NASH-CX Clinical Trial Top Line Results December 5, 2017 NASDAQ: GALT www.galectintherapeutics.com 2017 Galectin Therapeutics | NASDAQ: GALT For more information, see galectintherapeutics.com Exhibit 99.1
Forward Looking Statements This presentation contains, in addition to historical information, forward-looking statements within the meaning of the Private Securities Litigation Reform Act of 1995. These statements relate to future events or future performance and use words such as “may,” “estimate,” “could,” “expect” and others. They are based on our current expectations and are subject to factors and uncertainties which could cause actual results to differ materially from those described in the statements. These statements include those regarding the potential therapeutic benefits of our drugs and specifically the results of our NASH-CX clinical trial. Factors that could cause our actual performance to differ materially from those discussed in the forward-looking statements include, among others that: the data presented today represent a top line analysis, and there may be changes in the final clinical trial report due to further analysis of the full data set including additional statistical analysis; subsequent trials, if any, in whatever patient population chosen may fail to validate any positive results of our trial now concluded; future phases or future clinical studies could prove prohibitively time consuming and/or costly; plans regarding development, approval and marketing of any of our drugs are subject to change at any time based on the changing needs of our company as determined by management and regulatory agencies; strategies, personnel, and spending projections may change; due to the novel nature of our compounds, future phases of manufacturing scale-up and supporting chemical and physical characterizations for both trials and commercial purposes can be challenging and costly and there is no certainty this can be accomplished nor certainty it would acceptable to regulators; we may be unsuccessful in developing partnerships or other business relationships with other companies or obtaining capital that would allow us to further develop and/or fund any future studies or trials or sell or license our intellectual property; and, further, there is the uncertainty that any drug in development could obtain regulatory approval in any patient population. To date, we have incurred operating losses since our inception, and our future success may be impacted by our ability to manage costs and finance our continuing operations. For a discussion of additional factors impacting our business, see our Annual Report on Form 10-K for the year ended December 31, 2016, and our subsequent filings with the SEC. You should not place undue reliance on forward-looking statements. Although subsequent events may cause our views to change, we disclaim any obligation to update forward-looking statements.
