Filed Pursuant to Rule 424(b)(3)
Registration No. 333-177620
PROSPECTUS

IASIS Healthcare LLC
IASIS Capital Corporation
Offer to Exchange any and all of our outstanding unregistered 8.375% Senior Notes due 2019 for $850,000,000 aggregate principal amount of our new 8.375% Senior Notes due 2019 that have been registered under the Securities Act of 1933, as amended
Terms of the Exchange Offer
| | • | | We are offering to exchange any and all of our outstanding 8.375% Senior Notes due 2019 that were issued on May 3, 2011 (the “Old Notes”) for an equal amount of new 8.375% Senior Notes due 2019 (the “New Notes”, and together with the Old Notes, the “notes”). |
| | • | | The exchange offer expires at 5:00 p.m., New York City time, on December 12, 2011 (such date and time, the “Expiration Date”, unless we extend or terminate the exchange offer, in which case the “Expiration Date” will mean the latest date and time to which we extend the exchange offer). |
| | • | | Tenders of Old Notes may be withdrawn at any time prior to the Expiration Date. |
| | • | | All Old Notes that are validly tendered and not validly withdrawn will be exchanged. |
| | • | | The exchange of Old Notes for New Notes generally will not be a taxable exchange for U.S. federal income tax purposes. |
| | • | | We will not receive any proceeds from the exchange offer. |
| | • | | The terms of the New Notes to be issued in the exchange offer are substantially the same as the terms of the Old Notes, except that the offer of the New Notes is registered under the Securities Act of 1933, as amended (the “Securities Act”), and the New Notes have no transfer restrictions, rights to additional interest or registration rights. |
| | • | | The New Notes will not be listed on any securities exchange. A public market for the New Notes may not develop, which could make selling the New Notes difficult. |
Each broker-dealer that receives New Notes for its own account pursuant to the exchange offer must acknowledge that it will deliver a prospectus in connection with any resale of such New Notes. The letter of transmittal accompanying this prospectus states that by so acknowledging and by delivering a prospectus, a broker-dealer will not be deemed to admit that it is an “underwriter” within the meaning of the Securities Act. This prospectus, as it may be amended or supplemented from time to time, may be used by a
broker-dealer in connection with resales of New Notes received in exchange for Old Notes where such Old Notes were acquired by such broker-dealer as a result of market-making activities or other trading activities. Starting on the Expiration Date (as defined herein) and ending on the earlier of (i) 180 days from the date on which the Exchange Offer Registration Statement (as defined herein) is declared effective and (ii) the date on which a broker-dealer is no longer required to deliver a prospectus in connection with market-making or other trading activities, we will make this prospectus, as amended or supplemented, available to any broker-dealer for use in connection with any such resale. See “Plan of Distribution.”
Investing in the New Notes to be issued in the exchange offer involves certain risks. See “Risk Factors” beginning on page 20.
We are not making an offer to exchange the Old Notes in any jurisdiction where the offer is not permitted.
Neither the Securities and Exchange Commission (the “SEC”) nor any state securities commission has approved or disapproved of these securities or passed upon the adequacy or accuracy of this prospectus. Any representation to the contrary is a criminal offense.
The date of this prospectus is November 10, 2011.
TABLE OF CONTENTS
We have not authorized anyone to give any information or make any representation about the offering that is different from, or in addition to, that contained in this prospectus or the related registration statement. If you are in a jurisdiction where offers to sell, or solicitations of offers to purchase, the securities offered by this document are unlawful, or if you are a person to whom it is unlawful to direct these types of activities, then the offer presented in this document does not extend to you. The information contained in this document speaks only as of the date of this document unless the information specifically indicates that another date applies.
WHERE YOU CAN FIND MORE INFORMATION
We have filed with the SEC a registration statement on Form S-4 to register this exchange offer of the New Notes, which you can access on the SEC’s website at http://www.sec.gov. This prospectus, which forms part of the registration statement, does not contain all of the information included in that registration statement. For further information about us and about the New Notes offered in this prospectus, you should refer to the registration statement and its exhibits. You may read and copy any materials we file with the SEC at the public reference room maintained by the SEC at 100 F Street, N.E., Washington, D.C. 20549. You may obtain information on the operation of the public reference room by calling the SEC at 1-800-SEC-0330. These materials are also available to the public from the SEC’s website athttp://www.sec.gov.
1
MARKET AND INDUSTRY DATA
Certain market and industry data included in this prospectus has been obtained from third party sources that we believe to be reliable. Market estimates are calculated by using independent industry publications, government publications and third party forecasts in conjunction with our assumptions about our markets. We have not independently verified such third party information and cannot assure you of its accuracy or completeness. While we are not aware of any misstatements regarding any market, industry or similar data presented herein, such data involves risks and uncertainties and is subject to change based on various factors, including those discussed under the headings “Cautionary Note Regarding Forward-Looking Statements” and “Risk Factors” in this prospectus.
WEBSITES
The information contained on or that can be accessed through any of our websites is not incorporated in, and is not part of, this prospectus or the registration statement.
2
PROSPECTUS SUMMARY
This summary highlights significant aspects of our business and this exchange offer, but it is not complete and does not contain all of the information that you should consider before making your investment decision. You should carefully read this entire prospectus, including the information presented under the section entitled “Risk Factors” and the historical financial data and related notes before making an investment decision. This summary contains forward-looking statements that involve risks and uncertainties. Our actual results may differ significantly from the results discussed in the forward-looking statements as a result of certain factors, including those set forth under “Risk Factors” and “Cautionary Note Regarding Forward-Looking Statements.”
With respect to the discussion of the terms of the notes on the cover page, in the section entitled “Prospectus Summary—Summary of the Exchange Offer,” in the section entitled “Prospectus Summary—Summary of the New Notes” and in the section entitled “Description of Notes,” references to “we,” “us” or “our” include only IASIS Healthcare LLC and IASIS Capital Corporation (jointly, the “Issuers”) and not any other consolidated subsidiaries of the Issuers.
Company Overview
We are a leading owner and operator of acute care hospitals in high-growth urban and suburban markets. We are focused on delivering high-quality patient care by providing a broad range of services aimed at the needs of the individuals we serve, and by integrating our core strategies with our local physicians’ and clinicians’ practices. We continue to focus on expanding our footprint within our existing markets by establishing additional care delivery settings. At June 30, 2011, we owned or leased 18 acute care hospitals and one behavioral health hospital with a total of 4,362 licensed beds; we also operate several outpatient facilities and provide related services. For the nine months ended June 30, 2011, we generated consolidated net revenue and Adjusted EBITDA of $2,070.3 million and $228.0 million, respectively. We operate in the following regions:
| | | | | | | | |
Region Breakdown | | Licensed
Beds | | | Number of
Hospitals | |
Salt Lake City, Utah | | | 705 | | | | 4 | |
Phoenix, Arizona | | | 621 | | | | 4 | |
Tampa-St. Petersburg, Florida | | | 688 | | | | 3 | |
Five markets in Texas, including Houston and San Antonio | | | 1,935 | | | | 5 | |
Las Vegas, Nevada | | | 175 | | | | 1 | |
West Monroe, Louisiana | | | 223 | | | | 1 | |
Woodland Park, Colorado | | | 15 | | | | 1 | |
| | | | | | | | |
Total | | | 4,362 | | | | 19 | |
Our general, acute care hospital facilities offer a variety of medical and surgical services commonly available in hospitals, including emergency services, general surgery, internal medicine, cardiology, obstetrics, orthopedics, psychiatry and physical rehabilitation. In addition, our facilities provide outpatient and ancillary services including outpatient surgery, physical therapy, radiation therapy, diagnostic imaging and respiratory therapy.
We also own and operate Health Choice Arizona, Inc. (“Health Choice” or the “Plan”), a Medicaid and Medicare managed health plan in Phoenix that served over 197,000 members as of June 30, 2011.
Since 2001, following organic growth and the implementation of a number of operational initiatives, expansion projects and acquisitions, our financial performance has improved significantly. Adjusted EBITDA for the fiscal year ended September 30, 2010, was $290.8 million, representing a compound annual growth rate of 12.0%.
3
Industry Overview
We believe that the following healthcare trends will benefit well-positioned hospital companies:
Aging Population and Continued Growth in the Need for Healthcare Services. According to the U.S. Census Bureau, the U.S. population includes 40.2 million Americans aged 65 or older, which represents 13.0% of the total population. By the year 2030, the number of Americans aged 65 or older is expected to increase to 71.5 million, or 19.7% of the total population. Additionally, as a result of the increasing life expectancy of Americans, the number of people aged 85 years and older is expected to register a 57% increase by the year 2030.
Changes in the Delivery of Healthcare Services. We believe the U.S. healthcare system and the demand for healthcare services are evolving in ways that favor large-scale, comprehensive and integrated service networks. Specifically, we believe there are a number of initiatives that will continue to gain importance in the foreseeable future, including the introduction of value-based payment methodologies tied to performance, quality and coordination of care; implementation of integrated electronic health records (“EHR”) and information; and an increasing ability for patients and consumers to make choices about all aspects of healthcare. Due in large part to our investment in information technology and physician alignment strategies, we believe our company is well positioned to respond to these emerging trends and has the resources, expertise and flexibility necessary to adapt in a timely manner to the changing healthcare regulatory and reimbursement environment.
Impact of Health Reform Law. The recently enacted Patient Protection and Affordable Care Act, as amended by the Health Care and Education Reconciliation Act of 2010 (the “Health Reform Law”), will change how healthcare services are covered, delivered and reimbursed. It will do so through expanded coverage of uninsured individuals, significant reductions in the growth of Medicare program payments, material decreases in Medicare and Medicaid disproportionate share hospital (“DSH”) payments, and the establishment of programs where reimbursement is tied in part to quality and integration. The Health Reform Law is expected to expand health insurance coverage to approximately 32 to 34 million additional individuals through a combination of public program expansion and private sector health insurance reforms. We believe the expansion of private sector and Medicaid coverage will, over time, increase our reimbursement related to providing services to individuals who were previously uninsured. On the other hand, the reductions in the growth in Medicare payments and the decreases in DSH payments will adversely affect our government reimbursement. Because of the many variables involved, we are unable to predict the net impact of the Health Reform Law on us; however, we believe our experienced management team, emphasis on quality care and our diverse service offerings will enable us to capitalize on the opportunities presented by the Health Reform Law, as well as adapt in a timely manner to its challenges.
Competitive Strengths
We believe that the following competitive strengths will allow us to remain a leading owner and operator of acute care hospitals:
Diverse Portfolio of Hospitals. We currently operate 18 acute care hospitals and one behavioral health hospital in seven separate geographic regions. This broad geographic footprint diversifies our revenue base and payor mix, thus reducing our exposure to any one market or payor. For the nine months ended June 30, 2011, our largest geographic region accounted for less than 33% of our acute care related net revenue. In addition, at June 30, 2011, our hospitals had approximately 400 managed care contracts with no one commercial payor plan representing more than 10% of our total net patient revenue for the nine months ended June 30, 2011.
Well Positioned in Attractive, High-Growth Markets. We believe our hospitals are strategically positioned to capitalize on the positive demographic growth trends in the markets we serve. We believe our markets offer opportunities for significant revenue growth and margin expansion, since 15 of our 18 acute care hospitals operate in areas that have population growth rates above the national average.
4
Strong Return on Invested Capital. We maintain a disciplined approach to capital expenditures, strategically investing in our existing facilities and making key acquisitions in order to expand our range of services, increase patient volumes and grow our platform. We invest in projects based on a rigorous identification process that includes product line and market analysis, as well as evaluating the needs of our patients, physicians and the communities we serve. This process emphasizes investing in high-margin product lines within cardiology, surgery, outpatient imaging and other services. Since 2001, we have finished multiple expansion projects, built two new hospitals and made key acquisitions to grow our markets, including Glenwood Regional Medical Center (“Glenwood”) and Alliance Hospital in 2007, Brim Holdings, Inc. (“Brim”) in 2010 and St. Joseph Medical Center (“St. Joseph”) in 2011. In addition, our in-market capital investment strategies include the development and acquisition of healthcare delivery access points. These access points, which have expanded the reach of our hospital campuses, as well as improved overall business and payor mix, include outpatient imaging and surgery centers, urgent care facilities and physician clinics. We believe that the combination of our historical investments and our fiscal 2011 capital projects provide us with a strong growth opportunity.
Ability to Acquire and Integrate Acquisitions. We have a proven track record of successfully acquiring and integrating a variety of different types of healthcare delivery facilities. For example, in 2007, we acquired Glenwood, a 242-bed not-for-profit hospital, from the District of Ouachita Parish in West Monroe, Louisiana. Prior to the acquisition, the hospital was marginally profitable. In the four years under our ownership, we have made significant improvements in all aspects of the hospital’s operations and we have:
| | • | | Re-opened three nursing units that were closed prior to the acquisition; |
| | • | | Invested in upgrades in medical imaging and automated lab technology; |
| | • | | Expanded operating room capacity and services, including the area’s first hybrid operating room for cardiac catherizations; |
| | • | | Upgraded all facility information systems and converted to our standard patient accounting and clinical platform; |
| | • | | Established a successful hospitalist program; |
| | • | | Expanded the hospital’s healthcare delivery access points through acquisition of an outpatient surgical hospital and imaging center; |
| | • | | Opened a brand new facility that includes an urgent care center, imaging center and family care practice as a new patient access point; |
| | • | | Grown net revenue at a compounded annual growth rate of 7.0% from December 31, 2007 to December 31, 2010; and |
| | • | | Implemented operational efficiencies, which resulted in Adjusted EBITDA margin expansion in excess of growth in net revenue. |
Significant Investment in Integrated Information Systems. Since inception to June 30, 2011, we have invested over $125 million in integrated information systems implementing, across all of our operations, an advanced information systems platform that integrates our financial reporting, patient accounting, billing and clinical data systems. The infrastructure is in place to support the government’s healthcare information technology (“IT”) initiatives and integrated decision support reporting. We believe our information systems, which are scalable both in terms of adding new hospitals and adding new functionalities, allow us to enhance our facilities and maximize margins.
5
Proven and Committed Management Team Supported by Strong Equity Sponsorship. Our management team has extensive operational experience in managing both private and publicly traded hospital companies through periods of growth and consolidation. Our Chief Executive Officer and President, W. Carl Whitmer, has been with the Company since March 2000. Our management team is accustomed to operating under a leveraged capital structure, and has consistently demonstrated an ability to improve the operating performance and competitive position of our hospitals. We have also continued to strengthen local and regional management teams that enhance physician, employee and community relations. We will also continue to benefit from the sponsorship of TPG Capital, L.P. (“TPG Capital”), JLL Partners (“JLL”) and Trimaran Capital Partners (“Trimaran”).
Business Strategy
Our objective is to provide high-quality, cost-effective healthcare services to the communities we serve, while enhancing long-term growth and profitability that allows for the creation of value and opportunities for reinvestment. In order to achieve these objectives, we focus on the following elements, which we consider to be the key components of our business strategy:
Focus on Operational Excellence. We believe that a continuous focus on operational excellence sets the standard for managing all aspects of our business, including growth, quality and operating results. Our management team, which has extensive multi-facility operating experience, continually emphasizes the importance of operational excellence. We believe that in order to successfully achieve operational excellence we must concentrate on the following:
| | • | | Growing our presence in our existing markets; |
| | • | | Providing high-quality services to the communities we serve; |
| | • | | Achieving operational efficiencies and effective cost management in all aspects of patient care delivery; |
| | • | | Improving all aspects of the revenue cycle, including our processes for patient registration, such as patient qualification for financial assistance and point-of-service collections, billing, collections, and managed care contract compliance; and |
| | • | | Effectively deploying capital resources in a disciplined manner, including initiatives related to business development, growth, quality of care, information technology and plant maintenance. |
Provide High-Quality Services. The keys to providing high-quality services, which include patient safety, patient satisfaction and clinical quality, are at the center of success for our facilities. We strive each day to provide high-quality services at all of our facilities, as we believe the achievement of high-quality patient care results in the long-term growth of revenue and profitability. Our strategy for focusing on improving quality of care includes enhancing the patient care experience by:
| | • | | Attracting and retaining high-quality healthcare professionals; |
| | • | | Monitoring and tracking clinical performance and patient safety for numerous purposes, including the establishment of best practices; |
| | • | | Utilizing our advanced clinical information system, which provides more timely key clinical care data, to enable our hospitals to enhance patient safety, reduce medical errors through bar coding, increase staff time available for direct patient care and continue to achieve high-quality patient care outcomes; |
| | • | | Investing in our emergency rooms to improve patient flow, as well as quality and timeliness of care; |
6
| | • | | Utilizing our hospital medical management quality program to drive improvements in core management and allocation of resources, as well as quality and safety of care; and |
| | • | | Dedicating well-trained corporate and hospital resources to the improvement of patient care. |
Recruit and Employ Physicians to Meet Community Needs in Our Markets. We believe that a critical element to providing high-quality healthcare to the communities we serve is a comprehensive physician alignment strategy, which includes the continued investment in the employment, recruitment and retention of high-quality healthcare professionals. We believe the objective of attracting and retaining quality physicians is best accomplished by:
| | • | | Expanding the reach of our outpatient and other specialty services; |
| | • | | Equipping our hospitals with technologically advanced equipment, systems and platforms; |
| | • | | Focusing on community-based partnerships; |
| | • | | Enhancing physician convenience and access, including the development of medical office space on or near our hospital campuses; |
| | • | | Enabling physicians to remotely access clinical data through our advanced information systems, facilitating more convenient and timely patient care; and |
| | • | | Sponsoring training programs to educate physicians on advanced medical procedures. |
Utilize and Invest in Technology. We believe that technology is the key to improving clinical outcomes and quality of patient care. Since inception through June 30, 2011, we have spent over $300 million to equip our hospitals with cutting-edge clinical and health information technology. Our strategy to improve quality of care through investing in technology includes:
| | • | | Providing state of the art medical equipment and technology in our hospitals, including significant investment in sophisticated diagnostic equipment such as 64-slice CT scanners, MRIs, PET scanners and automated laboratories; |
| | • | | Utilizing our system-wide EHR information platform to connect all our hospitals and to provide comprehensive real time access to patient records and other information; |
| | • | | Providing a business intelligence system to enable real-time and effective decision making; |
| | • | | Investing in stronger physician partnerships by providing them with more advanced technology and platforms; and |
| | • | | Utilizing our information systems to track quality and patient outcomes. |
Pursue a Comprehensive Development Strategy. We will continue to assess opportunities to expand our regional and national presence. We believe the many factors currently affecting the healthcare industry will result in increased consolidation and business development opportunities across the industry, which we intend to actively pursue. We believe the successful pursuit of a comprehensive development strategy, including both the expansion of our national presence through the acquisition of hospitals in existing and new markets and a continued focus to capitalize on the opportunities in the communities we serve, will result in overall growth of our revenue and profitability. We believe that our existing markets will continue to benefit from strategic investments that expand the scope and reach of services provided through a variety of healthcare delivery access points. Our disciplined approach to enhancing our competitive position within our existing markets includes the development and expansion of profitable product lines, and the acquisition of new hospitals and other healthcare service providers, including outpatient and ancillary service centers and physician clinics.
7
Focus on Managed Care Relationships. We are focused on maintaining market-based relationships, as we believe that the broad geographic coverage of our hospitals in certain of the regions in which we operate, the expansion of our physician networks and our commitment to providing high-quality services increases our attractiveness to managed care plans in those areas. We believe these factors provide a platform that allows for negotiating reasonable terms with managed care plans, entering into contracts with additional managed care plans and aligning reimbursement with acuity of services.
Implement Operational Initiatives in Response to Healthcare Reform. In March 2010, President Obama signed the Health Reform Law into law. We believe that our consistent focus on quality and patient satisfaction programs, coupled with the significant investments we have made in information systems, positions us to respond promptly and effectively to the changes resulting from the Health Reform Law, as well as any additional reform initiatives at both the federal and state levels. Although we expect our business strategy to increase our patient volumes and reimbursement and allow us to control costs, certain risks could offset those increases to our net revenue and profitability.
Key Investors
TPG Capital is the global buyout group of TPG, a leading private investment firm founded in 1992 with more than $48 billion of assets under management and offices in San Francisco, Beijing, Fort Worth, Hong Kong, London, Luxembourg, Melbourne, Moscow, Mumbai, New York, Paris, Shanghai, Singapore and Tokyo. TPG Capital has extensive experience with global public and private investments executed through leveraged buyouts, recapitalizations, spinouts, growth investments, joint ventures and restructurings. Unless the context otherwise requires, references in this prospectus to “TPG” refer to TPG Partners III, L.P. and TPG Partners IV, L.P., the TPG Capital funds investing in the Company.
Founded in 1988 and headquartered in New York, New York, JLL is a leading private equity investment firm. Since inception, JLL has managed a series of private equity funds aggregating approximately $4.0 billion in committed capital. JLL’s healthcare investments, in addition to our company, have included PharmaNet, Patheon, OrNda Healthcorp, Kendall International, and AdvancePCS. JLL, through its predecessor funds, has been an investor in our company since its inception.
Trimaran is a private asset management firm, headquartered in New York, with assets under management and committed capital of approximately $2.7 billion. Since 1995, Trimaran has completed 59 private equity investments totaling over $1.6 billion of equity capital. Trimaran’s portfolio investments have included leveraged buyouts, build-ups, recapitalizations and growth investments in sectors such as manufacturing, healthcare, restaurants, retail, education, media, financial services, and utilities among others. Trimaran partners with outstanding management teams with the objective of creating long-term value.
8
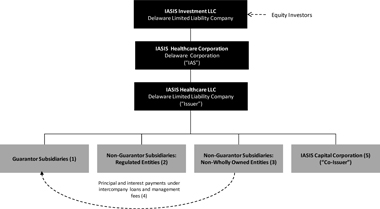
Organizational Structure
The following diagram summarizes our corporate structure:
Corporate Structure
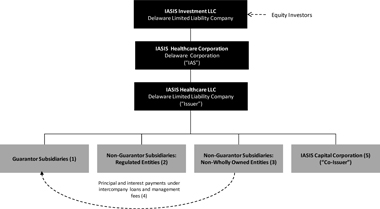
| (1) | Consists of 9 wholly owned hospitals. |
| (2) | Consists of 12 subsidiaries including Health Choice and other regulated hospital systems. |
| (3) | Consists of 7 non-wholly owned hospitals who serve as guarantors under the Senior Secured Credit Facilities. |
| (4) | All our consolidated Adjusted EBITDA comes from the non-guarantor subsidiaries. However, our guarantor subsidiaries hold unsubordinated promissory notes from the non-guarantor subsidiaries aggregating $665 million in principal amount as of June 30, 2011, under which the guarantor subsidiaries are entitled to principal and interest payments of $71 million annually. In addition, the non-guarantor subsidiaries are contractually obligated to pay the guarantor subsidiaries management fees. The management fee amount ranges from 2.0% to 2.5% of net revenue for the non-guarantor subsidiaries. For the nine months ended June 30, 2011, the non-guarantor subsidiaries paid $20 million in management fees. |
| (5) | Exists solely for the purpose of serving as co-issuer of the New Notes. |
9
Summary Of The Exchange Offer
The summary below describes the principal terms of the notes. Certain of the terms and conditions described below are subject to important limitations and exceptions. The “Description of Notes” section of this prospectus contains a more detailed description of the terms and conditions of the notes.
| | |
| Background | | On May 3, 2011, we issued $850,000,000 aggregate principal amount of the Old Notes in an unregistered offering. In connection with that offering, we entered into a registration rights agreement on May 3, 2011 (the “Registration Rights Agreement”) in which we agreed, among other things, to complete this exchange offer. Under the terms of the exchange offer, you are entitled to exchange the Old Notes for the New Notes evidencing the same indebtedness and with substantially similar terms. You should read the discussion under the heading “Description of Notes” for further information regarding the New Notes. |
| |
| The Exchange Offer | | We are offering to exchange, for each $1,000 aggregate principal amount of our Old Notes validly tendered and accepted, $1,000 aggregate principal amount of our New Notes. |
| |
| | We will not pay any accrued and unpaid interest on the Old Notes that we acquire in the exchange offer. Instead, interest on the New Notes will accrue from the most recent date to which interest has been paid or, if no interest has been paid, from and including May 3, 2011, the date of which we issued the Old Notes. |
| |
| | As of the date of this prospectus, $850,000,000 aggregate principal amount of the Old Notes are outstanding. |
| |
| Denominations of New Notes | | Tendering holders of the Old Notes must tender the Old Notes in minimum denominations of $2,000 and integral multiples of $1,000 in excess thereof. The New Notes will be issued in minimum denominations of $2,000 and integral multiples of $1,000 in excess thereof. |
| |
| Expiration Date | | The exchange offer will expire at 5:00 p.m., New York City time, on December 12, 2011, unless we extend or terminate the exchange offer in which case the “Expiration Date” will mean the latest date and time to which we extend the exchange offer. |
| |
| Settlement Date | | The settlement date of the exchange offer will be as soon as practicable after the Expiration Date of the exchange offer. |
| |
| Withdrawal of Tenders | | Tenders of the Old Notes may be withdrawn at any time prior to the Expiration Date. |
| |
| Conditions to the Exchange Offer | | Our obligation to consummate the exchange offer is subject to certain customary conditions, which we may assert or waive. See “Description of the Exchange Offer—Conditions to the Exchange Offer.” |
10
| | |
| Procedures for Tendering | | To participate in the exchange offer, you must follow the automatic tender offer program (“ATOP”), procedures established by The Depository Trust Company (“DTC”), for tendering the Old Notes held in book-entry form. The ATOP procedures require that the exchange agent receive, prior to the Expiration Date of the exchange offer, a computer-generated message known as an “agent’s message” that is transmitted through ATOP and that DTC confirm that: |
| |
| | • DTC has received instructions to exchange your Old Notes; and |
| |
| | • you agree to be bound by the terms of the letter of transmittal. |
| |
| | For more details, please read “Description of the Exchange Offer—Terms of the Exchange Offer” and “Description of the Exchange Offer—Procedures for Tendering.” If you elect to have the Old Notes exchanged pursuant to this exchange offer, you must properly tender your Old Notes prior to 5:00 p.m., New York City time, on the Expiration Date. All Old Notes validly tendered and not properly withdrawn will be accepted for exchange. The Old Notes may be exchanged only in minimum denominations of $2,000 and integral multiples of $1,000 in excess thereof. |
| |
| Consequences of Failure to Exchange | | If we complete the exchange offer and you do not participate in it, then: |
| |
| | • your Old Notes will continue to be subject to the existing restrictions upon their transfer; |
| |
| | • we will have no further obligation to provide for the registration under the Securities Act of those Old Notes except under certain limited circumstances; and |
| |
| | • the liquidity of the market for your Old Notes could be adversely affected. |
| |
| Taxation | | The exchange pursuant to the exchange offer generally will not be a taxable event for U.S. federal income tax purposes. See “Certain U.S. Federal Income Tax Considerations” in this prospectus. |
| |
| Use of Proceeds | | We will not receive any cash proceeds from the issuance of the New Notes in this exchange offer. |
| |
| Exchange Agent and Information Agent | | The Bank of New York Mellon Trust Company, N.A. is the exchange agent and the information agent for the exchange offer. |
11
Summary of the New Notes
The summary below describes the principal terms of the notes. Certain of the terms and conditions described below are subject to important limitations and exceptions. The “Description of Notes” section of this offering memorandum contains a more detailed description of the terms and conditions of the notes.
| | |
| Issuer | | IASIS Healthcare LLC (the “Company”). |
| |
| Co-Issuer | | IASIS Capital Corporation, a Delaware corporation and a wholly-owned subsidiary of the Issuer (together with the Issuer, the “Issuers”). |
| |
| Notes Offered | | $850,000,000 aggregate principal amount of 8.375% senior notes due 2019. |
| |
| Maturity Date | | The New Notes will mature on May 15, 2019. |
| |
| Interest | | Interest on the notes will accrue at a rate of 8.375% per annum starting from May 3, 2011. Interest on the notes will be payable semi-annually in cash in arrears on May 15 and November 15 of each year, commencing November 15, 2011. |
| |
| Guarantees | | The New Notes will be unconditionally guaranteed on a senior unsecured basis by certain of our current and future domestic wholly-owned subsidiaries. Subsidiaries constituting a material portion of our assets and operations, including all of our non-wholly owned subsidiaries, will not guarantee the notes. Certain of these non-guarantor subsidiaries guarantee our obligations under our $1,325 million outstanding senior secured credit facilities (the “Senior Secured Credit Facilities”). In addition, certain of these subsidiaries will be restricted subsidiaries and consequently we will have the ability to make additional investments in them. See “Description of Notes—Subsidiary Guarantees.” |
| |
| | Our non-guarantor subsidiaries accounted for approximately $1,507 million, or 72.8% of our consolidated net revenue for the nine months ended June 30, 2011, and approximately $2,101 million, or 78.2% of our consolidated total assets as of June 30, 2011. All our consolidated Adjusted EBITDA comes from the non-guarantor subsidiaries. However, our guarantor subsidiaries hold unsubordinated promissory notes from the non-guarantor subsidiaries aggregating $665 million in principal amount as of June 30, 2011, under which the guarantor subsidiaries are entitled to principal and interest payments of $71 million annually. In addition, the non-guarantor subsidiaries are contractually obligated to pay the guarantor subsidiaries management fees. The management fee amount ranges from 2.0% to 2.5% of net revenue for the non-guarantor subsidiaries. For the nine months ended June 30, 2011, the non-guarantor subsidiaries paid $20 million in management fees. |
12
| | |
| Ranking | | The New Notes and the guarantees will be general senior obligations of the Issuers and each guarantor and will: |
| | rank equally in right of payment to all our and each guarantor’s existing and future senior unsecured debt; |
| |
| | • rank senior in right of payment to our and each guarantor’s future debt that is expressly subordinated in right of payment to the notes and the guarantees; |
| |
| | • be effectively subordinated to our and each guarantor’s secured indebtedness, including indebtedness under the Senior Secured Credit Facilities, to the extent of the value of the collateral securing such indebtedness; and |
| |
| | • be structurally subordinate to the claims of creditors of the non-guarantor subsidiaries, including trade creditors, which will have to be satisfied before any of the assets of such subsidiaries would be available for distribution, upon a liquidation or otherwise, to us or a guarantor of the notes. |
| |
| | As of June 30, 2011, we have approximately $1,022 million of secured indebtedness outstanding under our Senior Secured Credit Facilities and an additional $300 million of borrowing capacity under the revolving portion of our Senior Secured Credit Facilities (before consideration of outstanding letters of credit totaling $85 million under the revolving portion of our Senior Secured Credit Facilities). |
| |
| Form and Denomination | | The New Notes will be issued in fully-registered form. The New Notes will be represented by one or more global notes, deposited with the trustee as custodian for DTC and registered in the name of Cede & Co., DTC’s nominee. Beneficial interests in the global notes will be shown on, and any transfers will be effective only through, records maintained by DTC and its participants. |
| |
| | The New Notes will be issued in minimum denominations of $2,000 and integral multiples of $1,000 in excess thereof. |
| |
| Optional Redemption | | We may redeem the New Notes, in whole or in part, at any time prior to May 15, 2014, at a price equal to 100% of the aggregate principal amount of the notes plus a “make-whole” premium and accrued and unpaid interest and special interest, if any, to but excluding the redemption date. We may redeem the New Notes, in whole or in part, at any time on or after May 15, 2014, at the redemption prices specified in “Description of Notes—Optional Redemption,” plus accrued and unpaid interest and special interest, if any, to but excluding the redemption date. In addition, we may redeem up to 35% of the New Notes before May 15, 2014, with the net cash proceeds from certain equity offerings at a |
13
| | |
| | redemption price equal to 108.375% of the aggregate principal amount of the New Notes plus accrued and unpaid interest and special interest, if any, to but excluding the redemption date if at least 65% of the aggregate principal amount of New Notes originally issued under the indenture remains outstanding after the redemption. See “Description of Notes—Optional Redemption.” |
| |
| Change of Control | | If we experience certain kinds of changes of control, we must offer to purchase the New Notes at 101% of their principal amount, plus accrued and unpaid interest and special interest, if any, to but excluding the repurchase date. For more details, see “Description of Notes — Repurchase at the Option of Holders — Change of Control.” |
| |
| Specified Change of Control | | Under certain circumstances, we will have the ability to make certain payments to facilitate a change of control transaction and to provide for the assumption of the New Notes by a new parent company resulting from such change of control transaction. See provisions relating to “Specified Change of Control” under “Description of Notes.” |
| |
| Certain Covenants | | The indenture will contain covenants that limit, among other things, our ability and the ability of our restricted subsidiaries to: • incur additional indebtedness or issue disqualified stock or preferred stock; • pay dividends or make other distributions on, redeem or repurchase our capital stock; • sell certain assets; • make certain loans and investments; • enter into certain transactions with affiliates; • incur liens on certain assets to secure debt; • impose restrictions on the ability of a subsidiary to pay dividends or make payments or distributions to us and our restricted subsidiaries; and • consolidate, merge or sell all or substantially all of our assets. These covenants are subject to important exceptions, limitations and qualifications. These covenants may not apply at any time after the New Notes achieve an investment grade rating. For more details, see “Description of Notes—Certain Covenants.” |
| |
| No Public Market | | The New Notes are a new issue of securities and will not be listed on any national securities exchange or included in any automated dealer quotation system. There is currently no established trading market for the New Notes and accordingly, there can be no assurance as to the development or liquidity of any market for the New Notes. |
14
| | |
| Governing Law | | The New Notes are governed by, and construed in accordance with, the internal laws of the State of New York. |
| |
| Book-Entry Depository | | The Depository Trust Company. |
| |
| Trustee | | The Bank of New York Mellon Trust Company, National Association. |
You should refer to the section entitled “Risk Factors” before investing in the New Notes.
15
Summary Consolidated Financial And Operating Data
The following tables set forth certain summary historical consolidated financial and operating data for the fiscal years ended September 30, 2008, 2009 and 2010, and the nine months ended June 30, 2010 and 2011. Our summary historical consolidated financial data for the fiscal years ended September 30, 2008, 2009 and 2010, was derived from our audited consolidated financial statements for each fiscal year presented, which is included elsewhere in this prospectus. The summary historical consolidated financial data for the nine months ended June 30, 2010 and 2011, was derived from our unaudited condensed consolidated financial statements and the notes thereto included elsewhere in this prospectus, which have been prepared on a basis consistent with our audited consolidated financial statements. Results of operations for interim periods are not necessarily indicative of the results that might be expected for any other interim period or for an entire year. Our historical results are not indicative of our future performance. The summary financial data presented below represent portions of our financial statements and are not complete. You should read this information in conjunction with “Selected Consolidated Financial and Other Data,” “Management’s Discussion and Analysis of Financial Condition and Results of Operations” and the annual consolidated and interim condensed consolidated financial statements and related notes included elsewhere in this prospectus.
Summary Financial Data
| | | | | | | | | | | | | | | | | | | | |
| | | Year Ended September 30, | | | Nine Months Ended | |
| | | | | | | | | | | | June 30, | |
| | | 2008 | | | 2009 | | | 2010 | | | 2010 | | | 2011 | |
| | | | | |
Statement of Operations Data (1): | | | | | | | | | | | | | | | | | | | | |
| | | | | |
Net revenue | | $ | 2,065,536 | | | $ | 2,361,972 | | | $ | 2,521,406 | | | $ | 1,891,467 | | | $ | 2,070,349 | |
| | | | | |
Costs and expenses: | | | | | | | | | | | | | | | | | | | | |
Salaries and benefits (2) | | | 632,109 | | | | 660,921 | | | | 686,303 | | | | 514,688 | | | | 597,063 | |
Supplies | | | 231,259 | | | | 250,573 | | | | 266,545 | | | | 200,167 | | | | 237,431 | |
Medical claims | | | 452,055 | | | | 592,760 | | | | 678,651 | | | | 510,692 | | | | 484,635 | |
Other operating expenses | | | 283,123 | | | | 325,735 | | | | 363,916 | | | | 266,854 | | | | 315,254 | |
Provision for bad debts | | | 161,936 | | | | 192,563 | | | | 197,680 | | | | 142,901 | | | | 175,100 | |
Rentals and leases | | | 36,633 | | | | 39,127 | | | | 39,955 | | | | 30,487 | | | | 34,229 | |
Interest expense, net | | | 75,665 | | | | 67,890 | | | | 66,810 | | | | 50,065 | | | | 60,984 | |
Depreciation and amortization | | | 96,741 | | | | 97,462 | | | | 96,106 | | | | 71,909 | | | | 74,942 | |
Management fees | | | 5,000 | | | | 5,000 | | | | 5,000 | | | | 3,750 | | | | 3,750 | |
Loss on extinguishment of debt | | | — | | | | — | | | | — | | | | — | | | | 23,075 | |
Impairment of goodwill (3) | | | — | | | | 64,639 | | | | — | | | | — | | | | — | |
Hurricane-related property damage (4) | | | 3,589 | | | | 938 | | | | — | | | | — | | | | — | |
| | | | | | | | | | | | | | | | | | | | |
Total costs and expenses | | | 1,978,110 | | | | 2,297,608 | | | | 2,400,966 | | | | 1,791,513 | | | | 2,006,463 | |
| | | | | | | | | | | | | | | | | | | | |
16
| | | | | | | | | | | | | | | | | | | | |
Earnings from continuing operations before gain (loss) on disposal of assets and income taxes | | | 87,426 | | | | 64,364 | | | | 120,440 | | | | 99,954 | | | | 63,886 | |
Gain (loss) on disposal of assets, net | | | (75 | ) | | | 1,465 | | | | 108 | | | | (206 | ) | | | 771 | |
Earnings from continuing operations before income taxes | | | 87,351 | | | | 65,829 | | | | 120,548 | | | | 99,748 | | | | 64,657 | |
Income tax expense | | | 35,325 | | | | 27,576 | | | | 44,715 | | | | 36,544 | | | | 24,078 | |
| | | | | | | | | | | | | | | | | | | | |
Net earnings from continuing operations | | | 52,026 | | | | 38,253 | | | | 75,833 | | | | 63,204 | | | | 40,579 | |
Earnings (loss) from discontinued operations, net of income taxes | | | (11,275 | ) | | | (176 | ) | | | (1,087 | ) | | | (363 | ) | | | (6,069 | ) |
| | | | | | | | | | | | | | | | | | | | |
Net earnings | | | 40,751 | | | | 38,077 | | | | 74,746 | | | | 62,841 | | | | 34,510 | |
Net earnings attributable to non-controlling interests | | | (4,437 | ) | | | (9,987 | ) | | | (8,279 | ) | | | (6,063 | ) | | | (6,201 | ) |
| | | | | | | | | | | | | | | | | | | | |
Net earnings attributable to IASIS Healthcare LLC | | $ | 36,314 | | | $ | 28,090 | | | $ | 66,467 | | | $ | 56,778 | | | $ | 28,309 | |
| | | | | | | | | | | | | | | | | | | | |
Balance Sheet and Other Financial Data (at end of period): | | | | | | | | | | | | | | | | | | | | |
Adjusted EBITDA | | $ | 264,832 | | | $ | 299,916 | | | $ | 290,843 | | | $ | 228,045 | | | $ | 228,001 | |
Cash and cash equivalents | | $ | 80,738 | | | $ | 206,528 | | | $ | 144,511 | | | $ | 130,160 | | | $ | 144,595 | |
| | | | | |
Total assets | | $ | 2,308,147 | | | $ | 2,357,204 | | | $ | 2,353,194 | | | $ | 2,299,461 | | | $ | 2,686,800 | |
| | | | | |
Long-term debt and capital lease obligations (including current portion) | | $ | 1,114,622 | | | $ | 1,059,837 | | | $ | 1,051,578 | | | $ | 1,053,185 | | | $ | 1,881,433 | |
Member’s equity | | $ | 714,507 | | | $ | 750,932 | | | $ | 702,135 | | | $ | 688,576 | | | $ | 115,342 | |
| (1) | Excludes Mesa General Hospital and Biltmore Surgery Center, where operations were discontinued effective May 31, 2008 and April 30, 2008, respectively. |
| (2) | Results for the year ended September 30, 2010, include $2 million in stock compensation expense related to the repurchase of certain equity by IAS. |
| (3) | Results for the year ended September 30, 2009, include a $64.6 million non-cash charge ($43.2 million after taxes) related to the impairment of goodwill in our Florida market. |
| (4) | Results for the years ended September 30, 2008 and 2009, included an adverse financial impact totaling $3.6 million and $938,000, respectively, before income taxes related to property damage sustained at The Medical Center of Southeast Texas, as a result of Hurricane Ike. |
17
Summary Operating Data
The following tables set forth certain unaudited operating data for each of the periods presented.
| | | | | | | | | | | | | | | | | | | | |
| | | Year Ended September 30, | | | Nine Months Ended | |
| | | | | | | | | | | | June 30, | |
| | | 2008 | | | 2009 | | | 2010 | | | 2010 | | | 2011 | |
| | | | | |
Acute Care (1): | | | | | | | | | | | | | | | | | | | | |
Number of acute care hospital facilities at end of period (2) | | | 15 | | | | 15 | | | | 15 | | | | 15 | | | | 18 | |
Licensed beds at end of period | | | 3,027 | | | | 3,162 | | | | 3,185 | | | | 3,185 | | | | 4,362 | |
Average length of stay (days) (3) | | | 4.7 | | | | 4.7 | | | | 4.8 | | | | 4.8 | | | | 4.9 | |
Occupancy rates (average beds in service) | | | 48.9 | % | | | 46.5 | % | | | 46.6 | % | | | 46.9 | % | | | 48.5 | % |
Admissions (4) | | | 101,302 | | | | 101,083 | | | | 101,798 | | | | 76,679 | | | | 84,469 | |
Adjusted admissions (5) | | | 165,819 | | | | 169,721 | | | | 170,812 | | | | 127,654 | | | | 144,066 | |
Patient days (6) | | | 471,853 | | | | 473,601 | | | | 489,274 | | | | 369,402 | | | | 416,365 | |
Adjusted patient days (5) | | | 741,466 | | | | 762,234 | | | | 790,958 | | | | 593,277 | | | | 682,948 | |
Net patient revenue per adjusted admission | | $ | 9,101 | | | $ | 9,703 | | | $ | 10,066 | | | $ | 10,118 | | | $ | 10,258 | |
Outpatient revenue as a % of gross patient revenue | | | 36.9 | % | | | 39.0 | % | | | 39.6 | % | | | 39.1 | % | | | 40.5 | % |
Health Choice: | | | | | | | | | | | | | | | | | | | | |
Medicaid covered lives | | | 142,193 | | | | 187,104 | | | | 194,095 | | | | 195,183 | | | | 193,277 | |
Dual-eligible lives (7) | | | 3,300 | | | | 3,659 | | | | 4,298 | | | | 4,256 | | | | 4,271 | |
Medical loss ratio (8) | | | 85.2 | % | | | 86.1 | % | | | 87.2 | % | | | 87.8 | % | | | 84.9 | % |
| (1) | Excludes Mesa General Hospital and Biltmore Surgery Center, where operations were discontinued effective May 31, 2008 and April 30, 2008, respectively. |
| (2) | Excludes St. Luke’s Behavioral Health Hospital. |
| (3) | Represents the average number of days that a patient stayed in our hospitals. |
| (4) | Represents the total number of patients admitted to our hospitals for stays in excess of 23 hours. Management and investors use this number as a general measure of inpatient volume. |
| (5) | Adjusted admissions and adjusted patient days are general measures of combined inpatient and outpatient volume. We compute adjusted admissions/patient days by multiplying admissions/patient days by gross patient revenue and then dividing that number by gross inpatient revenue. |
| (6) | Represents the number of days our beds were occupied by inpatients over the period. |
| (7) | Represents members eligible for Medicare and Medicaid benefits under Health Choice’s contract with the Centers for Medicare and Medicaid Services (“CMS”) to provide coverage as a Medicare Advantage Prescription Drug (“MAPD”) Special Needs Plan (“SNP”). |
| (8) | Represents medical claims expense as a percentage of premium revenue, including claims paid to our hospitals. |
18
| | | | | | | | | | | | | | | | | | | | |
| | | Fiscal Year Ended September 30, | | | Nine Months Ended
June 30, | |
| | | | | | | | | | | |
| | | 2008 | | | 2009 | | | 2010 | | | 2010 | | | 2011 | |
Adjusted EBITDA: | | | | | | | | | | | | | | | | | | | | |
Net earnings from continuing operations | | $ | 52,026 | | | $ | 38,253 | | | $ | 75,833 | | | $ | 63,204 | | | $ | 40,579 | |
Add: | | | | | | | | | | | | | | | | | | | | |
Interest expense, net | | | 75,665 | | | | 67,890 | | | | 66,810 | | | | 50,065 | | | | 60,984 | |
Income tax expense | | | 35,325 | | | | 27,576 | | | | 44,715 | | | | 36,544 | | | | 24,078 | |
Depreciation and amortization | | | 96,741 | | | | 97,462 | | | | 96,106 | | | | 71,909 | | | | 74,942 | |
| | | | | | | | | | | | | | | | | | | | |
EBITDA | | $ | 259,757 | | | $ | 231,181 | | | $ | 283,464 | | | $ | 221,722 | | | $ | 200,583 | |
Impairment of goodwill | | | — | | | | 64,639 | | | | — | | | | — | | | | — | |
Management fees | | | 5,000 | | | | 5,000 | | | | 5,000 | | | | 3,750 | | | | 3,750 | |
Loss (gain) on disposal of assets, net | | | 75 | | | | (1,465 | ) | | | (108 | ) | | | 206 | | | | (771 | ) |
Stock-based compensation | | | — | | | | 561 | | | | 2,487 | | | | 2,367 | | | | 1,364 | |
Loss on extinguishment of debt | | | — | | | | — | | | | — | | | | — | | | | 23,075 | |
| | | | | | | | | | | | | | | | | | | | |
Adjusted EBITDA | | $ | 264,832 | | | $ | 299,916 | | | $ | 290,843 | | | $ | 228,045 | | | $ | 228,001 | |
| | | | | | | | | | | | | | | | | | | | |
We have included discussion of Adjusted EBITDA, a non-GAAP financial measure, in this prospectus. Adjusted EBITDA represents net earnings from continuing operations before interest expense (net of interest income), income taxes, depreciation and amortization, management fees, loss (gain) on disposal of assets, as well as certain unusual or non-recurring items and other adjustments, such as stock-based compensation. We believe that the inclusion of certain adjustments in presenting Adjusted EBITDA are appropriate to provide additional information to investors about certain material non-cash items and about unusual or non-recurring items that we do not expect to continue in the future. We believe that the presentation of Adjusted EBITDA enhances an investor’s understanding of our financial performance. We believe that Adjusted EBITDA is a useful financial metric to assess our operating performance from period to period by excluding certain items that we believe are not representative of our core business. We believe that Adjusted EBITDA will provide investors with a useful tool for assessing the comparability between periods of our ability to generate cash from operations sufficient to pay taxes, to service debt and to undertake capital expenditures. We use Adjusted EBITDA for business planning purposes and in measuring our performance relative to that of our competitors.
The term Adjusted EBITDA is not defined under GAAP (generally accepted accounting principles in the United States), and is not a measure of net income, operating income or any other performance measure derived in accordance with GAAP, and is subject to important limitations. Our use of the term Adjusted EBITDA varies from others in our industry. For additional information regarding our use of Adjusted EBITDA, see “Selected Consolidated Financial and Other Data.” Adjusted EBITDA should not be considered as an alternative to net income, operating income or any other performance measures derived in accordance with GAAP as measures of operating performance or to operating cash flows as measures of liquidity.
Adjusted EBITDA has important limitations as an analytical tool and you should not consider it in isolation or as a substitute for analysis of our results as reported under GAAP. For example, Adjusted EBITDA, among other things:
| | • | | excludes certain tax payments that may represent a reduction in cash available to us; |
| | • | | does not reflect any cash capital expenditure requirements for the assets being depreciated and amortized that may have to be replaced in the future; |
| | • | | does not reflect changes in, or cash requirements for, our working capital needs; and |
| | • | | does not reflect the significant interest expense, or the cash requirements necessary to service interest or principal payments, on our debt. |
Adjusted EBITDA includes additional adjustments and exclusions, and should be read in conjunction with the explanations and reconciliations set forth in “Selected Consolidated Financial and Other Data.”
19
RISK FACTORS
Investing in the New Notes involves risk. You should consider carefully the risks and uncertainties described below, together with all of the other information in this prospectus, including the financial statements and the related notes included in this prospectus, before deciding to participate in the exchange offer and to invest in the New Notes. Any of the following risks could materially adversely affect our business, financial condition or results of operations. In such case, you may lose all or part of your original investment in the New Notes.
Risk Factors Relating to Our Business
If We Are Unable To Retain And Negotiate Reasonable Contracts With Managed Care Plans, Our Net Revenue May Be Reduced.
Our ability to obtain reasonable contracts with health maintenance organizations, preferred provider organizations and other managed care plans significantly affects the revenue and operating results of our hospitals. Revenue derived from health maintenance organizations, preferred provider organizations and other managed care plans accounted for 39.8%, 40.2%, 43.0% and 46.0% of our hospitals’ net patient revenue for the nine months ended June 30, 2011, and the years ended September 30, 2010, 2009 and 2008, respectively. Our hospitals have over 400 managed care contracts with no one commercial payor representing more than 10.0% of our net patient revenue. In most cases, we negotiate our managed care contracts annually as they come up for renewal at various times during the year. Further, many of these contracts are terminable by either party on relatively short notice. Our future success will depend, in part, on our ability to retain and renew our managed care contracts and enter into new managed care contracts on terms favorable to us. Other healthcare providers, including some with integrated health systems, provider networks, greater geographic coverage or a wider range of services, may impact our ability to enter into managed care contracts or negotiate increases in our reimbursement and other favorable terms and conditions. For example, some of our competitors may negotiate exclusivity provisions with managed care plans or otherwise restrict the ability of managed care companies to contract with us. In one region in which we operate, the largest healthcare provider organization controls one of the largest payor organizations and operates it primarily as a closed network. The patients enrolled in this integrated health system are largely unavailable to us. In addition, consolidation among managed care companies may reduce our ability to negotiate favorable contracts with such payors. It is not clear what impact, if any, the increased obligations on managed care and other payors imposed by the recently enacted Health Reform Law will have on our ability to negotiate reimbursement increases. If we are unable to retain and negotiate favorable contracts with managed care plans or experience reductions in payment increases or amounts received from nongovernmental payors, our revenues may be reduced.
We Are Unable to Predict The Impact Of The Health Reform Law, Which Represents Significant Change To The Healthcare Industry.
The Health Reform Law represents significant change across the healthcare industry. As enacted, the Health Reform Law will decrease the number of uninsured individuals by expanding coverage to additional individuals through a combination of public program expansion and private sector health insurance reforms. The Health Reform Law expands eligibility under existing Medicaid programs and subsidizes states that create non-Medicaid plans for certain residents that do not qualify for Medicaid. Further, the Health Reform Law requires states to establish health insurance exchanges to facilitate the purchase of health insurance by individuals and small businesses. It imposes financial penalties on individuals who fail to carry insurance coverage and certain employers that do not provide health insurance coverage. The Health Reform Law also establishes a number of health insurance market reforms, including a ban on lifetime limits and pre-existing condition exclusions, new benefit mandates, and increased dependent coverage. Although the expansion of health insurance coverage should increase revenues from providing care to certain previously uninsured individuals, many of these provisions of the Health Reform Law will not become effective until 2014 or later.
Numerous lawsuits have challenged the constitutionality of the Health Reform Law, and in particular the requirement for individuals to carry health insurance. Some federal courts have upheld the constitutionality of the Health Reform Law or dismissed cases on procedural grounds. Others have held unconstitutional the requirement that individuals maintain health insurance or pay a penalty and have either found the Health Reform Law void in its entirety or left the remainder of the law intact. Federal appellate courts are split on the constitutionality of the Health Reform Law, and it is anticipated that the issue will ultimately be decided by the Supreme Court.
20
The Health Reform Law could adversely affect our business and results of operations due to provisions of the Health Reform Law that are intended to reduce Medicare and Medicaid healthcare costs. Among other things, the Health Reform Law will reduce market basket updates, reduce Medicare and Medicaid DSH funding, and expand efforts to tie payments to quality and integration. Any decrease in payment rates or an increase in rates that is below our increase in costs may adversely affect our results of operations. The Health Reform Law also provides additional resources to combat fraud, waste, and abuse, including expansion of the Recovery Audit Contractor (“RAC”) program, which may result in increased costs for us to appeal or refund any alleged overpayments.
The Health Reform Law contains additional provisions intended to promote value-based purchasing. Effective July 1, 2011, the Health Reform Law prohibits the use of federal funds under the Medicaid program to reimburse providers for medical assistance provided to treat certain preventable adverse events, also known as hospital-acquired conditions (“HACs”). Further, effective in federal fiscal year 2013, hospitals with excessive readmissions for conditions designated by the U.S. Department of Health and Human Services (the “Department”) will receive reduced payments for all inpatient discharges, not just discharges relating to the conditions subject to the excessive readmission standard. Beginning in federal fiscal year 2015, hospitals that fall into the highest 25% of national risk-adjusted HAC rates for all hospitals in the previous year will receive a 1% reduction in their total Medicare payments. The Health Reform Law also requires the Department to implement a value-based purchasing system for hospitals that will provide incentive payments to hospitals that meet or exceed certain quality performance standards and that will be funded through decreases in the inpatient prospective payment system market basket updates to all hospitals beginning in federal fiscal year 2013.
As enacted, the Health Reform Law will change how healthcare services are covered, delivered, and reimbursed. Because of the many variables involved, we are unable to predict the net effect on our operations of the expected increases in insured individuals using our facilities, the reductions in government healthcare spending, and numerous other provisions in the Health Reform Law that may affect us. Furthermore, we are unable to predict how providers, payors, and other market participants will respond to the various reform provisions, many of which will not be implemented for several years. Legislative efforts may delay implementation of, repeal or amend the Health Reform Law. On January 19, 2011, the U.S. House of Representatives voted to repeal the Health Reform Law, but the U.S. Senate rejected this proposal. There may also be efforts to repeal specific provisions of the law. In addition, implementation of these provisions could be delayed or even blocked due to court challenges. Federal courts have issued conflicting rulings on the constitutionality of the Health Reform Law, in particular the requirement that individuals must have health insurance. Several federal appeals courts have granted expedited review of these cases. It is unclear how federal lawsuits challenging the constitutionality of the Health Reform Law will be resolved or what the impact will be of any resulting changes to the law.
Changes In Governmental Healthcare Programs May Reduce Our Revenues.
Governmental healthcare programs, principally Medicare and Medicaid, including managed Medicare and managed Medicaid, accounted for 47.5%, 47.6%, 45.9% and 44.9% of our hospitals’ net patient revenue for the nine months ended June 30, 2011, and the years ended September 30, 2010, 2009 and 2008, respectively. However, in recent years legislative and regulatory changes have limited, and in some cases reduced, the levels of payments that our hospitals receive for various services under the Medicare, Medicaid and other federal healthcare programs. The recently enacted Budget Control Act of 2011 (the “BCA”) provides for approximately $900 billion in deficit reduction, which is achieved by applying caps to federal discretionary spending, but not including Medicare and Medicaid programs. However, the BCA also provides for new spending on program integrity initiatives intended to reduce fraud and abuse under the Medicare program. Further, pursuant to the BCA, a bipartisan joint congressional committee has been created to identify at least $1.5 trillion in additional deficit reductions over ten years, and it is expected to consider entitlement program reforms including Medicare. If Congress does not enact deficit reductions greater than $1.2 trillion by January 15, 2012, the BCA requires automatic spending reductions of $1.2 trillion for federal fiscal years 2013 through 2021, minus any deficit reductions enacted by Congress and debt service costs. However, the percentage reduction for Medicare may not be more than 2% for a fiscal year, with a uniform percentage reduction across all Medicare programs. We are unable to predict how these spending reductions will be structured, or what other deficit reduction initiatives could be proposed by Congress.
21
The reductions required by the BCA are in addition to reductions that may be imposed by CMS and reductions mandated by the Health Reform Law. For example, CMS has completed its transition to the Medicare severity diagnosis-related group (“MS-DRG”) system, which represents a refinement to the pre-existing diagnosis-related group system. Future changes to the MS-DRG system could impact the margins we receive for certain services. Further, the Health Reform Law provides for material reductions in the growth of Medicare program spending, including reductions in Medicare market basket updates and Medicare DSH funding. CMS has issued a final rule that provides for a 1% increase in Medicare payments for inpatient hospital services in federal fiscal year 2012 compared to federal fiscal year 2011, after accounting for reductions required by the Health Reform Law and implementation of the MS-DRG system.
In some cases, commercial third-party payors and other payors, such as some state Medicaid programs, rely on all or portions of the Medicare MS-DRG system to determine payment rates, and therefore, adjustments that negatively impact Medicare payments may also negatively impact payments from Medicaid programs or commercial third-party payors and other payors.
In addition, from time to time, state legislatures consider measures to reform healthcare programs and coverage within their respective states. Because of economic conditions and other factors, a number of states are experiencing budget problems and have adopted or are considering legislation designed to reduce their Medicaid expenditures, including enrolling Medicaid recipients in managed care programs, reducing the number of Medicaid beneficiaries by implementing more stringent eligibility requirements and imposing additional taxes on hospitals to help finance or expand states’ Medicaid systems. The states in which we operate have decreased funding for healthcare programs or made other structural changes resulting in a reduction in Medicaid hospital rates in recent years. Additional Medicaid spending cuts may be implemented in the future in the states in which we operate, including reductions in supplemental Medicaid reimbursement programs. Our Texas hospitals participate in private supplemental Medicaid reimbursement programs that are structured to expand the community safety net by providing indigent healthcare services and result in additional revenues for participating hospitals. We cannot predict whether the Texas private supplemental Medicaid reimbursement programs will continue or guarantee that revenues recognized from the programs will not decrease. The Health Reform Law provides for significant expansion of the Medicaid program, but these changes are not required until 2014.
We believe that hospital operating margins across the country, including ours, have been and may continue to be under pressure because of limited pricing flexibility and growth in operating expenses in excess of the increase in payments under the Medicare and other governmental programs. Current or future healthcare reform efforts, additional changes in laws or regulations regarding government health programs, changes to structure and reimbursement rates of governmental health programs or other changes in the administration of government health programs could have a material, adverse effect on our financial position and results of operations.
Our Hospitals Face Competition For Patients From Other Hospitals And Healthcare Providers That Could Impact Patient Volume.
In general, the hospital industry is highly competitive. Our hospitals face competition for patients from other hospitals in our markets, large vertically integrated providers, large tertiary care centers and outpatient service providers that provide similar services to those provided by our hospitals. All of our facilities are located in geographic areas in which at least one other hospital provides services comparable to those offered by our hospitals. Some of the hospitals that compete with ours are owned by governmental agencies or not-for-profit corporations supported by endowments and charitable contributions and can finance capital expenditures and operations on a tax-exempt basis. In addition, the number of freestanding specialty hospitals, outpatient surgery centers and outpatient diagnostic centers has increased significantly in the areas in which we operate. Some of our competitors also have greater geographic coverage, offer a wider range of services or invest more capital or other resources than we do. If our competitors are able to achieve greater geographic coverage, improve access and convenience to physicians and patients, recruit physicians to provide competing services at their facilities, expand or improve their services or obtain more favorable managed care contracts, we may experience a decline in patient volume.
22
CMS publicizes performance data relating to quality measures that hospitals submit in connection with their Medicare reimbursement. Further, the Health Reform Law requires all hospitals annually to establish, update and make public a list of their standard charges for items and services. If any of our hospitals should achieve poor results (or results that are lower than our competitors) on these quality criteria, or if our standard charges are higher than those published by our competitors, our patient volumes could decline. In the future, other trends toward clinical transparency and value-based purchasing of healthcare services may have an adverse impact on our competitive position and patient volume.
If We Continue To Experience A Shift in Payor Mix From Commercial And Managed Care Payors To Self-Pay and Medicaid, Our Revenue and Results Of Operations Could Be Adversely Affected.
We have experienced a shift in our patient volumes and revenue from commercial and managed care payors to self-pay and Medicaid, including managed Medicaid. This has resulted in pressure on pricing and operating margins from expending the same amount of resources to provide patient care, but for less reimbursement. This shift is reflective of continued high unemployment and the resulting increases in states’ Medicaid rolls and the uninsured population. We believe the decline in managed care volume and revenue mix is not only indicative of the depressed labor market, but also utilization behavior of the insured population resulting from higher deductible and co-insurance plans implemented by employers, which, in turn, has resulted in the deferral of elective and non-emergent procedures. Given the high rate of unemployment and its impact on the economy, particularly in the markets we serve, we expect the increase in our self-pay and Medicaid payor mixes to continue until the U.S. economy experiences an economic recovery that includes job growth and a meaningful decline in unemployment.
If We Experience Further Growth In Volume And Revenue Related To Uncompensated Care, Our Financial Condition Or Results Of Operations Could Be Adversely Affected.
Like others in the hospital industry, we continue to experience high levels of uncompensated care, including charity care and bad debts. These elevated levels are driven by the number of uninsured and under-insured patients seeking care at our hospitals, the increased acuity levels at which these patients are presenting for treatment, primarily resulting from economic pressures and their related decisions to defer care, increasing healthcare costs and other factors beyond our control, such as increases in the amount of co-payments and deductibles as employers continue to pass more of these costs on to their employees. In addition, as a result of high unemployment and its continued impact on the economy, we believe that our hospitals may continue to experience high levels of or possibly growth in bad debts and charity care.
While the Health Reform Law seeks to decrease over time the number of uninsured individuals through expanding Medicaid and incentivizing employers to offer, and requiring individuals to carry, health insurance or be subject to penalties, these provisions, as enacted, generally will not become effective until January 1, 2014. Further, numerous lawsuits have challenged the constitutionality of the Health Reform Law, and in particular the requirement for individuals to carry health insurance. Federal appellate courts are split on the constitutionality of the Health Reform Law and implementation of the MS-DRG system. It is difficult to predict the full impact of the Health Reform Law due to the law’s complexity, lack of implementing regulations or interpretive guidance, gradual and potentially delayed implementation, pending court challenges and possible amendment or repeal, as well as our inability to foresee how individuals and businesses will respond to the choices afforded them under the law. We may continue to provide charity care to those who choose not to comply with the insurance requirements and undocumented aliens who are not permitted to enroll in a health insurance exchange or government healthcare programs.
Although we continue to seek ways of improving point of service collection efforts and implementing appropriate payment plans with our patients, if we continue to experience further growth in self-pay volume and revenue, including increased acuity levels and continued increases in co-payments and deductibles for insured patients, our results of operations could be adversely affected. Further, our ability to improve collections from self-pay patients may be limited by regulatory and investigatory initiatives, including private lawsuits directed at hospital charges and collection practices for uninsured and underinsured patients.
23
If We Are Unable To Attract And Retain Quality Medical Staffs, Our Financial Condition Or Results Of Operations Could Be Adversely Affected.
The success of our hospitals depends on the following factors, among others:
| | • | | the number and quality of the physicians on the medical staffs of our hospitals; |
| | • | | the admitting practices of those physicians; and |
| | • | | our maintenance of good relations with those physicians. |
Our efforts to attract and retain physicians are affected by our managed care contracting relationships, national shortages in some specialties, such as anesthesiology and radiology, the adequacy of our support personnel, the condition of our facilities and medical equipment, the availability of suitable medical office space and federal and state laws and regulations prohibiting financial relationships that may have the effect of inducing patient referrals.
In an effort to meet community needs in certain markets in which we operate, we have implemented a strategy to employ physicians, which has created an expansion of our employed physician base. The execution of a physician employment strategy includes increased salary costs, potential malpractice insurance coverage costs, risks of unsuccessful physician integration and difficulties associated with physician practice management. While we believe this strategy is consistent with industry trends, we cannot be assured of the long-term success of such a strategy.
Our Hospitals Face Competition For Staffing, Which May Increase Our Labor Costs And Reduce Profitability.
We compete with other healthcare providers in recruiting and retaining qualified management and staff personnel responsible for the day-to-day operations of each of our hospitals, including nurses and other non-physician healthcare professionals. In the past, the limited supply of nurses and other medical support personnel presented a significant operating issue. In part, due to the current economic environment, we have seen an improvement in the availability of nursing personnel and other skilled labor. If such a shortage were to occur again, it may require us to enhance wages and benefits to recruit and retain nurses and other medical support personnel and contract with more expensive temporary personnel. We also depend on the available labor pool of semi-skilled and unskilled employees in each of the markets in which we operate. Because a significant percentage of our revenue consists of fixed, prospective payments, our ability to pass along increased labor costs to third-party payors is constrained. Our failure to recruit and retain qualified management, nurses and other medical support personnel, or to control our labor costs could have a material adverse effect on our financial condition or results of operations.
If We Fail To Continually Enhance Our Hospitals With The Most Recent Technological Advances In Diagnostic And Surgical Equipment, Our Ability To Maintain And Expand Our Markets May Be Adversely Affected.
Technological advances with respect to computed axial tomography (“CT”), magnetic resonance imaging (“MRI”) and positron emission tomography (“PET”) equipment, as well as other equipment used in our facilities, are continually evolving. In an effort to compete with other healthcare providers, we must constantly evaluate our equipment needs and upgrade equipment as a result of technological improvements. If we fail to remain current with the technological advancements of the medical community, our volumes and revenue may be negatively impacted.
If We Fail To Comply With Extensive Laws And Government Regulations, We Could Suffer Penalties, Be Required To Alter Arrangements With Investors In Our Hospitals Or Be Required To Make Significant Changes To Our Operations.
The healthcare industry, including our company, is required to comply with extensive and complex laws and regulations at the federal, state and local government levels relating to, among other things:
| | • | | billing and coding for services and proper handling of overpayments; |
24
| | • | | classification of level of care provided, including proper classification of inpatient admissions, observation status and outpatient care; |
| | • | | relationships with physicians and other referral sources; |
| | • | | necessity and adequacy of medical care; |
| | • | | quality of medical equipment and services; |
| | • | | qualifications of medical and support personnel; |
| | • | | confidentiality, maintenance, data breach, identity theft and security issues associated with health related and personal information and medical records; |
| | • | | screening, stabilization and transfer of individuals who have emergency medical conditions; |
| | • | | licensure and certification; |
| | • | | hospital rate or budget review; |
| | • | | preparation and filing of cost reports; |
| | • | | activities regarding competitors; |
| | • | | operating policies and procedures; |
| | • | | addition of facilities and services; |
| | • | | provider-based reimbursement, including complying with requirements allowing multiple locations of a hospital to be billed under the hospital’s Medicare provider number; and |
| | • | | disclosures to patients, including disclosure of any physician ownership in a hospital. |
Because many of these laws and regulations are relatively new, we do not always have the benefit of significant regulatory or judicial interpretation of these laws and regulations. For that reason and because these laws and regulations are so complex, hospital companies face a risk of inadvertent violations. In the future, different interpretations or enforcement of these laws and regulations could subject our current or past practices to allegations of impropriety or illegality or could require us to make changes in our facilities, equipment, personnel, services, capital expenditure programs and operating expenses.
If we fail to comply with applicable laws and regulations, we could be subjected to liabilities, including:
| | • | | civil penalties, including the loss of our licenses to operate one or more of our facilities; and |
| | • | | exclusion of one or more of our facilities from participation in the Medicare, Medicaid and other federal and state healthcare programs. |
25
The Health Reform Law Imposes Significant New Restrictions On Hospitals That Have Physician Owners, Including Our Hospitals That Have Physician Owners.
Some of our hospitals have physician ownership pursuant to an exception to the “Stark Law” provision of the Social Security Act known as the “whole hospital exception.” However, the Health Reform Law significantly narrows the Stark Law’s whole hospital exception to apply only to hospitals that had physician ownership in place as of March 23, 2010, and a Medicare provider agreement effective as of December 31, 2010. On November 2, 2010, CMS issued a final rule implementing certain provisions of the amended whole hospital exception. While the amended whole hospital exception grandfathers certain existing physician-owned hospitals, including ours, it generally prohibits a grandfathered hospital from increasing its percentage of physician ownership beyond the aggregate level that was in place as of March 23, 2010. Further, subject to limited exceptions, a grandfathered physician-owned hospital may not increase its aggregate number of operating rooms, procedure rooms, and beds for which it is licensed beyond the number as of March 23, 2010.
The whole hospital exception, as amended, also contains additional disclosure requirements. For example, a grandfathered physician-owned hospital is required to submit an annual report to the Department listing each investor in the hospital, including all physician owners. In addition, grandfathered physician-owned hospitals must have procedures in place that require each referring physician owner to disclose to patients, with enough notice for the patient to make a meaningful decision regarding receipt of care, the physician’s ownership interest and, if applicable, any ownership interest held by the treating physician. A grandfathered physician-owned hospital also must disclose on its web site and in any public advertising the fact that it has physician ownership. The Health Reform Law requires grandfathered physician-owned hospitals to comply with these new requirements by September 23, 2011, and requires the Department to audit hospitals’ compliance beginning no later than May 1, 2012.
In light of the recently enacted restrictions on the whole hospital exception and limited interpretive guidance, it may be difficult for us to determine how the exception will apply to specific situations that may arise with our hospitals. If any of our hospitals fail to comply with the amended whole hospital exception, those hospitals could be found to be in violation of the Stark Law, and we could incur significant financial or other penalties.
Providers In The Healthcare Industry Have Been The Subject Of Federal And State Investigations, And We May Become Subject To Additional Investigations In The Future That Could Result In Significant Liabilities Or Penalties To Us.
Both federal and state government agencies have increased their focus on and coordination of civil and criminal enforcement efforts in the healthcare area. As a result, there are numerous ongoing investigations of hospital companies, as well as their executives and managers. The Office of Inspector General (“OIG”) and the U.S. Department of Justice (“DOJ”) have, from time to time, established national enforcement initiatives that focus on specific billing practices or other suspected areas of abuse. Further, under the federal False Claims Act (“FCA”), private parties have the right to bring “qui tam” whistleblower lawsuits against companies that submit false claims for payments to, or improperly retain overpayments from, the government. Some states have adopted similar state whistleblower and false claims provisions.
Federal and state investigations relate to a wide variety of routine healthcare operations including:
| | • | | cost reporting and billing practices; |
| | • | | financial arrangements with referral sources; |
| | • | | physician recruitment activities; |
| | • | | physician joint ventures; and |
| | • | | hospital charges and collection practices for self-pay patients. |
26
We engage in many of these and other activities that could be the subject of governmental investigations or inquiries from time to time. For example, we have significant Medicare and Medicaid billings, we have numerous financial arrangements with physicians who are referral sources to our hospitals and we have nine hospitals as of June 30, 2011, that have physician investors. In addition, our executives and managers, many of whom have worked at other healthcare companies that are or may become the subject of federal and state investigations and private litigation, may be included in governmental investigations or named as defendants in private litigation. Any additional investigations of us, our executives or our managers could result in significant liabilities or penalties to us, as well as adverse publicity.
In addition, governmental agencies and their agents, such as the Medicare Administrative Contractors, fiscal intermediaries and carriers, as well as the OIG, CMS and state Medicaid programs, conduct audits of our healthcare operations. Private payors may conduct similar audits, and we also perform internal audits and monitoring. Depending on the nature of the conduct found in such audits and whether the underlying conduct could be considered systemic, the resolution of these audits could have a material, adverse effect on our financial position, results of operations and liquidity.
CMS is implementing a nationwide RAC program as required by the Tax Relief and Health Care Act of 2006 and the Health Law Reform. Under the RAC program, CMS engages private contractors to conduct post-payment reviews to detect and correct improper payments in the Medicare program, and the contractors receive a contingency fee based on the amount of corrected, improper payments. The Health Reform Law expanded the RAC program’s scope to include other Medicare programs, including managed Medicare, effective December 31, 2010.
In addition, through the Deficit Reduction Act of 2005 (“DEFRA”), Congress has expanded the federal government’s involvement in fighting fraud, waste and abuse in the Medicaid program by creating the Medicaid Integrity Program. Under this program, CMS engages private contractors, referred to as MICs, to perform post-payment audits of Medicaid claims and identify overpayments. In addition, the Health Reform Law expanded the RAC program’s scope to include Medicaid claims, and a final rule released by CMS on September 14, 2011, requires states to implement Medicaid RAC programs by January 1, 2012. In addition to MICs and RACs, several other contractors and state Medicaid agencies have increased their review activities.
Any such audit or investigation could have a material adverse effect on the results of our operations.
We May Incur Material Fees, Costs And Expenses In Connection With the Qui Tam Action And Investigation of IAS.
On June 1, 2011, the United States District Court for the District of Arizona (the “District Court”) dismissed with prejudice the Third Amended Complaint filed by a qui tamrelator against IAS, our parent company, after thisqui tam action was remanded to the District Court by the Ninth Circuit. The qui tam action sought monetary damages and civil penalties under the FCA and included allegations that certain business practices related to physician relationships and the medical necessity of certain procedures resulted in the submission of claims for reimbursement in violation of the FCA. The case dates back to March 2005 and became the subject of a subpoena by the OIG in September 2005. In August 2007, the case was unsealed and the DOJ declined to intervene, and the action proceeded before the District Court. Thequi tam relator has filed a notice of appeal with respect to the dismissal with prejudice, and the appeal remains pending. If the qui tam appeal was to be resolved in a manner unfavorable to IAS, it could have a material adverse effect on our business, financial condition and results of operations, including exclusion from the Medicare and Medicaid programs. In addition, we may incur material fees, costs and expenses in connection with defending thequi tam action.
Compliance With Section 404 Of The Sarbanes-Oxley Act May Negatively Impact Our Results Of Operations And Failure To Comply May Subject The Company To Regulatory Scrutiny And A Loss Of Investors’ Confidence In Our Internal Control Over Financial Reporting.
We are required to perform an annual evaluation of our internal control over financial reporting and file management’s attestation with our annual report to comply with Section 404 of the Sarbanes-Oxley Act of 2002.
27
Compliance with all requirements and interpretive guidance associated with Section 404 of the Sarbanes-Oxley Act of 2002, and any changes in our internal control over financial reporting in response to our internal evaluations, may be expensive and time-consuming and may negatively impact our results of operations. In addition, we cannot assure you that we will be able to meet the annual required deadlines for compliance with Section 404. Any failure on our part to meet the required compliance deadlines may subject us to regulatory scrutiny and a loss of public confidence in our internal control over financial reporting.
A Failure Of Our Information Systems Would Adversely Affect Our Ability To Properly Manage Our Operations.
We rely on our advanced information systems and our ability to successfully use these systems in our operations. These systems are essential to the following areas of our business operations, among others:
| | • | | patient accounting, including billing and collection of net revenue; |
| | • | | financial, accounting, reporting and payroll; |
| | • | | laboratory, radiology and pharmacy systems; |
| | • | | materials and asset management; |
| | • | | negotiating, pricing and administering managed care contracts; and |
| | • | | monitoring quality of care and collecting data on quality measures necessary for full Medicare payment updates. |
If we are unable to use these systems effectively, we may experience delays in collection of net revenue and may not be able to properly manage our operations or oversee the compliance with laws or regulations.
If We Fail to Effectively and Timely Implement EHR Systems, Our Operations Could Be Adversely Affected.
As required by the American Recovery and Reinvestment Act of 2009 (“ARRA”), the Department has implemented an incentive payment program for eligible hospitals and healthcare professionals that adopt and meaningfully use certified EHR technology. If our hospitals and employed professionals are unable to meet the requirements for participation in the incentive payment program, we will not be eligible to receive incentive payments that could offset some of the costs of implementing EHR systems. Further, beginning in 2015, eligible hospitals and professionals that fail to demonstrate meaningful use of certified EHR technology will be subject to reduced payments from Medicare. Failure to implement EHR systems effectively and in a timely manner could have a material adverse effect on our financial position and results of operations.
Regional Economic Downturns Or Other Material Changes In The Economic Condition Could Cause Our Overall Business Results To Suffer.
The U.S. economy continues to experience the effects of a severe economic downturn. Depressed consumer spending and high unemployment rates continue to pressure many industries. During economic downturns, governmental entities often experience budgetary constraints as a result of increased costs and lower than expected tax collections. These budgetary constraints have resulted in decreased spending for health and human service programs, including Medicare, Medicaid and similar programs, which represent significant payor sources for our hospitals. Many states, including states in which we operate, have decreased funding for state healthcare programs or made other structural changes resulting in a reduction in Medicaid spending. Additional Medicaid spending cuts may be implemented in the future in the states in which we operate. Other risks we face from general economic weakness include patient decisions to postpone or cancel elective and non-emergent healthcare procedures, increases in the uninsured population and further difficulties in our collection of patient co-payment and deductible receivables.
28
Of our 18 acute care hospital facilities at June 30, 2011, four are located in Salt Lake City, three are located in Phoenix, three are located in Tampa-St. Petersburg, five are located in the state of Texas, one is located in Las Vegas, one is located in West Monroe, Louisiana and one is located in Woodland Park, Colorado. In addition, Health Choice and our behavioral health hospital facility are located in Phoenix. For the nine months ended June 30, 2011, our net revenue was generated as follows:
| | | | |
Health Choice | | | 28.1 | % |
Salt Lake City, Utah | | | 16.4 | % |
Phoenix, Arizona (excluding Health Choice) | | | 13.4 | % |
Five cities in Texas, including Houston and San Antonio | | | 23.5 | % |
Tampa-St. Petersburg, Florida | | | 8.3 | % |
Other | | | 10.3 | % |
Any material change in the current demographic, economic, competitive or regulatory conditions in any of these regions could adversely affect our overall business results because of the significance of our operations in each of these regions to our overall operating performance. Moreover, our business is not as diversified as some competing multi-facility healthcare companies and, therefore, is subject to greater market risks.
We May Be Subject To Liabilities Because Of Claims Brought Against Our Facilities.
Plaintiffs frequently bring actions against hospitals and other healthcare providers, alleging malpractice, product liability or other legal theories. Many of these actions involve large claims and significant defense costs. For example, certain other hospital companies have been subject to class-action claims in connection with their billing practices relating to uninsured patients or lawsuits alleging inappropriate classification of claims, for billing purposes, between observation and inpatient status.
We maintain professional malpractice liability insurance and general liability insurance in amounts we believe are sufficient to cover claims arising out of the operations of our facilities. Some of the claims could exceed the scope of the coverage in effect or coverage of particular claims or damages could be denied.
The volatility of professional liability insurance and, in some cases, the lack of availability of such insurance coverage, for physicians with privileges at our hospitals increases our risk of vicarious liability in cases where both our hospital and the uninsured or underinsured physician are named as co-defendants. As a result, we are subject to greater self-insured risk and may be required to fund claims out of our operating cash flow to a greater extent than currently required. We cannot assure you that we will be able to continue to obtain insurance coverage in the future or that such insurance coverage, if it is available, will be available on acceptable terms.
As of June 30, 2011, our self-insured retention for professional and general liability coverage is $5.0 million per claim, with an excess aggregate limit of $55.0 million, and maximum coverage under our insurance policies is $75.0 million.
If Health Choice’s Contract With the Arizona Health Care Cost Containment System Was Discontinued, Our Net Revenue And Profitability Would Be Adversely Affected.
Effective October 1, 2011, Health Choice has amended its contract with the Arizona Health Care Cost Containment System (“AHCCCS”), which now provides for a one-year term, with AHCCCS having the option to renew for an additional one-year period. The contract is terminable without cause on 90 days’ written notice or for cause upon written notice if we fail to comply with any term or condition of the contract or fail to take corrective action as required to comply with the terms of the contract. Additionally, AHCCCS can terminate our contract in the event of the unavailability of state or federal funding. If our contract with AHCCCS is terminated, our financial condition, cash flows and results of operations would be adversely affected.
29
If We Are Unable To Control Healthcare Costs At Health Choice, Our Profitability May Be Adversely Affected.
Health Choice derives its premium revenue through a contract with AHCCCS, which is the state agency that administers Arizona’s Medicaid program, and a contract with CMS for the MAPD SNP. For the nine months ended June 30, 2011, and the years ended September 30, 2010, 2009 and 2008, we derived 26.2%, 29.4%, 27.8% and 24.2%, respectively, of our consolidated net revenue from our contract with AHCCCS. AHCCCS and CMS set the capitated rates we receive at Health Choice which, in turn, subcontracts with physicians, hospitals and other healthcare providers to provide services to its enrollees. If we fail to effectively manage healthcare costs, these costs may exceed the payments we receive. Historically, our medical claims expense as a percentage of premium revenue has fluctuated. Our medical loss ratio for the nine months ended June 30, 2011, and the years ended September 30, 2010, 2009 and 2008, was 84.9%, 87.2%, 86.1% and 85.2%, respectively. Relatively small changes in these medical loss ratios can create significant changes in the profitability of Health Choice. Many factors can cause actual healthcare costs to exceed the capitated rates set by AHCCCS and CMS, including:
| | • | | our ability to contract with cost-effective healthcare providers; |
| | • | | the increased cost of individual healthcare services; |
| | • | | the type and number of individual healthcare services delivered; and |
| | • | | the occurrence of catastrophes, epidemics or other unforeseen occurrences. |
Although we have been able to manage medical claims expense through a variety of initiatives, we may not be able to continue to effectively manage medical claims expense in the future. Additionally, any future growth in members increases the risk associated with effectively managing health claims expense. If our medical claims expense increases, our financial condition or results of operations may be adversely affected.
If AHCCCS Significantly Alters The Payment Structure Of Its Contracts Or The Amount Of Premiums Paid To Us, Our Net Revenue And Profitability May Be Adversely Affected.
In response to state budgetary issues in Arizona, AHCCCS has taken steps to control its costs, including cuts in capitation premiums and the implementation of a risk-based or severity-adjusted payment methodology for all health plans. Capitation rates for each health plan and geographic service area are adjusted annually based on the severity of treatment episodes experienced by each plan’s membership compared to the average over a specified 12 month period. Adjustments are calculated using diagnosis codes and procedural information from medical and pharmacy claims data, in addition to member demographic information. Capitation rates are risk adjusted prospectively before the start of each contract year, and are not adjusted retroactively. Additionally, effective October 1, 2011, AHCCCS has implemented a tiered profit sharing plan, which will be administered through an annual reconciliation process with participating managed Medicaid health plans and will effectively limit our net profit margins. If AHCCCS continues to reduce capitation premium rates or makes further alterations to the payment structure of its contracts, our results of operations and cash flows may be adversely affected.
Significant Competition From Other Healthcare Companies And State Efforts To Regulate The Sale Of Not-For-Profit Hospitals May Affect Our Ability To Acquire Hospitals.
One element of our business strategy is to expand through selective acquisitions of hospitals in our existing markets and in new growing markets. We compete for acquisitions with other healthcare companies, some of which have greater competitive advantages or financial resources than us. Therefore, we may not be able to acquire hospitals on terms favorable to us or at all. Additionally, many states, including some where we have hospitals and others where we may in the future acquire hospitals, have adopted legislation regarding the sale or other disposition of hospitals operated by not-for-profit entities. In other states that do not have specific legislation, the attorneys general have demonstrated an interest in these transactions under their general obligations to protect charitable assets from waste. These legislative and administrative efforts focus primarily on the appropriate valuation of the assets divested and the use of the proceeds of the sale by the not-for-profit seller. These review and approval processes can add time to the closing of an acquisition of a not-for-profit hospital and future actions on the state level could seriously delay or even prevent our ability to acquire not-for-profit hospitals in the future.
30
Difficulties With The Integration Of Acquisitions May Disrupt Our Ongoing Operations.
We may, from time to time, evaluate strategic opportunities such as joint ventures and acquisitions that may be material. The process of integrating acquired hospitals may require a disproportionate amount of management’s time and attention, potentially distracting management from its other day-to-day responsibilities. In addition, poor integration of acquired facilities could cause interruptions to our business activities, including those of the acquired facilities. As a result, we may not realize all or any of the anticipated benefits of an acquisition and we may incur significant costs related to the acquisitions or integration of these facilities. In addition, we may acquire hospitals that have unknown or contingent liabilities, including liabilities for failure to comply with healthcare laws and regulations. Although we seek indemnification from prospective sellers covering these matters, we may nevertheless have material liabilities for past activities of acquired hospitals.
We Are Dependent On Key Personnel And The Loss Of One Or More Of Our Senior Management Team Or Local Management Personnel Could Have A Material Adverse Effect On Our Business.
Our business strongly depends upon the services and management experience of our senior management team. We depend on the ability of our senior management team and key employees to manage growth successfully and on our ability to attract and retain skilled employees. If any of our executive officers resign or otherwise are unable to serve, our management expertise and ability to deliver healthcare services efficiently and to effectively execute our business strategy could be diminished. If we fail to attract and retain managers at our hospitals and related facilities, our operations could be adversely effected. Moreover, we do not maintain key man life insurance policies on any of our officers.
Our Hospitals Are Subject To Potential Responsibilities And Costs Under Environmental Laws That Could Lead To Material Expenditures Or Liability.
We are subject to various federal, state and local environmental laws and regulations, including those relating to the protection of human health and the environment. We could incur substantial costs to maintain compliance with these laws and regulations. We could become the subject of future investigations, which could lead to fines or criminal penalties if we are found to be in violation of these laws and regulations. We also may be subject to requirements related to the remediation of substances that have been released into the environment at properties owned or operated by us or our predecessors or at properties where substances were sent for off-site treatment or disposal. These remediation requirements may be imposed without regard to fault, and liability for environmental remediation can be substantial.
To our knowledge, we have not been and are not currently the subject of any investigations relating to noncompliance with environmental laws and regulations. We maintain insurance coverage for third-party liability related to the storage tanks located at our facilities in the amount of $2.0 million per claim and $25.0 million in the aggregate.
If The Fair Value Of Our Reporting Units Declines, A Material Non-Cash Charge To Earnings From An Impairment Of Our Goodwill May Result.
At June 30, 2011, we had $836.7 million of goodwill recorded in our consolidated financial statements. We expect to recover the carrying value of this goodwill through our future cash flows.
On an ongoing basis, we evaluate, based on the fair value of our reporting units, whether the carrying value of our goodwill is impaired. If the carrying value of our goodwill is impaired, we may incur a material non-cash charge to earnings.
As a result of our annual impairment test during the year ended September 30, 2009, we recorded a $64.6 million non-cash charge to pre-tax earnings related to the impairment of goodwill in our Florida market. This impairment was due, in part, to limitations on our ability to expand in our Florida market as a result of certificate of need restrictions, as well as with high Medicare utilization and expanded managed care penetration. In addition, we had experienced changes in market conditions and the business mix in our Florida market, which negatively impacted operating results, producing trends that may not be temporary in nature. As a result, we wrote off all goodwill associated with our Florida market.
31
We Are Controlled By Our Principal Equity Sponsors.
We are controlled by our principal equity sponsors who have the ability to control our financial-related policies and decisions. For example, our principal equity sponsors could cause us to enter into transactions that, in their judgment, could enhance their equity investment, even though such transactions might reduce our cash flows or capital reserves. So long as our principal equity sponsors continue to own a significant amount of our equity interests, they will continue to be able to strongly influence and effectively control the decisions related to our company. Additionally, our principal equity sponsors may from time to time acquire and hold interests in businesses that compete directly or indirectly with us and, therefore, have interests that may conflict with the interests of our company.
Risk Factors Relating to the New Notes
Our Substantial Indebtedness Could Adversely Affect Our Financial Flexibility And Our Competitive Position.
We have a significant amount of indebtedness. As of June 30, 2011, we had $1,892 million of indebtedness outstanding, in addition to availability under the revolving portion of our Senior Secured Credit Facilities. Our substantial amount of indebtedness could have important consequences for you. For example, it could:
| | • | | make it more difficult for us to satisfy our obligations with respect to the notes; |
| | • | | increase our vulnerability to adverse economic and industry conditions; |
| | • | | expose us to fluctuations in the interest rate environment because the interest rates under our Senior Secured Credit Facilities will be variable; |
| | • | | require us to dedicate a substantial portion of our cash flow from operations to make payments on our indebtedness, thereby reducing the availability of our cash flow to fund working capital, capital expenditures and other general corporate purposes; |
| | • | | limit our flexibility in planning for, or reacting to, changes in the business and industry in which we operate; |
| | • | | restrict us from exploiting business opportunities; |
| | • | | make it more difficult to satisfy our financial obligations, including payments on the notes; |
| | • | | place us at a disadvantage compared to our competitors that have less debt; and |
| | • | | limit our ability to borrow additional funds for working capital, capital expenditures, acquisitions, debt service requirements, execution of our business strategy and other general corporate purposes or to refinance our existing debt. |
We, Including Our Subsidiaries, Have The Ability To Incur Substantially More Indebtedness, Including Senior Secured Indebtedness.
Subject to the restrictions in our Senior Secured Credit Facilities and the indenture governing the notes, we, including our subsidiaries, may incur significant additional indebtedness. As of June 30, 2011:
| | • | | we had $850 million of senior unsecured indebtedness under the notes; |
32
| | • | | we had $1,022 million of senior secured debt outstanding under our Senior Secured Credit Facilities; |
| | • | | subject to compliance with customary conditions, we had available to us $300 million (before consideration of outstanding letters of credit totaling $85 million under our revolving credit facility) under the revolving portion of our Senior Secured Credit Facilities, which, if borrowed, would be senior secured indebtedness; and |
| | • | | subject to our compliance with certain covenants and other conditions, including a senior secured leverage ratio, we had the option to request to borrow an unlimited amount of incremental term loans or increase our revolving credit commitments up to $375 million, which, if borrowed, would be senior secured indebtedness. |
Although the terms of our Senior Secured Credit Facilities and the indenture governing the notes contain restrictions on the incurrence of additional indebtedness, these restrictions are subject to a number of important exceptions, and indebtedness incurred in compliance with these restrictions could be substantial. If we and our restricted subsidiaries incur significant additional indebtedness, the related risks that we face could increase.
The Notes Will Be Unsecured And Will Be Effectively Subordinated To Our And The Guarantors’ Senior Secured Indebtedness To The Extent Of The Value Of The Collateral Securing Such Indebtedness And Indebtedness Of Non-Guarantor Subsidiaries.
Our obligations under the notes and the guarantors’ obligations under the guarantees of the notes will not be secured by any of our or our subsidiaries’ assets. As of June 30, 2011, we had $1,022 million of senior secured indebtedness outstanding under the term loan portion of the Senior Secured Credit Facilities and $300 million (before consideration of outstanding letters of credit totaling $85 million under our revolving credit facility) available to us under the revolving portion of our Senior Secured Credit Facilities. If we and the guarantors were to become insolvent or otherwise fail to make payments on the notes, holders of our and our guarantors’ secured obligations would be paid first to the extent of the value of the collateral securing such indebtedness and would receive payments from the assets securing such obligations before the holders of the notes would receive any payments. You may therefore not be fully repaid in the event we become insolvent or otherwise fail to make payments on the notes.
The notes will not be guaranteed by all of our subsidiaries. Subsidiaries constituting a material portion of our assets and operations, including all of our non-wholly owned subsidiaries, will not guarantee the notes. Our non-guarantor subsidiaries accounted for approximately $1,507 million, or 72.8% of our consolidated net revenue for the nine months ended June 30, 2011, and approximately $2,101 million, or 78.2% of our consolidated total assets as of June 30, 2011. All our consolidated Adjusted EBITDA comes from the non-guarantor subsidiaries. However, our guarantor subsidiaries hold unsubordinated promissory notes from the non-guarantor subsidiaries aggregating $665 million in principal amount as of June 30, 2011, under which the guarantor subsidiaries are entitled to principal and interest payments of $71 million annually. In addition, the non-guarantor subsidiaries are contractually obligated to pay the guarantor subsidiaries management fees. The management fee amount ranges from 2.0% to 2.5% of net revenue for the non-guarantor subsidiaries. For the nine months ended June 30, 2011, the non-guarantor subsidiaries paid $20 million in management fees. There can be no assurance that the non-guarantor subsidiaries will be able to make payments on the promissory notes or pay the management fees. In addition, the interest rates on the promissory notes may fluctuate, which could result in a decrease in the amount of annual payments to the guarantor subsidiaries.
Certain of these non-guarantor subsidiaries guaranteed and pledged their assets to secure our obligations under the Senior Secured Credit Facilities. In addition, certain of these subsidiaries are restricted subsidiaries and consequently we will have the ability to make additional investments in them. Claims of holders of the notes will be structurally subordinate to the claims of creditors of these non-guarantor subsidiaries, including trade creditors. All obligations of our non-guarantor subsidiaries will have to be satisfied before any of the assets of such subsidiaries would be available for distribution, upon liquidation or otherwise, to us or a guarantor of the notes.
33
We May Not Have The Ability To Raise The Funds Necessary To Finance The Change Of Control Offer Required By The Indenture Governing The Notes.
Upon the occurrence of a “change of control,” as defined in the indenture governing the notes, we must offer to buy back the notes at a price equal to 101% of the principal amount, together with any accrued and unpaid interest and special interest, if any, to but excluding the date of the repurchase. Our failure to purchase, or give notice of purchase of, the notes would be a default under the indenture governing the notes. See “Description of Notes—Repurchase at the Option of Holders—Change of Control.”
If a change of control occurs, it is possible that we may not have sufficient assets at the time of the change of control to make the required repurchase of notes or to satisfy all obligations under our credit facility and the indenture governing the notes. In order to satisfy our obligations, we could seek to refinance any or all of our outstanding indebtedness or seek to obtain a waiver from the lenders under our credit facility or the holders of the notes. We cannot assure you that we would be able to obtain a waiver or refinance our indebtedness on terms acceptable to us, if at all.
The Indenture Provides That Under Certain Circumstances We Will Have The Ability To Consummate A Change Of Control Transaction Notwithstanding The Limitations In Certain Of The Covenants In The Indenture That Would Otherwise Prohibit Being Able To Do So.
The indenture provides that if we consummate a change of control transaction in which, among other things, pro forma for such transaction our total leverage ratio would be no more than 5.75 to 1.00, we will have the ability to make restricted payments in order to facilitate the consummation of such change of control transaction, whether or not we would otherwise have the restricted payment capacity at such time. Our ability to utilize such provision will only be available one time and the indenture will also require that we make a customary change of control offer to holders of the notes. Under certain circumstances, following any such change of control transaction, we will have the right to replace the Issuers with a new parent company resulting from such transaction as the obligor under the notes. In addition, following any such assumption of the notes by a new parent company, subject to certain restrictions, we and our subsidiaries (including non-guarantor subsidiaries) will have the ability to guarantee, and pledge assets to secure, certain indebtedness of such parent and its subsidiaries and to satisfy the reporting requirements under the indenture by reporting at any new parent company. See provisions relating to “Specified Change of Control” under “Description of Notes.”
Our Indebtedness May Restrict Our Current And Future Operations, Which Could Adversely Affect Our Ability To Respond To Changes In Our Business And Manage Our Operations.
Agreements governing our indebtedness and the indenture governing the notes contain, and any future indebtedness may contain, a number of restrictive covenants that impose significant operating and financial restrictions on us and our restricted subsidiaries, including restrictions on our or our restricted subsidiaries’ ability to, among other things:
| | • | | incur additional indebtedness or issue disqualified stock or preferred stock; |
| | • | | pay dividends or make other distributions on, redeem or repurchase our capital stock; |
| | • | | make certain loans and investments; |
| | • | | enter into certain transactions with affiliates; |
| | • | | incur liens on certain assets to secure debt; |
| | • | | impose restrictions on the ability of a subsidiary to pay dividends or make payments or distributions to us and our restricted subsidiaries; or |
34
| | • | | consolidate, merge or sell all or substantially all of our assets. |
Our ability to comply with these agreements may be affected by events beyond our control, including prevailing economic, financial and industry conditions. These covenants could have an adverse effect on our business by limiting our ability to take advantage of financing, merger and acquisition or other corporate opportunities. The breach of any of these covenants or restrictions could result in a default under the indenture governing the notes or our Senior Secured Credit Facilities.
A failure by us or our subsidiaries to comply with the covenants contained in the agreements governing our indebtedness could result in an event of default under such indebtedness, which could adversely affect our ability to respond to changes in our business and manage our operations. Upon the occurrence of an event of default under any of the agreements governing our indebtedness, the lenders could elect to declare all amounts outstanding to be due and payable and exercise other remedies as set forth in the agreements. If any of our indebtedness were to be accelerated, there can be no assurance that our assets would be sufficient to repay this indebtedness in full, which could have a material adverse effect on our ability to continue to operate as a going concern.
To Service Our Indebtedness, We Will Require A Significant Amount Of Cash.
Our ability to generate cash depends on many factors beyond our control, and any failure to meet our debt service obligations could harm our business, financial condition and results of operations. Our ability to make payments on and to refinance our indebtedness, including the notes, and to fund working capital needs and planned capital expenditures will depend on our ability to generate cash in the future. This, to a certain extent, is subject to general economic, financial, competitive, business, legislative, regulatory and other factors that are beyond our control.
If our business does not generate sufficient cash flow from operations or if future borrowings are not available to us in an amount sufficient to enable us to pay our indebtedness, including the notes, or to fund our other liquidity needs, we may need to refinance all or a portion of our indebtedness, including the notes, on or before the maturity thereof, sell assets, reduce or delay capital investments or seek to raise additional capital, any of which could have a material adverse effect on our operations. In addition, we may not be able to effect any of these actions, if necessary, on commercially reasonable terms or at all. Our ability to restructure or refinance our indebtedness, including the notes, will depend on the condition of the capital markets and our financial condition at such time. Any refinancing of our debt could be at higher interest rates and may require us to comply with more onerous covenants, which could further restrict our business operations. The terms of existing or future debt instruments, including the indenture governing the notes, may limit or prevent us from taking any of these actions. In addition, any failure to make scheduled payments of interest and principal on our outstanding indebtedness would likely result in a reduction of our credit rating, which could harm our ability to incur additional indebtedness on commercially reasonable terms or at all. Our inability to generate sufficient cash flow to satisfy our debt service obligations, or to refinance or restructure our obligations on commercially reasonable terms or at all, would have an adverse effect, which could be material, on our business, financial condition and results of operations, as well as on our ability to satisfy our obligations in respect of the notes.
In addition, if we are unable to meet our debt service obligations under the notes, the holders of the notes would have the right following a cure period to cause the entire principal amount of the notes to become immediately due and payable. If the amounts outstanding under these instruments are accelerated, we cannot assure you that our assets will be sufficient to repay in full the money owed to our debt holders, including holders of the notes.
An Increase In Interest Rates Would Increase The Cost Of Servicing Our Debt And Could Reduce Our Profitability.
Borrowings under our Senior Secured Credit Facilities bear interest at variable rates. Interest rate changes will not affect the market value of any debt incurred under such facility, but could affect the amount of our interest payments, and accordingly, our future earnings and cash flows, assuming other factors are held constant. In the future, we may enter into interest rate hedging instruments in order to reduce our exposure to interest rate volatility; however, any hedging instruments we enter into may not fully mitigate our interest rate risk. As a result, an increase in interest rates, whether because of an increase in market interest rates or an increase in our own cost of borrowing, would increase the cost of servicing our debt and could materially reduce our profitability.
35
Our Failure To Comply With The Agreements Relating To Our Outstanding Indebtedness, Including As A Result Of Events Beyond Our Control, Could Result In An Event Of Default That Could Materially And Adversely Affect Our Results Of Operations And Our Financial Condition.
If there were an event of default under any of the agreements relating to our outstanding indebtedness, the holders of the defaulted debt could cause all amounts outstanding with respect to that debt to be due and payable immediately. Upon acceleration of certain of our other indebtedness, holders of the notes could declare all amounts outstanding under the notes immediately due and payable. We cannot assure you that our assets or cash flow would be sufficient to fully repay borrowings under our outstanding debt instruments if accelerated upon an event of default. Further, if we are unable to repay, refinance or restructure our secured debt, the holders of such debt could proceed against the collateral securing that indebtedness. In addition, any event of default or declaration of acceleration under one debt instrument could also result in an event of default under one or more of our other debt instruments. In addition, counterparties to some of our contracts material to our business may have the right to amend or terminate those contracts if we have an event of default or a declaration of acceleration under certain of our indebtedness, which could adversely affect our business, financial condition or results of operations.
Under Certain Circumstances A Court Could Cancel The Notes Or The Related Guarantees Under Fraudulent Conveyance Laws. If That Occurs, You May Not Receive Any Payments On The Notes.
Federal and state fraudulent transfer and conveyance statutes may apply to the issuance of the notes and the incurrence of the guarantees. Under federal bankruptcy law and comparable provisions of state fraudulent transfer or conveyance laws, which may vary from state to state, the notes or guarantees could be voided as a fraudulent transfer or conveyance if we or any of the guarantors, as applicable: (1) issued the notes or incurred the guarantees with the intent of hindering, delaying or defrauding creditors or (2) received less than reasonably equivalent value or fair consideration in return for either issuing the notes or incurring the guarantees and, in the case of (2) only, one of the following is also true at the time thereof:
| | • | | we or any of the guarantors, as applicable, were insolvent or rendered insolvent by reason of the issuance of the notes or the incurrence of the guarantees; |
| | • | | the issuance of the notes or the incurrence of the guarantees left us or any of the guarantors, as applicable, with an unreasonably small amount of capital to carry on the business; |
| | • | | we or any of the guarantors intended to, or believed that we or such guarantor would, incur debts beyond our or such guarantor’s ability to pay as they mature; or |
| | • | | we or any of the guarantors was a defendant in an action for money damages, or had a judgment for money damages docketed against us or such guarantor if, in either case, after final judgment, the judgment is unsatisfied. |
If a court were to find that the issuance of the notes or the incurrence of the guarantee was a fraudulent transfer or conveyance, the court could void the payment obligations under the notes or such guarantee or subordinate the notes or such guarantee to presently existing and future indebtedness of ours or of the related guarantor, or require the holders of the notes to repay any amounts received with respect to such guarantee. In the event of a finding that a fraudulent transfer or conveyance occurred, you may not receive any repayment on the notes. Further, the voidance of the notes could result in an event of default with respect to our and our subsidiaries’ other debt that could result in acceleration of such debt.
As a general matter, value is given for a transfer or an obligation if, in exchange for the transfer or obligation, property is transferred or an antecedent debt is secured or satisfied. A debtor will generally not be considered to have received value in connection with a debt offering if the debtor uses the proceeds of that offering to make a dividend payment or otherwise retire or redeem equity securities issued by the debtor. We cannot be certain as to the standards a court would use to determine whether
36
or not we or the guarantors were solvent at the relevant time or, regardless of the standard that a court uses, that the issuance of the notes and the guarantees would not be subordinated to our or any of our guarantors’ other debt.
Generally, an entity would be considered insolvent if, at the time it incurred debt:
| | • | | the sum of its debts, including contingent liabilities, was greater than the fair saleable value of all its assets; |
| | • | | the present fair saleable value of its assets was less than the amount that would be required to pay its probable liability on its existing debts and liabilities, including contingent liabilities, as they become absolute and mature; or |
| | • | | it could not pay its debts as they become due. |
If the guarantees were legally challenged, any guarantee could also be subject to the claim that, since the guarantee was incurred for our benefit, and only indirectly for the benefit of the guarantor, the obligations of the applicable guarantor were incurred for less than fair consideration. A court could thus void the obligations under the guarantees, subordinate them to the applicable guarantor’s other debt or take other action detrimental to the holders of the notes.
The indenture governing the notes contains a “savings clause” intended to limit each guarantor’s liability under its guarantee to the maximum amount that it could incur without causing the guarantee to be a fraudulent transfer under applicable law. There can be no assurance that this provision will be upheld as intended. In a recent case, the U.S. Bankruptcy Court in the Southern District of Florida found this kind of provision in that case to be ineffective, and held the guarantees to be fraudulent transfers and voided them in their entirety.
There Is No Established Trading Market For The Notes And You May Not Be Able To Sell The Notes Readily Or At All Or At Or Above The Price That You Paid.
The notes are a new issue of securities and there is no established trading market for them. We do not intend to apply for the notes to be listed on any securities exchange or to arrange for quotation on any automated dealer quotation system. The initial purchasers have advised us that they intend to make a market in the notes, but they are not obligated to do so and may discontinue any market making in the notes at any time, in their sole discretion. You may not be able to sell your notes at a particular time or at favorable prices. As a result, we cannot assure you as to the liquidity of any trading market for the notes. Accordingly, you may be required to bear the financial risk of your investment in the notes indefinitely. If a trading market were to develop, future trading prices of the notes may be volatile and will depend on many factors, including:
| | • | | our operating performance and financial condition; |
| | • | | the interest of securities dealers in making a market for them; |
| | • | | prevailing interest rates; and |
| | • | | the market for similar securities. |
In addition, the market for non-investment grade debt historically has been subject to disruptions that have caused substantial volatility in the prices of securities similar to the notes. The market for the notes, if any, may be subject to similar disruptions that could adversely affect their value.
We also cannot assure investors in the notes as to the level of liquidity in the trading market for the New Notes issued in exchange for the Old Notes in accordance with the exchange offer described in the “Description of the Exchange Offer” or, in the case of any noteholders that do not exchange their Old Notes in such exchange offer, the trading market for the Old Notes following completion of the exchange offer.
37
Our Principal Equity Holders’ Interests May Conflict With Yours.
TPG owns approximately 74.4% of the outstanding equity of IASIS Investment LLC (“IASIS Investment”) as of June 30, 2011. IASIS Investment is the majority stockholder of IAS, which owns 100% of our common interests. Accordingly, TPG has the ability to influence our policies and operations. TPG does not have any liability for any obligations under the notes, and its interests may not in all cases be aligned with your interests. For example, if we encounter financial difficulties or are unable to pay our debts as they mature, the interests of our equity holders might conflict with your interests as a noteholder. In addition, our equity holders may have an interest in pursuing acquisitions, divestitures, financings or other transactions that, in their judgment, could enhance their equity investments, even though such transactions might involve risks to you as a holder of the notes. Furthermore, TPG and its affiliates may in the future own businesses that directly or indirectly compete with us. TPG and its affiliates may pursue acquisition opportunities that may be complementary to our business, and as a result, those acquisition opportunities may not be available to us. For information concerning our arrangements with TPG, see “Certain Relationships and Related Party Transactions.”
The Lenders Under Our Senior Secured Credit Facilities Have The Discretion To Release Any Guarantors Under These Facilities In A Variety Of Circumstances, Which Will Cause Those Guarantors To Be Released From Their Guarantees Of The Notes.
While any obligations under our Senior Secured Credit Facilities remain outstanding, any guarantee of the notes may be released without action by, or consent of, any holder of the notes or the trustee under the indenture governing the notes, at the discretion of lenders under our Senior Secured Credit Facilities, if the related guarantor is no longer a guarantor of obligations under our Senior Secured Credit Facilities or any other indebtedness. See “Description of Notes.” The lenders under our Senior Secured Credit Facilities have the discretion to release the guarantees under our Senior Secured Credit Facilities in a variety of circumstances. Any of our subsidiaries that is released as a guarantor of our Senior Secured Credit Facilities will automatically be released as a guarantor of the notes. You will not have a claim as a creditor against any subsidiary that is no longer a guarantor of the notes, and the indebtedness and other liabilities, including trade payables, whether secured or unsecured, of those subsidiaries will effectively be senior to claims of noteholders.
Risks Related to the Exchange Offer
The Consummation Of The Exchange Offer May Not Occur.
We are not obligated to complete the exchange offer under certain circumstances. See “Description of the Exchange Offer—Conditions to the Exchange Offer.” Even if the exchange offer is completed, it may not be completed on the schedule described in this prospectus. Accordingly, holders participating in the exchange offer may have to wait longer than expected to receive their New Notes, during which time those holders of Old Notes will not be able to effect transfers of their Old Notes tendered in the exchange offer.
You May Be Required To Deliver Prospectuses And Comply With Other Requirements In Connection With Any Resale Of The New Notes.
If you tender your Old Notes for the purpose of participating in a distribution of the New Notes, you will be required to comply with the registration and prospectus delivery requirements of the Securities Act in connection with any resale of the New Notes. In addition, if you are a broker-dealer that receives New Notes for your own account in exchange for Old Notes that you acquired as a result of market-making activities or any other trading activities, you will be required to acknowledge that you will deliver a prospectus in connection with any resale of such New Notes.
38
Failure To Tender The Old Notes In The Exchange Offer May Affect Their Marketability And Will Substantially Limit, And May Effectively Eliminate, Opportunities To Sell Your Old Notes In The Future.
If the Old Notes are tendered and accepted in the exchange offer, the trading market, if any, for the untendered and tendered but unaccepted Old Notes will be adversely affected. Your failure to participate in the exchange offer will substantially limit, and may effectively eliminate, opportunities to sell your Old Notes in the future.
We issued the Old Notes in a private placement exempt from the registration requirements of the Securities Act. Accordingly, you may not offer, sell or otherwise transfer your Old Notes except in compliance with the registration requirements of the Securities Act and any other applicable securities laws, or pursuant to an exemption from the securities laws, or in a transaction not subject to the securities laws. If you do not exchange your Old Notes for the New Notes in the exchange offer, your Old Notes will continue to be subject to these transfer restrictions after the completion of the exchange offer. In addition, after the completion of the exchange offer, you will no longer be able to obligate us to register the Old Notes under the Securities Act.
39
CAUTIONARY NOTE REGARDING FORWARD-LOOKING STATEMENTS
Some of the statements made under the headings “Prospectus Summary” and elsewhere in this prospectus contain forward-looking statements within the meaning of the Private Securities Litigation Reform Act of 1995. Statements that are not historical facts, including statements about our beliefs and expectations, are forward-looking statements. Forward-looking statements are often characterized by the use of words such as “believes,” “estimates,” “expects,” “projects,” “may,” “intends,” “plans” or “anticipates,” or by discussions of strategy, plans or intentions. Such forward-looking statements involve known and unknown risks, uncertainties, assumptions and other important factors that could cause the actual results, performance or our achievements, or industry results, to differ materially from historical results, any future results or performance or achievements expressed or implied by such forward-looking statements. There are a number of risks and uncertainties that could cause our actual results to differ materially from the forward-looking statements contained in this prospectus. Further description of these risks and uncertainties and other important factors are set forth in “Risk Factors” herein, and include, but not limited to, such risks related to:
| | • | | our operating and growth strategy (including possible acquisitions and dispositions); |
| | • | | projections of our revenue and income or loss; |
| | • | | our capital expenditures; and |
There may be other factors of which we are currently unaware or that we deem immaterial that may cause our actual results to differ materially from the expectations we express in our forward-looking statements. Although we believe the assumptions underlying our forward-looking statements are reasonable, any of these assumptions, and, therefore, also the forward-looking statements based on these assumptions could themselves prove to be inaccurate.
Forward-looking statements are based on current plans, estimates, assumptions and projections, and therefore you should not place undue reliance on them. Forward-looking statements speak only as of the date they are made, and we undertake no obligation to update them publicly in light of new information or future events.
You should carefully consider the “Risk Factors” and subsequent public statements, or reports filed with or furnished to the SEC, before making any investment decision with respect to the notes. If any of these trends, risks, assumptions or uncertainties actually occurs or continues, our business, financial condition or operating results could be materially adversely affected, the trading prices of the notes could decline and you could lose all or part of your investment. All forward-looking statements attributable to us or persons acting on our behalf are expressly qualified in their entirety by this cautionary statement.
