Exhibit 99.1
Exhibit 99.1
Serving Families at Home Since 1979
The Pre-Acute Solution to the Post-Acute Problem.
JP Morgan Conference
January 12-15, 2015
Mark Heaney President and CEO Inna Berkovich Chief Information Officer
Darby Anderson Chief Business Development and Strategy Officer
Forward-Looking Statements
The following information contains, or may be deemed to contain, forward-looking statements. By their nature, forward-looking statements involve risks and uncertainties because they relate to events and depend on circumstances that may or may not occur in the future. The future results of Addus may vary from the results expressed in, or implied by, the following forward-looking statements, possibly to a material degree, and historical results may not be an indication of future performance. For a discussion of some of the important factors that could cause Addus’ results to differ from those expressed in, or implied by, the following forward-looking statements, please refer to Addus’ most recent Annual Report on Form 10-K, and its Quarterly Reports on Form 10-Q, each of which is available at www.SEC.gov, particularly the Sections entitled “Risk Factors.” Addus undertakes no obligation to update or revise any forward-looking statements, except as may be required by law.
Mission
It is the primary mission of Addus HomeCare to improve the health and well being of our consumers through the provision of quality, cost-effective home and community based services.
We will accomplish our goals by fostering an environment in which our employees enthusiastically support and advance our mission.
Reward for accomplishing our mission includes pride in our organization, contribution to the community and a reasonable profit.
3
Addus Profile
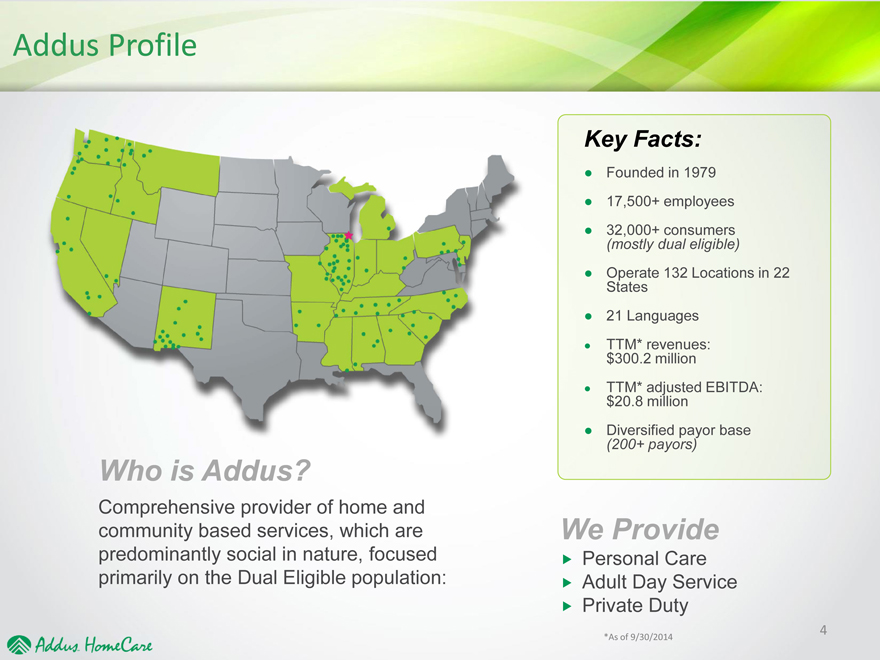
Who is Addus?
Comprehensive provider of home and community based services, which are predominantly social in nature, focused primarily on the Dual Eligible population:
Key Facts:
• Founded in 1979
• 17,500+ employees
• 32,000+ consumers
(mostly dual eligible)
• Operate 132 Locations in 22
States
• 21 Languages
• TTM* revenues:
$300.2 million
• TTM* adjusted EBITDA:
$20.8 million
• Diversified payor base
(200+ payors)
We Provide
? Personal Care
? Adult Day Service
? Private Duty
*As of 9/30/2014 4
Who We Serve….
