ContraFect January 2019 Differentiated, first-in-class anti-infectives for life-threatening, drug-resistant infections Exhibit 99.1

This presentation contains, and our officers and representatives may from time to time make, “forward-looking statements” within the meaning of the U.S. federal securities laws. Forward-looking statements can be identified by words such as “projects,” “may,” “will,” “could,” “would,” “should,” “believe,” “expect,” “target”, “anticipate,” “estimate,” “intend,” “plan,” “proposed”, “potential” or similar references to future periods. Examples of forward-looking statements in this presentation include, without limitation, statements made regarding ContraFect Corporation’s (“ContraFect”) therapeutic product candidates, including their ability to treat life-threatening, drug resistant infections, CF-301 properties and activity including but not limited to the ability of CF-301 used in addition to SOC antibiotics to significantly improve clinical success rates compared to SOC antibiotics alone, synergy with conventional antibiotics and clearance of biofilms, CF-301’s value proposition and product attributes, expectations regarding clinical outcomes and efficacy of CF-301, in vitro and in vivo study results, timing of the completion of clinical trials, ability to achieve Phase 2 study endpoints, CF-404’s ability to treat influenza, ContraFect’s CF-296, Gram-positive and Gram-negative lysins and other discovery programs, and related plans to advance into the clinic, and patent protection. Forward-looking statements are statements that are not historical facts, nor assurances of future performance. Instead, they are based on ContraFect’s current beliefs, expectations and assumptions regarding the future of its business, future plans, proposals, strategies, projections, anticipated events and trends, the economy and other future conditions. Because forward-looking statements relate to the future, they are subject to inherent risks, uncertainties and changes in circumstances that are difficult to predict and many of which are beyond ContraFect’s control, including those detailed in ContraFect's Quarterly Report on Form 10-Q for the quarter ended September 30, 2018 and other filings with the Securities and Exchange Commission (“SEC”). Actual results may differ from those set forth in the forward-looking statements. Important factors that could cause actual results to differ include, among others, the occurrence of any adverse events related to the discovery, development and commercialization of ContraFect’s product candidates such as unfavorable clinical trial results, insufficient supplies of drug products, the lack of regulatory approval, or the unsuccessful attainment or maintenance of patent protection. Any forward-looking statement made by ContraFect in this presentation is based only on information currently available and speaks only as of the date on which it is made. No representation or warranty is made as to the completeness or accuracy of the information provided in this presentation. Except as required by applicable law, ContraFect expressly disclaims any obligations