DEPARTMENT OF SOCIAL SERVICES
| Amendment Number: | 1 |
| Contract #: | 093-HUS-WCC-2 |
| Contract Period: | 07/01/2005 - 06/30/2007 |
| Contractor Name: | WELLCARE OF CONNECTICUT, INC. |
| Contractor Address: | 127 Washington Avenue, North Haven, CT 06473 |
Contract number 093-HUS-WCC-2 by and between the Department of Social Services (the "Department") and WELLCARE of CONNECTICUT, Inc. (the "Contractor") for the provision of services under the HUSKY A program is hereby amended as follows:
| 1. | Part II "GENERAL CONTRACT TERMS FOR MCOs" dated December 12, 2003 are deleted in their entirety and replaced with Part II "GENERAL CONTRACT TERMS FOR MCOs" pages 1 through 108 dated 05/01/07 attached hereto. |
| 2. | Appendices A through J are deleted in their entirety and replaced with the following appendices attached hereto; |
A. HUSKY B Covered Services
D. Provider Credentialing and Enrollment Requirements
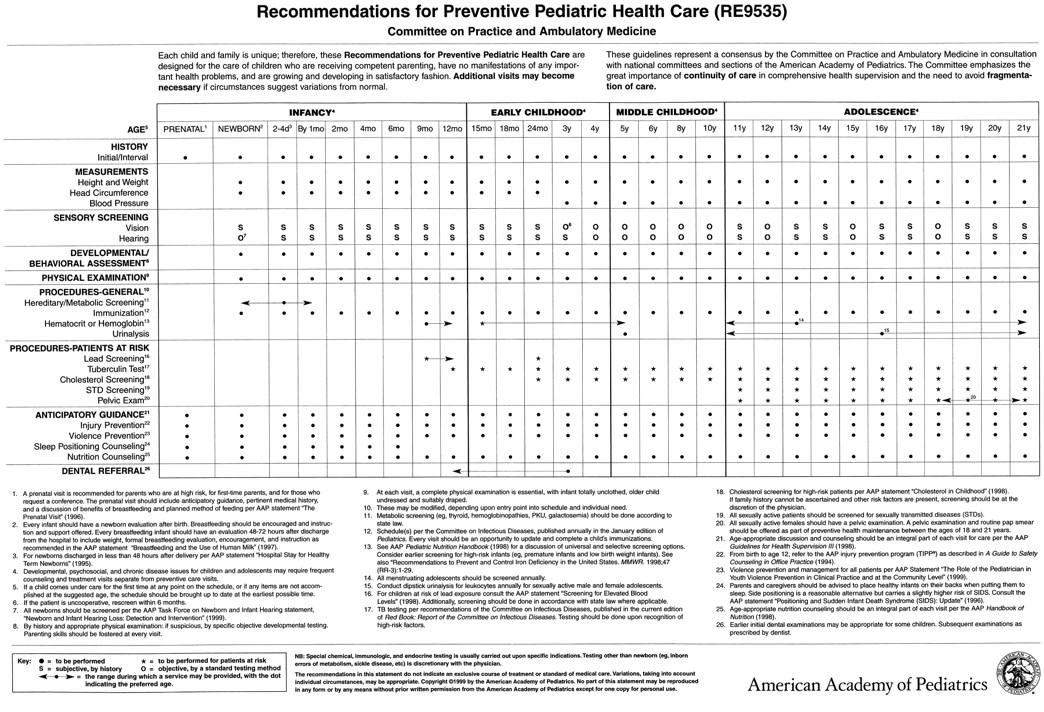
E. American Academy of Pediatrics - Recommendations for Preventative Pediatric Health Care
F. DSS Marketing Guidelines
G. Standards for Internal Quality Assurance Programs for Health Plans
H. Claims Inventory, Aging and Unaudited Quarterly Financial Reports
I. Capitation Payment Amount
J. Inpatient/Eligibility Recategorization Chart
L. BLANK - RESERVED FOR POSSIBLE FUTURE USE
M.BLANK - RESERVED FOR POSSIBLE FUTURE USE
N. HUSKY Behavioral Health Carve-Out Coverage and Coordination of Medical and Behavioral Services
O. CTBHP Master Covered Services Table
| 3. | Appendices A through H and J through O shall become effective upon the proper execution of this amendment by the Department and the Contractor. |
| 4. | Appendix I Capitation Payment Amount HUSKY B Capitation Rate shall be effective for the 07/01/06 - 06/30/07. |
| 5. | Pursuant to Public Act 07-1, An Act Concerning the State Contractor Contribution Ban and Gifts to State and Quasi-Public Agencies the Department must provide and each Contractor must acknowledge receipt of the State Elections Enforcement Commission's notice advising state contractors of state campaign contribution and solicitation prohibitions. Through the execution of this amendment the Department certifies that SEEC FORM 11 - NOTICE TO EXECUTIVE BRANCH STATE CONTRACTORS AND PROSPECTIVE STATE CONTRACTORS OF CAMPAIGN CONTRIBUTION AND SOLICITATION BAN has been provided to the Contractor and the Contractor acknowledges receipt of the same. |
ACCEPTANCES AND APPROVALS
This document constitutes an amendment to the above numbered contract. All provisions of that contract, except those explicitly changed or described above by this amendment, shall remain in full force and effect.
WELLCARE of CONNECTICUT, Inc. | Department of Social Services |
/s/ Todd Farha | 5/30/2007 | /s/ Michael P. Starkowski | 5/31/2007 |
| Signature (Authorized Official) | Date | Signature (Authorized Official) | Date |
| Todd Farha | President & CEO | Michael P. Starkowski | Commissioner |
| Typed Name (Authorized Official) | Title | Typed Name (Authorized Official) | Title |
Attorney General (as to form) Date
( ) This contract does not require the signature of the Attorney General pursuant to an agreement between the Department and the Office of the Attorney General dated: __________
PART I: STANDARD CONNECTICUT CONTRACT TERMS
PART II: GENERAL CONTRACT TERMS FOR MCOS
2. DELEGATIONS OF AUTHORITY
3. FUNCTIONS AND DUTIES OF THE MCO
3.01 Provision of Services
3.03 Gag Rules/Integrity of Professional Advice to Members
3.04 Coordination and Continuation of Care
3.07 Choice of Health Professional
3.09 Network Adequacy and Maximum Enrollment Levels
3.11 Provider Credentialing and Enrollment
3.12 Specialist Providers and the Referral Process
3.13 PCP and Specialist Selection, Scheduling and Capacity
3.14 Family Planning Access and Confidentiality
3.16 Mental Health and Substance Abuse Access
3.17 Children's Issues and Preventive Care and Services
3.18 Well-Care Services for Adolescents
3.22 Pre-Existing Conditions
3.24 Newborn Enrollment and Minimum Hospital Stays
3.25 Acute Care Hospitalization at Time of Enrollment or Disenrollment
3.27 Special Disenrollment
3.30 Information to Potential Members
3.31 DSS Marketing Guidelines
3.33 Quality Assessment and Performance Improvement
3.34 Inspection of Facilities
3.35 Examination of Records
3.38 Clinical Data Reporting
3.39 Utilization Management
3.42 Subcontracting for Services
3.43 Timely Payment of Claims
3.44 Insolvency Protection
4. MCO Responsibility Concerning Payments Made On Behalf Of The Member
4.1 Deductibles, Coinsurance, Annual Benefit Maximums, and Lifetime Benefit Maximums
4.2 Payments for Noncovered Services
4.3 Cost-Sharing Exemption for American Indian/Native American Children
4.5 Copayments Prohibited
4.6 Maximum Annual Limits for Copayments
4.8 Amount of Premium Paid
4.9 Billing and Collecting the Premium Payments
4.10 Notification of Premium Payments Due
4.11 Notification of Non-payment of the Premium Payments
4.12 Past Due Premium Payments Paid
4.13 Resumption of Services if the Child is Re-enrolled
4.14 Overpayment of Premium
4.15 Member Premium Share Paid by Another Entity
4.16 Tracking Premium Payments
4.17 Behavioral Health Payment Adjustment
5. LIMITED COVERAGE OF SOME GOODS AND SERVICES AND ALLOWANCES
5.01 Limited Coverage of Some Goods and Services
6. FUNCTIONS AND DUTIES OF THE DEPARTMENT
6.1 Eligibility Determinations
6.2 Ineligibility Determinations
6.3 Enrollment / Disenrollment
6.4 Lock-In / Open Enrollment
6.5 Capitation Payments to the MCO
6.6 Newborn Retroactive Adjustments
7. DECLARATIONS AND MISCELLANEOUS PROVISIONS
7.01 Competition not Restricted
7.02 Nonsegregated Facilities
7.04 Employment/Affirmative Action Clause
7.06 Independent Capacity
7.08 Freedom of Information
7.11 Financial Responsibilities of the MCO
7.12 Captilization and Reserves
7.13 Members Held Harmless
7.14 Compliance with Applicable Laws, Rules and Policies
7.15 Federal Requirements and Assurances
7.17 Statutory Requirements
7.18 Disclosure of Interlocking Relationships
7.19 DEPARTMENT'S Data Files
7.21 Executive Order Number 16
8. MCO RESPONSIBILITIES CONCERNING INTERNAL AND EXTERNAL APPEALS
8.1 MCO Responsibilities Concerning Internal and External Appeals and Notices of Denial
8.2 Internal Appeal Process Required
8.4 Internal Appeal Process
8.5 Written Appeal Decision
8.7 External Appeal Process through the DOI
8.8 Provider Appeal Process
9. CORRECTION ACTION AND CONTRACT TERMINATION
9.2 Settlement of Disputes
9.3 Administrative Errors
9.4 Suspension of New Enrollment
9.6 Payment Withhold, Class C Sanctions
9.7 Emergency Services Denials
9.8 Termination for Default
9.9 Termination for Mutual Convenience
9.10 Termination for Financial Instability of the MCO
9.11 Termination for Unavailability of Funds
9.12 Termination for Collusion in Price Determination
9.13 Termination Obligations of Contracting Parties
10.4 Correction of Deficiencies
10.5 This is not a Public Works Contract
Appendix A HUSKY B Covered Services | |
Appendix B HUSKY Plus-Behavioral Deleted | |
Appendix D Provider Credentialing and Enrollment Requirements; (same as HUSKY A) | |
Appendix E American Academy of Pediatrics - Recommendations for Preventive Pediatric Health Care | |
Appendix F DSS Marketing Guidelines; (same as HUSKY A) | |
Appendix G Standards for Internal Quality Assurance Programs for Health Plans; (same as HUSKY A) | |
Appendix H Claims Inventory, Aging and Unaudited Quarterly Financial Reports; (same as HUSKY A) | |
Appendix I Capitation Payment Amount | |
Appendix J Inpatient/Eligibility Recategorization Chart, (same as HUSKY A) | |
Appendix K Abortion Reporting. | |
Appendix N HUSKY (Behavioral Health Carve-Out Coverage and Coordination of Medical and Behavioral Services) (same as HUSKY A) | |
Appendix O CTBHP Master Covered Services Table (same as HUSKY A) | |
PART II: GENERAL CONTRACT TERMS FOR MCOs
As used throughout this contract, the following terms shall have the meanings set forth below.
MCO and/or provider practices that are inconsistent with sound fiscal, business, or medical practices, and result in an unnecessary cost to the HUSKY program, or the reimbursement for services that are not medically necessary or that fail to meet professionally recognized standards for health care, or a pattern of failing to provide medically necessary services required by this contract. Member practices that result in unnecessary cost to the HUSKY program, also constitute abuse.
Administrative Services Organization (ASO):
An organization providing utilization management, benefit information and intensive care management services within a centralized information system framework
The amount that a managed care organization (MCO) is responsible to pay a provider towards the cost of a limited covered benefit.
American Indian/Alaska Native (Al):
| 1) | A member of a Federally recognized Indian tribe, band, or group; |
| 2) | An Eskimo or Aleut other Alaska Native enrolled by the Secretary of the Interior pursuant to the Alaska Native Claims Settlement Act, 43 U.S.C. 1601 et seq.; or |
| 3) | A person who is considered by the Secretary of HHS to be an Indian for any purpose. |
Any of the following individuals who are applying for coverage under HUSKY B on behalf of a child, pursuant to Section 17b-290 of the Connecticut General Statutes:
| 1) | A natural parent, adoptive parent, legal guardian, caretaker relative, foster parent, or a stepparent who is over eighteen years of age and who lives with the child for whom he or she is applying; |
| 2) | A non-custodial parent who is under order of a court or family support magistrate to provide health insurance for his or her child; |
| 3) | A child who is eighteen (18) years of age who is applying on his or her own behalf or on behalf of a minor dependent with whom he or she lives; and |
| 4) | A child who is emancipated in accordance with the provisions of Sections 46b-150 to 46b-150e, inclusive, of the Connecticut General Statutes, who is applying on his or her own behalf or on behalf of a minor dependent with whom he or she lives. A child is an applicant until the child receives coverage under HUSKY B. |
Behavioral Health Partnership ("Partnership" or "BHP"):
An integrated behavioral health service system for HUSKY Part A and HUSKY Part B members, children enrolled in the Voluntary Services Program operated by the Department of Children and Families and may, at the discretion of the Commissioners of Children and Families and Social Services, include other children, adolescents, and families served by the Department of Children and Families
Behavioral Health Services:
Services that are necessary to diagnose, correct or diminish the adverse effects of a psychiatric or substance use disorder.
The amount paid per Member by the DEPARTMENT to each managed care organization (MCO) on a monthly basis.
The individualized monthly payment made by the DEPARTMENT to the MCO on behalf of Members.
For the purposes of the HUSKY B program, an individual under nineteen (19) years of age, as defined in Section 17b-290 of the Connecticut General Statutes.
Payment for part or all of the cost of health benefits coverage provided to targeted low-income children for the services listed at 42 CFR 457.402.
Preventive care and services that include periodic and well-child visits, routine immunizations, health screenings and routine laboratory tests.
Children with Special Health Care Needs:
Children at elevated risk for (biologic or acquired) chronic physical, developmental, behavioral, or emotional conditions and who also require health and related (not educational or recreational) services of a type and amount not usually required by children of the same age.
A bill for service(s) or goods, a line item of services or all services and/or goods for a recipient contained on one bill which can be processed without obtaining additional information from the provider of service(s) or a third party. A clean claim does not include a claim from a provider who is under investigation for fraud or abuse or a claim under review for medical necessity.
Centers for Medicare and Medicaid Services (CMS), formerly known as the Health Care Financing Administration (HCFA), a division within the United States Department of Health and Human Services.
The sharing of health care expenses by the insured and an insurer in a specified ratio, as defined in Section 17b-290 of the Connecticut General Statutes.
The Commissioner of the Department of Social Services, as defined in Section 17b-290 of the Connecticut General Statutes.
A written or oral communication from a Member expressing dissatisfaction with some aspect of the MCO's services.
A corporation, company, organization or person or their affiliates retained by the DEPARTMENT to provide assistance in administering the HUSKY B program, not the MCO or subcontractor.
The DEPARTMENT employee responsible for fulfilling the administrative responsibilities associated with this managed care project.
Those goods and services including limited benefits, which the MCO is required to provide Members under this contract.
A payment made by or on behalf of a Member for a specified covered benefit under HUSKY B, as defined in Section 17b-290 of the Connecticut General Statutes.
An arrangement made by or on behalf of a Member to pay a portion of the cost of health services and share costs with the DEPARTMENT and the MCO, which includes co-payments, premiums, deductibles and coinsurance, as defined in Section 17b-290 of the Connecticut General Statutes.
CPT Codes or Current Procedure Terminology:
A listing of descriptive terms and identifying codes for reporting medical services and procedures for a variety of uses, including billing of public and private health insurance programs. The codes are developed and published by the American Medical Association.
The date on which an application for the HUSKY B program is received by the DEPARTMENT or its agent, containing the applicant's signature.
Except where the term business day is expressly used, all references in this contract will be construed as calendar days.
The amount of out-of-pocket expenses that would be paid for health services by or on behalf of a Member before becoming payable by the insurer, as defined in Section 17b-290 of the Connecticut General Statutes.
The Department of Social Services (DSS), State of Connecticut.
DSM IV or Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition:
The current listing of descriptive terms and identifying codes for reporting a classification of mental and substance abuse disorders.
Durable Medical Equipment (DME):
Equipment furnished by a supplier or a home health agency that:
1) Can withstand repeated use;
2) Is primarily and customarily used to serve a medical purpose;
3) Generally is not useful to an individual in the absence of an illness or injury; and
4) Is appropriate for use in the home.
Emergency or Emergency Medical Condition:
A medical condition manifesting itself by acute symptoms of sufficient severity (including severe pain) such that a prudent layperson, who possesses an average knowledge of health and medicine, could reasonably expect the absence of immediate medical attention to result in placing the health of the individual (or with respect to a pregnant woman, the health of the woman or her unborn child) in serious jeopardy, serious impairment to body functions or serious dysfunction of any body organ or part.
Covered inpatient and outpatient services that are:
1) Furnished by a qualified provider and
2) Needed to evaluate or stabilize an emergency medical condition.
Such services shall include, but not be limited to, behavioral health and detoxification needed to evaluate or stabilize an emergency medical condition that is found to exist using the prudent layperson standard.
External Quality Review Organization (EQRO):
An entity responsible for conducting reviews of the quality outcomes, timeliness of the delivery of care, and access to items and services for which the MCO is responsible under this contract.
For the purposes of this contract, the family is defined as the household that includes the child and the following individuals who live with the child:
1) All of the child's siblings who are under nineteen (19) years of age, including full and half, and siblings who are HUSKY A Members;
2) Natural and adoptive parents of the child;
3) The spouse of the child; and
4) Stepparent and stepsiblings of the child, except when the inclusion of the stepparent and stepsiblings in the filing unit make the child ineligible for HUSKY B.
Federal Poverty Level (FPL):
The poverty guidelines updated annually in the Federal Register by the U.S. Department of Health & Human Services under authority of 42 U.S.C. Section 9902.
A list of selected Pharmaceuticals felt to be the most useful and cost effective for patient care, developed by a pharmacy and therapeutics committee at the MCO.
An MCO that is more than fifty (50) percent owned by Connecticut Federally Qualified Health Centers (FQHC), certified by the Department of Social Services to enroll HUSKY B Members.
| Intentional deception or misrepresentation, or reckless disregard or willful blindness, by a person or entity with the knowledge that the deception, misrepresentation, disregard or blindness could result in some unauthorized benefit to himself or some other person, including any act that constitutes fraud under applicable federal or state law. |
The ninety (90) day period of time, occurring from the date of onset of a lock-in period of the Member with the earliest date of enrollment in the MCO, during which time a family of which the Member is a part, shall have the opportunity to choose another MCO. Such period is contingent upon no Members of the family having previously been enrolled in the MCO chosen by the family.
The treatment plan that integrates the needed services from the benefit packages of the HUSKY B and the HUSKY Plus Physical programs when a medically eligible Member is concurrently receiving services from HUSKY B and the HUSKY Plus Physical programs.
Health Plan Employer Data and Information Set (HEDIS):
A standardized performance measurement tool that enables users to evaluate the quality of different MCOs based on the following categories: effectiveness of care; MCO stability; use of services; cost of care; informed health care choices; and MCO descriptive information.
The United States Department of Health and Human Services.
HUSKY, Part A, or HUSKY A:
For purposes of this contract, HUSKY PART A includes all those coverage groups previously covered in Connecticut Access, subject to expansion of eligibility groups pursuant to Section 17b-266 of the Connecticut General Statutes.
HUSKY Plan, Part B or HUSKY B:
The health insurance plan for children established pursuant to Title XXI of the Social Security Act, the provisions of Sections 17b-289 to 17b-303, inclusive, of the Connecticut General Statutes, and Section 16 of Public Act 97-1 of the October special session.
HUSKY Plus Physical Programs:
A supplemental physical health programs pursuant to Section 17b-294 of the Connecticut General Statutes, for medically eligible Members of the HUSKY B program in Income Bands 1 and 2, whose intensive physical health needs cannot be accommodated within the HUSKY Plan, Part B.
The International Classification of Disease, 9th Revision, Clinical Modification. A widely recognized system of disease classification developed and published by the National Center for Health Statistics.
A non-citizen or North American Indian born in Canada who is lawfully admitted into the United States for the express purpose of maintaining permanent residence.
As defined in Section 17b-290 of the Connecticut General Statutes. Income as calculated in the same manner as under the Medicaid program pursuant to Section 17b-261 of the Connecticut General Statutes.
Families with household incomes over 185% and up to and including 235% of the federal poverty level.
Families with household incomes over 235% and up to and including 300% of the
Families with household incomes over 300% of the federal poverty level.
In-network providers or network providers:
Providers who have contracted with the MCO to provide services to Members.
An establishment that furnishes food, shelter and some treatment or services to four (4) or more persons unrelated to the proprietor.
Goods and services that are covered only up to a specified dollar limit.
Limitations on Member changes of managed care organizations for a period of time, not to exceed twelve (12) months.
The period of time HUSKY B Members are not permitted to participate in an MCO due to nonpayment of a premium owed to the MCO in which they were enrolled.
Managed Care Organization (MCO):
The organization signing this agreement with the Department of Social Services.
Any communication from an MCO to a HUSKY B recipient who is not enrolled in that MCO, that can be reasonably interpreted as intended to influence the recipient to enroll or reenroll in that particular MCO or either to not enroll in, or disenroll from, another MCO.
Maximum Annual Aggregate Cost-sharing:
The maximum amount which the family is required to pay (out-of-pocket) for services under HUSKY B. These payments include co-payments and premiums.
The Connecticut Medical Assistance Program operated by the Connecticut Department of Social Services under Title XIX of the Federal Social Security Act, and related State and Federal rules and regulations.
Medical Appropriateness or Medically Appropriate:
Health care that is provided in a timely manner and meets professionally recognized standards of acceptable medical care; is delivered in the appropriate medical setting; and is the least costly of multiple, equally-effective alternative treatments or diagnostic modalities.
Medically Necessary or Medical Necessity:
Health care provided to correct or diminish the adverse effects of a medical condition or mental illness; to assist an individual in attaining or maintaining an optimal level of health; to diagnose a condition; or prevent a medical condition from occurring.
For the purposes of HUSKY B, a child who has been deemed eligible for the HUSKY B program pursuant to Section 17b-290 of the Connecticut General Statutes. For the purposes of this contract, Members of the HUSKY B program are enrollees as defined by Section 17b-290(11) of the Connecticut General Statutes.
National Committee on Quality Assurance (NCQA):
A not-for-profit organization that develops and defines quality and performance measures for managed care, thereby providing an external standard of accountability.
A person who is not a citizen of the United States.
A sixty (60) day period, which ends on the fifteenth (15th) of the last month of the lock-in period, during which time the applicant will be given the opportunity to change plans for any reason.
A provider that has not contracted with the MCO.
Automatic capitation payments generated by the DEPARTMENT or its agent based on enrollment.
Post-Stabilization Services:
Covered services related to an emergency medical condition that are provided after a Member is stabilized in order to maintain the stabilized condition, or under the circumstances described in 42 CFR 422.114(3), to improve or resolve the Member's condition.
Any required payment made by an individual to offset or pay in full the capitation rate under HUSKY B, as defined in Section 17b-290 of the Connecticut General Statutes.
Preventive Care and Services:
| 1) | Child preventive care, including periodic and interperiodic well-child visits, routine immunizations, health screenings and routine laboratory tests; |
| 2) | Prenatal care, including care of all complications of pregnancy; |
| 3) | Dare of newborn infants, including attendance at high-risk deliveries and normal newborn care; |
| 4) | WIC evaluations as applicable |
| 5) | Child abuse assessment required under Sections 17a-106a and 46-b-129a of the Connecticut General Statutes; |
| 6) | Preventive dental care for children; and |
| 7) | Periodicity schedules and reporting based on the standards specified by the American Academy of Pediatrics. |
Primary and Preventive Health Care Services:
The services of licensed health care professionals which are provided on an outpatient basis, including routine well-child visits; diagnosis and treatment of illness and injury; laboratory tests; diagnostic x-rays; prescription drugs; radiation therapy; chemotherapy; hemodialysis; emergency room services; and outpatient alcohol and substance abuse services.
Primary Care Provider (PCP):
A licensed health professional responsible for performing or directly supervising the primary care services of Members.
The process of obtaining prior approval as to the medical necessity or appropriateness of a service or plan of treatment.
The periodic determination of eligibility of the eligible beneficiary for HUSKY B performed by the DEPARTMENT or its agent.
The possibility of monetary loss or gain by the MCO resulting from service costs exceeding or being less than the capitation rates negotiated by the DEPARTMENT.
A symptomatic situation (such as a chronic back condition) for which the Member is seeking care, but for which treatment is neither of an emergency nor an urgent nature.
State Children's Health Insurance Program (SCHIP):
Services provided in accordance with Title XXI of the Social Security Act.
State-Funded HUSKY Plan, Part B or State-Funded HUSKY B:
A program which is funded solely by the State of Connecticut and which provides the same benefits as HUSKY B.
Any written agreement between the MCO and another party to fulfill any requirements of this contract.
A party contracting with the MCO to manage or arrange for one or more of the health care services provided by the MCO pursuant to this contract, but excluding services provided by a vendor.
For purposes of this contract, a state and federally funded program based at the Centers for Children with Special Health Care Needs at Connecticut Children's Medical Center and Yale Center for Children with Special Health Care.
The provisions of Title 42 United States Code Sections 1397aa et seg., providing funds to enable states to initiate and expand the provision of child health assistance to uninsured, low-income children.
Illnesses or injuries of a less serious nature than those constituting emergencies but for which treatment is required to prevent a serious deterioration in the Member's health and cannot be delayed without imposing undue risk on the Member's well-being until the Member is able to secure services from his/her regular physician(s).
Any party with which the MCO has subcontracted to provide administrative services or goods.
Routine physical examinations, immunizations and other preventive services that are not prompted by the presence of any adverse medical symptoms.
The federal Special Supplemental Food Program for Women, Infants and Children administered by the Department of Public Health, as defined in Section 17b-290 of the Connecticut General Statutes.
2. DELEGATIONS OF AUTHORITY
Connecticut's Department of Social Services is the single state agency responsible for administering the HUSKY B program. No delegation by either party in administering this contract shall relieve either party of responsibility for carrying out the terms of the contract.
3. FUNCTIONS AND DUTIES OF THE MCO The MCO agrees to the following duties.
3.01 Provision of Services
| a. | The MCO shall provide to Members enrolled under this contract, directly or through arrangements with others, all the covered services described in Appendix A of this contract. |
| b. | The MCO shall ensure that utilization management/review and coverage decisions concerning acute or chronic care services to each Member are made on an individualized basis in accordance with the contractual definitions for Medical Appropriateness or Medically Appropriate at Part II Section 1, Definitions. The MCO shall also ensure that its contracts with network providers requires that the decisions of network providers affecting the delivery of acute or chronic care services to Members are made in accordance with the contractual definitions for Medical Appropriateness or Medically Appropriate and Medically Necessary and Medical Necessity. |
| c. | The MCO shall require twenty-four (24) hour accessibility to qualified medical personnel to Members in need of urgent or emergency care. The MCO may provide such access to medical personnel through either: 1) a hotline staffed by physicians, physicians on-call or registered nurses; or 2) a PCP on-call system. Whether the MCO utilizes a hotline or PCPs on- call, Members shall gain access to medical personnel within thirty (30) minutes of their call. The MCO Member handbook and MCO taped telephone message shall instruct Members to go directly to an emergency room if the Member needs emergency care. If the Member needs urgent care and has not gained access to medical personnel within thirty (30) minutes, the Member shall be instructed to go to the emergency room. The DEPARTMENT will randomly monitor the availability of such access. |
| d. | Changes to HUSKY B covered services mandated by Federal or State law, or adopted by amendment to the State Plan for SCHIP, subsequent to the signing of this contract will not affect the contract services for the term of this contract, unless (1) agreed to by mutual consent of the DEPARTMENT and the MCO, or (2) unless the change is necessary to continue federal financial participation or due to action of a state or federal court of law. If SCHIP coverage were expanded to include new services, such services would be paid for outside the capitation rate through a |
separate financial arrangement with the MCO, which may include reimbursement to the MCO directly. The DEPARTMENT may opt to reimburse the MCO directly based on claims paid by the MCO. The rate of reimbursement will be negotiated between the DEPARTMENT and the MCO. If SCHIP covered services were changed to exclude services, the DEPARTMENT may determine that such services will no longer be covered under HUSKY B and the DEPARTMENT will propose a contract amendment to reduce the capitation rate accordingly.
In the event that the DEPARTMENT and the MCO are unable to agree on a contract amendment, the DEPARTMENT and the MCO shall negotiate a termination agreement to facilitate the transition of the MCO's Members to another MCO within a period of no less than ninety (90) days.
| a. | The MCO shall comply with all Federal and State laws relating to non-discrimination and equal employment opportunity, including but not necessarily limited to the Americans with Disabilities Act of 1990, 42 U.S.C. Section 12101 et seq.: 47 U.S.C. Section 225; 47 U.S.C. Section 611; Title VII of the Civil Rights Act of 1964, as amended, 42 U.S.C. Section 2000e; Title IX of the Education Amendments of 1972; Title VI of the Civil Rights Act, 42 U.S.C. 2000d et seq.: the Civil Rights Act of 1991; Section 504 of the Rehabilitation Act, 29 U.S.C. Section 794 et seq.: the Age Discrimination in Employment Act of 1975, 29 U.S.C. Sections 621-634; regulations issued pursuant to those Acts; and the provisions of Executive Order 11246 dated September 26, 1965 entitled "Equal Employment Opportunity" as amended by Federal Executive Order 11375, as supplemented in the United States Department of Labor Regulations (41 CFR pt. 60-1 et seq., Obligations of Contractors and Subcontractors). The MCO shall also comply with Sections 4a-60, 4a-61, 17b-520, 31-51d, 46a-64, 46a-71, 46a-75 and 46a-81 of the Connecticut General Statutes. |
The MCO shall also comply with the HCFA Civil Rights Compliance Policy, which mandates that all Members have equal access to the best health care, regardless of race, color, national origin, age, sex, or disability.
The HCFA Civil Rights Compliance Policy further mandates that the MCO shall ensure that its subcontractors and providers render services to Members in a non-discriminatory manner. The MCO shall also ensure that Members are not excluded from participation in or denied the benefits of the HUSKY programs because of prohibited discrimination.
The MCO acknowledges that in order to achieve the civil rights goals set forth in the HCFA Civil Rights Compliance Policy, CMS has committed itself to incorporating civil rights concerns into the culture of its agency and its programs and has asked all of its partners, including the DEPARTMENT and the MCO, to do the same. The MCO further
acknowledges that CMS will be including the following civil rights concerns into its regular program review and audit activities: collecting data on access to and participation of minority and disabled Members; furnishing information to Members, subcontractors, and providers about civil rights compliance; reviewing CMS publications, program regulations, and instructions to assure support for civil rights; and initiating orientation and training programs on civil rights. The MCO shall provide to the DEPARTMENT or to CMS upon request, any data or information regarding these civil rights concerns.
Within the resources available through the capitation rate, the MCO shall allocate financial resources to ensure equal access and prevent discrimination on the basis of race, color, national origin, age, sex, or disability.
| b. | Unless otherwise specified in this contract, the MCO shall provide covered services to HUSKY B Members under this contract in the same manner as those services are provided to other Members of the MCO, although delivery sites, covered services and provider payment levels may vary. The MCO shall ensure that the locations of facilities and practitioners providing health care services to Members are sufficient in terms of geographic convenience to low-income areas, handicapped accessibility and proximity to public transportation routes, where available. The MCO and its providers shall not discriminate among Members of HUSKY B and other Members of the MCO. |
3.03 Gag Rules/Integrity of Professional Advice to Members
The MCO shall comply with the provisions of Connecticut General Statutes Section 38a-478k concerning gag clauses, and with 42 CFR. 457.985, concerning the integrity of professional advice to Members, including interference with providers' advice to Members and information disclosure requirements related to physician incentive plans.
3.04 Coordination and Continuation of Care
| a. | The MCO shall have systems in place to provide well-managed patient care, which satisfies the DEPARTMENT that appropriate patient care is being provided, including at a minimum: |
| 1. | Management and integration of health care through a PCP, gatekeeper or other means. |
| 2. | Systems to assure referrals for medically necessary, specialty, secondary and tertiary care. |
| 3. | Systems to assure provision of care in emergency situations, including an education process to help assure that Members know where and how to obtain medically necessary care in emergency situations. |
| 4. | A system by which Members may obtain a covered service or services that the MCO does not provide or for which the MCO does not arrange because it would violate a religious or moral teaching of the religious institution or organization by which the MCO is owned, controlled, sponsored or affiliated. |
| 5. | Coordination and provision of well-child care services in accordance with the schedules for immunizations and periodicity of well-child care services as established by the DEPARTMENT and recommended by the American Academy of Pediatrics. |
| 6. | Coordinating with and providing a case manager to the HUSKY Pius Physical program, as indicated in Section 3.19 of this contract. |
| 7. | If notified, PCPs shall participate in the review and authorization of Individual Education Plans for Members receiving School Based Child Health services and Individual Family Service Plans for Members receiving services from the Birth to Three program. |
| 8. | The MCO shall coordinate Members' care with the Behavioral Health Partnership, as outlined in this Contract, including but not limited to section 3.16, and Appendix N. |
| a. | The MCO shall provide all emergency services twenty-four (24) hours each day, seven (7) days a week or arrange for the provision of said services twenty-four (24) hours each day, seven (7) days a week through its provider network. |
| b. | Emergency services shall be provided without regard to prior authorization or the emergency care provider's contractual relationship with the MCO. |
| c. | The MCO shall be responsible for payment for emergency department visits, including emergent and urgent visits and all associated charges billed by the facility, regardless of the Member's diagnosis. The Department and MCO will jointly develop audit procedures related to emergency department services when Members are admitted to the hospital and the primary diagnosis is behavioral. The Partnership shall be responsible for payment for the following: |
| 1. | Professional psychiatric services rendered in an emergency department by a community psychiatrist, if the psychiatrist is enrolled in the Medicaid program under either an individual provider or group provider number and bills the emergency facility under that provider number; and |
| 2. | Observation stays of 23 hours or less, billed as Revenue Center Code 762, with a primary behavioral health diagnosis. |
d. The MCO shall not limit the number of emergency visits.
| e. | The MCO shall cover emergency care services furnished to a Member by a provider whether or not the provider is a part of the Member's MCO provider network at the time of the service. |
| f. | The MCO shall cover emergency care services provided while the Member is out of the State of Connecticut, including emergency care incurred while outside the country. |
| g. | The MCO shall cover all services necessary to determine whether or not an emergency condition exists, even if it is later determined that the condition was not an emergency. |
| h. | The MCO may not retroactively deny a claim for an emergency screening examination because the condition, which appeared to be an emergency medical condition under the prudent layperson standard, turned out to be non-emergent in nature. |
| i. | The determination of whether the prudent layperson standard is met must be made on a case-by-case basis. The only exception to this general rule is that the MCO may approve coverage on the basis of an ICD-9 code. |
| j. | If the screening examination leads to a clinical determination by the examining physician that an actual emergency does not exist, then the nature and extent of payment liability will be based on whether the Member had acute symptoms under the prudent layperson standard at the time of presentation. |
| k. | Once the Member's condition is stabilized, the MCO may require authorization for a hospital admission or follow-up care. |
| I. | The MCO must cover post-stabilization services attendant to the primary presenting diagnosis that were either approved by the MCO or were delivered by the emergency service provider when the MCO failed to respond to a request for pre-approval of such services within one hour of the request to approve post-stabilization care, or could not be contacted for pre-approval. |
| m. | If there is a disagreement between a hospital and an MCO concerning whether the patient is stable enough for discharge or transfer from the emergency room, the judgment of the attending physician(s) actually caring for the Member at the treating facility prevails and is binding on the MCO. This subsection shall not apply to a disagreement concerning discharge or transfer following an inpatient admission. The MCO may establish arrangements with hospitals whereby the MCO may send one of its own physicians or may contract with appropriate physicians with appropriate emergency room privileges to assume the attending physician's responsibilities to stabilize, treat, and transfer the patient. |
| n. | When a Member's PCP or other plan representative instructs the Member to seek emergency care in-network or out-of-network, the MCO is responsible for payment for the screening examination and for other |
medically necessary emergency services, without regard to whether the patient meets the prudent layperson standard described above.
| o. | If a Member believes that a claim for emergency services has been inappropriately denied by the MCO, the Member may seek recourse through the MCO's internal appeal process and the Department of Insurance's (DOI) external review process pursuant to Section 8, MCO Responsibilities Concerning Notices of Action, Appeals and Administrative Hearings of this contract. |
| p. | When the MCO reimburses emergency services provided by an in-network provider, the rate of reimbursement will be subject to the contractual relationship that has been negotiated with said provider. When the MCO reimburses emergency services provided by an out-of-network provider within Connecticut, the rate of reimbursement will be the fees established by the DEPARTMENT for the Medicaid fee-for-service program. When the MCO reimburses emergency services provided by an out-of-network provider outside of Connecticut, the MCO may negotiate a rate of reimbursement with said provider. |
| q. | The MCO shall retain responsibility for payment for emergency medical transportation and associated charges, regardless of diagnosis. The MCO shall also retain responsibility for hospital-to-hospital ambulance transportation of members with a behavioral health condition. |
| r. | Effective January 1, 2007, when the MCO reimburses emergency services provided by an out-of-network provider whether within or outside Connecticut, the rate of reimbursement shall be limited to the fees established by the DEPARTMENT for the Medicaid fee-for-service program. |
| a. | The MCO shall serve Members statewide. The MCO shall ensure that its provider network includes access for each Member to PCPs, Obstetric/Gynecological Providers and mental-health-providers at a distance of no more than fifteen (15) miles for PCPs and Obstetric/Gynecological Providers and no more than twenty (20) miles for general dentists and mental health providers as measured by the Public Utility Commission. The MCO shall ensure that its provider network has the capacity to deliver or arrange for all the goods and services reimbursable under this contract. |
| b. | On a monthly basis, the MCO will provide the DEPARTMENT or its agent with a list of all contracted network providers. The list shall be in a format and contain such information as the DEPARTMENT may specify. |
Performance Measure: Geographic Access. The DEPARTMENT will randomly monitor geographic access by reviewing the mileage to the nearest town containing a PCP for every town in which the MCO has Members.