Summary: NASH-CX Clinical Trial Results in Patients with NASH Cirrhosis A statistically significant and clinically meaningful effect of GR-MD-02 was observed on the primary endpoint measurement of HVPG1 in the subgroup of NASH2 cirrhosis patients without esophageal varices (81 patients or 50% of total group), regardless of the severity of their baseline portal hypertension There was a positive trend in the total group of patients, but the difference did not reach statistical significance for this primary endpoint because there was more variability in HVPG measurements for patients with esophageal varices On liver biopsy, the entire study group of GR-MD-02 treated patients had a statistically significant improvement in hepatocyte ballooning, a measure of cell death and an important factor of NASH activity A statistically significant clinical outcome effect of GR-MD-02 treatment was observed on reducing the development of esophageal varices in patients without varices at baseline We believe this is the first large, randomized clinical trial of any drug to demonstrate a clinically meaningful improvement in portal hypertension or liver biopsy in patients with NASH cirrhosis 1 HVPG = Hepatic Venous Pressure Gradient 2 NASH = Non-Alcoholic Steatohepatitis
Background: Drug Development Program with GR-MD-02 GR-MD-02 is a galectin-3 inhibitor that reverses fibrosis, reduces cell death and inflammation, and decreases portal pressure of cirrhosis, in rodent models of NASH fibrosis1 and toxin-induced liver cirrhosis2 NASH3 is a chronic disease with progressive fibrosis that may lead to cirrhosis with portal hypertension and its consequent complications, and liver transplant or ultimately death The aim of the NASH-CX clinical trial was to evaluate the safety and efficacy of GR-MD-02 in patients with well-compensated NASH cirrhosis 1 Traber PG and Zomer E. PLOS ONE 2013;8:e83481 2 Traber PG, Chou H, Zomer E, Hong F, Klyosov A Fiel M-I, Friedman, SL. PLOS ONE 2013;8:e75361 3 NASH = Non-Alcoholic Steatohepatitis
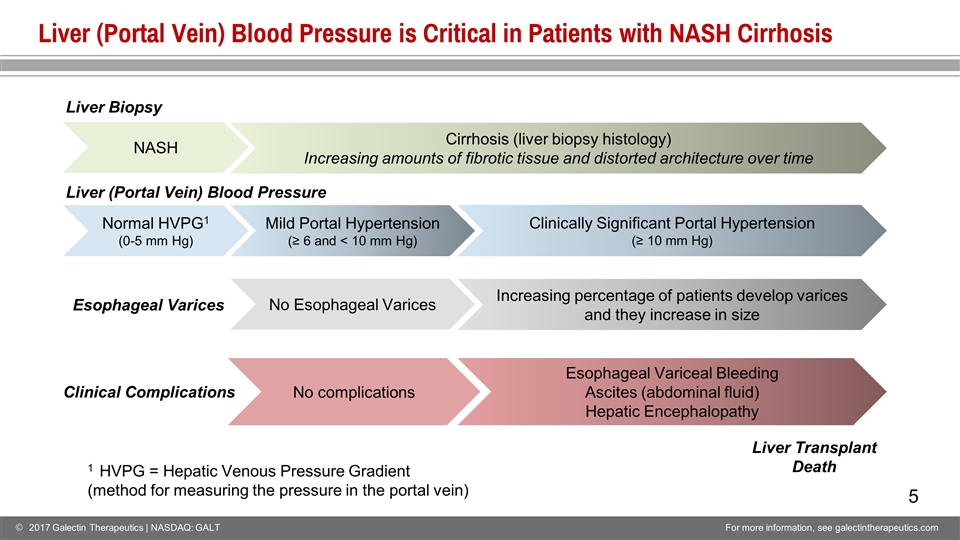
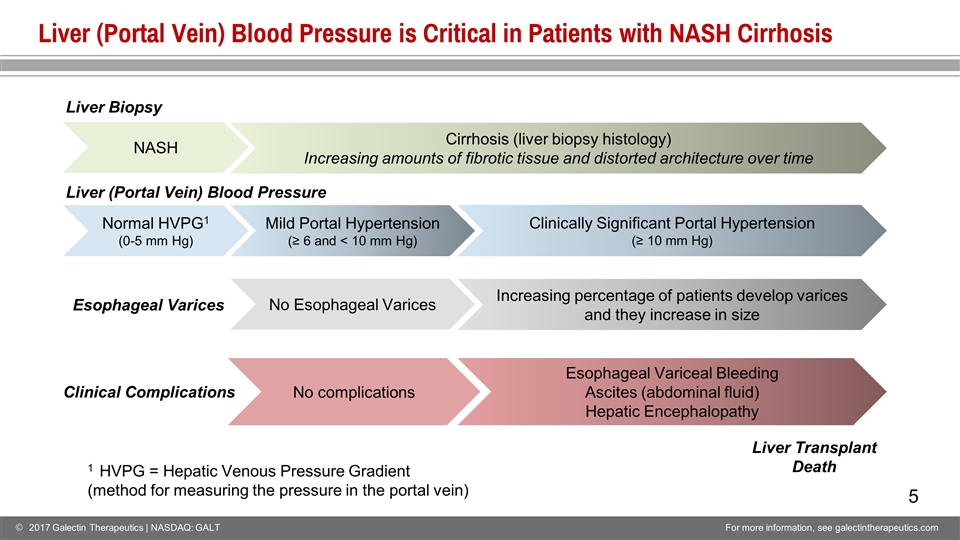