…The 5% who consume 50% of the Healthcare dollars
10,000 people a day turn 65 years old
Those baby boomers that live to 75 can expect to live at least 10 more years
In just 14 years, life expectancy has increased 2.4 years, meaning….…more elderly are living longer and, as they do, they become increasingly poor
5
Source: Pew Research Center, December 2010
Our Services
We serve high volume consumers of healthcare in their homes at the lowest
price point for hands-on care
We serve over 32,000 consumers—typically elderly, chronically ill or disabled, at risk of hospitalization or institutionalization
Our Homecare Aides assist with essential activities of daily living – without this help, consumers will go to a nursing home
Average duration of services is approximately 17 months per consumer
We see our consumers on average 45 hours per month
Addus average revenue per billable hour is $17.05
Substantial opportunity to integrate technology to leverage our low-cost care
6
Addus Dual AdvantageTM
The Very Front Line
No one knows more about the
member…
No one is in a better position to
positively affect health
outcomes…
Than the
Addus HomeCare
Aide.
7
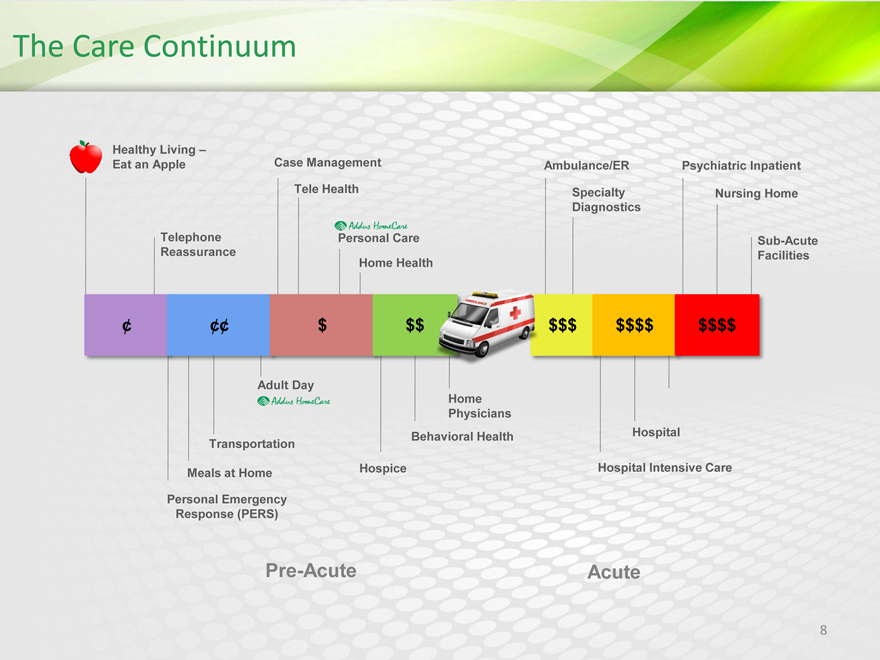
The Care Continuum
Healthy Living –
Eat an Apple Case Management Ambulance/ER Psychiatric Inpatient Tele Health Specialty Nursing Home Diagnostics
