from participating in Federal programs [42 CFR 455.104]. At a minimum, the following staff is required Key Staff:
| |
| a. | *Administrator/CEO/COO or their designee must be available during working hours to fulfill the responsibilities of the position and to oversee the entire operation of the Contractor. The Administrator shall devote sufficient time to the Contractor’s operations to ensure adherence to program requirements and timely responses to AHCCCS. |
| |
| b. | *Medical Director/CMO who is an Arizona-licensed physician. The Medical Director shall be actively involved in all-major clinical programs and QM and MM components of the Contractor. The Medical Director shall devote sufficient time to the Contractor’s operations to ensure timely medical decisions, including after-hours consultation as needed. |
| |
| c. | Chief Financial Officer/CFO who is available, full time, to fulfill the responsibilities of the position and to oversee the budget, accounting systems, and financial reporting implemented by the Contractor. |
| |
| d. | Pharmacy Director/Coordinator who is an Arizona licensed pharmacist or physician who oversees and administers the prescription drug and pharmacy benefits. The Pharmacy Coordinator/Director may be an employee or Contractor of the Plan. |
| |
| e. | Dental Director/Coordinator that is responsible for coordinating dental activities of the Contractor and providing required communication between the Contractor and AHCCCS. The Dental Director/Coordinator may be an employee or Contractor of the plan and must be a licensed dentist in Arizona if they are required to review or deny dental services. |
| |
| f. | *Compliance Officer who will implement and oversee the Contractor’s compliance program. The compliance officer shall be a management official, available to all employees, with designated and recognized authority to access records and make independent referrals to the AHCCCS Office of the Inspector General. See Section D, Paragraph 62, Corporate Compliance. |
43
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
| |
| g. | *Dispute and Appeal Manager who will manage and adjudicate member and provider disputes arising under the Grievance System including member grievances, appeals, and requests for hearing and provider claim disputes. |
| |
| h. | Business Continuity Planning Coordinator as noted in the ACOM Policy 104. |
| |
| i. | *Contract Compliance Officer who will serve as the primary point-of-contact for all Contractor operational issues. |
The primary functions of the Contract Compliance Officer may include but are not limited to:
| |
| ▪ | Coordinate the tracking and submission of all contract deliverables |
| |
| ▪ | Field and coordinate responses to AHCCCS inquiries |
| |
| ▪ | Coordinate the preparation and execution of contract requirements such as OFRS, random and periodic audits and ad hoc visits |
| |
| j. | *Quality Management Coordinator who is an Arizona-licensed registered nurse, physician or physician's assistant or a Certified Professional in Healthcare Quality (CPHQ) by the National Association for Health Care Quality (NAHQ) and/or Certified in Health Care Quality and Management (CHCQM) by the American Board of Quality Assurance and Utilization Review Providers. The QM Coordinator must have experience in quality management and quality improvement. |
The primary functions of the Quality Management Coordinator position are:
| |
| ▪ | Ensure individual and systemic quality of care |
| |
| ▪ | Integrate quality throughout the organization |
| |
| ▪ | Implement process improvement |
| |
| ▪ | Resolve, track and trend quality of care grievances |
| |
| ▪ | Ensure a credentialed provider network |
| |
| k. | Performance/Quality Improvement Coordinator who has a minimum qualification as a CPHQ or CHCQM or comparable education and experience in data and outcomes measurement. |
The primary functions of the Performance/Quality Improvement Coordinator are:
| |
| ▪ | Focus organizational efforts on improving clinical quality performance measures |
| |
| ▪ | Develop and implement performance improvement projects |
| |
| ▪ | Utilize data to develop intervention strategies to improve outcomes |
| |
| ▪ | Report quality improvement/performance outcomes |
| |
| l. | *Maternal Health/EPSDT (child health) Coordinator who is an Arizona licensed nurse, physician or physician's assistant; or have a Master's degree in health services, public health, health care administration or other related field, and/or a CPHQ or CHCQM. Staffing under this position should be sufficient to meet quality and performance measure goals. |
The primary functions of the MCH/EPSDT Coordinator are:
| |
| ▪ | Ensuring receipt of EPSDT services |
| |
| ▪ | Ensuring receipt of maternal and postpartum care |
| |
| ▪ | Promoting family planning services |
| |
| ▪ | Promoting preventive health strategies |
| |
| ▪ | Identification and coordination assistance for identified member needs |
| |
| ▪ | Interface with community partners |
| |
| m. | *Medical Management Coordinator who is an Arizona licensed registered nurse, physician or physician’s assistant if required to make medical necessity determinations; or have a Master’s degree in health services, health care administration, or business administration if not required to make medical necessity determination, who manages all required Medicaid management requirements under AHCCCS policies, Rules, and contract. |
The primary functions of the Medical Management Coordinator are:
| |
| ▪ | Ensure adoption and consistent application of appropriate inpatient and outpatient medical necessity criteria |
| |
| ▪ | Ensure appropriate concurrent review and discharge planning of inpatient stays is conducted |
| |
| ▪ | Develop, implement and monitor the provision of care coordination, disease management and case management functions |
44
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
| |
| ▪ | Monitor, analyze and implement appropriate interventions based on utilization data, including identifying and correcting over or under utilization of services |
| |
| ▪ | Monitor prior authorization functions and assure that decisions are made in a consistent manner based on clinical criteria and meet timeliness standards. |
45
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
| |
| n. | *Behavioral Health Coordinator who shall be a behavioral health professional as described in Health Services Rule R9-20. The Behavioral Health Coordinator shall devote sufficient time to ensure that the Contractor’s behavioral health referral and coordination activities are implemented per AHCCCS requirements. |
The primary functions of the Behavioral Health Coordinator are:
| |
| ▪ | Coordinate member behavioral care needs with the RBHA system |
| |
| ▪ | Develop processes to coordinate behavioral health care between PCPs and RBHAs |
| |
| ▪ | Participate in the identification of best practices for behavioral health in a primary care setting |
| |
| ▪ | Coordinate behavioral care with medically necessary services |
| |
| o. | Member Services Manager who shall coordinate communications with members; serve in the role of member advocate; coordinate issues with appropriate areas within the organization; resolve member inquiries/problems and meet standards for resolution, telephone abandonment rates and telephone hold times. |
| |
| p. | *Provider Services Manager and staff to coordinate communications between the Contractor and its subcontractors. There shall be sufficient Provider Services staff to enable providers to receive prompt resolution to their problems or inquiries and appropriate education about participation in the AHCCCS program and maintain a sufficient provider network. |
| |
| q. | Claims Administrator to develop, implement and administer a comprehensive claims processing system capable of paying claims in accordance with state and Federal requirements. |
The primary functions of the Claims Administrator are:
| |
| ▪ | Develop and implement claims processing systems capable of paying claims in accordance with state and Federal requirements |
| |
| ▪ | Develop processes for cost avoidance |
| |
| ▪ | Ensure minimization of claims recoupments |
| |
| ▪ | Meet claims processing timelines |
| |
| ▪ | Meet AHCCCS encounter reporting requirements |
| |
| r. | *Provider Claims Educator (full-time equivalent employee for a Contractor with over 100,000 members) The position is fully integrated with the Contractor’s grievance, claims processing, and provider relations systems and facilitates the exchange of information between these systems and providers |
The primary functions of the Provider Claims Educator are:
| |
| ▪ | Educate contracted and non-contracted providers (i.e.: professional and institutional) regarding appropriate claims submission requirements, coding updates, electronic claims transactions and electronic fund transfer, and available Contractor resources such as provider manuals, website, fee schedules, etc. |
| |
| ▪ | Interfaces with the Contractor’s call center to compile, analyze, and disseminate information from provider calls |
| |
| ▪ | Identifies trends and guides the development and implementation of strategies to improve provider satisfaction |
| |
| ▪ | Frequently communicates (i.e.: telephonic and on-site) with providers to assure the effective exchange of information and gain feedback regarding the extent to which providers are informed about appropriate claims submission practices |
Additional Required Staff
| |
| s. | Prior Authorization staff to authorize health care 24 hours per day, seven days per week. This staff shall include an Arizona-licensed nurse, physician or physician's assistant. The staff will work under the direction of an Arizona-licensed registered nurse, physician, or physician’s assistant. |
| |
| t. | *Concurrent Review staff to conduct inpatient concurrent review. This staff shall consist of an Arizona-licensed nurse, physician, or physician's assistant. The staff will work under the direction of an Arizona-licensed registered nurse, physician, or physician’s assistant. |
| |
| u. | *Clerical and Support staff to ensure proper functioning of the Contractor's operation. |
| |
| v. | Member Services staff there shall be sufficient Member Service staff to enable members to receive prompt resolution of their inquiries/problems. |
46
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
| |
| w. | *Provider Services staff There shall be sufficient Provider Services staff to enable providers to receive prompt responses and assistance (See Section D, Paragraph 29, Network Management, for more information). |
| |
| x. | Claims Processing staff there shall be sufficient, appropriately trained, Claim Processing staff to ensure the timely and accurate processing of original claims, resubmissions and overall adjudication of claims. |
| |
| y. | Encounter Processing staff there shall be sufficient, appropriately trained, Encounter Processing staff to ensure the timely and accurate processing and submission to AHCCCS of encounter data and reports. |
The Contractor must submit to the Division of Health Care Management the following items annually by October 15:
| |
| 1. | An organization chart complete with the “key staff” positions. The chart must include the person’s name, title and telephone number and portion of time allocated to each Medicaid contract and other lines of business. |
| |
| 2. | A functional organization chart of the key program areas, responsibilities and the areas which report to that position. |
| |
| 3. | A listing of all functions and their locations; and a list of any functions that have moved outside of the State of Arizona in the past contract year. |
Staff Training and Meeting Attendance
The Contractor shall ensure that all staff members have appropriate training, education, experience and orientation to fulfill the requirements of the position. AHCCCS may require additional staffing for a Contractor that has substantially failed to maintain compliance with any provision of this contract and/or AHCCCS policies.
The Contractor must provide initial and ongoing staff training that includes an overview of AHCCCS; AHCCCS Policy and Procedure Manuals; contract requirements and State and Federal requirements specific to individual job functions. The Contractor shall ensure that all staff members having contact with members or providers receive initial and ongoing training with regard to the appropriate identification and handling of quality of care/service concerns.
New and existing transportation, prior authorization and member services representatives must be trained in the geography of any/all GSA(s) in which the Contractor holds a contract and have access to mapping search engines (e.g. MapQuest, Yahoo Maps, Google Maps, etc) for the purposes of authorizing services in; recommending providers in; and transporting members to, the most geographically appropriate location.
The Contractor shall provide the appropriate staff representation for attendance and participation in meetings and/or events scheduled by AHCCCS. All meetings shall be considered mandatory unless otherwise indicated.
| |
| 19. | WRITTEN POLICIES, PROCEDURES AND JOB DESCRIPTIONS |
The Contractor shall develop and maintain written policies, procedures and job descriptions for each functional area of its plan, consistent in format and style. The Contractor shall maintain written guidelines for developing, reviewing and approving all policies, procedures and job descriptions. All policies and procedures shall be reviewed at least bi-annually to ensure that the Contractor's written policies reflect current practices. Reviewed policies shall be dated and signed by the Contractor's appropriate manager, coordinator, director or administrator. Minutes reflecting the review and approval of the policies by an appropriate committee are also acceptable documentation. All medical and quality management policies must be approved and signed by the Contractor's Medical Director. Job descriptions shall be reviewed at least bi-annually to ensure that current duties performed by the employee reflect written requirements.
47
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
Based on provider or member feedback, if AHCCCS deems a Contractor policy or process to be inefficient and/or place unnecessary burden on the members or providers, the Contractor will be required to work with AHCCCS to change the policy or procedure within a time period specified by AHCCCS.
The Contractor shall be accessible by phone for general member information during normal business hours. All enrolled members will have access to a toll free phone number. All informational materials, prepared by the Contractor, shall be approved by AHCCCS prior to distribution to members. The reading level and name of the evaluation methodology used should be included. The Contractor should refer to the ACOM Policy 404 for further information and requirements.
All materials shall be translated when the Contractor is aware that a language is spoken by 3,000 or 10%, whichever is less, of the Contractor’s members, who also have limited English proficiency (LEP).
All vital materials shall be translated when the Contractor is aware that a language is spoken by 1,000 or 5%, whichever is less, of the Contractor’s members, who also have LEP. Vital materials must include, at a minimum, Notices of Action, vital information from the Member Handbooks and consent forms.
All written notices informing members of their right to interpretation and translation services in a language shall be translated when the Contractor is aware that 1,000 or 5%, whichever is less, of the Contractor’s members speak that language and have LEP [42 CFR 438.10(c)(3)].
Oral interpretation services must be available and free of charge to all members regardless of the prevalence of the language. The Contractor must notify all members of their right to access oral interpretation services and how to access them. Refer to the ACOM Policy 404 [42 CFR 438.10(c)(4) and (5)].
The Contractor shall make every effort to ensure that all information prepared for distribution to members is written using an easily understood language and format and as further described in the AHCCCS Policy 404. Regardless of the format chosen by the Contractor, the member information must be printed in a type, style and size, which can easily be read by members with varying degrees of visual impairment. The Contractor must notify its members that alternative formats are available and how to access them [42 CFR 438.10(d)].
When there are program changes, notification shall be provided to the affected members at least 30 days before implementation.
| |
| I. | The Contractor shall produce and provide the following printed information to each member/representative or household within 12 business days of receipt of notification of the enrollment date [42 CFR 438.10(f)(3)]. The Contractor may provide the information in written format or via written notification that the Member Handbook information is available on the Contractor’s website per ACOM Policy 404 as applicable. |
| |
| II. | A Member Handbook which, at a minimum, shall include the items listed in the ACOM Policy 404. |
The Contractor shall review and update the Member Handbook at least once a year. The handbook must be submitted to AHCCCS, Division of Health Care Management for approval within four weeks of receiving the annual renewal amendment and upon any changes prior to distribution.
| |
| III. | A description of the Contractor’s provider network, which at a minimum, includes those items listed in the ACOM Policy 404. The Contractor may provide a description of the provider network in written format or via written notification that the information is available on the Contractor’s website per ACOM Policy 404 as applicable. |
48
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
The Contractor must give written notice about termination of a contracted provider, within 15 days after receipt or issuance of the termination notice, to each member who received their primary care from, or is seen on a regular basis by, the terminated provider. Affected members must be informed of any other changes in the network 30 days prior to the implementation date of the change [42 CFR 438.10(f)(4) and (5)]. The Contractor shall have information available for potential enrollees as described in the ACOM Policy 404.
The Contractor must develop and distribute, at a minimum, semi-annual newsletters during the contract year. The following types of information are to be contained in the newsletter at least annually:
| |
| • | Educational information on chronic illnesses and ways to self-manage care |
| |
| • | Reminders of flu shots and other prevention measures at appropriate times |
| |
| • | Cultural Competency, other than translation services |
| |
| • | Contractor specific issues (in each newsletter) |
| |
| • | Tobacco cessation information |
| |
| • | HIV/AIDS testing for pregnant women |
| |
| • | Other information as required by AHCCCS |
The Contractor shall ensure compliance with any applicable Federal and State laws that pertain to member rights and ensure that its staff and subcontractors take those rights into account when furnishing services to members.
The Contractor shall ensure that each member is guaranteed the right to request and receive one copy of the member’s medical record at no cost to the member and to request that the record be amended or corrected, as specified in 45 CFR Part 164.
The Contractor shall ensure that each member is free to exercise their rights and that the exercise of those rights does not adversely affect the way the Contractor or its subcontractors treat the member [42 CFR 438.100(c)]
The Contractor will, on an annual basis, inform all members of their right to request the following information [42 CFR 438.10(f)(6) and 42 CFR 438.100(a)(1) and (2)]:
| |
| a. | An updated Member Handbook at no cost to the member |
| |
| b. | The network description as described in the ACOM Policy 404 |
This information may be sent in a separate written communication or included with other written information such as in a member newsletter.
The Contractor may be required to perform its own annual general or focused member survey. All such Contractor surveys, along with a timeline for the project, shall be approved in advance by AHCCCS. The results and the analysis of the results shall be submitted to the AHCCCS, Division of Health Care Management, DHCM Operations Unit within 45 days of the completion of the project. AHCCCS may require inclusion of certain questions.
For non-AHCCCS required surveys, the Contractor shall provide AHCCCS notification 15 days prior to conducting any Contractor initiated member or provider survey. The notification must include a project scope statement, project timeline and a copy of the survey. The results and the analysis of the results of any Contractor initiated surveys shall be submitted to the DHCM Operations Unit within 45 days of the completion of the project.
49
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
AHCCCS may periodically conduct surveys of a representative sample of the Contractor's membership and providers. AHCCCS will consider suggestions from the Contractor for questions to be included in each survey. The results of these surveys, conducted by AHCCCS, will become public information and available to all interested parties on the AHCCCS website. The draft reports from the surveys will be shared with the Contractor prior to finalization. The Contractor will be responsible for reimbursing AHCCCS for the cost of these survey based on its share of AHCCCS enrollment.
At least quarterly, the Contractor is required to survey a sample of its membership that have received services to verify that services the Contractor paid for were delivered as outlined in the ACOM Policy 424 [42 CFR 455.20].
The Contractor shall have a Cultural Competency Plan which meets the requirements of the ACOM Policy 405. An annual assessment of the effectiveness of the plan, along with any modifications to the plan, must be submitted to the Division of Health Care Management, no later than 45 days after the start of each contract year. This plan should address all services and settings [42 CFR 438.206(c)(2)].
The Contractor shall ensure compliance with the Cultural Competency Plan and all requirements pertaining to Limited English Proficiency.
The member's medical record is the property of the provider who generates the record. Medical records include those maintained by PCPs or other providers as well as but not limited to those kept in placement settings such as nursing facilities, assisted living facilities and other home and community based providers. Each member is entitled to one copy of his or her medical record free of charge annually. The Contractor shall have written policies and procedures to maintain the confidentiality of all medical records.
The Contractor is responsible for ensuring that a medical record is established when information is received about a member. If the PCP has not yet seen the member, such information may be kept temporarily in an appropriately labeled file, in lieu of establishing a medical record, but must be associated with the member’s medical record as soon as one is established.
The Contractor shall have written policies and procedures for the maintenance of medical records so that those records are documented accurately and in a timely manner, are readily accessible, and permit prompt and systematic retrieval of information.
The Contractor shall have written standards for documentation on the medical record for legibility, accuracy and plan of care, which comply with the AMPM.
The Contractor shall have written plans for providing training and evaluating providers' compliance with the Contractor's medical records standards. Medical records shall be maintained in a detailed and comprehensive manner, which conforms to good professional medical practice, permits effective professional medical review and medical audit processes, and which facilitates an adequate system for follow‑up treatment. Medical records must be legible, signed and dated.
When a member changes PCPs, his or her medical records or copies of medical records must be forwarded to the new PCP within 10 business days from receipt of the request for transfer of the medical records.
50
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
AHCCCS is not required to obtain written approval from a member, before requesting the member's medical record from the PCP or any other agency. The Contractor may obtain a copy of a member's medical records without written approval of the member, if the reason for such request is directly related to the administration of the AHCCCS program. AHCCCS shall be afforded access to all members' medical records whether electronic or paper within 20 business days of receipt of request.
Information related to fraud and abuse may be released so long as protected HIV-related information is not disclosed (A.R.S. §36-664(I)).
The Contractor shall maintain policies and procedures addressing advanced directives for adult members that specify [42 CFR 422.128]:
| |
| 1. | Each contract or agreement with a hospital, nursing facility, home health agency, hospice or organization responsible for providing personal care, must comply with Federal and State law regarding advance directives for adult members [42 CFR 438.6(i)(1)]. Requirements include: |
| |
| a) | Maintaining written policies that address the rights of adult members to make decisions about medical care, including the right to accept or refuse medical care, and the right to execute an advance directive. If the agency/organization has a conscientious objection to carrying out an advance directive, it must be explained in policies. (A health care provider is not prohibited from making such objection when made pursuant to A.R.S. § 36-3205.C.1.) |
| |
| b) | Provide written information to adult members regarding an individual’s rights under State law to make decisions regarding medical care, and the health care provider's written policies concerning advance directives (including any conscientious objections) [42 CFR 438.6(i)(3)]. |
| |
| c) | Documenting in the member’s medical record whether or not the adult member has been provided the information and whether an advance directive has been executed. |
| |
| d) | Not discriminating against a member because of his or her decision to execute or not execute an advance directive, and not making it a condition for the provision of care. |
| |
| e) | Providing education to staff on issues concerning advance directives including notification of direct care providers of services, such as home health care and personal care, of any advanced directives executed by members to whom they are assigned to provide services. |
| |
| 2. | Contractors shall require subcontracted PCPs, which have agreements with the entities described in paragraph 1 above, to comply with the requirements of subparagraphs 1 (a) through (e) above. Contractors shall also encourage health care providers specified in subparagraph a. to provide a copy of the member’s executed advanced directive, or documentation of refusal, to the member’s PCP for inclusion in the member’s medical record. |
| |
| 3. | The Contractor shall provide written information to adult members that describe the following: |
| |
| a) | A member’s rights under State law, including a description of the applicable State law. |
| |
| b) | The organization’s policies respecting the implementation of those rights, including a statement of any limitation regarding the implementation of advance directives as a matter of conscience. |
| |
| c) | The member’s right to file complaints directly with AHCCCS. |
| |
| d) | Changes to State law as soon as possible, but no later than 90 days after the effective date of the change [42 CFR 438.6(i)(4)]. |
51
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
| |
| 25. | QUALITY MANAGEMENT (QM) |
The Contractor shall provide quality medical care and services to members, regardless of payer source or eligibility category. The Contractor shall promote improvement in the quality of care provided to enrolled members through established quality management and performance improvement processes. The Contractor shall execute processes to assess, plan, implement, evaluate, and as mandated report, quality management and performance improvement activities, as specified in the AMPM [42 CFR 438.240(a)(1) and (e)(2) and CFR 42 447.26]].
The Contractor must ensure that the Quality Management/Quality Improvement Unit within the organizational structure is separate and distinct from any other units or departments such as Medical Management. Contractors are expected to integrate quality management processes, such as tracking and trending of issues through all areas of the organization, with ultimate responsibility for quality management/quality improvement residing within the Quality Management Unit.
The Contractor quality assessment and performance improvement programs, at a minimum, shall comply with the requirements outlined in the AMPM and this Paragraph. In addition, 42 CFR 447.26 prohibits payment for Provider-Preventable Conditions that meet the definition of a Health Care-Acquired Condition (HCAC) or an Other Provider –Preventable Condition (OPPC) (refer to AMPM Chapter 900 requirements). If an HCAC or OPPC is identified, the Contractor must report the occurrence to AHCCCS and conduct a quality of care investigation.
A. Quality Management Program:
The Contractor shall have an ongoing quality management program for the services it furnishes to members that includes the requirements listed in AMPM Chapter 900 and the following:
| |
| 1. | A written Quality Assessment and Performance Improvement (QA/PI) plan, an evaluation of the previous year’s QA/PI program, and Quality Management Quarterly reports that address its strategies for performance improvement and conducting the quality management activities. |
| |
| 2. | QM/PI Program monitoring and evaluation activities that includes Peer Review and Quality Management Committees chaired by the Contractor’s Chief Medical Officer. |
| |
| 3. | Protection of medical records and any other personal health and enrollment information that identifies a particular member or subset of members in accordance with Federal and State privacy requirements. |
| |
| 4. | Member rights and responsibilities. |
| |
| 5. | Uniform provisional credentialing, initial credentialing, re-credentialing and organizational credential verification [42 CFR 438.206(b)(6)]. The Contractor shall demonstrate that its providers are credentialed and reviewed through the Contractor’s Credentialing Committee that is chaired by the Contractor’s Medical Director [42 CFR 438.214]. The Contractor should refer to the AMPM and Attachment F, Periodic Report Requirements, for reporting requirements. The process: |
| |
| a. | Shall follow a documented process for provisional credentialing, initial credentialing, re-credentialing and organizational credential verification of providers who have signed contracts or participation agreements with the Contractor; |
| |
| b. | Shall not discriminate against particular providers that serve high-risk populations or specialize in conditions that require costly treatment; |
| |
| c. | Shall not employ or contract with providers excluded from participation in Federal health care programs. |
| |
| 6. | Tracking and trending of member and provider issues, which includes investigation and analysis of quality of care issues, abuse, neglect and unexpected deaths. The resolution process must include: |
| |
| a. | Acknowledgement letter to the originator of the concern; |
| |
| b. | Documentation of all steps utilized during the investigation and resolution process; |
| |
| c. | Follow-up with the member to assist in ensuring immediate health care needs are met; |
52
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
| |
| d. | Closure/resolution letter that provides sufficient detail to ensure that the member has an understanding of the resolution of their issue, any responsibilities they have in ensuring all covered, medically necessary care needs are met, and a Contractor contact name/telephone number to call for assistance or to express any unresolved concerns; |
| |
| e. | Documentation of implemented corrective action plan(s) or action(s) taken to resolve the concern; |
| |
| f. | Analysis of the effectiveness of the interventions taken. |
| |
| 7. | Mechanisms to assess the quality and appropriateness of care furnished to members with special health care needs. |
| |
| 8. | Participation in community initiatives including applicable activities of the Medicare Quality Improvement Organization (QIO). |
| |
| 9. | Performance improvement programs including performance measures and performance improvement projects. |
B. Performance Improvement:
The Contractor’s quality management program shall be designed to achieve, through ongoing measurements and intervention, significant improvement, sustained over time, in the areas of clinical care and non-clinical care that are expected to have a favorable effect on health outcomes and member satisfaction. The Contractor must [42 CFR 438.240(b)(2) and (c)]:
| |
| 1. | Measure and report to the State its performance, using standard measures required by the State, or as required by CMS; |
| |
| 2. | Submit to the State data specified by the State, that enables the State to measure the Contractor’s performance; or |
| |
| 3. | Perform a combination of the activities. |
I. Performance Measures:
The Contractor shall comply with AHCCCS quality management requirements to improve performance for all AHCCCS established performance measures. Complete descriptions of the AHCCCS clinical quality Performance Measure can be found in the most recently published reports of acute care performance measures located on the AHCCCS website except the performance measure titled “EPSDT Participation”. AHCCCS bases the measurement of EPSDT Participation on the methodology established in CMS “Form 416” which can be found on the AHCCCS website at:
http://www.azahcccs.gov/reporting/quality/performancemeasures.aspx.
Contractors must comply with national performance measures and levels that may be identified and developed by the Centers for Medicare and Medicaid Services in consultation with AHCCCS and/or other relevant stakeholders. CMS has been working in partnership with states in developing core performance measures for Medicaid and CHIP programs. The current AHCCCS-established performance measures may be subject to change when these core measures are finalized and implemented.
AHCCCS intends to implement a hybrid methodology for collecting and reporting Performance Measure rates, as allowed by NCQA, for selected HEDIS measures. Contractors shall collect data from medical records and provide these data with supporting documentation, as instructed by AHCCCS, for each hybrid measure as requested. The number of records that each Contractor will be required to collect will be based on HEDIS sampling guidelines and may be affected by the Contractor’s previous rate for the measure being collected. AHCCCS may begin implementation of the hybrid methodology with the following measures: Adolescent Immunizations and Timeliness of Prenatal Care. AHCCCS may implement hybrid methodology for collecting and reporting additional measures in future contract years.
53
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
The Contractor must have in place a process for internal monitoring of Performance Measure rates, using a standard methodology established or adopted by AHCCCS, for each required Performance Measure. The Contractor’s Quality Assessment/Performance Improvement Program will report its performance on an ongoing basis to its Administration. It also will report this Performance Measure data to AHCCCS in conjunction with its Quarterly EPSDT Improvement and Adult Quarterly Monitoring Report.
The Contractor must meet AHCCCS stated Minimum Performance Standards for each population/eligibility category for which AHCCCS reports results. However, it is equally important that the Contractor continually improve performance measure outcomes from year to year. The Contractor shall strive to meet the goal established by AHCCCS.
Minimum Performance Standard – A Minimum Performance Standard (MPS) is the minimal expected level of performance by the Contractor. If a Contractor does not achieve this standard, the Contractor will be required to submit a corrective action plan and may be subject to a sanction of up to $100,000 dollars for each deficient measure.
Goal – If the Contractor has already met or exceeded the AHCCCS Minimum Performance Standard for any measure, the Contractor must strive to meet the established Goal for the measure(s). However, it is equally important that the Contractor continually improve performance measure outcomes from year to year.
A Contractor must show demonstrable and sustained improvement toward meeting AHCCCS Performance Standards. AHCCCS may impose sanctions on Contractors that do not show statistically significant improvement in a measure rate and require the Contractor to demonstrate that they are allocating increased administrative resources to improving rates for a particular measure or service area. AHCCCS also may require a corrective action plan and may sanction any Contractor that shows a statistically significant decrease in its rate, even if it meets or exceeds the Minimum Performance Standard.
An evidence-based corrective action plan must be received by AHCCCS within 30 days of receipt of notification of the deficiency from AHCCCS. This plan must be approved by AHCCCS prior to implementation. AHCCCS may conduct one or more follow-up on-site reviews to verify compliance with a corrective action plan.
All Performance Measures apply to all member populations [42 CFR 438.240(a)(2), (b)(2) and (c)]. AHCCCS may analyze and report results by line of business, by GSA or county, and/or applicable demographic factors.
AHCCCS has established standards for the measures listed below.
54
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
The following table identifies the Minimum Performance Standards (MPS) and Goals for each measure:
Acute Care Contractor Performance Standards
|
| | | |
| | | | |
| Performance Measure | Minimum Performance Standard | Goal (Healthy People Goals) | |
| Immunization of Two-year-olds | | | |
| 4:3:1:3:3:1 Series | 74% | 80% | |
| 4:3:1:3:3:1:4 Series | 68% | 80% | |
| Tdap- 4 doses | 85% | 90% | |
| Polio - 3 doses (*) | 90% | 90% | |
| MMR - 1 dose (*) | 90% | 90% | |
| Hib - 3 doses (*) | 86% | 90% | |
| HBV - 3 doses (*) | 90% | 90% | |
| Varicella - 1 dose (*) | 86% | 90% | |
| PCV – 4 doses (*) | 82% | 90% | |
| Adolescent Immunizations(1) | 54% | 90% | |
| Children’s Dental Visits 2 to 21 Years | 57% | 57% | |
| Well-child Visits 15 Months | 65% | 90% | |
| Well-child Visits 3 - 6 Years | 66% | 80% | |
| Adolescent Well-care Visits | 42% | 50% | |
| Children's Access to PCPs 12-24 Months | 93% | 97% | |
| Children's Access to PCPs 25 months-6 Years | 83% | 97% | |
| Children's Access to PCPs 7-11 Years | 83% | 97% | |
| Children's Access to PCPs 12-19 Years | 81% | 97% | |
| Timeliness of Prenatal Care | 80% | 90% | |
| Appropriate Medications for Asthma (2) | 86% | 93% | |
| Diabetes Care: Hb A1c Testing (2) | 77% | 89% | |
| Diabetes Care: Eye Exam (2) | 49% | 68% | |
| Diabetes Care: LDL-C Screening (2) | 70% | 91% | |
| EPSDT Participation | 68% | 80% | |
| EPSDT Dental Participation – Medicaid (2) |
46% |
54% | |
| EPSDT Dental Participation – KidsCare (2) |
52% |
60% | |
55
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
Notes:
Rates by Contractor for each measure will be compared with the MPS specified in the contract in effect during the measurement period. Thus, Performance Standards in the CYE 2012 contract apply to results calculated by AHCCCS based on the measurement period of CYE 2012.
Contractor Performance is evaluated annually on the AHCCCS-reported rate for each measure. Rates for measures that include only members less than 21 years of age are reported and evaluated separately for Title XIX and Title XXI eligibility groups.
The MPS is based on the most recent national HEDIS Medicaid mean reported by NCQA that is available or, if the most recent AHCCCS statewide average is greater than the national Medicaid mean, the MPS is based on the AHCCCS statewide average for Medicaid members.
Goals are based on Healthy People 2010 Objectives; if there was no comparable objective set for a particular measure, the most recent HEDIS 90th percentile rate for Medicaid plans nationally was used as the benchmark.
(*) AHCCCS will continue to measure and report results of these individual antigens; however, a Contractor may not be held accountable for specific Performance Standards unless AHCCCS determines that completion of a specific antigen or antigens is affecting overall completion of the childhood immunization series.
| |
| (1) | NCQA introduced a new measure of adolescent immunizations in HEDIS 2010, and national HEDIS and AHCCCS results for this measure have not been reported. The MPS is based on the National Immunization Survey (NIS) overall rate of 53.8% for one dose of meningococcal vaccine among 13-year-olds in 2009 (the rate for at least one dose of Td or Tdap was 70.5%). |
| |
| (2) | EPSDT Dental Participation Standards are based on the CMS-established goal that states improve their rates of children ages one through 20 enrolled in Medicaid or CHIP who received any preventive dental service by 10 percentage points over a five-year period. |
The Contractor shall participate in immunization audits, at intervals specified by AHCCCS, based on random sampling to verify the immunization status of members at 24 months of age and by 13 years of age. If records are missing for more than 5% of the Contractor’s final sample, the Contractor is subject to sanctions by AHCCCS. An External Quality Review Organization (EQRO) may conduct a study to validate the Contractor’s reported rates.