Liver (Portal Vein) Blood Pressure is Critical in Patients with NASH Cirrhosis Cirrhosis (liver biopsy histology) Increasing amounts of fibrotic tissue and distorted architecture over time Normal HVPG1 (0-5 mm Hg) Mild Portal Hypertension (≥ 6 and < 10 mm Hg) NASH Clinically Significant Portal Hypertension (≥ 10 mm Hg) Liver Biopsy Liver (Portal Vein) Blood Pressure No Esophageal Varices Esophageal Varices Increasing percentage of patients develop varices and they increase in size Clinical Complications Esophageal Variceal Bleeding Ascites (abdominal fluid) Hepatic Encephalopathy Liver Transplant Death No complications 1 HVPG = Hepatic Venous Pressure Gradient (method for measuring the pressure in the portal vein)
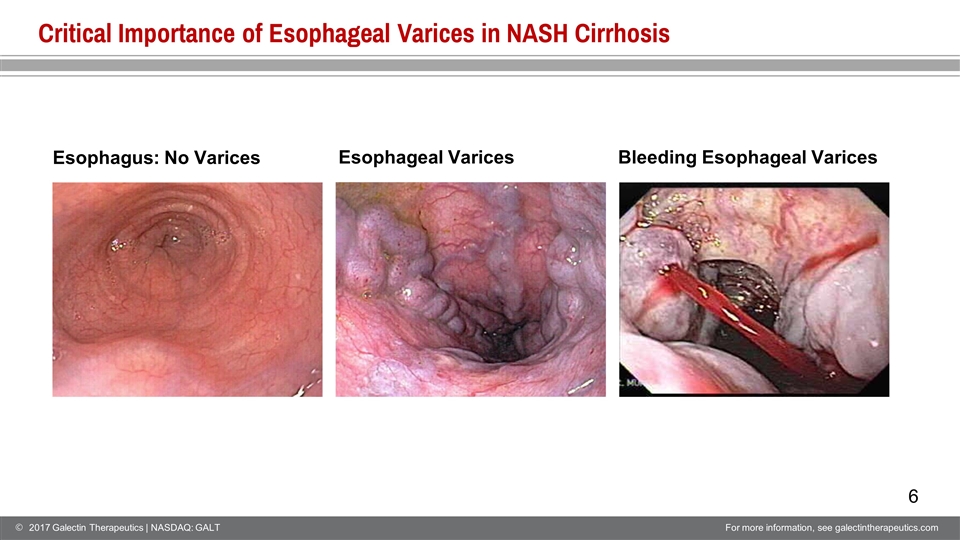
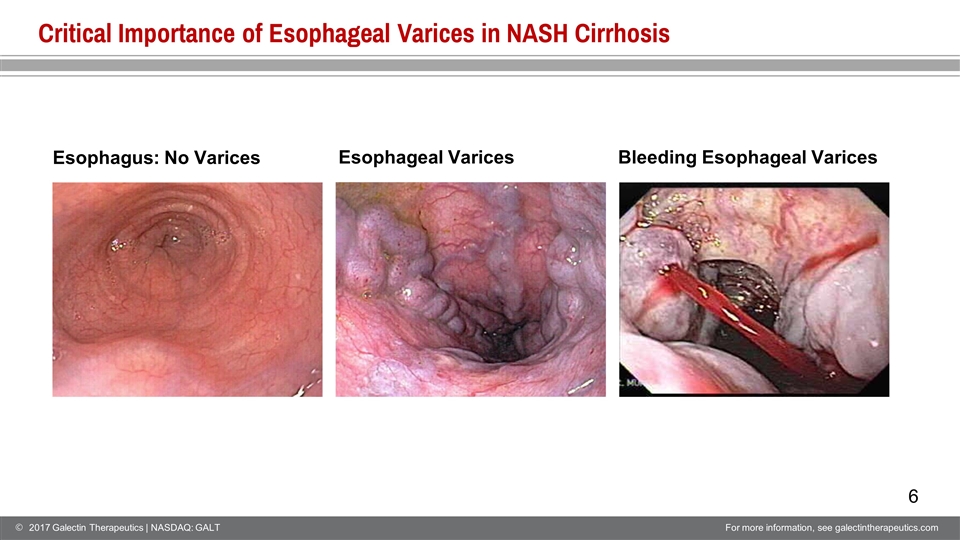
Critical Importance of Esophageal Varices in NASH Cirrhosis Esophagus: No Varices Esophageal Varices Bleeding Esophageal Varices
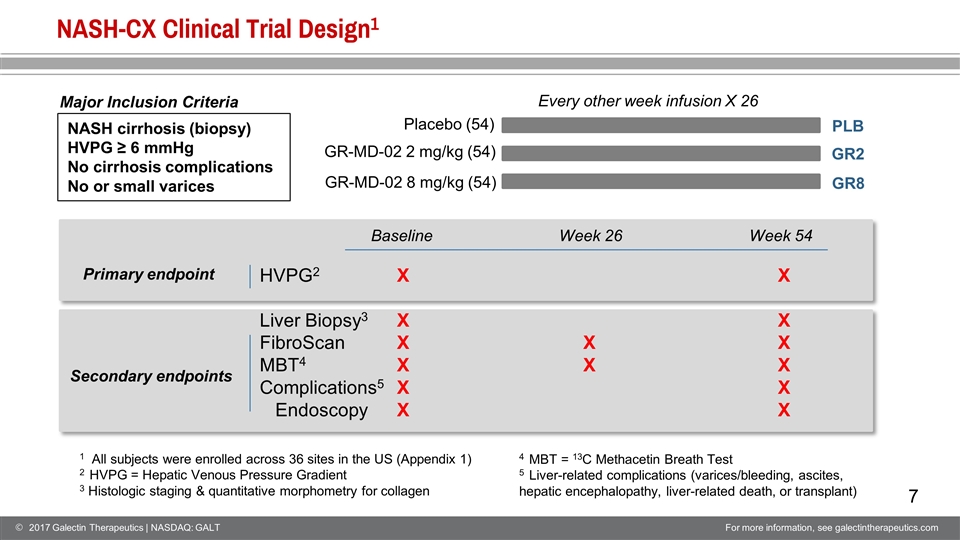
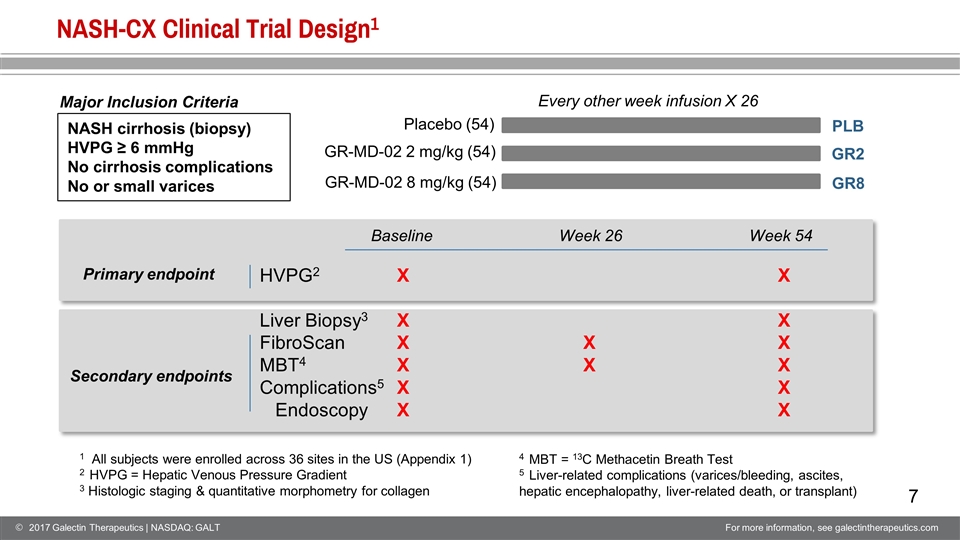
NASH-CX Clinical Trial Design1 Every other week infusion X 26 Placebo (54) GR-MD-02 2 mg/kg (54) GR-MD-02 8 mg/kg (54) NASH cirrhosis (biopsy) HVPG ≥ 6 mmHg No cirrhosis complications No or small varices HVPG2 Liver Biopsy3 FibroScan MBT4 Complications5 Endoscopy X X X X X X X X X X X X X X 1 All subjects were enrolled across 36 sites in the US (Appendix 1) 2 HVPG = Hepatic Venous Pressure Gradient 3 Histologic staging & quantitative morphometry for collagen Primary endpoint Secondary endpoints Baseline Week 26 Week 54 4 MBT = 13C Methacetin Breath Test 5 Liver-related complications (varices/bleeding, ascites, hepatic encephalopathy, liver-related death, or transplant) Major Inclusion Criteria PLB GR2 GR8
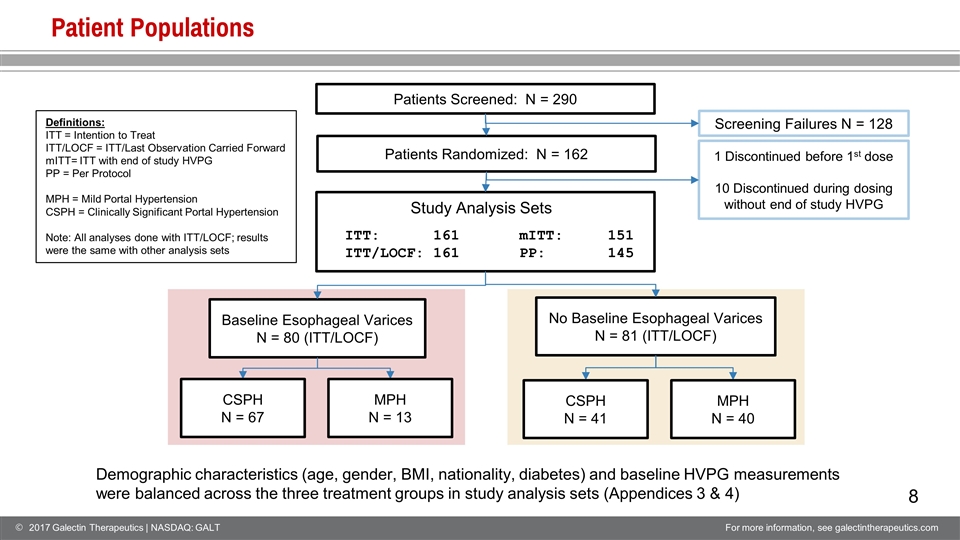
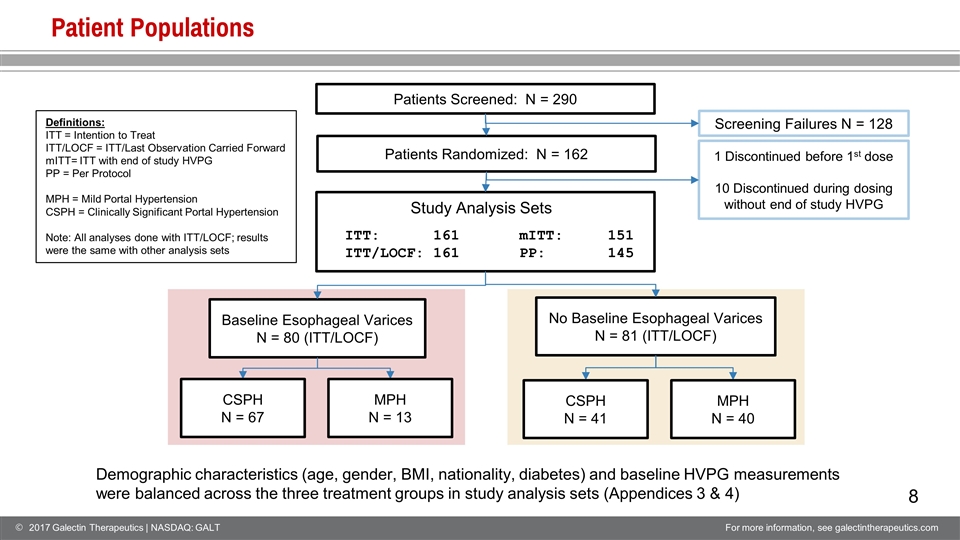
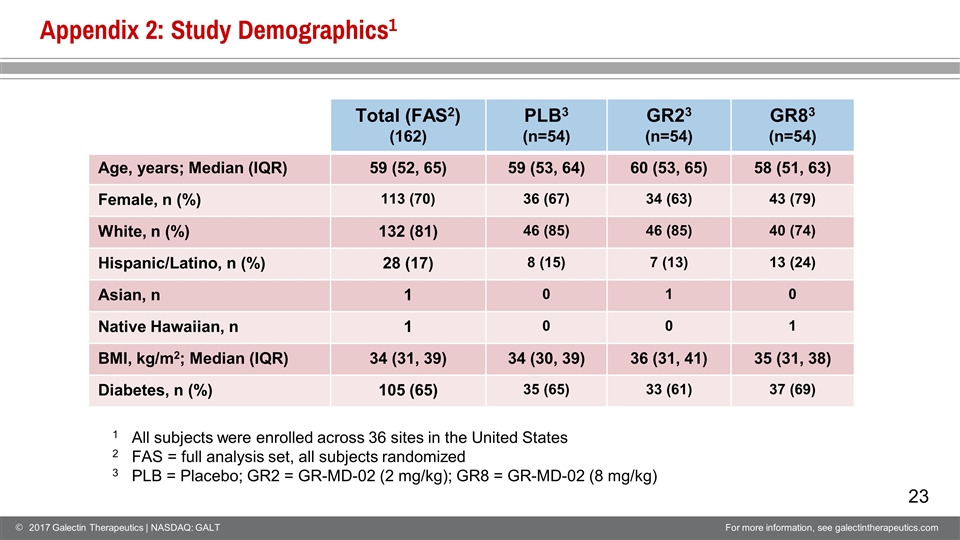
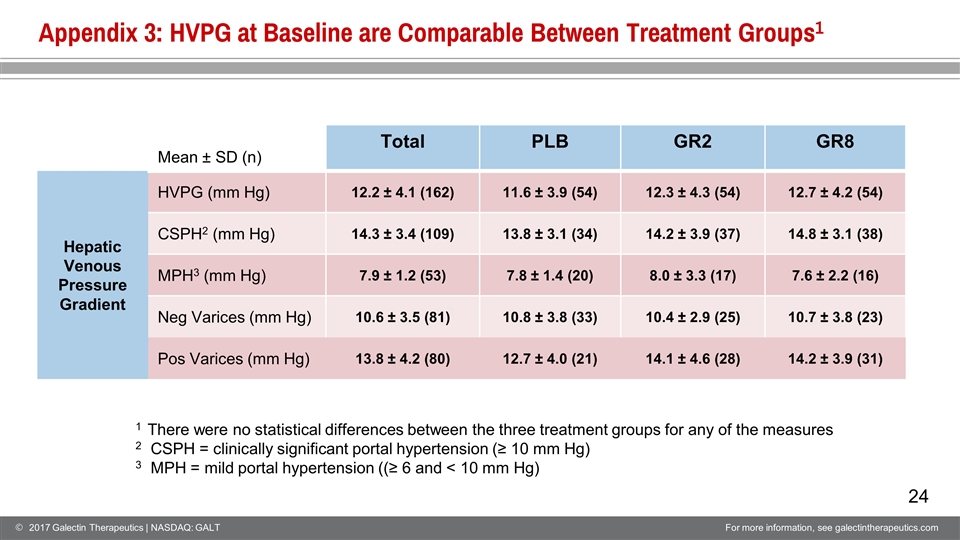
Patient Populations Patients Screened: N = 290 Screening Failures N = 128 Baseline Esophageal Varices N = 80 (ITT/LOCF) No Baseline Esophageal Varices N = 81 (ITT/LOCF) 1 Discontinued before 1st dose 10 Discontinued during dosing without end of study HVPG CSPH N = 67 MPH N = 13 CSPH N = 41 MPH N = 40 Patients Randomized: N = 162 Demographic characteristics (age, gender, BMI, nationality, diabetes) and baseline HVPG measurements were balanced across the three treatment groups in study analysis sets (Appendices 3 & 4) ITT: 161 ITT/LOCF: 161 mITT: 151 PP: 145 Definitions: ITT = Intention to Treat ITT/LOCF = ITT/Last Observation Carried Forward mITT= ITT with end of study HVPG PP = Per Protocol MPH = Mild Portal Hypertension CSPH = Clinically Significant Portal Hypertension Note: All analyses done with ITT/LOCF; results were the same with other analysis sets Study Analysis Sets
