PDS BIOTECHNOLOGY CORPORATION
FORM 10-K FOR THE YEAR ENDED DECEMBER 31, 2022
|
|
| PAGE |
| PART I |
|
|
| Item 1 | | 4 |
| Item 1A | | 43
|
| Item 1B | | 83
|
| Item 2 | | 83
|
| Item 3 | | 83
|
| Item 4 | | 83
|
| PART II |
|
|
| Item 5 | | 84
|
| Item 7 | | 85
|
| Item 7A | | 97
|
| Item 8 | | 97
|
| Item 9 | | 97
|
| Item 9A | | 97
|
| Item 9B | | 98
|
| Item 9C | | 98
|
| PART III |
|
|
| Item 10 | | 99
|
| Item 11 | | 99
|
| Item 12 | | 99
|
| Item 13 | | 99
|
| Item 14 | | 99
|
| PART IV |
|
|
| Item 15 | | 99
|
| Item 16 | | 99
|
|
| 103
|
Cautionary Note Regarding Forward-Looking Statements
This Annual Report on Form 10-K (this “Annual Report”) contains forward-looking statements (including within the meaning of Section 21E of the United States Securities Exchange Act of 1934, as amended, and Section 27A of the United States Securities Act of 1933, as amended) concerning the Company and other matters. These statements may discuss goals, intentions and expectations as to future plans, trends, events, results of operations or financial condition, or otherwise, based on current beliefs of the Company’s management, as well as assumptions made by, and information currently available to, management. Forward-looking statements generally include statements that are predictive in nature and depend upon or refer to future events or conditions, and include words such as “may,” “will,” “should,” “would,” “expect,” “anticipate,” “plan,” “likely,” “believe,” “estimate,” “project,” “intend,” “forecast,” “guidance”, “outlook” and other similar expressions among others. Forward-looking statements are based on current beliefs and assumptions that are subject to risks and uncertainties and are not guarantees of future performance. Actual results could differ materially from those contained in any forward-looking statement as a result of various factors, including, without limitation.
| ● | the Company’s ability to protect its intellectual property rights; |
| ● | the Company’s anticipated capital requirements, including the Company’s anticipated cash runway and the Company’s current expectations regarding its plans for future equity financings; |
| ● | the Company’s dependence on additional financing to fund its operations and complete the development and commercialization of its product candidates, and the risks that raising such additional capital may restrict the Company’s operations or require the Company to relinquish rights to the Company’s technologies or product candidates; |
| ● | the Company’s limited operating history in the Company’s current line of business, which makes it difficult to evaluate the Company’s prospects, the Company’s business plan or the likelihood of the Company’s successful implementation of such business plan; |
| ● | the timing for the Company or its partners to initiate the planned clinical trials for PDS0101, PDS0103, PDS0203, PDS0301 and other Versamune , Versamune plus PDS0301 and Infectimune based products and the future success of such trials; |
| ● | the successful implementation of the Company’s research and development programs and collaborations, including any collaboration studies concerning PDS0101, PDS0301, PDS0203 and other Versamune and Infectimune based products and the Company’s interpretation of the results and findings of such programs and collaborations and whether such results are sufficient to support the future success of the Company’s product candidates; |
| ● | the success, timing and cost of the Company’s ongoing clinical trials and anticipated clinical trials for the Company’s current product candidates, including statements regarding the timing of initiation, pace of enrollment and completion of the trials (including our ability to fully fund our disclosed clinical trials, which assumes no material changes to our currently projected expenses), futility analyses, presentations at conferences and data reported in an abstract, and receipt of interim results (including, without limitation, any preclinical results or data), which are not necessarily indicative of the final results of the Company’s ongoing clinical trials; |
| ● | expectations for the clinical and preclinical development, manufacturing, regulatory approval, and commercialization of our product candidates; |
| ● | any Company statements about its understanding of product candidates’ mechanisms of action and interpretation of preclinical and early clinical results from its clinical development programs and any collaboration studies; the acceptance by the market of the Company’s product candidates, if approved; |
| ● | the timing of and the Company’s ability to obtain and maintain U.S. Food and Drug Administration or other regulatory authority approval of, or other action with respect to, the Company’s product candidates; and |
| ● | other factors, including legislative, regulatory, political and economic developments not within the Company’s control, including unforeseen circumstances or other disruptions to normal business operations arising from or related to COVID-19 and those listed under Part II, Item 1A. Risk Factors. |
Any forward-looking statements in this Annual Report reflect our current views with respect to future events or to our future financial performance and involve known and unknown risks, uncertainties and other factors that may cause our actual results, performance or achievements to be materially different from any future results, performance or achievements expressed or implied by these forward-looking statements. Given these uncertainties, you should not place undue reliance on these forward-looking statements. Except as required by law, we assume no obligation to update or revise these forward-looking statements for any reason, whether as a result of new information, future events or otherwise.
In this Annual Report, unless otherwise stated or the context otherwise indicates, references to “PDS Biotech,” “the Company,” “we,” “us,” “our” and similar references refer to PDS Biotechnology Corporation, a Delaware corporation.
PART I
Unless the context requires otherwise, references in this report to “PDS Biotech,” “Company,” “we,” “us,” and “our” and similar designations refer to PDS Biotechnology Corporation and our subsidiary.
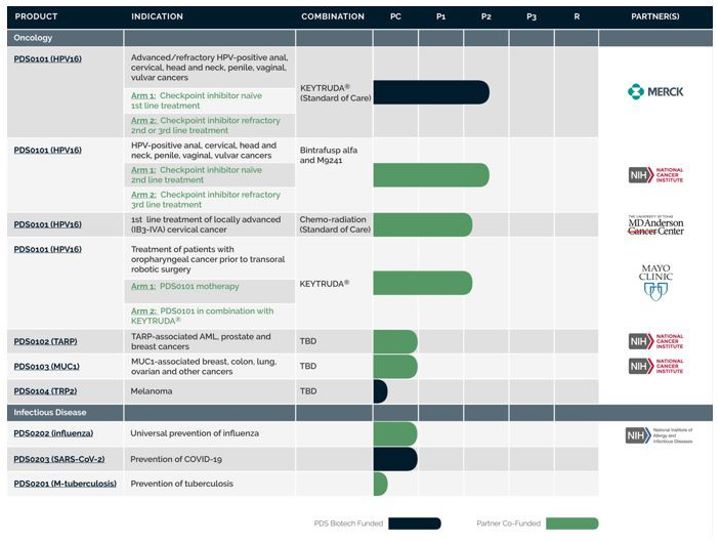
We are a clinical-stage immunotherapy company developing a growing pipeline of targeted cancer and infectious disease immunotherapies based on our proprietary Versamune®, Versamune plus IL-12 (PDS0301) and Infectimune™ T cell activating technology platforms. Our Versamune based products have demonstrated the potential to overcome the limitations of current immunotherapies by inducing, in vivo, large quantities of high-quality, potent polyfunctional CD4 helper and CD8 killer T cells. We have developed multiple therapies, based on combinations of Versamune and disease-specific antigens, designed to train the immune system to recognize diseased cells and effectively attack and destroy them. We continue to advance our pipeline of candidates to address a wide range of cancers including HPV-positive cancers (anal, cervical, head and neck, penile, vaginal, vulvar) and breast, colon, lung prostate and ovarian cancers. Our Infectimune based vaccines have demonstrated the potential to induce, not only robust and durable neutralizing antibody response, but also powerful T cell responses including long-lasting memory T cell responses. Our infectious disease candidates are of potential interest primarily for use in universal influenza vaccines.
In June 2022, two abstracts were presented at the 2022 American Society of Clinical Oncology Annual Meeting: Abstract number 6041, PDS0101 a novel type 1 interferon and CD8 T cell activating immunotherapy in combination with pembrolizumab in subjects with recurrent/metastatic HPV16-positive squamous cell carcinoma (HNSCC) and Abstract number 2518, Phase 2 evaluation of the combination of PDS0101, M9241, now PDS0301, and bintrafusp alfa with HPV16+ malignancies. Also in May 2022, we announced expansion of our VERSATILE-002 clinical trial into Europe and in June 2022, we announced the U.S. Food and Drug Administration (FDA) had granted Fast Track designation to our lead candidate PDS0101 in combination with Merck’s anti-PD-1 therapy, KEYTRUDA® (pembrolizumab). The FDA’s Fast Track designation is designed to aid in the development and to expedite the review of drug candidate applications that would potentially treat serious or life-threatening conditions. In order to receive Fast Track designation, a product must also demonstrate the potential to address an unmet medical need. Treatments granted this designation are given the opportunity to have more frequent meetings with the FDA throughout the entire dug development and review process, with the goal of moving promising new drugs more rapidly through the process. It also provides the opportunity to submit sections of a New Drug Application (NDA) or Biologics License Application (BLA) on a rolling basis, where the FDA may review portions of the NDA or BLA as they are received instead of waiting for the entire NDA or BLA submission. In addition, Fast Track designated products are eligible for priority review at the time of NDA or BLA submission. In October 2022, we announced the successful end-of-phase 2 meeting with the FDA, in which we received feedback on a number of points, including guidance on key elements of the clinical program that will support the submission of a Biologics License Application (BLA).
In July 2022, we announced the presentation of universal flu vaccine preclinical data for PDS0202 at the 41st American Society of Virology meeting: Abstract number 3733830, Infectimune™ enhances antibodies elicited by COBRA hemagglutinin influenza vaccine.
In November 2022, we announced the presentation of data from two Phase 2 clinical trials at the 37th Annual Meeting for the Society of Immunotherapy of Cancer (SITC): Abstract number 674, IMMUNOCERV, an ongoing Phase 2 trial combining PDS0101, an HPV-specific T cell immunotherapy, with chemotherapy and radiation for treatment of locally advanced cervical cancers and Abstract number 695, Immune correlates associated with clinical benefit in patients with immune checkpoint refractory HPV-associated malignancies treated with triple combination immunotherapy.
In January 2023, we announced the exclusive global license agreement with Merck KGaA, Darmstadt, Germany for the tumor targeting antibody conjugated IL-12, M9241 (formerly known as NHS-IL-12), which joined our pipeline as PDS0301. PDS0301 is a novel investigational tumor-targeting antibody conjugate of Interleukin 12 (IL-12) that enhances the proliferation, potency, infiltration and longevity of T cells in the tumor microenvironment and is designed to overcome tumor immune suppression utilizing a different mechanism from immune checkpoint inhibitors (ICI). The ownership of these two assets we believe will streamline the registrational process and a use of the combination of Versamune® and IL-12 is patented by PDS Biotech. In a Phase 2 National Cancer Institute (NCI)-led clinical trial in ICI refractory patients, the combination of PDS0101 and PDS0301 administered with an investigational bi-functional ICI resulted in a median overall survival of 21 months, which compares favorably to the historical median survival of 3-4 months seen with checkpoint inhibitors and best reported median survival to date with systemic therapy of 8.2 months in ICI refractory head and neck cancer.
In February 2023, we announced a successful completion of a Type B meeting with the FDA for the triple combination of PDS0101 and PDS0301 with an FDA-approved immune checkpoint inhibitor for the treatment of recurrent/metastatic, ICI refractory head and neck cancer that is positive for the human papilloma virus (HPV) type 16. In recent interactions with the FDA, we confirmed the required contents of a clinical protocol for the potential registrational trial.
The challenges to effective immunotherapy
The inability to generate adequate quantities of high-quality killer CD8 T cells, to minimize systemic toxicities, to overcome the immune system’s tolerance of the cancer and to generate immunological memory, all limit the clinical effectiveness of immunotherapies. On a fundamental biological or immunological level, one of the most significant challenges facing the industry is the development of simple and easy to administer therapies that can effectively treat cancer with minimal side effects. Suboptimal activation of killer CD8 T cells remains a key limitation of immunotherapies. Potential hurdles exist at various stages of the immunological process, including poor uptake of the antigen by the dendritic cells as well as inadequate processing and presentation of the tumor antigen into the correct immunological pathways.
Cancer Immunotherapy
Cancer immunotherapy is a form of cancer treatment that utilizes the power of the body’s own immune system to recognize, attack and eliminate cancer. The ultimate goal of cancer immunotherapy is to improve patient quality of life and to extend patient life by slowing down progression of the cancer, shrinkage of the tumors and in some cases eradication of the cancer. The body’s immune system is a complex, biological network designed to defend against germs, other microscopic invaders, and cancer cells. Once the immune system recognizes an organism or cell as foreign or dangerous, it begins a series of complex reactions to identify, target and eliminate them. This process of events is referred to as mounting an immune response. Cancer immunotherapy takes advantage of the fact that most cancer cells express unique proteins, also called tumor antigens, not normally expressed by healthy cells that can be recognized by the immune system as abnormal. Because the immune system is precise, for the most part, a resulting immune response can target these dangerous cancer cells exclusively while sparing healthy cells. However, the challenge remains that cancer cells are able by various mechanisms to evade the immune system’s surveillance, so the body becomes tolerant to them.
An ideal cancer immunotherapy should have the following attributes to maximize the opportunity for clinical effectiveness in patients. It should:
| ● | Stimulate both tumor-specific killer and helper T cells within the body |
| ● | Activate, arm and expand large numbers of T cells that recognize the tumor |
| ● | Alter or de-camouflage the tumor microenvironment (TME) to make the cancer more visible or susceptible to attack by the immune system |
| ● | Generate immune memory, so that if the cancer cells return, the immune system can recognize and eliminate them |
| ● | Optimize safety and tolerability by limiting systemic inflammation and toxicity |
As stated in the June 2019 issue of The Journal of Immunology, a leading peer-reviewed journal in the field of immunology, our Versamune platform possesses each of these attributes, inducing potent anti-tumor responses in preclinical studies. (Gandhapudi, et al., J. Immunology, June 2019; Rumfield et al, J. Journal for ImmunoTherapy of Cancer, May 2020). We believe our Versamune technology platform is unique in its ability to successfully encompass the mechanistic attributes required to induce a safe and effective anti-cancer immune response.
How does cancer immunotherapy work?
An important function of the body’s immune system is to scan for proteins not normally expressed in healthy tissue (antigens). Once an antigen has been identified as foreign, abnormal or dangerous, the antigen is presented to T cells, a type of white blood cell effective at eliminating cancer cells and infectious agents (e.g. bacteria and viruses). The presentation of an antigen to T cells is implemented primarily in the lymph nodes by specialized antigen presenting cells known as dendritic cells which are programmed specially to identify foreign antigens, process them and to present them to T cells. Unique proteins on the surface of dendritic cells, known as major histocompatibility complex (MHC) molecules, bind to the foreign antigen and display them on the cell surface for recognition by the appropriate T cells. Then, once presented, a sub-population of T cells known as the CD8 or killer T cells, are primed and respond to the specific foreign antigen by attacking and killing the cells containing the abnormal protein. Other T cell sub-populations, such as CD4 or helper T cells, are also critical in regulating immune responses.
Cells communicate via chemical signaling. For an immune response to be triggered and to be effective, important immune signaling pathways must be activated to enable the body to induce messenger proteins known as cytokines and chemokines. Some of these cytokines and chemokines serve both to activate and expand T cells and to arm the T cells with the appropriate cancer-killing function.
An effective cancer immunotherapy must modulate these complex processes, enhancing activation and producing robust expansion of the critically important high-quality, tumor-specific T cell populations, most notably CD8 killer cells. As will be reviewed in more detail in the section below, the ability to promote the induction of therapeutic quantities of high-quality tumor-targeting CD8 killer T cells within a patient’s own body has been a major limitation of cancer immunotherapy.
Production of adequate numbers of high-quality CD8 killer T cells alone, however, is insufficient to eradicate all cancer cells. One of the difficulties in treating cancer stems from the fact that cancer cells have the unique ability to evade the immune system; they camouflage themselves or suppress T cell attack by activating immune mechanisms that suppress the ability of T cells to detect or attack them. They accomplish this in part by increasing the population of immune suppressive cells, including cells known as regulatory T cells (Treg) as well as other cell types, within the tumor microenvironment. An effective immunotherapy must overcome the tumor’s immune suppressive mechanisms in order to successfully locate and attack the cancer cells.
Finally, cancers can be difficult to cure because they may recur even after successful initial treatment due to micro-metastatic (hidden) tumors that are not completely eradicated after treatment and that eventually expand. It is yet another task of the immune system to remain vigilant over a sustained period to mitigate the risk of recurrence. Such vigilance may be mediated by memory T cells which serve as the immune system’s long-term memory. To be durable and effective over an extended period after treatment, and to minimize the likelihood of cancer recurrence, an immunotherapy should enhance this immune function as well.
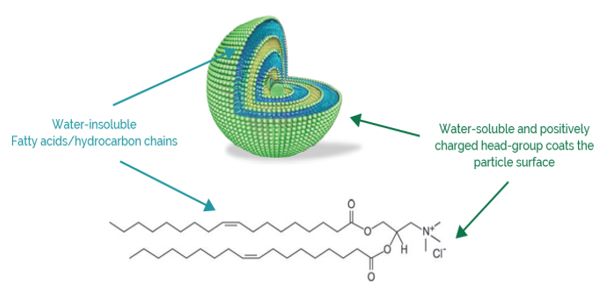
Versamune has shown the potential to overcome the challenges of immunotherapy
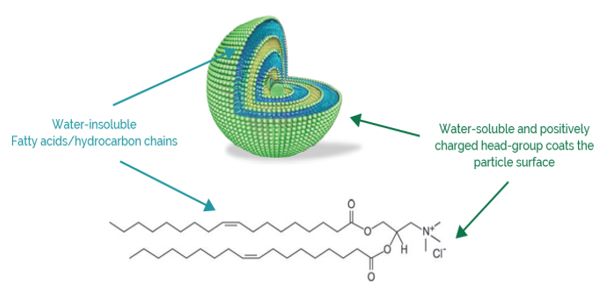
Versamune is a proprietary lipid nanoparticle and T cell activating platform designed to overcome the challenges of current immunotherapy and improve the treatment outcomes of patients with cancer. Versamune derived products are based on positively charged (cationic) and immune activating lipids that form spherical nanoparticles in aqueous media. These lipids include the R-enantiomer of 1,2-dioleoyl-e-trimethyl-ammonium-propane (R-DOTAP). Cationic lipids are positively charged molecules that have a water-soluble portion (head group) attached to a water insoluble tail. The water-soluble portion of the molecule has a positive charge and the water-insoluble portion is made up of hydrocarbon (also called fatty acid) chains. The nanoparticles, which are coated with a positive charge, are deliberately sized to mimic viruses, facilitating detection by the body’s immune system and uptake by dendritic cells.
To treat a specific cancer, the unique or overexpressed antigen found on the surface of the cancer cells is manufactured, then mixed with the Versamune nanoparticles to create a pharmaceutical product for simple subcutaneous injection.
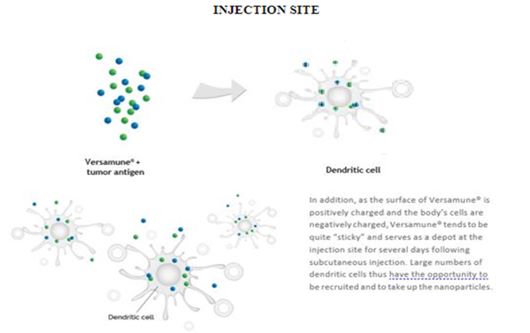
Versamune has the potential to promote dendritic cell update of antigens
One of the biggest challenges in developing a potent immunotherapy has been dendritic cell uptake. Versamune is designed specifically to be taken up by dendritic cells in the skin. As noted, Versamune nanoparticles are sized comparably to viruses normally taken up as part of the natural function of the dendritic cells, facilitating efficient uptake of the Versamune based immunotherapy. Studies evaluating the uptake of Versamune nanoparticles by dendritic cells and epithelial cells, found almost exclusive uptake by the dendritic cells. Four hours following a single subcutaneous injection, about 80% of the dendritic cells in the draining lymph node were found to have taken up the Versamune based immunotherapy.
Versamune has the potential to promote efficient antigen processing and T cell presentation
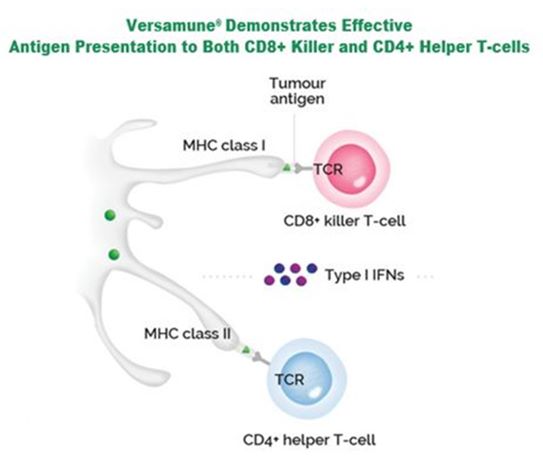
When dendritic cells take up Versamune nanoparticles they become activated, mature and begin recruiting additional dendritic cells. Once inside the dendritic cell, the tumor-associated antigen is released and processed into the requisite small peptides (pieces of protein) in the cell compartment known as the cytoplasm. An important potential advantage of Versamune is its ability to fuse with and destabilize endosomes in the cell, promoting efficient entry of the antigen into the cell compartment where processing can take place. Processed antigen is turned into peptides that then present in both the MHC class I and class II pathways. The MHC class I pathway is critical to programming CD8 killer T cells and the MHC class II pathway to programming CD4 helper T cells to recognize tumor antigens. When Versamune induced maturation occurs, the dendritic cells express costimulatory molecules on their surface, which facilitate the highly efficient uptake and presentation of antigens to the T cells. We believe this activity overcomes one of the most significant limitations of current immunotherapy development – the efficient priming of critical CD8 killer T cells against tumor antigens. Versamune has been demonstrated to promote presentation of antigens to CD4 helper cells as well.
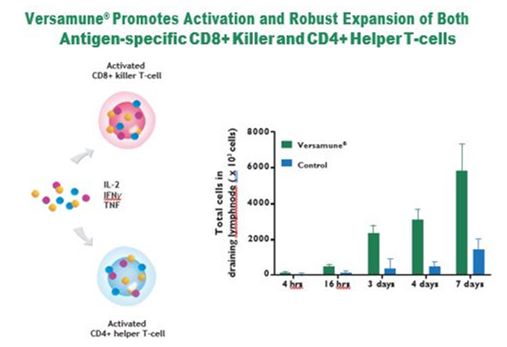
Versamune has the potential to promote efficient activation and robust expansion of high quality polyfunctional CD8 killer T cells and CD4 helper in Lymph Nodes
Ultimately mature dendritic cells migrate into lymph nodes, small glands located throughout the body containing white blood cells including T cells, where much of the key immunological activity pertaining to the priming and expansion of T cells takes place. In the lymph nodes, the dendritic cells present the tumor antigens to T cells resulting in activation or priming of the T cells to recognize the particular antigen expressed by the cancer. Importantly, Versamune has also demonstrated the potential to upregulate type I interferon genes (type I IFN), which are responsible for critical immunological processes. Upregulation of type I IFN induces an important immunological protein called CD69 that facilitates interactions between the dendritic cell and T cells in the lymph nodes.
Upregulation of type I IFN signaling also induces multiple immune messenger proteins called cytokines and chemokines that further signal T cells to infiltrate into the lymph nodes. Powerful activators of CD8 killer T cells, such as CCL2 and CXCL10 are documented to be induced by Versamune as well. As the Versamune induced production of chemokines appears to be restricted to the lymph nodes, the site of T cell activation, it provides for both superior activation and expansion of CD8 killer T cells. Localization of these immune messengers within the lymph nodes and their limited presence in the blood circulation enhances the safety of the Versamune based immunotherapies. Thus, through the versality of its mechanisms of action, as understood to date, we believe that Versamune may safely promote the efficient and robust expansion in-vivo of large numbers of highly potent (polyfunctional) CD8 killer T cells, both critical factors in developing a successful immunotherapy.
Versamune has the potential to overcome immune suppression
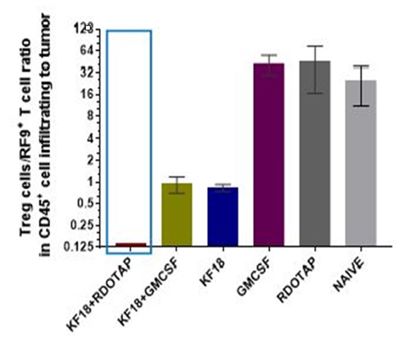
Regulatory T cells (Treg) are a sub-population of white blood cells normally responsible for recognizing normal healthy cells and for preventing autoimmune disease. In cancer however, they are utilized by the cancer cells to suppress immune detection. Versamune may contribute to significant alteration of the tumor microenvironment by dramatically reducing the Treg to killer CD8 T cell ratio thus making the tumors more susceptible to destruction by killer T cells. Preclinical studies have demonstrated that lowering the Treg to CD8 killer T cell ratio with polyfunctional CD8 killer and CD4 helper T cells promotes effective tumor lysis and regression. Overcoming a tumor’s immune tolerance and minimizing its ability to evade detection is a significant goal of a successful cancer immunotherapy that together with potent T cell induction may translate to enhanced tumor elimination.
In preclinical studies, Versamune (R-DOTAP) nanoparticles demonstrated a reduction in the Treg/CD8 T cell ratio
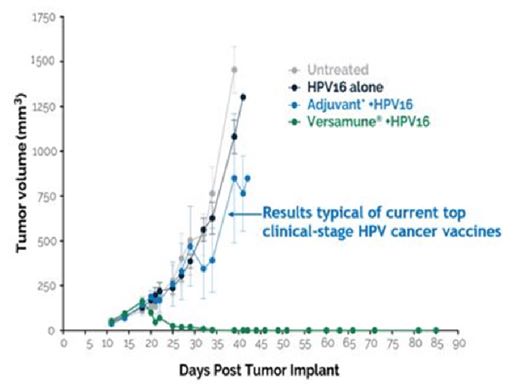
Results of Comparative Preclinical Testing of Versamune and Other Immunotherapies for the eradication of a Tumor
Using the tumor model, the Versamune based therapy was unique in its ability to reduce the tumor size and eventually completely regress the tumors. The results from the Versamune based treatment are attributed to its ability to induce: (i) powerful activation of the critical immunological signaling pathways, (ii) robust production of both CD8 killer and CD4 helper T cells, and (iii) the degradation of the tumor’s protective immune suppression mechanism.
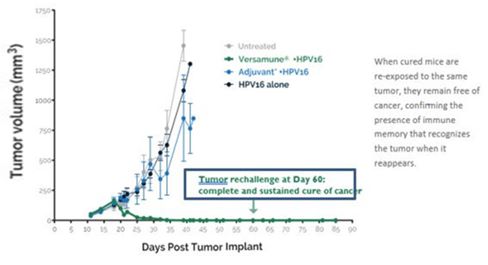
Versamune has the potential to induce Immune Memory
Memory T cells allow the body to maintain tumor-recognizing and attacking T cells for an extended period after treatment, with the ideal outcome of reducing cancer recurrence. Preliminary studies demonstrated that Versamune protected mice that had experienced tumor regression against tumor reestablishment even when the mice were reinjected with the same tumor cells. This sustained protection was evidence of immune memory: persistence of antigen-specific T cells to recognize tumor proteins associated with a particular cancer, as the animals were not protected against establishment of different tumors. Evidence of the potential for Versamune based immunotherapies to induce immune memory was also demonstrated in a Phase 1 clinical trial in humans.
Enhancing tumor-specific memory responses to monitor for tumor antigens and eradicate cancer cells well after initial treatment we believe provides potential for significant durable clinical benefit by possibly reducing the incidence of tumor recurrence and improving survival of patients.
Today, many cancer immunotherapies produce serious systemic autoimmune effects due to blockage of existing regulatory mechanisms such as the immune checkpoints as well as inflammatory toxicities due to the increased presence and spikes of cytokines in the blood circulation. We believe the mechanism of action of Versamune as well as its design have the potential to contribute to the localization of cytokines in the lymph nodes and specific targeting of CD8 killer T cells to antigens in tumor tissue. Therefore, the hypothesis is that Versamune based therapies may exhibit an improved and favorable safety profile compared to currently available treatments.
As noted, Versamune is injected subcutaneously (under the skin) and its mechanisms of action are localized primarily in the lymph nodes. Further supporting these observations are data demonstrating that negligible levels of Versamune induced cytokines were detected in the blood of mice. Very low quantities of Versamune were detected in the blood or in any organ outside of the lymph nodes.
Additionally, Versamune is broken down (hydrolyzed) in the body into fatty acids and excreted, showing in these preliminary studies that it could mitigate the potential for short- or long-term accumulation of the nanoparticles. These preclinical observations have been confirmed by early clinical data documenting that this localized and highly specific cascade of immune activity was associated with an absence of significant systemic toxicity at all doses tested. In a Phase 1 clinical trial designed to evaluate safety, all patients had transient swelling and redness at the injection site due to initiation of the immunological cascade at the injection site which cleared completely within 3-7 days and no dose-limiting toxicities or long-term safety concerns were observed. Similarly, in our ongoing Phase 2 trials in combination with other treatments, no dose-limiting toxicities or long-term safety concerns were attributed to PDS0101 since three of the four studies were initiated in 2020.
In choosing and designing a Versamune based therapy for development, careful attention is paid to selecting specific, appropriate antigens because, as described above, Versamune induces a strong T cell response to the antigen. All of the antigens currently being evaluated in combination with Versamune are present primarily in cancer cells which should therefore result in tumor-specific T cell attack, thereby minimizing off-target toxicity and potential destruction of healthy cells and tissue.
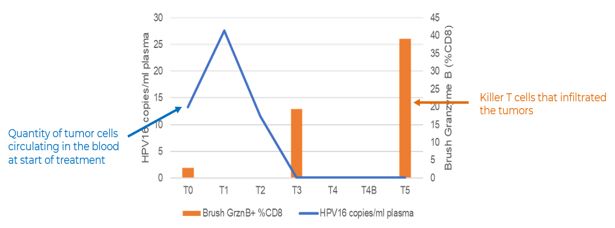
Versamune has the potential to minimize circulating tumor DNA (ctDNA)
ctDNA is tumor-derived fragmented DNA that is released into a person’s blood stream by cancerous cells and tumors. It can come from primary or metastatic cancer sites. We believe that the reduction of ctDNA, as a biomarker, has the potential to signify a potential reduction or elimination of cancer. As noted, we believe Versamune may safely promote the efficient and robust expansion in-vivo of large numbers of highly potent (polyfunctional) CD8 killer T cells. In MD Anderson led Phase 2 clinical trial, IMMUNOCERV, where the ctHPV 16 DNA biomarker measured in certain patients decreased in the blood by Day 170 (T5) as HPV16-specific killer T cells proliferated in the tumor microenvironment as seen in a representative patient in the chart below.
Versamune’ s potential as a cancer immunotherapy platform
The potential ability of Versamune to modulate and enhance numerous critical steps required for an effective immune response may provide additional opportunities to treat a variety of cancers. Further, its diverse mechanisms of action together with its favorable safety profile suggest therapeutic promise when used in combination with other treatment modalities or immunotherapies such as immune checkpoint inhibitors as well as in the single-agent monotherapy setting.
PDS0101: Human Papillomavirus (HPV)-Related Cancers
Despite the successful introduction of HPV preventive vaccines, HPV-related cancers remain a significant component of the global cancer burden. HPV infection occurs in both men and women and is associated with head and neck (oropharyngeal), cervical, anal, vaginal, vulvar and penile cancers.
PDS0101 is our lead Versamune based immunotherapy. PDS0101 combines Versamune with a mixture of short proteins (peptides) derived from the cancer-causing HPV16 viral protein. HPV16 is the most pervasive and difficult to treat HPV amongst the 13 different high-risk, cancer-causing HPV types. In a preclinical study in the most widely utilized animal HPV-cancer tumor model, PDS0101 uniquely induced complete regression of the tumors after a single sub-cutaneous injection. As a result of these data, a Phase 1 open-label, dose-escalation, proof of concept study of PDS0101 in women with cervical intraepithelial neoplasia (CIN) infected with high-risk HPV types. The data demonstrated that PDS0101 was immunologically active at all three doses studied, confirmed induction of high levels of active HPV-specific CD8 killer T cells, and was associated with clinical regression of the cervical lesions that often occurred rapidly. These results suggest that PDS0101 activated the critical mechanisms in humans resulting in potent T cells which target and effectively kill human HPV-positive cancer cells. All patients who experienced regression remained disease-free over the 2-year retrospective evaluation period, suggesting potential durability or memory of the immune response. The clinical data were presented at the 34th Annual Society for the Immunotherapy of Cancer Conference in November 2019 (Wood, et al., 2019). Based on these encouraging preclinical and human data, PDS0101 is being studied in multiple Phase 2 clinical studies in various HPV-related cancers one sponsored by the Company in collaboration Merck and three investigator-initiated trials being conducted by the National Cancer Institute (NCI), MD Anderson Cancer Center and Mayo Clinic. We believe the data presented from these Phase 2 clinical studies in 2022 demonstrated favorable results.
PDS0102: T cell receptor gamma Alternate Reading frame Protein (TARP)-Related Cancers
The TARP antigen is strongly associated with prostate and breast cancers. In the U.S. 450,000 patients are projected to be diagnosed with prostate or breast cancer this year. Approximately 90% of prostate cancers and 50% of breast cancers overexpress the TARP tumor antigen. In a human clinical trial, the NCI demonstrated that its proprietary TARP antigens were effectively recognized by the immune system in prostate cancer patients with PSA biochemical recurrence leading to a notable reduction in tumor growth rate. In preclinical studies, a dramatically enhanced TARP-specific killer T cell response was observed when our designed TARP antigens were combined with Versamune. As discussed further below, in November 2021, we entered into the NCI Patent License Agreement with the U.S. Department of Health and Human Services, as represented by the NCI of the National Institutes of Health (NIH). We obtained a nonexclusive worldwide license to the patent rights for NCI’s TARP to develop and commercialize TARP peptide-based therapies in combination with our Versamune technology for the treatment of acute myeloid leukemia, prostate and breast cancers. Preclinical development is ongoing.
PDS0103: Mucin-1 (MUC1)-Related Cancers
MUC1 is highly expressed in multiple solid tumor types and has been shown to be associated with drug resistance and poor disease prognosis. We are developing PDS0103, a Versamune based therapy in combination with novel, highly immunogenic, agonist epitopes of the MUC1 oncogenic C-terminal region to treat ovarian, breast, colorectal and lung cancers. In preclinical studies, a dramatically enhanced MUC1-specific killer T cell response was observed when the novel antigens were combined with Versamune. Preclinical development is ongoing.
Versamune has demonstrated immunological compatibility with a wide array of tumor and pathogenic antigens. While our current oncology pipeline pairs Versamune with 4 different tumor antigens, to address over 10 cancer types, more than 75 tumor antigens have been identified and reported. We believe that Versamune could work well with a wide range of identified tumor antigens and neoantigens. We are exploring the expansion of our Versamune based pipeline by pairing the technology with multiple tumor antigens to potentially develop additional product candidates.
Versamune based immunotherapies plus PDS0301 (IL-12) Platform as a cancer immunotherapy platform
PDS0301 (formerly known as NHS-IL-12 and M9241) is a novel investigational antibody conjugated (IgG1), tumor-targeting interleukin 12 (IL-12) immune-cytokine that enhances the proliferation, potency and longevity of T cells in the tumor microenvironment. Together with Versamune based immunotherapies PDS0301 works synergistically to promote a targeted T cell attack against cancers. As with Versamune, PDS0301 is given by a simple subcutaneous injection. Clinical data suggests the addition of PDS0301 to Versamune based immunotherapies may demonstrate significant disease control by shrinking tumors and/or prolonging life.
PDS0301 monotherapy has shown activation of an immune response and correlation with clinical benefit in metastatic solid tumors
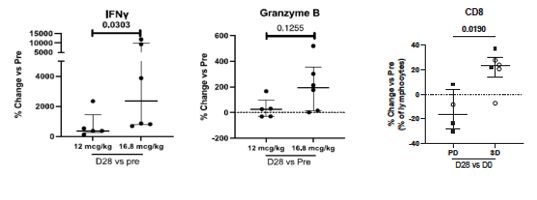
We believe PDS0301 monotherapy promotes therapeutically relevant immune responses, and stronger immune activation has been observed at higher doses. An analysis of patients at baseline and after PDS0301 monotherapy treatment documented in the graphs below. Interferon-gamma is associated with the induction of natural killer (NK) cells and T cells. Granzyme B is associated with the induction of active killer CD8 T cells. Importantly, higher levels of these CD8 T cells were associated with improved clinical outcomes. (Toney NJ et al. International Immunopharmacology 116 (2023) 109736).
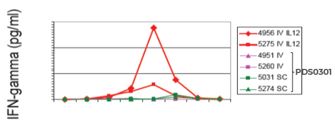
PDS0301 is differentiated from other IL-12s
PDS0301 is a novel immune-cytokine fusion protein composed of two molecules of IL-12 fused to each of the heavy-chains of a human IGg1 antibody. The IGg1 antibody targets the DNA/histones exposed in necrotic areas of solid tumors, thus delivering the IL-12 into the tumor and limiting its systemic accumulation. As seen in the chart below, PDS0301 shows low accumulation in blood circulation potentially promoting safety.
Infectimune has potential as an infectious disease vaccine platform
PDS Biotech has developed a second cationic platform that is being applied to the development of infectious disease vaccines and this specific formulation has been trademarked Infectimune. It has been formulated to activate the immune system to induce rapid and longer-lasting neutralizing antibody responses for improved protection against infectious pathogens. We believe it has the potential to induce T cell responses including memory T cell responses to provide the immune system with long-term memory and potential sustained protection against infectious pathogens over an extended period of time that may exceed traditional antibody-based protection. We believe it could provide safe and effective vaccines that are well tolerated by healthy individuals.
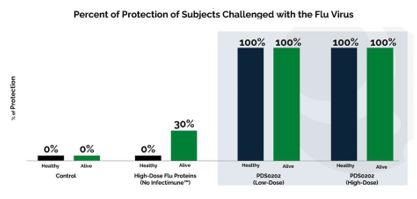
PDS0202: Universal influenza vaccine
According to the World Health Organization, influenza causes 3 to 5 million cases and approximately 290,000 to 650,000 deaths each year. Due to the existence of multiple strains of flu, a new seasonal flu vaccination is usually developed to provide protection against the strains predicted to be prevalent in an upcoming flu season. As a result, the protective efficacy of the current vaccines varies widely from season to season. We are developing a new generation of flu vaccines with the potential to provide long-lasting, and broad protection against multiple strains of the virus. We believe that the successful development of a universal flu vaccine could eliminate the need to create a vaccine to protect against each year’s predicted variants. Our Infectimune platform is combined with computationally optimized broadly reactive antigen (COBRA) to potentially provide longer lasting, more effective response to the influenza vaccine. The preclinical work is complete, and we are working to obtain nondilutive financing to fund the next steps in development. In the fourth quarter of 2021, we entered into a Patent License Agreement with the University of Georgia (UGA) which provides a nonexclusive license to the patent rights for UGA’s COBRA antigens to develop and commercialize a universal influenza vaccine worldwide. The UGA Patent License Agreement includes customary milestone payments and royalties. Initiation of preclinical work is dependent on obtaining nondilutive financing.
In February 2023, we announced preclinical Infectimune™ publication in peer reviewed journal Viruses showing unique induction of high levels of multifunctional CD4+ T cells capable of broadly protective functions compared to leading commercial vaccine technologies (Henson TR et al. Viruses 2023, 15, 538).
In February 2023, we announced a second preclinical Infectimune™ publication in peer reviewed journal Viruses showing complete protection in animal studies with PDS0202 a novel recombinant protein-based Universal flu vaccine (Gandhapudi SK et al. Viruses 2023, 15, 432).
PDS0201: Tuberculosis
PDS0201 combines the utility of the Versamune platform with bacillus Mycobacterium tuberculosis (M. tuberculosis) antigens. Tuberculosis (TB) is the leading cause of death from a single infectious agent and is caused by the M. tuberculosis, which is spread when people who are sick with TB expel bacteria into the air. About a quarter of the world’s population is infected with M. tuberculosis and thus at risk of developing TB disease. It has been reported that a total of 1.5 million people died from TB in 2020. Worldwide, TB is one of the top 10 causes of death and the leading cause from a single infectious agent (above HIV/AIDS). It is estimated that 10 million people fell ill with TB worldwide 5.7 million men, 3.2 million women and 1.1 million children. There were cases in all countries and age groups. Multidrug-resistant TB (MDR-TB) remains a public health crisis and a health security threat. The World Health Organization (WHO) estimates that there were 484,000 new cases with resistance to rifampicin – the most effective first-line drug, of which 78% had MDR-TB. WHO has identified TB as a global priority and is focused on eradication of the disease. The only licensed vaccine for prevention of TB disease was developed almost 100 years ago. PDS0201 is currently in preclinical development.
PDS0203: SARS-CoV-2 vaccine
Our Infectimune platform based COVID-19 vaccine combines our nanoparticle technology with a SARS-CoV-2 recombinant protein derived from the spike (S) protein. Notably, the protein in this fully synthetic vaccine includes conserved and non-mutating regions of the virus. The vaccine has demonstrated strong potential in preclinical studies to efficiently promote the induction of killer CD8 and helper CD4 helper T cells that recognize and induce immune responses against such non-mutating regions of the virus. The protein also includes regions of the spike protein that result in the induction of neutralizing antibodies.
In February 2023, PDS Biotech announced the publication of Infectimune based vaccines preclinical studies demonstrating complete protection against sickness after lethal challenge with live SARS-CoV-2 (Gandhapudi SK et al. Viruses 2023, 15, 432).
Versamune Development Strategy
The unique combination of high potency and excellent safety of the Versamune platform observed in preclinical studies was corroborated in the successfully-completed 12-patient PDS0101 monotherapy Phase 1/2a clinical trial. All patients were infected with cancer causing (high risk) strains of HPV, which are less likely to spontaneously regress. In September 2019, we reported retrospective clinical outcome data from this trial. Despite most of the patients being infected with multiple HPV strains including or excluding HPV 16, regression was seen in 8 out of 10 patients, with complete regression of pre-cancerous lesions documented in 6 out of 10 patients at their first post-treatment evaluation, which occurred within 1-3 months of completing treatment. In addition, the fact that no disease recurrence occurred over the two-year evaluation period strongly suggested a robust and durable therapeutic immune response due to the induction of T cells by PDS0101 administration that were clinically active. As a result of this information and the documentation in the trial of PDS0101’s ability to generate potent and biologically active CD8 T cells in-vivo, we focused our clinical strategy on areas of more severe unmet medical need in which PDS0101 is combined with other immune-modulating agents, including immune checkpoint inhibitors and standard of care e.g., chemoradiotherapy, to provide improved clinical benefit to patients.
We believe that rational design of combination immunotherapies using complementary agents that promote synergy with each other and reduce the potential for compounded toxicity will substantially enhance the potential for combination therapies to deliver improved clinical benefit for cancer patients. Based on our data, Versamune appears to activate an appropriate combination of immunological pathways to promote strong CD8 T cell induction while also altering the tumor microenvironment to make tumors more susceptible to T cell attack, which we believe makes it an ideal complement to immune checkpoint inhibitors and other immune-modulating agents by enhancing their potency as part of combination therapies. In addition, the differences in mechanism of action between Versamune and checkpoint inhibitors, as well as the initial demonstrated safety profile of Versamune, suggests that these combinations may be potentially much better tolerated by patients than other combination therapies involving immune checkpoint inhibitors and other cancer treatments such as immune-cytokines and chemotherapy.
VERSATILE-002: PDS0101 + KEYTRUDA®
In November 2020, our VERSATILE-002 Phase 2 clinical trial evaluating the combination of PDS0101 in combination with Merck’s anti-PD-1 therapy, KEYTRUDA® (pembrolizumab) which is the FDA-approved standard of care for first-line treatment of recurrent/ metastatic head and neck cancer opened and is actively recruiting patients. The clinical trial will evaluate the efficacy and safety of this therapeutic combination as a first-line treatment in patients with recurrent or metastatic head and neck cancer and high-risk human papillomavirus-16 (HPV16) infection.
In this PDS Biotech-sponsored trial, patients whose cancer has returned or spread following initial treatment, will be able to avoid chemotherapy and take this combination of two immuno-therapy drugs. Enrolling patients with more functional immune systems that have not been compromised by extensive chemotherapy may allow improved efficacy of the combination. Patients in the trial will receive a total of 5 cycles of combination therapy in the context of standard of care KEYTRUDA® therapy administered every three weeks until disease progression. The primary endpoint of VERSATILE-002 is the objective response rate – or ORR – at six months following initiation of treatment. There are two cohorts in the trial. Cohort 1 is for patients that are yet to be treated with an immune checkpoint inhibitor (ICI naïve) and cohort 2 which consists of patients that have failed immune checkpoint inhibitor therapy (ICI refractory).
In February 2022, we announced we had achieved the preliminary efficacy milestone of at least four or more objective responses of the first 17 patients in the ICI naïve arm that allowed that arm to proceed to full enrollment. We also announced detailed preliminary safety data which showed that the combination is well tolerated without evidence of enhanced or significant toxicity in the first 18 patients in the ICI naïve arm. We have completed enrollment in Stage 1 of the ICI refractory arm and are waiting for sufficient follow up to conduct the futility analysis.
In June 2022, we announced additional preliminary efficacy and safety data from this trial at the ASCO Annual Meeting (Weiss J et al. J Clin Oncol 40, 2022 (suppl 16; abstr 6041). The abstract provided preliminary data on 19 patients (safety) with available imaging data for 17 of the 19 patients (efficacy). Highlights from the abstract were as follows:
| ● | Response rates thus far (tumor shrinkage greater than 30%) seen in 7/17 (41.2%) patients in comparison to the published results of approximately 19% for approved ICI, used as monotherapy for recurrent or metastatic head and neck cancer, with 2 of the 7 having complete responses (CR) |
| ● | Stable disease (SD) was reported in 6/17 (35.3%) patients, with 4 of the 6 (67%) experiencing tumor shrinkage of less than 30% |
| ● | Clinical efficacy (ORR + SD) was seen in 13/17 (76.5%) patients |
| ● | Progressive/ongoing disease was reported in 4/17 (23.5%) patients |
| ● | Patients had received a median of 4/5 doses of PDS0101 (range 1-5) and 9/35 doses of KEYTRUDA® (range 1-18) |
| ● | There were no treatment-related adverse events greater than or equal to Grade 3 (N=19) |
| ● | No patients required dose interruption or reduction on the combination treatment |
| ● | No patients discontinued the combination treatment |
| ● | At 9 months of follow up (median not yet achieved): |
| ● | Progression free survival (PFS) rate was 55.2% |
| ● | Overall survival (OS) rate was 87.2% |
In May 2022, we announced the expansion of this trial into Europe and in June 2022, as described above, we received Fast Track designation for PDS0101 in combination with pembrolizumab.
In August 2022, we announced our independent Data Monitoring Committee (DMC) met and evaluated data from the first 43 patients and noted there were no Grade 3 or greater treatment-related adverse events attributed to the combination. The DMC recommended continuing the trial with no modifications.
In October 2022, we announced an end-of-phase 2 meeting with the FDA for PDS0101 in combination with KEYTRUDA®. We are currently evaluating the guidance on the key elements of the clinical program that will support the submission of a Biologics License Application for PDS0101.
