UNITED STATES
SECURITIES AND EXCHANGE COMMISSION
Washington, D.C. 20549
FORM 10-K
| x | ANNUAL REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 |
For the fiscal year ended December 31, 2006
Commission file number 001-32899
OR
| ¨ | TRANSITION REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 |
For the transition period from to
EASTERN INSURANCE HOLDINGS, INC.
| | |
| Incorporated in Pennsylvania | | I.R.S. Employer Identification No. |
25 Race Avenue, Lancaster, Pennsylvania 17603-3179 (717) 396-7095 | | 20-2653793 |
Securities registered pursuant to Section 12(b) of the Act:
| | |
| Title of Each Class | | Name of Each Exchange on Which Registered |
| Common Stock, No Par Value | | NASDAQ National Market |
Securities registered pursuant to Section 12(g) of the Act: None.
Indicate by check mark if the registrant is a well-known seasoned issuer, as defined in Rule 405 of the Securities Act: Yes ¨ No x
Indicate by check mark if the registrant is not required to file reports pursuant to Section 13 or 15(d) of the Act: Yes ¨ No x
Indicate by check mark whether the registrant: (1) has filed all reports required to be filed by Section 13 or 15(d) of the Securities Exchange Act of 1934 during the preceding 12 months (or for such shorter period that the registrant was required to file such reports), and (2) has been subject to such filing requirements for the past 90 days. Yes x No ¨
Indicate by check mark if disclosure of delinquent filers pursuant to Item 405 of Regulation S-K is not contained herein, and will not be contained, to the best of registrant’s knowledge, in definitive proxy or information statements incorporated by reference in Part III of this Form 10-K or any amendment to this Form 10-K. ¨
Indicate by check mark whether the registrant is a large accelerated filer, an accelerated filer, or a non-accelerated filer. See definition of “accelerated filer and large accelerated filer” in Rule 12b-2 of the Exchange Act. (Check one):
Large accelerated filer ¨ Accelerated filer ¨ Non-accelerated filer x
Indicate by check mark whether the registrant is a shell company (as defined in Rule 12b-2 of the Act): Yes ¨ No x
The aggregate market value of the common stock held by non-affiliates of the registrant, based on the closing price of the registrant on June 30, 2006, as reported by the NASDAQ National Market, was $113,793,293.
Indicate the number of shares outstanding of each of the registrant’s classes of common stock, as of the latest practicable date.
| | |
| Title of Each Class | | Number of Shares Outstanding as of March 28, 2007 |
| Common Stock, No Par Value | | 11,350,407 (Outstanding Shares) |
DOCUMENTS INCORPORATED BY REFERENCE
Portions of the Proxy Statement in connection with the 2007 Annual Meeting of Stockholders — Part III.
Table of Contents
Eastern Insurance Holdings, Inc. and Subsidiaries
PART I
Item 1 – Business
The results of operations of the workers’ compensation insurance, segregated portfolio cell reinsurance and specialty reinsurance segments for the period from June 17, 2006 to December 31, 2006 are included in the Company’s consolidated financial statements, as required by accounting principles generally accepted in the United States of America (“U.S. GAAP”). For purposes of this Item 1 – Business, the information provided for the workers’ compensation insurance, segregated portfolio cell reinsurance and specialty reinsurance segments represents the results of operations for the twelve months ended December 31, 2006, except as otherwise noted, as management believes this information is more useful for purposes of evaluating and understanding these segments and their historical financial results.
Our History and Overview
Eastern Insurance Holdings, Inc. (“EIHI”) is an insurance holding company offering workers’ compensation and group benefits insurance products and reinsurance products through its wholly-owned subsidiaries. EIHI was formed by Eastern Life and Health Insurance Company (“ELH”), formerly Educators Mutual Life Insurance Company, for the purpose of converting ELH from a mutual life and health insurance company to a stock life and health insurance company.
On June 16, 2006, EIHI completed its common stock offering and ELH completed its conversion from a mutual company to a stock company and became a wholly-owned subsidiary of EIHI. Immediately after the common stock offering and conversion, EIHI purchased all of the outstanding common stock of Eastern Holding Company, Ltd. (“EHC”) and its wholly-owned subsidiaries, Eastern Alliance Insurance Company (“Eastern Alliance”), Allied Eastern Indemnity Company (“Allied Eastern”), Employers Alliance, Inc. (“Employers Alliance”), Global Alliance Holdings, Ltd. (“Global Alliance”), Global Alliance Statutory Trust I (“Trust 1”), Eastern Services Corporation (“Eastern Services”), and Eastern Re Ltd., S.P.C. (“Eastern Re”). The stock offering, conversion, and acquisition of EHC are referred to as the “conversion/merger transaction” throughout the remainder of this document.
EIHI and its wholly-owned subsidiaries, EHC and ELH (collectively referred to as the “Company”), operate in five business segments: workers’ compensation insurance, segregated portfolio cell reinsurance, group benefits insurance, specialty reinsurance, and corporate/other.
Overview of Business Segments
The following discussion provides information on each of our business segments:
Workers’ Compensation Insurance. Workers’ compensation insurance is underwritten through Eastern Alliance and Allied Eastern, collectively referred to as Eastern Alliance Insurance Group, or EAIG. EAIG provides insurance coverage to employers, generally with 300 employees or less, in rural and suburban Pennsylvania, Maryland and Delaware. EAIG offers a complete line of workers’ compensation products to the marketplace including guaranteed cost policies, policyholder dividend policies, retrospectively-rated policies and large deductible policies. For the year ended December 31, 2006, EAIG had direct premiums written of $86.0 million. Because all of the premiums, losses and expenses generated by each company are shared through a pooling arrangement, EAIG can be viewed as a single entity for economic and segment reporting purposes.
Segregated Portfolio Cell Reinsurance. Eastern Re, a Cayman domiciled reinsurer, offers alternative market workers’ compensation solutions to individual companies, groups and associations (referred to as “segregated portfolio cell dividend participants”) through the creation of segregated portfolio cells. Eastern Re, a segregated portfolio company under Cayman Islands law, operates as a single legal
1
entity with segregated pools of assets, or segregated portfolio cells, that function as insurance companies within an insurance company. The pool of assets and associated liabilities of each segregated portfolio cell are solely for the benefit of the segregated portfolio cell dividend participants, and the pool of assets of one segregated portfolio cell are statutorily protected from the creditors of the others. This permits the Company to provide customers with a turn-key alternative markets solution that includes program design, fronting, claims administration, risk management, segregated portfolio cell rental, investment and segregated portfolio management services. The segregated portfolio cell structure provides dividend participants the opportunity to share in both underwriting profit and investment income derived from their respective segregated portfolio cell’s financial results.
Workers’ compensation insurance coverage is underwritten by EAIG through its alternative markets business unit and ceded 100% to each segregated portfolio cell at Eastern Re. As the primary insurer, EAIG receives a fronting fee generally based upon a percentage of direct premiums written. Eastern Re rents the segregated portfolio cell facilities to customers and receives a segregated portfolio cell rental fee, which is also based on a percentage of direct premiums written. Employers Alliance receives fees for claims administration and risk management services. For the year ended December 31, 2006, the segregated portfolio cell reinsurance segment had direct premiums written of $27.2 million and generated fee revenue to other business segments of $4.0 million. As of December 31, 2006, the segregated portfolio cells and dividend participants have provided EAIG with $37.6 million of irrevocable, unconditional letters of credit to secure unfunded liabilities and collateralize reserves for unpaid losses and loss adjustment expenses (“LAE”) and unearned premiums.
Group Benefits Insurance.Group benefits insurance is underwritten by ELH. The group benefits insurance products consist of dental, short-term and long-term disability, and term life, and may be structured (depending on customer requirements) as employer-paid or employee-paid programs, or some combination thereof. In typical plans, employers pay or supplement premium payments on behalf of their employees. Some plans allow for voluntary participation by employees of insured groups; in such cases, participating employees are solely responsible for paying their own premiums. ELH provides insurance coverage to employer groups, generally with 300 employees or less, primarily in the Mid-Atlantic, Southeast and Midwest regions of the continental United States.
Specialty Reinsurance. Specialty reinsurance is also underwritten through Eastern Re. Eastern Re assumes business through its participation in reinsurance treaties with an unaffiliated insurance company related to an underground storage tank insurance program, referred to as “EnviroGuard,” and a non-hazardous waste transportation product, referred to as “EIA Liability” (“EIA”). The EnviroGuard program provides coverage to underground tank owners for third party off-site bodily injury and property damage claims as well as clean-up coverage and first party on-site claims. The EIA program provides commercial automobile liability coverage for non-hazardous waste haulers.
Corporate/Other.The corporate/other segment includes the operations of Employers Alliance, EIHI, Eastern Holding Company, Ltd., Eastern Services, and Global Alliance. Employers Alliance provides claims administration and risk management services for self-insured workers’ compensation customers and property/casualty plans. Employers Alliance has 29 self-insured clients including a Fortune 500 company, municipal governments, hospital groups and Eastern Re’s segregated portfolio cells. For the year ended December 31, 2006, Employers Alliance had fee-based revenues of $3.0 million, including related business. EIHI, Eastern Holding Company, Ltd., Eastern Services and Global Alliance function primarily as coordinating and servicing units for the Company’s operating subsidiaries including general management, accounting and taxes, marketing and insurance risk management, borrowing activities, and general corporate expenses not allocated to the business segments. The corporate/other segment also includes the Company’s 10% interest in a segregated portfolio cell with an unaffiliated primary carrier that writes insurance coverage for sprinkler contractors.
2
Products
Workers’ Compensation Insurance
EAIG offers a complete line of workers’ compensation products to employers, generally with 300 employees or less, including guaranteed cost policies, policyholder dividend policies, retrospectively-rated policies, large deductible policies, and alternative market products. On a limited basis, EAIG also offers a commercial umbrella product to its workers’ compensation policyholders.
| | • | | Guaranteed cost policies. Guaranteed cost policies charge a fixed premium, which does not increase or decrease based upon loss experience during the policy period. For the year ended December 31, 2006, 55% of EAIG’s direct premiums written was derived from guaranteed cost policies. |
| | • | | Policyholder dividend policies. Policyholder dividend policies charge a fixed premium, but the customer may receive a dividend in the event of favorable loss experience during the policy period. EAIG generally restricts policyholder dividend plans to accounts with minimum annual premiums in excess of $20,000. For the year ended December 31, 2006, 9% of EAIG’s direct premiums written was derived from policyholder dividend policies. |
| | • | | Retrospectively-rated policies. Retrospectively-rated policies charge an initial premium that is subject to adjustment after the policy period expires, based upon the insured’s actual loss experience incurred during the policy period, subject to a minimum and maximum premium. These policies are typically subject to annual adjustment until all claims related to the policy year are closed. EAIG generally offers retrospectively-rated policies to employers with minimum annual premiums in excess of $150,000. For the year ended December 31, 2006, 3% of EAIG’s direct premiums written was derived from retrospectively-rated policies. |
| | • | | Large deductible policies. Large deductible policies generally result in a lower premium; however, the insured retains a greater share of the underwriting risk than under guaranteed cost or dividend paying policies, which reduces the risk to EAIG and further encourages loss control by the insured. The customer is contractually obligated to pay its own losses up to the amount of the deductible for each occurrence. The deductibles under these policies generally range from $250,000 to $300,000. EAIG generally offers large deductible policies to employers with annual premiums of $500,000 or higher. For the year ended December 31, 2006, less than 1% of EAIG’s direct premiums written was derived from large deductible policies. |
| | • | | Alternative market products. Alternative market products are offered to individual customers and trade associations. As described above in “Overview of Business Segments—Segregated Portfolio Cell Reinsurance,” EAIG issues a policy to an insured and cedes 100% of the premium written, less a ceding commission, to a segregated portfolio cell at Eastern Re. For the year ended December 31, 2006, 32% of EAIG’s direct premiums written was derived from alternative market products. |
Segregated Portfolio Cell Reinsurance
Segregated portfolio cells, or segregated cells or rent-a-captives, are all referred to as alternative market programs or products. The Company provides a variety of products to this marketplace, including program design, fronting, claims administration, investment management and cell rentals. Insurance coverage is underwritten (fronted) by EAIG and ceded 100% to the segregated portfolio cells at Eastern Re.
Group Benefits Insurance
ELH offers four primary products: dental insurance, short-term disability insurance, long-term disability insurance, and term life insurance.
| | • | | Dental Insurance.ELH’s dental plans include fee for service and managed care plans. Multiple variations of these products are available which offer different degrees of coverage, affordability |
3
| | and flexibility. Managed care plans utilize the networks of two unaffiliated dental Preferred Provider Organizations. Direct premiums written in the dental line totaled $19.5 million for the year ended December 31, 2006. |
| | • | | Short-Term Disability Insurance. ELH’s short-term disability plans pay flat weekly benefit amounts or a percentage of an individual claimant’s weekly earnings in the event of disability. Direct premiums written in the short-term disability line totaled $6.5 million for the year ended December 31, 2006. |
| | • | | Long-Term Disability Insurance. ELH’s long-term disability plans provide preset amounts or a preset percentage of an individual claimant’s monthly earnings in the event of disability. Direct premiums written in the long-term disability line totaled $4.1 million for the year ended December 31, 2006. |
| | • | | Term Life Insurance. ELH’s term life plans pay flat amounts or a multiple of an individual’s salary. Direct premiums written in the term life line totaled $5.9 million for the year ended December 31, 2006. |
Specialty Reinsurance
The specialty reinsurance segment does not directly underwrite any products. Rather, Eastern Re participates as a reinsurer in treaties with a large primary insurer for the EnviroGuard program and the EIA program. Eastern Re’s specialty reinsurance products are primarily marketed and distributed by Americana Program Underwriters, Inc. (“AmPro”). Lawrence Bitner, a Director of the Company, is an employee of AmPro and manages a significant portion of its program business. See Item 1A – Risk Factors, “All of the specialty reinsurance business of Eastern Re is controlled by one of our directors and is placed with one primary insurer and the loss of this business would adversely affect us.” Eastern Re had direct assumed premiums of $16.3 million for the year ended December 31, 2006.
Marketing and Distribution
Workers’ Compensation Insurance
The Company distributes its workers’ compensation products and services in Pennsylvania, Maryland and Delaware through a network of carefully chosen independent insurance producers. The following table segments the business, by state, for the year ended December 31, 2006 (dollars in thousands):
| | | | | | |
State | | Direct Premiums
Written | | Percentage | |
Pennsylvania | | $ | 83,675 | | 97.3 | % |
Delaware | | | 1,654 | | 1.9 | % |
Maryland | | | 678 | | 0.8 | % |
| | | | | | |
Total | | $ | 86,007 | | 100.0 | % |
| | | | | | |
The Company has its greatest representation and largest workers’ compensation premium volume in central Pennsylvania.
Producers are compensated through a fixed base commission plan with an opportunity for profit sharing depending on the producer’s premium volume and loss experience.
All current producers of the Company’s workers’ compensation products are encouraged to make a financial investment in EIHI. The Company strongly believes that a financial commitment by the producers to EIHI helps to align the interests of the Company and its producers.
The Company proactively manages its valued relationships with producers through a detailed producer management process. The process is driven by regular interaction and strong relationships between senior management of the Company and the principals of each producer. The primary components of the producer management process are:
| | • | | The Company carefully selects producers through a process that assesses financial results, market potential, business philosophy and reputation of the producer and its staff. Senior management of the Company approves all producer appointments following extensive meetings with the |
4
| | producer’s principals. Following the agreement to appoint, the Company’s Senior Vice President of Marketing and other key personnel conduct a formal orientation process focusing on the Company’s workers’ compensation products and services, dedicated service team and the joint business objectives of the Company and the producer. |
| | • | | The Company’s senior management team conducts annual business planning meetings with the producer’s principals to mutually agree upon the producer’s financial goals for the following year. Senior management and the underwriting staff conduct regular visits to monitor results and build relationships. |
| | • | | The Company has established an Agency Advisory Council to promote an active dialogue between the Company and its producer group. The Agency Advisory Council is comprised of six experienced insurance agency professionals. The Council meets twice a year to discuss such topics as market conditions, customer service, products, competition and areas of opportunity. In addition to the Agency Advisory Council, the Company has established a Select Business Focus Group with its producers. This group meets once a year to concentrate on issues that impact small workers’ compensation clients (under $20,000 in annual premium). |
| | • | | Producer management reports are distributed on a monthly basis, providing the producer with the data necessary to manage its relationship with the Company. |
The Company attempts to optimize the franchise value of an appointment for its approximate 47 workers’ compensation producers by limiting the number of appointments in identified marketing territories. As a result of this producer management strategy, the average direct premium written per agency contract was $1.8 million for the year ended December 31, 2006.
The Company’s ten largest producers in its workers’ compensation insurance segment accounted for 67.3% of its direct premiums written for the year ended December 31, 2006. The Company’s largest producer in its workers’ compensation insurance segment accounted for 23.3% of its direct premiums written for the year ended December 31, 2006. No other producer accounted for more than 10% of the Company’s direct premiums written in its workers’ compensation insurance segment for the year ended December 31, 2006.
Segregated Portfolio Cell Reinsurance
The distribution of policies that may be submitted to Eastern Re for consideration for reinsurance is substantially the same as that of the workers’ compensation insurance segment. The Company’s independent producers market the products to potential customer groups within the Company’s geographic target markets.
Group Benefits Insurance
The Company markets its group benefits insurance products through direct relationships with independent producers and general agencies, primarily in the Mid-Atlantic, Southeast, and Midwest regions of the continental United States. Prior to the sale of IBSi, ELH’s former general agency subsidiary, in October 2005, the Company’s group benefits insurance products were marketed primarily by IBSi. For the year ended December 31, 2005, IBSi accounted for more than 95% of the Company’s group benefits business.
IBSi continues to be a significant component of the Company’s group benefits insurance marketing and distribution strategy in the Southeast region, specifically North Carolina, South Carolina, and Virginia. During 2006, IBSi had the exclusive right to market the Company’s group benefits insurance products in these states. For the year ended December 31, 2006, the group benefits insurance segment’s direct premiums written in North Carolina, South Carolina, and Virginia totaled $14.3 million, which represented 40.0% of the group benefits insurance segment’s total direct premiums written.
IBSi’s exclusive right to market the Company’s group benefits insurance products in North Carolina, South Carolina, and Virginia expired as of December 31, 2006, except for IBSi’s relationships with its top 20 producers. IBSi continues to have exclusivity with respect to its top 20 producers in 2007.
5
For the year ended December 31, 2006, the group benefits insurance segment’s largest premium volumes were generated in Pennsylvania (38%), North Carolina (28%), Maryland (9%), South Carolina (6%), Virginia (6%), and Michigan (5%).
The Company provides sales, technical and educational training to its producers. Through ELH’s website, the Company provides its producers with online access to enrollment forms, product information, and online rate information for smaller groups (less than 10 people). These marketing efforts are further supported by the group benefits insurance segment’s claims and administrative philosophy, which emphasizes prompt and efficient service.
The Company provides its group benefits insurance producers with competitive compensation packages consisting of multiple commission levels, varying by product line and level of premium produced. As cost savings to the Company result when multiple product types are sold to a single group, incentive bonuses are offered to producers that reward such sales.
Specialty Reinsurance
Eastern Re does not engage in any marketing or distribution with respect to the specialty reinsurance segment. All marketing efforts are undertaken by AmPro, which develops programs for presentation to large primary insurers. Eastern Re’s Board of Directors considers analyses of historical loss information, market potential, and rate adequacy in determining whether to participate in each program.
Underwriting, Risk Management and Pricing
Workers’ Compensation Insurance
The Company’s workers’ compensation insurance segment is committed to an individual account underwriting strategy that is focused on selecting quality accounts. The goal of the workers’ compensation underwriting professionals is to select a diverse book of business with respect to risk classification, hazard level and geographic location. The Company expects to remain a rural underwriter focusing on territories, accounts and producers that generate acceptable underwriting margins.
The workers’ compensation underwriting strategy is focused on accounts with strong return to work and safety programs and low to middle hazard levels such as clerical office, light manufacturing, auto dealers and service industries. The Company writes workers’ compensation insurance in a total of 246 class codes with an average exposure base of $10.6 million.
For the year ended December 31, 2006, the average annual workers’ compensation traditional premium per policy was $18,686 and the average annual new premium per policy was $18,609.
Within the workers’ compensation underwriting operation, the Company operates a risk management unit, which delivers loss consulting services to the Company’s staff, producers and customers. The objective of the risk management operation is to protect the Company from catastrophic loss, reduce claims frequency and provide value added consulting services to insureds. The Company has expanded consulting services to include health and wellness, which supports injury prevention and mitigates claim expense. These services are provided at no additional cost to the insured and are services that differentiate the Company’s workers’ compensation products from its competitors. The risk management unit also provides risk pre-screening in support of the underwriting selection process.
Segregated Portfolio Cell Reinsurance
Underwriting and risk management services for the alternative market business are substantially the same as the Company’s traditional business, although a separate alternative markets unit has been formed for the delivery of services on a group program basis. The independent producers’ knowledge of the Company’s workers’ compensation product offerings is an important component in the offering of different product
6
proposals to customers, including the alternative market option. After successful completion of the underwriting process, if the risk is deemed to be an appropriate candidate for the alternative market, the risk is submitted to Eastern Re for consideration of intercompany reinsurance between EAIG and Eastern Re. In general, a pool of risks such as a trade group, or for similarly situated customers of an agency, are most appropriate for submission to the alternative markets unit. If a pool of risks is accepted by Eastern Re, reinsurance agreements and dividend participant agreements are executed, external reinsurance is bound and a segregated portfolio cell is established and presented to the Cayman Islands Monetary Authority for approval.
Group Benefits Insurance
The group benefits insurance underwriting department is responsible for managing the Company’s group benefits insurance book of business within established policies and procedures. The Company primarily underwrites small to medium size employer groups generally with 300 or less employees that fall within a low to moderate risk classification. Additionally, adequate levels of employee participation are required in order to underwrite a group. To limit exposure, the Company does not offer term life benefits in excess of $500,000 per claimant or long-term disability benefits in excess of $10,000 per month per claimant.
Pricing levels for the group benefits insurance products are developed based on the Company’s historical experience, as well as industry experience, and are periodically assessed for adequacy. Dental rates are evaluated on a quarterly basis, whereas short-term disability and term life rates are generally evaluated on an annual basis. Pricing for the long-term disability product is developed by the Company’s long-term disability reinsurer.
Account pricing is determined by the individual underwriter based on the level of risk, taking into consideration a group’s demographics and selected plan design.
Specialty Reinsurance
Eastern Re does not underwrite individual risks in the specialty reinsurance segment. Rather, Eastern Re examines specific program analytics and determines whether to enter into the reinsurance agreement with the primary insurer. The Company engages a third party to conduct an annual underwriting audit of the primary insurer’s underwriting function.
Claims
Workers’ Compensation Insurance
Workers’ compensation claims are handled by Employers Alliance. Employers Alliance focuses on early intervention and aggressive disability management, utilizing the professional services of medical case managers to supplement the expertise of in-house claims professionals when appropriate.
The Company believes in thorough education of its clients and their employees regarding the workers’ compensation law and workplace safety. The Company utilizes frequent communication with all parties as a means to maintain control of claims and minimize the influence of factors that increase costs such as attorney involvement and “doctor shopping.” The Company provides assistance and support to its clients in the implementation of physician panels and return to work programs.
The Company utilizes strategic vendor relationships rather than in-house personnel for services such as legal representation, private investigation, vocational rehabilitation and medical case management.
Medical cost management initiatives have been implemented with strategic vendors to reduce claim costs. Medical cost management services include preferred provider networks, physical therapy networks, a prescription drug program, and subrogation recovery.
The claims unit responsible for providing services to the workers’ compensation insurance segment is comprised of a supervisor, seven claim representatives, three claim analysts and one claim administrator. Each claim representative is assigned to a specific group of producers and their policyholders in order to facilitate teamwork and effective communication. In addition, this structure allows the team to develop extensive knowledge of specific geographic areas and customer operations.
7
In an effort to ensure aggressive management and quality outcomes on each claim, management closely monitors the pending caseloads and volume of new claim assignments for each claim representative. The Company’s strategy is to limit maximum caseloads to 125 open claims and an average of ten to twelve new claims per week for each claim representative.
The Company attempts to aggressively achieve final resolution of, and close, claims from prior accident years. The table below shows the number of workers’ compensation claims received and closed and open claims, by accident year, as of December 31, 2006.
Traditional Business
(Exclusive of Alternative Markets)
Open Claims (1)
| | | | | | | | | |
Accident Year | | Total Claims | | Open | | Closed | | % Closed | |
1998 | | 65 | | 0 | | 65 | | 100.0 | % |
1999 | | 205 | | 1 | | 204 | | 99.5 | % |
2000 | | 381 | | 0 | | 381 | | 100.0 | % |
2001 | | 594 | | 1 | | 593 | | 99.8 | % |
2002 | | 686 | | 8 | | 678 | | 98.8 | % |
2003 | | 690 | | 18 | | 672 | | 97.4 | % |
2004 | | 851 | | 51 | | 800 | | 94.0 | % |
2005 | | 794 | | 101 | | 693 | | 87.3 | % |
2006 | | 899 | | 347 | | 552 | | 61.4 | % |
| | | | | | | | | |
| | 5,165 | | 527 | | 4,638 | | 89.8 | % |
| | | | | | | | | |
| (1) | Excludes claims for medical only expenses because such claims are opened and closed in a short period of time. Excludes reinsured claims. |
The table below shows the number of open lost time claims for accident years 2005 and prior as of December 31, 2006 and 2005:
Traditional Business
(Exclusive of Alternative Markets)
Open Claims (1)
| | | | | | | | | |
Accident Year | | 12-31-06 Open | | 12-31-05 Open | | 2005 and Prior
Claims Closed
During 2006 | | % of 2005 Open Claims Closed During 2006 | |
1999 | | 1 | | 1 | | 0 | | 0.0 | % |
2000 | | 0 | | 2 | | 2 | | 100.0 | % |
2001 | | 1 | | 11 | | 10 | | 90.9 | % |
2002 | | 8 | | 22 | | 14 | | 63.6 | % |
2003 | | 18 | | 39 | | 21 | | 53.8 | % |
2004 | | 51 | | 101 | | 50 | | 49.5 | % |
2005 | | 101 | | 269 | | 168 | | 62.5 | % |
| | | | | | | | | |
| | 180 | | 445 | | 265 | | 59.6 | % |
| | | | | | | | | |
| (1) | Excludes claims for medical only expenses because such claims are opened and closed in a short period of time. Excludes reinsured claims. |
Segregated Portfolio Cell Reinsurance
Claims administration and risk management for the alternative market programs are performed by Employers Alliance. Each segregated portfolio cell at Eastern Re pays a fee to Employers Alliance for these services. This fee is included as part of the ceding commission in the reinsurance agreement between EAIG and Eastern Re.
8
Group Benefits Insurance
The group benefits insurance claims staff is responsible for investigating, processing and paying claims. Authority levels have been established for all individuals involved in the settlement of claims.
| | • | | Dental Claims. The Company’s dental claims department is comprised of experienced personnel who function within designated areas of expertise. The Company utilizes an independent dental peer review firm for claims outside of its employees’ areas of clinical expertise and to assist with benefit determination appeals. The Company’s dental claim examiners are able to review claimant x-rays and provider treatment notes online, reducing the time and expense associated with manual claims processing. In addition, the Company’s administrative software provides automated batch processing for basic claims, which allows examiners to devote greater attention to complex claims. Quality technicians are utilized to assess the accuracy of benefit determinations, with all examiners and analysts randomly audited on claims that exceed a set dollar amount. On average, dental claims are processed within two weeks of receipt by the Company. |
| | • | | Short-Term Disability Claims.Short-term disability claims are reviewed within 3 to 5 business days of their receipt. Lump sum benefit payments are offered for maternity claims. The short term disability claims review process may be supplemented by outside physicians who conduct independent medical examinations and provide peer review services to determine if claims are medically accurate. Following such a medical examination, the Company’s short-term disability claim examiners make the ultimate decision as to whether or not a claimant is disabled by measuring the results of the medical examination against the appropriate provisions in the disability insurance policy. |
| | • | | Long-Term Disability Claims. Since July 1, 2005, the Company has outsourced long term disability claims processing to Disability Reinsurance Management Services, Inc. (Disability RMS), which management believes has greater expertise and resources to administer such claims. |
| | • | | Term Life and Accidental Death & Dismemberment (“AD&D”) Claims.The manager of the life & disability claim department is responsible for the timely and accurate payment of term life and AD&D claims. Whenever death proceeds from an individual claimant’s policy exceed reinsurance limits, the Company’s life reinsurer participates in the benefit determination. |
Specialty Reinsurance
Neither Eastern Re nor any of its affiliates actively manages claims in the specialty reinsurance segment. Claims management is performed by the primary insurer. When the primary insurer sustains a loss, it invoices Eastern Re for its pro rata share of the loss. Eastern Re’s claims administration is limited to verification that the claim is a covered claim under the reinsurance contract between Eastern Re and the primary insurer. The Company engages a third party to conduct an annual audit of the primary insurer’s claim function.
Reinsurance
The Company’s insurance subsidiaries reinsure a portion of their loss exposure and pay to the reinsurers a portion of the premiums received on all policies reinsured. Insurance policies written by the Company’s insurance subsidiaries are reinsured with other insurance companies principally to:
| | • | | reduce net liability on individual risks; |
| | • | | mitigate the effect of individual loss occurrences (including catastrophic losses); |
| | • | | stabilize underwriting results; |
| | • | | increase underwriting capacity. |
9
Reinsurance does not legally discharge the Company from primary liability for the full amount due under the reinsured policies. However, the assuming reinsurer is obligated to reimburse the Company to the extent of the coverage ceded. As of December 31, 2006, the Company’s reinsurance recoverables, by segment, were as follows (in thousands):
| | | |
Segment | | Amount |
Workers’ compensation insurance | | $ | 3,856 |
Segregated portfolio cell reinsurance | | | 3,151 |
Group benefits insurance | | | 20,437 |
Specialty reinsurance | | | — |
Other | | | 81 |
| | | |
Total | | $ | 27,525 |
| | | |
The Company determines the amount and scope of reinsurance coverage to purchase each year based on a number of factors, including the evaluation of the risks accepted, consultations with reinsurance representatives and a review of market conditions, including the availability and pricing of reinsurance.
The Company monitors the solvency of its reinsurers through regular review of their financial statements and, if available, their A.M. Best financial strength ratings. The Company has experienced no difficulty collecting amounts due from reinsurers; however, the insolvency or inability of any reinsurer to meet its obligations could have a material adverse effect on the Company’s financial condition and results of operations.
Workers’ Compensation Insurance
The Company’s workers’ compensation traditional business is reinsured under an excess of loss arrangement with Lloyd’s of London and Aspen Insurance UK, Ltd., under which the Company retains the first $500,000 on each loss occurrence. Loss occurrences in excess of $500,000 are covered up to a maximum of $39.5 million per claim.
The following table sets forth the amounts recoverable from reinsurers for the Company’s workers’ compensation insurance segment as of December 31, 2006 (dollars in thousands):
| | | | | | | | | | | | |
Name | | Reinsurance
Recoverable | | A.M. Best Rating | | | Percentage of Shareholders’ Equity | | | Percentage of
Reinsurance
Recoverable | |
Lloyd’s of London | | $ | 2,372 | | A | | | 1.4 | % | | 8.6 | % |
St. Paul Reinsurance Company Ltd. | | | 52 | | NR-3 (1) | | | 0.0 | % | | 0.2 | % |
Alea London Ltd. | | | 463 | | NR-4 (2) | | | 0.3 | % | | 1.7 | % |
Aspen Insurance UK Ltd. | | | 954 | | A | | | 0.5 | % | | 3.5 | % |
Fairfield Insurance Company | | | 15 | | A | + | | 0.0 | % | | 0.1 | % |
| | | | | | | | | | | | |
| | $ | 3,856 | | | | | 2.2 | % | | 14.1 | % |
| | | | | | | | | | | | |
| (1) | Rating assigned to companies that are not rated by A.M. Best. |
| (2) | Rating assigned to companies that were assigned a rating by A.M. Best but requested that their ratings not be published because the companies disagree with A.M. Best’s rating conclusion. |
The commercial umbrella product is reinsured with American Re-Insurance Company under a 90% quota share arrangement up to $2.0 million and a 100% quota share arrangement in excess of $2.0 million up to a $5.0 million limit. Commercial umbrella policy limits are consistent with reinsurance limits.
Segregated Portfolio Cell Reinsurance
Intercompany Reinsurance Structure.Intercompany reinsurance agreements are the mechanisms by which premiums paid by alternative markets customers are ceded from EAIG to the segregated portfolio cells at Eastern Re. Each Eastern Re segregated portfolio cell has the following reinsurance agreements with EAIG:
10
| | • | | 100% Quota Share Reinsurance Agreements—Under this reinsurance agreement, EAIG cedes all premiums received from the specific customer to the respective segregated portfolio cell at Eastern Re and receives a ceding commission in return. Consistent with any policy issued by EAIG, the underlying risks within the program will dictate which company (Eastern Alliance or Allied Eastern) writes the policy. As with any reinsurance arrangement, the ultimate liability for the payment of claims resides with the primary insurance company. The ceding commission paid to EAIG by the segregated portfolio cell consists of charges customary to such arrangements including fronting fees, external reinsurance, producer’s commissions, premium taxes and assessments, claims administration and risk management services and segregated portfolio cell rental fees. In addition, the ceding commission compensates EAIG for the risk assumed under the aggregate excess reinsurance agreement described directly below. |
| | • | | Aggregate Excess Reinsurance Agreements—An aggregate excess reinsurance agreement exists between EAIG and each respective segregated portfolio cell whereby EAIG assumes 100% of aggregate losses over an aggregate attachment point (expressed as a percentage of direct premium written), with a maximum loss limit of $100,000. The attachment points for the aggregate excess reinsurance agreements average 89.0% of direct premium written. For example, in the case of a segregated portfolio cell with $1.0 million in assumed premium and an 89.0% attachment point, the segregated portfolio cell pays the first $890,000 in net losses and loss adjustment expenses, EAIG pays the next $100,000 in net losses and loss adjustment expenses and the external aggregate reinsurer (as described below) pays net losses and loss adjustment expenses beyond the initial $990,000 covered by the segregated portfolio cell and EAIG. |
External Reinsurance.Each segregated portfolio cell purchases external reinsurance coverage directly from Lloyd’s of London. The segregated portfolio cell purchases per occurrence coverage to cover severity of claims and aggregate reinsurance coverage to cover frequency of claims on its segregated portfolio cell business.
Per Occurrence Reinsurance Agreements.Per occurrence reinsurance agreements cover each segregated portfolio cell for a catastrophic claim resulting from one event with respect to its segregated portfolio cell business. The specific retentions for per occurrence coverage for segregated portfolio cells within Eastern Re range from $250,000 to $350,000, with limits ranging from $39.75 million to $39.65 million. For example, in the case of a segregated portfolio cell with a $300,000 retention that has a $3.0 million claim relating to the death of a covered employee, the segregated portfolio cell would cover the first $300,000 of the claim with the third party reinsurer paying the remaining $2.7 million in claims.
Aggregate Reinsurance Coverage.Aggregate reinsurance agreements cover the segregated portfolio cells for losses and loss adjustment expenses beyond the $100,000 aggregate coverage provided by EAIG. The need for this coverage would arise in the event of a series of losses as opposed to a single, catastrophic event. Aggregate reinsurance coverage purchased through Lloyd’s has ultimate loss limits of $1.0 million or $2.0 million, depending on the underlying risks. This external reinsurance combined with the aggregate coverage provided by EAIG provides aggregate loss limits for each segregated portfolio cell within Eastern Re ranging from $1.1 million to $2.1 million.
In addition to the reinsurance coverage on the segregated portfolio cell business, the dividend participants of each segregated portfolio cell provide a letter of credit for the most recent program year that is equal to the difference between the loss fund (amount of funds available to pay losses after deduction of ceding commission) and the aggregate attachment point of the reinsurance. This is sometimes called the GAP, or unfunded liability. As an example, if a program has $1.0 million of assumed premiums, a 40% ceding commission and a 90% aggregate attachment point, the letter of credit amount is $300,000 calculated as follows:
| | | |
Aggregate attachment point ($1,000,000 x .90) | | $ | 900,000 |
Loss fund ($1,000,000 – ($1,000,000 x .40) | | $ | 600,000 |
GAP | | $ | 300,000 |
11
The alternative market business involves services from several subsidiaries of the Company, which are paid out of the ceding commission. External costs are also paid out of the ceding commission. The flow of premium dollars is as follows:
| | • | | 100% of the direct premium written is ceded to the segregated portfolio cell at Eastern Re from EAIG. |
| | • | | In exchange for ceding the premium, EAIG is a ceding commission by the segregated portfolio cell equal to a percentage of the direct premium written. |
| | • | | The ceding commission is then typically allocated as follows: |
| | |
Fee Description | | Fee Recipient |
| Fronting fee | | EAIG |
| Producers’ commission | | Independent producer |
| Reinsurance | | Third party reinsurer (Lloyds) |
| Cell rental fee | | Eastern Re |
| Claims handling fee | | Employers Alliance |
| Risk management fee | | Employers Alliance |
| Premium and excise taxes | | State and offshore taxing authorities |
| | • | | The difference between the premium and the ceding commission is deposited in each respective segregated portfolio cell’s Cayman Island bank account to create the loss fund. |
The following table sets forth the amounts recoverable from reinsurers for the Company’s segregated portfolio cell reinsurance segment as of December 31, 2006 (dollars in thousands):
| | | | | | | | | | | |
Name | | Reinsurance
Recoverable | | A.M. Best Rating | | Percentage of Shareholders’ Equity | | | Percentage of
Reinsurance
Recoverable | |
Lloyd’s of London | | $ | 1,761 | | A | | 1.0 | % | | 6.4 | % |
St. Paul Reinsurance Company Ltd. | | | 12 | | NR-3 (1) | | 0.0 | % | | — | % |
Alea London Ltd. | | | 311 | | NR-4 (2) | | 0.2 | % | | 1.1 | % |
Aspen Insurance UK Ltd. | | | 1,067 | | A | | 0.6 | % | | 3.9 | % |
| | | | | | | | | | | |
| | $ | 3,151 | | | | 1.8 | % | | 11.4 | % |
| | | | | | | | | | | |
| (1) | Rating assigned to companies that are not rated by A.M. Best. |
| (2) | Rating assigned to companies that were assigned a rating by A.M. Best but requested that their ratings not be published because the companies disagree with A.M. Best’s rating conclusion. |
Group Benefits Insurance
The Company reinsures a portion of its long-term disability and term life business. There is currently no reinsurance coverage on the dental and short-term disability business.
The long-term disability product is reinsured under a quota-share arrangement with Union Security Insurance Company. Under the current quota-share arrangement, the Company retains 20% of the first $6,000 in monthly disability benefits on all new and renewal business sold on or after July 1, 2005. Monthly benefits in excess of $6,000 are 100% reinsured.
The term life product is reinsured under an excess of loss arrangement with Swiss Re Life & Health America, Inc. The Company retains the first $100,000 of each covered death claim and the first $50,000 of each covered AD & D claim.
12
The Company has a block of active disability claims that it has completely ceded to The Hartford Life and Accident Insurance Company. These claims arose out of long term disability policies that ELH formerly offered to selected professional associations. The largest of these policies terminated in April 1997 and all but two of the remaining active claims pursuant to such policies were acquired by The Hartford in 1999. The Hartford manages and pays all such claims without any involvement from the Company and provides any financial information required for the Company’s financial reporting purposes.
The following table sets forth the amounts recoverables from reinsurers for the Company’s group benefits insurance segment as of December 31, 2006 (dollars in thousands):
| | | | | | | | | | | |
Carrier | | Reinsurance
Recoverable | | A.M Best
Rating | | Percentage of
Shareholders’ Equity | | | Percentage of
Reinsurance
Recoverable | |
Hartford Life and Accident Insurance Company | | $ | 11,549 | | A+ | | 6.7 | % | | 42.0 | % |
Union Security Insurance Company (1) | | | 7,868 | | A | | 4.5 | % | | 28.6 | % |
Swiss Re Life and Health America, Inc. | | | 743 | | A+(2) | | 0.4 | % | | 2.7 | % |
United Teacher Associates Insurance Company | | | 256 | | A- | | 0.2 | % | | 0.9 | % |
Combined Insurance Company of America | | | 21 | | A | | — | | | 0.1 | % |
| | | | | | | | | | | |
| | $ | 20,437 | | | | 11.8 | % | | 74.3 | % |
| | | | | | | | | | | |
| (1) | Formerly, Fortis Benefits Insurance Company |
| (2) | Swiss Re Life and Health America, Inc. has been put on a negative outlook by A.M. Best. |
Specialty Reinsurance
Eastern Re acts as a reinsurer in the specialty reinsurance segment. None of the risks assumed by Eastern Re in this segment are further reinsured.
Loss and Loss Adjustment Expense Reserves
The Company estimates its reserves for unpaid losses and LAE as of the balance sheet date. The adequacy of the Company’s reserves is inherently uncertain and represents a significant risk to the business. The Company attempts to mitigate the uncertainty inherent in its reserves by continually reviewing loss cost trends, attempting to set premium rates that are adequate to cover anticipated future costs, and by professionally managing its claims administration function. Additionally, the Company attempts to minimize the estimation risk inherent in its reserves by employing actuarial techniques on a quarterly basis. Significant judgment is required in actuarial estimation to ascertain the relevance of historical payment and claim settlement patterns under current facts and circumstances. No assurance can be given as to whether the ultimate liability for unpaid losses and LAE will be more or less than the Company’s current estimates. While management believes that the assumptions underlying the amounts recorded for the reserves for unpaid losses and LAE as of December 31, 2006 are reasonable, the ultimate net liability may differ materially from the amount provided.
The following table provides a summary of the activity in the Company’s reserves for unpaid losses and LAE, excluding term life premium waiver reserves. The 2006 activity related to the workers’ compensation insurance, segregated portfolio cell reinsurance and specialty reinsurance segments is for the period from June 17, 2006 to December 31, 2006.
13
| | | | | | | | | | | | |
| | | 2006 | | | 2005 | | | 2004 | |
Balance, beginning of period | | $ | 38,729 | | | $ | 38,559 | | | $ | 41,326 | |
Reinsurance recoverables on unpaid losses and LAE | | | 23,911 | | | | 23,415 | | | | 24,464 | |
| | | | | | | | | | | | |
Net balance, beginning of period | | | 14,818 | | | | 15,144 | | | | 16,862 | |
Net reserves acquired as a result of EHC acquisition | | | 73,554 | | | | — | | | | — | |
Purchase accounting adjustments on acquisition date | | | 2,432 | | | | — | | | | — | |
Incurred related to: | | | | | | | | | | | | |
Current year | | | 54,104 | | | | 26,962 | | | | 28,340 | |
Prior year | | | (5,296 | ) | | | (269 | ) | | | (2,541 | ) |
| | | | | | | | | | | | |
Total incurred before purchase accounting adjustments | | | 48,808 | | | | 26,693 | | | | 25,799 | |
Purchase accounting adjustments | | | (538 | ) | | | — | | | | — | |
| | | | | | | | | | | | |
Total incurred | | | 48,270 | | | | 26,693 | | | | 25,799 | |
| | | | | | | | | | | | |
Paid related to: | | | | | | | | | | | | |
Current year | | | 28,609 | | | | 22,724 | | | | 23,264 | |
Prior year | | | 13,305 | | | | 4,295 | | | | 4,253 | |
| | | | | | | | | | | | |
Total paid | | | 41,914 | | | | 27,019 | | | | 27,517 | |
| | | | | | | | | | | | |
Net balance, end of period | | | 97,160 | | | | 14,818 | | | | 15,144 | |
Reinsurance recoverables on unpaid losses and LAE | | | 24,236 | | | | 23,911 | | | | 23,415 | |
| | | | | | | | | | | | |
Balance, end of period | | $ | 121,396 | | | $ | 38,729 | | | $ | 38,559 | |
| | | | | | | | | | | | |
Total reserves for unpaid losses and LAE | | $ | 126,467 | | | $ | 44,136 | | | $ | 43,384 | |
Less: Term life premium waiver reserves | | | 4,815 | | | | 5,333 | | | | 4,784 | |
Less: Other | | | 256 | | | | 74 | | | | 41 | |
| | | | | | | | | | | | |
Balance, end of period | | $ | 121,396 | | | $ | 38,729 | | | $ | 38,559 | |
| | | | | | | | | | | | |
The analysis in the following table presents the development of the Company’s reserves for unpaid losses and LAE. The first line in the table shows the liability for unpaid losses and LAE, net of reinsurance, as estimated at the end of each calendar year. The first section below that line shows the cumulative actual payments of loss and LAE, net of reinsurance, that relate to each year-end liability as they were paid at the end of subsequent annual periods. The next section shows revised estimates of the original unpaid amounts, net of reinsurance, that are based on the subsequent payments and re-estimates of the remaining unpaid liabilities. The next line shows the favorable or adverse development of the original estimates, net of reinsurance. Loss reserve development in this table is cumulative, the estimated favorable or adverse development for a particular year represents the cumulative amount by which all previous liabilities are currently estimated to have been over- or under-estimated. The “cumulative redundancy/(deficiency)” is as of December 31, 2006, which represents the difference between the latest reestimated liability and the amounts as originally estimated. A redundancy means the original estimate was higher than the current estimate; a deficiency means that the current estimate is higher than the original estimate.
