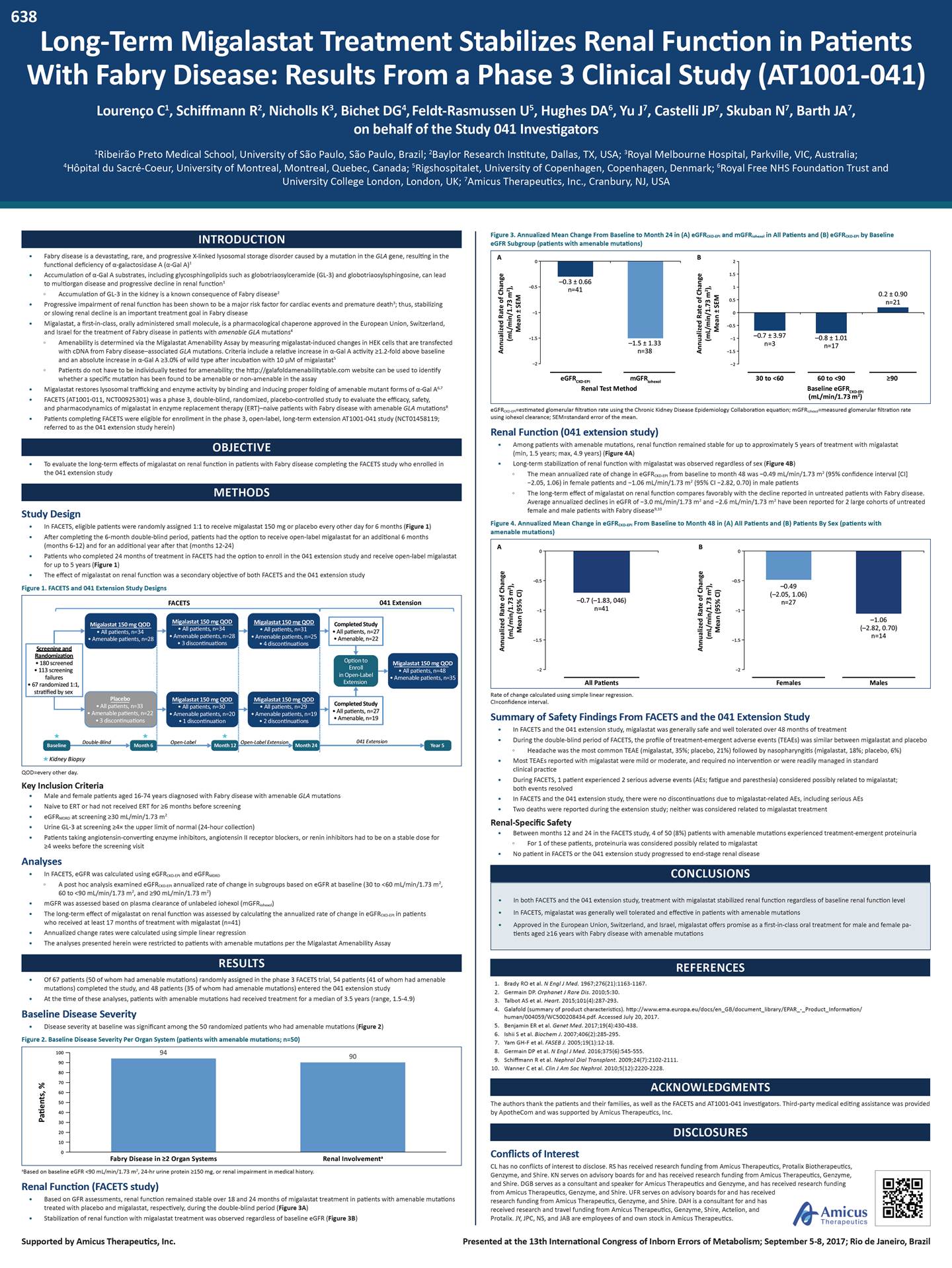
638 Long-Term Migalastat Treatment Stabilizes Renal Function in Patients With Fabry Disease: Results From a Phase 3 Clinical Study (AT1001-041) Lourenço C1, Schiffmann R2, Nicholls K3, Bichet DG4, Feldt-Rasmussen U5, Hughes DA6, Yu J7, Castelli JP7, Skuban N7, Barth JA7, on behalf of the Study 041 Investigators 1Ribeirão Preto Medical School, University of São Paulo, São Paulo, Brazil; 2Baylor Research Institute, Dallas, TX, USA; 3Royal Melbourne Hospital, Parkville, VIC, Australia; 4Hôpital du Sacré-Coeur, University of Montreal, Montreal, Quebec, Canada; 5Rigshospitalet, University of Copenhagen, Copenhagen, Denmark; 6Royal Free NHS Foundation Trust and University College London, London, UK; 7Amicus Therapeutics, Inc., Cranbury, NJ, USA Figure 3. Annualized Mean Change From Baseline to Month 24 in (A) eGFRCKD-EPI and mGFRiohexol in All Patients and (B) eGFRCKD-EPI by Baseline eGFR Subgroup (patients with amenable mutations) INTRODUCTION Fabry disease is a devastating, rare, and progressive X-linked lysosomal storage disorder caused by a mutation in the GLA gene, resulting in the functional deficiency of -galactosidase A (-Gal A)1 Accumulation of -Gal A substrates, including glycosphingolipids such as globotriaosylceramide (GL-3) and globotriaosylsphingosine, can lead to multiorgan disease and progressive decline in renal function1 • • Accumulation of GL-3 in the kidney is a known consequence of Fabry disease2 • Progressive impairment of renal function has been shown to be a major risk factor for cardiac events and premature death3; thus, stabilizing or slowing renal decline is an important treatment goal in Fabry disease Migalastat, a first-in-class, orally administered small molecule, is a pharmacological chaperone approved in the European Union, Switzerland, and Israel for the treatment of Fabry disease in patients with amenable GLA mutations4 • Amenability is determined via the Migalastat Amenability Assay by measuring migalastat-induced changes in HEK cells that are transfected with cDNA from Fabry disease–associated GLA mutations. Criteria include a relative increase in -Gal A activity 1.2-fold above baseline and an absolute increase in -Gal A 3.0% of wild type after incubation with 10 µM of migalastat5 Patients do not have to be individually tested for amenability; the http://galafoldamenabilitytable.com website can be used to identify whether a specific mutation has been found to be amenable or non-amenable in the assay • • Migalastat restores lysosomal trafficking and enzyme activity by binding and inducing proper folding of amenable mutant forms of -Gal A6,7 FACETS (AT1001-011, NCT00925301) was a phase 3, double-blind, randomized, placebo-controlled study to evaluate the efficacy, safety, and pharmacodynamics of migalastat in enzyme replacement therapy (ERT)–naive patients with Fabry disease with amenable GLA mutations8 Patients completing FACETS were eligible for enrollment in the phase 3, open-label, long-term extension AT1001-041 study (NCT01458119; referred to as the 041 extension study herein) eGFR =estimated glomerular filtration rate using the Chronic Kidney Disease Epidemiology Collaboration equation; mGFR =measured glomerular filtration rate CKD-EPI iohexol using iohexol clearance; SEM=standard error of the mean. • Renal Function (041 extension study) OBJECTIVE To evaluate the long-term effects of migalastat on renal function in patients with Fabry disease completing the FACETS study who enrolled in the 041 extension study • Among patients with amenable mutations, renal function remained stable for up to approximately 5 years of treatment with migalastat (min, 1.5 years; max, 4.9 years) (Figure 4A) Long-term stabilization of renal function with migalastat was observed regardless of sex (Figure 4B) • • The mean annualized rate of change in eGFRCKD-EPI from baseline to month 48 was -0.49 mL/min/1.73 m2 (95% confidence interval [CI] -2.05, 1.06) in female patients and -1.06 mL/min/1.73 m2 (95% CI -2.82, 0.70) in male patients The long-term effect of migalastat on renal function compares favorably with the decline reported in untreated patients with Fabry disease. Average annualized declines in eGFR of -3.0 mL/min/1.73 m2 and -2.6 mL/min/1.73 m2 have been reported for 2 large cohorts of untreated METHODS female and male patients with Fabry disease 9,10 Study Design Figure 4. Annualized Mean Change in eGFRCKD-EPI From Baseline to Month 48 in (A) All Patients and (B) Patients By Sex (patients with amenable mutations) • • In FACETS, eligible patients were randomly assigned 1:1 to receive migalastat 150 mg or placebo every other day for 6 months (Figure 1) After completing the 6-month double-blind period, patients had the option to receive open-label migalastat for an additional 6 months (months 6-12) and for an additional year after that (months 12-24) Patients who completed 24 months of treatment in FACETS had the option to enroll in the 041 extension study and receive open-label migalastat for up to 5 years (Figure 1) The effect of migalastat on renal function was a secondary objective of both FACETS and the 041 extension study 0 0 • • Figure 1. FACETS and 041 Extension Study Designs • All patients, n=34 • All patients, n=31 • All patients, n=34 uations uations patients, n=48 • 67 randomized 1:1, Rate of change calculated using simple linear regression. CI=confidence interval. Summary of Safety Findings From FACETS and the 041 Extension Study • Amenable patients, n=22 patients, n=20 patients, n=19 • • In FACETS and the 041 extension study, migalastat was generally safe and well tolerated over 48 months of treatment During the double-blind period of FACETS, the profile of treatment-emergent adverse events (TEAEs) was similar between migalastat and placebo Headache was the most common TEAE (migalastat, 35%; placebo, 21%) followed by nasopharyngitis (migalastat, 18%; placebo, 6%) • Most TEAEs reported with migalastat were mild or moderate, and required no intervention or were readily managed in standard clinical practice During FACETS, 1 patient experienced 2 serious adverse events (AEs; fatigue and paresthesia) considered possibly related to migalastat; both events resolved In FACETS and the 041 extension study, there were no discontinuations due to migalastat-related AEs, including serious AEs Two deaths were reported during the extension study; neither was considered related to migalastat treatment QOD=every other day. Key Inclusion Criteria • • • • • • Male and female patients aged 16-74 years diagnosed with Fabry disease with amenable GLA mutations Naive to ERT or had not received ERT for 6 months before screening eGFRMDRD at screening 30 mL/min/1.73 m2 Urine GL-3 at screening 4× the upper limit of normal (24-hour collection) Patients taking angiotensin-converting enzyme inhibitors, angiotensin II receptor blockers, or renin inhibitors had to be on a stable dose for 4 weeks before the screening visit • • Renal-Specific Safety • Between months 12 and 24 in the FACETS study, 4 of 50 (8%) patients with amenable mutations experienced treatment-emergent proteinuria For 1 of these patients, proteinuria was considered possibly related to migalastat • No patient in FACETS or the 041 extension study progressed to end-stage renal disease Analyses CONCLUSIONS • In FACETS, eGFR was calculated using eGFRCKD-EPI and eGFRMDRD A post hoc analysis examined eGFRCKD-EPI annualized rate of change in subgroups based on eGFR at baseline (30 to <60 mL/min/1.73 m2, 60 to <90 mL/min/1.73 m2, and 90 mL/min/1.73 m2) • • mGFR was assessed based on plasma clearance of unlabeled iohexol (mGFRiohexol) The long-term effect of migalastat on renal function was assessed by calculating the annualized rate of change in eGFRCKD-EPI in patients who received at least 17 months of treatment with migalastat (n=41) Annualized change rates were calculated using simple linear regression The analyses presented herein were restricted to patients with amenable mutations per the Migalastat Amenability Assay • • RESULTS Of 67 patients (50 of whom had amenable mutations) randomly assigned in the phase 3 FACETS trial, 54 patients (41 of whom had amenable mutations) completed the study, and 48 patients (35 of whom had amenable mutations) entered the 041 extension study At the time of these analyses, patients with amenable mutations had received treatment for a median of 3.5 years (range, 1.5-4.9) REFERENCES • 1. 2. 3. 4. Brady RO et al. N Engl J Med. 1967;276(21):1163-1167. Germain DP. Orphanet J Rare Dis. 2010;5:30. Talbot AS et al. Heart. 2015;101(4):287-293. Galafold (summary of product characteristics). http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/ human/004059/WC500208434.pdf. Accessed July 20, 2017. Benjamin ER et al. Genet Med. 2017;19(4):430-438. Ishii S et al. Biochem J. 2007;406(2):285-295. Yam GH-F et al. FASEB J. 2005;19(1):12-18. Germain DP et al. N Engl J Med. 2016;375(6):545-555. Schiffmann R et al. Nephrol Dial Transplant. 2009;24(7):2102-2111. Wanner C et al. Clin J Am Soc Nephrol. 2010;5(12):2220-2228. • Baseline Disease Severity 5. 6. 7. 8. 9. 