Percent Change from Baseline HVPG Data Expressed as Change in Absolute Value and Percent Change From Baseline Hepatic Venous Pressure Gradient 0 mmHg 5 mmHg 10 mmHg Normal Mild Portal Hypertension (MPH) Clinically Significant Portal Hypertension (CSPH) Many relevant clinical observations have been made based on percent change Clinical trials have shown that the lower threshold for a clinically significant change in HVPG, which has an effect on patient outcomes, ranges between 10% and 20% Change in Absolute Value (mm Hg) 10 ← 12 16 ← 18 10 ← 12 16 ← 18 6 ← 8 -2 -2 -2 6 ← 8 -25% -11% -17% Study Design Assumptions
HVPG Primary Endpoint: Total Patient Population1 (Mean baseline HVPG 12.2 mmHg) PLB GR2 GR8 8% -1% -2% There was a 0.8 mmHg and 10% difference between placebo and the GR8 treatment group, but the differences did not reach statistical significance n=54 n=53 n=54 Mean ± SEM Percent Change in HVPG from baseline to week 54 p=0.09 p=0.14 ANOVA ANCOVA with Bonferroni 1ITT with LOCF Absolute Change in HVPG from baseline to week 54 (mmHg) n=54 n=53 n=54 Mean ± SEM ns ns PLB GR2 GR8 Absolute change in HVPG (mm Hg) Percent change from baseline HVPG + 0.4 -0.2 -0.4 1ITT with LOCF
PLB GR2 GR8 Percent Change in HVPG from baseline to week 54 HVPG in NASH Cirrhosis Without Varices at Baseline1 (Mean baseline HVPG 10.6 mmHg) 12% -9.0% 0.5 % p=0.01 p=0.17 n=33 n=25 n=23 Mean ± SEM The drug effect was significantly dependent on the presence of varices at baseline (p<0.02). Analysis in the absence of baseline varices showed a statistically significant effect of GR2. ANCOVA 1ITT with LOCF Percent change from baseline HVPG ANOVA 1ITT with LOCF Absolute change in HVPG (mm Hg) p=0.01 p=0.37 PLB GR2 GR8 Absolute Change in HVPG from baseline to week 54 (mmHg) +0.8 -1.2 +0.2 n=33 n=25 n=23 Mean ± SEM
PLB GR2 GR8 Percent Change in HVPG from baseline to week 54 Mild Portal Hypertension Without Varices at Baseline1 (Mean baseline HVPG 7.8 mmHg) In the absence of varices and with mild portal hypertension, there was statistically significant treatment effect on HVPG in both dose groups ANCOVA 1ITT with LOCF Percent change from baseline HVPG ANOVA 1ITT with LOCF Absolute change in HVPG (mm Hg) p=0.07 PLB GR2 GR8 Absolute Change in HVPG from baseline to week 54 (mmHg) +1.8 -0.3 -0.4 n=16 n=12 n=12 Mean ± SEM p=0.04 n=16 n=12 n=12 Mean ± SEM p=0.04 p=0.04 25% -4% -3%
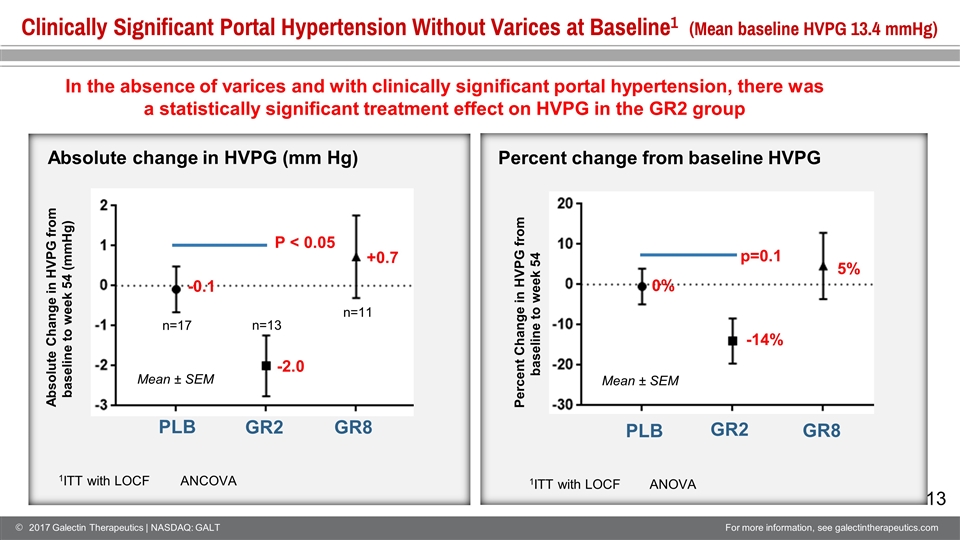
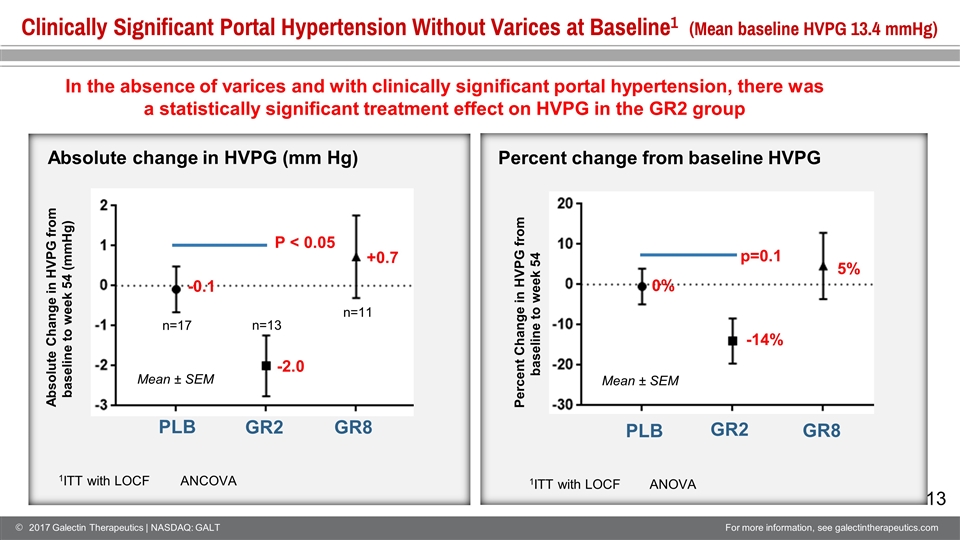