to publicly update any forward-looking statements, whether written or oral, that may be made from time to time, whether as a result of new information, future developments or otherwise. Audiences are cautioned that forward-looking statements or similar information are not guarantees of future performance and, accordingly, are expressly cautioned not to put undue reliance on forward-looking statements or similar information due to the inherent uncertainty therein. Forward Looking Statements

ContraFect is a clinical-stage biotech leading the development of differentiated, first-in-class biologics for the treatment of life-threatening and drug-resistant infections ©2019 ContraFect Corporation
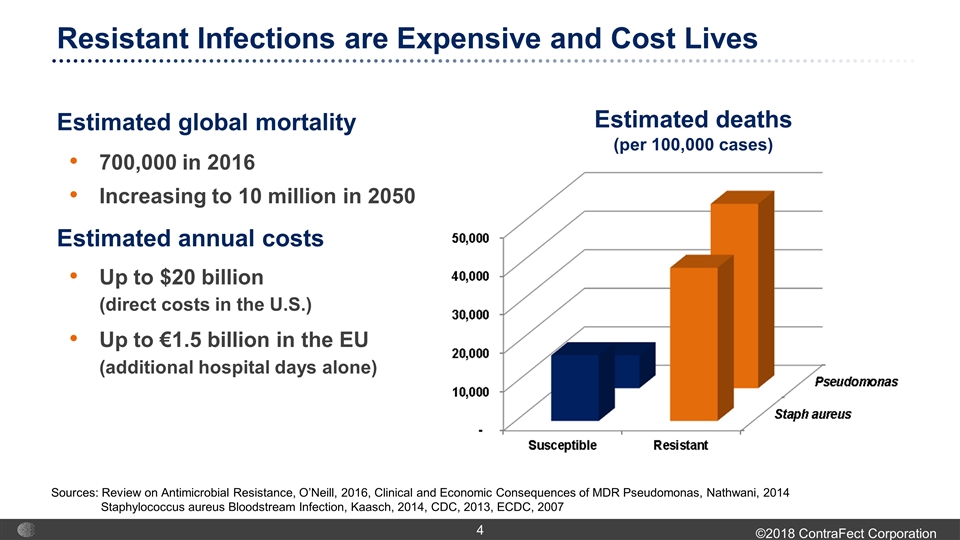
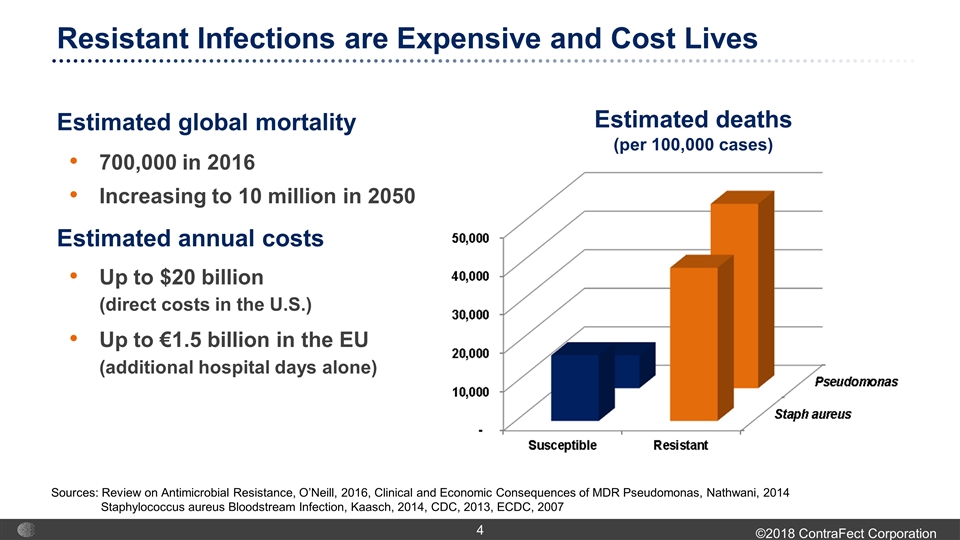
Resistant Infections are Expensive and Cost Lives Estimated deaths (per 100,000 cases) Estimated global mortality Estimated annual costs Up to $20 billion (direct costs in the U.S.) Up to €1.5 billion in the EU (additional hospital days alone) Sources: Review on Antimicrobial Resistance, O’Neill, 2016, Clinical and Economic Consequences of MDR Pseudomonas, Nathwani, 2014 Staphylococcus aureus Bloodstream Infection, Kaasch, 2014, CDC, 2013, ECDC, 2007 700,000 in 2016 Increasing to 10 million in 2050
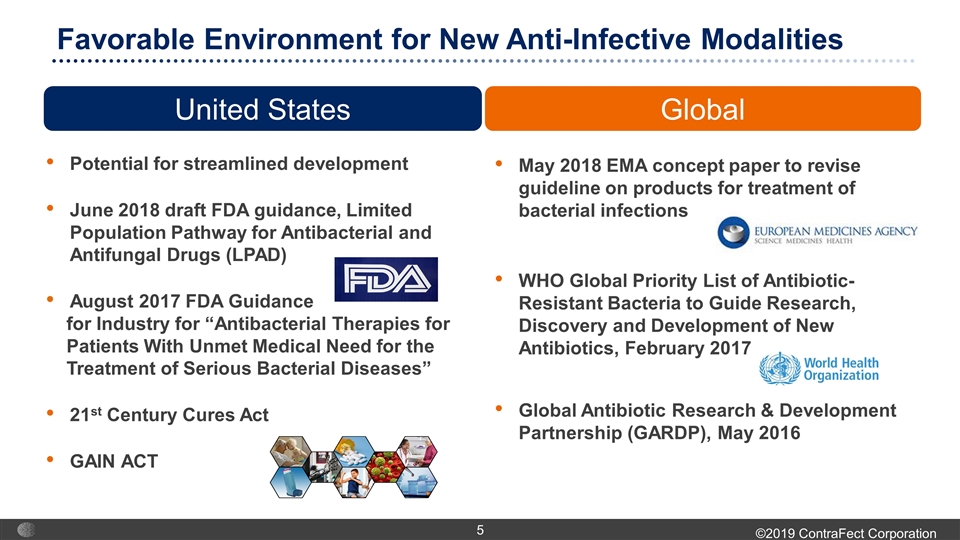
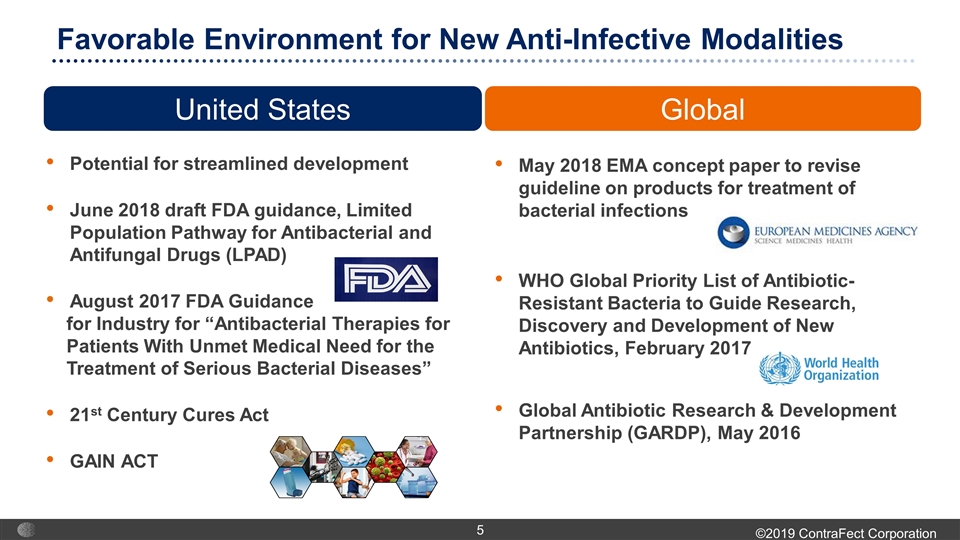
Potential for streamlined development June 2018 draft FDA guidance, Limited Population Pathway for Antibacterial and Antifungal Drugs (LPAD) August 2017 FDA Guidance for Industry for “Antibacterial Therapies for Patients With Unmet Medical Need for the Treatment of Serious Bacterial Diseases” 21st Century Cures Act GAIN ACT Favorable Environment for New Anti-Infective Modalities United States LEGISLATIVE Global May 2018 EMA concept paper to revise guideline on products for treatment of bacterial infections WHO Global Priority List of Antibiotic-Resistant Bacteria to Guide Research, Discovery and Development of New Antibiotics, February 2017 Global Antibiotic Research & Development Partnership (GARDP), May 2016

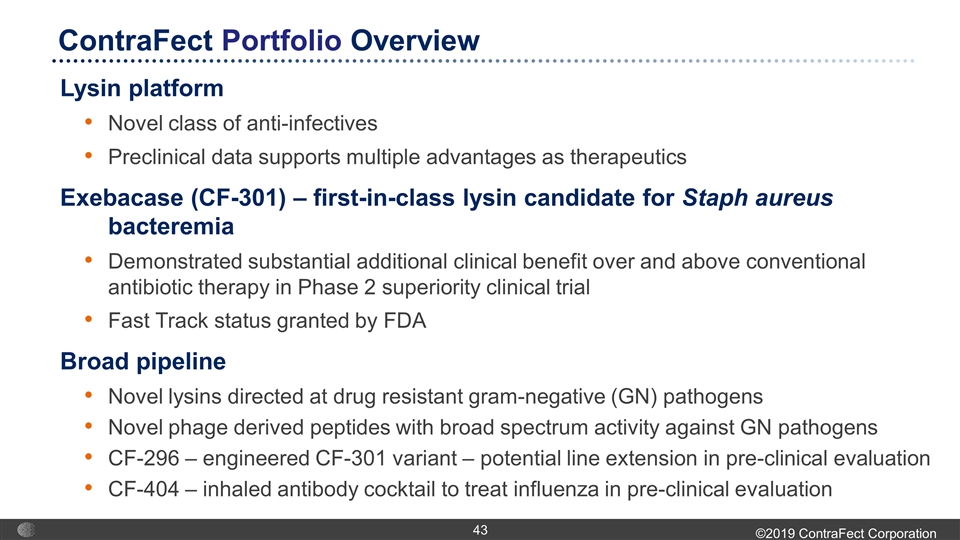
Lysin platform Novel class of anti-infectives Preclinical data supports multiple advantages as therapeutics Exebacase (CF-301) – first-in-class lysin candidate for Staph aureus bacteremia Demonstrated substantial additional clinical benefit over and above conventional antibiotic therapy in Phase 2 superiority clinical trial Fast Track status granted by FDA Broad pipeline Novel lysins directed at drug resistant gram-negative (GN) pathogens Novel phage derived peptides with broad spectrum activity against GN pathogens CF-296 – engineered CF-301 variant – potential line extension in pre-clinical evaluation CF-404 – inhaled antibody cocktail to treat influenza in pre-clinical evaluation ContraFect Portfolio Overview
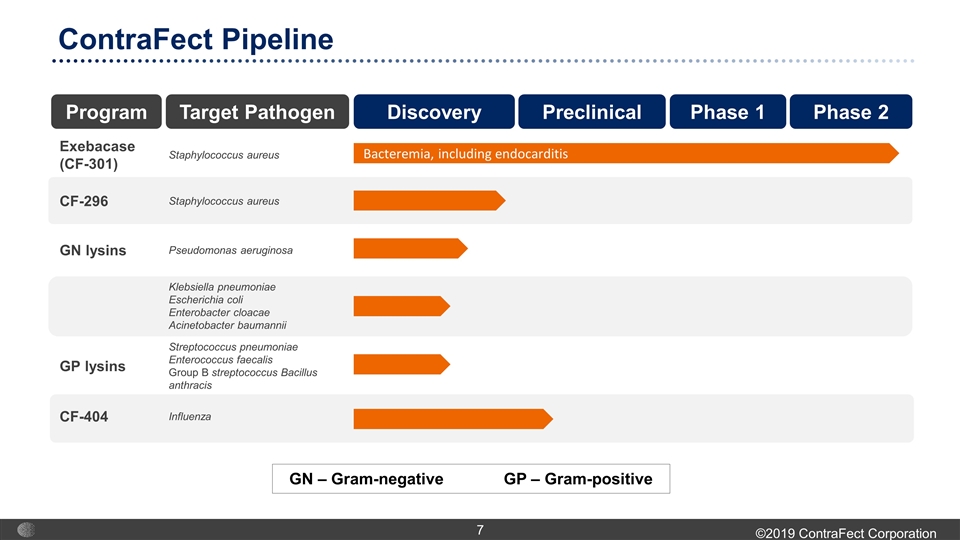
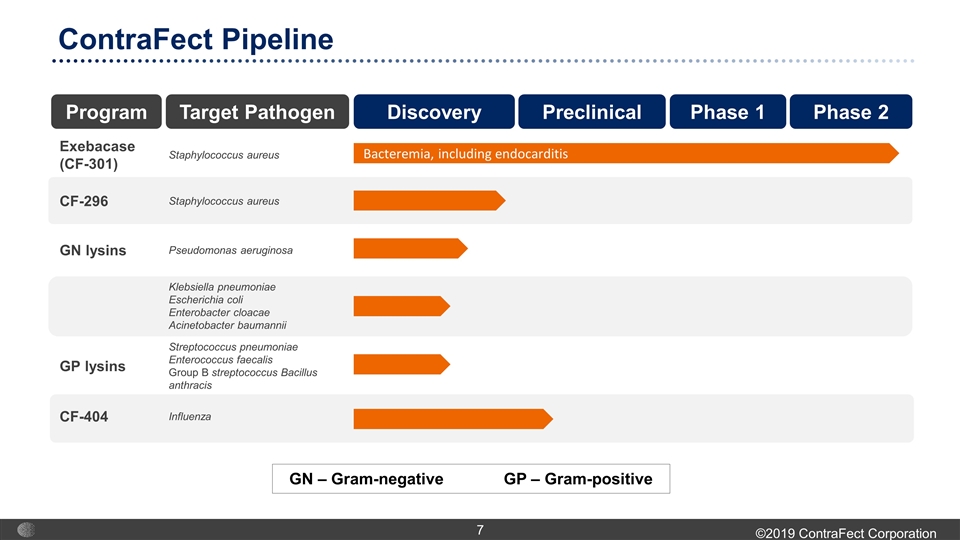