In addition, AHCCCS will measure and report the Contractor’s EPSDT Participation Rate, utilizing the CMS 416 methodology. The Contractor must take affirmative steps to increase EPSDT Participation rates, including the EPSDT Dental Participation Rate.
The Contractor must monitor rates for postpartum visits and low/very low birth weight deliveries and implement interventions as necessary to improve or sustain these rates. These activities will be monitored by AHCCCS during the Operational and Financial Review.
II. Performance Improvement Program:
The Contractor shall have an ongoing program of performance improvement projects (PIPs) that focus on clinical and non-clinical areas as specified in the AMPM, and that involve the following [42 CFR 438.240(b)(1) and (d)(1)]:
| |
| 1. | Measurement of performance using objective quality indicators |
| |
| 2. | Implementation of system interventions to achieve improvement in quality |
| |
| 3. | Evaluation of the effectiveness of the interventions |
| |
| 4. | Planning and initiation of activities for increasing or sustaining improvement |
56
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
PIPs are mandated by AHCCCS, but Contractors may self-select additional projects based on opportunities for improvement identified by internal data and information. The Contractor shall report the status and results of each project to AHCCCS as requested using the AHCCCS PIP Reporting Template included in the AMPM. Each performance improvement project must be completed in a reasonable time period so as to generally allow information on the success of performance improvement projects in the aggregate to produce new information on quality of care every year [42 CFR 438.240(d)(2)].
III. Data Collection Procedures:
When requested, the Contractor must submit data for standardized Performance Measures and/or Performance Improvement Projects as required by AHCCCS within specified timelines and according to AHCCCS procedures for collecting and reporting the data. The Contractor is responsible for collecting valid and reliable data and using qualified staff and personnel to collect the data. Data collected for Performance Measures and/or Performance Improvement Projects must be returned by the Contractor in the format and according to instructions from AHCCCS, by the due date specified. Any extension for additional time to collect and report data must be made in writing in advance of the initial due date and is subject to approval by AHCCCS. Failure to follow the data collection and reporting instructions that accompany the data request may result in sanctions imposed on the Contractor.
| |
| 26. | MEDICAL MANAGEMENT (MM) |
The Contractor shall implement processes to assess, plan, implement, evaluate, and as mandated, report Medical Management (MM) monitoring activities, as specified in the AMPM Chapter 1000. This shall include the Quarterly Inpatient Hospital Showings report, HIV Specialty Provider List, Transplant Report and Prior Authorization Requirements report as specified in the AMPM and Attachment F of this contract. The Contractor shall evaluate MM activities, as specified in the AMPM Chapter 1000, including:
| |
| 1. | Pharmacy Management; including the evaluation, reporting, analysis and interventions based on the data and reported through the MM Committee, which is chaired by the Contractor’s Chief Medical Officer. |
| |
| 2. | Prior authorization and Referral Management; for the processing of requests for initial and continuing authorizations of services the Contractor shall: |
| |
| a) | Have in effect mechanisms to ensure consistent application of review criteria for authorization decisions; |
| |
| b) | Consult with the requesting provider when appropriate [42 CFR 438.210(b)(2)]; |
| |
| c) | Monitor and ensure that all enrollees with special health care needs have direct access to care. |
| |
| d) | Review all prior authorization requirements for services, items or medications annually. The review will be reported through the MM Committee and will include the rationale for changes made to prior authorization requirements. A summary of the prior authorization requirement changes and the rationale for those changes must be included in the annual MM/UM Plan and Evaluation submission; and |
| |
| e) | Comply with all decision timelines as outlined in the ACOM and the AMPM |
| |
| 3. | Development and/or Adoption of Practice Guidelines [42 CFR 438.236(b)], that: |
| |
| a) | Are based on valid and reliable clinical evidence or a consensus of health care professionals in the particular field; |
| |
| b) | Consider the needs of the Contractor’s members; |
| |
| c) | Are adopted in consultation with contracting health care professionals; |
| |
| d) | Are reviewed and updated periodically as appropriate; |
| |
| e) | Are disseminated by the Contractor to all affected providers and, upon request, to enrollees and potential enrollees [42 CFR 438.236(c)]; and |
57
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
| |
| f) | Provide a basis for consistent decisions for utilization management, member education, coverage of services, and other areas to which the guidelines apply [42 CFR 438.236(d)]. |
| |
| a) | Consistent application of review criteria; Provide a basis for consistent decisions for utilization management, coverage of services, and other areas to which the guidelines apply; |
| |
| b) | Contractors must have policies and procedures in place that govern the process for proactive discharge planning when members have been admitted into acute care facilities. The intent of the discharge planning policy and procedure would be to increase the utilization management of inpatient admissions and decrease readmissions within 30 days of discharge;; and |
| |
| c) | In addition, 42 CFR 447.26 prohibits payment for Provider-Preventable Conditions that meet the definition of a Health Care-Acquired Condition (HCAC) or an Other Provider –Preventable Condition (OPPC) (refer to AMPM Chapter 1000 requirements). If an HCAC or OPPC is identified, the Contractor must report the occurrence to AHCCCS and conduct a quality of care investigation. |
| |
| 5. | Continuity and coordination of care; |
| |
| a. | Establish a process to ensure coordination of member care needs across the continuum based on early identification of health risk factors or special care needs; |
| |
| b. | Establish a process for timely and confidential communication of clinical information among providers; and |
| |
| c. | Must proactively provide care coordination for members who have multiple complaints regarding services or the AHCCCS Program. This includes, but is not limited to, members who do not meet the Contractor's criteria for case management. |
| |
| 6. | Monitoring and evaluation of over and/or under utilization of services [42 CFR 438-240(b)(3)]; |
| |
| 7. | Evaluation of new medical technologies, and new uses of existing technologies; and |
| |
| 8. | Disease Management or Chronic Care Program that reports results and provides for analysis of the program through the MM Committee. |
The Contractor shall have a process to report MM data and management activities through a MM Committee. The Contractor’s MM committee will analyze the data, make recommendations for action, monitor the effectiveness of actions and report these findings to the committee. The Contractor shall have in effect mechanisms to assess the quality and appropriateness of care furnished to members with special health care needs [42 CFR 438.240(b)(4)].
The Contractor will assess, monitor and report quarterly through the MM Committee medical decisions to assure compliance with timeliness, language, Notice of Action intent, and that the decisions comply with all Contractor coverage criteria. This includes quarterly evaluation of all Notice of Action decisions that are made by a subcontracted entity.
The Contractor shall maintain a written MM plan and work plan that addresses monitoring of MM activities (AMPM Chapter 1000). The plan and work plan must be submitted for review by AHCCCS Division of Health Care Management (DHCM) within timelines specified in Attachment F.
58
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
| |
| 27. | ADMINISTRATIVE PERFORMANCE STANDARDS |
This paragraph contains requirements for the Contractor’s Member Services, Provider Services and Claims Services telephonic performance; as well as the measurement of credentialing timeliness. All reported data is subject to validation through periodic audit and/or Operational and Financial Review.
Telephone Standards
The maximum allowable speed of answer (SOA) is 45 seconds. The SOA is defined as the on line wait time in seconds that the member/provider waits from the moment the call is connected in the Contractor’s phone switch until the call is picked up by a Contractor representative or Interactive Voice Recognition System (IVR). If the Contractor has IVR capabilities, callers must be given the choice of completing their call by IVR or by Contractor representative.
The Contractor shall meet the following standards for its member services and centralized provider telephone line statistics. All calls to the line shall be included in the measure.
| |
| a. | The Monthly Average Abandonment Rate shall be 5% or less; |
| |
| b. | First Contact Call Resolution shall be 70% or better; and |
| |
| c. | The Monthly Average Service Level shall be 75% or better. |
The Monthly Average Abandonment Rate (AR) is:
Number of calls abandoned in a 24-hour period
Total number of calls received in a 24-hour period
The ARs are then summed and divided by the number of days in the reporting period.
First Contact Call Resolution Rate (FCCR) is:
Number of calls received in 24-hour period for which no follow up communication or internal phone transfer is needed, divided by Total number of calls received in 24-hour period
The daily FCCRs are then summed and divided by the number of days in the reporting period.
The Monthly Average Service Level (MASL) is:
Calls answered within 45 seconds for the month reported
Total of month’s answered calls + month’s abandoned calls + (if available) month’s calls receiving a busy signal
Note: Do not use average daily service levels divided by the days in the reporting period.
On a monthly basis the measures are to be reported for both the Member Services and Provider telephone lines. For each of the Administrative Measures a. through c., the Contractor shall also report the number of days in the reporting period that the standard was not met. The Contractor shall include in the report the instances of down time for the centralized telephone lines, the dates of occurrence and the length of time they were out of service. The reports should be sent to the Contractor's assigned Operations and Compliance Officer in the DHCM Operations Unit of the Division of Health Care Management. The deadline for submission of the reports is the 15th day of the month following the reporting period (or the first business day following the 15th). Back up documentation for the report, to the level of measured segments in the 24-hour period, shall be retained for a
59
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
rolling 12-month period. AHCCCS may review the performance measure calculation procedures and source data for this report.
Credentialing Timeliness
The Contractor is required to process credentialing applications in a timely manner. To assess the timeliness of provisional and initial credentialing a Contractor will divide the number of complete applications processed (approved/denied) during the time period by the number of complete applications that were received during the time period, as follows:
Complete applications processed
Complete applications received
The standards for processing are listed by category below:
|
| | | | |
| Type of Credentialing | 14 days | 90 days | 120 days | 180 days |
| Provisional | 100% | | | |
| Initial | | 90% | 95% | 100% |
The Contractor will also report the following information with regard to all credentialing applications on a quarterly basis, as specified in Attachment F, Periodic Report Requirements:
| |
| 1. | Number of applications received |
| |
| 2. | Number of completed applications received (separated by type: provisional, initial) |
| |
| 3. | Number of completed provisional credentialing applications approved |
| |
| 4. | Number of completed provisional credentialing applications denied |
| |
| 5. | Number of initial credentialing applications approved |
| |
| 6. | Number of initial credentialing applications denied |
| |
| 7. | Number of initial (include provisional in this number) applications processed within 90, 120, 180 days |
The Contractor shall have in place a written grievance system process for subcontractors, enrollees and non-contracted providers, which define their rights regarding disputed matters with the Contractor. The Contractor’s grievance system for enrollees includes a grievance process (the procedures for addressing enrollee grievances), an appeals process and access to the state’s fair hearing process. The Contractor shall provide the appropriate personnel to establish implement and maintain the necessary functions related to the grievance systems process. Refer to Attachments H (1) and H (2) for Enrollee Grievance System and Provider Grievance System Standards and Policy, respectively.
The Contractor may delegate the grievance system process to subcontractors, however, the Contractor must ensure that the delegated entity complies with applicable Federal and State laws, regulations and policies, including, but not limited to 42 CFR Part 438 Subpart F. The Contractor shall remain responsible for compliance with all requirements. The Contractor shall also ensure that it timely provides written information to both enrollees and providers, which clearly explains the grievance system requirements. This information must include a description of: the right to a state fair hearing, the method for obtaining a state fair hearing, the Rules that govern representation at the hearing, the right to file grievances, appeals and claim disputes, the requirements and timeframes for filing grievances, appeals and claim disputes, the availability of assistance in the filing process, the toll-free numbers that the enrollee can use to file a grievance or appeal by phone, that benefits will continue when requested by the enrollee in an appeal or state fair hearing request concerning certain actions which are timely filed, that the enrollee
60
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
may be required to pay the cost of services furnished during the appeal/hearing process if the final decision is adverse to the enrollee, and that a provider may file an appeal on behalf of an enrollee with the enrollee’s written consent. Information to enrollees must meet cultural competency and limited English proficiency requirements as specified in Section D, Paragraph 18, Member Information, and Section D, Paragraph 20, Cultural Competency.
The Contractor shall be responsible to provide the necessary professional, paraprofessional and clerical services for the representation of the Contractor in all issues relating to the grievance system and any other matters arising under this contract which rise to the level of administrative hearing or a judicial proceeding. Unless there is an agreement with the State in advance, the Contractor shall be responsible for all attorney fees and costs awarded to the claimant in a judicial proceeding.
The Contractor will provide reports on the Grievance System as required in the AHCCCS Grievance System Reporting Guide available on the AHCCCS website.
The Contractor shall develop and maintain a provider network that is designed to support a medical home for members and sufficient to provide all covered services to AHCCCS members [42 CFR 438.206(b)(1)]. It shall ensure covered services are provided promptly and are reasonably accessible in terms of location and hours of operation [42 CFR 438.206(c)(1)(i) and (ii)]. There shall be sufficient personnel for the provision of covered services, including emergency medical care on a 24-hour-a-day, 7-days-a-week basis [42 CFR 438.206(c)(1)(iii)].
The network shall be sufficient to provide covered services within designated time and distance limits. For Maricopa and Pima Counties only, this includes a network such that 95% of its members residing within the boundary area of metropolitan Phoenix and Tucson do not have to travel more than 5 miles to visit a PCP, dentist or pharmacy. Additionally, a Contractor in Maricopa and/or Pima counties must have at least one contracted hospital in each of the service districts specified in Attachment B. In rural counties the Contractor must have a sufficient network of physicians to provide adequate inpatient and outpatient services to the Contractor’s members. For inpatient services Hospitalists may satisfy this requirement. See Attachment B for GSA specific requirements.
The Contractor is expected to design a network that provides a geographically convenient flow of patients among network providers. The provider network shall be designed to reflect the needs and service requirements of AHCCCS’ culturally and linguistically diverse member population. The Contractor shall design their provider networks to maximize the availability of community based primary care and specialty care access and that reduces utilization of emergency services, one day hospital admissions, hospital based outpatient surgeries when lower cost surgery centers are available, and hospitalization for preventable medical problems. The Contractor must provide a comprehensive provider network that ensures its membership has access at least equal to community norms. Services shall be as accessible to AHCCCS members in terms of timeliness, amount, duration and scope as those services are available to non-AHCCCS persons within the same service area [42 CFR 438.210(a)(2)]. The Contractor is expected to consider the full spectrum of care when developing its network. The Contractor is encouraged to have available non-emergent after-hours physician or primary care services within its network. The Contractor must also consider communities whose residents typically receive care in neighboring states/border communities. If the Contractor is unable to provide any services locally, it must notify AHCCCS and shall provide reasonable alternatives for members to access care. These alternatives must be approved by AHCCCS. If the Contractor’s network is unable to provide medically necessary services required under contract, the Contractor must adequately and timely cover these services through an out of network provider until a network provider is contracted. The Contractor and out of network provider must coordinate with respect to authorization and payment issues in these circumstances [42 CFR 438.206(b)(4) and (5)].
61
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
The Contractor must pay all AHCCCS registered Arizona Early Intervention Program (AzEIP) providers, regardless of their contract status with the Contractor, when Individual Family Service Plans identify and meet the requirement for medically necessary EPSDT covered services.
The Contractor is also encouraged to develop non-financial incentive programs to increase participation in its provider network.
AHCCCS is committed to workforce development and support of the medical residency and dental student training programs in the state of Arizona. AHCCCS expects the Contractor to support these efforts. AHCCCS encourages plans to contract with or otherwise support the many Graduate Medical Education (GME) Residency Training Programs currently operating in the state and to investigate opportunities for resident participation in Contractor medical management and committee activities. In the event of a contract termination between the Contractor and a Graduate Medical Education Residency Training Program or training site, the Contractor may not remove members from that program in such a manner as to harm the stability of the program. AHCCCS reserves the right to determine what constitutes risk to the program. Further, the Contractor must attempt to contract with graduating residents and providers that are opening new practices in, or relocating to, Arizona, especially in rural or underserved areas.
The Contractor shall not discriminate with respect to participation in the AHCCCS program, reimbursement or indemnification against any provider based solely on the provider’s type of licensure or certification [42 CFR 438.12(a)(1)]. In addition, the Contractor must not discriminate against particular providers that service high-risk populations or specialize in conditions that require costly treatment [42 CFR 438.214(c)]. This provision, however, does not prohibit the Contractor from limiting provider participation to the extent necessary to meet the needs of the Contractor’s members. This provision also does not interfere with measures established by the Contractor to control costs consistent with its responsibilities under this contract nor does it preclude the Contractor from using different reimbursement amounts for different specialists or for different practitioners in the same specialty [42 CFR 438.12(b)(1)]. If a Contractor declines to include individual or groups of providers in its network, it must give the affected providers timely written notice of the reason for its decision [42 CFR 438.12(a)(1)]. The Contractor may not include providers excluded from participation in Federal health care programs, under either section 1128 or section 1128A of the Social Security Act [42 CFR 438.214(d)].
See Attachment B, Minimum Network Requirements, for details on network requirements by Geographic Service Area.
Provider Network Development and Management Plan: The Contractor shall develop and maintain a provider network development and management plan, which ensures that the provision of covered services will occur as stated above. The requirements for the Network Development and Management Plan are found in the ACOM Policy 415 [42 CFR 438.207(b)]. This plan shall be updated annually and submitted to AHCCCS, Division of Health Care Management, 45 days from the start of each contract year.
| |
| 30. | PROVIDER AFFILIATION TRANSMISSION |
The Contractor must submit information quarterly regarding its provider network. This information must be submitted in the format described in the Provider Affiliation Transmission (PAT) User Manual on October 15, January 15, April 15, and July 15 of each contract year. The PAT User Manual may be found on the AHCCCS website.
The Contractor shall have policies on how the Contractor will [42 CFR 438.214(a)]:
62
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
| |
| a. | Communicate with the network regarding contractual and/or program changes and requirements; |
| |
| b. | Monitor network compliance with policies and Rules of AHCCCS and the Contractor, including compliance with all policies and procedures related to the grievance/appeal process and ensuring the member’s care is not compromised during the grievance/appeal process; |
| |
| c. | Evaluate the quality of services delivered by the network; |
| |
| d. | Provide or arrange for medically necessary covered services should the network become temporarily insufficient within the contracted service area; |
| |
| e. | Monitor the adequacy, accessibility and availability of its provider network to meet the needs of its members, including the provision of care to members with limited proficiency in English; |
| |
| f. | Recruit, select, credential, re-credential and contract with providers in a manner that incorporate quality management, utilization, office audits and provider profiling; |
| |
| g. | Provide training for its providers and maintain records of such training; |
| |
| h. | Track and trend provider inquiries/complaints/requests for information and take systemic action as necessary and appropriate, and |
| |
| i. | Ensure that provider calls are acknowledged within 3 business days of receipt, resolved and/or state the result communicated to the provider within 30 business days of receipt (this includes referrals from AHCCCS). |
Contractor policies shall be subject to approval by AHCCCS, Division of Health Care Management, and shall be monitored through operational audits.
Material Change to Operations and/or Provider Network
Operations: A material change to operations is defined as any change in overall business operations (i.e., policy, process, protocol, such as prior authorization or retrospective review) which affects, or can reasonably be foreseen to affect, the Contractor's ability to meet the performance standards as described in this contract. It also includes any change that would impact more than 5% of total membership and/or provider network in a specific GSA.
The Contractor must submit the request for approval of a material change to operations, including draft notification to affected members and providers, 60 days prior to the expected implementation of the change. The request should contain, at a minimum, information regarding the nature of the operational change; the reason for the change; methods of communication to be used; and the anticipated effective date. If AHCCCS does not respond to the Contractor within 30 days; the request and the notices are deemed approved. A material change in Contractor operations requires 30 days advance written notice to affected providers and members. The requirements regarding material changes to operations do not extend to contract negotiations between the Contractor and a provider.
The Contractor may be required to conduct meetings with providers to address issues (or to provide general information, technical assistance, etc.) related to Federal and State requirements, changes in policy, reimbursement matters, prior authorization and other matters as identified or requested by the AHCCCS.
Provider Network: All material changes in the Contractor's provider network must be approved in advance by AHCCCS, Division of Health Care Management. A material change to the provider network is defined as one which affects, or can reasonably be foreseen to affect, the Contractor's ability to meet the performance and network standards as described in this contract. It also includes any change that would cause more than 5% of members in the GSA to change the location where services are received or rendered. The Contractor must submit the request for approval of a material change in their provider network, including draft notification to affected members, 60 days prior to the expected implementation of the change. The request must include a description of any short-term gaps identified as a result of the change and the alternatives that will be used to fill them. If AHCCCS does not respond within 30 days the request and the notice are deemed approved. A material change in the Contractor’s provider network requires 30 days advance written notice to affected members. For emergency situations, AHCCCS will expedite the approval process.
63
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
The Contractor shall notify AHCCCS, Division of Health Care Management, within one business day of any unexpected changes that would impair its provider network [42 CFR 438.207 (c)]. This notification shall include (1) information about how the provider network change will affect the delivery of covered services, and (2) the Contractor's plans for maintaining the quality of member care, if the provider network change is likely to affect the delivery of covered services.
See Section D, Paragraph 55 regarding material changes by the Contractor that may impact capitation rates.
Contractors shall give hospitals and provider groups 90 days notice prior to a contract termination without cause. Contracts between the Contractor and single practioners are exempt from this requirement.
Homeless Clinics:
Contractors in Maricopa and Pima County must contract with homeless clinics at the AHCCCS Fee-for-Service rate for Primary Care services. Contracts must stipulate that:
1. Only those members that request a homeless clinic as a PCP may be assigned to them; and
2. Members assigned to a homeless clinic may be referred out-of-network for needed specialty services.
The Contractor must make resources available to assist homeless clinics with administrative issues such as obtaining Prior Authorization, and resolving claims issues.
AHCCCS will convene meetings, as necessary, with the Contractor and the homeless clinics to resolve administrative issues and perceived barriers to the homeless members receiving care. Representatives from the Contractor must attend these meetings.
| |
| 32. | PRIMARY CARE PROVIDER STANDARDS |
The Contractor shall include in its provider network a sufficient number of PCPs to meet the requirements of this contract. Health care providers designated by the Contractor as PCPs shall be licensed in Arizona as allopathic or osteopathic physicians who generally specialize in family practice, internal medicine, obstetrics, gynecology, or pediatrics; certified nurse practitioners or certified nurse midwives; or physician’s assistants [42 CFR 438.206(b)(2)].
The Contractor shall assess the PCP’s ability to meet AHCCCS appointment availability and other standards when determining the appropriate number of its members to be assigned to a PCP. The Contractor should also consider the PCP’s total panel size (i.e., AHCCCS and non-AHCCCS patients) when making this determination. AHCCCS members shall not comprise the majority of a PCP’s panel of patients. AHCCCS shall inform the Contractor when a PCP has a panel of more than 1,800 AHCCCS members (assigned by a single Contractor or multiple Contractors), to assist in the assessment of the size of their panel. This information will be provided on a quarterly basis. The Contractor will adjust the size of a PCP’s panel, as needed, for the PCP to meet AHCCCS appointment and clinical performance standards.
The Contractor shall have a system in place to monitor and ensure that each member is assigned to an individual PCP and that the Contractor’s data regarding PCP assignments is current. The Contractor is encouraged to assign members with complex medical conditions, who are age 12 and younger, to board certified pediatricians. PCP’s, with assigned members diagnosed with AIDS or as HIV positive, shall meet criteria and standards set forth in the AMPM.
The Contractor shall ensure that providers serving EPSDT-aged members utilize the AHCCCS-approved EPSDT Tracking forms and standardized developmental screening tools and are trained in the use of the tools. EPSDT-
64
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
aged members shall be assigned to providers who are trained on and who use AHCCCS approved developmental screening tools.
The Contractor shall offer members freedom of choice within its network in selecting a PCP consistent with 42 CFR 438.6(m) and 438.52(d) and this contract. The Contractor may restrict this choice when a member has shown an inability to form a relationship with a PCP, as evidenced by frequent changes, or when there is a medically necessary reason. When a new member has been assigned to the Contractor, the Contractor shall inform the member in writing of his enrollment and of his PCP assignment within 12 days of the Contractor's receipt of notification of assignment by AHCCCS. The Contractor shall include with the enrollment notification a list of all the Contractor's available PCPs, the process for changing the PCP assignment, should the member desire to do so, as well as the information required in the ACOM Policy 404. The Contractor shall confirm any PCP change in writing to the member. Members may make both their initial PCP selection and any subsequent PCP changes either verbally or in writing.
At a minimum, the Contractor shall hold the PCP responsible for the following activities [42 CFR 438.208(b)(1)]:
| |
| a. | Supervision, coordination and provision of care to each assigned member (except for children’s dental services when provided without a PCP referral; |
| |
| b. | Initiation of referrals for medically necessary specialty care; |
| |
| c. | Maintaining continuity of care for each assigned member; |
| |
| d. | Maintaining the member’s medical record, including documentation of all services provided to the member by the PCP, as well as any specialty or referral services including behavioral health; |
| |
| e. | Utilizing the AHCCCS approved EPSDT Tracking form; and |
| |
| f. | Providing clinical information regarding member’s health and medications to the treating provider (including behavioral health providers) within 10 business days of a request from the provider. |
| |
| g. | If serving children, for enrolling as a Vaccines for Children (VFC) provider, |
The Contractor shall establish and implement policies and procedures to monitor PCP activities and to ensure that PCPs are adequately notified of, and receive documentation regarding, specialty and referral services provided to assigned members by specialty physicians, and other health care professionals.
| |
| 33. | MATERNITY CARE PROVIDER STANDARDS |
The Contractor shall ensure that a maternity care provider is designated for each pregnant member for the duration of her pregnancy and postpartum care and that those maternity services are provided in accordance with the AMPM. The Contractor may include in its provider network the following maternity care providers:
| |
| a. | Arizona licensed allopathic and/or osteopathic physicians who are Obstetricians or general practice/family practice providers who provide maternity care services; |
| |
| d. | Certified Nurse Midwives; |
Pregnant members may choose, or be assigned, a PCP who provides obstetrical care. Such assignment shall be consistent with the freedom of choice requirements for selecting health care professionals while ensuring that the continuity of care is not compromised. Members receiving maternity services from a certified nurse midwife or a licensed midwife must also be assigned to a PCP for other health care and medical services. A certified nurse midwife may provide those primary care services that s/he is willing to provide and that the member elects to receive from the certified nurse midwife. Members receiving care from a certified nurse midwife may also elect
65
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
to receive some or all her primary care from the assigned PCP. Licensed midwives may not provide any additional medical services as primary care is not within their scope of practice.
All physicians and certified nurse midwives who perform deliveries shall have OB hospital privileges or a documented hospital coverage agreement for those practitioners performing deliveries in alternate settings. Certified midwives perform deliveries only in the member’s home. Labor and delivery services may also be provided in the member’s home by physicians, certified nurse practitioners and certified nurse midwives who include such services within their practice.
| |
| 34. | REFERRAL MANAGEMENT PROCEDURES AND STANDARDS |
The Contractor shall have adequate written procedures regarding referrals to specialists, to include, at a minimum, the following:
| |
| a. | Use of referral forms clearly identifying the Contractor |
| |
| b. | PCP referral shall be required for specialty physician services, except that women shall have direct access to in-network GYN providers, including physicians, physician assistants and nurse practitioners within the scope of their practice [42 CFR 438.206(b)(2)]. In addition, for members with special health care needs determined to need a specialized course of treatment or regular care monitoring, the Contractor must have a mechanism in place to allow such members to directly access a specialist (for example through a standing referral or an approved number of visits) as appropriate for the member’s condition and identified needs. Any waiver of this requirement by the Contractor must be approved in advance by AHCCCS. |
| |
| c. | Specialty physicians shall not begin a course of treatment for a medical condition other than that for which the member was referred, unless approved by the member’s PCP. |
| |
| d. | A process in place that ensures the member's PCP receives all specialist and consulting reports and a process to ensure PCP follow-up of all referrals including EPSDT referrals for behavioral health services. |
| |
| e. | A referral plan for any member who is about to lose eligibility and who requests information on low-cost or no-cost health care services. |
| |
| f. | Referral to Medicare Managed Care Plan |
| |
| g. | Allow for a second opinion from a qualified health care professional within the network, or if one is not available in network, arrange for the member to obtain one outside the network, at no cost to the member [42 CFR 438.206(b)(3)]. |
The Contractor shall comply with all applicable physician referral requirements and conditions defined in Sections 1903(s) and 1877 of the Social Security Act and their implementing regulations which include, but are not limited to, 42 CFR Part 411, Part 424, Part 435 and Part 455. Sections 1903(s) and 1877 of the Act prohibits physicians from making referrals for designated health services to health care entities with which the physician or a member of the physician’s family has a financial relationship. Designated health services include:
| |
| a. | Clinical laboratory services |
| |
| b. | Physical therapy services |
| |
| c. | Occupational therapy services |
| |
| e. | Radiation therapy services and supplies |
| |
| f. | Durable medical equipment and supplies |
| |
| g. | Parenteral and enteral nutrients, equipment and supplies |
| |
| h. | Prosthetics, orthotics and prosthetic devices and supplies |
| |
| j. | Outpatient prescription drugs |
| |
| k. | Inpatient and outpatient hospital services |
66
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
The Contractor shall monitor appointment availability utilizing the methodology found in the ACOM Policy 417 to ensure that the following standards are met:
For purposes of this section, "urgent" is defined as an acute, but not necessarily life-threatening disorder, which, if not attended to, could endanger the patient’s health. The Contractor shall have procedures in place that ensure the following standards are met.
67
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
For Primary Care Appointments, the Contractor shall be able to provide:
| |
| a. | Emergency PCP appointments - same day of request or within 24 hours of the member’s phone call or other notification |
| |
| b. | Urgent care PCP appointments - within 2 days of request |
| |
| c. | Routine care PCP appointments - within 21 days of request |
For specialty referrals, the Contractor shall be able to provide:
| |
| a. | Emergency appointments - within 24 hours of referral |
| |
| b. | Urgent care appointments - within 3 days of referral |
| |
| c. | Routine care appointments - within 45 days of referral |
For dental appointments, the Contractor shall be able to provide:
| |
| a. | Emergency appointments - within 24 hours of request |
| |
| b. | Urgent care appointments - within 3 days of request |
| |
| c. | Routine care appointments - within 45 days of request |
For maternity care, the Contractor shall be able to provide initial prenatal care appointments for enrolled pregnant members as follows:
| |
| a. | First trimester - within 14 days of request |
| |
| b. | Second trimester - within 7 days of request |
| |
| c. | Third trimester - within 3 days of request |
| |
| d. | High risk pregnancies - within 3 days of identification of high risk by the Contractor or maternity care provider, or immediately if an emergency exists |
For wait time in the office, the Contractor shall actively monitor and ensure that a member's waiting time for a scheduled appointment at the PCP’s or specialist’s office is no more than 45 minutes, except when the provider is unavailable due to an emergency.
For medically necessary non-emergent transportation, the Contractor shall require its transportation provider to schedule the transportation so that the member arrives on time for the appointment, but no sooner than one hour before the appointment; nor have to wait more than one hour after the conclusion of the treatment for transportation home; nor be picked up prior to the completion of treatment. Also see Section D, Paragraph 11, Special Health Care Needs. The Contractor must develop and implement a quarterly performance auditing protocol to evaluate compliance with the standards above for all subcontracted transportation vendors/brokers and require corrective action if standards are not met.
The Contractor must use the results of appointment standards monitoring to assure adequate appointment availability in order to reduce unnecessary emergency department utilization. The Contractor is also encouraged to contract with or employ the services of non-emergency facilities to address member non-emergency care issues occurring after regular office hours or on weekends.
The Contractor shall establish processes to monitor and reduce the appointment “no-show” rate by provider and service type. As best practices are identified, AHCCCS may require implementation by the Contractor.
The Contractor shall have written policies and procedures about educating its provider network regarding appointment time requirements. The Contractor must develop a corrective action plan when appointment standards
68
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
are not met; if appropriate, the corrective action plan should be developed in conjunction with the provider [42 CFR 438.206(c)(1)(iv), (v) and (vi)]. Appointment standards shall be included in the Provider Manual. The Contractor is encouraged to include the standards in the provider subcontracts.
| |
| 36. | FEDERALLY QUALIFIED HEALTH CENTERS (FQHCs) AND RURAL HEALTH CLINICS (RHCs) |
The Contractor is encouraged to use FQHCs/RHCs and FQHC Look-Alikes in Arizona to provide covered services. AHCCCS requires the Contractor to negotiate rates of payment with FQHCs/RHCs and FQHC Look-Alikes for non-pharmacy services that are comparable to the rates paid to providers that provide similar services. AHCCCS reserves the right to review a Contractor’s negotiated rates with an FQHC/RHC and FQHC Look-Alikes for reasonableness and to require adjustments when negotiated rates are found to be substantially less than those being paid to other, non-FQHC/RHC and FQHC Look-Alikes providers for comparable services.
For FQHC and FQHC Look-Alike pharmacies, all drugs identified in the 340B Drug Pricing Program are required to be billed at the lesser of: 1) the actual acquisition cost of the drug or 2) the 340B ceiling price. These drugs shall be reimbursed at the lesser of the two amounts above plus a dispensing fee. See AHCCCS Rule R9-22-710 (C) for further details.