PLB GR2 GR8 Percent Change in HVPG from baseline to week 54 Clinically Significant Portal Hypertension Without Varices at Baseline1 (Mean baseline HVPG 13.4 mmHg) Mean ± SEM In the absence of varices and with clinically significant portal hypertension, there was a statistically significant treatment effect on HVPG in the GR2 group ANCOVA 1ITT with LOCF Percent change from baseline HVPG ANOVA 1ITT with LOCF Absolute change in HVPG (mm Hg) P < 0.05 PLB GR2 GR8 Absolute Change in HVPG from baseline to week 54 (mmHg) -0.1 -2.0 +0.7 n=17 n=13 n=11 Mean ± SEM 0% -14% 5% p=0.1
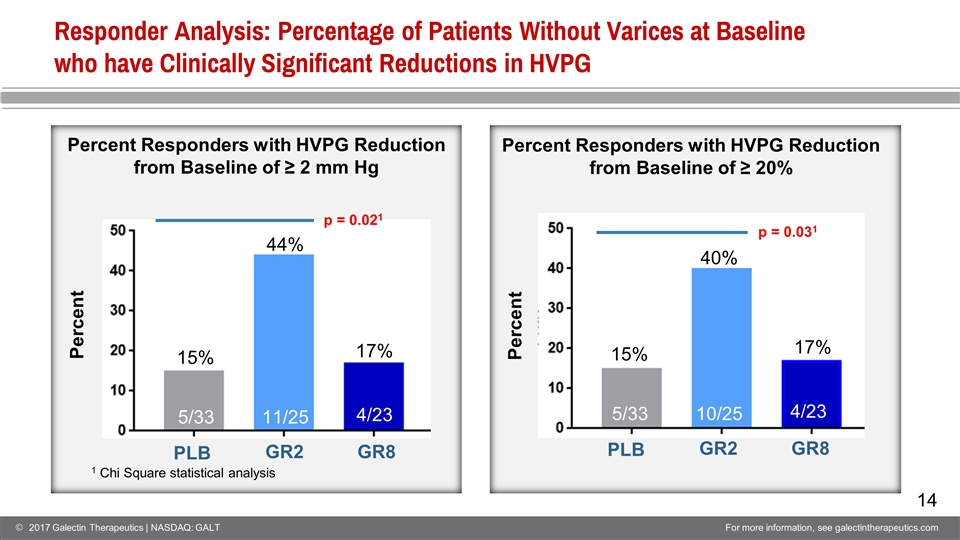
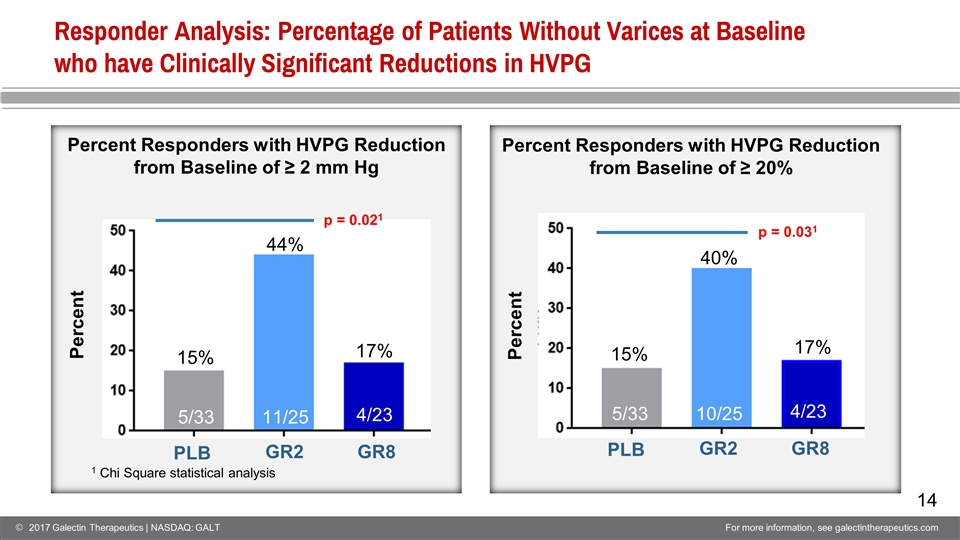
Responder Analysis: Percentage of Patients Without Varices at Baseline who have Clinically Significant Reductions in HVPG 1 Chi Square statistical analysis Percent 15% 44% 17% PLB GR2 GR8 p = 0.021 Percent Responders with HVPG Reduction from Baseline of ≥ 2 mm Hg Percent Responders with HVPG Reduction from Baseline of ≥ 20% 5/33 11/25 4/23 Percent 15% 40% 17% PLB GR2 GR8 p = 0.031 5/33 10/25 4/23
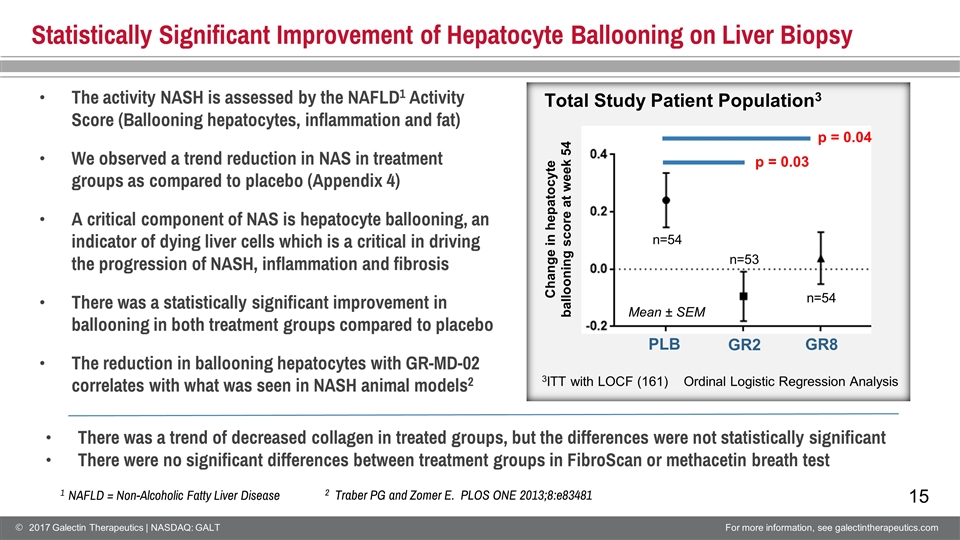
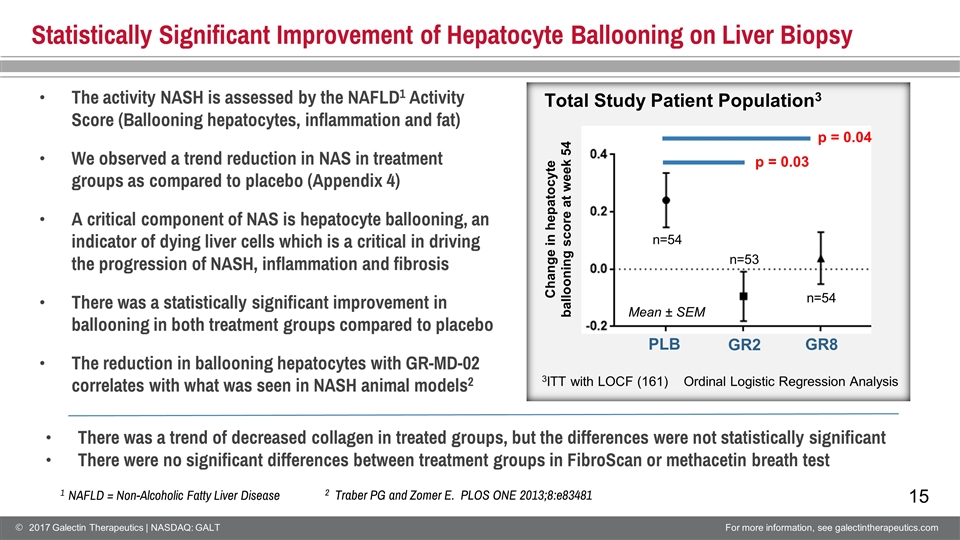
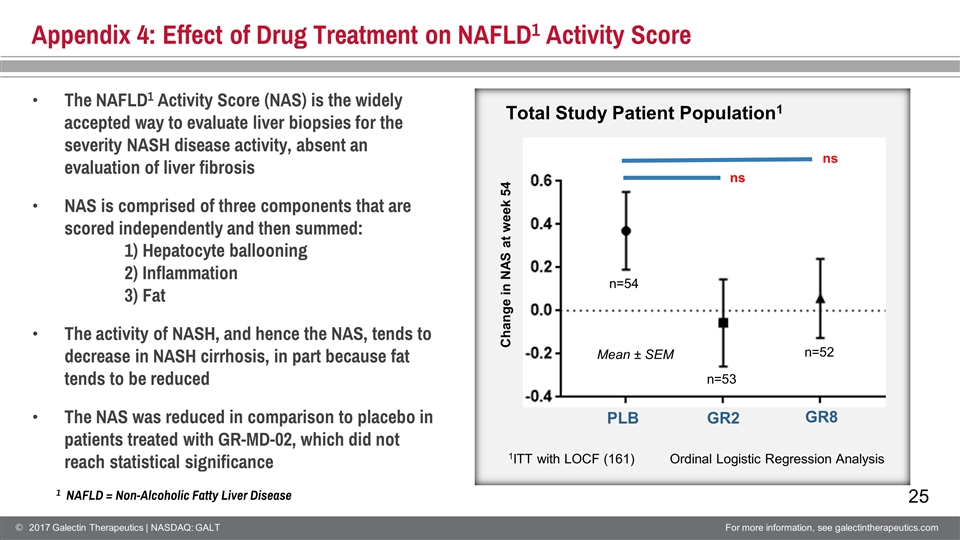
Statistically Significant Improvement of Hepatocyte Ballooning on Liver Biopsy PLB GR2 Change in hepatocyte ballooning score at week 54 The activity NASH is assessed by the NAFLD1 Activity Score (Ballooning hepatocytes, inflammation and fat) We observed a trend reduction in NAS in treatment groups as compared to placebo (Appendix 4) A critical component of NAS is hepatocyte ballooning, an indicator of dying liver cells which is a critical in driving the progression of NASH, inflammation and fibrosis There was a statistically significant improvement in ballooning in both treatment groups compared to placebo The reduction in ballooning hepatocytes with GR-MD-02 correlates with what was seen in NASH animal models2 Mean ± SEM n=54 n=54 There was a trend of decreased collagen in treated groups, but the differences were not statistically significant There were no significant differences between treatment groups in FibroScan or methacetin breath test GR8 n=53 Total Study Patient Population3 3ITT with LOCF (161) 2 Traber PG and Zomer E. PLOS ONE 2013;8:e83481 Ordinal Logistic Regression Analysis p = 0.03 p = 0.04 1 NAFLD = Non-Alcoholic Fatty Liver Disease
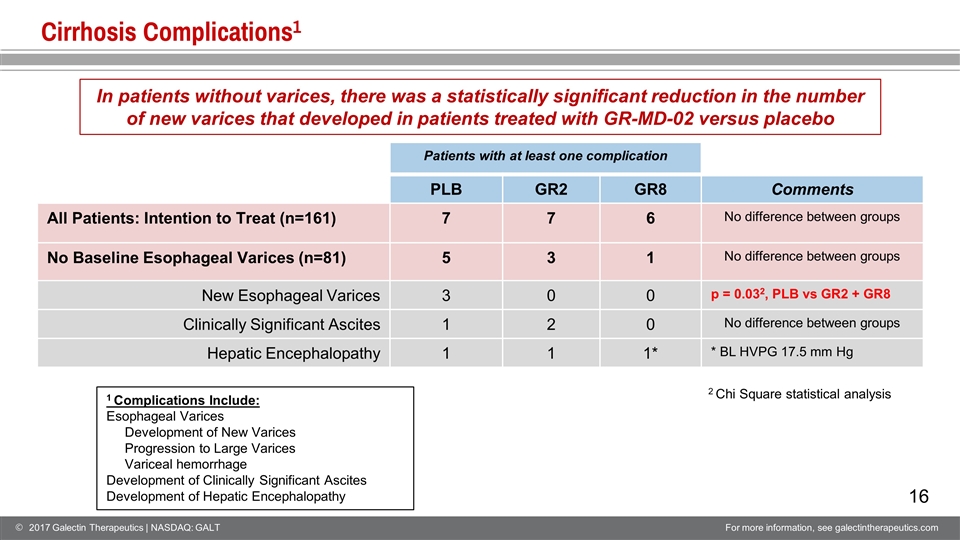
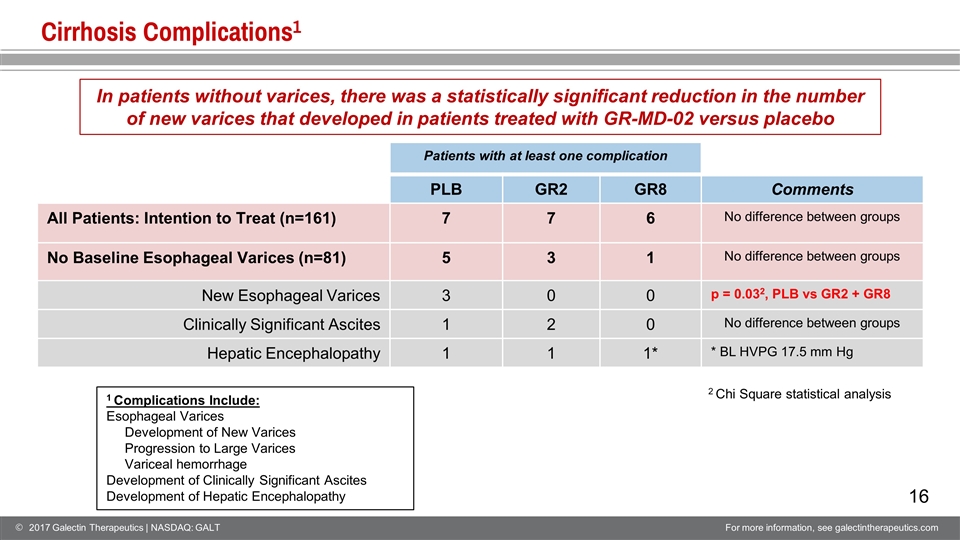
Cirrhosis Complications1 Patients with at least one complication PLB GR2 GR8 Comments All Patients: Intention to Treat (n=161) 7 7 6 No difference between groups No Baseline Esophageal Varices (n=81) 5 3 1 No difference between groups New Esophageal Varices 3 0 0 p = 0.032, PLB vs GR2 + GR8 Clinically Significant Ascites 1 2 0 No difference between groups Hepatic Encephalopathy 1 1 1* * BL HVPG 17.5 mm Hg 2 Chi Square statistical analysis In patients without varices, there was a statistically significant reduction in the number of new varices that developed in patients treated with GR-MD-02 versus placebo 1 Complications Include: Esophageal Varices Development of New Varices Progression to Large Varices Variceal hemorrhage Development of Clinically Significant Ascites Development of Hepatic Encephalopathy