10. • Disease severity at baseline was significant among the 50 randomized patients who had amenable mutations (Figure 2) Figure 2. Baseline Disease Severity Per Organ System (patients with amenable mutations; n=50) ACKNOWLEDGMENTS The authors thank the patients and their families, as well as the FACETS and AT1001-041 investigators. Third-party medical editing assistance was provided by ApotheCom and was supported by Amicus Therapeutics, Inc. DISCLOSURES Conflicts of Interest CL has no conflicts of interest to disclose. RS has received research funding from Amicus Therapeutics, Protalix Biotherapeutics, Genzyme, and Shire. KN serves on advisory boards for and has received research funding from Amicus Therapeutics, Genzyme, and Shire. DGB serves as a consultant and speaker for Amicus Therapeutics and Genzyme, and has received research funding from Amicus Therapeutics, Genzyme, and Shire. UFR serves on advisory boards for and has received research funding from Amicus Therapeutics, Genzyme, and Shire. DAH is a consultant for and has received research and travel funding from Amicus Therapeutics, Genzyme, Shire, Actelion, and Protalix. JY, JPC, NS, and JAB are employees of and own stock in Amicus Therapeutics. aBased on baseline eGFR <90 mL/min/1.73 m2, 24-hr urine protein 150 mg, or renal impairment in medical history. Renal Function (FACETS study) • Based on GFR assessments, renal function remained stable over 18 and 24 months of migalastat treatment in patients with amenable mutations treated with placebo and migalastat, respectively, during the double-blind period (Figure 3A) Stabilization of renal function with migalastat treatment was observed regardless of baseline eGFR (Figure 3B) • Supported by Amicus Therapeutics, Inc. Presented at the 13th International Congress of Inborn Errors of Metabolism; September 5-8, 2017; Rio de Janeiro, Brazil Patients, % Annualized Rate of Change (mL/min/1.73 m2), Mean ± SEM Annualized Rate of Change (mL/min/1.73 m2), Mean (95% Cl) Annualized Rate of Change (mL/min/1.73 m2), Mean ± SEM Annualized Rate of Change (mL/min/1.73 m2), Mean (95% Cl) 1009490 90 80 70 60 50 40 30 20 10 0 Fabry Disease in 2 Organ Systems Renal Involvementa •In both FACETS and the 041 extension study, treatment with migalastat stabilized renal function regardless of baseline renal function level •In FACETS, migalastat was generally well tolerated and effective in patients with amenable mutations •Approved in the European Union, Switzerland, and Israel, migalastat offers promise as a first-in-class oral treatment for male and female pa-tients aged 16 years with Fabry disease with amenable mutations FACETS 041 Extension Migalastat 150 mg QOD Migalastat 150 mg QOD Migalastat 150 mg QOD • Amenable patients, n=28patients, n=28patients, n=25 150 mg QOD patients, n=35 Placebo 150 mg QOD 150 mg QOD • All patients, n=33patients, n=30patients, n=29 • 3 discontinuationsdiscontinuationuations Baseline Double-BlindMonth 6Month 12Month 24Year 5 Kidney Biopsy Screening and Randomization • 180 screened • 113 screening failures stratified by sex Option toMigalastat Enroll• All in Open-Label• Amenable Extension 041 Extension Completed Study • All patients, n=27 • Amenable, n=19 • Amenable • 4 discontin Migalastat • All • Amenable • 2 discontin pen-Label Extension O • Amenable • 3 discontin Migalastat • All • Amenable • 1 Open-Label Completed Study • All patients, n=27 • Amenable, n=22 A B -0.5-0.5 -1-1 -1.5-1.5 -2-2 All Patients Females Males –0.49 (–2.05, 1.06) n=27 –1.06 (–2.82, 0.70) n=14 –0.7 (–1.83, 046) n=41 A B 02 1.5 -0.51 0.5 -10 -0.5 -1.5-1–0.8 ± 1.01 -1.5 -2-2 eGFRCKD-EPI mGFRiohexol 30 to <6060 to <90 90 Renal Test Method Baseline eGFRCKD-EPI (mL/min/1.73 m2) 0.2 ± 0.90 n=21 –0.7 ± 3.97 n=3n=17 –0.3 ± 0.66 n=41 –1.5 ± 1.33 n=38
636 Efficacy and Safety of Migalastat, an Oral Pharmacological Chaperone for Fabry Disease: Renal Findings From Two Randomized Phase 3 Studies (FACETS and ATTRACT) Jovanovic A1, Schiffmann R2, Nicholls K3, Feldt-Rasmussen U4, Giugliani R5, Bichet DG6, Hughes DA7, Jain V8, Yu J8, Castelli JP8, Skuban N8, Barth JA8 1Salford Royal Hospital and NHS Foundation Trust, Manchester, UK; 2Baylor Research Institute, Dallas, TX, USA; 3Royal Melbourne Hospital, Parkville, VIC, Australia; 4Rigshospitalet, University of Copenhagen, Copenhagen, Denmark; 5Medical Genetics Service, HCPA/UFRGS, Porto Alegre, Brazil; 6Hôpital du Sacré-Coeur, University of Montreal, Montreal, Quebec, Canada; 7Royal Free NHS Foundation Trust and University College London, London, UK; 8Amicus Therapeutics, Inc., Cranbury, NJ, USA Figure 5. Annualized Rate of Change in eGFRCKD-EPI at Month 18 by Baseline eGFR (ATTRACT; patients with amenable mutations) INTRODUCTION Fabry disease is a devastating, rare, and progressive X-linked lysosomal storage disorder caused by a mutation in the GLA gene, resulting in the functional deficiency of -galactosidase A (-Gal A)1 Accumulation of -Gal A substrates, including glycosphingolipids such as globotriaosylceramide (GL-3) and globotriaosylsphingosine (lyso-Gb3), can lead to multisystem disease and premature death1 Migalastat, a first-in-class, orally administered small molecule, is a pharmacologic chaperone approved in the European Union, Switzerland, and Israel for the treatment of Fabry disease in patients with amenable GLA mutations2 Migalastat restores lysosomal trafficking and enzyme activity by binding and inducing proper folding of amenable mutant forms of -Gal A1,3 As an orally administered small molecule, migalastat may obviate the need for lifelong biweekly agalsidase infusions or enzyme replacement therapy (ERT)4,5 RESULTS The FACETS and ATTRACT studies randomized 67 and 60 patients, respectively, of which 50 and 56 patients, respectively, had amenable mutations Patients in both studies had significant baseline disease severity • • • • 94% and 88% of patients in the FACETS and ATTRACT studies, respectively, had Fabry disease in 2 organ systems4,6 90% and 75% of patients in the FACETS and ATTRACT studies, respectively, had renal involvement4,6 • Disease Substrate • • In FACETS, migalastat treatment significantly reduced interstitial capillary GL-3 inclusions and lyso-Gb levels in patients with Fabry disease with amenable mutations6 3 • • In ATTRACT, plasma lyso-Gb3 levels remained low and stable following the switch from ERT to migalastat in patients with amenable mutations. Plasma lyso-Gb levels increased in 3 2 patients with non-amenable mutations following the switch from ERT to migalastat, but did not change in 2 patients with non-amenable mutations who remained on ERT4 Renal Function FACETS OBJECTIVE To summarize renal findings from 2 randomized phase 3 studies of migalastat in patients with Fabry disease • • From baseline to month 24, renal function was stable in patients with amenable mutations treated with migalastat in the FACETS study (Figure 3) Stabilization of renal function was observed regardless of baseline eGFR METHODS • Study Designs Figure 3. Annualized Mean Change From Baseline to Month 24 in (A) eGFR and mGFR CKD-EPI iohexol • FACETS (AT1001-011, NCT00925301) was a phase 3, double-blind, randomized, placebo-controlled study to evaluate the efficacy, safety, and pharmacodynamics of migalastat in patients with Fabry disease with amenable GLA mutations (Figure 1) ATTRACT (AT1001-012, NCT01218659) was a phase 3, randomized, open-label study to compare the efficacy and safety of migalastat and ERT in patients with Fabry disease with amenable GLA mutations who were previously treated with ERT (Figure 2) in All Patients and (B) eGFRCKD-EPI by Baseline eGFR (FACETS; patients with amenable mutations) • Figure 1. FACETS Study Design NA=not applicable. aInconclusive due to low n number. • In ATTRACT, renal function remained stable in patients with amenable mutations following 30 months of migalastat treatment using both GFR methods The mean annualized change from baseline to month 30 in eGFR was CKD-EPI -1.7 mL/min/1.73 m2 (95% CI, -2.7 to 0.8) (n=31) and in mGFRiohexol was -2.7 mL/min/1.73 m2 (95% CI, -4.8 to 0.7) (n=31) Summary of Safety Findings From FACETS and ATTRACT (AE) trends attributable to migalastat • All patients, n=33 • 3 discontinuations CKD-EPI iohexol • Treatment with migalastat was generally safe and well tolerated, with no adverse event • Most treatment-emergent AEs (TEAEs) reported with migalastat use were mild or moderate, and required no intervention or were readily managed in standard clinical practice The profile of TEAEs was similar between migalastat and placebo treatment, with headache the most commonly reported TEAE There were few serious AEs considered related to migalastat and no deaths during either study There were few discontinuations due to TEAEs, and most were related to underlying Fabry disease comorbidities Predefined renal AEs during the 18-month comparison stage of ATTRACT occurred in 24% and 33% of patients receiving migalastat and ERT, respectively 2 • • Extension • All patients, n=29 • All patients, n=31 • • No patients progressed to end-stage renal disease CONCLUSIONS Migalastat was generally well tolerated and effective in patients with amenable mutations in FACETS and ATTRACT In both FACETS and ATTRACT, treatment with migalastat stabilized renal function • Annualized rates based on the subset of patients who received at least 17 months of treatment with migalastat. eGFRCKD-EPI=estimated glomerular filtration rate using the Chronic Kidney Disease Epidemiology Collaboration equation; mGFRiohexol=measured glomerular filtration rate using iohexol clearance; SEM=standard error of the mean. ATTRACT • QOD=every other day. Figure 2. ATTRACT Study Design In ATTRACT, migalastat and ERT were shown to have comparable effects on renal function • Approved in the European Union, Switzerland, and Israel, migalastat offers promise as a first-in-class oral treatment for male and female patients aged 16 years with Fabry disease with amenable mutations • In the ATTRACT study, migalastat and ERT had comparable favorable effects on renal function at month 18 using both GFR methods (Figure 4) Migalastat stabilized renal function at 18 months regardless of baseline eGFR (Figure 5) REFERENCES Ishii S et al. Biochem J. 2007;406(2):285-295. Galafold (summary of product characteristics). http://www.ema.europa.eu/docs/en_GB/ document_library/EPAR_-_Product_Information/human/004059/WC500208434.pdf. Accessed August 1, 2017. Yam GH-F et al. FASEB J. 2005;19(1):12-18. Hughes DA et al. J Med Genet. 