For purposes of understanding the Company’s reserve estimation results for its current lines of business, the gross cumulative redundancy related to ELH’s former group medical business has been deducted from the total gross cumulative redundancy (deficiency) for all years presented.
14
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
Year Ended December 31, | |
| | | 1996 | | | 1997 | | | 1998 | | | 1999 | | | 2000 | | | 2001 | | | 2002 | | | 2003 | | | 2004 | | | 2005 | |
Reserve for unpaid losses and LAE, net of reinsurance | | $ | 22,276 | | | $ | 31,034 | | | $ | 31,883 | | | $ | 34,279 | | | $ | 38,156 | | | $ | 43,363 | | | $ | 49,871 | | | $ | 58,500 | | | $ | 74,430 | | | $ | 83,389 | |
Cumulative amount of liability paid through: | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
One year later | | | 10,109 | | | | 14,359 | | | | 13,913 | | | | 18,460 | | | | 21,248 | | | | 23,111 | | | | 23,399 | | | | 23,449 | | | | 24,178 | | | | 27,598 | |
Two years later | | | 10,857 | | | | 15,357 | | | | 15,745 | | | | 20,344 | | | | 25,890 | | | | 30,462 | | | | 34,122 | | | | 34,882 | | | | 37,688 | | | | — | |
Three years later | | | 11,473 | | | | 15,997 | | | | 16,555 | | | | 21,799 | | | | 29,330 | | | | 35,030 | | | | 39,742 | | | | 41,609 | | | | — | | | | — | |
Four years later | | | 11,939 | | | | 16,460 | | | | 17,201 | | | | 23,050 | | | | 31,022 | | | | 37,812 | | | | 43,186 | | | | — | | | | — | | | | — | |
Five years later | | | 12,283 | | | | 16,906 | | | | 17,860 | | | | 23,904 | | | | 32,834 | | | | 39,806 | | | | — | | | | — | | | | — | | | | — | |
Six years later | | | 12,659 | | | | 17,445 | | | | 18,443 | | | | 24,833 | | | | 34,194 | | | | — | | | | — | | | | — | | | | — | | | | — | |
Seven years later | | | 13,022 | | | | 17,952 | | | | 19,028 | | | | 25,580 | | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | |
Eight years later | | | 13,372 | | | | 18,456 | | | | 19,578 | | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | |
Nine years later | | | 13,779 | | | | 18,946 | | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | |
Ten years later | | | 14,184 | | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | |
| | | | | | | | | | |
Liability estimated as of: | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
One year later | | | 15,459 | | | | 20,819 | | | | 20,676 | | | | 27,881 | | | | 34,382 | | | | 39,782 | | | | 49,166 | | | | 57,373 | | | | 66,374 | | | | 77,411 | |
Two years later | | | 15,240 | | | | 20,576 | | | | 21,725 | | | | 29,004 | | | | 36,372 | | | | 43,030 | | | | 50,596 | | | | 57,462 | | | | 66,398 | | | | — | |
Three years later | | | 15,361 | | | | 20,646 | | | | 22,050 | | | | 28,406 | | | | 37,044 | | | | 44,741 | | | | 51,934 | | | | 57,612 | | | | — | | | | — | |
Four years later | | | 15,685 | | | | 20,970 | | | | 22,363 | | | | 28,604 | | | | 38,018 | | | | 45,931 | | | | 52,812 | | | | — | | | | — | | | | — | |
Five years later | | | 15,826 | | | | 21,270 | | | | 22,346 | | | | 29,133 | | | | 39,441 | | | | 46,640 | | | | — | | | | — | | | | — | | | | — | |
Six years later | | | 16,221 | | | | 21,348 | | | | 22,957 | | | | 29,827 | | | | 38,952 | | | | — | | | | — | | | | — | | | | — | | | | — | |
Seven years later | | | 16,069 | | | | 21,697 | | | | 23,325 | | | | 29,235 | | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | |
Eight years later | | | 16,359 | | | | 22,195 | | | | 22,835 | | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | |
Nine years later | | | 16,913 | | | | 21,894 | | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | |
Ten years later | | | 16,138 | | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | |
Cumulative total redundancy (deficiency) | | $ | 6,138 | | | $ | 9,140 | | | $ | 9,048 | | | $ | 5,044 | | | $ | (796 | ) | | $ | (3,277 | ) | | $ | (2,941 | ) | | $ | 888 | | | $ | 8,032 | | | $ | 5,978 | |
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
Gross liability - end of year | | | 23,296 | | | | 33,789 | | | | 35,593 | | | | 39,041 | | | | 44,141 | | | | 49,327 | | | | 57,955 | | | | 67,549 | | | | 84,555 | | | | 97,755 | |
Reinsurance recoverables | | | 1,020 | | | | 2,755 | | | | 3,710 | | | | 4,762 | | | | 5,985 | | | | 5,964 | | | | 8,084 | | | | 9,049 | | | | 10,125 | | | | 14,366 | |
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
Net liability - end of year | | $ | 22,276 | | | $ | 31,034 | | | $ | 31,883 | | | $ | 34,279 | | | $ | 38,156 | | | $ | 43,363 | | | $ | 49,871 | | | $ | 58,500 | | | $ | 74,430 | | | $ | 83,389 | |
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
Gross re-estimated liability - latest | | | 16,894 | | | | 23,205 | | | | 23,774 | | | | 31,021 | | | | 43,143 | | | | 51,772 | | | | 60,197 | | | | 65,189 | | | | 75,635 | | | | 88,455 | |
Re-estimated reinsurance recoverables - latest | | | 756 | | | | 1,311 | | | | 939 | | | | 1,786 | | | | 4,191 | | | | 5,132 | | | | 7,385 | | | | 7,577 | | | | 9,237 | | | | 11,044 | |
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
Net re-estimated liability - latest | | $ | 16,138 | | | $ | 21,894 | | | $ | 22,835 | | | $ | 29,235 | | | $ | 38,952 | | | $ | 46,640 | | | $ | 52,812 | | | $ | 57,612 | | | $ | 66,398 | | | $ | 77,411 | |
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
Gross cumulative redundancy (deficiency), including run-off group medical business | | $ | 6,402 | | | $ | 10,584 | | | $ | 11,819 | | | $ | 8,020 | | | $ | 998 | | | $ | (2,445 | ) | | $ | (2,242 | ) | | $ | 2,360 | | | $ | 8,920 | | | $ | 9,300 | |
Less: Gross cumulative redundancy related to run-off group medical business | | | (6,221 | ) | | | (7,885 | ) | | | (8,010 | ) | | | (5,201 | ) | | | (4,311 | ) | | | (6,314 | ) | | | (5,508 | ) | | | (1,937 | ) | | | (87 | ) | | | (45 | ) |
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
Gross cumulative redundancy (deficiency), excluding run-off group medical business | | $ | 181 | | | $ | 2,699 | | | $ | 3,809 | | | $ | 2,819 | | | $ | (3,313 | ) | | $ | (8,759 | ) | | $ | (7,750 | ) | | $ | 423 | | | $ | 8,833 | | | $ | 9,255 | |
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
Gross liability, end of year | | $ | 23,296 | | | $ | 33,789 | | | $ | 35,593 | | | $ | 39,041 | | | $ | 44,141 | | | $ | 49,327 | | | $ | 57,955 | | | $ | 67,549 | | | $ | 84,555 | | | $ | 97,755 | |
| | | | | | | | | | |
Professional group long-term disability reserves | | | 29,687 | | | | 30,611 | | | | 29,884 | | | | 27,443 | | | | 24,285 | | | | 21,843 | | | | 19,082 | | | | 18,921 | | | | 17,152 | | | | 16,330 | |
Term life premium waiver reserves | | | 2,360 | | | | 2,953 | | | | 3,257 | | | | 3,868 | | | | 4,474 | | | | 4,458 | | | | 4,305 | | | | 4,661 | | | | 4,783 | | | | 5,333 | |
Other | | | 512 | | | | 299 | | | | 125 | | | | 109 | | | | 74 | | | | 73 | | | | 52 | | | | 39 | | | | 41 | | | | 74 | |
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
Total reserves for unpaid losses and LAE | | $ | 55,855 | | | $ | 67,652 | | | $ | 68,859 | | | $ | 70,461 | | | $ | 72,974 | | | $ | 75,701 | | | $ | 81,394 | | | $ | 91,170 | | | $ | 106,531 | | | $ | 119,492 | |
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
Workers’ Compensation Insurance. The Company’s results of operations include a cumulative decrease in estimated incurred losses and LAE on its workers’ compensation line of business primarily related to accident years 2005, 2004, and 2003 of $3.3 million for the year ended December 31, 2006. The favorable development on prior accident years relates primarily to significant claim settlements during 2006 for amounts at, or less than, previously established case and incurred but not reported (“IBNR”) reserves.
Segregated Portfolio Cell Reinsurance. The Company’s results of operations in its segregated portfolio cell reinsurance segment included a decrease in estimated incurred losses and LAE primarily related to accident years 2005, 2004 and 2003 of $3.3 million for the year ended December 31, 2006. The favorable development on prior accident years relates primarily to significant claim settlements during 2006 for amounts at, or less than, previously established case and IBNR reserves. Any change in the reserves for unpaid losses and LAE in the segregated portfolio cell reinsurance segment is recorded to the segregated portfolio dividend payable/receivable account and would only impact the Company’s net income or shareholders’ equity if the Company was a segregated portfolio cell dividend participant.
Group Benefits Insurance.The Company’s results of operations for the year ended December 31, 2006 include favorable development on prior year reserves in the group benefits insurance segment. Favorable development in the dental and short-term disability lines totaled $533,000 and $337,000, respectively, which reflects better claim experience than anticipated at the time the liability was established. The Company’s results of operations also reflect the termination of prior year long-term disability claims totaling $2.2 million, which resulted from claimants returning to work, claimant death, or the termination of benefits in accordance with policy provisions.
Specialty Reinsurance. The Company’s results of operations included an increase in estimated incurred losses and LAE on its specialty reinsurance line of business related to prior accident years of $1.7 million for the year ended December 31, 2006. The unfavorable prior year development was the result of changes in estimates as losses emerged at a higher rate than had been originally anticipated when the reserves were estimated with respect to accident years 2005, 2004, 2003, and 2002. The evaluation of the reserve for unpaid losses and LAE related to the specialty reinsurance segment requires that loss development be estimated over an extended period of time. Because the primary insurer under these programs changed in 1999, historical loss data is insufficiently developed. Therefore, reliance has been placed on industry loss development patterns, adjusted based on the Company’s judgment, to reflect considerations particular to the exposure. The reliance on external benchmarks, while necessary, creates an additional element of uncertainty.
15
A.M. Best Rating
A.M. Best rates insurance companies based on factors of concern to policyholders. In evaluating a company’s financial and operating performance, A.M. Best reviews the company’s profitability, leverage and liquidity, its book of business, the adequacy and soundness of its reinsurance, the quality and estimated fair value of its assets, the adequacy of its reserves and surplus, its capital structure, the experience and competence of its management, and its marketing presence. A.M. Best ratings are intended to provide an independent opinion of an insurer’s ability to meet its obligations to its policyholders. Their evaluation is not directed at investors. In June 2006, A.M. Best assigned an “A-” financial strength rating to Eastern Alliance and Allied Eastern, and indicated a stable rating outlook. In August 2006, A.M. Best assigned an “A-” financial strength rating to Eastern Re. An “A-” (Excellent) financial strength rating is the fourth highest out of 16 rating classifications. The current “B++” (Very Good) financial strength rating assigned to ELH by A.M. Best was reaffirmed in June 2006. This rating is the fifth highest out of 16 rating classifications.
The financial strength ratings assigned by A.M. Best to the Company’s insurance subsidiaries are subject to periodic review and may be upgraded or downgraded by A.M. Best as a result of changes in the views of the rating agency or positive or adverse developments in the insurance subsidiaries’ financial conditions or results of operations.
Competition
The Company’s ability to compete successfully in its principal markets is dependent upon a number of factors, many of which are outside its control. Many of the Company’s business segments are subject to significant price competition. In addition to price, competition in the Company’s lines of insurance is based on quality of the products, quality and delivery of service, financial strength, ratings, distribution systems and technical expertise.
16
The property and casualty insurance market is highly competitive. The Company competes with stock insurance companies, mutual companies, local cooperatives and other underwriting organizations. In its workers’ compensation insurance segment, the Company considers its principal competitors to be PMA Capital Insurance Group, Erie Insurance Group, Guard Insurance Group, Penn National Insurance Company, Selective Insurance Group, Cincinnati Insurance Company, Lackawanna Insurance Group, and the Pennsylvania State Workers’ Insurance Fund. Certain of these competitors have higher A.M. Best financial strength ratings and substantially greater financial, technical and operating resources than the Company.
Group benefits insurance products are relatively inexpensive to develop and market, and as such are offered by hundreds of insurance carriers, including a number of financial services companies which are not considered members of the insurance industry. In its group benefits insurance segment, the Company’s principal competitors include Aetna, Inc., Assurant, Inc., Guardian Life Insurance Company and Metropolitan Life Insurance Company.
Investments
The Company’s investment portfolio consists of fixed income securities, equity securities, and other long-term investments in various limited partnerships. The management and accounting for the Company’s investment function is outsourced to third parties. The Company has established an investment policy, approved by the Finance/Investment Committee of the Board of Directors, which has been communicated to the Company’s external investment managers. In addition, the Company has hired an independent investment consultant to oversee the Company’s investment managers and to assist the Company in setting and monitoring its investment policy.
The Company’s investment objectives are:
| | • | | to meet insurance regulatory requirements; |
| | • | | to maintain adequate liquidity in its insurance subsidiaries; |
| | • | | to preserve capital through a well diversified, high quality investment portfolio; and |
| | • | | to maximize after tax income while generating competitive after tax total rates of return. |
The Company’s investments in fixed income and equity securities are classified as “available for sale” and are reported at estimated fair value, with changes in fair value reported as a component of accumulated other comprehensive income, net of applicable taxes. The Company periodically evaluates its investments for other-than-temporary impairment. At the time an investment is determined to be other-than-temporarily impaired, the Company records a realized loss in the consolidated statements of operations and comprehensive income (loss). Any subsequent increase in the investment’s market value would be reported as an unrealized gain.
The Company’s other long-term investments include interests in various limited partnerships. These limited partnerships are viewed as a means to enhance the diversification of the Company’s portfolio. The limited partnerships include a low volatility multi-strategy fund of funds and investments in two natural resource limited partnerships. We expect that these investments will provide long-term diversification benefits to the portfolio as they tend to have very little correlation to the fixed income markets. The Company also has made a small investment in a municipal bond based
17
limited partnership which complements its fixed income exposure. The Company accounts for its limited partnership investments under the equity method, with changes in the Company’s interest in the limited partnerships recorded in net investment income.
The Company evaluates the performance of its investments through the use of various industry benchmarks. Benchmarks have been selected for each investment manager and/or portfolio and are reviewed on a quarterly basis by management and the Company’s Finance/Investment Committee of the Board of Directors. For the year ended December 31, 2006, the Company’s taxable equivalent total return, net of management fees, was 5.59%, compared to the composite benchmark return of 5.06%. The Company’s portfolio benefited from its exposure to municipal bonds which exceeded return in most other investment grade fixed income sectors. In addition, the Company’s convertible securities manager significantly out-performed their benchmark.
The following table sets forth consolidated information concerning the Company’s investments as of December 31, 2006 and 2005 (in thousands).
| | | | | | | | | | | | |
| | | At December 31, |
| | | 2006 | | 2005 |
| | | Amortized
Cost | | Estimated
Fair Market
Value | | Amortized
Cost | | Estimated
Fair Market
Value |
U.S. Treasuries and government agencies | | $ | 18,434 | | $ | 18,913 | | $ | 6,798 | | $ | 7,162 |
State, municipalities and political subdivisions | | | 33,751 | | | 34,446 | | | 1,003 | | | 1,023 |
Foreign governments | | | 500 | | | 496 | | | 488 | | | 484 |
Corporate securities | | | 79,644 | | | 80,851 | | | 62,865 | | | 63,879 |
Mortgage-backed securities | | | 24,921 | | | 25,470 | | | 1,454 | | | 1,431 |
Collateralized mortgage obligations | | | 16,167 | | | 16,312 | | | — | | | — |
Asset-backed securities | | | 27,809 | | | 27,956 | | | — | | | — |
| | | | | | | | | | | | |
Total fixed income securities | | | 201,226 | | | 204,444 | | | 72,608 | | | 73,979 |
| | | | | | | | | | | | |
Equity securities | | | 17,027 | | | 18,219 | | | — | | | — |
Equity call options | | | 2,230 | | | 3,318 | | | 1,086 | | | 1,308 |
| | | | | | | | | | | | |
Total investments | | $ | 220,483 | | $ | 225,981 | | $ | 73,694 | | $ | 75,287 |
| | | | | | | | | | | | |
The following table shows the ratings distribution of the Company’s fixed income portfolio, excluding fixed income securities of the segregated portfolio cell reinsurance segment, as a percentage of the total market value of the fixed income portfolio as of December 31, 2006 (dollars in thousands).
| | | | | | |
| | | Total | | Percentage of
Total Market
Value | |
“AAA” | | $ | 101,588 | | 54.3 | % |
“AA” | | | 28,292 | | 15.2 | % |
“A” | | | 31,108 | | 16.7 | % |
“BBB” | | | 9,532 | | 5.1 | % |
Below Investment Grade | | | 1,802 | | 1.0 | % |
Not Rated | | | 14,383 | | 7.7 | % |
| | | | | | |
Total | | $ | 186,705 | | 100.0 | % |
| | | | | | |
18
The amortized cost and estimated fair value of fixed income securities, including the equity call option component of the Company’s convertible bond portfolio, as of December 31, 2006, by contractual maturity, are shown below. Expected maturities could differ from contractual maturities because borrowers may have the right to call or prepay obligations, with or without call or prepayment penalties (in thousands).
| | | | | | |
| | | Amortized
Cost | | Estimated
Fair Value |
Less than one year | | $ | 38,455 | | $ | 38,489 |
One through five years | | | 97,062 | | | 98,198 |
Five through ten years | | | 41,947 | | | 43,058 |
Greater than ten years | | | 25,992 | | | 28,017 |
| | | | | | |
Total fixed income securities | | $ | 203,456 | | $ | 207,762 |
| | | | | | |
The gross unrealized losses and estimated fair value of investments classified as available-for-sale securities by investment category and length of time an individual security is in a continuous unrealized loss position as of December 31, 2006 were as follows (in thousands):
| | | | | | | | | | | | | | | | | | | | | |
| | | Less Than 12 Months | | | 12 Months or More | | | Total | |
2006 | | Estimated
Fair
Value | | Gross Unrealized
Losses | | | Estimated
Fair
Value | | Gross Unrealized
Losses | | | Estimated
Fair
Value | | Gross Unrealized
Losses | |
U.S. Treasuries and government agencies | | $ | — | | $ | — | | | $ | 1,758 | | $ | (43 | ) | | $ | 1,758 | | $ | (43 | ) |
Foreign governments | | | — | | | — | | | | 496 | | | (4 | ) | | | 496 | | | (4 | ) |
States, municipalities, and political subdivisions | | | 3,355 | | | (10 | ) | | | — | | | — | | | | 3,355 | | | (10 | ) |
Corporate securities | | | 269 | | | (22 | ) | | | 8,177 | | | (230 | ) | | | 8,446 | | | (252 | ) |
Mortgage-backed securities | | | — | | | — | | | | — | | | — | | | | — | | | — | |
Collateralized mortgage obligations | | | 2,690 | | | (6 | ) | | | 469 | | | (12 | ) | | | 3,159 | | | (18 | ) |
Asset-backed securities | | | 3,533 | | | (8 | ) | | | 2,431 | | | (39 | ) | | | 5,964 | | | (47 | ) |
| | | | | | | | | | | | | | | | | | | | | |
Total fixed income securities | | | 9,847 | | | (46 | ) | | | 13,331 | | | (328 | ) | | | 23,178 | | | (374 | ) |
Equity securities | | | 2,509 | | | (101 | ) | | | — | | | — | | | | 2,509 | | | (101 | ) |
| | | | | | | | | | | | | | | | | | | | | |
Total investments | | $ | 12,356 | | $ | (147 | ) | | $ | 13,331 | | $ | (328 | ) | | $ | 25,687 | | $ | (475 | ) |
| | | | | | | | | | | | | | | | | | | | | |
Technology
The Company’s technology strategy is focused on utilizing vendor supplied components to address core system capabilities while utilizing its in-house staff to focus on vendor management, product integration, business intelligence and other business support functions. The Company’s technology strategy has several key components:
| | • | | Infrastructure. The Company is presently focused on the integration of pre-merger redundant systems and/or capabilities in the workers’ compensation and group benefits operations. In 2006, the general ledger and AP systems were combined and the previously separate networks were physically integrated. |
| | • | | Policy Administration. Central to the Company’s overall infrastructure are its policy administration systems. The workers’ compensation policy administration system is a Windows-based client server product provided by AGO Insurance Systems, Inc. The HIPPA compliant group benefits policy administration system is the Genelco system, provided by IBM, which runs on an AS400 platform. These policy administration systems provide the core capabilities needed to issue and administer our entire book of business. |
| | • | | Management Analysis and Reporting Software. The Company utilizes a comprehensive monthly report package as well as a web-based product which provides the ability to query and analyze real-time workers’ compensation underwriting, claim and financial data. Management utilizes this data on a real-time basis to analyze underwriting trends that help to assess the quality of the book |
19
| | of business and to review claim statistics, including frequency, severity, claim counts, and medical costs, among other things. This development was performed in-house utilizing the Company’s data warehouse and third party software. |
| | • | | eaport. - An internet policy administration system, eaport, was developed by Agencyport Insurance Services, Inc. and is designed to allow producers to submit workers compensation policies directly via the Internet. In 2006, the functionality was introduced, allowing producers to directly bind business via the internet. Eaport is designed to reduce the Company’s expenses associated with processing it workers’ compensation business by reducing underwriter involvement in policy submissions. The system enables the Company to control the growth of its underwriting staff, and makes it easier for producers to do business with the Company by allowing them to receive policy pricing indications and send submission information electronically. |
| | • | | Company Web sites. The Company operates three Web sites. The Company’s Corporate Web site (www.easterninsuranceholdings.com) provides investor relations information and news. EAIG’s Web site (www.eains.com) provides information and news regarding EAIG products and services, in addition to secured content accessible to producers and insureds. The secured sections include a risk management library that allows EAIG’s risk management personnel to disseminate safety information quickly and effectively to producers and insureds. ELH’s Web site (www.elhins.com) provides information and news regarding ELH products as well as access to an online group administration system. |
| | • | | Disaster Recovery.The Company’s disaster recovery and business continuity plans have been developed in conjunction with Agility Recovery Solutions (“Agility”), a provider of business continuity services, based in Charlotte, North Carolina. Agility provides mobile work facilities, telecommunications, computer equipment, generators and other services in the event of a disaster. Agility also provides a web based online service that houses the Company’s business continuity plan as well as other relevant information that might be needed in the event of a disaster. |
The Company’s technology systems are hosted in a physically secure data center located at the Company’s home offices in Lancaster, Pennsylvania.
Employees
As of December 31, 2006, the Company had 136 full time employees. None of the Company’s employees is represented by a union. The Company considers its relationship with its employees to be excellent.
Regulation
General
Insurance companies are subject to supervision and regulation in the jurisdictions in which they do business. Insurance authorities in each jurisdiction have broad administrative powers to administer statutes and regulations with respect to all aspects of the insurance business, including:
| | • | | approval of policy forms and premium rates; |
| | • | | mandating certain insurance benefits; |
20
| | • | | standards of solvency, including establishing statutory and risk-based capital requirements for statutory surplus; |
| | • | | classifying assets as admissible for purposes of determining statutory surplus; |
| | • | | licensing of insurers and their producers; |
| | • | | regulating unfair trade and claim practices, including through the imposition of restrictions on marketing and sales practices, distribution arrangements and payment of inducements; |
| | • | | restrictions on the nature, quality and concentration of investments; |
| | • | | assessments by guaranty and other associations; |
| | • | | restrictions on the ability of insurance companies to pay dividends; |
| | • | | restrictions on transactions between insurance companies and their affiliates; |
| | • | | restrictions on acquisitions and dispositions of insurance companies; |
| | • | | restrictions on the size of risks insurable under a single policy; |
| | • | | requiring deposits for the benefit of policyholders; |
| | • | | requiring certain methods of accounting; |
| | • | | periodic examinations of insurance company operations and finances; |
| | • | | reviewing claims practices; |
| | • | | prescribing the form and content of records of financial condition required to be filed; and |
| | • | | requiring reserves for unearned premiums, losses and other purposes. |
State insurance laws and regulations require insurance companies to file financial statements with insurance departments everywhere they do business, and the operations of insurance companies are subject to examination by those departments at any time. Eastern Alliance, Allied Eastern, and ELH prepare statutory financial statements in accordance with accounting practices and procedures prescribed or permitted by these departments.
Examinations
Examinations are conducted by the Pennsylvania Insurance Department (the “Insurance Department”) every three to five years. The Insurance Department’s last examinations of Eastern Alliance and ELH were as of December 31, 2001, and the last examination of Allied Eastern was as of April 22, 2002. These examinations did not result in any adjustments to the financial position of Eastern Alliance, Allied Eastern, or ELH. In addition, there were no substantive qualitative matters indicated in the examination reports that had a material adverse impact on the operations of Eastern Alliance, Allied Eastern, or ELH.
Risk-Based Capital Requirements
Pennsylvania imposes the NAIC risk-based capital requirements that require insurance companies to calculate and report information under a risk-based formula. These risk-based capital requirements attempt to measure statutory capital and surplus needs based on the risks in an insurance company’s mix
21
of products and investment portfolio. Under the formula, a company first determines its “authorized control level” risk-based capital. This authorized control level takes into account (i) the risk with respect to the insurer’s assets; (ii) the risk of adverse insurance experience with respect to the insurer’s liabilities and obligations; (iii) the interest rate risk with respect to the insurer’s business; and (iv) all other business and other relevant risks as are set forth in the risk-based capital instructions. An insurance company’s “total adjusted capital” is the sum of statutory capital and surplus and such other items as the risk-based capital instructions may provide. The formula is designed to allow state insurance regulators to identify weakly capitalized companies.
The requirements provide for four different levels of regulatory attention. The “company action level” is triggered if a company’s total adjusted capital is less than 2.0 times its authorized control level but greater than or equal to 1.5 times its authorized control level. At the company action level, a company must submit a comprehensive plan to the regulatory authority that discusses proposed corrective actions to improve its capital position. The “regulatory action level” is triggered if a company’s total adjusted capital is less than 1.5 times but greater than or equal to 1.0 times its authorized control level. At the regulatory action level, the regulatory authority will perform a special examination of the company and issue an order specifying corrective actions that must be followed. The “authorized control level” is triggered if a company’s total adjusted capital is less than 1.0 times but greater than or equal to 0.7 times its authorized control level. At the authorized control level, the regulatory authority may take any action it deems necessary, including placing the company under regulatory control. The “mandatory control level” is triggered if a company’s total adjusted capital is less than 0.7 times its authorized control level. At the mandatory control level, the regulatory authority is mandated to place the company under its control. As of December 31, 2006, the capital levels of Eastern Alliance, Allied Eastern, and ELH exceed risk-based capital requirements.
IRIS Ratios
The NAIC Insurance Regulatory Information System, or IRIS, is part of a collection of analytical tools designed to provide state insurance regulators with an integrated approach to screening and analyzing the financial condition of insurance companies operating in their respective states. IRIS is intended to assist state insurance regulators in targeting resources to those insurers in greatest need of regulatory attention. IRIS consists of two phases: statistical and analytical. In the statistical phase, the NAIC database generates key financial ratio results based on financial information obtained from insurers’ annual statutory statements. The analytical phase is a review of insurers’ annual statements, financial ratios and other automated solvency tools. The primary goal of the analytical phase is to identify companies that appear to require immediate regulatory attention. A ratio result falling outside the usual range of IRIS ratios is not considered a failing result; rather, unusual values are viewed as part of the regulatory early monitoring system. Furthermore, in some years, financially sound companies may have several ratios that temporarily deviate from the usual ranges.
The Company’s insurance subsidiaries, Eastern Alliance, Allied Eastern, and ELH, had the following IRIS ratios, which deviated from the usual ranges, as of and for the year ended December 31, 2006:
22
| | | | | | | | |
Subsidiary | | IRIS Ratio | | Usual
Range | | Actual
Results | | Reason for Unusual Result |
| Eastern Alliance | | Net Change in Adjusted Policyholders’ Surplus | | Less than 25% | | 28% | | Statutory net income for the year ended December 31, 2006. |
| | | | |
| Allied Eastern | | Investment Yield | | Greater than 3% | | 3% | | Due to the pooling arrangement with Eastern Alliance, Allied Eastern maintains a higher cash balance, which is invested at lower yields. |
| | | | |
| ELH | | Change in premium | | Greater than 10% decrease | | 14% decrease | | Change in distribution network at the end of 2005, which impacted sales and renewal retention in the first half of 2006. |
Market Conduct Regulation
State insurance laws and regulations include numerous provisions governing trade practices and the marketplace activities of insurers, including provisions governing the form and content of disclosure to consumers, illustrations, advertising, sales practices and complaint handling. State regulatory authorities generally enforce these provisions through periodic market conduct examinations. To our knowledge, Eastern Alliance, Allied Eastern, and ELH are currently in compliance with these provisions.
Sarbanes-Oxley Act of 2002
The Company is subject to the Sarbanes-Oxley Act of 2002, which implemented legislative reforms intended to address corporate and accounting fraud. Among other reforms, the Sarbanes-Oxley Act requires chief executive officers and chief financial officers, or their equivalent, to certify to the accuracy of periodic reports filed with the SEC, subject to civil and criminal penalties if they knowingly or willfully violate this certification requirement. The Sarbanes-Oxley Act also increases the oversight of, and codifies, certain requirements relating to audit committees of public companies and how they interact with the company’s auditors. Audit committee members must be independent and are barred from accepting consulting, advisory or other compensatory fees from the company. In addition, companies must disclose whether at least one member of the committee is a “financial expert,” as such term is defined by the SEC, and if not, why not. Pursuant to the Sarbanes-Oxley Act, the SEC has adopted rules requiring inclusion of an internal control report and assessment by management in the annual report to shareholders. The Sarbanes-Oxley Act requires the auditor that issues the audit report to attest to and report on management’s assessment of the company’s internal controls. EIHI will be subject to this provision as of and for the year ended December 31, 2007. We expect to incur significant costs in 2007 in order to become compliant with the requirements of the Sarbanes-Oxley Act.
Insurance Guaranty Funds
Many states have guaranty fund laws under which insurers doing business in the state can be assessed to fund policyholder liabilities of insolvent insurance companies. Pennsylvania and the other states in which our insurance companies do business have such laws. Under these laws, an insurer is subject to assessment depending upon its market share in the state of a given line of business. Eastern Alliance, Allied Eastern, and ELH establish reserves relating to insurance companies that are subject to insolvency proceedings when they are notified of assessments by the guaranty associations. We cannot predict the amount and timing of any future assessments under these laws.
Gramm-Leach-Bliley Act
The Gramm-Leach-Bliley Act facilitates affiliations among banks, securities firms and insurance companies. The ability of banks and securities firms to affiliate with insurers may increase the number, size and financial strength of our potential competitors.
23
As mandated by the Gramm-Leach-Bliley Act, states continue to promulgate and refine laws and regulations that require financial institutions, including insurance companies, to take steps to protect the privacy of certain consumer and customer information relating to products or services primarily for personal, family or household purposes. A recent NAIC initiative that affected the insurance industry was the adoption in 2000 of the Privacy of Consumer Financial and Health Information Model Regulation, which assisted states in promulgating regulations to comply with the Gramm-Leach-Bliley Act. In 2002, to further facilitate the implementation of the Gramm-Leach-Bliley Act, the NAIC adopted the Standards for Safeguarding Customer Information Model Regulation. Several states have now adopted similar provisions regarding the safeguarding of customer information. The Company has implemented procedures to comply with the Gramm-Leach-Bliley Act’s privacy requirements.
OFAC
The Treasury Department’s Office of Foreign Asset Control, or “OFAC,” maintains a list of Specifically Designated Nationals and Blocked Persons, or the “SDN List”. The SDN List identifies persons and entities that the government believes are associated with terrorists, rogue nations or drug traffickers. OFAC’s regulations prohibit insurers, among others, from doing business with persons or entities on the SDN List. If the insurer finds and confirms a match with the SDN List, the insurer must take steps to block or reject the transaction, notify the affected person and file a report with OFAC.
Cayman Islands Regulation
Eastern Re is organized and licensed as a Cayman Islands unrestricted Class B insurance company and is subject to regulation by the Cayman Islands Monetary Authority. Applicable laws and regulations govern the types of policies that Eastern Re can insure or reinsure, the amount of capital that it must maintain and the way it can be invested, and the payment of dividends without approval by the Cayman Islands Monetary Authority.
Holding Company Regulation
EIHI is registered as an insurance holding company under the Insurance Holding Company Act amendments to the Pennsylvania Insurance Code of 1921, as amended, and is subject to regulation and supervision by the Insurance Department. EIHI is required to annually file a report of its operations with, and is subject to examination by, the Insurance Department.
Each insurance company in a holding company system is required to register with the insurance supervisory agency of its state of domicile and furnish certain information. This includes information concerning the operations of companies within the holding company system that may materially affect the operations, management or financial condition of the insurers within the system. Pursuant to these laws, the respective insurance departments may examine insurance companies and their holding companies at any time, require disclosure of material transactions by insurance companies and their holding companies and require prior notice or approval of certain transactions, such as “extraordinary dividends” distributed by insurance companies.
All transactions within the holding company system affecting insurance companies and their holding companies must be fair and equitable. Notice of certain material transactions between insurance companies and any person or entity in their holding company system will be required to be given to the applicable insurance commissioner. In some states, certain transactions cannot be completed without the prior approval of the insurance commissioner.
Approval of the state insurance commissioner is required prior to any transaction affecting the control of an insurer domiciled in that state. In Pennsylvania, the acquisition of 10% or more of the outstanding capital stock of an insurer or its holding company is presumed to be a change in control. Pennsylvania law also prohibits any person from (i) making a tender offer for, or a request or invitation for tenders of, or seeking to acquire or acquiring any voting security of a Pennsylvania insurer if, after the acquisition, the person would be in control of the insurer, or (ii) effecting or attempting to effect an acquisition of control of or merger with a Pennsylvania insurer, unless the offer, request, invitation, acquisition, effectuation or attempt has received the prior approval of the Insurance Department.
24
Dividend Restrictions
EIHI’s ability to declare and pay dividends will depend in part on dividends received from Eastern Alliance, Allied Eastern, and ELH. The Pennsylvania Insurance Code regulates the distribution of dividends by insurance companies and states, in part, that dividends cannot exceed the greater of 10% of an insurance company’s statutory surplus as reported on the most recent annual statement filed with the Insurance Department or an insurance company’s net income for the period covered by such annual statement.
EIHI and its subsidiaries are prohibited from declaring or paying any dividends or other forms of distribution to EIHI for the three years after June 16, 2006, the effective date of the conversion/merger transaction, without the prior approval of the Pennsylvania Insurance Commissioner.
Note on Forward-Looking Statements
This document contains forward-looking statements, which can be identified by the use of such words as “estimate,” “project,” “believe,” “intend,” “anticipate,” “plan,” “seek,” “expect” and similar expressions. These forward-looking statements include:
| • | | statements of goals, intentions and expectations; |
| • | | statements regarding prospects and business strategy; and |
| • | | estimates of future costs, benefits and results. |
These forward-looking statements are subject to significant risks, assumptions and uncertainties, including, among other things, the factors discussed under the heading “Risk Factors” that could affect the actual outcome of future events.
All of these factors are difficult to predict and many are beyond our control. These important factors include those discussed under “Risk Factors” and those listed below:
| • | | the ability to carry out our business plans; |
| • | | future economic conditions in the regional and national markets in which we compete that are less favorable than expected; |
| • | | the effect of legislative, judicial, economic, demographic and regulatory events in the states in which we do business; |
| • | | the ability to obtain licenses and enter new markets successfully and capitalize on growth opportunities either through mergers or the expansion of our producer network; |
| • | | financial market conditions, including, but not limited to, changes in interest rates and the stock markets causing a reduction of investment income or investment gains, an acceleration of the amortization of deferred policy acquisition costs, reduction in the value of our investment portfolio or a reduction in the demand for our products; |
| • | | the impact of acts of terrorism and acts of war; |
| • | | the effects of terrorist related insurance legislation and laws; |
25
| • | | changes in general economic conditions, including inflation, unemployment, interest rates and other factors; |
| • | | the cost, availability and collectibility of reinsurance; |
| • | | estimates and adequacy of loss reserves and trends in losses and loss adjustment expenses; |
| • | | heightened competition, including specifically the intensification of price competition, increased underwriting capacity and the entry of new competitors and the development of new products by new and existing competitors; |
| • | | the effects of mergers, acquisitions and dispositions; |
| • | | changes in the coverage terms selected by insurance customers, including higher deductibles and lower limits; |
| • | | changes in the underwriting criteria that we use resulting from competitive pressures; |
| • | | our inability to obtain regulatory approval of, or to implement, premium rate increases; |
| • | | the potential impact on our reported net income that could result from the adoption of future accounting standards issued by the Financial Accounting Standards Board or other standard-setting bodies; |
| • | | our inability to carry out marketing and sales plans, including, among others, development of new products or changes to existing products and acceptance of the new or revised products in the market; |
| • | | unanticipated changes in industry trends and ratings assigned by nationally recognized rating organizations; |
| • | | adverse litigation or arbitration results; and |
| • | | adverse changes in applicable laws, regulations or rules governing insurance holding companies and insurance companies, and tax or accounting matters including limitations on premium levels, increases in minimum capital and reserves, and other financial viability requirements, and changes that affect the cost of, or demand for our products. |
Because forward-looking information is subject to various risks and uncertainties, actual results may differ materially from that expressed or implied by the forward-looking information. Therefore, we caution you not to place undue reliance on this forward-looking information.
All subsequent written and oral forward-looking information attributable to the Company or any person acting on our behalf is expressly qualified in its entirety by the cautionary statements contained or referred to in this section. We do not undertake any obligation to publicly release any revisions that may be made to any forward-looking statements.
Because of these and other uncertainties, our actual future results may be materially different from the results indicated by these forward-looking statements. The Company has no obligation to update or revise any forward-looking statements to reflect any changed assumptions, any unanticipated events or any changes in the future.
Item 1A – Risk Factors
Our business is subject to numerous risks and uncertainties, the outcome of which may impact future results of operations and financial condition. These risks are as follows:
26
Risk Factors Relating to Our Business
Our results may be adversely affected if our actual losses exceed our loss reserves.
The Company maintains loss reserves to cover estimated amounts needed to pay for insured losses and for the loss adjustment expenses necessary to settle claims with respect to insured events that have occurred, including events that have not yet been reported to us. Estimating the reserves for unpaid losses and LAE is a difficult and complex process involving many variables and subjective judgments; reserves do not represent an exact measure of liability. Accordingly, our loss reserves may prove to be inadequate to cover our actual losses. We regularly review our reserving techniques and our overall amount of reserves. We review historical data and consider the impact of various factors such as:
| • | | trends in claim frequency and severity; |
| • | | information regarding each claim for losses; |
| • | | legislative enactments, judicial decisions and legal developments regarding damages; and |
| • | | trends in general economic conditions, including inflation and levels of employment. |
If we determine that our reserves for unpaid losses and LAE are inadequate, we will have to increase them. This adjustment would reduce income during the period in which the adjustment is made, which could have a material adverse impact on our financial condition and results of operations. For additional information, see “Item 1 – Business, Loss and Loss Adjustment Expense Reserves.”
If we do not accurately establish our premium rates, our results of operations may be adversely affected.
In general, the premium rates for our insurance policies are established when coverage is initiated and therefore, before all of the underlying costs are known. Like other insurance companies, we rely on estimates and assumptions in setting our premium rates. Establishing adequate rates is necessary, together with investment income, to generate sufficient revenue to offset losses, loss adjustment expenses and other underwriting expenses and to earn a profit. If we fail to accurately assess the risks that we assume, we may fail to charge adequate premium rates to cover our losses and expenses, which could reduce our net income and cause us to become unprofitable. As a result, our actual costs for providing insurance coverage to our policyholders may be significantly higher than our premiums.
In order to set premium rates accurately, we must collect and properly analyze a substantial volume of data; develop, test, and apply appropriate rating formulae; closely monitor and recognize changes in trends; project both severity and frequency of losses with reasonable accuracy; and estimate customer retention. Customer retention means the amount of exposure a policyholder retains on any one risk or group of risks. The term may apply to an insurance policy, where the policyholder is an individual, family or business, or a reinsurance policy, where the policyholder is an insurance company. We must also implement our pricing accurately in accordance with our assumptions. For example, if we expand the geographic market in which we offer our workers’ compensation insurance products we may not price these products accurately or adequately. Our ability to undertake these efforts successfully, and as a result set premium rates accurately, is subject to a number of risks and uncertainties, including:
| • | | inaccurate assessment of new markets in which we have little or no prior experience; |
| • | | insufficient or unreliable data; |
| • | | incorrect or incomplete analysis of available data; |
27
| • | | uncertainties generally inherent in estimates and assumptions; |
| • | | our inability to implement appropriate rating formulae or other pricing methodologies; |
| • | | costs of ongoing medical treatment; |
| • | | our inability to accurately estimate customer retention, investment yields and the duration of our liability for losses and loss adjustment expenses; and |
| • | | unanticipated court decisions, legislation or regulatory action. |
Consequently, we could set our premium rates too low, which could negatively affect our results of operations and our profitability, or we could set our premium rates too high, which could reduce our ability to obtain new or retain existing business and lead to lower net premiums earned.
If we do not effectively manage the growth of our operations we may not be able to compete or operate profitably.
Our growth strategy includes enhancing our market share in our existing markets, entering new geographic markets, introducing new insurance products and programs, further developing our agency relationships, and pursuing merger and acquisition opportunities. Our strategy is subject to various risks, including risks associated with our ability to:
| • | | identify profitable new geographic markets to enter; |
| • | | obtain licenses in new states in which we wish to market and sell our products; |
| • | | successfully implement our underwriting, pricing, claims management, and product strategies over a larger operating region; |
| • | | properly design and price new and existing products and programs and reinsurance facilities; |
| • | | identify, train and retain qualified employees; |
| • | | identify, recruit and integrate new independent producers; |
| • | | formulate and execute a merger and acquisition strategy; and |
| • | | augment our internal monitoring and control systems as we expand our business. |
We also may encounter difficulties in the implementation of our growth strategies, including unanticipated expenditures. In addition, our growth strategies may result in us entering into markets or product lines in which we have little or no prior experience. Any such difficulties could result in diversion of senior management time and adversely affect our financial results.
All of the specialty reinsurance business of Eastern Re is controlled by one of our directors and is placed with one primary insurer and the loss of this business would adversely affect us.
The Company’s specialty reinsurance segment generates 100% of its premium revenue through reinsurance contracts with a large, primary insurer. This business is directly or indirectly managed by one producer, AmPro. Lawrence Bitner is a Director of the Company and the AmPro employee who produces the program business for the primary insurer and controls the placement of reinsurance contracts with Eastern Re. If the Company lost the goodwill of Mr. Bitner, Mr. Bitner could cause this business to be placed with another reinsurer and/or could cause the insurance policies to be written by a primary insurance carrier that would not purchase reinsurance coverage in respect of the business or would not place reinsurance with Eastern Re.
28
Our ability to manage our exposure to underwriting risks depends on the availability and cost of reinsurance coverage.
We use reinsurance arrangements to limit and manage the amount of risk we retain, to stabilize our underwriting results and to increase our underwriting capacity. Although we have not recently experienced difficulty in obtaining reinsurance at reasonable prices, the availability and cost of reinsurance is subject to current market conditions and may vary significantly over time. Any decrease in the amount of our reinsurance will increase our risk of loss. We may be unable to maintain our desired reinsurance coverage or to obtain other reinsurance coverage in adequate amounts and at favorable rates. If we are unable to renew our expiring coverage or obtain new coverage, it will be difficult for us to manage our underwriting risks and operate our business profitably.
It is also possible that the losses we experience on insured risks for which we have obtained reinsurance will exceed the coverage limits of the reinsurance. If the amount of our reinsurance coverage is insufficient, our insurance losses could increase substantially.
If our reinsurers do not pay our claims in a timely manner, we may incur losses.