3.07 Choice of Health Professional
The MCO must inform each Member about the full panel of participating providers in their network. To the extent possible and appropriate, the MCO must offer each Member covered under this contract the opportunity to choose among participating providers.
| a. | The MCO shall maintain a provider network capable of delivering or arranging for the delivery of all covered benefits to all Members. In addition, the MCO's provider network shall have the capacity to deliver or arrange for the delivery of all covered benefits reimbursable under this contract regardless of whether all the covered benefits are provided through direct provider contracts. The MCO shall submit a file of its most current provider network listing to the DEPARTMENT or its agent. The file shall be submitted, at a minimum, once a month in the format specified by the DEPARTMENT. |
| b. | The MCO shall notify the DEPARTMENT or its agent, in a timely manner, of any changes made in the MCO's provider network. The monthly file submitted to the DEPARTMENT or its agent should not contain any providers who are no longer in the MCO's network. The DEPARTMENT will randomly audit the provider network file for accuracy and completeness and take corrective action with the MCO if the provider network file fails to meet these requirements. |
3.09 Network Adequacy and Maximum Enrollment Levels
Primary Care Providers and Dentists
| a. | On a quarterly basis, except as otherwise specified the DEPARTMENT, the DEPARTMENT shall evaluate the adequacy of the MCO's provider network. Such evaluations shall use ratios of Members to specific types of providers based on fee-for-service experience in order to ensure that access in the MCO is at least equal to access experienced in the fee-for-service Medicaid program for a similar population. For each county the maximum ratio of Members to each provider type shall be: |
| 1. | Adult PCPs, including general practice specialists counted at 60.8%, internal medicine specialists counted at 88.9%, family practice specialists counted at 66.9%, nurse practitioners of the appropriate specialties, and physician assistants, 387 Members per provider; |
| 2. | Children's PCPs, including pediatric specialists counted at 100%, general practice specialists counted at 39.2%, internal medicine specialists counted at 11.1%, family practice specialists counted at 33.1%, nurse practitioners of the appropriate specialties, and physician assistants, 301 Members per provider; |
| 3. | Women's PCPs, including obstetrics and gynecology specialists, nurse midwives, and nurse practitioners of the appropriate specialty, 835 Members per provider; |
| 4. | Dental providers, including general and pediatric dentists counted at 100%, and dental hygienists counted at 50%, 486 Members per provider; and |
| b. | Based on the adequacy of the MCO's provider network, the DEPARTMENT may establish a maximum HUSKY (HUSKY A and B) enrollment level for all HUSKY Members for the MCO on a county-specific basis. The DEPARTMENT shall provide the MCO with written notification no less than thirty (30) days prior to the effective date of the maximum enrollment level. |
| c. | Subsequent to the establishment of this limit, if the MCO wishes to change its maximum enrollment level in a specific county, the MCO must notify the DEPARTMENT thirty (30) days prior to the desired effective date of the change. If the change is an increase, the MCO must demonstrate an increase in their provider network which would allow the MCO to serve additional HUSKY (combined A and B) Members. To do so the MCO must provide the DEPARTMENT with the signature pages from the executed provider contracts and/or signed letters of intent. The DEPARTMENT will not accept any other proof or documentation as evidence of a provider's participation in the MCO's provider network. The DEPARTMENT shall review the existence of additional capacity for confirmation no later than thirty (30) days following notice by the MCO. An increase will be effective the first of the month after the DEPARTMENT confirms additional capacity exists. |
| d. | In the event the DEPARTMENT deems that the MCO's provider network is not capable of accepting additional enrollments, the DEPARTMENT may exercise its rights under Section 9 of this contract, including but not limited to the rights under Section 9.04, Suspensions of New Enrollments. |
| e. | In addition to the network adequacy measures described in subsections (a) through (d) above, the DEPARTMENT shall measure access to specialists by examining and reviewing confirmed complaints received by the MCO, the Enrollment Broker, the DEPARTMENT and HUSKY Infoline and taking other steps as more fully described below: |
| 1. | For purposes of this section, a "complaint" shall be defined as dissatisfaction expressed by a Member, or their authorized representative, with the Member's ability to obtain an appointment with a specialist that will accommodate the member's medical needs within a reasonable timeframe or within a reasonable distance. |
| a) | Member requests for information or referrals to specialists within the MCO's network shall not constitute a complaint. |
| b) | The DEPARTMENT will count more than one complaint to different entities about a Member's inability to access a particular specialist, within the same timeframe, as one complaint. |
| c) | The DEPARTMENT will count as separate complaints when a Member complains about being unable to make appointments with more than one specialist. |
| 2. | The DEPARTMENT will refer to the MCO all complaints for resolution. |
| 3. | The DEPARTMENT will send the MCO a "Complaint Report" when it receives a certain number of confirmed access complaints from HUSKY A and HUSKY B members during a quarter regarding a particular specialty. |
| a) | The number of confirmed complaints that will initiate the DEPARTMENT'S sending a "Complaint Report" will be based on the MCOs HUSKY A membership factored by the ratio of one complaint per 10,000 members. |
| b) | For purposes of this section, a "confirmed complaint" means that the DEPARTMENT or another entity has received a complaint and the DEPARTMENT has confirmed that the MCO has not provided a specialist or dentist within a reasonable timeframe or within a reasonable distance from the Member's home, or both. |
| c) | In determining whether a complaint will be confirmed, the DEPARTMENT will consider a number of factors, including but not limited to: |
| 1) | The Member's PCP or other referring provider's medical opinion regarding how soon the Member should be seen by the specialist; |
| 2) | The severity of the Member's condition; |
| 3) | Nationally recognized standards of access, if any, with respect to the particular specialty; |
| 4) | Whether the access problem is related to a broader access or provider availability problem that is not within the MCO's control; |
| 5) | The MCO's diligence in attempting to address the Member's complaint; |
| 6) Whether both the Member and the MCO have reasonably attempted to obtain an appointment that will meet his or her medical needs. |
| 1. | In the event the DEPARTMENT deems that the MCO's provider network is not capable of accepting additional enrollments and lacks adequate access to providers as described in (a) through (d) above, the DEPARTMENT may exercise its rights under Section 7 of this contract, including but not limited to the rights under Section 7.04, Suspension of New Enrollments. |
| 2. | In the event the DEPARTMENT determines that it has received sufficient confirmed complaints regarding specialist access problems to initiate a statewide default enrollment freeze, The DEPARTMENT shall advise the MCO in the Complaint Report that it has received confirmed complaints and that it will impose a default enrollment freeze on the MCO in 30 days unless the MCO submits a satisfactory resolution of the access issue in a corrective action plan. |
| a) | The MCO, at its request, will have an opportunity to meet with the DEPARTMENT prior to the imposition of the default enrollment freeze; |
| b) | The DEPARTMENT will impose a default enrollment freeze statewide, for a minimum of three months. The default enrollment freeze will remain in effect until the DEPARTMENT determines that the access problem has been resolved to the DEPARTMENT'S satisfaction. |
| 3. | The MCO shall submit a corrective action plan to the DEPARTMENT when the DEPARTMENT formally notifies the MCO that the number of confirmed specialist complaints has passed the report threshold for that MCO during the reporting period. |
| 4. | If, subsequent to the DEPARTMENT'S approval of the corrective action plan, the network deficiency is not remedied within the time specified in the corrective action plan, or if the MCO does not develop a corrective action plan satisfactory to the DEPARTMENT, the DEPARTMENT may impose a strike towards a Class A sanction for each month the MCO fails to correct the deficiency, in accordance with Section 7.05. This sanction shall be in addition to any enrollment freeze imposed in accordance with (2) above. |
All provider contracts in the MCO'S provider network shall, at a minimum, include each of the following provisions:
| a. | MCO network providers serving HUSKY Members must meet the minimum requirements for participation in the HUSKY program stated in the Regulations of Connecticut State Agencies, Section 17b-262-522 - 17b-262-533, as applicable. |
| b. | MCO Members shall be held harmless, excluding appropriate cost-sharing for the costs of all HUSKY covered goods and services provided; |
| c. | Providers must provide evidence of and maintain adequate malpractice insurance. For physicians, the minimum malpractice coverage requirements are $1 million per individual episode and $3 million in the aggregate; |
| d. | Specific terms regarding provider reimbursement as specified in Timely Payment of Claims, Section 3.43 of this contract. |
| e. | Specific terms concerning each party's rights to terminate the contract; |
| f. | That any risk shifted to individual providers does not jeopardize access to care or appropriate service delivery; |
| g. | The exclusion of any provider that has been suspended from Medicare or a Medicaid program in any state; and |
| h. | For PCPs, the provision of "on-call" coverage through arrangements with other PCPs. |
3.11 Provider Credentialing and Enrollment
| a. | The MCO shall establish minimum credentialing criteria and shall formally re-credential all professional participating providers in their network at least once every two (2) years or such other time period as established by the NCQA. The MCO shall create and maintain a credentialing file for each participating provider that contains evidence that all credentialing requirements have been met. The file shall include copies of all relevant documentation including licenses, Drug Enforcement Agency (DEA) certificates and provider statements regarding lack of impairment. Credentialing files shall be subject to inspection by the DEPARTMENT or its agent. |
| b. | The MCO's credentialing and re-credentialing criteria for professional providers shall include at a minimum: |
| 1. | Appropriate license or certification as required by Connecticut law; |
| 2. | Verification that providers have not been suspended or terminated from participation in Medicare or the Medicaid program in any state; |
| 3. | Verification that providers of covered services meet minimum requirements for Medicaid participation; |
| 4. | Evidence of malpractice or liability insurance, as appropriate; |
| 5. | Board certification or eligibility, as appropriate; |
6. A current statement from the provider addressing:
| a) | Lack of impairment due to chemical dependency/drug abuse; |
| b) | Physical and mental health status; |
| c) | History of past or pending professional disciplinary actions, sanctions, or license limitations; |
| d) | Revocation and suspension of hospital privileges; and |
| e) | A history of malpractice claims. |
| 7. | Evidence of compliance with Clinical Laboratory Improvement Amendments of 1988 (CLIA), Public Law 100-578, 42 USC Section 1395aa et seg. and 42 CFR pt. 493 (as amended, 68 Fed. Reg. 3639-3714(2003)). |
| c. | The MCO may require more stringent credentialing criteria. Any other criteria shall be in addition to the minimum criteria set forth above. |
| d. | Additional MCO credentialing/recredentialing criteria for PCPs shall include, but not be limited to: |
| 1. | Adherence to the principles of Ethics of the American Medical Association, the American Osteopathic Association or other appropriate professional organization; |
| 2. | Ability to perform or directly supervise the ambulatory primary care services of Members; |
| 3. | Membership on the medical staff with admitting privileges to at least one accredited general hospital or an acceptable arrangement with a PCP with admitting privileges; |
4. | Continuing medical education credits; |
| 5. | A valid DEA certification; and |
| 6. | Assurances that any Advanced Practice Registered Nurse (APRN), Nurse Midwives or Physician Assistants are performing within the scope of their licensure. |
| e. | For purposes of credentialing and recredentialing, the MCO shall perform a check on all PCPs and other participating providers by contacting the National Practitioner Data Bank (NPDB). The DEPARTMENT will notify the MCO immediately if a provider under contract with the MCO is subsequently terminated or suspended from participation in the Medicare or Medicaid programs. Upon such notification from the DEPARTMENT or any other appropriate source, the MCO shall immediately act to terminate the provider from participation. |
| f. | The MCO may delegate credentialing functions to a subcontractor. The MCO is ultimately responsible and accountable to the DEPARTMENT for compliance with the credentialing requirements. The MCO shall demonstrate and document to the DEPARTMENT the MCO's significant |
oversight of its subcontractors performing any and all provider credentialing, including facility or delegated credentialing. The MCO and any such entity shall be required to cooperate in the performance of financial, quality or other audits conducted by the DEPARTMENT or its agent(s). Any subcontracted entity shall maintain a credentialing file for each participating provider, as set forth above.
| g. | The MCO must adhere to the additional credentialing requirements set forth in Appendix D. |
3.12 Specialist Providers and the Referral Process
| a. | The MCO shall contract with a sufficient number and mix of specialists so that the Member population's anticipated specialty care needs can be substantially met within the MCO's network of providers. The MCO will also be required to have a system to refer Members to out-of-network specialists if appropriate participating specialists are not available. The MCO shall make specialist referrals available to its Members when it is medically necessary and medically appropriate and shall assume all financial responsibility for any such referrals whether they are in-network or out-of-network. The MCO must have policies and written procedures for the coordination of care and the arrangement, tracking and documentation of all referrals to specialty providers. |
| b. | For Members enrolled in HUSKY Plus Physical, the MCO is required to coordinate the specialty care services and specialty provider referral process with the HUSKY Plus Physical programs to ensure access to care. Refer to Section 3.19 for specific guidance on the referral process. |
3.13 PCP and Specialist Selection, Scheduling and Capacity
| a. | The MCO shall provide Members with the opportunity to select a PCP within thirty (30) days of enrollment. The MCO shall assign a Member to a PCP when a Member fails to choose a PCP within thirty (30) days after being requested to do so. The assignment must be appropriate to the Member's age, gender, and residence. |
| b. | The MCO shall ensure that the PCPs in its network adhere to the following PCP scheduling practices: |
| 1. | Emergency cases shall be seen immediately or referred to an emergency facility; |
| 2. | Urgent cases shall be seen within forty-eight (48) hours of PCP notification; |
| 3. | Routine cases shall be seen within ten (10) days of PCP notification; |
| 4. | Well-care visits shall be scheduled within six (6) weeks of PCP notification; |
| 5. | All well-child visits, comprehensive health screens and immunizations shall be scheduled in accordance with the American Academy of Pediatrics' (AAP) periodicity schedule and the Advisory Committee on Immunization Practices (ACIP) immunization schedules; and |
| 6. | Waiting times at PCP sites are kept to a minimum. |
| c. | The MCO shall report quarterly on each PCP's panel size, group practice and hospital affiliations in a format specified by the DEPARTMENT. The DEPARTMENT will aggregate reports received from all MCOs for both HUSKY A and HUSKY B. In the event that the DEPARTMENT finds a PCP with more than 1,200 HUSKY (combined HUSKY A and HUSKY B) panel Members, the DEPARTMENT will notify the MCO if the PCP is part of the MCO's network. The DEPARTMENT expects that the MCO will take appropriate action to ensure that patient access to the MCO is assured. |
| d. | The MCO shall maintain a record of each Member's PCP assignments for a period of two (2) years. |
| e. | The MCO shall educate each Member on the benefits of a usual source of care. |
| f. | If the Member has not received any primary care services, the MCO shall contact the Member to encourage regular well-care visits. |
Performance Measure: PCP Appointment Availability. The DEPARTMENT or its agent will routinely monitor appointment availability as measured by b(1) through b(5) by using test cases to arrange appointments of various kinds with selected PCPs.
3.14 Family Planning Access and Confidentiality
| a. | The MCO shall notify and give each Member, including adolescents, the opportunity to use family planning services without requiring a referral or authorization. The MCO shall make a reasonable effort to subcontract with all local family planning clinics and providers, including those funded by Title X of the Public Health Services Act. |
| b. | The MCO shall keep family planning information and records for each individual patient confidential, even if the patient is a minor. |
| c. | Pursuant to federal law, 42 U.S.C. Section 1397ee(c)(1) and (7), 42 CFR 457.475 and the State of Connecticut's State Child Health Plan under Title XXI of the Social Security Act, ("the HUSKY Plan"), the DEPARTMENT may seek federal funding for abortions only if the pregnancy is the result of an act of rape or incest or necessary to save the life of the mother. The MCO shall cover all abortions that fall within these circumstances. |
| d. | The DEPARTMENT and the MCO shall enter into a separate contract for abortions that do not qualify for federal matching funds. |
The MCO shall not charge co-payments for any abortion.
Sanction: If the MCO fails to comply with the provisions in (c), and fails to accurately maintain and submit accurate records of those abortions which meet the federal definition for funding, the DEPARTMENT may impose a Class A sanction, pursuant to Section 9.05.
| a. | The MCO shall be responsible for payment for pharmacy services and all associated charges, regardless of a Member's diagnosis. The only exception is that the Partnership shall be responsible for methadone costs that are part of the bundled reimbursement for methadone maintenance and ambulatory detox providers. Prescribing behavioral health providers participating in the Partnership will follow the applicable pharmacy program requirements, including the formulary, of the MCO. These providers will provide the MCO with any clinical information needed to support requests for authorization or the preparation of summaries for administrative hearings. The MCO shall promptly inform the Department of any changes to its pharmacy program requirements. |
| b. | Pharmacies must be available and accessible on a statewide basis. The MCO shall: |
| 1. | Maintain a comprehensive provider network of pharmacies that will within available resources assure twenty-four (24) hour access to a full range of pharmaceutical goods and services; |
| 2. | Have established protocols to respond to urgent requests for medications; |
| 3. | Monitor and take steps to correct excessive utilization of regulated substances; |
| 4. | Have established protocols in place to assure the timely provision of pharmacy goods and to determine client eligibility and MCO affiliation services (by contacting the DEPARTMENT or its agent via telephone or fax) when there is a discrepancy between the information in the MCO's eligibility system and information given to the pharmacists by the Member, the Member's physician or other third party; and |
| 5. | Monitor quality assurance measures to assure that Member abuse of pharmacy benefits is corrected in a timely fashion. |
| b. | The MCO shall require that its provider network of pharmacies offers medically necessary goods and services to the MCO's Members. The |
MCO may have a drug management program that includes a prescription drug formulary. If the MCO has a drug formulary, the MCO shall have a prior authorization process to permit access at a minimum to all medically necessary and appropriate drugs covered for the Medicaid fee-for-service population. The MCO drug formulary must include only Food and Drug Administration approved drug products and be sufficiently broad enough in scope to meet the needs of the MCO's Members. The MCO drug formulary shall consist of a reasonable selection of drugs which do not require prior approval for each specific therapeutic drug class.
| c. | The MCO shall submit a copy of its formulary to the DEPARTMENT no later than thirty (30) days after the effective date of this contract. The MCO shall submit any subsequent deletions to the formulary to the DEPARTMENT thirty (30) days prior to making any change. The MCO shall also submit subsequent additions to the formulary immediately without seeking prior approval by the DEPARTMENT. The DEPARTMENT reserves the right to identify deficiencies in the content or operation of the formulary. In this instance, the MCO shall have thirty (30) days to address in writing the identified deficiencies to the DEPARTMENT'S satisfaction. The MCO may request to meet with the DEPARTMENT prior to the submission of the written response. |
| d. | The MCO shall ensure that Members using maintenance drugs (drugs usually prescribed to treat long-term or chronic conditions including, but not limited to, diabetes, arthritis and high blood pressure) are informed in advance, but no less than thirty (30) days in advance of any changes to the prescription drug formulary related to such maintenance drugs if the Member using the drug will not be able to continue using the drug without a new authorization. |
| e. | The MCO shall require that its provider network of pharmacies adheres to the provisions of Connecticut General Statutes Section 20-619 (b) and (c) related to generic substitutions. |
3.16 Mental Health and Substance Abuse Access
| a. | Except as otherwise identified in this section and this Contract, mental health and substance abuse services, for HUSKY A Members will be managed by the Connecticut Behavioral Health Partnership (CT-BHP) and paid for by the Department. The MCO shall coordinate services covered under this contract with the behavioral health services managed by the Partnership as outlined in Appendix X. |
| b. | The MCO may track utilization, including, but not limited to, primary care behavioral health, laboratory, behavioral health pharmacy, and transportation. The MCO shall bring any increases in the utilization trend for any of these services to the attention of the Department. |
| c. | If there is a conflict between the MCO and the BHP as to whether a Member's medical or behavioral health condition is primary, the MCO's |
medical director shall work with the BHP's medical director to reach a timely and mutually agreeable resolution. If the MCO and BMP are not able to reach a resolution, the Department will make a determination and the Department's determination shall be binding. Issues related to whether a Member's medical or behavioral health condition is primary must not delay timely medical necessity determinations. In these circumstances, the MCO must render a determination within the standard timeframe required under this contract or its policies and procedures.
| 1. | The MCO shall retain responsibility for all ancillary services such as laboratory, radiology, and medical equipment, devices and supplies regardless of diagnosis. |
| 2. | The MCO is not responsible for ancillary services that are part of the Department's all-inclusive rate for inpatient behavioral health services. |
e. | Co-Occuring Medical and Behavioral Health Conditions |
The MCO shall continue programs and procedures designed to support the identification of untreated behavioral health disorders in medical patients at risk for such disorders. The MCO shall:
| 1. | Contact the BMP ASO when co-management of a Member's care by the MCO and the BMP ASO is indicated, such as for persons with special physical health and behavioral health needs; |
| 2. | Respond to inquiries by the BMP ASO regarding the presence of medical co- morbidities; and |
| 3. | Coordinate with the BMP ASO, upon request. |
| 4. | Assign a key contact person in order to facilitate timely coordination with the ASO; and |
| 5. | Participate in medical/behavioral co-management meetings at least once a month, with the specific frequency to be determined by agreement between the MCO and the ASO. |
f. Freestanding Primary Care Clinics
The MCO shall be responsible for primary care and other services providing by primary care and medical clinics not affiliated with a hospital, regardless of diagnosis. The only exception is that the MCO shall not be responsible for behavioral health evaluation and treatment services billed un CPT codes 90801-90806, 90853, 90846, 90847 and 90862, when the Member has a primary behavioral health diagnosis and the services are provided by a licensed behavioral health professional.
| 1. | The MCO shall be responsible for management and payment of claims when home health services are required for the treatment of medical diagnoses alone and when home health services are required to treat both medical and behavioral diagnoses, but the medical diagnosis is primary. |
| 2. | The MCO shall also be responsible for authorization and payment of the medical component of claims if a Member has both medical and behavioral diagnoses, and the Member's medical treatment needs cannot be safely and effectively managed by the psychiatric nurse or aide. |
| 3. | the MCO shall manage and pay claims for home health physical therapy, occupational therapy, and speech therapy, regardless of diagnosis to the extent such services are otherwise covered under this contract. |
| 4. | The MCO shall be responsible for the management and payment of claims for home health services for Members with mental retardation when the Member does not also have a diagnosis of autism. |
h. | Hospital Inpatient Services. |
| 1. | The MCO will share responsibility for inpatient general hospital services with the BHP. |
| 2. | The MCO shall be responsible for management and payment of claims for inpatient general hospital services when the medical diagnosis is primary. The medical diagnosis is primary if both the Revenue Center Code and primary diagnosis are both medical. |
| 3. | The MCO shall also be responsible for professional services and other charges associated with primary medical diagnoses during a behavioral stay. |
| 4. | The MCO shall also be responsible for ancillary services associated with non-primary behavioral health diagnoses during a medical stay, as described in subsection a. of this section. |
| 5. | The MCO shall not be responsible for ancillary services that are included in the hospital's per diem inpatient behavioral health rate. |
| i. | Hospital Outpatient Clinic Services The MCO shall be responsible for all primary care and other medical services provided by hospital outpatient clinics, regardless of diagnosis, including all medical specialty services and all ancillary services. |
| j. | Long Term Care The MCO shall be responsible for all long term care services such as nursing homes and chronic disease hospitals, regardless of a Member's diagnosis. |
k. Primary Care Behavioral Health Services
| 1. | The MCO shall be responsible for all primary care services and all associated charges, regardless of diagnosis. Such responsibilities include: |
| a) | Behavioral health related prevention and anticipatory guidance; |
| b) | Screening for behavioral health disorders; |
| c) | Treatment of behavioral health disorders that the primary care physician concludes can be safely and appropriately treated in a primary care setting; |
| d) | Management of psychotropic medications, when the PCP determines it is safe and appropriate to do so, and in conjunction with treatment by a BMP non-medical behavioral health specialist when necessary; and |
| e) | Referral to a behavioral health specialist when the PCP concludes it is safe and appropriate to do so. |
| 2. | The BMP ASO will develop education and guidance for primary care physicians related to the provision of behavioral health services in primary care settings. The MCOs may participate with the ASO in the development of education and guidance or they will be provided the opportunity for review and comment. The education and guidance will address PCP prescribing with support and guidance from the ASO or referring clinic. The BMP ASO will make telephonic psychiatric consultation services available to primary care providers. Consultation may be initiated by any primary care provider that is seeking guidance on psychotropic prescribing for a HUSKY A or HUSKY B member. |
| 3. | The BHP ASO will work with the MCO and provider organizations to sponsor opportunities for joint training to promote effective coordination and collaboration. MCO policies and provider contracts must support the provision of behavioral health services by primary care providers and entry into coordination agreements with Enhanced Care Clinics established by the Department. |
I. School Based Health Center Services
The HUSKY MCOs will be responsible for primary care services provided by school-based health centers, regardless of diagnosis, but they will not be responsible for behavioral health assessment and treatment services billed under CPT codes 90801 - 90807, 90853, 90846 and 90847.
3.17 Children's Issues and Preventive Care and Services
The MCO shall ensure access to preventive care and services of the HUSKY B benefit package as follows:
| a. | The MCO shall provide preventive care and services consisting of the services described in this section and in accordance with the standards and schedules specified in Appendixes A and E. Any changes in the standards and schedule subsequent to the effective date of this contract shall be provided to the MCO sixty (60) days before the effective date of the change. The MCO shall not require prior authorization of preventive care and services. Preventive care and services consist of the following: |
1. Child preventive care consisting of:
| a). | Periodic well-child visits based on the schedule for such visits recommended by the American Academy of Pediatrics (AAP), see Appendix E, American Academy of Pediatrics Recommendations for Preventative Periodic Health Care; |
| b). | Office visits related to periodic well-child visits; |
| c). | Routine childhood immunizations based on the recommendations of the Advisory Committee on Immunization Practices (ACIP), see Appendix A; |
| d). | Health screenings; and |
| e). | Routine laboratory tests. |
| 2. | Prenatal Care, including care of all complications of pregnancy; |
| 3. | All healthy newborn inpatient physician visits, including routine inpatient and outpatient screenings and attendance at high-risk deliveries; |
| 4. | WIC evaluations, as applicable; |
| 5. | Child abuse assessments required under Sections 17a-106a and 46b-129a of the Connecticut General Statutes; |
| 6. | Preventive dental care based on the recommendations of the American Academy of Pediatric Dentistry (AAPD) and consisting of: |
a). Oral exams and prophylaxis;
b). Fluoride treatments;
c). Sealants, and
d). X-rays
| b. | The MCO shall provide office visits related to periodic well-child visits when medically necessary to determine the existence of a physical or mental illness or condition. The MCO shall not require prior authorization of such visits: |
| c. | The MCO shall provide periodic well-child visits that at a minimum, include: |
| 1. | A comprehensive health and developmental history (including assessment of both physical and mental health development and assessment of nutritional status); |
| 2. | A comprehensive unclothed or partially draped physical exam; |
| 3. | Appropriate immunizations as set forth in the ACIP recommendations and schedule at Appendix A; |
| 4. | Laboratory tests, as set forth in the AAP recommendations and schedule at Appendix E; |
| 5. | Vision and hearing screenings as set forth in the AAP schedule at Appendix E; |
| 6. | Dental assessments as set forth in the AAP recommendations and schedule at Appendix E; and |
| 7. | Health education, including anticipatory guidance. |
| d. | No later than sixty (60) days after enrollment in the plan and annually thereafter, the MCO shall use a combination of oral and written methods including methods for communicating with Members with limited English proficiency, Members who cannot read, and Members who are visually or hearing impaired, to: |
| 1. | Inform its Members about the availability of preventive care and services; |
| 2. | Inform its Members about the importance and benefits of preventive care and services; |
| 3. | Inform its Members about how to obtain preventive care and services; and |
| 4. | Inform its Members that assistance with scheduling appointments is available, and inform them how to obtain this assistance. |
The MCO shall require PCPs to obtain all available vaccines free of charge from the Department of Public Health under the state-funded Vaccines for Children program
3.18 Well-Care Services for Adolescents
On or before February 1, 2004, the MCO shall submit an action plan to improve the delivery of well-child care to adolescents. This plan shall include measures to increase the volume of well-child screenings provided to adolescent members and to improve the quality and the completeness of those screenings according to the guidelines provided by the American Academy of Pediatrics. Emphasis should be placed on improving health risk assessment and anticipatory guidance during these visits. Following the submission of these plans, the MCOs will meet with the department and representatives of other state agencies to develop a best practice model for the delivery of adolescent health care.
3.19 HUSKY PLUS: Physical
| 1. | HUSKY Plus Physical is a supplemental health insurance program that provides services to children whose intensive physical health care needs cannot be accommodated within the benefit package offered under HUSKY B. |
| 2. | HUSKY Plus Physical is administered by the Centers for Children with Special Health Care Needs at Connecticut Children's Medical Center. |
| 3. | HUSKY Plus Physical is available for children with intensive physical health care needs who are enrolled in HUSKY B and fall within income bands 1 and 2. HUSKY B Members who fall into income band 3 are excluded from the HUSKY Plus Physical program. |
| 4. | The MCO shall have final decision-making authority for those services for which they are at financial risk. The HUSKY Plus Physical program shall have final decision-making authority for those supplemental services for which they are at financial risk. The HUSKY Plus Physical program shall be the documented payor of last resort. |
| 5. | Any dispute between the participating MCO and the HUSKY Plus Physical program concerning the responsibility for reimbursement of a service authorized under the treatment plan shall be referred to the DEPARTMENT for resolution. |
| b. | MCO's Responsibility to Maximize HUSKY Plus Physical Services |
The MCO shall coordinate care with HUSKY Plus Physical so as to maximize the Member's coverage of special health needs. Such coordination shall include, but not be limited to, a monthly conference, either in person or by telephone or other interactive means, between the MCO case manager, the HUSKY Plus Physical case manager, and the Member or his/her representative.
c. HUSKY B MCO Case Management Responsibilities
| 1. | The HUSKY Plus Physical case management team will develop a global plan of care when a Member is receiving HUSKY Plus Physical services. A case manager with appropriate qualifications, credentials and decision-making authority shall be assigned by the MCO to the HUSKY Plus Physical case management team. |
| 2. | The global plan of care shall be based on the comprehensive diagnostic needs assessment, periodic reassessments, and treatment plans from the MCO and HUSKY Plus Physical programs providing services to the Member. |
| 3. | The global plan of care shall integrate HUSKY B services as set forth in Appendix A and HUSKY Plus services as set forth in Appendices B. The MCO shall be responsible for managing the utilization of HUSKY B services contained in the global plan of care. |
| 4. | The MCO case manager shall actively participate with the HUSKY Plus Physical case management team to ensure that all medically necessary HUSKY Plus Physical program services identified in the global plan of care, which are also covered in the HUSKY B benefit package, are exhausted first under HUSKY B. |
The MCO shall assign a liaison who will coordinate all communication related to disenrollment to the HUSKY Plus Physical programs.
| 1. | The MCO shall provide summary data reports to the DEPARTMENT or its agent in an agreed upon format on the utilization of physical health services for HUSKY Plus Physical Members on an as needed basis, but no more frequently. |
| 2. | The MCO shall designate a representative to the HUSKY Plus Physical Quality Assurance Subcommittees. |
Sanction: If the MCO fails to have a procedure to identify potential HUSKY Plus Physical Members or fails to assign a case manager to the HUSKY Plus Physical program, the DEPARTMENT may impose a strike towards a Class A sanction pursuant to Section 9.05.
| a. | In order to promote healthy birth outcomes, the MCO or its contracted providers shall: |
| 1. | Identify enrolled pregnant women as early as possible in the pregnancy; |
| 2. | Conduct prenatal risk assessments in order to identify high-risk pregnant women, arrange for specialized prenatal care and support services tailored to risk status, and begin care coordination that will continue throughout the pregnancy and early weeks postpartum; |
| 3. | Refer enrolled pregnant women to the WIC program, as applicable; |
| 4. | Offer case management services with obtaining prenatal care appointments, WIC services, as applicable, and other support services as necessary; |
| 5. | Offer prenatal health education materials and/or programs aimed at promoting health birth outcomes; |
| 6. | Offer HIV testing and counseling and all appropriate prophylaxis and treatment to all enrolled pregnant women; |
| 7. | Refer any pregnant Member who is actively abusing drugs or alcohol to the CT BMP ASO; and |
| 8. | Educate new mothers about the importance of the postpartum visit and well-baby care. |
Performance Measure: Early access to prenatal care: Percentage of enrolled women who had a live birth, who were continuously enrolled in the MCO for 280 days prior to delivery who had a prenatal visit on or between 176 to 280 days prior to delivery.
Performance Measure: Adequacy of prenatal care: Percentage of women with live births who were continuously enrolled during pregnancy who had more than eighty (80) percent of the prenatal visits recommended by the American College of Obstetrics and Gynecology, adjusted for gestational age at enrollment and delivery.
| a. | The MCO shall contract with a sufficient number of dentists throughout the state to assure access to oral health care. The MCO shall: |
| 1. | Maintain an adequate dental provider network throughout the state's eight (8) counties; |
| 2. | For the purpose of enrollment capacity a dental hygienist meeting the criteria of Connecticut General Statutes Section 20-1261 with two (2) years experience, working in an institution (other than hospital), a community health center, a group home or a school setting shall be counted as fifty (50) percent of a general dentist. If the MCO's provider network includes dental hygienists acting independently within their scope of practice to provide preventive services to Members, the MCO shall require that dental hygienists make appropriate referrals to in-network dentists for appropriate restorative and diagnostic services and treatment; |
| 3. | Implement a plan that includes a systematic approach for enhancing access to dental care through monitoring appointment availability, provision of training to providers around issues of cultural diversity and any other specialized programs; |
| 4. | Implement incentives and/or sanctions to ensure that access standards are met with respect to dental screens and appointment availability. The MCO shall ensure that the scheduling of a routine dental visit is six (6) weeks; |
| 5. | Certify that all dentists in the MCO's network shall take Members and that MCO's HUSKY Members shall be assured the same access to providers as non-HUSKY Members. Nothing in this |
section shall preclude the implementation of limits on panel size by providers;
| 6. | Implement procedures to provide all Members with the opportunity to choose a general dentist; |
| 7. | Educate Members about the importance of regular dental care, with a focus on accessing preventive care such as screenings and cleanings at least twice a year; and |
| 8. | Provide for sufficient access to dental services for different age groups. |
3.22 Pre-Existing Conditions
a. There is no exclusion for pre-existing conditions.
| b. | The MCO shall assume responsibility for all HUSKY B covered services as outlined in Appendix A for each Member as of the effective date of coverage under the contract. |
| a. | Prior authorization of services covered in the HUSKY B benefit package shall be determined by the MCO based on individual care plans, medical necessity and medical appropriateness, except that the following services in the benefit package shall not require prior authorization. |
1 Preventive care, including:
a) Periodic and well-child visits;
2 Preventive family planning services including:
a) Reproductive health exams;
| d) | Lab tests to detect the presence of conditions affecting reproductive health; and |
| e) | Screening, testing and treatment of pre and post-test counseling for sexually transmitted diseases and HIV, and |
f) Emergency ambulance services or emergency care.
| b. | Further details about HUSKY B prior authorization requirements are set forth in Appendix A. |
3.24 Newborn Enrollment and Minimum Hospital Stays
| a. | The MCO shall accept Membership of a newborn child as of the child's date of birth, if the application is submitted on behalf of the child with in thirty (30) days of the child's date of birth in accordance with C.G.S. 17b- 292(f). Additionally, the MCO shall be responsible for providing coverage of the benefit package beginning with the child's date of birth. |
| b. | The MCO shall comply with requirements of the Newborns' and Mothers' Health Protection Act of 1996 regarding requirements for minimum hospital stays for mothers and newborns in accordance with 45 CFR. 146.130 and 148.170. |
| c. | The MCO shall provide the newborn Member's family with reasonable notice of any premium to be paid for the first months of coverage, as provided by section 4.09. |
3.25 | Acute Care Hospitalization, Nursing Home or Chronic Disease Hospital Stay at Time of Enrollment or Disenrollment |
| a. | The MCO is responsible to ensure continuation of care for acute care requiring an inpatient stay at a hospital. |
| b. | The MCO shall be responsible for inpatient coverage as of the effective date of enrollment for newly enrolled HUSKY B Members who were uninsured. |
| c. | The MCO shall be responsible to provide continuing coverage for an inpatient hospital stay up to the point of discharge for any Member who was admitted as an inpatient in a hospital while enrolled in the MCO and is disenrolled from the MCO for any reason during the same inpatient stay, except as provided in paragraph g below. |
| d. | The continuation of care for the disenrolled Member shall only pertain to the daily inpatient rate charged by such hospital providing the Member's inpatient care. |
| e. | The MCO shall participate in and coordinate the discharge planning process with the MCO involved in the Member's care for Members who fall within sections b, c, and d above. |
| f. | As outlined in Appendix J, upon recategorization of a Member's eligibility from the HUSKY A to the HUSKY B program, the MCO shall provide continued coverage for an inpatient hospital stay as part of the HUSKY A coverage as of the effective date of the individual's enrollment into the MCO as a HUSKY B Member. In the instances where the inpatient stay was covered through the HUSKY A reinsurance program at the time of recategorization, the HUSKY A reinsurance ends effective the date of disenrollment of the individual as a HUSKY A Member. |
| g. | As outlined in Appendix J, upon recategorization of Members eligibility from the HUSKY B to the HUSKY A program, the MCO shall provide continued coverage for an inpatient hospital stay as part of the HUSKY A coverage as |
of the effective date of the individual's enrollment into the MCO as a HUSKY A Member. In the instances where the inpatient stay qualifies for HUSKY A reinsurance, the reinsurance day count starts with the individual's effective date of enrollment as a HUSKY A Member.
| a. | The MCO shall conduct continuous open enrollment during which the MCO shall accept recipients eligible for coverage under this contract. |
| b. | The MCO shall not discriminate in enrollment activities on the basis of health status or the recipient's need for health care services or on any other basis, and shall not attempt to discourage or delay enrollment with the MCO or encourage disenrollment from the MCO of eligible HUSKY B Members. |
| c. | If the MCO discovers that a Member's new or continued enrollment was in error, the MCO shall notify the DEPARTMENT or its agent within sixty (60) days of the discovery or sixty (60) days from the date that the MCO had the data to determine that the enrollment was in error, whichever occurs first. Disenrollment of the Member will be made retroactive to the month during which the Member's circumstances changed to cause ineligibility, or if the Member never met eligibility requirements, to the date of initial enrollment. Failure to notify the DEPARTMENT or its agent within the parameters defined in this section will result in the retention of the Member by the MCO for the erroneous retroactive period of enrollment. |
3.27 Special Disenrollment
| a. | The MCO may request in writing and the DEPARTMENT may approve disenrollment for specific persons when there is good cause. The request shall cite the specific event(s), date(s) and other pertinent information substantiating the MCO's request. Additionally, the MCO shall submit any other information concerning the MCO's request that the DEPARTMENT may require in order to make a determination in the case. |
b. Good cause is defined as a case in which a Member:
| 1. | Exhibits uncooperative or disruptive behavior. If, however, such behavior results from the Member's special needs, good cause may only be found if the Member's continued enrollment seriously impairs the MCO's ability to furnish services to either the particular Members; or |
| 2. | Permits others to use or loans his or her Membership card to others to obtain care or services. |
c. The following shall not constitute good cause:
1. Extensive or expensive health care needs;
2. A change in the member's health status;
3. The Member's diminished mental capacity; or
| 4. | Uncooperative or disruptive behavior related to a medical condition, except as described in b.1., above. |
| d. | The DEPARTMENT will notify an MCO prior to enrollment if a Member was previously disenrolled for cause from another MCO pursuant to this section. |
| a. | The MCO shall take appropriate measures to ensure adequate access to services by Members with limited English proficiency. These measures shall include, but not be limited to the promulgation and implementation of policies on linguistic accessibility for MCO staff, network providers and subcontractors; the identification of a single individual at the MCO for ensuring compliance with linguistic accessibility policies; identification of persons with limited English proficiency as soon as possible following enrollment; provisions for translation services; and the provision of a Member handbook, and information in languages other than English. |
| b. | Member educational materials must also be available in languages other than English and Spanish when more than five (5) percent of the MCO's HUSKY B Members served by the MCO speaks the alternative language, provided, however, this requirement shall not apply if the alternative language has no written form. The MCO may rely upon initial enrollment and monthly enrollment data from the DEPARTMENT or its agent to determine the percentage of Members who speak alternative languages. All Member educational materials must be made available in alternate formats to the visually impaired. |
| c. | The MCO shall also take appropriate measures to ensure access to services by persons with visual and hearing disabilities |
Sanction: For each documented instance of failure to provide appropriate linguistic accessibility to Members, the DEPARTMENT may impose a strike towards a Class A sanction pursuant to Section 9.
| a. | The MCO shall have in place an ongoing process of Member education which includes, but is not limited to, development of a Member handbook; provider directory; newsletter; and other Member educational materials. All written materials and correspondence to Members shall be culturally sensitive and written at no higher than a seventh grade reading level. All Member educational materials must be in both English and Spanish. |
| b. | The MCO shall mail the Member handbook and provider directory to Members within one week of enrollment notification. The Member handbook shall address and explain, at a minimum, the following: |
| 2. | Restrictions on services (including limitations and services not covered); |
| 3. | Prior authorization process; |
| 4. | Definition of and distinction between emergency care and urgent care; |
| 5. | Policies on the use of emergency and urgent care services including a phone number which can be used for assistance in obtaining emergency care; |
| 6. | How to access care twenty-four (24) hours; |
| 7. | Assistance locating an appropriate provider; |
| 8. | Member rights and responsibilities; |
| 9. | Member services, including hours of operation; |
| 10. | Enrollment, disenrollment and plan changes; |
| 11. | Procedures for selecting and changing PCP; |
| 12. | Availability of provider network directory and updates; |
| 13. | Limited liability for services from out-of-network providers; |
| 14. | Access and availability standards; |
| 15. | Special access and other MCO features of the health plan's program; |
| 16. | Family planning services; |
| 17. | Case management services targeted to Members as medically necessary and appropriate; |
| 20. | Maximum annual aggregate cost-sharing; |
| 22. | Involuntary disenrollments; |
| 23. | Appeals and complaints (internal MCO appeal process, external DOI appeal process); |
| 24. | Preventive health guidelines; and |
| 25. | Description of the drug formulary and prior approval process, if applicable. |
| 26. | Information on how to access services from the Partnership. |
| c. | All Member educational materials must be prior approved by the DEPARTMENT. Educational materials include, but are not limited to Member handbook; Membership card; introductory and other text language from the provider directory; and all communications to Members that include HUSKY B program information. The MCO must wait until receiving DEPARTMENT written approval or thirty (30) days from the date of submittal before disseminating educational materials to Members. |
| d. | The MCO must provide periodic updates to the handbook or inform Members, as needed, of changes to the Member information discussed above. The MCO shall update its Member handbook to incorporate all provisions and requirements of this contract within six (6) weeks of the effective date. The MCO shall distribute the Member handbook within six (6) weeks of receiving the DEPARTMENT'S written approval. |
| e. | The MCO shall maintain an adequately staffed Member Services Department to receive telephone calls from Members in order to answer Members' questions, respond to Members' complaints and resolve problems informally. |
| f. | The MCO shall identify to the DEPARTMENT the individual who is responsible for the performance of the Member Services Department. |
| g. | The MCO's Member Services Department shall include bilingual staff (Spanish and English) and translation services for non-English speaking Members. The MCO shall also make available translation services at provider sites either directly or through a contractual obligation with the service provider. |
| h. | The MCO shall require members of the Member Services Department to identify themselves to Members when responding to Members' questions or complaints. At a minimum, ninety (90) percent of all incoming calls shall be answered by a staff Member within the first minute and the call abandonment rate shall not exceed five (5) percent. The MCO shall submit call response and abandonment reports for the preceding six (6) month period to the DEPARTMENT upon request. |
| i. | When Members contact the Member Services Department to ask questions about, or complain about, the MCO's failure to respond promptly to a request for goods or services, or the denial, reduction, suspension or termination of goods or services, the MCO shall: attempt to resolve such concerns informally, and inform Members of the MCO's internal appeal process. |
| j. | The MCO shall maintain a log of complaints resolved informally, which shall be made available to the DEPARTMENT upon request, and which shall be a short dated summary of the problem, the response and the resolution. |
At the time of enrollment and at least annually thereafter, the MCO shall inform its Members of the procedural steps for filing an internal appeal and requesting an external review.
| k. | The MCO shall monitor and track PCP transfer requests and follow up on complaints made by Members as necessary. |
| l. | The MCO will participate in two (2) Member surveys. The first such survey will be an analysis of Members with special needs as defined by the DEPARTMENT after consultation with the Children's Health Council, EQRO, and the MCO, to be conducted at the DEPARTMENT'S expense. The survey will be developed and the sample will be chosen by the Children's Health Council, with input from the MCOs and the DEPARTMENT. The other survey will be an NCQA Consumer Assessment of Health Plans Survey (CAHPS) of combined HUSKY A and B Members using an independent vendor and paid for by the MCO. The MCO's CAHPS survey shall continue to include behavioral health questions. |
| m. | The MCO may provide outreach to its current Members at the time of the Member's renewal of eligibility. The outreach may involve special mailings or phone calls as reminders that the Member must complete the HUSKY renewal forms to ensure continued coverage. |
| n. | The MCO shall make appropriate referrals of Members who express the need for or may require behavioral health services to the Partnership. If a Member is in crisis, the MCO shall stay on the line with the member while connecting the Member with the Partnership. |
3.30 Information to Potential Members
| a. | The MCO shall, upon request, make the following information available to potential Members: |
| 1. | The identity, locations, qualifications and availability of MCO's network; |
| 2. | Rights and responsibilities of Members; |
| 4. | All covered items and services that are available either directly or indirectly or through referral and prior authorization. |
3.31 DSS Marketing Guidelines
The MCO may, at its option, market or promote their plan to potential members. All marketing and marketing related activities must be in compliance with the guidelines and restrictions as set forth in this section and Appendix D. DSS marketing restrictions apply to subcontractors and providers of care as well as to the MCOs. The MCO shall notify all its subcontractors and network providers of the DEPARTMENT'S marketing restrictions. The detailed marketing guidelines are set forth in Appendix D.
| a. | Prohibited Marketing Activities: Appendix D describes permitted and prohibited marketing activities that apply to all forms of communication, regardless of whether they are performed by the MCO directly, by its contracted providers, or its subcontractors: |
| b. | Any type of marketing activity that has not been clearly specified as permissible under the guidelines in Appendix D should be assumed to be prohibited. The MCO shall contact the DEPARTMENT for guidance and approval for any activity not clearly permissible under these guidelines. |
| c. | The MCO shall submit its annual marketing plan, revisions to the marketing plan and all marketing materials to the DEPARTMENT for approval. The DEPARTMENT will provide comments on the marketing materials to the MCO within thirty (30) days of receipt of the materials. MCOs, subcontractors and their providers must wait until receiving DSS written approval or 31 days from submission to the Department, if the Department has not responded by the 30th day before disseminating any such information to potential Members. DSS reserves the right to request revisions or changes in marketing materials at any time |
| d. | The MCO shall distribute marketing materials on a statewide basis. |
Sanction: If the MCO or its providers engage in inappropriate marketing activities, the DEPARTMENT may impose a sanction up to and including a Class C sanction pursuant to Section 9.05 as it deems appropriate.