2017;54(4):288-296. Linthorst GE et al. Kidney Int. 2004;66(4):1589-1595. Germain DP et al. N Engl J Med. 2016;375(6):545-555. • 1. 2. Figure 4. Annualized LS Mean Change in GFR From Baseline to Month 18 (ATTRACT; patients with amenable mutations) 3. 4. 5. 6. • 3 discontinuations ACKNOWLEDGMENTS The authors acknowledge the patients and their families, as well as the FACETS and ATTRACT investigators. Third-party medical editorial assistance was provided by ApotheCom and was supported by Amicus Therapeutics, Inc. Extension • Amenable treated patients, n=15 • Amenable treated patients, n=31 DISCLOSURE n=20 Conflicts of Interest AJ has no conflicts of interest to disclose. RS has received research funding from Amicus Therapeutics, Protalix Biotherapeutics, Shire, and Genzyme. KN serves on advisory boards for and has received research funding from Amicus Therapeutics, Genzyme, and Shire. UFR serves on advisory boards for and has received research funding from Amicus Therapeutics, Genzyme, and Shire. RG has received honoraria from Amicus Therapeutics, BioMarin, Sanofi-Genzyme, and Shire. DGB serves as a consultant and speaker for and has received funding from Amicus Therapeutics and Genzyme, and has received research funding from Shire. DAH is a consultant for and has received research and travel funding from Amicus Therapeutics, Shire, Genzyme, Actelion, and Protalix. VJ, JY, JPC, NS, and JAB are employees of and own stock in Amicus Therapeutics. ERT=enzyme replacement therapy. aProteinuria stratification: high (0.1 g/24 h); low (<0.1 g/24 h). Key Inclusion Criteria for FACETS and ATTRACT • Male and female patients aged 16-74 years diagnosed with Fabry disease with amenable GLA mutations Naive to ERT or had not received ERT for 6 months before screening (FACETS) Initiated treatment with ERT 12 months before baseline visit and had a stable ERT dose (at 80% labeled dose) for 3 months before baseline visit (ATTRACT) eGFRMDRD at screening 30 mL/min/1.73 m2 Urine GL-3 at screening 4× the upper limit of normal (24-hour collection) (FACETS) Patients taking angiotensin-converting enzyme inhibitors, angiotensin II receptor blockers, or renin inhibitors had to be on a stable dose for 4 weeks before the screening visit • • • • • LS means and 95% confidence intervals (CIs) based on analysis of covariance that includes treatment, baseline GFR, sex, age, and 24-hour urine protein. eGFR=estimated glomerular filtration rate; GFR, glomerular filtration rate; LS=least squares. Supported by Amicus Therapeutics, Inc. Presented at the 13th International Congress of Inborn Errors of Metabolism; September 5-8, 2017; Rio de Janeiro, Brazil Annualized LS Mean Change (mL/min/1.73 m2) Annualized Rate of Change (mL/min/1.73 m2), Mean ± SEM Annualized Rate of Change (mL/min/1.73 m2), Mean ± SEM Annualized Rate of Change (mL/min/1.73 m2), Mean ± SEM MigalastatERT eGFRCKD-EPI mGFRiohexol All Patients Baseline eGFR <90All Patients Baseline eGFR <90 0 -1 -2 -3 -4 -5 -6 -7 -8 -9 -10 Difference: 4.46 (95% CI -0.66, 9.57) Difference: 5.72 (95% CI -1.87, 13.30) -0.4 n=34 -1.03 n=18 Difference: 0.63-3.33 (95% CI -2.57, 3.83) n=20 -3.24-3.51 n=18 -4.35 n=34 Difference: -1.12 (95% CI -6.74, 4.51) -7.96 n=7 -9.05 n=8 Baseline ERT • Agalasidase alfa or agalasidase betaMigalastat 150 mg QOD Open-Label• 3 consents withdrawn prior to 1st dose• All treated patients, n=36 Randomized• All treated patients, n=21• Amenable treated patients, n=34 • Amenable treated patients, n=19• 2 discontinuations Month 18 Migalastat 150 mg QOD Migalastat 150 mg QOD Open-Label• All treated patients, n=15• All treated patients, n=33 • 3 discontinuations• 3 discontinuations Month 30 Option to Enroll in Open-Label Extension Completed Study: • All patients, n=12 • Amenable, n=12 Completed Study: • All patients, n=30 • Amenable, n=30 Completed Study: • All patients, n=34 • Amenable, n=32 • Declined extension, n=1 Completed Study: • All patients, n=18 • Amenable, n=16 • Declined extension, n=3 Screening and Randomization • 68 screened • 8 did not meet inclusion criteria • 60 randomized 1.5:1 • Stratified by sex and proteinuriaa Baseline Double-Blind150 mg QOD Month 6• Amenable patients, n=22•8 Open-LabelMigalastat 150 mg QOD Migalastat 150 mg QOD • All patients, n=30• All patients, n=34 • Amenable patients, n=20• Amenable patients, n=28 Month 12• 1 discontinuation• 3 discontinuations Open-LabelMigalastat 150 mg QOD Migalastat 150 mg QOD • Amenable patients, n=19• Amenable patients, n=25 Month 24• 2 discontinuations• 4 discontinuations Kidney Biopsy Option to Enroll in Open-Label Extension Completed Study: • All patients, n=27 • Amenable, n=22 Completed Study: • All patients, n=27 • Amenable, n=19 Plac ebo Screening and Randomization • 180 screened • 113 screening failures • 67 randomized 1:1, stratified by sex Migalastat • All patie Amenable p nts, n=34 atients, n=2 A 0 -0.5 -1 -1.5 -2 eGFR mGFR Renal Test Method B 1.5 1 0.5 0 -0.5 -1 -1.5 -2 30 to <6060 to <9090 Baseline eGFR (mL/min/1.73 m2) 0.2 ± 0.90 n=21 -0.7 ± 3.97-0.8 ± 1.01 n=3n=17 -0.3 ± 0.66 n=41 -1.5 ± 1.33 n=38 MigalastatERT 21.3 ± NA 0 -2 0 -4 -6 -8 -1060 to <9090 Baseline eGFR (mL/min/1.73 m2) n=1 -0.2 ± 1.25 n=18 -2.0 ± 0.57-2.1 ± 1.6 n=14n=11 -4.5 ± 2.68 n=2 -7.3 ± 6.01 n=7 30 to <60a

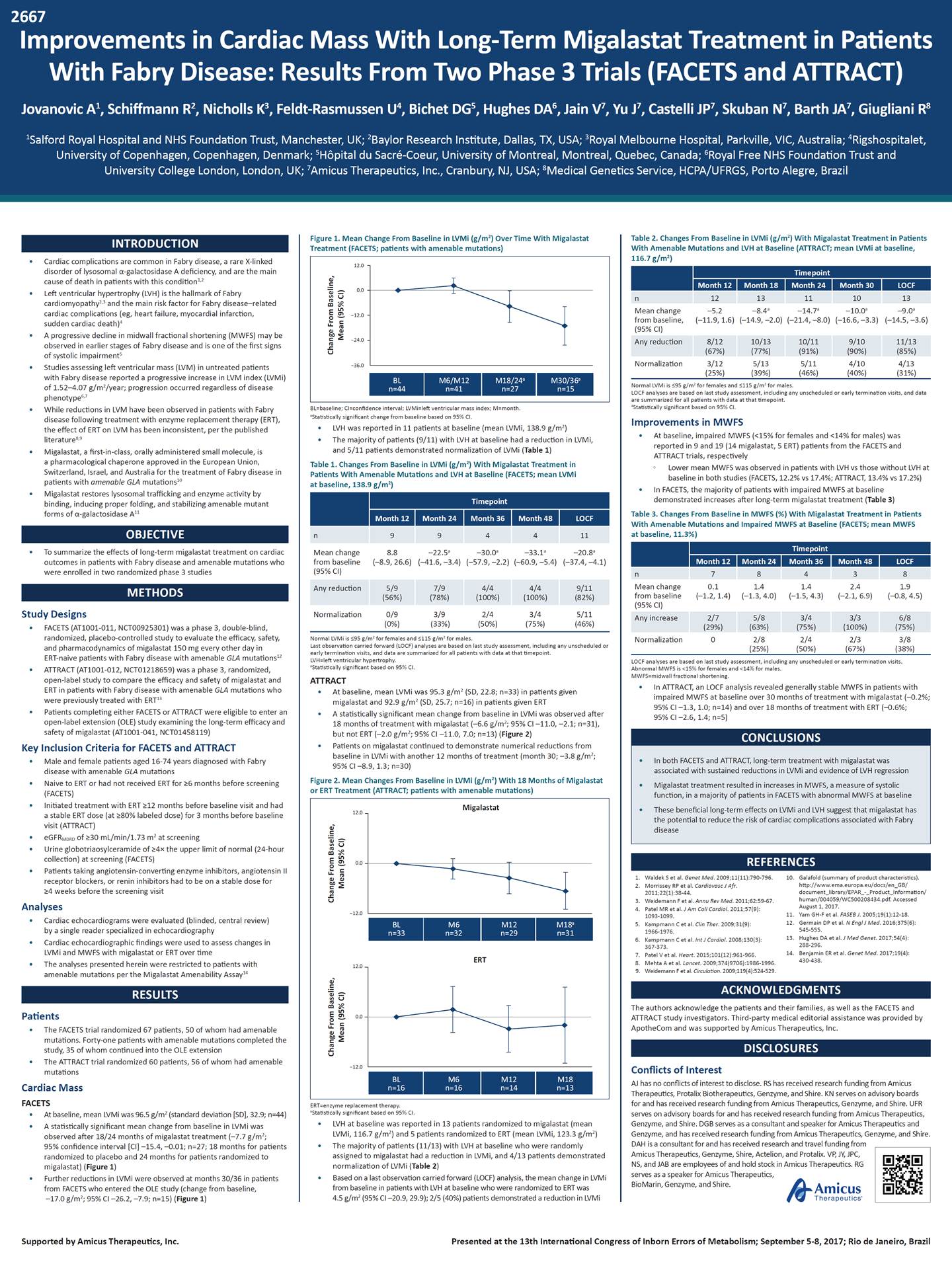
2667 Improvements in Cardiac Mass With Long-Term Migalastat Treatment in Patients With Fabry Disease: Results From Two Phase 3 Trials (FACETS and ATTRACT) Jovanovic A1, Schiffmann R2, Nicholls K3, Feldt-Rasmussen U4, Bichet DG5, Hughes DA6, Jain V7, Yu J7, Castelli JP7, Skuban N7, Barth JA7, Giugliani R8 1Salford Royal Hospital and NHS Foundation Trust, Manchester, UK; 2Baylor Research Institute, Dallas, TX, USA; 3Royal Melbourne Hospital, Parkville, VIC, Australia; 4Rigshospitalet, University of Copenhagen, Copenhagen, Denmark; 5Hôpital du Sacré-Coeur, University of Montreal, Montreal, Quebec, Canada; 6Royal Free NHS Foundation Trust and University College London, London, UK; 7Amicus Therapeutics, Inc., Cranbury, NJ, USA; 8Medical Genetics Service, HCPA/UFRGS, Porto Alegre, Brazil Figure 1. Mean Change From Baseline in LVMi (g/m ) Over Time With Migalastat Treatment (FACETS; patients with amenable mutations) 2 Table 2. Changes From Baseline in LVMi (g/m ) With Migalastat Treatment in Patients With Amenable Mutations and LVH at Baseline (ATTRACT; mean LVMi at baseline, 2 INTRODUCTION Cardiac complications are common in Fabry disease, a rare X-linked disorder of lysosomal -galactosidase A deficiency, and are the main cause of death in patients with this condition1,2 Left ventricular hypertrophy (LVH) is the hallmark of Fabry cardiomyopathy2,3 and the main risk factor for Fabry disease–related cardiac complications (eg, heart failure, myocardial infarction, sudden cardiac death)4 A progressive decline in midwall fractional shortening (MWFS) may be observed in earlier stages of Fabry disease and is one of the first signs of systolic impairment5 Studies assessing left ventricular mass (LVM) in untreated patients with Fabry disease reported a progressive increase in LVM index (LVMi) of 1.52–4.07 g/m2/year; progression occurred regardless of disease phenotype6,7 While reductions in LVM have been observed in patients with Fabry disease following treatment with enzyme replacement therapy (ERT), the effect of ERT on LVM has been inconsistent, per the published literature8,9 Migalastat, a first-in-class, orally administered small molecule, is a pharmacological chaperone approved in the European Union, Switzerland, Israel, and Australia for the treatment of Fabry disease in patients with amenable GLA mutations10 Migalastat restores lysosomal trafficking and enzyme activity by binding, inducing proper folding, and stabilizing amenable mutant forms of -galactosidase A11 116.7 g/m ) 2 • • Mean change from baseline, (95% CI) –5.2 (–11.9, 1.6) –8.4 a –14.7 a –10.0 a –9.0 a (–14.9, –2.0) (–21.4, –8.0) (–16.6, –3.3) (–14.5, –3.6) • Normalization 3/12 (25%) 5/13 (39%) 5/11 (46%) 