The Contractor is required to submit member information for Title XIX and Title XXI members for each FQHC/RHC/FQHC Look-Alikes on a quarterly basis to the AHCCCS Division of Health Care Management. AHCCCS may perform periodic audits of the member information submitted. Contractors should refer to the AHCCCS Reporting Guide for Acute Health Care Contractors for further guidance. The FQHCs/RHCs/FQHC Look-Alikes registered with AHCCCS are listed on the AHCCCS website (www.azahcccs.gov).
The Contractor shall develop, distribute and maintain a provider manual as described in the ACOM Policy 416.
The Contractor shall ensure that all of its subcontractors register with AHCCCS as an approved service provider. For specific requirements on Provider Registration refer to the AHCCCS website at http://www.azahcccs.gov/commercial/ProviderRegistration/registration.aspx .
The National Provider Identifier (NPI) is required on all claim submissions and subsequent encounters (from providers who are eligible for an NPI). The Contractor shall work with providers to obtain their NPI.
Except as otherwise required by law or as otherwise specified in a contract between a Contractor and a provider, the AHCCCS fee-for-service provisions referenced in the AHCCCS Provider Participation Agreement located on the AHCCCS website (e.g. billing requirements, coding standards, payment rates) are in force between the provider and Contractor.
The Contractor shall be legally responsible for contract performance whether or not subcontracts are used [42 CFR 438.230(a) and 434.6(c)]. No subcontract shall operate to terminate the legal responsibility of the Contractor to assure that all activities carried out by the subcontractor conform to the provisions of this contract. Subject to
69
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
such conditions, any function required to be provided by the Contractor pursuant to this contract may be subcontracted to a qualified person or organization. All such subcontracts must be in writing [42 CFR 438.6(l)]. See the ACOM Policy 203.
All subcontracts entered into by the Contractor are subject to prior review and written approval by AHCCCS, Division of Health Care Management, and shall incorporate by reference the applicable terms and conditions of this contract. The following types of Administrative Services subcontracts shall be submitted to AHCCCS, Division of Health Care Management for prior approval at least 60 days prior to the beginning date of the subcontract.
Administrative Services Subcontracts:
| |
| 1. | Delegated agreements that subcontract; |
| |
| a) | Any function related to the management of the contract with AHCCCS. Examples include member services, provider relations, quality management, medical management (e.g., prior authorization, concurrent review, issuance of denials or limited authorizations, member appeals, medical claims review, medical record review), |
| |
| b) | Claims processing, including pharmacy claims, |
| |
| c) | Credentialing including those for only primary source verification (CVO). |
| |
| 2. | All Management Service Agreements; |
| |
| 3. | All Service Level Agreements with any Division or Subsidiary of a corporate parent owner. |
AHCCCS may, at its discretion, communicate directly with the governing body or Parent Corporation of the Contractor regarding the performance of a subcontractor or Contractor respectively.
The Contractor shall maintain a fully executed original or electronic copy of all subcontracts, which shall be accessible to AHCCCS within two business days of request by AHCCCS. All requested subcontracts must have full disclosure of all terms and conditions and must fully disclose all financial or other requested information. Information may be designated as confidential but may not be withheld from AHCCCS as proprietary. Information designated as confidential may not be disclosed by AHCCCS without the prior written consent of the Contractor except as required by law. All subcontracts shall comply with the applicable provisions of Federal and State laws, regulations and policies.
Before entering into a subcontract which delegates duties or responsibilities to a subcontractor the Contractor must evaluate the prospective subcontractor’s ability to perform the activities to be delegated. If the Contractor delegates duties or responsibilities then the Contractor shall establish a written agreement that specifies the activities and reporting responsibilities delegated to the subcontractor. The written agreement shall also provide for revoking delegation or imposing other sanctions if the subcontractor’s performance is inadequate. In order to determine adequate performance, the Contractor shall monitor the subcontractor’s performance on an ongoing basis and subject it to formal review at least annually or more frequently if requested by AHCCCS. As a result of the performance review, any deficiencies must be communicated to the subcontractor in order to establish a corrective action plan. The results of the performance review and the correction plan shall be communicated to AHCCCS upon completion [42 CFR 438.230(b)].
A merger, reorganization or change in ownership of an Administrative Services subcontractor of the Contractor shall require a contract amendment and prior approval of AHCCCS.
The Contractor must submit the Administrative Services Annual Subcontractor Assignment and Evaluation Report (within 90 days from the start of the contract year) detailing any Contractor duties or responsibilities that have been subcontracted as described under Administrative Services Subcontracts previously in this section. The Administrative Services Annual Subcontractor Assignment and Evaluation Report will include the following:
70
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
| |
| • | Delegated duties and responsibilities |
| |
| • | Most recent review date of the duties, responsibilities and financial position of the subcontractor |
| |
| • | A comprehensive summary of the evaluation of the performance (operational and financial) of the subcontractor. The full report shall be made available upon request from AHCCCS. |
| |
| • | Next scheduled review date |
| |
| • | Identified areas of deficiency |
| |
| • | Corrective action plans as necessary |
The Contractor shall promptly inform AHCCCS, Division of Health Care Management, within 30 days if a subcontractor is in significant non-compliance that would affect their abilities to perform the duties and responsibilities of the subcontract. The Contractor will submit this in writing and provide the Corrective Action Plan and any measures taken by the Contractor to bring the subcontractor into compliance.
Provider Agreements:
The Contractor shall not include covenant-not-to-compete requirements in its provider agreements. Specifically, the Contractor shall not contract with a provider and require that the provider not provide services for any other AHCCCS Contractor. In addition, the Contractor shall not enter into subcontracts that contain compensation terms that discourage providers from serving any specific eligibility category.
The Contractor must enter into a written agreement with any provider (including out-of-state providers) the Contractor reasonably anticipates will be providing services at the request of the Contractor more than 25 times during the contract year. Exceptions to this requirement include the following:
| |
| 1. | If a provider who provides services more than 25 times during the contract year refuses to enter into a written agreement with the Contractor, the Contractor shall submit documentation of such refusal to AHCCCS, Division of Health Care Management within seven days of its final attempt to gain such agreement. |
| |
| 2. | If a provider performs emergency services such as an emergency room physician or an ambulance company, a written agreement is not required. |
| |
| 3. | Individual providers as detailed in the AMPM. |
| |
| 4. | Hospitals, as discussed in Section D, Paragraph 40, Hospital Subcontracting and Reimbursement. |
| |
| 5. | If a provider primarily performs services in an inpatient setting. |
| |
| 6. | If upon the Medical Director’s review, it is determined that the Contractor or members would not benefit by adding the provider to the contracted network. |
Any other exceptions to this requirement must be approved by AHCCCS, Division of Health Care Management. If AHCCCS does not respond within 30 days; the requested exception is deemed approved. The Contractor may request an expedited review and approval.
For all subcontracts in which the Contractor and Subcontractor have a capitated arrangement/risk sharing arrangement, the following provision must be included verbatim in every contract:
If the Subcontractor does not bill the Contractor (e.g., Subcontractor is capitated), the Subcontractor’s encounter data that is required to be submitted to the Contractor pursuant to contract is defined for these purposes as a “claim for payment”. The Subcontractor’s provision of any service results in a “claim for payment” regardless of whether there is any intention of payment. All said claims shall be subject to review under any and all fraud and abuse statutes, Rules and regulations, including but not limited to Arizona Revised Statute (A.R.S.) §36-2918.
71
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
All subcontracts must reference the provisions of Attachment A, Minimum Subcontract Provisions located on the AHCCCS website at http://www.azahcccs.gov/commercial/default.aspx . In addition, each subcontract must contain the following:
| |
| 1. | Full disclosure of the method and amount of compensation or other consideration to be received by the subcontractor. |
| |
| 2. | Identification of the name and address of the subcontractor. |
| |
| 3. | Identification of the population, to include patient capacity, to be covered by the subcontractor. |
| |
| 4. | The amount, duration and scope of medical services to be provided, and for which compensation will be paid. |
| |
| 5. | The term of the subcontract including beginning and ending dates, methods of extension, termination and re-negotiation. |
| |
| 6. | The specific duties of the subcontractor relating to coordination of benefits and determination of third‑party liability. |
| |
| 7. | A provision that the subcontractor agrees to identify Medicare and other third‑party liability coverage and to seek such Medicare or third party liability payment before submitting claims to the Contractor. |
| |
| 8. | A description of the subcontractor's patient, medical, dental and cost record keeping system. |
| |
| 9. | Specification that the subcontractor shall cooperate with quality management programs, and comply with the utilization control and review procedures specified in 42 CFR Part 456, as specified in the AMPM. |
| |
| 10. | A provision stating that a merger, reorganization or change in ownership of an Administrative Services subcontractor of the Contractor shall require a contract amendment and prior approval of AHCCCS. |
| |
| 11. | A provision that indicates that AHCCCS is responsible for enrollment, re‑enrollment and disenrollment of the covered population. |
| |
| 12. | A provision that the subcontractor shall be fully responsible for all tax obligations, Worker's Compensation Insurance, and all other applicable insurance coverage obligations which arise under this subcontract, for itself and its employees, and that AHCCCS shall have no responsibility or liability for any such taxes or insurance coverage. |
| |
| 13. | A provision that the subcontractor must obtain any necessary authorization from the Contractor or AHCCCS for services provided to eligible and/or enrolled members. |
| |
| 14. | A provision that the subcontractor must comply with encounter reporting and claims submission requirements as described in the subcontract. |
| |
| 15. | Provision(s) that allow the Contractor to suspend, deny, refuse to renew or terminate any subcontractor in accordance with the terms of this contract and applicable law and regulation. |
| |
| 16. | A provision that the subcontractor may provide the member with factual information, but is prohibited from recommending or steering a member in the member’s selection of a Contractor. |
| |
| 17. | A provision that compensation to individuals or entities that conduct utilization management and concurrent review activities is not structured so as to provide incentives for the individual or entity to deny, limit or discontinue medically necessary services to any enrollee [42 CFR 438.210(e)]. |
| |
| 40. | CLAIMS PAYMENT/HEALTH INFORMATION SYSTEM |
The Contractor shall develop and maintain a health information system that collects, analyzes, integrates, and reports data. The system shall provide information on areas including, but not limited to, service utilization, claim disputes and appeals [42 CFR 438.242(a)].
System Requirements:
The Contractor must have a health information system that integrates member demographic data, provider information, service provision, claims submission and reimbursement. This system must be capable of collecting, storing and producing information for the purposes of financial, medical and operational management.
The Contractor shall develop and maintain a HIPAA compliant claims processing and payment system capable of processing, cost avoiding and paying claims in accordance with A.R.S. §§ 36-2903 and 2904 and AHCCCS
72
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
Rules R9-22 Article 7. The system must be adaptable to updates in order to support future AHCCCS claims related policy requirements as needed.
The Contractor must include nationally recognized methodologies to correctly pay claims including but not limited to:
| |
| • | Medicaid Correct Coding Initiative (NCCI) for Professional, ASC and Outpatient services; |
| |
| • | Multiple Surgical Reductions; |
| |
| • | Global Day E & M Bundling. |
The Contractor claims payment system must be able to assess and/or apply t data related edits including but not limited to:
| |
| • | Benefit Package Variations; |
| |
| • | Adherence to AHCCCS Policy; |
| |
| • | Provider Qualifications; |
| |
| • | Member Eligibility and Enrollment; |
| |
| • | Over-Utilization Standards. |
This system must produce a remittance advice related to the Contractor’s payments and/or denials to providers and must include at a minimum:
| |
| • | An adequate description of all denials and adjustments; |
| |
| • | The reasons for such denials and adjustments; |
| |
| • | Application of COB and copays; |
| |
| • | Provider rights for claim disputes. |
The related remittance advice must be sent with the payment, unless the payment is made by electronic funds transfer (EFT). The remittance advice sent related to an EFT must be sent to the provider, no later than the date of the EFT.
General Claims Processing Requirements:
AHCCCS will require the Contractor to participate in an AHCCCS workgroup to develop uniform guidelines for standardizing hospital outpatient and outpatient provider claim requirements, including billing Rules and documentation requirements. The workgroup may be facilitated by an AHCCCS selected consultant. The Contractor will be held responsible for the cost of this project based on its share of AHCCCS enrollment.
Unless a shorter time period is specified in contract, the Contractor shall not pay a claim initially submitted more than six months after the date of service or pay a clean claim submitted more than 12 months after the date of service; except as directed by AHCCCS or otherwise noted in this contract. Claim payment requirements pertain to both contracted and non-contracted providers. The receipt date of the claim is the date stamp on the claim or the date electronically received. The receipt date is the day the claim is received at the Contractor’s specified claim mailing address. The paid date of the claim is the date on the check or other form of payment [42 CFR 447.45(d)]. Claims submission deadlines shall be calculated from the claim end date or the effective date of eligibility posting, whichever is later as stated in A.R.S. 36-2904.H.
Additionally, unless a subcontract specifies otherwise, a Contractor with 50,000 or more members at the end of the month that is being reported shall ensure that for each form type (Dental/Professional/Institutional), 95% of all clean claims are adjudicated within 30 days of receipt of the clean claim and 99% are adjudicated within 60 days of receipt of the clean claim. Unless a subcontract specifies otherwise, a Contractor with fewer than 50,000
73
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
members at the end of the month that is being reported shall ensure that for each form type (Dental/Professional/Institutional), 90% of all clean claims are adjudicated within 30 days of receipt of the clean claim and 99% are adjudicated within 60 days of receipt of the clean claim.
In accordance with the Deficit Reduction Act of 2005, Section 6085, Contractor is required to reimburse non-contracted emergency services providers at no more than the AHCCCS Fee-For-Service rate. This applies to in state as well as out of state providers.
In accordance with Arizona Revised Statute 36-2903 and 36-2904, in the absence of a written negotiated rate, Contractor is required to reimburse non-contracted non-emergent in state providers at the AHCCCS fee schedule and methodology, or pursuant to 36-2905.01, at 95% of the AHCCCS Fee-For-Service rates for urban hospital days. All payments are subject to other limitations that apply, such as provider registration, prior authorization, medical necessity, and covered service.
Effective for all non-hospital clean claims, in the absence of a contract specifying other late payment terms, a Contractor is required to pay interest on late payments. Late claims payments are those that are paid after 45 days of receipt of the clean claim (as defined in this contract). In grievance situations, interest shall be paid back to the date interest would have started to accrue beyond the applicable 45 day requirement. Interest shall be at the rate of 10% per annum, unless a different rate is stated in a written contract. In the absence of interest payment terms in a subcontract, interest shall accrue starting on the first day after a clean claim is contracted to be paid. For hospital clean claims, a slow payment penalty shall be paid in accordance with A.R.S. 2903.01. When interest is paid, the Contractor must report the interest as directed in the AHCCCS Encounter Manual.
Electronic Transactions:
The Contractor is required to accept and generate required HIPAA compliant electronic transactions from/to any provider interested and capable of electronic submission or electronic remittance receipt; and must be able to make claims payments via electronic funds transfer. In addition, the Contractor shall implement and meet the following milestone in order to make claims processing and payment more efficient and timely:
| |
| • | Receive and pay 60% of all claims (based on volume of actual claims excluding claims processed by Pharmacy Benefit Managers (PBMs)) electronically |
Recoupments:
The Contractor’s claims payment system, as well as its prior authorization and concurrent review process, must minimize the likelihood of having to recoup already-paid claims. Any individual recoupment in excess of $50,000 per provider within a contract year must be approved in advance by AHCCCS, DHCM Operations Unit. AHCCCS will respond within 30 days. AHCCCS must be notified of any cumulative recoupment greater than $50,000 per provider Tax Identification Number per contract year. A Contractor shall not recoup monies from a provider later than 12 months after the date of original payment on a clean claim, without prior approval from AHCCCS, as further described in the ACOM Policy 412. The Contractor is required to reimburse providers for previously denied or recouped claims if the provider was subsequently denied payment by the primary insurer based on timely filing limits or lack of prior authorization and the member failed to disclose additional insurance coverage other than AHCCCS.
The provider shall have 90 days from the date they become aware that payment will not be made, to submit a new claim with documentation from the primary insurer that payment will not be made. Documentation includes but is not limited to any of the following items establishing that the primary insurer has or would deny payment based on timely filing limits or lack of prior authorization; an EOB, policy or procedure, Provider Manual excerpt, etc.
74
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
The Contractor must void encounters for claims that are recouped in full. For recoupments that result in a reduced claim value or adjustments that result in an increased claim value, replacement encounters must be submitted. AHCCCS will validate the submission of applicable voids and replacement encounters upon completion of any approved recoupment that meets the qualifications of this section. All replaced or voided encounters must reach adjudicated status within 120 days of the approval of the recoupment. The Contractor should refer to the ACOM Policy 412 and AHCCCS Encounter Manual for further guidance.
Appeals:
If the Contractor or a Director's Decision reverses a decision to deny, limit, or delay authorization of services, and the member received the disputed services while an appeal was pending, the Contractor shall process a claim for payment from the provider in a manner consistent with the Contractor's or Director's Decision and applicable statutes, Rules, policies, and contract terms. The provider shall have 90 days from the date of the reversed decision to submit a clean claim to the Contractor for payment. For all claims submitted as a result of a reversed decision, the Contractor is prohibited from denying claims for untimeliness if they are submitted within the 90 day timeframe. Contractors are also prohibited from denying claims submitted as a result of a reversed decision because the member failed to request continuation of services during the appeals/hearing process: a member's failure to request continuation of services during the appeals/hearing process is not a valid basis to deny the claim.
System Related Reporting:
The Contractor shall submit a monthly Claims Dashboard as specified in the AHCCCS Claims Dashboard Reporting Guide.
AHCCCS may in the future require Contractors to review claim requirements, including billing Rules and documentation requirements, and submit a report to AHCCCS that will include the rationale for the requirements. AHCCCS shall determine and provide a format for the report.
System Changes and Upgrades:
The Contractor will ensure that changing or making major upgrades to the information systems affecting claims processing, or any other major business component, will be accompanied by a plan which includes a timeline, milestones, and adequate testing before implementation. At least six months before the anticipated implementation date, the Contractor shall provide the system change plan to AHCCCS for review and comment.
System Audits:
In support of this requirement, the Contractor may be required to have an independent audit of the Claims Payment/Health Information System. The Division of Health Care Management will monitor the scope of this audit, to include no less than a verification of contract information management (contract loading and auditing), claims processing and encounter submission processes. In addition to this requirement, the Contractor may be required in future contract years to initiate additional independent Claim System/Health Information System audit at the direction of AHCCCS. In the event of a system change or upgrade, the Contractor may be required to initiate an independent Claim System/Health Information System audit.
The Contractor shall develop and implement an internal claims audit function that will include the following:
| |
| • | Verification that provider contracts are loaded correctly |
| |
| • | Accuracy of payments against provider contract terms |
Audits of provider contract terms should be performed on a regular and periodic basis and consist of a random, statistically significant sampling of all contracts in effect at the time of the audit. The audit sampling methodology should be documented in policy, and the Contractor should review the contract loading of both large groups and individual practitioners at least once every five year period in addition to any time a contract change is initiated during that timeframe. The findings of the audits described above must be documented and any deficiencies noted in the resulting reports must be met with corrective action.
75
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
AHCCCS may at any time negotiate or contract on behalf of the Contractor and AHCCCS for specialized hospital and medical services. AHCCCS will consider existing Contractor resources in the development and execution of specialty contracts. AHCCCS may require the Contractor to modify its delivery network to accommodate the provisions of specialty contracts. AHCCCS may consider waiving this requirement in particular situations if such action is determined to be in the best interest of the State; however, in no case shall reimbursement exceeding that payable under the relevant AHCCCS specialty contract be considered in capitation rate development or risk sharing arrangements, including reinsurance.
During the term of specialty contracts, AHCCCS may act as an intermediary between the Contractor and specialty Contractors to enhance the cost effectiveness of service delivery, medical management, and adjudication of claims related to payments provided under specialty contracts shall remain the responsibility of the Contractor. AHCCCS may provide technical assistance prior to the implementation of any specialty contracts.
AHCCCS has specialty contracts, including but not limited to, transplant services, anti-hemophilic agents and pharmaceutical related services. AHCCCS shall provide at least 60 days advance written notice to the Contractor prior to the implementation of any specialty contract.
| |
| 42. | HOSPITAL SUBCONTRACTING AND REIMBURSEMENT |
Maricopa and Pima counties only: The Inpatient Hospital Reimbursement Program is defined in the Arizona Revised Statutes (A.R.S.) 36-2905.01, and requires hospital subcontracts to be negotiated between Contractors in Maricopa and Pima counties to establish reimbursement levels, terms and conditions. Subcontracts shall be negotiated by the Contractor and hospitals to cover operational concerns, such as timeliness of claims submission and payment, payment of discounts or penalties and legal resolution, which may, as an option, include establishing arbitration procedures. These negotiated subcontracts shall remain under close scrutiny by AHCCCS to insure availability of quality services within specific service districts, equity of related party interests and reasonableness of rates. The general provisions of this program encompass acute care hospital services and outpatient hospital services that result in an admission. The Contractor, upon request, shall make available to AHCCCS, all hospital subcontracts and amendments. For non-emergency patient-days, the Contractor shall ensure that at least 65% of its members use contracted hospitals. AHCCCS reserves the right to subsequently adjust the 65% standard. Further, if in AHCCCS’ judgment the number of non-emergency inpatient days at a particular non-contracted hospital becomes significant, AHCCCS may require a subcontract at that hospital. In accordance with R9-22-718, unless otherwise negotiated by both parties, the reimbursement for inpatient services, including outliers, provided at a non-contracted hospital shall be based on the rates as defined in A.R.S. § 36-2903.01, multiplied by 95%.
All counties EXCEPT Maricopa and Pima: The Contractor shall reimburse hospitals for member care in accordance with AHCCCS Rule 9 A.A.C. 22, Article 7. The Contractor is encouraged to obtain subcontracts with hospitals in all GSA’s. The Contractor, upon request, shall make available to AHCCCS, all hospital subcontracts and amendments.
For Out-of-State Hospitals: The Contractor shall reimburse out-of-state hospitals in accordance with AHCCCS Rule9 A.A.C.22, Article 7. A Contractor serving border communities (excluding Mexico) is strongly encouraged to establish contractual agreements with those out-of-state hospitals that are identified by GSA in Attachment B.
Outpatient hospital services: In the absence of a contract, the default payment rate for outpatient hospital services billed on a UB-04 will be based on the AHCCCS outpatient hospital fee schedule, rather than a hospital-specific cost-to-charge ratio (pursuant to ARS 36-2904).
76
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
Hospital Recoupments: The Contractor may conduct pre-payment and post-payment medical reviews of all hospital claims including outlier claims. Erroneously paid claims are subject to recoupment. If the Contractor fails to identify lack of medical necessity through concurrent review and/or pre-payment medical review, lack of medical necessity identified during post-payment medical review shall not constitute a basis for recoupment by the Contractor. See also Section D, Paragraph 38, Claims Payment/Health Information System. For a more complete description of the guidelines for hospital reimbursement, please consult the applicable statutes and Rules.
| |
| 43. | RESPONSIBILITY FOR NURSING FACILITY REIMBURSEMENT |
The Contractor shall provide medically necessary nursing facility services as outlined in Section D, Paragraph 10, Scope of Services. The Contractor shall also provide medically necessary nursing facility services for any enrolled member who has a pending ALTCS application who is currently residing in a nursing facility and is eligible for services provided under this contract. If the member becomes ALTCS eligible and is enrolled with an ALTCS Contractor before the end of the maximum 90 days per contract year of nursing facility coverage, the Contractor is only responsible for nursing facility reimbursement during the time the member is enrolled with the Contractor as shown in the PMMIS. Nursing facility services covered by another liable party (including Medicare) while the member is enrolled with the Contractor, shall be applied to the 90 day per contract year limitation.
The Contractor shall not deny nursing facility services when the member’s eligibility, including prior period coverage, had not been posted at the time of admission. In such situations the Contractor shall impose reasonable authorization requirements. There is no ALTCS enrollment, including prior period coverage that occurs concurrently with AHCCCS acute enrollment.
The Contractor shall notify the Assistant Director of the Division of Member Services, when a member has been residing in a nursing facility, alternative residential facility or receiving home and community based services for 45 days as specified in Section D, Paragraph 10, Scope of Services, under the heading Nursing Facility. This will allow AHCCCS time to follow-up on the status of the ALTCS application and to consider potential fee-for-service coverage if the stay goes beyond the 90 day per contract year maximum.
| |
| 44. | PHYSICIAN INCENTIVES/PAY FOR PERFORMANCE |
Physician Incentives
The reporting requirements under 42 CFR 417.479 have been suspended. No reporting to CMS is required until the suspension is lifted.
The Contractor must comply with all applicable physician incentive requirements and conditions defined in 42 CFR 417.479. These regulations prohibit physician incentive plans that directly or indirectly make payments to a doctor or a group as an inducement to limit or refuse medically necessary services to a member. The Contractor is required to disclose all physician incentive agreements to AHCCCS and to AHCCCS members who request them.
The Contractor shall not enter into contractual arrangements that place providers at significant financial risk as defined in 42 CFR 417.479 unless specifically approved in advance by the AHCCCS Division of Health Care Management. In order to obtain approval, the following must be submitted to the AHCCCS Division of Health Care Management 45 days prior to the implementation of the contract [42 CFR 438.6(g)]:
| |
| 1. | A complete copy of the contract |
| |
| 2. | A plan for the member satisfaction survey |
| |
| 3. | Details of the stop-loss protection provided |
77
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
| |
| 4. | A summary of the compensation arrangement that meets the substantial financial risk definition |
The Contractor shall disclose to AHCCCS the information on physician incentive plans listed in 42 CFR 417.479(h)(1) through 417.479(I) upon contract renewal, prior to initiation of a new contract, or upon request from AHCCCS or CMS.
The Contractor shall also comply with physician incentive plan requirements as set forth in 42 CFR 422.208, 422.210 and 438.6(h). These regulations apply to contract arrangements with subcontracted entities that provide utilization management services.
Transparency
AHCCCS programs will be in compliance with Federal and State transparency initiatives. AHCCCS may publicly report or make available any data, reports, analysis or outcomes related to Contractor activities, operations and/or performance. Public reporting may include, but is not limited to, the following components:
| |
| a) | Use of evidence based guidelines |
| |
| b) | Identification and publication of top performing Contractors |
| |
| c) | Identification and publication of top performing providers |
| |
| d) | Program pay for performance payouts |
| |
| e) | Mandated publication of guidelines |
| |
| f) | Mandated publication of outcomes |
| |
| g) | Identification of Centers of Excellence for specific conditions, procedures or member populations |
| |
| h) | Establishment of Return on Investment goals |
Any Contractor-selected and/or -developed pay for performance initiative that meets the requirements of 42 CFR 417.479 must be approved by AHCCCS Division of Health Care Management prior to implementation.
| |
| 45. | MANAGEMENT SERVICES AGREEMENT AND COST ALLOCATION PLAN |
If a Contractor has subcontracted for management services, the management service agreement must be approved in advance by AHCCCS, Division of Health Care Management. If there is a cost allocation plan as part of the management services agreement, it is subject to review by AHCCCS upon request. AHCCCS reserves the right to perform a thorough review of actual management fees charged and/or corporate allocations made.
If there is a change in ownership of the entity with which the Contractor has contracted for management services, AHCCCS must review and provide prior approval of the assignment of the subcontract to the new owner. AHCCCS may offer open enrollment to the members assigned to the Contractor should a change in ownership occur. AHCCCS will not permit two Contractors to utilize the same management service company in the same GSA.
The performance of management service subcontractors must be evaluated and included in the Annual Subcontractor Assignment and Evaluation Report required by Section D, Paragraph 37, Subcontracts and Attachment F: Periodic Report Requirements.
| |
| 48. | PERFORMANCE BOND OR BOND SUBSTITUTE |
78
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
In addition to the minimum capitalization requirements, the Contractor shall be required to establish and maintain a performance bond, in accordance with the ACOM Policy 306, to AHCCCS for as long as the Contractor has AHCCCS-related liabilities of $50,000 or more outstanding, or 15 months following the termination date of this contract, whichever is later, to guarantee: (1) payment of the Contractor's obligations to providers, and (2) performance by the Contractor of its obligations under this contract [42 CFR 438.116]. The Performance Bond shall be in a form acceptable to AHCCCS as described in the ACOM Policy 306 .
In the event of a default by the Contractor, AHCCCS shall, in addition to any other remedies it may have under this contract, obtain payment under the Performance Bond or substitute security for the purposes of the following:
| |
| 1. | Paying any damages sustained by providers, non-contracting providers and non-providers by reason of a breach of the Contractor's obligations under this contract; |
| |
| 2. | Reimbursing AHCCCS for any payments made by AHCCCS on behalf of the Contractor; and |
| |
| 3. | Reimbursing AHCCCS for any extraordinary administrative expenses incurred by reason of a breach of the Contractor's obligations under this contract, including, but not limited to, expenses incurred after termination of this contract for reasons other than the convenience of the State by AHCCCS. |
In the event AHCCCS agrees to accept substitute security in lieu of the security types outlined in the ACOM Policy 306, the Contractor agrees to execute any and all documents and perform any and all acts necessary to secure and enforce AHCCCS' security interest in such substitute security including, but not limited to, security agreements and necessary UCC filings pursuant to the Arizona Uniform Commercial Code. The Contractor must request acceptance from AHCCCS when a substitute security in lieu of the security types outlined in the ACOM Policy 306 is established. In the event such substitute security is agreed to and accepted by AHCCCS, the Contractor acknowledges that it has granted AHCCCS a security interest in such substitute security to secure performance of its obligations under this contract. The Contractor is solely responsible for establishing the credit-worthiness of all forms of substitute security. AHCCCS may, after written notice to the Contractor, withdraw its permission for substitute security, in which case the Contractor shall provide AHCCCS with a form of security described in the ACOM Policy 306.
The Contractor may not change the amount, duration or scope of the performance bond without prior written approval from AHCCCS, Division of Health Care Management. The Contractor shall not leverage the bond for another loan or create other creditors using the bond as security.
| |
| 49. | AMOUNT OF PERFORMANCE BOND |
The initial amount of the Performance Bond shall be equal to 80% of the total capitation payment expected to be paid to the Contractor in the first month of the contract year, or as determined by AHCCCS. The total capitation amount (including delivery supplement) excludes premium tax. This requirement must be satisfied by the Contractor no later than 30 days after notification by AHCCCS of the amount required. Thereafter, AHCCCS shall review the capitation amounts of the Contractor on a monthly basis to determine if the Performance Bond must be increased. The Contractor shall have 30 days following notification by AHCCCS to increase the amount of the Performance Bond. The Performance Bond amount that must be maintained after the contract term shall be sufficient to cover all outstanding liabilities and will be determined by AHCCCS. The Contractor may not change the amount of the performance bond without prior written approval from AHCCCS, Division of Health Care Management. Refer to the ACOM Policy 305 for more details.
| |
| 50. | ACCUMULATED FUND DEFICIT |
79
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
The Contractor and its owners must review for accumulated fund deficits on a quarterly and annual basis. In the event the Contractor has a fund deficit, the Contractor and its owners shall fund the deficit through capital contributions in a form acceptable to AHCCCS. The capital contributions must be for the period in which the deficit is reported and shall occur within 30 days of the financial statement due to AHCCCS. AHCCCS at its sole discretion may impose a different timeframe other than the 30 days required in this paragraph. AHCCCS may, at its option, impose enrollment caps in any or all GSA’s as a result of an accumulated deficit, even if unaudited.
| |
| 51. | ADVANCES, DISTRIBUTIONS, LOANS AND INVESTMENTS |
The Contractor shall not, without the prior approval of AHCCCS, make any advances, distributions, loans or loan guarantees to related parties or affiliates including another fund or line of business within its organization. The Contractor shall not, without prior approval of AHCCCS, make loans or advances to providers in excess of $50,000. All requests for prior approval are to be submitted to the AHCCCS Division of Health Care Management. Refer to the ACOM Policy 418 for further information.
| |
| 52. | FINANCIAL VIABILITY STANDARDS |
The Contractor must comply with the AHCCCS-established financial viability standards. On a quarterly basis, AHCCCS will review the following ratios with the purpose of monitoring the financial health of the Contractor: Current Ratio; Equity per Member; Medical Expense Ratio; and the Administrative Cost Percentage.
Sanctions may be imposed if the Contractor does not meet these financial viability standards. AHCCCS will take into account the Contractor’s unique programs for managing care and improving the heath status of members when analyzing medical expense and administrative ratio results. However, if a critical combination of the Financial Viability Standards, are not met, or if the Contractor’s experience differs significantly from other Contractors, additional monitoring, such as monthly reporting, may be required.
FINANCIAL VIABILITY STANDARDS
|
| |
| Current Ratio | Current assets divided by current liabilities. "Current assets" includes any long-term investments that can be converted to cash within 24 hours without significant penalty (i.e., greater than 20%).
Standard: At least 1.00
If current assets include a receivable from a parent company, the parent company must have liquid assets that support the amount of the inter-company loan. |
|
| |
| Equity per Member | Unrestricted equity, less on-balance sheet performance bond, divided by the number of non-SOBRA Family Planning Extension Services members enrolled at the end of the period.