Sanction: If the MCO engages in non-compliant marketing practices within one year of a marketing related sanction, the Department shall impose a Class C sanction of $25,000 for each determination of a marketing violation following the initial sanction episode.
Sanction: Each marketing sanction episode shall include a mandatory enrollment freeze of no less than three months in duration.
The MCO must routinely, but no less frequently than annually, remind and encourage Members to utilize benefits including physical examinations which are available and designed to prevent illness. The MCO shall keep a record of all activities it has conducted to satisfy this requirement.
3.33 Quality Assessment and Performance Improvement
| a. | The MCO is required to provide a quality level of care for all services, which it provides and for which it contracts. These services are expected to be medically necessary and may be provided by participating providers. The MCO shall implement a Quality Assessment and Performance |
Improvement program to assure the quality of care. The EQRO shall monitor the MCO's compliance with all requirements in this section.
| b. | The MCO shall comply with DEPARTMENT requirements concerning Quality Assessment and Performance Improvement set forth below. The MCO will develop and implement an internal Quality Assessment and Performance Improvement program consistent with the Quality Assessment and Performance Improvement program guidelines, as provided in Appendix G. |
| c. | The MCO must have a Quality Assessment and Performance Improvement system which: |
| 1. | Provides for review by appropriate health professionals of the processes followed in providing health services; |
| 2. | Provides for systematic data collection of performance and participant results; |
| 3. | Provides for interpretation of these data to the practitioners; |
| 4. | Provides for making needed changes; |
| 5. | Provides for the performance of at least one performance improvement project of the MCO's own choosing; |
| 6. | Provides for participation in at least one performance improvement project conducted by the EQRO; and |
| 7. | Has in effect mechanisms to detect both under utilization and over utilization of services. |
| d. | The MCO shall provide descriptive information on the operation, performance and success of its Quality Assessment and Performance Improvement system to the DEPARTMENT or its agent upon request. |
| e. | The MCO shall maintain and operate a Quality Assessment and Performance Improvement program which includes at least the following elements: |
| 1. | A quality assessment and performance improvement assurance plan; |
| 2. | A Quality Assessment and Performance Improvement Director who is responsible for the operation and success of the Quality Assessment and Performance Improvement Program. This person shall have adequate experience to ensure successful Quality Assessment and Performance Improvement, and shall be accountable for the Quality Assessment and Performance Improvement systems for all the MCO's providers, as well as the MCO's subcontractors; |
| 3. | The Quality Assessment and Performance Improvement Director shall spend an adequate proportion of time on Quality Assessment |
and Performance Improvement activities to ensure that a successful Quality Assessment and Performance Improvement Program will exist. Under the Quality Assessment and Performance Improvement program, there shall be access on an as-needed basis to the full compliment of health professions (e.g., pharmacy, physical therapy, nursing, etc.) and administrative staff. Oversight of the program shall be provided by a Quality Assessment and Performance Improvement committee which includes representatives from:
| a) | Variety of medical disciplines (e.g., medicine, surgery, mental health, etc.) and administrative staff; and |
b) Board of Directors of the MCO.
| 4. | The Quality Assessment and Performance Improvement committee shall be organized operationally within the MCO such that it can be responsible for all aspects of the Quality Assessment and Performance Improvement program. |
| 5. | Quality Assessment and Performance Improvement activities shall be sufficiently separate from Utilization Review activities, so that Quality Assessment and Performance Improvement activities can be distinctly identified as such. |
| 6. | The Quality Assessment and Performance Improvement activities of the MCO providers and subcontractors, if separate from the MCO's Quality Assessment and Performance Improvement activities shall be integrated into the overall MCO Quality Assessment and Performance Improvement program, and the MCO shall provide feedback to the providers/subcontractors regarding the operation of any such independent Quality Assessment and Performance Improvement effort. The MCO shall remain however, fully accountable for all Quality Assessment and Performance Improvement relative to its providers and subcontractors. |
| 7. | The Quality Assessment and Performance Improvement committee shall meet at least quarterly and produce written documentation of committee activities to be shared with the DEPARTMENT or its agent. |
| 8. | The results of the Quality Assessment and Performance Improvement activities shall be reported in writing at each meeting of the Board of Directors. |
| 9. | The MCO shall have a written procedure for following up on the results of Quality Assessment and Performance Improvement activities to determine success of implementation. Follow-up shall be documented in writing. |
| 10. | If the DEPARTMENT determines that a Quality Assessment and Performance Improvement plan does not meet the above requirements, the DEPARTMENT may provide the MCO with a model plan. The MCO agrees to modify its Quality Assessment and Performance Improvement plan based on negotiations with the DEPARTMENT. |
| 11. | The MCO shall monitor access to and quality of health care goods and services for its Member population, and, at a minimum, use this mechanism to capture and report all of the DEPARTMENT'S required utilization data. The MCO shall be subject to an annual medical audit by the DEPARTMENT'S EQRO and shall provide access to the data and records requested. |
| 12. | To the extent permitted under federal and state law, the MCO certifies that all data and records requested shall, upon reasonable notice, be made available to the DEPARTMENT or its agent. |
| 13. | The MCO will be an active participant in at least one of the EQRO's performance improvement focus studies each year. |
| 14. | The MCO must comply with external quality review that will be implemented by an organization contracted by the DEPARTMENT. This may include participating in the design of the external review, collecting data including, but not limited to, administrative and medical data, HEDIS measures, and/or making data available to the review organization. |
| 15. | The MCO must conduct at least one performance improvement project that includes the following: |
a) The project shall focus upon at one of the following areas:
1) Prevention and care of acute and chronic conditions;
3) Continuity and coordination of care;
4) Appeals and complaints; and
5) Access to and availability of services.
b). Measurement of performance using quality indicators that are:
2) Clearly and unambiguously defined;
3) Based on current clinical knowledge or health services research;
4) Valid and reliable;
5) Systematically collected; and
| 6) Capable of measuring outcomes such as changes in health status or Member satisfaction, or valid proxies of those outcomes. |
| c) | Implementation of system interventions to achieve quality improvement; |
| d) | Evaluation of the effectiveness of the interventions; |
| e) | Planning and initiation of activities for increasing or sustaining improvement; and |
| f) | Represent the entire population to which the quality indicator is relevant. |
| 16. | With the approval of the DEPARTMENT, the MCO may conduct performance improvement projects for the combined HUSKY A and HUSKY B population. |
| 17. | At the invitation of the Partnership, the MCO may, at its discretion, participate in a joint quality improvement initiative on an area of mutual concern. |
3.34 Inspection of Facilities
| a. | The MCO shall provide the State of Connecticut and any other legally authorized governmental entity, or their authorized representatives, the right to enter at all reasonable times the MCO's premises or other places, including the premises of any subcontractor, where work under this contract is performed to inspect, monitor or otherwise evaluate work performed pursuant to this contract. The MCO shall provide reasonable facilities and assistance for the safety and convenience of the persons performing those duties. The DEPARTMENT and its authorized agents will request access in advance in writing except in case of suspected fraud and abuse. |
| b. | In the event right of access is requested under this section, the MCO or subcontractor shall upon request provide and make available staff to assist in the audit or inspection effort, and provide adequate space on the premises to reasonably accommodate the State or Federal representatives conducting the audit or inspection effort. |
| c. | The MCO shall be given ten (10) business days to respond to any findings of an audit before the DEPARTMENT shall finalize its findings. All information so obtained will be accorded confidential treatment as provided under applicable law. |
3.35 Examination of Records
| a. | The MCO shall develop and keep such records as are required by law or other authority or as the DEPARTMENT determines are necessary or useful for assuring quality performance of this contract. The |
DEPARTMENT shall have an unqualified right of access to such records in accordance with Part II Section 3.34.
| b. | Upon non-renewal or termination of this contract, the MCO shall turn over or provide copies to the DEPARTMENT or to a designee of the DEPARTMENT all documents, files and records relating to persons receiving services and to the administration of this contract that the DEPARTMENT may request, in accordance with Part II Section 3.34. |
| c. | The MCO shall provide the DEPARTMENT and its authorized agents with reasonable access to records the MCO maintains for the purposes of this contract. The DEPARTMENT and its authorized agents will request access in writing except in cases of suspected fraud and abuse. The MCO must make all requested medical records available within thirty (30) days of the DEPARTMENT'S request. Any contract with a subcontractor must include a provision specifically authorizing access in accordance with the terms set forth in Part II 3.35. |
| d. | The MCO shall maintain the confidentiality of patients' records in conformance with this contract and state and federal statutes and regulations, including, but not limited to, the Health Insurance Portability and Accountability Act (HIPAA), 42 U.S.C. 1320d-2 et seq.. 45 CFR pts. 160 and 164, the Connecticut Insurance Information and Privacy Act, Section 38a-975 et secj. of the Connecticut General Statutes, and as applicable the Gramm-Leach-Bliley Act, 15 U.S.C. 6801 et seq. |
| e. | The MCO, for purposes of audit or investigation, shall provide the State of Connecticut, the Secretary of HHS and his/her designated agent, and any other legally authorized governmental entity or their authorized agents access to all the MCO's materials and information pertinent to the services provided under this contract and Member health claims and payment data, at any time, until the expiration of three (3) years from the completion date of this contract as extended. |
| f. | The State and its authorized agents may record any information and make copies of any materials necessary for the audit. |
| g. | Retention of Records: The MCO and its subcontractors shall retain financial records, supporting documents, statistical records and all other records supporting the services provided under this contract for a period of five (5) years from the completion date of this contract. The MCO shall make the records available at all reasonable times at the MCO's general offices. The DEPARTMENT and its authorized agents will request access in writing except in cases of suspected fraud and abuse. If any litigation, claim or audit is started before the expiration of the five (5) year period, the records must be retained until all litigation, claims or audit findings involving the records have been resolved.The MCO must make all requested records available within thirty (30) days of the DEPARTMENT'S request. |
| h. | The MCO shall not avoid costs for services covered in this contract by referring Members to publicly supported health care resources. |
| a. | In compliance with all state and federal law governing the privacy of individually identifiable health care information including the Health Insurance Portability and Accountability Act (HIPAA), 42 USC Sections 1320d-2 et seq.. 45 CFR pts. 160 and 164, the MCO shall establish a confidential, centralized record, for each Member, which includes information of all medical goods and services received. The MCO may delegate maintenance of the centralized medical record to the Member's PCP, provided however, that the record shall be made available upon request and reasonable notice, to the DEPARTMENT or its agent(s) at a centralized location. The medical record shall meet the DEPARTMENT'S medical record requirements as defined by the DEPARTMENT in its regulations, and shall comply with the requirements of the National Committee on Quality Assurance (NCQA) or other national accrediting body with a recognized expertise in managed care. The MCO shall establish a confidential, centralized record, which includes the medical record, for all Members including all goods and services received. The MCO may delegate maintenance of the centralized medical record to the Member's PCP, provided however, that the record shall be made available upon request and reasonable notice, to the DEPARTMENT or its agent(s) at a centralized location. The MCO or PCP shall maintain the medical records in compliance with all state and federal law governing the privacy of individually identifiable health care information including the Health Insurance Portability and Accountability Act (HIPAA), 42 U.S.C. 1320d-2 et seq.. 45 CFR pts. 160 and 164. The medical record shall meet the DEPARTMENT'S medical record requirements as defined by the DEPARTMENT in its regulations, and shall comply with the requirements of the NCQA. |
| b. | The MCO shall not turn over or provide documents, files and records pertaining to a Member to another health plan unless the Member has changed enrollment to the other plan and the MCO has been so notified by the DEPARTMENT or its agent. |
| c. | The MCO shall share information and provide copies of documents, files and records pertaining to a Member to the CT BHP ASO and any subcontractor upon the request of the Member, Department or ASO. |
In addition to and not in any way in limitation of the obligation of the contract, it is understood and agreed by the MCO that the MCO shall be held liable for any finally determined State or Federal audit exceptions and shall return to the
DEPARTMENT all payments made under the contract to which exception has been taken or which have been disallowed because of such an exception.
3.38 Clinical Data Reporting
| a. | Utilization Reporting: The MCO shall submit reports to the DEPARTMENT or its agent in the areas listed below. The purpose of the reports is to assist the DEPARTMENT in its efforts to assess and evaluate the performance of the HUSKY B program and the MCO. |
b. Utilization reports shall cover, but not be limited to, the following areas:
3. Maternal and prenatal care;
5. Inpatient and outpatient services;
| c. | The DEPARTMENT shall consult with the MCO, through a workgroup comprised of the DEPARTMENT, its agent, and MCO representatives that meets on a periodic basis, or as needed, to discuss the necessary data, methods of collecting the data, and the format and media for new reports or changes to existing reports. |
| d. | The MCO shall submit reports, which comply with the DEPARTMENT'S standards, to the DEPARTMENT or its agent. For each report the DEPARTMENT shall consider using any HEDIS standards promulgated by the NCQA which covers the same or similar subject matter. The DEPARTMENT reserves the right to modify HEDIS standards, or not use them at all, if in the DEPARTMENT'S judgment, the objectives of the HUSKY B program can be better served by using other methods. |
| e. | The DEPARTMENT or its agent, will choose a random sample of administrative and medical records each year, in order to measure utilization of services. The MCO will make required records available to the DEPARTMENT or agent, at a location upon reasonable notice. The agent shall review the records and report back to the DEPARTMENT on the extent to which the reporting measure results are validated through comparison with the records. Prior to making its report to the DEPARTMENT, its agent shall afford the MCO reasonable opportunity to suggest corrections to or comment upon the agent's findings. |
| f. | The DEPARTMENT shall provide the MCO with final specifications for submitting all reports no less than ninety (90) days before the reports are due. The MCO shall submit reports on a schedule to be determined by the DEPARTMENT, but not more frequently than quarterly. Before the beginning of each calendar year, the DEPARTMENT shall provide the MCO with a schedule of utilization reports, which shall be due that calendar year. Due dates for the reports shall be at the discretion of the DEPARTMENT, but not earlier than ninety (90) days after the end of the period that they cover. |
g. Daily and Monthly Reports
| 1. | The MCO shall provide to the BHP ASO daily and monthly reports and/or data as mutually agreed upon with the ASO regarding the following: |
a) Behavioral health emergency department visits;
b) Behavioral health emergency room recidivism;
c) Substance abuse and neonatal withdrawal;
d) Child and adolescent obesity and/or type II diabetes;
| 2. | The Department shall provide-specific behavioral health encounter data to the MCO upon request to support quality management activities and coordination. The format of the data extract will be consistent with the encounter data reporting format, or other format mutually agreed upon by the Department and the MCO. |
Sanction: Failure to comply with the above reporting requirements in a complete and timely manner may result in a strike towards a Class A sanction, pursuant to Section 9.05.
3.39 Utilization Management
| a. | The MCO and any subcontractor is required to be licensed by the Connecticut Department of Insurance as a utilization review company. The MCO may subcontract with a licensed utilization review company to perform some or all of the MCO's utilization management functions. |
| b. | If the MCO subcontracts for any portion of the utilization management function, the MCO shall provide a copy of any such subcontract to the DEPARTMENT and any such subcontract shall be subject to the provisions of Section 7.08 of this contract. The DEPARTMENT will review and approve the subcontract, subject to the provisions of Section 3.44, to ensure the appropriateness of the subcontractor's policies and procedures. The MCO is required to conduct regular and comprehensive monitoring of the utilization management subcontractor. |
| c. | The MCO and its subcontractors shall comply with the utilization review provisions of Connecticut General Statutes Section 38a-226c. |
| d. | If the MCO disagrees with a clinical management decision made by the BMP ASO, the MCO may raise the issue with the ASO on behalf of the Member and seek to resolve the issue informally prior to a scheduled administrative hearing. |
| a. | The MCO shall maintain for the purpose of this contract, an accounting system of procedures and practices that conforms to Generally Accepted Accounting Principles. |
| b. | The MCO shall permit audits or reviews by the DEPARTMENT and HHS or their agent(s), of the MCO's financial records related to the performance of this contract and the MCO's subcontrators' financial records related to the performance of this contract. In addition, the MCO will be required to provide Claims Aging Inventory Reports, Claims Turn Around Time Reports, cost, and other reports as outlined in sections (c) and (d) below or as directed by the DEPARTMENT. |
| c. | Reports specific to the MCO's HUSKY line of business shall be provided in formats developed by the DEPARTMENT. All reports described in Section 3.40 (c)(1) and 3.40(c)(2) shall contain separate sections for HUSKY A and B. It is anticipated that the requirements in this area will be modified to enable the DEPARTMENT to respond to inquiries that the DEPARTMENT receives regarding the financial status of the HUSKY program, to determine the relationship of capitation payments to actual appropriations for the program, and to allow for proper oversight of fiscal issues related to the managed care programs. The MCO will cooperate with the DEPARTMENT or its agent(s) to meet these objectives. The following is a list of required reports: |
| 1. | Audited financial reports per MCO HUSKY line of business. If the MCO is licensed as a health care center or insurance company, both the annual audited financial reports for the MCO and the audited financial reports per MCO HUSKY line of business shall be conducted and reported in accordance with C.G.S. Section 38a-54. If the MCO is not licensed as a health care center or insurance company, the annual audited financial reports for the MCO and the audited financial reports per MCO line of business shall be completed in accordance with generally accepted auditing principles. The MCO may elect to combine HUSKY A and HUSKY B in the audited financial statement. If this election is made, the MCO shall also submit the following: a separate unaudited income statement for HUSKY A and HUSKY B, which will be compared to the audited financial statement. |
| 2. | Unaudited financial reports, HUSKY line of business (formats shown in Appendix H). The reports shall be submitted quarterly, forty-five (45) days subsequent to the end of each quarter. Every line of the requested report must contain a dollar figure or an indication that said line is not applicable. |
| 3. | Annual and Quarterly Statements. If the MCO is licensed as a health care center or insurance company, the MCO is required to submit Annual and Quarterly Statements to the Department of Insurance in accordance with the C.G.S. Section 38a-53. One copy of each statement shall be submitted to the DEPARTMENT in accordance with Department of Insurance submittal schedule. |
| 4. | Claims Aging Inventory Report (format shown in Appendix H or any other format approved by the DEPARTMENT). The report will include all HUSKY claims outstanding as of the end of each quarter, by type of claim, claim status and aging categories. If a subcontractor is used to provide services and adjudicate claims or a vendor is used to adjudicate claims, the MCO is responsible for providing a claims aging report in the required format for each current or prior subcontractor who has claims outstanding. The Claims Aging Inventory reports will be submitted to the DEPARTMENT forty-five (45) days subsequent to the end of each quarter. |
| 5. | Claims Turn Around Time Report (format shown in Appendix H or any other format approved by the DEPARTMENT). For those claims processed in forty-six (46) or more days, indicate if interest was paid in accordance with the Section 3.43 of the contract. If a subcontractor is used to provide services and adjudicate claims or a vendor is used to adjudicate claims, the MCO is responsible for providing a Claims Turn Around Time Report for each current or prior subcontractor who has claims outstanding. The Claims Turn Around Time Report will be submitted to the DEPARTMENT forty- five (45) days subsequent to the end of each quarter. |
| d. | The MCO shall maintain accounting records in a manner which will enable the DEPARTMENT to easily audit and examine any books, documents, papers and records maintained in support of the contract. All such documents shall be made available to the DEPARTMENT at its request, and shall be clearly identifiable as pertaining to the contract. |
| e. | The MCO shall make available on request all financial reports required by the terms of any current contract with any other state agency(s) provided that said agency agrees that such information may be shared with the DEPARTMENT. |
3.41 Insurance
| a. | The MCO, its successors and assignees shall procure and maintain such insurance as is required by currently applicable federal and state law and regulation. Such insurance shall include, but not be limited to, the following: |
| 1. | Liability insurance (general, errors and omissions, and directors and officers coverage); |
| 2. | Fidelity bonding or coverage of persons entrusted with handling of funds; |
| 3. | Workers compensation; and |
| 4. | Unemployment insurance. |
| b. | The MCO shall name the State of Connecticut as an additional insured party under any insurance, except for professional liability, workers compensation, unemployment insurance, and fidelity bonding maintained for the purposes of this contract. However, the MCO shall name the State of Connecticut as either a loss payee or additional insured for fidelity bonding coverage. |
3.42 Subcontracting for Services
| a. | Licensed health care facilities, group practices and licensed health care professionals operating within the scope of their practice may contract with the MCO directly or indirectly through a subcontractor who directly contracts with the MCO. The MCO shall be held directly accountable and liable for all of the contractual provisions under this contract regardless of whether the MCO chooses to subcontract its responsibilities to a third party. No subcontract shall operate to terminate the legal responsibility of the MCO to assure that all activities carried out by the subcontractor conform to the provisions of this contract. Subcontracts shall not terminate the legal liability of the MCO under this contract. |
| b. | The MCO may subcontract for any function, excluding Member Services, covered by this contract, subject to the requirements of this contract. All subcontracts shall be in writing, shall include any general requirements of this contract that are appropriate to the services being provided, and shall assure that all delegated duties of the MCO under this contract are performed. All subcontracts shall also provide for the right of the DEPARTMENT or another governmental entity to enter the subcontractor's premises to inspect, monitor or otherwise evaluate the work being performed as a delegated duty of this contract, as specified in Section 3.33, Inspection of Facilities. |
| c. | With the exception of subcontracts specifically excluded by the DEPARTMENT, all subcontracts shall include verbatim the HUSKY B definitions of Medical Appropriateness/Medically Appropriate and Medically Necessary/Medical Necessity as set forth in the Definitions, Part II, Section 1 of this contract. All subcontracts shall require the use of these definitions by subcontractors in all requests for approval of coverage of goods or services made on behalf of HUSKY B Members. All subcontracts shall also provide that decisions concerning both acute and chronic care must be made according to these definitions. |
| d. | Within fifteen (15) days of the effective date of this contract the MCO shall provide the DEPARTMENT with a report of those functions under this contract that the MCO will be providing through subcontracts and copies of the contracts between the MCO and the subcontractor. Such report shall identify the names of the subcontractors, their addresses and a summary of the services they will be providing. If the MCO enters into any additional subcontracts after the MCO's initial compliance with this section, the MCO shall obtain the advance written approval of the DEPARTMENT. The MCO shall provide the DEPARTMENT with a draft of the proposed subcontract thirty (30) days in advance of the completion of the MCO's negotiation of such subcontract. In addition, amendments to any such subcontract, excluding those of a technical nature, shall require the pre-review and approval of the DEPARTMENT. |
| e. | All dental subcontracts, which include the payment of claims on behalf of HUSKY B Members for the provision of goods or services to HUSKY B Members shall require a performance bond, letter of credit, statement of financial reserves or payment withhold requirements. The performance bond, letter of credit, statement of financial reserves or payment withhold requirements shall be in a form to be mutually agreed upon by the MCO and the subcontractor. The amount of the performance bond shall be sufficient to ensure the completion of the subcontractor's claims processing and provider payment obligations under the subcontract in the event the contract between the MCO and the subcontractor is terminated. The MCO shall submit reports to the DEPARTMENT upon the DEPARTMENT'S request related to any payments made from the performance bonds or any payment withholds. |
| f. | All subcontracts shall include provisions for a well-organized transition in the event of termination of the subcontract for any reason. Such provisions shall ensure that an adequate provider network will be maintained at all times during any such transition period and that continuity of care is maintained for all Members. |
| g. | Prior to the approval by the DEPARTMENT of any subcontract with a dental subcontractor, the MCO shall submit a plan to the DEPARTMENT for the resolution of any outstanding claims submitted by providers to the MCO's previous dental subcontractor. Such plan shall meet the requirements described in subsection (h) below. |
| h. | In the event that a subcontract is terminated, the MCO shall submit a written transition plan to the DEPARTMENT sixty (60) days in advance of the scheduled termination. The transition plan shall include provisions concerning financial responsibility for the final settlement of provider claims and data reporting, which at a minimum must include a claims aging report prepared in accordance with Section 3.40 (c)(5) of this contract, with steps to ensure the resolution of the outstanding amounts. This plan shall be submitted prior to the DEPARTMENT'S approval. |
| i. | All subcontracts shall also include a provision that the MCO will withhold a portion of the final payment to the subcontractor, as a surety bond to ensure compliance under the terminated subcontract. |
| j. | The MCO shall have no right to and shall not assign, transfer or delegate this contract in its entirety, or any right or duty arising under this contract without the prior written approval of the DEPARTMENT. The DEPARTMENT in its discretion may grant such written approval of an assignment, transfer or delegation provided, however, that this paragraph shall not be construed to grant the MCO any right to such approval. |
3.43 Timely Payment of Claims
If the MCO or any other subcontractor or vendor who adjudicates claims fails to pay a clean claim within forty-five (45) days of receipt, or as otherwise stipulated by a provider contract, the MCO, vendor or subcontractor shall pay the provider the amount of such clean claims plus interest at the rate of fifteen (15) percent per annum or as stipulated by a provider contract. In accordance with Section 3.40 (c)(5), Financial Records, the MCO shall provide to the DEPARTMENT information related to interest paid beyond the forty-five (45) day timely filing limit, or as otherwise stipulated by provider contracts.
3.44 Insolvency Protection
The MCO must maintain protection against insolvency as required by the DEPARTMENT including demonstration of adequate initial capital and ongoing reserve contributions. The MCO must provide financial data to the DEPARTMENT in accordance with the DEPARTMENT'S required formats and timing.
| a. | The MCO shall not knowingly take any action or failure to take action that could result in an unauthorized benefit to the MCO, its employees, its subcontractors, its vendors, or to a Member. |
| b. | The MCO commits to preventing, detecting, investigating, and reporting potential fraud and abuse occurrences, and shall assist the DEPARTMENT and HHS in preventing and prosecuting fraud and abuse in the HUSKY B program. |
| c. | The MCO acknowledges that the DEPARTMENT and HHS, Office of the Inspector General, has the authority to impose civil monetary penalties on individuals and entities that submit false and fraudulent claims to the HUSKY B program. |
| d. | The MCO shall immediately notify the DEPARTMENT when it detects a situation of potential fraud or abuse, including, but not limited to, the following: |
| 1. | False statements, misrepresentation, concealment, failure to disclose, and conversion of benefits; |
| 2. | Any giving or seeking of kickbacks, rebates, or similar remuneration; |
| 3. | Charging or receiving reimbursement in excess of that provided by the DEPARTMENT; and |
| 4. | False statements or misrepresentation made by a provider, subcontractor, or Member in order to qualify for the HUSKY program. |
| e. | Upon written notification of the DEPARTMENT, the MCO shall cease any conduct that the DEPARTMENT or its agent deems to be abusive of the HUSKY program, and to take any corrective actions requested by the DEPARTMENT or its agent. |
| f. | The MCO attests to the truthfulness, accuracy, and completeness of all data submitted to the DEPARTMENT, based on the MCO's best knowledge, information, and belief. This data certification requirement includes encounter data and also applies to the MCO's subcontractors. |
| g. | The MCO shall establish a fraud and abuse plan, including, but not necessarily limited to, the following efforts: |
| 1. | Conducting regular reviews and audits of operations to guard against fraud and abuse; |
| 2. | Assessing and strengthening internal controls to ensure claims are submitted and payments are made properly; |
| 3. | Educating employees, providers, and subcontractors about fraud and abuse and how to report it; |
| 4. | Effectively organizing resources to respond to complaints of fraud and abuse; |
| 5. | Establishing procedures to process fraud and abuse complaints; and |
| 6. | Establishing procedures for reporting information to the DEPARTMENT. |
| h. | The MCO shall examine publicly available data, including but not limited to the HCFA Medicare/Medicaid Sanction Report and the HCFA website (http://www.oig.hhs.gov) to determine whether any potential or current employees, providers, or subcontractors have been suspended or excluded or terminated from the Medicare or Medicaid programs and shall |
comply with, and give effect to, any such suspension, exclusion, or termination in accordance with the requirements of state and federal law.
| i. | The MCO must provide full and complete information on the identity of each person or corporation with an ownership or controlling interest (five (5) percent) in the managed care plan, or any subcontractor in which the MCO has a five (5) percent or more ownership interest. |
| j. | The MCO must immediately provide full and complete information when it becomes aware of any employee or subcontractor who has been convicted of a civil or criminal offense related to that person's involvement under Medicare, Medicaid, or any other federal or state assistance program prior to entering into or renewing this contract. |
Sanction: The DEPARTMENT may impose a sanction up to an including a Class C sanction for the failure to comply with any provision of this section, or take any other action set forth in Section 9.05 of this contract, including terminating or refusing to renew this contract, or any other remedy allowed by federal or state law.
4. | MCO RESPONSIBILITY CONCERNING PAYMENTS MADE ON BEHALF OF THE MEMBER |
4.01 | Deductibles, Coinsurance, Annual Benefit Maximums, and Lifetime Benefit Maximums |
The MCO shall not apply deductibles, coinsurance, or annual or lifetime benefit maximums to any covered goods and services provided to Members in HUSKY B.
4.02 Payments for Non-covered Services
| a. | The MCO may allow a provider to charge for non-covered goods or services provided to a Member only if the parent or applicant knowingly elects to receive the goods or services and enters into an agreement in writing to pay for such goods or services prior to receiving them. For purposes of this section, non-covered services are services other than those described in Appendix A of this contract, services that are provided in the absence of appropriate authorization by the MCO, and services that are provided out-of-network unless otherwise specified in the contract or regulation. |
| b. | No payment made for non-covered services shall be considered cost- sharing for purposes of determining the family's maximum annual aggregate cost-sharing limit. |
4.03 | Cost-Sharing Exemption for American Indian/Alaskan Native Children |
| a. | Families of American Indian/ Alaskan Native (AI/AN) children who are Members of a Federally recognized tribe and who are in Income Band 1 or 2 are exempted from paying any cost sharing for HUSKY B. |
| b. | The DEPARTMENT or its agent will determine each AI/AN family's eligibility for HUSKY B and the appropriate Income Band, and will also determine whether or not a family's children qualify for the AI/AN cost- sharing exemption. The DEPARTMENT or its agent will then notify the MCO whether the Member is qualified for the exemption and the appropriate Income Band for the family. The MCO shall ensure that the family is not charged any premiums or co-payments for qualified AI/AN children as of the date the DEPARTMENT or its agent makes that determination. |
| c. | The MCO shall notify its providers and subcontractors of the AI/AN exemption from cost sharing. Member handbooks and information handouts developed by the MCO shall include information about the AI/AN exclusion from cost sharing. The MCO shall refer any Members who |
believe they qualify for the AI/AN exemption to the DEPARTMENT or its agent for a determination of their qualification.
| d. | The MCO shall provide all qualified AI/AN children in Income Bands 1 and 2 with Membership identification cards stating "no cost sharing" and the MCO shall inform their HUSKY B providers and subcontractors that children with Membership cards so noted shall not be charged any cost sharing. |
| e. | If the family has paid premiums and, co-payments or any other type of cost sharing for qualified AI/AN children, it is the responsibility of the MCO to repay their payments to the family within three (3) months of the MCO's determination that they were paid. It is the responsibility of the MCO to review the Member accounts quarterly to determine which families have paid premiums and/or co-payments or any other cost sharing for qualified AI/AN children. The quarterly review must be completed no later than fifteen (15) days after the end of each quarter. The MCO shall make the review available to the DEPARTMENT upon request. |
Sanction: If the MCO fails to repay the overpayment to the family within three (3) months of the determination that the cost sharing payment liability has been reached or if the MCO fails to exempt AI/AN children from cost sharing, the DEPARTMENT may impose a sanction up to and including a Class B sanction pursuant to Section 9.05.
| a. | The MCO shall allow providers to collect co-payments for the following goods and services only: |
1. Outpatient physician visits, except for well child visits;
5. Nurse practitioner visits;
11. Generic and brand name prescriptions; and
12. Non-emergency care provided in a hospital emergency department or urgent care facility, except for a condition such that a prudent
layperson, acting reasonably, would have believed that emergency medical treatment is needed.
b. The amounts of these co-payments are detailed in Appendix A.
4.05 Co-payments Prohibited No co-payment shall be charged for:
1. Ambulance for emergency medical conditions;
2. Durable medical equipment other than powered wheelchairs;
3. Emergency medical conditions; and
4. Family planning services, excluding oral contraceptives;
6. Hospice and short-term rehabilitation;
7. Inpatient hospital services;
8. Inpatient physician services;
9. Laboratory and x-ray services, including diagnostic and treatment radiology and ultrasound treatment;
10. Occupational therapy;11. Outpatient surgical visits;
13. Preadmission testing;
14. Preventive care and services, including all well-baby and well-child services as described in 42 CFR 457.520;
15. Prosthetic devices;18. The following dental services: oral exams, prophylaxis, x-rays, fillings, fluoride treatments, sealants, and oral surgery.
4.06 Maximum Annual Limits for Co-payments
| a. | The maximum annual limit for co-payments is $760 for families in Income Bands 1 and 2. |
| b. | Effective February 1, 2004, the maximum aggregate cost-sharing limit for co- payments will increase to $760 for families in Income Bands 1 and 2. For these families, the MCO shall not allow co-payments to be charged once the family has reached its maximum annual limit for co-payments. |
| c. | The maximum annual limit applies to the entire family regardless of the number of eligible children in such family who are enrolled in the MCO. |
| d. | The maximum annual limit applies to each eligibility period. The eligibility period is the one-year period following the Member's initial eligibility date or, for subsequent years, the one year-period following the anniversary of the initial eligibility date. |
| e. | It is the responsibility of the MCO to review the Member accounts at a minimum on a quarterly basis to determine which families have reached their maximum annual limit for co-payments. The review must be completed no later than fifteen (15) days after the end of each review period. The MCO shall make the review available to the DEPARTMENT upon request. |
| f. | If the family has paid more than the allowed limits for co-payments, it is the responsibility of the MCO to repay the overpayment to the family within three (3) months of the MCO's determination that the maximum annual limit for co-payments had been met. |
| g. | There is no maximum annual limit for co-payments for families in Income Band 3. |
Sanction: If the MCO fails to have an effective tracking system for the maximum annual co-payment provisions, the DEPARTMENT may impose a Class B sanction pursuant to Section 9.05.
4.07 Tracking Co-payments
| a. | The MCO shall establish and maintain a system to track the co-payments incurred by each family in Income Bands 1 and 2 in order to adhere to the requirements of the maximum annual aggregate cost-sharing limit for co- payments. The MCO shall require their providers and subcontractors to verify whether a family has reached the maximum annual limit for co-payments before charging a co-payment. |
| b. | The MCO shall carry over the tracking of the co-payment from one Income Band to the other within the annual period for families who move between Income Bands 1 and 2. For families moving within the annual period into Income Bands 1 or 2 from Income Band 3, the tracking begins with the enrollment in Income Band 1 or 2. |
| c. | If the Member is disenrolled due to nonpayment of premiums, the MCO shall maintain the tracked information on file for costs incurred through the date of disenrollment in the event the Member is re-enrolled after payment of the premium within the annual period. If the Member is re-enrolled within the annual period, the MCO will resume tracking the co-payments paid by the family throughout the remainder of the annual period. |
| d. | Families in Income Bands 1 and 2 shall not be charged co-payments once the maximum annual limits have been met. When a family in Income |
Bands 1 or 2 reaches the maximum annual limits for co-payments, the MCO shall inform the providers and subcontractors that the co-payment limit has been met, that the providers and subcontractors cannot charge further co-payments within the annual period, and the date when the annual period ends. The MCO shall provide this same information to the parent and the applicant.
| e. | The MCO shall send a monthly file to the DEPARTMENT or its agent showing the premiums and co-payments paid by the family. The DEPARTMENT or its agent will keep information regarding the amount of co-payments each family incurs within the annual period and if the children of the family disenroll and enroll in another MCO within the annual period, the DEPARTMENT or its agent will forward the family co-payment totals for the annual period to the new MCO. |
| f. | If a family believes it has reached the maximum annual limit for co- payments, it may request, in writing, that the MCO review the co- payments that have been paid by the family. The MCO shall then review the co-payments made by the family and respond to the family, in writing, within three (3) weeks of the date of the family's written request. If the family disagrees with the MCOs determination, the family may request, in writing, a review by the DEPARTMENT. The MCO and the family shall abide by the decision of the DEPARTMENT. The MCO shall include a summary of this right and the appropriate procedures to request the review in its Member Handbook. |
| g. | If the family has paid more than the allowed limits for co-payments, it is the responsibility of the MCO to repay the overpayment to the family within three (3) months of the determination that the maximum annual limit has been met. |
Sanction: Any one of the following may give rise to a strike toward a Class A Sanction pursuant to Section 9.05:
| a. | If the MCO fails to inform its subcontractors, providers, and the family when the family has met its maximum annual limit for co-payments; |
| b. | If the MCO fails to submit a file to the DEPARTMENT or its agent reporting on co-payment and premium amount of its Members within thirty (30) days of the close of the preceding month; or |
| c. | If the MCO fails to monitor the tracking system to determine if any family has reached the maximum annual limits. |
4.08 Amount of Premium Payment
| a. | The amount a family shall be required to pay in premium payments for the HUSKY B benefit package shall vary according to the family income. |
| b. | The premium charged and collected for families within Income Band 2 shall be $30 per month for families with one child or $50 per month for families with more than one child. |
| c. | The premium charged and collected for families in Income Bands 1, 2 and 3 will be the rate negotiated with the DEPARTMENT per month, per child |
| 1. | The premium for families in Income Bands 1 and 2 will be based on Medical coverage only |
| 2. | The premium for families in Income Bands 3 will be based on both Medical and Behavioral Health coverage. |
| d. | The premium provisions and amount are subject to change. The DEPARTMENT will give the MCO sixty (60) days advance notice of any premium changes unless a statutory change precludes such advance notice. |
4.09 Billing and Collecting the Premium Payments
| a. | The MCO shall bill the applicant or member for the premium payments and shall collect the premium payments. The applicant may be billed up to thirty (30) days in advance of the coverage period. The coverage period shall be no less than one month and no more than one year. The MCO shall offer all applicants or members the option of a schedule of monthly premium payments. The initial bill to new members may include billing for multiple months of membership to allow members the opportunity to make payments current to the first prospective coverage month. |
4.10 Notification of Premium Payments Due
The MCO shall provide the applicant or member with reasonable prior notice of any premiums to be paid. The notice shall contain: the amount of the premium due; the date the premium is due; the effective date of disenrollment in case of failure to pay the premium by the due date; information concerning lock-out if there is disenrollment for failure to pay the premium; an instruction for the applicant to immediately contact the DEPARTMENT or its agent if the applicant cannot pay the premium by the due date because of a decrease in family income or other changes in family circumstances; and any additional information required to be included in the notice by the DEPARTMENT.
Sanction: If the MCO fails to provide prior notice as required in this Section, the DEPARTMENT may impose a strike towards a Class A sanction pursuant to Section 9.05.
4.11 Notification of Non-payment of the Premium Payments
| a. | The MCO shall notify, in writing, the applicant or member and the custodial parent, if applicable, if a premium is not received by the due date. |
b. The notice shall contain:
1. The amount of the premium that is due;
2. The date the premium was due;
3. The effective date of disenrollment for failure to pay the premium;
4. Information concerning lock-out;
5. An instruction for the applicant to immediately contact the DEPARTMENT or its agent if the applicant cannot pay the premium by the due date because of a decrease in income or other change in family circumstances; and
6. Any additional information required to be included in the notice by the DEPARTMENT.
| b. | The MCO shall collaborate with the DEPARTMENT and its agent to establish billing and collection procedures. The MCO shall notify the Department or its agent pursuant to the agreed upon procedures if a premium is not received by the due date. |
Sanction: If the MCO fails to provide prior notice, as described above, or if the MCO fails to notify the DEPARTMENT or its agent of failure to pay a premium by the due date, the DEPARTMENT may impose a strike towards a Class A sanction pursuant to Section 9.05.
4.12 Past Due Premium Payments Paid
If the MCO receives premium payments after the Member has been disenrolled, the MCO shall notify the DEPARTMENT or its agent within fifteen (15) days of the receipt of the payment that the payment was received and when it was received.
Sanction: If the MCO fails to notify the DEPARTMENT or its agent as required in this Section, the DEPARTMENT may impose a sanction pursuant to Section 9.
4.13 Resumption of Services if the Child is Re-enrolled
If a child is re-enrolled in HUSKY B, the MCO shall resume providing goods and services to that child.
