UNITED STATES
SECURITIES AND EXCHANGE COMMISSION
Washington, D.C. 20549
FORM 10-K
ANNUAL REPORT PURSUANT TO SECTION 13 OR 15(d) OF
THE SECURITIES EXCHANGE ACT OF 1934
For the fiscal year ended December 31, 2016
Commission File Number: 001-36677
Diplomat Pharmacy, Inc.
(Exact name of registrant as specified in its charter)
Michigan |
| 38-2063100 |
(State or other jurisdiction of |
| (I.R.S. Employer |
incorporation or organization) |
| Identification Number) |
4100 S. Saginaw Street
Flint, Michigan 48507
(888) 720-4450
(Address, including zip code, and telephone number,
including area code, of registrant’s principal executive offices)
Not Applicable
(former name, former address and former fiscal year, if changed since last report)
Securities registered pursuant to Section 12(b) of the Act:
Title of Each Class |
| Name of Each Exchange on Which Registered |
Common Stock, no par value per share |
| New York Stock Exchange |
Securities registered pursuant to Section 12(g) of the Act:
None
Indicate by check mark if the registrant is a well-known seasoned issuer, as defined in Rule 405 of the Securities Act. Yes x No o
Indicate by check mark if the registrant is not required to file reports pursuant to Section 13 or Section 15(d) of the Act. Yes o No x
Indicate by check mark whether the registrant (1) has filed all reports required to be filed by Section 13 or 15(d) of the Securities Exchange Act of 1934 during the preceding 12 months (or for such shorter period that the registrant was required to file such reports), and (2) has been subject to such filing requirements for the past 90 days. Yes x No o
Indicate by check mark whether the registrant has submitted electronically and posted on its corporate Web site, if any, every Interactive Data File required to be submitted and posted pursuant to Rule 405 of Regulation S-T (§232.405 of this chapter) during the preceding 12 months (or for such shorter period that the registrant was required to submit and post such files). Yes x No o
Indicate by check mark if disclosure of delinquent filers pursuant to Item 405 of Regulation S-K (§ 229.405 of this chapter) is not contained herein, and will not be contained, to the best of registrant’s knowledge, in definitive proxy or information statements incorporated by reference in Part III of this Form 10-K or any amendment to this Form 10-K.o
Indicate by check mark whether the registrant is a large accelerated filer, an accelerated filer, a non-accelerated filer, or a smaller reporting company. See the definitions of “large accelerated filer,” “accelerated filer” and “smaller reporting company” in Rule 12b-2 of the Exchange Act.
Large accelerated filer | x | Accelerated filer | o | Non-accelerated filer | o | Smaller reporting company | o |
Indicate by check mark whether the registrant is a shell company (as defined in Rule 12b-2 of the Act). Yes o No x
The aggregate market value of the Registrant’s common stock held by non-affiliates of the Registrant was approximately $1.6 billion as of June 30, 2016 based on the reported last sale price as reported on the New York Stock Exchange on that date. Shares of the registrant’s Common Stock held by executive officers, directors and holders of 10 percent or more of the Common Stock outstanding have been excluded from this calculation because such persons may be deemed affiliates of the registrant; such exclusion does not reflect a determination that such persons are affiliates of the registrant for any other purpose.
The Registrant had 66,987,621 shares of Common Stock outstanding as of March 6, 2017.
DOCUMENTS INCORPORATED BY REFERENCE
Certain portions, as expressly described in this report, of the Registrant’s Proxy Statement for its 2017 Annual Meeting of Shareholders to be filed subsequently are incorporated by reference into Part III of this report.
DIPLOMAT PHARMACY, INC.
2016 ANNUAL REPORT ON FORM 10-K
Unless the context suggests otherwise, references in this Annual Report on Form 10-K to “Diplomat,” the “Company,” “we,” “us,” and “our” refer to Diplomat Pharmacy, Inc. and its consolidated subsidiaries.
Certain statements contained or incorporated in this Annual Report on Form 10-K which are not statements of historical fact constitute forward-looking statements within the meaning of the Private Securities Litigation Reform Act of 1995. These forward-looking statements are included throughout this Annual Report on Form 10-K, including under the headings entitled “Business,” “Risk Factors,” and “Management’s Discussion and Analysis of Financial Condition and Results of Operations,” and relate to matters such as our industry, business strategy, goals and expectations concerning our market position, future operations, margins, profitability, capital expenditures, liquidity and capital resources, and other financial and operating information. Words such as “anticipate,” “assume,” “believe,” “continue,” “could,” “estimate,” “expect,” “future,” “intend,” “may,” “plan,” “potential,” “predict,” “project,” “seek,” “should,” “will,” and similar terms and phrases, or the negative thereof, utilized in discussions of future operating or financial performance signify forward-looking statements.
The forward-looking statements contained in this Annual Report on Form 10-K are based on management’s good-faith belief and reasonable judgment based on current information, and these statements are qualified by important factors, many of which are beyond our control, that could cause our actual results to differ materially from those in the forward-looking statements, including changes in global, regional, or local economic, business, competitive, market, regulatory, and other factors, including those described in “Risk Factors.” Any forward-looking statement made by us speaks only as of the date of this report or the date specified in such forward-looking statement. We undertake no obligation to publicly update any forward-looking statement, whether as a result of new information, future developments, or otherwise, except as may be required by any applicable laws or regulations.
The following risks related to our business, among others, could cause actual results to differ materially from those described in the forward-looking statements:
· our ability to adapt to changes or trends within the specialty pharmacy industry;
· significant and increasing pricing pressure from third-party payors;
· the amount of direct and indirect remuneration fees, as well as the timing of assessing such fees and the non-transparent methodology used to calculate such fees;
· our relationships with key pharmaceutical manufacturers;
· bad publicity about, or market withdrawal of, specialty drugs we dispense;
· a significant increase in competition from a variety of companies in the health care industry;
· our ability to effectively execute our acquisition strategy or successfully integrate acquired businesses;
· fluctuations in operating results;
· our ability to expand the number of specialty drugs we dispense and related services;
· maintaining existing patients;
· increasing consolidation in the health care industry;
· managing our growth effectively;
· revenue concentration of the top specialty drugs we dispense;
· our ability to maintain relationships with a specified wholesaler and two pharmaceutical manufacturers, or other pharmaceutical manufacturers that become material to our business over time;
· security breaches or other failures or disruptions of our information technology and security systems, and significant costs required to oversee, maintain, and improve such systems;
· relationships with clinical experts and key thought leaders at physician groups and universities within the United States of America;
· dependence on our senior management and key employees, and managing recent turnover among key employees;
· potential disruption to our workforce and operations due to recent cost savings and restructuring initiatives;
· reliance on a single shipping provider;
· debt service obligations;
· our inability to identify and remediate any present or future material weaknesses in our internal control over financial reporting, which could impair our ability to produce accurate and timely financial statements;
· supply disruption of any of the specialty drugs we dispense;
· loss of orphan drug status for such specialty drugs we dispense;
· reductions of research, development, and marketing of specialty drugs;
· adverse impacts from environmental regulations, and health and safety laws and regulations, applicable to our business; and
· other factors set forth under “Risk Factors.”
Overview
We are the largest independent specialty pharmacy in the United States of America (“U.S.”), and are focused on improving the lives of patients with complex chronic diseases. We define our independence as our singular focus on specialty pharmacy services, independent of other operations such as pharmacy benefit management or managed care. Our patient-centric approach positions us at the center of the healthcare continuum for the treatment of complex chronic diseases through partnerships with patients, payors, pharmaceutical manufacturers, and physicians. We offer a broad range of innovative solutions to address the dispensing, delivery, dosing, and reimbursement of clinically intensive, high-cost specialty drugs. We were formed and incorporated in Michigan in 1975 by our Chief Executive Officer, Philip Hagerman, and his father, Dale, both trained pharmacists who transformed our business from a traditional pharmacy into a leading specialty pharmacy beginning in 2005. Diplomat opened its doors in 1975 as a neighborhood pharmacy with one essential tenet: “Take good care of patients and the rest falls into place.” Today, that tradition continues and we are focused on creating a culture that is highly committed to increasing adherence and improving therapy effectiveness.
Our core revenues are derived from the customized care management programs we deliver to our patients, including the dispensing of their specialty medications. We focus on specialty drugs that are typically administered on a recurring basis to treat patients with complex chronic diseases that require specialized handling and administration as part of their distribution process. We have expertise across a broad range of high-growth specialty therapeutic categories, including oncology, immunology, hepatitis, specialty infusion therapy, multiple sclerosis, and many other serious or long-term conditions.
Our comprehensive, patient-focused services ensure that patients receive a superior standard of care, including assistance with complicated medication therapies, refill processing, third-party funding support programs, side effect management, and adherence monitoring. We customize solutions for each patient based on the patient’s overall health, disease and family history, lifestyle, and financial means.
We have grown our business in recent years by strengthening our clinical expertise in key therapeutic categories, such as oncology, immunology, hepatitis, specialty infusion therapy, and multiple sclerosis, strengthening our relationships with patients, payors, pharmaceutical manufacturers, and physicians, and broadening the scope of our services to hospitals and health systems. While we will continue to focus on growing our business organically, we have completed several significant acquisitions in recent years and we may further opportunistically enhance our competitive position through complementary acquisitions in both existing and new markets. In June 2014, we acquired MedPro Rx, Inc. (“MedPro”), a specialty pharmacy focused on specialty infusion therapies including hemophilia and immune globulin. In April 2015, we acquired BioRx, LLC (“BioRx”), a highly specialized pharmacy and infusion services company that provides treatments for patients with ultra-orphan and rare, chronic diseases. In June 2015, we acquired Burman’s Apothecary, LLC (“Burman’s”), a provider of individualized patient care with a primary focus on hepatitis C. In June 2016, we acquired Valley Campus Pharmacy, Inc. doing business as TNH Advanced Specialty Pharmacy (“TNH”), a specialty pharmacy with a primary focus on oncology, hepatitis, and immunology.
Our services, together with our proactive engagement with pharmaceutical manufacturers early in the drug development process, have contributed to our current and growing access to limited distribution drugs, which we define as drugs that are only available for distribution by a select network of specialty pharmacies. Our inclusion in limited-distribution networks provides critical sources of revenue growth and provides a catalyst for our future growth.
As a part of our mission to improve patient care, we provide specialty pharmacy support services to a national network of retailers, as well as hospitals and health systems. Through many of these partners, we earn revenue by providing clinical and administrative support services on a fee-for-service basis to help them dispense specialty medications.
Specialty Pharmacy Industry
Specialty pharmacy services are a distinct form of pharmacy services that coordinate full-service patient care and complex disease management. Specialty pharmacy services are designed to take advantage of economies of scale by using standardized and efficient processes to deliver medications with customized handling, storage, and distribution requirements. Specialty pharmacies are also designed to improve clinical, adherence, and economic outcomes for patients with complex, often chronic, or rare conditions through a wide range of oral, injectable, inhalable, and infusible specialty pharmaceuticals.
Less acute, chronic conditions are generally treated with self-administered, oral, injectable, or inhalable specialty pharmaceuticals, but may also be administered by a physician or nurse. These pharmaceuticals can be distributed directly to the patient for at-home administration or to the patient’s physician for in-office administration. Several chronic, genetic conditions and orphan diseases are treated with infused pharmaceuticals via a more complex intravenous form of administration. These pharmaceuticals are dispensed under the supervision of a registered pharmacist, and the therapies are typically delivered to the patient for self-administration in the home or administration by a credentialed home-health care nurse or trained caregiver at home or in another care site. Many of the pharmaceuticals handled by specialty pharmacies require refrigeration during shipping, as well as special handling to prevent potency degradation. Patients receiving treatment usually require personalized counseling and education regarding their condition and treatment programs.
Specialty pharmacies primarily treat serious or chronic conditions such as cancer, hemophilia, hepatitis, immune deficiency disorders, multiple sclerosis, and neurological conditions. Retail pharmacies and other traditional distributors generally are designed to carry inventories of low-cost, high-volume products and therefore are not as well equipped to handle the high-cost, low-volume specialty pharmaceuticals that have specialized handling and administration requirements. In addition, those entities generally lack both the deep clinical expertise and the administrative and call center support functions necessary to effectively deliver specialty pharmacy services. As a result, specialty pharmaceuticals generally are provided by pharmacies that focus primarily on filling, labeling, and delivering oral, injectable, infusible, or inhalable pharmaceuticals and related medication and support services.
Segment Information
Our chief operating decision maker reviews our financial results in total when evaluating financial performance and for purposes of allocating resources. Therefore, we have determined that we operate in a single reportable segment — specialty pharmacy services.
Our Services
We provide specialty pharmacy services dedicated to servicing the needs of patients, while also providing clinical expertise, technology-driven innovation tools, and administrative efficiencies that support physicians, payors, pharmaceutical manufacturers, and retail pharmacies. We purchase specialty pharmaceuticals from manufacturers and wholesale distributors, fill prescriptions, and label, package, and deliver the pharmaceuticals to patients’ homes or physicians’ offices through contract couriers. We utilize our main Company-owned distribution facility and corporate headquarters, 19 smaller owned or leased regional facilities, and centralized clinical call centers to provide such services to all 50 states in the U.S. The services provided to our patients and other constituents described below are integral to securing the relationships that drive our revenue and prescription volumes, and are a central focus of our specialty pharmacy business. To successfully compete, we must provide value to each constituent in the specialty pharmacy industry.
Our value to constituents is based on our ability to provide broad specialty and limited-distribution product access, utilization management, high patient adherence rates, patient funding assistance, data management, outstanding patient and prescriber satisfaction rates, and direct and indirect cost savings. Further, we manage the high cost of specialty drugs by pursuing cost savings through channel management, utilization management, formulary management (i.e., the list of specialty drugs that will be reimbursed by a health plan or managed care organization), and waste minimization (including our split-fill program). Channel management is a strategy that includes targeting specialty medications covered under the medical benefit by payors and moving the coverage of these medications to the pharmacy benefit to take advantage of deeper discounts, rebates or more detailed reporting when available. Utilization management is the evaluation of the appropriateness, medical need, and efficiency of health care services, procedures, drugs, and facilities according to established criteria or guidelines and under the provisions of an applicable health benefits plan. Formulary management is an integrated patient care process which enables
physicians, pharmacists, and other health care professionals to work together to promote clinically sound, cost-effective medication therapy, and positive therapeutic effectiveness. A drug formulary, or preferred drug list, is a continually updated list of medications and related products supported by current evidence-based medicine, judgment of physicians, pharmacists, and other experts in the diagnosis and treatment of disease and preservation of health.
Our programs consist of the following business services:
· Specialty Drug Dispensing — For the years ended December 31, 2016, 2015, and 2014, we derived more than 99 percent of our revenue from the dispensing of drugs and the reporting of data associated with those dispenses to pharmaceutical manufacturers and other outside companies. The other services described below are included in our core business offerings and the overall payor reimbursement for dispensed drugs, rather than as separately reimbursable events. We are licensed to dispense prescriptions in all U.S. states and territories. Our business processes and dispensing solutions are well established and can provide specialty prescriptions to patients as required by the communicated “need by” date. All specialty prescriptions are verified by registered pharmacists for accuracy and appropriateness at two separate points in the dispensing process prior to shipping to the patient. Our specialty dispensing and distribution capabilities include package-tracking through contracted couriers, temperature controls, and signature confirmation upon delivery.
Our physical footprint has enabled us to develop a centralized infrastructure that we have successfully scaled to dispense to all U.S. states and territories. We have an advanced distribution center that enables us to ship medications nationwide as well as centralized clinical call centers that help us deliver localized services on a national scale. In addition to our headquarters and main distribution facility in Flint, Michigan, we operate 19 smaller regional facilities in Arizona, California, Connecticut, Florida, Illinois, Iowa, Maryland, Massachusetts, Michigan, Minnesota, North Carolina, Ohio, Pennsylvania, and Texas. We are fully accredited and licensed to conduct business in each state that requires such licensure. We primarily utilize UPS in the delivery of the specialty pharmaceutical products we dispense.
Specialty drug dispensing includes our specialty infusion pharmacy services. Our April 2015, June 2014, and December 2013 acquisitions of BioRx, MedPro, and AHF, respectively, expanded our specialty infusion pharmacy services. We provide individualized, patient-centric specialty infusion services to patients with bleeding disorders and other chronic conditions, while managing overall drug spend through factor utilization using dose management, assay management (which means ensuring that the prescribed amount is the dispensed amount), clinical and therapy education, intervention, and nursing support to advance better clinical effectiveness for patients. Specialty infusion drugs are high-cost, with intravenous or subcutaneous routes of administration, and can be managed at home or in a hospital or free-standing ambulatory infusion clinic, in a physician office, or through our extensive outsourced network of credentialed specialty nurses who administer medications in the patent’s home or at other sites of care. We estimate our drug reimbursement for specialty infusion patients is approximately 60 percent medical benefit and 40 percent pharmacy benefit.
Our specialty drug dispensing services include:
· Patient Care Coordination: Our proprietary patient care system coordinates and tracks patient adherence and safety. It is built around specific drug therapies and disease states for greater consistency of care using clinical algorithms. Each step of the patient’s treatment regimen is extensively researched based on various disease guideline publications. Our system automatically tracks all clinical interventions and activities and provides real-time access to patient information. Using this system, our patient care coordinators, including pharmacists, work with patients and prescribers to identify potential adherence failures and implement proactive plans to optimize treatment effectiveness.
· Clinical Services: Our pharmacists and nurses, with the assistance of our pharmacy technicians, provide clinically based drug therapy management programs for clients and patients. Pharmacists provide counseling on adherence and side-effect management. Our Clinical Help Desk includes
pharmacists, nurses, and pharmacy technicians. A pharmacist is available to patients and prescribers 24 hours per day, seven days per week, and nurses are available during regular business hours. Clinical pharmacists are responsible for high-level clinical interaction with patients and healthcare practitioners, including medication counseling and clinical advice. Our clinicians work with patients’ prescribers to identify adherence failures and to implement a proactive plan to achieve intended effectiveness. Our broader clinical and operations team has deep clinical expertise and includes more than 140 licensed pharmacists as of December 31, 2016.
· Compliance and Persistency Programs: Our drug-specific compliance and persistency programs support the needs of patients based on their therapy regimen. In some cases, a dedicated nurse proactively contacts patients at specific intervals of therapy to discuss precautions, side-effect management, medication administration, and refill procedures. Prior to every refill, we call patients to: verify the dose, dosing regimen, and shipping address; discuss side effects; and confirm that the patient is taking the medication appropriately. Aside from standard protocol, we initiate calls at critical points during the therapy to improve adherence. We also address non-compliance by offering enhanced patient education and communication through customized programs specific to the medications we provide.
· Patient Financial Assistance: Our funding specialists help patients navigate their benefits and find third-party financial assistance to address coverage deficiencies. We provide services to help patients understand and receive reimbursement benefits and we work with available co-pay assistance programs, including co-pay card enrollment and program management. We work with substantially all major commercial co-pay card programs. Our team also coordinates with many external charitable foundations and research grant organizations that help subsidize the cost of medications for patients. We also help patients access manufacturer patient assistance (free drug) programs when necessary and available. These programs result in increased access to specialty drug therapies for patients and increased revenues for us.
· Specialty Pharmacy Training/Consulting (Diplomat University): Diplomat University is our education and training department that educates both Diplomat employees and external professionals (including pharmacists, payors, pharmaceutical partners, and physicians) on topics unique to the specialty pharmacy industry. Our in-depth, ongoing training program promotes clinical competence and builds new skills, enabling employees to provide high-level care for our patients and improve overall business performance. Diplomat University also houses our quality assurance department, which focuses on programs that promote quality and patient safety. Diplomat University-produced materials have been used in trade conference materials, magazine articles, and business meetings, to explain the specialty pharmacy industry generally and the broad range of solutions we can provide.
· Benefits Investigation: Our standard procedures require that we conduct a benefits investigation for each patient we work with. In addition to processing test claims, our benefit specialists contact the appropriate pharmacy or medical benefit plan to verify coverage, deductibles, coinsurance, and out-of-pocket maximums. Our specialists provide all necessary coding for the prescribed therapy or service. Any prior authorization or predetermination requirements are defined at the time of the benefits investigation. Our standard procedures require an initial test adjudication upon receipt of the referral and require subsequent investigations under certain circumstances.
· Prior Authorization: Our prior authorization specialists, in coordination with the prescribing physician and their staff, contact the patient’s insurance plan and collect all necessary patient specific information, together with supporting documentation, to provide to the third-party payor to support reimbursement for the prescribed medication. If the required therapy is not listed on the third-party payor’s formulary, we compile the necessary information to file a formulary exception on behalf of the patient.
· Risk Evaluation and Mitigation Strategy (“REMS”): Our employees administer REMS protocols on all levels of risk mitigation, which is required by many pharmaceutical manufacturers
due to regulatory requirements. The U.S. Food and Drug Administration (“FDA”) requires REMS from certain manufacturers to ensure that the benefits of a drug or biological product outweigh its risks. Manufacturers are required to comply with specific FDA requirements that may include medication use guides, black box warnings / patient package insert language, and a communication plan to health care providers. As part of REMS protocols, manufacturers may also be required to comply with Elements to Assure Safe Use (“ETASU”) to mitigate a specific serious risk listed in the labeling of the drug, including specialized training and certifications, required dispensing locations, patient monitoring, and associated reporting. We have standard operating procedures in place to support all aspects of a REMS program, including REMS administration, REMS drug fulfillment, disease management, medication guide dispensing, and the ETASU specific to a pharmaceutical manufacturer’s program. We also partner with manufacturers to report and track Adverse Drug Events where required. Our patient care system has been designed to capture much of the information the pharmaceutical manufacturer must report to the FDA.
· Retail Specialty Services: Retail specialty services connect a retail pharmacy business to the specialty arena. Based on our broad industry experience, infrastructure, and unique treatment-tracking software, retail specialty services offer companies a strategic partner for clinical and administrative support services that help their business and their specialty patients achieve their optimal therapeutic effectiveness. Large retailers with pharmacies have access to many of the same specialty drugs we distribute, but lack the expertise and the infrastructure necessary to manage patients, payors, and physicians regarding these specialty drugs. Development of this infrastructure is very costly, time consuming, and requires trained clinical experts. Our retail specialty services fill this gap with our breadth of service expertise, which includes nearly every aspect of our specialty pharmacy business, other than purchasing the drugs, filling the prescriptions, and billing payors.
· Hospital and Health System Services: We provide clinical and administrative support services to hospitals and health systems that dispense specialty medications through their outpatient pharmacies. We partner with hospitals and health systems to assist with strategies and service delivery that is designed to maximize cost containment and improve efficiency and clinical effectiveness related to specialty pharmaceuticals. Our program also supports hospitals that are 340B covered entities through a contracted pharmacy strategy.
· Hub Services: We also offer hub services to capitalize on our expertise in providing the services described above and to compete with other hub service providers. Hub services generally are centralized management services for collaboration and efficiency among the key participants in the specialty pharmacy system (including patients, physicians, payors, pharmaceutical manufacturers, retail pharmacies, and other prescribers). To maintain client satisfaction and compliance, we keep certain information and software systems, infrastructure, and employees “firewalled” from our specialty pharmacy business to avoid commingling or favoring any specialty pharmacy (including ours) within the networks of the hub customers.
Constituent Relationships
Our patient-centric approach positions us at the center of the healthcare continuum for the treatment of complex chronic diseases through partnerships with patients, payors, pharmaceutical manufacturers, and physicians.
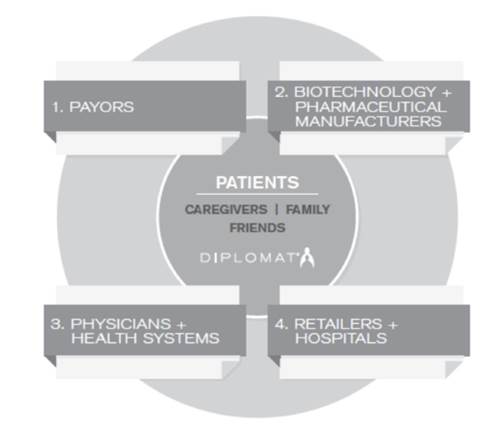
Our services provide value to our constituents in the following ways.
Patients
Our core focus is on patients. We help patients adhere to complex medication therapies, process refills, and manage any side effects and insurance concerns to ensure they get the best standard of care. The clinical efficacy of drug therapies, especially for chronic conditions, is typically enhanced when patients precisely follow the prescribed treatment regimens (including dosing and frequency). On the other hand, we believe, though we do not internally track, that medication non-adherence (i.e., patients not following the instructions for their medication or failing to finish taking their medication) can contribute to a substantial worsening of disease and, in some cases, accelerated mortality, which increases hospital and other health care costs. We have achieved patient adherence rates higher than 90 percent in each fiscal quarter of 2014, 2015, and 2016. We believe our high adherence rates are due in part to our patient training and education, adherence packaging, prophylactic starter kits, and nurse adherence calls. We also help identify third-party funding support programs to help cover expensive out-of-pocket costs.
We help manage patients’ complex disease states through counseling and education regarding their treatment and by providing ongoing monitoring and, in some cases, proactive follow-up contact to encourage patient adherence to their prescribed therapy. The goal of Diplomat’s patient care programs is to provide clinical services in a caring and supportive environment, optimize medication adherence, prevent disease progression, and improve therapeutic effectiveness. To accomplish this, Diplomat focuses on each patient and provides solutions related to medication access, tolerance, and adherence.
Diplomat provides patients with personalized medication programs and services for a variety of complex disease states, including the following:
· Oncology: Cancer therapy often involves the use of highly-toxic chemotherapy or oral oncolytic agents with a high incidence of adverse events. Our goals for these patients include providing the most effective therapy at the appropriate dose, adverse event management to ensure treatment can continue for as long as it is effective, and improving quality of life. Our clinicians strive to provide optimal treatment for these patients by providing high-touch proactive and reactive care, focusing on appropriate dosage and administration, adverse event management, and adherence monitoring.
· Immunology: Care of patients with autoimmune and/or inflammatory conditions generally involves the use of therapies aimed at slowing disease progression, reducing the rate of disease relapse, and managing disease symptoms. Goals for these patients include reducing the signs and symptoms of the disease, minimizing short- and long-term side effects and complications of the disease and therapy, and improving or normalizing quality of life. Our clinicians help these patients by providing clinical management, providing adverse event management support, proactively monitoring for adherence issues, and following up with prescribers in response to identified therapy issues.
· Hepatitis: Management of hepatitis C virus (“HCV”) infection involves appropriate therapy selection based on HCV genotype, the presence or absence of cirrhosis, transplant status, previous response to therapy, and whether or not the patient is co-infected with human immunodeficiency virus (“HIV”) or hepatitis B virus. Goals for these patients include achieving a sustained virologic response, decreasing the disease and therapy burden, and optimal adherence to therapy. Our clinicians ensure that HCV therapy regimens are complete and appropriate, provide adverse event management support, and follow-up with prescribers to ensure optimal therapy.
· Specialty Infusion Therapy: Several chronic, genetic conditions and orphan diseases are treated with infused pharmaceuticals with a more complex intravenous form of administration. These pharmaceuticals are prescribed for individuals including, but not limited to, the following conditions: alpha-1 antitrypsin deficiency; hemophilia; immune globulin and auto-immune deficiencies; hereditary angioedema; and lysosomal storage disorders. Patients are generally referred to specialty infusion pharmacy service providers by physicians or case managers. The medications are dispensed under the supervision of a registered pharmacist, and the therapy is typically delivered to the patient or caregiver for self-administration in the home or administration by a credentialed home-health care nurse or trained caregiver at home or in another care site.
· Multiple Sclerosis: Care for patients diagnosed with multiple sclerosis involves life-long support. Our goals for these patients include providing efficacious therapy to reduce the frequency of relapse and improving quality of life. Our clinicians ensure that patients are receiving the appropriate dose of therapy, provide adverse event counseling and management support, provide education on relapse mitigation strategies, and are available to respond to patient questions about therapy effectiveness and adverse events.
· Other Disease States: We also treat patients who have received organ transplants or who have HIV. Life-long therapy is essential for the prevention of organ rejection in transplant patients, and we seek to optimize adherence to therapy to decrease the likelihood of organ rejection. The management of HIV is complex and involves the use of highly active anti-retroviral therapy. Goals for our patients diagnosed with HIV include: achieving long-term, maximal suppression of viral load; preserving and improving immune system function (prevention of progression to acquired immunodeficiency syndrome); and prevention of the spread of HIV to others.
Payors
We partner with regional and mid-sized payors and independent pharmacy benefit managers (“PBM” or “PBMs”), on an exclusive or semi-exclusive basis, to improve clinical effectiveness and lower costs by managing high-risk members and implementing patient-focused specialty programs. Our electronic patient care platform, centered on
our disease-specific technology solution, is customized for each payor’s needs and is designed to improve efficiency and lower costs.
We offer payors access to limited distribution drugs and unique cost containment programs including split-fill programs, clinical management, and motivational interviewing techniques for improving adherence. We believe that medication non-adherence is the largest avoidable cost in specialty pharmacy because it contributes to a substantial worsening of disease resulting in significant increases to hospital and other health care costs, so our strong adherence rates provides a benefit to payors. For example, through our split-fill program of dispensing prescriptions with less than the typical 30-day supply, we promote more frequent direct intervention and tracking of patients and their therapies by our highly trained clinical experts. Our split-fill program focuses on medications that have a high discontinuation rate based on poor response, adverse effects, and non-compliance, to address potential waste as well as improve adherence to a prescribed therapy. We dispense a two-week supply when prescribed, and it is our policy to contact patients on the second and tenth days of therapy to verify patient tolerance. Once confirmed, we will dispense the remainder of that month’s supply. If not tolerated, we contact the prescriber to seek an alternate therapy.
We provide payors with a comprehensive approach to meeting their pharmacy service needs. Our specialty pharmacy services offer payors a cost effective solution for the distribution of specialty pharmaceuticals, generally directly to patients for self-administration. We manage high-risk members in the payors’ networks and assist with adherence to such members’ health plans to minimize waste in the purchase of specialty drugs and to optimize clinical effectiveness. We also provide access to a significant number of limited distribution drugs. Other services include coordinating care with the members’ physicians and payors, and providing clinical and adherence data to evaluate therapy effectiveness.
Pharmaceutical Manufacturers
Through the coverage and clinical expertise of our Company-owned, main distribution facility and 19 regional locations, some with retail capabilities and some with limited-to-moderate distribution capabilities, we provide pharmaceutical manufacturers with a strong distribution channel for their existing pharmaceutical products. In many cases, our national presence is critical to becoming a selected partner in the launch of new products. When providing new products to patients, we implement a monitoring program to encourage adherence to the prescribed therapy, and we provide valuable clinical information to the manufacturer to aid in their evaluation of product efficacy. We receive fees, which we record as revenue, from certain pharmaceutical manufacturers in return for providing them with clinical data.
We offer specialized and highly customized prescription programs for pharmaceutical companies to help them optimize and track patient adherence, which helps drive the clinical and commercial success of specialty drugs. In addition, we partner with pharmaceutical manufacturers early by helping them develop specialty pharmaceutical channel strategies as part of their commercial launch preparation.
We provide pharmaceutical manufacturers with a strong distribution channel for their existing pharmaceuticals and their new product launches. We implement patient monitoring programs that encourage adherence. We also provide drug trial assistance including product encapsulation and packaging.
The adherence rates that result from our patient-centered services described above directly benefit pharmaceutical manufacturers through clinically appropriate continued dispensing of their products to patients who might otherwise have failed to continue their prescribed therapies. In addition, the financial assistance and reimbursement management we provide to patients further drives pharmaceutical sales.
Pharmaceutical manufacturers frequently seek patient data on the efficacy and utilization of their products, which we currently provide in a de-identified format compliant with the Health Insurance Portability and Accountability Act of 1996 (“HIPAA”). This data provides valuable clinical information in the form of effectiveness and adherence data to manufacturers to aid in their evaluation of product efficacy. We continue to invest in new technologies that will enable us to better provide such analytical services.
We have also assisted emerging biotechnology pharmaceutical companies in their commercialization of new drugs. In cases where pharmaceutical companies have successful clinical trials but little commercialization experience, we
are engaged to formulate strategies to market to, educate, and fulfill the needs of patients, prescribers, and payors. We refer to this tailored, multifaceted approach as “channel strategies.” We believe that, in some cases, these engagements have led to exclusive rights to administer the products of these pharmaceutical companies or our inclusion in a small panel of authorized specialty pharmacies for limited distribution of drugs.
As of December 31, 2016, we have a portfolio of approximately 100 limited-distribution drugs, all of which are commercially available. We have historically earned access to many limited-distribution drugs, both at the time of their launch and post-launch. We actively monitor the drug pipeline and maintain dialogue with many of the major biotechnology and pharmaceutical manufacturers to identify opportunities in all pre-commercial stages of drug development. We believe that limited distribution is becoming the delivery system of choice for many drug manufacturers because it is conducive to smaller patient populations, facilitates high patient engagement, clinical expertise, and elevated focus on service, and because it allows for real-time patient-specific (albeit de-identified) data. We believe the trend toward limited distribution of specialty drugs will continue to expand, making strong representation in this area essential.
Physicians and Other Prescribers
Our team works with physician offices to manage prior-authorization and other managed care organization requirements, such as the denial and appeal process, to ensure that complicated administrative tasks do not impair the delivery of quality patient care. Additionally, we provide risk evaluation services, implement risk mitigation strategies, and collect patient adherence data to provide physicians and health systems with enhanced visibility.
Our singular focus on specialty pharmacy and complex chronic diseases has enabled us to develop strong relationships with clinical experts and thought leaders in key therapeutic categories, such as oncology, immunology, hepatitis, specialty infusion therapy, and multiple sclerosis. We leverage these relationships to gain greater visibility into future drug launches and to stay current on the latest advances in patient care.
We assist prescribers with personalized and intensive patient support by providing care management related to their patients’ pharmacy needs and improving patient adherence to therapy protocols. We eliminate the need for physicians to carry inventories of high-cost prescriptions by distributing medications directly to patients’ homes or, in rare cases, to physicians’ offices. We also assist physicians and their clinical and non-clinical staff members by performing many of the administratively intensive tasks associated with benefits investigations, prior authorizations, and other reimbursement-related matters. We bill payors directly, on the patient’s behalf, in nearly all cases. Further, we assist physicians by helping their patients manage the side effects of their therapies and by monitoring adherence. We also provide physicians with clinical updates and assist with managing the pipeline of potential new therapies.
Retail Pharmacies, Hospitals, and Health Systems
We provide clinical and administrative support services for our retail and hospital partners on a fee-for-service basis. Based on our broad industry experience, infrastructure, and treatment-tracking software, our specialty network solution provides customized clinical and administrative support services that help these partners and their specialty patients improve financial outcomes. These services are similar to those provided to payors with respect to their specialty pharmacy customers, except that we do not buy or dispense the specialty product or bill the payors. The services generally include patient engagement and adherence programs, reimbursement processing and patient funding programs, and general disease-state management services. These services constituted less than 1 percent of our revenues in each of the years ended December 31, 2016, 2015, and 2014.
We provide unique solutions to maximize cost containment, and improve efficiency and clinical effectiveness from specialty pharmaceuticals. Our programs also support hospitals that are 340B covered entities, which are organizations that provide access to reduced price prescription drugs to health care facilities in accordance with the federal 340B Drug Pricing Program and that have been certified by the U.S. Department of Health and Human Services (“HHS”), through a contracted pharmacy strategy.
Our Suppliers
We obtain the pharmaceuticals and medical supplies and equipment that we provide to our patients through pharmaceutical manufacturers, distributors, and group purchasing organizations. The majority of the pharmaceuticals that we purchase through distributors are available from multiple sources and are available in
sufficient quantities to meet our needs and the needs of our patients. However, some biotechnology drugs are only available through the manufacturer and may be subject to limits on distribution. In such cases, it is important for us to establish and maintain good working relationships with the manufacturer in order to ensure sufficient supply to meet our patients’ needs.
Most of the manufacturers of the pharmaceuticals we sell have the right to cancel their supply contracts with us without cause and after giving notice (generally 90 days or less). Specialty drug purchases from AmerisourceBergen, a drug wholesaler, Celgene Corporation (“Celgene”) and Pharmacyclics, Inc. (“Pharmacyclics”), pharmaceutical manufacturers from whom we purchase several drugs, represented 49 percent, 13 percent, and 10 percent, respectively, of cost of products sold in 2016, represented 50 percent, 12 percent, and 9 percent, respectively, of cost of products sold in 2015, and 57 percent, 15 percent, and 7 percent, respectively, of cost of products sold in 2014. We purchase large quantities from a single wholesaler to ease administration and leverage favorable pricing. In the event of a termination of our relationship with AmerisourceBergen, we believe there is typically at least one alternative drug wholesaler from whom we could source each non-limited-distribution drug we dispense. We further believe that we could replace the inventories without a material disruption to our operations. As for the specialty drugs we purchase from Celgene and Pharmacyclics, they are not available from any other source.
Billing and Significant Payors
We derive most of our revenue from contracts with third-party payors such as managed care organizations, insurance companies, self-insured employers, PBMs, and Medicare and Medicaid programs. We contract directly with some payors and PBMs or, in other cases, with third parties which in turn contract with payors and PBMs on our behalf. See “Constituent Relationships-Payors” for additional information on payors.