Exebacase (CF-301) Staphylococcus aureus CF-296 Staphylococcus aureus GN lysins Pseudomonas aeruginosa Klebsiella pneumoniae Escherichia coli Enterobacter cloacae Acinetobacter baumannii GP lysins Streptococcus pneumoniae Enterococcus faecalis Group B streptococcus Bacillus anthracis CF-404 Influenza Bacteremia, including endocarditis Program Target Pathogen Discovery Preclinical Phase 1 Phase 2 ContraFect Pipeline GN – Gram-negative GP – Gram-positive
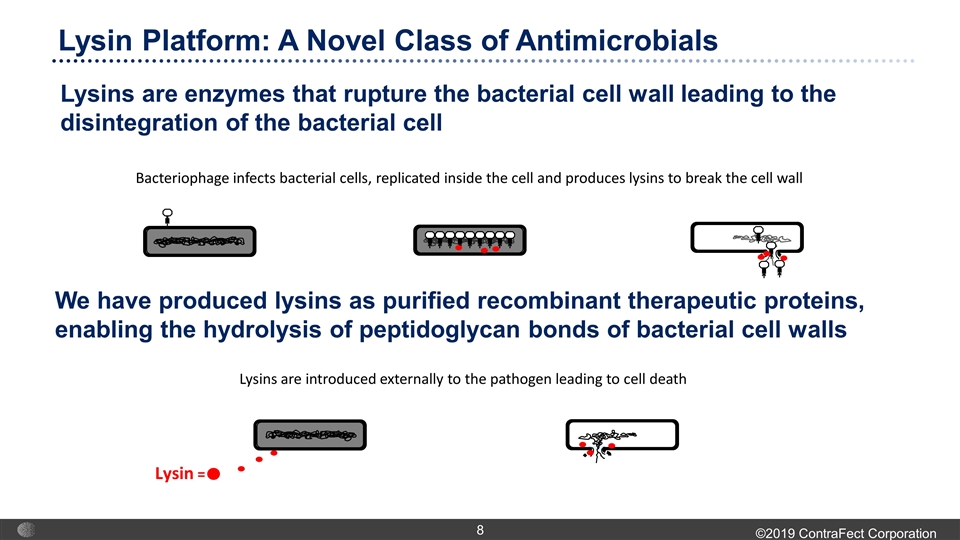
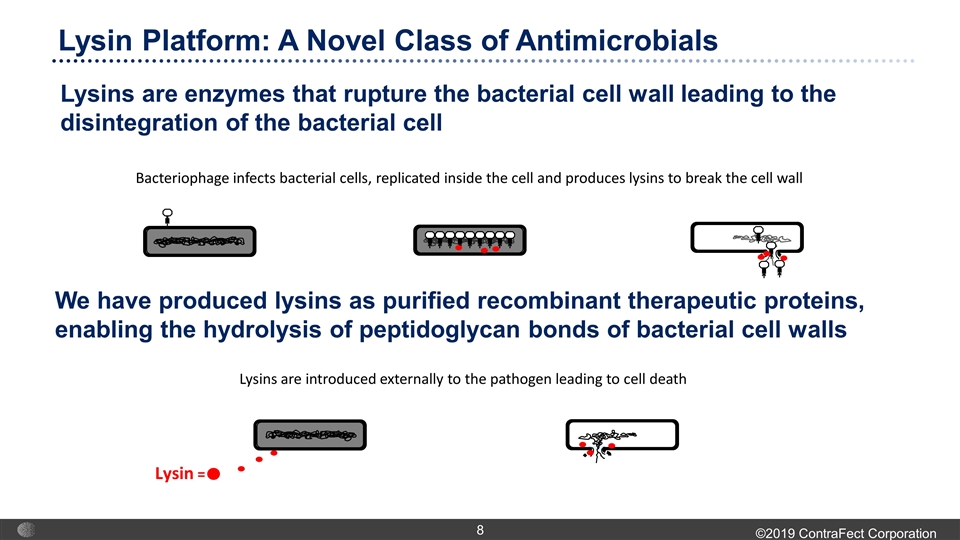
We have produced lysins as purified recombinant therapeutic proteins, enabling the hydrolysis of peptidoglycan bonds of bacterial cell walls Lysin Platform: A Novel Class of Antimicrobials Lysins are enzymes that rupture the bacterial cell wall leading to the disintegration of the bacterial cell Lysin = Bacteriophage infects bacterial cells, replicated inside the cell and produces lysins to break the cell wall Lysins are introduced externally to the pathogen leading to cell death
Synergy with conventional antibiotics Eradicates biofilms Low propensity for resistance Rapid, potent and targeted bactericidal activity Lysins: Hallmark Features of a New Class
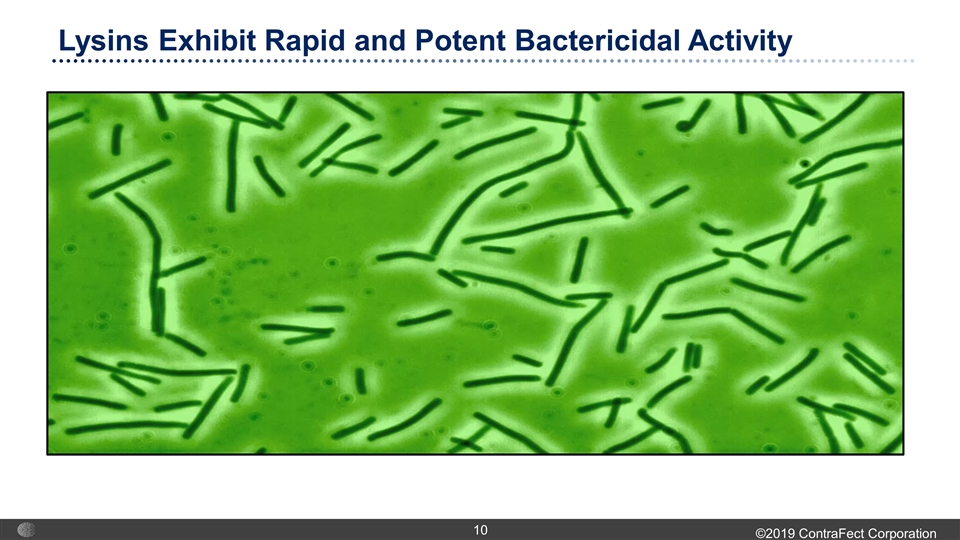
Lysins Exhibit Rapid and Potent Bactericidal Activity
Exebacase (CF-301) Novel, First-In-Class Anti-Infective for Staph aureus Bacteremia, Including Endocarditis
Exebacase (CF-301): First-in-Class Lysin Candidate Key attributes 26 kDa modular bacterial cell wall hydrolase enzyme Highly potent against Staph aureus, including antibiotic-resistant strains Rapid eradication of Staph biofilms Potent synergy with broad range of anti-staphylococcal antibiotics Clinical-stage program Ongoing Phase 2 superiority study Positive topline results overall and in key subgroups Demonstrated a robust safety and tolerability profile in patients Broad patent protection Patent with composition of matter claims expiring in 2032 Patent with method claims for killing all Staph strains expiring in 2032 Patent with method claims for disrupting or treating of Staph strain biofilms expiring in 2033
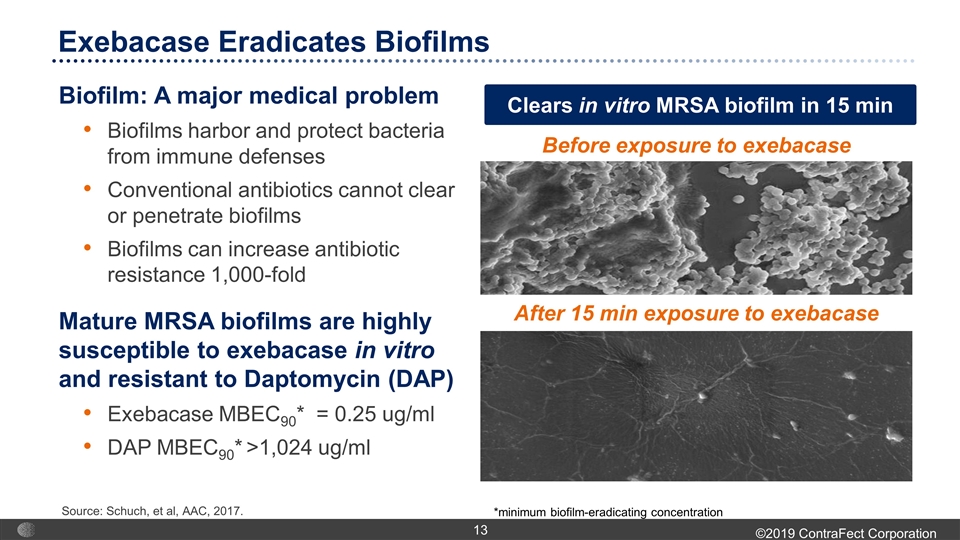
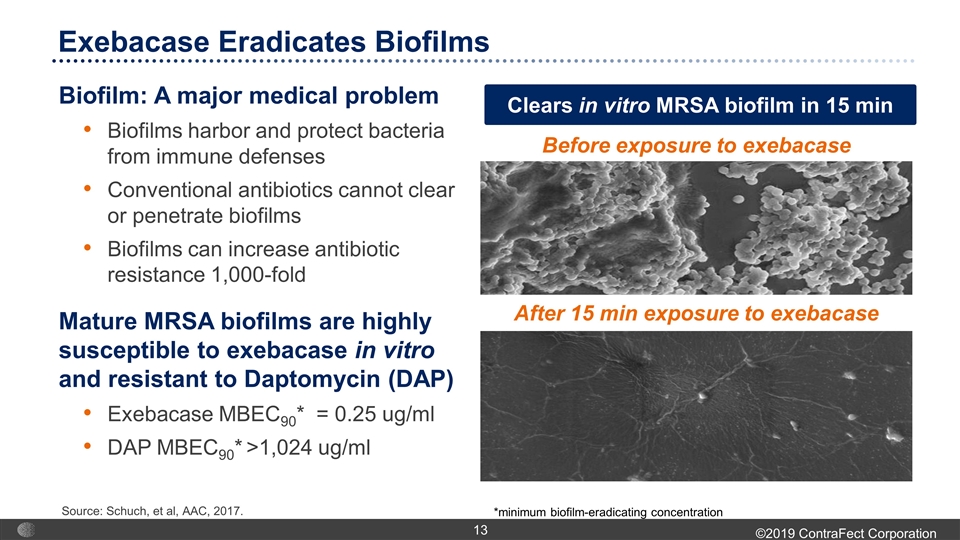
Before exposure to exebacase After 15 min exposure to exebacase *minimum biofilm-eradicating concentration Biofilm: A major medical problem Biofilms harbor and protect bacteria from immune defenses Conventional antibiotics cannot clear or penetrate biofilms Biofilms can increase antibiotic resistance 1,000-fold Mature MRSA biofilms are highly susceptible to exebacase in vitro and resistant to Daptomycin (DAP) Exebacase MBEC90* = 0.25 ug/ml DAP MBEC90* >1,024 ug/ml Exebacase Eradicates Biofilms Source: Schuch, et al, AAC, 2017. Clears in vitro MRSA biofilm in 15 min
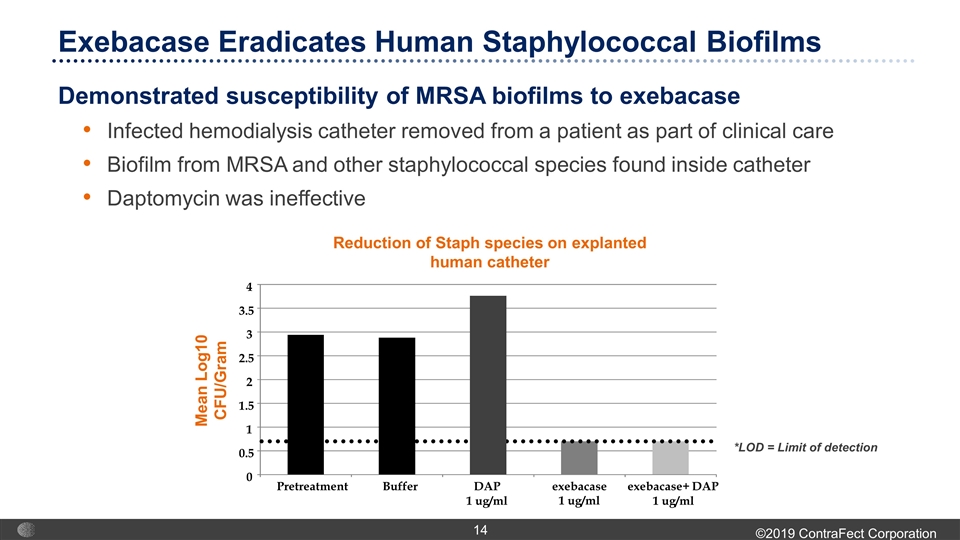
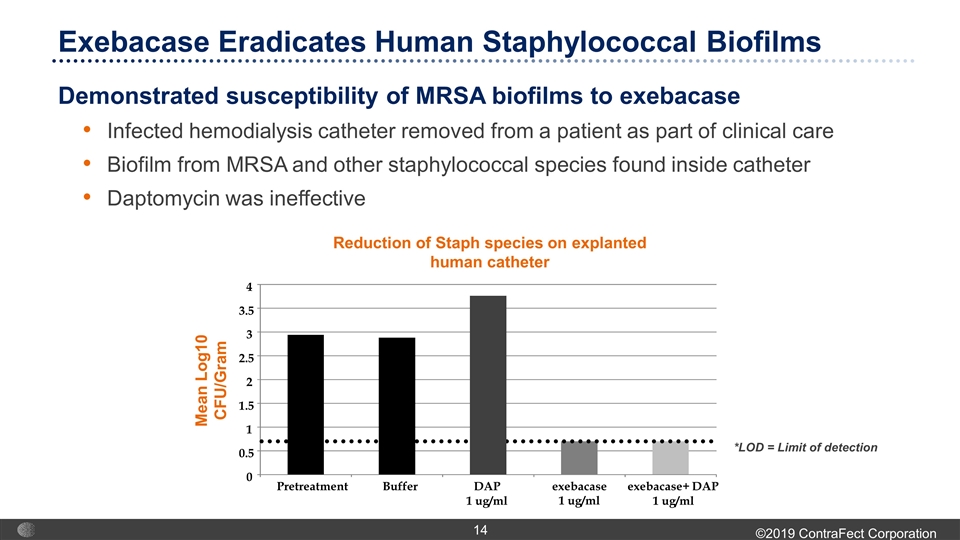
Demonstrated susceptibility of MRSA biofilms to exebacase Infected hemodialysis catheter removed from a patient as part of clinical care Biofilm from MRSA and other staphylococcal species found inside catheter Daptomycin was ineffective *LOD = Limit of detection Reduction of Staph species on explanted human catheter 0 0.5 1 1.5 2 2.5 3 3.5 4 Pretreatment Buffer DAP 1 ug/ml exebacase 1 ug/ml exebacase+ DAP 1 ug/ml Mean Log10 CFU/Gram Exebacase Eradicates Human Staphylococcal Biofilms
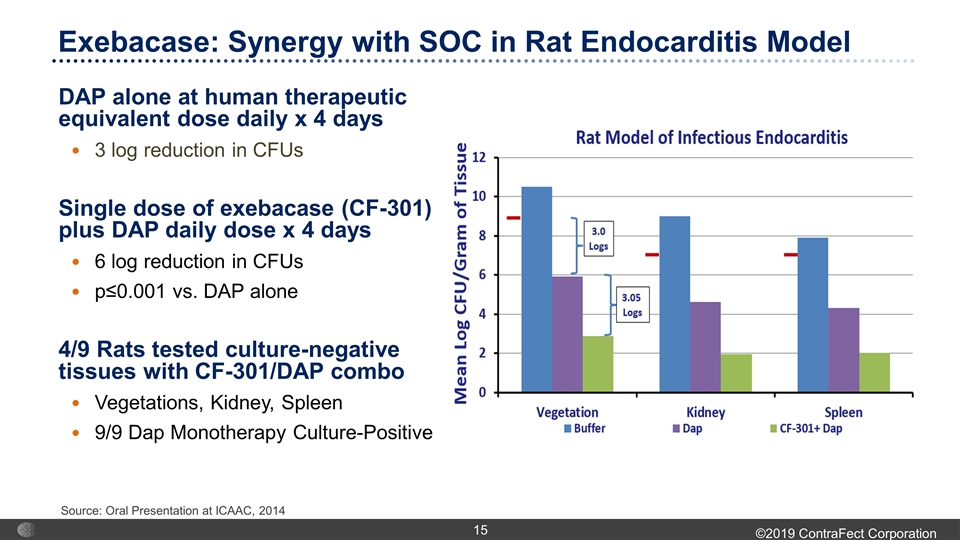
