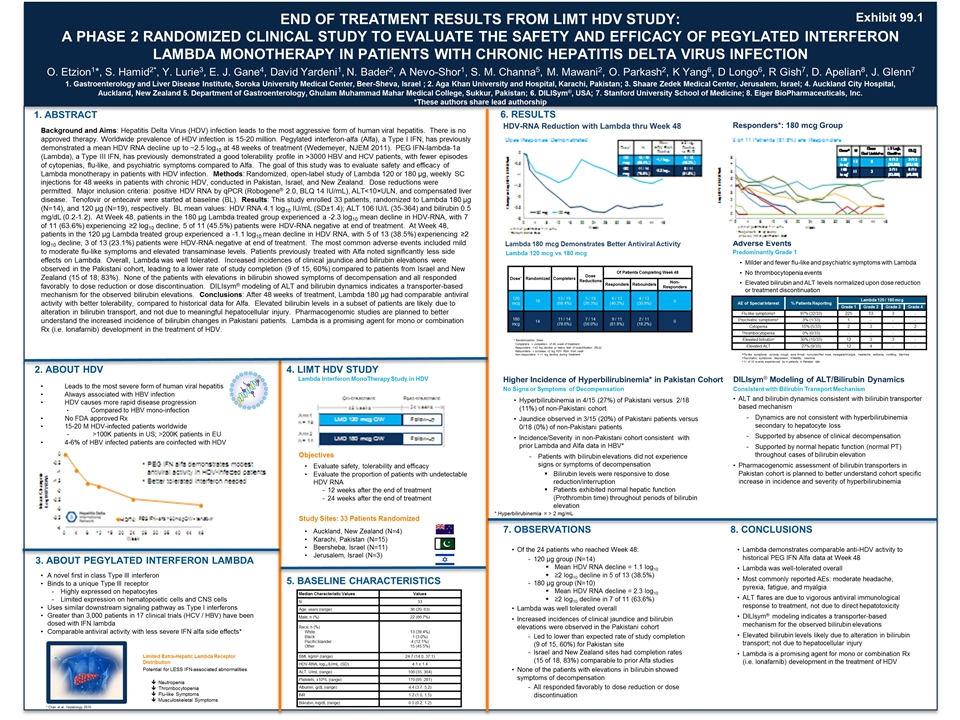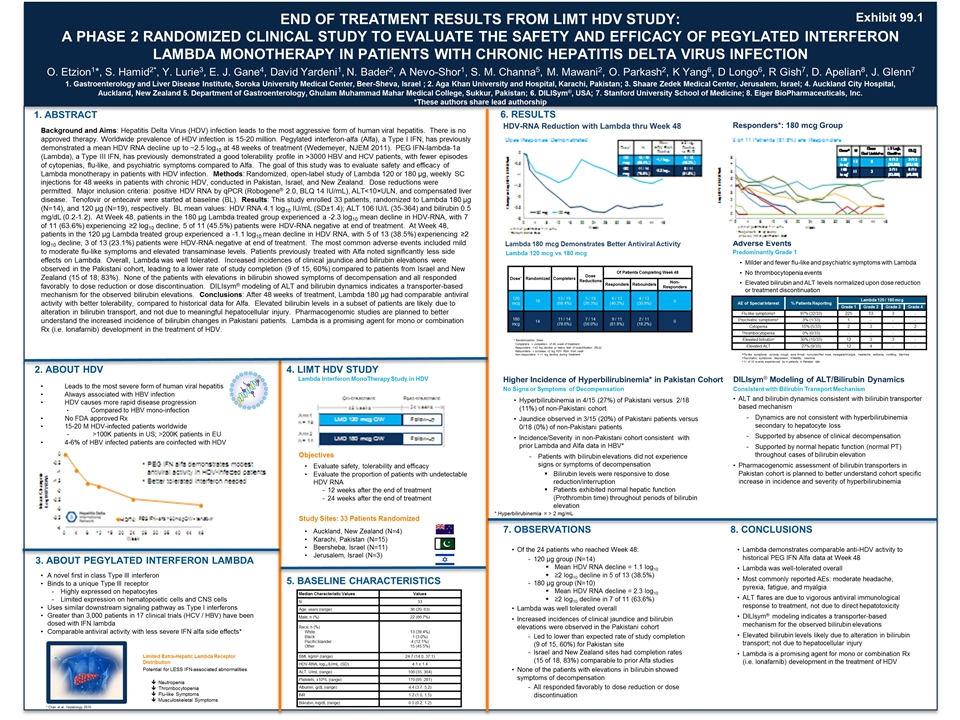
Consistent with Bilirubin Transporter Mechanism END OF TREATMENT RESULTS FROM LIMT HDV STUDY: A PHASE 2 RANDOMIZED CLINICAL STUDY TO EVALUATE THE SAFETY AND EFFICACY OF PEGYLATED INTERFERON LAMBDA MONOTHERAPY IN PATIENTS WITH CHRONIC HEPATITIS DELTA VIRUS INFECTION O. Etzion1*, S. Hamid2*, Y. Lurie3, E. J. Gane4, David Yardeni1, N. Bader2, A Nevo-Shor1, S. M. Channa5, M. Mawani2, O. Parkash2, K Yang6, D Longo6, R Gish7, D. Apelian8, J. Glenn7 1. Gastroenterology and Liver Disease Institute, Soroka University Medical Center, Beer-Sheva, Israel ; 2. Aga Khan University and Hospital, Karachi, Pakistan; 3. Shaare Zedek Medical Center, Jerusalem, Israel; 4. Auckland City Hospital, Auckland, New Zealand 5. Department of Gastroenterology, Ghulam Muhammad Mahar Medical College, Sukkur, Pakistan; 6. DILISym®, USA; 7. Stanford University School of Medicine; 8. Eiger BioPharmaceuticals, Inc. *These authors share lead authorship 1. ABSTRACT CONCLUSIONS Background and Aims: Hepatitis Delta Virus (HDV) infection leads to the most aggressive form of human viral hepatitis. There is no approved therapy. Worldwide prevalence of HDV infection is 15-20 million. Pegylated interferon-alfa (Alfa), a Type I IFN, has previously demonstrated a mean HDV RNA decline up to ~2.5 log10 at 48 weeks of treatment (Wedemeyer, NJEM 2011). PEG IFN-lambda-1a (Lambda), a Type III IFN, has previously demonstrated a good tolerability profile in >3000 HBV and HCV patients, with fewer episodes of cytopenias, flu-like, and psychiatric symptoms compared to Alfa. The goal of this study was to evaluate safety and efficacy of Lambda monotherapy in patients with HDV infection. Methods: Randomized, open-label study of Lambda 120 or 180 μg, weekly SC injections for 48 weeks in patients with chronic HDV, conducted in Pakistan, Israel, and New Zealand. Dose reductions were permitted. Major inclusion criteria: positive HDV RNA by qPCR (Robogene® 2.0, BLQ 14 IU/mL), ALT<10×ULN, and compensated liver disease. Tenofovir or entecavir were started at baseline (BL). Results: This study enrolled 33 patients, randomized to Lambda 180 μg (N=14), and 120 μg (N=19), respectively. BL mean values: HDV RNA 4.1 log10 IU/mL (SD±1.4); ALT 106 IU/L (35-364) and bilirubin 0.5 mg/dL (0.2-1.2). At Week 48, patients in the 180 μg Lambda treated group experienced a -2.3 log10 mean decline in HDV-RNA, with 7 of 11 (63.6%) experiencing ≥2 