We bill payors and track our accounts receivable through computerized billing systems. These systems allow our billing staff the flexibility to review and edit claims in the system before they are submitted to payors. For the great majority of our dispensing business, claims are submitted to payors electronically. We have extensive experience managing the coordination of benefits between commercial and government-sponsored plans. We participate with Medicare as a Durable Medical Equipment, Prosthetics, Orthotics and Supplies (“DMEPOS”) pharmacy supplier, and participate in Medicare Part D. A benefit coverage specialist reviews all Medicare coverage determinations to ensure that the appropriate benefit is being billed. Upon completion of all benefit verifications, we follow each plan’s guidelines to identify which plan is primary and secondary and submit the billing accordingly.
Our financial performance is highly dependent upon effective billing and collection practices. The process begins with an accurate and complete patient onboarding process, in which all critical information about the patient, the patient’s insurance, and the patient’s care needs is gathered. A critical part of this process is verification of insurance coverage and authorization from insurance to provide the required care, which typically takes place before we initiate services. An exception occurs when a patient referral is received outside of regular business hours, but we have an existing contractual relationship with the patient’s insurance carrier. In such cases, we provide the patient with sufficient drugs and services to last until the next business day, when the patient’s insurance coverage can be verified.
Sales and Marketing
Our sales and marketing efforts focus on three primary objectives: (1) establishing, maintaining, and strengthening relationships with pharmaceutical manufacturers to gain distribution access as they release new or improved products; (2) establishing, maintaining, and strengthening relationships with prescribers and key opinion leaders to obtain prescription referrals; and (3) building new relationships and expanding existing contracts with managed care organizations and other payors or PBMs. Our national and regional sales directors focus on establishing and expanding our contracts with managed care organizations, while our local account managers focus on maximizing value from these contracts by developing and maintaining relationships with local and regional referral sources, such as physicians, hospital discharge planners, other hospital personnel, health maintenance organizations, preferred provider organizations or other managed care organizations, and insurance companies. We also have a dedicated sales force, through a combination of internal (phone sales) and external (field sales) team members for scalability and efficiency, focused on maintaining and expanding our relationships with biotechnology drug manufacturers to establish our position as an exclusive, semi-exclusive, or participating provider. As of December 31, 2016, we had 202 sales employees, consisting of 85 centralized, mostly telephonic team members, and 117 team members working in the field in various U.S. regions.
Information Technology
Our information technology centers around a custom-developed scalable patient care system that provides real-time prescription and patient care status to us, prescribers, and contracted partners. Our technology allows us to track and report industry standard metrics on call center performance, dispensing, adherence, length of therapy, and persistency. We can also provide HIPAA-compliant reports that contain inventory data, prescription status, persistency, compliance, discontinuation, and payor data. In addition to reporting on patient and prescriber demographics, turnaround times, spend, and error reporting, we can also report on patient assessment data, clinical status, and other monitoring parameters. In 2014, we decided to in-source a substantial portion of our information technology development. We also use an off-the-shelf pharmacy software system for purposes of transmitting claims to payors. We have invested significantly in information technology in recent years to position us to improve cost efficiencies among us and our constituents and to provide additional services regarding the de-identified data we accumulate to take greater advantage of our relationships with data-driven pharmaceutical manufacturers.
Competition
There are a significant number of competitors that distribute specialty pharmacy drugs and provide related services, some of which have greater resources than we do. Many of the competitive segments in which we compete have experienced significant consolidation over the past few years, including 2016. Our competitors include: captive specialty pharmacies owned by PBMs; retail pharmacy chains and independent retail pharmacies; health plans; national, regional and niche specialty pharmacies; specialty infusion therapy companies; physician practices and hospital systems; and group purchasing organizations.
We are the largest independent specialty pharmacy in the U.S., with a market share of approximately 4 percent (based on 2016 revenues from pharmacy-dispensed specialty drugs). The three largest specialty pharmacies are divisions within CVS Caremark, Express Scripts, and Walgreens. We understand that a number of other traditionally non-specialty pharmacies with significant resources are attempting to build, acquire, or partner with specialty pharmacies due to the double-digit growth anticipated in spending on specialty prescription drugs compared to flat to low single-digit growth in spending on traditional prescription drugs. There are also many smaller specialty pharmacies and other entities in the healthcare industry that provide limited specialty pharmacy services that compete with us to a lesser extent. Some of these smaller entities, however, may be able to invest significant resources, through acquisition or otherwise, to compete with us on a larger scale.
Many of the retail pharmacies for whom we provide patient management services may acquire a competing specialty pharmacy business or start their own specialty pharmacy business and thereby become competitors. In addition, many of our PBM customers have their own specialty pharmacy businesses, and to the extent certain of our products can be obtained internally, these customers could cease doing business with us.
Governmental Regulation
The healthcare industry is subject to extensive regulation by a number of governmental entities at the federal, state, and local level. The industry is also subject to frequent regulatory change. Laws and regulations in the healthcare industry are extremely complex and, in many instances, the industry does not have the benefit of significant regulatory or judicial interpretation. Moreover, our business is impacted not only by those laws and regulations that are directly applicable to us, but also by certain laws and regulations that are applicable to our managed care and other clients. If we fail to comply with the laws and regulations directly applicable to our business, we could suffer civil and/or criminal penalties, and we could be excluded from participating in Medicare, Medicaid, and other federal and state healthcare programs, which would have an adverse impact on our business.
Professional Licensure
Pharmacists, nurses, and certain other healthcare professionals employed by us are required to be individually licensed or certified under applicable state law. We perform criminal, government exclusion, and other background checks on employees and take steps to ensure that our employees possess all necessary licenses and certifications, and we believe that our employees comply, in all material respects, with applicable licensure laws.
Pharmacy Licensing and Registration
State laws require that each of our pharmacy locations be appropriately licensed and/or registered to dispense pharmaceuticals in that state. We are licensed in all states that require such licensure and believe that we
substantially comply with all state licensing laws applicable to our business. Where required by law, we also have pharmacists licensed in all states in which we dispense.
Laws enforced by the U.S. Drug Enforcement Administration (“DEA”), as well as some similar state agencies, require our pharmacy locations to individually register to handle controlled substances, including prescription pharmaceuticals. A separate registration is required at each principal place of business where we dispense controlled substances. Federal and state laws also require that we follow specific labeling, reporting, and record-keeping requirements for controlled substances. We maintain DEA registrations for each of our facilities that require such registration and follow procedures intended to comply with all applicable federal and state requirements regarding controlled substances.
Food, Drug, and Cosmetic Act
Certain provisions of the federal Food, Drug, and Cosmetic Act govern the handling and distribution of pharmaceutical products. This law exempts many pharmaceuticals and medical devices from federal labeling and packaging requirements as long as they are not adulterated or misbranded and are dispensed in accordance with and pursuant to a valid prescription. We believe that we comply with all applicable requirements.
Fraud and Abuse Laws — Anti-Kickback Statute
The federal Anti-Kickback Statute prohibits individuals and entities from knowingly and willfully paying, offering, receiving, or soliciting money or anything else of value in order to induce the referral of patients or to induce a person to purchase, lease, order, arrange for, or recommend services or goods covered by Medicare, Medicaid, or other government healthcare programs. The federal courts have held that an arrangement violates the Anti-Kickback Statute if any one purpose of the remuneration is to induce the referral of patients covered by the Medicare or Medicaid programs, even if another purpose of the payment is to compensate an individual for rendered services. The Anti-Kickback Statute is broad and potentially covers many standard business arrangements. Violations can lead to significant penalties, including criminal fines of up to $25,000 per violation and/or five years imprisonment, civil monetary penalties of up to $50,000 per violation plus treble damages, and/or exclusion from participation in Medicare, Medicaid, and other federal government healthcare programs. In an effort to clarify the conduct prohibited by the Anti-Kickback Statute, the Office of the Inspector General of HHS (the “OIG”) publishes regulations that identify a limited number of safe harbors. Business arrangements that satisfy all of the elements of a safe harbor are immune from criminal enforcement or civil administrative actions. The Anti-Kickback Statute is an intent-based statute and the failure of a business relationship to satisfy all of the elements of a safe harbor does not, in and of itself, mean that the business relationship violates the Anti-Kickback Statute. The OIG, in its commentary to the safe harbor regulations, has recognized that many business arrangements that do not satisfy a safe harbor nonetheless operate without the type of abuses the Anti-Kickback Statute is designed to prevent. We attempt to structure our business relationships to satisfy an applicable safe harbor. However, in those situations where a business relationship does not fully satisfy the elements of a safe harbor, we attempt to satisfy as many elements of an applicable safe harbor as possible. The OIG is authorized to issue advisory opinions regarding the interpretation and applicability of the Anti-Kickback Statute, including whether an activity constitutes grounds for the imposition of civil or criminal sanctions.
A number of states have statutes and regulations that prohibit the same general types of conduct as those prohibited by the Anti-Kickback Statute described above. Some state anti-fraud and anti-kickback laws apply only to goods and services covered by Medicaid. Other state anti-fraud and anti-kickback laws apply to all healthcare goods and services, regardless of whether the source of payment is governmental or private. Where applicable, we attempt to structure our business relationships to comply with these statutes and regulations.
Fraud and Abuse Laws — False Claims Act
We are subject to state and federal laws that govern the submission of claims for reimbursement. These laws generally prohibit an individual or entity from knowingly and willfully presenting a claim or causing a claim to be presented for payment from a federal healthcare program that is false or fraudulent. The standard for “knowing and willful” may include conduct that amounts to a reckless disregard for the accuracy of information presented to payors. Penalties under these statutes include substantial civil and criminal fines, exclusion from the Medicare or Medicaid programs and imprisonment. One of the most prominent of these laws is the federal False Claims Act, which may be enforced by the federal government directly or by a private plaintiff by filing a qui tam lawsuit on the
government’s behalf. Under the False Claims Act, the government and private plaintiffs, if any, may recover monetary penalties in the amount of $5,500 to $11,000 per false claim, as well as an amount equal to three times the amount of damages sustained by the government as a result of the false claim. A number of states, including states in which we operate, have adopted their own false claims statutes as well as statutes that allow individuals to bring qui tam actions. In recent years, federal and state government authorities have launched several initiatives aimed at uncovering practices that violate false claims or fraudulent billing laws, and they have conducted numerous investigations of pharmaceutical manufacturers, PBMs, pharmacies, and health care providers with respect to false claims, fraudulent billing, and related matters. We believe that we have procedures in place to ensure the accuracy of our claims.
Ethics in Patient Referrals Law — Stark Law
The federal Stark Law generally prohibits a physician from making referrals for certain Designated Health Services, reimbursable by Medicare, to an entity with which the physician or an immediate family member has a financial relationship and prohibits the entity from presenting or causing to be presented claims to Medicare for those referred services, unless an exception applies. A financial relationship is generally defined as an ownership, investment, or compensation relationship. Designated Health Services include, but are not limited to, outpatient pharmaceuticals, parenteral and enteral nutrition products, home health services, durable medical equipment, physical and occupational therapy services, and inpatient and outpatient hospital services. Among other sanctions, a civil monetary penalty of up to $15,000 may be imposed for each bill or claim for a service a person knows or should know is for a service for which payment may not be made due to the Stark Law. Such persons or entities are also subject to exclusion from the Medicare and Medicaid programs. Any person or entity participating in a circumvention scheme to avoid the referral prohibitions is liable for a civil monetary penalty of up to $100,000. A $10,000 fine may be imposed for failure to comply with reporting requirements regarding an entity’s ownership, investment, and compensation arrangements for each day for which reporting is required to have been made under the Stark Law.
The Stark Law is a broad prohibition on certain business relationships, with detailed exceptions. However, unlike the Anti-Kickback Statute under which an activity may fall outside a safe harbor and still be lawful, a referral for Designated Health Services that does not fall within an exception is strictly prohibited by the Stark Law. We attempt to structure all of our relationships with physicians who make referrals to us in compliance with an applicable exception to the Stark Law.
In addition to the Stark Law, many of the states in which we operate have comparable restrictions on the ability of physicians to refer patients for certain services to entities with which they have a financial relationship. Certain of these state statutes mirror the Stark Law while others may be more restrictive. We attempt to structure all of our business relationships with physicians to comply with any applicable state self-referral laws.
HIPAA and Other Privacy and Confidentiality Legislation
Our activities involve the receipt, use, and disclosure of confidential health information, including disclosure of the confidential information to a patient’s health benefit plan, as permitted in accordance with applicable federal and state privacy laws. In addition, we use and disclose de-identified data for analytical and other purposes. Many state laws restrict the use and disclosure of confidential medical information, and similar new legislative and regulatory initiatives are underway at the state and federal levels.
HIPAA imposes extensive requirements on the way in which healthcare providers that engage in certain actions covered by HIPAA, as well as healthcare clearinghouses (each known as “covered entities”) and the persons or entities that create, receive, maintain, or transmit protected health information (“PHI”) on behalf of covered entities (known as “business associates”) and their use, disclosure and safeguarding of PHI, including requirements to protect the integrity, availability, and confidentiality of electronic PHI. Many of these obligations were expanded under the Health Information Technology for Economic and Clinical Health Act (“HITECH”), passed as part of the American Recovery and Reinvestment Act of 2009. In January 2013, the Office for Civil Rights of HHS issued a final rule under HITECH that makes significant changes to the privacy, security, breach notification, and enforcement regulations promulgated under HIPAA (the “Final Omnibus Rule”), and which generally took effect in September 2013. The Final Omnibus Rule enhances individual privacy protections, provides individuals new rights to their health information, and strengthens the government’s ability to enforce HIPAA.
The privacy regulations (the “Privacy Rule”) issued by the Office of Civil Rights of HHS pursuant to HIPAA give individuals the right to know how their PHI is used and disclosed, as well as the right to access, amend, and obtain information concerning certain disclosures of PHI. Covered entities, such as pharmacies and health plans, are required to provide a written Notice of Privacy Practices to individuals that describes how the entity uses and discloses PHI, and how individuals may exercise their rights with respect to their PHI. For most uses and disclosures of PHI other than for treatment, payment, healthcare operations, and certain public policy purposes, HIPAA generally requires that covered entities obtain a valid written individual authorization. In most cases, use or disclosure of PHI must be limited to the minimum necessary to achieve the purpose of the use or disclosure. The Final Omnibus Rule modifies the content of Notice of Privacy Practices in significant ways, requiring, among other things, statements informing individuals of their rights to receive notifications of any breaches of unsecured PHI and to restrict disclosures of PHI to a health plan where the individual pays out of pocket.
We are a covered entity under HIPAA in connection with our operation of specialty service pharmacies. To the extent that we provide services other than as a covered entity and we perform a function or activity, or provide a service to, a covered entity that involves PHI, the covered entity may be required to enter into a business associate agreement with us. Business associate agreements mandated by the Privacy Rule create a contractual obligation for us, as a business associate, to perform our duties for the applicable covered entity in compliance with the Privacy Rule. In addition, HITECH subjects us to certain aspects of the Privacy Rule and the HIPAA security regulations when we act as a business associate, including imposing direct liability on business associates for impermissible uses and disclosures of PHI and the failure to disclose PHI to the covered entity, the individual, or the individual’s designee (as specified in the business associate agreement), as necessary to satisfy a covered entity’s obligations with respect to an individual’s request for an electronic copy of PHI. The Final Omnibus Rule also extends the business associate provisions of HIPAA to subcontractors where the function, activity, or service delegated by the business associate to the subcontractor involves the creation, receipt, maintenance, or transmission of PHI. As such, business associates are required to enter into business associate agreements with subcontractors for services involving access to PHI and may be subject to civil monetary penalties for the acts and omissions of their subcontractors.
Importantly, the Final Omnibus Rule greatly expands the types of product- and service-related communications to patients or enrollees that will require individual authorizations by requiring individual authorization for all treatment and health care operations communications where the covered entity receives payment in exchange for the communication from or on behalf of a third-party whose product or service is being described. While the Office of Civil Rights of HHS has established limited exceptions to this rule where individual authorization is not required, the marketing provisions finalized in the Final Omnibus Rule could potentially have an adverse impact on our business and revenues.
If we fail to comply with HIPAA or our policies and procedures are not sufficient to prevent the unauthorized disclosure of PHI, we could be subject to liability, fines, and lawsuits under federal and state privacy laws, consumer protection statutes, and other laws. Criminal penalties and civil sanctions may be imposed for failing to comply with HIPAA standards either as a covered entity or business associate, and these penalties and sanctions have significantly increased under HITECH. In addition to imposing potential monetary penalties, HITECH also requires the Office of Civil Rights of HHS to conduct periodic compliance audits and empowers state attorneys general to bring actions in federal court for violations of HIPAA on behalf of state residents harmed by such violations. Several such actions have already been brought against both covered entities and at least one business associate, and continued enforcement actions are likely to occur in the future.
The transactions and code sets regulation promulgated under HIPAA requires that all covered entities that engage in certain electronic transactions, directly or through a third-party agent, use standardized formats and code sets. We, in our role as a business associate of a covered entity, must conduct such transactions in accordance with such transaction rule and related regulations that require the use of operating rules in connection with HIPAA transactions. In our role as a specialty pharmacy operator, we must also conduct such transactions in accordance with such regulations or engage a clearinghouse to process our covered transactions. HHS promulgated a National Provider Identifiers (“NPI”) Final Rule that requires covered entities to utilize NPIs in all standard transactions. NPIs replaced National Association of Boards of Pharmacy numbers for pharmacies, DEA numbers for physicians, and similar identifiers for other health care providers for purposes of identifying providers in connection with
HIPAA standard transactions. Covered entities may be excluded from federal health care programs for violating these regulations.
The security regulations issued pursuant to HIPAA mandate the use of administrative, physical, and technical safeguards to protect the confidentiality of electronic PHI. Such security rules apply to covered entities and business associates.
We must also comply with the “breach notification” regulations, which implement provisions of HITECH. In the case of a breach of “unsecured PHI,” covered entities must promptly notify affected individuals and the HHS Secretary, as well as the media in cases where a breach affects more than 500 individuals. Breaches affecting fewer than 500 individuals must be reported to the HHS Secretary on an annual basis. The regulations also require business associates of covered entities to notify the covered entity of such breaches by the business associate.
Final regulations governing the accounting of disclosures are forthcoming. The applicable proposed rule, if finalized, would require covered entities to develop systems to monitor and record: (1) which of their employees and business associates access an individual’s electronic PHI contained in a designated record set; (2) the time and date access occurs; and (3) the action taken during the access session (e.g., modification, deletion, viewing). The final regulations could impose significant burdens on covered entities and business associates.
The Health Reform Laws (as defined in “Health Reform Legislation” below) require the HHS Secretary to develop new health information technology standards that could require changes to our existing software products. For example, the statute requires the establishment of interoperable standards and protocols to facilitate electronic enrollment of individuals in federal and state health and human services programs and provides the government with authority to require incorporation of these standards and protocols in health information technology investments as a condition of receiving federal funds for such investments.
HIPAA generally preempts state laws, except when state laws are more protective of PHI or are more restrictive than HIPAA requirements. Therefore, to the extent states continue to enact more protective or restrictive legislation, we could be required to make significant changes to our business operations. In addition, independent of any statutory or regulatory restrictions, individual health plan clients could increase limitations on our use of medical information, which could prevent us from offering certain services.
Medicare Part D
The Medicare Part D program, which makes prescription drug coverage available to eligible Medicare beneficiaries, regulates various aspects of the provision of Medicare drug coverage, including enrollment, formularies, pharmacy networks, marketing, and claims processing. The Centers for Medicare & Medicaid Services (“CMS”) imposed restrictions and consent requirements for automatic prescription delivery programs, and further limited the circumstances under which Medicare Part D plans may recoup payments to pharmacies for claims that are subsequently determined not payable under Medicare Part D. CMS sanctions for non-compliance may include suspension of enrollment and even termination from the program.
The Medicare Part D program has undergone significant legislative and regulatory changes since its inception. Medicare Part D continues to attract a high degree of legislative and regulatory scrutiny, and applicable government rules and regulations continue to evolve. For example, CMS may issue regulations that limit the ability of Medicare Part D plans to establish preferred pharmacy networks. Accordingly, it is possible that legislative and regulatory developments and regulatory oversight could materially affect our Medicare Part D business or profitability.
Health Reform Legislation
Congress passed major health reform legislation, including the Patient Protection and Affordable Care Act, as amended by the Health Care and Education Reconciliation Act of 2010 (the “Health Reform Laws”). This legislation affects virtually every aspect of health care in the U.S. In addition to establishing the framework for every individual to have health coverage beginning in 2014, the Health Reform Laws enacted a number of significant health care reforms. President Donald Trump has stated his intentions to support the repeal and possible replacement of the Health Reform Laws during his term of office. While not all of these reforms, or their repeal or replacement, affect our business directly, they could affect the coverage and plan designs that are or will be provided by many of our health plan clients. As a result, these reforms, or their repeal or replacement, could impact many of
our services and business practices. There is considerable uncertainty as to the continuation of these reforms, their repeal, or their replacement.
Managed Care Reform
In addition to health reforms enacted by the Health Reform Laws, legislation has been considered, proposed, and/or enacted at the state level, aimed at providing additional rights and access to drugs to individuals enrolled in managed care plans. This legislation may impact the design and implementation of prescription drug benefit plans sponsored by our PBM health plan clients and/or the services we provide to them. Both the scope of the managed care reform proposals considered by state legislatures and reforms enacted by states to date vary greatly, and the scope of future legislation that may be enacted is uncertain.
21st Century Cures Act
The 21st Century Cures Act (“Cures Act”), enacted in December 2016, among other things implemented Average Sales Price pricing for Part B DME infusion drugs in January of 2017 and delayed payment for the home infusion services necessary to administer these drugs until January of 2021. Given our current understanding of the Cures Act, we do not believe that it will have a significant impact on our business.
Accreditations
We have and maintain accreditations from the following organizations:
· Accreditation Commission for Health Care (“ACHC”): Effective July 21, 2014, we hold specialty pharmacy and infusion pharmacy accreditations from the ACHC. Under such accreditation, the ACHC reviews and assesses our activities. Areas of focus include infusion pharmacy business, infusion pharmacy continuum of care, intravenous drug mixture preparation, administration, therapy monitoring, and client/patient counseling and education.
· American Society of Health-System Pharmacists (“ASHP”): Effective September 26, 2013, we hold a postgraduate year one pharmacy residency program accreditation from the ASHP. The ASHP reviews and evaluates our residency training program against established criteria to ensure that pharmacy residents are properly trained. The ASHP is a nationally recognized non-profit pharmacy association that has been accrediting pharmacy residency programs for more than 50 years.
· URAC: Effective January 1, 2013, we hold a URAC specialty pharmacy accreditation, a nationally recognized and rigorous accreditation that includes a thorough review of documentation, an on-site survey for verifying compliance standards, and final review by the URAC accreditation and executive committees.
· National Association of Boards of Pharmacy (“NABP”): Effective May 13, 2013, we hold a Verified-Accredited Wholesale Distributors® (“VAWD®”) accreditation from the NABP. This accreditation is designed for compliance with state and federal laws, for preventing counterfeit drugs from entering the U.S., and to protect patients from below-quality drug distribution by employing security and best practice standards for wholesale drug distribution. Effective July 23, 2012, we hold a DMEPOS accreditation from the NABP.
We hold a Verified Internet Pharmacy Practice Sites® (“VIPPS®”) accreditation, effective January 7, 2015 through January 6, 2018, from the NABP. This accreditation certifies that we comply with the licensing and inspection requirements of our state and each state to which we dispense pharmaceuticals. In addition, displaying the VIPPS® seal demonstrates NABP compliance with VIPPS® criteria including patient rights to privacy, authentication, and security of prescription orders, adherence to a recognized quality assurance policy, and provision of meaningful consultation between patients and pharmacists.
· Center for Pharmacy Practice Accreditation (“CPPA”): Effective January 4, 2016, we hold a CPPA certification. The CPPA recognizes pharmacies that practice efficient, high-quality patient care while promoting safe and effective medication management and distribution. With a focus on regulatory and organizational quality, the program ensures a superior level of pharmacy service to patients, prescribers, partners, and payors.
· Health Information Trust Alliance (“HITRUST”): Effective August 22, 2016, we hold a HITRUST Common Security Framework (“CSF”) certification. CSF certification through HITRUST places us in an limited group of organizations worldwide that have met industry-defined requirements and are appropriately managing risk. Incorporating a risk-based approach, the HITRUST CSF helps healthcare organizations comply with data privacy and security regulations through a comprehensive and flexible set
of prescriptive and scalable security controls. HITRUST CSF certification validates compliance with state and federal regulations, standards, and frameworks.
Intellectual Property
We rely on copyright, trademark, and trade secret laws, in addition to contractual restrictions, to establish and protect our proprietary rights. We have registered or applied to register a variety of our trademarks and service marks used throughout our business. DIPLOMAT SPECIALTY PHARMACY® and DIPLOMAT®, among others, are service marks registered with the U.S. Patent Trademark Office. In addition, we rely on unregistered common law trademark rights and unregistered copyrights under applicable U.S. law to distinguish and/or protect our services and branding. We believe that our trade names are becoming more recognized by many referral sources as representing a reliable, cost-effective source of specialty pharmacy services. We are not aware of any facts that could materially impact our continuing use of any of our intellectual property. We do not believe that the loss of copyrights, trademarks, or service marks would have a material adverse effect on our business.
Employees
As of December 31, 2016, we employed 1,827 persons, including 1,737 on a full-time basis and 90 persons on a part-time basis. Of our employees, 659 were corporate personnel and 1,168 were clinically focused. The majority of our part-time employees are clinicians due to the nature and timing of the services we provide. None of our employees are covered by collective bargaining agreements.
Executive Officers of the Registrant
The following table sets forth information regarding our executive officers (ages as of December 31, 2016):
Name |
| Age |
| Position |
|
Philip R. Hagerman |
| 64 |
| Chief Executive Officer, Chairman of the Board of Directors |
|
Paul N. Urick |
| 45 |
| President |
|
Gary Rice |
| 59 |
| Executive Vice President, Operations |
|
Philip R. Hagerman, RPh, has served as our chief executive officer, a director, and the chairman of the board of directors since 1991. Mr. Hagerman co-founded the Company with his father in 1975.
Paul N. Urick, RPh, became our president in November 2016. Mr. Urick works closely with Diplomat’s operations, clinical services, and sales teams, as well as industry partners. He has spent more than two decades building in-depth knowledge and key relationships in specialty pharmacy, managed markets, and integrated health systems. Mr. Urick served as vice president of Industry Relations, Pharmaceutical Account Management, and Payor Strategies upon our acquisition of Burman’s in June 2015. He was promoted to senior vice president in February 2016. In that role, he provided overall strategy and execution for all pharmaceutical and payor partners. Mr. Urick was president of managed markets and industry relations for Burman’s from September 2014 until its acquisition by us. Before that role, beginning May 2011, he served as senior vice president of pharmacy operations for Cigna Corporation, a healthcare company serving more than 15 million customers. He led Cigna’s internal PBM and home delivery operations. From 2004 to 2011, Mr. Urick was senior vice president of pharmacy services at Independence Blue Cross. During his tenure, he served as president for FutureScripts and FutureScripts Secure, two PBM companies he incorporated. In addition, Mr. Urick spent 10 years at Geisinger Health System, a leading integrated health services organization. There, he transformed and insourced PBM operations for Geisinger Health Plan. Mr. Urick is a member of the Academy of Managed Care Pharmacy, the National Association of Specialty Pharmacy, and other national associations.
Gary Rice became our executive vice president of operations in 2016 and is responsible for Diplomat’s core operational management. This position builds on his previous role as senior vice president of clinical, education, and human resources, in which he was responsible for Diplomat’s industry-leading clinical support services; education for patients and clients; and human resources department. Before joining Diplomat in June 2011, Mr. Rice was vice president of operations at ITSRx, where he provided operational and clinical leadership for the development of specialty and retail pharmacies. Mr. Rice also served as director of specialty clinical management for MedImpact Healthcare Systems Inc. Mr. Rice directed oncology strategy, specialty pharmacy sales management, the clinical guidance of specialty medication providers, and the clinical protocol development of 15 specialty therapy categories.
Before his time at MedImpact, he was vice president of retail and ancillary services and director of pharmaceutical services at the Kelsey-Seybold Clinic in Houston, Texas.
Available information
Our Internet address is diplomat.is and our investor relations website is located at ir.diplomat.is. We make available free of charge on our investor relations website under the heading “Financial and Filings” our Annual Reports on 10-K, Quarterly Reports on Form 10-Q, Current Reports on Form 8-K and amendments to those reports as soon as reasonably practicable after such materials are electronically filed with (or furnished to) the Securities and Exchange Commission (“SEC”). Information contained on our websites is not incorporated by reference into this Annual Report on Form 10-K. In addition, the SEC maintains an Internet site, sec.gov, that includes filings of and information about issuers that file electronically with the SEC.
Our business, prospects, financial condition, or operating results could be materially adversely affected by any of the risks and uncertainties set forth below, as well as in any amendments or updates reflected in subsequent filings with the SEC. In assessing these risks, you should also refer to the other information contained in this Annual Report on Form 10-K, including our consolidated financial statements and related notes.
Risks Related to Our Business and Industry
Our failure to anticipate or appropriately adapt to changes or trends within the specialty pharmacy industry could have a significant negative impact on our ability to compete successfully.
The specialty pharmacy industry is growing and evolving rapidly. Any significant shifts in the structure of the specialty pharmacy industry or the healthcare products and services industry in general could alter the industry dynamics and adversely affect our ability to attract or retain customers. These changes or trends could result from, among other things, a large intra- or inter-industry merger, a new entrant in the specialty pharmacy business, changes in the pricing or distribution model for specialty drugs, a slowdown in the biotechnology pharmaceutical pipeline in our areas of expertise, consolidation of shipping carriers, or the necessary changes or unintended consequences of the Health Reform Laws or future regulatory changes. Our failure to anticipate or appropriately adapt to any of these changes or trends, none of which are within our control, could have a significant negative impact on our competitive position and materially adversely affect our business.
Significant and increasing pressure from third-party payors to limit reimbursements and the impact of high-cost specialty drugs could materially adversely impact our profitability, results of operations, and financial condition.
The continued efforts of health maintenance organizations, managed care organizations, PBMs, government programs (such as Medicare, Medicaid and other federal and state funded programs), and other third-party payors to limit pharmacy reimbursements may adversely impact our profitability. While manufacturers have increased the price of drugs, payors have generally decreased reimbursement rates as a percentage of drug cost.
We expect pricing pressures from third-party payors to continue given the high and increasing costs of specialty drugs. In particular, we have recently declined to renew certain contracts with PBMs and other payors due to such pricing pressures. Given the significant competition in the industry, we have limited bargaining power to counter payor demands for reduced reimbursement rates. If we are unable negotiate for acceptable reimbursement rates or replace unfavorable contracts with new business on acceptable terms, our revenues and business could be adversely affected.
In response to rising specialty drug prices, payors may also demand that we provide additional services, enhanced service levels, and other cost savings to help mitigate the increase in drug costs. Additional services with minimal or no service fees would adversely impact our profitability. Since data-management technology and software make it challenging for us to prove specific cost savings to payors, we may be unable to demand additional service fees to offset the cost of additional services. Our inability or failure to demonstrate cost efficiencies could adversely impact a payor’s willingness to engage us, exclusively or at all, as a specialty pharmacy in the face of rising drug costs.
The amount of direct and indirect remuneration fees charged by payors, as well as the timing of assessing such fees and the non-transparent methodology in calculating such fees, may have a material adverse impact on our financial performance and, to the extent such fees are material, may limit our ability to provide accurate financial guidance for future periods.
Some payors charge certain direct and indirect remuneration fees (“DIR fees”), often calculated and charged several months after adjudication of a claim, which adversely impacts our profitability. DIR fees is a term used by CMS to address price concessions that ultimately impact the prescription drug costs of Medicare Part D plans, but are not captured at the point of sale; however, this term is used to capture a number of different type of fees assessed after adjudication of a claim. In particular, the methodology and transparency around how PBMs are applying these DIR fees changed materially in 2016 and the resulting significant DIR fees assessed in 2016 adversely impacted our financial performance and may continue to do so in the future. Further, the timing of assessments and non-transparent methodology in computing DIR fees may materially impact our ability to provide accurate financial guidance to investors and analysts, and may result in a future change in the estimated DIR fees we have recognized.
Changes in reimbursement rates from Medicare and Medicaid for the services we provide may cause our revenue and profitability to decline.
Reimbursement from government programs are subject to statutory and regulatory requirements, administrative rulings, interpretations of policy, implementation of reimbursement procedures, retroactive payment adjustments, governmental funding restrictions, changes to existing legislation, and the enactment of new legislation, all of which may materially affect the amount and timing of reimbursement payments to us. Changes to the way Medicare and Medicaid pay for our services may reduce our revenue and profitability on services provided to Medicare and Medicaid patients and increase our working capital requirements.
Since its inception in 2006, Medicare Part D has resulted in increased utilization and decreased pharmacy gross margin rates as higher margin business, such as cash and state Medicaid customers, migrated to Medicare Part D coverage. Further, as a result of the Health Reform Laws and changes to Medicare Part D, such as the elimination in 2013 of the tax deductibility of the retiree drug subsidy payment received by sponsors of retiree drug plans, our PBM clients could decide to discontinue providing prescription drug benefits to their Medicare-eligible members. To the extent this occurs, the adverse effects of increasing customer migration into Medicare Part D may outweigh the benefits we realize from growth of our Medicare Part D business.
If our relationship with any of our key pharmaceutical manufacturers deteriorates, or if we are unable to create new significant relationships with other pharmaceutical manufacturers, we could lose all or a significant portion of our access to existing and future specialty drugs.
In recent years, an increasing number of pharmaceutical manufacturers have attempted to significantly limit the number of pharmacies that may dispense their drugs. Out of a total of approximately 60,000 traditional and specialty pharmacies, these manufacturers increasingly limit access to their drugs to anywhere from one to 20 specialty pharmacies, to ensure they can manage a drug’s rollout, obtain real time data, and confirm the unique patient population’s receipt of the necessary services and support to remain adherent. There are a number of limited-distribution drugs to which we do not have access. In addition to directly providing significant revenues, access to limited-distribution drugs provides us with significant competitive advantages in developing relationships with payors and physicians, and our failure to continue obtaining access to new limited-distribution pharmaceuticals or losing our current access could have a material and adverse impact on our business.
We obtain access to limited-distribution drugs primarily from small to mid-size biotechnology companies, many of whom are bringing their first or second drug to market. We incur significant expense, time, and opportunity cost to educate and assist emerging small and mid-size biotechnology manufacturers in bringing these products to the marketplace without any guarantee of a successful drug launch or future sales. The failure to monetize these relationships could adversely impact our profitability and our prospects.
We also provide a significant amount of direct and indirect services for the benefit of our pharmaceutical manufacturer customers and our patients to gain access to specialty drugs, and our failure to provide services at optimal quality could result in losing access to existing and future drugs. In addition, we incur significant costs in providing these services and receive minimal service fees in return. If pharmaceutical manufacturers require significant additional services and products to obtain access to their drugs without a corresponding increase in service fees paid to us, our profitability could be adversely impacted.
We have limited contractual protections with pharmaceutical manufacturers and wholesalers that supply us with most of the pharmaceuticals that we distribute.
We dispense specialty pharmaceuticals that are supplied to us by a variety of manufacturers and wholesalers, many of which are our only source of that specific pharmaceutical. Our contracts with pharmaceutical manufacturers and wholesalers often provide us with, among other things:
· discounts on drugs we purchase to be dispensed from our specialty pharmacies;
· rebates and service fees; and
· access to limited-distribution specialty pharmaceuticals.
Our contracts with pharmaceutical manufacturers and wholesalers are generally for three years and are terminable on reasonably short notice by either party before or after the contract term. In addition, our contracts with wholesalers provide for purchase money security interests in products sold. If several of these contractual relationships are terminated or materially altered by the pharmaceutical manufacturers or wholesalers or if we are otherwise unable to renew these contracts or enter into similar contracts on favorable terms, we could lose a major source of the pharmaceuticals we dispense.
Our revenues, profitability, and cash flows may be negatively impacted if safety risks of a specialty drug are publicized or if a specialty drug is withdrawn from the market due to manufacturing or other issues.
Physicians may significantly reduce the numbers of prescriptions for a specialty drug with safety concerns or manufacturing issues. Additionally, negative press regarding a drug with a higher safety risk profile may result in reduced global consumer demand for such drug. Decreased utilization and demand of a specialty drug we distribute could materially and adversely impact our volumes, net revenues, profitability, and cash flows.
Many healthcare companies have a presence in the specialty pharmacy market, and we expect a significant increase in competition due to high growth anticipated in specialty drug spending, which could have a material and adverse impact on our business.
There are a significant number of competitors that provide one or more comprehensive services, including distribution, with respect to specialty pharmacy drugs, some of whom have greater resources than we do, including: PBMs; retail pharmacy chains and independent retail pharmacies; health plans; national, regional and niche specialty pharmacies; home and specialty infusion therapy companies; physician practices and hospital systems; and group purchasing organizations.
The three leading specialty pharmacies, which operate as divisions within each of Express Scripts, CVS Caremark and Walgreens, have significantly greater market share, resources, and purchasing power than we do. Express Scripts and CVS Caremark also benefit from their services as PBMs to a number of healthcare organizations, and CVS Caremark and Walgreens also benefit from their retail and urgent care locations. As we increase in scale and market share, we expect more direct competition for certain drugs, payor and patient access, and services from these three companies. Many of our constituents are well informed and can easily move between us and our competitors. These factors together with the impact of the competitive marketplace or other significant differentiating factors between us and our competitors may make it difficult for us to retain existing business.