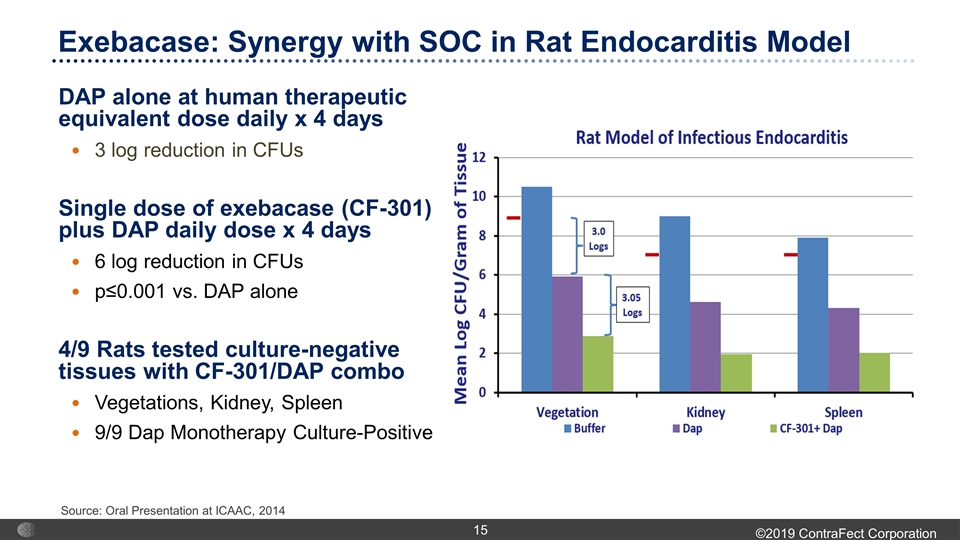
DAP alone at human therapeutic equivalent dose daily x 4 days 3 log reduction in CFUs Single dose of exebacase (CF-301) plus DAP daily dose x 4 days 6 log reduction in CFUs p≤0.001 vs. DAP alone 4/9 Rats tested culture-negative tissues with CF-301/DAP combo Vegetations, Kidney, Spleen 9/9 Dap Monotherapy Culture-Positive Source: Oral Presentation at ICAAC, 2014 Exebacase: Synergy with SOC in Rat Endocarditis Model
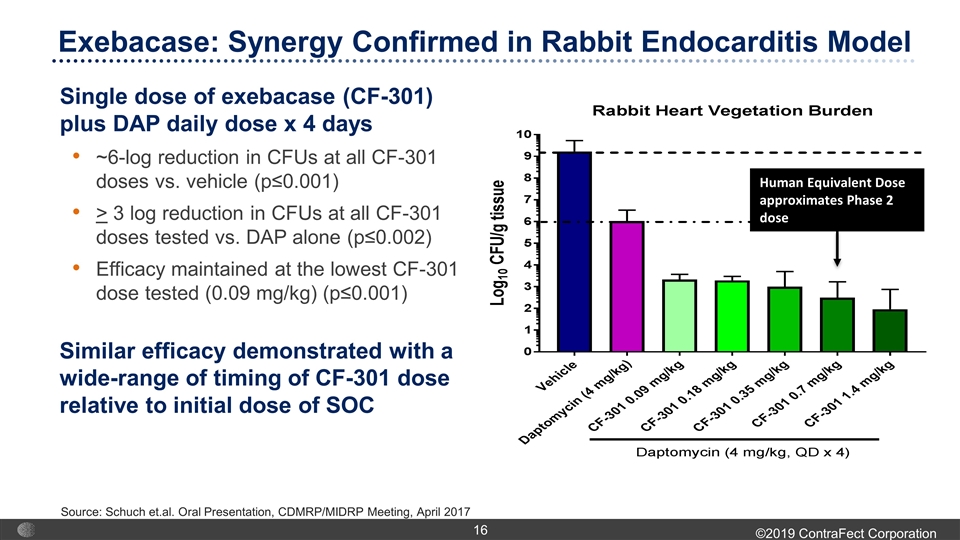
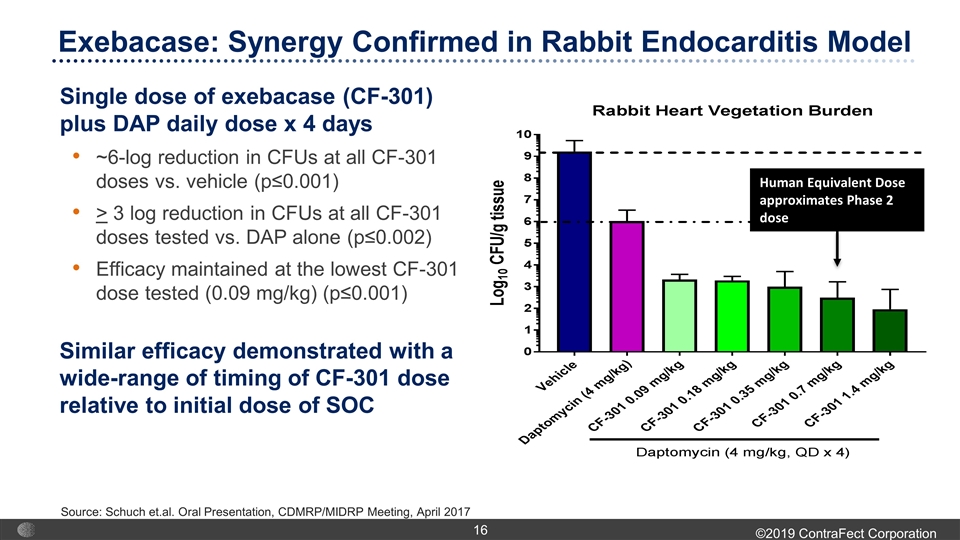
Single dose of exebacase (CF-301) plus DAP daily dose x 4 days ~6-log reduction in CFUs at all CF-301 doses vs. vehicle (p≤0.001) > 3 log reduction in CFUs at all CF-301 doses tested vs. DAP alone (p≤0.002) Efficacy maintained at the lowest CF-301 dose tested (0.09 mg/kg) (p≤0.001) Similar efficacy demonstrated with a wide-range of timing of CF-301 dose relative to initial dose of SOC Source: Schuch et.al. Oral Presentation, CDMRP/MIDRP Meeting, April 2017 Human Equivalent Dose approximates Phase 2 dose Exebacase: Synergy Confirmed in Rabbit Endocarditis Model
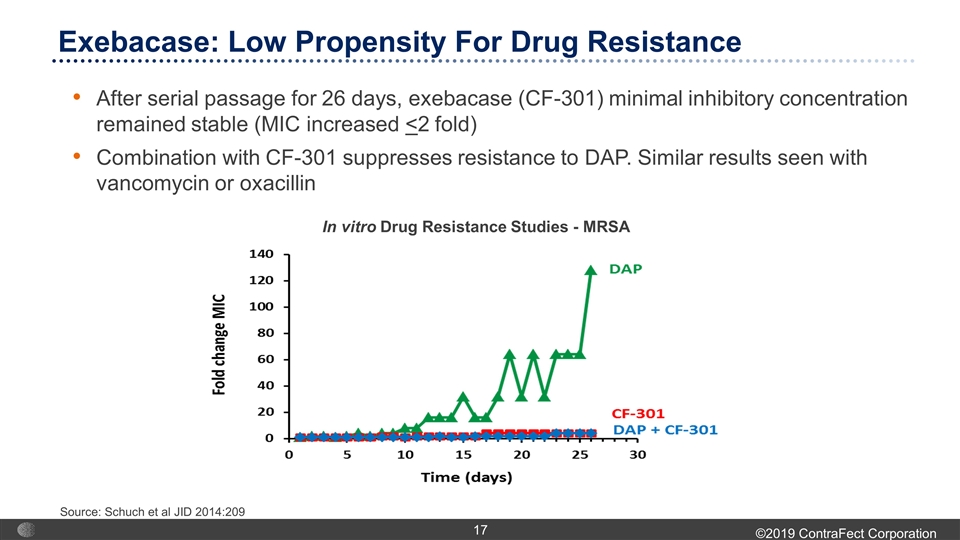
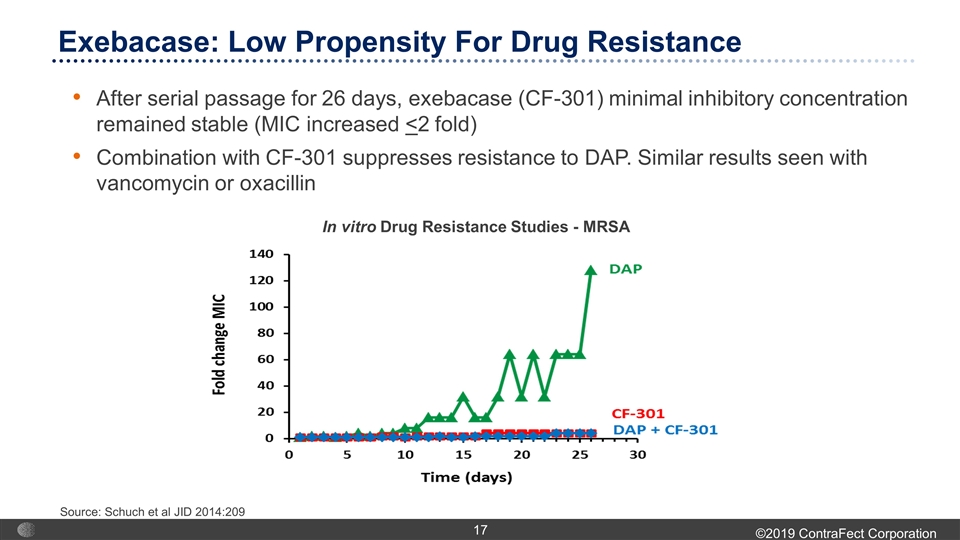
After serial passage for 26 days, exebacase (CF-301) minimal inhibitory concentration remained stable (MIC increased <2 fold) Combination with CF-301 suppresses resistance to DAP. Similar results seen with vancomycin or oxacillin Source: Schuch et al JID 2014:209 In vitro Drug Resistance Studies - MRSA Exebacase: Low Propensity For Drug Resistance
Single escalating IV dose, double-blind, placebo-controlled 20 healthy volunteers; 4 dosing cohorts (0.04, 0.12, 0.25, 0.40 mg/kg) Well tolerated; no clinical adverse safety signals No serious adverse events (AEs) No exebacase-related hypersensitivity AEs 5 non-serious AEs were mild, transient and resolved by end of study Exebacase - headache, contact dermatitis, allergic rhinitis Placebo - viral upper respiratory tract infection, viral infection 9 of 13 exebacase subjects developed anti-drug antibodies Complete or near complete resolution by Day 180 Well behaved pharmacokinetic (PK) profile Estimated effective exposures at 0.25 mg/kg dose Exebacase Demonstrated Safety and Tolerability in Phase 1
Staph aureus bacteremia and endocarditis patients have unmet need Approximately 200,000 hospitalizations per year in the US Clinical cure rates of <50% with current antibiotic therapy Mortality rates of at least 20% First antibacterial trial of its kind Endeavoring to improve clinical response rates over antibiotic treatment alone International, multi-center, randomized, double-blind, placebo-controlled trial for the treatment of Staph aureus bacteremia including endocarditis Comparison of response rates with exebacase used on top of antibiotics to antibiotics alone Primary study objectives Safety and tolerability of exebacase used in addition to antibiotics vs antibiotics alone Clinical outcome at Day 14 after study drug administration Phase 2: A ‘First-in-Patient’ Study with Superiority Design Source: AMR 2015 Data; 2012 GlobalData Market Research Report; Editor BWJ Mahy; Vol 6. Antimicrobial Resistance: Beyond the Breakpoint; Editor J. Todd Weber (US CDC) Klevens JAMA. 2007;298(15):1763-1771; Issues in Infectious Diseases; Fowler VG Jr, Boucher HW, Corey GR, et al. Daptomycin versus standard therapy for bacteremia and endocarditis caused by Staphylococcus aureus. N Engl J Med. 2006 Aug 17;355(7):653-65