40
SELECTED CONSOLIDATED FINANCIAL AND OTHER DATA
The following tables set forth our selected consolidated financial and other data for the fiscal years ended September 30, 2006, 2007, 2008, 2009 and 2010, and the nine months ended June 30, 2010 and 2011. The selected consolidated financial data for the fiscal year ended September 30, 2006 and 2007, was derived from our audited consolidated financial statements, adjusted for the retrospective impact on presentation of changes in accounting guidance related to non-controlling interests. Our selected consolidated financial data for the fiscal years ended September 30, 2008, 2009 and 2010, was derived from our audited consolidated financial statements for each fiscal year presented. The selected consolidated financial data for the nine months ended June 30, 2010 and 2011, was derived from our unaudited condensed consolidated financial statements, which have been prepared on a basis consistent with our audited consolidated financial statements. Results of operations for interim periods are not necessarily indicative of the results that might be expected for any other interim period or for an entire year. Our historical results are not indicative of our future performance. The selected consolidated financial data presented below represent portions of our financial statements and are not complete. You should read this information in conjunction with the annual consolidated and interim condensed consolidated financial statements and related notes and “Management’s Discussion and Analysis of Financial Condition and Results of Operations,” each of which is included elsewhere in this prospectus.
Selected Financial Data
| | | | | | | | | | | | | | | | | | | | | | | | | | | | |
| | | Year Ended September 30, | | | Nine Months Ended
June 30, | |
| | | 2006 | | | 2007 | | | 2008 | | | 2009 | | | 2010 | | | 2010 | | | 2011 | |
| | | | | | | |
Statement of Operations Data (1): | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
| | | | | | | |
Net revenue | | $ | 1,539,577 | | | $ | 1,766,079 | | | $ | 2,065,536 | | | $ | 2,361,972 | | | $ | 2,521,406 | | | $ | 1,891,467 | | | $ | 2,070,349 | |
| | | | | | | |
Costs and expenses: | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
Salaries and benefits (2) | | | 439,349 | | | | 533,792 | | | | 632,109 | | | | 660,921 | | | | 686,303 | | | | 514,688 | | | | 597,063 | |
Supplies | | | 167,616 | | | | 194,915 | | | | 231,259 | | | | 250,573 | | | | 266,545 | | | | 200,167 | | | | 237,431 | |
Medical claims | | | 347,217 | | | | 376,505 | | | | 452,055 | | | | 592,760 | | | | 678,651 | | | | 510,692 | | | | 484,635 | |
Other operating expenses | | | 223,946 | | | | 266,263 | | | | 283,123 | | | | 325,735 | | | | 363,916 | | | | 266,854 | | | | 315,254 | |
Provision for bad debts | | | 134,614 | | | | 136,233 | | | | 161,936 | | | | 192,563 | | | | 197,680 | | | | 142,901 | | | | 175,100 | |
Rentals and leases | | | 30,277 | | | | 31,546 | | | | 36,633 | | | | 39,127 | | | | 39,955 | | | | 30,487 | | | | 34,229 | |
Interest expense, net | | | 67,124 | | | | 71,206 | | | | 75,665 | | | | 67,890 | | | | 66,810 | | | | 50,065 | | | | 60,984 | |
Depreciation and amortization | | | 69,137 | | | | 75,388 | | | | 96,741 | | | | 97,462 | | | | 96,106 | | | | 71,909 | | | | 74,942 | |
Management fees | | | 4,189 | | | | 4,746 | | | | 5,000 | | | | 5,000 | | | | 5,000 | | | | 3,750 | | | | 3,750 | |
Loss on extinguishment of debt | | | — | | | | 6,229 | | | | — | | | | — | | | | — | | | | — | | | | 23,075 | |
Impairment of goodwill (3) | | | — | | | | — | | | | — | | | | 64,639 | | | | — | | | | — | | | | — | |
Business interruption insurance recoveries (4) | | | (8,974 | ) | | | (3,443 | ) | | | — | | | | — | | | | — | | | | — | | | | — | |
Hurricane-related property damage (5) | | | — | | | | — | | | | 3,589 | | | | 938 | | | | — | | | | — | | | | — | |
| | | | | | | | | | | | | | | | | | | | | | | | | | | | |
Total costs and expenses | | | 1,474,495 | | | | 1,693,380 | | | | 1,978,110 | | | | 2,297,608 | | | | 2,400,966 | | | | 1,791,513 | | | | 2,006,463 | |
| | | | | | | | | | | | | | | | | | | | | | | | | | | | |
41
| | | | | | | | | | | | | | | | | | | | | | | | | | | | |
Earnings from continuing operations before gain (loss) on disposal of assets and income taxes | | | 65,082 | | | | 72,699 | | | | 87,426 | | | | 64,364 | | | | 120,440 | | | | 99,954 | | | | 63,886 | |
Gain (loss) on disposal of assets, net | | | 913 | | | | (1,359 | ) | | | (75 | ) | | | 1,465 | | | | 108 | | | | (206 | ) | | | 771 | |
Earnings from continuing operations before income taxes | | | 65,995 | | | | 71,340 | | | | 87,351 | | | | 65,829 | | | | 120,548 | | | | 99,748 | | | | 64,657 | |
Income tax expense | | | 22,515 | | | | 25,909 | | | | 35,325 | | | | 27,576 | | | | 44,715 | | | | 36,544 | | | | 24,078 | |
| | | | | | | | | | | | | | | | | | | | | | | | | | | | |
Net earnings from continuing operations | | | 43,480 | | | | 45,431 | | | | 52,026 | | | | 38,253 | | | | 75,833 | | | | 63,204 | | | | 40,579 | |
Earnings (loss) from discontinued operations, net of income taxes | | | (385 | ) | | | 669 | | | | (11,275 | ) | | | (176 | ) | | | (1,087 | ) | | | (363 | ) | | | (6,069 | ) |
| | | | | | | | | | | | | | | | | | | | | | | | | | | | |
Net earnings | | | 43,095 | | | | 46,100 | | | | 40,751 | | | | 38,077 | | | | 74,746 | | | | 62,841 | | | | 34,510 | |
Net earnings attributable to non-controlling interests | | | (3,546 | ) | | | (4,496 | ) | | | (4,437 | ) | | | (9,987 | ) | | | (8,279 | ) | | | (6,063 | ) | | | (6,201 | ) |
| | | | | | | | | | | | | | | | | | | | | | | | | | | | |
Net earnings attributable to IASIS Healthcare LLC | | $ | 39,549 | | | $ | 41,604 | | | $ | 36,314 | | | $ | 28,090 | | | $ | 66,467 | | | $ | 56,778 | | | $ | 28,309 | |
| | | | | | | | | | | | | | | | | | | | | | | | | | | | |
Balance Sheet and Other Financial Data (at end of period): | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
Adjusted EBITDA | | $ | 205,532 | | | $ | 230,268 | | | $ | 264,832 | | | $ | 299,916 | | | $ | 290,843 | | | $ | 228,045 | | | $ | 228,001 | |
Cash and cash equivalents | | $ | 95,415 | | | $ | — | | | $ | 80,738 | | | $ | 206,528 | | | $ | 144,511 | | | $ | 130,160 | | | $ | 144,595 | |
Total assets | | $ | 1,967,835 | | | $ | 2,186,422 | | | $ | 2,308,147 | | | $ | 2,357,204 | | | $ | 2,353,194 | | | $ | 2,299,461 | | | $ | 2,686,800 | |
| | | | | | | |
Long-term debt and capital lease obligations (including current portion) | | $ | 896,945 | | | $ | 1,031,657 | | | $ | 1,114,622 | | | $ | 1,059,837 | | | $ | 1,051,578 | | | $ | 1,053,185 | | | $ | 1,881,433 | |
Member’s equity | | $ | 639,714 | | | $ | 674,732 | | | $ | 714,507 | | | $ | 750,932 | | | $ | 702,135 | | | $ | 688,576 | | | $ | 115,342 | |
| (1) | Excludes Mesa General Hospital and Biltmore Surgery Center, where operations were discontinued effective May 31, 2008 and April 30, 2008, respectively. |
| (2) | Results for the year ended September 30, 2010, include $2.0 million in stock compensation expense related to the repurchase of certain equity by IAS. |
| (3) | Results for the year ended September 30, 2009, include a $64.6 million non-cash charge ($43.2 million after taxes) related to the impairment of goodwill in our Florida market. |
| (4) | Results for the years ended September 30, 2006 and 2007, include $9.0 million and $3.4 million, respectively, of business interruption insurance recoveries received in connection with the temporary closure and disruption of operations at The Medical Center of Southeast Texas, as a result of Hurricane Rita. |
| (5) | Results for the years ended September 30, 2008 and 2009, included an adverse financial impact totaling $3.6 million and $938,000, respectively, before income taxes related to property damage sustained at The Medical Center of Southeast Texas, as a result of Hurricane Ike. |
42
Selected Operating Data
The following tables set forth certain unaudited operating data for each of the periods presented.
| | | | | | | | | | | | | | | | | | | | | | | | | | | | |
| | | Year Ended September 30, | | | Nine Months Ended
June 30, | |
| | | 2006 | | | 2007 | | | 2008 | | | 2009 | | | 2010 | | | 2010 | | | 2011 | |
Acute Care (1): | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
Number of acute care hospital facilities at end of period (2) | | | 14 | | | | 15 | | | | 15 | | | | 15 | | | | 15 | | | | 15 | | | | 18 | |
Licensed beds at end of period | | | 2,480 | | | | 3,011 | | | | 3,027 | | | | 3,162 | | | | 3,185 | | | | 3,185 | | | | 4,362 | |
Average length of stay (days) (3) | | | 4.6 | | | | 4.6 | | | | 4.7 | | | | 4.7 | | | | 4.8 | | | | 4.8 | | | | 4.9 | |
Occupancy rates (average beds in service) | | | 51.2 | % | | | 49.5 | % | | | 48.9 | % | | | 46.5 | % | | | 46.6 | % | | | 46.9 | % | | | 48.5 | % |
Admissions (4) | | | 82,862 | | | | 92,198 | | | | 101,302 | | | | 101,083 | | | | 101,798 | | | | 76,679 | | | | 84,469 | |
Adjusted admissions (5) | | | 137,703 | | | | 150,774 | | | | 165,819 | | | | 169,721 | | | | 170,812 | | | | 127,654 | | | | 144,066 | |
Patient days (6) | | | 383,175 | | | | 427,244 | | | | 471,853 | | | | 473,601 | | | | 489,274 | | | | 369,402 | | | | 416,365 | |
Adjusted patient days (5) | | | 612,058 | | | | 669,999 | | | | 741,466 | | | | 762,234 | | | | 790,958 | | | | 593,277 | | | | 682,948 | |
Net patient revenue per adjusted admission | | $ | 8,157 | | | $ | 8,639 | | | $ | 9,101 | | | $ | 9,703 | | | $ | 10,066 | | | $ | 10,118 | | | $ | 10,258 | |
Outpatient revenue as a % of gross patient revenue | | | 36.2 | % | | | 36.4 | % | | | 36.9 | % | | | 39.0 | % | | | 39.6 | % | | | 39.1 | % | | | 40.5 | % |
Health Choice: | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
Medicaid covered lives | | | 110,813 | | | | 122,437 | | | | 142,193 | | | | 187,104 | | | | 194,095 | | | | 195,183 | | | | 193,277 | |
Dual-eligible lives (7) | | | 3,937 | | | | 3,482 | | | | 3,300 | | | | 3,659 | | | | 4,298 | | | | 4,256 | | | | 4,271 | |
Medical loss ratio (8) | | | 87.2 | % | | | 85.2 | % | | | 85.2 | % | | | 86.1 | % | | | 87.2 | % | | | 87.8 | % | | | 84.9 | % |
| (1) | Excludes Mesa General Hospital and Biltmore Surgery Center, where operations were discontinued effective May 31, 2008 and April 30, 2008, respectively. |
| (2) | Excludes St. Luke’s Behavioral Health Hospital. |
| (3) | Represents the average number of days that a patient stayed in our hospitals. |
| (4) | Represents the total number of patients admitted to our hospitals for stays in excess of 23 hours. Management and investors use this number as a general measure of inpatient volume. |
| (5) | Adjusted admissions and adjusted patient days are general measures of combined inpatient and outpatient volume. We compute adjusted admissions/patient days by multiplying admissions/patient days by gross patient revenue and then dividing that number by gross inpatient revenue. |
| (6) | Represents the number of days our beds were occupied by inpatients over the period. |
| (7) | Represents members eligible for Medicare and Medicaid benefits under Health Choice’s contract with CMS to provide coverage as a MAPD SNP. |
| (8) | Represents medical claims expense as a percentage of premium revenue, including claims paid to our hospitals. |
43
| | | | | | | | | | | | | | | | | | | | | | | | | | | | |
| | | Fiscal Year Ended
September 30, | | | Nine Months Ended
June 30, | |
| | | 2006 | | | 2007 | | | 2008 | | | 2009 | | | 2010 | | | 2010 | | | 2011 | |
Adjusted EBITDA: | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
Net earnings from continuing operations | | $ | 43,480 | | | $ | 45,431 | | | $ | 52,026 | | | $ | 38,253 | | | $ | 75,833 | | | $ | 63,204 | | | $ | 40,579 | |
Add: | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
Interest expense, net | | | 67,124 | | | | 71,206 | | | | 75,665 | | | | 67,890 | | | | 66,810 | | | | 50,065 | | | | 60,984 | |
Income tax expense | | | 22,515 | | | | 25,909 | | | | 35,325 | | | | 27,576 | | | | 44,715 | | | | 36,544 | | | | 24,078 | |
Depreciation and amortization | | | 69,137 | | | | 75,388 | | | | 96,741 | | | | 97,462 | | | | 96,106 | | | | 71,909 | | | | 74,942 | |
| | | | | | | | | | | | | | | | | | | | | | | | | | | | |
EBITDA | | | 202,256 | | | $ | 217,934 | | | $ | 259,757 | | | $ | 231,181 | | | $ | 283,464 | | | $ | 221,722 | | | $ | 200,583 | |
Impairment of goodwill | | | — | | | | — | | | | — | | | | 64,639 | | | | — | | | | — | | | | — | |
Management fees | | | 4,189 | | | | 4,746 | | | | 5,000 | | | | 5,000 | | | | 5,000 | | | | 3,750 | | | | 3,750 | |
Loss (gain) on disposal of assets, net | | | (913 | ) | | | 1,359 | | | | 75 | | | | (1,465 | ) | | | (108 | ) | | | 206 | | | | (771 | ) |
Stock-based compensation | | | — | | | | — | | | | — | | | | 561 | | | | 2,487 | | | | 2,367 | | | | 1,364 | |
Loss on extinguishment of debt | | | — | | | | 6,229 | | | | — | | | | — | | | | — | | | | — | | | | 23,075 | |
| | | | | | | | | | | | | | | | | | | | | | | | | | | | |
Adjusted EBITDA | | $ | 205,532 | | | $ | 230,268 | | | $ | 264,832 | | | $ | 299,916 | | | $ | 290,843 | | | $ | 228,045 | | | $ | 228,001 | |
| | | | | | | | | | | | | | | | | | | | | | | | | | | | |
Adjusted EBITDA represents net earnings from continuing operations before interest expense, income tax expense, depreciation and amortization, stock-based compensation, impairment of goodwill, loss (gain) on disposal of assets, loss on extinguishment of debt and management fees. Management fees represent monitoring and advisory fees paid to affiliates of TPG, JLL and Trimaran. Management routinely calculates and communicates Adjusted EBITDA and believes that it is useful to investors because it is commonly used as an analytical indicator within the healthcare industry to evaluate hospital performance, allocate resources and measure leverage capacity and debt service ability. In addition, we use Adjusted EBITDA as a measure of performance for our business segments and for incentive compensation purposes. Adjusted EBITDA should not be considered as a measure of financial performance under GAAP, and the items excluded from Adjusted EBITDA are significant components in understanding and assessing financial performance. Adjusted EBITDA should not be considered in isolation or as an alternative to net earnings, cash flows generated by operating, investing, or financing activities or other financial statement data presented in the consolidated financial statements as an indicator of financial performance or liquidity. Adjusted EBITDA, as presented, differs from what is defined under our Senior Secured Credit Facilities and may not be comparable to similarly titled measures of other companies.
44
RATIO OF EARNINGS TO FIXED CHARGES
The following table sets forth our ratio of earnings to fixed charges for the years ended September 30, 2006, 2007, 2008, 2009 and 2010, and for the nine months ended June 30, 2010 and 2011. For the purpose of calculating the ratio of earnings to fixed charges, earnings are defined as earnings from continuing operations before income taxes plus fixed charges. Fixed charges are defined as interest expensed and capitalized, amortized premiums, discounts and capitalized expenses related to indebtedness and an estimate of the interest within rental expense.
| | | | | | | | | | | | | | | | | | | | | | | | | | | | |
| | | Year Ended September 30, | | | Nine Months Ended
June 30, | |
| | | 2006 | | | 2007 | | | 2008 | | | 2009 | | | 2010 | | | 2010 | | | 2011 | |
Ratio of earnings to fixed charges | | | 1.9x | | | | 1.8x | | | | 2.0x | | | | 1.8x | | | | 2.6x | | | | 2.8x | | | | 1.9x | |
45
MANAGEMENT’S DISCUSSION AND ANALYSIS OF FINANCIAL CONDITION AND RESULTS OF OPERATIONS
The following discussion and analysis of financial condition and results of operations should be read in conjunction with the “Selected Consolidated Financial and Other Data,” both our unaudited and audited consolidated financial statements and their related notes, and the other financial information appearing elsewhere in this prospectus. Data for the fiscal years ended September 30, 2008, 2009 and 2010, has been derived from our audited consolidated financial statements. Data for the nine months ended June 30, 2010 and 2011, has been derived from our unaudited condensed consolidated financial statements. This discussion contains forward-looking statements and involves numerous risks and uncertainties, including but not limited to those described in the "Risk Factors" section of this prospectus. Actual results may differ materially from those contained in any forward-looking statements. You should read "Cautionary Note Regarding Forward-Looking Statements" and "Risk Factors." References herein to “we,” “us,” “our” and “our company” are to IASIS Healthcare LLC and its subsidiaries, unless indicated otherwise. References to “IAS” are to IASIS Healthcare Corporation, our parent company.
Executive Overview
We are a leading owner and operator of medium-sized acute care hospitals in high-growth urban and suburban markets. We operate our hospitals with a strong community focus by offering and developing healthcare services targeted to the needs of the markets we serve, promoting strong relationships with physicians and working with local managed care plans. At June 30, 2011, we owned or leased 18 acute care hospital facilities and one behavioral health hospital facility, with a total of 4,362 licensed beds, located in seven regions:
| | • | | Tampa-St. Petersburg, Florida; |
| | • | | five cities in Texas, including Houston and San Antonio; |
| | • | | West Monroe, Louisiana; and |
| | • | | Woodland Park, Colorado. |
We also own and operate Health Choice, a Medicaid and Medicare managed health plan in Phoenix, Arizona, that serves over 197,000 members.
On May 3, 2011, we completed a transaction to refinance our then existing debt (the “Refinancing”). The Refinancing included $1.325 billion in new senior secured credit facilities and the issuance by us, together with our wholly owned subsidiary IASIS Capital Corporation (“IASIS Capital”), of $850.0 million aggregate principal amount of 8.375% senior notes due 2019. Proceeds from the Refinancing were used to refinance amounts outstanding under our then existing credit facilities; fund a cash tender offer to repurchase any and all of our $475.0 million aggregate principal amount of 8 3/4% senior subordinated notes due 2014; repay in full the senior paid-in-kind loans of IAS; pay fees and expenses associated with the Refinancing; and raise capital for general corporate purposes, including future acquisitions and strategic growth initiatives, as well as potential distributions to the equity holders of IAS. In connection with the Refinancing, we incurred a loss on extinguishment of debt totaling $23.1 million, along with an increase in interest costs primarily resulting from the additional outstanding debt associated with the transaction.
Effective May 1, 2011, we acquired a 79.1% equity ownership interest in St. Joseph in downtown Houston, Texas, in exchange for cash consideration of $156.8 million, subject to changes in net assets. In accordance with
46
the purchase agreement, independent investors, most of whom are physicians on the medical staff of St. Joseph, retained an aggregate 20.9% ownership interest in the hospital. St. Joseph is a 792-licensed bed acute care hospital facility that generates approximately $245.0 million in annual net revenue.
Effective October 1, 2010, we acquired Brim in a cash-for-stock transaction valued at $95.0 million, subject to changes in net working capital. Brim operates Wadley Regional Medical Center (“Wadley”), a 370-licensed bed acute care hospital facility in Texarkana, Texas, of which Brim owns a 72.7% equity interest, and Pikes Peak Regional Hospital, a 15-licensed bed critical access acute care hospital facility in Woodland Park, Colorado. Brim generates approximately $120.0 million in annual net revenue.
Significant Industry Trends
The following sections discuss recent trends that we believe are significant factors in our current and/or future operating results and cash flows. Certain of these trends apply to the entire acute care hospital industry, while others may apply to us more specifically. These trends could be short-term in nature or could require long-term attention and resources. While these trends may involve certain factors that are outside of our control, the extent to which these trends affect our hospitals and our ability to manage the impact of these trends play vital roles in our current and future success. In many cases, we are unable to predict what impact these trends, if any, will have on us.
The Impact of Health Reform
The Health Reform Law will change how healthcare services are covered, delivered, and reimbursed through expanded coverage of previously uninsured individuals and reduced government healthcare spending. In addition, as enacted, the law reforms certain aspects of health insurance, expands existing efforts to tie Medicare and Medicaid payments to performance and quality, places restrictions on physician-owned hospitals, and contains provisions intended to strengthen fraud and abuse enforcement. Because of the many variables involved, including the law’s complexity, lack of implementing regulations or interpretive guidance, gradual and potentially delayed implementation, pending efforts to repeal or amend portions of the Health Reform Law in the United States Congress and ongoing federal court cases challenging the constitutionality of the Health Reform Law, the impact of the Health Reform Law, including how individuals and businesses will respond to the new choice afforded them, is not yet fully known.
Payor Mix Shift
Like others in the hospital industry, we have experienced a shift in our patient volumes and revenue from commercial and managed care payors to self-pay and Medicaid, including managed Medicaid. This has resulted in pressures on pricing and operating margins created from expending the same amount of resources to provide patient care, but for less reimbursement. This shift is reflective of continued high unemployment and the resulting increases in states’ Medicaid rolls and the uninsured population. Additionally, we have recently experienced growth in our self-pay revenue, resulting in large part, from increased volume and acuity levels associated with uninsured patient decisions to defer non-emergent healthcare needs. We believe the decline in managed care volume and revenue mix is not only indicative of the depressed labor market, but also utilization behavior of the insured population resulting from higher deductible and co-insurance plans implemented by employers, which, in turn, has resulted in the deferral of elective and non-emergent procedures. Given the high rate of unemployment and its impact on the economy, particularly in the markets we serve, we expect the elevated levels in our self-pay and Medicaid payor mixes to continue until the U.S. economy experiences an economic recovery that includes job growth and a meaningful decline in unemployment.
State Medicaid Budgets
The states in which we operate have experienced budget constraints as a result of increased costs and lower than expected tax collections. Many states have experienced or project near term shortfalls in their budgets, and economic conditions may increase these budget pressures. Health and human services programs, including Medicaid and similar programs, represent a significant portion of state budgets. The states in which we operate, including Texas and Arizona, continue to respond to these budget concerns,
47
by decreasing funding for Medicaid and other healthcare programs or making structural changes that have resulted in a reduction in hospital reimbursement. In addition, many states are seeking waivers from CMS in order to implement or expand managed Medicaid programs. For example, Florida legislation has established a goal of statewide implementation of Medicaid managed care. On August 1, 2011, Florida submitted requests to CMS for approval of waivers, waiver amendments, and state plan amendments to implement two managed care Medicaid programs statewide for long-term care and all other healthcare services. It is uncertain whether or when CMS will approve Florida’s requests. Louisiana has requested a section 1115 Medicaid waiver from the federal government that, if approved, would result in an expansion of Medicaid managed care plans. The Texas legislature and the THHSC have recommended expanding Medicaid managed care enrollment in the state. On September 14, 2011, Texas received a letter indicating that CMS has reached agreement in principle on Texas’ plan to expand Medicaid managed care across the state and to create funding pools to finance hospital infrastructure and quality improvement programs.
In July 2011, in connection with the state’s reduced funding for Medicaid services in fiscal 2012, the Texas Health and Human Services Commission (“THHSC”) issued a final rule implementing a statewide acute care hospital inpatient Standard Dollar Amount (“SDA”) rate, along with an 8% reduction in Medicaid hospital outpatient reimbursement. The THHSC also rebased all MS-DRG relative weights concurrent with this SDA rate change. The new statewide SDA rate includes certain add-on adjustments for geographic wage-index, indirect medical education and trauma services. However, the new statewide SDA rate does not include add-on adjustments for higher acuity services, such as neonatal and other women’s services, which are utilized by a majority of the Medicaid patients we serve at our Texas hospitals.
Arizona’s budget for fiscal year 2011 included a reduction in funding for Medicaid through the elimination of Medicaid coverage for some services and a cut of up to 5% for all Medicaid providers, which began in April 2011. The Governor has signed the state’s fiscal 2012 budget legislation, which includes another 5% cut to provider reimbursement effective October 1, 2011, and a reduction of approximately 160,000 eligible Medicaid beneficiaries, which represents approximately 11.5% of the total Medicaid population in the state and includes approximately 100,000 childless adults. This reduction in eligible enrollees is to be accomplished over a twelve month period, beginning July 2011, through enrollment caps, attrition and more stringent eligibility requirements. While these structural changes to the Medicaid program have been included in Arizona’s approved fiscal 2012 budget, these changes require CMS approval under the confines of the Health Reform Law. On October 21, 2011, the state’s waiver was approved by CMS eliminating Medicaid coverage for the childless adults. However, CMS did not approve the enrollment freeze on the remaining 60,000 eligible beneficiaries, which represent families with income levels that fall between 75% and 100% of the federal poverty level. Other components of the waiver are still under review by CMS, including the 5% provider cuts that are to be effective October 1, 2011. Additionally, AHCCCS has implemented a tiered profit sharing plan, which will be administered through an annual reconciliation process with participating managed Medicaid health plans and will effectively limit our net profit margins for fiscal year 2012. If additional Medicaid spending cuts or other program changes are implemented in the future in Arizona or other states in which we operate, our revenue and earnings could be significantly impacted.
Value-Based Reimbursement
There is a trend in the healthcare industry towards value-based purchasing of healthcare services. These value-based purchasing programs include both public reporting and financial incentives tied to the quality and efficiency of care provided by facilities. The Health Reform Law expands the use of value-based purchasing initiatives in federal healthcare programs. We expect programs of this type to become more common in the healthcare industry.
Medicare requires providers to report certain quality measures in order to receive full reimbursement increases for inpatient and outpatient procedures that previously were awarded automatically. CMS has expanded, through a series of rulemakings, the number of patient care indicators that hospitals must report. Additionally, we anticipate that CMS will continue to expand the number of inpatient and outpatient quality measures. We have invested significant capital and resources in the implementation of our advanced clinical system that assists us in monitoring and reporting these quality measures. CMS makes the data submitted by hospitals, including our hospitals, public on its website.
Medicare no longer pays hospitals additional amounts for the treatment of certain preventable adverse events, also known as HACs, unless the conditions were present at admission. The Health Reform Law also prohibits the use of federal funds under the Medicaid program to reimburse providers for treating HACs. Further, beginning in federal fiscal year 2015, hospitals that rank in the worst 25% of all hospitals nationally for HACs in the previous year will receive reduced Medicare reimbursements. The Health Reform Law contains a number of other provisions that further tie reimbursement to quality and efficiency. For example, hospitals that have “excessive readmissions” for specified conditions will receive reduced reimbursement. In addition, the Health Reform Law requires the Department to implement a value-based purchasing program for inpatient hospital services. Beginning in federal fiscal
48
year 2013, the Department will reduce inpatient hospital payments for all discharges by a percentage specified by statute and pool the total amount collected from these reductions to fund payments to reward hospitals that meet or exceed certain quality performance standards established by the Department.
Many large commercial payors currently require providers to report quality data. Several commercial payors have announced that they will stop reimbursing hospitals for certain preventable adverse events. A number of state hospital associations have also announced policies addressing the waiver of patient bills for care related to a serious adverse event. In addition, managed care organizations may begin programs that condition payment on performance against specified measures. The quality measurement criteria used by commercial payors may be similar to or even more stringent than Medicare requirements.
We expect these trends towards value-based purchasing of healthcare services by Medicare and other payors to continue. Because of these trends, if we are unable to meet or exceed quality of care standards in our facilities, our operating results could be significantly impacted in the future.
Physician Alignment and Integration
In an effort to meet community needs and address coverage issues, we continue to seek alignment with physicians through various recruitment and employment strategies. Our ability to attract and retain skilled physicians to our hospitals is critical to our success and is affected by the quality of care at our hospitals. This is one reason we have taken significant steps in implementing our expanded quality of care initiatives. We believe intense efforts focusing on quality of care will enhance our ability to recruit and retain the skilled physicians necessary to make our hospitals successful.
We experience certain risks associated with the integration of medical staffs at our hospitals. As we continue to focus on our physician employment strategy, we face significant competition for skilled physicians in certain of our markets as more hospital providers adopt a physician staffing model approach, coupled with a general shortage of physicians across most specialties. This increased competition has resulted in efforts by managed care organizations to align with certain provider networks in the markets in which we operate. While we expect that employing physicians should provide relief on cost pressures associated with on-call coverage and other professional fees, we anticipate incurring additional labor and other start-up related costs as we continue the integration of employed physicians.
We also face risk from competition for outpatient business. We expect to mitigate this risk through continued focus on our physician employment strategy, the development of new access points of care, our commitment to capital investment in our hospitals, including updated technology and equipment, and our commitment to our quality of care initiatives that some competitors, including individual physicians or physician groups, may not be equipped to implement.
Uncompensated Care
Like others in the hospital industry, we continue to experience high levels of uncompensated care, including charity care and bad debts. These elevated levels are driven by the number of uninsured and under-insured patients seeking care at our hospitals, the increased acuity levels at which these patients are presenting for treatment, primarily resulting from economic pressures and their related decisions to defer care, increasing healthcare costs and other factors beyond our control, such as increases in the amount of co-payments and deductibles as employers continue to pass more of these costs on to their employees. In addition, as a result of high unemployment and its continued impact on the economy, we believe that our hospitals may continue to experience high levels of or possibly growth in bad debts and charity care. During the nine months ended June 30, 2011, our uncompensated care as a percentage of acute care revenue, which includes the impact of uninsured discounts and charity care, was 18.1%, compared to 16.0% in the prior year period.
We continue to monitor our self-pay admissions on a daily basis and continue to focus on the efficiency of our emergency rooms, point-of-service cash collections, Medicaid eligibility automation and process-flow improvements. While we continue to be successful at qualifying many uninsured patients for Medicaid or other third-party coverage, which has helped to alleviate some of the
49
pressure created from the growth in our uncompensated care, we have recently experienced a delay associated with the administrative functions of the Medicaid qualification process at the state levels. These delays are not indicative of eligibility issues, but rather staffing cut-backs as states continue working to address their budgetary issues.
We anticipate that if we experience further growth in uninsured volume and revenue over the near-term, including increased acuity levels and continued increases in co-payments and deductibles for insured patients, our uncompensated care will increase and our results of operations could be adversely affected.
The percentages of our insured and uninsured gross hospital receivables, net of discounts and contractual adjustments recorded at the time of billing (prior to allowances for contractual adjustments and doubtful accounts), are summarized as follows:
| | | | | | | | | | | | |
| | | September 30,
2009 | | | September 30,
2010 | | | June 30,
2011 | |
Insured receivables | | | 62.0 | % | | | 61.8 | % | | | 63.3 | % |
Uninsured receivables | | | 38.0 | % | | | 38.2 | % | | | 36.7 | % |
| | | | | | | | | | | | |
Total | | | 100.0 | % | | | 100.0 | % | | | 100.0 | % |
| | | | | | | | | | | | |
The percentages of our gross hospital receivables in summarized aging categories are as follows:
| | | | | | | | | | | | |
| | | September 30,
2009 | | | September 30,
2010 | | | June 30,
2011 | |
0 to 90 days | | | 69.4 | % | | | 71.9 | % | | | 70.3 | % |
91 to 180 days | | | 18.1 | % | | | 17.8 | % | | | 18.5 | % |
Over 180 days | | | 12.5 | % | | | 10.3 | % | | | 11.2 | % |
| | | | | | | | | | | | |
Total | | | 100.0 | % | | | 100.0 | % | | | 100.0 | % |
| | | | | | | | | | | | |
Revenue and Volume Trends
Net revenue for the nine months ended June 30, 2011, increased 9.5% to $2.1 billion, compared to $1.9 billion in the prior year period. Net revenue is comprised of acute care and premium revenue. Acute care revenue, which includes the impact of the Brim acquisition effective October 1, 2010 and the St. Joseph acquisition effective May 1, 2011, contributed $189.0 million to the increase in total net revenue for the nine months ended June 30, 2011, while premium revenue at Health Choice declined $10.1 million compared to the prior year period.
Acute Care Revenue
Acute care revenue is comprised of net patient revenue and other revenue. A large percentage of our hospitals’ net patient revenue consists of fixed payment, discounted sources, including Medicare, Medicaid and managed care organizations. Reimbursement for Medicare and Medicaid services are often fixed regardless of the cost incurred or the level of services provided. Similarly, a greater percentage of the managed care companies with which we contract reimburse providers on a fixed payment basis regardless of the costs incurred or the level of services provided. Net patient revenue is reported net of discounts and contractual adjustments. The contractual adjustments principally result from differences between the hospitals’ established charges and payment rates under Medicare, Medicaid and various managed care plans. Additionally, discounts and contractual adjustments result from our uninsured discount and charity care programs. Other revenue includes medical office building rental income and other miscellaneous revenue.
Certain of our acute care hospitals receive supplemental Medicaid reimbursement, including reimbursement from programs for participating private hospitals that enter into indigent care affiliation agreements with public hospitals or county governments in the state of Texas. Under the CMS-approved programs, affiliated hospitals, including our Texas hospitals, have expanded the community healthcare safety net by providing indigent healthcare services. Participation in indigent care affiliation agreements by our Texas hospitals has resulted in an increase in acute care revenue by virtue of the hospitals’ entitlement to supplemental Medicaid
50
inpatient reimbursement. Revenue recognized under these Texas private supplemental Medicaid reimbursement programs for the nine months ended June 30, 2011, was $60.2 million, compared to $60.1 million in the prior year period. The Texas private supplemental Medicaid reimbursement programs are currently being reviewed by the THHSC, which is seeking a waiver from CMS to replace the state’s current private supplemental reimbursement programs through the expansion of its managed Medicaid program. These efforts could result in the restructuring of the administration and funding of the private supplemental reimbursement programs. However, due to the uncertainty that the waiver request will be approved by CMS and the nature of ongoing deliberations with advocacy groups, we are unable to estimate the impact, if any, this will have on our revenue and earnings.
The ARRA provides for Medicare and Medicaid incentive payments beginning in calendar year 2011 for eligible hospitals and professionals that implement certified EHR technology and adopt the related meaningful use requirements. We will recognize revenues related to the Medicare or Medicaid incentive payments as we are able to complete attestations as to our eligible hospitals adopting, implementing or demonstrating meaningful use of certified EHR technology. We have recognized revenue of $8.1 million related to Medicaid incentive payments during the nine months ended June 30, 2011, which has helped to mitigate some of the pressure we have experienced resulting from the impact of recent Medicaid reimbursement cuts. We have incurred and will continue to incur both capital costs and operating expenses in order to implement our certified EHR technology and meet meaningful use requirements. These costs and expenses are projected to continue over all stages of our certified EHR technology and meaningful use implementation. As a result, the timing of the expense recognition will not correlate with the receipt of the incentive payments and the recognition of revenues. We have incurred operating expenses to implement our certified EHR technology and meet meaningful use requirements of approximately $3.1 million during the nine months ended June 30, 2011. There can be no assurance that we will be able to demonstrate meaningful use of certified EHR technology, and the failure to do so could have a material adverse effect on our results of operations.
Admissions increased 10.2% for the nine months ended June 30, 2011, compared to the prior year period. Adjusted admissions increased 12.9% for the nine months ended June 30, 2011, compared to the prior year period. On a same-facility basis, admissions declined 1.5% for the nine months ended June 30, 2011, compared to the prior year period, while adjusted admissions increased 0.4% for the nine months ended June 30, 2011, compared to the prior year period.
On a same-facility basis, our year-to-date inpatient volume has benefitted from an increase in surgeries, particularly inpatient procedures which increased 0.4% for the nine months ended June 30, 2011, and psychiatric services which increased 8.7% for the same period, each compared to the prior year period. However, hospital volumes continue to be negatively impacted, in part, by an overall industry-wide decline in obstetric related services, the impact of high unemployment and patient decisions to defer or cancel elective procedures, general primary care and other non-emergent healthcare procedures until their conditions become more acute, all resulting from the impact of the current economic environment. The deferral of non-emergent procedures has also been facilitated by an increase in the number of high deductible employer sponsored health plans, which ultimately shifts more of the medical cost responsibility onto the patient.
We believe our volumes over the long-term will grow as a result of our business strategies, including the strategic deployment of capital, the continued investment in our physician alignment strategy, the development of increased access points of care, including physician clinics, urgent care centers, outpatient imaging centers and ambulatory surgery centers, our increased marketing efforts to promote our commitment to quality and patient satisfaction, and the general aging of the population.
51
The sources of our net patient revenue by payor are summarized as follows:
| | | | | | | | | | | | | | | | | | | | |
| | | Year Ended
September 30, | | | Nine Months
Ended June 30, | |
| | | 2008 | | | 2009 | | | 2010 | | | 2010 | | | 2011 | |
Medicare | | | 23.4 | % | | | 22.7 | % | | | 23.4 | % | | | 23.4 | % | | | 24.6 | % |
Managed Medicare | | | 7.7 | % | | | 8.0 | % | | | 8.5 | % | | | 8.4 | % | | | 8.1 | % |
Medicaid and managed Medicaid | | | 13.8 | % | | | 15.2 | % | | | 15.7 | % | | | 15.2 | % | | | 14.8 | % |
Managed care | | | 46.0 | % | | | 43.0 | % | | | 40.2 | % | | | 40.7 | % | | | 39.8 | % |
Self-pay | | | 9.1 | % | | | 11.1 | % | | | 12.2 | % | | | 12.3 | % | | | 12.7 | % |
| | | | | | | | | | | | | | | | | | | | |
Total | | | 100.0 | % | | | 100.0 | % | | | 100.0 | % | | | 100.0 | % | | | 100.0 | % |
| | | | | | | | | | | | | | | | | | | | |
Our net patient revenue payor mix, as shown in the table above, has been impacted by our recent acquisitions, which include hospitals with higher Medicaid and managed Medicaid utilization and lower self-pay volume, as compared to our same-facility hospitals. The increase in our Medicaid and managed Medicaid patient mix has been offset by the impact of Medicaid rate cuts experienced in the states where we operate.
Net patient revenue per adjusted admission increased 1.4% for the nine months ended June 30, 2011, compared to the prior year period. On a same-facility basis, net patient revenue per adjusted admission increased 3.5% for the nine months ended June 30, 2011, compared to the prior year period. While our net patient revenue per adjusted admission continues to increase, we have experienced moderating rates of pricing growth resulting from the impact of high unemployment and other industry pressures, including elevated levels of Medicaid and managed Medicaid, which typically result in lower reimbursement on a per adjusted admission basis. As well, the impact of state budgetary issues on Medicaid funding has resulted in rate cuts to providers, which has caused a decline in pricing related to Medicaid and managed Medicaid volumes. As states continue working through their budgetary issues, any additional cuts to Medicaid funding would negatively impact our future pricing and earnings.
See “Business — Sources of Acute Care Revenue” and “Business — Government Regulation and Other Factors” included elsewhere in this prospectus, for a description of the types of payments we receive for services provided to patients enrolled in the traditional Medicare plan, managed Medicare plans, Medicaid plans, managed Medicaid plans and managed care plans. In those sections, we also discussed the unique reimbursement features of the traditional Medicare plan, including the annual Medicare regulatory updates published by CMS that impact reimbursement rates for services provided under the plan. The future potential impact to reimbursement for certain of these payors under the Health Reform Law is also addressed in these sections.
Premium Revenue
Premium revenue generated under the AHCCCS and CMS contracts with Health Choice represented 28.1% of our consolidated net revenue for the nine months ended June 30, 2011, compared to 31.2% in the prior year period. The decline in premium revenue as a percentage of our consolidated net revenue is primarily the result of the recent acquisitions in our acute care segment.
Most of the premium revenue at Health Choice is derived through a contract with AHCCCS to provide specified health services to qualified Medicaid enrollees through contracted providers. AHCCCS is the state agency that administers Arizona’s Medicaid program. The contract requires Health Choice to arrange for healthcare services for enrolled Medicaid patients in exchange for fixed monthly premiums, based upon negotiated per capita member rates, and supplemental payments from AHCCCS. Health Choice also contracts with CMS to provide coverage as a MAPD SNP. This contract allows Health Choice to offer Medicare and Part D drug benefit coverage to new and existing dual-eligible members (i.e., those that are eligible for Medicare and Medicaid). Effective for this 2011 plan year, SNPs are required to meet additional CMS requirements, including requirements relating to model of care, cost-sharing, disclosure of information and reporting of quality measures.
52
Critical Accounting Policies And Estimates
Our consolidated financial statements have been prepared in accordance with U.S. generally accepted accounting principles. In preparing our financial statements, we make estimates, judgments and assumptions that affect the reported amounts of assets and liabilities at the dates of the financial statements and the reported amounts of revenue and expenses during the reporting periods. Actual results could differ from those estimates.
We have determined an accounting estimate to be critical if: (1) the accounting estimate requires us to make assumptions about matters that were highly uncertain at the time the accounting estimate was made and (2) changes in the estimate would have a material impact on our financial condition or results of operations. There have been no changes in the nature of our critical accounting policies or the application of those policies during the nine months ended June 30, 2011, that would require update to these September 30, 2010 disclosures. There are other items within our financial statements that require estimation but are not deemed critical as defined herein. Changes in estimates used in these and other items could have a material impact on our financial statements.
Allowance for Doubtful Accounts.Our ability to collect outstanding receivables from third-party payors and patients is critical to our operating performance and cash flows. The primary collection risk lies with uninsured patient accounts or patient accounts for which primary insurance has paid but a patient portion remains outstanding. The provision for bad debts and the allowance for doubtful accounts relate primarily to amounts due directly from patients. Our estimation of the allowance for doubtful accounts is based primarily upon the type and age of the patient accounts receivable and the effectiveness of our collection efforts. Our policy is to reserve a portion of all self-pay receivables, including amounts due from the uninsured and amounts related to co-payments and deductibles, as these charges are recorded. We monitor our accounts receivable balances and the effectiveness of our reserve policies on a monthly basis and review various analytics to support the basis for our estimates. These efforts primarily consist of reviewing the following:
| | • | | Historical write-off and collection experience using a hindsight or look-back approach; |
| | • | | Revenue and volume trends by payor, particularly the self-pay components; |
| | • | | Changes in the aging and payor mix of accounts receivable, including increased focus on accounts due from the uninsured and accounts that represent co-payments and deductibles due from patients; |
| | • | | Cash collections as a percentage of net patient revenue less bad debt expense; |
| | • | | Trending of days revenue in accounts receivable; and |
| | • | | Various allowance coverage statistics. |
We regularly perform hindsight procedures to evaluate historical write-off and collection experience throughout the year to assist in determining the reasonableness of our process for estimating the allowance for doubtful accounts. We do not pursue collection of amounts related to patients who qualify for charity care under our guidelines. Charity care accounts are deducted from gross revenue and do not affect the provision for bad debts.
At September 30, 2010, our self-pay receivables, including amounts due from uninsured patients and co-payment and deductible amounts due from insured patients, were $160.7 million and our allowance for doubtful accounts was $125.4 million. Excluding third-party settlement balances, days revenue in accounts receivable were 43 days at September 30, 2010, compared to 49 days at September 30, 2009. For the year ended September 30, 2010, the provision for bad debts was 11.4% of acute care revenue, compared to 11.5% in the prior year. Significant changes in payor mix or business office operations could have a significant impact on the provision for bad debts, as well as our results of operations and cash flows.
Allowance for Contractual Discounts and Settlement Estimates.We derive a significant portion of our net patient revenue from Medicare, Medicaid and managed care payors that receive discounts from our standard charges. For the years ended September 30, 2010, 2009 and 2008, Medicare, Medicaid and managed care revenue together accounted for 87.8%, 88.9% and 90.9%, respectively, of our hospitals’ net patient revenue.
53
We estimate contractual discounts and allowances based upon payment terms outlined in our managed care contracts, by federal and state regulations for the Medicare and various Medicaid programs, and in accordance with terms of our uninsured discount program. Contractual discounts for most of our patient revenue are determined by an automated process that establishes the discount on a patient-by-patient basis. The payment terms or fee schedules for most payors have been entered into our patient accounting systems. Automated (system-generated) contractual discounts are recorded, at the time a patient account is billed, based upon the system-loaded payment terms. In certain instances for payors that are not significant or who have not entered into a contract with us, we make manual estimates in determining contractual allowances based upon historical collection rates. At the end of each month, we estimate contractual allowances for all unbilled accounts based on payor-specific six-month average contractual discount rates.
For governmental payors such as Medicare and Medicaid, we determine contractual discounts or allowances based upon the program’s reimbursement (payment) methodology (i.e. either prospectively determined or retrospectively determined based on costs as defined by the government payor). These contractual discounts are determined by an automated process in a manner similar to the process used for managed care revenue. Under prospective payment programs, we record contractual discounts based upon predetermined reimbursement rates. For retrospective cost-based revenues, which are less prevalent, we estimate contractual allowances based upon historical and current factors which are adjusted as necessary in future periods, when final settlements of filed cost reports are received. Net adjustments to estimated third-party payor settlements, also known as prior year contractuals, resulted in an increase in acute care revenue of $5.2 million, $3.2 million and $1.0 million for the years ended September 30, 2010, 2009 and 2008, respectively.
Management continually reviews the contractual estimation process to consider and incorporate updates to laws and regulations and the frequent changes in managed care contractual terms that result from contract renegotiations and renewals. All contractual adjustments, regardless of type of payor or method of calculation, are reviewed and compared to actual payment experience on an individual patient account basis. Discrepancies between expected and actual payments are reviewed, and as necessary, appropriate corrections to the patient accounts are made to reflect actual payments received. If a discrepancy exists between the payment terms loaded into the contract management system and the actual discount based on payments received, the system is updated accordingly to ensure appropriate discounting of future charges.
Additionally, we rely on other analytical tools to ensure our contractual discounts are reasonably estimated. These include, but are not limited to, monitoring of collection experience by payor, reviewing total patient collections as a percentage of net patient revenue (adjusted for the provision for bad debts) on a trailing twelve-month basis, gross to net patient revenue comparisons, contractual allowance metrics, etc. As well, patient accounts are continually reviewed to ensure all patient accounts reflect either system-generated discounts or estimated contractual allowances, as necessary.
Medicare and Medicaid regulations and various managed care contracts are often complex and may include multiple reimbursement mechanisms for different types of services provided in our healthcare facilities, requiring complex calculations and assumptions which are subject to interpretation. Additionally, the services authorized and provided and resulting reimbursement are often subject to interpretation. These interpretations sometimes result in payments that differ from our estimates. Additionally, updates to regulations and contract renegotiations occur frequently, necessitating continual review and assessment of the estimation process by management. We have made significant investments in our patient accounting information systems, human resources and internal controls, which we believe greatly reduces the likelihood of a significant variance occurring between the recorded and estimated contractual discounts. Given that most of our contractual discounts are pre-defined or contractually based, and as a result of continual internal monitoring processes and our use of analytical tools, we believe the aggregate differences between amounts recorded for initial contractual discounts and final contractual discounts resulting from payments received are not significant. Finally, we believe that having a wide variety and large number of managed care contracts that are subject to review and administration on a hospital-by-hospital basis minimizes the impact on the Company’s net revenue of any imprecision in recorded contractual discounts caused by the system-load of payment terms of a particular payor. We believe that our systems and processes, as well as other items discussed, provide reasonable assurance that any change in estimate related to contractual discounts is immaterial to our financial position, results of operations and cash flows.
54
Insurance Reserves. Given the nature of our operating environment, we may become subject to medical malpractice or workers compensation claims or lawsuits. We maintain third-party insurance coverage for individual malpractice and workers compensation claims to mitigate a portion of this risk. In addition, we maintain excess coverage limiting our exposure to an aggregate annual amount for claims. We estimate our reserve for self-insured professional and general liability and workers compensation risks using historical claims data, demographic factors, severity factors, current incident logs and other actuarial analysis. At September 30, 2010 and 2009, our professional and general liability accrual for asserted and unasserted claims was $41.6 million and $41.7 million, respectively. For the year ended September 30, 2010, our total premiums and self-insured retention cost for professional and general liability insurance was $23.4 million, compared with $25.5 million in the prior year.
The estimated accrual for medical malpractice and workers compensation claims could be significantly affected should current and future occurrences differ from historical claims trends. The estimation process is also complicated by the complexity and changing nature of tort reform in the states in which we operate. While we monitor current claims closely and consider outcomes when estimating our insurance accruals, the complexity of the claims and wide range of potential outcomes often hampers timely adjustments to the assumptions used in the estimates.
Valuations from our independent actuary for professional and general liability losses resulted in a change in related estimates for prior years which decreased professional and general liability expense by the following amounts (in millions):
| | | | |
Year ended September 30, 2010 | | $ | (2.6 | ) |
Year ended September 30, 2009 | | $ | (1.2 | ) |
Year ended September 30, 2008 | | $ | (6.8 | ) |
Our estimate of the reserve for professional and general liability claims is based upon actuarial calculations that are completed semi-annually. The changes in estimates noted above were recognized in the periods in which the independent actuarial calculations were received. The key assumptions underlying the development of our estimate (loss development, trends and increased limits factors) have not changed materially, as they are largely based upon professional liability insurance industry data published by the Insurance Services Office (“ISO”), a leading provider of data, underwriting, risk management and legal/regulatory services. The reductions in professional and general liability expense related to changes in prior year estimates reflected above for the years ended September 30, 2010, 2009 and 2008, are the result of better than expected claims experience as compared to the industry benchmarks for loss development included in the original actuarial estimate.
Sensitivity in the estimate of our professional and general liability claims reserve is reflected in various actuarial confidence levels. We utilize a statistical confidence level of 50% in developing our best estimate of the reserve for professional and general liability claims. Higher statistical confidence levels, while not representative of our best estimate, provide a range of reasonably likely outcomes upon resolution of the related claims. The following table outlines our reported reserve amounts compared to reserve levels established at the higher statistical confidence levels.
| | | | |
As reported at September 30, 2010 | | $ | 41.6 | |
75% Confidence Level | | $ | 48.2 | |
90% Confidence Level | | $ | 60.1 | |
Valuations from our independent actuary for workers’ compensation losses resulted in a change in related estimates for prior years which increased (decreased) workers’ compensation expense by the following amounts (in millions):
| | | | |
Year ended September 30, 2010 | | $ | 1.1 | |
Year ended September 30, 2009 | | $ | (0.5 | ) |
Year ended September 30, 2008 | | $ | 0.8 | |
55
Medical Claims Payable.Medical claims expense, including claims paid to our hospitals, was $690.5 million, $602.1 million and $461.6 million, or 87.2%, 86.1% and 85.2% of premium revenue, for the years ended September 30, 2010, 2009 and 2008, respectively. For the years ended September 30, 2010, 2009 and 2008, $11.8 million, $9.3 million and $9.6 million, respectively, of health plan payments made to hospitals and other healthcare entities owned by us for services provided to our enrollees were eliminated in consolidation.
The following table shows the components of the change in medical claims payable (in thousands):
| | | | | | | | |
| | | Year Ended
September 30,
2010 | | | Year Ended
September 30,
2009 | |
Medical claims payable as of October 1 | | $ | 113,519 | | | $ | 97,343 | |
Medical claims expense incurred during the year: | | | | | | | | |
Related to current year | | | 697,052 | | | | 620,153 | |
Related to prior years | | | (6,596 | ) | | | (18,077 | ) |
| | | | | | | | |
Total expenses | | | 690,456 | | | | 602,076 | |
Medical claims payments during the year: | | | | | | | | |
Related to current year | | | (587,292 | ) | | | (508,299 | ) |
Related to prior years | | | (105,310 | ) | | | (77,601 | ) |
| | | | | | | | |
Total payments | | | (692,602 | ) | | | (585,900 | ) |
| | | | | | | | |
Medical claims payable as of September 30 | | $ | 111,373 | | | $ | 113,519 | |
| | | | | | | | |
As reflected in the table above, medical claims expense for the year ended September 30, 2010, includes a $6.6 million reduction of medical costs related to prior years resulting from favorable development in the Medicaid and Medicare product lines of $6.4 million and $209,000, respectively. The favorable development is attributable to lower than anticipated medical costs. Medical claims expense for the year ended September 30, 2009, includes an $18.1 million reduction of medical costs related to prior years resulting from favorable development in the Medicaid and Medicare product lines of $15.5 million and $2.6 million, respectively. The favorable development is attributable to lower than anticipated medical costs and is offset, in part, by $10.8 million in reductions in premium revenue associated with settlements of various prior year program receivables.
We estimate our medical claims payable using historical claims experience (including severity and payment lag time) and other actuarial analysis including number of enrollees, age of enrollees and certain enrollee health indicators to predict the cost of healthcare services provided to enrollees during any given period. While management believes that its estimation methodology effectively captures trends in medical claims costs, actual payments could differ significantly from our estimates given changes in healthcare costs or adverse experience. For example, our medical claims payable is primarily composed of estimates related to the most recent three months and periods prior to the most recent three months. The claims trend factor, which is developed through a comprehensive analysis of claims incurred in prior months, is the most significant component used in developing the claims liability estimates for the most recent three months. The completion factor is an actuarial estimate, based upon historical experience, of the percentage of incurred claims during a given period that have been adjudicated as of the date of estimation. The completion factor is the most significant component used in developing the claims liability estimates for the periods prior to the most recent three months. The following table illustrates the sensitivity of our medical claims payable at September 30, 2010, and the estimated potential impact on our results of operations, to changes in these factors that management believes are reasonably likely based upon our historical experience and currently available information (dollars in thousands):
| | | | | | | | | | | | | | | | |
| Claims Trend Factor | | | | | Completion Factor | |
Increase (Decrease) in
Factor | | | Increase (Decrease) in
Medical Claims Payable | | | | | Increase (Decrease) in
Factor | | | Medical Claims Payable | |
| | (3.0 | )% | | $ | (4,363 | ) | | | | | 1.0 | % | | $ | (5,042 | ) |
| | (2.0 | ) | | | (2,908 | ) | | | | | 0.5 | | | | (2,524 | ) |
| | (1.0 | ) | | | (1,454 | ) | | | | | (0.5 | ) | | | 2,592 | |
| | 1.0 | | | | 1,454 | | | | | | (1.0 | ) | | | 5,190 | |
56
Goodwill and Other Intangibles.The accounting policies and estimates related to goodwill and other intangibles are considered critical because of the significant impact that impairment could have on our operating results. We record all assets and liabilities acquired in purchase acquisitions, including goodwill, indefinite-lived intangibles, and other intangibles, at fair value as required by Financial Accounting Standards Board (“FASB”) authoritative guidance regarding business combinations. Goodwill, which was $718.2 million at September 30, 2010, is not amortized but is subject to tests for impairment annually or more often if events or circumstances indicate it may be impaired. The initial recording of goodwill and other intangibles requires subjective judgments concerning estimates of the fair value of the acquired assets. An impairment loss is recorded to the extent that the carrying amount of goodwill exceeds its implied fair value. We did not record an impairment loss during the year ended September 30, 2010. During the year ended September 30, 2009, we recorded a $64.6 million non-cash charge ($43.2 million after tax) related to the impairment of goodwill in our Florida market. Other identifiable intangible assets, net of accumulated amortization, were $27.0 million at September 30, 2010, compared to $30.0 million in the prior year. These are amortized over their estimated useful lives and are evaluated for impairment if events and circumstances indicate a possible impairment. Such evaluation of other intangible assets is based on undiscounted cash flow projections. Estimated cash flows may extend far into the future and, by their nature, are difficult to determine over an extended timeframe. Factors that may significantly affect the estimates include, among others, competitive forces, customer behaviors and attrition, changes in revenue growth trends, cost structures and technology, and changes in discount rates and specific industry or market sector conditions. Other key judgments in accounting for intangibles include useful life and classification between goodwill and indefinite-lived intangibles or other intangibles which require amortization. See “Goodwill and Other Intangible Assets” in the Notes to Consolidated Financial Statements for additional information regarding intangible assets. To assist in assessing the impact of a goodwill or intangible asset impairment charge at September 30, 2010, we have $745.2 million of goodwill and intangible assets. The impact of a 5% impairment charge would result in a reduction in pre-tax income of $37.3 million.
Income Taxes. We estimate and record a valuation allowance to reduce deferred tax assets to the amount we believe is more likely than not to be realized in future periods based on all relevant information. We believe that future income as well as the reversal of deferred tax liabilities will enable us to realize the deferred tax assets we have recorded, net of the valuation allowance we have established.
Certain tax matters require interpretations of tax law that may be subject to future challenge and may not be upheld under tax audit. Significant judgment is required in determining and assessing the impact of such tax-related contingencies. Effective October 1, 2007, we adopted the provisions of FASB authoritative guidance regarding accounting for uncertainty in income taxes, which prescribes a recognition threshold and measurement attribute for the financial statement recognition and measurement of all tax positions accounted for in accordance with provisions of FASB authoritative guidance regarding accounting for income taxes. In addition, the provisions related to accounting for uncertainty in income taxes provides guidance on derecognition, classification, interest and penalties, accounting in interim periods, disclosure and transition. We applied these provisions to all tax positions upon initial adoption of this guidance. Only tax positions that meet the more-likely-than-not recognition threshold at the effective date, October 1, 2007, have been recognized in connection with these provisions.
The provisions regarding accounting for uncertainty in income taxes permits interest and penalties on underpayments of income taxes to be classified as interest expense, income tax expense, or another appropriate expense classification based on the accounting election of the company. Our policy is to classify interest and penalties as a component of income tax expense.
The estimates, judgments and assumptions used by us under “Allowance for Doubtful Accounts,” “Allowance for Contractual Discounts and Settlement Estimates,” “Insurance Reserves,” “Medical Claims Payable,” “Goodwill and Other Intangibles” and “Income Taxes” are, we believe, reasonable, but involve inherent uncertainties as described above, which may or may not be controllable by management. As a result, the accounting for such items could result in different amounts if management used different assumptions or if different conditions occur in future periods.
57
Results Of Operation Summary
Consolidated
The following table sets forth, for the periods indicated, results of consolidated operations expressed in dollar terms and as a percentage of net revenue. Such information has been derived from our audited consolidated and unaudited condensed consolidated statements of operations for each period presented.
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
| | | Year Ended September 30, | | | Nine Months Ended June 30, | |
| | | 2008 | | | 2009 | | | 2010 | | | 2010 | | | 2011 | |
($ in thousands) | | Amount | | | % | | | Amount | | | % | | | Amount | | | % | | | Amount | | | % | | | Amount | | | % | |
| | | | | | | | | | |
Net revenue: | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
| | | | | | | | | | |
Acute care revenue | | $ | 1,523,790 | | | | 73.8 | % | | $ | 1,662,469 | | | | 70.4 | % | | $ | 1,729,344 | | | | 68.6 | % | | $ | 1,300,445 | | | | 68.8 | % | | $ | 1,489,432 | | | | 71.9 | % |
Premium revenue | | | 541,746 | | | | 26.2 | % | | | 699,503 | | | | 29.6 | % | | | 792,062 | | | | 31.4 | % | | | 591,022 | | | | 31.2 | % | | | 580,917 | | | | 28.1 | % |
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
Total net revenue | | | 2,065,536 | | | | 100.0 | % | | | 2,361,972 | | | | 100.0 | % | | | 2,521,406 | | | | 100.0 | % | | | 1,891,467 | | | | 100.0 | % | | | 2,070,349 | | | | 100.0 | % |
| | | | | | | | | | |
Costs and expenses: | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
Salaries and benefits | | | 632,109 | | | | 30.6 | % | | | 660,921 | | | | 28.0 | % | | | 686,303 | | | | 27.2 | % | | | 514,688 | | | | 27.2 | % | | | 597,063 | | | | 28.8 | % |
Supplies | | | 231,259 | | | | 11.2 | % | | | 250,573 | | | | 10.6 | % | | | 266,545 | | | | 10.6 | % | | | 200,167 | | | | 10.6 | % | | | 237,431 | | | | 11.5 | % |
Medical claims | | | 452,055 | | | | 21.9 | % | | | 592,760 | | | | 25.1 | % | | | 678,651 | | | | 26.9 | % | | | 510,692 | | | | 27.0 | % | | | 484,635 | | | | 23.4 | % |
Other operating expenses | | | 283,123 | | | | 13.7 | % | | | 325,735 | | | | 13.8 | % | | | 363,916 | | | | 14.4 | % | | | 266,854 | | | | 14.1 | % | | | 315,254 | | | | 15.2 | % |
Provision for bad debts | | | 161,936 | | | | 7.8 | % | | | 192,563 | | | | 8.2 | % | | | 197,680 | | | | 7.9 | % | | | 142,901 | | | | 7.6 | % | | | 175,100 | | | | 8.5 | % |
Rentals and leases | | | 36,633 | | | | 1.8 | % | | | 39,127 | | | | 1.7 | % | | | 39,955 | | | | 1.6 | % | | | 30,487 | | | | 1.6 | % | | | 34,229 | | | | 1.7 | % |
Interest expense, net | | | 75,665 | | | | 3.7 | % | | | 67,890 | | | | 2.9 | % | | | 66,810 | | | | 2.6 | % | | | 50,065 | | | | 2.7 | % | | | 60,984 | | | | 2.9 | % |
Depreciation and amortization | | | 96,741 | | | | 4.7 | % | | | 97,462 | | | | 4.1 | % | | | 96,106 | | | | 3.8 | % | | | 71,909 | | | | 3.8 | % | | | 74,942 | | | | 3.6 | % |
Management fees | | | 5,000 | | | | 0.2 | % | | | 5,000 | | | | 0.2 | % | | | 5,000 | | | | 0.2 | % | | | 3,750 | | | | 0.2 | % | | | 3,750 | | | | 0.2 | % |
Impairment of goodwill | | | — | | | | — | | | | 64,639 | | | | 2.7 | % | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | |
Hurricane-related property damage | | | 3,589 | | | | 0.2 | % | | | 938 | | | | 0.0 | % | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | |
Loss on extinguishment of debt | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | 23,075 | | | | 1.1 | % |
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
| | | | | | | | | | |
Total costs and expenses | | | 1,978,110 | | | | 95.8 | % | | | 2,297,608 | | | | 97.3 | % | | | 2,400,966 | | | | 95.2 | % | | | 1,791,513 | | | | 94.8 | % | | | 2,006,463 | | | | 96.9 | % |
| | | | | | | | | | |
Earnings from continuing operations before gain (loss) on disposal of assets and income taxes | | | 87,426 | | | | 4.2 | % | | | 64,364 | | | | 2.7 | % | | | 120,440 | | | | 4.8 | % | | | 99,954 | | | | 5.2 | % | | | 63,886 | | | | 3.1 | % |
| | | | | | | | | | |
Gain (loss) on disposal of assets, net | | | (75 | ) | | | (0.0 | )% | | | 1,465 | | | | 0.1 | % | | | 108 | | | | 0.0 | % | | | (206 | ) | | | (0.0 | )% | | | 771 | | | | 0.0 | % |
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
| | | | | | | | | | |
Earnings from continuing operations before income taxes | | | 87,351 | | | | 4.2 | % | | | 65,829 | | | | 2.8 | % | | | 120,548 | | | | 4.8 | % | | | 99,748 | | | | 5.2 | % | | | 64,657 | | | | 3.1 | % |
| | | | | | | | | | |
Income tax expense | | | 35,325 | | | | 1.7 | % | | | 27,576 | | | | 1.2 | % | | | 44,715 | | | | 1.8 | % | | | 36,544 | | | | 1.9 | % | | | 24,078 | | | | 1.1 | % |
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
| | | | | | | | | | |
Net earnings from continuing operations | | | 52,026 | | | | 2.5 | % | | | 38,253 | | | | 1.6 | % | | | 75,833 | | | | 3.0 | % | | | 63,204 | | | | 3.3 | % | | | 40,579 | | | | 2.0 | % |
| | | | | | | | | | |
Loss from discontinued operations, net of income taxes | | | (11,275 | ) | | | (0.5 | )% | | | (176 | ) | | | (0.0 | )% | | | (1,087 | ) | | | (0.1 | )% | | | (363 | ) | | | (0.0 | )% | | | (6,069 | ) | | | (0.3 | )% |
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
| | | | | | | | | | |
Net earnings | | | 40,751 | | | | 2.0 | % | | | 38,077 | | | | 1.6 | % | | | 74,746 | | | | 2.9 | % | | | 62,841 | | | | 3.3 | % | | | 34,510 | | | | 1.7 | % |
| | | | | | | | | | |
Net earnings attributable to non-controlling interests | | | (4,437 | ) | | | (0.2 | )% | | | (9,987 | ) | | | (0.4 | )% | | | (8,279 | ) | | | (0.3 | )% | | | (6,063 | ) | | | (0.3 | )% | | | (6,201 | ) | | | (0.3 | )% |
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
| | | | | | | | | | |
Net earnings attributable to IASIS Healthcare LLC | | $ | 36,314 | | | | 1.8 | % | | $ | 28,090 | | | | 1.2 | % | | $ | 66,467 | | | | 2.6 | % | | $ | 56,778 | | | | 3.0 | % | | $ | 28,309 | | | | 1.4 | % |
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
58
Acute Care
The following table sets forth, for the periods indicated, results of our acute care operations expressed in dollar terms and as a percentage of acute care revenue. Such information has been derived from our audited consolidated and unaudited condensed consolidated statements of operations for each period presented.
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
| | | Year Ended September 30, | | | Nine Months Ended June 30, | |
| | | 2008 | | | 2009 | | | 2010 | | | 2010 | | | 2011 | |
($ in thousands) | | Amount | | | % | | | Amount | | | % | | | Amount | | | % | | | Amount | | | % | | | Amount | | | % | |
| | | | | | | | | | |
Net revenue: | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
| | | | | | | | | | |
Acute care revenue | | $ | 1,523,790 | | | | 99.4 | % | | $ | 1,662,469 | | | | 99.4 | % | | $ | 1,729,344 | | | | 99.3 | % | | $ | 1,300,445 | | | | 99.4 | % | | $ | 1,489,432 | | | | 99.4 | % |
Revenue between segments(1) | | | 9,594 | | | | 0.6 | % | | | 9,316 | | | | 0.6 | % | | | 11,805 | | | | 0.7 | % | | | 8,331 | | | | 0.6 | % | | | 8,532 | | | | 0.6 | % |
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
Total acute care revenue | | | 1,533,384 | | | | 100.0 | % | | | 1,671,785 | | | | 100.0 | % | | | 1,741,149 | | | | 100.0 | % | | | 1,308,776 | | | | 100.0 | % | | | 1,497,964 | | | | 100.0 | % |
Costs and expenses: | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
| | | | | | | | | | |
Salaries and benefits | | | 614,442 | | | | 40.1 | % | | | 641,893 | | | | 38.4 | % | | | 667,154 | | | | 38.3 | % | | | 500,283 | | | | 38.2 | % | | | 581,592 | | | | 38.8 | % |
| | | | | | | | | | |
Supplies | | | 231,001 | | | | 15.1 | % | | | 250,310 | | | | 15.0 | % | | | 266,347 | | | | 15.3 | % | | | 200,030 | | | | 15.3 | % | | | 237,274 | | | | 15.8 | % |
Other operating expenses | | | 264,814 | | | | 17.3 | % | | | 302,804 | | | | 18.1 | % | | | 339,304 | | | | 19.5 | % | | | 248,380 | | | | 19.0 | % | | | 295,913 | | | | 19.8 | % |
| | | | | | | | | | |
Provision for bad debts | | | 161,936 | | | | 10.6 | % | | | 192,563 | | | | 11.5 | % | | | 197,680 | | | | 11.4 | % | | | 142,901 | | | | 10.9 | % | | | 175,100 | | | | 11.7 | % |
Rentals and leases | | | 35,466 | | | | 2.3 | % | | | 37,563 | | | | 2.2 | % | | | 38,409 | | | | 2.2 | % | | | 29,334 | | | | 2.2 | % | | | 32,991 | | | | 2.2 | % |
Interest expense, net | | | 75,665 | | | | 4.9 | % | | | 67,890 | | | | 4.1 | % | | | 66,810 | | | | 3.8 | % | | | 50,065 | | | | 3.8 | % | | | 60,984 | | | | 4.1 | % |
Depreciation and amortization | | | 93,003 | | | | 6.0 | % | | | 94,014 | | | | 5.6 | % | | | 92,544 | | | | 5.3 | % | | | 69,240 | | | | 5.3 | % | | | 72,273 | | | | 4.8 | % |
Management fees | | | 5,000 | | | | 0.3 | % | | | 5,000 | | | | 0.3 | % | | | 5,000 | | | | 0.3 | % | | | 3,750 | | | | 0.3 | % | | | 3,750 | | | | 0.3 | % |
Impairment of goodwill | | | — | | | | — | | | | 64,639 | | | | 3.9 | % | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | |
Hurricane-related property damage | | | 3,589 | | | | 0.2 | % | | | 938 | | | | 0.1 | % | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | |
Loss on extinguishment of debt | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | 23,075 | | | | 1.5 | % |
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
Total costs and expenses | | | 1,484,916 | | | | 96.8 | % | | | 1,657,614 | | | | 99.2 | % | | | 1,673,248 | | | | 96.1 | % | | | 1,243,983 | | | | 95.0 | % | | | 1,482,952 | | | | 99.0 | % |
| | | | | | | | | | |
Earnings from continuing operations before gain (loss) on disposal of assets and income taxes | | | 48,468 | | | | 3.2 | % | | | 14,171 | | | | 0.8 | % | | | 67,901 | | | | 3.9 | % | | | 64,793 | | | | 5.0 | % | | | 15,012 | | | | 1.0 | % |
| | | | | | | | | | |
Gain (loss) on disposal of assets, net | | | (75 | ) | | | (0.0 | )% | | | 1,616 | | | | 0.1 | % | | | 108 | | | | 0.0 | % | | | (206 | ) | | | (0.0 | )% | | | 771 | | | | 0.1 | % |
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
| | | | | | | | | | |
Earnings from continuing operations before income taxes | | $ | 48,393 | | | | 3.2 | % | | $ | 15,787 | | | | 0.9 | % | | $ | 68,009 | | | | 3.9 | % | | $ | 64,587 | | | | 5.0 | % | | $ | 15,783 | | | | 1.1 | % |
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
| (1) | Revenue between segments is eliminated in our consolidated results. |
59
Nine Months Ended June 30, 2011 and 2010
Acute care revenue —Acute care revenue for the nine months ended June 30, 2011, was $1.5 billion, an increase of $189.2 million or 14.5%, compared to $1.3 billion in the prior year period. The increase in acute care revenue, which includes the impact of the Brim and St. Joseph acquisitions, is comprised of an increase in adjusted admissions of 12.9% and an increase in net patient revenue per adjusted admission of 1.4%.
Net adjustments to estimated third-party payor settlements, also known as prior year contractuals, resulted in an increase in acute care revenue of $2.2 million and $4.7 million for the nine months ended June 30, 2011 and 2010, respectively.
Salaries and benefits —Salaries and benefits expense for the nine months ended June 30, 2011, was $581.6 million, or 38.8% of acute care revenue, compared to $500.3 million, or 38.2% of acute care revenue in the prior year period. Included in the prior year period was $2.0 million of stock-based compensation incurred in connection with the repurchase of certain equity by our parent company. Also, included in the current year period was $1.3 million in severance related costs associated with the transition of our executive management. The remaining increase in our salaries and benefits expense as a percentage of acute care revenue is due to our recent acquisitions, which contributed an increase of 0.2%, and the expansion of our employed physician base, which requires additional investments in labor and other practice-related costs, including infrastructure and physician support staff.
Supplies —Supplies expense for the nine months ended June 30, 2011, was $237.3 million, or 15.8% of acute care revenue, compared to $200.0 million, or 15.3% of acute care revenue in the prior year period. The increase in supplies as a percentage of acute care revenue is primarily the result of a shift in the mix of our surgical volume to cases with more costly implant utilization, particularly in the area of orthopedics.
Other operating expenses —Other operating expenses for the nine months ended June 30, 2011, were $295.9 million, or 19.8% of acute care revenue, compared to $248.4 million, or 19.0% of acute care revenue in the prior year period. Included in the current year period was $3.1 million in settlement costs related to a terminated vendor contract for services provided from fiscal years 2006 to 2008 and $1.0 million in costs related to the start-up of our physician professional liability captive insurance program. Other operating expenses in the current year period also included a $948,000 increase in insurance expense resulting from changes in prior year actuarial estimates associated with our professional and general liability reserves, compared to a $1.9 million reduction in the prior year period. The remaining increase in our other operating expenses as a percentage of acute care revenue is primarily due to our recent acquisitions.
60
Provision for bad debts —Provision for bad debts for the nine months ended June 30, 2011, was $175.1 million, or 11.7% of acute care revenue, compared to $142.9 million, or 10.9% of acute care revenue in the prior year period. The increase in our provision for bad debts as a percentage of acute care revenue is due to an increase in self-pay volume and revenue, including related acuity levels, which have resulted primarily from patient decisions to defer non-emergent healthcare needs as a result of economic pressures and high unemployment.
Years Ended September 30, 2010 and 2009
Acute care revenue — Acute care revenue for the year ended September 30, 2010, was $1.7 billion, an increase of $69.4 million, or 4.1%, compared to $1.7 billion in the prior year. The increase in acute care revenue is comprised of an increase in adjusted admissions of 0.6% and an increase in net patient revenue per adjusted admission of 3.8%.
Salaries and benefits — Salaries and benefits expense for the year ended September 30, 2010, was $667.2 million, or 38.3% of acute care revenue, compared to $641.9 million, or 38.4% of acute care revenue in the prior year.
Supplies — Supplies expense for the year ended September 30, 2010, was $266.3 million, or 15.3% of acute care revenue, compared to $250.3 million, or 15.0% of acute care revenue, in the prior year. The increase in supplies as a percentage of acute care revenue is primarily the result of a shift in the mix of our surgical volume to cases with more costly implant utilization, such as certain cardiology and orthopedic procedures.
Other operating expenses — Other operating expenses for the year ended September 30, 2010, were $339.3 million, or 19.5% of acute care revenue, compared to $302.8 million, or 18.1% of acute care revenue in the prior year. Included in the current year were increased professional fees associated with our participation in the indigent care affiliation agreements in our Texas market. Excluding the impact of these indigent care affiliation agreements, other operating expenses as a percentage of acute care revenue were 16.7% for the year ended September 30, 2010, compared to 16.1% in the prior year. The remaining increase in other operating expenses as a percentage of acute care revenue in the current year period is impacted by a 0.3% increase in non-income related taxes, and a 0.4% increase in purchased services related to information technology costs and collection agency fees.
Provision for bad debts — Provision for bad debts for the year ended September 30, 2010, was $197.7 million, or 11.4% of acute care revenue, compared to $192.6 million, or 11.5% of acute care revenue in the prior year.
Earnings from continuing operations before income taxes — Earnings from continuing operations before income taxes increased $52.2 million to $68.0 million for the year ended September 30, 2010, compared to $15.8 million in the prior year. Earnings from continuing operations before income taxes for the year ended September 30, 2009, included the impact of a $64.6 million non-cash charge related to the impairment of goodwill in our Florida market.
Years Ended September 30, 2009 and 2008
Acute care revenue — Acute care revenue for the year ended September 30, 2009, was $1.7 billion, an increase of $138.4 million, or 9.0%, compared to $1.5 billion in the prior year. Approximately 2.1% of this increase is attributable to the increase in revenue associated with the supplemental Medicaid reimbursement programs in our Texas market. The remaining increase in acute care revenue of 6.9% is comprised of an increase in adjusted admissions of 2.4% and an increase in net patient revenue per adjusted admission of 4.4%, excluding the impact of supplemental Medicaid reimbursement.
Salaries and benefits — Salaries and benefits expense for the year ended September 30, 2009, was $641.9 million, or 38.4% of acute care revenue, compared to $614.4 million, or 40.1% of acute care revenue in the prior year. The decline in salaries and benefits expense as a percentage of acute care
61
revenue is attributable to a reduction in employee medical and pharmacy claims experience, primarily resulting from changes in our employee health plan design. Additionally, our nursing contract labor as a percentage of acute care revenue declined to 0.8% for the year ended September 30, 2009, compared to 1.2% in the prior year.
Other operating expenses — Other operating expenses for the year ended September 30, 2009, were $302.8 million, or 18.1% of acute care revenue, compared to $264.8 million, or 17.3% of acute care revenue in the prior year. The increase in other operating expenses as a percentage of acute care revenue was the result of additional professional fees incurred at our Texas hospitals to provide indigent care services during the current year, compared to the prior year.
Provision for bad debts — Provision for bad debts for the year ended September 30, 2009, was $192.6 million, or 11.5% of acute care revenue, compared to $161.9 million, or 10.6% of acute care revenue in the prior year. We believe, as a result of the prolonged economic recession and rising unemployment, we continue to experience an increase in self-pay volume and revenue, as well as increases in the amount of co-payments and deductibles passed on by employers to employees. For the year ended September 30, 2009, our self-pay admissions as a percentage of total admissions were 6.0%, compared to 5.2% in the prior year. These trends continue to be the main driver behind the increase in our provision for bad debts.
Interest expense, net — Interest expense, net of interest income, for the year ended September 30, 2009, was $67.9 million, compared to $75.7 million in the prior year. This decrease of $7.8 million was primarily due to the impact of lower LIBOR interest rates in the current year, compared to the prior year. The weighted average interest rate of outstanding borrowings under our senior secured credit facilities was 3.6% for the year ended September 30, 2009, compared to 5.6% in the prior year.
Impairment of goodwill — Impairment of goodwill for the year ended September 30, 2009, includes a $64.6 million non-cash charge related to our Florida market. We have experienced other than temporary changes in market conditions and the business mix of our Florida operations, which have negatively impacted operating results in this market. Accordingly, we have written off the goodwill associated with our Florida market.
Earnings from continuing operations before income taxes — Earnings from continuing operations before income taxes decreased $32.6 million to $15.8 million for the year ended September 30, 2009, compared to $48.4 million in the prior year. Earnings from continuing operations before income taxes for the year ended September 30, 2009, included the impact of a $64.6 million non-cash charge related to the impairment of goodwill in our Florida market.
Health Choice
The following table sets forth, for the periods indicated, results of our Health Choice operations expressed in dollar terms and as a percentage of premium revenue. Such information has been derived from our audited consolidated and unaudited condensed consolidated statements of operations for each period presented.
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
| | | Year Ended September 30, | | | Nine Months Ended June 30, | |
| | | 2008 | | | 2009 | | | 2010 | | | 2010 | | | 2011 | |
($ in thousands) | | Amount | | | % | | | Amount | | | % | | | Amount | | | % | | | Amount | | | % | | | Amount | | | % | |
Premium revenue: | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
| | | | | | | | | | |
Premium revenue | | $ | 541,746 | | | | 100.0 | % | | $ | 699,503 | | | | 100.0 | % | | $ | 792,062 | | | | 100.0 | % | | $ | 591,022 | | | | 100.0 | % | | $ | 580,917 | | | | 100.0 | % |
Costs and expenses: | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
| | | | | | | | | | |
Salaries and benefits | | | 17,667 | | | | 3.3 | % | | | 19,028 | | | | 2.7 | % | | | 19,149 | | | | 2.4 | % | | | 14,405 | | | | 2.4 | % | | | 15,471 | | | | 2.7 | % |
| | | | | | | | | | |
Supplies | | | 258 | | | | 0.0 | % | | | 263 | | | | 0.0 | % | | | 198 | | | | 0.0 | % | | | 137 | | | | 0.0 | % | | | 157 | | | | 0.0 | % |
| | | | | | | | | | |
Medical claims (1) | | | 461,649 | | | | 85.2 | % | | | 602,076 | | | | 86.1 | % | | | 690,456 | | | | 87.2 | % | | | 519,023 | | | | 87.8 | % | | | 493,167 | | | | 84.9 | % |
Other operating expenses | | | 18,309 | | | | 3.4 | % | | | 22,931 | | | | 3.3 | % | | | 24,612 | | | | 3.1 | % | | | 18,474 | | | | 3.2 | % | | | 19,341 | | | | 3.3 | % |
Rentals and leases | | | 1,167 | | | | 0.2 | % | | | 1,564 | | | | 0.2 | % | | | 1,546 | | | | 0.2 | % | | | 1,153 | | | | 0.2 | % | | | 1,238 | | | | 0.2 | % |
Depreciation and amortization | | | 3,738 | | | | 0.7 | % | | | 3,448 | | | | 0.5 | % | | | 3,562 | | | | 0.5 | % | | | 2,669 | | | | 0.5 | % | | | 2,669 | | | | 0.5 | % |
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
Total costs and expenses | | | 502,788 | | | | 92.8 | % | | | 649,310 | | | | 92.8 | % | | | 739,523 | | | | 93.4 | % | | | 555,861 | | | | 94.1 | % | | | 532,043 | | | | 91.6 | % |
| | | | | | | | | | |
Earnings before loss on disposal of assets | | | 38,958 | | | | 7.2 | % | | | 50,193 | | | | 7.2 | % | | | 52,539 | | | | 6.6 | % | | $ | 35,161 | | | | 5.9 | % | | $ | 48,874 | | | | 8.4 | % |
| | | | | | | | | | |
Loss on disposal of assets, net | | | — | | | | — | | | | (151 | ) | | | (0.0 | )% | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | |
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
| | | | | | | | | | |
Earnings before income taxes | | $ | 38,958 | | | | 7.2 | % | | $ | 50,042 | | | | 7.2 | % | | $ | 52,539 | | | | 6.6 | % | | $ | 35,161 | | | | 5.9 | % | | $ | 48,874 | | | | 8.4 | % |
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
| (1) | Medical claims paid to our hospitals of $9.6 million, $9.3 million and $11.8 million for the years ended September 30, 2008, 2009 and 2010, and $8.3 million and $8.5 million for the nine months ended June 30, 2010 and 2011, respectively, are eliminated in our consolidated results. |
62
Nine Months Ended June 30, 2011 and 2010
Premium revenue —Premium revenue was $580.9 million for the nine months ended June 30, 2011, a decrease of $10.1 or 1.7%, compared to $591.0 million in the prior year period. The decline in premium revenue is primarily due to a 5.0% reduction in capitation rates in our Medicaid product line, as a result of the provider cuts implemented by AHCCCS on April 1, 2011, and a 1.6% decline in related member months, compared to the prior year period.
Medical claims —Medical claims expense was $493.2 million for the nine months ended June 30, 2011, compared to $519.0 million in the prior year period. Medical claims expense as a percentage of premium revenue was 84.9% for the nine months ended June 30, 2011, compared to 87.8% in the prior year period. The decrease in medical claims as a percentage of premium revenue is primarily the result of declining medical claims costs, resulting from a general decline in medical utilization, AHCCCS provider payment reductions, and improvements in care management and other operational initiatives.
Years Ended September 30, 2010 and 2009
Premium revenue —Premium revenue was $792.1 million for the year ended September 30, 2010, an increase of $92.6 million or 13.2%, compared to $699.5 million in the prior year. The growth in premium revenue was due to a 14.4% increase in Medicaid member months resulting from increased enrollment in the state program, primarily attributable to the impact of high unemployment, partially offset by a 1.9% decline in Medicaid premium revenue on a per member per month basis.
Medical claims — Medical claims expense was $690.5 million for the year ended September 30, 2010, compared to $602.1 million in the prior year. Medical claims expense as a percentage of premium revenue was 87.2% for the year ended September 30, 2010, compared to 86.1% in the prior year. The increase in our medical claims expense as a percentage of premium revenue is primarily the result of an overall increase in medical costs on a per member per month basis, compared to the prior year, coupled with a 1.6% decline in overall premium revenue on a per member per month basis.
Years Ended September 30, 2009 and 2008
Premium revenue —Premium revenue was $699.5 million for the year ended September 30, 2009, an increase of $157.8 million or 29.1%, compared to $541.7 million in the prior year. The growth in premium revenue was attributable to a 31.6% increase in Medicaid enrollees, resulting from Health Choice’s new contract with AHCCCS and increased enrollment in the state program. In addition, Health Choice has implemented successful outreach efforts, especially in its new counties, which have helped to increase the number of covered lives.
63
Medical claims — Medical claims expense was $602.1 million for the year ended September 30, 2009, compared to $461.6 million in the prior year. Medical claims expense as a percentage of premium revenue was 86.1% for the year ended September 30, 2009, compared to 85.2% in the prior year. The increase in medical claims expense as a percentage of premium revenue is the result of AHCCCS’ implementation of a new risk based payment methodology, which has negatively affected premium revenue on a per member per month basis in the current year.
Income Taxes
The following discussion sets forth, for the periods indicated, the impact of income taxes on our consolidated results. Such information has been derived from our audited consolidated statements of operations.
Years Ended September 30, 2010 and 2009
Income tax expense — We recorded a provision for income taxes from continuing operations of $44.7 million, resulting in an effective tax rate of 37.1% for the year ended September 30, 2010, compared to $27.6 million, for an effective tax rate of 41.9% in the prior year. Our effective tax rate for the year ended September 30, 2009, was impacted by a non-deductible component of the $64.6 million non-cash charge related to the impairment of goodwill in our Florida market.
Years Ended September 30, 2009 and 2008
Income tax expense — We recorded a provision for income taxes from continuing operations of $27.6 million, resulting in an effective tax rate of 41.9% for the year ended September 30, 2009, compared to $35.3 million, for an effective tax rate of 40.4% in the prior year. The increase in our effective tax rate is the result of the impact of a non-deductible component of the $64.6 million non-cash charge related to the impairment of goodwill in our Florida market.
64
Liquidity And Capital Resources
Overview of Cash Flow Activities for the Nine Months Ended June 30, 2011 and 2010
Our cash flows are summarized as follows (in thousands):
| | | | | | | | |
| | | Nine Months Ended
June 30, | |
| | | 2010 | | | 2011 | |
Cash flows from operating activities | | $ | 113,915 | | | $ | 96,652 | |
Cash flows from investing activities | | $ | (51,559 | ) | | $ | (218,368 | ) |
Cash flows from financing activities | | $ | (138,724 | ) | | $ | 121,800 | |
Operating Activities
Operating cash flows decreased $17.3 million for the nine months ended June 30, 2011, compared to the prior year period. Our operating cash flows have been impacted by delays in payments from Medicaid and managed care organizations, as such payors implement administrative delays, including increased efforts related to utilization reviews.
At June 30, 2011, we had $229.7 million in net working capital, compared to $134.5 million at September 30, 2010. Net accounts receivable increased $86.7 million to $295.8 million at June 30, 2011, from $209.2 million at September 30, 2010. The increase in net working capital and net accounts receivable is primarily the result of the Brim and St. Joseph acquisitions. Excluding the impact of the Brim and St. Joseph acquisitions, our days revenue in accounts receivable at June 30, 2011, were 47, compared to 43 at September 30, 2010, and 45 at June 30, 2010.
Investing Activities
Capital expenditures for the nine months ended June 30, 2011, were $64.5 million, compared to $53.5 million in the prior year period.
During the nine months ended June 30, 2011, we paid $155.4 million for acquisitions, which included the acquisition of St. Joseph.
Financing Activities
During the nine months ended June 30, 2011, we completed our Refinancing which resulted in proceeds totaling $1.812 billion, net of creditors’ fees, original issue discounts and other transaction costs totaling $62.6 million. The Refinancing proceeds were used to repay $567.3 million in our then existing senior secured credit facilities and repurchase our previously outstanding $475.0 million aggregate principal amount of 8 3/4% senior subordinated notes due 2014, including $9.9 million in redemption premiums.
65
Also, as part of the Refinancing, we distributed $632.9 million to IAS, which is comprised of $402.9 million to fund the repayment of the IAS senior paid-in-kind loans and $230.0 million to be held for future acquisitions and strategic growth initiatives, as well as potential distributions to the equity holders of IAS.
During fiscal 2010, we distributed $125.0 million, net of a $1.8 million income tax benefit, to IAS to fund the repurchase of certain shares of its outstanding preferred stock and cancel certain vested rollover options to purchase its common stock. The holder of the IAS preferred stock is represented by an investor group led by TPG, JLL Partners and Trimaran Fund Management. The repurchase of preferred stock, which included accrued and outstanding dividends, and the cancellation of rollover options were funded by our excess cash on hand. The cancellation of the rollover options, which were associated with our 2004 recapitalization, resulted in the recognition of $2.0 million in stock-based compensation during the quarter ended March 31, 2010.
Capital Resources
As of June 30, 2011, we had the following debt arrangements:
| | • | | $1.325 billion senior secured credit facilities; and |
| | • | | $850.0 million in 8.375% senior notes due 2019. |
At June 30, 2011, amounts outstanding under our senior secured credit facilities consisted of $1.022 billion in term loans. In addition, we had $85.2 million in letters of credit outstanding under the revolving credit facility. The weighted average interest rate of outstanding borrowings under the senior secured credit facilities was 3.8% for the nine months ended June 30, 2011.
$1.325 Billion Senior Secured Credit Facilities
In connection with the Refinancing, we entered into a new senior credit agreement (the “Restated Credit Agreement”). The Restated Credit Agreement provides for senior secured financing of up to $1.325 billion consisting of (1) a $1.025 billion senior secured term loan facility with a seven-year maturity and (2) a $300.0 million senior secured revolving credit facility with a five-year maturity, of which up to $150.0 million may be utilized for the issuance of letters of credit (together, the “Senior Secured Credit Facilities”). Principal under the senior secured term loan facility is due in consecutive equal quarterly installments in an aggregate annual amount equal to 1% of the principal amount outstanding at the closing of the Refinancing, with the remaining balance due upon maturity of the senior secured term loan facility. The senior secured revolving credit facility does not require installment payments.
Borrowings under the senior secured term loan facility bear interest at a rate per annum equal to, at our option, either (1) a base rate (the “base rate”) determined by reference to the highest of (a) the federal funds rate plus 0.50%, (b) the prime rate of Bank of America, N.A. and (c) a one-month LIBOR rate, subject to a floor of 1.25%, plus 1.00%, in each case, plus a margin of 2.75% per annum or (2) the LIBOR rate for the interest period relevant to such borrowing, subject to a floor of 1.25%, plus a margin of 3.75% per annum. Borrowings under the senior secured revolving credit facility generally bear interest at a rate per annum equal to, at our option, either (1) the base rate plus a margin of 2.50% per annum, or (2) the LIBOR rate for the interest period relevant to such borrowing plus a margin of 3.50% per annum. In addition to paying interest on outstanding principal under the Senior Secured Credit Facilities, we will be required to pay a commitment fee on the unutilized commitments under the senior secured revolving credit facility, as well as pay customary letter of credit fees and agency fees.
The Senior Secured Credit Facilities are unconditionally guaranteed by IAS and certain of our subsidiaries (collectively, the “Credit Facility Guarantors”) and are required to be guaranteed by all of our future material wholly owned subsidiaries, subject to certain exceptions. All obligations under the Restated Credit Agreement are secured, subject to certain exceptions, by substantially all of our assets and the assets of the Credit Facility Guarantors, including (1) a pledge of 100% of our equity interests and that of the Credit Facility Guarantors, (2) mortgage liens on all of our material real property and that of the Credit Facility Guarantors, and (3) all proceeds of the foregoing.
66
The Restated Credit Agreement requires us to mandatorily prepay borrowings under the senior secured term loan facility with net cash proceeds of certain asset dispositions, following certain casualty events, following certain borrowings or debt issuances, and from a percentage of annual excess cash flow.
The Restated Credit Agreement contains certain restrictive covenants, including, among other things: (1) limitations on the incurrence of debt and liens; (2) limitations on investments other than, among other exceptions, certain acquisitions that meet certain conditions; (3) limitations on the sale of assets outside of the ordinary course of business; (5) limitations on dividends and distributions; and (6) limitations on transactions with affiliates, in each case, subject to certain exceptions. The Restated Credit Agreement also contains certain customary events of default, including, without limitation, a failure to make payments under the Senior Secured Credit Facilities, cross-defaults, certain bankruptcy events and certain change of control events.
8.375% Senior Notes due 2019
In connection with the Refinancing, we and IASIS Capital (together, the “Issuers”) issued $850.0 million aggregate principal amount of 8.375% senior notes due 2019 (the “Senior Notes”), which mature on May 15, 2019, pursuant to an indenture, dated as of May 3, 2011, among the Issuers and certain of the Issuers’ wholly owned domestic subsidiaries that guarantee the Senior Secured Credit Facilities (the “Notes Guarantors”) (the “Indenture”). The Indenture provides that the Senior Notes are general unsecured, senior obligations of the Issuers, and initially will be unconditionally guaranteed on a senior unsecured basis.
The Senior Notes bear interest at a rate of 8.375% per annum and will accrue from May 3, 2011. Interest on the Senior Notes is payable semi-annually, in cash in arrears, on May 15 and November 15 of each year, commencing on November 15, 2011.
We may redeem the Senior Notes, in whole or in part, at any time prior to May 15, 2014, at a price equal to 100% of the aggregate principal amount of the Senior Notes plus a “make-whole” premium and accrued and unpaid interest and special interest, if any, to but excluding the redemption date. In addition, we may redeem up to 35% of the Senior Notes before May 15, 2014, with the net cash proceeds from certain equity offerings at a redemption price equal to 108.375% of the aggregate principal amount of the Senior Notes plus accrued and unpaid interest and special interest, if any, to but excluding the redemption date, subject to compliance with certain conditions.
The Indenture contains covenants that limit our (and our restricted subsidiaries’) ability to, among other things: (1) incur additional indebtedness or liens or issue disqualified stock or preferred stock; (2) pay dividends or make other distributions on, redeem or repurchase our capital stock; (3) sell certain assets; (4) make certain loans and investments; (5) enter into certain transactions with affiliates; (5) impose restrictions on the ability of a subsidiary to pay dividends or make payments or distributions to us and our restricted subsidiaries; and (6) consolidate, merge or sell all or substantially all of our assets. These covenants are subject to a number of important limitations and exceptions.
The Indenture also provides for events of default, which, if any of them occurs, may permit or, in certain circumstances, require the principal, premium, if any, interest and any other monetary obligations on all the then outstanding Senior Notes to be due and payable immediately. If we experience certain kinds of changes of control, we must offer to purchase the Senior Notes at 101% of their principal amount, plus accrued and unpaid interest and special interest, if any, to but excluding the repurchase date. Under certain circumstances, we will have the ability to make certain payments to facilitate a change of control transaction and to provide for the assumption of the Senior Notes by a new parent company resulting from such change of control transaction. If such change of control transaction is facilitated, the Issuers will be released from all obligations under the Indenture and the Issuers and the trustee will execute a supplemental indenture effectuating such assumption and release.
67
Credit Ratings
The table below summarizes our corporate rating, as well as our credit ratings for the Senior Secured Credit Facilities and Senior Notes as of the date of this filing:
| | | | |
| | | Moody’s | | Standard
& Poors |
Corporate credit | | B2 | | B |
Senior secured term loan facility | | Ba3 | | B |
Senior secured revolving credit facility | | Ba3 | | BB- |
8.375% senior notes due 2019 | | Caa1 | | CCC+ |
| | |
Outlook | | Stable | | Stable |
Other
As of June 30, 2011, we are a party to interest rate swap agreements with Citibank, N.A. (“Citibank”) and Wells Fargo Bank, N.A. (“Wells Fargo”) (formerly Wachovia Bank, N.A.), as counterparties, with notional amounts totaling $200.0 million, in an effort to manage our exposure to floating interest rate risk on a portion of our variable rate debt. The arrangements with our counterparties include an interest rate swap agreement with a notional amount of $100.0 million maturing on February 29, 2012. Under these agreements, we are required to make monthly interest payments to our counterparties at fixed annual interest rate of 2.0%. Our counterparties are obligated to make monthly interest payments to us based upon the one-month LIBOR rate in effect over the term of the agreement.
Capital Expenditures
We plan to finance our proposed capital expenditures with cash generated from operations, borrowings under our Senior Secured Credit Facilities and other capital sources that may become available. We expect our capital expenditures for fiscal 2011 to be approximately $95.0 million, including the following significant expenditures:
| | • | | $25.0 million to $30.0 million for growth and new business projects; |
| | • | | $35.0 million to $40.0 million in replacement or maintenance related projects at our hospitals; and |
| | • | | $25.0 million in hardware and software costs related to information systems projects, including healthcare IT stimulus initiatives. |
Liquidity
We rely on cash generated from our operations as our primary source of liquidity, as well as available credit facilities, project and bank financings and the issuance of long-term debt. From time to time, we have also utilized operating lease transactions that are sometimes referred to as off-balance sheet arrangements. We expect that our future funding for working capital needs, capital expenditures, long-term debt repayments and other financing activities will continue to be provided from some or all of these sources. Each of our existing and projected sources of cash is impacted by operational and financial risks that influence the overall amount of cash generated and the capital available to us. For example, cash generated by our business operations may be impacted by, among other things, economic downturns, federal and state budget initiatives, weather-related catastrophes and adverse industry conditions. Our future liquidity will be impacted by our ability to access capital markets, which may be restricted due to our credit ratings, general market conditions, leverage capacity and by existing or future debt agreements. For a further discussion of risks that can impact our liquidity, see “Risk Factors” included elsewhere in this prospectus.
Including available cash at June 30, 2011, we have available liquidity as follows (in millions):
| | | | |
Cash and cash equivalents | | $ | 144.6 | |
Available capacity under our senior secured revolving credit facility | | | 214.8 | |
| | | | |
Net available liquidity at June 30, 2011 | | $ | 359.4 | |
| | | | |
68
Net available liquidity assumes 100% participation from all lenders currently participating in our senior secured revolving credit facility. In addition to our available liquidity, we expect to generate significant operating cash flows in fiscal 2011. We will also utilize proceeds from our financing activities as needed.
Based upon our current level of operations and anticipated growth, we believe we have sufficient liquidity to meet our cash requirements over the short-term (next 12 months) and over the next three years. In evaluating the sufficiency of our liquidity for both the short-term and long-term, we considered the expected cash flow to be generated by our operations, cash on hand and the available borrowings under our Senior Secured Credit Facilities, compared to our anticipated cash requirements for debt service, working capital, capital expenditures and the payment of taxes, as well as funding requirements for long-term liabilities.
We are unable at this time to extend our evaluation of the sufficiency of our liquidity beyond three years. We cannot assure you, however, that our operating performance will generate sufficient cash flow from operations or that future borrowings will be available under our Senior Secured Credit Facilities, or otherwise, to enable us to grow our business, service our indebtedness, or make anticipated capital expenditures and tax payments. For more information, see “Risk Factors” included elsewhere in this prospectus.
One element of our business strategy is to selectively pursue acquisitions and strategic alliances in existing and new markets. Any acquisitions or strategic alliances may result in the incurrence of, or assumption by us, of additional indebtedness. We continually assess our capital needs and may seek additional financing, including debt or equity as considered necessary to fund capital expenditures and potential acquisitions or for other corporate purposes. Our future operating performance and our ability to service or refinance our debt will be subject to future economic conditions and to financial, business and other factors, many of which are beyond our control. For more information, see “Risk Factors” included elsewhere in this prospectus.
Seasonality
The patient volumes and acute care revenue of our healthcare operations are subject to seasonal variations and generally are greater during the quarter ended March 31 than other quarters. These seasonal variations are caused by a number of factors, including seasonal cycles of illness, climate and weather conditions in our markets, vacation patterns of both patients and physicians and other factors relating to the timing of elective procedures.
Tabular Disclosure of Contractual Obligations
The following table reflects a summary of obligations and commitments outstanding including both the principal and interest portions of long-term debt and capital lease obligations at September 30, 2010.
| | | | | | | | | | | | | | | | | | | | |
| | | Payments Due By Period | |
| | | Less than
1 Year | | | 1-3
Years | | | 3-5
Years | | | More than
5 Years | | | Total | |
| | | (in millions) | |
Contractual Cash Obligations: | | | | | | | | | | | | | | | | | | | | |
Long-term debt, with interest (1) | | $ | 67.8 | | | $ | 408.5 | | | $ | 787.7 | | | $ | — | | | $ | 1,264.0 | |
Capital lease obligations, with interest | | | 0.9 | | | | 1.2 | | | | 1.1 | | | | 4.7 | | | | 7.9 | |
Medical claims | | | 111.4 | | | | — | | | | — | | | | — | | | | 111.4 | |
Operating leases | | | 28.5 | | | | 50.0 | | | | 38.5 | | | | 57.4 | | | | 174.4 | |
Estimated self-insurance liabilities | | | 7.7 | | | | 15.9 | | | | 21.4 | | | | — | | | | 45.0 | |
Purchase obligations | | | 30.8 | | | | 17.1 | | | | 0.2 | | | | — | | | | 48.1 | |
| | | | | | | | | | | | | | | | | | | | |
Subtotal | | $ | 247.1 | | | $ | 492.7 | | | $ | 848.9 | | | $ | 62.1 | | | $ | 1,650.8 | |
| | | | | | | | | | | | | | | | | | | | |
| | | | | | | | | | | | | | | | | | | | |
| | | Amount of Commitment Expiration Per Period | |
| | | Less than
1 Year | | | 1-3
Years | | | 3-5
Years | | | More than
5 Years | | | Total | |
| | | (in millions) | |
Other Commitments (2): | | | | | | | | | | | | | | | | | | | | |
Guarantees of surety bonds | | $ | 12.1 | | | $ | — | | | $ | — | | | $ | — | | | $ | 12.1 | |
Letters of credit | | | — | | | | 39.9 | | | | 41.4 | | | | — | | | | 81.3 | |
Other commitments | | | 4.8 | | | | — | | | | — | | | | — | | | | 4.8 | |
| | | | | | | | | | | | | | | | | | | | |
Subtotal | | | 16.9 | | | | 39.9 | | | | 41.4 | | | | — | | | | 98.2 | |
| | | | | | | | | | | | | | | | | | | | |
Total obligations and commitments | | $ | 264.0 | | | $ | 532.6 | | | $ | 890.3 | | | $ | 62.1 | | | $ | 1,749.0 | |
| | | | | | | | | | | | | | | | | | | | |
| (1) | We used 3.4%, the weighted average interest rate incurred on our senior secured credit facilities in fiscal 2010, which accrues actual interest at a variable rate. Actual interest will vary based on changes in interest rates. Included in the weighted average interest rate is the effect of our interest rate swap arrangements, which effectively converts $425.0 million of variable rate debt to fixed rate debt. |
| (2) | Excludes $11.7 million of unrecognized tax benefits and related interest that could result in a cash settlement, of which $9.2 million relates to timing differences between book and taxable income that may be offset by a reduction of cash tax obligations in future periods. We have not included these amounts in the above table as we cannot reliably estimate the amount and timing of payments related to these liabilities. |
69
BUSINESS
Company Overview
We are a leading owner and operator of medium-sized acute care hospitals in high-growth urban and suburban markets. We operate our hospitals with a strong community focus by offering and developing healthcare services targeted to the needs of the markets we serve, promoting strong relationships with physicians and working with local managed care plans. As of June 30, 2011, we owned or leased 18 acute care hospital facilities and one behavioral health hospital facility with a total of 4,362 licensed beds. We operate in the following regions:
| | • | | Tampa-St. Petersburg, Florida; |
| | • | | five cities in Texas, including Houston and San Antonio; |
| | • | | West Monroe, Louisiana; and |
| | • | | Woodland Park, Colorado. |
Our general, acute care hospital facilities offer a variety of medical and surgical services commonly available in hospitals, including emergency services, general surgery, internal medicine, cardiology, obstetrics, orthopedics, psychiatry and physical rehabilitation. In addition, our facilities provide outpatient and ancillary services including outpatient surgery, physical therapy, radiation therapy, diagnostic imaging and respiratory therapy.
We also own and operate Health Choice, a Medicaid and Medicare managed health plan in Phoenix that served over 197,000 members as of June 30, 2011.
Our principal executive offices are located at Dover Centre, 117 Seaboard Lane, Building E, Franklin, Tennessee 37067 and our telephone number at that address is (615) 844-2747. Our Internet website address is www.iasishealthcare.com. Information contained on our website is not part of this prospectus.
Industry Overview
Growth of Healthcare Spending
According to the CMS, U.S. healthcare expenditures were $2.3 trillion in 2008. CMS projects that total U.S. healthcare expenditures are expected to grow by 4.2% in 2011 and by an average of 6.3% annually from 2009 to 2019. As a result of this growth, total U.S. healthcare expenditures are estimated to be $4.6 trillion, or 19.6% of the total U.S. gross domestic product by 2019. The hospital services sector represents the single largest category of healthcare spending at $718.4 billion, or 30% of total healthcare spending in 2008. CMS expects continued increases in hospital services based on the aging of the U.S. population, advances in medical procedures, expansion of health coverage, increasing consumer demand for expanded medical services and increased prevalence of chronic conditions such as diabetes, heart disease and obesity. As a result, CMS projects the hospital services category to grow at an annual rate of at least 6.0% through 2018, and to continue as the largest category of healthcare spending.
According to the U.S Census Bureau, the U.S. population includes 40.2 million Americans aged 65 or older, which represents 13.0% of the total population. By the year 2030, the number of Americans aged 65 or older is expected to increase to 71.5 million, or 19.7% of the total population. Additionally, as a result of the increasing life expectancy of Americans, the number of people aged 85 years and older is also expected to increase by 57% by the year 2030.
Changes in the Delivery of Healthcare Services
We believe the U.S. healthcare system and the demand for healthcare services are evolving in ways that favor large-scale, comprehensive and integrated service networks. Specifically, we believe there are a number of initiatives that will continue to gain
70
importance in the foreseeable future, including: introduction of value-based payment methodologies tied to performance, quality and coordination of care, implementation of integrated EHR and information, and an increasing ability for patients and consumers to make choices about all aspects of healthcare. Due in large part to our investment in information technology and physician alignment strategies, we believe our company is well positioned to respond to these emerging trends and has the resources, expertise and flexibility necessary to adapt in a timely manner to the changing healthcare regulatory and reimbursement environment.
The Impact of Health Reform
The Health Reform Law will change how healthcare services are covered, delivered, and reimbursed through expanded coverage of previously uninsured individuals and reduced government healthcare spending. In addition, as enacted, the law reforms certain aspects of health insurance, expands existing efforts to tie Medicare and Medicaid payments to performance and quality, places restrictions on physician-owned hospitals, and contains provisions intended to strengthen fraud and abuse enforcement. Because of the many variables involved, including the law’s complexity, lack of implementing regulations or interpretive guidance, gradual and potentially delayed implementation, pending efforts to repeal or amend portions of the Health Reform Law in the United States Congress and ongoing federal court cases challenging the constitutionality of the Health Reform Law, the impact of the Health Reform Law, including how individuals and businesses will respond to the new choice afforded them, is not yet fully known.
Business Strategy
Our objective is to provide high-quality, cost-effective healthcare services to the communities we serve, while enhancing long-term growth and profitably that allows for the creation of value and opportunities for reinvestment. In order to achieve these objectives, we are focusing on the following elements, which we consider to be the key components of our business strategy:
Focus on Operational Excellence. We believe that a continuous focus on operational excellence sets the standard for managing all aspects of our business, including growth, quality and operating results. Our management team, which has extensive multi-facility operating experience, continually emphasizes the importance of operational excellence. We believe that in order to successfully achieve operational excellence we must focus on the following:
| | • | | growing our presence in our existing markets; |
| | • | | providing high-quality services to the communities we serve; |
| | • | | achieving operational efficiencies and effective cost management in all aspects of patient care delivery; |
| | • | | improving all aspects of the revenue cycle, including our processes for patient registration, such as patient qualification for financial assistance and point-of-service collections, billing, collections, and managed care contract compliance; and |
| | • | | effectively deploying capital resources in a disciplined manner, including initiatives related to business development, growth, quality of care, information technology and plant maintenance. |
Provide High-Quality Services. The keys to providing high-quality services, which include patient safety, patient satisfaction and clinical quality, are at the center of success for our facilities. We strive each day to provide high-quality services at all of our facilities, as we believe the achievement of high-quality care results in the long-term growth of revenue and profitability. Our strategy for focusing on improving quality of care includes enhancing the patient care experience by:
| | • | | attracting and retaining high-quality healthcare professionals; |
| | • | | monitoring and tracking clinical performance and patient safety for numerous purposes, including the establishment of best practices; |
71
| | • | | utilizing our advanced clinical information system, which provides more timely key clinical care data, to enable our hospitals to enhance patient safety, reduce medical errors through bar coding, increase staff time available for direct patient care and continue to achieve high quality patient care outcomes; |
| | • | | investing in our emergency rooms to improve patient flow, as well as quality and timeliness of care; |
| | • | | utilizing our hospital medical management quality program to drive improvements in core management and allocation of resources, as well as quality and safety of care; and |
| | • | | dedicating well-trained corporate and hospital resources to the improvement of patient care. |
Recruit and Employ Physicians to Meet Community Needs in Our Markets.We believe that a critical element to providing high quality healthcare to the communities we serve is a comprehensive physician alignment strategy, which includes the continued investment in the employment, recruitment and retention of high-quality healthcare professionals. We believe the objective of attracting and retaining quality physicians is best accomplished by:
| | • | | expanding the reach of our outpatient and other specialty services; |
| | • | | equipping our hospitals with technologically advanced equipment, systems and platforms; |
| | • | | enhancing physician convenience and access, including the development of medical office space on or near our hospital campuses; |
| | • | | enabling physicians to remotely access clinical data through our advanced information systems, facilitating more convenient and timely patient care; and |
| | • | | sponsoring training programs to educate physicians on advanced medical procedures. |
Utilize and Invest in Technology. We believe that technology is the key to improving clinical outcomes and quality of patient care. Since inception through June 30, 2011, we have spent over $300 million to equip our hospitals with cutting-edge clinical and health information technology. Our strategy to improve quality of care through investing in technology includes:
| | • | | Providing state of the art medical equipment and technology in our hospitals, including significant investment in sophisticated diagnostic equipment such as 64-slice CT scanners, MRIs, PET scanners and automated laboratories; |
| | • | | Utilizing our system-wide EHR information platform to connect all our hospitals and to provide comprehensive real time access to patient records and other information; |
| | • | | Providing a business intelligence system to enable real-time and effective decision making; |
| | • | | Investing in stronger physician partnerships by providing them with more advanced technology and platforms; and |
| | • | | Utilizing our information systems to track quality and patient outcomes. |
Pursue a Comprehensive Development Strategy. We will continue to assess opportunities to expand our regional and national presence. We believe the many factors currently affecting the healthcare industry will result in increased consolidation and business development opportunities across the industry, which we intend to actively pursue. We believe the successful pursuit of a comprehensive development strategy, including both the expansion of our national presence through the acquisition of hospitals in existing and new markets and a continued focus to capitalize on the opportunities in the communities we serve, will result in overall growth of our revenue and profitability. We believe that our existing markets will continue to benefit from strategic investments that expand the scope and reach of services provided through a variety of healthcare delivery access points. Our disciplined approach to enhancing our competitive position within our existing markets includes the development and expansion of profitable product lines, and the acquisition of new hospitals and other healthcare service providers, including outpatient and ancillary service centers and physician clinics.