4.14 Overpayment of Premium
| a. | The MCO shall not bill or collect premiums in excess of the monthly amounts set forth in Section 4.08. |
| b. | If the MCO has received more than the allowed premium rate, it is the responsibility of the MCO to repay the overpayment to the family within three (3) months ,or apply the excess to future coverage months, whichever is preferred by the applicant or member. |
Sanction: If the MCO fails to repay the overpayment to the family within three (3) months of the determination that the premium payment liability has been reached, the DEPARTMENT may impose a strike towards a Class A sanction pursuant to Section 9.05.
4.15 Member Premium Share Paid by Another Entity
The MCO may accept funds from private or tribal organizations for the purpose of subsidizing the payment of premiums. To ensure that the payment is not received from an employer attempting to shift coverage from the employer to the HUSKY B program, the MCO shall conduct periodic audits of received payments. The audits shall be conducted in accordance with DSS and MCO agreed upon criteria and schedule.
Sanction: If the MCO fails to conduct audits in accordance to the agreed upon criteria and schedule, the DEPARTMENT may impose sanctions up to and including a Class B sanction.
4.16 Tracking Premium Payments
| a. | The MCO shall establish and maintain a system to track the premium payments received for each family in Income Bands 1 and 2. |
| b. | The MCO shall cease tracking premium payments for families in Income Bands 1 and 2 who are moved into Income BandS when the move has been completed. For families moving into Income Band 1 or 2 from Income BandS, the tracking begins when the family moves into Income Band 1 or 2. |
| c. | The MCO shall send a monthly file to the DEPARTMENT or its agent showing the premiums and co-payments received for the family. The DEPARTMENT or its agent will maintain the information regarding the amount of premiums received for each family within the annual period and if the children of the family disenroll and then enroll in another MCO within the annual period, the DEPARTMENT or its agent will forward the family premium totals for the annual period to the new MCO. |
| d. | If a family believes it has overpaid premiums, it may request that the MCO review the premiums that have been paid by the family. This request shall be in writing. The MCO shall then review the premium payments made by the family and respond to the family, in writing, within three (3) weeks of the date of the family's written request. If the family disagrees with the MCO's determination, the family may request, in writing, a review by the DEPARTMENT. The MCO and family shall abide by the decision of the DEPARTMENT. The MCO shall include a summary of this right and the appropriate procedures to request the review in its Member Handbook. |
| e. | If the Member is disenrolled due to nonpayment of premiums, the MCO may cease tracking the premium payments, but will keep the tracked information on file in case the Member is re-enrolled after payment of the |
premium within the annual period. If the Member is re-enrolled the MCO shall resume tracking the premium payments paid, throughout the remainder of the annual period.
Sanction: If the MCO fails to comply with any of the provisions of this section, the DEPARTMENT may impose sanctions up to and including a Class B sanction pursuant to Section 9.05.
4.17 Behavioral Health Payment Adjustment
| a. | placeholder for the amount. |
| b. | The MCO shall serve as the single point of premium collection for Band 3 members by: |
| 1) | Collecting a single premium for both Medical and Behavioral Health coverage, and |
| 2) | Transferring to the Department on a quarterly basis the pro-rated Behavioral Health portion of the premium collected commencing with those Behavioral Health premiums collected on or after January 1, 2006. |
5. | LIMITED COVERAGE OF SOME GOODS AND SERVICES AND ALLOWANCES |
5.01 Limited Coverage of Some Benefits
| a. | Some goods and services are covered only up to a specified dollar limit, as set forth in Appendix A. This dollar limit is the allowance for which the MCO is responsible. If the Member decides to access these goods and services, the MCO must cover them up to the specified allowance. The Member's family is responsible for paying any remaining balance beyond the covered allowance. |
| b. | For the limited goods and services described in Appendix A, the MCO is responsible for ensuring that the Member's family is not charged the amount of the covered allowance. |
| c. | The amount a family pays toward the fee of the goods and services described in this section shall not be considered when calculating the maximum annual aggregate cost-sharing. |
6. FUNCTIONS AND DUTIES OF THE DEPARTMENT
6.01 Eligibility Determinations
The DEPARTMENT or its agent will determine the initial and ongoing eligibility for the HUSKY B program of each Member enrolled under this contract in accordance with the DEPARTMENT'S eligibility policies.
6.02 Ineligibility Determinations
The MCO shall inform the DEPARTMENT or its agent within thirty (30) days of its knowledge of information which may render a child ineligible for HUSKY B. The information that shall be reported to the DEPARTMENT or its agent includes age, residency, insurance status, and death.
6.03 Enrollment/Disenrollment
| a. | Enrollment, disenrollment and initial selection of PGP's Members will be handled by the DEPARTMENT through a contract with a central enrollment broker. |
| 1. | Coverage for new Members will be effective the first of the month |
| 2. | Coverage for disenrolled Members will terminate on the last day of the month. |
| 3. | Members remain continuously enrolled throughout the term of this contract, except in situations where clients change MCOs, become delinquent on their premium payments or lose their HUSKY B eligibility. |
| 4. | Disenrollments due to loss of eligibility become effective as of the last day of the month during which the Member's circumstances changed to cause ineligibility or, if the Member never met eligibility requirements, as of the date of initial enrollment. |
| 5. | The DEPARTMENT or its agent will notify the MCO of enrollments and disenrollments specific to the MCO via a daily data file. |
| 6. | The enrollments and disenrollments processed on any given day will be made available to the MCO via the data file the following day (i.e. after the daily overnight batching has been processed). |
| b. | In addition to the daily data file, a full file of all the Members will be made available on a monthly basis. Both the daily data file and the monthly full file can be accessed by the MCO electronically via dial-up. |
6.04 Lock-In/Open Enrollment
| a. | Upon enrollment into an MCO, Members will be locked-in to that MCO for a period of up to twelve (12) months. Members will not be allowed to change plan enrollment during the lock-in period except for good cause, as defined below. The lock-in period is subject to the following provisions: |
| 1. | The first ninety (90) days of enrollment into a new MCO will be designated as the free-look period during which time the Member may change plans. |
| 2. | The last sixty (60) days of the lock-in period will be an open enrollment period, during which time Members may change plans. |
| 3. | Plan changes made during the open enrollment period will go into effect on the first day of the month following the end of the lock-in period. |
| 4. | Members who do not change plans during the open enrollment period will continue the enrollment in the same MCO and be assigned to a new twelve (12) month lock-in period. |
| b. | The following shall constitute good cause for a Member to disenroll from the plan during the lock-in period. |
| 1. | Unfavorable resolution of a Member complaint adjudicated through the MCO's internal complaint process and continued dissatisfaction due to repeated incidents of any of the following: |
a) Documented long waiting times for appointments;
b) More than a forty-five (45) day wait for scheduling a well-care visit;
c) More than a two (2) business day wait for non-urgent, symptomatic office visit;
d) Unavailability of same day office visit or same day referral to an emergency provider for emergency care services;
e) Documented inaccessibility of MCO by phone or mail;
f) Phone calls not answered promptly;
g) Caller placed on hold for extended periods of time;
h) Phone messages and letters not responded to promptly; and i) Rude and demeaning treatment by MCO staff.
| 2. | Prior to pursuing the MCO's internal complaint process and without filing an appeal through the plan, dissatisfaction due to any of the following: |
| a) | Discriminatory treatment as documented in a complaint filed with the State of Connecticut, Commission on Human Rights and Opportunities (CHRO) or the DEPARTMENT'S Affirmative Action Division; |
| b) | PCP able to serve Member's specific individual needs (i.e. language or physical accessibility) is no longer participating with the MCO and there is no other suitable PCP within reasonable distance to the Member; or |
| c) | Member has a pending lawsuit against the MCO; verification of pending lawsuit must be provided. |
6.05 Capitation Payments to the MCO
| a. | In full consideration of contract services rendered by the MCO, the DEPARTMENT agrees to pay the MCO monthly payments based on the capitation rates specified in Appendix I. The DEPARTMENT will make the payments in the month following the month to which the capitation applies. |
| b. | Capitation payments to the MCO shall be based on a passive billing system. The MCO is not required to submit claims for the capitation billing for its HUSKY B Membership. |
| c. | Payments to the MCO shall be based on each month's enrollment data as determined by the DEPARTMENT or its agent. The DEPARTMENT or its agent will supply to the MCO, on a monthly basis a capitation roster, which includes all Members for whom capitation payments are made to the MCO. The MCO will be responsible for detecting any inconsistency between the capitation roster and the MCO Membership records. The MCO must notify the DEPARTMENT of any inconsistency between enrollment and payment data. The DEPARTMENT agrees to provide to the MCO information needed to determine the source of the inconsistency within sixty (60) working days after receiving written notice of the request to furnish such information. The DEPARTMENT will recoup overpayments or reimburse underpayments. The adjusted payment for each month of coverage shall be included in the next monthly capitation payment and roster. |
| d. | Any retrospective adjustments to prior capitation payments will be made in the form of an addition to or subtraction from the next month's capitation payment. |
| e. | In instances where enrollment is disputed the DEPARTMENT will be the final arbiter of Membership status and reserves the right to recover inappropriate capitation payments. Capitation payments for retroactive enrollment adjustments will made to the MCO pursuant to rules outlined in Section c, noted above. |
6.06 Newborn Retroactive Adjustments
a. | The DEPARTMENT shall determine the eligibility of a newborn child retroactively to the date of his or her birth, for an application filed within thirty (30) days following birth. |
| b. | For the purpose of determining the capitation payment to the MCO for the month in which the child was born, the effective date for such enrollment shall be the first of the month in which the child was born. |
The DEPARTMENT will make known to each MCO information which relates to pertinent statutes, regulations, policies, procedures, and guidelines affecting the operation of this contract. This information shall be available either through direct transmission to the MCO or by reference to public resource files accessible to the MCO personnel.
7. DECLARATIONS AND MISCELLANEOUS PROVISIONS
7.01 Competition Not Restricted
In signing this Contract, the MCO asserts that no attempt has been made or will be made by the MCO to induce any other person or firm to submit or not to submit an application for the purpose of restricting competition.
7.02 Non-segregated Facilities
| a. | The MCO certifies that it does not and will not maintain or provide for its employees any segregated facilities at any of its establishments; and that it does not permit its employees to perform their services at any location, under its control, where segregated facilities are maintained. As Contractor, the MCO agrees that a breach of this certification is a violation of Equal Opportunity in Federal employment. In addition, Contractor must comply with the Federal Executive Order 11246 entitled "Equal Employment Opportunity" as amended by Executive Order 11375 and as supplemented in the United States Department of Labor Regulations (41 CFR pt. 30). As used in this certification, the term "segregated facilities" includes any waiting rooms, restaurants and other eating areas, parking lots, drinking fountain, recreation or entertainment areas, transportation, and housing facilities provided for employees which are segregated on the basis of race, color, religion, or national origin, because of habit, local custom, national origin or otherwise. |
| b. | The MCO further agrees, (except where it has obtained identical certifications from proposed subcontractors for specific time periods) that it will obtain identical certifications from proposed subcontractors which are not exempt from the provisions for Equal Employment Opportunity; that it will retain such certifications in its files; and that it will forward a copy of this clause to such proposed subcontractors (except where the proposed subcontractors have submitted identical certifications for specific time periods). |
The MCO, its agents and employees, certify that no elected or appointed official or employee of the DEPARTMENT has or will benefit financially or materially from this contract. The contract may be terminated by the DEPARTMENT if it is determined that gratuities of any kind were either offered to or received by any of the aforementioned officials or employees of the MCO, its agent or employee.
7.04 Employment/Affirmative Action Clause
The MCO agrees to supply employment/affirmative action information as required for agency compliance with Title VI and VII of the Civil Rights Acts of 1964 and Connecticut General Statutes, Section 46a-68 and Section 46a-71.
| a. | The MCO agrees that all material and information, and particularly information relative to individual applicants or recipients of assistance through the DEPARTMENT, provided to the Contractor by the State or acquired by the Contractor in performance of the contract whether verbal, written, recorded magnetic media, cards or otherwise shall be regarded as confidential information and all necessary steps shall be taken by the Contractor to safeguard the confidentiality of such material or information in conformance with federal and state statutes and regulations. |
| b. | The MCO agrees not to release any information provided by the DEPARTMENT or providers or any information generated by the MCO without the express written consent of the Contract Administrator, except as specified in this contract and permitted by applicable state law. |
7.06 Independent Capacity
The MCO, its officers, employees, subcontractors, or any other agent of the Contractor in performance of this contract will act in an independent capacity and not as officers or employees of the State of Connecticut or of the DEPARTMENT.
Both parties agree to have specifically named liaisons at all times. These representatives of the parties will be the first contacts regarding any questions and problems which arise during implementation and operation of the contract.
7.08 Freedom of Information
Due regard will be given for the protection of proprietary information contained in all documents received by the DEPARTMENT; however, the MCO is aware that all materials associated with the contract are subject to the terms of the state Freedom of Information Act, Conn. Gen. Stat. Sections 1-200, et seq., and all rules, regulations and interpretations resulting there from. When materials are submitted by the MCO or a subcontractor to the DEPARTMENT and the MCO or subcontractor believes that the materials are proprietary or confidential in some way and that they should not be subject to disclosure pursuant to the Freedom of Information Act, it is not sufficient to protect the materials from disclosure for the MCO to state generally that the material is proprietary in nature and, therefore, not subject to release to third parties. If the MCO or the MCO or the subcontractor believes that any portions of the materials submitted to the DEPARTMENT are proprietary or confidential or constitute commercial of financial information, given in confidence, those portions or pages or sections the
MCO believes to be proprietary must be specifically identified as such. Convincing explanation and rationale sufficient to justify each claimed exemption from release, consistent with section 1-210 of the Connecticut General Statutes, must accompany the documents when they are submitted to the DEPARTMENT. The explanation and rationale must be stated in terms of the prospective harm to the MCO's or subcontractor's competitive position that would result if the identified materials were to be released and the reasons why the materials are legally exempt from release pursuant to the above-cited statute. The final administrative authority to release or exempt any or all material so identified by the MCO or subcontractor rests with the DEPARTMENT. The DEPARTMENT is not obligated to protect the confidentiality of materials or documents submitted to it by the MCO or the subcontractor if said materials or documents are not identified in accordance with the above-described procedure.
Except as specifically provided in any section of this contract, no covenant, condition, duty, obligation or undertaking contained in or made a part of the Contract shall be waived except by the written agreement of the parties, and forbearance or indulgence in any form or manner by the DEPARTMENT or the MCO in any regard whatsoever shall not constitute a waiver of the covenant, condition, duty, obligation or undertaking to be kept, performed, or discharged by the DEPARTMENT or the MCO; and not withstanding any such forbearance or indulgence, until complete performance or satisfaction of all such covenants, conditions, duties, obligations and undertakings, the DEPARTMENT or MCO shall have the right to invoke any remedy available under the contract, or under law or equity.
The MCO shall be excused from performance hereunderfor any period that is prevented from providing, arranging for, or paying for services as a result of a catastrophic occurrence or natural disaster including but not limited to an act of war, and excluding labor disputes.
7.11 Financial Responsibilities of the MCO
The MCO must maintain at all times financial reserves in accordance with the Connecticut Health Centers Act under Section 38a-175 et seq. of the Connecticut General Statutes, and with the requirements outlined in the DEPARTMENT'S Request for Application.
7.12 Capitalization and Reserves
| a. | The MCO shall comply with and maintain capitalization and reserves as required by the appropriate regulatory authority. |
| b. | If the MCO is licensed by the State of Connecticut, the MCO shall establish and maintain capitalization and reserves as required by the Connecticut DOI. |
| c. | If the MCO is majority-owned by federally qualified health centers (FQHCs) and not licensed by the State of Connecticut, the MCO will establish and maintain sequestere'd capital of $500,000 plus two (2) percent of ongoing annual capitation premiums. |
| 1. | These funds shall be placed in a restricted account for the duration of the FQHC plan's existence, to be accessed only in the event such funds are needed to meet unpaid claims liabilities. |
| 2. | This restricted account shall be established such that any withdrawals or transfers of funds will require signatures of authorized representatives of the FQHC plan and the DEPARTMENT. |
| 3. | The initial $500,000 must be deposited into the account by the beginning of the MCO's first enrollment period. |
| 4. | The MCO must make quarterly deposits into this account so that the account balance is equal to $500,000 plus two (2) percent of the premiums received during the preceding twelve (12) months. |
7.13 Members Held Harmless
The MCO shall not hold a Member liable for:
| a. | The debts of the MCO in the event of the MCO's insolvency; |
| b. | The cost of HUSKY B covered services provided pursuant to this contract, other than cost-sharing permitted under this contract, to the Member if the MCO or provider fails to receive payment; and/or |
| c. | Payments to a provider which exceed the amount that would be owed if the MCO directly provided the service. |
7.14 Compliance with Applicable Laws, Rules And Policies
The MCO in performing this contract shall comply with all applicable federal and state laws, regulations and written policies, including those pertaining to licensing.
7.15 Federal Requirements and Assurances
| 1. | The MCO shall comply with those federal requirements and assurances for recipients of federal grants provided in OMB Standard Form 424B (4-88) which are applicable to the MCO. The MCO is responsible for determining which requirements and |
assurances are applicable to the MCO. Copies of the form are available from the DEPARTMENT. The MCO shall comply with all applicable provisions of 45 CFR 74.48 and all applicable requirements of 45 CFR 74.48 Appendix A.
| 2. | The MCO shall provide for the compliance of any subcontractors with applicable federal requirements and assurances. |
| 1. | The MCO, as provided by 31 U.S.C. 1352 and 45 CFR 93.100 et seq.. shall not pay federally appropriated funds to any person for influencing or attempting to influence an officer or employee of any agency, a Member of the U.S. Congress, an officer or employee of the U.S. Congress or an employee of a Member of the U.S. Congress in connection with the awarding of any federal contract, the making of any cooperative agreement or the extension, continuation, renewal, amendment or modification of any federal contract, grant, loan or cooperative agreement. |
| 2. | The MCO shall submit to the DEPARTMENT a disclosure form as provided in 45 CFR 93.110 and Appendix B to 45 CFR Pt. 93, if any funds other than federally appropriated funds have been paid or will be paid to any person for influencing or attempting to influence an officer or employee of any agency, a Member of the U.S. Congress, an officer or employee of the U.S. Congress or an employee of a Member of the U.S. Congress in connection with this contract. |
c. Title XXI and SCHIP Regulations
The MCO shall comply with all applicable provisions of Title XXI of the Social Security Act and 42 CFR pt. 457
d. Clean Air and Water Acts
The MCO shall comply with all applicable standards, orders or regulations issued pursuant to the Clean Air Act as amended, 42 U.S.C. 7401, et seq. and the Federal Water Pollution Control Act as amended, 33 U.S.C. 1251 et seq.
The MCO shall comply with all applicable standards and policies relating to energy efficiency which are contained in the state energy plan issued in compliance with the federal Energy Policy and Conservation Act, 42 USC Sections 6231 - 6246. The MCO further covenants that no federally appropriated funds have been paid or will be paid on behalf of the DEPARTMENT or the contractor to any person for influencing or attempting to influence an officer or employee of any federal agency, a Member of Congress, an officer or employee of Congress, or an employee of a Member of Congress in connection with the awarding of any federal contract, the making of any federal grant, the making of any federal loan,
the entering into of any cooperative agreement, or the extension, continuation, renewal, amendment, or modification of any federal contract, grant, loan, or cooperative agreement. If any funds other than federally appropriated funds have been paid or will be paid to any person for influencing or attempting to influence an officer or employee of any federal agency, a Member of Congress, or an employee of a Member of Congress in connection with this contract, grant, loan, or cooperative agreement, the contractor shall complete and submit Standard Form - ILL, "Disclosure Form to Report Lobbying," in accordance with its instructions.
f. Maternity Access and Mental Health Parity
The MCO shall comply with the maternity access and mental health requirements of the Public Health Services Act, Title XXVII, Subpart 2, Part A, Section 2704, as added September 26, 1996, 42 U.S.C. Section 300gg-4, 300gg-5, and the implementing regulations at 45 CFR 146.136, insofar as such requirements apply to providers of group health insurance.
The MCO shall comply with the Civil Rights Act of 1964 (42 U.S.C. Section 2000d, et seq.). the Age Discrimination Act of 1975 (42 U.S.C. 6101, et sea.), the Americans with Disabilities Act of 1990 (42 U.S.C. Section 12101, etseg.) and Section 504 of the Rehabilitation Act of 1973, 29 U.S.C. Section 794, et seq.
Persons may not, on the grounds of race, color, national origin, creed, sex, religion, political ideas, marital status, age or disability be excluded from employment in, denied participation in, denied benefits or be otherwise subjected to discrimination under any program or activity connected with the implementation of this contract. The MCO shall use hiring processes that foster the employment and advancement of qualified persons with disabilities.
All hiring done in connection with this contract must be on the basis of merit qualifications genuinely related to competent performance of the particular occupational task. The MCO, in accordance with Federal Executive Order 11246, dated September 24, 1965 entitled "Equal Employment Opportunity", as amended by Federal Executive Order 11375 and as supplemented in the United States Department of Labor Regulations, 41 CFR Part 60-1, et seq., must provide for equal employment opportunities in its employment practices.
The MCO shall, in accordance with relevant laws, regulations and policies, protect the confidentiality of any material and information concerning an applicant for or recipient of services funded by the DEPARTMENT. Access to patient information, records, and data shall be limited to the purposes outlined in 42 CFR 434.6(a)(8). All requests for data or patient records for participation in studies, whether conducted by the MCO or outside parties, are subject to approval by the DEPARTMENT .
7.17 Statutory Requirements
| a. | State licensed MCO shall retain at all times during the period of this contract a valid Certificate of Authority issued by the State Commissioner of Insurance. |
| b. | The MCO shall adhere to the provisions of the Clinical Laboratory Improvement Amendments of 1988 (CLIA) Public Law 100-578, 42 USC Section 1395aa. |
7.18 Disclosure of Interlocking Relationships
An MCO which is not also a Federally-qualified Health Plan or a Competitive Medical Plan under the Public Health Service Act must report on request to the State, to the Secretary and the Inspector General of DHHS, and the Comptroller General, a description of transactions between the MCO and parties in interest including related parties as defined by federal and state law. Transactions that must be reported include: (a) any sale, exchange, or leasing of property; (b) any furnishing for consideration of goods, services or facilities (but not salaries paid to employees); and (c) any loans or extensions of credit.
7.19 DEPARTMENT'S Data Files
| a. | The DEPARTMENT'S data files and data contained therein shall be and remain the DEPARTMENT'S property and shall be returned to the DEPARTMENT by the MCO upon the termination of this contract at the DEPARTMENT'S request, except that any DEPARTMENT data files no longer required by the MCO to render services under this contract shall be returned upon such determination at the DEPARTMENT'S request. |
| b. | The DEPARTMENT'S data shall not be utilized by the MCO for any purpose other than that of rendering services to the DEPARTMENT under this contract, nor shall the DEPARTMENT'S data or any part thereof be disclosed, sold, assigned, leased or otherwise disposed of to third parties by the MCO unless there has been prior written DEPARTMENT approval. The MCO may disclose material and information to subcontractors and vendors, as necessary to fulfill the obligations of this contract. |
| c. | The DEPARTMENT shall have the right of access and use of any data files retained or created by the MCO for systems operation under this contract subject to the access procedures defined in Part II Section 3.34. |
| d. | The MCO shall establish and maintain at all times reasonable safeguards against the destruction, loss or alteration of the DEPARTMENT'S data and any other data in the possession of the MCO necessary to the performance of operations under this contract. |
| a. | The MCO agrees to indemnify, defend and hold harmless the State of Connecticut as well as all DEPARTMENTS, officers, agents and employees of the State from all claims, losses or suits accruing or resulting to any contractors, subcontractors, laborers and any person, firm or corporation who may be injured or damaged through the fault of the MCO in the performance of the contract. |
| b. | The MCO, at its own expense, shall defend any claims or suits which are brought against the DEPARTMENT or the State for the infringement of any patents, copyrights, or other proprietary rights arising from the MCO's or the State's use of any material or information prepared or developed by the MCO in conjunction with the performance of this contract; provided any such use by the State is expressly contemplated by this contract and approved by the MCO. |
| c. | The State, its DEPARTMENTS, officers, employees, contractors, and agents shall cooperate fully in the MCO's defense of any such claim or suit as directed by the MCO. The MCO shall, in any such suit, satisfy any damages for infringement assessed against the State or the DEPARTMENT, be it resolved by settlement negotiated by the MCO, final judgment of a court with jurisdiction after exhaustion of available appeals, consent decree, or any other manner approved by the MCO. |
7.21 Executive Order Number 16
This contract is subject to Executive Order No. 16 of Governor John G. Rowland promulgated August 4, 1999 and, as such, this contract may be cancelled, terminated or suspended by the State for violation of or noncompliance with said Executive Order No. 16. The parties to this contract, as part of the consideration hereof, agree that:
| a. | The MCO shall prohibit employees from bringing into the state work site, except as may be required as a condition of employment, any weapon or dangerous instrument as defined in b. |
| b. | Weapon means any firearm, including a BB gun, whether loaded or unloaded, any knife (excluding a small pen or pocket knife), including a switchblade or other knife having an automatic spring release device, a stiletto, any police baton or nightstick or any martial arts weapon or |
electronic defense weapon. Dangerous instrument means any instrument, article or substance that, under the circumstances, is capable of causing death or serious physical injury.
| c. | The MCO shall prohibit employees from using, attempting to use or threatening to use any such weapon or dangerous instrument in the state work site and employees shall be prohibited from causing or threatening to cause physical injury or death to any individual in the state work site. |
| d. | The MCO shall adopt the above prohibitions as work rules, violations of which shall subject the employee to disciplinary action up to and including discharge. The MCO shall insure that all employees are aware of such work rules. |
| e. | The MCO agrees that any subcontract it enters into in furtherance of the work to be performed hereunder shall contain the provisions (a) through (d). |
8. MCO RESPONSIBILITIES CONCERNING INTERNAL AND EXTERNAL APPEALS
8.01 | MCO Responsibilities Concerning Internal and External Appeals and Notices of Denial |
Members shall have the opportunity to request an internal appeal of a decision made by the MCO regarding the denial of goods and services covered in the basic benefit package. The MCO shall have an internal appeal process for receiving and acting upon these requests. This internal appeals process may consist of more than one level of review. In addition,, the MCO shall provide for an expedited internal appeals process as set forth in Section 8.06 below. The MCO shall also provide information to Members concerning the external appeal process available through the State of Connecticut Department of Insurance (DOI). The MCO shall also have a process for provider appeals, as set forth in Section 8.08.
8.02 Internal Appeal Process Required
| a. | The MCO shall have a timely and organized internal appeal process. The internal appeal process shall be available for resolution of disputes between the MCO or MCO subcontractors and Members concerning the denial of a request for goods and services covered under the HUSKY B benefit package. In addition the MCO shall provide for an expedited internal appeal process as set forth in Section 8.06 below. The MCO shall be responsible for ensuring compliance with the internal appeal process requirements set forth herein, whether the goods or services are denied by the MCO or one of its subcontractors. |
| b. | The MCO shall designate one primary and one back-up contact person for its internal appeal process. |
| a. | The MCO shall provide a written denial notice to the Member, which includes the MCO's denial decision as well as notice of the Member's right to appeal. The denial notice shall be sent to the Member's last known address. |
b. All denial notices shall clearly state or explain:
1. What goods and/or services are being denied;
2. The reasons for the denial;
3. The contract section that supports the denial;
| 4. | The address and toll-free number of the MCO's Member Services Department; |
| 5. | The Member's right to challenge the denial by filing an internal appeal with the MCO; |
| 6. | The procedure and timeframe for commencing each level of the MCO's internal appeals process, including the address to which any written request for appeal may be mailed; |
| 7. | The availability of expedited internal appeal; |
| 8. | The external appeal process available through the DOI; |
| 9. | Specifications and assistance as to the format in which the Member may file a request for an internal appeal. |
| 10. | That the Member will lose his or her right to challenge the denial with the MCO within sixty (60) days from the date the MCO mailed the denial notice; |
| 11. | That for each level of its appeals process, the MCO must issue a decision regarding an appeal no more than thirty (30) days following the date that the MCO receives the request for review |
| 12. | That the MCO must be responsive to questions which the Member may have about the denial; |
| 13. | That the Member may submit additional documentation or written material for the MCO's consideration; and |
| 14. | That the MCO's review may be based solely on information available to the MCO and its providers, unless the Member requests a meeting or the opportunity to submit additional information. |
8.04 Internal Appeal Process
| a. | The MCO shall develop written policies and procedures for each component of its internal appeals process. The MCO's policies and procedures must include the elements specified in this contract and must be approved by the DEPARTMENT in writing. The MCO shall not be excused from meeting the requirements for the policies, procedures and pending the DEPARTMENT'S written approval of these documents. |
| b. | The MCO shall maintain a record keeping system for each level of its appeal process, which shall include a copy of the Member's request for review, the response and the resolution, which the MCO shall make available to the DEPARTMENT upon request. |
| c. | The MCO shall clearly specify in its Member handbook/packet, the procedural steps and timeframes for each level of its internal appeals process and for filing an external appeal through the DOI. The MCO shall provide information on its internal appeals process and on the external DOI appeal process to providers and subcontractors, as it relates to Members. |
| d. | The MCO shall develop and make available to Members and potential Members appropriate alternative language versions of internal appeal materials, including but not limited to, the standard information contained in denial notices. Such materials shall be made available in Spanish, English and any other language(s) if more than five (5) percent of the MCO's Members in the State of Connecticut served by the MCO speak the alternative language. The MCO must submit such alternative language materials to the DEPARTMENT and the DEPARTMENT must approve any such materials in writing prior to use by the MCO. |
| e. | Internal appeals shall be filed by the applicant, the Member, the Member's authorized representative, or the Member's conservator. The Member Handbook shall state that requests for all levels of the internal appeals process shall be mailed or faxed to a single address. |
| f. | If the internal appeal contains a request for expedited review, the MCO shall follow the procedure described in Section 8.06 below. |
| g. | An individual or individuals having final decision-making authority shall conduct the final level of the MCO's review. One or more physicians who were not involved in the denial determination must decide any appeal arising from an action based on a determination of medical necessity. |
| h. | The MCO may decide an appeal on the basis of written documentation available to the MCO at the time of the request, unless the Member requests an opportunity to meet with the individual or individuals conducting the internal appeal on behalf of the MCO and/or requests the opportunity to submit additional written documentation or other written material. The MCO shall inform the Member that the MCO's review may be based solely on information available to the MCO and its providers, unless the Member requests a meeting or the opportunity to submit additional information. |
| i. | If the Member wishes to meet with the decisionmaker, the meeting may be held via telephone or at a location accessible to the Member. |
| j. | The MCO shall date stamp the form when it is received by the MCO. The postmark date on the denial notice envelope will be used to determine whether an appeal was timely filed. |
| a. | The MCO shall issue a written decision for each level of its internal appeals process. Each decision shall be mailed to the Member. The MCO shall send a copy of each decision to the DEPARTMENT. The appeal decision shall be sent no later than thirty (30) days from the date on which the MCO received the appeal. |
| b. | The MCO's written decision must include the Member's name and address; the provider's name and address; the MCO name and address; a complete statement of the MCO's findings and conclusions, including the |
section number and text of any statute or regulation that supports the decision; a clear statement of the MCO's disposition of the appeal; a statement that the Member has exhausted the MCO's internal appeal procedure concerning the denial at issue; and relevant information concerning the external appeals process available through the DOI, as described in Section 8.07, below.
| c. | For each level of its internal appeals process, the MCO shall issue a decision within thirty (30) days. If the MCO fails to issue a decision within thirty (30) days, the DEPARTMENT will deem the decision to be a denial and the Member may file an external appeal with the DOI, as more fully discussed in Section 8.07, below. |
| d. | The MCO shall include a copy of the HUSKY B Program - State of Connecticut - Insurance Department Request for External Appeal form approved by the DEPARTMENT with each written decision. |
| a. | Subject to Section 8.02 above, the internal appeals process must allow for expedited review. If a Member requests an expedited review, the MCO must determine within one business day of receipt of the request, whether to expedite the review or whether to perform the review according to the standard timeframes. |
| b. | An expedited review must be performed when the standard timeframes for determining an appeal could jeopardize the life or health of the Member or the Member's ability to regaining maximum functioning. The MCO must expedite its review in all cases in which such a review is requested by the Member's treating physician or primary care provider, functioning within his or her scope of practice as defined under state law, or by the DEPARTMENT. |
8.07 External Appeal Process through the DOI
| a. | A Member who has exhausted the internal appeal mechanisms of the MCO and is not satisfied with the outcome of the MCO's final decision may file an appeal with the DOI. |
| b. | The MCO shall include the following information concerning the DOI external appeal process in its member handbook: |
| 1. | If the Member has exhausted the MCO's internal appeals process and has received a final written decision from the MCO upholding the MCO's original denial of the good or service, the Member may file an external appeal with the DOI within thirty (30) days of receiving the final written appeal decision; |
| 2. | The Member may be required to file a filing fee for the DOI appeal. The DEPARTMENT shall pay the filing fee on behalf of any |
Member whose family economic filing unit income exceeds 185 percent of the federal poverty level but does not exceed 300 percent of the federal poverty level (Members in Income Bands 1 and 2). If the Member's family economic filing unit's income exceeds 300 percent of the federal poverty level (Income Band 3), the filing unit shall be responsible for the payment of the filing fee;
| 3. | The non-refundable filing fee for an external appeal through the DOI is $25; |
| 4. | The Member will be asked to submit certain information in support of his or her appeal request, including a photocopy of his or her HUSKY B enrollment card. The Member (or the Member's legal representative) will also be asked to sign a release of medical records; |
| 5. | The DOI will assign the appeal to an outside, independent entity. The reviewers will conduct a preliminary review and determine whether the appeal meets eligibility for review. The Member will be notified within five (5) business days of the DOI's receipt of the request whether the appeal has been accepted or denied for full review; |
| 6. | The MCO shall advise Members that they may obtain information about the external review process from the DOI, P.O. Box 816, Hartford, CT 06142 or at (860) 297-3862; and |
7. A copy of the DOI External Appeal Consumer Guide.
c. The MCO shall be bound by the DOI's external appeal decision.
8.08 Provider Appeal Process
| a. | The MCO shall have an internal appeal process through which a health care provider may grieve the MCO decision on behalf of a Member. The MCO shall provide information on the availability of this process to the providers in the MCO's network. |
| b. | The health care provider appeal process shall not include any appeal rights to the DEPARTMENT or any rights to an external appeal through the DOI. |
9. CORRECTIVE ACTION AND CONTRACT TERMINATION
| a. | A designated representative of the MCO and a designated representative of the DEPARTMENT shall meet on an annual basis, and as requested by either party, to review the performance of the MCO under this contract. Written minutes of such meetings shall be kept. In the event of any disagreement regarding the performance of services by the MCO under this contract, the designated representatives shall discuss the problem and shall negotiate in good faith in an effort to resolve the disagreement. |
| b. | In the event that no such resolution is achieved within a reasonable time, the matter shall be referred to the Contract Administrator as provided under Section 9.02, the Disputes clause of this contract. If the Contract Administrator determines that the MCO has failed to perform as measured against applicable contract provisions, the Contract Administrator may impose sanctions or any other penalty, set forth in this Section including the termination of this contract in whole or in part, as provided under this Section. |
9.02 Settlement of Disputes
Any dispute arising under the contract that is not disposed of by agreement shall be decided by the Contract Administrator whose decision shall be final and conclusive subject to any rights the MCO may have in a court of law. The foregoing shall not limit any right the MCO may have to present claims under Connecticut General Statutes Section 4-141 et. seq. or successor provisions regarding the Claims Commissioner, including without limitation Connecticut General Statutes Section 4-160 regarding authorization of actions. In connection with any appeal to the Contract Administrator under this paragraph, the MCO shall be afforded an opportunity to be heard and to offer evidence in support of its appeal. Pending final decision of a dispute, the MCO shall proceed diligently with the performance of the contract in accordance with the Contract Administrator's decision.
9.03 Administrative Errors
The MCO shall be liable for the actual amount of any costs in excess of $5,000 incurred by the DEPARTMENT as the result of any administrative error (e.g., submission of capitation, encounter or reinsurance data) of the MCO or its subcontractors. The DEPARTMENT may request a refund of, or recoup from subsequent capitation payments, the actual amount of such costs.
9.04 Suspension of New Enrollment
Whenever the DEPARTMENT determines that the MCO is out of compliance with this contract, unless corrective action is taken to the satisfaction of the DEPARTMENT, the DEPARTMENT may suspend enrollment of new Members under this contract. The DEPARTMENT, when exercising this option, must notify the MCO in writing of its intent to suspend new enrollment at least thirty (30) days prior to the beginning of the suspension period. The suspension period may be for any length of time specified by the DEPARTMENT, or may be indefinite. The suspension period may extend up to the contract expiration date as provided under PART I. (The DEPARTMENT may also notify existing Members of MCO non-compliance and provide an opportunity to disenroll from the MCO and to re-enroll in another MCO.)
It is agreed by the DEPARTMENT and the MCO that if by any means, including any report, filing, examination, audit, survey, inspection or investigation, the MCO is determined to be out of compliance with this contract, damage to the DEPARTMENT may or could result. Consequently, the MCO agrees that the DEPARTMENT may impose any of the following sanctions for noncompliance under this contract. Unless otherwise provided in this contract, sanctions imposed under this section shall be deducted from capitation payment or, at the discretion of the DEPARTMENT, paid directly to the DEPARTMENT.
a. Sanctions for Noncompliance
1. | Class A Sanctions. Three (3) Strikes. Sanctions Warranted After Three (3) Occurrences. |
For noncompliance of the contract which does not rise to the level warranting Class B sanctions as defined in subsection a (2) of this section or Class C sanctions as defined in subsection (b) of this section, including, but not limited to, those violations defined as Class A sanctions in any provision of this contract, the following course of action will be taken by the DEPARTMENT:
| a) | Each time the MCO fails to comply with the contract on an issue warranting a Class A sanction, the MCO receives a strike. |
| b) | The MCO will be notified each time a strike is imposed. After the third strike for the same contract provision a sanction may be imposed. If no specific time frame is set forth in any such contractual provision, the time frame is deemed to be the full length of the contract. |
| c) | The MCO will be notified in writing at least thirty (30) days in advance of any sanction being imposed and will be given an opportunity to meet with the DEPARTMENT to present its |
position as to the DEPARTMENT'S determination of a violation warranting a Class A sanction. At the DEPARTMENT'S discretion, a sanction will thereafter be imposed. Said sanction will be no more than $2,500 after the first three strikes. The next strike for noncompliance of the same contractual provision will result in a sanction of no more than $5,000 and any subsequent strike for noncompliance of the same contractual provision will result in a Class A sanction of no more than $10,000.