Demographics/Baseline Characteristics Were Balanced Majority of patients enrolled in the US (79%) Latin America, EU, Russia and Israel also enrolled patients A total of 121 patients randomized into the study Primary analysis group – microbiological intent-to-treat (mITT) population 116 patients with confirmed Staph aureus bacteremia/endocarditis who received study drug Average patient was age 56, caucasian and male (67.8% of the total population) Approximately one-third of patients had methicillin-resistant staph aureus (MRSA) and two-thirds of patients had methicillin-sensitive staph aureus (MSSA) Antibiotic treatment with vancomycin or daptomycin for MRSA and semi-synthetic penicillins or first generation cephalosporins for methicillin-sensitive Staph aureus was similar in treatment arms
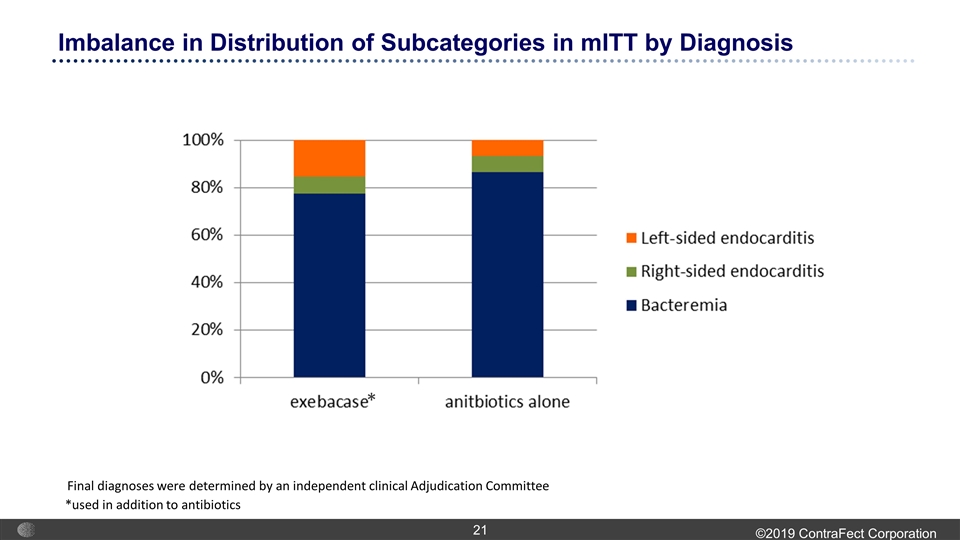
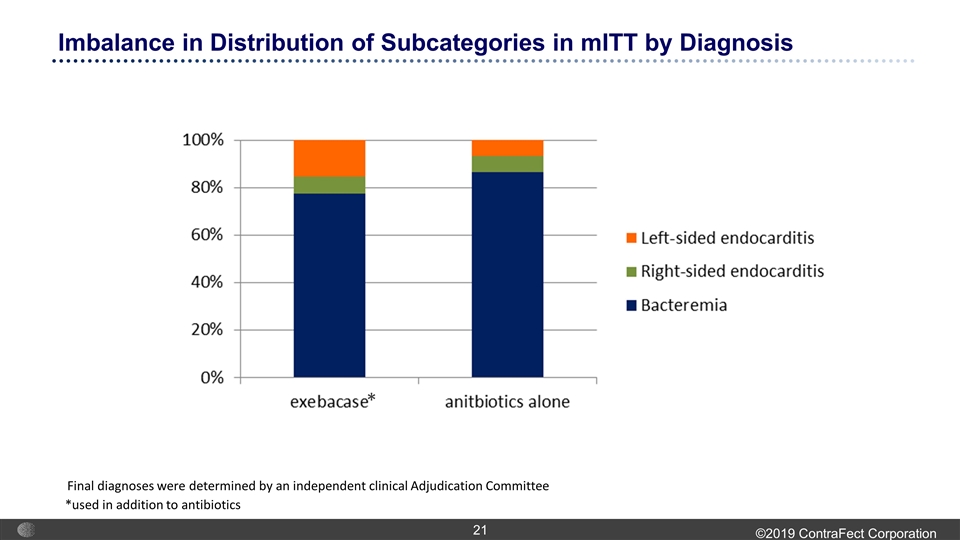
Imbalance in Distribution of Subcategories in mITT by Diagnosis *used in addition to antibiotics * Final diagnoses were determined by an independent clinical Adjudication Committee
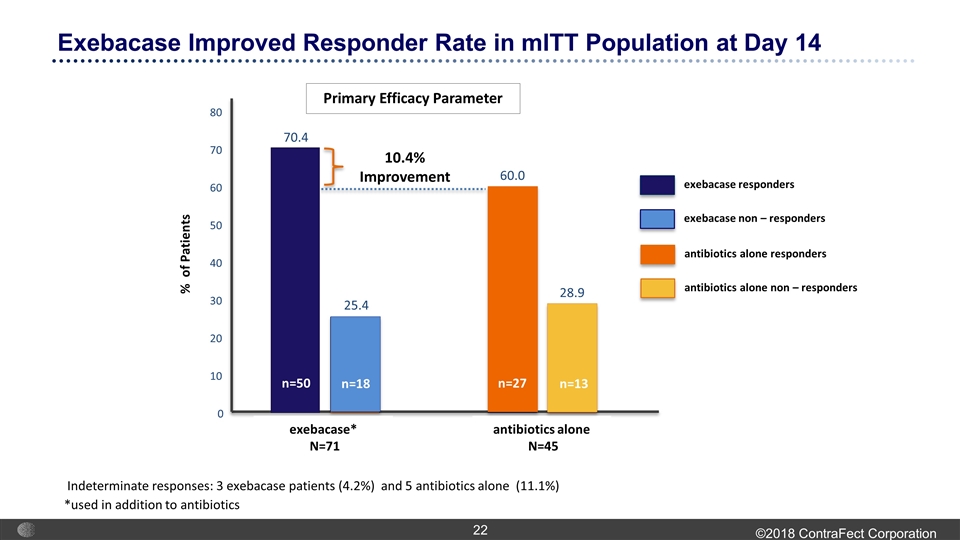
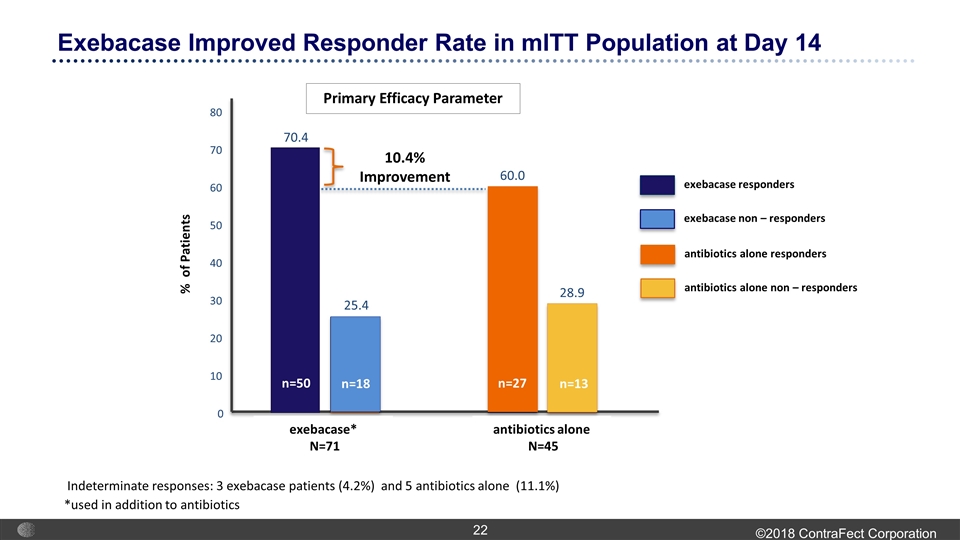
Exebacase Improved Responder Rate in mITT Population at Day 14 exebacase responders exebacase non – responders % of Patients antibiotics alone N=45 exebacase* N=71 10.4% Improvement 70.4 60.0 28.9 0 10 20 30 40 50 60 70 80 Indeterminate responses: 3 exebacase patients (4.2%) and 5 antibiotics alone (11.1%) 25.4 n=50 *used in addition to antibiotics Primary Efficacy Parameter n=18 antibiotics alone responders antibiotics alone non – responders n=27 n=13
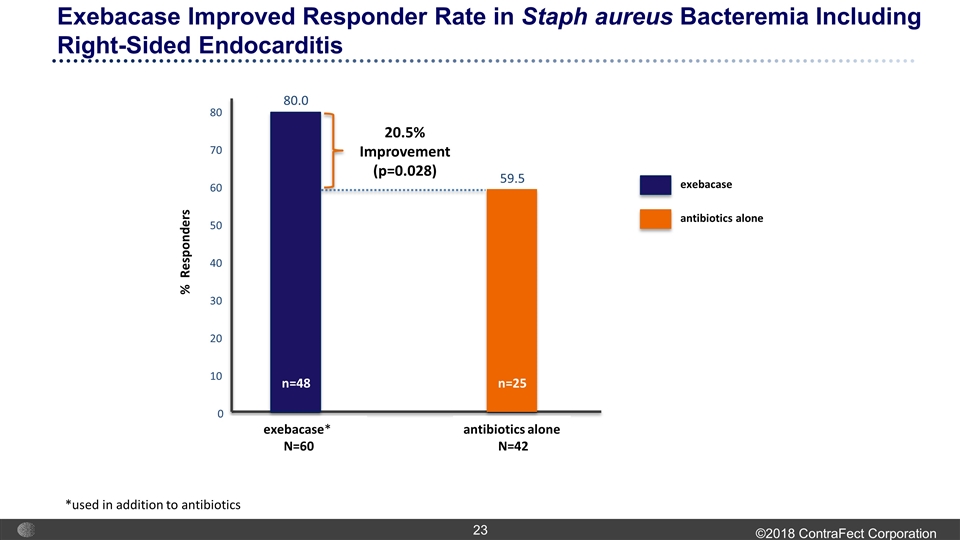
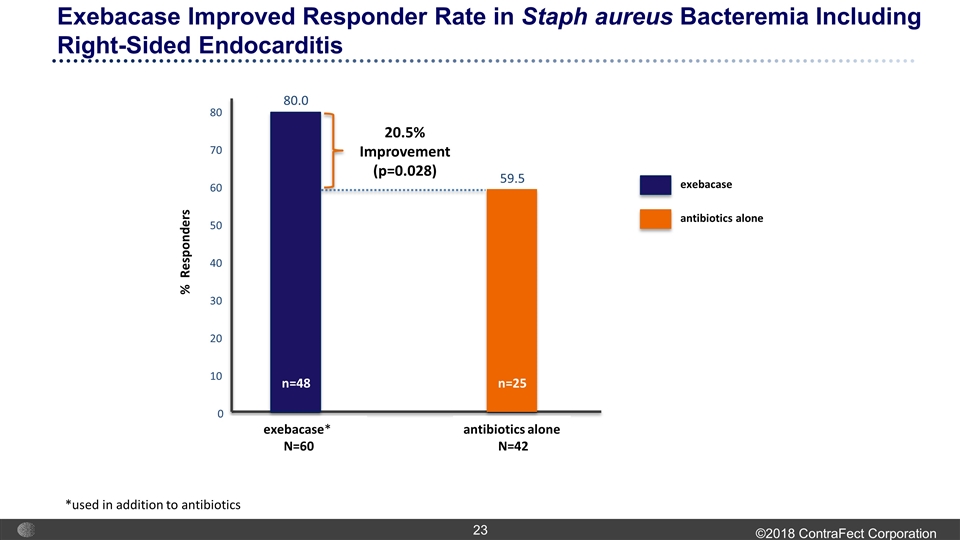
exebacase antibiotics alone antibiotics alone N=42 exebacase* N=60 20.5% Improvement (p=0.028) 80.0 59.5 0 10 20 30 40 50 60 70 80 N=18 N=13 n=25 n=48 Exebacase Improved Responder Rate in Staph aureus Bacteremia Including Right-Sided Endocarditis % Responders *used in addition to antibiotics
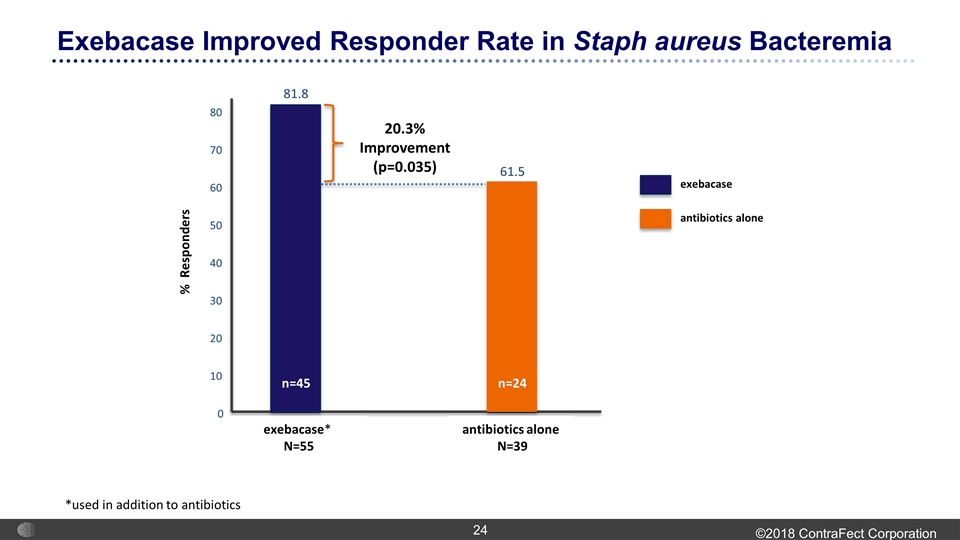
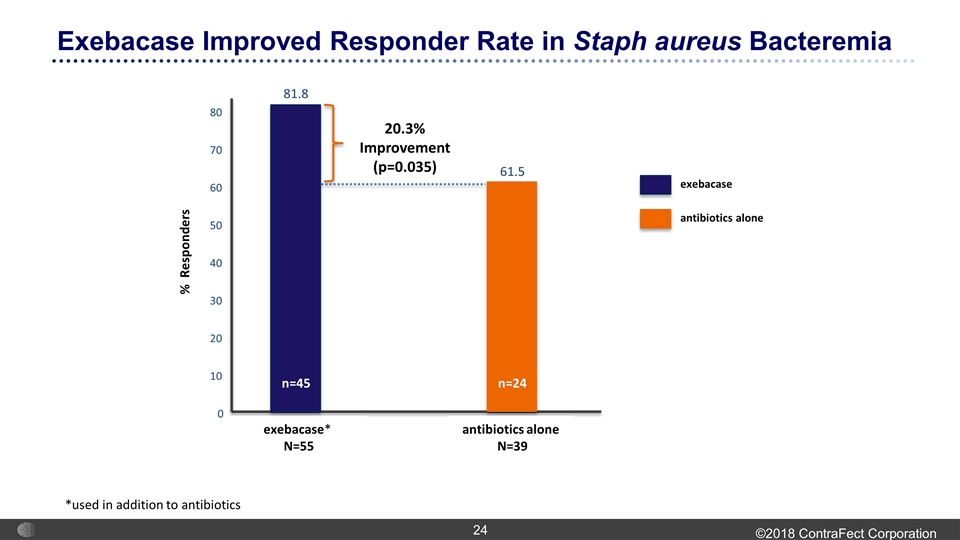
exebacase antibiotics alone antibiotics alone N=39 exebacase* N=55 20.3% Improvement (p=0.035) 81.8 61.5 0 10 20 30 40 50 60 70 80 N=18 N=13 n=24 n=45 Exebacase Improved Responder Rate in Staph aureus Bacteremia % Responders *used in addition to antibiotics
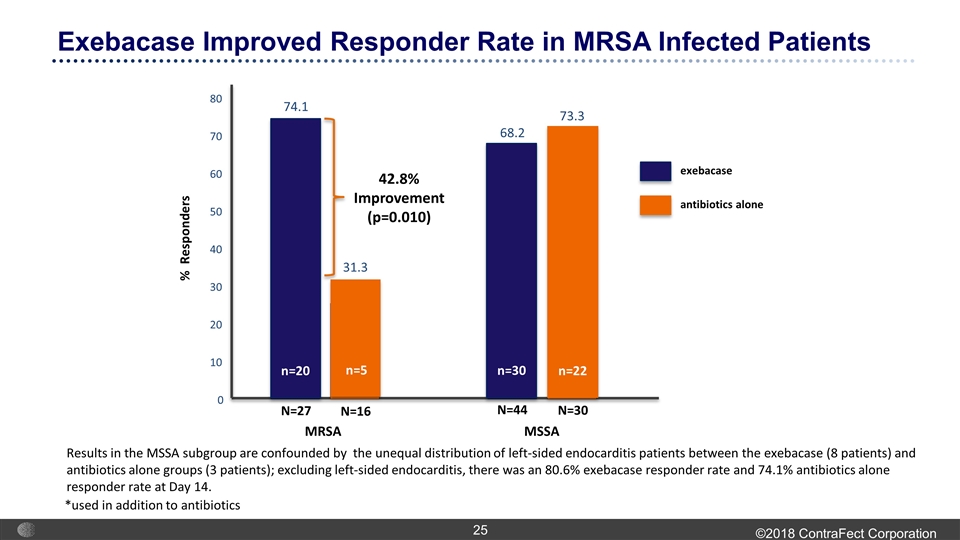
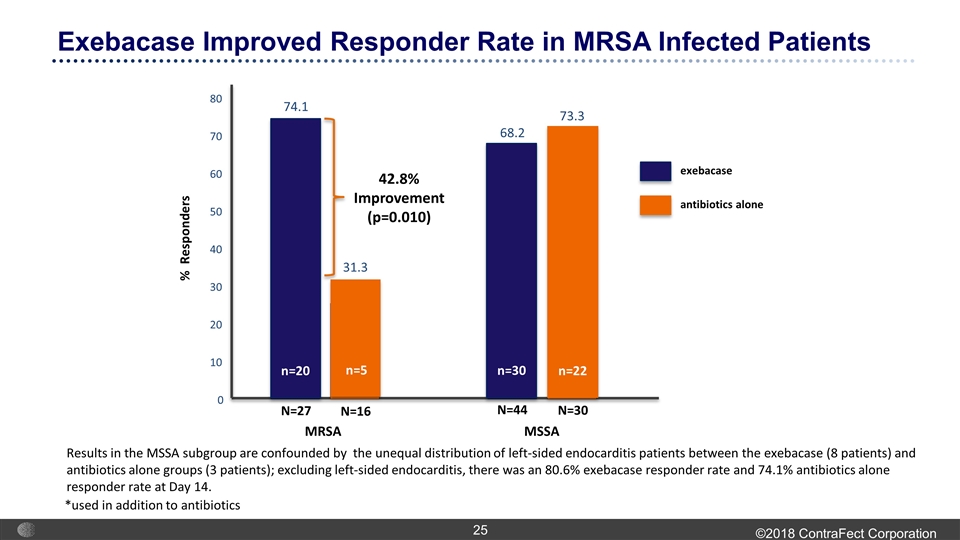
Exebacase Improved Responder Rate in MRSA Infected Patients MSSA MRSA 42.8% Improvement (p=0.010) 74.1 68.2 73.3 0 10 20 30 40 50 60 70 80 31.3 exebacase antibiotics alone Results in the MSSA subgroup are confounded by the unequal distribution of left-sided endocarditis patients between the exebacase (8 patients) and antibiotics alone groups (3 patients); excluding left-sided endocarditis, there was an 80.6% exebacase responder rate and 74.1% antibiotics alone responder rate at Day 14. N=27 N=16 N=44 N=30 % Responders *used in addition to antibiotics n=20 n=5 n=30 n=22