Standard: At least $150 for Contractors with enrollment < 100,000 $100 for Contractors with enrollment of 100,000+
Additional information regarding the Equity per Member requirement may be found in ACOM Policy 305. |
80
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
|
| |
| | |
| Medical Expense Ratio | Total medical expenses less TPL divided by the sum of total PPC and prospective capitation + Delivery Supplement + All Reconciliation Settlements + Reinsurance less premium tax
Standard: At least 85% |
| Administrative Cost Percentage | Total administrative expenses divided by the sum of total PPC and prospective capitation + Delivery Supplement + All Reconciliation Settlements + Reinsurance less premium tax
Standard: No greater than 10% |
| | |
The Contractor shall comply with all financial reporting requirements contained in Attachment F, Periodic Report Requirements and the AHCCCS Reporting Guide for Acute Health Care Contractors, a copy of which may be found on the AHCCCS website. The required reports are subject to change during the contract term and are summarized in Attachment F, Periodic Report Requirements.
| |
| 53. | SEPARATE INCORPORATION |
Within 60 days of contract award, a non-governmental Contractor shall have established a separate corporation for the purposes of this contract, whose sole activity is the performance of the requirements of this contract.
| |
| 54. | MERGER, REORGANIZATION AND CHANGE OF OWNERSHIP |
A proposed merger, reorganization or change in ownership of the Contractor shall require prior approval of AHCCCS and may require a contract amendment. AHCCCS may terminate this contract pursuant to Section D, Paragraph 1, Term of Contract and Option to Renew. If the Contractor does not obtain prior approval or AHCCCS determines that the change in ownership is not in the best interest of the State, AHCCCS may offer open enrollment to the members assigned to the Contractor should a change in ownership occur. AHCCCS will not permit one organization to own or manage more than one contract within the same program in the same GSA.
The Contractor must submit a detailed merger, reorganization and/or transition plan to AHCCCS, Division of Health Care Management, for review at least 60 days prior to the effective date of the proposed change. The purpose of the plan review is to ensure uninterrupted services to members, evaluate the new entity's ability to perform the contract requirements, ensure that services to members are not diminished and that major components of the organization and AHCCCS programs are not adversely affected by such merger, reorganization or change in ownership.
The method of compensation under this contract will be Prior Period Coverage (PPC) capitation, prospective capitation, delivery supplement, reinsurance and third party liability, as described and defined within this contract and appropriate laws, regulations or policies.
Actuaries establish the capitation rates using practices established by the Actuarial Standards Board. AHCCCS provides the following data to its actuaries for the purposes of rebasing and/or updating the capitation rates.
81
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
| |
| a. | Utilization and unit cost data derived from adjudicated encounters |
| |
| b. | Both audited and unaudited financial statements reported by the Contractor |
| |
| c. | Market basket inflation trends |
| |
| d. | AHCCCS fee-for-service schedule pricing adjustments |
| |
| e. | Programmatic or Medicaid covered service changes that affect reimbursement |
| |
| f. | Other changes to medical practices or administrative requirements that affect reimbursement |
AHCCCS adjusts its rates to best match payment to risk. This further ensures the actuarial basis for the capitation rates. The following are examples of risk factors that may be included.
| |
| a. | Reinsurance (as described in Section D, Paragraph 57) |
| |
| c. | Medicare enrollment for SSI members |
| |
| d. | Delivery supplemental payment |
| |
| e. | Geographic Service Area adjustments |
| |
| f. | Risk sharing arrangements for specific populations |
| |
| g. | Member specific statistics, e.g. member acuity, member choice, member diagnosis, etc. |
For services or pharmaceuticals, in instances in which AHCCCS has specialty contracts or legislation/policy limits the allowable reimbursement, the amount to be used in the capitation rate setting process and reconciliations will be the lesser of the contracted/mandated amount or the Contractor paid amount.
The above information is reviewed by AHCCCS’ actuaries in renewal years to determine if adjustments are necessary. A Contractor may cover services that are not covered under the State Plan; however those services are not included in the data provided to actuaries for setting capitation rates [42 CFR 438.6(e)].
AHCCCS will utilize a national episodic/diagnostic risk adjustment model that will be applied to all prospective capitation rates for all risk groups (excluding supplemental payments and SFP). For CYE 13, the capitation rate risk adjustment factors used for CYE12 will be applied for the CYE13 capitation rates.
Prospective Capitation: The Contractor will be paid capitation for all prospective member months, including partial member months. This capitation includes the cost of providing medically necessary covered services to members during the prospective period coverage.
Prior Period Coverage (PPC) Capitation: Except for SOBRA Family Planning, KidsCare and State Only Transplants, the Contractor will be paid capitation for all PPC member months, including partial member months. This capitation includes the cost of providing medically necessary covered services, excluding most behavioral health services, to members during prior period coverage. The PPC capitation rates will be set by AHCCCS and will be paid to the Contractor along with the prospective capitation described above. The Contractor will not receive PPC capitation for newborns of members who were enrolled at the time of delivery.
Reconciliation of Prospective Costs to Reimbursement: For CYE 13, AHCCCS will reconcile the Contractor’s prospective TANF, SOBRA, SSI w/Med, SSI w/o Med, SOBRA and SOBRA Family Planning medical cost expenses to prospective net capitation paid to the Contractor for the same population for dates of service October 1, 2012 through September 30, 2013. This reconciliation will limit the Contractor’s profits and losses as follows:
82
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
|
| | | | |
| Profit | MCO Share | State Share | Max MCO Profit | |
| <= 3% | 100% | —% | 3% | |
| >3% and <= 5% | 75% | 25% | 1.5% | |
| >5% and <= 7% | 50% | 50% | 1% | |
| >7% and <= 9% | 25% | 75% | 0.5% | |
| >9% | —% | 100% | —% | |
|
| | | | |
| Loss | MCO Share | State Share | Max MCO Loss | |
| <=3% | 100% | —% | 3% | |
| >3% and <=6% | 50% | 50% | 1.5% | |
| >6% | —% | 100% | —% | |
Adjudicated encounter data will be used to determine medical expenses. Refer to the ACOM Acute Program Tiered Prospective Reconciliation Policy for further details.
Reconciliation of PPC Costs to Reimbursement: AHCCCS will reconcile the Contractor’s PPC medical cost expenses to PPC capitation paid to the Contractor during the year. This reconciliation will limit the Contractor’s profits and losses to 2%. Any losses in excess of 2% will be reimbursed to the Contractor, and likewise, profits in excess of 2% will be recouped. Adjudicated encounter data will be used to determine medical expenses. Refer to the ACOM PPC Reconciliation Policy for further details.
Reconciliation of Prospective MED Costs to Reimbursement: Coverage for this population terminates September 30, 2011. There will be no reconciliation for CYE 13.
Reconciliation of Prospective non-MED Costs to Reimbursement: For CYE 13, AHCCCS will reconcile the Contractor’s prospective non-MED medical cost expenses to prospective non-MED net capitation paid to the Contractor for dates of service during the contract year being reconciled. This reconciliation will limit the Contractor’s profits and losses to 2%. Any losses in excess of 2% will be reimbursed to the Contractor, and likewise, profits in excess of 2% will be recouped. Adjudicated encounter data will be used to determine medical expenses. Refer to ACOM Policy 301A for further details.
For CYE 13 AHCCCS will reconcile the Contractor’s prospective non-MED medical cost expenses to prospective non-MED net capitation paid to the Contractor for dates of service during the contract year being reconciled. This reconciliation will limit the Contractor’s profits and losses to 2%. Any losses in excess of 2% will be reimbursed to the Contractor, and likewise, profits in excess of 2% will be recouped. Adjudicated encounter data will be used to determine medical expenses. Refer to ACOM Policy 301A for further details.
Delivery Supplement: When the Contractor has an enrolled woman who delivers during a prospective enrollment period, the Contractor will be entitled to a supplemental payment. Supplemental payments will not apply to women who deliver in a prior period coverage time period, or State Only Transplant members. AHCCCS reserves the right at any time during the term of this contract to adjust the amount of this payment for women who deliver at home.
State Only Transplants Option 1 and Option 2: The Contractor will only be paid capitation for an administrative component for those member months the member is enrolled with the Contractor. For Option 1 members the Contractor will be paid the administrative component up to a 12-month continuous period of extended eligibility. For Option 2 members the administrative component will be paid for the period of time the transplant is scheduled or performed. All medically necessary covered services will be reimbursed 100% with no deductible through
83
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
Reinsurance payments based on adjudicated encounters. Delivery supplement payments will not apply to women who deliver during the 12 month continuous period of extended eligibility specified as Option 1.
| |
| 56. | PAYMENTS TO CONTRACTORS |
Subject to the availability of funds, AHCCCS shall make payments to the Contractor in accordance with the terms of this contract provided that the Contractor’s performance is in compliance with the terms and conditions of this contract. Payment must comply with requirements of A.R.S. Title 36. AHCCCS reserves the option to make payments to the Contractor by wire or National Automated Clearing House Association (NACHA) transfer and will provide the Contractor at least 30 days notice prior to the effective date of any such change.
Where payments are made by electronic funds transfer, AHCCCS shall not be liable for any error or delay in transfer or indirect or consequential damages arising from the use of the electronic funds transfer process. Any charges or expenses imposed by the bank for transfers or related actions shall be borne by the Contractor. Except for adjustments made to correct errors in payment, and as otherwise specified in this section, any savings remaining to the Contractor as a result of favorable claims experience and efficiencies in service delivery at the end of the contract term may be kept by the Contractor.
All funds received by the Contractor pursuant to this contract shall be separately accounted for in accordance with generally accepted accounting principles.
Except for monies received from the collection of permitted copayments and third-party liabilities, the only source of payment to the Contractor for the services provided hereunder is from funds under the control of AHCCCS. An error discovered by the State, with or without an audit, in the amount of fees paid to the Contractor will be subject to adjustment or repayment by AHCCCS making a corresponding decrease in a current Contractor’s payment or by making an additional payment to the Contractor. When the Contractor identifies an overpayment, AHCCCS must be notified and reimbursed within 30 days of identification.
No payment due the Contractor by AHCCCS may be assigned or pledged by the Contractor. This section shall not prohibit AHCCCS at its sole option from making payment to a fiscal agent hired by the Contractor.
| |
| 57. | CAPITATION ADJUSTMENTS |
Except for changes made specifically in accordance with this contract, the rates set forth in Section B shall not be subject to re-negotiation or modification during the contract period. AHCCCS may, at its option, review the effect of a program changes, legislative requirements, Contractor experience, actuarial assumptions, and/or Contractor specific capitation factors to determine if a capitation adjustment is needed. In these instances the adjustment and assumptions will be discussed with the Contractor prior to modifying capitation rates. The Contractor may request a review of a program change if it believes the program change was not equitable; AHCCCS will not unreasonably withhold such a review.
The Contractor is responsible for notifying AHCCCS of program and/or expenditure changes initiated by the Contractor during the contract period that may result in material changes to the current or future capitation rates.
Contractor Default:
If the Contractor is in any manner in default in the performance of any obligation under this contract, AHCCCS may, at its option and in addition to other available remedies, adjust the amount of payment until there is satisfactory resolution of the default.
Change in Member Status:
84
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
The Contractor shall reimburse AHCCCS and/or AHCCCS may deduct from future monthly capitation for any portion of a month during which the Contractor was not at risk due to, for example:
| |
| b. | Inmate of a public institution |
| |
| c. | Duplicate capitation to the same Contractor |
| |
| d. | Adjustment based on change in member’s contract type |
85
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
Upon becoming aware that a member may be an inmate of a public institution, the Contractor must notify AHCCCS for an eligibility determination. Notifications must be sent via email to one of the following two email addresses as applicable:
For children under age 18: DMSJUVENILEIncarceration@azahcccs.gov
For adults age 18 and older: DMSADULTIncarceration@azahcccs.gov
Notifications must include:
Contractors do not need to report members incarcerated with the Arizona Department of Corrections.
Several Counties are submitting daily files of all inmates entering their jail and all inmates released. AHCCCS will match these files against the database of active AHCCCS members. AHCCCS members who become incarcerated will be disenrolled from their Contractor and placed in a “no-pay” status for the duration of their incarceration. Contractors will see the “IE” code for ineligible associated with the disenrollment. Upon release from jail, the member will be re-enrolled with their previous Contractor. A member is eligible for covered services until the effective date of the member’s “no-pay” status.
If a member is enrolled twice with the same Contractor, recoupment will be made as soon as the double capitation is identified. AHCCCS reserves the right to modify its policy on capitation recoupments at any time during the term of this contract.
| |
| 58. | MEMBER BILLING AND LIABILITY FOR PAYMENT |
AHCCCS registered providers may charge AHCCCS members for services which are excluded from AHCCCS coverage or which are provided in excess of AHCCCS limits according to the guidelines set forth in A.A.C R9-22-702.
The Contractor must ensure that members are not held liable for:
| |
| a. | The Contractor’s or any subcontractor’s debts in the event of Contractor’s or the subcontractor’s insolvency; |
| |
| b. | Covered services provided to the member except as permitted under R9-22-702; or, |
| |
| c. | Payments to the Contractor or any subcontractors for covered services furnished under a contract, referral or other arrangement, to the extent that those payments are in excess of the amount the member would owe if the Contractor or any subcontractor provided the services directly. |
Reinsurance is a stop-loss program provided by AHCCCS to the Contractor for the partial reimbursement of covered medical services, as described in this paragraph and incurred for a member beyond an annual deductible level. AHCCCS is self-insured for the reinsurance program and is characterized by an initial deductible level and a subsequent coinsurance percentage. The coinsurance percentage is the rate at which AHCCCS will reimburse the Contractor for covered services incurred above the deductible. The deductible is the responsibility of the
86
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
Contractor. Deductible levels are subject to change by AHCCCS during the term of this contract. Any change would have a corresponding impact on capitation rates. Refer to the AHCCCS Reinsurance Processing Manual for further details on the Reinsurance Program.
The following table represents deductible and coinsurance levels. The deductible level is based on the Contractor’s statewide AHCCCS acute care enrollment (not including SOBRA Family Planning Extension services) as of October 1st each contract year, as shown in the table below. AHCCCS may adjust the Contractor’s deductible level at the beginning of a contract year if the Contractor’s enrollment changes to the next enrollment level. These deductible levels are subject to change by AHCCCS during the term of this contract. Any change in deductible levels will have a corresponding impact on capitation rates.
|
| | |
| |
Annual Deductible | |
| Statewide Plan Enrollment | Regular Reinsurance |
Coinsurance |
| 0-34,999 | $20,000 | 75% |
| 35,000-49,999 | $35,000 | 75% |
| 50,000 and over | $50,000 | 75% |
For the contract year beginning October 1, 2011, Contractors will remain at the deductible level in place as of October 1, 2010.
|
| |
| Deductible at October 1, 2010 | Deductible for October 1, 2011 |
| $20,000 | $20,000 |
| $35,000 | $35,000 |
Annual deductible levels apply to all members except for State Only Transplant and SOBRA Family Planning members. Beginning October 1, 2012, and annually thereafter, each of the deductible levels above may increase by $5,000.
PPC expenses are not covered for any members under the reinsurance program unless they qualify under catastrophic or transplant reinsurance.
Reinsurance Case Types
For all reinsurance case types, For services or pharmaceuticals, in the instances in which AHCCCS has specialty contracts or legislation/policy limits the allowable reimbursement, the amount to be used in the computation of reinsurance will be the lesser of the contracted/mandated amount or the Contractor paid amount.
Regular Reinsurance: Regular reinsurance covers partial reimbursement of covered inpatient facility medical services. This coverage applies to prospective enrollment periods. See the table above for applicable deductible levels and coinsurance percentages. The coinsurance percent is the rate at which AHCCCS will reimburse the Contractor for covered inpatient costs incurred above the deductible. The deductible is the responsibility of the Contractor. In certain situations as outlined in the AHCCCS Reinsurance Processing Manual, per diem rates paid for nursing facility services provided within 30 days of an acute hospital stay, including room and board, provided in lieu of hospitalization for up to 90 days in any contract year shall be eligible for reinsurance coverage. Same-day admit-and-discharge services do not qualify for reinsurance.
87
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
Catastrophic Reinsurance: The Catastrophic Reinsurance program encompasses members receiving certain biotech drugs (listed below), and those members diagnosed with hemophilia, and non-DDAVP responding Von Willebrand’s Disease or Gaucher’s Disease. For additional detail and restrictions refer to the AHCCCS Reinsurance Processing Manual and the AMPM. There are no deductibles for catastrophic reinsurance cases. For member’s receiving Biotech drugs outside of the specific conditions mentioned in this paragraph, AHCCCS will reimburse at 85% of the cost of the drug only. For those members diagnosed with hemophilia, Von Willebrand’s Disease and Gaucher’s Disease, all medically necessary covered services provided during the contract year shall be eligible for reimbursement at 85% of the AHCCCS allowed amount or the Contractor’s paid amount, whichever is lower, depending on the subcap code. Reinsurance coverage for anti-hemophilic blood factors will be limited to 85% of the AHCCCS contracted amount or the Contractor’s paid amount, whichever is lower. All catastrophic claims are subject to medical review by AHCCCS.
AHCCCS holds a specialty contract for anti-hemophilic agents and related services for hemophilia. The Contractor may access anti-hemophilic agents and related pharmaceutical services for hemophilia or Von Willebrand’s under the terms and conditions of the specialty contract for members enrolled in their plans. In that instance, the Contractor is the authorizing payor. As such, the Contractor will provide prior authorization, care coordination, and reimbursement for all components covered under the contract for their members. A Contractor utilizing the contract will comply with the terms and conditions of the contract. A Contractor may use the AHCCCS contract or contract with a provider of their choice.
The Contractor must notify AHCCCS, Division of Health Care Management, Medical Management Unit, of cases identified for catastrophic reinsurance coverage within 30 days of initial diagnosis and/or enrollment with the Contractor, and annually within 30 days of the beginning of each contract year. Catastrophic reinsurance will be paid for a maximum 30-day retroactive period from the date of notification to AHCCCS. The determination of whether a case or type of case is catastrophic shall be made by the Director or designee based on the following criteria; 1) severity of medical condition, including prognosis; and 2) the average cost or average length of hospitalization and medical care, or both, in Arizona, for the type of case under consideration.
Hemophilia: Catastrophic reinsurance coverage is available for all members diagnosed with Hemophilia (ICD9 codes 286.0, 286.1, 286.2).
Von Willebrand’s Disease: Catastrophic reinsurance coverage is available for all members diagnosed with von Willebrand’s Disease who are non-DDAVP responders and dependent on Plasma Factor VIII.
Gaucher’s Disease: Catastrophic reinsurance is available for members diagnosed with Gaucher’s Disease classified as Type I and are dependent on enzyme replacement therapy.
Biotech Drugs Reinsurance: Catastrophic reinsurance is available to cover the cost of certain biotech drugs when medically necessary. These drugs, collectively referred to as Biotech Drugs, are the responsibility of the Contractor unless the members is CRS enrolled, the medications are related to the management of a CRS-covered condition, and CRS is providing coverage. Catastrophic reinsurance will cover the drug cost only. Refer to the AHCCCS Reinsurance Processing Manual. The Biotech Drugs covered under reinsurance may be reviewed by AHCCCS at the start of each contract year. AHCCCS reserves the right to require the use of a generic equivalent where applicable. AHCCCS will reimburse at the lesser of the Biotech Drug or its generic equivalent for reinsurance purposes.
Transplants Reinsurance: This program covers members who are eligible to receive covered major organ and tissue transplantation. Refer to the AMPM and the AHCCCS Reinsurance Processing Manual for covered services for organ and tissue transplants. Reinsurance coverage for transplants received at an AHCCCS contracted facility is paid at the lesser of 85% of the AHCCCS contract amount for the transplantation services rendered or 85% of the Contractor’s paid amount. Reinsurance coverage for transplants received at a non-AHCCCS contracted facility
88
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
is paid the lesser of 85% of the lowest AHCCCS contracted rate, for the same organ or tissue, or the Contractor paid amount. The AHCCCS contracted transplantation rates may be found on the AHCCCS website. The Contractor must notify AHCCCS Division of Health Care Management, Medical Management Unit when a member is referred to a transplant facility for evaluation for an AHCCCS-covered organ transplant. In order to qualify for reinsurance benefits, the notification must be received by AHCCCS Medical Management Unit within 30 days of referral to the transplant facility for evaluation.
If a Contractor intends to use an out of state transplant facility for a covered transplant and AHCCCS already holds an in state contract for that transplant type, the Contractor must obtain prior approval from the AHCCCS Medical Director. If no prior approval is obtained, and the Contractor incurs costs at the out of state facility, those costs will not be eligible for either transplant or regular reinsurance.
Option 1 and Option 2 Transplant Services: Reinsurance coverage for State Only Option 1 and Option 2 members (as described in Section D, Paragraph 2, Eligibility Categories) for transplants received at an AHCCCS contracted facility is paid at the lesser of 100% of the AHCCCS contract amount for the transplantation services rendered, or the Contractor paid amount, less the transplant share of cost. For transplants received at a facility not contracted with AHCCCS, payment is made at the lesser of 100% of the lowest AHCCCS contracted amount for the transplantation services rendered, or the Contractor paid amount, less the transplant share of cost. The AHCCCS contracted transplantation rates may be found on the AHCCCS website. When a member is referred to a transplant facility for an AHCCCS-covered organ transplant, the Contractor shall notify AHCCCS, Division of Health Care Management, Medical Management Unit as specified in the AMPM Chapter 300, Policy 310 Attachments A and B.
Option 1 Non-transplant Reinsurance: All medically necessary covered services provided to Option 1 members, unrelated to the transplant, shall be eligible for reimbursement, with no deductible, at 100% of the Contractor’s paid amount based on adjudicated encounters.
Other Reinsurance: For all reinsurance case types other than transplants, the Contractor will be reimbursed 100% for all medically necessary covered expenses provided in a contract year, after the Contractor paid amount in the reinsurance case reaches $650,000. It is the responsibility of the Contractor to notify AHCCCS, Division of Health Care Management, Reinsurance Supervisor, once a reinsurance case reaches $650,000. The Contractor is required to split encounters as necessary once the reinsurance case reaches $650,000. Failure to notify AHCCCS or failure to split and adjudicate encounters appropriately within 15 months from the end date or service will disqualify the related encounters for 100% reimbursement consideration.
Encounter Submission and Payments for Reinsurance
| |
| a) | Encounter Submission: All reinsurance associated encounters, except as provided below for “Disputed Matters” must reach a clean claim status within 15 months from the end date of service, or date of eligibility posting, whichever is later. |
Disputed Matters: For encounters which are the subject of a member appeal, provider claim dispute, or other legal action, including an informal resolution originating from a request for a formal claim dispute or member appeal, the Contractor has the longer of: 1) 90 days from the date of the final decision in that proceeding/action or 2) 15 months from the end date of service/date of eligibility posting to file the reinsurance claim AND for the reinsurance claim to reach clean claim status. Therefore, reinsurance claims for disputed matters will be considered timely if the Contractor files such claims in clean claim status no later than 90 days from the date of the final decision in that proceeding/action even though the 15 month deadline has expired.
89
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
Failure to submit encounters in clean claim status within the applicable timeframes specified above will result in the denial of reinsurance. The association of an encounter to a reinsurance case does not automatically qualify the encounter for reinsurance reimbursement.
The Contractor must void encounters for any claims that are recouped in full. For recoupments that result in a reduced claim value or any adjustments that result in an increased claim value, replacement encounters must be submitted. For replacement encounters resulting in an increased claim value, the replacement encounter must reach adjudicated status within 15 months of end date of service to receive additional reinsurance benefits. The Contractor should refer to Section D, Paragraph 65, Encounter Data Reporting, for encounter reporting requirements.
| |
| b) | Payment of Regular and Catastrophic Reinsurance Cases: AHCCCS will reimburse a Contractor for costs incurred in excess of the applicable deductible level, subject to coinsurance percentages and Medicare/TPL payment, less any applicable quick pay discounts, slow payment penalties and interest. Amounts in excess of the deductible level shall be paid based upon costs paid by the Contractor, minus the coinsurance and Medicare/TPL payment, unless the costs are paid under a subcapitated arrangement. In subcapitated arrangements, AHCCCS shall base reimbursement of reinsurance encounters on the lower of the AHCCCS allowed amount or the reported health plan paid amount, minus the coinsurance and Medicare/TPL payment and applicable quick pay discounts, slow payment penalties and interest. |
When a member with an annual enrollment choice changes Contractors within a contract year, for reinsurance purposes, no costs incurred for that member follow the member to the receiving Contractor. Encounters from the Contractor the member is leaving (for dates of service within the current contract year) will not be applied toward the receiving Contractor’s deductible level. For further details regarding this policy and other reinsurance policies refer to the AHCCCS Reinsurance Processing Manual.
| |
| c) | Payment of Transplant Reinsurance Cases: Reinsurance benefits are based upon the lower of the AHCCCS contract amount or the Contractor’s paid amount, subject to coinsurance percentages. The Contractor is required to submit all supporting encounters for transplant services. Reinsurance payments are linked to transplant encounter submissions. In order to receive reinsurance payment for transplant stages, billed amounts and health plan paid amounts for adjudicated encounters must agree with related claims and/or invoices. Timeliness for each stage payment will be calculated based on the latest adjudication date for the complete set of encounters related to the stage. Please refer to the AHCCCS Reinsurance Processing Manual for the appropriate billing of transplant services. |
Reinsurance Audits
AHCCCS may, at a later date, perform medical audits on reinsurance cases. Terms of the audit process will be disclosed prior to implementation of the audits and Contractors will be given appropriate advance notice.
| |
| 60. | COORDINATION OF BENEFITS |
Pursuant to Federal and State law, AHCCCS is the payer of last resort except under limited situations. This means AHCCCS shall be used as a source of payment for covered services only after all other sources of payment have been exhausted. The Contractor shall coordinate benefits in accordance with 42 CFR 433.135 et seq., ARS 36-2903, and A.A.C. R9-22-1001 et seq. so that costs for services otherwise payable by the Contractor are cost avoided or recovered from a liable party. The term “State” shall be interpreted to mean “Contractor” for purposes of complying with the Federal regulations referenced above. The Contractor may require subcontractors to be responsible for coordination of benefits for services provided pursuant to this contract.
90
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
The two methods used in the coordination of benefits are cost avoidance and post payment recovery. The Contractor shall use these methods as described in A.A.C. R9-22-1001 et seq. and Federal and State law. See also Section D, Paragraph 60, Medicare Services and Cost Sharing.
Cost Avoidance: The Contractor shall take reasonable measures to determine all legally liable parties. This refers to any individual, entity or program that is or may be liable to pay all or part of the expenditures for covered services. The Contractor shall cost-avoid a claim if it has established the probable existence of a liable party at the time the claim is filed. Establishing liability takes place when the Contractor receives confirmation that another party is, by statute, contract, or agreement, legally responsible for the payment of a claim for a healthcare item or service delivered to a member. If the probable existence of a party’s liability cannot be established the Contractor must adjudicate the claim. The Contractor must then utilize post payment recovery which is described in further detail below. If AHCCCS determines that the Contractor is not actively engaged in cost avoidance activities the Contractor shall be subject to sanctions in an amount not less than three times the amount that could have been cost avoided.
The Contractor shall not deny a claim for timeliness if the untimely claim submission results from a provider’s efforts to determine the extent of liability.
If a third party insurer other than Medicare requires the member to pay any copayment, coinsurance or deductible, the Contractor is responsible for making these payments under the method described below, even if the services are provided outside of the Contractor network.
A. If the provider is CONTRACTED with the Contractor:
The Contractor shall pay the lesser of the difference between:
1) The Primary Insurance Paid amount and the Primary Insurance rate, i.e., the member’s copayment required under the Primary Insurance
OR
2) The Primary Insurance Paid amount and the Contractor’s Contracted Rate
The lesser of methodology applies unless the Contractor’s contract with the provider requires a different payment scheme.
B. If the provider is NOT CONTRACTED with the Contractor:
The Contractor shall pay the lesser of the difference between:
1) The Primary Insurance Paid amount and the Primary Insurance Rate, i.e., the member’s copayment required under the Primary Insurance
OR
2) The Primary Insurance Paid amount and the AHCCCS Fee for Service Rate
Examples
91
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
|
| |
| | |
| Scenario 1 | |
| AHCCCS FFS Rate $50 | |
| Contractor Rate $55 | |
| Primary Insurance Rate $45 | |
| Primary Paid $30 | |
| | |
| Contractor Payment to Contracted Provider in this example | $15 (this is calculated from the lesser of: $45-$30 vs. $55 - $30) |
| Contractor Payment to Non Contracted Provider in this example | $15 (this is calculated from the lesser of: $45-30 vs. $50-30) |
92
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
|
| |
| | |
| Scenario 2 | |
| AHCCCS FFS Rate $50 | |
| Contractor Rate $55 | |
| Primary Insurance Rate $60 | |
| Primary Paid $40 | |
| | |
| Contractor Payment to Contracted Provider in this example | $15 (this is calculated from the lesser of: $60 - $40 vs. $55-$40) |
| Contractor Payment to Non Contracted Provider in this example | $10 (this is calculated from the lesser of: $60-$40 vs. $50-$40) |
| | |
| Scenario 3 | |
| AHCCCS FFS Rate $50 | |
| Contractor Rate $55 | |
| Primary Insurance Rate $70 | |
| Primary Paid $60 | |
| | |
| Contractor Payment to Contracted Provider in this example | $0 (this is calculated from the lesser of: $70 - $60 vs. $55-$60) |
| Contractor Payment to Non Contracted Provider in this example? | $0 (this is calculated from the lesser of: $70-$60 vs. $50-$60) |
If the Contractor refers the member for services to a third-party insurer, other than Medicare, and the insurer requires payment in advance of all copayments, coinsurance and deductibles, the Contractor must make such payments in advance.
Members with CRS condition: A member with private insurance or Medicare coverage is not required to utilize CRS. This includes members with Medicare whether they are enrolled in Medicare FFS or a Medicare Managed Care Plan. If the member uses the private insurance network for a CRS-covered condition, the Contractor is responsible for all applicable deductibles and copayments. If the member has Medicare coverage, the ACOM Policy 201 and Policy 202 shall apply. When the private insurance or Medicare is exhausted, or certain annual or lifetime limits are reached with respect to CRS-covered conditions, the Contractor shall refer the member to CRS for determination of eligibility. If the member with private insurance or Medicare chooses to enroll with CRS, CRS becomes the secondary payer responsible for all applicable deductibles and copayments. The Contractor is not responsible to provide services in instances when a member with a CRS covered condition who has no primary insurance or Medicare, refuses to participate in the CRS application process, or refuses to receive CRS covered services through the CRS program. The member may be billed by the provider in accordance with AHCCCS regulations regarding billing for unauthorized services.
Post-payment Recoveries: Post-payment recovery is necessary in cases where the Contractor has not established the probable existence of a liable party at the time services were rendered or paid for, or was unable to cost-avoid. The following sections set forth requirements for Contractor recovery actions including recoupment activities, other recoveries and total plan case requirements.
Recoupments: The Contractor must follow the protocols established in the ACOM Policy 412 . The Contractor must void encounters for claims that are recouped in full. For recoupments that result in an adjusted claim value, the Contractor must submit replacement encounters.
93
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
Other Recoveries: The Contractor shall identify the existence of potentially liable parties through the use of trauma code edits, utilizing diagnostic codes 800 to 999.9 (excluding code 994.6) external causes of injury codes E000 through E999, and other procedures. The Contractor shall not pursue recovery in the following circumstances, unless the case has been referred to the Contractor by AHCCCS or AHCCCS’ authorized representative:
|
| |
| Uninsured/underinsured motorist insurance | Restitution Recovery |
| First-and third-party liability insurance | Worker’s Compensation |
| Tort feasors, including casualty | Estate Recovery |
| Special Treatment Trust Recovery | |
Upon identification of any of the above situations, the Contractor shall promptly report any cases involving the above circumstances to AHCCCS’ authorized representative for determination of a “total plan” case. A total plan case is a case where payments for services rendered to the member are exclusively the responsibility of the Contractor; no reinsurance or fee-for-service payments are involved. By contrast, a “joint” case is one where fee-for-service payments and/or reinsurance payments are involved. In joint cases, the Contractor shall notify AHCCCS’ authorized representative within 10 business days of the identification of a liable party case with reinsurance or fee-for-service payments made by AHCCCS. Failure to report these cases may result in one of the remedies specified in Section D, Paragraph 72, Sanctions. The Contractor shall cooperate with AHCCCS’ authorized representative in all collection efforts.