Telephone Personal Care Sub-Acute Reassurance Home Health Facilities
¢ ¢¢ $ $$ $$$ $$$$ $$$$
Adult Day
Home Physicians
Behavioral Health Hospital Transportation
Hospice Hospital Intensive Care
Meals at Home
Personal Emergency Response (PERS)
Pre-Acute Acute
8
The Leader in Large, Highly Fragmented Industry
Only public pure-play home care provider
Approximately 20,000 home care agencies
Personal care market in excess of $60 billion
Home care proven effective in enabling consumers to remain safely and healthfully at home for as long as possible
Public policy shift to consolidate Medicare and Medicaid programs for 9 million dual-eligibles driving expansion of MCOs
9
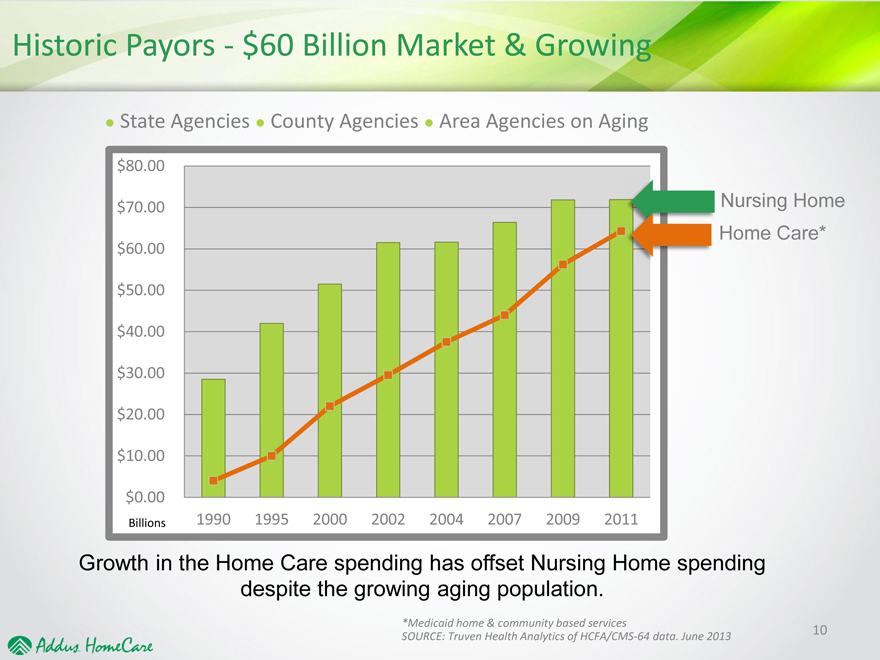
Historic Payors—$60 Billion Market & Growing
State Agencies County Agencies Area Agencies on Aging
$80.00
$70.00 Nursing Home
Home Care*
$60.00
$50.00
$40.00
$30.00
$20.00
$10.00
$0.00
Billions 1990 1995 2000 2002 2004 2007 2009 2011
Growth in the Home Care spending has offset Nursing Home spending
despite the growing aging population.
*Medicaid home & community based services
SOURCE: Truven Health Analytics of HCFA/CMS-64 data. June 2013 10
Strategies for Growth
Aging population Favor larger, more
Longer lifespan sophisticated,
Sales programs to increase providers
same store census • Require technology
De novo expansion int More
new markets comprehensive
