
ASH 2018 December 3, 2018 NASDAQ: BLUE Exhibit 99.1 Exhibit 99.1 ASH 2018 December 3, 2018 NASDAQ: BLUE
These slides and the accompanying oral presentation contain forward-looking statements and information. The use of words such as “may,” “might,” “will,” “should,” “expect,” “plan,” “anticipate,” “believe,” “estimate,” “project,” “intend,” “future,” “potential,” or “continue,” and other similar expressions are intended to identify forward-looking statements. For example, all statements we make regarding the initiation, timing, progress and results of our preclinical and clinical studies and our research and development programs, our ability to advance product candidates into, and successfully complete, clinical studies, and the timing or likelihood of regulatory filings and approvals are forward looking. All forward-looking statements are based on estimates and assumptions by our management that, although we believe to be reasonable, are inherently uncertain. All forward-looking statements are subject to risks and uncertainties that may cause actual results to differ materially from those that we expected. These statements are also subject to a number of material risks and uncertainties that are described in our most recent quarterly report on Form 10-Q, as well as our subsequent filings with the Securities and Exchange Commission. Any forward-looking statement speaks only as of the date on which it was made. We undertake no obligation to publicly update or revise any forward-looking statement, whether as a result of new information, future events or otherwise, except as required by law. Forward-Looking Statements Forward-Looking Statements These slides and the accompanying oral presentation contain forward-looking statements and information. The use of words such as “may,” “might,” “will,” “should,” “expect,” “plan,” “anticipate,” “believe,” “estimate,” “project,” “intend,” “future,” “potential,” or “continue,” and other similar expressions are intended to identify forward-looking statements. For example, all statements we make regarding the initiation, timing, progress and results of our preclinical and clinical studies and our research and development programs, our ability to advance product candidates into, and successfully complete, clinical studies, and the timing or likelihood of regulatory filings and approvals are forward looking. All forward-looking statements are based on estimates and assumptions by our management that, although we believe to be reasonable, are inherently uncertain. All forward-looking statements are subject to risks and uncertainties that may cause actual results to differ materially from those that we expected. These statements are also subject to a number of material risks and uncertainties that are described in our most recent quarterly report on Form 10-Q, as well as our subsequent filings with the Securities and Exchange Commission. Any forward-looking statement speaks only as of the date on which it was made. We undertake no obligation to publicly update or revise any forward-looking statement, whether as a result of new information, future events or otherwise, except as required by law. Nasdaq Blue 2
Agenda Liz Pingpank, director, investor relations, bluebird bio Nick Leschly, chief bluebird, bluebird bio David Davidson, M.D., chief medical officer, bluebird bio John Tisdale, M.D., National Heart, Lung and Blood Institute at the National Institutes of Health (NIH), Bethesda, MD Liviu Niculescu, M.D., Ph.D., SVP, global medical affairs, bluebird bio Nina Shah, M.D., University of California, San Francisco Nick Leschly, chief bluebird, bluebird bio Welcome Severe Genetic Diseases Multiple Myeloma Closing Agenda Welcome Liz Pingpank, director, investor relations, bluebird bio Nick Leschly, chief bluebird, bluebird bio Severe Genetic Diseases David Davidson, M.D., chief medical officer, bluebird bio John Tisdale, M.D., National Heart, Lung and Blood Institute at the National Institutes of Health (NIH), Bethesda, MD Multiple Myeloma Liviu Niculescu, M.D., Ph.D., SVP, global medical affairs, bluebird bio Nina Shah, M.D., University of California, San Francisco Closing Nick Leschly, chief bluebird, bluebird bio Nasdaq Blue
Welcome Nick Leschly, chief bluebird Welcome Nick Leschly, chief bluebird

Making Hope A Reality Making Hope A Reality

T H E G E N E T H E R A P Y P R O D U C T S C O M P A N Y LentiGlobin SCD Data-Driven Acceleration LentiGlobin TDT Potential First Approval (2019) Lenti-D CALD Potential First Approval (2020) bb2121 Multiple Myeloma Potential First Approval (2020) Products on the Market 2+ Additional Programs in the Clinic 4+ Programs Nearing Commercialization 2+ Patient Impact ∞ 2022 Vision on Track 2022 Vision on Track LentiGlobin TDT Potential First Approval (2019) LentiGlobin SCD Data-Driven Acceleration 2+ Products on the Market 2+ Programs Nearing Commercialization 4+ Additional Programs in the Clinic bb2121 Multiple Myeloma Potential First Approval (2020) Lenti-D CALD Potential First Approval (2020) THE GENE THERAPY PRODUCTS COMPANY Patient Impact
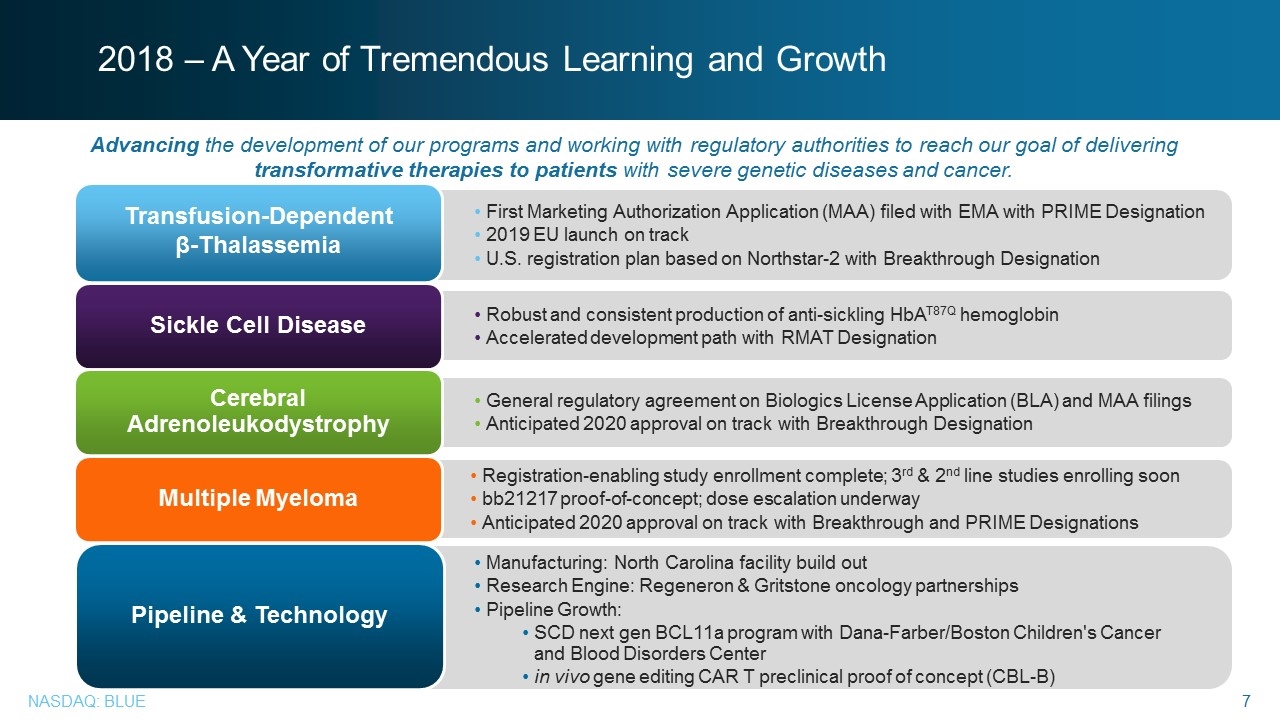
2018 – A Year of Tremendous Learning and Growth First Marketing Authorization Application (MAA) filed with EMA with PRIME Designation 2019 EU launch on track U.S. registration plan based on Northstar-2 with Breakthrough Designation Transfusion-Dependent β-Thalassemia Robust and consistent production of anti-sickling HbAT87Q hemoglobin Accelerated development path with RMAT Designation Sickle Cell Disease General regulatory agreement on Biologics License Application (BLA) and MAA filings Anticipated 2020 approval on track with Breakthrough Designation Cerebral Adrenoleukodystrophy Registration-enabling study enrollment complete; 3rd & 2nd line studies enrolling soon bb21217 proof-of-concept; dose escalation underway Anticipated 2020 approval on track with Breakthrough and PRIME Designations Multiple Myeloma Manufacturing: North Carolina facility build out Research Engine: Regeneron & Gritstone oncology partnerships Pipeline Growth: SCD next gen BCL11a program with Dana-Farber/Boston Children's Cancer and Blood Disorders Center in vivo gene editing CAR T preclinical proof of concept (CBL-B) Pipeline & Technology Advancing the development of our programs and working with regulatory authorities to reach our goal of delivering transformative therapies to patients with severe genetic diseases and cancer. 2018 – A Year of Tremendous Learning and Growth Advancing the development of our programs and working with regulatory authorities to reach our goal of delivering transformative therapies to patients with severe genetic diseases and cancer. Transfusion-Dependent β-Thalassemia First Marketing Authorization Application (MAA) filed with EMA with PRIME Designation 2019 EU launch on track U.S. registration plan based on Northstar-2 with Breakthrough Designation Sickle Cell Disease Robust and consistent production of anti-sickling HbAT87Q hemoglobin Accelerated development path with RMAT Designation Cerebral Adrenoleukodystrophy General regulatory agreement on Biologics License Application (BLA) and MAA filings Anticipated 2020 approval on track with Breakthrough Designation Multiple Myeloma Registration-enabling study enrollment complete; 3rd & 2nd line studies enrolling soon bb21217 proof-of-concept; dose escalation underway Anticipated 2020 approval on track with Breakthrough and PRIME Designations Pipeline & Technology Manufacturing: North Carolina facility build out Research Engine: Regeneron & Gritstone oncology partnerships Pipeline Growth: SCD next gen BCL11a program with Dana-Farber/Boston Children's Cancer and Blood Disorders Center in vivo gene editing CAR T preclinical proof of concept (CBL-B) Nasdaq Blue