Further, a number of other traditional pharmacies with significant resources are attempting to build, acquire, or partner with specialty pharmacies due to the double-digit growth anticipated in spending on specialty prescription drugs compared to flat to low-single digit growth in spending on traditional prescription drugs. There are also many smaller specialty pharmacies and other entities in the healthcare industry that provide limited specialty pharmacy services; while such entities presently compete with us to a lesser extent, they may be able to invest significant resources, through acquisition or otherwise, to compete with us on a larger scale.
Moreover, many of the retail and hospital pharmacies to which we provide patient management services may acquire a competing specialty pharmacy business or start their own specialty pharmacy business and thereby become competitors. In addition, many of our PBM customers have their own specialty pharmacy businesses, and to the extent certain of our products can be obtained internally, these customers could reduce or cease to do business with
us. Our failure to maintain and expand relationships with payors and PBM companies, who can effectively determine the pharmacy source for their members, could materially and adversely affect our competitive position and prospects.
Any increase in competition noted above could significantly increase the competition for limited-distribution drugs, reduce gross profit, and otherwise materially adversely affect our business, results of operations, financial condition, and prospects.
We may not be able to effectively execute our acquisition strategy or successfully integrate acquired businesses.
Organic growth has been paramount since we were founded, but we have completed five important acquisitions in recent years: American Homecare Federation, Inc. (December 2013); MedPro (June 2014); BioRx (April 2015); Burman’s (June 2015); and TNH (June 2016).
Any of the following risks associated with our recent or future acquisitions, individually or in aggregate, may have a material adverse effect on our business:
· difficulties in realizing anticipated financial or strategic benefits of such acquisition;
· diversion of capital from other uses;
· potential dilution of shareholder ownership if stock is used as consideration for the acquisition or if an equity offering is completed in connection with the financing of the acquisition;
· the risks related to increased indebtedness;
· significant capital expenditures may be required to integrate acquisition into our operations;
· disruption of our ongoing business or the ongoing acquired business, including impairment of existing relationships with our employees, distributors, suppliers, customers, or other constituents or those of the acquired companies;
· diversion of management’s attention and other resources from current operations, including potential strain on financial and managerial controls and reporting systems and procedures;
· difficulty in integrating acquired operations, including restructuring and realigning activities, personnel, technologies, and products, including the loss of key employees, distributors, suppliers, customers, or other constituents of the acquired businesses;
· difficulties in the assimilation of different cultures and practices, as well as in the assimilation of broad and geographically dispersed personnel and operations;
· inability to realize cost savings, sales increases, or other benefits that we anticipate from such acquisitions, either as to amount or in the expected time frame;
· assumption of known and unknown liabilities, some of which may be difficult or impossible to quantify; and
· non-cash impairment charges or other accounting charges relating to the acquired assets.
We will continue to review strategic acquisition opportunities that will enhance our market position, expand our expertise and drug access, add value to our constituents, and/or provide sufficient synergies. Strategic transactions, including the pursuit of such transactions, often require significant up-front costs and require significant resources and management attention. These significant up-front costs relate to the assessment, due diligence, negotiation, and execution of the transaction. We may also incur additional costs to retain key employees as well as transaction fees and costs related to executing our integration plans.
Our operating results may fluctuate significantly, which makes our future operating results difficult to predict and could cause our operating results to fall below expectations or our guidance.
Our quarterly and annual operating results, and in particular our revenues, have fluctuated in the past and may fluctuate significantly in the future. These fluctuations make it difficult for us to predict our future operating results. Our operating results may fluctuate due to a variety of factors, many of which are outside of our control and are difficult to predict, including the following:
· the launch timing for specialty drugs;
· the effect of the expiration of drug patents and the introduction of generic drugs;
· the demand for the specialty drugs to which we have access;
· whether our expected distribution share of drugs that come to market is properly estimated;
· whether revenues and margins on sales of drugs that come to market are properly estimated;
· expenditures that we will or may incur to acquire or develop additional capabilities;
· the timing of increases in drug costs by manufacturers;
· the amount of DIR fees and the timing for assessing us for such fees; and
· changes in the reimbursement policies of payors.
These factors, individually or in the aggregate, could result in large fluctuations and unpredictability in our quarterly and annual operating results. As a result, comparing our operating results on a period-to-period basis may not be meaningful. Investors should not rely on our past results as an indication of our future performance. This variability and unpredictability could also result in our failing to meet the expectations of industry or financial analysts or investors for any period.
Our ability to grow our specialty pharmacy business could be limited if we do not expand the number of drugs and treatments we offer or if we lose even a small percentage of our existing patients.
Our specialty pharmacy business focuses on complex and high cost medications that serve a relatively small patient population. Due to the limited patient populations utilizing the medications that our specialty pharmacy business handles, our future growth relies, in part, on expanding our base of drugs or penetration in certain treatment categories. Further, given our relatively high net sales and gross profit per prescription dispensed, a small percentage decrease in our patient base or reduction in demand for any reason for the medications we dispense could have a material adverse effect on our business.
Consolidation in the healthcare industry could materially adversely affect our business, financial condition, and results of operations.
Many healthcare industry participants are consolidating to create integrated healthcare delivery systems with significant market power and we expect such trend to continue. As provider networks and managed care organizations consolidate, thereby decreasing the number of market participants, competition to provide products and services like ours will become more intense, and the importance of establishing relationships with key industry participants will become greater. In addition, industry participants may try to use their increased market power to negotiate price reductions for our products and services. We expect that market demand, government regulation, third party reimbursement policies, and societal pressures will continue to cause the healthcare industry to evolve, potentially resulting in further business consolidations and alliances among the industry participants with whom we engage. If we are forced to reduce prices as a result of either an imbalance of market power or decreased demand for our products, revenue would be reduced, and we could become significantly less profitable.
Our future success depends upon our ability to maintain and manage our continued growth. If we are unable to manage our growth effectively, we may incur unexpected expenses and be unable to meet the demands of our customers and other constituents.
Over the past several years our business has grown significantly, and we aim to continue to expand the scope of our operations, both organically and through strategic acquisitions. Growth in our operations will place significant demands on our management, financial, and other resources. We cannot be certain that our current systems, procedures, controls, and space will adequately support expansion of our operations, and we may be unable to expand or upgrade our systems or infrastructure to accommodate future growth. Our future operating results will depend on the ability of our management and key employees to successfully maintain our independence and corporate culture, preserve the effectiveness of our high-touch patient care model, manage changing business conditions, and implement and improve our technical, administrative, financial control, and reporting systems. Our inability to finance future growth, manage future expansion, or hire and retain the personnel needed to manage our business successfully could have a material adverse effect on our business and prospects.
We generate a significant amount of revenue from certain specialty drugs we dispense.
Our three largest revenue producing specialty drugs we dispense represented 29 percent, 30 percent, and 28 percent of our revenues in 2016, 2015, and 2014, respectively, and our 10 largest revenue producing specialty drugs we dispense represented 51 percent, 55 percent, and 54 percent of our revenues in 2016, 2015, and 2014, respectively. In the event that the use of these specialty drugs were to decline due to clinical ineffectiveness or as a result of the introduction of more effective alternatives, and we are unable to obtain access to high growth alternative specialty drugs, our revenues would be adversely affected. Loss of revenues from our three largest revenue producing specialty drugs without access to alternative high growth specialty drugs could have a material adverse effect on our revenues in the short term.
We receive a significant amount of prescription drugs from one wholesaler and two manufacturers. The loss of any of these relationships could disrupt our business and adversely impact our revenues for one or more fiscal quarters.
Specialty drug purchases from AmerisourceBergen, a drug wholesaler, Celgene and Pharmacyclics, pharmaceutical manufacturers, represented 49 percent, 13 percent, and 10 percent, respectively, of cost of products sold in 2016, 50 percent, 12 percent, and 9 percent, respectively, of cost of products sold in 2015, and 57 percent, 15 percent, and 7 percent, respectively, of cost of products sold in 2014. Our amended contract with AmerisourceBergen expires September 30, 2018, and can be terminated by, among other things, either party’s material breach that continues for 30 days. The amended contract also commits us to a minimum purchase obligation per contract year of approximately $2.0 billion. Failure to meet this minimum purchase obligation would result in significant additional expense without corresponding revenues. The agreement also provides for negotiated discounts that differ by drug classification, and any permitted reclassification of products by AmerisourceBergen to a lower discount category could have an adverse impact on our gross profit. In addition, AmerisourceBergen has a long term relationship with one of the largest specialty pharmacy companies in the country, which could adversely impact our relationship with AmerisourceBergen. Our significant competitors may obtain better discounts from AmerisourceBergen or other wholesalers, which could impair our competitiveness.
Our amended agreement with Celgene expires June 30, 2017, and can be terminated by either party without cause upon 90 days prior written notice, or earlier in the event of a material breach. Unlike the specialty drugs we purchase from AmerisourceBergen, the specialty drugs we purchase from Celgene are not available from any other source.
Our agreement with Pharmacyclics automatically renews annually, and can be terminated by either party without cause upon 90 days prior written notice, or earlier in the event of a material breach. Unlike the specialty drugs we purchase from AmerisourceBergen, the specialty drugs we purchase from Pharmacyclics are not available from any other source.
The loss of any of these relationships, the failure by the suppliers to fulfill our purchase orders on a timely basis or at all, or a contractual dispute could significantly disrupt our business and adversely impact our revenues for one or more fiscal quarters. These agreements also limit our ability to distribute competing drugs, while allowing the supplier to distribute through other channels.
Security breaches or other failures or disruptions of our information technology systems, our information security systems, and our infrastructure to support our business and to protect the privacy and security of sensitive customer and business information could materially adversely affect our business.
Many aspects of our operations are dependent on our communications and information systems and the information collected, processed, stored, and handled by these systems. Throughout our operations, we receive, retain, and transmit certain highly confidential information, including personal health information, personally identifiable information, and other data that our customers and other constituents provide to purchase products or services, enroll in programs or services, register on our websites, interact with our personnel, or otherwise communicate with us. In addition, for these operations, we depend, in part, on the secure transmission of confidential information over public networks. Despite our security measures, our information technology and infrastructure may be vulnerable to attacks by hackers or breached due to employee error, malfeasance, or other disruptions. Although we have not historically experienced a major systems failure or security breach, our information systems are subject to damage or interruption from power outages, computer and telecommunications failures, computer viruses, and security breaches including credit card information breaches, vandalism, catastrophic events, and human error. Like most companies that conduct business in part over the internet, we rely on the availability and connectivity of the internet, which is out of our control.
A compromise of our information security controls or those of the businesses with whom we interact, which results in confidential information being accessed, obtained, damaged, or used by unauthorized or improper persons, could harm our reputation and expose us to regulatory actions and claims from patients, physicians, and other persons, any of which could adversely affect our business, brands, financial position, and results of operations. Moreover, a data security breach could require that we expend significant resources related to our information systems and infrastructure, subject us to investigations by various state or federal authorities, and distract management and other key personnel from performing their primary operational duties. Additionally, while certain data security breaches might not result in a material adverse effect on our business operations, breaches involving the exfiltration or unauthorized access to personally identifiable information of patients or other individuals can significantly impact such individuals, resulting in a loss of confidence in, or goodwill of, the Company. If our information systems are damaged, fail to work properly, or otherwise become unavailable, we may incur substantial costs to remediate, repair, or replace them, and we may experience a loss of critical information, customer disruptions, and interruptions or delays in our ability to perform essential functions and implement new and innovative services. In addition, compliance with changes in privacy and information security laws and standards may result in considerable expense due to increased investment in technology and the development of new operational processes. See also “Risks Related to Federal and State Laws and Regulations — Our business operations involve the substantial receipt and use of confidential health information concerning individuals. A failure to adequately protect such information may harm our reputation and subject us to significant liabilities, each of which could have a material adverse effect on our business.”
Our failure to maintain significant relationships or build new relationships with clinical experts and key thought leaders at U.S. physician groups and universities could result in a loss of existing patients, future referrals on existing and future drugs and pharmaceutical industry data, and could materially adversely impact our business and prospects.
We have developed significant relationships with clinical experts and key opinion leaders at physician groups and universities throughout the U.S. who are focused on oncology, immunology, hepatitis, specialty infusion therapy, and multiple sclerosis, involved in significant research projects related to specialty drugs, and who are high-volume prescribers of specialty drugs. Our failure to provide quality and timely services to such persons and their patients could impair our relationship, which could result in a loss of existing patients, future referrals on existing and future drugs and pharmaceutical industry data (including the anticipated drug pipeline), and therefore materially adversely impact our business and prospects.
A disruption in our operations could hurt our relations with our constituents and significantly impact our results of operations.
Our business is dependent on a number of different operations, products, and processes, many of which involve third parties. A disruption in our business operations could result from, among other things, contamination of drugs or a failure to maintain appropriate shipment and storage conditions, including maintenance of our coolers for products that require refrigeration, an error in order processing, the unavailability of services provided by our suppliers, vendors or shipping carriers, labor strikes, or unanticipated disruptions at our dispensing facilities, call centers, data
centers, or corporate facilities. Such disruptions or our failure to implement adequate business continuity and disaster recovery strategies could, temporarily or indefinitely, significantly reduce, or partially or totally eliminate our ability to process and dispense prescriptions and provide products and services to our partners, which could have a material adverse effect on our business and results of operations.
We are highly dependent on our senior management and key employees. Competition for our employees is intense, and we may not be able to attract and retain the highly skilled employees that we need to support our business and our anticipated future growth.
Our success largely depends on the skills, experience, and continued efforts of our management. In particular, our co-founder, chief executive officer and chairman of the board of directors, Philip Hagerman, has led our company throughout its history of more than 40 years. Further, we intend to grow the business significantly, which will depend on our ability to continue to attract, motivate, and retain highly qualified individuals in key management, pharmacist, nursing, and similar roles. Competition for senior management and other key personnel is intense, and the pool of suitable candidates is limited. In addition, the realization of the expected benefits from our recent, and potentially future, acquisitions will depend to some extent on our ability to retain key employees from the entities we have acquired or may acquire in the future. If we lose the services of one or more of our key employees, we may not be able to find a suitable replacement and our business could be materially adversely affected.
The integration of new key executives into our management team may interfere with our operations.
We have recently appointed new key executives, including our president and our vice president of operations, and we may expect to hire or promote additional key management team members, including a chief financial officer. These executives will be required to spend a significant amount of time on certain integration and transition efforts in addition to performing their regular duties and responsibilities. If we fail to complete these integrations and transitions in an efficient manner, or if we fail to provide sufficient incentives to motivate and retain our key executives, our business and prospects may suffer.
Our cost savings and restructuring initiatives may be disruptive to our workforce and operations and adversely affect our financial results.
In response to the business environment and to accomplish our strategic objectives, we have recently undertaken certain cost savings and restructuring initiatives across all sectors of our business. To the extent such initiatives involve workforce changes, such changes may temporarily reduce workforce productivity, which could be disruptive to our business and adversely affect our results of operations. In addition, we may not achieve or sustain the expected cost savings or other benefits of our restructuring plans, or do so within the expected time frame.
We rely heavily on a single shipping provider, and our business could be harmed if our shipping rates increase, our provider is unavailable, or our provider performs poorly and we are unable to successfully replace our shipping provider.
A substantial majority of the specialty drugs we dispense are shipped through UPS. We depend heavily on these shipping services for efficient and cost-effective delivery of our products.
The risks associated with our dependence on UPS include:
· any significant increase in shipping rates, including rate increases resulting from higher fuel prices;
· strikes or other service interruptions by UPS or by another carrier that could affect UPS;
· spoilage of high cost drugs during shipment, since our drugs often require special handling, such as refrigeration; and
· increased delivery errors by UPS, resulting in lost or stolen product.
In the event any of the foregoing occurs and we are unable to transition efficiently and effectively to a new provider, we could incur increased costs or experience a material disruption in our operations.
Our industry is highly litigious and future litigation or other proceedings could subject us to significant monetary damages or penalties or require us to change our business practices, which could impair our reputation and result in a material adverse effect on our business.
We are subject to risks relating to litigation, enforcement actions, regulatory proceedings, government inquiries and investigations, and other similar actions in connection with our business operations, including the dispensing of pharmaceutical products by our specialty and home delivery pharmacies, claims, and complaints related to the various regulations to which we are subject and services rendered in connection with our disease management activity. While we are currently not subject to any material litigation of this nature, such litigation is not unusual in our industry. Further, while certain costs are covered by insurance, we may incur uninsured costs related to the defense of such proceedings that could be material to our financial performance. In addition, as a public company, any material decline in the market price of our common stock may expose us to purported class action lawsuits that, even if unsuccessful, could be costly to defend or indemnify (to the extent not covered by insurance) and a distraction to management. See Item 3, “Legal Proceedings” for information regarding a purported class action against the Company and certain current and former executive officers.
Furthermore, unexpected volatility in insurance premiums or retention requirements or claims in excess of our insurance coverage could have a material adverse effect on our business and results of operations.
We have identified a material weakness in our internal control over financial reporting. If we fail to remediate this material weakness, our ability to produce accurate and timely financial statements could be impaired, which could adversely affect investor views of us and the value of our common stock.
As a public company, we are required to comply with the standards adopted by the Public Company Accounting Oversight Board in compliance with the requirements of Section 404 of the Sarbanes-Oxley Act of 2002, as amended, regarding internal control over financial reporting. In connection with our evaluation of compliance, we identified a material weakness in our internal control over financial reporting as of December 31, 2016. A “material weakness” is a deficiency, or a combination of deficiencies, in internal control over financial reporting such that there is a reasonable possibility that a material misstatement of our annual or interim financial statements will not be prevented or detected on a timely basis. During the fourth quarter of 2016, we have identified a material weakness in the operating effectiveness of our evaluation and review of recorded inventory balances. Specifically, at certain locations the initial costs used to value ending inventories were not correct and we did not initially identify all items necessary to accurately complete our inventory reconciliation. The remediation actions we are taking, and expect to take, include: additional testing of the pricing file utilized to cost physical inventory; and strengthening the depth and breadth of review of the inventory reconciliation by senior accounting and finance personnel. However, these steps will take time to fully integrate and confirm, and until the remediation steps are fully implemented and tested, the material weakness will continue to exist.
If we fail to remediate the identified material weakness or identify further material weaknesses, we may not be able to accurately report our financial results, prevent fraud, or file our periodic reports in a timely manner, which may cause investors to lose confidence in our reported financial information and may lead to a decline in our stock price. In addition, our failure to timely file our periodic reports could eventually result in the delisting of our common stock from the New York Stock Exchange, regulatory sanctions from the SEC, and/or the breach of covenants in our credit facilities or of any preferred equity or debt securities we may issue in the future, any of which could have a material adverse impact on our operations and your investment in our common stock.
Any debt service obligations will reduce the funds available for other business purposes, and the terms and covenants relating to our current and future indebtedness could adversely impact our financial performance and liquidity.
As of December 31, 2016, we had $111.0 million and $39.3 million in debt outstanding under our term loan and line of credit, respectively. As of such date, we could incur up to an additional $129.9 million in indebtedness under our line of credit. To the extent we incur significant debt in the future for acquisitions, capital expenditures, working capital, or otherwise, we will be subject to risks typically associated with debt financing, such as insufficient cash flow to meet required debt service payment obligations and the inability to refinance existing indebtedness.
In addition, our credit facility contains covenants requiring us to, among other things, provide financial and other information reporting, provide notice upon certain events, and maintain cash management arrangements. These covenants also place restrictions on our ability to incur additional indebtedness, pay dividends or make other distributions, redeem or repurchase capital stock, make investments and loans, and enter into certain transactions, including selling assets, engaging in mergers or acquisitions, or engaging in transactions with affiliates. If we fail to satisfy one or more of the covenants under our credit facility, we would be in default thereunder, and may be required to repay such debt with capital from other sources or otherwise not be able to draw down against our line of credit. Under such circumstances, other sources of capital may not be available to us on reasonable terms or at all.
Our business could be harmed if the supply of any of the specialty drugs we distribute becomes scarce or is disrupted.
Many specialty drugs are manufactured with ingredients that are susceptible to supply shortages. In particular, specialty drugs used to treat disease states such as hemophilia and autoimmune conditions can depend on supplies of donated blood, which may fluctuate. A supply shortage, or in rare cases, a complete cessation of manufacturing, of a specialty drug we distribute could materially and adversely impact our volumes, net revenues, profitability, and cash flows.
If some of the drugs that we provide lose their orphan drug status, we could face increased competition.
In order to encourage the development of drugs that might not otherwise be profitable for pharmaceutical companies, the FDA will occasionally grant certain drugs orphan status. When the FDA grants orphan status to a drug, it will not approve a second drug for the same treatment for a period of seven years unless the new drug is chemically different or clinically superior. Additionally, it is easier to gain marketing approval for an orphan drug, and there may be other financial incentives associated with the manufacturing and distribution of orphan drugs, such as extended exclusivity periods. Our business could be adversely affected by any challenges to or the expiration of a drug’s orphan status. The loss of such status, the approval of new drugs notwithstanding a drug’s orphan status, or the development of drugs that are superior to the orphan drugs we dispense could result in additional competition and adversely impact our business and results of operations.
Our business would be harmed if the pharmaceutical industry reduces research, development, and marketing of specialty drugs that are compatible with the services we provide.
Our business is highly dependent on continued research, development, and marketing expenditures of pharmaceutical companies, and the ability of those companies to develop, supply, and generate demand for specialty drugs that are compatible with the services we provide. Our business could be materially adversely affected if manufacturers fail to market and support existing drugs, research potential new treatments, or develop new drugs. Our business could also be harmed by any governmental or private initiative that would alter how drug manufacturers promote or sell products and services.
We support hospitals that participate in the 340B Drug Pricing Program (“340B Program”). In recent years, the 340B Program has faced increased scrutiny from Congress, federal agencies, and pharmaceutical manufacturers. In light of the publication or proposed regulatory guidance and future changes to the 340B Program, the revenues we derive from hospital services could be adversely impacted.
Our hospital program supports hospitals that are 340B covered entities pursuant to which such hospitals are able to purchase certain specialty drugs from pharmaceutical manufacturers at a discount for dispensing to eligible patients. In cases where the covered entity treats an insured patient with a discounted specialty drug, the federal government or the patient’s private insurance routinely reimburses the entity for the full price of the medication, and the entity is able to retain the difference between the reduced price it pays for the drug and the full amount for which it is reimbursed. In recent years, this practice and other aspects of the 340B Program have come under increased scrutiny. In August 2015, HHS published proposed 340B program guidance (the “Proposed Guidance”). The Proposed Guidance relates to program eligibility and registration, eligibility of drugs for purchase under 340B, patient eligibility to receive 340B drugs, requirements for covered entities, arrangements for contract pharmacies, manufacturer responsibilities, rebate options for HIV drug assistance programs, and program integrity. To address regulatory concerns with the risk of double discounting in the contract pharmacy setting, the Proposed Guidance provides that contract pharmacies will not dispense 340B drugs to certain Medicaid patients without a written agreement that describes a system to prevent duplicate discounts. In addition, the Proposed Guidance provides that (1) each covered entity is expected to conduct quarterly reviews and annual independent audits of each contract pharmacy location, and (2) any 340B Program violation detected through quarterly reviews or annual audits of a contract pharmacy should be disclosed to HHS.
Although we are not direct participants in the 340B Program and related services accounted for less than 0.1 percent of our revenues in each of the years ended December 31, 2016, 2015, and 2014, our involvement with hospitals that are covered entities could cause reputational harm as a result of increased controversy regarding the 340B Program. In addition, if hospitals decrease their utilization of the 340B Program, whether due to regulatory changes or increased scrutiny, such decrease would impact revenue from this business.
We may be unable to obtain or retain the right to use or successfully integrate third-party licenses in our technology-based products, which could limit the number and type of products we are able to offer our customers.
We rely on third-party licenses for some of the technology used in our products, and intend to continue licensing technologies from third parties. Most of these licenses can be renewed only by mutual consent and may be terminated if we breach the terms of the license and fail to cure the breach within a specified period of time. We may not be able to continue to obtain these licenses on commercially reasonable terms, or at all. Our inability to obtain or renew these licenses or find suitable alternatives could delay development of new products or prevent us from selling our existing products until suitable substitute technology can be identified, licensed, integrated, or developed by us. We cannot assure you as to when we would be able to do so, if at all.
Most of our third-party licenses are non-exclusive. Our competitors may obtain the right to use any of the technology covered by these licenses and use the technology to attempt to compete more effectively with us. In addition, our use of third-party technologies exposes us to risks associated with the integration of components from various sources into our products, such as unknown software errors or defects or unanticipated incompatibility with our systems and technologies, or unintended infringement resulting from the combination of intellectual property rights. Further, we are dependent on our vendors’ continued support of the technology we use. If a vendor chooses to discontinue or is unable to support a licensed technology, we may not be able to modify or adapt our products to fit other available technologies in a timely manner, if at all.
We outsource certain operations of our business to third-party vendors, which could leave us vulnerable to data security failures of third parties.
From time to time, like many similarly situated companies, we outsource certain operations to third-party vendors to achieve efficiencies. Such outsourced functions include payment processing, data center hosting and management, facilities management, etc. Although we expect our business partners to maintain the same vigilance as we do with respect to data security, we cannot control the operations of these third parties. While we engage in certain actions to reduce the exposure resulting from outsourcing, vulnerabilities in the information security infrastructure of our business partners could make us vulnerable to attacks or disruptions in service.
Possible changes in industry pricing benchmarks.
It is possible that the pharmaceutical industry or regulators may evaluate and/or develop an alternative pricing reference to replace average wholesale price (“AWP”), which is the pricing reference used for many pharmaceutical purchase agreements, retail network contracts, specialty payor agreements, and other contracts with third party payors in connection with the reimbursement of specialty drug payments. Future changes to the use of AWP or to other published pricing benchmarks used to establish pharmaceutical pricing, including changes in the basis for calculating reimbursement by federal and state health programs and/or other payors, could impact our pricing arrangements. The effect of these possible changes on our business cannot be predicted at this time.
Risks Related to Federal and State Laws and Regulations
We operate in a highly regulated industry and must comply with a significant number of complex and evolving requirements. Changes in state and federal government regulations could restrict our ability to conduct our business and cause us to incur significant costs.
The marketing, sale, and purchase of pharmaceuticals and medical supplies and provision of healthcare services generally are extensively regulated by federal and state governments. In addition, other aspects of our business are also subject to government regulation. The applicable regulatory framework is complex, and the laws are very broad in scope. Many of these laws remain open to interpretation and have not been addressed by substantive court decisions. Accordingly, we cannot assure you that our interpretation would prevail or that one or more government agencies will not interpret the applicable laws and regulations differently. Changes in the law or new interpretations of existing law can have a dramatic effect on our operations, our cost of doing business, and the amount of reimbursement we receive from governmental third-party payors such as Medicare and Medicaid.
Some of the healthcare laws and regulations that apply to our activities include:
· The federal Anti-Kickback Statute prohibits individuals and entities from knowingly and willfully paying, offering, receiving or soliciting money or anything else of value in order to induce the referral of patients, or to induce a person to purchase, lease, order, arrange for, or recommend services or goods covered in whole or in part by Medicare, Medicaid, or other government healthcare programs. The Anti-Kickback Statute is an intent-based statute and the failure of a business arrangement to satisfy all elements of a safe harbor will not necessarily render the arrangement illegal, but it may subject that arrangement to increased scrutiny by enforcement authorities. Any violation of the Anti-Kickback Statute can lead to significant penalties, including criminal penalties, civil fines, and exclusion from participation in Medicare and Medicaid.
· The Stark Law prohibits physicians from making referrals to any entity with which the physicians or their immediate family members have a “financial relationship” (i.e., an ownership, investment, or compensation relationship) for the furnishing of certain Designated Health Services that are reimbursable under Medicare, and prohibits the entity from presenting or causing to be presented claims to Medicare for those referred services, unless an exception applies. The Stark Law is a broad prohibition on certain business relationships, with detailed exceptions. However, unlike the Anti-Kickback Statute under which an activity may fall outside a safe harbor and still be lawful, a referral for Designated Health Services that does not fall within an exception is strictly prohibited by the Stark Law. A violation of the Stark Law is punishable by civil sanctions, including significant fines and exclusion from participation in Medicare and Medicaid.
· HIPAA and HITECH provide federal privacy protections for individually identifiable health information. See “Our business operations involve the substantial receipt and use of confidential health information concerning individuals. A failure to adequately protect any of this information could result in severe harm to our reputation and subject us to significant liabilities, each of which could have a material adverse effect on our business.” below.
· Pharmacies and pharmacists must obtain state licenses to operate and dispense pharmaceuticals. If we are unable to maintain our licenses or if states place burdensome restrictions or limitations on non-resident pharmacies, this could limit or affect our ability to operate in some states.
· Federal and state investigations and enforcement actions continue to focus on the health care industry, scrutinizing a wide range of items such as joint venture arrangements, referral and billing practices, product discount arrangements, home health care services, dissemination of confidential patient information, clinical drug research trials, and gifts for patients.
Legislative or regulatory policies in the U.S. designed to manage healthcare costs or alter healthcare financing practices or changes to government policies in general may adversely impact our business and results of operations.
From time to time, legislative and/or regulatory proposals are made in the U.S. which seek to manage the cost of healthcare, including prescription drug cost. Such proposals include changes in reimbursement rates, restrictions on rebates and discounts, restrictions on access or therapeutic substitution, limits on more efficient delivery channels, taxes on goods and services, price controls on prescription drugs, and other significant healthcare reform proposals, including their repeal or replacement. Further, more exacting regulatory policies and requirements specific to the specialty pharmacy sector may cause a rise in costs, labor, and time to meet all such requirements. We are unable to predict whether any such policies or proposals will be enacted, or the specific terms thereof. Certain of these policies or proposals, if enacted, could have a material adverse impact on our business.
Our business operations involve the substantial receipt and use of confidential health information concerning individuals. A failure to adequately protect any of this information could result in severe harm to our reputation and subject us to significant liabilities, each of which could have a material adverse effect on our business.
Most of our activities involve the receipt or use of PHI concerning individuals. We also use aggregated and de-identified data for research and analysis purposes, and in some cases, provide access to such de-identified data to pharmaceutical manufacturers, payors, and third-party data aggregators and analysts. We believe our de-identified data is proprietary and we expect our future operations will include additional services regarding the de-identified data we accumulate to take greater advantage of our relationships with data-driven pharmaceutical manufacturers.
There is substantial regulation at the federal and state levels addressing the use, disclosure, and security of patient identifiable health information. At the federal level, HIPAA and the regulations issued thereunder impose extensive requirements governing the transmission, use, and disclosure of health information by all participants in health care delivery, including physicians, hospitals, insurers, and other payors. Many of these obligations were expanded under HITECH, passed as part of the American Recovery and Reinvestment Act of 2009. Failure to comply with standards issued pursuant to federal or state statutes or regulations may result in criminal penalties and civil sanctions. In addition to regulating privacy of individual health information, HIPAA includes several anti-fraud and abuse laws, extends criminal penalties to private health care benefit programs and, in addition to Medicare and Medicaid, to other federal health care programs, and expands the Office of Inspector General’s authority to exclude persons and entities from participating in the Medicare and Medicaid programs. Further, future regulations and legislation that severely restrict or prohibit our use of patient identifiable or other information could limit our ability to use information critical to the operation of our business. If we violate a patient’s privacy or are found to have violated any federal or state statute or regulation with regard to confidentiality or dissemination or use of PHI, we could be liable for significant damages, fines, or penalties and suffer severe reputational harm, each of which could have a material adverse effect on our business, results of operations, and prospects. These risks may become more prominent as we provide additional services related to our de-identified data.
Our business operations involve communication with patients, for which certain federal and state laws exist. Violations of these laws could result in substantial statutory penalties and other sanctions.
Certain federal and state laws, such as the Telephone Consumer Protection Act, give the Federal Trade Communication, Federal Communications Commission, and state attorneys general the ability to regulate, and bring enforcement actions relating to, telemarketing practices and certain automated outbound contacts such as phone calls, texts, or emails. Under certain circumstances, these laws may provide consumers with a private right of action. Violations of these laws could result in substantial statutory penalties and other sanctions.
Our business, financial position, and operations could be adversely affected by environmental regulations, and health and safety laws and regulations applicable to our business.
Certain federal, state, and local environmental regulations and health and safety laws and regulations are applicable to our business, including the management of hazardous substances, storage, and transportation of possible hazardous materials, and various other disclosure and procedure requirements that may be promulgated by the Occupational Safety and Health Administration or the Environmental Protection Agency that may apply to our operations. Violations of these laws and regulations could result in substantial statutory penalties, sanctions, and, in certain circumstances, a private right of action by consumers, employees, or the general public.
There remains considerable uncertainty as to the full impact of the Health Reform Laws on our business.
Many of the structural changes enacted by the Health Reform Laws were implemented in 2014; however, much of the applicable regulations and sub-regulatory guidance are subject to being repealed or replaced. There is considerable uncertainty as to the impact of Health Reform Laws (and their potential repeal or replacement) on our business.
Risks Related to Governance Matters
Certain provisions of our corporate governance documents and Michigan law could discourage, delay, or prevent a merger or acquisition at a premium price.
Our amended and restated articles of incorporation and bylaws contain provisions that may make the acquisition of our Company more difficult without the approval of our Board of Directors. These include provisions that, among other things:
· permit the Board to issue up to 10,000,000 shares of preferred stock, with any rights, preferences, and privileges as they may determine (including the right to approve an acquisition or other change in control);
· provide that the authorized number of directors may be fixed only by the Board in accordance with our amended and restated bylaws;
· do not provide for cumulative voting rights (therefore allowing the holders of a majority of the shares entitled to vote in any election of directors to elect all of the directors standing for election);
· divide our Board into three staggered classes;
· provide that all vacancies and newly created directorships may be filled by the affirmative vote of a majority of directors then in office, even if less than a quorum;
· prohibit removal of directors without cause;
· prohibit shareholders from calling special meetings of shareholders;
· requires unanimous consent for shareholders to take action by written consent without approval of the action by our Board;
· provide that shareholders seeking to present proposals before a meeting of shareholders or to nominate candidates for election as directors at a meeting of shareholders must provide advance notice in writing and also comply with specified requirements related to the form and content of a shareholder’s notice;
· require at least 80 percent supermajority shareholder approval to alter, amend, or repeal certain provisions of our amended and restated articles of incorporation; and
· require at least 80 percent supermajority shareholder approval in order for shareholders to adopt, amend, or repeal our amended and restated bylaws.
These provisions may frustrate or prevent any attempts by our shareholders to replace or remove our current management by making it more difficult for shareholders to replace members of the Board of Directors, which is responsible for appointing members of our management. Any matters requiring the approval of our shareholders will be significantly impacted by the Hagerman family (as defined below), which may have interests that differ from those of our other shareholders. See “Philip Hagerman, our chairman and chief executive officer, and his immediate family have significant influence on the outcome of matters submitted for shareholder approval and they may have interests that differ from those of our other shareholders.”
In addition, the award agreements for outstanding stock options under our 2007 Option Plan generally provide that all unvested options will immediately vest upon a change in control. The 2014 Omnibus Plan permits the Board of Directors or a committee thereof to accelerate, vest, or cause the restrictions to lapse with respect to outstanding equity awards in the event of, or immediately prior to, a change in control. Although our more recent form of option awards contain “double trigger” vesting, such vesting or acceleration of earlier awards could discourage the acquisition of our Company.
We could also become subject to certain anti-takeover provisions under Michigan law which may discourage, delay or prevent someone from acquiring us or merging with us, whether or not an acquisition or merger is desired by or beneficial to our shareholders. If a corporation’s board of directors chooses to “opt-in” to certain provisions of Michigan Law, such corporation may not, in general, engage in a business combination with any beneficial owner, directly or indirectly, of 10 percent of the corporation’s outstanding voting shares unless the holder has held the shares for five years or more or, among other things, the board of directors has approved the business combination. Our Board of Directors has not elected to be subject to this provision, but could do so in the future. Any provision of our amended and restated articles of incorporation or bylaws or Michigan law that has the effect of delaying or deterring a change in control could limit the opportunity for our shareholders to receive a premium for their shares, and could also affect the price that some investors are willing to pay for our common stock otherwise.
Philip Hagerman, our chairman and chief executive officer, has significant influence on the outcome of matters submitted for shareholder approval and he may have interests that differ from those of our other shareholders.
Philip Hagerman and various trusts affiliated with or for the benefit of Philip Hagerman or his wife (the “Hagerman family”) beneficially own approximately 29.8 percent of our common stock as of March 6, 2017. Therefore, the Hagerman family will continue to have significant influence over the outcome of votes on all matters requiring approval by shareholders, including the election of directors, the adoption of amendments to our articles of incorporation and bylaws, and approval of a sale of the Company and other significant corporate transactions. Furthermore, the interests of the Hagerman family may be different than the interests of other shareholders. This concentration of voting power could also have the effect of delaying, deterring, or preventing a change in control or other business combination that might otherwise be beneficial to our shareholders.
ITEM 1.B. UNRESOLVED STAFF COMMENTS
Not applicable.
We own a 599,383 square foot distribution facility in Flint, Michigan, which also contains our corporate headquarters. We believe that our headquarters and the other facilities described below are suitable and adequate for our current business needs.