4/10 (40%) 4/13 (31%) • Normal LVMi is 95 g/m2 for females and 115 g/m2 for males. LOCF analyses are based on last study assessment, including any unscheduled or early termination visits, and data are summarized for all patients with data at that timepoint. aStatistically significant based on 95% CI. Improvements in MWFS BL=baseline; CI=confidence interval; LVMi=left ventricular mass index; M=month. aStatistically significant change from baseline based on 95% CI. • • • LVH was reported in 11 patients at baseline (mean LVMi, 138.9 g/m2) The majority of patients (9/11) with LVH at baseline had a reduction in LVMi, and 5/11 patients demonstrated normalization of LVMi (Table 1) • At baseline, impaired MWFS (<15% for females and <14% for males) was reported in 9 and 19 (14 migalastat, 5 ERT) patients from the FACETS and ATTRACT trials, respectively • Table 1. Changes From Baseline in LVMi (g/m2) With Migalastat Treatment in Patients With Amenable Mutations and LVH at Baseline (FACETS; mean LVMi at baseline, 138.9 g/m2) Lower mean MWFS was observed in patients with LVH vs those without LVH at baseline in both studies (FACETS, 12.2% vs 17.4%; ATTRACT, 13.4% vs 17.2%) • In FACETS, the majority of patients with impaired MWFS at baseline demonstrated increases after long-term migalastat treatment (Table 3) • Table 3. Changes From Baseline in MWFS (%) With Migalastat Treatment in Patients With Amenable Mutations and Impaired MWFS at Baseline (FACETS; mean MWFS at baseline, 11.3%) OBJECTIVE To summarize the effects of long-term migalastat treatment on cardiac outcomes in patients with Fabry disease and amenable mutations who were enrolled in two randomized phase 3 studies • Mean change from baseline (95% CI) 8.8 (–8.9, 26.6) –22.5a (–41.6, –3.4) –30.0a (–57.9, –2.2) –33.1a (–60.9, –5.4) –20.8a (–37.4, –4.1) Mean change from baseline (95% CI) 0.1 (–1.2, 1.4) 1.4 (–1.3, 4.0) 1.4 (–1.5, 4.3) 2.4 (–2.1, 6.9) 1.9 (–0.8, 4.5) METHODS Study Designs Normalization 0/9 (0%) 3/9 (33%) 2/4 (50%) 3/4 (75%) 5/11 (46%) • FACETS (AT1001-011, NCT00925301) was a phase 3, double-blind, randomized, placebo-controlled study to evaluate the efficacy, safety, and pharmacodynamics of migalastat 150 mg every other day in ERT-naive patients with Fabry disease with amenable GLA mutations12 ATTRACT (AT1001-012, NCT01218659) was a phase 3, randomized, open-label study to compare the efficacy and safety of migalastat and ERT in patients with Fabry disease with amenable GLA mutations who were previously treated with ERT13 Patients completing either FACETS or ATTRACT were eligible to enter an open-label extension (OLE) study examining the long-term efficacy and safety of migalastat (AT1001-041, NCT01458119) Normal LVMi is 95 g/m2 for females and 115 g/m2 for males. Last observation carried forward (LOCF) analyses are based on last study assessment, including any unscheduled or early termination visits, and data are summarized for all patients with data at that timepoint. LVH=left ventricular hypertrophy. aStatistically significant based on 95% CI. ATTRACT Normalization 0 2/8 (25%) 2/4 (50%) 2/3 (67%) 3/8 (38%) LOCF analyses are based on last study assessment, including any unscheduled or early termination visits. Abnormal MWFS is <15% for females and <14% for males. MWFS=midwall fractional shortening. • • In ATTRACT, an LOCF analysis revealed generally stable MWFS in patients with impaired MWFS at baseline over 30 months of treatment with migalastat (–0.2%; 95% CI –1.3, 1.0; n=14) and over 18 months of treatment with ERT (–0.6%; 95% CI –2.6, 1.4; n=5) • At baseline, mean LVMi was 95.3 g/m2 (SD, 22.8; n=33) in patients given migalastat and 92.9 g/m2 (SD, 25.7; n=16) in patients given ERT A statistically significant mean change from baseline in LVMi was observed after 18 months of treatment with migalastat (–6.6 g/m2; 95% CI –11.0, –2.1; n=31), but not ERT (–2.0 g/m2; 95% CI –11.0, 7.0; n=13) (Figure 2) Patients on migalastat continued to demonstrate numerical reductions from • • CONCLUSIONS • Key Inclusion Criteria for FACETS and ATTRACT baseline in LVMi with another 12 months of treatment (month 30; –3.8 g/m ; 95% CI –8.9, 1.3; n=30) 2 • Male and female patients aged 16-74 years diagnosed with Fabry disease with amenable GLA mutations Naive to ERT or had not received ERT for 6 months before screening (FACETS) Initiated treatment with ERT 12 months before baseline visit and had a stable ERT dose (at 80% labeled dose) for 3 months before baseline visit (ATTRACT) eGFRMDRD of 30 mL/min/1.73 m2 at screening Urine globotriaosylceramide of 4× the upper limit of normal (24-hour collection) at screening (FACETS) Patients taking angiotensin-converting enzyme inhibitors, angiotensin II receptor blockers, or renin inhibitors had to be on a stable dose for 4 weeks before the screening visit Figure 2. Mean Changes From Baseline in LVMi (g/m2) With 18 Months of Migalastat or ERT Treatment (ATTRACT; patients with amenable mutations) • • • • REFERENCES • 1. 2. Waldek S et al. Genet Med. 2009;11(11):790-796. Morrissey RP et al. Cardiovasc J Afr. 2011;22(1):38-44. Weidemann F et al. Annu Rev Med. 2011;62:59-67. Patel MR et al. J Am Coll Cardiol. 2011;57(9): 1093-1099. Kampmann C et al. Clin Ther. 2009;31(9): 1966-1976. Kampmann C et al. Int J Cardiol. 2008;130(3): 367-373. Patel V et al. Heart. 2015;101(12):961-966. Mehta A et al. Lancet. 2009;374(9706):1986-1996. Weidemann F et al. Circulation. 2009;119(4):524-529. 10. Galafold (summary of product characteristics). http://www.ema.europa.eu/docs/en_GB/ document_library/EPAR_-_Product_Information/ human/004059/WC500208434.pdf. Accessed August 1, 2017. Yam GH-F et al. FASEB J. 2005;19(1):12-18. Germain DP et al. N Engl J Med. 2016;375(6): 545-555. Hughes DA et al. J Med Genet. 2017;54(4): 288-296. Benjamin ER et al. Genet Med. 2017;19(4): 430-438. 3. 4. Analyses 11. 12. • Cardiac echocardiograms were evaluated (blinded, central review) by a single reader specialized in echocardiography Cardiac echocardiographic findings were used to assess changes in LVMi and MWFS with migalastat or ERT over time The analyses presented herein were restricted to patients with amenable mutations per the Migalastat Amenability Assay14 5. 13. 6. • 14. 7. 8. 9. • ACKNOWLEDGMENTS The authors acknowledge the patients and their families, as well as the FACETS and ATTRACT study investigators. Third-party medical editorial assistance was provided by ApotheCom and was supported by Amicus Therapeutics, Inc. RESULTS Patients • The FACETS trial randomized 67 patients, 50 of whom had amenable mutations. Forty-one patients with amenable mutations completed the study, 35 of whom continued into the OLE extension The ATTRACT trial randomized 60 patients, 56 of whom had amenable mutations DISCLOSURES • Conflicts of Interest AJ has no conflicts of interest to disclose. RS has received research funding from Amicus Therapeutics, Protalix Biotherapeutics, Genzyme, and Shire. KN serves on advisory boards for and has received research funding from Amicus Therapeutics, Genzyme, and Shire. UFR serves on advisory boards for and has received research funding from Amicus Therapeutics, Genzyme, and Shire. DGB serves as a consultant and speaker for Amicus Therapeutics and Genzyme, and has received research funding from Amicus Therapeutics, Genzyme, and Shire. Cardiac Mass FACETS ERT=enzyme replacement therapy. aStatistically significant based on 95% CI. • • At baseline, mean LVMi was 96.5 g/m2 (standard deviation [SD], 32.9; n=44) A statistically significant mean change from baseline in LVMi was observed after 18/24 months of migalastat treatment (–7.7 g/m2; 95% confidence interval [CI] –15.4, –0.01; n=27; 18 months for patients randomized to placebo and 24 months for patients randomized to migalastat) (Figure 1) Further reductions in LVMi were observed at months 30/36 in patients from FACETS who entered the OLE study (change from baseline, –17.0 g/m2; 95% CI –26.2, –7.9; n=15) (Figure 1) • LVH at baseline was reported in 13 patients randomized to migalastat (mean LVMi, 116.7 g/m2) and 5 patients randomized to ERT (mean LVMi, 123.3 g/m2) The majority of patients (11/13) with LVH at baseline who were randomly assigned to migalastat had a reduction in LVMi, and 4/13 patients demonstrated normalization of LVMi (Table 2) Based on a last observation carried forward (LOCF) analysis, the mean change in LVMi from baseline in patients with LVH at baseline who were randomized to ERT was 4.5 g/m2 (95% CI –20.9, 29.9); 2/5 (40%) patients demonstrated a reduction in LVMi DAH is a consultant for and has received research and travel funding from Amicus Therapeutics, Genzyme, Shire, Actelion, and Protalix. VP, JY, JPC, NS, and JAB are employees of and hold stock in Amicus Therapeutics. RG serves as a speaker for Amicus Therapeutics, BioMarin, Genzyme, and Shire. • • • Supported by Amicus Therapeutics, Inc. Presented at the 13th International Congress of Inborn Errors of Metabolism; September 5-8, 2017; Rio de Janeiro, Brazil Change From Baseline, Mean (95% CI) Change From Baseline, Mean (95% CI) Change From Baseline, Mean (95% CI) Migalastat 12.0 0.0 -12.0 12.0ERT 0.0 -12.0 BL n=16 M6 n=16 M12 n=14 M18 n=13 BL n=33 M6 n=32 M12 n=29 M18a n=31 •In both FACETS and ATTRACT, long-term treatment with migalastat was associated with sustained reductions in LVMi and evidence of LVH regression •Migalastat treatment resulted in increases in MWFS, a measure of systolic function, in a majority of patients in FACETS with abnormal MWFS at baseline •These beneficial long-term effects on LVMi and LVH suggest that migalastat has the potential to reduce the risk of cardiac complications associated with Fabry disease Any increase2/75/83/43/36/8 (29%)(63%)(75%)(100%)(75%) Any reduction5/97/94/44/49/11 (56%)(78%)(100%)(100%)(82%) Timepoint Month 12 Month 24 Month 36 Month 48 LOCF n78438 Timepoint Month 12 Month 24 Month 36 Month 48 LOCF n994411 Any reduction8/1210/1310/119/10 (67%)(77%)(91%)(90%) 11/13 (85%) Timepoint Month 12 Month 18 Month 24 Month 30 LOCF n1213111013 12.0 0.0 -12.0 -24.0 -36.0 BL n=44 M6/M12 n=41 M18/24a n=27 M30/36a n=15