National Cancer Institute: PDS0101+ M9241 (now PDS0301) +Bintrafusp Alfa
In June 2020, the first patient was dosed under a PDS0101 Cooperative Research and Development Agreement (CRADA), in the NCI led Phase 2 investigator-initiated trial evaluating PDS0101 with an IgG1 IL-12 (M9241), now PDS0301, and M7824 (Bintrafusp Alfa), which is owned by EMD Serono (Merck KGaA) in patients with advanced/refractory HPV-associated cancers who have failed prior treatment. In February 2021, we announced that the NCI’s Phase 2 clinical trial of PDS0101 for the treatment of advanced/refractory HPV-associated cancers achieved its preliminary objective response target in patients naïve to immune checkpoint inhibitors (ICI) which allowed for full enrollment of approximately 20 patients in this group. In addition, based on promising results in the ICI naïve arm, the trial was amended to allow enrollment of a separate cohort of ICI-refractory patients for assessment of safety and activity of the triple combination. Preliminary efficacy assessment of the triple combination in this added group of 20 ICI refractory patients is ongoing. The NCI recently achieved the intended enrollment objective of 30 patients in the ICI refractory arm of the trial. The trial has enrolled 45 patients and enrollment in the trial will continue until the total enrollment of 56 patients is achieved.
Preclinical study results arising from this CRADA were recently published in the Journal for ImmunoTherapy of Cancer, Immunomodulation to enhance the efficacy of an HPV therapeutic vaccine (Journal for ImmunoTherapy of Cancer 2020;8:e000612. doi:10.1136/ jitc-2020-000612), indicating that PDS0101 generated both HPV-specific T cells and an associated antitumor response when used as a monotherapy. When PDS0101 was combined with two other novel clinical-stage anti-cancer agents, Bintrafusp Alfa and M9241, now PDS0301, the preclinical data suggested that all three therapeutic agents worked synergistically to provide superior tumor T cell responses and subsequent tumor regression when compared to any of the agents alone or the 2-component combinations. If the published preclinical data demonstrating powerful activity of the triple combination is successfully confirmed in the ongoing Phase 2 trial, this triple combination could form the basis of a unique platform providing improved cancer treatments across multiple cancers.
In June 2021, at the American Society of Clinical Oncology (ASCO) conference the NCI announced interim data in this trial which included, data in both ICI naïve and refractory patients (Strauss J et al. J Clin Oncol 39, 2021 [suppl 15; abstr 2502]). In the ICI naïve group 83% (5/6) of patients had an objective response, and 1 subject had achieved a complete response with no evidence of disease. 100% of the ICI naïve patients were alive at a median duration of 8 months. In the ICI refractory group 42% (5/12) of patients had an objective response, and 1 subject had achieved a complete response with no evidence of disease. 10/12 (83%) of ICI refractory patients were alive at a median duration of 8 months. An update provided in January 2022 showed as of December 31, 2021, that >40 subjects had been recruited into the trial and 30 HPV16-positive patients had been evaluated. The median survival of all patients (3:1 ICI refractor to naïve) was 12 months and progressing. The historical survival of ICI naïve and ICI refractory advanced HPV-associated cancers when treated with ICI are 7-11 months and 3-4 months, respectively, best reported median survival to date with systemic therapy of 8.2 months in ICI refractory head and neck cancer.
In June 2022, at the 2022 ASCO Annual Meeting, the NCI provided an update to the preliminary data presented at the 2021 meeting (Strauss J et al. J Clin Oncol 40, 2022 [suppl 16; abstr 2518]). This included data from 30 patients and highlights were as follows:
| ● | Objective response (OR = >30% tumor reduction) was seen in 88% (7/8) of patients with ICI-naive disease; 4/7 (57%) patients’ responses are ongoing (median 17 months). |
| ● | With ICI refractory patients: PDS0301 dosing appears to affect response rates, with 5/8 (63%) patients receiving PDS0301 at 16.8 mcg/kg achieving an OR compared to 1/14 (7%) patients who received PDS0301 at 8 mcg/kg achieving an OR; 4/6 (67%) patients’ responses are ongoing (median 12 months). |
| ● | Tumor reduction was seen in 45% (10/22) of patients with ICI-refractory disease, including patients receiving high or low dose PDS0301. |
| ● | In ICI refractory patients treated with high or low dose PDS0301, survival outcomes were similar (p=0.96 by Kaplan Meier analysis). At a median of 12 months of follow up 17/22 (77%) of patients were alive. |
| ● | In ICI naïve patients 6/8 (75%) were alive at median 17 months of follow up. |
| ● | Similar OR and survival were seen across all types of HPV16-positive cancers. |
| ● | Preliminary safety data: 13/30 (43%) of patients experienced Grade 3 treatment-related adverse events (AEs), and 2/30 patients (7%) experienced Grade 4 AEs. There were no grade 5 treatment-related AEs. |
| ● | We believe the study results to date strongly suggest, in agreement with the published preclinical studies, that all 3 drugs contribute to the clinical outcomes. |
In September 2022, we announced, in agreement with the NCI, that the ICI refractory patients had been selected as the preferred treatment group in the on-going PDS0101-based triple combination therapy in advanced HPV-positive cancers and the trial was closed to further enrollment given the ICI refractory arm has been fully recruited.
In October 2022, we announced expanded interim data as follows:
| ● | Survival data: 66% (19/29) of HPV16-positive ICI refractory patients in the cohort were alive at a median follow up of 16 months. |
| ● | Safety profile: 48% (24/50) patients experienced Grade 3 treatment-related adverse events (AEs), and 4% (2/50) patients experienced Grade 4 AEs. There were no Grade 3 treatment-related AEs. |
| ● | HPV16-positive ICI naïve patients: 75% (6/8) were alive at a median follow up of 25 months and 38% (3/8) of responders had a complete response. |
In December 2022, we announced expanded interim data as follows:
| ● | Median OS is 21 months in 29 checkpoint inhibitor refractory patients who received the triple combination. The reported historical median OS in patients with ICI refractory disease is 3-4 months seen with checkpoint inhibitors and best reported median survival to date with systemic therapy of 8.2 months in ICI refractory head and neck cancer. |
| ● | In ICI naïve subjects, 75% remain alive at a median follow-up of 27 months. As a result, median OS has not yet been reached. Historically median OS for similar patients with platinum experienced ICI naïve disease is 7-11 months. |
| ● | Objective response rate (ORR) in ICI refractory patients who received the optimal dose of the triple combination is 63% (5/8). In current approaches ORR is reported to be less than 10%. |
| ● | ORR in ICI naïve patients with the triple combination is 88%. In current approaches ORR is reported to be less than 25% with FDA-approved ICIs in HPV-associated cancers. |
| ● | Safety data have not changed since October’s update. 48% (24/50) of patients experienced Grade 3 (moderate) treatment-related adverse events (AEs), and 4% (2/50) patients experienced Grade 4 (severe) AEs, compared with approximately 70% of patients receiving the combination of ICIs and chemotherapy reporting Grade 3 and higher treatment-related AEs. |
In February 2023, we announced the successful completion of a Type B meeting with the FDA for the combination therapy of PDS0101, PDS0301, and an FDA-approved immune checkpoint inhibitor for the treatment of recurrent/metastatic HPV-positive ICI-refractory head and neck cancer. We confirmed the required contents of the study design for a potential registration of the combination.
MD Anderson Cancer Center (IMMUNOCERV): PDS0101+ Chemoradiotherapy
In October 2020, another PDS0101 Phase 2 IIT was initiated with The University of Texas MD Anderson Cancer Center and is actively recruiting patients. This clinical trial is investigating the safety and anti-tumor efficacy of PDS0101 in combination with standard-of-care chemo-radiotherapy, or CRT, and their correlation with critical immunological biomarkers in patients with locally advanced cervical cancer. We believe that Versamune has strong T cell induction has the potential to enhance efficacy of the current standard of care CRT treatment in this indication. Enrollment rate in this trial had been negatively impacted by the COVID-19 pandemic and enrollment is on-going.
In November 2022, we announced data from this trial was included in a poster presentation at the 2022 SITC Annual Meeting which included the following:
| ● | 9 of the 17 patients had completed a Day 170 post-treatment Positron Emission Tomography, Computed Tomography (PET CT) scan to assess the status of the cancer. This included 78% (7/9) of treated patients with advanced cervical cancer (FIGO stage III or IV). |
| ● | 100% (9/9) of patients treated with the combination of PDS0101 and CRT had an objective response. |
| ● | 89% (8/9) of patients treated with the combination of PDS0101 and CRT demonstrated a complete response (CR) on Day 170 by PET CT. One patient who received 3 of the 5 scheduled doses of PDS0101 showed signs of residual disease. One patient who had a CR died from an event unrelated to either their underlying disease or treatment. |
| ● | 1-year disease-free survival and 1-year overall survival of 89% (8/9) in patients treated with the combination of PDS0101 and CRT. |
| ● | As previously reported, data confirm PDS0101 treatment activates HPV16-specific CD8 T cells. This increase was not seen in patients who did not receive PDS0101. The increase in HPV16-specific T cells generated by the treatment is positively correlated with tumor cell death, suggesting cytotoxic CD8 T cells are important mediators of antigen-specific immunity. |
| ● | The data affirm that PDS0101 activates Type 1 interferon pathway in humans, mimicking the mechanism previously demonstrated in preclinical studies in animal models. |
| ● | Toxicity of PDS0101 remains limited to low-grade local injection site reactions. |
Mayo Clinic: PDS0101 Monotherapy and in combination with KEYTRUDA®
In February 2022 we announced the initiation of an Investigator-Initiated Trial (ITT), MC200710, for PDS0101 alone or in combination with the immune checkpoint inhibitor, KEYTRUDA®, in patients with HPV-associated oropharyngeal cancer (HPV(+)OPSCC) at high risk of recurrence. The trial is being led by Drs. David Routman, Katharine Price, Kathryn Van Abel, and Ashish Chintakuntlawar at Mayo Clinic, a nationally and internationally recognized center of excellence for the treatment of head and neck cancers. We believe that this trial not only broadens our addressable patient population of those affected by the increasing incidence of HPV(+)OPSCC, but also allows us to better understand the activity of PDS0101 alone or in combination with KEYTRUDA® in earlier stages of disease. This trial is currently open for enrollment.
In this trial treatment will be administered before patients proceed to transoral robotic surgery (TORS) with curative intent. Treatment in this setting is referred to as neoadjuvant treatment. PDS0101 has been shown to induce killer T cells that target and kill HPV-positive cancers, either alone or in combination with ICIs in preclinical studies, and in combination in clinical studies of patients with advanced recurrent/metastatic HPV-associated cancers. This trial will explore whether PDS0101 with or without checkpoint inhibition may increase HPV-specific anti-tumor responses, potentially resulting in tumor shrinkage, pathologic regression, and decreases in circulating tumor DNA (ctDNA).
PDS0102 is an investigational immunotherapy utilizing tumor-associated and immunologically active T cell receptor gamma alternate reading framed protein (TARP) from the NCI. PDS0102 is designed to treat TARP-associated cancers including, acute myeloid leukemia (AML), prostate and breast cancer. In our preclinical work, the administration of PDS0102, the Versamuine+TARP antigen combination led to the induction of large numbers of tumor targeted killer T cells. In addition, the TARP tumor antigen alone has already been studied at the NCI in men with prostate cancer and been shown to be safe, immunogenic with slowing tumor growth rates (NCT00972309). We are evaluating the next steps in the clinical development of PDS0102 and are seeking nondilutive financings to move to human trials.
PDS0103
In April 2020, the above mentioned, PDS-NCI CRADA was expanded beyond PDS0101 to include clinical and preclinical development of PDS0103. PDS0103 is an investigational immunotherapy owned by us and designed to treat cancers associated with the mucin 1, or MUC1, oncogenic protein. These include cancers such as ovarian, breast, colorectal and lung cancers. PDS0103 combines Versamune with novel highly immunogenic agonist epitopes of MUC1 developed by the NCI and licensed by PDS. PDS0103 is currently in late preclinical development.
MUC1 is highly expressed in several types of cancer and has been shown to be associated with drug resistance and poor disease prognosis in breast, colorectal, lung and ovarian cancers, for which PDS0103 is being developed. Expression of MUC1 is often associated with poor disease prognosis, due in part to drug resistance. In preclinical studies, and similarly to PDS0101, PDS0103 demonstrated the ability to generate powerful MUC1-specific CD8 killer T cells. In the first quarter of 2022, we held a pre-IND meeting with the FDA on PDS0103. Our primary goal is commercialization of PDS0101, and allocation of resources to implement an earlier than planned start of a registrational trial may delay PDS0103 initiation.
Infectimune Development Strategy
Based on the promising data recently announced with the universal seasonal flu vaccine and the current focus of the NIAID in developing more effective flu vaccines, we have decided to opportunistically focus our near-term infectious disease activities to align with the interests of the NIAID Collaborative Influenza Vaccine Innovation Centers (CIVICs) program. This will involve development of a universal seasonal flu vaccine and the potential development of a universal pandemic influenza vaccine based on similar computationally designed antigens as have shown promise with Infectimune.
In July 2022, we announced the presentation of universal flu vaccine preclinical data for PDS0202 at the 41st American Society of Virology meeting: Abstract number 3733830, Infectimune™ enhances antibodies elicited by COBRA hemagglutinin influenza vaccine. We are evaluating the next steps in the clinical development and funding for PDS0202.
PDS0202; Universal Flu
Based on the key characteristics of Infectimune we are progressing development of PDS0202, a universal influenza vaccine candidate, which combines Infectimune with novel Computationally Optimized Broadly Reactive (COBRA) influenza vaccine antigens designed by renowned influenza expert Dr. Ted Ross and licensed from the University of Georgia. PDS0202 preclinical development was supported by an agreement with the NIAID CIVICs, program, with a goal of progressing into a human clinical trial with nondilutive financing. Preclinical development studies were performed at three sites: our Princeton, NJ laboratories, The University of Kentucky School of Medicine, and the CIVICs Center for Influenza Vaccine Research for High-Risk Populations. The data produced in the preclinical showed significant levels of hemagglutinin inhibition (HAI) titer levels when utilizing PDS0202 as compared to COBRA antigens alone ranging from 28x to 62x on various strains of the H1N1 influenza virus.
The preclinical data also showed all animals in the control group when challenged by the flu virus became sick and died while all animals treated with either a 3mcg (high dose) or .012mcg (low dose) of PDS0102 remained alive and healthy.
We are seeking nondilutive financing for the next stage of clinical development.
PDS0203 is being designed with the goal to potentially provide long-term and broad protection against infection from COVID-19 and its potential mutations, based on the understood potential of Infectimune to prime the immune system to generate both antibodies for near term protection and T cell responses for long term protection against pathogens. Preclinical data of studies performed at the University of Kentucky indicates that PDS0203 elicits the induction of highly active and potent virus-specific CD8 killer and CD4 helper T cells within 14 days of treatment. The study also showed induction of the long-lasting virus-specific memory T cells necessary for longer term protection. A 30-45-fold increase in COVID-19 specific T cells was observed by Day 14 when compared to the vaccine without Versamune. These preclinical studies also indicated induction of strong anti-SARS-CoV-2 neutralizing antibodies within 14 days, with a 20-25-fold increase when compared to the vaccine without Versamune.
As previously noted, the results highlighted above for Infectimune based PDS0202 and PDS0203 were published in the peer reviewed journal Viruses in February 2023: preclinical studies demonstrating complete protection against sickness after lethal challenge with live SARS-CoV-2 or influenza viruses (Gandhapudi SK et al. Viruses 2023, 15, 432) and dramatically enhanced CD4 T cell responses to recombinant influenza proteins compared to leading commercial vaccine adjuvants (Henson TR et al. Viruses 2023, 15, 538).
Since our inception we have devoted substantially all our resources to developing our Versamune and Infectimune platforms and our Versamune and Infectimune based products, advancing preclinical programs, conducting clinical trials, manufacturing PDS0101 for clinical trials, and providing general and administrative support. We have funded our operations primarily from the issuance of common stock. We have not generated any product revenue to date. We have never been profitable and have incurred net losses in each year since our inception.
Our future funding requirements will depend on many factors, including the following:
| ● | the timing and costs of our planned clinical trials; |
| ● | the timing and costs of our planned preclinical studies of our Versamune, Versamune plus PDS0301 and Infectimune based products; |
| ● | the outcome, timing and costs of seeking regulatory approvals; |
| ● | ability to repay debt financings including interest payments; |
| ● | the terms and timing of any future collaborations, licensing, consulting or other arrangements that we may enter into; |
| ● | the amount and timing of any payments we may be required to make in connection with the licensing, filing, prosecution, maintenance, defense and enforcement of any patents or patent applications or other intellectual property rights; and |
| ● | the extent to which we license or acquire other products and technologies. |
Leadership
We are led by a team of executives and directors with significant experience in drug discovery, development and commercialization. Our founder and CEO Frank Bedu-Addo has been responsible for developing and launching products for KBI BioPharma Inc., Schering-Plough, Merck, Elan Corporation, and the National Cancer Institute. Our other co-founder and Chief Scientific Officer, Dr. Gregory Conn has more than 35 years of drug-development experience, including development of antiviral and anticancer drugs through to commercialization. Our Chief Medical Officer, Dr. Lauren V. Wood has over 30 years of translational clinical research experience and held senior positions at the National Cancer Institute Center for Cancer Research. Our Chief Financial Officer, Matthew Hill has over 25 years of experience in finance and held prior roles as Chief Financial Officer and in operational leadership roles at several public life science companies.
We are supported by scientific leaders in the field of vaccine development and oncology. Dr. Lisa Rohan, one of our founders, is Chair of the Scientific Advisory Board. She is a professor in the department of Pharmaceutical Sciences at the University of Pittsburgh where she also holds appointments in the Department of Obstetrics, Gynecology and Reproductive Sciences in the School of Medicine and the Clinical Translational Science Institute. Dr. Mark Einstein, Professor and Chair in the Department of OB/ GYN & Women’s Heath at Rutgers University Medical School is an expert in HPV-related pathogenesis, therapy and prevention of lower anogenital tract and gynecologic cancers. He is an active leader for management guidelines and translating clinical study and translational data for the World Health Organization, American Cancer Society, Society of Gynecologic Oncology and the American College of Obstetrics and Gynecology. Dr. Neil D. Gross, Department of Head and Neck Surgery, Division of Surgery, The University of Texas MD Anderson Cancer Center. Dr. Jon Wigginton, President, Research and Development Bright Peak Therapeutics and former President of Society for Immunotherapy of Cancer. Professor Leaf Huang, one of our founders, is a Distinguished Professor of Pharmaco-engineering and Molecular Pharmaceutics at the Eshelman School of Pharmacy, University of North Carolina at Chapel Hill pioneered the liposome design and manufacture of cationic lipid vector nanoparticles as a delivery system for cDNA, mRNA, siRNA, proteins and peptides for tumor growth inhibition and for vaccines in treating cancer and infectious diseases. Dr. Olivera Finn is a Distinguished Professor of Immunology at the University of Pittsburgh School of Medicine and she discovered the MUC1 antigen. Our Principal Investigator for the PDS0101 Head and Neck Trial with KEYTRUDA® for first-line treatment of recurrent/ metastatic Head and Neck Cancer is Dr. Jared Weiss, Associate Professor of Medicine, University of North Carolina Lineberger Comprehensive Cancer Center, who is an expert in head and neck thoracic oncology with a focus on immunotherapeutic approaches for these diseases.
Facilities & Manufacturing and Commercial Scale Up
Product candidates using our Versamune, Versamune plus PDS0301 and Infectimune development platforms are manufactured using a readily scalable, fill-finish process with well-defined and reproducible operations. We do not own or operate cGMP compliant manufacturing facilities to produce any of our product candidates and we do not have plans to develop our own manufacturing operations in the foreseeable future. We currently rely on third-party contract manufacturing organizations to produce the amounts of our product candidates necessary for our preclinical research and clinical studies. As part of the manufacture and design process for our product candidates, we rely on internal, scientific and manufacturing know-how and trade secrets and the know-how and trade secrets of third-party manufacturers. We currently employ internal resources to manage our manufacturing contractors.
Our research and development activities are located at the Princeton Innovation Center BioLabs, 303A College Road East, Princeton, NJ 08540, which provides first-rate development facilities for biotech companies. All animal toxicology and efficacy testing are done via third party contracts and collaborations to provide maximum flexibility and to minimize operational costs and overhead. This approach allows for independent validation of our data, and we believe it has historically been a cost-efficient way to progress our development programs.
We do not intend to incur the costs of building, staffing and maintaining manufacturing facilities in the near term. Our management team has formulation, manufacturing and operations expertise, including past senior executive management roles in contract drug development and manufacturing. Our management team plans to utilize its expertise and knowledge to identify suitable alternative contract manufacturers who will be capable of efficiently manufacturing our products.
For our lead product candidate, PDS0101, we continue to progress our ongoing Phase 2 clinical trials. This process is described further under “U.S. Product Development Process.” The final protocols for all Phase 2 clinical trials were submitted to the FDA prior to trial initiation and information for all three trials are on www.clinicaltrials.gov. To conform to the FDA electronic Common Technical Document format requirement and submission of the cGMP material that will be used in the Phase 2 trials for PDS0101, we submitted a Chemistry, Manufacturing, and Controls amendment to our IND application, related to our Phase 2 studies with PDS0101 to the FDA in 2020.
In addition, the next step for PDS0101, in our most advanced Phase 2 clinical trial, VERSATILE-002, will be transitioning into Phase 3 clinical development called VERSATILE-003, where we plan to file an amended IND in the third quarter 2023 to enter into a registrational trial by the end of the year.
We anticipate that we would seek marketing authorization from the FDA for our product candidates through the Biologics License Application pathway, under Section 351(a) of the Public Health Service Act. This process and the requirements are described further under “U.S. Product Development Process.”
For our earlier stage, preclinical product candidates PDS0102 and PDS0103, we plan to work to develop data with the goal of progressing to an IND submission in 2023 and progressing clinical development to first-in-human trials with these products. We have engaged with the FDA and received useful initial feedback on the clinical trial design for the PDS0103 program and this information will influence our strategy for regulatory submissions and the protocol development.
Intellectual Property
Patents
We seek to maintain high barriers to entry around our product candidates and the markets in which they are utilized by using a multiple layered approach to our patents, patent applications, substantial know-how and trade secrets related to the Versamune, Versamune plus PDS0301, and Infectimune platforms. We strive to protect and enhance the proprietary technology, inventions and improvements that are commercially important to our business, including seeking, maintaining, and defending patent rights. We also rely on trade secrets relating to our platforms and on know-how, continuing technological innovation to develop, strengthen and maintain its proprietary position in the vaccine field. In addition, we rely on regulatory protection afforded through data exclusivity, market exclusivity and patent term extensions where available. We also utilize trademark protection for our company name and we expect to do so for products and/or services as they are marketed.
We have developed numerous patents and patent applications and owns substantial know-how and trade secrets related to our Versamune platform. As of December 31, 2022, PDS holds seven (7) U.S. patents with granted claims directed to its platform technology and nineteen (19) pending U.S. patent applications. These issued patents will expire in 2026, 2029, 2031 and 2033. Should the more recently submitted patent applications currently in prosecution be issued, these will expire in 2033 through 2043 assuming no patent term extensions are granted. As of March 1, 2023, PDS holds seventy-one (71) issued foreign patents and thirty-eight (38) pending or published foreign patent applications. Most of our international issued patents are issued in multiple countries including Europe, Japan and Australia, and all of which cover compositions of matter and methods of use related to its platform technology. These issued patents will expire in 2028-2037, or later if patent term extension applies. Most recently, the USPTO allowed two (2) applications methods of use related to our Versamune platform technology which when granted will run until November 2036. Included in the patents above is a patent protecting the use of Versamune plus PDS0301.
Licensed Patents
We have an exclusive worldwide license from Merck & Cie to (R)-DOTAP and its crystal forms, manufacturing methods, and pharmaceutical compositions using the compounds., which are owned by Merck Patent GmbH, for use in our immunotherapy compositions and immunotherapies. Merck & Cie has informed us that it has rights to license these patent families through an intra-company agreement with Merck Patent GmbH. These licensed patents are significant to the Versamune, Versamune plus PDS0301 and Infectimune platforms, as they are directed to an important ingredient utilized in the Versamune product.
We have licensed patented antigens from the US government for use worldwide in our cationic lipid immunotherapies. We have licensed T cell receptor gamma alternate reading frame protein (“TARP”) from the National Cancer Institute (“NCI”) to develop and commercialize TARP peptide-based therapies in combination with our Versamune technology and any other of our proprietary technologies for prostate and breast cancers and Acute Myeloid Leukemia. These patents are directed to immunogenic peptides and peptide Derivatives for the treatment of prostate and breast cancer treatment and multi-epitope TARP peptide vaccines and Uses Thereof. These antigens are incorporated in PDS0102 with Versamune. We have licensed novel and highly immunogenic agonist epitopes of mucin-1 (“MUC1”) developed by the National Cancer Institute. MUC1 is highly expressed in multiple solid tumors and has been shown to be associated with drug resistance and poor disease prognosis in breast, colorectal, lung and ovarian cancers, for which PDS0103 is being developed. We have granted patents and are pursuing additional patents that cover compositions and methods of use of cationic lipid immunotherapies with each of the licensed technologies.
We entered into a non-exclusive agreement to license COBRA universal influenza antigens with the University of Georgia Research Foundation to develop, manufacture and use COBRA antigens in a clinical trial for a universal influenza vaccine worldwide. These antigens are developed by Dr. Ted Ross at the University of Georgia. We believe that the combination of these antigens with our proprietary Infectimune technology, representing PDS0202, has the potential to induce a broad immune response as a universal flu vaccine, based on preclinical development studies performed to date.
Exclusive License Agreement
On December 30, 2022, we entered into a License Agreement (the “Merck KGaA License”), with Merck KGaA, Darmstadt, Germany, pursuant to which Merck KGaA, Darmstadt, Germany granted us an exclusive (even as to Merk KGaA), worldwide, sublicensable, milestone and royalty-bearing right and license to certain patent rights and certain related data (the “Licensed Technology”) to develop, manufacture, use, commercialize and otherwise exploit any product containing NHS-IL12 fusion protein known as M9241 (the “Compound”). Merck KGaA, Darmstadt, Germany retains the right under the Licensed Technology in connection with certain existing collaborations between Merck KGaA, Darmstadt, Germany and academic institutions to allow such academic institutions to exercise their rights granted under such collaborations. We agreed to use commercially reasonable efforts to develop, manufacture and commercialize at least one pharmaceutical preparation, substance, or formulation, comprising or employing, the Compound (the “Product”).
In consideration for the rights granted by Merck KGaA, Darmstadt, Germany, we (i) made a one-time up-front cash payment of $5.0 million to Merck KGaA, Darmstadt, Germany, and (ii) entered into a Share Transfer Agreement dated December 30, 2022 (the “Share Transfer Agreement”), pursuant to which we issued 378,787 shares of our common stock (the “Shares”) to Merck KGaA, Darmstadt, Germany in a private placement for an aggregate value of $5.0 million, as measured by the closing price of our common stock on the Nasdaq Capital Market as of December 30, 2022.
Pursuant to the Merck KGaA License Agreement, we agreed to make (i) development and first commercial sale milestone payments totaling up to $11 million upon the achievement of certain milestones, including the dosing of the fifth patient in a Phase 3 trial of the Product and first commercial sale of the Product for a first and second indications in a major market, and (ii) up to $105 million upon achieving certain aggregate sales levels of the Product.
We also agreed to pay Merck KGaA, Darmstadt, Germany a royalty of 10% on aggregate net sales of Product as specified in the Merck KGaA License Agreement on a Product-by-Product and country-by-country basis until the later of: (i) ten years after the first commercial sale of a Product in a given country; and (ii) the expiration or invalidation of the licensed patents covering the Compound or Product in such country (collectively, the “Royalty Term”). The royalty rate is subject to reduction in that event that a Product is not covered by a valid patent claim, a biosimilar to the Compound or the Product comes on the market in a particular country, or if we obtain a license to any intellectual property owned or controlled by a third-party which but for such license would be infringed by making, using or selling the Compound.
The Merck KGaA License Agreement will expire on a Product-by-Product and country-by-country basis upon expiration of the last-to-expire Royalty Term for such Product. On expiration (but not earlier termination), we will have a fully paid-up, royalty-free, non-exclusive, transferable, perpetual and irrevocable license under the licensed patent rights and related data to develop, manufacture, use, commercialize and otherwise exploit the Compound. Either party may terminate the Merck KGaA License Agreement for the other party’s material breach following a cure period. The Merck KGaA License Agreement may not be terminated upon certain insolvency events relating to us. We may terminate the License Agreement for any reason upon ninety days written notice to Merck KGaA, Darmstadt, Germany. The Merck KGaA License Agreement also includes indemnification obligations of each party.
Trade Secrets and Other Proprietary Information
In contrast to patent protection or regulatory exclusivities, trade secret protection is a form of intellectual property that does not require disclosure of the subject information as part of the process, but instead depends on maintaining the subject information as strictly confidential. Companies may in some circumstances rely on trade secrets to protect certain aspects of their proprietary know-how and technological advances, especially where they do not believe patent protection is appropriate or obtainable. Trade secret protection depends in part on confidentiality agreements with employees, consultants, outside scientific collaborators, sponsored researchers and other advisors that prohibit disclosure of designated proprietary information. Trade secrets can be difficult to protect. Confidentiality agreements may not succeed in preventing a person or parties from disclosing confidential information, and in that event the rights of the trade secret holder are subject to the viability of an adequate remedy at law, typically under state law modeled on the Uniform Trade Secrets Protection Act, to stop, mitigate or compensate for the unauthorized disclosure of confidential information. Costly and time-consuming litigation could be necessary to enforce and determine the scope of the proprietary rights. Finally, there is always at least some risk that others may independently discover the trade secrets and proprietary information.
Material License Agreements and Research and Development Agreements
Patent License Agreements with National Institutes of Health.
Effective January 5, 2015, we entered into a Patent License Agreement (the “Patent License Agreement”) as Amended by First Amendment to Patent License Agreement (“First Amendment”) of August 5, 2015, with an agency within the Department of Health and Human Services (“HHS”), pursuant to which NIH granted PDS a nonexclusive license to certain patent rights for the development of a therapeutic cancer vaccine specifically in combination with PDS’s proprietary Versamune technology for ovarian, breast, colon and lung cancers. The Patent License Agreement expires when the last licensed patent expires if the Patent License Agreement is not terminated prior to that date. NIH may terminate the Patent License Agreement if PDS is in default in the performance of any material obligation under the Patent License Agreement. PDS may unilaterally terminate the Patent License Agreement in any country or territory upon sixty (60) days written notice.
Under the Patent License Agreement and First Amendment PDS agreed to pay NIH: (a) a noncreditable, nonrefundable royalty in the amount of $30,000 upon execution of the Patent License Agreement; (b) a noncreditable, nonrefundable royalty in the amount of $60,000 upon execution of the First Amendment to Patent License Agreement (c) a nonrefundable minimum annual royalty of $5,000; (d) earned royalties of two percent (2%) on net sales, reducible by a half percent (0.5%) for any earned royalties PDS must pay to third parties; (e) benchmark royalties as follows: (i) $25,000 upon successful completion of each Phase 2 Clinical Studies of a licensed product for breast, colon, lung or ovarian cancer within each licensed territory; (ii) $50,000 upon initiation of the first Phase 3 Clinical Trial of a licensed product for breast, colon, lung or ovarian cancer within each licensed territory; (iii) $750,000 upon the first commercial sale in the licensed territory utilizing and/or directed to licensed product(s) and/or licensed process(es) within the licensed patent rights for breast, colon, lung or ovarian cancer; and (f) additional sublicensing royalties for each sublicense required to be approved by NIH of four percent (4%) on the fair market value of any consideration received for granting such sublicense.
Effective as November 5, 2021, we entered into a Patent License Agreement (the “NCI Patent License Agreement”) with the U.S. Department of Health and Human Services, as represented by NCI of NIH. Pursuant to the NCI Patent License Agreement, we obtained a nonexclusive, worldwide license to the patent rights for TARP to develop and commercialize TARP peptide-based therapies in combination with the Versamune technology and any other of our proprietary technologies for prostate and breast cancers and Acute Myeloid Leukemia. The NCI Patent License Agreement expires when the last licensed patent expires if the Patent License Agreement is not terminated prior to that date. NCI may terminate the Patent License Agreement if we are in default in the performance of any material obligation under the Patent License Agreement. We may unilaterally terminate the NCI Patent License Agreement in any country or territory upon sixty (60) days written notice. Under the NCI Patent License Agreement, we agreed to pay NCI certain non-creditable, nonrefundable license issue royalties, unreimbursed patent expenses for the licensed patent rights, a nonrefundable minimum annual royalty, earned royalties as a percentage of net sales and benchmark royalties.
DOTAP Chloride Enantiomer License Agreement with Merck Eprova AG.
Effective November 1, 2008, we entered into a DOTAP Chloride Enantiomer License (the “DOTAP License Agreement”) with Merck Eprova AG (“EPRO”), pursuant to which we obtained an exclusive license from EPRO technology to undertake development of products relating to the R-enantiomer and S-enantiomer of DOTAP Chloride for worldwide commercialization in a composition and method of inducing an immune response in a subject by administering at least one cationic lipid with or without an antigen. The DOTAP License Agreement expires on a licensed product-by-licensed product and country-by-country basis until the expiration of the obligation to pay royalties applicable to such licensed product in such country. We have the right to unilaterally terminate the DOTAP License Agreement (in its entirety or on a licensed product-by-licensed product or country-by-country basis) at any time for any reason upon prior written notice.
Cooperative Research and Development Agreement for Intramural-PHS Clinical Research with The U.S. Department of Health and Human Services.
Effective February 2, 2016, we entered into a Cooperative Research and Development Agreement (the “CRADA”) with the U.S. Department of Health and Human Services, as represented by the National Cancer Institute (“NCI”), pursuant to which the parties agreed to perform certain research and development activities as defined by the exhibited Research Plan. The principal goal of the CRADA is to determine whether our Versamune immunotherapeutic technology will be effective for enhancing delivery of cancer vaccines or viral vaccines or other immunotherapies developed by the Vaccine Branch, Center for Cancer Research, NCI, in mouse models and in human clinical studies. The CRADA provides for development, testing and studies to be conducted in conjunction with the Vaccine Branch involving Versamune and Multi-epitope (ME) T cell receptor gamma alternate reading frame protein peptide (TARP) to develop a treatment for prostate cancer using autologous dendritic cells and co- administered locally with ME TARP peptides co-formulated with Versamune immunotherapeutic technology in a non-cellular vaccine platform.
The term of the CRADA is five (5) years, starting February 2, 2016. Pursuant to Appendix A, PDS agreed to provide up to $1,000,000 but no less than $500,000 during the first year of the CRADA and up to $1,000,000 but no less than $750,000 per year for the remaining years of the CRADA for NCI to use in connection with acquiring technical, statistical, and administrative support for the clinical research activities, as well as to pay for supplies and travel expenses and, upon consent of the parties, to acquire support for a postdoctoral research fellow to conduct additional preclinical studies. The CRADA may be terminated by either party at any time by mutual written consent. Either party may unilaterally terminate the CRADA at any time by providing sixty (60) days written notice. If we terminate prior to the completion of all approved or active study protocol(s) pursuant to the CRADA, we must supply enough study test product to complete these study protocol(s) unless termination is for safety reasons. If the CRADA is mutually or unilaterally terminated by us before its expiration, we must pay non-cancellable obligations for personnel for a period of six (6) months after the termination date or until the expiration date of the CRADA, whichever is sooner. If we suspend development on the test article without the transfer of its active development efforts, assets, and obligations to a third party within ninety (90) days of discontinuation, NCI may continue development. In such event, we must transfer all information necessary to enable NCI to contract for the manufacture of the test article and grant NCI a nonexclusive, irrevocable, worldwide, paid-up license regarding same.
Cost Reimbursement Agreement with University of Kentucky Research Foundation - I. with University of Kentucky Research Foundation - I.
Effective November 1, 2015, we entered into an annual Research Agreement (the “Cost Reimbursement Agreement”) with the University of Kentucky Research Foundation (“UKRF”), pursuant to which UKRF agreed to test PDS’s preclinical and clinical-stage formulations based on HPV, TARP, MUC1, Melanoma antigens as specified more fully in the statement of work. The Cost Reimbursement Agreement has been renewed annually, and was renewed on July 1, 2021, for an anticipated cost of $404,502. The agreement terminates on June 30, 2022, unless extended by written mutual agreement of parties or is terminated by one of the parties. Either party may terminate the Cost Reimbursement Agreement for any reason with thirty (30) days written notice.
Cost Reimbursement and Sponsored Agreement with University of Kentucky Research Foundation - II.
Effective November 1, 2015, we entered into an annual Research Agreement (the “Cost Reimbursement Agreement”) with the University of Kentucky Research Foundation (“UKRF”), pursuant to which UKRF agreed to test PDS’s preclinical and clinical-stage formulations based on HPV, TARP, MUC1, Melanoma antigens as specified more fully in the statement of work. The Cost Reimbursement Agreement has been renewed annually, and was renewed on July 1, 2021, for an anticipated cost of $13,998. The agreement terminates on June 30, 2022, unless extended by written mutual agreement of parties or is terminated by one of the parties. Either party may terminate the Cost Reimbursement Agreement for any reason with thirty (30) days written notice.
Clinical Trial Collaboration and Supply Agreement with MSD International GmbH.
Effective May 19, 2017, we entered into a Clinical Trial Collaboration and Supply Agreement (the “CTCSA”) with MSD International GmbH (“Merck”) pursuant to which we and Merck agreed to collaborate in a Phase 2 clinical trial to evaluate the safety, and preliminary efficacy of the concomitant and/or sequenced administration of the combination of a Merck compound (i.e., pembrolizumab, a humanized anti-human PD-1 monoclonal antibody) and our compound (i.e., PDS0101, a cationic lipid-based therapeutic vaccine combining HPV peptides) in treatment of patients with recurrent or metastatic head and neck cancer and high-risk human papillomavirus-16 (HPV 16) infection. The term of the CTCSA commenced on May 19, 2017 and will continue until the earlier of (i) delivery of the final study report and (ii) Study Completion (i.e., upon database lock of the Study results), or until terminated by either party. In the event the CTCSA is terminated by Merck upon a material breach by PDS, PDS must reimburse Merck for its direct manufacturing costs, such as manufacturing fees, raw materials, direct labor, freight and duty, factory overhead costs and its indirect manufacturing costs, such as allocations of indirect factory overhead and site support costs. This agreement was amended on October 28, 2019 to reflect the trial will be for first in line treatment of disease.
On October 28, 2019, we entered into an amendment to the clinical trial collaboration agreement with Merck to evaluate the combination of our lead Versamune based immunotherapy, PDS0101, with Merck’s anti-PD-1 therapy, KEYTRUDA® (pembrolizumab), in a Phase 2 clinical trial. The modification to the clinical trial design to evaluate PDS0101 in combination with KEYTRUDA® as first-line treatment comes as a result of Merck’s approval by the FDA on June 10, 2019 for first line treatment of patients with metastatic or unresectable recurrent HNSCC using KEYTRUDA® in combination with platinum and fluorouracil (FU) for all patients and as a single agent for patients whose tumors express PD-L1 as determined by an FDA-approved test. The trial was initiated in November of 2020 to evaluate the efficacy and safety of the combination as a first-line treatment in patients with recurrent or metastatic head and neck cancer and high-risk human papillomavirus-16 (HPV16) infection.
Other Research and Development Agreements
Cooperative Research and Development Agreement for Intramural-PHS Clinical Research with The U.S. Department of Health and Human Services.
Effective April 22, 2019, PDS entered into a Cooperative Research and Development Agreement (the “CRADA”) with the U.S. Department of Health and Human Services, as represented by the National Cancer Institute (“NCI”), pursuant to which the parties agreed to perform certain research and development activities as defined by the exhibited Research Plan. Under the agreement, PDS will collaborate with the NCI’s Genitourinary Malignancies Branch (GMB) and Laboratory of Tumor Immunology and Biology (LTIB) with plans to conduct a Phase 2 clinical trial evaluating PDS0101 with novel immune-modulating agents M7824 and NHS-IL12 being studied at NCI as part of a CRADA with EMD serono (Merck KGaA). The Phase 2 clinical trial was initiated in June of 2020. The CRADA also involves preclinical evaluation of PDS0101 in combination with other therapeutic modalities upon the mutual agreement of both parties. In April 2020, this agreement was amended to include PDS0103, in preclinical and clinical development for treatment of ovarian, breast, colorectal and lung cancers.
The term of the CRADA is five (5) years, starting April 22, 2019. Pursuant to Appendix A, we agreed to provide $110,000 annually, the first payment of which is to be made on the first anniversary the of the CRADA Effective date or upon the initiation of a Phase 2 clinical trial as the NIH Clinical Center, whichever comes first for NCI to use in connection with acquiring technical, statistical, and administrative support for the clinical research activities, as well as to pay for supplies and travel expenses and infrastructure costs. The CRADA may be terminated by either party at any time by mutual written consent. Either party may unilaterally terminate the CRADA at any time by providing sixty (60) days written notice. If we terminate prior to the completion of all approved or active study protocol(s) pursuant to the CRADA, we must supply enough study test product to complete these study protocol(s) unless termination is for safety reasons. If the CRADA is mutually or unilaterally terminated by PDS before its expiration, we must pay non-cancellable obligations for personnel for a period of six (6) months after the termination date or until the expiration date of the CRADA, whichever is sooner. If we suspend development on the test article without the transfer of its active development efforts, assets, and obligations to a third party within ninety (90) days of discontinuation, NCI may continue development. In such event, we must transfer all information necessary to enable NCI to contract for the manufacture of the test article and grant NCI a nonexclusive, irrevocable, worldwide, paid-up license regarding same.
Option to License with the University of Georgia Research Foundation of Georgia Research Foundation
On October 25, 2021, we entered into a non-exclusive agreement to license Computationally Optimized Broadly Reactive Antigen (COBRA) with the University of Georgia Research Foundation. This agreement allows us to develop, manufacture and use COBRA antigens in a clinical trial for a universal influenza vaccine worldwide. The term of the agreement extends twelve months after initiation of first Phase 1 clinical trial and may be extended upon agreement of the parties. We may convert the option to a full agreement any time prior to the conclusion of the term.
Competition
The biotechnology and pharmaceutical industries are characterized by intense competition to develop new technologies and proprietary products. We are aware of various established companies, including major pharmaceutical companies, broadly engaged in immunotherapies and vaccines in research and development that may compete directly with the products we are developing including Jansen Pharmaceuticals (part of J&J), Sanofi-Aventis, GlaxoSmithKline plc, Merck and Pfizer, among others. In addition, there are many development-stage biotechnology companies in various immunotherapy and vaccine development including, but not limited to Inovio, Advaxis, Kite Pharma, Hookipa, Moderna, ZIOPHARM Oncology, Heat Biologics, Harpoon Therapeutics, Oncosec Medical, BioNTech, Osivax, Medicago, Vaxart, and Flugen. If one or more of these companies is successful in developing their technologies, it could materially impact our business.
While we believe that the Versamune, Versamune plus PDS0301 and Infectimune platforms provide us with competitive advantages, we face competition from many different sources, including biotechnology and pharmaceutical companies, academic institutions, government agencies, as well as public and private research institutions. Any products that we may commercialize will have to compete with existing products and therapies as well as new products and immunotherapies that may become available in the future.
We anticipate that it will face intense and increasing competition as new immunotherapies enter the market and advanced technologies become available. PDS Biotech expects any products that it develops and commercializes to compete based on, among other things, efficacy, safety, convenience of administration and delivery, price, availability of therapeutics, the level of generic competition and the availability of reimbursement from government and other third-party payors. PDS Biotech’s competitors may obtain FDA or other regulatory approval for their products more rapidly than it may obtain approval for its products, which could result in our competitors establishing a strong market position before it is able to enter the market. In addition, our ability to compete may be affected in many cases by insurers or other third-party payors seeking to encourage the use of generic products.
Government Regulation and Product Approval
Federal, state and local government authorities in the United States and in other countries extensively regulate, among other things, the research, development, testing, manufacturing, quality control, approval, labeling, packaging, storage, record-keeping, promotion, advertising, distribution, post-approval monitoring and reporting, marketing and export and import of biological and pharmaceutical products such as those we are developing. Our product candidates must be approved by the FDA before they may be legally marketed in the United States and by the appropriate foreign regulatory agency before they may be legally marketed in foreign countries. Generally, its activities in other countries will be subject to regulation that is similar in nature and scope as that imposed in the United States. The process for obtaining regulatory marketing approvals and the subsequent compliance with appropriate federal, state, local and foreign statutes and regulations require the expenditure of substantial time and financial resources.
U.S. Product Development Process
In the United States, the FDA regulates biological drug products under the Federal Food, Drug and Cosmetic Act, or FDCA, and the Public Health Service Act, or PHSA, and implementing regulations. Products are also subject to certain other federal, state and local statutes and regulations. The process of obtaining regulatory approvals and the subsequent compliance with appropriate federal, state, local and foreign statutes and regulations requires the expenditure of substantial time and financial resources. Failure to comply with the applicable U.S. requirements at any time during the product development process, approval process or post-approval, may subject an applicant to administrative or judicial action. FDA decisions or enforcement actions could include, among other actions, refusal to approve pending applications, withdrawal of an approval, a clinical hold, warning letters, product recalls or withdrawals from the market, product seizures, total or partial suspension of production or distribution injunctions, fines, refusals of government contracts, restitution, disgorgement or civil or criminal penalties. Any agency or judicial enforcement action could have a material adverse effect on PDS.
The process required by the FDA before a biological drug product may be marketed In the United States generally involves the following:
| ● | completion of nonclinical laboratory tests and animal studies according to good laboratory practice regulations, or GLP, and applicable requirements for the humane use of laboratory animals or other applicable regulations; |
| ● | submission to the FDA of an investigational new drug application, or an IND, which must become effective before human clinical studies may begin; |
| ● | approval by an independent institutional review board, or IRB, representing each clinical site before each clinical may be initiated; |
| ● | performance of adequate and well-controlled human clinical studies according to the FDA’s regulations commonly referred to as good clinical practice, or GCP, and any additional requirements for the protection of human research subjects and their health information, to establish the safety and efficacy of the proposed biological product for its intended use; |
| ● | submission to the FDA of a Biologics License Application, or BLA, for marketing approval that meets applicable requirements to ensure the continued safety, purity, and potency/efficacy of the product that is the subject of the BLA based on results of nonclinical testing and clinical studies (including among other things clinical data, chemistry, and manufacturing and controls (CMC) data); |
| ● | review by an FDA advisory committee, where appropriate or if applicable; |
| ● | satisfactory completion of an FDA inspection of the manufacturing facility or facilities where the biological product, or components thereof, are produced, to assess compliance with cGMP, and to assure that the facilities, methods and controls are adequate to preserve the biological product’s identity, strength, quality and purity; |
| ● | pre-approval inspection by the FDA of the sponsor (or any third party service providers) relative to oversight of clinical studies, clinical trial sites that generated the data in support of the BLA, and any manufacturing facilities to assure compliance with GCPs and the integrity of clinical data; |
| ● | FDA review and approval, or licensure, of the BLA; and |
| ● | Compliance with any post-approval requirements, including the potential requirement to implement a Risk Evaluation and Mitigation Strategy, or REMS, and the potential requirement to conduct post-approval studies |
Satisfaction of FDA pre-market approval requirements typically takes many years and the actual time required may vary substantially based upon the type, complexity, and novelty of the product candidate or disease. A clinical hold may occur at any time during the life of an IND and may affect one or more specific trials or all trials conducted under the IND. The testing and approval process requires substantial time, effort, and financial resources.