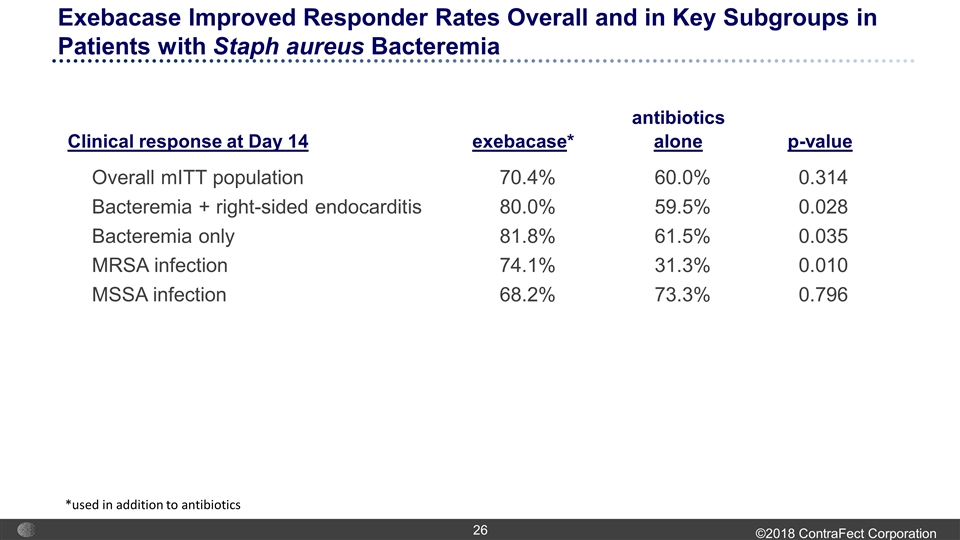
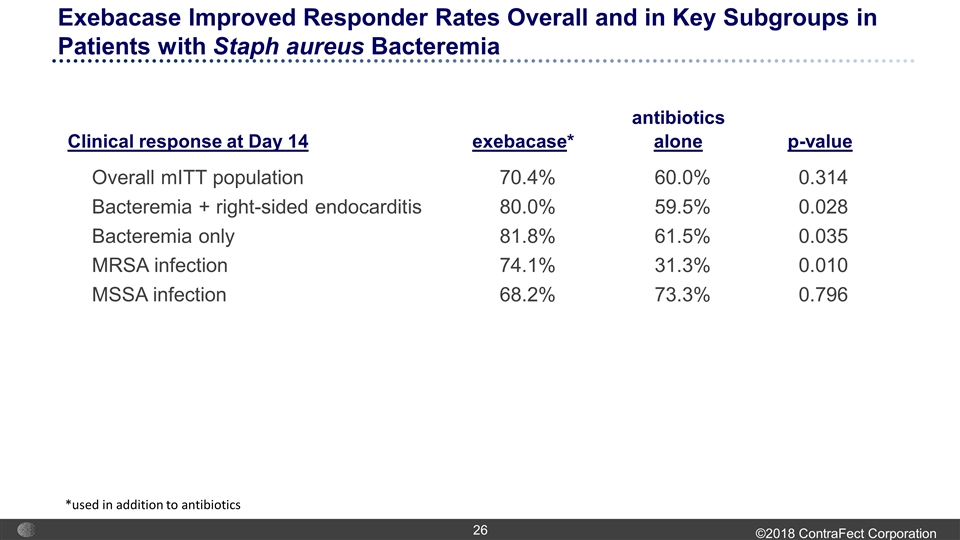
antibiotics Clinical response at Day 14 exebacase* alone p-value Overall mITT population 70.4% 60.0% 0.314 Bacteremia + right-sided endocarditis 80.0% 59.5% 0.028 Bacteremia only 81.8% 61.5% 0.035 MRSA infection 74.1% 31.3% 0.010 MSSA infection 68.2% 73.3% 0.796 Exebacase Improved Responder Rates Overall and in Key Subgroups in Patients with Staph aureus Bacteremia *used in addition to antibiotics
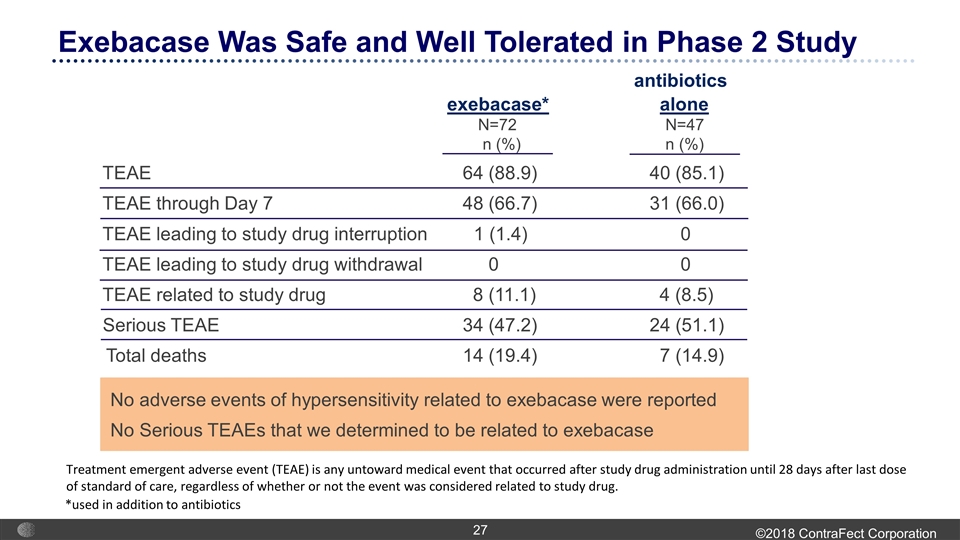
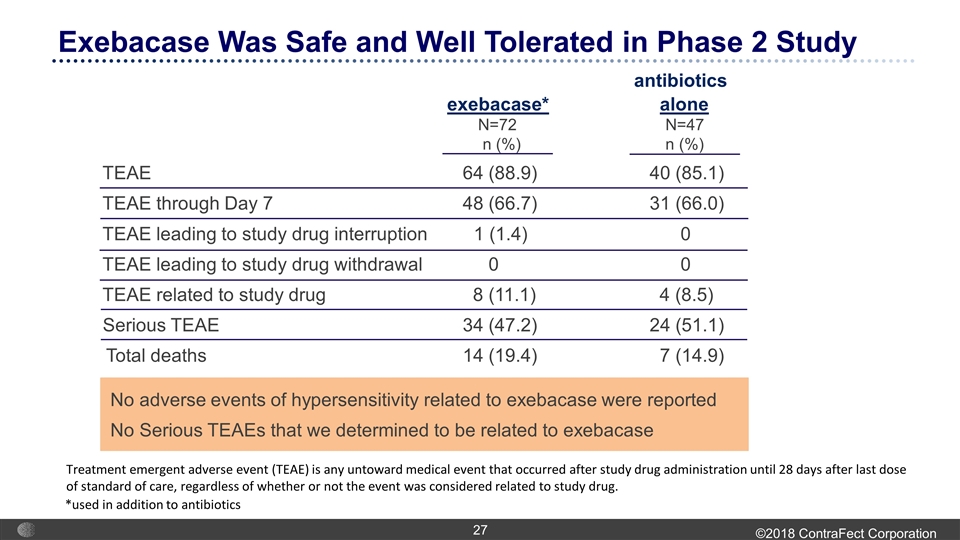
Exebacase Was Safe and Well Tolerated in Phase 2 Study Treatment emergent adverse event (TEAE) is any untoward medical event that occurred after study drug administration until 28 days after last dose of standard of care, regardless of whether or not the event was considered related to study drug. *used in addition to antibiotics No adverse events of hypersensitivity related to exebacase were reported No Serious TEAEs that we determined to be related to exebacase antibiotics exebacase* alone N=72 N=47 n (%) n (%) TEAE 64 (88.9) 40 (85.1) TEAE through Day 7 48 (66.7) 31 (66.0) TEAE leading to study drug interruption 1 (1.4) 0 TEAE leading to study drug withdrawal 0 0 TEAE related to study drug 8 (11.1) 4 (8.5) Serious TEAE 34 (47.2) 24 (51.1) Total deaths 14 (19.4) 7 (14.9)
First-in-Patient Phase 2 study with positive efficacy signals and robust safety and tolerability profile Identified Phase 3 study population with exebacase responder rates that were 20% higher than antibiotics alone Staph aureus bacteremia including right-sided endocarditis First non-traditional antimicrobial agent to demonstrate substantial additional clinical benefit over conventional antibiotic therapy alone Establishes clinical Proof of Concept for lysins as therapeutic agents Underscores our opportunity to address Gram-negative pathogens with our proprietary lysins Supports our plans to aggressively advance our portfolio of Gram-negative lysins into the clinic First Step to a Potential New Treatment Paradigm for Patients with Serious, Life-Threatening Bacterial Infections
GN Lysins Combating Multi-Drug Resistant Gram-Negative Infections Based on Novel Lysin Platform
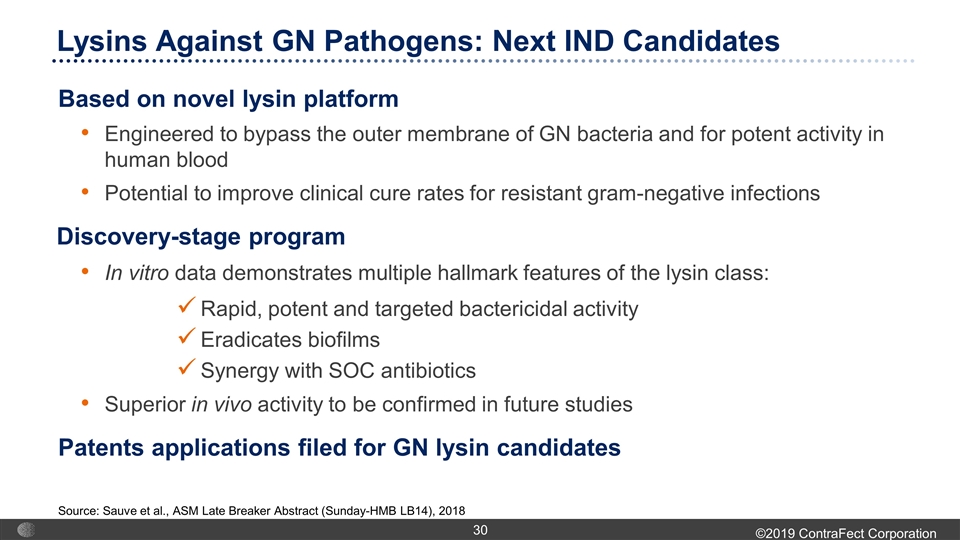
Lysins Against GN Pathogens: Next IND Candidates Based on novel lysin platform Engineered to bypass the outer membrane of GN bacteria and for potent activity in human blood Potential to improve clinical cure rates for resistant gram-negative infections Discovery-stage program In vitro data demonstrates multiple hallmark features of the lysin class: Rapid, potent and targeted bactericidal activity Eradicates biofilms Synergy with SOC antibiotics Superior in vivo activity to be confirmed in future studies Patents applications filed for GN lysin candidates Source: Sauve et al., ASM Late Breaker Abstract (Sunday-HMB LB14), 2018
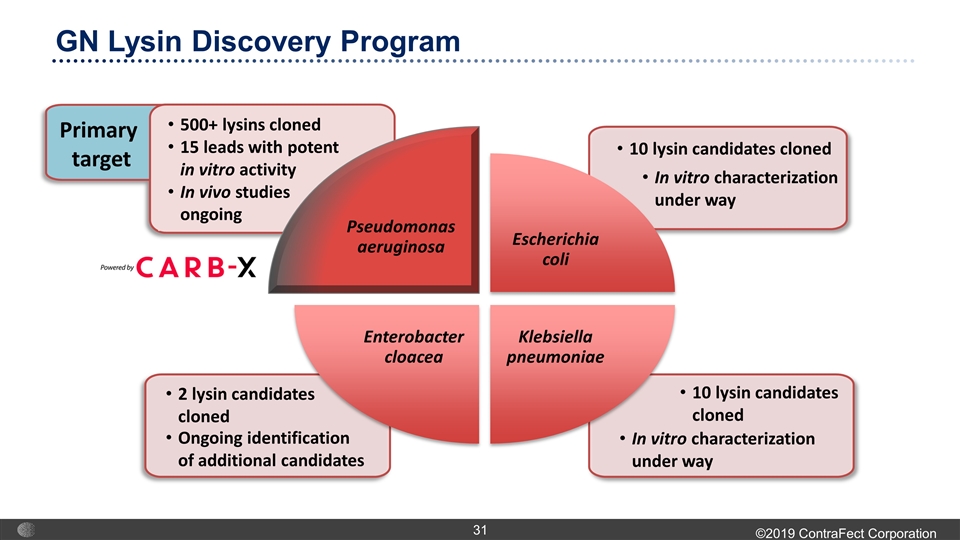
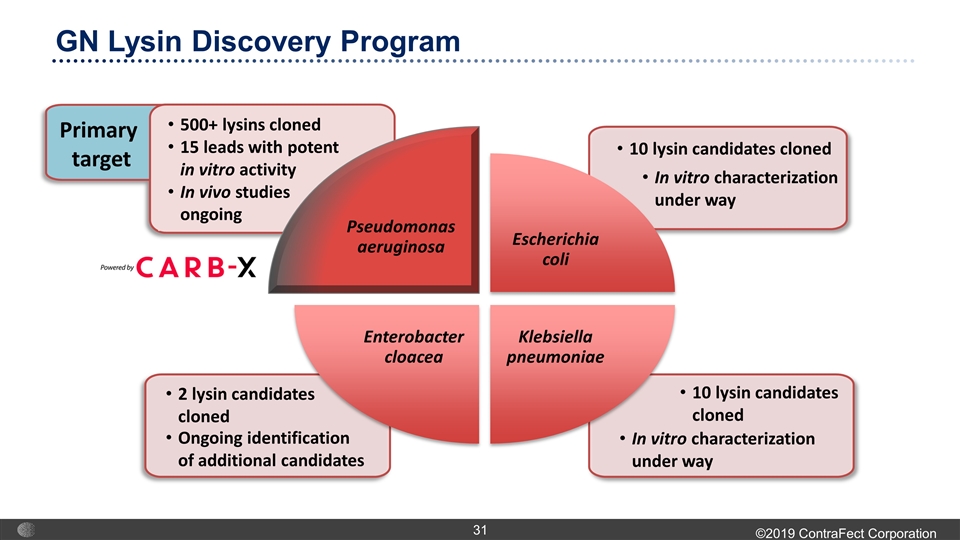