2. | Class B Sanctions. Sanctions Warranted Upon Single Occurrence. |
For noncompliance with the contract which does not warrant the imposition of Class C sanctions as defined in subsection (b) of this section, including, but not limited to, those violations defined as Class B sanctions in any provision of this contract, the following course of action will be taken by the DEPARTMENT:
a) The DEPARTMENT may impose a sanction at the DEPARTMENT'S discretion if, after at least thirty (30) days notice to the MCO and an opportunity to meet with the DEPARTMENT to present the MCO's position as to the DEPARTMENT'S determination of a violation warranting a Class B sanction, the DEPARTMENT determines that the MCO has failed to meet a performance measure which merits the imposition of a Class B sanction not to exceed $10,000.
| b. | Class C Sanctions. Sanctions Related to Noncompliance Potentially Resulting in Harm to an Individual Member |
| 1. | The DEPARTMENT may impose a Class C sanction on the MCO for noncompliance potentially resulting in harm to an individual Member, including, but not limited to, the following: |
| a) | Failing to substantially authorize medically necessary items and services that are covered (under law or under this contract) to be provided to a Member covered under this contract, up to any applicable allowance; |
| b) | Imposing a premium or copay on Members in excess of that specifically permitted under provisions of the contract; |
| c) | Discriminating among Members on the basis of their health status or requirements for health care services, including expulsion or refusal to re-enroll an individual, except as permitted by law or under this contract, or engaging in any practice that would reasonably be expected to have the effect of denying or discouraging enrollment with the MCO by eligible individuals whose medical condition or history indicates a need for substantial future medical services; |
| d) | Misrepresenting or falsifying information that is furnished to the Secretary, the DEPARTMENT, Member, potential Member, or a health care provider; and |
| e) | Distributing directly or through any agent or independent contractor marketing materials containing false or misleading information. |
| 2. | Class C sanctions for noncompliance with the contract under this subsection includes the following: |
| a) | Withholding the next month's capitation payment to the MCO in full or in part; |
| b) | Assessment of liquidated damages: |
| 1) | For each determination that the MCO fails to substantially provide medically necessary services, not more than $25,000; |
| 2) | For each determination that the MCO discriminates among Members on the basis of their health status or requirements for health care services or engages in any practice that has the effect of denying or discouraging enrollment with the MCO by eligible individuals based on their medical condition or history that indicates a need for substantial future medical services, or the MCO misrepresents or falsifies information furnished to the Secretary, DEPARTMENT, Member, potential Member or health care provider, not more than $100,000; |
| 3) | For each determination that the MCO has discriminated among Members or engaged in any practice that has denied or discouraged enrollment, $15,000 for each individual not enrolled as a result of the practice up to a total of $100,000; for a determination that the MCO has imposed premiums or co-payments on Members in excess of the premiums or co- payments permitted, double the excess amount. The excess amount charged in such a circumstance must be deducted from the penalty and returned to the Member concerned; |
| c) | Freeze on new enrollment and/or alter the current enrollment; or |
| d) | Appointment of temporary management upon a finding by the DEPARTMENT that there is continued egregious behavior by the MCO or there is a substantial risk to the health of the Members. After a finding pursuant to this subsection, Members enrolled with the MCO must be permitted to terminate enrollment without cause and the MCO shall be responsible for notification of such right to terminate enrollment. Nothing in this subsection shall preclude the DEPARTMENT from proceeding under the termination provisions of the contract rather than |
appointing temporary management. If however, the DEPARTMENT chooses not to first terminate the contract and repeated violations occur, the DEPARTMENT must than appoint temporary management of the MCO and allow individuals to disenroll without cause.
| 3. | Prior to imposition of any Class C sanction, the MCO will be notified at least thirty (30) days in advance and provided, at a minimum, an opportunity to meet with the DEPARTMENT to present its position as to the DEPARTMENT'S determination of a violation warranting a Class C Sanction. For any contract violation under this subsection, at the DEPARTMENT'S discretion, the MCO may be permitted to submit a corrective action plan within twenty (20) days of the notice to the MCO of the violation. Immediate compliance (within thirty (30) days) under any such corrective action plan may result in the imposition of a lesser sanction on the MCO. If any sanction issued under this subsection is equivalent to termination of the contract, the MCO shall be offered a hearing to contest the imposition of such a sanction. |
| 1. | Notwithstanding the provisions of this section, failure to provide required services will place the MCO in default of this contract, and the remedies in this section are not a substitute for other remedies for default which the DEPARTMENT may impose as set forth in this contract. |
| 2. | The imposition of any sanction under this section does not preclude the DEPARTMENT from obtaining any other legal relief to which it may be entitled pursuant to state or federal law. |
9.06 Payment Withhold, Class C Sanctions
| a. | The DEPARTMENT may withhold capitation payments from the MCO as provided in Section 9.05 or terminate the contract for cause. Cause shall include, but not be limited to: |
| 1. | Use of funds and/or personnel for purposes other than those described in the HUSKY B program and this contract and |
| 2. | If a civil action or suit if federal or state court involving allegations of health fraud of violation of 18 U.S.C. Section 1961 et seq is brought on behalf of the DEPARTMENT. |
| b. | Whenever the DEPARTMENT determines that the MCO has failed to provide one or more of the medically necessary contract services required, the DEPARTMENT may withhold an estimated portion of the MCO's capitation payment in subsequent months, such withhold to be equal to the amount of money the DEPARTMENT expects to pay for such services, plus any administrative costs involved. The MCO may not elect |
to withhold any required services in order to receive adjusted payment levels. Failure to provide required services will place the MCO in default of this contract, and the remedies in this section are not a substitute for other remedies for default which the DEPARTMENT may impose as set forth in this contract. The MCO shall be given at least seven (7) days written notice prior to the withholding of any capitation payment.
| c. | When it withholds payments under this section, the DEPARTMENT must submit to the MCO a list of the Members for whom payment is being withheld, the nature of service(s) denied, and payments the DEPARTMENT must make to provide medically necessary services. When all payments have been made by the DEPARTMENT for the MCO contracted services, the DEPARTMENT will reconcile the estimated withhold against actual payments. |
| d. | The DEPARTMENT may also adjust payment levels accordingly if the MCO has failed to maintain or make available any records or reports required under this contract which the DEPARTMENT needs to determine whether the MCO is providing required contract services. The MCO will be given at least thirty (30) days notice prior to taking any action set forth in this paragraph. |
9.07 Emergency Services Denials
If the MCO has a pattern of inappropriately denying payments for emergency services as defined in Part II, Definitions, it may be subject to suspension of new enrollments, withholding of capitation payments, contract termination, or refusal to contract in a future time period. This applies not only to cases where the DEPARTMENT has ordered payment after appeal, but also to cases where no appeal has been made (i.e., the DEPARTMENT is knowledgeable about documented abuse from other sources.)
9.08 Termination For Default
| a. | The DEPARTMENT may terminate performance of work under this contract in whole, or in part, whenever the MCO materially defaults in performance of this contract and fails to cure such default or make progress satisfactory to the DEPARTMENT toward contract performance within a period of thirty (30) days (or such longer period as the DEPARTMENT may allow). Such termination shall be referred to herein as "Termination for Default." |
| b. | If after notice of termination of the contract for default, it is determined by the DEPARTMENT or a court that the MCO was not in default, the notice of termination shall be deemed to have been rescinded and the contract reinstated for the balance of the term. |
| c. | In the event the DEPARTMENT terminates the contract in full or in part as provided in this clause, the DEPARTMENT may procure services similar |
to those terminated, and the MCO shall be liable to the DEPARTMENT for any excess costs for such similar services for any calendar month for which the MCO has been paid to provide services to HUSKY B Members. In addition, the MCO shall be liable to the DEPARTMENT for administrative costs incurred by the DEPARTMENT in procuring such similar services. Provided, however, that the MCO shall not be liable for any excess costs or administrative costs if the failure to perform the contract arises out of causes beyond the control and without error or negligence of the MCO or any of its subcontractors.
| d. | In the event of a termination for default, the MCO shall be financially responsible for Members in the current month at the applicable capitation rate. |
| e. | The rights and remedies of the DEPARTMENT provided in this clause shall not be exclusive and are in addition to any other rights and remedies provided by law or under this contract. |
| f. | In addition to the termination rights under Part I Section 8, the MCO may terminate this contract on ninety (90) days written notice in the event that the DEPARTMENT fails to (a) pay capitation claims in accordance with Part II Section 6.05 and Part III Section 3.01 of this contract (b) provide eligibility or enrollment/disenrollment information and shall fail to cure such default or make progress satisfactory to the MCO within a period of sixty (60) days of such default. |
9.09 Termination for Mutual Convenience
The DEPARTMENT and the MCO may terminate this contract at any time if both parties mutually agree in writing to termination. At least sixty (60) days shall be allowed. The effective date must be the first day of a month. The MCO shall, upon such mutual agreement being reached, be paid at the capitation rate for enrolled Members through the termination of the contract.
9.10 Termination for Financial Instability of the MCO
In the event of financial instability of the MCO, the DEPARTMENT shall have the right to terminate the contract upon the same terms and conditions as a Termination for Default.
9.11 Termination for Unavailability of Funds
| a. | The DEPARTMENT at its discretion may terminate at any time the whole or any part of this contract or modify the terms of the contract if federal or state funding for the contract or for the HUSKY B program as a whole is reduced or terminated for any reason. Modification of the contract includes, but is not limited to, reduction of the rates or amounts of consideration, reducing services covered by the MCO or the alteration of the manner of the performance in order to reduce expenditures under the |
contract. Whenever possible, the MCO will be given thirty (30) days notification of termination.
| b, | In the event of a reduction in the appropriation from the state or federal budget for the Division of Health Care Financing of the Department of Social Services or an across-the-board budget reduction affecting the Department of Social Services, the DEPARTMENT may either re negotiate this contract or terminate with thirty (30) days' written notice. Any reduction in the capitation rates that is agreed upon by the parties or any subsequent termination of this contract by the DEPARTMENT in accordance with this provision shall only affect capitation payments or portions thereof for covered services purchased on or after the effective date of any such reduction or termination. Should the DEPARTMENT elect to renegotiate the contract, the DEPARTMENT will provide the MCO with those contract modifications, including capitation rate revisions, it would deem acceptable. |
| c. | The MCO shall have the right not to extend the contract if the new contract terms are deemed to be insufficient notwithstanding any other provision of this contract. The MCO shall have a minimum of sixty (60) days to notify the DEPARTMENT regarding its desire to accept new terms. If the new capitation rates and any other contract modifications are not established at least sixty (60) days prior to the expiration of the initial or extension agreement, the DEPARTMENT will reimburse the MCO at the higher of the new or current capitation rates for that period during which the new contract period had commenced and the MCO's 60-day determination and notification period had not been completed, and the MCO will be held to the terms of the executed contract. |
9.12 Termination for Collusion in Price Determination
| a. | In competitive bidding markets, the MCO has previously certified that the prices presented in its proposal were arrived at independently, without consultation, communication, or agreement with any other bidder for the purpose of restricting competition; that, unless otherwise required by law, the prices quoted have not been knowingly disclosed by the MCO, prior to bid opening, directly or indirectly to any other bidder or to any competitor; and that no attempt has been made by the MCO to induce any other person or firm to submit or not to submit a proposal for the purpose of restricting competition. |
| b. | In the event that such action is proven, the DEPARTMENT shall have the right to terminate this contract upon the same terms and conditions as a Termination for Default. |
9.13 Termination Obligations of Contracting Parties
| A | The MCO shall be provided the opportunity for a hearing prior to any termination of this contract pursuant to any provision of this contact. The |
DEPARTMENT may notify Members of the MCO and permit such Members to disenroll immediately without cause during the hearing process.
| b. | Upon contract termination, the MCO shall allow the DEPARTMENT, its agents and representatives full access to the MCO's facilities and records to arrange the orderly transfer of the contracted activities. These records include the information necessary for the reimbursement of any outstanding HUSKY B claims. |
| c. | If this contract is terminated for any reason other than default by the MCO: |
| 1. | The MCO shall ensure that an adequate provider network will be maintained at all times during the transition period and that continuity of care is maintained for all Members; |
| 2. | The MCO shall submit a written transition plan to the DEPARTMENT sixty (60) days in advance of the scheduled termination; |
| 3. | The DEPARTMENT shall be responsible for notifying all Members of the date of termination and process by which the Members will continue to receive services; |
| 4. | The DEPARTMENT shall be responsible for all expenses relating to said notification; |
| 5. | The MCO shall notify all providers and be responsible for all expenses related to such notification; and |
| 6. | The DEPARTMENT shall withhold a portion, not to exceed $100,000, of the last month's capitation payment as a surety bond for a six (6) month period to ensure compliance under the contract. |
Waiver of any default shall not be deemed to be a waiver of any subsequent default. Waiver of breach of any provision of the contract shall not be deemed to be a waiver of any other or subsequent breach and shall not be construed to be a modification of the terms of the contract unless stated to be such in writing, signed by an authorized representative of the DEPARTMENT, and attached to the original contract.
If any provision of this procurement or the resultant contract is declared or found to be illegal, unenforceable, or void, then both parties shall be relieved of all obligations under that provision. The remainder of this procurement or the resultant contract shall be enforced to the fullest extent permitted by law.
This contract is subject to review for form and substance by and will not become effective until it is approved by the DEPARTMENT.
10.03 Order of Precedence
This contract shall be read together to achieve one harmonious whole. However, should any irreconcilable conflict arise between Part I and Part II of this contract, Part II shall prevail.
10.04 Correction of Deficiencies
This contract does not release the MCO from its obligation to correct any and all outstanding certification deficiencies. Failure to correct all outstanding material deficiencies may cause the MCO to be determined in Default of this contract.
10.05 This is not a Public Works Contract
The DEPARTMENT and the MCO as parties to this purchase of service Contract mutually covenant, acknowledge and agree that this contract does not constitute and shall not be construed to constitute a public works contract. The DEPARTMENT and the MCO's mutual agreement that this contract is not a public works contract shall have full force and effect on Part I Section 32 and other Sections of this contract as applicable.
HUSKY B - APPENDIX A: Covered Benefits
Benefit Features | HUSKY Coverage | |
Outpatient Physician Visits | $5 co-pay | * |
Preventive Care | No co-pay Periodic and well child visits, immunizations, WIC evaluations as applicable, and prenatal care covered in full with $5 co-pay on other visits. Periodicity schedule and reporting based on the American Academy of Pediatrics (AAP) as amended from time to time: Age Category # of Exams Birth to Age 1 6 exams Ages 1-5 6 exams Ages 6-10 1 exam every 2 years Ages 11-19 1 exam every year. Immunization schedule per the Advisory Committee on Immunization Practices (ACIP), as amended from time to time. As of January 1, 2001, the schedule is as follows: Age CategoryVaccine Type BirthHepatitis B-1st dose 1-4 monthsHepatitis B-2nd dose 2 monthsDiphtheria, Tetanus, Pertussis (DTP) 1st dose; Haemophilus Influenza Type B (hib)-1st dose; Polio (OVP)-1st dose 4 monthsDiphtheria, Tetanus, Pertussis (DTP) 2nd dose; Haemophilus Influenza Type B (hib)- 2nd dose; Polio (OVP)- 2nd dose 6 monthsDiphtheria, Tetanus, Pertussis (DTP) 3rd dose; Haemophilus Influenza Type B (hib)-3rd dose 6-12 monthsHepatitis B-3rd dose; Polio (OVP)-3rd dose 12-15 monthsHaemophilus Influenza Type B (hib)-3rd dose; Measles, Mumps, Rubella (MMR)-1st dose 12-18 monthsChicken Pox (Var)-single dose; Diphtheria, Tetanus, Pertussis (DTP) 4th dose 4-6 yearsDiphtheria, Tetanus, Pertussis (DTP) 5th dose; Measles, Mumps, Rubella (MMR)-2nd dose; Polio (OVP)-4th dose 11-12 yearsTetanus Diphtheria (Td) Influenza: Every year beginning at 6 months for children who have serious long-term health problems such as heart disease, lung disease, kidney disease, metabolic disease, diabetes, asthma, anemia, and/or are on long term aspirin treatment Pneumococcal: Vaccinate children 2 years and older who are at risk of pneumococcal disease or its complications | * |
Family Planning | 100% Family Planning Services include: Reproductive health exams; Patient Counseling; Patient Education; Lab tests to detect the presence of conditions affecting reproductive health; Screening, testing and treatment; Pre and post-test counseling for sexually transmitted diseases and HIV; Abortions that are necessary to save the life of the mother or if the pregnancy resulted from rape or incest or if pregnancy resulted from rape or incest and other medically necessary abortions as defined in Section 3.14 of the contract. | |
| Preventative Family Planning Services | 100% | * |
| Oral Contraceptives | $5 co-pay (included in prescription drugs) | * |
Inpatient Physician | 100% | * |
Inpatient Hospital | 100% | |
Outpatient Surgical Facility | 100% | |
Ambulance | 100% if determined to be an emergency in accordance with state law | |
Pre-Admission /Continued Stay | Arranged through provider. | |
Prescription Drug | $3 co-pay on generics $5 co-pay on oral contraceptives $6 co-pay on brand-name formularies | * |
Short Term Rehabilitation | 100% For conditions where significant improvement is expected within 60 days including: Physical Therapy; Speech Therapy; Occupational Therapy; and Skilled Nursing Care (excludes private duty nursing) | |
Home Health Care | 100% Includes Disposable medical supplies for homebound members Excludes: Custodial care, homemaker care or care that may be provided in a medical office, hospital or skilled nursing facility and offered to the member is such setting. | |
Hospice | 100% provided to members who are diagnosed as having a terminal illness with a life expectancy of six months or less. Covered care includes Nursing care; Physical therapy, Speech therapy, and Occupational therapy; Medical social services; Home health aides and homemakers; Medical supplies; Drugs; Appliances; DME; Physician services; Short-term inpatient care, including respite care and care for pain control and acute and chronic symptom management; services of volunteers and other benefits when ordered by a physician. Limitations on short-term therapies do not apply. | |
Long Term: Rehabilitation; Physical Therapy; Skilled Nursing Care | Not covered under HUSKY B. Supplemental coverage available under HUSKY Plus Physical for medically eligible children. | |
Lab and X-Ray | 100% | |
Pre-Admission Testing | 100% | |
Emergency Care | 100% if determined to be an emergency in accordance with state law. $25 co-pay if determined a non-emergency. $25 co-pay waived if the patient is admitted. | * |
Durable Medical Equipment (DME) | DME means equipment that is furnished by a supplier or home health agency that: 1.can withstand repeated use; 2.is primarily and customarily used to serve a medical purpose; 3.is generally not useful to an individual in the absence of an illness or injury; and 4.is appropriate for use in the home 100 % covered except DME does not include: · Power wheelchairs for members who are eligible for HUSKY Plus Physical; · Devices not medical in natures such as: · whirlpools, · saunas, · elevators, · vans, · van lifts, · home convenience items (e.g., air cleaners, filtration units and related apparatus, exercise bicycles and other types of exercise equipment), · insulin injectors, · non-rigid appliances and supplies, such as, sheets, self-help devices, experimental or investigational research equipment, and · items for personal comfort and or usefulness to the member’s household. Supplemental coverage available under HUSKY Plus Physical for medically eligible children. | |
Hearing Aids | Hearing aids for children twelve years of age or younger, limited to $1,000.00 within a 24-month period. Supplemental coverage available under HUSKY Plus for medically eligible children | |
Prosthetics | 100% Includes: Devices whether worn anatomically or surgically implanted, which replace all or part of a body organ or structure and which correct, strengthen or provide necessary support to the body will be covered when medically necessary. Excludes: Orthopedic shoes, foot orthotics, wigs or hairpieces. Supplemental coverage available under HUSKY Plus Physical for medically eligible children | |
Eye Care Eye Exams | 5$ co-pay | * |
Hearing Exam | $5 co-pay | * |
Nurse Midwives | $5 co-pay (except for preventative services) | * |
Nurse Practitioners | $5 co-pay (except for preventative services) | * |
Podiatrists | $5 co-pay | * |
Chiropractors | $5 co-pay | * |
Naturopaths | $5 co-pay | * |
Dental | 100% Dental Services include: Exams, 1 every 6 months; X-rays, Fillings; Fluoride Treatments; Oral Surgery | * |
Limited Benefits
Benefit Features | HUSKY Coverage | |
Eye Care Eyeglass frames and lenses or contact lenses | Once every 2 consecutive eligibility periods with an allowance of $100 toward the purchase of these goods. The optical hardware must be provided without charge under the following conditions: (i)One pair of contact lenses every 2 consecutive eligibility periods when such lenses are determined to be the primary and the best method for aiding the member vision and the lenses are not needed solely for the correction of vision; (ii)Eyeglass frames and lenses and contact lenses that are determined to be medically necessary after eye surgery, the initial pair only; and (iii)Contact lenses, as needed, for the treatment of Keratonconus. | |
Dental Orthodontia | $725 allowance per orthodontia case. | |
| Bridges or crowns; root canals; full or partial dentures; or extractions | $50 allowance per procedure, per member but no more than an aggregate allowance for all such procedures of $250 per eligibility period. | |
Contraceptives Intruterine Devices (IUD) and insertion of the IUD | $50 allowance per member | * |
| Internally implantable time-release devices and their insertion | $50 allowance per member | * |
| Time-released contraceptive injections | $15 allowance per member per injection | * |
Nutritional Formulas | 100% Limited to medically necessary amino acid modified preparations and low protein modified food products for the treatment of inherited metabolic diseases when ordered by a participating physician | * |
Annual co-payments cannot exceed $760/$1350 (Income Band 1/Income Band 2) including premiums, per year.
`Note: Prior authorization may be required by the MCO unless otherwise noted by an asterisk (*). Co-payment not required for preventive services.
EXCLUSIONS AND LIMITATIONS
| 1. | Services and/or procedures considered to be of an unproven, experimental, or research nature or cosmetic, social, habilitative, vocational, recreational, or educational. |
| 2. | Services in excess of those deemed medically necessary to treat the patient’s condition. |
| 3. | Services for a condition that is not medical in nature. |
| 4. | Devices required by third parties, such as school or employment physicals, physicals for summer camp, enrollment in health, athletic, or similar clubs, premarital blood work or physicals, or physicals required by insurance companies or court ordered alcohol or drug abuse course. |
| 5. | Cosmetic and reconstructive surgery is excluded, except when surgery is required for: |
| a) | reconstructive surgery in connection with the treatment of malignant tumors or other destructive pathology that causes dysfunction; |
| b) | reduction mammoplasty in females when Medically Necessary and breast surgery in males only in cases of suspected malignancy. Surgery must be necessary to achieve normal physical or bodily function. |
| 6. | Routine foot care rendered: |
| a) | in the examination, treatment or removal of all or part of corns, callosities, hypertrophy or hyperplasia of the skin or subcutaneous tissues of the foot. |
| b) | in the cutting, trimming or other non-operative partial removal of toenails, except when Medically Necessary in the treatment of neuro-circulatory conditions. |
| 7. | Evaluation, treatment and procedures related to, and performance of, sex-change operations. |
| 8. | Surgical treatment or hospitalization for the treatment of morbid obesity except where prior authorized Medically Necessary. |
| 9. | Care, treatment, procedures, services or supplies that are primarily for dietary control including, but not limited to, any exercise weight reduction programs, whether formal or informal, and whether or not recommended by an In-network Physician or Out-of-Network Physician. |
| 10. | Acupuncture, biofeedback, or hypnosis. |
| 11. | Treatment at pain clinics unless determined to be Medically Necessary. |
| 12. | Ambulatory blood pressure monitoring. |
| 13. | Any court order for testing, diagnosis, care, or treatment deemed not Medically Necessary. |
`Note: Prior authorization may be required by the MCO unless otherwise noted by an asterisk (*). Co-payment not required for preventive services.
Appendix B
Husky Plus Behavioral - Deleted
Appendix C
HUSKY Plus
HUSKY PLUS
SUPPLEMENTAL INSURANCE COVERAGE
On October 29, 1997, the Connecticut legislature authorized the establishment of the HUSKY, Part B and HUSKY Plus insurance programs to provide health care coverage for uninsured children pursuant to Title XXI of the Social Security Act. HUSKY, Part A is the program for children’s coverage under Title XIX of the Social Security Act. The HUSKY Plus program was originally comprised of two supplemental health insurance programs to provide services to children whose intensive medical and/or behavioral health needs cannot be accommodated within the basic benefit package offered under HUSKY, Part B. Effective January 1, 2006 the supplemental health insurance program that covered children with intensive behavioral health needs, HUSKY Plus Behavioral (HPB) was eliminated. Emergency mobile, case management, and rehabilitative services previously covered under HPB are now covered under the core HUSKY B benefit package (see Sec. 6.2 and Appendix 6.1). This appendix only addresses the HUSKY Plus Physical program, the program designed to provide coverage to children with intensive physical health needs. General Features of the HUSKY Plus Physical Program
The HUSKY Plus Physical (HPP) Plan is a supplemental benefit package for children who are eligible for and enrolled in HUSKY, Part B, with household incomes under 300% of the federal poverty limit (Income bands 1 and 2 only). Children may not apply for coverage under HUSKY Plus unless they have already been determined to be eligible under HUSKY, Part B, and have enrolled in HUSKY, Part B.
Children who are eligible under HPP will be dually eligible. That is, children who are determined to be eligible under HPP will continue to receive benefits under HUSKY, Part B, including those physical health services for their special needs diagnoses or conditions that are covered under Part B.
As described below, these services will be coordinated by a case management/treatment team composed of case managers from both HUSKY, Part B and one or both of the HUSKY Plus Physical plan, which will maximize the coordination of benefits under both plans and other sources of coverage through federal, state and private support. The case management/treatment team will need to coordinate the development of the Global Plan of Care (GPC) so that services included do not replicate special education services authorized under an Individual Education Plan (I.E.P.) or Individualized Family Service Plan (I.F.S.P.).
In the event that the child is eligible for HUSKY, Part B and HPP, the case management team leader of HPP will need to coordinate with the HUSKY, Part B case manager to assure that the HPP GPC’s complements services provided under HUSKY, Part B.
However, ultimate utilization management decisions will rest with the utilization managers of the plan that is financially at risk; i.e., HUSKY, Part B utilization managers will have final decision making authority for those services for which they are at risk and HPP utilization managers will have the decision making authority for those supplemental services included in their benefit package.
In the event there is a dispute between the participating HUSKY, Part B managed care plan and the HPP concerning the responsibility for reimbursement of a service authorized under the treatment plan, the dispute will be referred to the Commissioner (or his/her designee) for resolution.
Eligible children will be able to receive services under both the basic and one or both supplemental benefit package simultaneously in order to allow both plans to provide services to the child to the fullest extent possible in the least restrictive setting.
HPP services may supplement HUSKY, Part B services once a child has exhausted his or her annual benefit limits under Part B. However, HPP will always be the payer of last resort. The case management/treatment team will always look to exhaust all medically necessary coverage benefits under HUSKY, Part B, including conversion options when appropriate, before these services are supplanted or replaced by services available under HPP .
II. HUSKY Plus Plan for Children with Special Physical Health Care Needs
Program Administration
The HUSKY Plus Plan for Children with Special Physical Health Care Needs (HPP) will be administered by the Connecticut Children’s Medical Center. The advisory committee established by the Department of Public Health for Title V of the Social Security Act will be the Steering Committee for the HPP plan along with representatives from the Departments of Social Services (DSS) and Children and Families (DCF). The Steering Committee shall be named the Steering and Advisory Committee for Children with Special Health Care Needs and HUSKY Plus Physical (SASH).
Eligibility
Children enrolled in HUSKY, Part B, Income Bands 1 and 2, who have intensive physical health needs that cannot be met within the Part B benefit package will be eligible for supplemental services under the HPP plan if they meet the clinical eligibility standard. The clinical eligibility standard is based on diagnostic and/or acuity criteria and shall be the same as those for the Title V program currently operating in the state.
Clinical eligibility will be determined:
| 1. | By documentation of clinical information which meets the “Medical Eligibility Criteria” of the Department of Public Health Title V Program; or |
| 2. | By meeting the approved definition of Children with Special Health Needs with documentation of clinical evidence. The definition adopted by the Steering Committee but subject to change is as follows: |
“Children with Special Health Care Needs are those who have or are at elevated risk for (biologic or acquired) chronic physical or developmental conditions and who also require health and related (not educational and not recreational) services of a type and amount not usually required by children of the same age (beyond Connecticut’s EPSDT periodicity schedule). The age of eligibility is birth to 18 years, but may include those to age 21 (for those determined eligible before age 18) for purposes of transition to adult services.” . In addition, eligibility for HPP will end at age 19, when eligibility for HUSKY, Part B also ends.
For the purposes of determining acuity of a child who meets the Medical Eligibility Criteria or who may qualify as a Child with Special Health Care Needs, the HPP Center will use the Children with Special Health Care Needs Screening Tool, or others as approved by the Department (See attached).
Referral and Application Process
Children who may be at risk may be identified by their parents, their primary care provider, or another provider in the HUSKY, Part B Plan in which the child is enrolled. Referral made by made in writing or by telephone by any of the above parties. However, the application process for HPP will be coordinated by the HUSKY, Part B Plan.
Children will be assessed for eligibility consistent with the practices and procedures currently in place under the Title V Program.
Covered Services
All children determined eligible for HPP will receive care coordination, advocacy, family support and case management services as well as comprehensive multidisciplinary evaluation once a year and up to 3 follow-up visits per year with members of the multidisciplinary group as needed. In addition, the range of services will include the following to the extent that they are not covered under the HUSKY, Part B benefit package:
· | Adaptive Seating, Specialized: One evaluation, fabrication and completion per year. Fees are inclusive of one adjustment every 2 weeks until family is satisfied. |
· | Audiometry: Includes BAER, OAE; two per year. |
· | Cast Room: Cast room visits as necessary to maintain integrity of cast or to implement treatment plan. |
· | Diagnostic Imaging (i.e., MRI, CT): |
· | Durable Medical Equipment: Exclusive of the basic HUSKY B plan and include items that assist in the activities of daily living |
· | EEG/telemetry: Two per year. |
· | EKG/Holter: Two per year. |
· | Emergency Care: Exclusive of the basic plan; directly related to condition that qualifies child for HPP. |
| · | Gait Analysis: One per year. |
| · | General Dental, Orthodontic: Only for children who have malocclusive disorders or periodontal disease resulting from their underlying qualifying condition or related treatment. |
| · | Hearing Aids: One (or one pair) analog hearing aid(s) as prescribed per year; One (or one pair) digital hearing aid(s) as prescribed every 5 years |
· | Home Health Aide: Total of ten hours/week |
· | Medical and Surgical Supplies |
· | Medical Nutrition Services |
· | Medical 23 Hour and Day Surgery |
· | Occupational, Physical and Speech Therapies |
| · | Orthotic Devices: No more than one a year or one pair per year per prescribed type, including all delivery fees, fittings and adjustments. |
· | Pharmacy: Over the Counter medications will be covered if medically necessary and directly related to the condition that qualifies the child for the program. Prior authorization by DSS required. |
· | Physician Fees for Inpatient Care: Visits must be requested as consultations by the admitting physician and be specifically related to the qualifying condition. |
· | Physician Fees for Outpatient Care: Covered as per care plan. |
· | Prosthetics/Prosthetic Devices: No more than one per year including all delivery fees, fittings and adjustments/repairs. Excludes myoelectric devices. |
· | Pulmonary Function Testing: One per year. |
· | Skilled Intermittent Nursing: One visit per day for evaluation, treatment, and education. Must be provided by a licensed home health agency. |
· | Sleep Study/Polysomography: One per year. |
· | Special Nutritional Formulas or Supplements/ PKU Foods: Nutritional habilitative and/or rehabilitative sustenance of a type or amount not usually required by children. Prescribed by an authorized professional within acceptable standards of the American Dietetic Association. |
· | Transportation: 2 round trips per year to any health care appointment by ambulance, chair-vans and/or other licensed medical transportation for non-emergent visits. |
· | Wheelchairs: One new manual wheelchair no more than every three years. One new motorized wheelchair no more than every five years. |
This list may be revised from time to time as recommended by the Steering Committee and approved by the Department.
Service Providers
The Connecticut Children’s Medical Center will serve as the coordinating organization. but services will be provided by the entities under contract to provide Title V services.
Service Utilization Management
Service utilization will be managed through a clear definition of medical necessity. “Medical Necessity” or “medically necessary” is defined as health care provided to correct or diminish the adverse effects of a medical condition or mental illness; to assist an individual in attaining or maintaining an optimal level of health; to diagnose a condition; or prevent a medical condition from occurring.
All services will be subject to prior authorization by the utilization management staff at the Connecticut Children’s Medical Center. These decisions will be subject to the process for Grievances and Appeals (see below).
Coordination of HPP Services with HUSKY, Part B
In order to ensure that HPP will be the documented payer of last resort, the HPP Center shall assign each enrollee with a case manager and provide care coordination services. The HPP case manager shall coordinate with the HUSKY, Part B case manager to ensure that all medically necessary HPP covered services identified in the global plan of care (GPC), which are also covered in the HUSKY, Part B basic benefit package, are exhausted first under HUSKY, Part B.
The HPP Center shall designate a Lead Case Manager who will be responsible for convening a case management/treatment team that will develop an individualized GPC for each enrollee. The case management/treatment team may be composed of, but not limited to, the enrollee or enrollee’s parent(s), treating clinicians and/or providers, the HUSKY, Part B Case Manager, and the Lead Case Manager. The case management/treatment team will coordinate the development of the GPC so that covered services included in the GPC do not replicate special education services authorized under an I.E.P. or I.F.S.P.
In the event that the enrollee is also eligible for HPB, the case management/treatment team shall include the case manager from HPB. The case management/treatment team shall develop a GPC that integrates services from HUSKY, Part B, HPP and HPB as appropriate.
Global Plan of Care (GPC)
HPP will ensure that the case management/treatment team completes the GPC for each enrollee within 30 days of the date of eligibility determination. The case management/treatment team on at least a semi-annual basis will reassess the GPC. The GPC will be based on the comprehensive need assessment, periodic reassessments, and treatment plans from the HUSKY, Part B Plan and HPP Contractor providing services to the child. The GPC will include medical management recommendations reflecting the level of involvement of the HPP staff and the scope of clinical practice of the clinical staff, estimates of the need and frequency of specific clinical services and a designation of who is responsible for the specific elements of the GPC.
The GPC will be mailed or faxed to the enrollee’s HUSKY, Part B Plan and to the child’s primary care physician. A written copy of the GPC will be kept on file at HPP, as part of the child’s case file.
Program Quality
Both HPP will be reviewed annually by an external quality review organization (EQRO) pursuant to the goals identified in the Title XXI State Plan. Pursuant to this review, the Commissioner will submit a report to the Governor and the General Assembly on the HUSKY Plus Programs which will include an evaluation of the special health outcome and access measures identified for HUSKY Plus enrollees.
In addition, the Department will review the HPP Center at least annually. Based on the EQRO report and the Department review, recommendations for program quality improvement will be identified. Corrective action plans and quality improvement projects will be initiated by the Centers in conjunction with the Department.
Grievance and Appeals Process
In accordance with 42 CFR 457 part(s) 1120 – 1180, a HUSKY Plus applicant has the right to request an administrative review regarding a decision made on their HUSKY Plus application. Whenever possible, HPP will attempt to resolve grievances informally. However, parents and providers will be encouraged and supported in the filing of appeals without fear of compromised service. A copy of the appeals procedure, written in a manner easily understood by the lay public, will be distributed to every family at the time of their application to HPP.
The state ensures that all enrollees and applicants receive timely written notice of any determinations required to be subject to review, as outlined below. Written notices at each level include the reasons for the determination, an explanation of applicable rights to review of that determination, the standard and expedited time frames for review, the manner in which a review can be requested, and the circumstances under which enrollment may continue pending review. However, the State will not provide an opportunity for review of a matter if the sole basis for the decision is a provision in this plan or in federal or State law requiring automatic change in eligibility, enrollment, or a change in coverage under the health benefits package that affects all applicants or enrollees or a group of applicants or enrollees without regard to their individual circumstances.
The following decisions can be appealed through the grievance process:
| · | Denial of eligibility for Income Bands One and Two only; |
| · | Failure to make a determination of eligibility within 21 days of application; |
| · | Suspension or termination of enrollment in HPP for enrollees enrolled in Income Band One or Income Band Two of HUSKY B; |
| · | Delay, denial, reduction, suspension or termination of goods or services, including determination regarding level of services; |
| · | Failure to approve, furnish or provide payment for services in a timely manner; |
| · | Medical necessity of a type of service or setting; and |
While an appeal regarding suspension or termination of eligibility or enrollment is being considered, the enrollee will remain eligible for HPP and their goods and/or services will be continued until the grievance is decided, so long as the enrollee remains in Income Band 1 and 2. An enrollee who has been enrolled in Income Band 3 of the HUSKY B program shall be disenrolled from HPP.
While an appeal regarding delay, denial, reduction, suspension or termination of goods and/or services is being considered, the enrollee will continue to receive such goods and/or services until the appeal is decided, so long as the child remains in Income Band 1 or 2.
Applicants or enrollees requesting to review their files or other information relevant to the appeal review will be provided access to their files at a mutually convenient date and time, but no later than four days prior to the decision being issued. Additionally, the State will ensure that applicants or enrollees have opportunities to represent themselves or have representatives of their choosing in the review process, and to fully participate in the review process.
The grievance and appeals process will have three levels of appeal: the first to HPP’s medical director (who was not involved in the prior decision), the second to a sub-group of the Steering Committee, and the third to the Commissioner.
Whenever a decision is made regarding an enrollee’s eligibility, enrollment or goods and/or services, a letter is sent from the HPP Center to the parent describing the decision. Letters, which deny, reduce, suspend or terminate eligibility or enrollment, or goods and/or services (as listed above), will also include a one page Appeal Form and a copy of the Appeals Procedure Summary. To begin the appeals process, the parent or provider should complete the Appeals Form. The form should be mailed or delivered to the HPP Center but must be received by the Center within 45 days of the date of the letter describing the decision that is being appealed.
Level One Appeal:
The HPP Center will send a letter that acknowledges receipt of the appeal form to the parent or provider. The letter will identify a HPP staff member as the Appeals Manager. The Appeals Manager will track the appeal, act as the contact person for questions and updates, and will attempt to resolve the appeal within ten days. If the appeal is resolved to the satisfaction of the parent or provider by the Appeals Manager, a letter will be sent describing the resolution, and there will be no further action. If the appeal cannot be resolved at this level, the Appeals Subcommittee will review the appeal.
Level Two Appeal:
The Appeals Subcommittee of the Steering and Advisory Committee for Children with Special Health Care Needs and HUSKY Plus Physical (SASH) for HPP has three members, one each from:
| · | The Department of Social Services (DSS) |
| · | The Department of Public Health (DPH) and |
| · | The Connecticut Children’s Medical Center |
No one directly involved in the decision being appealed will be a member of this subcommittee. The Appeals Manager is not a member of this subcommittee but will attend to provide needed information.
A letter will be sent to the parent or provider that gives the time and date of the Appeals Subcommittee meeting. The meeting will be scheduled to occur within ten business days of receipt of the written appeal. The parent or provider may reschedule this meeting, for any reason, once. However, the Appeals Committee meeting must occur within 25 business days of the receipt of the appeal.
The parent or provider may bring support persons to the Appeals Subcommittee meeting, including legal counsel, a person with special knowledge or training with respect to the problems of the enrollee, and one or two individuals for support.
In the Appeals Subcommittee, the Appeals Manager will present the appeal; along with any documents involved in the initial decision. The Appeals Manager will also present a summary of the efforts to this point to resolve the appeal. The parent, provider or accompanying support persons may also present arguments and documents, which support the appeal. Once all appeal arguments are completed, the Appeals Subcommittee will either make a decision regarding the appeal, or if necessary, continue the case until more information is obtained or until documents are reviewed. The Appeals Subcommittee must render a final decision no later than 30 days from the date of the Appeals Subcommittee meeting. The Appeals Subcommittee chairperson will send the parent or provider a letter describing the Appeal Committee’s decision no later than 30 days from the date of the Appeals Subcommittee meeting.
Level Three Appeal:
If the parent or provider does not agree with the Appeal Subcommittee’s decision, he/she may continue the appeal process by writing a letter to the Commissioner of the Department of Social Services (DSS) or designee. In this case, the parent or provider must send a copy of the original Appeal Form, the Appeals Subcommittee letter and any other pertinent documents to the Commissioner or designee within ten business days of the date of the Appeals Subcommittee letter. The Appeals Manager will continue to help the parent or provider with this next step. The DSS Commissioner or designee shall make a determination and provide a written decision to the parent no later than 90 days from the initial request date.
If the enrollee has been enrolled in the HPP program and is found to be ineligible for HPP, and this decision is appealed, the enrollee will continue to be eligible for HPP services so long as the child remains eligible for and enrolled in HUSKY, Part B, Income Bands 1 and 2, until the appeal process is completed. Enrollees of HUSKY, Part B who are in Income Band 3 are not eligible for the HUSKY Plus Program and shall be immediately disenrolled from HPP
Expedited Appeal:
Pursuant to 42 CFR 457.1160, the appeal process for HPP must allow for expedited review. This process applies to both eligibility and enrollment matters as well as for goods and/or services. If an enrollee requests an expedited review, HPP must determine within one business day of receipt of the request, whether to expedite the review or whether to perform the review according to the standard timeframes. The review may be expedited if the Medical Director of HPP determines that the standard time frame could seriously jeopardize life or health or ability to attain, maintain or regain maximum function. If the Medical Director of HPP determines that the appeal should be expedited, the Level One review must be completed within 72 hours of receipt of the appeal request by HPP. A Level Two review of an expedited appeal must be completed within 72 hours after completion of the Level One review. An expedited Level Three review must be completed within 72 hours after completion of the Level Two expedited review. The above timeframe may be extended upon request of the parent up to a maximum of 14 days.
Appenndix D
Provider Credentialing and Enrollment Requirements
HUSKY B
PROVIDER CREDENTIALING AND ENROLLMENT REQUIREMENTS
1. Provider Credentialing, and Enrollment Distinction
Provider Credentialing and provider enrollment are separate and distinct processes in the HUSKY Programs. However, credentialing and enrollment are linked in that these requirements affect direct service providers as well as the manner in which MCOs submit provider network information to the Department of Social Services.
2. Credentialing Definition
For the purpose of the HUSKY programs, the term credentialing means the requirements for provider participation specified in the contracts between the Department of Social Services (DSS or the Department) and the MCO (Part II, 3.11, Provider Credentialing and Enrollment). In this section of the contract, the Department specifies the minimum criteria that the MCOs must require for provider participation in a health plan. The MCOs must ensure that their providers meet the Department's credentialing requirements.
3. Other Sources Credentialing
Credentialing is sometimes used to refer to a variety of requirements or entities, which issue credentialing standards. Examples include: the MCO's individual credentialing requirements; the managed care subcontractor's credentialing requirements; an accreditation organization requirements, such as the National Committee on Quality Assurance (NCQA); the licensure process; a trade organization or association such as the Joint Commission on Accreditation of Health Organizations (JCAHO).
4. DSS Requirements and Other Credentialing Sources
DSS credentialing requirements represent the minimum criteria for provider participation in a health plan. The Department will allow flexibility to the MCOs to use more stringent criteria, particularly as it concerns quality level of care for clients. While the MCOs may require additional, more stringent criteria, the Department is concerned with the impact on access to care. Therefore, DSS expects the MCOs to balance the need for stringent credentialing standards with the need to assure accessibility and continuity of care.
5. Delegated Credentialing
The contract between the Department and the MCOs permits the plan to delegate credentialing of individual providers to a facility. However, the MCO is ultimately responsible and accountable to DSS for compliance with the Department's credentialing requirements.
For the purpose of HUSKY, delegated credentialing means that the MCO entrusts the Department's credentialing requirements to another entity. MCOs delegate credentialing to a variety of entities depending on the nature of the services and the type of provider.
In delegated credentialing, the MCO remains responsible to DSS to verify and monitor compliance with the Department's credentialing requirements. The Department views delegated credentialing as a form of subcontract, therefore, similar oversight issues arise in the performance of the credentialing requirements. The Department requires the plans to demonstrate and document to DSS the plan's strong oversight of its delegated credentialing facilities. (Part II, Section 3.41 in B 3.44 in A, Subcontracting for Services).
6. Implications of Delegated Credentialing
In some instances, the MCO credentials the individual provider directly or delegates credentialing of the providers to the following entities:
| · | A subcontractor providing specific services (e.g., dental care); |
| · | A credentialing subcontractor; or |
| · | A facility (e.g., a freestanding clinic or hospital) |
The relationship between the MCO and the delegated entity as well as the interplay with various credentialing requirements may take any number of configurations. Currently, the Department reiterates that the MCO may delegate credentialing of individual providers to a facility (e.g., a school based health center, freestanding clinic or hospital). However, the Department emphasizes that the MCO is ultimately responsible and accountable to DSS for compliance with all of the Department's credentialing requirements.