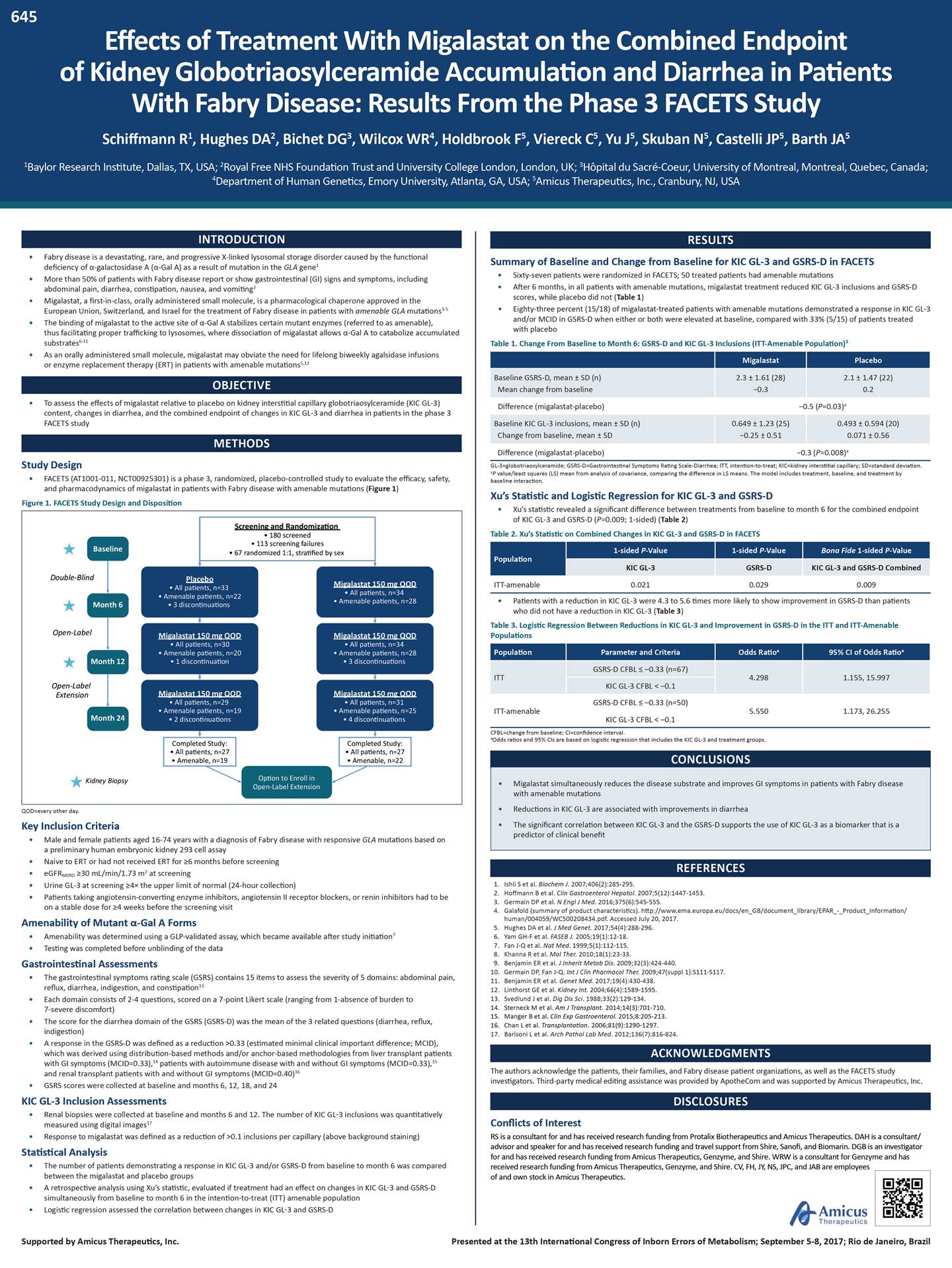
645 Effects of Treatment With Migalastat on the Combined Endpoint of Kidney Globotriaosylceramide Accumulation and Diarrhea in Patients With Fabry Disease: Results From the Phase 3 FACETS Study Schiffmann R1, Hughes DA2, Bichet DG3, Wilcox WR4, Holdbrook F5, Viereck C5, Yu J5, Skuban N5, Castelli JP5, Barth JA5 1Baylor Research Institute, Dallas, TX, USA; 2Royal Free NHS Foundation Trust and University College London, London, UK; 3Hôpital du Sacré-Coeur, University of Montreal, Montreal, Quebec, Canada; 4Department of Human Genetics, Emory University, Atlanta, GA, USA; 5Amicus Therapeutics, Inc., Cranbury, NJ, USA INTRODUCTION Fabry disease is a devastating, rare, and progressive X-linked lysosomal storage disorder caused by the functional deficiency of -galactosidase A (-Gal A) as a result of mutation in the GLA gene1 More than 50% of patients with Fabry disease report or show gastrointestinal (GI) signs and symptoms, including abdominal pain, diarrhea, constipation, nausea, and vomiting2 Migalastat, a first-in-class, orally administered small molecule, is a pharmacological chaperone approved in the European Union, Switzerland, and Israel for the treatment of Fabry disease in patients with amenable GLA mutations3-5 The binding of migalastat to the active site of -Gal A stabilizes certain mutant enzymes (referred to as amenable), thus facilitating proper trafficking to lysosomes, where dissociation of migalastat allows -Gal A to catabolize accumulated substrates6-11 As an orally administered small molecule, migalastat may obviate the need for lifelong biweekly agalsidase infusions or enzyme replacement therapy (ERT) in patients with amenable mutations5,12 RESULTS Summary of Baseline and Change from Baseline for KIC GL-3 and GSRS-D in FACETS • • • Sixty-seven patients were randomized in FACETS; 50 treated patients had amenable mutations After 6 months, in all patients with amenable mutations, migalastat treatment reduced KIC GL-3 inclusions and GSRS-D scores, while placebo did not (Table 1) Eighty-three percent (15/18) of migalastat-treated patients with amenable mutations demonstrated a response in KIC GL-3 and/or MCID in GSRS-D when either or both were elevated at baseline, compared with 33% (5/15) of patients treated with placebo • • • • Table 1. Change From Baseline to Month 6: GSRS-D and KIC GL-3 Inclusions (ITT-Amenable Population)3 • OBJECTIVE To assess the effects of migalastat relative to placebo on kidney interstitial capillary globotriaosylceramide (KIC GL-3) content, changes in diarrhea, and the combined endpoint of changes in KIC GL-3 and diarrhea in patients in the phase 3 FACETS study • Difference (migalastat-placebo) -0.5 (P=0.03)a METHODS -0.3 (P=0.008)a Difference (migalastat-placebo) Study Design GL-3=globotriaosylceramide; GSRS-D=Gastrointestinal Symptoms Rating Scale-Diarrhea; ITT, intention-to-treat; KIC=kidney interstitial capillary; SD=standard deviation. aP value/least squares (LS) mean from analysis of covariance, comparing the difference in LS means. The model includes treatment, baseline, and treatment by baseline interaction. Xu’s Statistic and Logistic Regression for KIC GL-3 and GSRS-D • FACETS (AT1001-011, NCT00925301) is a phase 3, randomized, placebo-controlled study to evaluate the efficacy, safety, and pharmacodynamics of migalastat in patients with Fabry disease with amenable mutations (Figure 1) Figure 1. FACETS Study Design and Disposition • Xu’s statistic revealed a significant difference between treatments from baseline to month 6 for the combined endpoint of KIC GL-3 and GSRS-D (P=0.009; 1-sided) (Table 2) Table 2. Xu’s Statistic on Combined Changes in KIC GL-3 and GSRS-D in FACETS ITT-amenable 0.021 0.029 0.009 • Amenable patients, n=22 • Patients with a reduction in KIC GL-3 were 4.3 to 5.6 times more likely to show improvement in GSRS-D than patients who did not have a reduction in KIC GL-3 (Table 3) Table 3. Logistic Regression Between Reductions in KIC GL-3 and Improvement in GSRS-D in the ITT and ITT-Amenable Populations ITT 4.298 1.155, 15.997 Migalastat 150 mg QOD Migalastat 150 mg QOD Extension GSRS-D CFBL –0.33 (n=50) KIC GL-3 CFBL < –0.1 ITT-amenable 5.550 1.173, 26.255 CFBL=change from baseline; CI=confidence interval. aOdds ratios and 95% CIs are based on logistic regression that includes the KIC GL-3 and treatment groups. CONCLUSIONS with amenable mutations QOD=every other day. Key Inclusion Criteria • Male and female patients aged 16-74 years with a diagnosis of Fabry disease with responsive GLA mutations based on a preliminary human embryonic kidney 293 cell assay Naive to ERT or had not received ERT for 6 months before screening eGFRMDRD 30 mL/min/1.73 m2 at screening Urine GL-3 at screening 4× the upper limit of normal (24-hour collection) Patients taking angiotensin-converting enzyme inhibitors, angiotensin II receptor blockers, or renin inhibitors had to be on a stable dose for 4 weeks before the screening visit • • • • REFERENCES 1. 2. 3. 4. Ishii S et al. Biochem J. 2007;406(2):285-295. Hoffmann B et al. Clin Gastroenterol Hepatol. 2007;5(12):1447-1453. Germain DP et al. N Engl J Med. 2016;375(6):545-555. Galafold (summary of product characteristics). http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/ human/004059/WC500208434.pdf. Accessed July 20, 2017. Hughes DA et al. J Med Genet. 2017;54(4):288-296. Yam GH-F et al. FASEB J. 2005;19(1):12-18. Fan J-Q et al. Nat Med. 1999;5(1):112-115. Khanna R et al. Mol Ther. 2010;18(1):23-33. Benjamin ER et al. J Inherit Metab Dis. 2009;32(3):424-440. Germain DP, Fan J-Q. Int J Clin Pharmacol Ther. 2009;47(suppl 1):S111-S117. Benjamin ER et al. Genet Med. 2017;19(4):430-438. Linthorst GE et al. Kidney Int. 2004;66(4):1589-1595. Svedlund J et al. Dig Dis Sci. 1988;33(2):129-134. Sterneck M et al. Am J Transplant. 2014;14(3):701-710. Manger B et al. Clin Exp Gastroenterol. 2015;8:205-213. Chan L et al. Transplantation. 2006;81(9):1290-1297. Barisoni L et al. Arch Pathol Lab Med. 2012;136(7):816-824. Amenability of Mutant -Gal A Forms 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. • • Amenability was determined using a GLP-validated assay, which became available after study initiation7 Testing was completed before unblinding of the data Gastrointestinal Assessments • The gastrointestinal symptoms rating scale (GSRS) contains 15 items to assess the severity of 5 domains: abdominal pain, reflux, diarrhea, indigestion, and constipation13 Each domain consists of 2-4 questions, scored on a 7-point Likert scale (ranging from 1-absence of burden to 7-severe discomfort) The score for the diarrhea domain of the GSRS (GSRS-D) was the mean of the 3 related questions (diarrhea, reflux, indigestion) A response in the GSRS-D was defined as a reduction >0.33 (estimated minimal clinical important difference; MCID), which was derived using distribution-based methods and/or anchor-based methodologies from liver transplant patients with GI symptoms (MCID=0.33),14 patients with autoimmune disease with and without GI symptoms (MCID=0.33),15 and renal transplant patients with and without GI symptoms (MCID=0.40)16 GSRS scores were collected at baseline and months 6, 12, 18, and 24 • • • ACKNOWLEDGMENTS The authors acknowledge the patients, their families, and Fabry disease patient organizations, as well as the FACETS study investigators. Third-party medical editing assistance was provided by ApotheCom and was supported by Amicus Therapeutics, Inc. • DISCLOSURES KIC GL-3 Inclusion Assessments • Renal biopsies were collected at baseline and months 6 and 12. The number of KIC GL-3 inclusions was quantitatively measured using digital images17 Response to migalastat was defined as a reduction of >0.1 inclusions per capillary (above background staining) Conflicts of Interest RS is a consultant for and has received research funding from Protalix Biotherapeutics and Amicus Therapeutics. DAH is a consultant/ advisor and speaker for and has received research funding and travel support from Shire, Sanofi, and Biomarin. DGB is an investigator for and has received research funding from Amicus Therapeutics, Genzyme, and Shire. WRW is a consultant for Genzyme and has • Statistical Analysis • The number of patients demonstrating a response in KIC GL-3 and/or GSRS-D from