Preclinical studies
Before testing any product candidate in humans, the product enters the preclinical testing stage. Preclinical tests, also referred to as nonclinical studies, include laboratory evaluations of product chemistry, toxicity and formulation, as well as in vitro and animal studies to assess the potential safety and activity of the product candidate for initial testing in humans and to establish a rationale for therapeutic use. The conduct of the preclinical tests must comply with federal regulations and requirements including GLP. The clinical study sponsor must submit the results of the preclinical tests, together with manufacturing information, analytical data, any available clinical data or literature and a proposed clinical protocol, to the FDA as part of the IND. Some preclinical testing may continue even after the IND is submitted. The results of preclinical studies and early clinical studies of product candidates with small patient populations may not be predictive of the results of later-stage clinical studies or the results once the applicable clinical studies are completed.
The IND and IRB processes
An IND is an exemption from the FDCA that allows an unapproved drug to be shipped in interstate commerce for use in an investigational clinical trial and a request for FDA authorization to administer an investigational drug to humans. Such authorization must be secured prior to interstate shipment and administration of any new drug that is not the subject of an approved NDA or BLA. In support of a request for an IND, a sponsor must submit, among other things, a protocol for each clinical trial and any subsequent protocol amendments must be submitted to the FDA as part of the IND. The sponsor may be a company seeking to develop the drug or, as in the case of an investigator-initiated trial, the sponsor may be an investigator who is conducting the trial. In addition, the results of the preclinical tests, together with manufacturing information, analytical data, any available clinical data or literature and plans for clinical trials, among other things, are submitted to the FDA as part of an IND. The FDA requires a 30-day waiting period after the filing of each IND before clinical trials may begin. This waiting period is designed to allow the FDA to review the IND to determine whether human research subjects will be exposed to unreasonable health risks. The IND automatically becomes effective 30 days after receipt by the FDA, unless the FDA raises concerns or questions regarding the proposed clinical studies and places the study on a clinical hold within that 30-day time period. In such a case, the IND sponsor and the FDA must resolve any outstanding concerns before the clinical study can begin. The FDA may also impose clinical holds on a biological product candidate at any time before or during clinical studies due to safety concerns or non-compliance. If the FDA imposes a clinical hold, studies may not recommence without FDA authorization and then only under terms authorized by the FDA. Accordingly, PDS cannot be sure that submission of an IND will result in the FDA allowing clinical studies to begin, or that, once begun, issues will not arise that suspend or terminate such studies.
Following commencement of a clinical trial under an IND, the FDA may also place a clinical hold or partial clinical hold on that trial. A clinical hold is an order issued by the FDA to the sponsor to delay a proposed clinical investigation or to suspend an ongoing investigation. A partial clinical hold is a delay or suspension of only part of the clinical work requested under the IND. For example, a specific protocol or part of a protocol is not allowed to proceed, while other protocols may do so. No more than 30 days after imposition of a clinical hold or partial clinical hold, the FDA will provide the sponsor a written explanation of the basis for the hold. Following issuance of a clinical hold or partial clinical hold, an investigation may only resume after the FDA has notified the sponsor that the investigation may proceed. The FDA will base that determination on information provided by the sponsor correcting the deficiencies previously cited or otherwise satisfying the FDA that the investigation can proceed.
A sponsor may choose, but is not required, to conduct a foreign clinical study under an IND. When a foreign clinical study is conducted under an IND, all IND requirements must be met unless waived. When the foreign clinical study is not conducted under an IND, the sponsor must ensure that the study complies with certain FDA regulatory requirements in order to use the study as support for an IND or application for marketing approval. Specifically, FDA has promulgated regulations governing the acceptance of foreign clinical trials not conducted under an IND, establishing that such studies will be accepted as support for an IND or application for marketing approval if the study was conducted in accordance with GCP, including review and approval by an independent ethics committee, or IEC, and use of proper procedures for obtaining informed consent from subjects, and the FDA is able to validate the data from the study through an on-site inspection if FDA deems such inspection necessary. The GCP requirements encompass both ethical and data integrity standards for clinical studies. The FDA’s regulations are intended to help ensure the protection of human subjects enrolled in non-IND foreign clinical trials, as well as the quality and integrity of the resulting data. They further help ensure that non-IND foreign studies are conducted in a manner comparable to that required for IND studies. If a marketing application is based solely on foreign clinical data, the FDA requires that the foreign data be applicable to the U.S. population and U.S. medical practice; the studies must have been performed by clinical investigators of recognized competence; and the FDA must be able to validate the data through an on-site inspection or other appropriate means, if the FDA deems such an inspection to be necessary.
In addition to the foregoing IND requirements, an IRB representing each institution participating in the clinical trial must review and approve the plan for any clinical trial before it commences at that institution, and the IRB must conduct continuing review and reapprove the study at least annually. The IRB must review and approve, among other things, the study protocol and informed consent information to be provided to study subjects. An IRB must operate in compliance with FDA regulations. An IRB can suspend or terminate approval of a clinical trial at its institution, or an institution it represents, if the clinical trial is not being conducted in accordance with the IRB’s requirements or if the product candidate has been associated with unexpected serious harm to patients. A separate submission to the existing IND must be made for each successive clinical trial conducted during product development, as well as amendments to previously submitted clinical trials. Further, an independent IRB for each institution participating in the clinical trial must review and approve the plan for any clinical trial, its informed consent form, and other communications to study subjects before the clinical trial commences at that site. The IRB must continue to oversee the clinical trial while it is being conducted, including any changes to the study plans.
Additionally, some trials are overseen by an independent group of qualified experts organized by the trial sponsor, known as a data safety monitoring board or committee. This group provides authorization for whether or not a trial may move forward at designated check points based on access that only the group maintains to available data from the study. Suspension or termination of development during any phase of clinical trials can occur if it is determined that the participants or patients are being exposed to an unacceptable health risk. Other reasons for suspension or termination may be made by us based on evolving business objectives and/or competitive climate.
Information about certain clinical trials must be submitted within specific timeframes to the National Institutes of Health, or NIH, for public dissemination on its ClinicalTrials.gov website.
Human clinical trials in support of an NDA or BLA
Clinical trials involve the administration of the biological product candidate to volunteers or patients under the supervision of qualified investigators, generally physicians not employed by or under the trial sponsor’s control, in accordance with GCP requirements, which include, among other things, the requirement that all research subjects provide their informed consent in writing before their participation in any clinical trial. Clinical trials are conducted under protocols detailing, among other things, the objectives of the clinical trial, dosing procedures, subject selection (for example, inclusion and exclusion criteria), and the parameters to be used to monitor subject safety, including stopping rules that assure a clinical trial will be stopped if certain adverse events should occur. Each protocol and any amendments to the protocol must be submitted to the FDA as part of the IND and require IRB approval. Human clinical trials are typically conducted in three sequential phases that may overlap or be combined:
| ● | Phase 1. The biological product is initially introduced into healthy human subjects and tested for safety. In the case of some products for severe or life-threatening diseases, especially when the product may be too inherently toxic to ethically administer to healthy volunteers, the initial human testing is often conducted in seriously ill subjects. These studies are designed to test the safety, dosage tolerance, absorption, metabolism and pharmacologic actions of the investigational product in humans, the side effects associated with increasing doses, and, if possible, to gain early evidence of Effectiveness. |
| ● | Phase 2. The biological product is evaluated in a limited patient population to identify possible adverse effects and safety risks, to preliminarily evaluate the efficacy of the product for specific targeted diseases and to determine dosage tolerance, optimal dosage and dosing schedule. Multiple Phase 2 clinical studies may be conducted to obtain information prior to beginning larger and more expensive Phase 3 clinical studies. |
| ● | Phase 3. The biological product is administered to an expanded patient population, generally at geographically dispersed clinical trial sites, in well-controlled clinical trials to generate enough data to statistically evaluate the dosage, clinical efficacy, potency, and safety of the product for approval, to establish the overall risk to benefit ratio of the product and provide an adequate basis for product labeling. |
| ● | Phase 4. Post-approval studies, which are conducted following initial approval, are typically conducted to gain additional experience and data from treatment of patients in the intended therapeutic indication. |
Although these are the typical phases of progression, and characteristics of the phases of a clinical development program, certain expedited programs allow for variations that could support a marketing application based on surrogate endpoints, intermediate clinical endpoints, or single-arm as opposed to comparative or placebo-controlled studies (for example, FDA could rely on well-controlled Phase 2 studies for evidence of effectiveness under certain circumstances).
During all phases of clinical development, regulatory agencies require extensive monitoring and auditing of all clinical activities, clinical data, and clinical trial investigators. Annual progress reports detailing the results of the clinical trials must be submitted to the FDA. Written IND safety reports must be promptly submitted to the FDA and the investigators of potential safety risks, from clinical trials or any other source, including for serious and unexpected adverse events and serious and unexpected suspected adverse reactions, any findings from other studies suggesting a significant risk in humans exposed to the drug, tests in laboratory animals or in vitro testing that suggest a significant risk for human subjects, or any clinically important increase in the rate of a serious suspected adverse reaction over that listed in the protocol or investigator brochure. The sponsor must submit an IND safety report within 15 calendar days after the sponsor determines that the information qualifies for reporting. The sponsor also must notify the FDA of any unexpected fatal or life-threatening suspected adverse reaction as soon as possible but no later than within seven calendar days after the sponsor’s initial receipt of the information. Phase 1, Phase 2 and Phase 3 clinical trials may not be completed successfully within any specified period, if at all. The FDA, the sponsor or its data safety monitoring board, or DSMB, which receives special access to unblinded data during the clinical trial, may suspend or terminate a clinical trial at any time on various grounds, including a finding that the research subjects are being exposed to an unacceptable health risk or no demonstration of efficacy. Similarly, an IRB can suspend or terminate approval of a clinical trial at its institution if the clinical trial is not being conducted in accordance with the IRB’s requirements or if the biological product has been associated with unexpected serious harm to subjects. The FDA will typically inspect one or more clinical sites to assure compliance with GCP and the integrity of the clinical data submitted.
Information about certain clinical trials must be submitted within specific timeframes to the National Institutes of Health, or NIH, for public dissemination on their ClinicalTrials.gov website, and other jurisdictions have similar laws that may apply.
Concurrently with clinical trials, companies usually complete additional studies and must also develop additional information about the physical characteristics of the biological product as well as finalize a process for manufacturing the product in commercial quantities in accordance with cGMP requirements. To help reduce the risk of the introduction of adventitious agents with use of biological products, the PHSA emphasizes the importance of manufacturing controls for products whose attributes cannot be precisely defined. The manufacturing process must be capable of consistently producing quality batches of the product candidate and, among other criteria, the sponsor must develop methods for testing the identity, strength, quality, potency and purity of the final biological product. Additionally, appropriate packaging must be selected and tested, and stability studies must be conducted to demonstrate that the biological product candidate does not undergo unacceptable deterioration over its shelf life.
U.S. Review and Approval Processes
After the completion of clinical trials of a biological product, FDA approval of a BLA must be obtained before commercial marketing of the biological product. The BLA must include results of product development, laboratory and animal studies, human trials, information on the manufacture and composition of the product, proposed labeling and other relevant information. The testing and approval processes require substantial time and effort and there can be no assurance that the FDA will accept the BLA for filing and, even if filed, that any approval will be granted on a timely basis, if at all.
Under the Prescription Drug User Fee Act, or PDUFA, as amended, each BLA must be accompanied by a significant application fee. For approved drugs, including BLA-licensed biological products, PDUFA also imposes an annual PDUFA program fee. The FDA adjusts the PDUFA user fees on an annual basis. Under federal law, the submission of BLAs requiring clinical data is additionally subject to an application user fee, which for federal fiscal year 2023 is $3,242,026. The sponsor of an approved BLA is also subject to annual program fees, which for fiscal year 2023 are $393,933 per eligible product. Fee waivers or reductions are available in certain circumstances, including a waiver of the application fee for the first application filed by a small business. No user fees are assessed on BLAs for products designated as orphan drugs unless the application for the product also includes a non-orphan indication.
Within 60 days following submission of the application, the FDA reviews a BLA submitted to determine if it is substantially complete before the agency accepts it for filing. The FDA may refuse to file any BLA that it deems incomplete or not properly reviewable at the time of submission and may request additional information. In this event, the BLA must be resubmitted with the additional information. The resubmitted application also is subject to review before the FDA accepts it for filing. Once the submission is accepted for filing, the FDA begins an in-depth substantive review of the BLA. The FDA has agreed to specified performance goals in the review process of BLAs. Most such applications are meant to be reviewed within ten months from the filing date, and most applications for “priority review” products are meant to be reviewed within six months of the filing date. The review process and the PDUFA goal date may be extended by the FDA for three additional months to consider new information or clarification provided by the applicant to address an outstanding deficiency identified by the FDA following the original submission.
The FDA reviews the BLA to determine, among other things, whether the proposed product is safe, potent, and/or effective for its intended use, and has an acceptable purity profile, and whether the product is being manufactured in accordance with cGMP to assure and preserve the product’s identity, safety, strength, quality, potency and purity. The FDA may refer an application to an advisory committee for review, evaluation and recommendation as to whether the application should be approved, and applications for new molecular entities and original BLAs are generally discussed at advisory committee meetings unless the FDA determines that this type of consultation is not needed under the circumstances. The FDA is not bound by the recommendations of an advisory committee, but it considers such recommendations carefully when making decisions.
During the biological product approval process, the FDA also will determine whether a Risk Evaluation and Mitigation Strategy, or REMS, is necessary to assure the safe use of the biological product. To determine whether a REMS is needed, the FDA will consider the size of the population likely to use the product, seriousness of the disease, expected benefit of the product, expected duration of treatment, and seriousness of known or potential adverse events. REMS can include medication guides, physician communication plans for healthcare professionals, and elements to assure safe use, or EYASU. EYASU may include, but are not limited to, special training or certification for prescribing or dispending, dispensing only under certain circumstances, special monitoring, and the use of patient registries. The FDA may require a REMS before approval or post-approval if it becomes aware of a serious risk associated with the use of a product. If the FDA concludes a REMS is needed, the sponsor of the BLA must submit a proposed REMS. The FDA will not approve a BLA without a REMS, if required. The requirement for a REMS can materially affect the potential market and profitability of a product.
Before approving a BLA, the FDA will typically inspect the facilities at which the product is manufactured. These pre-licensing inspections may cover all facilities associated with a BLA submission, including component manufacturing, finished product manufacturing, and control testing laboratories. The FDA will not approve the product unless it is satisfied that the manufacturing establishments and processes supporting the BLA meet the appropriate requirements and comply with the applicable regulations (including cGMP requirements and adequate assurance for consistent commercial production of the product within required specifications). Additionally, before approving a BLA, the FDA will typically conduct a pre-approval inspection of regulated participants in clinical trials (for example, the sponsor, investigators responsible for specific sites, and CROs) to assure that the clinical trials were conducted in compliance with the IND and GCP requirements. To assure cGMP and GCP compliance, an applicant must incur significant expenditure of time, money and effort in the areas of training, record keeping, production, and quality control.
Notwithstanding the submission of relevant data and information, the FDA may ultimately decide that the BLA does not satisfy its regulatory criteria for approval and deny approval. Data obtained from clinical studies are not always conclusive and the FDA may interpret data differently than PDS interprets the same data. If the agency decides not to approve the BLA in its present form, the FDA will issue a complete response letter that describes all of the specific deficiencies in the BLA identified by the FDA. The deficiencies identified may be minor, for example, requiring labeling changes, or major, for example, requiring additional clinical studies. Additionally, the complete response letter may include recommended actions that the applicant might take to place the application in a condition for approval. If a complete response letter is issued, the applicant may either resubmit the BLA, addressing all of the deficiencies identified in the letter, or withdraw the application. Even if the submission is re-submitted with additional information, the FDA ultimately may decide that the application does not satisfy the regulatory criteria for approval.
If a product receives regulatory approval, the approval may be significantly limited to specific diseases and dosages or the indications for use may otherwise be limited, which could restrict the commercial value of the product.
Further, the FDA may require that certain contraindications, warnings or precautions be included in the product labeling. The FDA may impose restrictions and conditions on product distribution, prescribing, or dispensing in the form of a risk management plan, or otherwise limit the scope of any approval. In addition, the FDA may require post marketing clinical studies, sometimes referred to as Phase 4 clinical studies, designed to further assess a biological product’s safety and effectiveness, and testing and surveillance programs to monitor the safety of approved products that have been commercialized. The FDA may prevent or limit further marketing of a product based on the results of post-market studies or surveillance programs. After approval, many types of changes to the approved product, such as adding new indications, manufacturing changes and additional labeling claims, are subject to further testing requirements and FDA review and approval.
In addition, under the Pediatric Research Equity Act, a BLA or supplement to a BLA for a new indication, dosage form, dosage regimen, or route of administration must contain data that are adequate to assess the safety and effectiveness of the product for the claimed indications in all relevant pediatric subpopulations and to support dosing and administration for each pediatric subpopulation for which the product is safe and effective. The FDA may, on its own initiative or at the request of the applicant, grant deferrals for submission of some or all pediatric data until after approval of the product for use in adults, or full or partial waivers from the pediatric data requirements.
Fast track, breakthrough therapy and priority review designations
The FDA is authorized to designate certain products for expedited review if they are intended to address an unmet medical need in the treatment of a serious or life-threatening disease or condition. These programs are referred to as fast track designation, breakthrough therapy designation and priority review designation. In May 2014, the FDA published a final Guidance for Industry titled “Expedited Programs for Serious Conditions-Drugs and Biologics,” which provides guidance on the FDA programs that are intended to facilitate and expedite development and review of new product candidates as well as threshold criteria generally applicable to concluding that a product candidate is a candidate for these expedited development and review programs.
Specifically, the FDA may designate a product for Fast Track review if it is intended, whether alone or in combination with one or more other products, for the treatment of a serious or life-threatening disease or condition, and it demonstrates the potential to address unmet medical needs for such a disease or condition. For Fast Track products, sponsors may have greater interactions with the FDA and the FDA may initiate review of sections of a Fast Track product’s application before the application is complete. This rolling review may be available if the FDA determines, after preliminary evaluation of clinical data submitted by the sponsor, that a Fast Track product may be effective. The sponsor must also provide, and the FDA must approve, a schedule for the submission of the remaining information and the sponsor must pay applicable user fees. However, the FDA’s time period goal for reviewing a Fast Track application does not begin until the last section of the application is submitted. In addition, the Fast Track designation may be withdrawn by the FDA if the FDA believes that the designation is no longer supported by data emerging in the clinical trial process.
Second, a product may be designated as a Breakthrough Therapy if it is intended, either alone or in combination with one or more other products, to treat a serious or life-threatening disease or condition and preliminary clinical evidence indicates that the product may demonstrate substantial improvement over existing therapies on one or more clinically significant endpoints, such as substantial treatment effects observed early in clinical development. The FDA may take certain actions with respect to Breakthrough Therapies, including holding meetings with the sponsor throughout the development process; providing timely advice to the product sponsor regarding development and approval; involving more senior staff in the review process; assigning a cross-disciplinary project lead for the review team; and taking other steps to design the clinical trials in an efficient manner.
Third, the FDA may designate a product for priority review if it is a product that treats a serious condition and, if approved, would provide a significant improvement in safety or effectiveness. The FDA determines, on a case-by-case basis, whether the proposed product represents a significant improvement when compared with other available therapies. Significant improvement may be illustrated by evidence of increased effectiveness in the treatment of a condition, elimination or substantial reduction of a treatment-limiting product reaction, documented enhancement of patient compliance that may lead to improvement in serious outcomes, and evidence of safety and effectiveness in a new subpopulation. A priority designation is intended to direct overall attention and resources to the evaluation of such applications, and to shorten the FDA’s goal for taking action on a marketing application from ten months to six months.
Accelerated approval pathway
The FDA may grant accelerated approval to a drug for a serious or life-threatening condition that provides meaningful therapeutic advantage to patients over existing treatments based upon a determination that the drug has an effect on a surrogate endpoint that is reasonably likely to predict clinical benefit. The FDA may also grant accelerated approval for such a condition when the product has an effect on an intermediate clinical endpoint that can be measured earlier than an effect on irreversible morbidity or mortality, or IMM, and that is reasonably likely to predict an effect on irreversible morbidity or mortality or other clinical benefit, taking into account the severity, rarity or prevalence of the condition and the availability or lack of alternative treatments. Drugs granted accelerated approval must meet the same statutory standards for safety and effectiveness as those granted traditional approval.
For the purposes of accelerated approval, a surrogate endpoint is a marker, such as a laboratory measurement, radiographic image, physical sign or other measure that is thought to predict clinical benefit, but is not itself a measure of clinical benefit. Surrogate endpoints can often be measured more easily or more rapidly than clinical endpoints. An intermediate clinical endpoint is a measurement of a therapeutic effect that is considered reasonably likely to predict the clinical benefit of a drug, such as an effect on IMM. The FDA has limited experience with accelerated approvals based on intermediate clinical endpoints, but has indicated that such endpoints generally may support accelerated approval where the therapeutic effect measured by the endpoint is not itself a clinical benefit and basis for traditional approval, if there is a basis for concluding that the therapeutic effect is reasonably likely to predict the ultimate clinical benefit of a drug.
The accelerated approval pathway is most often used in settings in which the course of a disease is long and an extended period of time is required to measure the intended clinical benefit of a drug, even if the effect on the surrogate or intermediate clinical endpoint occurs rapidly. Thus, accelerated approval has been used extensively in the development and approval of drugs for treatment of a variety of cancers in which the goal of therapy is generally to improve survival or decrease morbidity and the duration of the typical disease course requires lengthy and sometimes large trials to demonstrate a clinical or survival benefit.
The accelerated approval pathway is contingent on a sponsor’s agreement to conduct, in a diligent manner, additional post-approval confirmatory studies to verify and describe the drug’s clinical benefit. As a result, a drug candidate approved on this basis is subject to rigorous post-marketing compliance requirements, including the completion of Phase 4 or post-approval clinical trials to confirm the effect on the clinical endpoint. Failure to conduct required post-approval studies, or confirm a clinical benefit during post-marketing studies, would allow the FDA to withdraw the drug from the market on an expedited basis. All promotional materials for drug candidates approved under accelerated regulations are subject to prior review by the FDA.
Even if a product qualifies for one or more of these programs, the FDA may later decide that the product no longer meets the conditions for qualification or decide that the time period for FDA review or approval will not be shortened. In addition, the manufacturer of an investigational drug for a serious or life-threatening disease is required to make available, such as by posting on its website, its policy on responding to requests for expanded access. Furthermore, fast track designation, breakthrough therapy designation, accelerated approval and priority review do not change the standards for approval and may not ultimately expedite the development or approval process.
Post-Approval Requirements
Any products for which PDS receives FDA approvals are subject to continuing regulation by the FDA, including, among other things, record-keeping requirements, reporting of adverse experiences with the product, providing the FDA with updated safety and efficacy information, product sampling and distribution requirements, and complying with FDA promotion and advertising requirements, which include, among others, standards for direct-to-consumer advertising, restrictions on promoting products for uses or in patient populations that are not described in the product’s approved uses or consistent with the approved labeling, known as ‘off-label’ use, limitations on industry-sponsored scientific and educational activities, and requirements for promotional activities involving the internet. Although physicians may prescribe legally available products for off-label uses, if the physicians deem to be appropriate in their professional medical judgment, manufacturers may not market or promote such off-label uses. Recent court decisions have impacted the FDA’s enforcement activity regarding off-label promotion in light of First Amendment considerations; however, there are still significant risks in this area in part due to the potential False Claims Act exposure. Further, the FDA has not materially changed its position on off-label promotion following legal setbacks on First Amendment grounds and the DOJ has consistently asserted in FCA briefings that “speech that serves as a conduit for violations of the law is not constitutionally protected.”
After approval, most changes to the approved product, such as adding new indications or other labeling claims, are subject to prior FDA review and approval. There also are continuing, annual user fee requirements for any marketed products and the establishments at which such products are manufactured, as well as new application fees for supplemental applications with clinical data.
In addition, quality control and manufacturing procedures must continue to conform to applicable manufacturing requirements after approval to ensure the long-term stability of the product. cGMP regulations require among other things, quality control and quality assurance as well as the corresponding maintenance of records and documentation and the obligation to investigate and correct any deviations from cGMP. Manufacturers and other entities involved in the manufacture and distribution of approved products are required to register their establishments with the FDA and certain state agencies and are subject to periodic unannounced inspections by the FDA and certain state agencies for compliance with cGMP and other laws. Accordingly, manufacturers must continue to expend time, money, and effort in the area of production and quality control to maintain cGMP compliance. Discovery of problems with a product after approval may result in restrictions on a product, manufacturer, or holder of an approved BLA, including, among other things, recall or withdrawal of the product from the market. In addition, changes to the manufacturing process are strictly regulated, and depending on the significance of the change, may require prior FDA approval before being implemented. Other types of changes to the approved product, such as adding new indications and claims, are also subject to further FDA review and approval.
The Drug Supply Chain Security Act, or DSCSA imposes obligations on manufacturers of prescription biopharmaceutical products for commercial distribution, regulating the distribution of the products at the federal level, and sets certain standards for federal or state registration and compliance of entities in the supply chain (manufacturers and repackagers, wholesale distributors, third-party logistics providers, and dispensers). The DSCSA preempts certain previously enacted state pedigree laws and the pedigree requirements of the Prescription Drug Marketing Act, or PDMA. Trading partners within the drug supply chain must now ensure certain product tracing requirements are met that they are doing business with other authorized trading partners; and they are required to exchange transaction information, transaction history, and transaction statements. Product identifier information (an aspect of the product tracing scheme) is also now required. The DSCSA requirements, development of standards, and the system for product tracing have been and will continue to be phased in over a period of years. The distribution of product samples continues to be regulated under the PDMA, and some states also impose regulations on drug sample distribution.
Once an approval is granted, the FDA may withdraw the approval if compliance with regulatory requirements and standards is not maintained or if problems occur after the product reaches the market. Later discovery of previously unknown problems with a product, including AEs of unanticipated severity or frequency, or with manufacturing processes, or failure to comply with regulatory requirements, may result in revisions to the approved labeling to add new safety information; imposition of post-market studies or clinical trials to assess new safety risks; or imposition of distribution or other restrictions under a REMS program. Other potential consequences include, among other things:
| ● | restrictions on the marketing or manufacturing of the product, including total or partial suspension of production, complete withdrawal of the product from the market or product recalls; |
| ● | fines, warning or untitled letters or holds on post-approval clinical trials; |
| ● | refusal of the FDA to approve pending BLAs or supplements to approved BLAs, or suspension or revocation of product license approvals; |
| ● | product seizure or detention, or refusal to permit the import or export of products; or |
| ● | injunctions or the imposition of civil or criminal penalties. |
In addition, the distribution of prescription drug products is subject to the Prescription Drug Marketing Act, or PDMA, which regulates the distribution of drugs and drug samples at the federal level, and sets minimum standards for the registration and regulation of drug distributors by the states. Both the PDMA and state laws limit the distribution of prescription drug product samples and impose requirements to ensure accountability in distribution.
Failure to comply with any of the FDA’s requirements could result in significant adverse enforcement actions. These include a variety of administrative or judicial sanctions, such as refusal to approve pending applications, license suspension or revocation, withdrawal of an approval, imposition of a clinical hold or termination of clinical trials, warning letters, untitled letters, modification of promotional materials or labeling, product recalls, product seizures or detentions, refusal to allow imports or exports, total or partial suspension of production or distribution, debarment, injunctions, fines, consent decrees, corporate integrity agreements, refusals of government contracts and new orders under existing contracts, exclusion from participation in federal and state healthcare programs, restitution, disgorgement or civil or criminal penalties, including fines and imprisonment. It is also possible that failure to comply with the FDA’s requirements relating to the promotion of prescription drugs may lead to investigations alleging violations of federal and state healthcare fraud and abuse and other laws, as well as state consumer protection laws. Any of these sanctions could result in adverse publicity, among other adverse consequences.
The FDA also may require post-marketing testing, known as Phase 4 testing, and surveillance to monitor the effects of an approved product. Discovery of previously unknown problems with a product or the failure to comply with applicable FDA requirements can have negative consequences, including adverse publicity, judicial or administrative enforcement, warning letters from the FDA, mandated corrective advertising or communications with doctors, and civil or criminal penalties, among others. Newly discovered or developed safety or effectiveness data may require changes to a product’s approved labeling, including the addition of new warnings and contraindications, and also may require the implementation of other risk management measures. Also, new government requirements, including those resulting from new legislation, may be established, or the FDA’s policies may change, which could delay or prevent regulatory approval of its product candidates under development.
Regulatory Exclusivities Applicable to Biologics and Related Matters
Abbreviated Licensure Pathway for Biosimilars: The Biologics Price Competition and Innovation Act of 2009 (BPCIA) amended the PHSA to create an abbreviated approval pathway for “biosimilar” biologics, that is, those shown to be highly similar to an already-FDA-licensed reference biologic. The abbreviated approval process for biosimilars under the BPCIA is similar in concept to the Abbreviated New Drug Application (“ANDA”) for generic small molecule drugs established by the Drug Price Competition and Patent Term Restoration Act of 1984 (“Hatch-Waxman”) amendments to the FDCA. As with Hatch-Waxman, the goal of the BPCIA was to increase access to lower-priced versions of drugs, while balancing the need to continue incentivizing innovation in drug development. Biosimilarity is defined to mean that the proposed biologic is highly similar to the reference product notwithstanding minor differences in clinically inactive components and that there are no clinically meaningful differences between the biological product and the reference product in terms of the safety, purity and potency of the product. Further, a biosimilar may be determined to be “interchangeable” with the reference product, in which case the biosimilar may be substituted for the reference product under state substitution laws, similar to the way generic small molecule drugs are substituted. The higher standard of interchangeability requires a showing that the biosimilar is expected to produce the same clinical result as the reference biologic in any given patient, and further that the risk to the patient in terms of safety, purity, and/or potency pf switching between the biosimilar and the reference product is no more than using the reference product without switching.
Regulatory Exclusivities Applicable to Biologics Under the BPCIA: The BPCIA established certain regulatory exclusivities that provide reference biologics with prescribed periods of time during which competing biosimilars or interchangeable biosimilars may not be approved or may not be marketed. Once its BLA is approved (“date of first licensure) the reference biologic is entitled to a period of four years after its date of first licensure during which time FDA is prohibited from accepting a marketing application that would seek approval of any products that are biosimilar to the branded product. In addition, the reference biologic is entitled to a period of 12 years after its date of first licensure during which time FDA is prohibited from approving marketing applications for any products that are biosimilar to the branded product. In addition, the first interchangeable biosimilar may be entitled to a period of one year after its date of first licensure, or other periods keyed to the outcome of patent litigation if instituted, during which FDA is prohibited from finding that any other biosimilars are interchangeable to the same reference biologic. The reference biologic may also be entitled to regulatory exclusivity under other statutory provisions that apply to biologics and small molecule drugs.
Orphan Drug Exclusivity: Under the Orphan Drug Act, the FDA may designate a drug product as an “orphan drug” if it is intended to treat a rare disease or condition (generally meaning that it affects fewer than 200,000 individuals in the United States, or more in cases in which there is no reasonable expectation that the cost of developing and making a drug product available in the United States for treatment of the disease or condition will be recovered from sales of the product). A company must request orphan product designation before submitting an NDA. If the request is granted, the FDA will disclose the identity of the therapeutic agent and its potential use. Orphan product designation does not convey any advantage in or shorten the duration of the regulatory review and approval process. Among the other benefits of orphan drug designation are tax credits for certain research and an exemption from the NDA or BLA application fee. The FDA may revoke orphan drug designation, and if it does, it will publicize that the drug is no longer designated as an orphan drug.
If the sponsor of a product with orphan designation receives the first FDA approval for that drug for the disease or condition for which it has such designation or for a select indication or use within the rare disease or condition for which it was designated, the product generally will receive orphan product exclusivity. Orphan product exclusivity means that the FDA may not approve any other applications for the same product for the same indication for seven years, except in certain limited circumstances. If a drug or drug product designated as an orphan product ultimately receives marketing approval for an indication broader than what was designated in its orphan product application, it may not be entitled to exclusivity. Orphan drug exclusivity, however, could also block the approval of one of our therapeutic candidates for seven years if a competitor obtains orphan drug designation and FDA approval of the same therapeutic candidate for the same condition or disease as our orphan-designated drug.
Orphan exclusivity will not bar approval of another product under certain circumstances, including if a subsequent product with the same active ingredient for the same indication is shown to be clinically superior to the approved product on the basis of greater efficacy or safety, or providing a major contribution to patient care, or if the company with orphan drug exclusivity is not able to meet market demand. Further, the FDA may approve more than one product for the same orphan indication or disease as long as the products contain different active ingredients. Moreover, competitors may receive approval of different products for the indication for which the orphan product has exclusivity or obtain approval for the same product but for a different indication for which the orphan product has exclusivity.
In addition, as the FDA has interpreted the Orphan Drug Act, even if a previously approved same drug does not have unexpired orphan exclusivity, a demonstration of clinical superiority is required for a subsequent marketing application for the same orphan-designated drug for the same disease or condition to be awarded a 7-year period of orphan exclusivity upon marketing approval. In recent years, there have been multiple legal challenges to this FDA interpretation, and in August 2017, Congress amended the orphan drug provisions of the FDCA through enactment of the FDA Reauthorization Act of 2017 to codify FDA’s longstanding interpretation. Section 527 of the FDCA now expressly provides that if a sponsor of an orphan-designated drug that is otherwise the same as an already approved drug for the same rare disease or condition is seeking orphan exclusivity, FDA shall require such sponsor, to demonstrate that such drug is clinically superior to any already approved or licensed drug that is the same drug in order to obtain orphan drug exclusivity.
In September 2021, the United States Court of Appeals for the Eleventh Circuit decided in Catalyst Pharmaceuticals, Inc. v. FDA that the FDA’s interpretation of orphan drug exclusivity “for the same drug for the same disease or condition” as meaning the same “use or indication” was inappropriately narrow. This decision had the potential to significantly broaden the scope of orphan drug exclusivity for drugs that receive marketing approval for orphan indications that are narrower than their orphan-designated conditions in the United States. On January 24, 2023, the FDA issued a statement to address the uncertainty created by the circuit court’s decision in Catalyst. This notification announced that, at this time, in matters beyond the scope of that court order (i.e., ordering the FDA to set aside its approval of the specific drug at issue), the FDA intends to continue to apply its existing regulations tying orphan-drug exclusivity to the uses or indications for which the orphan drug was approved. We cannot guarantee which rules and interpretations will be governing going forward in different situations, that the FDA will maintain this current position, or that other judicial actions will not impact the FDA’s application of the Orphan Drug Act.
Pediatric Study Requirements and Pediatric Exclusivity: Under the Best Pharmaceuticals for Children Act (BPCA), a sponsor qualifies for “pediatric exclusivity” if it complies with a Written Request (WR) issued by FDA for pediatric studies. The sponsor may apply to FDA to issue a WR. Pediatric exclusivity operates by adding six months of exclusivity on to the end of the latest-expiring form of exclusivity and may apply to patent rights or to FDA regulatory exclusivities. To qualify for pediatric exclusivity, at least one of those rights must still be currently in force at the time FDA approves the pediatric studies.
Under the Pediatric Research Equity Act of 2003, an NDA, BLA, or supplement thereto must contain data that are adequate to assess the safety and effectiveness of the drug product for the claimed indications in all relevant pediatric subpopulations, and to support dosing and administration for each pediatric subpopulation for which the product is safe and effective. With enactment of the Food and Drug Administration Safety and Innovation Act of 2012 (FDASIA), sponsors must also submit pediatric study plans prior to the assessment data.
Those plans must contain an outline of the proposed pediatric study or studies the applicant plans to conduct, including study objectives and design, any deferral or waiver requests, and other information required by regulation. The applicant, the FDA, and the FDA’s internal review committee must then review the information submitted, consult with each other, and agree upon a final plan. The FDA or the applicant may request an amendment to the plan at any time.
The FDA may, on its own initiative or at the request of the applicant, grant deferrals for submission of some or all pediatric data until after approval of the product for use in adults, or full or partial waivers from the pediatric data requirements. Additional requirements and procedures relating to deferral requests and requests for extension of deferrals are contained in FDASIA. Unless otherwise required by regulation, the pediatric data requirements do not apply to products with orphan designation.
Patent Term Extensions: Patents have a limited lifespan. In most countries, including the U.S., the standard expiration of a patent is 20 years from the effective filing date. Various extensions of patent terms may be available in certain circumstances, for example where there are delays in obtaining FDA regulatory approvals that result in a reduction of the period of time during which we could market a product under patent protection. In the U.S., a patent claiming a new drug product may be eligible for a limited patent term extension under the Hatch-Waxman Act, which permits a patent restoration of up to five years for patent term lost during product development and the FDA regulatory review. The restoration period granted is typically one-half the time between the effective date of an IND and the submission date of an NDA less any time the applicant did not act with due diligence during the period, plus the time between the submission date of an NDA and the ultimate approval date less any time the applicant did not act with due diligence during the period. Patent term restoration cannot be used to extend the remaining term of a patent past a total of 14 years from the product’s approval date. Only one patent applicable to an approved drug product is eligible for the extension, only those claims covering the approved drug, a method for using it, or a method for manufacturing it may be extended, and the application for the extension must be submitted prior to the expiration of the patent in question. A patent that covers multiple drugs for which approval is sought can only be extended in connection with one of the approvals. The USPTO reviews and approves the application for any patent term extension or restoration in consultation with the FDA. Similar provisions are available in Europe and other foreign jurisdictions to extend the term of a patent that covers an approved drug. In the future, if and when our products receive FDA approval, we expect to apply for patent term extensions on patents covering those products. We plan to seek patent term extensions to any of our issued patents in any jurisdiction where these are available, however there is no guarantee that the applicable authorities, including the FDA in the United States, will agree with our assessment of whether such extensions should be granted, and if granted, the length of such extensions. For more information regarding the risks related to our intellectual property, see “Risk Factors—Risks Related to Our Intellectual Property.”.
Other U.S. Healthcare Laws and Compliance Requirements
In the United States, PDS’s activities are potentially subject to regulation, either directly or indirectly, by various federal, state and local authorities in addition to the FDA, including but not limited to, the Centers for Medicare and Medicaid Services, or CMS, other divisions of the U.S. Department of Health and Human Services, for instance the Office of Inspector General (OIG), the U.S. Department of Justice (DOJ), and individual U.S. Attorney offices within the DOJ, and state and local governments. For example, sales, marketing and scientific/educational grant programs must comply with the anti-fraud and abuse provisions of the Social Security Act, the criminal provisions of the Health Insurance Portability and Accountability Act of 1996 (HIPAA), the federal Anti-Kickback Statute, the federal false claims laws, the physician payment transparency laws, and similar state laws, each as amended. The compliance and enforcement landscape, and related risk, is informed by government enforcement precedent and settlement history, Advisory Opinions, and Special Fraud Alerts. Our approach to compliance may evolve over time in light of these types of developments.
The federal Anti-Kickback Statute prohibits, among other things, any person or entity, from knowingly and willfully offering, paying, soliciting or receiving any remuneration, directly or indirectly, overtly or covertly, in cash or in kind, to induce or in return for purchasing, leasing, ordering or arranging for the purchase, lease or order of any item or service reimbursable under Medicare, Medicaid or other federal healthcare programs. The term remuneration has been interpreted broadly to include anything of value. The Anti-Kickback Statute has been interpreted to apply to arrangements between pharmaceutical manufacturers on one hand and prescribers, purchasers, and formulary managers on the other. There are a number of statutory exceptions and regulatory safe harbors protecting some common activities from prosecution. The exceptions and safe harbors are drawn narrowly and practices that involve remuneration that may be alleged to be intended to induce prescribing, purchasing or recommending may be subject to scrutiny if they do not qualify for an exception or safe harbor. Failure to meet all of the requirements of a particular applicable statutory exception or regulatory safe harbor, however, does not make the conduct per se illegal under the Anti-Kickback Statute. Instead, the legality of the arrangement will be evaluated on a case-by-case basis based on a cumulative review of all of its facts and circumstances. PDS’s practices may not in all cases meet all of the criteria for protection under a statutory exception or regulatory safe harbor. The lack of uniform court interpretation of the Anti-Kickback Statute combined with emerging, novel enforcement theories, makes compliance with the law difficult. The potential safe harbors available are subject to change through legislative and regulatory action, and we may decide to adjust our business practices or be subject to heightened scrutiny as a result. Violations of the federal Anti-Kickback Statute can result in significant criminal fines, exclusion from participation in Medicare and Medicaid and follow-on civil litigation, among other things, for both entities and individuals.
Additionally, the intent standard under the Anti-Kickback Statute was amended by the Affordable Care Act to a stricter standard such that a person or entity no longer needs to have actual knowledge of the statute or specific intent to violate it in order to have committed a violation. In addition, the Affordable Care Act codified case law that a claim including items or services resulting from a violation of the federal Anti-Kickback Statute constitutes a per se false or fraudulent claim for purposes of the federal False Claims Act, as discussed below.
The Criminal Healthcare Fraud statute, 18 U.S.C. § 1347 prohibits knowingly and willfully executing a scheme to defraud any healthcare benefit program, including private third-party payers. Federal criminal law at 18 U.S.C. § 1001, among other sections, prohibits knowingly and willfully falsifying, concealing or covering up a material fact or making any materially false, fictitious or fraudulent statement in connection with the delivery of or payment for healthcare benefits, items or services.
The civil monetary penalties statute imposes penalties against any person or entity that, among other things, is determined to have presented or caused to be presented a claim to a federal health program that the person knows or should know is for an item or service that was not provided as claimed or is false or fraudulent. The Federal Civil Monetary Penalties Law authorizes the imposition of substantial civil monetary penalties against an entity, such as a pharmaceutical manufacturer, that engages in activities including, among others (1) knowingly presenting, or causing to be presented, a claim for services not provided as claimed or that is otherwise false or fraudulent in any way; (2) arranging for or contracting with an individual or entity that is excluded from participation in federal healthcare programs to provide items or services reimbursable by a federal healthcare program; (3) violations of the federal Anti-Kickback Statute; or (4) failing to report and return a known overpayment.
The federal False Claims Act prohibits, among other things, any person or entity from knowingly presenting, or causing to be presented, a false claim for payment to, or approval by, the federal government or knowingly making, using, or causing to be made or used a false record or statement material to a false or fraudulent claim to the federal government. The qui tam provisions of the False Claims Act and similar state laws allow a private individual to bring civil actions on behalf of the federal or state government and to share in any monetary recovery. As a result of a modification made by the Fraud Enforcement and Recovery Act of 2009, a claim includes “any request or demand” for money or property presented to the U.S. government, whether directly or indirectly. Recently, several pharmaceutical and other healthcare companies have been prosecuted under these laws for allegedly providing free product to customers with the expectation that the customers would bill federal programs for the product.
Other companies have been prosecuted for causing false claims to be submitted because of the companies’ marketing of the product for unapproved, and thus non-reimbursable, uses.
HIPAA created new federal criminal statutes that prohibit knowingly and willfully executing, or attempting to execute, a scheme to defraud or to obtain, by means of false or fraudulent pretenses, representations or promises, any money or property owned by, or under the control or custody of, any healthcare benefit program, including private third-party payors and knowingly and willfully falsifying, concealing or covering up by trick, scheme or device, a material fact or making any materially false, fictitious or fraudulent statement in connection with the delivery of or payment for healthcare benefits, items or services. Similar to the federal Anti-Kickback Statute, a person or entity does not need to have actual knowledge of the statute or specific intent to violate it in order to have committed a violation.
Also, many states have enacted similar fraud and abuse statutes or regulations that apply to items and services reimbursed under Medicaid and other state programs, or, in several states, apply regardless of the payor, even extending to self-pay items and services.
PDS may be subject to data privacy and security regulations by both the federal government and the states in which it conducts its business. We are not a covered entity under HIPAA and have not functioned as a business associate under HIPAA that would cause the HIPAA Security Rule and provisions of the Privacy Rule to apply directly to us as a business associate. To the extent that we ever function in a business associate capacity, HIPAA, as amended by the HITECH Act, and its respective implementing regulations, including the final omnibus rule published on January 25, 2013, imposes requirements relating to the privacy, security and transmission of individually identifiable health information. Following enactment of the HITECH Act, HIPAA’s privacy and security standards now directly apply to business associates of covered entities that receive or obtain protected health information in connection with providing a service on behalf of a covered entity. HITECH also created four new tiers of civil monetary penalties, gave state attorneys general new authority to file civil actions for damages or injunctions in federal courts to enforce the federal HIPAA laws and seek attorneys’ fees and costs associated with pursuing federal civil actions. In addition, state laws govern the privacy and security of health information in specified circumstances, many of which differ from each other in significant ways, and may apply more broadly thus complicating compliance efforts (for example, California recently enacted legislation — the California Consumer Privacy Act, or CCPA — which went into effect on January 1, 2020 and among other things, creates new data privacy obligations for covered companies and provides new privacy rights to California residents, including the right to opt out of certain disclosures of their information, and creates a private right of action with statutory damages for certain data breaches. The CCPA was recently amended by the California Privacy Rights Act, or CPRA, expanding certain consumer rights such as the right to know. It remains unclear what, if any, additional modifications will be made to these laws by the California legislature or how these laws will be interpreted and enforced. The potential effects of the CCPA and CPRA and implementing regulations are significant and may cause us to incur substantial costs and expenses to comply.
Even for entities that are not deemed “covered entities” or “business associates” under HIPAA, according to the United States Federal Trade Commission, or the FTC, failing to take appropriate steps to keep consumers’ personal information secure constitutes unfair acts or practices in or affecting commerce in violation of Section 5(a) of the Federal Trade Commission Act, or the FTCA, 15 USC § 45(a). The FTC expects a company’s data security measures to be reasonable and appropriate in light of the sensitivity and volume of consumer information it holds, the size and complexity of its business, and the cost of available tools to improve security and reduce vulnerabilities. Medical data is considered sensitive data that merits stronger safeguards. The FTC’s guidance for appropriately securing consumers’ personal information is similar to what is required by the HIPAA Security Rule. The FTC’s authority under Section 5 is concurrent with HIPAA’s jurisdiction and with any action taken under state law.
Additionally, the Federal Physician Payments Sunshine Act under the Affordable Care Act, and its implementing regulations, require that certain manufacturers of drugs, devices, biological and medical supplies for which payment is available under Medicare, Medicaid or the Children’s Health Insurance Program, with certain exceptions, report information related to certain payments or other transfers of value made or distributed to physicians and teaching hospitals, or to entities or individuals at the request of, or designated on behalf of, the physicians and teaching hospitals and to report annually certain ownership and investment interests held by physicians and their immediate family members. Failure to submit timely, accurately, and completely the required information may result in civil monetary penalties of up to an aggregate of $150,000 per year and up to an aggregate of $1 million per year for “knowing failures”. In 2022 the Sunshine Act reporting will be extended to payments and transfers of value to physician assistants, nurse practitioners, and other mid-level practitioners (with reporting requirements going into effect in 2022 for payments made in 2021). Certain states also mandate implementation of compliance programs, impose restrictions on pharmaceutical manufacturer marketing practices and/or require the tracking and reporting of gifts, compensation and other remuneration to healthcare providers and entities.