7. Oversight of Delegated Credentialing
The Department requires the MCO to demonstrate strong oversight of their delegated credentialing facilities, as with any subcontract. - Therefore, the Department reiterates that these arrangements are subject to the Department's review and approval. For the purpose of delegated credentialing, the MCOs must provide assurances to DSS at a minimum of the following:
| • | The MCO and the delegated entity should clearly identify in detail each party's responsibility for credentialing of providers. |
| • | The Department's credentialing requirements should be clearly identified as well as each party's role in adhering to these requirements. |
| • | The *credentialing files must be available to the plan in order to perform its oversight of the credentialing requirements. The Department must also have adequate access to credentialing files for the purposes of administering the managed care contracts. |
(DSS/MCO HUSKY A Contract, Part II, Section 3.45 “Subcontracting for Services” and in HUSKY B Section 3.42 “Subcontracting for Services”.)
8. Provider Enrollment Clarifications
For the purpose of HUSKY, the Department refers to provider enrollment as the process of capturing information on providers participating with MCOs contracted by DSS to provide services to clients. This process results in a profile of an MCO's provider network. The MCOs submit the provider network information to DSS via the Department's agent on a continuous basis. The Department utilizes the provider network information to facilitate the administration of managed care contracts and- the Medicaid program.
Provider enrollment information serves the following purposes:
| a) | To evaluate each MCO's service area and access to services which areused to establish enrollment ceiling or cap (currently summarized by plan submittals of provider tables); |
| b) | To provide accurate infori-nation to clients for the purpose of client enrollment in an MCO; and |
| c) | To maintain each plan's provider network information consistent with the provider directory. |
Based on the previous discussion of credentialing, the Department clarifies the relationship between credentialing or delegated credentialing and provider enrollment as follows:
| a) | Enrollment for purposes of cap determination. |
| • | The MCO must credential and enroll individual providers when the providers are counted towards the member enrollment ceiling. |
| • | DSS credentialing requirements and provider enrollment processes also apply to individual providers in a facility when the individual provider is included in the count for cap determination. |
| • | The MCO may delegate credentialing of individual providers to a facility (e.g., a clinic or hospital) and enroll the facility as such. In this case, -neither the facility nor the individual providers are provided in the count for cap determination. |
b) Enrollment for purposes of accurate information to clients
| · | The MCO must enroll and credential individual providers as well as facilities in order to maintain accurate and updated information on the providers participating with a health plan. The provider network information is used by the Department's enrollment broker during enrollment. |
| · | The Department stresses the importance of maintaining provider network information accurate and up-to-date. It is crucial that clients should have access to provider network information during the MCO select-ion process. |
c) Enrollment for purposes of inclusion in the provider network directory.
| • | The MCO must credential and enroll individual providers when the providers are included and listed as individual providers in the health plan's provider directory. |
| • | DSS credentialing requirements and provider enrollment processes also apply to individual providers in a facility when the individual provider is included and listed in the provider directory. |
| • | If the 14CO delegates credeintialing of individual providers to a facility and enrolls the facility, the facility is included and listed in the provider directory. The facility's individual providers are listed in the provider directory. The facility's providers are not listed in the provider directory. |
9. | Specific Issues and DSS Credentialing Requirements |
The MCO or the delegated credentialing entity is responsible for the determination and verification that the provider meets the minimum requirements for Medicaid participation. The MCO or its -subcontractors may not delegate this provision to the Department nor require providers to enroll or participate in fee-for-service Medicaid to fulfill the requirement. While the Department encourages the MCO to contract with traditional and existing Medicaid providers, Medicaid participation in itself is not a requirement of the HUSKY contracts.
| b) | Allied Health Professional Licensed Clinics or Hospitals |
The Department pays freestanding clinics participating in the Medicaid program for a variety of services. In Connecticut, clinic services include for example, medical services, well-child care, dental care, mental health and substance abuse services, rehabilitation services and other services. Clinic providers must meet federal and state requirements for participation in the Medicaid program. In accordance with Title 42 of the Code of Federal Regulations, Part 440.90 and Section 171 of the Medical Services Policy of the Connecticut Medical Assistance Program, clinic services are provided by or under the direction or a physician, dentist or psychiatrist.
The physician direction requirement means that the free-standing clinic's services may be provided by the clinic's allied health professionals whether or not the physician is physically present at the time that the services are provided. An allied health professional is further defined as an individual, employed in a clinic, who is qualified by special education and training, skills, and experience in providing care and treatment. The clinic is staffed by physicians and allied health professionals who are directly involved in the facility's programs. The allied health professionals provide services under the direction of a physician who is a licensed practitioner performing within the scope of his/her practice.
Based on the Department's definition of clinic services, the services provided by allied health professionals are included under the terms of the contracts between the Department and the MCOs.
As with all services, clinic services must be properly credentialed according to the Department's requirements, including licensure and certification standards. Allied health professionals may have licensure or certification requirements, such as Certified Addition Counselors or Licensed Social Workers. In accordance with the Department's definition, other allied health professions may qualify by virtue of their skills or experience and must function under the direction of a physician. In this case- the directing physician, as opposed to the allied health professional, is subject to the credentialing requirements as well as provider enrollment. The MCO may credential the physician directly or may delegate credentialing.
The Department's provisions for credentialing, delegated and provider enrollment would remain in effect for the directing physician (please refer to Section 8, Provider Enrollment Clarifications).
| c) | NCQA Standards and DSS requirements |
While NCQA standards do not address credentialing of allied health professionals, services provided by allied health professionals may qualify for reimbursement by virtue of their skills or experience, however, the allied health professionals must function under the direction of a physician. In this case, the directing physician is subject to the credentialing requirements.
Appendix E
American Academy of Pediatrics - Recommendations for Preventive Pediatric Health Care
Appendix F
DSS Marketing Guidelines
Appendix F
Detailed Marketing Guidelines
1) General HUSKY marketing materials
Marketing materials are defined as all media, including brochures and leaflets; newspaper, magazine, radio, television, billboard and yellow pages advertisements; and presentation materials used by MCO representatives.
The DEPARTMENT will not restrict the MCO's general communications to the public. However, the MCO must obtain prior approval from the DEPARTMENT prior to any written material or advertisement that is mailed to, distributed to, or aimed at HUSKY recipients or individuals potentially eligible for HUSKY, specifically, material that mentions Medicaid, Medical Assistance, Title XIX, Title XXI State Children's Health Insurance Program (SCHIP) or HUSKY. Examples of HUSKY-specific materials would be those which are in any way targeted to HUSKY populations (such as billboards or bus posters disproportionately located in low-income neighborhoods); those that mention the MCO's HUSKY product name; or those that contain language or information specifically designed to attract HUSKY enrollment.
2) General MCO marketing/advertising
All MCO-specific marketing activities for the HUSKY population, as defined above, and all marketing materials /advertising put forth by HUSKY-only MCO require DEPARTMENT prior approval.
In determining whether to approve a particular marketing activity, the DEPARTMENT will apply a variety of criteria, including, but not limited to:
| a) | Accuracy: The content of the material must be accurate. Any information that is deemed inaccurate will be disallowed. |
| b) | Misleading references to the MCO's positive attributes: Misleading information will be disallowed even if it is accurate. For example, the MCO may seek to advertise that its health care services are free to its Medicaid (HUSKY A) Members. In this situation, DEPARTMENT would disallow the language since this could be construed by Members as being a particular advantage of the plan (e.g. they might believe they would have to pay for health services if they chose another MCO or remained in fee-for-service). |
| c) | Threatening Messages: MCOs shall not imply that the managed care program or the failure to join a particular MCO would endanger the Member's health status, personal dignity, or the opportunity to succeed in various aspects of their lives. MCOs are strictly prohibited from creating threatening implications about the State's mandatory assignment process for HUSKY A Members or other aspects of the HUSKY A or HUSKY B programs. |
| d) | MCO's Legitimate Strengths: MCOs may differentiate themselves by promoting their legitimate positive attributes. |
3) MCO advertising at provider care sites
Promotional and health education materials at care delivery sites (including patient waiting areas) are permitted, subject to prior DEPARTMENT content approval. MCO member services staff may provide member services (e.g. face-to-face member education) at provider care sites, however, face-to-face meetings, for purposes of marketing, at care delivery sites between individual Members and MCO staff are not permitted.
4) MCO advertising in DEPARTMENT eligibility offices
MCOs may make their materials available at DEPARTMENT offices only through the DEPARTMENT or its agent. This restriction applies to all eligibility offices, including those based in hospitals. MCO marketing staff and provider staff are not permitted to solicit Member enrollment by positioning themselves at or near eligibility offices. Note that the only face-to-face marketing activities allowed are those directly permitted under items #5, #7, #11 and #12 of these guidelines. All other face-to-face marketing activities are prohibited.
5) Provider communications with HUSKY patients about MCO options
DEPARTMENT marketing restrictions apply to the MCO's participating providers as well as to the MCOs. MCOs must notify all of their participating providers of the DEPARTMENT marketing restrictions and provide them with a copy of this document.
Each provider entity is allowed to notify its patients of the HUSKY-certified MCOs it participates in, and to explain that the patients must enroll in one of these MCOs if they wish to preserve their existing relationship. This must be done through written materials prior-approved by DEPARTMENT, and must be distributed to HUSKY patients without regard to health status. Providers must not indicate a preference between the MCOs in which they participate.
6) Member-initiated telephone conversations with MCOS and providers
These conversations are permitted and do not require prior approval by the DEPARTMENT, but information given to potential Members, during such telephone conversation must be in accordance with the DEPARTMENT's marketing guidelines. However, telephone conversations must be initiated by the potential Member, not by the MCO staff (or provider staff). MCOs and providers may return calls to Members and potential Members when Members and potential Members leave a message requesting that this occur.
7) Member-initiated one-on-one meetings with MCO staff prior to enrollment
Such meetings, when requested by the Member, are permitted but may not occur at a participating provider's care delivery site or at the Member's residence. These meetings must occur at the MCO's offices or another mutually-agreed upon public location. All verbal interaction with the Member must be in compliance with the DEPARTMENT's marketing guidelines.
8) Mailings by MCO in response to Member requests
MCO mailings are permitted in response to Member verbal or written requests for information. The content of such mailings must be prior-approved by the DEPARTMENT. MCOs may include gifts of nominal value (unit cost less than $2, e.g. magnets, pens, bags, jar grippers, etc.) in these mailings.
9) Unsolicited MCO mailings
MCOs are permitted to send unsolicited mailings. The content of such mailings must be prior-approved by DEPARTMENT. In addition, the target audiences must be prior-approved by DEPARTMENT, and the MCOs must explain how they obtained the list of names, addresses and phone numbers.
10) Telemarketing
Telemarketing is not a permitted marketing activity
11) MCO group meetings held at MCO
These meetings must be prior approved by the DEPARTMENT. The MCO may not notify prospective Members until DEPARTMENT prior approval has been obtained
12) MCO group meetings held in public facilities, churches, health fairs, or other community sites
These are permitted activities as long as DEPARTMENT approved materials are utilized in the presentations and the DEPARTMENT's marketing guidelines are followed. The DEPARTMENT reserves the right to monitor such meetings on an ad hoc basis. MCOs are required to notify the DEPARTMENT sufficiently in advance to allow DEPARTMENT representatives to attend such meetings in order to monitor MCO activities if desired. As soon as the MCO has scheduled these activities, the DEPARTMENT should be notified.
13) MCO group meetings held in private clubs or homes
These activities are prohibited. The only permitted group meetings are those described under items #11 and #12.
14) Individual solicitation, residences
MCO (and provider) staff are not permitted to visit potential Members at their places of residence for purposes of explaining MCO features and promoting enrollment. This prohibition is absolute, and applies even in situations where
the potential Member desires and/or requests a home visit. MCO staff can visit Member homes after enrollment becomes effective, as part of their orientation/education efforts.
15) Gifts, cash incentives, or rebates to potential Members and members.
MCOs (and their providers) are prohibited from disseminating gift items, except those of a nominal value (pens, key chains, magnets, etc.), to potential Members. DEPARTMENT-approved written materials may also be disseminated to prospective Members along with similar nominal value gifts. MCOs may give items of nominal value (unit cost less than $2), with their logo on it, to persons (potential Members and others) attending health fairs, presentations at community forums organized through or other sanctioned events, with DEPARTMENT approval. Such items would include magnets, pens, bags, plastic band-aid dispensers, etc. Pre-approved nominal value items may also be included with new Member information packets.
16) Gifts to Members for specific health-related events
Gifts to Members are allowed for medically "good" behavior (e.g. baby T-shirt showing immunization schedule once a woman completes targeted series of prenatal visits). All such gifts, including any written materials included with them (or on them), must be prior-approved by the DEPARTMENT. The criteria for providing such gifts must also be prior-approved by DEPARTMENT. MCOs must not provide gifts in any situations other than those that have been prior-approved by DEPARTMENT. Additional DEPARTMENT prior approval is required for all additional uses of the gift items or for new gifts.
The DEPARTMENT may approve magnets, phone labels, and other nominal items that reinforce a MCO's care coordination programs (e.g. through advertising the Member Services hotline and/or the PCP office phone number). All such items must be prior-approved by the DEPARTMENT. The criteria for disseminating this information must also be prior-approved, although the DEPARTMENT is likely to be amenable to the MCOs' inclusion of this information in "welcome" packets sent to new Members.
Health education videos are also allowed, but must be prior-approved by DEPARTMENT.
17) Phoning by Members from health care provider locations
Providers may provide the use of a phone to potential HUSKY Members or HUSKY Members subject to the following restrictions:
| a) | MCO or provider staff may not coach or instruct the caller; |
| b) | Privacy must be given to the MEMBER during their phone conversation with the HUSKY application and enrollment center. |
18) | Non-alcoholic beverages and light refreshments for potential Members at meetings |
Non-alcoholic beverages and light refreshments are permitted at DEPARTMENT approved group meetings.
19. | Use of HUSKY Name; HUSKY Logo and Mandatory Language Requirements |
MCOs will be allowed use of the HUSKY logo and name for use in their marketing materials, subject to the following:
| a) | must be used in conjunction with the following language unless alternative language has been prior approved by the DEPARTMENT. HUSKY gives families the freedom of choice to enroll in one of several participating health plans. Toll-free information: 1-877-CT-HUSKY; |
| b) | the above mandatory language must be placed in the vicinity of the HUSKY logo; and |
| c) | the font size for the HUSKY phone number cannot be smaller than the MCOs member services phone number. |
| | Type of Marketing Activity | Permitted | Not Permitted | Permitted With DEPARTMENT Approval |
| 1 | General HUSKY marketing materials | | | X |
| 2 | General, MCO advertising/marketing | | | X |
| 3 | MCO advertising in provider care sites | | | X |
| 4 | MCO advertising in all DEPARTMENT- eligibility offices, including hospital-based (Must be made available only through the DEPARTMENT or its agent) | | | X |
| 5 | Provider communications with Medicaid patients about MCO options | | | X |
| 6 | Member-initiated telephone conversations with MCO and Provider staff | X | | |
| 7 | Member-initiated one-on-one meetings with MCO staff prior to enrollment | X | | |
| 8 | Mailings by MCO in response to Member requests | | | X |
| 9 | Unsolicited MCO mailings to Members | | | X |
| 10 | Telemarketing | | X | |
| 11 | MCO group meetings, held at MCO | | | X |
| 12 | MCO group meetings held in public facilities such as churches, health fairs, WIC program or other community sites | | | X |
| 13 | MCO group meetings held in private clubs or homes | | X | |
| 14 | Individual solicitation at residences | | X | |
| 15 | Items of nominal value along with written information about the MCO or general health education information to potential Members (given at such places as health fairs, community forums or other events approved by the Department) or included in new Member information packets. | | | X |
| 16 | Gifts to Members (e.g. baby T-shirt showing immunization schedule) based on specific health events unrelated to enrollment | | | X |
| 17 | Phoning by Members from health care provider locations | X | | |
| 18 | Non-alcoholic beverages and light refreshments (e.g. fruit, cookies) for potential Members at meetings (may not mention refreshments in advertisements for meetings) | X | | |
Appendix G
Standards for Internal Quality Assurance Programs for Health Plans
STANDARDS FOR INTERNAL QUALITY ASSURANCE PROGRAMS FOR HEALTH PLANS
Standard I: | Written QAP Description |
The organization has a written description of its Quality Assurance Program (QAP). This written description meets the following criteria:
A. | Goals and objectives - There is a written description of the QA program with detailed goals and annually developed objectives that outline the program structure and design and include a timetable for implementation and accomplishment. |
B. Scope
| 1. | The scope of the QAP is comprehensive, addressing both the quality of clinical care and quality of non-clinical aspects of services, such as and including: availability, accessibility, coordination, and continuity of care. |
| 2. | The QAP methodology provides for review of the entire range of care provided by the organization, by assuring that all demographic groups, care settings (e.g. inpatient, ambulatory, [including care provided in private practice offices] and home care), and types of services (e.g. preventive, primary, specialty care and ancillary) are included in the scope of the review. This review should be carried out over multiple review periods and not on just a concurrent basis. |
C. | Specific activities - The written description specifies quality of care studies and other activities to be undertaken over a prescribed period of time, and methodologies and organizational arrangements to be used to accomplish them. Individuals responsible for the studies and other activities are clearly identified and are appropriate. |
D. | Continuous activity - The written description provides for continuous performance of the activities, including tracking of issues over time. |
| E. | Provider review - The QAP provides: |
| 1. | Review by physicians and other health professionals of the process followed in the provision of health services; |
| 2. | Feedback to health professionals and health plan staff regarding performance and patient results. |
F. | Focus on health outcomes - The QAP methodology addresses health outcomes to the extent consistent with existing technology. |
Standard II: | Systematic Process of Quality Assessment and Improvement |
The QAP objectively and systematically monitors and evaluates the quality and appropriateness of care and service provided members, through quality of care studies and related activities, and pursues opportunities for improvement on an ongoing basis.
| A. | Specification of clinical or health services delivery areas to be monitored |
| 1. | Monitoring and evaluation of clinical issues reflects the population served by the health plan, in terms of age groups, disease categories, and special risk status. |
| 2. | For the Medicaid population, the QAP monitors and evaluates at a minimum, care and services in certain priority areas of concern selected by the State. It is recommended that these be taken from among those identified by the Health | Care Financing Administration's (HCFA's) Medicaid Bureau and jointly determined by the State and the Managed Care Organization (MCO). |
| 3. | At its discretion and/or as required by the State Medicaid agency, the MCO's QAP also monitors and evaluates other aspects of care and service. |
B. Use of quality indicators
Quality indicators are measurable variables relating to a specified clinical or health services delivery area, which are reviewed over a period of time to monitor the process of outcomes of care delivered in that area.
| 1. | The MCO identifies and uses quality indicators that are measurable, objective, and based on current knowledge and clinical experiences. |
| 2. | For the priority area selected by the State from the HCFA Medicaid Bureau's list of priority clinical and health service delivery areas of concern, the MCO monitors and evaluates quality of care through studies, which include, but are not limited to, the quality indicators also specified by the HCFA Medicaid Bureau. |
| 3. | Methods and frequency of data collection are appropriate and sufficient to detect need for program change. |
C. Use of clinical care standards/practice guidelines
| 1. | The QAP studies and other activities monitor quality of care against clinical care or health services delivery standards or practice guidelines specified for each area identified. |
| 2. | The clinical standards/practice guidelines are based on reasonable scientific evidence and are developed or reviewed by plan providers. |
| 3. | The clinical standards/practice guidelines focus on the process and outcomes of health care delivery, as well as access to care. |
| 4. | A mechanism is in place for continuously updating the standards/practice guidelines. |
| 5. | The clinical standards/practice guidelines shall be included in provider manuals developed for use by HMO providers or otherwise disseminated to the providers as they are adopted. |
| 6. | The clinical standards/practice guidelines address preventive health services. |
| 7. | The clinical standards/practice guidelines are developed for the full spectrum of populations enrolled in the plan. |
| 8. | The QAP shall use these clinical standards/practice guidelines to evaluate the quality of care provided by the MCO's providers, whether the providers are organized in groups, as individuals, as IPAs, or in a combination thereof. |
D. | Analysis of clinical care and related services |
| 1. | Appropriate clinicians monitor and evaluate quality through review of individual cases where there are questions about care and through studies analyzing patterns of clinical care and related service. For quality issues identified in the QAP's targeted clinical areas, the analysis includes the identified quality indicators and uses clinical care standards or practice guidelines. |
| 2. | Mulitdisciplinary teams are used, where indicated, to analyze and address system issues. |
| 3. | For the D.1. and D.2. above, clinical and related services requiring improvement are identified. |
| E. | | Implementation of remedial/corrective actions |
| | | The QAP includes written procedures for taking appropriate remedial action whenever, as determined under the QAP, inappropriate or substandard services are furnished, or services that should have been furnished were not. These written remedial/corrective action procedures include: |
| 1. | Specification of the types of problems requiring remedial/corrective action. |
| 2. | Specification of the person(s) or body responsible for making the final determinations regarding quality problems. |
| 3. | Specific actions to be taken. |
| 4. | Provision of feedback to appropriate health professionals, providers and staff. |
| 5. | The schedule and accountability for implementing corrective actions. |
| 6. | The approach to modify the corrective action if improvements do not occur. |
| 7. | Procedures for terminating the affiliation with the physician, or other health professional or provider. |
F. | Assessment of effectiveness of corrective actions |
| 1. | As actions are taken to improve care, there is monitoring and evaluation of corrective actions to assure that appropriate changes have been made. In addition, changes in practice patterns are tracked. | |
| 2. | The MCO assures follow-up on identified issues to ensure that actions for improvement have been effective. | |
G. | Evaluation of continuity and effectiveness of the QAP |
| 1. | The MCO conducts a regular and periodic examination of the scope and content of the QAP to ensure that it covers all types of services in all settings, as specified in standard I-B-2. | | |
| 2. | At the end of each year, a written report on the QAP is prepared which addresses: QA studies and other activities completed, trending of clinical and services indicators and other performance data; demonstrated improvements in quality; areas of deficiency and recommendations for corrective action; and an evaluation of the overall effectiveness of the QAP |
| 3. | There is evidence that QA activities have contributed to significant improvements in the care and services delivered to members. |
Standard III: | Accountability to the Governing Body |
The QA committee is accountable to the governing body of the managed care organization. The governing body should be the board of directors, or a committee of senior management may be designated in instances in which the board's participation with QA issues is not direct. There is evidence of a formally designated structure, accountability at the highest levels of the organization, and ongoing and/or continuous oversight of the QA program. Responsibilities of the Governing Board for monitoring, evaluating, and making improvements to care include:
A. | Oversight of the QAP - There is documentation that the governing body has approved the overall QAP and the annual QAP. |
B. | Oversight of entity - The Governing Body has formally designated an accountable entity or entities within the organization to provide oversight of QA, or has formally decided to provide such oversight as a committee of the whole. |
C. | QAP progress reports - The Governing body routinely receives written reports from the QAP describing actions taken, progress in meeting QA objectives, and improvements made. |
D. | Annual QAP review - The Governing Body formally reviews on a periodic basis (but no less frequently than annually) a written report on the QAP which includes: studies undertaken, results, subsequent actions, and aggregate data on utilization and quality of services rendered, to assess the QAP's continuity, effectiveness and current acceptability. |
E. | Program modification - Upon receipt of regular written reports from the QAP delineating actions taken and improvements made, the Governing Body takes actions when appropriate and directs that the operational QAP be modified on an ongoing basis to accommodate review findings and issues of concern within the MCO. Minutes of the meetings of the Governing Board demonstrate that the Board has directed and followed up on necessary actions pertaining to QA. |
Standard IV: | Active QA Committee |
The QAP delineates an identifiable structure responsible for performing QA functions within the MCO. The committee or other structure has:
A. | Regular meetings - The structure/committee meets on a regular basis with specified frequency to oversee QAP activities. This frequency is sufficient to demonstrate that the structure/committee is following up on all findings and required actions, but in no case are such meetings less frequent than quarterly. |
B. | Established parameters for operating -The role, structure and function of the structure/committee are specified. |
C. | Documentation - There are contemporaneous records documenting the structure's/committee's activities, findings, recommendations and actions. |
D. | Accountability - The QAP committee is accountable to the Governing Body and reports to it (or its designee) on a scheduled basis on activities, findings, recommendations and actions. |
E. | Membership - There is active participation in the QA committee from health plan providers, who are representative of the composition of the health plan's providers. |
Standard V: | QAP Supervision |
There is a designated senior executive who is responsible for program implementation. The organization's Medical Director has substantial involvement in QA activities.
Standard VI: | Adequate Resources |
The QAP has sufficient material resources, and staff with the necessary education, experience, or training; to effectively carry out its specified activities.
Standard VII: | Provider Participation in the QAP |
| A. | Participating physicians and other providers are kept informed about the written QA plan. |
| B. | The MCO includes in all its provider contracts and employment agreements, for both physicians and nonphysician providers, a requirement securing cooperation with the QAP. |
| C. | Contracts specify that hospitals, physicians, and other contractors will allow the MCO access to the medical records of their members. |
Standard VIII: | Delegation of QAP Activities |
The MCO remains accountable for all QAP functions, even if certain functions are delegated to other entities. If the MCO delegates any QA activities to contractors.
| A. | There is a written description of delegated activities; the delegate's accountability for these activities; and the frequency of reporting to the MCO. |
| B. | The MCO has written procedures for monitoring the implementation of the delegated functions and for verifying the actual quality of care being provided. |
| C. | There is evidence of continuous and ongoing evaluation of delegated activities, including approval of quality improvement plans and regular specified reports. |
Standard IX: | Enrollee Rights and Responsibilities |
The MCO demonstrates a commitment to treating members in a manner that acknowledges their rights and responsibilities.
| A. | | Written policy on enrollee rights |
| | | The MCO has a written policy that recognizes the following rights of members: |
| 1. | To be treated with respect, and recognition of their dignity and need for privacy; |
| 2. | To be provided with information about the MCO, its services, the practitioners providing care, and members' rights and responsibilities; |
| 3. | To be able to choose primary care practitioners, within the limits of the plan network, including the right to refuse care from specific practitioners; |
| 4. | To participate in decision-making regarding their health care; |
| 5. | To voice grievances about the MCO or care provided; |
| 6. | To formulate advance directives; and |
| 7. | To have access to his/her medical records on accordance with applicable Federal and State laws. |
B. | Written policy enrollee responsibilities - The MCO has a written policy that addresses members' responsibility for cooperating with those providing health care services. This written policy addresses members' responsibility for: |
| 1. | Providing, to the extent possible, information needed by professional staff in caring for the member; and |
| 2. | Following instructions and guidelines given by those providing health care services. |
C. | Communication of policies to providers - A copy of the organization's policies on members' rights and responsibilities is provided to all participating providers. |
D. | Communication of policies to enrollees/members - Upon enrollment, members are provided a written statement that includes information on the following: |
| 1. | Rights and responsibilities of members; |
| 2. | Benefits and services included and excluded as a condition of memberships, and how to obtain them, including a description of: |
| a. | Any special benefit provisions (example, co-payment, higher deductibles, rejection of claim) that may apply to service obtained outside the system; and |
| b. | The procedures for obtaining out-of-area coverage; |
| 3. | Provisions for after-hours and emergency coverage; |
| 4. | The organization's policy on referrals for specialty care; |
| 5. | Charges to members, if applicable, including: |
| a. | Policy on payment of charges; and |
| b. | Co-payment and fees for which the member is responsible. |
| 6. | Procedures for notifying those members affected by the termination or change in any benefit services, or service delivery office/site; |
| 7. | Procedures for appealing decisions adversely affecting the members' coverage, benefits, or relationship with the organization; |
| 8. | Procedures for changing practitioners; |
| 9. | Procedures for disenrollment; and |
| 10. | Procedures for voicing complaints and/or grievances and for recommending changes in policies and services. |
E. | Enrollee/member grievance procedures - The organization has a system(s) linked to the QAP, for resolving members' complaints and formal grievances. This system includes: |
| 1. | Procedures for registering and responding to complaints and grievances in a timely fashion (organizations should establish and monitor standards for timeliness); | |
| 2. | Documentation of the substance of the complaint or grievances, and actions taken; |
| 3. | Procedures to ensure a resolution of the compliant or grievance; |
| 4. | Aggregation and analysis of complaint and grievance data and use of the data for quality improvement; and |
| 5. | An appeal process for grievances. |
F. | Enrollee/member suggestions - Opportunity is provided for members to offer suggestions for changes in policies and procedures. |
G. | Steps to assure accessibility of services - The MCO takes steps to promote accessibility of services offered to members. These steps include: |
| 1. | The points of access to primary care, specialty care and hospital services are identified for members; |
| 2. | At a minimum, members are given information about: |
| a. | How to obtain services during regularly hours of operation |
| b. | How to obtain emergency and after-hours care; and |
| c. | How to obtain the names, qualifications, and titles of the professionals providing and/or responsible for their care. |
H. | Written information for members |
| 1. | Member information is written in prose that is readable and easily understood; and |
| 2. | Written information is available, as needed, in the languages of the major population groups served. A "major" population group is one which represents at least 10% of plan's membership. |
I. | Confidentiality of patient information - The MCO acts to ensure that the confidentiality of the specified patient information and records is protected. |
| 1. | The MCO has established in writing, and enforced, policies and procedures on confidentiality of medical records. |
| 2. | The MCO ensures that patient care offices/sites have implemented mechanisms that guard against the unauthorized or inadvertent disclosure of confidential information to persons outside of the medical care organization. |
| 3. | The MCO shall hold confidential information obtained by its personnel about enrollees related to their examination, care and treatment and shall not divulge it without the enrollee's authorization, unless: |
| b. | it is necessary to coordinate the patient's care with physicians, hospitals, or other health care entities, or to coordinate insurance or other matters pertaining to payment; or |
| c. | it is necessary in compelling circumstances to protect the health or safety of an individual. |
| 4. | Any release of information in response to a court order is reported to the patient in a timely manner; and |
| 5. | Enrollee records may be disclosed, whether or not authorized by the enrollee, to qualified personnel for the purpose of conducting scientific research, but these personnel may not identify, directly or indirectly, any individual enrollee in any report of the research or otherwise disclose participant identity in any manner. |
J. | Treatment of minors - The MCO has written policies regarding the appropriate treatment of minors. |
K. | Assessment of member satisfaction - The MCO conducts periodic surveys of member satisfaction with its services. |
| 1. | The surveys include content on perceived problems in the quality, accessibility and availability of care. |
| 2. | The surveys assess at least a sample of: |
| b. | Medicaid member requests to change practitioners and/or facilities; and |
| c. | Disenrollment by Medicaid members. |
| 3. | As a results of the surveys, the organization: |
| a. | Identifies and investigates sources of dissatisfaction; |
| b. | Outlines action steps to follow-up on the findings; and |
| c. | Informs practitioners and providers of assessment results. |
| 4. | The MCO reevaluates the effects of the above activities. |
Standard X: | Standards for Availability and Accessibility |
The MCO has established standards for access (e.g. to routine, urgent and emergency care; telephone appointments; advice; and member service lines). Performance on these on these dimensions of access are assessed against the standards.
Standard XI: | Medical Records Standards |
A. | Accessibility and availability of medical records - The MCO shall include provision in provider contracts for appropriate access to the medical records of its enrollees for purposes of quality reviews conducted by the Secretary, State Medicaid agencies, or agents thereof. |
B. | Record keeping - Medical records may be on paper or electronic. The plan takes steps to promote maintenance of medical records in a legible, current, detailed, organized and comprehensive manner that permits effective patient care and quality review as follows: |
| 1. | Medical records standards- The MCO sets standards for medical records. The records reflect all aspects of patient care, including ancillary services. These standards shall at a minimum, include requirements for: |
| a. | Patient identification information - Each page or electronic file in the record contains the patient's name or patient ID number. |
| b. | Personal/biographical data - Personal/biographical data includes: age, sex, address; employer; home and work telephone numbers; and martial status. |
| c. | Entry date - All entries are dated. |
| d. | Provider identification - All entries are identified as to author. |
| e. | Legibility - The record is legible to someone other than the writer. Any record judged illegible by one physician reviewer should be evaluated by a second reviewer. |
| f. | Allergies - Medication allergies and adverse reactions are prominently noted on the record. Absence of allergies (no known allergies-NKA) is noted in an easily recognizable location. |
| g. | Past medical history - (for patients seen 3 or more times) Past medical history is easily identified including serious accidents, operations, illnesses. For children, past medical history relates to prenatal care and birth. |
| h. | Immunizations- For pediatric records (ages 12 and under) there is a completed immunization record or a notation that immunizations are up-to-date. |
| k. | Identification of current problems - Significant illness, medical conditions and health maintenance concerns are identified in the medical record. |
| l. | Smoking/ETOH/substance abuse - Notation concerning cigarettes and alcohol use and substance abuse is present (for patients 12 years and over and seen three or more times). Abbreviations and symbols may be appropriate. |
| m. | Consultations, referral and specialist reports - Notes from consultations are in the record. Consultation, lab, and x-ray reports filed in the chart have the ordering physicians initials or other documentation signifying review. Consultation and significantly abnormal lab and imaging study results have an explicit notation in the record and follow-up plans. |
| o. | Hospital discharge summaries - Discharge summaries are included as part of the medical record for (1) all hospital admissions which occur while the patient is enrolled in the MCO and (2) prior admissions as necessary. |
| p. | Advance directives - For medical records of adults, the medical record documents whether or not the individual has executed an advance directive. An advance directive is a written instruction such as a living will or durable power of attorney for health care relating to the provision of health care when the individual is incapacitated. |
| 2. | Patient visit data - Documentation of individual encounters must provide adequate evidence of, at a minimum; |
| a. | History and physical examination - Appropriate subjective and objective information is obtained for the presenting complaints. |
| d. | Therapies and other prescribed regimens; and |
| e. | Follow-up - Encounter forms or notes have a notation, when indicated, concerning follow-up care, call, or visit. Specific time to return is noted in weeks, months, or PRN. Unresolved problems from previous visits are addressed in subsequent visits. |
| f. | Referrals and results thereof; and |
| g. | All other aspects of patient care, including ancillary services. |
| 1. | The MCO has a system (record review process) to assess the content of medical records for legibility, organization, completion and conformance to its standards. |
| 2. | The record assessment system addresses documentation of the items listed in B, above. |
Standard XII: | Utilization Review |
| A. | Written program description- The MCO has a written utilization management program description which includes, at a minimum, procedures to evaluate medical necessity, criteria used, and approve the provision of medical information sources and the process used to review services | . |
| B. | Scope - The program has mechanisms to detect underutilization as well as overutilization. |
| C. | Preauthorization and concurrent review - For MCO with preauthorization or concurrent review programs: |
| 1. | Preauthorization and concurrent review decisions are supervised by qualified medical professionals; |
| 2. | Efforts are made to obtain all necessary information, including pertinent clinical information, and consult with the treating physician as appropriate; |
| 3. | The reasons for decisions are clearly documented and available to the member. |
| 4. | There are well-publicized and readily available appeals mechanisms for both providers and patients. Notification of a denial includes a description of how file an appeal; |
| 5. | Decisions and appeals are made in a timely manner as required by the exigencies of the situation; |
| 6. | There are mechanisms to evaluate the effects of the program using data on member satisfaction, provider satisfaction or other appropriate; and |
| 7. | If the MCO delegates responsibilities for utilization management, it has mechanisms to ensure that these standards are met by the delegate. |
Standard XIII: | Continuity of Care System |
The MCO has put a basic system in place which promotes continuity of care and case management.
Standard XIV: | QAP Documentation |
A. | Scope - The MCO shall document that it is monitoring the quality of care across all services and all treatment modalities, according to its written QAP. |
B. | Maintenance and availability of documentation - The MCO must maintain and make available to the State, and upon request to the Secretary of HHS, studies, reports, appropriate, concerning the activities and corrective actions. |
Standard XV: | Coordination of QA Activity with other Management Activity |
The findings, conclusions, recommendations, actions taken, and results of actions taken as a result of QA activity, are documented and reported to appropriate individuals within the MCO and through established QA channels.
| A. | QA information is used in recredentialing, recontracting, and/or annual performance evaluations. | |
| B. | QA activities are coordinated with other performance monitoring activities, including utilization management, risk management, and resolution and monitoring of member complaints and grievances. |
| C. | There is a linkage between QA and other management functions of the MCO, such as: network changes, benefit redesign, medical management systems, practice feedback to providers, patient education and member services. |
Appendix H
Claims Inventory, Aging and Unaudited Quarterly Financial Reports
HUSKY B Appendix H
(document 1 of 5)
Report #1
HUSKY A & B Unprocessed Claims in Dollars
Plan Name | | | | | | | |
Qtr. Ending: | | | | | | | |
| | | | | | | | |
Claim Type | Claims In Process During Qtr. (In Dollars) (1) | | | |
| | 1-30 Days | 31-45 Days | 46-60 Days | 61-90 Days | 91-120 Days | >120 Days | Total Claims Outstanding At The End Of The Qtr. |
| UB92 Claims | | | | | | | |
| HCFA 1500 Claims | | | | | | | |
Subtotal MCO Claims | | | | | | | |
| Pharmacy | | | | | | | |
| Dental | | | | | | | |
| Vision | | | | | | | |
Subtotal Vendor Claims | | | | | | | |
Total | | | | | | | |
| | | | | | | | |
Claim Type | Unpaid Adjudicated Claims (In Dollars) (2) | | | | |
| | 1-30 Days | 31-45 Days | 46-60 Days | 61-90 Days | 91-120 Days | >120 Days | Total Unpaid Adjudicated Claims (In Dollars) At The End Of The Qtr. |
| UB92 Claims | | | | | | | |
| HCFA 1500 Claims | | | | | | | |
Subtotal MCO Claims | | | | | | | |
| Pharmacy | | | | | | | |
| Dental | | | | | | | |
| Vision | | | | | | | |
Subtotal Vendor Claims | | | | | | | |
Total | | | | | | | |
| | | | | | | | |
1. Claims in process-all claims that are in a pending status (data, medical, COB edits) and require review by a claim examiner prior to being released for adjudication. Because the final pay amount is unknown, the amounts are recorded at the billed amount |
2. Unpaid adjudicated claims-claims which have been adjudicated and have a known pay amount, however, a check has not been issued for these claims. Because the final pay amount is known, the amounts are recorded using net amount + withhold. |
| | | | | | | | |
| UB92 - In general these claim forms represent hospital based claims (inpatient and outpatient). | | | |
| HCFA 1500 - These claim forms are used for outpatient services provided by non-hospital facilities. | | | |
| | | | | | | | |
Other items to note about report #1 and #2: | | | | | | |
* If a claim does not include the information specified in Bulletin HC-56 it is rejected. This claim would not appear in the inventory after it was rejected. |
| * A claim could contain all of the information specified by Bulletin HC-56, but it is incorrect. In this instance it could have been included in the pending claims prior to identifying it as a claim with incorrect data. Examples of incorrect data would be using a discontinued code. |
| * If a claim is submitted for a service which requires prior authorization, but none if found by the MCO, it is denied. | | |
| At the point of denial the claim would be excluded from the report. | | | | | |
| * The pending claims could include duplicates which have not been identified by the MCO. If a duplicate is identified, one is paid and | |
| all of the duplicates are rejected. | | | | | | | |
* The pending category may include claims which have been pended for a medical records review. As per the guidelines in Bulleting HC-56, if additional information is needed from the provider, the MCO has 30 days to request additional information. After the information is received, the MCO has 30 days to pay the claim without interest. |
| * If a claim is denied and subsequently reversed on appeal, the clock would start on the date of the appeal determination. | | |
* If a credit balance exists for a provider, the time to process the claim is still measured. To the extent that processing exceeds 45 days it would accrue interest as any other claim would. |
| If a rejected or denied claim is subsequently resubmitted, it would take on a new claim number. The clock would begin from the date of re-submissions. | |
| The only time a processed claim is re-opened is for an adjustment to amount paid. | | | | | |
HUSKY B Appendix H
document 2 of 5)
Report #2
HUSKY A & B Volume of Unprocessed Claims
Plan Name | | | | | | | |
Qtr. Ending: | | | | | | | |
| | | | | | | | |
Claim Type | Claims In Process During Qtr. (# of claims) (1) | | | Total Claims In Process During Qtr. |
| | 01-30 Days | 31-45 Days | 46-60 Days | 61-90 Days | 91-120 Days | >120 Days | |
| UB92 Claims | | | | | | | |
| HCFA 1500 Claims | | | | | | | |
Subtotal MCO Claims | | | | | | | |
| Pharmacy | | | | | | | |
| Dental | | | | | | | |
| Vision | | | | | | | |
Subtotal Vendor Claims | | | | | | | |
Total | | | | | | | |
| | | | | | | | |
| | | | | | | | |
Claim Type | Unpaid Adjudicated Claims (# of claims) (2) | | | Total Unpaid Adjudicated Claims (# of claims) At The End Of The Qtr. |
| | 01-30 Days | 31-45 Days | 46-60 Days | 61-90 Days | 91-120 Days | >120 Days | |
| UB92 Claims | | | | | | | |
| HCFA 1500 Claims | | | | | | | |
Subtotal MCO Claims | | | | | | | |
| Pharmacy | | | | | | | |
| Dental | | | | | | | |
| Vision | | | | | | | |
Subtotal Vendor Claims | | | | | | | |
Total | | | | | | | |
| | | | | | | | |
Claim Type | Total Unprocessed And Unpaid Adjudicated Claims (3) | | | Total Unprocessed & Unpaid Adjudicated Claims |
| | 01-30 Days | 31-45 Days | 46-60 Days | 61-90 Days | 91-120 Days | >120 Days | |
| UB92 Claims | | | | | | | |
| HCFA 1500 Claims | | | | | | | |
Subtotal MCO Claims | | | | | | | |
| Pharmacy | | | | | | | |
| Dental | | | | | | | |
| Vision | | | | | | | |
Subtotal Vendor Claims | | | | | | | |
Total | | | | | | | |
| | | | | | | | |
| EQUAL OR Less than 45 Days | Greater than 45 Days |
| | | |
MCO Claims | % | % |
| Pharmacy | % | % |
| Dental | % | % |
| Vision | % | % |
Mental Health
| % | % |
| Total | % | % |
| | | | | | | | |
Claim Type | Estimated Claims Received but not in system (# of claims) (4) | | |
| | 01-30 Days | 31-45 Days | 46-60 Days | 61-90 Days | 91-120 Days | >120 Days | Total Claims Received But Not In System |
| UB92 Claims | | | | | | | |
| HCFA 1500 Claims | | | | | | | |
Subtotal MCO Claims | | | | | | | |
| Pharmacy | | | | | | | |
| Dental | | | | | | | |
| Vision | | | | | | | |
Mental Health
| | | | | | | |
Subtotal Vendor Claims | | | | | | | |
Total | | | | | | | |
| | | | | | | | |
| | | | | | | | |
| | | | | | | | |
Tick Mark Legend: | | | | | | | |
| | | | | | | | |
1. Claims in process-all claims that are in a pending status (data, medical, COB edits) and require review by a claim examiner prior to being released for adjudication. |
| | | | | | |
2. Unpaid adjudicated claims-claims which have been adjudicated and have a known pay amount, however, a check has not been issued for these claims. | |
| | | | | | |
3. Total of estimated claims in process, and unpaid adjudicated claims. | | | |
| 4. Estimated claims received but not in system-includes any claim that has been received and not input in the system(I.e. claims in the mailroom). |
HUSKY B Appendix H
(document 3 of 5)
Report #3
HUSKY A & B Turn Around Time - Claims Processed
Plan Name | | | | | | | |
Qtr. Ending: | | | | | | | |
| | | | | | | | |
Claim Type | Paper Claims Processed During Qtr. | | | | | |
| | 01-30 Days | 31-45 Days | 46-60 Days | 61-90 Days | 91-120 Days | >120 Days | Total Paper Claims Processed During Qtr. |
| UB92 Claims | | | | | | | |
| HCFA 1500 Claims | | | | | | | |
Subtotal MCO Claims | | | | | | | |
| Pharmacy | | | | | | | |
| Dental | | | | | | | |
| Vision | | | | | | | |
Subtotal Vendor Claims | | | | | | | |
Total | | | | | | | |
| | | | | | | | |
Claim Type | Electronic Claims Processed During Qtr. | | | | | |
| | 01-30 Days | 31-45 Days | 46-60 Days | 61-90 Days | 91-120 Days | >120 Days | Total Electronic Claims Processed During Qtr. |
| UB92 Claims | | | | | | | |
| HCFA 1500 Claims | | | | | | | |
Subtotal MCO Claims | | | | | | | |
| Pharmacy | | | | | | | |
| Dental | | | | | | | |
| Vision | | | | | | | |
Subtotal Vendor Claims | | | | | | | |
Total | | | | | | | |
| | | | | | | | |
Claim Type | Total Paper and Electronic Claims Processed During Qtr. | | | | |
| | 01-30 Days | 31-45 Days | 46-60 Days | 61-90 Days | 91-120 Days | >120 Days | Total Paper & Electronic Claims Processed During Qtr. |
| UB92 Claims | | | | | | | |
| HCFA 1500 Claims | | | | | | | |
Subtotal MCO Claims | | | | | | | |
| Pharmacy | | | | | | | |
| Dental | | | | | | | |
| Vision | | | | | | | |
Subtotal Vendor Claims | | | | | | | |
Total | | | | | | | |
| | | | | | | | |
Turn Around Statistics | EQUAL OR Less than 45 Days | Greater than 45 Days |
| | | |
MCO Claims | % | % |
| Pharmacy | % | % |
| Dental | % | % |
| Vision | % | % |
Mental Health
| % | % |
| Total | % | % |
Note: This report includes only paid claims, therefore it excludes denied claims.