Business development offerings
with traditional payors • Expect health
Adult Day expansion outcomes
Product diversification Risk based contracts
o Tele-monitoring
o Risk assessments
o Platform for small
providers
• 20,000 Mostly small agencies
• Changing market
• Mounting regulatory pressure
• Industry consolidation
11
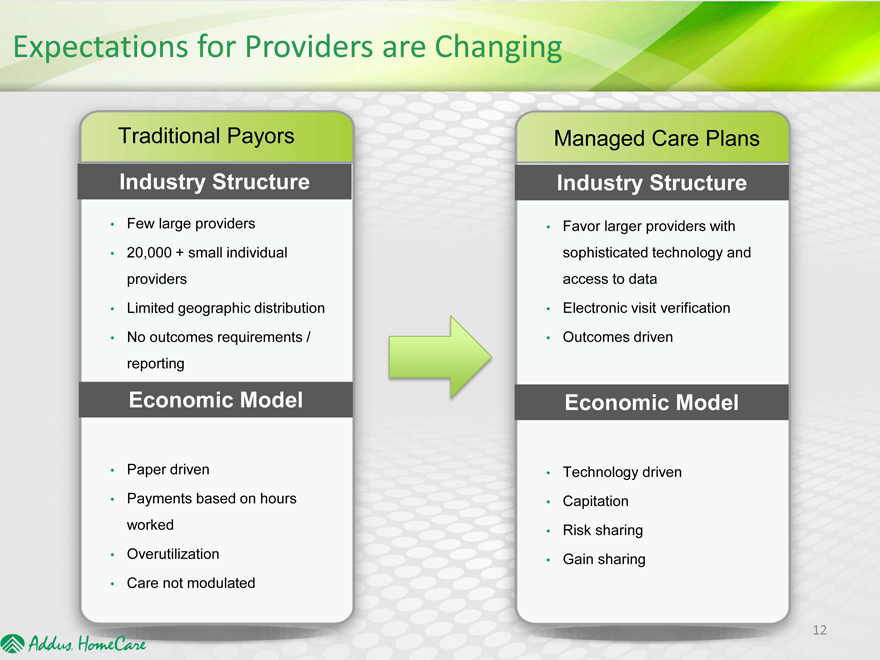
Expectations for Providers are Changing
Traditional Payors
Industry Structure
Few large providers
20,000 + small individual
providers
Limited geographic distribution
No outcomes requirements /
reporting
Economic Model
Paper driven
Payments based on hours
worked
Overutilization
Care not modulated
Managed Care Plans
Industry Structure
Favor larger providers with
sophisticated technology and
access to data
Electronic visit verification
Outcomes driven
Economic Model
Technology driven
Capitation
Risk sharing
Gain sharing
12
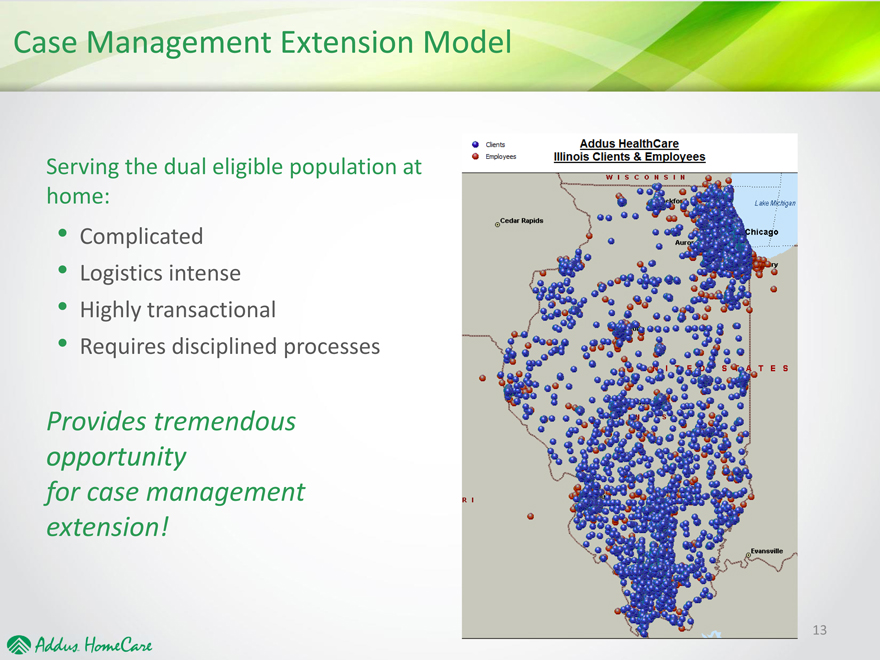
Case Management Extension Model
Serving the dual eligible population at
home:
Complicated
Logistics intense
Highly transactionvbal
Requires disciplined processes
Provides tremendous
opportunity
for case management
extension!
Addus Dual Advantage™ — The New Paradigm
The Addus Advantage coordinated care model
By Enabling members to live safely and healthfully at home as long as possible we add value for any provider/payer at financial risk