In order to distribute products commercially, PDS must also comply with state laws that require the registration of manufacturers and wholesale distributors of drug and biological products in a state, including, in certain states, manufacturers and distributors who ship products into the state even if such manufacturers or distributors have no place of business within the state. Several states have enacted legislation requiring pharmaceutical and biotechnology companies to establish marketing compliance programs, file periodic reports with the state, make periodic public disclosures on sales, marketing, pricing, clinical studies and other activities, and/or register their sales representatives, as well as to prohibit pharmacies and other healthcare entities from providing certain physician prescribing data to pharmaceutical and biotechnology companies for use in sales and marketing, and to prohibit certain other sales and marketing practices. All of PDS’s activities are potentially subject to federal and state consumer protection and unfair competition laws.
We expect that one or more of our products, if approved, may be eligible for coverage under Medicare, the federal health care program that provides health care benefits to the aged and disabled, including coverage for outpatient services and supplies, such as certain drug products, that are medically necessary to treat a beneficiary’s health condition. In addition, one or more of our products, if approved, may be covered and reimbursed under other federal health care programs, such as Medicaid and the 340B Drug Pricing Program. The Medicaid Drug Rebate Program requires pharmaceutical manufacturers to enter into and have in effect a national rebate agreement with the Secretary of the Department of Health and Human Services and pay quarterly rebates based on utilization of a manufacturer’s covered outpatient drugs under the program as a condition for states to receive federal matching funds for a manufacturer’s covered outpatient drugs furnished to Medicaid patients and in order for payment to be available for a manufacturer’s drugs under Medicare Part B. Pharmaceutical manufacturers are also required to participate in the 340B Drug Pricing Program in order for payment to be available for a manufacturer’s drugs under Medicaid and Medicare Part B. Under the 340B Drug Pricing Program, a manufacturer must charge no more than the 340B “ceiling price” for its covered outpatient drugs purchased by statutorily defined covered entities that participate in the program.
In addition, federal law requires that, in order for payment to be available for a manufacturer’s drugs under Medicaid and Medicare Part B, as well as to be purchased by certain federal agencies and grantees, it must also participate in the Department of Veterans Affairs (“VA”) Federal Supply Schedule (“FSS”) pricing program. To participate, manufacturers are required to enter into an FSS contract and other agreements with the VA for their covered drugs. Under these agreements, manufacturers must make their covered drugs available to the “Big Four” federal agencies— the VA, the Department of Defense (“DoD”), the Public Health Service (including the Indian Health Service), and the Coast Guard—at pricing that is capped pursuant to a statutory federal ceiling price, or FCP, formula. The FCP is based on a weighted average non-federal average manufacturer price, which manufacturers are required to report on a quarterly and annual basis to the VA. Further, pursuant to regulations issued by the DoD to implement Section 703 of the National Defense Authorization Act for Fiscal Year 2008, manufacturers may enter into an agreement with the Defense Health Agency (DHA) under which they agree to honor “Big Four” pricing for their covered drugs when they are dispensed to TRICARE beneficiaries by TRICARE retail network pharmacies.
As part of the requirements to participate in these government programs, many pharmaceutical manufacturers must calculate and report certain price reporting metrics to the government, such as average manufacturer price, best price, average sales price, and non-federal average manufacturer price. The calculations can be complex and are often subject to interpretation by manufacturers, governmental or regulatory agencies and the courts. Governmental agencies may also make changes in program interpretations, requirements, or conditions of participation, some of which may have implications for amounts previously estimated or paid. Any failure to comply with these price reporting and rebate payment obligations, when applicable, could negatively impact our financial results. Civil monetary penalties can be applied if a manufacturer is found to have knowingly submitted any false price information to the government, if a manufacturer is found to have made a misrepresentation in the reporting of its average sales price, or if a manufacturer fails to submit the required price data on a timely basis. Such conduct also could be grounds for CMS to terminate a manufacturer’s Medicaid drug rebate agreement, in which case federal payments may not be available under Medicaid or Medicare Part B for a manufacturer’s covered outpatient drugs and may provide a basis for other potential liability under other federal laws such as the False Claims Act.
Efforts to ensure that our business arrangements with third parties will comply with applicable healthcare laws and regulations will involve substantial costs. It is possible that governmental authorities will conclude that our business practices may not comply with current or future statutes, regulations, guidance, case law or other applicable law. If our operations are found to be in violation of any of these laws or any other governmental regulations that may apply to us, we may be subject to significant civil, criminal and administrative penalties, damages, fines, individual imprisonment, exclusion from participation in federal health care programs, such as Medicare and Medicaid, disgorgement, reputational harm, additional oversight and reporting obligations pursuant to a corporate integrity agreement or similar agreement to resolve allegations of non-compliance with applicable laws and regulations, and the curtailment or restructuring of our operations, any of which could adversely affect our ability to market our products, if approved, and adversely impact our financial results. Although effective compliance programs can mitigate the risk of investigation and prosecution for violations of these laws and regulations, these risks cannot be eliminated entirely. Any action against us for an alleged or suspected violation could cause us to incur significant legal expenses and could divert our management’s attention from the operation of our business, even if our defense is successful. If any of the physicians or other healthcare providers or entities with whom we expect to do business is found not to be in compliance with applicable laws, it may be costly to us in terms of money, time and resources, and they may be subject to criminal, civil or administrative sanctions, including exclusions from government-funded healthcare programs.
The scope and enforcement of each of these laws is uncertain and subject to rapid change in the current environment of healthcare reform, especially in light of the lack of applicable precedent and regulations. Federal and state enforcement bodies have recently increased their scrutiny of interactions between pharmaceutical companies and providers and patients, which has led to a number of investigations, prosecutions, convictions and settlements in the industry. Ensuring that business arrangements with third parties comply with applicable healthcare laws, as well as responding to possible investigations by government authorities, can be time- and resource-consuming and can divert management’s attention from the business, even if investigators ultimately find that no violation has occurred.
If PDS operations are found to be in violation of any of the federal and state healthcare laws described above or any other governmental regulations that apply to it, PDS may be subject to penalties, including without limitation, civil, criminal and/or administrative penalties; damages; fines; disgorgement; exclusion from participation in government programs, such as Medicare and Medicaid; injunctions; private “qui tam” actions brought by individual whistleblowers in the name of the government, or refusal to allow it to enter into government contracts; contractual damages; reputational harm; administrative burdens; diminished profits and future earnings; and the curtailment or restructuring of its operations; any of which could adversely affect PDS’s ability to operate its business and its results of operations.
In addition to the laws discussed above, we may see more stringent state and federal privacy legislation in the future, as the increased cyber-attacks during the COVID-19 pandemic have heightened attention to data privacy and security in the U.S. and other jurisdictions. We cannot predict where new legislation might arise, the scope of such legislation, or the potential impact to our business and operations.
Coverage, Pricing and Reimbursement
Significant uncertainty exists as to the coverage and reimbursement status of any product candidates for which PDS obtains regulatory approval. In the United States and markets in other countries, sales of any products for which PDS receives regulatory approval for commercial sale will depend, in part, on the extent to which third-party payors provide coverage, and establish adequate reimbursement levels for such products. In the United States, third-party payors include federal and state healthcare programs, private managed care providers, health insurers and other organizations. The process for determining whether a third-party payor will provide coverage for a product may be separate from the process for setting the price of a product or for establishing the reimbursement rate that such a payor will pay for the product. Third-party payors may limit coverage to specific products on an approved list, also known as a formulary, which might not include all of the FDA-approved products for a particular indication. Third-party payors are increasingly challenging the price, examining the medical necessity and reviewing the cost-effectiveness of medical products, therapies and services, in addition to questioning their safety and efficacy. PDS may need to conduct expensive pharmaco-economic studies in order to demonstrate the medical necessity and cost-effectiveness of its tablet product candidates, in addition to the costs required to obtain the FDA approvals. PDS’s product candidates may not be considered medically necessary or cost-effective. A payor’s decision to provide coverage for a product does not imply that an adequate reimbursement rate will be approved. No uniform policy requirement for coverage and reimbursement exists among third-party payors in the United States, which causes significant uncertainty related to the insurance coverage and reimbursement of newly approved products, and the procedures which may utilize such newly approved products. Further, one payor’s determination to provide coverage for a product does not assure that other payors will also provide coverage for the product. Therefore, coverage and reimbursement can differ significantly from payor to payor and health care provider to health care provider. As a result, the coverage determination process is often a time-consuming and costly process that requires the provision of scientific and clinical support for the use of new products to each payor separately, with no assurance that coverage and adequate reimbursement will be applied consistently or obtained in the first instance. Adequate third-party reimbursement may not be available to enable PDS to maintain price levels sufficient to realize an appropriate return on its investment in product development.
Different pricing and reimbursement schemes exist in other countries. Some jurisdictions operate positive and negative list systems under which products may only be marketed once a reimbursement price has been agreed. To obtain reimbursement or pricing approval, some of these countries may require the completion of clinical studies that compare the cost-effectiveness of a particular product candidate to currently available therapies. Other countries allow companies to fix their own prices for medicines, but monitor and control company profits. The downward pressure on health care costs has become very intense. As a result, increasingly high barriers are being erected to the entry of new products. In addition, in some countries, cross-border imports from low-priced markets exert a commercial pressure on pricing within a country.
The marketability of any product candidates for which it receives regulatory approval for commercial sale may suffer if the government and third-party payors fail to provide adequate coverage and reimbursement, or require onerous prior approvals or other restricted access. In addition, emphasis on managed care in the United States has increased and PDS expects the pressure on healthcare pricing will continue to increase. Coverage policies and third-party reimbursement rates may change at any time. Even if favorable coverage and reimbursement status is attained for one or more products for which PDS receives regulatory approval, less favorable coverage policies and reimbursement rates may be implemented in the future.
There may be significant delays in obtaining coverage and reimbursement for newly approved products, and coverage may be more limited than the purposes for which the product is approved by the FDA. Moreover, eligibility for coverage and reimbursement does not imply that a product, or the procedures which utilize such product, will be paid for in all cases or at a rate which the health care providers who purchase those products will find cost effective. Additionally, we expect pricing pressures in connection with the sale of any of our product candidates due to the trend toward managed healthcare, the increasing influence of health maintenance organizations, and additional legislative changes.
We cannot be sure that coverage and reimbursement will be available for any product that we commercialize, or the procedures which utilize such product, and, if reimbursement is available, what the level of reimbursement will be. Coverage and reimbursement may impact the demand for, or the price of, any product candidate for which we obtain marketing approval. If coverage and reimbursement are not available or reimbursement is available only to limited levels, we may not successfully commercialize any product candidate for which we obtain marketing approval.
U.S. Healthcare Reform
In recent years, there have been numerous initiatives on the federal and state levels in the United States for comprehensive reforms. In the United States and some foreign jurisdictions, there have been and continue to be a number of legislative and regulatory changes and proposed changes regarding the healthcare system that could prevent or delay marketing approval of our product candidates, restrict or regulate post-approval activities and affect our ability, or the ability of our future collaborators, to effectively sell any drugs for which we, or they, obtain marketing approval. We expect that current laws, as well as other healthcare reform measures that may be adopted in the future, may result in more rigorous coverage criteria and additional downward pressure on the price that we, or our future collaborators, may receive for any approved drugs. For example, the Patient Protection and Affordable Care Act, as amended by the Health Care and Education Reconciliation Act (collectively, “PPACA”) has substantially changed and continues to impact healthcare financing and delivery by both government payors and private insurers. Among the PPACA provisions of importance to the pharmaceutical industry, in addition to those otherwise described above, are the following:
| ● | an annual, nondeductible fee on any entity that manufactures or imports specified branded prescription drugs and biologic agents, apportioned among these entities according to their market share in certain federal programs identified in the PPACA; |
| ● | expansion of beneficiary eligibility criteria for Medicaid programs by, among other things, allowing states to offer Medicaid coverage to certain individuals with income at or below 138% of the federal poverty level, thereby potentially increasing manufacturers’ Medicaid rebate liability; |
| ● | expansion of manufacturers’ rebate liability under the Medicaid Drug Rebate Program by increasing the minimum rebate for both branded and generic drugs and revising the definition of “average manufacturer price” for calculating and reporting Medicaid drug rebates on outpatient prescription drug prices; |
| ● | extension of manufacturers’ Medicaid rebate liability to covered drugs dispensed to individuals who are enrolled in Medicaid managed care organizations; |
| ● | a separate methodology by which rebates owed by manufacturers under the Medicaid Drug Rebate Program are calculated for drugs that are inhaled, infused, instilled, implanted or injected; |
| ● | expansion of the types of entities eligible for the 340B drug discount program; |
| ● | establishment of the Medicare Part D coverage gap discount program that, as a condition for the manufacturers outpatient drugs to be covered under Medicare Part D, requires manufacturers to provide a now 70% point-of-sale-discount off the negotiated price of applicable brand drugs to eligible beneficiaries during their coverage gap period; |
| ● | establishment of the Center for Medicare and Medicaid Innovation within the Centers for Medicare and Medicaid Services to test innovative payment and service delivery models to lower Medicare and Medicaid spending, potentially including prescription drug spending; |
| ● | creation of the Patient-Centered Outcomes Research Institute to oversee, identify priorities in, and conduct comparative clinical effectiveness research, along with funding for such research; |
| ● | reporting of certain financial arrangements between manufacturers of drugs, biologics, devices, and medical supplies and physicians and teaching hospitals under the Physician Payments Sunshine Act; and |
| ● | annual reporting of certain information regarding drug samples that manufacturers and distributors provide to licensed practitioners. |
The framework of the PPACA continues to evolve as a result of executive, legislative, regulatory, and administrative developments that have challenged the law and contribute to legal uncertainty that could affect the profitability of our products. While Congress has not enacted legislation to comprehensively repeal the PPACA, legislation affecting the PPACA has been signed into law, including the elimination, effective January 1, 2019, of the tax-based shared responsibility payment imposed by the PPACA on certain individuals who fail to maintain qualifying health coverage for all or part of a year, which is commonly referred to as the “individual mandate.” In December 2018, a federal district court in Texas ruled that the PPACA’s individual mandate, without the penalty that was eliminated effective January 1, 2019, was unconstitutional and could not be severed from the PPACA. As a result, the court ruled the remaining provisions of the PPACA were also invalid. The Fifth Circuit Court of Appeals affirmed the district court’s ruling that the individual mandate was unconstitutional, but it remanded the case back to the district court for further analysis of whether the mandate could be severed from the PPACA (i.e., whether the entire PPACA was therefore also unconstitutional). On June 17, 2021, the U.S. Supreme Court dismissed this challenge without specifically ruling on the constitutionality of the PPACA.
Effective January 1, 2019, the Bipartisan Budget Act of 2018, among other things, further amended portions of the Social Security Act implemented as part of the PPACA to increase from 50% to 70% the point-of-sale discount that pharmaceutical manufacturers participating in the Coverage Gap Discount Program must provide to eligible Medicare Part D beneficiaries during the coverage gap phase of the Part D benefit, commonly referred to as the “donut hole,” and to reduce standard beneficiary cost sharing in the coverage gap from 30% to 25% in most Medicare Part D plans. In addition, the Further Consolidated Appropriations Act of 2020, signed into law December 20, 2019, fully repealed the PPACA’s “Cadillac Tax” on certain high-cost employer-sponsored insurance plans (for tax years beginning after December 31, 2019), the annual fee imposed on certain health insurance providers based on market share (for calendar year 2021), and the medical device excise tax on non-exempt medical devices (for sales after December 31, 2019). In the future, there may be additional challenges and/or amendments to the PPACA. It remains to be seen precisely what any new legislation will provide, when or if it will be enacted, and what impact it will have on the availability and cost of healthcare items and services, including drug products.
In addition, other legislative changes have been proposed and adopted since the PPACA was enacted. For example, the Budget Control Act of 2011, among other things, resulted in reductions in payments to Medicare providers of 2% per fiscal year, which went into effect on April 1, 2013 and, due to subsequent legislation, will remain in effect through 2031, with the exception of a temporary suspension of the payment reduction from May 1, 2020 through March 31, 2022 due to the coronavirus pandemic. Sequestration will start again on April 1, 2022. From April 1, 2022 to June 30, 2022, payment for Medicare fee-for-service claims will be adjusted downwards by 1%; beginning on July 1, 2022, the payment will be adjusted downwards by 2%. In addition, on March 11, 2021, President Biden signed the American Rescue Plan Act of 2021 into law, which eliminates the statutory Medicaid drug rebate cap, currently set at 100% of a drug’s average manufacturer price, for single source and innovator multiple source drugs, beginning January 1, 2024. Further, the American Taxpayer Relief Act of 2012, among other things, reduced CMS payments to several providers, including hospitals, and increased the statute of limitations period for the government to recover Medicare overpayments to providers from three to five years. These legislative changes may result in additional reductions in Medicare and other healthcare funding and otherwise affect the prices we may obtain for any of our product candidates for which we may obtain regulatory approval or the frequency with which any such product candidate is prescribed or used.
Recently, the cost of prescription pharmaceuticals has been the subject of considerable discussion in the United States. Congress considered and passed legislation, and the former Trump administration pursued several regulatory reforms to further increase transparency around prices and price increases, lower out-of-pocket costs for consumers, and decrease spending on prescription drugs by government programs. Congress also continued to conduct inquiries into the prescription drug industry’s pricing practices. While several proposed reform measures will require Congress to pass legislation to become effective, Congress and the Biden administration have each indicated that it will continue to seek new legislative and/or administrative measures to address prescription drug costs. The Biden administration has taken several recent executive actions that signal changes in policy from the prior administration. For example, on July 9, 2021, President Biden signed an executive order to promote competition in the US economy that included several initiatives addressing prescription drugs. Among other provisions, the executive order directed the Secretary of HHS to issue a report to the White House within 45 days that includes a plan to, among other things, reduce prices for prescription drugs, including prices paid by the federal government for such drugs. In response to the Executive Order, on September 9, 2021, HHS issued a Comprehensive Plan for Addressing High Drug Prices that identified potential legislative policies and administrative tools that Congress and the agency can pursue in order to make drug prices more affordable and equitable, improve and promote competition throughout the prescription drug industry, and foster scientific innovation. Additionally, on February 2, 2022, the Biden Administration signaled its continued commitment to the Cancer Moonshot initiative, which was initially launched in 2016. In its recent announcement, the administration noted that its new goals under the initiative include addressing inequities in order to ensure broader access to cutting-edge cancer therapeutics and investing in a robust pipeline for new treatments. At the state level, legislatures are increasingly passing legislation and states are implementing regulations designed to control spending on and patient out-of-pocket costs for drug products. Implementation of cost containment measures or other healthcare reforms that affect the pricing and/or availability of drug products may impact our ability to generate revenue, attain or maintain profitability, or commercialize products for which we may receive regulatory approval in the future.
Most recently, on August 16, 2022 the Inflation Reduction Act of 2022, or IRA was signed into law. Among other things, the IRA requires manufacturers of certain drugs to engage in price negotiations with Medicare (beginning in 2026), with prices that can be negotiated subject to a cap; imposes rebates under Medicare Part B and Medicare Part D to penalize price increases that outpace inflation (first due in 2023); and replaces the Part D coverage gap discount program with a new discounting program (beginning in 2025). The IRA permits the Secretary of the Department of Health and Human Services (HHS) to implement many of these provisions through guidance, as opposed to regulation, for the initial years. For that and other reasons, it is currently unclear how the IRA will be effectuated, and the impact of the IRA on the pharmaceutical industry cannot yet be fully determined.
We expect that these and other healthcare reform measures that may be adopted in the future may result in more rigorous coverage criteria and/or new payment methodologies, and place additional downward pressure on the price that we receive for any approved product and/or the level of reimbursement physicians and other healthcare providers receive for administering any approved product we might bring to market. Reductions in reimbursement levels and imposition of more rigorous coverage criteria or new payment methodologies may negatively impact the prices we receive or the frequency with which our products are prescribed or administered. Any coverage or reimbursement policies instituted by Medicare or other federal health care programs may result in similar policies from private payors. The implementation of cost containment measures or other healthcare reforms may affect our ability to generate revenue, attain or maintain profitability, or commercialize our drug candidates. We expect that additional state and federal healthcare reform measures will be adopted in the future, any of which could limit the amounts that federal and state governments will pay for healthcare products and services, which could result in reduced demand for our drug candidates or additional pricing pressures.
At the state level, legislatures have increasingly passed legislation and implemented regulations designed to control pharmaceutical and biological product pricing, including price or patient reimbursement constraints, discounts, restrictions on certain product access and marketing cost disclosure and transparency measures, and, in some cases, designed to encourage importation from other countries and bulk purchasing. In addition, regional health care authorities and individual hospitals are increasingly using bidding procedures to determine what pharmaceutical products and which suppliers will be included in their prescription drug and other health care programs. These measures could reduce the ultimate demand for our products or put pressure on our product pricing. We expect that additional state healthcare reform measures will be adopted in the future, which could limit the amounts that state governments will pay for healthcare products and services and result in additional pricing pressures. The boom in state laws targeting drug pricing is unprecedented and the requirements are not uniform from state to state, creating additional compliance and commercialization challenges for manufacturers. If PDS is able to obtain marketing approval for one or more of our products, our revenue and future profitability could be negatively affected if these or other inquiries were to result in legislative or regulatory proposals that limit our ability to increase the prices of any products for which we obtain marketing approval.
Foreign Regulation
In order to market any product outside of the United States, we would need to comply with numerous and varying regulatory requirements of other countries and jurisdictions regarding quality, safety and efficacy and governing, among other things, clinical studies, marketing authorization, commercial sales and distribution of its products. Whether or not PDS obtains FDA approval for a product, it would need to obtain the necessary approvals by the comparable foreign regulatory authorities before it can commence clinical studies or marketing of the product in foreign countries and jurisdictions. Although many of the issues discussed above with respect to the United States apply similarly in the context of the European Union, the approval process varies between countries and jurisdictions and can involve additional product testing and additional administrative review periods. The time required to obtain approval in other countries and jurisdictions might differ from and be longer than that required to obtain FDA approval. Regulatory approval in one country or jurisdiction does not ensure regulatory approval in another, but a failure or delay in obtaining regulatory approval in one country or jurisdiction may negatively impact the regulatory process in others.
European Union member states and other foreign jurisdictions, including Switzerland, have adopted data protection laws and regulations which impose significant compliance obligations. Moreover, the collection and use of personal health data in the European Union, which was formerly governed by the provisions of the European Union Data Protection Directive, was replaced with the European Union General Data Protection Regulation, or the GDPR, in May 2018. The GDPR, which is wide-ranging in scope, imposes several requirements relating to the consent of the individuals to whom the personal data relates, the information provided to the individuals, the security and confidentiality of the personal data, data breach notification and the use of third-party processors in connection with the processing of personal data. The GDPR also imposes strict rules on the transfer of personal data out of the European Union to the United States, provides an enforcement authority and imposes large penalties for noncompliance, including the potential for fines of up to €20 million or 4% of the annual global revenues of the noncompliant company, whichever is greater. The recent implementation of the GDPR has increased our responsibility and liability in relation to personal data that we process, including in clinical trials, and we may in the future be required to put in place additional mechanisms to ensure compliance with the GDPR, which could divert management’s attention and increase our cost of doing business. In addition, new regulation or legislative actions regarding data privacy and security (together with applicable industry standards) may increase our costs of doing business. In this regard, we expect that there will continue to be new proposed laws, regulations and industry standards relating to privacy and data protection in the United States, the European Union and other jurisdictions, and we cannot determine the impact such future laws, regulations and standards may have on our business.
Employees and Human Capital Management
Our management team possesses considerable experience in drug development research, manufacturing, clinical development and regulatory matters. PDS’ virtual operating strategy of collaborating with scientific and clinical experts in cancer immunology, tumor immunology and gynecological oncology provides additional considerable experience in immunotherapy development, clinical design and execution. We have no collective bargaining agreements with our employees and we have not experienced any work stoppages.
As of December 31, 2022, we had 26 employees, all of which were full time employees. Our employees are highly skilled, and many hold advanced degrees. We consider our relationship with our employees to be good. Our future performance depends significantly upon the continued service of our key scientific, technical, and senior management personnel and our continued ability to attract and retain highly skilled employees. We provide our employees with market salaries and bonuses, opportunities for equity ownership, development programs that enable continued learning and growth and a robust employment package that promotes well-being across all aspects of their lives. In addition to salaries, these programs include potential annual discretionary bonuses, stock awards, a 401(k) plan, healthcare and insurance benefits, health savings and flexible spending accounts, paid time off, family leave, and flexible work schedules, among other benefits.
Environmental Regulations
We believe we are compliant in all material respects with applicable environmental laws. Presently, we do not anticipate such compliance will have a material effect on capital expenditures, earnings, or our competitive position with respect to any of our operations.
The risks described below may not be the only ones relating to our company. Additional risks that we currently believe are immaterial may also impair our business operations. Our business, financial conditions and future prospects and the trading price of our common stock could be harmed as a result of any of these risks. Investors should also refer to the other information contained or incorporated by reference in this Annual Report on Form 10-K, including our financial statements and related notes, and our other filings from time to time with the Securities and Exchange Commission or SEC.
Risk Factors Summary
Our business is subject to a number of risks and uncertainties, including those risks discussed at length below. These risks include, among others, the following principal risk factors that make an investment in our company speculative or risky. You are encouraged to carefully review our full discussion of the material risk factors relevant to an investment in our business, which follows the brief bulleted list of our principal risk factors set forth below:
| ● | We have incurred significant losses since our inception and expect to continue to incur significant losses for the foreseeable future and may never achieve or maintain profitability. |
| ● | We are dependent on the success of our Versamune and Infectimune products, which are still in early-stage clinical development, and if our Versamune and Infectimune products do not receive regulatory approval or are not successfully commercialized, our business may be harmed. |
| ● | We have a limited operating history and have never generated any product revenue. |
| ● | We will require additional capital to fund our operations, , and if we fail to obtain necessary financing, we may not be able to complete the development and commercialization of our Versamune and Infectimune based products. |
| ● | Raising additional funds by issuing securities may cause dilution to existing stockholders and raising funds through lending and licensing arrangements may restrict our operations or require us to relinquish proprietary rights. |
| ● | We will need to expand our organization, and may experience difficulties in managing this growth, which could disrupt operations. |
| ● | Our employees, independent contractors, principal investigators, consultants, commercial collaborators, service providers and other vendors may engage in misconduct or other improper activities, including noncompliance with regulatory standards and requirements, which could have an adverse effect on our results of operations. |
| ● | If we fail to maintain an effective system of internal control over financial reporting in the future, we may not be able to accurately report our financial condition, results of operations or cash flows, which may adversely affect investor confidence in us and, as a result, the value of our common stock. Further, we continue to incur significant increased costs as a result of operating as a public company, and our management is required to devote substantial time to compliance initiatives. |
| ● | Our business and operations would suffer, and could be negatively affected, in the event of system failures or cyberattacks. |
| ● | Periodic reporting requirements under the Exchange Act and compliance with the Sarbanes-Oxley Act of 2002, including establishing and maintaining acceptable internal control over financial reporting, are costly and may increase substantially and, as a smaller reporting company, we may take advantage of reduced reporting requirements which may make our common stock less attractive to investors. |
| ● | Clinical trials are very expensive, time-consuming, difficult to design and implement and involve an uncertain outcome, and if they fail to demonstrate safety and efficacy to the satisfaction of the FDA, or similar regulatory authorities, we will be unable to commercialize PDS0101 and other Versamune and Infectimune based products. |
| ● | Enrollment and retention of subjects in clinical trials is an expensive and time-consuming process and could be made more difficult or rendered impossible by multiple factors outside our control. |
| ● | We face significant competition from other biotechnology and pharmaceutical companies, and our operating results will suffer if we fail to compete effectively. |
| ● | Our product candidates are in various stages of development and we will not be able to commercialize our product candidates if our preclinical studies do not produce successful results and/or our clinical trials do not demonstrate the safety and efficacy of our product candidates; early results and early understanding of product candidate potential may not be predictive of later success. |
| ● | We have no manufacturing, sales, marketing or distribution capability and we must rely upon third parties for such. |
| ● | If we are unable to establish sales, marketing and distribution capabilities either on our own or in collaboration with third parties, we may not be successful in commercializing PDS0101 and our other product candidates, if approved. |
| ● | If we obtain approval to commercialize PDS0101 and other candidates outside of the United States, a variety of risks associated with international operations could harm our business. |
| ● | Recently enacted and future healthcare legislation, regulations, and policy initiatives may increase the difficulty and cost for us to obtain marketing approval of and commercialize PDS0101 and our other product candidates and affect the prices we may obtain and our profitability. |
| ● | We rely, and intend to continue to rely, on third parties to conduct our clinical trials and perform some of our research and preclinical studies. If these third parties do not satisfactorily carry out their contractual duties, fail to comply with applicable regulatory requirements or do not meet expected deadlines, our development programs may be delayed or subject to increased costs or we may be unable to obtain regulatory approval, each of which may have an adverse effect on our business, financial condition, results of operations and prospects. |
| ● | Our stock price is expected to be volatile, and the market price of our common stock may drop in the future. |
| ● | We may expend our limited resources to pursue a particular product candidate or indication and fail to capitalize on product candidates or indications that may be more profitable or for which there is a greater likelihood of success. |
| ● | If we are unable to establish or manage strategic collaborations in the future, our revenue and drug development may be limited. |
| ● | Our business could be adversely affected by the effects of health epidemics, pandemics, or outbreaks of infectious diseases, including the recent COVID-19 pandemic, in regions where we or third parties on which we rely have significant manufacturing facilities, concentrations of clinical trial sites or other business operations. The COVID-19 pandemic could materially affect our operations, including at our headquarters in New Jersey, and at our clinical trial sites, as well as the business or operations of our manufacturers, CROs or other third parties with whom we conduct business. |
| ● | If we are unable to obtain and/or maintain patent protection for our Versamune, Versamune plus PDS0301 platforms, PDS0101, or other Versamune based Products or if the scope of the patent protection obtained is not sufficiently broad, we may not be able to compete effectively in our markets. |
| ● | We may be involved in lawsuits to protect or enforce our patents, the patents of our licensors or our other intellectual property rights, or defend our products and methods against the property rights of others, which could be expensive, time consuming and unsuccessful. |
| ● | If we fail to comply with federal and state healthcare regulatory laws, including in our relationships with healthcare providers and customers and third-party payors, we could face criminal prosecution and sanctions, substantial civil penalties, damages, fines, disgorgement, exclusion from participation in governmental healthcare programs, contractual damages, reputational harm, and the curtailment of our operations, any of which could harm our business. |
| ● | Our effective tax rate may increase in the future, including as a result of tax legislation changes, which may have a material adverse effect on our business, financial condition and results of operations. |
Risks Related to Our Business, Financial Position and Capital Requirements
We have a limited operating history and have never generated any product revenue.
We have no products approved for sale. We are a clinical-stage biopharmaceutical company with a limited operating history. Our operations to date have been limited to organizing our company and developing the Versamune platform and related immunotherapy product candidates that incorporate the technology of our Versamune platform. We have not yet successfully completed a large-scale, pivotal clinical trial, obtained marketing approval, manufactured Versamune at commercial scale, or conducted sales and marketing activities that will be necessary to successfully commercialize our Versamune products. Consequently, predictions about our future success or viability may not be as accurate as they could be if we had a longer operating history or a history of successfully developing and commercializing immunotherapies.
Our product candidates will require additional clinical development, evaluation of clinical, preclinical and manufacturing activities, marketing approval in multiple jurisdictions, substantial investment and significant marketing efforts before we generate any revenues from product sales. We are not permitted to market or promote any of our product candidates before we receive marketing approval from the FDA and comparable foreign regulatory authorities, and we may never receive such marketing approvals.
Our ability to generate revenue and achieve and maintain profitability will depend upon our ability to successfully complete the development of our Versamune based oncology products PDS0101, PDS0102, PDS0103, PDS0104, or PDS0301 and Infectimune to treat infectious diseases and to obtain the necessary regulatory approvals. We have never generated any product revenue and have no immunotherapy candidate in late-stage clinical development or approved for commercial sale.
Even if we receive regulatory approval for the sale of the Versamune, Versamune plus PDS0301 and Infectimune Products, we do not know when we will begin to generate revenue from PDS0101 or other products, if at all. Our ability to generate revenue depends on a number of factors, including our ability to:
| ● | set an acceptable price for Versamune based immunotherapy candidates, including the Versamune Products, and obtain coverage and adequate reimbursement from third-party payors; |
| ● | establish sales, marketing, manufacturing and distribution systems; |
| ● | add operational, financial and management information systems and personnel, including personnel to support our clinical, manufacturing and planned future clinical development and commercialization efforts and operations as a public company; |
| ● | develop manufacturing capabilities for bulk materials and manufacture commercial quantities of PDS0101 and other Versamune Products at acceptable cost levels; |
| ● | achieve broad market acceptance of PDS0101 and other Versamune, Versamune plus PDS0301 and Infectimune based-products in the medical community and with third-party payors and consumers; |
| ● | attract and retain an experienced management and advisory team; |
| ● | launch commercial sales of PDS0101 and other Versamune, Versamune plus PDS0301 and Infectimune based-products, whether alone or in collaboration with others; and |
| ● | maintain, expand and protect our intellectual property portfolio. |
Because of the numerous risks and uncertainties associated with immunotherapy development and manufacturing, we are unable to predict the timing or amount of increased development expenses, or when we will be able to achieve or maintain profitability, if at all. Our expenses could increase beyond expectations if we are required by the U.S. Food and Drug Administration, or FDA, or comparable non-U.S. regulatory authorities, to perform studies or clinical trials in addition to those we currently anticipate. Even if PDS0101 is approved for commercial sale, we anticipate incurring significant costs associated with the commercial launch of and the related commercial-scale manufacturing requirements for PDS0101 and other Versamune and Infectimune products. If we cannot successfully execute on any of the factors listed above, our business may not succeed, and your investment will be adversely affected.
We have incurred significant losses since our inception and expect to continue to incur significant losses for the foreseeable future and may never achieve or maintain profitability.
We have never generated any product revenues and expect to continue to incur substantial and increasing losses as we continue to develop PDS0101 and other Versamune and Infectimune based products. None of our products have been approved for marketing in the United States and may never receive such approval. As a result, we are uncertain when or if we will achieve profitability and, if so, whether we will be able to sustain it. Our ability to generate revenue and achieve profitability is dependent on our ability to complete development, obtain necessary regulatory approvals, and have our products manufactured and successfully marketed. We cannot assure you that we will be profitable even if we successfully commercialize PDS0101 or other Versamune and Infectimune based products. If we successfully obtain regulatory approval to market PDS0101, our revenues will be dependent, in part, upon, the size of the markets in the territories for which regulatory approval is received, the number of competitors in such markets for the approved indication, and the price at which we can offer our products. If the indication approved by regulatory authorities is narrower than we expect, or the treatment population is narrowed by competition, physician choice or treatment guidelines, we may not generate significant revenue from sales of our products, even if approved. Even if we do achieve profitability, we may not be able to sustain or increase profitability on a quarterly or annual basis. If we fail to become and remain profitable the market price of our common stock and our ability to raise capital and continue operations will be adversely affected.
We expect research and development expenses to increase significantly for PDS0101 and other Versamune and Infectimune based products. In addition, even if we obtain regulatory approval, significant sales and marketing expenses will be required to commercialize our products. As a result, we expect to continue to incur significant and increasing operating losses and negative cash flows for the foreseeable future. These losses have had and will continue to have an adverse effect on our financial position and working capital. As of December 31, 2022 and 2021, we had an accumulated deficit of $101.6 and $60.7 million, respectively.
We are dependent on the success of our Versamune and Infectimune products, which are still in early-stage clinical development, and if our Versamune and Infectimune products do not receive regulatory approval or are not successfully commercialized, our business may be harmed.
PDS0101 is only in mid clinical development, and as a consequence, it is too early to determine whether the Versamune and Infectimune based products will ever be approved for commercial sale or be marketable. We expect that a substantial portion of our efforts and expenditures over the next few years will be devoted to PDS0101 and other Versamune and Infectimune based products. Accordingly, our business currently depends heavily on the successful development, regulatory approval and commercialization of PDS0101. PDS0101 may not receive regulatory approval or be successfully commercialized even if regulatory approval is received. The research, testing, manufacturing, labeling, approval, sale, marketing and distribution of PDS0101 is and will remain subject to extensive regulation by the FDA and other regulatory authorities in the United States and other countries that each have differing regulations. We are not permitted to market PDS0101 in the United States until it receives approval of a biologics license application, or BLA, from the FDA, or in any foreign countries until it receives the requisite approval from such countries. To date, we have only completed Phase 1/2a clinical trials for certain applications of PDS0101. As a result, we have not submitted a BLA to the FDA or comparable applications to other regulatory authorities and do not expect to be in a position to do so for the foreseeable future. Obtaining approval of a BLA is an extensive, lengthy, expensive and inherently uncertain process, and the FDA may delay, limit or deny approval of PDS0101 for many reasons, including:
| ● | we may not be able to demonstrate that PDS0101 is safe and effective to the satisfaction of the FDA; |
| ● | the FDA may not agree that the completed Phase 2 clinical trials of PDS0101 satisfy the FDA’s requirements and may require us to conduct additional testing; |
| ● | the results of our future clinical trials may not meet the level of statistical or clinical significance required by the FDA for marketing approval; |
| ● | the FDA may disagree with the number, design, size, conduct or implementation of one or more of our clinical trials; |
| ● | the contract research organizations, or CROs, that we retain to conduct clinical trials may take actions outside of our control that materially and adversely impact our clinical trials; |
| ● | the FDA may not find the data from our preclinical studies and clinical trials sufficient to demonstrate that the clinical and other benefits of PDS0101 outweigh the safety risks; |
| ● | the FDA may disagree with our interpretation of data from our preclinical studies and clinical trials; |
| ● | the FDA may not accept data generated at our clinical trial sites; |
| ● | if our BLA is reviewed by an advisory committee, the FDA may have difficulties scheduling an advisory committee meeting in a timely manner or the advisory committee may recommend against approval of our application or may recommend that the FDA require, as a condition of approval, additional preclinical studies or clinical trials, limitations on approved labeling or distribution and use restrictions; |
| ● | the FDA may require development of a risk evaluation and mitigation strategy, or REMS, as a condition of approval; |
| ● | the FDA may identify deficiencies in our manufacturing processes or facilities; or |
| ● | the FDA may change its approval policies or adopt new regulations. |
We will require additional capital to fund our operations, and if we fail to obtain necessary financing, we may not be able to complete the development and commercialization of our Versamune and Infectimune based products.
We expect to spend substantial amounts to complete the development of, seek regulatory approvals for and commercialize PDS0101. Even with our current cash reserves, we will require substantial additional capital to complete the development and potential commercialization of PDS0101 and the development of other Versamune and Infectimune based products. If we are unable to raise capital or find appropriate partnering or licensing collaborations or other nondilutive financing, when needed or on acceptable terms, if at all, we could be forced to delay, reduce or eliminate one or more of our development programs or any future commercialization efforts. In addition, attempting to secure additional financing may divert the time and attention of our management from day-to-day activities and harm our development efforts.
Based upon our current operating plan, we believe that our cash reserves will be sufficient to fund our operating expenses and capital expenditure requirements for at least the next 24 months from the date of this report. Our estimate as to what we will be able to accomplish is based on assumptions that may prove to be inaccurate, and we could exhaust our available capital resources sooner than is currently expected. Because the length of time and activities associated with successful development of PDS0101 is highly uncertain, we are unable to estimate the actual funds we will require for development and any approved marketing and commercialization activities. Our future funding requirements, both near and long-term, will depend on many factors, including, but not limited to:
| ● | the initiation, progress, timing, costs and results of our planned clinical trials; |
| ● | the outcome, timing and cost of meeting regulatory requirements established by the FDA and other comparable foreign regulatory authorities; |
| ● | the cost of filing, prosecuting, defending and enforcing our patent claims and other intellectual property rights; |
| ● | the cost of defending potential intellectual property disputes, including any patent infringement actions brought by third parties against us now or in the future; |
| ● | the effect of competing technological and market developments; |
| ● | the cost of establishing sales, marketing and distribution capabilities in regions where we choose to commercialize PDS0101 on our own; and |
| ● | the initiation, progress, timing and results of the commercialization of PDS0101, if approved, for commercial sale. |
Additional funding may not be available on acceptable terms, or at all. If we are unable to raise additional capital in sufficient amounts or on terms acceptable to us, we may have to significantly delay, scale back or discontinue the development or commercialization of PDS0101 or potentially discontinue operations. In July 2019, we entered into a common stock purchase agreement, or the Aspire Purchase Agreement, with Aspire Capital, which provides that, upon the terms and subject to the conditions and limitations set forth therein, at our discretion, Aspire Capital is committed to purchase up to an aggregate of $20.0 million of shares of our common stock, or the Purchased Shares, over the 30-month term of the Aspire Purchase Agreement. We may sell an aggregate of 1,034,979 shares of our common stock (which represented 19.99% of the Company’s outstanding shares of common stock on the date of the Aspire Purchase Agreement) without stockholder approval. We may sell additional shares of our common stock above the 19.99% limit provided that (i) we obtain stockholder approval or (ii) stockholder approval has not been obtained at any time the 1,034,979 share limitation is reached and at all times thereafter the average price paid for all shares issued under the Aspire Purchase Agreement, is equal to or greater than $5.76, which was the consolidated closing bid price of our common stock on July 26, 2019. On July 29, 2019, we issued 100,654 shares of our common stock to Aspire Capital, as consideration for entering into the Aspire Purchase Agreement, which we refer to as the Commitment Shares. As of December 31, 2022, no Purchase Shares have been sold to Aspire Capital under the Aspire Purchase Agreement. The Aspire Purchase Agreement expired in January 2022 and we raised no capital under the Aspire Purchase Agreement.
Raising additional funds by issuing securities may cause dilution to existing stockholders and raising funds through lending and licensing arrangements may restrict our operations or require us to relinquish proprietary rights.
We expect that significant additional capital will be needed in the future to continue our planned operations. Until such time, if ever, as we can generate substantial product revenues, we expect to finance our cash needs through a combination of equity offerings, debt financings, strategic alliances and license and development agreements in connection with any collaborations. In February 2020, we completed an underwritten public offering, in which we sold 10,000,000 shares of common stock at a public offering price of $1.30 per share. The shares sold included 769,230 shares issued upon the exercise by the underwriter of its option to purchase additional shares at the public offering price. We received gross proceeds of approximately $13 million and net proceeds of approximately $11.9 million after deducting underwriting discounts and commissions. In July 2020, we filed a shelf registration statement, or the 2020 Shelf Registration Statement, with the SEC, for the issuance of common stock, preferred stock, warrants, rights, debt securities and units, which we refer to collectively as the Shelf Securities, up to an aggregate amount of $100 million. The 2020 Shelf Registration Statement was declared effective on July 31, 2020. The 2020 Registration Statement was terminated upon effectiveness of the 2022 Registration Statement (as discussed below). On August 13, 2020, we sold 6,900,000 shares of our common stock at a public offering price of $2.75 per share pursuant to the 2020 Shelf Registration Statement, which includes 900,000 shares issued upon the exercise by the underwriter of its option to purchase additional shares at the public offering price, minus underwriting discounts and commissions. We received gross proceeds of approximately $19.0 million and net proceeds of approximately $17.1 million, after deducting underwriting discounts and offering expenses. In June 2021, we completed an underwritten public offering in which we sold 6,088,235 shares of common stock at a public offering price of $8.50 per share pursuant to the 2020 Shelf Registration Statement, which includes 794,117 shares issued upon the exercise by the underwriter of its option to purchase additional shares at the public offering price, minus underwriting discounts and commissions. We received gross proceeds of approximately $51.7 million and net proceeds of approximately $48.5 million, after deducting underwriting discounts and offering expenses.
In August 2022, we filed a shelf registration statement, or the 2022 Shelf Registration Statement, with the SEC for the issuance of common stock, preferred stock, warrants, rights, debt securities, and units up to an aggregate amount of $150 million, $50 million of which covers the offer, issuance and sale by the Company of its common stock under the Sales Agreement (as discussed below). The 2022 Shelf Registration Statement was declared effective on September 2, 2022. In August 2022, we entered into an At Market Issuance Sales Agreement, or the Sales Agreement, with B. Riley Securities, Inc. and BTIG, LLC, each an Agent and collectively the Agents, with respect to an at-the-market offering program under which we may offer and sell, from time to time at our sole discretion, shares of our common stock, having an aggregate offering price of up to $50.0 million, or the Placement Shares, through or to the Agents, as sales agents or principals. Upon delivery of a placement notice and subject to the terms and conditions of the Sales Agreement, the Agents may sell the Placement Shares by any method permitted by law deemed to be an “at the market” offering as defined in Rule 415 of the Securities Act of 1933, as amended, including, without limitation, sales made through The Nasdaq Capital Market or on any other existing trading market for our common stock. The Agents will use commercially reasonable efforts to sell the Placement Shares from time to time, based upon our instructions (including any price, time or size limits or other customary parameters or conditions we may impose). We will pay the Agents a commission equal to three percent (3%) of the gross sales proceeds of any Placement Shares sold through the Agents under the Sales Agreement, and also has provided the Agents with customary indemnification and contribution rights. We are not obligated to make any sales of our common stock under the Sales Agreement. The offering of Placement Shares pursuant to the Sales Agreement will terminate upon the earlier of (i) the sale of all Placement Shares subject to the Sales Agreement or (ii) termination of the Sales Agreement in accordance with its terms. For the year ended December 31, 2022, we sold 1,238,491 shares of our common stock for a net value of $9.9 million pursuant to the Sales Agreement. In the first quarter of 2023, we sold 553,293 shares of our common stock for a net value of $ 4.6 million pursuant to the Sales Agreement.
To the extent that we raise additional capital by issuing equity securities, our existing stockholders’ ownership may experience substantial dilution, and the terms of these securities may include liquidation or other preferences that adversely affect your rights as a common stockholder. Debt financing and preferred equity financing, if available, may involve agreements that include covenants limiting or restricting our ability to take specific actions, such as incurring additional debt, making capital expenditures, declaring dividends, creating liens, redeeming our stock or making investments.
If we raise additional funds through collaborations, strategic alliances or marketing, distribution or licensing arrangements with third parties, we may have to relinquish valuable rights to our technologies, future revenue streams, research programs or Versamune Products or grant licenses on terms that may not be favorable to us. If we are unable to raise additional funds through equity or debt financings when needed, or through collaborations, strategic alliances or marketing, distribution or licensing arrangements with third parties on acceptable terms, we may be required to delay, limit, reduce or terminate our PDS0101 development or future commercialization efforts or grant rights to develop and market other Versamune and Infectimune products that we would otherwise develop and market.
Our operating activities may be restricted as a result of covenants related to the outstanding indebtedness under our venture loan and security agreement with Horizon and we may be required to repay the outstanding indebtedness in an event of default, which could have a materially adverse effect on our business.
In August 2022, we entered into a Venture Loan and Security Agreement, or the Loan Agreement, for separate term loans of up to an aggregate amount of $35.0 million, with Horizon Technology Finance Corporation, or Horizon, in its capacity as a lender and collateral agent for itself and the other financial institutions that from time to time become parties to the Loan Agreement, collectively referred to as the Lenders, secured by a by a security interest in all of our respective rights, title, interests, claims and demands in, to and under all of our respective properties and other assets, subject to limited exceptions and excluding our intellectual property. The Loan Agreement contains various covenants that limit our ability to engage in specified types of transactions. These covenants limit our ability to, among other things, sell, transfer, lease or dispose of certain assets; incur indebtedness; encumber or permit liens on certain assets; make certain investments; make certain restricted payments, including paying dividends on, or repurchasing or making distributions with respect to, our common stock; and enter into certain transactions with affiliates. Our business may be adversely affected by these restrictions on our ability to operate our business. A breach of any of the covenants under the Loan Agreement could result in a default. Upon the occurrence of an event of default, the Lenders could elect to declare all amounts outstanding, if any, to be immediately due and payable. If there are any amounts outstanding that we are unable to repay, the Lenders could proceed against the collateral granted to them to secure such indebtedness.