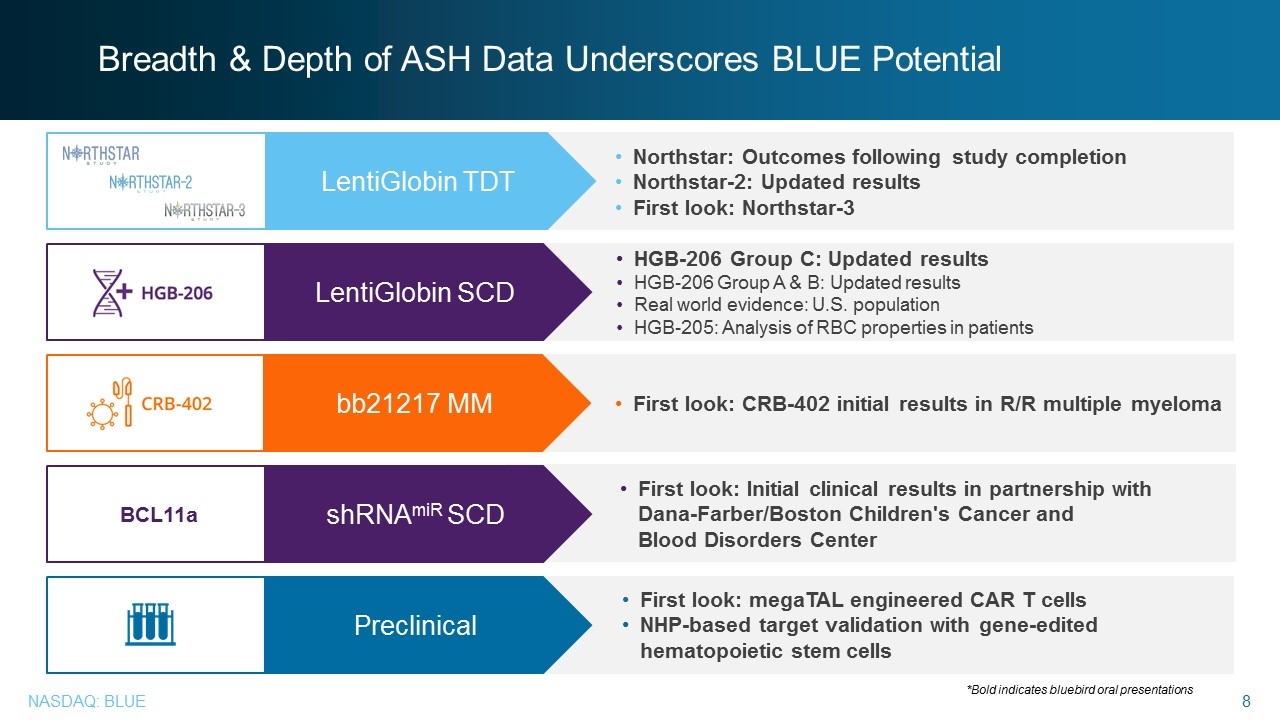
Breadth & Depth of ASH Data Underscores BLUE Potential HGB-206 Group C: Updated results HGB-206 Group A & B: Updated results Real world evidence: U.S. population HGB-205: Analysis of RBC properties in patients LentiGlobin SCD First look: CRB-402 initial results in R/R multiple myeloma bb21217 MM BCL11a First look: Initial clinical results in partnership with Dana-Farber/Boston Children's Cancer and Blood Disorders Center shRNAmiR SCD First look: megaTAL engineered CAR T cells NHP-based target validation with gene-edited hematopoietic stem cells Preclinical *Bold indicates bluebird oral presentations Northstar: Outcomes following study completion Northstar-2: Updated results First look: Northstar-3 LentiGlobin TDT Breadth & Depth of ASH Data Underscores BLUE Potential LentiGlobin TDT Northstar: Outcomes following study completion Northstar-2: Updated results First look: Northstar-3 LentiGlobin SCD HGB-206 Group C: Updated results HGB-206 Group A & B: Updated results Real world evidence: U.S. population HGB-205: Analysis of RBC properties in patients bb21217 MM First look: CRB-402 initial results in R/R multiple myeloma shRNAmiR SCD First look: Initial clinical results in partnership with Dana-Farber/Boston Children's Cancer and Blood Disorders Center Preclinical NHPFirst look: megaTAL engineered CAR T cells -based target validation with gene-edited hematopoietic stem cells Bold indicates bluebird oral presentationsNasdaq Blue 8
Transfusion-Dependent β-Thalassemia and Sickle Cell Disease David Davidson, M.D., chief medical officer, bluebird bio Transfusion-Dependent β-Thalassemia and Sickle Cell Disease David Davidson, M.D., chief medical officer, bluebird bio Nasdaq 9
Transfusion-Dependent β-Thalassemia (TDT) Inherited blood disease that requires lifelong, frequent blood transfusions and iron reduction therapy PROGRAM OVERVIEW Filed MAA with European Medicines Agency General regulatory agreement with FDA for BLA filing Studies ongoing: Northstar-2 (HGB-207) Northstar-3 (HGB-212) HGB-205 Long-term follow-up: LTF-303 Transfusion-Dependent β-Thalassemia (TDT) Inherited blood disease that requires lifelong, frequent blood transfusions and iron reduction therapy PROGRAM OVERVIEW Filed MAA with European Medicines Agency General regulatory agreement with FDA for BLA filing Studies ongoing: Northstar-2 (HGB-207) Northstar-3 (HGB-212) HGB-205 Long-term follow-up: LTF-303 Nasdaq Blue 10
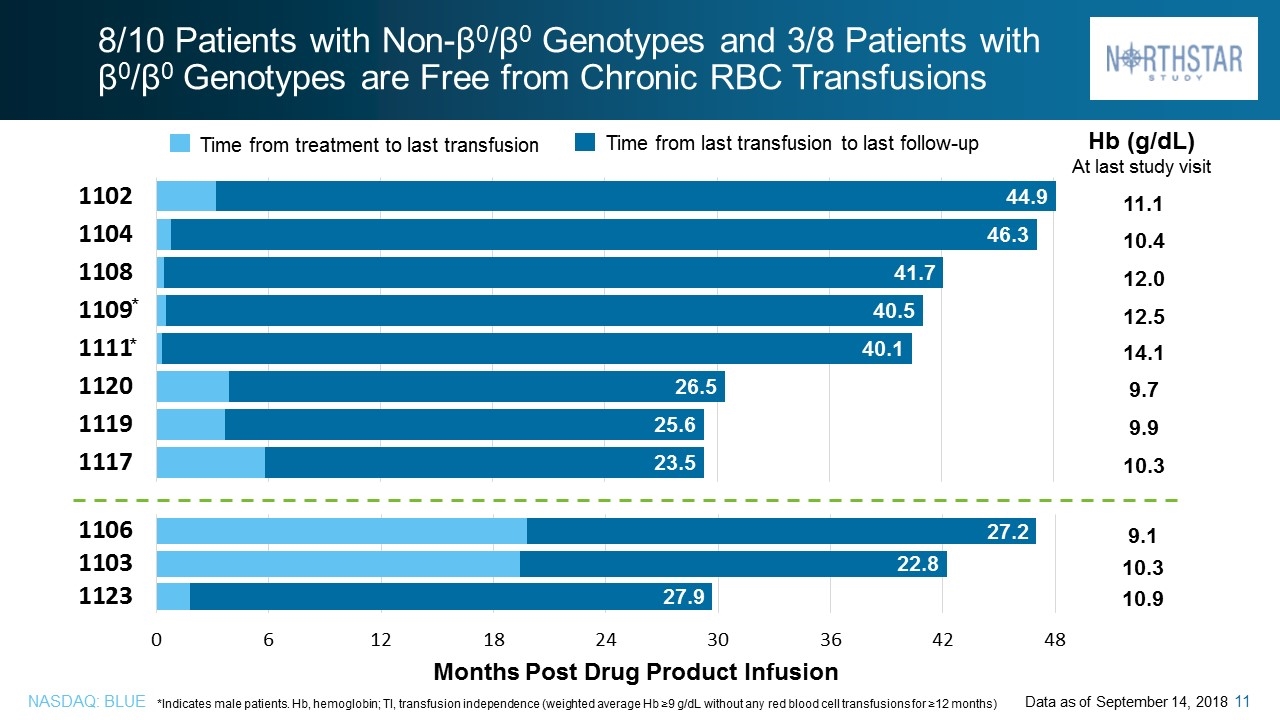
8/10 Patients with Non-β0/β0 Genotypes and 3/8 Patients with β0/β0 Genotypes are Free from Chronic RBC Transfusions 11.1 10.4 12.0 12.5 14.1 9.7 9.9 10.3 Time from treatment to last transfusion Time from last transfusion to last follow-up 9.1 10.3 10.9 Hb (g/dL) At last study visit Months Post Drug Product Infusion Data as of September 14, 2018 *Indicates male patients. Hb, hemoglobin; TI, transfusion independence (weighted average Hb ≥9 g/dL without any red blood cell transfusions for ≥12 months) 8/10 Patients with Non-β0/β0 Genotypes and 3/8 Patients with β0/β0 Genotypes are Free from Chronic RBC Transfusions Time from treatment to last transfusion Time from last transfusion to last follow-up Hb (g/dL) At last study visit Months Post Drug Product Infusion *Indicates male patients. Hb, hemoglobin; TI, transfusion independence (weighted average Hb ≥9 g/dL without any red blood cell transfusions for ≥12 months) Data as of September 14, 2018 Nasdaq Blue 11
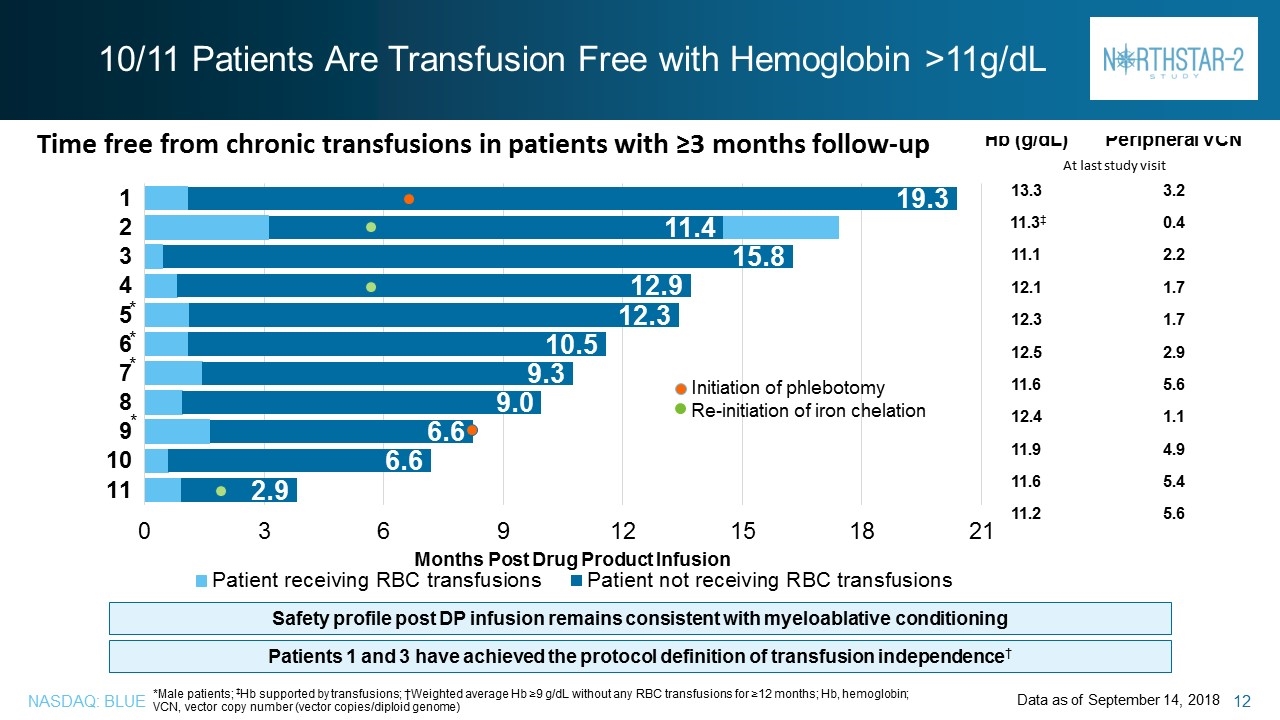
10/11 Patients Are Transfusion Free with Hemoglobin >11g/dL *Male patients; ‡Hb supported by transfusions; †Weighted average Hb ≥9 g/dL without any RBC transfusions for ≥12 months; Hb, hemoglobin; VCN, vector copy number (vector copies/diploid genome) Data as of September 14, 2018 Time free from chronic transfusions in patients with ≥3 months follow-up * * * * Safety profile post DP infusion remains consistent with myeloablative conditioning Patients 1 and 3 have achieved the protocol definition of transfusion independence† Hb (g/dL) Peripheral VCN At last study visit 13.3 3.2 11.3‡ 0.4 11.1 2.2 12.1 1.7 12.3 1.7 12.5 2.9 11.6 5.6 12.4 1.1 11.9 4.9 11.6 5.4 11.2 5.6 Initiation of phlebotomy Re-initiation of iron chelation 10/11 Patients Are Transfusion Free with Hemoglobin >11g/dL Time free from chronic transfusions in patients with ≥3 months follow-up Hb (g/dL) Peripheral VCN At last study visit Months Post Drug Product Infusion Safety profile post DP infusion remains consistent with myeloablative conditioning Patients 1 and 3 have achieved the protocol definition of transfusion independence† *Male patients; ‡Hb supported by transfusions; †Weighted average Hb ≥9 g/dL without any RBC transfusions for ≥12 months; Hb, hemoglobin; VCN, vector copy number (vector copies/diploid genome) Data as of September 14, 2018 Nasdaq Blue 12
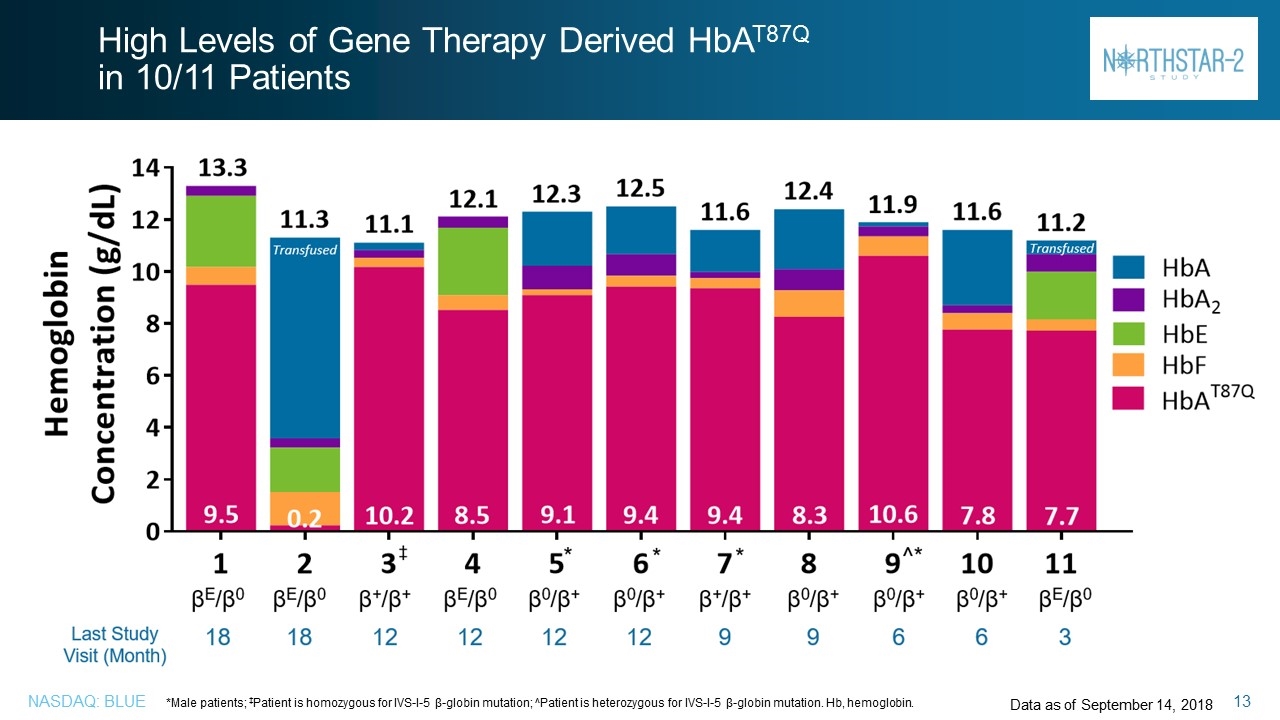
High Levels of Gene Therapy Derived HbAT87Q in 10/11 Patients *Male patients; ‡Patient is homozygous for IVS-I-5 β-globin mutation; ^Patient is heterozygous for IVS-I-5 β-globin mutation. Hb, hemoglobin. Transfused Data as of September 14, 2018 Transfused High Levels of Gene Therapy Derived HbAT87Q in 10/11 Patients *Male patients; ‡Patient is homozygous for IVS-I-5 β-globin mutation; ^Patient is heterozygous for IVS-I-5 β-globin mutation. Hb, hemoglobin. Data as of September 14, 2018 Nasdaq Blue 13
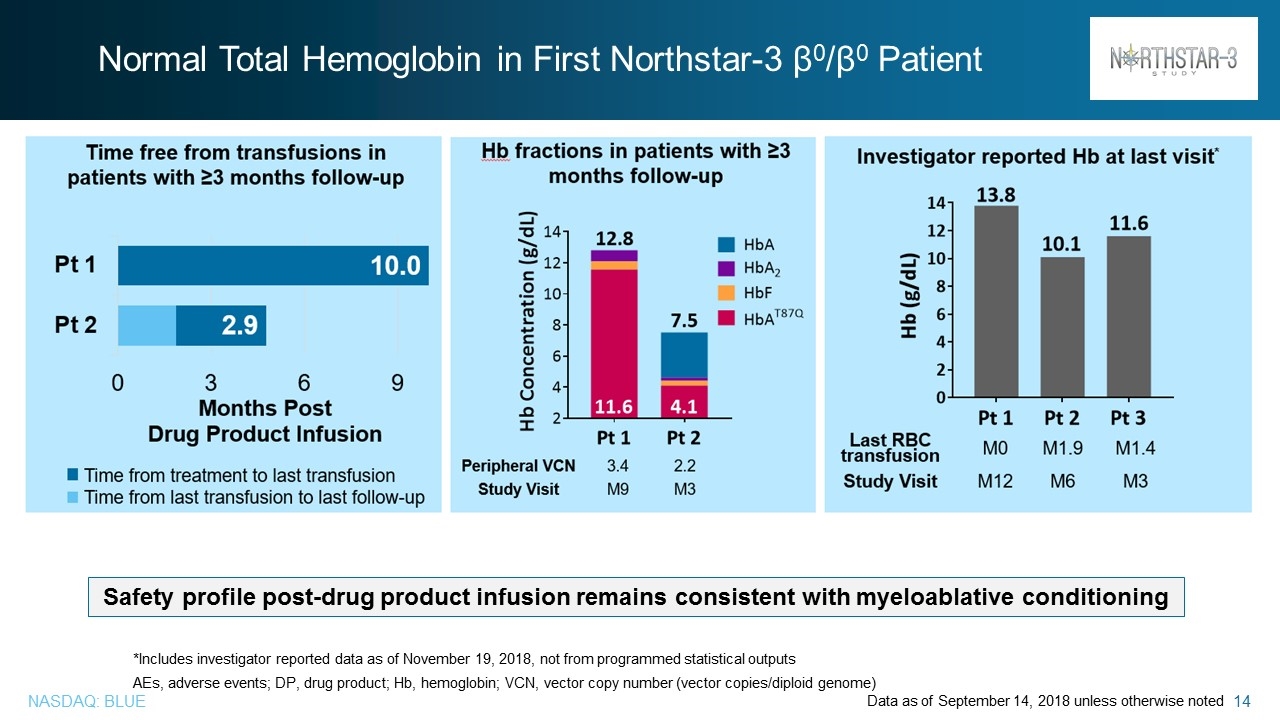
Normal Total Hemoglobin in First Northstar-3 β0/β0 Patient Data as of September 14, 2018 unless otherwise noted *Includes investigator reported data as of November 19, 2018, not from programmed statistical outputs AEs, adverse events; DP, drug product; Hb, hemoglobin; VCN, vector copy number (vector copies/diploid genome) Safety profile post-drug product infusion remains consistent with myeloablative conditioning Normal Total Hemoglobin in First Northstar-3 β0/β0 Patient Safety profile post-drug product infusion remains consistent with myeloablative conditioning *Includes investigator reported data as of November 19, 2018, not from programmed statistical outputs AEs, adverse events; DP, drug product; Hb, hemoglobin; VCN, vector copy number (vector copies/diploid genome) Data as of September 14, 2018 unless otherwise noted Nasdaq Blue 14
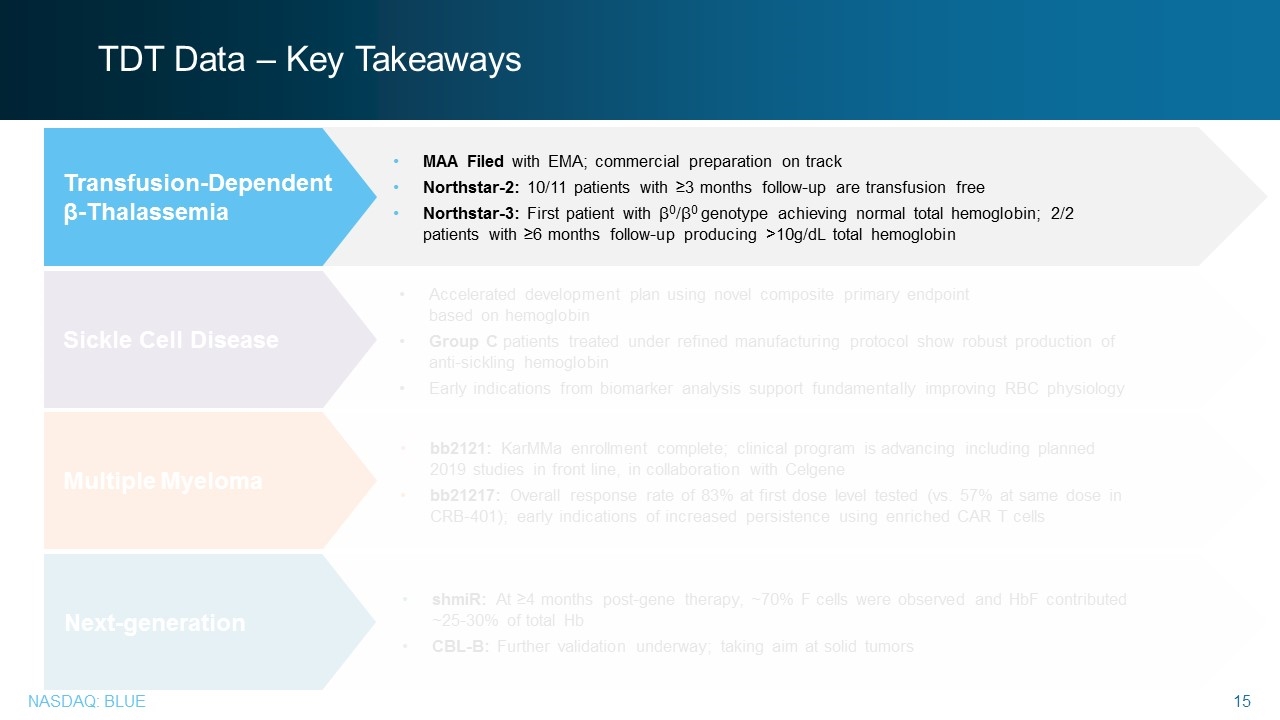
TDT Data – Key Takeaways bb2121: KarMMa enrollment complete; clinical program is advancing including planned 2019 studies in front line, in collaboration with Celgene bb21217: Overall response rate of 83% at first dose level tested (vs. 57% at same dose in CRB-401); early indications of increased persistence using enriched CAR T cells shmiR: At ≥4 months post-gene therapy, ~70% F cells were observed and HbF contributed ~25-30% of total Hb CBL-B: Further validation underway; taking aim at solid tumors Multiple Myeloma Next-generation MAA Filed with EMA; commercial preparation on track Northstar-2: 10/11 patients with ≥3 months follow-up are transfusion free Northstar-3: First patient with β0/β0 genotype achieving normal total hemoglobin; 2/2 patients with ≥6 months follow-up producing >10g/dL total hemoglobin Transfusion-Dependent β-Thalassemia Accelerated development plan using novel composite primary endpoint based on hemoglobin Group C patients treated under refined manufacturing protocol show robust production of anti-sickling hemoglobin Early indications from biomarker analysis support fundamentally improving RBC physiology Sickle Cell Disease TDT Data – Key Takeaways Transfusion-Dependent β-Thalassemia MAA Filed with EMA; commercial preparation on track Northstar-2: 10/11 patients with ≥3 months follow-up are transfusion free Northstar-3: First patient with β0/β0 genotype achieving normal total hemoglobin; 2/2 patients with ≥6 months follow-up producing >10g/dL total hemoglobin Nasdaq Blue 15