Focus on Managed Care Relationships. We are focused on maintaining market-based relationships, as we believe that the broad geographic coverage of our hospitals in certain of the regions in which we operate, the expansion of our physician networks and our commitment to providing high-quality services increases our attractiveness to managed care plans in those areas. We believe these factors provide a platform that allows for negotiating reasonable terms with managed care plans, entering into contracts with additional managed care plans and aligning reimbursement with acuity of services.
Implement Operational Initiatives in Response to Healthcare Reform. In March 2010, President Obama signed the Health Reform Law into law. We believe that our consistent focus on quality and patient satisfaction programs, coupled with the significant investments we have made in information systems, positions us to respond promptly and effectively to the changes resulting from the Health Reform Law, as well as any additional reform initiatives at both the federal and state levels.
72
Although we expect our business strategy to increase our patient volumes and reimbursement and allow us to control costs, certain risk factors could offset those increases to our net revenue and profitability. Please see “Risk Factors” for a discussion of risk factors affecting our business.
Our Markets
The following includes a discussion of the acute care operations in certain of our markets.
Salt Lake City, Utah
We operate four acute care hospital facilities with a total of 705 licensed beds in the Salt Lake City area, which has consistently been a very competitive environment. We believe that our hospitals in this market benefit from attractive strategic locations, participate in a more favorable reimbursement environment and possess significant opportunity to capture additional market share. For the nine months ended June 30, 2011, we generated 22.8% of our total acute care revenue in this market.
Our strategy to capitalize on these elements focuses on providing high-quality patient care, a disciplined deployment of capital and the expansion of our footprint by developing a more extensive network of services, including outpatient services and the implementation of a comprehensive physician employment strategy. In response to this strategy, we have completed various capital projects at our facilities in this market over the past five years, including patient tower expansion projects at Jordan Valley Medical Center and Davis Hospital and Medical Center, as well as emergency room and intensive care unit expansions at Salt Lake Regional Medical Center. These projects have provided increased bed capacity, as well as additional capacity for women’s and neonatal services, inpatient and outpatient surgery, including cardiac catheterization services, intensive care, emergency rooms, pediatric services, inpatient psychiatric and various diagnostic services, along with upgraded imaging technology.
Phoenix, Arizona
We operate three acute care hospital facilities and one behavioral health hospital facility with a total of 621 licensed beds in the Phoenix area, which has historically experienced high population growth. We have made strategic investments in this market, which have focused on capturing market share through expansion of various service lines, as well as capacity. For the nine months ended June 30, 2011, exclusive of Health Choice, we generated 18.6% of our total acute care revenue in this market.
Since its opening in July 2007, Mountain Vista Medical Center (“Mountain Vista”) has already become a state-of-the-art market leader. With the expanded capacity provided by Mountain Vista, as well as our continued focus on profitable product lines in our other facilities, such as outpatient imaging, psychiatric and orthopedic services, we believe we can continue to achieve growth in this market.
We have also implemented a physician employment strategy in our Arizona market. Our strategy focuses on enhancing our physician specialty and emergency room coverage and is allowing our hospitals to more effectively meet the needs of the communities we serve.
Texas
We operate five acute care hospital facilities with a total of 1,935 licensed beds in Houston, San Antonio, Odessa, Texarkana and Port Arthur, Texas. We believe our facilities in Texas benefit from the lack of a single dominant competitor in their service areas. For the nine months ended June 30, 2011, we generated 32.7% of our total acute care revenue in this market.
Effective May 1, 2011, we acquired St. Joseph, a 792-licensed bed acute care hospital facility located in downtown Houston, Texas. St. Joseph benefits from a partnership with independent investors, most of whom are physicians on the medical staff of St. Joseph, which retained an aggregate 20.9% ownership interest in the hospital. St. Joseph provides a full range of general, acute care medical and surgical inpatient and outpatient services including cardiology and cardiovascular surgery, cancer, intensive/critical care, emergency, neurosurgery, imaging, orthopedics, neonatal intensive care and a full-service women’s program, as well as sub-acute services such as psychiatric and rehabilitation units.
73
On October 1, 2010, through the acquisition of Brim, we acquired Wadley, a 370 licensed bed acute care hospital facility located in Texarkana, Texas, that serves a surrounding population of approximately 275,000, with one primary competitor. Additionally, Wadley benefits from existing market share opportunities and a strategic partnership with physician investors. Wadley’s services include a full range of medical and surgical specialties such as internal medicine, family practice, cardiology, cardiovascular surgery, urology, neurology, pulmonology, orthopedics, gastroenterology, radiology and women’s services. The facility is fully equipped with a 24-bed trauma-ready emergency department, eight general operating rooms, two open-heart operating rooms, two cardiac catheterization labs, a gastro-intestinal lab and a 23-bed outpatient surgery pavilion.
Our strategic focus in our Texas market is centered on providing high-quality patient care, developing a more extensive network of primary care physicians, including expansion of our physician employment strategy, extending the reach of our outpatient business, including both surgical and imaging services, and continuing to expand profitable product lines within our higher acuity service lines, including neurosurgery, cardiology and cardio-thoracic services, neonatology and other surgical services. In recent years, we have completed various growth capital projects in our Texas market that we believe provide the basis for future success in this market.
Tampa-St. Petersburg, Florida
We operate three acute care hospital facilities with a total of 688 licensed beds in the Tampa-St. Petersburg area. As a result of a large Medicare population, high managed care penetration and state restrictions regarding the expansion of operations, the operating environment in Florida can be more challenging than other markets in which we operate. Certain material capital projects, including the addition of new beds or services, require regulatory approval under Florida’s certificate of need program, which restricts our ability to expand operations in this market. Despite these limitations, we believe we can maintain our competitive position in the Tampa-St. Petersburg market through maintaining and improving quality of services and continuing our focus on profitable product lines, such as orthopedic, psychiatric, bariatric, outpatient imaging and non-invasive radio-surgery services. For the nine months ended June 30, 2011, we generated 11.6% of our total acute care revenue in this market.
West Monroe, Louisiana
We operate Glenwood with a total of 223 licensed beds, in West Monroe, Louisiana, which we believe benefits from a strong market position, opportunities for strategic growth of profitable product lines and a lower than average rate of self-pay utilization. For the nine months ended June 30, 2011, we generated 7.0% of our total acute care revenue in this market.
Our strategic focus for growth in the market is exemplified in our capital spending during the first four years of our ownership, which has included renovations, expansion and other various capital projects at Glenwood, with an emphasis on expanding the hospital’s cardiovascular program, expanding and renovating operating rooms, and purchasing new diagnostic imaging, automated laboratory systems and other equipment. In addition to our capital projects, as part of our effort to more effectively serve the community in which Glenwood operates, we have improved the facility’s hospitalist program, expanded emergency room coverage and re-opened the inpatient psychiatric program.
Glenwood also owns a majority ownership interest in Ouachita Community Hospital (“Ouachita”), a ten-bed surgical hospital located in West Monroe, Louisiana. We believe this strategic acquisition has provided additional surgical capacity and allowed us to expand our market presence.
In connection with these strategic initiatives and capital investments, we believe our focus on providing high-quality patient care, and our efforts to expand the reach of our physician network in this market, will result in capturing additional market share.
74
Our Properties
As of June 30, 2011, we operate 18 acute care hospital facilities and one behavioral health hospital facility. We own 16 and lease three of our hospital facilities. Nine of our acute care hospitals have third-party investors. The following table contains information concerning our hospitals.
| | | | | | | | |
| Hospitals | | City | | | Beds | |
Utah | | | | | | | | |
Davis Hospital & Medical Center (1) | | | Layton | | | | 225 | |
Jordan Valley Medical Center (2) | | | West Jordan | | | | 183 | |
Pioneer Valley Hospital (3) | | | West Valley City | | | | 139 | |
Salt Lake Regional Medical Center (4) | | | Salt Lake City | | | | 158 | |
Arizona | | | | | | | | |
Mountain Vista Medical Center (5) | | | Mesa | | | | 178 | |
St. Luke’s Medical Center (6) | | | Phoenix | | | | 232 | |
St. Luke’s Behavioral Health Hospital | | | Phoenix | | | | 124 | |
Tempe St. Luke’s Hospital (7) | | | Tempe | | | | 87 | |
Texas | | | | | | | | |
Odessa Regional Medical Center (8) | | | Odessa | | | | 222 | |
Southwest General Hospital (9) | | | San Antonio | | | | 327 | |
St. Joseph Medical Center (10) | | | Houston | | | | 792 | |
The Medical Center of Southeast Texas (11) | | | Port Arthur | | | | 224 | |
Wadley Regional Medical Center (12) | | | Texarkana | | | | 370 | |
Florida | | | | | | | | |
Memorial Hospital of Tampa | | | Tampa | | | | 180 | |
Palms of Pasadena Hospital | | | St. Petersburg | | | | 307 | |
Town & Country Hospital | | | Tampa | | | | 201 | |
Louisiana | | | | | | | | |
Glenwood Regional Medical Center (13) | | | West Monroe | | | | 223 | |
Colorado | | | | | | | | |
Pikes Peak Regional Hospital (14) | | | Woodland Park | | | | 15 | |
Nevada | | | | | | | | |
North Vista Hospital | | | Las Vegas | | | | 175 | |
| | |
Total | | | | | | | 4,362 | |
| (1) | Owned by a limited partnership in which we own a 96.2% interest. |
| (2) | On July 1, 2007, Jordan Valley Medical Center acquired Pioneer Valley Hospital, a wholly-owned subsidiary of IASIS. The combined entity is owned by a limited partnership in which we own a 95.6% interest. |
| (3) | A separate campus of Jordan Valley Medical Center, which is leased under an agreement that expires on January 31, 2019. We have options to extend the term of the lease through January 31, 2039. |
| (4) | Owned by a limited partnership in which we own a 98.1% interest. |
| (5) | Owned by a limited partnership in which we own a 90.8% interest. |
| (6) | On September 28, 2007, St. Luke’s Medical Center acquired Tempe St. Luke’s Hospital, a wholly-owned subsidiary of IASIS. |
| (7) | A separate campus of St. Luke’s Medical Center. |
| (8) | Owned by a limited partnership in which we own an 88.4% interest. |
| (9) | Owned by a limited partnership in which we own a 93.9% interest. |
| (10) | Owned by a limited liability corporation in which we own a 79.1% interest. |
| (11) | Owned by a limited partnership in which we own an 88.0% interest. |
| (12) | Wadley is leased under an agreement that contains unlimited successive renewal options, at our discretion. The operations are owned by a limited liability company in which we own a 72.7% interest. |
| (13) | Includes Ouachita, a surgical hospital with 10 licensed beds. |
| (14) | Pikes Peak Regional Hospital is leased under an agreement that expires on September 11, 2017, and is subject to three five year renewal periods at our option. |
75
We also operate and lease medical office buildings in conjunction with our hospitals. These office buildings are occupied primarily by physicians who practice at our hospitals.
Hospital Operations
At each hospital we operate, we have implemented policies and procedures to improve the hospital’s operating and financial performance. A hospital’s local management team is generally comprised of a chief executive officer, chief financial officer and chief nursing officer. Local management teams, in consultation with our corporate staff, develop annual operating plans setting forth quality and patient satisfaction goals, revenue growth and operating profit strategies. These strategies can include the expansion of services offered by the hospital, market development to improve community access to care, the recruitment and employment of physicians in each community plans to enhance quality of care and improvements in operating efficiencies to reduce costs. We believe that the competence, skills and experience of the management team at each hospital is critical to the hospital’s success because of its role in executing the hospital’s operating plan. Our performance-based compensation program for each local management team is based upon the achievement of qualitative and quantitative goals set forth in the annual operating plan. Our hospital management teams are advised by boards of trustees that include members of hospital medical staffs, as well as community leaders. Each board of trustees establishes policies concerning medical, professional and ethical practices, monitors such practices and is responsible for ensuring that these practices conform to established standards.
Factors that affect demand for our services include:
| | • | | local economic conditions; |
| | • | | the geographic location of our hospital facilities and their convenience for patients and physicians; |
| | • | | our participation in managed care programs; |
| | • | | utilization management practices of managed care plans; |
| | • | | consolidation of managed care payors; |
| | • | | strategic investment and improvements in healthcare access points; |
| | • | | capital investment at our facilities; |
| | • | | the quality of our medical staff; |
| | • | | competition from other healthcare providers; |
| | • | | the size of and growth in local population; and |
| | • | | improved treatment protocols as a result of advances in medical technology and pharmacology. |
76
We believe that the ability of our hospitals to meet the healthcare needs of their communities is determined by the:
| | • | | level of physician support; |
| | • | | availability of nurses and other healthcare professionals; |
| | • | | quality, skills and compassion of our employees; |
| | • | | breadth of our services; |
| | • | | physical capacity and level of technological advancement at our facilities; and |
| | • | | emphasis on quality of care. |
We continually evaluate our services with the intention of improving quality of care, expanding our profitable lines of business and improving our business mix. We use our advanced information systems to perform detailed clinical process reviews, product line margin analyses and monitor the profitability of the services provided at our facilities. We employ these analyses to capitalize on price and volume trends through the expansion and improvement of certain services. We use our information systems to monitor patient care and other quality of care assessment activities on a continuing basis.
Competition
Our facilities and related businesses operate in competitive environments. A number of factors affect our competitive position, including:
| | • | | the local economies in which we operate; |
| | • | | decline in tourism in our service areas; |
| | • | | our managed care contracting relationships; |
| | • | | the number, availability, quality and specialties of physicians, nurses and other healthcare professionals; |
| | • | | the scope, breadth and quality of services; |
| | • | | the reputation of our facilities and physicians; |
| | • | | growth in hospital capacity and healthcare access points in the markets we serve; |
| | • | | the physical condition of our facilities and medical equipment; |
| | • | | the location of our facilities and availability of physician office space; |
| | • | | certificate of need restrictions, where applicable; |
| | • | | the availability of parking or proximity to public transportation; |
| | • | | accumulation, access and interpretation of publicly reported quality indicators; |
| | • | | growth in outpatient service providers; |
| | • | | charges for services; and |
77
| | • | | the geographic coverage of our hospitals in the regions in which we operate. |
We currently face competition from established, not-for-profit healthcare companies, investor-owned hospital companies, large tertiary care centers, specialty hospitals and outpatient service providers, such as surgery centers and imaging centers. In addition, some of our hospitals operate in regions with vertically integrated healthcare providers that include both payors and healthcare providers, which could affect our ability to obtain managed care contracts. We continue to encounter increased competition from specialty hospitals, outpatient service providers, not-for-profit healthcare companies and companies, like ours, that consolidate hospitals and healthcare companies in specific geographic markets. Continued consolidation in the healthcare industry will be a leading contributing factor to increased competition in markets in which we already have a presence and in markets we may enter in the future.
Another factor in the competitive position of a hospital is the ability of its management to obtain contracts with purchasers of group healthcare services. The importance of obtaining managed care contracts continues as private and government payors and others turn to managed care organizations to help control rising healthcare costs. Most of our markets have experienced significant managed care penetration, along with consolidation of major managed care plans. The revenue and operating results of our hospitals are significantly affected by our hospitals’ ability to negotiate reasonable contracts with managed care plans. Health maintenance organizations and preferred provider organizations use managed care contracts to encourage patients to use certain hospitals in exchange for discounts from the hospitals’ established charges. Traditional health insurers also contain costs through similar contracts with hospitals.
An additional competitive factor is whether a hospital is part of a local hospital network, as well as the scope and quality of services offered by the network compared to competing networks. A hospital that is part of a network offering a broad range of services in a wide geographic area is more likely to obtain more favorable managed care contracts. On an ongoing basis, we evaluate changing circumstances in each geographic area in which we operate. We may position ourselves to compete in these managed care markets by forming our own, or joining with others to form, local hospital networks.
As we continue to focus on our physician employment strategy, we face significant competition for skilled physicians in certain of our markets, as more providers are adopting a physician staffing model approach, coupled with a general shortage of physicians across most specialties, especially primary care. This increased competition has resulted in efforts by managed care organizations to align with certain provider networks in the markets in which we operate. While we anticipate that our physician employment strategy will help us compete more effectively in our markets, we are unable to provide any assurance regarding the success of our strategy.
Health Choice
Health Choice is a prepaid Medicaid and Medicare managed health plan in the Phoenix, Arizona area. Premium revenue is generated through capitated contracts whereby the Plan provides healthcare services in exchange for fixed periodic payments from the AHCCCS and CMS. Most premium revenue at Health Choice is derived through its contract with AHCCCS to provide specified health services to qualified Medicaid enrollees through contracted providers. AHCCCS is the state agency that administers Arizona’s Medicaid program. The contract requires Health Choice to arrange for healthcare services for enrolled Medicaid patients in exchange for fixed monthly premiums, based upon negotiated per capita member rates, and supplemental payments from AHCCCS. Capitation payments received by Health Choice are recognized as revenue in the month that members are entitled to healthcare services.
In connection with our contract effective October 1, 2008, AHCCCS implemented a risk-based or severity-adjusted payment methodology for all health plans. Capitation rates for each health plan and geographic service area are adjusted annually based on the severity of treatment episodes experienced by each plan’s membership compared to the average over a specified 12 month period. Adjustments are calculated using diagnosis codes and procedural information from medical and pharmacy claims data, in addition to member demographic information. Capitation rates are risk adjusted prospectively before the start of each contract year, and are not adjusted retroactively.
78
The Plan receives reinsurance and other supplemental payments from AHCCCS for healthcare costs that exceed stated amounts at a rate ranging from 75% to 100% of qualified healthcare costs in excess of stated levels of up to $35,000 per claim, depending on the eligibility classification of the member. Qualified costs must be incurred during the contract year and are the lesser of the amount paid by the Plan or the AHCCCS fee schedule. Reinsurance recoveries are recognized under the contract with AHCCCS when healthcare costs exceed stated amounts as provided under the contract, including estimates of such costs at the end of each accounting period.
Health Choice’s amended contract with AHCCCS, which was effective October 1, 2011, provides for a one-year term, with AHCCCS having the option to renew for an additional one-year period. The contract, which continued our state-wide presence, covers Medicaid members in the following Arizona counties: Apache, Coconino, Maricopa, Mohave, Navajo, Pima, Yuma, La Paz and Santa Cruz.
Health Choice also contracts with CMS to provide coverage as a MAPD SNP. This contract allows Health Choice to offer Medicare and Part D drug benefit coverage to new and existing dual eligible members (i.e. those that are eligible for Medicare and Medicaid). The contract with CMS includes successive one-year renewal options at the discretion of CMS. CMS has notified Health Choice that it is exercising its option to extend the contract through December 31, 2012. Under current law, CMS’ authority to designate SNPs has been extended through December 31, 2013. Additionally, SNPs are required to meet additional CMS requirements, including requirements relating to model of care, cost-sharing, disclosure of information, and reporting of quality measures.
Health Choice is subject to state and federal laws and regulations, and CMS and AHCCCS have the right to audit Health Choice to determine the plan’s compliance with such standards. Health Choice is required to file periodic reports with CMS and AHCCCS and to meet certain financial viability standards. Health Choice also must provide its enrollees with certain mandated benefits and must meet certain quality assurance and improvement requirements. Health Choice must also comply with the electronic transactions regulations and privacy and security standards of the Health Insurance Portability and Accountability Act of 1996 (“HIPAA”).
The federal anti-kickback statute has been interpreted to prohibit the payment, solicitation, offering or receipt of any form of remuneration in return for the referral of federal healthcare program patients or any item or service that is reimbursed, in whole or in part, by any federal healthcare program. Similar anti-kickback statutes have been adopted in Arizona, which apply regardless of the source of reimbursement. The Department has adopted safe harbor regulations specifying the following relationships and activities that are deemed not to violate the federal anti-kickback statute that specifically relate to managed care:
| | • | | waivers by health maintenance organizations of Medicare and Medicaid beneficiaries’ obligation to pay cost-sharing amounts or to provide other incentives in order to attract Medicare and Medicaid enrollees; |
| | • | | certain discounts offered to prepaid health plans by contracting providers; |
| | • | | certain price reductions offered to eligible managed care organizations; and |
| | • | | certain price reductions offered by contractors with substantial financial risk to managed care organizations. |
We believe that the incentives offered by Health Choice to its Medicaid and Medicare enrollees and the discounts it receives from contracting healthcare providers satisfy the requirements of the safe harbor regulations. However, failure to satisfy each criterion of the applicable safe harbor does not mean that the arrangement constitutes a violation of the law; rather the safe harbor regulations provide that the arrangement must be analyzed on the basis of its specific facts and circumstances. We believe that Health Choice’s arrangements comply in all material respects with the federal anti-kickback statute and similar Arizona statutes.
79
Sources of Acute Care Revenue
Acute care revenue is comprised of net patient revenue and other revenue. A large percentage of our hospitals’ net patient revenue consists of fixed payment from discounted sources, including Medicare, Medicaid and managed care organizations. Reimbursement for Medicare and Medicaid services are often fixed regardless of the cost incurred or the level of services provided. Similarly, various managed care companies with which we contract reimburse providers on a fixed payment basis regardless of the costs incurred or the level of services provided. Net patient revenue is reported net of discounts and contractual adjustments. Contractual adjustments principally result from differences between the hospitals’ established charges and payment rates under Medicare, Medicaid and various managed care plans. Additionally, discounts and contractual adjustments result from our uninsured discount and charity care programs. Other revenue includes medical office building rental income and other miscellaneous revenue.
We receive payment for patient services primarily from:
| | • | | the federal government, primarily under the Medicare program; |
| | • | | state Medicaid programs, including managed Medicaid plans; |
| | • | | managed care payors, including health maintenance organizations, preferred provider organizations and managed Medicare plans; and |
| | • | | individual patients and private insurers. |
The following table presents the approximate percentages of our hospitals’ net patient revenue from these sources:
| | | | | | | | | | | | | | | | |
| Payor Source | | Year Ended September 30, | | | Nine Months
Ended June 30, | |
| | 2008 | | | 2009 | | | 2010 | | | 2011 | |
Medicare | | | 23.4 | % | | | 22.7 | % | | | 23.4 | % | | | 24.6 | % |
Managed Medicare | | | 7.7 | % | | | 8.0 | % | | | 8.5 | % | | | 8.1 | % |
Medicaid and managed Medicaid | | | 13.8 | % | | | 15.2 | % | | | 15.7 | % | | | 14.8 | % |
Managed care | | | 46.0 | % | | | 43.0 | % | | | 40.2 | % | | | 39.8 | % |
Self-pay | | | 9.1 | % | | | 11.1 | % | | | 12.2 | % | | | 12.7 | % |
| | | | | | | | | | | | | | | | |
Total(1) | | | 100.0 | % | | | 100.0 | % | | | 100.0 | % | | | 100.0 | % |
| | | | | | | | | | | | | | | | |
| (1) | For the years ended September 30, 2008, 2009 and 2010, and the nine months ended June 30, 2011, net patient revenue comprised 73.8%, 70.4%, 68.6% and 71.9%, respectively, of our consolidated net revenue. |
Medicare is a federal program that provides hospital and medical insurance benefits to persons age 65 and over, some disabled persons and persons with Lou Gehrig’s Disease and end-stage renal disease. All of our hospitals are certified as providers of Medicare services. Under the Medicare program, acute care hospitals receive reimbursement under a prospective payment system for inpatient and outpatient hospital services. Currently, certain types of facilities are exempt or partially exempt from the prospective payment system methodology, including children’s hospitals, cancer hospitals and critical access hospitals. Hospitals and units exempt from the prospective payment system are reimbursed on a reasonable cost-based system, subject to cost limits.
Our hospitals offer discounts from established charges to managed care plans if they are large group purchasers of healthcare services. Additionally, we offer discounts to all uninsured patients receiving healthcare services who do not qualify for assistance under state Medicaid, other federal or state assistance plans or charity care. These discount programs generally limit our ability to increase net patient revenue in response to increasing costs. Patients generally are not responsible for any difference between established hospital charges and amounts reimbursed for such services under Medicare, Medicaid, health maintenance organizations, preferred provider organizations or private insurance plans. Patients generally are responsible for services not covered by these plans, along with exclusions, deductibles or co-insurance features of their coverage. Collecting amounts due from patients is
80
more difficult than collecting from governmental programs, managed care plans or private insurers. Increases in the population of uninsured individuals, changes in the states’ indigent and Medicaid eligibility requirements, continued efforts by employers to pass more out-of pocket healthcare costs to employees in the form of increased co-payments and deductibles, and the effects of the current economic environment, have resulted in increased levels of uncompensated care.
Medicare
Inpatient Acute Care
Under the inpatient prospective payment system, a hospital receives a fixed payment based on the patient’s assigned MS-DRG. In federal fiscal year 2009, CMS completed a two-year transition to full implementation of MS-DRGs to replace the previously used Medicare diagnosis related groups in an effort to better recognize severity of illness in Medicare payment rates. The MS-DRG system classifies categories of illnesses according to the estimated intensity of hospital resources necessary to furnish care for each principal diagnosis. The MS-DRG rates for acute care hospitals are based upon a statistically normal distribution of severity. The MS-DRG payments do not consider a specific hospital’s actual costs but are adjusted for geographic area wage differentials. Inpatient capital costs for acute care hospitals are reimbursed on a prospective system based on diagnosis related group weights multiplied by geographically adjusted federal weights. When treatments for patients fall well outside the normal distribution, providers may receive additional payments known as outlier payments. For federal fiscal year 2012, CMS has established an outlier threshold of $22,385.
The MS-DRG rates are adjusted each federal fiscal year and have been affected by federal legislation. The index used to adjust the MS-DRG rates, known as the “market basket index,” gives consideration to the inflation experienced by hospitals and entities outside of the healthcare industry in purchasing goods and services. In past years, the percentage increases to the MS-DRG rates have been lower than the percentage increases in the costs of goods and services purchased by hospitals. For federal fiscal year 2011, CMS updated the MS-DRG rates by a market basket of 2.35%, representing the full market basket of 2.6% reduced by 0.25% as required by the Health Reform Law. CMS issued a final rule for federal fiscal year 2012 that updates the MS-DRG rates by a market basket of 2.9%, which represents the full market basket of 3.0% reduced by 0.1% as required by the Health Reform Law. The Health Reform Law provides for additional reductions to the inpatient prospective payment system market basket update, as well as other payment adjustments, in future years as discussed below and in the section entitled “Government Regulation and Other Factors—Healthcare Reform.”
In federal fiscal years 2008 and 2009, CMS reduced payments to hospitals through a documentation and coding adjustment intended to account for coding and classification changes under the new MS-DRG system that were unrelated to changes in patient case mix. In addition, Congress gave CMS the ability to determine retrospectively whether the documentation and coding adjustment levels for federal fiscal years 2008 and 2009 were adequate to account for changes in payments not related to changes in patient case mix. CMS did not impose an adjustment for federal fiscal year 2010, but announced its intent to impose reductions to payments in federal fiscal years 2011 and 2012 because of what CMS has determined to be an inadequate adjustment in federal fiscal year 2008. In federal fiscal year 2011, CMS implemented a documentation and coding adjustment of negative 2.9%, which when combined with the market basket increase of 2.35%, results in a net decrease of 0.55% to MS-DRG rates. CMS noted that this documentation and coding reduction was only half of the full recoupment of 5.8% needed to offset its estimations of excess payments in 2008 and 2009. For federal fiscal year 2012, CMS issued a final rule that will result in a net increase of 1.0% for federal fiscal year 2012. This increase reflects the 2.9% market basket increase, a prospective documentation and coding adjustment of negative 2.0%, a multi-factor productivity adjustment of negative 1.0%, and a 1.1% increase in light of a January 2011 court decision. In addition, CMS intends to make an additional negative 1.9% documentation and coding adjustment in future years, but has not specified when the adjustment will be made.
Quality of care provided is becoming an increasingly important factor in Medicare reimbursement. Hospitals must submit data for certain patient care indicators to the Secretary of the Department in order to receive MS-DRG increases at the full market basket. Those hospitals not submitting the required data will receive an increase in payment equal to the market basket minus two percentage points. In federal fiscal year 2011, CMS required hospitals to report 55 quality measures to receive the full market basket update in federal fiscal year 2012. In federal fiscal year 2012, CMS will retire four quality measures and suspend data collection on four other quality measures. CMS has indicated that hospitals will be required to report 76 quality measures in federal fiscal year 2013 for the federal fiscal year 2014 and 2015 payment determinations. We currently have the ability to monitor our compliance with the quality indicators and intend to submit the quality data required to receive the full market basket pricing update when appropriate.
81
Beginning in federal fiscal year 2009, Medicare does not pay hospitals additional amounts for the treatment of certain preventable adverse events, also known as HACs, unless the conditions were present at admission. Currently, there are ten categories of conditions on the list of HACs. DEFRA provides that CMS may revise the list of conditions from time to time. In 2009, CMS announced three National Coverage Determinations (“NCDs”) that prohibit Medicare reimbursement for erroneous surgical procedures performed on an inpatient or outpatient basis. These three erroneous surgical procedures are in addition to the HACs designated by regulation. The Health Reform Law contains additional measures to further tie Medicare payments to performance and quality as discussed below in the section entitled “Government Regulation and Other Factors—Healthcare Reform.”
Outpatient
CMS reimburses hospital outpatient services and certain Medicare Part B services furnished to hospital inpatients that have no Part A coverage on a prospective payment system basis. CMS uses fee schedules to pay for physical, occupational and speech therapies, durable medical equipment, clinical diagnostic laboratory services and nonimplantable orthotics and prosthetics.
All services paid under the prospective payment system for hospital outpatient services are classified into groups called ambulatory payment classifications or “APCs.” Services in each APC are similar clinically and in terms of the resources they require. A payment rate is established for each APC. For calendar year 2011, CMS updated the market basket by 2.35%, representing the full market basket of 2.6%, reduced by 0.25% as required by the Health Reform Law. CMS has issued a proposed rule that, if finalized, would increase the market basket for calendar year 2012 by 1.5%, which includes the full market basket of 2.8%, a negative 1.2% multifactor productivity adjustment and a negative 0.1% adjustment required by the Health Reform Law. The Health Reform Law provides for additional reductions to the outpatient prospective payment system market basket update, as well as other payment adjustments, in future years as discussed below in the section entitled “Government Regulation and Other Factors—Healthcare Reform.”
Hospitals must submit quality data regarding 15 measures relating to outpatient care in calendar year 2011 in order to receive the full market basket increase under the outpatient prospective payment system in calendar year 2012. In calendar year 2012, hospitals will be required to submit quality data regarding 23 measures relating to outpatient care in order to receive the full market basket increase for outpatient payments in calendar year 2013. Hospitals that fail to submit such data will receive the market basket update minus two percentage points for the outpatient prospective payment system.
Rehabilitation
Inpatient rehabilitation hospitals and designated units are reimbursed under a prospective payment system. Under this prospective payment system, patients are classified into case mix groups based upon impairment, age, co-morbidities and functional capability. Inpatient rehabilitation facilities are paid a predetermined amount per discharge that reflects the patient’s case mix group and is adjusted for area wage levels, low-income patients, rural areas and high-cost outliers. For federal fiscal year 2011, CMS updated the market basket by 2.25%, representing the full market basket of 2.5% reduced by 0.25% as required by the Health Reform Law. For federal fiscal year 2012, CMS has issued a final rule updating inpatient rehabilitation payment rates by 2.2%, which reflects a 2.9% market basket increase, a negative 1.0% productivity adjustment, a 0.1% reduction required by the Health Reform Law, and a 0.4% increase resulting from an update to the outlier threshold amount. The Health Reform Law provides for additional reductions to the inpatient rehabilitation facility prospective payment system market basket update, as well as other payment adjustments, in future years as discussed below in the section entitled “Government Regulation and Other Factors—Healthcare Reform.”
82
In order to qualify for classification as an inpatient rehabilitation facility, at least 60% of the facility’s inpatient population during the most recent 12-month cost reporting period must have required intensive rehabilitation services for one or more of 13 specified conditions. Effective January 1, 2010, inpatient rehabilitation facilities must meet additional coverage criteria, including patient selection and care requirements relating to pre-admission screenings, post-admission evaluations, ongoing coordination of care and involvement of rehabilitation physicians. As of June 30, 2011, we operated nine inpatient rehabilitation units within our hospitals.
Psychiatric
Inpatient psychiatric facilities are paid based on a prospective payment system. Under this prospective payment system, inpatient psychiatric facilities receive a federal per diem base rate that is based on the sum of the average routine operating, ancillary and capital costs for each patient day of psychiatric care in an inpatient psychiatric facility, adjusted for budget neutrality. This federal per diem base rate is further adjusted to reflect certain patient and facility characteristics, including patient age, certain diagnostic related groups, facility wage index adjustment, and facility rural location. The payment rates are adjusted annually on a July 1 update cycle. Inpatient psychiatric facilities receive additional outlier payments for cases in which estimated costs for the case exceed an adjusted threshold amount plus the total adjusted payment amount for the stay. For rate year 2011, CMS updated the market basket by 2.15%, representing the full market basket of 2.4% reduced by 0.25% as required by the Health Reform Law. For rate year 2012, which began on July 1, 2011, CMS increased inpatient psychiatric payment rates by 2.95%, which includes a market basket increase of 3.2% and a 0.25% reduction required by the Health Reform Law. CMS anticipates an additional aggregate $10 million decrease in payments due to an adjustment to the outlier threshold in rate year 2012. Rate year 2012 will be a 15-month period in order to transition to a federal fiscal year update period, which will begin October 1, 2012. The Health Reform Law provides for additional reductions to the inpatient psychiatric facility prospective payment system market basket update, as well as other payment adjustments, in future years as discussed below in the section entitled “Government Regulation and Other Factors—Healthcare Reform.” As of June 30, 2011, we operated one behavioral health hospital facility and six specially designated psychiatric units that are subject to these rules.
Physician Services Reimbursement
Physician services are reimbursed under the physician fee schedule (“PFS”) system, under which CMS has assigned a national relative value unit (“RVU”) to most medical procedures and services that reflects the various resources required by a physician to provide the services relative to all other services. Each RVU is calculated based on a combination of work required in terms of time and intensity of effort for the service, practice expense (overhead) attributable to the service and malpractice insurance expense attributable to the service. These three elements are each modified by a geographic adjustment factor to account for local practice costs then aggregated. The aggregated amount is multiplied by a conversion factor that accounts for inflation and targeted growth in Medicare expenditures (as calculated by the sustainable growth rate (“SGR”)) to arrive at the payment amount for each service. While RVUs for various services may change in a given year, any alterations are required by statute to be virtually budget neutral, such that total payments made under the PFS may not differ by more than $20 million from what payments would have been if adjustments were not made.
The PFS rates are adjusted each year, and reductions in both current and future payments are anticipated. The SGR formula, mandated by statute, is intended to control growth in aggregate Medicare expenditures for physicians’ services. Since 2003, Congress has passed multiple legislative acts delaying application of the SGR to the PFS. For calendar year 2011, CMS issued a final rule applying the SGR in a manner that would have resulted in an aggregate reduction of 24.9% to all physician payments under the PFS, but Congress passed legislation postponing the cut from December 1, 2010 until January 1, 2012. We cannot predict whether Congress will intervene to prevent this reduction to payments in the future. Barring delay or repeal of the SGR by Congress, Medicare payments to physicians are scheduled to be cut by nearly 30% effective January 1, 2012.
83
Ambulatory Surgery Centers
CMS reimburses ambulatory surgical centers (“ASC”) using a predetermined fee schedule. Reimbursements for ASC overhead costs are limited to no more than the overhead costs paid to hospital outpatient departments under the Medicare hospital outpatient prospective payment system. Effective January 1, 2008, CMS issued final regulations that change payment for procedures performed in an ASC. Under this rule, ASC payment groups increased from nine clinically disparate payment groups to over 200 APCs used under the outpatient prospective payment system for these surgical services. In addition, CMS significantly expanded the types of procedures that may be performed in ASCs. More Medicare procedures that are now performed in hospitals, such as ours, may be moved to ASCs, potentially reducing surgical volume in our hospitals.
Recovery Audit Contractors
The Medicare Modernization Act established the RAC three-year demonstration program. Under this program, CMS contracted with third-parties to conduct post-payment reviews on a contingency fee basis to detect and correct improper payments in the Medicare program. The Tax Relief and Health Care Act of 2006 made the RAC program permanent and mandated its nationwide expansion by 2010. CMS has awarded contracts to four RACs that have implemented the permanent RAC program on a nationwide basis.
Managed Medicare
Managed Medicare plans represent arrangements where CMS contracts with private companies to provide members with Medicare Part A, Part B and Part D benefits. Managed Medicare plans can be structured as health maintenance organizations, preferred provider organizations, or private fee-for-service plans. The Medicare program allows beneficiaries to choose enrollment in certain managed Medicare plans. Legislative changes in 2003 increased reimbursement to managed Medicare plans and limited, to some extent, the financial risk to the companies offering the plans. Following these changes, the number of beneficiaries choosing to receive their Medicare benefits through such plans has increased. However, the Health Reform Law provides for reductions to managed Medicare plan payments beginning in 2010 that will result in managed Medicare per capita premium payments becoming equal, on average, to traditional Medicare payments. The Health Reform Law also expanded the RAC program to include managed Medicare by December 31, 2010.
Medicaid
Medicaid programs are jointly funded by federal and state governments and are administered by states under an approved plan that provides hospital and other healthcare benefits to qualifying individuals who are unable to afford care. All of our hospitals are certified as providers of Medicaid services. State Medicaid programs may use a prospective payment system, cost-based payment system or other payment methodology for hospital services. However, Medicaid reimbursement is often less than a hospital’s cost of services. In addition, the Health Reform Law prohibits the use of federal funds under the Medicaid program to reimburse providers for medical assistance provided to treat certain HACs. The statutory effective date for the prohibition of use of federal Medicaid funds to pay for treatment of HACs is July 1, 2011, but CMS has announced that it will delay enforcement until July 1, 2012. In a final rule released June 1, 2011, CMS authorizes states to add additional provider-preventable conditions to the list of HACs for which Medicaid reimbursement will not be allowed.
The federal government and many states from time to time consider altering the level of Medicaid funding or expanding Medicaid benefits in a manner that could adversely affect future levels of Medicaid reimbursement received by our hospitals. Additionally, the states in which we operate have experienced budget constraints as a result of increased costs and lower than expected tax collections. Many states have experienced or projected shortfalls in their budgets, and economic conditions may increase these budget pressures. Health and human services programs, including Medicaid and similar programs, represent a significant portion of state budgets. The states in which we operate have responded to these budget concerns by decreasing funding for healthcare programs or making structural changes that have resulted or may result in a reduction to Medicaid hospital revenues. Additional Medicaid spending cuts or other program changes may be implemented in the future in the states in which we operate. However, effective March 23, 2010, the Health Reform Law generally requires states at least to maintain Medicaid eligibility standards established prior to the enactment of the law until January 1, 2014 for adults and until October 1, 2019 for children. The Health Reform Law also requires states to significantly expand their Medicaid program coverage by 2014.
84
ARRA allocated approximately $87.0 billion to temporarily increase the share of program costs paid by the federal government to fund each state’s Medicaid program. Although initially scheduled to expire at the end of 2010, Congress allocated additional funds to extend this increased federal funding to states through June 2011. Although these increased funds provided a benefit to state Medicaid programs by temporarily helping to avoid more extensive program and reimbursement cuts, the expiration of the increased federal funding may now result in significant reductions to states’ Medicaid programs.
Through DEFRA, Congress has expanded the federal government’s involvement in fighting fraud, waste and abuse in the Medicaid program by creating the Medicaid Integrity Program. Among other things, this legislation requires CMS to employ private contractors, referred to as Medicaid Integrity Contractors (“MICs”), to perform reviews and post-payment audits of Medicaid claims and identify overpayments. MICs are assigned to five geographic jurisdictions and have commenced audits of Medicaid providers in several states in each jurisdiction. The Health Reform Law increases federal funding for the MIC program for federal fiscal year 2011 and later years. In addition to MICs, several other contractors and state Medicaid agencies have increased their review activities. The Health Reform Law also expands the RAC program’s scope to include Medicaid claims, and a final rule released by CMS on September 14, 2011, requires states to implement Medicaid RAC programs by January 1, 2012.
Private Supplemental Medicaid Reimbursement Programs
Certain of our acute care hospitals receive supplemental Medicaid reimbursement, including reimbursement from programs for participating private hospitals that enter into indigent care affiliation agreements with public hospitals or county governments in the state of Texas. Under the CMS-approved programs, affiliated hospitals, including our Texas hospitals, have expanded the community healthcare safety net by providing indigent healthcare services. Participation in indigent care affiliation agreements by our Texas hospitals has resulted in an increase in acute care revenue by virtue of the hospitals’ entitlement to supplemental Medicaid inpatient reimbursement. It is unclear whether our revenues from these programs will be adversely affected as the provisions of the Health Reform Law are implemented.
Managed Medicaid
Managed Medicaid programs represent arrangements in which states contract with one or more entities for patient enrollment, care management and claims adjudication. The states usually do not give up program responsibilities for financing, eligibility criteria and core benefit plan design. We generally contract directly with one of the designated entities, usually a managed care organization. The provisions of these programs are state-specific.
As state governments seek to control the cost of their Medicaid programs, enrollment in managed Medicaid plans, including states in which we operate, has increased in recent years. For example, Florida legislation has established a goal of statewide implementation of Medicaid managed care. On August 1, 2011, Florida submitted requests to CMS for approval of waivers, waiver amendments, and state plan amendments to implement two managed care Medicaid programs statewide for long-term care and all other healthcare services. It is uncertain whether or when CMS will approve Florida’s requests. Louisiana has requested a section 1115 Medicaid waiver from the federal government that, if approved, would result in an expansion of Medicaid managed care plans. The Texas legislature and the THHSC have recommended expanding Medicaid managed care enrollment in the state. On September 14, 2011, Texas received a letter indicating that CMS has reached agreement in principle on Texas’ plan to expand Medicaid managed care across the state and to create funding pools to finance hospital infrastructure and quality improvement programs. In the future there may be additional expansion of managed Medicaid plans in the states in which we operate, and economic conditions or budgetary pressures may result in reductions in premium payments to these plans.
Disproportionate Share Hospital Payments
In addition to making payments for services provided directly to beneficiaries, Medicare makes additional payments to hospitals that treat a disproportionately large number of low-income patients (Medicaid and Medicare patients eligible to receive Supplemental Security Income). DSH payments are determined annually based on certain statistical information required by the
85
Department and are calculated as a percentage addition to MS-DRG payments. The primary method used by a hospital to qualify for Medicare DSH payments is a complex statutory formula that results in a DSH percentage that is applied to payments on MS-DRGs. Hospitals that provide care to a disproportionately high number of low-income patients may also receive Medicaid DSH payments. The federal government distributes federal Medicaid DSH funds to each state based on a statutory formula. The states then distribute the DSH funding among qualifying hospitals. States have broad discretion to define which hospitals qualify for Medicaid DSH payments and the amount of such payments.
Annual Cost Reports
All hospitals participating in the Medicare and Medicaid programs, whether paid on a reasonable cost basis or under a prospective payment system, are required to meet specific financial reporting requirements. Federal regulations require submission of annual cost reports identifying medical costs and expenses associated with the services provided by each hospital to Medicare beneficiaries and Medicaid recipients. These annual cost reports are subject to routine audits, which may result in adjustments to the amounts ultimately determined to be due to us under these reimbursement programs. The audit process may take several years to reach the final determination of allowable amounts under the programs. Providers also have the right of appeal, and it is common to contest issues raised in audits of prior years’ reports.
Cost reports filed by our facilities generally remain open for three years after the notice of program reimbursement date. If any of our facilities are found to have been in violation of federal or state laws relating to preparing and filing of Medicare or Medicaid cost reports, whether prior to or after our ownership of these facilities, we and our facilities could be subject to substantial monetary fines, civil and criminal penalties and exclusion from participation in the Medicare and Medicaid programs. If an allegation is lodged against one of our facilities for a violation occurring during the time period before we owned the facility, we may have indemnification rights against the former owner of the facility for any damages we may incur based on negotiated indemnification and hold harmless provisions in the transaction documents. However, we offer no assurances that any such matter would be covered by indemnification, or if covered, that such indemnification would be adequate to cover any potential losses, fines and penalties. Additionally, we offer no assurances that the former owner would have the financial ability to satisfy indemnification claims.
Managed Care
Managed care payors, including health maintenance organizations and preferred provider organizations, are organizations that provide insurance coverage and a network of healthcare providers to members for a fixed monthly premium. To control costs, these organizations typically contract with hospitals and other providers for discounted prices, review medical services to ensure that no unnecessary services are provided, and market providers within their networks to patients. A significant percentage of our overall payor mix is commercial managed care. We generally receive lower payments from commercial managed care payors than from traditional commercial/indemnity insurers for similar services.
Commercial Insurance
Our hospitals provide services to a decreasing number of individuals covered by traditional private healthcare insurance. Private insurance carriers make direct payments to hospitals or, in some cases, reimburse their policy holders, based upon negotiated discounts from the particular hospital’s established charges and the particular coverage provided in the insurance policy.
Commercial insurers are continuing efforts to limit the payments for hospital services by adopting discounted payment mechanisms, including prospective payment or diagnosis related group-based payment systems, for more inpatient and outpatient services. In addition, commercial insurers increasingly are implementing quality requirements and refusing to pay for serious adverse events, similar to Medicare. To the extent that these efforts are successful, hospitals may receive reduced levels of reimbursement.
86
Charity Care
In the ordinary course of business, we provide care without charge to patients who are financially unable to pay for the healthcare services they receive. Because we do not pursue collection of amounts determined to qualify as charity care, they are not reported in net revenue. We currently record revenue deductions for patient accounts that meet our guidelines for charity care. We provide charity care to patients with income levels below 200% of the federal poverty level (“FPL”). Additionally, at all of our hospitals, a sliding scale of reduced rates is offered to all uninsured patients, who are not covered through federal, state or private insurance, with incomes between 200% and 400% of the FPL.
Government Regulation and Other Factors
A framework of extremely complex federal and state laws, rules and regulations governs the healthcare industry and, for many provisions, there is little history of regulatory or judicial interpretation upon which to rely.
Healthcare Reform
The Health Reform Law, as enacted, will change how healthcare services are covered, delivered and reimbursed through expanded coverage of uninsured individuals, reduced growth in Medicare program spending, reductions in Medicare and Medicaid DSH payments, and the establishment of programs where reimbursement is tied to quality and integration. In addition, the new law reforms certain aspects of health insurance, expands existing efforts to tie Medicare and Medicaid payments to performance and quality and contains provisions intended to strengthen fraud and abuse enforcement. Numerous lawsuits have challenged the constitutionality of the Health Reform Law. Some federal courts have upheld the constitutionality of the Health Reform Law or dismissed cases on procedural grounds. Others have held unconstitutional the requirement that individuals maintain health insurance or pay a penalty and have either found the Health Reform Law void in its entirety or left the remainder of the law intact. Federal appellate courts are split on the constitutionality of the Health Reform Law, and it is anticipated that the issue will ultimately be decided by the Supreme Court.
Expanded Coverage
Based on estimates of the Congressional Budget Office (“CBO”) and CMS, by 2019, the Health Reform Law, as enacted, will expand coverage to 32 to 34 million additional individuals (resulting in coverage of an estimated 94% of the legal U.S. population). This increased coverage will occur through a combination of public program expansion and private sector health insurance and other reforms.
Medicaid Expansion. The primary public program coverage expansion will occur through changes in Medicaid, and to a lesser extent, expansion of the Children’s Health Insurance Program (“CHIP”). The most significant changes will expand the categories of individuals eligible for Medicaid coverage and permit individuals with relatively higher incomes to qualify. The federal government reimburses the majority of a state’s Medicaid expenses, and it conditions its payment on the state meeting certain requirements. The federal government currently requires that states provide coverage for only limited categories of low-income adults under 65 years old (e.g., women who are pregnant and the blind or disabled). In addition, the income level required for individuals and families to qualify for Medicaid varies widely from state to state.
The Health Reform Law materially changes the requirements for Medicaid eligibility. Commencing January 1, 2014, all state Medicaid programs are required to provide, and the federal government will subsidize, Medicaid coverage to virtually all adults under 65 years old with incomes at or under 133% of the FPL. This expansion will create a minimum Medicaid eligibility threshold that is uniform across states. Further, the Health Reform Law also requires states to apply a “5% income disregard” to the Medicaid eligibility standard, so that Medicaid eligibility will effectively be extended to those with incomes up to 138% of the FPL. These new eligibility requirements will expand Medicaid and CHIP coverage by an estimated 16 to 18 million people nationwide. A disproportionately large percentage of the new Medicaid coverage is likely to be in states that currently have relatively low income eligibility requirements.
As Medicaid is a joint federal and state program, the federal government provides states with “matching funds” in a defined percentage, known as the federal medical assistance percentage (“FMAP”). Beginning in 2014, states will receive an enhanced FMAP for the individuals enrolled in Medicaid pursuant to the Health Reform Law. The FMAP percentage is as follows: 100% for calendar years 2014 through 2016; 95% for 2017; 94% in 2018; 93% in 2019; and 90% in 2020 and thereafter.
87
The Health Reform Law also provides that the federal government will subsidize states that create non-Medicaid plans for residents whose incomes are greater than 133% of the FPL but do not exceed 200% of the FPL. Approved state plans will be eligible to receive federal funding. The amount of that funding per individual will be equal to 95% of subsidies that would have been provided for that individual had he or she enrolled in a health plan offered through one of the Exchanges, as discussed below.
Historically, states often have attempted to reduce Medicaid spending by limiting benefits and tightening Medicaid eligibility requirements. Effective March 23, 2010, the Health Reform Law requires states to at least maintain Medicaid eligibility standards established prior to the enactment of the law for adults until January 1, 2014, and for children until October 1, 2019. States with budget deficits may, however, seek exemptions from this requirement, but only to address eligibility standards that apply to adults making more than 133% of the FPL.
Private Sector Expansion. The expansion of health coverage through the private sector as a result of the Health Reform Law, as enacted, will occur through new requirements on health insurers, employers and individuals. Commencing January 1, 2014, health insurance companies will be prohibited from imposing annual coverage limits, dropping coverage, excluding persons based upon pre-existing conditions or denying coverage for any individual who is willing to pay the premiums for such coverage. Effective January 1, 2011, each health plan must keep its annual non-medical costs lower than 15% of premium revenue for the group market and lower than 20% in the small group and individual markets or rebate its enrollees the amount spent in excess of the percentage. In addition, effective September 23, 2010, health insurers are not permitted to deny coverage to children based upon a pre-existing condition and must allow dependent care coverage for children up to 26 years old.
Larger employers will be subject to new requirements and incentives to provide health insurance benefits to their full-time employees. Effective January 1, 2014, employers with 50 or more employees that do not offer health insurance will be held subject to a penalty if an employee obtains coverage through an Exchange and that coverage is subsidized by the government. The employer penalties will range from $2,000 to $3,000 per employee, subject to certain thresholds and conditions.
As enacted, the Health Reform Law uses various means to induce individuals who do not have health insurance to obtain coverage. By January 1, 2014, individuals will be required to maintain health insurance for a minimum defined set of benefits or pay a tax penalty. The penalty in most cases is $95 in 2014, $325 in 2015, $695 in 2016, and indexed to a cost of living adjustment in subsequent years. The Internal Revenue Service (“IRS”), in consultation with the Department, is responsible for enforcing the tax penalty, although the Health Reform Law limits the availability of certain IRS enforcement mechanisms. In addition, for individuals and families below 400% of the FPL, the cost of obtaining health insurance will be subsidized by the federal government. Those with lower incomes will be eligible to receive greater subsidies. It is anticipated that those at the lowest income levels will have the majority of their premiums subsidized by the federal government, in some cases in excess of 95% of the premium amount.
To facilitate the purchase of health insurance by individuals and small employers, each state must establish an Exchange by January 1, 2014. Based on CBO and CMS estimates, between 29 and 31 million individuals will obtain their health insurance coverage through an Exchange by 2019. Of that amount, an estimated 16 million will be individuals who were previously uninsured, and 13 to 15 million will be individuals who switched from their prior insurance coverage to a plan obtained through the Exchange. The Health Reform Law requires that the Exchanges be designed to make the process of evaluating, comparing and acquiring coverage simple for consumers. For example, each state’s Exchange must maintain an internet website through which consumers may access health plan ratings that are assigned by the state based on quality and price, view governmental health program eligibility requirements and calculate the actual cost of health coverage. Health insurers participating in the Exchange must offer a set of minimum benefits to be defined by the Department and may offer more benefits. Health insurers must offer at least two, and up to five, levels of plans that vary by the percentage of medical expenses that must be paid by the enrollee. These levels are referred to as platinum, gold, silver, bronze and catastrophic plans, with gold and silver being the two mandatory levels of plans. Each level of plan must require the enrollee to share the following percentages of medical expenses up to the deductible/co-payment limit: platinum,
88
10%; gold, 20%; silver, 30%; bronze, 40%; and catastrophic, 100%. Health insurers may establish varying deductible/co-payment levels, up to the statutory maximum (estimated to be between $6,000 and $7,000 for an individual). The health insurers must cover 100% of the amount of medical expenses in excess of the deductible/co-payment limit. For example, an individual making 100% to 200% of the FPL will have co-payments and deductibles reduced to about one-third of the amount payable by those with the same plan with incomes at or above 400% of the FPL.
Public Program Spending
The Health Reform Law provides for Medicare, Medicaid and other federal healthcare program spending reductions between 2010 and 2019. The CBO estimates that these will include $156 billion in Medicare fee-for-service market basket and productivity reimbursement reductions for all providers, the majority of which will come from hospitals; CMS sets this estimate at $233 billion. The CBO estimates also include an additional $36 billion in reductions of Medicare and Medicaid DSH funding ($22 billion for Medicare and $14 billion for Medicaid). CMS estimates include an additional $64 billion in reductions of Medicare and Medicaid DSH funding, with $50 billion of the reductions coming from Medicare.
Payments for Hospitals and ASCs
Inpatient Market Basket and Productivity Adjustment. Under the Medicare program, hospitals receive reimbursement under a prospective payment system for general, acute care hospital inpatient services. CMS establishes fixed prospective payment system payment amounts per inpatient discharge based on the patient’s assigned MS-DRG. These MS-DRG rates are updated each federal fiscal year, which begins October 1, using the market basket, which takes into account inflation experienced by hospitals and other entities outside the healthcare industry in purchasing goods and services.
The Health Reform Law provides for three types of annual reductions in the market basket. The first is a general reduction of a specified percentage each federal fiscal year starting in 2010 and extending through 2019. These reductions are as follows: federal fiscal year 2010, 0.25% for discharges occurring on or after April 1, 2010; 2011, 0.25%; 2012, 0.1%; 2013, 0.1%; 2014, 0.3%; 2015, 0.2%; 2016, 0.2%; 2017, 0.75%; 2018, 0.75%; and 2019, 0.75%.
The second type of reduction to the market basket is a “productivity adjustment” that will be implemented by the Department beginning in federal fiscal year 2012. The amount of that reduction will be the projected nationwide productivity gains over the preceding 10 years. To determine the projection, the Department will use the Bureau of Labor Statistics (“BLS”) 10-year moving average of changes in specified economy-wide productivity (the BLS data is typically a few years old). The Health Reform Law does not contain guidelines for the Department to use in projecting the productivity figure. For federal fiscal year 2012, CMS has announced a negative 1.0% productivity adjustment to the market basket. CMS estimates that the combined market basket and productivity adjustments will reduce Medicare payments under the inpatient prospective payment system by $112.6 billion from 2010 to 2019.
The third type of reduction is in connection with the value-based purchasing program discussed in more detail below. Beginning in federal fiscal year 2013, CMS will reduce the inpatient prospective payment system payment amount for all discharges by the following: 1% for 2013; 1.25% for 2014; 1.5% for 2015; 1.75% for 2016; and 2% for 2017 and subsequent years. For each federal fiscal year, the total amount collected from these reductions will be pooled and used to fund payments to hospitals that satisfy certain quality metrics. While some or all of these reductions may be recovered if a hospital satisfies these quality metrics, the recovery amounts may be delayed.
If the aggregate of the three market basket reductions described above is more than the annual market basket adjustments made to account for inflation, there will be a reduction in the MS-DRG rates paid to hospitals. For example, if market basket increases to account for inflation would result in a 2% market basket update and the aggregate Health Reform Law market basket adjustments would result in a 3% reduction, then the rates paid to a hospital for inpatient services would be 1% less than rates paid for the same services in the prior year.
89
Quality-Based Payment Adjustments and Reductions for Inpatient Services. The Health Reform Law establishes or expands three provisions to promote value-based purchasing and to link payments to quality and efficiency. First, in federal fiscal year 2013, the Department is directed to implement a value-based purchasing program for inpatient hospital services. This program will reward hospitals that meet certain quality performance standards established by the Department. The Health Reform Law provides the Department considerable discretion over the value-based purchasing program. On April 29, 2011, CMS issued a final rule establishing the value-based purchasing program for hospital inpatient services. Under this final rule, CMS will distribute an estimated $850 million to hospitals based on their overall performance on a set of quality measures that have been linked to improved clinical processes of care and patient satisfaction. For payments in federal fiscal year 2013, hospitals will be scored based on a weighted average of patient experience scores using the Hospital Consumer Assessment of Healthcare Providers and Systems survey and 12 clinical process-of-care measures. CMS will score each hospital based on achievement (relative to other hospitals) and improvement ranges (relative to the hospital’s own past performance) for each applicable measure. Because the Health Reform Law provides that the pool will be fully distributed, hospitals that meet or exceed the quality performance standards set by the Department will receive greater reimbursement under the value-based purchasing program than they would have otherwise. On the other hand, hospitals that do not achieve the necessary quality performance will receive reduced Medicare inpatient hospital payments. CMS will notify each hospital of the amount of its value-based incentive payment for fiscal year 2013 on November 1, 2012.
Second, beginning in federal fiscal year 2013, inpatient payments will be reduced if a hospital experiences “excessive readmissions” within a 30-day period of discharge for heart attack, heart failure, pneumonia or other conditions that may be designated by CMS at a future time. Hospitals with what CMS defines as “excessive readmissions” for these conditions will receive reduced payments for all inpatient discharges, not just discharges relating to the conditions subject to the excessive readmission standard. Each hospital’s performance will be publicly reported by CMS. On August 1, 2011, CMS issued a final rule implementing portions of this program but indicated that it will issue additional policies with respect to excessive readmissions, including the specific payment adjustment methodology, in future rulemakings.
Third, reimbursement will be reduced based on a facility’s HAC rates. A HAC is a condition that is acquired by a patient while admitted as an inpatient in a hospital, such as a surgical site infection. Beginning in federal fiscal year 2015, hospitals that rank in the worst 25% nationally of HACs for all hospitals in the previous year will receive a 1% reduction in their total Medicare payments. In addition, the Health Reform Law prohibits the use of federal funds under the Medicaid program to reimburse providers for medical services provided to treat HACs. In a final rule released June 1, 2011, CMS authorizes states to add additional provider-preventable conditions to the list of HACs for which Medicaid reimbursement will not be allowed. Although the statutory effective date for the prohibition of use of federal Medicaid funds to pay for treatment of HACs is July 1, 2011, CMS will delay enforcement until July 1, 2012.
Outpatient Market Basket and Productivity Adjustment. Hospital outpatient services paid under the prospective payment system are classified into APCs. The APC payment rates are updated each calendar year based on the market basket. The first two market basket changes outlined above —the general reduction and the productivity adjustment —apply to outpatient services as well as inpatient services, although these are applied on a calendar year basis. The percentage changes specified in the Health Reform Law summarized above as the general reduction for inpatients —e.g., 0.2% in 2015 —are the same for outpatients. CMS estimates that the combined market basket and productivity adjustments will reduce Medicare payments under the outpatient prospective payment system by $26.3 billion from 2010 to 2019.
Inpatient Rehabilitation Hospitals and Units. The first two market basket changes outlined above for inpatient services—the general reduction and the productivity adjustment—also apply to inpatient rehabilitation services. The percentage changes specified in the Health Reform Law summarized above as the general reduction for inpatients—e.g., 0.2% in 2015—are the same for rehabilitation inpatients. CMS estimates that the combined market basket and productivity adjustments will reduce Medicare payments under the inpatient rehabilitation facilities prospective payment system by $5.7 billion from 2010 to 2019. The Health Reform Law requires each inpatient rehabilitation facility to report certain quality measures to the Department or receive a two percentage point reduction to the market basket update beginning with the market basket update for federal fiscal year 2014. In a final rule issued on July 29, 2011, CMS announced two quality measures that must be reported to receive the full market basket update in federal fiscal year 2014 and indicated that a third quality measure is under development.
90
Inpatient Psychiatric Facilities. The first two market basket changes outlined above for inpatient services—the general reduction and the productivity adjustment—also apply to inpatient psychiatric services. The percentage changes specified in the Health Reform Law summarized above as the general reduction for inpatients—e.g., 0.2% in 2015—are the same for psychiatric inpatients, although these are applied on a rate year basis. However, effective October 1, 2012, CMS will switch from a July 1 through June 30 rate year to a federal fiscal year for inpatient psychiatric facility rate updates. CMS estimates that the combined market basket and productivity adjustments will reduce Medicare payments under the inpatient psychiatric facilities prospective payment system by $4.3 billion from 2010 to 2019.
Medicare and Medicaid Disproportionate Share Hospital Payments. The Medicare DSH program provides for additional payments to hospitals that treat a disproportionate share of low-income patients. Under the Health Reform Law, beginning in federal fiscal year 2014, Medicare DSH payments will be reduced to 25% of the amount they otherwise would have been absent the new law. The remaining 75% of the amount that would otherwise be paid under Medicare DSH will be effectively pooled, and this pool will be reduced further each year by a formula that reflects reductions in the national level of uninsured who are under 65 years of age. In other words, the greater the level of coverage for the uninsured nationally, the more the Medicare DSH payment pool will be reduced. Each hospital will then be paid, out of the reduced DSH payment pool, an amount allocated based upon its level of uncompensated care.
It is difficult to predict the full impact of the Medicare DSH reductions. The CBO estimates that the Health Reform Law will result in $22 billion in reductions to Medicare DSH payments between 2010 and 2019, but CMS estimates reimbursement reductions totaling $50 billion during that same time period. The Health Reform Law does not mandate what data source the Department must use to determine the reduction, if any, in the uninsured population nationally. In addition, the Health Reform Law does not contain a definition of “uncompensated care.” As a result, it is unclear how a hospital’s share of the Medicare DSH payment pool will be calculated. CMS could use the definition of “uncompensated care” used in connection with hospital cost reports.
However, in July 2009, CMS proposed material revisions to the definition of “uncompensated care” used for cost report purposes. Those revisions would exclude certain significant costs that had historically been covered, such as unreimbursed costs of Medicaid services. CMS has not issued a final rule, and the Health Reform Law does not require the Department to use this definition, even if finalized, for DSH purposes. How CMS ultimately defines “uncompensated care” for purposes of these DSH funding provisions could have a material effect on a hospital’s Medicare DSH reimbursements.
In addition to Medicare DSH funding, hospitals that provide care to a disproportionately high number of low-income patients may receive Medicaid DSH payments. The federal government distributes federal Medicaid DSH funds to each state based on a statutory formula. The states then distribute the DSH funding among qualifying hospitals. Although federal Medicaid law defines some level of hospitals that must receive Medicaid DSH funding, states have broad discretion to define additional hospitals that also may qualify for Medicaid DSH payments and the amount of such payments. The Health Reform Law will reduce funding for the Medicaid DSH hospital program in federal fiscal years 2014 through 2020 by the following amounts: 2014, $500 million; 2015, $600 million; 2016, $600 million; 2017, $1.8 billion; 2018, $5 billion; 2019, $5.6 billion; and 2020, $4 billion. How such cuts are allocated among the states, and how the states allocate these cuts among providers, have yet to be determined.
Accountable Care Organizations. The Health Reform Law requires the Department to establish a Medicare Shared Savings Program that promotes accountability and coordination of care through the creation of Accountable Care Organizations (“ACOs”). Beginning no later than January 1, 2012, the program will allow providers (including hospitals), physicians and other designated professionals and suppliers to form ACOs and voluntarily work together to invest in infrastructure and redesign delivery processes to achieve high quality and efficient delivery of services. The program is intended to produce savings as a result of improved quality and operational efficiency. ACOs that achieve quality performance standards established by the Department will be eligible to share in a portion of the amounts saved by the Medicare program. The Department has significant discretion to determine key elements of the program, including what steps providers must take to be considered an ACO, how to decide if Medicare program savings have occurred and what portion of such savings will be paid to ACOs. In addition, the Department will determine to what degree hospitals, physicians and other eligible participants will be able to form and operate an ACO without violating certain existing laws, including
91
the federal Civil Monetary Penalty Law, the anti-kickback statute and the Stark Law. However, the Health Reform Law does not authorize the Department to waive other laws that may impact the ability of hospitals and other eligible participants to participate in ACOs.
Bundled Payment Pilot Programs. The Health Reform Law requires the Department to establish a five-year, voluntary national bundled payment pilot program for Medicare services beginning no later than January 1, 2013. Under the program, providers would agree to receive one payment for services provided to Medicare patients for certain medical conditions or episodes of care. The Department will have the discretion to determine how the program will function. For example, the Department will determine what medical conditions will be included in the program and the amount of the payment for each condition. In addition, the Health Reform Law provides for a five-year bundled payment pilot program for Medicaid services to begin January 1, 2012. The Department will select up to eight states to participate based on the potential to lower costs under the Medicaid program while improving care. State programs may target particular categories of beneficiaries, selected diagnoses or geographic regions of the state. The selected state programs will provide one payment for both hospital and physician services provided to Medicaid patients for certain episodes of inpatient care. For both pilot programs, the Department will determine the relationship between the programs and restrictions in certain existing laws, including the federal Civil Monetary Penalty Law, the anti-kickback statute, the Stark Law and the HIPAA privacy, security and transaction standard requirements. However, the Health Reform Law does not authorize the Department to waive other laws that may impact the ability of hospitals and other eligible participants to participate in the pilot programs, such as antitrust laws.
Ambulatory Surgery Centers. The Health Reform Law reduces reimbursement for ASCs through a productivity adjustment to the market basket similar to the productivity adjustment for inpatient and outpatient hospital services, beginning in federal fiscal year 2011. Further, on April 18, 2011, as required by the Health Reform Law, the Department reported to Congress on its plan for implementing a value-based purchasing program for ASCs. The Department recommends a phased-in timeframe for implementation and anticipates proposing an ASC quality measure reporting program in 2012 that provides for a reduction in annual payment updates for an ASC that fails to report on quality measures.
Medicare Managed Care (Medicare Advantage or “MA”). Under the MA program, the federal government contracts with private health plans to provide inpatient and outpatient benefits to beneficiaries who enroll in such plans. Nationally, approximately 24% of Medicare beneficiaries have elected to enroll in MA plans. Effective in 2014, the Health Reform Law requires MA plans to keep annual administrative costs lower than 15% of annual premium revenue. The Health Reform Law reduces, over a three year period, premium payments to the MA Plans such that CMS’ managed care per capita premium payments are, on average, equal to traditional Medicare. As a result of these changes, the CBO and CMS, respectively, estimate that payments to MA plans will be reduced by $138 to $145 billion between 2010 and 2019. These reductions to MA plan premium payments may cause some plans to raise premiums or limit benefits, which in turn might cause some Medicare beneficiaries to terminate their MA coverage and enroll in traditional Medicare. However, CMS has indicated that MA premium rates are expected to decrease in 2012 relative to 2011 and that enrollment in MA plans is forecast to increase in 2012.
Physician-owned Hospitals. The Health Reform Law prohibits newly created physician-owned hospitals from billing for Medicare patients referred by their physician owners. As a result, the new law effectively prevents the formation of physician-owned hospitals after December 31, 2010. While the new law grandfathers existing physician-owned hospitals, including our facilities that have physician ownership, it does not allow these hospitals to increase the percentage of physician ownership and significantly restricts their ability to expand services.
Program Integrity and Fraud and Abuse
The Health Reform Law makes several significant changes to healthcare fraud and abuse laws, provides additional enforcement tools to the government, increases cooperation between agencies by establishing mechanisms for the sharing of information and enhances criminal and administrative penalties for non-compliance. For example, the Health Reform Law: (1) provides $350 million in increased federal funding over 10 years to fight healthcare fraud, waste and abuse; (2) expands the scope of the RAC program to include MA plans and Medicaid; (3) authorizes the Department, in consultation with the OIG, to suspend Medicare and Medicaid payments to a provider of services or a supplier “pending an investigation of a credible allegation of fraud;”
92
(4) provides Medicare contractors with additional flexibility to conduct random prepayment reviews; and (5) tightens up the requirements for returning overpayments made by governmental health programs and expands the FCA liability to include failure to report and return an overpayment within 60 days of identifying the overpayment or by the date a corresponding cost report is due, whichever is later.
Impact of Health Reform Law on Our Company
The expansion of health insurance coverage under the Health Reform Law may result in a material increase in the number of patients using our facilities who have either private or public program coverage. In addition, a disproportionately large percentage of the new Medicaid coverage is likely to be in states that currently have relatively low income eligibility requirements. Further, the Health Reform Law provides for a value-based purchasing program, the establishment of ACOs and bundled payment pilot programs, which will create possible sources of additional revenue.
However, it is difficult to predict the potential amount of additional revenue resulting from these elements of the Health Reform Law, because of uncertainty surrounding a number of material factors, including the following:
| | • | | how many previously uninsured individuals will obtain coverage as a result of the Health Reform Law (while the CBO estimates 32 million, CMS estimates almost 34 million; both agencies made a number of assumptions to derive that figure, including how many individuals will ignore substantial subsidies and decide to pay the penalty rather than obtain health insurance and what percentage of people in the future will meet the new Medicaid income eligibility requirements); |
| | • | | what percentage of the newly insured patients will be covered under the Medicaid program and what percentage will be covered by private health insurers; |
| | • | | the extent to which states will enroll new Medicaid participants in managed care programs; |
| | • | | the pace at which insurance coverage expands, including the pace of different types of coverage expansion; |
| | • | | the change, if any, in the volume of inpatient and outpatient hospital services that are sought by and provided to previously uninsured individuals; |
| | • | | the rate paid to hospitals by private payors for newly covered individuals, including those covered through the newly created Exchanges and those who might be covered under the Medicaid program under contracts with the state; |
| | • | | the rate paid by state governments under the Medicaid program for newly covered individuals; |
| | • | | the effect of the value-based purchasing program on our hospitals’ revenue and the effects of other quality programs that will be implemented; |
| | • | | the percentage of individuals in the Exchanges who select the high deductible plans, since health insurers offering those kinds of products have traditionally sought to pay lower rates to hospitals; |
| | • | | whether the net effect of the Health Reform Law, including the prohibition on excluding individuals based on pre-existing conditions, the requirement to keep medical costs lower than a specified percentage of premium revenue, other health insurance reforms and the annual fee applied to all health insurers, will put pressure on the profitability of health insurers, which in turn might cause them to seek to reduce payments to hospitals with respect to both newly insured individuals and their existing business; and |
| | • | | the possibility that implementation of provisions expanding health insurance coverage will be delayed or even blocked due to court challenges or revised or eliminated as a result of court challenges and efforts to repeal or |
93
| | amend the new law. Numerous lawsuits have challenged the constitutionality of the Health Reform Law. Some federal courts have upheld the constitutionality of the Health Reform Law or dismissed cases on procedural grounds. Others have held unconstitutional the requirement that individuals maintain health insurance or pay a penalty and have either found the Health Reform Law void in its entirety or left the remainder of the law intact. Federal appellate courts are split on the constitutionality of the Health Reform Law, and it is anticipated that the issue will ultimately be decided by the Supreme Court. |
On the other hand, the Health Reform Law provides for significant reductions in the growth of Medicare spending, reductions in Medicare and Medicaid DSH payments and the establishment of programs where reimbursement is tied to quality and integration. Reductions in Medicare and Medicaid spending may significantly impact our business and could offset any positive effects of the Health Reform Law. It is difficult to predict the amount of potential revenue reductions resulting from reduced Medicare and Medicaid spending because of uncertainty regarding a number of material factors, including the following:
| | • | | the amount of overall revenues we will generate from Medicare and Medicaid business when the reductions are implemented; |
| | • | | whether reductions required by the Health Reform Law will be changed by statute or judicial decision prior to becoming effective; |
| | • | | the size of the Health Reform Law’s annual productivity adjustment to the market basket in future years; |
| | • | | the amount of the Medicare DSH reductions that will be made, commencing in federal fiscal year 2014; |
| | • | | the allocation to our hospitals of the Medicaid DSH reductions, commencing in federal fiscal year 2014; |
| | • | | what the losses in revenues will be, if any, from the Health Reform Law’s quality initiatives; |
| | • | | how successful ACOs will be at coordinating care and reducing costs; |
| | • | | the scope and nature of potential changes to Medicare reimbursement methods, such as an emphasis on bundling payments or coordination of care programs; |
| | • | | whether our revenues from private supplemental Medicaid reimbursement programs will be adversely affected, because there may be fewer indigent, non-Medicaid patients for whom we provide services pursuant to these programs; and |
| | • | | reductions to Medicare payments that CMS may impose for “excessive readmissions.” |
Because of the many variables involved, we are unable to predict the net effect of the expected increases in insured individuals using our facilities, the reductions in Medicare spending, including Medicare and Medicaid DSH funding, and numerous other provisions in the Health Reform Law that may affect our business. Further, it is unclear how federal lawsuits challenging the constitutionality of the Health Reform Law will be resolved or what the impact will be of any resulting changes to the law. For example, should the requirement that individuals maintain health insurance ultimately be deemed unconstitutional but the prohibition on health insurers excluding coverage due to pre-existing conditions be maintained, significant disruption to the health insurance industry could result, which could impact our revenues and operations.
Licensure, Certification and Accreditation
Healthcare facility construction and operation is subject to federal, state and local regulations relating to the adequacy of medical care, equipment, personnel, operating policies and procedures, fire prevention, rate-setting and compliance with building
94
codes and environmental protection laws. Our facilities also are subject to periodic inspection by governmental and other authorities to assure continued compliance with the various standards necessary for licensing and accreditation. We believe that all of our operating healthcare facilities are properly licensed under appropriate state healthcare laws, but we cannot assure you that government agencies or other entities enforcing licensure requirements would find our facilities in compliance with such requirements.
All of our operating hospitals are certified under the Medicare program and are accredited by either The Joint Commission or Det Norske Veritas (“DNV”), the effect of which is to permit the facilities to participate in the Medicare and Medicaid programs. If any facility loses its accreditation by either The Joint Commission or DNV, as applicable, the facility would be subject to state surveys, potentially be subject to increased scrutiny by CMS and likely lose payment from non-government payors. We intend to conduct our operations in compliance with current applicable federal, state, local and independent review body regulations and standards, but we cannot assure you that government agencies or other entities enforcing such requirements would find our facilities in compliance with such requirements. Licensure, certification, or accreditation requirements also may require notification or approval in the event of certain transfers or changes in ownership or organization. Requirements for licensure, certification and accreditation are subject to change and, in order to remain qualified, we may need to make changes in our facilities, equipment, personnel and services.
CMS recently has announced an initiative to require all Medicare-certified providers and suppliers that have enrolled prior to March 25, 2011, to revalidate their Medicare enrollment records by March 2013 in order for CMS to implement new screening criteria mandated by the Health Reform Law. Pursuant to this initiative, Medicare contractors will send mandatory revalidation requests to all affected providers and suppliers, including to our facilities, and our facilities will have a limited time to respond to the requests. We believe that we are in a position to promptly comply with any mandatory revalidation requests, but failure to timely revalidate Medicare enrollment records for our facilities could result in deactivation or termination of our facilities’ Medicare enrollment, which could adversely affect our business.
Utilization Review
Federal law contains numerous provisions designed to ensure that services rendered by hospitals to Medicare and Medicaid patients meet professionally recognized standards and are medically necessary and that claims for reimbursement are properly filed. These provisions include a requirement that a sampling of admissions of Medicare and Medicaid patients be reviewed by quality improvement organizations that analyze the appropriateness of Medicare and Medicaid patient admissions and discharges, quality of care provided, validity of diagnosis related group classifications and appropriateness of cases of extraordinary length of stay or cost. Quality improvement organizations may deny payment for services provided, assess fines and recommend to the Department that a provider not in substantial compliance with the standards of the quality improvement organization be excluded from participation in the Medicare program. Most non-governmental managed care organizations also require utilization review.
Federal and State Fraud and Abuse Provisions
Participation in any federal healthcare program, like Medicare, is regulated heavily by statute and regulation. If a hospital provider fails to substantially comply with the numerous conditions of participation in the Medicare or Medicaid program or performs specific prohibited acts, the hospital’s participation in the Medicare and Medicaid programs may be terminated or civil or criminal penalties may be imposed upon it under provisions of the Social Security Act and other statutes.
Among these statutes is a section of the Social Security Act known as the federal anti-kickback statute. This law prohibits providers and others from soliciting, receiving, offering or paying, directly or indirectly, any remuneration with the intent of generating referrals or orders for services or items covered by a federal healthcare program. Courts have interpreted this law broadly and held that there is a violation of the anti-kickback statute if just one purpose of the remuneration is to generate referrals, even if there are other lawful purposes. The Health Reform Law further provides that knowledge of the law or intent to violate the law is not required to establish a violation of the anti-kickback statute.
95
The OIG has published final safe harbor regulations that outline categories of activities that are deemed protected from prosecution under the anti-kickback statute. Currently there are safe harbors for various arrangements and activities, including the following: investment interests, space rental, equipment rental, practitioner recruitment, personal services and management contracts, sale of practice, referral services, warranties, discounts, employees, group purchasing organizations, waiver of beneficiary coinsurance and deductible amounts, managed care arrangements, obstetrical malpractice insurance subsidies, investments in group practices, ambulatory surgery centers, and referral agreements for specialty services.
The fact that conduct or a business arrangement does not fall within a safe harbor does not automatically render the conduct or business arrangement illegal under the anti-kickback statute. The conduct or business arrangement, however, does risk increased scrutiny by government enforcement authorities. We may be less willing than some of our competitors to take actions or enter into business arrangements that do not clearly satisfy the safe harbors. As a result, this unwillingness may put us at a competitive disadvantage.
The OIG, among other regulatory agencies, is responsible for identifying and eliminating fraud, abuse and waste. The OIG carries out this mission through a nationwide program of audits, investigations and inspections. In order to provide guidance to healthcare providers, the OIG has from time to time issued “fraud alerts” that, although they do not have the force of law, identify features of a transaction that may indicate that the transaction could violate the anti-kickback statute or other federal healthcare laws. The OIG has identified several incentive arrangements as potential violations, including:
| | • | | payment of any incentive by the hospital when a physician refers a patient to the hospital; |
| | • | | use of free or significantly discounted office space or equipment for physicians in facilities usually located close to the hospital; |
| | • | | provision of free or significantly discounted billing, nursing, or other staff services; |
| | • | | free training for a physician’s office staff, including management and laboratory techniques; |
| | • | | guarantees that provide that, if the physician’s income fails to reach a predetermined level, the hospital will pay any portion of the remainder; |
| | • | | low-interest or interest-free loans, or loans that may be forgiven if a physician refers patients to the hospital; |
| | • | | payment of the costs of a physician’s travel and expenses for conferences or a physician’s continuing education courses; |
| | • | | coverage on the hospital’s group health insurance plans at an inappropriately low cost to the physician; |
| | • | | rental of space in physician offices, at other than fair market value terms, by persons or entities to which physicians refer; |
| | • | | payment for services that require few, if any, substantive duties by the physician, or payment for services in excess of the fair market value of the services rendered; or |
| | • | | “gainsharing,” the practice of giving physicians a share of any reduction in a hospital’s costs for patient care attributable in part to the physician’s efforts. |
In addition to issuing fraud alerts, the OIG from time to time issues compliance program guidance for certain types of healthcare providers. In January 2005, the OIG issued supplemental compliance program guidance for hospitals. In the supplemental compliance guidance, the OIG identifies areas of potential risk of liability under federal fraud and abuse statutes and regulations. These areas of risk include compensation arrangements with physicians, recruitment arrangements with physicians and joint venture relationships with physicians. The OIG recommends structuring arrangements to fit squarely within a safe harbor.
96
We have a variety of financial relationships with physicians who refer patients to our hospitals. As of June 30,2011, physicians own interests in nine of our full service acute care hospitals. We also have other joint venture relationships with physicians and contracts with physicians providing for a variety of financial arrangements, including employment contracts, leases and professional service agreements. We provide financial incentives to recruit physicians to relocate to communities served by our hospitals, including minimum cash collections guarantees and forgiveness of repayment obligations. Although we have established policies and procedures to ensure that our arrangements with physicians comply with current law and available interpretations, we cannot assure you that regulatory authorities that enforce these laws will not determine that some of these arrangements violate the anti-kickback statute or other applicable laws. Violation of the anti-kickback statute is a felony, and such a determination could subject us to liabilities under the Social Security Act, including criminal penalties of imprisonment or fines, civil penalties up to $50,000, damages up to three times the total amount of the improper payment to the referral source and exclusion from participation in Medicare, Medicaid or other federal healthcare programs, any of which could have a material adverse effect on our business, financial condition or results of operations.
The Social Security Act also imposes criminal and civil penalties for submitting false claims to Medicare and Medicaid. False claims include, but are not limited to, billing for services not rendered, misrepresenting actual services rendered in order to obtain higher reimbursement and cost report fraud. Like the anti-kickback statute, these provisions are very broad. Further, the Social Security Act contains civil penalties for conduct including improper coding and billing for unnecessary goods and services. Pursuant to the Health Reform Law, civil penalties may be imposed for the failure to report and return an overpayment within 60 days of identifying the overpayment or by the date a corresponding cost report is due, whichever is later. To avoid liability, providers must, among other things, carefully and accurately code claims for reimbursement, as well as accurately prepare cost reports.
Some of these provisions, including the federal Civil Monetary Penalty Law, require a lower burden of proof than other fraud and abuse laws, including the federal anti-kickback statute. Civil monetary penalties that may be imposed under the federal Civil Monetary Penalty Law range from $10,000 to $50,000 per act, and in some cases may result in penalties of up to three times the remuneration offered, paid, solicited or received. In addition, a violator may be subject to exclusion from federal and state healthcare programs. Federal and state governments increasingly use the federal Civil Monetary Penalty Law, especially where they believe they cannot meet the higher burden of proof requirements under the federal anti-kickback statute.
HIPAA broadened the scope of the fraud and abuse laws by adding several criminal provisions for healthcare fraud offenses that apply to all health benefit programs. This act also created new enforcement mechanisms to combat fraud and abuse, including the Medicare Integrity Program and an incentive program under which individuals can receive up to $1,000 for providing information on Medicare fraud and abuse that leads to the recovery of at least $100 of Medicare funds. In addition, federal enforcement officials now have the ability to exclude from Medicare and Medicaid any investors, officers and managing employees associated with business entities that have committed healthcare fraud. Additionally, this act establishes a violation for the payment of inducements to Medicare or Medicaid beneficiaries in order to influence those beneficiaries to order or receive services from a particular provider or practitioner.
The Social Security Act also includes a provision commonly known as the “Stark Law.” This law prohibits physicians from referring Medicare and Medicaid patients to entities with which they or any of their immediate family members have a financial relationship for the provision of certain designated health services that are reimbursable by Medicare or Medicaid, including inpatient and outpatient hospital services. The law also prohibits the entity from billing the Medicare program for any items or services that stem from a prohibited referral. Sanctions for violating the Stark Law include civil monetary penalties up to $15,000 per item or service improperly billed and exclusion from the federal healthcare programs. There are a number of exceptions to the self-referral prohibition, including an exception for a physician’s ownership interest in an entire hospital, although the Health Reform Law significantly restricts this exception. There are also exceptions for many of the customary financial arrangements between physicians and providers, including employment contracts, leases, professional services agreements, non-cash gifts having a value less than $359 (effective for calendar year 2011) and recruitment agreements. Unlike safe harbors under the anti-kickback statute, with which compliance is voluntary, an arrangement must comply with every requirement of the appropriate Stark Law exception or the arrangement is in violation of the Stark Law. Further, intent does not have to be proven to establish a violation of the Stark Law.
97
Through a series of rulemakings, CMS has issued final regulations implementing the Stark Law. Additional changes to these regulations, which became effective October 1, 2009, further restrict the types of arrangements that hospitals and physicians may enter, including restrictions on certain leases, percentage compensation arrangements, and agreements under which a hospital purchases services under arrangements. While these regulations help clarify the requirements of the exceptions to the Stark Law, it is unclear how the government will interpret many of these exceptions for enforcement purposes. CMS has indicated that it is considering additional changes to the Stark Law regulations. We cannot assure you that the arrangements entered into by us and our hospitals will be found to be in compliance with the Stark Law, as it ultimately may be implemented or interpreted.
Historically the Stark Law has contained an exception, commonly referred to as the whole hospital exception, allowing physicians to own an interest in an entire hospital, as opposed to an interest in a hospital department. However, the Health Reform Law significantly narrows the Stark Law’s whole hospital exception. Specifically, the whole hospital exception is available only to hospitals that had physician ownership in place as of March 23, 2010, and a Medicare provider agreement effective as of December 31, 2010. Thus, the Health Reform Law effectively prevents the formation of new physician-owned hospitals. On November 2, 2010, CMS issued a final rule implementing certain provisions of the amended whole hospital exception. While the amended whole hospital exception grandfathers certain existing physician-owned hospitals, including ours, it generally prohibits a grandfathered hospital from increasing its aggregate percentage of physician ownership beyond the aggregate level that was in place as of March 23, 2010. Further, subject to limited exceptions, a grandfathered physician-owned hospital may not increase its aggregate number of operating rooms, procedure rooms, and beds for which it is licensed beyond the number as of March 23, 2010.
The whole hospital exception, as amended, also contains additional disclosure requirements. For example, a grandfathered physician-owned hospital is required to submit an annual report to the Department listing each investor in the hospital, including all physician owners. In addition, grandfathered physician-owned hospitals must have procedures in place that require each referring physician owner to disclose to patients, with enough notice for the patient to make a meaningful decision regarding receipt of care, the physician’s ownership interest and, if applicable, any ownership interest held by the treating physician. A grandfathered physician-owned hospital also must disclose on its web site and in any public advertising the fact that it has physician ownership. The Health Reform Law requires grandfathered physician-owned hospitals to comply with these new requirements by September 23, 2011, and requires the Department to audit hospitals’ compliance beginning no later than May 1, 2012.
In addition to the restrictions and disclosure requirements applicable to physician-owned hospitals set forth in the Health Reform Law, CMS regulations require physician-owned hospitals and their physician owners to disclose certain ownership information to patients. Physician-owned hospitals that receive referrals from physician owners must disclose in writing to patients that such hospitals are owned by physicians and that patients may receive a list of the hospitals’ physician investors upon request. Additionally, a physician-owned hospital must require all physician owners who are members of the hospital’s medical staff to agree, as a condition of continued medical staff membership or admitting privileges, to disclose in writing to all patients whom they refer to the hospital their (or an immediate family member’s) ownership interest in the hospital. A hospital is considered to be physician-owned if any physician, or an immediate family member of a physician, holds debt, stock or other types of investment in the hospital or in any owner of the hospital, excluding physician ownership through publicly traded securities that meet certain conditions. If a hospital fails to comply with these regulations, the hospital could lose its Medicare provider agreement and be unable to participate in Medicare.
Sanctions for violating the Stark Law include denial of payment, civil monetary penalties of up to $15,000 per claim submitted and exclusion from the federal healthcare programs. The statute also provides for a penalty of up to $100,000 for a scheme intended to circumvent the Stark Law prohibitions.
Evolving interpretations of current, or the adoption of new, federal or state laws or regulations could affect many of the arrangements entered into by each of our hospitals. In addition, law enforcement authorities, including the OIG, the courts and Congress are increasing scrutiny of arrangements between healthcare providers and potential referral sources to ensure that the
98
arrangements are not designed as a mechanism to improperly pay for patient referrals or other business. Investigators also have demonstrated a willingness to look behind the formalities of a business transaction to determine the underlying purpose of payments between healthcare providers and potential referral sources.
Many of the states in which we operate also have adopted laws that prohibit payments to physicians in exchange for referrals similar to the federal anti-kickback statute or that otherwise prohibit fraud and abuse activities. Many states also have passed self-referral legislation similar to the Stark Law, prohibiting the referral of patients to entities with which the physician has a financial relationship. Often these state laws are broad in scope and may apply regardless of the source of payment for care. These statutes typically provide criminal and civil penalties, as well as loss of licensure. Little precedent exists for the interpretation or enforcement of these state laws.
Our operations could be adversely affected by the failure of our arrangements to comply with the anti-kickback statute, the Stark Law, billing laws and regulations, current state laws or other legislation or regulations in these areas adopted in the future. We are unable to predict whether other legislation or regulations at the federal or state level in any of these areas will be adopted, what form such legislation or regulations may take or how they may affect our operations. We are continuing to enter into new financial arrangements with physicians and other providers in a manner structured to comply in all material respects with these laws. We cannot assure you, however, that governmental officials responsible for enforcing these laws or whistleblowers will not assert that we are in violation of them or that such statutes or regulations ultimately will be interpreted by the courts in a manner consistent with our interpretation.
The Federal False Claims Act and Similar State Laws
Another trend affecting the healthcare industry today is the increased use of the FCA and, in particular, actions being brought by individuals on the government’s behalf under the FCA’s “qui tam” or whistleblower provisions. Whistleblower provisions allow private individuals to bring actions on behalf of the government alleging that the defendant has defrauded the federal government. If the government intervenes in the action and prevails, the party filing the initial complaint may share in any settlement or judgment. If the government does not intervene in the action, the whistleblower plaintiff may pursue the action independently and may receive a larger share of any settlement or judgment. When a private party brings aqui tamaction under the FCA, the defendant generally will not be made aware of the lawsuit until the government commences its own investigation or makes a determination whether it will intervene. Further, every entity that receives at least $5.0 million annually in Medicaid payments must have written policies for all employees, contractors or agents, providing detailed information about false claims, false statements and whistleblower protections under certain federal laws, including the FCA, and similar state laws.
When a defendant is determined by a court of law to be liable under the FCA, the defendant must pay three times the actual damages sustained by the government, plus mandatory civil penalties of between $5,500 to $11,000 for each separate false claim. Settlements entered into prior to litigation usually involve a less severe calculation of damages. There are many potential bases for liability under the FCA. Liability often arises when an entity knowingly submits a false claim for reimbursement to the federal government. The FCA broadly defines the term “knowingly.” Although simple negligence will not give rise to liability under the FCA, submitting a claim with reckless disregard to its truth or falsity can constitute “knowingly” submitting a false claim and result in liability. In some cases, whistleblowers, the federal government and courts have taken the position that providers that allegedly have violated other statutes, such as the anti-kickback statute or the Stark Law, have thereby submitted false claims under the FCA. The Health Reform Law clarifies this issue with respect to the anti-kickback statute by providing that submission of a claim for an item or service generated in violation of the anti-kickback statute constitutes a false or fraudulent claim under the FCA. The Fraud Enforcement and Recovery Act of 2009 expanded the scope of the FCA by, among other things, creating liability for knowingly and improperly avoiding repayment of an overpayment received from the government and broadening protections for whistleblowers. Under the Health Reform Law, the FCA is implicated by the knowing failure to report and return an overpayment within 60 days of identifying the overpayment or by the date a corresponding cost report is due, whichever is later. Further, the FCA will cover payments involving federal funds in connection with the new health insurance exchanges to be created pursuant to the Health Reform Law.
99
A number of states, including states in which we operate, have adopted their own false claims provisions as well as their own whistleblower provisions whereby a private party may file a civil lawsuit in state court. DEFRA creates an incentive for states to enact false claims laws that are comparable to the FCA. From time to time, companies in the healthcare industry, including ours, may be subject to actions under the FCA or similar state laws.
Corporate Practice of Medicine/Fee Splitting
Certain of the states in which we operate have laws that prohibit unlicensed persons or business entities, including corporations, from employing physicians or laws that prohibit certain direct or indirect payments or fee-splitting arrangements between physicians and unlicensed persons or business entities. Possible sanctions for violations of these restrictions include loss of a physician’s license, civil and criminal penalties and rescission of business arrangements that may violate these restrictions. These statutes vary from state to state, are often vague and seldom have been interpreted by the courts or regulatory agencies. Although we exercise care to structure our arrangements with healthcare providers to comply with relevant state laws, we cannot assure you that governmental officials responsible for enforcing these laws will not assert that we, or transactions in which we are involved, are in violation of such laws, or that such laws ultimately will be interpreted by the courts in a manner consistent with our interpretations.
HIPAA Administrative Simplification and Privacy and Security Requirements
HIPAA requires the use of uniform electronic data transmission standards for healthcare claims and payment transactions submitted or received electronically. These provisions are intended to encourage electronic commerce in the healthcare industry. The Department has established electronic data transmission standards that all healthcare providers must use when submitting or receiving certain healthcare transactions electronically. In addition, HIPAA requires that each provider use a National Provider Identifier. In January 2009, CMS published a final rule making changes to the formats used for certain electronic transactions and requiring the use of updated standard code sets for certain diagnoses and procedures known as ICD-10 code sets. Although use of the ICD-10 code sets is not mandatory until October 1, 2013, we will be modifying our payment systems and processes to prepare for their implementation. Use of the ICD-10 code sets will require significant changes; however, we believe that the cost of compliance with these regulations has not had and is not expected to have a material adverse effect on our business, financial position or results of operations. The Health Reform law requires the Department to adopt standards for additional electronic transactions and to establish operating rules to promote uniformity in the implementation of each standardized electronic transaction.
As required by HIPAA, the Department has issued privacy and security regulations that extensively regulate the use and disclosure of individually identifiable health-related information and require healthcare providers to implement administrative, physical and technical practices to protect the security of individually identifiable health information that is electronically maintained or transmitted. ARRA broadens the scope of the HIPAA privacy and security regulations. In addition, ARRA extends the application of certain provisions of the security and privacy regulations to business associates (entities that handle identifiable health-related information on behalf of covered entities) and subjects business associates to civil and criminal penalties for violation of the regulations. On July 14, 2010, the Department issued a proposed rule that would implement these ARRA provisions. If finalized, these changes would likely require amendments to existing agreements with business associates and would subject business associates and their subcontractors to direct liability under the HIPAA privacy and security regulations. We have developed and utilize a HIPAA compliance plan as part of our effort to comply with HIPAA privacy and security requirements. The privacy regulations and security regulations have and will continue to impose significant costs on our facilities in order to comply with these standards.
As required by ARRA, the Department published an interim final rule on August 24, 2009, that requires covered entities to report breaches of unsecured protected health information to affected individuals without unreasonable delay, but not to exceed 60 days of discovery of the breach by the covered entity or its agents. Notification must also be made to the Department and, in certain situations involving large breaches, to the media. Various state laws and regulations may also require us to notify affected individuals in the event of a data breach involving individually identifiable information.
100
Violations of the HIPAA privacy and security regulations may result in civil and criminal penalties, and ARRA has strengthened the enforcement provisions of HIPAA, which may result in increased enforcement activity. Under ARRA, the Department is required to conduct periodic compliance audits of covered entities and their business associates. ARRA broadens the applicability of the criminal penalty provisions to employees of covered entities and requires the Department to impose penalties for violations resulting from willful neglect. ARRA significantly increases the amount of the civil penalties, with penalties of up to $50,000 per violation for a maximum civil penalty of $1,500,000 in a calendar year for violations of the same requirement. Further, ARRA authorizes state attorneys general to bring civil actions seeking either injunction or damages in response to violations of HIPAA privacy and security regulations that threaten the privacy of state residents.
Our facilities also are subject to any federal or state privacy-related laws that are more restrictive than the privacy regulations issued under HIPAA. These laws vary, may impose additional obligations and could impose additional penalties.
There are numerous other laws and legislative and regulatory initiatives at the federal and state levels addressing privacy and security concerns. For example, in 2007, the Federal Trade Commission issued a final rule requiring financial institutions and creditors, which arguably included hospitals and other healthcare providers, to implement written identity theft prevention programs to detect, prevent, and mitigate identity theft in connection with certain accounts. The Federal Trade Commission delayed enforcement of this rule until December 31, 2010. In addition, on December 18, 2010, the Red Flag Program Clarification Act of 2010 became law, restricting the definition of a “creditor.” This law may exempt many hospitals from complying with the rule.
The Emergency Medical Treatment and Active Labor Act
The federal Emergency Medical Treatment and Active Labor Act (“EMTALA”) was adopted by Congress in response to reports of a widespread hospital emergency room practice of “patient dumping.” At the time of the enactment, patient dumping was considered to have occurred when a hospital capable of providing the needed care sent a patient to another facility or simply turned the patient away based on such patient’s inability to pay for his or her care. The law imposes requirements upon physicians, hospitals and other facilities that provide emergency medical services. Such requirements pertain to what care must be provided to anyone who comes to such facilities seeking care before they may be transferred to another facility or otherwise denied care. The government broadly interprets the law to cover situations in which patients do not actually present to a hospital’s emergency department, but present to a hospital-based clinic that treats emergency medical conditions on an urgent basis or are transported in a hospital-owned ambulance, subject to certain exceptions. At least one court has interpreted the law also to apply to a hospital that has been notified of a patient’s pending arrival in a non-hospital owned ambulance. Sanctions for violations of this statute include termination of a hospital’s Medicare provider agreement, exclusion of a physician from participation in Medicare and Medicaid programs and civil money penalties. In addition, the law creates private civil remedies that enable an individual who suffers personal harm as a direct result of a violation of the law, and a medical facility that suffers a financial loss as a direct result of another participating hospital’s violation of the law, to sue the offending hospital for damages and equitable relief. We can give no assurance that governmental officials responsible for enforcing the law, individuals or other medical facilities will not assert from time to time that our facilities are in violation of this statute.
Conversion Legislation
Many states have enacted or are considering enacting laws affecting the conversion or sale of not-for-profit hospitals. These laws generally include provisions relating to attorney general approval, advance notification and community involvement. In addition, attorneys general in states without specific conversion legislation may exercise authority over these transactions based upon existing law. In many states, there has been an increased interest in the oversight of not-for-profit conversions. The adoption of conversion legislation and the increased review of not-for-profit hospital conversions may increase the cost and difficulty or prevent the completion of transactions with or acquisitions of not-for-profit organizations in various states.
101
Healthcare Industry Investigations
Significant media and public attention has focused in recent years on the hospital industry. Recently, increased attention has been paid by government investigators as well as private parties pursuing civil lawsuits to the amounts charged by hospitals to uninsured and indigent patients and the related collection practices of hospitals. Other current areas of interest include hospitals with high Medicare outlier payments and recruitment arrangements with physicians. Further, there are numerous ongoing federal and state investigations regarding multiple issues that have targeted hospital companies as well as their executives and managers. We have substantial Medicare, Medicaid and other governmental billings, which could result in heightened scrutiny of our operations. We continue to monitor these and all other aspects of our business and have developed a compliance program to assist us in gaining comfort that our business practices are consistent with both legal principles and current industry standards. However, because the law in this area is complex and constantly evolving, we cannot assure you that government investigations will not result in interpretations that are inconsistent with industry practices, including ours. In public statements surrounding current investigations, governmental authorities have taken positions on a number of issues, including some for which little official interpretation previously has been available, that appear to be inconsistent with practices that have been common within the industry and that previously have not been challenged in this manner. In some instances, government investigations that have in the past been conducted under the civil provisions of federal law may now be conducted as criminal investigations. Additionally, the federal government has indicated that it plans to expand its use of civil monetary penalties and Medicare program exclusions to focus on those in the healthcare industry who accept kickbacks or present false claims, in addition to the federal government’s continuing efforts to focus on the companies that offer or pay kickbacks. Failure to comply with applicable laws and regulations could subject us to significant regulatory action, including fines, penalties and exclusion from the Medicare and Medicaid programs.
Many current healthcare investigations are national initiatives in which federal agencies target an entire segment of the healthcare industry. One example is the federal government’s initiative regarding hospital providers’ improper requests for separate payments for services rendered to a patient on an outpatient basis within three days prior to the patient’s admission to the hospital, where reimbursement for such services is included as part of the reimbursement for services furnished during an inpatient stay. In particular, the government has targeted all hospital providers to ensure conformity with this reimbursement rule. Further, the federal government continues to investigate Medicare overpayments to prospective payment hospitals that incorrectly report transfers of patients to other prospective payment system hospitals as discharges. We are aware that prior to our acquisition of them, several of our hospitals were contacted in relation to certain government investigations that were targeted at an entire segment of the healthcare industry. Although we take the position that, under the terms of the acquisition agreements, the prior owners of these hospitals retained any liability resulting from these government investigations, we cannot assure you that the prior owners’ resolution of these matters or failure to resolve these matters, in the event that any resolution was deemed necessary, will not have a material adverse effect on our operations.
The Health Reform Law allocates $350.0 million of additional federal funding over 10 years to fight healthcare fraud, waste and abuse, including $95.0 million for federal fiscal year 2011, $55.0 million for federal fiscal year 2012 and additional increased funding through 2016. In addition, government agencies and their agents, including MACs, may conduct audits of our healthcare operations. Private payors may conduct similar audits, and we also perform internal audits and monitoring.
Certificates of Need
In some states, the construction of new facilities, acquisition of existing facilities or addition of new beds or services may be subject to review by state regulatory agencies under a certificate of need program. Florida and Nevada are the only states in which we currently operate that require approval of acute care hospitals under a certificate of need program. These laws generally require appropriate state agency determination of public need and approval prior to the addition of beds or services or other capital expenditures. Failure to obtain necessary state approval can result in the inability to expand facilities, add services and complete an acquisition or change ownership. Further, violation may result in the imposition of civil sanctions or the revocation of a facility’s license.
102
Environmental Matters
We are subject to various federal, state and local environmental laws and regulations, including those relating to the protection of human health and the environment. The principal environmental requirements applicable to our operations relate to:
| | • | | the proper handling and disposal of medical waste, hazardous waste and low-level radioactive medical waste; |
| | • | | the proper use, storage and handling of mercury and other hazardous materials; |
| | • | | underground and above-ground storage tanks; |
| | • | | management of hydraulic fluid or oil associated with elevators, chiller units or other equipment; |
| | • | | management of asbestos-containing materials or lead-based paint present or likely to be present at some locations; and |
| | • | | air emission permits and standards for boilers or other equipment. |
We do not expect our obligations under these or other applicable environmental laws and requirements to have a material effect on us. In the course of our operations, we may also identify other circumstances at our facilities, such as water intrusion or the presence of mold or fungus, which warrant action, and we can and do incur additional costs to address those circumstances. Under various environmental laws, we may also be required to clean up or contribute to the cost of cleaning up substances that have been released to the environment either at properties owned or operated by us or our predecessors or at properties to which substances from our operations were sent for off-site treatment or disposal. These remediation obligations may be imposed without regard to fault, and liability for environmental remediation can be substantial. While we cannot predict whether or to what extent we might be held responsible for such cleanup costs in the future, at present we have not identified any significant cleanup costs or liabilities that are expected to have a material effect on us.
Professional and General Liability Insurance
As is typical in the healthcare industry, we are subject to claims and legal actions by patients in the ordinary course of business. To cover these claims, we maintain professional malpractice liability insurance and general liability insurance in amounts that we believe to be sufficient for our operations, including our employed physicians, although some claims may exceed the scope of the coverage in effect. We also maintain umbrella coverage. Losses up to our self-insured retentions and any losses incurred in excess of amounts maintained under such insurance will be funded from working capital.
For fiscal 2011, our self-insured retention for professional and general liability coverage remains unchanged at $5.0 million per claim, with an excess aggregate limit of $55.0 million, and maximum coverage under our insurance policies of $75.0 million. Our self-insurance reserves for estimated claims incurred but not yet reported is based upon estimates determined by third-party actuaries. Funding for the self-insured retention of such claims is derived from operating cash flows. We cannot assure you that this insurance will continue to be available at reasonable prices that will allow us to maintain adequate levels of coverage. We also cannot assure you that our cash flow will be adequate to provide for professional and general liability claims in the future.
Our Information Systems
We use a common information systems platform across all of our hospitals. We use McKesson’s clinical, patient accounting, laboratory, radiology and decision support software and Lawson’s financial application and enterprise resource planning software. We use other vendors for specialized information systems needs for our decision support, emergency and radiology departments.
Our information systems are essential to the following areas of our business operations, among others:
| | • | | patient accounting, including billing and collection of net revenue; |
103
| | • | | financial, accounting, reporting and payroll; |
| | • | | laboratory, radiology and pharmacy systems; |
| | • | | materials and asset management; |
| | • | | negotiating, pricing and administering our managed care contracts; and |
| | • | | monitoring of quality of care and collecting data on quality measures necessary for full Medicare payment updates. |
Utilizing a common information systems platform across all our hospitals allows us to:
| | • | | enhance patient safety, automate medication administration and increase staff time available for direct patient care; |
| | • | | optimize staffing levels according to patient volumes, acuity and seasonal needs at each facility; |
| | • | | perform product line analyses; |
| | • | | continue to meet or exceed quality of care indicators on a current basis; |
| | • | | effectively monitor registration, billing, collections, managed care contract compliance and all other aspects of our revenue cycle; |
| | • | | control supply costs by complying with our group purchasing organization contract; and |
| | • | | effectively monitor financial results. |
The cost of maintaining our information systems has increased significantly in recent years. Information systems maintenance expense increased $2.4 million to $8.7 million for the nine months ended June 30, 2011, as compared to the prior year. We expect the trend of increased maintenance costs in this area to continue in the future.
ARRA included approximately $26.0 billion in funding for various healthcare IT initiatives, including incentives for hospitals and physicians to implement EHR - compatible systems. Implementation of these IT initiatives has been divided into three stages, with stage 1 requiring satisfaction in the 2012 year. Stage 1 requires providers and physicians to meet “meaningful use” standards, which include electronically capturing health information in structured format, tracking key clinical conditions for coordination of care purposes, implementing clinical decision support tools to facilitate disease and medication management, using EHRs to engage patients and families, and reporting clinical quality measures and public health information. We have currently spent a total of $16.6 million towards meeting the meaningful use standards. Though additional investments in hardware and software will be required, we believe our historical capital investments in advanced clinicals and other information systems, as well as quality of care programs, provides a solid platform to build upon for timely compliance with the healthcare IT requirements of ARRA.
Employees and Medical Staff
As of June 30, 2011, we had 14,235 employees, including 4,444 part-time employees. We consider our employee relations to be good. We recruit and retain nurses and medical support personnel by creating a desirable, professional work environment, providing competitive wages, benefits and long-term incentives, and providing career development and other training programs. In order to supplement our current employee base, we have expanded our relationship with local colleges and universities, including our sponsorship of nursing scholarship programs, in our markets.
104
Our hospitals are staffed by licensed physicians who have been admitted to the medical staff of our individual hospitals. Any licensed physician may apply to be admitted to the medical staff of any of our hospitals, but admission to the staff must be approved by each hospital’s medical staff and the appropriate governing board of the hospital in accordance with established credentialing criteria. In an effort to meet community needs in certain markets in which we operate, we have implemented a strategy of employing physicians, with an emphasis on those practicing within certain specialties. While we believe this strategy is consistent with industry trends, we cannot be assured of the long-term success of such a strategy, which includes related integration of physician practice management.
Compliance Program
Our compliance program is designed to ensure that we maintain high standards of conduct in the operation of our business and implement policies and procedures so that employees act in compliance with all applicable laws, regulations and company policies. The organizational structure of our compliance program includes a compliance committee of our board of directors, a corporate management compliance committee and local management compliance committees at each of our hospitals. These committees have the oversight responsibility for the effective development and implementation of our program. Our Vice President of Ethics and Business Practices, who reports directly to our Chief Executive Officer and to the compliance committee of our board of directors, serves as Chief Compliance Officer and is charged with direct responsibility for the development and implementation of our compliance program. Other features of our compliance program include the designation of a Regional Compliance Officer for each of our hospitals, periodic ethics and compliance training and effectiveness reviews, the development and implementation of policies and procedures, including a mechanism for employees to report, without fear of retaliation, any suspected legal or ethical violations. See “Risk Factors.”
105
PROPERTIES
Information with respect to our hospitals and other healthcare related properties can be found in this prospectus under the caption, “Business—Our Properties.”
Additionally, our principal executive offices in Franklin, Tennessee are located in approximately 42,000 square feet of office space. Our office space is leased pursuant to a contract which expires on December 31, 2020. Our principal executive offices, hospitals and other facilities are suitable for their respective uses and generally are adequate for our present needs.
LEGAL PROCEEDINGS
On June 1, 2011, the District Court dismissed with prejudice the Third Amended Complaint filed by a qui tamrelator against IAS, our parent company, after thisqui tam action was remanded to the District Court by the Ninth Circuit. The qui tam action sought monetary damages and civil penalties under the FCA and included allegations that certain business practices related to physician relationships and the medical necessity of certain procedures resulted in the submission of claims for reimbursement in violation of the FCA. The case dates back to March 2005 and became the subject of a subpoena by the OIG in September 2005. In August 2007, the case was unsealed and the DOJ declined to intervene, and the action proceeded before the District Court. Thequi tam relator has filed a notice of appeal with respect to the dismissal with prejudice, and the appeal remains pending. If the qui tam appeal was to be resolved in a manner unfavorable to IAS, it could have a material adverse effect on our business, financial condition and results of operations, including exclusion from the Medicare and Medicaid programs. In addition, we may incur material fees, costs and expenses in connection with defending thequi tam action.
Our facilities obtain clinical and administrative services from a variety of vendors. One vendor, a medical practice that furnished cardiac catheterization services under contractual arrangements at Mesa General Hospital and St. Luke’s Medical Center through March 31, 2008 and May 31, 2008, respectively, asserted that, because of deferred fee adjustments that it claims were due under these arrangements, it was owed additional amounts for services rendered since April 1, 2006 at both facilities. We were unable to reach an agreement with the vendor with respect to the amount of the fee adjustment, if any, that was contractually required, nor with respect to an appropriate methodology for determining such amount. On September 30, 2008, the vendor filed a state court complaint for an aggregate adjustment in excess of the amount we had accrued, in addition to certain tort claims. On March 20, 2009, we filed a Motion to Dismiss and in the alternative to Compel Arbitration. On July 27, 2009, the court granted our Motion to Compel Arbitration on the grounds that the issues are to be determined by binding arbitration. On December 24, 2010, after conducting the arbitration hearing, the arbitration panel issued its decision rejecting the fees sought by the vendor, but did not adopt the fees we proposed. The arbitration panel rendered its judgment on the fair market value of the vendor’s services at a point between the amounts the two parties argued were owed. On July 22, 2011, we paid $15.0 million to discharge the liability resulting from the arbitration panel’s decision, which includes all amounts required to be paid with respect to the fair market value compensation for services rendered by the vendor, prejudgment interest and its attorneys’ fees, but excludes consideration of amounts that may be recoverable by us from our insurance carrier with respect to our attorneys fees above our insurance limits. The payment of this claim brings this arbitration dispute to a final resolution.
CHANGES IN AND DISAGREEMENTS WITH ACCOUNTANTS ON ACCOUNTING OR FINANCIAL DISCLOSURE
None.
106
QUANTITATIVE AND QUALITATIVE DISCLOSURES ABOUT MARKET RISK
We are subject to market risk from exposure to changes in interest rates based on our financing, investing and cash management activities. At June 30, 2011, the following components of our Senior Secured Credit Facilities bear interest at variable rates at specified margins above either the agent bank’s alternate base rate or the LIBOR rate: (i) a $1.025 billion, seven-year term loan; and (ii) a $300.0 million, five-year revolving credit facility. As of June 30, 2011, we had outstanding variable rate debt of $1.022 billion.