Our future success depends on our ability to retain executive officers and attract, retain and motivate qualified personnel.
We are highly dependent on our executive officers and the other principal members of the executive and scientific teams, particularly our President and Chief Executive Officer, Dr. Frank K. Bedu-Addo, our Chief Medical Officer, Dr. Lauren Wood, our Chief Financial Officer, Mr. Matthew Hill and our Chief Scientific Officer, Dr. Gregory L. Conn. The loss of the services of any of our senior executive officers could impede the achievement of our research, development and commercialization objectives. We do not maintain “key person” insurance for any executive officer or employee.
Recruiting and retaining qualified scientific, clinical, and operational personnel is also critical to our success. We may not be able to attract and retain these personnel on acceptable terms given the competition among numerous pharmaceutical and biotechnology companies for similar personnel. we also experience competition for the hiring of scientific and clinical personnel from universities and research institutions. Our industry has experienced an increasing rate of turnover of management and scientific personnel in recent years. In addition, we rely on consultants and advisors, including scientific and clinical advisors, to assist us in devising our research and development and commercialization strategy. Our consultants and advisors may be employed by third parties and have commitments under consulting or advisory contracts with other entities that may limit their availability to advance our strategic objectives. If any of these advisors or consultants can no longer dedicate a sufficient amount of time to the company, our business may be harmed
If we fail to obtain or maintain adequate coverage and reimbursement for PDS0101, our ability to generate revenue could be limited.
The availability and extent of reimbursement by governmental and private payors is essential for most patients to be able to afford expensive treatments. Sales of any of PDS0101 that receive marketing approval will depend substantially, both in the United States and internationally, on the extent to which the costs of PDS0101 will be paid by health maintenance, managed care, pharmacy benefit and similar healthcare management organizations, or reimbursed by government health administration authorities, private health coverage insurers and other third-party payors. If reimbursement is not available, or is available only on a limited basis, we may not be able to successfully commercialize PDS0101. Even if coverage is provided, the approved reimbursement amount may not be high enough to allow us to establish or maintain adequate pricing that will allow it to realize a sufficient return on our investment.
Outside the United States, international operations are generally subject to extensive governmental price controls and other market regulations, and we believe the increasing emphasis on cost-containment initiatives in Europe, Canada and other countries may cause us to price PDS0101 on less favorable terms than we currently anticipate. In many countries, particularly the countries of the European Union, the prices of medical products are subject to varying price control mechanisms as part of national health systems. In these countries, pricing negotiations with governmental authorities can take considerable time after the receipt of marketing approval for a product. To obtain reimbursement or pricing approval in some countries, we may be required to conduct a clinical trial that compares the cost-effectiveness of PDS0101 to other available therapies. In general, the prices of products under such systems are substantially lower than in the United States. Other countries allow companies to fix their own prices for products, but monitor and control company profits. Additional foreign price controls or other changes in pricing regulation could restrict the amount that we are able to charge for PDS0101. Accordingly, in markets outside the United States, the reimbursement for our products may be reduced compared with the United States and may be insufficient to generate commercially reasonable revenues and profits.
Moreover, increasing efforts by governmental and third-party payors, in the United States and internationally, to cap or reduce healthcare costs may cause such organizations to limit both coverage and level of reimbursement for newly approved products and, as a result, they may not cover or provide adequate payment for PDS0101. We expect to experience pricing pressures in connection with the sale of PDS0101 due to the trend toward managed healthcare, the increasing influence of health maintenance organizations and additional legislative changes. The downward pressure on healthcare costs in general, particularly prescription drugs and surgical procedures and other treatments, has become very intense. As a result, increasingly high barriers are being erected to the entry of new products into the healthcare market.
The Inflation Reduction Act, referred to as the IRA, was recently signed into law by President Biden, which makes significant changes to how drugs are covered and paid for under the Medicare program, including the creation of financial penalties for drugs whose prices rise faster than the rate of inflation, redesign of the Medicare Part D program to require manufacturers to bear more of the liability for certain drug benefits, and government price-setting for certain Medicare Part D drugs, starting in 2026, and Medicare Part B drugs starting in 2028. We have evaluated, and will continue to evaluate, the effect of the IRA on our business. At this time, we do not expect the IRA to have a material effect
We are unable to predict the future course of federal or state healthcare legislation in the United States directed at broadening the availability of healthcare and containing or lowering the cost of healthcare. The ACA and any further changes in the law or regulatory framework that reduce our revenue or increase our costs could also have a material and adverse effect on our business, financial condition and results of operations.
Even if any of our product candidates receive marketing approval, they may fail to achieve the degree of market acceptance by physicians, patients, healthcare payors and others in the medical community necessary for commercial success.
If any of our product candidates receive marketing approval, they may nonetheless fail to gain sufficient market acceptance by physicians, patients, healthcare payors and others in the medical community. For example, current cancer treatments like chemotherapy and radiation therapy are well-established in the medical community, and doctors may continue to rely on these treatments. If our product candidates do not achieve an adequate level of acceptance, we may not generate significant revenues from sales of drugs and we may not become profitable. The degree of market acceptance of our product candidates, if approved for commercial sale, will depend on a number of factors, including:
| ● | the efficacy and safety of the product; |
| ● | the potential advantages of the product compared to alternative therapies; |
| ● | the prevalence and severity of any side effects; |
| ● | whether the product is designated under physician and other provider treatment guidelines as a first-, second- or third-line therapy; |
| ● | our ability, or the ability of any future collaborators, to offer the product for sale at competitive prices; |
| ● | the product’s convenience and ease of administration for patients and healthcare practitioners compared to alternative treatments; |
| ● | the willingness of the target patient population to try, and of physicians to prescribe, the product; |
| ● | limitations or warnings, including distribution or use restrictions and safety information contained in the product’s approved labeling; |
| ● | the strength of sales, marketing and distribution support; |
| ● | changes in the standard of care for the targeted indications for the product; and |
| ● | the availability of coverage by, and the amount of reimbursement from, government payors, managed care plans and other third-party payors. |
We will need to expand our organization, and may experience difficulties in managing this growth, which could disrupt operations.
Our future financial performance and our ability to commercialize PDS0101 and compete effectively will depend, in part, on our ability to effectively manage any future growth. As of December 31, 2022, we had 26 employees and 3 consultants. We expect to hire additional employees for our managerial, clinical, scientific and engineering, operational, manufacturing, sales and marketing teams. We may have operational difficulties in connection with identifying, hiring and integrating new personnel. Future growth would impose significant additional responsibilities on our management, including the need to identify, recruit, maintain, motivate and integrate additional employees, consultants and contractors. Also, our management may need to divert a disproportionate amount of our attention away from our day-to-day activities and devote a substantial amount of time to managing these growth activities. We may not be able to effectively manage the expansion of our operations, which may result in weaknesses in our infrastructure, give rise to operational mistakes, loss of business opportunities, loss of employees and reduced productivity among remaining employees. Our expected growth could require significant capital expenditures and may divert financial resources from other projects, such as the development of PDS0101. If we are unable to effectively manage our growth, our expenses may increase more than expected, our ability to generate and/or grow revenues could be reduced, and we may not be able to implement our business strategy.
Many of the other pharmaceutical companies that we compete against for qualified personnel and consultants have greater financial and other resources, different risk profiles and a longer history in the industry than us. They also may provide more diverse opportunities and better chances for career advancement. Some of these characteristics may be more appealing to high-quality candidates and consultants than what it has to offer. If we are unable to continue to attract and retain high-quality personnel and consultants, the rate and success at which we can select and develop PDS0101 and our business will be limited.
Our employees, independent contractors, principal investigators, consultants, commercial collaborators, service providers and other vendors may engage in misconduct or other improper activities, including noncompliance with regulatory standards and requirements, which could have an adverse effect on our results of operations.
We are exposed to the risk that our employees and contractors, including principal investigators, consultants, commercial collaborators, service providers and other vendors may engage in fraudulent or other illegal activity. Misconduct by these parties could include intentional, reckless and/or negligent conduct or other unauthorized activities that violate the laws and regulations of the FDA and other similar regulatory bodies, including those laws that require the reporting of true, complete and accurate information to such regulatory bodies, manufacturing standards, federal and state healthcare fraud and abuse and health regulatory laws and other similar foreign fraudulent misconduct laws, or laws that require the true, complete and accurate reporting of financial information or data. Misconduct by these parties may also involve the improper use or misrepresentation of information obtained in the course of clinical trials, which could result in regulatory sanctions and serious harm to our reputation. It is not always possible to identify and deter third-party misconduct, and the precautions we take to detect and prevent this activity may not be effective in controlling unknown or unmanaged risks or losses or in protecting us from governmental investigations or other actions or lawsuits stemming from a failure to be in compliance with such laws or regulations. If any such actions are instituted against us, and we are not successful in defending ourselves or asserting our rights, those actions could have a significant impact on our business and financial results, including the imposition of significant civil, criminal and administrative penalties, damages, monetary fines, possible exclusion from participation in Medicare, Medicaid and other federal healthcare programs, reputational harm, diminished profits and future earnings, and curtailment of our operations, any of which could adversely affect our ability to operate our business and our results of operations.
Our business and operations would suffer, and could be negatively affected, in the event of system failures or cyberattacks
Our computer systems and those of our service providers, including our CROs, are vulnerable to damage from computer viruses, unauthorized access, natural disasters, terrorism, war and telecommunication and electrical failures. If such an event were to occur and cause interruptions in our or their operations, it could result in a material disruption of our development programs. For example, the loss of preclinical or clinical trial data from completed, ongoing or planned trials could result in delays in our regulatory approval efforts and significantly increase our costs to recover or reproduce the data. To the extent that any disruption or security breach were to result in a loss of or damage to data or applications, or inappropriate disclosure of personal, confidential or proprietary information, we could incur liability and the further development of PDS0101 could be delayed.
A cyberattack or similar incident could occur and result in information theft, data corruption, operational disruption, damage to our reputation or financial loss. Our industry has become increasingly dependent on digital technologies to conduct certain development and financial activities. Our technologies, systems, networks, or other proprietary information, and those of our vendors, suppliers and other business partners, may become the target of cyberattacks or information security breaches that could result in the unauthorized release, gathering, monitoring, misuse, loss or destruction of proprietary and other information, or could otherwise lead to the disruption of our business operations. Cyberattacks are becoming more sophisticated and certain cyber incidents, such as surveillance, may remain undetected for an extended period and could lead to disruptions in critical systems or the unauthorized release of confidential or otherwise protected information. These events could lead to financial loss from remedial actions, loss of business, disruption of operations, damage to our reputation or potential liability. Our systems and insurance coverage for protecting against cybersecurity risks may not be sufficient. Further, as cyberattacks continue to evolve, we may be required to expend significant additional resources to continue to modify or enhance our protective measures or to investigate and remediate any vulnerability to cyberattacks.
Our failure to comply with international data protection laws and regulations could lead to government enforcement actions and significant penalties against us, and adversely impact our operating results.
EU member states and other foreign jurisdictions, including Switzerland, have adopted data protection laws and regulations which impose significant compliance obligations. Moreover, the collection and use of personal health data in the EU, which was formerly governed by the provisions of the EU Data Protection Directive, was replaced with the EU General Data Protection Regulation, or the GDPR, in May 2018. The GDPR, which is wide-ranging in scope, imposes several requirements relating to the consent of the individuals to whom the personal data relates, the information provided to the individuals, the security and confidentiality of the personal data, data breach notification and the use of third-party processors in connection with the processing of personal data. The GDPR also imposes strict rules on the transfer of personal data out of the EU to the U.S., provides an enforcement authority and imposes large penalties for noncompliance, including the potential for fines of up to €20 million or 4% of the annual global revenues of the noncompliant company, whichever is greater. The GDPR requirements apply not only to third-party transactions, but also to transfers of information between us and our subsidiary, including employee information. The recent implementation of the GDPR has increased our responsibility and liability in relation to personal data that we process, including in clinical trials, and we may in the future be required to put in place additional mechanisms to ensure compliance with the GDPR, which could divert management’s attention and increase our cost of doing business. In addition, new regulation or legislative actions regarding data privacy and security (together with applicable industry standards) may increase our costs of doing business. In this regard, we expect that there will continue to be new proposed laws, regulations and industry standards relating to privacy and data protection in the United States, the EU and other jurisdictions, and we cannot determine the impact such future laws, regulations and standards may have on our business.
Our failure to comply with state and/or national data protection laws and regulations could lead to government enforcement actions and significant penalties against us, and adversely impact our operating results.
There are numerous other laws and legislative and regulatory initiatives at the federal and state levels addressing privacy and security concerns, and some state privacy laws apply more broadly than the Health Insurance Portability and Accountability Act, or HIPAA, and associated regulations. For example, California recently enacted legislation – the California Consumer Privacy Act, or CCPA – which went into effect January 1, 2020. The CCPA, among other things, creates new data privacy obligations for covered companies and provides new privacy rights to California residents, including the right to opt out of certain disclosures of their information. The CCPA also creates a private right of action with statutory damages for certain data breaches, thereby potentially increasing risks associated with a data breach. The CCPA was recently amended by the California Privacy Rights Act, or CPRA, expanding certain consumer rights such as the right to know. It remains unclear what, if any, additional modifications will be made to these laws by the California legislature or how these laws will be interpreted and enforced. The potential effects of the CCPA and CPRA and implementing regulations are significant and may cause us to incur substantial costs and expenses to comply.
If we fail to maintain an effective system of internal control over financial reporting in the future, we may not be able to accurately report our financial condition, results of operations or cash flows, which may adversely affect investor confidence in us and, as a result, the value of our common stock. Further, we continue to incur significant increased costs as a result of operating as a public company, and our management is required to devote substantial time to compliance initiatives.
As a public company, we continue to incur significant legal, accounting and other expenses that we did not incur as a private company. In addition, the Sarbanes-Oxley Act, as well as rules subsequently implemented by the SEC and Nasdaq, impose various requirements on public companies, including requiring establishment and maintenance of effective disclosure controls and internal control over financial reporting and changes in corporate governance practices. Our management and other personnel devote a substantial amount of time to these compliance initiatives. Moreover, these rules and regulations have increased our legal and financial compliance costs and have made some activities more time-consuming and costly.
Effective internal controls over financial reporting are necessary for us to provide reliable financial reports and, together with adequate disclosure controls and procedures, are designed to prevent fraud. Any failure to implement required new or improved controls, or difficulties encountered in their implementation, could cause us to fail to meet our reporting obligations. In addition, any testing by us conducted in connection with Section 404 of the Sarbanes-Oxley Act, may reveal deficiencies in our internal control over financial reporting that are deemed to be material weaknesses or that may require prospective or retroactive changes to our financial statements or identify other areas for further attention or improvement. If we are unable to conclude that our internal control over financial reporting is effective, or if our independent registered public accounting firm determines we have a material weakness or significant deficiency in our internal control over financial reporting once that firm begins its Section 404 reviews or becomes aware of either during the conduct of an audit, we could lose investor confidence in the accuracy and completeness of our financial reports, the market price of our common stock could decline, and we could be subject to sanctions or investigations by the Nasdaq Capital Market, the SEC or other regulatory authorities. Failure to remedy any material weakness in our internal control over financial reporting, or to implement or maintain other effective control systems required of public companies, could also restrict our future access to the capital markets.
Periodic reporting requirements under the Exchange Act and compliance with the Sarbanes-Oxley Act of 2002, including establishing and maintaining acceptable internal control over financial reporting, are costly and may increase substantially and, as a smaller reporting company, we may take advantage of reduced reporting requirements which may make our common stock less attractive to investors.
We are subject to the periodic reporting requirements of the Securities Exchange Act of 1934, as amended, or the Exchange Act. Our disclosure controls and procedures are designed to reasonably assure that information required to be disclosed by us in reports we file or submit under the Exchange Act is accumulated and communicated to management, recorded, processed, summarized and reported within the time periods specified in the rules and forms of the SEC. We believe that any disclosure controls and procedures or internal controls and procedures, no matter how well conceived and operated, can provide only reasonable, not absolute, assurance that the objectives of the control system are met. Our management and other personnel devote a substantial amount of time to these compliance initiatives. Moreover, these rules and regulations have increased our legal and financial compliance costs and will make some activities more time-consuming and costly.
In addition, the Sarbanes-Oxley Act requires, among other things, that we maintain effective disclosure controls and procedures and internal control over financial reporting. In particular, Section 404 of the Sarbanes-Oxley Act will require us to perform system and process evaluation and testing of our internal control over financial reporting to allow management to report on, and our independent registered public accounting firm to attest to, the effectiveness of our internal control over financial reporting. We are currently a “smaller reporting company,” but we will cease to be a smaller reporting company if we have a non-affiliate public float in excess of $250 million and annual revenues in excess of $100 million, or a non-affiliate public float in excess of $700 million, determined on an annual basis. As a smaller reporting company, we could take advantage of certain reduced governance and disclosure requirements, including not being required to comply with the auditor attestation requirements in the assessment of our internal control over financial reporting. As a result, investors and others may be less comfortable with the effectiveness of our internal controls and the risk that material weaknesses or other deficiencies in internal controls go undetected may increase. In addition, as a smaller reporting company, we take advantage of our ability to provide certain other less comprehensive disclosures in our SEC filings, including, among other things, providing only two years of audited financial statements in annual reports and simplified executive compensation disclosures. Consequently, it may be more challenging for investors to analyze our results of operations and financial prospects, as the information we provide to stockholders may be different from what one might receive from other public companies.
Risks Related to Clinical Development, Regulatory Approval and Commercialization
Clinical trials are very expensive, time-consuming, difficult to design and implement and involve an uncertain outcome, and if they fail to demonstrate safety and efficacy to the satisfaction of the FDA, or similar regulatory authorities, we will be unable to commercialize PDS0101 and other Versamune and Infectimune based products.
PDS0101 is still in early-stage clinical development and will require extensive additional clinical testing before we are prepared to submit a BLA for regulatory approval for any indication or for any other treatment regime. We cannot predict with any certainty if or when it might submit a BLA for regulatory approval for PDS0101 and other Versamune based products or whether any such BLAs will be approved by the FDA. Human clinical trials are very expensive and difficult to design and implement, in part because they are subject to rigorous regulatory requirements. For instance, the FDA may not agree with our proposed endpoints for any clinical trial we propose, which may delay the commencement of our clinical trials. The clinical trial process is also time-consuming. We estimate that the clinical trials we need to conduct to be in a position to submit BLAs for PDS0101 will take several years to complete. We cannot predict the timeline for review of submissions to any regulatory authorities or when any of our product candidates will receive marketing approval, if at all. The timeline for regulatory approval can be affected by a variety of factors, including, budget and funding levels, agency staffing, and statutory, regulatory and policy changes.
Furthermore, failure can occur at any stage of the trials, and we could encounter problems that cause us to abandon or repeat clinical trials. In later stages of clinical trials, PDS0101 may fail to show the desired safety and efficacy traits despite having progressed through preclinical studies and initial clinical trials, and the results of current clinical trials of PDS0101 therefore may not be predictive of the results of our continued or planned Phase 2 and 3 trials. A number of companies in the biopharmaceutical industry have suffered significant setbacks in advanced clinical trials due to lack of efficacy or adverse safety profiles, notwithstanding promising results in earlier stages of clinical trials.
Moreover, preclinical and clinical data are often susceptible to multiple interpretations and analyses. Many companies that have believed their immunotherapies performed satisfactorily in preclinical studies and clinical trials have nonetheless failed to obtain marketing approval of their products. Success in preclinical testing and early clinical trials does not ensure that later clinical trials, which involve many more subjects and different indications than we have studied in Phase 2 clinical trials to date, and the results of later clinical trials may not replicate the results of prior clinical trials and preclinical testing. In particular, the small number of patients in our planned early clinical trials may make the results of these trials less predictive of the outcome of later clinical trials.
Product development costs will also increase if we experience delays in testing or in receiving marketing approvals. We do not know whether any clinical trials will begin as planned, will need to be restructured or will be completed on schedule, or at all. Significant clinical trial delays also could shorten any periods during which we may have the exclusive right to commercialize PDS0101, could allow our competitors to bring products to market before we do, and could impair our ability to successfully commercialize PDS0101, any of which may harm our business and results of operations.
Clinical drug development is a lengthy and expensive process, with an uncertain outcome. If clinical trials of our product candidates fail to demonstrate safety and efficacy to the satisfaction of regulatory authorities or do not otherwise produce positive results, we may incur additional costs, experience delays in completing, or ultimately be unable to complete, the development of our product candidates or be unable to obtain marketing approval.
Before obtaining marketing approval from regulatory authorities for the sale of our product candidates, we must complete preclinical development and then conduct extensive clinical trials to demonstrate the safety and efficacy of our product candidates. Clinical testing is expensive, difficult to design and implement, can take many years to complete and is uncertain as to outcome. A failure of one or more clinical trials can occur at any stage of testing. The outcome of preclinical studies and early-stage clinical trials may not be predictive of the success of later clinical trials, and interim results of a clinical trial do not necessarily predict final results.
Moreover, preclinical and clinical data are often susceptible to varying interpretations and analyses, and many companies that have believed their product candidates performed satisfactorily in preclinical studies and clinical trials have nonetheless failed to obtain marketing approval of their drugs.
We do not know whether ongoing clinical trials will be completed on schedule or at all, or whether future clinical trials will begin on time, need to be redesigned, enroll patients on time or be completed on schedule, if at all. Clinical trials can be delayed for a variety of reasons, including delays related to:
| ● | obtaining regulatory authorization to commence a trial; |
| ● | reaching agreement on acceptable terms with prospective contract research organizations, or CROs, and clinical trial sites, the terms of which can be subject to extensive negotiation and may vary significantly among different CROs and clinical trial sites; |
| ● | obtaining institutional review board or ethics committee approval at each clinical trial site; |
| ● | recruiting suitable patients to participate in a trial; |
| ● | the impact of COVID-19 on patient screening, patient enrollment, and follow-up; |
| ● | patients failing to comply with the clinical trial protocol or dropping out of a trial; |
| ● | clinical trial sites failing to comply with the clinical trial protocol or dropping out of a trial; |
| ● | addressing any conflicts with new or existing laws or regulations; |
| ● | the need to add new clinical trial sites; |
| ● | manufacturing sufficient quantities of product candidate for use in clinical trials and ensuring clinical trial material is provided to clinical sites in a timely manner; or |
| ● | obtaining advice from regulatory authorities regarding the statistical analysis plan to be used to evaluate the clinical trial data or other trial design issues. |
We may experience numerous unforeseen events during, or as a result of, clinical trials that could delay or prevent our ability to receive marketing approval or commercialize our product candidates, including:
| ● | we may receive feedback from regulatory authorities that requires us to modify the design of our clinical trials; |
| ● | clinical trials of our product candidates may produce negative or inconclusive results, and we may decide, or regulators may require us, to conduct additional clinical trials or abandon drug development programs; |
| ● | the number of patients required for clinical trials of our product candidates may be larger than we anticipate, enrollment in these clinical trials may be slower than we anticipate or participants may drop out of these clinical trials at a higher rate than we anticipate; |
| ● | our third-party contractors, including our CROs, may fail to comply with regulatory requirements or meet their contractual obligations to us in a timely manner, or at all; |
| ● | we, our investigators, or any of the overseeing IRBs or ethics committees might decide to suspend or terminate clinical trials of our product candidates for various reasons, including non-compliance with regulatory requirements, a finding that our product candidates have undesirable side effects or other unexpected characteristics, or a finding that the participants are being exposed to unacceptable health risks; |
| ● | the cost of clinical trials of our product candidates may be greater than we anticipate; |
| ● | the supply or quality of our product candidates or other materials necessary to conduct clinical trials of our product candidates may be insufficient or inadequate; |
| ● | regulators may revise the requirements for approving our product candidates, or such requirements may not be as we anticipate; and |
| ● | any future collaborators that conduct clinical trials may face any of the above issues and may conduct clinical trials in ways they view as advantageous to them but that are suboptimal for us. |
If we are required to conduct additional clinical trials or other testing of our product candidates beyond those that we currently contemplate, if we are unable to successfully complete clinical trials of our product candidates or other testing, if the results of these trials or tests are not positive or are insufficiently positive to support marketing approval, or if there are safety concerns, we may:
| ● | be delayed in obtaining marketing approval for our product candidates or not obtain marketing approval at all; |
| ● | obtain marketing approval in some countries and not in others; |
| ● | obtain marketing approval for indications or patient populations that are narrower or more limited in scope than intended or desired; |
| ● | obtain marketing approval subject to significant use or distribution restrictions or with labeling that includes significant safety warnings, including boxed warnings; |
| ● | be subject to additional post-marketing testing requirements; or |
| ● | have the drug removed from the market after obtaining marketing approval. |
Our drug development costs will also increase if we experience delays in testing or marketing approvals. We do not know whether clinical trials will begin as planned, will need to be restructured or will be completed on schedule, or at all. Furthermore, we rely on third-party CROs and clinical trial sites to ensure the proper and timely conduct of our clinical trials, and while we have agreements governing their committed activities, we have limited influence over their actual performance. Significant clinical trial delays also could shorten any periods during which we may have the exclusive right to commercialize our product candidates or allow our competitors to bring drugs to market before we do and impair our ability to successfully commercialize our product candidates and may harm our business and results of operations.
Enrollment and retention of subjects in clinical trials is an expensive and time-consuming process and could be made more difficult or rendered impossible by multiple factors outside our control.
We may encounter delays in enrolling, or be unable to enroll, a sufficient number of participants to complete any of our clinical trials. Once enrolled, we may be unable to retain a sufficient number of participants to complete any of our trials. Late-stage clinical trials of PDS0101 may require the enrollment and retention of large numbers of subjects. Subject enrollment and retention in clinical trials depends on many factors, including the size of the subject population, the nature of the trial protocol, the existing body of safety and efficacy data with respect to the study drug, the number and nature of competing treatments and ongoing clinical trials of competing drugs for the same indication, patients’ and clinicians’ perceived risks and benefits of the product candidate under study the proximity of subjects to clinical sites and the eligibility criteria for the study. Moreover, the current pandemic is negatively impacting enrollment in many oncology clinical trials.
Furthermore, any negative results we may report in clinical trials of PDS0101 may make it difficult or impossible to recruit and retain participants in other clinical trials of PDS0101. Delays or failures in planned subject enrollment or retention may result in increased costs, program delays or both, which could have a harmful effect on our ability to develop PDS0101, or could render further development impractical. In addition, we expect to rely on CROs and clinical trial sites to ensure proper and timely conduct of our future clinical trials and, while we intend to enter into agreements governing their services, we will be limited in our ability to compel their actual performance in compliance with applicable regulations. Enforcement actions brought against these third parties may cause further delays and expenses related to our clinical development programs.
Our inability to enroll a sufficient number of patients for our clinical trials would result in significant delays or may require us to abandon one or more clinical trials altogether. Enrollment delays in our clinical trials may result in increased development costs for our product candidates, which would cause the value of our company to decline and limit our ability to obtain additional financing.
The successful development of immunotherapies is highly uncertain.
Successful development of immunotherapies is highly uncertain and is dependent on numerous factors, many of which are beyond our control. Immunotherapies that appear promising in the early phases of development may fail to reach, or be delayed in reaching, the market for several reasons including: preclinical study results that may show the immunotherapy to be less effective than desired (e.g., the study failed to meet its primary objectives) or to have harmful or problematic side effects; clinical study results that may show the immunotherapy to be less effective than expected (e.g., the study failed to meet its primary endpoint) or to have unacceptable side effects; failure to receive the necessary regulatory approvals or a delay in receiving such approvals. Among other things, such delays may be caused by slow enrollment in clinical studies, length of time to achieve study endpoints, delays in receiving the necessary products or supplies for the conduct of clinical or preclinical trials, additional time requirements for data analysis, or Biologics License Application preparation, discussions with the FDA, an FDA request for additional preclinical or clinical data, FDA delays in inspecting manufacturing establishments, failure to receive FDA approval for manufacturing processes or facilities, or unexpected safety or manufacturing issues; manufacturing costs, formulation issues, pricing or reimbursement issues, or other factors that make the immunotherapy uneconomical; and the proprietary rights of others and their competing products and technologies that may prevent the immunotherapy from being commercialized. Success in preclinical and early and interim clinical studies does not ensure that large-scale clinical studies will be successful. Clinical results are frequently susceptible to varying interpretations that may delay, limit or prevent regulatory approvals. The length of time necessary to complete clinical studies and to submit an application for marketing approval for a final decision by a regulatory authority varies significantly from one immunotherapy to the next and may be difficult to predict. Even if our product candidates are approved, they may be subject to limitations on the indicated uses and populations for which they may be marketed. They may also be subject to other conditions of approval, may contain significant safety warnings, including boxed warnings, contraindications, and precautions, may not be approved with label statements necessary or desirable for successful commercialization, or may contain requirements for costly post-market testing and surveillance, or other requirements, including the submission of a REMS, to monitor the safety or efficacy of the products. If we do not receive FDA approval for, and successfully commercialize our product candidates, we will not be able to generate revenue from these product candidates in the United States in the foreseeable future, or at all. Any significant delays in obtaining approval for and commercializing our product candidates will have a material adverse impact on our business and financial condition.
In addition, the success of our products will depend on several factors, including the following:
| ● | successful initiation, successful patient enrollment and timely completion of clinical trials of these products; |
| ● | successful initiation and successful patient enrollment and completion of additional clinical trials, for our product candidates; |
| ● | the impact of COVID-19 on our operations, ability to conduct clinical trials and on the ability of our regulators to review and approve our product candidates; |
| ● | our ability to demonstrate our products’ safety, tolerability and efficacy to the FDA or any comparable foreign regulatory authority for marketing approval; |
| ● | timely receipt of marketing approvals for our products; |
| ● | obtaining and maintaining patent protection, trade secret protection and regulatory exclusivity, both in the United States and internationally; |
| ● | successfully defending and enforcing our rights in our intellectual property portfolio; |
| ● | avoiding and successfully defending against any claims that we have infringed, misappropriated or otherwise violated any intellectual property of any third party; |
| ● | the performance of our future collaborators, if any; |
| ● | the extent of, and our ability to timely complete, any required post-marketing approval commitments imposed by FDA or other applicable regulatory authorities; |
| ● | establishment of supply arrangements with third-party raw materials and drug product suppliers and manufacturers who are able to manufacture clinical trial and commercial quantities of our products and their components and to develop, validate and maintain a commercially viable manufacturing process that is compliant with current good manufacturing practices, or cGMP, at a scale sufficient to meet anticipated demand and over time enable us to reduce our cost of manufacturing; |
| ● | establishment of scaled production arrangements with third-party manufacturers to obtain finished products that are compliant with cGMP and appropriately packaged for sale; |
| ● | successful launch of commercial sales following any marketing approval; |
| ● | a continued acceptable safety profile following any marketing approval; |
| ● | commercial acceptance by patients, the medical community and third-party payors; |
| ● | the availability of coverage and adequate reimbursement and pricing by third-party payors and government authorities; |
| ● | the availability, perceived advantages, relative cost, relative safety and relative efficacy of alternative and competing treatments; and |
| ● | our ability to compete with other therapies. |
We do not have complete control over many of these factors, including certain aspects of clinical development and the regulatory submission process, potential threats to our intellectual property rights and the manufacturing, marketing, distribution and sales efforts of any future collaborator. Accordingly, we cannot assure you that we will ever be able to generate revenue through the sale of our product candidates. If we are not successful in commercializing our products, or are significantly delayed in doing so, our business will be materially harmed.
We may not be able to file INDs or IND amendments to commence additional clinical trials on the timelines we expect, and even if we are able to, the FDA may not permit us to proceed.
We may not be able to file INDs for our future product candidates on the timelines we expect. For example, we may experience manufacturing delays or other delays with IND-enabling studies. Moreover, we cannot be sure that submission of an IND will result in the FDA allowing further clinical trials to begin, or that, once begun, issues will not arise that lead FDA, IRBs, or other authorities to suspend, terminate, or require changes to our clinical trials. Additionally, even if such regulatory and other authorities agree with the design and implementation of the clinical trials set forth in an IND, we cannot guarantee that such regulatory authorities will not change their requirements in the future. These considerations also apply to new clinical trials or changes to existing clinical trials we may submit as amendments to existing INDs or to a new IND. Any failure to file INDs on the timelines we expect or to obtain regulatory clearance or approvals for our trials may prevent us from completing our clinical trials or commercializing our products on a timely basis, if at all.
We face significant competition from other biotechnology and pharmaceutical companies, and our operating results will suffer if we fail to compete effectively.
The biotechnology and biopharmaceutical industries are characterized by rapid technological developments and a high degree of competition. As a result, PDS0101 or other Versamune and Infectimune based products could become obsolete before we recoup any portion of our related research and development and commercialization expenses. Competition in the biopharmaceutical industry is based significantly on scientific and technological factors. These factors include the availability of patent and other protection for technology and products, the ability to commercialize technological developments and the ability to obtain governmental approval for testing, manufacturing and marketing. We compete with specialized biopharmaceutical firms in the United States, Europe and elsewhere, as well as a growing number of large pharmaceutical companies that are applying biotechnology to their operations. Many biopharmaceutical companies have focused their development efforts in the human therapeutics area, including cancer. Many major pharmaceutical companies have developed or acquired internal biotechnology capabilities or made commercial arrangements with other biopharmaceutical companies. These companies, as well as academic institutions and governmental agencies and private research organizations, also compete with us in recruiting and retaining highly qualified scientific personnel and consultants. Our ability to compete successfully with other companies in the pharmaceutical field will also depend to a considerable degree on the continuing availability of capital to us.
We are aware of certain investigational new drugs under development or approved products by competitors that are used for the prevention, diagnosis, or treatment of certain diseases we have targeted for drug development. Various companies are developing biopharmaceutical products that have the potential to directly compete with PDS0101 even though their approach to may be different. We believe our top clinical-stage competitors pursuing cancer immunotherapies and/or vaccines for infectious diseases include, but not limited to Jansen Pharmaceuticals (part of J&J), Sanofi-Aventis, GlaxoSmithKline plc, Merck and Pfizer, Inovio, Advaxis, Kite Pharma, Hookipa, Moderna, ZIOPHARM Oncology, Heat Biologics, Harpoon Therapeutics, Oncosec Medical, BioNTech, Osivax, Medicago, Vaxart, and Flugen. Many of these companies have substantially greater financial, marketing, and human resources than we do (including, in some cases, substantially greater experience in clinical testing, manufacturing, and marketing of pharmaceutical products). If one or more of these companies is successful in developing their technologies, it could materially impact our business. We also experience competition in the development of our immunotherapies from universities and other research institutions and competes with others in acquiring technology from such universities and institutions.
Competition may increase further as a result of advances in the commercial applicability of technologies and greater availability of capital for investment in these industries. Our competitors may succeed in developing, acquiring or licensing, on an exclusive basis, drugs that are more effective or less costly than PDS0101 or our other Versamune and Infectimune based products.
We will face competition from other drugs currently approved or that will be approved in the future for the treatment of the other cancers and infectious diseases we are currently targeting. Therefore, our ability to compete successfully will depend largely on our ability to:
| ● | develop and commercialize immunotherapies that are superior to other alternatives in the market; |
| ● | demonstrate through our clinical trials that PDS0101 is differentiated from existing and future therapies; |
| ● | attract qualified scientific, immunotherapy development and commercial personnel; |
| ● | obtain additional patent or other proprietary protection for PDS0101 and other Versamune and Infectimune-based products; |
| ● | obtain required regulatory approvals; |
| ● | obtain coverage and adequate reimbursement from, and negotiate competitive pricing with, third-party payors; and |
| ● | successfully develop and commercialize, independently or with collaborators, new applications for PDS0101 or immunotherapies. |
The availability of our competitors’ immunotherapies and other treatments could limit the demand, and the price we are able to charge, for PDS0101. The inability to compete with existing or subsequently introduced immunotherapies and other treatments would have an adverse impact on our business, financial condition and prospects.
Established pharmaceutical companies may invest heavily to accelerate discovery and development of novel compounds or to license novel compounds that could make PDS0101 less competitive. In addition, any new immunotherapy that competes with an approved treatment must demonstrate compelling advantages in efficacy, convenience, tolerability and safety in order to overcome price competition and to be commercially successful. Accordingly, our competitors may succeed in obtaining patent protection, discovering, developing, receiving the FDA’s approval for or commercializing medicines before we do, which would have an adverse impact on our business and results of operations.
PDS0101 may cause adverse effects or have other properties that could delay or prevent its regulatory approval or limit the scope of any approved label or market acceptance.
Adverse events caused by PDS0101 could cause reviewing entities, clinical trial sites or regulatory authorities to interrupt, delay or halt clinical trials and could result in the denial of regulatory approval. If clinical trials for PDS0101 report an unacceptable frequency or severity of adverse events, our ability to obtain regulatory approval for PDS0101 may be negatively impacted.
Furthermore, if PDS0101 is approved and then causes serious or unexpected side effects, a number of potentially significant negative consequences could result, including:
| ● | regulatory authorities may withdraw their approval of PDS0101 or impose restrictions on its distribution or other risk management measures; |
| ● | regulatory authorities may require the addition of labeling statements, such as warnings or contraindications; |
| ● | we may be required to change the way PDS0101 is administered or to conduct additional clinical trials; |
| ● | we could be sued and held liable for injuries sustained by patients; |
| ● | we could elect to discontinue the sale of PDS0101; |
| ● | our entire Versamune and Infectimune-based pipeline could be then put at risk; and |
| ● | our reputation may suffer. |
Any of these events could prevent us from achieving or maintaining market acceptance of PDS0101 and could substantially increase the costs of commercialization.
In addition, if any of our product candidates are associated with adverse events or undesirable side effects or have properties that are unexpected, our trials could be suspended or terminated and the FDA or comparable foreign regulatory authorities could order us to cease further development of or deny approval of our product candidates for any or all targeted indications. We, or any future collaborators, may abandon development or limit development of that product candidate to certain uses or subpopulations in which the undesirable side effects or other characteristics are less prevalent, less severe or more acceptable from a risk-benefit perspective. Drug-related side effects could affect patient recruitment or the ability of enrolled patients to complete the trial or result in potential product liability claims. Any of these occurrences may harm our business, results of operations, financial condition and prospects significantly.
If we are not able to obtain, or if there are delays in obtaining, required regulatory approvals, we will not be able to commercialize, or will be delayed in commercializing, PDS0101, and our ability to generate revenue will be impaired.
PDS0101 and the activities associated with its development and commercialization, including its design, testing, manufacture, safety, efficacy, recordkeeping, labeling, storage, approval, advertising, promotion, sale and distribution, are subject to comprehensive regulation by the FDA and other regulatory agencies in the United States and by comparable authorities in other countries. Failure to obtain marketing approval for PDS0101 will prevent us from commercializing PDS0101. We have not received approval to market PDS0101 from regulatory authorities in any jurisdiction. We have only limited experience in filing and supporting the applications necessary to gain marketing approvals and expect to rely on CROs to assist us in this process. Securing regulatory approval requires the submission of extensive preclinical and clinical data and supporting information to the various regulatory authorities for each therapeutic indication to establish the safety and efficacy of PDS0101. Securing regulatory approval also requires the submission of information about the product manufacturing process to, and inspection of manufacturing facilities by, the relevant regulatory authority. PDS0101 may not be effective, may be only moderately effective or may prove to have undesirable or unintended side effects, toxicities or other characteristics that may preclude it from obtaining marketing approval or prevent or limit commercial use.
The process of obtaining marketing approvals, both in the United States and elsewhere, is expensive, may take many years and can vary substantially based upon a variety of factors. We cannot assure you that we will ever obtain any marketing approvals in any jurisdiction. Changes in marketing approval policies during the development period, changes in or the enactment of additional statutes or regulations or changes in regulatory review for each submitted product application may cause delays in the approval or rejection of an application. The FDA and comparable authorities in other countries have substantial discretion in the approval process and may refuse to accept any application or may decide that our data is insufficient for approval and require additional preclinical or other studies, and clinical trials. In addition, varying interpretations of the data obtained from preclinical testing and clinical trials could delay, limit or prevent marketing approval of PDS0101. Additionally, any marketing approval we ultimately obtain may be limited or subject to restrictions or post-approval commitments that render the approved product not commercially viable.
If any of our product candidates receives marketing approval and we, or others, later discover that the drug is less effective than previously believed or causes undesirable side effects that were not previously identified, our ability, or that of any future collaborators, to market the drug could be compromised.
Clinical trials of our product candidates must be conducted in carefully defined subsets of patients who have agreed to enter into clinical trials. Consequently, it is possible that our clinical trials, or those of any future collaborator, may indicate an apparent positive effect of a product candidate that is greater than the actual positive effect, if any, or alternatively fail to identify undesirable side effects. If one or more of our product candidates receives marketing approval and we, or others, discover that the drug is less effective than previously believed or causes undesirable side effects that were not previously identified, a number of potentially significant negative consequences could result, including:
| ● | regulatory authorities may withdraw their approval of the drug or seize the drug; |
| ● | we, or any future collaborators, may be required to recall the drug, change the way the drug is administered or conduct additional clinical trials; |
| ● | additional restrictions may be imposed on the marketing of, or the manufacturing processes for, the particular drug; |
| ● | we may be subject to fines, injunctions or the imposition of civil or criminal penalties; |
| ● | regulatory authorities may require the addition of labeling statements, such as a “black box” warning or a contraindication; |
| ● | we, or any future collaborators, may be required to create a Medication Guide outlining the risks of the previously unidentified side effects for distribution to patients; |
| ● | we, or any future collaborators, could be sued and held liable for harm caused to patients; |
| ● | the drug may become less competitive in the marketplace; and |
| ● | our reputation may suffer. |
Any of these events could have a material and adverse effect on our operations and business and could adversely impact our stock price.
We rely, and intend to continue to rely, on third parties to conduct our clinical trials and perform some of our research and preclinical studies. If these third parties do not satisfactorily carry out their contractual duties, fail to comply with applicable regulatory requirements or do not meet expected deadlines, our development programs may be delayed or subject to increased costs or we may be unable to obtain regulatory approval, each of which may have an adverse effect on our business, financial condition, results of operations and prospects.
There is no guarantee that any such CROs, clinical trial investigators or other third parties on which we rely will devote adequate time and resources to our development activities or perform as contractually required. If any of these third parties fail to meet expected deadlines, adhere to our clinical protocols or meet regulatory requirements, otherwise perform in a substandard manner, or terminate their engagements with us, the timelines for our development programs may be extended or delayed or our development activities may be suspended or terminated. If our clinical trial site terminates for any reason, we may experience the loss of follow-up information on subjects enrolled in such clinical trial unless we are able to transfer those subjects to another qualified clinical trial site, which may be difficult or impossible. In addition, certain of our scientific advisors or consultants who receive compensation from us are clinical trial investigators for our clinical trial. Although we believe our existing relationships are within the FDA’s guidelines, if these relationships and any related compensation result in perceived or actual conflicts of interest, or the FDA concludes that the financial relationship may have affected the interpretation of the trial, the integrity of the data generated at the applicable clinical trial site may be questioned and the utility of the clinical trial itself may be jeopardized, which could result in the delay or rejection of any marketing application we submit by the FDA. Any such delay or rejection could prevent us from commercializing PDS0101 or any other product candidates.
Even if we obtain FDA approval in the United States, we may never obtain approval for or commercialize PDS0101 in any other jurisdiction, which would limit our ability to realize each product’s full market potential.
In order to market PDS0101 in a particular jurisdiction, we must establish and comply with numerous and varying regulatory requirements on a country-by-country basis regarding safety and efficacy. Approval by the FDA in the United States does not ensure approval by regulatory authorities in other countries or jurisdictions.
In addition, clinical trials conducted in one country may not be accepted by regulatory authorities in other countries, and regulatory approval in one country does not guarantee regulatory approval in any other country. Approval processes vary among countries and can involve additional testing and validation and additional administrative review periods. Seeking foreign regulatory approval could result in difficulties and costs for us and require additional preclinical studies or clinical trials that could be costly and time consuming. Regulatory requirements can vary widely from country to country and could delay or prevent the introduction of PDS0101 in those countries. PDS0101 is not approved for sale in any jurisdiction, including in international markets, and we do not have experience in obtaining regulatory approval in international markets. If we fail to comply with regulatory requirements in international markets or to obtain and maintain required approvals, or if regulatory approvals in international markets are delayed, our target market will be reduced.
Interim, topline and preliminary data from our clinical trials that we announce or publish from time to time may change as more subject data become available and are subject to audit and verification procedures that could result in material changes in the final data.
From time to time, we may publicly disclose interim, topline or preliminary data from our sponsored or investigator initiated clinical trials, such as preliminary topline results which are based on a preliminary analysis of then-available data, and the results and related findings and conclusions are subject to change following a full analysis of all data related to the particular trial. We also make assumptions, estimations, calculations and conclusions as part of our analyses of data, and we may not have received or had the opportunity to fully and carefully evaluate all data. In addition, we may report preliminary analyses of only certain endpoints rather than all endpoints. As a result, the interim, topline or preliminary results that we report may differ from future results of the same trials, or different conclusions or considerations may qualify such results, once additional data have been received and fully evaluated. Topline data also remain subject to audit and verification procedures that may result in the final data being materially different from the preliminary data we previously published. As a result, interim, topline and preliminary data should be viewed with caution until the final data are available. We may also disclose interim data from our clinical trials. Interim data from clinical trials that we may complete are subject to the risk that one or more of the clinical outcomes may materially change as subject enrollment continues and more subject data become available. Adverse differences between interim, topline or preliminary data and final data could significantly harm our reputation and business prospects. Further, disclosure of interim, topline or preliminary data by us or by our competitors could result in volatility in the price of our common stock.
Further, others, including regulatory agencies, may not accept or agree with our assumptions, estimates, calculations, conclusions or analyses or may interpret or weigh the importance of data differently, which could impact the potential of the particular program, the likelihood of marketing approval or commercialization of the particular drug candidate, any approved product, and our company in general. In addition, the information we choose to publicly disclose regarding a particular study or clinical trial is derived from information that is typically extensive, and you or others may not agree with what we determine is material or otherwise appropriate information to include in our disclosure, and any information we determine not to disclose may ultimately be deemed significant with respect to future decisions, conclusions, views, activities or otherwise regarding a particular program, drug candidate or our business.
If the interim, topline or preliminary data that we report differ from actual results, or if others, including regulatory authorities, disagree with the conclusions reached, our ability to pursue strategic alternatives, including identifying and consummating transactions with third-party partners, to further develop, obtain marketing approval for and/or commercialize our drug candidates may be harmed, which could harm our business, operating results, prospects or financial condition.
The outcome of preclinical testing and early clinical trials may not be predictive of the success of later clinical trials, interim results of a clinical trial do not necessarily predict final results, and the results of our clinical trials may not satisfy the requirements of the FDA or comparable foreign regulatory authorities.
We currently have no drugs approved for sale and we cannot guarantee that we will ever have marketable drugs. Clinical failure can occur at any stage of clinical development. Clinical trials may produce negative or inconclusive results, and we or any future collaborators may decide, or regulators may require us, to conduct additional clinical trials or preclinical studies. We will be required to demonstrate with substantial evidence through adequate and well-controlled clinical trials that our product candidates are safe and effective for use in treating specific conditions in order to obtain marketing approvals for their commercial sale. Success in preclinical studies and early-stage clinical trials does not mean that future larger registration clinical trials will be successful because product candidates in later-stage clinical trials may fail to demonstrate safety and efficacy to the satisfaction of the FDA and non-U.S. regulatory authorities despite having progressed through preclinical studies and early-stage clinical trials. Product candidates that have shown promising results in preclinical studies and early-stage clinical trials may still suffer significant setbacks in subsequent registration clinical trials. Additionally, the outcome of preclinical studies and early-stage clinical trials may not be predictive of the success of later-stage clinical trials.