The following table lists information regarding each of our major properties as of December 31, 2016:
Location |
| Square |
| Facility Description |
| Owned/Leased |
|
Flint, MI |
| 599,383 |
| Headquarters and main distribution facility |
| Owned |
|
Cincinnati, OH |
| 15,147 |
| Specialty pharmacy |
| Leased (expires Jun. 30, 2025) |
|
Boothwyn, PA |
| 11,400 |
| Specialty and retail pharmacy |
| Leased (expires Oct. 31, 2026) |
|
Flint, MI |
| 10,366 |
| Specialty and wholesale pharmacy |
| Owned |
|
Cincinnati, OH |
| 8,205 |
| Office space |
| Leased (expires May 31, 2025) |
|
Cincinnati, OH |
| 8,100 |
| Office space |
| Leased (expires Mar. 31, 2017) |
|
Ontario, CA |
| 7,280 |
| Specialty pharmacy |
| Leased (expires Mar. 14, 2020) |
|
Urbandale, IA |
| 7,050 |
| Specialty pharmacy |
| Leased (expires Apr. 30, 2021) |
|
Flint, MI |
| 7,000 |
| Specialty and retail pharmacy |
| Owned |
|
Greensboro, NC |
| 7,000 |
| Specialty pharmacy |
| Leased (expires Apr. 30, 2024) |
|
Carlsbad, CA |
| 6,589 |
| Specialty pharmacy |
| Leased (expires Nov. 20, 2017) |
|
Raleigh, NC |
| 6,032 |
| Office space |
| Leased (expires Jun. 30, 2019) |
|
Raleigh, NC |
| 5,872 |
| Specialty pharmacy and office space |
| Leased (expires Nov. 30, 2018) |
|
Scottsdale, AZ |
| 5,792 |
| Specialty pharmacy |
| Leased (expires Jun. 9, 2021) |
|
Van Nuys, CA |
| 5,747 |
| Specialty pharmacy and office space |
| Leased (expires Nov. 30, 2018) |
|
Cincinnati, OH |
| 5,710 |
| Office space |
| Leased (expires Sep. 30, 2019) |
|
Beltsville, MD |
| 5,625 |
| Specialty pharmacy |
| Leased (expires Mar. 31, 2022) |
|
Woburn, MA |
| 4,734 |
| Specialty pharmacy |
| Leased (expires Nov. 30, 2017) |
|
Enfield, CT |
| 4,664 |
| Specialty pharmacy |
| Leased (expires Dec. 17, 2018) |
|
Richardson, TX |
| 4,147 |
| Specialty pharmacy |
| Leased (expires Jul. 31, 2021) |
|
Buffalo Grove, IL |
| 3,408 |
| Specialty pharmacy |
| Leased (expires May 31, 2021) |
|
Ft. Lauderdale, FL |
| 2,665 |
| Specialty and retail pharmacy |
| Leased (expires Mar. 31, 2018) |
|
The Company leases an additional 22 facilities (ranging from 400 square feet to 2,000 square feet) in the mid-Atlantic and southeast regions of the U.S. for use as specialty infusion suites. The majority of these specialty infusion suite leases have one-year terms and automatically renew for additional one-year terms unless either party gives written notice of termination.
On November 10, 2016, a putative class action complaint was filed in the U.S. District Court for the Eastern District of Michigan against Diplomat Pharmacy, Inc. and certain officers of the Company. The complaint alleges violations of Sections 10(b) and 20(a) of the Securities Exchange Act of 1934 in connection with public filings made between October 9, 2014 and November 2, 2016 (the “potential class period”). The plaintiff seeks to represent a class of shareholders who purchased stock in the potential class period. The complaint seeks unspecified monetary damages and other relief. The Company believes the complaint and allegations to be without merit and intends to vigorously defend itself against these actions. The Company is unable at this time to determine whether the outcome of the litigation would have a material impact on our results of operations, financial condition, or cash flows.
In addition, our business of providing specialized pharmacy services and other related services may subject us to litigation and liability for damages in the ordinary course of business. Although the results of litigation and claims cannot be predicted, we believe there are no legal proceedings, the outcome of which, if determined adversely to us,
would individually or in the aggregate be reasonably expected to have a material adverse effect on our business, financial position, cash flows, or results of operations.
ITEM 4. MINE SAFETY DISCLOSURES
Not applicable.
ITEM 5. MARKET FOR REGISTRANT’S COMMON EQUITY, RELATED STOCKHOLDER MATTERS AND ISSUER PURCHASES OF EQUITY SECURITIES
Market Information
The following table sets forth for the periods indicated the high and low closing sale prices per share of our common stock as reported on the New York Stock Exchange:
|
| 2016 |
| 2015 |
| ||||||||
Quarter |
| High |
| Low |
| High |
| Low |
| ||||
|
|
|
|
|
|
|
|
|
| ||||
First |
| $ | 35.62 |
| $ | 25.21 |
| $ | 34.63 |
| $ | 22.41 |
|
Second |
| $ | 35.00 |
| $ | 28.14 |
| $ | 47.04 |
| $ | 32.87 |
|
Third |
| $ | 37.76 |
| $ | 27.00 |
| $ | 51.31 |
| $ | 27.06 |
|
Fourth |
| $ | 29.06 |
| $ | 12.50 |
| $ | 36.19 |
| $ | 24.39 |
|
On March 6, 2017, we had 66,987,621 shares of common stock, no par value, outstanding and 43 holders of record of our common stock. A substantially greater number of holders are beneficial owners whose shares are held of record by banks, brokers and other nominees. The transfer agent and registrar for our common stock is Computershare Trust Company, N.A.
Dividends
We currently expect to retain all future earnings, if any, for use in the operation and expansion of our business. Any determination to declare and pay cash dividends on our common stock in the future will be made at the discretion of our Board of Directors and will depend on our results of operations, financial performance and condition, capital requirements, contractual restrictions under our credit facility, restrictions imposed by applicable law, and other factors that our Board of Directors may deem relevant. We do not anticipate paying cash dividends on our common stock for the foreseeable future.
Issuer Purchases of Equity Securities
There have been no repurchases of our common stock either on the open market or by private transaction during the quarter ended December 31, 2016.
Performance Graph
The following graph compares the total cumulative stockholder return on our common stock with the total cumulative return of the S&P 500 Index and the S&P Small Cap 600 Index during the period commencing on October 10, 2014, the initial trading day of our common stock, and ending on December 31, 2016. The graph assumes that $100 was invested at the beginning of the period in our common stock and in each of the comparative indices, and the reinvestment of any dividends. Historical stock price performance should not be relied upon as an indication of future stock price performance.
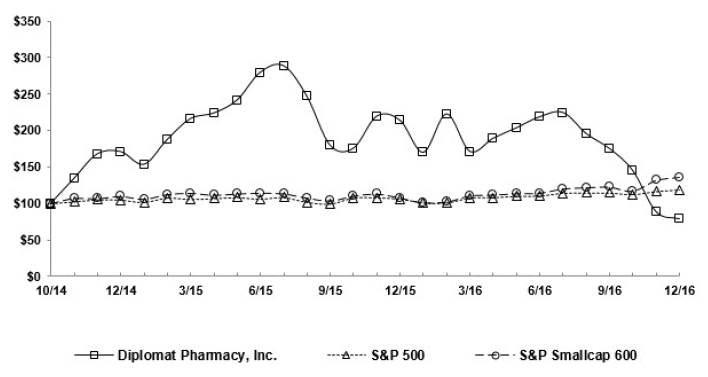
ITEM 6. SELECTED FINANCIAL DATA
The following selected financial data should be read in conjunction with the information under “Item 7. Management’s Discussion and Analysis of Financial Condition and Results of Operations” and our consolidated financial statements and related notes in “Item 8. Financial Statements and Supplementary Data” of this Annual Report on Form 10-K.
|
| Year Ended December 31, |
| |||||||||||||
|
| 2016 |
| 2015 |
| 2014 |
| 2013 |
| 2012 |
| |||||
|
| (Dollars in thousands, except per share amounts) |
| |||||||||||||
Consolidated Statements of Operations Data |
|
|
|
|
|
|
|
|
|
|
| |||||
Net sales |
| $ | 4,410,388 |
| $ | 3,366,631 |
| $ | 2,214,956 |
| $ | 1,515,139 |
| $ | 1,126,943 |
|
Cost of products sold |
| (4,085,560 | ) | (3,103,392 | ) | (2,074,817 | ) | (1,426,112 | ) | (1,057,608 | ) | |||||
Gross profit |
| 324,828 |
| 263,239 |
| 140,139 |
| 89,027 |
| 69,335 |
| |||||
Selling, general, and administrative expenses |
| (277,751 | ) | (217,302 | ) | (127,556 | ) | (77,944 | ) | (64,392 | ) | |||||
Income from operations |
| 47,077 |
| 45,937 |
| 12,583 |
| 11,083 |
| 4,943 |
| |||||
Other (expense) income: |
|
|
|
|
|
|
|
|
|
|
| |||||
Interest expense |
| (6,573 | ) | (5,239 | ) | (2,528 | ) | (1,996 | ) | (1,086 | ) | |||||
Equity loss and impairment of non-consolidated entities |
| (4,659 | ) | — |
| (6,208 | ) | (1,055 | ) | (267 | ) | |||||
Change in fair value of redeemable common shares |
| — |
| — |
| 9,073 |
| (34,348 | ) | (6,566 | ) | |||||
Termination of existing stock redemption agreement |
| — |
| — |
| (4,842 | ) | — |
| — |
| |||||
Other |
| 370 |
| 308 |
| 1,128 |
| 196 |
| 337 |
| |||||
Total other expense |
| (10,862 | ) | (4,931 | ) | (3,377 | ) | (37,203 | ) | (7,582 | ) | |||||
Income (loss) before income taxes |
| 36,215 |
| 41,006 |
| 9,206 |
| (26,120 | ) | (2,639 | ) | |||||
Income tax expense |
| (11,195 | ) | (16,234 | ) | (4,655 | ) | — |
| — |
| |||||
Net income (loss) |
| 25,020 |
| 24,772 |
| 4,551 |
| (26,120 | ) | (2,639 | ) | |||||
Less net loss attributable to noncontrolling interest |
| (3,253 | ) | (1,004 | ) | (225 | ) | — |
| — |
| |||||
Net income (loss) attributable to Diplomat Pharmacy, Inc. |
| 28,273 |
| 25,776 |
| 4,776 |
| (26,120 | ) | (2,639 | ) | |||||
Net income allocable to preferred shareholders |
| — |
| — |
| 458 |
| — |
| — |
| |||||
Net income (loss) allocable to common shareholders |
| $ | 28,273 |
| $ | 25,776 |
| $ | 4,318 |
| $ | (26,120 | ) | $ | (2,639 | ) |
|
|
|
|
|
|
|
|
|
|
|
| |||||
Net income (loss) per common share: |
|
|
|
|
|
|
|
|
|
|
| |||||
Basic |
| $ | 0.43 |
| $ | 0.42 |
| $ | 0.12 |
| $ | (0.79 | ) | $ | (0.08 | ) |
Diluted |
| $ | 0.42 |
| $ | 0.41 |
| $ | 0.11 |
| $ | (0.79 | ) | $ | (0.08 | ) |
|
|
|
|
|
|
|
|
|
|
|
| |||||
Weighted average common shares outstanding: |
|
|
|
|
|
|
|
|
|
|
| |||||
Basic |
| 65,970,396 |
| 60,730,133 |
| 36,012,592 |
| 33,141,500 |
| 33,141,500 |
| |||||
Diluted |
| 68,047,723 |
| 63,096,951 |
| 38,553,995 |
| 33,141,500 |
| 33,141,500 |
| |||||
|
| As of December 31, |
| |||||||||||||
|
| 2016 |
| 2015 |
| 2014 |
| 2013 |
| 2012 |
| |||||
|
| (Dollars in thousands) |
| |||||||||||||
Consolidated Balance Sheet Data |
|
|
|
|
|
|
|
|
|
|
| |||||
Total assets |
| $ | 1,107,947 |
| $ | 1,001,579 |
| $ | 390,086 |
| $ | 211,777 |
| $ | 139,595 |
|
Total debt |
| 150,255 |
| 117,000 |
| — |
| 88,164 |
| 63,102 |
| |||||
Total shareholders’ equity (deficit) |
| 613,724 |
| 515,546 |
| 168,727 |
| (77,782 | ) | (51,562 | ) | |||||
|
| Year Ended December 31, |
| |||||||||||||
|
| 2016 |
| 2015 |
| 2014 |
| 2013 |
| 2012 |
| |||||
|
| (Per prescription information in dollars) |
| |||||||||||||
Other Data (unaudited) |
|
|
|
|
|
|
|
|
|
|
| |||||
Prescriptions dispensed |
| 981,000 |
| 911,000 |
| 797,000 |
| 722,000 |
| 680,000 |
| |||||
Prescriptions serviced (not dispensed) |
| 177,000 |
| 282,000 |
| 212,000 |
| 208,000 |
| 118,000 |
| |||||
Total prescriptions |
| 1,158,000 |
| 1,193,000 |
| 1,009,000 |
| 930,000 |
| 798,000 |
| |||||
|
|
|
|
|
|
|
|
|
|
|
| |||||
Net sales per prescription dispensed |
| $ | 4,487 |
| $ | 3,683 |
| $ | 2,770 |
| $ | 2,090 |
| $ | 1,652 |
|
Gross profit per prescription dispensed |
| $ | 325 |
| $ | 280 |
| $ | 167 |
| $ | 116 |
| $ | 97 |
|
Net sales per prescription serviced (not dispensed) |
| $ | 36 |
| $ | 29 |
| $ | 27 |
| $ | 27 |
| $ | 29 |
|
Gross profit per prescription serviced (not dispensed) |
| $ | 36 |
| $ | 29 |
| $ | 27 |
| $ | 27 |
| $ | 29 |
|
ITEM 7. MANAGEMENT’S DISCUSSION AND ANALYSIS OF FINANCIAL CONDITION AND RESULTS OF OPERATIONS
(Dollars in thousands, except per share, per patient, and per prescription data)
Overview
We are the largest independent specialty pharmacy in the U.S., and are focused on improving the lives of patients with complex chronic diseases. Our patient-centric approach positions us at the center of the healthcare continuum for treatment of complex chronic diseases through partnerships with patients, payors, pharmaceutical manufacturers, and physicians. We offer a broad range of innovative solutions to address the dispensing, delivery, dosing, and reimbursement of clinically intensive, high-cost specialty drugs (many of which can cost more than $100,000 per patient, per year). We have expertise across a broad range of high-growth specialty therapeutic categories, including oncology, immunology, hepatitis, specialty infusion therapy, multiple sclerosis, and many other serious or long-term conditions. We dispense to patients in all 50 states and U.S. territories through our advanced distribution centers and manage centralized clinical call centers to deliver localized services on a national scale. We were founded in 1975 by our chief executive officer, Philip Hagerman, and his father, Dale, both trained pharmacists who transformed our business from a traditional pharmacy into a leading specialty pharmacy beginning in 2005.
Our core revenues are derived from the customized care management programs we deliver to our patients, including the dispensing of their specialty medications. Because our core therapeutic disease states generally require multiyear or lifelong therapy, our singular focus on complex chronic diseases helps drive recurring revenues and sustainable growth. Our revenue growth is primarily driven by new drugs coming to market, new indications for existing drugs, volume growth with current clients, and the addition of new clients. For the years ended December 31, 2016, 2015 and 2014, we derived more than 99 percent of our revenue from the dispensing of drugs and the reporting of data associated with those dispenses to pharmaceutical manufacturers and other outside companies.
Our recent and historical revenue growth has largely been driven by our position as a leader in the oncology, immunology, hepatitis, specialty infusion, and multiple sclerosis therapeutic categories. For the years ended December 31, 2016, 2015, and 2014, we generated approximately 93 percent, 92 percent, and 90 percent, respectively, of our revenues in these categories.
We expect our revenue growth to continue to be driven by a highly visible and recurring base of prescription volume and revenues, favorable demographic trends, advanced clinical developments, expanding drug pipelines, earlier detection of chronic diseases, improved access to medical care, mix shift toward higher-cost specialty drugs, and manufacturer price increases. In addition, we believe our expanding breadth of services, our growing penetration with new customers, and our access to limited-distribution drugs will help us achieve sustainable revenue growth in the future. Further, we believe that limited distribution is becoming the delivery system of choice for many specialty drug manufacturers because it is conducive to smaller patient populations, facilitates high patient engagement, clinical expertise, and elevated focus on service, and because it allows for real-time patient-specific (albeit de-identified) data. Accordingly, we believe our current portfolio of approximately 100 limited-distribution drugs, all of which are commercially available, is important to our revenue growth.
We also provide specialty pharmacy support services to a national network of retailers and independent hospital groups, as well as hospitals and health systems. Through many of these partners, we earn revenue by providing clinical and administrative support services on a fee-for-service basis to help them dispense specialty medications. Our other revenue in 2016, 2015, and 2014 was derived from these services provided to retail and hospital pharmacy partners.
As a result of our clinical expertise and our ability to expand scope of services, demand for our services has grown, which, along with acquisition activity, has driven growth in revenue. Net sales for the years ended December 31, 2016, 2015, and 2014, were $4,410,388, $3,366,631, and $2,214,956, respectively. Our net income attributable to Diplomat for the years ended December 31, 2016, 2015, and 2014 was $28,273, $25,776, and $4,776, respectively.
Recent Development
TNH Acquisition
On June 1, 2016, we acquired all of the outstanding equity interests of TNH for a total acquisition price of $78,422, excluding related acquisition costs. Included in the total acquisition price is $68,915 in cash and 324,244 restricted shares of our common stock, fair valued at $9,507 as of the acquisition date. TNH, a specialty pharmacy based in Van Nuys, California, provides medication management programs for individuals with complex chronic diseases, including oncology, hepatitis, and immunology. We acquired TNH to expand our existing business, enhance our proprietary technology, and increase our geographic presence, particularly in California and Texas.
Key Performance Metrics
We regularly review a number of metrics, including the following key metrics, to evaluate our business, measure our performance, identify trends, formulate financial projections, and make strategic decisions:
|
| Year Ended December 31, |
| |||||||
|
| 2016 |
| 2015 |
| 2014 |
| |||
Prescriptions dispensed |
| 981,000 |
| 911,000 |
| 797,000 |
| |||
Prescriptions serviced (not dispensed) ) |
| 177,000 |
| 282,000 |
| 212,000 |
| |||
Total prescriptions |
| 1,158,000 |
| 1,193,000 |
| 1,009,000 |
| |||
|
|
|
|
|
|
|
| |||
Net sales per prescription dispensed |
| $ | 4,487 |
| $ | 3,683 |
| $ | 2,770 |
|
Gross profit per prescription dispensed |
| $ | 325 |
| $ | 280 |
| $ | 167 |
|
Net sales per prescription serviced (not dispensed) |
| $ | 36 |
| $ | 29 |
| $ | 27 |
|
Gross profit per prescription serviced (not dispensed) |
| $ | 36 |
| $ | 29 |
| $ | 27 |
|
Prescription Data (rounded to the nearest thousand)
Prescriptions dispensed represent prescriptions filled and dispensed by Diplomat to patients or, in rare cases, to physicians. Prescriptions serviced (not dispensed) represent prescriptions filled and dispensed by a third-party (non-Diplomat) pharmacy, including unaffiliated retailers and health systems, as well as those for which we provide support services required to assist these patients and pharmacies through the complexity of filling specialty medications and those for which we earn a fee.
Our volume for the year ended December 31, 2016 was 1,158,000 prescriptions dispensed or serviced, a 3 percent decrease compared to 1,193,000 prescriptions dispensed or serviced for the year ended December 31, 2015. The volume decrease was due to a decrease in prescriptions serviced for retailers, the loss of non-specialty dispenses resulting from the sale of our compounding business in September 2015, and a business decision to exit dispensing certain high-volume, but low-profit, drugs. These volume decreases were partially offset by the contribution of our BioRx, Burman’s, and TNH acquisitions, new drugs to the market or newly dispensed by us, growth in patients from current payors and physician practices, and the addition of patients from new payors and physician practices.
Our volume for the year ended December 31, 2015 was 1,193,000 prescriptions dispensed or serviced, an 18 percent increase compared to 1,009,000 prescriptions dispensed or serviced for the year ended December 31, 2014. The volume increase was due to new drugs to the market or newly dispensed by us, growth in patients from current payors and physician practices, growth in prescriptions serviced for retailers, the addition of patients from new payors and physician practices, as well as the contribution of our BioRx, Burman’s, and MedPro acquisitions. These volume increases were partially offset by the loss of non-specialty dispenses resulting from the decision to close our Grand Rapids facility in November 2014 and the impact of the sale of our compounding business in September 2015.
Other Metrics
Other key metrics used in analyzing our business are net sales per prescription dispensed, gross profit per prescription dispensed, net sales per prescription serviced (not dispensed), and gross profit per prescription serviced (not dispensed).
Net sales per prescription dispensed represent total prescription revenue from prescriptions dispensed by Diplomat divided by the number of prescriptions dispensed by Diplomat. Gross profit per prescription dispensed represents gross profit from prescriptions dispensed by Diplomat divided by the number of prescriptions dispensed by Diplomat. Total prescription revenue from prescriptions dispensed includes all revenue collected from patients, third-party payors, and various patient assistance programs, as well as revenue collected from pharmaceutical manufacturers for data and other services directly tied to the actual dispensing of their drug(s). Gross profit represents total prescription revenue from prescriptions dispensed less the cost of the drugs purchased, including performance-related rebates paid by manufacturers to us, which are recorded as a reduction to cost of products sold.
Net sales per prescription serviced (not dispensed) represent total prescription revenue from prescriptions serviced divided by the number of prescriptions serviced for the non-Diplomat pharmacies. Gross profit per prescription serviced (not dispensed) is equal to net sales per prescription serviced because there is no cost of drug associated with such transactions. Total prescription revenue from prescriptions serviced includes revenue collected from partner pharmacies, including retailers and health systems, for support services rendered to their patients.
Components of Results of Operations
Net Sales
Revenue for a dispensed prescription is recognized at the time of shipment for home delivery and at prescription adjudication (which approximates the fill date) for patient pick-up at open-door or retail pharmacy locations. We can earn revenue from multiple sources for any one claim, including the primary insurance plan, the secondary insurance plan, the tertiary insurance plan, the patient copay, and patient assistance programs. Prescription revenue also includes revenue from pharmaceutical manufacturers and other outside companies for data reporting or additional services rendered for dispensed prescriptions. Service revenue is primarily derived from fees earned by us from retail and hospital pharmacies for patient support that is provided by us to those non-Diplomat pharmacies to dispense specialty drugs to patients. The retail and hospital pharmacies dispense the drug and pay us a service fee for clinically and administratively servicing their patients.
Cost of Products Sold
Cost of products sold represents the purchase price of the drugs that we ultimately dispense. These drugs are purchased directly from the manufacturer or from an authorized wholesaler and the purchase price is negotiated with the selling entity. In general, period-over-period percentage changes in cost of products sold will move directionally with period-over-period percentage changes in net sales for prescription dispensing transactions. This is due to the mathematical relationship between AWP and wholesale acquisition cost (“WAC”), where most commonly AWP equals WAC multiplied by 1.20, and our contractual relationships to purchase at a discount off WAC and receive reimbursement at a discount off AWP. The discounts off AWP and WAC that we receive vary significantly by drug and by contract. Rebates we receive from manufacturers are reflected as reductions to cost of products sold when they are earned.
Selling, General, and Administrative Expenses (“SG&A”)
Our operating expenses primarily consist of employee and employee-related costs, outbound prescription drug transportation and logistics costs, and amortization expense from definite-lived intangible assets associated with our acquired entities. Our employee and employee-related costs relate to both our patient-facing personnel and our non-patient-facing support and administrative personnel. Other operating expenses consist of occupancy and other indirect costs, insurance costs, professional fees, and other general overhead expenses. We expect that general and administrative expenses will continue to increase as we incur additional expenses related to our growth.
Other Expense
Other expense primarily consists of interest expense associated with our debt, equity losses and impairments of non-consolidated entities, and tax credits.
Income Tax Expense
On January 23, 2014, we converted from an S corporation to a C corporation. Prior to this date, our historical financial statements reflect our results as an S corporation.
RESULTS OF OPERATIONS
The following table provides consolidated statements of operations data for each of the years presented:
|
| Year Ended December 31, |
| |||||||
|
| 2016 |
| 2015 |
| 2014 |
| |||
Net sales |
| $ | 4,410,388 |
| $ | 3,366,631 |
| $ | 2,214,956 |
|
Cost of products sold |
| (4,085,560 | ) | (3,103,392 | ) | (2,074,817 | ) | |||
Gross profit |
| 324,828 |
| 263,239 |
| 140,139 |
| |||
SG&A |
| (277,751 | ) | (217,302 | ) | (127,556 | ) | |||
Income from operations |
| 47,077 |
| 45,937 |
| 12,583 |
| |||
Other (expense) income: |
|
|
|
|
|
|
| |||
Interest expense |
| (6,573 | ) | (5,239 | ) | (2,528 | ) | |||
Equity loss and impairment of non-consolidated entities |
| (4,659 | ) | — |
| (6,208 | ) | |||
Change in fair value of redeemable common shares |
| — |
| — |
| 9,073 |
| |||
Termination of existing stock redemption agreement |
| — |
| — |
| (4,842 | ) | |||
Other |
| 370 |
| 308 |
| 1,128 |
| |||
Total other expense |
| (10,862 | ) | (4,931 | ) | (3,377 | ) | |||
Income before income taxes |
| 36,215 |
| 41,006 |
| 9,206 |
| |||
Income tax expense |
| (11,195 | ) | (16,234 | ) | (4,655 | ) | |||
Net income |
| 25,020 |
| 24,772 |
| 4,551 |
| |||
Less net loss attributable to noncontrolling interest |
| (3,253 | ) | (1,004 | ) | (225 | ) | |||
Net income attributable to Diplomat Pharmacy, Inc. |
| 28,273 |
| 25,776 |
| 4,776 |
| |||
Net income allocable to preferred shareholders |
| — |
| — |
| 458 |
| |||
Net income allocable to common shareholders |
| $ | 28,273 |
| $ | 25,776 |
| $ | 4,318 |
|
Year Ended December 31, 2016 vs. Year Ended December 31, 2015
Net Sales
Net sales for the year ended December 31, 2016 were $4,410,388, a $1,043,757 or 31 percent increase, compared to $3,366,631 for the year ended December 31, 2015. The increase was primarily the result of organic growth, including approximately $256,000 of additional revenue from drugs that were new to the market in 2016 and approximately $241,000 from the impact of price increases. The remaining organic growth was primarily the result of a more favorable mix of those drugs that existed a year ago, partially offset by a shift in hepatitis C drug mix from those drugs that existed a year ago to new drugs and increased DIR fees. BioRx, Burman’s, and TNH, combined, contributed approximately $476,000 to the increase.
Cost of Products Sold
Cost of products sold for the year ended December 31, 2016 was $4,085,560, a $982,168 or 32 percent increase, compared to $3,103,392 for the year ended December 31, 2015. The increase was primarily the result of the same factors that drove the increase in our net sales over the same period. Cost of products sold was 92.6 percent and 92.2
percent of net sales for the years ended December 31, 2016 and 2015, respectively. The reduction in gross margin from 7.8 percent to 7.4 percent for the years ended December 31, 2015 and 2016, respectively, was primarily due to: a continued shift in mix towards higher priced but lower percent margin drugs, including the impact of TNH; lower growth and lower margins in our specialty infusion therapeutic category; increased DIR fees; the September 2015 sale of our low profit, but high margin, compounding business; and the recognition of a $2,407 inventory loss due to a cooler failure at one of our pharmacy locations during the fourth quarter of 2016.
SG&A
SG&A for the year ended December 31, 2016 were $277,751, a $60,449 increase, compared to $217,302 for the year ended December 31, 2015. Total employee cost increased by $35,974 and includes the employee expense for our acquired entities. The increased employee expense was primarily attributable to the 8 percent increase in dispensed prescription volume, combined with the increased clinical and administrative complexity associated with our mix of business. We also experienced a $13,925 increase in amortization expense from definite-lived intangible assets associated with our acquired entities, a $4,804 impairment expense to fully impair the definite-lived intangible assets associated with Primrose Healthcare, LLC (“Primrose”), a $3,544 increase in bad debt expense, and a $1,250 early termination fee associated with a software licensing agreement. The remaining increase was in all other SG&A to support our growth including software licenses, travel, freight, and other miscellaneous expenses. These increases were partially offset by a $15,590 decrease in the change in fair value of contingent consideration related to our acquisitions. As a percent of net sales, SG&A, excluding the change in fair value of contingent consideration and the Primrose impairment, accounted for 6.4 percent of net sales for the year ended December 31, 2016 compared to 6.3 percent for the year ended December 31, 2015.
Other Expense
Other expense for the years ended December 31, 2016 and 2015 was $10,862 and $4,931, respectively. We recognized a $4,659 impairment during the year ended December 31, 2016 to write down our cost method investment in Physician Resource Management, Inc. (“PRM”) to net realizable value. Interest expense increased by $1,334 as Term Loan A was outstanding for all of 2016 versus only nine months of 2015.
Income Tax Expense
Income tax expense for the years ended December 31, 2016 and 2015 was $11,195 and $16,234, respectively, resulting in effective tax rates of 31 percent and 40 percent, respectively. Income tax expense for the year ended December 31, 2016 included the recognition of excess tax benefits, which favorably impacted the 2016 effective tax rate by 11 percent (see Note 3 to our consolidated financial statements, included in Item 8 of this report).
Year Ended December 31, 2015 vs. Year Ended December 31, 2014
Net Sales
Net sales for the year ended December 31, 2015 were $3,366,631, a $1,151,675 or 52 percent increase, compared to $2,214,956 for the year ended December 31, 2014. The increase was primarily the result of organic growth, including approximately $453,000 from increased volume and a more favorable mix of those drugs that existed a year ago, approximately $136,000 from the impact of price increases, and approximately $103,000 of additional revenue from drugs that were new to the market in 2015. BioRx, Burman’s and MedPro, combined, contributed approximately $460,000 to the increase.
Cost of Products Sold
Cost of products sold for the year ended December 31, 2015 was $3,103,392, a $1,028,575 or 50 percent increase, compared to $2,074,817 for the year ended December 31, 2014. The increase was primarily the result of the same factors that drove the increase in our net sales over the same period. Cost of products sold was 92.2 percent and 93.7 percent of net sales for the years ended December 31, 2015 and 2014, respectively. The gross margin improvement from 6.3 percent to 7.8 percent for the years ended December 31, 2014 and 2015, respectively, was primarily due to
drug mix changes, including the impact of BioRx, Burman’s and MedPro, as well as the impact of increased pharma dollars, and, to a lesser extent, manufacturer price increases.
SG&A
SG&A for the year ended December 31, 2015 were $217,302, an $89,746 increase, compared to $127,556 for the year ended December 31, 2014. Total employee cost increased by $44,104 and includes the employee expense for our acquired entities. The increased employee expense was primarily attributable to the 18 percent increase in dispensed and serviced prescription volume, combined with the increased clinical and administrative complexity associated with our mix of business. Amortization expense from definite-lived intangible assets associated with our acquired entities increased $22,045. The remaining increase was in all other SG&A to support our growth including public company requirements, consulting fees, software licenses, travel, freight, and other miscellaneous expenses. As a percent of net sales, SG&A, excluding acquisition-related amortization and the change in fair value of contingent consideration, accounted for 5.5 percent of net sales for the year ended December 31, 2015 compared to 5.3 percent for the year ended December 31, 2014. This increase was primarily attributable to the more clinically intensive businesses we have acquired and the additional operating expense associated with servicing those patients, partially offset by operating efficiencies.
Other Expense
Other expense for the year ended December 31, 2015 was $4,931, compared to $3,377 for the year ended December 31, 2014. Interest expense increased by $2,711 due to increased borrowings during 2015. This increase was partially offset by the net impact of 2014 non-operating activities that were not applicable in 2015 (change in fair value of redeemable shares, termination of existing stock redemption agreement, and equity loss and impairment of non-consolidated entity).
Income Tax Expense
On January 23, 2014, we converted our income tax status from an S corporation to a C corporation. Since such conversion date, we bear income taxes which had previously been borne by our shareholders. Accordingly, on that date, we recorded a net deferred income tax liability of $2,965 and a charge to income tax expense for the same amount. Income tax expense for the years ended December 31, 2015 and 2014 was $16,234 and $4,655, respectively, resulting in effective tax rates of 40 percent and 51 percent, respectively.
Liquidity and Capital Resources
Our primary uses of cash include funding our ongoing working capital needs, business acquisitions, acquiring and maintaining property and equipment and internal use software, and debt service. Our primary source of liquidity for our working capital is cash flows generated from operations. At various times during the course of the year, we may be in an operating cash usage position, which may require us to use our short-term borrowings. We continuously monitor our working capital position and associated cash requirements and explore opportunities to more effectively manage our inventory and capital spending. As of December 31, 2016 and 2015, we had $7,953 and $27,600, respectively, of cash and cash equivalents. Our cash balances fluctuate based on working capital needs and the timing of sweeping available cash each day to pay down any outstanding balance on our line of credit, which was $39,255 and $0 at December 31, 2016 and 2015, respectively. Our available liquidity under our line of credit was $129,908 and $166,691 at December 31, 2016 and 2015, respectively.
We believe that funds generated from operations, cash and cash equivalents on hand, and available borrowing capacity under our credit facility will be sufficient to meet our working capital and capital expenditure requirements for at least the next 12 months. We may enhance our competitive position through additional complementary acquisitions in both existing and new markets. Therefore, from time to time, we may access the equity or debt markets to raise additional funds to finance acquisitions or otherwise on a strategic basis.
The following table provides cash flow data for each of the years presented:
|
| Year Ended December 31, |
| |||||||
|
| 2016 |
| 2015 |
| 2014 |
| |||
Net cash provided by (used in) operating activities |
| $ | 31,326 |
| $ | 29,447 |
| $ | (9,568 | ) |
Net cash used in investing activities |
| (85,967 | ) | (311,573 | ) | (66,084 | ) | |||
Net cash provided by financing activities |
| 34,994 |
| 291,769 |
| 84,500 |
| |||
Net (decrease) increase in cash and cash equivalents |
| $ | (19,647 | ) | $ | 9,643 |
| $ | 8,848 |
|
Cash Flows from Operating Activities
Cash flows from operating activities consists of net income, adjusted for noncash items, and changes in various working capital items, including accounts receivable, inventories, accounts payable, and other assets/liabilities.
The $1,879 increase in cash provided by operating activities for the year ended December 31, 2016 compared to the year ended December 31, 2015 was due to a $248 increase in net income and a $51,784 increase in noncash adjustments to net income, partially offset by a $50,153 increase in net working capital outflows.
The $39,015 increase in cash flow associated with operating activities for the year ended December 31, 2015 compared to the year ended December 31, 2014 was due to a $20,221 increase in net income, a $17,930 decrease in net working capital outflows, and an $864 increase in noncash adjustments to net income.
Cash Flows from Investing Activities
Our primary investing activities have consisted of business acquisitions, labor expenditures associated with capitalized software for internal use, investments in non-consolidated entities, capital expenditures to purchase computer equipment, software, furniture and fixtures, as well as building improvements to support the expansion of our infrastructure and workforce. As our business grows, our capital expenditures and our investment activity may continue to increase.
The $225,606 decrease in cash used in investing activities during the year ended December 31, 2016 compared to the year ended December 31, 2015 was primarily related to a $226,340 decrease in cash used to acquire businesses.
The $245,489 increase in cash used in investing activities during the year ended December 31, 2015 compared to the year ended December 31, 2014 was primarily related to a $241,897 increase in cash used to acquire businesses.
Cash Flows from Financing Activities
Our primary financing activities have consisted of proceeds from capital stock offerings, payments made to repurchase capital stock and stock options, debt borrowings and repayments, payment of debt issuance costs, and proceeds from stock option exercises.
The $256,775 decrease in cash provided by financing activities during the year ended December 31, 2016 compared to the year ended December 31, 2015 was primarily related to the non-recurrence of the following 2015 activities: $187,988 in net proceeds from our follow-on public offering and $120,000 in proceeds from the Term Loan A component of our credit facility (described below), partially offset by $36,298 in payments made to repurchase stock options.
The $207,269 increase in cash provided by financing activities during the year ended December 31, 2015 compared to the year ended December 31, 2014 was primarily related to $120,000 in proceeds from entering into our Term Loan A on April 1, 2015, $10,341 in 2015 proceeds from issuance of stock upon stock option exercises, $62,622 of net payments on the line of credit in 2014, and the following changes in year-over-year activities: $26,502 decrease in the repurchase of stock and stock options; and $22,542 decrease in payments on long-term debt; partially offset by a $44,267 decrease in net proceeds from capital stock offerings.
Excess Tax Benefits Related to Share-Based Awards
For accounting principles generally accepted in the U.S. (“U.S. GAAP”) purposes, share-based compensation expense associated with stock options is based upon recognition of the grant date fair value over the vesting period of the option. For income tax purposes, share-based compensation tax deductions associated with nonqualified stock option exercises and repurchases are based upon the difference between the stock price and the exercise price at time of exercise or repurchase. Prior to our January 1, 2016 adoption of Financial Accounting Standards Board’s Accounting Standards Update No. 2016-09, Compensation — Stock Compensation (Topic 718): Improvements to Employee Share-Based Payment Accounting (“ASU 2016-09”) (see Note 3 to our consolidated financial statements, included in Item 8 of this report), in instances where share-based compensation expense for income tax purposes was in excess of share-based compensation expense for U.S. GAAP purposes, which had predominately been the case for us, U.S. GAAP required that the tax benefit associated with this excess expense be recorded to shareholders’ equity to the extent that it reduced cash taxes payable. During the years ended December 31, 2015 and 2014, we recorded excess tax benefits related to share-based awards of $20,805 and $3,689, respectively, as increases to shareholders’ equity.