We have managed our market exposure to changes in interest rates by converting $200.0 million of our variable rate debt to fixed rate debt through the use of interest rate swap agreements. Our interest rate swaps provide for a total notional amount of $200.0 million through February 29, 2012, at a rate of 2.0% in accordance with the terms of the specific agreements. Our interest rate swap agreements expose us to credit risk in the event of non-performance by our counterparties, Citibank and Wells Fargo. However, we do not anticipate non-performance by Citibank or Wells Fargo.
Although changes in the alternate base rate or the LIBOR rate would affect the cost of funds borrowed in the future, we believe the effect, if any, of reasonably possible near-term changes in interest rates on our remaining variable rate debt or our consolidated financial position, results of operations or cash flows would not be material. Holding other variables constant, including levels of indebtedness, a 0.125% increase in current interest rates would have no estimated impact on pre-tax earnings and cash flows for the next twelve month period given the 1.25% LIBOR floor that exists in our Senior Secured Credit Facilities.
We currently believe we have adequate liquidity to fund operations during the near term through the generation of operating cash flows, cash on hand and access to the revolving credit portion of our Senior Secured Credit Facilities. Our ability to borrow funds under our senior secured revolving credit facility is subject to the financial viability of the participating financial institutions. While we do not anticipate any of our current lenders defaulting on their obligations, we are unable to provide assurance that any particular lender will not default at a future date.
107
DIRECTORS, EXECUTIVE OFFICERS AND CORPORATE GOVERNANCE
The following table sets forth the name, age and position of the directors and executive officers of IAS and executive officers of IASIS. See “Certain Relationships and Related Transactions.”
| | | | | | |
| Name | | Age | | | Position |
W. Carl Whitmer | | | 47 | | | Director, Chief Executive Officer and President |
Phillip J. Mazzuca | | | 52 | | | Chief Operating Officer |
John M. Doyle | | | 51 | | | Chief Financial Officer |
Frank A. Coyle | | | 47 | | | Secretary and General Counsel |
James Moake | | | 42 | | | Operations Chief Financial Officer |
Paul Jenson | | | 63 | | | Executive Vice President |
Richard Gonzalez | | | 60 | | | President, Texas and Louisiana Markets |
Matt Tulin | | | 45 | | | Chief Financial Officer, Utah Market |
Shane Wells | | | 42 | | | Chief Financial Officer, Arizona and Nevada Markets |
Bashar Abunaser | | | 43 | | | Corporate Operations Controller and Chief Financial Officer, Florida, Texas and Louisiana Markets |
Peter Stanos | | | 48 | | | Vice President, Ethics and Business Practices |
Carolyn Rose | | | 62 | | | Chief Executive Officer, Health Choice Arizona, Inc. |
David R. White | | | 64 | | | Chairman of the Board |
Jonathan J. Coslet | | | 47 | | | Director |
David Dupree | | | 58 | | | Director |
Kirk E. Gorman | | | 61 | | | Director |
Greg Kranias | | | 34 | | | Director |
Todd B. Sisitsky | | | 40 | | | Director |
Paul S. Levy | | | 64 | | | Director |
Jeffrey C. Lightcap | | | 52 | | | Director |
Sharad Mansukani | | | 42 | | | Director |
W. Carl Whitmerbecame a Director of IAS in April 2010. He has served as President since April 2010 and was appointed Chief Executive Officer in November 2010. Prior to that time, he served as Chief Financial Officer since November 2001 and Vice President and Treasurer from March 2000 to October 2001. Prior to joining our company, Mr. Whitmer served various roles including Vice President of Finance and Treasurer and Chief Financial Officer of PhyCor Inc., where he was employed from July 1994 through February 2000. Mr. Whitmer’s responsibilities at PhyCor included acquisitions, capital planning and management, investor relations, treasury management and external financial reporting. Prior to joining PhyCor Inc., Mr. Whitmer served as a Senior Manager with the accounting firm of KPMG LLP, where he was employed from July 1986 to July 1994. Mr. Whitmer also serves on the board of directors, including the audit committee, of Fenwall, Inc.
Phillip J. Mazzucawas appointed Chief Operating Officer in October 2010. Prior to joining our company, Mr. Mazzuca served as President and Chief Executive Officer of Brim Holdings, Inc., for the past two years. Prior to joining Brim Holdings, Inc., Mr. Mazzuca served for three years as the Executive Vice President and Chief Operating Officer of Charlotte, North Carolina-based MedCath Corporation, where he oversaw the company’s hospital operations. Starting in 1999, he spent six years at IASIS, rising to Division President for the Texas and Florida markets. In previous years, he served in operations leadership roles for a number of hospitals and hospital companies, including Chief Executive Officer of hospitals in several states including Alabama, California, Illinois and Virginia.
108
John M. Doylehas served as Chief Financial Officer since April 2010. Prior to that time, he served as Vice President and Chief Accounting Officer since July 2006 and Vice President and Treasurer from April 2006 to July 2006. Prior to joining our company, Mr. Doyle was a Senior Manager at Ernst & Young LLP from February 1997 until March 2002 and at KPMG LLP from August 1994 to January 1997, where he specialized in healthcare audit and business advisory services, including mergers and acquisitions. In addition, from October 1991 to August 1994, Mr. Doyle was the Chief Financial Officer for two community hospitals in East Tennessee and North Carolina.
Frank A. Coylehas been Secretary and General Counsel since October 1999. From August 1998 until October 1999, Mr. Coyle served as Secretary and General Counsel of a company formed by members of our management that was merged into one of our subsidiaries. Mr. Coyle served from May 1995 to August 1998 as Assistant Vice President Development in Physician Services and in-house Development Counsel for Columbia/HCA. From May 1990 to May 1995, Mr. Coyle was an attorney with Baker, Worthington, Crossley, Stansberry & Woolf where his work included mergers, acquisitions, securities transactions, not-for-profit representation and formation of Tennessee health maintenance organizations.
James Moakehas served as Operations Chief Financial Officer since February 2005. Prior to that time, he has served as a Division Chief Financial Officer since March 2003. From November 2002 to March 2003, Mr. Moake served as Operations Controller. Prior to joining our company, from March 2000 to November 2002, he served as the Chief Financial Officer for two regional medical centers of Province Healthcare Corporation. Mr. Moake served as the Chief Financial Officer of HMA, Inc.’s Community Hospital of Lancaster (PA) from July 1999 to March 2000 and the Assistant Chief Financial Officer of HMA, Inc.’s Biloxi Regional Medical Center (MS) from June 1998 to June 1999. From December 1994 to May 1998, he served as the Chief Financial Officer of Grant Regional Health Center, Inc. in Wisconsin.
Paul Jensonhas served as the Executive Vice President —Western Region since April 1, 2008. Prior to that time, Mr. Jenson served as President of the Arizona Market from July 1, 2007 and had also served as the President of the Nevada Market since October 1, 2007. From April 1, 2005 to July 1, 2007, his position was Chief Executive Officer of St. Luke’s Medical Center, St. Luke’s Behavioral Health Center and Biltmore Surgery Center in Phoenix, Arizona. Prior to joining our company, Mr. Jenson worked for HCA Inc. for 14 years with his last position being Chief Executive Officer of HCA-Brunswick Community Hospital from September 2002 until April 2005. Mr. Jenson has a background of 40 years of experience in healthcare management in locations throughout the United States.
Richard Gonzalezhas served as President of the Texas and Louisiana markets since December 2008. In addition, he has served as Chief Executive Officer of Southwest General Hospital since April 2003. Prior to joining our company, Mr. Gonzalez held numerous healthcare leadership positions in the United States and Mexico since 1975, including, most recently, as Chief Financial Officer of The Methodist Hospital in Houston, Texas.
Matt Tulinhas served as Chief Financial Officer of the Utah market since April 2009. Prior to that time, Mr. Tulin served as Chief Financial Officer over finance and operations, from 2006 to 2009, for NEA Baptist Memorial Hospital, formally Triad Healthcare then Community Health Systems, a joint venture syndication health system over two acute care facilities. From 2004 to 2006, Mr. Tulin served as Chief Financial Officer at two LifePoint Hospitals, Southern Tennessee Medical Center in Winchester, Tennessee and Emerald Hodgson Hospital in Sewanee, Tennessee.
Shane Wells has served as Chief Financial Officer of the Arizona and Nevada markets since April 2011. Prior to rejoining our company, Mr. Wells served as a Regional Finance Director for AnesthiaCare, the anesthesia contract management services division of EmCare, Inc. Mr. Wells’ previous experience at our company included serving as Chief Financial Officer of the Texas, Florida, Louisiana and Nevada markets from 2006 to 2008. Prior to joining our company, Mr. Wells was a hospital Chief Financial Officer with Health Management Associates, Inc.
Bashar Abunaseris serving as the Corporate Operations Controller and the Chief Financial Officer of the Florida, Texas and Louisiana markets. Prior to that time, Mr. Abunaser served as Director of Financial Operations at SunLink Health Systems, Inc. from August 2006 to December 2007 and as Chief Financial Officer at two SunLink hospitals, Chestatee Regional Hospital in Dahlonega, Georgia and Missouri Southern Healthcare in Dexter, Missouri, from September 2003 to August 2006.
Peter Stanoshas served as Vice President, Ethics & Business Practices since April 2003. Prior to that time, he served as Regional Director Clinical Operations for our Utah market since July 2002. Prior to joining our company, from May 2000 until July 2002, Mr. Stanos was employed by Province Healthcare Corporation as Chief Quality Officer of Havasu Regional Medical Center and as Regional Director of Quality and Resource Management. From 1997 until 2000, Mr. Stanos was employed by HCA and Triad Hospitals, Inc. as an Associate Administrator
109
and Director of Quality and Resource Management, Materials, Pharmacy and Risk Management. Prior to joining HCA, Mr. Stanos served as Regional Director of several healthcare companies, as well as an independent healthcare consultant.
Carolyn Rosehas served as Chief Executive Officer of Health Choice since 1999. From 1983 to 1999, Ms. Rose held a number of senior management positions in the managed healthcare industry. Ms. Rose served as Executive Director/CEO for several large indigent practice associations, as well as serving as a principal and partner in a consulting firm specializing in managed care and hospital consolidations.
David R. Whitecurrently serves as Chairman of the Board of Directors of IAS. Mr. White served as Chief Executive Officer of IAS from December 1, 2000 to October 2010 and President of IAS from May 2001 through May 2004. Mr. White served as President and Chief Executive Officer of LifeTrust, an assisted living company, from November 1998 until November 2000. From June 1994 to September 1998, Mr. White served as President of the Atlantic Group at Columbia/HCA, where he was responsible for 45 hospitals located in nine states. Previously, Mr. White was Executive Vice President and Chief Operating Officer at Community Health Systems, Inc., a for-profit hospital management company that operated approximately 20 acute-care hospitals.
Jonathan J. Cosletbecame a Director of IAS in June 2004. Mr. Coslet is a Senior Partner of TPG Capital. Mr. Coslet is also a member of the firm’s Investment Committee and Management Committee. Prior to joining TPG Capital in 1993, Mr. Coslet was in the Investment Banking Department of Donaldson, Lufkin & Jenrette, specializing in leveraged acquisitions and high yield finance from 1991 to 1993. Mr. Coslet serves on the boards of directors of The Neiman Marcus Group, Inc., PETCO Animal Supplies, Inc., Biomet, Inc., Quintiles Transnational Corp. and Caesars Entertainment Corporation.
David Dupreebecame a director of IAS in April 2007. Mr. Dupree has been Managing Director and Chief Executive Officer of The Halifax Group since 1999. Prior to co-founding Halifax, Mr. Dupree was a Managing Director and Partner with The Carlyle Group, where he was primarily responsible for investments in healthcare and related sectors. Prior to joining The Carlyle Group in 1992, Mr. Dupree was a Principal in corporate finance with Montgomery Securities. Mr. Dupree also serves as a Director of Primo Water Corporation, a supplier of bottled water dispensers, and a Director Emeritus of Whole Foods Market, Inc., a natural and organic foods supermarket company where he served as Director from 1997 until 2008.
Kirk E. Gormanwas appointed a Director of IAS in August 2004. Mr. Gorman currently serves as Senior Vice President and Chief Financial Officer of Jefferson Health System, a not-for-profit health system based in Radnor, Pennsylvania, which he joined in October 2003. Prior to joining Jefferson Health System, Mr. Gorman served as Senior Vice President and Chief Financial Officer of Universal Health Services, Inc., a public hospital company based in Pennsylvania, from 1987 to February 2003. Mr. Gorman also has 13 years of experience in the banking industry and served as Senior Vice President of Mellon Bank prior to his work in the healthcare industry. Mr. Gorman serves as a Director of Cardionet Inc., the leading provider of mobile cardiac outpatient telemetry. Mr. Gorman served as a Director of Care Investment Trust, a real estate investment and finance company, from 2007 to 2009.
Greg Kraniasbecame a Director of IAS effective May 25, 2010. Mr. Kranias serves as a Principal at TPG Capital. Prior to joining TPG Capital in 2005, Mr. Kranias worked at the private equity firm Forstmann Little & Company. Before joining Forstmann Little & Company in 2001, Mr. Kranias was an investment banker with Goldman, Sachs & Co. Mr. Kranias is involved with the investment by affiliates of Caesars Entertainment Corporation. He received his M.B.A. from the Stanford Graduate School of Business and his A.B. from Harvard College, where he graduated Phi Beta Kappa.
Todd B. Sisitsky became a Director of IAS in June 2004. Mr. Sisitsky is a Partner of TPG Capital, where he leads the firm’s investment activities in the healthcare services, pharmaceutical and medical device sectors. In addition to our company, he played leadership roles in connection with investments by TPG and its affiliates in Aptalis Pharma, Biomet, Inc., Fenwal Transfusion Therapies, Surgical Care Affiliates, LLC, HealthScope and IMS Health and serves on the board of directors of each of these companies. Prior to joining TPG Capital in 2003, Mr. Sisitsky worked at Forstmann Little & Company and Oak Hill Capital Partners.
110
Paul S. Levyhas been a Director of IAS since October 1999. Mr. Levy is a Senior Managing Director of JLL Partners, Inc., which he founded in 1988. Mr. Levy serves as a director of several companies, including Builders FirstSource, Inc., Medical Card Systems, Inc., Patheon Inc., PGT Inc. and PharmaNet Development Group, Inc.
Jeffrey C. Lightcaphas been a Director of IAS since October 1999. Since October 2006, Mr. Lightcap has been a Senior Managing Director of HealthCor Group. Prior to joining HealthCor Group, Mr. Lightcap was a Senior Managing Director at JLL Partners, Inc., which he joined in June 1997. From February 1993 to May 1997, Mr. Lightcap was a Managing Director at Merrill Lynch & Co., Inc., where he was the head of leveraged buyout firm coverage for the mergers and acquisitions group.
Sharad Mansukanibecame a Director of IAS in April 2005. Dr. Mansukani serves as a senior advisor of TPG Capital, and serves on the faculty at both the University of Pennsylvania and Temple University School of Medicine. Dr. Mansukani previously served as a senior advisor to the Administrator of CMS from 2003 to 2005, and as Senior Vice President and Chief Medical Officer of Health Partners, a non-profit Medicaid and Medicare health plan owned at the time by Philadelphia-area hospitals. Dr. Mansukani completed a residency and fellowship in ophthalmology at the University of Pennsylvania School of Medicine and a fellowship in quality management and managed care at the Wharton School of Business. Dr. Mansukani also serves as a Director of Healthspring, Inc.
Director Qualifications
The certificate of incorporation and by-laws of IAS provide that its board of directors will consist of not less than three nor more than 15 members, the exact number of which shall be determined by the board of directors in a resolution. The directors are elected at the annual meeting of stockholders for one-year terms and until their successors are duly elected and qualified.
Pursuant to the limited liability company operating agreement of IASIS Investment, JLL is entitled to nominate two directors to IAS’ board of directors. TPG is entitled to nominate the remaining directors. Messrs. Levy and Lightcap serve on IAS’ board of directors as designees of JLL. The remaining directors serve as designees of TPG.
When considering whether the directors and nominees have the experience, qualifications, attributes and skills, taken as a whole, to enable the board of directors to satisfy its oversight responsibilities effectively in light of the Company’s business and structure, the board of directors focused primarily on the information discussed in each of the directors’ biographical information set forth above.
Each of the directors possesses high ethical standards, acts with integrity, and exercises careful, mature judgment. Each is committed to employing their skills and abilities to aid the long-term interests of the stakeholders of the Company. In addition, our directors are knowledgeable and experienced in one or more business, governmental, or civic endeavors, which further qualifies them for service as members of the board of directors. Alignment with our stockholders is important in building value at the Company over time.
As a group, the non-management directors possess experience in owning and managing enterprises like the Company and are familiar with corporate finance, strategic business planning activities and issues involving stakeholders more generally.
The management directors bring leadership, extensive business, operating, financial, legal and policy experience, and knowledge of our Company and the Company’s industry, to the board of directors. In addition, the management directors bring their broad strategic vision for our Company to the board of directors.
Audit Committee Financial Expert
The current members of our audit committee are Messrs. Sisitsky, Lightcap and Gorman. IAS’ board of directors has determined that Todd Sisitsky is an “audit committee financial expert” as that term is defined in Item 401(h) of Regulation S-K promulgated by the SEC.
111
EXECUTIVE COMPENSATION
Compensation Discussion and Analysis
Executive Summary
This section discusses the principles underlying our executive compensation policies and decisions. It provides qualitative information regarding the manner in which compensation is earned by our executive officers and places in context the data presented in the tables that follow. In addition, in this section, we address the compensation paid or awarded during fiscal 2010 to the following executive officers: David R. White, our Chairman and Chief Executive Officer through October 31, 2010; W. Carl Whitmer, our President and effective November 1, 2010, our Chief Executive Officer (who also acted as our Chief Financial Officer during part of fiscal 2010), John M. Doyle, our Chief Financial Officer (who also acted as our Chief Accounting Officer during part of fiscal 2010; and three other executive officers who were our three other most highly compensated executive officers in fiscal 2010, as follows: Sandra McRee, our Chief Operating Officer through October 31, 2010; Frank Coyle, our Secretary and General Counsel, and Carolyn Rose, Chief Executive Officer of Health Choice. We refer to these six executive officers as our “named executive officers”.
During fiscal 2010, as part of a leadership transition at the Company, Mr. White and Ms. McRee announced their respective retirements, effective after fiscal 2010. Mr. White will continue as Chairman of the Board of Directors and Ms. McRee will take on the position of Vice Chair of the Board of Directors. During fiscal 2010, Mr. Whitmer was promoted from Chief Financial Officer to President and Mr. Doyle was promoted from Chief Accounting Officer to Chief Financial Officer. Mr. Whitmer also became our Chief Executive Officer effective November 1, 2010.
On June 22, 2004, an investor group led by TPG acquired IAS through a merger. In order to effect the acquisition, the investor group established IASIS Investment LLC (“IASIS Investment”), and a wholly owned subsidiary of IASIS Investment, which merged with and into IAS. In the merger, IAS issued shares of common and preferred stock to IASIS Investment, which is the sole stockholder of IAS after giving effect to the merger. Prior to the merger, IAS contributed substantially all of its assets and liabilities to IASIS in exchange for all of the equity interests in IASIS. As a result, IAS is a holding company, IASIS is a limited liability company consisting of 100% common interests owned by IAS and IAS’s operations are conducted by IASIS and its subsidiaries. We refer to the merger, the related financing transactions and the applications of the proceeds from the financing transactions as the “Transactions.” As discussed in more detail below, various aspects of named executive officer compensation were negotiated and determined at the time of the Transactions. In addition, since the equity of our company is owned entirely by a group of sophisticated investment funds who also control our board of directors, our compensation structure is largely driven by these investment funds that rely heavily upon their experience and expertise. Our Compensation Committee (the “Committee”) is made up of three individuals, our Chief Executive Officer, two directors of IAS, one of whom serves as a representative of JLL Partners and one of whom is designated by TPG who represents our equity investors and chairs the Committee.
The Committee’s compensation philosophy is to align the interests of the executive officers with those of the investors while encouraging long-term executive retention. Furthermore, the Committee believes that our ability to grow and be successful in the long-term is enhanced by a comprehensive compensation program that includes different types of incentives for attracting, motivating and retaining executives and rewarding outstanding service, including awards that link compensation to applicable performance measures. Under the Committee’s direction and supervision, we have developed and implemented compensation policies, plans and programs designed to enhance the quality of healthcare services delivered by our hospitals and increase investor value by closely aligning the financial interests of our named executive officers with those of our investors.
As discussed in more detail in the following pages, the compensation structure utilizes not only base salary to compensate our executives competitively, but also heavily relies on annual and long-term incentive compensation to attract and retain highly qualified executives and motivate them to perform to the best of their abilities. In years of outstanding achievement, the Committee believes that our named executive officers should be properly rewarded for their respective contributions to our success through a combination of incentive-based cash and equity-based awards.
112
The Executive Compensation Process
The Compensation Committee
The Committee oversees our executive compensation program. The Committee’s responsibilities include, but are not limited to, the following:
| | • | | Reviewing and approving our compensation philosophy; |
| | • | | Determining executive compensation levels; |
| | • | | Annually reviewing and assessing performance goals and objectives for all executive officers, with particular emphasis with respect to the Chief Executive Officer, the Chief Operating Officer and the Chief Financial Officer; and |
| | • | | Determining short-term and long-term incentive compensation for all executive officers with particular emphasis with respect to the Chief Executive Officer, the Chief Operating Officer and the Chief Financial Officer. |
Mr. Coslet, the TPG designee on the Committee, makes all decisions with respect to the compensation of the Chief Executive Officer. Annually, the non-executive directors of the board of directors evaluate the performance of the Chief Executive Officer and that evaluation is then communicated to the Chief Executive Officer by Mr. Coslet. The Chief Executive Officer recommends to Mr. Coslet compensation decisions for our Chief Operating Officer and our Chief Financial Officer, respectively. Our Chief Executive Officer and Mr. Coslet discuss these recommendations in detail before reaching a final decision. With respect to the other named executive officers, our Chief Executive Officer is generally responsible for conducting reviews and making compensation decisions.
During our fiscal year ended September 30, 2010, the Committee did not rely on the advice or reports of any external compensation consultant in making compensation decisions. As TPG Capital has substantial experience and expertise in executive compensation and in some cases internally employs compensation experts, the Committee may from time to time rely upon such experience, expertise and experts.
Our Chief Executive Officer, a member of the board of directors of IAS, is also a member of the Committee and, as discussed above, plays an important role in many compensation decisions. Other named executive officers also attend the Committee meetings and participate only as and if required by the Committee. As discussed above, the Chief Executive Officer does not participate on behalf of the Committee or the board of directors in decisions regarding his own compensation. Any discussion by the Committee regarding compensation for the Chief Executive Officer or other named executive officers is conducted by the Committee in executive session without such persons in attendance.
Benchmarking Process
The Committee’s process for determining executive compensation is straightforward and, in part, involves consideration of the highly competitive market for executives in the healthcare industry, including review of compensation levels of comparable companies. Management prepares for the Committee informal schedules that compare our cash compensation to the cash compensation offered by certain comparable companies in the acute hospital industry that file such information with the SEC. These comparisons are part of the total mix of information used to annually evaluate base salary, short-term incentive compensation and total cash compensation. The Committee may also, from time to time, rely on analysis performed by TPG Capital that compares the compensation of our executive officers with that of other portfolio companies or private equity backed companies in general. Since one of the objectives of our compensation program is to consistently reward and retain top performers, compensation will also vary depending on individual and company performance.
113
Pay for Performance
The Company emphasizes aligning compensation with performance. With respect to our named executive officers, the primary factor that is utilized in structuring annual compensation, including payouts under the short-term incentive plan, is Adjusted EBITDA (as such term is defined in Note 17 to our consolidated financial statements) compared to our company budget for the previous year. Other factors that may in the Committee’s discretion be considered in certain years include:
| | • | | Adjusted EBITDA year over year growth; |
| | • | | Peer group comparisons including comparisons of net revenue growth, expense margins and return on capital; |
| | • | | Individual, company or division performance including certain core performance measures; |
| | • | | Promotion of an effective, company-wide program that fosters a culture of legal compliance; and |
| | • | | Response to unusual or extreme events. |
Another component of the Company’s pay for performance compensation philosophy is the significant equity holdings of the named executive officers. Certain named executive officers were granted common stock options at the time of the Transactions and also rolled over equity. As shown in the compensation tables below, the Company paid approximately $6.1 million to certain named executive officers during fiscal 2010 to cancel remaining vested rollover options to purchase its common stock.
Internal Pay Equity
Internal pay equity is not a material factor with respect to the Committee’s compensation decisions. The Committee believes that the variation in compensation among the named executive officers is reasonable in light of each executive’s experience, contribution and importance to the Company.
Components of the Executive Compensation Program
Employment Agreements
During the process of completing the Transactions, TPG and the other equity investors entered into negotiations regarding employment agreements with Mr. White, Mr. Whitmer and Ms. McRee. The employment agreements that resulted were heavily negotiated and were largely influenced by the experience and expertise of TPG and the other equity holders as well as the executive’s previous performance and familiarity with the business. The resulting employment agreements established the foundation of the Company’s compensation structure with respect to Mr. White, Mr. Whitmer and Ms. McRee. Mr. Whitmer entered into a new negotiated employment agreement upon his promotion to President during fiscal 2010. Mr. Doyle entered into a negotiated employment agreement upon his promotion to Chief Financial Officer during the year. Ms. Rose entered into an agreement for severance benefits and restrictive covenants upon being hired by IASIS in March 2001. Mr. Coyle does not have an employment agreement.
Base Salary
Base salary represents the fixed component of our named executive officers’ compensation and is intended to compensate the executive for competence in the executive role. The Committee attempts to maintain base salaries at competitive levels while also reserving a substantial portion of compensation for the other compensation elements that are directly related to company performance.
114
The Committee annually reviews and adjusts base salaries of the Chief Executive Officer, Chief Operating Officer and Chief Financial Officer. The Chief Executive Officer approves all base salary increases for other named executive officers. Any base salary increase during this annual process is generally intended to compensate the executive for exceptional performance or contributions, cost of living increases, changes in responsibility, and changes in the competitive landscape. Base salaries may also be adjusted at any time during the year if Mr. Coslet, the Committee, or the Chief Executive Officer, as relevant, finds it necessary or advisable to maintain a competitive level or to compensate an individual for increased responsibility. Mr. White and Ms. McRee did not receive a base compensation increase during the year. Effective April 23, 2010, in connection with their respective promotions, Mr. Whitmer received a base compensation increase from $534,871 to $650,000 and Mr. Doyle received a base compensation increase from $260,000 to $400,000. Mr. Coyle and Ms. Rose did not receive a base compensation increase during the year.
Short-Term Incentive Compensation
Our named executive officers have the opportunity to earn cash incentive awards based upon the level of achievement of financial performance metrics. The range of potential payouts for Mr. White, Mr. Whitmer, Ms. McRee and Mr. Doyle are set forth in their employment agreements and, as discussed above, were highly negotiated. Mr. Coyle and Ms. Rose have target and maximum bonus levels that have been approved by the Chief Executive Officer as representing a competitive level and significantly aligning the interests of these executive officers with those of the investors.
Before the end of the first quarter of the relevant fiscal year, the Company, with the input of members of the board of directors and the investors, establishes target levels for Adjusted EBITDA (as such term is defined in Note 17 to our consolidated financial statements) and other operating metrics such as revenue growth and free cash flow that are used both for compensation and budgeting purposes. Our performance during the year versus the Adjusted EBITDA target levels is the primary factor in calculating the short-term incentive compensation paid to the named executive officers. The Committee has chosen Adjusted EBITDA as the primary financial metric used to calculate short term incentive compensation payouts because it believes it provides an effective measure of our company’s financial health and the creation of long-term equity value.
Annual incentive target awards to our named executive officers vary depending on the Company’s performance against the target levels for Adjusted EBITDA and other operating metrics, as follows:
Annual Incentive Target Award Ranges (as a Percentage of Base Salary) for Fiscal 2010
| | | | | | | | | | | | |
| | | Threshold | | | Target | | | Maximum | |
David R. White | | | 20 | % | | | 100 | % | | | 200 | % |
W. Carl Whitmer(1) | | | 10 | % | | | 75 | % | | | 150 | % |
Sandra K. McRee | | | 10 | % | | | 50 | % | | | 100 | % |
John M. Doyle(2) | | | 10 | % | | | 50 | % | | | 100 | % |
Frank A. Coyle | | | — | | | | 35 | % | | | 35 | % |
Carolyn Rose | | | — | | | | 35 | % | | | 75 | % |
| (1) | For the time period prior to his promotion to President on April 23, 2010, Mr. Whitmer’s Target award was 50% and his Maximum award was 100%. |
| (2) | For the time period prior to his promotion to Chief Financial Officer on April 23, 2010, Mr. Doyle’s Target award was 35% and his Maximum award was 50%. |
While the primary factor in calculating short-term incentive compensation payouts for Mr. White, Mr. Whitmer, Ms. McRee and Mr. Doyle is Adjusted EBITDA, Mr. Coslet or the Committee, as relevant, may consider, in its discretion, other factors in awarding annual incentive compensation to these individuals, including:
| | • | | Adjusted EBITDA year over year growth; |
115
| | • | | Peer group comparisons including comparisons of net revenue growth, expense margins and return on capital; |
| | • | | Individual, company or division performance including certain core performance measures; |
| | • | | Promotion of an effective, company-wide program that fosters a culture of legal compliance; and |
| | • | | Response to unusual or extreme events. |
While the primary factor in calculating short-term incentive compensation payouts for Mr. Coyle and Ms. Rose is also Adjusted EBITDA and the awards are generally either paid or not paid based upon meeting the budgeted level, payouts for Mr. White, Mr. Whitmer, Ms. McRee and Mr. Doyle may consider quality and customer service metrics, cash collections, certain operational and individual goals, as well as any of the factors listed above, in either adjusting the level of payout or whether a payout is made.
In fiscal 2010, the Adjusted EBITDA target was the primary factor considered in awarding payment under the short-term incentive plan to the named executive officers. However, Mr. Coslet and the Committee, as relevant, also considered individual achievements, our company’s free cash flow financial performance to budget and the company’s overall financial performance compared to peer companies. As a result of the Company not achieving target levels for Adjusted EBITDA and other factors, Mr. White, Mr. Whitmer, Ms. McRee, Mr. Doyle or Mr. Coyle were not granted an award,. The Committee granted an award at 75%, the maximum target level, to Ms. Rose based on the targets and goals achieved at Health Choice.
Long-Term Incentive Compensation
Our executive officer compensation has a substantial equity component as we believe superior equity investors’ returns are achieved through a culture that focuses on long-term performance by our named executive officers and other key associates. By providing our executives with an equity stake in the Company, we are better able to align the interests of our named executive officers and our equity holders. At the time of the Transactions, certain named executive officers each received common stock options granted under the 2004 Option Plan and rolled over certain equity. As shown in the compensation tables below, the Company paid approximately $6.1 million to certain named executive officers during fiscal 2010 to cancel vested rollover options to purchase its common stock.
IAS also maintains the IAS 2004 Stock Option Plan and from time to time may grant additional options to the named executive officers pursuant to this plan. In making long-term equity incentive grants to the named executive officers, certain factors are considered, including but not limited to, the present ownership levels of the named executive officers and the level of the executive’s total compensation package compared to peer companies. It is the responsibility of Mr. Coslet to recommend grants to the Committee for the Chief Executive Officer, the Chief Executive Officer to recommend grants to the Committee for the Chief Operating Officer and Chief Financial Officer, and the Chief Executive Officer, Chief Operating Officer or Chief Financial Officer to recommend grants to the Committee for any other named executive officers. No grants were made to the named executive officers in fiscal 2010.
Generally, the exercise price of an option grant is set at the fair market value of a share of the common stock as of the grant date, as determined by the IAS board of directors in good faith and, as necessary, supplemented and supported by an independent third party valuation. We have no formal practices regarding the timing of option grants.
116
Due to our current equity structure, an optionee is expected at the time of grant to enter into an agreement that will generally provide that for the 90-day period following the later of (i) a termination of employment or (ii) six months and one day following the date that shares of common stock were acquired pursuant to the exercise of the option, we have the right to repurchase each share then owned by the participant at fair value, as determined in good faith by the IAS board of directors.
Non-qualified Executive Savings Plan
We provide certain of our employees a non-qualified executive savings plan. The plan is a voluntary, tax-deferred savings vehicle that is available to those employees earning a minimum base salary ($115,000 in 2010). The executive savings plan was implemented in order to assist in the recruitment and retention of key executives by providing the ability to defer additional pre-tax compensation in excess of the limits allowed by the Company’s 401(k) plan.
An eligible employee must contribute the maximum allowed by law to the IASIS 401(k) plan in order to participate in the nonqualified executive savings plan. There are two types of deferrals available under the plan: excess deferrals and additional deferrals. Excess deferrals are contributions that are deposited into the non-qualified executive savings plan because either (a) the participant’s earnings have exceeded $250,000 and/or (b) the participant’s deferrals into the 401(k) plan have reached a dollar limit stipulated by the IRS ($16,500 in 2010). Excess deferrals are automatically deposited into the nonqualified executive savings plan if these limits are reached. Employed physician excess deferrals are not matched. Executive excess deferrals are matched at the same rate as contributions to the 401(k) plan. There is a five-year service requirement for participants to vest in the IASIS excess matching contributions. Currently, none of the named executive officers participates in the plan.
Additional deferrals are contributions to the non-qualified executive savings plan that are independent of a participant’s 401(k) contribution election. These contributions are voluntary and are capped according to applicable IRS guidelines for such a plan.
The non-qualified executive savings plan offers a range of investment options that act as “benchmark funds.” Benchmark funds are defined as the investment fund or funds used to represent the performance and current deemed balance of a participant’s nonqualified account, which is considered a notional deferred compensation account. Contributions become part of our general assets. Investment options under the non-qualified executive savings plan are the same as those available under the IASIS 401(k) plan.
Severance and Change in Control Agreements
Messrs. White and Whitmer and Ms. McRee entered into employment agreements in connection with the Transactions, which agreements provide, among other things, for each executive’s rights upon a termination of employment. Mr. Whitmer entered into a new negotiated employment agreement upon his promotion to President during fiscal 2010. Mr. Doyle entered into a negotiated employment agreement upon his promotion to Chief Financial Officer during fiscal 2010. Ms. Rose entered into an agreement for severance benefits and restrictive covenants in March 2001, which provides for her rights upon a termination of employment. We believe that reasonable and appropriate severance and change in control benefits are appropriate in order to be competitive in our executive retention efforts. In agreeing to these benefits, the board of directors recognized that it may be difficult for such executives to find comparable employment within a short period of time. In addition, the board of directors recognized that formalized severance and change in control arrangements are common benefits offered by employers competing for similar senior executive talent. Information regarding applicable payments under such agreements for the named executive officers is provided under “Narrative Disclosure to Summary Compensation Table and Grants of Plan-Based Awards Table” and “Potential Payments Upon Termination or Change in Control.”
Perquisites
From time to time we agree to provide certain executives with perquisites. We provide these perquisites on a limited basis in order to attract key talent and to enhance business efficiency. We believe these perquisites are in line with market practice. For fiscal 2010, we provided the named executive officers with the following perquisite:
Group term life insurance premiums.We paid insurance premiums with respect to group term life insurance for the named executive officers.
117
Impact of Tax and Accounting Rules
The forms of our executive compensation are largely dictated by our capital structure and have not been designed to achieve any particular accounting treatment. We do take tax considerations into account, both to avoid tax disadvantages, and obtain tax advantages where reasonably possible consistent with our compensation goals. Certain tax advantages for our executives benefit us by reducing the overall compensation we must pay to provide the same after-tax income to our executives. Thus, our severance pay plans are designed to take account of and avoid “parachute” excise taxes under Section 280G of the Internal Revenue Code. Since we currently have no publicly traded equity interests, we are not currently subject to the $1,000,000 limitation on deductions for certain executive compensation under Section 162(m) of the Internal Revenue Code, though that rule will be considered if our equity interests become publicly traded. Incentives paid to executives under our annual incentive plan are taxable at the time paid to our executives.
Recovery of Certain Awards
We do not have a formal policy for recovery of annual incentives paid on the basis of financial results which are subsequently restated. Under the Sarbanes-Oxley Act, our Chief Executive Officer and Chief Financial Officer must forfeit incentive compensation paid on the basis of previously issued financial statements for which they were responsible and which have to be restated due to such officers’ actions. If the situation arises, we would consider our course of action in light of the particular facts and circumstances, including the culpability of the individuals involved.
118
Summary Compensation Table — Fiscal 2010
The following table sets forth, for the fiscal year ended September 30, 2010, the compensation earned by the Principal Executive Officer and Principal Financial Officer. Both Mr. Whitmer and Mr. Doyle served as our Principle Financial Officer during fiscal 2010. The table also sets forth the compensation earned by our other three most highly compensated executive officers during 2010. We refer to these persons as our named executive officers. For 2010, “Salary” accounted for approximately 31.5% of the total compensation of the named executives, “Option Awards” accounted for approximately 66.0% of total compensation, and all other compensation accounted for approximately 2.5% of total compensation. There are no above-market or preferential earnings on deferred compensation. Consequently, the table does not include earnings on deferred amounts. None of the named executive officers is eligible for pension benefits as we do not have a defined benefit program.
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
Name and Principal Position | | Year | | | Salary
($) | | | Bonus
($) | | | Option
Awards
($)(1) | | | Non-Equity
Incentive Plan
Compensation
($)(2) | | | Change in
Pension Value
and
Nonqualified
Deferred
Compensation
Earnings ($) | | | All Other
Compensation
($) | | | Total ($) | |
| | | | | | | | |
David R. White (3) | | | 2010 | | | | 808,500 | | | | — | | | | 2,466,992 | | | | — | | | | — | | | | 9,628 | | | | 3,285,120 | |
Chairman of the Board & | | | 2009 | | | | 808,500 | | | | — | | | | 16,374 | | | | 1,617,000 | | | | — | | | | 9,628 | | | | 2,451,502 | |
Chief Executive Officer | | | 2008 | | | | 808,500 | | | | — | | | | — | | | | — | | | | — | | | | 9,474 | | | | 817,974 | |
| | | | | | | | |
W. Carl Whitmer (3) | | | 2010 | | | | 585,458 | | | | — | | | | 1,438,157 | | | | — | | | | — | | | | 7,945 | | | | 2,031,560 | |
President | | | 2009 | | | | 534,871 | | | | — | | | | 6,264 | | | | 534,871 | | | | — | | | | 7,879 | | | | 1,083,885 | |
| | | 2008 | | | | 521,620 | | | | — | | | | — | | | | — | | | | — | | | | 8,638 | | | | 530,258 | |
| | | | | | | | |
Sandra K. McRee (3) | | | 2010 | | | | 600,000 | | | | — | | | | 1,809,865 | | | | — | | | | — | | | | 7,242 | | | | 2,417,107 | |
Chief Operating Officer | | | 2009 | | | | 600,000 | | | | — | | | | 6,264 | | | | 600,000 | | | | — | | | | 7,242 | | | | 1,213,506 | |
| | | 2008 | | | | 585,135 | | | | — | | | | — | | | | — | | | | — | | | | 8,142 | | | | 593,277 | |
| | | | | | | | |
John M. Doyle | | | 2010 | | | | 321,515 | | | | — | | | | 150,453 | | | | — | | | | — | | | | 9,179 | | | | 481,147 | |
Chief Financial Officer | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
| | | | | | | | |
Frank A. Coyle | | | 2010 | | | | 339,570 | | | | — | | | | 221,255 | | | | — | | | | — | | | | 7,640 | | | | 568,465 | |
Secretary and General Counsel | | | 2009 | | | | 339,570 | | | | — | | | | 5,693 | | | | 118,850 | | | | — | | | | 7,596 | | | | 471,709 | |
| | | 2008 | | | | 337,097 | | | | — | | | | — | | | | — | | | | — | | | | 7,098 | | | | 344,195 | |
| | | | | | | | |
Carolyn Rose | | | 2010 | | | | 245,000 | | | | — | | | | — | | | | 180,000 | | | | — | | | | 7,057 | | | | 432,057 | |
Chief Executive Officer — | | | 2009 | | | | 245,000 | | | | — | | | | 13,208 | | | | 158,400 | | | | — | | | | 8,498 | | | | 425,106 | |
Health Choice | | | 2008 | | | | 240,000 | | | | — | | | | — | | | | 236,250 | | | | — | | | | 9,551 | | | | 485,801 | |
| 1. | For 2010, amount represents the incremental fair value paid for canceled vested rollover options to purchase common stock. For 2009, represents the proportionate amount of the total value of option awards recognized as an expense during fiscal 2009 for financial accounting purposes under the provision of FASB authoritative guidance regarding accounting for share-based payments, disregarding for this purpose estimated forfeitures related to service-based vesting conditions. Compensation expense is equal to the grant date fair value of the options estimated using the Black-Scholes-Merton model as amortized over the requisite service periods. See Note 2 to our consolidated financial statements, “Significant Accounting Policies” for additional information. |
| 2. | Represents compensation to the named executive officers made pursuant to the Company’s short-term incentive bonus plan. |
| 3. | Mr. White acted as Chief Executive Officer through October 31, 2010 and currently serves as Chairman of the Board. Mr. Whitmer currently acts as President and became Chief Executive Officer effective November 1, 2010. Ms. McRee acted as Chief Operating Officer through October 31, 2010 and currently serves as Vice Chair of the Board. |
119
Grants of Plan-Based Awards in Fiscal Year 2010
| | | | | | | | | | | | |
| | | Estimated Future Payouts Under
Non-Equity Incentive Plan Awards(1) | |
Name of Executive | | Threshold
($) | | | Target
($) | | | Maximum
($) | |
David R White | | | 161,700 | | | | 808,500 | | | | 1,617,000 | |
W. Carl Whitmer | | | 58,546 | | | | 292,729 | | | | 585,458 | |
Sandra K. McRee | | | 60,000 | | | | 300,000 | | | | 600,000 | |
John M. Doyle | | | 32,152 | | | | 160,758 | | | | 321,515 | |
Frank A. Coyle | | | — | | | | 118,850 | | | | 118,850 | |
Carolyn Rose | | | — | | | | 85,750 | | | | 183,750 | |
| | | | | | | | | | | | |
| | | Future Payouts Under
Equity Incentive Plan Awards(2) | |
Name of Executive | | All Other
Option
Awards:
Number of
Securities
Underlying
Options
(#) | | | Exercise or
Base Price
of Option
Awards
($/Sh) | | | Grant date
fair
value of
stock and
option
awards
($) | |
David R White | | | 60,658 | | | | 8.75 | | | | 2,466,992 | |
Sandra K. McRee | | | 44,501 | | | | 8.75 | | | | 1,809,865 | |
W. Carl Whitmer | | | 35,361 | | | | 8.75 | | | | 1,438,157 | |
Frank A. Coyle | | | 5,440 | | | | 8.75 | | | | 221,255 | |
John M. Doyle | | | 3,699 | | | | 8.75 | | | | 150,453 | |
| 1. | Awards made under the 2010 Short Term Incentive Plan. |
| 2. | Amounts are for cancelled option awards that were paid at $49.42 per share during fiscal 2010. |
Narrative Disclosure to Summary Compensation Table and Grants of Plan-Based Awards Table
Employment Agreements
On May 4, 2004, we entered into employment agreements with Mr. White, Ms. McRee and Mr. Whitmer that commenced upon the consummation of the Transactions. Mr. White is entitled to receive an annual target bonus of up to 100% of his base salary and an annual maximum bonus of up to 200% of his base salary based upon the achievement of certain performance objectives set annually by the IAS board of directors. Ms. McRee is also are entitled to receive an annual target bonus of up to 50% of her base salary and an annual maximum bonus of up to 100% of her base salary based upon the achievement of certain performance objectives set annually by the IAS board of directors. The base salaries of Mr. White, Ms. McRee and Mr. Whitmer have been increased over time from the initial amounts set forth in such agreements pursuant to the process discussed below.
Effective April 2010, upon his promotion to President, Mr. Whitmer entered into a new negotiated employment agreement. Under the terms of the employment agreement, Mr. Whitmer was entitled to an initial base salary of $650,000 per year during the period in which he served as President of the Company and is entitled to $750,000 per year during the period in which he serves as Chief Executive Officer of the Company. In addition, Mr. Whitmer was also entitled to receive an annual cash target bonus of 75% of his base salary and an annual cash maximum bonus of 150% of his base salary during the period in which he served as the Company’s President and is entitled to an annual cash target bonus of 100% of his base salary and an annual cash maximum bonus of 200% of his base salary during the period in which he serves as the Company’s Chief Executive Officer, in each case based upon the achievement of certain performance objectives set annually by the IAS board of directors. In October 2010, pursuant to the employment agreement, Mr. Whitmer was also granted an option to purchase 88,500 of the total outstanding common stock of IAS at fair market value on the date of grant, and, upon his promotion to Chief Executive Officer, an option to purchase an additional 88,500 of the total outstanding common stock of IAS at fair market value on the date of grant, in each case under the terms of the related grant agreement and the IAS 2004 Stock Option Plan.
120
Also in April 2010, Mr. Doyle entered into a negotiated employment agreement upon his promotion to Chief Financial Officer. Under the terms of the employment agreement, Mr. Doyle is entitled to an initial base salary of $400,000 per year. Mr. Doyle is also entitled to receive an annual cash target bonus of 50% of his base salary and an annual cash maximum bonus of 100% of his base salary based upon the achievement of certain performance objectives set annually by the IAS board of directors. In October 2010, pursuant to the terms of the employment agreement, Mr. Doyle was also granted an option to purchase 62,000 shares of common stock of the IAS at fair market value on the date of grant and under the terms of the related grant agreement and the IAS 2004 Stock Option Plan.
On March 1, 2001, we entered into an agreement for severance benefits and restrictive covenants with Ms. Rose. Although Ms. Rose’s agreement does not provide for an initial base salary, it does provide for amounts to be paid to her upon certain termination events. Ms. Rose is also entitled to participate in a short-term compensation program on similar terms to the other executive officers and as described below.
The 2004 Stock Option Plan
All outstanding options were granted pursuant to the IAS 2004 Stock Option Plan. Generally, the exercise price of the options will equal the fair market value of a share of the common stock as of the grant date as determined by the IAS board of directors. Upon a change in control, the options will become 100% vested if the participant’s employment is terminated without “cause” or by the participant for good reason within the 2-year period immediately following such change in control. On a termination of a participant’s employment outside the change in control context, unvested options automatically expire and vested options expire on the earlier of (i) the commencement of business on the date the employment is terminated for “cause”; (ii) 90 days after the date employment is terminated for any reason other than cause, death or disability; (iii) one year after the date employment is terminated by reason of death or disability; or (iv) the 10th anniversary of the grant date for such option.
In connection with the plan, each participant is expected to enter into an agreement that will generally provide that for the 90-day period following the later of (i) a termination of employment or (ii) six months and one day following the date that shares of common stock were acquired pursuant to the exercise of the option, we have the right to repurchase each share then owned by the participant at fair value, as determined in good faith by the IAS board of directors.
The maximum number of shares of IAS common stock that may be issued pursuant to options granted under the plan is 2,625,975.
The terms and conditions applicable to options are set forth by the Committee in each individual option agreement. However, no option granted under this plan may expire later than ten years from its date of grant. In addition, the Committee may not grant incentive stock options to any person who is not our employee on the date of the grant, and the exercise price of an incentive stock option cannot be less than the fair market value of a share of IAS common stock on the date of its grant. The exercise price of an incentive stock option granted to a stockholder who owns at the time of the grant shares of IAS common stock with more than 10% of the total combined voting power of all classes of IAS capital stock cannot be less than 110% of the fair market value of a share of IAS common stock on the date of the grant and the exercise period shall not exceed five years from the date of the grant. Furthermore, the aggregate fair market value of the shares of IAS common stock for which incentive stock options granted under this plan or any other stock option plan, determined as of the date of grant, that become exercisable for the first time by any person during any calendar year may not exceed $100,000. Any incentive stock options granted in excess of this limitation will be treated for all purposes as non-qualified stock options. As of September 30, 2010, we had no incentive stock options outstanding under the 2004 Stock Option Plan.
The IAS board of directors may amend this plan at any time for any reason subject to the stockholders approval to the extent necessary to meet the requirements of applicable law. However, no amendment can adversely affect an optionee’s right under a previously granted option without the consent of the optionee. Unless terminated earlier by the board of directors, this plan will terminate by its terms effective June 22, 2014, although previously granted options may be exercised after plan termination in accordance with the terms of the plan as in effect upon termination.
As of September 30, 2010, options to purchase a total of 1,687,329 shares had been granted and were outstanding under this plan, of which 1,374,620 were then vested and exercisable.
121
Outstanding Equity Awards at Fiscal 2010 Year-End
The following table summarizes the outstanding equity awards held by each named executive officer at September 30, 2010.
| | | Unexercisable | | | | Unexercisable | | | | Unexercisable | | | | Unexercisable | |
| | | Option Awards | |
Name | | Number of Securities
Underlying Unexercised
Options (#)
Exercisable | | | Number of Securities
Underlying Unexercised
Options (#)
Unexercisable | | | Option
Exercise
Price
($) | | | Option
Expiration
Date | |
| (a) | | (b) | | | (c) | | | (d) | | | (e) | |
David R. White | | | 292,000 | | | | — | | | | 20.00 | | | | 6/23/14 | |
| | | 194,000 | | | | — | | | | 20.00 | | | | 3/22/15 | |
| | | 5,000 | | | | — | | | | 35.68 | | | | 4/1/16 | |
| | | 2,875 | | | | 8,625 | | | | 34.75 | | | | 10/2/18 | |
Sandra K. McRee | | | 116,800 | | | | — | | | | 20.00 | | | | 6/23/14 | |
| | | 85,200 | | | | — | | | | 20.00 | | | | 3/22/15 | |
| | | 2,600 | | | | 650 | | | | 35.68 | | | | 4/1/16 | |
| | | 1,100 | | | | 4,400 | | | | 34.75 | | | | 10/2/18 | |
W. Carl Whitmer | | | 116,800 | | | | — | | | | 20.00 | | | | 6/23/14 | |
| | | 85,200 | | | | — | | | | 20.00 | | | | 3/22/15 | |
| | | 2,600 | | | | 650 | | | | 35.68 | | | | 4/1/16 | |
| | | 1,100 | | | | 4,400 | | | | 34.75 | | | | 10/2/18 | |
John M. Doyle | | | 18,300 | | | | — | | | | 20.00 | | | | 9/9/14 | |
| | | 6,700 | | | | — | | | | 20.00 | | | | 3/22/15 | |
| | | 10,400 | | | | 2,600 | | | | 35.68 | | | | 4/1/16 | |
| | | 4,800 | | | | 7,200 | | | | 34.75 | | | | 10/2/18 | |
Frank A. Coyle | | | 30,000 | | | | — | | | | 20.00 | | | | 9/9/14 | |
| | | 30,000 | | | | — | | | | 20.00 | | | | 3/22/15 | |
| | | 8,000 | | | | 2,000 | | | | 35.68 | | | | 4/1/16 | |
| | | 1,000 | | | | 4,000 | | | | 34.75 | | | | 10/2/18 | |
Carolyn Rose | | | 7,000 | | | | — | | | | 20.00 | | | | 9/9/14 | |
| | | 1,120 | | | | 280 | | | | 35.68 | | | | 4/1/16 | |
| | | 2,320 | | | | 9,280 | | | | 34.75 | | | | 10/2/18 | |
Option Award Vesting Schedule for David R. White
| | |
Grant Date | | Vesting Schedule |
6/23/2004 | | 25% vests each year for four years from date of grant |
3/22/2005 | | 25% vests each year for four years from date of grant |
4/1/2006 | | 25% vests each year for four years from date of grant |
10/2/2008 | | 25% vests each year for four years from date of grant |
Option Award Vesting Schedule
Named Executive Officers except David R. White
| | |
Grant Date | | Vesting Schedule |
6/23/2004 | | 20% vests each year for five years from date of grant |
9/9/2004 | | 20% vests each year for five years from date of grant |
3/22/2005 | | 20% vests each year for five years from date of grant |
4/1/2006 | | 20% vests each year for five years from date of grant |
10/2/2008 | | 20% vests each year for five years from date of grant |
122
Pension Benefits
We maintain a 401(k) plan as previously discussed in the Compensation Discussion and Analysis. We do not maintain any defined benefit plans.
Nonqualified Deferred Compensation for Fiscal 2010
We introduced our non-qualified executive savings plan July 1, 2006. The plan is a voluntary, tax-deferred savings vehicle that is available to those employees, including physicians, earning a minimum base salary ($250,000 in 2010). The executive savings plan was implemented in order to contribute to the recruitment and retention of key executives by providing the ability to defer additional pre-tax compensation in excess of the limits allowed by our 401(k) plan.
An eligible employee must contribute the maximum allowed by law to the IASIS 401(k) Retirement Savings Plan in order to participate in the non-qualified executive savings plan. There are two types of deferrals available under the plan: excess deferrals and additional deferrals. Excess deferrals are contributions that are deposited into the non-qualified executive savings plan because either (a) the participant’s earnings have exceeded $245,000 and/or (b) the participant’s deferrals into the 401(k) retirement plan have reached a dollar limit stipulated by the IRS ($16,500 in 2010). Excess deferrals are automatically deposited into the nonqualified executive savings plan if these limits are reached. Physician excess deferrals are not matched. Executive excess deferrals are matched at the same rate as contributions to the 401(k) Retirement Savings Plan. There is a five-year service requirement for participants to vest in the IASIS excess matching contributions. Currently, none of the named executive officers participates in the plan.
Additional deferrals are contributions to the non-qualified executive savings plan that are independent of a participant’s 401(k) contribution election. These contributions are voluntary and are capped according to applicable IRS guidelines for such a plan.
The non-qualified executive savings plan offers a range of investment options that act as “benchmark funds.” Benchmark funds are defined as the investment fund or funds used to represent the performance and current deemed balance of a participant’s nonqualified account, which is considered a notional deferred compensation account. Contributions become part of our general assets. Investment options under the non-qualified executive savings plan are the same as those available under the IASIS 401(k) plan.
Employment Agreements
Messrs. White and Whitmer and Mrs. McRee entered into employment agreements in connection with the Transactions. Mr. Whitmer entered into a new negotiated employment agreement upon his promotion to President during the year. Mr. Doyle entered into a negotiated employment agreement upon his promotion to Chief Financial Officer during the year. Ms. Rose entered into an agreement for severance benefits and restrictive covenants in March, 2001. Mr. Coyle does not have an employment agreement. Information regarding these employment agreements is provided under “Narrative Disclosure to Summary Compensation Table and Grants of Plan-Based Awards Table” and “Potential Payments Upon Termination or Change of Control.”
Potential Payments Upon Termination or Change in Control
The Employment Agreements
Messrs. White, Whitmer and Doyle and Ms. McRee have employment agreements in place that require payment upon certain termination events including, in certain circumstances, a change of control. Ms. Rose has an agreement for severance benefits and restrictive covenants in place that require payment upon certain termination events. As previously stated, Mr. Coyle does not have an employment agreement.
123
Death
The employment agreements provide that the respective estates of Mr. White, Mr. Whitmer, Ms. McRee and Mr. Doyle will receive the following upon the death of such named executive officer:
(i) all base salary and benefits to be paid or provided to the executive through the date of death;
(ii) a severance amount equal to the executive’s base salary at the then-current rate of base salary with respect to Mr. White, Ms. McRee and Mr. Doyle;
(iii) with respect to Mr. Whitmer, an amount equal to the sum of executive’s base salary at the then-current rate of base salary and the annual cash target bonus;
(iv) to the extent applicable, an amount equal to the pro rata bonus;
(v) in the event that the executive’s spouse or heirs are entitled to receive a payment with respect to the pro rata bonus, they will also be entitled to an additional severance amount equal to one hundred percent (100%) of the pro rata bonus with respect to Mr. White and Ms. McRee;
(vi) the company will also provide the executive’s eligible dependents continued health and medical benefits through the date one year after the date of death; the company may satisfy this obligation by paying such dependents’ health and medical continuation coverage (“COBRA”) premium payments (with the dependents paying the portion of such COBRA payments that the executive was required to pay with respect to such dependents prior to the date of death) with respect to Mr. White, Ms. McRee and Mr. Whitmer; and
(vii) additionally, all of the executive’s options to purchase shares of capital stock of IAS which are unvested as of the date of death but otherwise scheduled to vest on the first vesting date scheduled to occur following the date of death, will immediately vest and become exercisable while all remaining unvested options will terminate as of the date of death. Where the executive’s spouse or heirs are entitled to receive a payment with respect to the pro rata bonus, all of the vested options must be exercised by the executive’s spouse or heirs within two years following the date of death or they will terminate with respect to Mr. White and Ms. McRee. If the executive’s spouse or heirs are not entitled to receive a payment with respect to the pro rata bonus, all of the vested options must be exercised by the executive’s spouse or heirs within one year following the date of death or they will terminate with respect to Mr. White and Ms. McRee. With respect to Mr. Whitmer and Mr. Doyle, all of the vested options must be exercised within the earlier of (i) the tenth anniversary of the date the options were granted or (ii) two years in the case of Mr. Whitmer, and one year, in the case of Mr. Doyle, following the date of death.
Disability
The employment agreements provide that Mr. White, Mr. Whitmer, Ms. McRee and Mr. Doyle will receive the following upon the disability of such named executive officer:
(i) all base salary and benefits to be paid or provided to the executive through the date of disability;
(ii) with respect to Mr. White, Ms. McRee and Mr. Whitmer, a severance amount equal to the executive’s base salary at the then-current rate of base salary provided, however, that in the event the date of termination is the date of delivery of the final required physician’s opinion that the executive will be disabled for 6 consecutive months, the payment with respect to base salary, together with all base salary paid to the executive following the first date that the executive was disabled will equal one hundred and fifty percent (150%) of the executive’s base salary and; provided, further, that amounts payable to the executive must be reduced by the proceeds of any short or long-term disability payments to which the executive may be entitled during such period under policies maintained at the expense of the Company;
(iii) with respect to Mr. Whitmer, an amount equal to 100% of his annual cash target bonus;
124
(iv) to the extent applicable, an amount equal to the pro rata bonus; if the executive is eligible for such a pro rata bonus, the executive is also entitled to an additional severance amount equal to the pro rata bonus;
(v) with respect to Mr. White, Ms. McRee and Mr. Whitmer, the Company will pay for the executive and his eligible dependents’ continued health and medical benefits through the date one year after the date of termination (provided, however, that in the event that the date of termination is the date of delivery of the final physician’s opinion referred to above, the Company will provide health and medical benefits through the date that is eighteen (18) months following the first date that Executive was unable to perform his duties; the Company may satisfy this obligation by paying COBRA premium payments with respect to the executive and his eligible dependents (with the executive paying the portion of such COBRA payments that executive was required to pay prior to the date of termination); and
(vi) additionally, all of the executive’s options to purchase shares of capital stock of IAS which are unvested as of the date of termination but otherwise scheduled to vest on the first vesting date scheduled to occur following the date of termination, will immediately vest and become exercisable while all remaining unvested options will terminate as of the date of termination. Where the executive is entitled to receive a payment with respect to the pro rata bonus, all of the vested options must be exercised by the executive within two years following the date of termination or the options will terminate with respect to Mr. White and Ms. McRee. If the executive is not entitled to receive a payment with respect to the pro rata bonus, all of the vested options must be exercised by the executive within one year following the date of termination or the options will terminate with respect to Mr. White and Ms. McRee. With respect to Mr. Whitmer and Mr. Doyle, all of the vested options must be exercised within the earlier of (i) the tenth anniversary of the date the options were granted or (ii) two years, in the case of Mr. Whitmer, and one year, in the case of Mr. Doyle, from the date of disability.
The agreement for severance benefits and restrictive covenants for Ms. Rose does not address this scenario.
Termination by the Company for Cause
Upon termination for cause, the executive will be entitled to receive all base salary and benefits to be paid or provided to the executive through the date of termination.
By the Company without Cause
The employment agreements provide that Mr. White, Mr. Whitmer, Ms. McRee and Mr. Doyle will receive the following upon the termination by the Company without cause of such named executive officer:
(i) all base salary and benefits to be paid or provided to the executive through the date of termination;
(ii) with respect to Mr. White and Ms. McRee, a severance amount equal to two hundred percent (200%) of the executive’s base salary at the then-current rate of base salary;
(iii) with respect to Mr. Whitmer and Mr. Doyle, an amount equal to the sum of (i) two hundred percent (200%), in the case of Mr. Whitmer, and one hundred fifty percent (150%) in the case of Mr. Doyle, of the executive’s base salary at the then current rate of base salary and (ii) the annual cash target bonus;
(iv) to the extent applicable, an amount equal to the pro rata bonus,
(v) with respect to Mr. White and Ms. McRee, in the event that the executive is entitled to receive a payment with respect to the pro rata bonus, an additional severance amount equal to two hundred percent (200%) of the pro rata bonus;
(vi) a lump sum payment equal to the then present value of all major medical, disability and life insurance coverage through the date two years (eighteen months with respect to Mr. Doyle) after the date of termination, provided that under such circumstances the executive shall make all COBRA premium payments on his own behalf; and
125
(vii) additionally, all of the executive’s options to purchase shares of capital stock of IAS which are unvested as of the date of termination but otherwise scheduled to vest on the first vesting date scheduled to occur following the date of termination, will immediately vest and become exercisable while all remaining unvested options will terminate as of the date of termination. Where the executive is entitled to receive a payment with respect to the pro rata bonus, all of the vested options must be exercised by the executive within two years following the date of termination or the options will terminate with respect to Mr. White and Ms. McRee. If the executive is not entitled to receive a payment with respect to the pro rata bonus, all of the vested options must be exercised by the executive within one year following the date of termination or the options will terminate with respect to Mr. White and Ms. McRee. With respect to Mr. Whitmer and Mr. Doyle, all of the vested options must be exercised within the earlier of (i) the tenth anniversary of the date the options were granted or (ii) two years, in the case of Mr. Whitmer, and one year, in the case of Mr. Doyle, following the date of termination.
The agreement for severance benefits and restrictive covenants for Ms. Rose provides that she will receive the following upon her termination by the Company without cause:
(i) the monthly base salary at the time of termination for a period of nine consecutive months;
(ii) an amount equal to all unused sick leave, vacation time and/or paid time off; and
(iii) additional consideration of $2,500 to provide with outplacement assistance.
By the Executive for Good Reason
The employment agreements provide that Mr. White, Mr. Whitmer, Ms. McRee and Mr. Doyle will receive the following upon the resignation by such executive for good reason:
(i) all base salary and benefits to be paid or provided to the executive through the date of Termination;
(ii) with respect to Mr. White and Ms. McRee, an amount equal to two hundred percent (200%) of the executive’s base salary at the then-current rate of base salary;
(iii) with respect to Mr. Whitmer and Mr. Doyle, an amount equal to the sum of (i) two hundred percent (200%), in the case of Mr. Whitmer, and one hundred fifty percent (150%), in the case of Mr. Doyle, of the executive’s base salary at the then current rate of base salary and (ii) the annual cash target bonus;
(iv) to the extent applicable, an amount equal to the pro rata bonus;
(v) with respect to Mr. White and Ms. McRee in the event that the executive is entitled to receive a payment with respect to the pro rata bonus, an additional severance amount equal to two hundred percent (200%) of the pro rata bonus;
(vi) a lump sum payment equal to the then present value of all major medical, disability and life insurance coverage through the date two years (eighteen months with respect to Mr. Doyle) after the date of termination, provided that under such circumstances the executive shall make all COBRA premium payments on his own behalf; and
(vii) additionally, all of the executive’s options to purchase shares of capital stock of IAS which are unvested as of the date of termination but otherwise scheduled to vest on the first vesting date scheduled to occur following the date of termination, will immediately vest and become exercisable while all remaining unvested options will terminate as of the date of termination. Where the executive is entitled to receive a payment with respect to the pro rata bonus, all of the vested options must be exercised by the executive within two years following the date of termination or the options will terminate with respect to Mr. White and Ms. McRee. If the executive is not entitled to receive a payment with respect to the pro rata bonus, all of the vested options must be exercised by the executive within one year following the date of termination or the options will terminate with respect to Mr. White and Ms. McRee. With respect to Mr. Whitmer and
126
Mr. Doyle, all of the vested options must be exercised within the earlier of (i) the tenth anniversary of the date the options were granted or (ii) two years, in the case of Mr. Whitmer, and one year, in the case of Mr. Doyle, following the date of termination.
Ms. Rose’s agreement for severance benefits and restrictive covenants provides that she will receive the following upon the event of her resignation for good reason:
(i) the monthly base salary at the time of termination for a period of nine consecutive months;
(ii) an amount equal to all unused sick leave, vacation time and/or paid time off; and
(iii) additional consideration of $2,500 to provide with outplacement assistance.
By the Executive without Good Reason or the Executive’s Failure to Extend the Employment Term
Upon termination for good reason, the executive will be entitled to receive all base salary and benefits to be paid or provided to the executive through the date of termination.
Definition of Good Reason
Each of the following events shall constitute “good reason” for resignation for purposes of the employment agreements of Mr. White, Mr. Whitmer, Ms. McRee and Mr. Doyle:
(i) with respect to Mr. White, Ms. McRee and Mr. Whitmer, the one-year anniversary of the date of any Change of Control (as defined below) unless the acquirer is in the healthcare facilities business, in which case the one-year anniversary will be reduced to six months after the date of the Change of Control;
(ii) the removal of the executive from or the failure to elect or re-elect the executive to his or her respective positions within the company or on the board (other than a removal or failure to elect Mr. White as Chairman after an initial public offering, and provided that the appointment of a non-executive chairman following a transaction or a Change of Control will not constitute grounds for good reason);
(iii) with respect to Mr. Whitmer and Mr. White only, the removal of or the failure to elect Mr. White to the board of directors;
(iv) any material reduction in duties of the respective executive or any assignment materially inconsistent with his or her position;
(v) any breach by the company of the respective employment agreement; and
(vi) with respect to Mr. Whitmer only, any failure to promote Mr. Whitmer to Chief Executive Officer within 90 days after the retirement of Mr. White.
Each of the following events shall constitute “good reason” for resignation for Ms. Rose only:
(i) the removal of or failure to re-elect Ms. Rose to the position of Chief Executive Officer of Health Choice;
(ii) any material reduction by the Company of Ms. Rose’s duties or responsibilities or the assignment to Ms. Rose of duties materially inconsistent with such position;
(iii) any material breach by the Company of the agreement for severance benefits and restrictive covenants; and
(iv) resignation within 12 months after the date of any Change in Control (as defined below).
127
The Company’s Failure to Extend the Employment Term
The employment agreements provide that Mr. White, Mr. Whitmer, Ms. McRee and Mr. Doyle will receive the following upon the Company’s failure to the extend the employment term:
(i) all base salary and benefits to be paid or provided to the executive through the date of death;
(ii) with respect to Mr. White and Ms. McRee a severance amount equal to the executive’s base salary at the then-current rate of base salary;
(iii) with respect to Mr. Whitmer and Mr. Doyle, an amount equal to the sum of (i) the executive’s base salary at the then current rate of base salary and (ii) the annual cash target bonus;
(iv) to the extent applicable, an amount equal to the pro rata bonus;
(v) with respect to Mr. White and Ms. McRee, in the event that the executive is entitled to receive a payment with respect to the pro rata bonus, an additional severance amount equal to one hundred percent (100%) of the pro rata bonus;
(vi) a lump sum payment equal to the then present value of all major medical, disability and life insurance coverage through the date one year after the date of termination, provided that under such circumstances the executive shall make all COBRA premium payments on his own behalf; and
(vii) additionally, all of the executive’s options to purchase shares of capital stock of IAS which are unvested as of the date of termination but otherwise scheduled to vest on the first vesting date scheduled to occur following the date of termination, will immediately vest and become exercisable while all remaining unvested options will terminate as of the date of termination. Where the executive is entitled to receive a payment with respect to the pro rata bonus, all of the vested options must be exercised by the executive within two years following the date of termination or the options will terminate with respect to Mr. White and Ms. McRee. If the executive is not entitled to receive a payment with respect to the pro rata bonus, all of the vested options must be exercised by the executive within one year following the date of termination or the options will terminate with respect to Mr. White and Ms. McRee. With respect to Mr. Whitmer and Mr. Doyle, all of the vested options must be exercised within the earlier of (i) the tenth anniversary of the date the options were granted and (ii) two years, in the case of Mr. Whitmer, and one year, in the case of Mr. Doyle, following the date of termination.
Definition of Change of Control
The employment agreements of Mr. White, Mr. Whitmer and Ms. McRee define a change of control as any transaction where a person or group of persons (other than the present private equity investors in the Company or their affiliates):
(i) acquire a majority interest in IAS or IASIS Investment LLC, its parent; or
(ii) acquire all or substantially all of the assets of IAS or IASIS Investment LLC, its parent; or
The initial public offering of IAS shares or any secondary offering of such shares will not constitute a change of control.
The agreement for severance benefits and restrictive covenants for Ms. Rose defines a change of control as any transaction where a person or group of persons other than IAS directly or indirectly acquires beneficially or of record, more than 50% of the outstanding voting securities of Health Choice or upon a sale of all or substantially all of the assets of Health Choice.
128
In addition, the employment agreements contain non-competition and non-solicitation provisions pursuant to which Mr. White, Mr. Whitmer, Ms. McRee and Mr. Doyle will not compete with IAS or its subsidiaries within 25 miles of the location of any hospital we manage for two years (eighteen months with respect to Mr. Doyle) following the date of termination of such person’s employment. The agreements provide that during this time such person will not solicit or recruit our business partners and employees, respectively. Ms. Rose’s agreement for severance benefits and restrictive covenants contains non-competition provisions pursuant to which Ms. Rose will not compete with Health Choice, without prior consent of the Company, for a period of 15 months following a voluntary termination of Ms. Rose or a termination by the Company for cause.
In certain circumstances following a change of control, IAS has agreed to compensate Mr. White in the event any payment under his employment agreement is subject to an excise tax under Section 4999 of the Internal Revenue Code.
IAS 2004 Stock Option Plan
Vesting Date of Options
Each stock option grant agreement must indicate the date or conditions under which the option will become exercisable. However, unless otherwise provided in a participant’s stock option grant agreement, if within the two-year period following a Change of Control the executive’s employment is:
(i) terminated by the company or its Affiliates without cause; or
(ii) terminated by the executive with good reason,
all of the executive’s options granted hereunder shall immediately become vested and exercisable.
Definition of Change of Control
The IAS 2004 Stock Option Plan defines Change of Control in substantially the same way as the employment agreements of Messrs. White and Whitmer and Ms. McRee.
Definition of Good Reason
The IAS 2004 Stock Option Plan defines good reason as:
(i) a material reduction in an executive’s duties and responsibilities other than a change in such executive’s duties and responsibilities that results from becoming part of a larger organization following a Change of Control,
(ii) a decrease in an executive’s base salary or benefits other than a decrease in benefits that applies to all employees of the company otherwise eligible to participate in the affected plan, or
(iii) a relocation of an executive’s primary work location more than 50 miles from the executive’s primary work location, as in effect immediately before a Change of Control, without written consent.
Definition of Cause
The IAS 2004 Stock Option Plan defines termination with cause as the termination of the executive’s employment because of:
(i) dishonesty in the performance of such executive’s duties;
(ii) the executive’s willful misconduct in connection with such executive’s duties or any act or omission which is materially injurious to the financial condition or business reputation of the Company or any of its subsidiaries or affiliates;
129
(iii) a breach by an executive of the participant’s duty of loyalty to the Company and its affiliates;
(iv) the executive’s unauthorized removal from the premises of the Company of any document (in any medium or form) relating to the company or the customers of the company; or (v) the commission by the executive of any felony or other serious crime involving moral turpitude.
Summary of Payments Made Upon Termination or a Change of Control
The following tables describe the potential payments and benefits under our compensation and benefit plans and arrangements to which Messrs. White, Whitmer, Doyle, Ms. McRee and Ms. Rose would be entitled upon a termination of their employment under their employment agreements. In accordance with SEC disclosure rules, dollar amounts below assume a termination of employment on September 30, 2010 (the last business day of our last completed fiscal year).
| | | 000000000 | | | | 000000000 | | | | 000000000 | | | | 000000000 | | | | 000000000 | | | | 000000000 | | | | 000000000 | | | | 000000000 | |
David R. White | | Involuntary
Termination
Without
Cause ($) | | | Involuntary
Termination
For Cause
($) | | | Resignation
($) | | | Resignation
For Good
Reason
($) | | | Retirement
($) | | | Death
($) | | | Disability
($) | | | Change
In
Control
($) | |
Cash severance | | | 1,617,000 | | | | — | | | | — | | | | 1,617,000 | | | | — | | | | 808,500 | | | | 1,212,750 | | | | 1,617,000 | |
Health and welfare continuation | | | 27,248 | | | | — | | | | — | | | | 27,248 | | | | — | | | | 27,248 | | | | 27,248 | | | | 27,248 | |
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
Total | | | 1,644,248 | | | | — | | | | — | | | | 1,644,248 | | | | — | | | | 835,748 | | | | 1,239,998 | | | | 1,644,248 | |
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
| | | 000000000 | | | | 000000000 | | | | 000000000 | | | | 000000000 | | | | 000000000 | | | | 000000000 | | | | 000000000 | | | | 000000000 | |
| | | | | | | | |
Sandra K. McRee | | Involuntary
Termination
Without
Cause | | | Involuntary
Termination
For Cause | | | Resignation | | | Resignation
For Good
Reason | | | Retirement | | | Death | | | Disability | | | Change
In
Control | |
Cash severance | | | 1,200,000 | | | | — | | | | — | | | | 1,200,000 | | | | — | | | | 600,000 | | | | 900,000 | | | | 1,200,000 | |
Health and welfare continuation | | | 25,656 | | | | — | | | | — | | | | 25,656 | | | | — | | | | 25,656 | | | | 25,656 | | | | 25,656 | |
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
Total | | | 1,225,656 | | | | — | | | | — | | | | 1,225,656 | | | | — | | | | 625,656 | | | | 925,656 | | | | 1,225,656 | |
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
| | | 000000000 | | | | 000000000 | | | | 000000000 | | | | 000000000 | | | | 000000000 | | | | 000000000 | | | | 000000000 | | | | 000000000 | |
| | | | | | | | |
W. Carl Whitmer | | Involuntary
Termination
Without
Cause | | | Involuntary
Termination
For Cause | | | Resignation | | | Resignation
For Good
Reason | | | Retirement | | | Death | | | Disability | | | Change
In
Control | |
Cash severance | | | 1,170,916 | | | | — | | | | — | | | | 1,170,916 | | | | — | | | | 585,458 | | | | 878,187 | | | | 1,170,916 | |
Health and welfare continuation | | | 37,878 | | | | — | | | | — | | | | 37,878 | | | | — | | | | 37,878 | | | | 37,878 | | | | 37,878 | |
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
Total | | | 1,208,794 | | | | — | | | | — | | | | 1,208,794 | | | | — | | | | 623,336 | | | | 916,065 | | | | 1,208,794 | |
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
| | | 000000000 | | | | 000000000 | | | | 000000000 | | | | 000000000 | | | | 000000000 | | | | 000000000 | | | | 000000000 | | | | 000000000 | |
| | | | | | | | |
John M. Doyle | | Involuntary
Termination
Without
Cause | | | Involuntary
Termination
For Cause | | | Resignation | | | Resignation
For Good
Reason | | | Retirement | | | Death | | | Disability | | | Change
In
Control | |
Cash severance | | | 482,273 | | | | — | | | | — | | | | 482,273 | | | | — | | | | 321,515 | | | | 482,273 | | | | — | |
Health and welfare continuation | | | 37,605 | | | | — | | | | — | | | | 37,605 | | | | — | | | | 37,605 | | | | 37,605 | | | | — | |
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
Total | | | 519,878 | | | | — | | | | — | | | | 519,878 | | | | — | | | | 359,120 | | | | 519,878 | | | | — | |
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
| | | 000000000 | | | | 000000000 | | | | 000000000 | | | | 000000000 | | | | 000000000 | | | | 000000000 | | | | 000000000 | | | | 000000000 | |
| | | | | | | | |
Carolyn Rose | | Involuntary
Termination
Without
Cause | | | Involuntary
Termination
For Cause | | | Resignation | | | Resignation
For Good
Reason | | | Retirement | | | Death | | | Disability | | | Change
In
Control | |
Cash severance | | | 183,750 | | | | — | | | | — | | | | 183,750 | | | | — | | | | — | | | | — | | | | 183,750 | |
Health and welfare continuation | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | |
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
Total | | | 183,750 | | | | — | | | | — | | | | 183,750 | | | | — | | | | — | | | | — | | | | 183,750 | |
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
130
Director Compensation for Fiscal 2010
The following table provides compensation information for the year ended September 30, 2010.
| | | | | | | | | | | | | | | | | | | | |
Name | | Fees
Earned
or Paid
in
Cash
($) | | | Stock
Awards
($) | | | Option
Awards
($) | | | All Other
Compensation
($) | | | Total
($) | |
Jonathan J. Coslet | | | — | | | | — | | | | — | | | | — | | | | — | |
David Dupree | | | — | | | | — | | | | — | | | | — | | | | — | |
Kirk E. Gorman | | | 37,500 | | | | — | | | | — | | | | — | | | | 37,500 | |
Greg Kranias | | | — | | | | — | | | | — | | | | — | | | | — | |
Todd B. Sisitsky | | | — | | | | — | | | | — | | | | — | | | | — | |
Paul S. Levy | | | — | | | | — | | | | — | | | | — | | | | — | |
Jeffrey C. Lightcap | | | — | | | | — | | | | — | | | | — | | | | — | |
Sharad Mansukani | | | 37,500 | | | | — | | | | — | | | | — | | | | 37,500 | |
| | | | | | | | |
Name | | Aggregate
Options
Held
at Fiscal
Year End | | | Aggregate
Stock
Awards
Held
at Fiscal
Year End | |
Jonathan J. Coslet | | | — | | | | — | |
David Dupree | | | — | | | | — | |
Kirk E. Gorman | | | 3,319 | | | | 3,319 | |
Greg Kranias | | | — | | | | — | |
Todd B. Sisitsky | | | — | | | | — | |
Paul S. Levy | | | — | | | | — | |
Jeffrey C. Lightcap | | | — | | | | — | |
Sharad Mansukani | | | 3,082 | | | | 3,082 | |
On February 14, 2005, pursuant to a Director Compensation and Restricted Share Award Agreement, IAS granted Kirk Gorman options to purchase 1,175 shares of IAS’s common stock and committed to grant Mr. Gorman, on each of the first, second, third and fourth anniversaries of the grant date, provided that he is still a director, options to purchase a number of shares valued at $18,750 based on the fair market value of the common stock as determined on each such anniversary. These grants were made pursuant to the form of stock option grant agreement under the IAS 2004 Stock Option Plan. In addition, IAS entered into a Director Compensation and Restricted Share Award Agreement with Mr. Gorman on the grant date. Pursuant to such Director Compensation and Restricted Share Award Agreement, IAS agreed to pay Mr. Gorman cash compensation of $9,375 for the fiscal quarter ended December 31, 2004 and annual cash compensation of $37,500 for the remaining term (five years or until the date on which, for any reason, Mr. Gorman no longer serves as a director of the company) in equal quarterly installments, in consideration for his services as a member of IAS’s board of directors. IAS also granted Mr. Gorman 1,175 shares of restricted common stock on the grant date and committed to grant Mr. Gorman, on each of the first, second, third and fourth anniversaries of the grant date, provided that he is still a director, restricted common stock valued at $18,750 based on the fair market value of the common stock as determined on each such anniversary.
On April 14, 2005, IAS granted Sharad Mansukani options to purchase 938 shares of IAS’s common stock and committed to grant Dr. Mansukani, on each of the first, second, third and fourth anniversaries of the grant date, provided that he is still a director, options to purchase a number of shares of common stock valued at $18,750 based on the fair market value of the common stock on each such anniversary. These grants were made pursuant to the form of stock option grant agreement under the IAS 2004 Stock Option Plan. In addition, IAS entered into a Director Compensation and Restricted Share Award Agreement with Dr. Mansukani on the grant date. Pursuant to such Director Compensation and Restricted Share Award Agreement, IAS agreed to pay Dr. Mansukani annual cash compensation of $37,500 for the term (five years or until the date on which, for any reason, Dr. Mansukani no longer serves as a director of the Company) of the Director Compensation and Restricted Share Award Agreement, payable in equal quarterly installments, in consideration for his services as a member of IAS’s board of directors. IAS also granted Dr. Mansukani 938 shares of restricted common stock on the grant date and committed to grant Dr. Mansukani, on each of the first, second, third and fourth anniversaries of the grant date, provided that he is still a director, restricted common stock valued at $18,750 based on the fair market value of the common stock on each such anniversary.
131
Currently, IAS’s other directors do not receive any compensation for their services. IAS does, however, reimburse them for travel expenses and other out-of-pocket costs incurred in connection with attendance at board of directors and committee meetings.
Committee Interlocks and Insider Participation
During fiscal 2010, the Committee was composed of David R. White, Jonathan J. Coslet and Jeffrey C. Lightcap. Mr. White currently serves as our Chairman and served as our Chief Executive Officer until November 1, 2010. Officer. Mr. Coslet has never been an officer of IAS. Mr. Lightcap is currently a Director of IAS.
132
SECURITY OWNERSHIP OF CERTAIN BENEFICIAL OWNERS AND MANAGEMENT AND RELATED STOCKHOLDER MATTERS
Equity Compensation Plans
The table below sets forth the following information as of September 30, 2010 with respect to IAS’ equity compensation plans (including individual compensation arrangements) under which its equity securities are authorized for issuance, aggregated by (i) all compensation plans previously approved by IAS’ security holders and (ii) all compensation plans not previously approved by IAS’ security holders:
| | • | | the number of securities to be issued upon the exercise of outstanding options; |
| | • | | the weighted-average exercise price of the outstanding options; and |
| | • | | the number of securities remaining available for future issuance under the plans. |
The IAS 2004 Stock Option Plan has been approved by its stockholders. IAS has not issued any warrants or other rights to purchase its equity securities.
| | | | | | | | | | | | |
Plan Category | | Number of
Securities to be
Issued Upon
Exercise of
Outstanding Options | | | Weighted-average
Exercise
Price of
Outstanding
Options | | | Remaining Available for
Future Issuance Under
Equity Compensation
Plans (excluding securities
reflected in the first column) | |
Equity compensation plans approved by security holders (1) | | | 1,686,329 | | | $ | 24.58 | | | | 939,646 | |
Equity compensation plans not approved by security holders | | | — | | | | — | | | | — | |
| | | | | | | | | | | | |
Total | | | 1,686,329 | | | $ | 24.58 | | | | 939,646 | |
| | | | | | | | | | | | |
| (1) | Consists of 1,686,329 shares of common stock to be issued upon exercise of options issued under IAS’ 2004 Stock Option Plan, with exercise prices ranging from $20.00 to $35.68 per share. Of the 2,625,975 shares of common stock currently authorized for issuance under the 2004 Stock Option Plan, 939,646 shares remain available for future issuance. |
Beneficial Ownership of Common Stock
IASIS is a limited liability company consisting of 100% common interests owned by IAS. IAS’ outstanding shares consist of one class of common stock and one class of preferred stock, and 99.9% of the outstanding common stock and 100% of the outstanding preferred stock is owned by IASIS Investment. The outstanding equity interest of IASIS Investment is held 74.4% by TPG, 18.8% by JLL and 6.8% by Trimaran.
The following table presents information as of December 21, 2010, regarding ownership of shares of IAS common stock and preferred stock by each person known to be a holder of more than 5% of IAS common stock and preferred stock, the members of the IAS board of directors, each executive officer named in the summary compensation table and all current directors and executive officers as a group.
When reviewing the following table, you should be aware that the amounts and percentage of common stock and preferred stock beneficially owned are reported on the basis of regulations of the SEC governing the determination of beneficial ownership of securities. Under the rules of the SEC, a person is deemed to be a “beneficial owner” of a security if that person has or shares “voting power,” which includes the power to vote or to direct the voting of such security, or “investment power,” which includes the power to dispose of or to direct the disposition of such security. A person is also deemed to be a beneficial owner of any securities of which that person has a right to acquire beneficial ownership within 60 days.
133
Unless otherwise indicated, the address of each person listed below is 117 Seaboard Lane, Building E, Franklin, Tennessee 37067.
| | | 0000000000 | | | | 0000000000 | | | | 0000000000 | | | | 0000000000 | |
Beneficial Owners | | Preferred
Shares
Beneficially
Owned | | | Common
Shares
Beneficially
Owned (a) | | | Percentage of
Preferred
Shares Beneficially
Owned | | | Percentage of
Common
Shares Beneficially
Owned | |
IASIS Investment (b)(c) | | | 17,989 | | | | 14,600,000 | | | | 100.0 | % | | | 99.9 | % |
David R. White | | | — | | | | 497,250 | | | | * | | | | * | |
Sandra K. McRee | | | — | | | | 206,800 | | | | * | | | | * | |
W. Carl Whitmer | | | — | | | | 206,800 | | | | * | | | | * | |
John M. Doyle | | | — | | | | 40,200 | | | | * | | | | * | |
Frank A. Coyle | | | — | | | | 70,000 | | | | * | | | | * | |
Carolyn Rose | | | — | | | | 12,760 | | | | * | | | | * | |
| | | 0000000000 | | | | 0000000000 | | | | 0000000000 | | | | 0000000000 | |
Beneficial Owners | | Preferred
Shares
Beneficially
Owned | | | Common
Shares
Beneficially
Owned (a) | | | Percentage of
Preferred
Shares Beneficially
Owned | | | Percentage of
Common
Shares Beneficially
Owned | |
Jonathan J. Coslet (d) | | | — | | | | — | | | | — | | | | — | |
David Dupree | | | — | | | | — | | | | — | | | | — | |
Kirk E. Gorman | | | — | | | | 5,562 | (e) | | | * | | | | * | |
Greg Kranias (d) | | | — | | | | — | | | | — | | | | — | |
Todd B. Sisitsky (d) | | | — | | | | — | | | | — | | | | — | |
Paul S. Levy (f) | | | 3,382 | | | | 2,744,800 | | | | 18.8 | % | | | 18.8 | % |
Jeffrey C. Lightcap | | | — | | | | — | | | | — | | | | — | |
Sharad Mansukani (g) | | | — | | | | 5,088 | (e) | | | * | | | | * | |
Current directors and executive officers as a group (21 persons) | | | 17,989 | | | | 1,126,815 | | | | 100.0 | % | | | 100.0 | % |
| (a) | The following shares of common stock subject to options currently exercisable or exercisable within 60 days of December 21, 2010, include: Mr. White, 497,250; Ms. McRee, 206,800; Mr. Whitmer, 206,800; Mr. Doyle, 140,200; Mr. Coyle, 70,000; Ms. Rose, 12,760; and all current directors and executive officers as a group (21 persons), 1,126,815. |
| (b) | The membership interests of IASIS Investment are owned as follows: the TPG Funds (as defined below), 74.4%, JLL, 18.8%, and Trimaran, 6.8%. |
| (c) | The membership interests (the “TPG Membership Interests”) owned by the TPG Funds (as defined below) reflect an aggregate of the following: (i) 199,045 membership units beneficially owned by TPG IASIS III LLC, a Delaware limited liability company (“TPG IASIS III”), whose sole member is TPG Partners III, L.P., a Delaware limited partnership, whose general partner is TPG GenPar III, L.P., a Delaware limited partnership, whose general partner is TPG Advisors III, Inc., a Delaware corporation (“Advisors III”), (ii) 318,507 membership units beneficially owned by TPG IASIS IV LLC (“TPG IASIS IV”), whose sole member is TPG Partners IV, L.P., a Delaware limited partnership (“Partners IV”), whose general partner is TPG GenPar IV, L.P., a Delaware limited partnership, whose general partner is TPG GenPar IV Advisors, LLC, a Delaware limited liability company, whose sole member is TPG Holdings I, L.P., a Delaware limited partnership, whose general partner is TPG Holdings I-A, LLC, a Delaware limited liability company, whose sole member is TPG Group Holdings (SBS), L.P., a Delaware limited partnership, whose general partner is TPG Group Holdings (SBS) Advisors, Inc., a Delaware corporation (“Group Advisors”), (iii) 193,201 membership units beneficially owned by TPG IASIS Co-Invest I LLC, a Delaware limited liability company (“TPG Co-Invest I”), whose managing member is Partners IV, and (iv) 32,398 membership units beneficially owned by TPG IASIS Co-Invest II LLC, a Delaware limited liability company (“TPG Co-Invest II”, and together with TPG IASIS III, TPG IASIS IV and TPG Co-Invest I, the “TPG Funds”), whose managing member is Partners IV. David Bonderman and James G. Coulter are directors, officers and sole shareholders of Advisors III and Group Advisors and may therefore be deemed to be the beneficial owners of the TPG Membership Interests. The address of Messrs. Bonderman and Coulter is c/o TPG Capital, 301 Commerce Street, Suite 3300, Fort Worth, TX 76102. The TPG Funds have the right to designate four out of the seven directors of IASIS Investment (collectively, the “TPG Directors”) and each TPG Director shall have three votes. |
| (d) | Jonathan J. Coslet and Todd B. Sisitsky are each partners and Greg Kranias is a Principal of TPG Capital, which is an affiliate of the TPG Funds. None of Messrs. Coslet, Sisitsky or Kranias has voting or investment power over and each disclaims beneficial ownership of the TPG Membership Interests. The address of Messrs. Coslet, Sisitsky and Kranias is c/o TPG Capital, 301 Commerce Street, Suite 3300, Fort Worth, TX 76102. |
| (e) | Represents shares of restricted stock and options currently or exercisable within 60 days of December 21, 2010, granted to Messrs. Gorman and Mansukani pursuant to Director Compensation and Restricted Stock Award Agreements. |
| (f) | Mr. Levy is a senior managing director of JLL Partners, Inc. which, through its controlling interest in JLL, which owns 18.8% of IASIS Investment, may be deemed to beneficially own 18.8% of the shares of preferred stock and common stock owned by IASIS Investment. Accordingly, Mr. Levy may be deemed to beneficially own 18.8% of the shares of preferred stock and common stock owned by IASIS Investment. |
| (g) | Sharad Mansukani is a senior advisor of TPG Capital, which is an affiliate of the TPG Funds. Mr. Mansukani has no voting or investment power over and disclaims beneficial ownership of the TPG Membership Interests. The address of Mr. Mansukani is c/o TPG Capital, 301 Commerce Street, Suite 3300, Fort Worth, TX 76102. |
All of the membership interests in IASIS are pledged to our lenders as security for our obligations under our senior secured credit facilities. In the event of a default under our senior secured credit facilities, our lenders would have the right to foreclose on such membership interests, which would result in a change of control of our company.
134
CERTAIN RELATIONSHIPS AND RELATED PARTY TRANSACTIONS
IASIS Investment Limited Liability Company Operating Agreement
TPG is party to a limited liability company operating agreement of IASIS Investment LLC with Trimaran and JLL. TPG, JLL and Trimaran hold approximately 74.4%, 18.8% and 6.8%, respectively, of the equity interests of IASIS Investment LLC. TPG is the managing member of IASIS Investment LLC.
The board of directors has not made a determination as to whether each director is “independent” because all of the members of our board have been appointed by our equity sponsors. Pursuant to the limited liability company operating agreement of IASIS Investment LLC, JLL is entitled to nominate two directors to the IAS board of directors. TPG is entitled to nominate the remaining directors. Messrs. Levy and Lightcap serve on the IAS board of directors as designees of JLL. The remaining directors serve as designees of TPG. The right of JLL to nominate two directors is subject to its ownership percentage in IASIS Investment LLC remaining at or above 9.4%. In the event JLL’s ownership percentage in IASIS Investment LLC falls below 9.4%, but is at least 4.7%, JLL will have the right to nominate one director. If JLL’s ownership percentage falls below 4.7%, it will not have the right to nominate any directors. The agreement also places certain restrictions on the transfer of membership interests in IASIS Investment LLC. JLL and Trimaran have the right to participate in certain dispositions by TPG and can be required to participate on the same terms in any sale by TPG in excess of a specified percentage of its collective interest.
We have no securities listed for trading on a national securities exchange or in an automated inter-dealer quotation system of a national securities association, which have requirements that a majority of directors be independent. We do not believe any of our directors would be considered independent under the New York Stock Exchange’s definition of independence.
Investor Rights Agreement
IASIS Investment is the majority stockholder of IAS, which owns 100% of the common interests of IASIS. IASIS Investment is party to an investor rights agreement with IAS. Pursuant to this agreement, IASIS Investment can cause IAS to register its interests in IAS under the Securities Act and to maintain a shelf registration statement effective with respect to such interests. IASIS Investment is also entitled to participate on a pro rata basis in any registration of our equity interests under the Securities Act that IAS may undertake. The agreement also grants IASIS Investment preemptive rights over certain additional issuances of equity securities by IAS.
Management Services Agreement
We entered into a management services agreement with affiliates of TPG, JLL and Trimaran. The management services agreement provides that in exchange for consulting and management advisory services that will be provided to us by the investors, we will pay an aggregate monitoring fee of 0.25% of budgeted net revenue up to a maximum of $5 million per fiscal year to these parties (or certain of their respective affiliates) and reimburse them for their reasonable disbursements and out-of-pocket expenses. This monitoring fee will be subordinated to the notes in the event of a bankruptcy of the company. For each of the years ended September 30, 2010, 2009 and 2008, we paid $5.0 million in monitoring fees under the management services agreement.
Income Tax Allocations
The Company and some of its subsidiaries are included in IAS’ consolidated filing group for U.S. federal income tax purposes, as well as in certain state and local income tax returns that include IAS. With respect to tax returns for any taxable period in which the Company or any of its subsidiaries are included in a tax return filing with IAS, the amount of taxes to be paid by the Company is determined, subject to some adjustments, as if it and its subsidiaries filed their own tax returns excluding IAS.
135
Policy on Transactions with Related Persons
On an annual basis, each director, director nominee and executive officer is required to complete a Director and Officer’s Questionnaire that requires disclosure of any transaction in which the director or executive officer has a direct or indirect material interest and in which the company participates and the amount involved exceeds $120,000. The board has not adopted a formal policy for the review, approval or ratification of such transactions. However, pursuant to the company’s corporate code of ethics, executive officers may not participate in, or benefit from, a related party transaction without the approval of the Company’s compliance officer. During fiscal year 2010, there were no transactions between our company and a related person requiring disclosure under applicable securities laws.
During fiscal year 2010, there were no transactions between our company and a related person requiring disclosure under applicable securities laws.
136
DESCRIPTION OF THE EXCHANGE OFFER
Purpose of the Exchange Offer
On May 3, 2011, we issued $850,000,000 aggregate principal amount of Old Notes. In connection with that issuance, we entered into a Registration Rights Agreement on May 3, 2011. Pursuant to the Registration Rights Agreement, we agreed that we would:
| | • | | file a registration statement (the “Exchange Offer Registration Statement”) covering an offer to the Holders of Old Notes to exchange all Old Notes for New Notes on or prior to 180 days after the closing of the offering of the Old Notes; |
| | • | | cause the Exchange Offer Registration Statement to become effective on or prior to 270 days after the closing of the offering of Old Notes; |
| | • | | commence the Exchange Offer as soon as reasonably practicable after the Exchange Offer Registration Statement is declared effective by the SEC, and |
| | • | | complete the registered exchange offer not later than 30 days after the effective date of the Exchange offer Registration Statement. |
Upon the effectiveness of the Exchange Offer Registration Statement of which this prospectus is a part, we will offer the New Notes in exchange for the Old Notes. We filed a copy of the Registration Rights Agreement as an exhibit to the Exchange Offer Registration Statement.
Resale of the New Notes
We are making the exchange offer in reliance on the position of the staff of the SEC as set forth in interpretive letters addressed to other parties in other transactions. For further information on the SEC’s position, seeExxon Capital Holdings Corporation, available May 13, 1988,Morgan Stanley & Co. Incorporated, available June 5, 1991 andShearman & Sterling, available July 2, 1993, and other interpretive letters to similar effect. We have not sought our own interpretive letter, however, and we cannot assure you that the staff would make a similar determination with respect to the exchange offer as it has in interpretive letters to other parties. Based on these interpretations by the staff, we believe that the New Notes issued under the exchange offer may be offered for resale, resold or otherwise transferred by you, without further compliance with the registration and prospectus delivery provisions of the Securities Act, so long as you:
| | (1) | are acquiring the New Notes in the ordinary course of your business; |
| | (2) | are not participating in, and do not intend to participate in, a distribution of the New Notes within the meaning of the Securities Act and have no arrangement or understanding with any person to participate in a distribution of the New Notes within the meaning of the Securities Act; |
| | (3) | are not a broker-dealer who acquired the Old Notes directly from us; and |
| | (4) | are not an “affiliate” of ours, within the meaning of Rule 405 of the Securities Act. |
By tendering the Old Notes in exchange for New Notes, you will be required to represent to us that each of the above statements applies to you. If you are participating in or intend to participate in, a distribution of the New Notes, or have any arrangement or understanding with any person to participate in a distribution of the New Notes to be acquired in this exchange offer, you may be deemed to have received restricted securities and may not rely on the applicable interpretations of the staff of the SEC. If you are so deemed, you will have to comply with the registration and prospectus delivery requirements of the Securities Act in connection with any secondary resale transaction.
Each broker-dealer that receives New Notes for its own account in exchange for Old Notes, where the Old Notes were acquired by the broker-dealer as a result of market-making activities or other trading activities, must acknowledge that it will deliver a prospectus in connection with any resale of the New Notes. The letter of transmittal states that by so acknowledging and by delivering a prospectus, a broker-dealer will not be deemed to admit that it is an “underwriter” within the meaning of the Securities Act. A broker-dealer may use this prospectus, as it may be amended or supplemented from time to time, in connection with resales of
137
New Notes received in exchange for Old Notes which the broker-dealer acquired as a result of market-making or other trading activities. See “Plan of Distribution.”
The exchange offer is not being made to, nor will we accept tenders for exchange from, holders of Old Notes in any jurisdiction in which the exchange offer or the acceptance of it would not be in compliance with the securities or blue sky laws of such jurisdiction.
Terms of the Exchange Offer
Upon the terms and subject to the conditions set forth in this prospectus and the letter of transmittal, we will accept any and all Old Notes validly tendered and not withdrawn prior to 5:00 p.m., New York City time, on the Expiration Date. We will issue $1,000 principal amount of New Notes in exchange for each $1,000 principal amount of Old Notes validly tendered and accepted pursuant to the exchange offer.
We will not pay any accrued and unpaid interest on the Old Notes that we acquire in the exchange offer. Instead, interest on the New Notes will accrue from the most recent date to which interest has been paid or, if no interest has been paid, from and including May 3, 2011, the date on which we issued the Old Notes.
Tendering holders of Old Notes must tender Old Notes in minimum denominations of $2,000, and integral multiples of $1,000 in excess thereof. New Notes will be issued in minimum denominations of $2,000 and integral multiples of $1,000 in excess thereof.
The terms of the New Notes are identical in all material respects to the terms of the Old Notes, except that:
| | (1) | we have registered the New Notes under the Securities Act and therefore these notes will not bear legends restricting their transfer, and |
| | (2) | specified rights under the Registration Rights Agreement, including the provisions providing for payment of additional interest in specified circumstances relating to the exchange offer, will be eliminated for all the Notes. |
The New Notes will evidence the same debt as the Old Notes. The New Notes will be issued under the same indenture and will be entitled to the same benefits under that indenture as the Old Notes being exchanged. As of the date of this prospectus, approximately $850,000,000 aggregate principal amount of the Old Notes are outstanding. Old Notes accepted for exchange will be retired and cancelled and not reissued.
Except as described under “Form, Book-Entry Procedures and Transfer,” we will issue the New Notes in the form of one or more global notes registered in the name of DTC or its nominee, and each beneficial owner’s interest in it will be transferable in book-entry form through DTC.
We will conduct the exchange offer in accordance with the applicable requirements of the Securities Act and the Exchange Act, and the rules and regulations of the SEC thereunder.
We will be considered to have accepted validly tendered Old Notes if and when we have given oral or written notice to that effect to the exchange agent. The exchange agent will act as agent for the tendering holders for the purposes of receiving the New Notes from us.
If we do not accept any tendered Old Notes for exchange because of an invalid tender, the occurrence of the other events described in this prospectus or otherwise, we will return these Old Notes, without expense, to the tendering holder as soon as practicable after the Expiration Date of the exchange offer.
Holders who tender Old Notes will not be required to pay brokerage commissions or fees or, subject to the instructions in the letter of transmittal, transfer taxes on exchange of Old Notes in connection with the exchange offer. We will pay all charges and expenses, other than certain applicable taxes in certain circumstances, in connection with the exchange offer. See “—Other Fees and Expenses” and “—Transfer Taxes.”
138
If we successfully complete the exchange offer, any Old Notes which holders do not tender or which we do not accept in the exchange offer will remain outstanding and continue to accrue interest. The holders of Old Notes after the exchange offer in general will not have further rights under the Registration Rights Agreement, including registration rights and any rights to additional interest. Holders wishing to transfer the Old Notes would have to rely on exemptions from the registration requirements of the Securities Act.
Expiration Date; Extensions; Amendments; Termination
For purposes of the exchange offer, the term “Expiration Date” means 5:00 p.m., New York City time, on December 12, 2011, subject to our right to extend that time and date in our sole discretion, in which case the Expiration Date means the latest time and date to which the exchange offer is extended.
We reserve the right, in our sole discretion, by giving oral or written notice to the exchange agent, to:
| | • | | extend the exchange offer; |
| | • | | terminate the exchange offer if a condition to our obligation to exchange Old Notes for New Notes is not satisfied or waived on or prior to the Expiration Date; and |
| | • | | amend the exchange offer. |
If the exchange offer is amended in a manner that we determine constitutes a material change, we will extend the exchange offer for a period of two to ten business days, depending upon the significance of the amendment and the manner of disclosure to the holders, if the exchange offer would otherwise have expired during that two to ten business day period.
We will notify holders of the Old Notes of any extension, amendment or termination of the exchange offer by press release or other public announcement. We will announce any extension of the Expiration Date no later than 9:00 a.m., New York City time, on the first business day after the previously scheduled Expiration Date. We have no other obligation to publish, advertise or otherwise communicate any information about any extension, amendment or termination.
Settlement Date
We will deliver the New Notes on the settlement date, which will be as soon as practicable after the Expiration Date of the exchange offer. We will not be obligated to deliver New Notes unless the exchange offer is consummated.
Conditions to the Exchange Offer
Notwithstanding any other provision of the exchange offer, we will not be required to accept for exchange, or to issue New Notes in exchange for, any Old Notes and may terminate or amend the exchange offer if at any time before the expiration of the exchange offer, we determine (i) that the exchange offer violates applicable law, any applicable interpretation of the staff of the SEC or any order of any governmental agency or court of competent jurisdiction; (ii) an action or proceeding shall have been instituted or threatened in any court or by any governmental agency which might materially impair our ability to proceed with the exchange offer or a material adverse development shall have occurred in any existing action or proceeding with respect to us; or (iii) all governmental approvals that we deem necessary for the consummation of the exchange offer have not been obtained.
The foregoing conditions are for our sole benefit and may be asserted by us regardless of the circumstances giving rise to any such condition or may be waived by us in whole or in part at any time and from time to time. The failure by us at any time to exercise any of the foregoing rights shall not be deemed a waiver of any of those rights and each of those rights shall be deemed an ongoing right which may be asserted at any time and from time to time. Any determination made by us concerning an event, development or circumstance described or referred to above will be conclusive and binding.
If any of the foregoing conditions are not satisfied, we may, at any time on or prior to the Expiration Date:
| | • | | terminate the exchange offer and return all tendered Old Notes to the respective tendering holders; |
139
| | • | | modify, extend or otherwise amend the exchange offer and retain all tendered Old Notes until the Expiration Date, as extended, subject, however, to the withdrawal rights of holders; or |
| | • | | to the extent lawful, waive the unsatisfied conditions with respect to the exchange offer and accept all Old Notes tendered and not previously validly withdrawn. |
In addition, we will not accept for exchange any Old Notes tendered, and no New Notes will be issued in exchange for those Old Notes, if at such time any stop order shall be threatened or in effect with respect to the Exchange Offer Registration Statement or with respect to the qualification of the indenture governing the New Notes under the Trust Indenture Act of 1939, as amended.
Effect of Tender
Any tender by a holder, and our subsequent acceptance of that tender, of Old Notes will constitute a binding agreement between that holder and us upon the terms and subject to the conditions of the exchange offer described in this prospectus and in the letter of transmittal. The acceptance of the exchange offer by a tendering holder of Old Notes will constitute the agreement by that holder to deliver good and marketable title to the tendered Old Notes, free and clear of any and all liens, restrictions, charges, pledges, security interests, encumbrances or rights of any kind of third parties.
Letter of Transmittal; Representations, Warranties and Covenants of Holders of Old Notes
Upon agreement to the terms of the letter of transmittal pursuant to an agent’s message, a holder, or the beneficial holder of Old Notes on behalf of which the holder has tendered, will, subject to that holder’s ability to withdraw its tender, and subject to the terms and conditions of the exchange offer generally, thereby:
| | (1) | irrevocably sell, assign and transfer to or upon our order or the order of our nominee all right, title and interest in and to, and any and all claims in respect of or arising or having arisen as a result of the holder’s status as a holder of, all Old Notes tendered thereby, such that thereafter the holder shall have no contractual or other rights or claims in law or equity against us or any fiduciary, trustee, fiscal agent or other person connected with the Old Notes arising under, from or in connection with those Old Notes; |
| | (2) | waive any and all rights with respect to the Old Notes tendered thereby, including, without limitation, any existing or past defaults and their consequences in respect of those Old Notes; and |
| | (3) | release and discharge us and the trustee for the Old Notes from any and all claims the holder may have, now or in the future, arising out of or related to the Old Notes tendered thereby, including, without limitation, any claims that the holder is entitled to receive additional principal or interest payments with respect to the Old Notes tendered thereby, other than as expressly provided in this prospectus and in the letter of transmittal, or to participate in any redemption or defeasance of the Old Notes tendered thereby. |
In addition, by tendering Old Notes in the exchange offer, each holder of Old Notes will represent, warrant and agree that:
| | (1) | it has received and reviewed this prospectus; |
| | (2) | it is the beneficial owner (as defined below) of, or a duly authorized representative of one or more beneficial owners of, the Old Notes tendered thereby, and it has full power and authority to execute the letter of transmittal; |
| | (3) | the Old Notes being tendered thereby were owned as of the date of tender, free and clear of any liens, charges, claims, encumbrances, interests and restrictions of any kind, and we will acquire good, indefeasible and unencumbered title to those Old Notes, free and clear of all liens, charges, claims, encumbrances, interests and restrictions of any kind, when we accept the same; |
140
| | (4) | it will not sell, pledge, hypothecate or otherwise encumber or transfer any Old Notes tendered thereby from the date of the letter of transmittal, and any purported sale, pledge, hypothecation or other encumbrance or transfer will be void and of no effect; |
| | (5) | in evaluating the exchange offer and in making its decision whether to participate in the exchange offer by tendering its Old Notes, it has made its own independent appraisal of the matters referred to in this prospectus and the letter of transmittal and in any related communications and it is not relying on any statement, representation or warranty, express or implied, made to it by us, the information agent or the exchange agent, other than those contained in this prospectus, as amended or supplemented through the Expiration Date; |
| | (6) | the execution and delivery of the letter of transmittal shall constitute an undertaking to execute any further documents and give any further assurances that may be required in connection with any of the foregoing, in each case on and subject to the terms and conditions described or referred to in this prospectus; |
| | (7) | the agreement to the terms of the letter of transmittal pursuant to an agent’s message shall, subject to the terms and conditions of the exchange offer, constitute the irrevocable appointment of the exchange agent as its attorney and agent and an irrevocable instruction to that attorney and agent to complete and execute all or any forms of transfer and other documents at the discretion of that attorney and agent in relation to the Old Notes tendered thereby in favor of us or any other person or persons as we may direct and to deliver those forms of transfer and other documents in the attorney’s and agent’s discretion and the certificates and other documents of title relating to the registration of Old Notes and to execute all other documents and to do all other acts and things as may be in the opinion of that attorney or agent necessary or expedient for the purpose of, or in connection with, the acceptance of the exchange offer, and to vest in us or our nominees those Old Notes; |
| | (8) | the terms and conditions of the exchange offer shall be deemed to be incorporated in, and form a part of, the letter of transmittal, which shall be read and construed accordingly; |
| | (9) | it is acquiring the New Notes in the ordinary course of its business; |
| | (10) | it is not participating in, and does not intend to participate in, a distribution of the New Notes within the meaning of the Securities Act and has no arrangement or understanding with any person to participate in a distribution of the New Notes within the meaning of the Securities Act; |
| | (11) | it is not a broker-dealer who acquired the Old Notes directly from us; and |
| | (12) | it is not an “affiliate” of ours, within the meaning of Rule 405 of the Securities Act. |
The representations, warranties and agreements of a holder tendering Old Notes will be deemed to be repeated and reconfirmed on and as of the Expiration Date and the settlement date. For purposes of this prospectus, the “beneficial owner” of any Old Notes means any holder that exercises investment discretion with respect to those Old Notes.
Absence of Dissenters’ Rights
Holders of the Old Notes do not have any appraisal or dissenters’ rights in connection with the exchange offer.
Acceptance of Old Notes for Exchange and Delivery of New Notes
On the settlement date, New Notes to be issued in exchange for Old Notes in the exchange offer, if consummated, will be delivered in book-entry form.
141
We will be deemed to accept validly tendered Old Notes that have not been validly withdrawn as provided in this prospectus when, and if, we give oral or written notice of acceptance to the exchange agent. Subject to the terms and conditions of the exchange offer, delivery of the New Notes will be made by the exchange agent on the settlement date following receipt of that notice. The exchange agent will act as agent for tendering holders of Old Notes for the purpose of receiving Old Notes and transmitting New Notes as of the settlement date. If any tendered Old Notes are not accepted for any reason described in the terms and conditions of the exchange offer, such unaccepted Old Notes will be returned without expense to the tendering holders as promptly as practicable after the expiration or termination of the exchange offer.
Procedures for Tendering
To participate in the exchange offer, you must properly tender your Old Notes to the exchange agent as described below. We will only issue New Notes in exchange for Old Notes that you timely and properly tender. Therefore, you should allow sufficient time to ensure timely delivery of the Old Notes, and you should follow carefully the instructions on how to tender your Old Notes. It is your responsibility to properly tender your Old Notes. We have the right to waive any defects. However, we are not required to waive defects, and neither we, nor the exchange agent is required to notify you of defects in your tender.
If you have any questions or need help in exchanging your Old Notes, please contact the exchange agent at the address or telephone numbers set forth below.
All of the Old Notes were issued in book-entry form, and all of the Old Notes are currently represented by global certificates registered in the name of Cede & Co., the nominee of DTC. We have confirmed with DTC that the Old Notes may be tendered using DTC’s automatic tender offer program, or ATOP. The exchange agent will establish an account with DTC for purposes of the exchange offer promptly after the commencement of the exchange offer, and DTC participants may electronically transmit their acceptance of the exchange offer by causing DTC to transfer their Old Notes to the exchange agent using the ATOP procedures. In connection with the transfer, DTC will send an “agent’s message” to the exchange agent. The agent’s message will state that DTC has received instructions from the participant to tender Old Notes and that the participant agrees to be bound by the terms of the letter of transmittal.