We are subject to credit risk with respect to the reinsurers with whom we deal because buying reinsurance does not relieve us of our liability to policyholders. The Company had net reinsurance recoverables of $27.5 million as of December 31, 2006. If our reinsurers are not capable of fulfilling their financial obligations to us, our insurance losses would increase, which would negatively affect our financial condition and results of operations.
A reduction in ELH’s A.M. Best rating or our inability to increase ELH’s A.M. Best rating could affect our ability to write new business or renew existing business in our group benefits insurance segment.
Ratings assigned by A.M. Best are an important factor influencing the competitive position of insurance companies. ELH holds a financial strength rating of “B++” (Very Good) by A.M. Best, the fifth highest rating out of 16 classifications. A.M. Best ratings represent independent opinions of financial strength and ability to meet obligations to policyholders and are not directed toward the protection of investors. Financial strength ratings are used by producers and customers as a means of assessing the financial strength and quality of insurers. A downgrade of ELH’s financial strength rating could severely limit or prevent us from writing desirable business or from renewing existing business in our group benefits insurance segment.
Our investment performance may suffer as a result of adverse capital market developments, which may affect our financial results and ability to conduct business.
We invest the premiums we receive from policyholders until cash is needed to pay insured claims or other expenses. As of December 31, 2006, the Company had investments of $237.6 million. For the year ended December 31, 2006, the Company had $9.0 million of net investment income, representing 10.3% of its total revenues. Our investments are subject to a variety of investment risks, including risks relating to general economic conditions, market volatility, interest rate fluctuations, liquidity risk and credit risk. In particular, an unexpected increase in the volume or severity of claims may force us to liquidate securities, which may cause us to incur capital losses. If we do not structure the duration of our investments to match our insurance and reinsurance liabilities, we may be forced to liquidate investments prior to maturity at a significant loss to cover such payments. Investment losses could significantly decrease our asset base and statutory surplus, thereby affecting our ability to conduct business.
29
Our revenues may fluctuate with changes in interest rates.
Our investment portfolio contains a significant amount of fixed-income securities, including bonds, mortgage-backed securities (“MBSs”), collateralized mortgage obligations (“CMOs”), and asset-backed securities. The market values of all of our investments fluctuate depending on economic and political conditions and other factors beyond our control. The market values of our fixed-income securities are particularly sensitive to changes in interest rates.
For example, if interest rates rise, fixed-income investments generally will decrease in value. If interest rates decline, these investments generally will increase in value, except for MBSs, which may decline due to higher prepayments on the mortgages underlying the securities.
As of December 31, 2006, MBSs, including CMOs, constituted 18.5% of the market value of the Company’s investment portfolio. MBSs and CMOs are subject to prepayment risks that vary with, among other things, interest rates. During periods of declining interest rates, MBSs generally prepay faster as the underlying mortgages are prepaid and/or refinanced by the borrowers in order to take advantage of lower interest rates. MBSs that have an amortized cost that is greater than par (i.e., purchased at a premium) may incur a reduction in yield or a loss as a result of prepayments. In addition, during such periods, we generally will be unable to reinvest the proceeds of any prepayment at comparable yields. Conversely, during periods of rising interest rates, the frequency of prepayments generally decreases, and we may receive interest payments that are below the then prevailing interest rate for longer than expected. MBSs that have an amortized cost that is less than par (i.e., purchased at a discount) may incur a decrease in yield or a loss as a result of slower prepayments.
If we fail to comply with insurance industry regulations, or if those regulations become more burdensome, we may not be able to operate profitably.
Our insurance subsidiaries are regulated by government agencies in the states in which we do business, and we must comply with a number of state and federal laws and regulations. Most insurance regulations are intended to protect the interests of insureds rather than those of shareholders and other investors. These regulations, generally administered by the department of insurance in each state in which we do business, relate to, among other things:
| • | | approval of policy forms and premium rates; |
| • | | mandating certain insurance benefits; |
| • | | standards of solvency, including establishing statutory and risk-based capital requirements for statutory surplus; |
| • | | classifying assets as admissible for purposes of determining statutory surplus; |
| • | | licensing of insurers and their producers; |
| • | | regulating unfair trade and claim practices, including through the imposition of restrictions on marketing and sales practices, distribution arrangements and payment of inducements; |
| • | | restrictions on the nature, quality and concentration of investments; |
| • | | assessments by guaranty funds, second injury funds and other associations including residual risk pools; |
| • | | restrictions on the ability of our insurance company subsidiaries to pay dividends to us; |
| • | | restrictions on transactions between our insurance company subsidiaries and their affiliates; |
30
| • | | restrictions on acquisitions and dispositions of insurance companies; |
| • | | restrictions on the size of risks insurable under a single policy; |
| • | | requiring deposits for the benefit of policyholders; |
| • | | requiring certain methods of accounting; |
| • | | periodic examinations of our operations and finances; |
| • | | reviewing claims administration practices; |
| • | | prescribing the form and content of records of financial condition required to be filed; and |
| • | | requiring reserves for unearned premiums, losses and other purposes. |
If we fail to comply with these laws and regulations, state insurance departments can exercise a range of remedies from the imposition of fines to being placed in rehabilitation or liquidation. State insurance departments also conduct periodic examinations of the affairs of insurance companies and require the filing of annual and other reports relating to financial condition, holding company issues and other matters. These regulatory requirements may adversely affect or inhibit our ability to achieve some or all of our business objectives.
Part of our strategy includes expanded licensing and product filings for the Company. Regulatory authorities, however, have broad discretion to deny or revoke licenses for various reasons, including the violation of regulations. If we do not have or obtain the requisite licenses and approvals or do not comply with applicable regulatory requirements, insurance regulatory authorities could preclude or temporarily suspend us from carrying on some or all of our activities, including our expansion objectives, or otherwise penalize us. Furthermore, changes in the level of regulation of the insurance industry or changes in laws or regulations or interpretations of such laws and regulations by regulatory authorities could adversely affect our ability to operate our business.
We are subject to various accounting and financial requirements established by the NAIC. Eastern Re is subject to the laws of the Cayman Islands and regulations promulgated by the Cayman Islands Monetary Authority. Failure to comply with these laws, regulations and requirements could result in consequences ranging from a regulatory examination to a regulatory takeover of one or more of our insurance subsidiaries. This would make our business less profitable. In addition, state regulators and the NAIC continually re-examine existing laws and regulations, with an emphasis on insurance company solvency issues and fair treatment of policyholders. Insurance laws and regulations could change or additional restrictions could be imposed that are more burdensome and make our business less profitable. Because these laws and regulations are for the protection of policyholders, any changes may not be in your best interest as a shareholder.
Compliance with applicable laws and regulations is time consuming and personnel-intensive, and changes in these laws and regulations may materially increase our direct and indirect compliance and other expenses of doing business, thus adversely affecting our financial condition and results of operations.
Acts of terrorism could negatively affect our business and our financial condition.
Under our workers’ compensation policies, we are required to provide workers’ compensation benefits for losses resulting from certain acts of terrorism. The impact of any terrorist act is unpredictable, and the ultimate impact on us will depend upon the nature, extent, location and timing of such an act. Any such impact could be material.
31
The Terrorism Risk Insurance Act of 2002 (the “Terrorism Act”) is effective through December 31, 2007. The Terrorism Act may provide us with reinsurance protection under certain circumstances and subject to certain limitations. The Secretary of the Treasury must declare the act to be a “certified act of terrorism” for it to be covered under this federal program. The definition of terrorism for purposes of the Terrorism Act excludes domestic acts of terrorism or acts of terrorism committed in the course of a war declared by Congress. No federal compensation will be paid under the Terrorism Act unless aggregate insured losses from the act for the entire insurance industry exceed $100.0 million for terrorism losses occurring in 2007. Each insurance company is responsible for a deductible based on a percentage of the direct earned premiums of its affiliated group in the previous calendar year for commercial lines policies (except for certain excluded lines such as commercial auto) covering risk in the United States. This deductible amount is 20.0% of such premiums for losses occurring in 2007. For losses in excess of the deductible, the federal government will reimburse 85% of the insurer’s loss occurring in 2007.
Notwithstanding the protection provided by reinsurance and the Terrorism Act, the risk of severe losses to us from acts of terrorism has not been eliminated. The Company’s reinsurance treaties include various exclusions limiting its reinsurers’ obligation to cover losses caused by acts of terrorism. Accordingly, events constituting acts of terrorism may not be covered by, or may exceed the capacity of, our reinsurance and could adversely affect our business and financial condition. In addition, the Terrorism Act is set to expire on December 31, 2007, If this law is not extended, reinsurance for losses arising from terrorism may be unavailable or prohibitively expensive, and we may be further exposed to material losses arising from acts of terrorism.
The group benefits insurance and workers’ compensation insurance markets in which we operate are highly competitive.
Competition in these markets is based on many factors. These factors include the perceived financial strength of the insurer, premiums charged, policy terms and conditions, services provided, reputation, financial ratings assigned by independent rating agencies and the experience of the insurer in the line of insurance to be written. The Company’s insurance subsidiaries compete with stock insurance companies, mutual companies, local cooperatives and other underwriting organizations. Our principal competitors in the group benefits market include Aetna, Inc., Assurant, Inc., Guardian Life Insurance Company, and Metropolitan Life Insurance Company. Our principal competitors in the workers’ compensation insurance market include PMA Capital Insurance Group, Erie Insurance Group, Guard Insurance Group, Penn National Insurance Company, Selective Insurance Group, Cincinnati Insurance Company, Lackawanna Insurance Group, and the Pennsylvania State Workers’ Insurance Fund. Many of these competitors have higher ratings and substantially greater financial, technical and operating resources than we have. The group benefits and workers’ compensation lines of insurance are subject to significant price competition. If competitors price their products aggressively, our ability to grow or renew our business may be adversely affected. We pay producers on a commission basis to produce business. Some competitors may offer higher commissions to independent producers or offer insurance at lower premium rates through the use of salaried personnel or other distribution methods that do not rely on independent producers. Increased competition could adversely affect our ability to attract and retain business and thereby reduce our profits from operations.
We could be adversely affected by the loss of our key personnel.
The success of our business is dependent, to a large extent, on the efforts of certain key managers, in particular, Bruce M. Eckert, our Chief Executive Officer, Michael L. Boguski, our President and Chief Operating Officer, Kevin M. Shook, our Treasurer and Chief Financial Officer, Robert A. Gilpin, our Senior Vice President of Marketing, and Suzanne M. Emmet, our Senior Vice President of Claims. We have employment agreements with each of Messrs. Eckert, Boguski, Shook, Gilpin, and Ms. Emmet, which contain covenants not to compete. We do not maintain key man life insurance on any of these executives. The loss of key personnel could prevent us from fully implementing our business strategy and could significantly and negatively affect our financial condition and results of operations. As we continue
32
to grow, we will need to recruit and retain additional qualified management personnel, and our ability to do so will depend upon a number of factors, such as our results of operations and prospects and the level of competition then prevailing in the market for qualified personnel. The current market for qualified insurance personnel is highly competitive.
Our results of operations may be adversely affected by any loss of business from key producers and by the creditworthiness of our producers.
Our products are marketed by independent producers. Other insurance companies compete with the Company for the services and allegiance of these producers. Because they are independent, these producers are not obligated to direct business to the Company and may choose to direct business to our competitors, or may direct less desirable risks to us. The Company’s ten largest producers in its workers’ compensation insurance segment accounted for 67.3% of its direct premiums written for the year ended December 31, 2006. The Company’s largest producer in its workers’ compensation insurance segment accounted for 23.3% of direct premiums written for the year ended December 31, 2006. No other producer accounted for more than 10% of direct premiums written in the Company’s workers’ compensation insurance segment for the year ended December 31, 2006. No independent producer accounted for more than 5% of the Company’s group benefits insurance direct premiums written for the year ended December 31, 2006. As a result of the sale of IBSiin 2005, the Company’s group benefits insurance segment continues to be dependent on IBSi marketing its group benefits products to IBSi’s producers in North Carolina, South Carolina, and Virginia. If IBSi is unsuccessful in maintaining its existing relationships with key independent producers in these states, the Company’s group benefits insurance direct premiums written could be adversely impacted. If premium volume produced by any of the Company’s large producers were to decrease significantly, it would have a material adverse effect on us.
In addition, in accordance with industry practice, our customers sometimes pay the premiums for their policies to producers for payment to us. These premiums are considered paid when received by the producer and, thereafter, the customer is no longer liable to us for those amounts, whether or not we have actually received the premiums from the producer. Consequently, we assume a degree of credit risk associated with our reliance on producers in connection with the collection of insurance premiums.
Because the Company’s workers’ compensation insurance business is concentrated in Pennsylvania, the Company is subject to local economic risks as well as to changes in the regulatory and legal climate in Pennsylvania.
Almost all of the Company’s workers’ compensation premium volume is produced in Pennsylvania. The Company’s workers’ compensation insurance business is affected by the economic health of Pennsylvania for two principal reasons. First, premium growth is dependent upon payroll growth, which, in turn, is affected by economic conditions. Second, losses and loss adjustment expenses can increase in weak economic conditions because it is more difficult to return injured workers to the job when employers are otherwise reducing payrolls. Finally, as predominantly a single state insurer, the Company can be adversely affected by any material change in Pennsylvania law or regulation or any Pennsylvania court decision affecting workers’ compensation carriers generally.
The group benefits insurance segment’s premium volume could decline if the coinsurance arrangement with London Life Re is terminated.
In order to mitigate the impact of the April 2003 downgrade of ELH by A.M. Best from a financial strength rating of “A-” to “B++”, ELH entered into a coinsurance agreement with London Life Reinsurance Company effective October 1, 2003, and a companion stop loss reinsurance agreement with London Life International Reinsurance Corporation (an affiliate of London Life Reinsurance Company). Under the coinsurance agreement, London Life has reinsured all of ELH’s liability on claims under ELH’s in-force insurance policies written or renewed after October 1, 2003. London Life, in turn, is reinsured for these benefit costs by London Life International. ELH, in turn, reinsures London Life
33
International against loss on this business pursuant to the stop loss reinsurance agreement. The transaction is purposely circular so that all risk of loss on ELH’s in-force business will remain with ELH so long as it remains solvent. If, however, ELH were to become insolvent, then London Life would be required to pay ELH the full amount of the reinsured benefit costs under the coinsurance agreement, but London Life International would have only a subordinated claim as a general creditor for reimbursement under the stop loss agreement. Notwithstanding this arrangement, if ELH were to become insolvent, depending on the extent of its liabilities, there can be no assurance that the payment by London Life will be sufficient to allow ELH to fund the claims of its policyholders and certificateholders.
London Life receives a quarterly fee of the greater of $15,000 or 25% times the product of .0012 and the annualized premium of the in-force policies of ELH that are subject to this arrangement. ELH also must maintain assets in a trust account for London Life’s benefit having a value equal to no less than 105% of statutory claim reserves on the reinsured business. ELH can terminate the coinsurance agreement at any time and immediately recapture the reinsured business and the assets in the trust. London Life can terminate the coinsurance agreement on ninety (90) days’ prior notice to ELH. However, if ELH’s A.M. Best rating falls below “B”, its surplus falls below a level specified in the coinsurance agreement, or it is the subject of regulatory action, London Life can terminate the coinsurance agreement immediately. In any event, the coinsurance agreement would remain in-force for insurance policies sold or renewed by ELH prior to the termination date, but only until the earlier of the policy termination date or the next renewal date.
Future changes in financial accounting standards or practices or existing tax laws may adversely affect our reported results of operations.
Financial accounting standards in the United States are constantly under review and may be changed from time to time. We would be required to apply these changes when adopted. Once implemented, these changes could materially affect our results of operations and/or the way in which such results of operations are reported. Similarly, we are subject to taxation in the United States and a number of state jurisdictions. Rates of taxation, definitions of income, exclusions from income, and other tax policies are subject to change over time. Eastern Re is domiciled in the Cayman Islands. Changes in Cayman Islands tax laws could have a material impact on Eastern Re and our consolidated results of operations.
Proposals to federally regulate the insurance business could affect our business.
Currently, the U.S. federal government does not directly regulate the insurance business. However, federal legislation and administrative policies in several areas can significantly and adversely affect insurance companies. These areas include financial services regulation, securities regulation, pension regulation, privacy, tort reform legislation and taxation. In addition, various forms of directed federal regulation of insurance have been proposed. These proposals include the State Modernization and Regulatory Transparency Act, which would maintain state-based regulation of insurance but would affect state regulation of certain aspects of the insurance business, including rates, producer and company licensing, and market conduct examinations. We cannot predict whether this or other proposals will be adopted, or what impact, if any, such proposals or, if enacted, such laws may have on our business, financial condition or results of operations.
Risk Factors Relating to Our Common Stock
Directors and management could effectively control certain situations that may be viewed as contrary to your interests.
The extent of management’s control over the Company is related to the following factors:
| • | | Directors and management own approximately 25% of the Company’s outstanding stock as of December 31, 2006. |
34
| • | | The employee stock ownership plan (“ESOP”) owns 6.6%, or 747,500 shares, of the Company’s outstanding stock as of December 31, 2006. The shares held by the ESOP will be voted in the manner directed by the ESOP participants. |
| • | | We have implemented a stock compensation plan pursuant to which shares of restricted stock and stock options will be issued to certain of our directors, officers and employees. |
As a result of these factors, the company’s Directors and management could acquire, directly or indirectly, a substantial equity interest in the Company. If all members of management were to act together as a group, they could have a significant influence over the outcome of the election of directors and any other shareholder vote. Therefore, management might have the power to take actions that nonaffiliated shareholders may deem to be contrary to the shareholders’ best interests.
Provisions in our articles and bylaws and statutory provisions may serve to entrench management and also may discourage takeover attempts that you may believe are in your best interests.
We are subject to provisions of Pennsylvania corporate and insurance law that hinder a change of control. Pennsylvania law requires the Insurance Department’s prior approval of a change of control of an insurance holding company. Under Pennsylvania law, the acquisition of 10% or more of the outstanding capital stock of an insurer or its holding company is presumed to be a change in control. Approval by the Insurance Department may be withheld even if the transaction would be in the shareholders’ best interest if, among other things, the Insurance Department determines that the transaction would be detrimental to policyholders.
Our articles of incorporation and bylaws also contain provisions that may discourage a change in control. These provisions include:
| • | | the prohibition of ownership and voting of shares having in excess of 10% of the total voting power of the outstanding stock of the Company for a period of three years after the conversion; |
| • | | a classified Board of Directors divided into three classes serving for successive terms of three years each; |
| • | | a provision that the Board of Directors has the authority to issue shares of authorized but unissued common stock and preferred stock and to establish the terms of any one or more series of preferred stock, including voting rights, without additional shareholder approval; |
| • | | the prohibition of cumulative voting in the election of directors; |
| • | | the requirement that nominations for the election of directors made by shareholders and any shareholder proposals for inclusion on the agenda at any annual meeting must be made by notice (in writing) delivered or mailed to us not less than 90 days or more than 120 days prior to the meeting; |
| • | | the provision that, for a period of three years, any merger, consolidation, sale of assets or similar transaction involving the Company requires the affirmative vote of shareholders entitled to cast at least 66 2/3% of the votes which all shareholders are entitled to cast, unless the transaction is approved in advance by 66 2/3% of the members of the Board of Directors; |
| • | | the prohibition of shareholder action without a meeting and the prohibition of shareholders being able to call a special meeting; |
35
| • | | the requirement that certain provisions of our articles of incorporation can only be amended by an affirmative vote of shareholders entitled to cast at least 80% of all votes that shareholders are entitled to cast, unless approved by an affirmative vote of at least 80% of the members of the Board of Directors; and |
| • | | the requirement that certain provisions of our bylaws can only be amended by an affirmative vote of shareholders entitled to cast at least 66 2/3%, or in certain cases 80%, of all votes that shareholders are entitled to cast. |
These provisions may serve to entrench management and may discourage a takeover attempt that you may consider to be in your best interest or in which you would receive a substantial premium over the current market price. These provisions may make it extremely difficult for any one person or group of affiliated persons to acquire voting control of the Company, with the result that it may be extremely difficult to bring about a change in the Board of Directors or management. Some of these provisions also may perpetuate present management because of the additional time required to cause a change in the control of the board. Other provisions make it difficult for shareholders owning less than a majority of the voting stock to be able to elect even a single director.
Provisions of the Pennsylvania Business Corporation Law, which we refer to as the PBCL, that are applicable to publicly traded companies provide, among other things, that we may not engage in a business combination with an “interested shareholder” during the five-year period after the interested shareholder became such, except under certain specified circumstances. Under the PBCL an interested shareholder is generally a holder of 20% or more of our voting stock. The PBCL also contains provisions providing for the ability of shareholders to object to the acquisition by a person, or group of persons acting in concert, of 20% or more of our outstanding voting securities and to demand that they be paid a cash payment for the fair value of their shares from the controlling person or group.
If our insurance subsidiaries are not sufficiently profitable, our ability to pay dividends will be limited by regulatory restrictions.
Our domestic insurance subsidiaries’ ability to pay dividends to the Company is limited by the insurance laws and regulations of Pennsylvania. The maximum dividend that the domestic insurance entities may pay without prior approval from the Insurance Department is limited to the greater of 10% of statutory surplus or 100% of statutory net income for the most recently filed annual statement. In addition, EIHI and its subsidiaries are prohibited from declaring or paying any dividends or other forms of distribution for the three years after June 16, 2006, the effective date of the conversion/merger transaction, without the prior approval of the Pennsylvania Insurance Commissioner. Eastern Re must receive approval from the Cayman Islands Monetary Authority before it can pay any dividend to the Company.
Item 1B – Unresolved Staff Comments
Not applicable.
Item 2 – Properties
The Company’s corporate headquarters are located at 25 Race Avenue in Lancaster, Pennsylvania. The Company leases approximately 48,841 square feet of office space at this location under a 15-year lease entered into in February 2002. Monthly lease payments are subject to an annual increase based upon the consumer price index for the first five years and are subject to negotiation thereafter based on market conditions. The Company has a 5% interest in the limited partnership that owns the building.
36
Item 3 – Legal Proceedings
The Company is, from time to time, involved in legal proceedings that arise in the ordinary course of business. We believe we have sufficient loss reserves and reinsurance to cover claims under insurance policies issued by us. Although there can be no assurance as to the ultimate disposition of these matters, we do not believe, based upon the information available at this time, that any current pending legal proceedings, individually or in the aggregate, will have a material adverse effect on our business, financial condition, or results of operations.
Item 4 – Submission of Matters to a Vote of Security Holders
A special meeting of the shareholders (“Special Meeting”) of the Company was held on December 18, 2006. At the Special Meeting, the shareholders of the Company approved the Eastern Insurance Holdings, Inc. 2006 Stock Incentive Plan (“2006 Plan”). Eligible shareholders of the Company were entitled to cast 11,350,407 votes at the meeting. There were present at the Special Meeting, in person or by proxy, shareholders who were entitled to cast 8,368,239 votes, or 73.7% of the total number of votes which all shareholders were entitled to cast at the Special Meeting. Of the 8,368,239 votes cast, 7,578,632 voted for approval of the 2006 Plan, 758,158 voted against approval of the 2006 Plan and 31,449 withheld.
PART II
Item 5 – Market for Registrant’s Common Equity, Related Stockholder Matters and Issuer Purchases of Equity Securities
The no par value common stock trades on the NASDAQ National Market under the symbol “EIHI”. As of March 28, 2007, there were 665 registered holders of record of our common stock.
The Company does not currently pay a dividend. Any payment of dividends in the future on the common stock is subject to determination and declaration by the Company’s Board of Directors, who will take into consideration the Company’s financial condition, results of operations and future prospects. Additionally, the Company is prohibited from declaring or paying any dividends during the three years following the conversion/merger transaction, unless such dividends are approved by the Insurance Department.
Information regarding restrictions and limitations on the payment of cash dividends can be found in Item 7, “Management’s Discussion and Analysis of Financial Condition and Results of Operations” in the “Financial Condition, Liquidity and Capital Resources” section.
The table below sets forth the high and low sales prices of our common stock for each quarterly period as reported by the NASDAQ for the period from June 19, 2006 to December 31, 2006.
| | | | | | |
| | | Low | | High |
Period from June 19, 2006 to June 30, 2006 | | $ | 11.41 | | $ | 12.80 |
3rd quarter 2006 | | $ | 12.70 | | $ | 14.95 |
4th quarter 2006 | | $ | 14.01 | | $ | 15.02 |
Set forth below is a line graph comparing the dollar change in the cumulative total shareholder return on the Company’s common stock from June 19, 2006, the day in which trading commenced on the NASDAQ National Market, to December 31, 2006 as compared to the cumulative total return of the NASDAQ Composite Index and the cumulative total return of the SNL Insurance Underwriter Index. The chart depicts the value on December 31, 2006 of a $100 investment made on June 19, 2006.
37
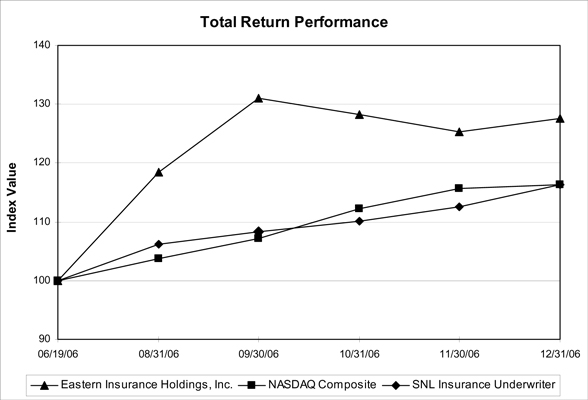
| | | | | | | | | | | | |
| | | Period Ending |
Index | | 06/19/06 | | 08/31/06 | | 09/30/06 | | 10/31/06 | | 11/30/06 | | 12/31/06 |
Eastern Insurance Holdings, Inc. | | 100.00 | | 118.40 | | 130.94 | | 128.31 | | 125.33 | | 127.61 |
NASDAQ Composite | | 100.00 | | 103.72 | | 107.22 | | 112.24 | | 115.61 | | 116.32 |
SNL Insurance Underwriter | | 100.00 | | 106.10 | | 108.25 | | 110.04 | | 112.50 | | 116.30 |
Note: The above results reflect the change in the Company’s stock price, based on the opening price of $11.40 per share on June 19, 2006. The offering price of the Company’s common stock was $10.00 per share.
Item 6 – Selected Financial Data
The following table sets forth selected historical financial information for the Company for the years ended and as of the dates indicated. This information comes from the Company’s consolidated financial statements. The information presented for the year ended December 31, 2006 includes the results of ELH for the entire year and the results of EIHI and EHC and its subsidiaries for the period from June 17, 2006 to December 31, 2006. The information presented as of December 31, 2005, 2004, 2003 and 2002 and for the years then ended represents the financial condition and results of operations of ELH for the respective periods. You should read the following selected financial information along with the information contained in this annual report, including Part II, Item 7 of this annual report entitled “Management’s Discussion and Analysis of Financial Condition and Results of Operations” and the consolidated financial statements and related notes and the reports of the independent registered public accounting firm included in Part II, Item 8 and elsewhere in this report. These historical results are not necessarily indicative of results to be expected from any future period.
38
| | | | | | | | | | | | | | | | | | | | |
| | | At or for the Years Ended December 31, | |
| | | 2006 | | | 2005 | | | 2004 | | | 2003 | | | 2002 | |
Income Statement Data: | | | | | | | | | | | | | | | | | | | | |
Direct premiums written | | $ | 75,011 | | | $ | 40,994 | | | $ | 40,790 | | | $ | 43,911 | | | $ | 98,139 | |
Reinsurance premiums assumed | | | 17,836 | | | | — | | | | — | | | | — | | | | — | |
Net premiums written | | | 67,529 | | | | 38,700 | | | | 39,070 | | | | 41,678 | | | | 94,863 | |
| | | | | |
Net premiums earned | | $ | 74,919 | | | $ | 38,702 | | | $ | 39,057 | | | $ | 41,714 | | | $ | 94,875 | |
Investment income, net of expenses | | | 8,992 | | | | 3,815 | | | | 3,724 | | | | 4,361 | | | | 5,645 | |
Net realized investment gains | | | 2,757 | | | | 445 | | | | 1,271 | | | | 662 | | | | 461 | |
Other revenue | | | 313 | | | | 1,066 | | | | 946 | | | | 978 | | | | 230 | |
| | | | | | | | | | | | | | | | | | | | |
Total revenue | | $ | 86,981 | | | $ | 44,028 | | | $ | 44,998 | | | $ | 47,715 | | | $ | 101,211 | |
| | | | | | | | | | | | | | | | | | | | |
Expenses: | | | | | | | | | | | | | | | | | | | | |
Losses and loss adjustment expenses incurred | | $ | 47,913 | | | $ | 27,090 | | | $ | 25,932 | | | $ | 25,379 | | | $ | 75,899 | |
Acquisition and other underwriting expenses | | | 5,941 | | | | 5,452 | | | | 5,670 | | | | 5,575 | | | | 9,855 | |
Other expenses | | | 15,690 | | | | 9,674 | | | | 10,601 | | | | 14,615 | | | | 18,748 | |
Amortization of intangibles | | | 1,088 | | | | — | | | | — | | | | — | | | | — | |
Policyholder dividend expense | | | 239 | | | | — | | | | — | | | | — | | | | — | |
Segregated portfolio dividend expense (1) | | | 2,890 | | | | — | | | | — | | | | — | | | | — | |
| | | | | | | | | | | | | | | | | | | | |
Total expenses | | $ | 73,761 | | | $ | 42,216 | | | $ | 42,203 | | | $ | 45,569 | | | $ | 104,502 | |
| | | | | | | | | | | | | | | | | | | | |
Income (loss) before income taxes | | $ | 13,220 | | | $ | 1,812 | | | $ | 2,795 | | | $ | 2,146 | | | $ | (3,291 | ) |
Income taxes (benefit) | | | 4,942 | | | | 685 | | | | 1,012 | | | | 709 | | | | (1,061 | ) |
| | | | | | | | | | | | | | | | | | | | |
Net income (loss) | | $ | 8,278 | | | $ | 1,127 | | | $ | 1,783 | | | $ | 1,437 | | | $ | (2,230 | ) |
| | | | | | | | | | | | | | | | | | | | |
Selected Balance Sheet Data (at period end): | | | | | | | | | | | | | | | | | | | | |
Total investments and cash | | $ | 288,288 | | | $ | 82,319 | | | $ | 85,168 | | | $ | 85,252 | | | $ | 92,796 | |
Total assets | | | 368,206 | | | | 111,225 | | | | 111,673 | | | | 113,854 | | | | 123,520 | |
Reserves for unpaid losses and loss adjustment expenses | | | 126,467 | | | | 44,137 | | | | 43,384 | | | | 46,026 | | | | 55,139 | |
Unearned premiums | | | 34,599 | | | | 95 | | | | 98 | | | | 88 | | | | 122 | |
Total liabilities | | | 194,462 | | | | 49,116 | | | | 49,132 | | | | 51,498 | | | | 62,367 | |
Total equity | | | 173,744 | | | | 62,109 | | | | 62,541 | | | | 62,355 | | | | 61,154 | |
| | | | | |
U.S. GAAP Ratios: | | | | | | | | | | | | | | | | | | | | |
Loss ratio (2) | | | 64.0 | % | | | 70.0 | % | | | 66.4 | % | | | 60.8 | % | | | 80.0 | % |
Expense ratio (3) | | | 34.5 | % | | | 39.1 | % | | | 41.7 | % | | | 48.4 | % | | | 30.1 | % |
Combined ratio (4) | | | 98.5 | % | | | 109.1 | % | | | 108.1 | % | | | 109.2 | % | | | 110.1 | % |
| | | | | |
Per-share Data: | | | | | | | | | | | | | | | | | | | | |
Basic earnings per share | | $ | 0.67 | | | | N/A | | | | N/A | | | | N/A | | | | N/A | |
Diluted earnings per share | | $ | 0.65 | | | | N/A | | | | N/A | | | | N/A | | | | N/A | |
| | | | | |
Weighted Average Shares: | | | | | | | | | | | | | | | | | | | | |
Basic | | | 10,623,182 | | | | N/A | | | | N/A | | | | N/A | | | | N/A | |
Diluted | | | 10,929,281 | | | | N/A | | | | N/A | | | | N/A | | | | N/A | |
| (1) | The segregated portfolio dividend expense represents the change in accrual for the dividend that may be payable to the segregated portfolio dividend participants. |
| (2) | Calculated by dividing losses and loss adjustment expenses incurred by net premiums earned. |
| (3) | Calculated by dividing the sum of acquisition and other underwriting expenses, other expenses, amortization of intangibles, policyholder dividend expense, and segregated portfolio dividend expense by net premiums earned. |
| (4) | The sum of the loss and loss adjustment expense ratio and expense ratio. |
Item 7 – Management’s Discussion and Analysis of Financial Condition and Results of Operations
Overview
The Company is an insurance holding company offering workers’ compensation and group benefits insurance products and reinsurance products through its wholly-owned subsidiaries. As a result of the acquisition of EHC on June 16, 2006, the Company’s consolidated results of operations for the year ended December 31, 2006 include the results of operations of the Company’s workers’ compensation insurance, segregated portfolio cell reinsurance, and specialty reinsurance segments from June 17, 2006 to December 31, 2006 and the results of operations of the Company’s group benefits insurance segment for the year ended December 31, 2006. The Company’s results of operations for the year ended December 31, 2005 represent the results of operations of the Company’s group benefits insurance segment and ELH’s former general agency operations segment, which is included in corporate/other. The corporate/other segment for the year ended December 31, 2006 includes the results of operations of Employers Alliance, EIHI, Eastern Holding Company, Ltd., Eastern Services, and Global Alliance from June 17, 2006 to December 31, 2006 and the results of operations of ELH’s corporate activity and group medical run-off operations for the year ended December 31, 2006.
39
Marketplace Conditions and Trends
Workers’ Compensation Insurance.The property and casualty insurance industry is affected by recurring industry cycles known as “hard” and “soft” markets. Since EAIG began operations in 1997 and continuing into 2001, EAIG operated in a soft market cycle, which is generally considered an adverse industry cycle in the property and casualty insurance industry. A soft cycle is characterized by intense competition resulting in lower pricing and increased commissions paid to distribution sources in order to compete for business. Management believes that a hard market began in 2001. A hard market, generally considered a beneficial industry trend, is characterized by reduced competition that results in higher pricing and lower commissions paid to acquire business. The hard market conditions significantly intensified after the September 11, 2001 terrorist attacks. Management believes that a soft market commenced in 2005, as evidenced by increased competition. During 2006, the workers’ compensation insurance segment experienced renewal rate decreases of 6.1%.
Although 2001 signified the beginning of the hard market, it also was the beginning of an economic downturn. The economic downturn increased unemployment, which generally has a negative impact on workers’ compensation loss results. The two components of a worker’s compensation claim are medical and indemnity. The medical component of a claim is the amount paid to treat work-related injuries, while the indemnity portion of a claim is the amount of lost time wages that are paid to an employee as a result of work absenteeism related to an injury that was sustained while operating in the scope of employment. In a favorable economy, an employer may have a better chance of offering an injured worker modified duty, relieving the workers’ compensation insurer of some or all of the indemnity exposure. If an employer is unable to take an injured employee back to work or offer modified duty positions, the indemnity portion of the workers’ compensation claim will result an increased expense to the insurer.
Segregated Portfolio Cell Reinsurance. Workers’ compensation insurance business that is assumed by the segregated portfolio cells of Eastern Re is underwritten by EAIG through its alternative markets business unit and ceded 100% to the respective segregated portfolio cell. Market conditions and trends are substantially the same as those noted in the workers’ compensation insurance segment above.
Group Benefits Insurance.The group benefits insurance market is highly competitive. The Company has experienced significant price competition from other carriers, which can be attributed to a number of factors including, but not limited to, new carriers which enter markets with lower prices to gain market share and financially larger carriers that are able to compete on price. In addition to price, the group benefits insurance market is highly competitive with respect to new products and/or new features for existing products. The competitiveness of the marketplace has a significant impact on the Company’s ability to generate new sales as well as retain existing business. The Company continuously monitors its key markets with respect to price and products through active discussions with its independent producers. In addition, the Company enhanced its renewal process by proactively working with its independent producers to retain business which management considers to be favorable.
Specialty Reinsurance. Eastern Re participates as a reinsurer in quota share reinsurance treaties with a large primary insurer in the EnviroGuard and EIA programs. Both products are specialty niche products that have minimal marketplace information.
Principal Revenue and Expense Items
The Company derives its revenue primarily from net premiums earned, including assumed premiums earned, net investment income and net realized investment gains.
Direct and net premiums written. Direct premiums written is the sum of both direct premiums and assumed premiums before the effect of ceded reinsurance. Net premiums written is the difference between direct premiums written and premiums ceded or paid to reinsurers (ceded premiums written). In the specialty reinsurance segment, assumed premiums are premiums that are received from another company under a reinsurance agreement, which are reported to the Company directly from the broker on a quarterly basis. In the segregated portfolio cell reinsurance segment, assumed premiums are derived from insurance contracts written by EAIG and ceded to the segregated portfolio cells at Eastern Re.
40
Net premiums earned.Net premiums earned are the earned portion of the Company’s net premiums written. Direct premiums written include all premiums billed during a specified policy period.
Premiums are earned over the term of the related policies. At the end of each accounting period, the portion of the premiums that are not yet earned are included in unearned premiums and are realized as revenue in subsequent periods over the remaining term of the policy. The Company’s workers’ compensation policies typically have a term of twelve months. Thus, for example, for a policy that is written on July 1, 2006, one-half of the premiums would be earned in 2006 and the other half would be earned in 2007. Workers’ compensation premiums are determined based upon the payroll of the insured, the applicable premium rates and, where applicable, an experience based modification factor. An audit of the policyholders’ records is conducted after policy expiration, to make a final determination of applicable premiums. Included with net premiums earned is an estimate for earned but unbilled final audit premiums. The Company can estimate earned but unbilled premiums because it keeps track, by policy, of how much additional premium is billed in final audit invoices as a percentage to estimate the probable additional amount that it has earned but not yet billed as of the balance sheet date. The majority of the Company’s group benefits insurance policies are billed on a monthly basis with premiums being earned in the month in which coverage is provided. As a result, there is minimal unearned premium related to the group benefits insurance policies as of the balance sheet date.
Net investment income and realized gains and losses on investments. The Company invests its surplus and the funds supporting its insurance liabilities (including unearned premiums and unpaid losses and loss adjustment expenses) in cash, cash equivalents, fixed income securities, equity securities, and other long-term investments. Investment income includes interest earned on invested assets. Realized gains and losses on invested assets are reported separately from net investment income. The Company recognizes realized gains when invested assets are sold for an amount greater than their cost or amortized cost (in the case of fixed income securities) and recognizes realized losses when investment securities are written down as a result of an other than temporary impairment or sold for an amount less than their cost or amortized cost.
Other revenue. Other revenue includes claim administration and risk management fees earned by Employers Alliance and cell rental fees earned by the specialty reinsurance segment. There are other revenue items that the Company recognizes on a segmental basis that are eliminated in consolidation. Such items consist primarily of fees paid by the segregated portfolio cells to other entities within the consolidated group. The segregated portfolio cells recognize an expense for such items (included as part of its ceding commission) and a corresponding revenue item is recognized by the affiliate providing the service. For segment reporting purposes, such revenue items primarily include fronting fees paid by the segregated portfolio cells to EAIG, claims administration and risk management fees paid by the segregated portfolio cells to Employers Alliance and cell rental fees paid by the segregated portfolio cells to Eastern Re. For segment reporting purposes, such fees are recognized ratably over the period in which the service is provided, which generally corresponds to the earned portion of net premiums written for the underlying policies.
The Company’s expenses consist primarily of:
Losses and loss adjustment expenses.Losses and loss adjustment expenses represent the largest expense item and include: (1) claim payments made, (2) estimates for future claim payments and changes in those estimates for prior periods, and (3) costs associated with investigating, defending and adjusting claims.
Acquisition and other underwriting expenses.In the workers’ compensation and group benefits insurance segments, expenses incurred to underwrite risks are referred to as acquisition and other underwriting expenses, which consist of commission expenses, premium taxes and fees and other underwriting expenses incurred in acquiring, writing and administering the Company’s business as well as required payments to the Pennsylvania Workers’ Compensation Security Fund (the “Security Fund”). The Security Fund assesses workers’ compensation insurers doing business in Pennsylvania for the purpose of providing funds to cover obligations to policyholders of insolvent insurance companies. In the specialty reinsurance and segregated portfolio cell reinsurance segments, acquisition and other underwriting expenses consist of ceding commissions earned under the respective reinsurance agreements. Ceding commissions received by EAIG are netted against other underwriting expenses.
41
Other expenses.Other expenses consist of general administrative expenses such as salaries, rent, office supplies, depreciation and all other operating expenses not otherwise classified separately. Other expenses also include interest expense related primarily to the Company’s junior subordinated debt.
Income tax expense. EIHI and certain of its subsidiaries pay federal, state and local income taxes. Income tax expense includes an amount for both current and deferred income taxes. Current income tax expense includes an amount for the Company’s current year federal income tax liability and any adjustments related to differences between the prior year federal income tax estimate and the actual income tax expense reported in the tax return. Deferred tax expense represents the change in the Company’s net deferred tax asset, exclusive of the tax effect related to changes in unrealized gains and losses in the Company’s investment portfolio and changes in the unrecognized amounts related to the Company’s benefit plan liabilities.
Key Financial Measures
The Company evaluates its insurance operations by monitoring certain key measures of growth and profitability. The Company measures growth by monitoring changes in direct premiums written and net premiums written. The Company measures underwriting profitability by examining loss, expense and combined ratios. On a segmental basis, the Company measures a segment’s operating results by examining net income and return on average equity.
Loss ratio.The loss ratio is the ratio (expressed as a percentage) of losses and loss adjustment expenses incurred to net premiums earned and measures the underwriting profitability of a company’s insurance business. The Company measures the loss ratio on an accident year and calendar year loss basis to measure underwriting profitability. An accident year loss ratio measures losses and loss adjustment expenses for insured events occurring in a particular year, regardless of when they are reported, as a percentage of net premiums earned during that year. A calendar year loss ratio measures losses and loss adjustment expenses for insured events occurring during a particular year and the change in loss reserves from prior accident years as a percentage of net premiums earned during that year.
Expense ratio. The expense ratio is the ratio (expressed as a percentage) equal to the sum of the acquisition and other underwriting expenses and other expenses to net premiums earned, and measures the Company’s operational efficiency in producing, underwriting and administering its insurance business.
Combined ratio.The combined ratio is the sum of the loss ratio and the expense ratio and measures the Company’s overall underwriting profit. If the combined ratio is below 100%, the Company is making an underwriting profit. If the Company’s combined ratio is at or above 100%, the Company is not profitable without investment income and may not be profitable if investment income is insufficient.
Net premiums written to statutory surplus ratio.The net premiums written to statutory surplus ratio represents the ratio of net premiums written to statutory surplus. This ratio measures the Company’s insurance subsidiaries exposure to pricing errors in its current book of business. The higher the ratio, the greater the impact on surplus should pricing prove inadequate.
Net income and return on average equity.The Company uses net income to measure its profits and return on average equity to measure its effectiveness in utilizing shareholders’ equity to generate net income. In determining return on average equity for a given year, net income is divided by the average of the beginning and ending shareholders’ equity for that year.
Critical Accounting Policies and Estimates
The preparation of financial statements in accordance with U.S. GAAP requires both the use of estimates and judgment relative to the application of appropriate accounting policies. The Company is required to make estimates and assumptions in certain circumstances that affect amounts reported in the consolidated financial statements and related footnotes. The Company evaluates these estimates and assumptions on an
42
on-going basis based on historical developments, market conditions, industry trends and other information that is believed to be reasonable under the circumstances. There can be no assurance that actual results will conform to the estimates and assumptions and that reported results of operations will not be materially adversely affected by the need to make accounting adjustments to reflect changes in these estimates and assumptions from time to time. The Company believes the following policies are the most sensitive to estimates and judgments.
Reserves for Unpaid Losses and Loss Adjustment Expenses
The Company establishes reserves for unpaid losses and LAE for its workers’ compensation, segregated portfolio cell reinsurance, group benefits insurance, and specialty reinsurance products, which are estimates of future payments of reported and unreported claims for losses and related expenses. The adequacy of the Company’s reserves for unpaid losses and LAE are inherently uncertain because the ultimate amount that the Company may pay under many of the claims incurred as of the balance sheet date will not be known for many years. Establishing reserves continues to be a complex and imprecise process, requiring the use of informed estimates and judgments. The Company’s estimates and judgments may be revised as additional experience and other data becomes available and are reviewed, as new or improved methodologies are developed, or as current laws change. Any such revisions could result in future changes in estimates of losses or reinsurance recoverables and would be reflected in the Company’s results of operations in the period in which the estimates are changed. Estimating the ultimate claims liability is necessarily a complex and judgmental process inasmuch as the amounts are based on management’s informed estimates and judgments using data currently available. If ultimate losses, net of reinsurance, prove to be substantially higher than the amounts recorded as of December 31, 2006, the related adjustments could have a material adverse effect on the Company’s financial condition, results of operations or liquidity.