Prior to our adoption of ASU 2016-09, U.S. GAAP also required that excess tax benefits related to share-based awards be reported as a decrease to cash flows from operating activities and as an increase to cash flows from financing activities. We reported $20,805 and $3,689 of excess tax benefits related to share-based awards as decreases to cash flows from operating activities and as increases to cash flows from financing activities for the years ended December 31, 2015 and 2014, respectively.
Debt
On July 20, 2012, we entered into a credit facility (“facility”) with Capital One that provided for borrowings under a line of credit of up to $60,000. In 2013, the facility was amended to increase the commitment under the line of credit to $85,000. In June 2014, the facility was further amended to increase the commitment under the line of credit to $120,000. On April 1, 2015, in connection with the BioRx acquisition, we entered into a Second Amended and Restated Credit Agreement with Capital One, as agent and as a lender, the other lenders party thereto, and the other credit parties party thereto, providing for an increase in our line of credit to $175,000, a fully drawn Term Loan A for $120,000, and a deferred draw term loan for an additional $25,000 (“credit facility”). The credit facility also extended the maturity date to April 1, 2020. The credit facility provides for the issuance of letters of credit up to $10,000 and swingline loans up to $15,000, the issuance and incurrence of which will reduce the availability of the line of credit. The credit facility is guaranteed by substantially all of our subsidiaries and is collateralized by substantially all of our and our subsidiaries’ respective assets, with certain exceptions. In addition, we have pledged the equity of substantially all of our subsidiaries as security for the obligations under the credit facility. We add newly acquired subsidiaries promptly for purposes of, among other things, the guarantor, collateralization, and pledge provisions of the credit facility. We are required to maintain a depository bank account where money is collected and swept directly to the line of credit. We had $111,000 and $117,000 outstanding on Term Loan A at December 31, 2016 and 2015, respectively. Under our line of credit, we had weighted average borrowings of $11,986 and $12,022 and maximum borrowings of $82,683 and $78,866 during the years ended December 31, 2016 and 2015, respectively. We had $39,255 and $0 outstanding on our line of credit as of December 31, 2016 and 2015, respectively. We had $129,908 and $166,691 available to borrow on our line of credit at December 31, 2016 and 2015, respectively.
At December 31, 2016, our Term Loan A interest rate options were (i) LIBOR (as defined) plus 2.50 percent or (ii) Base Rate (as defined) plus 1.50 percent, and our line of credit and swingline loan interest rate options were (i) LIBOR (as defined) plus 2.00 percent or (ii) Base Rate (as defined) plus 1.00 percent. Our Term Loan A interest rate was 3.13 percent and 2.74 percent at December 31, 2016 and 2015, respectively. Our line of credit interest rate was 4.50 percent at December 31, 2016. In addition, we are charged a monthly unused commitment fee ranging from 0.25 percent to 0.50 percent on our average unused daily balance on our $175,000 line of credit and from 0.50 percent to 0.75 percent on our $25,000 deferred draw term loan.
During 2015, we incurred deferred financing costs of $5,055 associated with the credit facility, which were capitalized. These costs, along with previously unamortized deferred debt issuance costs are being amortized to interest expense over the term of the credit facility.
The credit facility contains certain financial and non-financial covenants. We were in compliance with all such covenants as of December 31, 2016 and 2015.
Contractual Obligations
Our contractual obligations, including estimated payments due by year, as of December 31, 2016 are as follows:
|
| 2017 |
| 2018 |
| 2019 |
| 2020 |
| 2021 |
| Thereafter |
| Total |
| |||||||
Long-term debt |
| $ | 7,500 |
| $ | 9,000 |
| $ | 10,500 |
| $ | 84,000 |
| $ | — |
| $ | — |
| $ | 111,000 |
|
Line of credit |
| 39,255 |
| — |
| — |
| — |
| — |
| — |
| 39,255 |
| |||||||
Interest payments |
| 4,265 |
| 3,943 |
| 3,643 |
| 842 |
| — |
| — |
| 12,693 |
| |||||||
Operating leases |
| 1,761 |
| 1,679 |
| 958 |
| 704 |
| 572 |
| 1,559 |
| 7,233 |
| |||||||
Total |
| $ | 52,781 |
| $ | 14,622 |
| $ | 15,101 |
| $ | 85,546 |
| $ | 572 |
| $ | 1,559 |
| $ | 170,181 |
|
We purchase a large portion of our prescription drug inventory from AmerisourceBergen. In October 2016, we amended our contract with AmerisourceBergen, which now expires on September 30, 2018. The amended contract commits us to a minimum purchase obligation of approximately $2,000,000 per contract year. We fully expect to meet this requirement.
Off-Balance Sheet Arrangements
During the periods presented, we did not have any relationships with unconsolidated entities or financial partnerships, such as entities often referred to as structured finance or special purpose entities, which would have been established for the purpose of facilitating off-balance sheet arrangements or other contractually narrow or limited purposes.
Critical Accounting Policies
The accompanying consolidated financial statements, included under Item 8 of this report, have been prepared in conformity with U.S. GAAP and, accordingly, our significant accounting policies have been disclosed in Note 3 to the consolidated financial statements. Certain of our accounting policies require the application of significant judgment by our management in selecting the appropriate assumptions for calculating financial estimates. These policies require the most difficult, subjective, or complex judgments that our management makes in the preparation of the consolidated financial statements. We consider an accounting estimate to be critical if: (i) the estimates involve matters that are highly uncertain at the time the accounting estimate is made; and (ii) different estimates or changes to estimates could have a material impact on the reported financial position, changes in financial position, or results of operations.
When more than one accounting principle, or the method of its application, is generally accepted, our management selects the principle or method that it considers to be the most appropriate given the specific circumstances. Application of these accounting principles requires our management to make estimates about future resolution of existing uncertainties. Estimates are typically based upon historical experience, current trends, contractual documentation, and other information, as appropriate. Due to the inherent uncertainty involving estimates, actual results reported in the future may differ from those estimates. In preparing these financial statements, our management has made its best estimate and judgments of the amounts and disclosures included in the financial statements, giving due regard to materiality. Such critical accounting estimates are discussed below.
Revenue Recognition
We recognize revenue from prescription drug sales for home delivery at the time the drugs are shipped. At the time of shipment, we have performed substantially all of our obligations under our payor contracts and do not experience
a significant level of returns or reshipments. Revenues from dispensing specialty prescriptions that are picked up by customers at an open door or retail pharmacy location are recorded at prescription adjudication, which approximates fill date. We recognize revenue from service, data, and consulting services when the services have been performed and the earnings process is therefore complete. Sales taxes are presented on a net basis (excluded from revenues and costs).
We accrue an estimate of fees, including DIR fees, which are assessed or expected to be assessed by payors at some point after adjudication of a claim, as a reduction at the time revenue is recognized. Changes in our estimate of such fees are recorded when the change becomes known.
Business Combinations
The assets acquired and liabilities assumed in a business combination, including identifiable intangible assets, are based on their estimated fair values as of the acquisition date. The excess of purchase price over the estimated fair value of the net tangible and identifiable intangible assets acquired is recorded as goodwill. The allocation of the purchase price requires management to make significant estimates in determining the fair values of assets acquired and liabilities assumed, especially with respect to intangible assets. These estimates are based on information obtained from management of the acquired companies and historical experience and are generally made with the assistance of an independent valuation firm. These estimates can include, but are not limited to, the cash flows that an asset is expected to generate in the future, and the cost savings expected to be derived from acquiring an asset. When an acquisition involves contingent consideration, we recognize a liability equal to the fair value of the contingent consideration obligation as of the acquisition date. The estimate of fair value of a contingent consideration obligation requires subjective assumptions to be made regarding future business results, discount rates, and probabilities assigned to various potential business result scenarios.
These estimates are inherently uncertain and unpredictable, and, if different estimates were used, the purchase price for the acquisition could be allocated to the acquired assets and liabilities differently from the allocation that we have made. In addition, unanticipated events and circumstances may occur which affect the accuracy or validity of such estimates, and, if such events occur, we may be required to record a charge against the value ascribed to an acquired asset or an increase in the amounts recorded for assumed liabilities.
Goodwill
Goodwill is reviewed for impairment annually during the fourth quarter, or more frequently if indicators of impairment exist. Goodwill impairment testing involves a comparison of the estimated fair value of a reporting unit to its respective carrying amount, which may be performed utilizing either a qualitative or quantitative assessment. A reporting unit is defined as an operating segment or one level below an operating segment. The qualitative assessment evaluates various events and circumstances, such as macro-economic conditions, industry and market conditions, cost factors, relevant events, and financial trends that may impact a reporting unit’s fair value. If it is determined that the estimated fair value of the reporting unit is more likely than not less than the carrying amount, including goodwill, a quantitative assessment is required. Otherwise, no further analysis is necessary.
If a quantitative assessment is performed, step one is to determine the fair value of a reporting unit and then compare its fair value to its carrying value. A reporting unit’s fair value is determined based upon consideration of various valuation methodologies, including the income approach which utilizes projected future cash flows discounted at rates commensurate with the risks involved, and multiples of current and future earnings. If the fair value of a reporting unit is less than its carrying amount, an indication of goodwill impairment exists and step two of the quantitative assessment is required. Under step two, a goodwill impairment loss is recognized for any excess of the carrying amount of a reporting unit’s goodwill over the implied fair value of that goodwill. The implied fair value of goodwill is determined by allocating the fair value of a reporting unit in a manner similar to a purchase price allocation and the residual fair value after this allocation is the implied fair value of the reporting unit goodwill.
A significant amount of judgment is involved in determining if an indicator of goodwill impairment has occurred. Such indicators may include, among others: a significant decline in expected future cash flows; a significant adverse change in legal factors or in the business climate; unanticipated competition; and the testing for recoverability of a
significant asset group within a reporting unit. Our goodwill impairment analysis also includes a comparison of the aggregate estimated fair value of all reporting units to our total market capitalization. Therefore, our stock may trade below our book value and a significant and sustained decline in our stock price and market capitalization could result in goodwill impairment charges. Any adverse change in these factors could have a significant impact on the recoverability of these assets and could have a material impact on our consolidated financial statements.
The income approach used to test our reporting units includes the projection of estimated operating results and cash flows, discounted using a weighted-average cost of capital (“WACC”) that reflects current market conditions appropriate to each reporting unit. Such projections contain management’s best estimates of economic and market conditions over the projected period, including growth rates in revenues and costs and best estimates of future expected changes in operating margins and cash expenditures. Other significant assumptions and estimates used in the income approach include terminal value growth rates, future estimates of capital expenditures, and changes in future working capital requirements. In addition, the WACC utilized to discount estimated future cash flows is sensitive to changes in interest rates and other market rates in place at the time the assessment is performed. Future changes in our estimates or assumptions or in interest rates could have a significant impact on the estimated fair value of reporting units and result in a goodwill impairment charge that could be material to our consolidated financial statements.
We performed a quantitative assessment during the fourth quarter of 2016. The following table contains our step one results:
|
| Fair Value |
| Goodwill |
| |
Reporting unit 1 |
| 30 | % | $ | 216,385 |
|
Reporting unit 2 |
| 11 | % | 100,231 |
| |
|
|
|
| $ | 316,616 |
|
The market price of our common stock experienced significant fluctuations during 2016. Our market capitalization significantly exceeded our total book value for most of 2016 and as of our annual impairment test date. However, continued fluctuations could result in our market capitalization dropping below book value. A significant and sustained decline in our common stock price and market capitalization could result in a goodwill impairment charge that could be material to our consolidated financial statements. See the New Accounting Pronouncements section of Note 3 to our consolidated financial statements, included in Item 8 of this report, regarding the simplification of the goodwill impairment test that we intend to early adopt on January 1, 2017.
Long-Lived Assets
Long-lived assets, such as capitalized software for internal use, property and equipment, and definite-lived intangible assets, are reviewed for impairment whenever events or changes in circumstances indicate that the related carrying amounts may not be recoverable. In assessing long-lived assets for impairment, assets are grouped with other assets and liabilities at the lowest level for which identifiable cash flows are largely independent of the cash flows of other assets and liabilities. If circumstances require a long-lived asset or asset group to be tested for possible impairment, we compare the undiscounted cash flows expected to be generated by that asset or asset group to its carrying amount. If the carrying amount of the long-lived asset or asset group is not recoverable on an undiscounted cash flow basis, an impairment charge is recognized to the extent that the carrying amount exceeds its fair value. Fair values of long-lived assets are determined through various techniques, such as applying probability weighted, expected present value calculations to the estimated future cash flows using assumptions a market participant would utilize, or through the use of a third-party independent appraiser or valuation specialist.
Allowance for Doubtful Accounts
We maintain an allowance for doubtful accounts that reduces receivables to amounts that we expect to be collected. In estimating this allowance, we consider overall economic conditions, historical and anticipated customer
performance, historical experience with write-offs, and the level of past due accounts. Our general policy for uncollectible accounts, if not reserved through specific examination procedures, is to reserve based upon the aging categories of accounts receivable. Account balances are charged off against the allowance after all means of collection have been exhausted and the potential for recovery is considered remote.
Share-Based Compensation
We grant stock options to key employees, which are accounted for as equity awards. The exercise price of a granted stock option is equal to the closing market stock price of the underlying common share as of the date the option is granted. Options generally become exercisable in installments of 25 percent per year, beginning on the first anniversary of the grant date and each of the three anniversaries thereafter, and have a maximum term of 10 years. Certain stock option grants have performance-based conditions, which require the satisfaction of one-year revenue and Adjusted EBITDA goals prior to vesting. We use the Black-Scholes-Merton option pricing model to determine the grant date fair value of options.
We expense the grant date fair values of our employee stock options over their respective vesting periods on a straight-line basis. Estimating grant date fair values for employee stock options requires management to make assumptions regarding expected volatility of the underlying shares, the risk-free rate over the expected life of the stock options, and the length of time in years that the granted options are expected to be outstanding. Due to our limited history as a public company, expected volatility is based on an implied volatility for a group of industry-relevant healthcare companies as of the measurement date. Risk-free rate is determined based upon U.S. Treasury rates over the estimated expected option lives. Expected dividend yield is zero as we do not anticipate declaring a dividend during the expected term of the options. Expected option life is calculated using the simplified method (the midpoint between the end of the vesting period and the end of the maximum term) because we do not have sufficient historical exercise data to provide a reasonable basis upon which to estimate the expected term due to the limited period of time such awards have been outstanding. If actual results differ significantly from these estimates and assumptions, particularly in relation to management’s estimation of volatility which requires the most judgment due to our limited history as a public entity, share-based compensation expense, primarily with respect to future share-based awards, could be materially impacted.
We grant restricted stock awards to non-employee directors. Such restricted stock fully vests on the first anniversary of the grant date. The grant date fair value of a restricted stock award is determined by the closing market price of our common stock as of the date of grant. We expense the grant date fair values of restricted stock over the one year vesting period on a straight-line basis.
Income Taxes
We account for income taxes under the asset and liability method. Deferred tax assets and liabilities are recognized for the future tax consequences attributable to differences between the financial statement carrying amounts of existing assets and liabilities and their respective tax bases and operating loss and tax credit carryforwards. Deferred tax assets and liabilities are measured using enacted tax rates expected to apply to taxable income in the years in which those temporary differences are expected to be recovered or settled. The effect on deferred tax assets and liabilities of a change in tax rates is recognized in income in the period that includes the enactment date. We provide a valuation allowance against net deferred tax assets unless, based upon the available evidence, it is more likely than not that the deferred tax assets will be realized.
Prior to January 23, 2014, we had elected to be taxed under the provisions of Subchapter S of the Internal Revenue Code. Under these provisions, we did not pay federal corporate income taxes on our taxable income. Instead, the shareholders were liable for individual federal income taxes on their respective shares of our taxable income. Distributions were made periodically to our shareholders to the extent needed to cover their income tax liability based on our taxable income.
We prepare and file tax returns based on interpretations of tax laws and regulations. In the normal course of business, our tax returns are subject to examination by various taxing authorities. Such examinations may result in future tax and interest assessments by these taxing authorities. In determining our tax provision for financial reporting purposes, we establish a reserve for examination, based on their technical merits. That is, for reporting
purposes, we only recognize tax benefits taken on the tax return if we believe it is more likely than not that such tax positions would be sustained. There is considerable judgment involved in determining whether it is more likely than not that such tax positions would be sustained. As of both December 31, 2016 and 2015, we had unrecognized tax benefits of $268; all of which, if recognized, would reduce both tax expense and the effective tax rate.
We adjust our tax reserve estimates periodically because of ongoing examinations by, and settlements with, varying taxing authorities, as well as changes in tax laws, regulations, and interpretations. The consolidated tax provision of any given year includes adjustments to prior year income tax accruals and related estimated interest charges that are considered appropriate. Our policy is to recognize, when applicable, interest and penalties on uncertain income tax positions as part of income tax expense.
Recently Issued Accounting Standards to be Implemented
See Note 3 to our consolidated financial statements, included in Item 8 of this report.
ITEM 7A. QUANTITATIVE AND QUALITATIVE DISCLOSURES ABOUT MARKET RISK
Our operations are solely in the U.S. and U.S. territories and are exposed to market risks in the ordinary course of our business. These risks primarily include interest rate and certain exposure, as well as risks relating to changes in the general economic conditions in the U.S. We are exposed to interest rate fluctuations with regard to future issuances of fixed-rate debt, and existing and future issuances of floating-rate debt. Primary exposures include the U.S. Prime Rate and LIBOR related to debt outstanding under our credit facility. In the past, we used interest rate swaps to reduce the volatility of our financing costs and to achieve a desired proportion of fixed and floating-rate debt. We did not use these interest rate swaps for trading or other speculative purposes. We currently are not using any interest rate swaps, but may in the future. A 100 basis-point increase in 2016 interest rates would have decreased our 2016 pre-tax income by approximately $1.3 million.
ITEM 8. FINANCIAL STATEMENTS AND SUPPLEMENTARY DATA
MANAGEMENT’S REPORT ON INTERNAL CONTROL OVER FINANCIAL REPORTING
We are responsible for establishing and maintaining adequate internal control over financial reporting. Our Company’s internal control over financial reporting includes those policies and procedures that pertain to the Company’s ability to record, process, summarize, and report a system of internal accounting controls and procedures to provide reasonable assurance, at an appropriate cost/benefit relationship, that the unauthorized acquisition, use, or disposition of assets are prevented or timely detected and that transactions are authorized, recorded, and reported properly to permit the preparation of financial statements in accordance with generally accepted accounting principles in the United States of America and receipt and expenditures are duly authorized. Management of the Company is required to assess the effectiveness of the Company’s internal control over financial reporting as of December 31, 2016.
As allowed pursuant to guidance from the Securities and Exchange Commission (which states that management may omit an assessment of an acquired business’ internal control over financial reporting from its assessment of internal control over financial reporting for a period not to exceed one year), our assessment of and conclusion on the effectiveness of internal control over financial reporting did not include the internal controls of Valley Campus Pharmacy, Inc., doing business as TNH Advanced Specialty Pharmacy (“TNH”), which was acquired on June 1, 2016, and which is included in the consolidated balance sheet of Diplomat Pharmacy, Inc. as of December 31, 2016, and the related consolidated statements of operations, cash flows, and changes in shareholders’ equity for the year then ended. From June 1, 2016 through December 31, 2016, TNH’s net sales represented approximately 6 percent of consolidated net sales for the year ended December 31, 2016. As of December 31, 2016, TNH’s total assets represented approximately 10 percent of consolidated total assets.
We conducted an assessment of the effectiveness of our internal controls over financial reporting based on the criteria set forth in Internal Control-Integrated Framework issued by the Committee of Sponsoring Organizations of the Treadway Commission (2013 Framework). This evaluation included review of the documentation, evaluation of the design effectiveness, and testing of the operating effectiveness of controls. Our system of internal control over financial reporting is enhanced by written policies and procedures and a written Code of Conduct adopted by our Company’s Board of Directors, applicable to all employees of our Company. In addition, we have an internal Disclosure Committee, which performs a separate review of our disclosure controls and procedures. There are inherent limitations in the effectiveness of any system of internal controls over financial reporting.
Based on our assessment, we concluded that the Company’s internal control over financial reporting was not effective as of December 31, 2016.
A material weakness is a deficiency, or combination of deficiencies, in internal control over financial reporting such that there is a reasonable possibility that a material misstatement of the Company's annual or interim financial statements will not be prevented or detected on a timely basis. During the fourth quarter of 2016, we have identified a material weakness in the operating effectiveness of our evaluation and review of recorded inventory balances. Specifically, at certain locations the initial costs used to value ending inventories were not correct and we did not initially identify all items necessary to accurately complete our inventory reconciliation.
Management is actively implementing a remediation plan to ensure that deficiencies contributing to the material weakness are remediated such that these controls will operate effectively, which includes steps to strengthen our inventory costing and reconciliation controls. The remediation actions we are taking, and expect to take, include: additional testing of the pricing file utilized to cost physical inventories; and strengthening the depth and breadth of review of the inventory reconciliation by senior accounting and finance personnel.
The Company has concluded that these remediation efforts will represent significant improvements to our internal control over financial reporting. The Company has started to implement these steps, however, some of these steps will take time to fully integrate and confirm the effectiveness and sustainability of such procedures. Additional controls may also be required over time. Until the remediation steps set forth above are fully implemented and tested, the material weakness described above will continue to exist.
BDO USA, LLP, the Company’s independent registered public accounting firm, that audited the Company’s consolidated financial statements included in this annual report on Form 10-K also audited the Company’s system of internal control over financial reporting. The accompanying reports of BDO USA, LLP are based upon audits conducted in accordance with the standards of the Public Company Accounting Oversight Board (United States).
REPORT OF INDEPENDENT REGISTERED PUBLIC ACCOUNTING FIRM
Board of Directors and Shareholders
Diplomat Pharmacy, Inc.
Flint, Michigan
We have audited Diplomat Pharmacy, Inc.’s internal control over financial reporting as of December 31, 2016, based on criteria established in Internal Control — Integrated Framework (2013) issued by the Committee of Sponsoring Organizations of the Treadway Commission (the COSO criteria). Diplomat Pharmacy, Inc.’s management is responsible for maintaining effective internal control over financial reporting and for its assessment of the effectiveness of internal control over financial reporting, included in the accompanying “Item 8, Management’s Report on Internal Control Over Financial Reporting.” Our responsibility is to express an opinion on the company’s internal control over financial reporting based on our audit.
We conducted our audit in accordance with the standards of the Public Company Accounting Oversight Board (United States). Those standards require that we plan and perform the audit to obtain reasonable assurance about whether effective internal control over financial reporting was maintained in all material respects. Our audit included obtaining an understanding of internal control over financial reporting, assessing the risk that a material weakness exists, and testing and evaluating the design and operating effectiveness of internal control based on the assessed risk. Our audit also included performing such other procedures as we considered necessary in the circumstances. We believe that our audit provides a reasonable basis for our opinion.
A company’s internal control over financial reporting is a process designed to provide reasonable assurance regarding the reliability of financial reporting and the preparation of financial statements for external purposes in accordance with generally accepted accounting principles. A company’s internal control over financial reporting includes those policies and procedures that: (1) pertain to the maintenance of records that, in reasonable detail, accurately and fairly reflect the transactions and dispositions of the assets of the company; (2) provide reasonable assurance that transactions are recorded as necessary to permit preparation of financial statements in accordance with generally accepted accounting principles, and that receipts and expenditures of the company are being made only in accordance with authorizations of management and directors of the company; and (3) provide reasonable assurance regarding prevention or timely detection of unauthorized acquisition, use, or disposition of the company’s assets that could have a material effect on the financial statements.
Because of its inherent limitations, internal control over financial reporting may not prevent or detect misstatements. Also, projections of any evaluation of effectiveness to future periods are subject to the risk that controls may become inadequate because of changes in conditions, or that the degree of compliance with the policies or procedures may deteriorate.
A material weakness is a deficiency, or a combination of deficiencies, in internal control over financial reporting, such that there is a reasonable possibility that a material misstatement of the company’s annual or interim financial statements will not be prevented or detected on a timely basis. The following material weakness has been identified and described in management's assessment. The Company identified a material weakness in the operating effectiveness of its evaluation and review of recorded inventory balances. Specifically, at certain locations the initial costs used to value the Company’s ending inventories were not correct and the Company did not initially identify all items necessary to accurately complete its inventory reconciliation. This material weakness was considered in determining the nature, timing, and extent of audit tests applied in our audit of the 2016 financial statements, and this report does not affect our report dated March 8, 2017 on those financial statements.
As indicated in the accompanying “Item 8, Management’s Report on Internal Control Over Financial Reporting”, management’s assessment of and conclusion on the effectiveness of internal control over financial reporting did not include the internal controls of Valley Campus Pharmacy, Inc., doing business as TNH Advanced Specialty Pharmacy (“TNH”), and which is included in the consolidated balance sheet of Diplomat Pharmacy, Inc. as of December 31, 2016, and the related consolidated statements of operations, cash flows, and changes in shareholders’ equity for the year then ended. From June 1, 2016 through December 31, 2016, TNH’s combined net sales represented approximately 6 percent of consolidated net sales for the year ended December 31, 2016. As of December 31, 2016, TNH’s total assets represented approximately 10 percent of consolidated total assets. Management did not assess the effectiveness of internal control over financial reporting of TNH because of the timing of this acquisition, which was completed on June 1, 2016. Our audit of internal control over financial reporting of Diplomat Pharmacy, Inc. also did not include an evaluation of the internal control over financial reporting of TNH.
In our opinion, Diplomat Pharmacy, Inc. did not maintain, in all material respects, effective internal control over financial reporting as of December 31, 2016, based on the COSO criteria.
We do not express an opinion or any other form of assurance on management’s statements referring to any corrective actions taken by the Company after the date of management’s assessment.
We also have audited, in accordance with the standards of the Public Company Accounting Oversight Board (United States), the consolidated balance sheets of Diplomat Pharmacy, Inc. as of December 31, 2016 and 2015 and the related consolidated statements of operations, cash flows, and changes in shareholders’ equity (deficit) for each of the three years in the period ended December 31, 2016 and our report dated March 8, 2017 expressed an unqualified opinion thereon.
/s/ BDO USA, LLP |
|
|
|
Troy, Michigan |
|
March 8, 2017 |
|
REPORT OF INDEPENDENT REGISTERED PUBLIC ACCOUNTING FIRM
Board of Directors and Shareholders
Diplomat Pharmacy, Inc.
Flint, Michigan
We have audited the accompanying consolidated balance sheets of Diplomat Pharmacy, Inc. as of December 31, 2016 and 2015 and the related consolidated statements of operations, cash flows, and changes in shareholders’ equity (deficit) for each of the three years in the period ended December 31, 2016. These financial statements are the responsibility of the Company’s management. Our responsibility is to express an opinion on these financial statements based on our audits.
We conducted our audits in accordance with the standards of the Public Company Accounting Oversight Board (United States). Those standards require that we plan and perform the audit to obtain reasonable assurance about whether the financial statements are free of material misstatement. An audit includes examining, on a test basis, evidence supporting the amounts and disclosures in the financial statements, assessing the accounting principles used, and significant estimates made by management, as well as evaluating the overall financial statement presentation. We believe that our audits provide a reasonable basis for our opinion.
In our opinion, the consolidated financial statements referred to above present fairly, in all material respects, the financial position of Diplomat Pharmacy, Inc. at December 31, 2016 and 2015, and the results of its operations and its cash flows for each of the three years in the period ended December 31, 2016, in conformity with accounting principles generally accepted in the United States of America.
We also have audited, in accordance with the standards of the Public Company Accounting Oversight Board (United States), Diplomat Pharmacy, Inc.’s internal control over financial reporting as of December 31, 2016, based on criteria established in Internal Control — Integrated Framework (2013) issued by the Committee of Sponsoring Organizations of the Treadway Commission (COSO) and our report dated March 8, 2017 expressed an adverse opinion thereon.
/s/ BDO USA, LLP |
|
|
|
Troy, Michigan |
|
March 8, 2017 |
|
DIPLOMAT PHARMACY, INC.
Consolidated Balance Sheets
(Dollars in thousands)
|
| December 31, |
| December 31, |
| ||
ASSETS |
|
|
|
|
| ||
Current assets: |
|
|
|
|
| ||
Cash and equivalents |
| $ | 7,953 |
| $ | 27,600 |
|
Accounts receivable, net |
| 275,568 |
| 254,682 |
| ||
Inventories |
| 215,351 |
| 165,950 |
| ||
Deferred income taxes |
| 14,703 |
| 5,311 |
| ||
Prepaid expenses and other current assets |
| 6,235 |
| 7,427 |
| ||
Total current assets |
| 519,810 |
| 460,970 |
| ||
|
|
|
|
|
| ||
Property and equipment, net |
| 20,372 |
| 16,538 |
| ||
Capitalized software for internal use, net |
| 50,247 |
| 37,250 |
| ||
Goodwill |
| 316,616 |
| 256,318 |
| ||
Definite-lived intangible assets, net |
| 199,862 |
| 224,644 |
| ||
Investment in non-consolidated entity |
| 300 |
| 4,959 |
| ||
Other noncurrent assets |
| 740 |
| 900 |
| ||
|
|
|
|
|
| ||
Total assets |
| $ | 1,107,947 |
| $ | 1,001,579 |
|
|
|
|
|
|
| ||
LIABILITIES AND SHAREHOLDERS’ EQUITY |
|
|
|
|
| ||
Current liabilities: |
|
|
|
|
| ||
Accounts payable |
| $ | 320,684 |
| $ | 296,587 |
|
Borrowings on line of credit |
| 39,255 |
| — |
| ||
Short-term debt, including current portion of long-term debt |
| 7,500 |
| 6,000 |
| ||
Accrued expenses: |
|
|
|
|
| ||
Compensation and benefits |
| 5,674 |
| 5,563 |
| ||
Contingent consideration |
| — |
| 52,665 |
| ||
Other |
| 12,233 |
| 11,087 |
| ||
Total current liabilities |
| 385,346 |
| 371,902 |
| ||
|
|
|
|
|
| ||
Long-term debt, less current portion |
| 100,184 |
| 106,706 |
| ||
Deferred income taxes |
| 8,693 |
| 7,425 |
| ||
Total liabilities |
| 494,223 |
| 486,033 |
| ||
|
|
|
|
|
| ||
Commitments and contingencies |
|
|
|
|
| ||
|
|
|
|
|
| ||
Shareholders’ equity: |
|
|
|
|
| ||
Preferred stock (10,000,000 shares authorized; none issued and outstanding) |
| — |
| — |
| ||
Common stock (no par value; 590,000,000 shares authorized; 66,764,999 and 64,523,864 shares issued and outstanding at December 31, 2016 and 2015, respectively) |
| 503,828 |
| 451,620 |
| ||
Additional paid-in capital |
| 33,268 |
| 29,221 |
| ||
Retained earnings |
| 76,306 |
| 31,130 |
| ||
Total Diplomat Pharmacy shareholders’ equity |
| 613,402 |
| 511,971 |
| ||
Noncontrolling interests |
| 322 |
| 3,575 |
| ||
Total shareholders’ equity |
| 613,724 |
| 515,546 |
| ||
|
|
|
|
|
| ||
Total liabilities and shareholders’ equity |
| $ | 1,107,947 |
| $ | 1,001,579 |
|
See accompanying notes to consolidated financial statements.
DIPLOMAT PHARMACY, INC.
Consolidated Statements of Operations
(Dollars in thousands, except per share amounts)
|
| Year Ended December 31, |
| |||||||
|
| 2016 |
| 2015 |
| 2014 |
| |||
Net sales |
| $ | 4,410,388 |
| $ | 3,366,631 |
| $ | 2,214,956 |
|
Cost of products sold |
| (4,085,560 | ) | (3,103,392 | ) | (2,074,817 | ) | |||
Gross profit |
| 324,828 |
| 263,239 |
| 140,139 |
| |||
Selling, general, and administrative expenses |
| (277,751 | ) | (217,302 | ) | (127,556 | ) | |||
Income from operations |
| 47,077 |
| 45,937 |
| 12,583 |
| |||
Other (expense) income: |
|
|
|
|
|
|
| |||
Interest expense |
| (6,573 | ) | (5,239 | ) | (2,528 | ) | |||
Equity loss and impairment of non-consolidated entities |
| (4,659 | ) | — |
| (6,208 | ) | |||
Change in fair value of redeemable common shares |
| — |
| — |
| 9,073 |
| |||
Termination of existing stock redemption agreement |
| — |
| — |
| (4,842 | ) | |||
Other |
| 370 |
| 308 |
| 1,128 |
| |||
Total other expense |
| (10,862 | ) | (4,931 | ) | (3,377 | ) | |||
Income before income taxes |
| 36,215 |
| 41,006 |
| 9,206 |
| |||
Income tax expense |
| (11,195 | ) | (16,234 | ) | (4,655 | ) | |||
Net income |
| 25,020 |
| 24,772 |
| 4,551 |
| |||
Less net loss attributable to noncontrolling interest |
| (3,253 | ) | (1,004 | ) | (225 | ) | |||
Net income attributable to Diplomat Pharmacy, Inc. |
| 28,273 |
| 25,776 |
| 4,776 |
| |||
Net income allocable to preferred shareholders |
| — |
| — |
| 458 |
| |||
Net income allocable to common shareholders |
| $ | 28,273 |
| $ | 25,776 |
| $ | 4,318 |
|
|
|
|
|
|
|
|
| |||
Net income per common share: |
|
|
|
|
|
|
| |||
Basic |
| $ | 0.43 |
| $ | 0.42 |
| $ | 0.12 |
|
Diluted |
| $ | 0.42 |
| $ | 0.41 |
| $ | 0.11 |
|
|
|
|
|
|
|
|
| |||
Weighted average common shares outstanding: |
|
|
|
|
|
|
| |||
Basic |
| 65,970,396 |
| 60,730,133 |
| 36,012,592 |
| |||
Diluted |
| 68,047,723 |
| 63,096,951 |
| 38,553,995 |
| |||
See accompanying notes to consolidated financial statements.
DIPLOMAT PHARMACY, INC.
Consolidated Statements of Cash Flows
(Dollars in thousands)
|
| Year Ended December 31, |
| |||||||
|
| 2016 |
| 2015 |
| 2014 |
| |||
Cash flows from operating activities: |
|
|
|
|
|
|
| |||
Net income |
| $ | 25,020 |
| $ | 24,772 |
| $ | 4,551 |
|
Adjustments to reconcile net income to net cash provided by (used in) operating activities: |
|
|
|
|
|
|
| |||
Depreciation and amortization |
| 50,045 |
| 30,841 |
| 8,139 |
| |||
Net provision for doubtful accounts |
| 9,534 |
| 5,990 |
| 4,045 |
| |||
Changes in fair value of contingent consideration |
| (8,922 | ) | 6,724 |
| 6,121 |
| |||
Contingent consideration payments |
| (4,174 | ) | (3,738 | ) | — |
| |||
Deferred income tax expense (benefit) |
| 8,779 |
| (4,615 | ) | (1,295 | ) | |||
Share-based compensation expense |
| 5,412 |
| 3,936 |
| 2,871 |
| |||
Impairment expense |
| 4,804 |
| 150 |
| — |
| |||
Equity loss and impairment of non-consolidated entities |
| 4,659 |
| — |
| 6,208 |
| |||
Amortization of debt issuance costs |
| 1,176 |
| 963 |
| 366 |
| |||
Excess tax benefits related to share-based awards |
| — |
| (20,805 | ) | (3,689 | ) | |||
Change in fair value of redeemable common shares |
| — |
| — |
| (9,073 | ) | |||
Termination of existing stock redemption agreement |
| — |
| — |
| 4,842 |
| |||
Other |
| 2 |
| 85 |
| 132 |
| |||
Changes in operating assets and liabilities, net of business acquisitions: |
|
|
|
|
|
|
| |||
Accounts receivable |
| (15,128 | ) | (50,771 | ) | (43,130 | ) | |||
Inventories |
| (44,342 | ) | (41,657 | ) | (50,334 | ) | |||
Accounts payable |
| (5,906 | ) | 43,202 |
| 56,505 |
| |||
Other assets and liabilities |
| 367 |
| 34,370 |
| 4,173 |
| |||
Net cash provided by (used in) operating activities |
| 31,326 |
| 29,447 |
| (9,568 | ) | |||
|
|
|
|
|
|
|
| |||
Cash flows from investing activities: |
|
|
|
|
|
|
| |||
Payments to acquire businesses, net of cash acquired |
| (67,156 | ) | (293,496 | ) | (51,599 | ) | |||
Expenditures for capitalized software for internal use |
| (12,595 | ) | (12,021 | ) | (9,470 | ) | |||
Expenditures for property and equipment |
| (6,217 | ) | (4,624 | ) | (1,487 | ) | |||
Capital investments in and loans to non-consolidated entities |
| — |
| (1,459 | ) | (4,000 | ) | |||
Other |
| 1 |
| 27 |
| 472 |
| |||
Net cash used in investing activities |
| (85,967 | ) | (311,573 | ) | (66,084 | ) | |||
|
|
|
|
|
|
|
| |||
Cash flows from financing activities: |
|
|
|
|
|
|
| |||
Net proceeds from (payments on) line of credit |
| 39,255 |
| — |
| (62,622 | ) | |||
Payments on long-term debt |
| (6,000 | ) | (3,000 | ) | (25,542 | ) | |||
Proceeds from issuance of stock upon stock option exercises |
| 4,448 |
| 10,341 |
| — |
| |||
Contingent consideration payments |
| (2,681 | ) | (3,012 | ) | — |
| |||
Payments of debt issuance costs |
| (28 | ) | (5,055 | ) | (480 | ) | |||
Proceeds from public offering, net of transaction costs |
| — |
| 187,988 |
| 130,440 |
| |||
Proceeds from long-term debt |
| — |
| 120,000 |
| — |
| |||
Payments made to repurchase stock options |
| — |
| (36,298 | ) | (9,400 | ) | |||
Excess tax benefits related to share-based awards |
| — |
| 20,805 |
| 3,689 |
| |||
Proceeds from sale of preferred stock, net of transaction costs |
| — |
| — |
| 101,815 |
| |||
Payments made to repurchase common stock |
| — |
| — |
| (53,400 | ) | |||
Net cash provided by financing activities |
| 34,994 |
| 291,769 |
| 84,500 |
| |||
|
|
|
|
|
|
|
| |||
Net (decrease) increase in cash and equivalents |
| (19,647 | ) | 9,643 |
| 8,848 |
| |||
|
|
|
|
|
|
|
| |||
Cash and equivalents at beginning of year |
| 27,600 |
| 17,957 |
| 9,109 |
| |||
|
|
|
|
|
|
|
| |||
Cash and equivalents at end of year |
| $ | 7,953 |
| $ | 27,600 |
| $ | 17,957 |
|
|
|
|
|
|
|
|
| |||
Supplemental disclosures of cash flow information: |
|
|
|
|
|
|
| |||
Cash paid for interest |
| $ | 5,273 |
| $ | 3,949 |
| $ | 2,248 |
|
Cash paid for income taxes |
| 728 |
| 351 |
| 5,924 |
| |||
See accompanying notes to condensed consolidated financial statements.