In addition, the design of a clinical trial can determine whether its results will support approval of a drug and flaws in the design of a clinical trial may not become apparent until the clinical trial is well advanced. We have limited experience in designing clinical trials and may be unable to design and conduct a clinical trial to support marketing approval. Further, if our product candidates are found to be unsafe or lack efficacy, we will not be able to obtain marketing approval for them and our business would be harmed. A number of companies in the pharmaceutical industry, including those with greater resources and experience than us, have suffered significant setbacks in advanced clinical trials, even after obtaining promising results in preclinical studies and earlier clinical trials.
In some instances, there can be significant variability in safety and efficacy results between different clinical trials of the same product candidate due to numerous factors, including changes in trial protocols, differences in size and type of the patient populations, differences in and adherence to the dosing regimen and other trial protocols and the rate of dropout among clinical trial participants. We do not know whether any clinical trials we may conduct will demonstrate consistent or adequate efficacy and safety sufficient to obtain marketing approval to market our product candidates.
In addition, in the event that an adverse safety issue, clinical hold, or other adverse finding occurs in one of our clinical trials, that event could adversely affect any other clinical trials for the same product candidate. An adverse safety issue or other adverse finding in a clinical trial conducted by a third party with a similar mechanism of action could adversely affect clinical trials involving our product candidates.
Further, our product candidates may not be approved even if they achieve their primary endpoints in clinical trials, including registration trials. The FDA or comparable foreign regulatory authorities may disagree with our trial design and our interpretation of data from preclinical studies and clinical trials. In addition, any of these regulatory authorities may change requirements for the approval of a product candidate even after reviewing and providing comments or advice on a protocol for a pivotal clinical trial that has the potential to result in approval by the FDA or comparable foreign regulatory authorities. In addition, any of these regulatory authorities may also approve a product candidate for fewer or more limited indications than we request or may grant approval contingent on the performance of costly post-marketing clinical trials. In addition, the FDA or other comparable foreign regulatory authorities may not approve the labeling claims that we believe would be necessary or desirable for the successful commercialization of our product candidates.
Before obtaining marketing approvals for the commercial sale of any product candidate for a target indication, we must demonstrate with substantial evidence gathered in preclinical studies and adequate and well-controlled clinical trials, and, with respect to approval in the United States, to the satisfaction of the FDA and elsewhere to the satisfaction of other comparable foreign regulatory authorities, that the product candidate is safe and effective for use for that target indication. There is no assurance that the FDA or other comparable foreign regulatory authorities will consider our future clinical trials to be sufficient to serve as the basis for approval of one of our product candidates for any indication. The FDA and other comparable foreign regulatory authorities retain broad discretion in evaluating the results of our clinical trials and in determining whether the results demonstrate that a product candidate is safe and effective. If we are required to conduct additional clinical trials of a product candidate than we expect prior to its approval, we will need substantial additional funds and there is no assurance that the results of any such additional clinical trials will be sufficient for approval.
Our product candidates are in various stages of development and we will not be able to commercialize our product candidates if our preclinical studies do not produce successful results and/or our clinical trials do not demonstrate the safety and efficacy of our product candidates; early results and early understanding of product candidate potential may not be predictive of later success.
Our oncology and infectious disease product candidates are susceptible to the risks of failure inherent at any stage of product development, including the occurrence of unexpected or unacceptable adverse events or the failure to demonstrate efficacy in clinical trials. Clinical development is expensive and can take many years to complete, and its outcome is inherently uncertain.
The results of preclinical studies, preliminary study results, and early clinical trials of our product candidates may not be predictive of the results of later-stage clinical trials. Our product candidates may not perform as we expect, may ultimately have a different or no impact than expected, may have a different mechanism of action than we initially understand or that we expect in humans, and may not ultimately prove to be safe and effective.
Preliminary and final results from preclinical studies and early-stage trials, and trials in compounds that we believe are similar to ours, may not be representative of results that are found in larger, controlled, blinded, and longer-term studies. Product candidates may fail at any stage of preclinical or clinical development. Product candidates may fail to show the desired safety and efficacy traits even if they have progressed through preclinical studies or initial clinical trials. Preclinical studies and clinical trials may also reveal unfavorable product candidate characteristics, including safety concerns. A number of companies in the biopharmaceutical industry have suffered significant setbacks in clinical trials, notwithstanding promising results in earlier preclinical studies or clinical trials or promising mechanisms of action. In some instances, there can be significant variability in safety or efficacy results between different clinical trials of the same product candidate due to numerous factors, including changes in trial procedures set forth in protocols, differences in the size and type of the patient populations, changes in and adherence to the clinical trial protocols and the rate of dropout among clinical trial participants. Moreover, should there be an issue with the design of a clinical trial, our results may be impacted. We may not discover such a flaw until the clinical trial is at an advanced stage.
We may also experience numerous unforeseen events during, or as a result of, clinical trials that could delay or prevent our ability to receive marketing approval or commercialize our product candidates. There may be emerging new data or regulatory questions or disagreements regarding interpretations of data and results at any stage. For example, the FDA or comparable foreign regulatory authorities may disagree with our study design, including endpoints, or our interpretation of data from preclinical studies and clinical trials or find that a product candidate’s benefits do not outweigh its safety risks.
Even if we obtain regulatory approval, we will still face extensive ongoing regulatory requirements and PDS0101 and other candidates may face future development and regulatory difficulties.
Marketing of PDS0101, if approved, along with the manufacturing processes, post- approval clinical data, labeling, packaging, distribution, adverse event reporting, storage, recordkeeping, export, import, advertising and promotional activities for PDS0101, among other things, will be subject to extensive and ongoing requirements of and review by the FDA and other regulatory authorities. These requirements include submissions of safety, efficacy and other post-marketing information and reports, establishment registration and drug listing requirements, continued compliance with current Good Manufacturing Practice, or cGMP, requirements relating to manufacturing, quality control, quality assurance and corresponding maintenance of records and documents, requirements regarding the distribution of samples to physicians and recordkeeping and current Good Clinical Practice, or cGCP requirements for any clinical trials that we conduct post-approval. Even if marketing approval of PDS0101 is granted, the approval may be subject to limitations on the indicated uses for which PDS0101 may be marketed or to the conditions of approval. If PDS0101 receives marketing approval, an accompanying label may limit the approved use of PDS0101, which could limit sales.
The FDA may also impose requirements for costly post-marketing studies or clinical trials and surveillance to monitor the safety and/or efficacy of PDS0101. The FDA closely regulates the post-approval marketing and promotion of drugs to ensure drugs are marketed only for the approved indications and in accordance with the provisions of the approved labeling. The FDA imposes stringent restrictions on manufacturers’ communications regarding off-label use and if we promote or otherwise market PDS0101 for indications other than those for which it is approved, we may be subject to certain enforcement actions. Violations of the Federal Food, Drug, and Cosmetic Act relating to the promotion of prescription biopharmaceutical products may lead to FDA enforcement actions and investigations alleging violations of federal and state health care fraud and abuse laws, as well as state consumer protection laws.
In addition, later discovery of previously unknown adverse events or other problems with PDS0101, manufacturers or manufacturing processes, or failure to comply with regulatory requirements, may yield various results, including:
| ● | restrictions on manufacturing PDS0101; |
| ● | restrictions on the labeling or marketing of PDS0101; |
| ● | restrictions on PDS0101 distribution or use; |
| ● | requirements to conduct post-marketing studies or clinical trials; |
| ● | suspension of any of our ongoing clinical trials; |
| ● | withdrawal of PDS0101 from the market; |
| ● | refusal to approve pending applications or supplements to approved applications that we submit; |
| ● | fines, restitution or disgorgement of profits or revenues; |
| ● | suspension or withdrawal of marketing approvals; |
| ● | refusal to permit the import or export of PDS0101; |
| ● | injunctions or the imposition of civil or criminal penalties. |
Any government investigation of alleged violations of law could require us to expend significant time and resources in response and could generate negative publicity. Any failure to comply with ongoing regulatory requirements may significantly and adversely affect our ability to commercialize and generate revenue from our product candidates, if approved. If regulatory sanctions are applied or if regulatory approval is withdrawn, the value of our company and our operating results will be adversely affected.
The regulatory requirements and policies may change, and additional government regulations may be enacted for which we may also be required to comply. We cannot predict the likelihood, nature or extent of government regulation that may arise from future legislation or administrative action, either in the United States or in other countries. If we or any future collaboration partner are not able to maintain regulatory compliance, we or such collaboration partner, as applicable, may face government enforcement action and our business will suffer. Moreover, our or our future collaborators’ ability to market any future drugs could be limited, which could adversely affect our ability to achieve or sustain profitability. Further, the cost of compliance with post-approval regulations may have a negative effect on our operating results and financial condition.
Even if PDS0101 receives licensure, it may fail to achieve market acceptance by physicians, patients, third-party payors or others in the medical community necessary for commercial success.
If PDS0101 receives marketing approval, it may nonetheless fail to gain sufficient market acceptance by physicians, patients, third-party payors and others in the medical community. If PDS0101 does not achieve an adequate level of acceptance, we may not generate significant revenues and become profitable. The degree of market acceptance, if approved for commercial sale, will depend on a number of factors, including but not limited to:
| ● | the efficacy and potential advantages compared to alternative treatments; |
| ● | effectiveness of sales and marketing efforts; |
| ● | the cost of treatment in relation to alternative treatments; |
| ● | our ability to offer PDS0101 for sale at competitive prices; |
| ● | the convenience and ease of administration compared to alternative treatments; |
| ● | the willingness of the target patient population to try new therapies and of physicians to prescribe these therapies; |
| ● | the willingness of the medical community to offer customers PDS0101 in addition to or in the place of other immunotherapies; |
| ● | the strength of marketing and distribution support; |
| ● | the availability of third-party coverage and adequate reimbursement; |
| ● | whether the product is designated under physician and other provided treatment guidelines as a first, second, or third line therapy; |
| ● | the prevalence and severity of any side effects; and |
| ● | any restrictions on the use of PDS0101 together with other medications. |
Because we expect sales of PDS0101, if approved, to generate substantially all of our revenues for the foreseeable future, the failure of PDS0101 to achieve market acceptance would harm our business and could require us to seek additional financing sooner than we otherwise plan.
We may expend our limited resources to pursue a particular product candidate or indication and fail to capitalize on product candidates or indications that may be more profitable or for which there is a greater likelihood of success.
Because we have limited financial and managerial resources, we are initially developing our lead product candidate, PDS0101 and the other Versamune and Infectimune based products. As a result, we may forego or delay pursuit of opportunities with other product candidates or for other indications that later prove to have greater commercial potential. Our resource allocation decisions may cause us to fail to timely capitalize on viable commercial products or profitable market opportunities. Our spending on current and future research and development programs and product candidates for specific indications may not yield any commercially viable products. If we do not accurately evaluate the commercial potential or target market for a particular product candidate, we may relinquish valuable rights to that product candidate through collaboration, licensing or other royalty arrangements in cases in which it would have been more advantageous for us to retain sole development and commercialization rights to such product candidate.
If we fail to comply with federal and state healthcare regulatory laws, including in our relationships with healthcare providers and customers and third-party payors, we could face criminal prosecution and sanctions, substantial civil penalties, damages, fines, disgorgement, exclusion from participation in governmental healthcare programs, contractual damages, reputational harm, and the curtailment of our operations, any of which could harm our business.
Although we do not provide healthcare services or submit claims for third-party reimbursement, we are subject to healthcare fraud and abuse regulation and enforcement by federal and state governments, which could significantly impact our business, particularly if and when we commercialize any product candidates and if and when payment becomes available from payors for our products. Additionally, our future arrangements with third-party payors and customers may expose us to broadly applicable fraud and abuse and other healthcare laws and regulations that may constrain the business or financial arrangements and relationships through which we market, sell and distribute our medicines for which we obtain marketing approval. The laws that may affect our ability to operate include, but are not limited to:
The Federal Anti-Kickback Statute (AKS), which prohibits, among other things, persons and entities from knowingly and willfully soliciting, receiving, offering, or paying remuneration, directly or indirectly, in cash or in kind, in exchange for or to induce either the referral of an individual for, or the purchase, lease, order or recommendation of, any good, facility, item or service for which payment may be made, in whole or in part, under federal healthcare programs such as Medicare and Medicaid. The Affordable Care Act, among other things, amended the intent requirements of the federal AKS. A person or entity can now be found guilty of violating the AKS without actual knowledge of the statute or specific intent to violate it. In addition, the Affordable Care Act provides that a claim including items or services resulting from a violation of the federal AKS constitutes a false or fraudulent claim for purposes of the FCA.
The False Claims Act’s civil provisions, which prohibit, among other things, individuals or entities from knowingly presenting, or causing to be presented, claims for payment from Medicare, Medicaid or other third-party payors that are false or fraudulent; knowingly making using, or causing to be made or used, a false record or statement to get a false or fraudulent claim paid or approved by the government; or knowingly making, using, or causing to be made or used, a false record or statement to avoid, decrease or conceal an obligation to pay money to the federal government. Intent to deceive is not required to establish liability under the civil False Claims Act.
The False Claims Act’s criminal provisions, which imposes criminal fines or imprisonment against individuals or entities who make or present a claim to the government knowing such claim to be false, fictitious or fraudulent.
The federal Health Insurance Portability and Accountability Act of 1996, or HIPAA, as amended, prohibits, among other actions, executing or attempting to execute, a scheme to defraud or to obtain, by means of false or fraudulent pretenses, representations, or promises, any of the money or property owned by, or under the custody or control of, a healthcare benefit program, regardless of whether the payor is public or private, knowingly and willfully embezzling or stealing from a health care benefit program, willfully obstructing a criminal investigation of a health care offense, and knowingly and willfully falsifying, concealing, or covering up by any trick or device a material fact or making any materially false statements in connection with the delivery of, or payment for, healthcare benefits, items, or services relating to healthcare matters.
HIPAA, as amended by the HITECH Act, and its respective implementing regulations, now makes HIPAA’s privacy and security standards directly applicable to business associates independent contractors or agents of covered entities that receive or obtain protected health information in connection with providing a service on behalf of a covered entity.
Section 5(a) of the Federal Trade Commission Act, or the FTCA, 15 USC § 45(a), given that even for entities that are not deemed “covered entities” or “business associates” under HIPAA, according to the United States Federal Trade Commission, or the FTC, failing to take appropriate steps to keep consumers’ personal information secure constitutes unfair acts or practices in or affecting commerce in violation of its laws. The FTC expects a company’s data security measures to be reasonable and appropriate in light of the sensitivity and volume of consumer information it holds, the size and complexity of its business, and the cost of available tools to improve security and reduce vulnerabilities. Medical data is considered sensitive data that merits stronger safeguards. The FTC’s guidance for appropriately securing consumers’ personal information is similar to what is required by the HIPAA Security Rule.
The federal ”Sunshine” and “Open Payments” requirements under the Patient Protection and Affordable Care Act, as amended by the Health Care Education Reconciliation Act, or collectively, the Affordable Care Act, which require certain manufacturers of drugs, devices, biologics, and medical supplies to report annually to the U.S. Department of Health and Human Services information related to payments and other transfers of value to physicians, other healthcare providers, and teaching hospitals, and ownership and investment interests held by physicians and other healthcare providers and their immediate family members. Failure to submit timely, accurately, and completely the required information may result in civil monetary penalties of up to an aggregate of $150,000 per year and up to an aggregate of $1 million per year for “knowing failures.” In 2022 the Sunshine Act was extended to payments and transfers of value to physician assistants, nurse practitioners, and other mid-level practitioners (with reporting requirements going into effect in 2022 for payments made in 2021). In addition, Section 6004 of the ACA requires annual reporting of information about drug samples that manufacturers and authorized distributors provide to healthcare providers.
State law equivalents of each of the above federal laws and state laws otherwise addressing the pharmaceutical and healthcare industries, such as anti-kickback and false claims laws that may apply to sales or marketing arrangements and claims involving healthcare items or services reimbursed by any third-party payor, including commercial insurers, and in some cases that may apply regardless of payor, i.e., even if reimbursement is not available; state laws that require pharmaceutical companies to comply with the pharmaceutical industry’s voluntary compliance guidelines (the PhRMA Code) and the relevant compliance program guidance promulgated by the federal government (HHS-OIG), or otherwise prohibit, restrict or impose tracking and disclosure requirements related to payments, gifts, or others remuneration that may be made to healthcare providers and other potential referral sources, or marketing practices to such persons and entities or drug pricing information; data privacy and security laws and regulations in foreign jurisdictions that may be more stringent than those in the United States (such as the European Union, which adopted the General Data Protection Regulation, which became effective in May 2018) and state laws governing the privacy and security of information in certain circumstances, many of which differ from each other in significant ways and may not have the same effect, and may apply more broadly than HIPAA, thus complicating compliance efforts.
In our business, healthcare providers, physicians and third-party payors will play a primary role in the recommendation and prescription of our product candidates, if approved for marketing. Moreover, while we do not plan to submit claims and our customers will make the ultimate decision on how to submit claims, from time to time, we may provide reimbursement guidance to our customers. Current or future arrangements with physicians and other healthcare providers and customers, and third-party payors, may expose us to broadly applicable fraud and abuse and other healthcare laws and regulations that may constrain the business or financial arrangements and relationships through which we market, sell and distribute our medicines for which we obtain marketing approval. If a government authority were to conclude that we provided improper advice to our customers or encouraged the submission of false claims for reimbursement or failed to comply with government price reporting requirements, or engaged in off-label promotion of products, we could face action by government authorities. Any violations of these laws, or any action against us for violation of these laws, even if we successfully defend against it, could result in a material adverse effect on our reputation, business, results of operations and financial condition.
We have entered into consulting and employment arrangements with individuals, physicians and other healthcare providers. While we have worked to structure our arrangements to comply with applicable laws, because of the complex and far-reaching nature of these laws, regulatory agencies may view these transactions as prohibited arrangements that must be restructured, or discontinued, or for which we could be subject to other significant penalties. We could be adversely affected if regulatory agencies interpret our financial relationships with providers who serve as clinical investigators in our clinical trials, or influence the ordering of and use our products to be in violation of applicable laws.
The scope and enforcement of each of these laws is uncertain and subject to rapid change in the current environment of healthcare reform, especially in light of the lack of applicable precedent and regulations. Federal and state enforcement bodies have recently increased their scrutiny of interactions between healthcare companies and healthcare providers, which has led to a number of investigations, prosecutions, convictions and settlements in the healthcare industry.
Responding to investigations can be time- and resource-consuming and can divert management’s attention from the business. Additionally, as a result of these investigations, healthcare providers and entities may have to agree to additional onerous compliance and reporting requirements as part of a consent decree or corporate integrity agreement. Any such investigation or settlement could increase our costs or otherwise have an adverse effect on our business.
Even if we are able to commercialize any product candidate, such product candidate may become subject to unfavorable pricing regulations, third-party coverage and reimbursement policies or healthcare reform initiatives, which could harm our business.
The regulations that govern marketing approval, pricing, coverage and reimbursement for new drugs vary widely from country to country. Some countries require approval of the sale price of a drug before it can be marketed. In many countries, the pricing review period begins after marketing approval is granted. In some foreign markets, prescription pharmaceutical pricing remains subject to continuing governmental control even after initial approval is granted. As a result, we might obtain marketing approval for a product in a particular country, but then be subject to price regulations that delay our commercial launch of the product, possibly for lengthy time periods, and negatively impact the revenues we are able to generate from the sale of the product in that country. Adverse pricing limitations may hinder our ability to recoup our investment in one or more product candidates, even if our product candidates obtain marketing approval.
Our ability to commercialize any products successfully also will depend in part on the extent to which reimbursement and coverage for these products and related treatments will be available from government authorities, private health insurers and other organizations, and if reimbursement and coverage is available, the level of reimbursement and coverage. Government authorities and third-party payors, such as private health insurers and health maintenance organizations, decide which medications they will pay for and establish reimbursement levels. A primary trend in the healthcare industry in the United States and elsewhere is cost containment. Government authorities and third-party payors have attempted to control costs by limiting coverage and the amount of reimbursement for particular medications. Increasingly, the third-party payors who reimburse patients or healthcare providers, such as government and private insurance plans, are requiring that drug companies provide them with predetermined discounts from list prices, and are seeking to reduce the prices charged or the amounts reimbursed for medical products. We cannot be sure that coverage and reimbursement will be available for any drug that we commercialize and, if coverage and reimbursement are available, we cannot be sure as to the level of reimbursement. Reimbursement may impact the demand for, or the price of, any product candidate for which we obtain marketing approval. If reimbursement is not available or is available only to limited levels, we may not be able to successfully commercialize any product candidate for which we obtain marketing approval.
There may be significant delays in obtaining reimbursement for newly approved drugs, and coverage may be more limited than the purposes for which the drug is approved by the FDA or comparable foreign regulatory authorities. Moreover, eligibility for reimbursement does not imply that any drug will be reimbursed in all cases or at a rate that covers our costs, including research, development, manufacture, sale and distribution. Interim reimbursement levels for new drugs, if applicable, may also not be sufficient to cover our costs and may not be made permanent. Reimbursement rates may vary according to the use of the drug and the clinical setting in which it is used, may be based on reimbursement levels already set for lower cost drugs, may be incorporated into existing payments for other items or services and may reflect budgetary constraints or imperfections in Medicare data. Net prices for drugs may be reduced by mandatory discounts or rebates required by government healthcare programs or private payors and by any future relaxation of laws that presently restrict imports of drugs from countries where they may be sold at lower prices than in the United States. Third-party payors often rely upon Medicare coverage policy and payment limitations in setting their own reimbursement rates. Our inability to promptly obtain coverage and adequate reimbursement rates from both government-funded and private payors for new products that we develop and for which we obtain marketing approval could have a material adverse effect on our operating results, our ability to raise capital needed to commercialize products and our overall financial condition.
Product liability lawsuits against us could cause us to incur substantial liabilities and could limit the commercialization of PDS0101.
We face an inherent risk of product liability exposure related to the testing of PDS0101 in human clinical trials and will face an even greater risk if we commercially sell any products that we may develop after approval. Regardless of merit or eventual outcome, liability claims may result in:
| ● | decreased demand for PDS0101 or other immunotherapies that we may develop; |
| ● | injury to our reputation and significant negative media attention; |
| ● | withdrawal of clinical trial participants; |
| ● | significant costs to defend any related litigation; |
| ● | substantial monetary awards to trial subjects or patients; |
| ● | the inability to commercialize any products we may develop. |
Although we maintain product liability insurance coverage in the amount of up to $10 million per claim and $10 million in the aggregate, it may not be adequate to cover all liabilities that it may incur. We anticipate that we will need to increase our insurance coverage as we continue clinical trials and if we successfully commercialize any products. Insurance coverage is increasingly expensive. We may not be able to maintain insurance coverage at a reasonable cost or in an amount adequate to satisfy any liability that may arise.
If we are unable to establish sales, marketing and distribution capabilities either on our own or in collaboration with third parties, we may not be successful in commercializing PDS0101 and other product candidates, if approved.
We do not have any infrastructure for the sales, marketing or distribution of PDS0101 or other product candidates, and the cost of establishing and maintaining such an organization may exceed the cost-effectiveness of doing so. In order to market PDS0101 or other product candidates, we must build our sales, distribution, marketing, managerial and other non-technical capabilities or make arrangements with third parties to perform these services. To achieve commercial success for PDS0101 or other product candidates, we will need either our own, or a third party’s, sales and marketing organization. There are significant expenses and risks involved with creating teams for, or contracting for, sales, marketing and distribution capabilities. Any failure or delay in the development of our sales, marketing and distribution capabilities, either internally or in collaboration with third parties, could delay the launch of PDS0101 or other product candidates, which would adversely affect commercialization.
We may be competing with many companies that currently have extensive and well-funded marketing and sales operations. Without an internal team or the support of a third-party to perform marketing and sales functions, we may be unable to compete successfully against these more established companies.
If we obtain approval to commercialize PDS0101 or other product candidates outside of the United States, a variety of risks associated with international operations could harm our business.
If PDS0101 or other product candidates is approved for commercialization, we may enter into agreements with third parties to market them in certain jurisdictions outside the United States. We expect that we will be subject to additional risks related to international operations or entering into international business relationships, including:
| ● | different regulatory requirements for drug approvals and rules governing drug commercialization in foreign countries; |
| ● | reduced protection for intellectual property rights; |
| ● | unexpected changes in tariffs, trade barriers and regulatory requirements; |
| ● | economic weakness, including inflation, or political instability in particular foreign economies and markets; |
| ● | compliance with tax, employment, immigration and labor laws for employees living or traveling abroad; |
| ● | foreign reimbursement, pricing and insurance regimes; |
| ● | foreign currency fluctuations, which could result in increased operating expenses and reduced revenues, and other obligations incident to doing business in another country; |
| ● | workforce uncertainty in countries where labor unrest is more common than in the United States; |
| ● | potential noncompliance with the U.S. Foreign Corrupt Practices Act, the U.K. Bribery Act 2010 and similar anti-bribery and anticorruption laws in other jurisdictions; |
| ● | shortages resulting from any events affecting raw material supply or manufacturing capabilities abroad; and |
| ● | business interruptions resulting from geopolitical actions, including war and terrorism, or natural disasters including earthquakes, typhoons, floods and fires. |
We have no prior experience in these areas. In addition, there are complex regulatory, tax, labor and other legal requirements imposed by both the European Union and many of the individual countries in Europe with which we will need to comply.
Recently enacted and future healthcare legislation, regulations, and policy initiatives may increase the difficulty and cost for us to obtain marketing approval of and commercialize PDS0101 or other product candidates and affect the prices we may obtain and our profitability.
In the United States and some foreign jurisdictions, there have been a number of legislative and regulatory changes and proposed changes regarding the healthcare system that could, among other things, prevent or delay marketing approval of PDS0101 and our other product candidates, restrict or regulate post-approval activities and affect our ability to profitably sell PDS0101 and other product candidates.
For example, in March 2010, the Affordable Care Act, or ACA, was enacted to broaden access to health insurance, reduce or constrain the growth of healthcare spending, enhance remedies against fraud and abuse, add new transparency requirements for health care and health insurance industries, impose new taxes and fees on the health industry and impose additional health policy reforms. Since its enactment, there have been judicial, executive and Congressional challenges to certain aspects of the ACA. On June 17, 2021, the U.S. Supreme Court dismissed the most recent judicial challenge to ACA brought by several states without specifically ruling on the constitutionality of the Act. Prior to the Supreme Court’s decision, President Biden issued an executive order to initiate a special enrollment period from February 15, 2021 through August 15, 2021 for purposes of obtaining health insurance coverage through the ACA marketplace. The executive order also instructed certain governmental agencies to review and reconsider their existing policies and rules that limit access to healthcare, including among others, reexamining Medicaid demonstration projects and waiver programs that include work requirements, and policies that create unnecessary barriers to obtaining access to health insurance coverage through Medicaid or the ACA. It is unclear how other healthcare reform measures of the Biden administration or other efforts, if any, to challenge, repeal or replace the ACA will impact health care laws and regulations or our business.
As another example, the Drug Supply Chain Security Act imposes obligations on manufacturers of prescription biopharmaceuticals in finished dosage forms for commercial distribution. We have not yet adopted the significant measures that will be required to comply with this law. We are not sure whether additional legislative changes will be enacted, or whether the current regulations, guidance or interpretations will be changed, or what the impact of such changes on our business, if any, may be.
We expect that additional state and federal healthcare reform measures will be adopted in the future, any of which could limit the amounts that federal and state governments will pay for immunotherapies, which could result in reduced demand for PDS0101 and other product candidates or additional pricing pressures.
Risks Related to Our Dependence on Third Parties
We have no manufacturing, sales, marketing or distribution capability and we must rely upon third parties for such.
We currently have agreements with various third-party manufacturing facilities for production of our products for research and development and testing purposes. We depend on third-party manufacturers to supply our preclinical and clinical materials and will be reliant on a third-party manufacturer to produce PDS0101 on a commercial scale, should that product receive regulatory approval. Third-party manufacturers must be able to meet our deadlines and adhere to quality standards and specifications. Our predominant reliance on third parties for the manufacture of PDS0101 and all of our Versamune and Infectimune based products creates a dependency that could severely disrupt our research and development, clinical testing, and sales and marketing efforts if the source of such supply proves to be unreliable or unavailable. There is no assurance that any third-party manufacturers will be able to meet commercialized scale production requirements in a timely manner or in accordance with applicable standards or cGMP.
We expect to rely on third-party manufacturers or third-party collaborators for the manufacture of our product candidates for commercial supply of any of our product candidates for which we or any of our future collaborators obtain marketing approval. We may be unable to establish any agreements with third-party manufacturers or to do so on acceptable terms. Even if we are able to establish agreements with third-party manufacturers, reliance on third-party manufacturers entails additional risks, including:
| ● | the possible failure of the third party to manufacture our product candidate according to our schedule, or at all, including if our third-party contractors give greater priority to the supply of other products over our product candidates or otherwise do not satisfactorily perform according to the terms of the agreements between us and them; |
| ● | the possible termination or nonrenewal of agreements by our third-party contractors at a time that is costly or inconvenient for us; |
| ● | the possible breach by the third-party contractors of our agreements with them; |
| ● | the failure of third-party contractors to comply with applicable regulatory requirements; |
| ● | the possible failure of the third party to manufacture our product candidates according to our specifications; |
| ● | the impact of COVID-19 on the facilities of our manufacturers and their supply lines; |
| ● | the possible mislabeling of clinical supplies, potentially resulting in issues including the wrong dose amounts being supplied or active drug or placebo not being properly identified; |
| ● | the possibility of clinical supplies not being delivered to clinical sites on time, leading to clinical trial interruptions, or of drug supplies not being distributed to commercial vendors in a timely manner, resulting in lost sales; and |
| ● | the possible misappropriation of our proprietary information, including our trade secrets and know-how. |
The facilities used by our contract manufacturers to manufacture our product candidates must be approved by the FDA or the EMA pursuant to inspections that will be conducted after we submit our BLA to the FDA or our MAA to the EMA. We do not have complete control over all aspects of the manufacturing process of, and are dependent on, our contract manufacturing partners for compliance with cGMP regulations for manufacturing both active drug substances and finished drug products. Third-party manufacturers may not be able to comply with cGMP regulations or similar regulatory requirements outside of the United States. If our contract manufacturers cannot successfully manufacture material that conforms to our specifications and the strict regulatory requirements of the FDA or comparable foreign regulatory bodies, they will not be able to secure and/or maintain marketing approval for their manufacturing facilities. In addition, we do not have complete control over the ability of our contract manufacturers to maintain adequate quality control, quality assurance and qualified personnel. If the FDA, the EMA or a comparable foreign regulatory authority does not approve these facilities for the manufacture of our product candidates or if it withdraws any such approval in the future, we may need to find alternative manufacturing facilities, which would significantly impact our ability to develop, obtain marketing approval for or market our product candidates, if approved.
Our failure, or the failure of our third-party manufacturers, to comply with applicable regulations could result in sanctions being imposed on us, including fines, injunctions, civil penalties, delays, suspension or withdrawal of approvals, license revocation, seizures or recalls of product candidates or drugs, operating restrictions and criminal prosecutions, any of which could significantly and adversely affect supplies of our product candidates and harm our business and results of operations.
Any drugs that we may develop may compete with other product candidates and drugs for access to manufacturing facilities. There are a limited number of manufacturers that operate under cGMP regulations and that might be capable of manufacturing for us.
Any performance failure on the part of our existing or future manufacturers could delay clinical development or marketing approval.
We do not currently have arrangements in place for redundant supply of the components of our product candidates. If our current contract manufacturer cannot perform as agreed, we may be required to replace that manufacturer. Although we believe that there are several potential alternative manufacturers who could manufacture our product candidates, we may incur added costs and delays in identifying and qualifying any such replacement.
Our current and anticipated future dependence upon others for the manufacture of our product candidates or drugs may adversely affect our future profit margins and our ability to commercialize any drugs that receive marketing approval on a timely and competitive basis.
We intend to rely on third parties to conduct, supervise and monitor our clinical trials, and if those third parties perform in an unsatisfactory manner, it may harm our business.
We intend to rely on CROs and clinical trial sites to ensure the proper and timely conduct of our clinical trials, and we expect to have limited influence over their actual performance.
We intend to rely upon CROs to monitor and manage data for our clinical programs. We expect to control only certain aspects of our CROs’ activities. Nevertheless, we will be responsible for ensuring that each of our studies is conducted in accordance with the applicable protocol, legal, regulatory and scientific standards and our reliance on the CROs does not relieve us of our regulatory responsibilities.
We and our CROs will be required to comply with the Good Laboratory Practices and GCPs, which are regulations and guidelines enforced by the FDA and are also required by the Competent Authorities of the Member States of the European Economic Area and comparable foreign regulatory authorities in the form of International Conference on Harmonization guidelines for our products. The Regulatory authorities enforce GCPs through periodic inspections of trial sponsors, principal investigators and clinical trial sites. If we or our CROs fail to comply with GCPs, the clinical data generated in our clinical trials may be deemed unreliable and the FDA or comparable foreign regulatory authorities may require us to perform additional clinical trials before approving our marketing applications. Accordingly, if our CROs fail to comply with these regulations or fail to recruit a sufficient number of subjects, we may be required to repeat clinical trials, which would delay the regulatory approval process.
Our CROs will not be our employees, and we will not control whether or not they devote sufficient time and resources to our future clinical and nonclinical programs. These CROs may also have relationships with other commercial entities, including our competitors, for whom they may also be conducting clinical trials, or other drug development activities which could harm our competitive position. We face the risk of potential unauthorized disclosure or misappropriation of our intellectual property by CROs, which may reduce our trade secret protection and allow our potential competitors to access and exploit our proprietary technology. If our CROs do not successfully carry out their contractual duties or obligations, fail to meet expected deadlines, or if the quality or accuracy of the clinical data they obtain is compromised due to the failure to adhere to our clinical protocols or regulatory requirements or for any other reasons, our clinical trials may be extended, delayed or terminated, and we may not be able to obtain regulatory approval for, or successfully commercialize PDS0101. As a result, our financial results and the commercial prospects for PDS0101 would be harmed, our costs could increase, and our ability to generate revenues could be delayed.
If our relationship with these CROs terminate, we may not be able to enter into arrangements with alternative CROs or do so on commercially reasonable terms. Switching or adding additional CROs involves substantial cost and requires management time and focus. In addition, there is a natural transition period when a new CRO commences work. As a result, delays occur, which can materially impact our ability to meet our desired clinical development timelines. Though we intend to carefully manage our relationships with our CROs, there can be no assurance that we will not encounter challenges or delays in the future or that these delays or challenges will not have an adverse impact on our business, financial condition and prospects.
If we are unable to establish or manage strategic collaborations in the future, our revenue and drug development may be limited.
Our strategy may include potential reliance upon strategic collaborations for marketing and commercialization of PDS0101 and other Versamune, Versamune plus PDS0301 and Infectimune Products. We also rely on strategic collaborations for research, development, marketing and commercialization for PDS0101 and other Versamune Products. We have also been heavily reliant upon third party outsourcing for our clinical trials execution and production of drug supplies for use in clinical trials.
Establishing strategic collaborations is difficult and time-consuming. Our discussions with potential collaborators may not lead to the establishment of collaborations on favorable terms, if at all. We face significant competition in seeking appropriate collaborators. Whether we reach a definitive agreement for a collaboration will depend, among other things, upon our assessment of the collaborator’s resources and expertise, the terms and conditions of the proposed collaboration and the proposed collaborator’s evaluation of a number of factors. Those factors may include the design or results of clinical trials, the likelihood of approval by the FDA or similar regulatory authorities outside the United States, the potential market for PDS0101 and other Versamune and Versamune plus PDS0301 Products, the costs and complexities of manufacturing and delivering PDS0101 and other Versamune and Versamune plus PDS0301 Products to patients, the potential of competing products, the existence of uncertainty with respect to our ownership of technology, which can exist if there is a challenge to such ownership without regard to the merits of the challenge and industry and market conditions generally. The collaborator may also consider alternative immunotherapies for similar indications that may be available to collaborate on and whether such a collaboration could be more attractive than the one with us for PDS0101 and other Versamune and Versamune plus PDS0301 Products.
Our current collaborations, as well as any future new collaborations, may never result in the successful development or commercialization of PDS0101 and other Versamune, Versamune plus PDS0301 and Infectimune Products or the generation of sales revenue. To the extent that we have entered or will enter into co-promotion or other collaborative arrangements, PDS0101 and other Versamune and Versamune plus PDS0301 Products revenues are likely to be lower than if we directly marketed and sold any products that we develop.
Management of our relationships with our collaborators will require:
| ● | significant time and effort from our management team; |
| ● | financial funding to support said collaboration; |
| ● | coordination of our research and development programs with the research and development priorities of our collaborators; and |
| ● | effective allocation of our resources to multiple projects. |
If we continue to enter into research and development collaborations, our success will in part depend on the performance of our collaborators. We will not directly control the amount or timing of resources devoted by our collaborators to activities related to PDS0101 and other Versamune and Versamune plus PDS0301 Products. Our collaborators may not commit sufficient resources to our research and development programs or the commercialization, marketing or distribution of PDS0101 and other Versamune and Versamune plus PDS0301 Products. If any collaborator fails to commit sufficient resources, our preclinical or clinical development programs related to this collaboration could be delayed or terminated. Also, our collaborators may pursue existing or other development-stage products or alternative technologies in preference to those being developed in collaboration with us. If we fail to make required milestone or royalty payments to our collaborators or to observe other obligations in our agreements with them, our collaborators may have the right to terminate those agreements. Additionally, our collaborators may seek to renegotiate agreements we have entered into, or may disagree with us about the terms and implementation of these agreements. If collaborators disagree with us about the terms or implementation of our agreements, we may face legal claims that may involve considerable expense and could negatively affect our financial results.
We enter into various contracts in the normal course of our business in which we agree to indemnify the other party to the contract. In the event we have to perform under these indemnification provisions, it could have a material adverse effect on our business, financial condition and results of operations.
In the normal course of business, we periodically enter into academic, commercial, service, collaboration, licensing, consulting and other agreements that contain indemnification provisions. With respect to our academic and other research agreements, we typically agree to indemnify the institution and related parties from losses arising from claims relating to the products, processes or services made, used, sold or performed pursuant to the agreements for which we have secured licenses, and from claims arising from our or our sub licensees’ exercise of rights under the agreement. With respect to our commercial agreements, we have agreed to indemnify our vendors from any third-party product liability claims that could result from the production, use or consumption of the product, as well as for alleged infringements of any patent or other intellectual property right by a third party. With respect to consultants, we typically agree to indemnify them from claims arising from the good faith performance of their services.
Should our obligation under an indemnification provision exceed applicable insurance coverage or if we were denied insurance coverage or not covered by insurance, our business, financial condition and results of operations could be adversely affected. Similarly, if we are relying on a collaborator or other third party to indemnify us and the collaborator or other third party is denied insurance coverage or otherwise does not have assets available to indemnify us, our business, financial condition and results of operations could be adversely affected.
The failure of third parties to meet their contractual, regulatory, and other obligations could adversely affect our business.
We rely on suppliers, vendors, outsourcing partners, consultants, alliance partners and other third parties to research, develop, manufacture and commercialize our products and manage certain parts of our business. Using these third parties poses a number of risks, such as:
| ● | they may not perform to our standards or legal requirements; |
| ● | they may not produce reliable results; |
| ● | they may not perform in a timely manner; |
| ● | they may not maintain confidentiality of our proprietary information; |
| ● | disputes may arise with respect to ownership of rights to technology developed with our partners, and those disputes may be resolved against us; and |
| ● | disagreements could cause delays in, or termination of, the research, development or commercialization of our products or result in litigation or arbitration. |
Moreover, some third parties are located in markets subject to political and social risk, corruption, infrastructure problems and natural disasters, in addition to country-specific privacy and data security risk given current legal and regulatory environments. Failure of third parties to meet their contractual, regulatory, legal and other obligations may materially affect our business.
Our business could be adversely affected by the effects of health epidemics, pandemics, or outbreaks of infectious diseases, including the recent COVID-19 pandemic, in regions where we or third parties on which we rely have significant manufacturing facilities, concentrations of clinical trial sites or other business operations. The COVID-19 pandemic could materially affect our operations, including at our headquarters in New Jersey, and at our clinical trial sites, as well as the business or operations of our manufacturers, CROs or other third parties with whom we conduct business.
Our business could be adversely affected by health epidemics in regions where we have concentrations of clinical trial sites or other business operations and could cause significant disruption in the operations of third-party manufacturers and CROs upon whom we rely.
As a result of the COVID-19 outbreak, or similar pandemics, and related “shelter in place” orders and other public health guidance measures, we have and may in the future experience disruptions that materially and adversely impact our clinical trials, business, financial condition and results of operations. Potential disruptions include but are not limited to:
| ● | delays or difficulties in enrolling patients in our clinical trials; |
| ● | delays or difficulties in initiating or expanding clinical trials, including delays or difficulties with clinical site initiation and recruiting clinical site investigators and clinical site staff; |
| ● | increased rates of patients withdrawing from our clinical trials following enrollment as a result of contracting COVID-19 or other health conditions or being forced to quarantine; |
| ● | diversion of healthcare resources away from the conduct of clinical trials, including the diversion of hospitals serving as our clinical trial sites and hospital staff supporting the conduct of our clinical trials; |
| ● | interruption of key clinical trial activities, such as clinical trial site data monitoring, due to limitations on travel imposed or recommended by federal or state governments, employers and others or interruption of clinical trial subject visits and study procedures, which may impact the integrity of subject data and clinical study endpoints; |
| ● | interruption or delays in the operations of the FDA or other regulatory authorities, which may impact review and approval timelines; |
| ● | delays or disruptions in preclinical experiments and investigational new drug application-enabling studies due to restrictions of on-site staff and unforeseen circumstances at contract research organizations and vendors; |
| ● | interruption of, or delays in receiving, supplies of our product candidates from our contract manufacturing organizations due to staffing shortages, production slowdowns or stoppages and disruptions in delivery systems; |
| ● | limitations on our ability to recruit and hire key personnel due to our inability to meet with candidates because of travel restrictions and “shelter in place” orders; |
| ● | limitations on employee resources that would otherwise be focused on the conduct of our preclinical studies and clinical trials, including because of sickness of employees or their families or the desire of employees to avoid contact with large groups of people; and |
| ● | interruption or delays to our sourced discovery and clinical activities. |
Risks Related to Our Intellectual Property
If we are unable to obtain and/or maintain patent protection for our Versamune, Versamune plus PDS0301 platforms, PDS0101, or other Versamune based Products or if the scope of the patent protection obtained is not sufficiently broad, we may not be able to compete effectively in our markets.
We rely upon a combination of patents, trade secret protection and confidentiality agreements to protect the intellectual property related to Versamune. Our success depends in large part on our ability to obtain and maintain patent protection in the United States and other countries. We seek to protect our proprietary position by filing patent applications in the United States and abroad related to Versamune, Versamune plus PDS0301 and Infectimune based products. The patent prosecution process is expensive and time-consuming, and we may not be able to file and prosecute all necessary or desirable patent applications at a reasonable cost or in a timely manner.
It is also possible that we will fail to identify patentable aspects of our research and development output before it is too late to obtain patent protection. The patent applications that we own or license may fail to result in issued patents with claims that cover Versamune, Versamune plus PDS0301 and Infectimune based products or applications in the United States or in other countries. There is no assurance that all potentially relevant prior art relating, which can invalidate a patent or prevent a patent from issuing from a pending patent application is known to us. Even if patents do successfully issue, third parties may challenge their validity, enforceability or scope, which may result in such patents being narrowed, invalidated, or held unenforceable. Any successful challenge to these patents or any other patents owned by or licensed to us could deprive us of rights necessary for the successful commercialization of PDS0101 and other Versamune, Versamune plus PDS0301 and Infectimune based products that we may develop. Further, if we encounter delays in regulatory approvals, the period of time during which we could exclusively market PDS0101 and other Versamune, Versamune plus PDS0301 and Infectimune based products under patent protection could be reduced.
The patent position of biotechnology and pharmaceutical companies generally is highly uncertain, involves complex legal and factual questions and has in recent years been the subject of much litigation. In addition, the laws of foreign countries may not protect our rights to the same extent as the laws of the United States. For example, European patent law restricts the patentability of methods of treatment of the human body more than U.S. law does. Publications of discoveries in scientific literature often lag behind the actual discoveries, and patent applications in the United States and other jurisdictions are typically not published until 18 months after filing, or in some cases not at all. Therefore, we cannot know with certainty whether we were the first to make the inventions claimed in our owned or licensed patents or pending patent applications, or that we were the first to file for patent protection of such inventions. As a result, the issuance, scope, validity, enforceability and commercial value of our patent rights are highly uncertain. Our pending and future patent applications may not result in patents being issued which protect PDS0101 or other Versamune, Versamune plus PDS0301 and Infectimune based products, in whole or in part, or which effectively prevent others from commercializing competitive technologies and immunotherapies. Changes in either the patent laws or interpretation of the patent laws in the United States and other countries may diminish the value of our patents or narrow the scope of our patent protection. Recent Russian Federal Law, No. 46-FZ of March 8, 2022, allows the Russian Government to designate goods for which IP rights are exempted and this rule applies to all IP rights, including trademarks and this rule may affect our IP in the Russian Federation. There is no guidance on how broadly this rule will be applied, though the rule appears to be limited only to the year 2022.
Moreover, we may be subject to a third-party pre-issuance submission of prior art to the U.S. Patent Office, or become involved in derivation, reexamination, inter parties review, post-grant review or interference proceedings challenging its patent rights or the patent rights of others. In other countries, we may be subject to or become involved in opposition proceedings challenging our patent rights or the patent rights of others. An adverse determination in any such submission or proceeding could reduce the scope of, or invalidate, our patent rights, allow third parties to commercialize our technology or immunotherapies and compete directly with us, without payment to us, or result in our inability to manufacture or commercialize PDS0101 without infringing third- party patent rights. In addition, if the breadth or strength of protection provided by our patents and patent applications is threatened, it could dissuade companies from collaborating with us to license, develop or commercialize PDS0101 and other Versamune, Versamune plus PDS0301 and Infectimune based products.
The issuance of a patent is not conclusive as to our inventorship, scope, validity or enforceability, and our owned and licensed patents may be challenged in the courts or patent offices in the United States and abroad. Such challenges may result in patent claims being narrowed, invalidated or held unenforceable, in whole or in part, which could limit our ability to stop others from using or commercializing similar or identical technology and immunotherapies, or limit the duration of the patent protection of our technology and immunotherapies. Moreover, patents have a limited lifespan. In the United States and other countries, the natural expiration of a patent is generally 20 years after it is filed. Various extensions may be available; however, the life of a patent, and the protection it affords, is limited. Without patent protection for PDS0101 and other Versamune, Versamune plus PDS0301 and Infectimune based products, we may be open to competition from generic versions of PDS0101 or other similar products using our technology. Given the amount of time required for the development, testing and regulatory review of new immunotherapy candidates, patents protecting such candidates might expire before or shortly after such candidates are commercialized. As a result, our owned and licensed patent portfolio may not provide us with sufficient rights to exclude others from commercializing immunotherapies similar or identical to ours.