By using the ATOP procedures to exchange Old Notes, you will not be required to deliver a letter of transmittal to the exchange agent. However, you will be bound by its terms just as if you had signed it.
Determinations Under the Exchange Offer. We will determine in our sole discretion all questions as to the validity, form, eligibility, time of receipt, acceptance of tendered Old Notes and withdrawal of tendered Old Notes. Our determination will be final and binding. We reserve the absolute right to reject any Old Notes not properly tendered or any Old Notes our acceptance of which would, in the opinion of our counsel, be unlawful. We also reserve the right to waive any defect, irregularities or conditions of tender as to particular Old Notes. Our interpretation of the terms and conditions of the exchange offer, including the instructions in the letter of transmittal, will be final and binding on all parties. Unless waived, all defects or irregularities in connection with tenders of Old Notes must be cured within such time as we shall determine. Although we intend to notify holders of defects or irregularities with respect to tenders of Old Notes, neither we, the information agent, the exchange agent nor any other person will incur any liability for failure to give such notification. Tenders of Old Notes will not be deemed made until such defects or irregularities have been cured or waived. Any Old Notes received by the exchange agent that are not properly tendered and as to which the defects or irregularities have not been cured or waived will be returned to the tendering holder as soon as practicable after the Expiration Date of the exchange.
When We Will Issue New Notes. In all cases, we will issue New Notes for Old Notes that we have accepted for exchange under the exchange offer only after the exchange agent receives, prior to 5:00 p.m., New York City time, on the Expiration Date:
| | • | | a book-entry confirmation of such number of Old Notes into the exchange agent’s account at DTC; and |
| | • | | a properly transmitted agent’s message. |
Return of Old Notes Not Accepted or Exchanged. If we do not accept any tendered Old Notes for exchange or if Old Notes are submitted for a greater principal amount than the holder desires to exchange, the unaccepted or non-exchanged Old Notes will
142
be returned without expense to their tendering holder. Such non-exchanged Old Notes will be credited to an account maintained with DTC. These actions will occur as promptly as practicable after the expiration or termination of the exchange offer.
Participating Broker-Dealers. Each broker-dealer that receives New Notes for its own account in exchange for Old Notes, where those Old Notes were acquired by such broker-dealer as a result of market-making activities or other trading activities, must acknowledge that it will deliver a prospectus in connection with any resale of those New Notes. See “Plan of Distribution.”
Withdrawal of Tenders
Tenders of Old Notes may be withdrawn at any time prior to 5:00 p.m., New York City time, on the Expiration Date.
For a withdrawal to be effective, you must comply with the appropriate ATOP procedures. Any notice of withdrawal must specify the name and number of the account at DTC to be credited with withdrawn Old Notes and otherwise comply with the ATOP procedures.
We will determine all questions as to the validity, form, eligibility and time of receipt of a notice of withdrawal. Our determination shall be final and binding on all parties. We will deem any Old Notes so withdrawn not to have been validly tendered for exchange for purposes of the exchange offer.
Any Old Notes that have been tendered for exchange but that are not exchanged for any reason will be credited to an account maintained with DTC for the Old Notes. This return or crediting will take place as soon as practicable after withdrawal, rejection of tender, expiration or termination of the exchange offer. You may retender properly withdrawn Old Notes by following the procedures described under “—Procedures for Tendering” above at any time on or prior to the Expiration Date of the exchange offer.
Exchange Agent and Information Agent
The Bank of New York Mellon has been appointed as the exchange agent and the information agent for the exchange offer. All correspondence in connection with the exchange offer should be sent or delivered by each holder of Old Notes, or a beneficial owner’s commercial bank, broker, dealer, trust company or other nominee, to the exchange agent at:
The Bank of New York Mellon Trust Company, N.A.
900 Ashwood Parkway, Suite 425
Atlanta, Georgia 30338
Facsimile: 770-698-5195
Questions concerning tender procedures and requests for additional copies of this prospectus or the letter of transmittal should be directed to the information agent at the address or fax number listed above. Holders of Old Notes may also contact their commercial bank, broker, dealer, trust company or other nominee for assistance concerning the exchange offer. We will pay the exchange agent and information agent reasonable and customary fees for its services and will reimburse it for its reasonable out-of-pocket expenses.
Announcements
We may make any announcement required pursuant to the terms of this prospectus or required by the Exchange Act or the rules promulgated thereunder through a reasonable press release or other public announcement in our sole discretion; provided, that, if any such announcement is made by issuing a press release to Business Wire, such announcement shall be reasonable and sufficient.
Other Fees and Expenses
We will bear the expenses of soliciting tenders of the Old Notes. The principal solicitation is being made by mail. Additional solicitations may, however, be made by e-mail, facsimile transmission, telephone or in person by the information agent as well as our officers and other employees and those of our affiliates.
143
We have not retained any dealer-manager in connection with this exchange offer and will not make any payments to broker-dealers or others soliciting acceptances of the exchange offer. However, we will pay the exchange agent reasonable and customary fees for its services and will reimburse it for its reasonable out-of-pocket expenses.
Tendering holders of Old Notes will not be required to pay any fee or commission to the exchange agent. If, however, a tendering holder handles the transaction through its commercial bank, broker, dealer, trust company or other institution, that holder may be required to pay brokerage fees or commissions.
Transfer Taxes
Holders who tender their Old Notes for exchange will not be obligated to pay any transfer taxes in connection with that tender or exchange, except that holders who instruct us to register New Notes in the name of, or request that Old Notes not tendered or not accepted in the exchange offer be returned to, a person other than the registered tendering holder will be responsible for the payment of any applicable transfer tax on those Old Notes.
Consequences of Failure to Exchange
Holders of Old Notes who do not exchange their Old Notes for New Notes under this exchange offer will remain subject to the restrictions on transfer applicable in the Old Notes (i) as set forth in the legend printed on the Old Notes as a consequence of the issuance of the Old Notes pursuant to exemptions from, or in transactions not subject to, the registration requirements of the Securities Act and applicable state securities laws and (ii) otherwise as set forth in the prospectus distributed in connection with the private offering of the Old Notes.
Any Old Notes not tendered by their holders in exchange for New Notes in this exchange offer will not retain any rights under the Registration Rights Agreement (except in certain limited circumstances). See “—Resale Registration Statement; Additional Interest.”
In general, you may not offer or sell the Old Notes unless they are registered under the Securities Act, or if the offer or sale is exempt from the registration requirements of the Securities Act and applicable state securities laws. We do not intend to register resales of the Old Notes under the Securities Act. Based on interpretations of the SEC staff, New Notes issued pursuant to this exchange offer may be offered for resale, resold or otherwise transferred by their holders (other than any such holder that is our “affiliate” within the meaning of Rule 405 under the Securities Act) without compliance with the registration and prospectus delivery provisions of the Securities Act, provided that the holders acquired the New Notes in the ordinary course of business and the holders are not engaged in, have no arrangement with any person to participate in, and do not intend to engage in, any public distribution of the New Notes to be acquired in this exchange offer. Any holder who tenders in this exchange offer and is engaged in, has an arrangement with any person to participate in, or intends to engage in, any public distribution of the New Notes (i) may not rely on the applicable interpretations of the SEC and (ii) must comply with the registration and prospectus delivery requirements of the Securities Act in connection with a secondary resale transaction.
Resale Registration Statement; Additional Interest
Under the Registration Rights Agreement, we have agreed that if:
| | (1) | any change in law or applicable interpretations of the staff of the SEC do not permit us to effect the exchange offer; |
| | (2) | for any other reason the exchange offer is not completed within 270 days after the closing of the offering of the Old Notes; |
| | (3) | any holder of the Notes notifies us that: |
| | (a) | it is prohibited by law or SEC policy from participating in the exchange offer; or |
144
| | (b) | it may not resell the New Notes acquired by it in the exchange offer to the public without delivering a prospectus and the prospectus contained in the Exchange Offer Registration Statement is not appropriate or available for such resales; or |
| | (c) | it is a broker-dealer (“Participating Broker-Dealer”) receiving New Notes in the exchange offer and owns Notes acquired directly from us or an affiliate of ours; |
then we will (a) file a registration statement (the “Shelf Registration Statement”) covering resales of the Notes (1) the 180th day after the date on which the Company determines that it is not required to file the Exchange Offer Registration Statement, (2) the 180th day after the date on which the Company receives notice of a request from a holder of transfer restricted securities, and (3) the 270th day after the Closing Date (or if such 270th day is not a Business Day, the next succeeding Business Day); (b) use our commercially reasonable efforts to cause the Shelf Registration Statement to be declared effective under the Securities Act on or before the 270th day after the closing of the offering of the Old Notes and (c) use our reasonable best efforts to keep the Shelf Registration Statement effective for a period of two years after the Expiration Date, or such earlier date on which (a) such Notes covered by the Shelf Registration Statement have been sold, or (b) all Notes covered by such Shelf Registration Statement are distributed to the public pursuant to Rule 144. We will, in the event a Shelf Registration Statement is filed, among other things, provide to each holder for whom such Shelf Registration Statement was filed copies of the prospectus which is a part of the Shelf Registration Statement, notify each such holder when the Shelf Registration Statement has become effective and take certain other actions as are required to permit unrestricted resales of the Notes. A holder selling Old Notes or New Notes pursuant to the Shelf Registration Statement generally would be required to be named as a selling security holder in the related prospectus and to deliver a prospectus to purchasers, and will be subject to certain of the civil liability provisions under the Securities Act in connection with such sales and will be bound by the provisions of the Registration Rights Agreement which are applicable to such holder (including certain indemnification obligations).
The Registration Rights Agreement further provides that in the event that either (i) the Exchange Offer Registration Statement or the Shelf Registration Statement is not filed on or prior to the date specified for such filing in the Registration Rights Agreement, (ii) the Exchange Offer is not completed prior to 30 days after the effective date of the Exchange Offer Registration Statement, (iii) the Exchange Offer Registration Statement or the the Shelf Registration Statement have not become effective on or prior to the date specified for effectiveness in the Registration Rights Agreement or the Exchange Offer Registration Statement or (iv) the Shelf Registration Statement ceases to be effective or this prospectus ceases to be usable, the interest rate on the Old Notes will be increased by (x) 0.25% per annum for the first 90-day period immediately following and (y) an additional 0.25% per annum with respect to each subsequent 90 day period thereafter, in each case until the Exchange Offer is completed or the Shelf Registration Statement, if required, becomes effective or is no longer required or this prospectus becomes usable, up to a maximum increase of 1.00% per annum.
Other
Participation in this exchange offer is voluntary, and you should carefully consider whether to participate. You are urged to consult your financial and tax advisors in making your own decision as to what action to take.
145
DESCRIPTION OF NOTES
You can find the definitions of certain terms used in this description under the subheading “Certain Definitions.” In this description, (1) the term “Company” refers only to IASIS Healthcare LLC and not to any of its subsidiaries, (2) the term “IASIS Capital” refers to IASIS Capital Corporation, a wholly owned subsidiary of the Company with nominal assets which conducts no operations, (3) the term “Issuers” refers to the Company and IASIS Capital and (iv) the term “Notes” refers to the Old Notes and any New Notes issued in exchange hereunder.
The Issuers issued the old Notes, and will issue the New Notes under an indenture, dated as of May 3, 2011, among the Issuers, the Guarantors and The Bank of New York Mellon Trust Company, N.A., as trustee. The terms of the notes will include those stated in the indenture and those made part of the indenture by reference to the Trust Indenture Act of 1939, as amended.
The following description is a summary of the material provisions of the indenture. It does not restate those agreements in their entirety. We urge you to read the indenture because it, and not this description, defines your rights as holders of the notes. A copy of the indenture is available as set forth below under “—Additional Information.”
The registered holder of a note will be treated as the owner of it for all purposes. Only registered holders will have rights under the indenture.
Brief Description of Notes and the Subsidiary Guarantees
The Notes
The notes:
| | • | | will be senior unsecured obligations of the Issuers; |
| | • | | will be pari passu in right of payment to all existing and future senior Indebtedness of the Issuers, including borrowings under the Credit Agreement; |
| | • | | will be senior in right of payment to all existing and future Subordinated Indebtedness of the Issuers; |
| | • | | will be effectively subordinated to any secured Indebtedness of the Issuers (including Borrowings under the Credit Agreement) to the extent of the assets securing such Indebtedness; and |
| | • | | will be unconditionally guaranteed by each of the Guarantors on a senior basis. |
The Subsidiary Guarantees
The notes will be guaranteed by all of the Company’s current Wholly-Owned Domestic Subsidiaries other than the Non-Guarantor Subsidiaries. Future Wholly-Owned Domestic Subsidiaries (other than Non-Guarantor Subsidiaries) that are guarantors under the Credit Agreement will also become guarantors of the notes. Non-Guarantor Subsidiaries include Domestic Subsidiaries that are guarantors under the Credit Agreement but are not wholly-owned and thus do not guarantee the notes.
The guarantee of each Guarantor of the notes:
| | • | | will be a senior unsecured obligation of that Guarantor; |
| | • | | will be pari passu in right of payment to all existing and future senior Indebtedness of that Guarantor, including guarantees of Indebtedness under the Credit Agreement; |
146
| | • | | will be senior in right of payment with all existing and future Subordinated Indebtedness of that Guarantor; and |
| | • | | will be effectively subordinated to any secured Indebtedness of such Guarantor (including such Guarantor’s guarantee of Indebtedness under the Credit Agreement) to the extent of the assets securing such Indebtedness. |
The Non-Guarantor Subsidiaries will not guarantee the notes. The Non-Guarantor Subsidiaries constitute a significant portion of our Total Assets and account for all of our Consolidated Adjusted EBITDA. In the event of a bankruptcy, liquidation or reorganization of any of the Non-Guarantor Subsidiaries, the Non-Guarantor Subsidiaries will pay the holders of their debt and their trade creditors before they will be able to distribute any of their assets to us. As a result, the notes will be effectively subordinated in right of payment to all Indebtedness and other liabilities and commitments (including trade payables and lease obligations) of the Non-Guarantor Subsidiaries. The Non-Guarantor Subsidiaries generated $1,507 million or 72.8% of our consolidated net revenue in the nine months ended June 30, 2011, and held $2,101 million or 78.2% of our consolidated assets as of June 30, 2011. As of June 30, 2011, the Non-Guarantor Subsidiaries would have had approximately $396 million of trade payables, lease obligations and other liabilities (excluding (1) debt owing to the Company and its Subsidiaries and (2) borrowings under the Credit Agreement guaranteed by certain Non-Guarantor Subsidiaries) assuming consummation of the Transactions. All our Consolidated Adjusted EBITDA comes from the Non-Guarantor Subsidiaries. However, the Guarantor subsidiaries have unsubordinated promissory notes from certain Non-Guarantor Subsidiaries aggregating $665 million in principal amount as of June 30, 2011, under which the guarantors are entitled to principal and interest payments of $71 million annually. In addition, the non-guarantor subsidiaries are contractually obligated to pay the guarantor subsidiaries management fees. The management fee amount ranges from 2.0% to 2.5% of net revenue for the non-guarantor subsidiaries. For the nine months ended June 30, 2011, the non-guarantor subsidiaries paid $20 million in management fees. See “Risk Factors—Risk Factors Relating to the Notes—The Notes Will Be Unsecured And Will Be Effectively Subordinated To Our And The Guarantors’ Senior Secured Indebtedness To The Extent Of The Value Of The Collateral And Indebtedness Of Non-Guarantor Subsidiaries.” For more detail about the revenues and assets of certain of our Non-Guarantor Subsidiaries, see our condensed consolidated financial statements included elsewhere in this prospectus.
As of the date of the indenture, Health Choice Arizona, Inc., Brim Healthcare of Texas, LLC (d/b/a Wadley Regional Medical Center), Texarkana Regional Healthcare Network, Harpeth Insurance Limited, NLV Healthcare Development, LP, Permian Premier Health Services, Inc., Permian Basin Clinical Services, Inc., Indigent Care Services of Permian Basin, Inc., IASIS Healthcare Foundation, SET Physicians, Southwest Physicians of San Antonio, Odessa Regional Hospital, LP, The Medical Center of Southeast Texas, LP, Southwest General Hospital, LP, Mountain Vista Medical Center, LP, Jordan Valley Medical Center, LP, Davis Hospital & Medical Center, LP and Salt Lake Regional Medical Center, LP will be Non-Guarantor Subsidiaries. In addition, other Subsidiaries of the Company may become Non-Guarantor Subsidiaries. See the definition of “Non-Guarantor Subsidiaries” under “—Certain Definitions” below.
As of the date of the indenture, the following Non-Guarantor Subsidiaries have guaranteed, and pledged their assets to secure, the Company’s obligations under the Credit Agreement: Odessa Regional Hospital, LP, The Medical Center of Southeast Texas, LP, Southwest General Hospital, LP, Mountain Vista Medical Center, LP, Jordan Valley Medical Center, LP, Davis Hospital & Medical Center, LP, and Salt Lake Regional Medical Center, LP. These Non-Guarantor Subsidiaries generated $792.4 million, or 38.3%, of our consolidated net revenue in the nine months ended June 30, 2011, and held $1,414 million, or 52.6%, of our consolidated assets as of June 30, 2011. As of June 30, 2011, these Non-Guarantor Subsidiaries would have had approximately $81 million of trade payables, lease obligations and other liabilities (excluding (1) debt owing to the Company and its Subsidiaries and (2) borrowings under the Credit Agreement guaranteed by certain Non-Guarantor Subsidiaries) assuming consummation of the Transactions. There may in the future be other Non-Guarantor Subsidiaries that will guarantee, and pledge their assets to secure, the Company’s obligations under the Credit Agreement. See the definition of “Non-Guarantor Subsidiaries” under “—Certain Definitions” below.
As of the date of the indenture, all of our Subsidiaries will be “Restricted Subsidiaries.” However, under the circumstances described below under the caption “—Certain Covenants—Designation of Restricted and Unrestricted Subsidiaries,” we will be permitted to designate certain of our Subsidiaries as “Unrestricted Subsidiaries.” Our Unrestricted Subsidiaries will not be subject to many of the restrictive covenants in the indenture. Our Unrestricted Subsidiaries will not guarantee the notes.
147
Principal, Maturity and Interest
We issued $850.0 million in aggregate principal amount of note. We may issue additional notes under the indenture from time to time. Any issuance of additional notes is subject to all of the covenants in the indenture, including the covenant described below under the caption “—Certain Covenants—Incurrence of Indebtedness and Issuance of Disqualified Stock and Preferred Stock.” The notes and any additional notes subsequently issued under the indenture will be treated as a single class for all purposes under the indenture, including, without limitation, waivers, amendments, redemptions and offers to purchase. We will issue notes in denominations of $2,000 and integral multiples of $1,000. The notes will mature on May 15, 2019.
Interest on the notes will accrue at the rate of 8.375% per annum and will be payable semiannually in arrears on May 15 and November 15, commencing on November 15, 2011. Interest on overdue principal, interest and Special Interest, if any, will accrue at a rate that is 1% higher than the then applicable interest rate on the notes. The Issuers will make each interest payment to the holders of record on the immediately preceding May 1 or November 1.
Interest on the notes will accrue from the date of original issuance or, if interest has already been paid, from the date it was most recently paid. Interest will be computed on the basis of a 360-day year comprised of twelve 30-day months.
Methods of Receiving Payments on the Notes
All payments on the notes will be made at the office or agency of the paying agent and registrar within the City and State of New York unless the Issuers elect to make interest payments by check mailed to the noteholders at their address set forth in the register of holders.
Paying Agent and Registrar for the Notes
The trustee will initially act as paying agent and registrar. The Issuers may change the paying agent or registrar without prior notice to the holders of the notes.
Transfer and Exchange
A holder may transfer or exchange notes in accordance with the provisions of the indenture. The registrar and the trustee may require a holder, among other things, to furnish appropriate endorsements and transfer documents in connection with a transfer of notes. Holders will be required to pay all taxes due on transfer. The Issuers will not be required to transfer or exchange any note selected for redemption. Also, the Issuers will not be required to transfer or exchange any note for a period of 15 days before a selection of notes to be redeemed.
Subsidiary Guarantees
The notes will be guaranteed on a senior basis by each of the Company’s current Wholly-Owned Domestic Subsidiaries, other than the Non-Guarantor Subsidiaries, as long as they remain Restricted Subsidiaries. Future Wholly-Owned Domestic Subsidiaries (other than Non-Guarantor Subsidiaries) that are guarantors under the Credit Agreement and that are Wholly-Owned Subsidiaries will also become guarantors of the notes. Non-Guarantor Subsidiaries include Domestic Subsidiaries that are guarantors under the Credit Agreement but are not wholly-owned and thus do not guarantee the notes. The Subsidiary Guarantees will be joint and several obligations of the Guarantors. The obligations of each Guarantor under its Subsidiary Guarantee will be limited as necessary to prevent that Subsidiary Guarantee from constituting a fraudulent conveyance under applicable law. See “Risk Factors—Risks Relating to the Notes—Under Certain Circumstances A Court Could Cancel The Notes Or The Related Guarantees Under Fraudulent Conveyance Laws. If That Occurs, You May Not Receive Any Payments On The Notes.”
148
A Guarantor may not sell or otherwise dispose of all or substantially all of its assets to, or consolidate with or merge with or into (whether or not such Guarantor is the surviving Person) another Person, other than the Company, IASIS Capital or another Guarantor, unless:
| | (1) | immediately after giving effect to that transaction, no Default or Event of Default exists; and |
| | (a) | the Person (if other than the Company, IASIS Capital or a Guarantor) acquiring the property in any such sale or disposition or the Person (if other than the Company, IASIS Capital or a Guarantor) formed by or surviving any such consolidation or merger assumes all the obligations of that Guarantor under the indenture, its Subsidiary Guarantee and the registration rights agreement pursuant to a supplemental indenture satisfactory to the trustee; or |
| | (b) | the Net Proceeds of such sale or other disposition are applied in accordance with the applicable provisions of the indenture. |
The Subsidiary Guarantee of a Guarantor will be released:
| | (1) | in connection with any sale or other disposition of all or substantially all of the assets of that Guarantor (including by way of merger or consolidation) to a Person that is not (either before or after giving effect to such transaction) the Company or a Restricted Subsidiary of the Company, if the sale or other disposition does not violate the “Asset Sale” provisions of the indenture; |
| | (2) | in connection with any sale or other disposition of all of the Capital Stock of that Guarantor to a Person that is not (either before or after giving effect to such transaction) the Company or a Restricted Subsidiary of the Company, if the sale or other disposition does not violate the “Asset Sale” provisions of the indenture; |
| | (3) | if the Company designates any Restricted Subsidiary that is a Guarantor to be an Unrestricted Subsidiary in accordance with the applicable provisions of the indenture; |
| | (4) | if that Guarantor is released from its guarantee under the Credit Agreement; |
| | (5) | if that Guarantor is designated as a Non-Guarantor Subsidiary in accordance with the definition of Non-Guarantor Subsidiary; |
| | (6) | upon legal defeasance or satisfaction and discharge of the indenture as provided below under the captions “—Legal Defeasance and Covenant Defeasance” and “—Satisfaction and Discharge”; or |
| | (7) | upon delivery of a Covenant Termination Event Notice pursuant to a Covenant Termination Event. |
If any Guarantor is released from its Subsidiary Guarantee, any of its Subsidiaries that are Guarantors will be released from their Subsidiary Guarantees, if any.
See “—Repurchase at the Option of Holders—Asset Sales.
Optional Redemption
At any time prior to May 15, 2014, the Issuers may, on any one or more occasions, redeem up to 35% of the aggregate principal amount of notes issued under the indenture at a redemption price of 108.375% of the principal amount, plus accrued and unpaid interest and Special Interest, if any, to the redemption date, with the net cash proceeds of one or more Equity Offerings by the Issuers or a contribution to the common equity capital of the Company from the net proceeds of one or more Equity Offerings by a
149
direct or indirect parent of the Company (in each case, other than Excluded Contributions and the net proceeds of a sale of Designated Preferred Stock);provided that:
| | (1) | at least 65% of the aggregate principal amount of notes originally issued under the indenture (excluding notes held by the Company and its Subsidiaries) remains outstanding immediately after the occurrence of such redemption; and |
| | (2) | the redemption occurs within 90 days of the date of the closing of such Equity Offering or equity contribution. |
At any time prior to May 15, 2014, the Issuers may redeem all or a part of the notes, at a redemption price equal to 100% of the principal amount of the notes redeemed plus the Applicable Premium as of, and accrued and unpaid interest and Special Interest, if any, to, but excluding, the date of redemption (the “Redemption Date”), subject to the rights of Holders of record of notes on the relevant record date to receive interest due on the relevant interest payment date.
On or after May 15, 2014, the Issuers may redeem all or a part of the notes upon not less than 30 nor more than 60 days’ notice, at the redemption prices (expressed as percentages of principal amount) set forth below plus accrued and unpaid interest and Special Interest, if any, on the notes redeemed, to but excluding the applicable redemption date, if redeemed during the twelve-month period beginning on May 15 of the years indicated below, subject to the rights of holders of notes on the relevant record date to receive interest on the relevant interest payment date:
| | | | |
Year | | Percentage | |
2014 | | | 106.281 | % |
2015 | | | 104.188 | % |
2016 | | | 102.094 | % |
2017 and thereafter | | | 100 | % |
Unless the Issuers default in the payment of the redemption price, interest will cease to accrue on the notes or portions thereof called for redemption on the applicable redemption date.
Mandatory Redemption
The Issuers are not required to make mandatory redemption or sinking fund payments with respect to the notes.
Repurchase at the Option of Holders
Change of Control
The indenture will provide that if a Change of Control occurs after the date of the indenture, unless, prior to the time the Issuers are required to make a Change of Control Offer (as defined below), the Issuers have previously or concurrently mailed a redemption notice with respect to all the outstanding notes as described under “Optional Redemption” or “Satisfaction and Discharge,” the Issuers will make an offer to purchase all of the notes pursuant to the offer described below (the “Change of Control Offer”) at a price in cash (the “Change of Control Payment”) equal to 101% of the aggregate principal amount thereof plus accrued and unpaid interest and Special Interest, if any, to, but excluding, the date of purchase, subject to the right of holders of record on the relevant record date to receive interest due on the relevant interest payment date. Within 30 days following any Change of Control, the Issuers will send notice of such Change of Control Offer by first class mail, with a copy to the trustee, to each holder of notes to the address of such holder appearing in the security register with a copy to the trustee or otherwise in accordance with the procedures of DTC, with the following information:
| | (1) | that a Change of Control Offer is being made pursuant to the covenant entitled “Change of Control,” and that all notes properly tendered pursuant to such Change of Control Offer will be accepted for payment by the Issuer; |
150
| | (2) | the purchase price and the purchase date, which will be no earlier than 30 days nor later than 60 days from the date such notice is mailed (the “Change of Control Payment Date”); |
| | (3) | that any note not properly tendered will remain outstanding and continue to accrue interest; |
| | (4) | that, unless the Issuer defaults in the payment of the Change of Control Payment, all notes accepted for payment pursuant to the Change of Control Offer will cease to accrue interest on the Change of Control Payment Date; |
| | (5) | that holders electing to have any notes purchased pursuant to a Change of Control Offer will be required to surrender such notes, with the form entitled “Option of holder to Elect Purchase” on the reverse of such notes completed, to the paying agent specified in the notice at the address specified in the notice prior to the close of business on the third Business Day preceding the Change of Control Payment Date; |
| | (6) | that holders will be entitled to withdraw their tendered notes and their election to require the Issuer to purchase such notes; provided that the paying agent receives, not later than the expiration time of the Change of Control Offer, a telegram, telex, facsimile transmission or letter setting forth the name of the holder of the notes, the principal amount of notes tendered for purchase, and a statement that such holder is withdrawing its tendered notes and its election to have such notes purchased; |
| | (7) | that if a holder requests that only a portion of a note held by it be purchased, such holder will be issued a New Note equal in principal amount to the unpurchased portion of the note surrendered. The unpurchased portion of the New Note must be equal to $2,000 or an integral multiple of $1,000 in excess thereof; |
| | (8) | if such notice is delivered prior to the occurrence of a Change of Control, stating that the Change of Control Offer is conditional on the occurrence of such Change of Control; and |
| | (9) | the other instructions, as determined by us, consistent with the covenant hereunder, that a holder must follow. |
While the notes are in global form and the Issuer makes an offer to purchase all of the notes pursuant to the Change of Control Offer, a holder may exercise its option to elect for the purchase of the notes through the facilities of DTC, subject to its rules and regulations.
The Issuers will comply with the requirements of Rule 14e-1 under the Exchange Act and any other securities laws and regulations thereunder to the extent those laws and regulations are applicable in connection with the repurchase of the notes as a result of a Change of Control. To the extent that the provisions of any securities laws or regulations conflict with the Change of Control provisions of the indenture, the Issuers will comply with the applicable securities laws and regulations and will not be deemed to have breached their obligations under the Change of Control provisions of the indenture by virtue of such compliance.
On the Change of Control Payment Date, the Issuers will, to the extent lawful:
| | (1) | accept for payment all notes or portions of notes properly tendered pursuant to the Change of Control Offer; |
| | (2) | deposit with the paying agent an amount equal to the Change of Control Payment in respect of all notes or portions of notes properly tendered; and |
151
| | (3) | deliver or cause to be delivered to the trustee the notes properly accepted together with an officer’s certificate stating the aggregate principal amount of notes or portions of notes being purchased by the Issuers. |
The paying agent will promptly mail to each holder of notes properly tendered the Change of Control Payment for such notes, and the trustee will promptly authenticate and mail (or cause to be transferred by book entry) to each holder a new note equal in principal amount to any unpurchased portion of the notes surrendered, if any. The Issuers will publicly announce the results of the Change of Control Offer on or as soon as practicable after the Change of Control Payment Date.
The Credit Agreement will limit, and future credit agreements or other agreements relating to Indebtedness to which the Issuers (or one of their affiliates) becomes a party may prohibit or limit, the Issuers from purchasing any notes as a result of a Change of Control. In the event a Change of Control occurs at a time when the Issuers are contractually prohibited from purchasing the notes, the Issuers could seek the consent of their lenders to permit the purchase of the notes or could attempt to refinance the borrowings that contain such prohibition. If the Issuers do not obtain such consent or repay such borrowings, the Issuers will remain contractually prohibited from purchasing the notes. In such case, the Issuers’ failure to purchase tendered notes would constitute a Default under the indenture.
The Credit Agreement will provide that certain change of control events with respect to the Issuers would constitute a default thereunder (including a Change of Control under the indenture). If we experience a change of control event that triggers a default under our Credit Agreement, we could seek a waiver of such default or seek to refinance our Credit Agreement. In the event we do not obtain such a waiver or refinance the Credit Agreement, such default could result in amounts outstanding under our Credit Agreement being declared due and payable. Our ability to pay cash to the holders of notes following the occurrence of a Change of Control may be limited by our then existing financial resources. Therefore, sufficient funds may not be available when necessary to make any required repurchases of the notes.
The provisions described above that require the Issuers to make a Change of Control Offer following a Change of Control will be applicable whether or not any other provisions of the indenture are applicable. Except as described above with respect to a Change of Control, the indenture does not contain provisions that permit the holders of the notes to require that the Issuers repurchase or redeem the notes in the event of a takeover, recapitalization or similar transaction.
The Issuers will not be required to make a Change of Control Offer upon a Change of Control if (1) a third party makes the Change of Control Offer in the manner, at the times and otherwise in compliance with the requirements set forth in the indenture applicable to a Change of Control Offer made by the Issuers and purchases all notes properly tendered and not withdrawn under the Change of Control Offer or (2) notice of redemption has been given pursuant to the indenture as described above under the caption “—Optional Redemption,” unless and until there is a default in payment of the applicable redemption price. Notwithstanding anything to the contrary herein, a Change of Control Offer may be made in advance of a Change of Control, conditional upon such Change of Control, if a definitive agreement is in place for the Change of Control at the time of the making of such Change of Control Offer.
The definition of Change of Control includes a phrase relating to the direct or indirect sale, lease, transfer, conveyance or other disposition of “all or substantially all” of the properties or assets of the Company and its Subsidiaries taken as a whole. Although there is a limited body of case law interpreting the phrase “substantially all,” there is no precise established definition of the phrase under applicable law. Accordingly, the ability of a holder of notes to require the Issuers to repurchase its notes as a result of a sale, lease, transfer, conveyance or other disposition of less than all of the assets of the Company and its Subsidiaries taken as a whole to another Person or group may be uncertain.
Specified Change of Control
In connection with a Specified Change of Control, the Company may, by notice to the trustee identifying the Specified Change of Control Parent and the Specified Change of Control Parent Assumption Date, elect to effect a Specified Change of Control Parent Assumption. If such election is made, on the Specified Change of Control Assumption Date, the Specified Change of Control
152
Parent Assumption shall occur, and the Issuers shall be released from all of their obligations under the indenture. The Issuers and the trustee shall execute a supplemental indenture effectuating such assumption and release.
Asset Sales
The Company will not, and will not permit any of its Restricted Subsidiaries to, consummate an Asset Sale unless:
| | (1) | the Company (or the Restricted Subsidiary, as the case may be) receives consideration at the time of the Asset Sale at least equal to the Fair Market Value of the assets or Equity Interests issued or sold or otherwise disposed of; and |
| | (2) | at least 75% of the consideration received in the Asset Sale by the Company or such Restricted Subsidiary is in the form of cash other than in the case where the Company or such Restricted Subsidiary is undertaking a Hospital Swap. For purposes of this provision, each of the following will be deemed to be cash: |
| | (b) | any liabilities, as shown on the Company’s most recent consolidated balance sheet, of the Company or any Restricted Subsidiary (other than contingent liabilities and liabilities that are by their terms subordinated to the notes or any Subsidiary Guarantee) that are assumed by the transferee of any such assets pursuant to a customary novation agreement that releases the Company or such Restricted Subsidiary from further liability; |
| | (c) | any securities, notes or other obligations received by the Company or any such Restricted Subsidiary from such transferee that are converted by the Company or such Restricted Subsidiary into cash within 180 days of receipt, to the extent of the cash received in that conversion; |
| | (d) | any Designated Noncash Consideration the Fair Market Value of which, when taken together with all other Designated Noncash Consideration received pursuant to this clause (d) (and not subsequently converted into Cash Equivalents that are treated as Net Proceeds of an Asset Sale), does not exceed $40.0 million since the date of the indenture, with the Fair Market Value of each item of Designated Noncash Consideration being measured at the time received and without giving effect to subsequent changes in value; and |
| | (e) | any stock or assets of the kind referred to in clauses (2) or (4) of the third paragraph of this covenant. |
Notwithstanding the foregoing, the 75% limitation referred to in clause (2) above shall not apply to any Asset Sale in which the cash or Cash Equivalents portion of the consideration received therefrom, determined in accordance with the foregoing provision, is equal to or greater than what the after-tax proceeds would have been had such Asset Sale complied with the aforementioned 75% limitation.
Within 365 days after the receipt of any Net Proceeds from an Asset Sale, the Company (or the applicable Restricted Subsidiary, as the case may be) may apply such Net Proceeds at its option:
| | (x) | Obligations under a Credit Facility to the extent such Obligations were incurred under paragraph (1) of the definition of “Permitted Debt” (as defined under the caption “—Incurrence of Indebtedness and Issuance of Disqualified Stock and Preferred Stock”) and to correspondingly reduce any outstanding commitments with respect thereto or other Indebtedness secured by the assets subject to such Asset Sale; |
153
| | (y) | Obligations under the notes or any other Pari Passu Indebtedness of the Issuers or any Restricted Subsidiary (and, in the case of other Pari Passu Indebtedness, to correspondingly reduce any outstanding commitments with respect thereto, if applicable); provided that if the Issuers or any Restricted Subsidiary shall so repay any such other Pari Passu Indebtedness, the Issuers will reduce Obligations under the notes on a pro rata basis by, at its option, (A) redeeming notes as described under “—Optional Redemption,” (B) making an offer (in accordance with the procedures set forth below for an Asset Sale Offer) to all holders to purchase their notes at 100% of the principal amount thereof, plus the amount of accrued but unpaid interest, if any, thereon up to the principal amount of notes to be repurchased or (C) purchasing notes through privately negotiated transactions or open market purchases, at a price equal to or higher than 100% of the principal amount thereof, in a manner that complies with the indenture and applicable securities law; or |
| | (z) | Indebtedness of a Restricted Subsidiary that is not a Guarantor, other than Indebtedness owed to the Issuers or another Restricted Subsidiary; |
| | (2) | to acquire all or substantially all of the assets of, or any Capital Stock of, another Permitted Business, if, after giving effect to any such acquisition of Capital Stock, the Permitted Business is or becomes a Restricted Subsidiary of the Company; |
| | (3) | to make a capital expenditure; or |
| | (4) | to acquire Additional Assets, |
provided that the requirements of clauses (2) through (4) above shall be extended by an additional 180 days if an agreement (including a lease, whether a capital lease or an operating lease) committing to make the acquisitions or expenditures referred to therein is entered into by the Company or its Restricted Subsidiary within 365 days after the receipt of such Net Proceeds and such Net Proceeds are applied in accordance with such agreement.
Pending the final application of any Net Proceeds, the Company may temporarily reduce revolving credit borrowings or otherwise invest the Net Proceeds in any manner that is not prohibited by the indenture.
Any Net Proceeds from Asset Sales that are not applied or invested as provided in the third paragraph of this covenant will constitute “Excess Proceeds.” When the aggregate amount of Excess Proceeds exceeds $25.0 million, within ten business days thereof, the Company will make an Asset Sale Offer to all holders of notes and if the Company elects (or is required by the terms of such other pari passu Indebtedness), all holders of other Indebtedness that is pari passu with the notes (an “Asset Sale Offer”) to purchase the maximum aggregate principal amount of notes and such pari passu Indebtedness, in denominations of $2,000 initial principal amount and multiples of $1,000 thereafter, that may be purchased out of the Excess Proceeds at an offer price in cash in an amount equal to 100% of the principal amount thereof, or, in the case of Pari Passu Indebtedness represented by securities sold at a discount, the amount of the accreted value thereof at such time, plus accrued and unpaid interest and Special Interest, if any, to the date fixed for the closing of such offer, in accordance with the procedures set forth in the indenture. In the event that the Company or a Restricted Subsidiary prepays any Pari Passu Indebtedness that is outstanding under a revolving credit or other committed loan facility pursuant to an Asset Sale Offer, the Company or such Restricted Subsidiary shall cause the related loan commitment to be reduced in an amount equal to the principal amount so prepaid. If any Excess Proceeds remain after consummation of an Asset Sale Offer, the Company may use those Excess Proceeds for any purpose not otherwise prohibited by the indenture. If the aggregate principal amount of notes and other pari passu Indebtedness tendered into such Asset Sale Offer exceeds the amount of Excess Proceeds, the trustee will select the notes and such other pari passu Indebtedness to be purchased on a pro rata basis. Upon completion of each Asset Sale Offer, the amount of Excess Proceeds will be reset at zero.
154
The Company will comply with the requirements of Rule 14e-1 under the Exchange Act and any other securities laws and regulations thereunder to the extent those laws and regulations are applicable in connection with each repurchase of notes pursuant to an Asset Sale Offer. To the extent that the provisions of any securities laws or regulations conflict with the Asset Sale provisions of the indenture, the Company will comply with the applicable securities laws and regulations and will not be deemed to have breached its obligations under the Asset Sale provisions of the indenture by virtue of such compliance.
The Credit Agreement limits, and future credit agreements or other agreements relating to Indebtedness to which the Issuers (or one of their affiliates) become a party may prohibit or limit, the Issuers from purchasing any notes pursuant to this Asset Sales covenant. In the event the Issuers are contractually prohibited from purchasing the notes, the Issuers could seek the consent of their lenders to the purchase of the notes or could attempt to refinance the borrowings that contain such prohibition. If the Issuers do not obtain such consent or repay such borrowings, they will remain contractually prohibited from purchasing the notes. In such case, the Issuers’ failure to purchase tendered notes would constitute a Default under the indenture.
Selection and Notice
If less than all of the notes are to be redeemed at any time, the trustee will select notes for redemption on a pro rata basis unless otherwise required by law or applicable stock exchange requirements.
No notes of $2,000 or less can be redeemed in part. Notices of redemption will be mailed by first class mail at least 30 but not more than 60 days before the redemption date to each holder of notes to be redeemed at its registered address, except that redemption notices may be mailed more than 60 days prior to a redemption date if the notice is issued in connection with a defeasance of the notes or a satisfaction and discharge of the indenture. Notices of redemption may not be conditional.
If any note is to be redeemed in part only, the notice of redemption that relates to that note will state the portion of the principal amount of that note that is to be redeemed. A new note in principal amount equal to the unredeemed portion of the original note will be issued in the name of the holder of notes upon cancellation of the original note. Notes called for redemption become due on the date fixed for redemption. On and after the redemption date, interest ceases to accrue on notes or portions of notes called for redemption.
Certain Covenants
Set forth below are summaries of certain covenants contained in the indenture and that will be operative after the date of the indenture.
At any time after the notes have received Investment Grade Ratings from both Rating Agencies (a “Covenant Termination Event”), upon notice by the Company to the trustee certifying that a Covenant Termination Event has occurred and that at the time of the giving of such notice no Default has occurred and is continuing under the indenture (a “Covenant Termination Event Notice”), the Issuers and the Restricted Subsidiaries will not thereafter be subject to the following provisions of the indenture:
| | (1) | “—Restricted Payments”; |
| | (2) | “—Incurrence of Indebtedness and Issuance of Disqualified Stock and Preferred Stock”; |
| | (3) | “—Dividend and Other Payment Restrictions Affecting Restricted Subsidiaries”; |
| | (4) | “Repurchase at the Option of Holders—Asset Sales”; |
| | (5) | clause (4) of the first paragraph of “Merger, Consolidation or Sale of Assets”; |
| | (6) | “—Transactions with Affiliates”; and |
155
| | (7) | any provision contained in “—Designation of Restricted and Unrestricted Subsidiaries”, requiring compliance with any test for the incurrence of Indebtedness. |
Upon the delivery of a Covenant Termination Event Notice, the Guarantees of the Guarantors will also be released.
Restricted Payments
The Company will not, and will not permit any of its Restricted Subsidiaries to, directly or indirectly:
| | (A) | declare or pay any dividend or make any other payment or distribution on account of the Company’s or any of its Restricted Subsidiaries’ Equity Interests (including, without limitation, any payment in connection with any merger or consolidation involving the Company or any of its Restricted Subsidiaries) or to the direct or indirect holders of the Company’s or any of its Restricted Subsidiaries’ Equity Interests in their capacity as such (other than dividends or distributions payable in Equity Interests (other than Disqualified Stock) of the Company);provided that the repurchase, redemption or other acquisition or retirement for value of any Equity Interests of a Restricted Subsidiary of the Company shall not constitute a Restricted Payment; |
| | (B) | purchase, redeem or otherwise acquire or retire for value (including, without limitation, in connection with any merger or consolidation involving the Company) any Equity Interests of the Company or any direct or indirect parent of the Company; |
| | (C) | make any payment on or with respect to, or purchase, redeem, defease or otherwise acquire or retire for value any Subordinated Indebtedness of the Company or any Guarantor (excluding any intercompany Indebtedness between or among the Company and any of its Restricted Subsidiaries), except (i) a payment of interest or principal at the Stated Maturity thereof or (ii) the purchase, repurchase or other acquisition of any such Subordinated Indebtedness purchased in anticipation of satisfying a sinking fund obligation, principal installment or payment at final maturity, in each case within one year of the date of acquisition; or |
| | (D) | make any Restricted Investment; |
(all such payments and other actions set forth in these clauses (A) through (D) above being collectively referred to as “Restricted Payments”), unless, at the time of and after giving effect to such Restricted Payment:
| | (1) | no Default or Event of Default has occurred and is continuing or would occur as a consequence of such Restricted Payment; |
| | (2) | the Company would, at the time of such Restricted Payment and after giving pro forma effect thereto as if such Restricted Payment had been made at the beginning of the applicable four-quarter period, have been permitted to incur at least $1.00 of additional Indebtedness pursuant to the Fixed Charge Coverage Ratio test set forth in the first paragraph of the covenant described below under the caption “—Incurrence of Indebtedness and Issuance of Disqualified Stock and Preferred Stock”; and |
| | (3) | such Restricted Payment, together with the aggregate amount of all other Restricted Payments made by the Company and its Restricted Subsidiaries since the date of the indenture (excluding Restricted Payments permitted by clauses (2), (3), (4), (5), (6), (7), (8), (9), (10), (12), (13), (14), (15), (16) and (17) of the next succeeding paragraph), is less than the sum, without duplication, of: |
| | (a) | 50% of the Consolidated Net Income of the Company for the period (taken as one accounting period) from April 1, 2011 to the end of the Company’s most recently ended fiscal quarter for which internal financial statements are available at the time of such Restricted Payment (or, if such Consolidated Net Income for such period is a deficit, less 100% of such deficit);plus |
156
| | (b) | 100% of the aggregate Qualified Proceeds received by the Company since the date of the indenture as a contribution to its common equity capital or from the issue or sale of Equity Interests of the Company (other than Disqualified Stock, Excluded Contributions and the net proceeds from a sale of Designated Preferred Stock) or from the issue or sale of convertible or exchangeable Disqualified Stock or convertible or exchangeable debt securities of the Company that have been converted into or exchanged for such Equity Interests (other than Equity Interests (or Disqualified Stock or debt securities) sold to a Subsidiary of the Company);plus |
| | (c) | to the extent not already included in Consolidated Net Income, 100% of the aggregate Qualified Proceeds from (A) the sale or other disposition (other than to the Company or a Restricted Subsidiary) of any Restricted Investment that was made after the date of the indenture and (B) repurchases, redemptions and repayments of such Restricted Investments and the receipt of any dividends or distributions from such Restricted Investments;plus |
| | (d) | to the extent that any Unrestricted Subsidiary of the Company designated as such after the date of the indenture is redesignated as a Restricted Subsidiary after the date of the indenture, the Fair Market Value of the Company’s Investment in such Subsidiary as of the date of such redesignation;plus |
| | (e) | in the event the Company and/or any Restricted Subsidiary of the Company makes any Investment in a Person that, as a result of or in connection with such Investment, becomes a Restricted Subsidiary of the Company, an amount equal to the existing Investment of the Company and/or any of its Restricted Subsidiaries in such Person that was previously treated as a Restricted Payment. |
The sum of all amounts under clauses (a) through (e) above are hereinafter referred to as the “Cumulative Buildup Basket.” Upon consummation of a Specified Change of Control transaction pursuant to which a Restricted Payment is made pursuant to clause (19) of the immediately succeeding paragraph, the Cumulative Buildup Basket, if positive immediately prior to such Specified Change of Control transaction, shall be reset to zero. In the event of a Specified Change of Control Parent Assumption, the Cumulative Buildup Basket shall be calculated on a consolidated basis as to the Specified Change of Control Parent and its Restricted Subsidiaries; provided, however that the Cumulative Buildup Basket shall not give effect to any amounts attributable to the Specified Change of Control Parent and its subsidiaries (other than the Company and its Restricted Subsidiaries) prior to the date of such Specified Change of Control transaction.
The preceding provisions will not prohibit:
| | (1) | the payment of any dividend or other distribution or the consummation of any irrevocable redemption within 60 days after the date of declaration of the dividend or giving of the redemption notice, as the case may be, if at the date of declaration or notice, the dividend or redemption payment would have complied with the provisions of the indenture; |
| | (2) | the making of any Restricted Payment in exchange for, or out of the net cash proceeds of the substantially concurrent sale (other than to a Restricted Subsidiary of the Company) of, Equity Interests of the Company (other than Disqualified Stock) or from the substantially concurrent contribution of common equity capital to the Company; provided that the amount of any such net cash proceeds that are utilized for any such Restricted Payment will be excluded from clause (3)(b) of the preceding paragraph; |
157
| | (3) | the repurchase, redemption, defeasance or other acquisition or retirement for value of Subordinated Indebtedness of the Company or any Guarantor with the net cash proceeds from a substantially concurrent incurrence of Permitted Refinancing Indebtedness; |
| | (4) | the declaration and payment of regularly scheduled or accrued dividends to holders of any class or series of Disqualified Stock of the Company or any Restricted Subsidiary of the Company issued on or after the date of the indenture in accordance with the provisions of the covenant described below under the caption “—Incurrence of Indebtedness and Issuance of Disqualified Stock and Preferred Stock”; |
| | (5) | the repurchase, redemption or other acquisition or retirement for value of Disqualified Stock of the Company or any Restricted Subsidiary of the Company made by exchange for, or out of the proceeds of the substantially concurrent sale of Replacement Preferred Stock that is permitted to be incurred pursuant to the covenant described below under “—Incurrence of Indebtedness and Issuance of Disqualified Stock and Preferred Stock”; |
| | (6) | the payment of any dividend or other distributions to holders of any class or series of Designated Preferred Stock (other than Disqualified Stock) issued by the Company after the date of the indenture; |
| | (7) | the payment of any dividend (or any similar distribution) by a Restricted Subsidiary of the Company to the holders of its Equity Interests on a pro rata basis; |
| | (8) | the repurchase, redemption or other acquisition or retirement for value of any Equity Interests of the Company or any Restricted Subsidiary of the Company held by any current or former officer, director, employee or consultant of the Company or any of its Restricted Subsidiaries, and any dividend payment or other distribution by the Company or a Restricted Subsidiary to a direct or indirect parent holding company of the Company utilized for the repurchase, redemption or other acquisition or retirement for value of any Equity Interests of such direct or indirect parent holding company held by any current or former officer, director, employee or consultant of the Company or any of its Restricted Subsidiaries, in each case, pursuant to any equity subscription agreement, stock option agreement, shareholders’ agreement or similar agreement or benefit plan of any kind; provided that the aggregate price paid for all such repurchased, redeemed, acquired or retired Equity Interests may not exceed $15.0 million in any fiscal year (it being understood, however, that unused amounts permitted to be paid pursuant to this proviso are available to be carried over to subsequent fiscal years); provided further that such amount in any fiscal year may be increased by an amount not to exceed: |
| | (a) | the cash proceeds from the sale of Equity Interests of the Company and, to the extent contributed to the Company as common equity capital, Equity Interests of the Company’s direct or indirect parent entities, in each case to members of management, directors or consultants of the Company, any of its Subsidiaries or any of its direct or indirect parent entities that occurs after the date of the indenture, to the extent the cash proceeds from the sale of such Equity Interests have not otherwise been applied to the payment of Restricted Payments by virtue of clause (3)(b) of the preceding paragraph, and excluding Excluded Contributions;plus |
| | (b) | the cash proceeds of key man life insurance policies received by the Company and its Restricted Subsidiaries after the date of the indenture;less |
| | (c) | the amount of any Restricted Payments previously made pursuant to clauses (a) and (b) of this clause (8); |
and provided further that cancellation of Indebtedness owing to the Company from members of management, directors or consultants of the Company or any of its Restricted Subsidiaries, or any direct or indirect parent holding company of the Company, in connection
158
with a repurchase of Equity Interests of the Company or any direct or indirect parent holding company of the Company will not be deemed to constitute a Restricted Payment for purposes of this covenant or any other provision of the indenture;
| | (9) | the repurchase of Equity Interests deemed to occur upon the exercise of options, rights or warrants to the extent such Equity Interests represent a portion of the exercise price of those options, rights or warrants; |
| | (10) | the repurchase, redemption, defeasance or other acquisition or retirement for value of Subordinated Indebtedness of the Company or any Guarantor with any Excess Proceeds that remain after consummation of an Asset Sale Offer; |
| | (11) | so long as no Default has occurred and is continuing or would be caused thereby, after the occurrence of a Change of Control and within 60 days after the completion of the offer to repurchase the notes pursuant to the covenant described above under “—Repurchase at the Option of Holders—Change of Control” (including the purchase of the notes tendered), any purchase or redemption of Subordinated Indebtedness required pursuant to the terms thereof as a result of such Change of Control at a purchase or redemption price not to exceed 101% of the outstanding principal amount thereof, plus any accrued and unpaid interest; provided, however, the Company would be able to incur at least $1.00 of additional Indebtedness pursuant to the Fixed Charge Coverage Ratio test set forth in the first paragraph of the covenant described below under the Caption “—Incurrence of Indebtedness and Issuance of Disqualified Stock and Preferred Stock” below after giving pro forma effect to such Restricted Payment; |
| | (12) | cash payments in lieu of fractional shares issuable as dividends on preferred stock or upon the conversion of any convertible debt securities of the Company or any of its Restricted Subsidiaries; |
| | (13) | Permitted Payments to Parent; |
| | (14) | so long as no default has occurred and is continuing or would be caused thereby, the payment: |
| | (a) | by the Company or any Restricted Subsidiary to any direct or indirect parent of the Company, which payment is used by the Person receiving such payment, following the first initial public offering of common Equity Interests by such Person, to pay dividends of up to 6% per annum of the net proceeds received by such Person in such public offering that are contributed to the Company as common equity capital; or |
| | (b) | by the Company, following the first initial public offering of common Equity Interests by the Company, to pay dividends of up to 6% per annum of the net proceeds received by the Company in such public offering; (excluding, in the case of both clause (a) and clause (b), public offerings of common Equity Interests registered on Form S-8 and any other public sale to the extent the proceeds thereof are Excluded Contributions); |
| | (15) | Investments that are made with Excluded Contributions; |
| | (16) | distributions or payments of Receivables Fees; |
| | (17) | all payments made or to be made in connection with the application of the proceeds of this offering and the related Transactions as described under the caption “Certain Relationships and Related Party Transactions” in this prospectus, including all payments contemplated by the definition of Transactions; |
| | (18) | so long as no Default has occurred and is continuing or would be caused thereby, other Restricted Payments in an aggregate amount not to exceed $100.0 million since the date of the indenture; and |
159
| | (19) | dividends or other payments or distributions on account of Equity Interests of the Company or any of its Restricted Subsidiaries or of any counterparty to a Specified Change of Control transaction, or the purchase, redemption or other acquisition or retirement for value of any Equity Interests of the Company or any of its Restricted Subsidiaries or of any counterparty to a Specified Change of Control transaction, in each case, made as part of a Specified Change of Control transaction. |
The amount of all Restricted Payments (other than cash) will be the Fair Market Value on the date of the Restricted Payment of the asset(s) or securities proposed to be transferred or issued by the Company or such Restricted Subsidiary, as the case may be, pursuant to the Restricted Payment. The Fair Market Value of any assets or securities that are required to be valued by this covenant will be determined by the Board of Directors of the Company whose resolution with respect thereto will be delivered to the trustee.
For purposes of determining compliance with the provisions set forth above, in the event that a Restricted Payment meets the criteria of more than one of the types of Restricted Payments described in the above clauses, the Company, in its sole discretion, may order and classify, and from time to time may reorder and reclassify, such Restricted Payment if it would have been permitted at the time such Restricted Payment was made and at the time of any such reclassification.
Incurrence of Indebtedness and Issuance of Disqualified Stock and Preferred Stock
The Company will not, and will not permit any of its Restricted Subsidiaries to, directly or indirectly, create, incur, issue, assume, guarantee or otherwise become directly or indirectly liable, contingently or otherwise, with respect to (collectively, “incur”) any Indebtedness (including Acquired Debt), and the Company will not issue any Disqualified Stock and will not permit any of its Restricted Subsidiaries to issue any shares of preferred stock; provided, however, that the Issuers and the Guarantors may incur Indebtedness (including Acquired Debt) or issue Disqualified Stock or preferred stock, if the Fixed Charge Coverage Ratio for the Company’s most recently ended four full fiscal quarters for which internal financial statements are available immediately preceding the date on which such additional Indebtedness is incurred or such Disqualified Stock or such preferred stock is issued, as the case may be, would have been at least 2.0 to 1, determined on a pro forma basis (including a pro forma application of the net proceeds therefrom), as if the additional Indebtedness had been incurred or the Disqualified Stock or the preferred stock had been issued, as the case may be, at the beginning of such four-quarter period.
The first paragraph of this covenant will not prohibit the incurrence of any of the following items of Indebtedness or the issuance of any of the following items of Disqualified Stock or preferred stock (collectively, “Permitted Debt”):
| | (1) | the incurrence by the Company, IASIS Capital and/or any Restricted Subsidiary (and the Guarantee thereof by the Guarantors, IASIS Capital and the Non-Guarantor Subsidiaries) of Indebtedness under the Credit Agreement and other Credit Facilities entered into after the date of the Credit Agreement in an aggregate principal amount at any one time outstanding under this clause (1) (with letters of credit being deemed to have a principal amount equal to the maximum potential liability of the Company and its Restricted Subsidiaries thereunder) not to exceed the greater of (x) $1,325 million and (y) the aggregate principal amount of Indebtedness that may be incurred such that (i) the Consolidated Secured Debt Ratio (at the time of incurrence and after giving pro forma effect thereto with such pro forma adjustments to Consolidated Total Indebtedness and Consolidated Adjusted EBITDA as are appropriate and consistent with the pro forma adjustment provisions set forth in the definition of “Fixed Charge Coverage Ratio”) would not exceed 3.75 to 1.00 and (ii) the Fixed Charge Coverage Ratio for the Company’s most recently ended four full fiscal quarters for which internal financial statements are available immediately preceding the date on which such additional Indebtedness is incurred would have been at least 2.0 to 1, determined on a pro forma basis (including a pro forma application of the net proceeds therefrom), as if the additional Indebtedness had been incurred at the beginning of such four-quarter period, less the aggregate amount of all Net Proceeds of Asset Sales applied by the Company or any of its Restricted Subsidiaries since the date of the indenture to repay any term Indebtedness under a Credit Facility or to repay any revolving credit Indebtedness under a Credit Facility and effect a corresponding commitment reduction thereunder pursuant to the covenant described above under the |
160
| | caption “—Repurchase at the Option of Holders—Asset Sales”; provided that any amount of Indebtedness incurred pursuant to this clause (1) in excess of $1,325 million may be incurred only under the Credit Agreement; |
| | (2) | the incurrence by the Company and its Restricted Subsidiaries of the Existing Indebtedness (other than Indebtedness described in clauses (1) and (3)); |
| | (3) | the incurrence by the Issuers and the Guarantors of Indebtedness represented by the notes to be issued on the date of the indenture, replacement notes in respect thereof, if any, and the related Subsidiary Guarantees and the Exchange Notes and related Subsidiary Guarantees to be issued pursuant to the registration rights agreement; |
| | (4) | the incurrence or issuance by the Company or any of its Restricted Subsidiaries of Indebtedness (including Capital Lease Obligations), Disqualified Stock or preferred stock, in each case, incurred or issued for the purpose of financing all or any part of the purchase price or cost of design, construction, lease, installation or improvement of property, plant or equipment used or useful in a Permitted Business, in an aggregate principal amount, including all Permitted Refinancing Indebtedness and Replacement Preferred Stock incurred to renew, refund, refinance, replace, defease or discharge any Indebtedness incurred pursuant to this clause (4), not to exceed the greater of $75.0 million and 3% of Total Assets at any time outstanding; |
| | (5) | the incurrence by the Company or any of its Restricted Subsidiaries of Permitted Refinancing Indebtedness or Replacement Preferred Stock in exchange for, or the net proceeds of which are used to renew, refund, refinance, replace, defease or discharge any Indebtedness (other than intercompany Indebtedness) or any Disqualified Stock or preferred stock that was permitted by the indenture to be incurred under the first paragraph of this covenant or clauses (2), (3), (4), (5), (13), (15), (18), (19) or (21) of this paragraph; |
| | (6) | the incurrence by the Company or any of its Restricted Subsidiaries of intercompany Indebtedness between or among the Company and any of its Restricted Subsidiaries; provided,however, that: |
| | (a) | if the Company or any Guarantor is the obligor on such Indebtedness and the payee is not the Company or a Guarantor, such Indebtedness must be unsecured and expressly subordinated to the prior payment in full in cash of all Obligations then due with respect to the notes, in the case of the Company or the Subsidiary Guarantee, in the case of a Guarantor, except to the extent such subordination would violate a material contract as in effect on the date of the indenture or is not permitted pursuant to applicable laws, rules or regulations; and |
| | (b) | (i) any subsequent issuance or transfer of Equity Interests that results in any such Indebtedness being held by a Person other than the Company or a Restricted Subsidiary of the Company and (ii) any sale or other transfer of any such Indebtedness to a Person that is not either the Company or a Restricted Subsidiary of the Company, will be deemed, in each case, to constitute a new incurrence of such Indebtedness by the Company or such Restricted Subsidiary, as the case may be, which new incurrence is not permitted by this clause (6); |
| | (7) | the issuance by any of the Company’s Restricted Subsidiaries to the Company or to any of its Restricted Subsidiaries of shares of preferred stock; provided, however, that: |
| | (a) | any subsequent issuance or transfer of Equity Interests that results in any such preferred stock being held by a Person other than the Company or a Restricted Subsidiary of the Company; and |
161
| | (b) | any sale or other transfer of any such preferred stock to a Person that is not either the Company or a Restricted Subsidiary of the Company will be deemed, in each case, to constitute a new issuance of such preferred stock by such Restricted Subsidiary which new issuance is not permitted by this clause (7); |
| | (8) | the incurrence by the Company or any of its Restricted Subsidiaries of Hedging Obligations in the ordinary course of business; |
| | (a) | by the Issuers or any of the Guarantors of Indebtedness of the Company or a Restricted Subsidiary of the Company that was permitted to be incurred by another provision of this covenant; |
provided that if the Indebtedness being guaranteed is subordinated to or pari passu with the notes, then the guarantee shall be subordinated or pari passu, as applicable, to the same extent as the Indebtedness guaranteed;
| | (b) | by any Restricted Subsidiary that is not a Guarantor of Indebtedness of a Restricted Subsidiary that is not a Guarantor; and |
| | (c) | by the Issuers or any Restricted Subsidiary of Indebtedness of the Specified Change of Control Parent or its Subsidiaries (other than debt securities issued in a capital markets transaction); provided that the Fixed Charge Coverage Ratio for the Company’s most recently ended four full fiscal quarters for which internal financial statements are available immediately preceding the date on which such guarantee is incurred would have been at least 2.0 to 1, determined on a pro forma basis (including a pro forma application of the net proceeds therefrom), as if such guarantee had been incurred at the beginning of such four-quarter period; |
| | (10) | the incurrence by the Company or any of its Restricted Subsidiaries of Indebtedness in respect of workers’ compensation claims, self-insurance obligations, bankers’ acceptances, letters of credit, performance bonds, surety bonds, appeal bonds or other similar bonds in the ordinary course of business; provided, however, that upon the drawing of letters of credit for reimbursement obligations, including with respect to workers’ compensation claims, or the incurrence of other Indebtedness with respect to reimbursement type obligations regarding workers’ compensation claims, such obligations are reimbursed within 30 days following such drawing or incurrence; |
| | (11) | the incurrence by the Company or any of its Restricted Subsidiaries of Indebtedness arising from the honoring by a bank or other financial institution of a check, draft or similar instrument inadvertently (except in the case of daylight overdrafts) drawn against insufficient funds in the ordinary course of business, so long as such Indebtedness is extinguished within five business days; |
| | (12) | the incurrence of Indebtedness arising from agreements of the Company or a Restricted Subsidiary providing for indemnification, adjustment of purchase price, holdback, contingency payment obligations or similar obligations, in each case, incurred or assumed in connection with the disposition or acquisition of any business, assets or Capital Stock of the Company or any Restricted Subsidiary; |
| | (13) | the incurrence of Indebtedness or the issuance of any Disqualified Stock or preferred stock by any Non-Guarantor Subsidiary of the Company, in an amount not to exceed $30.0 million at any time outstanding; provided that after giving effect to such incurrence or issuance, the Company would be permitted to incur at least $1.00 of additional Indebtedness pursuant to the Fixed Charge Coverage Ratio test set forth in the first paragraph of this covenant; |
162
| | (14) | the incurrence of Indebtedness resulting from endorsements of negotiable instruments for collection in the ordinary course of business; |
| | (15) | Indebtedness, Disqualified Stock or preferred stock of Persons that are acquired by the Company or any Restricted Subsidiary (including by way of merger or consolidation) in accordance with the terms of the indenture; provided that such Indebtedness, Disqualified Stock or preferred stock is not incurred in contemplation of such acquisition or merger; and provided further that after giving effect to such acquisition or merger, either |
| | (a) | the Company would be permitted to incur at least $1.00 of additional Indebtedness pursuant to the Fixed Charge Coverage Ratio; or |
| | (b) | the Company’s Fixed Charge Coverage Ratio after giving pro forma effect to such acquisition or merger would be greater than the Company’s actual Fixed Charge Coverage Ratio immediately prior to such acquisition or merger; |
| | (16) | Indebtedness of the Company or a Restricted Subsidiary in respect of netting services, overdraft protection and otherwise in connection with deposit accounts; provided that such Indebtedness remains outstanding for ten business days or less; |
| | (17) | Physician Support Obligations incurred by the Company or any of its Restricted Subsidiaries; |
| | (18) | the incurrence by a Receivables Subsidiary of Indebtedness in a Qualified Receivables Transaction; |
| | (19) | the incurrence or issuance by the Company or any of its Restricted Subsidiaries of additional Indebtedness, Disqualified Stock or preferred stock in an aggregate principal amount (or accreted value or liquidation preference, as applicable) at any time outstanding, including all Permitted Refinancing Indebtedness and all Replacement Preferred Stock incurred to renew, refund, refinance, replace, defease or discharge any Indebtedness, Disqualified Stock and preferred stock incurred or issued pursuant to this clause (19), not to exceed the greater of $125.0 million and 5% of Total Assets; |
| | (20) | Indebtedness incurred on behalf of or representing Guarantees of Indebtedness of joint ventures of the Company or any Restricted Subsidiaries not in excess of $50.0 million at any time outstanding; and |
| | (21) | in the event of a Specified Change of Control Parent Assumption, Indebtedness, Disqualified Stock or preferred stock of the Specified Change of Control Parent or any of its Restricted Subsidiaries (except to the extent incurred in connection with such Specified Change of Control Transaction); provided that the Specified Change of Control Parent would, on the date of such transaction after giving pro forma effect thereto and any related financing, be permitted to incur at least $1.00 of additional Indebtedness pursuant to the Fixed Charge Coverage Ratio test set forth in the first paragraph of the covenant described above under the caption “—Incurrence of Indebtedness and Issuance of Disqualified Stock and Preferred Stock” or have a Fixed Charge Coverage Ratio that is greater than the actual Fixed Charge Coverage Ratio of the Company immediately prior to such transaction. |
For purposes of determining compliance with this “Incurrence of Indebtedness and Issuance of Disqualified Stock and Preferred Stock” covenant, in the event that an item of proposed Indebtedness meets the criteria of more than one of the categories of Permitted Debt described in clauses (1) through (21) above, or is entitled to be incurred pursuant to the first paragraph of this covenant, the Company will be permitted to classify such item of Indebtedness on the date of its incurrence, or later reclassify all or a portion of such item of Indebtedness, in any manner that complies with this covenant. Indebtedness under the Credit Agreement outstanding on the date on which notes are first issued and authenticated under the indenture will be deemed to have been incurred on such date in reliance on the exception provided by clause (1) of the definition of Permitted Debt above. The accrual of interest, the
163
accretion or amortization of original issue discount, the payment of interest on any Indebtedness in the form of additional Indebtedness with the same terms, the reclassification of preferred stock as Indebtedness due to a change in accounting principles, and the payment of dividends on Disqualified Stock or preferred stock in the form of additional shares of the same class of Disqualified Stock or preferred stock will not be deemed to be an incurrence of Indebtedness or an issuance of Disqualified Stock or preferred stock for purposes of this covenant; provided, in each such case, that the amount thereof is included in Fixed Charges of the Company as accrued (other than the reclassification of preferred stock as Indebtedness due to a change in accounting principles).
The amount of any Indebtedness outstanding as of any date will be:
| | (1) | the accreted value of the Indebtedness, in the case of any Indebtedness issued with original issue discount; |
| | (2) | the principal amount of the Indebtedness, in the case of any other Indebtedness; and |
| | (3) | in respect of Indebtedness of another Person secured by a Lien on the assets of the specified Person, the lesser of: |
| | (a) | the Fair Market Value of such assets at the date of determination; and |
| | (b) | the amount of the Indebtedness of the other Person. |
Liens
The Company will not, and will not permit any of its Restricted Subsidiaries to create, incur, assume or otherwise cause or suffer to exist or become effective any Lien of any kind (other than Permitted Liens) securing Indebtedness upon any of their property or assets, now owned or hereafter acquired, or any income or profits therefrom unless all payments due under the indenture and the notes (or a Guarantee in the case of Liens of a Guarantor) are secured on an equal and ratable basis with the obligations so secured until such time as such obligations are no longer secured by a Lien.
Dividend and Other Payment Restrictions Affecting Restricted Subsidiaries
The Company will not, and will not permit any of its Restricted Subsidiaries to, directly or indirectly, create or permit to exist or become effective any consensual encumbrance or restriction on the ability of any Restricted Subsidiary to:
| | (1) | pay dividends or make any other distributions on its Capital Stock to the Company or any of its Restricted Subsidiaries, or with respect to any other interest or participation in, or measured by, its profits, or pay any indebtedness owed to the Company or any of its Restricted Subsidiaries; |
| | (2) | make loans or advances to the Company or any of its Restricted Subsidiaries; or |
| | (3) | sell, lease or transfer any of its properties or assets to the Company or any of its Restricted Subsidiaries. |
However, the preceding restrictions will not apply to encumbrances or restrictions existing under or by reason of:
| | (1) | agreements governing Existing Indebtedness and Credit Facilities as in effect on the date of the indenture and any amendments, restatements, modifications, renewals, increases, supplements, refundings, replacements or refinancings of those agreements; provided that the amendments, restatements, modifications, renewals, increases, supplements, refundings, replacements or refinancings are not materially more restrictive, taken as a whole, with respect to such dividend and other payment restrictions than those contained in those agreements on the date of the indenture; |
164
| | (2) | the indenture, the notes and the Subsidiary Guarantees; |
| | (3) | applicable law, rule, regulation or order; |
| | (4) | any instrument governing Indebtedness or Capital Stock of a Restricted Subsidiary acquired by the Company or any of its Restricted Subsidiaries as in effect at the time of such acquisition (except to the extent such Indebtedness or Capital Stock was incurred in connection with or in contemplation of such acquisition), which encumbrance or restriction is not applicable to any Person, or the properties or assets of any Person, other than the Person or any of its Subsidiaries, or the property or assets of the Person or any of its Subsidiaries, so acquired;provided that, in the case of Indebtedness, such Indebtedness was permitted by the terms of the indenture to be incurred; |
| | (5) | customary non-assignment provisions in contracts and licenses entered into in the ordinary course of business; |
| | (6) | customary restrictions in leases (including capital leases), security agreements or mortgages or other purchase money obligations for property acquired in the ordinary course of business that impose restrictions on the property purchased or leased of the nature described in clause (3) of the preceding paragraph; |
| | (7) | any agreement for the sale or other disposition of all or substantially all the Capital Stock or the assets of a Restricted Subsidiary that restricts distributions by that Restricted Subsidiary pending the sale or other disposition; |
| | (8) | Permitted Refinancing Indebtedness; provided that the restrictions contained in the agreements governing such Permitted Refinancing Indebtedness are not materially more restrictive, taken as a whole, than those contained in the agreements governing the Indebtedness being refinanced; |
| | (9) | Liens permitted to be incurred under the provisions of the covenant described above under the caption “—Liens” that limit the right of the debtor to dispose of the assets subject to such Liens; |
| | (10) | provisions limiting the disposition or distribution of assets or property in joint venture agreements, asset sale agreements, sale-leaseback agreements, stock sale agreements and other similar agreements, which limitation is applicable only to the assets that are the subject of such agreements; |
| | (11) | restrictions on cash or other deposits or net worth imposed by customers under contracts entered into in the ordinary course of business; |
| | (12) | customary provisions imposed on the transfer of copyrighted or patented materials; |
| | (13) | customary provisions restricting dispositions of real property interests set forth in any reciprocal easement agreements of the Company or any Restricted Subsidiary; |
| | (14) | Indebtedness or other contractual requirements of a Receivables Subsidiary in connection with a Qualified Receivables Transaction; provided that such restrictions apply only to such Receivables Subsidiary; |
| | (15) | contracts entered into in the ordinary course of business, not relating to any Indebtedness, and that do not, individually or in the aggregate, detract from the value of property or assets of the Company or any Restricted Subsidiary of the Company in any manner material to the Company or any Restricted Subsidiary of the Company; |
165
| | (16) | restrictions on the transfer of property or assets required by any regulatory authority having jurisdiction over the Company or any Restricted Subsidiary of the Company or any of their businesses; |
| | (17) | restrictions arising in connection with Indebtedness permitted under the indenture of a Restricted Subsidiary that is not a Guarantor; |
| | (18) | restrictions arising in connection with Permitted Liens; and |
| | (19) | in the event of a Specified Change of Control Parent Assumption, any instrument governing Indebtedness or Capital Stock of the Specified Change of Control Parent or any of its Restricted Subsidiaries (as in effect at the time of such Specified Change of Control transaction) except to the extent such Indebtedness or Capital Stock was incurred in connection with or in contemplation of such Specified Change of Control transaction. |
Merger, Consolidation or Sale of Assets
The Company will not, directly or indirectly: (1) consolidate or merge with or into another Person (whether or not the Company is the surviving corporation); or (2) sell, assign, transfer, convey or otherwise dispose of all or substantially all of the properties or assets of the Company and its Restricted Subsidiaries taken as a whole, in one or more related transactions, to another Person, unless:
| | (1) | either: (a) the Company is the surviving entity; or (b) the Person formed by or surviving any such consolidation or merger (if other than the Company) or to which such sale, assignment, transfer, conveyance or other disposition has been made is an entity organized or existing under the laws of the United States, any state of the United States or the District of Columbia; |
| | (2) | the Person formed by or surviving any such consolidation or merger (if other than the Company) or the Person to which such sale, assignment, transfer, conveyance or other disposition has been made assumes all the obligations of the Company under the notes, the indenture and the registration rights agreement pursuant to agreements reasonably satisfactory to the trustee;provided, however, that at all times, a corporation organized and existing under the laws of the United States of America, any State thereof or the District of Columbia must be a co-issuer or the issuer of the notes; |
| | (3) | immediately after such transaction, no Default or Event of Default exists; and |
| | (4) | the Company or the Person formed by or surviving any such consolidation or merger (if other than the Company), or to which such sale, assignment, transfer, conveyance or other disposition has been made would, on the date of such transaction after giving pro forma effect thereto and any related financing transactions as if the same had occurred at the beginning of the applicable four-quarter period: |
| | (a) | be permitted to incur at least $1.00 of additional Indebtedness pursuant to the Fixed Charge Coverage Ratio test set forth in the first paragraph of the covenant described above under the caption “—Incurrence of Indebtedness and Issuance of Disqualified Stock and Preferred Stock” or |
| | (b) | have a Fixed Charge Coverage Ratio that is greater than the actual Fixed Charge Coverage Ratio of the Company immediately prior to such transaction. |
In addition, the Company will not, directly or indirectly, lease all or substantially all of the properties and assets of it and its Restricted Subsidiaries taken as a whole, in one or more related transactions, to any other Person.
This “Merger, Consolidation or Sale of Assets” covenant will not apply to:
| | (1) | a merger of the Company with an Affiliate solely for the purpose of reincorporating the Company in another jurisdiction or any other transaction the sole purpose of which is to reorganize the Company as a corporation; |
166
| | (2) | any consolidation or merger, or any sale, assignment, transfer, conveyance, lease or other disposition of assets between or among the Company and its Restricted Subsidiaries; and |
| | (3) | transfers of accounts receivable and related assets of the type specified in the definition of Qualified Receivables Transaction (or a fractional undivided interest therein) by a Receivables Subsidiary in a Qualified Receivables Transaction. |
Transactions with Affiliates
The Company will not, and will not permit any of its Restricted Subsidiaries to, make any payment to, or sell, lease, transfer or otherwise dispose of any of its properties or assets to, or purchase any property or assets from, or enter into or make or amend any transaction, contract, agreement, understanding, loan, advance or guarantee with, or for the benefit of, any Affiliate of the Company involving aggregate consideration in excess of $10.0 million (each, an “Affiliate Transaction”), unless:
| | (1) | the Affiliate Transaction is on terms that, taken as a whole, are not materially less favorable to the Company or the relevant Restricted Subsidiary than those that would have been obtained in a comparable transaction by the Company or such Restricted Subsidiary with an unrelated Person; and |
| | (2) | the Company delivers to the trustee, with respect to any Affiliate Transaction or series of related Affiliate Transactions involving aggregate consideration in excess of $20.0 million, a resolution of the Board of Directors of the Company set forth in an officers’ certificate certifying that such Affiliate Transaction complies with this covenant and that such Affiliate Transaction has been approved by a majority of the members of the Board of Directors of the Company. |
The following items will not be deemed to be Affiliate Transactions and, therefore, will not be subject to the provisions of the prior paragraph:
| | (1) | any employment agreement, employee benefit plan, officer or director indemnification agreement or any similar arrangement entered into by the Company or any of its Restricted Subsidiaries in the ordinary course of business and payments pursuant thereto; |
| | (2) | transactions between or among the Company and/or its Restricted Subsidiaries or any entity that becomes a Restricted Subsidiary as a result of such transaction; |
| | (3) | transactions with a Person (other than an Unrestricted Subsidiary of the Company) that is an Affiliate of the Company solely because the Company owns, directly or through a Restricted Subsidiary, an Equity Interest in, or controls, such Person; |
| | (4) | payment of reasonable directors’ fees; |
| | (5) | any issuance of Equity Interests (other than Disqualified Stock) of the Company to Affiliates of the Company; |
| | (6) | Permitted Investments or Restricted Payments that do not violate the provisions of the indenture described above under the caption “—Restricted Payments”; |
| | (7) | payment of fees and the reimbursement of other expenses to the Permitted Holders in connection with the Transactions on the terms as described above under the caption “Certain Relationships and Related Party Transactions”; |
167
| | (8) | payment of Subordinated Management Fees in each fiscal year not in excess of the lesser of (x) 0.25% of the Company’s net revenue as reflected on the budget prepared for such fiscal year by the management of the Company and approved by the Board of Directors of the Company and (y) $5.0 million, pursuant to the Management Services Agreement as in effect on the date of the indenture and as described above under the caption “Certain Relationships and Related Party Transactions” in this prospectus and the reimbursement of all other expenses; |
| | (9) | loans (or cancellation of loans) or advances to employees in the ordinary course of business; |
| | (10) | transactions with customers, suppliers, contractors, joint venture partners or purchasers or sellers of goods or services, in each case which are in the ordinary course of business (including, without limitation, pursuant to joint venture agreements) and otherwise in compliance with the terms of the indenture, and which are fair to the Company or its Restricted Subsidiaries, as applicable, in the reasonable determination of the Board of Directors, chief executive officer or chief financial officer of the Company or its Restricted Subsidiaries, as applicable, or are on terms at least as favorable as might reasonably have been obtained at such time from an unaffiliated party; |
| | (11) | the existence of, or the performance by the Company or any Restricted Subsidiary of their obligations under the terms of, any stockholders agreement, partnership agreement or limited liability company agreement (including any registration rights agreement or purchase agreement related thereto) to which it is a party as of the date of the indenture as described above under the caption “Certain Relationships and Related Party Transactions” and any similar agreements which it may enter into thereafter; provided, however, that the existence of, or the performance by the Company or any Restricted Subsidiary of obligations under any future amendment to any such existing agreement or under any similar agreement entered into after the date of the indenture will only be permitted by this clause to the extent that the terms of any such amendment or new agreement, taken as a whole, are not materially disadvantageous to the holders of the notes, as determined in good faith by the Board of Directors, chief executive officer or chief financial officer of the Company; |
| | (12) | the Transactions, including all payments made or to be made in connection with the Transactions as described under the caption “Certain Relationships and Related Party Transactions;” |
| | (13) | any Qualified Receivables Transaction; |
| | (14) | Permitted Payments to Parent; |
| | (15) | any management, financial advisory, financing, underwriting or placement services or any other investment banking, banking or similar services involving the Company and any of its Restricted Subsidiaries (including without limitation any payments in cash, Equity Interests or other consideration made by the Company or any of its Restricted Subsidiaries in connection therewith) on the one hand and the Permitted Holders on the other hand, which services (and payments and other transactions in connection therewith) are approved by a majority of the members of the Board of Directors of the Company in good faith; |
| | (16) | the issuance of Equity Interests (other than Disqualified Stock) in the Company or any Restricted Subsidiary for compensation purposes; |
| | (17) | intellectual property licenses in the ordinary course of business; |
| | (18) | Existing Indebtedness and any other obligations pursuant to an agreement existing on the date of the indenture, including any amendment thereto (so long as such amendment is not disadvantageous to the holders of the notes in any material respect); |
168
| | (19) | payments by the Company or any of its Restricted Subsidiaries of reasonable insurance premiums to, and any borrowings from, any Insurance Subsidiary, in each case on terms that are no less favorable to the Company or such Restricted Subsidiary than those that would have been obtained in a comparable arm’s-length transaction by the Company or such Restricted Subsidiary with a Person that is not an Affiliate of the Company; and |
| | (20) | (x) the guarantee by the Company or any of its Restricted Subsidiaries of the Indebtedness of any parent company of the Company that becomes the parent company of the Company in a Change of Control transaction consummated in accordance with the indenture, or of any Indebtedness of Subsidiaries of such parent company; provided that such guarantee was permitted by the terms of the indenture to be incurred and (y) the granting by the Company or any of its Restricted Subsidiaries of any Liens to secure such Indebtedness or such guarantee;provided that such Liens are permitted to be incurred under the indenture. |
Business Activities
The Company will not, and will not permit any of its Restricted Subsidiaries to, engage in any business other than Permitted Businesses, except to such extent as would not be material to the Company and its Restricted Subsidiaries taken as a whole.
Additional Subsidiary Guarantees
If the Company or any of its Restricted Subsidiaries, acquires or creates another Subsidiary, other than a Non-Guarantor Subsidiary, after the date of the indenture that guarantees Indebtedness under the Credit Agreement, then that newly acquired or created Subsidiary will become a Guarantor and execute a supplemental indenture and deliver an opinion of counsel satisfactory to the trustee within 30 business days of the date on which it was acquired or created.
Designation of Restricted and Unrestricted Subsidiaries
The Board of Directors of the Company may designate any Restricted Subsidiary to be an Unrestricted Subsidiary if that designation would not cause a Default. If a Restricted Subsidiary is designated as an Unrestricted Subsidiary, the aggregate Fair Market Value of all outstanding Investments owned by the Company and its Restricted Subsidiaries in the Subsidiary designated as an Unrestricted Subsidiary will be deemed to be an Investment made as of the time of the designation and will reduce the amount available for Restricted Payments under the covenant described above under the caption “—Restricted Payments” or under one or more clauses of the definition of Permitted Investments, as determined by the Company. That designation will only be permitted if the Investment would be permitted at that time and if the Restricted Subsidiary otherwise meets the definition of an Unrestricted Subsidiary. The Board of Directors of the Company may redesignate any Unrestricted Subsidiary to be a Restricted Subsidiary if that redesignation would not cause a Default and either: (1) the Issuers could incur at least $1.00 of additional Indebtedness pursuant to the Fixed Charge Coverage Ratio test described in the first paragraph under “—Incurrence of Indebtedness and Issuance of Disqualified Stock and Preferred Stock” or (2) the Fixed Charge Coverage Ratio for the Issuers and the Restricted Subsidiaries would be greater than such ratio for the Issuers and the Restricted Subsidiaries immediately prior to such designation, in each case on a pro forma basis taking into account such designation.
Any designation of a Subsidiary of the Company as an Unrestricted Subsidiary will be evidenced to the trustee by filing with the trustee a certified copy of a resolution of the Board of Directors of the Company giving effect to such designation and an officers’ certificate certifying that such designation complied with the preceding conditions and was permitted by the covenant described above under the caption “—Restricted Payments.” If, at any time, any Unrestricted Subsidiary would fail to meet the preceding requirements as an Unrestricted Subsidiary, it will thereafter cease to be an Unrestricted Subsidiary for purposes of the indenture and any Indebtedness of such Subsidiary will be deemed to be incurred by a Restricted Subsidiary of the Company as of such date and, if such Indebtedness is not permitted to be incurred as of such date under the covenant described under the caption “—Incurrence of Indebtedness and Issuance of Disqualified Stock and Preferred Stock,” the Company will be in default of such covenant. The Board of Directors of the Company may at any time designate any Unrestricted Subsidiary to be a Restricted
169
Subsidiary of the Company; providedthat such designation will be deemed to be an incurrence of Indebtedness by a Restricted Subsidiary of the Company of any outstanding Indebtedness of such Unrestricted Subsidiary, and such designation will only be permitted if (1) such Indebtedness is permitted under the covenant described under the caption “—Incurrence of Indebtedness and Issuance of Disqualified Stock and Preferred Stock,” and (2) no Default or Event of Default would be in existence following such designation.
Payments for Consent
The Company will not, and will not permit any of its Restricted Subsidiaries to, directly or indirectly, pay or cause to be paid any consideration to or for the benefit of any holder of notes for or as an inducement to any consent, waiver or amendment of any of the terms or provisions of the indenture or the notes unless such consideration is offered to be paid and is paid to all holders of the notes that consent, waive or agree to amend in the time frame set forth in the solicitation documents relating to such consent, waiver or agreement.
Existence of Corporate Co-Issuer
The Company will always maintain a Wholly Owned Subsidiary that is a Restricted Subsidiary of the Company organized as a corporation under the laws of the United States of America, any State thereof or the District of Columbia that will serve as a co-issuer of the notes unless the Company is itself a corporation under the laws of the United States of America, any State thereof or the District of Columbia.
Reports
Whether or not required by the rules and regulations of the SEC, so long as any notes are outstanding, the Company will furnish to the holders of notes or to the trustee with instructions to furnish to the holders of notes, within 45 days after the end of each of the first three fiscal quarters of each fiscal year commencing with the fiscal quarter ended March 31, 2011 or (in the case of annual financial information) within 90 days after the end of each fiscal year, all quarterly and annual financial information that would be required to be contained in a filing with the SEC on Forms 10-Q and 10-K if the Company were required to file such Forms, including a “Management’s Discussion and Analysis of Financial Condition and Results of Operations” and, with respect to the annual information only, a report on the annual financial statements by the Company’s certified independent accountants.
In addition, whether or not required by the SEC, the Company will file a copy of all of the information and reports referred to above with the SEC for public availability within the time periods specified above (unless the SEC will not accept such a filing) and make such information available to securities analysts and prospective investors upon request.
If in the event of a Specified Change of Control Parent Assumption, the Specified Change of Control Parent assuming the Company’s obligations hereunder does not regularly file reports with the SEC at the time of the Specified Change of Control Assumption Date and has ongoing material operations, the Specified Change of Control Parent shall not be required to file reports with the SEC until the date that is 180 days after the Specified Change of Control Parent Assumption, but shall otherwise be required during such 180-day period to comply with the reporting obligations contained in the prior paragraphs by posting any such reports on information on a website made available to all holders.
In addition, Company will:
| | (1) | hold a quarterly conference call to discuss the information contained in the annual and quarterly reports required under the first paragraph of this covenant (the “Financial Reports”) not later than five business days from the time the Company furnishes such reports to the Trustee; and |
| | (2) | no fewer than three business days prior to the date of the conference call required to be held in accordance with clause (1) above, issue a press release to the appropriate U.S. wire services announcing the time and date of such conference call and directing the beneficial owners of, and prospective investors in, the Notes and securities analysts to contact an individual at the Company (for whom contact information shall be provided in such press release) to obtain the Financial Reports and information on how to access such conference call. |
170
If, at any time after consummation of the exchange offer contemplated by the registration rights agreement, the Company is no longer subject to the periodic reporting requirements of the Exchange Act for any reason, the Company will nevertheless continue filing the reports specified in the preceding paragraphs of this covenant with the SEC within the time periods specified above unless the SEC will not accept such a filing. The Company will not take any action for the purpose of causing the SEC not to accept any such filings. If, notwithstanding the foregoing, the SEC will not accept the Company’s filings for any reason, the Company will post the reports referred to in the preceding paragraphs on its website within the time periods that would apply if the Company were required to file those reports with the SEC.
In addition, the Company and the Guarantors agree that, for so long as any notes remain outstanding, if at any time they are not required to file with the SEC the reports required by the preceding paragraphs, they will furnish to the holders of notes and to securities analysts and prospective investors, upon their request, the information required to be delivered pursuant to Rule 144A(d)(4) under the Securities Act.
The indenture will permit the Issuers to satisfy their obligations in this covenant with respect to financial information relating to the Issuers by furnishing financial information relating to any direct or indirect parent company of the Company (which shall be permitted, subject to compliance with the indenture, at any time, at the Issuers’ sole discretion); provided that either (x) a Covenant Termination Event has occurred; or (y) such parent company is a Guarantor of the notes and, if such parent company has material operations other than through its ownership of the Company, such reports shall be accompanied by consolidating information that explains in reasonable detail the differences between the information relating to such parent and its subsidiaries that are not guarantors of the notes, on the one hand, and the information relating to the Issuers and their Restricted Subsidiaries on the other hand.
Events of Default and Remedies
Each of the following is an Event of Default:
| | (1) | default for 30 days in the payment when due of interest on, or Special Interest, if any, with respect to, the notes; |
| | (2) | default in the payment when due (at maturity, upon redemption, acceleration or otherwise) of the principal of, or premium, if any, on, the notes; |
| | (3) | failure by the Company or any of its Restricted Subsidiaries to comply with the provisions described above under the caption “—Certain Covenants—Merger, Consolidation or Sale of Assets”; |
| | (4) | failure by the Company or any of its Restricted Subsidiaries for 60 days after notice to the Company by the trustee or the holders of at least 25% in aggregate principal amount of the notes then outstanding voting as a single class to comply with any of the other agreements in the indenture; |
| | (5) | default under any mortgage, indenture or instrument under which there may be issued or by which there may be secured or evidenced any Indebtedness for money borrowed by the Company or any of its Significant Subsidiaries (or the payment of which is guaranteed by the Company or any of its Significant Subsidiaries), whether such Indebtedness or Guarantee now exists, or is created after the date of the indenture, if that default: |
| | (a) | is caused by a failure to pay principal at the final Stated Maturity of such Indebtedness (a “Payment Default”); or |
171
| | (b) | results in the acceleration of such Indebtedness prior to its express maturity, |
and, in each case, the principal amount of such Indebtedness, together with the principal amount of any other such Indebtedness under which there has been a Payment Default or the maturity of which has been so accelerated, aggregates $30.0 million or more;
| | (6) | with respect to any judgment or decree for the payment of money (net of any amount covered by insurance issued by a reputable and creditworthy insurer that has not contested coverage or reserved rights with respect to an underlying claim) in excess of $30.0 million or its foreign currency equivalent against the Company or any Restricted Subsidiary, the failure by the Company or such Restricted Subsidiary, as applicable, to pay such judgment or decree, which |
| | (7) | judgment or decree has remained outstanding for a period of 60 days after such judgment or decree became final and nonappealable without being paid, discharged, waived or stayed; except as permitted by the indenture, any Subsidiary Guarantee of any Significant Subsidiary is declared to be unenforceable or invalid by any final and nonappealable judgment or decree or ceases for any reason to be in full force and effect, or any Guarantor, that is a Significant Subsidiary or any Person acting on behalf of any Guarantor that is a Significant Subsidiary denies or disaffirms its obligations in writing under its Subsidiary Guarantee and such Default continues for 10 days after receipt of the notice specified in the indenture; and |
| | (8) | certain events of bankruptcy or insolvency described in the indenture with respect to either Issuer or any Subsidiary that is a Significant Subsidiary. |
In the case of an Event of Default arising from certain events of bankruptcy or insolvency, with respect to either Issuer or any Restricted Subsidiary of the Company that is a Significant Subsidiary, all outstanding notes will become due and payable immediately without further action or notice. If any other Event of Default occurs and is continuing, the trustee or the holders of at least 25% in aggregate principal amount of the then outstanding notes may declare all the notes to be due and payable immediately.
Subject to certain limitations, holders of a majority in aggregate principal amount of the then outstanding notes may direct the trustee in its exercise of any trust or power. The trustee may withhold from holders of the notes notice of any continuing Default or Event of Default if it determines that withholding notice is in their interest, except a Default or Event of Default relating to the payment of principal, interest or premium or Special Interest, if any.
Subject to the provisions of the indenture relating to the duties of the trustee, in case an Event of Default occurs and is continuing, the trustee will be under no obligation to exercise any of the rights or powers under the indenture at the request or direction of any holders of notes unless such holders have offered to the trustee reasonable indemnity or security against any loss, liability or expense. Except to enforce the right to receive payment of principal, premium, if any, or interest or Special Interest, if any, when due, no holder of a note may pursue any remedy with respect to the indenture or the notes unless:
| | (1) | such holder has previously given the trustee notice that an Event of Default is continuing; |
| | (2) | holders of at least 25% in aggregate principal amount of the then outstanding notes have requested the trustee to pursue the remedy; |
| | (3) | such holders have offered the trustee reasonable security or indemnity against any loss, liability or expense; |
| | (4) | the trustee has not complied with such request within 60 days after the receipt of the request and the offer of security or indemnity; and |
172
| | (5) | holders of a majority in aggregate principal amount of the then outstanding notes have not given the trustee a direction inconsistent with such request within such 60-day period. |
The holders of a majority in aggregate principal amount of the then outstanding notes by notice to the trustee may, on behalf of the holders of all of the notes, rescind an acceleration or waive any existing Default or Event of Default and its consequences under the indenture except a continuing Default or Event of Default in the payment of interest or premium or Special Interest, if any, on, or the principal of, the notes.
The Issuers are required to deliver to the trustee annually a statement regarding compliance with the indenture. Upon becoming aware of any Default or Event of Default, the Issuers are required to deliver to the trustee within 30 days a statement specifying such Default or Event of Default.
No Personal Liability of Directors, Officers, Employees and Stockholders
No director, officer, employee, incorporator, stockholder, member or other holder of Equity Interests of the Issuers or any Guarantor, as such, will have any liability for any obligations of the Issuers or the Guarantors under the notes, the indenture, the Subsidiary Guarantees or for any claim based on, in respect of, or by reason of, such obligations or their creation. Each holder of notes by accepting a note waives and releases all such liability. The waiver and release are part of the consideration for issuance of the notes. The waiver may not be effective to waive liabilities under the federal securities laws.
Legal Defeasance and Covenant Defeasance
The Issuers may at any time, elect to have all of their obligations discharged with respect to the outstanding notes and all obligations of the Guarantors discharged with respect to their Subsidiary Guarantees (“Legal Defeasance”) except for:
| | (1) | the rights of holders of outstanding notes to receive payments in respect of the principal of, or interest or premium and Special Interest, if any, on, such notes when such payments are due from the trust referred to below; |
| | (2) | the Issuers’ obligations with respect to the notes concerning issuing temporary notes, registration of notes, mutilated, destroyed, lost or stolen notes and the maintenance of an office or agency for payment and money for security payments held in trust; |
| | (3) | the rights, powers, trusts, duties and immunities of the trustee, and the Issuers’ and the Guarantors’ obligations in connection therewith; and |
| | (4) | the Legal Defeasance provisions of the indenture. |
In addition, the Issuers may, at their option and at any time, elect to have the obligations of the Issuers and the Guarantors released (“Covenant Defeasance”) with respect to the covenants described under “—Repurchase at the Option of Holders—Change of Control,” “—Repurchase at the Option of Holders— Asset Sales” and “Certain Covenants” and with respect to certain Events of Default (including bankruptcy default with respect to Significant Subsidiaries, cross-default and judgment default) and thereafter any omission to comply with those covenants will not constitute a Default or Event of Default with respect to the notes. In the event Covenant Defeasance occurs, certain events (not including non-payment and bankruptcy, receivership, rehabilitation and insolvency events with respect to the Issuers) described under “—Events of Default and Remedies” will no longer constitute an Event of Default with respect to the notes.
In order to exercise either Legal Defeasance or Covenant Defeasance:
| | (1) | the Issuers must irrevocably deposit with the trustee, in trust, for the benefit of the holders of the notes, cash in U.S. dollars, non-callable Government Securities, or a combination of cash in U.S. dollars and non-callable Government Securities, in amounts as will be sufficient, in the opinion of a nationally recognized investment |
173
| | bank, appraisal firm or firm of independent public accountants, to pay the principal of, or interest and premium and Special Interest, if any, on, the outstanding notes on the stated date for payment thereof or on the applicable redemption date, as the case may be, and the Issuers must specify whether the notes are being defeased to such stated date for payment or to a particular redemption date; |
| | (2) | in the case of Legal Defeasance, the Issuers must deliver to the trustee an opinion of counsel reasonably acceptable to the trustee confirming that (a) the Issuers have received from, or there has been published by, the Internal Revenue Service a ruling or (b) since the date of the indenture, there has been a change in the applicable federal income tax law, in either case to the effect that, and based thereon such opinion of counsel will confirm that, the holders of the outstanding notes will not recognize income, gain or loss for federal income tax purposes as a result of such Legal Defeasance and will be subject to federal income tax on the same amounts, in the same manner and at the same times as would have been the case if such Legal Defeasance had not occurred; |
| | (3) | in the case of Covenant Defeasance, the Issuers must deliver to the trustee an opinion of counsel reasonably acceptable to the trustee confirming that the holders of the outstanding notes will not recognize income, gain or loss for federal income tax purposes as a result of such Covenant Defeasance and will be subject to federal income tax on the same amounts, in the same manner and at the same times as would have been the case if such Covenant Defeasance had not occurred; |
| | (4) | such Legal Defeasance or Covenant Defeasance will not result in a breach or violation of, or constitute a default under, any material agreement (including, without limitation, the Credit Agreement) or instrument (other than the indenture) to which the Company or any of its Subsidiaries is a party or by which the Company or any of its Subsidiaries is bound; |
| | (5) | the Issuers must deliver to the trustee an officers’ certificate stating that the deposit was not made by the Issuers with the intent of preferring the holders of notes over the other creditors of the Issuers with the intent of defeating, hindering, delaying or defrauding any creditors of the Issuers or others; and |
| | (6) | the Issuers must deliver to the trustee an officers’ certificate and an opinion of counsel, each stating that all conditions precedent relating to the Legal Defeasance or the Covenant Defeasance have been complied with. |
Amendment, Supplement and Waiver
Except as provided in the next two succeeding paragraphs, the indenture or the notes or the Subsidiary Guarantees may be amended or supplemented with the consent of the holders of at least a majority in aggregate principal amount of the notes then outstanding (including, without limitation, consents obtained in connection with a purchase of, or tender offer or exchange offer for, notes), and any existing Default or Event of Default or compliance with any provision of the indenture or the notes or the Subsidiary Guarantees may be waived with the consent of the holders of a majority in aggregate principal amount of the then outstanding notes (including, without limitation, consents obtained in connection with a purchase of, or tender offer or exchange offer for, notes).
Without the consent of each holder of notes affected, an amendment, supplement or waiver may not (with respect to any notes held by a non-consenting holder):
| | (1) | reduce the principal amount of notes whose holders must consent to an amendment, supplement or waiver; |
| | (2) | reduce the principal of or change the fixed maturity of any note or alter the provisions with respect to the redemption of the notes (other than provisions relating to the covenants described above under the caption “—Repurchase at the Option of Holders”); |
174
| | (3) | reduce the rate of or change the time for payment of interest, including default interest, on any note; |
| | (4) | waive a Default or Event of Default in the payment of principal of, or interest or premium, or Special Interest, if any, on, the notes (except a rescission of acceleration of the notes by the holders of at least a majority in aggregate principal amount of the then outstanding notes and a waiver of the payment default that resulted from such acceleration); |
| | (5) | make any note payable in money other than that stated in the notes; |
| | (6) | make any change in the provisions of the indenture relating to waivers of past Defaults or the rights of holders of notes to receive payments of principal of, or interest or premium or Special Interest, if any, on, the notes; |
| | (7) | waive a redemption payment with respect to any note (other than a payment required by one of the covenants described above under the caption “—Repurchase at the Option of Holders”); |
| | (8) | release any Guarantor from any of its obligations under its Subsidiary Guarantee or the indenture, except in accordance with the terms of the indenture; |
| | (9) | impair the right of any holder of the notes to receive payment of principal of, or interest on such holder’s notes on or after the due dates therefor or to institute suit for the enforcement of any payment on or with respect to such holder’s notes; or |
| | (10) | make any change to or modify the ranking of any such note or related Guarantee that would adversely affect the holders of the notes; or |
| | (11) | make any change in the preceding amendment and waiver provisions. |
Notwithstanding the preceding, without the consent of any holder of notes, the Issuers, the Guarantors and the trustee may amend or supplement the indenture or the notes or the Subsidiary Guarantees:
| | (1) | to cure any ambiguity, defect or inconsistency; |
| | (2) | to provide for uncertificated notes in addition to or in place of certificated notes; |
| | (3) | to provide for the assumption of the Company’s or a Guarantor’s obligations to holders of notes and Subsidiary Guarantees in the case of a merger or consolidation or sale of all or substantially all of the Company’s or such Guarantor’s assets or a Specified Change of Control, as applicable and the corresponding release of the Issuers’ obligations under the Indenture; |
| | (4) | to make any change that would provide any additional rights or benefits (including the addition of collateral) to the holders of notes or that does not adversely affect the legal rights under the indenture of any such holder; |
| | (5) | to comply with requirements of the SEC in order to effect or maintain the qualification of the indenture under the Trust Indenture Act; |
| | (6) | to conform the text of the indenture, the Subsidiary Guarantees or the notes to any provision of this Description of Notes; |
| | (7) | to provide for the issuance of additional notes in accordance with the limitations set forth in the indenture as of the date of the indenture; |
175
| | (8) | to allow any Guarantor to execute a supplemental indenture and/or a Subsidiary Guarantee with respect to the notes; or |
| | (9) | to issue the Exchange Notes. |
Satisfaction and Discharge
The indenture will be discharged and will cease to be of further effect as to all notes issued thereunder, when:
| | (a) | all notes that have been authenticated, except lost, stolen or destroyed notes that have been replaced or paid and notes for whose payment money has been deposited in trust and thereafter repaid to the Issuers, have been delivered to the trustee for cancellation; or |
| | (b) | all notes that have not been delivered to the trustee for cancellation have become due and payable by reason of the mailing of a notice of redemption or otherwise or will become due and payable within one year and the Issuers or any Guarantor has irrevocably deposited or caused to be deposited with the trustee as trust funds in trust solely for the benefit of the holders, cash in U.S. dollars, non-callable Government Securities, or a combination of cash in U.S. dollars and noncallable Government Securities, in amounts as will be sufficient, without consideration of any reinvestment of interest, to pay and discharge the entire Indebtedness on the notes not delivered to the trustee for cancellation for principal, premium and Special Interest, if any, and accrued interest to the date of maturity or redemption; |
| | (2) | no Default or Event of Default has occurred and is continuing on the date of the deposit (other than a Default or Event of Default resulting from the borrowing of funds to be applied to such deposit) and the deposit will not result in a breach or violation of, or constitute a default under, any other instrument to which the Issuers or any Guarantor is a party or by which the Issuers or any Guarantor is bound; |
| | (3) | the Issuers or any Guarantor has paid or caused to be paid all sums payable by it under the indenture; and |
| | (4) | the Issuers have delivered irrevocable instructions to the trustee under the indenture to apply the deposited money toward the payment of the notes at maturity or on the redemption date, as the case may be. |
In addition, the Issuers must deliver an officers’ certificate and an opinion of counsel to the trustee stating that all conditions precedent to satisfaction and discharge have been satisfied.
Concerning the Trustee
If the trustee becomes a creditor of the Issuers or any Guarantor, the indenture limits the right of the trustee to obtain payment of claims in certain cases, or to realize on certain property received in respect of any such claim as security or otherwise. The trustee will be permitted to engage in other transactions; however, if it acquires any conflicting interest it must eliminate such conflict within 90 days, apply to the SEC for permission to continue as trustee (if the indenture has been qualified under the Trust Indenture Act) or resign.
The holders of a majority in aggregate principal amount of the then outstanding notes will have the right to direct the time, method and place of conducting any proceeding for exercising any remedy available to the trustee, subject to certain exceptions. The indenture provides that in case an Event of Default occurs and is continuing, the trustee will be required, in the exercise of its power, to use the degree of care of a prudent man in the conduct of his own affairs. Subject to such provisions, the trustee will be under no
176
obligation to exercise any of its rights or powers under the indenture at the request of any holder of notes, unless such holder has offered to the trustee security and indemnity satisfactory to it against any loss, liability or expense.
Additional Information
Anyone who receives this prospectus may obtain a copy of the indenture and registration rights agreement without charge by writing to IASIS Healthcare LLC, 117 Seaboard Lane, Building E, Franklin, Tennessee 37067, Attention: Chief Financial Officer.
The New Notes will be issued in fully registered global form. The New Notes initially will be represented by one or more global certificates without interest coupons (the “global notes”). The global notes will be deposited upon issuance with the trustee as custodian for DTC and registered in the name of DTC or its nominee for credit to the accounts of direct or indirect participants in DTC, as described below under “—Depositary Procedures.”
Form, Book-Entry Procedures and Transfer
General
The global notes will be deposited on behalf of the acquirers of the New Notes for credit to the respective accounts of the acquirers or to such other accounts as they may direct. Except as described below, the global notes may be transferred, in whole and not in part, only to another nominee of DTC or to a successor of DTC or its nominee. Beneficial interests in the global notes may not be exchanged for the New Notes in certificated form except in the limited circumstances described below under “—Exchange of Book-Entry Notes for Certificated Notes.”
Transfers of beneficial interests in the global notes will be subject to the applicable rules and procedures of DTC and its direct or indirect participants, which may change from time to time.
Depositary Procedures
The following description of the operations and procedures of DTC is provided solely as a matter of convenience. These operations and procedures are solely within the control of the respective settlement systems and are subject to changes by them. We take no responsibility for these operations and procedures and urge investors to contact the systems or their participants directly to discuss these matters.
DTC has advised us that it is:
| | • | | a limited purpose trust company organized under the New York State Banking Law; |
| | • | | a “banking organization” within the meaning of the New York State Banking Law; |
| | • | | a member of the U.S. Federal Reserve System; |
| | • | | a “clearing corporation” within the meaning of the New York Uniform Commercial Code; and |
| | • | | a “clearing agency” registered under Section 17A of the Exchange Act. |
DTC was created to hold securities for its participating organizations (collectively, the “participants”) and facilitate the clearance and settlement of transactions in those securities between participants through electronic book-entry changes in accounts of its participants. The participants include securities brokers and dealers, banks, trust companies, clearing corporations and certain other organizations. Access to DTC’s system is also available to other entities such as banks, brokers, dealers and trust companies that clear through or maintain a custodial relationship with a participant, either directly or indirectly (collectively, the “indirect participants”). Persons who are not participants may beneficially own securities held by or on behalf of DTC only through participants or indirect
177
participants. DTC has no knowledge of the identity of beneficial owners of securities held by or on behalf of DTC. DTC’s records reflect only the identity of participants to whose accounts securities are credited. The ownership interests and transfer of ownership interests of each beneficial owner of each security held by or on behalf of DTC are recorded on the records of the participants and indirect participants.
DTC has also advised us that, pursuant to procedures established by DTC, ownership of interests in the global notes will be shown on, and the transfer of ownership of such interest will be effected only through, records maintained by DTC (with respect to the participants) or by the participants and the indirect participants (with respect to other owners of beneficial interests in the global notes).
Investors in the global notes may hold their interests therein directly through DTC if they are participants in such system or indirectly through organizations that are participants or indirect participants in such system. All interests in the global notes will be subject to the procedures and requirements of DTC. The laws of some states
require that certain persons take physical delivery of certificates evidencing securities they own. Consequently, the ability to transfer beneficial interests in the global notes to such persons will be limited to that extent. Because DTC can act only on behalf of participants, which in turn act on behalf of indirect participants, the ability of beneficial owners of interests in the global notes to pledge such interests to persons or entities that do not participate in the DTC system, or otherwise take actions in respect of such interests, may be affected by the lack of a physical certificate evidencing such interests.
Except as described below, owners of interests in the global notes will not have New Notes registered in their names, will not receive physical delivery of the New Notes in certificated form and will not be considered the registered owners or holders thereof under the indenture for any purpose.
Payments in respect of the principal of and premium, if any, and interest on the global notes registered in the name of DTC or its nominee will be payable by the trustee (or the paying agent if other than the trustee) to DTC in its capacity as the registered holder under the indenture. We and the trustee will treat the persons in whose names the New Notes, including the global notes, are registered as the owners thereof for the purpose of receiving such payments and for any and all other purposes whatsoever. Consequently, none of us, the trustee or any agent of ours or the trustee has or will have any responsibility or liability for:
| | • | | any aspect of DTC’s records or any participant’s or indirect participant’s records relating to or payments made on account of beneficial ownership interests in the global notes, or for maintaining, supervising or reviewing any of DTC’s records or any participant’s or indirect participant’s records relating to the beneficial ownership interests in the global notes; or |
| | • | | any other matter relating to the actions and practices of DTC or any of its participants or indirect participants. |
DTC has advised us that its current practice, upon receipt of any payment in respect of securities such as the New Notes (including principal and interest), is to credit the accounts of the relevant participants with the payment on the payment date in amounts proportionate to their respective holdings in the principal amount of the relevant security as shown on the records of DTC, unless DTC has reason to believe it will not receive payment on such payment date. Payments by the participants and the indirect participants to the beneficial owners of New Notes will be governed by standing instructions and customary practices and will be the responsibility of the participants or the indirect participants and will not be the responsibility of DTC, the trustee or us. Neither we nor the trustee will be liable for any delay by DTC or any of its participants in identifying the beneficial owners of the New Notes, and we and the trustee may conclusively rely on and will be protected in relying on instructions from DTC or its nominee for all purposes.
Interests in the global notes are expected to be eligible to trade in DTC’s Same-Day Funds Settlement System and secondary market trading activity in such interests will therefore settle in immediately available funds, subject in all cases to the rules and procedures of DTC and its participants.
178
DTC has advised us that it will take any action permitted to be taken by a holder of New Notes only at the direction of one or more participants to whose account with DTC interests in the global notes are credited and only in respect of such portion of the aggregate principal amount of the New Notes as to which such participant or participants has or have given such direction.
Although DTC has agreed to the foregoing procedures to facilitate transfers of interests in the global notes among participants in DTC, it is under no obligation to perform or to continue to perform such procedures, and the procedures may be discontinued at any time. Neither we nor the trustee will have any responsibility for the
performance by DTC or its participants or indirect participants of their respective obligations under the rules and procedures governing their operations.
The information in this section concerning DTC and its book-entry system has been obtained from sources that we believe to be reliable, but we take no responsibility for the accuracy thereof.
Exchange of Book-Entry Notes for Certificated Notes
If (i) DTC is at any time unwilling or unable to continue as depositary and a successor depositary is not appointed by us within 90 days, (ii) DTC has ceased to be a clearing agency registered under the Exchange Act, (iii) we, at our option, notify the trustee in writing that we elect to cause the issuance of the notes in the form of certificated notes, or (iv) an Event of Default has occurred and is continuing, upon request by the holders of the notes, we will issue notes in certificated form in exchange for global securities. The indenture permits us to determine at any time and in our sole discretion that notes shall no longer be represented by global securities. DTC has advised us that, under its current practices, it would notify its participants of our request, but will only withdraw beneficial interests from the global security at the request of each DTC participant. We would issue definitive certificates in exchange for any beneficial interests withdrawn.