Workers’ Compensation Insurance
On a quarterly basis, the Company prepares actuarial analyses to assess the reasonableness of the recorded reserves for unpaid losses and LAE in its workers’ compensation insurance segment. These actuarial analyses incorporate various methodologies, including paid loss development, incurred loss development and a combination of other actuarial methodologies that incorporate characteristics of incurred and paid methodologies combined with a review of the Company’s exposure base. The recorded amount in each accident year is then compared to the results of these methodologies, with consideration being given to the age of the accident year. As accident years mature, the various methodologies generally produce consistent loss estimates. For more recent accident years, the methodologies produce results that are not as consistent. Accordingly, more emphasis is placed on supplementing the methodologies in more recent accident years with trends in exposure base, medical expense inflation, general inflation, severity, and claim counts, among other things.
The Company’s reserves for unpaid losses and LAE in its workers’ compensation insurance segment as of December 31, 2006 are summarized below (in thousands):
| | | | |
| | | Workers’
Compensation
Insurance | |
Case reserves | | $ | 18,057 | |
Case incurred development, IBNR and unallocated loss adjustment expense reserves | | | 25,910 | |
Amount of discount | | | (2,183 | ) |
| | | | |
Net reserves before reinsurance recoverables and purchase accounting | | | 41,784 | |
Reinsurance recoverables on unpaid losses and LAE | | | 1,475 | |
Purchase accounting adjustments | | | 1,699 | |
| | | | |
Reserves for unpaid losses and LAE | | $ | 44,958 | |
| | | | |
In its workers’ compensation segment, the Company records reserves for estimated losses under insurance policies and for loss adjustment expenses related to the investigation and settlement of policy claims. The Company’s reserves for unpaid losses and LAE represent the estimated cost of reported and unreported losses and LAE incurred and unpaid at a given point in time. In establishing its workers’ compensation
43
reserves, the Company uses loss discounting, which involves recognizing the time value of money and offsetting estimates of future payments by future expected investment income. For claims reported in the workers’ compensation insurance and segregated portfolio cell reinsurance segments, claims are administered by Employers Alliance.
When a claim is reported, the Company’s claims adjusters establish a case reserve, which consists of anticipated medical costs, indemnity costs and certain defense and cost containment expenses that the Company refers to as allocated loss adjustment expenses, or ALAE. At any point in time, the amount paid on a claim, plus the case reserve for future amounts to be paid, represents the claims adjuster’s estimate at that time of the total cost of the claim, or the case incurred amount. The case reserve for each reported claim is based upon various factors, including:
| | • | | severity of the injury or damage; |
| | • | | age and occupation of the injured employee; |
| | • | | estimated length of temporary disability; |
| | • | | anticipated permanent disability; |
| | • | | expected medical procedures, costs and duration; |
| | • | | knowledge of the circumstances surrounding the claim; |
| | • | | insurance policy provisions, including coverage, related to the claim; |
| | • | | jurisdiction of the occurrence; and |
| | • | | other benefits defined by applicable statute. |
The case incurred amount can vary over time due to changes in expectations with respect to medical treatment and outcome, length and degree of disability, employment availability and wage levels and judicial determinations. As changes occur, the case incurred amount is adjusted. The initial estimate of the case incurred amount can vary significantly from the amount ultimately paid, especially in circumstances involving severe injuries with comprehensive medical treatment. Changes in case incurred amounts, or case incurred development, is an important component of the Company’s historical claim data.
In addition to case reserves, the Company establishes loss and ALAE reserves on an aggregate basis for case incurred development and IBNR claims. Case incurred development and IBNR reserves are primarily intended to provide for aggregate changes in preexisting case incurred amounts and, secondarily, as the unpaid cost of IBNR claims for which an initial case reserve has not been established.
The third component of the Company’s reserves for unpaid losses and LAE is unallocated loss adjustment expense, or ULAE. The Company’s ULAE reserve is established for the costs of future unallocated loss adjustment expenses for known and unknown claims. The Company’s ULAE reserve covers primarily the estimated cost of administering claims.
In estimating case incurred development and IBNR reserves, the Company performs most of its detailed analysis on a net of reinsurance basis, and then considers expected recoveries in arriving at its recorded amounts for unpaid losses and LAE. To estimate such reserves, the Company relies primarily on the analysis of claims in its 10-year workers’ compensation insurance history. Using standard actuarial methods, the Company estimates reserves based on historical patterns of case development, payment patterns, mix of business, premium rates charged, case reserving adequacy, operational changes, adjustment philosophy and severity and duration trends. However, the number of variables and judgments involved in establishing reserve estimates, combined with some random variation in loss development patterns, results in uncertainty regarding projected ultimate losses. As a result, the Company’s ultimate liability for losses and LAE may be more or less than its reserve estimate.
44
To estimate reserves, the Company stratifies its data using variations of the following different categorizations of claims:
| | • | | All loss and loss adjustment expense data developed together; |
| | • | | Lost time claims developed independently; |
| | • | | Medical only claims developed independently; |
| | • | | The indemnity portion of lost time claims developed independently; |
| | • | | The medical portion of a lost time claim and medical only claims developed together; and |
| | • | | Loss adjustment expenses developed independently. |
The term “developed together” refers to the summation of the claims data for a particular data stratification. For example, “All loss and loss adjustment expense data developed together” represents all loss and loss adjustment expense data of the Company, regardless of medical, indemnity or expense components, developed together using the historical data for this particular data stratification. The term “developed independently” refers to a specific data element. For example, “The indemnity portion of lost time claims developed independently” represents the development of the indemnity portion of a claim separately using historical data for this particular type of claim. Developing claims using different data stratifications allows the Company to identify trends for a specific group of claims that would not necessarily be readily identifiable if the data were included with other types of claim information. For example, developing the medical portion of a claim separately may allow the Company to identify a medical inflation trend that may not have been evident if it had been included with indemnity claim information. The combination of the different data stratifications and standard actuarial methods, including the following, produce different actuarial indications for the Company to evaluate:
Incurred Loss Development Method. The incurred (case incurred) loss development method relies on the assumption that, at any given state of maturity, ultimate losses can be predicted by multiplying cumulative reported losses (paid losses plus case reserves) by a cumulative development factor. The validity of the results of this method depends on the stability of claim reporting and settlement rates, as well as the consistency of case reserve levels. Case reserves do not have to be adequately stated for this method to be effective; they only need to have a fairly consistent level of adequacy at all stages of maturity. “Age-to-age” loss development factors (“LDFs”) are calculated to measure the relative development of an accident year from one maturity point to the next.
Paid Loss Development Method. The paid loss development method is mechanically identical to the incurred loss development method described above. The paid method does not rely on case reserves or claim reporting patterns in making projections. The validity of the results from using a paid loss development approach can be affected by many conditions, such as internal claim department processing changes, legal changes or variations in a company’s mix of business from one year to the next. Also, since the percentage of losses paid for immature years is often low, development factors are more volatile. A small variation in the number of claims paid can have a leveraging effect that can lead to significant changes in estimated ultimate liability for losses and loss adjustment expenses. Therefore, ultimate values for immature accident years are often based on alternative estimation techniques.
Bornhuetter-Ferguson Methodology. The Bornhuetter-Ferguson expected loss projection method based on reported loss data relies on the assumption that remaining unreported losses are a function of the total expected ultimate losses rather than a function of the currently reported losses. The expected ultimate losses in this analysis are based on historical results, adjusted for known pricing changes and inflationary trends. The expected ultimate losses are multiplied by the unreported percentage to
45
produce expected unreported losses. The unreported percentage is calculated as one minus the reciprocal of the selected cumulative incurred LDFs. Finally, the unreported losses are added to the current reported losses to produce ultimate losses. The Bornhuetter-Ferguson method is most useful as an alternative to other models for immature accident years. For these immature accident years, the amounts reported or paid may be small and unstable and therefore not predictive of future development. Therefore, future development is assumed to follow an expected pattern that is supported by more stable historical data or by emerging trends. This method is also useful when changing reporting patterns distort historical development of losses.
The Bornhuetter-Ferguson method can also be applied with paid losses.
In estimating ULAE reserves, the Company reviews past adjustment expenses in relation to paid claims and estimated future costs based on expected claims activity and duration. The sum of the Company’s net loss and ALAE reserve, and ULAE reserves is its total net reserve for unpaid losses and LAE.
In determining management’s best estimate, the Company considers the various accident year loss indications produced by the actuarial methods. Considering the results of the methods, the inherent strengths and weaknesses of each method as described above, as well as other statistical information such as ultimate loss ratios, ultimate loss to exposure ratios and average ultimate claim values, the Company determines and records its best estimate of unpaid losses and ALAE. Management believes its best estimate of recorded reserves for unpaid losses and LAE is representative of the inherent uncertainty surrounding reserving for a long-tail line of business such as workers’ compensation as well as the relative immature accident year historical experience of its workers’ compensation insurance segment, which completed its first full year of operations in 1998.
As of December 31, 2006, the Company’s best estimate of its ultimate liability for losses and LAE, net of amounts recoverable from reinsurers and before purchase accounting adjustments, for its workers’ compensation insurance segment was $41.8 million. This amount was determined based on methods which were viewed to be better predictors than other methods.
Given the long reporting and paid development patterns, the tail factors used to project actual current losses to ultimate losses for claims covered by the Company’s workers’ compensation policies require considerable judgment. Management believes that its selected tail factors represent the most likely loss development based on historical loss payment patterns as well as the current legal and economic environment. The actual tail factor could vary from the tail factor selected. Following is a sensitivity analysis of the Company’s workers’ compensation reserves to reasonably likely changes in the tail factors used to project actual current losses to ultimate losses (dollars in thousands):
| | | | | | | | | | | |
Change in Tail Factor Assumption | | Increase (Decrease)
in Net Reserves | | | Impact on Net
Income | | | Percentage of
Shareholders’
Equity | |
20 basis point increase | | $ | 2,277 | | | $ | (1,480 | ) | | -0.9 | % |
10 basis point increase | | $ | 1,145 | | | $ | (744 | ) | | -0.4 | % |
10 basis point decrease | | $ | (1,157 | ) | | $ | 752 | | | 0.4 | % |
20 basis point decrease | | $ | (2,327 | ) | | $ | 1,513 | | | 0.9 | % |
The estimates above rely on substantial judgment. There is inherent uncertainty in estimating reserves for unpaid losses and LAE. It is possible that the actual losses and loss adjustment expenses incurred may vary significantly from the Company’s estimates.
Segregated Portfolio Cell Reinsurance
The Company’s reserves for unpaid losses and LAE in its segregated portfolio cell reinsurance segment as of December 31, 2006 are summarized below (in thousands):
46
| | | | |
| | | Segregated
Portfolio Cell
Reinsurance | |
Case reserves | | $ | 8,216 | |
Case incurred development, IBNR and unallocated loss adjustment expense reserves | | | 13,992 | |
Amount of discount | | | (1,125 | ) |
| | | | |
Net reserves before reinsurance recoverables and purchase accounting | | | 21,083 | |
Reinsurance recoverables on unpaid losses and LAE | | | 2,893 | |
Purchase accounting adjustments | | | (97 | ) |
| | | | |
Reserves for unpaid losses and loss adjustment expenses | | $ | 23,879 | |
| | | | |
The Company estimates and records reserves for its segregated portfolio cell reinsurance segment in the same manner as for its workers’ compensation insurance segment.
The reporting and paid loss development patterns in the segregated portfolio cell reinsurance segment are also consistent with that of the workers’ compensation insurance segment. Accordingly, the tail factors used to project actual current losses to ultimate losses for claims covered in the Company’s segregated portfolio cell reinsurance segment require considerable judgment. The difference between total revenue for the segregated portfolio cell reinsurance segment for each period and the sum of losses and loss adjustment expenses, underwriting expenses, policyholder dividend expenses and other expenses is accrued as a segregated portfolio dividend expense. Accordingly, any change in the reserve for unpaid losses and LAE is recorded to the segregated portfolio dividend payable / receivable account and would only impact the Company’s net income or shareholders’ equity if it were a segregated portfolio cell dividend participant.
Group Benefits
The reserves for unpaid losses and LAE includes an estimate of future amounts for reported but unpaid and IBNR claims related to the Company’s dental, long-term disability, short-term disability and term life products, as well as an estimate of the costs associated with investigating, processing and paying the related claims.
The Company utilizes a number of methodologies, explained below, to estimate its reserves for unpaid losses in its group benefits insurance segment. These methods include the lag factor development, loss ratio, and tabular reserve methods.
Lag Factor Development Method. The lag factor development method is used to estimate the reserve for insurance products that are “short-tail” by nature, in which claims related to the products are settled shortly after they are reported by the insured. The method uses historical paid claims data to estimate the reserve for claims in the course of settlement (reported claims) and IBNR claims. The method involves the use of a claim model, or a loss triangle, in which paid claims data is aggregated into categories based on the dates on which the claims in question were incurred and paid. Data in the loss triangle is reviewed to evaluate historical claim payment patterns. A point estimate is then determined based on the historical claim payment patterns.
Loss Ratio Method. The loss ratio method involves the use of historical loss ratios to estimate the reserve for unpaid claims and claims payable. Under the loss ratio method, the reserve is determined by multiplying the selected loss ratio, which is based on historical loss ratio trends, by the amount of net earned premium or the in-force premium at the valuation date.
Tabular Reserve Method. The tabular reserve method is used to estimate the reserve for insurance products that are longer tail by nature and for which the claim payment patterns are relatively predictable. Under the tabular reserve method, the reserve for reported but unpaid claims is estimated using industry-standard valuation tables (for long-term disability claims, the Company uses the 1987 Commissioners Group Disability Table; for life premium waiver claims, the Company uses the 1970 Intercompany Group Life Disability Table). These tables incorporate expected death and recovery rate assumptions (based on an insured’s age and length of disability) that impact the reserve for unpaid claims.
The Company’s reserves for unpaid losses and LAE in its group benefits insurance segment, by line business, as of December 31, 2006 and 2005, were as follows (in thousands):
| | | | | | |
| | | 2006 | | 2005 |
Dental | | $ | 1,634 | | $ | 1,976 |
Short-term disability | | | 1,141 | | | 1,155 |
Long-term disability | | | 9,210 | | | 10,511 |
Term life | | | 5,310 | | | 6,115 |
Other | | | 245 | | | 256 |
| | | | | | |
Net reserves for unpaid losses and LAE | | | 17,540 | | | 20,013 |
Reinsurance recoverable on unpaid losses and LAE | | | 20,289 | | | 24,123 |
| | | | | | |
Reserves for unpaid losses and LAE | | $ | 37,829 | | $ | 44,136 |
| | | | | | |
47
Dental Reserves
The dental reserves represent the Company’s estimate of future amounts due on in-process and IBNR dental claims. The Company estimates its dental reserves using a combination of the lag factor development method and the loss ratio method, which results in the development of a point estimate. The loss ratio method is applied to the last three months (or most recent quarter), based on recent loss ratio trends. The Company’s reserving methodology takes into consideration the immaturity of the most recent quarter’s paid claim runout. Therefore, the recorded dental reserve represents a point estimate plus an amount for adverse development, equal to 10% of the point estimate. The most significant assumptions used in estimating the dental reserves include the selection of claim completion factors and ultimate loss ratios. Completion factors are selected based on the average for the past twelve months and are applied to all periods prior to the most recent three months. An ultimate loss ratio is applied to the most recent three months based on recent trends. Due to the small size of the Company’s dental block of business, the ultimate loss ratios on a monthly basis can be quite volatile. The Company evaluated the impact to its recorded dental reserves by adjusting the loss ratios for the most recent three months by 100, 200 and 300 basis points above and below the selected loss ratios. The results of this analysis are shown in the table below (dollars in thousands):
| | | | | | | | | |
| | | Net Increase
(Decrease)
in Reserves | | Impact on
Net Income | | Percentage of
Shareholders’
Equity | |
300 basis point increase | | $ | 171 | | $ | (111) | | -0.1 | % |
200 basis point increase | | $ | 113 | | $ | (73) | | 0.0 | % |
100 basis point increase | | $ | 57 | | $ | (37) | | 0.0 | % |
100 basis point increase | | $ | (56) | | $ | 36 | | 0.0 | % |
200 basis point increase | | $ | (113) | | $ | 113 | | 0.0 | % |
300 basis point increase | | $ | (171) | | $ | 111 | | 0.1 | % |
Short-Term Disability Reserves
The short-term disability reserves represent the Company’s estimate of future amounts due on in-process and IBNR short-term disability claims. The short-term disability reserve is determined using the lag factor development method, which results in the calculation of a point estimate. The inherent limitation of the lag factor development method is that the more recent incurral periods are relatively immature and the historical claim payment patterns may not be representative of the most recent claim experience. The Company takes this into consideration in its reserving process; therefore, the recorded short-term disability reserve represents the point estimate plus an amount for adverse development, equal to 10% of the point estimate. For the most recent incurral months, which usually consist of the last three months, the reserve is estimated by applying a loss ratio to the respective months’ net premiums earned. The most significant assumptions used in estimating the short-term disability reserve include the selection of claim completion factors and ultimate loss ratios. Completion factors are selected based on the average for the past twelve months and are applied to all periods prior to the most recent three months. An ultimate loss ratio is applied to the most recent three months based on recent trends. Due to the small size of the Company’s short-term disability block of business, the ultimate loss ratios on a monthly basis can be quite volatile. The Company evaluated the impact to its recorded short-term disability reserves by adjusting the loss ratios for the most recent three months by 100, 200 and 300 basis points above and below the selected loss ratios. The results of this analysis are shown in the table below (dollars in thousands):
| | | | | | | | | |
| | | Net Increase
(Decrease)
in Reserves | | Impact on
Net Income | | Percentage of
Shareholders’
Equity | |
300 basis point increase | | $ | 58 | | $ | (37) | | 0.0 | % |
200 basis point increase | | $ | 38 | | $ | (25) | | 0.0 | % |
100 basis point increase | | $ | 20 | | $ | (13) | | 0.0 | % |
100 basis point increase | | $ | (20) | | $ | 13 | | 0.0 | % |
200 basis point increase | | $ | (39) | | $ | 25 | | 0.0 | % |
300 basis point increase | | $ | (59) | | $ | 38 | | 0.0 | % |
Long-Term Disability Reserves
The long-term disability tabular reserve represents the Company’s estimate of future amounts due on reported long-term disability claims. The Company establishes a reserve at the time a long-term disability claim is reported using the 1987 Commissioners Group Disability Table. Due to the long-term nature of long-term disability claims, management discounts the liability using an interest rate that reflects the estimated investment return in the Company’s group benefits insurance segment that will be earned over the expected life of the claim. In establishing the discount rate, the Company’s management evaluates the current interest rate environment at the end of each year and, if necessary, adjusts the interest rate for the following year based on the expected rate of return on new investments. The discount rates for claims incurred in 2006, 2005 and 2004 were 4.75%, 4.25%, and 3.09%, respectively. A lower discount rate results in a higher claim reserve and an increase in losses and loss adjustment expenses, whereas a higher discount rate results in a lower claim reserve and a decrease in losses and loss adjustment expenses. The reserve established represents the present value of expected future claim payments based on the terms of the underlying long-term disability insurance contract. With the exception of the discount rate, the assumptions that impact the reserve amount, such as recovery, morbidity and mortality rates, are embedded in the table. The long-term disability IBNR reserve is estimated on a policy-by-policy basis, taking into consideration the average monthly premium, the policy elimination period, and an expected loss ratio.
The impact to the long-term disability tabular reserve, net income and shareholders’ equity due to an increase or decrease in the discount rate of 10 basis points, 25 basis points, and 50 basis points is shown below (dollars in thousands):
48
| | | | | | | | | | | |
| | | Net Increase
(Decrease)
in Reserves | | | Impact on
Net Income | | | Percentage of
Shareholders’
Equity | |
50 basis point increase | | $ | (402 | ) | | $ | 261 | | | 0.2 | % |
25 basis point increase | | $ | (203 | ) | | $ | 132 | | | — | |
10 basis point increase | | $ | (82 | ) | | $ | 53 | | | — | |
10 basis point decrease | | $ | 83 | | | $ | (54 | ) | | — | |
25 basis point decrease | | $ | 209 | | | $ | (136 | ) | | — | |
50 basis point decrease | | $ | 424 | | | $ | (276 | ) | | -0.2 | % |
Term Life Reserves
Term life reserves consist of reported but unpaid and IBNR claims on the Company’s term life product, as well as a life premium waiver reserve. Reported but unpaid life claims represent those claims reported to the Company as of the balance sheet date for which payment has not yet been made. Term life IBNR claims are estimated based on historical patterns of losses incurred as a percent of in-force premium as of the balance sheet date.
The term life reported claim reserve represents the Company’s liability for reported but unpaid death benefits and AD & D claims. The reserve is based on the death benefit of the underlying term life insurance contract.
The term life IBNR claim reserve represents the Company’s estimate of future amounts to be paid under existing term life insurance contracts for insured deaths and dismemberments that have occurred but not yet been reported. The Company estimates the term life IBNR claim reserve by applying a reserve factor to the current in-force volume of life insurance and AD & D benefits, resulting in the development of a point estimate. The reserve factor is based on past experience and is evaluated against actual results on an annual basis for reasonableness. The reserve factor selected as of December 31, 2006 was based on the average actual reserve factor for the past three years, which management believes produces the best indication of the Company’s expected term life IBNR claims.
Life premium waiver reserves represent the present value of future life insurance benefits under those term life policies for which the premiums have been waived due to the insured’s disability. The Company establishes a reserve at the time the insured’s disability is reported using the 1970 Intercompany Group Life Disability Table. Life premium waiver reserves are calculated using the tabular reserve method. Due to the long-term nature of premium waiver claims, the reserve is discounted using a rate of 3%, which is built into the standard valuation table. The assumptions that impact the reserve amount, including the discount rate, are embedded in the table.
The term life premium waiver IBNR reserve represents the Company’s estimate of unreported premium waiver claims. The Company utilizes the lag factor development method to estimate the number of unreported premium waiver claims and then applies the number of estimated outstanding claims to an average reserve amount, resulting in the development of a point estimate. The most significant assumptions used in estimating the premium waiver IBNR reserve are the completion factors and the estimated average reserve amount. As of December 31, 2006, the selected completion factors were based on a combination of the 3- and 5-year averages and the average reserve amount was based on the last three years’ reported premium waiver claims.
The following table presents the impact to the premium waiver IBNR reserve, net income, and shareholders’ equity of a change in the selected completion factor and average reserve assumptions:
49
| | | | | | | | | | | |
| | | Net Increase
(Decrease)
in Reserves | | | Impact on
Net Income | | | Percentage of
Shareholders’
Equity | |
3-year average completion factors | | $ | (290 | ) | | $ | 189 | | | 0.1 | % |
5-year average completion factors | | $ | 291 | | | $ | (189 | ) | | -0.1 | % |
| | | |
Lowest average reserve amount | | $ | (102 | ) | | $ | 66 | | | — | |
Highest average reserve amount | | $ | 159 | | | $ | (103 | ) | | -0.1 | % |
Specialty Reinsurance
With respect to the specialty reinsurance segment, numerous internal and external factors will affect the ultimate settlements of future claims including, but not necessarily limited to, changes in the cost of environmental remediation, impacts of relevant federal or state legislation, changes in technology and the resulting impact on costs, and reliance on ceding companies to handle claims and remit proper loss information in a timely manner. Reserving for assumed reinsurance requires evaluating loss information received from the ceding company. On a quarterly basis, Eastern Re receives a statement from the ceding company which includes premium and loss settlement activity for the period with corresponding reserves as established by the ceding company. Claims reported to the ceding company by insureds are entered into its claim system and ceded to Eastern Re on a quarterly basis. The claim information received from the ceding company is compiled into loss development triangles. Generally accepted actuarial methodologies, supplemented by judgment where appropriate, are used to develop the appropriate IBNR reserves for Eastern Re. Each quarter the Company compares its actual reported losses for the quarter, and cumulative reported losses since the most recently completed reserve study, to expected reported losses for the respective period, which may result in the Company increasing its losses and loss adjustment expenses, and its corresponding loss reserves in that quarter. This information is used as a tool in the judgmental process by which management assesses the overall adequacy of the reserves for unpaid losses and loss adjustment expenses at Eastern Re. The evaluation of the reserves for unpaid losses and LAE related to the Company’s specialty reinsurance programs requires that loss development be estimated over an extended period of time. Because the primary insurer under this program changed in 1999 and the claims management philosophy of the two primary insurers differed, historical loss data for years prior to 1999 is not very useful. Therefore, reliance has been placed on industry loss development patterns, adjusted to reflect considerations particular to the exposure. The reliance on external benchmarks, while necessary, creates an additional element of uncertainty.
The Company’s reserves for unpaid losses and LAE in its specialty reinsurance segment as of December 31, 2006 are summarized below (in thousands):
| | | |
| | | Specialty
Reinsurance |
Case reserves | | $ | 8,985 |
Case incurred development, IBNR and unallocated loss adjustment expense reserves | | | 10,523 |
Amount of discount | | | — |
| | | |
Net reserves before purchase accounting | | | 19,508 |
Purchase accounting adjustments | | | 293 |
| | | |
Reserves for unpaid losses and loss adjustment expenses | | $ | 19,801 |
| | | |
In its specialty reinsurance segment, the Company categorizes unpaid losses and loss adjustment expenses into case reserves and IBNR reserves. Case reserves represent unpaid losses reported by the ceding company. The Company updates its reserve estimates on a quarterly basis using information received from its cedants.
The Company analyzes its ultimate losses and loss adjustment expenses for specialty reinsurance after consideration of the loss experience on each treaty for each underwriting year on a quarterly basis. The
50
methodologies that the Company employs include, but may not be limited to, paid loss development methods and incurred loss development methods similar to those described in the workers’ compensation insurance and segregated portfolio cell reinsurance segments above.
In applying these methods, the Company evaluates loss development trends by underwriting year to determine various assumptions that are required as inputs in the actuarial methodologies it employs. These typically involve the analysis of historical loss development trends by underwriting year. In addition, the Company utilizes external or internal benchmark sources of information for which it does not have sufficient loss development data to calculate credible trends. The evaluation of the reserve for unpaid losses and LAE related to the specialty reinsurance segment requires that loss development be estimated over an extended period of time.
The Company relies on information provided by ceding companies regarding premiums and reported claims, and then uses that data as a key input to estimate unpaid losses and loss adjustment expenses. Since the Company relies on claims information reported by ceding companies, the estimation of unpaid losses and loss adjustment expenses for specialty reinsurance includes certain risks and uncertainties that do not exist with its other segments, and include, but are not necessarily limited to, the following:
| | • | | The reported claims information could be inaccurate, and/or could be subject to significant reporting lags. Such potential inaccuracies or reporting lags would increase the risk of reserve estimation error. |
| | • | | A significant amount of time can lapse between the assumption of risk, occurrence of a loss event, the reporting of the event to an insurance company, often referred to as the primary company or cedant, the subsequent reporting to the reinsurance company, referred to as the reinsurer, and the ultimate payment of the claim on the loss event by the reinsurer. |
| | • | | Because the primary insurer under these programs changed in 1999, historical loss data is insufficiently developed. Therefore, reliance has been placed on industry loss development patterns adjusted, based on the management’s judgment, to reflect considerations particular to the exposure. The reliance on external benchmarks, while necessary, creates an additional element of uncertainty. |
Claims reported to the ceding company by insureds are entered into the ceding company’s claim system and ceded to the specialty reinsurance segment on a quarterly basis. The Company mitigates the above risk by engaging an independent third party to perform periodic claims reviews of the ceding companies’ detailed claim reports to ensure reported claims information appears to be reasonably accurate and timely.
As of December 31, 2006, the Company’s best estimate of its ultimate liability for unpaid losses and loss adjustment expenses, before purchase accounting adjustments, for its specialty reinsurance segment was $19.5 million. This amount was determined based on methods which were viewed to be better predictors than other methods.
The evaluation of the reserves for unpaid losses and LAE in the specialty reinsurance segment requires that loss development be estimated over an extended period of time without the benefit of credible historical loss development patterns. As the historical loss development data lacks credibility, reliance has been placed on loss development patterns based on industry loss development patterns judgmentally adjusted to reflect considerations particular to the exposure. The reliance on external benchmarks, while necessary, creates an additional element of uncertainty. Following is a sensitivity analysis of the reserves for unpaid losses and LAE to reasonably likely changes in industry loss development factors used to project current losses to ultimate losses (in thousands):
| | | | | | | | | | | |
Change in Industry Loss Development Factors | | Increase (Decrease)
in Net Loss Reserves | | | Impact on Net
Income | | | Percentage of
Shareholders’
Equity | |
100 basis point increase | | $ | 2,011 | | | $ | (1,307 | ) | | -0.8 | % |
75 basis point increase | | $ | 1,524 | | | $ | (991 | ) | | -0.6 | % |
50 basis point increase | | $ | 1,026 | | | $ | (667 | ) | | -0.4 | % |
25 basis point increase | | $ | 519 | | | $ | (337 | ) | | -0.2 | % |
25 basis point decrease | | $ | (530 | ) | | $ | 345 | | | 0.2 | % |
50 basis point decrease | | $ | (1,074 | ) | | $ | 698 | | | 0.4 | % |
75 basis point decrease | | $ | (1,630 | ) | | $ | 1,060 | | | 0.6 | % |
100 basis point decrease | | $ | (2,201 | ) | | $ | 1,431 | | | 0.8 | % |
51
While management believes that the assumptions underlying the amounts recorded for the reserves for unpaid losses and LAE as of December 31, 2006 are reasonable, the ultimate net liability may differ materially from the amount period.
“Other Than Temporary” Investment Impairments
Unrealized investment gains or losses on investments carried at fair value, net of applicable income taxes, are reflected directly in shareholders’ equity as a component of comprehensive income (loss) and, accordingly, have no effect on net income. When, in the opinion of management, a decline in the fair value of an investment below its cost or amortized cost is considered to be “other-than-temporary,” such investment is written-down to its fair value. The amount written-down is recorded in earnings as a realized loss on investments. Generally, the determination of other-than-temporary impairment includes, in addition to other relevant factors, a presumption that if the market value is below cost by a significant amount for a period of time, a write-down is necessary. Notwithstanding this presumption, the determination of other-than-temporary impairment requires judgment about future prospects for an investment and is therefore a matter of inherent uncertainty. For the year ended December 31, 2006, the Company did not experience any declines in investment securities that were determined to be other-than-temporary. Adverse investment market conditions, or poor operating results of underlying investments, could result in impairment charges in the future. The Company generally applies the following standards in determining whether the decline in fair value of an investment is other-than-temporary:
Equity securities. If an equity security has a market value below 80% of cost and remains below 80% of cost for more than three months, a review of the financial condition and prospects of the company is performed to determine if the decline in market value is other-than-temporary. A specific determination is made for any such security. Other equity securities in an unrealized loss position not meeting these quantitative thresholds are evaluated considering the magnitude and reasons for the decline and the prospects for the fair value of the securities to recover in the near term. If the decline in market value is determined to be other-than-temporary, then the cost basis of the security is written down to realizable value and the amount of the write down is accounted for as a realized loss.
Fixed income securities. A fixed income security generally is written down if the Company is unable to hold or otherwise intends to sell a security with an unrealized loss, or if it is probable that it will be unable to collect all amounts due according to the contractual terms of the security. A fixed income security is reviewed for collectibility if any of the following situations occur:
| | • | | A review of the financial condition and prospects of the issuer indicates that the security should be evaluated; |
| | • | | Moody’s or Standard & Poor’s rate the security below investment grade; or |
| | • | | The security has a market value below 80% of amortized cost due to deterioration in credit quality. |
Deferred Acquisition Costs
Certain direct policy acquisition costs consisting of commissions, premium taxes, fronting fees and certain other direct underwriting costs are deferred and amortized as the underlying policy premiums are earned. As of December 31, 2006, deferred policy acquisition costs and the related unearned premium reserves in the Company’s workers’ compensation insurance, segregated portfolio cell reinsurance, and specialty reinsurance segments were as follows (in thousands):
52
| | | |
Workers’ compensation insurance segment: | | | |
Deferred policy acquisition costs | | $ | 1,232 |
Unearned premium reserves | | $ | 20,596 |
| |
Segregated portfolio cell reinsurance segment: | | | |
Deferred policy acquisition costs | | $ | 1,496 |
Unearned premium reserves | | $ | 6,330 |
| |
Specialty reinsurance segment: | | | |
Deferred policy acquisition costs | | $ | 1,773 |
Unearned premium reserves | | $ | 6,854 |
Acquisition costs of the group benefits insurance segment are not capitalized and deferred as the group benefits insurance policies are cancelable and not guaranteed renewable. In addition, the group benefits insurance policies provide coverage on a month-to-month basis with most policies’ coverage effective on the first of each month. As a result, most of the premiums are earned as of the balance sheet date and all direct expenses related to the issuance or renewal of policies are recognized when incurred.
Deferred Income Taxes
The temporary differences between the tax and book bases of assets and liabilities are recorded as deferred income taxes. Management evaluates the recoverability of the net deferred tax asset based on historical trends of generating taxable income or losses, as well as expectations of future taxable income or loss. As of December 31, 2006, the Company recorded a net deferred tax asset of $2.7 million. Management expects that the net deferred tax asset is fully recoverable. If this assumption were to change, any amount of the net deferred tax asset that the Company could not expect to recover would be provided for as an allowance and would be reflected as an increase in income tax expense in the period in which it was established.
Reinsurance Recoverables
Amounts recoverable from Company’s reinsurers are estimated in a manner consistent with the reserves for unpaid losses and LAE associated with the reinsured policy. Amounts paid for reinsurance contracts are expensed over the contract period during which insured events are covered by the reinsurance contracts. Reinsurance balances recoverable on paid and unpaid loss and loss adjustment expenses are reported separately as assets, instead of being netted with the appropriate liabilities, because reinsurance does not relieve the Company of its legal liability to its policyholders. Reinsurance balances recoverable are subject to credit risk associated with the particular reinsurer. Additionally, the same uncertainties associated with estimating unpaid losses and loss adjustment expenses affect the estimates for the ceded portion of these liabilities. The Company continually monitors the financial condition of its reinsurers.
53
Recent Accounting Pronouncements
SFAS 158
In September 2006, the Financial Accounting Standards Board (“FASB”) issued SFAS 158, “Employers’ Accounting for Defined Benefit Pension and Other Postretirement Plans, an amendment to FASB Statements No. 87, 88, 106, and 132(R)”. SFAS 158 requires employers to recognize the funded status of a benefit plan in its statement of financial position, with changes in the funded status occurring during the year reported as a component of other comprehensive income or loss. The funded status of a benefit plan represents the difference between plan assets at fair value and the benefit obligation. For defined benefit pension plans and postretirement benefit plans, the benefit obligation is the projected benefit obligation and accumulated postretirement benefit obligation, respectively. In addition to the above changes, SFAS 158 requires that plan assets and benefit obligations be measured as of the date of an employer’s fiscal year-end. The recognition and disclosure provisions of SFAS 158 are effective for fiscal years ending December 31, 2006. The requirement to measure plan assets and benefit obligations as of the end of an employer’s fiscal year-end is effective for fiscal years ending after December 31, 2008. As a result of adopting SFAS 158 effective December 31, 2006, the prepaid asset related to our defined benefit pension plan increased $287,000 and our liability related to our defined benefit postretirement plan decreased $364,000, resulting in an increase to accumulated other comprehensive income of $423,000, net of tax.
SFAS 157
In September 2006, the FASB issued SFAS 157, “Fair Value Measurements”. SFAS 157 clarifies the definition of fair value for purposes of financial reporting, specifies the methods to be used to measure fair value, and requires expanded disclosures related to fair value and financial instruments measured at fair value. SFAS 157 is effective for financial statements issued for fiscal years beginning after November 15, 2007. Early application is encouraged, provided an entity has not yet issued financial statements for the fiscal year, including interim financial statements. Management is currently evaluating the impact of SFAS 157 on its current fair value disclosures. The Company expects that the adoption of SFAS 157 will not have a material effect on its consolidated financial condition or results of operations.
FIN 48
In July 2006, the FASB issued FASB Interpretation No. 48, “Accounting for Uncertainty in Income Taxes – an interpretation of FASB Statement No. 109” (“FIN 48”), which provides criteria for the recognition, measurement, presentation and disclosure of uncertain tax positions. A tax benefit from an uncertain position may be recognized only if it is “more likely than not” that the position is sustainable based on its technical merits. The provisions of FIN 48 are effective for fiscal years beginning after December 15, 2006. The Company expects that the adoption of FIN 48 will not have a material effect on its consolidated financial condition or results of operations.
SFAS 155
In February 2006, the FASB issued SFAS 155, “Accounting for Certain Hybrid Financial Instruments, an amendment of FASB Statements No. 133 and 140”. SFAS 155 amends the accounting requirements for certain financial instruments covered by FASB Statements No. 133 and 140, including financial instruments containing embedded derivatives. SFAS 155 amends FASB Statement No. 133 by permitting fair value remeasurement of any hybrid financial instrument that contains an embedded derivative. Under current accounting guidance contained in FASB Statement No. 133, embedded derivatives must be bifurcated from their host contract and accounted for separately. SFAS 155 is effective for all financial instruments acquired, issued or subject to a remeasurement event occurring after the beginning of an entity’s first fiscal year that begins after September 15, 2006. The fair value election for hybrid financial instruments may also be applied upon adoption of SFAS 155 to those hybrid financial instruments held by an entity and bifurcated under FASB Statement No. 133 prior to the adoption of SFAS 155. Any difference between the total carrying amount of the individual components of an existing bifurcated hybrid financial instrument and the fair value of the combined hybrid financial instrument must be recognized as a cumulative effect adjustment to beginning retained earnings. Restatement of prior periods is prohibited. The Company currently holds convertible debt securities that require bifurcation under FASB Statement No. 133. The Company expects that the adoption of SFAS 155 will not have a material effect on its consolidated financial condition or results of operations.
54
SOP 05-1
In September 2005, the American Institute of Certified Public Accountants (“AICPA”) released Statement of Position 05-1, “Accounting by Insurance Enterprises for Deferred Acquisition Costs in Connection With Modifications or Exchanges of Insurance Contracts” (“SOP 05-1”). SOP 05-1 requires identification of transactions that result in a substantial change in an insurance contract. Transactions subject to review include internal contract exchanges, contract modifications via amendment, rider or endorsement, and elections of benefits, features or rights contained within the contract. If determined that a substantial change has occurred, the related unamortized deferred policy acquisition costs, unearned premiums and other related balances must be written off. The Company will adopt SOP 05-1 on January 1, 2007. The Company expects that the adoption of SOP 05-1 will not have a material effect on its consolidated financial condition or results of operations.
55
YEAR ENDED DECEMBER 31, 2006 COMPARED TO YEAR ENDED DECEMBER 31, 2005
RESULTS OF OPERATIONS
The components of consolidated revenue were as follows for the year ended December 31, 2006 and 2005 (in thousands):
| | | | | | |
| | | 2006 | | 2005 |
Net premiums written | | $ | 67,529 | | $ | 38,700 |
| | | | | | |
Net premiums earned | | $ | 74,919 | | $ | 38,702 |
Net investment income | | | 8,992 | | | 3,815 |
Net realized investment gains | | | 2,757 | | | 445 |
Other revenue | | | 313 | | | 1,066 |
| | | | | | |
Consolidated revenue | | $ | 86,981 | | $ | 44,028 |
| | | | | | |
The increase in consolidated revenue reflects the acquisition of EHC on June 16, 2006. The increase in net investment income reflects the increase in cash and investments, which increased from $82.2 million at December 31, 2005 to $288.3 million at December 31, 2006, as a result of the initial public offering and the acquisition of EHC. Other revenue for the year ended December 31, 2006 represents fees from the Company’s third party administration operations and cell rental fees from the Company’s specialty reinsurance segment for the period from June 17, 2006 to December 31, 2006. Other revenue for the year ended December 31, 2005 represents sales and marketing fees earned by ELH’s former general agency operations segment.
The components of consolidated net income, by segment, for the year ended December 31, 2006 and 2005 were as follows (in thousands):
| | | | | | | | |
| | | 2006 | | | 2005 | |
Workers’ compensation insurance | | $ | 5,318 | | | $ | — | |
Segregated portfolio cell reinsurance | | | — | | | | — | |
Group benefits insurance | | | 4,587 | | | | 1,987 | |
Specialty reinsurance | | | (489 | ) | | | — | |
Corporate/other | | | (1,138 | ) | | | (860 | ) |
| | | | | | | | |
Consolidated net income | | $ | 8,278 | | | $ | 1,127 | |
| | | | | | | | |
The increase in consolidated net income reflects the acquisition of EHC on June 16, 2006. The corporate/other segment results for the year ended December 31, 2006 include the results of operations of Employers Alliance, EIHI, Eastern Holding Company, Ltd., Eastern Services, Global Alliance, and the Company’s corporate activities for the period from June 17, 2006 to December 31, 2006, and ELH’s group medical insurance run-off operations and corporate activities for the year ended December 31, 2006. The corporate/other segment results for the year ended December 31, 2005 include the results of operations of ELH’s former general agency operations and corporate activities, and the group medical insurance run-off operations.
Consolidated net income for the year ended December 31, 2006 includes the impact of purchase accounting adjustments that reduced net income by $2.2 million, including reductions in the workers’ compensation insurance and specialty reinsurance segments of $2.4 million and $647,000, respectively, and a decrease in the net loss in the corporate/other segment of $801,000.
WORKERS’ COMPENSATION INSURANCE
The workers’ compensation insurance segment consists of the operating results of EAIG. Summarized financial results of the workers’ compensation insurance segment are as follows for the period from June 17, 2006 to December 31, 2006 (in thousands):
56
| | | | |
| | | 2006 | |
Revenue: | | | | |
Direct premiums written | | $ | 34,031 | |
Reinsurance premiums assumed | | | 143 | |
Ceded premiums written | | | (12,073 | ) |
| | | | |
Net premiums written | | | 22,101 | |
| |
Change in unearned premiums | | | 2,047 | |
| | | | |
Net premiums earned | | | 24,148 | |
| |
Net investment income | | | 2,225 | |
Net realized investment gains | | | 586 | |
| | | | |
Total revenue | | $ | 26,959 | |
| | | | |
Expenses: | | | | |
Loss and loss adjustment expenses | | $ | 15,162 | |
Acquisition and other underwriting expenses | | | (40 | ) |
Other expenses | | | 3,724 | |
Policyholder dividend expense | | | 239 | |
| | | | |
Total expenses | | $ | 19,085 | |
| | | | |
Income before income taxes | | | 7,874 | |
| |
Income tax expense | | | 2,556 | |
| | | | |
Net income | | $ | 5,318 | |
| | | | |
Net Income
Net income reflects an after-tax charge of $2.4 million related to the amortization of purchase accounting adjustments, favorable loss reserve development on prior accident years of $1.4 million and a $567,000 reduction in the accrual for the Security Fund assessment.
Premiums
Direct premiums written for the period from June 17, 2006 to December 31, 2006 were $34.0 million. Direct premiums written for traditional business and alternative markets were $27.1 million and $6.9 million for the period from June 17, 2006 to December 31, 2006, respectively. Direct written premiums include the impact of 2006 renewal rate decreases of 6.1%, a premium renewal retention rate of 85.4% and a reduction for purchase accounting adjustments of $5.1 million. Audit premiums of $1.6 million were also included in direct premiums written for the period from June 17, 2006 to December 31, 2006.
Net premiums written for the period from June 17, 2006 to December 31, 2006 were $22.1 million. Net premiums written include traditional production, net of external reinsurance, because alternative markets business is ceded 100% to the segregated portfolio cell reinsurance segment.
Losses and Loss Adjustment Expenses
The workers’ compensation ratios were as follows for the period from June 17, 2006 to December 31, 2006:
| | | |
| | | 2006 | |
Loss and loss adjustment expense ratio | | 62.8 | % |
Expense ratio | | 15.3 | % |
Policyholders’ dividend ratio | | 1.0 | % |
| | | |
Combined ratio | | 79.1 | % |
| | | |
Loss and loss adjustment expenses were reduced by the amortization of purchase accounting adjustments of $484,000. The accident period loss and loss adjustment expense ratio was 62.1% for the period from June 17, 2006 to December 31, 2006. The calendar period loss and loss adjustment expense
57
ratio was 62.8% for the period from June 17, 2006 to December 31, 2006, including 9.2 points related to purchase accounting adjustments. Favorable loss reserve development on prior accident years of $2.1 million was recorded for the period from June 17, 2006 to December 31, 2006. The favorable loss and loss adjustment expense reserve development relates primarily to a decrease in the prior accident period loss development factors used to estimate loss and loss adjustment expenses. The decrease in prior accident period loss development factors relates primarily to significant prior year claim settlements during 2006 for amounts at, or less than, previously established case and IBNR reserves. This decrease had the effect of lowering loss development factors as of December 31, 2006. For the period from July 1, 2006 to December 31, 2006, the Company closed 95, or 22.5%, of the 423 open lost time claims as of December 31, 2005. In the aggregate, the claims were closed at amounts lower than the provision established for claims incurred but not reported. Management believes that the realization of the benefits of its return-to-work controls implemented in 2003 coupled with strong economies in its underwriting territories during 2006 enabled it to record loss and loss adjustment expenses that were lower than the amount reserved for claim settlements. For the period from June 17, 2006 to December 31, 2006, there were no claims that exceeded the Company’s $500,000 reinsurance retention.