We may have limited foreign intellectual property rights and may not be able to protect our intellectual property rights throughout the world.
We may have limited intellectual property rights outside the U.S. Filing, prosecuting and defending patents on product candidates in all countries throughout the world would be prohibitively expensive, and our intellectual property rights in some countries outside the U.S. can be less extensive than those in the U.S. In addition, the laws of some foreign countries do not protect intellectual property rights to the same extent as federal and state laws in the U.S. Consequently, we may not be able to prevent third parties from practicing our inventions in all countries outside the U.S., or from selling or importing products made using our inventions in and into the U.S. or other jurisdictions. Competitors may use our technologies in jurisdictions where we have not obtained patent protection to develop their own products and further, may export otherwise infringing products to territories where we have patent protection, but enforcement is not as strong as that in the U.S. These products may compete with our products and our patents or other intellectual property rights may not be effective or sufficient to prevent them from competing. Many companies have encountered significant problems in protecting and defending intellectual property rights in foreign jurisdictions. The legal systems of certain countries, particularly certain developing countries, do not favor the enforcement of patents, trade secrets and other intellectual property protection, particularly those relating to biopharmaceutical products, which could make it difficult for us to stop the infringement of our patents or marketing of competing products in violation of our proprietary rights generally. Proceedings to enforce our patent rights in foreign jurisdictions could result in substantial costs and divert our efforts and attention from other aspects of our business, could put our patents at risk of being invalidated or interpreted narrowly and our patent applications at risk of not issuing and could provoke third parties to assert claims against us. We may not prevail in any lawsuits that we initiate, and the damages or other remedies awarded, if any, may not be commercially meaningful. Accordingly, our efforts to enforce our intellectual property rights around the world may be inadequate to obtain a significant commercial advantage from the intellectual property that we develop or license.
We may be involved in lawsuits to protect or enforce our patents, the patents of our licensors or our other intellectual property rights, or defend our products and methods against the property rights of others, which could be expensive, time consuming and unsuccessful.
Competitors may infringe or otherwise violate our patents, the patents of our licensors or our other intellectual property rights. To counter infringement or unauthorized use, we may be required to file legal claims, which can be expensive and time-consuming. In addition, in an infringement proceeding, a court may decide that a patent of ours or our licensors is not valid or is unenforceable, or may refuse to stop the other party from using the technology at issue on the grounds that such patents do not cover the technology in question. An adverse result in any litigation or defense proceedings could put one or more of our patents at risk of being invalidated or interpreted narrowly and could put our patent applications at risk of not issuing. The initiation of a claim against a third-party may also cause the third-party to bring counter claims against us, such as claims asserting that our patents are invalid or unenforceable. In patent litigation in the United States, defendant counterclaims alleging invalidity or unenforceability are commonplace. Grounds for a validity challenge could be an alleged failure to meet any of several statutory requirements, including lack of novelty, obviousness, non-enablement or lack of statutory subject matter. Grounds for an unenforceability assertion could be an allegation that someone connected with prosecution of the patent withheld relevant material information from the USPTO, or made a materially misleading statement, during prosecution. Third parties may also raise similar validity claims before the USPTO in post-grant proceedings such as inter partes review, or post-grant review, or oppositions or similar proceedings outside the United States, in parallel with litigation or even outside the context of litigation. The outcome following legal assertions of invalidity and unenforceability is unpredictable. We cannot be certain that there is no invalidating prior art, of which we and the patent examiner were unaware during prosecution. For the patents and patent applications that we have licensed, we may have limited or no right to participate in the defense of any licensed patents against challenge by a third-party. If a defendant were to prevail on a legal assertion of invalidity or unenforceability, we would lose at least part, and perhaps all, of any future patent protection on PDS0101 and other Versamune, Versamune plus PDS0301 and Infectimune based products. Such a loss of patent protection could harm our business.
We may also face claims that our products infringe patents that our competitors hold. Claims for alleged infringement and any resulting lawsuit, if successful, could subject us to significant liability for damages and invalidations of our proprietary rights. Any such lawsuit, regardless of our success, would likely be time consuming and expensive to resolve and would divert management time and attention. Any potential intellectual property litigation could also force us to do one or more of the following: (a) stop selling our products; (b) obtain a license(s), from the owner of any asserted intellectual property, to sell or use the relevant technology, which license may not be available on reasonable terms, or at all; or (c) redesign our products to avoid using the relevant technology.
We may not be able to prevent, alone or with our licensors, misappropriation of our intellectual property rights, particularly in countries where the laws may not protect those rights as fully as in the United States. Our business could be harmed if in litigation the prevailing party does not offer us a license on commercially reasonable terms. Any litigation or other proceedings to enforce our intellectual property rights may fail, and even if successful, may result in substantial costs and distract our management and other employees.
Furthermore, because of the substantial amount of discovery required in connection with intellectual property litigation, there is a risk that some of our confidential information could be compromised by disclosure during this type of litigation. There could also be public announcements of the results of hearings, motions or other interim proceedings or developments. If securities analysts or investors perceive these results to be negative, it could have an adverse effect on the price of our common stock.
Changes in patent law in the United States and other jurisdictions could diminish the value of patents in general, thereby impairing our ability to protect our products.
As is the case with other biotechnology companies, our success is heavily dependent on intellectual property, particularly patents. Obtaining and enforcing patents in the biotechnology industry involves both technological and legal complexity, and is therefore costly, time-consuming and inherently uncertain. Patent reform legislation in the United States and in other jurisdictions could increase those uncertainties and costs.
The United States has enacted and implemented wide-ranging patent reform legislation. The United States Supreme Court has ruled on several patent cases in recent years, either narrowing the scope of patent protection available in certain circumstances or weakening the rights of patent owners in certain situations. In addition to increasing uncertainty with regard to our ability to obtain patents in the future, this combination of events has created uncertainty with respect to the value of patents, once obtained. Depending on actions by the U.S. Congress, the federal courts, and the USPTO, the laws and regulations governing patents could change in unpredictable ways that would weaken our ability to obtain new patents or to enforce patents that we have licensed or that we might obtain in the future.
We may not be able to protect our intellectual property rights throughout the world, which could impair our business.
Filing, prosecuting and defending patents covering Versamune, Versamune plus PDS0301 and Infectimune based products throughout the world would be prohibitively expensive. Competitors may use our technologies in jurisdictions where we have not obtained patent protection to develop their own immunotherapies and, further, may export otherwise infringing immunotherapies to territories where we may obtain patent protection, but where patent enforcement is not as strong as that in the United States. These immunotherapies may compete with PDS0101 in jurisdictions where we do not have any issued or licensed patents and any future patent claims or other intellectual property rights may not be effective or sufficient to prevent them from so competing.
Many countries, including European Union countries, India, Japan and China, have compulsory licensing laws under which a patent owner may be compelled under specified circumstances to grant licenses to third parties. In those countries, we may have limited remedies if patents are infringed or if we are compelled to grant a license to a third party, which could materially diminish the value of those patents. This could limit our ability to pursue strategic alternatives, including identifying and consummating transactions with potential third-party partners, to further develop, obtain marketing approval for and/or commercialize our drug candidates, and consequently our potential revenue opportunities. Accordingly, our efforts to enforce our intellectual property rights around the world may be inadequate to obtain a significant commercial advantage from the intellectual property that we develop or license.
Our reliance on third parties requires us to share our trade secrets, which increases the possibility that a competitor will discover them or that our trade secrets will be misappropriated or disclosed.
We seek to protect our proprietary technology in part by entering into confidentiality agreements with third parties and, if applicable, material transfer agreements, consulting agreements or other similar agreements with our advisors, employees, third-party contractors and consultants prior to beginning research or disclosing proprietary information. These agreements typically limit the rights of the third parties to use or disclose our confidential information, including our trade secrets. Despite the contractual provisions employed when working with third parties, the need to share trade secrets and other confidential information increases the risk that such trade secrets become known by our competitors, are inadvertently incorporated into the technology of others, or are disclosed or used in violation of these agreements. Given that our proprietary position is based, in part, on our know-how and trade secrets, a competitor’s discovery of our trade secrets or other unauthorized use or disclosure would impair our competitive position and may have an adverse effect on our business and results of operations.
In addition, these agreements typically restrict the ability of our advisors, employees, third-party contractors and consultants to publish data potentially relating to our trade secrets, although our agreements may contain certain limited publication rights. Despite our efforts to protect our trade secrets, our competitors may discover our trade secrets, either through breach of our agreements with third parties, independent development or publication of information by any of our third-party collaborators. A competitor’s discovery of our trade secrets would impair our competitive position and have an adverse impact on our business.
We may be subject to claims that our employees, consultants or independent contractors have wrongfully used or disclosed confidential information of third parties.
We have received confidential and proprietary information from third parties and our employees and contractors. In addition, we employ or may employ individuals who were previously employed at other biotechnology or pharmaceutical companies. We may be subject to claims that we or our employees, consultants or independent contractors have inadvertently or otherwise used or disclosed confidential information of these third parties or our employees’ former employers. Litigation may be necessary to defend against or pursue these claims. Even if we are successful in resolving these claims, litigation could result in substantial cost and be a distraction to our management and employees.
General Market Risk Factors
Our stock price is expected to be volatile, and the market price of our common stock may drop in the future.
The market price of our common stock may be subject to significant fluctuations in the future. Market prices for securities of early-stage pharmaceutical, biotechnology and other life sciences companies have historically been particularly volatile. Some of the factors that may cause the market price of our common stock to fluctuate include:
| ● | the ability of us and our partners to develop product candidates and conduct clinical trials that demonstrate such product candidates are safe and effective; |
| ● | the ability of us or our partners to obtain regulatory approvals for product candidates, and delays or failures to obtain such approvals; |
| ● | failure of any of our product candidates to demonstrate safety and efficacy, receive regulatory approval and achieve commercial success; |
| ● | failure by us to maintain our existing third-party license, manufacturing and supply agreements; |
| ● | impact of COVID-19 and its variants on business operations and clinical trials; |
| ● | failure by us or our licensors to prosecute, maintain, or enforce our intellectual property rights; |
| ● | changes in laws or regulations applicable to our product candidates; |
| ● | any inability to obtain adequate supply of product candidates or the inability to do so at acceptable prices; |
| ● | adverse regulatory authority decisions; |
| ● | introduction of new or competing products by our competitors; |
| ● | failure to meet or exceed financial and development projections we may provide to the public; |
| ● | the perception of the pharmaceutical industry by the public, legislatures, regulators and the investment community; |
| ● | announcements of significant acquisitions, strategic partnerships, joint ventures, or capital commitments by us or our competitors; |
| ● | disputes or other developments relating to proprietary rights, including patents, litigation matters, and our ability to obtain intellectual property protection for our technologies; |
| ● | additions or departures of key personnel; |
| ● | significant lawsuits, including intellectual property or stockholder litigation; |
| ● | if securities or industry analysts do not publish research or reports about us, or if they issue an adverse or misleading opinions regarding our business and stock; |
| ● | if large short positions are taken in our stock and or negative reports are provided, whether they are based in fact or otherwise; |
| ● | changes in the market valuations of similar companies; |
| ● | general market or macroeconomic conditions; |
| ● | sales of our common stock by us or our stockholders in the future; |
| ● | trading volume of our common stock; |
| ● | adverse publicity relating to our markets generally, including with respect to other products and potential products in such markets; |
| ● | changes in the structure of health care payment systems; and |
| ● | period-to-period fluctuations in our financial results. |
Moreover, the stock markets in general have experienced substantial volatility that has often been unrelated to the operating performance of individual companies. These broad market fluctuations may also adversely affect the trading price of our common stock.
In the past, following periods of volatility in the market price of a company’s securities, stockholders have often instituted class action securities litigation against those companies. Such litigation, if instituted, could result in substantial costs and diversion of management attention and resources, which could significantly harm our profitability and reputation.
We are required to meet the Nasdaq Capital Market’s continued listing requirements and other Nasdaq rules, and if we fail to meet such rules and requirements, we may be subject to delisting. Delisting could negatively affect the price of our common stock, which could make it more difficult for us to sell securities in a future financing or for you to sell our common stock.
We are required to meet the continued listing requirements of the Nasdaq Capital Market and other Nasdaq rules, including those regarding director independence and independent committee requirements, minimum stockholders’ equity, minimum share price and certain other corporate governance requirements. In particular, we are required to maintain a minimum bid price for our listed common stock of $1.00 per share. If we do not meet these continued listing requirements, our common stock could be delisted. Delisting from the Nasdaq Capital Market would cause us to pursue eligibility for trading of these securities on other markets or exchanges, including the OTC BB or QB markets, or on the OTC “pink sheets.” In such case, our stockholders’ ability to trade, or obtain quotations of the market value of our common stock would be severely limited because of lower trading volumes and transaction delays. These factors could contribute to lower prices and larger spreads in the bid and ask prices of our securities. There can be no assurance that our securities, if delisted from the Nasdaq Capital Market in the future, would be listed on a national securities exchange, a national quotation service, the OTC markets or the pink sheets. Delisting from the Nasdaq Capital Market, or even the issuance of a notice of potential delisting, would also result in negative publicity, make it more difficult for us to raise additional capital, cause us to lose eligibility to register the sale or resale of our shares on Form S-3 and the automatic exemption from registration under state securities laws for exchange-listed securities, adversely affect the market liquidity of our securities, decrease securities analysts’ coverage of us or diminish investor, supplier and employee confidence.
We do not anticipate that we will pay any cash dividends in the foreseeable future.
We currently expect to retain our future earnings, if any, to fund the development and growth of our business. As a result, capital appreciation, if any, of our company will be the sole source of our stockholders’ gain, if any, for the foreseeable future.
Future sales of shares by existing stockholders could cause our stock price to decline.
If our existing stockholders sell, or indicate an intention to sell, substantial amounts of our common stock in the public market after certain legal restrictions on resale lapse, the trading price of our common stock could decline. As of December 31, 2022, we had 30,170,317 shares of common stock outstanding. Approximately 28,794,124 of such shares are freely tradable, without restriction, in the public market. Approximately 1,376,193 of such shares of common stock are held by directors, executive officers and other affiliates and will be subject to volume limitations under Rule 144 under the Securities Act and various vesting agreements.
Because the Merger resulted in an ownership change under Section 382 of the Code for Edge, pre-merger U.S. net operating loss carryforwards and certain other tax attributes will be subject to limitations.
On March 15, 2019, we, then operating as Edge Therapeutics, Inc., or Edge, completed a reverse merger with privately held PDS Biotechnology Corporation, or Private PDS, pursuant to and in accordance with the terms of the Agreement and Plan of Merger and Reorganization, dated as of November 23, 2018, as amended on January 24, 2019, by and among us, Echos Merger Sub, a wholly-owned subsidiary of Edge, or Merger Sub, and Private PDS, whereby Private PDS merged with and into Merger Sub, with Private PDS surviving as our wholly-owned subsidiary, which we refer to as the Merger. In connection with and immediately following completion of the Merger, we changed our corporate name from Edge Therapeutics, Inc. to PDS Biotechnology Corporation, and Private PDS changed its name to PDS Operating Corporation.
As of December 31, 2018, prior to completion of the Merger, Edge had federal and state net operating loss carryforwards, or NOLs, of $128.6 million and $27.1 million, respectively, due to prior period losses. If a corporation undergoes an “ownership change” within the meaning of Section 382 of the Code, the corporation’s U.S. net operating loss carryforwards and certain other tax attributes arising from before the ownership change are subject to limitations on use after the ownership change. In general, an ownership change occurs if there is a cumulative change in the corporation’s equity ownership by certain stockholders that exceeds fifty percentage points over a rolling three-year period. Similar rules may apply under state and foreign tax laws. We believe that Edge may have already undergone one or more ownership changes prior to the Merger. However, the Merger also resulted in an ownership change for Edge and, accordingly, Edge’s U.S. net operating loss carryforwards and certain other tax attributes available to us are subject to limitations on their use.
Our effective tax rate may increase in the future, including as a result of tax legislation changes, which may have a material adverse effect on our business, financial condition and results of operations.
Our effective tax rate may be impacted by changes in or interpretations of tax laws in the United States or in any given jurisdiction in which we operate, utilization of or limitations on our ability to utilize any tax credit carry-forwards, changes in geographical allocation of revenue and expense and changes in management’s assessment of matters such as our ability to realize the value of deferred tax assets.
In particular, the U.S. government may enact significant changes to the taxation of business entities including, among others, an increase in the corporate income tax rate, the imposition of minimum taxes or surtaxes on certain types of income, significant changes to the taxation of income derived from international operations, and an addition of further limitations on the deductibility of business interest. While certain draft legislation has been publicly released and is under development in Congress at this time, the likelihood of these changes being enacted or implemented is unclear.
Our effective tax rate could also increase due to several factors, including:
| ● | changes in tax rates, tax treaties, and regulations or the interpretation of them; |
| ● | changes to our assessment about our ability to realize deferred tax assets that are based on estimates of our future results, the prudence and feasibility of possible tax planning strategies, and the economic and political environments in which we do business; |
| ● | the outcome of any future tax audits, examinations, or administrative appeals; and |
| ● | the effects of any acquisitions. |
There can be no assurance that our effective income tax rate will not change in future periods. Accordingly, if our effective tax rate were to increase, it may have a material adverse effect on our business, financial condition and results of operations.
Anti-takeover provisions under Delaware law could make an acquisition more difficult and may prevent attempts by our stockholders to replace or remove our current or future management.
Because we are incorporated in Delaware, our company is governed by the provisions of Section 203 of the DGCL, which prohibits stockholders owning in excess of 15% of our voting stock from merging or combining with us. Although we believe these provisions collectively will provide for an opportunity to receive higher bids by requiring potential acquirors to negotiate with our board of directors, they would apply even if the offer may be considered beneficial by some stockholders. In addition, these provisions may frustrate or prevent any attempts by our stockholders to replace or remove then current management by making it more difficult for stockholders to replace members of the board of directors, which is responsible for appointing the members of management.
Our eighth amended and restated certificate of incorporation, as amended, provides that, unless we consent to the selection of an alternative forum, the Court of Chancery of the State of Delaware is the sole and exclusive forum, to the fullest extent permitted by law, for: (a) any derivative action or proceeding brought on our behalf; (b) any action asserting a claim of breach of a fiduciary duty owed by any of our directors, officers or other employees to us or our stockholders; (c) any action asserting a claim arising pursuant to the DGCL, our eighth amended and restated certificate of incorporation, as amended, or our amended and restated bylaws; or (d) any action asserting a claim against us governed by the internal affairs doctrine. This choice of forum provision does not preclude or contract the scope of exclusive federal or concurrent jurisdiction for any actions brought under the Securities Act or the Exchange Act. Accordingly, our exclusive forum provision will not relieve us of our duties to comply with the federal securities laws and the rules and regulations thereunder, and our stockholders will not be deemed to have waived our compliance with these laws, rules and regulations.
Any person or entity purchasing or otherwise acquiring any interest in any of our securities shall be deemed to have notice of and consented to these provisions. These exclusive-forum provisions may limit a stockholder’s ability to bring a claim in a judicial forum of its’ choosing for disputes with us or our directors, officers or other employees, which may discourage lawsuits against us and our directors, officers and other employees.
If a court were to find the choice of forum provision contained in our eighth amended and restated certificate of incorporation, as amended, to be inapplicable or unenforceable in an action, we may incur additional costs associated with resolving such action in other jurisdictions, which could harm our business, results of operations, and financial condition. Even if we are successful in defending against these claims, litigation could result in substantial costs and be a distraction to management and other employees.
Provisions in our amended and restated bylaws could limit our stockholders’ ability to obtain a favorable judicial forum for disputes with us or our directors, officers or employees.
Our amended and restated bylaws provide that, unless we consent in writing to the selection of an alternative forum, the federal district courts of the U.S. shall be the exclusive forum for the resolution of any complaint asserting a cause of action under the Securities Act. This provision limits the ability of our stockholders to bring claims under the Securities Act in any court other than the U.S. federal courts, which ultimately may disadvantage our stockholders or be cost prohibitive. Notwithstanding the foregoing, there is uncertainty as to whether a court (other than state courts in the State of Delaware, which have recently upheld the validity of such a provision) would enforce such a provision and whether investors can waive compliance with the federal securities laws and the rules and regulations thereunder. Furthermore, the exclusive forum provision only applies to claims brought under the Securities Act and does not apply to actions arising under the Exchange Act, which is already subject to federal courts as the exclusive forum.
If a court were to find these provisions of our amended and restated bylaws inapplicable to, or unenforceable in respect of, one or more of the specified types of actions or proceedings, we may incur additional costs associated with resolving such matters in other jurisdictions, which could adversely affect our business, results of operations and financial condition. Even if we are successful in defending against these claims, litigation could result in substantial costs and be a distraction to management and other employees.
We are currently operating in a period of economic uncertainty and capital markets disruption, which has been significantly impacted by geopolitical instability, an ongoing military conflict between Russia and Ukraine, and record inflation. Our business, financial condition and results of operations could be materially adversely affected by any negative impact on the global economy and capital markets resulting from the conflict in Ukraine, geopolitical tensions, or record inflation.
We are exposed to the risk of changes in social, geopolitical, legal, and economic conditions. The global economy has been, and may continue to be, negatively impacted by Russia’s invasion of Ukraine. As a result of Russia’s invasion of Ukraine, the United States, the European Union, the United Kingdom, and other G7 countries, among other countries, have imposed substantial financial and economic sanctions on certain industry sectors and parties in Russia. Broad restrictions on exports to Russia have also been imposed. These measures include: (i) comprehensive financial sanctions against major Russian banks; (ii) additional designations of Russian individuals with significant business interests and government connections; (iii) designations of individuals and entities involved in Russian military activities; and (iv) enhanced export controls and trade sanctions limiting Russia’s ability to import various goods.
Although the length and impact of the ongoing military conflict is highly unpredictable, the conflict in Ukraine has led to market disruptions, including significant volatility in commodity prices, credit markets, as well as supply chain interruptions, which has contributed to record inflation globally. In addition, the ongoing Russian military actions and the resulting sanctions could continue to adversely affect the global economy and financial markets and lead to instability and lack of liquidity in capital markets, potentially making it more difficult for us to obtain additional funds. We are continuing to monitor inflation, the situation in Ukraine and global capital markets and assessing its potential impact on our business.
Furthermore, because of current geopolitical tensions, the Biden administration has recently signed multiple executive orders regarding China. One particular executive order titled Advancing Biotechnology and Biomanufacturing Innovation for a Sustainable, Safe, and Secure American Bioeconomy, signed on September 12, 2022, will likely impact the pharmaceutical industry to encourage U.S. domestic manufacturing of pharmaceutical products. Any additional executive orders regarding or potential sanctions on China could materially impact our manufacturing partners.
To date, our business has not been materially impacted by the ongoing military conflict between Russian and Ukraine, geopolitical tensions, or record inflation, it is impossible to predict the extent to which our operations will be impacted in the short and long term, or the ways in which such matters may impact our business. The extent and duration of the conflict in Ukraine, geopolitical tensions, record inflation and resulting market disruptions are impossible to predict but could be substantial. Any such disruptions may also magnify the impact of other risks described herein.
Our results of operations and liquidity needs could be materially affected by market fluctuations and general economic conditions.
Our results of operations could be materially affected by economic conditions generally, both in the United States and elsewhere around the world. Concerns over inflation, energy costs, geopolitical issues, and the availability and cost of credit have in the past and may continue to contribute to increase volatility and diminished expectations of the economy and markets going forward. Market upheavals may have an adverse effect on us. In the event of a market downturn, our results of operations could be adversely affected. Our future cost of equity or debt capital and access to the capital markets could be adversely affected, and our stock price could decline. There may be disruption or delay in the performance of our third-party contractors and suppliers. If our contractors, suppliers and partners are unable to satisfy their contractual obligations, our business could suffer.
Adverse developments affecting the financial services industry, such as actual events or concerns involving liquidity, defaults or non-performance by financial institutions or transactional counterparties, could adversely affect our current and projected business operations and our financial condition and results of operations.
Actual events involving limited liquidity, defaults, non-performance or other adverse developments that affect financial institutions, transactional counterparties or other companies in the financial services industry or the financial services industry generally, or concerns or rumors about any events of these kinds or other similar risks, have in the past and may in the future lead to market-wide liquidity problems. For example, on March 10, 2023, Silicon Valley Bank, or SVB, was closed by the California Department of Financial Protection and Innovation, which appointed the Federal Deposit Insurance Corporation, or the FDIC, as receiver. Similarly, on March 12, 2023, Signature Bank and Silvergate Capital Corp. were each swept into receivership. Although a statement by the Department of the Treasury, the Federal Reserve and the FDIC stated that all depositors of SVB would have access to all of their money after only one business day of closure, including funds held in uninsured deposit accounts, borrowers under credit agreements, letters of credit and certain other financial instruments with SVB, Signature Bank or any other financial institution that is placed into receivership by the FDIC may be unable to access undrawn amounts thereunder. If any of our counterparties to any such instruments were to be placed into receivership, we may be unable to access such funds. In addition, if any parties with whom we conduct business are unable to access funds pursuant to such instruments or lending arrangements with such a financial institution, such parties’ ability to pay their obligations to us or to enter into new commercial arrangements requiring additional payments to us could be adversely affected. In this regard, counterparties to SVB credit agreements and arrangements, and third parties such as beneficiaries of letters of credit (among others), may experience direct impacts from the closure of SVB and uncertainty remains over liquidity concerns in the broader financial services industry. Similar impacts have occurred in the past, such as during the 2008-2010 financial crisis.
Inflation and rapid increases in interest rates have led to a decline in the trading value of previously issued government securities with interest rates below current market interest rates. Although the U.S. Department of Treasury, FDIC and Federal Reserve Board have announced a program to provide up to $25 billion of loans to financial institutions secured by certain of such government securities held by financial institutions to mitigate the risk of potential losses on the sale of such instruments, widespread demands for customer withdrawals or other liquidity needs of financial institutions for immediately liquidity may exceed the capacity of such program. There is no guarantee that the U.S. Department of Treasury, FDIC and Federal Reserve Board will provide access to uninsured funds in the future in the event of the closure of other banks or financial institutions, or that they would do so in a timely fashion.
Although we assess our banking relationships as we believe necessary or appropriate, our access to funding sources and other credit arrangements in amounts adequate to finance or capitalize our current and projected future business operations could be significantly impaired by factors that affect us, the financial institutions with which we have arrangements directly, or the financial services industry or economy in general. These factors could include, among others, events such as liquidity constraints or failures, the ability to perform obligations under various types of financial, credit or liquidity agreements or arrangements, disruptions or instability in the financial services industry or financial markets, or concerns or negative expectations about the prospects for companies in the financial services industry. These factors could involve financial institutions or financial services industry companies with which we have financial or business relationships, but could also include factors involving financial markets or the financial services industry generally.
In addition, investor concerns regarding the U.S. or international financial systems could result in less favorable commercial financing terms, including higher interest rates or costs and tighter financial and operating covenants, or systemic limitations on access to credit and liquidity sources, thereby making it more difficult for us to acquire financing on acceptable terms or at all. Any decline in available funding or access to our cash and liquidity resources could, among other risks, adversely impact our ability to meet our operating expenses, financial obligations or fulfill our other obligations, result in breaches of our financial and/or contractual obligations or result in violations of federal or state wage and hour laws. Any of these impacts, or any other impacts resulting from the factors described above or other related or similar factors not described above, could have material adverse impacts on our liquidity and our current and/or projected business operations and financial condition and results of operations.
In addition, any further deterioration in the macroeconomic economy or financial services industry could lead to losses or defaults by parties with whom we conduct business, which in turn, could have a material adverse effect on our current and/or projected business operations and results of operations and financial condition. For example, a party with whom we conduct business may fail to make payments when due, default under their agreements with us, become insolvent or declare bankruptcy. Any bankruptcy or insolvency, or the failure to make payments when due, of any counterparty of ours, or the loss of any significant relationships, could result in material losses to us and may material adverse impacts on our business.
| ITEM 1B. | Unresolved Staff Comments |
None.
We maintain a month-to-month lease for our research facilities at the Princeton Innovation Center BioLabs located at 303A College Road E, Princeton, NJ 08540.
On March 10, 2020, we entered into a sublease agreement, effective as of March 5, 2020, to occupy our corporate and executive office located at 25B Vreeland Road, Suite 300, Florham Park, NJ. The sublease commenced on May 1, 2020 and continues for a term of approximately forty (40) months with an option to renew through October 31, 2027. On March 17, 2020, the master lessor provided its consent to the sublease in accordance with the terms of the sublease. This lease will expire in August of 2023.
We believe our current facilities are suitable and adequate to meet our current needs.
The information in Note 11 to the Consolidated Financial Statements contained in Part IV, Item 15 of this Annual Report on Form 10-K is incorporated herein by reference. There are no matters which constitute material pending legal proceedings to which we are a party other than those incorporated into this item by reference from Note 11 to our Consolidated Financial Statements for the year ended December 31, 2022 contained in this Annual Report on Form 10-K.
| ITEM 4. | Mine Safety Disclosures |
Not applicable.
PART II
| ITEM 5. | Market for Registrant’s Common Equity, Related Stockholder Matters and Issuer Purchases of Equity Securities |
Our common stock is listed on the Nasdaq Capital Market under the symbol “PDSB”.
Holders
As of March 16, 2023, there were 44 stockholders of record, which excludes stockholders whose shares were held in nominee or street name by brokers.
We have never declared or paid any cash dividends on our common stock and do not anticipate paying any cash dividends in the foreseeable future. Any future determination to pay dividends will be at the discretion of our board of directors, subject to applicable laws, and will depend on a number of factors, including our financial condition, results of operations, capital requirements, contractual restrictions, general business conditions, and any other factors that our board may deem relevant.
Equity Compensation Plans
Information regarding our equity compensation plans is incorporated by reference from the information in our Proxy Statement for our 2023 Annual Meeting of Stockholders, which we will file with the SEC within 120 days after the end of the fiscal year to which this Annual Report on Form 10-K relates.
Issuer Purchases of Equity Securities
We did not purchase any of our registered equity securities during the period covered by this Annual Report.
| ITEM 7. | Management’s Discussion and Analysis of Financial Condition and Results of Operations |
You should read the following discussion and analysis of our financial condition and results of operations together with our consolidated financial statements and related notes appearing elsewhere in this Annual Report. In addition to historical information, this discussion and analysis contains forward-looking statements that involve risks, uncertainties and assumptions. Our actual results may differ materially from those anticipated in these forward-looking statements as a result of certain factors. We discuss factors that we believe could cause or contribute to these differences below and elsewhere in this Annual Report, including those set forth under Item 1A. “Risk Factors” and under “Forward-Looking Statements” in this Annual Report.
Introduction to PDS Biotechnology Corporation
We are a clinical-stage immunotherapy company developing a growing pipeline of targeted cancer and infectious disease immunotherapies based on our proprietary Versamune®, Versamune plus PDS0301 and Infectimune™ T cell activating technology platforms. Our Versamune based products have demonstrated the potential to overcome the limitations of current immunotherapies by inducing, in vivo, large quantities of high-quality, potent polyfunctional CD4 helper and CD8 killer T cells. We have developed multiple therapies, based on combinations of Versamune and disease-specific antigens, designed to train the immune system to recognize diseased cells and effectively attack and destroy them. We continue to advance our pipeline of candidates to address a wide range of cancers including HPV-positive cancers (anal, cervical, head and neck, penile, vaginal, vulvar) and breast, colon, lung prostate and ovarian cancers. Our Infectimune -based vaccines have demonstrated the potential to induce, not only robust and durable neutralizing antibody response, but also powerful T cell responses including long-lasting memory T cell responses. Our infectious disease candidates are of potential interest primarily for use in universal influenza vaccines.
In June 2022, two abstracts were presented at the 2022 American Society of Clinical Oncology Annual Meeting: Abstract number 6041, PDS0101 a novel type 1 interferon and CD8 T cell activating immunotherapy in combination with pembrolizumab in subjects with recurrent/metastatic HPV16-positive squamous cell carcinoma (HNSCC) and Abstract number 2518, Phase 2 evaluation of the combination of PDS0101, M9241, now PDS0301, and bintrafusp alfa with HPV16+malignancies. Also in May 2022, we announced expansion of our VERSATILE-002 clinical trial into Europe and in June 2022, we announced the U.S. Food and Drug Administration (the “FDA”) had granted Fast Track designation to our lead candidate, PDS0101 in combination with Merck’s anti-PD-1 therapy, KEYTRUDA® (pembrolizumab). The FDA’s Fast Track designation is designed to aid in the development and to expedite the review of drug candidate applications that would potentially treat serious or life-threatening conditions. In order to receive Fast Track designation, a product must also demonstrate the potential to address an unmet medical need. Treatments granted this designation are given the opportunity to have more frequent meetings with the FDA throughout the entire dug development and review process, with the goal of moving promising new drugs more rapidly through the process. It also provides the opportunity to submit sections of a New Drug Application (the “NDA”) on a rolling basis, where the FDA may review portions of the NDA as they are received instead of waiting for the entire NDA submission. In addition, Fast Track designated products are eligible for priority review at the time of NDA or Biologics License Application submission. In October 2023, we announced the successful end-of-phase 2 meeting with the FDA including guidance on key elements of the clinical program that will support the submission of a Biologics License Application (BLA).
In July 2022, we announced the presentation of universal flu vaccine preclinical data for PDS0202 at the 41st American Society of Virology meeting: Abstract number 3733830, Infectimune™ enhances antibodies elicited by COBRA hemagglutinin influenza vaccine.
In November 2022, we announced the presentation of data from two Phase 2 clinical trials at the 37th Annual Meeting for the Society of Immunotherapy of Cancer (SITC): Abstract number 674, IMMUNOCERV, an ongoing Phase 2 trial combining PDS0101, an HPV-specific T cell immunotherapy, with chemotherapy and radiation for treatment of locally advanced cervical cancers and abstract number 695, Immune correlates associated with clinical benefit in patients with checkpoint refractory HPV-associated malignancies treated with triple combination immunotherapy.
In January 2023, we announced the exclusive global license agreement with Merck KGaA, Darmstadt, Germany for the tumor targeting antibody conjugated IL-12, M9241, which joined our pipeline as PDS0301. PDS0301 is a novel investigational tumor-targeting fusion protein of Interleukin 12 that enhances the proliferation, potency, infiltration and longevity of T cells in the tumor microenvironment and is designed to overcome tumor immune suppression utilizing a different mechanism from immune checkpoint inhibitors (ICI). The ownership of these two assets we believe will streamline the registrational process and as use of the combination of Versamune® and an IgG1 IL-12 is patented by PDS Biotech. In a Phase 2 National Cancer Institute (NCI)-led clinical trial in ICI refractory patients, the combination of PDS0101 and PDS0301 administered with an investigational bi-functional ICI resulted in a median overall survival of 21 months, which compares favorably to the historical median survival of 3-4 months seen with checkpoint inhibitors and best reported median survival to date with systemic therapy of 8.2 months in ICI refractory head and neck cancer.
In February 2023, we announced a successful completion of a Type B meeting with the FDA for the triple combination of PDS0101 and PDS0301 with an FDA-approved immune checkpoint inhibitor for the treatment of recurrent/metastatic, ICI refractory head and neck cancer that is positive for the human papilloma virus (HPV) type 16. In recent interactions with the FDA, we confirmed the required contents of a clinical protocol for the potential registrational trial.
VERSATILE-002: PDS0101 + KEYTRUDA®
In November 2020, our VERSATILE-002 Phase 2 clinical trial evaluating the combination of PDS0101 in combination with Merck’s anti-PD-1 therapy, KEYTRUDA® (pembrolizumab) which is the FDA-approved standard of care for first-line treatment of recurrent/ metastatic head and neck cancer commenced and is actively recruiting patients. The clinical trial will evaluate the efficacy and safety of this therapeutic combination as a first-line treatment in patients with recurrent or metastatic head and neck cancer and high-risk human papillomavirus-16 (HPV16) infection.
In this PDS Biotech-sponsored trial patients whose cancer has returned or spread following initial treatment will be treated with the combination of PDS0101 and KEYTRUDA® to evaluate if the addition of PDS0101 might improve the efficacy reported in published studies of KEYTRUDA® alone. Patients in the trial will receive a total of 5 cycles of combination therapy in the context of standard of care KEYTRUDA® therapy administered every three weeks until disease progression. The primary endpoint of VERSATILE-002 is the objective response rate– or ORR – at six months following initiation of treatment. There are two cohorts in the trial. Cohort 1 is for patients who have yet to be treated with a immune checkpoint inhibitor (ICI naïve) and cohort 2 which consists of patients who have failed immune checkpoint inhibitor therapy (ICI refractory).
In February 2022, we announced we had achieved the preliminary efficacy milestone of at least four or more objective responses of the first 17 patients in the ICI naïve arm that allowed that arm to proceed to full enrollment. We also announced detailed preliminary safety data which showed that the combination is well tolerated without evidence of enhanced or significant toxicity in the first 18 patients in the ICI naïve arm. We have completed enrollment in Stage 1 of the ICI refractory arm and are waiting for sufficient follow up to conduct the futility analysis.
In June 2022, we announced additional preliminary efficacy and safety data from this trial at the ASCO Annual Meeting (Weiss J et al. J Clin Oncol 40, 2022 (suppl 16; abstr 6041). The abstract provided preliminary data on 19 patients (safety) with available imaging data for 17 of the 19 patients (efficacy). Highlights from the abstract were as follows:
| ● | Response rates thus far (tumor shrinkage greater than 30%) seen in 7/17 (41.2%) patients in comparison to the published results of approximately 19% for approved ICIs, used as monotherapy for recurrent or metastatic head and neck cancer, with 2 of the 7 having complete responses (CR) |
| ● | Stable disease (SD) was reported in 6/17 (35.3%) patients, with 4 of the 6 (67%) experiencing tumor shrinkage of less than 30% |
| ● | Clinical efficacy (ORR + SD) was seen in 13/17 (76.5%) patients |
| ● | Progressive/ongoing disease was reported in 4/17 (23.5%) patients |
| ● | Patients had received a median of 4/5 doses of PDS0101 (range 1-5) and 9/35 doses of KEYTRUDA® (range 1-18) |
| ● | There were no treatment-related adverse events greater than or equal to Grade 3 (N=19) |
| ● | No patients required dose interruption or reduction on the combination treatment |
| ● | No patients discontinued the combination treatment |
| ● | At 9 months of follow up (median not yet achieved): |
| ● | Progression free survival (PFS) rate was 55.2% |
| ● | Overall survival (OS) rate was 87.2% |
| ● | no control or comparative studies have been conducted between ICIs and PDS0101 |
In May 2022, we announced the expansion of this trial into Europe and in June 2022, as described above, we received Fast Track designation for PDS0101 in combination with pembrolizumab.
In August 2022, we announced our independent Data Monitoring Committee (DMC) met and evaluated data from 43 patients and noted there were no Grade 3 or greater treatment-related adverse events attributed to the combination. The DMC recommended continuing the trial with no modifications.
In October 2022, we announced an end-of-phase 2 meeting with the FDA for PDS0101 in combination with KEYTRUDA®. We are currently evaluating the guidance on the key elements of the clinical program that will support the submission of a Biologics License Application for PDS0101.
In December 2022, we announced completion of the first stage of enrollment in the ICI refractory arm. Cohort follow-up is in progress that will permit a futility analysis to determine progression to stage 2 enrollment.
National Cancer Institute: PDS0101+ M9241 (now PDS0301) +Bintrafusp Alfa
In June 2020, the first patient was dosed under a PDS0101 Cooperative Research and Development Agreement (CRADA), in the NCI led Phase 2 investigator initiated trial evaluating PDS0101 with an IgG1 IL-12 (M9241), now PDS0301, and M7824 (Bintrafusp alfa), which is owned by EMD Serono (Merck KGaA) in patients with advanced/refractory HPV-positive cancers who have failed prior treatment. In February 2021, we announced that the NCI’s Phase 2 clinical trial of PDS0101 for the treatment of advanced/refractory HPV-positive cancers had achieved its preliminary objective response target in patients naïve to check point inhibitors which allowed for full enrollment of approximately 20 patients in this group. In addition, based on promising results in the ICI naïve arm, the trial was amended to allow enrollment of a separate cohort of ICI-refractory patients for assessment of safety and activity of the triple combination. Preliminary efficacy assessment of the triple combination in this added group of 20 ICI refractory patients is ongoing.
Preclinical study results arising from this CRADA were published in the Journal for ImmunoTherapy of Cancer, Immunomodulation to enhance the efficacy of an HPV therapeutic vaccine (Journal for ImmunoTherapy of Cancer2020;8:e000612. doi:10.1136/ jitc-2020-000612), indicating that PDS0101 generated both HPV-specific T cells and an associated antitumor response when used as a monotherapy. When PDS0101 was combined with two other novel clinical-stage anti-cancer agents, Bintrafusp Alfa and M9241, now PDS0301, the preclinical data suggested that all three therapeutic agents worked synergistically to provide superior tumor T cell responses and subsequent tumor regression when compared to any of the agents alone or the 2-component combinations. If the published preclinical data demonstrating powerful activity of the triple combination is successfully confirmed in the ongoing Phase 2 trial, this triple combination could form the basis of a unique platform providing improved cancer treatments across multiple cancers.
In June 2021, at the American Society of Clinical Oncology (ASCO) conference the NCI announced interim data in this trial which included, data in both ICI naïve and refractory patients. In the ICI naïve group 83% (5/6) of patients had an objective response, and 1 subject had achieved a complete response with no evidence of disease. 100% of the ICI naïve patients were alive at a median duration of 8 months. In the ICI refractory group 42% (5/12) of patients had an objective response, and 1 subject had achieved a complete response with no evidence of disease. 10/12 (83%) of ICI refractory patients were alive at a median duration of 8 months. An update provided in January 2022 showed as of December 31, 2021, that >40 subjects had been recruited into the trial and 30 HPV16-positive patients had been evaluated. The median survival of all patients (3:1 ICI refractor to naïve) was 12 months and progressing. The historical survival of ICI naïve and ICI refractory advanced HPV-positive cancers when treated with ICI are 7-11 months and 3-4 months, respectively, and best reported median survival to date with systemic therapy of 8.2 months in ICI refractory head and neck cancer.
In June 2022, at the 2022 ASCO Annual Meeting, the NCI provided an update to the preliminary data presented at the 2021 meeting (Strauss J et al. J Clin Oncol 40, 2022 [suppl 16; abstr 2518]). This included data from 30 patients and highlights were as follows:
| ● | Objective response (OR = > 30% tumor reduction) was seen in 88% (7/8) of patients with ICI-naive disease; 4/7 (57%) patients’ responses are ongoing (median 17 months). |
| ● | With ICI refractory patients: PDS0301 dosing appears to affect response rates, with 5/8 (63%) patients receiving PDS0301 at 16.8 mcg/kg achieving an OR compared to 1/14 (7%) patients who received PDS0301 at 8 mcg/kg achieving an OR; 4/6 (67%) patients’ responses are ongoing (median 12 months). |
| ● | Tumor reduction was seen in 45% (10/22) of patients with ICI-refractory disease, including patients receiving high or low dose PDS0301. |
| ● | In ICI refractory patients treated with high or low dose PDS0301, survival outcomes were similar (p=0.96 by Kaplan Meier analysis). At a median of 12 months of follow up 17/22 (77%) of patients were alive. |
| ● | In ICI naïve patients 6/8 (75%) were alive at median 17 months of follow up. |
| ● | Similar OR and survival were seen across all types of HPV16-positive cancers. |
| ● | Preliminary safety data: 13/30 (43%) of patients experienced Grade 3 treatment-related adverse events (AEs), and 2/30 patients (7%) experienced Grade 4 AEs. There were no grade 5 treatment-related AEs. |
| ● | The study results to date strongly suggest, in agreement with the published preclinical studies, that all 3 drugs contribute to the clinical outcomes. |
In September 2022, we announced, in agreement with the NCI, that the ICI refractory patients had been selected as the preferred treatment group in the on-going PDS0101 based triple combination therapy in advanced HPV-positive cancers and the trial was closed to further enrollment given the ICI refractory arm has been fully recruited.
In October 2022, we announced expanded interim data as follows:
| ● | Survival data: 66% (19/29) of HPV16-positive ICI refractory patients in the cohort were alive at a median follow up of 16 months |
| ● | Safety profile: 48% (24/50) patients experienced Grade 3 treatment-related adverse events (AEs), and 4% (2/50) patients experienced Grade 4 AEs. There were no Grade 3 treatment-related AEs. |
| ● | HPV16-positive ICI naïve patients: 75% (6/8) were alive at a median follow up of 25 months and 38% (3/8) of responders had a complete response. |
In December 2022, we announced expanded interim data as follows:
| ● | Median OS is 21 months in 29 checkpoint inhibitor refractory patients who received the triple combination. The reported historical median OS in patients with ICI refractory disease is 3-4 months seen with checkpoint inhibitors and best reported median survival to date with systemic therapy of 8.2 months in ICI refractory head and neck cancer. |
| ● | In ICI naïve subjects, 75% remain alive at a median follow-up of 27 months. As a result, median OS has not yet been reached. Historically median OS for similar patients with platinum experienced ICI naïve disease is 7-11 months. |
| ● | Objective response rate (ORR) in ICI refractory patients who received the optimal dose of the triple combination is 63% (5/8). In current approaches ORR is reported to be less than 10%. |
| ● | ORR in ICI naïve patients with the triple combination is 88%. In current approaches ORR is reported to be less than 25% with FDA-approved ICIs in HPV-associated cancers. |
| ● | Safety data have not changed since October’s update. 48% (24/50) of patients experienced Grade 3 (moderate) treatment-related adverse events (AEs), and 4% (2/50) patients experienced Grade 4 (severe) AEs, compared with approximately 70% of patients receiving the combination of ICIs and chemotherapy reporting Grade 3 and higher treatment-related AEs |
In February 2023, we announced the successful completion of a Type B meeting with the FDA for the combination therapy of PDS0101, PDS0301, and an FDA-approved immune checkpoint inhibitor for the treatment of recurrent/metastatic HPV-positive ICI-refractory head and neck cancer. We confirmed the required contents of the study design for a potential registration of the combination.
MD Anderson Cancer Center (IMMUNOCERV): PDS0101+ Chemoradiotherapy
In October 2020, another PDS0101 Phase 2 IIT was initiated with The University of Texas MD Anderson Cancer Center and is actively recruiting patients. This clinical trial is investigating the safety and anti-tumor efficacy of PDS0101 in combination with standard-of-care chemo-radiotherapy, or CRT, and their correlation with critical immunological biomarkers in patients with locally advanced cervical cancer. We believe Versamune has strong T cell induction has the potential to meaningfully enhance efficacy of the current standard of care CRT treatment in this indication. Enrollment in this trial is on-going.