Certain Definitions
Set forth below are certain defined terms used in the indenture. Reference is made to the indenture for a full disclosure of all defined terms used therein, as well as any other capitalized terms used herein for which no definition is provided.
“2004 Transactions” means the acquisition in 2004 by the Permitted Holders of the business then being conducted by a predecessor of the Company, including the financing of the acquisition, the refinancing of Indebtedness then existing, and all financings, contributions and other transactions related thereto.
“Acquired Debt” means, with respect to any specified Person:
| | (1) | Indebtedness of any other Person existing at the time such other Person is merged with or into or became a Restricted Subsidiary of such specified Person, whether or not such Indebtedness is incurred in connection with, or in contemplation of, such other Person merging with or into, or becoming a Restricted Subsidiary of, such specified Person; and |
| | (2) | Indebtedness secured by a Lien encumbering any asset acquired by such specified Person. |
“Additional Assets” means any property or assets (other than Indebtedness and Capital Stock) to be used by the Company or a Restricted Subsidiary in a Permitted Business.
“Affiliate” of any specified Person means any other Person directly or indirectly controlling or controlled by or under direct or indirect common control with such specified Person. For purposes of this definition, “control,” as used with respect to any Person, means the possession, directly or indirectly, of the power to direct or cause the direction of the management or policies of such Person, whether through the ownership of voting securities, by agreement or otherwise. No Person in whom a Receivables Subsidiary makes an Investment in connection with a Qualified Receivables Transaction will be deemed to be an Affiliate of the Company or any of its Subsidiaries solely by reason of such Investment.
179
“Applicable Premium” means, with respect to any note on any Redemption Date, the greater of:
| | (1) | 1.0% of the principal amount of such note; and |
| | (2) | the excess, if any, of (a) the present value at such redemption date of (i) the redemption price (such redemption price being set forth in the table appearing above under the caption “Optional Redemption”) of such note at May 15, 2014, plus (ii) all required interest payments due on such note (excluding accrued but unpaid interest to the Redemption Date) to but excluding May 15, 2014, computed using a discount rate equal to the Treasury Rate as of such Redemption Date plus 50 basis points; over (b) the principal amount of such note. |
“Asset Sale” means:
| | (1) | the sale, lease (other than operating leases), conveyance or other disposition of any assets or rights outside of the ordinary course of business; provided that the sale, lease, conveyance or other disposition of all or substantially all of the assets of the Company and its Restricted Subsidiaries taken as a whole will be governed by the provisions of the indenture described above under the caption “—Repurchase at the Option of Holders—Change of Control” and/or the provisions described above under the caption “—Certain Covenants—Merger, Consolidation or Sale of Assets” and not by the provisions of the Asset Sale covenant; and |
| | (2) | the issuance of Equity Interests in any of the Company’s Restricted Subsidiaries or the sale of Equity Interests in any of its Subsidiaries (other than directors’ qualifying Equity Interests or Equity Interests required by applicable law to be held by a Person other than the Company or a Restricted Subsidiary). |
Notwithstanding the preceding, none of the following items will be deemed to be an Asset Sale:
| | (1) | any single transaction or series of related transactions that involves assets having a Fair Market Value of less than $10.0 million; |
| | (2) | a transfer of assets between or among the Company and its Restricted Subsidiaries; |
| | (3) | an issuance of Equity Interests by a Restricted Subsidiary of the Company to the Company or to a Restricted Subsidiary of the Company; |
| | (4) | the sale or lease of products, services or accounts receivable (including at a discount) in the ordinary course of business and any sale or other disposition of damaged, worn-out, negligible, surplus or obsolete assets in the ordinary course of business; |
| | (5) | the sale or other disposition of Cash Equivalents; |
| | (6) | a Restricted Payment that does not violate the covenant described above under the caption “—Certain Covenants—Restricted Payments” or a Permitted Investment; |
| | (7) | a sale and leaseback transaction with respect to any assets within 180 days of the acquisition of such assets; |
| | (8) | any exchange of like-kind property of the type described in Section 1031 of the Code for use in a Permitted Business; |
180
| | (9) | the sale or disposition of any assets or property received as a result of a foreclosure by the Company or any of its Restricted Subsidiaries on any secured Investment or any other transfer of title with respect to any secured Investment in default; |
| | (10) | the licensing of intellectual property in the ordinary course of business or in accordance with industry practice; |
| | (11) | the sale, lease, conveyance, disposition or other transfer of (a) the Capital Stock of, or any Investment in, any Unrestricted Subsidiary or (b) Permitted Investments made pursuant to clause (15) of the definition thereof; |
| | (12) | surrender or waiver of contract rights or the settlement, release or surrender of contract, tort or other claims of any kind; |
| | (13) | leases or subleases to third persons in the ordinary course of business that do not interfere in any material respect with the business of the Company or any of its Restricted Subsidiaries; |
| | (14) | sales of accounts receivable and related assets of the type specified in the definition of Qualified Receivables Transaction to a Receivables Subsidiary for the Fair Market Value thereof, less amounts required to be established as reserves and customary discounts pursuant to contractual agreements with entities that are not Affiliates of the Company entered into as part of a Qualified Receivables Transactions; and |
| | (15) | transfers of accounts receivable and related assets of the type specified in the definition of Qualified Receivables Transaction (or a fractional undivided interest therein) by a Receivables Subsidiary in a Qualified Receivables Transaction. |
“Beneficial Owner” has the meaning assigned to such term in Rule 13d-3 and Rule 13d-5 under the Exchange Act, except that in calculating the beneficial ownership of any particular “person” (as that term is used in Section 13(d)(3) of the Exchange Act), such “person” will be deemed to have beneficial ownership of all securities that such “person” has the right to acquire by conversion or exercise of other securities, whether such right is currently exercisable or is exercisable only after the passage of time.
“Board of Directors” means:
| | (1) | with respect to a corporation, the board of directors of the corporation or any committee thereof duly authorized to act on behalf of such board; |
| | (2) | with respect to a partnership, the Board of Directors of the general partner of the partnership; |
| | (3) | with respect to a limited liability company, the managing member or members or any controlling committee of managing members thereof; and |
| | (4) | with respect to any other Person, the board or committee of such Person serving a similar function. |
“Capital Lease Obligation” means, at the time any determination is to be made, the amount of the liability in respect of a capital lease that would at that time be required to be capitalized on a balance sheet prepared in accordance with GAAP, and the Stated Maturity thereof shall be the date of the last payment of rent or any other amount due under such lease prior to the first date upon which such lease may be prepaid by the lessee without payment of a penalty.
“Capital Stock” means:
| | (1) | in the case of a corporation, corporate stock; |
181
| | (2) | in the case of an association or business entity, any and all shares, interests, participations, rights or other equivalents (however designated) of corporate stock; |
| | (3) | in the case of a partnership or limited liability company, partnership interests (whether general or limited) or membership interests; and |
| | (4) | any other interest or participation that confers on a Person the right to receive a share of the profits and losses of, or distributions of assets of, the issuing Person, but excluding from all of the foregoing any debt securities convertible into Capital Stock, whether or not such debt securities include any right of participation with Capital Stock. |
“Cash Equivalents” means:
| | (5) | United States dollars or any other currencies held from time to time in the ordinary course of business; |
| | (6) | securities issued or directly and fully and unconditionally guaranteed or insured by the United States government or any agency or instrumentality thereof the securities of which are unconditionally guaranteed as a full faith and credit obligation of such government with maturities of 24 months or less from the date of acquisition; |
| | (7) | certificates of deposit, time deposits and eurodollar time deposits with maturities of two years or less from the date of acquisition, bankers’ acceptances with maturities not exceeding two years and overnight bank deposits, in each case with any domestic commercial bank having capital and surplus of not less than $250,000,000; |
| | (8) | repurchase obligations for underlying securities of the types described in clauses (2), (3) and (7) entered into with any financial institution meeting the qualifications specified in clause (3) above; |
| | (9) | commercial paper rated at least P-1 by Moody’s or at least A-1 by S&P (or, if at any time neither Moody’s nor S&P shall be rating such obligations, an equivalent rating from another nationally recognized statistical rating agency selected by the Company) and in each case maturing within 24 months after the date of creation thereof and Indebtedness or preferred stock issued by Persons with a rating of “A” or higher from S&P or “A2” or higher from Moody’s with maturities of 24 months or less from the date of acquisition; |
| | (10) | marketable short-term money market and similar funds either having (A) assets in excess of $250,000,000 or (B) a rating of at least P-2 or A-2 from either Moody’s or S&P, respectively (or, if at any time neither Moody’s nor S&P shall be rating such obligations, an equivalent rating from another nationally recognized statistical rating agency selected by the Company); |
| | (11) | readily marketable direct obligations issued by any state, commonwealth or territory of the United States or any political subdivision or taxing authority thereof having an Investment Grade Rating from either Moody’s or S&P (or, if at any time neither Moody’s nor S&P shall be rating such obligations, an equivalent rating from another nationally recognized statistical rating agency selected by the Company) with maturities of 24 months or less from the date of acquisition; |
| | (12) | readily marketable direct obligations issued by any foreign government or any political subdivision or public instrumentality thereof, in each case having an Investment Grade Rating from either Moody’s or S&P (or, if at any time neither Moody’s nor S&P shall be rating such obligations, an equivalent rating from another nationally recognized statistical rating agency selected by the Company) with maturities of 24 months or less from the date of acquisition; and |
| | (13) | investment funds investing at least 90% of their assets in securities of the types described in clauses (1) through (8) above. |
182
“Change of Control” means the occurrence of any of the following:
| | (1) | the direct or indirect sale, lease, transfer, conveyance or other disposition (other than by way of merger or consolidation), in one or a series of related transactions, of all or substantially all of the properties or assets of the Company and its Subsidiaries taken as a whole to any “person” (as that term is used in Section 13(d) of the Exchange Act) other than Permitted Holders; |
| | (2) | the adoption of a plan relating to the liquidation or dissolution of the Company (other than a plan with respect to the Company adopted solely for the purpose of reorganizing the Company as a corporation); or |
| | (3) | the Issuers become aware of (by way of a report or any other filing pursuant to Section 13(d) of the Exchange Act, proxy, vote, written notice or otherwise) the acquisition by (A) any Person (other than any Permitted Holder) or (B) Persons (other than any Permitted Holder) that are together a group (within the meaning of Section 13(d)(3) or Section 14(d)(2) of the Exchange Act, or any successor provision), including any such group acting for the purpose of acquiring, holding or disposing of securities (within the meaning of Rule 13d-5(b)(1) under the Exchange Act), in a single transaction or in a related series of transactions, by way of merger, consolidation or other business combination or purchase of beneficial ownership (within the meaning of Rule 13d-3 under the Exchange Act, or any successor provision) of more than 50.0% of the total voting power of the Voting Stock of the Company directly or indirectly through any of its direct or indirect parent holding companies; provided that a Change of Control shall not be deemed to have occurred solely as a result of the Issuers becoming Subsidiaries of any direct or indirect parent holding companies so long as no Person or Persons that are together a group (within the meaning of Section 13(d)(3) or Section 14(d)(2) of the Exchange Act, or any successor provision), including any such group acting for the purpose of acquiring, holding or disposing of securities (within the meaning of Rule 13d-5(b)(1) under the Exchange Act), in a single transaction or in a related series of transactions, by way of merger, consolidation or other business combination or purchase of beneficial ownership (within the meaning of Rule 13d-3 under the Exchange Act, or any successor provision), in each case other than the Permitted Holders owns or holds, directly or indirectly, more than 50.0% of the total voting power of the ultimate parent holding company. |
“Consolidated Adjusted EBITDA” means, with respect to any specified Person for any period (the “Measurement Period”), the Consolidated Net Income of such Person for such period plus, without duplication and to the extent deducted in determining such Consolidated Net Income, the amounts for such period of:
| | (1) | the Fixed Charges of such Person and its Restricted Subsidiaries for the Measurement Period;plus |
| | (2) | the consolidated income tax expense of such Person and its Restricted Subsidiaries for the Measurement Period;plus |
| | (3) | the consolidated depreciation expense of such Person and its Restricted Subsidiaries for the Measurement Period;plus |
| | (4) | the consolidated amortization expense of such Person and its Restricted Subsidiaries for the Measurement Period;plus |
| | (5) | Subordinated Management Fees paid and permitted to be paid under the terms of the indenture plus reasonable out-of-pocket expenses incurred, in each case, during the Measurement Period pursuant to the Management Services Agreement as described above under the caption “Certain Relationships and Related Party Transactions”;plus |
| | (6) | fees, costs and expenses paid or payable in cash by the Company or any of its Subsidiaries during the Measurement Period in connection with the Transactions;plus |
183
| | (7) | other non-cash expenses and charges for the Measurement Period reducing Consolidated Net Income (excluding any such non-cash item to the extent representing an accrual or reserve for potential cash items in any future period or amortization of a prepaid cash item that was paid in a prior period);plus |
| | (8) | any non-recurring out-of-pocket expenses or charges for the Measurement Period relating to any offering of Equity Interests by the Company or any direct or indirect parent of the Company, any Asset Sale, Investment or merger, recapitalization or acquisition or disposition transactions made by the Company or any of its Restricted Subsidiaries, or any Indebtedness incurred, repaid, refinanced or amended by the Company or any of its Restricted Subsidiaries (in each case, whether or not successful and whether before or after the issuance of the notes);plus |
| | (9) | Consolidated Net Income attributable to minority interests of a Restricted Subsidiary that is not a Wholly Owned Subsidiary;plus |
| | (10) | to the extent deducted from the calculation of Consolidated Net Income, payments made pursuant to clause (1) of the definition of “Permitted Payments to Parent”;minus |
| | (11) | without duplication, other non-cash items (other than the accrual of revenue in accordance with GAAP consistently applied in the ordinary course of business) increasing Consolidated Net Income for the Measurement Period (excluding any such non-cash item to the extent it represents the reversal of an accrual or reserve for potential cash item in any prior period). |
“Consolidated Net Income” means, with respect to any specified Person for any period, the aggregate of the Net Income of such Person and its Restricted Subsidiaries for such period, on a consolidated basis, determined in accordance with GAAP; provided that:
| | (1) | the Net Income (but not loss) of any Person that is not a Restricted Subsidiary or that is accounted for by the equity method of accounting will be included only to the extent of the amount of dividends or similar distributions paid in cash to the specified Person or a Restricted Subsidiary of the Person; |
| | (2) | solely for the purpose of determining the amount available for Restricted Payments under clause (3)(a) of the first paragraph of “—Certain Covenants—Restricted Payments,” the Net Income of any Restricted Subsidiary will be excluded to the extent that the declaration or payment of dividends or other distributions by that Restricted Subsidiary of that Net Income is not at the date of determination permitted without any prior governmental approval (that has not been obtained) or, directly or indirectly, by operation of the terms of its charter or any agreement, instrument, judgment, decree, order, statute, rule or governmental regulation applicable to that Restricted Subsidiary or its stockholders; |
| | (3) | the cumulative effect of a change in accounting principles will be excluded; |
| | (4) | the amortization of any premiums, fees or expenses incurred in connection with the 2004 Transactions or subsequent acquisition transactions or the Transactions or any amounts required or permitted by Accounting Principles Board Opinions Nos. 16 (including non-cash write-ups and non-cash charges relating to inventory and fixed assets, in each case arising in connection with the 2004 Transactions or subsequent acquisition transactions or the Transactions) and 17 (including non-cash charges relating to intangibles and goodwill) and any net after-tax income or loss (less fees and expenses or charges relating thereto attributable to the early extinguishment of indebtedness, in each case in connection with the 2004 Transactions or subsequent acquisition transactions or the Transactions, will be excluded; |
184
| | (5) | any increase in amortization or depreciation or any one-time non-cash charges resulting from purchase accounting in connection with any acquisition that is consummated after the date of the indenture shall be excluded; |
| | (6) | any gain or loss, together with any related provision for taxes on such gain or loss, realized in connection with: (a) any Asset Sale; or (b) the disposition of any securities by such Person or any of its Restricted Subsidiaries or the extinguishment of any Indebtedness of such Person or any of its Restricted Subsidiaries will be excluded; |
| | (7) | any extraordinary gain or loss, together with any related provision for taxes on such extraordinary gain or loss will be excluded; |
| | (8) | income or losses attributable to discontinued operations (including, without limitation, operations disposed during such period whether or not such operations were classified as discontinued) will be excluded; |
| | (9) | all non-recurring or unusual gains and losses and all restructuring charges will be excluded; |
| | (10) | any non-cash charges attributable to applying the purchase method of accounting in accordance with GAAP will be excluded; |
| | (11) | an amount equal to the payments actually made to Holdings pursuant to clause (1) of the definition of Permitted Payments to Parent in respect of the net taxable income allocated by the Company to Holdings for such period shall be excluded as though such amounts had been paid as income taxes directly by the Company; and |
| | (12) | all non-cash charges relating to employee benefit or other management or stock compensation plans of the Company or a Restricted Subsidiary (excluding any such non-cash charge to the extent that it represents an accrual of or reserve for cash expenses in any future period or amortization of a prepaid cash expense incurred in a prior period) will be excluded to the extent that such non-cash charges are deducted in computing such Consolidated Net Income; provided,further that if the Company or any Restricted Subsidiary of the Company makes a cash payment in respect of such non-cash charge in any period, such cash payment will (without duplication) be deducted from the Consolidated Net Income of the Company for such period. |
“Consolidated Secured Debt Ratio” means, as of the date of determination, the ratio of (a) the Consolidated Total Indebtedness of the Issuers and their Restricted Subsidiaries as of the end of the most recent fiscal quarter for which internal financial statements are available that is secured by a Lien to (b) Consolidated Adjusted EBITDA of the Issuers and their Restricted Subsidiaries for the most recently ended four fiscal quarters ending immediately prior to such date for which internal financial statements are available, in each case with such pro forma adjustments to Consolidated Total Indebtedness and Consolidated Adjusted EBITDA as are appropriate and consistent with the pro forma adjustment provisions set forth in the definition of “Fixed Charge Coverage Ratio.”
“Consolidated Total Indebtedness” means, as at any date of determination, an amount equal to (a) the sum of (1) the aggregate amount of all outstanding Indebtedness of the Issuers and their Restricted Subsidiaries on a consolidated basis consisting of Indebtedness for borrowed money, Obligations in respect of Capital Lease Obligations and debt obligations evidenced by promissory notes and similar instruments, as determined in accordance with GAAP (but excluding the effects of any discounting of Indebtedness resulting from the application of purchase accounting in connection with the 2004 Transactions or any permitted acquisition under the indenture) and (2) the aggregate amount of all outstanding Disqualified Stock of the Issuers and all Preferred Stock of its Restricted Subsidiaries on a consolidated basis, with the amount of such Disqualified Stock and preferred stock equal to the greater of their respective voluntary or involuntary liquidation preferences and maximum fixed repurchase prices, in each case determined on a consolidated basis in accordance with GAAP minus (b) the lesser of (x) the aggregate amount of cash and Cash Equivalents (in each case, free and clear of all Liens, other than nonconsensual Liens permitted by “—Certain Covenants— Liens”) included in the consolidated balance sheet of the Issuers and the Restricted Subsidiaries as of such date and (y) $100.0 million; provided that
185
Consolidated Total Indebtedness shall not include Indebtedness in respect of (i) any Qualified Receivables Transaction, (ii) letters of credit, except to the extent of unreimbursed amounts thereunder, (iii) Unrestricted Subsidiaries and (iv) Hedging Obligations. For purposes hereof, the “maximum fixed repurchase price” of any Disqualified Stock or Preferred Stock that does not have a fixed repurchase price shall be calculated in accordance with the terms of such Disqualified Stock or preferred stock as if such Disqualified Stock or preferred stock were purchased on any date on which Consolidated Total Indebtedness shall be required to be determined pursuant to the indenture, and if such price is based upon, or measured by, the fair market value of such Disqualified Stock or preferred stock, such fair market value shall be determined reasonably and in good faith by the Issuers.
“Credit Agreement” means that certain Credit Agreement, dated as of the date of the indenture, by and among the Company, as borrower, Holdings, certain subsidiaries of the Company, Bank of America, N.A., as administrative agent, and various lenders providing for up to $1,025.0 million of term loan to be drawn on the closing date and $300.0 million of revolving credit borrowings, including any related notes, Guarantees, collateral documents, instruments and agreements executed in connection therewith, and, in each case, as amended, restated, modified, renewed, refunded, replaced (whether upon or after termination or otherwise) or refinanced by any other Indebtedness (including by means of sales of debt securities and including any amendment, restatement, modification, renewal, refunding, replacement or refinancing that increases the amount borrowed thereunder or extends the maturity thereof) in whole or in part from time to time.
“Credit Facilities” means, one or more debt facilities (including, without limitation, the Credit Agreement) or commercial paper facilities, in each case, with banks or other institutional lenders providing for revolving credit loans, term loans, receivables financing (including through the sale of receivables to such lenders or to special purpose entities formed to borrow from such lenders against such receivables) or letters of credit or any other Indebtedness, in each case, as amended, restated, modified, renewed, refunded, replaced (whether upon or after termination or otherwise) or refinanced (including by means of sales of debt securities and including any amendment, restatement, modification, renewal, refunding, replacement or refinancing that increases the amount borrowed thereunder or extends the maturity thereof) in whole or in part from time to time.
“Default” means any event that is, or with the passage of time or the giving of notice or both would be, an Event of Default.
“Designated Noncash Consideration” means any non-cash consideration received by the Company or a Restricted Subsidiary in connection with an Asset Sale that is designated as Designated Noncash Consideration pursuant to an officers’ certificate, executed by the president and the principal financial officer of the Company.
“Designated Preferred Stock” means preferred stock of the Company (other than Disqualified Stock), that is issued for cash (other than to a Restricted Subsidiary) and is so designated as Designated Preferred Stock, pursuant to an officers’ certificate executed on the date of such issuance.
“Disqualified Stock” means any Capital Stock that, by its terms (or by the terms of any security into which it is convertible, or for which it is exchangeable, in each case, at the option of the holder of the Capital Stock), or upon the happening of any event, matures or is mandatorily redeemable, pursuant to a sinking fund obligation or otherwise, or redeemable at the option of the holder of the Capital Stock, in whole or in part, on or prior to the date that is 90 days after the date on which the notes mature. Notwithstanding the preceding sentence, (x) any Capital Stock that would constitute Disqualified Stock solely because the holders of the Capital Stock have the right to require the Company or the Subsidiary that issued such Capital Stock to repurchase such Capital Stock upon the occurrence of a change of control or an asset sale will not constitute Disqualified Stock, (y) any Capital Stock that would constitute Disqualified Stock solely as a result of any redemption feature that is conditioned upon, and subject to, compliance with the covenant described above under “—Certain Covenants—Restricted Payments” will not constitute Disqualified Stock and (z) any Capital Stock issued to any plan for the benefit of employees will not constitute Disqualified Stock solely because it may be required to be repurchased by the Company or the Subsidiary that issued such Capital Stock in order to satisfy applicable statutory or regulatory obligations. The amount of Disqualified Stock deemed to be outstanding at any time for purposes of the indenture will be the maximum amount that the Company and its Restricted Subsidiaries may become obligated to pay upon the maturity of, or pursuant to any mandatory redemption provisions of, such Disqualified Stock, exclusive of accrued dividends.
186
“Domestic Subsidiary” means any Restricted Subsidiary of the Company that was formed under the laws of the United States or any state of the United States or the District of Columbia or that guarantees any Indebtedness of the Company under the Credit Agreement.
“Equity Interests” means Capital Stock and all warrants, options or other rights to acquire Capital Stock (but excluding any debt security that is convertible into, or exchangeable for, Capital Stock).
“Equity Offering” means a public or private offering of Qualified Capital Stock of the Company or a direct or indirect parent of the Company.
“Exchange Offer” has the meaning set forth for such term in the registration rights agreement.
“Exchange Notes” means the notes issued in the Exchange Offer pursuant to the registration rights agreement.
“Excluded Contributions” means net cash proceeds, marketable securities or Qualified Proceeds received by the Company from (i) contributions to its common equity capital and (ii) the sale (other than to a Subsidiary of the Company or to any management equity plan or stock option plan or any other management or employee benefit plan or agreement of the Company) of Equity Interests (other than Disqualified Stock and Designated Preferred Stock) of the Company, in each case designated as Excluded Contributions pursuant to an officers’ certificate on the date such capital contributions are made or the date such Equity Interests are sold, as the case may be, that are excluded from the calculation set forth in clause (3) of the first paragraph under “—Certain Covenants—Restricted Payments.”
“Existing Indebtedness” means Indebtedness existing on the date of the indenture, plus interest accruing thereon.
“Fair Market Value” means the value that would be paid by a willing buyer to an unaffiliated willing seller in a transaction not involving distress or necessity of either party, determined in good faith by the Board of Directors, chief executive officer or chief financial officer of the Company (unless otherwise provided in the indenture).
“Fixed Charge Coverage Ratio” means with respect to any specified Person for any period, the ratio of the Consolidated Adjusted EBITDA of such Person for such period to the Fixed Charges of such Person for such period. In the event that the specified Person or any of its Restricted Subsidiaries incurs, assumes, guarantees, repays, repurchases, redeems, defeases or otherwise discharges any Indebtedness (other than ordinary working capital borrowings) or issues, repurchases or redeems preferred stock or Disqualified Stock subsequent to the commencement of the period for which the Fixed Charge Coverage Ratio is being calculated and on or prior to the date on which the event for which the calculation of the Fixed Charge Coverage Ratio is made (the “Calculation Date”), then the Fixed Charge Coverage Ratio will be calculated giving pro forma effect to such incurrence, assumption, Guarantee, repayment, repurchase, redemption, defeasance or other discharge of Indebtedness, or such issuance, repurchase or redemption of preferred stock or Disqualified Stock, and the use of the proceeds therefrom, as if the same had occurred at the beginning of the applicable four-quarter reference period.
In addition, for purposes of calculating the Fixed Charge Coverage Ratio:
| | (1) | Investments, acquisitions, mergers, consolidations and dispositions that have been made by the specified Person or any of its Restricted Subsidiaries, or any Person or any of its Restricted Subsidiaries acquired by, merged or consolidated with the specified Person or any of its Restricted Subsidiaries, and including any related financing transactions and including increases in ownership of Restricted Subsidiaries, during the four-quarter reference period or subsequent to such reference period and on or prior to the Calculation Date will be given pro forma effect, including giving effect to Pro Forma Cost Savings, as if they had occurred on the first day of the four-quarter reference period; |
187
| | (2) | the Consolidated Adjusted EBITDA attributable to discontinued operations, as determined in accordance with GAAP, and operations or businesses (and ownership interests therein) disposed of prior to the Calculation Date, will be excluded; |
| | (3) | the Fixed Charges attributable to discontinued operations, as determined in accordance with GAAP, and operations or businesses (and ownership interests therein) disposed of prior to the Calculation Date, will be excluded, but only to the extent that the obligations giving rise to such Fixed Charges will not be obligations of the specified Person or any of its Restricted Subsidiaries following the Calculation Date; |
| | (4) | any Person that is a Restricted Subsidiary on the Calculation Date will be deemed to have been a Restricted Subsidiary at all times during such four-quarter period; |
| | (5) | any Person that is not a Restricted Subsidiary on the Calculation Date will be deemed not to have been a Restricted Subsidiary at any time during such four-quarter period; and |
| | (6) | if any Indebtedness bears a floating rate of interest, the interest expense on such Indebtedness will be calculated as if the rate in effect on the Calculation Date had been the applicable rate for the entire period (taking into account any Hedging Obligation applicable to such Indebtedness). |
For purposes of this definition, whenever pro forma effect is given to a transaction, the pro forma calculations shall be made in good faith by a responsible financial or accounting officer of the Company. For purposes of determining whether any Indebtedness constituting a Guarantee may be incurred, the interest on the Indebtedness to be guaranteed shall be included in calculating the Fixed Charge Coverage Ratio on a pro forma basis. Interest on a Capitalized Lease Obligation shall be deemed to accrue at an interest rate reasonably determined by a responsible financial or accounting officer of the Company to be the rate of interest implicit in such Capitalized Lease Obligation in accordance with GAAP. For purposes of making the computation referred to above, interest on any Indebtedness under a revolving credit facility computed on a pro forma basis shall be computed based upon the average daily balance of such Indebtedness during the applicable period. Interest on Indebtedness that may optionally be determined at an interest rate based upon a factor of a prime or similar rate, a eurocurrency interbank offered rate, or other rate, shall be deemed to have been based upon the rate actually chosen, or, if none, then based upon such optional rate chosen as the Company may designate.
“Fixed Charges” means, with respect to any specified Person for any period, the sum, without duplication, of:
| | (1) | the consolidated interest expense of such Person and its Restricted Subsidiaries for such period, net of interest income, whether paid or accrued, including, without limitation, original issue discount, non-cash interest payments, the interest component of any deferred payment obligations, the interest component of all payments associated with Capital Lease Obligations, commissions, discounts and other fees and charges incurred in respect of letter of credit or bankers’ acceptance financings, and net of the effect of all cash payments made or received pursuant to Hedging Obligations in respect of interest rates, and excluding amortization of deferred financing costs;plus |
| | (2) | any interest on Indebtedness of another Person that is guaranteed by such Person or one of its Restricted Subsidiaries or secured by a Lien on assets of such Person or one of its Restricted Subsidiaries, but only to the extent that such Guarantee or Lien is called upon;plus |
| | (3) | all cash dividends, paid on any series of preferred stock of such Person or any of its Restricted Subsidiaries (other than to the Company or a Restricted Subsidiary of the Company), |
in each case, determined on a consolidated basis in accordance with GAAP.
188
“GAAP” means generally accepted accounting principles set forth in the opinions and pronouncements of the Accounting Principles Board of the American Institute of Certified Public Accountants and statements and pronouncements of the Financial Accounting Standards Board or in such other statements by such other entity as have been approved by a significant segment of the accounting profession, which are in effect on the date of the indenture.
“Government Securities” means direct obligations of, or obligations guaranteed by, the United States of America (including any agency or instrumentality thereof) and the payment for which the United States pledges its full faith and credit.
“Guarantee” means a guarantee other than by endorsement of negotiable instruments for collection in the ordinary course of business, direct or indirect, in any manner including, without limitation, by way of a pledge of assets or through letters of credit or reimbursement agreements in respect thereof, of all or any part of any Indebtedness (whether arising by virtue of partnership arrangements, or by agreements to keep-well, to purchase assets, goods, securities or services, to take or pay or to maintain financial statement conditions or otherwise).
“Guarantors” means each Restricted Subsidiary of the Company that executes a Subsidiary Guarantee in accordance with the provisions of the indenture, and their respective successors and assigns, in each case, until the Subsidiary Guarantee of such Person has been released in accordance with the provisions of the indenture.
“Hedging Obligations” means, with respect to any specified Person, the obligations of such Person under:
| | (1) | interest rate swap agreements (whether from fixed to floating or from floating to fixed), interest rate cap agreements and interest rate collar agreements; |
| | (2) | other agreements or arrangements designed to manage interest rates or interest rate risk; and |
| | (3) | other agreements or arrangements designed to protect such Person against fluctuations in currency exchange rates or commodity prices. |
“Holdings” means IASIS Healthcare Corporation, a Delaware corporation.
“Holdings Loans” means the senior unsecured payment-in-kind loans borrowed by Holdings on April 27, 2007 pursuant to that certain credit agreement dated as of April 27, 2007, among Holdings, the lenders party thereto and Banc of America Bridge LLC, as administrative agent, and including any additional loans outstanding thereunder as a result of the payment-in-kind of interest.
“Hospital” means a hospital, outpatient clinic, long-term care facility, medical office building or other facility, business or other asset that is used or useful in or related to the provision of healthcare services.
“Hospital Investment Program” means, with respect to any Subsidiary of the Company, substantially all of the assets of which consist of one or more Hospitals, an offering by such Subsidiary for the sale or issuance of Equity Interests in such Subsidiary to any Hospital Investment Program Participants; provided that
| | (i) | after giving effect to such sale or issuance with respect to any Subsidiary, the Company directly or indirectly controls such Subsidiary and owns at least 65% of the economic interests of such Subsidiary, |
| | (ii) | each such sale or issuance shall be for an amount at least equal to the Fair Market Value thereof, |
| | (iii) | each such sale results in consideration at least 75% of which shall be in the form of cash (for such purpose, taking into account the amount of cash, the principal amount of any promissory notes and the Fair Market Value of any other consideration), |
189
| | (iv) | the cash and Cash Equivalents received in connection therewith are treated as aggregate cash proceeds in respect of an Asset Sale, and |
| | (v) | each Hospital Investment Program Participant acknowledges in writing that the documentation governing the notes restricts the ability of such Subsidiary to make distributions to such Hospital Investment Program Participant. |
“Hospital Investment Program Participants” means, with respect to any Hospital, Persons interested in such Hospital including physicians, administrators and other Persons in the community in which such Hospital is located.
“Hospital Swap” means an exchange of assets by the Company or a Restricted Subsidiary for one or more Hospitals and/or one or more Related Businesses or for 100% of the Capital Stock of any Person owning or operating one or more Hospitals and/or one or more Related Businesses and, to the extent necessary to equalize the value of the assets being exchanged, the receipt or payment of cash by the Company or a Restricted Subsidiary; provided that cash received by the Company or a Restricted Subsidiary does not exceed 20% of the sum of the amount of the cash and the Fair Market Value of the Capital Stock or assets received by the Company or a Restricted Subsidiary in such transaction, unless such excess cash over the aforementioned 20% threshold is treated as aggregate cash proceeds in respect of an Asset Sale.
“Indebtedness” means, with respect to any specified Person, the principal and premium (if any) of any indebtedness of such Person (excluding accrued expenses and trade payables), whether or not contingent:
| | (1) | in respect of borrowed money; |
| | (2) | evidenced by bonds, notes, debentures or similar instruments or letters of credit (or reimbursement agreements in respect thereof) (other than letters of credit issued in respect of trade payables); |
| | (3) | in respect of banker’s acceptances; |
| | (4) | representing Capital Lease Obligations; |
| | (5) | representing the balance deferred and unpaid of the purchase price of any property or services due more than twelve months after such property is acquired or such services are completed (except any such balance that constitutes a trade payable or similar obligation to a trade creditor); or |
| | (6) | representing the net obligations under any Hedging Obligations, |
if and to the extent any of the preceding items (other than letters of credit, and Hedging Obligations) would appear as a liability upon a balance sheet of the specified Person prepared in accordance with GAAP. In addition, the term “Indebtedness” includes all Indebtedness of others secured by a Lien on any asset of the specified Person (whether or not such Indebtedness is assumed by the specified Person) and, to the extent not otherwise included, the Guarantee by the specified Person of any Indebtedness of any other Person.
“Insurance Subsidiary” means a Subsidiary of the Company or a Restricted Subsidiary established for the purpose of insuring (1) the healthcare businesses or facilities owned or operated by the Company or any Subsidiary of the Company or (2) any physician employed by or on the medical staff of any such business or facility.
“Investment Grade Rating” means a rating equal to or higher than Baa3 (or the equivalent) by Moody’s and BBB- (or the equivalent) by S&P, or an equivalent rating by any other Rating Agency.
“Investments” means, with respect to any Person, all direct or indirect investments by such Person in other Persons (including Affiliates) in the forms of loans (including Guarantees or other obligations), advances or capital contributions (excluding commission, travel, relocation and similar advances to officers and employees made in the ordinary course of business), purchases or other acquisitions for consideration of Indebtedness, Equity Interests or other securities, together with all items that are or would be
190
classified as investments on a balance sheet prepared in accordance with GAAP. If the Company or any Restricted Subsidiary of the Company sells or otherwise disposes of any Equity Interests of any direct or indirect Restricted Subsidiary of the Company such that, after giving effect to any such sale or disposition, such Person is no longer a Subsidiary of the Company, the Company will be deemed to have made an Investment on the date of any such sale or disposition equal to the Fair Market Value of the Company’s Investments in such Subsidiary that were not sold or disposed of in an amount determined as provided in the penultimate paragraph of the covenant described above under the caption “—Certain Covenants—Restricted Payments.” The acquisition by the Company or any Restricted Subsidiary of the Company of a Person that holds an Investment in a third Person will be deemed to be an Investment by the Company or such Restricted Subsidiary in such third Person in an amount equal to the Fair Market Value of the Investments held by the acquired Person in such third Person in an amount determined as provided in the penultimate paragraph of the covenant described above under the caption “—Certain Covenants—Restricted Payments.” The outstanding amount of any Investment shall be the original cost thereof, reduced by all returns on such Investment (including dividends, interest, distributions, returns of principal and profits on sale).
“Lien” means, with respect to any asset, any mortgage, lien, pledge, charge, security interest or encumbrance of any kind in respect of such asset, whether or not filed, recorded or otherwise perfected under applicable law, including any conditional sale or other title retention agreement, any lease in the nature thereof, any option or other agreement to sell or give a security interest in and any filing of or agreement to give any financing statement under the Uniform Commercial Code (or equivalent statutes) of any jurisdiction, except in connection with any Qualified Receivables Transaction.
“Management Services Agreement” means the Management Services Agreement as in effect on June 22, 2004, as described under the caption “Certain Relationships and Related Party Transactions.”
“Net Income” means, with respect to any specified Person, the net income (loss) of such Person, determined in accordance with GAAP and before any reduction in respect of preferred stock dividends.
“Net Proceeds” means the aggregate cash proceeds received by the Company or any of its Restricted Subsidiaries in respect of any Asset Sale (including, without limitation, any cash received upon the sale or other disposition of any non-cash consideration received in any Asset Sale), net of the direct costs relating to such Asset Sale, including, without limitation, legal, accounting and investment banking fees, payments made in order to obtain a necessary consent or required by applicable law, and sales commissions, and any relocation expenses incurred as a result of the Asset Sale, taxes paid or payable as a result of the Asset Sale, including taxes resulting from the transfer of the proceeds of such Asset Sale to the Company, in each case, after taking into account:
| | (1) | any available tax credits or deductions and any tax sharing arrangements; |
| | (2) | amounts required to be applied to the repayment of Indebtedness secured by a Lien on the asset or assets that were the subject of such Asset Sale; |
| | (3) | any reserve for adjustment in respect of the sale price of such asset or assets established in accordance with GAAP; |
| | (4) | any reserve for adjustment in respect of any liabilities associated with the asset disposed of in such transaction and retained by the Company or any Restricted Subsidiary after such sale or other disposition thereof; |
| | (5) | any distributions and other payments required to be made to minority interest holders in Subsidiaries or joint ventures as a result of such Asset Sale; and |
| | (6) | in the event that a Restricted Subsidiary consummates an Asset Sale and makes a pro rata payment of dividends to all of its stockholders from any cash proceeds of such Asset Sale, the amount of dividends paid to any stockholder other than the Company or any other Restricted Subsidiary, |
191
provided that any net proceeds of an Asset Sale by a Non-Guarantor Subsidiary that are subject to restrictions on repatriation to the Company will not be considered Net Proceeds for so long as such proceeds are subject to such restrictions.
“Non-Guarantor Subsidiaries” means (v) any Unrestricted Subsidiary, (w) Health Choice Arizona, Inc., Brim Healthcare of Texas, LLC (d/b/a Wadley Regional Medical Center), Texarkana Regional Healthcare Network, Harpeth Insurance Limited, NLV Healthcare Development, LP, Permian Premier Health Services, Inc., Permian Basin Clinical Services, Inc., Indigent Care Services of Permian Basin, Inc., IASIS Healthcare Foundation, SET Physicians, Southwest Physicians of San Antonio, Odessa Regional Hospital, LP, The Medical Center of Southeast Texas, LP, Southwest General Hospital, LP, Mountain Vista Medical Center, LP, Jordan Valley Medical Center, LP, Davis Hospital & Medical Center, LP and Salt Lake Regional Medical Center, LP, (x) any Receivables Subsidiary, (y) any Subsidiary of the Company that does not guarantee the Company’s Obligations under the Credit Agreement and (z) in addition to the foregoing, any other nonWholly-Owned Subsidiary of the Company. The Board of Directors of the Company may designate any Restricted Subsidiary as a Non-Guarantor Subsidiary by filing with the trustee a certified copy of a resolution of such Board of Directors giving effect to such designation and an officers’ certificate certifying as to the applicable clause of the definition of Non-Guarantor Subsidiaries that warrants such designation. In addition, if a Guarantor that is a guarantor under the Credit Agreement is released from its guarantee of the Credit Agreement, it will be automatically released from its guarantee of the notes and will be a Non-Guarantor Subsidiary.
“Non-Recourse Debt” means Indebtedness:
| | (1) | as to which neither the Company nor any of its Restricted Subsidiaries (a) provides credit support of any kind (including any undertaking, agreement or instrument that would constitute Indebtedness), (b) is directly or indirectly liable as a guarantor or otherwise, or (c) constitutes the lender; |
| | (2) | no default with respect to which (including any rights that the holders of the Indebtedness may have to take enforcement action against an Unrestricted Subsidiary) would permit upon notice, lapse of time or both any holder of any other Indebtedness of the Company or any of its Restricted Subsidiaries to declare a default on such other Indebtedness or cause the payment of such other Indebtedness to be accelerated or payable prior to its Stated Maturity; and |
| | (3) | as to which the lenders have been notified in writing or have agreed in writing (in the agreement relating thereto or otherwise) that they will not have any recourse to the stock or assets of the Company or any of its Restricted Subsidiaries. |
“Obligations” means any principal, interest, penalties, fees, indemnifications, reimbursements, damages and other liabilities payable under the documentation governing any Indebtedness.
“Pari Passu Indebtedness” means:
| | (1) | all Indebtedness of the Issuers or any Guarantor outstanding under the Credit Agreement or under any other Credit Facilities (including post-petition interest at the rate provided in the documentation with respect thereto, whether or not allowed as a claim in any bankruptcy proceeding), and all Hedging Obligations and Treasury Management Obligations with respect thereto; |
| | (2) | any other Indebtedness of the Issuers or any Guarantor permitted to be incurred under the terms of the indenture, unless the instrument under which such Indebtedness is incurred expressly provides that it is subordinated in right of payment to the notes or any Subsidiary Guarantee; and |
| | (3) | all Obligations with respect to the items listed in the preceding clauses (1) and (2). |
Notwithstanding anything to the contrary in the preceding, Pari Passu Indebtedness will not include:
| | (1) | any intercompany Indebtedness of the Issuers or any of their Subsidiaries to the Company or any of its Affiliates; |
192
| | (3) | the portion of any Indebtedness that is incurred in violation of the indenture (but only to the extent so incurred); provided that Indebtedness outstanding under Credit Facilities will not cease to be Pari Passu Indebtedness as a result of this clause (4) if the lenders or agents thereunder obtained a representation from the Company or any of its Subsidiaries on the date such Indebtedness was incurred to the effect that such Indebtedness was not prohibited by the indenture; or |
| | (4) | Indebtedness which is classified as non-recourse in accordance with GAAP or any unsecured claim arising in respect thereof by reason of the application of Section 1111(b)(1) of the Bankruptcy Code. |
“Permitted Business” means (i) any business engaged in by the Company or any of its Restricted Subsidiaries on the date of the original issuance of the notes, (ii) any business or other activities that are reasonably similar, ancillary, complementary or related to, or a reasonable extension, development or expansion of, the businesses in which the Company and its Restricted Subsidiaries are engaged on the date of original issuance of the notes and (iii) any business in the healthcare industry.
“Permitted Holders” means (i) TPG Partners IV, L.P., JLL Partners Fund IV, L.P., Trimaran Fund Management, L.L.C. and their respective Affiliates, but not including any portfolio companies of any of the foregoing and (ii) any group (within the meaning of Section 13(d)(3) or Section 14(d)(2) of the Exchange Act or any successor provision) of which any of the foregoing beneficially own more than 50.0% of the total voting power of the aggregate Voting Stock of the Company held by such group.
“Permitted Investments” means:
| | (1) | any Investment in the Company or in a Restricted Subsidiary of the Company; provided that any Investment in a Non-Guarantor Subsidiary by either Issuer or a Guarantor shall be evidenced by (A) a certificate, or other evidence of equity, in the case of any Investment in the form of equity or (B) a note, or other evidence of Indebtedness, in the case of any Investment in the form of Indebtedness, in each case, issued to and held by such Issuer or Guarantor, as applicable, except to the extent of the Fair Market Value of assets received by such Issuer or Guarantor, as applicable, in respect of such Investment; |
| | (2) | any Investment in Cash Equivalents; |
| | (3) | any Investment by the Company or any Restricted Subsidiary of the Company in a Person, if as a result of such Investment: |
| | (a) | such Person becomes a Restricted Subsidiary of the Company; or |
| | (b) | such Person, in one transaction or a series of transactions, is merged, consolidated or amalgamated with or into, or transfers or conveys substantially all of its assets to, or is liquidated into, the Company or a Restricted Subsidiary of the Company; |
| | (4) | any Investment made as a result of the receipt of non-cash consideration from an Asset Sale that was made pursuant to and in compliance with the covenant described above under the caption “—Repurchase at the Option of Holders—Asset Sales”; |
| | (5) | any Investment solely in exchange for the issuance of Equity Interests (other than Disqualified Stock) of the Company; |
193
| | (6) | any Investments received in compromise, settlement or resolution of (A) obligations of trade creditors or customers that were incurred in the ordinary course of business of the Company or any of its Restricted Subsidiaries, including pursuant to any plan of reorganization or similar arrangement upon the bankruptcy or insolvency of any trade creditor or customer, (B) litigation, arbitration or other disputes with Persons who are not Affiliates or (C) as a result of a foreclosure by the Company or any Restricted Subsidiary with respect to any secured Investment or other transfer of title with respect to any secured Investment in default; |
| | (7) | Investments represented by Hedging Obligations; |
| | (8) | any Investment in payroll, travel and similar advances to cover business-related travel expenses, moving expenses or other similar expenses, in each case incurred in the ordinary course of business; |
| | (9) | Investments in receivables owing to the Company or any Restricted Subsidiary if created or acquired in the ordinary course of business and payable or dischargeable in accordance with customary trade terms; provided, however, that such trade terms may include such concessionary trade terms as the Company or any such Restricted Subsidiary deems reasonable under the circumstances; |
| | (10) | Investments in prepaid expenses, negotiable instruments held for collection and lease, utility and workers compensation, performance and similar deposits entered into as a result of the operations of the business in the ordinary course of business; |
| | (11) | obligations of one or more officers or other employees of the Company or any of its Restricted Subsidiaries in connection with such officer’s or employee’s acquisition of shares of common stock of the Company so long as no cash or other assets are paid by the Company or any of its Restricted Subsidiaries to such officers or employees in connection with the acquisition of any such obligations; |
| | (12) | loans or advances to and guarantees provided for the benefit of employees made in the ordinary course of business of the Company or the Restricted Subsidiary of the Company in an aggregate principal amount not to exceed $12.5 million at any one time outstanding; |
| | (13) | Investments existing as of the date of the indenture or made pursuant to a binding commitment existing on the date hereof or an Investment consisting of any extension, modification or renewal of any Investment existing as of the date of the indenture (excluding any such extension, modification or renewal involving additional advances, contributions or other investments of cash or property or other increases thereof unless it is a result of the accrual or accretion of interest or original issue discount or payment-in-kind pursuant to the terms, as of the date of the indenture, of the original Investment so extended, modified or renewed); |
| | (14) | repurchases of the notes; |
| | (15) | other Investments in any Person having an aggregate Fair Market Value (measured on the date each such Investment was made and without giving effect to subsequent changes in value), when taken together with all other Investments made pursuant to this clause (15) that are at the time outstanding not to exceed the greater of $125.0 million and 5% of Total Assets; provided,however, that if any Investment pursuant to this clause (15) is made in any Person that is not a Restricted Subsidiary of the Company at the date of the making of such Investment and such Person becomes a Restricted Subsidiary of the Company after such date, such Investment shall thereafter be deemed to have been made pursuant to clause (1) above and shall cease to have been made pursuant to this clause (15) for so long as such Person continues to be a Restricted Subsidiary (it being understood that if such Person thereafter ceases to be a Restricted Subsidiary of the Company, such Investment will again be deemed to have been made pursuant to this clause (15)); |
194
| | (16) | the acquisition by a Receivables Subsidiary in connection with a Qualified Receivables Transaction of Equity Interests of a trust or other Person established by such Receivables Subsidiary to effect such Qualified Receivables Transaction; and any other Investment by the Company or a Subsidiary of the Company in a Receivables Subsidiary or any Investment by a Receivables Subsidiary in any other Person in connection with a Qualified Receivables Transaction customary for such transactions; |
| | (17) | Investments in connection with Hospital Swaps; |
| | (18) | Physician Support Obligations; |
| | (19) | Investments in an Insurance Subsidiary in an amount that does not exceed the minimum amount of capital required under the laws of the jurisdiction in which the Insurance Subsidiary is formed plus the amount of any reasonable general corporate and overhead expenses of such Insurance Subsidiary, and any Investment by such Insurance Subsidiary that is a legal investment for an insurance company under the laws of the jurisdiction in which the Insurance Subsidiary is formed and made in the ordinary course of business and rated in one of the four highest rating categories; |
| | (20) | Investments in Health Choice Arizona, Inc. required to be made under applicable laws, rules and regulations or pursuant to contractual obligations of the Company or a Subsidiary with the Arizona Health Care Cost Containment System as in effect on the date of the indenture; |
| | (21) | Investments consisting of repurchase or redemptions of Capital Stock of Subsidiaries sold or issued in connection with the Company’s Hospital Investment Program and (ii) Investments in joint ventures to the extent required by, or made pursuant to, customary buy/sell arrangements between the joint venture parties set forth in the joint venture arrangements and similar binding arrangements; and |
| | (22) | additional investments in Unrestricted Subsidiaries and/or joint ventures of the Company or any Restricted Subsidiary existing on the date of the indenture in an aggregate amount not to exceed $50.0 million. |
“Permitted Liens” means:
| | (1) | Liens in favor of the Issuers or the Guarantors; |
| | (2) | Liens on property or assets of a Person, plus renewals and extensions of such Liens, existing at the time such Person is merged with or into, consolidated with or acquired by the Company or any Subsidiary of the Company; provided that such Liens were in existence prior to the contemplation of such merger, consolidation or acquisition and do not extend to any assets other than those of the Person merged into, consolidated with or acquired by the Company or such Subsidiary, and other than pursuant to customary after-acquired property clauses; |
| | (3) | Liens on property (including Capital Stock) existing at the time of acquisition of the property by the Company or any Restricted Subsidiary of the Company; provided that such Liens were in existence prior to, such acquisition, and not incurred in contemplation of, such acquisition; |
| | (4) | Liens (including deposits and pledges) to secure the performance of public or statutory obligations, progress payments, surety or appeal bonds, performance bonds or other obligations of a like nature incurred in the ordinary course of business; |
195
| | (5) | Liens to secure Indebtedness (including Capital Lease Obligations) permitted by clause (4) of the second paragraph of the covenant entitled “—Certain Covenants—Incurrence of Indebtedness and Issuance of Disqualified Stock and Preferred Stock” covering only the assets acquired, constructed or improved with or financed by such Indebtedness, and additions, accessions, improvements and replacements and customary deposits in connection therewith;provided that individual financings of equipment provided by one lender may be cross collateralized to other financings of equipment provided by such lender; |
| | (6) | Liens existing on the date of the indenture (other than Liens securing the Credit Agreement), plus renewals and extensions of such Liens; |
| | (7) | Liens for taxes, assessments or governmental charges or claims that are not yet delinquent or that are being contested in good faith by appropriate proceedings promptly instituted and diligently concluded; provided that any reserve or other appropriate provision as is required in conformity with GAAP has been made therefor; |
| | (8) | Liens imposed by law, such as carriers’, warehousemen’s, landlord’s, materialmen’s, laborers’, employees’, suppliers’ and mechanics’ Liens, in each case, incurred in the ordinary course of business; |
| | (9) | survey exceptions, title defects, encumbrances, easements or reservations of, or rights of others for, licenses, rights-of-way, sewers, electric lines, telegraph and telephone lines and other similar purposes, or zoning or other restrictions as to the use of real property that do not materially interfere with the ordinary conduct of the business of the Company and its Subsidiaries, taken as a whole; |
| | (10) | Liens created for the benefit of (or to secure) the notes (or the Subsidiary Guarantees); |
| | (11) | Liens to secure any Permitted Refinancing Indebtedness permitted to be incurred under the indenture; provided, however, that: |
| | (a) | the new Lien shall be limited to all or part of the same property and assets that secured or, under the written agreements pursuant to which the original Lien arose, could secure the original Indebtedness (plus improvements and accessions to, such property or proceeds or distributions thereof); and |
| | (b) | the Indebtedness secured by the new Lien is not increased to any amount greater than the sum of (x) the outstanding principal amount, or, if greater, committed amount, of the Permitted Refinancing Indebtedness and (y) an amount necessary to pay any fees and expenses, including premiums, related to such renewal, refunding, refinancing, replacement, defeasance or discharge; |
| | (12) | Liens incurred in connection with a Qualified Receivables Transaction (which, in the case of the Company and its Restricted Subsidiaries (other than Receivables Subsidiaries) shall be limited to receivables and related assets referred to in the definition of Qualified Receivables Transaction); |
| | (13) | Liens incurred in the ordinary course of business of the Company or any Subsidiary of the Company with respect to obligations that do not exceed $75.0 million at any one time outstanding; |
| | (14) | security for the payment of workers’ compensation, unemployment insurance, other social security benefits or other insurance-related obligations (including, but not limited to, in respect of deductibles, self-insured retention amounts and premiums and adjustments thereto) entered into in the ordinary course of business; |
196
| | (15) | deposits or pledges in connection with bids, tenders, leases and contracts (other than contracts for the payment of money), and Liens arising from conditional sale, title retention, consignment and similar arrangements, in each case entered into in the ordinary course of business; |
| | (16) | zoning restrictions, easements, licenses, reservations, provisions, encroachments, encumbrances, protrusion permits, servitudes, covenants, conditions, waivers, restrictions on the use of property or minor irregularities of title (and with respect to leasehold interests, mortgages, obligations, liens and other encumbrances incurred, created, assumed or permitted to exist and arising by, through or under a landlord or owner of the leased property, with or without consent of the lessee), in each case, not materially interfering with the ordinary conduct of the business of the Company and its Subsidiaries, taken as a whole; |
| | (17) | leases, subleases, licenses or sublicenses to third parties entered into in the ordinary course of business; |
| | (18) | Liens securing Hedging Obligations and cash management obligations; |
| | (19) | Liens arising out of judgments, decrees, orders or awards in respect of which the Company shall in good faith be prosecuting an appeal or proceedings for review which appeal or proceedings shall not have been finally terminated, or if the period within which such appeal or proceedings may be initiated shall not have expired; |
| | (20) | Liens on Capital Stock of an Unrestricted Subsidiary that secure Indebtedness or other obligation of such Unrestricted Subsidiary; |
| | (21) | Liens on assets of Restricted Subsidiaries that are not Guarantors securing Indebtedness in an aggregate principal amount not to exceed $50.0 million; |
| | (22) | Liens on the assets of Non-Guarantor Subsidiaries securing Indebtedness of the Company or the Restricted Subsidiaries that were permitted by the terms of the indenture to be incurred; and |
| | (23) | Liens securing Indebtedness under one or more Credit Facilities or other pari passu Indebtedness permitted to be incurred pursuant to the covenant described under “—Certain Covenants— Incurrence of Indebtedness and Issuance of Disqualified Stock and Preferred Stock” in an amount not to exceed the greater of (i) the amount of Indebtedness permitted to be incurred pursuant to clause (1) under “—Certain Covenants—Incurrence of Indebtedness and Issuance of Disqualified Stock and Preferred Stock” and (ii) the amount of Indebtedness such that the Consolidated Secured Debt Ratio (at the time of incurrence of such Indebtedness after giving pro forma effect thereto in a manner consistent with the calculation of the Fixed Charge Coverage Ratio) would not be greater than 3.75 to 1.00. |
“Permitted Payments to Parent” means
| | (1) | payments, directly or indirectly, to Holdings to be used by Holdings to pay (x) consolidated, combined or similar Federal, state and local taxes payable by Holdings and directly attributable to (or arising as a result of) the operations of the Company and its Subsidiaries and (y) franchise or similar taxes and fees of Holdings required to maintain Holdings’ corporate existence and other taxes; provided, that: |
| | (a) | the amount of such dividends, distributions or advances paid shall not exceed the amount (x) that would be due with respect to a consolidated, combined or similar Federal, state or local tax return that included the Company and its Subsidiaries if the Company were a corporation for Federal, state and local tax purposes plus (y) the actual amount of such franchise or similar taxes and fees of Holdings required to maintain Holdings’ corporate existence and other taxes, each as applicable; and |
197
| | (b) | such payments are used by Holdings for such purposes within 90 days of the receipt of such payments; and |
| | (2) | payments, directly or indirectly, to Holdings if the proceeds thereof are used to pay general corporate and overhead expenses (including salaries and other compensation of employees) incurred in the ordinary course of its business or of the business of its parent holding company as a direct or indirect holding company for the Company. |
“Permitted Refinancing Indebtedness” means any Indebtedness of the Company or any of its Restricted Subsidiaries issued in exchange for, or the net proceeds of which are used to extend, renew, refund, refinance, replace, defease or discharge other Indebtedness of the Company or any of its Restricted Subsidiaries (other than intercompany Indebtedness); provided that:
| | (1) | the principal amount (or accreted value, if applicable) of such Permitted Refinancing Indebtedness does not exceed the principal amount (or accreted value, if applicable) of the Indebtedness extended, renewed, refunded, refinanced, replaced, defeased or discharged (plus all accrued interest on the Indebtedness and the amount of all fees, commissions, discounts and expenses, including premiums, incurred in connection therewith); |
| | (2) | either (a) such Permitted Refinancing Indebtedness has a final maturity date later than the final maturity date of, and has a Weighted Average Life to Maturity equal to or greater than the Weighted Average Life to Maturity of, the Indebtedness being extended, renewed, refunded, refinanced, replaced, defeased or discharged or (b) all scheduled payments on or in respect of such Permitted Refinancing Indebtedness (other than interest payments) shall be at least 91 days following the final scheduled maturity of the notes; and if such Indebtedness is Pari Passu Indebtedness and has a final stated maturity later than the final stated maturity of the notes, such Permitted Refinancing Indebtedness has a final stated maturity later than the final maturity of the notes; |
| | (3) | if the Indebtedness being extended, renewed, refunded, refinanced, replaced, defeased or discharged is subordinated in right of payment to the notes, such Permitted Refinancing Indebtedness is subordinated in right of payment to the notes on terms at least as favorable to the holders of notes as those contained in the documentation governing the Indebtedness being extended, renewed, refunded, refinanced, replaced, defeased or discharged; and |
| | (4) | such Indebtedness is incurred |
| | (a) | by the Company or by the Restricted Subsidiary who is the obligor on the Indebtedness being renewed, refunded, refinanced, replaced, defeased or discharged; |
| | (b) | by any Guarantor if the obligor on the Indebtedness being renewed, refunded, refinanced, replaced, defeased or discharged is a Guarantor; or |
| | (c) | by any Non-Guarantor Subsidiary if the obligor on the Indebtedness being renewed, refunded, refinanced, replaced, defeased or discharged is a Non-Guarantor Subsidiary. |
“Person” means any individual, corporation, partnership, joint venture, association, joint-stock company, trust, unincorporated organization, limited liability company or government or other entity.
“Physician Support Obligation” means a loan to or on behalf of, or a guarantee of indebtedness of, a physician or healthcare professional providing service to patients in the service area of a Hospital or other health care facility operated by the Company or any of its Restricted Subsidiaries made or given by the Company or any Subsidiary of the Company (a) in the ordinary course of its business and (b) pursuant to a written agreement having a period not to exceed five years.
198
“Pro Forma Cost Savings” means, with respect to any period, the reduction in net costs and related adjustments that (i) were directly attributable to an acquisition, merger, consolidation or disposition that occurred during the four-quarter reference period or subsequent to the four-quarter reference period and on or prior to the Calculation Date and calculated on a basis that is consistent with Regulation S-X under the Securities Act as in effect and applied as of the date of the indenture or (ii) have been realized or for which the steps necessary for realization have been taken or are reasonably expected to be taken within 12 months following any such acquisition and, in the case of each of (i) and (ii), are described, as provided below, in an officers’ certificate, as if all such reductions in costs had been effected as of the beginning of such period. Pro Forma Cost Savings described above shall be accompanied by an officers’ certificate delivered to the trustee from the Company’s chief financial officer that outlines the specific actions taken or to be taken, the net cost savings achieved or to be achieved from each such action.
“Qualified Capital Stock” means any Capital Stock that is not Disqualified Stock.
“Qualified Proceeds” means any of the following or any combination of the following:
| | (2) | the Fair Market Value of assets that are used or useful in the Permitted Business; and |
| | (3) | the Fair Market Value of the Capital Stock of any Person engaged primarily in a Permitted Business if, in connection with the receipt by the Company or any of its Restricted Subsidiaries of such Capital Stock, such Person becomes a Restricted Subsidiary or such Person is merged or consolidated into the Company or any Restricted Subsidiary; |
provided that Qualified Proceeds shall not include Excluded Contributions.
“Qualified Receivables Transaction” means any transaction or series of transactions entered into by the Company or any of its Subsidiaries pursuant to which the Company or any of its Subsidiaries sells, conveys or otherwise transfers, or grants a security interest, to:
| | (1) | a Receivables Subsidiary (in the case of a transfer by the Company or any of its Subsidiaries, which transfer may be effected through the Company or one or more of its Subsidiaries); and |
| | (2) | if applicable, any other Person (in the case of a transfer by a Receivables Subsidiary), |
in each case, in any accounts receivable (including health care insurance receivables), instruments, chattel paper, general intangibles and similar assets (whether now existing or arising in the future, the “Receivables”) of the Company or any of its Subsidiaries, and any assets related thereto, including, without limitation, all collateral securing such Receivables, all contracts, contract rights and all guarantees or other obligations in respect of such Receivables, proceeds of such Receivables and any other assets, which are customarily transferred or in respect of which security interests are customarily granted in connection with receivables financings and asset securitization transactions of such type, together with any related transactions customarily entered into in a receivables financings and asset securitizations, including servicing arrangements.
“Rating Agencies” mean Moody’s and S&P or if Moody’s or S&P or both shall not make a rating on the notes publicly available, a nationally recognized statistical rating agency or agencies, as the case may be, selected by the Issuer (as certified by a Board Resolution) which shall be substituted for Moody’s or S&P or both, as the case may be.
“Receivables Fees” means distributions or payments made directly or by means of discounts with respect to any participation interest issued or sold in connection with, and other fees paid to a Person that is not a Restricted Subsidiary in connection with, any Qualified Receivables Transaction.
199
“Receivables Subsidiary” means a Subsidiary of the Company which engages in no activities other than in connection with the financing of accounts receivable and in businesses related or ancillary thereto and that is designated by the Board of Directors of the Company (as provided below) as a Receivables Subsidiary (A) no portion of the Indebtedness or any other Obligations (contingent or otherwise) of which:
| | (1) | is guaranteed by the Company or any Subsidiary of the Company (excluding guarantees of Obligations (other than the principal of, and interest on, Indebtedness) pursuant to representations, warranties, covenants and indemnities entered into in the ordinary course of business in connection with a Qualified Receivables Transaction); |
| | (2) | is recourse to or obligates the Company or any Subsidiary of the Company in any way other than pursuant to representations, warranties, covenants and indemnities customarily entered into in connection with a Qualified Receivables Transaction; or |
| | (3) | subjects any property or asset of the Company or any Subsidiary of the Company (other than accounts receivable and related assets as provided in the definition of Qualified Receivables Transaction), directly or indirectly, contingently or otherwise, to the satisfaction thereof, other than pursuant to representations, warranties, covenants and indemnities customarily entered into in connection with a Qualified Receivables Transaction; and |
(B) with which neither the Company nor any Subsidiary of the Company has any material contract, agreement, arrangement or understanding other than on terms no less favorable to the Company or such Subsidiary than those that might be obtained at the time from Persons who are not Affiliates of the Company, other than as may be customary in a Qualified Receivables Transaction including for fees payable in the ordinary course of business in connection with servicing accounts receivable; and (C) with which neither the Company nor any Subsidiary of the Company has any obligation to maintain or preserve such Subsidiary’s financial condition or cause such Subsidiary to achieve certain levels of operating results. Any such designation by the Board of Directors of the Company will be evidenced to the Trustee by filing with the Trustee a certified copy of the resolution of the Board of Directors of the Company giving effect to such designation and an officers’ certificate certifying that such designation complied with the foregoing conditions.
“Related Business” means a healthcare business affiliated or associated with a Hospital or any business related or ancillary to the provision of healthcare services or information or the investment in, or the management, leasing or operation of, a Hospital.
“Replacement Preferred Stock” means any Disqualified Stock or preferred stock of the Company or any of its Restricted Subsidiaries issued in exchange for, or the net proceeds of which are used to renew, refund, refinance, replace or discharge any other preferred stock of the Company or any of its Restricted Subsidiaries (other than intercompany preferred stock); provided that such Replacement Preferred Stock is issued by the Company or by the Restricted Subsidiary who is the issuer of the preferred stock being renewed, refunded, refinanced, replaced or discharged.
“Restricted Investment” means an Investment other than a Permitted Investment.
“Restricted Subsidiary” of a Person means any Subsidiary of the referent Person that is not an Unrestricted Subsidiary. In the event of a Specified Change of Control Parent Assumption, the Company shall be a Restricted Subsidiary.
“Significant Subsidiary” means any Subsidiary that would be a “significant subsidiary” as defined in Article 1, Rule 1-02 of Regulation S-X, promulgated pursuant to the Securities Act, as such Regulation is in effect on the date of the indenture.
“Special Interest” means all special interest then owing pursuant to the registration rights agreement.
200
“Specified Change of Control” means a Change of Control transaction in which the following conditions are satisfied: (i) the Issuers shall comply with the provisions of the Indenture applicable to a Change of Control, including the making of a Change of Control Offer except as otherwise provided under “—Repurchase at the Option of Holders—Change of Control”, (ii) to the extent such transaction involves a merger with or the acquisition by another Person with ongoing material operations, such person is a Permitted Business or a Related Business, (iii) after giving pro forma effect to the Specified Change of Control and any related financing transactions (including any incurrence of Indebtedness with respect thereto), with such pro forma adjustments to Consolidated Total Indebtedness and Consolidated Adjusted EBITDA as are appropriate and consistent with the pro forma adjustment provisions set forth in the definition of “Fixed Charge Coverage Ratio”, the Total Leverage Ratio of the Company and its Restricted Subsidiaries would not exceed 5.75 to 1.0, (iv) no Default or Event of Default is continuing or would result from the Specified Change of Control and (v) such transaction is designated as a Specified Change of Control pursuant to an officers’ certificate on or prior to the date such Specified Change of Control occurs certifying as to the applicable conditions set forth in clauses (i) through (iv) of this definition; provided, however that no more than one Change of Control transaction may be designated and treated as a Specified Change of Control under the indenture.
“Specified Change of Control Parent” means any person as to which the Company is a Restricted Subsidiary as a result of a Specified Change of Control.
“Specified Change of Control Parent Assumption” means the irrevocable assumption by a Specified Change of Control Parent of all of the obligations of the Company in the indenture in connection with and upon the consummation of a Specified Change of Control; provided, however, that such assumption may only be made if, after giving pro forma effect to the Specified Change of Control and any related financing transactions, the Specified Change of Control Parent would meet the conditions described in clause (1)(b), (2), (3) and (4) of the first paragraph contained under the covenant “—Merger, Consolidation or Sale of Assets” (assuming for this purpose that the Specified Change of Control Parent were the surviving corporation in a merger with the Company).
“Specified Change of Control Parent Assumption Date” means the date of occurrence of a Specified Change of Control Parent Assumption, as designated by the Company; provided, however, that such date may not be later than 180 days after the occurrence of the Specified Change of Control.
“Stated Maturity” means, with respect to any installment of interest or principal on any series of Indebtedness, the date on which the payment of interest or principal was scheduled to be paid in the documentation governing such Indebtedness as of the date of the indenture, and will not include any contingent obligations to repay, redeem or repurchase any such interest or principal prior to the date originally scheduled for the payment thereof.
“Subordinated Indebtedness” means
| | (a) | with respect to the Issuers, any Indebtedness of such Issuer which is by its terms subordinated in right of payment to the notes, and |
| | (b) | with respect to any Guarantor, any Indebtedness of such Guarantor which is by its terms subordinated in right of payment to the Guarantee of such Guarantor under the indenture. |
“Subordinated Management Fees” means the management fees payable pursuant to the Management Services Agreement which in the event of a bankruptcy of the Company shall be subordinated to the prior payment in full, in cash, of all Obligations due in respect of the notes (including interest after the commencement of any bankruptcy proceeding at the rate specified in the notes) and payment of which shall be suspended during the continuance of a payment default in respect of the notes
“Subsidiary” means, with respect to any specified Person:
| | (1) | any corporation, association or other business entity of which more than 50% of the total voting power of shares of Capital Stock entitled (without regard to the occurrence of any contingency and |
201
| | after giving effect to any voting agreement or stockholders’ agreement that effectively transfers voting power) to vote in the election of directors, managers or trustees of the corporation, association or other business entity is at the time owned or controlled, directly or indirectly, by that Person or one or more of the other Subsidiaries of that Person (or a combination thereof); and |
| | (2) | any partnership (a) the sole general partner or the managing general partner of which is such Person or a Subsidiary of such Person or (b) the only general partners of which are that Person or one or more Subsidiaries of that Person (or any combination thereof). |
“Subsidiary Guarantee” means the Guarantee by each Guarantor of the Issuers’ obligations under the indenture and the notes, executed pursuant to the provisions of the indenture.
“Total Assets” means the total consolidated assets of the Company and its Restricted Subsidiaries as set forth on the most recent consolidated balance sheet of the Company and its Restricted Subsidiaries.
“Total Leverage Ratio” means, as of the date of determination, the ratio of (a) Consolidated Total Indebtedness of the Issuers and their Restricted Subsidiaries as of the end of the most recent fiscal quarter for which internal financial statements are available to (b) Consolidated Adjusted EBITDA of the Issuers and their Restricted Subsidiaries for the most recently ended four fiscal quarters ending immediately prior to such date for which internal financial statements are available, in each case with such pro forma adjustments to Consolidated Total Indebtedness and Consolidated Adjusted EBITDA as are appropriate and consistent with the pro forma adjustment provisions set forth in the definition of “Fixed Charge Coverage Ratio.”
“Transactions” means, collectively, the transactions contemplated by the indenture and the Credit Agreement, including the borrowings under the Credit Agreement and the offering of the notes, the consummation of a cash tender offer for or redemption of all outstanding 8 3/4% Senior Subordinated Notes due 2014 of the Issuers, the Restricted Payment to Holdings to fund the repayment of the Holdings Loans, other Restricted Payments to Holdings in an amount not to exceed $233,000,000, the consummation of any other transactions in connection with the foregoing and the payment of the fees and expenses incurred in connection with any of the foregoing.
“Treasury Management Obligations” means obligations under any agreement governing the provision of treasury or cash management services, including deposit accounts, funds transfer, automated clearinghouse, zero balance accounts, returned check concentration, controlled disbursement, lockbox, account reconciliation and reporting and trade finance services. Treasury Management Obligations shall not constitute Indebtedness.
“Treasury Rate” means, as of any redemption date, the yield to maturity as of such redemption date of United States Treasury securities with a constant maturity (as compiled and published in the most recent Federal Reserve Statistical Release H.15 (519) that has become publicly available at least two Business Days prior to the redemption date (or, if such Statistical Release is no longer published, any publicly available source of similar market data)) most nearly equal to the period from the redemption date to May 15, 2014;provided that if the period from the redemption date to May 15, 2014 is less than one year, the weekly average yield on actively traded United States Treasury securities adjusted to a constant maturity of one year will be used.
“Unrestricted Subsidiary” means any Subsidiary of the Company and any Subsidiary of an Unrestricted Subsidiary that is designated by the Board of Directors of the Company as an Unrestricted Subsidiary pursuant to a resolution of the Board of Directors, but only to the extent that such Subsidiary:
| | (1) | has no Indebtedness other than Non-Recourse Debt; |
| | (2) | except as permitted by the covenant described above under the caption “—Certain Covenants— Transactions with Affiliates,” is not party to any agreement, contract, arrangement or understanding with the Company or any Restricted Subsidiary of the Company unless the terms of any such agreement, contract, arrangement or understanding are no less favorable to the Company or such Restricted Subsidiary than those that might be obtained at the time from Persons who are not Affiliates of the Company; |
202
| | (3) | is a Person with respect to which neither the Company nor any of its Restricted Subsidiaries has any direct or indirect obligation (a) to subscribe for additional Equity Interests or (b) to maintain or preserve such Person’s financial condition or to cause such Person to achieve any specified levels of operating results; and |
| | (4) | has not guaranteed or otherwise directly or indirectly provided credit support for any Indebtedness of the Company or any of its Restricted Subsidiaries, except in the case of clauses (3) and (4), to the extent: |
| | (A) | that the Company or such Restricted Subsidiary could otherwise provide such a guarantee or incur such Indebtedness (other than as Permitted Debt) as described above under the caption “—Certain Covenants—Incurrence of Indebtedness and Issuance of Disqualified Stock and Preferred Stock”, and |
| | (B) | the provision of such guarantee and the incurrence of such indebtedness otherwise would be permitted as described above under the caption “—Certain Covenants—Restricted Payments.” |
“Voting Stock” of any specified Person as of any date means the Capital Stock of such Person that is at the time entitled to vote in the election of the Board of Directors of such Person.
“Weighted Average Life to Maturity” means, when applied to any Indebtedness at any date, the number of years obtained by dividing:
| | (1) | the sum of the products obtained by multiplying (a) the amount of each then remaining installment, sinking fund, serial maturity or other required payments of principal, including payment at final maturity, in respect of the Indebtedness, by (b) the number of years (calculated to the nearest one-twelfth) that will elapse between such date and the making of such payment; by |
| | (2) | the then outstanding principal amount of such Indebtedness. |
“Wholly-Owned Domestic Subsidiary” means a Domestic Subsidiary that is a Wholly-Owned Subsidiary of the Company.
“Wholly Owned Subsidiary” of any specified Person means a Subsidiary of such Person all of the outstanding Capital Stock or other ownership interest of which (other than directors’ qualifying shares) will as that time be owned by such Person or by one or more Wholly Owned Subsidiaries of such person.
203
CERTAIN UNITED STATES FEDERAL INCOME TAX CONSIDERATIONS
The following is a summary of certain U.S. federal income tax considerations of the exchange offer and the ownership and disposition of New Notes issued pursuant to the exchange offer. This summary does not describe all of the tax consequences that may be relevant to you in light of your particular circumstances. For example, it does not address considerations that may be relevant to you if you are an investor that is subject to special tax rules such as banks, thrifts, real estate investment trusts, regulated investment companies, insurance companies, dealers in securities or currencies, traders in securities electing to mark to market, tax-exempt investors, controlled foreign corporations, passive foreign investment companies, or U.S. expatriates. It also does not discuss Notes held as part of a hedge, straddle, conversion, “synthetic security” or other integrated transaction. This summary addresses only holders that purchased the Old Notes in connection with their original issue from the initial purchaser at the issue price (i.e., the first price at which a substantial amount of notes is sold for money, other than to bondhouses, brokers or similar persons acting in the capacity of underwriters, placement agents or wholesalers), that acquire the New Notes in this exchange offer and that held the Old Notes as capital assets for U.S. federal income tax purposes. It does not include any description of any alternative minimum tax consequences, federal estate tax consequences or the tax laws of any state or local government or of any foreign government that may be applicable to the Notes. Prospective holders should consult their tax advisors as to the particular tax consequences to them of the exchange offer, and holding and disposing of the New Notes.
This summary is based upon the Internal Revenue Code of 1986, as amended (the “Code”), Treasury regulations, Internal Revenue Service (“IRS”) rulings and pronouncements and administrative and judicial decisions currently in effect, all of which are subject to change (possibly with retroactive effect) or possible differing interpretations.
If an entity treated as a partnership for U.S. federal income tax purposes is a holder, the tax treatment of a partner in the partnership will generally depend upon the status of the partner and the activities of the partnership. A holder that is a partnership, and partners in such a partnership, should consult their own tax advisors regarding the tax consequences of the exchange offer, and holding and disposing of the New Notes.
U.S. Holders
For the purposes of this summary, you are a “U.S. Holder” if you are a beneficial owner of the Notes and, for U.S. federal income tax purposes:
| | • | | You are an individual who is a citizen or resident of the United States; |
| | • | | You are a corporation or other entity taxable as a corporation under U.S. federal income tax laws created or organized in or under the laws of the United States, any state thereof or the District of Columbia; |
| | • | | You are an estate the income of which is includable in gross income for U.S. federal income tax purposes regardless of its source; or |
| | • | | You are a trust whose administration is subject to the primary supervision of a U.S. court and which has one or more U.S. persons who have the authority to control all substantial decisions of the trust or a trust that was in existence on August 20, 1996, was treated as a U.S. person prior to such date and has elected to continue to be treated as a U.S. person. |
Tax Consequences to U.S. Holders who Participate in the Exchange Offer
Neither the registration of the exchange offer pursuant to our obligations under the registration rights agreement nor the receipt of New Notes in exchange for Old Notes will constitute a taxable event to U.S. Holders for U.S. federal income tax purposes. U.S. Holders will retain the tax basis in the New Notes they had in the Old Notes, and the holding period for the New Notes will include the holding period for the Old Notes before such Old Notes were registered.
204
Payments of Interest
Interest on a New Note will generally be taxable to a U.S. Holder as ordinary income at the time it is paid or accrued in accordance with the U.S. Holder’s regular method of accounting for U.S. federal income tax purposes.
Sale, Redemption or Other Disposition
Subject to the discussion below in “—Specified Change of Control Parent Assumption,” a U.S. Holder will recognize taxable gain or loss on the sale, redemption, retirement or other taxable disposition of a New Note. The amount of gain or loss recognized will generally equal the difference between the amount received for the New Note (less amounts attributable to accrued but unpaid interest, which will be taxable as interest income to the extent not previously included in income by the U.S. Holder) and the adjusted tax basis of the New Note. A U.S. Holder’s adjusted tax basis in a New Note will generally be the cost of the corresponding Old Note. Any such gain or loss will generally constitute capital gain or loss and will be long-term capital gain or loss if the U.S. Holder held the Note for more than one year. Certain non-corporate U.S. Holders (including individuals) generally are eligible for preferential rates of U.S. federal income taxation in respect of long-term capital gains. The deductibility of capital losses is subject to certain limitations.
Specified Change of Control Parent Assumption
In the event of a Specified Change of Control Parent Assumption, the Specified Change of Control Parent would assume all obligations of the Company with respect to the New Notes. It is possible that a Specified Change of Control Parent Assumption would result in a “deemed exchange” of the New Notes for U.S. federal income tax purposes, depending on the form of the related Specified Change of Control and certain other factors. If there were a deemed exchange of the New Notes, U.S. Holders would generally recognize taxable gain or loss equal to the difference between: (x) the “issue price” of the “modified” New Notes deemed issued by the Specified Change of Control Parent, and (y) the holders’ tax basis in the “unmodified” New Notes (as defined above in “—Sale, Redemption or Other Disposition”). The issue price of the modified New Notes will depend on whether or not the unmodified New Notes or the modified New Notes are treated as “publicly traded” for specified U.S. tax purposes. If either the modified New Notes or the unmodified New Notes are publicly traded, the issue price will generally be equal to the New Notes’ fair market value at the time of the exchange. If neither the modified New Notes nor the unmodified New Notes are publicly traded at the time of the assumption, the issue price will generally be equal to the New Notes’ principal amount. Whether notes are publicly traded may be subject to some uncertainty. If the issue price of the modified New Notes is less than the New Notes’ principal amount by more than a de minimis amount, then the difference between the issue price and the principal amount would be treated as original issue discount, and U.S. Holders would be required to accrue such original issue discount as ordinary income over the remaining life of the New Notes (regardless of such U.S. Holders’ method of tax accounting). U.S. Holders are urged to consult their tax advisors as to the consequences of a Specified Change of Control Parent Assumption.
Backup Withholding Tax and Information Reporting
In general, U.S. Holders may be subject to information reporting on payments of interest and the proceeds of the sale, exchange, retirement or other disposition of the New Notes. Backup withholding generally will not apply to payments made to a U.S. Holder unless the holder fails to provide the appropriate certification on IRS Form W-9 or otherwise does not provide evidence of exempt status. Any amount paid as backup withholding will be creditable against the U.S. Holder’s U.S. federal income tax liability, and may entitle such U.S. Holder to a refund, provided that the required information is timely furnished to the IRS.
Non-U.S. Holders
You are a “Non-U.S. Holder” if you are a beneficial owner of the Notes and are neither a U.S. Holder nor an entity classified as a partnership for U.S. federal income tax purposes.
Tax Consequences to Non-U.S. Holders Who Participate in the Exchange Offer
Neither the registration of the exchange offer pursuant to our obligations under the Registration Rights Agreement nor the receipt of New Notes in exchange for Old Notes will be a taxable event to Non-U.S. Holders for U.S. federal income tax purposes. Non-U.S. Holders will recognize income in respect of the New Notes at the same time and in the same amounts as they would have recognized such income in respect of the Old Notes had the exchange offer not occurred.
205
U.S. federal income tax purposes. Non-U.S. Holders will recognize income in respect of the New Notes at the same time and in the same amounts as they would have recognized such income in respect of the Old Notes had the exchange offer not occurred.
Payments of Interest
If you are a Non-U.S. Holder, you will not be subject to U.S. federal withholding tax on payments of interest that are not effectively connected with a trade or business within the United States conducted by you, provided that you (a) do not actually or constructively own 10% or more of the combined voting power of all classes of IASIS Capital Corporation’s stock and are not a controlled foreign corporation related to IASIS Capital Corporation through actual or constructive equity ownership, and (b) have provided a properly completed form W-8BEN or other IRS Form W-8, signed under penalties of perjury, establishing your status as a Non-U.S. Holder (or you satisfy certain documentary evidence requirements for establishing that you are a Non-U.S. Holder).
If the foregoing requirements are not met, the payments of interest that are not effectively connected with a U.S. trade or business will be subject to 30% U.S. federal withholding tax (or lower applicable treaty rate, provided certain certification requirements are met).
Sale, Redemption or Other Disposition
If you are a Non-U.S. Holder, you will not be subject to U.S. federal income tax or withholding tax on gain realized on the sale, exchange, redemption or other disposition of the New Notes (including a “deemed exchange” of the New Notes as described in “—U.S. Holders—Specified Change of Control Parent Assumption”) unless:
| | • | | Such gain is effectively connected with your conduct of a trade or business in the United States, in which case such gain will be taxed as described below; or |
| | • | | You are an individual holder present in the United States for 183 days or more in the taxable year of the disposition and certain other conditions are met, in which case you will be subject to 30% (or a lower applicable treaty rate) U.S. federal income tax on such gain (net of certain U.S. source losses). |
Any payment with respect to the sale, exchange, redemption or other disposition that is attributable to accrued interest will be subject to tax as described under “—Payments of Interest” above.
Effectively Connected Income
If the payment of interest or gain from the sale or other disposition of the New Notes is effectively connected with your conduct of a U.S. trade or business, you generally will be subject to U.S. federal income tax on the gain or income on a net income basis in the same manner as if you were a U.S. person unless an applicable income tax treaty provides otherwise. If you are a foreign corporation, you also may be subject to a “branch profits tax” equal to 30% of your effectively connected earnings and profits for the taxable year, subject to certain adjustments, unless you qualify for a lower rate under an applicable income tax treaty.
Specified Change of Control Parent Assumption After March 18, 2012
If a Specified Change of Control Parent Assumption were to occur after March 18, 2012, and it resulted in a deemed exchange (as described in “—U.S. Holders—Specified Change of Control Parent Assumption”), then payments of interest on the New Notes made to a Non-U.S. Holder (or a U.S. Holder holding New Notes through certain non-U.S. intermediaries (a “foreign financial institution”)) after December 31, 2013, and the gross proceeds from the disposition of New Notes by such Holder after December 31, 2014, generally would be subject to a withholding tax of 30 percent under the Foreign Account Tax Compliance provisions of the Hiring Incentives to Restore Employment Act (“FATCA”) unless the Holder (and/or the foreign financial institution through which the Holder holds its New Notes) has provided any required information with respect to its direct and indirect U.S. owners and investors and satisfied certain other requirements. The IRS has issued no regulations and only very limited interim guidance regarding the information that would be required to be reported, the content of the agreement that a foreign financial institution would be required to enter into with the IRS, or the procedures that would be required to be followed in order to comply with FATCA. Holders are encouraged to consult with their own tax advisors regarding the possible implications of FATCA on a Specified Change of Control Parent Assumption.
206
Backup Withholding Tax and Information Reporting
In general, payments of interest and the proceeds of the sale, exchange, retirement or other disposition of the New Notes (and the amount of tax withheld with respect to such payments, if any) payable by a U.S. paying agent or other U.S. intermediary to a Non-U.S. Holder will be subject to information reporting. Copies of the information returns reporting such payments (and withholding, if any) may also be made available to the tax authorities in the country in which the Non-U.S. Holder resides under the provisions of an applicable income tax treaty. Backup withholding generally will not apply to payments made to a Non-U.S. Holder unless the holder fails to provide the certification on IRS Form W-8BEN (or IRS Form W-8ECI, if applicable) or otherwise does not provide evidence of exempt status. Any amount paid as backup withholding will be creditable against the Non-U.S. Holder’s U.S. federal income tax liability, and may entitle such Non-U.S. Holder to a refund, provided that the required information is timely furnished to the IRS.
207
PLAN OF DISTRIBUTION
Each broker-dealer that receives New Notes for its own account pursuant to the exchange offer must acknowledge that it will deliver a prospectus in connection with any resale of such New Notes. This prospectus, as it may be amended or supplemented from time to time, may be used by a broker-dealer in connection with resales of New Notes received in exchange for Old Notes, where such Old Notes were acquired as a result of market-making activities or other trading activities. Starting on the Expiration Date and ending on the close of business on the earlier of (i) 180 days from the date on which the Exchange Offer Registration Statement is declared effective and (ii) the date on which a broker-dealer is no longer required to deliver a prospectus in connection with market-making or other trading activities, we will make this prospectus, as amended or supplemented, available to any broker-dealer for use in connection with any such resale. In addition, until the date that is 90 days from the date of original issuance of the New Notes, all dealers effecting transactions in the New Notes may be required to deliver a prospectus.
We will not receive any proceeds from any sale of New Notes by broker-dealers. New Notes received by broker-dealers for their own account pursuant to the exchange offer may be sold from time to time in one or more transactions in the over-the-counter market, in negotiated transactions, through the writing of options on the New Notes or a combination of such methods of resale, at market prices prevailing at the time of resale, at prices related to such prevailing market prices or negotiated prices. Any such resale may be made directly to purchasers or to or through brokers or dealers who may receive compensation in the form of commissions or concessions from any such broker-dealer and/or the purchasers of any such New Notes. Any broker-dealer that resells New Notes that were received by it for its own account pursuant to the exchange offer and any broker or dealer that participates in a distribution of such New Notes may be deemed to be an “underwriter” within the meaning of the Securities Act and any profit of any such resale of New Notes and any commissions or concessions received by any such persons may be deemed to be underwriting compensation under the Securities Act. The letter of transmittal states that by acknowledging that it will deliver and by delivering a prospectus, a broker-dealer will not be deemed to admit that it is an “underwriter” within the meaning of the Securities Act.
For a period of 180 days from the date on which the Exchange Offer Registration Statement is declared effective, we will promptly send additional copies of this prospectus and any amendment or supplement to this prospectus to any broker-dealer that requests such documents in the letter of transmittal. We have agreed to pay all expenses incident to the exchange offer (including the expenses of one counsel for the holders of the Notes) other than commissions or concessions of any brokers or dealers and will indemnify the holders of the Notes (including any broker-dealers) against certain liabilities, including liabilities under the Securities Act.
USE OF PROCEEDS
We will not receive any proceeds from the issuance of New Notes in the exchange offer. In consideration for issuing the New Notes, we will receive Old Notes in like principal amount. The Old Notes surrendered in exchange for the New Notes will be retired and cancelled.
LEGAL MATTERS
The validity of the New Notes and the related guarantees will be passed upon for us by Cleary Gottlieb Steen & Hamilton LLP, New York, New York and Christopher Y. Chi, Esq., Assistant Vice President, Legal Counsel of the Issuers.
EXPERTS
The consolidated financial statements of IASIS Healthcare LLC at September 30, 2010 and 2009, and for each of the three years in the period ended September 30, 2010, appearing in this Prospectus and Registration Statement have been audited by Ernst & Young LLP, independent registered public accounting firm, as set forth in their report thereon appearing elsewhere herein, and are included in reliance upon such report given on the authority of such firm as experts in accounting and auditing.
208
INDEX TO CONSOLIDATED FINANCIAL STATEMENTS
Unaudited Condensed Consolidated Historical Financial Data
for the Quarters and Nine Months Ended June 30, 2011 and 2010
IASIS Healthcare LLC
Audited Consolidated Historical Financial Data
for the Years Ended September 30, 2010, 2009 and 2008
IASIS Healthcare LLC
F-1
IASIS HEALTHCARE LLC
CONDENSED CONSOLIDATED BALANCE SHEETS
(In Thousands)
| | | | | | | | |
| | | June 30,
2011 | | | September 30,
2010 | |
| | | (Unaudited) | | | | |
| ASSETS | | | | | | | | |
| | |
Current assets | | | | | | | | |
Cash and cash equivalents | | $ | 144,595 | | | $ | 144,511 | |
Accounts receivable, less allowance for doubtful accounts of $145,092 and $125,406 at June 30, 2011 and September 30, 2010, respectively | | | 295,823 | | | | 209,173 | |
Inventories | | | 65,446 | | | | 53,842 | |
Deferred income taxes | | | 31,565 | | | | 15,881 | |
Prepaid expenses and other current assets | | | 88,404 | | | | 65,340 | |
| | | | | | | | |
Total current assets | | | 625,833 | | | | 488,747 | |
| | |
Property and equipment, net | | | 1,129,151 | | | | 985,291 | |
Goodwill | | | 836,688 | | | | 718,243 | |
Other intangible assets, net | | | 33,385 | | | | 27,000 | |
Deposit for acquisition | | | — | | | | 97,891 | |
Other assets, net | | | 61,743 | | | | 36,022 | |
| | | | | | | | |
Total assets | | $ | 2,686,800 | | | $ | 2,353,194 | |
| | |
| LIABILITIES AND EQUITY | | | | | | | | |
| | |
Current liabilities | | | | | | | | |
Accounts payable | | $ | 108,667 | | | $ | 78,931 | |
Salaries and benefits payable | | | 65,046 | | | | 38,110 | |
Accrued interest payable | | | 11,994 | | | | 12,536 | |
Medical claims payable | | | 99,530 | | | | 111,373 | |
Other accrued expenses and other current liabilities | | | 96,913 | | | | 106,614 | |
Current portion of long-term debt and capital lease obligations | | | 13,973 | | | | 6,691 | |
| | | | | | | | |
Total current liabilities | | | 396,123 | | | | 354,255 | |
| | |
Long-term debt and capital lease obligations | | | 1,867,460 | | | | 1,044,887 | |
Deferred income taxes | | | 118,380 | | | | 109,272 | |
Other long-term liabilities | | | 82,218 | | | | 60,162 | |
| | |
Non-controlling interests with redemption rights | | | 97,443 | | | | 72,112 | |
| | |
Equity | | | | | | | | |
Member’s equity | | | 115,342 | | | | 702,135 | |
Non-controlling interests | | | 9,834 | | | | 10,371 | |
| | | | | | | | |
Total equity | | | 125,176 | | | | 712,506 | |
| | | | | | | | |
Total liabilities and equity | | $ | 2,686,800 | | | $ | 2,353,194 | |
| | | | | | | | |
See accompanying notes.
F-2
IASIS HEALTHCARE LLC
CONDENSED CONSOLIDATED STATEMENTS OF OPERATIONS (UNAUDITED)
(In Thousands)
| | | | | | | | | | | | | | | | |
| | | Quarter Ended
June 30, | | | Nine Months Ended
June 30, | |
| | | 2011 | | | 2010 | | | 2011 | | | 2010 | |
Net revenue | | | | | | | | | | | | | | | | |
Acute care revenue | | $ | 529,844 | | | $ | 438,211 | | | $ | 1,489,432 | | | $ | 1,300,445 | |
Premium revenue | | | 188,765 | | | | 199,777 | | | | 580,917 | | | | 591,022 | |
| | | | | | | | | | | | | | | | |
Total net revenue | | | 718,609 | | | | 637,988 | | | | 2,070,349 | | | | 1,891,467 | |
Costs and expenses | | | | | | | | | | | | | | | | |
Salaries and benefits (includes stock-based compensation of $330, $118, $1,364 and $2,367, respectively) | | | 211,114 | | | | 170,035 | | | | 597,063 | | | | 514,688 | |
Supplies | | | 83,071 | | | | 66,333 | | | | 237,431 | | | | 200,167 | |
Medical claims | | | 155,885 | | | | 172,031 | | | | 484,635 | | | | 510,692 | |
Other operating expenses | | | 114,778 | | | | 93,579 | | | | 315,254 | | | | 266,854 | |
Provision for bad debts | | | 60,685 | | | | 49,416 | | | | 175,100 | | | | 142,901 | |
Rentals and leases | | | 11,774 | | | | 10,067 | | | | 34,229 | | | | 30,487 | |
Interest expense, net | | | 27,597 | | | | 16,711 | | | | 60,984 | | | | 50,065 | |
Depreciation and amortization | | | 26,312 | | | | 24,007 | | | | 74,942 | | | | 71,909 | |
Management fees | | | 1,250 | | | | 1,250 | | | | 3,750 | | | | 3,750 | |
Loss on extinguishment of debt | | | 23,075 | | | | — | | | | 23,075 | | | | — | |
| | | | | | | | | | | | | | | | |
Total costs and expenses | | | 715,541 | | | | 603,429 | | | | 2,006,463 | | | | 1,791,513 | |
| | | | |
Earnings from continuing operations before gain (loss) on disposal of assets and income taxes | | | 3,068 | | | | 34,559 | | | | 63,886 | | | | 99,954 | |
Gain (loss) on disposal of assets, net | | | (114 | ) | | | (149 | ) | | | 771 | | | | (206 | ) |
| | | | | | | | | | | | | | | | |
| | | | |
Earnings from continuing operations before income taxes | | | 2,954 | | | | 34,410 | | | | 64,657 | | | | 99,748 | |
Income tax expense | | | 1,389 | | | | 12,683 | | | | 24,078 | | | | 36,544 | |
| | | | | | | | | | | | | | | | |
| | | | |
Net earnings from continuing operations | | | 1,565 | | | | 21,727 | | | | 40,579 | | | | 63,204 | |
Loss from discontinued operations, net of income taxes | | | (15 | ) | | | (384 | ) | | | (6,069 | ) | | | (363 | ) |
| | | | | | | | | | | | | | | | |
| | | | |
Net earnings | | | 1,550 | | | | 21,343 | | | | 34,510 | | | | 62,841 | |
Net earnings attributable to non-controlling interests | | | (2,013 | ) | | | (2,002 | ) | | | (6,201 | ) | | | (6,063 | ) |
| | | | | | | | | | | | | | | | |
| | | | |
Net earnings (loss) attributable to IASIS Healthcare LLC | | $ | (463 | ) | | $ | 19,341 | | | $ | 28,309 | | | $ | 56,778 | |
| | | | | | | | | | | | | | | | |
See accompanying notes.
F-3
IASIS HEALTHCARE LLC
CONDENSED CONSOLIDATED STATEMENT OF EQUITY (UNAUDITED)
(In Thousands)
| | | | | | | | | | | | | | | | | | |
| | | Non-controlling
Interests with
Redemption
Rights | | | | | Member’s
Equity | | | Non-controlling
Interests | | | Total
Equity | |
Balance at September 30, 2010 | | $ | 72,112 | | | | | $ | 702,135 | | | $ | 10,371 | | | $ | 712,506 | |
Net earnings | | | 6,144 | | | | | | 28,309 | | | | 57 | | | | 28,366 | |
Distributions to non-controlling interests | | | (7,308 | ) | | | | | — | | | | (87 | ) | | | (87 | ) |
Repurchase of non-controlling interests | | | (307 | ) | | | | | — | | | | (507 | ) | | | (507 | ) |
Acquisition related adjustments to redemption value of non-controlling interests with redemption rights | | | 34,303 | | | | | | — | | | | — | | | | — | |
Stock-based compensation | | | — | | | | | | 1,364 | | | | — | | | | 1,364 | |
Other comprehensive income | | | — | | | | | | 1,698 | | | | — | | | | 1,698 | |
Contribution from parent company related to tax benefit from Holdings Senior PIK Loans interest | | | — | | | | | | 7,201 | | | | — | | | | 7,201 | |
Distributions to parent company in connection with refinancing | | | — | | | | | | (632,866 | ) | | | — | | | | (632,866 | ) |
Adjustment to redemption value of non-controlling interests with redemption rights | | | (7,501 | ) | | | | | 7,501 | | | | — | | | | 7,501 | |
| | | | | | | | | | | | | | | | | | |
Balance at June 30, 2011 | | $ | 97,443 | | | | | $ | 115,342 | | | $ | 9,834 | | | $ | 125,176 | |
| | | | | | | | | | | | | | | | | | |
See accompanying notes.
F-4
IASIS HEALTHCARE LLC
CONDENSED CONSOLIDATED STATEMENTS OF CASH FLOWS (UNAUDITED)
(In Thousands)
| | | | | | | | |
| | | Nine Months Ended
June 30, | |
| | | 2011 | | | 2010 | |
Cash flows from operating activities | | | | | | | | |
Net earnings | | $ | 34,510 | | | $ | 62,841 | |
Adjustments to reconcile net earnings to net cash provided by operating activities: | | | | | | | | |
Depreciation and amortization | | | 74,942 | | | | 71,909 | |
Amortization of loan costs | | | 4,319 | | | | 2,356 | |
Stock-based compensation | | | 1,364 | | | | 2,367 | |
Deferred income taxes | | | 899 | | | | 23,839 | |
Income tax benefit from stock-based compensation | | | — | | | | (1,770 | ) |
Income tax benefit from parent company interest | | | 7,201 | | | | 4,989 | |
Fair value change in interest rate swaps | | | (695 | ) | | | — | |
Loss (gain) on disposal of assets, net | | | (771 | ) | | | 206 | |
Loss from discontinued operations, net | | | 6,069 | | | | 363 | |
Loss on extinguishment of debt | | | 23,075 | | | | — | |
Changes in operating assets and liabilities, net of the effect of acquisitions and dispositions: | | | | | | | | |
Accounts receivable, net | | | (32,494 | ) | | | 9,154 | |
Inventories, prepaid expenses and other current assets | | | (13,572 | ) | | | (74,909 | ) |
Accounts payable, other accrued expenses and other accrued liabilities | | | (11,455 | ) | | | 13,137 | |
| | | | | | | | |
Net cash provided by operating activities — continuing operations | | | 93,392 | | | | 114,482 | |
Net cash provided by (used in) operating activities — discontinued operations | | | 3,260 | | | | (567 | ) |
| | | | | | | | |
Net cash provided by operating activities | | | 96,652 | | | | 113,915 | |
| | | | | | | | |
| | |
Cash flows from investing activities | | | | | | | | |
Purchases of property and equipment, net | | | (64,475 | ) | | | (53,465 | ) |
Cash paid for acquisitions, net | | | (155,428 | ) | | | — | |
Proceeds from sale of assets | | | 150 | | | | 50 | |
Change in other assets, net | | | 1,385 | | | | 1,856 | |
| | | | | | | | |
Net cash used in investing activities | | | (218,368 | ) | | | (51,559 | ) |
| | | | | | | | |
| | |
Cash flows from financing activities | | | | | | | | |
Proceeds from refinancing | | | 1,863,730 | | | | — | |
Payment of debt and capital lease obligations | | | (1,049,547 | ) | | | (6,772 | ) |
Debt financing costs incurred | | | (51,308 | ) | | | — | |
Distributions to parent company | | | (632,866 | ) | | | (124,962 | ) |
Distributions to non-controlling interests | | | (7,395 | ) | | | (6,921 | ) |
Costs paid for the repurchase of non-controlling interests | | | (814 | ) | | | (69 | ) |
| | | | | | | | |
Net cash provided by (used in) financing activities | | | 121,800 | | | | (138,724 | ) |
| | | | | | | | |
| | |
Change in cash and cash equivalents | | | 84 | | | | (76,368 | ) |
Cash and cash equivalents at beginning of period | | | 144,511 | | | | 206,528 | |
| | | | | | | | |
Cash and cash equivalents at end of period | | $ | 144,595 | | | $ | 130,160 | |
| | | | | | | | |
| | |
Supplemental disclosure of cash flow information | | | | | | | | |
Cash paid for interest | | $ | 58,283 | | | $ | 58,145 | |
| | | | | | | | |
Cash paid for income taxes, net | | $ | 17,587 | | | $ | 7,513 | |
| | | | | | | | |
| | |
Supplemental disclosure of non-cash investing and financing activities | | | | | | | | |
Capital lease obligations resulting from acquisitions | | $ | 9,559 | | | $ | — | |
| | | | | | | | |
See accompanying notes.
F-5
IASIS HEALTHCARE LLC
NOTES TO CONDENSED CONSOLIDATED FINANCIAL STATEMENTS (UNAUDITED)
1. ORGANIZATION AND BASIS OF PRESENTATION
The unaudited condensed consolidated financial statements as of and for the quarters and nine months ended June 30, 2011 and 2010, reflect the financial position, results of operations and cash flows of IASIS Healthcare LLC (“IASIS” or the “Company”). The Company’s sole member and parent company is IASIS Healthcare Corporation (“Holdings” or “IAS”).
IASIS owns and operates medium-sized acute care hospitals in high-growth urban and suburban markets. At June 30, 2011, the Company owned or leased 18 acute care hospital facilities and one behavioral health hospital facility, with a total of 4,362 licensed beds, located in seven regions:
| | • | | Tampa-St. Petersburg, Florida; |
| | • | | five cities in Texas, including Houston and San Antonio; |
| | • | | West Monroe, Louisiana; and |
| | • | | Woodland Park, Colorado. |
The Company also owns and operates Health Choice Arizona, Inc. (“Health Choice” or the “Plan”), a Medicaid and Medicare managed health plan in Phoenix, Arizona.
The unaudited condensed consolidated financial statements have been prepared in accordance with U.S. generally accepted accounting principles (“GAAP”) for interim financial reporting and in accordance with Rule 10-01 of Regulation S-X. Accordingly, they do not include all of the information and notes required by GAAP for complete financial statements. The condensed consolidated balance sheet of the Company at September 30, 2010, has been derived from the audited consolidated financial statements at that date, but does not include all of the information and notes required by GAAP for complete financial statements. For further information, refer to the consolidated financial statements and footnotes thereto included in the Company’s Annual Report on Form 10-K for the fiscal year ended September 30, 2010.
In the opinion of management, the accompanying unaudited condensed consolidated financial statements contain all material adjustments (consisting of normal recurring items) necessary for a fair presentation of results for the interim periods presented. The results of operations for any interim period are not necessarily indicative of results for the full year.
Principles of Consolidation
The unaudited condensed consolidated financial statements include all subsidiaries and entities under common control of the Company. Control is generally defined by the Company as ownership of a majority of the voting interest of an entity. In addition, control is demonstrated in most instances when the Company is the sole general partner in a limited partnership. Significant intercompany transactions have been eliminated.
F-6
IASIS HEALTHCARE LLC
NOTES TO CONDENSED CONSOLIDATED FINANCIAL STATEMENTS (UNAUDITED)
Use of Estimates
The preparation of the financial statements in conformity with GAAP requires management to make estimates and assumptions that affect the amounts reported in the accompanying unaudited condensed consolidated financial statements and notes. Actual results could differ from those estimates.
Reclassifications
Certain prior year amounts have been reclassified to conform to the current year presentation. These reclassifications have no impact on the Company’s total assets or total liabilities and equity.
General and Administrative
The majority of the Company’s expenses are “cost of revenue” items. Costs that could be classified as “general and administrative” by the Company would include the IASIS corporate office costs, which were $12.7 million and $7.7 million for the quarters ended June 30, 2011 and 2010, respectively, and $33.5 million and $27.0 million for the nine months ended June 30, 2011 and 2010, respectively.
Subsequent Events Consideration
The Company has evaluated its financial statements and disclosures for the impact of subsequent events up to the date of filing its quarterly report on Form 10-Q with the Securities and Exchange Commission.
2. LONG-TERM DEBT AND CAPITAL LEASE OBLIGATIONS
On May 3, 2011, the Company completed a transaction to refinance its then existing debt (the “Refinancing”). The Refinancing included $1.325 billion in new senior secured credit facilities and the issuance by the Company, together with its wholly owned subsidiary IASIS Capital Corporation (“IASIS Capital”), of $850.0 million aggregate principal amount of 8.375% senior notes due 2019 (the “Senior Notes”). Proceeds from the Refinancing were used to refinance amounts outstanding under the Company’s then existing credit facilities; fund a cash tender offer to repurchase any and all of the Company’s $475.0 million aggregate principal amount of 8 3/4% senior subordinated notes due 2014; repay in full the Holdings Senior Paid-in-Kind (“PIK”) Loans held at IAS; pay fees and expenses associated with the Refinancing; and raise capital for general corporate purposes.
As part of the Refinancing, the Company distributed $632.9 million to IAS, which is comprised of $402.9 million to fund the repayment of the Holdings Senior PIK Loans, including interest that had accrued to the principal balance of the loans totaling $102.9 million, and $230.0 million to be held for future acquisitions and strategic growth initiatives, as well as potential distributions to the equity holders of IAS.
Long-term debt and capital lease obligations consist of the following (in thousands):
| | | | | | | | |
| | | June 30,
2011 | | | September 30,
2010 | |
Senior secured term loan facility | | $ | 1,017,435 | | | $ | 570,260 | |
Senior Notes | | | 843,983 | | | | — | |
8 3/4% senior subordinated notes due 2014 | | | — | | | | 475,000 | |
Capital leases and other obligations | | | 20,015 | | | | 6,318 | |
| | | | | | | | |
| | |
| | | 1,881,433 | | | | 1,051,578 | |
| | |
Less current maturities | | | 13,973 | | | | 6,691 | |
| | | | | | | | |
| | $ | 1,867,460 | | | $ | 1,044,887 | |
| | | | | | | | |
F-7
IASIS HEALTHCARE LLC
NOTES TO CONDENSED CONSOLIDATED FINANCIAL STATEMENTS (UNAUDITED)
As of June 30, 2011, the senior secured term loan facility balance reflects an original issue discount (“OID”) of $5.0 million, which is net of accumulated amortization of $122,000. The Senior Notes balance reflects an OID of $6.0 million, which is net of accumulated amortization of $128,000.
In connection with the refinancing, the company incurred a loss on extinguishment of debt totaling $23.1 million, which is included in the accompanying unaudited condensed consolidated statements of operations for the quarter and nine months ended June 30, 2011. The loss on extinguishment of debt included the write-off of $8.3 million in existing deferred financing costs, $4.9 million in creditor fees and $9.9 million in redemption premiums associated with the repurchase of the 8 3/4% senior subordinated notes due 2014. Additionally, the company incurred 36.5 million in creditor fees and other related costs that have been included in other assets in the accompanying unaudited condensed consolidated balance sheet at June 30, 2011.
$1.325 Billion Senior Secured Credit Facilities
In connection with the Refinancing, the Company entered into a new senior credit agreement (the “Restated Credit Agreement”). The Restated Credit Agreement provides for senior secured financing of up to $1.325 billion consisting of (1) a $1.025 billion senior secured term loan facility with a seven-year maturity and (2) a $300.0 million senior secured revolving credit facility with a five-year maturity, of which up to $150.0 million may be utilized for the issuance of letters of credit (together, the “Senior Secured Credit Facilities”). Principal under the senior secured term loan facility is due in consecutive equal quarterly installments in an aggregate annual amount equal to 1% of the principal amount outstanding at the closing of the Refinancing, with the remaining balance due upon maturity of the senior secured term loan facility. The senior secured revolving credit facility does not require installment payments.
Borrowings under the senior secured term loan facility bear interest at a rate per annum equal to, at the Company’s option, either (1) a base rate (the “base rate”) determined by reference to the highest of (a) the federal funds rate plus 0.50%, (b) the prime rate of Bank of America, N.A. and (c) a one-month LIBOR rate, subject to a floor of 1.25%, plus 1.00%, in each case, plus a margin of 2.75% per annum or (2) the LIBOR rate for the interest period relevant to such borrowing, subject to a floor of 1.25%, plus a margin of 3.75% per annum. Borrowings under the senior secured revolving credit facility generally bear interest at a rate per annum equal to, at the Company’s option, either (1) the base rate plus a margin of 2.50% per annum, or (2) the LIBOR rate for the interest period relevant to such borrowing plus a margin of 3.50% per annum. In addition to paying interest on outstanding principal under the Senior Secured Credit Facilities, the Company will be required to pay a commitment fee on the unutilized commitments under the senior secured revolving credit facility, as well as pay customary letter of credit fees and agency fees.
The Senior Secured Credit Facilities are unconditionally guaranteed by IAS and certain subsidiaries of the Company (collectively, the “Credit Facility Guarantors”) and are required to be guaranteed by all future material wholly-owned subsidiaries of the Company, subject to certain exceptions. All obligations under the Restated Credit Agreement are secured, subject to certain exceptions, by substantially all of the Company’s assets and the assets of the Credit Facility Guarantors, including (1) a pledge of 100% of the equity interests of the Company and the Credit Facility Guarantors, (2) mortgage liens on all of the Company’s material real property and that of the Credit Facility Guarantors, and (3) all proceeds of the foregoing.
The Restated Credit Agreement requires the Company to mandatorily prepay borrowings under the senior secured term loan facility with net cash proceeds of certain asset dispositions, following certain casualty events, following certain borrowings or debt issuances, and from a percentage of annual excess cash flow.
The Restated Credit Agreement contains certain restrictive covenants, including, among other things: (1) limitations on the incurrence of debt and liens; (2) limitations on investments other than, among other exceptions,
F-8
IASIS HEALTHCARE LLC
NOTES TO CONDENSED CONSOLIDATED FINANCIAL STATEMENTS (UNAUDITED)
certain acquisitions that meet certain conditions; (3) limitations on the sale of assets outside of the ordinary course of business; (5) limitations on dividends and distributions; and (6) limitations on transactions with affiliates, in each case, subject to certain exceptions. The Restated Credit Agreement also contains certain customary events of default, including, without limitation, a failure to make payments under the Senior Secured Credit Facilities, cross-defaults, certain bankruptcy events and certain change of control events.