Total Plan Case Requirements: In “total plan” cases, the Contractor is responsible for performing all research, investigation, the mandatory filing of initial liens on cases that exceed $250, lien amendments, lien releases, and payment of other related costs in accordance with A.R.S. 36-2915 and A.R.S. 36-2916. The Contractor shall use the AHCCCS-approved casualty recovery correspondence when filing liens and when corresponding to others in regard to casualty recovery. The Contractor may retain up to 100% of its recovery collections if all of the following conditions exist:
| |
| a. | Total collections received do not exceed the total amount of the Contractor’s financial liability for the member; |
| |
| b. | There are no payments made by AHCCCS related to fee-for-service, reinsurance or administrative costs (i.e., lien filing , etc.); and, |
| |
| c. | Such recovery is not prohibited by state or Federal law. |
Prior to negotiating a settlement on a total plan case, the Contractor shall notify AHCCCS to ensure that there is no reinsurance or fee-for-service payment that has been made by AHCCCS. Failure to report these cases prior to negotiating a settlement amount may result in one of the remedies specified in Section D, Paragraph 72, Sanctions.
Total Plan Cases: The Contractor shall report settlement information to AHCCCS, utilizing the AHCCCS-approved casualty recovery Notification of Settlement form, within 10 business days from the settlement date. Failure to report these cases may result in one of the remedies specified in Section D, Paragraph 72, Sanctions.
Joint Cases: AHCCCS’ authorized representative is responsible for performing all research, investigation and payment of lien-related costs, subsequent to the referral of any and all relevant case information to AHCCCS’ authorized representative by the Contractor. In joint cases, AHCCCS’ authorized representative is also responsible for negotiating and acting in the best interest of all parties to obtain a reasonable settlement and may compromise a settlement in order to maximize overall reimbursement, net of legal and other costs. The Contractor will be responsible for their prorated share of the contingency fee. The Contractor’s share of the contingency fee will be deducted from the settlement proceeds prior to AHCCCS remitting the settlement to the Contractor.
94
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
Other Reporting Requirements:
If a Contractor discovers the probable existence of a liable party that is not known to AHCCCS, or any change in coverage, the Contractor must report the information to the AHCCCS contracted vendor not later than 10 days from the date of discovery. Notification by the Contractor must occur electronically through the Third Party Leads submission process. Refer to AHCCCS Technical Interface Guidelines at:
http://www.azahcccs.gov/commercial/ContractorResources/manuals/TIG/HealthPlan/TPLleads.aspx.
Failure to report these cases may result in one of the remedies specified in Section D, Paragraph 72, and Sanctions.
Upon AHCCCS’ request, the Contractor shall provide an electronic extract of the Casualty cases, including open and closed cases. Data elements include, but are not limited to: the member’s first and last name; AHCCCS ID; date of incident; claimed amount; paid/recovered amount; and case status. The AHCCCS TPL Section shall provide the format and reporting schedule for this information to the Contractor. AHCCCS will provide the Contractor with a file of all other coverage information, for the purpose of updating the Contractor’s files, as described in the AHCCCS Technical Interface Guidelines.
Title XXI (KidsCare), BCCTP, and SOBRA Family Planning: Eligibility for KidsCare, BCCTP, and SOBRA Family Planning benefits require that the applicant/member not be enrolled with any other creditable health insurance plan. If the Contractor becomes aware of any such coverage, the Contractor shall notify AHCCCS immediately. AHCCCS will determine if the other insurance meets the creditable coverage definition in A.R.S. 36-2982(G).
Cost Avoidance/Recovery Report:
The Contractor shall report on a quarterly basis a summary of their cost avoidance/recovery activity. The report shall be submitted in a format as specified in the AHCCCS Program Integrity Reporting Guide.
Contract Termination: Upon termination of this contract, the Contractor will complete the existing third party liability cases or make any necessary arrangements to transfer the cases to AHCCCS’ authorized TPL representative.
The Contractor is required to apply copayments as per ACOM Policy 431 and other direction by AHCCCS. Most of the AHCCCS members remain exempt from copayments while others are subject to optional or mandatory copayments. Those populations exempt or subject to optional copayments may not be denied services for the inability to pay the copayment [42 CFR 438.108]. However, for those populations subject to mandatory copayments services may be denied for the inability to pay the copayment.
| |
| 62. | MEDICARE SERVICES AND COST SHARING |
AHCCCS has members enrolled who are eligible for both Medicaid and Medicare. These members are referred to as “dual eligibles”. Generally, Contractors are responsible for payment of Medicare coinsurance and/or deductibles for covered services provided to dual eligible members within the Contractor’s network. However, there are different cost-sharing responsibilities that apply to dual eligible members based on a variety of factors. Unless prior approval is obtained from AHCCCS, the Contractor must limit their cost sharing responsibility according to ACOM Policy 201 and Policy 202. Contractors shall have no cost sharing obligation if the Medicare payment exceeds what the Contractor would have paid for the same service of a non-Medicare member. Please refer to Section D, Paragraph 10, Scope of Services, for information regarding prescription medication for Medicare Part D.
95
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
Dual eligible members shall have choice of all providers in the network and shall not be restricted to those that accept Medicare.
When a person with Medicare who is also eligible for Medicaid (dual eligible) is in a medical institution that is funded by Medicaid for a full calendar month, the dual eligible person is not required to pay copayments for their Medicare covered prescription medications for the remainder of the calendar year To ensure appropriate information is communicated for these members to the Centers for Medicare and Medicaid Services (CMS), the Contractor must, using the approved form, notify the AHCCCS Member Database Management Administration (MDMA), via fax at (602) 253-4807 as soon as it determines that a dual eligible person is expected to be in a medical institution that is funded by Medicaid for a full calendar month, regardless of the status of the dual eligible person’s Medicare lifetime or annual benefits. This includes:
| |
| a. | Members who have Medicare part “B” only; |
| |
| b. | Members who have used their Medicare part “A” life time inpatient benefit; |
| |
| c. | Members who are in a continuous placement in a single medical institution or any combination of continuous placements in a medical institution. |
For purposes of the medical institution notification, medical institutions are defined as acute hospitals, psychiatric hospital – Non IMD, psychiatric hospital – IMD, residential treatment center – Non IMD, residential treatment center – IMD, skilled nursing facilities, and Intermediate Care Facilities for persons with intellectual disabilities.
The Contractor shall submit all proposed marketing and outreach materials and events that will involve the general public to the AHCCCS Marketing Committee for prior approval in accordance with the AHCCCS Rules and the ACOM Policy 101, a copy of which is available on the AHCCCS Website www.azahcccs.gov [42 CFR 438.104]. The Contractor must have signed contracts with hospitals, PCPs, specialists, pharmacies, dentists, and pharmacies in order for them to be included in marketing materials. Marketing materials that have received prior approval must be resubmitted to the Division of Health Care Management every two years for re-approval.
In accordance with A.R.S. Section 36-2918.01, and AHCCCS Contractor Operation Manual (ACOM), Chapter 100, Contractors and their subcontractors and providers are required to immediately notify the AHCCCS Office of Inspector General (OIG) regarding any suspected fraud or abuse [42 CFR 455.17] The Contractor agrees to immediately (within 10 business days of discovery) inform the OIG in writing of instances of suspected fraud or abuse [42 CFR 455.1(a)(1)] by completing the confidential AHCCCS Referral for Preliminary Investigation form. This shall include acts of suspected fraud or abuse that were resolved internally but involved AHCCCS funds, contractors, or subcontractors.
As stated in A.R.S. Section 13-2310, incorporated herein by reference, any person who knowingly obtains any benefit by means of false or fraudulent pretenses, representations, promises, or material omissions is guilty of a Class 2 felony.
The Contractor agrees to permit and cooperate with any onsite review. A review by the OIG may be conducted without notice and for the purpose of ensuring program compliance. The Contractor also agrees to respond to electronic, telephonic or written requests for information within the timeframe specified by AHCCCS. The Contractor agrees to provide documents, including original documents, to representatives of the OIG upon request.
96
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
The OIG shall allow a reasonable time for the Contractor to copy the requested documents, not to exceed 20 business days from the date of the OIG request.
The Contractor shall be in compliance with 42 CFR 438.608. The Contractor must have a mandatory compliance program, supported by other administrative procedures, that is designed to guard against fraud and abuse. The Contractor shall have written criteria for selecting a Compliance Officer and job description that clearly outlines the responsibilities and authority of the position. The Compliance Officer shall have the authority to assess records and independently refer suspected member fraud, provider fraud and member abuse cases to the OIG or other duly authorized enforcement agencies.
The compliance program shall be designed to both prevent and detect suspected fraud or abuse. The compliance program must include:
| |
| 1. | Written policies, procedures, and standards of conduct that articulates the organization’s commitment to and processes for complying with all applicable Federal and State standards. |
| |
| 2. | The written designation of a compliance committee who are accountable to the Contractor’s top management. |
| |
| 3. | The Compliance Officer must be an onsite management official who reports directly to the Contractor’s top management. Any exceptions must be approved by AHCCCS. |
| |
| 4. | Effective training and education. |
| |
| 5. | Effective lines of communication between the compliance officer and the organization’s employees. |
| |
| 6. | Enforcement of standards through well-publicized disciplinary guidelines. |
| |
| 7. | Provision for internal monitoring and auditing. |
| |
| 8. | Provision for prompt response to problems detected. |
| |
| 9. | A Compliance Committee which shall be made up of, at a minimum, the Compliance Officer, a budgetary official and other executive officials with the authority to commit resources. The Compliance Committee will assist the Compliance Officer in monitoring, reviewing and assessing the effectiveness of the compliance program and timeliness of reporting. |
| |
| 10. | Pursuant to the Deficit Reduction Act of 2005 (DRA), Contractors, as a condition for receiving payments shall establish written policies for employees detailing: |
a. The Federal False Claims Act provisions;
b. The administrative remedies for false claims and statements;
c. Any state laws relating to civil or criminal penalties for false claims and statements;
d. The whistleblower protections under such laws.
11. The Contractor must establish a process for training existing staff and new hires on the compliance program and on the items in section 10. All training must be conducted in such a manner that can be verified by AHCCCS.
12. The Contractor must require, through documented policies and subsequent contract amendments, that providers train their staff on the following aspects of the Federal False Claims Act provisions:
a. The administrative remedies for false claims and statements;
b. Any state laws relating to civil or criminal penalties for false claims and statements;
c. The whistleblower protections under such laws.
| |
| 13. | The Contractor must notify AHCCCS of any CMS compliance issues related to HIPAA transaction and code set complaints or sanctions. |
Once the Contractor has referred a suspected case of fraud or abuse to AHCCCS, the Contractor shall take no action to recoup or otherwise offset any suspected overpayments until AHCCCS provides written notice to the Contractor that the fraud or abuse case has been closed or otherwise dispositioned. At that time, and after conducting a cost benefit analysis to determine if such action is warranted, the Contractor should attempt to recover any overpayments identified. The OIG shall be advised of the final disposition of the research and advised of actions, if any, taken by the Contractor.
97
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
In addition the Contractor must furnish to AHCCCS or CMS within 35 days of receiving the request, full and complete information, pertaining to business transactions (42 CFR 455.105):
| |
| • | The ownership of any subcontractor with whom the Contractor has had business transaction totaling more than $25,000 during the two month period ending on the date of request; and |
| |
| • | Any significant business transactions between the Contractor and wholly owned supplier, or between the Contractor and any subcontractor ending on the date of the request. |
In the event that AHCCCS-OIG, either through a civil monetary penalty, a global civil settlement or judgment, or any other form of civil action, receives a monetary recovery from an entity, the entirety of such monetary recovery belongs exclusively to AHCCCS and the Contractor has no claim to any portion of this recovery. Furthermore, the Contractor is fully subrogated to AHCCCS for all civil recoveries.
Disclosure on Ownership Information and Control (42 CFR 455.104)(SMDL09-001)
| |
| A. | The Contractor must provide the following information to AHCCCS: |
| |
| 1. | (a) The Name and Address of any person (individual or corporation) with an ownership or control interest in the Contractor. The address for corporate entities must include as applicable primary business address, every business location, and P.O. Box address; |
(b) The Date of Birth and Social Security Numbers of any person with an ownership or control interest in the Contractor;
(c) The Tax Identification Number of any corporation with an ownership or control interest in the Contractor;
| |
| 2. | Whether the person (individual or corporation) with an ownership or control interest in the Contractor is related to another person with ownership or control interest in the Contractor as a spouse, parent, child, or sibling; or whether the person (individual or corporation) with an ownership or control interest in any subcontractor of the Contractor has a 5% or more interest is related to another person with ownership or control interest in the Contractor as a spouse, parent, child, or sibling; |
| |
| 3. | The name of any other disclosing entity as defined in 42 CFR 455.101 in which an owner of the Contractor has an ownership or control interest; |
| |
| 4. | The Name, Address, Date of Birth and Social Security Number of any managing employee of the Contractor as defined in 42 CFR 455.101. |
The Contractor shall provide the above-listed information to AHCCCS at any of the following times:
| |
| 1. | Upon the Contractor submitting the proposal in accordance with the State’s procurement process; |
| |
| 2. | Upon the Contractor executing the contract with the State; |
| |
| 3. | Upon renewal or extension of the contract; |
| |
| 4. | Within 35 days after any change in ownership of the Contractor. |
| |
| B. | The Contractor shall also, with regard to its subcontracted providers and fiscal agents, obtain the following information regarding ownership and control: |
98
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
1.(a) The Name and Address of any person (individual or corporation) with an ownership or control interest in the subcontracted Provider or Fiscal Agent. The address for corporate entities must include as applicable primary business address, every business location, and P.O. Box address;
(b) The Date of Birth and Social Security Numbers of any person with an ownership or control interest in the subcontracted provider or fiscal agent;
| |
| (c) | The Tax Identification Number of any corporation with an ownership or control interest in the subcontracted provider or fiscal agent; |
| |
| 2. | Whether the person (individual or corporation) with an ownership or control interest in the subcontracted provider or fiscal agent is related to another person with ownership or control interest in the subcontracted provider or fiscal agent as a spouse, parent, child, or sibling; or whether the person (individual or corporation) with an ownership or control interest in any subcontractor of the subcontracted provider or fiscal agent has a 5% or more interest is related to another person with ownership or control interest in the subcontracted provider or fiscal agent as a spouse, parent, child, or sibling; |
| |
| 3. | The name of any other disclosing entity as defined in 42 CFR 455.101 in which an owner of the subcontracted provider or fiscal agent has an ownership or control interest; |
| |
| 4. | The Name, Address, Date of Birth and Social Security Number of any managing employee of the subcontracted provider or fiscal agent as defined in 42 CFR 455.101. |
Disclosure of Information on Persons Convicted of Crimes (42 CFR 455.101; 106; 436) (SMDL09-001)
The Contractor must identify all persons associated with the Contractor and its subcontracted providers and fiscal agents with an ownership or control interest or managing employee interest and determine if they have been convicted of a criminal offense related to that person’s involvement in any program under Medicare, Medicaid, or the Title XX services program. The Contractor shall, on a monthly basis, confirm the identity and determine the exclusion status through routine checks of:
A. Social Security Administration DEATH MASTER FILE
B. The National Plan and Provider Enumeration System (NPPES)
C. The List of Excluded Individuals (LEIE)
D. The Excluded Parties List (EPLS)
E. Any other databases directed by AHCCCS or CMS
The Contractor must immediately notify AHCCCS of any person who has been excluded through these checks.
The results of the Disclosure on Ownership Information and Control and the Disclosure of Information on Persons Convicted of Crimes shall be held by the Contractor. The Contractor shall submit an annual attestation that the above-listed information has been requested and obtained from its contracted providers and fiscal agents. Refer to Attachment F, Chart of Deliverables for further information. Upon request, the Contractor shall provide AHCCCS with the above-listed information.
The Contractor shall maintain records relating to covered services and expenditures including reports to AHCCCS and documentation used in the preparation of reports to AHCCCS. The Contractor shall comply with all specifications for record keeping established by AHCCCS. All records shall be maintained to the extent and in such detail as required by AHCCCS Rules and policies. Records shall include but not be limited to financial
99
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
statements, records relating to the quality of care, medical records, prescription files and other records specified by AHCCCS.
The Contractor agrees to make available, at all reasonable times during the term of this contract, any of its records for inspection, audit or reproduction by any authorized representative of AHCCCS, State or Federal government. The Contractor shall be responsible for any costs associated with the reproduction of requested information.
The Contractor shall preserve and make available all records for a period of five years from the date of final payment under this contract.
HIPAA related documents must be retained for a period of six years per 45 CFR 164.530(j)(2).
If this contract is completely or partially terminated, the records relating to the work terminated shall be preserved and made available for a period of five years from the date of any such termination. Records which relate to grievances, disputes, litigation or the settlement of claims arising out of the performance of this contract, or costs and expenses of this contract to which exception has been taken by AHCCCS, shall be retained by the Contractor for a period of five years after the date of final disposition or resolution thereof.
| |
| 66. | DATA EXCHANGE REQUIREMENTS |
The Contractor is authorized to exchange data with AHCCCS relating to the information requirements of this contract and as required to support the data elements to be provided to AHCCCS in the formats prescribed by AHCCCS, which include formats prescribed by the Health Insurance Portability and Accountability Act (HIPAA). Details for the formats may be found in the HIPAA Transaction Companion Guides & Trading Partner Agreements, the AHCCCS Encounter Manual and in the AHCCCS Technical Interface Guidelines, available on the AHCCCS website.
The information so recorded and submitted to AHCCCS shall be in accordance with all procedures, policies, Rules, or statutes in effect during the term of this contract. If any of these procedures, policies, Rules, regulations or statutes are hereinafter changed, both parties agree to conform to these changes following appropriate notification by AHCCCS.
The Contractor is responsible for any incorrect data, delayed submission or payment (to the Contractor or its subcontractors), and/or penalty applied due to any error, omission, deletion, or erroneous insert caused by Contractor-submitted data. Any data that does not meet the standards required by AHCCCS shall not be accepted by AHCCCS.
The Contractor is responsible for identifying any inconsistencies immediately upon receipt of data from AHCCCS. If any unreported inconsistencies are subsequently discovered, the Contractor shall be responsible for the necessary adjustments to correct its records at its own expense.
The Contractor shall accept from AHCCCS original evidence of eligibility and enrollment in a form appropriate for electronic data exchange. Upon request by AHCCCS, the Contractor shall provide to AHCCCS updated date-sensitive PCP assignments in a form appropriate for electronic data exchange.
The Contractor shall be provided with a Contractor-specific security code for use in all data transmissions made in accordance with contract requirements. Each data transmission by the Contractor shall include the Contractor's security code. The Contractor agrees that by use of its security code, it certifies that any data transmitted is accurate and truthful, to the best of the Contractor's Chief Executive Officer, Chief Financial Officer or designee’s knowledge [42 CFR 438.606]. The Contractor further agrees to indemnify and hold harmless the State of Arizona and AHCCCS from any and all claims or liabilities, including but not limited to consequential damages,
100
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
reimbursements or erroneous billings and reimbursements of attorney fees incurred as a consequence of any error, omission, deletion or erroneous insert caused by the Contractor in the submitted input data. Neither the State of Arizona nor AHCCCS shall be responsible for any incorrect or delayed payment to the Contractor’s AHCCCS services providers (subcontractors) resulting from such error, omission, deletion, or erroneous input data caused by the Contractor in the submission of AHCCCS claims.
The costs of software changes are included in administrative costs paid to the Contractor. There is no separate payment for software changes. A PMMIS systems contact will be assigned after contract award. AHCCCS will work with the Contractor as they evaluate Electronic Data Interchange options.
Health Insurance Portability and Accountability Act (HIPAA):
The Contractor shall comply with the Administrative Simplification requirements of Subpart F of the HIPAA of 1996 (Public Law 107-191, 110 Statutes 1936) and all Federal regulations implementing that Subpart that are applicable to the operations of the Contractor by the dates required by the implementing Federal regulations as well as all subsequent requirements and regulations as published.
HIPAA Privacy and Security:
The Contractor is required to a have HIPAA security audit performed by an independent third party. The initial audits must be conducted at contract award (prior to the first exchange of AHCCCS data) and annually thereafter, and must include a review of Contractor compliance with all security and privacy requirements. The annual audit report must be submitted to AHCCCS within 90 days of the start of the contract year.
The audit must include a review of Contractor policies and procedures to verify that appropriate security and privacy requirements have been adequately incorporated into the Contractors business practices, and the use of automated and/or manual scans of the production processing systems to validate compliance.
The audit must result in a findings report and as necessary a remediation plan, detailing all issues and discrepancies between the security requirements and the Contractors policies, practices and systems. The remediation plan must also include timelines for corrective actions related to all issues or discrepancies identified. The findings report and remediation plan must be submitted to AHCCCS for review and approval. AHCCCS will verify that the required audit has been completed and the appropriate approved remediation plans are in place and being followed as part of Operational and Financial Reviews.
| |
| 67. | ENCOUNTER DATA REPORTING |
Encounter Submissions
Complete, accurate and timely reporting of encounter data is crucial to the success of the AHCCCS program. AHCCCS uses encounter data to pay reinsurance benefits, set fee-for-service and capitation rates, determine reconciliation amounts, determine disproportionate share payments to hospitals, and to determine compliance with performance standards. The Contractor shall submit encounter data to AHCCCS for all services for which the Contractor incurred a financial liability and claims for services eligible for processing by the Contractor where no financial liability was incurred including services provided during prior period coverage. This requirement is a condition of the CMS grant award [42 CFR 438.242(b)(1)][42 CFR 455.1 (a)(2)].
A Contractor shall prepare, review, verify, certify, and submit, encounters for consideration to AHCCCS. Upon submission, the Contractor certifies that the services listed were actually rendered. The encounters must be submitted in the format prescribed by AHCCCS.
Encounter data must be provided to AHCCCS as outlined in the X12 and NCPDP Transaction Companion Guides & Trading Partner Agreements and the AHCCCS Encounter Manual and should be received by AHCCCS no later than 240 days after the end of the month in which the service was rendered, or the effective date of the enrollment
101
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
with the Contractor, whichever date is later. Requirements for encounter data are described in the AHCCCS Encounter Manual and the AHCCCS Encounter Companion Guides.
To support Federal Drug Rebate processing, pharmacy related encounter data must be provided to AHCCCS no later than 30 days after the end of the quarter in which the pharmaceutical item was dispensed. For the purposes of this requirement, pharmacy encounter data is defined as retail pharmacy encounters until such time AHCCCS expands Federal Drug Rebate processing to include all other pharmaceuticals reported on professional and outpatient facility encounters.
The Contractor will be assessed sanctions for noncompliance with encounter submission requirements.
Encounter Reporting
The Contractor must produce reports for the purposes of tracking, trending, reporting process improvement and monitoring submissions of encounters and encounter revisions. The Contractor will submit these reports to AHCCCS as required per the AHCCCS Encounter Manual.
At least twice each month, AHCCCS provides the Contractor with full replacement files containing provider and medical coding information. These files should be used by the Contractor to ensure accurate Encounter Reporting. Refer to the AHCCCS Encounter Manual for further information.
Encounter Corrections
Contractors are required to monitor and resolve pended encounters, encounters denied by AHCCCS, and encounters voided and voided/replaced. AHCCCS has established encounter performance standards as detailed in the AHCCCS Encounter Manual. In addition to adjudicated approved encounters, pended, denied and voided encounters affect completeness, accuracy and timeliness rates. Rates below the established standards (pended encounters that have pended for more than 120 days), or poor encounter performance overall, may result in Corrective Action Plans and/or sanctions.
Contractors are required to submit replacement or voided encounters in the event that claims are subsequently corrected following the initial encounter submission. This includes corrections as a result of inaccuracies identified by fraud and abuse audits or investigations conducted by AHCCCS or the Contractor. The Contractor must void encounters for claims that are recouped in full. For recoupments that result in a reduced claim value or adjustments that result in an increased claim value, replacement encounters must be submitted. For those recoupments requiring approval from AHCCCS, replacement encounters must be submitted within 120 days of the recoupment approval from AHCCCS. Refer to the AHCCCS Encounter Manual for instructions regarding the submission of corrected encounters.
Encounter Validation Studies
Per the CMS requirement, AHCCCS will conduct encounter validation studies of the Contractor’s encounter submissions, and may sanction the Contractor and/or require a corrective action plan for noncompliance with encounter submission requirements. The purpose of encounter validation studies is to compare recorded utilization information from a medical record or other source with the Contractor’s submitted encounter data. Any and all covered services may be validated as part of these studies. The criteria used in encounter validation studies may include timeliness, correctness and omission of encounters. Refer to the AHCCCS Data Validation Technical Document for further information.
AHCCCS may revise study methodology, timelines, and sanction amounts based on agency review or as a result of consultations with CMS. The Contractor will be notified in writing of any significant change in study methodology.
102
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
| |
| 68. | ENROLLMENT AND CAPITATION TRANSACTION UPDATES |
AHCCCS produces daily enrollment transaction updates identifying new members and changes to existing members' demographic, eligibility and enrollment data, which the Contractor shall use to update its member records. The daily enrollment transaction update, that is run immediately prior to the monthly enrollment and capitation transaction, is referred to as the "last daily" and will contain all rate code changes made for the prospective month, as well as any new enrollments and disenrollments as of the 1st of the prospective month.
AHCCCS also produces a daily Manual Payment Transaction, which identifies enrollment or disenrollment activity that was not included on the daily enrollment transaction update due to internal edits. The Contractor shall use the Manual Payment Transaction in addition to the daily enrollment transaction update to update its member records.
A weekly capitation transaction will be produced to provide the Contractor with member-level capitation payment information. This file will show changes to the prospective capitation payments, as sent in the monthly file, resulting from enrollment changes that occur after the monthly file is produced. This file will also identify mass adjustments to and/or manual capitation payments that occurred at AHCCCS after the monthly file is produced.
On a monthly basis AHCCCS provides the Contractor with an electronic file of all Acute members who must complete a review of their eligibility in order to maintain enrollment with the Contractor. AHCCCS strongly encourages the Contractor to utilize this file to support member retention efforts.
The monthly enrollment and monthly capitation transaction updates are generally produced two days before the end of every month. The update will identify the total active population for the Contractor as of the first day of the next month. These updates contain the information used by AHCCCS to produce the monthly capitation payment for the next month. The Contractor must reconcile their member files with the AHCCCS monthly update. After reconciling the monthly update information, the Contractor will record the results of the reconciliation, which will be made available upon request, and will resume posting daily updates beginning with the last two days of the month. The last two daily updates are different from the regular daily updates in that they pay and/or recoup capitation into the next month. If the Contractor detects an error through the monthly update process, the Contractor shall notify AHCCCS, Information Services Division.
Refer to Section D, Paragraph 64, Data Exchange Requirements, for further information.
| |
| 69. | PERIODIC REPORT REQUIREMENTS |
AHCCCS, under the terms and conditions of its CMS grant award, requires periodic reports, encounter data and other information from the Contractor. The submission of late, inaccurate, or otherwise incomplete reports shall constitute failure to report subject to the penalty provisions described in Section D, Paragraph 72, Sanctions and Attachment F, Periodic Report Requirements.
Standards applied for determining adequacy of required reports are as follows [42 CFR 438.242(b)(2)]:
| |
| a. | Timeliness: Reports or other required data shall be received on or before scheduled due dates. |
| |
| b. | Accuracy: Reports or other required data shall be prepared in strict conformity with appropriate authoritative sources and/or AHCCCS defined standards. |
| |
| c. | Completeness: All required information shall be fully disclosed in a manner that is both responsive and pertinent to report intent with no material omissions. |
103
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
The Contractor shall comply with all reporting requirements contained in this contract. AHCCCS requirements regarding reports, report content and frequency of submission of reports are subject to change at any time during the term of the contract. The Contractor shall comply with all changes specified by AHCCCS. The Contractor shall be responsible for continued reporting beyond the term of the contract.
| |
| 70. | REQUESTS FOR INFORMATION |
AHCCCS may, at any time during the term of this contract, request financial or other information from the Contractor. Responses shall fully disclose all financial or other information requested. Information may be designated as confidential but may not be withheld from AHCCCS as proprietary. Information designated as confidential may not be disclosed by AHCCCS without the prior written consent of the Contractor except as required by law. Upon receipt of such requests for information, the Contractor shall provide complete information to AHCCCS as requested no later than 30 days after the receipt of the request unless otherwise specified in the request itself.
If the Contractor believes the requested information is confidential and may not be disclosed to third parties, the Contractor shall provide a detailed statement to AHCCCS, within the timeframe designated by AHCCCS, setting forth the reasons why the information is confidential and describing the specific harm or injury that would result from disclosure. In the event that AHCCCS withholds information from a third party as a result of the Contractor's statement, the Contractor shall be responsible for all costs associated with the nondisclosure, including but not limited to legal fees and costs.
| |
| 71. | DISSEMINATION OF INFORMATION |
Upon request, the Contractor shall assist AHCCCS in the dissemination of information prepared by AHCCCS or the Federal government to its members. The cost of such dissemination shall be borne by the Contractor. All advertisements, publications and printed materials that are produced by the Contractor and refer to covered services shall state that such services are funded under contract with AHCCCS.
| |
| 72. | OPERATIONAL AND FINANCIAL READINESS REVIEWS |
AHCCCS may conduct Operational and Financial Readiness Reviews on the Contractor and will, subject to the availability of resources, provide technical assistance as appropriate. The Readiness Review will be conducted prior to the start of business. The purpose of a Readiness Review is to assess Contractor’s readiness and ability to provide covered services to members at the start of the contract year. The Contractor will be permitted to commence operations only if the Readiness Review factors are met to AHCCCS' satisfaction.
| |
| 73. | OPERATIONAL AND FINANCIAL REVIEWS |
In accordance with CMS requirements, AHCCCS Rule 9 A.A.C.22 Article 5, AHCCCS, or an independent agent, will conduct periodic operational and financial reviews for the purpose of (but not limited to) identifying best practices and ensuring program compliance [42 CFR 438.204]. The type and duration of the review will be solely at the discretion of AHCCCS. The reviews will identify areas where improvements can be made and make recommendations accordingly, monitor the Contractor's progress towards implementing mandated programs and provide the Contractor with technical assistance if necessary.
Except in cases where advance notice is not possible or advance notice may render the review less useful, AHCCCS will give the Contractor at least three weeks advance notice of the date of the scheduled Operational and Financial
104
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
Review. AHCCCS reserves the right to conduct reviews without notice. AHCCCS may conduct a review without notice in the event the Contractor undergoes a merger, reorganization, changes ownership or makes changes in three or more key staff positions within a 12-month period, or to investigate complaints received by AHCCCS. The Contractor shall comply with all other medical audit provisions as required by AHCCCS.
AHCCCS may request, at the expense of the Contractor, to conduct on-site reviews of functions performed at out of state locations. AHCCCS will coordinate travel arrangements and accommodations with the Contractor at their request.
In preparation for the reviews, the Contractor shall cooperate fully with AHCCCS and the AHCCCS Review Team by forwarding in advance such policies, procedures, job descriptions, contracts, records, logs and other material that AHCCCS may request. Any documents not requested in advance by AHCCCS shall be made available upon request of the Review Team during the course of the review. Contractor personnel as identified in advance shall be available to the Review Team at all times during AHCCCS review activities. Should the review be conducted on-site, the Contractor shall provide the Review Team with appropriate workspace, access to a telephone, electrical outlets, internet access and privacy for conferences.
The Contractor will be furnished a copy of the draft Operational and Financial Review report and given an opportunity to comment on any review findings prior to AHCCCS issuing the final report. Recommendations, made by the Review Team to bring the Contractor into compliance with Federal, State, AHCCCS, and/or contract requirements, must be implemented by the Contractor. Modifications to the corrective action plan must be approved in advance by AHCCCS. Unannounced follow-up reviews may be conducted at any time after the initial Operational and Financial Review to determine the Contractor's progress in implementing recommendations and achieving compliance. Review findings may be used in the scoring of subsequent bid proposals submitted by the Contractor.
The Contractor shall not distribute or otherwise make available the Operational and Financial Review Tool, draft Operational and Financial Review Report nor final report to other AHCCCS Contractors.
In addition to the annual Operational and Financial Review AHCCCS may conduct unannounced site visits to monitor contractual requirements and performance as needed.
In accordance with applicable Federal and State regulations, AHCCCS Rules R9-22-606, ACOM Policy 408 and the terms of this contract. AHCCCS may impose sanctions, including buy not limited to: temporary management of the Contractor; monetary penalties; suspension of enrollment; withholding of payments; and suspension, refusal to renew, or termination of the contract or any related subcontracts. [42 CFR 422.208, 42 CFR 438.700, 702, 704 and 45 CFR 92.36(i)(1) 45 CFR 74.48]. Written notice will be provided to the Contractor specifying the sanction to be imposed, the grounds for such sanction and either the length of suspension or the amount of capitation to be withheld. The Contractor may dispute the decision to impose a sanction in accordance with the process outlined in A.A.C. 9-34-401 et seq.