(document 5 of 6)
Appendix H
Unaudited Quarterly Financial Reports
| | Current Assets: | Current Year | Previous Year |
| 1 | Cash and Cash Equivalents | | |
| 2 | Short-Term Investments | | |
| 3 | Premiums Receivable | | |
| 4 | Investment Income Receivables | | |
| 5 | Health Care receivables | | |
| 6 | Amounts Due from Affiliates | | |
| 7 | Aggregate Write-Ins for Current Assets | | |
| 8 | TOTAL CURRENT ASSETS (items 1-7) | | |
| | | | |
| | Other Assets | | |
| 9 | Restricted Cash and Other Assets | | |
| 10 | Long Term Investments | | |
| 11 | Amounts Due from Affiliates | | |
| 12 | Aggregate Write-Ins for Other Assets | | |
| 13 | TOTAL OTHER ASSETS (items 9-12) | | |
| | | | |
| | Property and Equipment | | |
| 14 | Land, building and Improvements | | |
| 15 | Furniture and Equipment | | |
| 16 | Leasehold Improvements | | |
| 17 | Aggreate Write-Ins for Other Equipment | | |
| 18 | TOTAL PROPERTY (items 7-14) | | |
| 19 | TOTAL ASSETS 9items 8, 13, and 18) | | |
| | | | |
| | Details of Write-Ins Aggregated at item 7 for Current Assets | | |
| 701 | | | |
| 702 | | | |
| 703 | | | |
| 704 | | | |
| 705 | | | |
| 798 | Summary of remaining write-ins for item 7 from overflow page | | |
| 799 | TOTALS: (items 701 through 705 plus 798 page 2, item 7) | | |
| | | | |
| | Details of Write-Ins Aggregated at item 12 for Other Assets | | |
| 1201 | | | |
| 1202 | | | |
| 1203 | | | |
| 1204 | | | |
| 1205 | | | |
| 1298 | Summary of remaining write-ins for item 12 from overflow page | |
| 1299 | TOTALS: (items 1201 through 1205 plus 1298 page 2, item 12) | |
| | | | |
| | Details of Write-Ins Aggregated at item 17 for Other Equipment | |
| 1701 | | | |
| 1702 | | | |
| 1703 | | | |
| 1704 | | | |
| 1705 | | | |
(document 5 of 6)
Appendix H
Unaudited Quarterly Financial Reports
| 1798 | Summary of remaining write-ins for item 17 from overflow page | |
| 1799 | TOTALS: (items 1701 through 1705 plus 1798 page 2, item 17) | |
| | | | |
| | Current Liabilities | | |
| 1 | Accounts Payable (Schedule G) | | |
| 2 | Claims Payable (Reported and Unreported) (Schedule H) | | |
| 3 | Accrued Medical Incentive Pool (Schedule H) | | |
| 4 | Unearned Premiums | | |
| 5 | Amounts Due to Affiliates (Schedule J) | | |
| 6 | | | |
| 7 | Aggregate Write-Ins for Current Liabilities | | |
| 8 | TOTAL CURRENT LIABILITIES (items 1-7) | | |
| | | | |
| | Other Liabilities | | |
| 9 | Loans and Notes Payable (Schedule I) | | |
| 10 | Amounts Due to Affiliates (Schedule J) | | |
| 11 | Aggregate Write-Ins for Other Liabilities | | |
| 12 | TOTAL OTHER LIABILITIES (items 9-11) | | |
| 13 | TOTAL LIABILITIES (items 8 and 12) | | |
| | | | |
| | Net Worth | | |
| 14 | Common Stock | | |
| 15 | Preferred Stock | | |
| 16 | Paid in Surplus | | |
| 17 | Contributed Capital | | |
| 18 | Surplus Notes (Schedule K) | | |
| 19 | Contingency Reserves | | |
| 20 | Retained Earnings/Fund Balance | | |
| 21 | Aggregate Write-Ins for Other Net Worth Items | | |
| 22 | TOTAL NET WORTH (items 13 and 22) | | |
| 23 | TOTAL LIABILITIES AND NET WORTH (items 13 and 22) | | |
| | | | |
| | Details of Write-Ins Aggregated at item 7 for Current Liabilities | |
| 701 | Payroll and Related Liabilities | | |
| 702 | Accrued Audit and Actuarial Fees | | |
| 703 | | | |
| 704 | | | |
| 705 | | | |
| 798 | Summary of Remaining Write-Ins for item 7 from overflow page | |
| 799 | TOTALS (items 0701 through 0705 plus 0798 Page 3, item 7) | | |
| | | | |
| | Details of Write-Ins Aggregated at item 11 for Other Liabilities | | |
| 1101 | | | |
| 1102 | | | |
| 1103 | | | |
| 1104 | | | |
| 1105 | | | |
| 1198 | Summary of remaining write-ins for item 11 from overflow page | |
| 1199 | TOTALS: (items 1101 through 1105 plus 1198 page 3, item 11) | |
| | | | |
| | Details of Write-Ins Aggregated at item 21 for Other Net Worth Items | |
| 2101 | | | |
(document 5 of 6)
Appendix H
Unaudited Quarterly Financial Reports
| 2102 | | | |
| 2103 | | | |
| 2104 | | | |
| 2105 | | | |
| 2198 | Summary of remaining write-ins for item 21 from overflow page | |
| 2199 | TOTALS: (items 2101 through 2105 plus 2198 page 3, item 21) | |
| | | | |
| | Member months | | |
| | Revenues | | |
| 1 | Premium | | |
| 2 | Fee-For-Service | | |
| 3 | Title XVIII - Medicare | | |
| 4 | Title XIX - Medicaid | | |
| 5 | Investment | | |
| 6 | Aggregate Write-Ins for Other Revenues | | |
| 7 | TOTAL REVENUES (items 1-6) | | |
| | | | |
| | Expenses | | |
| 8 | Medical and Hospital | | |
| 9 | Other Professional Services | | |
| 10 | Outside Referrals | | |
| 11 | Emergency Room and Out-of-Area | | |
| 12 | Occupancy, Depreciation and Amortization | | |
| 13 | Inpatient | | |
| 14 | Incentive Pool and Withhold Adjustments | | |
| 15 | Aggregate Write-Ins for other Medical and Hospital Expenses | | |
| 16 | Subtotal (items 8-15) | | |
| 17 | Reinsurance Expenses of Net of Recoveries | | |
| | | | |
| | Less | | |
| 18 | Copayments | | |
| 19 | COB and Subrogation | | |
| 20 | Subtotal (items 18 and 19) | | |
| 21 | Total Medical and Hospital (items 16 and 17 less 20) | | |
| | | | |
| | Administration | | |
| 22 | Compensation | | |
| 23 | Interest Expense | | |
| 24 | Occupancy, Depreciation and Amortization | | |
| 25 | Marketing | | |
| 26 | Aggregate Write-Ins for Other Administration Expenses | | |
| 27 | TOTAL ADMINISTRATION (items 22-26) | | |
| 28 | TOTAL EXPENSES (items 21 and 27) | | |
| 29 | Income (LOSS) (item 21 and 27) | | |
| 30 | Cumulative Effect of Accountin Change) | | |
| 31 | Provision for Federal Income Taxes | | |
| 32 | NET INCOME (item 29, less items 30 and 31) | | |
| | | | |
| | Details or Write-Ins Aggregated at item 6 for other Revenues | | |
| 601 | Other Income | | |
| 602 | | | |
| 603 | | | |
(document 5 of 6)
Appendix H
Unaudited Quarterly Financial Reports
| 604 | | | |
| 605 | | | |
| 698 | Summary of remaining write-ins for item 6 from overflow page | | |
| 699 | TOTALS: (items 601 through 605 plus 698 page 4, item 6) | | |
| | | | |
| | Member months | | |
| | Details of Write-Ins Aggregated at Item 6 for Other Revenues | | |
| 1501 | Drugs | | |
| 1502 | Outpatient | | |
| 1503 | | | |
| 1504 | | | |
| 1505 | | | |
| 1598 | Summary of remaining write-ins for item 15 from overflow page | |
| | | | |
| | Details of Write-Ins Aggregated at Item 26 for Other Administration Expenses | |
| 2601 | MGMT Fee Income - SWWA | | |
| 2602 | MGMTFee Expense GOHS | | |
| 2603 | Other Administration Expense | | |
| 2604 | MGMT Fee Expense Corp. | | |
| 2605 | Accrued Audit and Actuarial Expense | | |
| 2698 | Summary of remaining write-Ins for item 26 from ovrflow page | | |
| 2699 | TOTALS (items 2601 through 2605 plus 2698) (page 4, item 26) | |
Appendix I
Capitation Payment Amount
SFY 2007 Rates for Husky B Band 1 & 2
Includes BHP Carve out, 3.88% Rate Increase, Hosp Adjustment and Dental Adjustment
| | (Hardcoded) SFY 2007 Rate |
| FirstChoice | $155.73 |
Appendix J
Inpatient / Eligibility Recategorization Chart
HUSKY B - Appendix J HUSKY A & B Medical Acute Care Primary Inpatient/Eligibility Recategorization Changes |
| | | | | |
| Description | Admitting MCO | New/Continued MCO | Responsible Entity |
| HUSKY A, different MCO | A1 | A2 | A1 | |
| HUSKY A to FFS | A1 | FFS | FFS | |
| HUSKY A to HUSKY B, same MCO | A1 | B1 | A1 | |
| HUSKY A to HUSKY B, different MCO | A1 | B2 | A1 | |
| HUSKY B, different MCO | B1 | B2 | B1 | |
HUSKY A to disenrolled due to loss of eligibility (Out of Program) | A1 | x | A1 | |
HUSKY B to disenrolled due to loss of eligibility (Out of Program) | B1 | x | B1 | |
HUSKY B to A (Same MCO, different coverage) | B1 | A1 | A1 | |
HUSKY B to A (different MCO, different coverage) | B1 | A2 | A2 | |
| HUSKY B to FFS | B1 | FFS | FFS | |
| Code | | | | |
| A1 = HUSKY A, MCO #1 | | | | |
| A2 = HUSKY A, MCO #2 | | | | |
| B1 = HUSKY B, MCO #1 | | | | |
| B2 = HUSKY B, MCO #2 | | | | |
| FFS = Fee-for-service | | | | |
x= Disenrolled due to loss of eligibility | | | | |
Appendix K
Abortion Reporting
HUSKY B Non-Hyde Amendment Abortions
Name of MCO: ___________________________
Quarter Ended: ___________________________
This report shall include all abortions that do not meet the HYDE Amendment criteria, and that are paid by the MCO during the quarter (e.g. July 1 - September 30). These reports shall be submitted by the 15th of the month following the end of the quarter (e.g. October 15). The reports shall be submitted in hard copy, as well as electronically to Lee Voghel, Division of Fiscal Analysis.
| Date of Service | CPT Code | Medicaid Recipient ID# | Provider ID# | Provider Name | Date Paid | Amount Paid |
| | | | Total | | | |
I hereby certify that to the best of my knowledge the information contained herein is true and accurate.
Signature:
Printed Name:
Title:
Date:
Appendix L
Blank
Reserved for Possible Future Use
Appendix M
Blank
Reserved for Possible Future Use
APPENDIX N
HUSKY BEHAVIORAL HEALTH CARE-OUT COVERAGE
AND COORDINATION OF MEDICAL AND BEHAVIORAL SERVICES
HUSKY A - 05/07 - Appendix N
Coverage and Coordination of Medical and Behavioral Services
DEPARTMENT OF SOCIAL SERVICES DEPARTMENT OF CHILDREN AND FAMILIES
| |
| |
Co-Occurring Medical and Behavioral Health Conditions - Screening, Referral, and Coordination | |
Freestanding Medical/Primary Care Clinics | |
| |
Hospital Emergency Department | |
Hospital Inpatient Services | |
Hospital Outpatient Clinic Services | |
| |
| |
| |
| |
| |
Multi-Disciplinary Examinations | |
| |
| |
| |
| |
Primary Care Behavioral Health Services | |
| |
| |
School-Based Health Center Services | |
| |
State of Connecticut Page 2 01/26/06
The purpose of this document is to outline the policies according to which the HUSKY MCOs and the Behavioral Health Partnership (BHP) will share responsibility for providing covered services to HUSKY A and B enrollees after HUSKY behavioral health benefits are carved out and administered under a contract with the BHP Administrative Service Organization ("BHP ASO"). After the carve-out, the Managed Care Organizations that participate in HUSKY A and B ("HUSKY MCOs") will be responsible for providing services for medical conditions and BHP will be responsible for providing services for behavioral health conditions. The BHP ASO will provide member services, provider relations services, utilization management, intensive care management, quality management and other management services to facilitate the provision of timely, effective, and coordinated services under the BHP. The BHP ASO will not be responsible for contracting with providers or maintaining a provider network. Behavioral health providers will be required to enroll in the Department of Social Services' Connecticut Medical Assistance Program Network (CMAP). With the exception of DCF funded residential services, claims will be processed by the Department of Social Services' Medicaid vendor, Electronic Data Systems (EDS).
This document is intended to summarize the coverage responsibilities and coordination responsibilities for each of the major service areas as established by the HUSKY BH carve-out transition planning workgroup. In addition to this document, which is intended for use as an amendment or attachment to the ASO and MCO contracts, each of the HUSKY MCOs will develop a coordination agreement with the BHP ASO. The coordination agreements will further elaborate the coordination protocols with special attention to the areas noted below and to the key contacts and workflows particular to each MCO.
HUSKY MCOs will retain responsibility for all ancillary services such as laboratory, radiology, and medical equipment, devices and supplies regardless of diagnosis. However, laboratory costs for methadone chemistry (quantitative analysis) will be covered under the BHP when they are part of the bundled reimbursement for methadone maintenance providers. The HUSKY MCOs may track and trend laboratory utilization as part of coordination with the BHP ASO. In addition, the MCOs will address any increases in the utilization trend with The Department of Social Services.
State of Connecticut Page 3 01/26/06
Co-Occurring Medical and Behavioral Health Conditions - Screening, Referral, and Coordination
The HUSKY MCOs currently have programs and procedures designed to support the identification of untreated behavioral health disorders in medical patients at risk for such disorders. Such procedures may be carried out by medical service providers or by the MCO through the utilization management, case management and quality management processes. The MCOs will be expected to continue such activities in order to foster early and effective treatment of behavioral health disorders, including those disorders that could affect compliance with and the effectiveness of medical interventions.
Both the HUSKY MCOs and the BHP ASO will be required to communicate and coordinate as necessary to ensure the effective coordination of medical and behavioral health benefits. The HUSKY MCOs will contact the BHP ASO when co-management is indicated (including BH hospital emergency department visits), such as for persons with special physical health and behavioral health needs; will respond to inquiries by the BHP ASO regarding the presence of medical co-morbidities; and will coordinate with the BHP ASO when invited to do so. Conversely, the BHP ASO will contact the HUSKY MCOs when co-management is indicated; will respond to inquiries by the HUSKY MCOs regarding the presence of behavioral co-morbidities; and will coordinate with the HUSKY MCOs when invited to do so.
Both the BHP ASO and the MCOs will assign key contacts in order to facilitate timely coordination. In addition, it is anticipated that the BHP ASO's intensive care management department will be able to accept warm-line transfers as necessary from the HUSKY MCO case management departments to facilitate timely co-management.
The BHP ASO will convene Medical/Behavioral Co-Management meetings at least once a month with each HUSKY MCO. The frequency of the meetings will be by agreement between the BHP ASO and each HUSKY MCO. The purpose of the meeting will be to ensure appropriate management of clients with co-occurring medical and behavioral health conditions. Cases discussed between the BHP ASO and the MCO will include all levels of behavioral health and medical care. Furthermore, the BHP ASO and the HUSKY MCOs shall provide reports in advance of the meetings on the cases to be reviewed.
The HUSKY MCOs and the BHP ASO will from time to time make a determination as to whether a client's medical or behavioral health condition is primary. If there is a conflicting determination as to whether medical or behavioral health is primary, the respective medical directors will work together toward a timely and mutually agreeable resolution. At the request of either party, the Department of Social Services will make a determination as to the whether medical or behavioral health is primary and that determination shall be binding.
State of Connecticut Page 4 01/26/06
Freestanding Medical/Primary Care Clinics
The HUSKY MCOs will be responsible for primary care and other medical services provided by freestanding primary care/medical clinics regardless of diagnosis except for behavioral health evaluation and treatment services billed under CPT codes 90801-90806, 90853, 90846, 90847, and 90862 with a primary behavioral health diagnosis and only when provided by a licensed behavioral health professional.
HUSKY MCOs and BHP will share responsibility for covering home health services. The coordination agreements will include language that details procedures for resolving coverage responsibility issues. Home health coordination will be based on the following guidelines:
The HUSKY MCOs will be responsible for management and payment of claims when home health services are required for the treatment of medical diagnoses alone and when home health services are required to treat both medical and behavioral diagnoses, but the medical diagnosis is primary. If the individual's behavioral health treatment needs cannot be safely and effectively managed by the medical nurse and/or aide, the home care agency will be required to provide psychiatric nursing and/or aide services separately authorized and paid for under the BHP.
BHP will be responsible for management and payment of claims when home health services are required for the treatment of behavioral diagnoses alone (ICD 9: 291-316) and when home health services are required to treat both medical and behavioral diagnoses, but the behavioral diagnosis is primary. If the individual's medical treatment needs cannot be safely and effectively managed by the psychiatric nurse and/or aide, then the home care agency will be required to provide medical nursing and/or aide services separately authorized and paid for by the HUSKY MCOs.
The following table summarizes this policy:
| |
| Behavioral diagnosis only |
Medical and behavioral diagnoses, Med primary | Behavioral and medical diagnoses, Behavioral primary |
Medical component only, when medical and behavioral diagnoses are present and behavioral health needs cannot be effectively managed by the medical nurse and/or aide. | Behavioral component only, when behavioral and medical diagnoses are present and medical needs cannot be effectively managed by the medical nurse and/or aide. |
In addition, HUSKY MCOs will manage and pay claims for home health physical therapy, occupational therapy, and speech therapy services regardless of diagnosis.
State of Connecticut Page 5 01/26/06
When physical therapy, occupational therapy, and speech therapy services occur alongside home health behavioral health services, the home health care agency will be required to get authorization from and submit claims to the both the HUSKY MCO and to Electronic Data Systems (EDS), the claims vendor for the BHP.
The above policy will require that providers and management entities make decisions as to whether a medical or behavioral diagnosis is primary. This determination will be made at the time the service is presented for authorization. The determination will be based on the diagnosis that is the principal focus of the services — typically the one that requires the most time and/or expertise. A rebuttable presumption shall be made that the primary diagnosis is psychiatric if a psychiatrist makes the referral. The following examples should help in determining the issue of primary diagnosis:
| • | In general, if a recipient is receiving home health behavioral health services and at some point requires home health services for a medical condition, the behavioral health diagnosis remains primary if the medical treatment needs can be safely and effectively managed by the nurse that is providing the behavioral health services. If the medical condition requires treatment by a medical nurse, and the medical nurse is able to safely assume responsibility for the behavioral condition, then the medical diagnosis becomes primary. |
| • | Similarly, if a recipient is receiving home health medical services and at some point requires home health behavioral services for a behavioral condition, the medical diagnosis remains primary if the behavioral health treatment needs can be safely and effectively managed by the nurse that is providing the medical services. If the behavioral condition requires treatment by a psychiatric nurse, and the psychiatric nurse is able to safely assume responsibility for the medical condition, then the behavioral diagnosis becomes primary. |
If, at some point, separate nurses or aides are required to provide the behavioral and medical services, then the nurse and/or aide treating the medical condition must obtain authorization and payment from the HUSKY MCO and the nurse and/or aide treating the behavioral health condition must obtain authorization and payment under the BHP.
In some cases, a recipient will not require treatment for both a medical and behavioral condition at every visit. For example, a recipient may require two visits per day for his or her medical condition, but only one visit per day for the behavioral health condition, hi this case, the medical condition ought to be billed as primary for both visits. Conversely, if a recipient requires two visits per day for his or her behavioral condition, but only one visit per day for the medical condition, the behavioral condition ought to be billed as primary for both visits.
Finally, the primary reason for a visit may change from medical to behavioral or visa versa in the course of home health treatment. If this change occurs at the time of re-authorization, the home health care agency should pursue a new authorization from the entity with responsibility for the new condition for which home health care is required. If
State of Connecticut Page 6 01/26/06
the change in primary diagnosis occurs during an authorized episode of care, the home health care agency should discontinue services under the preceding authorization and pursue a new authorization from the entity with responsibility for the services going forward. If the HUSKY MCO reviews a request for authorization and believes that the primary has changed from medical to behavioral health, the MCO should direct the home care agency to pursue authorization through the BHP ASO. The converse is also true. If the primary is not apparent, the clinical reviewers from the BHP ASO and the MCO should confer and come to agreement.
Data provided by the HUSKY MCOs suggests that there are a modest number of clients with diagnoses of autism or mental retardation receiving home health services and that more than half of these clients have mixed diagnoses that could complicate management and billing. BHP will be responsible for the management and payment of claims when home health services are required for the treatment of autism, whether on its own or co-morbid with mental retardation. For those members with these dual diagnoses, providers will be directed to obtain authorization from the BHP ASO and to bill EDS with autism primary. The HUSKY MCOs will retain responsibility for mental retardation alone. BHP will also be responsible for management and payment of claims when home health services are required for the treatment of both autism and medical disorders, when the medical disorder can be safely and effectively managed by the psychiatric nurse and/or aide. If the individual's medical treatment needs are so significant that they cannot be safely and effectively managed by the psychiatric nurse and/or aide, then the home care agency will be required to provide medical nursing and/or aide services separately authorized and paid for by the HUSKY MCOs.
All home health care agencies operating in Connecticut are enrolled in the Connecticut Medical Assistance Program (CMAP) network and may, at their discretion, provide behavioral health home health services to HUSKY recipients. In contrast, the HUSKY MCOs may contract with only a subset of the CMAP providers. This means that there may be times when a client is in treatment for a behavioral health condition with a CMAP provider that is not participating with a HUSKY MCO. If this client develops a co-occurring medical disorder that is secondary and can be managed by the psychiatric home care nurse, BHP will continue to be responsible for management and payment of claims. If, however, the patient's medical disorder becomes primary and thus the responsibility of the HUSKY MCO, the HUSKY MCO can elect to continue to use the home care provider as an out of network provider, or the HUSKY MCO can, at its discretion, transition the care to a participating home care provider. The client's best interest will be a factor in this determination. The MCOs and BHP ASO will be expected to create coordination agreements to expedite the proper handling of such cases.
Hospital Emergency Department
The HUSKY MCOs will assume responsibility for emergency department services, including emergent and urgent visits and all associated charges billed by the facility, regardless of diagnosis. Professional psychiatric services rendered in an emergency department by a community psychiatrist will be reimbursed by the BHP if the psychiatrist
State of Connecticut Page 7 01/26/06
is enrolled in CMAP as an independent solo or group practitioner and bills under the solo or group practice ID. The BHP will be responsible for observation stays of 23 hours or less (RCC 762) with a primary behavioral health diagnosis. The HUSKY MCOs and the Department will implement audit procedures to ensure that hospitals do not bill HUSKY MCOs for emergency department services when patients are admitted to the hospital and behavioral health is primary. The HUSKY MCOs may track and trend Emergency Department utilization for behavioral health. The MCOs will address any increase in the utilization trend with the Departments.
Hospital Inpatient Services
In order to assure appropriate coordination and communication, the coordination agreements will include specific language detailing processes and procedures for concurrent communication and the process for handling co-occurring medical and behavioral health hospital inpatient conditions. In addition, the agreements will include specific language on the procedures for resolving coverage related issues when the ASO and MCOs disagree. Coordination will be based on the following guidelines:
BHP will be responsible for all psychiatric hospital services and all associated charges billed by a psychiatric hospital, regardless of diagnosis. The rate is all-inclusive so there will be no reimbursement for professional services rendered by community-based consulting physicians.
HUSKY MCOs and BHP will share responsibility for covering inpatient general hospital services. The HUSKY MCOs will be responsible for management and payment of claims for inpatient general hospital services when the medical diagnosis is primary. Medical would be considered primary when the billed RCC and the primary diagnosis are both medical.
During a medical stay, BHP will be responsible for professional services associated with behavioral health diagnoses. The admitting physician will be responsible for coordinating medical orders for any necessary behavioral health services with the BHP ASO. Other ancillary charges associated with non-primary behavioral health diagnoses shall remain the responsibility of the HUSKY MCOs, as described in the ancillary services section of this document.
BHP will be responsible for management and payment of claims for inpatient general hospital services when the behavioral diagnosis is primary. The behavioral diagnosis will be considered primary when the billed RCC and the primary diagnosis are both behavioral or when the billed RCC is medical, but the primary diagnosis on the claim form is behavioral. During a behavioral stay, the HUSKY MCOs will be responsible for professional services and other charges associated with primary medical diagnoses.
State of Connecticut Page 8 01/26/06
| o When an admission to a general hospital is initially medical, but the reason for continued admission becomes behavioral, responsibility for management and payment of claims will transition to BHP. When the hospital admission is no longer medically necessary for the medical diagnosis, the HUSKY MCO ceases to be responsible for management and payment. The BHP ASO will monitor the timeliness of transfer from a medical unit to a psychiatric unit when the primary diagnosis changes from medical to behavioral health. |
The following table summarizes this policy:
Inpatient Payment for Primary Diagnosis | | Professional Services Paid for Secondary Diagnosis |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
Hospital Outpatient Clinic Services
BHP will be responsible for all outpatient psychiatric clinic, intensive outpatient, extended day treatment, and partial hospitalization services provided by general and psychiatric hospitals for the evaluation and treatment of behavioral health disorders. BHP will also cover evaluation and treatment services related to a non-behavioral health diagnosis if the billing code is psychiatric as outlined in the covered services grid.
The HUSKY MCOs will be responsible for all primary care and other medical services provided by hospital medical clinics regardless of diagnosis including all medical specialty services and all ancillary services.
HUSKY Plus Behavioral services (intensive in-home psychiatric services) will be included in the HUSKY B benefit package. The ASO will manage access to these services under the carve-out.
The HUSKY MCOs will be responsible for all long term care services (i.e., nursing homes, chronic disease hospitals) regardless of diagnosis. These services are seldom
State of Connecticut Page 9 01/26/06
required for the treatment of clients with primary behavioral health disorders under the HUSKY program. The admission of a client with a primary behavioral health disorder must be by mutual agreement of the BHP ASO and the HUSKY MCO in which the client is enrolled.
DSS currently exempts any long-term care client from managed care the first of the month in which the client's stay exceeds 90 days. DSS will consider early exemption for clients with a primary behavioral health diagnosis if DSS were provided with adequate notice when such clients are admitted to long-term care.
The BHP ASO will have its own member services department with a dedicated toll free phone number. The member services staff will provide non-clinical information to recipients and when appropriate provide immediate access to clinical staff for care related assistance. The member services staff will respond to all calls directed to the member services line and it is expected will have the ability to accept warm-line transfers from the HUSKY MCOs. The HUSKY MCOs will replace references to existing BH subcontractors on member materials with the new BHP ASO name and member services phone number, wherever such references occur. Branch logic for the DSS' 1-877-CTHUSKY number will be modified to incorporate the ASO member services line as an option for callers that require BHP related assistance.
The MCOs will continue to conduct welcome calls to new members. At the time of the welcome call, the HUSKY MCO member services representative will provide the member with information on how to access the BHP ASO.
HUSKY MCO member services departments will occasionally receive calls from members who are requesting BH services. In addition, BH issues may emerge in the course of a welcoming call. The member may screen positive for behavioral health issues and express an interest in discussing further or have clear behavioral health issues and need a referral. In either case, the member service representative can affect a warm-line transfer to the ASO member services department, take the member's information and fax this information to the ASO for follow-up, or provide the member with the telephone number for the BHP ASO.
If the client is in crisis, the MCO member services representative should follow the MCO's protocols for handling crisis calls. The BHP ASO will have the capacity to accept warm-line transfer of such crisis calls when, at the discretion of the MCO, such transfer is appropriate.
BHP will be responsible for all Mental Health Clinic Services regardless of diagnosis including routine outpatient services and all diagnostic and treatment services billed as intensive outpatient treatment, extended day treatment, and partial hospitalization
State of Connecticut Page 10 01/26/06
treatment. BHP will also cover evaluation and treatment services related to a medical diagnosis such as psychological testing for a client with traumatic brain injury.
BHP will be responsible for reimbursing methadone clinics for methadone maintenance services provided to HUSKY enrollees. All methadone maintenance services for which the source of service is the methadone maintenance clinic are included in the Department's bundled rate with methadone maintenance clinics. The MCOs will cover all methadone maintenance laboratory services when billed by an independent laboratory
Multi-Disciplinary Examinations
The MCOs will be responsible for contracting with DCF certified Multi-Disciplinary Examination providers and for covering all components of the DCF Multi-Disciplinary Examinations including behavioral health evaluation services (e.g., 90801, 96110). .
The HUSKY MCOs will be responsible for issuing notices of action for medical review decisions and the BHP ASO will be responsible for issuing notices of action for behavioral health review decisions. The HUSKY MCOs will issue notices of action to the client and the provider, but will not issue a notice to the BHP ASO. Similarly, the BHP ASO will issue notices of action to the client and the provider, but will not issue a notice to the HUSKY MCO.
In preparation for a fair hearing, the Department of Social Services will work with the Department's contractor that issued the notice to prepare the Department's case. Typically, the ASO will not be involved in an MCO related fair hearing and the MCO will not be involved in an ASO related fair hearing. However, when a client has co-morbid medical and behavioral health conditions and the action affects both conditions, then both the MCO and the ASO may be involved in preparation for the fair hearing.
If a HUSKY MCO or one of its providers disagrees with a clinical management decision made by the BHP ASO, the HUSKY MCO is encouraged to raise the issue with the ASO on behalf of the client and to resolve the issue informally prior to the scheduled fair hearing. The converse is also true. If the issue remains unresolved, DSS will review the issue with the HUSKY MCO and the ASO and make a determination as to whether DSS supports the decision of the contractor that issued the notice. If DSS supports the contractor that issued the notice, the matter will proceed to fair hearing.
The HUSKY MCOs may at times refer a client or provider to the BHP ASO because the primary presenting condition is behavioral health rather than medical. The HUSKY MCO's determination that a condition is behavioral health rather than medical shall not constitute grounds for issuing a notice of action. The converse is true for the BHP ASO.
State of Connecticut Page 11 01/26/06
The HUSKY MCO may at times issue a notice of action for a prescription written by a CMAP enrolled behavioral health prescribing provider. In such instances, the HUSKY MCO will be expected to send notice of action to the client and to the prescribing provider.
In order to support coordination and communication regarding operational issues such as claims payment, the Departments will host a monthly meeting with the BHP ASO and the HUSKY MCOs.
The HUSKY MCOs currently provide outreach to members to assist them with accessing necessary services. The MCOs will continue to provide outreach to members to assist them with accessing medical services. For example, they may reach out to members to connect them to a primary care provider or to ensure necessary follow-up after a medical hospitalization. If an MCO's outreach worker identifies a member with a behavioral health issue, the worker may, at the MCO's discretion, provide information to the member on how to access behavioral health services via the ASO or facilitate a direct referral.
The BHP ASO will conduct extensive outreach focused on connecting clients to behavioral health care when clients are experiencing barriers to care. They will also make efforts to ensure a connection to care after discharge from a hospital or residential treatment center. If in the course of outreach the BHP ASO identifies a member with a significant medical issue, the ASO may provide information to the member on how to access necessary medical services through the MCO or the member's primary care provider or facilitate a direct referral.
The HUSKY MCOs will assume responsibility for all pharmacy services and all associated charges, regardless of diagnosis. However, methadone costs that are part of the bundled reimbursement for methadone maintenance and ambulatory detox providers will be covered under BHP. Methadone maintenance providers and ambulatory detox providers are responsible for supplying and dispensing methadone and these costs are covered by the BHP as part of an all-inclusive rate.
Each HUSKY MCO maintains its own pharmacy program with distinct formularies, drug utilization review requirements, and prior authorization requirements. Under BHP, the Departments will have contracts with prescribing behavioral health providers and these providers will be required to follow the pharmacy program requirements of the HUSKY MCO in which the member is enrolled as well as other applicable Medicaid program
State of Connecticut Page 12 01/26/06
requirements. BHP prescribing providers include psychiatrists, psychiatric nurses, freestanding behavioral health clinics, and hospitals.
DSS disseminates all policy transmittals and provider bulletins for CMAP providers through EDS. The ASO will not have a role in communications of this type. DSS will issue a provider bulletin to all enrolled prescribing providers prior to the carve-out date in order to apprise the providers of the pharmacy program requirements of each MCO and remind providers of the HUSKY program's temporary supply rules. DSS will require that providers adhere to each MCOs pharmacy program requirements and provide MCOs with any clinical information necessary to support requests for authorization or the preparation of clinical summaries for the purpose of fair hearings.
Subsequently, the MCOs must notify DSS of changes to its pharmacy program requirements. DSS will in turn use the provider bulletin process to notify CMAP providers of such changes within 30 days of the effective date. The Departments prefer that DSS manage such pharmacy program communications since it will have a complete and up-to-date file of enrolled prescribing providers. This new communication process should resolve some of the pharmacy program communication issues that currently exist in the HUSKY program. Specifically, among some HUSKY MCOs, certain providers such as freestanding behavioral health clinics are not included in routine pharmacy program communications issued by the MCO. Under the carve-out, all providers will be apprised of the requirements of all HUSKY MCOs. The initial provider bulletin pertaining to pharmacy will provide each MCO's web address where pharmacy program requirements are available.
The BHP ASO will fully cooperate with the MCOs and work closely with the MCOs to ensure compliance with the pharmacy programs of the individual MCOs. The BHP ASO will work closely with the MCOs to monitor pharmacy utilization and, if necessary, cooperate with the MCOs in conducting targeted provider education or training related to prescribing. DSS will require that its prescribing providers participate in quality initiatives and targeted pharmacy education and training conducted by the HUSKY MCOs for the purpose of improving prescribing practices and/or adherence to pharmacy program requirements. If the HUSKY MCOs encounter a behavioral health provider who engages in persistent misconduct related to psychiatric prescribing, the matter should be referred to DSS for investigation.
The HUSKY MCOs may track and trend behavioral health pharmacy utilization and address any increase in the utilization trend with the Departments. DSS will continue to review each MCO's compliance with pharmacy contract provisions and new DSS staff will meet with each MCO to familiarize themselves with each MCO formulary/pharmacy process and available data in order to be prepared to work with the MCOs on reporting specs.
Primary Care Behavioral Health Services
The HUSKY MCOs will retain responsibility for all primary care services and all associated charges, regardless of diagnosis. These responsibilities include:
State of Connecticut Page 13 01/26/06
1. behavioral health related prevention and anticipatory guidance;
2. screening for behavioral health disorders;
| 3. | treatment of behavioral health disorders that the primary care physician concludes can be safely and appropriately treated in a primary care setting; |
| 4. | management of psychotropic medications, when the primary care physician concludes it is safe and appropriate to do so, in conjunction with treatment by a BHP non-medical behavioral health specialist when necessary; and |
| 5. | referral to a behavioral health specialist when the primary care physician concludes that it is safe and appropriate to do so. |
The BHP ASO will develop education and guidance for primary care physicians related to the provision of behavioral health services in primary care settings. At their discretion, the HUSKY MCOs can collaborate with the ASO in the development of education and guidance or they will be provided the opportunity to review and comment. The education and guidance will address PCP prescribing with support and guidance from the ASO or referring clinic, in circumstances when the PCP is comfortable with this responsibility. The BHP ASO will make telephonic psychiatric consultation services available to primary care providers. Consultation may be initiated by any primary care provider that is seeking guidance on psychotropic prescribing for a HUSKY A, HUSKY B, or Voluntary Services enrollee.
To promote effective coordination and collaboration, the BHP ASO will work with interested HUSKY MCOs and provider organizations to sponsor opportunities for joint training. HUSKY MCO policies and provider contracts must permit the provision of behavioral health services by primary care providers; however, the MCOs will not be expected to provide education and training to improve ability of primary care providers to provide these services.
The HUSKY MCOs may track and trend primary care behavioral health utilization. The MCOs will address any increase in the utilization trend with the Departments.
The BHP ASO will be required to conduct at least three quality improvement initiatives each year. For the second year of the contract, the ASO will invite the HUSKY MCOs to participate in a joint quality improvement initiative focused on an area of mutual concern. Each MCO may participate at its discretion. The Departments will determine during the second year of the project whether to ask the BHP ASO to propose an additional joint quality improvement initiative with the MCOs during the third year of its contract.
The BHP ASO will provide a weekly census report on all behavioral health inpatient stays identifying those with co-occurring medical and behavioral health conditions. In
State of Connecticut Page 14 01/26/06
addition, the reports in Exhibit E of the BHP ASO contract will also be made available to the MCOs upon request.
The MCOs will provide daily and monthly reports and/or data as mutually agreed upon to the BHP ASO regarding i) behavioral health emergency department visits, ii) behavioral health emergency room recidivism, iii) substance abuse & neonatal withdrawal, iv) child/adolescent obesity and/or type II diabetes, v) sickle cell report, vi) eating disorders report, and vii) medical detox.
The Departments will also make MCO specific behavioral health encounter data available to the MCOs upon request to support quality management activities and coordination. The format of the data extract will be consistent with the encounter data reporting format, or other format mutually agreed upon by the Departments and the MCO.
The HUSKY MCOs will identify BH NEMT data versus medical NEMT data in their NEMT reporting to DSS. In addition, the HUSKY MCOs will track and trend NEMT complaints related to BH visits separately from NEMT complaints related to medical visits. The BHP ASO will also compile NEMT related complaints, although these complaints will be forwarded to the HUSKY MCOs for resolution.
The MCOs will continue to include behavioral health access in their CAHPS survey and report this information to the Departments.
School-Based Health Center Services
In general, BHP will be responsible for reimbursing school-based health centers for behavioral health diagnostic and treatment services (CPT 90801-90807, 90853, 90846, and 90847) provided to students with a behavioral health diagnosis. The HUSKY MCOs will be responsible for primary care services provided by school-based health centers, regardless of diagnosis, but they will not be responsible for behavioral health assessment and treatment services billed under CPT codes 90801-90807, 90853, 90846, and 90847. The following narrative provides additional background and a rationale for this arrangement.