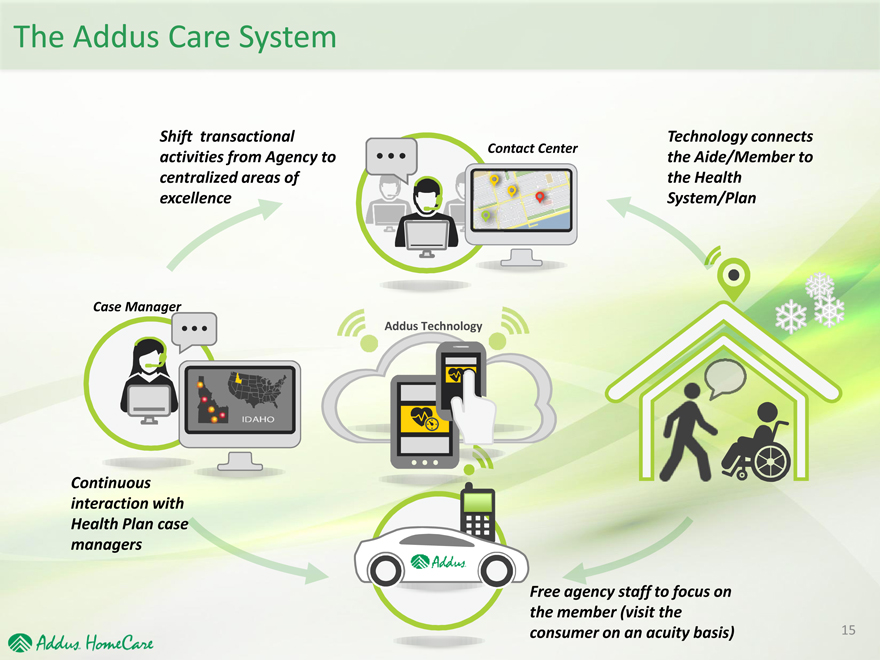
The Addus Care System
Shift transactional activities from Agency to centralized areas of excellence
Contact Center
Technology connects the Aide/Member to the Health System/Plan
Case Manager
Addus Technology
Continuous
interaction with
Health Plan case
managers
Free agency staff to focus on the member (visit the consumer on an acuity basis)
Driving Outcomes
Services We Provide
Activities of Daily Living Needs
Driving to
Doctor Visits
Personal Hygiene
Nutrition/Meal Prep
Errands/Shopping
Home Safety Assessment
Member Engagement
Because we’re always there
Observe & Report
Photo Documentation
Real-time Patient
Condition Monitoring
and Early Intervention
Outcomes
Early Intervention and Compliance
Weight Mgmt &
Medication Compliance
Nutrition
Stay At Home
Reduced
Hospitalizations/Nursing
Homes
Fall Prevention
16
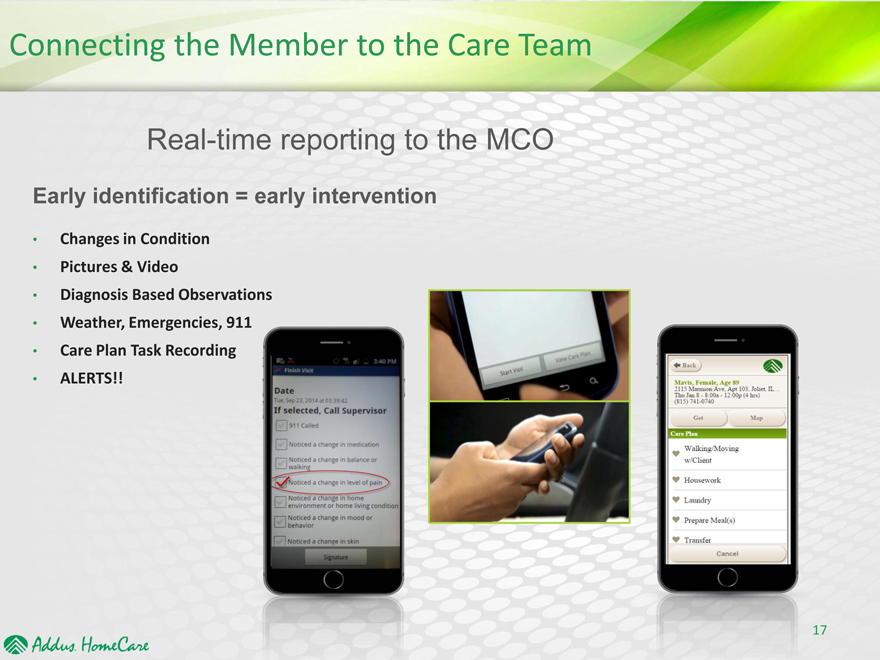
Connecting the Member to the Care Team
Real-time reporting to the MCO
Early identification = early intervention
Changes in Condition
Pictures & Video
Diagnosis Based Observations
Weather, Emergencies, 911
Care Plan Task Recording
ALERTS!!
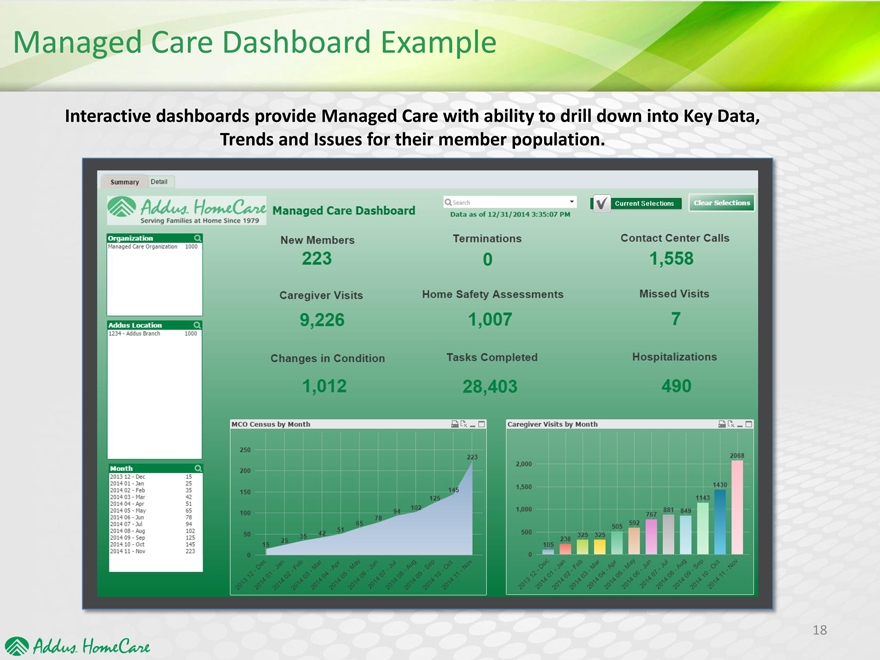
Managed Care Dashboard Example
Interactive dashboards provide Managed Care with ability to drill down into Key Data, Trends and Issues for their member population.