Intermediate sanctions may be imposed, but are not limited to the following actions:
| |
| a. | Substantial failure to provide medically necessary services that the Contractor is required to provide under the terms of this contract to its enrolled members. |
| |
| b. | Imposition of premiums or charges in excess of the amount allowed under the AHCCCS 1115 Waiver. |
| |
| c. | Discrimination of members on the basis of their health status of need for health care services. |
| |
| d. | Misrepresentation or falsification of information furnished to CMS or AHCCCS. |
| |
| e. | Misrepresentation or falsification of information furnished to an enrollee, potential enrollee, or provider. |
105
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
| |
| f. | Failure to comply with the requirement for physician incentive plan as delineated in Section D, Paragraph 42, Physician Incentives/Pay for Performance. |
| |
| g. | Distribution directly, or indirectly through any agent or independent Contractor, of marketing materials that have not been approved by AHCCCS or that contain false or materially misleading information. |
| |
| h. | Failure to meet AHCCCS Financial Viability Standards. |
| |
| i. | Material deficiencies in the Contractor’s provider network. |
| |
| j. | Failure to meet quality of care and quality management requirements. |
| |
| k. | Failure to meet AHCCCS encounter standards. |
| |
| l. | Violation of other applicable State or Federal laws or regulations. |
| |
| m. | Failure to fund accumulated deficit in a timely manner. |
| |
| n. | Failure to increase the Performance Bond in a timely manner. |
| |
| o. | Failure to comply with any provisions contained in this contract. |
| |
| p. | Failure to report third party liability cases as described in Section D, Paragraph 58, Coordination of Benefits. |
| |
| q. | Submitting late, incomplete or inaccurate deliverables. |
AHCCCS may impose the following types of intermediate sanctions:
| |
| a. | Civil monetary penalties. |
| |
| b. | Appointment of temporary management for a Contractor as provided in 42 CFR 438.706 and |
A.R.S. §36-2903 (M).
| |
| c. | Granting members the right to terminate enrollment without cause and notifying the affected members of their right to disenroll [42 CFR 438.702(a)(3)]. |
| |
| d. | Suspension of all new enrollments, including auto assignments after the effective date of the sanction. |
| |
| e. | Suspension of payment for recipients enrolled after the effective date of the sanction until CMS or AHCCCS is satisfied that the reason for imposition of the sanction no longer exists and is not likely to recur. |
| |
| f. | Additional sanctions allowed under statute or regulation that address areas of noncompliance. |
Cure Notice Process:
Prior to the imposition of a sanction for non-compliance, AHCCCS may provide a written cure notice to the Contractor regarding the details of the non-compliance. If a notice to cure is provided to the Contractor, the cure notice will specify the period of time during which the Contractor must bring its performance back into compliance with contract requirements. If, at the end of the specified time period, the Contractor has complied with the cure notice requirements, AHCCCS will not impose a sanction. If, however, the Contractor has not complied with the cure notice requirements, AHCCCS may proceed with the imposition of sanctions.
Refer to ACOM Policy 408 for details.
Automatic Sanctions: AHCCCS will assess the sanctions listed in Attachment F, Periodic Reporting Requirements on deliverables listed under DHCM Operations, Clinical Quality Management and Medical Management that are not received by 5:00 PM on the due date indicated. If the due date falls on a weekend or a State Holiday, sanctions will be assessed on deliverables not received by 5:00 PM on the next business day.
| |
| 75. | BUSINESS CONTINUITY AND RECOVERY PLAN |
The Contractor shall develop a Business Continuity and Recovery Plan as detailed in the ACOM Policy 104, to deal with unexpected events that may affect its ability to adequately serve members. This plan shall, at a minimum, include planning and training for:
| |
| • | Electronic/telephonic failure at the Contractor's main place of business |
| |
| • | Complete loss of use of the main site and satellite offices out of state |
| |
| • | Loss of primary computer system/records |
106
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
| |
| • | Communication between the Contractor and AHCCCS in the event of a business disruption |
The Business Continuity and Recovery Plan shall be updated annually. The Contractor shall submit a summary of the plan to AHCCCS 15 days after the start of the contract year. All staff shall be trained and familiar with the Plan.
| |
| 76. | TECHNOLOGICAL ADVANCEMENT |
The Contractor must have a website with links to the information as described in ACOM Policy 404 and 416.
107
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
| |
| 77. | PENDING LEGISLATION / OTHER ISSUES |
The following constitute pending items that may be resolved after the issuance of this contract. Any program changes due to the resolution of the issues will be reflected in future amendments to the contract. Capitation rates may also be adjusted to reflect the financial impact of program changes. The items in this paragraph are subject to change and should not be considered all-inclusive.
Federal and State Legislation: AHCCCS and its Contractors are subject to legislative mandates that may result in changes to the program. AHCCCS will either amend the contract or incorporate changes in policies incorporated in the contract by reference.
Health Information Technology for Economic and Clinical Health Act (HITECH):
In February 2009, as part of the Federal stimulus package, Congress enacted the Health Information Technology for Economic and Clinical Health Act (HITECH). The legislation included a number of provisions designed to encourage the adoption and use of health information technology including electronic health records (EHRs) and the development of a health information exchange (HIE) infrastructure. The underlying rationale for the Act is the belief that the adoption on a nationwide basis would reduce total spending on health care by diminishing the number of inappropriate tests and procedures, reducing paperwork and administrative overhead, and decreasing the number of adverse events resulting from medical errors.
The Health Information Technology for Economic and Clinical Health Act (HITECH) includes provisions designed to encourage the adoption and use of health information technology including electronic health records (EHRs), e-prescribing and the development of a health information exchange (HIE) infrastructure. AHCCCS and its Contractors support these new evolving technologies, designed to create efficiencies and improve effectiveness of care resulting in improved patient satisfaction with the health care experience, the provision of optimal care outcomes and cost efficiencies.
To further the integration of technology based solutions and the meaningful use of electronic health records within provider offices, AHCCCS anticipates increasing opportunities for providers and Contractors to utilize technological functions for processes that are necessary to meet Medicaid requirements. Expanding the adoption may reduce total spending on health care by diminishing the number of inappropriate tests and procedures, reducing paperwork and administrative overhead, and decreasing the number of adverse events resulting from medical errors. Contractors will actively participate in offering information and providing provider support and education to further expand provider adoption and use of health information technology. It is AHCCCS' expectation that Contractors review operational processes to reduce provider hassle factors by implementing technological solutions for those providers utilizing electronic health records and to incentivize providers to implement and meaningfully use health information technology as a standard of doing business with the AHCCCS program. AHCCCS also anticipates establishing minimum standards, goals and requirements related to operational areas where improved efficiencies or effectiveness could be achieved. AHCCCS anticipates expanding utilization of health information technology as it relates to health care management and Contractor deliverables in the following, but not limited to, areas:
| |
| • | Pharmacy, including but not limited to polypharmacy |
| |
| • | Coordination with community services |
108
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION D: PROGRAM REQUIREMENTS Contract/RFP No. YH09-0001
| |
| • | Performance improvement projects |
| |
| • | Quality of care review processes |
Patient Protection and Affordable Care Act:
The Contractor shall comply with the sections of the Patient Protection and Affordable Care Act upheld by the United States Supreme Court. Effective January 1, 2013, the Contractor will utilize the published AHCCCS primary care services fee schedule for AHCCCS identified primary care providers and select primary care services and meet all other requirements as stipulated. Contracts and capitation rates will be amended as necessary for January 1, 2013.
[END OF SECTION D]
109
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION E: CONTRACT TERMS AND CONDITIONS Contract/RFP No. YH09-0001
SECTION E: CONTRACT TERMS AND CONDITIONS
Arizona Law - The law of Arizona applies to this contract including, where applicable, the Uniform Commercial Code, as adopted in the State of Arizona.
Implied Contract Terms - Each provision of law and any terms required by law to be in this contract are a part of this contract as if fully stated in it.
This contract is issued under the authority of the Contracting Officer who signed this contract. Changes to the contract, including the addition of work or materials, the revision of payment terms, or the substitution of work or materials, directed by an unauthorized state employee or made unilaterally by the Contractor are violations of the contract and of applicable law. Such changes, including unauthorized written contract amendments, shall be void and without effect, and the Contractor shall not be entitled to any claim under this contract based on those changes.
The parties to this contract shall be bound by all terms and conditions contained herein. For interpreting such terms and conditions the following sources shall have precedence in descending order: The Constitution and laws of the United States and applicable Federal regulations; the terms of the CMS 1115 waiver for the State of Arizona; the Constitution and laws of Arizona, and applicable State Rules; the terms of this contract including any attachments, executed amendments and modifications; and AHCCCS policies and procedures.
| |
| 4) | CONTRACT INTERPRETATION AND AMENDMENT |
No Parole Evidence - This contract is intended by the parties as a final and complete expression of their agreement. No course of prior dealings between the parties and no usage of the trade shall supplement or explain any term used in this contract.
No Waiver - Either party's failure to insist on strict performance of any term or condition of the contract shall not be deemed a waiver of that term or condition even if the party accepting or acquiescing in the non-conforming performance knows of the nature of the performance and fails to object to it.
Written Contract Amendments - The contract shall be modified only through a written contract amendment within the scope of the contract signed by the procurement officer on behalf of the State and signed by a duly authorized representative of the Contractor.
The provisions of this contract are severable to the extent that any provision or application held to be invalid shall not affect any other provision or application of the contract, which may remain in effect without the invalid provision, or application.
| |
| 6) | RELATIONSHIP OF PARTIES |
The Contractor under this contract is an independent Contractor. Neither party to this contract shall be deemed to be the employee or agent of the other party to the contract.
| |
| 7) | ASSIGNMENT AND DELEGATION |
The Contractor shall not assign any rights nor delegate all of the duties under this contract. Delegation of less than all of the duties under this contract must conform to the requirements of Section D, Subcontracts.
110
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION E: CONTRACT TERMS AND CONDITIONS Contract/RFP No. YH09-0001
Contractor/Vendor Indemnification (Not Public Agency)
The parties to this contract agree that the State of Arizona, its departments, agencies, boards and commissions shall be indemnified and held harmless by the Contractor for the vicarious liability of the State as a result of entering into this contract. The Contractor agrees to indemnify, defend, and hold harmless the State from and against any and all claims, losses, liability, costs, and expenses, including attorney’s fees and costs, arising out of litigation against AHCCCS including, but not limited to, class action lawsuits challenging actions by the Contractor. The requirement for indemnification applies irrespective of whether or not the Contractor is a party to the lawsuit. Each Contractor shall indemnify the State, on a pro rata basis based on population, attorney’s fees and costs awarded against the State as well as the attorney’s fees and costs incurred by the State in defending the lawsuit. The Contractor shall also indemnify AHCCCS, on a pro rata basis based on population, the administrative expenses incurred by AHCCCS to address Contractor deficiencies arising out of the litigation. The parties further agree that the State of Arizona, its departments, agencies, boards and commissions shall be responsible for its own negligence and/or willful misconduct. Each party to this contract is responsible for its own negligence and/or willful misconduct.
Contractor/Vendor Indemnification (Public Agency)
Each party (“as indemnitor”) agrees to indemnify, defend, and hold harmless the other party (“as indemnitee”) from and against any and all claims, losses, liability, costs, or expenses (including reasonable attorney’s fees) (hereinafter collectively referred to as ‘claims’) arising out of bodily injury of any person (including death) or property damage but only to the extent that such claims which result in vicarious/derivative liability to the indemnitee, are caused by the act, omission, negligence, misconduct, or other fault of the indemnitor, its officers, officials, agents, employees, or volunteers.
| |
| 9) | INDEMNIFICATION -- PATENT AND COPYRIGHT |
To the extent permitted by applicable law, the Contractor shall defend, indemnify and hold harmless the State against any liability including costs and expenses for infringement of any patent, trademark or copyright arising out of contract performance or use by the State of materials furnished or work performed under this contract. The State shall reasonably notify the Contractor of any claim for which it may be liable under this paragraph.
| |
| 10) | COMPLIANCE WITH APPLICABLE LAWS, RULES AND REGULATIONS |
The Contractor shall comply with all applicable Federal and State laws and regulations including Title VI of the Civil Rights Act of 1964; Title IX of the Education Amendments of 1972 (regarding education programs and activities); the Age Discrimination Act of 1975; the Rehabilitation Act of 1973 (regarding education programs and activities), and the Americans with Disabilities Act; EEO provisions; Copeland Anti-Kickback Act; Davis-Bacon Act; Contract Work Hours and Safety Standards; Rights to Inventions Made Under a Contract or Agreement; Clean Air Act and Federal Water Pollution Control Act; Byrd Anti-Lobbying Amendment. The Contractor shall maintain all applicable licenses and permits.
| |
| 11) | ADVERTISING AND PROMOTION OF CONTRACT |
The Contractor shall not advertise or publish information for commercial benefit concerning this contract without the prior written approval of the Contracting Officer.
| |
| 12) | THIRD PARTY ANTITRUST VIOLATIONS |
The Contractor assigns to the State any claim for overcharges resulting from antitrust violations to the extent that those violations concern materials or services supplied by third parties to the Contractor toward fulfillment of this contract.
111
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION E: CONTRACT TERMS AND CONDITIONS Contract/RFP No. YH09-0001
If AHCCCS, in good faith, has reason to believe that the Contractor does not intend to perform or is unable to continue to perform under this contract, the procurement officer may demand in writing that the Contractor give a written assurance of intent to perform. The demand shall be sent to the Contractor by certified mail, return receipt required. Failure by the Contractor to provide written assurance within the number of days specified in the demand may, at the State's option, be the basis for terminating the contract.
| |
| 14) | TERMINATION FOR CONFLICT OF INTEREST |
AHCCCS may cancel this contract without penalty or further obligation if any person significantly involved in initiating, negotiating, securing, drafting or creating the contract on behalf of AHCCCS is, or becomes at any time while the contract or any extension of the contract is in effect, an employee of, or a consultant to, any other party to this contract with respect to the subject matter of the contract. The cancellation shall be effective when the Contractor receives written notice of the cancellation unless the notice specifies a later time.
If the Contractor is a political subdivision of the State, it may also cancel this contract as provided by A.R.S. 38-511.
AHCCCS may, by written notice to the Contractor, immediately terminate this contract if it determines that employment or a gratuity was offered or made by the Contractor or a representative of the Contractor to any officer or employee of the State for the purpose of influencing the outcome of the procurement or securing the contract, an amendment to the contract, or favorable treatment concerning the contract, including the making of any determination or decision about contract performance. AHCCCS, in addition to any other rights or remedies, shall be entitled to recover exemplary damages in the amount of three times the value of the gratuity offered by the Contractor.
| |
| 16) | SUSPENSION OR DEBARMENT |
The Contractor shall not employ, consult, subcontract or enter into any agreement for Title XIX services with any person or entity who is debarred, suspended or otherwise excluded from Federal procurement activity or from participating in non-procurement activities under regulations issued under Executive Order No. 12549 [42 CFR 438.610(a) and (b) or under guidelines implementing Executive Order 12549. This prohibition extends to any entity which employs, consults, subcontracts with or otherwise reimburses for services any person substantially involved in the management of another entity which is debarred, suspended or otherwise excluded from Federal procurement activity. The Contractor is obligated to screen all employees and contractors to determine whether any of them have been excluded from participation in Federal health care programs. You can search the HHS-OIG website by the names of any individuals. The database can be accessed at http://www.oig.hhs.gov/fraud/exclusions.asp.
The Contractor shall not retain as a director, officer, partner or owner of 5% or more of the Contractor entity, any person, or affiliate of such a person, who is debarred, suspended or otherwise excluded from Federal procurement activity.
AHCCCS may, by written notice to the Contractor, immediately terminate this contract if it determines that the Contractor has been debarred, suspended or otherwise lawfully prohibited from participating in any public procurement activity.
| |
| 17) | TERMINATION FOR CONVENIENCE |
AHCCCS reserves the right to terminate the contract in whole or in part at any time for the convenience of the State without penalty or recourse. The Contracting Officer shall give written notice, by certified mail, of the termination, at least 90 days before the effective date of the termination. Upon receipt of written notice, the Contractor shall stop all work, as directed in the notice, notify all subcontractors of the effective date of the termination and minimize all further costs to the State. In the event of termination under this paragraph, all
112
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION E: CONTRACT TERMS AND CONDITIONS Contract/RFP No. YH09-0001
documents, data and reports prepared by the Contractor under the contract shall become the property of and be delivered to AHCCCS. The Contractor shall be entitled to receive just and equitable compensation for work in progress, work completed and materials accepted before the effective date of the termination.
| |
| 18) | TEMPORARY MANAGEMENT/OPERATION OF A CONTRACTOR AND TERMINATION |
Temporary Management and Operation of a Contractor: Pursuant to the Medicaid Managed Care Regulations, 42 CFR 438.700 et seq. and State Law ARS §36-2903, AHCCCS is authorized to impose temporary management for a Contractor under certain conditions. Under Federal law, temporary management may be imposed if AHCCCS determines that there is continued egregious behavior by the Contractor, including but not limited to the following: substantial failure to provide medically necessary services the Contractor is required to provide; imposition on enrollees premiums or charges that exceed those permitted by AHCCCS; discrimination among enrollees on the basis of health status or need for health care services; misrepresentation or falsification of information to AHCCCS or CMS; misrepresentation or falsification of information furnished to an enrollee or provider; distribution of marketing materials that have not been approved by AHCCCS or that are false or misleading; or behavior contrary to any requirements of Sections 1903(m) or 1932 of the Social Security Act. Temporary management may also be imposed if AHCCCS determines that there is substantial risk to enrollees’ health or that temporary management is necessary to ensure the health of enrollees while the Contractor is correcting the deficiencies noted above or until there is an orderly transition or reorganization of the Contractor. Under Federal law, temporary management is mandatory if AHCCCS determines that the Contractor has repeatedly failed to meet substantive requirements in Sections 1903(m) or 1932 of the Social Security Act. In these situations, AHCCCS shall not delay imposition of temporary management to provide a hearing before imposing this sanction.
State law ARS §36-2903 authorizes AHCCCS to operate a Contractor as specified in this contract. In addition to the bases specified in 42 CFR 438.700 et seq., AHCCCS may directly operate the Contractor if, in the judgment of AHCCCS, the Contractor's performance is in material breach of the contract or the Contractor is insolvent. Under these circumstances, AHCCCS may directly operate the Contractor to assure delivery of care to members enrolled with the Contractor until cure by the Contractor of its breach, by demonstrated financial solvency or until the successful transition of those members to other Contractors. Prior to operation of the Contractor by AHCCCS pursuant to state statute, the Contractor shall have the opportunity for a hearing. If AHCCCS determines that emergency action is required, operation of the Contractor may take place prior to hearing. Operation by AHCCCS shall occur only as long as it is necessary to assure delivery of uninterrupted care to members, to accomplish orderly transition of those members to other Contractors, or until the Contractor reorganizes or otherwise corrects contract performance failure.
If AHCCCS undertakes direct operation of the Contractor, AHCCCS, through designees appointed by the Director, shall be vested with full and exclusive power of management and control of the Contractor as necessary to ensure the uninterrupted care to persons and accomplish the orderly transition of persons to a new or existing Contractor, or until the Contractor corrects the contract Performance failure to the satisfaction of AHCCCS. AHCCCS shall have the power to employ any necessary assistants, to execute any instrument in the name of the Contractor, to commence, defend and conduct in its name any action or proceeding in which the Contractor may be a party; such powers shall only apply with respect to activities occurring after AHCCCS undertakes direct operation of the Contractor in connection with this Section.
All reasonable expenses of AHCCCS related to the direct operation of the Contractor, including attorney fees, cost of preliminary or other audits of the Contractor and expenses related to the management of any office or other assets of the Contractor, shall be paid by the Contractor or withheld from payment due from AHCCCS to the Contractor.
Termination: AHCCCS reserves the right to terminate this contract in whole or in part due to the failure of the Contractor to comply with any term or condition of the contract and as authorized by Medicaid Managed Care Regulations and 42 CFR 438.708. If the Contractor is providing services under more than one contract with AHCCCS, AHCCCS may deem unsatisfactory performance under one contract to be cause to require the Contractor to provide assurance of performance under any and all other contracts. In such situations, AHCCCS reserves the right to seek remedies under both actual and anticipatory breaches of contract if adequate assurance
113
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION E: CONTRACT TERMS AND CONDITIONS Contract/RFP No. YH09-0001
of performance is not received. The Contracting Officer shall mail written notice of the termination and the reason(s) for it to the Contractor by certified mail, return receipt requested. Pursuant to Medicaid Managed Care Regulations and 42 CFR 438.708, AHCCCS shall provide the Contractor with a pre-termination hearing before termination of the contract.
Upon termination, all documents, data, and reports prepared by the Contractor under the contract shall become the property of and be delivered to AHCCCS on demand.
AHCCCS may, upon termination of this contract, procure on terms and in the manner that it deems appropriate, materials or services to replace those under this contract. The Contractor shall be liable for any excess costs incurred by AHCCCS in re-procuring the materials or services.
| |
| 19) | TERMINATION - AVAILABILITY OF FUNDS |
Availability of Funds for the current State fiscal year. Should the State Legislature enter back into session and reduce the appropriations or for any reason and these goods or services are not funded, the State may take any of the following actions:
| |
| a. | Accept a decrease in price offered by the Contractor; |
| |
| b. | Cancel the contract; or |
| |
| c. | Cancel the contract and re-solicit the requirements. |
Funds are not presently available for performance under this contract beyond the current fiscal year. No legal liability on the part of AHCCCS for any payment may arise under this contract until funds are made available for performance of this contract.
Notwithstanding any other provision in the Agreement, this Agreement may be terminated by AHCCCS, if, for any reason, there are not sufficient appropriated and available monies for the purpose of maintaining this Agreement. In the event of such termination, the Contractor shall have no further obligation to AHCCCS.
AHCCCS shall be entitled to offset against any sums due the Contractor, any expenses or costs incurred by AHCCCS, or damages assessed by AHCCCS concerning the Contractor’s non-conforming performance or failure to perform the contract, including but not limited to expenses, costs and damages.
| |
| 21) | NON-EXCLUSIVE REMEDIES |
The rights and the remedies of AHCCCS under this contract are not exclusive.
In accordance with ARS 41-1461 et seq. and Executive Order 2009-09, the Contractor shall provide equal employment opportunities for all persons, regardless of race, color, religion, creed, sex, age, national origin, disability or political affiliation. The Contractor shall comply with the Americans with Disabilities Act.
The effective date of this contract shall be the Offer and Acceptance date referenced on page 1 of this contract.
A certificate of insurance naming the State of Arizona and AHCCCS as the "additional insured" must be submitted to AHCCCS within 10 days of notification of contract award and prior to commencement of any services under this contract. This insurance shall be provided by carriers rated as "A+" or higher by the A.M. Best Rating Service. The following types and levels of insurance coverage are required for this contract:
| |
| a. | Commercial General Liability: Provides coverage of at least $1,000,000 for each occurrence for bodily injury and property damage to others as a result of accidents on the premises of or as the result of operations of the Contractor. |
114
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION E: CONTRACT TERMS AND CONDITIONS Contract/RFP No. YH09-0001
| |
| b. | Commercial Automobile Liability: Provides coverage of at least $1,000,000 for each occurrence for bodily injury and property damage to others resulting from accidents caused by vehicles operated by the Contractor. |
| |
| c. | Workers Compensation: Provides coverage to employees of the Contractor for injuries sustained in the course of their employment. Coverage must meet the obligations imposed by Federal and State statutes and must also include Employer's Liability minimum coverage of $100,000. Evidence of qualified self-insured status will also be considered. |
| |
| d. | Professional Liability (if applicable): Provides coverage for alleged professional misconduct or lack of ordinary skills in the performance of a professional act of service. |
The above coverage may be evidenced by either one of the following:
| |
| a. | The State of Arizona Certificate of Insurance: This is a form with the special conditions required by the contract already pre-printed on the form. The Contractor's agent or broker must fill in the pertinent policy information and ensure the required special conditions are included in the Contractor's policy. |
| |
| b. | The Accord form: This standard insurance industry certificate of insurance does not contain the pre-printed special conditions required by this contract. These conditions must be entered on the certificate by the agent or broker and read as follows: |
The State of Arizona and Arizona Health Care Cost Containment System are hereby added as additional insureds. Coverage afforded under this Certificate shall be primary and any insurance carried by the State or any of its agencies, boards, departments or commissions shall be in excess of that provided by the insured Contractor. No policy shall expire, be canceled or materially changed without 30 days written notice to the State. This Certificate is not valid unless countersigned by an authorized representative of the insurance company.
| |
| c. | If the Contractor is insured pursuant to A.R.S. § 11-981, the Insurance provisions required by the contract are satisfied. |
Contract claims and disputes shall be adjudicated in accordance with State Law, AHCCCS Rules and this contract.
Except as provided by 9 A.A.C. Chapter 22, Article 6, the exclusive manner for the Contractor to assert any dispute against AHCCCS shall be in accordance with the process outlined in 9 A.A.C. Chapter 34and ARS §36-2903.01. All disputes except as provided under 9 A.A.C. Chapter 22, Article 6 shall be filed in writing and be received by AHCCCS no later than 60 days from the date of the disputed notice. All disputes shall state the factual and legal basis for the dispute. Pending the final resolution of any disputes involving this contract, the Contractor shall proceed with performance of this contract in accordance with AHCCCS' instructions, unless AHCCCS specifically, in writing, requests termination or a temporary suspension of performance.
| |
| 26) | RIGHT TO INSPECT PLANT OR PLACE OF BUSINESS |
AHCCCS may, at reasonable times, inspect the part of the plant or place of business of the Contractor or subcontractor that is related to the performance of this contract, in accordance with A.R.S. §41‑2547.
| |
| 27) | INCORPORATION BY REFERENCE |
This solicitation and all attachments and amendments, the Contractor's proposal, best and final offer accepted by AHCCCS, and any approved subcontracts are hereby incorporated by reference into the contract.
| |
| 28) | COVENANT AGAINST CONTINGENT FEES |
The Contractor warrants that no person or agency has been employed or retained to solicit or secure this contract upon an agreement or understanding for a commission, percentage, brokerage or contingent fee. For violation of this warranty, AHCCCS shall have the right to annul this contract without liability.
115
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION E: CONTRACT TERMS AND CONDITIONS Contract/RFP No. YH09-0001
AHCCCS may at any time, by written notice to the Contractor, make changes within the general scope of this contract. If any such change causes an increase or decrease in the cost of, or the time required for, performance of any part of the work under this contract, the Contractor may assert its right to an adjustment in compensation paid under this contract. The Contractor must assert its right to such adjustment within 30 days from the date of receipt of the change notice. Any dispute or disagreement caused by such notice shall constitute a dispute within the meaning of Section E, Disputes, and be administered accordingly.
When AHCCCS issues an amendment to modify the contract, the provisions of such amendment will be deemed to have been accepted 60 days after the date of mailing by AHCCCS, even if the amendment has not been signed by the Contractor, unless within that time the Contractor notifies AHCCCS in writing that it refuses to sign the amendment. If the Contractor provides such notification, AHCCCS will initiate termination proceedings.
Firm Fixed-Price stated as capitated per member per month, except as otherwise provided.
| |
| 31) | AMERICANS WITH DISABILITIES ACT |
People with disabilities may request special accommodations such as interpreters, alternative formats or assistance with physical accessibility. Requests for special accommodations must be made with at least three days prior notice by contacting the Solicitation Contact person.
The Contractor warrants that all services provided under this contract will conform to the requirements stated herein. AHCCCS' acceptance of services provided by the Contractor shall not relieve the Contractor from its obligations under this warranty. In addition to its other remedies, AHCCCS may, at the Contractor's expense, require prompt correction of any services failing to meet the Contractor's warranty herein. Services corrected by the Contractor shall be subject to all of the provisions of this contract in the manner and to the same extent as the services originally furnished.
| |
| 33) | NO GUARANTEED QUANTITIES |
AHCCCS does not guarantee the Contractor any minimum or maximum quantity of services or goods to be provided under this contract.
The Contractor shall not undertake any work that represents a potential conflict of interest, or which is not in the best interest of AHCCCS or the State without prior written approval by AHCCCS. The Contractor shall fully and completely disclose any situation that may present a conflict of interest. If the Contractor is now performing or elects to perform during the term of this contract any services for any AHCCCS Contractor, provider or Contractor or an entity owning or controlling same, the Contractor shall disclose this relationship prior to accepting any assignment involving such party.
| |
| 35) | CONFIDENTIALITY AND DISCLOSURE OF CONFIDENTIAL INFORMATION |
The Contractor shall safeguard confidential information in accordance with Federal and State laws and regulations, including but not limited to, 42 CFR 431 Subpart F, , A.R.S. §§36-107, 36-2903 (for Acute). 36-2932 (for ALTCS), 41-1959, and 46-135, the Health Insurance Portability and Accountability Act (Public Law 107-191 Statutes 1936), 45 CFR parts 160 and 164, and AHCCCS Rules.
The Contractor shall establish and maintain procedures and controls that are acceptable to AHCCCS for the purpose of assuring that no information contained in its records or obtained from AHCCCS or others carrying out its functions under the contract shall be used or disclosed by its agents, officers or employees, except as required to efficiently perform duties under the contract. Except as required or permitted by law, the Contractor also agrees that any information pertaining to individual persons shall not be divulged other than to employees
116
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION E: CONTRACT TERMS AND CONDITIONS Contract/RFP No. YH09-0001
or officers of the Contractor as needed for the performance of duties under the contract, unless otherwise agreed to, in writing, by AHCCCS.
The Contractor shall not, without prior written approval from AHCCCS, either during or after the performance of the services required by this contract, use, other than for such performance, or disclose to any person other than AHCCCS personnel with a need to know, any information, data, material, or exhibits created, developed, produced, or otherwise obtained during the course of the work required by this contract. This nondisclosure requirement shall also pertain to any information contained in reports, documents, or other records furnished to the Contractor by AHCCCS.
| |
| 36) | COOPERATION WITH OTHER CONTRACTORS |
AHCCCS may award other contracts for additional work related to this contract and Contractor shall fully cooperate with such other contractors and AHCCCS employees or designated agents The Contractor shall not commit or permit any act which will interfere with the performance of work by any other Contractor or by AHCCCS employees.
| |
| 37) | ASSIGNMENT OF CONTRACT AND BANKRUPTCY |
This contract is voidable and subject to immediate cancellation by AHCCCS upon the Contractor becoming insolvent or filing proceedings in bankruptcy or reorganization under the United States Code, or assigning rights or obligations under this contract without the prior written consent of AHCCCS.
| |
| 38) | OWNERSHIP OF INFORMATION AND DATA |
Materials, reports and other deliverables created under this contract are the sole property of AHCCCS. The Contractor is not entitled to any rights to those materials and may not transfer any rights to anyone else. Except as necessary to carry out the requirements of this contract, as otherwise allowed under this contract, or as required by law, the Contractor shall not use or release data, information or materials, reports, or deliverables derived from that data or information without the prior written consent of AHCCCS. Data, information and reports collected or prepared by the Contractor in the course of performing its duties and obligations under this contract shall not be used by the Contractor for any independent project of the Contractor or publicized by the Contractor without the prior written permission of AHCCCS. Subject to applicable state and Federal laws and regulations, AHCCCS shall have full and complete rights to reproduce, duplicate, disclose and otherwise use all such information.
At the termination of the contract, the Contractor shall make available all such data to AHCCCS within 30 days following termination of the contract or such longer period as approved by AHCCCS, Office of the Director. For purposes of this subsection, the term “data” shall not include member medical records.
Except as otherwise provided in this section, if any copyrightable or patentable material is developed by the Contractor in the course of performance of this contract, the Federal government, AHCCCS and the State of Arizona shall have a royalty‑free, nonexclusive, and irrevocable right to reproduce, publish, or otherwise use, and to authorize others to use, the work for state or Federal government purposes. The Contractor shall additionally be subject to the applicable provisions of 45 CFR Part 92.
| |
| 39) | AUDITS AND INSPECTIONS |
The Contractor shall comply with all provisions specified in applicable A.R.S. 35-214 and 35-215 and AHCCCS Rules and AHCCCS policies and procedures relating to the audit of the Contractor's records and the inspection of the Contractor's facilities. The Contractor shall fully cooperate with AHCCCS staff and allow them reasonable access to the Contractor's staff, subcontractors, members, and records [42 CFR 438.6(g)].
At any time during the term of this contract, and five (5) years thereafter unless a longer time is otherwise required by law, the Contractor's or any subcontractor's books and records shall be subject to audit by AHCCCS and, where applicable, the Federal government, to the extent that the books and records relate to the performance of the contract or subcontracts [42 CFR 438.242(b)(3)].
117
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION E: CONTRACT TERMS AND CONDITIONS Contract/RFP No. YH09-0001
AHCCCS, or its duly authorized agents, and the Federal government may evaluate through on-site inspection or other means, the quality, appropriateness and timeliness of services performed under this contract.
No funds paid to the Contractor by AHCCCS, or interest earned thereon, shall be used for the purpose of influencing or attempting to influence an officer or employee of any Federal or State agency, a member of the United States Congress or State Legislature, an officer or employee of a member of the United States Congress or State Legislature in connection with awarding of any Federal or State contract, the making of any Federal or State grant, the making of any Federal or State loan, the entering into of any cooperative agreement, and the extension, continuation, renewal, amendment or modification of any Federal or State contract, grant, loan, or cooperative agreement. The Contractor shall disclose if any funds paid to the Contractor by AHCCCS have been used or will be used to influence the persons and entities indicated above and will assist AHCCCS in making such disclosures to CMS.
The parties agree that jurisdiction over any action arising out of or relating to this contract shall be brought or filed in a court of competent jurisdiction located in the State of Arizona.