baseline to month 6 was compared between the migalastat and placebo groups A retrospective analysis using Xu’s statistic, evaluated if treatment had an effect on changes in KIC GL-3 and GSRS-D simultaneously from baseline to month 6 in the intention-to-treat (ITT) amenable population Logistic regression assessed the correlation between changes in KIC GL-3 and GSRS-D received research funding from Amicus Therapeutics, Genzyme, and Shire. CV, FH, JY, NS, JPC, and JAB are employees of and own stock in Amicus Therapeutics. • • Supported by Amicus Therapeutics, Inc. Presented at the 13th International Congress of Inborn Errors of Metabolism; September 5-8, 2017; Rio de Janeiro, Brazil •Migalastat simultaneously reduces the disease substrate and improves GI symptoms in patients with Fabry disease •Reductions in KIC GL-3 are associated with improvements in diarrhea •The significant correlation between KIC GL-3 and the GSRS-D supports the use of KIC GL-3 as a biomarker that is a predictor of clinical benefit PopulationParameter and CriteriaOdds Ratioa95% CI of Odds Ratioa GSRS-D CFBL –0.33 (n=67) KIC GL-3 CFBL < –0.1 Population 1-sided P-Value1-sided P-ValueBona Fide 1-sided P-Value KIC GL-3GSRS-DKIC GL-3 and GSRS-D Combined Baseline Double-Blind • All patients, n=33150 mg QOD Month 6• 3 discontinuations Open-LabelMigalastat 150 mg QOD Migalastat 150 mg QOD • All patients, n=30• All patients, n=34 • Amenable patients, n=20• Amenable patients, n=28 Month 12• 1 discontinuation• 3 discontinuations Open-Label • All patients, n=29• All patients, n=31 • Amenable patients, n=19• Amenable patients, n=25 Month 24• 2 discontinuations• 4 discontinuations Kidney BiopsyOption to Enroll in Open-Label Extension Completed Study: • All patients, n=27 • Amenable, n=22 Completed Study: • All patients, n=27 • Amenable, n=19 Migalastat • All patie • Amenable p nts, n=34 atients, n=28 Plac ebo Screening and Randomization • 180 screened • 113 screening failures • 67 randomized 1:1, stratified by sex Baseline KIC GL-3 inclusions, mean ± SD (n)0.649 ± 1.23 (25)0.493 ± 0.594 (20) Change from baseline, mean ± SD-0.25 ± 0.510.071 ± 0.56 MigalastatPlacebo Baseline GSRS-D, mean ± SD (n)2.3 ± 1.61 (28)2.1 ± 1.47 (22) Mean change from baseline-0.30.2
644 Response of Patients With Fabry Disease With the Amenable GLA Mutation p.N215S to Treatment With Migalastat Feldt-Rasmussen U1, Nicholls K2, Shankar SP3,a, Sunder-Plassmann G4, Bichet DG5, Schiffmann R6, Viereck C7, Skuban N7, Yu J7, Castelli JP7, Barth JA7, Hughes DA8 1Rigshospitalet, University of Copenhagen, Copenhagen, Denmark; 2Royal Melbourne Hospital, Parkville, VIC, Australia; 3Department of Human Genetics, Emory University School of Medicine, Atlanta, GA; 4Division of Nephrology and Dialysis, Department of Medicine III, Medical University of Vienna, Vienna, Austria; 5Hôpital du Sacré-Coeur, University of Montreal, Montreal, Quebec, Canada; 6Baylor Research Institute, Dallas, TX, USA; 7Amicus Therapeutics, Inc., Cranbury, NJ, USA; 8Royal Free NHS Foundation Trust and University College London, London, UK aCurrently at University of California Davis, Davis, CA, USA Figure 3. Change from Baseline to Month 18 in Patients With the p.N215S Mutation and All Patients Randomized to Migalastat at Baseline INTRODUCTION Fabry disease is a devastating, rare, and progressive X-linked lysosomal storage disorder caused by mutations in the GLA gene, resulting in the deficient activity of -galactosidase A (-Gal A)1,2 Accumulation of -Gal A substrates can lead to functional impairments in the kidney, heart, and brain and premature death1,2 Renal dysfunction progresses over time in a majority of male patients with Fabry disease, and can lead to end-stage renal disease. However, cardiac disease is currently the main cause of death in patients with Fabry disease2 Migalastat, a first-in-class, orally administered small molecule, is a pharmacological chaperone approved in the European Union for the treatment of Fabry disease in adults and adolescents aged >16 years with amenable GLA mutations3-5 Migalastat restores lysosomal trafficking and enzyme activity by binding, inducing proper folding, and stabilizing amenable mutant forms of -Gal A1,6 As an orally administered small molecule, migalastat may obviate the need for lifelong biweekly agalsidase infusions or enzyme replacement therapy (ERT) in patients with amenable mutations3-5,7 p.N215S, often referred to as a “cardiac genetic variant”,8 is a common GLA mutation observed in Fabry disease. In general, the p.N215S phenotype is associated with higher plasma enzyme activity, older age of symptom onset, and significant cardiac disease. It is also less associated with expression of the early symptoms typically seen with severe classical disease. However, more research is needed to better understand p.N215S phenotypic expression9,10 RESULTS Patient disposition is summarized in Figure 1 The ITT amenable population consisted of 53/57 (34 migalastat; 19 ERT) patients 10 patients in the ITT amenable population had the p.N215S mutation; 7 were randomized to migalastat, while 3 remained on ERT • • • • • CKD-EPI iohexol 3 Baseline Disease Severity and Characteristics • • Age, plasma globotriaosylsphingosine (lyso-Gb3), and eGFR at baseline were similar between patients in the p.N215S population and all patients in the ITT-amenable population. However, consistent with the literature, patients with the p.N215S mutation had higher median LVMi and had lower median 24-hour protein urine at baseline compared with all patients in the ITT-amenable population (Tables 1 and 2) 5/7 migalastat-treated patients and 1/3 ERT-treated patients with the p.N215S mutation had left ventricular hypertrophy at baseline A greater proportion of patients with the p.N215S mutation had cardiac disease at baseline than all patients (80% vs 52%). Patients with the p.N215S mutation had disease involvement in multiple organs/systems, including renal, central nervous system, and gastrointestinal but not angiokeratoma or corneal whorling (Figure 2) • • • • • • Table 1. Individual Baseline Characteristics of Patients With the p.N215S Mutation 3 2 OBJECTIVE To assess the efficacy of migalastat in a subset of patients with Fabry disease with the amenable p.N215S mutation relative to all patients with Fabry disease with amenable mutations during the first 18 months of the phase 3 ATTRACT study 1 Migalastat 60 2 2 8.61 125 0 78 • 3 Migalastat 64 7 5 5.18 95 99 88 Data are graphed as median (center line), first/third quartiles (box perimeter), and min/max (error bars). CI=confidence interval; mGFRiohexol=measured GFR using iohexol clearance; SEM=standard error of the mean. METHODS • Individual treatment outcomes for the 3 patients with the p.N215S mutation treated with ERT are listed in Table 3 5 ERT 57 6 6 8.89 121 0 97 Table 3. Individual Change From Baseline to Month 18 in Renal Function, Cardiac Mass, and Substrate Level in p.N215S Patients Treated With ERT Study Design label, 30-month study comparing the efficacy and safety of migalastat and ERT in patients with Fabry disease with amenable GLA mutations who were previously treated with ERT (Figure 1) • ATTRACT (AT1001-012, NCT01218659) is a phase 3, randomized, open-6 ERT 39 9 9 1.47 70 619 103 • The intention-to-treat (ITT) amenable population consisted of patients with amenable mutations based on the Good Laboratory Practice Human Embryonic Kidney 293 cells (GLP-HEK) assay11 Patients completing ATTRACT were eligible to enter open-label extensions (OLE) examining the long-term safety and efficacy of migalastat (NCT01458119 and NCT02194985) 8 Migalastat 70 6 4 4.64 105 0 72 • 6 -0.8 -7.9 -7.7 0 10 Migalastat 59 4 2 3.47 98 265 89 eGFRCKD-EPI=estimated glomerular filtration rate using the Chronic Kidney Disease Epidemiology Collaboration; LVMi=left ventricular mass index; lyso-Gb3=globotriaosylsphingosine; N/A=not available. aConfounded by ERT. Table 2. Group Baseline Characteristics of Patients With the p.N215S Mutation and All Patients Randomized to Migalastat at Baseline Figure 1. ATTRACT Study Design and Disposition CONCLUSIONS Characteristic (n=10) (n=36) Years since diagnosis 5.50 (2, 9) 4.50 (1, 43) LVMi (g/m2) 100.0 (55, 138) 90.14 (63.56, 165.73)c eGFRCKD-EPI (mL/min/1.73 m2) 85.50 (72, 113) 85.91 (51.33, 145.12) REFERENCES Ishii S et al. Biochem J. 2007;406(2):285-295. Waldek S et al. Genet Med. 2009;11(11):790-796. Germain DP et al. N Engl J Med. 2016;375(6):545-555. Galafold (summary of product characteristics). http://www.ema.europa.eu/docs/en_GB/document_ library/EPAR_-Product_Information/human/004059/WC500208434.pdf. Accessed July 20, 2017. Hughes DA et al. J Med Genet. 2017;54(4)288-296. Yam GH-F et al. FASEB J. 2005;19(1):12-18. Linthorst GE et al. Kidney Int. 2004;66(4):1589-1595. Patel V et al. Heart. 2015;101(12):961-966. Thomas A et al. Mol Gen Metab. 2015;114(2):S113. Germain DP et al. Mol Gen Metab. 2016;117(2):S48-S49. Benjamin ER et al. Genet Med. 2017;19(4):430-438. Tennankore K et al. Presented at the 39th Annual Meeting of the Canadian Society of Nephrology; 2007; Halifax, NS, Canada. Weidemann F et al. J Am Soc Nephrol. 