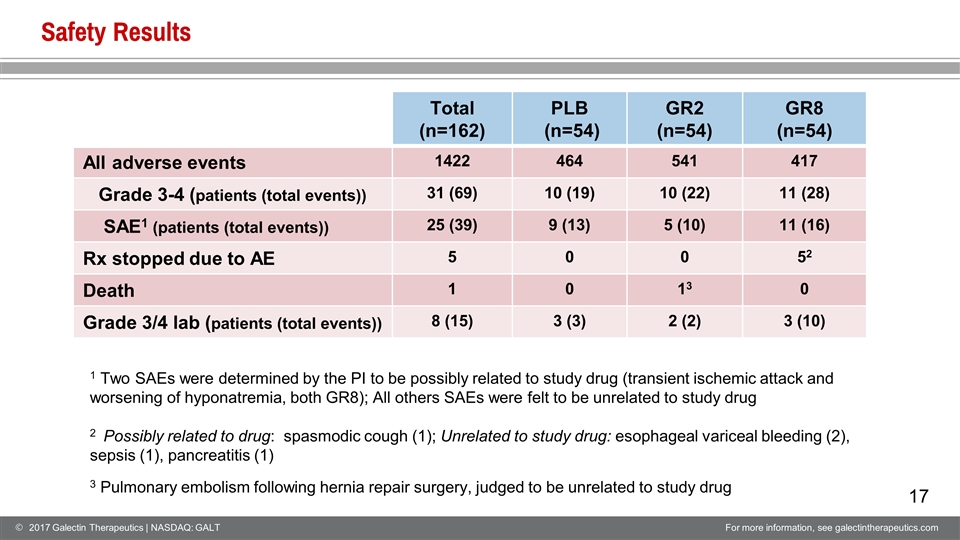
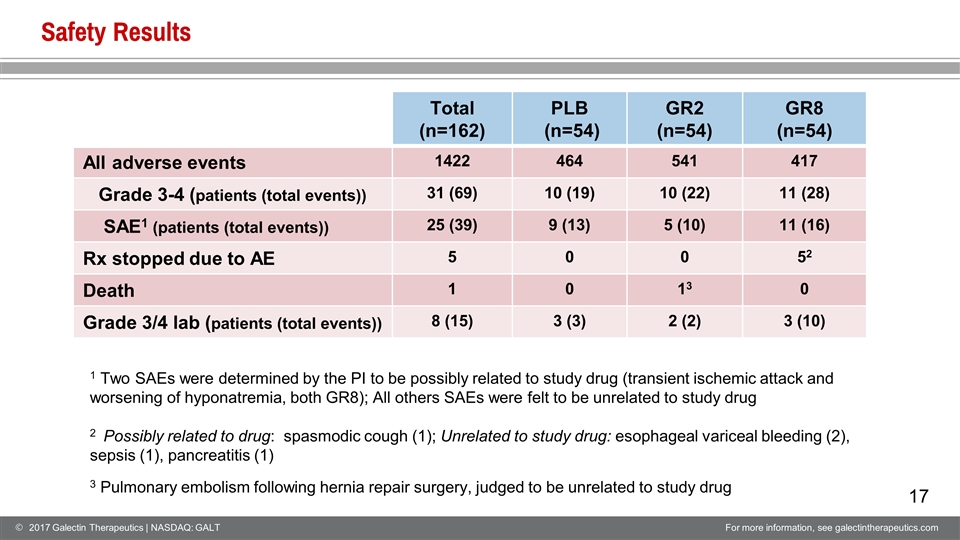
Safety Results Total (n=162) PLB (n=54) GR2 (n=54) GR8 (n=54) All adverse events 1422 464 541 417 Grade 3-4 (patients (total events)) 31 (69) 10 (19) 10 (22) 11 (28) SAE1 (patients (total events)) 25 (39) 9 (13) 5 (10) 11 (16) Rx stopped due to AE 5 0 0 52 Death 1 0 13 0 Grade 3/4 lab (patients (total events)) 8 (15) 3 (3) 2 (2) 3 (10) 1 Two SAEs were determined by the PI to be possibly related to study drug (transient ischemic attack and worsening of hyponatremia, both GR8); All others SAEs were felt to be unrelated to study drug 2 Possibly related to drug: spasmodic cough (1); Unrelated to study drug: esophageal variceal bleeding (2), sepsis (1), pancreatitis (1) 3 Pulmonary embolism following hernia repair surgery, judged to be unrelated to study drug
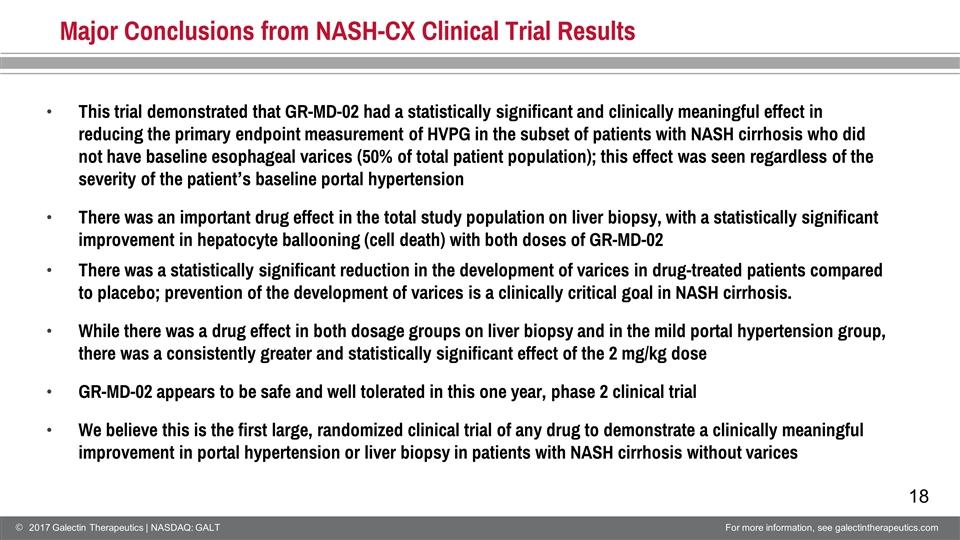
Major Conclusions from NASH-CX Clinical Trial Results This trial demonstrated that GR-MD-02 had a statistically significant and clinically meaningful effect in reducing the primary endpoint measurement of HVPG in the subset of patients with NASH cirrhosis who did not have baseline esophageal varices (50% of total patient population); this effect was seen regardless of the severity of the patient’s baseline portal hypertension There was an important drug effect in the total study population on liver biopsy, with a statistically significant improvement in hepatocyte ballooning (cell death) with both doses of GR-MD-02 There was a statistically significant reduction in the development of varices in drug-treated patients compared to placebo; prevention of the development of varices is a clinically critical goal in NASH cirrhosis. While there was a drug effect in both dosage groups on liver biopsy and in the mild portal hypertension group, there was a consistently greater and statistically significant effect of the 2 mg/kg dose GR-MD-02 appears to be safe and well tolerated in this one year, phase 2 clinical trial We believe this is the first large, randomized clinical trial of any drug to demonstrate a clinically meaningful improvement in portal hypertension or liver biopsy in patients with NASH cirrhosis without varices
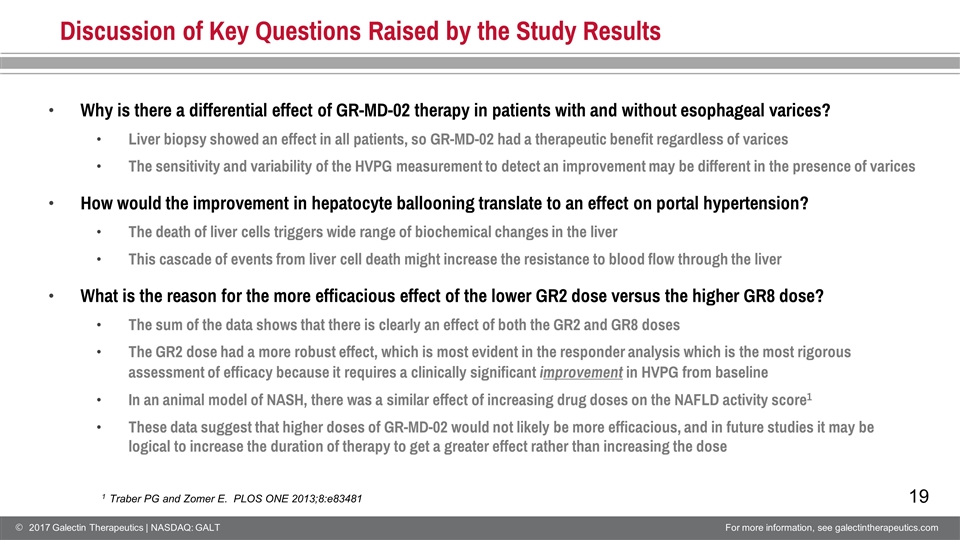