The Contractor shall certify that financial and encounter data submitted to AHCCCS is complete, accurate and truthful. Certification of financial and encounter data must be submitted concurrently with the data. Certification may be provided by the Contractor CEO, CFO or an individual who is delegated authority to sign for, and who report directly to the CEO or CFO [42 CFR 438.604 et seq.].
| |
| 43) | OFF-SHORE PERFORMANCE OF WORK PROHIBITED |
Any services that are described in the specifications or scope of work that directly serve the State of Arizona or its clients and involve access to secure or sensitive data or personal client data shall be performed within the defined territories of the United States. Unless specifically stated otherwise in the specifications, this paragraph does not apply to indirect or 'overhead’ services, redundant back-up services or services that are incidental to the performance of the contract. This provision applies to work performed by subcontractors at all tiers.
| |
| 44) | FEDERAL IMMIGRATION AND NATIONALITY ACT |
The Contractor shall comply with all Federal, State and local immigration laws and regulations relating to the immigration status of their employees during the term of the contract. Further, the Contractor shall flow down this requirement to all subcontractors utilized during the term of the contract. The State shall retain the right to perform random audits of Contractor and subcontractor records or to inspect papers of any employee thereof to ensure compliance. Should the State determine that the Contractor and/or any subcontractors be found noncompliant, he State may pursue all remedies allowed by law, including, but not limited to; suspension of work, termination of the contract for default and suspension and/or debarment of the Contractor.
In order to receive payment under any resulting contract, the Contractor shall have a current IRS W-9 Form on file with the State of Arizona.
| |
| 46) | CONTINUATION OF PERFORMANCE THROUGH TERMINATION |
The Contractor shall continue to perform, in accordance with the requirements of the contract, up to the date of termination and as directed in the termination notice.
In accordance with A.R.S 41-4401, the Contractor warrants compliance with all Federal immigration laws and regulations relating to employees and warrants its compliance with Section A.R.S. 23-214, Subsection A.
118
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION E: CONTRACT TERMS AND CONDITIONS Contract/RFP No. YH09-0001
In accordance with A.R.S. 35-391 and A.R.S. 35-393, Contractor certifies that the Contractor does not have scrutinized business operations in Sudan or Iran
[END OF SECTION E]
119
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION F: RESERVED Contract/RFP No. YH09-0001
SECTION F: RESERVED
120
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION G: RESERVED Contract/RFP No. YH09-0001
SECTION G: RESERVED
121
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION H: RESERVED Contract/RFP No. YH09-0001
SECTION H: RESERVED
122
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION I: RESERVED Contract/RFP No. YH09-0001
SECTION I: RESERVED
123
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
SECTION J: LIST OF ATTACHMENTS Contract/RFP No. YH09-0001
SECTION J: LIST OF ATTACHMENTS
Attachment A: RESERVED
Attachment B: Geographic Service Area; Minimum Network Requirements
Attachment C: RESERVED
Attachment D: Sample Letter of Intent: Network Submission Requirements
Attachment E: RESERVED
Attachment F: Periodic Reporting Requirements
Attachment G: Auto-Assignment Algorithm
Attachment H: Grievance System Standards and Policy
Attachment I: RESERVED
Attachment J: RESERVED
Attachment K: RESERVED
124
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
ATTACHMENT A: RESERVED Contract/RFP No. YH09-0001
ATTACHMENT A: RESERVED
The Minimum Subcontract Provisions document is available on the AHCCCS Website at:
http://www.azahcccs.gov/commercial/default.aspx
125
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
ATTACHMENT A: RESERVED Contract/RFP No. YH09-0001
ATTACHMENT B: MINIMUM NETWORK STANDARDS (By Geographic Service Area)
INSTRUCTIONS:
Contractors shall have in place an adequate network of providers capable of meeting contract requirements. The information that follows describes the minimum network requirements by Geographic Service Area (GSA).
In some GSAs there are required service sites located outside of the geographical boundary of a GSA. The reason for this relates to practical access to care. In certain instances, a member must travel a much greater distance to receive services within their assigned GSA, than if the member were not allowed to receive services in an adjoining Border Community.
Split zip codes occur in some counties. Split zip codes are those which straddle two different counties. Enrollment for members residing in these zip codes is based upon the county and GSA to which the entire zip code has been assigned by AHCCCS. The Contractor shall be responsible for providing services to members residing in the entire zip code that is assigned to the GSA for which the Contractor has agreed to provide services. The split zip codes GSA assignments are as follows:
|
| | | |
| ZIP CODE | SPLIT BETWEEN THESE COUNTIES | COUNTY ASSIGNED TO | ASSIGNED GSA |
| 85140 | Pinal and Maricopa | Maricopa | 12 |
| 85120 | Pinal and Maricopa | Maricopa | 12 |
| 85142 | Pinal and Maricopa | Maricopa | 12 |
| 85192 | Gila and Pinal | Gila | 8 |
| 85342 | Yavapai and Maricopa | Maricopa | 12 |
| 85358 | Yavapai and Maricopa | Maricopa | 12 |
| 85390 | Yavapai and Maricopa | Maricopa | 12 |
| 85643 | Graham and Cochise | Cochise | 14 |
| 85645 | Pima and Santa Cruz | Santa Cruz | 10 |
| 85943 | Apache and Navajo | Navajo | 4 |
| 86336 | Coconino and Yavapai | Yavapai | 6 |
| 86351 | Coconino and Yavapai | Coconino | 4 |
| 86434 | Mohave and Yavapai | Yavapai | 6 |
| 86340 | Coconino and Yavapai | Yavapai | 6 |
| 85143 | Pinal and Maricopa | Maricopa | 12 |
If outpatient specialty services (OB, family planning, and pediatrics) are not included in the primary care provider contract, at least one subcontract is required for each of these specialties in the service sites specified.
In Tucson (GSA 10) and Metropolitan Phoenix (GSA 12), the Contractor must have a network that is able to provide PCP, dental and pharmacy services so that members do not need to travel more than 5 miles from their residence. The Contractor must also obtain at least one hospital contract in each service district listed on the Hospitals in Phoenix and Tucson Metropolitan area pages within this section, respectively. Metropolitan Phoenix is further defined on the Minimum Network Standard page specific to GSA # 12.
126
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
ATTACHMENT A: RESERVED Contract/RFP No. YH09-0001
At a minimum, the Contractor shall have contracts with physicians with admitting and treatment privileges at each hospital in its network.
For the remaining GSAs and areas not included in the Phoenix or Tucson Metropolitan Areas, the Contractor is required to obtain contracts with Physician(s) with admission and treatment privileges in the communities identified under Hospitals on the Minimum Network Standard page specific to each GSA. The Contractor must have a network that is able to provide PCP, dental and pharmacy services in each of the communities identified on the Minimum Network Standard Page specific to each GSA.
Provider categories required at various service delivery sites included in the Service Area Minimum Network Standards are indicated as follows:
H Hospitals
P Primary Care Providers (physicians, certified nurse practitioners and physician assistants)
D Dentists
Ph Pharmacies
127
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
ATTACHMENT A: RESERVED Contract/RFP No. YH09-0001
HOSPITALS IN PHOENIX METROPOLITAN AREA (By service district, by zip code)
DISTRICT 1
85006 Banner Good Samaritan Medical Center
85281 St. Luke’s Medical Center
85008 Maricopa Medical Center
85013 St. Joseph’s Hospital Phoenix
85020 John C. Lincoln Hospital – North Mountain
DISTRICT 2
85015 Phoenix Baptist Hospital
85027 John C. Lincoln Hospital – Deer Valley
85037 Banner Estrella Medical Center
85306 Banner Thunderbird Medical Center
85308 Arrowhead Community Hospital
85338 West Valley Hospital
85351 Banner Boswell Medical Center
85375 Banner Del E. Webb Medical Center
85031 Maryvale Hospital Medical Center
DISTRICT 3
85031 Paradise Valley Hospital
85054 Mayo Clinic Hospital
85251 Scottsdale Healthcare – Osborn
85261 Scottsdale Healthcare – Shea
85255 Scottsdale Healthcare – Thompson Peak
DISTRICT 4
85201 Arizona Regional Medical Center
85202 Banner Desert Medical Center
85206 Banner Baywood Medical Center
85224 Chandler Regional Hospital
85281 Tempe St. Luke’s Hospital
85296 Mercy Gilbert Medical Center
85234 Banner Gateway Medical Center
85209 Mountain Vista Medical Center
85140 Banner Ironwood Medical Center
128
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
ATTACHMENT A: RESERVED Contract/RFP No. YH09-0001
HOSPITALS IN TUCSON METROPOLITAN AREA (By service district, by zip code)
DISTRICT 1
85719 University Medical Center
85741 Northwest Medical Center
85745 Carondelet St. Mary’s Hospital
85775 Northwest Medical Center Oro Valley
DISTRICT 2
85711 Carondelet St. Joseph’s Hospital
85717 Tucson Medical Center
85713 University Physicians Hospital at Kino Campus
129
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
ATTACHMENT A: RESERVED Contract/RFP No. YH09-0001
130
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
ATTACHMENT A: RESERVED Contract/RFP No. YH09-0001
131
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
ATTACHMENT A: RESERVED Contract/RFP No. YH09-0001
132
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
ATTACHMENT A: RESERVED Contract/RFP No. YH09-0001
133
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
ATTACHMENT A: RESERVED Contract/RFP No. YH09-0001
134
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
ATTACHMENT A: RESERVED Contract/RFP No. YH09-0001
135
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
ATTACHMENT A: RESERVED Contract/RFP No. YH09-0001
136
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
ATTACHMENT C: RESERVED Contract/RFP No. YH09-0001
ATTACHMENT C: RESERVED
137
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
ATTACHMENT D: SAMPLE LETTER OF INTENT Contract/RFP No. YH09-0001
ATTACHMENT D: SAMPLE LETTER OF INTENT
The following information is provided as early notification for Offerors’ benefit. However, complete instructions regarding this Letter of Intent will be provided when the RFP is released. Only instructions included in the RFP are considered official. Do not send completed Letter of Intent to AHCCCS at this time.
Letter of Intent Instructions
The following is the mandated format for the Arizona Health Care Cost Containment System, contract Year Ending 2007 Letter of Intent (LOI). It is to be used to show a provider’s intention to enter into a contract with an Offeror. No alterations or changes are permitted, except for shaded areas which identify the Offeror. The Offeror may print the form on its letterhead or insert its name or logo in the box at the top of the forms. The completed LOI or an executed contract will be acceptable evidence of an Offeror’s proposed network.
If a provider has multiple sites that offer identical services, only one LOI should be signed, with additional service site information (items 1 to 6) attached to the LOI. If services differ between sites, a separate LOI must be obtained for each service site.
If a representative signs an LOI on behalf of a provider, evidence of authority for the representative must be available upon request.
138
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
ATTACHMENT D: SAMPLE LETTER OF INTENT Contract/RFP No. YH09-0001
OFFEROR’S LOGO
Please do not sign this Letter of Intent unless you seriously intend to enter into negotiations with the Offeror mentioned below and understand that the Arizona Health Care Cost Containment System (AHCCCS) requires all contracts to include Minimum Subcontract Provisions as listed at http://www.azahcccs.gov/Contracting/BidderLib_Acute.asp.
No alterations or changes are permitted, except for shaded areas which identify the Offeror. This letter is subject to verification by AHCCCS.
The provider signing below is willing to enter into contract negotiations with (Offeror’s name), for provision of covered services to AHCCCS members enrolled with (Offeror’s name). This provider intends to sign a contract with (Offeror’s name) if (Offeror’s name) is awarded an AHCCCS contract beginning October 1, 2008 in the provider’s service area and an acceptable agreement can be reached between the provider and (Offeror’s name). Signing this Letter of Intent does not obligate the provider to sign a contract with (Offeror’s name) however, please do not sign this Letter of Intent unless you seriously intend to enter into negotiations with the above mentioned health plan.
The following information is furnished by the provider:
1. NATIONAL PROVIDER IDENTIFICATION NUMBER (NPI) or AHCCCS PROVIDER IDENTIFICATION NUMBER _____________________________________________________________
2. PROVIDER’S PRINTED NAME ____________________________________________________________
3. ADDRESS (where services will be provided) ___________________________________________________
_________________________________________________ZIP CODE________________________________
4. COUNTY ________________ 5. TELEPHONE ________________ 6. FAX _________________________
___ Please check here if additional service site information is attached to the Letter of Intent
7. CHECK ALL THAT APPLY
___ A. Primary Care Physician ___ Family Practice
___ General Practice
___ Pediatrics
___ Internal Medicine
Services: ___ EPSDT
___ OB
___ B. Primary Care Nurse Practitioner ___ Family Practice
___ Adult
139
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
ATTACHMENT D: SAMPLE LETTER OF INTENT Contract/RFP No. YH09-0001
___ Pediatrics
___ Midwife
Services: ___ EPSDT
___ OB
___ C. Primary Care Physician’s Assistant
Services: ___ EPSDT
___ OB
___ D. Physician – Specialist – (Specify)_____________________________________________________
___ E. Hospital
___ F. Urgent Care Facility
___ G. Pharmacy
___ H. Laboratory
___ I. Medical Imaging
___ J. Medically Necessary Transportation
___ K. Nursing Facility
___ L. Dentist
___ M. Therapy (Specify Physical Therapy, Occupational Therapy, Speech, Respiratory) ______________
________________________________________________________________________________
___ N. Behavioral Health Provider (Specify) __________________________________________________
___ O. Durable Medical Equipment
___ P. Home Health Agency
___ Q. Other (Please Specify)______________________________________________________________
8. LANGUAGES SPOKEN BY THE PROVIDER (OTHER THAN ENGLISH) _____________________
__________________________________________________________________________
9. NAME OF HOSPITAL(S) WHERE PHYSICIAN HAS ADMITTING PRIVILEGES ______________
______________________________________________________________________________________
NOTICE TO PROVIDERS: This Letter of Intent will be used by AHCCCS in its bid evaluation and contract award process. You should only sign this Letter of Intent if you intend to enter into contract negotiations with (Offeror’s name) should they receive a contract award. If you are signing on behalf of a physician, please provide evidence of your authority to do so.
Do not return completed Letter of Intent to AHCCCS. Completed Letter of Intent needs to be returned to (Offeror’s name).
10. PROVIDER’S SIGNATURE ____________________________________DATE _______________
11. PRINTED NAME OF SIGNER _________________________________TITLE _______________
140
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
ATTACHMENT D: SAMPLE LETTER OF INTENT Contract/RFP No. YH09-0001
OFFEROR’S LOGO
ADDITIONAL SERVICE SITES:
1. NATIONAL PROVIDER IDENTIFICATION NUMBER (NPI) or AHCCCS PROVIDER IDENTIFICATION NUMBER _____________________________________________________________
2. PROVIDER’S PRINTED NAME ____________________________________________________________
3. ADDRESS (where services will be provided) ___________________________________________________
_________________________________________________ZIP CODE________________________________
4. COUNTY ________________ 5. TELEPHONE ________________ 6. FAX _________________________
3. ADDRESS (where services will be provided) ___________________________________________________
_________________________________________________ZIP CODE________________________________
4. COUNTY ________________ 5. TELEPHONE ________________ 6. FAX _________________________
3. ADDRESS (where services will be provided) ___________________________________________________
_________________________________________________ZIP CODE________________________________
4. COUNTY ________________ 5. TELEPHONE ________________ 6. FAX _________________________
3. ADDRESS (where services will be provided) ___________________________________________________
_________________________________________________ZIP CODE________________________________
4. COUNTY ________________ 5. TELEPHONE ________________ 6. FAX _________________________
141
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
ATTACHMENT D: SAMPLE LETTER OF INTENT Contract/RFP No. YH09-0001
3. ADDRESS (where services will be provided) ___________________________________________________
_________________________________________________ZIP CODE________________________________
4. COUNTY ________________ 5. TELEPHONE ________________ 6. FAX _________________________
3. ADDRESS (where services will be provided) ___________________________________________________
_________________________________________________ZIP CODE________________________________
4. COUNTY ________________ 5. TELEPHONE ________________ 6. FAX _________________________
142
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
ATTACHMENT E: RESERVED Contract/RFP No. YH09-0001
ATTACHMENT E: RESERVED
143
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
ATTACHMENT F: PERIODIC REPORT REQUIREMENTS Contract/RFP No. YH09-0001
ATTACHMENT F: CONTRACTORS CHART OF DELIVERABLES
The following table is a summary of the periodic reporting requirements for the Contractor and is subject to change at any time during the term of the contract. The table is presented for convenience only and should not be construed to limit the Contractor’s responsibilities in any manner. Content for all deliverables is subject to review. AHCCCS may assess sanctions if it is determined that late, inaccurate or incomplete data is submitted.
The deliverables listed below are due by 5:00 PM on the due date indicated, if the due date falls on a weekend or a State Holiday the due date is 5:00 PM on the next business day.
If a Contractor is in compliance with the contractual standards on the deliverables below marked with an asterisk (*), for a period of three consecutive months, the Contractor may request to submit data on a quarterly basis. However, if the Contractor is non-compliant with any standard on the deliverable or AHCCCS has concerns during the reporting quarter, the Contractor must immediately begin to submit on a monthly basis until three consecutive months of compliance are achieved.
144
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
ATTACHMENT F: PERIODIC REPORT REQUIREMENTS Contract/RFP No. YH09-0001
|
| | | | |
| REPORT | WHEN DUE | SOURCE/REFERENCE | SEND TO: | SUBMITTED VIA |
| DHCM Finance | | | | |
| Monthly Financial Reporting Package | 30 days after the end of the month, only when required by AHCCCS | Reporting Guide For Acute Health Care Contractors | Finance Manager | FTP server with email notification |
| Quarterly Financial Reporting Package | 60 days after the end of each quarter | Reporting Guide For Acute Health Care Contractors | Finance Manager | FTP server with email notification |
| FQHC Member Information | 60 days after the end of each quarter | Reporting Guide For Acute Health Care Contractors; Section D, Paragraph 34 | Finance Manager | FTP server with email notification |
| Draft Annual Financial Reporting Package | 90 days after the end of each fiscal year | Reporting Guide For Acute Health Care Contractors | Finance Manager | FTP server with email notification |
| Final Annual Financial Reporting Package | 120 days after the end of each fiscal year | Reporting Guide For Acute Health Care Contractors | Finance Manager | FTP server with email notification |
| Advances/Loans/Equity Distributions | Submit for approval prior to effective date | Section D, Paragraph 49; | Finance Manager | FTP server with email notification |
| Premium Tax Reporting | March 15th, June 15th, September 15th , December 15th | ACOM Policy 304 | Finance Manager | FTP server with email notification |
Quarterly Verification of Receipt of Paid Services (Section D, ¶66 and ACOM Policy 424) | Due the 15th day after the end of the quarter that follows the reporting quarter Oct. – Dec. due April 15 Jan. – March due July 15 April – June due Oct. 15 July – Sept. due Jan. 15 | Section D, Paragraph 19 and ACOM Policy 424 | Finance Manager | FTP server with email notification |
| Quarterly Cost Avoidance/Recovery Report | Due 45 days after the reporting quarter Oct - Dec due Feb 14 Jan – March due May 15 Apr – June due August 14 July – Sept due Nov 14 | Section D, ¶58 and Program Integrity Reporting Guide | Finance Manager | FTP server with email notification |
145
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
ATTACHMENT F: PERIODIC REPORT REQUIREMENTS Contract/RFP No. YH09-0001
|
| | | | |
| REPORT | WHEN DUE | SOURCE/REFERENCE | SEND TO: | SUBMITTED VIA |
| DHCM Data Analysis and Research | | | | |
| Corrected Pended Encounter Data | Monthly, according to established schedule | Encounter Manual | Encounter Administrator | FTP server with email notification |
| New Day Encounter | Monthly, according to established schedule | Encounter Manual | Encounter Administrator | FTP server with email notification |
| Medical Records for Data Validation | 90 days after the request received from AHCCCS | Data Validation User Manual | Encounter Administrator | FTP server with email notification |
| Encounter Submission and Tracking | Quarterly, 15 days after the end of each quarter | Section D, ¶ 65 and Encounter Manual | DHCM, Encounter Administrator | FTP server with email notification |
|
| | | | |
| REPORT | WHEN DUE | SOURCE/REFERENCE | SEND TO: | SUBMITTED VIA |
| Office of Inspector General | | | | |
| Provider Fraud/Abuse Report | Within 10 days of discovery | Section D, Paragraph 62 | Office of Inspector General | Secure email or web portal |
| Eligible Person Fraud/Abuse Report | Within 10 days of discovery | Section D, Paragraph 62 | Office of Inspector General | Secure email or web portal |
146
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
ATTACHMENT F: PERIODIC REPORT REQUIREMENTS Contract/RFP No. YH09-0001
|
| | | | |
| REPORT | WHEN DUE | SOURCE/REFERENCE | SEND TO: | SUBMITTED VIA |
| DBF Contracts & Purchasing | | | | |
| Third Party Liability Reporting | Within 10 days of discovery | Section D, Paragraph 58 | AHCCCS TPL Administrator | Third Party Leads Submission File |
AHCCCS will assess the following sanctions on the deliverables listed below, under DHCM Operations, Clinical Quality Management and Medical Management that are not received by 5:00 PM on the due date indicated, if the due date falls on a weekend or a State Holiday, sanctions will be assessed on deliverables not received by 5:00 PM on the next business day.
Late Deliverables
1st time “late” sanction/ 1-10 days: $5,000
1st time “late” sanction/ 11-20 days: $10,000
1st time “late” sanction/ over 21 days: $15,000
2nd time “late” sanction/ 1-10 days: $10,000
2nd time “late” sanction/ 11-20 days: $20,000
2nd time “late” sanction/over 21 days: $30,000
3rd time “late” sanction/ 1-10 days: $20,000
3rd time “late” sanction/ 11-20 days: $40,000
3rd time “late” sanction/over 21 days: $60,000
The sanctions outlined above are deliverable specific. For example, if the Contractor submits its claims dashboard five days late in January, a $5,000 sanction will be assessed. The next month, if the Contractor submits its administrative measures five days late, it will be assessed a 1st time late sanction of $5,000. However if the Contractor submits the claims dashboard five days late again in March AHCCCS will asses a 2nd time late sanction of $10,000.
|
| | | | |
| REPORT | WHEN DUE | SOURCE/REFERENCE | SEND TO: | SUBMITTED VIA |
| DHCM Operations | | | | |
| Annual Subcontractor Assignment and Evaluation Report | 90 days after the beginning of the contract year | Section D, Paragraph 37; Section D, Paragraph 43 | Operations and Compliance Officer | FTP server with email notification |
| Provider Affiliation Transmission | 15 days after the end of each quarter | Provider Affiliation Transmission Manual, submitted to PMMIS Provider-to-Contractor FTP | Operations and Compliance Officer | FTP server with email notification |
| * Claims Dashboard | 15th day of each month following the reporting period | Section D, Paragraph 38; Claims Dashboard Reporting Guide | Operations and Compliance Officer | FTP server with email notification |
| Subcontracts | As required by contract | Section D, Paragraph 37; ACOM Policy 106 | Operations and Compliance Officer | FTP server with email notification |
147
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
ATTACHMENT F: PERIODIC REPORT REQUIREMENTS Contract/RFP No. YH09-0001
|
| | | | |
| Third Party Administrator subcontracts | 60 days prior to the effective date of the subcontract | Section D, Paragraph 37; ACOM Policy 106 | Operations and Compliance Officer | FTP server with email notification |
| Provider Advances | As required by Policy | ACOM Policy 418 | Operations and Compliance Officer | FTP server with email notification |
| Claim recoupments >$50,000 | Upon identification by Contractor | Section D, Paragraph 38; ACOM Policy 412 | Operations and Compliance Officer | FTP server with email notification |
| * Administrative Measures | 15th day of each month following the reporting period | Section D, Paragraph 25 | Operations and Compliance Officer | FTP server with email notification |
| Grievance System Report | First Day of 2nd Month Following Month Being Reported | Section D, Paragraph 26; Grievance System Reporting Guide | Operations and Compliance Officer | FTP server with email notification |
| Provider Network Development and Management Plan | 45 days after the first day of a new contract year | Section D, Paragraph 27; ACOM Policy 415 | Operations and Compliance Officer | FTP server with email notification |
| Quarterly Provider Terminations Due To Rates | 15 days after the end of each quarter | ACOM Policy 415 | Operations and Compliance Officer | FTP server with email notification |
| Cultural Competency Plan | 45 days after the first day of a new contract year | ACOM Policy 405 | Operations and Compliance Officer | FTP server with email notification |
| Business Continuity and Recovery Plan | 15 days after the beginning of each contract year | ACOM Policy 104 | Operations and Compliance Officer | FTP server with email notification |
| Marketing Attestation Statement | 45 days after the beginning of each contract year | ACOM Policy 101 | Operations and Compliance Officer | FTP server with email notification |
| Marketing and Outreach Materials | 30 days prior to dissemination | ACOM Policy 101 | Marketing Committee Chairperson | FTP server with email notification |
| Member Handbook | Within 4 weeks of receiving annual amendment and upon any changes prior to distribution. | Section D, Paragraph 18; ACOM Policy 404 | Operations and Compliance Officer | FTP server with email notification |
| Annual Website Certification | Within 45 days after the beginning of the contract year | Section D, Paragraph 18; ACOM Policy 404 | Operations and Compliance Officer | FTP server with email notification |
| Provider Network – Material Change | Submit change for approval prior to effective date | Section D, Paragraph 29; ACOM Policy 416 | Operations and Compliance Officer | FTP server with email notification |
| Provider Network – Unexpected change | Within one business day | Section D, Paragraph 29 | Operations and Compliance Officer | FTP server with email notification |
148
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
ATTACHMENT F: PERIODIC REPORT REQUIREMENTS Contract/RFP No. YH09-0001
|
| | | | |
| REPORT | WHEN DUE | SOURCE/REFERENCE | SEND TO: | SUBMITTED VIA |
| System Change Plan | Six months prior to implementation | Section D, Paragraph 38 | Operations and Compliance Officer | FTP server with email notification |
Organizational Chart with “Key Staff” positions | October 15th | Section D, Paragraph 16 | Operations and Compliance Officer | FTP server with email notification |
Key Staff Demographics for Staff listed in a., b. & c. (Section D, ¶25) | October 15th | Section D, Paragraph 16 | Valarie Noor, HC Health Program Manager III, OIG/Provider Relations; MD 4500, 701 E. Jefferson, Phoenix, AZ 85034 | Hardcopy |
Functional Organizational Chart with key program areas, responsibilities and reporting lines. | October 15th | Section D, Paragraph 16 | Operations and Compliance Officer | FTP server with email notification |
| Key Position Change | Within 7 days after an employee leaves and as soon as new hire has taken place | Section D, Paragraph 16 | Operations and Compliance Officer | FTP server with email notification |
| Staff functions located outside of Arizona | October 15th | Section D, Paragraph 16 | Operations and Compliance Officer | FTP server with email notification |
| Annual HIPAA Security and Privacy Audit Review | 90 days after the beginning of the contract year | Section D, Paragraph 64 | Operations and Compliance Officer | FTP server with email notification |
Attestation of Disclosure Information of: Ownership & Control and Persons Convicted of a Crime | October 15 | Section D, Paragraph 62 | Operations and Compliance Officer | FTP server with email notification |
149
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
ATTACHMENT F: PERIODIC REPORT REQUIREMENTS Contract/RFP No. YH09-0001
|
| | | | |
| REPORT | WHEN DUE | SOURCE/REFERENCE | SEND TO: | SUBMITTED VIA |
| DHCM Clinical Quality Management | | | | |
| EPSDT Annual Monitoring Report | Annually on December 15th | Section D, Paragraph 10, Scope of Services, AMPM Chapter 400 | Clinical Quality Management Unit (DHCM) | FTP server with email notification |
| EPSDT Improvement and Adult Quarterly Monitoring Report (Template must be used) | 15 days after the end of each quarter | Section D, Paragraph 23, Scope of Services, AMPM Chapter 400 See Suspension list for specific items being suspended | Clinical Quality Management Unit (DHCM) | FTP server with email notification |
| Quality Assessment/Performance Improvement Plan and Evaluation (Checklist to be submitted with Document) | Annually on December 15th | AMPM Chapter 900 | Clinical Quality Management Unit (DHCM) | FTP server with email notification |
| Credentialing Quarterly Report | 30 days after the end of each quarter | Section D, Paragraph 25 | Clinical Quality Management Unit (DHCM) | FTP server with email notification |
| Monthly Pregnancy Termination Report | End of the month following the pregnancy termination | AMPM Chapter 400 | Clinical Quality Management Unit (DHCM) | Secure email to CQM Administrator or fax to 602-417-4162 |
| Maternity Care Plan | Annually on December 15th | AMPM Chapter 400 | Clinical Quality Management Unit (DHCM) | FTP server with email notification |
| Stillbirth Report | Immediately following procedure | AMPM Chapter 400 | Clinical Quality Management Unit (DHCM) | Secure email to CQM Administrator or fax to 602-417-4162 |
| Semi-annual report of number of pregnant women who are HIV/AIDS positive | 30 days after the reporting periods of: [10/1 through 9/30] & [4/1 through 9/30] | AMPM Chapter 400 | Clinical Quality Management Unit (DHCM) | FTP server with email notification |
| Performance Improvement Project Baseline Report (Standardized format to be utilized) | Annually on December 15th | AMPM Chapter 900 | Clinical Quality Management Unit (DHCM) | FTP server with email notification |
150
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
ATTACHMENT F: PERIODIC REPORT REQUIREMENTS Contract/RFP No. YH09-0001
|
| | | | |
| REPORT | WHEN DUE | SOURCE/REFERENCE | SEND TO: | SUBMITTED VIA |
| DHCM Clinical Quality Management | | | | |
| Performance Improvement Project Re-measurement Report (Standardized format to be utilized) | Annually on December 15th | AMPM Chapter 900 | Clinical Quality Management Unit (DHCM) | FTP server with email notification |
| Performance Improvement Project Final Report (Standardized format to be utilized) | Within 180 days of the end of the project, as defined in the project proposal approved by AHCCCS DHCM | AMPM Chapter 900 | Clinical Quality Management Unit (DHCM) | FTP server with email notification |
| QM Quarterly Report | 45 Days after the end of each quarter | Section D, Paragraph 23 | Clinical Quality Management Unit (DHCM) | FTP server with email notification |
| Pediatric Immunization Audit | As requested | Section D, Paragraph 23 | Clinical Quality Management Unit (DHCM) | FTP server with email notification |
|
| | | | |
| REPORT | WHEN DUE | SOURCE/REFERENCE | SEND TO: | SUBMITTED VIA |
| DHCM Medical Management | | | | |
| Quarterly Inpatient Hospital Showing | 15 days after the end of each quarter | State Medicaid Manual and the AMPM Chapter 1000 | Medical Management Unit (DHCM) | FTP server with email notification |
| MM/UM Plan and Evaluation | Annually on December 15th | AMPM Chapter 1000 | Medical Management Unit (DHCM) | FTP server with email notification |
| UM Quarterly Report | 60 Days after the end of each quarter | Section D, Paragraph 24 (Suspended) | Medical Management Unit (DHCM) | FTP server with email notification |
| HIV Specialty Provider List | Annually, on December 15th | AMPM Chapter 300 | Medical Management Unit (DHCM) (DHCM) | FTP server with email notification |
| Transplant Report | 15 days after the end of each quarter | AMPM Chapter 1000 | Medical Management Unit (DHCM) | FTP server with email notification |
151
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
ATTACHMENT F: PERIODIC REPORT REQUIREMENTS Contract/RFP No. YH09-0001
|
| | | | |
| REPORT | WHEN DUE | SOURCE/REFERENCE | SEND TO: | SUBMITTED VIA |
| DHCM Medical Management | | | | |
| Non-Transplant and Catastrophic Reinsurance covered Diseases | Annually, within 30 days of the beginning of the contract year and when newly enrolled in the plan or newly diagnosed. | Section D, Paragraph 57 | Medical Management Unit (DHCM) | FTP server with email notification |
Suspensions and Modifications
The following describes suspensions and modifications made during the current contract or renewal period with limited application. The following suspensions and modifications will be in effect for the period from October 1, 2012 through September 30, 2013. These changes do not serve to remove the requirement for the Contractor to collect, analyze, and respond to the internal monitoring mechanisms that support compliance with contractual and statutory requirements but serve only to condense deliverable requirements in order to ease administrative burden.
Suspensions
Suspensions will be defined as a complete temporary release from the deliverable requirement as presented in contract for the term shown in this Attachment.
Section D, Paragraph 23, Quality Management
Certain requirements contained in the EPSDT Quarterly Report are being suspended. The reporting requirements are being reduced by suspending the PEDS tracking and Obesity Tracking reporting in the EPSDT Quarterly Report are suspended.
Section D, Paragraph 24, Medical Management
The Medical Management UM Quarterly Report is suspended.