DIPLOMAT PHARMACY, INC.
Consolidated Statement of Changes in Shareholders’ Equity (Deficit)
(Dollars in thousands)
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Total |
|
|
|
|
| ||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Retained |
| Diplomat |
|
|
|
|
| ||||||||
|
| Common Stock |
| Additional |
| Earnings |
| Pharmacy, Inc. |
|
|
| Total |
| ||||||||||||||||||
|
| Class A |
| Class B |
| No Par |
| Paid-In |
| (Accumulated |
| Shareholders’ |
| Noncontrolling |
| Shareholders’ |
| ||||||||||||||
|
| Shares |
| Amount |
| Shares |
| Amount |
| Shares |
| Amount |
| Capital |
| Deficit) |
| Equity (Deficit) |
| Interest |
| Equity (Deficit) |
| ||||||||
Balance at January 1, 2014 |
| 1,657,500 |
| $ | — |
| 31,492,500 |
| $ | 4 |
| — |
| — |
| $ | 4,186 |
| $ | (81,972 | ) | $ | (77,782 | ) | $ | — |
| $ | (77,782 | ) | |
Net income (loss) |
| — |
| — |
| — |
| — |
| — |
| — |
| — |
| 4,776 |
| 4,776 |
| (225 | ) | 4,551 |
| ||||||||
Reclassification of S Corporation accumulated deficit |
| — |
| — |
| — |
| — |
| — |
| — |
| (82,550 | ) | 82,550 |
| — |
| — |
| — |
| ||||||||
Repurchase of shares of common stock |
| — |
| — |
| (2,850,407 | ) | — |
| — |
| — |
| (47,726 | ) | — |
| (47,726 | ) | — |
| (47,726 | ) | ||||||||
Removal of common stock redemption features |
| — |
| — |
| 425,000 |
| — |
| — |
| — |
| 7,116 |
| — |
| 7,116 |
| — |
| 7,116 |
| ||||||||
Repurchase of stock options |
| — |
| — |
| — |
| — |
| — |
| — |
| (9,400 | ) | — |
| (9,400 | ) | — |
| (9,400 | ) | ||||||||
Issuance of shares of Class B common stock as partial consideration of MedPro Rx, Inc. aquisition |
| — |
| — |
| 716,695 |
| — |
| — |
| — |
| 12,000 |
| — |
| 12,000 |
| — |
| 12,000 |
| ||||||||
Issuance of shares of Class B common stock in connection with termination of existing stock redemption agreement |
| — |
| — |
| 372,486 |
| — |
| — |
| — |
| 4,842 |
| — |
| 4,842 |
| — |
| 4,842 |
| ||||||||
Capital investment in subsidiary by noncontrolling shareholders |
| — |
| — |
| — |
| — |
| — |
| — |
| — |
| — |
| — |
| 4,804 |
| 4,804 |
| ||||||||
Share-based compensation expense |
| — |
| — |
| — |
| — |
| — |
| — |
| 2,871 |
| — |
| 2,871 |
| — |
| 2,871 |
| ||||||||
Excess tax benefits related to share-based awards |
| — |
| — |
| — |
| — |
| — |
| — |
| 3,689 |
| — |
| 3,689 |
| — |
| 3,689 |
| ||||||||
Proceeds from initial public offering, net of issuance costs |
| — |
| — |
| — |
| — |
| 11,000,000 |
| — |
| 130,440 |
| — |
| 130,440 |
| — |
| 130,440 |
| ||||||||
Conversion of capital stock into new shares: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| ||||||||
Redeemable common stock |
| — |
| — |
| — |
| — |
| 2,423,616 |
| 31,507 |
| — |
| — |
| 31,507 |
| — |
| 31,507 |
| ||||||||
Series A Preferred Stock |
| — |
| — |
| — |
| — |
| 6,211,356 |
| 101,815 |
| — |
| — |
| 101,815 |
| — |
| 101,815 |
| ||||||||
Class A and B common stock |
| (1,657,500 | ) | — |
| (30,156,274 | ) | (4 | ) | 31,813,774 |
| 4 |
| — |
| — |
| — |
| — |
| — |
| ||||||||
Reclassification of capital |
| — |
| — |
| — |
| — |
| — |
| 15,575 |
| (15,575 | ) | — |
| — |
| — |
| — |
| ||||||||
Restricted stock awards |
| — |
| — |
| — |
| — |
| 8,277 |
| — |
| — |
| — |
| — |
| — |
| — |
| ||||||||
Balance at December 31, 2014 |
| — |
| — |
| — |
| — |
| 51,457,023 |
| 148,901 |
| 9,893 |
| 5,354 |
| 164,148 |
| 4,579 |
| 168,727 |
| ||||||||
Net income (loss) |
| — |
| — |
| — |
| — |
| — |
| — |
| — |
| 25,776 |
| 25,776 |
| (1,004 | ) | 24,772 |
| ||||||||
Proceeds from follow-on public offering, net of issuance costs |
| — |
| — |
| — |
| — |
| 6,821,125 |
| 187,988 |
| — |
| — |
| 187,988 |
| — |
| 187,988 |
| ||||||||
Repurchase of stock options |
| — |
| — |
| — |
| — |
| — |
| (34,194 | ) | (2,104 | ) | — |
| (36,298 | ) | — |
| (36,298 | ) | ||||||||
Issuance of shares of no par common stock as partial consideration of BioRx, LLC aquisition |
| — |
| — |
| — |
| — |
| 4,038,853 |
| 125,697 |
| — |
| — |
| 125,697 |
| — |
| 125,697 |
| ||||||||
Issuance of shares of no par common stock as partial consideration of Burman’s Apothecary, LLC aquisition |
| — |
| — |
| — |
| — |
| 253,036 |
| 9,578 |
| — |
| — |
| 9,578 |
| — |
| 9,578 |
| ||||||||
Stock issued upon stock option exercises |
| — |
| — |
| — |
| — |
| 1,943,022 |
| 13,650 |
| (3,309 | ) | — |
| 10,341 |
| — |
| 10,341 |
| ||||||||
Excess tax benefits related to share-based awards |
| — |
| — |
| — |
| — |
| — |
| — |
| 20,805 |
| — |
| 20,805 |
| — |
| 20,805 |
| ||||||||
Share-based compensation expense |
| — |
| — |
| — |
| — |
| — |
| — |
| 3,936 |
| — |
| 3,936 |
| — |
| 3,936 |
| ||||||||
Restricted stock awards |
| — |
| — |
| — |
| — |
| 10,805 |
| — |
| — |
| — |
| — |
| — |
| — |
| ||||||||
Balance at December 31, 2015 |
| — |
| — |
| — |
| — |
| 64,523,864 |
| 451,620 |
| 29,221 |
| 31,130 |
| 511,971 |
| 3,575 |
| 515,546 |
| ||||||||
Adoption of ASU 2016-09 (Note 3) |
| — |
| — |
| — |
| — |
| — |
| — |
| — |
| 16,903 |
| 16,903 |
|
|
| 16,903 |
| ||||||||
Net income (loss) |
| — |
| — |
| — |
| — |
| — |
| — |
| — |
| 28,273 |
| 28,273 |
| (3,253 | ) | 25,020 |
| ||||||||
Issuance of shares of no par common stock upon full contingent consideration payout |
| — |
| — |
| — |
| — |
| 1,346,282 |
| 36,888 |
| — |
| — |
| 36,888 |
| — |
| 36,888 |
| ||||||||
Issuance of shares of no par common stock as partial consideration of Valley Campus Pharmacy, Inc. aquisition |
| — |
| — |
| — |
| — |
| 324,244 |
| 9,507 |
| — |
| — |
| 9,507 |
| — |
| 9,507 |
| ||||||||
Stock issued upon stock option exercises |
| — |
| — |
| — |
| — |
| 564,844 |
| 5,813 |
| (1,365 | ) | — |
| 4,448 |
| — |
| 4,448 |
| ||||||||
Share-based compensation expense |
| — |
| — |
| — |
| — |
| — |
| — |
| 5,412 |
| — |
| 5,412 |
| — |
| 5,412 |
| ||||||||
Restricted stock awards |
| — |
| — |
| — |
| — |
| 5,765 |
| — |
| — |
| — |
| — |
| — |
| — |
| ||||||||
Balance at December 31, 2016 |
| — |
| $ | — |
| — |
| $ | — |
| 66,764,999 |
| $ | 503,828 |
| $ | 33,268 |
| $ | 76,306 |
| $ | 613,402 |
| $ | 322 |
| $ | 613,724 |
|
See accompanying notes to consolidated financial statements.
DIPLOMAT PHARMACY, INC.
Notes to Consolidated Financial Statements
(Dollars in thousands, except per share amounts)
1. DESCRIPTION OF BUSINESS
Diplomat Pharmacy, Inc. and its consolidated subsidiaries (the “Company”) operate a specialty pharmacy business that stocks, dispenses, and distributes prescriptions for various biotechnology and specialty pharmaceutical manufacturers. Its primary focus is on medication management programs for individuals with complex chronic diseases. Disease states covered include oncology, immunology, hepatitis, specialty infusion therapy, multiple sclerosis, and many other serious or long-term conditions. The Company has its corporate headquarters and main distribution facility in Flint, Michigan, and operates 19 other pharmacy locations in Arizona, California, Connecticut, Florida, Illinois, Iowa, Maryland, Massachusetts, Michigan, Minnesota, North Carolina, Ohio, Pennsylvania, and Texas. The Company also has centralized call centers to effectively deliver services to customers located in all 50 states in the United States of America (“U.S.”) and U.S. territories.
Initial Public Offering
In October 2014, the Company completed its initial public offering (“IPO”), in which 15,333,333 shares of common stock were sold at a public offering price of $13.00 per share. The Company sold 11,000,000 shares of common stock, and certain existing shareholders sold 4,333,333 shares of common stock. The Company did not receive any proceeds from the sale of common stock by the existing shareholders. The Company received net proceeds of $130,440 after deducting underwriting discounts and commissions of $9,652, and other offering expenses of $2,908. Proceeds of $80,458 were used to repay existing indebtedness to certain current or former shareholders and employees ($19,824), and borrowings under the line of credit ($60,634). The remaining proceeds were used for working capital and other general corporate purposes.
Immediately prior to the closing of the IPO, each share of the Company’s then-outstanding capital stock converted into one share of its newly-authorized shares of no par value common stock. Refer to notes 15, 16, and 17.
Follow-On Public Offering
In March 2015, the Company completed a public equity offering, in which 9,821,125 shares of common stock were sold at $29.00 per share. The Company sold 6,821,125 shares of common stock, and certain existing shareholders sold 3,000,000 shares of common stock. The Company did not receive any proceeds from the sale of common stock by the existing shareholders. The Company received net proceeds of $187,988 after deducting underwriting discounts and commissions of $9,141, and other offering expenses of $685. The Company used $36,298 of the net proceeds to repurchase options to purchase common stock held by a number of current and former employees, including certain executive officers, with the remainder of the proceeds used to pay a portion of the cash consideration for the BioRx, LLC (“BioRx”) acquisition (Note 4). The purchase price for each stock option repurchased was based on the public offering price per share, net of the underwriting discount and each individual’s exercise price.
2. BASIS OF PRESENTATION
The accompanying consolidated financial statements have been prepared in accordance with accounting principles generally accepted in the U.S. (“U.S. GAAP”) and the applicable rules and regulations of the Securities and Exchange Commission (“SEC”).
Stock Split
In October 2014, immediately prior to the completion of the IPO, the Board of Directors declared and approved a 8,500-for-one stock split, effected in the form of a stock dividend, on each share of common stock outstanding to the
common shareholders of record. Accordingly, all share and per share amounts in these consolidated financial statements and notes thereto, were adjusted, where applicable, to reflect the stock split on a retroactive basis.
Effect of Conversion from S Corporation to C Corporation
On January 23, 2014, the Company converted its income tax status from an S corporation to a C corporation. Accordingly, on that date, the Company recorded a net deferred income tax liability of $2,965 and a charge to income tax expense for the same amount. The Company reclassified its accumulated deficit, inclusive of the net deferred tax liability adjustment, into additional paid-in capital on the date of conversion.
Reclassifications
Certain items in the prior periods’ financial statements have been reclassified to conform to the current presentation.
3. SUMMARY OF SIGNIFICANT ACCOUNTING POLICIES
Principles of Consolidation
The consolidated financial statements include the accounts of Diplomat Pharmacy, Inc., its wholly owned subsidiaries, and a 51 percent owned subsidiary, formed in August 2014, which the Company controls. The Company also owns a 25 percent interest in a non-consolidated entity which is accounted for under the equity method of accounting since the Company does not control the entity but has the ability to exercise significant influence over its operating and financial policies. This equity method investment was fully impaired during the fourth quarter of 2014 (Note 9). An investment in an entity in which the Company owns less than 20 percent and does not have the ability to exercise significant influence is accounted for under the cost method. This cost method investment was impaired during the fourth quarter of 2016 (Note 9).
Noncontrolling interest in a consolidated subsidiary in the consolidated balance sheets represents the minority shareholders’ proportionate share of the equity in such subsidiary. Consolidated net income (loss) is allocated to the Company and noncontrolling interests (i.e., minority shareholders) in proportion to their percentage ownership.
All intercompany transactions and balances have been eliminated in consolidation.
Use of Estimates
The preparation of financial statements in conformity with U.S. GAAP requires management to make estimates and assumptions that affect the amounts reported therein. Due to the inherent uncertainty involved in making estimates, actual results reported in future periods may be based upon amounts that differ from these estimates.
Concentrations of Risk
Financial instruments which potentially subject the Company to concentrations of credit risk consist principally of cash on deposit with banks or other financial institutions and trade accounts receivable.
A federal program provides non-interest bearing cash balances insurance coverage up to $250 per depositor at each financial institution. The Company’s cash balances may exceed federally insured limits.
Concentration of credit risk with respect to trade accounts receivable is limited by the large number of patients comprising the Company’s customer base and their dispersion across multiple payors and multiple geographic areas. No single payor customer accounted for more than 10 percent of net sales for any period presented or trade accounts receivable at December 31, 2016 and 2015.
The Company purchases a significant portion of its prescription drug inventory from AmerisourceBergen, a prescription drug wholesaler. These purchases accounted for approximately 49 percent, 50 percent, and 57 percent of cost of products sold for the years ended December 31, 2016, 2015, and 2014, respectively. The Company has
alternative vendors available if necessary. See Note 14 for discussion of the Company’s minimum purchase obligation with AmerisourceBergen.
The Company purchases certain prescription drugs from Celgene Corporation (“Celgene”) and Pharmacyclics, Inc. (“Pharmacyclics”), drug manufacturers. Purchases from Celgene and Pharmacyclics accounted for approximately 13 percent and 10 percent, 12 percent and 9 percent, and 15 percent and 7 percent of cost of products sold for the years ended December 31, 2016, 2015, and 2014, respectively, with no minimum purchase obligation. The specialty drugs that the Company purchases from Celgene and Pharmacyclics are not available from any other source.
Cash Equivalents
The Company considers all highly liquid investments with maturities of three months or less from the date of purchase to be cash equivalents.
Accounts Receivable, net
Trade accounts receivable are stated at the invoiced amount. Trade accounts receivable primarily include amounts from third-party pharmacy benefit managers and insurance providers and are based on contracted prices. Trade accounts receivable are unsecured and require no collateral. Trade accounts receivable terms vary by payor, but generally are due within 30 days after the sale of the product or performance of the service.
The Company maintains an allowance for doubtful accounts that reduces receivables to amounts that are expected to be collected. In estimating the allowance, management considers factors such as current overall economic conditions, historical and anticipated customer performance, historical experience with write-offs, and the level of past due accounts. The Company’s general policy for uncollectible accounts, if not reserved through specific examination procedures, is to reserve based upon the aging categories of accounts receivable. Account balances are charged off against the allowance after all means of collection have been exhausted and the potential for recovery is considered remote.
Activity in the allowance for doubtful accounts was as follows:
|
| Year Ended December 31, |
| |||||||
|
| 2016 |
| 2015 |
| 2014 |
| |||
Beginning balance |
| $ | (8,123 | ) | $ | (3,043 | ) | $ | (849 | ) |
Charged to expense |
| (9,534 | ) | (5,990 | ) | (4,045 | ) | |||
Write-offs, net of recoveries |
| 2,400 |
| 910 |
| 1,851 |
| |||
Ending balance |
| $ | (15,257 | ) | $ | (8,123 | ) | $ | (3,043 | ) |
Inventories
Inventories consist of prescription and over-the-counter medications and are stated at the lower of cost or market. Cost is determined using the first-in, first-out method. Prescription medications are returnable to the Company’s vendors and fully refundable before six months of expiration, and any remaining expired medication is relieved from inventory on a quarterly basis.
Property and Equipment, net
Property and equipment are stated at cost less accumulated depreciation. Depreciation is generally computed on a straight-line basis over the estimated useful lives of the assets. The costs of leasehold improvements are depreciated either over the life of the improvement or the lease term, whichever is shorter. For income tax purposes, accelerated methods of depreciation are generally used. Significant improvements are capitalized, and disposed or replaced property is written off. Maintenance and repairs are charged to expense in the period they are incurred. When items of property or equipment are sold or retired, the related cost and accumulated depreciation are removed from the accounts, and any gain or loss is included in earnings.
Capitalized Software for Internal Use, net
The Company capitalizes certain development costs primarily related to a custom-developed, proprietary, scalable patient care system. The Company expenses the costs incurred during the preliminary project stage, and capitalizes the direct development costs, including the associated payroll and related costs for employees and outside contractors working on development, during the application development stage. The Company monitors development on an ongoing basis and capitalizes the costs of any major improvements or that result in significant additional functionality.
Capitalized internal use software costs are amortized on a straight-line basis over the estimated useful lives of the assets, generally three to five years. For income tax purposes, accelerated methods of amortization are generally used. Management evaluates the useful lives of these assets on an annual basis.
Definite-Lived Intangible Assets, net
Definite-lived intangible assets consist of assets related to acquisitions and are amortized over their estimated useful lives using an accelerated method for patient and physician relationships, and the straight line method for the remaining intangible assets.
Long-Lived Assets
Long-lived assets, such as property and equipment, capitalized software for internal use, and definite-lived intangible assets, are reviewed for impairment whenever events or changes in circumstances indicate that the carrying amount of an asset may not be recoverable. If circumstances require a long-lived asset or asset group to be tested for possible impairment, the Company compares the undiscounted cash flows expected to be generated by that asset or asset group to its carrying amount. If the carrying amount of the long-lived asset or asset group is not recoverable on an undiscounted cash flow basis, an impairment charge is recognized to the extent that the carrying amount exceeds fair value. Fair values of long-lived assets are determined through various techniques, such as applying probability weighted, expected present value calculations to the estimated future cash flows using assumptions a market participant would utilize, or through the use of a third-party independent appraiser or valuation specialist.
Goodwill
Goodwill represents the excess acquisition cost of an acquired entity over the estimated fair values of the net tangible assets and the identifiable intangible assets acquired. Goodwill is not amortized, but rather is reviewed for impairment annually during the fourth quarter, or more frequently if facts or circumstances indicate that the carrying value may not be recoverable.
An entity has the option to perform a qualitative assessment to determine whether it is more-likely-than-not that the fair value of the reporting unit is less than its carrying amount prior to performing a quantitative impairment test. The qualitative assessment evaluates various events and circumstances, such as macro-economic conditions, industry and market conditions, cost factors, relevant events and financial trends that may impact a reporting unit’s fair value. If it is determined that the estimated fair value of the reporting unit is more-likely-than-not less than its carrying amount, including goodwill, a quantitative assessment is required. Otherwise, no further analysis is necessary.
If a quantitative assessment is performed, step one is to compare a reporting unit’s fair value to its carrying value. A reporting unit’s fair value is determined based upon consideration of various valuation methodologies, including the income approach which utilizes projected future cash flows discounted at rates commensurate with the risks involved, and multiples of current and future earnings. If the fair value of a reporting unit is less than its carrying amount, an indication of goodwill impairment exists and the Company must perform step two of the quantitative assessment. Under step two, a goodwill impairment loss is recognized for any excess of the carrying amount of a reporting unit’s goodwill over the implied fair value of that goodwill. The implied fair value of goodwill is determined by allocating the fair value of a reporting unit in a manner similar to a purchase price allocation and the residual fair value after this allocation is the implied fair value of the reporting unit goodwill.
See the New Accounting Pronouncements section of this Note regarding the simplification of the goodwill impairment test that the Company intends to early adopt on January 1, 2017.
Debt Issuance Costs
Costs incurred related to the issuance of the Company’s credit facility were deferred and are being amortized to interest expense over the term of the agreement.
Revenue Recognition
The Company recognizes revenue from prescription drug sales for home delivery at the time the drugs are shipped. At the time of shipment, the Company has performed substantially all of its obligations under its payor contracts and does not experience a significant level of returns or reshipments. Revenues from dispensing specialty prescriptions that are picked up by patients at an open-door or retail pharmacy location are recorded at prescription adjudication, which approximates the fill date. Sales taxes are presented on a net basis (excluded from revenues and costs). Revenues generated from prescription drug sales were $4,386,643, $3,346,652, and $2,202,299 for the years ended December 31, 2016, 2015, and 2014, respectively.
The Company accrues an estimate of fees, including direct and indirect remuneration fees (“DIR fees”), which are assessed or expected to be assessed by payors at some point after adjudication of a claim, as a reduction at the time revenue is recognized. Changes in the Company’s estimate of such fees are recorded when the change becomes known.
The Company recognizes revenue from service, data, and consulting services when the services have been performed and the earnings process is therefore complete. Revenues generated from service, data, and consulting services were $23,745, $19,979, and $12,657 for the years ended December 31, 2016, 2015, and 2014, respectively.
The Company derived its revenue from the following therapeutic classes:
|
| Year Ended December 31, |
| |||||||
|
| 2016 |
| 2015 |
| 2014 |
| |||
Oncology |
| $ | 2,102,130 |
| $ | 1,432,091 |
| $ | 1,068,751 |
|
Immunology(1) |
| 644,173 |
| 510,708 |
| 438,145 |
| |||
Hepatitis |
| 583,751 |
| 520,771 |
| <10 | % | |||
Specialty Infusion |
| 505,240 |
| 374,884 |
| <10 | % | |||
Multiple Sclerosis |
| <10 | % | <10 | % | 226,805 |
| |||
Other (none greater than 10% in the period) |
| 575,094 |
| 528,177 |
| 481,255 |
| |||
Total revenue |
| $ | 4,410,388 |
| $ | 3,366,631 |
| $ | 2,214,956 |
|
(1) Includes drugs dispensed to treat arthritis, Crohn’s disease and psoriasis.
Shipping and Handling Costs
Shipping and handling costs are not billed to patients; therefore, there are no shipping and handling revenues. The Company recognizes shipping and handling costs as incurred as a component of “Selling, general and administrative expenses” and were $15,144, $13,899, and $12,269 for the years ended December 31, 2016, 2015, and 2014, respectively.
Advertising and Marketing Costs
Advertising and marketing costs are expensed as incurred and were $3,868, $3,553, and $1,174 for the years ended December 31, 2016, 2015, and 2014, respectively.
Defined Contribution Savings Plans
The Company maintains certain defined contribution savings plans for eligible employees. The total expenses attributable to the Company’s defined contribution savings plans were $2,665, $1,877, and $1,179 for the years ended December 31, 2016, 2015, and 2014, respectively.
Share-Based Compensation
The Company grants stock options to key employees, which are accounted for as equity awards. The exercise price of a granted stock option is equal to the closing market stock price of the underlying common share on the date the option is granted. The grant date fair value of these awards is measured using the Black-Scholes-Merton option pricing model. Stock options generally become exercisable in installments of 25 percent per year, beginning on the first anniversary of the grant date and each of the three anniversaries thereafter, and have a maximum term of ten years. Certain stock option grants have performance-based conditions, which require the satisfaction of one-year revenue and Adjusted EBITDA goals prior to vesting. The Company expenses the grant date fair value of its stock options over their respective vesting periods on a straight-line basis.
The Company grants restricted stock awards to non-employee directors, which are accounted for as equity awards. Such restricted stock fully vests on the first anniversary of the grant date. The grant date fair value of a restricted stock award is determined by the closing market price of the Company’s common stock as of the date of grant. The grant date fair value of restricted stock is expensed over the vesting period on a straight-line basis.
Income Taxes
Income taxes are accounted for under the asset and liability method. Deferred tax assets and liabilities are recognized for the future tax consequences attributable to differences between the financial statement carrying amounts of existing assets and liabilities and their respective tax bases and operating loss and tax credit carryforwards. Deferred tax assets and liabilities are measured using enacted tax rates expected to apply to taxable income in the years in which those temporary differences are expected to be recovered or settled. The effect on deferred tax assets and liabilities of a change in tax rates is recognized in income in the period that includes the enactment date. The Company provides a valuation allowance against net deferred tax assets unless, based upon the available evidence, it is more likely than not that the deferred tax assets will be realized.
The Company records interest and penalties related to tax uncertainties as income tax expense. Based on management’s evaluation, the Company concluded there were no significant uncertain tax positions requiring recognition in its consolidated financial statements.
Prior to January 23, 2014, the Company had elected to be taxed under the provisions of Subchapter S of the Internal Revenue Code. Under these provisions, the Company did not pay federal corporate income taxes on its taxable income. Instead, the shareholders were liable for individual federal income taxes on their respective shares of the Company’s taxable income. Distributions were made periodically to the Company’s shareholders to the extent needed to cover their income tax liability based on the Company’s taxable income.
Segment Information
The Company’s chief operating decision maker reviews the financial results of the Company in total when evaluating financial performance and for purposes of allocating resources. The Company has thus determined that it operates in a single reportable segment — specialty pharmacy services.
Accounting Standards Update (“ASU”) Adoption — Debt Issuance Cost Presentation
In April 2015, the Financial Accounting Standards Board (“FASB”) issued ASU No. 2015-03, Interest — Imputation of Interest (Subtopic 835-30): Simplifying the Presentation of Debt Issuance Costs (“ASU 2015-03”), and, in August 2015, the FASB issued ASU No. 2015-15, Interest — Imputation of Interest (Subtopic 835-30): Presentation and Subsequent Measurement of Debt Issuance Costs Associated with Line-of-Credit Arrangements - Amendments to SEC Paragraphs Pursuant to Staff Announcement at June 18, 2015 EITF Meeting (“ASU 2015-15”). ASU 2015-03
required that debt issuance costs related to a recognized debt liability be presented in the balance sheet as a direct deduction from the carrying amount of that debt liability, consistent with debt discounts. ASU 2015-15 then clarified that the SEC staff would not object to debt issuance costs related to a line-of-credit arrangement being presented as an asset on the balance sheet, regardless of whether there are any outstanding borrowings on the line-of-credit arrangement. These ASUs were effective for annual periods beginning after December 15, 2015, and for interim periods within those annual periods. Upon adoption, these ASUs were to be applied on a retrospective basis and disclosed as a change in an accounting principle.
Effective January 1, 2016, the Company adopted the accounting guidance contained within ASU 2015-03 and 2015-15. The following December 31, 2015 consolidated balance sheet line items were adjusted due to this adoption:
|
| As |
|
|
|
|
| |||
|
| Previously |
|
|
|
|
| |||
|
| Reported |
| Adjustment |
| As Adjusted |
| |||
Other noncurrent assets |
| $ | 5,194 |
| $ | (4,294 | ) | $ | 900 |
|
Total assets |
| 1,005,873 |
| (4,294 | ) | 1,001,579 |
| |||
Long-term debt, less current portion |
| 111,000 |
| (4,294 | ) | 106,706 |
| |||
Total liabilities |
| 490,327 |
| (4,294 | ) | 486,033 |
| |||
Total liabilities and shareholders’ equity |
| 1,005,873 |
| (4,294 | ) | 1,001,579 |
| |||
Debt issuance costs of $550 and $719 related to the Company’s line of credit arrangement remained classified within “Other noncurrent assets” as of December 31, 2016 and 2015, respectively.
ASU Adoption — Employee Share-Based Payment Accounting
In March 2016, the FASB issued ASU No. 2016-09, Compensation — Stock Compensation (Topic 718): Improvements to Employee Share-Based Payment Accounting (“ASU 2016-09”). The intent of ASU 2016-09 is to simplify several aspects of the accounting for employee share-based payment award transactions, including: recognition of excess tax benefits irrespective of whether the benefit reduces taxes payable in the current period; recognition of excess tax benefits as a reduction to income taxes on the statement of operations; changes to the determination of award classification as being either an equity or liability award; and the cessation of classifying excess tax benefits as a decrease to operating cash flows and as an increase to financing cash flows on the statement of cash flows. ASU 2016-09 is effective for annual periods beginning on or after December 15, 2016, including interim periods within those annual periods. Early adoption is permitted.
Effective January 1, 2016, the Company adopted the accounting guidance contained within ASU 2016-09. As a result, the Company recorded a $16,903 current deferred tax asset and a $16,903 increase to retained earnings on January 1, 2016 to recognize the Company’s excess tax benefits that existed as of December 31, 2015 (modified retrospective application). Beginning January 1, 2016, the Company recognizes all newly arising excess tax benefits as a reduction to income tax expense in its consolidated statement of operations, which resulted in the Company’s recognition of $4,148 in benefits to income tax expense during the year ended December 31, 2016. Also beginning January 1, 2016, the Company elected the prospective transition method such that excess tax benefits will no longer be reflected as a decrease to cash flows from operating activities and as an increase to cash flows from financing activities on the consolidated statement of cash flows. Finally, effective January 1, 2016, the Company elected to account for share-based compensation forfeitures when they occur. There was no impact of this election because prior to the adoption the Company did not have adequate historical information to estimate forfeitures. No prior period amounts have been adjusted as a result of the adoption of ASU 2016-09.
ASU Adoption — Transition to the Equity Method of Accounting
In March 2016, the FASB issued ASU No. 2016-07, Investments — Equity Method and Joint Ventures (Topic 323): Simplifying the Transition to the Equity Method of Accounting (“ASU 2016-07”), eliminating the requirement that when an investment qualifies for use of the equity method as a result of an increase in the level of ownership interest or degree of influence, an investor must adjust the investment, results of operations, and retained earnings retroactively on a step-by-step basis as if the equity method had been in effect during all previous periods that the investment had been held. Instead, ASU 2016-07 requires that the equity method investor add the cost of acquiring
the additional interest in the investee to the current basis of the investor’s previously held interest and adopt the equity method of accounting as of the date the investment qualifies for equity method accounting. Therefore, upon qualifying for the equity method of accounting, no retroactive adjustment of the investment is required. ASU 2016-07 is effective for annual periods beginning on or after December 15, 2016, including interim periods within those annual periods. Early adoption is permitted.
Effective January 1, 2016, the Company adopted the accounting guidance contained within ASU 2016-07. There was no impact to the Company’s consolidated financial statements as a result of this adoption.
New Accounting Pronouncements
In May 2014, the FASB issued ASU No. 2014-09, Revenue from Contracts with Customers (Topic 606) (“ASU 2014-09”), which will supersede the existing revenue recognition guidance under U.S. GAAP. The new standard focuses on creating a single source of revenue guidance for revenue arising from contracts with customers for all industries. The objective of the new standard is for companies to recognize revenue when it transfers the promised goods or services to its customers at an amount that represents what the company expects to be entitled to in exchange for those goods or services. In July 2015, the FASB issued ASU No. 2015-14, Revenue from Contracts with Customers (Topic 606) Deferral of the Effective Date, which deferred the effective date of ASU 2014-09 by one year to annual reporting periods beginning after December 15, 2017 for public entities, though early adoption is permitted. ASU 2014-09 permits two methods of adoption: retrospectively to each prior reporting period presented (full retrospective method), or retrospectively with the cumulative effect of initially applying the guidance recognized at the date of initial application (cumulative catch-up transition method). The Company currently anticipates adopting ASU 2014-09 using the cumulative catch-up transition method. The Company continues to assess the impact that the adoption of ASU 2014-09 will have on its consolidated financial statements and/or notes thereto, although the Company does not expect the impact to be significant.
In July 2015, the FASB issued ASU No. 2015-11, Inventory (Topic 330): Simplifying the Measurement of Inventory, requiring that inventory be measured at the lower of cost and net realizable value. Net realizable value is defined as estimated selling price in the ordinary course of business, less reasonably predictable costs of completion, disposal, and transportation. This ASU is effective for annual periods beginning on or after December 15, 2016, including interim periods within those annual periods. The Company does not expect the adoption of this guidance to have a significant impact on its consolidated financial statements and/or notes thereto.
In November 2015, the FASB issued ASU No. 2015-17, Income Taxes (Topic 740): Balance Sheet Classification of Deferred Taxes, eliminating the current requirement for companies to present deferred tax assets and liabilities as current and noncurrent. Instead, companies will be required to classify all deferred tax assets and liabilities as noncurrent. This ASU is effective for annual periods beginning on or after December 15, 2016, including interim periods within those annual periods, and can be adopted either prospectively or retrospectively. The adoption of this guidance will result in a balance sheet reclassification and require related disclosure revisions in the Company’s consolidated financial statements and notes thereto.
In February 2016, the FASB issued ASU No. 2016-02, Leases (Topic 842), requiring lessees to recognize a right-of-use asset and a lease liability for all leases (with the exception of short-term leases) at the lease commencement date. This ASU is effective for annual periods beginning on or after December 15, 2018, including interim periods within those annual periods. Early adoption is permitted. The Company is currently evaluating the impact that the adoption of this guidance will have on its consolidated financial statements and/or notes thereto.
In January 2017, the FASB issued ASU No. 2017-04, Intangibles — Goodwill and Other (Topic 350): Simplifying the Test for Goodwill Impairment (“ASU 2017-04”), which eliminates Step two from the goodwill impairment test. Instead, an entity should perform its annual, or interim, goodwill impairment test by comparing the fair value of a reporting unit with its carrying amount. An entity should recognize an impairment charge for the amount by which the carrying amount exceeds the reporting unit’s fair value; however, the loss recognized should not exceed the total amount of goodwill allocated to that reporting unit. This ASU is effective for an entity’s annual or any interim goodwill impairment tests in fiscal years beginning after December 15, 2019. Early adoption is permitted. The Company intends to adopt the accounting guidance contained within ASU 2017-04 effective January 1, 2017. The Company anticipates no immediate impact on its consolidated financial statements as a result of this adoption.
4. BUSINESS ACQUISITIONS
The Company accounts for its business acquisitions using the acquisition method as required by FASB Accounting Standards Codification Topic 805, Business Combinations. The Company ascribes significant value to the synergies and other benefits that do not meet the recognition criteria of acquired identifiable intangible assets. Accordingly, the value of these components is included within goodwill. The Company’s business acquisitions described below, except for one subsidiary of BioRx, were treated as asset purchases for income tax purposes and the related goodwill resulting from these business acquisitions is deductible for income tax purposes. The results of operations for acquired businesses are included in the Company’s consolidated financial statements from their respective acquisition dates.
The assets acquired and liabilities assumed in the business combinations described below, including identifiable intangible assets, were based on their estimated fair values as of the acquisition date. The excess of purchase price over the estimated fair value of the net tangible and identifiable intangible assets acquired was recorded as goodwill. The allocation of the purchase price required management to make significant estimates in determining the fair values of assets acquired and liabilities assumed, especially with respect to identifiable intangible assets. These estimated fair values were based on information obtained from management of the acquired companies and historical experience and, with respect to the long-lived tangible and intangible assets, were made with the assistance of an independent valuation firm. These estimates included, but were not limited to, the cash flows that an asset is expected to generate in the future, and the cost savings expected to be derived from acquiring an asset, discounted at rates commensurate with the risks and uncertainties involved. For acquisitions that involved contingent consideration, the Company recognized a liability equal to the fair value of the contingent consideration obligation as of the acquisition date. The estimate of fair value of a contingent consideration obligation required subjective assumptions regarding future business results, discount rates, and probabilities assigned to various potential business result scenarios.