Sickle Cell Disease Development Plan Sickle Cell Disease Development Plan Nasdaq Blue 16
Sickle Cell Disease (SCD) Severe blood disorder that causes anemia, frequent pain crises and shortened lifespan Global annual birth incidence ~ 300,000 – 400,000 Mean age of death in the U.S. is 44 years1 PROGRAM OVERVIEW Plan to pursue accelerated development path based on hematological primary endpoint Phase 3 study to begin in 2019 HGB-206 amended and Group C expanded Source: Global Genes 1Paulukonis et al, California’s Sickle Cell Data Collection Cohort, 2005-2015* ASH 2017* Sickle Cell Disease (SCD) Severe blood disorder that causes anemia, frequent pain crises and shortened lifespan Global annual birth incidence ~ 300,000 – 400,000 Mean age of death in the U.S. is 44 years1 PROGRAM OVERVIEW Plan to pursue accelerated development path based on hematological primary endpoint Phase 3 study to begin in 2019 HGB-206 amended and Group C expanded Nasdaq Blue 17
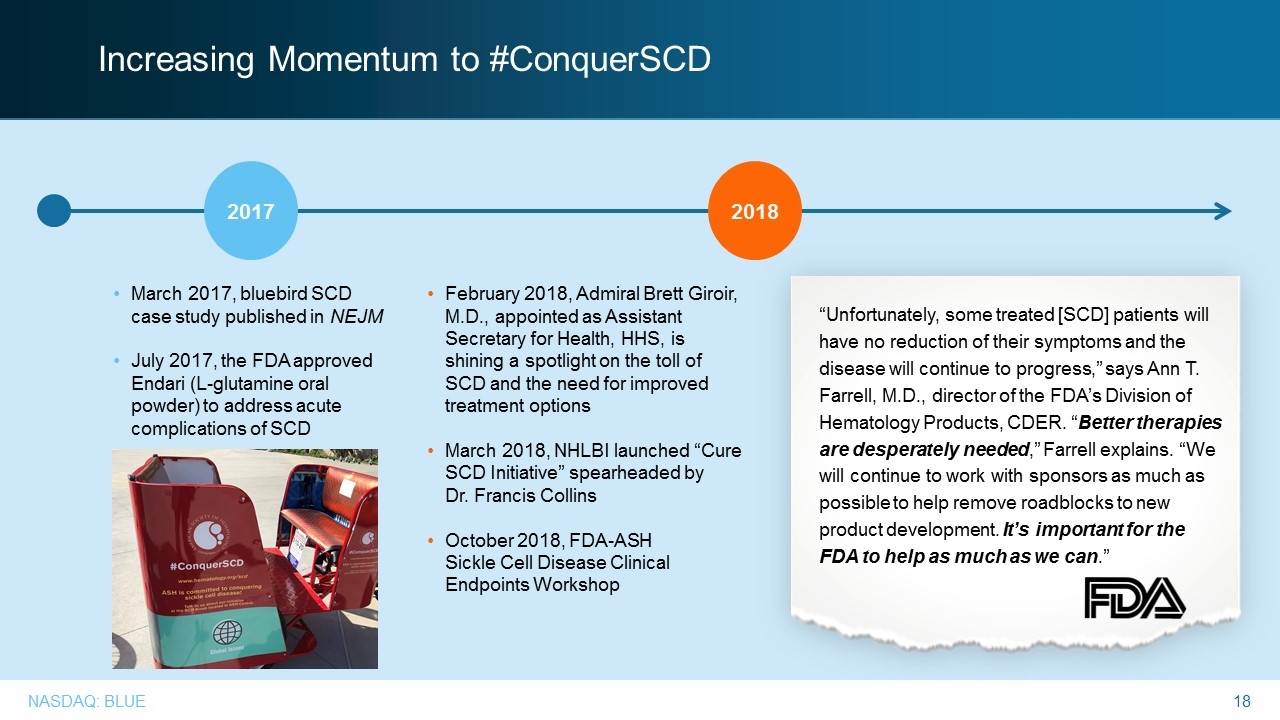
Increasing Momentum to #ConquerSCD “Unfortunately, some treated [SCD] patients will have no reduction of their symptoms and the disease will continue to progress,” says Ann T. Farrell, M.D., director of the FDA’s Division of Hematology Products, CDER. “Better therapies are desperately needed,” Farrell explains. “We will continue to work with sponsors as much as possible to help remove roadblocks to new product development. It’s important for the FDA to help as much as we can.” 2017 2018 March 2017, bluebird SCD case study published in NEJM July 2017, the FDA approved Endari (L-glutamine oral powder) to address acute complications of SCD February 2018, Admiral Brett Giroir, M.D., appointed as Assistant Secretary for Health, HHS, is shining a spotlight on the toll of SCD and the need for improved treatment options March 2018, NHLBI launched “Cure SCD Initiative” spearheaded by Dr. Francis Collins October 2018, FDA-ASH Sickle Cell Disease Clinical Endpoints Workshop Increasing Momentum to #ConquerSCD 2017 2018 March 2017, bluebird SCD case study published in NEJM July 2017, the FDA approved Endari (L-glutamine oral powder) to address acute complications of SCD February 2018, Admiral Brett Giroir, M.D., appointed as Assistant Secretary for Health, HHS, is shining a spotlight on the toll of SCD and the need for improved treatment options March 2018, NHLBI launched “Cure SCD Initiative” spearheaded by Dr. Francis Collins October 2018, FDA-ASH Sickle Cell Disease Clinical Endpoints Workshop Unfortunately, some treated [SCD] patients will have no reduction of their symptoms and the disease will continue to progress,” says Ann T. Farrell, M.D., director of the FDA’s Division of Hematology Products, CDER. “Better therapies are desperately needed,” Farrell explains. “We will continue to work with sponsors as much as possible to help remove roadblocks to new product development. It’s important for the FDA to help as much as we can.” Nasdaq Blue 18
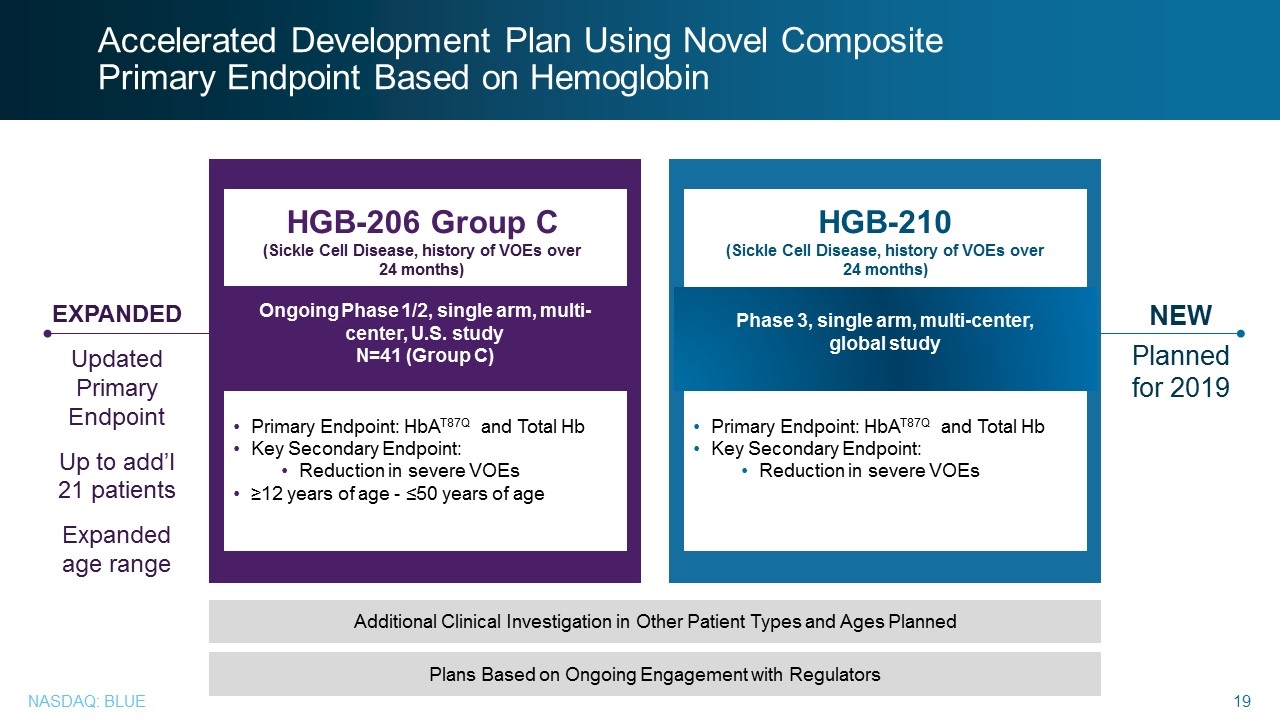
Ongoing Phase 1/2, single arm, multi-center, U.S. study N=41 (Group C) Primary Endpoint: HbAT87Q and Total Hb Key Secondary Endpoint: Reduction in severe VOEs ≥12 years of age - ≤50 years of age Phase 1/2, single-center in France N=7 (4 β-thalassemia) HGB-205 (Transfusion-dependent b-thalassemia & severe sickle cell disease) All thalassemia subjects dosed as of Sep 2015 2 year study duration; last β-thalassemia subject visit ≈Sep 2017 Phase 3, single arm, multi-center, global study HGB-210 (Sickle Cell Disease, history of VOEs over 24 months) Primary Endpoint: HbAT87Q and Total Hb Key Secondary Endpoint: Reduction in severe VOEs HGB-206 Group C (Sickle Cell Disease, history of VOEs over 24 months) Accelerated Development Plan Using Novel Composite Primary Endpoint Based on Hemoglobin NEW Planned for 2019 EXPANDED Updated Primary Endpoint Up to add’l 21 patients Expanded age range Additional Clinical Investigation in Other Patient Types and Ages Planned Plans Based on Ongoing Engagement with Regulators Accelerated Development Plan Using Novel Composite Primary Endpoint Based on Hemoglobin EXPANDED Updated Primary Endpoint Up to add’l 21 patients Expanded age range HGB-206 Group C (Sickle Cell Disease, history of VOEs over 24 months) Ongoing Phase 1/2, single arm, multi-center, U.S. study N=41 (Group C) Primary Endpoint: HbAT87Q and Total Hb Key Secondary Endpoint: Reduction in severe VOEs ≥12 years of age - ≤50 years of age HGB-210 (Sickle Cell Disease, history of VOEs over 24 months) Phase 3, single arm, multi-center, global study Primary Endpoint: HbAT87Q and Total Hb Key Secondary Endpoint: Reduction in severe VOEs NEW Planned for 2019 Additional Clinical Investigation in Other Patient Types and Ages Planned Plans Based on Ongoing Engagement with Regulators Nasdaq Blue 19
Sickle Cell Disease John Tisdale, M.D., National Heart, Lung and Blood Institute at the NIH, Bethesda, MD Sickle Cell Disease John Tisdale, M.D., National Heart, Lung and Blood Institute at the NIH, Bethesda, MD Nasdaq Blue 20
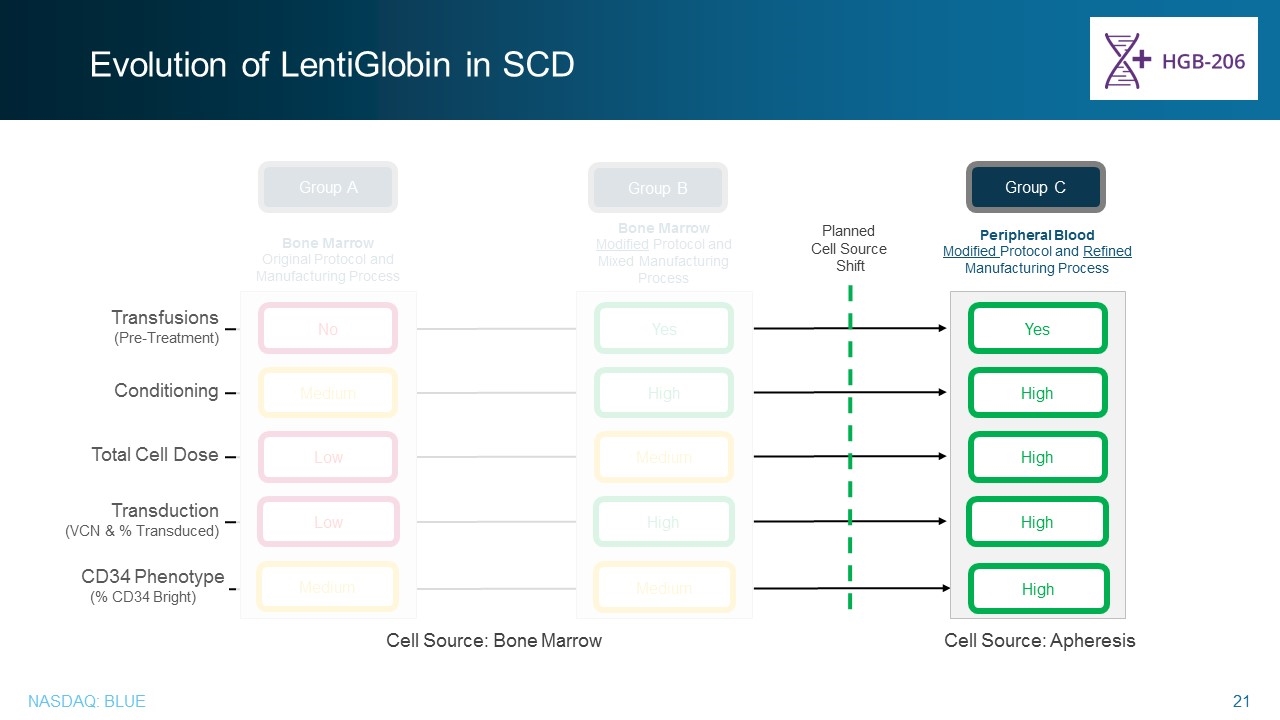
Evolution of LentiGlobin in SCD Peripheral Blood Modified Protocol and Refined Manufacturing Process Group C High High High Yes Transfusions (Pre-Treatment) Conditioning Total Cell Dose Transduction (VCN & % Transduced) Planned Cell Source Shift Cell Source: Apheresis Cell Source: Bone Marrow High CD34 Phenotype (% CD34 Bright) Bone Marrow Original Protocol and Manufacturing Process Medium Low Low Group A Medium No Bone Marrow Modified Protocol and Mixed Manufacturing Process High Medium High Group B Medium Yes Evolution of LentiGlobin in SCD Transfusions (Pre-Treatment) Conditioning Total Cell Dose Transduction (VCN & % Transduced) CD34 Phenotype (% CD34 Bright) Planned Cell Source Shift Group C Peripheral Blood Modified Protocol and Refined Manufacturing Process Cell Source: Bone Marrow Cell Source: Apheresis Nasdaq Blue 21
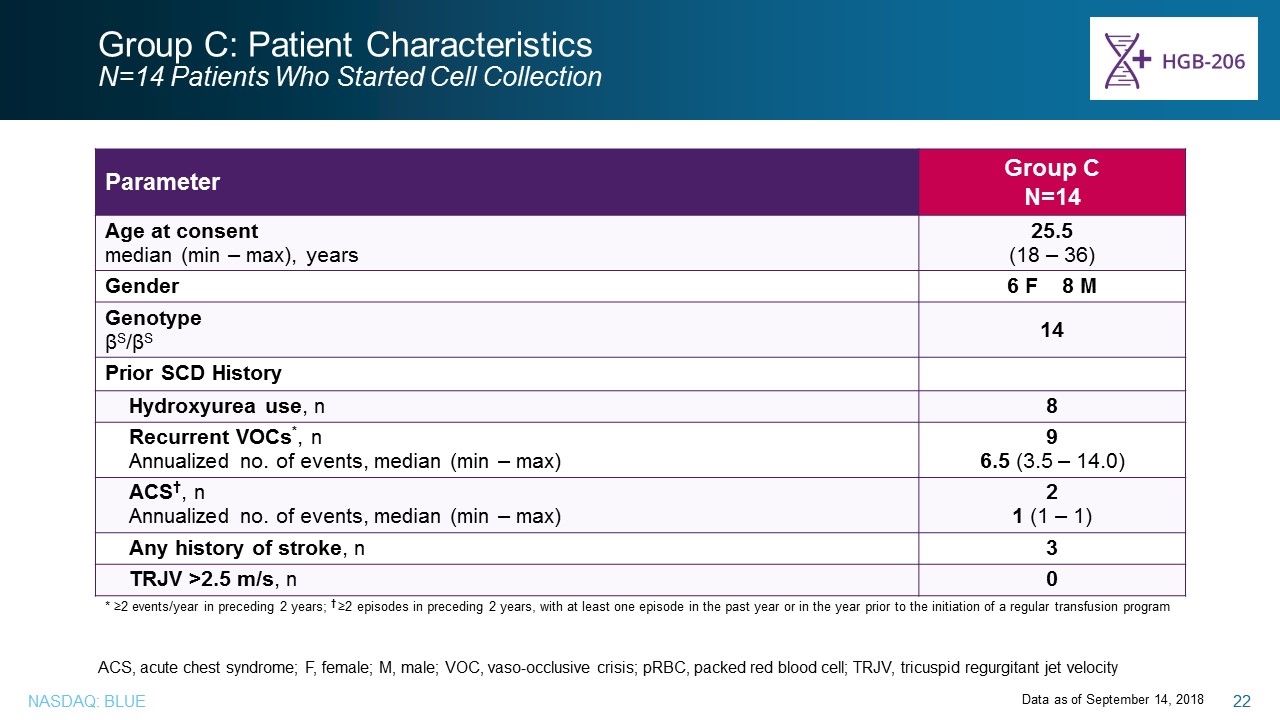
Group C: Patient Characteristics N=14 Patients Who Started Cell Collection Parameter Group C N=14 Age at consent median (min – max), years 25.5 (18 – 36) Gender 6 F 8 M Genotype βS/βS 14 Prior SCD History Hydroxyurea use, n 8 Recurrent VOCs*, n Annualized no. of events, median (min – max) 9 6.5 (3.5 – 14.0) ACS†, n Annualized no. of events, median (min – max) 2 1 (1 – 1) Any history of stroke, n 3 TRJV >2.5 m/s, n 0 * ≥2 events/year in preceding 2 years; † ≥2 episodes in preceding 2 years, with at least one episode in the past year or in the year prior to the initiation of a regular transfusion program Data as of September 14, 2018 ACS, acute chest syndrome; F, female; M, male; VOC, vaso-occlusive crisis; pRBC, packed red blood cell; TRJV, tricuspid regurgitant jet velocity Group C: Patient Characteristics N=14 Patients Who Started Cell Collection Parameter Group C N=14 Age at consent median (min – max), years 25.5 (18 – 36) Gender 6 F 8 M Genotype βS/βS 14 Prior SCD History Hydroxyurea use, n 8 Recurrent VOCs*, n Annualized no. of events, median (min – max) 9 6.5 (3.5 – 14.0) ACS†, n 2 1 (1 – 1) Annualized no. of events, median (min – max) Any history of stroke, n 3 TRJV >2.5 m/s, n 0 * ≥2 events/year in preceding 2 years; † ≥2 episodes in preceding 2 years, with at least one episode in the past year or in the year prior to the initiation of a regular transfusion program ACS, acute chest syndrome; F, female; M, male; VOC, vaso-occlusive crisis; pRBC, packed red blood cell; TRJV, tricuspid regurgitant jet velocity Data as of September 14, 2018 Nasdaq Blue 22
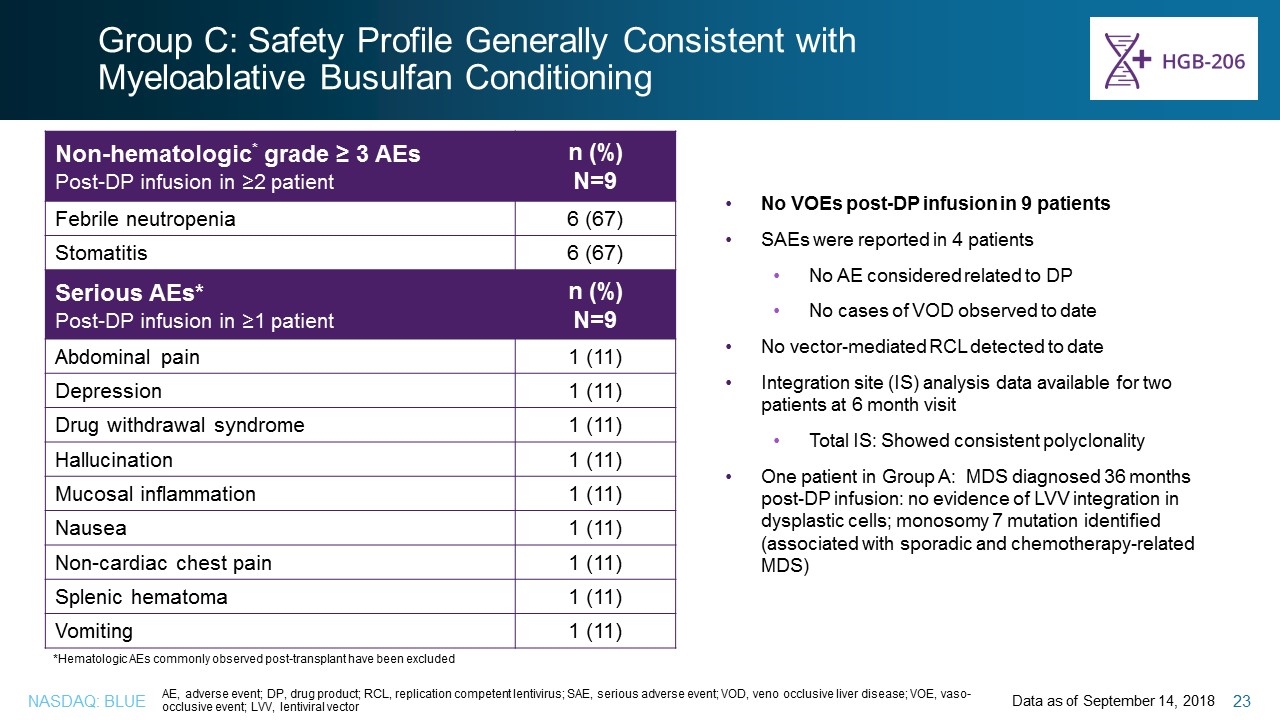