Acquisition and Other Underwriting Expenses
Acquisition and other underwriting expenses for the period from June 17, 2006 to December 31, 2006 were $(40,000) and include a reduction for purchase accounting adjustments of $968,000 and a decrease of $872,000 related to management’s estimate that the Security Fund will not be making an assessment in 2007 based on 2006 direct written premium. Acquisition and other underwriting expenses consist primarily of agent commissions and premium taxes. Offsetting acquisition and other underwriting expenses are fee-based revenue from Alternative Market writings. Other expenses were $3.7 million for the period from June 17, 2006 to December 31, 2006. The expense ratio was 15.3% for the period from June 17, 2006 to December 31, 2006.
Policyholder Dividends
Policyholder dividends were $239,000 for the period from June 17, 2006 to December 31, 2006. Dividends represent payments to customers who purchased participating policies that produced favorable loss ratios. In 2006, 9.1% of all policies were written on a dividend policy basis.
Net Investment Income
Net investment income was $2.2 million for the period from June 17, 2006 to December 31, 2006.
Net Realized Gains
For the period from June 17, 2006 to December 31, 2006, net realized gains were $586,000 and related primarily to sales activity on equity securities.
Tax Expense
For the period from June 17, 2006 to December 31, 2006, tax expense totaled $2.6 million. The effective tax rate for the period from June 17, 2006 to December 31, 2006 was 32.5%. The primary difference between the statutory tax rate of 35.0% and the effective tax rate relates to tax exempt income recorded for the period from June 17, 2006 to December 31, 2006.
58
SEGREGATED PORTFOLIO CELL REINSURANCE
Summarized financial results of the segregated portfolio cell reinsurance segment are as follows for the period from June 17, 2006 to December 31, 2006 (in thousands):
| | | | |
| | | 2006 | |
Revenue: | | | | |
Reinsurance premiums assumed | | $ | 6,896 | |
Ceded premiums written | | | (671 | ) |
| | | | |
Net premiums written | | | 6,225 | |
Change in unearned premiums | | | 5,581 | |
| | | | |
Net premiums earned | | | 11,806 | |
Net investment income | | | 588 | |
Net realized investment gains | | | 365 | |
| | | | |
Total revenue | | $ | 12,759 | |
| | | | |
Expenses: | | | | |
Loss and loss adjustment expenses | | $ | 5,892 | |
Acquisition and other underwriting expenses | | | 2,746 | |
Other expenses | | | 106 | |
Segregated portfolio dividend expense (1) | | | 4,015 | |
| | | | |
Total expenses | | $ | 12,759 | |
| | | | |
Net income (1) | | $ | 0 | |
| | | | |
| (1) | The workers’ compensation insurance, specialty reinsurance and corporate/other segments provide services to the segregated portfolio cell reinsurance segment. The fees paid by the segregated portfolio cell reinsurance segment for these services are included in the revenue of the segment providing the service. The segregated portfolio cell reinsurance segment records the fees associated with these services as ceding expense, which is included in its underwriting expenses. The difference between total revenue for the segregated portfolio cell reinsurance segment for each period and the sum of losses and loss adjustment expenses, acquisition and other underwriting expenses, policyholder dividend expenses and other expenses is accrued as a segregated portfolio dividend expense. As a result, the segregated portfolio cell reinsurance segment has no net income for any period presented in this table. |
Premiums
Reinsurance premiums assumed were $6.9 million for the period from June 17, 2006 to December 31, 2006. Reinsurance premiums assumed include the impact of 2006 renewal rate decreases of 3.8%, a premium renewal retention rate of 85.0% and a reduction for purchase accounting adjustments of $2.4 million. Audit premiums of $312,000 were also included in reinsurance premiums assumed for the period from June 17, 2006 to December 31, 2006.
Net premiums written for the period from June 17, 2006 to December 31, 2006 were $6.2 million and include an increase of $1.0 million related to purchase accounting adjustments.
Losses and Loss Adjustment Expenses
The Company’s segregated portfolio cell ratios were as follows for the period from June 17, 2006 to December 31, 2006:
| | | |
| | | 2006 | |
Loss and loss adjustment expense ratio | | 49.9 | % |
Expense ratio | | 24.2 | % |
| | | |
Combined ratio | | 74.1 | % |
| | | |
59
Loss and loss adjustment expenses were $6.0 million for the period from June 17, 2006 to December 31, 2006. The calendar period loss and loss adjustment expense ratio was 49.9% in 2006, including 4.6 points related to purchase accounting adjustments recorded to net premiums earned and loss and loss adjustment expenses.
Acquisition and Other Underwriting Expenses
Acquisition and other underwriting expenses were $2.7 million for the period from June 17, 2006 to December 31, 2006 and include a reduction of $1.5 million for purchase accounting adjustments. Underwriting expenses consist of the ceding commissions due under the reinsurance agreements with Eastern Alliance and/or Allied Eastern. Other expenses consist primarily of accounting, banking and legal fees. The expense ratio of 24.2% for the period from June 17, 2006 to December 31, 2006 includes a reduction of 8.4 points related to purchase accounting adjustments. The expense ratio, without regard to the aforementioned purchase accounting adjustments, is consistent with the contractual ceding commissions for this period.
Segregated Portfolio Dividend Expense
Segregated portfolio dividend expense was $4.0 million for the period from June 17, 2006 to December 31, 2006. The segregated portfolio dividend expense represents the amount of net income or loss in a specific period that may be payable to the segregated portfolio dividend participants.
GROUP BENEFITS INSURANCE
The following table represents the operations of the group benefits insurance segment for the years ended December 31, 2006 and 2005 (in thousands):
| | | | | | |
| | | 2006 | | 2005 |
Revenue: | | | | | | |
Net premiums earned | | $ | 33,451 | | $ | 38,702 |
Net investment income | | | 3,669 | | | 3,546 |
Net realized investment gains | | | 1,972 | | | 232 |
| | | | | | |
Total revenue | | | 39,092 | | | 42,480 |
| | | | | | |
Expenses: | | | | | | |
Loss and loss adjustment expenses | | | 20,600 | | | 27,132 |
Acquisition and other underwriting expenses | | | 5,072 | | | 6,659 |
Other expenses | | | 6,336 | | | 5,740 |
| | | | | | |
Total expenses | | | 32,008 | | | 39,531 |
| | | | | | |
Income before income taxes | | | 7,084 | | | 2,949 |
| | |
Income tax expense | | | 2,497 | | | 962 |
| | | | | | |
Net income | | $ | 4,587 | | $ | 1,987 |
| | | | | | |
Net Income
The increase in net income primarily reflects the decrease in the loss ratio and an increase in net realized investment gains, offset by the decrease in net premiums earned and an increase in other expenses. The improvement in the loss ratio primarily reflects better experience in the dental, long-term disability and term life lines of business. Net realized investment gains included proceeds of $716,000 from the sale of common stock previously written down to $0 and the change in the fair value of equity call options during 2006. The decrease in net premiums earned reflects the decline in new business sales and the decline in renewal retention during the first six months of 2006. During the fourth quarter of 2005, ELH recognized an after-tax gain of $967,000 related to its postretirement medical and life insurance benefits plan, which reduced other expenses in that period.
60
Premiums
The decrease in net premiums earned reflects the aforementioned decline in new business sales and renewal retention. New business sales totaled $3.6 million for the year ended December 31, 2006, compared to $6.2 million for the year ended December 31, 2005. Renewal retention declined 5.2 percentage points for the first six months of 2006, which adversely impacted net premiums earned for the remainder of the year.
Net premiums earned, by line of business, for the years ended December 31, 2006 and 2005 were as follows (in thousands):
| | | | | | |
| | | 2006 | | 2005 |
Dental | | $ | 19,482 | | $ | 23,570 |
Short-term disability | | | 6,459 | | | 6,672 |
Long-term disability | | | 1,906 | | | 2,395 |
Term life | | | 5,604 | | | 6,065 |
| | | | | | |
Total | | $ | 33,451 | | $ | 38,702 |
| | | | | | |
Net Investment Income
The increase in net investment income primarily reflects an increase in the equity interest in limited partnership investments.
Net Realized Investment Gains
The increase in net realized investment gains primarily reflects the aforementioned change in the fair value of equity call options and the gain on the common stock sale, which totaled $716,000. The change in the fair value of equity call options increased $608,000 for the year ended December 31, 2006, compared to a decrease of $367,000 for the same period in 2005.
Losses and Loss Adjustment Expenses
The decrease in losses and loss adjustment expenses reflects the improved loss experience and favorable development in the dental, long-term disability and term life lines of business, and the decrease in net premiums earned. The calendar period loss ratios, by line of business, for the years ended December 31, 2006 and 2005 were as follows:
| | | | | | |
| | | 2006 | | | 2005 | |
Dental | | 63.4 | % | | 67.3 | % |
Short-term disability | | 75.1 | % | | 74.2 | % |
Long-term disability | | 23.4 | % | | 79.6 | % |
Term life | | 52.0 | % | | 71.2 | % |
| | |
Total group benefits | | 61.6 | % | | 70.1 | % |
Dental
The decrease in the calendar period dental loss ratio reflects the improvement in the accident year loss ratio and favorable development on prior year reserves. The accident year loss ratio was 66.2% and 69.8% in 2006 and 2005, respectively, which reflects renewal rate increases, lower claim frequency, and the termination of business with higher loss experience. During 2006, management began to more closely monitor the renewal rate actions, focusing on retaining more profitable business at renewal and terminating less profitable business through renewal rate actions. As a result of these efforts, the loss ratio on retained business was 61.9%, compared to a loss ratio of 79.2% on terminated business. Favorable development on prior year reserves reduced the calendar year loss ratio by 2.8 percentage points in 2006, compared to 2.5 percentage points in 2005.
61
Short-term Disability
The increase in the calendar period short-term disability reflects an increase in the accident period loss ratio, offset by offset by favorable development on prior year reserves. The accident period loss ratio was 80.3% and 77.4% in 2006 and 2005, respectively. The increase in the accident period loss ratio reflects increased claim frequency and severity, offset by renewal rate increases. Favorable development on prior year reserves reduced the calendar year loss ratio by 5.2 percentage points in 2006, compared to 3.2 percentage points in 2005.
Long-term Disability
The improvement in the long-term disability loss ratio reflects lower claim frequency and severity and the termination of prior year claims. As a result of the decrease in the long-term disability claim retention, from a 50% coinsurance to a 20% coinsurance effective July 1, 2005, the termination of prior year claim reserves at a 50% coinsurance had a favorable impact on the 2006 calendar year loss ratio.
Term Life
The decrease in the term life loss ratio reflects favorable development on the prior year death benefit IBNR reserve, a 54.1% decrease in premium waiver claim frequency and favorable reserve development related to the termination of prior year premium waiver claims. The favorable development on the prior year death benefit IBNR reserve reflects lower than expected reported death benefit claims. For the year ended December 31, 2006, there were only 16 reported premium waiver claims, with total reserves of $394,000, compared to 38 reported premium waiver claims, with total reserves of $852,000, for the same period in 2005. Terminated premium waiver claim reserves totaled $552,000 for the year ended December 31, 2006, compared to terminated reserves of $264,000 for the same period in 2005.
Acquisition and Other Underwriting Expenses
The decrease in acquisition and other underwriting expenses reflects the decline in net premiums earned and the elimination of sales and marketing fees paid to IBSiin Pennsylvania, Maryland and Delaware. Acquisition and other underwriting expenses totaled 14.1% and 16.2% of direct premiums written in 2006 and 2005, respectively. The decrease of 2.1% primarily reflects the reduction in sales and marketing fees.
Other Expenses
The increase in other expenses primarily reflects the aforementioned gain recognized in 2005. Excluding the gain, other expenses would have decreased $869,000, which reflects management’s expense reduction efforts.
Tax Expense
The increase in income tax expense reflects the improvement in pre-tax income and the increase in the effective tax rate from 32.6% in 2005 to 35.2% in 2006. The 2005 effective tax rate reflects the release of a valuation allowance related to tax credits totaling $227,000. The tax credits were fully utilized in 2006. In addition, ELH’s statutory tax rate increased from 34% in 2005 to 35% in 2006 as a result of the Company’s acquisition of EHC.
SPECIALTY REINSURANCE
Summarized financial results of the specialty reinsurance segment are as follows for the period from June 17, 2006 to December 31, 2006 (in thousands):
62
| | | | |
| | | 2006 | |
Revenue: | | | | |
Reinsurance premiums assumed | | $ | 5,775 | |
| |
Change in unearned premiums | | | (261 | ) |
| | | | |
Net premiums earned | | $ | 5,514 | |
| |
Net investment income | | | 1,032 | |
Net realized investment gains | | | 15 | |
Other revenue | | | 177 | |
| | | | |
Total revenue | | $ | 6,738 | |
| | | | |
Expenses: | | | | |
Loss and loss adjustment expenses | | $ | 6,292 | |
Acquisition and other underwriting expenses | | | 789 | |
Other expenses | | | 411 | |
| | | | |
Total expenses | | $ | 7,492 | |
| | | | |
Loss before income taxes | | | (754 | ) |
Income tax benefit | | | (265 | ) |
| | | | |
Net loss | | $ | (489 | ) |
| | | | |
Net Loss
The net loss includes an after-tax charge of $647,000 related to the amortization of purchase accounting adjustments and an increase in the frequency and severity of reported claims by the ceding company, which resulted in an increase in the 2006 accident year loss and LAE ratio and after-tax unfavorable loss reserve development of $894,000.
Premiums
Reinsurance premiums assumed by line of business were as follows for the period from June 17, 2006 to December 31, 2006 (in thousands):
| | | | |
| | | 2006 | |
EnviroGuard | | $ | 5,993 | |
EIA liability | | | 2,403 | |
Purchase accounting adjustments | | | (2,621 | ) |
| | | | |
Total reinsurance premiums assumed | | $ | 5,775 | |
| | | | |
Reinsurance premiums assumed include a reduction for purchase accounting adjustments of $2.6 million.
Losses and Loss Adjustment Expenses
The Company’s specialty reinsurance ratios were as follows for the period from June 17, 2006 to December 31, 2006:
63
| | | |
| | | 2006 | |
Loss and loss adjustment expense ratio | | 114.1 | % |
Expense ratio | | 21.8 | % |
| | | |
Combined ratio | | 135.9 | % |
| | | |
Loss and loss adjustment expenses were $6.3 million for the period from June 17, 2006 to December 31, 2006. The calendar period loss and loss adjustment expense ratio was 114.1% in 2006, including 37.1 points related to purchase accounting adjustments recorded to net premiums earned and loss and loss adjustment expenses. The loss ratio included an increase in claims reported from the ceding company, which resulted in an increase in the 2006 accident year loss ratio and unfavorable loss reserve development on prior accident years of $894,000 or 16.2 percentage loss ratio points. The accident year loss ratio increased to 54.2% during the period from June 17, 2006 to December 31, 2006 resulting in the recording of additional loss and loss adjustment expenses of $977,000 or 17.7 percentage loss ratio points for the period from June 17, 2006 to December 31, 2006.
Acquisition and Other Underwriting Expenses
Acquisition and other underwriting expenses for the period from June 17, 2006 to December 31, 2006 were $789,000 and include a reduction for purchase accounting adjustments of $1.7 million. As part of its quota share reinsurance agreement with the primary insurer, Eastern Re pays the primary insurer a ceding commission based on assumed premiums. For the period from June 17, 2006 to December 31, 2006, the ceding commission paid to the primary insurer was 30.0%. Other expenses of $411,000 were incurred for the period from June 17, 2006 to December 31, 2006. Other expenses consist primarily of accounting, banking, management services and legal fees.
Net Investment Income
Net investment income was $1.0 million for the period from June 17, 2006 to December 31, 2006.
Net Realized Investment Gains
For the period from June 17, 2006 to December 31, 2006, net realized investment gains were $15,000.
Tax Benefit
Income tax benefit was $265,000 for the period from June 17, 2006 to December 31, 2006. The effective tax rate for the period from June 17, 2006 to December 31, 2006 was 35.1%. Specialty reinsurance is underwritten by Eastern Re, a Cayman domiciled reinsurer. Eastern Re has received an undertaking from the Cayman Islands government exempting them from all local income, profits and capital gains taxes until February 14, 2026. Eastern Re has remained a Cayman Islands corporation after the acquisition of EHC, however, it is now controlled indirectly by the Company, which is a Pennsylvania corporation. As a result, under applicable federal income tax laws and regulations, Eastern Re is deemed a controlled foreign corporation and its income after June 16, 2006 is subject to United States federal income taxes.
CORPORATE/OTHER
The corporate/other segment results for the year ended December 31, 2006 include the results of operations of Employers Alliance, EIHI, Eastern Holding Company, Ltd., Eastern Services, and Global Alliance for the period from June 17, 2006 to December 31, 2006, and ELH’s group medical insurance run-off operations and corporate activities for the year ended December 31, 2006. This segment also includes certain eliminations necessary to reconcile the segment information to the consolidated statements of operations. For the year ended December 31, 2005, the corporate/other segment consists of the results of operations of ELH’s former general agency operations, group medical insurance run-off operations, and certain corporate activities of ELH.
64
YEAR ENDED DECEMBER 31, 2005 COMPARED TO YEAR ENDED DECEMBER 31, 2004
The following discussion of the Company’s results of operations for the years ended December 31, 2005 and 2004 reflects the results of operations of ELH, including ELH’s former general agency operations, IBSi. IBSi’s results of operations are included in the corporate/other segment.
RESULTS OF OPERATIONS
The major components of consolidated revenue were as follows for the years ended December 31, 2005 and 2004 (in thousands):
| | | | | | |
| | | 2005 | | 2004 |
Net premiums written | | $ | 38,700 | | $ | 39,070 |
| | | | | | |
Net premiums earned | | $ | 38,702 | | $ | 39,057 |
Net investment income | | | 3,815 | | | 3,724 |
Net realized investment gains | | | 445 | | | 1,271 |
Other revenue | | | 1,066 | | | 946 |
| | | | | | |
Consolidated revenue | | $ | 44,028 | | $ | 44,998 |
| | | | | | |
The decrease in consolidated revenue primarily reflects a reduction in net premiums earned totaling $355,000 and a reduction in net realized investment gains totaling $826,000. Net premiums earned in 2004 includes the release of a reinsurance premium payable totaling $284,000 under ELH’s group medical reinsurance agreement that never materialized. The decrease in net realized investment gains primarily reflects changes in the estimated fair value of the equity call option component of ELH’s convertible bond portfolio, from a gain in 2004 totaling $217,000 to a loss in 2005 totaling $367,000. In addition, an other than temporary impairment charge totaling $104,000 was recognized in 2005. There were no impairments in 2004.
The components of consolidated net income, by segment, for the years ended December 31, 2005 and 2004 were as follows (in thousands):
| | | | | | | |
| | | 2005 | | | 2004 |
Group benefits insurance | | $ | 1,987 | | | $ | 1,673 |
Corporate/other | | | (860 | ) | | | 110 |
| | | | | | | |
Consolidated net income | | $ | 1,127 | | | $ | 1,783 |
| | | | | | | |
The decrease in consolidated net income reflects the impact of certain unusual items, including conversion/merger expenses totaling $877,000, a charge for one-time termination benefits totaling $580,000, and a charge related to ELH’s defined benefit pension plan totaling $294,000. These items were offset by a net after-tax reduction in the Company’s benefit plan liabilities totaling $773,000 and the release of loss reserves in the dental and short-term disability lines of business totaling $692,000. The decrease in consolidated net income from 2004 to 2005 was also impacted by the release of loss reserves totaling $1.6 million related to the run-off of ELH’s group medical insurance business in 2004.
Group Benefits Insurance
The following table represents the operations of the group benefits insurance segment for the years ended December 31, 2005 and 2004 (in thousands):
65
| | | | | | |
| | | 2005 | | 2004 |
Revenue: | | | | | | |
Net premiums earned | | $ | 38,702 | | $ | 38,753 |
Net investment income | | | 3,546 | | | 3,617 |
Net realized investment gains | | | 232 | | | 1,255 |
| | | | | | |
Total revenue | | | 42,480 | | | 43,625 |
| | | | | | |
Expenses: | | | | | | |
Loss and loss adjustment expenses | | | 27,132 | | | 27,543 |
Acquisition and other underwriting expenses | | | 6,659 | | | 6,954 |
Other expenses | | | 5,740 | | | 6,540 |
| | | | | | |
Total expenses | | | 39,531 | | | 41,037 |
| | | | | | |
Income before income taxes | | | 2,949 | | | 2,588 |
| | |
Income tax expense | | | 962 | | | 915 |
| | | | | | |
Net income | | $ | 1,987 | | $ | 1,673 |
| | | | | | |
Net Income
The increase in net income primarily reflects a decrease in losses and loss adjustment expenses and the net after-tax reduction in the pension and postretirement liabilities, partially offset by a decrease in net realized investment gains.
Premiums
The decrease in net premiums earned primarily reflects higher ceded premiums related to the Company’s long-term disability reinsurance arrangement effective July 1, 2005 and an increase in the lapse rate from 2004 to 2005. Net premiums earned in the dental line of business decreased $716,000, or 2.9%, from $24.3 million in 2004 to $23.6 million in 2005, primarily reflecting a 7.2% increase in the lapse rate, from 27.1% in 2004 to 34.3% in 2005. The decrease in dental premiums was offset by an increase in short-term disability premiums totaling $659,000, from $6.0 million in 2004 to $6.7 million in 2005, primarily reflecting a 9.1% increase in certificate months and average renewal rate increases of 9.3%.
Net premiums earned, by line of business, for the years ended December 31, 2005 and 2004 were as follows (in thousands):
| | | | | | |
| | | 2005 | | 2004 |
Dental | | $ | 23,570 | | $ | 24,286 |
Short-term disability | | | 6,672 | | | 6,013 |
Long-term disability | | | 2,395 | | | 2,419 |
Term life | | | 6,065 | | | 6,035 |
| | | | | | |
Total | | $ | 38,702 | | $ | 38,753 |
| | | | | | |
Net Investment Income
The decrease in net investment income primarily reflects the reinvestment of proceeds from maturities of higher coupon bonds in bonds with lower yields.
Net Realized Investment Gains
The decrease in net realized investment gains primarily reflects the change in the fair value of equity call options during 2005 totaling $367,000, compared to an increase during 2004 totaling $217,000. In addition, the 2004 net realized gains included the sale of certain previously impaired securities that had recovered a portion of their fair value and were sold at a gain.
66
Losses and Loss Adjustment Expenses
The decrease in losses and loss adjustment expenses primarily reflects reserve releases in the dental and short-term disability lines totaling $637,000 and $55,000, respectively. Losses and loss adjustment expenses in the disability lines increased $969,000, from $6.0 million in 2004 to $6.9 million in 2005, while term life losses and loss adjustment expenses increased $364,000, from $4.0 million in 2004 to $4.3 million in 2005. Claim frequency increased 6.7% and 6.9% in the short-term disability and long-term disability lines, respectively, while long-term disability claim severity increased 11.4%. The increase in term life losses and loss adjustment expenses primarily reflects increasing claim frequency and severity related to premium waiver claims, offset by a decrease in frequency and severity related to death claims. The increase in losses and loss adjustment expenses in the disability and term life lines was offset by a decrease in losses and loss adjustment expenses in the dental line totaling $1.7 million, from $17.6 million in 2004 to $15.9 million in 2005. In addition to the reserve releases, the decrease in dental losses and loss adjustment expenses reflects a decrease in dental premiums and claim frequency, offset by an increase in claim severity. Dental claim frequency decreased 4.4%, while claim severity increased 5.5%.
The loss ratios, by line of business, were as follows for the years ended December 31, 2005 and 2004:
| | | | | | |
| | | 2005 | | | 2004 | |
Dental | | 67.3 | % | | 72.6 | % |
Short-term disability | | 74.2 | % | | 71.9 | % |
Long-term disability | | 79.6 | % | | 67.7 | % |
Term life | | 71.2 | % | | 65.6 | % |
| | |
Total group benefits | | 70.1 | % | | 71.1 | % |
The group benefits loss ratio decreased 1.0%, from 71.1% in 2004 to 70.1% in 2005. Excluding the impact of the dental and short-term disability reserve releases, the loss ratio increased 0.8%, to 71.9%, from 2004 to 2005. Excluding the effect of the reserve release, the dental loss ratio decreased 2.5% from 2004 to 2005, which primarily reflects an increase in premium per certificate of 6.1%, offset by an increase in claims per certificate of 2.4%. The short-term disability loss ratio continued to increase in 2005, primarily as a result of the aforementioned increase in claim frequency. Claims per certificate in the short-term disability line increased 6.1%, while premiums per certificate increased only 1.8%. The increase in the long-term disability primarily reflects the impact of claim reserve releases totaling $370,000 in 2004, while the increase in the term life loss ratio primarily reflects the increased claim frequency and severity related to premium waiver claims.
Acquisition and Other Underwriting Expenses
The decrease in acquisition and other underwriting expenses from 2004 to 2005 primarily reflects a prior year premium tax return adjustment recorded in 2004, which increased other expenses.
Other Expenses
The decrease in other expenses primarily reflects the reduction in the postretirement liability totaling $1.5 million, partially offset by the additional pension expense totaling $294,000 and the absorption of certain expenses, including office rent and information technology, that were previously allocated to IBSi.
Tax Expense
The increase in income tax expense reflects the increase in pre-tax income, offset by a decrease in the effective tax rate. The effective tax rate was 32.6% in 2005, compared to 35.4% in 2004. The decrease in the effective tax rate from 2004 to 2005 reflects the release of the prior year valuation allowance totaling $227,000 related to low income housing credits, offset by a prior year tax return adjustment totaling $183,000.
67
Financial Position
December 31, 2006 compared to December 31, 2005.Total assets were $368.2 million as of December 31, 2006, compared to $111.2 million as of December 31, 2005. The increase reflects the proceeds from the initial public offering and the acquisition of EHC.
Total liabilities were $194.5 million as of December 31, 2006, compared to $49.1 million as of December 31, 2005. The increase primarily reflects the acquisition of EHC.
Total shareholders’ equity was $173.7 million as of December 31, 2006, compared to $62.1 million as of December 31, 2005. The increase primarily reflects the proceeds from the initial public offering and the acquisition of EHC.
Liquidity and Capital Resources
Liquidity is a measure of an entity’s ability to secure sufficient cash to meet its contractual obligations and operating needs. The Company’s principal sources of funds are underwriting operations, investment income and proceeds from sales and maturities of investments. The Company’s primary use of funds is to pay claims and operating expenses and to purchase investments.
The Company’s investment portfolio is structured so that investments mature periodically over time in reasonable relation to current expectations of future claim payments. The Company’s investment portfolio as of December 31, 2006 had an effective duration of 2.40 years. Currently, claim payments are made from positive cash flow from operations, but the Company also invests excess cash in securities with appropriate maturity dates matched against anticipated future claim payments. As these securities mature, the Company intends to invest any excess funds with appropriate durations to match expected future claim payments.
The Company and its subsidiaries also have lines of credit available to provide additional liquidity if needed. The Company has a $2.6 million line of credit and Eastern Re has a $30 million letter of credit facility if needed to secure obligations to reinsurers.
On May 15, 2003, Global Alliance Statutory Trust I, a business trust subsidiary formed by Global Alliance, issued $8.0 million of fixed/floating rate trust preferred securities. These securities have a thirty-year maturity, with a provision that allows the trust, at the direction of Global Alliance, to call these securities at par after five years from the date of issuance. Cash distributions will be paid quarterly in arrears at a rate of 7.35% for a period of five years and will float thereafter at 410 basis points over the three-month London Inter-Bank Offer Rate. The Company guarantees all obligations of the trust with respect to distributions and payments of these securities. Proceeds from the sale of these securities by the trust were used to acquire $8.0 million of fixed/floating rate junior subordinated debt issued by Global Alliance. This debt has the same terms with respect to maturity, payments, and distributions as the fixed/floating rate trust preferred securities issued by the trust.
The Company’s ability to manage liquidity results, in part, from the purchase of reinsurance to protect the Company against severe claims and catastrophic events. See “Item 1 – Business, Reinsurance.”
Our domestic insurance subsidiaries’ ability to pay dividends to the Company is limited by the insurance laws and regulations of Pennsylvania. The maximum annual dividends that the domestic insurance entities may pay without prior approval from the Department is limited to the greater of 10% of statutory surplus or 100% of statutory net income for the most recently filed annual statement. In addition, EIHI and its subsidiaries are prohibited from declaring or paying any dividends or other forms of distribution for the three years after June 16, 2006, the effective date of the conversion/merger transaction, without the prior approval of the Pennsylvania Insurance Commissioner. Eastern Re must receive approval from the Cayman Islands Monetary Authority before it can pay any dividend to the Company.
68
Cash Flows
The primary sources of cash flows for the Company are net premiums written, investment income, and proceeds from the sale or maturity of investments. The major components of cash flow are as follows for the years ended December 31, 2006, 2005, and 2004 (in thousands):
| | | | | | | | | | | | |
| | | December 31, | |
| | | 2006 | | | 2005 | | | 2004 | |
Cash provided by (used in) operating activities | | $ | 17,909 | | | $ | (847 | ) | | $ | 1,175 | |
Cash used in investing activities | | | (32,304 | ) | | | (5,414 | ) | | | (7,077 | ) |
Cash provided by financing activities | | | 60,399 | | | | — | | | | — | |
Cash Flows for Years Ended December 31, 2006 and 2005.The increase in net cash from operating activities reflects the acquisition of EHC and the improvement in the group benefits insurance segment operating results.
The increase in net cash used in investing activities reflects the acquisition of EHC and the investment of excess cash in the group benefits segment that was held during the prior year for purposes of paying expenses related to the conversion/merger transaction.
The net cash from financing activities reflects the net proceeds received from the initial public offering, net of related expenses.
Cash Flows for Years Ended December 31, 2005 and December 31, 2004. The decrease in net cash from operating activities primarily reflects the payment of transaction expenses totaling $2.3 million.
The decrease in net cash from investing activities primarily reflects a decrease in investment purchases of $8.1 million, offset by a decrease in investment sales and maturities of $6.7 million. The Company’s 2004 investment purchases included the investment of excess cash totaling $9.0 million in fixed income securities, as well as the investment of $2 million in a hedge fund. The decrease in investment sales and maturities from 2004 to 2005 primarily reflects the repositioning of the fixed income portfolio during 2004, as well as higher volume of maturities in 2004.
Contractual Commitments
The following table summarizes information about contractual obligations and commercial commitments. The minimum payments under these agreements as of December 31, 2006 were as follows (in thousands):
| | | | | | | | | | | | | | | |
| | | Payments Due By Period |
| | | Total | | Less than
1 year | | 1-3 years | | 4-5 years | | After 5 years |
Long term debt obligations: | | | | | | | | | | | | | | | |
Junior subordinated debentures (1) | | $ | 23,514 | | $ | 588 | | $ | 1,764 | | $ | 1,176 | | $ | 19,986 |
| | | | | | | | | | | | | | | |
Total long term debt obligations | | $ | 23,514 | | $ | 588 | | $ | 1,764 | | $ | 1,176 | | $ | 19,986 |
| | | | | |
Real estate lease obligation | | | 9,171 | | | 742 | | | 1,535 | | | 1,607 | | | 5,287 |
Loss reserves | | | 126,467 | | | 46,240 | | | 47,614 | | | 12,781 | | | 19,832 |
| | | | | | | | | | | | | | | |
Total contractual obligations | | $ | 159,152 | | $ | 47,570 | | $ | 50,913 | | $ | 15,564 | | $ | 45,105 |
| | | | | | | | | | | | | | | |
| (1) | Amounts include interest payments associated with the debt issued to related party trust using applicable interest rates as of December 31, 2006. In connection with the adoption of FIN 46R, the Company does not consolidate the trust established in connection with the issuance of its trust preferred securities. As a result, the Company reports as a component of long-term debt the junior subordinated debenture that its subsidiary, Global Alliance, pays to the trust. For a discussion of the circumstances in which the Company’s subordinated debt may be subject to acceleration, please see “Liquidity and Capital Resources.” |
The loss reserves payments due by period in the table above are based upon the loss and loss expense reserves estimates as of December 31, 2006, and actuarial estimates of expected payout patterns by line of business. As a result, our calculation of loss reserve payments due by period is subject to the same uncertainties associated with determining the level of reserves and to the additional uncertainties arising from the difficulty of predicting when claims (including claims that have not yet been reported to us) will
69
be paid. For a discussion of our reserving process, see “Item 1 – Business, Loss and Loss Adjustment Expense Reserves.” Actual payments of loss and loss adjustment expenses by period will vary, perhaps materially, from the above table to the extent that current estimates of loss reserves vary from actual ultimate claims amounts and as a result of variations between expected and actual payout patterns.
Off-Balance Sheet Arrangements
As of December 31, 2006, the Company has no off-balance sheet arrangements that have or are reasonably likely to have a current or future effect on the Company’s financial condition, changes in financial condition, revenues or expenses, results of operations, liquidity, capital expenditures or capital resources.
Item 7A – Quantitative and Qualitative Disclosures About Market Risk
Market risk is the potential economic loss principally arising from adverse changes in the fair value of financial instruments. The major components of market risk affecting the Company are credit risk, interest rate risk, and equity risk.
Credit Risk. Credit risk is the potential economic loss principally arising from adverse changes in the financial condition of a specific debt issuer. The Company addresses this risk by investing primarily in fixed-income securities which are rated “A” or higher by Standard & Poor’s. The Company also independently, and through the Company’s outside investment manager, monitors the financial condition of all of the issuers of fixed-income securities in the portfolio. To limit the Company’s exposure to risk, the Company employs diversification rules that limit the credit exposure to any single issuer or business sector.
Interest Rate Risk.The Company had fixed-income investments with a fair value of $204.4 million at December 31, 2006, that are subject to interest rate risk. The Company manages the exposure to interest rate risk through an asset/liability matching and capital management process. In the management of this risk, the characteristics of duration, credit and variability of cash flows are critical elements. These risks are assessed regularly and balanced within the context of the Company’s liability and capital position.
The table below summarizes the Company’s interest rate risk. It illustrates the sensitivity of the fair value of the Company’s fixed-income portfolio, including the equity call option component of the Company’s convertible bond portfolio, to selected hypothetical changes in interest rates as of December 31, 2006. The selected scenarios are not predictions of future events, but rather illustrate the effect that such events may have on the fair value of the Company’s fixed-income portfolio and shareholders’ equity (dollars in thousands).
| | | | | | | | | | |
Hypothetical Change in Interest Rates | | Estimated Change in
Fair Value | | | Estimated
Fair Value | | Hypothetical
Percentage Increase
(Decrease) in
Shareholders’ Equity | |
200 basis point increase | | $ | (13,523 | ) | | $ | 194,239 | | (7.8 | )% |
100 basis point increase | | | (6,713 | ) | | | 201,049 | | (3.9 | )% |
50 basis increase | | | (3,335 | ) | | | 204,427 | | (1.9 | )% |
No change | | | — | | | | 207,762 | | — | |
50 basis point decrease | | | 3,263 | | | | 211,025 | | 1.9 | % |
100 basis point decrease | | | 6,468 | | | | 214,230 | | 3.7 | % |
200 basis point decrease | | | 12,822 | | | | 220,584 | | 7.4 | % |
Equity Risk.Equity risk is the risk that the Company may incur economic loss due to adverse changes in equity prices. The Company’s exposure to changes in equity prices primarily results from its holdings of exchange traded funds and other equities. The Company’s portfolio of equity securities is carried on the balance sheet at fair value. Since only a small percentage of the Company’s assets are invested in equity securities, the Company does not believe that its exposure to equity price risk is significant.
70
Impact of Inflation
Inflation rates may impact the Company’s financial condition and operating results in several ways. Fluctuations in rates of inflation influence interest rates, which in turn affect the market value of the investment portfolio and yields on new investments. Inflation also affects the portion of losses and loss reserves that relates to hospital and medical expenses and property claims and loss adjustment expenses, but not the portion of losses and loss reserves that relates to workers’ compensation indemnity payments for lost wages, which are fixed by statute. Adjustments for inflationary effects are included as part of the continual review of loss reserve estimates. Increased costs are considered in setting premium rates, and this is particularly important in the health care area where hospital and medical inflation rates have exceeded general inflation rates. Operating expenses, including payrolls, are affected to a certain degree by the inflation rate.
71
Item 8 – Financial Statements and Supplementary Data
Report of Independent Registered Public Accounting Firm
To the Board of Directors and Shareholders
of Eastern Insurance Holdings, Inc.:
In our opinion, the consolidated financial statements listed in the accompanying index present fairly, in all material respects, the financial position of Eastern Insurance Holdings, Inc. and its subsidiaries at December 31, 2006, and the results of their operations and their cash flows for the year ended December 31, 2006 in conformity with accounting principles generally accepted in the United States of America. In addition, in our opinion, the financial statement schedules listed in the index appearing under Item 15 present fairly, in all material respects, the information set forth therein as of and for the year ended December 31, 2006 when read in conjunction with the related consolidated financial statements. These financial statements and financial statement schedules are the responsibility of the Company’s management. Our responsibility is to express an opinion on these financial statements and financial statement schedules based on our audit. We conducted our audit of these statements in accordance with the standards of the Public Company Accounting Oversight Board (United States). Those standards require that we plan and perform the audit to obtain reasonable assurance about whether the financial statements are free of material misstatement. An audit includes examining, on a test basis, evidence supporting the amounts and disclosures in the financial statements, assessing the accounting principles used and significant estimates made by management, and evaluating the overall financial statement presentation.

PricewaterhouseCoopers LLP
Philadelphia, Pennsylvania
March 30, 2007
72
Report of Independent Registered Public Accounting Firm
Board of Directors
Eastern Insurance Holdings, Inc. and Subsidiaries
Lancaster, Pennsylvania
We have audited the accompanying consolidated balance sheet of Eastern Insurance Holdings, Inc. and subsidiaries (formerly Educators Mutual Life Insurance Company) (the Company) as of December 31, 2005 and the related consolidated statements of operations and comprehensive income (loss) changes in shareholders’ equity, and cash flows for each of the two years in the period ended December 31, 2005. These consolidated financial statements are the responsibility of the Company’s management. Our responsibility is to express an opinion on these consolidated financial statements based on our audits.
We conducted our audits in accordance with the standards of the Public Company Accounting Oversight Board (United States). Those standards require that we plan and perform the audit to obtain reasonable assurance about whether the consolidated financial statements are free of material misstatement. The Company is not required to have, nor were we engaged to perform, an audit of its internal control over financial reporting. Our audits included consideration of internal control over financial reporting as a basis for designing audit procedures that are appropriate in the circumstances, but not for the purpose of expressing an opinion on the effectiveness of the Company’s internal control over financial reporting. Accordingly, we express no such opinion. An audit includes examining, on a test basis, evidence supporting the amounts and disclosures in the consolidated financial statements. An audit also includes assessing the accounting principles used and significant estimates made by management, as well as evaluating the overall financial statement presentation. We believe that our audits provide a reasonable basis for our opinion.
In our opinion, the 2005 and 2004 consolidated financial statements referred to above present fairly, in all material respects, the financial position of Eastern Insurance Holdings, Inc. and subsidiaries as of December 31, 2005 and the results of their operations and their cash flows for each of the two years in the period ended December 31, 2005 in conformity with accounting principles generally accepted in the United States of America.
/s/ Beard Miller Company LLP
Beard Miller Company LLP
Harrisburg, Pennsylvania
March 24, 2006
73
EASTERN INSURANCE HOLDINGS, INC. AND SUBSIDIARIES
CONSOLIDATED BALANCE SHEETS
(In thousands, except share and per share data)
| | | | | | | |
| | | December 31, 2006 | | | December 31, 2005 |
ASSETS | | | | | | | |
| | |
Investments: | | | | | | | |
Fixed income securities, at estimated fair value (amortized cost, $201,226; $72,608) | | $ | 204,444 | | | $ | 73,979 |
Equity securities, at estimated fair value (cost, $17,027) | | | 18,219 | | | | — |
Equity call options, at estimated fair value (cost, $2,230; $1,086) | | | 3,318 | | | | 1,308 |
Other long-term investments | | | 11,604 | | | | 2,333 |
| | | | | | | |
Total investments | | | 237,585 | | | | 77,620 |
| | |
Cash and cash equivalents | | | 50,703 | | | | 4,699 |
Accrued investment income | | | 2,236 | | | | 930 |
Premiums receivable (net of allowance, $558; $2) | | | 23,225 | | | | 87 |
Reinsurance recoverable on paid and unpaid losses and loss adjustment expenses | | | 27,525 | | | | 24,461 |
Deferred acquisition costs | | | 4,501 | | | | — |
Deferred income taxes, net | | | 2,696 | | | | 946 |
Intangible assets | | | 8,110 | | | | — |
Goodwill | | | 5,140 | | | | — |
Other assets | | | 6,485 | | | | 2,482 |
| | | | | | | |
Total assets | | $ | 368,206 | | | $ | 111,225 |
| | | | | | | |
LIABILITIES | | | | | | | |
| | |
Reserves for unpaid losses and loss adjustment expenses | | $ | 126,467 | | | $ | 44,136 |
Unearned premium reserves | | | 33,860 | | | | 95 |
Advance premium | | | 1,755 | | | | 1,241 |
Accounts payable and accrued expenses | | | 7,927 | | | | 2,473 |
Ceded reinsurance balances payable | | | 5,623 | | | | 216 |
Benefit plan liabilities | | | 324 | | | | 777 |
Dividends payable | | | 8,560 | | | | — |
Federal income taxes payable | | | 1,902 | | | | 178 |
Junior subordinated debentures | | | 8,044 | | | | — |
| | | | | | | |
Total liabilities | | | 194,462 | | | $ | 49,116 |
| | | | | | | |
Commitments and contingencies (Note 15) | | | | | | | |
| | |
SHAREHOLDERS’ EQUITY | | | | | | | |
| | |
Series A preferred stock, par value $0, auth. shares – 5,000,000; no shares issued and outstanding | | | — | | | | — |
Common capital stock, par value $0, auth. shares – 20,000,000; issued and outstanding - 11,350,407 | | | — | | | | — |
Unearned ESOP compensation | | | (7,101 | ) | | | — |
Additional paid in capital | | | 108,502 | | | | — |
Retained earnings | | | 69,483 | | | | 61,205 |
Accumulated other comprehensive income, net | | | 2,860 | | | | 904 |
| | | | | | | |
Total shareholders’ equity | | | 173,744 | | | | 62,109 |
| | | | | | | |
Total liabilities and shareholders’ equity | | $ | 368,206 | | | $ | 111,225 |
| | | | | | | |
See accompanying notes to consolidated financial statements.
74
EASTERN INSURANCE HOLDINGS, INC. AND SUBSIDIARIES
CONSOLIDATED STATEMENTS OF OPERATIONS
AND COMPREHENSIVE INCOME (LOSS)
(In thousands, except per share data)
| | | | | | | | | | | |
| | | For the Years Ended December 31, | |
| | | 2006 | | 2005 | | | 2004 | |
REVENUE | | | | | | | | | | | |
Net premiums earned | | $ | 74,919 | | $ | 38,702 | | | $ | 39,057 | |
Net investment income | | | 8,992 | | | 3,815 | | | | 3,724 | |
Net realized investment gains | | | 2,757 | | | 445 | | | | 1,271 | |
Other revenue | | | 313 | | | 1,066 | | | | 946 | |
| | | | | | | | | | | |
Total revenue | | | 86,981 | | | 44,028 | | | | 44,998 | |
| | | | | | | | | | | |
EXPENSES | | | | | | | | | | | |
Losses and loss adjustment expenses incurred | | | 47,913 | | | 27,090 | | | | 25,932 | |
Acquisition and other underwriting expenses | | | 5,941 | | | 5,452 | | | | 5,670 | |
Other expenses | | | 15,690 | | | 9,674 | | | | 10,601 | |
Amortization of intangibles | | | 1,088 | | | — | | | | — | |
Policyholder dividend expense | | | 239 | | | — | | | | — | |
Segregated portfolio dividend expense | | | 2,890 | | | — | | | | — | |
| | | | | | | | | | | |
Total expenses | | | 73,761 | | | 42,216 | | | | 42,203 | |
| | | | | | | | | | | |
Income before income taxes | | | 13,220 | | | 1,812 | | | | 2,795 | |
Income tax expense | | | 4,942 | | | 685 | | | | 1,012 | |
| | | | | | | | | | | |
Net income | | $ | 8,278 | | $ | 1,127 | | | $ | 1,783 | |
| | | | | | | | | | | |
Other comprehensive income (loss) | | | | | | | | | | | |
Unrealized holding gains (losses) arising during period, net of tax | | | 1,902 | | | (1,162 | ) | | | (903 | ) |
Less: Reclassification adjustment for gains included in net income, net of tax of $198, $204, and $358 | | | 369 | | | 397 | | | | 695 | |
| | | | | | | | | | | |
Other comprehensive income (loss) | | | 1,533 | | | (1,559 | ) | | | (1,598 | ) |
| | | | | | | | | | | |
Comprehensive income (loss) | | $ | 9,811 | | $ | (432 | ) | | $ | 185 | |
| | | | | | | | | | | |
| | | |
| | | For the Period
from June 17, 2006
to December 31, 2006 |
Earnings per share (See Note 6): | | | |
Net income after conversion and acquisition | | $ | 7,142 |
Basic earnings per share after conversion and acquisition | | $ | 0.67 |
Diluted earnings per share after conversion and acquisition | | $ | 0.65 |
See accompanying notes to consolidated financial statements.