2014;25(4):837-849. Data are represented as median (min, max). aConfounded by ERT. bn=32. cn=33. Figure 2. Organ System Involvement at Baselinea 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. ERT=enzyme replacement therapy; QOD=every other day. aProteinuria stratification: high (0.1 g/24 h); low (<0.1 g/24 h). Key Inclusion Criteria • Male and female patients aged 16-74 years diagnosed with Fabry disease with responsive GLA mutations based on a preliminary GLP-HEK 293 cell assay Treatment initiation with ERT 12 months before baseline visit and stable ERT dose (at 80% labeled dose) for 3 months before baseline visit eGFRMDRD at screening 30 mL/min/1.73 m2 Patients taking angiotensin-converting enzyme inhibitors, angiotensin II receptor blockers, or renin inhibitors had to be on a stable dose for 4 weeks before the screening visit 13. • ACKNOWLEDGMENTS The authors acknowledge the patients, their families, and Fabry disease patient organizations, as well as the ATTRACT study investigators. Third-party medical editing assistance was provided by ApotheCom and was supported by Amicus Therapeutics, Inc. • • DISCLOSURES Amenability of Mutant -Gal A Forms • Amenability was determined using a GLP-validated assay, which became available after study initiation11 Testing was completed before unblinding of the data CNS=central nervous system; GI=gastrointestinal. aAngiokeratoma, corneal whorling, neuropathic pain, and GI symptoms were based on medical history findings. bRenal involvement was based on medical history or baseline eGFR <90 mL/min/1.73 m2 and 24-hour protein 150 mg. cCardiac involvement included previous cardiac event (based on medical history), left ventricular hypertrophy, or conduction abnormality (eg, tachycardia, ST-segment abnormality) based on medical history finding or baseline assessment of LVMi. dCNS involvement was based on medical history (stroke/transient ischemic attack, tinnitus/hearing loss). Change from Baseline to Month 18 Conflicts of Interest UF-R is an advisor for and has received research funding from Amicus Therapeutics, Genzyme/Sanofi, and Shire. KN has received research funding from Genzyme/Sanofi. SPS has received honoraria and travel support from Amicus Therapeutics, Biomarin, Genzyme/Sanofi, Protalix Biotherapeutics, Pfizer, and Shire. GS-P has received fees from Amicus Therapeutics, Genzyme/Sanofi, and Shire HGT. DGB is an investigator for and has received research funding from Amicus Therapeutics, Genzyme, and Shire. RS is a consultant for and has received research funding from Protalix Biotherapeutics and Amicus Therapeutics. CV, NS, JY, JPC, and JAB are employees of and own stock in Amicus Therapeutics. DAH is a consultant/advisor and speaker for and has received research funding and travel support from Shire, Sanofi, and Biomarin. • Renal Assessments • • • eGFRCKD-EPI was assessed at baseline and at months 1, 3, 6, 9, 12, 15, and 18 mGFRiohexol was assessed at baseline and at months 6, 12, and 18 The long-term effect of migalastat on renal activity was assessed by calculating the annualized rates of change for each patient using the slope of the linear regression between the observed values and the assessment times • The median change from baseline to month 18 for eGFRCKD-EPI, mGFRiohexol, LVMi, and plasma lyso-Gb3 was similar between migalastat-treated patients with the p.N215S mutation and all migalastat-treated patients in the ITT-amenable population (Figure 3) In patients with the p.N215S mutation, 5/7 migalastat-treated patients and 1/3 ERT-treated patients achieved a decrease in LVMi There was a reduction in median GFR and stabilization of plasma lyso-Gb3 in migalastat-treated patients with and without the p.N215S mutation; there was a small range across measured outcomes in patients with the p.N215S mutation Patients with the p.N215S mutation had a response to treatment similar to that of all migalastat-treated patients in ATTRACT Cardiac Assessments 2D or M-mode every 6 months through blinded, centralized evaluation (Cardiocore, Rockville, MD, USA) • • Left ventricular mass index (LVMi) was measured by echocardiography using • • The long-term effect of migalastat on LVMi was assessed by calculating the change from baseline to the last available time point and the 95% confidence interval for each patient • Supported by Amicus Therapeutics, Inc. Presented at the 13th International Congress of Inborn Errors of Metabolism; September 5-8, 2017; Rio de Janeiro, Brazil Patients Reporting Fabry Disease by Organ System, % Median Change From Baseline to Month 18 Patients With the p.N215S Mutation All Migalastat-Treated Patients 90 80 70 60 50 40 30 20 10 0 or Involvmentb Involvmentc Involvmentd Pain Symptoms Corneal Whorling 52 71 80 64 75 70 52 20 61 40 50 0 Angiokeratoma Renal Cardiac CNS Neuropathic GI 24-hr urine protein (mg)72.00 (0, 619)129 (0, 2282) Plasma lyso-Gb3a (nmol/L)4.91 (1.47, 8.89)6.345 (0.80, 59.07)b p.N215S PatientsAll Patients Age59.50 (23, 70)54 (18,70) •Following 18 months of treatment with migalastat in the phase 3 ATTRACT study, a majority of patients with Fabry disease with the p.N215S mutation had a response similar to that of all migalastat-treated patients and demonstrated a decrease in LVMi •The small reduction in eGFR in this ERT-experienced population is noteworthy based on data in the literature demonstrating a worsening of renal function over 12-15 months after stopping ERT treatment12 or reducing ERT dose13 •Migalastat may offer promise as an oral treatment alternative for male and female patients with Fabry disease with amenable mutations, including those with the p.N215S mutation Baseline ERT • Agalasidase alfa or agalasidase betaMigalastat 150 mg QOD Open-Label• 3 consents withdrawn prior to 1st dose• All treated patients, n=36 Randomized• All treated patients, n=21• Amenable treated patients, n=34 • Amenable treated patients, n=19• 2 discontinuations • 3 discontinuations Month 18 Migalastat 150 mg QOD Migalastat 150 mg QOD Open-Label• All treated patients, n=15• All treated patients, n=33 Extension• Amenable treated patients, n=15• Amenable treated patients, n=31 • 3 discontinuations• 3 discontinuations Month 30 Option to Enroll in Open-Label Extension Completed Study: • All patients, n=12 • Amenable, n=12 Completed Study: • All patients, n=30 • Amenable, n=30 Completed Study: • All patients, n=34 • Amenable, n=32 • Declined extension, n=1 Completed Study: • All patients, n=18 • Amenable, n=16 • Declined extension, n=3 Screening and Randomization • 68 screened • 8 did not meet inclusion criteria • 60 randomized 1.5:1 • Stratified by sex and proteinuriaa 7-1.9-3.8-7.6-0.1 9Migalastat63422.31100078 7ERT23651.735545113 Plasma Lyso-Gb3 PatienteGFRCKD-EPI AnnualizedmGFRiohexol Annualized LVMi Change FromChange From p.N215S IDRate of Change FromRate of Change FromBaseline toBaseline to Baseline to Month 18Baseline to Month 18Month 18Month 18 50.4-1.722.72 Females 4Migalastat64446.2313813078 2Migalastat595N/A7.19N/A11983 PatientPlasma p.N215S TreatmentAgeYears Since Years Since Lyso-Gb a LVMi24-hr UrineeGFRCKD-EPI ID(years) Diagnosis Start of ERT (nmol/L) (g/m ) Protein (mg) (mL/min/1.73 m2) Males Migalastat-Treated Patients With the p.N215S Mutation All Migalastat-Treated Patients eGFR mGFR LVMi Lyso-Gb 20 20 40 30 15 0 20 20 10 -10 0 5 10 -20 -20 0 0 -5 -30 -40 -10 -40 -60 -10 CKD-EPI iohexol 3 Baseline to Month 18 Mean ± SEM (95% CI) eGFR Annualized Rate mGFR Annualized Rate Plasma Lyso-Gb of Change From of Change From LVMi Change From Change From Baseline Baseline to Month 18 Baseline to Month 18 to Month 18 p.N215S Treated with Migalastat (n=7) All Migalastat-Treated Patients (n=34) p.N215S Treated with Migalastat (n=7) All Migalastat-Treated Patients (n=34) p.N215S Treated with Migalastat (n=6) All Migalastat-Treated Patients (n=31) p.N215S Treated with Migalastat (n=7) All Migalastat-Treated Patients (n=30) 0.05 ± 1.42 (-3.42, 3.52) -0.40 ± 0.93 (-2.27, 1.48) -1.92 ± 1.86 (-6.48, 2.64) -4.35 ± 1.64 (-7.65, -1.06) -5.10 ± 2.44 (-11.38, 1.18) -6.58 ± 2.17 (-11.01, -2.15) 0.23 ± 0.42 (-0.80, 1.25) -1.68 ± 1.03 (-0.42, -3.77) Median (min, max) -1.13 (-4.73, 6.38) -1.29 (-6.97, 15.82) -4.11 (-7.57, 5.27) -3.23 (-28.77, 9.45) -3.08 (-15.6, 1.67) -7.74 (-40.72, 28.43) 0.52 (-1.10, 2.07) 0.54 (-2.27, 28.30)