Group C: Safety Profile Generally Consistent with Myeloablative Busulfan Conditioning Data as of September 14, 2018 Non-hematologic* grade ≥ 3 AEs Post-DP infusion in ≥2 patient n (%) N=9 Febrile neutropenia 6 (67) Stomatitis 6 (67) Serious AEs* Post-DP infusion in ≥1 patient n (%) N=9 Abdominal pain 1 (11) Depression 1 (11) Drug withdrawal syndrome 1 (11) Hallucination 1 (11) Mucosal inflammation 1 (11) Nausea 1 (11) Non-cardiac chest pain 1 (11) Splenic hematoma 1 (11) Vomiting 1 (11) AE, adverse event; DP, drug product; RCL, replication competent lentivirus; SAE, serious adverse event; VOD, veno occlusive liver disease; VOE, vaso-occlusive event; LVV, lentiviral vector *Hematologic AEs commonly observed post-transplant have been excluded No VOEs post-DP infusion in 9 patients SAEs were reported in 4 patients No AE considered related to DP No cases of VOD observed to date No vector-mediated RCL detected to date Integration site (IS) analysis data available for two patients at 6 month visit Total IS: Showed consistent polyclonality One patient in Group A: MDS diagnosed 36 months post-DP infusion: no evidence of LVV integration in dysplastic cells; monosomy 7 mutation identified (associated with sporadic and chemotherapy-related MDS) Group C: Safety Profile Generally Consistent with Myeloablative Busulfan Conditioning Non-hematologic* grade ≥ 3 AEs Post-DP infusion in ≥2 patient n (%) N=9 Febrile neutropenia 6 (67) Stomatitis 6 (67) Serious AEs* Post-DP infusion in ≥1 patient n (%) N=9 Abdominal pain 1 (11) Depression 1 (11) Drug withdrawal syndrome 1 (11) Hallucination 1 (11) Mucosal inflammation 1 (11) Nausea 1 (11) Non-cardiac chest pain 1 (11) 1 (11) Splenic hematoma 1 (11) Vomiting 1 (11) No VOEs post-DP infusion in 9 patients SAEs were reported in 4 patients No AE considered related to DP No cases of VOD observed to date No vector-mediated RCL detected to date Integration site (IS) analysis data available for two patients at 6 month visit Total IS: Showed consistent polyclonality One patient in Group A: MDS diagnosed 36 months post-DP infusion: no evidence of LVV integration in dysplastic cells; monosomy 7 mutation identified (associated with sporadic and chemotherapy-related MDS) *Hematologic AEs commonly observed post-transplant have been excluded AE, adverse event; DP, drug product; RCL, replication competent lentivirus; SAE, serious adverse event; VOD, veno occlusive liver disease; VOE, vaso-occlusive event; LVV, lentiviral vector Data as of September 14, 2018 Nasdaq Blue 23
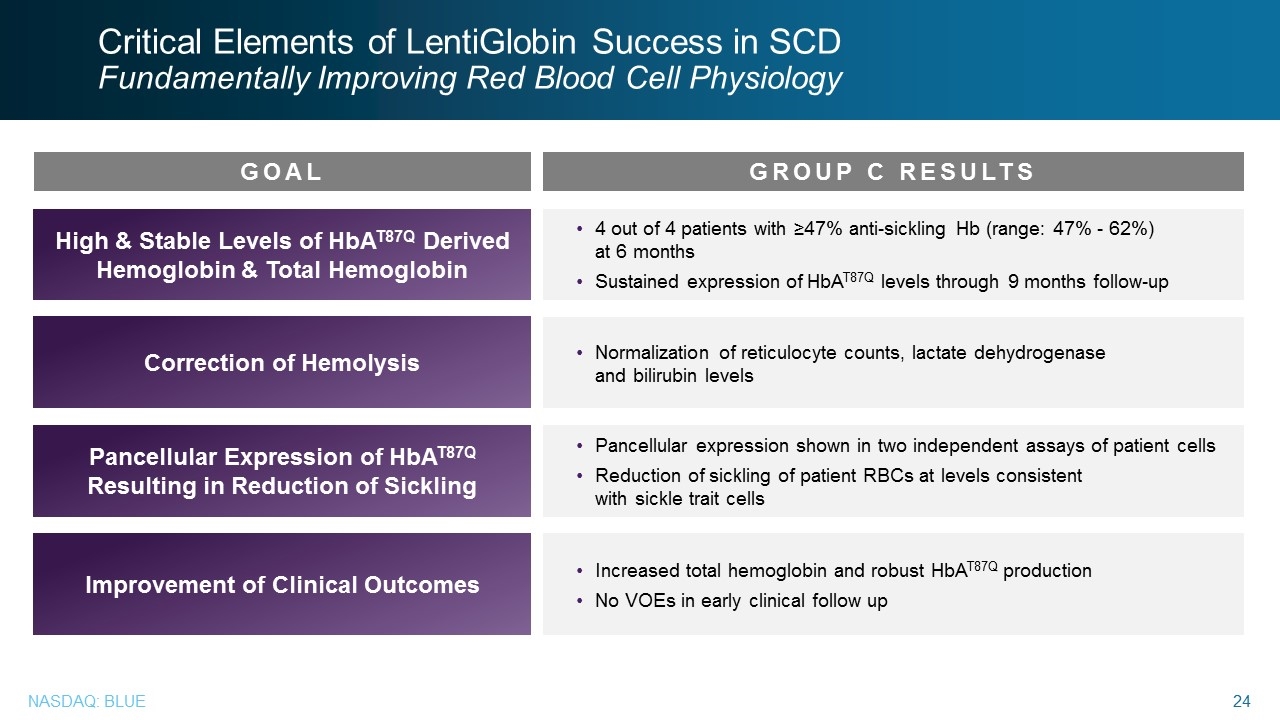
Critical Elements of LentiGlobin Success in SCD Fundamentally Improving Red Blood Cell Physiology 4 out of 4 patients with ≥47% anti-sickling Hb (range: 47% - 62%) at 6 months Sustained expression of HbAT87Q levels through 9 months follow-up High & Stable Levels of HbAT87Q Derived Hemoglobin & Total Hemoglobin Correction of Hemolysis Pancellular Expression of HbAT87Q Resulting in Reduction of Sickling Normalization of reticulocyte counts, lactate dehydrogenase and bilirubin levels Pancellular expression shown in two independent assays of patient cells Reduction of sickling of patient RBCs at levels consistent with sickle trait cells Increased total hemoglobin and robust HbAT87Q production No VOEs in early clinical follow up Improvement of Clinical Outcomes GOAL GROUP C RESULTS
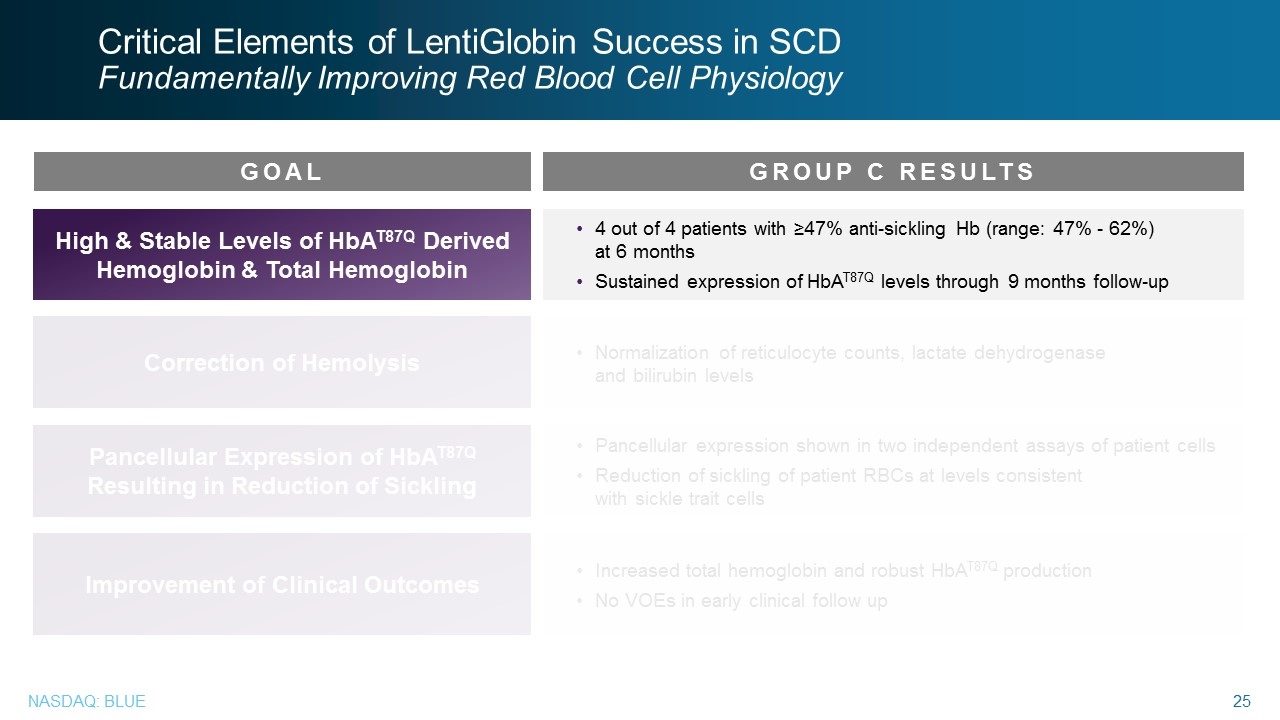
Critical Elements of LentiGlobin Success in SCD Fundamentally Improving Red Blood Cell Physiology 4 out of 4 patients with ≥47% anti-sickling Hb (range: 47% - 62%) at 6 months Sustained expression of HbAT87Q levels through 9 months follow-up High & Stable Levels of HbAT87Q Derived Hemoglobin & Total Hemoglobin Correction of Hemolysis Pancellular Expression of HbAT87Q Resulting in Reduction of Sickling Normalization of reticulocyte counts, lactate dehydrogenase and bilirubin levels Pancellular expression shown in two independent assays of patient cells Reduction of sickling of patient RBCs at levels consistent with sickle trait cells Increased total hemoglobin and robust HbAT87Q production No VOEs in early clinical follow up Improvement of Clinical Outcomes GOAL GROUP C RESULTS Critical Elements of LentiGlobin Success in SCD Fundamentally Improving Red Blood Cell Physiology GOAL High & Stable Levels of HbAT87Q Derived Hemoglobin & Total Hemoglobin Correction of Hemolysis Pancellular Expression of HbAT87Q Resulting in Reduction of Sickling Improvement of Clinical Outcomes GROUP C RESULTS 4 out of 4 patients with ≥47% anti-sickling Hb (range: 47% - 62%) at 6 months Sustained expression of HbAT87Q levels through 9 months follow-up Normalization of reticulocyte counts, lactate dehydrogenase and bilirubin levels Pancellular expression shown in two independent assays of patient cells Reduction of sickling of patient RBCs at levels consistent with sickle trait cells Increased total hemoglobin and robust HbAT87Q production No VOEs in early clinical follow up
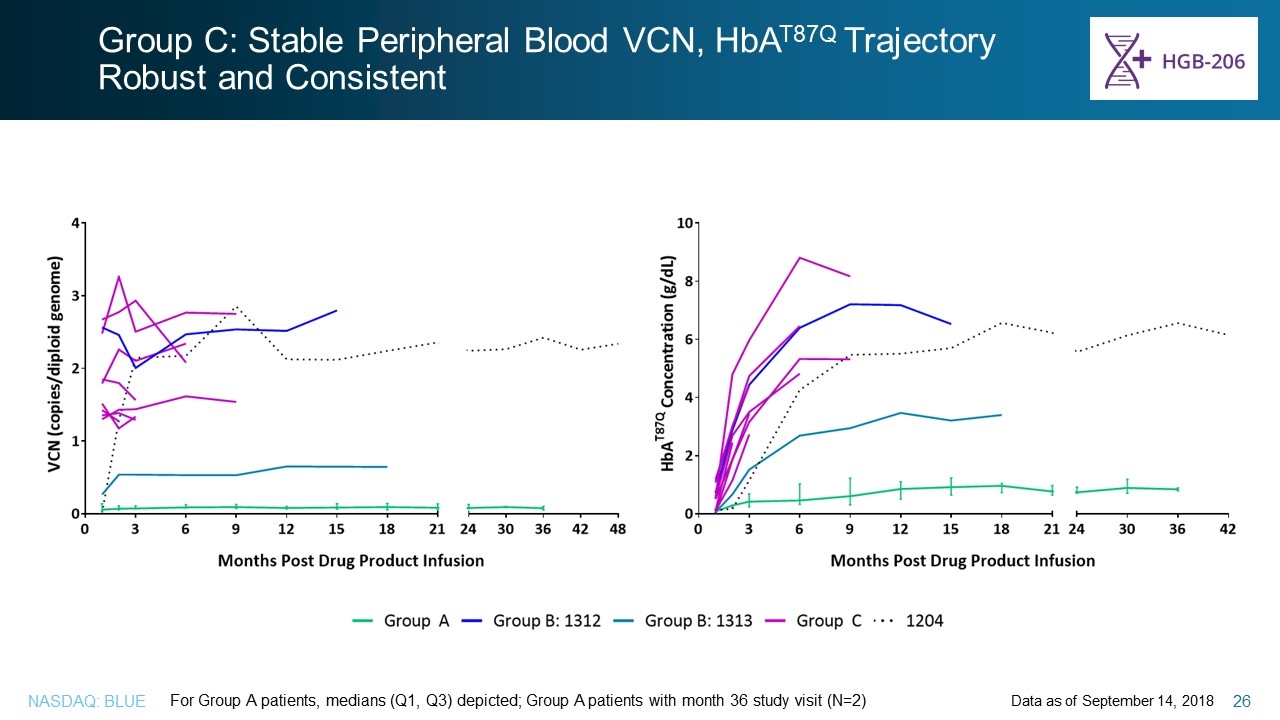
Group C: Stable Peripheral Blood VCN, HbAT87Q Trajectory Robust and Consistent Data as of September 14, 2018 For Group A patients, medians (Q1, Q3) depicted; Group A patients with month 36 study visit (N=2) Group C: Stable Peripheral Blood VCN, HbAT87Q Trajectory Robust and Consistent For Group A patients, medians (Q1, Q3) depicted; Group A patients with month 36 study visit (N=2) Data as of September 14, 2018
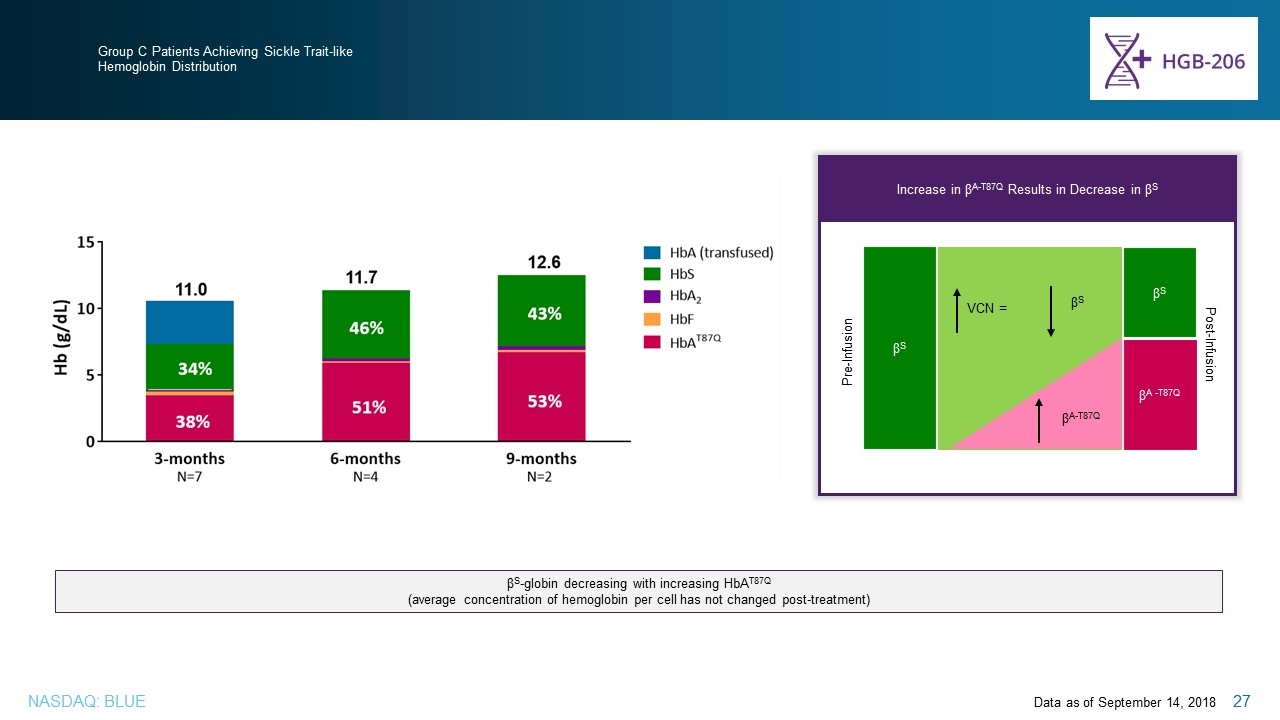
Group C Patients Achieving Sickle Trait-like Hemoglobin Distribution Data as of September 14, 2018 βS-globin decreasing with increasing HbAT87Q (average concentration of hemoglobin per cell has not changed post-treatment) Increase in βA-T87Q Results in Decrease in βS βS βA -T87Q βS Pre-Infusion Post-Infusion 34% 51% 38% 46% 53% 43% βS VCN = βA-T87Q Group C Patients Achieving Sickle Trait-like Hemoglobin Distribution Increase in βA-T87Q Results in Decrease in βS Pre-Infusion Post-Infusion βS VCN = βS βA-T87Q βS βA -T87Q βS-globin decreasing with increasing HbAT87Q (average concentration of hemoglobin per cell has not changed post-treatment)
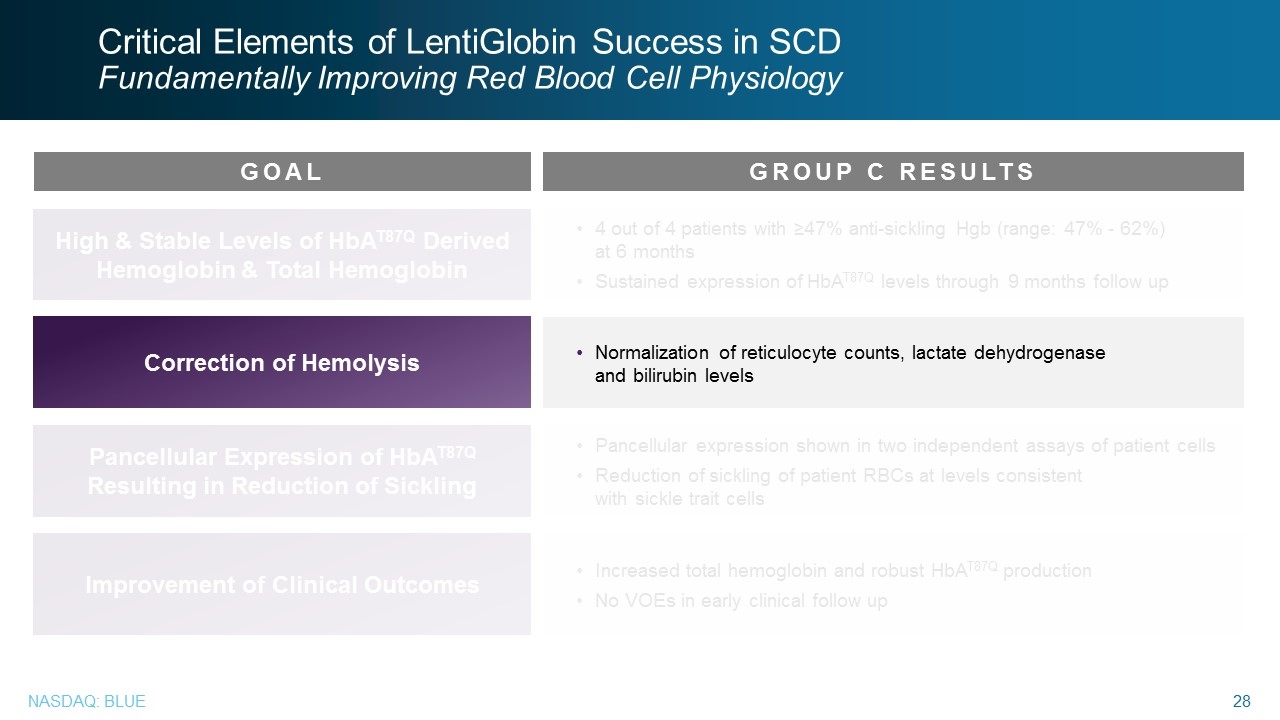
Critical Elements of LentiGlobin Success in SCD Fundamentally Improving Red Blood Cell Physiology 4 out of 4 patients with ≥47% anti-sickling Hgb (range: 47% - 62%) at 6 months Sustained expression of HbAT87Q levels through 9 months follow up High & Stable Levels of HbAT87Q Derived Hemoglobin & Total Hemoglobin Correction of Hemolysis Pancellular Expression of HbAT87Q Resulting in Reduction of Sickling Normalization of reticulocyte counts, lactate dehydrogenase and bilirubin levels Pancellular expression shown in two independent assays of patient cells Reduction of sickling of patient RBCs at levels consistent with sickle trait cells Increased total hemoglobin and robust HbAT87Q production No VOEs in early clinical follow up Improvement of Clinical Outcomes GOAL GROUP C RESULTS Critical Elements of LentiGlobin Success in SCD Fundamentally Improving Red Blood Cell Physiology GOAL Correction of Hemolysis GROUP C RESULTS Normalization of reticulocyte counts, lactate dehydrogenase and bilirubin levels
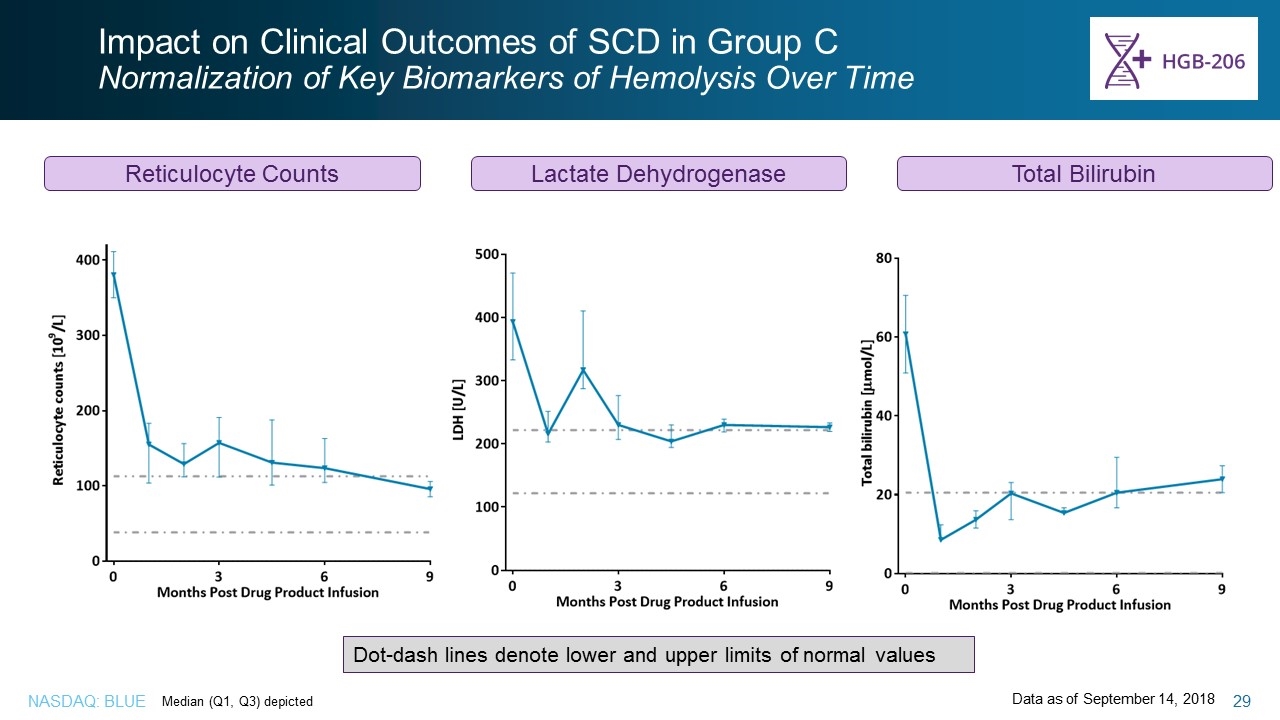
Impact on Clinical Outcomes of SCD in Group C Normalization of Key Biomarkers of Hemolysis Over Time Reticulocyte Counts Lactate Dehydrogenase Median (Q1, Q3) depicted Dot-dash lines denote lower and upper limits of normal values Data as of September 14, 2018 Total Bilirubin Impact on Clinical Outcomes of SCD in Group C Normalization of Key Biomarkers of Hemolysis Over Time Reticulocyte Counts Lactate Dehydrogenase Total Bilirubin Dot-dash lines denote lower and upper limits of normal values Median (Q1, Q3) depicted Data as of September 14, 2018
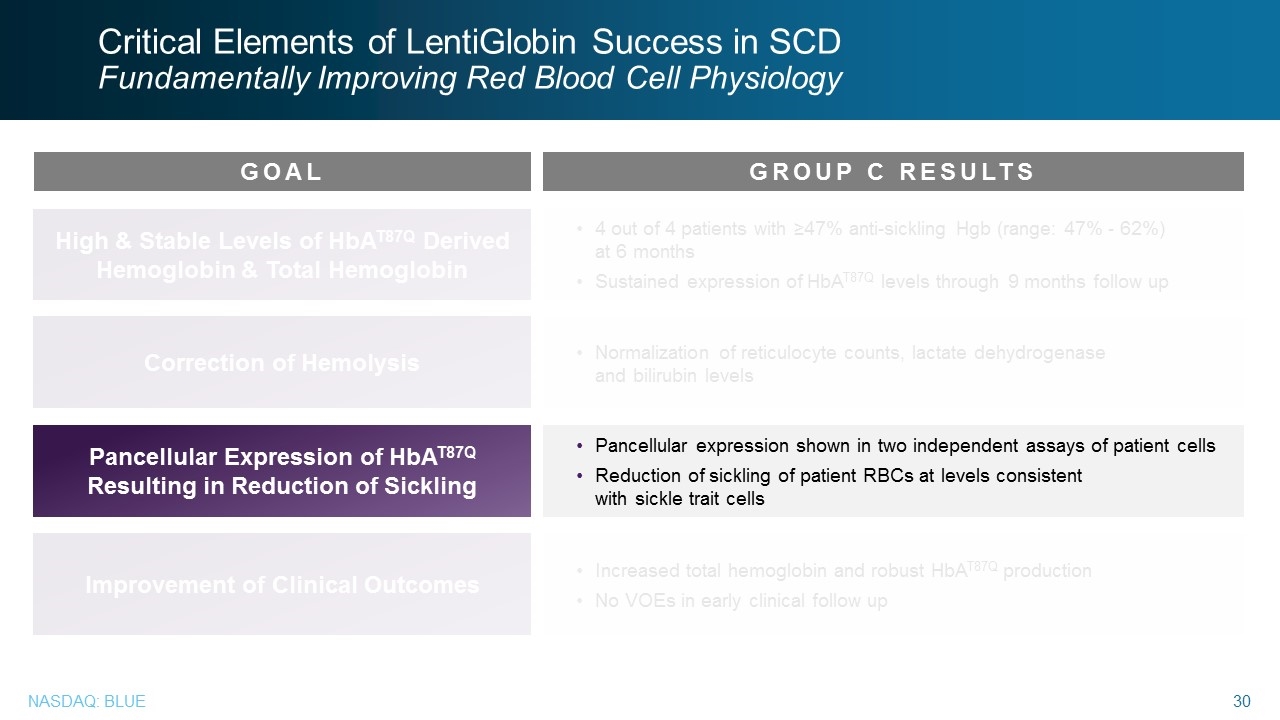