log10 decline, 5 of 11 (45.5%) patients were HDV-RNA negative at end of treatment. At Week 48, patients in the 120 μg Lambda treated group experienced a -1.1 log10 mean decline in HDV RNA, with 5 of 13 (38.5%) experiencing ≥2 log10 decline, 3 of 13 (23.1%) patients were HDV-RNA negative at end of treatment. The most common adverse events included mild to moderate flu-like symptoms and elevated transaminase levels. Patients previously treated with Alfa noted significantly less side effects on Lambda. Overall, Lambda was well tolerated. Increased incidences of clinical jaundice and bilirubin elevations were observed in the Pakistani cohort, leading to a lower rate of study completion (9 of 15, 60%) compared to patients from Israel and New Zealand (15 of 18; 83%). None of the patients with elevations in bilirubin showed symptoms of decompensation and all responded favorably to dose reduction or dose discontinuation. DILIsym® modeling of ALT and bilirubin dynamics indicates a transporter-based mechanism for the observed bilirubin elevations. Conclusions: After 48 weeks of treatment, Lambda 180 μg had comparable antiviral activity with better tolerability, compared to historical data for Alfa. Elevated bilirubin levels in a subset of patients are likely due to alteration in bilirubin transport, and not due to meaningful hepatocellular injury. Pharmacogenomic studies are planned to better understand the increased incidence of bilirubin changes in Pakistani patients. Lambda is a promising agent for mono or combination Rx (i.e. lonafarnib) development in the treatment of HDV. 2. ABOUT HDV 3. ABOUT PEGYLATED INTERFERON LAMBDA 4. LIMT HDV STUDY 5. BASELINE CHARACTERISTICS Leads to the most severe form of human viral hepatitis Always associated with HBV infection HDV causes more rapid disease progression Compared to HBV mono-infection No FDA approved Rx 15-20 M HDV-infected patients worldwide >100K patients in US; >200K patients in EU 4-6% of HBV infected patients are coinfected with HDV A novel first in class Type III interferon Binds to a unique Type III receptor Highly expressed on hepatocytes Limited expression on hematopoietic cells and CNS cells Uses similar downstream signaling pathway as Type I interferons Greater than 3,000 patients in 17 clinical trials (HCV / HBV) have been dosed with IFN lambda Comparable antiviral activity with less severe IFN alfa side effects* Limited Extra-Hepatic Lambda Receptor Distribution Potential for LESS