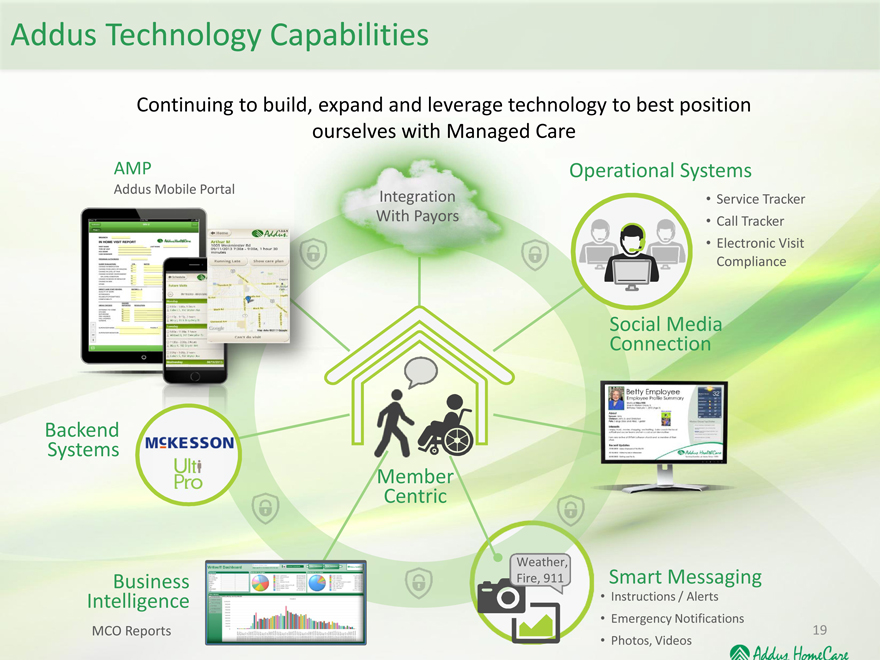
Addus Technology Capabilities
Continuing to build, expand and leverage technology to best position
ourselves with Managed Care
AMP Operational Systems
Addus Mobile Portal Integration • Service Tracker
With Payors • Call Tracker
• Electronic Visit
Compliance
Social Media
Connection
Backend
Systems
Member
Centric
Weather,
Business Fire, 911 Smart Messaging
Intelligence • Instructions / Alerts
• Emergency Notifications
MCO Reports
• Photos, Videos
19
Compelling Investment Considerations
Favorable demographic trends for growth
We serve a high utilization/high risk population (the 5% who use 50%)
Health care is moving to home based care away from acute based care
To manage this population we have to treat the consumer, at home, with people and
technology
Managed care is assuming management of this population and will favor larger, more
sophisticated, technology and outcome driven, risk taking organizations
Largest public, pure play, home care company with significant geographic footprint
Our model is easily replicable and scalable
We have made significant technology investments and are an operating laboratory for