8.375% Senior Notes due 2019
In connection with the Refinancing, the Company and IASIS Capital (together, the “Issuers”) issued the Senior Notes, which mature on May 15, 2019, pursuant to an indenture, dated as of May 3, 2011, among the Issuers and certain of the Issuers’ wholly owned domestic subsidiaries that guarantee the Senior Secured Credit Facilities (the “Notes Guarantors”) (the “Indenture”). The Indenture provides that the Senior Notes are general unsecured, senior obligations of the Issuers, and initially will be unconditionally guaranteed on a senior unsecured basis.
The Senior Notes bear interest at a rate of 8.375% per annum and will accrue from May 3, 2011. Interest on the Senior Notes is payable semi-annually, in cash in arrears, on May 15 and November 15 of each year, commencing on November 15, 2011.
The Company may redeem the Senior Notes, in whole or in part, at any time prior to May 15, 2014, at a price equal to 100% of the aggregate principal amount of the Senior Notes plus a “make-whole” premium and accrued and unpaid interest and special interest, if any, to but excluding the redemption date. In addition, the Company may redeem up to 35% of the Senior Notes before May 15, 2014, with the net cash proceeds from certain equity offerings at a redemption price equal to 108.375% of the aggregate principal amount of the Senior Notes plus accrued and unpaid interest and special interest, if any, to but excluding the redemption date, subject to compliance with certain conditions.
The Indenture contains covenants that limit the Company’s (and its restricted subsidiaries’) ability to, among other things: (1) incur additional indebtedness or liens or issue disqualified stock or preferred stock; (2) pay dividends or make other distributions on, redeem or repurchase the Company’s capital stock; (3) sell certain assets; (4) make certain loans and investments; (5) enter into certain transactions with affiliates; (5) impose restrictions on the ability of a subsidiary to pay dividends or make payments or distributions to the Company and its restricted subsidiaries; and (6) consolidate, merge or sell all or substantially all of the Company’s assets. These covenants are subject to a number of important limitations and exceptions.
The Indenture also provides for events of default, which, if any of them occurs, may permit or, in certain circumstances, require the principal, premium, if any, interest and any other monetary obligations on all the then outstanding Senior Notes to be due and payable immediately. If the Company experiences certain kinds of changes of control, it must offer to purchase the Senior Notes at 101% of their principal amount, plus accrued and unpaid interest and special interest, if any, to but excluding the repurchase date. Under certain circumstances, the Company will have the ability to make certain payments to facilitate a change of control transaction and to provide for the assumption of the Senior Notes by a new parent company resulting from such change of control transaction. If such change of control transaction is facilitated, the Issuers will be released from all obligations under the Indenture and the Issuers and the trustee will execute a supplemental indenture effectuating such assumption and release.
Registration Rights Agreement
In connection with the issuance of the Senior Notes, the Company entered into a registration rights agreement (the “Registration Rights Agreement”) that provides holders of the Senior Notes certain rights relating to registration of the Senior Notes under the Securities Act of 1933, as amended (the “Securities Act”).
Pursuant to the Registration Rights Agreement, the Company will file the Exchange Offer Registration Statement on or prior to 180 days after the issuance of the Senior Notes, enabling noteholders to exchange the privately placed notes for publicly registered notes with substantially identical terms; use commercially reasonable efforts to cause the Exchange Offer Registration Statement to become effective on or prior to 270 days after the closing of the offering; and use commercially reasonable efforts to consummate the exchange offer within 30 business days after the effective date of the Exchange Offer Registration Statement, or longer if required by the federal securities laws.
F-9
IASIS HEALTHCARE LLC
NOTES TO CONDENSED CONSOLIDATED FINANCIAL STATEMENTS (UNAUDITED)
If the Company fails to comply with any of the requirements described above or if the shelf registration statement or the Exchange Offer Registration statement is declared effective but thereafter ceases to be effective or usable (in either case, a “Registration Default”), the annual interest rate borne by the Senior Notes will be increased by 0.25% per annum during the 90-day period immediately following such Registration Default and will increase by 0.25% per annum at the end of each subsequent 90-day period, but in no event shall such increase exceed 1.00% per annum.
3. INTEREST RATE SWAPS
Effective March 2, 2009, the Company executed interest rate swap agreements with Citibank, N.A. and Wachovia Bank, N.A. (currently Wells Fargo Bank, N.A.), as counterparties, with notional amounts totaling $425.0 million, of which $225.0 million expired on February 28, 2011. As of June 30, 2011, two interest rate swap agreements remain in effect with each agreement having a notional amount of $100.0 million expiring on February 29, 2012. The Company entered into its interest rate swap arrangements to mitigate the floating interest rate risk on a portion of its outstanding variable rate debt. Under the remaining agreements, the Company is required to make monthly fixed rate payments to the counterparties, as calculated on the notional amounts, at an annual fixed rate of 2.0%. The counterparties are obligated to make monthly floating rate payments to the Company based on the one-month LIBOR rate.
The Company accounts for its interest rate swaps in accordance with the provisions of Financial Accounting Standards Board (“FASB”) authoritative guidance regarding accounting for derivative instruments and hedging activities, which also includes enhanced disclosure requirements. In accordance with these provisions, the Company has designated its interest rate swaps as a cash flow hedge instrument. The Company assesses the effectiveness of its cash flow hedge on a quarterly basis, with any ineffectiveness being measured using the hypothetical derivative method. The Company completed an assessment of its cash flow hedge during the quarters and nine months ended June 30, 2011 and 2010, and determined that the hedge was effective for all periods except the quarter ended June 30, 2011. The hedging ineffectiveness during the quarter ended June 30, 2011, was a result of the Refinancing which established a LIBOR floor applicable to borrowings under the Senior Secured Credit Facilities, the source of the Company’s variable rate debt. Accordingly, a gain resulting from the $695,000 change in fair value of the Company’s interest rate swaps since March 31, 2011, the last period that the hedge was deemed effective, has been reflected as a component of interest expense in the accompanying unaudited condensed consolidated statement of operations. No gain or loss has been reflected in the accompanying unaudited condensed consolidated statements of operations for the periods that the cash flow hedge was determined to be effective.
The Company applies the provisions of FASB authoritative guidance regarding fair value measurements, which provides a single definition of fair value, establishes a framework for measuring fair value, and expands disclosures concerning fair value measurements. The Company applies these provisions to the valuation and disclosure of its interest rates swaps. This authoritative guidance establishes a three-tier fair value hierarchy, which prioritizes the inputs used in measuring fair value. These tiers include: (i) Level 1, which is defined as quoted prices in active markets that can be accessed at the measurement date; (ii) Level 2, which is defined as inputs other than quoted prices in active markets that are observable, either directly or indirectly; and (iii) Level 3, which is defined as unobservable inputs resulting from the existence of little or no market data, therefore potentially requiring an entity to develop its own assumptions.
The Company determines the fair value of its interest rate swaps in a manner consistent with that used by market participants in pricing hedging instruments, which includes using a discounted cash flow analysis based upon the terms of the agreements, the impact of the one-month forward LIBOR curve and an evaluation of credit risk. Given the use of observable market assumptions and the consideration of credit risk, the Company has categorized the valuation of its interest rate swaps as Level 2.
The fair value of the Company’s interest rate swaps at June 30, 2011 and September 30, 2010, reflect liability balances of $2.3 million and $5.7 million, respectively, and are included in other long-term liabilities in the
F-10
IASIS HEALTHCARE LLC
NOTES TO CONDENSED CONSOLIDATED FINANCIAL STATEMENTS (UNAUDITED)
accompanying unaudited condensed consolidated balance sheets. The fair value of the Company’s interest rate swaps reflects a liability because the effect of the forward LIBOR curve on future interest payments results in less interest due to the Company under the variable rate component included in the interest rate swap agreements, as compared to the amount due the Company’s counterparties under the fixed interest rate component. Any change in the fair value of the Company’s interest rate swaps, net of income taxes, from inception to March 31, 2011, is included in accumulated other comprehensive loss as a component of member’s equity in the accompanying unaudited condensed consolidated balance sheets. Any change in fair value since March 31, 2011, has been included as a component of interest expense in the accompanying unaudited condensed consolidated statement of operations, as previously described.
4. ACQUISITIONS
Effective May 1, 2011, the Company acquired a 79.1% equity ownership interest in St. Joseph Medical Center (“St. Joseph”), a 792-licensed bed acute care hospital facility located in downtown Houston, Texas, in exchange for cash consideration of $156.8 million, subject to changes in net assets. In accordance with the purchase agreement, independent investors, most of whom are physicians on the medical staff of St. Joseph, retained an aggregate 20.9% ownership interest in the hospital. This acquisition was accounted for as a business combination, which requires the Company to allocate the purchase price to assets acquired or liabilities assumed based on their fair values. The excess of the purchase price allocation over those fair values is recorded as goodwill. The Company is currently working with third party valuation experts to finalize the valuation of acquired assets; therefore, the fair values as recorded in the accompanying unaudited condensed consolidated balance sheet at June 30, 2011, have been estimated based upon the most accurate information available, and are subject to adjustment once the valuation is completed.
Effective October 1, 2010, the Company acquired Brim Holdings, Inc. (“Brim”) in a cash-for-stock transaction valued at $95.0 million, subject to changes in net working capital. Brim operates Wadley Regional Medical Center (“Wadley”), a 370-licensed bed acute care hospital facility located in Texarkana, Texas, and Pikes Peak Regional Hospital, a 15-licensed bed critical access acute care hospital facility, in Woodland Park, Colorado, through operating lease agreements with separate parties. The Brim acquisition was accounted for as a business combination; therefore, the Company allocated the purchase price of these facilities to the assets acquired or liabilities assumed based on their fair values. The excess of the purchase price allocation over those fair values was recorded as goodwill. The Company’s third-party valuation of acquired assets has been finalized, and the appropriate fair values have been reflected in the accompanying unaudited condensed consolidated balance sheet at June 30, 2011.
5. GOODWILL
The following table presents the changes in the carrying amount of goodwill (in thousands):
| | | | | | | | | | | | |
| | | Acute
Care | | | Health
Choice | | | Total | |
Balance at September 30, 2010 | | $ | 712,486 | | | $ | 5,757 | | | $ | 718,243 | |
Brim acquisition | | | 78,451 | | | | — | | | | 78,451 | |
St. Joseph acquisition | | | 34,692 | | | | — | | | | 34,692 | |
Other acquisitions | | | 5,302 | | | | — | | | | 5,302 | |
| | | | | | | | | | | | |
Balance at June 30, 2011 | | $ | 830,931 | | | $ | 5,757 | | | $ | 836,688 | |
| | | | | | | | | | | | |
See Note 4 for more information regarding the fair value assessment of acquired assets and assumed liabilities.
F-11
IASIS HEALTHCARE LLC
NOTES TO CONDENSED CONSOLIDATED FINANCIAL STATEMENTS (UNAUDITED)
6. COMPREHENSIVE INCOME
Comprehensive income consists of two components: net earnings and other comprehensive income. Other comprehensive income refers to revenues, expenses, gains and losses that under the FASB authoritative guidance related to accounting for comprehensive income are recorded as elements of equity, but are excluded from net earnings. The following table presents the components of comprehensive income, net of income taxes (in thousands):
| | | | | | | | | | | | | | | | |
| | | Quarter Ended
June 30, | | | Nine Months Ended
June 30, | |
| | | 2011 | | | 2010 | | | 2011 | | | 2010 | |
Net earnings | | $ | 1,550 | | | $ | 21,343 | | | $ | 34,510 | | | $ | 62,841 | |
Change in fair value of interest rate swaps | | | — | | | | 56 | | | | 2,708 | | | | (1,092 | ) |
Change in income tax expense (benefit) | | | — | | | | (21 | ) | | | (1,010 | ) | | | 407 | |
| | | | | | | | | | | | | | | | |
| | | | |
Comprehensive income | | $ | 1,550 | | | $ | 21,378 | | | $ | 36,208 | | | $ | 62,156 | |
| | | | | | | | | | | | | | | | |
As a result of the Company’s cash flow hedge being deemed ineffective during the quarter ended June 30, 2011, the change in fair value of the Company’s interest rate swaps since March 31, 2011, is included as a component of interest expense in the accompanying unaudited condensed consolidated statement of operations.
The components of accumulated other comprehensive loss, net of income taxes, are as follows (in thousands):
| | | | | | | | |
| | | June 30,
2011 | | | September 30,
2010 | |
Fair value of interest rate swaps | | $ | (2,999 | ) | | $ | (5,707 | ) |
Income tax benefit | | | 1,118 | | | | 2,128 | |
| | | | | | | | |
| | |
Accumulated other comprehensive loss | | $ | (1,881 | ) | | $ | (3,579 | ) |
| | | | | | | | |
The fair value of the Company’s interest rate swaps included as a component of accumulated other comprehensive loss in the table above represents the fair value as of March 31, 2011, the last period the cash flow hedge was deemed effective.
7. DISTRIBUTION TO PARENT
As part of the Refinancing, the Company distributed $632.9 million to IAS, $402.9 million to fund the repayment of the Holdings Senior PIK Loans, which included interest that had accrued to the principal balance of the loans totaling $102.9 million, and $230.0 million to be held for future acquisitions and strategic growth initiatives, as well as potential distributions to the equity holders of IAS.
During fiscal 2010, the Company distributed $125.0 million, net of a $1.8 million income tax benefit, to IAS to fund the repurchase of certain shares of its outstanding preferred stock and cancel certain vested rollover options to purchase its common stock. The holder of the IAS preferred stock is represented by an investor group led by TPG, JLL Partners and Trimaran Fund Management. The repurchase of preferred stock, which included accrued and outstanding dividends, and the cancellation of rollover options, were funded by the Company’s excess cash on hand. The cancellation of the rollover options, which were associated with the Company’s 2004 recapitalization, resulted in the Company recognizing $2.0 million in stock-based compensation during the quarter ended March 31, 2010.
8. COMMITMENTS AND CONTINGENCIES
Net Revenue
The calculation of appropriate payments from the Medicare and Medicaid programs, as well as terms governing agreements with other third-party payors, is complex and subject to interpretation. Final determination of amounts earned under the
F-12
IASIS HEALTHCARE LLC
NOTES TO CONDENSED CONSOLIDATED FINANCIAL STATEMENTS (UNAUDITED)
Medicare and Medicaid programs often occurs subsequent to the year in which services are rendered because of audits by the programs, rights of appeal and the application of numerous technical provisions. In the opinion of management, adequate provision has been made for adjustments that may result from such routine audits and appeals.
Professional, General and Workers’ Compensation Liability Risks
The Company is subject to claims and legal actions in the ordinary course of business, including but not limited to claims relating to patient treatment and personal injuries. To cover these types of claims, the Company maintains professional and general liability insurance in excess of self-insured retentions through a commercial insurance carrier in amounts that the Company believes to be sufficient for its operations, although, potentially, some claims may exceed the scope of coverage in effect. Plaintiffs in these matters may request punitive or other damages that may not be covered by insurance. The Company is currently not a party to any such proceedings that, in the Company’s opinion, would have a material adverse effect on the Company’s business, financial condition or results of operations. The Company expenses an estimate of the costs it expects to incur under the self-insured retention exposure for professional and general liability claims using historical claims data, demographic factors, severity factors, current incident logs and other actuarial analysis. At June 30, 2011 and September 30, 2010, the Company’s professional and general liability accrual for asserted and unasserted claims totaled $65.2 million and $41.6 million, respectively. The semi-annual valuations from the Company’s independent actuary for professional and general liability losses resulted in a change in related estimates for prior periods which increased insurance expense by $948,000 during the nine months ended June 30, 2011, compared to a decrease of $1.9 million during the same prior year period. No changes were reflected in the quarters ended June 30, 2011 and 2010.
The Company is subject to claims and legal actions in the ordinary course of business relating to workers’ compensation matters. To cover these types of claims, the Company maintains workers’ compensation insurance coverage with a self-insured retention. The Company accrues the costs of workers’ compensation claims based upon estimates derived from its claims experience. The semi-annual valuations from the Company’s independent actuary for workers’ compensation losses resulted in a change in related estimates for prior periods which increased benefits expense by $1.2 million and $801,000 during the nine months ended June 30, 2011 and 2010, respectively. No changes were reflected in the quarters ended June 30, 2011 and 2010.
Health Choice
Health Choice has entered into capitated contracts whereby the Plan provides managed healthcare services in exchange for fixed periodic and supplemental payments from the Arizona Health Care Cost Containment System (“AHCCCS”) and the Centers for Medicare & Medicaid Services (“CMS”). These services are provided regardless of the actual costs incurred to provide these services. The Company receives reinsurance and other supplemental payments from AHCCCS to cover certain costs of healthcare services that exceed certain thresholds. The Company believes that current capitated payments received, together with reinsurance and other supplemental payments, are sufficient to pay for the services Health Choice is obligated to deliver. As of June 30, 2011, the Company has provided a performance guaranty in the form of letters of credit totaling $48.3 million for the benefit of AHCCCS to support Health Choice’s obligations under its contract to provide and pay for the healthcare services. The amount of the performance guaranty is generally based, in part, upon the membership in the Plan and the related capitation revenue paid to Health Choice.
Acquisitions
The Company has acquired and in the future may choose to acquire businesses with prior operating histories. Such businesses may have unknown or contingent liabilities, including liabilities for failure to comply with healthcare laws and regulations, such as billing and reimbursement, fraud and abuse and similar anti-referral laws. Although the Company has procedures designed to conform business practices to its policies following the completion of any acquisition, there can be no assurance that the Company will not become liable for previous activities of prior owners that may later be asserted to be improper by private plaintiffs or government agencies. Although the Company generally seeks to obtain indemnification from prospective sellers covering such matters, there can be no assurance that any such matter will be covered by indemnification, or if covered, that such indemnification will be adequate to cover potential losses and fines.
F-13
IASIS HEALTHCARE LLC
NOTES TO CONDENSED CONSOLIDATED FINANCIAL STATEMENTS (UNAUDITED)
Other
On March 31, 2008, the United States District Court for the District of Arizona (“District Court”) dismissed with prejudice thequi tamcomplaint against IAS, our parent company. Thequi tam action sought monetary damages and civil penalties under the federal False Claims Act (“FCA”) and included allegations that certain business practices related to physician relationships and the medical necessity of certain procedures resulted in the submission of claims for reimbursement in violation of the FCA. The case dates back to March 2005 and became the subject of a subpoena by the Office of Inspector General in September 2005. In August 2007, the case was unsealed and the U.S. Department of Justice (“DOJ”) declined to intervene. The District Court dismissed the case from the bench at the conclusion of oral arguments on IAS’ motion to dismiss. On April 21, 2008, the District Court issued a written order dismissing the case with prejudice and entering formal judgment for IAS and denying as moot IAS’ motions related to the relator’s misappropriation of information subject to a claim of attorney-client privilege by IAS. Both parties appealed. On August 12, 2010, United States Court of Appeals for the Ninth Circuit reversed the District Court’s dismissal of thequi tamcomplaint and the District Court’s denial of IAS’ motions concerning the relator’s misappropriation of documents and ordered that thequi tamrelator be allowed leave to file a Third Amended Complaint and for the District Court to consider IAS’ motions concerning the relator’s misappropriation of documents. The District Court ordered thequi tamrelator to file his Third Amended Complaint by November 22, 2010, and set a schedule for the filing of motions related to the relator’s misappropriation of documents. On October 20, 2010, thequi tamrelator filed a motion to transfer this action to the United States District Court for the Eastern District of Texas. On November 22, 2010, the relator filed his Third Amended Complaint. On January 3, 2011, IAS filed its renewed motion for sanctions concerning the relator’s misappropriation of documents and, on January 14, 2011, IAS filed its motion to dismiss the relator’s Third Amended Complaint. On May 4, 2011, the District Court in Arizona heard oral arguments on all pending motions, including IAS’ motion to dismiss and renewed motions for sanctions and the relator’s motion to transfer the action to the United States District Court for the Eastern District of Texas. On June 1, 2011, the District Court in Arizona issued a written order dismissing the relator’s Third Amended Complaint with prejudice. The order also denied the relator’s motion to transfer the case to the Eastern District of Texas, finding that the relator was “attempting to engage in forum shopping,” and denied the relator’s request for leave to further amend the complaint. The District Court expressly reserved decision on the collateral issue of sanctions against the relator and, preliminary to further briefing on IAS’ pending motion for sanctions, directed the relator to return all documents withheld to IAS within 20 days. IAS continues its vigorous pursuit of sanctions and other remedies against the relator related to the misappropriation and misuse of information subject to a claim of attorney-client privilege by IAS. Oral argument on IAS’ pending motion for sanctions currently is set for August 26, 2011. The District Court’s dismissal of this lawsuit with prejudice is appealable and the relator filed a notice of appeal on June 28, 2011. While the District Court’s order in favor of IAS should effectively bring to an end the relator’squi tamlitigation in the District Court that has been pending since March 2005, if the appeal of the District Court’s ruling was resolved in a manner unfavorable to IAS, it could have a material adverse effect on the Company’s business, financial condition and results of operations, including exclusion from the Medicare and Medicaid programs. In addition, the Company may incur material fees, costs and expenses in connection with defending thequi tamaction.
The Company’s facilities obtain clinical and administrative services from a variety of vendors. One vendor, a medical practice that furnished cardiac catheterization services under contractual arrangements at Mesa General Hospital and St. Luke’s Medical Center through March 31, 2008 and May 31, 2008, respectively, asserted that, because of deferred fee adjustments that it claims were due under these arrangements, it was owed additional amounts for services rendered since April 1, 2006 at both facilities. The Company and the vendor were unable to reach an agreement with respect to the amount of the fee adjustment, if any, that was contractually required, nor with respect to an appropriate methodology for determining such amount. On September 30, 2008, the vendor filed a state court complaint for an aggregate adjustment in excess of the amount accrued by the Company, in addition to certain tort claims. On March 20, 2009, the Company filed a Motion to Dismiss and in the alternative to Compel Arbitration. On July 27, 2009, the court granted the Company’s Motion to Compel Arbitration on the grounds that the issues are to be determined by binding arbitration. On December 24, 2010, after conducting the arbitration hearing, the arbitration panel issued its decision rejecting the fees sought by the vendor, but did not adopt the fees proposed by the Company. The arbitration panel rendered its judgment on the fair market value of the vendor’s services at a point between the amounts the two parties argued were owed. On July 22, 2011, the Company paid $15.0 million to discharge the liability resulting from the arbitration panel’s decision, which includes all amounts required to be paid with respect to the fair market value compensation for services rendered by the vendor, pre-judgment
F-14
IASIS HEALTHCARE LLC
NOTES TO CONDENSED CONSOLIDATED FINANCIAL STATEMENTS (UNAUDITED)
interest and its attorneys’ fees, but excludes consideration of amounts that may be recoverable by the Company from its insurance carrier with respect to the Company’s attorneys fees above its insurance limits. The payment of this claim brings this arbitration dispute to a final resolution.
In November 2010, the DOJ sent a letter to IAS requesting a 12-month tolling agreement in connection with an investigation into Medicare claims submitted by the Company’s hospitals in connection with the implantation of implantable cardioverter defibrillators (“ICDs”) from 2003 through November 2010. At that time, neither the precise number of procedures, number of claims nor the hospitals involved were identified by the DOJ. The Company understands that the government is conducting a national initiative with respect to ICD procedures involving a number of healthcare providers and is seeking information in order to determine if ICD implantation procedures were performed in accordance with Medicare coverage requirements. On January 11, 2011, IAS entered into the tolling agreement with the DOJ and, subsequently, the DOJ has provided IAS with a list of 194 procedures involving ICDs at 14 hospitals which are the subject of further medical necessity review by the DOJ. The Company is cooperating fully with the government and, to date, the DOJ has not asserted any claim against the Company’s hospitals.
9. RECENTLY ISSUED ACCOUNTING PRONOUNCEMENTS
In July 2011, the FASB issued Accounting Standards Update (“ASU”) 2011-7, “Health Care Entities” (Topic 954):Presentation and Disclosure of Patient Service Revenue, Provision for Bad Debts, and the Allowance for Doubtful Accounts for Certain Health Care Entities. ASU 2011-7 requires healthcare organizations to present their provision for doubtful accounts related to patient service revenue as a deduction from revenue, similar to contractual discounts. In addition, all healthcare organizations will be required to provide certain disclosures designed to help users understand how contractual discounts and bad debts affect recorded revenue in both interim and annual financial statements. ASU 2011-7 is required to be applied retrospectively and is effective for public companies for fiscal years, and interim periods within those years, beginning December 15, 2011, with early adoption permitted. ASU 2011-7 is effective for the Company’s fiscal year beginning October 1, 2012, and is not expected to significantly impact the Company’s financial position, results of operations or cash flows, although it will change the presentation of the Company’s revenues on its statements of operations, as well as requiring additional disclosures.
In December 2010, the FASB issued ASU No. 2010-29, “Business Combinations” (Topic 805):Disclosure of Supplementary Pro Forma Information for Business Combinations. ASU 2010-29 clarifies that, if a reporting entity presents comparative financial statements, the pro forma revenue and earnings of the combined entity should be reported as though the business combinations that occurred during the current year had occurred as of the beginning of the comparable prior annual reporting period. The ASU is effective prospectively for business combinations for which the acquisition date is on or after the beginning of the first annual reporting period beginning on or after December 15, 2010. ASU No. 2010-29 is effective for the Company’s fiscal year beginning October 1, 2011, with early adoption permitted, and is an accounting principle which clarifies disclosure requirements, and is not expected to significantly impact the Company’s financial statement disclosures.
In December 2010, the FASB issued ASU No. 2010-28, “Intangibles—Goodwill and Other” (Topic 350):When to Perform Step 2 of the Goodwill Impairment Test for Reporting Units with Zero or Negative Carrying Amounts. ASU 2010-28 requires Step 2 of the impairment test be performed in circumstances where the carrying amount of a reporting unit is zero or negative and there are qualitative factors that indicate it is more likely than not that a goodwill impairment exists. The ASU is effective for fiscal years, and interim periods within those years, beginning after December 15, 2010. ASU 2010-28 is effective for the Company’s fiscal year beginning October 1, 2011, and is not expected to significantly impact the Company’s financial position, results of operations or cash flows.
In August 2010, the FASB issued ASU No. 2010-24, “Health Care Entities” (Topic 954):Presentation of Insurance Claims and Related Insurance Recoveries. This ASU eliminates the practice of netting claim liabilities with expected related insurance recoveries for balance sheet presentation. Claim liabilities are to be determined with no regard for recoveries and presented gross. Expected recoveries are presented separately. ASU 2010-24 is effective for fiscal years, and interim periods within those years, beginning after December 15, 2010. ASU 2010-24 is effective for the Company’s fiscal year beginning October 1, 2011, and is not expected to significantly impact the Company’s financial position, results of operations or cash flows.
F-15
IASIS HEALTHCARE LLC
NOTES TO CONDENSED CONSOLIDATED FINANCIAL STATEMENTS (UNAUDITED)
In August 2010, the FASB issued ASU No. 2010-23, “Health Care Entities” (Topic 954):Measuring Charity Care for Disclosure. Due to the lack of comparability existing as a result of the use of either revenue or cost as the basis for disclosure of charity care, this ASU standardizes cost as the basis for charity care disclosures and specifies the elements of cost to be used in charity care disclosures. ASU 2010-23 is effective for the Company’s fiscal year beginning October 1, 2011, and is not expected to significantly impact the Company’s financial statement disclosures.
10. SEGMENT AND GEOGRAPHIC INFORMATION
The Company’s acute care hospitals and related healthcare businesses are similar in their activities and the economic environments in which they operate (i.e. urban and suburban markets). Accordingly, the Company’s reportable operating segments consist of (1) acute care hospitals and related healthcare businesses, collectively “Acute Care”, and (2) Health Choice. The following is a financial summary by business segment for the periods indicated (in thousands):
| | | | | | | | | | | | | | | | |
| | | For the Quarter Ended June 30, 2011 | |
| | | Acute
Care | | | Health Choice | | | Eliminations | | | Consolidated | |
Acute care revenue | | $ | 529,844 | | | $ | — | | | $ | — | | | $ | 529,844 | |
Premium revenue | | | — | | | | 188,765 | | | | — | | | | 188,765 | |
Revenue between segments | | | 3,065 | | | | — | | | | (3,065 | ) | | | — | |
| | | | | | | | | | | | | | | | |
Net revenue | | | 532,909 | | | | 188,765 | | | | (3,065 | ) | | | 718,609 | |
| | | | |
Salaries and benefits (excludes stock-based compensation) | | | 205,509 | | | | 5,275 | | | | — | | | | 210,784 | |
Supplies | | | 83,010 | | | | 61 | | | | — | | | | 83,071 | |
Medical claims | | | — | | | | 158,950 | | | | (3,065 | ) | | | 155,885 | |
Other operating expenses | | | 108,658 | | | | 6,120 | | | | — | | | | 114,778 | |
Provision for bad debts | | | 60,685 | | | | — | | | | — | | | | 60,685 | |
Rentals and leases | | | 11,378 | | | | 396 | | | | — | | | | 11,774 | |
| | | | | | | | | | | | | | | | |
Adjusted EBITDA(1) | | | 63,669 | | | | 17,963 | | | | — | | | | 81,632 | |
| | | | |
Interest expense, net | | | 27,597 | | | | — | | | | — | | | | 27,597 | |
Depreciation and amortization | | | 25,425 | | | | 887 | | | | — | | | | 26,312 | |
Stock-based compensation | | | 330 | | | | — | | | | — | | | | 330 | |
Management fees | | | 1,250 | | | | — | | | | — | | | | 1,250 | |
Loss on extinguishment of debt | | | 23,075 | | | | — | | | | — | | | | 23,075 | |
| | | | | | | | | | | | | | | | |
Earnings (loss) from continuing operations before loss on disposal of assets and income taxes | | | (14,008 | ) | | | 17,076 | | | | — | | | | 3,068 | |
Loss on disposal of assets, net | | | (114 | ) | | | — | | | | — | | | | (114 | ) |
| | | | | | | | | | | | | | | | |
Earnings (loss) from continuing operations before income taxes | | $ | (14,122 | ) | | $ | 17,076 | | | $ | — | | | $ | 2,954 | |
| | | | | | | | | | | | | | | | |
F-16
IASIS HEALTHCARE LLC
NOTES TO CONDENSED CONSOLIDATED FINANCIAL STATEMENTS (UNAUDITED)
| | | | | | | | | | | | | | | | |
| | | For the Quarter Ended June 30, 2010 | |
| | | Acute
Care | | | Health Choice | | | Eliminations | | | Consolidated | |
Acute care revenue | | $ | 438,211 | | | $ | — | | | $ | — | | | $ | 438,211 | |
Premium revenue | | | — | | | | 199,777 | | | | — | | | | 199,777 | |
Revenue between segments | | | 2,319 | | | | — | | | | (2,319 | ) | | | — | |
| | | | | | | | | | | | | | | | |
Net revenue | | | 440,530 | | | | 199,777 | | | | (2,319 | ) | | | 637,988 | |
| | | | |
Salaries and benefits (excludes stock-based compensation) | | | 165,051 | | | | 4,866 | | | | — | | | | 169,917 | |
Supplies | | | 66,293 | | | | 40 | | | | — | | | | 66,333 | |
Medical claims | | | — | | | | 174,350 | | | | (2,319 | ) | | | 172,031 | |
Other operating expenses | | | 87,451 | | | | 6,128 | | | | — | | | | 93,579 | |
Provision for bad debts | | | 49,416 | | | | — | | | | — | | | | 49,416 | |
Rentals and leases | | | 9,650 | | | | 417 | | | | — | | | | 10,067 | |
| | | | | | | | | | | | | | | | |
Adjusted EBITDA(1) | | | 62,669 | | | | 13,976 | | | | — | | | | 76,645 | |
| | | | |
Interest expense, net | | | 16,711 | | | | — | | | | — | | | | 16,711 | |
Depreciation and amortization | | | 23,115 | | | | 892 | | | | — | | | | 24,007 | |
Stock-based compensation | | | 118 | | | | — | | | | — | | | | 118 | |
Management fees | | | 1,250 | | | | — | | | | — | | | | 1,250 | |
| | | | | | | | | | | | | | | | |
Earnings from continuing operations before loss on disposal of assets and income taxes | | | 21,475 | | | | 13,084 | | | | — | | | | 34,559 | |
Loss on disposal of assets, net | | | (149 | ) | | | — | | | | — | | | | (149 | ) |
| | | | | | | | | | | | | | | | |
Earnings from continuing operations before income taxes | | $ | 21,326 | | | $ | 13,084 | | | $ | — | | | $ | 34,410 | |
| | | | | | | | | | | | | | | | |
F-17
IASIS HEALTHCARE LLC
NOTES TO CONDENSED CONSOLIDATED FINANCIAL STATEMENTS (UNAUDITED)
| | | | | | | | | | | | | | | | |
| | | For the Nine Months Ended June 30, 2011 | |
| | | Acute
Care | | | Health Choice | | | Eliminations | | | Consolidated | |
Acute care revenue | | $ | 1,489,432 | | | $ | — | | | $ | — | | | $ | 1,489,432 | |
Premium revenue | | | — | | | | 580,917 | | | | — | | | | 580,917 | |
Revenue between segments | | | 8,532 | | | | — | | | | (8,532 | ) | | | — | |
| | | | | | | | | | | | | | | | |
| | | | |
Net revenue | | | 1,497,964 | | | | 580,917 | | | | (8,532 | ) | | | 2,070,349 | |
| | | | |
Salaries and benefits (excludes stock-based compensation) | | | 580,228 | | | | 15,471 | | | | — | | | | 595,699 | |
Supplies | | | 237,274 | | | | 157 | | | | — | | | | 237,431 | |
Medical claims | | | — | | | | 493,167 | | | | (8,532 | ) | | | 484,635 | |
Other operating expenses | | | 295,913 | | | | 19,341 | | | | — | | | | 315,254 | |
Provision for bad debts | | | 175,100 | | | | — | | | | — | | | | 175,100 | |
Rentals and leases | | | 32,991 | | | | 1,238 | | | | — | | | | 34,229 | |
| | | | | | | | | | | | | | | | |
Adjusted EBITDA(1) | | | 176,458 | | | | 51,543 | | | | — | | | | 228,001 | |
| | | | |
Interest expense, net | | | 60,984 | | | | — | | | | — | | | | 60,984 | |
Depreciation and amortization | | | 72,273 | | | | 2,669 | | | | — | | | | 74,942 | |
Stock-based compensation | | | 1,364 | | | | — | | | | — | | | | 1,364 | |
Management fees | | | 3,750 | | | | — | | | | — | | | | 3,750 | |
Loss on extinguishment of debt | | | 23,075 | | | | — | | | | — | | | | 23,075 | |
| | | | | | | | | | | | | | | | |
Earnings from continuing operations before gain on disposal of assets and income taxes | | | 15,012 | | | | 48,874 | | | | — | | | | 63,886 | |
Gain on disposal of assets, net | | | 771 | | | | — | | | | — | | | | 771 | |
| | | | | | | | | | | | | | | | |
Earnings from continuing operations before income taxes | | $ | 15,783 | | | $ | 48,874 | | | $ | — | | | $ | 64,657 | |
| | | | | | | | | | | | | | | | |
Segment assets | | $ | 2,368,758 | | | $ | 318,042 | | | | | | | $ | 2,686,800 | |
| | | | | | | | | | | | | | | | |
Capital expenditures | | $ | 64,104 | | | $ | 371 | | | | | | | $ | 64,475 | |
| | | | | | | | | | | | | | | | |
Goodwill | | $ | 830,931 | | | $ | 5,757 | | | | | | | $ | 836,688 | |
| | | | | | | | | | | | | | | | |
F-18
IASIS HEALTHCARE LLC
NOTES TO CONDENSED CONSOLIDATED FINANCIAL STATEMENTS (UNAUDITED)
| | | | | | | | | | | | | | | | |
| | | For the Nine Months Ended June 30, 2010 | |
| | | Acute
Care | | | Health Choice | | | Eliminations | | | Consolidated | |
Acute care revenue | | $ | 1,300,445 | | | $ | — | | | $ | — | | | $ | 1,300,445 | |
Premium revenue | | | — | | | | 591,022 | | | | — | | | | 591,022 | |
Revenue between segments | | | 8,331 | | | | — | | | | (8,331 | ) | | | — | |
| | | | | | | | | | | | | | | | |
Net revenue | | | 1,308,776 | | | | 591,022 | | | | (8,331 | ) | | | 1,891,467 | |
| | | | |
Salaries and benefits (excludes stock-based compensation) | | | 497,916 | | | | 14,405 | | | | — | | | | 512,321 | |
Supplies | | | 200,030 | | | | 137 | | | | — | | | | 200,167 | |
Medical claims | | | — | | | | 519,023 | | | | (8,331 | ) | | | 510,692 | |
Other operating expenses | | | 248,380 | | | | 18,474 | | | | — | | | | 266,854 | |
Provision for bad debts | | | 142,901 | | | | — | | | | — | | | | 142,901 | |
Rentals and leases | | | 29,334 | | | | 1,153 | | | | — | | | | 30,487 | |
| | | | | | | | | | | | | | | | |
Adjusted EBITDA(1) | | | 190,215 | | | | 37,830 | | | | — | | | | 228,045 | |
| | | | |
Interest expense, net | | | 50,065 | | | | — | | | | — | | | | 50,065 | |
Depreciation and amortization | | | 69,240 | | | | 2,669 | | | | — | | | | 71,909 | |
Stock-based compensation | | | 2,367 | | | | — | | | | — | | | | 2,367 | |
Management fees | | | 3,750 | | | | — | | | | — | | | | 3,750 | |
| | | | | | | | | | | | | | | | |
Earnings from continuing operations before loss on disposal of assets and income taxes | | | 64,793 | | | | 35,161 | | | | — | | | | 99,954 | |
Loss on disposal of assets, net | | | (206 | ) | | | — | | | | — | | | | (206 | ) |
| | | | | | | | | | | | | | | | |
Earnings from continuing operations before income taxes | | $ | 64,587 | | | $ | 35,161 | | | $ | — | | | $ | 99,748 | |
| | | | | | | | | | | | | | | | |
Segment assets | | $ | 2,006,311 | | | $ | 293,150 | | | | | | | $ | 2,299,461 | |
| | | | | | | | | | | | | | | | |
Capital expenditures | | $ | 53,288 | | | $ | 177 | | | | | | | $ | 53,465 | |
| | | | | | | | | | | | | | | | |
Goodwill | | $ | 712,163 | | | $ | 5,757 | | | | | | | $ | 717,920 | |
| | | | | | | | | | | | | | | | |
F-19
IASIS HEALTHCARE LLC
NOTES TO CONDENSED CONSOLIDATED FINANCIAL STATEMENTS (UNAUDITED)
| (1) | Adjusted EBITDA represents net earnings from continuing operations before interest expense, income tax expense, depreciation and amortization, stock-based compensation, gain (loss) on disposal of assets, loss on extinguishment of debt and management fees. Management fees represent monitoring and advisory fees paid to affiliates of TPG, JLL and Trimaran. Management routinely calculates and communicates adjusted EBITDA and believes that it is useful to investors because it is commonly used as an analytical indicator within the healthcare industry to evaluate hospital performance, allocate resources and measure leverage capacity and debt service ability. In addition, the Company uses adjusted EBITDA as a measure of performance for its business segments and for incentive compensation purposes. Adjusted EBITDA should not be considered as a measure of financial performance under GAAP, and the items excluded from adjusted EBITDA are significant components in understanding and assessing financial performance. Adjusted EBITDA should not be considered in isolation or as an alternative to net earnings, cash flows generated by operating, investing, or financing activities or other financial statement data presented in the condensed consolidated financial statements as an indicator of financial performance or liquidity. Adjusted EBITDA, as presented, differs from what is defined under the Company’s senior secured credit facilities and may not be comparable to similarly titled measures of other companies. |
11. SUPPLEMENTAL CONDENSED CONSOLIDATING FINANCIAL INFORMATION
Similar to the 8 3/4% senior subordinated notes that were refinanced on May 3, 2011, the Senior Notes described in Note 2 are fully and unconditionally guaranteed on a joint and several basis by all of the Company’s existing domestic subsidiaries, other than non-guarantor subsidiaries which include Health Choice and the Company’s non-wholly owned subsidiaries. The guarantees are subject to customary release provisions set forth in the Indenture for the Senior Notes and are described in this prospectus under the heading “Description of Notes—Subsidiary Guarantees.”
Effective October 1, 2010, the operations and net assets of Wadley, acquired as part of the Brim acquisition, are included in the subsidiary non-guarantor information in the following summarized unaudited condensed consolidating financial statements.
Effective May 1, 2011, the operations and net assets of St. Joseph are included in the subsidiary non-guarantor information in the following summarized unaudited condensed consolidating financial statements.
Summarized condensed consolidating balance sheets at June 30, 2011 and September 30, 2010, condensed consolidating statements of operations for the quarters and nine months ended June 30, 2011 and 2010, and condensed consolidating statements of cash flows for the nine months ended June 30, 2011 and 2010, for the Company, segregating the parent company issuer, the subsidiary guarantors, the subsidiary non-guarantors and eliminations, are found below. Prior year amounts have been reclassified to conform to the current year presentation.
F-20
IASIS HEALTHCARE LLC
NOTES TO CONDENSED CONSOLIDATED FINANCIAL STATEMENTS (UNAUDITED)
IASIS Healthcare LLC
Condensed Consolidating Balance Sheet (unaudited)
June 30, 2011
(in thousands)
| | | | | | | | | | | | | | | | | | | | |
| | | Parent
Issuer | | | Subsidiary
Guarantors | | | Subsidiary
Non-Guarantors | | | Eliminations | | | Condensed
Consolidated | |
Assets | | | | | | | | | | | | | | | | | | | | |
Current assets: | | | | | | | | | | | | | | | | | | | | |
Cash and cash equivalents | | $ | — | | | $ | 136,874 | | | $ | 7,721 | | | $ | — | | | $ | 144,595 | |
Accounts receivable, net | | | — | | | | 109,608 | | | | 186,215 | | | | — | | | | 295,823 | |
Inventories | | | — | | | | 24,015 | | | | 41,431 | | | | — | | | | 65,446 | |
Deferred income taxes | | | 31,565 | | | | — | | | | — | | | | — | | | | 31,565 | |
Prepaid expenses and other current assets | | | — | | | | 33,823 | | | | 54,581 | | | | — | | | | 88,404 | |
| | | | | | | | | | | | | | | | | | | | |
Total current assets | | | 31,565 | | | | 304,320 | | | | 289,948 | | | | — | | | | 625,833 | |
| | | | | |
Property and equipment, net | | | — | | | | 347,698 | | | | 781,453 | | | | — | | | | 1,129,151 | |
Intercompany | | | — | | | | (269,735 | ) | | | 269,735 | | | | — | | | | — | |
Net investment in and advances to subsidiaries | | | 2,030,278 | | | | — | | | | — | | | | (2,030,278 | ) | | | — | |
Goodwill | | | 7,701 | | | | 99,663 | | | | 729,324 | | | | — | | | | 836,688 | |
Other intangible assets, net | | | — | | | | 8,635 | | | | 24,750 | | | | — | | | | 33,385 | |
Other assets, net | | | 37,589 | | | | (24,978 | ) | | | 49,132 | | | | — | | | | 61,743 | |
| | | | | | | | | | | | | | | | | | | | |
Total assets | | $ | 2,107,133 | | | $ | 465,603 | | | $ | 2,144,342 | | | $ | (2,030,278 | ) | | $ | 2,686,800 | |
| | | | | | | | | | | | | | | | | | | | |
| | | | | |
Liabilities and Equity | | | | | | | | | | | | | | | | | | | | |
Current liabilities: | | | | | | | | | | | | | | | | | | | | |
Accounts payable | | $ | — | | | $ | 31,947 | | | $ | 76,720 | | | $ | — | | | $ | 108,667 | |
Salaries and benefits payable | | | — | | | | 30,372 | | | | 34,674 | | | | — | | | | 65,046 | |
Accrued interest payable | | | 11,994 | | | | (3,222 | ) | | | 3,222 | | | | — | | | | 11,994 | |
Medical claims payable | | | — | | | | — | | | | 99,530 | | | | — | | | | 99,530 | |
Other accrued expenses and other current liabilities | | | — | | | | 42,216 | | | | 54,697 | | | | — | | | | 96,913 | |
Current portion of long-term debt and capital lease obligations | | | 10,250 | | | | 3,723 | | | | 25,036 | | | | (25,036 | ) | | | 13,973 | |
| | | | | | | | | | | | | | | | | | | | |
Total current liabilities | | | 22,244 | | | | 105,036 | | | | 293,879 | | | | (25,036 | ) | | | 396,123 | |
| | | | | |
Long-term debt and capital lease obligations | | | 1,851,167 | | | | 16,293 | | | | 674,685 | | | | (674,685 | ) | | | 1,867,460 | |
Deferred income taxes | | | 118,380 | | | | — | | | | — | | | | — | | | | 118,380 | |
Other long-term liabilities | | | — | | | | 81,593 | | | | 625 | | | | — | | | | 82,218 | |
| | | | | | | | | | | | | | | | | | | | |
Total liabilities | | | 1,991,791 | | | | 202,922 | | | | 969,189 | | | | (699,721 | ) | | | 2,464,181 | |
| | | | | |
Non-controlling interests with redemption rights | | | — | | | | 97,443 | | | | — | | | | — | | | | 97,443 | |
| | | | | | | | | | | | | | | | | | | | |
| | | | | |
Equity: | | | | | | | | | | | | | | | | | | | | |
Member’s equity | | | 115,342 | | | | 155,404 | | | | 1,175,153 | | | | (1,330,557 | ) | | | 115,342 | |
Non-controlling interests | | | — | | | | 9,834 | | | | — | | | | — | | | | 9,834 | |
| | | | | | | | | | | | | | | | | | | | |
| | | | | |
Total equity | | | 115,342 | | | | 165,238 | | | | 1,175,153 | | | | (1,330,557 | ) | | | 125,176 | |
| | | | | | | | | | | | | | | | | | | | |
Total liabilities and equity | | $ | 2,107,133 | | | $ | 465,603 | | | $ | 2,144,342 | | | $ | (2,030,278 | ) | | $ | 2,686,800 | |
| | | | | | | | | | | | | | | | | | | | |
F-21
IASIS HEALTHCARE LLC
NOTES TO CONDENSED CONSOLIDATED FINANCIAL STATEMENTS (UNAUDITED)
IASIS Healthcare LLC
Condensed Consolidating Balance Sheet
September 30, 2010
(in thousands)
| | | | | | | | | | | | | | | | | | | | |
| | | Parent
Issuer | | | Subsidiary
Guarantors | | | Subsidiary
Non-Guarantors | | | Eliminations | | | Condensed
Consolidated | |
Assets | | | | | | | | | | | | | | | | | | | | |
Current assets: | | | | | | | | | | | | | | | | | | | | |
Cash and cash equivalents | | $ | — | | | $ | 143,599 | | | $ | 912 | | | $ | — | | | $ | 144,511 | |
Accounts receivable, net | | | — | | | | 81,649 | | | | 127,524 | | | | — | | | | 209,173 | |
Inventories | | | — | | | | 22,793 | | | | 31,049 | | | | — | | | | 53,842 | |
Deferred income taxes | | | 15,881 | | | | — | | | | — | | | | — | | | | 15,881 | |
Prepaid expenses and other current assets | | | — | | | | 23,577 | | | | 41,763 | | | | — | | | | 65,340 | |
| | | | | | | | | | | | | | | | | | | | |
Total current assets | | | 15,881 | | | | 271,618 | | | | 201,248 | | | | — | | | | 488,747 | |
| | | | | |
Property and equipment, net | | | — | | | | 351,265 | | | | 634,026 | | | | — | | | | 985,291 | |
Intercompany | | | — | | | | (297,257 | ) | | | 297,257 | | | | — | | | | — | |
Net investment in and advances to subsidiaries | | | 1,823,973 | | | | — | | | | — | | | | (1,823,973 | ) | | | — | |
Goodwill | | | 17,331 | | | | 65,504 | | | | 635,408 | | | | — | | | | 718,243 | |
Other intangible assets, net | | | — | | | | — | | | | 27,000 | | | | — | | | | 27,000 | |
Deposit for acquisition | | | — | | | | 97,891 | | | | — | | | | — | | | | 97,891 | |
Other assets, net | | | 12,018 | | | | 17,967 | | | | 6,037 | | | | — | | | | 36,022 | |
| | | | | | | | | | | | | | | | | | | | |
Total assets | | $ | 1,869,203 | | | $ | 506,988 | | | $ | 1,800,976 | | | $ | (1,823,973 | ) | | $ | 2,353,194 | |
| | | | | | | | | | | | | | | | | | | | |
| | | | | |
Liabilities and Equity | | | | | | | | | | | | | | | | | | | | |
Current liabilities: | | | | | | | | | | | | | | | | | | | | |
Accounts payable | | $ | — | | | $ | 32,400 | | | $ | 46,531 | | | $ | — | | | $ | 78,931 | |
Salaries and benefits payable | | | — | | | | 19,916 | | | | 18,194 | | | | — | | | | 38,110 | |
Accrued interest payable | | | 12,536 | | | | (3,237 | ) | | | 3,237 | | | | — | | | | 12,536 | |
Medical claims payable | | | — | | | | — | | | | 111,373 | | | | — | | | | 111,373 | |
Other accrued expenses and other current liabilities | | | — | | | | 32,326 | | | | 74,288 | | | | — | | | | 106,614 | |
Current portion of long-term debt and capital lease obligations | | | 5,890 | | | | 801 | | | | 20,570 | | | | (20,570 | ) | | | 6,691 | |
| | | | | | | | | | | | | | | | | | | | |
Total current liabilities | | | 18,426 | | | | 82,206 | | | | 274,193 | | | | (20,570 | ) | | | 354,255 | |
| | | | | |
Long-term debt and capital lease obligations | | | 1,039,370 | | | | 5,517 | | | | 547,170 | | | | (547,170 | ) | | | 1,044,887 | |
Deferred income taxes | | | 109,272 | | | | — | | | | — | | | | — | | | | 109,272 | |
Other long-term liabilities | | | — | | | | 59,527 | | | | 635 | | | | — | | | | 60,162 | |
| | | | | | | | | | | | | | | | | | | | |
Total liabilities | | | 1,167,068 | | | | 147,250 | | | | 821,998 | | | | (567,740 | ) | | | 1,568,576 | |
| | | | | |
Non-controlling interests with redemption rights | | | — | | | | 72,112 | | | | — | | | | — | | | | 72,112 | |
| | | | | |
Equity: | | | | | | | | | | | | | | | | | | | | |
Member’s equity | | | 702,135 | | | | 277,255 | | | | 978,978 | | | | (1,256,233 | ) | | | 702,135 | |
Non-controlling interests | | | — | | | | 10,371 | | | | — | | | | — | | | | 10,371 | |
| | | | | | | | | | | | | | | | | | | | |
| | | | | |
Total equity | | | 702,135 | | | | 287,626 | | | | 978,978 | | | | (1,256,233 | ) | | | 712,506 | |
| | | | | | | | | | | | | | | | | | | | |
Total liabilities and equity | | $ | 1,869,203 | | | $ | 506,988 | | | $ | 1,800,976 | | | $ | (1,823,973 | ) | | $ | 2,353,194 | |
| | | | | | | | | | | | | | | | | | | | |
F-22
IASIS HEALTHCARE LLC
NOTES TO CONDENSED CONSOLIDATED FINANCIAL STATEMENTS (UNAUDITED)
IASIS Healthcare LLC
Condensed Consolidating Statement of Operations (unaudited)
For the Quarter Ended June 30, 2011
(in thousands)
| | | | | | | | | | | | | | | | | | | | |
| | | Parent
Issuer | | | Subsidiary
Guarantors | | | Subsidiary
Non-Guarantors | | | Eliminations | | | Condensed
Consolidated | |
Net revenue | | | | | | | | | | | | | | | | | | | | |
Acute care revenue | | $ | — | | | $ | 192,609 | | | $ | 340,300 | | | $ | (3,065 | ) | | $ | 529,844 | |
Premium revenue | | | — | | | | — | | | | 188,765 | | | | — | | | | 188,765 | |
| | | | | | | | | | | | | | | | | | | | |
Total net revenue | | | — | | | | 192,609 | | | | 529,065 | | | | (3,065 | ) | | | 718,609 | |
| | | | | |
Costs and expenses | | | | | | | | | | | | | | | | | | | | |
Salaries and benefits | | | — | | | | 95,012 | | | | 116,102 | | | | — | | | | 211,114 | |
Supplies | | | — | | | | 32,413 | | | | 50,658 | | | | — | | | | 83,071 | |
Medical claims | | | — | | | | — | | | | 158,950 | | | | (3,065 | ) | | | 155,885 | |
Other operating expenses | | | — | | | | 35,306 | | | | 79,472 | | | | — | | | | 114,778 | |
Provision for bad debts | | | — | | | | 24,538 | | | | 36,147 | | | | — | | | | 60,685 | |
Rentals and leases | | | — | | | | 4,842 | | | | 6,932 | | | | — | | | | 11,774 | |
Interest expense, net | | | 27,597 | | | | — | | | | 12,002 | | | | (12,002 | ) | | | 27,597 | |
Depreciation and amortization | | | — | | | | 10,429 | | | | 15,883 | | | | — | | | | 26,312 | |
Management fees | | | 1,250 | | | | (7,313 | ) | | | 7,313 | | | | — | | | | 1,250 | |
Loss on extinguishment of debt | | | 23,075 | | | | — | | | | — | | | | — | | | | 23,075 | |
Equity in earnings of affiliates | | | (39,530 | ) | | | — | | | | — | | | | 39,530 | | | | — | |
| | | | | | | | | | | | | | | | | | | | |
Total costs and expenses | | | 12,392 | | | | 195,227 | | | | 483,459 | | | | 24,463 | | | | 715,541 | |
| | | | | |
Earnings (loss) from continuing operations before loss on disposal of assets and income taxes | | | (12,392 | ) | | | (2,618 | ) | | | 45,606 | | | | (27,528 | ) | | | 3,068 | |
Loss on disposal of assets, net | | | — | | | | (72 | ) | | | (42 | ) | | | — | | | | (114 | ) |
| | | | | | | | | | | | | | | | | | | | |
| | | | | |
Earnings (loss) from continuing operations before income taxes | | | (12,392 | ) | | | (2,690 | ) | | | 45,564 | | | | (27,528 | ) | | | 2,954 | |
Income tax expense | | | 82 | | | | — | | | | 1,307 | | | | — | | | | 1,389 | |
| | | | | | | | | | | | | | | | | | | | |
| | | | | |
Net earnings (loss) from continuing operations | | | (12,474 | ) | | | (2,690 | ) | | | 44,257 | | | | (27,528 | ) | | | 1,565 | |
Earnings (loss) from discontinued operations, net of income taxes | | | 9 | | | | (23 | ) | | | (1 | ) | | | — | | | | (15 | ) |
| | | | | | | | | | | | | | | | | | | | |
| | | | | |
Net earnings (loss) | | | (12,465 | ) | | | (2,713 | ) | | | 44,256 | | | | (27,528 | ) | | | 1,550 | |
Net earnings attributable to non-controlling interests | | | — | | | | (2,013 | ) | | | — | | | | — | | | | (2,013 | ) |
| | | | | | | | | | | | | | | | | | | | |
| | | | | |
Net earnings (loss) attributable to IASIS Healthcare LLC | | $ | (12,465 | ) | | $ | (4,726 | ) | | $ | 44,256 | | | $ | (27,528 | ) | | $ | (463 | ) |
| | | | | | | | | | | | | | | | | | | | |
F-23
IASIS HEALTHCARE LLC
NOTES TO CONDENSED CONSOLIDATED FINANCIAL STATEMENTS (UNAUDITED)
IASIS Healthcare LLC
Condensed Consolidating Statement of Operations (unaudited)
For the Quarter Ended June 30, 2010
(in thousands)
| | | | | | | | | | | | | | | | | | | | |
| | | Parent
Issuer | | | Subsidiary
Guarantors | | | Subsidiary
Non-Guarantors | | | Eliminations | | | Condensed
Consolidated | |
Net revenue | | | | | | | | | | | | | | | | | | | | |
Acute care revenue | | $ | — | | | $ | 170,905 | | | $ | 269,625 | | | $ | (2,319 | ) | | $ | 438,211 | |
Premium revenue | | | — | | | | — | | | | 199,777 | | | | — | | | | 199,777 | |
| | | | | | | | | | | | | | | | | | | | |
Total net revenue | | | — | | | | 170,905 | | | | 469,402 | | | | (2,319 | ) | | | 637,988 | |
| | | | | |
Costs and expenses | | | | | | | | | | | | | | | | | | | | |
Salaries and benefits | | | — | | | | 86,937 | | | | 83,098 | | | | — | | | | 170,035 | |
Supplies | | | — | | | | 27,907 | | | | 38,426 | | | | — | | | | 66,333 | |
Medical claims | | | — | | | | — | | | | 174,350 | | | | (2,319 | ) | | | 172,031 | |
Other operating expenses | | | — | | | | 29,185 | | | | 64,394 | | | | — | | | | 93,579 | |
Provision for bad debts | | | — | | | | 21,589 | | | | 27,827 | | | | — | | | | 49,416 | |
Rentals and leases | | | — | | | | 4,268 | | | | 5,799 | | | | — | | | | 10,067 | |
Interest expense, net | | | 16,711 | | | | — | | | | 10,507 | | | | (10,507 | ) | | | 16,711 | |
Depreciation and amortization | | | — | | | | 10,271 | | | | 13,736 | | | | — | | | | 24,007 | |
Management fees | | | 1,250 | | | | (5,759 | ) | | | 5,759 | | | | — | | | | 1,250 | |
Equity in earnings of affiliates | | | (39,249 | ) | | | — | | | | — | | | | 39,249 | | | | — | |
| | | | | | | | | | | | | | | | | | | | |
Total costs and expenses | | | (21,288 | ) | | | 174,398 | | | | 423,896 | | | | 26,423 | | | | 603,429 | |
| | | | | |
Earnings (loss) from continuing operations before loss on disposal of assets and income taxes | | | 21,288 | | | | (3,493 | ) | | | 45,506 | | | | (28,742 | ) | | | 34,559 | |
Loss on disposal of assets, net | | | — | | | | (31 | ) | | | (118 | ) | | | — | | | | (149 | ) |
| | | | | | | | | | | | | | | | | | | | |
| | | | | |
Earnings (loss) from continuing operations before income taxes | | | 21,288 | | | | (3,524 | ) | | | 45,388 | | | | (28,742 | ) | | | 34,410 | |
Income tax expense | | | 12,683 | | | | — | | | | — | | | | — | | | | 12,683 | |
| | | | | | | | | | | | | | | | | | | | |
| | | | | |
Net earnings (loss) from continuing operations | | | 8,605 | | | | (3,524 | ) | | | 45,388 | | | | (28,742 | ) | | | 21,727 | |
Earnings (loss) from discontinued operations, net of income taxes | | | 229 | | | | (608 | ) | | | (5 | ) | | | — | | | | (384 | ) |
| | | | | | | | | | | | | | | | | | | | |
| | | | | |
Net earnings (loss) | | | 8,834 | | | | (4,132 | ) | | | 45,383 | | | | (28,742 | ) | | | 21,343 | |
Net earnings attributable to non-controlling interests | | | — | | | | (2,002 | ) | | | — | | | | — | | | | (2,002 | ) |
| | | | | | | | | | | | | | | | | | | | |
| | | | | |
Net earnings (loss) attributable to IASIS Healthcare LLC | | $ | 8,834 | | | $ | (6,134 | ) | | $ | 45,383 | | | $ | (28,742 | ) | | $ | 19,341 | |
| | | | | | | | | | | | | | | | | | | | |
F-24
IASIS HEALTHCARE LLC
NOTES TO CONDENSED CONSOLIDATED FINANCIAL STATEMENTS (UNAUDITED)
IASIS Healthcare LLC
Condensed Consolidating Statement of Operations (unaudited)
For the Nine Months Ended June 30, 2011
(in thousands)
| | | | | | | | | | | | | | | | | | | | |
| | | Parent
Issuer | | | Subsidiary
Guarantors | | | Subsidiary
Non-Guarantors | | | Eliminations | | | Condensed
Consolidated | |
Net revenue | | | | | | | | | | | | | | | | | | | | |
Acute care revenue | | $ | — | | | $ | 565,412 | | | $ | 932,552 | | | $ | (8,532 | ) | | $ | 1,489,432 | |
Premium revenue | | | — | | | | — | | | | 580,917 | | | | — | | | | 580,917 | |
| | | | | | | | | | | | | | | | | | | | |
Total net revenue | | | — | | | | 565,412 | | | | 1,513,469 | | | | (8,532 | ) | | | 2,070,349 | |
| | | | | |
Costs and expenses | | | | | | | | | | | | | | | | | | | | |
Salaries and benefits | | | — | | | | 283,860 | | | | 313,203 | | | | — | | | | 597,063 | |
Supplies | | | — | | | | 94,713 | | | | 142,718 | | | | — | | | | 237,431 | |
Medical claims | | | — | | | | — | | | | 493,167 | | | | (8,532 | ) | | | 484,635 | |
Other operating expenses | | | — | | | | 101,805 | | | | 213,449 | | | | — | | | | 315,254 | |
Provision for bad debts | | | — | | | | 72,180 | | | | 102,920 | | | | — | | | | 175,100 | |
Rentals and leases | | | — | | | | 14,167 | | | | 20,062 | | | | — | | | | 34,229 | |
Interest expense, net | | | 60,984 | | | | — | | | | 32,937 | | | | (32,937 | ) | | | 60,984 | |
Depreciation and amortization | | | — | | | | 30,376 | | | | 44,566 | | | | — | | | | 74,942 | |
Management fees | | | 3,750 | | | | (19,900 | ) | | | 19,900 | | | | — | | | | 3,750 | |
Loss on extinguishment of debt | | | 23,075 | | | | — | | | | — | | | | — | | | | 23,075 | |
Equity in earnings of affiliates | | | (102,349 | ) | | | — | | | | — | | | | 102,349 | | | | — | |
| | | | | | | | | | | | | | | | | | | | |
Total costs and expenses | | | (14,540 | ) | | | 577,201 | | | | 1,382,922 | | | | 60,880 | | | | 2,006,463 | |
| | | | | |
Earnings (loss) from continuing operations before gain on disposal of assets and income taxes | | | 14,540 | | | | (11,789 | ) | | | 130,547 | | | | (69,412 | ) | | | 63,886 | |
Gain on disposal of assets, net | | | — | | | | 420 | | | | 351 | | | | — | | | | 771 | |
| | | | | | | | | | | | | | | | | | | | |
| | | | | |
Earnings (loss) from continuing operations before income taxes | | | 14,540 | | | | (11,369 | ) | | | 130,898 | | | | (69,412 | ) | | | 64,657 | |
Income tax expense | | | 22,771 | | | | — | | | | 1,307 | | | | — | | | | 24,078 | |
| | | | | | | | | | | | | | | | | | | | |
| | | | | |
Net earnings (loss) from continuing operations | | | (8,231 | ) | | | (11,369 | ) | | | 129,591 | | | | (69,412 | ) | | | 40,579 | |
Earnings (loss) from discontinued operations, net of income taxes | | | 3,603 | | | | (9,612 | ) | | | (60 | ) | | | — | | | | (6,069 | ) |
| | | | | | | | | | | | | | | | | | | | |
| | | | | |
Net earnings (loss) | | | (4,628 | ) | | | (20,981 | ) | | | 129,531 | | | | (69,412 | ) | | | 34,510 | |
Net earnings attributable to non-controlling interests | | | — | | | | (6,201 | ) | | | — | | | | — | | | | (6,201 | ) |
| | | | | | | | | | | | | | | | | | | | |
| | | | | |
Net earnings (loss) attributable to IASIS Healthcare LLC | | $ | (4,628 | ) | | $ | (27,182 | ) | | $ | 129,531 | | | $ | (69,412 | ) | | $ | 28,309 | |
| | | | | | | | | | | | | | | | | | | | |
F-25
IASIS HEALTHCARE LLC
NOTES TO CONDENSED CONSOLIDATED FINANCIAL STATEMENTS (UNAUDITED)
IASIS Healthcare LLC
Condensed Consolidating Statement of Operations (unaudited)
For the Nine Months Ended June 30, 2010
(in thousands)
| | | | | | | | | | | | | | | | | | | | |
| | | Parent
Issuer | | | Subsidiary
Guarantors | | | Subsidiary
Non-Guarantors | | | Eliminations | | | Condensed
Consolidated | |
Net revenue | | | | | | | | | | | | | | | | | | | | |
Acute care revenue | | $ | — | | | $ | 517,001 | | | $ | 791,775 | | | $ | (8,331 | ) | | $ | 1,300,445 | |
Premium revenue | | | — | | | | — | | | | 591,022 | | | | — | | | | 591,022 | |
| | | | | | | | | | | | | | | | | | | | |
Total net revenue | | | — | | | | 517,001 | | | | 1,382,797 | | | | (8,331 | ) | | | 1,891,467 | |
| | | | | |
Costs and expenses | | | | | | | | | | | | | | | | | | | | |
Salaries and benefits | | | — | | | | 261,713 | | | | 252,975 | | | | — | | | | 514,688 | |
Supplies | | | — | | | | 84,049 | | | | 116,118 | | | | — | | | | 200,167 | |
Medical claims | | | — | | | | | | | | 519,023 | | | | (8,331 | ) | | | 510,692 | |
Other operating expenses | | | — | | | | 86,414 | | | | 180,440 | | | | — | | | | 266,854 | |
Provision for bad debts | | | — | | | | 65,352 | | | | 77,549 | | | | — | | | | 142,901 | |
Rentals and leases | | | | | | | 12,750 | | | | 17,737 | | | | — | | | | 30,487 | |
Interest expense, net | | | 50,065 | | | | — | | | | 30,886 | | | | (30,886 | ) | | | 50,065 | |
Depreciation and amortization | | | | | | | 30,129 | | | | 41,780 | | | | — | | | | 71,909 | |
Management fees | | | 3,750 | | | | (17,075 | ) | | | 17,075 | | | | — | | | | 3,750 | |
Equity in earnings of affiliates | | | (116,035 | ) | | | | | | | | | | | 116,035 | | | | — | |
| | | | | | | | | | | | | | | | | | | | |
Total costs and expenses | | | (62,220 | ) | | | 523,332 | | | | 1,253,583 | | | | 76,818 | | | | 1,791,513 | |
| | | | | |
Earnings (loss) from continuing operations before gain (loss) on disposal of assets and income taxes | | | 62,220 | | | | (6,331 | ) | | | 129,214 | | | | (85,149 | ) | | | 99,954 | |
Gain (loss) on disposal of assets, net | | | — | | | | 28 | | | | (234 | ) | | | — | | | | (206 | ) |
| | | | | | | | | | | | | | | | | | | | |
Earnings (loss) from continuing operations before income taxes | | | 62,220 | | | | (6,303 | ) | | | 128,980 | | | | (85,149 | ) | | | 99,748 | |
Income tax expense | | | 36,544 | | | | — | | | | — | | | | — | | | | 36,544 | |
| | | | | | | | | | | | | | | | | | | | |
| | | | | |
Net earnings (loss) from continuing operations | | | 25,676 | | | | (6,303 | ) | | | 128,980 | | | | (85,149 | ) | | | 63,204 | |
Earnings (loss) from discontinued operations, net of income taxes | | | 216 | | | | (571 | ) | | | (8 | ) | | | — | | | | (363 | ) |
| | | | | | | | | | | | | | | | | | | | |
| | | | | |
Net earnings (loss) | | | 25,892 | | | | (6,874 | ) | | | 128,972 | | | | (85,149 | ) | | | 62,841 | |
Net earnings attributable to non-controlling interests | | | — | | | | (6,063 | ) | | | — | | | | — | | | | (6,063 | ) |
| | | | | | | | | | | | | | | | | | | | |
| | | | | |
Net earnings (loss) attributable to IASIS Healthcare LLC | | $ | 25,892 | | | $ | (12,937 | ) | | $ | 128,972 | | | $ | (85,149 | ) | | $ | 56,778 | |
| | | | | | | | | | | | | | | | | | | | |
F-26
IASIS HEALTHCARE LLC
NOTES TO CONDENSED CONSOLIDATED FINANCIAL STATEMENTS (UNAUDITED)
IASIS Healthcare LLC
Condensed Consolidating Statement of Cash Flows (unaudited)
For the Nine Months Ended June 30, 2011
(in thousands)
| | | | | | | | | | | | | | | | | | | | |
| | | Parent
Issuer | | | Subsidiary
Guarantors | | | Subsidiary
Non-Guarantors | | | Eliminations | | | Condensed
Consolidated | |
Cash flows from operating activities | | | | | | | | | | | | | | | | | | | | |
Net earnings (loss) | | $ | (4,628 | ) | | $ | (20,981 | ) | | $ | 129,531 | | | $ | (69,412 | ) | | $ | 34,510 | |
Adjustments to reconcile net earnings (loss) to net cash provided by (used in) operating activities: | | | | | | | | | | | | | | | | | | | | |
Depreciation and amortization | | | — | | | | 30,376 | | | | 44,566 | | | | — | | | | 74,942 | |
Amortization of loan costs | | | 4,319 | | | | — | | | | — | | | | — | | | | 4,319 | |
Stock-based compensation | | | 1,364 | | | | — | | | | — | | | | — | | | | 1,364 | |
Deferred income taxes | | | 899 | | | | — | | | | — | | | | — | | | | 899 | |
Income tax benefit from parent company interest | | | 7,201 | | | | — | | | | — | | | | — | | | | 7,201 | |
Fair value change in interest rate swaps | | | (695 | ) | | | — | | | | — | | | | — | | | | (695 | ) |
Gain on disposal of assets, net | | | — | | | | (420 | ) | | | (351 | ) | | | — | | | | (771 | ) |
Loss (earnings) from discontinued operations, net | | | (3,603 | ) | | | 9,612 | | | | 60 | | | | — | | | | 6,069 | |
Loss on extinguishment of debt | | | 23,075 | | | | — | | | | — | | | | — | | | | 23,075 | |
Equity in earnings of affiliates | | | (102,349 | ) | | | — | | | | — | | | | 102,349 | | | | — | |
Changes in operating assets and liabilities, net of the effect of acquisitions and dispositions: | | | | | | | | | | | | | | | | | | | | |
Accounts receivable, net | | | — | | | | (25,039 | ) | | | (7,455 | ) | | | — | | | | (32,494 | ) |
Inventories, prepaid expenses and other current assets | | | — | | | | (39,764 | ) | | | 26,192 | | | | — | | | | (13,572 | ) |
Accounts payable, other accrued expenses and other accrued liabilities | | | (542 | ) | | | 41,615 | | | | (52,528 | ) | | | — | | | | (11,455 | ) |
| | | | | | | | | | | | | | | | | | | | |
Net cash provided by (used in) operating activities — continuing operations | | | (74,959 | ) | | | (4,601 | ) | | | 140,015 | | | | 32,937 | | | | 93,392 | |
Net cash provided by (used in) operating activities — discontinued operations | | | 3,603 | | | | (343 | ) | | | — | | | | — | | | | 3,260 | |
| | | | | | | | | | | | | | | | | | | | |
Net cash provided by (used in) operating activities | | | (71,356 | ) | | | (4,944 | ) | | | 140,015 | | | | 32,937 | | | | 96,652 | |
| | | | | | | | | | | | | | | | | | | | |
| | | | | |
Cash flows from investing activities | | | | | | | | | | | | | | | | | | | | |
Purchases of property and equipment, net | | | — | | | | (29,328 | ) | | | (35,147 | ) | | | — | | | | (64,475 | ) |
Cash paid for acquisitions, net | | | — | | | | (154,022 | ) | | | (1,406 | ) | | | — | | | | (155,428 | ) |
Proceeds from sale of assets | | | — | | | | 12 | | | | 138 | | | | — | | | | 150 | |
Change in other assets, net | | | — | | | | (4,689 | ) | | | 6,074 | | | | — | | | | 1,385 | |
| | | | | | | | | | | | | | | | | | | | |
Net cash used in investing activities | | | — | | | | (188,027 | ) | | | (30,341 | ) | | | — | | | | (218,368 | ) |
| | | | | | | | | | | | | | | | | | | | |
| | | | | |
Cash flows from financing activities | | | | | | | | | | | | | | | | | | | | |
Proceeds from refinancing | | | 1,863,730 | | | | — | | | | — | | | | — | | | | 1,863,730 | |
Payment of debt and capital lease obligations | | | (1,048,034 | ) | | | — | | | | (1,513 | ) | | | — | | | | (1,049,547 | ) |
Debt financing costs incurred | | | (51,308 | ) | | | — | | | | — | | | | — | | | | (51,308 | ) |
Distributions to parent company in connection with refinancing | | | (632,866 | ) | | | — | | | | — | | | | — | | | | (632,866 | ) |
Distributions to non-controlling interests | | | — | | | | (7,395 | ) | | | — | | | | — | | | | (7,395 | ) |
Costs paid for repurchase of non-controlling interests | | | — | | | | (814 | ) | | | — | | | | — | | | | (814 | ) |
Change in intercompany balances with affiliates, net | | | (60,166 | ) | | | 194,455 | | | | (101,352 | ) | | | (32,937 | ) | | | — | |
| | | | | | | | | | | | | | | | | | | | |
| | | | | |
Net cash provided by (used in) financing activities | | | 71,356 | | | | 186,246 | | | | (102,865 | ) | | | (32,937 | ) | | | 121,800 | |
| | | | | | | | | | | | | | | | | | | | |
| | | | | |
Change in cash and cash equivalents | | | — | | | | (6,725 | ) | | | 6,809 | | | | — | | | | 84 | |
Cash and cash equivalents at beginning of period | | | — | | | | 143,599 | | | | 912 | | | | — | | | | 144,511 | |
| | | | | | | | | | | | | | | | | | | | |
| | | | | |
Cash and cash equivalents at end of period | | $ | — | | | $ | 136,874 | | | $ | 7,721 | | | $ | — | | | $ | 144,595 | |
| | | | | | | | | | | | | | | | | | | | |
F-27
IASIS HEALTHCARE LLC
NOTES TO CONDENSED CONSOLIDATED FINANCIAL STATEMENTS (UNAUDITED)
IASIS Healthcare LLC
Condensed Consolidating Statement of Cash Flows (unaudited)
For the Nine Months Ended June 30, 2010
(in thousands)
| | | | | | | | | | | | | | | | | | | | |
| | | Subsidiary
Parent
Issuer | | | Subsidiary
Guarantors | | | Condensed
Non-Guarantors | | | Eliminations | | | Consolidated | |
Cash flows from operating activities | | | | | | | | | | | | | | | | | | | | |
Net earnings (loss) | | $ | 25,892 | | | $ | (6,874 | ) | | $ | 128,972 | | | $ | (85,149 | ) | | $ | 62,841 | |
Adjustments to reconcile net earnings (loss) to net cash provided by (used in) operating activities: | | | | | | | | | | | | | | | | | | | | |
Depreciation and amortization | | | — | | | | 30,129 | | | | 41,780 | | | | — | | | | 71,909 | |
Amortization of loan costs | | | 2,356 | | | | — | | | | — | | | | — | | | | 2,356 | |
Stock-based compensation | | | 2,367 | | | | — | | | | — | | | | — | | | | 2,367 | |
Deferred income taxes | | | 23,839 | | | | — | | | | — | | | | — | | | | 23,839 | |
Income tax benefit from stock-based compensation | | | (1,770 | ) | | | — | | | | — | | | | — | | | | (1,770 | ) |
Income tax benefit from parent company interest | | | 4,989 | | | | — | | | | — | | | | — | | | | 4,989 | |
Loss (gain) on disposal of assets, net | | | — | | | | (28 | ) | | | 234 | | | | — | | | | 206 | |
Loss (earnings) from discontinued operations, net | | | (216 | ) | | | 571 | | | | 8 | | | | — | | | | 363 | |
Equity in earnings of affiliates | | | (116,035 | ) | | | — | | | | — | | | | 116,035 | | | | — | |
Changes in operating assets and liabilities, net of the effect of dispositions: | | | | | | | | | | | | | | | | | | | | |
Accounts receivable, net | | | — | | | | 1,385 | | | | 7,769 | | | | — | | | | 9,154 | |
Inventories, prepaid expenses and other current assets | | | — | | | | (3,798 | ) | | | (71,111 | ) | | | — | | | | (74,909 | ) |
Accounts payable, other accrued expenses and other accrued liabilities | | | (8,613 | ) | | | 13,557 | | | | 8,193 | | | | — | | | | 13,137 | |
| | | | | | | | | | | | | | | | | | | | |
Net cash provided by (used in) operating activities — continuing operations | | | (67,191 | ) | | | 34,942 | | | | 115,845 | | | | 30,886 | | | | 114,482 | |
Net cash used in operating activities — discontinued operations | | | (216 | ) | | | (351 | ) | | | — | | | | — | | | | (567 | ) |
| | | | | | | | | | | | | | | | | | | | |
Net cash provided by (used in) operating activities | | | (67,407 | ) | | | 34,591 | | | | 115,845 | | | | 30,886 | | | | 113,915 | |
| | | | | | | | | | | | | | | | | | | | |
| | | | | |
Cash flows from investing activities | | | | | | | | | | | | | | | | | | | | |
Purchases of property and equipment, net | | | — | | | | (31,626 | ) | | | (21,839 | ) | | | — | | | | (53,465 | ) |
Proceeds from sale of assets | | | — | | | | 19 | | | | 31 | | | | — | | | | 50 | |
Change in other assets, net | | | — | | | | 1,960 | | | | (104 | ) | | | — | | | | 1,856 | |
| | | | | | | | | | | | | | | | | | | | |
Net cash used in investing activities | | | — | | | | (29,647 | ) | | | (21,912 | ) | | | — | | | | (51,559 | ) |
| | | | | | | | | | | | | | | | | | | | |
| | | | | | | | | | | | | | | | | | | | |
Cash flows from financing activities | | | | | | | | | | | | | | | | | | | | |
Payment of debt and capital lease obligations | | | (6,079 | ) | | | — | | | | (693 | ) | | | — | | | | (6,772 | ) |
Distribution to parent company in connection with the repurchase of equity, net | | | (124,962 | ) | | | — | | | | — | | | | — | | | | (124,962 | ) |
Distributions to non-controlling interests | | | — | | | | (179 | ) | | | (6,742 | ) | | | — | | | | (6,921 | ) |
Costs paid for repurchase of non-controlling interests | | | — | | | | (69 | ) | | | — | | | | — | | | | (69 | ) |
Change in intercompany balances with affiliates, net | | | 198,448 | | | | (81,064 | ) | | | (86,498 | ) | | | (30,886 | ) | | | — | |
| | | | | | | | | | | | | | | | | | | | |
Net cash provided by (used in) financing activities | | | 67,407 | | | | (81,312 | ) | | | (93,933 | ) | | | (30,886 | ) | | | (138,724 | ) |
| | | | | | | | | | | | | | | | | | | | |
Change in cash and cash equivalents | | | — | | | | (76,368 | ) | | | — | | | | — | | | | (76,368 | ) |
Cash and cash equivalents at beginning of period | | | — | | | | 206,331 | | | | 197 | | | | — | | | | 206,528 | |
| | | | | | | | | | | | | | | | | | | | |
Cash and cash equivalents at end of period | | $ | — | | | $ | 129,963 | | | $ | 197 | | | $ | — | | | $ | 130,160 | |
| | | | | | | | | | | | | | | | | | | | |
F-28
Report of Independent Registered Public Accounting Firm
To the Board of Directors of
IASIS Healthcare Corporation, sole member of IASIS Healthcare LLC
We have audited the accompanying consolidated balance sheets of IASIS Healthcare LLC as of September 30, 2010 and 2009, and the related consolidated statements of operations, equity and cash flows for each of the three years in the period ended September 30, 2010. These financial statements are the responsibility of the Company’s management. Our responsibility is to express an opinion on these financial statements based on our audits.
We conducted our audits in accordance with the standards of the Public Company Accounting Oversight Board (United States). Those standards require that we plan and perform the audit to obtain reasonable assurance about whether the financial statements are free of material misstatement. We were not engaged to perform an audit of the Company’s internal control over financial reporting. Our audits included consideration of internal control over financial reporting as a basis for designing audit procedures that are appropriate in the circumstances, but not for the purpose of expressing an opinion on the effectiveness of the Company’s internal control over financial reporting. Accordingly, we express no such opinion. An audit also includes examining, on a test basis, evidence supporting the amounts and disclosures in the financial statements, assessing the accounting principles used and significant estimates made by management, and evaluating the overall financial statement presentation. We believe that our audits provide a reasonable basis for our opinion.
In our opinion, the financial statements referred to above present fairly, in all material respects, the consolidated financial position of IASIS Healthcare LLC at September 30, 2010 and 2009, and the consolidated results of its operations and its cash flows for each of the three years in the period ended September 30, 2010, in conformity with U.S. generally accepted accounting principles.
As discussed in Note 2 to the consolidated financial statements, the Company changed its accounting and disclosure for noncontrolling interests with the adoption of the guidance originally issued in FASB Statement No. 160,Noncontrolling Interests in Consolidated Financial Statements (codified in FASB ASC Topic 810,Consolidation) effective October 1, 2009.
|
| /s/ Ernst & Young LLP |
|
| Nashville, Tennessee |
| December 21, 2010 |
F-29
IASIS HEALTHCARE LLC
CONSOLIDATED BALANCE SHEETS
(In thousands)
| | | | | | | | |
| | | September 30,
2010 | | | September 30,
2009 | |
| ASSETS | | | | | | | | |
Current assets: | | | | | | | | |
Cash and cash equivalents | | $ | 144,511 | | | $ | 206,528 | |
Accounts receivable, less allowance for doubtful accounts of $125,406 and $126,132 at September 30, 2010 and 2009, respectively | | | 209,173 | | | | 230,198 | |
Inventories | | | 53,842 | | | | 50,492 | |
Deferred income taxes | | | 15,881 | | | | 39,038 | |
Prepaid expenses and other current assets | | | 65,340 | | | | 49,453 | |
| | | | | | | | |
Total current assets | | | 488,747 | | | | 575,709 | |
| | |
Property and equipment, net | | | 985,291 | | | | 997,353 | |
Goodwill | | | 718,243 | | | | 717,920 | |
Other intangible assets, net | | | 27,000 | | | | 30,000 | |
Deposit for acquisition | | | 97,891 | | | | — | |
Other assets, net | | | 36,022 | | | | 36,222 | |
| | | | | | | | |
Total assets | | $ | 2,353,194 | | | $ | 2,357,204 | |
| | | | | | | | |
| | |
| LIABILITIES AND EQUITY | | | | | | | | |
| | |
Current liabilities: | | | | | | | | |
Accounts payable | | $ | 78,931 | | | $ | 68,552 | |
Salaries and benefits payable | | | 38,110 | | | | 42,548 | |
Accrued interest payable | | | 12,536 | | | | 12,511 | |
Medical claims payable | | | 111,373 | | | | 113,519 | |
Other accrued expenses and other current liabilities | | | 106,614 | | | | 65,701 | |
Current portion of long-term debt and capital lease obligations | | | 6,691 | | | | 8,366 | |
| | | | | | | | |
Total current liabilities | | | 354,255 | | | | 311,197 | |
| | |
Long-term debt and capital lease obligations | | | 1,044,887 | | | | 1,051,471 | |
Deferred income taxes | | | 109,272 | | | | 106,425 | |
Other long-term liabilities | | | 60,162 | | | | 54,222 | |
| | |
Non-controlling interests with redemption rights | | | 72,112 | | | | 72,527 | |
| | |
Equity: | | | | | | | | |
Member’s equity | | | 702,135 | | | | 750,932 | |
Non-controlling interests | | | 10,371 | | | | 10,430 | |
| | | | | | | | |
Total equity | | | 712,506 | | | | 761,362 | |
| | | | | | | | |
Total liabilities and equity | | $ | 2,353,194 | | | $ | 2,357,204 | |
| | | | | | | | |
See accompanying notes.
F-30
IASIS HEALTHCARE LLC
CONSOLIDATED STATEMENTS OF OPERATIONS
(In thousands)
| | | | | | | | | | | | |
| | | Year Ended
September 30,
2010 | | | Year Ended
September 30,
2009 | | | Year Ended
September 30,
2008 | |
Net revenue: | | | | | | | | | | | | |
Acute care revenue | | $ | 1,729,344 | | | $ | 1,662,469 | | | $ | 1,523,790 | |
Premium revenue | | | 792,062 | | | | 699,503 | | | | 541,746 | |
| | | | | | | | | | | | |
Total net revenue | | | 2,521,406 | | | | 2,361,972 | | | | 2,065,536 | |
| | | |
Costs and expenses: | | | | | | | | | | | | |
Salaries and benefits | | | 686,303 | | | | 660,921 | | | | 632,109 | |
Supplies | | | 266,545 | | | | 250,573 | | | | 231,259 | |
Medical claims | | | 678,651 | | | | 592,760 | | | | 452,055 | |
Other operating expenses | | | 363,916 | | | | 325,735 | | | | 283,123 | |
Provision for bad debts | | | 197,680 | | | | 192,563 | | | | 161,936 | |
Rentals and leases | | | 39,955 | | | | 39,127 | | | | 36,633 | |
Interest expense, net | | | 66,810 | | | | 67,890 | | | | 75,665 | |
Depreciation and amortization | | | 96,106 | | | | 97,462 | | | | 96,741 | |
Management fees | | | 5,000 | | | | 5,000 | | | | 5,000 | |
Impairment of goodwill | | | — | | | | 64,639 | | | | — | |
Hurricane-related property damage | | | — | | | | 938 | | | | 3,589 | |
| | | | | | | | | | | | |
Total costs and expenses | | | 2,400,966 | | | | 2,297,608 | | | | 1,978,110 | |
| | | |
Earnings from continuing operations before gain (loss) on disposal of assets and income taxes | | | 120,440 | | | | 64,364 | | | | 87,426 | |
Gain (loss) on disposal of assets, net | | | 108 | | | | 1,465 | | | | (75 | ) |
| | | | | | | | | | | | |
| | | |
Earnings from continuing operations before income taxes | | | 120,548 | | | | 65,829 | | | | 87,351 | |
Income tax expense | | | 44,715 | | | | 27,576 | | | | 35,325 | |
| | | | | | | | | | | | |
| | | |
Net earnings from continuing operations | | | 75,833 | | | | 38,253 | | | | 52,026 | |
Loss from discontinued operations, net of income taxes | | | (1,087 | ) | | | (176 | ) | | | (11,275 | ) |
| | | | | | | | | | | | |
| | | |
Net earnings | | | 74,746 | | | | 38,077 | | | | 40,751 | |
Net earnings attributable to non-controlling interests | | | (8,279 | ) | | | (9,987 | ) | | | (4,437 | ) |
| | | | | | | | | | | | |
| | | |
Net earnings attributable to IASIS Healthcare LLC | | $ | 66,467 | | | $ | 28,090 | | | $ | 36,314 | |
| | | | | | | | | | | | |
See accompanying notes.
F-31
IASIS HEALTHCARE LLC
CONSOLIDATED STATEMENTS OF EQUITY
(In thousands)
| | | | | | | | | | | | | | | | |
| | | Non-controlling
Interests with
Redemption
Rights | | | Member’s
Equity | | | Non-controlling
Interests | | | Total
Equity | |
| | | | |
Balance at September 30, 2007 (as previously reported) | | $ | — | | | $ | 691,514 | | | $ | — | | | $ | 691,514 | |
| | | | |
Adjustment to non-controlling interests from adoption of FASB authoritative guidance | | | 44,134 | | | | (16,782 | ) | | | 8,604 | | | | (8,178 | ) |
| | | | | | | | | | | | | | | | |
| | | | |
Balance at September 30, 2007 (as adjusted) | | | 44,134 | | | | 674,732 | | | | 8,604 | | | | 683,336 | |
Net earnings | | | 4,285 | | | | 36,314 | | | | 152 | | | | 36,466 | |
Distributions to non-controlling interests | | | (5,313 | ) | | | — | | | | (172 | ) | | | (172 | ) |
Proceeds from the sale of non-controlling interests | | | 15,872 | | | | — | | | | — | | | | — | |
Repurchases of non-controlling interests | | | (802 | ) | | | — | | | | — | | | | — | |
Non-controlling interests in acquisition of Ouachita | | | — | | | | — | | | | 1,897 | | | | 1,897 | |
Tax effect of adoption of FASB income tax guidance | | | — | | | | (59 | ) | | | — | | | | (59 | ) |
Adjustment to redemption value of non-controlling interests with redemption rights | | | (3,520 | ) | | | 3,520 | | | | — | | | | 3,520 | |
| | | | | | | | | | | | | | | | |
| | | | |
Balance at September 30, 2008 | | | 54,656 | | | | 714,507 | | | | 10,481 | | | | 724,988 | |
Net earnings | | | 9,769 | | | | 28,090 | | | | 218 | | | | 28,308 | |
Distributions to non-controlling interests | | | (6,481 | ) | | | — | | | | (269 | ) | | | (269 | ) |
Repurchases of non-controlling interests | | | (1,379 | ) | | | — | | | | — | | | | — | |
Conversion of non-controlling interests to note payable | | | (691 | ) | | | — | | | | — | | | | — | |
Stock compensation | | | — | | | | 561 | | | | — | | | | 561 | |
Other comprehensive loss | | | — | | | | (2,926 | ) | | | — | | | | (2,926 | ) |
Income tax benefit resulting from exercise of employee stock options | | | — | | | | 9 | | | | — | | | | 9 | |
Contribution from parent company related to tax benefit from Holdings Senior PIK Loans interest | | | — | | | | 27,344 | | | | — | | | | 27,344 | |
Adjustment to redemption value of non-controlling interests with redemption rights | | | 16,653 | | | | (16,653 | ) | | | — | | | | (16,653 | ) |
| | | | | | | | | | | | | | | | |
| | | | |
Balance at September 30, 2009 | | | 72,527 | | | | 750,932 | | | | 10,430 | | | | 761,362 | |
Net earnings | | | 8,144 | | | | 66,467 | | | | 135 | | | | 66,602 | |
Distributions to non-controlling interests | | | (8,790 | ) | | | — | | | | (194 | ) | | | (194 | ) |
Repurchases of non-controlling interests | | | (459 | ) | | | — | | | | — | | | | — | |
Stock compensation | | | — | | | | 2,487 | | | | — | | | | 2,487 | |
Other comprehensive loss | | | — | | | | (653 | ) | | | — | | | | (653 | ) |
Distribution to parent company in connection with the repurchase of equity, net | | | — | | | | (124,962 | ) | | | — | | | | (124,962 | ) |
Contribution from parent company related to tax benefit from Holdings Senior PIK Loans interest | | | — | | | | 8,554 | | | | — | | | | 8,554 | |
Adjustment to redemption value of non-controlling interests with redemption rights | | | 690 | | | | (690 | ) | | | — | | | | (690 | ) |
| | | | | | | | | | | | | | | | |
| | | | |
Balance at September 30, 2010 | | $ | 72,112 | | | $ | 702,135 | | | $ | 10,371 | | | $ | 712,506 | |
| | | | | | | | | | | | | | | | |
See accompanying notes.
F-32
IASIS HEALTHCARE LLC
CONSOLIDATED STATEMENTS OF CASH FLOWS
(In thousands)
| | | | | | | | | | | | |
| | | Year Ended
September 30,
2010 | | | Year Ended
September 30,
2009 | | | Year Ended
September 30,
2008 | |
Cash flows from operating activities: | | | | | | | | | | | | |
Net earnings | | $ | 74,746 | | | $ | 38,077 | | | $ | 40,751 | |
Adjustments to reconcile net earnings to net cash provided by operating activities: | | | | | | | | | | | | |
Depreciation and amortization | | | 96,106 | | | | 97,462 | | | | 96,741 | |
Amortization of loan costs | | | 3,163 | | | | 3,029 | | | | 2,913 | |
Stock compensation costs | | | 2,487 | | | | 561 | | | | — | |
Deferred income taxes | | | 30,473 | | | | (5,572 | ) | | | 19,368 | |
Income tax benefit from stock compensation | | | (1,770 | ) | | | — | | | | — | |
Income tax benefit from parent company interest | | | 8,554 | | | | 27,344 | | | | — | |
Loss (gain) on disposal of assets, net | | | (108 | ) | | | (1,465 | ) | | | 75 | |
Loss from discontinued operations | | | 1,087 | | | | 176 | | | | 11,275 | |
Impairment of goodwill | | | — | | | | 64,639 | | | | — | |
Hurricane-related property damage | | | — | | | | 938 | | | | 3,589 | |
Changes in operating assets and liabilities, net of the effect of acquisitions and dispositions: | | | | | | | | | | | | |
Accounts receivable, net | | | 21,279 | | | | (7,302 | ) | | | 17,131 | |
Inventories, prepaid expenses and other current assets | | | (19,227 | ) | | | 6,728 | | | | (21,361 | ) |
Accounts payable, other accrued expenses and other accrued liabilities | | | 41,957 | | | | 45,884 | | | | (29,419 | ) |
| | | | | | | | | | | | |
Net cash provided by operating activities — continuing operations | | | 258,747 | | | | 270,499 | | | | 141,063 | |
Net cash provided by (used in) operating activities — discontinued operations | | | (1,508 | ) | | | 1,472 | | | | 2,313 | |
| | | | | | | | | | | | |
Net cash provided by operating activities | | | 257,239 | | | | 271,971 | | | | 143,376 | |
| | | | | | | | | | | | |
| | | |
Cash flows from investing activities: | | | | | | | | | | | | |
Purchases of property and equipment | | | (81,268 | ) | | | (87,720 | ) | | | (137,415 | ) |
Cash paid for acquisitions | | | (98,305 | ) | | | (1,941 | ) | | | (16,821 | ) |
Proceeds from sale of assets | | | 57 | | | | 5,252 | | | | 360 | |
Change in other assets | | | 3,043 | | | | 1,823 | | | | 4,613 | |
| | | | | | | | | | | | |
Net cash used in investing activities — continuing operations | | | (176,473 | ) | | | (82,586 | ) | | | (149,263 | ) |
Net cash provided by (used in) investing activities — discontinued operations | | | — | | | | 10 | | | | (1,017 | ) |
| | | | | | | | | | | | |
Net cash used in investing activities | | | (176,473 | ) | | | (82,576 | ) | | | (150,280 | ) |
| | | | | | | | | | | | |
| | | |
Cash flows from financing activities: | | | | | | | | | | | | |
Payment of debt and capital lease obligations | | | (8,378 | ) | | | (55,476 | ) | | | (306,611 | ) |
Proceeds from debt borrowings | | | — | | | | — | | | | 384,978 | |
Distribution to parent company in connection with the repurchase of equity, net | | | (124,962 | ) | | | — | | | | — | |
Distributions to non-controlling interests | | | (8,984 | ) | | | (6,750 | ) | | | (5,485 | ) |
Proceeds received from sale (costs paid for repurchase) of non-controlling interests, net | | | (459 | ) | | | (1,379 | ) | | | 15,070 | |
Other | | | — | | | | — | | | | 192 | |
| | | | | | | | | | | | |
Net cash provided by (used in) financing activities — continuing operations | | | (142,783 | ) | | | (63,605 | ) | | | 88,144 | |
Net cash used in financing activities — discontinued operations | | | — | | | | — | | | | (502 | ) |
| | | | | | | | | | | | |
Net cash provided by (used in) financing activities | | | (142,783 | ) | | | (63,605 | ) | | | 87,642 | |
| | | | | | | | | | | | |
Change in cash and cash equivalents | | | (62,017 | ) | | | 125,790 | | | | 80,738 | |
Cash and cash equivalents at beginning of period | | | 206,528 | | | | 80,738 | | | | — | |
| | | | | | | | | | | | |
Cash and cash equivalents at end of period | | $ | 144,511 | | | $ | 206,528 | | | $ | 80,738 | |
| | | | | | | | | | | | |
| | | |
Supplemental disclosure of cash flow information: | | | | | | | | | | | | |
Cash paid for interest | | $ | 63,762 | | | $ | 66,136 | | | $ | 83,126 | |
| | | | | | | | | | | | |
Cash paid (received) for income taxes, net | | $ | 13,528 | | | $ | 4,104 | | | $ | (925 | ) |
| | | | | | | | | | | | |
| | | |
Supplemental schedule of noncash investing and financing activities: | | | | | | | | | | | | |
Capital lease obligations resulting from acquisitions | | $ | — | | | $ | — | | | $ | 4,849 | |
| | | | | | | | | | | | |
See accompanying notes.
F-33
IASIS HEALTHCARE LLC
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS
| 1. | ORGANIZATION AND BASIS OF PRESENTATION |
Organization
IASIS Healthcare LLC (“IASIS” or the “Company”) owns and operates medium-sized acute care hospitals in high-growth urban and suburban markets. At September 30, 2010, the Company owned or leased 15 acute care hospital facilities and one behavioral health hospital facility, with a total of 3,185 licensed beds, located in six regions:
| | • | | Tampa-St. Petersburg, Florida; |
| | • | | three cities in Texas, including San Antonio; |
| | • | | West Monroe, Louisiana. |
The Company also owns and operates Health Choice Arizona, Inc. (“Health Choice” or the “Plan”), a Medicaid and Medicare managed health plan in Phoenix.
Principles of Consolidation
The consolidated financial statements include all subsidiaries and entities under common control of the Company. Control is generally defined by the Company as ownership of a majority of the voting interest of an entity. In addition, control is demonstrated in instances when the Company is the sole general partner in a limited partnership. Significant intercompany transactions have been eliminated.
Use of Estimates
The preparation of the financial statements in conformity with U.S. generally accepted accounting principles (“GAAP”) requires management to make estimates and assumptions that affect the amounts reported in the accompanying audited consolidated financial statements and notes. Actual results could differ from those estimates.
Reclassifications
Certain prior year amounts have been reclassified to conform to the current year presentation. These reclassifications have no impact on the Company’s total assets or total liabilities and equity.
General and Administrative
The majority of the Company’s expenses are “cost of revenue” items. Costs that could be classified as “general and administrative” by the Company would include the IASIS corporate office costs, which were $39.2 million, $45.6 million and $50.5 million, for the years ended September 30, 2010, 2009 and 2008, respectively.
F-34
IASIS HEALTHCARE LLC
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (CONTINUED)
Subsequent Events Consideration
The Company has evaluated its financial statements and disclosures for the impact of subsequent events up to the date of filing its annual report on Form 10-K with the Securities and Exchange Commission.
| 2. | SIGNIFICANT ACCOUNTING POLICIES |
Net Revenue
Acute Care Revenue
The Company’s healthcare facilities have entered into agreements with third-party payors, including government programs and managed care health plans, under which the facilities are paid based upon established charges, the cost of providing services, predetermined rates per diagnosis, fixed per diem rates or discounts from established charges. Additionally, the Company offers discounts through its uninsured discount program to all uninsured patients receiving healthcare services who do not qualify for assistance under state Medicaid, other federal or state assistance plans, or charity care.
Net patient revenue is reported at the estimated net realizable amounts from third-party payors and others for services rendered, including estimated retroactive adjustments under reimbursement agreements with third-party payors. Retroactive adjustments are accrued on an estimated basis in the period the related services are rendered and are adjusted, if necessary, in future periods when final settlements are determined. Net adjustments to estimated third-party payor settlements (“prior year contractuals”) resulted in an increase in net revenue of $5.2 million, $3.2 million and $1.0 million for the years ended September 30, 2010, 2009 and 2008, respectively.
In the ordinary course of business, the Company provides care without charge to patients who are financially unable to pay for the healthcare services they receive. Because the Company does not pursue collection of amounts determined to qualify as charity care, they are not reported in net revenue. The Company currently records revenue deductions for patient accounts that meet its guidelines for charity care. The Company provides charity care to patients with income levels below 200% of the federal poverty level (“FPL”). Additionally, at all of the Company’s hospitals, a sliding scale of reduced rates is offered to uninsured patients, who are not covered through federal, state or private insurance, with incomes between 200% and 400% of the FPL. Charity care deductions based on gross charges for the years ended September 30, 2010, 2009 and 2008 were $37.9 million, $38.6 million and $37.7 million, respectively.
Premium Revenue
Health Choice is a prepaid Medicaid and Medicare managed health plan that derives most of its revenue through a contract with the Arizona Health Care Cost Containment System (“AHCCCS”) to provide specified health services to qualified Medicaid enrollees through contracted providers. AHCCCS is the state agency that administers Arizona’s Medicaid program. The contract requires the Plan to arrange for healthcare services for enrolled Medicaid patients in exchange for fixed monthly premiums, based upon negotiated per capita member rates, and supplemental payments from AHCCCS. Capitation payments received by Health Choice are recognized as revenue in the month that members are entitled to healthcare services.
The Plan receives reinsurance and other supplemental payments from AHCCCS for healthcare costs that exceed stated amounts at a rate ranging from 75% to 100% of qualified healthcare costs in excess of stated levels of up to $35,000 per claim, depending on the eligibility classification of the member. Qualified costs must be incurred during the contract year and are the lesser of the amount paid by the Plan or the AHCCCS fee schedule. Reinsurance recoveries are recognized under the contract with AHCCCS when healthcare costs exceed stated amounts as provided under the contract, including estimates of such costs at the end of each accounting period.
Effective October 1, 2008, Health Choice began its current contract with AHCCCS, which provides for a three-year term, with AHCCCS having the option to renew for two additional one-year periods. The contract is terminable without cause on 90 days’ written notice or for cause upon written notice if the Company fails to comply with any term or condition of the contract or fails
F-35
IASIS HEALTHCARE LLC
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (CONTINUED)
to take corrective action as required to comply with the terms of the contract. Additionally, AHCCCS can terminate the contract in the event of the unavailability of state or federal funding.
Health Choice also provides coverage as a Medicare Advantage Prescription Drug (“MAPD”) Special Needs Plan (“SNP”) provider pursuant to its contract with the Centers for Medicare and Medicaid Services (“CMS”). The SNP allows Health Choice to offer Medicare and Part D drug benefit coverage for new and existing dual-eligible members, or those that are eligible for Medicare and Medicaid. The contract with CMS includes successive one-year renewal options at the discretion of CMS and is terminable without cause on 90 days’ written notice or for cause upon written notice if the Company fails to comply with any term or condition of the contract or fails to take corrective action as required to comply with the terms of the contract. Health Choice has received notification that CMS is exercising its option to extend its contract through December 31, 2011.
The Plan subcontracts with hospitals, physicians and other medical providers within Arizona and surrounding states to provide services to its Medicaid enrollees in Apache, Coconino, Maricopa, Mohave, Navajo, Pima, Yuma, LaPaz and Santa Cruz counties, and to its Medicare enrollees in Maricopa, Pima, Pinal, Coconino, Apache and Navajo counties. These services are provided regardless of the actual costs incurred to provide these services.
Cash and Cash Equivalents
The Company considers highly liquid investments with original maturities of three months or less to be cash equivalents. The Company maintains its cash and cash equivalents balances primarily with high credit quality financial institutions. The Company manages its credit exposure by placing its investments in United States Treasury securities or other high quality securities, and by periodically evaluating the relative credit standing of the financial institution.
Accounts Receivable
The Company receives payments for services rendered from federal and state agencies (under the Medicare, Medicaid and TRICARE programs), managed care health plans, including Medicare and Medicaid managed health plans, commercial insurance companies, employers and patients. During the years ended September 30, 2010, 2009 and 2008, 47.6%, 45.9% and 44.9%, respectively, of the Company’s net patient revenue related to patients participating in the Medicare and Medicaid programs, including Medicare and Medicaid managed health plans. The Company recognizes that revenue and receivables from government agencies are significant to its operations, but does not believe that there is significant credit risks associated with these government agencies. The Company believes that concentration of credit risk from other payors is limited due to the number of patients and payors.
Net Medicare settlement receivables estimated at September 30, 2010 and 2009, totaled $1.3 million and $6.3 million, respectively, are included in accounts receivable in the accompanying consolidated balance sheets.
Allowance for Doubtful Accounts
The Company’s estimation of the allowance for doubtful accounts is based primarily upon the type and age of the patient accounts receivable and the effectiveness of the Company’s collection efforts. The Company’s policy is to reserve a portion of all self-pay receivables, including amounts due from the uninsured and amounts related to co-payments and deductibles, as these charges are recorded. On a monthly basis, the Company reviews its accounts receivable balances, the effectiveness of the Company’s reserve policies and various analytics to support the basis for its estimates. These efforts primarily consist of reviewing the following:
| | • | | Historical write-off and collection experience using a hindsight or look-back approach; |
| | • | | Revenue and volume trends by payor, particularly the self-pay components; |
F-36
IASIS HEALTHCARE LLC
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (CONTINUED)
| | • | | Changes in the aging and payor mix of accounts receivable, including increased focus on accounts due from the uninsured and accounts that represent co-payments and deductibles due from patients; |
| | • | | Cash collections as a percentage of net patient revenue less bad debt expense; |
| | • | | Trending of days revenue in accounts receivable; and |
| | • | | Various allowance coverage statistics. |
The Company regularly performs hindsight procedures to evaluate historical write-off and collection experience throughout the year to assist in determining the reasonableness of its process for estimating the allowance for doubtful accounts.
Inventories
Inventories, principally medical supplies, implants and pharmaceuticals, are stated at the lower of average cost or market.
Long-lived Assets
The primary components of the Company’s long-lived assets are discussed below. When events, circumstances or operating results indicate that the carrying values of certain long-lived assets and related identifiable intangible assets (excluding goodwill) that are expected to be held and used might be impaired under the provisions of Financial Accounting Standards Board (“FASB”) authoritative guidance regarding accounting for the impairment or disposal of long-lived assets, the Company considers the recoverability of assets to be held and used by comparing the carrying amount of the assets to the undiscounted value of future net cash flows expected to be generated by the assets. If assets are identified as impaired, the impairment is measured by the amount by which the carrying amount of the assets exceeds the fair value of the assets as determined by independent appraisals or estimates of discounted future cash flows. Assets to be disposed of are reported at the lower of the carrying amount or fair value less costs to sell.
Property and Equipment
Property and equipment are stated at cost. Routine maintenance and repairs are charged to expense as incurred. Expenditures that increase capacities or extend useful lives are capitalized. Buildings and improvements are depreciated over estimated useful lives ranging generally from 14 to 40 years. Estimated useful lives of equipment vary generally from 3 to 25 years. Leasehold improvements are amortized on a straight-line basis over the lesser of the terms of the respective leases or their estimated useful lives. Depreciation expense, including amortization of assets capitalized under capital leases, is computed using the straight-line method and was $93.1 million, $94.5 million and $93.7 million for the years ended September 30, 2010, 2009 and 2008, respectively. In connection with certain construction projects, the Company capitalized interest totaling $1.2 million and $1.4 million for the years ended September 30, 2009 and 2008, respectively. No amounts were capitalized in the year ended September 30, 2010.
Goodwill and Other Intangible Assets
See Note 10 for the values of goodwill and other intangible assets assigned to each business segment. Intangible assets are evaluated for impairment if events and circumstances indicate a possible impairment.
Goodwill is not amortized but is subject to annual tests for impairment or more often if events or circumstances indicate it may be impaired. An impairment loss is recorded to the extent that the carrying amount of goodwill exceeds its implied fair value. The Company completed its annual impairment test of goodwill during fiscal 2010, noting no impairment. During fiscal 2009, the Company’s testing of goodwill indicated impairment of goodwill associated with its Florida market. See Note 10 for more details.
F-37
IASIS HEALTHCARE LLC
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (CONTINUED)
Other Assets
Other assets consist primarily of costs associated with the issuance of debt, which are amortized over the life of the related debt. Amortization of deferred financing costs is included in interest expense and totaled $3.2 million, $3.0 million and $2.9 million for the years ended September 30, 2010, 2009 and 2008, respectively. Deferred financing costs, net of accumulated amortization, totaled $12.0 million and $15.2 million at September 30, 2010 and 2009, respectively.
Insurance Reserves
The Company estimates its reserve for self-insured professional and general liability and workers compensation risks using historical claims data, demographic factors, severity factors, current incident logs and other actuarial analysis.
Income Taxes
The Company accounts for income taxes under the asset and liability method in accordance with FASB authoritative guidance regarding accounting for income taxes and its related uncertainty. This approach requires the recognition of deferred tax assets and liabilities for the expected future tax consequences of temporary differences between the carrying amounts and the tax bases of assets and liabilities. Deferred tax assets and liabilities are measured using enacted tax rates expected to apply when the temporary differences are expected to reverse. The Company assesses the likelihood that deferred tax assets will be recovered from future taxable income to determine whether a valuation allowance should be established.
Non-controlling Interests in Consolidated Entities
Effective October 1, 2009, the Company adopted the provisions of FASB authoritative guidance regarding non-controlling interests in consolidated financial statements. The guidance requires the Company to clearly identify and present ownership interests in subsidiaries held by parties other than the Company in the consolidated financial statements within the equity section. It also requires the amounts of consolidated net earnings attributable to the Company and to the non-controlling interests to be clearly identified and presented on the face of the consolidated statements of operations.
The Company consolidates seven subsidiaries with non-controlling interests that include third-party partners that own limited partnership units with certain redemption features. The redeemable limited partnership units require the Company to buy back the units upon the occurrence of certain events at the fair value of the units. In addition, the limited partnership agreements for all of the limited partnerships provide the limited partners with put rights which allow the units to be sold back to the Company, subject to certain limitations, at the fair value of the units. According to the limited partnership agreements, the fair value of the units is generally calculated as the product of the most current audited fiscal period’s EBITDA (earnings before interest, taxes, depreciation, amortization and management fees) and a fixed multiple, less any long-term debt of the entity. The majority of these put rights require an initial holding period of six years after purchase, at which point the holder of the redeemable limited partnership units may put back to the Company 20% of such holder’s units. Each succeeding year, the number of vested redeemable units will increase by 20% until the end of the tenth year after the initial investment, at which point 100% of the units may be put back to the Company. Under no circumstances shall the Company be required to repurchase more than 25% of the total vested redeemable limited partnership units in any fiscal year. The equity attributable to these interests has been classified as non-controlling interests with redemption rights in the accompanying consolidated balance sheets.
Medical Claims Payable
Monthly capitation payments made by Health Choice to physicians and other healthcare providers are expensed in the month services are contracted to be performed. Claims expense for non-capitated arrangements is accrued as services are rendered by hospitals, physicians and other healthcare providers during the year.
F-38
IASIS HEALTHCARE LLC
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (CONTINUED)
Medical claims payable related to Health Choice includes claims received but not paid and an estimate of claims incurred but not reported. Incurred but not reported claims are estimated using a combination of historical claims experience (including severity and payment lag time) and other actuarial analysis, including number of enrollees, age of enrollees and certain enrollee health indicators, to predict the cost of healthcare services provided to enrollees during any given period. While management believes that its estimation methodology effectively captures trends in medical claims costs, actual payments could differ significantly from estimates given changes in the healthcare cost structure or adverse experience.