Discussion of Key Questions Raised by the Study Results Why is there a differential effect of GR-MD-02 therapy in patients with and without esophageal varices? Liver biopsy showed an effect in all patients, so GR-MD-02 had a therapeutic benefit regardless of varices The sensitivity and variability of the HVPG measurement to detect an improvement may be different in the presence of varices How would the improvement in hepatocyte ballooning translate to an effect on portal hypertension? The death of liver cells triggers wide range of biochemical changes in the liver This cascade of events from liver cell death might increase the resistance to blood flow through the liver What is the reason for the more efficacious effect of the lower GR2 dose versus the higher GR8 dose? The sum of the data shows that there is clearly an effect of both the GR2 and GR8 doses The GR2 dose had a more robust effect, which is most evident in the responder analysis which is the most rigorous assessment of efficacy because it requires a clinically significant improvement in HVPG from baseline In an animal model of NASH, there was a similar effect of increasing drug doses on the NAFLD activity score1 These data suggest that higher doses of GR-MD-02 would not likely be more efficacious, and in future studies it may be logical to increase the duration of therapy to get a greater effect rather than increasing the dose 1 Traber PG and Zomer E. PLOS ONE 2013;8:e83481
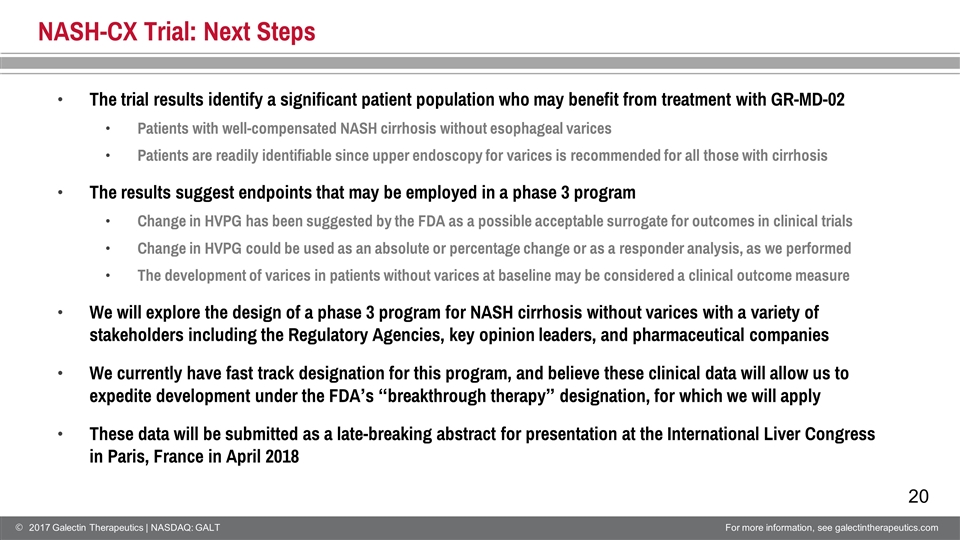
NASH-CX Trial: Next Steps The trial results identify a significant patient population who may benefit from treatment with GR-MD-02 Patients with well-compensated NASH cirrhosis without esophageal varices Patients are readily identifiable since upper endoscopy for varices is recommended for all those with cirrhosis The results suggest endpoints that may be employed in a phase 3 program Change in HVPG has been suggested by the FDA as a possible acceptable surrogate for outcomes in clinical trials Change in HVPG could be used as an absolute or percentage change or as a responder analysis, as we performed The development of varices in patients without varices at baseline may be considered a clinical outcome measure We will explore the design of a phase 3 program for NASH cirrhosis without varices with a variety of stakeholders including the Regulatory Agencies, key opinion leaders, and pharmaceutical companies We currently have fast track designation for this program, and believe these clinical data will allow us to expedite development under the FDA’s “breakthrough therapy” designation, for which we will apply These data will be submitted as a late-breaking abstract for presentation at the International Liver Congress in Paris, France in April 2018

