Exhibit 99.2
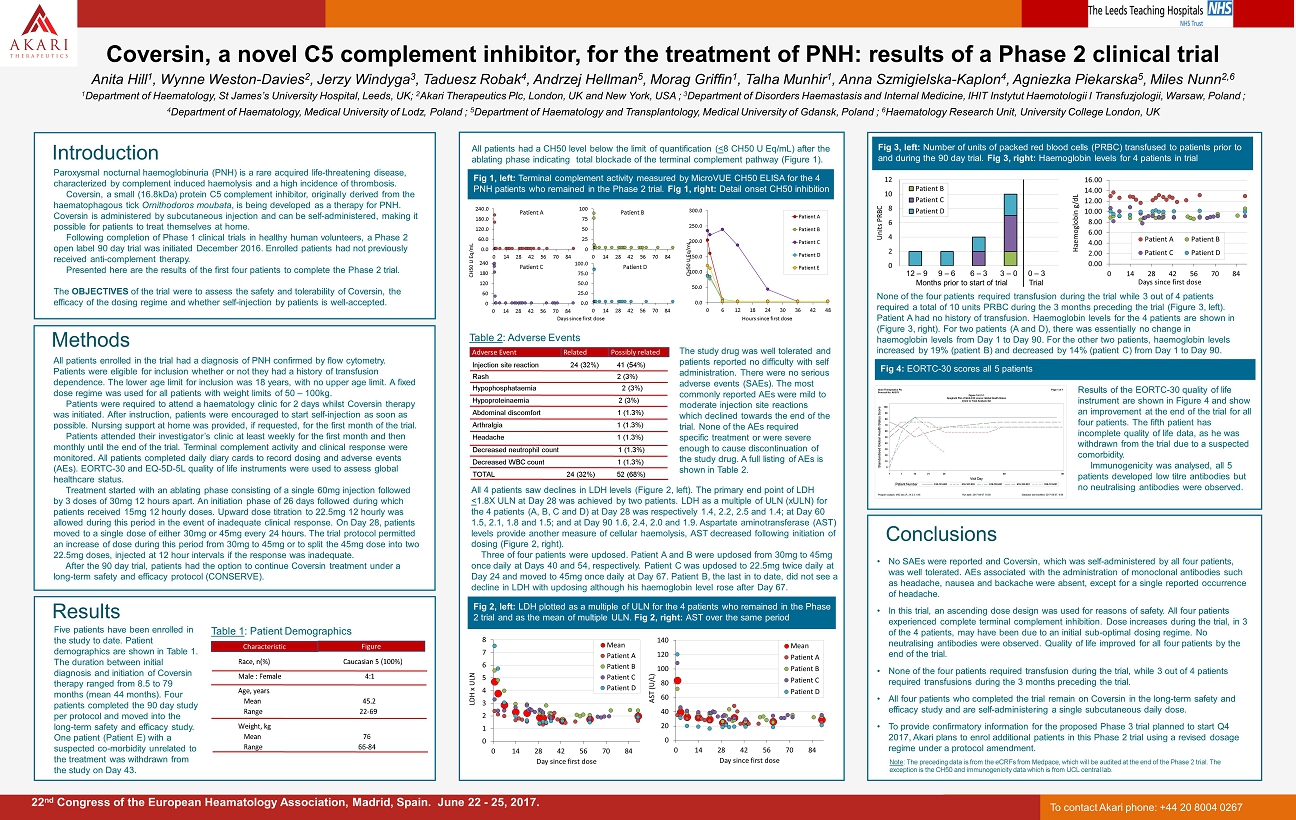
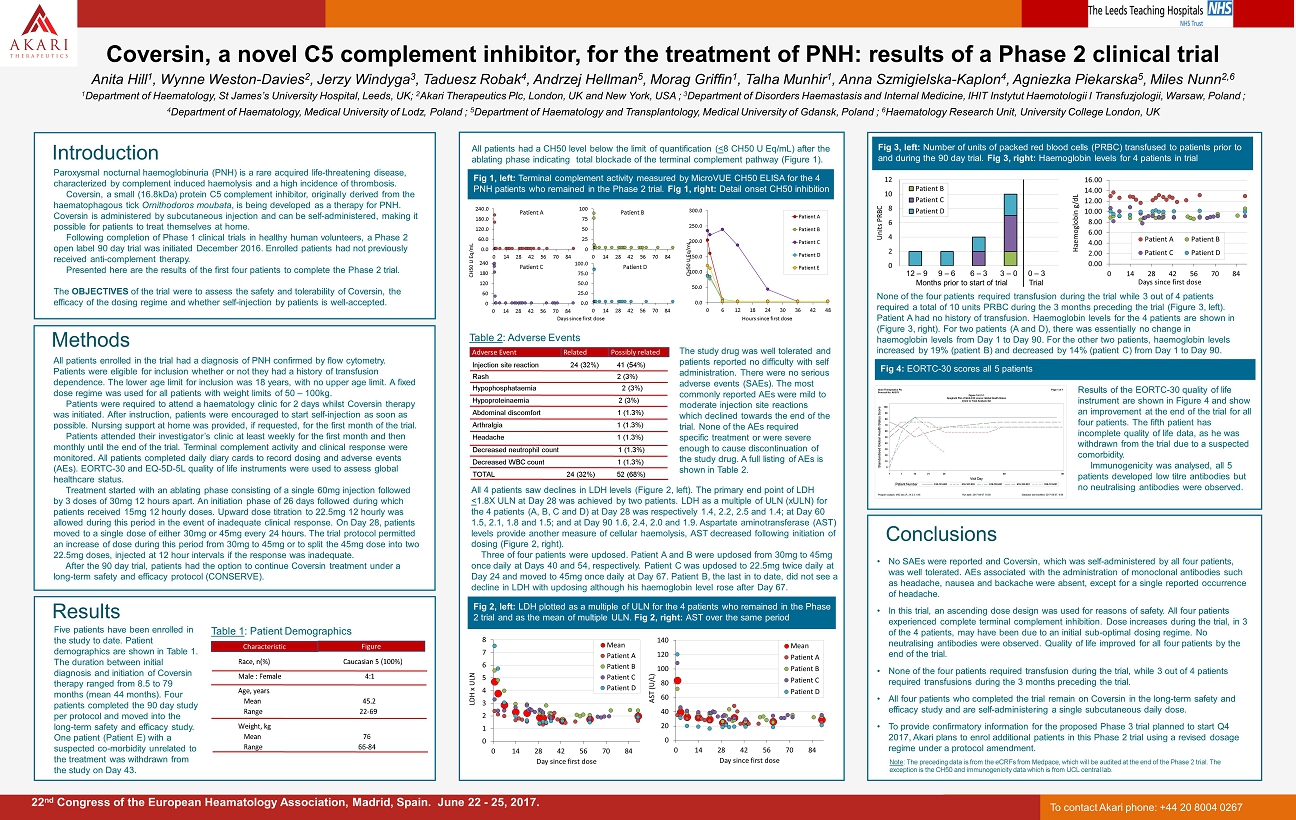
• No SAEs were reported and Coversin , which was self - administered by all four patients, was well tolerated. AEs associated with the administration of monoclonal antibodies such as headache, nausea and backache were absent, except for a single reported occurrence of headache. • In this trial, an ascending dose design was used for reasons of safety. All four patients experienced complete terminal complement inhibition. Dose increases during the trial, in 3 of the 4 patients, may have been due to an initial sub - optimal dosing regime. No neutralising antibodies were observed. Quality of life improved for all four patients by the end of the trial. • None of the four patients required transfusion during the trial, while 3 out of 4 patients required transfusions during the 3 months preceding the trial .. • All four patients who completed the trial remain on Coversin in the long - term safety and efficacy study and are self - administering a single subcutaneous daily dose. • To provide confirmatory information for the proposed Phase 3 trial planned to start Q4 2017, Akari plans to enrol additional patients in this Phase 2 trial using a revised dosage regime under a protocol amendment. Introduction Coversin , a novel C5 complement inhibitor, for the treatment of PNH: results of a Phase 2 clinical trial Anita Hill 1 , Wynne Weston - Davies 2 , Jerzy Windyga 3 , Taduesz Robak 4 , Andrzej Hellman 5 , Morag Griffin 1 , Talha Munhir 1 , Anna Szmigielska - Kaplon 4 , Agniezka Piekarska 5 , Miles Nunn 2,6 1 Department of Haematology , St James’s University Hospital , Leeds, UK; 2 Akari Therapeutics Plc , London, UK and New York, USA ; 3 Department of Disorders Haemastasis and Internal Medicine, IHIT Instytut Haemotologii I Transfuzjologii , Warsaw, Poland ; 4 Department of Haematology , Medical University of Lodz, Poland ; 5 Department of Haematology and Transplantology , Medical University of Gdansk, Poland ; 6 Haematology Research Unit, University College London, UK 22 nd Congress of the European Heamatology Association, Madrid, Spain. June 22 - 25, 2017. Methods Conclusions All patients enrolled in the trial had a diagnosis of PNH confirmed by flow cytometry. Patients were eligible for inclusion whether or not they had a history of transfusion dependence. The lower age limit for inclusion was 18 years, with no upper age limit. A fixed dose regime was used