Critical Elements of LentiGlobin Success in SCD Fundamentally Improving Red Blood Cell Physiology 4 out of 4 patients with ≥47% anti-sickling Hgb (range: 47% - 62%) at 6 months Sustained expression of HbAT87Q levels through 9 months follow up High & Stable Levels of HbAT87Q Derived Hemoglobin & Total Hemoglobin Correction of Hemolysis Pancellular Expression of HbAT87Q Resulting in Reduction of Sickling Normalization of reticulocyte counts, lactate dehydrogenase and bilirubin levels Pancellular expression shown in two independent assays of patient cells Reduction of sickling of patient RBCs at levels consistent with sickle trait cells Increased total hemoglobin and robust HbAT87Q production No VOEs in early clinical follow up Improvement of Clinical Outcomes GOAL GROUP C RESULTS Critical Elements of LentiGlobin Success in SCD Fundamentally Improving Red Blood Cell Physiology GOAL Pancellular Expression of HbAT87Q Resulting in Reduction of Sickling GROUP C RESULTS Pancellular expression shown in two independent assays of patient cells Reduction of sickling of patient RBCs at levels consistent with sickle trait cells
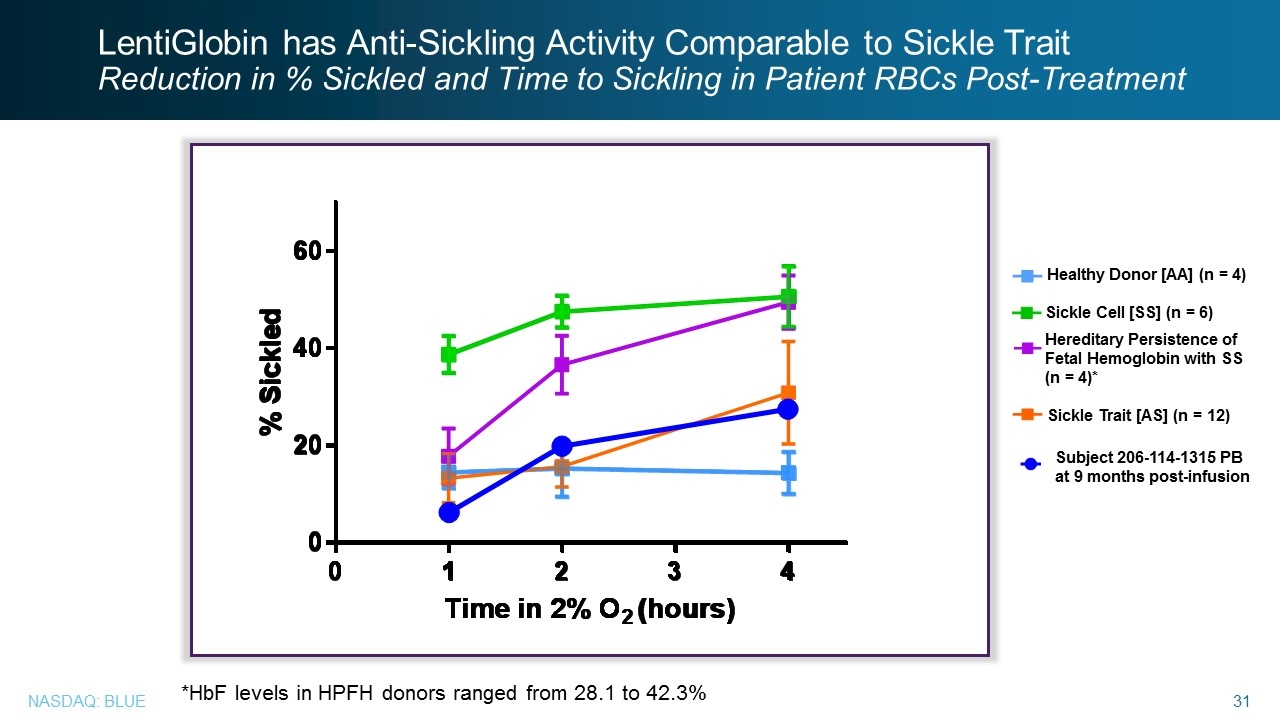
Healthy Donor [AA] (n = 4) Sickle Trait [AS] (n = 12) Sickle Cell [SS] (n = 6) Hereditary Persistence of Fetal Hemoglobin with SS (n = 4)* *HbF levels in HPFH donors ranged from 28.1 to 42.3% Subject 206-114-1315 PB at 9 months post-infusion LentiGlobin has Anti-Sickling Activity Comparable to Sickle Trait Reduction in % Sickled and Time to Sickling in Patient RBCs Post-Treatment LentiGlobin has Anti-Sickling Activity Comparable to Sickle Trait Reduction in % Sickled and Time to Sickling in Patient RBCs Post-Treatment Healthy Donor [AA] (n = 4) Sickle Cell [SS] (n = 6) Hereditary Persistence of Fetal Hemoglobin with SS (n = 4)* Sickle Trait [AS] (n = 12) Subject 206-114-1315 PB at 9 months post-infusion *HbF levels in HPFH donors ranged from 28.1 to 42.3%
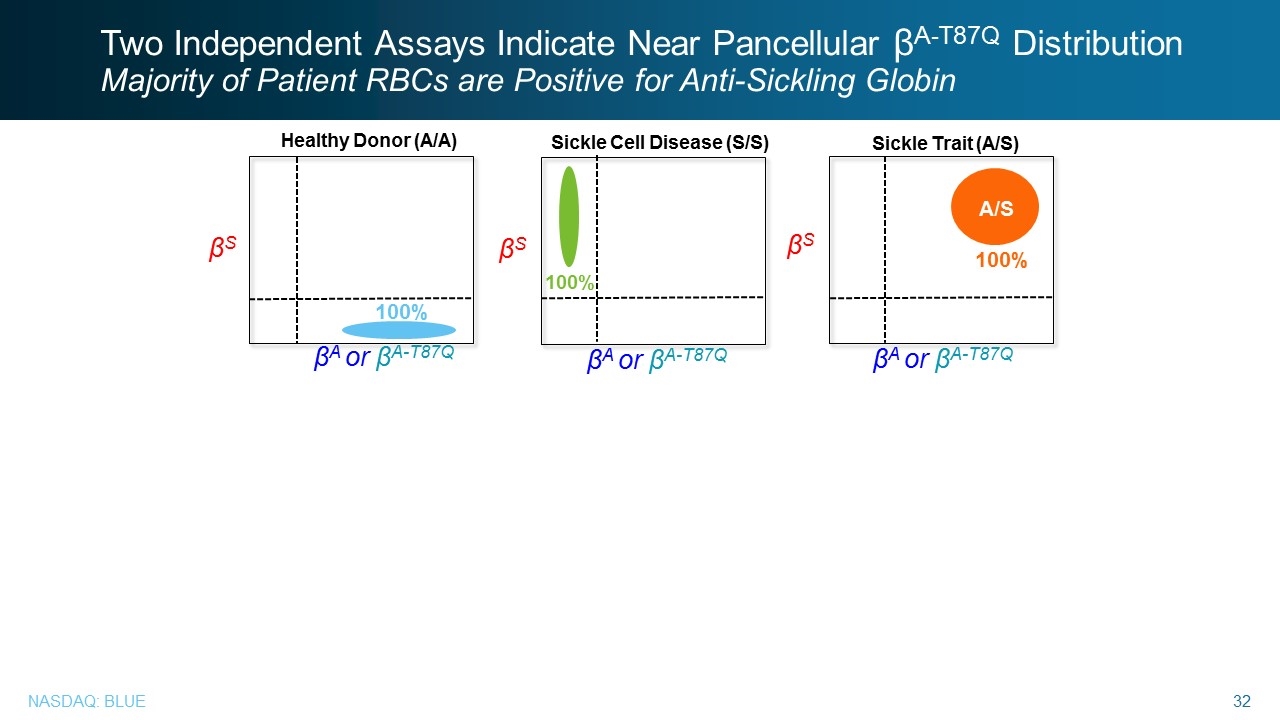
Two Independent Assays Indicate Near Pancellular βA-T87Q Distribution Majority of Patient RBCs are Positive for Anti-Sickling Globin βS Healthy Donor (A/A) βS Sickle Cell Disease (S/S) βS βA or βA-T87Q 100% 100% A/S 100% Sickle Trait (A/S) βA or βA-T87Q βA or βA-T87Q Two Independent Assays Indicate Near Pancellular βA-T87Q Distribution Majority of Patient RBCs are Positive for Anti-Sickling Globin Healthy Donor (A/A) βA or βA-T87Q βS 100 % Sickle Cell Disease (S/S) βA or βA-T87Q βS 100 % Sickle Trait (A/S) βA or βA-T87Q βS A/S 100%
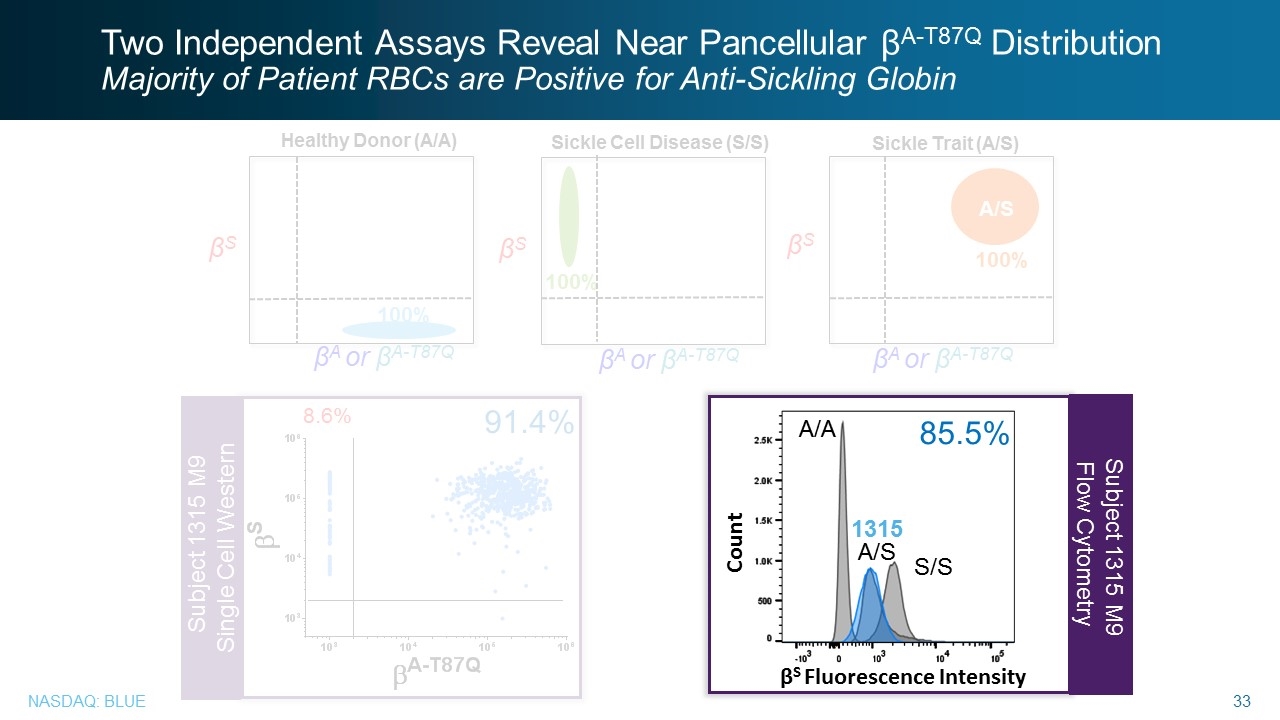
Two Independent Assays Reveal Near Pancellular βA-T87Q Distribution Majority of Patient RBCs are Positive for Anti-Sickling Globin 8.6% 91.4% Subject 1315 M9 Single Cell Western Subject 1315 M9 Flow Cytometry βS Healthy Donor (A/A) βS Sickle Cell Disease (S/S) βS βA or βA-T87Q 100% 100% A/S 100% Sickle Trait (A/S) βA or βA-T87Q βA or βA-T87Q βS Fluorescence Intensity Count S/S A/S A/A 1315 85.5% Two Independent Assays Reveal Near Pancellular βA-T87Q Distribution Majority of Patient RBCs are Positive for Anti-Sickling Globin Subject 1315 M9 Flow Cytometry Count A/A 85.5% 1315 A/S S/S βS Fluorescence Intensity
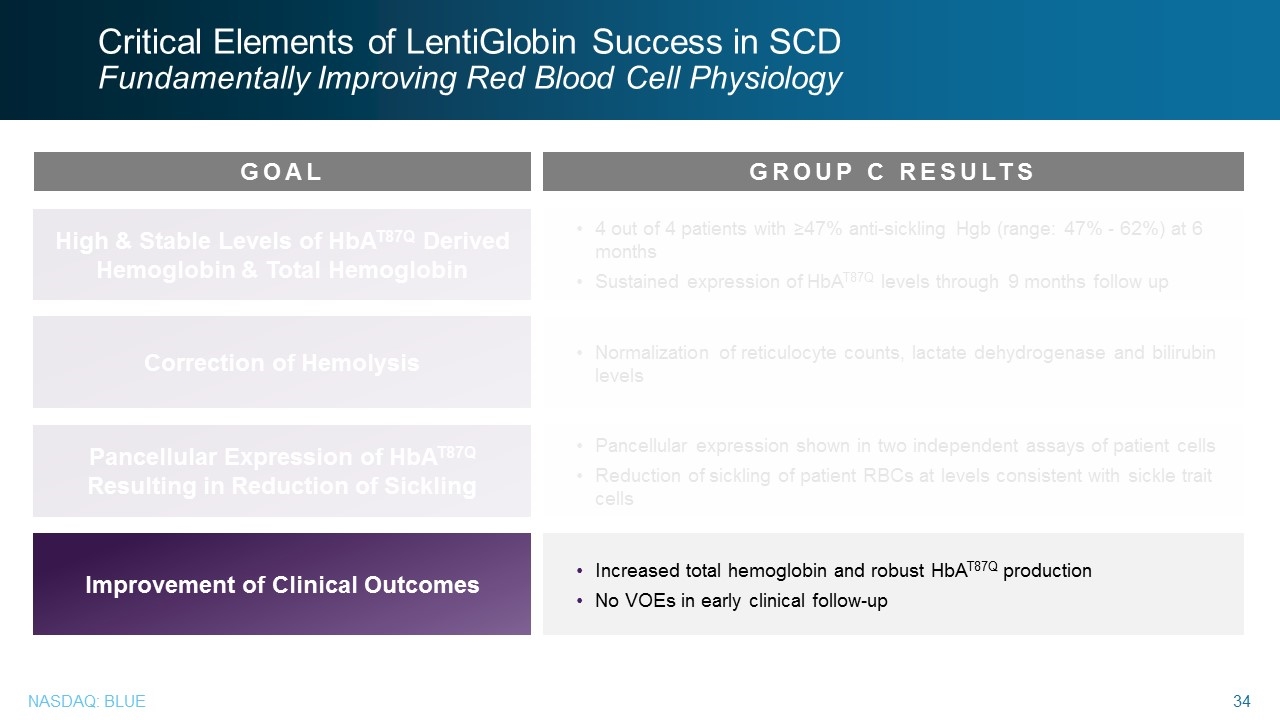
Critical Elements of LentiGlobin Success in SCD Fundamentally Improving Red Blood Cell Physiology 4 out of 4 patients with ≥47% anti-sickling Hgb (range: 47% - 62%) at 6 months Sustained expression of HbAT87Q levels through 9 months follow up High & Stable Levels of HbAT87Q Derived Hemoglobin & Total Hemoglobin Correction of Hemolysis Pancellular Expression of HbAT87Q Resulting in Reduction of Sickling Normalization of reticulocyte counts, lactate dehydrogenase and bilirubin levels Pancellular expression shown in two independent assays of patient cells Reduction of sickling of patient RBCs at levels consistent with sickle trait cells Increased total hemoglobin and robust HbAT87Q production No VOEs in early clinical follow-up Improvement of Clinical Outcomes GOAL GROUP C RESULTS Critical Elements of LentiGlobin Success in SCD Fundamentally Improving Red Blood Cell Physiology GOAL Improvement of Clinical Outcomes GROUP C RESULTS Improvement of Clinical Outcomes Increased total hemoglobin and robust HbAT87Q production No VOEs in early clinical follow-up
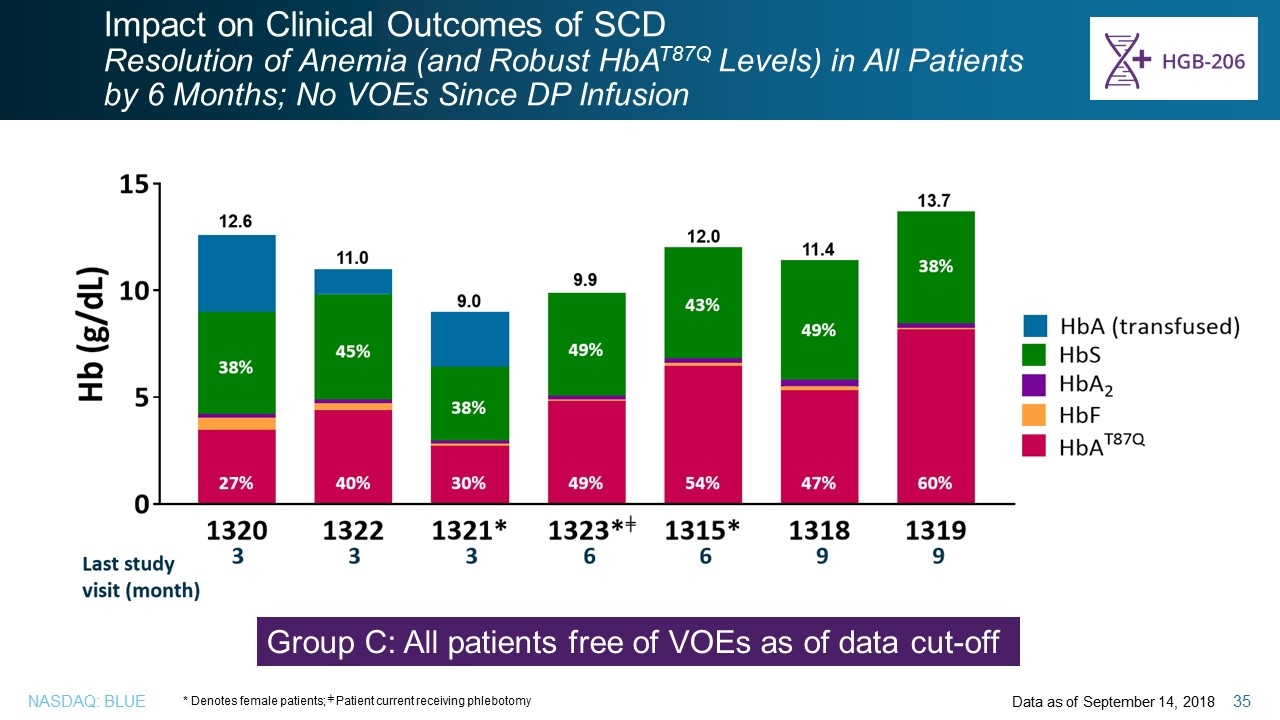
Impact on Clinical Outcomes of SCD Resolution of Anemia (and Robust HbAT87Q Levels) in All Patients by 6 Months; No VOEs Since DP Infusion Data as of September 14, 2018 * Denotes female patients; ╪ Patient current receiving phlebotomy Group C: All patients free of VOEs as of data cut-off Impact on Clinical Outcomes of SCD Resolution of Anemia (and Robust HbAT87Q Levels) in All Patients by 6 Months; No VOEs Since DP Infusion Group C: All patients free of VOEs as of data cut-off * Denotes female patients; ╪ Patient current receiving phlebotomy Data as of September 14, 2018
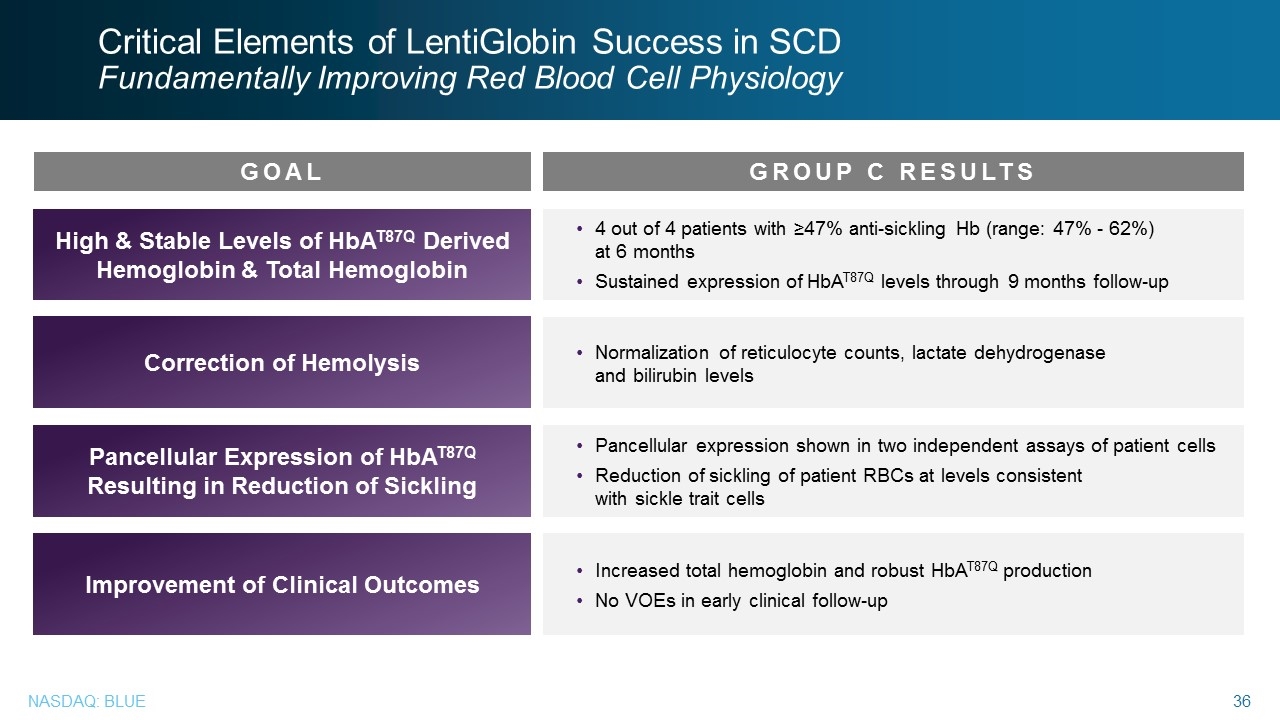
Critical Elements of LentiGlobin Success in SCD Fundamentally Improving Red Blood Cell Physiology 4 out of 4 patients with ≥47% anti-sickling Hb (range: 47% - 62%) at 6 months Sustained expression of HbAT87Q levels through 9 months follow-up High & Stable Levels of HbAT87Q Derived Hemoglobin & Total Hemoglobin Correction of Hemolysis Pancellular Expression of HbAT87Q Resulting in Reduction of Sickling Normalization of reticulocyte counts, lactate dehydrogenase and bilirubin levels Pancellular expression shown in two independent assays of patient cells Reduction of sickling of patient RBCs at levels consistent with sickle trait cells Increased total hemoglobin and robust HbAT87Q production No VOEs in early clinical follow-up Improvement of Clinical Outcomes GOAL GROUP C RESULTS Critical Elements of LentiGlobin Success in SCD Fundamentally Improving Red Blood Cell Physiology GOAL High & Stable Levels of HbAT87Q Derived Hemoglobin & Total Hemoglobin Correction of Hemolysis Pancellular Expression of HbAT87Q Resulting in Reduction of Sickling Improvement of Clinical Outcomes GROUP C RESULTS 4 out of 4 patients with ≥47% anti-sickling Hb (range: 47% - 62%) at 6 months Sustained expression of HbAT87Q levels through 9 months follow-up Normalization of reticulocyte counts, lactate dehydrogenase and bilirubin levels Pancellular expression shown in two independent assays of patient cells Reduction of sickling of patient RBCs at levels consistent with sickle trait cells Increased total hemoglobin and robust HbAT87Q production No VOEs in early clinical follow-up
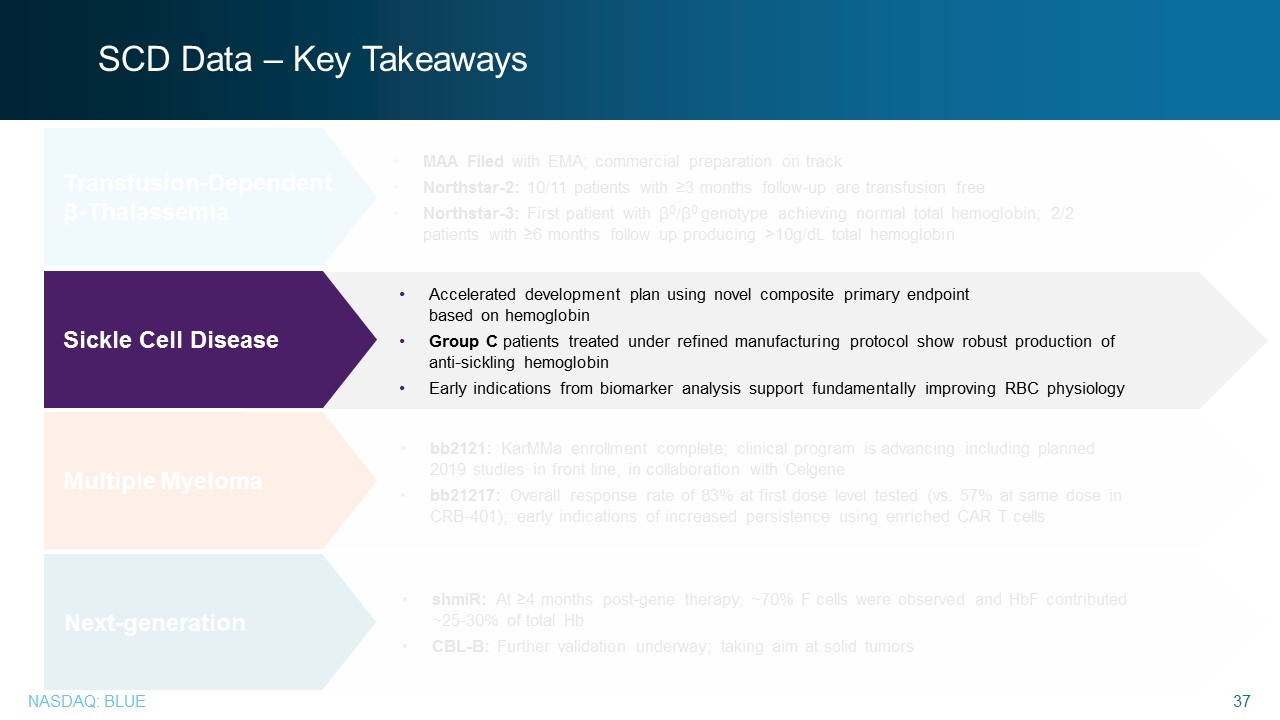
SCD Data – Key Takeaways bb2121: KarMMa enrollment complete; clinical program is advancing including planned 2019 studies in front line, in collaboration with Celgene bb21217: Overall response rate of 83% at first dose level tested (vs. 57% at same dose in CRB-401); early indications of increased persistence using enriched CAR T cells shmiR: At ≥4 months post-gene therapy, ~70% F cells were observed and HbF contributed ~25-30% of total Hb CBL-B: Further validation underway; taking aim at solid tumors Multiple Myeloma Next-generation MAA Filed with EMA; commercial preparation on track Northstar-2: 10/11 patients with ≥3 months follow-up are transfusion free Northstar-3: First patient with β0/β0 genotype achieving normal total hemoglobin; 2/2 patients with ≥6 months follow up producing >10g/dL total hemoglobin Transfusion-Dependent β-Thalassemia Accelerated development plan using novel composite primary endpoint based on hemoglobin Group C patients treated under refined manufacturing protocol show robust production of anti-sickling hemoglobin Early indications from biomarker analysis support fundamentally improving RBC physiology Sickle Cell Disease
Multiple Myeloma Liviu Niculescu, M.D., Ph.D., SVP, global medical affairs, bluebird bio Multiple Myeloma Liviu Niculescu, M.D., Ph.D., SVP, global medical affairs, bluebird bio