School-based health centers currently provide a range of general health and behavioral health services that are reimbursable under the HUSKY program. All of these school-based health centers are licensed by the Department of Public Health, either as freestanding outpatient clinics or as satellites under a hospital license. Under these licenses, clinics can provide general medical services as well as behavioral health services.
School-based health centers vary in their degree of expertise in the provision of behavioral health services. Some school-based health centers provide prevention and counseling for students with emotional or behavioral issues and bill for those services using general primary care prevention and counseling codes, often without a behavioral
State of Connecticut Page 15 01/26/06
health diagnosis. Those primary care and preventive counseling services that are currently covered under the MCO contracts with individual School-Based Health Centers will continue to be the responsibility of the HUSKY MCOs.
Other school-based health centers have taken steps to develop their behavioral health services including relying on licensed behavioral health practitioners and/or affiliation agreements with local outpatient child psychiatric clinic that provide clinical staff, consultation, or oversight. If the school-based health center provides behavioral health diagnostic and treatment services, these services will be the responsibility of the BHP ASO. The school-based health center must enroll as a CMAP provider in order to be reimbursed for those services under BHP.
In some cases, the behavioral health component of the school-based health center's services is provided under the license of an outpatient child psychiatric clinic. In this case, the outpatient child psychiatric clinic will be enrolled as a CMAP provider and the services provided will be reimbursable as behavioral health clinic services under BHP.
All of the HUSKY MCOs will continue to provide transportation for HUSKY A enrollees with behavioral health disorders for behavioral health services that are covered under Medicaid. Specifically, the MCOs will continue to be responsible for transportation to hospitals, clinics, and independent professionals for routine outpatient, extended day treatment, intensive outpatient, partial hospitalization, detoxification, methadone maintenance, and inpatient psychiatric services. The MCOs will also be responsible for services that might be covered under EPSDT. For example, case management services are not included in the Connecticut Medicaid state plan, but they are covered under EPSDT when medically necessary. Although case management does not necessarily require transportation to a facility, if transportation to a facility were necessary for a case management encounter, the MCOs would be responsible for providing it. These policies under BHP are simply a continuation of current HUSKY A program policies.
The MCOs will not be responsible for transportation for non-Medicaid services such as respite, or DCF funded services that are designed to come to the client including care coordination, emergency mobile psychiatric services, home-based services, and therapeutic mentoring.
The transportation benefit for behavioral health visits will continue to be subject to the same policies and procedures applicable to other HUSKY A covered services. The Departments will issue a member services handbook that indicates that transportation services are covered for HUSKY A enrollees and that such services will be covered by the HUSKY MCO with which the member is enrolled. The handbook will indicate that the MCO specific transportation policies apply, that HUSKY MCO recipients should refer to their HUSKY member handbook for details, and arrange for transportation directly with their HUSKY MCO transportation broker.
State of Connecticut Page 16 01/26/06
The ASO will make referrals to the closest appropriate providers (typically 3 names will be given upon request) and avoid referrals to facilities and offices outside of a 25-30 mile radius unless circumstances require otherwise. The ASO is not required to review provider distance from the member when responding to requests for authorization. The transportation brokers will assess all requests for transportation when contacted by the member and it will be up to the transportation broker and the MCO to apply coverage limitations as appropriate when contacted by the member. In most cases, the transportation broker and/or the MCO will be able to make decisions about whether to authorize transportation to the non-closest provider or to a provider that is outside of the 25-30 mile radius by working directly with the member. However, the ASO will be required to respond to inquiries from the MCO or transportation broker if additional information is needed to support authorization of a transportation request.
The HUSKY MCOs will also retain responsibility for all Emergency Medical Transportation and associated charges, regardless of diagnosis, and hospital-to-hospital ambulance transportation of members with a behavioral health condition.
The BHP ASO is expected to work closely with the MCOs to monitor transportation utilization and, if necessary, cooperate with the MCOs in conducting targeted provider education or training related to the appropriate use of transportation services. The HUSKY MCOs may track and trend utilization of transportation to behavioral health facilities. Any increases in the utilization trend will be addressed with the Departments.
State of Connecticut Page 17 01/26/06
CTBHP Master Covered Services Table
| CTBHP Covered Services Table Revised July 31,2006 |
HUSKY A and B Appendix O - CT BHP Master Covered Services Table - September 2006 |
| 1 = HUSKY MCO - All diagnoses |
| |
| 3= BHP for Primary Diagnoses 291-316, HUSKY MCO all other diagnoses |
| | |
| | | |
| General Hospital Inpatient | |
| | |
| Room & Board- Private -Med/Surg/Gyn | |
| Room & Board- Private -OB | |
| Room & Board- Private -Pediatric | |
| Room & Board - Private - Psychiatric | |
| Room & Board- Private -Hospice | |
| Room & Board - Private - Detox | |
| Room & Board- Private -Oncology | |
| Room & Board- Private -Rehab | |
| Room & Board- Private -Other | |
| Room & Board-Semi-Private/2 Bed | |
| Room & Board-Semi-Private/ 2 Bed- Med/Surg/Gyn | |
| Room & Board-Semi-Private/ 2 Bed -OB | |
| Room & Board-Semi-Private/ 2 Bed-Pediatric | |
| Room & Board - Semi-Private/2 Bed - Psychiatric | |
| Room & Board-Semi-Private/ 2 Bed-Hospice | |
| Room & Board - Semi-Private/2 Bed - Detox | |
| Room & Board-Semi-Private/ 2 Bed-Oncology | |
| Room & Board-Semi-Private/ 2 Bed-Rehab | |
| Room & Board-Semi-Private/ 2 Bed-Other | |
| Room & Board-Semi-Private/3-4 Bed | |
| Room & Board-Semi-Private/3-4 Bed- Med/Surg/Gyn | |
| Room & Board-Semi-Private/3-4 Bed-OB | |
| Room & Board-Semi-Private/3-4 Bed-Pediatric | |
| Room & Board - Semi-Private/3-4 Bed - Psychiatric | |
| Room & Board-Semi-Private/3-4 Bed-Hospice | |
| Room & Board - Semi-Private/3-4 Bed - Detox | |
| Room & Board-Semi-Private/3-4 Bed-Oncology | |
| Room & Board-Semi-Private/3-4 Bed-Rehab | |
| Room & Board-Semi-Private/3-4 Bed-Other | |
| Room & Board-Private-Deluxe | |
| Room & Board-Private-Deluxe- Med/Surg/Gyn | |
| Room & Board-Private - Deluxe-OB | |
| Room & Board-Private - Deluxe-Pediatric | |
| Room & Board - Private - Deluxe - Psychiatric | |
| Room & Board-Private - Deluxe-Hospice | |
| Room & Board - Private - Deluxe - Detox | |
| Room & Board-Private - Deluxe-Oncology | |
| Room & Board-Private - Deluxe-Rehab | |
| Room & Board-Private - Deluxe-Other | |
| | |
| Room & Board - Ward - Med/Surg/ Gyn | |
| | |
| Room & Board - Ward - Pediatric | |
| Room & Board - Ward - Psychiatric | |
| Room & Board - Ward - Hospice | |
| Room & Board - Ward - Detox | |
| Room & Board - Ward - Oncology | |
| Room & Board - Ward - Rehab | |
| Room & Board - Ward - Other | |
| | |
| Other Room & Board - Sterile Environment | |
| Other Room & Board - Self Care | |
| Other Room & Board - Other | |
| | |
| Room & Board- Nursery - Newborn | |
| Room & Board- Nursery - Premature | |
| Room & Board- Nursery - Neonatal ICU | |
| Room & Board- Nursery - Other | |
1 of 11 HUSKY A B Appendix O - BHP Master Covered Services Table 05/01/07]
| CTBHP Covered Services Table Revised July 31, 2006 |
| | HUSKY A and B Appendix 0 - CT BHP Master Covered Services Table - September 2006 | |
| 1= HUSKY MCO - All diagnoses | |
| | |
| 3= BHP for Primary Diagnoses 291-316, HUSKY MCO all other diagnoses | |
| | | |
| | |
| | |
| Intensive Care - Surgical | |
| | |
| Intensive Care - Pediatric | |
| Intensive Care - Psychiatric | |
| Intensive Care - Post ICU | |
| Intensive Care - Burn Treatment | |
| | |
| | |
| | |
| Coronary Care - Myocardial Infarction | |
| Coronary Care - Pulmonary | |
| Coronary Care - Heart Transplant | |
| | |
| | |
| Late discharge/Medically necessary | |
| | Note: MCOs cover alcohol detoxification on a medical floor. | |
| General Hospital Emergency Department | |
| Emergency Room General Classification | |
| EMTALA Emergency Medical Screening Services | |
| Emergency Room Beyond EMTALA Screening | |
| | |
| | |
| | |
| Professional Fee - Emergency Department | |
| | | |
| General Hospital Outpatient | |
| | |
| | |
| Psychiatric Services General (Evaluation) | |
| Electroconvulsive Therapy** | |
| Intensive Outpatient Services - Psychiatric | |
| Intensive Outpatient Services - Chemical Dependency | |
| Community Behavioral Health Program (Day Treatment) | |
| | |
| | |
| | |
| | |
| Psychiatric Service - Testing | |
| | |
| Professional Fees-Psychiatric | |
| | |
| | Note: Includes outpatient provided by special care hospitals (e.g., Gaylord) | |
| | "MCOs pay for all professional services charges (e.g., anesthesiologist) regardless of diagnosis, except psychiatrist charges. | |
| Psychiatric Hospital Inpatient (includes Riverview, CVH) | |
| All inclusive room and board plus ancillary | |
| Room and Board-Psychiatric | |
| Room & Board - Semi-Private/2 Bed - Detox | |
| Room & Board-Semi-Private/ 2 Bed-Rehab | |
| | |
| Late discharge/Medically necessary | |
| | | |
| Psychiatric Hospital Outpatient | |
| | |
| | |
| Psychiatric Services General (Evaluation) | |
| Electroconvulsive Therapy | |
| Intensive Outpatient Services ^psychiatric | |
| Intensive Outpatient Services - Chemical Dependency | |
2 of 11 HUSKY A B Appendix 0 - BHP Master Covered Services Table 05/01/07]
| CTBHP Covered Services Table Revised July 31, 2006 |
HUSKY A and B Appendix O - CT BHP Master Covered Services Table - September 2006 |
| 1= HUSKY MCO -All diagnoses |
| |
| 3= BHP for Primary Diagnoses 291-316, HUSKY MCO all other diagnoses |
| | |
| Community Behavioral Health Program (Day Treatment) | |
| Partial Hospital-More Intensive | |
| Psychiatric Service-Individual Therapy | |
| Psychiatric Service-Group Therapy | |
| Psychiatric Service-Family Therapy | |
| Psychiatric Service-Testing | |
| | |
| | "MCOs pay for all professional services charges (e.g., anesthesiologist) regardless of diagnosis, except psychiatrist charges. | |
| Alcohol and Drug Abuse Center (Non-hospital Inpatient Detox) | |
| Acute Detoxification (residential program inpatient) | |
| | | |
| Alcohol and Drug Abuse Center (Ambulatory Detoxification) | |
| Ambulatory Detoxification | |
| | | |
| | |
| Psychiatric health facility service, per diem | |
| | | |
| | |
| DCF Funded residential facility | |
| | | |
| | |
| | |
| | |
| Inpatient hospital reserve | |
| | |
| | Note: Includes inpatient at special care hospitals. | |
| | |
| Psychiatric Diagnostic Interview | |
| Interactive Psychiatric Diagnostic Interview | |
| Individual Psychotherapy- Office or other Outpatient (20-30 min) | |
| Individual Psychotherapy-Office or other Outpatient (20-30 min) with medical evaluation and management services | |
| Individual Psychotherapy-Office or other Outpatient (45-50 min) | |
| Individual Psychotherapy-Office or other Outpatient (45-50 min) with medical evaluation and management services | |
| Individual Psychotherapy-Office or other Outpatient (75-80 min) | |
| Individual Psychotherapy-Office or other Outpatient (75-80 min) with medical evaluation and management services | |
| Interactive Individual Psychotherapy-Office or other Outpatient (20-30 min) | |
| Interactive Individual Psychotherapy-Office or other Outpatient (20-30 min) with medical evaluation and management services | |
| Interactive Individual Psychotherapy-Office or other Outpatient (45-50 min) | |
| Interactive Individual Psychotherapy-Office or other Outpatient (45-50 min) with medical evaluation and management services | |
| Interactive Individual Psychotherapy-Office or other Outpatient (75-80 min) | |
| Interactive Individual Psychotherapy-Office or other Outpatient (75-80 min) with medical evaluation and management services | |
| Family Psychotherapy (without the patient present) | |
| Family Psychotherapy (conjoint psychotherapy) (with the patient present) | |
| Multi-group family psychotherapy | |
| | |
| Interactive group psychotherapy | |
| | |
| Interpretation or explanation of results of psychiatric or other medical examinations and procedures or other accumulated data to family or other responsible persons. | |
| Psychological testing, per hour | |
| Developmental testing and report, limited | |
| Developmental testing and report, extended | |
| Neuropsychological testing battery, per hour | |
| Intensive Outpatient-Substance Dependence* | |
| Mental health partial hospitalization, treatment, less than 24 hours (CMHC)* | |
| | |
| Partial Hospitalization (non-CMHC)* | |
3 of 11 HUSKY A B Appendix O - BHP Master Covered Services Table 05/01/07]
| CTBHP Covered Services Table Revised July 31,2006 |
HUSKY A and B Appendix O - CT BMP Master Covered Services Table - September 2006 |
| 1= HUSKY MCO - All diagnoses |
| |
| 3= BHP for Primary Diagnoses 291-316, HUSKY MCO all other diagnoses |
| | |
| Therapeutic Behavioral Services, per 15 minutes (IICAPS, MST, MDFT, FFT, FST, HVS) (Clients under 21 only) | |
| Targeted case management, each 15 minutes (part of home-based services only - IICAPS, MST, MDFT, FFT, FST, HVS) (Clients under 21 only) | |
| Jnjection, Haloperidol, up to 5 mg | |
| Injection, Haloperidol decanoate, per 50 mg^ | |
| Injection, Fluphenazine decanoate, up to 25 mg | |
| Brief office visit for the sole purpose of monitoring or changing drug prescriptions used in the treatment of mental psychoneurotic and personality disorders | |
| Intensive Outpatient-Mental Health | |
| Emergency mobile mental health service, follow-up (Clients under 21 only) | |
| Emergency mobile mental health service, initial evaluation (Clients under 21 only) | |
| Case Management - Coordination of health care services - each 15 min. | |
| Community_psychiatric supportive treatment program, per diem | |
| Ambulatory setting, substance abuse treatment or detoxification services | |
| | 'Coverage restricted to providers approved by DSS to provide this service | |
| | *** Coverage restricted to providers certified by DCF to provide this service | |
| | ""Coverage restricted to providers licensed by DCF to provide this service | |
| | | |
| FQHC Mental Health Clinic | |
| Psychiatric Diagnostic Interview | |
| Interactive Psychiatric Diagnostic Interview | |
| Individual Psychotherapy- Office or other Outpatient (20-30 min) | |
| Individual Psychotherapy-Office or other Outpatient (20-30 min) with medical evaluation and management services | |
| Individual Psychotherapy-Office or other Outpatient (45-50 min) | |
| Individual Psychotherapy-Office or other Outpatient (45-50 min) with medical evaluation and management services | |
| Individual Psychotherapy-Office or other Outpatient (75-80 min) | |
| Individual Psychotherapy-Office or other Outpatient (75-80 min) with medical evaluation and management services | |
| Interactive Individual Psychotherapy-Office or other Outpatient (20-30 min) | |
| Interactive Individual Psychotherapy-Office or other Outpatient (20-30 min) with medical evaluation and management services | |
| Interactive Individual Psychotherapy-Office or other Outpatient (45-50 min) | |
| Interactive Individual Psychotherapy-Office or other Outpatient (45-50 min) with medical evaluation and management services | |
| Interactive Individual Psychotherapy-Office or other Outpatient (75-80 min) | |
| Interactive Individual Psychotherapy-Office or other Outpatient (75-80 min) with medical evaluation and management services | |
| Family Psychotherapy (without the patient present) | |
| Family Psychotherapy (conjoint psychotherapy) (with the patient present) | |
| Multi-group family psychotherapy | |
| | |
| Interactive group psychotherapy | |
| | |
| Interpretation or explanation of results of psychiatric or other medical examinations and procedures or other accumulated data to family or other responsible persons. | |
| Psychological testing, per hour | |
| Developmental testing and report, limited | |
| Developmental testing and report, extended | |
| Neuropsychological testing battery, per hour | |
| Intensive Outpatient-Substance Dependence* | |
| | |
| Partial Hospitalization (non-CMHC)* | |
| Injection, Haloperidol, up to 5 mg | |
| Injection, Haloperidol decanoate, per 50 mg | |
| Injection, Fluphenazine decanoate, up to 25 mg | |
| Brief office visit for the sole purpose of monitoring or changing drug prescriptions used in the treatment of mental psychoneurotic and personality disorders | |
| Intensive Outpatient-Mental Health | |
| Emergency mobile mental health service, follow-up (Clients under 21 only) | |
| Emergency mobile mental health service, initial evaluation (Clients under 21 only) | |
| Clinic visit/encounter all-inclusive (For use by FQHC MH Clinics) | |
4 of 11 HUSKY A B Appendix O - BHP Master Covered Services Table 05/01/07]
| CTBHP Covered Services Table Revised July 31, 2006 |
| | HUSKY A and B Appendix O - CT BHP Master Covered Services Table - September 2006 | |
| 1= HUSKY MCO - All diagnoses | |
| | |
| 3= BHP for Primary Diagnoses 291-316, HUSKY MCO all other diagnoses | |
| | | |
| Community psychiatric supportive treatment program, per diem | |
| Ambulatory setting, substance abuse treatment or detoxification services | |
| | 'Coverage restricted to providers approved by DSS to provide this service | |
| | | |
| | |
| Psychiatric Diagnostic Interview | |
| Individual Psychotherapy- Office or other Outpatient (20-30 min) | |
| Individual Psychotherapy-Office or other Outpatient (20-30 min) with medical evaluation and management services | |
| Individual Psychotherapy-Office or other Outpatient (45-50 min) | |
| Individual Psychotherapy-Office or other Outpatient (45-50 min) with medical evaluation and management services | |
| Individual Psychotherapy-Office or other Outpatient (75-80 min) | |
| Individual Psychotherapy-Office or other Outpatient (75-80 min) with medical evaluation and management services | |
| Family psychotherapy (without the patient present) | |
| Family psychotherapy (conjoint) | |
| | |
| Interactive Group therapy | |
| Neuropsychological testing battery, per hour | |
| | |
| | | |
| School-Based Health Centers (Freestanding Medical Clinic) | |
| Therapeutic or diagnostic injection; subcutaneous or intramuscular | |
| Therapeutic or diagnostic injection; intra-arterial | |
| Therapeutic or diagnostic injection; intravenous | |
| Psychiatric Diagnostic Interview | |
| Individual psychotherapy (20-30 min) | |
| Individual Psychotherapy-Office or other Outpatient (45-50 min) | |
| Family psychotherapy (without the patient present) | |
| Family psychotherapy (conjoint psychotherapy w/patient present) | |
| Group psychotherapy (other than of a multiple-family group) | |
| Office or other outpatient visit for the evaluation and management of an established patient, that may not require the presence of a physician. (Typically 5 minutes) | |
| Office or other outpatient visit for the evaluation and management of an established patient, which requires at least two of these three components: problem focused history; problem focused examination; straightforward medical decision-making. (Typically 10 minutes face-to-face) | |
| Office or other outpatient visit for the evaluation and management of an established patient, which requires at least two of these three components: expanded problem focused history; expanded problem focused examination; medical decision making of low complexity. (Typically 15 minutes face-to-face) | |
| Office or other outpatient visit for the evaluation and management of an established patient, which requires at least two of these three components: detailed history; detailed examination; medical decision making of moderate complexity (Typically 25 minutes face-to-face) | |
| Office or other outpatient visit for the evaluation and management of an established patient, which requires at least two of these three components: comprehensive history; comprehensive examination; medical decision making of high complexity (Typically 40 minutes face-to-face) | |
| | |
| | | |
| School-Based Health Centers (FQHC Medical Clinic) | |
| Therapeutic or diagnostic injection; subcutaneous or intramuscular | |
| Therapeutic or diagnostic injection; intra-arterial | |
| Therapeutic or diagnostic injection; intravenous | |
| Psychiatric Diagnostic Interview | |
| Individual psychotherapy (20-30 min) | |
| Individual Psychotherapy-Office or other Outpatient (45-50 min) | |
| Family psychotherapy (without the patient present) | |
| Family psychotherapy (conjoint psychotherapy w/patient present) | |
| Group psychotherapy (other than of a multiple-family group) | |
| Clinic visit/encounter all-inclusive (For use by FQHC Clinics) | |
| Office or other outpatient visit for the evaluation and management of an established patient, that may not require the presence of a physician. (Typically 5 minutes) | |
5 of 11 HUSKY A B Appendix O - BHP Master Covered Services Table 05/01/07]
| CTBHP Covered Services Table Revised July 31, 2006 |
HUSKY A and B Appendix O - CT BHP Master Covered Services Table - September 2006 |
| 1 = HUSKY MCO - All diagnoses |
| |
| 3= BHP for Primary Diagnoses 291-316, HUSKY MCO all other diagnoses |
| | |
| Office or other outpatient visit for the evaluation and management of an established patient, which requires at least two of these three components: problem focused history; problem focused examination; straightforward medical decision-making. (Typically 10 minutes face-to-face) | |
| Office or other outpatient visit for the evaluation and management of an established patient, which requires at least two of these three components: expanded problem focused history; expanded problem focused examination; medical decision making of low complexity. (Typically 15 minutes face-to-face) | |
| Office or other outpatient visit for the evaluation and management of an established patient, which requires at least two of these three components: detailed history; detailed examination; medical decision making of moderate complexity (Typically 25 minutes face-to-face) | |
| Office or other outpatient visit for the evaluation and management of an established patient, which requires at least two of these three components: comprehensive history; comprehensive examination; medical decision making of high complexity (Typically 40 minutes face-to-face) | |
| | |
| | | |
| | |
| Methadone service; rate includes all services for which the source of service is the methadone maintenance clinic. | |
| | | |
| MD, DO and APRN other than Psychiatrist or Psychiatric APRN | |
| Anesthesia for electroconvulsive therapy | |
| Drug screen, qualitative, chromatographic method, each procedure | |
| Urinalysis, by dip stick or tablet reagent, non-automated, with microscopy | |
| Methadone chemistry (quantitative analysis) | |
| Therapeutic or diagnostic injection; subcutaneous or intramuscular | |
| Therapeutic or diagnostic injection; intra-arterial | |
| Therapeutic or diagnostic injection; intravenous | |
| | |
| Office or other outpatient visit for the evaluation and management of an established patient, that may not require the presence of a physician. (Typically 5 minutes) | |
| Office or other outpatient visit for the evaluation and management of an established patient, which requires at least two of these three components: problem focused history; problem focused examination; straightforward medical decision making (Typically 10 minutes face-to-face) | |
| Office or other outpatient visit for the evaluation and management of an established patient, which requires at least two of these three components: expanded problem focused history; expanded problem focused examination; medical decision making of low complexity. (Typically 15 minutes face-to-face) | |
| Office or other outpatient visit for the evaluation and management of an established patient, which requires at least two of these three components: detailed history; detailed examination; medical decision making of moderate complexity (Typically 25 minutes face-to-face) | |
| Office or other outpatient visit for the evaluation and management of an established patient, which requires at least two of these three components: comprehensive history; comprehensive examination; medical decision making of high complexity (Typically 40 minutes face-to-face) | |
| | |
| | | |
| | |
| | |
| Interactive Diagnostic Interview | |
| Individual Psychotherapy-Office or other Outpatient (20-30 min) | |
| Individual Psychotherapy-Office or other Outpatient (20-30 min) with medical evaluation and management services | |
| Individual Psychotherapy-Office or other Outpatient (45-50 min) | |
| Individual Psychotherapy-Office or other Outpatient (45-50 min) with medical evaluation and management services | |
| Individual Psychotherapy-Office or other Outpatient (75-80 min) | |
| Individual PsychotherapyjOffice or other Outpatient (75-80 min) with medical evaluation and management services | |
| Interactive Individual Psychotherapy-Office or other Outpatient (20-30 min) | |
| Interactive Individual Psychotherapy-Office or other Outpatient (20-30 min) with medical evaluation and management services | |
| Interactive Individual Psychotherapy-Office or other Outpatient (45-50 min) | |
| Interactive Individual Psychotherapy-Office or other Outpatient (45-50 min) with medical evaluation and management services | |
| Interactive Individual Psychotherapy-Office or other Outpatient (75-80 min) | |
| Interactive Individual Psychotherapy-Office or other Outpatient (75-80 min) with medical evaluation and management services | |
6 of 11 HUSKY A B Appendix O - BHP Master Covered Services Table 05/01/07]
| CTBHP Covered Services Table Revised July 31, 2006 |
| | HUSKY A and B Apjoejrdixjg^CT BMP Master Covered Services Table - September 2006 | |
| 1 = HUSKY MCO - All diagnoses | |
| | |
| 3= BHP for Primary Diagnoses 291-316, HUSKY MCO all other diagnoses | |
| | | |
| Individual Psychotherapy-Facility Based (20-30 min) | |
| 90816 with medical evaluation and management | |
| Individual psychotherapy, insight oriented 45-50 minutes | |
| 90818 with medical evaluation and management | |
| Individual Psychotherapy-Facility Based (75-80 min) | |
| Individual Psychotherapy-Facility Based (75-80 min) with med management | |
| Interactive Individual Psychotherapy-Facility Based (20-30 min) | |
| Interactive Individual Psychotherapy-Facility Based (20-30 min) med management | |
| Interactive Individual Psychotherapy-Facility Based (45-50 min) | |
| Interactive Individual Psychotherapy-Facility Based (45-50 min) med management | |
| Interactive Individual Psychotherapy-Facility Based (75-80 min) | |
| Interactive Individual Psychotherapy-Facility Based (75-80 min) med management | |
| Family Psychotherapy (without the patient present) | |
| Family Psychotherapy (conjoint) | |
| Multi-group family psychotherapy | |
| | |
| Interactive Group psychotherapy | |
| Pharmacological management, including prescription, use, and review of medication with no more than minimal medical psychotherapy | |
| Narcosynthesis for Psychiatric Diagnostic and Therapeutic purposes | |
| Electroconvulsive therapy (including necessary monitoring); single seizure | |
| Individual psychophysiological therapy incorporating biofeedback training (20-30 min) | |
| Individual psychophysiological therapy incorporating biofeedback training (45-50 min) | |
| | |
| Interpretation or explanation of results of psychiatric or other medical examinations and procedures or other accumulated data to family or other responsible persons. | |
| Psychological testing, per hour | |
| Developmental testing with report | |
| Developmental testing, extended | |
| Neuropsychological testing battery, per hour | |
| Office or other outpatient visit, 10 minutes, new patient | |
| Office or other outpatient visit, 20 minutes, new patient | |
| Office or other outpatient visit, 30 minutes, new patient | |
| Office or other outpatient visit, 45 minutes, new patient | |
| Office or other outpatient visit, 60 minutes, new patient | |
| Office or other outpatient visit, 5 minutes, established patient | |
| Office or other outpatient visit, 10 minutes, established patient | |
| Office or other outpatient visit, 15 minutes, established patient | |
| Office or other outpatient visit, 25 minutes, established patient | |
| Office or other outpatient visit, 40 minutes, established patient | |
| Observation care discharge | |
| Initial observation care, low severity | |
| Initial observation care, moderate severity | |
| Initial observation care, high severity | |
| Inpatient hospital care, 30 minutes | |
| Inpatient hospital care, 50 minutes | |
| Inpatient hospital care, 70 minutes | |
| Subsequent hospital care, 15 minutes | |
| Subsequent hospital care, 25 minutes | |
| Subsequent hospital care, 35 minutes | |
| Observation of inpatient hospital care, low severity | |
| Observation of inpatient hospital care, moderate severity | |
| Observation of inpatient hospital care, high severity | |
| Hospital discharge day management 30 minutes or less | |
| Hospital discharge day management more than 30 minutes | |
| Office consultation for a new or established patient, approximately 15 minutes | |
| Office consultation for a new or established patient, approximately 30 minutes | |
| Office consultation for a new or established patient, approximately 40 minutes | |
| Office consultation for a new or established patient, approximately 60 minutes | |
| Office consultation for a new or established patient, approximately 80 minutes | |
| Initial inpatient consultation, 20 minutes | |
7 of 11 HUSKY A B Appendix O - BHP Master Covered Services Table 05/01/07]
| CTBHP Covered Services Table Revised July 31, 2006 |
| | HUSKY A and B Appendix 0 - CT BHP Master Covered Services Table - September 2006 | |
| 1= HUSKY MCO - All diagnoses | |
| | |
| 3= BHP for Primary Diagnoses 291-316, HUSKY MCO all other diagnoses | |
| | | |
| Initial inpatient consultation, 40 minutes | |
| Initial inpatient consultation, 55 minutes | |
| Initial inpatient consultation, 80 minutes | |
| Initial inpatient consultation, 110 minutes | |
| Confirmatory consultation, limited or minor | |
| Confirmatory consultation, low severity | |
| Confirmatory consultation, moderate severity | |
| Confirmatoryjjonsultation, moderate to high severity | |
| Confirmatory consultation, high severity | |
| Emergency department visit, minor severity | |
| Emergency department visit, low to moderate severity | |
| Emergency department visit, moderate severity | |
| Emergency department visit, high severity | |
| Emergency department visit, high severity with significant threat | |
| Injection, Haloperidol, up to 5 mg | |
| Injection, Haloperidol decanoate, per 50 mg | |
| Injection, Fluphenazine decanoate, up to 25 mg | |
| Brief office visit for the sole purpose of monitoring or changing prescriptions used in the treatment of mental psychoneurotic or personality disorders | |
| Case Management - Coordination of health care services - each 15 min. | |
| | |
| | | |
| | |
| | |
| Interactive Diagnostic Interview | |
| Individual Psychotherapy-Office or other Outpatient (20-30 min) | |
| Individual Psychotherapy-Office or other Outpatient (20-30 min) with medical evaluation and management services | |
| Individual Psychotherapy-Office or other Outpatient (45-50 min) | |
| Individual Psychotherapy-Office or other Outpatient (45-50 min) with medical evaluation and management services | |
| Individual Psychotherapy-Office or other Outpatient (75-80 min) | |
| Individual Psychotherapy-Office or other Outpatient (75-80 min) with medical evaluation and management services | |
| Interactive Individual Psychotherapy-Office or other Outpatient (20-30 min) | |
| Interactive Individual Psychotherapy-Office or other Outpatient (20-30 min) with medical evaluation and management services | |
| Interactive Individual Psychotherapy-Office or other Outpatient (45-50 min) | |
| Interactive Individual Psychotherapy-Office or other Outpatient (45-50 min) with medical evaluation and management services | |
| Interactive Individual Psychotherapy-Office or other Outpatient (75-80 min) | |
| Interactive Individual Psychotherapy-Office or other Outpatient (75-80 min) with medical evaluation and management services | |
| Individual Psychotherapy-Facility Based (20-30 min) | |
| 90816 with medical evaluation and management | |
| Individual psychotherapy, insight oriented 45-50 minutes | |
| 90818 with medical evaluation and management | |
| Individual Psychotherapy-Facility Based (75-80 min) | |
| Individual Psychotherapy-Facility Based (75-80 min) with med management | |
| Interactive Individual Psychotherapy-Facility Based (20-30 min) | |
| Interactive Individual Psychotherapy-Facility Based (20-30 min) med management | |
| Interactive Individual Psychotherapy-Facility Based (45-50 min) | |
| Interactive Individual Psychotherapy-Facility Based (45-50 min) med management | |
| Interactive Individual Psychotherapy-Facility Based (75-80 min) | |
| Interactive Individual Psychotherapy-Facility Based (75-80 min) med management | |
| Family Psychotherapy (without the patient present) | |
| Family Psychotherapy (conjoint) | |
| Multi-group family psychotherapy | |
| | |
| Interactive Group psychotherapy | |
| Pharmacological management, including prescription, use, and review of medication with no more than minimal medical psychotherapy | |
| Narcosynthesis for Psychiatric Diagnostic and Therapeutic purposes | |
8 of 11 HUSKY A B Appendix 0 - BHP Master Covered Services Table 05/01/07]
| CTBHP Covered Services Table Revised July 31,2006 |
| | HUSKY A and B Appendix O - CT BHP Master Covered Services Table - September 2006 | |
| 1= HUSKY MCO - All diagnoses | |
| | |
| 3= BHP for Primary Diagnoses 291-316, HUSKY MCO all other diagnoses | |
| | | |
| Electroconvulsive therapy (including necessary monitoring); single seizure | |
| Individual psychophysiological therapy incorporating biofeedback training (20-30 min) | |
| Individual psychophysiological therapy incorporating biofeedback training (45-50 min) | |
| | |
| Interpretation or explanation of results of psychiatric or other medical examinations and procedures or other accumulated data to family or other responsible persons. | |
| Psychological testing, per hour | |
| Developmental testing with report | |
| Developmental testing, extended | |
| Neuropsychological testing battery, per hour | |
| Office or other outpatient visit, 10 minutes, new patient | |
| Office or other outpatient visit, 20 minutes, new patient | |
| Office or other outpatient visit, 30 minutes, new patient | |
| Office or other outpatient visit, 45 minutes, new patient | |
| Office or other outpatient visit, 60 minutes, new patient | |
| Office or other outpatient visit, 5 minutes, established patient | |
| Office or other outpatient visit, 10 minutes, established patient | |
| Office or other outpatient visit, 15 minutes, established patient | |
| Office or other outpatient visit, 25 minutes, established patient | |
| Office or other outpatient visit, 40 minutes, established patient | |
| Observation care discharge | |
| Initial observation care, low severity | |
| Initial observation care, moderate severity | |
| Initial observation care, high severity | |
| Inpatient hospital care, 30 minutes | |
| Inpatient hospital care, 50 minutes | |
| Inpatient hospital care, 70 minutes | |
| Subsequent hospital care, 15 minutes | |
| Subsequent hospital care, 25 minutes | |
| Subsequent hospital care, 35 minutes | |
| Observation of inpatient hospital care, low severity | |
| Observation of inpatient hospital care, moderate severity | |
| Observation of inpatient hospital care, high severity | |
| Hospital discharge day management 30 minutes or less | |
| Hospital discharge day management more than 30 minutes | |
| Office consultation for a new or established patient, approximately 15 minutes | |
| Office consultation for a new or established patient, approximately 30 minutes | |
| Office consultation for a new or established patient, approximately 40 minutes | |
| Office consultation for a new or established patient, approximately 60 minutes | |
| Office consultation for a new or established patient, approximately 80 minutes | |
| Initial inpatient consultation, 20 minutes | |
| Initial inpatient consultation, 40 minutes | |
| Initial inpatient consultation, 55 minutes | |
| Initial inpatient consultation, 80 minutes | |
| Initial inpatient consultation, 110 minutes | |
| Confirmatory consultation, limited or minor | |
| Confirmatory consultation, low severity | |
| Confirmatory consultation, moderate severity | |
| Confirmatory consultation, moderate to high severity | |
| Confirmatory consultation, high severity | |
| Emergency department visit, minor severity | |
| Emergency department visit, low to moderate severity | |
| Emergency department visit, moderate severity | |
| Emergency department visit, high severity | |
| Emergency department visit, high severity with significant threat | |
| Injection, Haloperidol, up to 5 mg | |
| Injection, Haloperidol decanoate, per 50 mg | |
| Injection, Fluphenazine decanoate, up to 25 mg | |
| Brief office visit for the sole purpose of monitoring or changing prescriptions used in the treatment of mental psychoneurotic or personality disorders | |
| Case Management - Coordination of health care services - each 15 min. | |
9 of 11 HUSKY A B Appendix O - BHP Master Covered Services Table 05/01/07]
| CTBHP Covered Services Table Revised July 31, 2006 |
HUSKY A and B Appendix O;- CT BMP Master Covered Services Table | |
| 1= HUSKY MCO - All diagnoses |
| |
| 3= BMP for Primary Diagnoses 291-316, HUSKY MCO all other diagnoses | |
| | | |
| | |
| | | |
| Psychologist and Psychologist Group | |
| | |
| Interactive Diagnostic Interview | |
| Individual Psychotherapy-Office or other Outpatient (20-30 min) | |
| Individual Psychotherapy-Office or other Outpatient (45-50 min) | |
| Individual Psychotherapy-Office or other Outpatient (75-80 min) | |
| Interactive Individual Psychotherapy-Office or other Outpatient (20-30 min) | |
| Interactive Individual Psychotherapy-Office or other Outpatient (45-50 min) | |
| Interactive Individual Psychotherapy-Office or other Outpatient (75-80 min) | |
| Individual Psychotherapy-Facility Based (20-30 min) | |
| Individual psychotherapy, insight oriented 45-50 minutes | |
| Individual Psychotherapy-Facility Based (75-80 min) | |
| Interactive Individual Psychotherapy-Facility Based (20-30 min) | |
| Interactive Individual Psychotherapy-Facility Based (45-50 min) | |
| Interactive Individual Psychotherapy-Facility Based (75-80 min) | |
| Family Psychotherapy (without the patient present) | |
| Family Psychotherapy (conjoint) | |
| Multi-group family psychotherapy | |
| | |
| Interactive Group psychotherapy | | |
| Individual psychophysiological therapy incorporating biofeedback training (20-30 | | |
| Individual psychophysiological therapy incorporating biofeedback training (45-50 | | |
| | | |
| Interpretation or explanation of results of psychiatric or other medical examinations and procedures or other accumulated data to family or other responsible persons. . | |
| Psychological testing, per hour | |
| Developmental testing with report | |
| Developmental testing, extended | |
| Neuropsychological testing battery, per hour | |
| Case Management - Coordination of health care services - each 15 min. | |
| | | |
| | | |
| Independent Practice Behavioral Health Professional (LCSW, LMFT, LPC, LADC) | |
| | |
| Interactive Diagnostic Interview | |
| Individual Psychotherapy-Office or other Outpatient (20-30 min) | |
| Individual Psychotherapy-Office or other Outpatient (45-50 min) | |
| Individual Psychotherapy-Office or other Outpatient (75-80 min) | |
| Interactive Individual Psychotherapy-Office or other Outpatient (20-30 min) | |
| Interactive Individual Psychotherapy-Office or other Outpatient (45-50 min) | |
| Interactive Individual Psychotherapy-Office or other Outpatient (75-80 min) | |
| Individual Psychotherapy-Facility Based (20-30 min) | |
| Individual psychotherapy, insight oriented 45-50 minutes | |
| Individual Psychotherapy-Facility Based (75-80 min) | |
| Interactive Individual Psychotherapy-Facility Based (20-30 min) | |
| Interactive Individual Psychotherapy-Facility Based (45-50 min) | |
| Interactive Individual Psychotherapy-Facility Based (75-80 min) | |
| Family Psychotherapy (without the patient present) | |
| Family Psychotherapy (conjoint) | |
| Multi-group family psychotherapy | | |
| | | |
| Interactive Group psychotherapy | |
| Individual psychophysiological therapy incorporating biofeedback training (20-30 | | |
| Individual psychophysiological therapy incorporating biofeedback training (45-50 | | |
| | |
| Interpretation or explanation of results of psychiatric or other medical examinations and procedures or other accumulated data to family or other responsible persons. | |
| Developmental testing with report | |
10 of 11 HUSKY A B Appendix O - BMP Master Covered Services Table 05/01/07]
| CTBHP Covered Services Table Revised July 31, 2006 |
| | HUSKY A and B Appendix O - CT BMP Master Covered Services Table - September 2006 | |
| 1= HUSKY MCO - All diagnoses | |
| | |
| 3= BMP for Primary Diagnoses 291-316, HUSKY MCO all other diagnoses | |
| | | |
| Developmental testing, extended | |
| Case Management - Coordination of health care services - each 15 min. | |
| | | |
| Home Health Care Agencies | |
| | |
| | |
| Physical Therapy Evaluation | |
| | |
| Occupational Therapy Evaluation | |
| | |
| Speech Therapy Evaluation | |
| Services of a qualified nursing aide, up to 15 minutes | |
| Nursing care, in the home by an RN, per hour | |
| Nursing Care, in the home by an LPN, per hour | |
| Nursing Assessment/Evaluation | |
| RN Services, up to 15 minutes | |
| LPN/LVN services, up to 15 minutes | |
| Administration of oral, intramuscular and/or subcutaneous medication by health care agency/professional, per visit | |
| | *BHP covers home health services for children with autism including when autism is co-morbid with mental retardation. | |
| Independent Occupational Therapist | |
| | |
| | | |
| Independent Physical Therapist | |
| | |
| | | |
| | |
| | |
| | | |
| Emergency Medical Transportation | |
| | |
| | | |
| Independent Laboratory Services | |
| Drug screen, qualitative, chromatographic method, each procedure | |
| Urinalysis, by dip stick or tablet reagent, non-automated, with microscopy | |
| Methadone chemistry (quantitative analysis) | |
| | |
| | | |
| | |
| | |
| | | |
| | |
| Psychosocial Rehabilitation services, per 15 minutes | |
| Therapeutic Behavioral Services, per 15 minutes (IICAPS, MST, MDFT, FFT, FST, HBV) (Clients under 21 only) | |
| Targeted case management, each 15 minutes (part of home-based services only - IICAPS, MST, MDFT, FFT, FST, HBV) (Clients under 21 only) | |
| Activity Therapy, per 15 minutes (Therapeutic Mentoring/Behavioral Management Service) (Clients under 21 only) | |
| | "'Coverage restricted to providers certified by DCF to provide this service | |
| | ""Coverage restricted to providers licensed by DCF to provide this service | |
11 of 11 HUSKY A B Appendix 0 - BHP Master Covered Services Table 05/01/07]