for all patients with weight limits of 50 – 100kg. Patients were required to attend a haematology clinic for 2 days whilst Coversin therapy was initiated . After instruction, patients were encouraged to start self - injection as soon as possible. Nursing support at home was provided, if requested, for the first month of the trial. Patients attended their investigator’s clinic at least weekly for the first month and then monthly until the end of the trial. Terminal complement activity and clinical response were monitored. All patients completed daily diary cards to record dosing and adverse events (AEs). EORTC - 30 and EQ - 5D - 5L quality of life instruments were used to assess global healthcare status. Treatment started with an ablating phase consisting of a single 60mg injection followed by 3 doses of 30mg 12 hours apart. An initiation phase of 26 days followed during which patients received 15mg 12 hourly doses. Upward dose titration to 22.5mg 12 hourly was allowed during this period in the event of inadequate clinical response. On Day 28, patients moved to a single dose of either 30mg or 45mg every 24 hours. The trial protocol permitted an increase of dose during this period from 30mg to 45mg or to split the 45mg dose into two 22.5mg doses, injected at 12 hour intervals if the response was inadequate. After the 90 day trial, patients had the option to continue Coversin treatment under a long - term safety and efficacy protocol (CONSERVE). Fig 2 , left: LDH plotted as a multiple of ULN for the 4 patients who remained in the Phase 2 trial and as the mean of multiple ULN. Fig 2, right: AST over the same period 0 1 2 3 4 5 6 7 8 0 14 28 42 56 70 84 LDH x ULN Day since first dose Mean Patient A Patient B Patient C Patient D Fig 1, left: Terminal complement activity measured by MicroVUE CH50 ELISA for the 4 PNH patients who remained in the Phase 2 trial. Fig 1, right: Detail onset CH50 inhibition 0.0 60.0 120.0 180.0 240.0 0 14 28 42 56 70 84 0 60 120 180 240 0 14 28 42 56 70 84 CH50 U Eq /mL 0.0 25.0 50.0 75.0 100.0 0 14 28 42 56 70 84 Patient A Patient B Patient C Patient D Days since first dose 0.0 50.0 100.0 150.0 200.0 250.0 300.0 0 6 12 18 24 30 36 42 48 CH50 U Eq/mL Hours since first dose Patient A Patient B Patient C Patient D Patient E 0 25 50 75 100 0 14 28 42 56 70 84 0 20 40 60 80 100 120 140 0 14 28 42 56 70 84 AST (U/L) Day since first dose Mean Patient A Patient B Patient C Patient D Fig 3 , left: Number of units of packed