Valley Campus Pharmacy, Inc.
On June 1, 2016, the Company acquired Valley Campus Pharmacy, Inc., doing business as TNH Advanced Specialty Pharmacy (“TNH”). TNH, a specialty pharmacy based in Van Nuys, California, provides medication management programs for individuals with complex chronic diseases, including oncology, hepatitis, and immunology. The Company acquired TNH to expand its existing business, enhance its proprietary technology, and increase its geographic presence, particularly in California and Texas. The following table summarizes the consideration transferred to acquire TNH:
Cash |
| $ | 68,915 |
|
324,244 restricted common shares |
| 9,507 |
| |
|
| $ | 78,422 |
|
The above share consideration at closing is based on 324,244 shares, in accordance with the purchase agreement, multiplied by the per share closing market price of the Company’s common stock as of May 31, 2016 ($32.58), and multiplied by 90 percent to account for the restricted nature of the shares.
Approximately $3,800 of the purchase consideration was deposited into an escrow account to be held for two years after the closing date to satisfy any indemnification claims that may be made by the Company.
The Company incurred acquisition-related costs of $410 which were charged to “Selling, general and administrative expenses” during the year ended December 31, 2016.
The following table summarizes the preliminary fair values of identifiable assets acquired and liabilities assumed at the acquisition date:
Cash |
| $ | 2,114 |
|
Accounts receivable |
| 16,271 |
| |
Inventories |
| 4,740 |
| |
Prepaid expenses and other current assets |
| 46 |
| |
Property and equipment |
| 200 |
| |
Capitalized software for internal use |
| 14,000 |
| |
Definite-lived intangible assets |
| 13,890 |
| |
Other noncurrent assets |
| 21 |
| |
Accounts payable |
| (29,773 | ) | |
Accrued expenses — compensation and benefits |
| (400 | ) | |
Accrued expenses — other |
| (1,962 | ) | |
Total identifiable net assets |
| 19,147 |
| |
Goodwill |
| 59,275 |
| |
|
| $ | 78,422 |
|
Definite-lived intangible assets that were acquired and their respective useful lives are as follows:
|
| Useful |
| Amount |
| |
Physician relationships |
| 10 years |
| $ | 7,700 |
|
Noncompete employment agreements |
| 5 years |
| 4,490 |
| |
Trade names and trademarks |
| 1 year |
| 1,700 |
| |
|
|
|
| $ | 13,890 |
|
Burman’s Apothecary, LLC
On June 19, 2015, the Company acquired all of the outstanding equity interests of Burman’s Apothecary, LLC (“Burman’s”). Burman’s, located in the greater Philadelphia area of Pennsylvania, is a provider of individualized patient care with a primary focus on those infected with the hepatitis C virus. The Company acquired Burman’s to expand its existing hepatitis business, enhance its proprietary technology, and increase its national presence. The following table summarizes the consideration transferred to acquire Burman’s:
Cash |
| $ | 77,416 |
|
253,036 restricted common shares |
| 9,578 |
| |
|
| $ | 86,994 |
|
The above share consideration is based on 253,036 shares, as computed in accordance with the purchase agreement, multiplied by the per share closing market price of the Company’s common stock as of June 18, 2015 ($42.06), and multiplied by 90 percent to account for the restricted nature of the shares.
Approximately $5,000 of the purchase consideration was deposited into an escrow account to be held for two years after the closing date to satisfy any indemnification claims that may be made by the Company.
The Company incurred acquisition-related costs of $860 which were charged to “Selling, general and administrative expenses” during the year ended December 31, 2015.
The following table summarizes the fair values of identifiable assets acquired and liabilities assumed at the acquisition date:
Accounts receivable |
| $ | 17,109 |
|
Inventories |
| 8,064 |
| |
Prepaid expenses and other current assets |
| 7,513 |
| |
Property and equipment |
| 88 |
| |
Capitalized software for internal use |
| 17,000 |
| |
Definite-lived intangible assets |
| 22,200 |
| |
Accounts payable |
| (25,761 | ) | |
Accrued expenses — compensation and benefits |
| (169 | ) | |
Accrued expenses — other |
| (6 | ) | |
Total identifiable net assets |
| 46,038 |
| |
Goodwill |
| 40,956 |
| |
|
| $ | 86,994 |
|
Definite-lived intangible assets that were acquired and their respective useful lives are as follows:
|
| Useful |
| Amount |
| |
Physician relationships |
| 10 years |
| $ | 14,000 |
|
Noncompete employment agreements |
| 5 years |
| 5,500 |
| |
Favorable supply agreement |
| 1 year |
| 2,700 |
| |
|
|
|
| $ | 22,200 |
|
BioRx
On April 1, 2015, the Company acquired BioRx, a highly specialized pharmacy and infusion services company based in Cincinnati, Ohio. BioRx provides treatments for patients with ultra-orphan and rare, chronic diseases — predominately administered in the home and often via intravenous infusion. The Company acquired BioRx to expand its existing specialty infusion business and increase its national presence. The following table summarizes the consideration transferred to acquire BioRx:
Cash |
| $ | 217,024 |
|
4,038,853 restricted common shares |
| 125,697 |
| |
Contingent consideration at fair value |
| 41,000 |
| |
|
| $ | 383,721 |
|
The above share consideration at closing is based on 4,038,853 shares, in accordance with the purchase agreement, multiplied by the per share closing market price of the Company’s common stock as of March 31, 2015 ($34.58), and multiplied by 90 percent to account for the restricted nature of the shares.
The purchase price included a contingent consideration arrangement that required the Company to issue up to 1,350,309 shares of its restricted common stock, as computed in accordance with the purchase agreement, to the former holders of BioRx’s equity interests based upon the achievement of a certain earnings before interest, taxes, depreciation, and amortization target in the 12-month period ending March 31, 2016. An independent valuation firm assisted with the Company’s determination of the fair value of the contingent consideration utilizing a Monte Carlo simulation. The fair value of the contingent consideration liability was $46,208 as of December 31, 2015. The Company issued 1,346,282 shares of its common stock, with a fair value of $36,888, along with $104 in cash, in full payout of the contingent consideration arrangement in April 2016.
Approximately $10,000 of the purchase consideration was deposited into an escrow account to be held for two years after the closing date to satisfy any indemnification claims made by the Company.
The Company incurred acquisition-related costs of $1,398 which were charged to “Selling, general and administrative expenses” during the year ended December 31, 2015.
The following table summarizes the fair values of identifiable assets acquired and liabilities assumed at the acquisition date:
Cash and cash equivalents |
| $ | 1,786 |
|
Accounts receivable |
| 37,716 |
| |
Inventories |
| 5,546 |
| |
Deferred income taxes |
| 715 |
| |
Prepaid expenses and other current assets |
| 287 |
| |
Property and equipment |
| 494 |
| |
Definite-lived intangible assets |
| 181,700 |
| |
Other noncurrent assets |
| 163 |
| |
Accounts payable |
| (25,088 | ) | |
Accrued expenses — compensation and benefits |
| (1,653 | ) | |
Accrued expenses — other |
| (852 | ) | |
Deferred income taxes |
| (8,495 | ) | |
Total identifiable net assets |
| 192,319 |
| |
Goodwill |
| 191,402 |
| |
|
| $ | 383,721 |
|
Definite-lived intangible assets that were acquired and their respective useful lives are as follows:
|
| Useful |
| Amount |
| |
Patient relationships |
| 10 years |
| $ | 130,000 |
|
Noncompete employment agreements |
| 5 years |
| 39,700 |
| |
Trade names and trademarks |
| 8 years |
| 12,000 |
| |
|
|
|
| $ | 181,700 |
|
MedPro Rx, Inc.
On June 27, 2014, the Company acquired all of the authorized, issued, and outstanding shares of capital stock of MedPro Rx, Inc. (“MedPro”). MedPro, based in Raleigh, North Carolina, is a specialty pharmacy focused on specialty infusion therapies including hemophilia and immune globulin. The Company acquired MedPro to expand its existing specialty infusion business and increase its presence in the mid-Atlantic and Southern regions of the U.S.
The Company did not acquire MedPro’s affiliate from which MedPro leased certain operating and other facilities. Instead, the Company, commensurate with the acquisition, entered into a five-year external lease agreement for the facilities on similar terms. As the Company does not direct the significant activities of the lessor, it is not consolidated into the Company’s financial statements.
The following table summarizes the consideration transferred to acquire MedPro:
Cash |
| $ | 52,267 |
|
716,695 restricted common shares |
| 12,000 |
| |
Contingent consideration at fair value |
| 4,270 |
| |
|
| $ | 68,537 |
|
The purchase price includes a contingent consideration arrangement that required the Company to pay the former owners an additional payout based upon the achievement of certain revenue and gross profit targets in each of the 12-month periods ending June 30, 2015 and 2016. The maximum payout of contingent consideration was $11,500. Based upon MedPro’s actual results for the 12-month periods ended June 30, 2015 and 2016, the Company paid the maximum payout of $5,750 during both the third quarter of 2015 and 2016.
Approximately $3,500 of the purchase consideration was deposited into an escrow account to be held for two years after the closing date to satisfy any of the Company’s indemnification claims. The full amount was released to the seller from escrow during the third quarter of 2016.
The Company incurred acquisition-related costs of $825 which were charged to “Selling, general and administrative expenses” during the year ended December 31, 2014.
The following table summarizes the fair values of identifiable assets acquired and liabilities assumed at the acquisition date:
Cash and cash equivalents |
| $ | 668 |
|
Accounts receivable |
| 9,050 |
| |
Inventories |
| 3,819 |
| |
Prepaid expenses and other current assets |
| 204 |
| |
Property and equipment |
| 697 |
| |
Capitalized software for internal use |
| 25 |
| |
Definite-lived intangible assets |
| 37,099 |
| |
Accounts payable |
| (3,638 | ) | |
Accrued expenses — compensation and benefits |
| (157 | ) | |
Accrued expenses — other |
| (865 | ) | |
Total identifiable net assets |
| 46,902 |
| |
Goodwill |
| 21,635 |
| |
|
| $ | 68,537 |
|
Definite-lived intangible assets that were acquired and their respective useful lives are as follows:
|
| Useful |
| Amount |
| |
Patient relationships |
| 7 years |
| $ | 24,000 |
|
Trade names and trademarks |
| 10 years |
| 8,700 |
| |
Noncompete employment agreements |
| 5 years |
| 4,399 |
| |
|
|
|
| $ | 37,099 |
|
Pro Forma Operating Results
The following 2016 unaudited pro forma summary presents consolidated financial information as if the TNH acquisition had occurred on January 1, 2015. The following 2015 unaudited pro forma summary presents consolidated financial information as if the TNH acquisition had occurred on January 1, 2015 and the BioRx and Burman’s acquisitions had occurred on January 1, 2014. The unaudited pro forma results reflect certain adjustments related to the acquisitions, such as amortization expense resulting from intangible assets acquired and adjustments to reflect the Company’s borrowings and tax rates. Accordingly, such pro forma operating results were prepared for comparative purposes only and do not purport to be indicative of what would have occurred had the acquisitions been made as of the as if dates or of results that may occur in the future.
|
| Year Ended December 31, |
| ||||
|
| 2016 |
| 2015 |
| ||
Net sales |
| $ | 4,613,181 |
| $ | 4,047,540 |
|
Net income attributable to Diplomat Pharmacy, Inc. |
| $ | 28,990 |
| $ | 34,168 |
|
Net income per common share — basic |
| $ | 0.44 |
| $ | 0.54 |
|
Net income per common share — diluted |
| $ | 0.43 |
| $ | 0.52 |
|
5. FAIR VALUE MEASUREMENTS
The Company utilizes valuation techniques that maximize the use of observable inputs and minimize the use of unobservable inputs to the extent possible. Fair value is defined as the amount that would be received to sell an asset or paid to transfer a liability in an orderly transaction between market participants at the measurement date. As such, fair value is a market-based measurement that should be determined based upon assumptions that market participants would use in pricing an asset or liability. As a basis for considering such assumptions, a three-tier fair value hierarchy was established, which prioritizes the inputs used in measuring fair value as follows:
Level 1: Observable inputs such as quoted prices in active markets;
Level 2: Inputs, other than quoted prices in active markets, that are observable either directly or indirectly; and
Level 3: Unobservable inputs in which there is little or no market data, which require the reporting entity to develop its own assumptions.
An asset or liability’s fair value measurement level within the fair value hierarchy is based on the lowest level of any input that is significant to the fair value measurement. Valuation techniques used need to maximize the use of observable inputs and minimize the use of unobservable inputs.
Assets and liabilities measured at fair value are based on one or more of the following three valuation techniques:
A. Market approach: Prices and other relevant information generated by market transactions involving identical or comparable assets or liabilities.
B. Cost approach: Amount that would be required to replace the service capacity of an asset (replacement cost).
C. Income approach: Techniques to convert future amounts to a single present amount based upon market expectations (including present value techniques, option-pricing and excess earnings models).
The following table presents the placement in the fair value hierarchy of assets and liabilities that were measured and disclosed at fair value on a recurring basis at December 31, 2015:
|
| Asset / |
|
|
| Valuation |
| ||
|
| (Liability) |
| Level 3 |
| Technique |
| ||
Contingent consideration |
| $ | (52,665 | ) | $ | (52,665 | ) | C |
|
The following table sets forth a roll forward of the Level 3 measurements:
|
| Contingent |
| |
Balance at January 1, 2014 |
| $ | (1,300 | ) |
MedPro acquisition |
| (4,270 | ) | |
Change in fair value — American Homecare Federation, Inc. (“AHF”) and MedPro |
| (6,121 | ) | |
Balance at December 31, 2014 |
| (11,691 | ) | |
BioRx acquisition |
| (41,000 | ) | |
Change in fair value — AHF, BioRx, and MedPro |
| (6,724 | ) | |
Payments — AHF and MedPro |
| 6,750 |
| |
Balance at December 31, 2015 |
| (52,665 | ) | |
Change in fair value — BioRx and MedPro |
| 8,922 |
| |
Payments — AHF, BioRx, and MedPro |
| 43,743 |
| |
Balance at December 31, 2016 |
| $ | — |
|
The carrying amounts of the Company’s financial instruments — consisting primarily of cash and cash equivalents, accounts receivable, accounts payable, and other liabilities — approximate their estimated fair values due to the relative short-term nature of the amounts. The carrying amount of debt approximates fair value due to variable interest rates at customary terms and rates the Company could obtain in current financing.
6. PROPERTY AND EQUIPMENT
Property and equipment consisted of the following:
|
|
|
| December 31, |
| ||||
|
| Useful Life |
| 2016 |
| 2015 |
| ||
Land |
| — |
| $ | 332 |
| $ | 332 |
|
Buildings |
| 40 years |
| 10,007 |
| 9,331 |
| ||
Leasehold improvements |
| 5 - 15 years* |
| 1,644 |
| 1,142 |
| ||
Equipment and fixtures |
| 5 - 10 years |
| 12,178 |
| 9,369 |
| ||
Computer equipment |
| 3 - 5 years |
| 6,657 |
| 3,912 |
| ||
Construction in progress |
|
|
| 485 |
| 519 |
| ||
|
|
|
| 31,303 |
| 24,605 |
| ||
Accumulated depreciation |
|
|
| (10,931 | ) | (8,067 | ) | ||
|
|
|
| $ | 20,372 |
| $ | 16,538 |
|
* Unless applicable lease term is shorter.
Depreciation expense for the years ended December 31, 2016, 2015, and 2014 was $3,075, $2,071, and $1,474, respectively.
7. CAPITALIZED SOFTWARE FOR INTERNAL USE
Capitalized software, consisting of software acquired and developed internally, was comprised as follows:
|
|
|
| December 31, |
| ||||
|
| Useful Life |
| 2016 |
| 2015 |
| ||
Capitalized software for internal use |
| 3 - 5 years |
| $ | 74,471 |
| $ | 33,213 |
|
Construction in progress |
|
|
| 1,994 |
| 17,409 |
| ||
|
|
|
| 76,465 |
| 50,622 |
| ||
Accumulated amortization |
|
|
| (26,218 | ) | (13,372 | ) | ||
|
|
|
| $ | 50,247 |
| $ | 37,250 |
|
Amortization expense for the years ended December 31, 2016, 2015, and 2014 was $13,102, $4,541, and $2,635, respectively. Estimated future amortization expense is as follows:
2017 |
| $ | 21,440 |
|
2018 |
| 21,273 |
| |
2019 |
| 7,202 |
| |
2020 |
| 332 |
| |
|
| $ | 50,247 |
|
8. GOODWILL AND DEFINITE-LIVED INTANGIBLE ASSETS
The following table sets forth a roll forward of goodwill:
Balance at January 1, 2014 |
| $ | 1,537 |
|
MedPro acquisition |
| 21,635 |
| |
Miscellaneous |
| (24 | ) | |
Balance at December 31, 2014 |
| 23,148 |
| |
BioRx acquisition |
| 191,402 |
| |
Burman’s acquisition |
| 40,956 |
| |
Miscellaneous |
| 812 |
| |
Balance at December 31, 2015 |
| 256,318 |
| |
TNH acquisition |
| 59,275 |
| |
Miscellaneous |
| 1,023 |
| |
Balance at December 31, 2016 |
| $ | 316,616 |
|
Definite-lived intangible assets consisted of the following:
|
| December 31, 2016 |
| December 31, 2015 |
| ||||||||||||||
|
| Gross |
| Accumulated |
| Net |
| Gross |
| Accumulated |
| Net |
| ||||||
Patient relationships |
| $ | 159,100 |
| $ | (31,445 | ) | $ | 127,655 |
| $ | 159,100 |
| $ | (15,217 | ) | $ | 143,883 |
|
Noncompete employment agreements |
| 54,689 |
| (18,674 | ) | 36,015 |
| 50,199 |
| (8,111 | ) | 42,088 |
| ||||||
Physician relationships |
| 21,700 |
| (2,831 | ) | 18,869 |
| 14,000 |
| (758 | ) | 13,242 |
| ||||||
Trade names and trademarks |
| 23,800 |
| (6,477 | ) | 17,323 |
| 22,100 |
| (2,710 | ) | 19,390 |
| ||||||
Software licensing agreement |
| 2,647 |
| (2,647 | ) | — |
| 2,647 |
| — |
| 2,647 |
| ||||||
Intellectual property |
| 2,157 |
| (2,157 | ) | — |
| 2,157 |
| — |
| 2,157 |
| ||||||
Favorable supply agreement |
| 2,700 |
| (2,700 | ) | — |
| 2,700 |
| (1,463 | ) | 1,237 |
| ||||||
|
| $ | 266,793 |
| $ | (66,931 | ) | $ | 199,862 |
| $ | 252,903 |
| $ | (28,259 | ) | $ | 224,644 |
|
Amortization expense for the years ended December 31, 2016, 2015, and 2014 was $33,868, $24,229, and $4,030, respectively. As of December 31, 2016, the weighted average remaining useful lives for the net carrying amounts of patient relationships, noncompete employment agreements, physician relationships, and trade names and trademarks are 7.8 years, 3.4 years, 6.6 years, and 2.8 years, respectively. Estimated future amortization expense is as follows:
2017 |
| $ | 37,690 |
|
2018 |
| 36,465 |
| |
2019 |
| 35,253 |
| |
2020 |
| 24,459 |
| |
2021 |
| 20,251 |
| |
Thereafter |
| 45,744 |
| |
|
| $ | 199,862 |
|
On August 28, 2014, the Company and two unrelated third party entities entered into a contribution agreement to form a new company, Primrose Healthcare, LLC (“Primrose”). Primrose functions as a management company, managing a network of physicians and medical professionals providing continuum care for patients infected with the hepatitis C virus. The Company contributed $5,000 for its 51 percent ownership interest, of which $2,000 and $3,000 were contributed during the years ended December 31, 2015 and 2014, respectively. The unrelated third party entities contributed a software licensing agreement valued at $2,647 and intellectual property valued at $2,157. During the third quarter of 2016, primarily due to updated projections of continuing losses into the foreseeable future, the Company fully impaired Primrose’s intangible assets. The $4,804 impairment is contained within “Selling, general and administrative expenses” for the year ended December 31, 2016. Primrose’s post-impairment balance sheet consists primarily of cash and cash equivalents as of December 31, 2016.
9. INVESTMENTS IN NON-CONSOLIDATED ENTITIES
Ageology
In October 2011, the Company purchased a 25 percent minority interest in WorkSmart MD, LLC, also known as Ageology, for $5,000 of cash consideration, which was paid in installments during 2011, 2012, and 2013. No further payments or other commitments are required as of December 31, 2016. Because the Company does not direct the activities that most significantly impact the economic performance of Ageology, management has determined that the Company is not its primary beneficiary.
Ageology is an anti-aging physician network dedicated to nutrition, fitness, and hormones, and has created a commercial software product for anti-aging physician practices that became a saleable product during the latter half of 2014. The Company accounted for Ageology under the equity method, as it has significant influence over its operations. The Company’s portion of Ageology’s net loss for the year ended December 31, 2014 was $1,339.
During January 2014, the Company entered into a $500, 8 percent per annum interest bearing secured promissory note receivable from Ageology. During November and December 2013, the Company entered into two $1,000 6 percent per annum interest-bearing promissory notes receivable from Ageology. The notes are secured by all personal property and fixtures owned by Ageology. These notes are due on demand. In addition, in transactions unrelated to the Company, an affiliated entity of the Company’s chief executive officer has personally invested $15,250 in Ageology as of December 31, 2016.
During the fourth quarter of 2014, the Company reassessed the recoverability of its investment in Ageology. Based upon this assessment, it was determined that a full impairment was warranted, primarily due to updated projections of continuing losses into the foreseeable future. The $4,869 impairment is contained within “Equity loss and impairment of non-consolidated entities” for the year ended December 31, 2014.
Physician Resource Management, Inc.
In December 2014, the Company invested $3,500 in Physician Resource Management, Inc. (“PRM”) in exchange for a 15.0 percent equity position. In October 2015, the Company invested an additional $1,459, which increased its equity position in PRM to 19.9 percent. The Company accounted for this investment under the cost method, as the Company does not have significant influence over its operations. In transactions unrelated to the Company, the Company’s chief executive officer has personally invested $250 in PRM through December 31, 2016.
During January 2017, PRM completed the planned sale of its primary asset. Based upon the terms of the sales agreement, the Company anticipates that it will receive approximately $300 in proceeds from this sale. The Company recognized a $4,659 impairment, which is contained within “Equity loss and impairment of non-consolidated entities,” for the year ended December 31, 2016 to write its cost method investment in PRM to net realizable value.
10. DEBT
On July 20, 2012, the Company entered into a credit facility (“facility”) with Capital One, as agent and lender, along with other lenders and credit parties, that provided for borrowings under a line of credit of up to $60,000. In 2013, the facility was amended to increase the commitment under the line of credit to $85,000. In June 2014, the facility was further amended to increase the commitment under the line of credit to $120,000. On April 1, 2015, in connection with the BioRx acquisition, the Company entered into a Second Amended and Restated Credit Agreement with Capital One, as agent and as a lender, the other lenders party thereto, and the other credit parties party thereto, providing for an increase in the Company’s line of credit to $175,000, a fully drawn Term Loan A for $120,000, and a deferred draw term loan for an additional $25,000 (“credit facility”). The credit facility also extended the maturity date to April 1, 2020. The credit facility provides for the issuance of letters of credit up to $10,000 and swingline loans up to $15,000, the issuance and incurrence of which will reduce the availability of the line of credit. The credit facility is guaranteed by substantially all of the Company’s subsidiaries and is collateralized by substantially all of the Company’s and its subsidiaries’ respective assets, with certain exceptions. In addition, the Company has pledged the equity of substantially all of its subsidiaries as security for the obligations under the credit facility. The Company adds newly acquired subsidiaries promptly for purposes of, among other things, the guarantor, collateralization, and pledge provisions of the credit facility. The Company is required to maintain a depository bank account where money is collected and swept directly to the line of credit. Under its line of credit, the Company had weighted average borrowings of $11,986 and $12,022, and maximum borrowings of $82,683 and $78,866 during the years ended December 31, 2016 and 2015, respectively. The Company had $111,000 and $117,000 outstanding on Term Loan A as of December 31, 2016 and 2015, respectively. Unamortized debt issuance costs of $3,316 and $4,294 as of December 31, 2016 and 2015, respectively, are presented in the consolidated balance sheets as direct deductions from the outstanding debt balances (Note 3). The Company had $39,255 and $0 outstanding on its line of credit as of December 31, 2016 and 2015, respectively. The Company had $129,908 and $166,691 available to borrow on its line of credit at December 31, 2016 and 2015, respectively.
At December 31, 2016, the Company’s Term Loan A interest rate options were (i) LIBOR (as defined) plus 2.50 percent or (ii) Base Rate (as defined) plus 1.50 percent, and the Company’s line of credit and swingline loan interest rate options were (i) LIBOR (as defined) plus 2.00 percent or (ii) Base Rate (as defined) plus 1.00 percent. The Company’s Term Loan A interest rate was 3.13 percent and 2.74 percent at December 31, 2016 and 2015, respectively. The Company’s line of credit interest rate was 4.50 percent at December 31, 2016. In addition, the Company is charged a monthly unused commitment fee ranging from 0.25 percent to 0.50 percent on its average unused daily balance on its $175,000 line of credit and from 0.50 percent to 0.75 percent on its $25,000 deferred draw term loan.
During 2015, the Company incurred deferred financing costs of $5,055 associated with the credit facility, which were capitalized. These costs, along with previously unamortized deferred debt issuance costs, are being amortized to interest expense over the term of the credit facility.
The credit facility contains certain financial and non-financial covenants. The Company was in compliance with all such covenants as of December 31, 2016 and 2015.
The Company has the following contractual debt obligations outstanding associated with Term Loan A at December 31, 2016:
2017 |
| $ | 7,500 |
|
2018 |
| 9,000 |
| |
2019 |
| 10,500 |
| |
2020 |
| 84,000 |
| |
|
| $ | 111,000 |
|
The Company recognized related party interest expense of $781 for the year ended December 31, 2014. In October 2014, the Company repaid all of its outstanding borrowings, including related party note payables, with proceeds received from its IPO.
11. SHARE-BASED COMPENSATION
Stock Options
Effective October 2014, the Company established the 2014 Omnibus Incentive Plan (“2014 Plan”), which permits the granting of stock options, stock appreciation rights, restricted stock awards, and other stock-based awards. The 2014 Plan initially authorized up to 4,000,000 shares of common stock for awards to be issued to employees, directors, or consultants of the Company, and each fiscal year, the number of shares reserved for issuance under the plan automatically increases by an amount equal to 2 percent of the total number of outstanding shares of common stock as of the beginning of such fiscal year. The stock-based awards will be issued at no less than the market price on the date the awards are granted. Under the 2014 Plan, the Company granted service-based awards of 1,165,000, 893,896, and 982,000 options to purchase common stock to key employees during the years ended December 31, 2016 and 2015 and the fourth quarter of 2014, respectively. The options become exercisable in installments of 25 percent per year, beginning on the first anniversary of the grant date and each of the three anniversaries thereafter, and have a maximum term of 10 years. The Company also granted performance-based awards of 381,532 and 391,043 options to purchase common stock to key employees under the 2014 Plan during the years ended December 31, 2016 and 2015, respectively, that are earned based upon the Company’s performance relative to specified revenue and adjusted earnings before interest, taxes, depreciation, and amortization goals corresponding to the year in which granted. None of the performance-based awards granted during 2016 were earned and, therefore, no share-based compensation expense was recorded for these awards in 2016. All but 2,084 of the performance-based awards granted during 2015 were earned. The earned options vest in four installments of 25%, with the first installment vesting upon Audit Committee confirmation of the satisfaction of the applicable performance goals, and the remaining installments vesting annually thereafter. These options also have a maximum term of 10 years.
The Company’s 2007 Stock Option Plan, as amended (“2007 Plan”), authorized the granting of stock options to employees, directors, or consultants at no less than the market price on the date the option was granted. Options generally become exercisable in installments of 25 percent per year, beginning on the first anniversary of the grant date and each of the three anniversaries thereafter, and have a maximum term of 10 years. No further awards will be granted under the 2007 Plan. All outstanding awards previously granted under the 2007 Plan, including those granted in 2014, will continue to be governed by their existing terms.
The Company recorded share-based compensation expense associated with stock options of $5,073, $3,748, and $2,846 for the years ended December 31, 2016, 2015, and 2014, respectively.
At December 31, 2016, the total compensation cost related to non-vested options not yet recognized was $13,042, which will be recognized over a weighted average period of 1.5 years, assuming all employees complete their respective service periods for vesting of the options.
A summary of the Company’s stock option activity for the years ended December 31, 2014, 2015, and 2016 is as follows:
|
|
|
|
|
| Weighted |
|
|
| ||
|
|
|
| Weighted |
| Average |
|
|
| ||
|
|
|
| Average |
| Remaining |
| Aggregate |
| ||
|
| Number |
| Exercise |
| Contractual |
| Intrinsic |
| ||
|
| of Options |
| Price |
| Life |
| Value |
| ||
|
|
|
|
|
| (In years) |
|
|
| ||
Outstanding at January 1, 2014 |
| 6,657,504 |
| $ | 4.30 |
| 7.0 |
| $ | 69,732 |
|
Granted |
| 1,867,588 |
| 14.77 |
|
|
|
|
| ||
Repurchased |
| (1,307,761 | ) | 9.39 |
|
|
|
|
| ||
Outstanding at December 31, 2014 |
| 7,217,331 |
| 7.54 |
| 6.9 |
| 142,262 |
| ||
Granted |
| 1,284,939 |
| 39.11 |
|
|
|
|
| ||
Repurchased |
| (1,641,387 | ) | 5.44 |
|
|
|
|
| ||
Exercised |
| (1,943,022 | ) | 5.32 |
|
|
|
|
| ||
Expired/cancelled |
| (803,176 | ) | 16.59 |
|
|
|
|
| ||
Outstanding at December 31, 2015 |
| 4,114,685 |
| 17.53 |
| 7.7 |
| 76,567 |
| ||
Granted |
| 1,546,532 |
| 22.64 |
|
|
|
|
| ||
Exercised |
| (564,844 | ) | 7.87 |
|
|
|
|
| ||
Expired/cancelled |
| (683,032 | ) | 27.41 |
|
|
|
|
| ||
Outstanding at December 31, 2016 |
| 4,413,341 |
| $ | 19.02 |
| 7.0 |
| $ | 11,558 |
|
|
|
|
|
|
|
|
|
|
| ||
Exercisable at December 31, 2016 |
| 2,005,925 |
| $ | 11.56 |
| 4.6 |
| $ | 10,385 |
|
The total intrinsic value of options exercised/repurchased during the years ended December 31, 2016, 2015, and 2014 was $13,048, $103,317, and $9,400, respectively.
The weighted average grant-date fair value of options granted during the years ended December 31, 2016, 2015, and 2014 was $6.34, $11.84, and $3.37, respectively. The grant-date fair value of each option award was estimated using the Black-Scholes-Merton option-pricing model using the assumptions set forth in the following table:
|
| Year Ended December 31, |
| ||||
|
| 2016 |
| 2015 |
| 2014 |
|
Exercise price |
| $14.40 - $36.60 |
| $27.80 - $48.72 |
| $13.00 - $16.74 |
|
Expected volatility |
| 23.90% - 24.76% |
| 25.12% - 26.70% |
| 23.2% - 24.3% |
|
Expected dividend yield |
| 0% |
| 0% |
| 0% |
|
Risk-free rate for expected term |
| 1.23% - 2.06% |
| 1.53% - 2.01% |
| 1.82% - 1.85% |
|
Expected term (in years) |
| 6.25 |
| 6.25 |
| 6.25 |
|
Estimating grant date fair values for employee stock options requires management to make assumptions regarding the current value of the Company’s common shares (prior to IPO closing), expected volatility of value of those underlying shares, the risk-free rate over the expected life of the stock options, and the length of time in years that the granted options are expected to be outstanding. Prior to the closing of the IPO, the Company estimated its common share fair value using the income approach and market approach using the market comparable method. Due to the Company’s limited history as a public company, expected volatility is based on an implied volatility for a group of industry-relevant healthcare companies as of the measurement date. Risk-free rate is determined based upon U.S. Treasury rates over the estimated expected option lives. Expected dividend yield is zero, as the Company does not anticipate that any dividends will be declared during the expected term of the options. The expected term of options granted is calculated using the simplified method (the midpoint between the end of the vesting period and the end of the maximum term) because the Company does not have sufficient historical exercise data to provide a reasonable basis upon which to estimate the expected term due to the limited period of time its awards have been outstanding. If actual results differ significantly from these estimates and assumptions, share-based compensation expense, primarily with respect to future share-based awards, could be materially impacted.
In March 2015, the Company repurchased vested stock options to buy 1,641,387 shares of common stock from certain current employees, including certain executive officers, for cash consideration totaling $36,298. All repurchased stock options were granted under the Company’s 2007 Stock Option Plan. No incremental compensation expense was recognized as a result of these repurchases.
In May 2014, the Company entered into a Stock Option Redemption Agreement with a former executive whereby the Company repurchased vested stock options to buy 884,000 shares of common stock for the cash purchase price of $4,000. No incremental compensation expense was recognized as a result of this repurchase.
In April 2014, the Company repurchased vested stock options to buy 183,993 shares of common stock from certain current employees for cash consideration, totaling $2,300. No incremental compensation expense was recognized as a result of these repurchases.
In January 2014, the Company repurchased vested stock options to buy 239,768 shares of common stock from certain current employees for cash consideration, totaling $3,100. No incremental compensation expense was recognized as a result of these repurchases.
For U.S. GAAP purposes, share-based compensation expense associated with stock options is based upon recognition of the grant date fair value over the vesting period of the option. For income tax purposes, share-based compensation tax deductions associated with nonqualified stock option exercises and repurchases are based upon the difference between the stock price and the exercise price at time of exercise or repurchase. Prior to the Company’s adoption of ASU 2016-09 (Note 3), in instances where share-based compensation expense for income tax purposes was in excess of share-based compensation expense for U.S. GAAP purposes, which has predominately been the case for the Company, U.S. GAAP required that the tax benefit associated with this excess expense be recorded to shareholders’ equity to the extent that it reduced cash taxes payable. During the years ended December 31, 2015 and 2014, the Company recorded excess tax benefits related to share-based awards of $20,805 and $3,689, respectively, as increases to shareholders’ equity.
Prior to the Company’s adoption of ASU 2016-09 (Note 3), U.S. GAAP also required that excess tax benefits related to share-based awards be reported as a decrease to cash flows from operating activities and as an increase to cash flows from financing activities. The Company reported $20,805 and $3,689 of excess tax benefits related to share-based awards as decreases to cash flows from operating activities and as increases to cash flows from financing activities for the years ended December 31, 2015 and 2014, respectively.
Restricted Stock Awards
Under the 2014 Plan, the Company issued restricted stock awards to non-employee directors. The value of the restricted stock awards was determined by the market value of the Company’s common stock at the date of grant. The value of the restricted stock awards is recorded as compensation expense on a straight-line basis over the vesting period, which is one year.
The Company recorded share-based compensation expense associated with restricted stock awards of $339, $188, and $25 for the years ended December 31, 2016, 2015, and 2014, respectively. At December 31, 2016, the total compensation cost related to non-vested restricted stock awards not yet recognized was $79, which will be recognized during 2017, assuming the non-employee directors complete their service period for vesting of the restricted stock awards.
A summary of the Company’s restricted stock award activity for the years ended December 31, 2014, 2015, and 2016 is as follows:
|
| Number |
| Weighted |
| |
|
| of Shares |
| Average |
| |
|
| Subject to |
| Grant Date |
| |
|
| Restriction |
| Fair Value |
| |
Nonvested at January 1, 2014 |
| — |
| $ | — |
|
Granted |
| 8,277 |
| 18.12 |
| |
Nonvested at December 31, 2014 |
| 8,277 |
| 18.12 |
| |
Granted |
| 10,805 |
| 26.60 |
| |
Vested |
| (8,277 | ) | 18.12 |
| |
Nonvested at December 31, 2015 |
| 10,805 |
| $ | 26.60 |
|
Granted |
| 5,765 |
| 32.97 |
| |
Vested |
| (10,805 | ) | 26.60 |
| |
Nonvested at December 31, 2016 |
| 5,765 |
| $ | 32.97 |
|
12. INCOME TAXES
As disclosed in Note 2, the Company converted its income tax status from an S corporation to a C corporation on January 23, 2014. Accordingly, on that date, the Company recorded a net deferred income tax liability of $2,965 and a corresponding charge to deferred income tax expense.