GN Lysin Discovery Program Escherichia coli Klebsiella pneumoniae Enterobacter cloacea 2 lysin candidates cloned 10 lysin candidates cloned 10 lysin candidates cloned 500+ lysins cloned 15 leads with potent in vitro activity In vivo studies ongoing Primary target In vitro characterization under way In vitro characterization under way Ongoing identification of additional candidates Pseudomonas aeruginosa
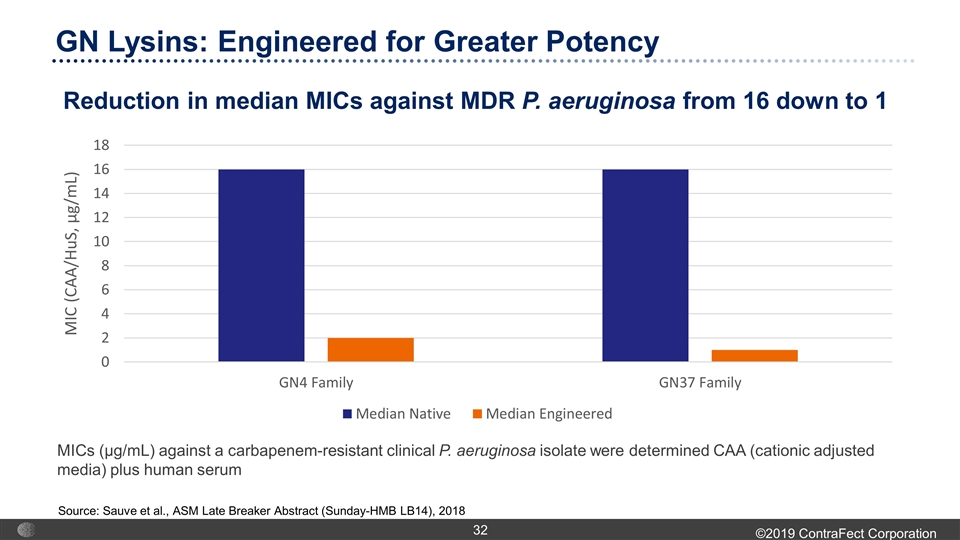
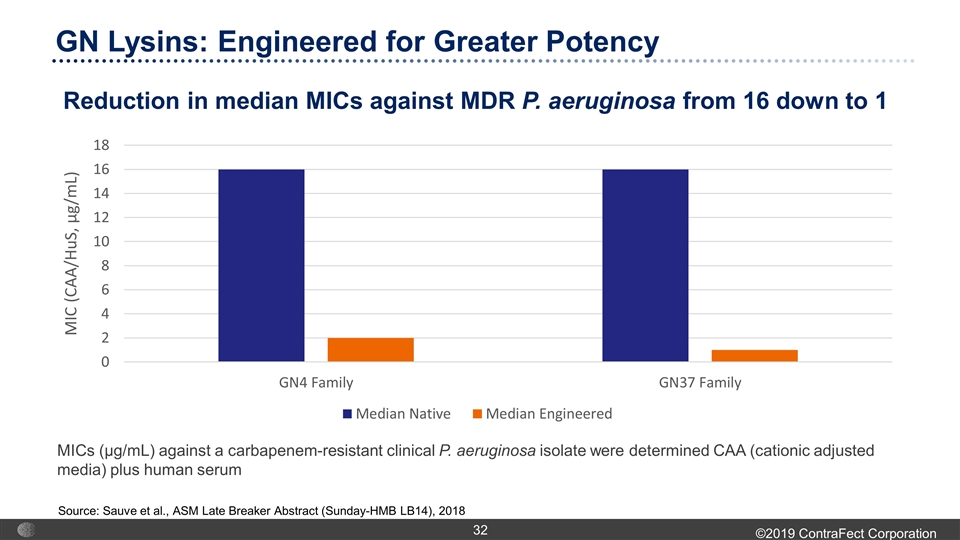
GN Lysins: Engineered for Greater Potency MICs (µg/mL) against a carbapenem-resistant clinical P. aeruginosa isolate were determined CAA (cationic adjusted media) plus human serum Reduction in median MICs against MDR P. aeruginosa from 16 down to 1 Source: Sauve et al., ASM Late Breaker Abstract (Sunday-HMB LB14), 2018
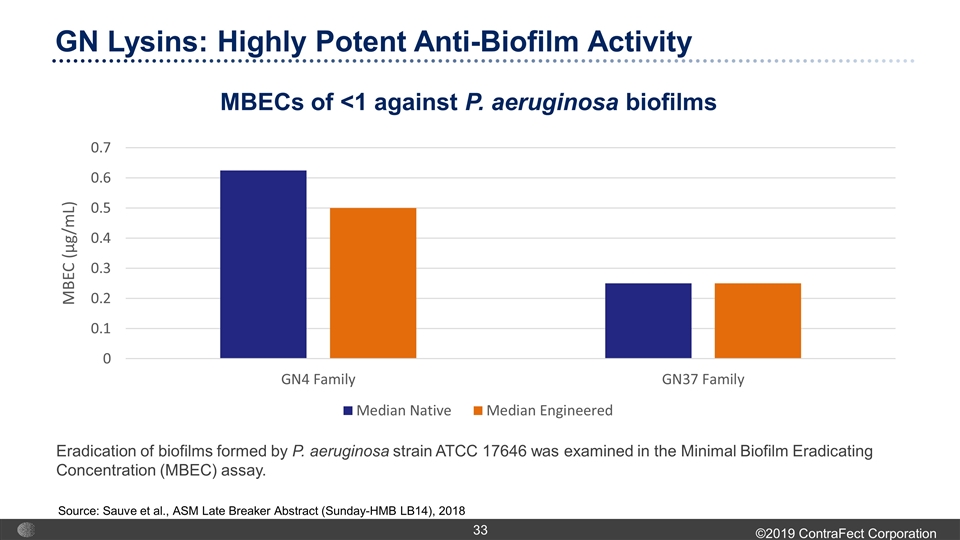
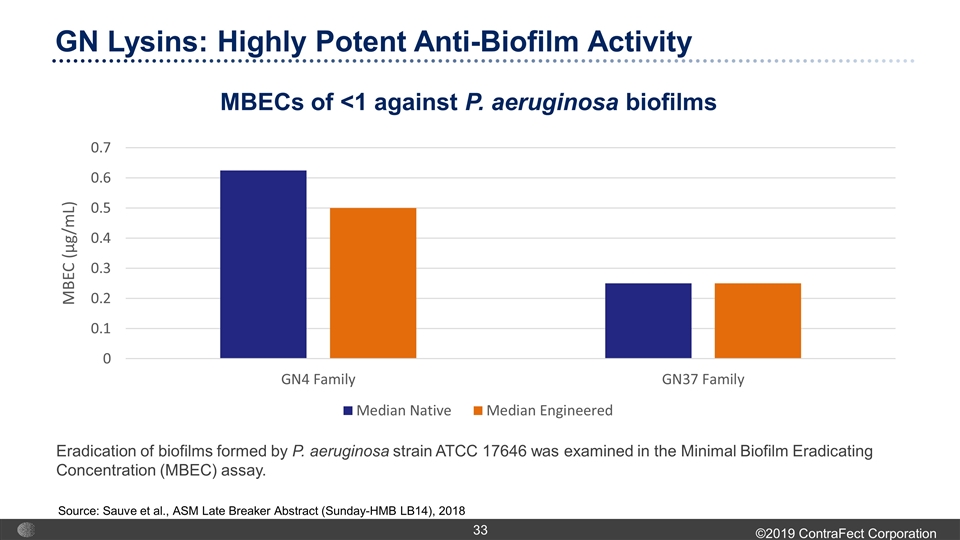
GN Lysins: Highly Potent Anti-Biofilm Activity Eradication of biofilms formed by P. aeruginosa strain ATCC 17646 was examined in the Minimal Biofilm Eradicating Concentration (MBEC) assay. MBECs of <1 against P. aeruginosa biofilms Source: Sauve et al., ASM Late Breaker Abstract (Sunday-HMB LB14), 2018
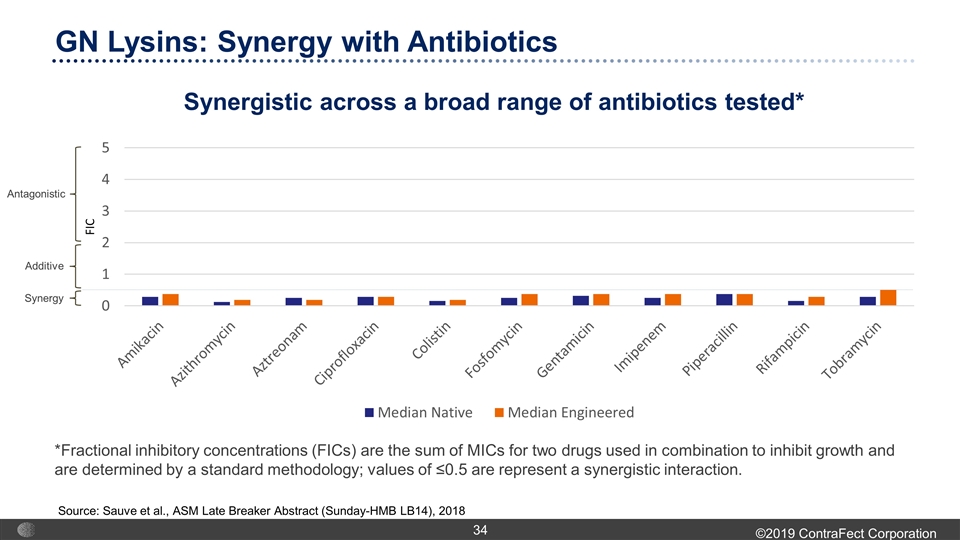
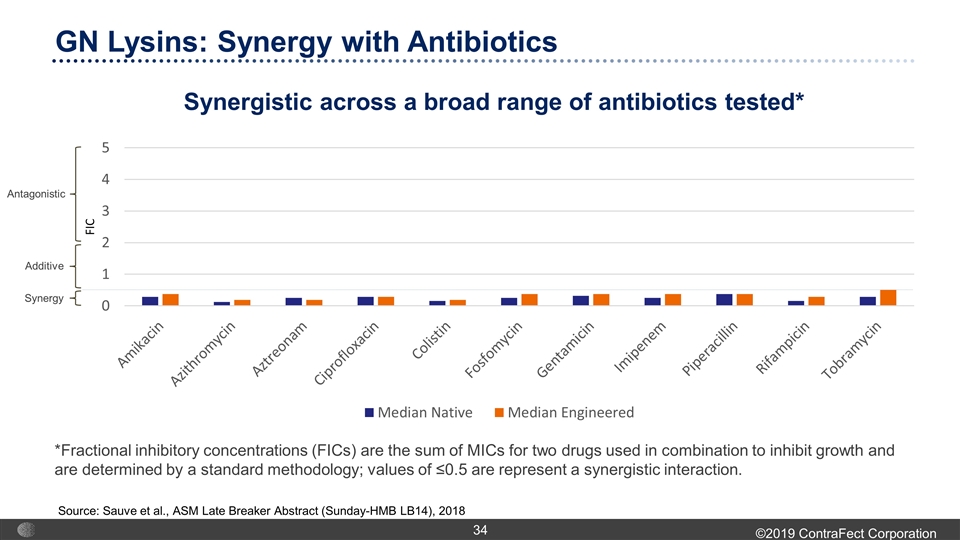
GN Lysins: Synergy with Antibiotics Synergistic across a broad range of antibiotics tested* *Fractional inhibitory concentrations (FICs) are the sum of MICs for two drugs used in combination to inhibit growth and are determined by a standard methodology; values of ≤0.5 are represent a synergistic interaction. Source: Sauve et al., ASM Late Breaker Abstract (Sunday-HMB LB14), 2018 Synergy Additive Antagonistic
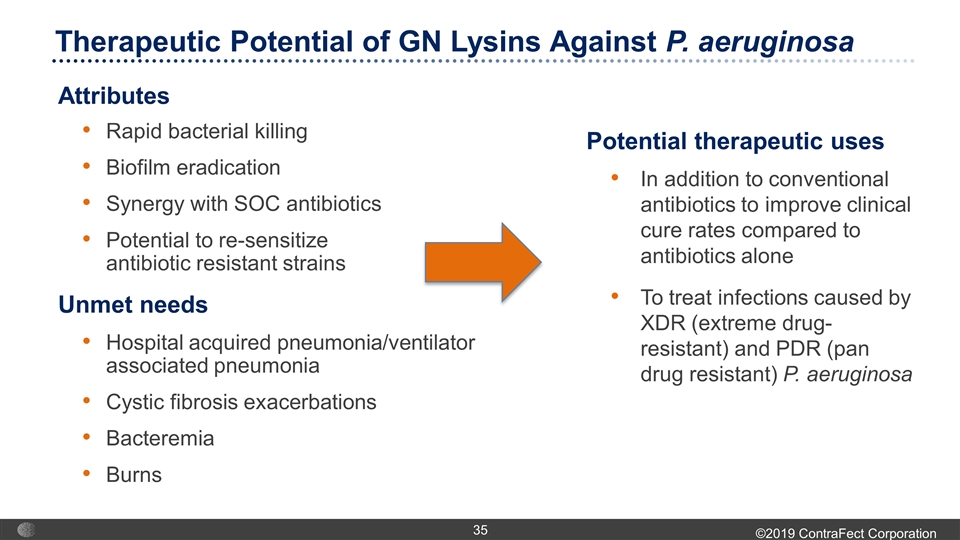
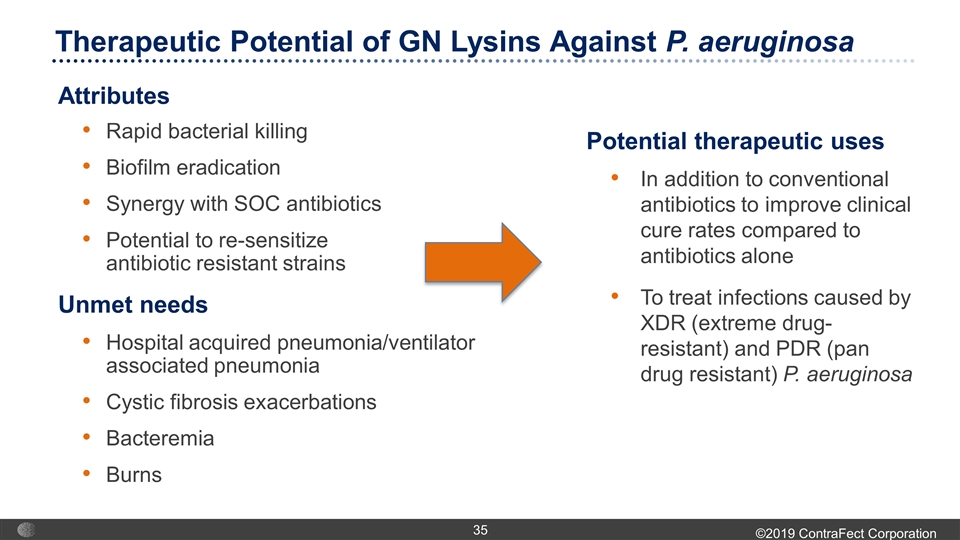
Attributes Rapid bacterial killing Biofilm eradication Synergy with SOC antibiotics Potential to re-sensitize antibiotic resistant strains Therapeutic Potential of GN Lysins Against P. aeruginosa Potential therapeutic uses In addition to conventional antibiotics to improve clinical cure rates compared to antibiotics alone To treat infections caused by XDR (extreme drug-resistant) and PDR (pan drug resistant) P. aeruginosa Unmet needs Hospital acquired pneumonia/ventilator associated pneumonia Cystic fibrosis exacerbations Bacteremia Burns
CF-404 Inhaled Combination of mAbs for Influenza
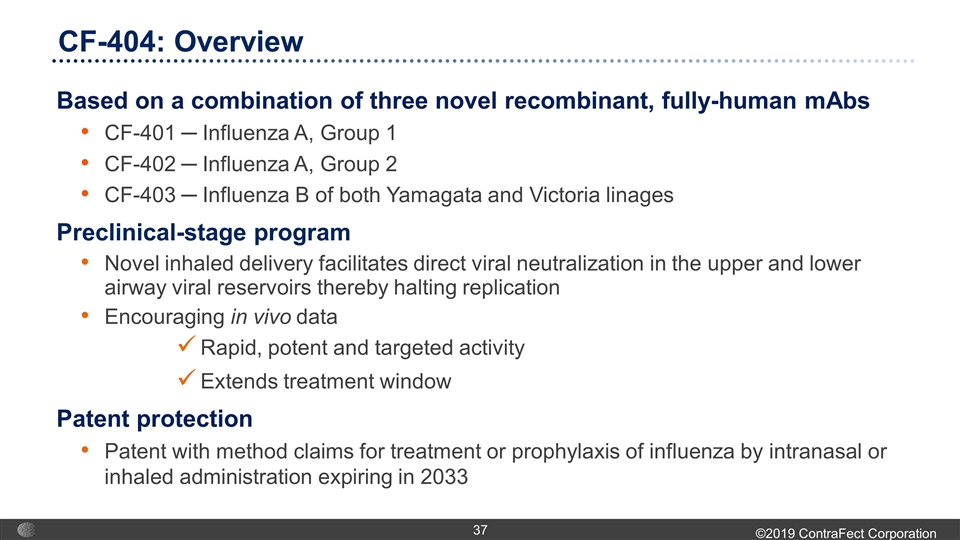
Based on a combination of three novel recombinant, fully-human mAbs CF-401 ─ Influenza A, Group 1 CF-402 ─ Influenza A, Group 2 CF-403 ─ Influenza B of both Yamagata and Victoria linages Preclinical-stage program Novel inhaled delivery facilitates direct viral neutralization in the upper and lower airway viral reservoirs thereby halting replication Encouraging in vivo data Rapid, potent and targeted activity Extends treatment window Patent protection Patent with method claims for treatment or prophylaxis of influenza by intranasal or inhaled administration expiring in 2033 CF-404: Overview
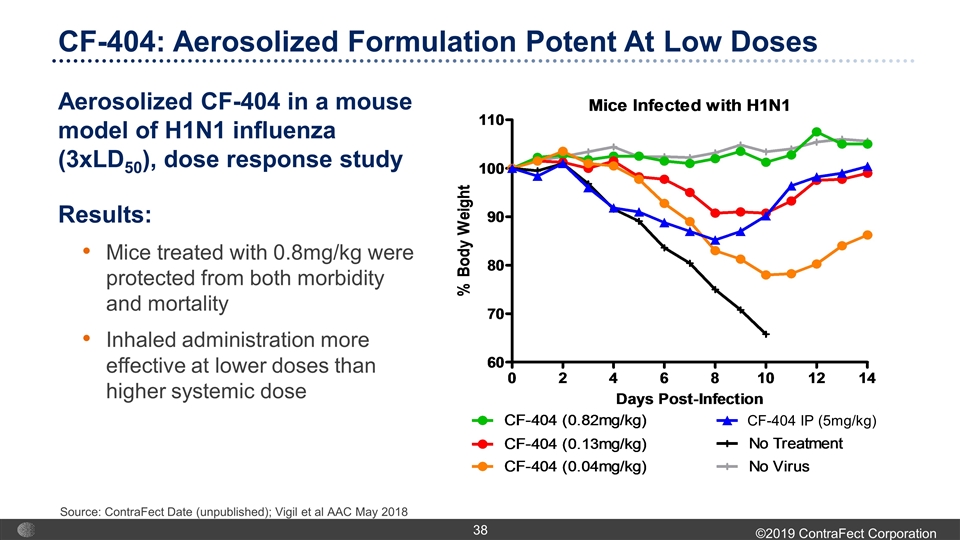
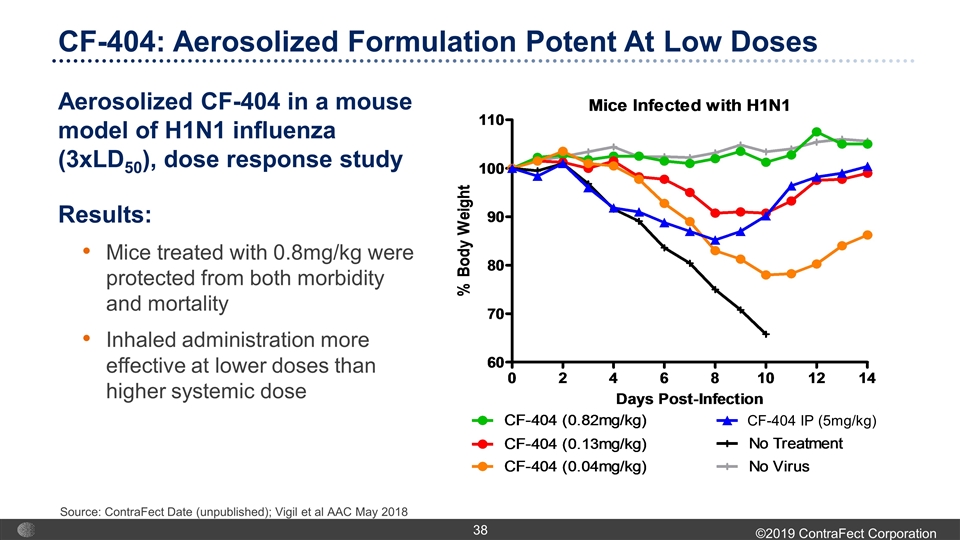