IFN-associated abnormalities Neutropenia Thrombocytopenia Flu-like Symptoms Musculoskeletal Symptoms Evaluate safety, tolerability and efficacy Evaluate the proportion of patients with undetectable HDV RNA 12 weeks after the end of treatment 24 weeks after the end of treatment Median Characteristic Values Values N 33 Age, years (range) 36 (20, 63) Male, n (%) 22 (66.7%) Race, n (%) White Black Pacific Islander Other 13 (39.4%) 1 (3.0%) 4 (12.1%) 15 (45.5%) BMI, kg/m2 (range) 24.7 (14.0, 37.1) HDV-RNA, log10 IU/mL (SD) 4.1 ± 1.4 ALT, U/mL (range) 106 (35, 364) Platelets, x109/L (range) 170 (95, 281) Albumin, g/dL (range) 4.4 (3.7, 5.2) INR 1.2 (1.0, 1.5) Bilirubin, mg/dL (range) 0.5 (0.2, 1.2) HDV-RNA Reduction with Lambda thru Week 48 Dose* Randomized Completers Dose Reductions Of Patients Completing Week 48 Responders Rebounders Non-Responders 120 mcg 19 13 / 19 (68.4%) 5 / 19 (26.3%) 6 / 13 (46.2%) 4 / 13 (30.8%) 0 180 mcg 14 11 / 14 (78.6%) 7 / 14 (50.0%) 9 / 11 (81.8%) 2 / 11 (18.2%) 0 a Flu-like symptoms: pyrexia, cough, sore throat, runny/stuffed nose, myalgia/arthralgia, headache, asthenia, vomiting, diarrhea b Psychiatric symptoms: depression, irritability, insomnia c 11 of 18 events experienced by 4 patients in Pakistan site AE of Special Interest % Patients Reporting Lambda 120 / 180 mcg Grade 1 Grade 2 Grade 3 Grade 4 Flu-like symptomsa 97% (32/33) 225 53 3 - Psychiatric symptomsb 3% (1/33) 1 - - - Cytopenia 15% (5/33) 2 3 - 2 Thrombocytopenia 0% (0/33) - - - - Elevated bilirubinc 30% (10/33) 12 3 3 - Elevated ALT 27% (9/33) 12 4 - - Adverse Events Higher Incidence of Hyperbilirubinemia* in Pakistan Cohort Hyperbilirubinemia in 4/15 (27%) of Pakistani versus 2/18 (11%) of non-Pakistani cohort Jaundice observed in 3/15 (20%) of Pakistani patients versus 0/18 (0%) of non-Pakistani patients Incidence/Severity in non-Pakistani cohort consistent with prior Lambda and Alfa data in HBV* Patients with bilirubin elevations did not experience signs or symptoms of decompensation Bilirubin levels were responsive to dose reduction/interruption Patients exhibited normal hepatic function (Prothrombin time) throughout periods of bilirubin elevation DILIsym® Modeling of ALT/Bilirubin Dynamics ALT and bilirubin dynamics consistent with bilirubin transporter based mechanism Dynamics are not consistent with hyperbilirubinemia secondary to hepatocyte loss Supported by absence of clinical decompensation Supported by normal hepatic function (normal PT) throughout