Multiple Myeloma A lethal blood cancer that often infiltrates the bone marrow causing anemia, kidney failure, immune problems and bone fractures BCMA PROGRAM OVERVIEW bb2121: Enrollment in KarMMa registration-enabling study complete (N=140) Additional studies advancing: KarMMa-2 in 2nd line Phase 2 study enrolling soon KarMMa-3 in 3rd line+ Phase 3 study enrolling soon Opportunities for bb2121 in newly diagnosed MM including high risk, transplant ineligible and transplant eligible vs. transplant under evaluation Multiple Myeloma A lethal blood cancer that often infiltrates the bone marrow causing anemia, kidney failure, immune problems and bone fractures BCMA PROGRAM OVERVIEW bb2121: Enrollment in KarMMa registration-enabling study complete (N=140) Additional studies advancing: KarMMa-2 in 2nd line Phase 2 study enrolling soon KarMMa-3 in 3rd line+ Phase 3 study enrolling soon Opportunities for bb2121 in newly diagnosed MM including high risk, transplant ineligible and transplant eligible vs. transplant under evaluation
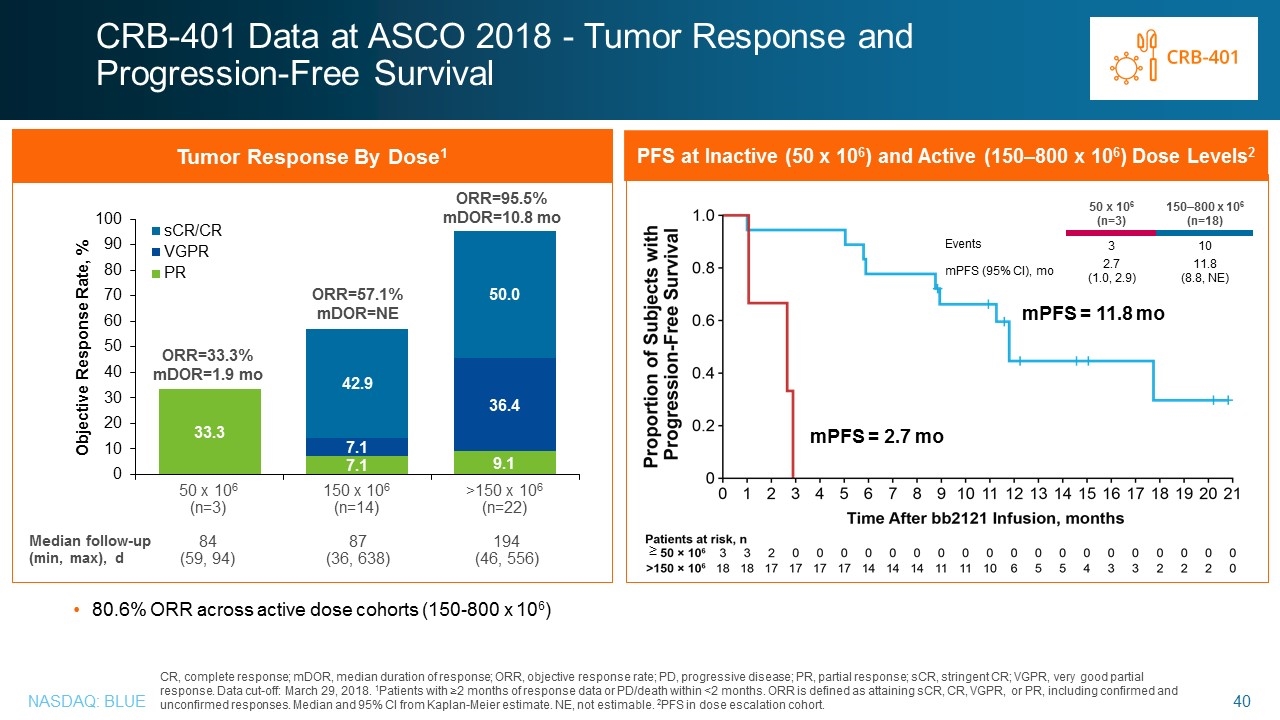
CR, complete response; mDOR, median duration of response; ORR, objective response rate; PD, progressive disease; PR, partial response; sCR, stringent CR; VGPR, very good partial response. Data cut-off: March 29, 2018. 1Patients with ≥2 months of response data or PD/death within <2 months. ORR is defined as attaining sCR, CR, VGPR, or PR, including confirmed and unconfirmed responses. Median and 95% CI from Kaplan-Meier estimate. NE, not estimable. 2PFS in dose escalation cohort. Tumor Response By Dose1 ORR=33.3% mDOR=1.9 mo ORR=57.1% mDOR=NE 150 x 106 (n=14) >150 x 106 (n=22) 50 x 106 (n=3) ORR=95.5% mDOR=10.8 mo Median follow-up (min, max), d 87 (36, 638) 84 (59, 94) 194 (46, 556) CRB-401 Data at ASCO 2018 - Tumor Response and Progression-Free Survival 80.6% ORR across active dose cohorts (150-800 x 106) PFS at Inactive (50 x 106) and Active (150–800 x 106) Dose Levels2 50 x 106 (n=3) 150–800 x 106 (n=18) Events 3 10 mPFS (95% CI), mo 2.7 (1.0, 2.9) 11.8 (8.8, NE) mPFS = 2.7 mo mPFS = 11.8 mo ≥ Data at ASCO 2018 - Tumor Response and Progression-Free Survival Tumor Response By Dose1 Objective Response Rate, % ORR=33.3% mDOR=1.9 mo ORR=57.1% mDOR=NE ORR=95.5% mDOR=10.8 mo 50 x 106 (n=3) 150 x 106 (n=14) >150 x 106 (n=22) Median follow-up (min, max), d 84 (59, 94) 87 (36, 638) 194 (46, 556) PFS at Inactive (50 x 106) and Active (150–800 x 106) Dose Levels2 50 x 106 (n=3) 150–800 x 106 (n=18) Events 3 10 mPFS (95% CI), mo (1.0, 2.9) (8.8, NE) mPFS = 2.7 mo 80.6% ORR across active dose cohorts (150-800 x 106) CR, complete response; mDOR, median duration of response; ORR, objective response rate; PD, progressive disease; PR, partial response; sCR, stringent CR; VGPR, very good partial response. Data cut-off: March 29, 2018. 1Patients with ≥2 months of response data or PD/death within <2 months. ORR is defined as attaining sCR, CR, VGPR, or PR, including confirmed and unconfirmed responses. Median and 95% CI from Kaplan-Meier estimate. NE, not estimable. 2PFS in dose escalation cohort.
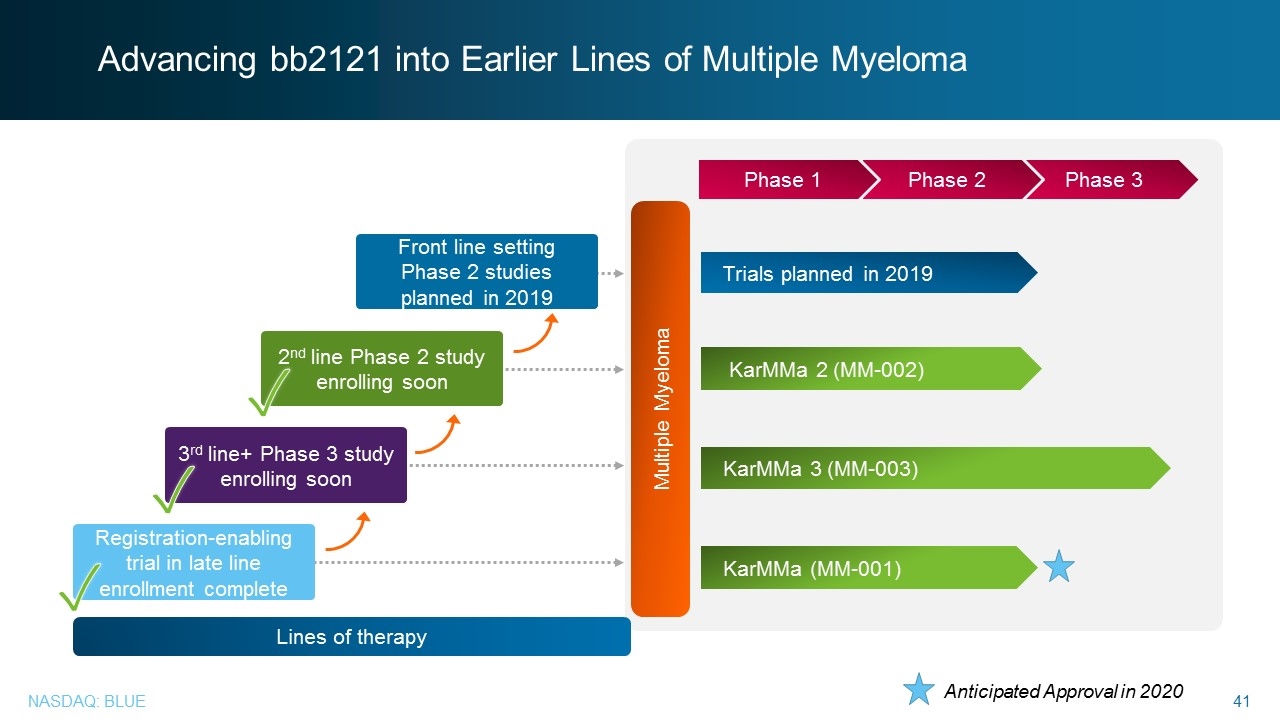
Advancing bb2121 into Earlier Lines of Multiple Myeloma Multiple Myeloma Trials planned in 2019 KarMMa 3 (MM-003) KarMMa 2 (MM-002) KarMMa (MM-001) Phase 3 Phase 2 Phase 1 Registration-enabling trial in late line enrollment complete Front line setting Phase 2 studies planned in 2019 3rd line+ Phase 3 study enrolling soon 2nd line Phase 2 study enrolling soon ✓ Lines of therapy Anticipated Approval in 2020 ✓ ✓ Advancing bb2121 into Earlier Lines of Multiple Myeloma Front line setting Phase 2 studies planned in 2019 2nd line Phase 2 study enrolling soon 3rd line+ Phase 3 study enrolling soon Registration-enabling trial in late line enrollment complete Lines of therapy Phase 1 Phase 2 Phase 3 Trials planned in 2019 KarMMa 2 (MM-002) KarMMa 3 (MM-003) KarMMa (MM-001) Anticipated Approval in 2020
Multiple Myeloma: bb21217 Nina Shah, M.D., University of California, San Francisco Multiple Myeloma: bb21217 Nina Shah, M.D., University of California, San Francisco
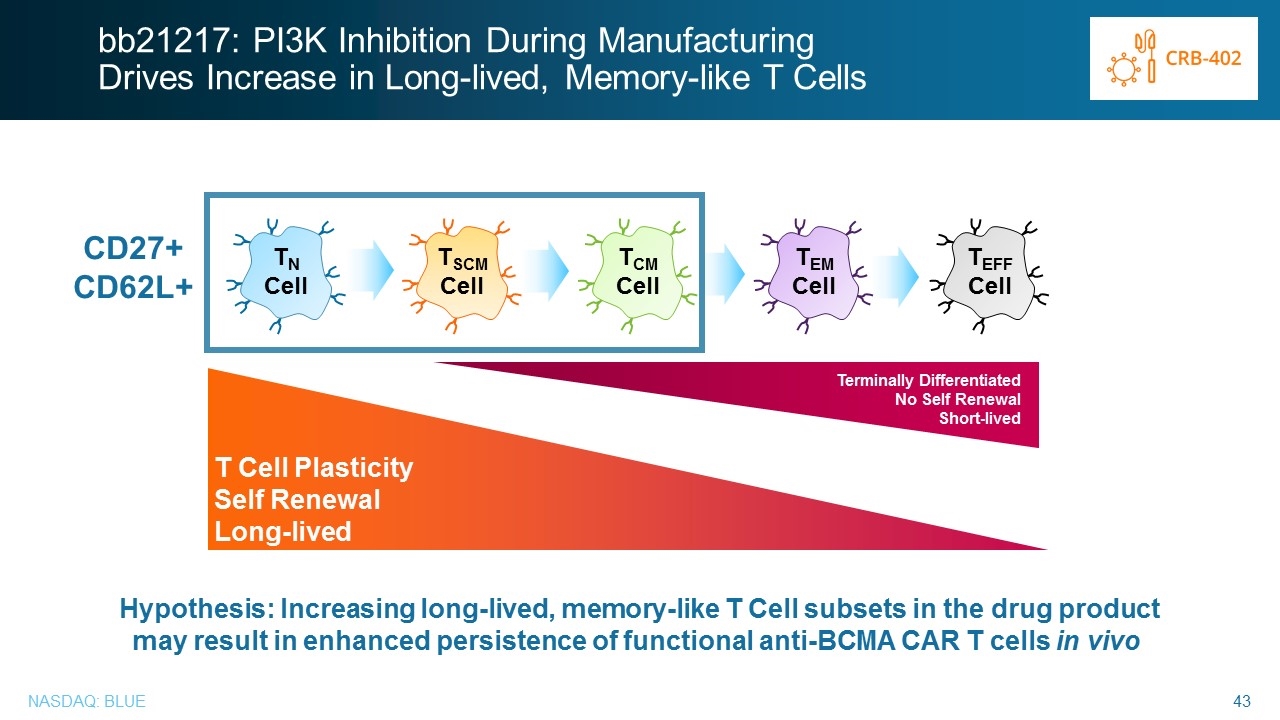
Hypothesis: Increasing long-lived, memory-like T Cell subsets in the drug product may result in enhanced persistence of functional anti-BCMA CAR T cells in vivo TN Cell TSCM Cell TCM Cell TEM Cell TEFF Cell T Cell Plasticity Self Renewal Long-lived Terminally Differentiated No Self Renewal Short-lived bb21217: PI3K Inhibition During Manufacturing Drives Increase in Long-lived, Memory-like T Cells CD27+ CD62L+ bb21217: PI3K Inhibition During Manufacturing Drives Increase in Long-lived, Memory-like T Cells CD27+ CD62L+ TN Cell TSCM Cell TCM Cell TEM Cell TEFF Cell Terminally Differentiated No Self Renewal Short-lived T Cell Plasticity Self Renewal Long-lived Hypothesis: Increasing long-lived, memory-like T Cell subsets in the drug product may result in enhanced persistence of functional anti-BCMA CAR T cells in vivo
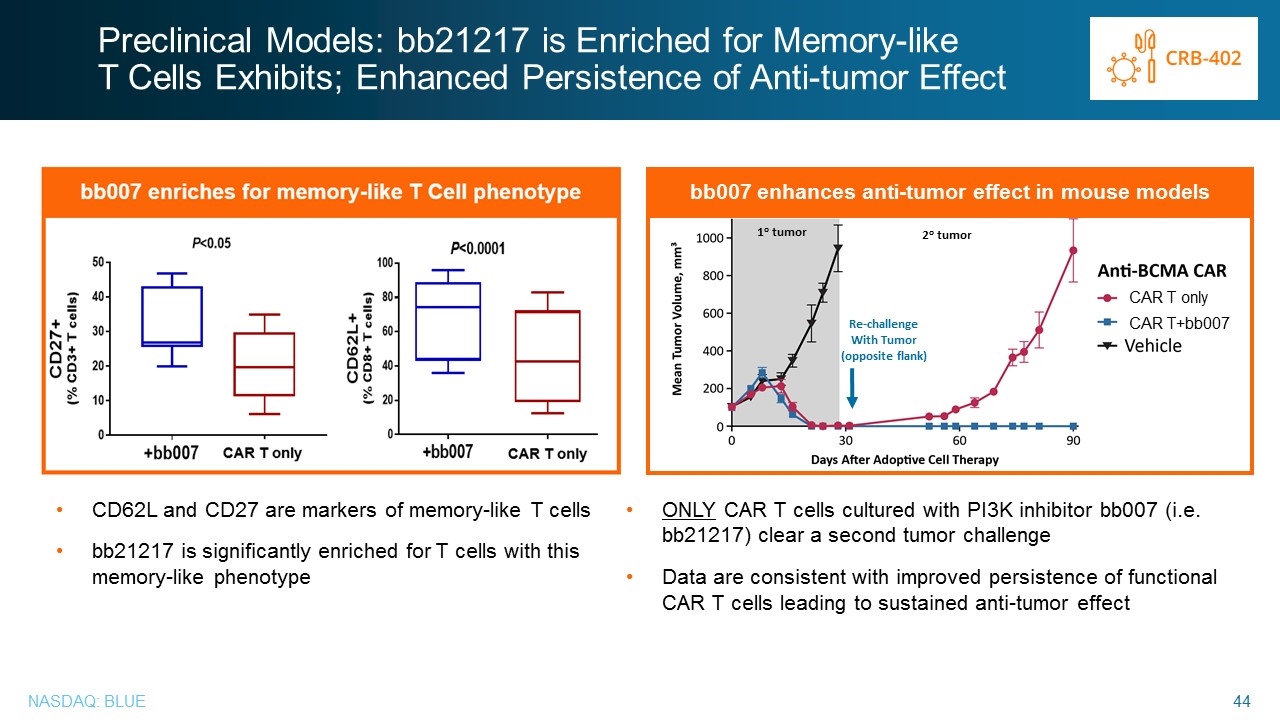
Preclinical Models: bb21217 is Enriched for Memory-like T Cells Exhibits; Enhanced Persistence of Anti-tumor Effect CD62L and CD27 are markers of memory-like T cells bb21217 is significantly enriched for T cells with this memory-like phenotype bb007 enhances anti-tumor effect in mouse models ONLY CAR T cells cultured with PI3K inhibitor bb007 (i.e. bb21217) clear a second tumor challenge Data are consistent with improved persistence of functional CAR T cells leading to sustained anti-tumor effect Re-challenge With Tumor (opposite flank) 1o tumor 2o tumor CAR T only CAR T+bb007 Preclinical Models: bb21217 is Enriched for Memory-like T Cells Exhibits; Enhanced Persistence of Anti-tumor Effect bb007 enhances anti-tumor effect in mouse models Re-challenge With Tumor (opposite flank) 2o tumor CAR T only CAR T+bb007 CD62L and CD27 are markers of memory-like T cells bb21217 is significantly enriched for T cells with this memory-like phenotype ONLY CAR T cells cultured with PI3K inhibitor bb007 (i.e. bb21217) clear a second tumor challenge Data are consistent with improved persistence of functional CAR T cells leading to sustained anti-tumor effect
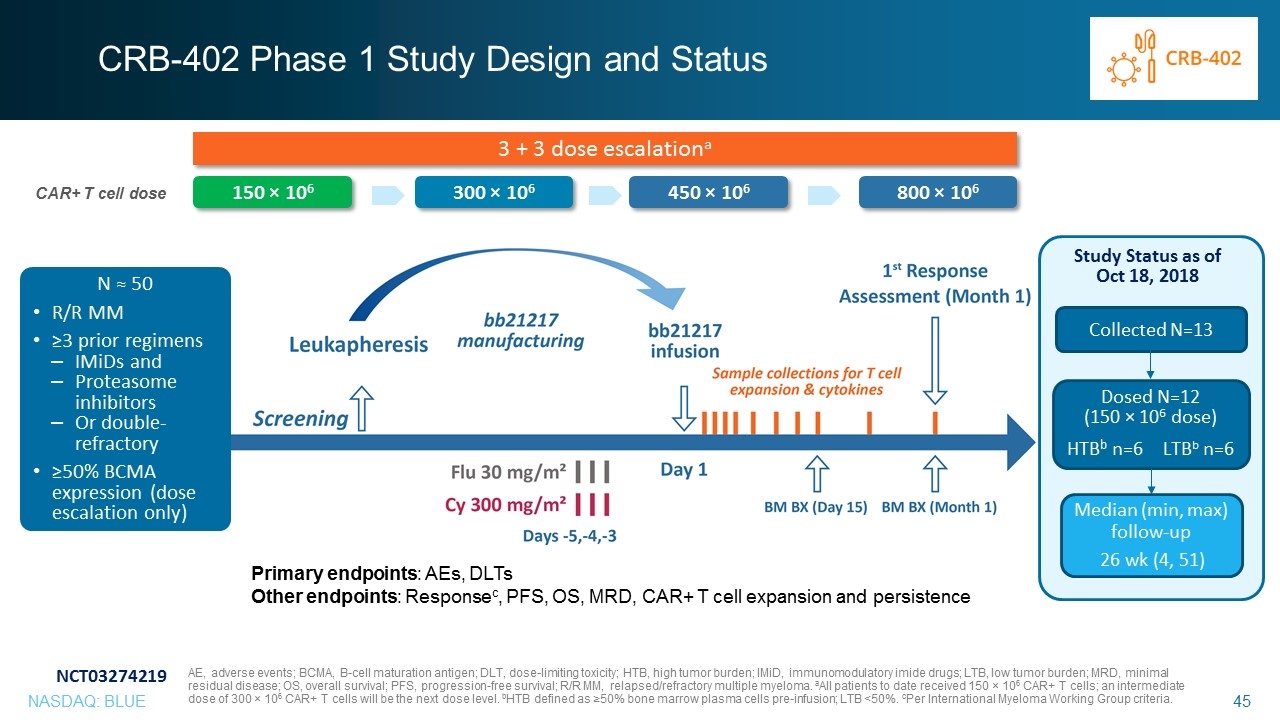
CRB-402 Phase 1 Study Design and Status 3 + 3 dose escalationa 300 × 106 450 × 106 800 × 106 150 × 106 Collected N=13 Dosed N=12 (150 × 106 dose) HTBb n=6LTBb n=6 Study Status as of Oct 18, 2018 Median (min, max) follow-up 26 wk (4, 51) Primary endpoints: AEs, DLTs Other endpoints: Responsec, PFS, OS, MRD, CAR+ T cell expansion and persistence N ≈ 50 R/R MM ≥3 prior regimens IMiDs and Proteasome inhibitors Or double-refractory ≥50% BCMA expression (dose escalation only) NCT03274219 AE, adverse events; BCMA, B-cell maturation antigen; DLT, dose-limiting toxicity; HTB, high tumor burden; IMiD, immunomodulatory imide drugs; LTB, low tumor burden; MRD, minimal residual disease; OS, overall survival; PFS, progression-free survival; R/R MM, relapsed/refractory multiple myeloma. aAll patients to date received 150 × 106 CAR+ T cells; an intermediate dose of 300 × 106 CAR+ T cells will be the next dose level. bHTB defined as ≥50% bone marrow plasma cells pre-infusion; LTB <50%. cPer International Myeloma Working Group criteria. CAR+ T cell dose CRB-402 Phase 1 Study Design and Status 3 + 3 dose escalationa CAR+ T cell dose 150 × 106 300 × 106 450 × 106 800 × 106 N ≈ 50 R/R MM ≥3 prior regimens IMiDs and Proteasome inhibitors Or double-refractory ≥50% BCMA expression (dose escalation only) Study Status as of Oct 18, 2018 Collected N=13 Dosed N=12 (150 × 106 dose) HTBb n=6 LTBb n=6 Median (min, max) follow-up 26 wk (4, 51) Primary endpoints: AEs, DLTs Other endpoints: Responsec, PFS, OS, MRD, CAR+ T cell expansion and persistence NCT03274219 AE, adverse events; BCMA, B-cell maturation antigen; DLT, dose-limiting toxicity; HTB, high tumor burden; IMiD, immunomodulatory imide drugs; LTB, low tumor burden; MRD, minimal residual disease; OS, overall survival; PFS, progression-free survival; R/R MM, relapsed/refractory multiple myeloma. aAll patients to date received 150 × 106 CAR+ T cells; an intermediate dose of 300 × 106 CAR+ T cells will be the next dose level. bHTB defined as ≥50% bone marrow plasma cells pre-infusion; LTB <50%. cPer International Myeloma Working Group criteria