future development
We have a solid record and reputation
20
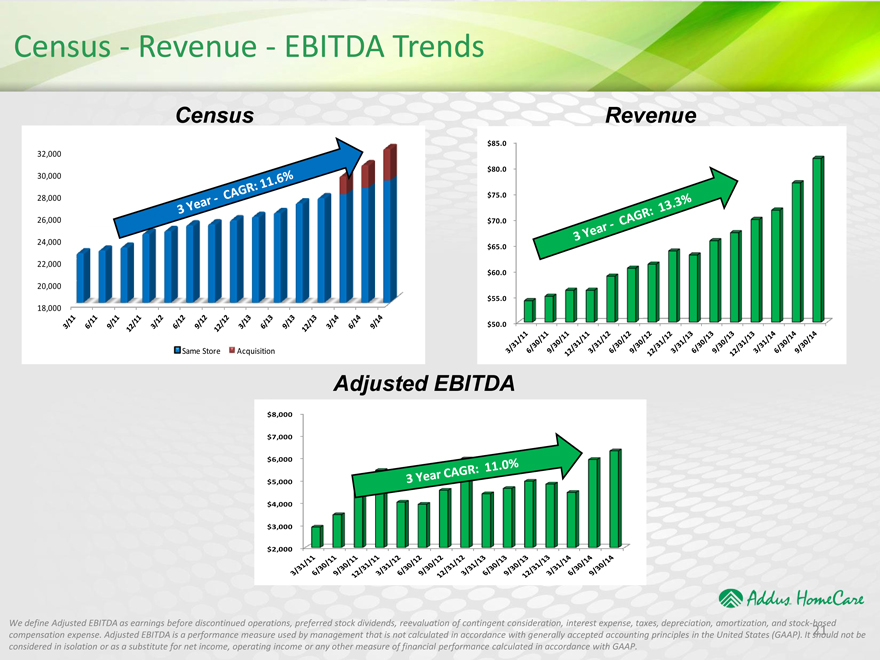
Census—Revenue—EBITDA Trends
Census
32,000
30,000
28,000
26,000
24,000
22,000
20,000
18,000
Same Store Acquisition
Revenue
$ 85.0
$ 80.0
$ 75.0
$ 70.0
$ 65.0
$ 60.0
$ 55.0
$ 50.0
Adjusted EBITDA
$ 8,000
$ 7,000
$ 6,000
$ 5,000
$ 4,000
$ 3,000
$ 2,000
We define Adjusted EBITDA as earnings before discontinued operations, preferred stock dividends, reevaluation of contingent consideration, interest expense, taxes, depreciation, amortization, and stock-based
compensation expense. Adjusted EBITDA is a performa
ce measure used by management that is not calculated in accordance with generally accepted accounting principles in the United States (GAAP). It should not be
considered in isolation or as a substitute for net income
operating income r any other measure of financial performance calculated in accordance with GAAP.
21
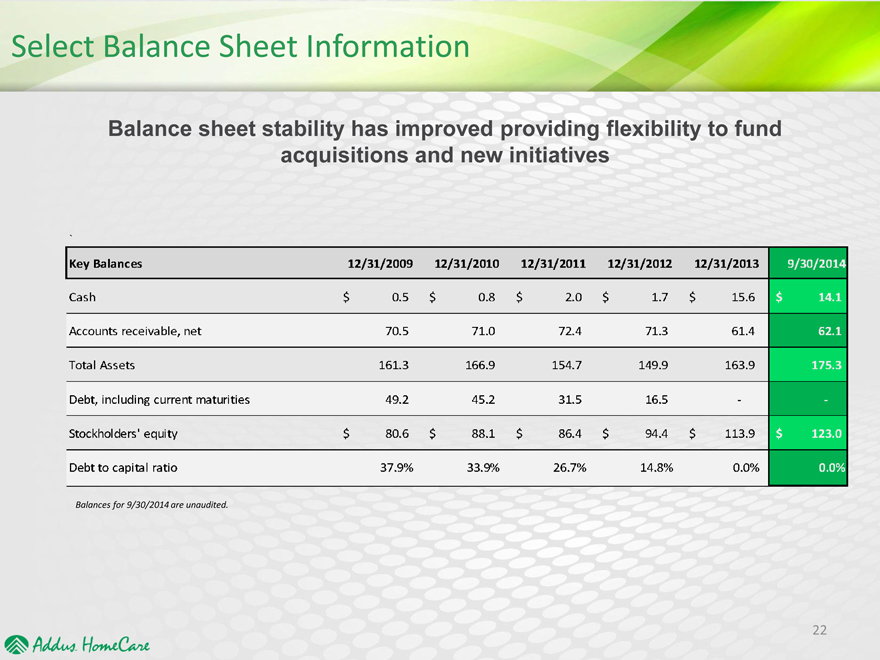
Select Balance Sheet Information
Balance sheet stability has improved providing flexibility to fund acquisitions and new initiatives