The following table shows the components of the change in medical claims payable (in thousands):
| | | | | | | | |
| | | Year Ended
September 30,
2010 | | | Year Ended
September 30,
2009 | |
| | |
Medical claims payable as of October 1 | | $ | 113,519 | | | $ | 97,343 | |
Medical claims expense incurred during the year: | | | | | | | | |
Related to current year | | | 697,052 | | | | 620,153 | |
Related to prior years | | | (6,596 | ) | | | (18,077 | ) |
| | | | | | | | |
Total expenses | | | 690,456 | | | | 602,076 | |
| | | | | | | | |
| | |
Medical claims payments during the year: | | | | | | | | |
Related to current year | | | (587,292 | ) | | | (508,299 | ) |
Related to prior years | | | (105,310 | ) | | | (77,601 | ) |
| | | | | | | | |
Total payments | | | (692,602 | ) | | | (585,900 | ) |
| | | | | | | | |
| | |
Medical claims payable as of September 30 | | $ | 111,373 | | | $ | 113,519 | |
| | | | | | | | |
As reflected in the table above, medical claims expense for the year ended September 30, 2010, includes a $6.6 million reduction of medical costs related to prior years resulting from favorable development in the Medicaid and Medicare product lines of $6.4 million and $209,000, respectively. The favorable development is attributable to lower than anticipated medical costs. Medical claims expense for the year ended September 30, 2009, includes an $18.1 million reduction of medical costs related to prior years resulting from favorable development in the Medicaid and Medicare product lines of $15.5 million and $2.6 million, respectively. The favorable development is attributable to lower than anticipated medical costs and is offset, in part, by $10.8 million in reductions in premium revenue associated with settlements of various prior year program receivables. Additional adjustments to prior year estimates may be necessary in future periods as more information becomes available.
Health Choice has experienced an increase in the number of lives served by the plan. Enrollment in Health Choice at September 30, 2010 and 2009, was 198,393 and 190,763, respectively.
Stock Based Compensation
Although IASIS has no stock option plan or outstanding stock options, the Company, through its parent, IASIS Healthcare Corporation (“IAS”), grants stock options for a fixed number of common shares to employees. The Company accounts for this stock-based incentive plan under the measurement and recognition provisions of FASB authoritative guidance regarding share-based payments (“Share-Based Payments Guidance”). Accordingly, the Company has not recognized any compensation expense for the stock options granted prior to October 1, 2006, as the exercise price of the options equaled, or was greater than, the market value of the underlying stock on the date of grant.
For stock options granted on or after October 1, 2006, the Company applies the fair value recognition provisions of the Share-Based Payments Guidance, requiring all share-based payments to employees, including grants of employee stock options, to be recognized in the income statement based on their fair values. In accordance with the provisions of the Share-Based Payments Guidance, the Company uses the Black-Scholes-Merton model in determining the fair value of its share-based payments. The fair value of compensation costs will be amortized on a straight-line basis over the requisite service periods of the awards, generally equal to the awards’ vesting periods.
F-39
IASIS HEALTHCARE LLC
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (CONTINUED)
Fair Value of Financial Instruments
Cash and cash equivalents, accounts receivable, accounts payable and accrued liabilities are reflected in the accompanying consolidated financial statements at amounts that approximate fair value because of the short-term nature of these instruments. The fair value of the Company’s capital lease obligations also approximate carrying value as they bear interest at current market rates. The estimated fair values of the Company’s 8 3/4% senior subordinated notes due 2014 (the “8 3/4% notes”) and senior secured credit facilities were $485.7 million and $570.3 million, respectively, at September 30, 2010, based upon quoted market prices at that date.
Management Services Agreement
The Company is party to a management services agreement with affiliates of TPG, JLL Partners and Trimaran Fund Management. The management services agreement provides that in exchange for consulting and management advisory services that will be provided to the Company by the investors, the Company will pay an aggregate monitoring fee of 0.25% of budgeted net revenue up to a maximum of $5.0 million per fiscal year to these parties (or certain of their respective affiliates) and reimburse them for their reasonable disbursements and out-of-pocket expenses. This monitoring fee is divided among the parties in proportion to their relative ownership percentages in IASIS Investment LLC, parent company and majority stockholder of IAS. The monitoring fee will be subordinated to the senior subordinated notes in the event of a bankruptcy of the Company. The management services agreement does not have a stated term. Pursuant to the provisions of the management services agreement, the Company has agreed to indemnify the investors (or certain of their respective affiliates) in certain situations arising from or relating to the agreement, the investors’ investment in the securities of IAS or any related transactions or the operations of the investors, except for losses that arise on account of the investors’ negligence or willful misconduct. For each of the three years ended September 30, 2010, 2009 and 2008, the Company paid $5.0 million in monitoring fees under the management services agreement.
Recently Issued Accounting Pronouncements
The Company has adopted the new FASB authoritative guidance regarding business combinations, which applies prospectively to business combinations for which the acquisition date is on or after the beginning of the first annual reporting period beginning on or after December 15, 2008. This new guidance establishes principles and requirements for recognition and measurement of items acquired during a business combination, as well as certain disclosure requirements in the financial statements. The adoption of these provisions did not impact the Company’s results of operations or financial position; however, it is anticipated to have a material effect on the Company’s accounting for future acquisitions.
F-40
IASIS HEALTHCARE LLC
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (CONTINUED)
| 3. | LONG-TERM DEBT AND CAPITAL LEASE OBLIGATIONS |
Long-term debt and capital lease obligations consist of the following (in thousands):
| | | | | | | | |
| | | September 30,
2010 | | | September 30,
2009 | |
| | |
Senior secured credit facilities | | $ | 570,260 | | | $ | 576,150 | |
Senior subordinated notes | | | 475,000 | | | | 475,000 | |
Capital leases and other obligations | | | 6,318 | | | | 8,687 | |
| | | | | | | | |
| | | 1,051,578 | | | | 1,059,837 | |
Less current maturities | | | 6,691 | | | | 8,366 | |
| | | | | | | | |
| | $ | 1,044,887 | | | $ | 1,051,471 | |
| | | | | | | | |
Senior Secured Credit Facilities
The $854.0 million senior secured credit facilities include: (i) a senior secured term loan of $439.0 million; (ii) a senior secured delayed draw term loan of $150.0 million; (iii) a senior secured revolving credit facility of $225.0 million, which includes a $100.0 million sub-limit for letters of credit; and (iv) a senior secured synthetic letter of credit facility of $40.0 million. All facilities mature on March 15, 2014, except for the revolving credit facility, which matures on April 27, 2013. The term loans bear interest at an annual rate of LIBOR plus 2.00% or, at the Company’s option, the administrative agent’s base rate plus 1.00%. The revolving loans bear interest at an annual rate of LIBOR plus an applicable margin ranging from 1.25% to 1.75% or, at the Company’s option, the administrative agent’s base rate plus an applicable margin ranging from 0.25% to 0.75%, such rate in each case depending on the Company’s senior secured leverage ratio. A commitment fee ranging from 0.375% to 0.5% per annum is charged on the undrawn portion of the senior secured revolving credit facility and is payable in arrears.
Principal under the senior secured term loan is due in 24 consecutive equal quarterly installments in an aggregate annual amount equal to 1.0% of the original principal amount ($439.0 million) during the first six years thereof, with the balance payable in four equal installments in year seven. Principal under the senior secured delayed draw term loan is due in equal quarterly installments in an aggregate annual amount equal to 1.0% of the original principal amount ($150.0 million) until March 31, 2013, with the balance payable in four equal installments during the final year of the loan. Unless terminated earlier, the senior secured revolving credit facility has a single maturity of six years. The senior secured credit facilities are also subject to mandatory prepayment under specific circumstances, including a portion of excess cash flow, a portion of the net proceeds from an initial public offering, asset sales, debt issuances and specified casualty events, each subject to various exceptions.
The senior secured credit facilities are (i) secured by a first mortgage and lien on the real property and related personal and intellectual property of the Company and pledges of equity interests in the entities that own such properties and (ii) guaranteed by certain of the Company’s subsidiaries.
In addition, the senior secured credit facilities contain certain covenants which, among other things, limit the incurrence of additional indebtedness, investments, dividends, transactions with affiliates, asset sales, acquisitions, mergers and consolidations, liens and encumbrances and other matters customarily restricted in such agreements.
At September 30, 2010, amounts outstanding under the Company’s senior secured credit facilities consisted of a $423.6 million term loan and a $146.7 million delayed draw term loan. In addition, the Company had $39.9 million and $41.4 million in letters of credit outstanding under the synthetic letter of credit facility and the revolving credit facility, respectively. The weighted average interest rate of outstanding borrowings under the senior secured credit facilities was 3.4% and 3.6% for the years ended September 30, 2010 and 2009, respectively.
F-41
IASIS HEALTHCARE LLC
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (CONTINUED)
8 3/4% Senior Subordinated Notes
The Company, together with its wholly-owned subsidiary, IASIS Capital Corporation, a holding company with no assets or operations, as issuers, have outstanding $475.0 million aggregate principal amount of 8 3/4% notes. The 8 3/4% notes are general unsecured senior subordinated obligations and are subordinated in right of payment to all existing and future senior debt of the Company. The Company’s existing domestic subsidiaries, other than certain non-guarantor subsidiaries, which include Health Choice and the Company’s non-wholly owned subsidiaries, are guarantors of the 8 3/4% notes. The 8 3/4% notes are effectively subordinated to all of the issuers’ and the guarantors’ secured debt to the extent of the value of the assets securing the debt and are structurally subordinated to all liabilities and commitments (including trade payables and capital lease obligations) of the Company’s subsidiaries that are not guarantors of the 8 3/4% notes.
Holdings Senior Paid-in-Kind Loans
IAS has outstanding unsecured Senior Paid-in-Kind (“PIK”) Loans, which were used to repurchase certain preferred equity from its stockholders in fiscal 2007. The Senior PIK Loans mature June 15, 2014, and bear interest at an annual rate equal to LIBOR plus 5.25%. At September 30, 2010, the outstanding balance of the Senior PIK Loans was $389.8 million, which includes $89.8 million of interest that has accrued to the principal of these loans since the date of issuance, and is recorded in the financial statements of IAS. In June 2012, the Senior PIK Loans, which rank behind the Company’s existing debt, will convert to cash-pay, at which time all accrued interest becomes payable. In the event the Senior PIK Loans are not refinanced before their maturity, it is anticipated that principle and interest will be funded by the cash flows of the Company.
Effective March 2, 2009, the Company executed interest rate swap transactions with Citibank, N.A. and Wachovia Bank, N.A., as counterparties, with notional amounts totaling $425.0 million. The arrangements with each counterparty include two interest rate swap agreements, one with a notional amount of $112.5 million maturing on February 28, 2011 and one with a notional amount of $100.0 million maturing on February 29, 2012. The Company entered into these interest rate swap arrangements to mitigate the floating interest rate risk on a portion of its outstanding variable rate debt. Under these agreements, the Company is required to make monthly fixed rate payments to the counterparties, as calculated on the applicable notional amounts, at annual fixed rates, which range from 1.5% to 2.0% depending upon the agreement. The counterparties are obligated to make monthly floating rate payments to the Company based on the one-month LIBOR rate for the same referenced notional amount.
| | | | |
Date Range | | Total Notional
Amounts | |
| | | (in thousands) | |
| |
Expiring on February 28, 2011 | | $ | 225,000 | |
Expiring on February 29, 2012 | | $ | 200,000 | |
The Company accounts for its interest rate swaps in accordance with the provisions of FASB authoritative guidance regarding accounting for derivative instruments and hedging activities, which also includes enhanced disclosure requirements. In accordance with these provisions, the Company has designated its interest rate swaps as cash flow hedge instruments. The Company assesses the effectiveness of these cash flow hedges on a quarterly basis, with any ineffectiveness being measured using the hypothetical derivative method. The Company completed an assessment of its cash flow hedge instruments during the years ended September 30, 2010 and 2009, and determined its hedging instruments to be highly effective in all periods. Accordingly, no gain or loss resulting from hedging ineffectiveness is reflected in the Company’s accompanying consolidated statements of operations.
The Company applies the provisions of FASB authoritative guidance regarding fair value measurements, which provides a single definition of fair value, establishes a framework for measuring fair value, and expands disclosures concerning fair value measurements. The Company applies these provisions to the valuation and disclosure of its interest rate swaps. This authoritative guidance establishes a three-tier fair value hierarchy, which prioritizes the inputs used in measuring fair value. These tiers include: (i) Level 1, which is defined as quoted prices in active markets that can be accessed at the measurement date; (ii) Level 2, which is
F-42
IASIS HEALTHCARE LLC
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (CONTINUED)
defined as inputs other than quoted prices in active markets that are observable, either directly or indirectly; and (iii) Level 3, which is defined as unobservable inputs resulting from the existence of little or no market data, therefore potentially requiring an entity to develop its own assumptions.
The Company determines the fair value of its interest rate swaps in a manner consistent with that used by market participants in pricing hedging instruments, which includes using a discounted cash flow analysis based upon the terms of the agreements, the impact of the one-month forward LIBOR curve and an evaluation of credit risk. Given the use of observable market assumptions and the consideration of credit risk, the Company has categorized the valuation of its interest rate swaps as Level 2.
The fair value of the Company’s interest rate swaps at September 30, 2010 and 2009, reflect liability balances of $5.7 million and $4.7 million, respectively, and are included in other long-term liabilities in the accompanying consolidated balance sheets. The fair value of the Company’s interest rate swaps reflects a liability because the effect of the forward LIBOR curve on future interest payments results in less interest due to the Company under the variable rate component included in the interest rate swap agreements, as compared to the amount due the Company’s counterparties under the fixed interest rate component. Any change in the fair value of the Company’s interest rate swaps, net of income taxes, is included in other comprehensive loss as a component of member’s equity in the accompanying consolidated balance sheets.
Comprehensive income consists of two components: net earnings and other comprehensive income. Other comprehensive income refers to revenues, expenses, gains and losses that under the FASB authoritative guidance related to accounting for comprehensive income are recorded as elements of equity, but are excluded from net earnings. The following table presents the components of comprehensive income, net of income taxes (in thousands):
| | | | | | | | |
| | | Year Ended
September 30,
2010 | | | Year Ended
September 30,
2009 | |
| | |
Net earnings | | $ | 74,746 | | | $ | 38,077 | |
Change in fair value of interest rate swaps | | | (1,045 | ) | | | (4,660 | ) |
Change in income tax benefit | | | 392 | | | | 1,734 | |
| | | | | | | | |
| | |
Comprehensive income | | $ | 74,093 | | | $ | 35,151 | |
| | | | | | | | |
The components of accumulated other comprehensive loss, net of income taxes, are as follows (in thousands):
| | | | | | | | |
| | | September 30,
2010 | | | September 30,
2009 | |
| | |
Fair value of interest rate swaps | | $ | (5,707 | ) | | $ | (4,662 | ) |
Income tax benefit | | | 2,128 | | | | 1,736 | |
| | | | | | | | |
| | |
Accumulated other comprehensive loss | | $ | (3,579 | ) | | $ | (2,926 | ) |
| | | | | | | | |
During the year ended September 30, 2010, the Company distributed $125.0 million, net of a $1.8 million income tax benefit, to IAS to fund the repurchase of certain shares of its outstanding preferred stock and cancel certain vested rollover options to purchase its common stock. The holder of the IAS preferred stock is represented by an investor group led by TPG, JLL Partners and Trimaran Fund Management. The repurchase of preferred stock, which included accrued and outstanding dividends, and the cancellation of rollover options were funded by the Company’s excess cash on hand.
F-43
IASIS HEALTHCARE LLC
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (CONTINUED)
Effective October 1, 2010, the Company purchased Brim Holdings, Inc. (“Brim”) in a cash-for-stock transaction valued at $95.0 million, subject to changes in net working capital. Brim operates Wadley Regional Medical Center, a 370 licensed bed acute care hospital facility located in Texarkana, Texas, and Pikes Peak Regional Hospital, a 15 licensed bed critical access acute care hospital facility, in Woodland Park, Colorado. In connection with the Company’s agreement to purchase Brim, the Company made an agent fund deposit of $97.9 million, which is included in long-term assets in the accompanying consolidated balance sheet as of September 30, 2010.
Effective February 1, 2008, IASIS Glenwood Regional Medical Center, LP, a wholly-owned subsidiary of the Company, purchased a majority ownership interest in Ouachita Community Hospital, a ten-bed surgical hospital located in West Monroe, Louisiana. The purchase price for the majority ownership interest included $16.8 million in cash.
| 8. | DISCONTINUED OPERATIONS |
The Company’s lease agreements to operate Mesa General Hospital (“Mesa General”), located in Mesa, Arizona, and Biltmore Surgery Center (“Biltmore”), located in Phoenix, Arizona, expired by their terms on July 31, 2008 and September 30, 2008, respectively. The Company discontinued services at Mesa General on May 31, 2008, and Biltmore on April 30, 2008. The operating results of Mesa General and Biltmore are classified in the Company’s accompanying consolidated financial statements as discontinued operations. The following table sets forth the components of discontinued operations (in thousands):
| | | | | | | | | | | | |
| | | Year Ended
September 30,
2010 | | | Year Ended
September 30,
2009 | | | Year Ended
September 30,
2008 | |
| | | |
Total net revenue | | $ | 77 | | | $ | 974 | | | $ | 49,974 | |
| | | |
Operating expenses | | | 1,814 | | | | 1,256 | | | | 64,648 | |
Loss on disposal of assets | | | — | | | | — | | | | 3,928 | |
Income tax benefit | | | (650 | ) | | | (106 | ) | | | (7,327 | ) |
| | | | | | | | | | | | |
| | | |
Loss from discontinued operations, net of income taxes | | $ | (1,087 | ) | | $ | (176 | ) | | $ | (11,275 | ) |
| | | | | | | | | | | | |
The Company allocated to discontinued operations interest expense of $2.5 million for the year ended September 30, 2008. The allocation of interest expense to discontinued operations was based on the ratio of disposed net assets of Mesa General and Biltmore to the sum of total net assets of the Company plus the Company’s total outstanding debt.
Income taxes allocated to the discontinued operations resulted in related effective tax rates of 37.4%, 37.6% and 39.4% for the years ended September 30, 2010, 2009 and 2008, respectively.
Property and equipment consist of the following (in thousands):
| | | | | | | | |
| | | September 30,
2010 | | | September 30,
2009 | |
| | |
Land | | $ | 102,969 | | | $ | 102,499 | |
Buildings and improvements | | | 811,569 | | | | 792,467 | |
Equipment | | | 556,353 | | | | 500,450 | |
| | | | | | | | |
| | | 1,470,891 | | | | 1,395,416 | |
Less accumulated depreciation and amortization | | | (501,952 | ) | | | (414,572 | ) |
| | | | | | | | |
| | | 968,939 | | | | 980,844 | |
Construction-in-progress | | | 16,352 | | | | 16,509 | |
| | | | | | | | |
| | $ | 985,291 | | | $ | 997,353 | |
| | | | | | | | |
F-44
IASIS HEALTHCARE LLC
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (CONTINUED)
Included in property and equipment are assets acquired under capital leases of $4.7 million and $4.6 million, net of accumulated amortization of $2.6 million and $3.4 million, at September 30, 2010 and 2009, respectively.
| 10. | GOODWILL AND OTHER INTANGIBLE ASSETS |
The following table presents the changes in the carrying amount of goodwill (in thousands):
| | | | | | | | | | | | |
| | | Acute Care | | | Health Choice | | | Total | |
| | | |
Balance at September 30, 2008 | | $ | 774,842 | | | $ | 5,757 | | | $ | 780,599 | |
Impairment of Florida market goodwill | | | (64,639 | ) | | | — | | | | (64,639 | ) |
Other acquisitions | | | 1,960 | | | | — | | | | 1,960 | |
| | | | | | | | | | | | |
Balance at September 30, 2009 | | | 712,163 | | | | 5,757 | | | | 717,920 | |
Other acquisitions | | | 323 | | | | — | | | | 323 | |
| | | | | | | | | | | | |
Balance at September 30, 2010 | | $ | 712,486 | | | $ | 5,757 | | | $ | 718,243 | |
| | | | | | | | | | | | |
For the year ended September 30, 2010, as a result of the Company’s annual impairment testing, the Company has determined all remaining goodwill and long-lived assets to be recoverable. For the year ended September 30, 2009, as a result of the Company’s annual impairment testing, the Company recorded a $64.6 million non-cash charge ($43.2 million after tax) for the impairment of goodwill related to its Florida market.
Other intangible assets consist solely of Health Choice’s contract with AHCCCS, which is amortized over a period of 15 years, the contract’s estimated useful life, including assumed renewal periods. The gross intangible value originally assigned to the contract was $45.0 million. The Company expects amortization expense for this intangible asset to be $3.0 million per year over the estimated life of the contract. Amortization of this intangible asset is included in depreciation and amortization expense in the accompanying consolidated statement of operations and totaled $3.0 million for each of the years ended September 30, 2010, 2009 and 2008. Net other intangible assets included in the accompanying consolidated balance sheets at September 30, 2010 and 2009, totaled $27.0 million and $30.0 million, respectively.
Common Interests of IASIS
As of September 30, 2010, all of the common interests of IASIS were owned by IAS, its sole member.
Management Rollover Options
In 2004, an investor group led by TPG acquired IAS, the parent company of IASIS. Prior to the acquisition, IAS maintained the IASIS 2000 Stock Option Plan. In connection with the acquisition, certain holders of 299,900 of in-the-money common stock options elected to rollover and convert such options into fully vested options to purchase an aggregate 3,263 shares of preferred stock, with an exercise price of $437.48 per share, and an aggregate 163,150 shares of common stock, with an exercise price of $8.75 per share. All of the other outstanding options under the IASIS 2000 Stock Option Plan were cancelled upon consummation of the acquisition and the plan was terminated.
F-45
IASIS HEALTHCARE LLC
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (CONTINUED)
In connection with the issuance of the Senior PIK Loans in fiscal 2007, the preferred rollover options were cancelled in exchange for a cash payment equal to the excess of the accreted value of the preferred stock over the exercise price of $437.48 per share.
During the year ended September 30, 2010, the Company paid $4.9 million, net of a $1.8 million income tax benefit, to cancel the 163,150 vested rollover options to purchase its common stock. The cancellation of the rollover options resulted in the Company recognizing $2.0 million in stock compensation expense during the year ended September 30, 2010.
2004 Stock Option Plan
The IAS 2004 Stock Option Plan (the “2004 Stock Option Plan”) was established to promote the Company’s interests by providing additional incentives to its key employees, directors, service providers and consultants. The options granted under the plan represent the right to purchase IAS common stock upon exercise. Each option shall be identified as either an incentive stock option or a non-qualified stock option. The plan was adopted by the board of directors and majority stockholder of IAS in June 2004. The maximum number of shares of IAS common stock that may be issued pursuant to options granted under the 2004 Stock Option Plan is 2,625,975. The options become exercisable over a period not to exceed five years after the date of grant, subject to earlier vesting provisions as provided for in the 2004 Stock Option Plan. All options granted under the 2004 Stock Option Plan expire no later than 10 years from the respective dates of grant. At September 30, 2010, there were 939,646 options available for grant.
F-46
IASIS HEALTHCARE LLC
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (CONTINUED)
Information regarding the Company’s stock option activity is summarized below:
| | | | | | | | | | | | | | | | | | | | | | | | |
| | | 2004 Stock Option Plan | | | Rollover Options | |
| | | Options | | | Option
Price
Per Share | | | Weighted
Average
Exercise
Price | | | Options | | | Option
Price
Per Share | | | Weighted
Average
Exercise
Price | |
| | | | | | |
Options outstanding at September 30, 2007 | | | 1,491,125 | | | $ | 20.00-$35.68 | | | $ | 22.09 | | | | 163,150 | | | $ | 8.75 | | | $ | 8.75 | |
| | | | | | | | | | | | | | | | | | | | | | | | |
Granted | | | 1,080 | | | $ | 34.75 | | | $ | 34.75 | | | | — | | | | — | | | | — | |
Exercised | | | (9,600 | ) | | $ | 20.00 | | | $ | 20.00 | | | | — | | | | — | | | | — | |
Cancelled/forfeited | | | (80,720 | ) | | $ | 20.00-$35.68 | | | $ | 26.04 | | | | — | | | | — | | | | — | |
| | | | | | | | | | | | | | | | | | | | | | | | |
Options outstanding at September 30, 2008 | | | 1,401,885 | | | $ | 20.00-$35.68 | | | $ | 21.82 | | | | 163,150 | | | $ | 8.75 | | | $ | 8.75 | |
| | | | | | | | | | | | | | | | | | | | | | | | |
Granted | | | 477,700 | | | $ | 34.75 | | | $ | 34.75 | | | | — | | | | — | | | | — | |
Exercised | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | |
Cancelled/forfeited | | | (119,410 | ) | | $ | 20.00-$35.68 | | | $ | 31.17 | | | | — | | | | — | | | | — | |
| | | | | | | | | | | | | | | | | | | | | | | | |
Options outstanding at September 30, 2009 | | | 1,760,175 | | | $ | 20.00-$35.68 | | | $ | 24.70 | | | | 163,150 | | | $ | 8.75 | | | $ | 8.75 | |
| | | | | | | | | | | | | | | | | | | | | | | | |
Granted | | | 45,000 | | | $ | 34.75-$45.66 | | | $ | 43.24 | | | | — | | | | — | | | | — | |
Exercised | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | |
Cancelled/forfeited | | | (118,846 | ) | | $ | 20.00-$35.68 | | | $ | 33.38 | | | | (163,150 | ) | | | 8.75 | | | | 8.75 | |
| | | | | | | | | | | | | | | | | | | | | | | | |
Options outstanding at September 30, 2010 | | | 1,686,329 | | | $ | 20.00-$45.66 | | | $ | 24.58 | | | | — | | | | — | | | | — | |
| | | | | | | | | | | | | | | | | | | | | | | | |
Options exercisable at September 30, 2010 | | | 1,374,620 | | | $ | 20.00-$35.68 | | | $ | 21.98 | | | | — | | | $ | — | | | $ | — | |
| | | | | | | | | | | | | | | | | | | | | | | | |
The following table provides information regarding assumptions used in the fair value measurement for options granted on or after October 1, 2006.
| | | | |
| | | Options Granted
On or After
October 1, 2006 | |
| |
Risk-free interest | | | 3.1 | % |
Dividend yield | | | 0.0 | % |
Volatility | | | 35.0 | % |
Expected option life | | | 7.3 years | |
For options granted on or after October 1, 2006, the Company used the Black-Scholes-Merton valuation model in determining the fair value measurement. Volatility for such options was estimated based on the historical stock price information of certain peer group companies for a period of time equal to the expected option life period.
Income tax expense on earnings from continuing operations consists of the following (in thousands):
| | | | | | | | | | | | |
| | | Year Ended
September 30,
2010 | | | Year Ended
September 30,
2009 | | | Year Ended
September 30,
2008 | |
| | | |
Current: | | | | | | | | | | | | |
Federal | | $ | 11,439 | | | $ | 28,220 | | | $ | 12,631 | |
State | | | 2,803 | | | | 4,933 | | | | 3,326 | |
Deferred: | | | | | | | | | | | | |
Federal | | | 26,750 | | | | (5,092 | ) | | | 15,522 | |
State | | | 3,723 | | | | (485 | ) | | | 3,846 | |
| | | | | | | | | | | | |
| | $ | 44,715 | | | $ | 27,576 | | | $ | 35,325 | |
| | | | | | | | | | | | |
F-47
IASIS HEALTHCARE LLC
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (CONTINUED)
A reconciliation of the federal statutory rate to the effective income tax rate applied to earnings from continuing operations before income taxes is as follows (in thousands):
| | | | | | | | | | | | |
| | | Year Ended
September 30,
2010 | | | Year Ended
September 30,
2009 | | | Year Ended
September 30,
2008 | |
| | | |
Federal statutory rate | | $ | 35.0 | % | | $ | 35.0 | % | | $ | 35.0 | % |
State income taxes, net of federal income tax benefit | | | 3.5 | | | | 4.4 | | | | 5.3 | |
Non-deductible goodwill impairment charges | | | — | | | | 3.8 | | | | — | |
Other non-deductible expenses | | | 0.2 | | | | 0.8 | | | | 0.5 | |
Income attributable to non-controlling interests | | | (2.4 | ) | | | (5.3 | ) | | | (1.8 | ) |
Change in valuation allowance charged to federal income tax expense | | | 0.4 | | | | 2.4 | | | | 1.1 | |
Other items, net | | | 0.4 | | | | 0.8 | | | | 0.3 | |
| | | | | | | | | | | | |
Income tax expense | | $ | 37.1 | % | | $ | 41.9 | % | | $ | 40.4 | % |
| | | | | | | | | | | | |
A summary of the items comprising deferred tax assets and liabilities is as follows (in thousands):
| | | | | | | | | | | | | | | | |
| | | September 30, 2010 | | | September 30, 2009 | |
| | | Assets | | | Liabilities | | | Assets | | | Liabilities | |
| | | | |
Depreciation and fixed asset basis differences | | $ | — | | | $ | 76,706 | | | $ | — | | | $ | 77,743 | |
Amortization and intangible asset basis differences | | | — | | | | 66,092 | | | | — | | | | 55,721 | |
Allowance for doubtful accounts | | | 8,424 | | | | — | | | | 30,769 | | | | — | |
Professional liability | | | 15,350 | | | | — | | | | 15,561 | | | | — | |
Accrued expenses and other liabilities | | | 18,617 | | | | — | | | | 14,625 | | | | — | |
Deductible carryforwards and credits | | | 10,221 | | | | — | | | | 9,861 | | | | — | |
Other, net | | | 6,325 | | | | — | | | | 3,841 | | | | — | |
Valuation allowance | | | (9,530 | ) | | | — | | | | (8,580 | ) | | | — | |
| | | | | | | | | | | | | | | | |
Total | | $ | 49,407 | | | $ | 142,798 | | | $ | 66,077 | | | $ | 133,464 | |
| | | | | | | | | | | | | | | | |
Net current deferred tax assets of $15.9 million and $39.0 million and net non-current deferred tax liabilities of $109.3 million and $106.4 million are included in the accompanying consolidated balance sheets at September 30, 2010 and 2009, respectively. The Company had a net income tax receivable of $6.6 million included in other current assets at September 30, 2010, and a net income tax payable of $3.4 million included in other current liabilities at September 30, 2009.
The Company and some of its subsidiaries are included in IAS’ consolidated filing group for U.S. federal income tax purposes, as well as in certain state and local income tax returns that include IAS. With respect to tax returns for any taxable period in which the Company or any of its subsidiaries are included in a tax return filing with IAS, the amount of taxes to be paid by the Company is determined, subject to some adjustments, as if it and its subsidiaries filed their own tax returns excluding IAS. Member’s equity in the accompanying consolidated balance sheets as of September 30, 2010 and 2009, include $35.9 million and $27.3 million, respectively, in capital contributions representing cumulative tax benefits generated by IAS and utilized by the Company in the combined tax return filings, for which IAS did not require cash settlement from the Company.
The Company maintains a valuation allowance for deferred tax assets it believes may not be utilized. The valuation allowance increased by $900,000 and $2.9 million during the years ended September 30, 2010 and 2009, respectively. The increases in the valuation allowance for both years relate to the generation of net operating loss carryforwards by certain subsidiaries excluded from the IAS consolidated federal income tax return, as well as state net operating loss carryforwards that may not ultimately be utilized.
As of September 30, 2010, federal net operating loss carryforwards were available to offset $12.1 million of future taxable income generated by subsidiaries of the Company that are excluded from the IAS consolidated return. A valuation allowance has been
F-48
IASIS HEALTHCARE LLC
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (CONTINUED)
established against $10.3 million of these carryforwards, which expire between 2026 and 2030. State net operating losses in the amount of $149.8 million were also available, but largely offset by a valuation allowance. The state net operating loss carryforwards expire between 2018 and 2030.
The Company adopted the provisions of FASB authoritative guidance regarding accounting for uncertainty in income taxes, on October 1, 2007. As a result, the Company recorded a liability for unrecognized tax benefits of $8.1 million, and reduced deferred tax assets for federal and state net operating losses generated by uncertain tax deductions by $9.9 million as of October 1, 2007.
The liability for unrecognized tax benefits included in the accompanying consolidated balance sheets was $11.7 million, including accrued interest of $319,000 at September 30, 2010, and $7.8 million, including accrued interest of $122,000 at September 30, 2009. An additional $6.2 million and $5.9 million of unrecognized tax benefits are reflected as a reduction to deferred tax assets for state net operating losses generated by uncertain tax deductions as of September 30, 2010 and 2009, respectively. Of the total unrecognized tax benefits at September 30, 2010, $2.3 million (net of the tax benefit on state taxes and interest) represents the amount of unrecognized tax and interest that, if recognized, would favorably impact the Company’s effective income tax rate. The remainder of the unrecognized tax positions consist of items for which the uncertainty relates only to the timing of the deductibility, and state net operating loss carryforwards for which ultimate recognition would result in the creation of an offsetting valuation allowance due to the unlikelihood of future taxable income in that state.
A summary of activity of the Company’s total amounts of unrecognized tax benefits is as follows (in thousands):
| | | | | | | | | | | | |
| | | Year Ended
September 30,
2010 | | | Year Ended
September 30,
2009 | | | Year Ended
September 30,
2008 | |
| | | |
Unrecognized tax benefits at October 1 | | $ | 13,638 | | | $ | 15,550 | | | $ | 17,942 | |
Additions resulting from tax positions taken in a prior period | | | — | | | | 14 | | | | 937 | |
Reductions resulting from tax positions taken in a prior period | | | (1,700 | ) | | | (3,171 | ) | | | (6,258 | ) |
Additions resulting from tax positions taken in the current period | | | 5,596 | | | | 1,965 | | | | 2,929 | |
Reductions resulting from lapse of statute of limitations | | | — | | | | (720 | ) | | | — | |
| | | | | | | | | | | | |
Unrecognized tax benefits at September 30 | | $ | 17,534 | | | $ | 13,638 | | | $ | 15,550 | |
| | | | | | | | | | | | |
The Company’s policy is to classify interest and penalties as a component of income tax expense. Interest expense totaling $129,000 and $146,000 (net of related tax benefits) is included in income tax expense for the years ended September 30, 2010 and 2008, respectively. Income tax expense for the year ended September 30, 2009, has been reduced by $122,000 due to a decrease in accrued interest payable in connection with uncertain tax positions (net of related tax benefits).
The Company’s tax years 2007 and beyond remain open to examination by U.S. federal and state taxing authorities. It is reasonably possible that unrecognized tax benefits could significantly increase or decrease within the next twelve months. However, the Company is currently unable to estimate the range of any possible change.
| 14. | COMMITMENTS AND CONTINGENCIES |
Net Revenue
The calculation of appropriate payments from the Medicare and Medicaid programs, including supplemental Medicaid reimbursement, as well as terms governing agreements with other third-party payors are complex and subject to interpretation. Final determination of amounts earned under the Medicare and Medicaid programs often occurs subsequent to the year in which services are rendered because of audits by the programs, rights of appeal and the application of numerous technical provisions. In the opinion of management, adequate provision has been made for adjustments that may result from such routine audits and appeals.
F-49
IASIS HEALTHCARE LLC
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (CONTINUED)
Professional, General and Workers’ Compensation Liability Risks
The Company is subject to claims and legal actions in the ordinary course of business, including claims relating to patient treatment and personal injuries. To cover these types of claims, the Company maintains professional and general liability insurance in excess of self-insured retentions through a commercial insurance carrier in amounts that the Company believes to be sufficient for its operations, although, potentially, some claims may exceed the scope of coverage in effect. Plaintiffs in these matters may request punitive or other damages that may not be covered by insurance. The Company is currently not a party to any such proceedings that, in the Company’s opinion, would have a material adverse effect on the Company’s business, financial condition or results of operations. The Company expenses an estimate of the costs it expects to incur under the self-insured retention exposure for professional and general liability claims using historical claims data, demographic factors, severity factors, current incident logs and other actuarial analysis. At September 30, 2010 and 2009, the Company’s professional and general liability accrual for asserted and unasserted claims totaled $41.6 million and $41.7 million, respectively. The semi-annual valuations from the Company’s independent actuary for professional and general liability losses resulted in a change related to estimates for prior years which decreased professional and general liability expense by $2.6 million, $1.2 million and $6.8 million during the years ended September 30, 2010, 2009 and 2008, respectively.
The Company is subject to claims and legal actions in the ordinary course of business relative to workers’ compensation. To cover these types of claims, the Company maintains workers’ compensation insurance coverage with a self-insured retention. The Company accrues costs of workers’ compensation claims based upon estimates derived from its claims experience. The semi-annual valuations from the Company’s independent actuary for workers’ compensation losses resulted in a change related to estimates for prior years which increased workers’ compensation expense by $1.1 million during the year ended September 30, 2010, decreased workers’ compensation expense by $526,000, during the year ended September 30, 2009, and increased workers’ compensation expense by $759,000 during the year ended September 30, 2008.
Health Choice
Health Choice has entered into capitated contracts whereby the Plan provides healthcare services in exchange for fixed periodic and supplemental payments from the AHCCCS and CMS. These services are provided regardless of the actual costs incurred to provide these services. The Company receives reinsurance and other supplemental payments from AHCCCS to cover certain costs of healthcare services that exceed certain thresholds. The Company believes the capitated payments, together with reinsurance and other supplemental payments are sufficient to pay for the services Health Choice is obligated to deliver. As of September 30, 2010, the Company has provided a performance guaranty in the form of letters of credit totaling $48.3 million for the benefit of AHCCCS to support its obligations under the Health Choice contract to provide and pay for the healthcare services. The amount of the performance guaranty is generally based in part upon the membership in the Plan and the related capitation revenue paid to Health Choice.
Acquisitions
The Company has acquired and in the future may choose to acquire businesses with prior operating histories. Such businesses may have unknown or contingent liabilities, including liabilities for failure to comply with healthcare laws and regulations, such as billing and reimbursement, fraud and abuse and similar anti-referral laws. Although the Company has procedures designed to conform business practices to its policies following the completion of any acquisition, there can be no assurance that the Company will not become liable for previous activities of prior owners that may later be asserted to be improper by private plaintiffs or government agencies. Although the Company generally seeks to obtain indemnification from prospective sellers covering such matters, there can be no assurance that any such matter will be covered by indemnification, or if covered, that such indemnification will be adequate to cover potential losses and fines.
F-50
IASIS HEALTHCARE LLC
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (CONTINUED)
Other
On March 31, 2008, the United States District Court for the District of Arizona (the “District Court”) dismissed with prejudice thequi tam complaint against IAS. The qui tam action sought monetary damages and civil penalties under the federal False Claims Act (“FCA”) and included allegations that certain business practices related to physician relationships and the medical necessity of certain procedures resulted in the submission of claims for reimbursement in violation of the FCA. The case dates back to March 2005 and became the subject of a subpoena by the Office of Inspector General (“OIG”) in September 2005. In August 2007, the case was unsealed and the U.S. Department of Justice declined to intervene. The District Court dismissed the case from the bench at the conclusion of oral arguments on IAS’ motion to dismiss. On April 21, 2008, the District Court issued a written order dismissing the case with prejudice and entering formal judgment for IAS and denying as moot IAS’ motions related to the relator’s misappropriation of information subject to a claim of attorney-client privilege by IAS. Both parties appealed. On August 12, 2010, United States Court of Appeals for the Ninth Circuit reversed the District Court’s dismissal of thequi tam complaint and the District Court’s denial of IAS’ motions concerning relator’s misappropriation of documents and ordered that thequi tam relator be allowed leave to file a Third Amended Complaint and for the District Court to consider IAS’ motions concerning relator’s misappropriation of documents. The District Court ordered thequi tam relator to file his Third Amended Complaint by November 22, 2010, and set a schedule for the filing of motions related to the relator’s misappropriation of documents. On October 20, 2010, thequi tam relator filed a motion to transfer this action to the United States District Court for the Eastern District of Texas. That motion remains pending. On November 22, 2010, the relator filed his Third Amended Complaint. IAS anticipates filing a motion to dismiss the Third Amended Complaint and motions concerning the relator’s misappropriation of documents. If thequi tam action was to be resolved in a manner unfavorable to us, it could have a material adverse effect on our business, financial condition and results of operations, including exclusion from the Medicare and Medicaid programs. In addition, we may incur material fees, costs and expenses in connection with defending thequi tam action.
F-51
IASIS HEALTHCARE LLC
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (CONTINUED)
The Company leases various buildings, office space and equipment under capital and operating lease agreements. These leases expire at various times and have various renewal options.
The Company is a party to an amended facility lease with a 15 year term that expires in January 31, 2019, and includes options to extend the term of the lease through January 31, 2039. The annual cost under this agreement is $6.4 million, payable in monthly installments. Future minimum lease payments at September 30, 2010, are as follows (in thousands):
| | | | | | | | |
| | | Capital
Leases | | | Operating
Leases | |
| | |
2011 | | $ | 933 | | | $ | 28,525 | |
2012 | | | 652 | | | | 25,766 | |
2013 | | | 562 | | | | 24,254 | |
2014 | | | 562 | | | | 20,769 | |
2015 | | | 562 | | | | 17,713 | |
Thereafter | | | 4,679 | | | | 57,380 | |
| | | | | | | | |
Total minimum lease payments | | $ | 7,950 | | | $ | 174,407 | |
| | | | | | | | |
Amount representing interest (at rates ranging from 4.4% to 11.0%) | | | 3,374 | | | | | |
| | | | | | | | |
Present value of net minimum lease payments (including $649 classified as current) | | $ | 4,576 | | | | | |
| | | | | | | | |
Aggregate future minimum rentals to be received under noncancellable subleases as of September 30, 2010, were $6.8 million.
Substantially all employees who are employed by the Company or its subsidiaries, upon qualification, are eligible to participate in a defined contribution 401(k) plan (the “Retirement Plan”). Employees who elect to participate generally make contributions from 1% to 20% of their eligible compensation, and the Company matches, at its discretion, such contributions up to a maximum percentage. Generally, employees immediately vest 100% in their own contributions and vest in the employer portion of contributions over a period not to exceed five years. Company contributions to the Retirement Plan were $6.7 million, $5.7 million and $5.0 million for the years ended September 30, 2010, 2009 and 2008, respectively.
F-52
IASIS HEALTHCARE LLC
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (CONTINUED)
| 17. | SEGMENT AND GEOGRAPHIC INFORMATION |
The Company’s acute care hospitals and related healthcare businesses are similar in their activities and the economic environments in which they operate (i.e., urban and suburban markets). Accordingly, the Company’s reportable operating segments consist of (1) acute care hospitals and related healthcare businesses, collectively, and (2) Health Choice. The following is a financial summary by business segment for the periods indicated (in thousands):
| | | | | | | | | | | | | | | | |
| | | For the Year Ended September 30, 2010 | |
| | | Acute Care | | | Health Choice | | | Eliminations | | | Consolidated | |
| | | | |
Acute care revenue | | $ | 1,729,344 | | | $ | — | | | $ | — | | | $ | 1,729,344 | |
Premium revenue | | | — | | | | 792,062 | | | | — | | | | 792,062 | |
Revenue between segments | | | 11,805 | | | | — | | | | (11,805 | ) | | | — | |
| | | | | | | | | | | | | | | | |
Total net revenue | | | 1,741,149 | | | | 792,062 | | | | (11,805 | ) | | | 2,521,406 | |
| | | | |
Salaries and benefits (excludes stock compensation) | | | 664,667 | | | | 19,149 | | | | — | | | | 683,816 | |
Supplies | | | 266,347 | | | | 198 | | | | — | | | | 266,545 | |
Medical claims | | | — | | | | 690,456 | | | | (11,805 | ) | | | 678,651 | |
Other operating expenses | | | 339,304 | | | | 24,612 | | | | — | | | | 363,916 | |
Provision for bad debts | | | 197,680 | | | | — | | | | — | | | | 197,680 | |
Rentals and leases | | | 38,409 | | | | 1,546 | | | | — | | | | 39,955 | |
| | | | | | | | | | | | | | | | |
Adjusted EBITDA(1) | | | 234,742 | | | | 56,101 | | | | — | | | | 290,843 | |
| | | | |
Interest expense, net | | | 66,810 | | | | — | | | | — | | | | 66,810 | |
Depreciation and amortization | | | 92,544 | | | | 3,562 | | | | — | | | | 96,106 | |
Stock compensation | | | 2,487 | | | | — | | | | — | | | | 2,487 | |
Management fees | | | 5,000 | | | | — | | | | — | | | | 5,000 | |
| | | | | | | | | | | | | | | | |
Earnings from continuing operations before gain on disposal of assets and income taxes | | | 67,901 | | | | 52,539 | | | | — | | | | 120,440 | |
Gain on disposal of assets, net | | | 108 | | | | — | | | | — | | | | 108 | |
| | | | | | | | | | | | | | | | |
Earnings from continuing operations before income taxes | | $ | 68,009 | | | $ | 52,539 | | | $ | — | | | $ | 120,548 | |
| | | | | | | | | | | | | | | | |
| | | | |
Segment assets | | $ | 2,032,246 | | | $ | 320,948 | | | | | | | $ | 2,353,194 | |
| | | | | | | | | | | | | | | | |
| | | | |
Capital expenditures | | $ | 80,966 | | | $ | 302 | | | | | | | $ | 81,268 | |
| | | | | | | | | | | | | | | | |
| | | | |
Goodwill | | $ | 712,486 | | | $ | 5,757 | | | | | | | $ | 718,243 | |
| | | | | | | | | | | | | | | | |
F-53
IASIS HEALTHCARE LLC
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (CONTINUED)
| | | | | | | | | | | | | | | | |
| | | For the Year Ended September 30, 2009 | |
| | | Acute Care | | | Health Choice | | | Eliminations | | | Consolidated | |
| | | | |
Acute care revenue | | $ | 1,662,469 | | | $ | — | | | $ | — | | | $ | 1,662,469 | |
Premium revenue | | | — | | | | 699,503 | | | | — | | | | 699,503 | |
Revenue between segments | | | 9,316 | | | | — | | | | (9,316 | ) | | | — | |
| | | | | | | | | | | | | | | | |
Total net revenue | | | 1,671,785 | | | | 699,503 | | | | (9,316 | ) | | | 2,361,972 | |
| | | | |
Salaries and benefits (excludes stock compensation) | | | 641,332 | | | | 19,028 | | | | — | | | | 660,360 | |
Supplies | | | 250,310 | | | | 263 | | | | — | | | | 250,573 | |
Medical claims | | | — | | | | 602,076 | | | | (9,316 | ) | | | 592,760 | |
Other operating expenses | | | 302,804 | | | | 22,931 | | | | — | | | | 325,735 | |
Provision for bad debts | | | 192,563 | | | | — | | | | — | | | | 192,563 | |
Rentals and leases | | | 37,563 | | | | 1,564 | | | | — | | | | 39,127 | |
Hurricane-related property damage | | | 938 | | | | — | | | | — | | | | 938 | |
| | | | | | | | | | | | | | | | |
Adjusted EBITDA(1) | | | 246,275 | | | | 53,641 | | | | — | | | | 299,916 | |
| | | | |
Interest expense, net | | | 67,890 | | | | — | | | | — | | | | 67,890 | |
Depreciation and amortization | | | 94,014 | | | | 3,448 | | | | — | | | | 97,462 | |
Stock compensation | | | 561 | | | | — | | | | — | | | | 561 | |
Impairment of goodwill | | | 64,639 | | | | — | | | | — | | | | 64,639 | |
Management fees | | | 5,000 | | | | — | | | | — | | | | 5,000 | |
| | | | | | | | | | | | | | | | |
Earnings from continuing operations before gain (loss) on disposal of assets and income taxes | | | 14,171 | | | | 50,193 | | | | — | | | | 64,364 | |
Gain (loss) on disposal of assets, net | | | 1,616 | | | | (151 | ) | | | — | | | | 1,465 | |
| | | | | | | | | | | | | | | | |
Earnings from continuing operations before income taxes | | $ | 15,787 | | | $ | 50,042 | | | $ | — | | | $ | 65,829 | |
| | | | | | | | | | | | | | | | |
| | | | |
Segment assets | | $ | 2,109,422 | | | $ | 247,782 | | | | | | | $ | 2,357,204 | |
| | | | | | | | | | | | | | | | |
| | | | |
Capital expenditures | | $ | 86,875 | | | $ | 845 | | | | | | | $ | 87,720 | |
| | | | | | | | | | | | | | | | |
| | | | |
Goodwill | | $ | 712,163 | | | $ | 5,757 | | | | | | | $ | 717,920 | |
| | | | | | | | | | | | | | | | |
F-54
IASIS HEALTHCARE LLC
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (CONTINUED)
| | | | | | | | | | | | | | | | |
| | | For the Year Ended September 30, 2008 | |
| | | Acute Care | | | Health Choice | | | Eliminations | | | Consolidated | |
| | | | |
Acute care revenue | | $ | 1,523,790 | | | $ | — | | | $ | — | | | $ | 1,523,790 | |
Premium revenue | | | — | | | | 541,746 | | | | — | | | | 541,746 | |
Revenue between segments | | | 9,594 | | | | — | | | | (9,594 | ) | | | — | |
| | | | | | | | | | | | | | | | |
Total net revenue | | | 1,533,384 | | | | 541,746 | | | | (9,594 | ) | | | 2,065,536 | |
| | | | |
Salaries and benefits | | | 614,442 | | | | 17,667 | | | | — | | | | 632,109 | |
Supplies | | | 231,001 | | | | 258 | | | | — | | | | 231,259 | |
Medical claims | | | — | | | | 461,649 | | | | (9,594 | ) | | | 452,055 | |
Other operating expenses | | | 264,814 | | | | 18,309 | | | | — | | | | 283,123 | |
Provision for bad debts | | | 161,936 | | | | — | | | | — | | | | 161,936 | |
Rentals and leases | | | 35,466 | | | | 1,167 | | | | — | | | | 36,633 | |
Hurricane-related property damage | | | 3,589 | | | | — | | | | — | | | | 3,589 | |
| | | | | | | | | | | | | | | | |
Adjusted EBITDA(1) | | | 222,136 | | | | 42,696 | | | | — | | | | 264,832 | |
| | | | |
Interest expense, net | | | 75,665 | | | | — | | | | — | | | | 75,665 | |
Depreciation and amortization | | | 93,003 | | | | 3,738 | | | | — | | | | 96,741 | |
Management fees | | | 5,000 | | | | — | | | | — | | | | 5,000 | |
| | | | | | | | | | | | | | | | |
Earnings from continuing operations before loss on disposal of assets and income taxes | | | 48,468 | | | | 38,958 | | | | — | | | | 87,426 | |
Loss on disposal of assets, net | | | (75 | ) | | | — | | | | — | | | | (75 | ) |
| | | | | | | | | | | | | | | | |
Earnings from continuing operations before income taxes | | $ | 48,393 | | | $ | 38,958 | | | $ | — | | | $ | 87,351 | |
| | | | | | | | | | | | | | | | |
| | | | |
Segment assets | | $ | 2,123,069 | | | $ | 185,078 | | | | | | | $ | 2,308,147 | |
| | | | | | | | | | | | | | | | |
| | | | |
Capital expenditures | | $ | 136,425 | | | $ | 990 | | | | | | | $ | 137,415 | |
| | | | | | | | | | | | | | | | |
| | | | |
Goodwill | | $ | 774,842 | | | $ | 5,757 | | | | | | | $ | 780,599 | |
| | | | | | | | | | | | | | | | |
| (1) | Adjusted EBITDA represents net earnings from continuing operations before interest expense, income tax expense, depreciation and amortization, stock compensation, impairment of goodwill, gain (loss) on disposal of assets and management fees. Management fees represent monitoring and advisory fees paid to affiliates of TPG, JLL and Trimaran. Management routinely calculates and communicates adjusted EBITDA and believes that it is useful to investors because it is commonly used as an analytical indicator within the healthcare industry to evaluate hospital performance, allocate resources and measure leverage capacity and debt service ability. In addition, the Company uses adjusted EBITDA as a measure of performance for its business segments and for incentive compensation purposes. Adjusted EBITDA should not be considered as a measure of financial performance under GAAP, and the items excluded from adjusted EBITDA are significant components in understanding and assessing financial performance. Adjusted EBITDA should not be considered in isolation or as an alternative to net earnings, cash flows generated by operating, investing, or financing activities or other financial statement data presented in the consolidated financial statements as an indicator of financial performance or liquidity. Adjusted EBITDA, as presented, differs from what is defined under the Company’s senior secured credit facilities and may not be comparable to similarly titled measures of other companies. |
F-55
IASIS HEALTHCARE LLC
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (CONTINUED)
| 18. | ACCRUED EXPENSES AND OTHER CURRENT LIABILITIES |
A summary of accrued expenses and other current liabilities consists of the following (in thousands):
| | | | | | | | |
| | | September 30,
2010 | | | September 30,
2009 | |
| | |
Employee health insurance payable | | $ | 8,265 | | | $ | 9,183 | |
Accrued property taxes | | | 11,645 | | | | 10,496 | |
Health Choice program settlements payable | | | 56,487 | | | | 13,720 | |
Other | | | 30,217 | | | | 32,302 | |
| | | | | | | | |
| | $ | 106,614 | | | $ | 65,701 | |
| | | | | | | | |
| 19. | ALLOWANCE FOR DOUBTFUL ACCOUNTS |
A summary of activity in the Company’s allowance for doubtful accounts is as follows (in thousands):
| | | | | | | | | | | | | | | | | | | | |
| | | Beginning
Balance | | | Provision
for Bad
Debts | | | Other (1) | | | Accounts
Written
Off, Net of
Recoveries | | | Ending
Balance | |
| | | | | |
Year Ended September 30, 2008 | | $ | 97,829 | | | | 161,936 | | | | 6,782 | | | | (158,092 | ) | | $ | 108,455 | |
Year Ended September 30, 2009 | | $ | 108,455 | | | | 192,563 | | | | 641 | | | | (175,527 | ) | | $ | 126,132 | |
Year Ended September 30, 2010 | | $ | 126,132 | | | | 197,680 | | | | — | | | | (198,406 | ) | | $ | 125,406 | |
| (1) | Represents provision for bad debts recorded at facilities which are now included in discontinued operations. |
The provision for bad debts increased $30.6 million during the year ended September 30, 2009, primarily as a result of increases in self-pay volume and revenue.
| 20. | IMPACT OF HURRICANE ACTIVITY |
The Medical Center of Southeast Texas, the Company’s hospital located in Port Arthur, Texas, was damaged during Hurricane Ike in September 2008. The hospital sustained roof and water intrusion damage. The majority of services at the hospital became operational during October of 2008. The Company’s results from operations include hurricane-related property damage of $938,000 and $3.6 million for the years ended September 30, 2009 and 2008, respectively.
| 21. | SUPPLEMENTAL CONDENSED CONSOLIDATING FINANCIAL INFORMATION |
The 8 3/4% notes described in Note 3 are fully and unconditionally guaranteed on a joint and several basis by all of the Company’s existing domestic subsidiaries, other than non-guarantor subsidiaries which include Health Choice and the Company’s non-wholly owned subsidiaries.
Effective February 1, 2008, Salt Lake Regional Medical Center, LP (“Salt Lake”) sold limited partner units representing, in the aggregate, a 92.2% ownership in Salt Lake. As a result, the Company’s ownership interest in Salt Lake was reduced to 97.8%. Salt Lake is included in the condensed consolidating financial statements as a subsidiary non-guarantor.
Summarized condensed consolidating balance sheets at September 30, 2010 and 2009, condensed consolidating statements of operations and cash flows for the years ended September 30, 2010, 2009 and 2008, for the Company, segregating the parent company issuer, the subsidiary guarantors, the subsidiary non-guarantors and eliminations, are found below. Prior year amounts have been reclassified to conform to the current year presentation.
F-56
IASIS HEALTHCARE LLC
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (CONTINUED)
IASIS Healthcare LLC
Condensed Consolidating Balance Sheet
September 30, 2010
(in thousands)
| | | | | | | | | | | | | | | | | | | | |
| | | Parent
Issuer | | | Subsidiary
Guarantors | | | Subsidiary
Non-Guarantors | | | Eliminations | | | Condensed
Consolidated | |
| Assets | | | | | | | | | | | | | | | | | | | | |
Current assets: | | | | | | | | | | | | | | | | | | | | |
Cash and cash equivalents | | $ | — | | | $ | 143,599 | | | $ | 912 | | | $ | — | | | $ | 144,511 | |
Accounts receivable, net | | | — | | | | 81,649 | | | | 127,524 | | | | — | | | | 209,173 | |
Inventories | | | — | | | | 22,793 | | | | 31,049 | | | | — | | | | 53,842 | |
Deferred income taxes | | | 15,881 | | | | — | | | | — | | | | — | | | | 15,881 | |
Prepaid expenses and other current assets | | | — | | | | 23,577 | | | | 41,763 | | | | — | | | | 65,340 | |
| | | | | | | | | | | | | | | | | | | | |
Total current assets | | | 15,881 | | | | 271,618 | | | | 201,248 | | | | — | | | | 488,747 | |
| | | | | |
Property and equipment, net | | | — | | | | 351,265 | | | | 634,026 | | | | — | | | | 985,291 | |
Intercompany | | | — | | | | (297,257 | ) | | | 297,257 | | | | — | | | | — | |
Net investment in and advances to subsidiaries | | | 1,823,973 | | | | — | | | | — | | | | (1,823,973 | ) | | | — | |
Goodwill | | | 17,331 | | | | 65,504 | | | | 635,408 | | | | — | | | | 718,243 | |
Other intangible assets, net | | | — | | | | — | | | | 27,000 | | | | — | | | | 27,000 | |
Deposit for acquisition | | | — | | | | 97,891 | | | | — | | | | — | | | | 97,891 | |
Other assets, net | | | 12,018 | | | | 17,967 | | | | 6,037 | | | | — | | | | 36,022 | |
| | | | | | | | | | | | | | | | | | | | |
Total assets | | $ | 1,869,203 | | | $ | 506,988 | | | $ | 1,800,976 | | | $ | (1,823,973 | ) | | $ | 2,353,194 | |
| | | | | | | | | | | | | | | | | | | | |
| | | | | |
| Liabilities and Equity | | | | | | | | | | | | | | | | | | | | |
Current liabilities: | | | | | | | | | | | | | | | | | | | | |
Accounts payable | | $ | — | | | $ | 32,400 | | | $ | 46,531 | | | $ | — | | | $ | 78,931 | |
Salaries and benefits payable | | | — | | | | 19,916 | | | | 18,194 | | | | — | | | | 38,110 | |
Accrued interest payable | | | 12,536 | | | | (3,237 | ) | | | 3,237 | | | | — | | | | 12,536 | |
Medical claims payable | | | — | | | | — | | | | 111,373 | | | | — | | | | 111,373 | |
Other accrued expenses and other current liabilities | | | — | | | | 32,326 | | | | 74,288 | | | | — | | | | 106,614 | |
Current portion of long-term debt and capital lease obligations | | | 5,890 | | | | 801 | | | | 20,570 | | | | (20,570 | ) | | | 6,691 | |
| | | | | | | | | | | | | | | | | | | | |
Total current liabilities | | | 18,426 | | | | 82,206 | | | | 274,193 | | | | (20,570 | ) | | | 354,255 | |
| | | | | |
Long-term debt and capital lease obligations | | | 1,039,370 | | | | 5,517 | | | | 547,170 | | | | (547,170 | ) | | | 1,044,887 | |
Deferred income taxes | | | 109,272 | | | | — | | | | — | | | | — | | | | 109,272 | |
Other long-term liabilities | | | — | | | | 59,527 | | | | 635 | | | | — | | | | 60,162 | |
| | | | | | | | | | | | | | | | | | | | |
Total liabilities | | | 1,167,068 | | | | 147,250 | | | | 821,998 | | | | (567,740 | ) | | | 1,568,576 | |
| | | | | |
Non-controlling interests with redemption rights | | | — | | | | 72,112 | | | | — | | | | — | | | | 72,112 | |
| | | | | |
Equity: | | | | | | | | | | | | | | | | | | | | |
Member’s equity | | | 702,135 | | | | 277,255 | | | | 978,978 | | | | (1,256,233 | ) | | | 702,135 | |
Non-controlling interests | | | — | | | | 10,371 | | | | — | | | | — | | | | 10,371 | |
| | | | | | | | | | | | | | | | | | | | |
| | | | | |
Total equity | | | 702,135 | | | | 287,626 | | | | 978,978 | | | | (1,256,233 | ) | | | 712,506 | |
| | | | | | | | | | | | | | | | | | | | |
Total liabilities and equity | | $ | 1,869,203 | | | $ | 506,988 | | | $ | 1,800,976 | | | $ | (1,823,973 | ) | | $ | 2,353,194 | |
| | | | | | | | | | | | | | | | | | | | |
F-57
IASIS HEALTHCARE LLC
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (CONTINUED)
IASIS Healthcare LLC
Condensed Consolidating Balance Sheet
September 30, 2009
(in thousands)
| | | | | | | | | | | | | | | | | | | | |
| | | Parent
Issuer | | | Subsidiary
Guarantors | | | Subsidiary
Non-Guarantors | | | Eliminations | | | Condensed
Consolidated | |
| Assets | | | | | | | | | | | | | | | | | | | | |
Current assets: | | | | | | | | | | | | | | | | | | | | |
Cash and cash equivalents | | $ | — | | | $ | 206,331 | | | $ | 197 | | | $ | — | | | $ | 206,528 | |
Accounts receivable, net | | | — | | | | 90,883 | | | | 139,315 | | | | — | | | | 230,198 | |
Inventories | | | — | | | | 22,405 | | | | 28,087 | | | | — | | | | 50,492 | |
Deferred income taxes | | | 39,038 | | | | — | | | | — | | | | — | | | | 39,038 | |
Prepaid expenses and other current assets | | | — | | | | 15,521 | | | | 33,932 | | | | — | | | | 49,453 | |
| | | | | | | | | | | | | | | | | | | | |
Total current assets | | | 39,038 | | | | 335,140 | | | | 201,531 | | | | — | | | | 575,709 | |
| | | | | |
Property and equipment, net | | | — | | | | 347,657 | | | | 649,696 | | | | — | | | | 997,353 | |
Intercompany | | | — | | | | (243,956 | ) | | | 243,956 | | | | — | | | | — | |
Net investment in and advances to subsidiaries | | | 1,851,008 | | | | — | | | | — | | | | (1,851,008 | ) | | | — | |
Goodwill | | | 17,331 | | | | 67,445 | | | | 633,144 | | | | — | | | | 717,920 | |
Other intangible assets, net | | | — | | | | — | | | | 30,000 | | | | — | | | | 30,000 | |
Other assets, net | | | 15,182 | | | | 16,780 | | | | 4,260 | | | | — | | | | 36,222 | |
| | | | | | | | | | | | | | | | | | | | |
Total assets | | $ | 1,922,559 | | | $ | 523,066 | | | $ | 1,762,587 | | | $ | (1,851,008 | ) | | $ | 2,357,204 | |
| | | | | | | | | | | | | | | | | | | | |
| | | | | |
| Liabilities and Equity | | | | | | | | | | | | | | | | | | | | |
Current liabilities: | | | | | | | | | | | | | | | | | | | | |
Accounts payable | | $ | — | | | $ | 25,269 | | | $ | 43,283 | | | $ | — | | | $ | 68,552 | |
Salaries and benefits payable | | | — | | | | 25,008 | | | | 17,540 | | | | — | | | | 42,548 | |
Accrued interest payable | | | 12,511 | | | | (3,239 | ) | | | 3,239 | | | | — | | | | 12,511 | |
Medical claims payable | | | — | | | | — | | | | 113,519 | | | | — | | | | 113,519 | |
Other accrued expenses and other current liabilities | | | — | | | | 39,559 | | | | 26,142 | | | | — | | | | 65,701 | |
Current portion of long-term debt and capital lease obligations | | | 7,431 | | | | 935 | | | | 20,614 | | | | (20,614 | ) | | | 8,366 | |
| | | | | | | | | | | | | | | | | | | | |
Total current liabilities | | | 19,942 | | | | 87,532 | | | | 224,337 | | | | (20,614 | ) | | | 311,197 | |
| | | | | |
Long-term debt and capital lease obligations | | | 1,045,260 | | | | 6,211 | | | | 566,980 | | | | (566,980 | ) | | | 1,051,471 | |
Deferred income taxes | | | 106,425 | | | | — | | | | — | | | | — | | | | 106,425 | |
Other long-term liabilities | | | — | | | | 53,577 | | | | 645 | | | | — | | | | 54,222 | |
| | | | | | | | | | | | | | | | | | | | |
Total liabilities | | | 1,171,627 | | | | 147,320 | | | | 791,962 | | | | (587,594 | ) | | | 1,523,315 | |
| | | | | |
Non-controlling interests with redemption rights | | | — | | | | 72,527 | | | | — | | | | — | | | | 72,527 | |
| | | | | |
Equity: | | | | | | | | | | | | | | | | | | | | |
Member’s equity | | | 750,932 | | | | 292,789 | | | | 970,625 | | | | (1,263,414 | ) | | | 750,932 | |
Non-controlling interests | | | — | | | | 10,430 | | | | — | | | | — | | | | 10,430 | |
| | | | | | | | | | | | | | | | | | | | |
| | | | | |
Total equity | | | 750,932 | | | | 303,219 | | | | 970,625 | | | | (1,263,414 | ) | | | 761,362 | |
| | | | | | | | | | | | | | | | | | | | |
Total liabilities and equity | | $ | 1,922,559 | | | $ | 523,066 | | | $ | 1,762,587 | | | $ | (1,851,008 | ) | | $ | 2,357,204 | |
| | | | | | | | | | | | | | | | | | | | |
F-58
IASIS HEALTHCARE LLC
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (CONTINUED)
IASIS Healthcare LLC
Condensed Consolidating Statement of Operations
(in thousands)
| | | | | | | | | | | | | | | | | | | | |
| | | For the Year Ended September 30, 2010 | |
| | | Parent
Issuer | | | Subsidiary
Guarantors | | | Subsidiary
Non-Guarantors | | | Eliminations | | | Condensed
Consolidated | |
Net revenue: | | | | | | | | | | | | | | | | | | | | |
Acute care revenue | | $ | — | | | $ | 685,244 | | | $ | 1,055,905 | | | $ | (11,805 | ) | | $ | 1,729,344 | |
Premium revenue | | | — | | | | — | | | | 792,062 | | | | — | | | | 792,062 | |
| | | | | | | | | | | | | | | | | | | | |
Total net revenue | | | — | | | | 685,244 | | | | 1,847,967 | | | | (11,805 | ) | | | 2,521,406 | |
| | | | | |
Costs and expenses: | | | | | | | | | | | | | | | | | | | | |
Salaries and benefits | | | — | | | | 351,792 | | | | 334,511 | | | | — | | | | 686,303 | |
Supplies | | | — | | | | 111,777 | | | | 154,768 | | | | — | | | | 266,545 | |
Medical claims | | | — | | | | — | | | | 690,456 | | | | (11,805 | ) | | | 678,651 | |
Other operating expenses | | | — | | | | 121,522 | | | | 242,394 | | | | — | | | | 363,916 | |
Provision for bad debts | | | — | | | | 90,564 | | | | 107,116 | | | | — | | | | 197,680 | |
Rentals and leases | | | — | | | | 16,736 | | | | 23,219 | | | | — | | | | 39,955 | |
Interest expense, net | | | 66,810 | | | | — | | | | 41,270 | | | | (41,270 | ) | | | 66,810 | |
Depreciation and amortization | | | — | | | | 40,762 | | | | 55,344 | | | | — | | | | 96,106 | |
Management fees | | | 5,000 | | | | (22,831 | ) | | | 22,831 | | | | — | | | | 5,000 | |
Equity in earnings of affiliates | | | (139,647 | ) | | | — | | | | — | | | | 139,647 | | | | — | |
| | | | | | | | | | | | | | | | | | | | |
Total costs and expenses | | | (67,837 | ) | | | 710,322 | | | | 1,671,909 | | | | 86,572 | | | | 2,400,966 | |
| | | | | |
Earnings (loss) from continuing operations before gain (loss) on disposal of assets and income taxes | | | 67,837 | | | | (25,078 | ) | | | 176,058 | | | | (98,377 | ) | | | 120,440 | |
Gain (loss) on disposal of assets, net | | | — | | | | 273 | | | | (165 | ) | | | — | | | | 108 | |
| | | | | | | | | | | | | | | | | | | | |
| | | | | |
Earnings (loss) from continuing operations before income taxes | | | 67,837 | | | | (24,805 | ) | | | 175,893 | | | | (98,377 | ) | | | 120,548 | |
Income tax expense | | | 43,290 | | | | — | | | | 1,425 | | | | — | | | | 44,715 | |
| | | | | | | | | | | | | | | | | | | | |
| | | | | |
Net earnings (loss) from continuing operations | | | 24,547 | | | | (24,805 | ) | | | 174,468 | | | | (98,377 | ) | | | 75,833 | |
Earnings (loss) from discontinued operations, net of income taxes | | | 650 | | | | (1,731 | ) | | | (6 | ) | | | — | | | | (1,087 | ) |
| | | | | | | | | | | | | | | | | | | | |
| | | | | |
Net earnings (loss) | | | 25,197 | | | | (26,536 | ) | | | 174,462 | | | | (98,377 | ) | | | 74,746 | |
Net earnings attributable to non-controlling interests | | | — | | | | (8,279 | ) | | | — | | | | — | | | | (8,279 | ) |
| | | | | | | | | | | | | | | | | | | | |
| | | | | |
Net earnings (loss) attributable to IASIS Healthcare LLC | | $ | 25,197 | | | $ | (34,815 | ) | | $ | 174,462 | | | $ | (98,377 | ) | | $ | 66,467 | |
| | | | | | | | | | | | | | | | | | | | |
F-59
IASIS HEALTHCARE LLC
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (CONTINUED)
IASIS Healthcare LLC
Condensed Consolidating Statement of Operations
(in thousands)
| | | | | | | | | | | | | | | | | | | | |
| | | For the Year Ended September 30, 2009 | |
| | | Parent
Issuer | | | Subsidiary
Guarantors | | | Subsidiary
Non-Guarantors | | | Eliminations | | | Condensed
Consolidated | |
Net revenue: | | | | | | | | | | | | | | | | | | | | |
Acute care revenue | | $ | — | | | $ | 656,913 | | | $ | 1,014,872 | | | $ | (9,316 | ) | | $ | 1,662,469 | |
Premium revenue | | | — | | | | — | | | | 699,503 | | | | — | | | | 699,503 | |
| | | | | | | | | | | | | | | | | | | | |
Total net revenue | | | — | | | | 656,913 | | | | 1,714,375 | | | | (9,316 | ) | | | 2,361,972 | |
| | | | | |
Costs and expenses: | | | | | | | | | | | | | | | | | | | | |
Salaries and benefits | | | — | | | | 336,687 | | | | 324,234 | | | | — | | | | 660,921 | |
Supplies | | | — | | | | 103,587 | | | | 146,986 | | | | — | | | | 250,573 | |
Medical claims | | | — | | | | — | | | | 602,076 | | | | (9,316 | ) | | | 592,760 | |
Other operating expenses | | | — | | | | 121,597 | | | | 204,138 | | | | — | | | | 325,735 | |
Provision for bad debts | | | — | | | | 94,662 | | | | 97,901 | | | | — | | | | 192,563 | |
Rentals and leases | | | — | | | | 16,138 | | | | 22,989 | | | | — | | | | 39,127 | |
Interest expense, net | | | 67,890 | | | | — | | | | 43,063 | | | | (43,063 | ) | | | 67,890 | |
Depreciation and amortization | | | — | | | | 42,492 | | | | 54,970 | | | | — | | | | 97,462 | |
Management fees | | | 5,000 | | | | (21,862 | ) | | | 21,862 | | | | — | | | | 5,000 | |
Impairment of goodwill | | | — | | | | 64,639 | | | | — | | | | — | | | | 64,639 | |
Hurricane-related property damage | | | — | | | | — | | | | 938 | | | | — | | | | 938 | |
Equity in earnings of affiliates | | | (84,640 | ) | | | — | | | | — | | | | 84,640 | | | | — | |
| | | | | | | | | | | | | | | | | | | | |
Total costs and expenses | | | (11,750 | ) | | | 757,940 | | | | 1,519,157 | | | | 32,261 | | | | 2,297,608 | |
| | | | | |
Earnings (loss) from continuing operations before gain (loss) on disposal of assets and income taxes | | | 11,750 | | | | (101,027 | ) | | | 195,218 | | | | (41,577 | ) | | | 64,364 | |
Gain (loss) on disposal of assets, net | | | — | | | | 1,598 | | | | (133 | ) | | | — | | | | 1,465 | |
| | | | | | | | | | | | | | | | | | | | |
| | | | | |
Earnings (loss) from continuing operations before income taxes | | | 11,750 | | | | (99,429 | ) | | | 195,085 | | | | (41,577 | ) | | | 65,829 | |
Income tax expense | | | 26,829 | | | | — | | | | 747 | | | | — | | | | 27,576 | |
| | | | | | | | | | | | | | | | | | | | |
| | | | | |
Net earnings (loss) from continuing operations | | | (15,079 | ) | | | (99,429 | ) | | | 194,338 | | | | (41,577 | ) | | | 38,253 | |
Earnings (loss) from discontinued operations, net of income taxes | | | 106 | | | | (310 | ) | | | 28 | | | | — | | | | (176 | ) |
| | | | | | | | | | | | | | | | | | | | |
| | | | | |
Net earnings (loss) | | | (14,973 | ) | | | (99,739 | ) | | | 194,366 | | | | (41,577 | ) | | | 38,077 | |
Net earnings attributable to non-controlling interests | | | — | | | | (9,987 | ) | | | — | | | | — | | | | (9,987 | ) |
| | | | | | | | | | | | | | | | | | | | |
| | | | | |
Net earnings (loss) attributable to IASIS Healthcare LLC | | $ | (14,973 | ) | | $ | (109,726 | ) | | $ | 194,366 | | | $ | (41,577 | ) | | $ | 28,090 | |
| | | | | | | | | | | | | | | | | | | | |
F-60
IASIS HEALTHCARE LLC
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (CONTINUED)
IASIS Healthcare LLC
Condensed Consolidating Statement of Operations
(in thousands)
| | | | | | | | | | | | | | | | | | | | |
| | | For the Year Ended September 30, 2008 | |
| | | Parent
Issuer | | | Subsidiary
Guarantors | | | Subsidiary
Non-Guarantors | | | Eliminations | | | Condensed
Consolidated | |
Net revenue: | | | | | | | | | | | | | | | | | | | | |
Acute care revenue | | $ | — | | | $ | 637,773 | | | $ | 895,611 | | | $ | (9,594 | ) | | $ | 1,523,790 | |
Premium revenue | | | — | | | | — | | | | 541,746 | | | | — | | | | 541,746 | |
| | | | | | | | | | | | | | | | | | | | |
Total net revenue | | | — | | | | 637,773 | | | | 1,437,357 | | | | (9,594 | ) | | | 2,065,536 | |
| | | | | |
Costs and expenses: | | | | | | | | | | | | | | | | | | | | |
Salaries and benefits | | | — | | | | 319,243 | | | | 312,866 | | | | — | | | | 632,109 | |
Supplies | | | — | | | | 104,698 | | | | 126,561 | | | | — | | | | 231,259 | |
Medical claims | | | — | | | | — | | | | 461,649 | | | | (9,594 | ) | | | 452,055 | |
Other operating expenses | | | — | | | | 111,781 | | | | 171,342 | | | | — | | | | 283,123 | |
Provision for bad debts | | | — | | | | 80,139 | | | | 81,797 | | | | — | | | | 161,936 | |
Rentals and leases | | | — | | | | 14,891 | | | | 21,742 | | | | — | | | | 36,633 | |
Interest expense, net | | | 75,665 | | | | — | | | | 54,716 | | | | (54,716 | ) | | | 75,665 | |
Depreciation and amortization | | | — | | | | 42,721 | | | | 54,020 | | | | — | | | | 96,741 | |
Management fees | | | 5,000 | | | | (19,337 | ) | | | 19,337 | | | | — | | | | 5,000 | |
Hurricane-related property damage | | | — | | | | — | | | | 3,589 | | | | — | | | | 3,589 | |
Equity in earnings of affiliates | | | (91,476 | ) | | | — | | | | — | | | | 91,476 | | | | — | |
| | | | | | | | | | | | | | | | | | | | |
Total costs and expenses | | | (10,811 | ) | | | 654,136 | | | | 1,307,619 | | | | 27,166 | | | | 1,978,110 | |
| | | | | |
Earnings (loss) from continuing operations before gain (loss) on disposal of assets and income taxes | | | 10,811 | | | | (16,363 | ) | | | 129,738 | | | | (36,760 | ) | | | 87,426 | |
Gain (loss) on disposal of assets, net | | | — | | | | (81 | ) | | | 6 | | | | — | | | | (75 | ) |
| | | | | | | | | | | | | | | | | | | | |
| | | | | |
Earnings (loss) from continuing operations before income taxes | | | 10,811 | | | | (16,444 | ) | | | 129,744 | | | | (36,760 | ) | | | 87,351 | |
Income tax expense | | | 34,996 | | | | — | | | | 329 | | | | — | | | | 35,325 | |
| | | | | | | | | | | | | | | | | | | | |
| | | | | |
Net earnings (loss) from continuing operations | | | (24,185 | ) | | | (16,444 | ) | | | 129,415 | | | | (36,760 | ) | | | 52,026 | |
Earnings (loss) from discontinued operations, net of income taxes | | | 5,783 | | | | (12,257 | ) | | | (4,801 | ) | | | — | | | | (11,275 | ) |
| | | | | | | | | | | | | | | | | | | | |
| | | | | |
Net earnings (loss) | | | (18,402 | ) | | | (28,701 | ) | | | 124,614 | | | | (36,760 | ) | | | 40,751 | |
Net earnings attributable to non-controlling interests | | | — | | | | (4,437 | ) | | | — | | | | — | | | | (4,437 | ) |
| | | | | | | | | | | | | | | | | | | | |
| | | | | |
Net earnings (loss) attributable to IASIS Healthcare LLC | | $ | (18,402 | ) | | $ | (33,138 | ) | | $ | 124,614 | | | $ | (36,760 | ) | | $ | 36,314 | |
| | | | | | | | | | | | | | | | | | | | |
F-61
IASIS HEALTHCARE LLC
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (CONTINUED)
IASIS Healthcare LLC
Condensed Consolidating Statement of Cash Flows
(in thousands)
| | | | | | | | | | | | | | | | | | | | |
| | | For the Year Ended September 30, 2010 | |
| | | Parent
Issuer | | | Subsidiary
Guarantors | | | Subsidiary
Non-Guarantors | | | Eliminations | | | Condensed
Consolidated | |
Cash flows from operating activities | | | | | | | | | | | | | | | | | | | | |
Net earnings (loss) | | $ | 25,197 | | | $ | (26,536 | ) | | $ | 174,462 | | | $ | (98,377 | ) | | $ | 74,746 | |
Adjustments to reconcile net earnings (loss) to net cash provided by (used in) operating activities: | | | | | | | | | | | | | | | | | | | | |
Depreciation and amortization | | | — | | | | 40,762 | | | | 55,344 | | | | — | | | | 96,106 | |
Amortization of loan costs | | | 3,163 | | | | — | | | | — | | | | — | | | | 3,163 | |
Stock compensation costs | | | 2,487 | | | | — | | | | — | | | | — | | | | 2,487 | |
Deferred income taxes | | | 30,473 | | | | — | | | | — | | | | — | | | | 30,473 | |
Income tax benefit from stock compensation | | | (1,770 | ) | | | — | | | | — | | | | — | | | | (1,770 | ) |
Income tax benefit from parent company interest | | | 8,554 | | | | — | | | | — | | | | — | | | | 8,554 | |
Loss (gain) on disposal of assets | | | — | | | | (273 | ) | | | 165 | | | | — | | | | (108 | ) |
Loss (earnings) from discontinued operations | | | (650 | ) | | | 1,731 | | | | 6 | | | | — | | | | 1,087 | |
Equity in earnings of affiliates | | | (139,647 | ) | | | — | | | | — | | | | 139,647 | | | | — | |
Changes in operating assets and liabilities, net of the effect of acquisitions and dispositions: | | | | | | | | | | | | | | | | | | | | |
Accounts receivable, net | | | — | | | | 9,488 | | | | 11,791 | | | | — | | | | 21,279 | |
Inventories, prepaid expenses and other current assets | | | — | | | | (8,423 | ) | | | (10,804 | ) | | | — | | | | (19,227 | ) |
Accounts payable, other accrued expenses and other accrued liabilities | | | 1,795 | | | | 11,108 | | | | 29,054 | | | | — | | | | 41,957 | |
| | | | | | | | | | | | | | | | | | | | |
Net cash provided by (used in) operating activities — continuing operations | | | (70,398 | ) | | | 27,857 | | | | 260,018 | | | | 41,270 | | | | 258,747 | |
Net cash used in operating activities — discontinued operations | | | (216 | ) | | | (1,292 | ) | | | — | | | | — | | | | (1,508 | ) |
| | | | | | | | | | | | | | | | | | | | |
Net cash provided by (used in) operating activities | | | (70,614 | ) | | | 26,565 | | | | 260,018 | | | | 41,270 | | | | 257,239 | |
| | | | | | | | | | | | | | | | | | | | |
| | | | | |
Cash flows from investing activities | | | | | | | | | | | | | | | | | | | | |
Purchases of property and equipment | | | — | | | | (44,246 | ) | | | (37,022 | ) | | | — | | | | (81,268 | ) |
Cash paid for acquisitions | | | — | | | | (97,891 | ) | | | (414 | ) | | | — | | | | (98,305 | ) |
Proceeds from sale of assets | | | — | | | | 20 | | | | 37 | | | | — | | | | 57 | |
Change in other assets | | | — | | | | 4,247 | | | | (1,204 | ) | | | — | | | | 3,043 | |
| | | | | | | | | | | | | | | | | | | | |
Net cash used in investing activities | | | — | | | | (137,870 | ) | | | (38,603 | ) | | | — | | | | (176,473 | ) |
| | | | | | | | | | | | | | | | | | | | |
| | | | | |
Cash flows from financing activities | | | | | | | | | | | | | | | | | | | | |
Payment of debt and capital lease obligations | | | (7,521 | ) | | | (43 | ) | | | (814 | ) | | | — | | | | (8,378 | ) |
Distribution to parent company in connection with the repurchase of equity, net | | | (124,962 | ) | | | — | | | | — | | | | — | | | | (124,962 | ) |
Distributions to non-controlling interests | | | — | | | | (194 | ) | | | (8,790 | ) | | | — | | | | (8,984 | ) |
Costs paid for repurchase of non-controlling interests | | | — | | | | (459 | ) | | | — | | | | — | | | | (459 | ) |
Change in intercompany balances with affiliates, net | | | 49,269 | | | | 49,269 | | | | (211,096 | ) | | | (41,270 | ) | | | — | |
| | | | | | | | | | | | | | | | | | | | |
Net cash provided by (used in) financing activities | | | 70,614 | | | | 48,573 | | | | (220,700 | ) | | | (41,270 | ) | | | (142,783 | ) |
| | | | | | | | | | | | | | | | | | | | |
Change in cash and cash equivalents | | | — | | | | (62,732 | ) | | | 715 | | | | — | | | | (62,017 | ) |
Cash and cash equivalents at beginning of period | | | — | | | | 206,331 | | | | 197 | | | | — | | | | 206,528 | |
| | | | | | | | | | | | | | | | | | | | |
Cash and cash equivalents at end of period | | $ | — | | | $ | 143,599 | | | $ | 912 | | | $ | — | | | $ | 144,511 | |
| | | | | | | | | | | | | | | | | | | | |
F-62
IASIS HEALTHCARE LLC
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (CONTINUED)
IASIS Healthcare LLC
Condensed Consolidating Statement of Cash Flows
(in thousands)
| | | | | | | | | | | | | | | | | | | | |
| | | For the Year Ended September 30, 2009 | |
| | | Parent
Issuer | | | Subsidiary
Guarantors | | | Subsidiary
Non-Guarantors | | | Eliminations | | | Condensed
Consolidated | |
Cash flows from operating activities | | | | | | | | | | | | | | | | | | | | |
Net earnings (loss) | | $ | (14,973 | ) | | $ | (99,739 | ) | | $ | 194,366 | | | $ | (41,577 | ) | | $ | 38,077 | |
Adjustments to reconcile net earnings (loss) to net cash provided by (used in) operating activities: | | | | | | | | | | | | | | | | | | | | |
Loss (earnings) from discontinued operations | | | (106 | ) | | | 310 | | | | (28 | ) | | | — | | | | 176 | |
Depreciation and amortization | | | — | | | | 42,492 | | | | 54,970 | | | | — | | | | 97,462 | |
Amortization of loan costs | | | 3,029 | | | | — | | | | — | | | | — | | | | 3,029 | |
Income tax benefit from parent company interest | | | 27,344 | | | | — | | | | — | | | | — | | | | 27,344 | |
Deferred income taxes | | | (5,572 | ) | | | — | | | | — | | | | — | | | | (5,572 | ) |
Loss (gain) on disposal of assets | | | — | | | | (1,598 | ) | | | 133 | | | | — | | | | (1,465 | ) |
Impairment of goodwill | | | — | | | | 64,639 | | | | — | | | | — | | | | 64,639 | |
Hurricane-related property damage | | | — | | | | — | | | | 938 | | | | — | | | | 938 | |
Stock compensation costs | | | 561 | | | | — | | | | — | | | | — | | | | 561 | |
Equity in earnings of affiliates | | | (84,640 | ) | | | — | | | | — | | | | 84,640 | | | | — | |
Changes in operating assets and liabilities, net of the effect of acquisitions and dispositions: | | | | | | | | | | | | | | | | | | | | |
Accounts receivable, net | | | — | | | | 9,319 | | | | (16,621 | ) | | | — | | | | (7,302 | ) |
Inventories, prepaid expenses and other current assets | | | — | | | | 1,179 | | | | 5,549 | | | | — | | | | 6,728 | |
Accounts payable, other accrued expenses and other accrued liabilities | | | 51 | | | | 30,220 | | | | 15,613 | | | | — | | | | 45,884 | |
| | | | | | | | | | | | | | | | | | | | |
Net cash provided by (used in) operating activities — continuing operations | | | (74,306 | ) | | | 46,822 | | | | 254,920 | | | | 43,063 | | | | 270,499 | |
Net cash provided by (used in) operating activities — discontinued operations | | | (106 | ) | | | 1,739 | | | | (161 | ) | | | — | | | | 1,472 | |
| | | | | | | | | | | | | | | | | | | | |
Net cash provided by (used in) operating activities | | | (74,412 | ) | | | 48,561 | | | | 254,759 | | | | 43,063 | | | | 271,971 | |
| | | | | | | | | | | | | | | | | | | | |
| | | | | |
Cash flows from investing activities | | | | | | | | | | | | | | | | | | | | |
Purchases of property and equipment | | | — | | | | (24,965 | ) | | | (62,755 | ) | | | — | | | | (87,720 | ) |
Cash paid for acquisitions | | | — | | | | (1,941 | ) | | | — | | | | — | | | | (1,941 | ) |
Proceeds from sale of assets | | | — | | | | 3,018 | | | | 2,234 | | | | — | | | | 5,252 | |
Change in other assets | | | — | | | | (654 | ) | | | 2,477 | | | | — | | | | 1,823 | |
| | | | | | | | | | | | | | | | | | | | |
Net cash used in investing activities — continuing operations | | | — | | | | (24,542 | ) | | | (58,044 | ) | | | — | | | | (82,586 | ) |
Net cash provided by investing activities — discontinued operations | | | — | | | | 10 | | | | — | | | | — | | | | 10 | |
| | | | | | | | | | | | | | | | | | | | |
Net cash used in investing activities | | | — | | | | (24,532 | ) | | | (58,044 | ) | | | — | | | | (82,576 | ) |
| | | | | | | | | | | | | | | | | | | | |
| | | | | |
Cash flows from financing activities | | | | | | | | | | | | | | | | | | | | |
Payment of debt and capital lease obligations | | | (55,015 | ) | | | — | | | | (461 | ) | | | — | | | | (55,476 | ) |
Distributions to non-controlling interests | | | — | | | | (269 | ) | | | (6,481 | ) | | | — | | | | (6,750 | ) |
Costs paid for repurchase of non-controlling interests | | | — | | | | (1,379 | ) | | | — | | | | — | | | | (1,379 | ) |
Change in intercompany balances with affiliates, net | | | 129,427 | | | | 103,614 | | | | (189,978 | ) | | | (43,063 | ) | | | — | |
| | | | | | | | | | | | | | | | | | | | |
Net cash provided by (used in) financing activities | | | 74,412 | | | | 101,966 | | | | (196,920 | ) | | | (43,063 | ) | | | (63,605 | ) |
| | | | | | | | | | | | | | | | | | | | |
Change in cash and cash equivalents | | | — | | | | 125,995 | | | | (205 | ) | | | — | | | | 125,790 | |
Cash and cash equivalents at beginning of period | | | — | | | | 80,336 | | | | 402 | | | | — | | | | 80,738 | |
| | | | | | | | | | | | | | | | | | | | |
Cash and cash equivalents at end of period | | $ | — | | | $ | 206,331 | | | $ | 197 | | | $ | — | | | $ | 206,528 | |
| | | | | | | | | | | | | | | | | | | | |
F-63
IASIS HEALTHCARE LLC
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS (CONTINUED)
IASIS Healthcare LLC
Condensed Consolidating Statement of Cash Flows
(in thousands)
| | | | | | | | | | | | | | | | | | | | |
| | | For the Year Ended September 30, 2008 | |
| | | Parent
Issuer | | | Subsidiary
Guarantors | | | Subsidiary
Non-Guarantors | | | Eliminations | | | Condensed
Consolidated | |
| | | | | |
Cash flows from operating activities | | | | | | | | | | | | | | | | | | | | |
Net earnings (loss) | | $ | (18,402 | ) | | $ | (28,701 | ) | | $ | 124,614 | | | $ | (36,760 | ) | | $ | 40,751 | |
Adjustments to reconcile net earnings (loss) to net cash provided by (used in) operating activities: | | | | | | | | | | | | | | | | | | | | |
Loss (earnings) from discontinued operations | | | (5,783 | ) | | | 12,257 | | | | 4,801 | | | | — | | | | 11,275 | |
Depreciation and amortization | | | — | | | | 42,721 | | | | 54,020 | | | | — | | | | 96,741 | |
Amortization of loan costs | | | 2,913 | | | | — | | | | — | | | | — | | | | 2,913 | |
Deferred income taxes | | | 19,368 | | | | — | | | | — | | | | — | | | | 19,368 | |
Loss (gain) on disposal of assets | | | — | | | | 81 | | | | (6 | ) | | | — | | | | 75 | |
Hurricane-related property damage | | | — | | | | — | | | | 3,589 | | | | — | | | | 3,589 | |
Equity in earnings of affiliates | | | (91,476 | ) | | | — | | | | — | | | | 91,476 | | | | — | |
Changes in operating assets and liabilities, net of the effect of acquisitions and dispositions: | | | | | | | | | | | | | | | | | | | | |
Accounts receivable, net | | | — | | | | 23,114 | | | | (5,983 | ) | | | — | | | | 17,131 | |
Inventories, prepaid expenses and other current assets | | | — | | | | 2,328 | | | | (23,689 | ) | | | — | | | | (21,361 | ) |
Accounts payable, other accrued expenses and other accrued liabilities | | | (10,947 | ) | | | (13,040 | ) | | | (5,432 | ) | | | — | | | | (29,419 | ) |
| | | | | | | | | | | | | | | | | | | | |
Net cash provided by (used in) operating activities — continuing operations | | | (104,327 | ) | | | 38,760 | | | | 151,914 | | | | 54,716 | | | | 141,063 | |
Net cash provided by (used in) operating activities — discontinued operations | | | 5,783 | | | | (884 | ) | | | (2,586 | ) | | | — | | | | 2,313 | |
Net cash provided by (used in) operating activities | | | (98,544 | ) | | | 37,876 | | | | 149,328 | | | | 54,716 | | | | 143,376 | |
| | | | | | | | | | | | | | | | | | | | |
| | | | | |
Cash flows from investing activities | | | | | | | | | | | | | | | | | | | | |
Purchases of property and equipment | | | — | | | | (45,109 | ) | | | (92,306 | ) | | | — | | | | (137,415 | ) |
Cash paid for acquisitions | | | — | | | | (16,799 | ) | | | (22 | ) | | | — | | | | (16,821 | ) |
Proceeds from sale of assets | | | — | | | | 94 | | | | 266 | | | | — | | | | 360 | |
Change in other assets | | | — | | | | 5,226 | | | | (613 | ) | | | — | | | | 4,613 | |
| | | | | | | | | | | | | | | | | | | | |
Net cash used in investing activities — continuing operations | | | — | | | | (56,588 | ) | | | (92,675 | ) | | | — | | | | (149,263 | ) |
Net cash provided by (used in) investing activities — discontinued operations | | | — | | | | (1,040 | ) | | | 23 | | | | — | | | | (1,017 | ) |
| | | | | | | | | | | | | | | | | | | | |
Net cash used in investing activities | | | — | | | | (57,628 | ) | | | (92,652 | ) | | | — | | | | (150,280 | ) |
| | | | | | | | | | | | | | | | | | | | |
| | | | | |
Cash flows from financing activities | | | | | | | | | | | | | | | | | | | | |
Payment of debt and capital lease obligations | | | (303,190 | ) | | | (849 | ) | | | (2,572 | ) | | | — | | | | (306,611 | ) |
Proceeds from debt borrowings | | | 384,978 | | | | — | | | | — | | | | — | | | | 384,978 | |
Distributions to non-controlling interests | | | — | | | | (172 | ) | | | (5,313 | ) | | | — | | | | (5,485 | ) |
Proceeds received from sale of non-controlling interests, net | | | — | | | | 15,070 | | | | — | | | | — | | | | 15,070 | |
Other | | | 192 | | | | — | | | | — | | | | — | | | | 192 | |
Change in intercompany balances with affiliates, net | | | 16,564 | | | | 90,593 | | | | (52,441 | ) | | | (54,716 | ) | | | — | |
| | | | | | | | | | | | | | | | | | | | |
Net cash provided by (used in) financing activities — continuing operations | | | 98,544 | | | | 104,642 | | | | (60,326 | ) | | | (54,716 | ) | | | 88,144 | |
Net cash used in financing activities — discontinued operations | | | — | | | | (502 | ) | | | — | | | | — | | | | (502 | ) |
| | | | | | | | | | | | | | | | | | | | |
Net cash provided by (used in) financing activities | | | 98,544 | | | | 104,140 | | | | (60,326 | ) | | | (54,716 | ) | | | 87,642 | |
| | | | | | | | | | | | | | | | | | | | |
Change in cash and cash equivalents | | | — | | | | 84,388 | | | | (3,650 | ) | | | — | | | | 80,738 | |
Cash and cash equivalents at beginning of period | | | — | | | | (4,052 | ) | | | 4,052 | | | | — | | | | — | |
| | | | | | | | | | | | | | | | | | | | |
Cash and cash equivalents at end of period | | $ | — | | | $ | 80,336 | | | $ | 402 | | | $ | — | | | $ | 80,738 | |
| | | | | | | | | | | | | | | | | | | | |
F-64
Annex A
THIS DOCUMENT IS IMPORTANT AND REQUIRES YOUR IMMEDIATE ATTENTION. If you are in any doubt as to the action to be taken, you should immediately consult your broker, bank manager, lawyer, accountant, investment advisor or other professional adviser.
LETTER OF TRANSMITTAL
Relating to
IASIS Healthcare LLC and IASIS Capital Corporation
Offer to Exchange
any and all of their outstanding unregistered 8.375% Senior Notes due 2019 (CUSIP Nos. 45072PAC6 and
U45827AB5) for $850,000,000 aggregate principal amount of their new 8.375% Senior Notes due 2019 that
have been registered under the Securities Act of 1933, as amended (the “Securities Act”)
This document relates to the exchange offer (the “Exchange Offer”) made by IASIS Healthcare LLC and IASIS Capital Corporation (the “Issuers”) to exchange any and all of their unregistered $850,000,000 8.375% Senior Notes due 2019 (the “Old Notes”) for new 8.375% Senior Notes due 2019 (the “New Notes”) that have been registered under the Securities Act. The Exchange Offer is described in the Prospectus dated November 10, 2011 (the “Prospectus”) and in this letter of transmittal (this “Letter of Transmittal”). All terms and conditions contained in, or otherwise referred to in, the Prospectus are deemed to be incorporated in, and form a part of, this Letter of Transmittal. Therefore you are urged to read carefully the Prospectus and the items referred to therein. The terms and conditions contained in the Prospectus, together with the terms and conditions governing this Letter of Transmittal and the instructions herein, are collectively referred to herein as the “terms and conditions.”
The Exchange Offer will expire at 5:00 p.m., New York City time, on December 12, 2011, unless extended by the Issuers (such date and time, as they may be extended, the “Expiration Date”). Tendered Old Notes may be withdrawn at any time prior to the expiration of the Exchange Offer.
Upon the satisfaction or waiver of the conditions to the acceptance of the Old Notes set forth in the Prospectus under “Description of the Exchange Offer—Conditions to the Exchange Offer,” the Issuers will accept for settlement the Old Notes that have been validly tendered (and not subsequently validly withdrawn). This acceptance date is referred to as the “Acceptance Date.” The Issuers will deliver the New Notes on a date (the “Settlement Date”) as soon as practicable after the Expiration Date.
The Exchange Agent for the Exchange Offer is:
The Bank of New York Mellon Trust Company, National Association
| | | | |
Registered & Certified Mail: | | Regular Mail or Courier: | | In Person by Hand Only: |
The Bank of New York Mellon Trust Company | | The Bank of New York Mellon Trust Company | | The Bank of New York Mellon Trust Company |
Corporate Trust Operations – Reorganization Unit | | Corporate Trust Operations – Reorganization Unit | | Corporate Trust Operations – Reorganization Unit |
| 101 Barclay Street | | 101 Barclay Street | | 101 Barclay Street Floor 7 East |
| New York, NY 10286 | | New York, NY 10286 | | New York, NY 10286 |
| Attn.: David Mauer | | Attn.: David Mauer | | Attn.: David Mauer |
or
By Facsimile Transmission:
(212) 298-1915
Attention: Corporate Trust Operations; Attn. of David Mauer
or
By Telephone:
(212) 815-3687
A-1
This Letter of Transmittal is to be used by holders of the Old Notes. Tender of the Old Notes is to be made using the Automated Tender Offer Program (“ATOP”) of The Depository Trust Company (“DTC”) pursuant to the procedures set forth in the Prospectus under the caption “Description of the Exchange Offer—Procedures for Tendering.” DTC participants that are accepting the Exchange Offer must transmit their acceptance to DTC, which will verify the acceptance and execute a book-entry delivery to the Exchange Agent’s DTC account. DTC will then send a computer-generated message known as an “agent’s message” to the Exchange Agent for its acceptance. For you to validly tender your Old Notes in the Exchange Offer, the Exchange Agent must receive, prior to the Expiration Date, an agent’s message under the ATOP procedures that confirms that:
| | • | | DTC has received your instructions to tender your Old Notes; and |
| | • | | You agree to be bound by the terms of this Letter of Transmittal. |
By using the ATOP procedures to tender the Old Notes, you will not be required to deliver this Letter of Transmittal to the Exchange Agent. However, you will be bound by its terms, and you will be deemed to have made the acknowledgments and the representations and warranties it contains, just as if you had signed it.
The New Notes will be issued in full exchange for the Old Notes in the Exchange Offer, if consummated, on the Settlement Date and will be delivered in book-entry form.
A-2
Please read the accompanying instructions carefully.
Ladies and Gentlemen:
Upon the terms and subject to the conditions of the Exchange Offer, the undersigned hereby tenders to the Issuer the aggregate principal amount of Old Notes credited by the undersigned to the Exchange Agent’s account at DTC using ATOP.
The undersigned understands that validly tendered Old Notes (or defectively tendered Old Notes with respect to which the Issuer has waived such defect or caused such defect to be waived) will be deemed to have been accepted by the Issuer if, as and when the Issuer gives oral or written notice thereof to the Exchange Agent. The undersigned understands that, subject to the terms and conditions, the Old Notes properly tendered and accepted (and not validly withdrawn) in accordance with the terms and conditions will be exchanged for the New Notes. The undersigned understands that, under certain circumstances, the Issuer may not be required to accept any of the Old Notes tendered (including any such Old Notes tendered after the Expiration Date). If any Old Notes are not accepted for exchange for any reason (or if the Old Notes are validly withdrawn), such Old Notes will be returned, without expense, to the undersigned’s account at DTC or such other account as designated herein, pursuant to the book-entry transfer procedures described in the Prospectus, as promptly as practicable after the expiration or termination of the Exchange Offer.
By tendering the Old Notes in the Exchange Offer, the undersigned acknowledges that the Exchange Offer is being made based upon the Issuer’s understanding of an interpretation by the staff of the Securities and Exchange Commission (the “SEC”) as set forth in no-action letters issued to other parties, includingExxon Capital Holdings Corporation, SEC No-Action Letter (available May 13, 1988),Morgan Stanley & Co. Incorporated, SEC No-Action Letter (available June 5, 1991) andShearman & Sterling, SEC No-Action Letter (available July 2, 1993), that the New Notes issued in exchange for the Old Notes pursuant to the Exchange Offer may be offered for resale, resold and otherwise transferred by each holder thereof (other than a broker-dealer who acquires such New Notes directly from the Issuer for resale pursuant to Rule 144A under the Securities Act or any other available exemption under the Securities Act or any such holder that is an “affiliate” of the Issuer within the meaning of Rule 405 under the Securities Act), without compliance with the registration and prospectus delivery provisions of the Securities Act, provided that such New Notes are acquired in the ordinary course of such holder’s business and such holder is not engaged in, and does not intend to engage in, a distribution of such New Notes and has no arrangement with any person to participate in the distribution of such New Notes. If the undersigned is not a broker-dealer, the undersigned represents that it acquires the New Notes in the ordinary course of its business, it is not engaged in, and does not intend to engage in, a distribution of the New Notes and it has no arrangements or understandings with any person to participate in a distribution of the New Notes. If the undersigned is a broker-dealer that will receive the New Notes for its own account in exchange for the Old Notes, it represents that the Old Notes to be exchanged for the New Notes were acquired by it as a result of market-making activities or other trading activities and acknowledges that it will deliver a prospectus in connection with any resale of such New Notes; however, by so acknowledging and by delivering a prospectus, the undersigned will not be deemed to admit that it is an “underwriter” within the meaning of the Securities Act.
Upon agreement to the terms of this Letter of Transmittal pursuant to an agent’s message, the undersigned, or the beneficial holder of the Old Notes on behalf of which the undersigned has tendered, will, subject to that holder’s ability to withdraw its tender, and subject to the terms and conditions of the Exchange Offer generally, hereby:
| | • | | irrevocably sell, assign and transfer to or upon the order of the Issuer or their nominee all right, title and interest in and to, and any and all claims in respect of or arising or having arisen as a result of the undersigned’s status as a holder of, all Old Notes tendered hereby, such that thereafter it shall have no contractual or other rights or claims in law or equity against the Issuer or any fiduciary, trustee, fiscal agent or other person connected with the Old Notes arising under, from or in connection with such Old Notes; |
| | • | | waive any and all rights with respect to the Old Notes tendered hereby, including, without limitation, any existing or past defaults and their consequences in respect of such Old Notes; and |
A-3
| | • | | release and discharge the Issuer, the Guarantors and The Bank of New York Mellon Trust Company, National Association, as the trustee for the Old Notes from any and all claims the undersigned may have, now or in the future, arising out of or related to the Old Notes tendered hereby, including, without limitation, any claims that the undersigned is entitled to receive additional principal or interest payments with respect to the Old Notes tendered hereby, other than as expressly provided in the Prospectus and in this Letter of Transmittal, or to participate in any redemption or defeasance of the Old Notes tendered hereby. |
The undersigned understands that tenders of the Old Notes pursuant to the procedures described in the Prospectus and in this Letter of Transmittal and acceptance of such Old Notes by the Issuer will, following such acceptance, constitute a binding agreement between the undersigned and the Issuer upon the terms and conditions.
By tendering the Old Notes in the Exchange Offer, the undersigned represents, warrants and agrees that:
| | • | | it has received and reviewed the Prospectus; |
| | • | | it is the beneficial owner (as defined below) of, or a duly authorized representative of one or more beneficial owners of, the Old Notes tendered hereby, and it has full power and authority to execute this Letter of Transmittal; |
| | • | | the Old Notes being tendered hereby were owned as of the date of tender, free and clear of any liens, charges, claims, encumbrances, interests and restrictions of any kind, and the Issuer will acquire good, indefeasible and unencumbered title to such Old Notes, free and clear of all liens, charges, claims, encumbrances, interests and restrictions of any kind, when the Issuer accepts the same; |
| | • | | it will not sell, pledge, hypothecate or otherwise encumber or transfer any Old Notes tendered hereby from the date of this Letter of Transmittal, and any purported sale, pledge, hypothecation or other encumbrance or transfer will be void and of no effect; |
| | • | | in evaluating the Exchange Offer and in making its decision whether to participate in the Exchange Offer by tendering its Old Notes, the undersigned has made its own independent appraisal of the matters referred to in the Prospectus and this Letter of Transmittal and in any related communications and it is not relying on any statement, representation or warranty, express or implied, made to such holder by the Issuer or the Exchange Agent, other than those contained in the Prospectus, as amended or supplemented through the Expiration Date; |
| | • | | the execution and delivery of this Letter of Transmittal shall constitute an undertaking to execute any further documents and give any further assurances that may be required in connection with any of the foregoing, in each case on and subject to the terms and conditions described or referred to in the Prospectus; |
| | • | | the agreement to the terms of this Letter of Transmittal pursuant to an agent’s message shall, subject to the terms and conditions of the Exchange Offer, constitute the irrevocable appointment of the Exchange Agent as its attorney and agent and an irrevocable instruction to such attorney and agent to complete and execute all or any forms of transfer and other documents at the discretion of that attorney and agent in relation to the Old Notes tendered hereby in favor of the Issuer or any other person or persons as the Issuer may direct and to deliver such forms of transfer and other documents in the attorney’s and agent’s discretion and the certificates and other documents of title relating to the registration of such Old Notes and to execute all other documents and to do all other acts and things as may be in the opinion of that attorney or agent necessary or expedient for the purpose of, or in connection with, the acceptance of the Exchange Offer, and to vest in the Issuer or their nominees such Old Notes; |
| | • | | the terms and conditions of the Exchange Offer shall be deemed to be incorporated in, and form a part of, this Letter of Transmittal, which shall be read and construed accordingly; |
A-4
| | • | | it is acquiring the New Notes in the ordinary course of its business; |
| | • | | it is not participating in, and does not intend to participate in, a distribution of the New Notes within the meaning of the Securities Act and has no arrangement or understanding with any person to participate in a distribution of the New Notes within the meaning of the Securities Act; |
| | • | | it is not a broker-dealer who acquired the Old Notes directly from the Issuer; and |
| | • | | it is not an “affiliate” of the Issuer, within the meaning of Rule 405 of the Securities Act. |
The representations, warranties and agreements of a holder tendering the Old Notes shall be deemed to be repeated and reconfirmed on and as of the Expiration Date and the Settlement Date. For purposes of this Letter of Transmittal, the “beneficial owner” of any Old Notes means any holder that exercises investment discretion with respect to such Old Notes.
The undersigned understands that tenders may not be withdrawn at any time after the Expiration Date, except as set forth in the Prospectus, unless the Exchange Offer is amended with changes to the terms and conditions that are, in the reasonable judgment of the Issuer, materially adverse to the tendering holders, in which case tenders may be withdrawn under the conditions described in the extension.
If the Exchange Offer is amended in a manner determined by the Issuer to constitute a material change, the Issuer will extend the Exchange Offer for a period of two to ten business days, depending on the significance of the amendment and the manner of disclosure to such holders, if the Exchange Offer would otherwise have expired during such two to ten business day period.
All authority conferred or agreed to be conferred in this Letter of Transmittal and every obligation of the undersigned hereunder shall be binding upon the undersigned’s successors, assigns, heirs, executors, administrators, trustees in bankruptcy and legal representatives of the undersigned and shall not be affected by, and shall survive, the death or incapacity of the undersigned.
Name:
Amount Tendered (if less than all):
Address:
Name of Tendering Institution:
Account Number:
Transaction Code Number:
By crediting the Old Notes to the Exchange Agent’s account at DTC using ATOP and by complying with applicable ATOP procedures with respect to the Exchange Offer, the participant in DTC confirms on behalf of itself and the beneficial owners of such Old Notes all provisions of this Letter of Transmittal (including all representations and warranties) applicable to it and such beneficial owner as fully as if it had completed the information required herein and executed and transmitted this Letter of Transmittal to the Exchange Agent.
A-5
INSTRUCTIONS FORMING PART OF
THE TERMS AND CONDITIONS OF THE EXCHANGE OFFER
| | 1. | Book-Entry Confirmations |
Any confirmation of a book-entry transfer to the Exchange Agent’s account at DTC of the Old Notes tendered by book-entry transfer, as well as an agent’s message, and any other documents required by this Letter of Transmittal, must be received by the Exchange Agent at its address set forth on the cover page of this Letter of Transmittal prior to the Expiration Date.
The Issuer will determine in their sole discretion all questions as to the validity, form, eligibility, time of receipt, acceptance of tendered Old Notes and withdrawal of tendered Old Notes. The Issuer’s determination will be final and binding. The Issuer reserves the absolute right to reject any Old Notes not properly tendered or any acceptance of the Old Notes that would, in the opinion of its counsel, be unlawful. The Issuer also reserves the right to waive any defect, irregularities or conditions of tender as to particular Old Notes. The Issuer’s interpretation of the terms and conditions of the Exchange Offer, including the instructions in this Letter of Transmittal, will be final and binding on all parties. Unless waived, all defects or irregularities in connection with tenders of the Old Notes must be cured within such time as the Issuer shall determine. Although the Issuer intends to notify holders of defects or irregularities with respect to tenders of the Old Notes, none of the Issuer, the Exchange Agent and any other person will incur any liability for failure to give such notification. Tenders of the Old Notes will not be deemed made until such defects or irregularities have been cured or waived. Any Old Notes received by the Exchange Agent that are not properly tendered and as to which the defects or irregularities have not been cured or waived will be returned to the tendering holder through the facilities of DTC as soon as practicable after the Expiration Date.
The Issuer reserves the absolute right to waive, in whole or part, at any time or from time to time, any of the conditions to the Exchange Offer set forth in the Prospectus or in this Letter of Transmittal.
No alternative, conditional, irregular or contingent tender of the Old Notes will be accepted.
Requests for assistance regarding the Prospectus or this Letter of Transmittal may be directed to the Exchange Agent at the address, telephone numbers or fax number set forth on the cover page of this Letter of Transmittal. Holders may also contact their commercial bank, broker, dealer, trust company or other nominee for assistance concerning the Exchange Offer.
Tenders of the Old Notes may be withdrawn at any time prior to the Expiration Date. For a withdrawal to be effective you must comply with the appropriate ATOP procedures. Any notice of withdrawal must specify the name and number of the account at DTC to be credited with withdrawn Old Notes and otherwise comply with the ATOP procedures. For more information, see the section of the Prospectus entitled “Description of the Exchange Offer—Withdrawal of Tenders.”
Holders who tender their Old Notes for exchange will not be obligated to pay any transfer taxes in connection with that tender or exchange, except that holders who instruct the Issuer to register the New Notes in the name of, or request that the Old Notes not tendered or not accepted in the Exchange Offer be returned to, a person other than the registered tendering holder will be responsible for the payment of any applicable transfer tax on those Old Notes.
A-6
IMPORTANT: BY USING THE ATOP PROCEDURES TO TENDER THE OLD NOTES, YOU WILL NOT BE REQUIRED TO DELIVER THIS LETTER OF TRANSMITTAL TO THE EXCHANGE AGENT. HOWEVER, YOU WILL BE BOUND BY ITS TERMS, AND YOU WILL BE DEEMED TO HAVE MADE THE ACKNOWLEDGMENTS AND THE REPRESENTATIONS AND WARRANTIES IT CONTAINS, JUST AS IF YOU HAD SIGNED IT.
A-7