75
EASTERN INSURANCE HOLDINGS, INC. AND SUBSIDIARIES
CONSOLIDATED STATEMENTS OF CHANGES IN SHAREHOLDERS’ EQUITY
For the Years Ended December 31, 2006, 2005 and 2004
(In thousands, except share data)
| | | | | | | | | | | | | | | | | | | | | | | | | |
| | | Outstanding Shares | | | | | | | | | | | | | | | |
| | | Series A
Preferred
Stock | | Common Capital
Stock | | Common
Capital
Stock | | Unearned
ESOP
Compensation | | | Additional
Paid-In
Capital | | Retained
Earnings | | Accumulated
Other
Comprehensive
Income,
Net of Taxes | | | Total | |
Balance, January 1, 2004 | | — | | — | | $ | — | | $ | — | | | $ | — | | $ | 58,295 | | $ | 4,061 | | | $ | 62,356 | |
Net income | | — | | — | | | — | | | — | | | | — | | | 1,783 | | | — | | | | 1,783 | |
Other comprehensive loss, net of tax | | — | | — | | | — | | | — | | | | — | | | — | | | (1,598 | ) | | | (1,598 | ) |
| | | | | | | | | | | | | | | | | | | | | | | | | |
Balance, December 31, 2004 | | — | | — | | | — | | | — | | | | — | | | 60,078 | | | 2,463 | | | | 62,541 | |
Net income | | — | | — | | | — | | | — | | | | — | | | 1,127 | | | — | | | | 1,127 | |
Other comprehensive loss, net of tax | | — | | — | | | — | | | — | | | | — | | | — | | | (1,559 | ) | | | (1,559 | ) |
| | | | | | | | | | | | | | | | | | | | | | | | | |
Balance, December 31, 2005 | | — | | — | | | — | | | — | | | | — | | | 61,205 | | | 904 | | | | 62,109 | |
Net proceeds from stock offering | | — | | 7,475,000 | | | — | | | — | | | | 69,597 | | | — | | | — | | | | 69,597 | |
Unearned ESOP compensation | | —�� | | — | | | — | | | (7,475 | ) | | | — | | | — | | | — | | | | (7,475 | ) |
ESOP shares released | | — | | | | | — | | | 374 | | | | 151 | | | — | | | — | | | | 525 | |
Issuance of common stock | | — | | 3,875,407 | | | — | | | — | | | | 38,754 | | | — | | | — | | | | 38,754 | |
Net income | | — | | — | | | — | | | — | | | | — | | | 8,278 | | | — | | | | 8,278 | |
Other comprehensive income, net of tax | | — | | — | | | — | | | — | | | | — | | | — | | | 1,533 | | | | 1,533 | |
Adoption of SFAS 158 | | — | | — | | | — | | | — | | | | — | | | — | | | 423 | | | | 423 | |
| | | | | | | | | | | | | | | | | | | | | | | | | |
Balance, December 31, 2006 | | — | | 11,350,407 | | $ | — | | $ | (7,101 | ) | | $ | 108,502 | | $ | 69,483 | | $ | 2,860 | | | $ | 173,744 | |
| | | | | | | | | | | | | | | | | | | | | | | | | |
See accompanying notes to consolidated financial statements.
76
EASTERN INSURANCE HOLDINGS, INC. AND SUBSIDIARIES
CONSOLIDATED STATEMENTS OF CASH FLOWS
For the Years Ended December 31, 2006, 2005 and 2004
(In thousands)
| | | | | | | | | | | | |
| | | 2006 | | | 2005 | | | 2004 | |
Cash flows from operating activities: | | | | | | | | | | | | |
Net income | | $ | 8,278 | | | $ | 1,127 | | | $ | 1,783 | |
Adjustments to reconcile net income to net cash provided by (used in) operating activities: | | | | | | | | | | | | |
Depreciation and amortization | | | 263 | | | | 222 | | | | 448 | |
Amortization of bond premium/discount | | | 516 | | | | 167 | | | | 148 | |
Gain on sale of investments | | | (1,920 | ) | | | (706 | ) | | | (1,054 | ) |
Other than temporary investment impairments | | | — | | | | 104 | | | | — | |
Unrealized (gain) loss on equity call options | | | (837 | ) | | | 367 | | | | (217 | ) |
Gain on sale of interest of IBSi | | | — | | | | (210 | ) | | | — | |
Equity in income of limited partnerships | | | (236 | ) | | | (100 | ) | | | (65 | ) |
Loss on disposal of property and equipment | | | 19 | | | | 32 | | | | 27 | |
Loss on impairment of property and equipment and software | | | — | | | | — | | | | 81 | |
Recognition of deferred gain on sale of building | | | (287 | ) | | | (116 | ) | | | (116 | ) |
Deferred tax (benefit) provision | | | (243 | ) | | | 344 | | | | 789 | |
Stock compensation | | | 525 | | | | — | | | | — | |
Intangible asset amortization | | | 1,088 | | | | — | | | | — | |
Changes in assets and liabilities: | | | | | | | | | | | | |
Accrued investment income | | | 101 | | | | 91 | | | | 152 | |
Premiums receivable | | | 5,084 | | | | (33 | ) | | | 26 | |
Reinsurance recoverable on paid and unpaid losses and loss adjustment expenses | | | 4,024 | | | | (682 | ) | | | 1,043 | |
Deferred acquisition costs | | | (4,501 | ) | | | — | | | | — | |
Other assets | | | (394 | ) | | | (1,555 | ) | | | 255 | |
Reserves for unpaid losses and loss adjustment expenses | | | 985 | | | | 753 | | | | (2,626 | ) |
Unearned and advance premium | | | 4,275 | | | | 105 | �� | | | 205 | |
Ceded reinsurance balances payable | | | (1,081 | ) | | | 44 | | | | (313 | ) |
Accounts payable and accrued expenses | | | 185 | | | | 809 | | | | (78 | ) |
Benefit plan liabilities | | | (88 | ) | | | (1,349 | ) | | | (10 | ) |
Federal income taxes recoverable/payable | | | 1,703 | | | | 120 | | | | 168 | |
Dividends payable | | | 450 | | | | — | | | | — | |
Other liabilities | | | — | | | | (381 | ) | | | 529 | |
| | | | | | | | | | | | |
Net cash provided by (used in) operating activities | | | 17,909 | | | | (847 | ) | | | 1,175 | |
| | | | | | | | | | | | |
Cash flows from investing activities: | | | | | | | | | | | | |
Purchase of fixed income securities | | | (63,783 | ) | | | (18,982 | ) | | | (27,112 | ) |
Purchase of equity securities | | | (15,666 | ) | | | — | | | | — | |
Purchase of other long-term investments | | | (7,860 | ) | | | — | | | | — | |
Proceeds from sale of fixed income securities | | | 42,443 | | | | 6,166 | | | | 9,030 | |
Proceeds from maturities/calls of fixed income securities | | | 19,699 | | | | 7,097 | | | | 10,901 | |
Proceeds from the sale of equity securities | | | 6,855 | | | | — | | | | — | |
Proceeds from sale of other long-term investments | | | 550 | | | | — | | | | — | |
Change in unsettled investment purchases and sales | | | (352 | ) | | | — | | | | — | |
Acquisition of Eastern Holding Company, Ltd., net of cash received | | | (14,149 | ) | | | — | | | | — | |
Net proceeds from sale of interest in IBSi | | | — | | | | 210 | | | | — | |
Principal payments received on mortgage loans | | | 18 | | | | 112 | | | | 132 | |
Purchase of equipment, net | | | (59 | ) | | | (17 | ) | | | (28 | ) |
| | | | | | | | | | | | |
Net cash used in investing activities | | | (32,304 | ) | | | (5,414 | ) | | | (7,077 | ) |
| | | | | | | | | | | | |
Cash flows from financing activities: | | | | | | | | | | | | |
Proceeds from initial public offering, net of expenses | | | 62,122 | | | | — | | | | — | |
Repayment of long-term debt | | | (1,723 | ) | | | — | | | | — | |
| | | | | | | | | | | | |
Net cash provided by financing activities | | | 60,399 | | | | — | | | | — | |
| | | | | | | | | | | | |
Net increase (decrease) in cash and cash equivalents | | | 46,004 | | | | (6,261 | ) | | | (5,902 | ) |
Cash and cash equivalents, beginning of period | | | 4,699 | | | | 10,960 | | | | 16,862 | |
| | | | | | | | | | | | |
Cash and cash equivalents, end of period | | $ | 50,703 | | | $ | 4,699 | | | $ | 10,960 | |
| | | | | | | | | | | | |
Supplemental disclosure of cash flow information: | | | | | | | | | | | | |
Cash paid for income taxes | | $ | 7,163 | | | $ | 200 | | | $ | 278 | |
Cash paid for interest | | $ | 324 | | | $ | — | | | $ | — | |
See accompanying notes to consolidated financial statements
77
Eastern Insurance Holdings, Inc. and Subsidiaries
Notes to Consolidated Financial Statements
(Dollars in thousands except share and per share data)
1. Background and Nature of Operations
Eastern Insurance Holdings, Inc. (“EIHI”) was formed by Eastern Life and Health Insurance Company (“ELH”), formerly Educators Mutual Life Insurance Company, for the purpose of converting from a mutual life and health insurance company to a stock life and health insurance company. On June 16, 2006, EIHI completed its common stock offering and ELH completed its conversion from a mutual company to a stock company and became a wholly-owned subsidiary of EIHI. In the common stock offering, EIHI sold 7,475,000 shares of its common stock at a price of $10.00 per share, raising gross proceeds of $74.8 million. Direct expenses of the offering were $5.2 million and were recorded as a direct reduction of additional paid-in capital in the accompanying consolidated balance sheet as of December 31, 2006.
Immediately after the common stock offering and conversion, EIHI purchased all of the outstanding common stock of Eastern Holding Company, Ltd. (“EHC”) for a purchase price of $78.9 million (See Note 3).
EIHI is an insurance holding company offering workers’ compensation and group benefits insurance products through its wholly-owned subsidiaries. The accompanying consolidated financial statements include the accounts of EIHI and its wholly-owned subsidiaries (collectively, the “Company”), EHC and ELH, and EHC’s wholly-owned subsidiaries, Eastern Services Corporation (“Eastern Services”), Global Alliance Holdings, Ltd. (“Global Alliance”), Global Alliance Statutory Trust I (“Trust I”), Eastern Alliance Insurance Company (“Eastern Alliance”), Allied Eastern Indemnity Company (“Allied Eastern”), Eastern Re Ltd., S.P.C. (“Eastern Re”), and Employers Alliance, Inc. (“Employers Alliance”).
Effective June 16, 2006, EHC was redomesticated from the Cayman Islands to the United States of America. As a result of the redomestication, EHC and Eastern Re are subject to federal income tax on a prospective basis.
The Company operates in five segments: workers’ compensation insurance, group benefits insurance, specialty reinsurance, segregated portfolio cell reinsurance, and corporate/other.
Workers’ Compensation Insurance
Workers’ compensation insurance is underwritten through Eastern Alliance and Allied Eastern, both Pennsylvania domiciled insurance companies, which provide workers’ compensation insurance coverage to small and medium sized businesses in rural and suburban Pennsylvania, Maryland and Delaware.
Segregated Portfolio Cell Reinsurance
The Company provides a variety of services to self-insured workers’ compensation plans including program design, fronting, claims adjusting, investment management and cell rental services at Eastern Re. The primary insurance coverage for the segregated portfolio cell programs is underwritten by Eastern Alliance and Allied Eastern and ceded 100% to Eastern Re.
Group Benefits Insurance
Group benefits insurance, which includes the Company’s dental, short and long-term disability, and term life insurance products are underwritten through ELH. The group benefits insurance products are primarily marketed to small and medium sized businesses. ELH is licensed to write business in 41 jurisdictions in the United States. ELH is currently actively writing business in 16 jurisdictions, primarily in the Mid-Atlantic, Southeast, and Midwest regions of the United States.
Specialty Reinsurance
Specialty reinsurance is underwritten through Eastern Re, a Cayman domiciled reinsurer. Eastern Re assumes business through its participation in reinsurance treaties with an unaffiliated insurance company related to an underground storage tank program and a non-hazardous waste transportation product.
78
Corporate/Other
The corporate/other segment consists of the operating results of Employers Alliance, the Company’s third party administrator, which provides claims adjusting and risk management services to self-insured workers’ compensation and property and casualty plans. This segment also includes the operations of EIHI, EHC, Eastern Services and Global Alliance, the run-off operations of ELH’s group medical insurance operations, and certain eliminations necessary to reconcile the segment information to the consolidated statements of operations and comprehensive income (loss). Prior to January 1, 2006, the corporate/other segment included the operating results of IBSi, ELH’s former general agency operation. IBSi was sold by ELH on October 31, 2005 (See Note 14).
These segments are more fully described in Note 13.
2. Significant Accounting Policies
Basis of Presentation
The accompanying consolidated financial statements have been prepared in accordance with accounting principles generally accepted in the United States of America (“GAAP”).
All inter-company transactions and related account balances have been eliminated in consolidation.
Certain amounts in the prior year consolidated financial statements have been reclassified to conform to the current year presentation.
Use of Estimates
The preparation of the consolidated financial statements requires management to make estimates and assumptions that affect the amount of reported assets and liabilities and disclosures of contingent assets and liabilities as of the date of the consolidated financial statements and the reported amounts of revenue and expenses during the reporting period. The most significant estimates in the consolidated financial statements include reserves for unpaid losses and loss adjustment expenses, earned but unbilled premium, deferred acquisition costs, return premiums under reinsurance contracts, current and deferred income taxes, and benefit plan liabilities. Actual results could differ from these estimates.
Cash and Cash Equivalents
The Company considers all investments with original maturity dates of three months or less to be cash equivalents for purposes of the consolidated statements of cash flows. The carrying amount of cash equivalents approximates their fair value.
Investments
Fixed Income Securities
The Company’s investments in fixed income securities are classified as available-for-sale and are carried at estimated fair value, with unrealized gains and losses reported in accumulated other comprehensive income (loss), net of tax. Fixed income securities include publicly traded and private placement bonds, including convertible bonds. The estimated fair value of publicly traded bonds is determined based on quoted market prices obtained through an independent pricing service or independent broker. The estimated fair value of private placement bonds is determined using valuation models, taking into consideration the securities’ coupon rate, maturity date, and other pertinent features.
Premiums or discounts are amortized using the effective interest method. Realized gains or losses are based on amortized cost and are computed using the specific identification method. The Company monitors its fixed income securities for unrealized losses that appear to be other-than-temporary. The Company performs a detailed review of these securities to determine the underlying cause of the unrealized loss and whether the security is impaired. At the time a security is determined to be other-than- temporarily impaired, the Company reduces the book value of the security to the estimated fair value and records a realized loss in the consolidated statements of operations and comprehensive income (loss). Any subsequent increase in the security’s estimated fair value would be reported as an unrealized gain.
79
Equity Securities
The Company’s investments in equity securities are classified as available-for-sale and are carried at estimated fair value, with unrealized gains and losses reported in accumulated other comprehensive income (loss), net of tax. The estimated fair value of equity securities is determined based on quoted market prices obtained through an independent pricing service or independent broker.
Realized gains or losses are based on cost and are computed using the specific identification method. The Company monitors its equity securities for unrealized losses that appear to be other-than-temporary. The Company performs a detailed review of these securities to determine the underlying cause of the unrealized loss and whether the security is impaired. At the time a security is determined to be other-than-temporarily impaired, the Company reduces the cost of the security to the estimated fair value and records a realized loss in the consolidated statements of operations and comprehensive income (loss). Any subsequent increase in the security’s estimated fair value would be reported as an unrealized gain.
Equity Call Options
Equity call options represent the estimated fair value of the stock options embedded in the Company’s convertible bond portfolio. The estimated fair value of the fixed income component of the convertible bond is included in fixed income securities. The estimated fair value of equity call options is determined by deducting the theoretical bond value (which is determined using spread information on non-convertible issues from the same issuer) from the estimated fair value of the convertible bond (which is determined based on quoted market prices obtained through an independent pricing service). The equity call option is considered an embedded derivative and changes in the estimated fair value of the equity call options are reported as realized gains or losses in the consolidated statements of operations and comprehensive income (loss).
Other Long-Term Investments
Other long-term investments consist of investments in limited partnerships and mortgage loans on real estate.
Investments in limited partnerships are reported in the consolidated financial statements using the equity method. Changes in the value of the Company’s proportionate share of its limited partnership investments are included in net investment income in the consolidated statements of operations and comprehensive income (loss).
Mortgage loans on real estate are carried at their unpaid principal balance.
Premiums
Premiums generated by the Company’s workers’ compensation insurance segment, including estimates of additional premiums resulting from audits of insureds’ records, are generally recognized as written upon inception of the policy. Premiums written are primarily earned on a daily pro rata basis over the terms of the policies to which they relate. Accordingly, unearned premiums represent the portion of premiums written which is applicable to the unexpired portion of the policies in force. Workers’ compensation premiums are determined based upon the payroll of the insured, the applicable premium rates and, where applicable, an experience based modification factor. An audit of the policyholders’ records is conducted after policy expiration to make a final determination of applicable premiums. Included in net premiums earned is an estimate for earned but unbilled final audit premiums. The Company estimates earned but unbilled premiums by tracking, by policy, how much additional premium is billed in final audit invoices as a percentage of payroll exposure to estimate the probable additional amount that it has earned, but not yet billed, as of the balance sheet date. Earned but unbilled premiums accrued as of December 31, 2006, and included in net premiums earned, totaled $1.5 million.
Premiums generated by the Company’s group benefits insurance segment are generally billed on a monthly basis with premiums being earned in the month in which the coverage is provided. Unearned premiums represent those premiums that have been received but for which the coverage period has not expired. Advance premiums represent those premiums that have been received in advance of the coverage period. Premiums receivable represent only those premiums that have been billed to policyholders for coverage periods through the balance sheet date.
80
Reinsurance premiums assumed by the Company’s specialty reinsurance segment are estimated based on information provided by the ceding companies. The information used in establishing these estimates is reviewed and subsequent adjustments are recorded in the period in which they are reported. These premiums are earned over the terms of the related reinsurance contracts.
Other Revenue
Other revenue for the year ended December 31, 2006 primarily consists of service revenues related to claims adjusting and risk management services provided by Employers Alliance. Claims adjusting and risk management service revenue is earned over the term of the related contracts in proportion to the actual services rendered.
Other revenue for the years ended December 31, 2005 and 2004 consists of sales and marketing fees earned by IBSiunder contracts with unaffiliated insurance carriers. Prior to the sale of IBSi, sales and marketing fees were generally recognized as revenue in the period in which the insurance policy was effective. IBSi also earned bonus revenue for meeting agreed-upon production levels with certain external carriers. Bonus revenue was estimated and accrued in the period in which the agreed-upon production levels were met.
Losses and Loss Adjustment Expenses
A liability is established for the estimated unpaid losses and loss adjustment expenses (“LAE”) of the Company’s workers’ compensation insurance segment under the terms of, and with respect to, its policies and agreements and includes amounts determined on the basis of claims adjusters’ evaluations and an amount based on past experience for losses incurred but not reported.
The Company discounts its reserves for unpaid losses and LAE for workers’ compensation claims on a non-tabular basis, using a discount rate of 3%, based upon regulatory guidelines. The reserves for unpaid losses and LAE have been reduced for the effects of discounting by approximately $3.3 million as of December 31, 2006.
A liability is established for the estimated unpaid losses and loss adjustment expenses of the Company’s group benefits insurance segment as follows:
| | • | | The liability for reported but unpaid long-term disability claims is calculated using the 1987 Commissioners Group Disability Table. The long-term disability reserves are discounted based on the expected rate of return of ELH’s fixed income portfolio in the year that the claim was incurred. The discount rate for claims incurred in 2006 and 2005 was 4.75% and 4.25%, respectively. The liability for incurred but not reported claims is estimated on a policy-by-policy basis, taking into consideration average monthly premium, policy elimination periods, and an expected loss ratio. |
| | • | | The liability for reported but unpaid and incurred but not reported dental and short-term disability claims is estimated using statistical claim development models, taking into consideration historical claim severity and frequency patterns and changes in benefit structures that may impact the amount at which claims are ultimately settled. For the most recent incurral months, which usually consist of the last three months, the liability is estimated by applying an expected loss ratio to net premiums earned, less claim payments through the balance sheet date. |
| | • | | The liability for reported but unpaid term life claims represent those claims reported to the Company as of the balance sheet date for which payment has not yet been made. Term life incurred but not reported claims are estimated based on historical patterns of claims incurred as a percent of in-force premium as of the balance sheet date. |
| | • | | The liability for life premium waiver reserves represents the present value of future life insurance benefits under those term life insurance policies for which premium has been waived due to the |
81
insured’s disability. The liability for life premium waiver reserves is calculated using the 1970 Intercompany Group Life Disability Table. The liability for life premium waiver reserves is discounted using a rate of 3%, which is built into the valuation table.
A liability is established for the estimated unpaid losses and LAE of the Company’s specialty reinsurance segment based on information provided by the ceding company. Premiums and reported claims data provided by the ceding company is utilized by management to estimate the ultimate losses and LAE, including an amount for incurred but not reported claims.
The methods used to estimate the reserves for unpaid losses and loss adjustment expenses are reviewed periodically and any adjustments resulting therefrom are reflected in current operations.
Management believes that its reserves for unpaid losses and loss adjustment expenses is adequate as of December 31, 2006. However, estimating the ultimate liability is necessarily a complex and judgmental process inasmuch as the amounts are based on management’s informed estimates and judgments using data currently available. If the Company’s ultimate losses, net of reinsurance, prove to differ substantially from the amounts recorded as of December 31, 2006, the related adjustments could have a material adverse effect on the Company’s financial condition, results of operations or liquidity.
Reinsurance
In the ordinary course of business, the Company assumes and cedes reinsurance with other insurance companies. These arrangements provide greater diversification of business and minimize the net loss potential arising from large claims. Ceded reinsurance contracts do not relieve the Company of its obligation to its insureds. Premiums and claims under the Company’s reinsurance contracts are accounted for on a basis consistent with those used in accounting for the underlying policies reinsured and the terms of the reinsurance contracts. The Company has certain reinsurance contracts that provide for return premium based on the actual loss experience of the written and reinsured business. The Company estimates the amounts to be recorded for return premium based on the terms set forth in the reinsurance agreements and the expected loss experience.
The reinsurance recoverable for unpaid losses and LAE includes the balances due from reinsurance companies for unpaid losses and LAE that are expected to be recovered from reinsurers, based on contracts in force.
Policy Acquisition Costs
Policy acquisition costs consist primarily of commissions and premium taxes that vary with and are primarily related to the production of premium. Policy acquisition costs are deferred and amortized over the period in which the related premiums are earned. Deferred acquisition costs are limited to the estimated amounts recoverable after providing for losses and loss adjustment expenses that are expected to be incurred based upon historical and current experience. Anticipated investment income is considered in determining recoverability.
The Company’s group benefits insurance policies are cancelable and are not guaranteed renewable. In addition, the group benefits insurance policies provide coverage on a month-to-month basis with most policies’ coverage effective on the first of each month. As a result, most of the Company’s group benefits insurance premiums are earned as of the balance sheet date. Based on the nature of the Company’s group benefits insurance policies, costs related to the acquisition of new and renewal business are expensed as incurred.
Amortization of policy acquisition costs totaled $1.9 million for the year ended December 31, 2006. There were no deferred acquisition costs or related amortization in 2005 or 2004.
Income Taxes
Deferred tax assets and liabilities are determined based on differences between the financial reporting and tax basis of assets and liabilities and are measured using enacted tax rates and laws that are expected to be in effect when the difference is reversed. A valuation allowance is recorded against gross deferred tax assets if it is more likely than not that all or some portion of the benefits related to the deferred tax assets will not be realized.
82
Eastern Alliance, Allied Eastern and ELH are not subject to state income taxes; rather, they are subject to state premium tax in the jurisdictions in which they write business. Employers Alliance and Eastern Services are subject to Pennsylvania state income tax.
Eastern Re is an exempt entity under the Companies Law of the Cayman Islands; however, Eastern Re’s earnings and profits are subject to federal income tax for earnings subsequent to June 16, 2006, as a result of the redomestication of EHC.
Policyholder Dividends
Eastern Alliance and Allied Eastern issue certain workers’ compensation insurance policies with dividend payment features. These policyholders share in the operating results of their respective policies in the form of dividends. Dividends to policyholders are accrued during the period in which the related premiums are earned and are determined based on the terms of the individual policies.
Property and Equipment
Property and equipment, including expenditures for significant improvements and purchased software, is carried at cost less accumulated depreciation and amortization. Maintenance, repairs and minor improvements are expensed as incurred. When property and equipment is retired or otherwise disposed of, the cost and related accumulated depreciation are removed from the accounts and any resulting gain or loss is included in operations. Depreciation is computed under the straight-line method. The estimated useful lives of property and equipment range from 3-7 years. Accumulated depreciation and amortization expense totaled $6,038 and $5,652 as of December 31, 2006 and 2005, respectively. Depreciation and amortization expense totaled $263, $222, and $448 for the years ended December 31, 2006, 2005 and 2004, respectively.
Property, equipment and software are reviewed for impairment whenever changes in circumstances indicate that the carrying value of such assets may not be recoverable. Impairment losses are recognized to the extent the carrying amount of the asset exceeds the undiscounted cash flows expected to result from the use of the asset and its eventual disposal. There were no impairments recorded in 2006 or 2005. The Company recorded an impairment loss related to the write-down of certain property, equipment and software totaling $81 in 2004, which is included in other expenses in the consolidated statements of operations and comprehensive income (loss).
Assessments
Eastern Alliance and Allied Eastern are subject to state guaranty fund assessments in the Commonwealth of Pennsylvania, which provide for the payment of covered claims or to meet other insurance obligations from insurance company insolvencies. The Company’s assessments consist primarily of charges from the Workers’ Compensation Security Fund of Pennsylvania (“Security Fund”). The Security Fund serves as a guaranty fund to provide claim payments for those workers entitled to workers’ compensation benefits when the insurance company originally providing the benefits was placed into liquidation by a court. Security Fund assessments are established on an actuarial basis to provide an amount sufficient to pay the outstanding and anticipated claims in a timely manner, to meet the costs of the Pennsylvania Insurance Department to administer the fund and to maintain a minimum balance in the fund of $500 million. If the Security Fund determines that the balance in the Security Fund is less than $500 million based on the actuarial study, then an assessment equal to one percent of direct written premium is made to all companies licensed to write workers’ compensation in Pennsylvania. Eastern Alliance and Allied Eastern recognize a liability and the related expense for the assessments when premiums covered under the Security Fund are written; when an assessment from the Security Fund has been imposed or it is probable that an assessment will be imposed; and the amount of the assessment is reasonably estimable. The Company has not recorded an assessment for the year ended December 31, 2006, as an assessment is not expected in 2007 on direct premium written in 2006.
Goodwill and Intangible Assets
Goodwill represents the excess of cost over the fair value of net assets of businesses acquired. Goodwill and other intangible assets acquired in a purchase business combination and determined to have an indefinite useful life are not amortized, but are instead tested for impairment at least annually. Intangible
83
assets with estimable useful lives are amortized over their respective estimated useful lives to their estimated residual values, and reviewed for impairment in accordance with Statement of Financial Accounting Standards No. 144 (“SFAS 144”), “Accounting for Impairment or Disposal of Long-Lived Assets.”
Employee Stock Ownership Plan
The Company recognizes compensation expense related to its employee stock ownership plan (“ESOP”) equal to the product of the number of shares earned, or committed to be released, during the period, and the average price of the Company’s common stock during the period. The estimated fair value of unearned ESOP shares is calculated based on the average price of the Company’s common stock for the period. For purposes of calculating earnings per share, the Company includes the weighted average of ESOP shares committed to be released for the period.
Concentrations of Credit Risk
Financial instruments, which potentially expose the Company to concentrations of credit risk, consist primarily of cash and cash equivalents, investments, premiums receivable, and amounts recoverable from reinsurers.
The Company’s investment policy limits the amount of securities that can be held in any one issuer or any one industry. Therefore, the Company believes there are no significant concentrations of credit risk related to its investment portfolio.
Comprehensive Income (Loss)
Comprehensive income (loss) includes all changes in shareholders’ equity during the reporting period. Other comprehensive income (loss) includes those revenues, expenses, gains and losses that are included in comprehensive income (loss), but not net income.
Cash Flow Information
Purchases and sales or maturities of short-term investments are recorded net for purposes of the consolidated statements of cash flows and are included with fixed income securities.
Recent Accounting Pronouncements
SFAS 158
In September 2006, the Financial Accounting Standards Board (“FASB”) issued SFAS 158, “Employers’ Accounting for Defined Benefit Pension and Other Postretirement Plans, an amendment to FASB Statements No. 87, 88, 106, and 132(R)”. SFAS 158 requires employers to recognize the funded status of a benefit plan in its statement of financial position, with changes in the funded status occurring during the year reported as a component of other comprehensive income or loss. The funded status of a benefit plan represents the difference between plan assets at fair value and the benefit obligation. For defined benefit pension plans and postretirement benefit plans, the benefit obligation is the projected benefit obligation and accumulated postretirement benefit obligation, respectively. In addition to the above changes, SFAS 158 requires that plan assets and benefit obligations be measured as of the date of an employer’s fiscal year-end. The recognition and disclosure provisions of SFAS 158 are effective for fiscal years ending December 31, 2006. The requirement to measure plan assets and benefit obligations as of the end of an employer’s fiscal year-end is effective for fiscal years ending after December 31, 2008. As a result of adopting SFAS 158 effective December 31, 2006, the prepaid asset related to our defined benefit pension plan increased $287 and our liability related to our defined benefit postretirement plan decreased $364, resulting in an increase to accumulated other comprehensive income of $423, net of tax.
The incremental effect of adopting SFAS 158 on the Company’s consolidated balance sheet as of December 31, 2006 is shown in the table below (in thousands). The adoption of SFAS 158 had no effect on the Company’s consolidated statement of operations and comprehensive income (loss) for the year ended December 31, 2006.
84
| | | | | | | | | | |
| | | Before Application
of SFAS 158 | | Adjustments | | | After Application
of SFAS 158 |
Other assets | | $ | 6,198 | | $ | 287 | | | $ | 6,485 |
Total assets | | | 367,919 | | | 287 | | | | 368,206 |
Benefit plan liabilities | | | 688 | | | (364 | ) | | | 324 |
Total liabilities | | | 194,826 | | | (364 | ) | | | 194,462 |
Accumulated OCI | | | 2,209 | | | 651 | | | | 2,860 |
Total shareholders’ equity | | | 173,093 | | | 651 | | | | 173,744 |
Total liabilities and shareholders’ equity | | | 367,919 | | | 287 | | | | 368,206 |
SFAS 157
In September 2006, the FASB issued SFAS 157, “Fair Value Measurements”. SFAS 157 clarifies the definition of fair value for purposes of financial reporting, specifies the methods to be used to measure fair value, and requires expanded disclosures related to fair value and financial instruments measured at fair value. SFAS 157 is effective for financial statements issued for fiscal years beginning after November 15, 2007. Early application is encouraged, provided an entity has not yet issued financial statements for the fiscal year, including interim financial statements. Management is currently evaluating the impact of SFAS 157 on its current fair value disclosures. The Company expects that the adoption of SFAS 157 will not have a material effect on its consolidated financial condition or results of operations.
FIN 48
In July 2006, the FASB issued FASB Interpretation No. 48, “Accounting for Uncertainty in Income Taxes – an interpretation of FASB Statement No. 109” (“FIN 48”), which provides criteria for the recognition, measurement, presentation and disclosure of uncertain tax positions. A tax benefit from an uncertain position may be recognized only if it is “more likely than not” that the position is sustainable based on its technical merits. The provisions of FIN 48 are effective for fiscal years beginning after December 15, 2006. The Company expects that the adoption of FIN 48 will not have a material effect on its consolidated financial condition or results of operations.
SFAS 155
In February 2006, the FASB issued SFAS 155, “Accounting for Certain Hybrid Financial Instruments, an amendment of FASB Statements No. 133 and 140”. SFAS 155 amends the accounting requirements for certain financial instruments covered by FASB Statements No. 133 and 140, including financial instruments containing embedded derivatives. SFAS 155 amends FASB Statement No. 133 by permitting fair value remeasurement of any hybrid financial instrument that contains an embedded derivative. Under current accounting guidance contained in FASB Statement No. 133, embedded derivatives must be bifurcated from their host contract and accounted for separately. SFAS 155 is effective for all financial instruments acquired, issued or subject to a remeasurement event occurring after the beginning of an entity’s first fiscal year that begins after September 15, 2006. The fair value election for hybrid financial instruments may also be applied upon adoption of SFAS 155 to those hybrid financial instruments held by an entity and bifurcated under FASB Statement No. 133 prior to the adoption of SFAS 155. Any difference between the total carrying amount of the individual components of an existing bifurcated hybrid financial instrument and the fair value of the combined hybrid financial instrument must be recognized as a cumulative effect adjustment to beginning retained earnings. Restatement of prior periods is prohibited. The Company currently holds convertible debt securities that require bifurcation under FASB Statement No. 133. The Company expects that the adoption of SFAS 155 will not have a material effect on its consolidated financial condition or results of operations.
SOP 05-1
In September 2005, the American Institute of Certified Public Accountants (“AICPA”) released Statement of Position 05-1, “Accounting by Insurance Enterprises for Deferred Acquisition Costs in Connection With Modifications or Exchanges of Insurance Contracts” (“SOP 05-1”). SOP 05-1 requires identification of transactions that result in a substantial change in an insurance contract. Transactions subject to review include internal contract exchanges, contract modifications via amendment, rider or endorsement, and elections of benefits, features or rights contained within the contract. If determined that
85
a substantial change has occurred, the related unamortized deferred policy acquisition costs, unearned premiums and other related balances must be written off. The Company will adopt SOP 05-1 on January 1, 2007. The Company expects that the adoption of SOP 05-1 will not have a material effect on its consolidated financial condition or results of operations.
3. Acquisition of EHC
On June 16, 2006, the Company acquired all of the outstanding common stock of EHC for a purchase price of $78.9 million, which consisted of the Company issuing 3,875,407 shares of its $10.00 common stock and paying cash of $40.2 million to the EHC’s shareholders. The excess of the purchase price over the net fair value of the assets and liabilities acquired was $14.3 million, consisting of identifiable intangible assets of $9.2 million and goodwill of $5.1 million. Direct expenses incurred in connection with the acquisition of EHC were $636. In connection with the acquisition of EHC, the purchase price was allocated to the estimated fair values of the acquired assets and liabilities as follows (in thousands):
| | | |
| | | (Unaudited)
June 16,
2006 |
ASSETS | | | |
| |
Investments and cash | | $ | 162,251 |
Accrued investment income | | | 1,405 |
Premiums receivable | | | 28,391 |
Reinsurance recoverable on paid and unpaid losses and loss adjustment expenses | | | 7,253 |
Deferred income taxes, net | | | 2,317 |
Deferred acquisition costs | | | — |
Prepaid reinsurance | | | — |
Other assets | | | 4,879 |
| | | |
Total assets | | $ | 206,496 |
| | | |
LIABILITIES | | | |
| |
Reserves for unpaid losses and loss adjustment expenses | | $ | 81,346 |
Unearned premium reserves | | | 30,004 |
Accounts payable and accrued expenses | | | 12,017 |
Dividends payable | | | 4,585 |
Shareholder dividend payable | | | 3,522 |
Loans payable | | | 1,750 |
Junior subordinated debentures | | | 8,044 |
| | | |
Total liabilities | | $ | 141,268 |
| | | |
Estimated fair value of net assets acquired | | $ | 65,228 |
| | | |
Purchase price for EHC | | $ | 78,929 |
Direct acquisition expenses | | | 636 |
| | | |
Adjusted purchase price for EHC | | | 79,565 |
Estimated fair value of net assets acquired | | | 65,228 |
| | | |
Excess of adjusted purchase price over the net fair value of assets and liabilities acquired | | $ | 14,337 |
| | | |
The transaction was accounted for using the purchase method of accounting in accordance with SFAS 141, “Business Combinations”.
In connection with the acquisition of EHC, the assets and liabilities acquired by EIHI were adjusted to fair value. The most significant adjustments were as follows:
The fair value of the reserve for unpaid losses and loss adjustment expenses was estimated by discounting the gross reserves and applying a risk margin to the gross reserves. EIHI discounted the reserve for unpaid losses and loss adjustment expenses based on the present value of the expected underlying cash flows using a risk-free interest rate, which approximated the U.S. Treasury rate on the acquisition date. The discounting pattern was developed by EIHI based on historical loss data. A risk margin was applied to the
86
discounted reserve for unpaid losses and loss adjustment expenses to reflect management’s estimate of the cost EHC would incur to reinsure the full amount of its unpaid losses and loss adjustment expenses with a third-party reinsurer. This risk margin was based upon management’s assessment of the inherent uncertainty in reserving for unpaid losses and loss adjustment expenses and their knowledge of the reinsurance marketplace. As a result of these adjustments, the reserve for unpaid losses and loss adjustment expenses was increased by $2.4 million as of June 16, 2006.
As of the acquisition date, EIHI adjusted EHC’s net unearned premium reserves to fair value by (1) discounting the unearned premium reserves and (2) applying a risk margin to the unearned premium reserves. EIHI discounted the unearned premium reserves based on the present value of the expected underlying cash flows using a risk-free interest rate, which approximated the U.S. Treasury rate on the acquisition date. The discounting pattern was developed by EIHI based on historical loss data. As a result of these adjustments, unearned premium reserves were reduced by $12.9 million as of June 16, 2006.
Acquisition and other underwriting expenses were decreased by $6.8 million as of June 16, 2006 to exclude deferred acquisition costs. Deferred acquisition costs consisting primarily of commissions and premium taxes, which vary with and are primarily related to the production of new business, are deferred and amortized to achieve a matching of revenue and expenses.
The following tables present unaudited pro forma income statement information for the years ended December 31, 2006 and 2005 as if the stock offering, conversion and acquisition of EHC had taken place on January 1, 2006 and 2005, respectively (in thousands, except share and per share data):
| | | | | | |
| | | (Unaudited) Pro Forma Years Ended December 31, 2006 and 2005 |
| | | 2006 | | 2005 |
Revenue: | | | | | | |
Net premiums earned | | $ | 113,148 | | $ | 109,517 |
Net investment income | | | 10,483 | | | 8,395 |
Net realized investment gains | | | 3,356 | | | 615 |
Other revenue | | | 581 | | | 1,721 |
| | | | | | |
Total revenue | | | 127,568 | | | 120,248 |
| | | | | | |
Expenses: | | | | | | |
Losses and loss adjustment expenses incurred | | | 70,317 | | | 68,370 |
Acquisition and other underwriting expenses | | | 10,176 | | | 9,084 |
Other expenses | | | 22,445 | | | 21,887 |
Amortization of intangibles | | | 2,004 | | | 2,004 |
Policyholder dividend expense | | | 406 | | | 223 |
Segregated portfolio dividend expense | | | 3,998 | | | 962 |
| | | | | | |
Total expenses | | | 109,346 | | | 102,530 |
| | | | | | |
Income before income taxes | | | 18,222 | | | 17,718 |
Income tax expense | | | 7,173 | | | 6,906 |
| | | | | | |
Net income | | $ | 11,049 | | $ | 10,812 |
| | | | | | |
Earnings per share (EPS): | | | | | | |
Basic shares outstanding | | | 10,640,282 | | | 10,640,282 |
Basis EPS | | $ | 1.04 | | $ | 1.02 |
| | |
Diluted shares outstanding | | | 10,946,381 | | | 10,946,381 |
Diluted EPS | | $ | 1.01 | | $ | 0.99 |
87
4. Non-Cash Investing and Financing Activities
The Company issued 747,500 shares of its common stock to the ESOP for $7.5 million. The Company issued a loan to the ESOP in the amount of $7.5 million for the purchase of the common stock. The issuance of the loan to the ESOP and the related purchase of the Company’s common stock by the ESOP are considered non-cash transactions for purposes of the statement of cash flows. As such, the net proceeds received as a result of the Company’s stock offering of $69.6 million is reflected net of the proceeds from the shares purchased by the ESOP of $7.5 million, or $62.1 million, in the statement of cash flows for year ended December 31, 2006.
5. Intangible Assets
The acquisition of EHC resulted in the identification of certain intangible assets. The allocation of the purchase price in excess of the fair value of the Company’s net assets acquired to intangible assets totaled $9.2 million. As of December 31, 2006, intangible assets consisted of the following (in thousands):
| | | | | | | | |
Intangible Assets with Finite Life | | Balance | | Accumulated
Amortization | | Amortization
Period |
Agency relationships | | $ | 1,584 | | $ | 165 | | 15 years |
Renewal rights | | | 5,476 | | | 923 | | 15 years |
| | | | | | | | |
| | $ | 7,060 | | $ | 1,088 | | |
| | | | | | | | |
| | | |
Intangible Assets with Indefinite Life | | | | | | |
State insurance licenses | | | 1,050 | | | | | |
| | | | | | | | |
Total intangible assets | | $ | 8,110 | | | | | |
| | | | | | | | |
Amortization expense totaled $1.1 million for the year ended December 31, 2006. The estimated aggregated amortization expense for each of the next five years is as follows (in thousands):
| | | |
2007 | | $ | 1,738 |
2008 | | | 1,312 |
2009 | | | 993 |
2010 | | | 753 |
2011 | | | 572 |
| | | |
Total | | $ | 5,368 |
| | | |
6. Earnings Per Share
The conversion, stock offering and the acquisition of EHC resulted in the issuance of common shares of the Company on June 16, 2006. Basic earnings per share are computed by dividing the net income for the period from June 17, 2006 to December 31, 2006 by the weighted average number of shares outstanding. Diluted earnings per share are computed by dividing net income for the period from June 17, 2006 to December 31, 2006 by the weighted average number of shares outstanding for the period, including dilutive potential common shares outstanding for the period. Stock warrants of 306,099 have been included as dilutive potential common shares outstanding. There were no anti-dilutive stock warrants or options as of December 31, 2006. Consolidated net income, basic shares outstanding, diluted shares outstanding, basic earnings per share and diluted earnings per share for the period from June 17, 2006 to December 31, 2006 were as follows (in thousands, except share and per share data):
| | | |
| | | For the Period from June 17, 2006 to December 31, 2006 |
Consolidated net income | | $ | 7,142 |
Basic shares outstanding | | | 10,623,182 |
Diluted shares outstanding | | | 10,929,281 |
Basic earnings per share | | $ | 0.67 |
Diluted earnings per share | | $ | 0.65 |
88
7. Statutory Financial Information
The Company’s domestic insurance subsidiaries, Eastern Alliance, Allied Eastern and ELH, prepare statutory-basis financial statements in accordance with accounting practices prescribed or permitted by the Insurance Department of the Commonwealth of Pennsylvania (the “Insurance Department”). The Insurance Department requires that insurance companies domiciled in the Commonwealth prepare their statutory-basis financial statements in accordance with the National Association of Insurance Commissioners’ (“NAIC”)Accounting Practices and Proceduresmanual, subject to any deviations prescribed or permitted by the Commonwealth’s insurance commissioner (“SAP”).
Permitted statutory accounting practices encompass all accounting practices that are not prescribed; such practices differ from state to state, may differ from company to company within a state, and may change in the future. The reserves for unpaid losses and loss adjustment expenses of Eastern Alliance and Allied Eastern are discounted on both a tabular and non-tabular basis. The discounting of workers’ compensation indemnity reserves on a tabular basis is a prescribed practice by the NAIC. The discounting of other workers’ compensation reserves on a non-tabular basis is a permitted practice by the Insurance Department. The non-tabular discounting of other workers’ compensation reserves increased Eastern Alliance’s and Allied Eastern’s statutory surplus by $1,239 and $180, respectively, as of December 31, 2006 and by $1,079 and $148, respectively, as of December 31, 2005. The non-tabular discounting of other workers’ compensation reserves increased (decreased) Eastern Alliance’s statutory net income by $176, $(32), and $(126) and increased (decreased) Allied Eastern’s statutory net income by $34, $(11), and $75 for the years ended December 31, 2006, 2005, and 2004, respectively. ELH did not have any permitted practices for the years ended December 31, 2006, 2005, or 2004.