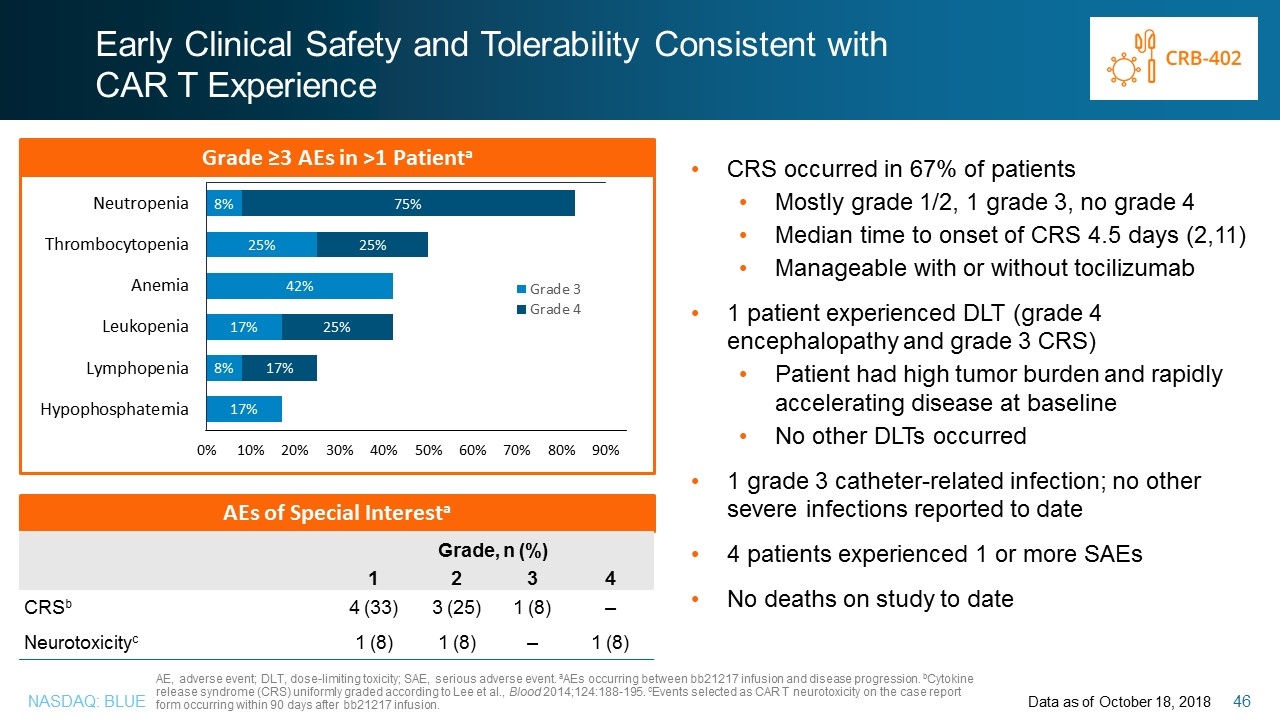
Early Clinical Safety and Tolerability Consistent with CAR T Experience CRS occurred in 67% of patients Mostly grade 1/2, 1 grade 3, no grade 4 Median time to onset of CRS 4.5 days (2,11) Manageable with or without tocilizumab 1 patient experienced DLT (grade 4 encephalopathy and grade 3 CRS) Patient had high tumor burden and rapidly accelerating disease at baseline No other DLTs occurred 1 grade 3 catheter-related infection; no other severe infections reported to date 4 patients experienced 1 or more SAEs No deaths on study to date Data as of October 18, 2018 AE, adverse event; DLT, dose-limiting toxicity; SAE, serious adverse event. aAEs occurring between bb21217 infusion and disease progression. bCytokine release syndrome (CRS) uniformly graded according to Lee et al., Blood 2014;124:188-195. cEvents selected as CAR T neurotoxicity on the case report form occurring within 90 days after bb21217 infusion. Grade ≥3 AEs in >1 Patienta AEs of Special Interesta Grade, n (%) 1 2 3 4 CRSb 4 (33) 3 (25) 1 (8) – Neurotoxicityc 1 (8) 1 (8) – 1 (8) Early Clinical Safety and Tolerability Consistent with CAR T Experience Grade ≥3 AEs in >1 Patienta 8% 75% 25% Grade, n (%) CRSb 1 2 3 4 4 (33) 3 (25) 1 (8) – Neurotoxicityc 1 (8) 1 (8) – 1 (8) CRS occurred in 67% of patients Mostly grade 1/2, 1 grade 3, no grade 4 Median time to onset of CRS 4.5 days (2,11) Manageable with or without tocilizumab 1 patient experienced DLT (grade 4 encephalopathy and grade 3 CRS) Patient had high tumor burden and rapidly accelerating disease at baseline No other DLTs occurred 1 grade 3 catheter-related infection; no other severe infections reported to date 4 patients experienced 1 or more SAEs No deaths on study to date AE, adverse event; DLT, dose-limiting toxicity; SAE, serious adverse event. aAEs occurring between bb21217 infusion and disease progression. bCytokine release syndrome (CRS) uniformly graded according to Lee et al., Blood 2014;124:188-195. cEvents selected as CAR T neurotoxicity on the case report form occurring within 90 days after bb21217 infusion. Data as of October 18, 2018
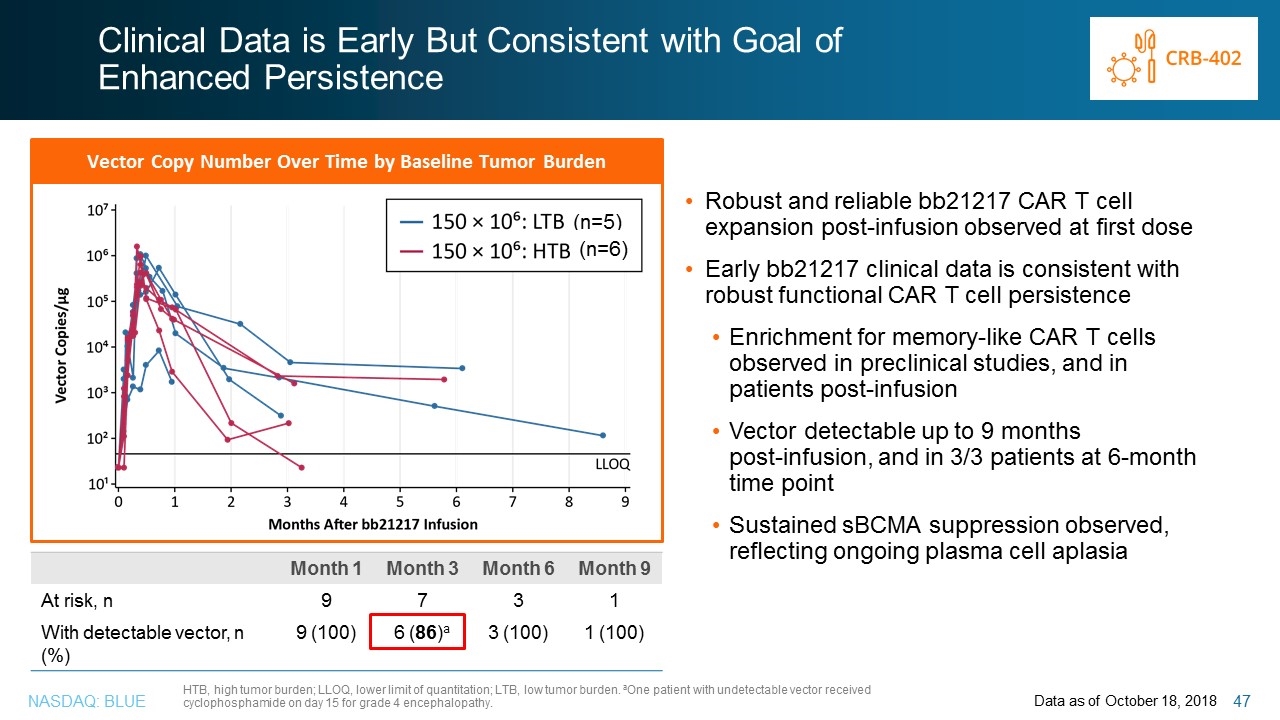
Clinical Data is Early But Consistent with Goal of Enhanced Persistence Robust and reliable bb21217 CAR T cell expansion post-infusion observed at first dose Early bb21217 clinical data is consistent with robust functional CAR T cell persistence Enrichment for memory-like CAR T cells observed in preclinical studies, and in patients post-infusion Vector detectable up to 9 months post-infusion, and in 3/3 patients at 6-month time point Sustained sBCMA suppression observed, reflecting ongoing plasma cell aplasia Data as of October 18, 2018 Month 1 Month 3 Month 6 Month 9 At risk, n 9 7 3 1 With detectable vector, n (%) 9 (100) 6 (86)a 3 (100) 1 (100) Vector Copy Number Over Time by Baseline Tumor Burden (n=5) (n=6) HTB, high tumor burden; LLOQ, lower limit of quantitation; LTB, low tumor burden. aOne patient with undetectable vector received cyclophosphamide on day 15 for grade 4 encephalopathy. Clinical Data is Early But Consistent with Goal of Enhanced Persistence Vector Copy Number Over Time by Baseline Tumor Burden Month 1 Month 3 Month 9 At risk, n 9 7 3 1 With detectable vector, n (%) 9 (100) 6 (86)a 3 (100) 1 (100) Robust and reliable bb21217 CAR T cell expansion post-infusion observed at first dose Early bb21217 clinical data is consistent with robust functional CAR T cell persistence Enrichment for memory-like CAR T cells observed in preclinical studies, and in patients post-infusion Vector detectable up to 9 months post-infusion, and in 3/3 patients at 6-month time point Sustained sBCMA suppression observed, reflecting ongoing plasma cell aplasia HTB, high tumor burden; LLOQ, lower limit of quantitation; LTB, low tumor burden. aOne patient with undetectable vector received cyclophosphamide on day 15 for grade 4 encephalopathy. Data as of October 18, 2018
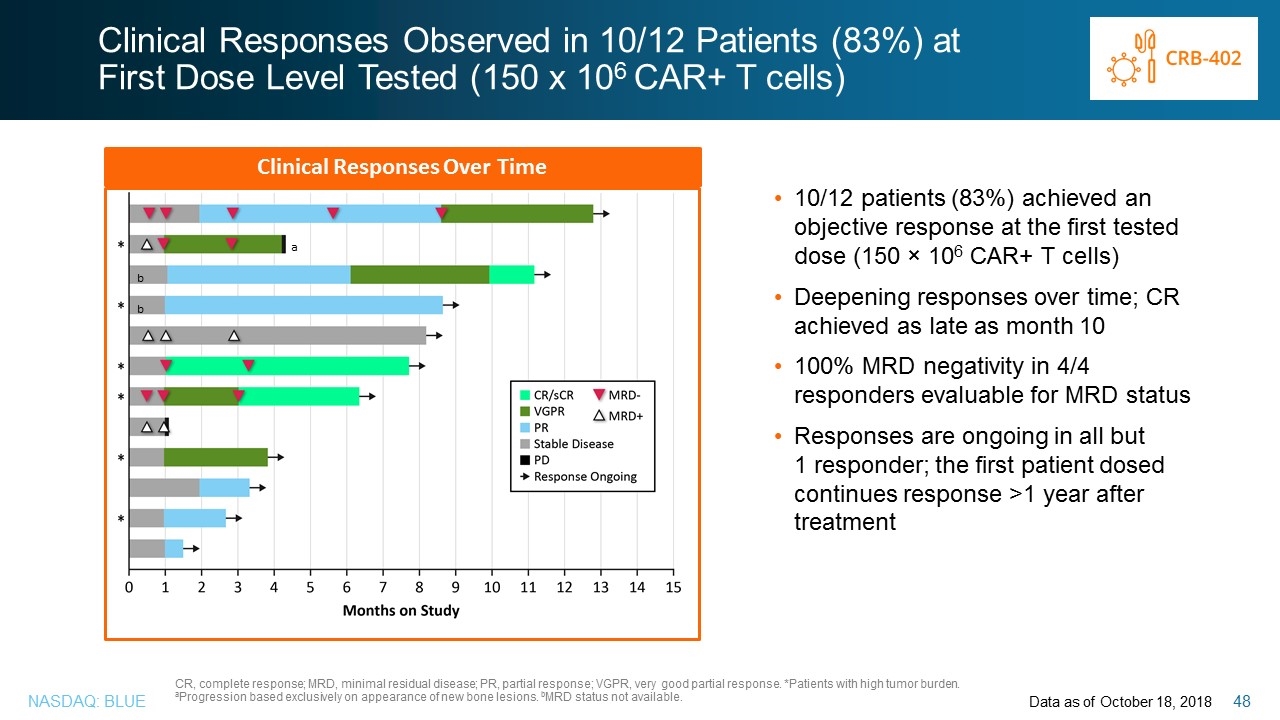
Clinical Responses Observed in 10/12 Patients (83%) at First Dose Level Tested (150 x 106 CAR+ T cells) Data as of October 18, 2018 b b a Clinical Responses Over Time CR, complete response; MRD, minimal residual disease; PR, partial response; VGPR, very good partial response. *Patients with high tumor burden. aProgression based exclusively on appearance of new bone lesions. bMRD status not available. 10/12 patients (83%) achieved an objective response at the first tested dose (150 × 106 CAR+ T cells) Deepening responses over time; CR achieved as late as month 10 100% MRD negativity in 4/4 responders evaluable for MRD status Responses are ongoing in all but 1 responder; the first patient dosed continues response >1 year after treatment Clinical Responses Observed in 10/12 Patients (83%) at First Dose Level Tested (150 x 106 CAR+ T cells) Clinical Responses Over Time 10/12 patients (83%) achieved an objective response at the first tested dose (150 × 106 CAR+ T cells) Deepening responses over time; CR achieved as late as month 10 100% MRD negativity in 4/4 responders evaluable for MRD status Responses are ongoing in all but 1 responder; the first patient dosed continues response >1 year after treatment CR, complete response; MRD, minimal residual disease; PR, partial response; VGPR, very good partial response. *Patients with high tumor burden. aProgression based exclusively on appearance of new bone lesions. bMRD status not available. Data as of October 18, 2018
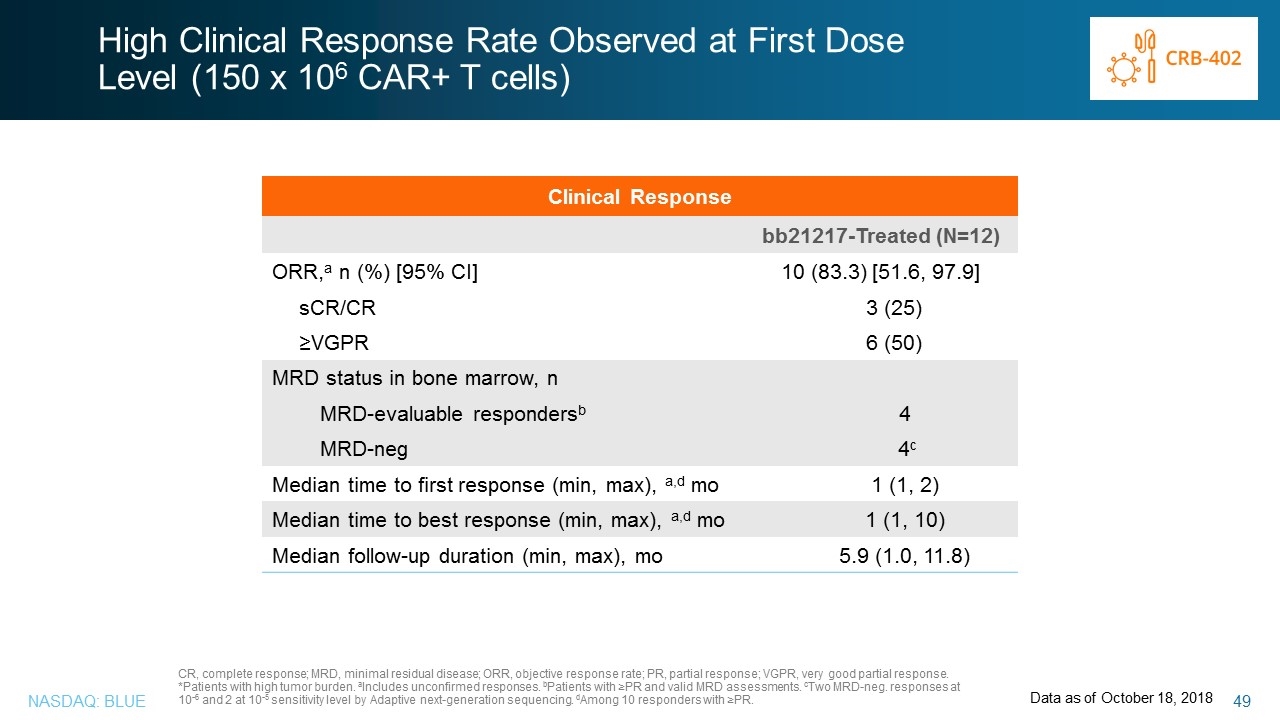
High Clinical Response Rate Observed at First Dose Level (150 x 106 CAR+ T cells) Clinical Response bb21217-Treated (N=12) ORR,a n (%) [95% CI] 10 (83.3) [51.6, 97.9] sCR/CR 3 (25) ≥VGPR 6 (50) MRD status in bone marrow, n MRD-evaluable respondersb 4 MRD-neg 4c Median time to first response (min, max), a,d mo 1 (1, 2) Median time to best response (min, max), a,d mo 1 (1, 10) Median follow-up duration (min, max), mo 5.9 (1.0, 11.8) CR, complete response; MRD, minimal residual disease; ORR, objective response rate; PR, partial response; VGPR, very good partial response. *Patients with high tumor burden. aIncludes unconfirmed responses. bPatients with ≥PR and valid MRD assessments. cTwo MRD-neg. responses at 10-6 and 2 at 10-5 sensitivity level by Adaptive next-generation sequencing. dAmong 10 responders with ≥PR. Data as of October 18, 2018 High Clinical Response Rate Observed at First Dose Level (150 x 106 CAR+ T cells) Clinical Response ORR,a n (%) [95% CI] sCR/CR ≥VGPR MRD status in bone marrow, n MRD-evaluable respondersb MRD-neg Median time to first response (min, max), a,d mo Median time to best response (min, max), a,d mo Median follow-up duration (min, max), mo 10 (83.3) [51.6, 97.9] 3 (25) 6 (50) 4 4c 1 (1, 2) 1 (1, 10) 5.9 (1.0, 11.8) CR, complete response; MRD, minimal residual disease; ORR, objective response rate; PR, partial response; VGPR, very good partial response. *Patients with high tumor burden. aIncludes unconfirmed responses. bPatients with ≥PR and valid MRD assessments. cTwo MRD-neg. responses at 10-6 and 2 at 10-5 sensitivity level by Adaptive next-generation sequencing. dAmong 10 responders with ≥PR. Data as of October 18, 2018