In November 2022, we announced data from this trial was included in a poster presentation at the 2022 SITC Annual Meeting which included the following:
| ● | 9 of the 17 patients had completed a Day 170 post-treatment Positron Emission Tomography, Computed Tomography (PET CT) scan to assess the status of the cancer. This included 78% (7/9) of treated patients with advanced cervical cancer (FIGO stage III or IV). |
| ● | 100% (9/9) of patients treated with the combination of PDS0101 and CRT had an objective response. |
| ● | 89% (8/9) of patients treated with the combination of PDS0101 and CRT demonstrated a complete response (CR) on Day 170 by PET CT. One patient who received 3 of the 5 scheduled doses of PDS0101 showed signs of residual disease. One patient who had a CR died from an event unrelated to either their underlying disease or treatment. |
| ● | 1-year disease-free survival and 1-year overall survival of 89% (8/9) in patients treated with the combination of PDS0101 and CRT |
| ● | As previously reported, data confirm PDS0101 treatment activates HPV16-specific CD8 T cells. This increase was not seen in patients who did not receive PDS0101. The increase in HPV16-specific T cells generated by the treatment is positively correlated with tumor cell death, suggesting cytotoxic CD8 T cells are important mediators of antigen-specific immunity. |
| ● | The data affirm that PDS0101 activates Type 1 interferon pathway in humans, mimicking the mechanism previously demonstrated in preclinical studies in animal models |
| ● | Toxicity of PDS0101 remains limited to low-grade local injection site reactions. |
Mayo Clinic: PDS0101 Monotherapy and in combination with KEYTRUDA
In February 2022 we announced the initiation of another ITT, MC200710, for PDS0101 alone or in combination with the check point inhibitor, KEYTRUDA®, in patients with HPV-positive oropharyngeal cancer(HPV(+)OPSCC) at high risk of recurrence. The trial is being led by Drs. David Routman, Katharine Price, Kathryn Van Abel, and Ashish Chintakuntlawar at Mayo Clinic, a nationally and internationally recognized center of excellence for the treatment of head and neck cancers. We believe that this trial not only broadens our addressable patient population of those affected by the increasing incidence of HPV(+)OPSCC, but also allows us to better understand the activity of PDS0101 alone or in combination with KEYTRUDA® in earlier stages of disease. This trial is currently open for enrollment.
In this trial treatment will be administered before patients proceed to transoral robotic surgery (TORS) with curative intent. Treatment in this setting is referred to as neoadjuvant treatment. PDS0101 has been shown to induce CD8 killer T cells that target and kill HPV-positive cancers, either alone or in combination with checkpoint inhibitors in preclinical studies, and in combination in clinical studies of patients with advanced recurrent/metastatic HPV-positive cancers. This trial will explore whether PDS0101 with or without checkpoint inhibition may increase HPV-specific anti-tumor responses, potentially resulting in tumor shrinkage, pathologic regression, and decreases in circulating tumor DNA (ctDNA).
Other Versamune® -Based Products in Development:
PDS0102
PDS0102 is an investigational immunotherapy utilizing tumor-associated and immunologically active T cell receptor gamma alternate reading framed protein (TARP) from the NCI. PDS0102 is designed to treat TARP-positive cancers including, acute myeloid leukemia (AML), prostate and breast cancer. In our preclinical work, the administration of PDS0102, the Versamuine+TARP antigen combination led to the induction of large numbers of polyfunctional tumor targeted killer T cells. In addition, the TARP tumor antigen alone has already been studied at the NCI in men with prostate cancer and been shown to be safe, immunogenic with slowing tumor growth rates (NCT00972309). We are evaluating the next steps in the clinical development of PDS0102 and are seeking nondilutive funding to progress to human trials.
In April 2020, the above mentioned, PDS Biotech-NCI CRADA was expanded beyond PDS0101 to include clinical and preclinical development of PDS0103. PDS0103 is an investigational immune therapy owned by us and designed to treat cancers associated with the mucin-1, or MUC1, oncogenic protein. These include cancers such as ovarian, breast, colorectal and lung cancers. PDS0103 combines Versamune with novel highly immunogenic agonist epitopes of MUC1 developed by the NCI and licensed by PDS. PDS0103 is currently in late preclinical development.
MUC1 is highly expressed in several types of cancer and has been shown to be associated with drug resistance and poor disease prognosis in breast, colorectal, lung and ovarian cancers, for which PDS0103 is being developed. Expression of MUC1 is often associated with poor disease prognosis, due in part to drug resistance. In preclinical studies, and similarly to PDS0101, PDS0103 demonstrated the ability to generate powerful MUC1-specific CD8 killer T cells. In the first quarter of 2022, we held a pre-IND meeting with the FDA on PDS0103 and prepared to submit our IND package in the first half of 2023. However, the actual submission date may potentially be impacted by the outcome of our meetings with the FDA on the timing of a pivotal trial for PDS0101. Our primary goal is commercialization of PDS0101, and allocation of resources to implement an earlier than planned start of a registrational trial may delay PDS0103 initiation.
Infectimune Development Strategy
We believe that the key differentiating attributes of the Infectimune platform technology are strong induction of CD8 and CD4 T cells as well as antibodies which can be leveraged to improve treatment and preventive options in several infectious disease indications. In January 2022 we announced preclinical data on our universal flu program sponsored by the National Institute of Allergy and Infectious Disease (NIAID) demonstrating the potential of the Infectimune technology with computationally designed influenza proteins developed by the laboratory of Dr. Ted Ross at the University of Georgia to generate broadly protective anti-influenza immune responses across multiple strains of influenza. This data has provided a unique opportunity to highlight Infectimune’s potentially transformative utility in the development of more broadly effective and longer lasting protective vaccines. Current preventive and prophylactic vaccine approaches and technologies predominantly focus on creating strong induction of antibody responses. However, the induction of T cell responses, in addition to antibody responses, provides more durable and broad protection against infectious diseases.
Based on the promising data recently announced with the universal seasonal flu vaccine and the current focus of the NIAID in developing more effective flu vaccines, we have decided to opportunistically focus our near-term infectious disease activities to align with the interests of the NIAID Collaborative Influenza Vaccine Innovation Centers (CIVICs) program. This will involve development of a universal seasonal flu vaccine and the potential development of a universal pandemic influenza vaccine based on similar computationally designed antigens as have shown promise with Infectimune.
In July 2022, we announced the presentation of universal flu vaccine preclinical data for PDS0202 at the 41st American Society of Virology meeting: Abstract number 3733830, Infectimune enhances antibodies elicited by COBRA hemagglutinin influenza vaccine. We are evaluating the next steps in the clinical development and funding for PDS0202.
The results for Infectimune based PDS0202 and PDS0203 were published in the peer reviewed journal Viruses in February 2023: preclinical studies demonstrating complete protection against sickness after lethal challenge with live SARS-CoV-2 or influenza viruses (Gandhapudi SK et al. Viruses 2023, 15, 432) and dramatically enhanced CD4 T cell responses to recombinant influenza proteins compared to leading commercial vaccine adjuvants (Henson TR et al. Viruses 2023, 15, 538).
Our current pipeline of Versamune and Infectimune based therapies is as follows:
We have never been profitable and have incurred net losses in each year since inception. Our net losses were $40.9 million, and $16.9 million for the years ended December 31, 2022 and 2021, respectively. As of December 31, 2022, we had an accumulated deficit of $101.6 million. Substantially all of our net losses have resulted from costs incurred in connection with our research and development programs and from general and administrative costs associated with these operations.
As of December 31, 2022, we had $73.8 million in cash and cash equivalents.
Our future funding requirements will depend on many factors, including the following:
| ● | the timing and costs of our planned clinical trials; |
| ● | the timing and costs of our planned preclinical studies of our Versamune platform; |
| ● | the outcome, timing and costs of seeking regulatory approvals; |
| ● | the terms and timing of any future collaborations, licensing, consulting or other arrangements that we may enter into; |
| ● | the amount and timing of any payments we may be required to make in connection with the licensing, filing, prosecution, maintenance, defense and enforcement of any patents or patent applications or other intellectual property rights; and |
| ● | the extent to which we license or acquire other products and technologies. |
Selected Financial Operations Overview
Revenue
We have not generated any revenues from commercial product sales and do not expect to generate any such revenue in the near future. We may, but there are no assurances that we will, generate revenue in the future from a combination of research and development payments, license fees and other upfront payments or milestone payments.
Research and Development Expenses
Research and development expenses include employee-related expenses, costs to acquire license rights to use certain technology in our research and development projects, costs of acquiring, developing and manufacturing clinical trial materials, as well as fees paid to consultants and various entities that perform certain research and testing on our behalf. Costs for certain development activities, such as clinical trials, are recognized based on an evaluation of the progress to completion of specific tasks using data such as patient enrollment, clinical site activations or information provided by vendors on their actual costs incurred. Payments for these activities are based on the terms of the individual arrangements, which may differ from the pattern of costs incurred, and are reflected in the consolidated financial statements as prepaid or accrued expenses. Costs incurred in connection with research and development activities are expensed as incurred.
We expect that our research and development expenses will increase significantly over the next several years as we advance our Versamune based immuno-oncology, or I-O, candidates into and through clinical trials, pursues regulatory approval of our injectable Versamune candidates and prepare for a possible commercial launch, all of which will also require a significant investment in contract and internal manufacturing and inventory related costs.
The process of conducting human clinical trials necessary to obtain regulatory approval is costly and time consuming. We may never succeed in achieving marketing approval for our injectable I-O candidates. The probability of successful commercialization of our I-O candidates may be affected by numerous factors, including clinical data obtained in future trials, competition, manufacturing capability and commercial viability. As a result, we are unable to determine the duration and completion costs of our research and development projects or when and to what extent we will generate revenue from the commercialization and sale of any of our product candidates.
The following table summarizes our research and development expenses incurred for the periods indicated (in thousands):
| | | Year Ended December 31, | |
| | | 2022 | | | 2021 | |
| PDS projects | | $ | 12,468 | | | $ | 6,173 | |
| Clinical consulting | | | 378 | | | | 732 | |
| Cost of license rights | | | 10,000 | | | | - | |
| Salaries and other costs | | | 6,586 | | | | 4,349 | |
| Total | | $ | 29,431 | | | $ | 11,254 | |
General and Administrative Expenses
General and administrative expenses consist primarily of salaries and related benefits, including stock-based compensation, related to our executive, finance, legal, business development and support functions. Other general and administrative expenses include travel expenses, professional fees for auditing, tax and legal services and facility-related costs.
Interest Income (Expense), net
Interest income (expense), net consists of interest income earned from bank deposits and interest expense consists of interest paid on outstanding debt plus amortization of the debt discount and interest from capital leases. These amounts will fluctuate based on changes to the interest rate environment.
Critical Accounting Policies
Our accounting policies are more fully described in Note 2 to the consolidated financial statements included in this Annual Report on Form 10-K. As described in Note 2, the preparation of these financial statements requires us to make estimates and assumptions that affect the reported amounts of assets and liabilities and the disclosure of contingent assets and liabilities at the date of the financial statements, as well as the reported revenue generated and expenses incurred during the reporting periods. Our estimates are based on our historical experience and on various market specific and other relevant assumptions that we believe are reasonable under the circumstances, the results of which form the basis for making judgments about the carrying value of assets and liabilities that are not readily apparent from other sources. Estimates are assessed each period and updated to reflect current information. Actual results may differ from these estimates. We believe that the following discussion addresses our most critical accounting policies, which are those that are most important to the portrayal of our financial condition and results of operations and require management’s most difficult, subjective and complex judgments.
We file U.S. federal income tax returns and New Jersey state tax returns. Our deferred tax assets are primarily comprised of federal and state tax net operating losses and tax credit carryforwards and are recorded using enacted tax rates expected to be in effect in the years in which these temporary differences are expected to be utilized. At December 31, 2022, we had federal net operating losses, or NOLs, carryforwards of approximately $119.3 million, $30.0 million of which expire at various dates between 2028 and 2037, losses generated in 2018 or later of $78.7 million will carry forward indefinitely. At December 31, 2022, we had federal research and development credits carryforwards of approximately $1.7 million. We may be subject to the net operating loss utilization provisions of Section 382 of the Internal Revenue Code. The effect of an ownership change would be the imposition of an annual limitation on the use of NOL carryforwards attributable to periods before the change. The amount of the annual limitation depends upon our value immediately before the ownership change, changes to our capital during a specified period prior to the change, and the federal published interest rate. Although we have not completed an analysis under Section 382 of the Code, it is likely that the utilization of the NOLs will be limited.
Accrued Clinical Expenses
When preparing our financial statements, we are required to estimate our accrued clinical expenses. This process involves reviewing open contracts and communicating with our personnel to identify services that have been performed on our behalf and estimating the level of service performed and the associated cost incurred for the service when we have not yet been invoiced or otherwise notified of actual cost. If we underestimate or overestimate the cost associated with a trial or service at a given point in time, adjustments to research and development expenses may be necessary in future periods. Historically, our estimated accrued clinical expenses have approximated actual expense incurred.
Stock-based Compensation
We estimate the fair value of our stock-based option awards to employees, directors and non-employees using the Black-Scholes option-pricing model, which requires the following assumptions: (1) the expected volatility of our stock is based on volatilities of a peer group of similar companies in the biotechnology industry whose share prices are publicly available, (2) the expected term of the award is based on the simplified method, which is the midpoint between the requisite service period and the contractual term of the option, as we have a limited history of being a public company to develop reasonable expectations about future exercise patterns and employment duration for our options, (3) the risk-free interest rate based on U.S. Treasury notes with a term approximating the expected life of the option and (4) expected dividend yield of 0, since we have never paid cash dividends and have no present intention to pay cash dividends.
Results of Operations
Comparison of the Years Ended December 31, 2022 and 2021
| | | Year Ended December 31, | | | Increase (Decrease) | |
| | | 2022 | | | 2021 | | | $ | | |
| % | |
| | | (in thousands) | | | | | | | | |
| Operating expenses: | | | | | | | | | | | | | |
| Research and development expenses | | $ | 29,431 | | | $ | 11,254 | | | $ | 18,177 | | | | 162 | % |
| General and administrative expenses | | | 12,241 | | | | 10,185 | | | | 2,056 | | | | 20 | % |
| Total operating expenses | | | 41,672 | | | | 21,439 | | | | 20,233 | | | | 94 | % |
| Loss from operations | | | (41,672 | ) | | | (21,439 | ) | | | (20,233 | ) | | | 94 | % |
| Interest income (expense), net | | | (381 | ) | | | 4 | | | | (385 | ) | | | (9,625 | )% |
| Benefit from income taxes | | | 1,199 | | | | 4,516 | | | | (3,317 | ) | | | (73 | )% |
| Net loss and comprehensive loss | | $ | (40,855 | ) | | $ | (16,918 | ) | | $ | (23,937 | ) | | | 141 | % |
Research and Development Expenses
For the year ended December 31, 2022, research and development expenses increased to approximately $29.4 million compared to approximately $11.3 million for the year ended December 31, 2021. The increase of $18.2 million was primarily attributable to an increase in personnel costs of $2.3 million, clinical costs of $2.3 million, quality and manufacturing costs of $3.6 million and $10 million for the rights to PDS0301 from Merck KGaA, Darmstadt Germany. Of the $10 million, $5 million was in cash and the balance in shares of the Company’s common stock.
General and Administrative Expenses
For the year ended December 31, 2022, general and administrative expenses increased to approximately $12.2 million compared to approximately $10.2 million for the year ended December 31, 2021. The $2.0 million increase was primarily attributable to an increase in personnel costs of $1.3 million and an increase in professional fees of $0.7 million.
Interest Income (Expense), net
For the year ended December 31, 2022, interest expense, net was $0.4 million compared to an immaterial amount of interest income for the year ended December 31, 2021. The increase in interest expense for the year ended December 31, 2022 was $1.3 million of interest expense primarily related to the note payable partially offset by $0.9 million of interest income from interest earned on bank balances during the year.
Benefit from Income Taxes
Income tax benefit was $1.2 million for the year ended December 31, 2022 as compared to $4.5 million for the prior year ended December 31, 2021. A decrease of $3.3 million was due to a smaller portion of the accumulated Net Operating Losses ( NOL) through 2021 available for sale through our NJ tax benefits pursuant to the New Jersey Technology Business Tax Certificate Transfer Net Operating Loss program.
Liquidity and Capital Resources
In May 2021, we received approximately $4.5 million from the net sale of tax benefits to an unrelated, profitable New Jersey corporation pursuant our participation in the New Jersey Technology Business Tax Certificate Transfer Net Operating Loss (NOL) program for State Fiscal Year 2020.
In June 2021, we sold 6,088,235 shares of common stock at a public offering price of $8.50 per share pursuant to the 2020 Shelf Registration Statement, which includes 794,117 shares issued upon the exercise by the underwriter of its option to purchase additional shares at the public offering price, minus underwriting discounts and commissions. We received gross proceeds of approximately $51.7 million and net proceeds of approximately $48.5 million, after deducting underwriting discounts and offering expenses.
In April 2022, we received approximately $1.2 million from the net sale of tax benefits to an unrelated, profitable New Jersey corporation pursuant our participation in the New Jersey Technology Business Tax Certificate Transfer NOL program for State Fiscal Year 2020.
In August 2022, we filed a shelf registration statement, or the 2022 Shelf Registration Statement, with the SEC for the issuance of common stock, preferred stock, warrants, rights, debt securities, and units, which the Company refers to collectively as the Shelf Securities, up to an aggregate amount of $150 million, $50 million of which covers the offer, issuance and sale by the Company of its common stock under the Sales Agreement (as discussed below). The 2022 Shelf Registration Statement was declared effective on September 2, 2022.
In August 2022, we entered into an At Market Issuance Sales Agreement, or the Sales Agreement, with B. Riley Securities, Inc. and BTIG, LLC, each an Agent and collectively the Agents, with respect to an at-the-market offering program under which we may offer and sell, from time to time at our sole discretion, shares of our common stock, having an aggregate offering price of up to $50.0 million, or the Placement Shares, through or to the Agents, as sales agents or principals. Upon delivery of a placement notice and subject to the terms and conditions of the Sales Agreement, the Agents may sell the Placement Shares by any method permitted by law deemed to be an “at the market” offering as defined in Rule 415 of the Securities Act of 1933, as amended, including, without limitation, sales made through The Nasdaq Capital Market or on any other existing trading market for our common stock. The Agents will use commercially reasonable efforts to sell the Placement Shares from time to time, based upon our instructions (including any price, time or size limits or other customary parameters or conditions we may impose). We will pay the Agents a commission equal to three percent (3%) of the gross sales proceeds of any Placement Shares sold through the Agents under the Sales Agreement, and also has provided the Agents with customary indemnification and contribution rights. We are not obligated to make any sales of our common stock under the Sales Agreement. The offering of Placement Shares pursuant to the Sales Agreement will terminate upon the earlier of (i) the sale of all Placement Shares subject to the Sales Agreement or (ii) termination of the Sales Agreement in accordance with its terms. For the year ended December 31, 2022, we sold 1,238,491 shares of our common stock for a net value of $9.9 million pursuant to the Sales Agreement. In the first quarter 2023, we sold 553,293 shares of our common stock for a net value of $4.6 million pursuant to the Sales Agreement.
In August 2022, we entered into a venture loan and security agreement, or the Loan and Security Agreement, with Horizon Technology Finance Corporation, as lender and collateral agent for itself and the other lenders. The Loan and Security Agreement provides for the following 6 separate and independent term loans: (a) a term loan in the amount of $7,500,000, or Loan A, (b) a term loan in the amount of $10,000,000, or Loan B, (c) a term loan in the amount of $3,750,000, or Loan C, (d) a term loan in the amount of $3,750,000, or Loan D, (e) a term loan in the amount of $5,000,000, or Loan E, and (f) a term loan in the amount of $5,000,000, or Loan F, (with each of Loan A, Loan B, Loan C, Loan D, Loan E, and Loan F, individually a Loan and, collectively, the Loans). Loan A, Loan B, Loan C, and Loan D were delivered to us on August 24, 2022. In total, we received $24.6 million in net proceeds. Loan E and Loan F are uncommitted Loans that may be advanced by the lenders upon their discretion prior to July 31, 2023 upon the satisfaction of certain agreed upon conditions precedent. We may only use the proceeds of the Loans for working capital or general corporate purposes. Each Loan matures on the 48-month anniversary following the applicable funding date unless accelerated pursuant to agreed upon events of default. The principal balance of each Loan bears a floating interest. The interest rate is calculated initially and, thereafter, each calendar month as the sum of (a) the per annum rate of interest from time to time published in The Wall Street Journal as contemplated by the Loan and Security Agreement, or any successor publication thereto, as the “prime rate” then in effect, plus (b) 5.75%; provided that, in the event such rate of interest is less than 4.00%, such rate shall be deemed to be 4.00% for purposes of calculating the interest rate.
Interest is payable on a monthly basis based on each Loan principal amount outstanding the preceding month. We, at our option upon at least ten (10) business days’ written notice to the lenders, may prepay all (and not less than all) of the outstanding Loan by simultaneously paying to each lender an amount equal to (i) any accrued and unpaid interest on the outstanding principal balance of the Loans; plus (ii) an amount equal to (A) if such Loan is prepaid on or before the Loan Amortization Date (as defined in the Loan and Security Agreement) applicable to such Loan, 3% of the then outstanding principal balance of such Loan, (B) if such Loan is prepaid after the Loan Amortization Date applicable to such Loan, but on or before the date that is 12 months after such Loan Amortization Date, 2% of the then outstanding principal balance of such Loan, or (C) if such Loan is prepaid more than 12 months after the Loan Amortization Date but prior to the stated maturity date applicable to such Loan, 1% of the then outstanding principal balance of such Loan; plus (iii) the outstanding principal balance of such Loan; plus (iv) all other sums, if any, that shall have become due and payable thereunder. No prepayment premium will be applied to any outstanding balance of any Loan paid on the stated maturity date.
In connection with the Loan and Security Agreement, we issued Horizon Technology Finance Corporation and Powerscourt Investments XXV, LP warrants to purchase an aggregate total of 381,625 shares of the Company’s common stock at an initial exercise price of $3.6685 per share. Each warrant is classified as equity and is exercisable at any time for a period beginning on the date of grant and ending on the earlier of (A) 10 years from the date of grant, and (B) the closing of (A) (i) the sale, lease, exchange, conveyance or other disposition of all or substantially all of the our property or business, or (ii) its merger into or consolidation with any other corporation (other than a wholly-owned subsidiary of the Company), or any transaction (including a merger or other reorganization) or series of related transactions, in which more than 50% of the voting power of the Company is disposed of, in each case, for cash or for marketable securities meeting certain requirements as described in the applicable warrants. The key assumptions used in Black-Scholes option pricing model were (i) expected term of 10 years, (ii) a risk-free rate of 3.11%, (iii) expected volatility of 93.8%, (iv) and no estimated dividend yield.
As of December 31, 2022, we had $73.8 million of cash and cash equivalents. Our primary uses of cash are to fund operating expenses, primarily research and development expenditures. Cash used to fund operating expenses is impacted by the timing of when we pay these expenses, as reflected in the change in our outstanding accounts payable and accrued expenses.
We evaluated whether there are any conditions and events, considered in the aggregate, that raise substantial doubt about our ability to continue as a going concern within one year beyond the filing of this Annual Report on Form 10-K. Our budgeted cash requirements in 2023 and beyond include expenses related to continuing development and clinical studies. Based on our available cash resources and cash flow projections as of the date the consolidated financial statements were available for issuance, we believe there are sufficient funds to continue operations and research and development programs into the third quarter of 2024.
We plan to continue to fund our operations and capital funding needs through existing cash and additional equity and/or debt financing. However, we cannot be certain that additional financing will be available when needed or that, if available, financing will be obtained on terms favorable to us or our existing stockholders. We may also enter into government funding programs and consider selectively partnering for clinical development and commercialization. The sale of additional equity would result in additional dilution to our stockholders. Incurring debt financing would result in debt service obligations, and the instruments governing such debt could provide for operating and financing covenants that would restrict our operations. If we are unable to raise additional capital in sufficient amounts or on acceptable terms, we may be required to delay, limit, reduce, or terminate our product development or future commercialization efforts or grant rights to develop and market immunotherapies that we would otherwise prefer to develop and market ourselves. Any of these actions could harm our business, results of operations and prospects.
Cash flows
The following table shows a summary of our cash flows for each of the years indicated (in thousands):
| | | Year Ended December 31, | |
| | | 2022 | | | 2021 | |
| Net cash used in operating activities | | $ | (25,710 | ) | | $ | (12,486 | ) |
| Net cash provided by financing activities | | | 34,287 | | | | 48,889 | |
| Net increase in cash | | $ | 8,577 | | | $ | 36,403 | |
Net Cash Used in Operating Activities
Net cash used in operating activities was $25.7 million and $12.5 million for the years ended December 31, 2022 and 2021, respectively. The increase in cash used in operating activities of $13.2 million is primarily due to the increase in net loss of $23.9 million, reduced by the non-cash stock- based compensation expense of $1.1 and the value of the shares issued for the Merck licensing agreement of $5.0 million, offset by an increase in prepaid expenses of $1.0 million, and increase in accrued expenses of $5.7 million.
Net Cash Provided by Financing Activities
Net cash provided by financing activities for the year ended December 31, 2022 was primarily due to the receipt of net proceeds from the issuance of the note payable of $24.6 and the issuance of common stock of $9.9 million.
Net cash provided by financing activities for the year ended December 31, 2021 was primarily due to the receipt of net proceeds from the issuance of common stock of $48.5 million.
Operating Capital Requirements
To date, we have not generated any product revenue. We do not know when, or if, we will generate any product revenue and we do not expect to generate significant product revenue unless and until we obtain regulatory approval and commercialize one of our current or future product candidates. We anticipate that we will continue to generate losses for the foreseeable future, and we expect the losses to increase as we continue the development of, and seek regulatory approvals for, our tablet vaccine candidates, and begin to commercialize any approved vaccine candidates. We are subject to all of the risks incident to the development of new products, and may encounter unforeseen expenses, difficulties, complications, delays and other unknown factors that may harm our business. We expect to incur additional costs associated with operating as a public company and anticipate that we will need substantial additional funding in connection with our continuing operations.
We evaluated whether there are any conditions and events, considered in the aggregate, that raise substantial doubt about our ability to continue as a going concern within one year beyond the filing of this Annual Report. Our budgeted cash requirements in 2023 and beyond include expenses related to continuing development and clinical studies. We believe that our existing cash and cash equivalents as of December 31, 2022
are sufficient to continue operations and research and development programs into the third quarter of 2024. Until we can generate significant cash from our operations, we expect to continue to fund our operations with available financial resources.
We have based our projections of operating capital requirements on assumptions that may prove to be incorrect and we may use all of our available capital resources sooner than we expect. Because of the numerous risks and uncertainties associated with research, development and commercialization of pharmaceutical products, we are unable to estimate the exact amount of our operating capital requirements. Our future funding requirements will depend on many factors, including, but not limited to:
| ● | the initiation, progress, timing, costs and results of our planned clinical trials; |
| ● | the effects of health epidemics, pandemics, or outbreaks of infectious diseases, on our business operations, financial condition, results of operations and cash flows; |
| ● | the outcome, timing and cost of meeting regulatory requirements established by the U.S. Food and Drug Administration, or FDA, the European Medicines Agency, or EMA, and other comparable foreign regulatory authorities; |
| ● | the cost of filing, prosecuting, defending and enforcing our patent claims and other intellectual property rights; |
| ● | the cost of defending potential intellectual property disputes, including patent infringement actions brought by third parties against us now or in the future; |
| ● | the effect of competing technological and market developments; |
| ● | the cost of establishing sales, marketing and distribution capabilities in regions where we choose to commercialize our tablet vaccines on our own; and |
| ● | the initiation, progress, timing and results of our commercialization of our tablet vaccine candidates, if approved, for commercial sale. |
Please see the section titled “Risk Factors” elsewhere in this Annual Report on Form 10-K for additional risks associated with our operations.
Purchase Commitments
We have no material non-cancelable purchase commitments with service providers as we have generally contracted on a cancelable, purchase order basis.
Off-Balance Sheet Arrangements
We did not have during the periods presented, and we do not currently have, any off-balance sheet arrangements, as defined in the rules and regulations of the SEC.
Smaller Reporting Company
As of January 1, 2021, we are no longer an “emerging growth company,” as defined in the Jumpstart Our Business Startups Act of 2012, or the JOBS Act. However, we remain a “smaller reporting company,” as defined in Rule 12b-2 under the Securities Exchange Act of 1934, as amended. We will cease to be a smaller reporting company if we have a non-affiliate public float in excess of $250 million and annual revenues in excess of $100 million, or a non-affiliate public float in excess of $700 million, determined on an annual basis. Even though we no longer qualify as an emerging growth company, we may still qualify as a smaller reporting company. As a smaller reporting company, we are permitted and intend to rely on exemptions from certain disclosure requirements that are applicable to other public companies that are not smaller reporting companies. These exemptions include:
| ● | being permitted to provide only two years of audited consolidated financial statements in this Annual Report on Form 10-K, with correspondingly reduced “Management’s Discussion and Analysis of Financial Condition and Results of Operations” disclosure; |
| ● | reduced disclosure obligations regarding executive compensation; |
| ● | not being required to furnish a contractual obligations table in “Management’s Discussion and Analysis of Financial Condition and Results of Operations”; and |
| ● | not being required to furnish a stock performance graph in our annual report. |
We expect to continue to take advantage of some or all of the available exemptions.
| ITEM 7A. | Quantitative and qualitative disclosures about market risk |
Interest Rate Risk
We are exposed to market risk related changes in interest rates. As of December 31, 2022, our cash equivalents consisted of bank deposits and money market accounts. Our primary exposure to market risk is interest income sensitivity, which is affected by changes in the general level of U.S. interest rates. However, historical fluctuations in interest income have not been significant for us.
Inflation Risk
Inflation generally affects us by increasing our cost of labor and pricing of contracts. We do not believe that inflation has had a material effect on our business, financial condition, or results of operations during the year ended December 31, 2022.
| ITEM 8. | Financial Statements and Supplementary Data |
The financial statements required to be filed pursuant to this Item 8 are appended to this report. An index of those financial statements is found in Item 15.
| ITEM 9. | Changes in and Disagreements with Accountants on Accounting and Financial Disclosure |
None.
| ITEM 9A. | Controls and Procedures |
Limitations of Internal Control System
Because of the inherent limitations in a cost-effective control system, no evaluation of internal control over financial reporting can provide absolute assurance that misstatements due to error or fraud will not occur or that all control issues and instances of fraud, if any, within our company have been detected. Therefore, even those systems determined to be effective can provide only reasonable assurance with respect to financial statement preparation and presentation. Management does not expect that our disclosure controls and procedures or our internal control over financial reporting will prevent or detect all errors and all fraud.
Evaluation of Disclosure Controls and Procedures
Our management, with the participation of our Chief Executive Officer and Chief Financial Officer, has evaluated the effectiveness of the design and operation of our disclosure controls and procedures, (as such term is defined in Rules 13a-15(e) and 15d-15(e) under the Securities Exchange Act of 1934 (the “Exchange Act”)), as of December 31, 2022. Based on that evaluation, management has concluded that, as of such date, our disclosure controls and procedures were effective at the reasonable assurance level.
We maintain disclosure controls and procedures that are designed to ensure that information required to be disclosed by us in reports that we file or submit under the Exchange Act is recorded, processed, summarized, and reported within the time periods specified in SEC rules and forms, and that such information is accumulated and communicated to our management, including our Chief Executive Officer and Chief Financial Officer, as appropriate, to allow timely decisions regarding required disclosure.
In designing and evaluating our disclosure controls and procedures, management recognized that disclosure controls and procedures, no matter how well conceived and operated, can provide only reasonable, not absolute, assurance that the objectives of the disclosure controls and procedures are met. Additionally, in designing disclosure controls and procedures, our management necessarily was required to apply its judgment in evaluating the cost-benefit relationship of possible disclosure controls and procedures. The design of any disclosure controls and procedures also is based in part upon certain assumptions about the likelihood of future events, and there can be no assurance that any design will succeed in achieving its stated goals under all potential future conditions
Management’s Report on Internal Control over Financial Reporting
Our Management is responsible for establishing and maintaining adequate internal control over financial reporting as defined in Rules 13a-15(f) and 15d-15(f) under the Exchange Act. Our management conducted an assessment of the effectiveness of our internal control over financial reporting based on the framework established in the 2013 Internal Control-Integrated Framework issued by the Committee of Sponsoring Organizations of the Treadway Commission (COSO). Based on this assessment, our management has determined that our internal control over financial reporting was effective as of December 31, 2022.
Changes in Internal Control over Financial Reporting
There has been no change in our internal control over financial reporting in our most recent fiscal quarter that has materially affected, or is reasonably likely to materially affect, our internal control over financial reporting.
| ITEM 9B. | Other Information |
Not applicable.
| ITEM 9C. | Disclosure Regarding Foreign Jurisdictions that Prevent Inspections. |
Not applicable.
PART III
Certain information required by Part III is omitted from this Annual Report on Form 10-K because we will file a definitive Proxy Statement for the Annual Meeting of Stockholders pursuant to Regulation 14A of the Securities Exchange Act of 1934 (the Proxy Statement), not later than 120 days after the end of the fiscal year covered by this Annual Report on Form 10-K, and the applicable information included in the Proxy Statement is incorporated herein by reference.
| ITEM 10. | Directors, Executive Officers and Corporate Governance |
The information required by this Item is incorporated herein by reference to the Proxy Statement.
| ITEM 11. | Executive Compensation |
The information required by this Item is incorporated herein by reference to the Proxy Statement.
| ITEM 12. | Security Ownership of Certain Beneficial Owners and Management and Related Stockholder Matters |
The information required by this Item is incorporated herein by reference to the Proxy Statement.
| ITEM 13. | Certain Relationships and Related Transactions, and Director Independence |
The information required by this Item is incorporated herein by reference to the Proxy Statement.
| ITEM 14. | Principal Accounting Fees and Services |
The information required by this Item is incorporated herein by reference to the Proxy Statement.
PART IV
| ITEM 15. | Exhibits, Financial Statement Schedules |
| (a) | The following documents are filed as part of this report: |
The information concerning our consolidated financial statements, and Report of Independent Registered Public Accounting Firm required by this Item is incorporated by reference herein to the section of this Annual Report on Form 10-K in Item 8, entitled “(PCAOB ID 185) Financial Statements and Supplementary Data”.
| (2) | Financial Statement Schedules: |
All schedules have been omitted because the required information is not present or not present in amounts sufficient to require submission of the schedules, or because the information required is shown in the financial statements or the notes thereto.
The list of exhibits required by Item 601 of Regulation S-K is set forth in the Exhibit Index immediately preceding the signature page to this Annual Report on Form 10-K and is incorporated herein by reference.
| ITEM 16. | Form 10-K Summary |
We may voluntarily include a summary of information required by Form 10-K under this Item 16. We have elected not to include such summary information.
Exhibit Number | Exhibit Description |
| Agreement and Plan of Merger and Reorganization, dated November 23, 2018, by and among Edge Therapeutics, Inc., Echos Merger Sub, Inc. and PDS Biotechnology Corporation (filed as Exhibit 2.1 to the Company’s Current Report on Form 8-K filed on November 26, 2018, and incorporated by reference herein). |
| | |
| Amendment No. 1 to Agreement and Plan of Merger and Reorganization, dated January 24, 2019, by and among Edge Therapeutics, Inc., Echos Merger Sub, Inc. and PDS Biotechnology Corporation (filed as Exhibit 2.1 to the Company’s Current Report on Form 8-K filed on January 30, 2019, and incorporated by reference herein). |
| | |
| Eighth Amended and Restated Certificate of Incorporation of Edge Therapeutics, Inc. (filed as Exhibit 3.1 to the Company’s Current Report on Form 8-K filed on October 6, 2015, and incorporated by reference herein). |
| | |
| Third Amended and Restated Bylaws of PDS Biotechnology Corporation (filed as Exhibit 3.1 to the Company’s Current Report on Form 8-K filed on March 15, 2022, and incorporated by reference herein). |
| | |
| Certificate of Amendment to Amended and Restated Certificate of Incorporation (filed as Exhibit 3.1 to the Company’s Current Report on Form 8-K on March 18, 2019, and incorporated by reference herein). |
| | |
| Certificate of Amendment to Amended and Restated Certificate of Incorporation (filed as Exhibit 3.2 to the Company’s Current Report on Form 8-K on March 18, 2019, and incorporated by reference herein). |
| | |
| Form of Certificate of Common Stock (filed as Exhibit 4.1 to the Company’s Pre-Effective Amendment No. 1 to the registration statement on Form S-1 (File No. 333- 206416) filed on September 21, 2015, and incorporated by reference herein). |
| | |
| Description of Securities (filed as Exhibit 4.10 to the Company’s Annual Report on Form 10-K filed on March 27, 2020, and incorporated by reference herein). |
| | |
| Form of Indenture (filed as Exhibit 4.3 to the Company’s registration statement on Form S-3 (File No. 333-267041) on August 24, 2022, and incorporated by reference herein). |
| | |
| Form of Warrant issued under the Venture Loan and Security Agreement, dated August 24, 2022 (filed as Exhibit 10.1 to the Company’s Quarterly Report on Form 10-Q on November 14, 2022, and incorporated by reference herein). |
| | |
| Venture Loan and Security Agreement, dated August 24, 2022, by and among Horizon Technology Finance Corporation, as a lender and collateral agent, Powerscourt Investments XXV, LP, as a lender, PDS Operating Corporation, as a guarantor, and PDS Biotechnology Corporation, as borrower (filed as Exhibit 10.2 to the Company’s Quarterly Report on Form 10-Q on November 14, 2022, and incorporated by reference herein). |
| | |
| Clinical Trial Collaboration and Supply Agreement, dated May 19, 2017, by and between PDS Biotechnology Corporation and MSD International GmbH (filed as Exhibit 10.24 to the Company’s Registration Statement on Form S-4/A on January 25, 2019, and incorporated by reference herein). |
| | |
| Patent License Agreement, dated January 5, 2015, by and between PDS Biotechnology Corporation and National Institutes of Health, as amended by First Amendment, dated August 5, 2015 (filed as Exhibit 10.25 to the Company’s Registration Statement on Form S-4/A on January 25, 2019, and incorporated by reference herein). |
| | |
10.5
| Cost Reimbursement Agreement, dated November 1, 2015, by and between PDS Biotechnology Corporation and University of Kentucky Research Foundation (filed as Exhibit 10.26 to the Company’s Registration Statement on Form S-4/A on January 25, 2019, and incorporated by reference herein). |
| | |
| Cost Reimbursement Agreement, dated November 1, 2015, by and between PDS Biotechnology Corporation and University of Kentucky Research Foundation (filed as Exhibit 10.27 to the Company’s Registration Statement on Form S-4/A on January 25, 2019, and incorporated by reference herein). |
| | |
| Public Health Service Cooperative Research & Development Agreement for Intramural-PHS Clinical Research, dated effective as of February 2, 2015, by and between the National Cancer Institute and PDS Biotechnology Corporation (filed as Exhibit 10.28 to the Company’s Registration Statement on Form S-4/A on January 25, 2019, and incorporated by reference herein). |
| DOTAP Chloride Enantiomer License Agreement effective November 1, 2008, between Merck Eprova AG and PDS Biotechnology Corporation (filed as Exhibit 10.29 to the Company’s Registration Statement on Form S-4/A on January 25, 2019, and incorporated by reference herein). |
| | |
| License Agreement dated as of December 30, 2022 by and between Merck KGaA, Darmstadt, Germany and PDS Biotechnology Corporation. |
| | |
| Share Transfer Agreement by and between PDS Biotechnology Corporation and Merck KGaA, Darmstadt, Germany. (filed as Exhibit 10.1 to the Company’s Current Report on Form 8-K on January 3, 2023, and incorporated by reference herein). |
| | |
| PDS Biotechnology 2010 Equity Incentive Plan, and forms of agreement thereunder (filed as Exhibit 10.2 to the Company’s Registration Statement on Form S-1/A on September 21, 2015, and incorporated by reference herein). |
| | |
| Second Amended and Restated PDS Biotechnology Corporation 2014 Equity Incentive Plan (filed as Exhibit 10.3 to the Company’s Current Report on Form 8-K on December 9, 2020, and incorporated by reference herein). |
| | |
| Employee Stock Option Agreement under the Second Amended and Restated PDS Biotechnology Corporation 2014 Equity Incentive Plan (filed as Exhibit 10.4 to the Company’s Current Report on Form 8-K filed on December 9, 2020, and incorporated by reference herein). |
| | |
| PDS Biotechnology Corporation 2009 Stock Option Plan, as amended (filed as Exhibit 99.1 to the Company’s Registration Statement on Form S-8 on June 4, 2019, and incorporated by reference herein). |
| | |
| PDS Biotechnology Corporation 2018 Stock Option Plan (filed as Exhibit 99.2 to the Company’s Registration Statement on Form S-8 on June 4, 2019, and incorporated by reference herein). |
| | |
| Form of PDS Biotechnology Corporation Option Agreement for 2009 Stock Option Plan, as amended (filed as Exhibit 99.3 to the Company’s Registration Statement on Form S-8 on June 4, 2019, and incorporated by reference herein). |
| | |
| Form of PDS Biotechnology Corporation Option Agreement for 2018 Stock Incentive Plan (filed as Exhibit 99.4 to the Company’s Registration Statement on Form S-8 on June 4, 2019, and incorporated by reference herein). |
| | |
| PDS Biotechnology Corporation 2019 Inducement Plan, as amended (filed as Exhibit 10.1 to the Company’s Current Report on Form 8-K filed on May 18, 2022, and incorporated by reference herein). |
| | |
| Form of Stock Option Grant Notice and Stock Option Agreement under the 2019 Inducement Plan (filed as Exhibit 10.2 to the Company’s Current Report on Form 8-K on June 20, 2019, and incorporated by reference herein). |
| | |
| Form of Indemnification Agreement for officers and directors (filed as Exhibit 10.9 to the Company’s Registration Statement on Form S-1 on August 14, 2015, and incorporated by reference herein). |
| | |
| Common Stock Purchase Agreement, dated July 29, 2019, by and among the Company and Aspire Capital Fund, LLC (filed as Exhibit 10.1 to the Company’s Current Report on Form 8-K on July 30, 2019, and incorporated by reference herein). |
| | |
| Sublease Agreement, effective as of March 5, 2020, by and between PDS Biotechnology Corporation and COWI North America, Inc. (filed as Exhibit 10.37 to the Company’s Annual Report on Form 10-K filed on March 27, 2020, and incorporated by reference herein). |
| | |
| Patent License Agreement dated as of November 5, 2021, by and between PDS Biotechnology Corporation and the U.S. Department of Health and Human Services, as represented by the National Cancer Institute (filed as Exhibit 10.19 to the Company’s Annual Report on Form 10-K filed on March 31, 2022, and incorporated by reference herein). |
| | |
| Option Agreement with University of Georgia Research Foundation, Inc. effective as of October 25, 2021 (filed as Exhibit 10.20 to the Company’s Annual Report on Form 10-K filed on March 31, 2022, and incorporated by reference herein). |
| PDS Biotechnology Corporation Change of Control Severance Plan effective as of March 14, 2022 (filed as Exhibit 10.21 to the Company’s Annual Report on Form 10-K filed on March 31, 2022, and incorporated by reference herein) |
| | |
| Amended and Restated Executive Employment Agreement by and between Frank K. Bedu-Addo and PDS Biotechnology Corporation, effective as of March 14, 2022 (filed as Exhibit 10.22 to the Company’s Annual Report on Form 10-K filed on March 31, 2022, and incorporated by reference herein). |
| | |
| Executive Employment Agreement by and between Gregory Conn, Ph.D. and PDS Biotechnology Corporation, effective as of March 14, 2022 (filed as Exhibit 10.23 to the Company’s Annual Report on Form 10-K filed on March 31, 2022, and incorporated by reference herein). |
| | |
| Executive Employment Agreement by and between Matthew Hill and PDS Biotechnology Corporation, effective as of March 14, 2022(filed as Exhibit 10.24 to the Company’s Annual Report on Form 10-K filed on March 31, 2022, and incorporated by reference herein). |
| | |
| Executive Employment Agreement by and between Lauren V. Wood, M.D. and PDS Biotechnology Corporation, effective as of March 14, 2022 (filed as Exhibit 10.25 to the Company’s Annual Report on Form 10-K filed on March 31, 2022, and incorporated by reference herein). |
| | |
| Executive Employment Agreement by and between Spencer Brown and PDS Biotechnology Corporation, effective as of June 1, 2022 (filed as Exhibit 10.1 to the Company’s Quarterly Report on Form 10-Q filed on August 8, 2022, and incorporated herein by reference). |
| | |
| Subsidiary of PDS Biotechnology Corporation. |
| | |
| Consent of KPMG LLP. |
| | |
| Principal Executive Officer’s Certifications Pursuant to Section 302 of the Sarbanes-Oxley Act of 2002. |
| | |
| Principal Financial Officer’s Certifications Pursuant to Section 302 of the Sarbanes-Oxley Act of 2002. |
| | |
| Certification Pursuant to Section 906 of the Sarbanes-Oxley Act of 2002 (furnished herewith). |
| | |
| Certification Pursuant to Section 906 of the Sarbanes-Oxley Act of 2002 (furnished herewith). |
| | |
101.INS* | Inline XBRL Instance Document (the instance document does not appear in the Interactive Data File because its XBRL tags are embedded within the Inline XBRL document) |
| | |
101.SCH* | Inline XBRL Taxonomy Extension Schema Document |
| | |
101.CAL* | Inline XBRL Taxonomy Extension Calculation Linkbase Document |
| | |
| 101.DEF* | Inline XBRL Taxonomy Extension Definition Linkbase Document |
| | |
| 101.LAB* | Inline XBRL Taxonomy Extension Label Linkbase Document |
| | |
| 101.PRE* | Inline XBRL Taxonomy Extension Presentation Linkbase Document |
| | |
| 104 | Cover Page Interactive Data File (formatted as inline XBRL and contained in Exhibit 101) |
| + | Indicates management contract or compensatory plan. |
| * | Filed herewith unless otherwise indicated as furnished herewith. |
| ** | Confidential Treatment has been requested with respect to certain portions of this Exhibit. Omitted portions have been filed separately with the Securities and Exchange Commission. |
| ++ | Certain portions of this exhibit have been redacted pursuant to Item 601(b)(10)(iv) of Regulation S-K. |
Pursuant to the requirements of the Section 13 or 15(d) of the Securities Exchange Act of 1934, the Registrant has duly caused this Form 10-K to be signed on its behalf by the undersigned, thereunto duly authorized.
| | PDS Biotechnology Corporation |
| | |
| March 28, 2023 | By: | /s/ Frank Bedu-Addo |
| | | Frank Bedu-Addo, Ph.D. |
| | | President and Chief Executive Officer |
| | | |
| March 28, 2023 | By: | /s/ Matthew Hill |
| | | Matthew Hill |
| | | Chief Financial Officer |
Pursuant to the requirements of the Securities Exchange Act of 1934, this Form 10-K has been signed by the following persons in the capacities indicated below and on the dates indicated:
| Signature | | Title | | Date |
| | | | | |
| /s/ Frank Bedu-Addo | | President and Chief Executive Officer and Director | | March 28, 2023 |
| Frank Bedu-Addo, Ph.D. | | (Principal Executive Officer) | | |
| | | | | |
| /s/ Matthew Hill | | Chief Financial Officer | | March 28, 2023 |
| Matthew Hill | | (Principal Financial and Accounting Officer) | | |
| | | | | |
| /s/ Gregory Freitag | | Director | | March 28, 2023 |
| Gregory Freitag J.D., CPA | | | | |
| | | | | |
| /s/ Stephen Glover | | Director | | March 28, 2023 |
| Stephen Glover | | | | |
| | | | | |
| /s/ Sir Richard Sykes | | Director | | March 28, 2023 |
| Sir Richard Sykes | | | | |
| | | | | |
| /s/ Kamil Ali-Jackson | | Director | | March 28, 2023 |
| Kamil Ali-Jackson | | | | |
| | | | | |
| /s/ Otis W. Brawley | | Director | | March 28, 2023 |
| Otis W. Brawley | | | | |
| | | | | |
| /s/ Ilian Iliev | | Director | | March 28, 2023 |
| Ilian Iliev | | | | |