The principal differences between GAAP and SAP relate to the carrying value of fixed income securities, deferred acquisition costs, deferred income taxes, dividends payable, benefit plan liabilities, the non-admissibility of certain assets for SAP purposes, and the reporting of reserves for unpaid losses and loss adjustment expenses and the related reinsurance recoverables on a gross versus net basis.
Financial Information
The statutory surplus and statutory net income (loss) of Eastern Alliance, Allied Eastern, and ELH as of December 31, 2006 and 2005 and for the years ended December 31, 2006, 2005, and 2004 was as follows (in thousands):
| | | | | | | | | | | | | | | | |
| | | Statutory Surplus as of December 31, | | Net Income (Loss) for the Year Ended December 31, |
| | | 2006 | | 2005 | | 2006 | | 2005 | | | 2004 |
Eastern Alliance | | $ | 48,358 | | $ | 36,352 | | $ | 9,798 | | $ | 11,249 | | | $ | 2,973 |
Allied Eastern | | $ | 7,460 | | $ | 5,789 | | $ | 1,336 | | $ | 1,730 | | | $ | 622 |
ELH | | $ | 60,244 | | $ | 57,003 | | $ | 2,955 | | $ | (9,500 | ) | | $ | 2,225 |
The statutory net loss of ELH for the year ended December 31, 2005 included the recognition of a realized loss on the sale of IBSi, totaling $10.3 million. Under SAP, the equity in income or loss of affiliates is recorded directly to statutory surplus as an unrealized gain or loss. As a result of the sale of IBSi, the cumulative unrealized loss was reclassified to a realized loss. There was no impact to statutory surplus as a result of this transaction.
Risk-Based Capital
Risk-based capital is designed to measure the acceptable amount of capital an insurer should have based on the inherent risks of the insurer’s business. Insurers failing to meet adequate capital levels may be subject to insurance department scrutiny and ultimately rehabilitation or liquidation. Based on established standards, Eastern Alliance, Allied Eastern, and ELH maintained statutory-basis surplus in excess of minimum prescribed risk-based capital requirements at December 31, 2006.
Dividend Restrictions
The ability of Eastern Alliance, Allied Eastern and ELH to pay dividends to EIHI is limited by the laws and regulations of Pennsylvania. The maximum annual dividends that EIHI’s insurance subsidiaries may pay without the prior approval from the Insurance Department is limited to the greater of 10% of statutory surplus or 100% of statutory net income for the most recently filed annual statement. For the three years subsequent to June 16, 2006, the effective date of the common stock offering, conversion of ELH, and acquisition of EHC, Eastern Alliance, Allied Eastern and ELH are prohibited from declaring or paying any dividends or other forms of distribution without the prior approval of the Pennsylvania Insurance Commissioner.
89
8. Investments
The following tables provide the amortized cost and estimated fair value of the Company’s investments as of December 31, 2006 and 2005 (in thousands):
| | | | | | | | | | | | | |
2006 | | Cost or
Amortized
Cost | | Gross
Unrealized
Gains | | Gross
Unrealized
Losses | | | Estimated
Fair Value |
U.S. Treasuries and government agencies | | $ | 18,434 | | $ | 522 | | $ | (43 | ) | | $ | 18,913 |
Foreign governments | | | 500 | | | — | | | (4 | ) | | | 496 |
States, municipalities, and political subdivisions | | | 33,751 | | | 705 | | | (10 | ) | | | 34,446 |
Corporate securities | | | 79,644 | | | 1,459 | | | (252 | ) | | | 80,851 |
Mortgage-backed securities | | | 24,921 | | | 549 | | | — | | | | 25,470 |
Collateralized mortgage obligations | | | 16,167 | | | 163 | | | (18 | ) | | | 16,312 |
Asset-backed securities | | | 27,809 | | | 194 | | | (47 | ) | | | 27,956 |
| | | | | | | | | | | | | |
Total fixed income securities | | | 201,226 | | | 3,592 | | | (374 | ) | | | 204,444 |
| | | | |
Equity securities | | | 17,027 | | | 1,293 | | | (101 | ) | | | 18,219 |
Equity call options | | | 2,230 | | | 1,309 | | | (221 | ) | | | 3,318 |
| | | | | | | | | | | | | |
Total investments | | $ | 220,483 | | $ | 6,194 | | $ | (696 | ) | | $ | 225,981 |
| | | | | | | | | | | | | |
| | | | | | | | | | | | | |
2005 | | Cost or
Amortized
Cost | | Gross
Unrealized
Gains | | Gross
Unrealized
Losses | | | Estimated
Fair
Value |
U.S. Treasuries and government agencies | | $ | 6,798 | | $ | 446 | | $ | (82 | ) | | $ | 7,162 |
Foreign governments | | | 488 | | | — | | | (4 | ) | | | 484 |
States, municipalities, and political subdivisions | | | 1,003 | | | 26 | | | (6 | ) | | | 1,023 |
Corporate | | | 62,865 | | | 1,418 | | | (404 | ) | | | 63,879 |
Mortgage-backed | | | 1,454 | | | — | | | (23 | ) | | | 1,431 |
| | | | | | | | | | | | | |
Total fixed income securities | | | 72,608 | | | 1,890 | | | (519 | ) | | | 73,979 |
Equity call options | | | 1,086 | | | 441 | | | (219 | ) | | | 1,308 |
| | | | | | | | | | | | | |
Total | | $ | 73,694 | | $ | 2,331 | | $ | (738 | ) | | $ | 75,287 |
| | | | | | | | | | | | | |
For the years ended December 31, 2006, 2005, and 2004, the change in the estimated fair value of equity call options included in net realized investment gains in the consolidated statements of operations and comprehensive income (loss) totaled $837, $(367), and $217, respectively.
Certain insurance departments in the states in which the Company is licensed to do business require a deposit in the event the Company would become insolvent. In order to satisfy these requirements, the Company had fixed income securities with an estimated fair value of $5,462 and $2,951 on deposit with various insurance departments as of December 31, 2006 and 2005, respectively.
The amortized cost and estimated fair value of fixed income securities, including the equity call option component of the Company’s convertible bond portfolio, as of December 31, 2006, by contractual maturity, are shown below (in thousands). Expected maturities could differ from contractual maturities because borrowers may have the right to call or prepay obligations, with or without call or prepayment penalties.
| | | | | | |
| | | Amortized
Cost | | Estimated
Fair Value |
Less than one year | | $ | 38,455 | | $ | 38,489 |
One through five years | | | 97,062 | | | 98,198 |
Five through ten years | | | 41,947 | | | 43,058 |
Greater than ten years | | | 25,992 | | | 28,017 |
| | | | | | |
Total | | $ | 203,456 | | $ | 207,762 |
| | | | | | |
The gross unrealized losses and estimated fair value of investments classified as available-for-sale securities by investment category and length of time an individual security has been in a continuous unrealized position as of December 31, 2006 and 2005 are as follows (in thousands):
90
| | | | | | | | | | | | | | | | | | | | | |
| | | Less Than 12 Months | | | 12 Months or More | | | Total | |
2006 | | Estimated
Fair
Value | | Gross Unrealized
Losses | | | Estimated
Fair
Value | | Gross Unrealized
Losses | | | Estimated
Fair
Value | | Gross Unrealized
Losses | |
U.S. Treasuries and government agencies | | $ | — | | $ | — | | | $ | 1,758 | | $ | (43 | ) | | $ | 1,758 | | $ | (43 | ) |
Foreign governments | | | — | | | — | | | | 496 | | | (4 | ) | | | 496 | | | (4 | ) |
States, municipalities, and political subdivisions | | | 3,355 | | | (10 | ) | | | — | | | — | | | | 3,355 | | | (10 | ) |
Corporate securities | | | 269 | | | (22 | ) | | | 8,177 | | | (230 | ) | | | 8,446 | | | (252 | ) |
Mortgage-backed securities | | | — | | | — | | | | — | | | — | | | | — | | | — | |
Collateralized mortgage obligations | | | 2,690 | | | (6 | ) | | | 469 | | | (12 | ) | | | 3,159 | | | (18 | ) |
Asset-backed securities | | | 3,533 | | | (8 | ) | | | 2,431 | | | (39 | ) | | | 5,964 | | | (47 | ) |
| | | | | | | | | | | | | | | | | | | | | |
Total fixed income securities | | | 9,847 | | | (46 | ) | | | 13,331 | | | (328 | ) | | | 23,178 | | | (374 | ) |
| | | | | | |
Equity securities | | | 2,509 | | | (101 | ) | | | — | | | — | | | | 2,509 | | | (101 | ) |
| | | | | | | | | | | | | | | | | | | | | |
Total investments | | $ | 12,356 | | $ | (147 | ) | | $ | 13,331 | | $ | (328 | ) | | $ | 25,687 | | $ | (475 | ) |
| | | | | | | | | | | | | | | | | | | | | |
| | | | | | | | | | | | | | | | | | | | | |
| | | Less Than 12 Months | | | 12 Months or More | | | Total | |
2005 | | Estimated
Fair
Value | | Unrealized
Losses | | | Estimated
Fair
Value | | Unrealized
Losses | | | Estimated
Fair
Value | | Unrealized
Losses | |
U.S. Treasuries and government agencies | | $ | 1,729 | | $ | (14 | ) | | $ | 2,982 | | | (68 | ) | | $ | 4711 | | $ | (82 | ) |
Foreign governments | | | — | | | — | | | | 484 | | | (4 | ) | | | 484 | | | (4 | ) |
States, municipalities, and political subdivisions | | | 506 | | | (6 | ) | | | — | | | — | | | | 506 | | | (6 | ) |
Corporate | | | 13,087 | | | (119 | ) | | | 10,839 | | | (285 | ) | | | 23,926 | | | (404 | ) |
Mortgage-backed | | | 1,431 | | | (23 | ) | | | — | | | — | | | | 1,431 | | | (23 | ) |
| | | | | | | | | | | | | | | | | | | | | |
Total investments | | $ | 16,753 | | $ | (162 | ) | | $ | 14,305 | | $ | (357 | ) | | $ | 31,058 | | $ | (519 | ) |
| | | | | | | | | | | | | | | | | | | | | |
| | | | | | | | | | | | | | | | | | | | | |
As of December 31, 2006, the Company held 51 fixed income securities with gross unrealized losses totaling $374. Management has evaluated the unrealized losses related to those fixed income securities and determined that they are primarily due to a fluctuation in interest rates and not attributable to credit risk factors. For investments in fixed income securities, losses in the estimated fair values are viewed as temporary if the security can be held to maturity and it is reasonable to assume that the issuer will be able to service the debt, both as to principal and interest. Management believes that the current carrying value of these investments will be realized and that the Company has the ability and intent to hold them until that time.
As of December 31, 2006, the Company held 16 equity securities with gross unrealized losses totaling $101. All of the equity securities have been in an unrealized loss position for less than twelve months and management has determined, based on an evaluation of these securities, that the decline in value is other-than-temporary as of December 31, 2006.
Proceeds from the sale of fixed income securities totaled $44,771, $6,166, and $9,030 for the years ended December 31, 2006, 2005, and 2004, respectively. Proceeds from the sale of equity securities totaled $4,588, $0, and $0 for the years ended December 31, 2006, 2005, and 2004, respectively.
The gross realized gains and gross realized losses recognized by the Company as a result of the sale of investments were as follows for the years ended December 31, 2006, 2005, and 2004 (in thousands):
91
| | | | | | | | | | | | | | | |
2006 | | Fixed
Income
Securities | | | Equity
Securities | | | Other
Invested
Assets | | Total | |
Gross realized gains | | $ | 655 | | | $ | 1,272 | | | $ | 81 | | $ | 2,008 | |
Gross realized losses | | | (65 | ) | | | (23 | ) | | | — | | | (88 | ) |
| | | | | | | | | | | | | | | |
Net realized gains | | $ | 590 | | | $ | 1,249 | | | $ | 81 | | $ | 1,920 | |
| | | | | | | | | | | | | | | |
| | | | |
2005 | | Fixed
Income
Securities | | | Equity
Securities | | | Other
Invested
Assets | | Total | |
Gross realized gains | | $ | 754 | | | $ | — | | | $ | — | | $ | 754 | |
Gross realized losses | | | (48 | ) | | | — | | | | — | | | (48 | ) |
| | | | | | | | | | | | | | | |
Net realized gains | | $ | 706 | | | $ | — | | | $ | — | | $ | 706 | |
| | | | | | | | | | | | | | | |
| | | | |
2004 | | Fixed
Income
Securities | | | Equity
Securities | | | Other
Invested
Assets | | Total | |
Gross realized gains | | $ | 1,161 | | | $ | — | | | $ | — | | $ | 1,161 | |
Gross realized losses | | | (107 | ) | | | — | | | | — | | | (107 | ) |
| | | | | | | | | | | | | | | |
Net realized gains | | $ | 1,054 | | | $ | — | | | $ | — | | $ | 1,054 | |
| | | | | | | | | | | | | | | |
During 2005, the Company recorded a realized loss totaling $104 related to the impairment of a fixed income security. There were no impairments of fixed income securities recorded during 2006 or 2004.
The change in the Company’s net unrealized gains and losses for the years ended December 31, 2006, 2005, and 2004 was as follows (in thousands):
| | | | | | | | | | | | |
2006 | | Fixed
Income
Securities | | | Equity
Securities | | | Total | |
Change in unrealized gains and losses, gross of tax | | $ | 1,850 | | | $ | 529 | | | $ | 2,379 | |
Tax effect | | | (661 | ) | | | (185 | ) | | | (846 | ) |
| | | | | | | | | | | | |
Change in net unrealized gains and losses | | $ | 1,189 | | | $ | 344 | | | $ | 1,533 | |
| | | | | | | | | | | | |
| | | |
2005 | | Fixed
Income
Securities | | | Equity
Securities | | | Total | |
Change in unrealized gains and losses, gross of tax | | $ | (2,362 | ) | | $ | — | | | $ | (2,362 | ) |
Tax effect | | | 803 | | | | — | | | | 803 | |
| | | | | | | | | | | | |
Change in net unrealized gains and losses | | $ | (1,559 | ) | | $ | — | | | $ | (1,559 | ) |
| | | | | | | | | | | | |
| | | |
2004 | | Fixed
Income
Securities | | | Equity
Securities | | | Total | |
Change in unrealized gains and losses, gross of tax | | $ | (2,421 | ) | | $ | — | | | $ | (2,421 | ) |
Tax effect | | | 823 | | | | — | | | | 823 | |
| | | | | | | | | | | | |
Change in net unrealized gains and losses | | $ | (1,598 | ) | | $ | — | | | $ | (1,598 | ) |
| | | | | | | | | | | | |
92
Net investment income for the years ended December 31, 2006, 2005, and 2004 was as follows (in thousands):
| | | | | | | | | | | | |
| | | 2006 | | | 2005 | | | 2004 | |
Fixed income securities | | $ | 7,192 | | | $ | 3,621 | | | $ | 3,673 | |
Equity securities | | | 36 | | | | — | | | | — | |
Short-term investments | | | 1,865 | | | | 303 | | | | 221 | |
Equity in income of limited partnership investments | | | 236 | | | | 100 | | | | 65 | |
Other | | | 30 | | | | 6 | | | | 18 | |
| | | | | | | | | | | | |
Gross investment income | | | 9,359 | | | | 4,030 | | | | 3,977 | |
Investment expenses | | | (367 | ) | | | (215 | ) | | | (253 | ) |
| | | | | | | | | | | | |
Net investment income | | $ | 8,992 | | | $ | 3,815 | | | $ | 3,724 | |
| | | | | | | | | | | | |
9. Reserves for Unpaid Losses and Loss Adjustment Expenses
The following table provides a summary of the activity in the Company’s reserves for unpaid losses and loss adjustment expenses, excluding term life premium waiver reserves, for the years ended December 31, 2006, 2005, and 2004 (in thousands):
| | | | | | | | | | | | |
| | | 2006 | | | 2005 | | | 2004 | |
Balance, beginning of period | | $ | 38,729 | | | $ | 38,559 | | | $ | 41,326 | |
Reinsurance recoverables on unpaid losses and LAE | | | 23,911 | | | | 23,415 | | | | 24,464 | |
| | | | | | | | | | | | |
Net balance, beginning of period | | | 14,818 | | | | 15,144 | | | | 16,862 | |
Net reserves acquired as a result of EHC acquisition | | | 73,554 | | | | — | | | | — | |
Purchase accounting adjustments on acquisition date | | | 2,432 | | | | — | | | | — | |
Incurred related to: | | | | | | | | | | | | |
Current year | | | 54,104 | | | | 26,962 | | | | 28,340 | |
Prior year | | | (5,296 | ) | | | (269 | ) | | | (2,541 | ) |
| | | | | | | | | | | | |
Total incurred before purchase accounting adjustments | | | 48,808 | | | | 26,693 | | | | 25,799 | |
Purchase accounting adjustments | | | (538 | ) | | | — | | | | — | |
| | | | | | | | | | | | |
Total incurred | | | 48,270 | | | | 26,693 | | | | 25,799 | |
Paid related to: | | | | | | | | | | | | |
Current year | | | 28,609 | | | | 22,724 | | | | 23,264 | |
Prior year | | | 13,305 | | | | 4,295 | | | | 4,253 | |
| | | | | | | | | | | | |
Total paid | | | 41,914 | | | | 27,019 | | | | 27,517 | |
| | | | | | | | | | | | |
Net balance, end of period | | | 97,160 | | | | 14,818 | | | | 15,144 | |
Reinsurance recoverables on unpaid losses and LAE | | | 24,236 | | | | 23,911 | | | | 23,415 | |
| | | | | | | | | | | | |
Balance, end of period | | $ | 121,396 | | | $ | 38,729 | | | $ | 38,559 | |
| | | | | | | | | | | | |
Total reserves for unpaid for losses and loss adjustment expenses | | $ | 126,467 | | | $ | 44,136 | | | $ | 43,384 | |
Less: Term life premium waiver reserves | | | 4,815 | | | | 5,333 | | | | 4,784 | |
Less: Other | | | 256 | | | | 74 | | | | 41 | |
| | | | | | | | | | | | |
Balance, end of period | | $ | 121,396 | | | $ | 38,729 | | | $ | 38,559 | |
| | | | | | | | | | | | |
Incurred losses by segment were as follows for the year ended December 31, 2006 (in thousands):
| | | | | | | | | | | | | | | | | | | |
| | | Workers’
Compensation
Insurance
Segment | | | Segregated
Portfolio Cell
Reinsurance
Segment | | | Group
Benefits
Insurance
Segment | | | Specialty
Reinsurance
Segment | | Total | |
Incurred related to: | | | | | | | | | | | | | | | | | | | |
Current year, gross of discount | | $ | 17,941 | | | $ | 8,184 | | | $ | 23,487 | | | $ | 5,372 | | $ | 54,984 | |
Current period discount | | | (568 | ) | | | (312 | ) | | | — | | | | — | | | (880 | ) |
Prior year, gross of discount | | | (2,050 | ) | | | (2,088 | ) | | | (2,563 | ) | | | 894 | | | (5,807 | ) |
Accretion of prior period discount | | | 323 | | | | 188 | | | | — | | | | — | | | 511 | |
| | | | | | | | | | | | | | | | | | | |
Total incurred before purchase accounting adjustments | | | 15,646 | | | | 5,972 | | | | 20,924 | | | | 6,266 | | | 48,808 | |
Purchase accounting adjustments | | | (484 | ) | | | (80 | ) | | | — | | | | 26 | | | (538 | ) |
| | | | | | | | | | | | | | | | | | | |
Total incurred | | $ | 15,162 | | | $ | 5,892 | | | $ | 20,924 | | | $ | 6,292 | | $ | 48,270 | |
| | | | | | | | | | | | | | | | | | | |
Workers’ Compensation Insurance. The Company’s results of operations include a cumulative decrease in estimated incurred losses and LAE on its workers’ compensation line of business primarily related to accident years 2005, 2004, and 2003 of $2.1 million for the year ended December 31, 2006. The favorable development on prior accident years relates primarily to significant claim settlements during 2006 for amounts at, or less than, previously established case and IBNR reserves.
Segregated Portfolio Cell Reinsurance. The Company’s results of operations in its segregated portfolio cell reinsurance segment included a decrease in estimated incurred losses and LAE primarily related to accident years 2005, 2004 and 2003 of $2.1 million for the year ended December 31, 2006. The favorable development on prior accident years relates primarily to significant claim settlements during 2006 for amounts at, or less than, previously established case and IBNR reserves. Any change in the reserves for unpaid losses and LAE in the segregated portfolio cell reinsurance segment is recorded to the segregated portfolio dividend payable/receivable account and would only impact the Company’s net income or shareholders’ equity if the Company was a segregated portfolio cell dividend participant.
Group Benefits Insurance.The Company’s results of operations for the year ended December 31, 2006 include favorable development on prior year reserves in the group benefits insurance segment. Favorable development in the dental and short-term disability lines totaled $533 and $337, respectively, which reflects better claim experience than anticipated at the time the liability was established. The Company’s results of operations also reflect the termination of prior year long-term disability claims totaling $2.2 million, which resulted from claimants returning to work, claimant death, or the termination of benefits in accordance with policy provisions.
Specialty Reinsurance. The Company’s results of operations included an increase in estimated incurred losses and LAE on its specialty reinsurance line of business related to prior accident years of $894 for the year ended December 31, 2006. The unfavorable prior year development was the result of changes in estimates as losses emerged at a higher rate than had been originally anticipated when the reserves were estimated with respect to accident years 2005, 2004, 2003, and 2002. The evaluation of the reserve for unpaid losses and LAE related to the specialty reinsurance segment requires that loss development be estimated over an extended period of time. Because the primary insurer under these programs changed in 1999, historical loss data is insufficiently developed. Therefore, reliance has been placed on industry loss development patterns, adjusted based on the Company’s judgment, to reflect considerations particular to the exposure. The reliance on external benchmarks, while necessary, creates an additional element of uncertainty.
93
10. Reinsurance
The Company purchases reinsurance to manage its loss exposure. Although reinsurance agreements contractually obligate the Company’s reinsurers to reimburse the Company for the agreed upon portion of its gross paid losses, they do not discharge the primary liability of the Company.
The following table provides a summary of the Company’s premiums on a direct, assumed, ceded, and net basis for the years ended December 31, 2006, 2005, and 2004 (in thousands):
| | | | | | | | | | | | | | | | | | | | | | | | |
| | | 2006 | | | 2005 | | | 2004 | |
| | | Written | | | Earned | | | Written | | | Earned | | | Written | | | Earned | |
Direct premiums | | $ | 75,011 | | | $ | 67,446 | | | $ | 40,994 | | | $ | 40,996 | | | $ | 40,790 | | | $ | 40,780 | |
Assumed premiums | | | 17,836 | | | | 23,250 | | | | — | | | | — | | | | — | | | | — | |
Ceded premiums | | | (16,242 | ) | | | (6,701 | ) | | | (2,294 | ) | | | (2,294 | ) | | | (1,720 | ) | | | (1,723 | ) |
| | | | | | | | | | | | | | | | | | | | | | | | |
Net premiums before purchase accounting | | | 76,605 | | | | 83,995 | | | | 38,700 | | | | 38,702 | | | | 39,070 | | | | 39,057 | |
Purchase accounting adjustment | | | (9,076 | ) | | | (9,076 | ) | | | — | | | | — | | | | — | | | | — | |
| | | | | | | | | | | | | | | | | | | | | | | | |
Net premiums | | $ | 67,529 | | | $ | 74,919 | | | $ | 38,700 | | | $ | 38,702 | | | $ | 39,070 | | | $ | 39,057 | |
| | | | | | | | | | | | | | | | | | | | | | | | |
The following table provides a summary of the Company’s losses and loss adjustment expenses incurred on a direct, assumed, ceded and net basis for the years ended December 31, 2006, 2005, and 2004 (in thousands):
| | | | | | | | | | | | |
| | | 2006 | | | 2005 | | | 2004 | |
Direct losses and LAE incurred | | $ | 33,510 | | | $ | 28,875 | | | $ | 26,572 | |
Assumed losses and LAE incurred | | | 12,926 | | | | — | | | | — | |
Ceded losses and LAE incurred | | | 2,015 | | | | (1,785 | ) | | | (640 | ) |
| | | | | | | | | | | | |
Net losses and LAE incurred before purchase accounting | | | 48,451 | | | | 27,090 | | | | 25,932 | |
Purchase accounting adjustment | | | (538 | ) | | | — | | | | — | |
| | | | | | | | | | | | |
Net losses and LAE | | $ | 47,913 | | | $ | 27,090 | | | $ | 25,932 | |
| | | | | | | | | | | | |
Effective October 1, 2003, ELH entered into a coinsurance agreement with London Life Reinsurance Company (LLRC), under which ELH cedes 100% of its group benefits insurance business written or renewed on or after the effective date to LLRC. Concurrent upon entering into the coinsurance agreement, LLRC retroceded the business assumed from ELH to its affiliate, London Life International Reinsurance Corporation (LLIRC). Under a stop loss reinsurance agreement with LLIRC, ELH reinsures LLIRC against any net loss on the reinsured business. As a result of the above transactions, the Company retains 100% of the insurance risk on business written and renewed by ELH, on and after the effective date. Therefore, the arrangement does not transfer insurance risk and, accordingly, is not accounted for as reinsurance. The Company recognized fees totaling $60 in each of the years ended December 31, 2006, 2005 and 2004, related to these agreements, which are included in other expenses in the consolidated statements of operations and comprehensive income (loss). In addition, ELH is required to maintain a trust deposit equal to 105% of statutory reserves at the end of each calendar quarter. As of December 31, 2006, ELH was required to maintain a trust deposit of at least $8.6 million. The actual trust deposit totaled $10.8 million as of December 31, 2006.
ELH entered into a coinsurance agreement in 1999, under which it ceded an existing block of outstanding claims related to a program that provided long-term disability coverage to certain professional associations. The Company recorded a reinsurance recoverable totaling $11,549 and $15,366 at December 31, 2006 and 2005, related to this block of ceded claims.
94
11. Income Taxes
The components of the income tax provision for the years ended December 31, 2006, 2005, and 2004 are as follows (in thousands):
| | | | | | | | | | |
| | | 2006 | | | 2005 | | 2004 |
Current tax expense | | $ | 5,185 | | | $ | 341 | | $ | 223 |
Deferred tax expense | | | 849 | | | | 344 | | | 789 |
| | | | | | | | | | |
Income tax expense before purchase accounting | | $ | 6,034 | | | $ | 685 | | $ | 1,012 |
Purchase accounting adjustment | | | (1,092 | ) | | | — | | | — |
| | | | | | | | | | |
Income tax expense | | $ | 4,942 | | | $ | 685 | | | 1,012 |
| | | | | | | | | | |
In addition to the income tax provision, the net deferred tax asset increased by $132, $803, and $823 in 2006, 2005, and 2004, respectively, as a result of changes in the unrealized gains and losses on the Company’s fixed income and equity securities. The tax effect of these items is recorded directly to accumulated other comprehensive income, which is a component of equity.
The provision for income taxes for the years ended December 31, 2006, 2005, and 2004 is as follows (in thousands):
| | | | | | | | | | | |
| | | 2006 | | | 2005 | | | 2004 |
Income tax expense at statutory rate | | $ | 5,719 | | | $ | 616 | | | $ | 951 |
Prior year tax return adjustment | | | 208 | | | | 200 | | | | — |
Non-deductible intangible asset amortization | | | 381 | | | | — | | | | — |
Non-deductible transaction expenses | | | 109 | | | | 74 | | | | — |
Tax-exempt interest | | | (174 | ) | | | — | | | | — |
Reduction of valuation allowance | | | — | | | | (227 | ) | | | — |
Release of contingency reserve | | | (162 | ) | | | — | | | | — |
ESOP compensation expense | | | 53 | | | | — | | | | — |
Other | | | (100 | ) | | | 22 | | | | 61 |
| | | | | | | | | | | |
Income tax expense before purchase accounting adjustment | | | 6,034 | | | | 685 | | | | 1,012 |
Purchase accounting adjustment | | | (1,092 | ) | | | — | | | | — |
| | | | | | | | | | | |
Income tax expense | | $ | 4,942 | | | $ | 685 | | | $ | 1,012 |
| | | | | | | | | | | |
95
The components of the net deferred tax asset as of December 31, 2006 and 2005 are as follows (in thousands):
| | | | | | |
| | | 2006 | | 2005 |
Deferred tax assets: | | | | | | |
Postretirement liability | | $ | 114 | | $ | 264 |
Reserve discounting | | | 2,367 | | | 95 |
DAC tax | | | 324 | | | 106 |
Unearned/advance premiums | | | 2,231 | | | 76 |
Policyholder dividends | | | 209 | | | — |
Allowance for doubtful accounts | | | 204 | | | — |
Accrued liabilities | | | 402 | | | 197 |
Alternative minimum tax credits | | | — | | | 541 |
Low income housing credits | | | — | | | 41 |
Other | | | 255 | | | 443 |
| | | | | | |
Total deferred tax assets | | | 6,106 | | | 1,763 |
| | | | | | |
| | |
Deferred tax liabilities: | | | | | | |
Unrealized gain on investments | | | 334 | | | 466 |
Deferred acquisition costs | | | 1,423 | | | — |
Depreciation and amortization | | | 114 | | | 148 |
Unrealized gains on equity call options | | | 411 | | | 76 |
Equity income in limited partnerships | | | 1,035 | | | 92 |
Pension asset | | | 212 | | | 29 |
Other | | | 45 | | | 6 |
| | | | | | |
Total deferred tax liabilities | | | 3,574 | | | 817 |
| | | | | | |
Net deferred tax asset before purchase accounting | | | 2,532 | | | 946 |
Purchase accounting adjustment | | | 164 | | | — |
| | | | | | |
Net deferred tax asset | | $ | 2,696 | | $ | 946 |
| | | | | | |
As of December 31, 2006, the net deferred tax asset has not been reduced by a valuation allowance because management believes that, while it is not assured, it is more likely than not that the Company will generate sufficient future taxable income to utilize these net future tax deductions. The amount of the net deferred tax asset considered realizable, however, could be materially reduced in the near term if estimates of future taxable income in the years in which the differences are expected to reverse are decreased.
12. Employee Benefit Plans
ESOP
The Company sponsors an ESOP, which was established as a result of the conversion of ELH from a mutual company to a stock company. Eligible employees generally include those employees who have reached the age of 21 and have completed one year of service. All employees that were employed by EHC or ELH on June 16, 2006 were determined to have met the eligibility requirements on that date. ESOP shares are allocated to participants based on the ratio of their individual compensation during the plan year to the total compensation of eligible employees during the plan year.
The Company issued 747,500 shares of its common stock to the ESOP on June 16, 2006, and the ESOP signed a promissory note in the amount of $7.5 million for the purchase of the shares, which is due in ten equal installments, with interest accruing annually at 4%. Shares purchased are held in a suspense account for allocation among participating employees as the loan is repaid.
Shares committed to be released and stock compensation expense for the period from June 17, 2006 to December 31, 2006 were as follows:
96
| | | |
| | | For the Period from June 17, 2006 to December 31, 2006 |
Shares committed to be released | | | 37,375 |
Stock compensation expense | | $ | 525,000 |
As of December 31, 2006, the estimated fair value of unearned ESOP shares were $10.3 million.
Other Benefit Plans
ELH sponsors a non-contributory defined benefit pension plan (the “pension plan”) covering substantially all of its employees. On May 17, 2005, ELH’s Board of Directors approved the freezing of the pension plan effective December 31, 2005. ELH also sponsors a defined benefit postretirement plan (the “postretirement plan”), which provides certain health care and life insurance benefits for retired employees. Current employees of ELH may become eligible for these benefits if they reach retirement age while working for ELH and meet certain years of service levels prior to January 1, 2015. Life insurance benefits are set at 100% of an employee’s annual salary at the time of retirement, up to a maximum of $175,000, and are reduced to $10 by age 70.
Pension costs are funded to the limits specified by the Employee Retirement Income Security Act of 1974, as amended. From time to time, the Company may contribute additional amounts to the pension plan as it deems appropriate, subject to funding limitations. Based on the funded status of the pension plan at December 31, 2006, the Company is not required to make a contribution in 2007 and does not anticipate making a contribution. The Company does anticipate making a contribution to the postretirement plan in 2007 totaling approximately $65 to cover the Company’s portion of retirees’ healthcare premiums.
The Company uses a measurement date of December 31 for its plans.
A reconciliation of changes in the benefit obligation, fair value of plan assets and funded status of the pension plan and the postretirement plan at December 31, 2006 and 2005 is as follows (in thousands):
| | | | | | | | | | | | | | | | |
| | | Pension Plan | | | Postretirement Plan | |
| | | 2006 | | | 2005 | | | 2006 | | | 2005 | |
Change in benefit obligation: | | | | | | | | | | | | | | | | |
Benefit obligation at beginning of year | | $ | 9,502 | | | $ | 10,490 | | | $ | 469 | | | $ | 2,909 | |
Service cost | | | — | | | | 404 | | | | — | | | | 21 | |
Interest cost | | | 511 | | | | 592 | | | | 22 | | | | 162 | |
Participant contributions | | | — | | | | — | | | | 63 | | | | 56 | |
Actuarial gain | | | (156 | ) | | | (34 | ) | | | (78 | ) | | | (246 | ) |
Settlement gain | | | — | | | | — | | | | — | | | | (2,239 | ) |
Benefits paid | | | (522 | ) | | | (561 | ) | | | (152 | ) | | | (194 | ) |
Other | | | — | | | | (1,389 | ) | | | — | | | | — | |
| | | | | | | | | | | | | | | | |
Benefit obligation at end of year | | | 9,335 | | | | 9,502 | | | | 324 | | | | 469 | |
| | | | |
Change in plan assets: | | | | | | | | | | | | | | | | |
Fair value of plan assets at beginning of year | | | 9,561 | | | | 9,293 | | | | — | | | | — | |
Actual return on plan assets | | | 791 | | | | 379 | | | | — | | | | — | |
Employer contributions | | | 110 | | | | 450 | | | | 89 | | | | 138 | |
Participant contributions | | | — | | | | — | | | | 63 | | | | 56 | |
Benefits paid | | | (522 | ) | | | (561 | ) | | | (152 | ) | | | (194 | ) |
| | | | | | | | | | | | | | | | |
Fair value of plan assets at end of year | | | 9,940 | | | | 9,561 | | | | — | | | | — | |
| | | | |
Funded status: | | | | | | | | | | | | | | | | |
Funded status | | | (605 | ) | | | (59 | ) | | | 324 | | | | 469 | |
Unrecognized net actuarial (gain) loss | | | — | | | | (41 | ) | | | — | | | | 307 | |
Unrecognized transition obligation | | | — | | | | 15 | | | | — | | | | — | |
Unrecognized prior service cost | | | — | | | | — | | | | — | | | | — | |
| | | | | | | | | | | | | | | | |
(Prepaid) accrued benefit plan (assets) liabilities | | $ | (605 | ) | | $ | (85 | ) | | $ | 324 | | | $ | 776 | |
| | | | | | | | | | | | | | | | |
97
As of December 31, 2006, the following amounts related to the pension plan and postretirement plan have been included in accumulated other comprehensive income (AOCI) (in thousands):
| | | | | | | | |
| | | Pension
Plan | | | Postretirement
Plan | |
Net actuarial gain | | $ | (275 | ) | | $ | (364 | ) |
Net transition asset | | | (12 | ) | | | — | |
| | | | | | | | |
Total before taxes | | | (287 | ) | | | (364 | ) |
Tax effect | | | 100 | | | | 128 | |
| | | | | | | | |
Net amount included in AOCI | | $ | (187 | ) | | $ | (236 | ) |
| | | | | | | | |
The amounts included in AOCI that are expected to be recognized in 2007 are as follows (in thousands):
| | | | | | | | |
| | | Pension
Plan | | | Postretirement
Plan | |
Net actuarial gain | | $ | — | | | $ | (28 | ) |
Net transition asset | | | (2 | ) | | | — | |
| | | | | | | | |
Total | | $ | (2 | ) | | $ | (28 | ) |
| | | | | | | | |
As a result of freezing the pension plan at December 31, 2005, the Company recognized a decrease in its pension plan benefit obligation totaling $1,468. This decrease was offset by an increase in the benefit plan obligation and related net periodic benefit cost totaling $79 as a result of fully vesting plan participants that were involuntarily terminated by the Company during 2005. The Company also incurred additional net periodic benefit cost in 2005 totaling $215 related to the recognition of prior service cost as a result of freezing the pension plan. During 2004, the Company increased its net periodic benefit cost by $58 as a result of fully vesting plan participants that were involuntarily terminated by the Company in the 2003 plan year.
During 2005, the Company’s Board of Directors approved an amendment to the postretirement plan, which passes a portion of the healthcare premium costs to the retirees beginning with the 2006 plan year. The amendment requires retirees to contribute one-third of the healthcare premium in 2006, with the retiree contribution increasing to two-thirds in 2007 and 100% in 2008. As a result of this amendment, the Company recorded a settlement gain totaling $2,239 that reduced the postretirement obligation as of December 31, 2005. The settlement resulted in a reduction to the net periodic benefit cost in 2005 totaling $1,465.
The accumulated benefit obligation of the pension plan at December 31, 2006 and 2005 was $9,335 and $9,502, respectively, and the accumulated benefit obligation of the postretirement plan was $324 and $469, respectively.
Benefits paid totaled $522, $561, and $518 for the pension plan and $152, $194, and $203 for the postretirement plan for the years ended December 31, 2006, 2005, and 2004, respectively. The estimated future benefits to be paid over the next ten years are as follows (in thousands):
| | | | | | |
| | | Pension
Plan | | Postretirement
Plan |
2007 | | $ | 440 | | $ | 65 |
2008 | | | 470 | | | 26 |
2009 | | | 530 | | | 26 |
2010 | | | 530 | | | 25 |
2011 | | | 540 | | | 25 |
2012-2016 | | | 3,530 | | | 114 |
| | | | | | |
Total | | $ | 6,040 | | $ | 281 |
| | | | | | |
98
The pension plan’s assets were comprised of the following at December 31, 2006 and 2005 (in thousands):
| | | | | | |
| | | 2006 | | 2005 |
Equity securities | | $ | 4,016 | | $ | 3,468 |
Fixed income securities | | | 5,924 | | | 6,093 |
| | | | | | |
Total | | $ | 9,940 | | $ | 9,561 |
| | | | | | |
The primary investment objective of the pension plan is to achieve maximum rates of return commensurate with safety of principal. The pension plan asset allocation is reviewed annually to determine whether the portfolio mix is within an acceptable range of the target allocation. Target asset allocations are based on asset and liability studies with the goal to enhance the expected return of the pension plan portfolio while maintaining acceptable levels of risk. The target asset allocation for the portfolio is 35% equity securities and 65% fixed income securities.
Historical and future expected returns of multiple asset classes were analyzed to develop a risk-free real rate of return and risk premiums for each asset class. The overall rate for each asset class was developed by combining a long-term inflation component, the risk-free real rate of return, and the associated risk premium. A weighted average rate was developed based on those overall rates and the target asset allocation of the pension plan.
The assumptions used in the measurement of the Company’s benefit obligation are shown in the following table:
| | | | | | | | | | | | |
| | | Pension Plan | | | Postretirement Plan | |
| | | 2006 | | | 2005 | | | 2006 | | | 2005 | |
Weighted average discount rate | | 5.60 | % | | 5.50 | % | | 5.60 | % | | 5.50 | % |
Rate of increase in compensation levels | | N/A | | | N/A | | | 3.50 | % | | 3.50 | % |
The following table provides the components of net periodic benefit cost for the pension plan and the postretirement plan for the years ending December 31, 2006, 2005, and 2004 (in thousands):
| | | | | | | | | | | | | | | | | | | | | | | |
| | | Pension Plan | | | Postretirement Plan |
| | | 2006 | | | 2005 | | | 2004 | | | 2006 | | | 2005 | | | 2004 |
Service cost | | $ | — | | | $ | 404 | | | $ | 394 | | | $ | — | | | $ | 21 | | | $ | 16 |
Interest cost | | | 511 | | | | 592 | | | | 575 | | | | 22 | | | | 162 | | | | 150 |
Expected return on plan assets | | | (631 | ) | | | (596 | ) | | | (561 | ) | | | — | | | | — | | | | — |
Recognized net actuarial gain | | | — | | | | 23 | | | | 15 | | | | (21 | ) | | | 71 | | | | 27 |
Amortization of transition obligation | | | (3 | ) | | | (3 | ) | | | (3 | ) | | | — | | | | — | | | | — |
Amortization of prior service cost | | | — | | | | 12 | | | | 12 | | | | — | | | | — | | | | — |
Other | | | — | | | | 294 | | | | 58 | | | | — | | | | (1,465 | ) | | | — |
| | | | | | | | | | | | | | | | | | | | | | | |
Net periodic benefit cost | | $ | (123 | ) | | $ | 726 | | | $ | 490 | | | $ | 1 | | | $ | (1,211 | ) | | $ | 193 |
| | | | | | | | | | | | | | | | | | | | | | | |
The assumptions used in the measurement of the Company’s net periodic benefit cost for the pension plan and the postretirement plan are shown in the following table:
| | | | | | | | | | | | | | | | | | |
| | | Pension Plan | | | Postretirement Plan | |
| | | 2006 | | | 2005 | | | 2004 | | | 2006 | | | 2005 | | | 2004 | |
Weighted average discount rate | | 5.50 | % | | 5.75 | % | | 6.00 | % | | 5.50 | % | | 5.75 | % | | 6.00 | % |
Expected long-term rate of return on plan assets | | 6.75 | % | | 6.50 | % | | 6.50 | % | | N/A | | | N/A | | | N/A | |
Rate of increase in compensation levels | | N/A | | | 4.50 | % | | 5.00 | % | | 3.50 | % | | 4.50 | % | | 5.00 | % |
At December 31, 2006, the assumed healthcare cost trend rate used in the estimate of the postretirement benefit plan obligation was 9.00% for those participants under age 65, with the rate decreasing to 5.00% in 2011 and thereafter. The assumed healthcare cost trend rate used for those participants over age 65 was 8.00%, with the rate decreasing to 4.00% in 2011 and thereafter.
99
Assumed healthcare cost trend rates are a significant assumption in the development of postretirement medical plan liabilities. As a result of the amendment to the Company’s postretirement plan that transfers 100% of the healthcare premium contribution to the retirees on January 1, 2008, the assumed healthcare cost trend does not have a material impact on the Company’s benefit obligation or net periodic benefit cost at December 31, 2006.
Eastern Alliance and ELH also sponsor defined contribution plans covering their respective eligible employees. The Company’s contributions to the defined contribution plan for the years ended December 31, 2006, 2005, and 2004 totaled $131, $108, and $120, respectively.
13. Segment Information
The Company’s current operations are organized into the five following business segments. As a result of the acquisition of EHC, the Company has three new business segments: worker’s compensation insurance, segregated portfolio cell reinsurance and specialty reinsurance. In addition, the Company’s prior year segment information has been restated to reflect the sale of IBSi and the completion of the group medical run-off operations, both of which are included in the corporate/other segment for the years ended December 31, 2005 and 2004.
Workers’ Compensation Insurance
Workers’ compensation insurance is underwritten through Eastern Alliance and Allied Eastern, both Pennsylvania domiciled insurance companies, which provide insurance coverage to small and medium sized businesses in rural and suburban Pennsylvania, Maryland and Delaware. Eastern Alliance and Allied Eastern offer a complete line of workers’ compensation products, including guaranteed cost and loss sensitive products. Under the guaranteed cost program, the prospective workers’ compensation policy premium is determined at the beginning of the policy period based on estimated payroll. The loss sensitive products offer the opportunity of returning a portion of the policyholder’s premium in the form of a dividend based upon loss experience. Eastern Alliance and Allied Eastern distribute their products and services through a network of independent agents. Fronting fees earned by Eastern Alliance and Allied Eastern on the segregated portfolio cell reinsurance business are reported in the workers’ compensation insurance segment.
Segregated Portfolio Cell Reinsurance
The Company provides a variety of services to self-insured workers’ compensation plans including program design, fronting, claims adjusting, investment management, and cell rental services at Eastern Re. The primary insurance coverage for the segregated portfolio cell program is underwritten by Eastern Alliance and Allied Eastern and ceded 100% to Eastern Re. The cell rental structure provides the segregated portfolio dividend participants the opportunity to retain control of both underwriting profit and investment income derived from the insurance programs. Eastern Re currently provides cell rental facilities and Eastern Alliance and Allied Eastern provide fronting services to 11 customers. Upon termination of the respective agreements with the customers and after settlement of the ultimate liabilities due under the various programs, the segregated portfolio dividend participants are entitled to receive a profit participation dividend payment from Eastern Re for the remaining underwriting profit, if any, under the cell rental programs. Fronting fees earned by Eastern Alliance and Allied Eastern on the segregated portfolio cell reinsurance business are reported in the workers’ compensation insurance segment. Outstanding loss reserves and unearned premiums under the segregated portfolio cell programs are collateralized by letters of credit provided by the segregated portfolio dividend participants.