cases of bilirubin elevation Pharmacogenomic assessment of bilirubin transporters in Pakistan cohort is planned to better understand cohort specific increase in incidence and severity of hyperbilirubinemia Of the 24 patients who reached Week 48: 120 μg group (N=14) Mean HDV RNA decline = 1.1 log10 ≥2 log10 decline in 5 of 13 (38.5%) 180 μg group (N=10) Mean HDV RNA decline = 2.3 log10 ≥2 log10 decline in 7 of 11 (63.6%) Lambda was well tolerated overall Increased incidences of clinical jaundice and bilirubin elevations were observed in the Pakistani cohort Led to lower than expected rate of study completion (9 of 15, 60%) for Pakistan site Israel and New Zealand sites had completion rates (15 of 18, 83%) comparable to prior Alfa studies None of the patients with elevations in bilirubin showed symptoms of decompensation All responded favorably to dose reduction or dose discontinuation Lambda demonstrates comparable anti-HDV activity to historical PEG IFN Alfa data at Week 48 Lambda was well-tolerated overall Most commonly reported AEs: moderate headache, pyrexia, fatigue, and myalgia ALT flares are due to vigorous antiviral immunological response to treatment, not due to direct hepatotoxicity DILIsym® modeling indicates a transporter-based mechanism for the observed bilirubin elevations Elevated bilirubin levels likely due to alteration in bilirubin transport; not due to hepatocellular injury Lambda is a promising agent for mono or combination Rx (i.e. lonafarnib) development in the treatment of HDV 6. RESULTS Responders*: 180 mcg Group 7. OBSERVATIONS 8. CONCLUSIONS Milder and fewer flu-like and psychiatric symptoms with Lambda No thrombocytopenia events Elevated bilirubin and ALT levels normalized upon dose reduction or treatment discontinuation Lambda 180 mcg Demonstrates Better Antiviral Activity Consistent with Bilirubin Transport Mechanism Objectives Study Sites: 33 Patients Randomized Auckland, New Zealand (N=4) Karachi, Pakistan (N=15) Beersheba, Israel (N=11) Jerusalem, Israel (N=3) Lambda Interferon MonoTherapy Study in HDV Predominantly Grade 1 Lambda 120 mcg vs 180 mcg No Signs or Symptoms of Decompensation * Hyperbilirubinemia = > 2 mg/mL Completers = completion of 48 week of treatment Responders = ≥2 log decline or below limit of quantification (BLQ) Rebounders = increase >2 log HDV RNA from nadir Non-responders = <1 log decline during treatment * Randomization Dose * Chan et al, Hepatology 2016 Exhibit 99.1 Exhibit 99.1