Section D, Paragraph 38, Claims Payment/Health Information System
Independent Audits of Claims Payment/Health Information Systems
152
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
ATTACHMENT F: PERIODIC REPORT REQUIREMENTS Contract/RFP No. YH09-0001
Attachment F, Periodic Reporting Requirements
|
| | | | |
| REPORT | WHEN DUE | SOURCE/REFERENCE | SEND TO: | SUBMITTED VIA |
| DHCM Medical Management | | | | |
| UM Quarterly Report | 60 Days after the end of each quarter | Section D, Paragraph 24 | DHCM/MM | FTP server with email notification |
Modifications
Modifications will be defined as a reduction in the frequency or content of a deliverable requirement that will remain in place throughout the temporary term shown in this Attachment.
There are no modifications at this time.
153
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
ATTACHMENT G: AUTO-ASSIGNMENT ALGORITHM Contract/RFP No. YH09-0001
ATTACHMENT G: AUTO-ASSIGNMENT ALGORITHM
Members who have the right to choose, but do not exercise this right, will be assigned to a Contractor through an auto-assignment algorithm. The algorithm is a mathematical formula used to distribute members to the various Contractors in a manner that is consistent with AHCCCS goals.
With the exception of an enhanced auto-assignment algorithm that may be in effect at the start of a new contract cycle (October 1, 2008) for a three to six month period, the auto-assignment algorithm calculation details are as follows:
The algorithm employs a data table and a formula to assign cases (a case may be a member or a household of members) to Contractors using the target percentages developed. The algorithm data table consists of all the geographic service areas (GSA) in the state, all Contractors serving each GSA, and the target percentages by risk group within each GSA.
The Contractor farthest away from its target percentage within a GSA and risk group, the largest negative difference, is assigned the next case for that GSA. The equation used is:
(t/T) – P = d
t = The total members assigned to the GSA, per risk group category, for the Contractor
T = The total members assigned to the GSA, per risk group category, all Contractors combined
P = The target percentage of members per risk group for the Contractor
d = The difference
The algorithm is calculated after each assignment to give a new difference for each Contractor. When more than one Contractor has the same difference, and their differences are greater than all other Contractors, the Contractor with the lowest Health Plan I.D. Number will be assigned the case.
Assignment by the algorithm applies to:
| |
| 1. | Members who are newly eligible to the AHCCCS program that did not choose a Contractor within the prescribed time limits. |
| |
| 2. | Members whose assigned health plan is no longer available after the member moves to a new GSA and did not choose a new Contractor within the prescribed time limits. |
All Contractors, within a given geographic service area (GSA) and for each risk group, will have a placement in the algorithm and will receive members accordingly. A Contractor with a more favorable target percentage in the algorithm will receive proportionally more members. Conversely, a Contractor with a lower target percentage in the algorithm will receive proportionally fewer members. The initial algorithm formula favors Contractors with both lower awarded capitation rates and higher scores on the Program Component of the proposal.
In future contract years, AHCCCS may adjust the auto-assignment algorithm in consideration of Contractors’ clinical performance measure results when calculating target percentages. Ranking in the algorithm may be weighted based on the number of Performance Measures for which a Contractor is meeting the current AHCCCS Minimum Performance Standard (MPS) as a percentage of the total number of measures utilized in the calculation. AHCCCS will determine the Performance Measures used to evaluate Contractor performance and apply the criterion universally when making the adjustment.
154
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
ATTACHMENT G: AUTO-ASSIGNMENT ALGORITHM Contract/RFP No. YH09-0001
Development of the Target Percentages for CYE 09 through CYE 12
Beginning in CYE ’09, the algorithm target percentages will be developed using the methodology described below, subject to the enhanced algorithm described below, if applicable. However, for subsequent years, AHCCCS reserves the right to change the algorithm methodology to assure assignments are made in the best interest of the AHCCCS program and the State.
A Contractor’s placement in the algorithm is based upon the following two factors, which are weighted as follows:
|
| | |
| # | Factor | Weighting |
| 1 | The Contractor’s final awarded capitation rate from AHCCCS. | 50% |
| 2 | The Contractor’s score on the Program component of the proposal. | 50% |
Points will be assigned to each Contractor by risk group by GSA. Based on the rankings of the final awarded capitation rates and the final Program component scores, each Contractor will be assigned a number of points for each of these two components separately using the table below:
TABLE OF POINTS FOR FACTORS #1 (LOWEST CAPITATION RATE) AND #2 (HIGHEST PROGRAM SCORE)
|
| | | | | | |
| Number of Awards in GSA |
1st Place | 2nd Place | 3rd Place | 4th Place | 5th Place | 6th Place |
| 2 | 60 | 40 | | | | |
| 3 | 44 | 32 | 24 | | | |
| 4 | 35 | 28 | 22 | 15 | | |
| 5 | 30 | 25 | 20 | 15 | 10 | |
| 6 | 26 | 23 | 19 | 15 | 11 | 6 |
Two or more Contractors that have equal final awarded capitation rates or Program component scores in a GSA for the same risk group will be given an equal percentage of the points for all of the positions held by the tied Contractors combined.
The points awarded for the two components will be combined as follows to give the target percentage for each Contractor by GSA by risk group:
Final Awarded Capitation Rate (.50) + Program Component Score (.50) = TARGET PERCENTAGE
Development of the Target Percentages for CYE 13
A Contractor’s placement in the algorithm for CYE 13 will be based upon the following two factors, which are weighted as follows:
|
| | |
| # | Factor | Weighting |
| 1 | The Contractor’s final awarded capitation rate from AHCCCS. | 50% |
| 2 | The Contractor’s percent of all Clinical Quality Performance Measures for which no sanctions are applied for the measurement period of CYE 2011. | 50% |
155
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
ATTACHMENT G: AUTO-ASSIGNMENT ALGORITHM Contract/RFP No. YH09-0001
Points will be assigned to each Contractor by risk group by GSA. Based on the rankings of the final awarded capitation rates and the Clinical Quality Performance Measure results, each Contractor will be assigned a number of points for each of these two components separately using the table below:
TABLE OF POINTS FOR FACTORS #1 (LOWEST CAPITATION RATE) AND #2 (CLINICAL QUALITY PREFORMANCE MEASURES)
|
| | | | | | |
| Number of Awards in GSA for Factor #1 and Factor #2 |
1st Place | 2nd Place | 3rd Place | 4th Place | 5th Place | 6th Place |
| 2 | 60 | 40 | | | | |
| 3 | 44 | 32 | 24 | | | |
| 4 | 35 | 28 | 22 | 15 | | |
| 5 | 30 | 25 | 20 | 15 | 10 | |
| 6 | 26 | 23 | 19 | 15 | 11 | 6 |
Two or more Contractors that have equal final awarded capitation rates in a GSA for the same risk group or equal Clinical Quality Performance Measure results will be given an equal percentage of the points for all of the positions held by the tied Contractors combined.
The points awarded for the two components will be combined as follows to give the target percentage for each Contractor by GSA by risk group:
Final Awarded Capitation Rate (.50) + Clinical Quality Performance Measure results (.50) = TARGET PERCENTAGE
Enrollment Considerations
AHCCCS will favor new and small Contractors in each GSA with increased auto-assignment. A new Contractor is defined as a Contractor new to the AHCCCS program or an incumbent Contractor that is new to a GSA. Small Contractors will be determined based on enrollment as of May 1, 2008. A small Contractor is defined by GSA and has a membership level as delineated in the following table:
|
| |
| County/GSA | GSA-specific Enrollment Threshold |
| Maricopa – GSA 12 | <50,000 |
| Pima County Only | <30,000 |
| Rural GSAs (including Santa Cruz County) | less than or equal to 45% of enrollment in the entire GSA as of May 1, 2008 |
156
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
ATTACHMENT G: AUTO-ASSIGNMENT ALGORITHM Contract/RFP No. YH09-0001
Conversion Group Auto-Assignment
Members who are enrolled as of June 30, 2008 in an Exiting Contractor (Conversion Group) will be assigned to new and small Contractors within their GSA, effective October 1, 2008 via the conversion auto-assignment algorithm. These members will be allowed to remain with the Contractor to which they were auto-assigned or to choose a different Contractor by August 31, 2008 from any of the incumbent or new Contractors in the GSA that are effective October 1, 2008. These members will again have an opportunity to change Contractors from October 1, 2008 until November 30, 2008 in order to provide them with the choice of any incumbent or new Contractors.
If the number of members in the Conversion Group in a GSA is enough to bring all new and small Contractors within the GSA above the thresholds listed in the table above, the conversion auto-assignment algorithm will be applied until all of the new and small Contractors reach the thresholds. The remaining members of the Conversion Group will be auto-assigned to all Contractors in the GSA according to the initial algorithm methodology based on awarded capitation rates and Program Component scores.
If the number of Conversion Group members in a GSA is not enough to bring all new and small Contractors within the GSA above the thresholds listed in the table above, an enhanced auto-assignment will be utilized to bring all new and small Contractors as close to equal as possible, without reducing any Contractor size.
In a rural GSA, if both Contractors are new to AHCCCS, the Conversion Group members will be auto-assigned approximately equally between the two Contractors.
For details on member choice of Contractors for the months of July, August and September 2008, see Section I. For members being auto-assigned in July 2008, the algorithm will be based on the CYE 08 contract. For members auto-assigned during August and September 2008, the algorithm will be based on the CYE 08 contract with exiting Contractors in each GSA excluded, except in family continuity, newborn enrollment, and 90-day re-enrollment situations. For GSAs in which all Contractors are exiting, the CYE 08 algorithm will remain in effect through September 30, 2008.
Post-Conversion Auto-Assignment
For purposes of determining the enhanced algorithm, new Contractors and Continuing Contractors still below the thresholds on September 1, 2008 will receive members under the enhanced auto-assign algorithm beginning October 1, 2008. The enhanced algorithm will continue to favor those Contractors below the threshold, for at least three months but no longer than six months, regardless of their membership level during or at the end of the time period. In this situation, the plans not qualifying for the enhanced auto-assignment algorithm will not receive any members via auto-assignment for the time period. After the three to six month time period, the algorithm will revert to the initial methodology based on final awarded capitation and Program Component score and all Contractors will again be included in the algorithm.
All efforts will be made to auto-assign members based on the methodology and thresholds above, however amounts may not be exact due to issues such as family continuity, newborns, 90-day re-enrollment etc.
157
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
ATTACHMENT H: GRIEVANCE SYSTEM AND STANDARDS Contract/RFP No. YH09-0001
ATTACHMENT H(1): ENROLLEE GRIEVANCE SYSTEM STANDARDS AND POLICY
The Contractor shall have a written policy delineating its Grievance System which shall be in accordance with applicable Federal and State laws, regulations and policies, including, but not limited to 42 CFR Part 438 Subpart F. The Contractor shall provide the AHCCCS Grievance System Reporting Guide to all providers and subcontractors at the time of contract. The Contractor shall also furnish this information to enrollees within a reasonable time after the Contractor receives notice of the enrollment. Additionally, the Contractor shall provide written notification of any significant change in this policy at least 30 days before the intended effective date of the change.
The written information provided to enrollees describing the Grievance System including the grievance process, the appeals process, enrollee rights, the grievance system requirements and timeframes, shall be in each prevalent non-English language occurring within the Contractor’s service area and in an easily understood language and format. The Contractor shall inform enrollees that oral interpretation services are available in any language, that additional information is available in prevalent non-English languages upon request and how enrollees may obtain this information.
Written documents, including but not limited to the Notice of Action, the Notice of Appeal Resolution, Notice of Extension for Resolution, and Notice of Extension of Notice of Action shall be translated in the enrollee’s language if information is received by the Contractor, orally or in writing, indicating that the enrollee has a limited English proficiency. Otherwise, these documents shall be translated in the prevalent non-English language(s) or shall contain information in the prevalent non-English language(s) advising the enrollee that the information is available in the prevalent non-English language(s) and in alternative formats along with an explanation of how enrollees may obtain this information. This information must be in large, bold print appearing in a prominent location on the first page of the document.
At a minimum, the Contractor’s Grievance System Standards and Policy shall specify:
| |
| 1. | That the Contractor shall maintain records of all grievances, appeals and requests for hearing. |
| |
| 2. | Information explaining the grievance, appeal, and fair hearing procedures and timeframes. This information shall include a description of the circumstances when there is a right to a hearing, the method for obtaining a hearing, the requirements which govern representation at the hearing, the right to file grievance and appeals and the requirements and timeframes for filing a grievance, appeal, or request for hearing. |
| |
| 3. | The availability of assistance in the filing process and the Contractor’s toll-free numbers that an enrollee can use to file a grievance or appeal by phone if requested by the enrollee. |
| |
| 4. | That the Contractor shall acknowledge receipt of each grievance and appeal. For Appeals, the Contractor shall acknowledge receipt of standard appeals in writing within five business days of receipt and within one business day of receipt of expedited appeals. |
| |
| 5. | That the Contractor shall permit both oral and written appeals and grievances and that oral inquiries appealing an action are treated as appeals. |
| |
| 6. | That the Contractor shall ensure that individuals who make decisions regarding grievances and appeals are individuals not involved in any previous level of review or decision making and that individuals who make decisions regarding: 1) appeals of denials based on lack of medical necessity, 2) a grievance regarding denial of expedited resolution of an appeal or 3) grievances or appeals |
158
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
ATTACHMENT H: GRIEVANCE SYSTEM AND STANDARDS Contract/RFP No. YH09-0001
involving clinical issues are health care professionals as defined in 42 CFR 438.2 with the appropriate clinical expertise in treating the enrollee’s condition or disease.
| |
| 7. | The resolution timeframes for standard appeals and expedited appeals may be extended up to 14 days if the enrollee requests the extension or if the Contractor establishes a need for additional information and that the delay is in the enrollee’s interest. |
| |
| 8. | That if the Contractor extends the timeframe for resolution of an appeal when not requested by the enrollee, the Contractor shall provide the enrollee with written notice of the reason for the delay. |
| |
| 9. | The definition of grievance as a member’s expression of dissatisfaction with any aspect of their care, other than the appeal of actions. |
| |
| 10. | That an enrollee must file a grievance with the Contractor and that the enrollee is not permitted to file a grievance directly with AHCCCS. |
| |
| 11. | That the Contractor must dispose of each grievance in accordance with theAHCCCS Grievance System Reporting Guide, but in no case shall the timeframe exceed 90 days. |
| |
| 12. | The definition of action as the [42 CFR 438.400(b)]: |
| |
| a. | Denial or limited authorization of a requested service, including the type or level of service; |
| |
| b. | Reduction, suspension, or termination of a previously authorized service; |
| |
| c. | Denial, in whole or in part, of payment for a service; |
| |
| d. | Failure to provide services in a timely manner; |
| |
| e. | Failure to act within the timeframes required for standard and expedited resolution of appeals and standard disposition of grievances; or |
| |
| f. | Denial of a rural enrollee’s request to obtain services outside the Contractor’s network under 42 CFR 438.52(b)(2)(ii), when the Contractor is the only Contractor in the rural area. |
| |
| 13. | The definition of a service authorization request as an enrollee’s request for the provision of a service [42 CFR 431.201]. |
| |
| 14. | The definition of appeal as the request for review of an action, as defined above. |
| |
| 15. | Information explaining that a provider acting on behalf of an enrollee and with the enrollee’s written consent, may file an appeal. |
| |
| 16. | That an enrollee may file an appeal of: 1) the denial or limited authorization of a requested service including the type or level of service, 2) the reduction, suspension or termination of a previously authorized service, 3) the denial in whole or in part of payment for service, 4) the failure to provide services in a timely manner, 5) the failure of the Contractor to comply with the timeframes for dispositions of grievances and appeals and 6) the denial of a rural enrollee’s request to obtain services outside the Contractor’s network under 42 CFR 438.52(b)(2)(ii) when the Contractor is the only Contractor in the rural area. |
| |
| 17. | The definition of a standard authorization request. For standard authorization decisions, the Contractor must provide a Notice of Action to the enrollee as expeditiously as the enrollee’s health condition requires, but not later than 14 days following the receipt of the authorization request with a possible extension of up to 14 days if the enrollee or provider requests an extension or if the Contractor establishes a need for additional information and delay is in the enrollee’s best interest [42 CFR 438.210(d)(1)]. The Notice of Action must comply with the advance notice requirements when there is a termination or reduction of a previously |
159
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
ATTACHMENT H: GRIEVANCE SYSTEM AND STANDARDS Contract/RFP No. YH09-0001
authorized service OR when there is a denial of an authorization request and the physician asserts that the requested service/treatment is a necessary continuation of a previously authorized service.
| |
| 18. | The definition of an expedited authorization request. For expedited authorization decisions, the Contractor must provide a Notice of Action to the enrollee as expeditiously as the enrollee’s health condition requires, but not later than three business days following the receipt of the authorization request with a possible extension of up to 14 days if the enrollee or provider requests an extension or if the Contractor establishes a need for additional information and delay is in the enrollee’s interest [42 CFR 438.210(d)(2)]. |
| |
| 19. | That the Notice of Action for a service authorization decision not made within the standard or expedited timeframes, whichever is applicable, will be made on the date that the timeframes expire. If the Contractor extends the timeframe to make a standard or expedited authorization decision, the Contractor must give the enrollee written notice of the reason to extend the timeframe and inform the enrollee of the right to file a grievance if the enrollee disagrees with the decision. The Contractor must issue and carry out its decision as expeditiously as the enrollee’s health condition requires and no later than the date the extension expires. |
| |
| 20. | That the Contractor shall notify the requesting provider of the decision to deny or reduce a service authorization request. The notice to the provider must be written. |
| |
| 21. | The definition of a standard appeal and that the Contractor shall resolve standard appeals no later than 30 days from the date of receipt of the appeal unless an extension is in effect. If a Notice of Appeal Resolution is not completed when the timeframe expires, the member’s appeal shall be considered to be denied by the Contractor, and the member can file a request for hearing. |
| |
| 22. | The definition of an expedited appeal and that the Contractor shall resolve all expedited appeals not later than three business days from the date the Contractor receives the appeal (unless an extension is in effect) where the Contractor determines (for a request from the enrollee), or the provider (in making the request on the enrollee’s behalf indicates) that the standard resolution timeframe could seriously jeopardize the enrollee’s life or health or ability to attain, maintain or regain maximum function. The Contractor shall make reasonable efforts to provide oral notice to an enrollee regarding an expedited resolution appeal. If a Notice of Appeal Resolution is not completed when the timeframe expires, the member’s appeal shall be considered to be denied by the Contractor, and the member can file a request for hearing. |
| |
| 23. | That if the Contractor denies a request for expedited resolution, it must transfer the appeal to the 30-day timeframe for a standard appeal. The Contractor must make reasonable efforts to give the enrollee prompt oral notice and follow-up within two days with a written notice of the denial of expedited resolution. |
| |
| 24. | That an enrollee shall be given 60 days from the date of the Contractor’s Notice of Action to file an appeal. |
| |
| 25. | That the Contractor shall mail a Notice of Action: 1) at least 10 days before the date of a termination, suspension or reduction of previously authorized AHCCCS services, except as provided in (a)-(e) below; 2) at least five days before the date of action in the case of suspected fraud; 3) at the time of any action affecting the claim when there has been a denial of payment for a service, in whole or in part; 4) within 14 days from receipt of a standard service authorization request and within three business days from receipt of an expedited service authorization request, unless an extension is in effect. For service authorization decisions, the Contractor shall also ensure that the Notice of Action provides the enrollee with advance notice and the right to request continued benefits for all terminations and reductions of a previously authorized service and for denials when the physician asserts that the requested service/treatment which has been denied is a necessary continuation of a previously authorized service. As described below, the Contractor may elect to mail a Notice of Action no later than the date of action when: |
| |
| a) | The Contractor receives notification of the death of an enrollee; |
160
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
ATTACHMENT H: GRIEVANCE SYSTEM AND STANDARDS Contract/RFP No. YH09-0001
| |
| b) | The enrollee signs a written statement requesting service termination or gives information requiring termination or reduction of services (which indicates understanding that the termination or reduction will be the result of supplying that information); |
| |
| c) | The enrollee is admitted to an institution where he is ineligible for further services; |
| |
| d) | The enrollee’s address is unknown and mail directed to the enrollee has no forwarding address; |
| |
| e) | The enrollee has been accepted for Medicaid in another local jurisdiction. |
| |
| 26. | That the Contractor include, as parties to the appeal, the enrollee, the enrollee’s legal representative, or the legal representative of a deceased enrollee’s estate. |
| |
| 27. | That the Notice of Action must explain: 1) the action the Contractor has taken or intends to take, 2) the reasons for the action, 3) the enrollee’s right to file an appeal with the Contractor, 4) the procedures for exercising these rights, 5) circumstances when expedited resolution is available and how to request it and 6) the enrollee’s right to receive continued benefits pending resolution of the appeal, how to request continued benefits and the circumstances under which the enrollee may be required to pay for the cost of these services. The Notice of Action shall comply with ACOM Policy 414. |
| |
| 28. | That benefits shall continue until a hearing decision is rendered if: 1) the enrollee files an appeal before the later of a) 10 days from the mailing of the Notice of Action or b) the intended date of the Contractor’s action, 2) a) the appeal involves the termination, suspension, or reduction of a previously authorized course of treatment or b) the appeal involves a denial and the physician asserts that the requested service/treatment is a necessary continuation of a previously authorized service, 3) the services were ordered by an authorized provider and 4) the enrollee requests a continuation of benefits. |
For purposes of this paragraph, benefits shall be continued based on the authorization which was in place prior to the denial, termination, reduction, or suspension which has been appealed.
| |
| 29. | That for appeals, the Contractor provides the enrollee a reasonable opportunity to present evidence and allegations of fact or law in person and in writing and that the Contractor informs the enrollee of the limited time available in cases involving expedited resolution. |
| |
| 30. | That for appeals, the Contractor provides the enrollee and his representative the opportunity before and during the appeals process to examine the enrollee’s case file including medical records and other documents considered during the appeals process. |
| |
| 31. | That the Contractor must ensure that punitive action is not taken against a provider who either requests an expedited resolution or supports an enrollee’s appeal. |
| |
| 32. | That the Contractor shall provide written Notice of Appeal Resolution to the enrollee and the enrollee’s representative or the representative of the deceased enrollee’s estate which must contain: 1) the results of the resolution process, including the legal citations or authorities supporting the determination, and the date it was completed, and 2) for appeals not resolved wholly in favor of enrollees: a) the enrollee’s right to request a State fair hearing (including the requirement that the enrollee must file the request for a hearing in writing) no later than 30 days after the date the enrollee receives the Contractor’s notice of appeal resolution and how to do so, b) the right to receive continued benefits pending the hearing and how to request continuation of benefits and c) information explaining that the enrollee may be held liable for the cost of benefits if the hearing decision upholds the Contractor. |
| |
| 33. | That the Contractor continues extended benefits originally provided to the enrollee until any of the following occurs: 1) the enrollee withdraws appeal, 2) the enrollee has not specifically requested continued benefits |
161
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
ATTACHMENT H: GRIEVANCE SYSTEM AND STANDARDS Contract/RFP No. YH09-0001
pending a hearing decision within 10 days of the Contractor mailing of the appeal resolution notice, or 3) AHCCCS issues a state fair hearing decision adverse to the enrollee.
| |
| 34. | That if the enrollee files a request for hearing the Contractor must ensure that the case file and all supporting documentation is received by the AHCCCS Office of Administrative Legal Services (OALS) as specified by OALS. The file provided by the Contractor must contain a cover letter that includes: |
| |
| b. | Enrollee’s AHCCCS I.D. number |
| |
| d. | Enrollee’s phone number (if applicable) |
| |
| e. | Date of receipt of the appeal |
| |
| f. | Summary of the Contractor’s actions undertaken to resolve the appeal and summary of the appeal resolution |
| |
| 35. | The following material shall be included in the file sent by the Contractor: |
| |
| a. | The Enrollee’s written request for hearing |
| |
| b. | Copies of the entire appeal file which includes all supporting documentation including Pertinent findings and medical records |
| |
| c. | The Contractor’s Notice of Appeal Resolution |
| |
| d. | Other information relevant to the resolution of the appeal |
| |
| 36. | That if the Contractor or the State fair hearing decision reverses a decision to deny, limit or delay services not furnished during the appeal or the pendency of the hearing process, the Contractor shall authorize or provide the services promptly and as expeditiously as the enrollee's health condition requires irrespective of whether the Contractor contests the decision. |
| |
| 37. | That if the Contractor or State fair hearing decision reverses a decision to deny authorization of services and the disputed services were received pending appeal, the Contractor shall pay for those services, as specified in policy and/or regulation. |
| |
| 38. | That if the Contractor or the Director's Decision reverses a decision to deny, limit, or delay authorization of services, and the member received the disputed services while the appeal was pending, the Contractor shall process a claim for payment from the provider in a manner consistent with the Contractor's or Director's Decision and applicable statutes, Rules, policies, and contract terms. The provider shall have 90 days from the date of the reversed decision to submit a clean claim to the Contractor for payment. For all claims submitted as a result of a reversed decision, the Contractor is prohibited from denying claims for untimeliness if they are submitted within the 90 day timeframe. Contractors are also prohibited from denying claims submitted as a result of a reversed decision because the member failed to request continuation of services during the appeals/hearing process: a member's failure to request continuation of services during the appeals/hearing process is not a valid basis to deny the claim. |
| |
| 39. | That if the Contractor or State fair hearing decision upholds a decision to deny authorization of services and the disputed services were received pending appeal, the Contractor may recover the cost of those services from the enrollee. |
162
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
ATTACHMENT H: GRIEVANCE SYSTEM AND STANDARDS Contract/RFP No. YH09-0001
ATTACHMENT H(2): PROVIDER CLAIM DISPUTE STANDARDS AND POLICY
The Contractor shall have in place a written claim dispute policy for providers. The policy shall be in accordance with applicable Federal and State laws, regulations and policies. The claim dispute policy shall include the following provisions:
| |
| 1. | The Provider Claim Dispute Policy shall be provided to all subcontractors at the time of contract. For providers without a contract, the claim dispute policy may be mailed with a remittance advice, provided the remittance is sent within 45 days of receipt of a claim. |
| |
| 2. | The Provider Claim Dispute Policy must specify that all claim disputes challenging claim payments, denials or recoupments must be filed in writing with the Contractor no later than 12 months from the date of service, 12 months after the date of eligibility posting or within 60 days after the payment, denial or recoupment of a timely claim submission, whichever is later. |
| |
| 3. | Specific individuals are appointed with authority to require corrective action and with requisite experience to administer the claim dispute process. |
| |
| 4. | A log is maintained for all claim disputes containing sufficient information to identify the Complainant, date of receipt, nature of the claim dispute and the date the claim dispute is resolved. Separate logs must be maintained for provider and behavioral health recipient claim disputes. |
| |
| 5. | Within five business days of receipt, the Complainant is informed by letter that the claim dispute has been received. |
| |
| 6. | Each claim dispute is thoroughly investigated using the applicable statutory, regulatory, contractual and policy provisions, ensuring that facts are obtained from all parties. |
| |
| 7. | All documentation received by the Contractor during the claim dispute process is dated upon receipt. |
| |
| 8. | All claim disputes are filed in a secure designated area and are retained for five years following the Contractor’s decision, the AHCCCS’ decision, judicial appeal or close of the claim dispute, whichever is later, unless otherwise provided by law. |
| |
| 9. | A copy of the Contractor’s Notice of Decision (hereafter referred to as Decision) shall be mailed to all parties no later than 30 days after the provider files a claim dispute with the Contractor, unless the provider and Contractor agree to a longer period. The Decision must include and describe in detail, the following: |
| |
| a. | The nature of the claim dispute |
| |
| c. | The reasons supporting the Contractor’s Decision, including references to applicable statute, Rule, applicable contractual provisions, policy and procedure |
| |
| d. | the Provider’s right to request a hearing by filing a written request for hearing to the Contractor no later than 30 days after the date the Provider receives the Contractor’s decision. |
| |
| e. | If the claim dispute is overturned, the requirement that the Contractor shall reprocess and pay the claim(s) in a manner consistent with the decision within 15 business days of the date of the Decision. |
| |
| 10. | If the Provider files a written request for hearing, the Contractor must ensure that all supporting documentation is received by the AHCCCS Office Administrative Legal Services (OALS), no later than |
163
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
ATTACHMENT H: GRIEVANCE SYSTEM AND STANDARDS Contract/RFP No. YH09-0001
five business days from the date the Contractor receives the provider’s written hearing request. The file sent by the Contractor must contain a cover letter that includes:
| |
| c. | Member’s Name and AHCCCS Identification Number |
| |
| d. | Provider’s phone number (if applicable) |
| |
| e. | The date of receipt of claim dispute |
| |
| f. | A summary of the Contractor’s actions undertaken to resolve the claim dispute and basis of the determination |
| |
| 11. | The following material shall be included in the file sent by the Contractor: |
| |
| a. | Written request for hearing filed by the Provider |
| |
| b. | Copies of the entire file which includes pertinent records; and the Contractor’s Decision |
| |
| c. | Other information relevant to the Notice of Decision of the claim dispute |
| |
| 12. | If the Contractor’s decision regarding a claim dispute is reversed through the appeal process, the Contractor shall reprocess and pay the claim (s) in a manner consistent with the decision within 15 business days of the date of the Decision. |
164
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
ATTACHMENT I: RESERVED Contract/RFP No. YH09-0001
ATTACHMENT I: RESERVED
165
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
ATTACHMENT J: RESERVED Contract/RFP No. YH09-0001
ATTACHMENT J: RESERVED
166
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
ATTACHMENT J(2): RESERVED Contract/RFP No. YH09-0001
ATTACHMENT J(2): RESERVED
167
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
ATTACHMENT K: RESERVED Contract/RFP No. YH09-0001
ATTACHMENT K: RESERVED
168
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012
ARIZONA HEALTH CARE COST CONTAINMENT SYSTEM
Phoenix Health Plan
10/01/12-9/30/13
|
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
| | TANF | TANF | TANF | TANF | TANF | SSI | SSI | | Maternity Delivery Supplement | |
| | <1, M/F | 1-13, M/F | 14-44, F | 14-44, M | 45+, M/F | W/Med | W/o Med | SFP | Non-Med |
Title XIX and KidsCare Rates1: | | | | | | | | | | |
| 4 Apache/Coconino/Mohave/Navajo | $ | 513.10 |
| $ | 106.54 |
| $ | 241.87 |
| $ | 165.40 |
| $ | 384.15 |
| $ | 99.01 |
| $ | 770.74 |
| $ | 13.37 |
| $ | 5,639.96 |
| $ | 416.41 |
|
| 6 Yavapai | $ | 450.81 |
| $ | 116.47 |
| $ | 282.27 |
| $ | 178.23 |
| $ | 401.28 |
| $ | 104.90 |
| $ | 870.13 |
| $ | 14.75 |
| $ | 6,703.78 |
| $ | 462.12 |
|
| 8 Gila/Pinal | $ | 480.06 |
| $ | 104.09 |
| $ | 262.85 |
| $ | 161.14 |
| $ | 430.57 |
| $ | 116.18 |
| $ | 702.66 |
| $ | 12.36 |
| $ | 6,366.34 |
| $ | 452.44 |
|
| 10 Pima | $ | 452.26 |
| $ | 86.38 |
| $ | 190.68 |
| $ | 116.16 |
| $ | 294.30 |
| $ | 93.65 |
| $ | 666.94 |
| $ | 15.06 |
| $ | 5,998.75 |
| $ | 324.48 |
|
| 12 Maricopa | $ | 506.70 |
| $ | 106.45 |
| $ | 218.74 |
| $ | 140.38 |
| $ | 379.21 |
| $ | 145.15 |
| $ | 694.52 |
| $ | 14.34 |
| $ | 6,167.47 |
| $ | 386.47 |
|
|
| | | | | | | | | | | | | | |
| | TANF | TANF | TANF | TANF | TANF | SSI | SSI |
| | <1, M/F | 1-13, M/F | 14-44, F | 14-44, M | 45+, M/F | W/Med | W/o Med |
| PPC Rates: | | | | | | | |
| 4 Apache/Coconino/Mohave/Navajo | 920.18 |
| 42.22 |
| 222.71 |
| 142.73 |
| 418.18 |
| 113.16 |
| 424.99 |
|
| 6 Yavapai | 881.60 |
| 63.27 |
| 214.71 |
| 206.87 |
| 341.07 |
| 135.94 |
| 394.98 |
|
| 8 Gila/Pinal | 883.05 |
| 65.30 |
| 199.35 |
| 157.02 |
| 295.34 |
| 99.48 |
| 418.09 |
|
| 10 Pima | 1,030.43 |
| 51.43 |
| 165.16 |
| 127.28 |
| 360.06 |
| 108.05 |
| 319.51 |
|
| 12 Maricopa | 953.45 |
| 57.64 |
| 188.92 |
| 163.37 |
| 273.63 |
| 121.19 |
| 366.17 |
|
|
| | | | |
| PPC Rates: | Option 1 Transplant | Option 2 Transplant |
| 4 Apache/Coconino/Mohave/Navajo | 16.50 |
| 16.50 |
|
| 6 Yavapai | 16.50 |
| 16.50 |
|
| 8 Gila/Pinal | 16.50 |
| 16.50 |
|
| 10 Pima | 16.50 |
| 16.50 |
|
| 12 Maricopa | 16.50 |
| 16.50 |
|
169
CYE ‘13 Acute Care Contract
Revised 9-26-2012 Effective 10-01-2012