Promising Early Data with Next-Generation Anti-BCMA CAR T bb21217 demonstrated promising early clinical activity in heavily pretreated patients with relapsed/refractory multiple myeloma at first dose level tested 83% ORR with 90% of responses ongoing Elimination of MRD in the bone marrow of all 4 evaluable responders Early indications of increased persistence using enriched CAR T cells Safety profile appears consistent with known toxicities of CAR T cell therapies Dose escalation is ongoing Promising Early Data with Next-Generation Anti-BCMA CAR T bb21217 demonstrated promising early clinical activity in heavily pretreated patients with relapsed/refractory multiple myeloma at first dose level tested 83% ORR with 90% of responses ongoing Elimination of MRD in the bone marrow of all 4 evaluable responders Early indications of increased persistence using enriched CAR T cells Safety profile appears consistent with known toxicities of CAR T cell therapies Dose escalation is ongoing
BCMA Data – Key Takeaways bb2121: KarMMa enrollment complete; clinical program is advancing including planned 2019 studies in front line, in collaboration with Celgene bb21217: Overall response rate of 83% at first dose level tested (vs. 57% at same dose in CRB-401); early indications of increased persistence using enriched CAR T cells shmiR: At ≥4 months post-gene therapy, ~70% F cells were observed and HbF contributed ~25-30% of total Hb CBL-B: Further validation underway; taking aim at solid tumors Multiple Myeloma Next-generation MAA Filed with EMA; commercial preparation on track Northstar-2: 10/11 patients with ≥3 months follow-up are transfusion free Northstar-3: First patient with β0/β0 genotype achieving normal total hemoglobin; 2/2 patients with ≥6 months follow up producing >10g/dL total hemoglobin Transfusion-Dependent β-Thalassemia Accelerated development plan using novel composite primary endpoint based on hemoglobin Group C patients treated under refined manufacturing protocol show robust production of anti-sickling hemoglobin Early indications from biomarker analysis support fundamentally improving RBC physiology Sickle Cell Disease BCMA Data – Key Takeaways Multiple Myeloma bb2121: KarMMa enrollment complete; clinical program is advancing including planned 2019 studies in front line, in collaboration with Celgene bb21217: Overall response rate of 83% at first dose level tested (vs. 57% at same dose in CRB-401); early indications of increased persistence using enriched CAR T cells
ASH Highlights: Next Generation Programs / Platforms First clinical demonstration of the potential to genetically manipulate HbF levels through BCL11a Novel LVV expressing a shRNAmiR to knock down BCL11a at the level exclusively in erythroid cells Robust knock down of BCL11a observed in patient cells At ≥4 months post-gene therapy, ~70% F cells were observed and HbF contributed ~25-30% of total Hb Example of bbb’s T cell enhancement technologies aimed at delivering transformative outcomes for solid tumors bbb megaTAL technology used to efficiently and specifically knockout CBL-B in CAR T cells via gene editing Increases cytokine production in response to tumor cells in vitro Enhances anti-tumor activity of CAR T cells in a mouse xenograft model Flipping the Switch: Initial Results of Genetic Targeting of the Fetal to Adult Globin Switch in Sickle Cell Patients Esrick et al. (Abstract #801) Knockout of CBL-B Greatly Enhances Anti-Tumor Activity of CAR T Cells Hooper et al. (Abstract #338) ASH Highlights: Next Generation Programs / Platforms First clinical demonstration of the potential to genetically manipulate HbF levels through BCL11a Novel LVV expressing a shRNAmiR to knock down BCL11a at the level exclusively in erythroid cells Robust knock down of BCL11a observed in patient cells At ≥4 months post-gene therapy, ~70% F cells were observed and HbF contributed ~25-30% of total Hb Flipping the Switch: Initial Results of Genetic Targeting of the Fetal to Adult Globin Switch in Sickle Cell Patients Esrick et al. (Abstract #801) Example of bbb’s T cell enhancement technologies aimed at delivering transformative outcomes for solid tumors bbb megaTAL technology used to efficiently and specifically knockout CBL-B in CAR T cells via gene editing Increases cytokine production in response to tumor cells in vitro Enhances anti-tumor activity of CAR T cells in a mouse xenograft model Knockout of CBL-B Greatly Enhances Anti-Tumor Activity of CAR T Cells Hooper et al. (Abstract #338)
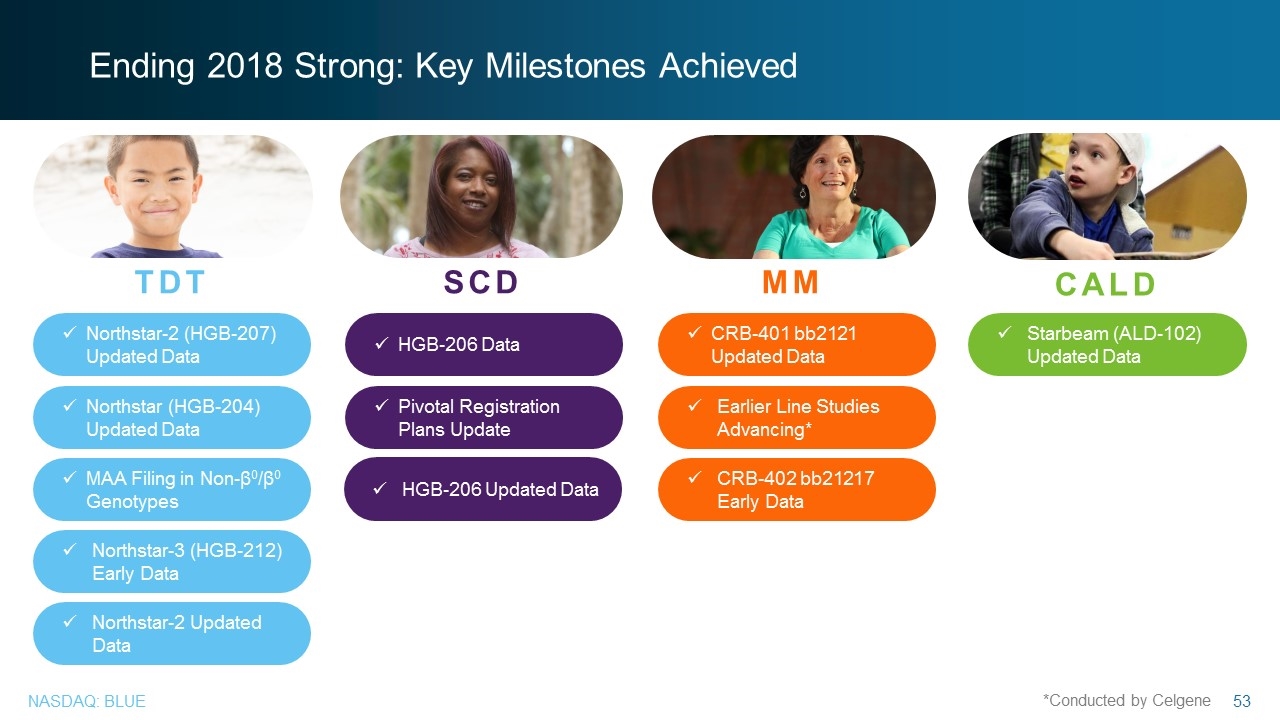
Ending 2018 Strong: Key Milestones Achieved TDT SCD MM CALD Pivotal Registration Plans Update Northstar-3 (HGB-212) Early Data MAA Filing in Non-β0/β0 Genotypes Earlier Line Studies Advancing* CRB-402 bb21217 Early Data Northstar-2 (HGB-207) Updated Data HGB-206 Data CRB-401 bb2121 Updated Data Starbeam (ALD-102) Updated Data Northstar-2 Updated Data Northstar (HGB-204) Updated Data *Conducted by Celgene HGB-206 Updated Data Ending 2018 Strong: Key Milestones Achieved TDT Northstar-2 (HGB-207) Updated Data Northstar (HGB-204) Updated Data MAA Filing in Non-β0/β0 Genotypes Northstar-3 (HGB-212) Early Data Northstar-2 Updated Data SCD HGB-206 Data Pivotal Registration Plans Update HGB-206 Updated Data MM CRB-401 bb2121 Updated Data Earlier Line Studies Advancing* CRB-402 bb21217 Early Data CALD Starbeam (ALD-102) Updated Data

Q & A Q & A
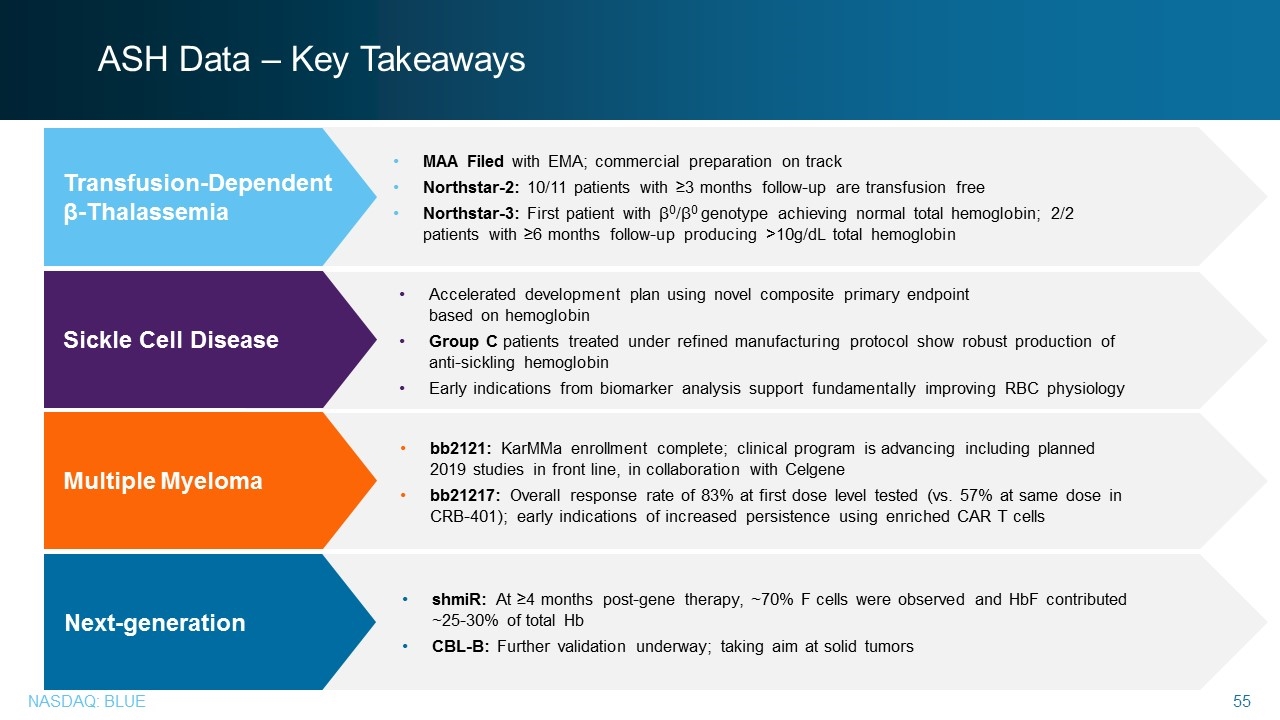
ASH Data – Key Takeaways bb2121: KarMMa enrollment complete; clinical program is advancing including planned 2019 studies in front line, in collaboration with Celgene bb21217: Overall response rate of 83% at first dose level tested (vs. 57% at same dose in CRB-401); early indications of increased persistence using enriched CAR T cells shmiR: At ≥4 months post-gene therapy, ~70% F cells were observed and HbF contributed ~25-30% of total Hb CBL-B: Further validation underway; taking aim at solid tumors Multiple Myeloma Next-generation MAA Filed with EMA; commercial preparation on track Northstar-2: 10/11 patients with ≥3 months follow-up are transfusion free Northstar-3: First patient with β0/β0 genotype achieving normal total hemoglobin; 2/2 patients with ≥6 months follow-up producing >10g/dL total hemoglobin Transfusion-Dependent β-Thalassemia Accelerated development plan using novel composite primary endpoint based on hemoglobin Group C patients treated under refined manufacturing protocol show robust production of anti-sickling hemoglobin Early indications from biomarker analysis support fundamentally improving RBC physiology Sickle Cell Disease ASH Data – Key Takeaways Transfusion-Dependent β-Thalassemia MAA Filed with EMA; commercial preparation on track Northstar-2: 10/11 patients with ≥3 months follow-up are transfusion free Northstar-3: First patient with β0/β0 genotype achieving normal total hemoglobin; 2/2 patients with ≥6 months follow-up producing >10g/dL total hemoglobin Sickle Cell Disease Accelerated development plan using novel composite primary endpoint based on hemoglobin Group C patients treated under refined manufacturing protocol show robust production of anti-sickling hemoglobin Early indications from biomarker analysis support fundamentally improving RBC physiology Multiple Myeloma bb2121: KarMMa enrollment complete; clinical program is advancing including planned 2019 studies in front line, in collaboration with Celgene bb21217: Overall response rate of 83% at first dose level tested (vs. 57% at same dose in CRB-401); early indications of increased persistence using enriched CAR T cells Next-generation shmiR: At ≥4 months post-gene therapy, ~70% F cells were observed and HbF contributed ~25-30% of total Hb CBL-B: Further validation underway; taking aim at solid tumors