Aerosolized CF-404 in a mouse model of H1N1 influenza (3xLD50), dose response study Results: Mice treated with 0.8mg/kg were protected from both morbidity and mortality Inhaled administration more effective at lower doses than higher systemic dose CF-404 IP (5mg/kg) CF-404: Aerosolized Formulation Potent At Low Doses Source: ContraFect Date (unpublished); Vigil et al AAC May 2018
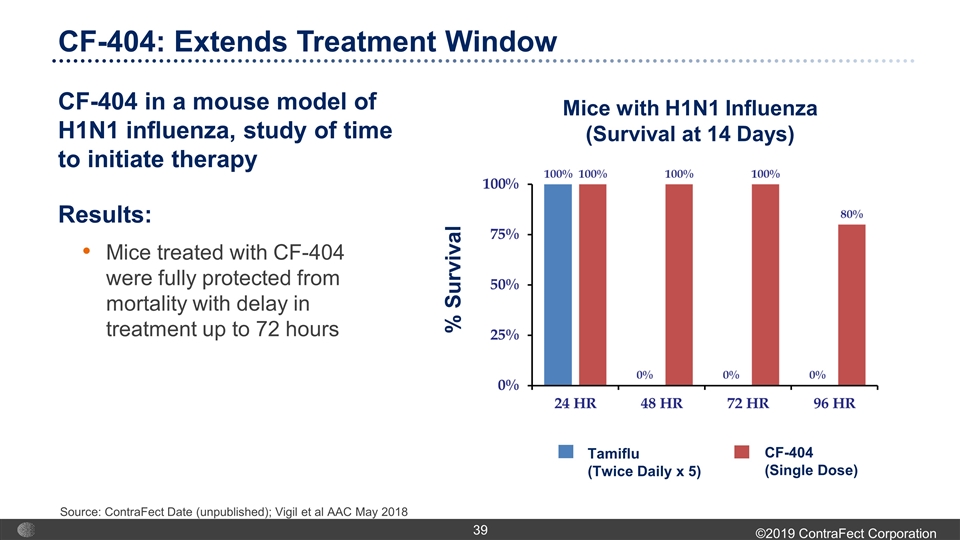
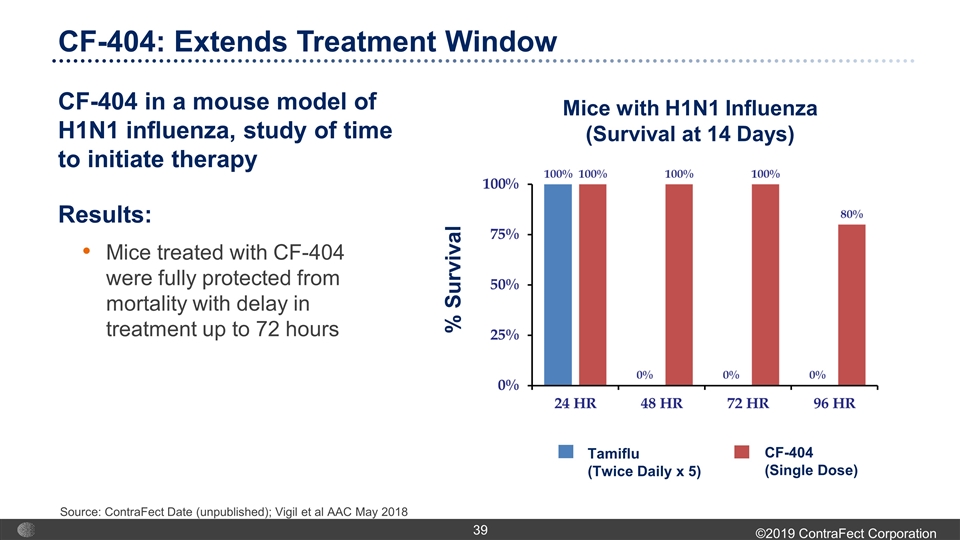
% Survival Tamiflu (Twice Daily x 5) CF-404 (Single Dose) Mice with H1N1 Influenza (Survival at 14 Days) CF-404: Extends Treatment Window CF-404 in a mouse model of H1N1 influenza, study of time to initiate therapy Results: Mice treated with CF-404 were fully protected from mortality with delay in treatment up to 72 hours Source: ContraFect Date (unpublished); Vigil et al AAC May 2018
Corporate Information
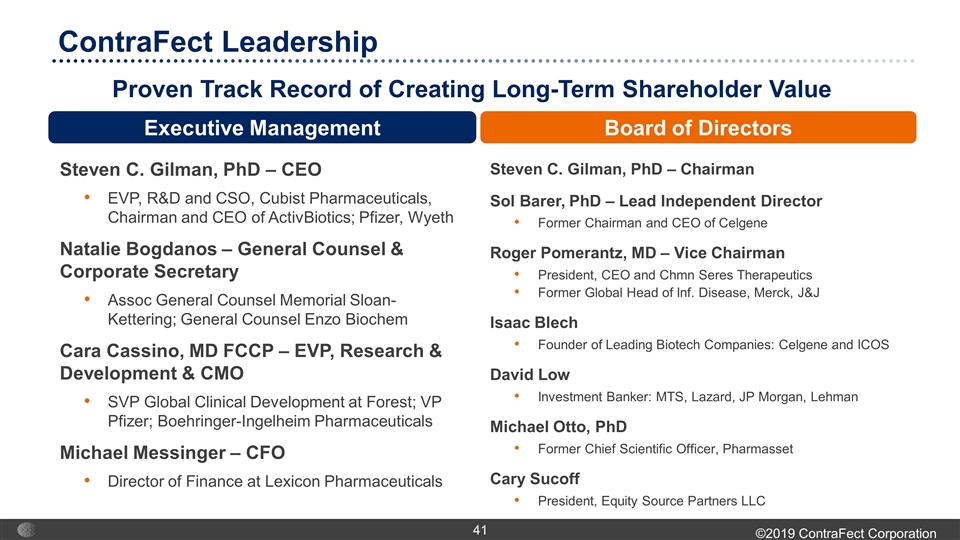
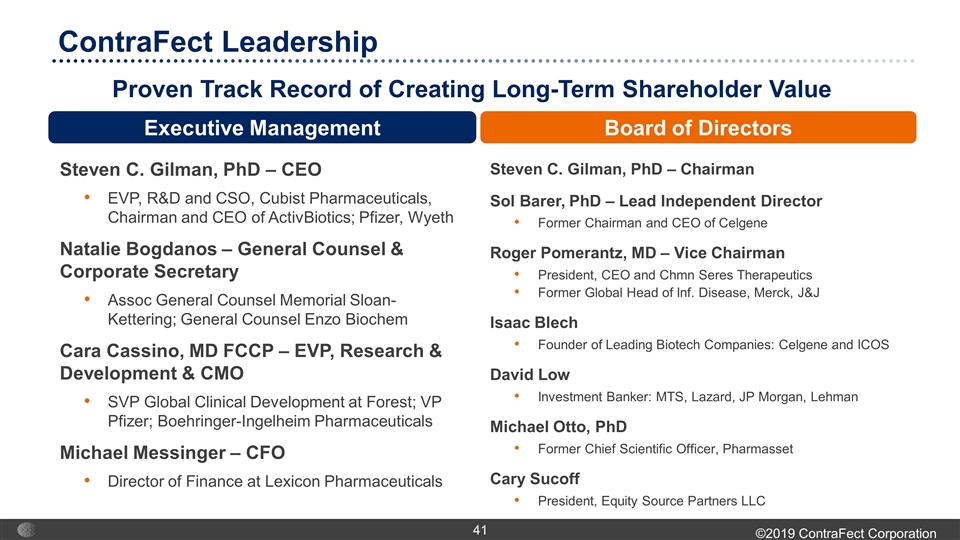
ContraFect Leadership Proven Track Record of Creating Long-Term Shareholder Value Steven C. Gilman, PhD – Chairman Sol Barer, PhD – Lead Independent Director Former Chairman and CEO of Celgene Roger Pomerantz, MD – Vice Chairman President, CEO and Chmn Seres Therapeutics Former Global Head of Inf. Disease, Merck, J&J Isaac Blech Founder of Leading Biotech Companies: Celgene and ICOS David Low Investment Banker: MTS, Lazard, JP Morgan, Lehman Michael Otto, PhD Former Chief Scientific Officer, Pharmasset Cary Sucoff President, Equity Source Partners LLC Steven C. Gilman, PhD – CEO EVP, R&D and CSO, Cubist Pharmaceuticals, Chairman and CEO of ActivBiotics; Pfizer, Wyeth Natalie Bogdanos – General Counsel & Corporate Secretary Assoc General Counsel Memorial Sloan-Kettering; General Counsel Enzo Biochem Cara Cassino, MD FCCP – EVP, Research & Development & CMO SVP Global Clinical Development at Forest; VP Pfizer; Boehringer-Ingelheim Pharmaceuticals Michael Messinger – CFO Director of Finance at Lexicon Pharmaceuticals Executive Management Board of Directors
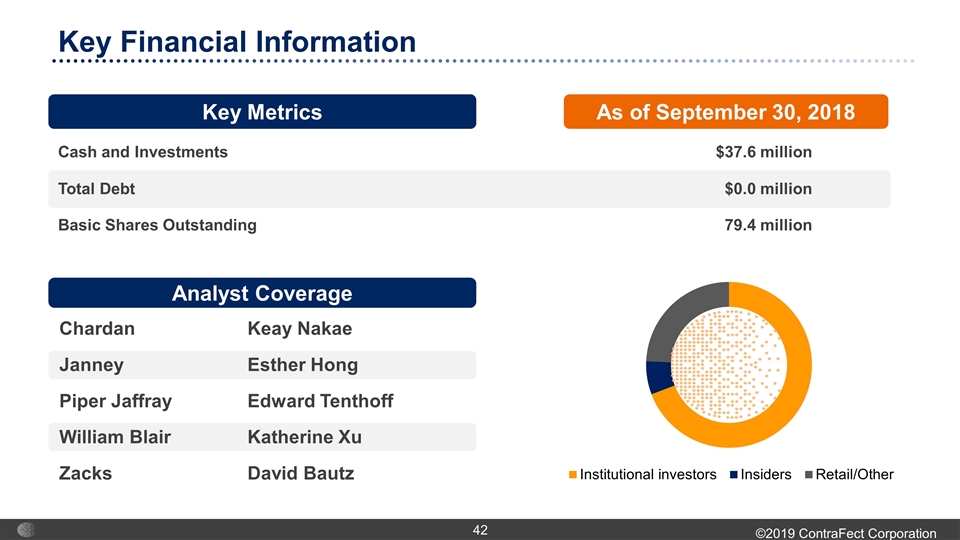
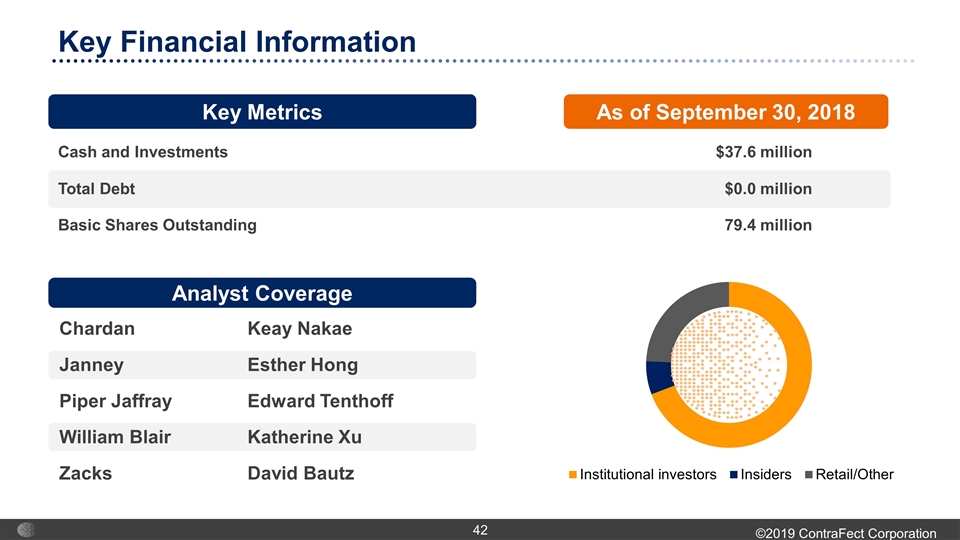
Cash and Investments $37.6 million Total Debt $0.0 million Basic Shares Outstanding 79.4 million Key Financial Information Key Metrics As of September 30, 2018 Analyst Coverage Chardan Keay Nakae JanneyEsther Hong Piper JaffrayEdward Tenthoff William BlairKatherine Xu ZacksDavid Bautz
Lysin platform Novel class of anti-infectives Preclinical data supports multiple advantages as therapeutics Exebacase (CF-301) – first-in-class lysin candidate for Staph aureus bacteremia Demonstrated substantial additional clinical benefit over and above conventional antibiotic therapy in Phase 2 superiority clinical trial Fast Track status granted by FDA Broad pipeline Novel lysins directed at drug resistant gram-negative (GN) pathogens Novel phage derived peptides with broad spectrum activity against GN pathogens CF-296 – engineered CF-301 variant – potential line extension in pre-clinical evaluation CF-404 – inhaled antibody cocktail to treat influenza in pre-clinical evaluation ContraFect Portfolio Overview

ContraFect Corporation NASDAQ: CFRX First in class anti-infectives for life-threatening, drug-resistant infections