red blood cells (PRBC) transfused to patients prior to and during the 90 day trial. Fig 3, right: Haemoglobin levels for 4 patients in trial 0 2 4 6 8 10 12 Units PRBC Patient B Patient C Patient D None of the four patients required transfusion during the trial while 3 out of 4 patients required a total of 10 units PRBC during the 3 months preceding the trial (Figure 3, left). Patient A had no history of transfusion. Haemoglobin levels for the 4 patients are shown in (Figure 3, right). For two patients (A and D), there was essentially no change in haemoglobin levels from Day 1 to Day 90. For the other two patients, haemoglobin levels increased by 19% (patient B) and decreased by 14 % (patient C) from Day 1 to Day 90. Results Table 1 : Patient Demographics Five patients have been enrolled in the study to date. Patient demographics are shown in Table 1. The duration between initial diagnosis and initiation of Coversin therapy ranged from 8.5 to 79 months (mean 44 months). Four patients completed the 90 day study per protocol and moved into the long - term safety and efficacy study. One patient (Patient E ) with a suspected co - morbidity unrelated to the treatment was withdrawn from the study on Day 43 . The study drug was well tolerated and patients reported no difficulty with self administration. There were no serious adverse events ( SAEs). The most commonly reported AE s were mild to moderate injection site reactions which declined towards the end of the trial. None of the AEs required specific treatment or were severe enough to cause discontinuation of the study drug. A full listing of AEs is shown in Table 2. Adverse Event Related Table 2 : Adverse Events Possibly related Injection site reaction 24 (32%) 41 (54%) Rash 2 (3%) Hypophosphataemia 2 (3%) Hypoproteinaemia 2 (3%) Abdominal discomfort 1 (1.3%) Arthralgia 1 (1.3%) Headache 1 (1.3%) Decreased neutrophil count 1 (1.3%) Decreased WBC count 1 (1.3%) TOTAL 24 (32%) 52 (68%) Results of the EORTC - 30 quality of life instrument are shown in Figure 4 and show an improvement at the end of the trial for all four patients. The fifth patient has incomplete quality of life data, as he was withdrawn from the trial due to a suspected comorbidity. Immunogenicity was analysed, all 5 patients developed low titre antibodies but no neutralising antibodies were observed . 