Appendix NASDAQ: GALT www.galectintherapeutics.com 2017 Galectin Therapeutics | NASDAQ: GALT For more information, see galectintherapeutics.com
22 Appendix 1: Deep Gratitude to Patient Volunteers and Clinical Study Sites
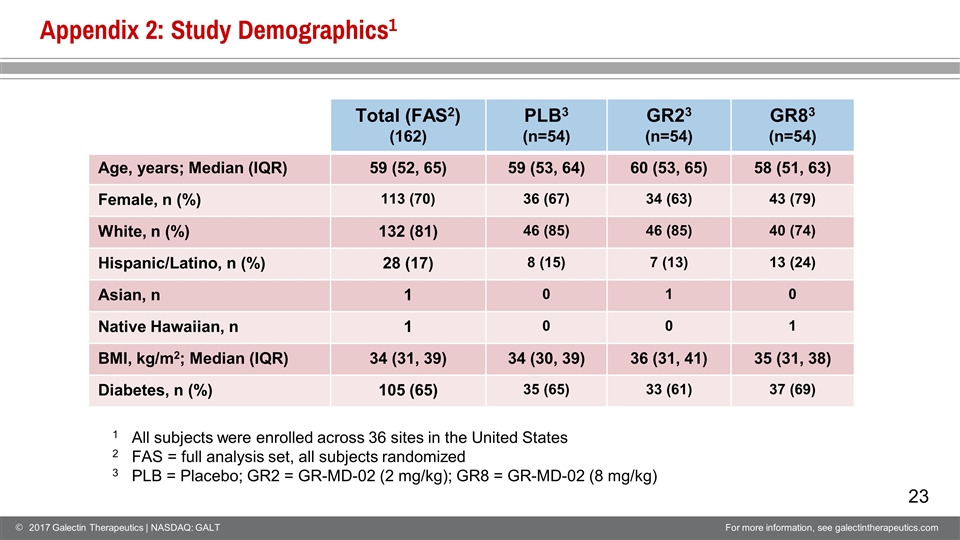
Appendix 2: Study Demographics1 Total (FAS2) (162) PLB3 (n=54) GR23 (n=54) GR83 (n=54) Age, years; Median (IQR) 59 (52, 65) 59 (53, 64) 60 (53, 65) 58 (51, 63) Female, n (%) 113 (70) 36 (67) 34 (63) 43 (79) White, n (%) 132 (81) 46 (85) 46 (85) 40 (74) Hispanic/Latino, n (%) 28 (17) 8 (15) 7 (13) 13 (24) Asian, n 1 0 1 0 Native Hawaiian, n 1 0 0 1 BMI, kg/m2; Median (IQR) 34 (31, 39) 34 (30, 39) 36 (31, 41) 35 (31, 38) Diabetes, n (%) 105 (65) 35 (65) 33 (61) 37 (69) 1 All subjects were enrolled across 36 sites in the United States 2 FAS = full analysis set, all subjects randomized 3 PLB = Placebo; GR2 = GR-MD-02 (2 mg/kg); GR8 = GR-MD-02 (8 mg/kg)
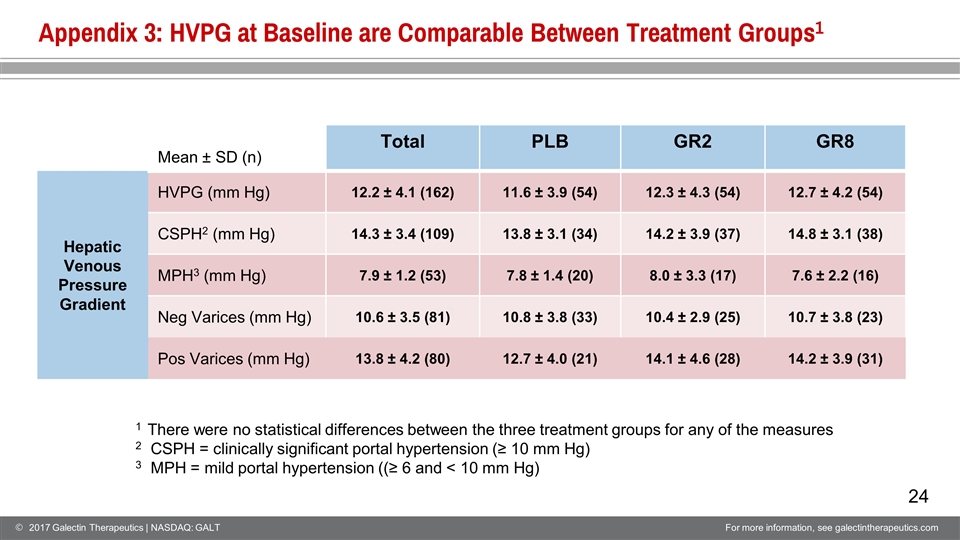
Appendix 3: HVPG at Baseline are Comparable Between Treatment Groups1 Mean ± SD (n) Total PLB GR2 GR8 Hepatic Venous Pressure Gradient HVPG (mm Hg) 12.2 ± 4.1 (162) 11.6 ± 3.9 (54) 12.3 ± 4.3 (54) 12.7 ± 4.2 (54) CSPH2 (mm Hg) 14.3 ± 3.4 (109) 13.8 ± 3.1 (34) 14.2 ± 3.9 (37) 14.8 ± 3.1 (38) MPH3 (mm Hg) 7.9 ± 1.2 (53) 7.8 ± 1.4 (20) 8.0 ± 3.3 (17) 7.6 ± 2.2 (16) Neg Varices (mm Hg) 10.6 ± 3.5 (81) 10.8 ± 3.8 (33) 10.4 ± 2.9 (25) 10.7 ± 3.8 (23) Pos Varices (mm Hg) 13.8 ± 4.2 (80) 12.7 ± 4.0 (21) 14.1 ± 4.6 (28) 14.2 ± 3.9 (31) 1 There were no statistical differences between the three treatment groups for any of the measures 2 CSPH = clinically significant portal hypertension (≥ 10 mm Hg) 3 MPH = mild portal hypertension ((≥ 6 and < 10 mm Hg)
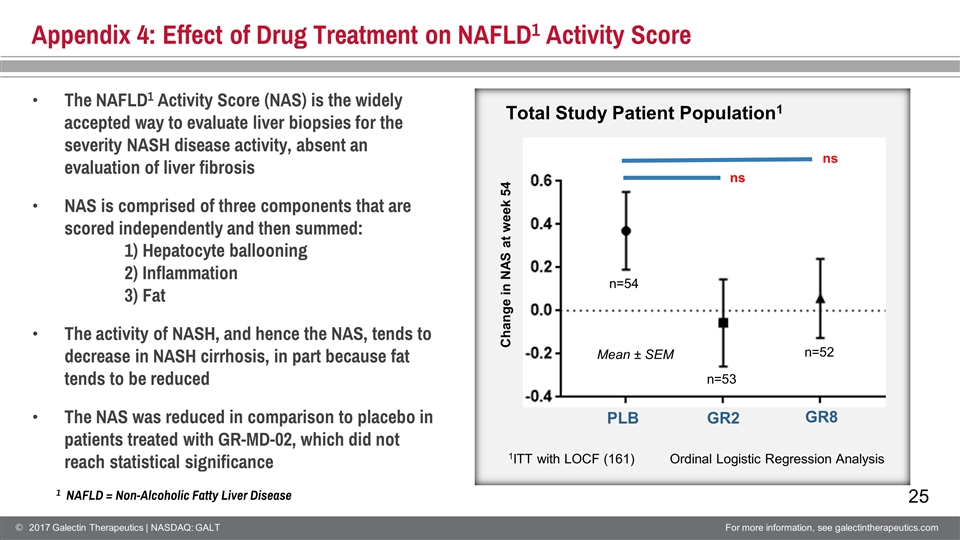
Appendix 4: Effect of Drug Treatment on NAFLD1 Activity Score ns PLB GR2 Change in NAS at week 54 The NAFLD1 Activity Score (NAS) is the widely accepted way to evaluate liver biopsies for the severity NASH disease activity, absent an evaluation of liver fibrosis NAS is comprised of three components that are scored independently and then summed: 1) Hepatocyte ballooning 2) Inflammation3) Fat The activity of NASH, and hence the NAS, tends to decrease in NASH cirrhosis, in part because fat tends to be reduced The NAS was reduced in comparison to placebo in patients treated with GR-MD-02, which did not reach statistical significance Ordinal Logistic Regression Analysis Mean ± SEM n=54 n=52 GR8 n=53 ns Total Study Patient Population1 1ITT with LOCF (161) 1 NAFLD = Non-Alcoholic Fatty Liver Disease