2576 A Next-Generation Enzyme Replacement Therapy for Fabry Disease: Co-formulation of a Proprietary Recombinant Human -Galactosidase A With a Pharmacological Chaperone Demonstrates Greater Substrate Reduction Than Agalsidase Beta in Mice Xu S, Schilling A, Gomez N, Frascella M, Garcia A, Hamler R, Ellsworth D, Soska R, Nair A, Della Valle MC, Feng J, Manger H, Valenzano KJ, Do H, Gotschall R, Khanna R Amicus Therapeutics, Inc., Cranbury, NJ, USA ATB101/AT1001 Co-Formulation Increases -Gal A Activities in Tissues of Gla KO Mice Figure 3. ATB101/AT1001 Co-Formulation Improves Plasma Lyso-Gb3 Reduction in Gla KO Mice Over Standard of Care Figure 5. INTRODUCTION Fabry disease is an X-linked lysosomal storage disorder caused by a deficiency in -galactosidase A (-Gal A) activity, leading to progressive accumulation of lysosomal globotriaosylceramide (GL-3) in multiple tissues While enzyme replacement therapy (ERT) with manufactured human -Gal A, namely agalsidase beta and agalsidase alfa, has brought many therapeutic benefits to patients, the infused enzymes have potential limitations, including low physical stability, short circulating half-lives in blood, and variable uptake into different disease-relevant tissues, that may impact efficacy and tolerability Previously, we demonstrated that the pharmacological chaperone AT1001 (migalastat) improves the pharmacological properties of the manufactured enzymes via binding and stabilization A proprietary recombinant human -Gal A (rh-Gal A), ATB101, has recently been developed and is co-formulated with AT1001 (designated as ATB101/AT1001). The co-formulated ATB101/AT1001 as a single intravenously administered product is aimed to improve the pharmacological properties of the enzyme and result in improved substrate clearance compared with the standard of care. This concept was tested in preclinical studies using a Fabry mouse model (Gla knockout [KO]) • • 15 • • RESULTS AT1001 Stabilizes ATB101 In Vitro Figure 1. 800 0.4 0.2 3 40 50 60 70 80 3 The thermal stability of ATB101 was assessed using a fluorescence-based thermal performed in the absence and presence of 10 and 100 µM AT1001 at pH 7.4 and maximum fluorescence in each sample. As expected for any lysosomal enzyme at previously for patients with Fabry disease, a strong correlation (p<0.0001) pH resulted in a concentration-dependent stabilization of ATB101, with 10 µM CONCLUSIONS AT1001 Co-Formulation Increases the Circulating Levels of ATB101 in Gla KO Mice Figure 2. ATB101/AT1001 Co-Formulation Improves the Tissue GL-3 Reduction in Gla KO Mice Over Standard of Care Figure 4. 900 300 Low Dose 60 0.5 1.0 1.5 2.0 6 12182430 Vehicle Agalsidase beta Agalsidase beta ATB101/AT1001 1000 80 80 600 0.5 1.0 1.5 2.0 18 24 30 0.51.01.52.0 18 24 30 (1 mg/kg) (10 mg/kg) REFERENCES Flanagan JJ et al. Hum Mutat. 2009;30(12):1683-1692. Benjamin ER et al. Mol Ther. 2012;20(4):717-726. Germain DP et al. N Engl J Med. 2016;375(6):545-555. 1. 2. 3. 3000 2000 ACKNOWLEDGMENTS Third-party medical editorial assistance was provided by ApotheCom and was supported by Amicus Therapeutics, Inc. DISCLOSURES Conflicts of Interest All of the authors are employees of and hold stock in Amicus Therapeutics, Inc. Supported by Amicus Therapeutics, Inc. Presented at the 13th International Congress of Inborn Errors of Metabolism; September 5-8, 2017; Rio de Janeiro, Brazil % of Cmax Activity (corresponding group) % of Cmax Activity (corresponding group) SYPRO Orange Fluorescence (normalized) % of Cmax Activity (corresponding group) GL-3 (µg/g tissue) GL-3 (µg/g tissue) GL-3 (µg/g tissue) -Gal A Activity (nmol/mg protein/hr) -Gal A Activity (nmol/mg protein/hr) -Gal A Activity (nmol/mg protein/hr) Kidney GL-3 (µg/g tissue) Lyso-Gb3 (ng/mL) Heart 600 150 100 50 0 (1 mg/kg)(10 mg/kg) Kidney 800 400 200 0 VehicleAgalsidase betaAgalsidase betaATB101/AT1001 Skin 2500 600 450 300 150 0 VehicleAgalsidase betaAgalsidase betaATB101/AT1001 (1 mg/kg)(10 mg/kg) Approximately 16-week-old male Gla KO mice (n=8/group) were given 2 biweekly IV bolus administrations of either 1 or 10 mg/kg of agalsidase beta or co-formulation of AT1001 with <10 mg/kg ATB101 (ATB101/AT1001). Disease-relevant tissues were collected 7 days after the last administration and GL-3 levels were determined by liquid chromatography coupled to tandem mass spectrometry (LC-MS/MS). In all tissues tested, ATB101/AT1001 co-formulation achieved GL-3 reduction that was significantly greater (p<0.05) than agalsidase beta 1 mg/kg (standard of care). Importantly, the GL-3 reduction with ATB101/ AT1001 co-formulation reached or exceeded the reduction seen with agalsidase beta 10 mg/kg, demonstrating substantially superior substrate clearance compared with the current standard of care. 120 100High Dose 80Mid Dose 40 20 0 Time (hours) 120120 100100 Low DoseMid Dose 60+AT100160+AT1001 4040 2020 00 Time (hours) Time (hours) Approximately 6-month-old male Gla KO mice (n=5/group) were given a single intravenous (IV) bolus administration of low-, mid-, or high-dose (up to 10 mg/ kg) ATB101 alone or ATB101 co-formulated with AT1001 (ATB101/AT1001) at low or mid enzyme dose. Blood samples were collected from each mouse using serial mandibular bleeds at 5 minutes, 15 minutes, 30 minutes, 1 hour, 2 hours, and 24 hours after IV administration, and -Gal A activity in plasma was determined using an enzymatic method with 4-MU-galactopyranoside (4MU-Gal) as the substrate. The plasma activity was used to determine pharmacokinetic parameters using GraphPad version 6. For each group, the averaged activity of each timepoint was normalized to the averaged peak plasma -gal A activity (Cmax) of the corresponding group, and a plot was made using the normalized activity and the nominal time. The half-life of ATB101 activity following each dosing regimen was calculated using a one-phase decay model. The fitted curves are shown in the graphs, and the calculated half-lives are summarized in the table. When administered alone, ATB101 showed dose-dependent, nonlinear pharmacokinetics, as the half-lives increased with increasing doses. Co-formulation with AT1001 increased circulating -Gal A activity levels, with an up to 2.3-fold increase in ATB101 half-life. N/A=not applicable; PK=pharmacokinetics. Half Life, Hours Low Dose Mid Dose High Dose ATB101 alone 0.19 0.26 0.61 ATB101/AT1001 0.44 0.49 N/A Fold increase compared with enzyme alone 2.3 1.9 N/A PK of ATB101 ± AT1001 PK of ATB101 alone •AT1001 increased the physical stability of a proprietary rh-Gal A, ATB101, currently in nonclinical development •In mice, following IV administration, ATB101 showed dose-dependent, nonlinear pharmacokinetics, as the half-lives increased with increasing doses. Upon co-formulation with AT1001, the half-life of active ATB101 in plasma increased up to 2.3-fold compared with enzyme alone •In Gla KO mice, co-formulated ATB101/AT1001 led to substantially increased -Gal A activity in disease-relevant tissues compared with enzyme alone •Importantly, under a repeat IV administration regimen, co-formulated ATB101/AT1001 achieved robust GL-3 reduction in kidney, heart, and skin tissues, reaching or even exceeding the levels achieved with 10 mg/kg agalsidase beta (i.e. 10× the standard-of-care dose) In plasma, a similar effect on the lyso-Gb3 levels was observed, and levels correlated well with kidney GL-3 •Collectively, these results indicate that ATB101/AT1001 co-formulation increases the stability of the enzyme, resulting in substantially greater substrate reduction in preclinical models compared with the current standard therapy. Therefore, ATB101/AT1001 co-formulation represents a promising next-generation treatment for Fabry disease that warrants further investigation 1.2 1.0 0.8 0.6 10 µM AT1001 100 µM AT1001 0.0 Temperature (°C) denaturation assay as described previously.1,2 The thermal stability scans were in the absence of AT1001 at pH 5.2. Data were normalized to the minimum and neutral pH, ATB101 was also significantly less stable (melting temperature [Tm]=48.9°C) than at acidic pH (Tm=57.8°C). Co-incubation with AT1001 at neutral AT1001 shifting the Tm to 54.6°C, and 100 µM AT1001 shifting the Tm to 58.4°C. The latter was similar to the Tm observed for ATB101 alone at acidic pH. ATB101 pH 7.4 ATB101 pH 7.4 + ATB101 pH 7.4 + ATB101 pH 5.2 Heart 10 5 0 ATB101++ AT1001+ Kidney 2.0 1.5 1.0 0.5 0.0 ATB101++ AT1001+ Skin 100 80 60 40 20 0 ATB101++ AT1001+ Approximately 16-week-old male Gla KO mice (n=8/group) were given 2 biweekly IV bolus administrations of either ATB101 alone (<10 mg/kg) or ATB101/AT1001. Seven days after the final drug administration, the -Gal A activity in disease-relevant tissues was measured using an enzymatic method with 4MU-Gal as the substrate. Co-formulation with AT1001 substantially increased -Gal A activity in all tissues measured compared with enzyme alone. -Gal A Activity (nmol/mg protein/hr) (standard deviation) Heart Kidney Skin ATB101 alone 1.9 (0.7) 0.7 (0.2) 7.2 (7.3) ATB101/AT1001 6.7 (4.1) 1.4 (0.5) 30.1 (50.5) Fold increase compared with enzyme alone 3.6 2.0 4.2 Plasma Lyso-Gb3 500 400 300 100 50 0 VehicleAgalsidase betaAgalsidase betaATB101/AT1001 (1 mg/kg) (10 mg/kg) Correlation (Kidney GL-3 vs Plasma Lyso-Gb3) 1000 Vehicle Agalsidase beta (1 mg/kg) Agalsidase beta (10 mg/kg) 600ATB101/AT1001 400 200 0 Plasma Lyso-Gb3 (ng/mL) In the same study described in Figure 4, plasma samples were collected 7 days after the last administration, and levels of globotriaosylsphingosine (lyso-Gb ), an important biomarker for Fabry disease severity, were determined by LC-MS/MS. ATB101/AT1001 co-formulation achieved plasma lyso-Gb reduction that was significantly better (p<0.05) than agalsidase beta 1 mg/kg and similar to the effects seen with agalsidase beta 10 mg/kg, once again demonstrating substantially superior efficacy compared with the current standard of care. Plasma lyso-Gb3 levels were correlated with kidney GL-3 (the most severely affected tissue in Fabry disease) using GraphPad version 6. As reported 3 between plasma lyso-Gb3 and kidney GL-3 was observed, indicating the utility and reliability of testing plasma lyso-Gb3 in preclinical studies.