12 – 9 9 – 6 6 – 3 3 – 0 0 – 3 Months prior to start of trial Trial Paroxysmal nocturnal haemoglobinuria (PNH) is a rare acquired life - threatening disease, characterized by complement induced haemolysis and a high incidence of thrombosis. Coversin , a small (16.8kDa) protein C5 complement inhibitor, originally derived from the haematophagous tick Ornithodoros moubata , is being developed as a therapy for PNH. Coversin is administered by subcutaneous injection and can be self - administered, making it possible for patients to treat themselves at home. Following completion of Phase 1 clinical trials in healthy human volunteers, a Phase 2 open label 90 day trial was initiated December 2016. Enrolled patients had not previously received anti - complement therapy. Presented here are the results of the first four patients to complete the Phase 2 trial. The OBJECTIVES of the trial were to assess the safety and tolerability of Coversin , the efficacy of the dosing regime and whether self - injection by patients is well - accepted . All patients had a CH50 level below the limit of quantification ( < 8 CH50 U Eq /mL) after the ablating phase indicating total blockade of the terminal complement pathway (Figure 1). All 4 patients saw declines in LDH levels (Figure 2, left). The primary end point of LDH < 1.8X ULN at Day 28 was achieved by two patients. LDH as a multiple of ULN ( xULN ) for the 4 patients (A, B, C and D) at Day 28 was respectively 1.4, 2.2, 2.5 and 1.4; at Day 60 1.5, 2.1, 1.8 and 1.5; and at Day 90 1.6, 2.4, 2.0 and 1.9. Aspartate aminotransferase (AST) levels provide another measure of cellular haemolysis, AST decreased following initiation of dosing (Figure 2, right ). Three of four patients were updosed . P atient A and B were updosed from 30mg to 45mg once daily at Days 40 and 54, respectively . Patient C was updosed to 22.5mg twice daily at Day 24 and moved to 45mg once daily at Day 67. Patient B, the last in to date, did not see a decline in LDH with updosing although his haemoglobin level rose after Day 67. 0.00 2.00 4.00 6.00 8.00 10.00 12.00 14.00 16.00 0 14 28 42 56 70 84 Haemoglobin g/dL Days since first dose Patient A Patient B Patient C Patient D Fig 4: EORTC - 30 scores all 5 patients Note : The preceding data is from the eCRFs from Medpace , which will be audited at the end of the Phase 2 trial. The exception is the CH50 and immunogenicity data which is from UCL central lab. To contact Akari phone: +44 20 8004 0267 Characteristic Figure Race, n(%) Caucasian 5 (100%) Male : Female 4:1 Age, years Mean 45.2 Range 22-69 Weight, kg Mean 76 Range 66-84