Group Benefits Insurance
Group benefits insurance, which includes dental, short and long-term disability, and term life insurance products are underwritten through ELH. The group benefits insurance products are primarily marketed to small and medium sized businesses. ELH is licensed to write business in 41 jurisdictions in the United States. ELH is currently actively writing business in 16 jurisdictions, primarily in the Mid-Atlantic, Southeast, and Midwest regions of the United States. ELH distributes its products through a network of independent producers.
100
Specialty Reinsurance
Specialty reinsurance is underwritten through Eastern Re. Eastern Re assumes business through its participation in reinsurance treaties with an unaffiliated insurance company related to an underground storage tank insurance program, referred to as “EnviroGuard,” and a non-hazardous waste transportation product, referred to as “EIA liability” (“EIA”). The EnviroGuard program provides coverage to underground tank owners for third party off-site bodily injury and property damage claims as well as clean-up coverage and first party on-site claims. The EIA program provides commercial automobile liability coverage for non-hazardous waste haulers.
Corporate/Other
The corporate/other segment consists of the operating results of Employers Alliance, the Company’s third party administrator, which provides claims adjusting and risk management services to self-insured workers’ compensation and property and casualty plans. This segment also includes the operations of the Company, Eastern Services and Global Alliance, the run-off operations of ELH’s group medical insurance operations, and certain eliminations necessary to reconcile the segment information to the consolidated statements of operations and comprehensive income (loss). Prior to January, 1, 2006, the corporate/other segment also included the operating results of ELH’s general agency operations, IBSi.
The following table represents the segment results for the year ended December 31, 2006 (in thousands):
| | | | | | | | | | | | | | | | | | | | | |
| | | Workers’
Compensation
Insurance | | | Segregated
Portfolio Cell
Reinsurance | | Group
Benefits
Insurance | | Specialty
Reinsurance | | | Corporate/
Other | | | Total |
Revenue: | | | | | | | | | | | | | | | | | | | | | |
Net premiums earned | | $ | 24,148 | | | $ | 11,806 | | $ | 33,451 | | $ | 5,514 | | | $ | — | | | $ | 74,919 |
Net investment income | | | 2,225 | | | | 588 | | | 3,669 | | | 1,032 | | | | 1,478 | | | | 8,992 |
Net realized investment gains (losses) | | | 586 | | | | 365 | | | 1,972 | | | 15 | | | | (181 | ) | | | 2,757 |
Other revenue | | | — | | | | — | | | — | | | 177 | | | | 136 | | | | 313 |
| | | | | | | | | | | | | | | | | | | | | |
Total revenue | | | 26,959 | | | | 12,759 | | | 39,092 | | | 6,738 | | | | 1,433 | | | | 86,981 |
| | | | | | | | | | | | | | | | | | | | | |
Expenses: | | | | | | | | | | | | | | | | | | | | | |
Loss and loss adjustment expenses incurred | | | 15,162 | | | | 5,892 | | | 20,600 | | | 6,292 | | | | (33 | ) | | | 47,913 |
Acquisition and other underwriting expenses | | | (40 | ) | | | 2,746 | | | 5,072 | | | 789 | | | | (2,626 | ) | | | 5,941 |
Other expenses | | | 3,724 | | | | 106 | | | 6,336 | | | 411 | | | | 5,113 | | | | 15,690 |
Amortization of intangibles | | | — | | | | — | | | — | | | — | | | | 1,088 | | | | 1,088 |
Policyholder dividend expense | | | 239 | | | | — | | | — | | | — | | | | — | | | | 239 |
Segregated portfolio dividend expense | | | — | | | | 4,015 | | | — | | | — | | | | (1,125 | ) | | | 2,890 |
| | | | | | | | | | | | | | | | | | | | | |
Total expenses | | | 19,085 | | | | 12,759 | | | 32,008 | | | 7,492 | | | | 2,417 | | | | 73,761 |
| | | | | | | | | | | | | | | | | | | | | |
Income before income taxes | | | 7,874 | | | | — | | | 7,084 | | | (754 | ) | | | (984 | ) | | | 13,220 |
Income tax expense | | | 2,556 | | | | — | | | 2,497 | | | (265 | ) | | | 154 | | | | 4,942 |
| | | | | | | | | | | | | | | | | | | | | |
Net income (loss) | | $ | 5,318 | | | $ | — | | $ | 4,587 | | $ | (489 | ) | | $ | (1,138 | ) | | $ | 8,278 |
| | | | | | | | | | | | | | | | | | | | | |
Total assets | | $ | 171,662 | | | $ | 41,451 | | $ | 108,650 | | $ | 44,999 | | | $ | 1,444 | | | $ | 368,206 |
| | | | | | | | | | | | | | | | | | | | | |
101
The following table represents the segment results for the year ended December 31, 2005, which reflects the results of operations of ELH (in thousands):
| | | | | | | | | | |
| | | Year Ended December 31, 2005 |
| | | Group
Benefits
Insurance | | Corporate /
Other | | | Total |
Revenue: | | | | | | | | | | |
Net premiums earned | | | 38,702 | | | — | | | | 38,702 |
Net investment income | | | 3,546 | | | 269 | | | | 3,815 |
Net realized investment gains | | | 232 | | | 213 | | | | 445 |
Other revenue | | | — | | | 1,066 | | | | 1,066 |
| | | | | | | | | | |
Total revenue | | | 42,480 | | | 1,548 | | | | 44,028 |
| | | | | | | | | | |
Expenses: | | | | | | | | | | |
Losses and loss adjustment expenses incurred | | | 27,132 | | | (42 | ) | | | 27,090 |
Acquisition and other underwriting expenses | | | 6,659 | | | (1,207 | ) | | | 5,452 |
Other expenses | | | 5,740 | | | 3,934 | | | | 9,674 |
| | | | | | | | | | |
Total expenses | | | 39,531 | | | 2,685 | | | | 42,216 |
| | | | | | | | | | |
Income (loss) before income taxes | | | 2,949 | | | (1,137 | ) | | | 1,812 |
Income tax expense (benefit) | | | 962 | | | (277 | ) | | | 685 |
| | | | | | | | | | |
Net income (loss) | | | 1,987 | | | (860 | ) | | | 1,127 |
| | | | | | | | | | |
Total assets | | $ | 111,125 | | $ | 100 | | | $ | 111,225 |
| | | | | | | | | | |
The following table represents the segment results for the year ended December 31, 2004, which reflects the results of operations of ELH (in thousands):
| | | | | | | | | | |
| | | Group
Benefits
Insurance | | Corporate /
Other | | | Total |
Revenue: | | | | | | | | | | |
Net premiums earned | | | 38,753 | | | 304 | | | | 39,057 |
Net investment income | | | 3,617 | | | 107 | | | | 3,724 |
Net realized investment gains | | | 1,255 | | | 16 | | | | 1,271 |
Other revenue | | | — | | | 946 | | | | 946 |
| | | | | | | | | | |
Total revenue | | | 43,625 | | | 1,373 | | | | 44,998 |
| | | | | | | | | | |
Expenses: | | | | | | | | | | |
Losses and loss adjustment expenses incurred | | | 27,543 | | | (1,611 | ) | | | 25,932 |
Acquisition and other underwriting expenses | | | 6,954 | | | (1,284 | ) | | | 5,670 |
Other expenses | | | 6,540 | | | 4,061 | | | | 10,601 |
| | | | | | | | | | |
Total expenses | | | 41,037 | | | 1,166 | | | | 42,203 |
| | | | | | | | | | |
Income (loss) before income taxes | | | 2,588 | | | 207 | | | | 2,795 |
Income tax expense (benefit) | | | 915 | | | 97 | | | | 1,012 |
| | | | | | | | | | |
Net income (loss) | | | 1,673 | | | 110 | | | | 1,783 |
| | | | | | | | | | |
Total assets | | $ | 106,485 | | $ | 5,188 | | | $ | 111,673 |
| | | | | | | | | | |
14. Sale of IBSiInterest
On October 31, 2005, ELH entered into a Membership Purchase Agreement (the “Agreement”) for the sale of its interest in IBSi to IBSi’s Vice President of Sales, an IBSi Regional Sales Director, and an unaffiliated third party (collectively referred to as the “purchasers”). The sale was completed through a cash purchase of $300, subject to certain purchase price adjustments. Prior to the sale, all inter-company
102
balances between ELH and IBSi were settled, and any remaining assets and liabilities of IBSi, excluding certain furniture and equipment, became the property of ELH. As a result of the sale, ELH recognized a net gain totaling $210. Under the terms of the Agreement, the purchasers received certain furniture and equipment owned by IBSi, totaling $5, and have the exclusive right to market ELH’s group benefits products in North and South Carolina and Virginia from October 31, 2005 through December 31, 2006. ELH may market its group benefits products directly to independent producers in the aforementioned states beginning on January 1, 2007; however, ELH is prohibited from marketing its products through IBSi’s top twenty producers in 2007, and in 2008, subject to IBSi meeting certain production goals. IBSi also has the right to market ELH’s products in other states in which IBSi operates, with the exception of Pennsylvania and Maryland. Subsequent to the sale, ELH markets and sells its group benefits products through direct relationships with its independent producers in Pennsylvania and Maryland. The net assets transferred from IBSi to ELH, as a result of the sale, totaled $4.7 million.
15. Commitments and Contingencies
Lease Commitments
The Company leases its home office building under a 15-year, non-cancelable lease with a related party through February 2017. The base monthly lease payment is subject to an annual increase based upon the consumer price index. Minimum monthly lease commitments for the remainder of the lease term are as follows (in thousands):
| | | |
2007 | | $ | 742 |
2008 | | | 759 |
2009 | | | 776 |
2010 | | | 794 |
2011 | | | 813 |
2012 thereafter | | | 5,287 |
| | | |
Total | | $ | 9,171 |
| | | |
Rent expense totaled $533, $254, and $254 for the years ended December 31, 2006, 2005 and 2004, respectively.
Prior to October 31, 2006, ELH leased its office building under a multi-year sale-leaseback agreement entered into in June 2001. The term of the lease was seven years, ending on June 30, 2008. On March 20, 2006, ELH entered into a Lease Termination Agreement with the landlord of its office building to terminate the current operating lease upon ELH vacating the building and moving to its new office space. ELH moved to its new office space on October 27, 2006. Under the terms of the Lease Termination Agreement, ELH paid the landlord $394. The impact of the termination payment on ELH’s results of operations was reduced by the recognition of the remaining deferred gain, related to the sale-leaseback agreement, on October 31, 2006, totaling $191. For the year ended December 31, 2006, ELH recognized a charge of $203 related to the lease termination. This expense is included in other expenses in the consolidated statement of operations and comprehensive income (loss) for the year ended December 31, 2006. As a result of ELH’s move, the monthly lease payments increased from $32 per month to approximately $58 per month beginning in November 2006.
16. Junior Subordinated Debentures
On May 15, 2003, Trust I, a business trust subsidiary formed by Global Alliance, issued $8.0 million of fixed/floating rate trust preferred securities. These securities have a thirty-year maturity, with a provision that allows the Company to call these securities at par after five years from the date of issuance. Cash distributions will be paid quarterly in arrears at a rate of 7.35% for a period of five years and will float thereafter at 410 basis points over three-month London Interbank Offered Rates. The Company guarantees all obligations of the Trust I with respect to distributions and payments of these securities.
Proceeds from the sale of these securities by the Trust I were used to acquire $8.0 million of Floating/Fixed Rate Junior Subordinated Deferrable Interest Rate Debentures issued by the Company. These debentures have the same terms with respect to maturity, payments, and distributions, as the fixed/floating rate trust preferred securities issued by the Trust I.
103
17. Subsequent Event - Stock-Based Compensation:
The Company adopted the Eastern Insurance Holdings, Inc. 2006 Stock Incentive Plan (the Plan) on December 18, 2006. Awards under the Plan may be made in the form of incentive stock options, nonqualified stock options, restricted stock or any combination to employees and non-employee Directors. The Plan limits to 299,000 the number of shares that may be awarded as restricted stock, and to 747,500 the number of shares for which incentive stock options may be granted. The total number of shares authorized in the plan is 1,046,500 shares, with an annual increase equal to 1% of the shares outstanding at the end of the previous year, with a corresponding proportional annual increase in the number of shares that can be issued as restricted stock. The Plan provides that stock options and restricted stock awards may include vesting restrictions and performance criteria at the discretion of the Compensation Committee of the Board of Directors. The term of options may not exceed ten years for incentive stock options, and ten years and 1 month for nonqualified stock options, and the option price may not be less than fair market value on the date of grant. On December 18, 2006, the Company authorized the grant of 616,688 stock options and 246,675 restricted stock awards on January 3, 2007. The exercise price for the stock options was $14.35 on January 3, 2007. The 2007 grants have a vesting period of 5 years on restricted stock, incentive stock options, and nonqualified stock options.
18. Quarterly Financial Data (Unaudited, in thousands, except per share data)
| | | | | | | | | | | | |
2006 | | March 31 | | June 30 | | September 30 | | December 31 |
Total Revenue | | $ | 10,522 | | $ | 11,898 | | $ | 30,542 | | $ | 34,019 |
Income from operations | | | 1,156 | | | 1,189 | | | 4,015 | | | 6,860 |
Net income | | | 695 | | | 752 | | | 2,302 | | | 4,529 |
Basic earnings per share | | | N/A | | $ | 0.03 | | $ | 0.22 | | $ | 0.43 |
Diluted earnings per share | | | N/A | | $ | 0.03 | | $ | 0.21 | | $ | 0.41 |
The basic and diluted earnings per share for the quarter ended June 30, 2006 was computed based on the Company’s net income for the period from June 17, 2006 to June 30, 2006.
| | | | | | | | | | | | | | |
2005 | | March 31 | | | June 30 | | | September 30 | | December 31 |
Total Revenue | | $ | 10,805 | | | $ | 11,176 | | | $ | 11,387 | | $ | 10,660 |
(Loss) income from operations | | | (1,034 | ) | | | (397 | ) | | | 1,215 | | | 2,028 |
Net (loss) income | | | (791 | ) | | | (322 | ) | | | 611 | | | 1,629 |
104
Item 9 – Changes in and Disagreements with Accountants on Accounting and Financial Disclosure
None.
Item 9A – Controls and Procedures
Disclosure Controls and Procedures
The Company’s management, with the participation of the Company’s Chief Executive Officer and Chief Financial Officer, has evaluated the effectiveness of the Company’s disclosure controls and procedures (as such term is defined in Rules 13a-15(e) and 15d-15(e) under the Securities Exchange Act of 1934, as amended (the “Exchange Act”)) as of the end of the period covered by this report. Based on such evaluation, the Company’s Chief Executive Officer and Chief Financial Officer have concluded that, as of the end of such period, the Company’s disclosure controls and procedures are effective in recording, processing, summarizing and reporting, on a timely basis, information required to be disclosed by the Company in the reports that it files or submits under the Exchange Act and are effective in ensuring that information required to be disclosed by the Company in the reports that it files or submits under the Exchange Act is accumulated and communicated to the Company’s management, including the Company’s Chief Executive Officer and Chief Financial Officer, as appropriate to allow timely decisions regarding required disclosure.
Management’s Report on Internal Control Over Financial Reporting
Not applicable. The Company is not subject to the internal control reporting requirement as of December 31, 2006. The Company will be subject to this requirement effective December 31, 2007.
Item 9B – Other Information
None.
PART III
Item 10 – Directors and Officers of the Registrant
Incorporated by reference from the Company’s 2007 Proxy Statement.
Item 11 – Executive Compensation
Incorporated by reference from the Company’s 2007 Proxy Statement.
Item 12 – Security Ownership of Certain Beneficial Owners and Management and Related Stockholder Matters
Incorporated by reference from the Company’s 2007 Proxy Statement.
Item 13 – Certain Relationships and Related Transactions
Incorporated by reference from the Company’s 2007 Proxy Statement.
105
Item 14 – Principal Accountant Fees and Services
Incorporated by reference from the Company’s 2007 Proxy Statement.
106
PART IV
Item 15 – Exhibits, Financial Statement Schedules.
| (a) (1) | Financial Statements. |
The following consolidated financial statements are filed as part of this report in Item 8:
| | |
Consolidated Financial Statements | | |
Consolidated Balance Sheets as of December 31, 2006 and 2005 | | |
Consolidated Statements of Operations and Comprehensive Income (Loss) for Years Ended December 31, 2006, 2005 and 2004 | | |
Consolidated Statements of Changes in Shareholders’ Equity for Years Ended December 31, 2006, 2005 and 2004 | | |
Consolidated Statements of Cash Flows for Years Ended December 31, 2006, 2005 and 2004 | | |
Notes to Consolidated Financial Statements | | |
| | (2) | Financial Statement Schedules. |
The following consolidated financial statement schedules for the years 2006, 2005 and 2004 are submitted herewith:
Schedule I - Summary of Investments
Schedule II - Condensed Financial Information of Parent Company
Schedule III - Supplementary Schedule Information
Schedule IV - Reinsurance
Schedule VI - Supplemental Information
The information required by Schedule V - Allowance for Uncollectible Premiums and Other Receivables has been included within the consolidated financial statements or notes thereto.
| | |
Exhibit
Number | | Description |
| |
| 2.1 | | Plan of Conversion from Mutual to Stock Organization of Educators Mutual Life Insurance Company adopted March 17, 2005, as amended June 9, 2005. (Incorporated by reference from Exhibit 2.1 to the Eastern Insurance Holdings, Inc. Registration Statement No. 333-128913 on Form S-1) |
| |
| 2.2 | | Agreement and Plan of Reorganization dated March 17, 2005, between and among Educators Mutual Life Insurance Company, Eastern Insurance Holdings, Inc., and Eastern Holding Company, Ltd. (Incorporated by reference from Exhibit 2.2 to the Eastern Insurance Holdings, Inc. Registration Statement No. 333-131215 on Form S-4) |
| |
| 3.1 | | Articles of Incorporation of Eastern Insurance Holdings, Inc. (Incorporated by reference from Exhibit 3.1 to the Eastern Insurance Holdings, Inc. Registration Statement No. 333-128913 on Form S-1) |
| |
| 3.2 | | Bylaws of Eastern Insurance Holdings, Inc. (Incorporated by reference from Exhibit 3.2 to the Eastern Insurance Holdings, Inc. Registration Statement No. 333-128913 on Form S-1) |
| |
| 4.1 | | Form of Stock Certificate of Eastern Insurance Holdings, Inc. (Incorporated by reference from Exhibit 4.1 to the Eastern Insurance Holdings, Inc. Registration Statement No. 333-128913 on Form S-1) |
| |
| 10.1 | | Transition Agreement, dated March 4, 2005, between Educators Insurance Company and Alex T. Schneebacher (Incorporated by reference from Exhibit 10.1 to the Eastern Insurance Holdings, Inc. Registration Statement No. 333-128913 on Form S-1) |
| |
| 10.2 | | Employee Stock Ownership Plan of Eastern Insurance Holdings, Inc. (Incorporated by reference from Exhibit 10.2 to the Eastern Insurance Holdings, Inc. Registration Statement No. 333-128913 on Form S-1) |
| |
| 10.3 | | Stock Compensation Plan of Eastern Insurance Holdings, Inc. (Incorporated by reference from Exhibit 10.3 to the Eastern Insurance Holdings, Inc. Registration Statement No. 333-128913 on Form S-1) |
107
| | |
| |
| 10.4 | | Employment Agreement, dated March 17, 2005, between Eastern Holding Company, Ltd. and Bruce M. Eckert (Incorporated by reference from Exhibit 10.4 to the Eastern Insurance Holdings, Inc. Registration Statement No. 333-128913 on Form S-1) |
| |
| 10.5 | | Employment Agreement, dated March 17, 2005, between Eastern Holding Company, Ltd. and Michael L. Boguski (Incorporated by reference from Exhibit 10.5 to the Eastern Insurance Holdings, Inc. Registration Statement No. 333-128913 on Form S-1) |
| |
| 10.6 | | Employment Agreement, dated March 17, 2005, between Eastern Holding Company, Ltd. and Kevin M. Shook (Incorporated by reference from Exhibit 10.6 to the Eastern Insurance Holdings, Inc. Registration Statement No. 333-128913 on Form S-1) |
| |
| 10.7 | | Employment Agreement, dated March 17, 2005, between Eastern Holding Company, Ltd. and Robert A. Gilpin (Incorporated by reference from Exhibit 10.7 to the Eastern Insurance Holdings, Inc. Registration Statement No. 333-128913 on Form S-1) |
| |
| 10.8 | | Employment Agreement, dated March 17, 2005, between Eastern Holding Company, Ltd. and Suzanne M. Emmet (Incorporated by reference from Exhibit 10.8 to the Eastern Insurance Holdings, Inc. Registration Statement No. 333-128913 on Form S-1) |
| |
| 10.9 | | Coinsurance Agreement, effective October 1, 2003, between Educators Mutual Life Insurance Company and London Life Reinsurance Company (Incorporated by reference from Exhibit 10.10 to the Eastern Insurance Holdings, Inc. Registration Statement No. 333-128913 on Form S-1) |
| |
| 10.10 | | Agreement of Sale for IBSi(Incorporated by reference from Exhibit 10.26 to the Eastern Insurance Holdings, Inc. Registration Statement No. 333-128913 on Form S-1) |
| |
| 10.11 | | Officer Retention Agreement dated March 4, 2005, between M. Christine Gimber and Educators Mutual Life Insurance Company (Incorporated by reference from Exhibit 10.27 to the Eastern Insurance Holdings, Inc. Registration Statement No. 333-128913 on Form S-1) |
| |
| 10.12 | | Eastern Insurance Holdings, Inc. 2006 Stock Incentive Plan (filed herewith) |
| |
| 14.1 | | Code of Ethics (filed herewith) |
| |
| 21.1 | | Subsidiaries of Eastern Insurance Holdings, Inc. (Incorporated by reference from Exhibit 21 to the Eastern Insurance Holdings, Inc. Registration Statement No. 333-128913 on Form S-1) |
| |
| 31.1 | | Certification of Chief Executive Officer in accordance with Section 302 of the Sarbanes-Oxley Act of 2002 (filed herewith) |
| |
| 31.2 | | Certification of Chief Financial Officer in accordance with Section 302 of the Sarbanes-Oxley Act of 2002 (filed herewith) |
| |
| 32.1 | | Certification of Chief Executive Officer in accordance with Section 906 of the Sarbanes-Oxley Act of 2002 (filed herewith) |
| |
| 32.2 | | Certification of Chief Financial Officer in accordance with Section 906 of the Sarbanes-Oxley Act of 2002 (filed herewith) |
108
SIGNATURES
Pursuant to the requirements of Section 13 or 15(d) of the Securities Exchange Act of 1934, the registrant has duly caused this report to be signed on its behalf by the undersigned, thereunto duly authorized.
| | |
| EASTERN INSURANCE HOLDINGS, INC. |
| |
| By: | | /s/ Kevin M. Shook |
| | Kevin M. Shook, Chief Financial Officer |
Pursuant to the requirements of the Securities Exchange Act of 1934, this report has been signed by the following persons in the capacities indicated on the date indicated:
| | | | |
Signature | | | | |
| | |
/s/ Bruce M. Eckert Bruce M. Eckert | | Chief Executive Officer (Principal Executive Officer) and Director | | March___, 2007 |
| | |
/s/ Kevin M. Shook Kevin M. Shook | | Treasurer and Chief Financial Officer (Principal Financial and Accounting Officer) | | March___, 2007 |
| | |
/s/ Robert M. McAlaine Robert M. McAlaine | | Chairman and Director | | March___, 2007 |
| | |
/s/ Lawrence W. Bitner Lawrence W. Bitner | | Director | | March___, 2007 |
| | |
/s/ Paul R. Burke Paul R. Burke | | Director | | March___, 2007 |
| | |
/s/ Ronald L. King Ronald L. King | | Director | | March___, 2007 |
| | |
/s/ Scott C. Penwell Scott C. Penwell | | Director | | March___, 2007 |
| | |
/s/ John O. Shirk John O. Shirk | | Director | | March___, 2007 |
| | |
/s/ W. Lloyd Snyder III W. Lloyd Snyder III | | Director | | March___, 2007 |
| | |
/s/ Richard Stevens III Richard Stevens III | | Director | | March___, 2007 |
| | |
/s/ Charles H. Vetterlein, Jr. Charles H. Vetterlein, Jr. | | Director | | March___, 2007 |
| | |
/s/ James L. Zech James L. Zech | | Director | | March___, 2007 |
109
EXHIBIT INDEX
| | |
Exhibit
Number | | Description |
| |
| 2.1 | | Plan of Conversion from Mutual to Stock Organization of Educators Mutual Life Insurance Company adopted March 17, 2005, as amended June 9, 2005. (Incorporated by reference from Exhibit 2.1 to the Eastern Insurance Holdings, Inc. Registration Statement No. 333-128913 on Form S-1) |
| |
| 2.2 | | Agreement and Plan of Reorganization dated March 17, 2005, between and among Educators Mutual Life Insurance Company, Eastern Insurance Holdings, Inc., and Eastern Holding Company, Ltd. (Incorporated by reference from Exhibit 2.2 to the Eastern Insurance Holdings, Inc. Registration Statement No. 333-131215 on Form S-4) |
| |
| 3.1 | | Articles of Incorporation of Eastern Insurance Holdings, Inc. (Incorporated by reference from Exhibit 3.1 to the Eastern Insurance Holdings, Inc. Registration Statement No. 333-128913 on Form S-1) |
| |
| 3.2 | | Bylaws of Eastern Insurance Holdings, Inc. (Incorporated by reference from Exhibit 3.2 to the Eastern Insurance Holdings, Inc. Registration Statement No. 333-128913 on Form S-1) |
| |
| 4.1 | | Form of Stock Certificate of Eastern Insurance Holdings, Inc. (Incorporated by reference from Exhibit 4.1 to the Eastern Insurance Holdings, Inc. Registration Statement No. 333-128913 on Form S-1) |
| |
| 10.1 | | Transition Agreement, dated March 4, 2005, between Educators Insurance Company and Alex T. Schneebacher (Incorporated by reference from Exhibit 10.1 to the Eastern Insurance Holdings, Inc. Registration Statement No. 333-128913 on Form S-1) |
| |
| 10.2 | | Employee Stock Ownership Plan of Eastern Insurance Holdings, Inc. (Incorporated by reference from Exhibit 10.2 to the Eastern Insurance Holdings, Inc. Registration Statement No. 333-128913 on Form S-1) |
| |
| 10.3 | | Stock Compensation Plan of Eastern Insurance Holdings, Inc. (Incorporated by reference from Exhibit 10.3 to the Eastern Insurance Holdings, Inc. Registration Statement No. 333-128913 on Form S-1) |
| |
| 10.4 | | Employment Agreement, dated March 17, 2005, between Eastern Holding Company, Ltd. and Bruce M. Eckert (Incorporated by reference from Exhibit 10.4 to the Eastern Insurance Holdings, Inc. Registration Statement No. 333-128913 on Form S-1) |
| |
| 10.5 | | Employment Agreement, dated March 17, 2005, between Eastern Holding Company, Ltd. and Michael L. Boguski (Incorporated by reference from Exhibit 10.5 to the Eastern Insurance Holdings, Inc. Registration Statement No. 333-128913 on Form S-1) |
| |
| 10.6 | | Employment Agreement, dated March 17, 2005, between Eastern Holding Company, Ltd. and Kevin M. Shook (Incorporated by reference from Exhibit 10.6 to the Eastern Insurance Holdings, Inc. Registration Statement No. 333-128913 on Form S-1) |
| |
| 10.7 | | Employment Agreement, dated March 17, 2005, between Eastern Holding Company, Ltd. and Robert A. Gilpin (Incorporated by reference from Exhibit 10.7 to the Eastern Insurance Holdings, Inc. Registration Statement No. 333-128913 on Form S-1) |
| |
| 10.8 | | Employment Agreement, dated March 17, 2005, between Eastern Holding Company, Ltd. and Suzanne M. Emmet (Incorporated by reference from Exhibit 10.8 to the Eastern Insurance Holdings, Inc. Registration Statement No. 333-128913 on Form S-1) |
| |
| 10.9 | | Coinsurance Agreement, effective October 1, 2003, between Educators Mutual Life Insurance Company and London Life Reinsurance Company (Incorporated by reference from Exhibit 10.10 to the Eastern Insurance Holdings, Inc. Registration Statement No. 333-128913 on Form S-1) |
| |
| 10.10 | | Agreement of Sale for IBSi(Incorporated by reference from Exhibit 10.26 to the Eastern Insurance Holdings, Inc. Registration Statement No. 333-128913 on Form S-1) |
110
| | |
| |
| 10.11 | | Officer Retention Agreement dated March 4, 2005, between M. Christine Gimber and Educators Mutual Life Insurance Company (Incorporated by reference from Exhibit 10.27 to the Eastern Insurance Holdings, Inc. Registration Statement No. 333-128913 on Form S-1) |
| |
| 10.12 | | Eastern Insurance Holdings, Inc. 2006 Stock Incentive Plan (filed herewith) |
| |
| 14.1 | | Code of Ethics (filed herewith) |
| |
| 21.1 | | Subsidiaries of Eastern Insurance Holdings, Inc. (Incorporated by reference from Exhibit 21 to the Eastern Insurance Holdings, Inc. Registration Statement No. 333-128913 on Form S-1) |
| |
| 31.1 | | Certification of Chief Executive Officer in accordance with Section 302 of the Sarbanes-Oxley Act of 2002 (filed herewith) |
| |
| 31.2 | | Certification of Chief Financial Officer in accordance with Section 302 of the Sarbanes-Oxley Act of 2002 (filed herewith) |
| |
| 32.1 | | Certification of Chief Executive Officer in accordance with Section 906 of the Sarbanes-Oxley Act of 2002 (filed herewith) |
| |
| 32.2 | | Certification of Chief Financial Officer in accordance with Section 906 of the Sarbanes-Oxley Act of 2002 (filed herewith) |
111
Report of Independent Registered Public Accounting Firm
Board of Directors
Eastern Insurance Holdings, Inc. and Subsidiaries
Lancaster, Pennsylvania
We have audited the consolidated financial statements of Eastern Insurance Holdings, Inc. and subsidiaries (formerly Educators Mutual Life Insurance Company) (the Company) as of December 31, 2005 and for each of the two years in the period ended December 31, 2005 and have issued our report thereon dated March 24, 2006; such report is included elsewhere in the Form 10-K. We have also audited the 2005 and 2004 consolidated financial statement schedules of the Company listed in Item 15. These consolidated financial statement schedules are the responsibility of the Company’s management. Our responsibility is to express an opinion based on our audits. In our opinion, such financial statement schedules, when considered in relation to the basic consolidated financial statements taken as a whole, present fairly, in all material respects, the information set forth herein.
/s/ Beard Miller Company LLP
Beard Miller Company LLP
Harrisburg, Pennsylvania
March 24, 2006
112
Eastern Insurance Holdings, Inc. and Subsidiaries
Schedule I — Summary of Investments — Other than
Investments in Related Parties as of December 31, 2006
| | | | | | | | | |
Column A | | Column B | | Column C | | Column D |
Type of Investment | | Cost | | Market
Value | | Balance Sheet |
| | | (Dollars in thousands) |
Fixed maturities: | | | | | | | | | |
Bonds: | | | | | | | | | |
United States Government and government agencies and authorities | | $ | 18,434 | | $ | 18,913 | | $ | 18,913 |
States, municipalities and political subdivisions | | | 33,751 | | | 34,446 | | | 34,446 |
Foreign governments | | | 500 | | | 496 | | | 496 |
Public utilities | | | 5,336 | | | 5,350 | | | 5,350 |
Convertibles and bonds with warrants attached | | | 11,830 | | | 13,545 | | | 13,545 |
All other corporate bonds | | | 133,605 | | | 135,012 | | | 135,012 |
| | | | | | | | | |
Total bonds | | | 203,456 | | | 207,762 | | | 207,762 |
Redeemable preferred stock | | | — | | | — | | | — |
| | | | | | | | | |
Total fixed maturities | | | 203,456 | | | 207,762 | | | 207,762 |
| | | | | | | | | |
Equity securities: | | | | | | | | | |
Common stocks: | | | | | | | | | |
Public utilities | | | 4 | | | 5 | | | 5 |
Banks, trust and insurance companies | | | 419 | | | 453 | | | 453 |
Industrial, miscellaneous and all other | | | 16,604 | | | 17,761 | | | 17,761 |
Non-redeemable preferred stocks | | | — | | | — | | | — |
| | | | | | | | | |
Total equity securities | | | 17,027 | | | 18,219 | | | 18,219 |
| | | | | | | | | |
Other long-term investments | | | 9,994 | | | 11,604 | | | 11,604 |
| | | | | | | | | |
Total investments | | $ | 230,477 | | $ | 237,585 | | $ | 237,585 |
| | | | | | | | | |
See accompanying report of independent registered public accounting firm.
113
Eastern Insurance Holdings, Inc.
Schedule II — Condensed Financial Information Of Parent Company
Condensed Balance Sheet
December 31, 2006
(In thousands, except share data)
| | | | |
| | | 2006 | |
ASSETS | | | | |
Investment in common stock of subsidiaries (equity method) | | $ | 141,590 | |
Cash and cash equivalents | | | 19,589 | |
Intangible assets | | | 8,110 | |
Goodwill | | | 5,140 | |
Other assets | | | 515 | |
| | | | |
Total assets | | $ | 174,944 | |
| | | | |
LIABILITIES AND STOCKHOLDERS’ EQUITY | | | | |
Liabilities: | | | | |
Accounts payable and accrued expenses | | $ | 207 | |
Deferred tax liability, net | | | 110 | |
Federal income taxes payable | | | 97 | |
Due to subsidiaries, net | | | 786 | |
| | | | |
Total liabilities | | | 1,200 | |
| | | | |
Equity: | | | | |
Series A preferred stock, no par value, authorized 5,000,000 shares, no shares issued and outstanding | | | — | |
Common stock, no par value, authorized 20,000,000 shares,11,350,407 shares issued and outstanding | | | — | |
Unearned ESOP compensation | | | (7,101 | ) |
Additional paid-in capital | | | 108,502 | |
Accumulated other comprehensive income: | | | | |
Unrealized gains in investments, net of deferred income taxes | | | 2,437 | |
Unrecognized benefit plan gains | | | 423 | |
Retained Earnings | | | 69,483 | |
| | | | |
Total stockholders’ equity | | | 173,744 | |
| | | | |
Total liabilities and stockholders’ equity | | $ | 174,944 | |
| | | | |
See accompanying report of independent registered public accounting firm.
114
Eastern Insurance Holdings, Inc.
Schedule II — Condensed Financial Information Of Parent Company
Condensed Statement of Earnings
For the Period from June 17, 2006 to December 31, 2006
(In thousands)
| | | | |
| | | 2006 | |
Revenue | | | | |
Investment income, net of expenses | | $ | 720 | |
| | | | |
Total revenue | | | 720 | |
| | | | |
Expenses: | | | | |
Other expenses | | | 1,412 | |
Amortization of intangibles | | | 1,088 | |
| | | | |
Total expenses | | | 2,500 | |
| | | | |
Loss before income tax expense | | | (1,780 | ) |
Income tax expense | | | 227 | |
| | | | |
Loss before equity in income of subsidiaries | | | (2,007 | ) |
Equity in income of subsidiaries | | | 10,285 | |
| | | | |
Net income | | $ | 8,278 | |
| | | | |
See accompanying report of independent registered public accounting firm.
115
Eastern Insurance Holdings, Inc
Schedule II — Condensed Financial Information Of Parent Company
Condensed Statements of Cash Flows
For the Years ended December 31, 2006
(In thousands)
| | | | |
| | | 2006 | |
Cash flows from operating activities: | | | | |
Net income | | $ | 8,278 | |
Adjustments to reconcile net income to net cash used in operating activities: | | | | |
Equity in undistributed income of subsidiaries | | | (10,285 | ) |
Stock compensation | | | 525 | |
Intangible asset amortization | | | 1,088 | |
Deferred income tax provision | | | 130 | |
Other | | | (1,731 | ) |
| | | | |
Net cash used in operating activities | | | (1,995 | ) |
| | | | |
Cash flows from investing activities: | | | | |
Acquisition of EHC | | | (38,496 | ) |
Capital contributions to subsidiaries | | | (4,130 | ) |
Dividend from ELH | | | 2,100 | |
Other | | | (12 | ) |
| | | | |
Net cash used in investing activities | | | (40,538 | ) |
| | | | |
Cash flows from financing activities: | | | | |
Proceeds from initial public offering, net of expenses | | | 62,122 | |
| | | | |
Net cash provided by financing activities | | | 62,122 | |
| | | | |
Net increase in cash and cash equivalents | | | 19,589 | |
Cash and cash equivalents at beginning of period | | | — | |
| | | | |
Cash and cash equivalents at end of period | | $ | 19,589 | |
| | | | |
Cash paid during the year for: | | | | |
Interest | | $ | — | |
Income taxes | | $ | — | |
See accompanying report of independent registered public accounting firm.
116
Eastern Insurance Holdings, Inc. and Subsidiaries
Schedule III — Supplementary Schedule Information
(In thousands)
| | | | | | | | | | | | | | | |
Column A | | Column B | | Column C | | Column D | | Column E | | Column F |
| | | Deferred
Policy
Acquisition
Costs | | Future Policy
Benefits,
Losses, Claims,
and Loss
Expenses | | Unearned
Premiums | | Other Policy
Claims and
Benefits
Payable | | Premium
Revenue |
December 31, 2006 | | | | | | | | | | | | | | | |
Workers’ compensation insurance | | $ | 1,232 | | $ | 44,958 | | $ | 20,596 | | $ | — | | $ | 24,148 |
Group benefits insurance | | | — | | | 37,584 | | | 80 | | | — | | | 33,451 |
Specialty reinsurance | | | 1,773 | | | 23,879 | | | 6,854 | | | — | | | 5,514 |
Segregated portfolio cell reinsurance | | | 1,496 | | | 19,801 | | | 6,330 | | | — | | | 11,806 |
Corporate and other | | | — | | | 245 | | | — | | | — | | | — |
| | | | | | | | | | | | | | | |
Total | | $ | 4,501 | | $ | 126,467 | | $ | 33,860 | | $ | — | | $ | 74,919 |
| | | | | | | | | | | | | | | |
December 31, 2005 | | | | | | | | | | | | | | | |
Group benefits insurance | | $ | — | | $ | 43,880 | | $ | 95 | | $ | — | | $ | 38,702 |
Corporate and other | | | — | | | 256 | | | — | | | — | | | — |
| | | | | | | | | | | | | | | |
Total | | $ | — | | $ | 44,136 | | $ | 95 | | $ | | | $ | 38,702 |
| | | | | | | | | | | | | | | |
December 31, 2004 | | | | | | | | | | | | | | | |
Group benefits insurance | | $ | — | | $ | 43,139 | | $ | 98 | | $ | — | | $ | 38,753 |
Corporate and other | | | — | | | 245 | | | — | | | — | | | 304 |
| | | | | | | | | | | | | | | |
Total | | $ | — | | $ | 43,384 | | $ | 98 | | $ | — | | $ | 39,057 |
| | | | | | | | | | | | | | | |
| | | | | | | | | | | | | | | | |
| | | Column G | | Column H | | | Column I | | Column J | | Column K |
| | | Net
Investment
Income | | Benefits,
Claims, Losses
and Settlement
Expenses | | | Amortization
and DPAC | | Other
Operating
Expenses | | Premiums
Written |
December 31, 2006 | | | | | | | | | | | | | | | | |
Workers’ compensation insurance | | $ | 2,225 | | $ | 15,162 | | | $ | 707 | | $ | 3,724 | | $ | 22,101 |
Group benefits insurance | | | 3,669 | | | 20,600 | | | | — | | | 6,336 | | | 33,428 |
Specialty reinsurance | | | 1,032 | | | 6,292 | | | | 1,266 | | | 411 | | | 5,775 |
Segregated portfolio cell reinsurance | | | 588 | | | 5,892 | | | | 830 | | | 106 | | | 6,225 |
Corporate and other | | | 1,478 | | | (33 | ) | | | — | | | 5,113 | | | — |
| | | | | | | | | | | | | | | | |
Total | | $ | 8,992 | | $ | 47,913 | | | $ | 2,803 | | $ | 15,690 | | $ | 67,529 |
| | | | | | | | | | | | | | | | |
December 31, 2005 | | | | | | | | | | | | | | | | |
Group benefits insurance | | $ | 3,546 | | $ | 27,132 | | | $ | — | | $ | 12,399 | | $ | 38,700 |
Corporate and other | | | 269 | | | (42 | ) | | | — | | | 2,727 | | | — |
| | | | | | | | | | | | | | | | |
Total | | $ | 3,815 | | $ | 27,090 | | | $ | — | | $ | 15,126 | | $ | 38,700 |
| | | | | | | | | | | | | | | | |
December 31, 2004 | | | | | | | | | | | | | | | | |
Group benefits insurance | | $ | 3,617 | | $ | 27,543 | | | $ | — | | $ | 13,494 | | $ | 39,070 |
Corporate and other | | | 107 | | | (1,611 | ) | | | — | | | 2,777 | | | — |
| | | | | | | | | | | | | | | | |
Total | | $ | 3,724 | | $ | 25,932 | | | $ | — | | $ | 16,271 | | $ | 39,070 |
| | | | | | | | | | | | | | | | |
See accompanying report of independent registered public accounting firm.
117
Eastern Insurance Holdings, Inc. and Subsidiaries
Schedule IV — Reinsurance
For the years ended December 31, 2006, 2005 and 2004
(In thousands)
| | | | | | | | | | | | | | | |
Column A | | Column B | | Column C | | Column D | | Column E | | Column F | |
| | | Gross
Amount | | Ceded to
Other
Companies | | Assumed
from Other
Companies | | Net Amount | | Percentage
of Amount
Assumed to
Net | |
Premiums Earned | | | | | | | | | | | | | | | |
For the year ended December 31, 2006 | | | | | | | | | | | | | | | |
Life insurance in force | | $ | 1,676,349 | | $ | 76,194 | | $ | — | | $ | 1,600,155 | | 0 | % |
| | | | | |
Premiums: | | | | | | | | | | | | | | | |
Life insurance | | $ | 5,852 | | $ | 248 | | $ | — | | $ | 5,604 | | 0 | % |
Accident and health insurance | | $ | 30,076 | | $ | 2,230 | | $ | — | | $ | 27,846 | | 0 | % |
Property and liability insurance | | $ | 26,451 | | $ | 4,223 | | $ | 19,241 | | $ | 41,469 | | 46.4 | % |
For the year ended December 31, 2005 | | | | | | | | | | | | | | | |
Life insurance in force | | $ | 1,800,055 | | $ | 76,172 | | $ | — | | $ | 1,723,833 | | 0 | % |
| | | | | |
Premiums: | | | | | | | | | | | | | | | |
Life insurance | | $ | 6,342 | | $ | 277 | | $ | — | | $ | 6,065 | | 0 | % |
Accident and health insurance | | $ | 34,654 | | $ | 2,017 | | $ | — | | $ | 32,637 | | 0 | % |
For the year ended December 31, 2004 | | | | | | | | | | | | | | | |
Life insurance in force | | $ | 1,849,132 | | $ | 74,930 | | $ | — | | $ | 1,774,202 | | 0 | % |
| | | | | |
Premiums: | | | | | | | | | | | | | | | |
Life insurance | | $ | 6,251 | | $ | 216 | | $ | — | | $ | 6,035 | | 0 | % |
Accident and health insurance | | $ | 34,529 | | $ | 1,507 | | $ | — | | $ | 33,022 | | 0 | % |
See accompanying report of independent registered public accounting firm.
118
Eastern Insurance Holdings, Inc.
Schedule VI — Supplemental Information
For the year ended December 31, 2006
| | | | | | | | | | | | | | | | | | |
Column A | | Column B | | Column C | | Column D | | Column E | | Column F | | Column G |
| Affiliation with Registrant | | Deferred
Policy
Acquisition
Costs | | Reserve for
Losses and
Loss Adj.
Expenses | | Discount if
any Deducted
in Column C | | Unearned
Premiums | | Net Earned
Premiums | | Net
Investment
Income |
| | | (Dollars in thousands) |
Year ended December 31, 2006 | | $ | 1,232 | | $ | 44,958 | | $ | 2,183 | | $ | 20,596 | | $ | 24,148 | | $ | 2,225 |
| | | | | | | | | | | | | | | | |
| | | Column H Losses and LAE
Incurred | | | Column I | | Column J | | Column K |
| | | Current
Period | | Prior
Year | | | Amortization
of DPAC | | Paid Losses and
Adjustment
Expenses | | Net Written
Premiums |
| | | (Dollars in thousands) |
Year ended December 31, 2006 | | $ | 16,888 | | $ | (1,727 | ) | | $ | 707 | | $ | 11,418 | | $ | 22,101 |
See accompanying report of independent registered public accounting firm.
119