Significant components of the expense for income taxes for the years ended December 31, 2016 and 2015 and for the period from January 23, 2014 to December 31, 2014 are as follows:
|
| 2016 |
| 2015 |
| 2014 |
| |||
Current: |
|
|
|
|
|
|
| |||
Federal |
| $ | (703 | ) | $ | (17,592 | ) | $ | (4,752 | ) |
State and local |
| (1,713 | ) | (3,257 | ) | (1,198 | ) | |||
Total current |
| (2,416 | ) | (20,849 | ) | (5,950 | ) | |||
|
|
|
|
|
|
|
| |||
Deferred: |
|
|
|
|
|
|
| |||
Federal |
| (7,989 | ) | 4,061 |
| 1,087 |
| |||
State and local |
| (790 | ) | 554 |
| 208 |
| |||
Total deferred |
| (8,779 | ) | 4,615 |
| 1,295 |
| |||
|
|
|
|
|
|
|
| |||
|
| $ | (11,195 | ) | $ | (16,234 | ) | $ | (4,655 | ) |
The reconciliation of income taxes computed at the U.S. federal statutory tax rate to income tax expense is as follows:
|
| Year Ended December 31, |
| |||||||
|
| 2016 |
| 2015 |
| 2014 |
| |||
Income tax expense at U.S. statutory rate |
| $ | (12,675 | ) | $ | (14,352 | ) | $ | (3,222 | ) |
Tax effect from: |
|
|
|
|
|
|
| |||
Excess tax benefits (Note 3) |
| 4,148 |
| — |
| — |
| |||
State income taxes, net of federal benefit |
| (1,904 | ) | (1,563 | ) | (351 | ) | |||
Loss on noncontrolling interest |
| (1,138 | ) | (351 | ) | (79 | ) | |||
Change in fair value of redeemable common shares |
| — |
| — |
| 3,176 |
| |||
Adoption of C corporation status |
| — |
| — |
| (2,965 | ) | |||
Termination of existing stock redemption agreement |
| — |
| — |
| (1,695 | ) | |||
Earnings while a S corporation |
| — |
| — |
| 499 |
| |||
Other |
| 374 |
| 32 |
| (18 | ) | |||
Income tax expense |
| $ | (11,195 | ) | $ | (16,234 | ) | $ | (4,655 | ) |
Significant components of deferred tax assets and liabilities are as follows:
|
| December 31, |
| ||||
|
| 2016 |
| 2015 |
| ||
Deferred tax assets: |
|
|
|
|
| ||
Allowance for doubtful accounts |
| $ | 8,861 |
| $ | 3,728 |
|
Net operating loss and credit carryforwards |
| 6,383 |
| — |
| ||
Compensation and benefits |
| 3,598 |
| 3,638 |
| ||
Investments |
| 1,101 |
| — |
| ||
Other temporary differences |
| 1,014 |
| 429 |
| ||
Total deferred tax assets |
| 20,957 |
| 7,795 |
| ||
|
|
|
|
|
| ||
Deferred tax liabilities: |
|
|
|
|
| ||
Property and intangible assets |
| (13,825 | ) | (8,550 | ) | ||
Prepaid expenses and other current assets |
| (1,122 | ) | (870 | ) | ||
Other temporary differences |
| — |
| (489 | ) | ||
Total deferred tax liabilities |
| (14,947 | ) | (9,909 | ) | ||
|
|
|
|
|
| ||
Net deferred tax assets (liabilities) |
| $ | 6,010 |
| $ | (2,114 | ) |
At December 31, 2016, the Company had $11,779 of federal and $45,769 of state and local gross net operating loss carry-forwards. The federal gross net operating loss carry-forwards expire in 2036. The state and local gross net operating loss carry-forwards expire at various times through 2036. At December 31, 2016, the Company has alternative minimum tax credit carry-forwards of $676, which have no expiration.
The Company prepares and files tax returns based on interpretations of tax laws and regulations. In the normal course of business, the Company’s tax returns are subject to examination by various taxing authorities. Such examinations may result in future tax and interest assessments by these taxing authorities. In determining the Company’s tax provision for financial reporting purposes, the Company establishes a reserve for uncertain income tax positions unless it is determined to be more likely than not that such tax positions would be sustained upon examination, based on their technical merits. That is, for financial reporting purposes, the Company only recognizes a tax benefit taken on its tax return if it believes it is more likely than not that such tax position would be sustained. There is considerable judgment involved in determining whether it is more likely than not that such tax positions would be sustained.
As of both December 31, 2016 and 2015, the Company had unrecognized tax benefits of $268; all of which, if recognized, would reduce both tax expense and the effective tax rate. The following table sets forth a roll forward of the Company’s unrecognized tax benefits:
|
| Year Ended |
| ||||
|
| December 31, |
| ||||
|
| 2016 |
| 2015 |
| ||
Balance at January 1 |
| $ | 268 |
| $ | — |
|
Additions for tax positions of prior years |
| — |
| 268 |
| ||
Balance at December 31 |
| $ | 268 |
| $ | 268 |
|
The Company would adjust its tax reserve estimates periodically because of ongoing examinations by, and settlements with, varying taxing authorities, as well as changes in tax laws, regulations, and interpretations. The consolidated tax provision of any given year includes adjustments to prior year income tax accruals and related estimated interest charges that are considered appropriate. The Company’s 2015 and 2014 C corporation tax returns are open to examination by U.S. federal, state, and local taxing authorities.
13. INCOME PER COMMON SHARE
For the period January 23, 2014 through October 9, 2014, the Company computed net income per common share using the two-class method as its Redeemable Series A Preferred Stock met the definition of a participating security and thereby shared in the net income or loss of the Company on a ratable basis with the common shareholders. The preferred stock’s portion of net income for the year ended December 31, 2014 was 10 percent. Concurrent with the closing of the Company’s IPO, all outstanding Redeemable Series A Preferred Stock converted into Class C Voting Common Stock, which then immediately converted into no par common stock.
Basic income per common share is computed by dividing net income allocable to common shareholders by the weighted average number of common shares outstanding during the period. Diluted income per common share further includes any common shares available to be issued upon: exercise of outstanding service-based stock options; exercise of outstanding performance-based stock options for which all performance conditions were satisfied; and satisfaction of all contingent consideration performance conditions; and conversion of preferred stock, along with the vesting of restricted stock, if such inclusions would be dilutive.
The following table sets forth the computation of basic and diluted income per common share:
|
| Year Ended December 31, |
| |||||||
|
| 2016 |
| 2015 |
| 2014 |
| |||
Numerator: |
|
|
|
|
|
|
| |||
Net income attributable to Diplomat Pharmacy, Inc. |
| $ | 28,273 |
| $ | 25,776 |
| $ | 4,776 |
|
Less: income attributable to preferred shareholders |
| — |
| — |
| 458 |
| |||
Net income attributable to common shareholders |
| 28,273 |
| 25,776 |
| 4,318 |
| |||
|
|
|
|
|
|
|
| |||
Denominator: |
|
|
|
|
|
|
| |||
Weighted average common shares outstanding, basic |
| 65,970,396 |
| 60,730,133 |
| 36,012,592 |
| |||
Weighted average dilutive effect of stock options and restricted stock awards |
| 1,739,750 |
| 2,029,241 |
| 2,541,403 |
| |||
Weighted average dilutive effect of contingent consideration |
| 337,577 |
| 337,577 |
| — |
| |||
Weighted average common shares outstanding, diluted |
| 68,047,723 |
| 63,096,951 |
| 38,553,995 |
| |||
|
|
|
|
|
|
|
| |||
Net income per share attributable to common shareholders: |
|
|
|
|
|
|
| |||
Basic |
| $ | 0.43 |
| $ | 0.42 |
| $ | 0.12 |
|
Diluted |
| $ | 0.42 |
| $ | 0.41 |
| $ | 0.11 |
|
Stock options to purchase a weighted average of 1,542,064, 649,564, and 485,122 common shares were excluded from the computation of diluted weighted average common shares outstanding for the years ended December 31, 2016, 2015, and 2014, respectively, as inclusion of such options would be anti-dilutive. Performance-based stock options to purchase up to a weighted average of 291,277, 410,452, and 799,067 common shares were excluded from the computation of diluted weighted average common shares outstanding for the years ended December 31, 2016, 2015, and 2014, respectively, as all performance conditions were not satisfied at some/all quarter-end periods within the respective years. Contingent consideration to issue a weighted average of 1,012,732 common shares was excluded in the computation of diluted weighted average common shares outstanding for the year ended December 31, 2015, as all performance conditions were not satisfied until the quarter ended December 31, 2015.
All outstanding restricted stock awards were dilutive for the years ended December 31, 2016, 2015, and 2014.
The effect of all Redeemable Series A Preferred Stock were excluded from the computation of diluted weighted average common shares outstanding for the year ended December 31, 2014 as inclusion would be anti-dilutive.
14. COMMITMENTS AND CONTINGENCIES
Legal Proceedings
The Company is subject to claims and lawsuits that arise primarily in the ordinary course of business. In addition, on November 10, 2016, a putative class action complaint was filed in the U.S. District Court for the Eastern District of Michigan against Diplomat Pharmacy, Inc. and certain officers of the Company. The complaint alleges violations of Sections 10(b) and 20(a) of the Securities Exchange Act of 1934 in connection with public filings made between October 9, 2014 and November 2, 2016 (the “potential class period”). The plaintiff seeks to represent a class of shareholders who purchased stock in the potential class period. The complaint seeks unspecified monetary damages and other relief. The Company believes the complaint and allegations to be without merit and intends to vigorously defend itself against these actions. The Company is unable at this time to determine whether the outcome of the litigation would have a material impact on its results of operations, financial condition, or cash flows. In the opinion of management, the disposition or ultimate resolution of all other currently known claims and lawsuits will not have a material adverse effect on the Company’s consolidated financial position, results of operations, or liquidity.
Purchase Commitments
In October 2016, the Company amended its contract with AmerisourceBergen. This amended contract commits the Company to a minimum purchase obligation of approximately $2,000,000 per contract year and extended the contract expiration date to September 30, 2018. The Company fully expects to meet this requirement.
Lease Commitments
The Company leases multiple pharmacy and distribution facilities and office equipment under various operating lease agreements expiring through September 2026. Total rental expense under operating leases for the years ended December 31, 2016, 2015, and 2014 was $4,179, $3,295, and $2,241, respectively, exclusive of property taxes, insurance, and other occupancy costs generally payable by the Company.
Future minimum payments under non-cancelable operating leases with initial or remaining terms in excess of one year as of December 31, 2016 are as follows:
2017 |
| $ | 1,761 |
|
2018 |
| 1,679 |
| |
2019 |
| 958 |
| |
2020 |
| 704 |
| |
2021 |
| 572 |
| |
Thereafter |
| 1,559 |
| |
|
| $ | 7,233 |
|
15. SHAREHOLDERS’ EQUITY (DEFICIT) AND NONCONTROLLING INTERESTS
Capital Stock
Effective September 2014, the Company amended its Certificate of Incorporation to change its authorized capital stock to consist of (i) 590 million shares of common stock, no par value, of which 66,764,999 shares were issued and outstanding as of December 31, 2016, and (ii) 10 million authorized shares of preferred stock.
In January 2014, the Company’s authorized capital stock consisted of (i) 42,500,000 shares of Class A Voting Common Stock, (ii) 807,500,000 shares of Class B Nonvoting Common Stock, (iii) 2,992,000 shares of Class C Voting Stock, and (iv) 2,992,000 of Series A Preferred Stock. On March 31, 2014, pursuant to the Second Amended and Restated Articles of Incorporation, the Company’s authorized capital stock was amended further to provide for a total of 6,222,000 shares of Redeemable Series A Preferred Stock and 6,222,000 shares of Class C Voting Stock.
Prior to January 2014, the Company’s authorized capital stock consisted of 42,500,000 shares of Class A Voting Common Stock and 807,500,000 of Class B Nonvoting Common Stock.
No Par, Common Stock
In October 2014, the Company issued and sold 11,000,000 shares of its no par common stock and certain existing shareholders sold 4,333,333 shares in its IPO at an offering price of $13.00 per share. The Company received net proceeds of $130,440 after deducting underwriting discounts and commissions of $9,652, and other offering expenses of $2,908. The Company did not receive any proceeds from the sale of common stock by the existing shareholders. Immediately prior to the closing of the IPO, each share of the then outstanding shares of capital stock totaling 40,448,744 shares converted into one share of no par common stock. Accordingly, $15,575 of previously contributed capital was reclassified into common stock leaving only accumulated stock-based compensation and related excess tax benefits in the additional paid-in capital account.
Holders of common stock are entitled to one vote per share and to receive dividends. The holders have no preemptive, conversion, or subscription rights, and there are no redemption or sinking fund provisions with respect to such shares. Common stock is subordinate to the preferred stock as described below with respect to dividend rights or rights upon liquidation, winding up, and dissolution of the Company.
Class A, B, and C Common Stock
Prior to the closing of the IPO, each class of common stock had equal and identical rights, preferences, and limitations, other than voting. The Class B common stock did not have any voting rights, but Class A and Class C had 20 votes per share and one vote per share, respectively.
In August 2014, the Company issued 372,486 shares of Class B Nonvoting Common Stock to a non-employee relative (and associated trusts) of the Company’s chief executive officer, in connection with the termination of an existing Stock Redemption Agreement. The Company recorded a charge of $4,842 during the year ended December 31, 2014 to “Termination of existing stock redemption agreement” in the consolidated statement of operations upon issuance of the shares. The value of the issued shares was based on the Company’s IPO price of $13.00 per share.
In June 2014, the Company issued 716,695 shares of Class B Nonvoting Common Stock, valued at $12,000, in connection with its acquisition of MedPro. Refer to Note 4.
Upon the closing of the IPO, the Class A, Class B, and Class C common shares were converted into shares of the Company’s no par value common stock on a one-for-one basis.
Preferred Stock
The Company’s authorized capital stock includes 10 million shares of preferred stock. The shares of preferred stock may be divided into and issued in one or more series. The Board of Directors is authorized to issue preferred stock from time to time in one or more series, with such designations and such relative voting, dividend, liquidation, and other rights, preferences, and limitations as may be adopted by the Board of Directors. No shares of preferred stock were issued or outstanding as of December 31, 2016.
Noncontrolling Interest
Noncontrolling interest in a consolidated subsidiary in the consolidated balance sheets represents minority stockholders’ proportionate share of the equity in Primrose.
16. MANDATORILY REDEEMABLE COMMON SHARES
Upon the closing of the Company’s IPO, 2,423,616 shares of redeemable common stock outstanding were converted into shares of no par value common stock on a one-for-one basis.
Several years prior to its IPO, the Company issued 11,050,000 shares of common stock to two shareholders that had certain redemption features which provided that upon the death of the shareholder or termination of his employment from the Company, all such outstanding shares owned by such shareholder would immediately be deemed to be offered for sale to the Company at an agreed-upon price meant to represent the then-current fair value of such shares. Due to this repurchase feature, the Company would be required to purchase the shares. Pursuant to this provision, the common shares were deemed to be mandatorily redeemable and, as such, were required to be reflected as a liability at their period-end estimated fair value. Changes in fair value were reflected as “Changes in fair value of redeemable common shares” on the consolidated statement of operations. Fair value was determined based on good faith estimates of the Company’s Board of Directors, in some cases with the assistance of independent third party valuations of the Company. At January 1, 2014, 3,187,500 shares of these mandatorily redeemable common stock were outstanding.
The Company redeemed 143,339 common shares in exchange for cash of $2,400 pursuant to a Stock Redemption Agreement, dated January 2014.
The Company redeemed 195,545 common shares in exchange for cash of $3,274 pursuant to a Stock Redemption Agreement, dated April 2014.
In June 2014, the holder of 425,000 redeemable common shares transferred them into a separate trust. On such date, the redemption provisions on the transferred shares were terminated and the fair value of the common shares of $7,116 was reclassified from liabilities to shareholders’ equity.
17. REDEEMABLE SERIES A PREFERRED STOCK
Upon the closing of the Company’s IPO, the shares of Redeemable Series A Preferred Stock outstanding were converted into shares of Class C Voting Common Stock on a one-for-one basis. The shares of Class C Voting Common Stock were then immediately converted into shares of no par value common stock on a one-for-one basis.
Prior to the Company’s IPO, the Redeemable Series A Preferred Stock had a zero coupon rate, optional redemption rights, and liquidation preferences. The Redeemable Series A Preferred Stock was also convertible into Class C Voting Common Stock at any time at the option of the holder on a one-for-one basis, subject to certain adjustments. The initial conversion price per share for Redeemable Series A Preferred Stock was the original issue price, subject to adjustment, as defined. The Redeemable Series A Preferred Stock was entitled to vote as if converted into Class C Voting Common Stock. The Redeemable Series A Preferred Stock automatically converted into Class C Voting Common Stock upon either (i) a qualified common stock public offering, as defined, or (ii) an affirmative vote of the majority of the Redeemable Series A Preferred Stock.
The holders of the Redeemable Series A Preferred Stock, upon an affirmative vote of the majority, could have demanded redemption of all outstanding shares of Redeemable Series A Preferred Stock anytime on or after the earlier of (i) January 23, 2021, (ii) such time as the Company’s aggregate market price, as defined, was equal to or greater than $5,000,000, and (iii) such time as certain changes were made to the Company’s Board of Directors, certain executive officers, and/or certain controlling shareholders. The redemption price was payable in cash and would be the greater of the original issuance price plus all declared but unpaid dividends and fair market value, as defined. Due to these redemption features, the Redeemable Series A Preferred Stock was reflected outside of permanent equity on the consolidated balance sheet. Upon a liquidation event, as defined, the Redeemable Series A
Preferred stockholders were entitled to receive the greater of (i) the sum of the original issuance price plus a 15 percent return compounded annually and (ii) the amount they would receive upon the liquidation had the Redeemable Series A Preferred Stock converted into Class C Voting Common Stock on the liquidation date.
In January 2014, the Company entered into a Redeemable Series A Preferred Stock Purchase Agreement with certain funds of T. Rowe Price Associates, Inc. (“T. Rowe”) under which the Company issued to T. Rowe 2,986,229 shares of Redeemable Series A Preferred Stock at a purchase price of $16.74 per share. The Company used $20,000 of this $50,000 investment for general corporate purposes, inclusive of fees associated with this transaction, and the remaining $30,000 was distributed to holders of common stock including 143,339 redeemable shares ($26,900) and holders of options to acquire common stock ($3,100) (Note 11).
In April 2014, the Company entered into a Redeemable Series A Preferred Stock Purchase Agreement with certain funds of Janus Capital Management LLC (“Janus”) under which the Company issued to Janus 3,225,127 shares of Redeemable Series A Preferred Stock at a purchase price of $16.74 per share. The Company used $25,200 of this $54,000 investment for general corporate purposes, inclusive of fees associated with this transaction, and the remaining $28,800 was distributed to holders of common stock including 195,545 redeemable shares ($26,500) and holders of options to acquire common stock ($2,300) (Note 11).
18. SUBSEQUENT EVENT
On February 1, 2017, the Company acquired Affinity Biotech, Inc., a specialty pharmacy and infusion services company based in Houston, TX that provides treatments and nursing services for patients with hemophilia. Under the terms of the agreement, Diplomat transferred cash consideration of approximately $16,000, with an additional payout of up to $4,000 based upon the achievement of a certain earnings before interest, taxes, depreciation, and amortization target in the 12-month period ending January 31, 2018.
19. SELECTED QUARTERLY FINANCIAL DATA (UNAUDITED)
The following table presents selected quarterly financial data for each of the quarters in the years ended December 31, 2016 and 2015:
|
| For the 2016 Quarter Ended |
| ||||||||||
|
| March 31 |
| June 30 |
| September 30 |
| December 31 |
| ||||
Net sales |
| $ | 995,870 |
| $ | 1,088,506 |
| $ | 1,181,173 |
| $ | 1,144,838 |
|
Gross profit |
| 79,238 |
| 83,270 |
| 78,512 |
| 83,808 |
| ||||
Income (loss) before income taxes |
| 23,717 |
| 12,438 |
| (408 | ) | 468 |
| ||||
Net income (loss) |
| 15,183 |
| 8,293 |
| 2,828 |
| (1,284 | ) | ||||
Net income (loss) attributable to Diplomat |
| 15,429 |
| 8,534 |
| 5,408 |
| (1,098 | ) | ||||
Basic income (loss) per common share |
| 0.24 |
| 0.13 |
| 0.08 |
| (0.02 | ) | ||||
Diluted income (loss) per common share |
| 0.23 |
| 0.13 |
| 0.08 |
| (0.02 | ) | ||||
|
| For the 2015 Quarter Ended |
| ||||||||||
|
| March 31 |
| June 30 |
| September 30 |
| December 31 |
| ||||
Net sales |
| $ | 624,883 |
| $ | 808,011 |
| $ | 946,913 |
| $ | 986,823 |
|
Gross profit |
| 41,142 |
| 69,669 |
| 75,763 |
| 76,665 |
| ||||
Income before income taxes |
| 4,622 |
| 5,367 |
| 25,451 |
| 5,564 |
| ||||
Net income |
| 2,672 |
| 3,113 |
| 15,683 |
| 3,304 |
| ||||
Net income attributable to Diplomat |
| 2,858 |
| 3,390 |
| 15,961 |
| 3,566 |
| ||||
Basic income per common share |
| 0.06 |
| 0.05 |
| 0.25 |
| 0.06 |
| ||||
Diluted income per common share |
| 0.05 |
| 0.05 |
| 0.24 |
| 0.05 |
| ||||
The Company’s results were impacted by the following:
· Quarter ended December 31, 2016: The Company recognized a $4,659 impairment of its cost method investment in PRM (Note 9).
· Quarter ended September 30, 2016: The Company was assessed and recorded approximately $8,000 in additional DIR fees, of which approximately $4,000 were retroactive DIR fees that increased its previous estimates by approximately $1,700 and $2,300 for the first and second quarters of 2016, respectively. The Company recognized a $4,804 impairment of its Primrose intangible assets (Note 8), partially offset by $2,354 which was the noncontrolling interests’ allocation of the recognized impairment. The Company recognized $3,076 in excess tax benefits (Note 3).
· Quarter ended March 31, 2016: The Company recognized a $9,071 change in the fair value of contingent consideration, primarily due to a reduction in its BioRx contingent consideration liability caused by a decrease in the Company’s stock price.
· Quarter ended December 31, 2015: The Company recognized a $(8,384) change in the fair value of contingent consideration, primarily due to an increase in its BioRx contingent consideration liability caused by an increase in the Company’s stock price.
· Quarter ended September 30, 2015: The Company recognized a $6,829 change in the fair value of contingent consideration, primarily due to a reduction in its BioRx contingent consideration liability caused by a decrease in the Company’s stock price.
ITEM 9. CHANGES IN AND DISAGREEMENTS WITH ACCOUNTANTS ON ACCOUNTING AND FINANCIAL DISCLOSURE
None
ITEM 9A. CONTROLS AND PROCEDURES
Limitations on Controls
A control system, no matter how well conceived and operated, can provide only reasonable, not absolute, assurance that the objectives of the control system are met. Further, the design of a control system must reflect the fact that there are resource constraints, and the benefits of controls must be considered relative to their costs. Because of the inherent limitations in all control systems, no evaluation of controls can provide absolute assurance that all control issues and instances of fraud, if any, within the Company have been detected.
Disclosure Controls and Procedures
We maintain disclosure controls and procedures designed to provide reasonable assurance that information required to be disclosed in our reports that we file or submit under the Securities Exchange Act of 1934, as amended (the “Exchange Act”), is recorded, processed, summarized, and reported within the specified time periods in the rules and forms of the Securities and Exchange Commission, and that such information is accumulated and communicated to our management, including our chief executive officer and principal financial officer, as appropriate, to allow timely decisions regarding required disclosure.
Our management, with the participation of the chief executive officer and the principal financial officer, evaluated the effectiveness of our disclosure controls and procedures (as defined in Rule 13a-15(e) or 15(d)-15(e) promulgated under the Exchange Act) as of December 31, 2016. Based on these evaluations, the chief executive officer and the principal financial officer concluded that our disclosure controls and procedures required by paragraph (b) of Rule 13a-15 or 15d-15 were not effective as of December 31, 2016 as a result of the material weakness discussed below.
Management’s Report on Internal Control over Financial Reporting and Attestation Report of the Registered Public Accounting Firm
A material weakness is a deficiency, or combination of deficiencies, in internal control over financial reporting such that there is a reasonable possibility that a material misstatement of the Company's annual or interim financial statements will not be prevented or detected on a timely basis. During the fourth quarter of 2016, we identified a material weakness in the operating effectiveness of our evaluation and review of recorded inventory balances. Specifically, at certain locations the initial costs used to value ending inventories were not correct and we did not initially identify all items necessary to accurately complete our inventory reconciliation.
As a result of the material weakness noted above, we completed additional substantive procedures prior to filing this Annual Report on Form 10-K for the year ended December 31, 2016. Based on these procedures, management believes that our consolidated financial statements included in this Annual Report on Form 10-K have been prepared in accordance with generally accepted accounting principles. Our chief executive officer and principal financial officer have certified that, based on each such officer’s knowledge, the financial statements, and other financial information included in this Annual Report on Form 10-K, fairly present in all material respects our financial condition, results of operations, and cash flows as of, and for, the periods presented in this Annual Report on Form 10-K. There was no adjustment required as a result of this material weakness. In addition, we have developed a remediation plan for this material weakness, which is described below.
Pursuant to Section 404 of the Sarbanes-Oxley Act of 2002, we included within this Form 10-K Management’s Report on Internal Control over Financial Reporting as of December 31, 2016. Our independent registered public accounting firm also attested to, and reported on, the Company’s Internal Control over Financial Reporting, which report expressed an adverse opinion on the effectiveness of our internal controls over financial reporting as of December 31, 2016. Management’s report and the independent registered public accounting firm’s report are included in Item 8 of this Form 10-K.
Changes in Internal Control over Financial Reporting
Except for the control deficiencies discussed above that have been assessed as a material weakness as of December 31, 2016, there were no changes in our internal control over financial reporting (as defined in Rule 13a-15(f) of the Exchange Act) that occurred during the fourth quarter of 2016 that have materially affected, or are reasonably likely to materially affect, our internal control over financial reporting.
Remediation Plan
Management is actively implementing a remediation plan to ensure that deficiencies contributing to the material weakness are remediated such that these controls will operate effectively, which includes steps to strengthen our inventory costing and reconciliation controls. The remediation actions we are taking, and expect to take, include: additional testing of the pricing file utilized to cost physical inventory; and strengthening the depth and breadth of review of the inventory reconciliation by senior accounting and finance personnel.
We believe that these actions, and the improvements we expect to achieve as a result, will effectively remediate the material weakness. However, until the remediated controls operate for a sufficient period of time and management has concluded, through testing, that these controls are operating effectively, the material weakness in our internal controls over financial reporting will not be considered remediated. We expect that the remediation of this material weakness will be completed in fiscal 2017.
None
ITEM 10. DIRECTORS, EXECUTIVE OFFICERS AND CORPORATE GOVERANCE
The information required by this item is set forth under the following captions in our proxy statement to be filed with respect to the 2017 annual meeting of shareholders (the “Proxy Statement”), all of which is incorporated herein by reference: “Proposal No. 1 — Election of Directors,” “Board Matters — The Board of Directors,” “Board Matters — Committees of the Board,” “Board Matters — Corporate Governance,” “Certain Relationships and Related Person Transactions,” “Additional Information — Section 16(a) Beneficial Ownership Reporting Compliance,” and “Additional Information — Requirements for Submission of Shareholder Proposals and Nominations for 2018 Annual Meeting.”
ITEM 11. EXECUTIVE COMPENSATION
The information required by this item is set forth under the following captions in our Proxy Statement, all of which is incorporated herein by reference: “Compensation Discussion and Analysis,” “Named Executive Officer Compensation Tables,” “Board Matters — Director Compensation,” “Compensation Committee Interlocks and Insider Participation,” and “Compensation Committee Report.”
ITEM 12. SECURITY OWNERSHIP OF CERTAIN BENEFICIAL OWNERS AND MANAGEMENT AND RELATED STOCKHOLDER MATTERS
The information required by this item is set forth under the following captions in our Proxy Statement, all of which is incorporated herein by reference: “Additional Information — Equity Compensation Plans” and “Security Ownership of Certain Beneficial Owners and Management.”
ITEM 13. CERTAIN RELATIONSHIPS AND RELATED TRANSACTIONS, AND DIRECTORS INDEPENDENCE
The information required by this item is set forth under the following captions in our Proxy Statement, all of which is incorporated herein by reference: “Certain Relationships and Related Person Transactions” and “Proposal No. 1 — Election of Directors — Director Independence.”
ITEM 14. PRINCIPAL ACCOUNTANT FEES AND SERVICES
The information required by this item is set forth under the following captions in our Proxy Statement, which is incorporated herein by reference: “Audit Committee Matters.”
ITEM 15. EXHIBITS AND FINANCIAL STATEMENT SCHEDULES
1. Financial Statements
The financial statements of the Company filed in this Annual Report on Form 10-K are listed in Part II, Item 8.
2. Financial Statement Schedules
All financial statement schedules have been omitted because they are not required or applicable under instructions contained in Regulation S-X or because the information called for is shown in the financial statements and notes thereto.
3. Exhibits
The exhibits required to be filed as part of this Annual Report on Form 10-K are listed in the attached Exhibit Index.
None
Pursuant to the requirements of Section 13 or 15(d) of the Securities Exchange Act of 1934, the Registrant has duly caused this report to be signed on its behalf by the undersigned, thereunto duly authorized.
| DIPLOMAT PHARMACY, INC. | |
| (Registrant) | |
|
|
|
|
|
|
| By: | /s/ ROBIN JOHNSON |
|
| Robin Johnson |
|
| Vice President, Finance |
|
| (Principal Financial Officer and |
|
| Principal Accounting Officer) |
Date: March 8, 2017
Pursuant to the requirements of the Securities Exchange Act of 1934, this report has been signed below as of March 8, 2017 by the following persons on behalf of the registrant and in the capacities indicated.
/s/ PHILIP R. HAGERMAN | Chief Executive Officer, Chairman of the Board |
Philip R. Hagerman | Of Directors (Principal Executive Officer) |
|
|
/s/ ROBIN JOHNSON | Vice President, Finance |
Robin Johnson | (Principal Financial Officer and Principal |
| Accounting Officer) |
|
|
/s/ GARY W. KADLEC | Director |
Gary W. Kadlec |
|
|
|
/s/ DAVID DREYER | Director |
David Dreyer |
|
|
|
/s/ KENNETH O. KLEPPER | Director |
Kenneth O. Klepper |
|
|
|
/s/ SHAWN CLINE TOMASELLO | Director |
Shawn Cline Tomasello |
|
|
|
/s/ BENJAMIN WOLIN | Director |
Benjamin Wolin |
|
|
|
|
|
|
| Incorporated by reference | ||||||
Exhibit |
| Exhibit description |
| Filed/Furnished |
| Form |
| Period |
| Exhibit |
| Filing |
|
|
|
|
|
|
|
|
|
|
|
|
|
2.1** |
| Membership Interest Purchase Agreement, dated June 19, 2015, by and among Diplomat, Burman’s Apothecary, L.L.C., and the other parties named therein |
|
|
| 8-K |
|
|
| 2.1 |
| 06/22/15 |
|
|
|
|
|
|
|
|
|
|
|
|
|
3.1 |
| Third Amended and Restated Articles of Incorporation |
|
|
| S-1/A |
|
|
| 3.1 |
| 09/17/14 |
|
|
|
|
|
|
|
|
|
|
|
|
|
3.2 |
| Amended and Restated Bylaws |
|
|
| S-1/A |
|
|
| 3.2 |
| 09/17/14 |
|
|
|
|
|
|
|
|
|
|
|
|
|
4.1 |
| Form of Common Stock Certificate |
|
|
| S-1/A |
|
|
| 4.1 |
| 09/11/14 |
|
|
|
|
|
|
|
|
|
|
|
|
|
4.2 |
| Diplomat Pharmacy, Inc. First Amended and Restated Investors’ Rights Agreement, dated March 31, 2014, by and among Diplomat and various funds of T. Rowe Price Associates, Inc. and Janus Capital Management, LLC |
|
|
| S-1 |
|
|
| 4.2 |
| 07/03/14 |
|
|
|
|
|
|
|
|
|
|
|
|
|
4.3 |
| Registration Rights Agreement, dated April 1, 2015, by and among Diplomat and each shareholder named therein |
|
|
| 8-K |
|
|
| 4 |
| 04/06/15 |
|
|
|
|
|
|
|
|
|
|
|
|
|
10.1* |
| Diplomat Pharmacy, Inc. 2007 Option Plan |
|
|
| S-1 |
|
|
| 10.4 |
| 07/03/14 |
|
|
|
|
|
|
|
|
|
|
|
|
|
10.2* |
| Form of Amended and Restated 2007 Option Plan Grant Agreement |
|
|
| S-1 |
|
|
| 10.5 |
| 07/03/14 |
|
|
|
|
|
|
|
|
|
|
|
|
|
10.3* |
| Form of 2007 Option Plan Grant (Performance-Based) Agreement |
|
|
| S-1/A |
|
|
| 10.6 |
| 09/11/14 |
|
|
|
|
|
|
|
|
|
|
|
|
|
10.4* |
| Diplomat Pharmacy, Inc. 2014 Omnibus Incentive Plan |
|
|
| S-1/A |
|
|
| 10.7 |
| 09/29/14 |
|
|
|
|
|
|
|
|
|
|
|
|
|
10.5* |
| Form of Stock Option Award Agreement (Time-Based) (2014 Omnibus Incentive Plan) |
|
|
| S-1/A |
|
|
| 10.11 |
| 10/03/14 |
|
|
|
|
|
|
|
|
|
|
|
|
|
10.6* |
| Form of Restricted Stock Award Agreement (2014 Omnibus Incentive Plan) |
|
|
| S-1/A |
|
|
| 10.12 |
| 10/03/14 |
|
|
|
|
|
|
|
|
|
|
|
|
|
10.7* |
| Form of Stock Option Award Agreement (Performance-Based) (2014 Omnibus Incentive Plan) |
|
|
| 8-K |
|
|
| 10.1 |
| 06/09/15 |
|
|
|
|
|
|
|
|
|
|
|
|
|
10.8* |
| Form of Restricted Stock Award Agreement (Non-Employee Directors) (2014 Omnibus Incentive Plan) |
|
|
| 10-Q |
| 09/30/15 |
| 10.3 |
| 11/04/15 |
|
|
|
|
|
| Incorporated by reference | ||||||
Exhibit |
| Exhibit description |
| Filed/Furnished |
| Form |
| Period |
| Exhibit |
| Filing |
10.9* |
| Form of Stock Option Award Agreement (Time-Based) (2014 Omnibus Incentive Plan) |
|
|
| 8-K |
|
|
| 10.1 |
| 12/09/16 |
|
|
|
|
|
|
|
|
|
|
|
|
|
10.10.1† |
| Pharmacy Distribution and Services Agreement, dated July 1, 2013, by and between Celgene Corporation and Diplomat |
|
|
| S-1/A |
|
|
| 10.8.1 |
| 08/19/14 |
|
|
|
|
|
|
|
|
|
|
|
|
|
10.10.2† |
| First Amendment to Pharmacy Distribution and Services Agreement, dated July 8, 2013, by and between Celgene Corporation and Diplomat |
|
|
| S-1/A |
|
|
| 10.8.2 |
| 08/19/14 |
|
|
|
|
|
|
|
|
|
|
|
|
|
10.10.3† |
| Adoption and Amendment of Pharmacy Distribution and Services Agreement, dated March 21, 2014, by and between Celgene Corporation and Diplomat |
|
|
| S-1/A |
|
|
| 10.8.3 |
| 08/19/14 |
|
|
|
|
|
|
|
|
|
|
|
|
|
10.10.4† |
| Amendment to Pharmacy Distribution and Services Agreement, executed October 19, 2015 and effective as of June 1, 2016, by and between Diplomat and Celgene Corporation |
|
|
| 10-K |
| 12/31/15 |
| 10.18 |
| 02/29/16 |
|
|
|
|
|
|
|
|
|
|
|
|
|
10.11.1† |
| Prime Vendor Agreement, dated January 1, 2012, by and among AmerisourceBergen Drug Corporation, Diplomat and its subsidiaries named therein |
|
|
| S-1/A |
|
|
| 10.9.1 |
| 08/19/14 |
|
|
|
|
|
|
|
|
|
|
|
|
|
10.11.2 |
| First Amendment to Prime Vendor Agreement, dated July 20, 2012, by and among AmerisourceBergen Drug Corporation, Diplomat and its subsidiaries named therein |
|
|
| S-1/A |
|
|
| 10.9.2 |
| 08/19/14 |
|
|
|
|
|
|
|
|
|
|
|
|
|
10.11.3† |
| Second Amendment to Prime Vendor Agreement, effective August 1, 2015, by and among Diplomat, AmerisourceBergen Drug Corporation, and each Company subsidiary named therein |
|
|
| 8-K |
|
|
| 10.1 |
| 09/15/15 |
|
|
|
|
|
|
|
|
|
|
|
|
|
10.11.4† |
| Third Amendment to Prime Vendor Agreement, effective October 1, 2016, by and among AmerisourceBergen Drug Corporation and the Company subsidiaries named therein |
|
|
| 8-K |
|
|
| 10.1 |
| 10/06/16 |
|
|
|
|
|
|
|
|
|
|
|
|
|
10.12 |
| Joinder Agreement, dated November 1, 2015, by and among AmerisourceBergen Drug Corporation, Diplomat and the Diplomat subsidiaries named therein |
|
|
| 10-K |
| 12/31/15 |
| 10.20 |
| 02/29/16 |
|
|
|
|
|
| Incorporated by reference | ||||||
Exhibit |
| Exhibit description |
| Filed/Furnished |
| Form |
| Period |
| Exhibit |
| Filing |
10.13 |
| Second Amended and Restated Credit Agreement, dated April 1, 2015, by and among Diplomat, each party thereto designated as a credit party, General Electric Capital Corporation, as agent and as lender, and the lenders from time to time party thereto |
|
|
| 8-K |
|
|
| 10.1 |
| 04/06/15 |
|
|
|
|
|
|
|
|
|
|
|
|
|
10.14 |
| Second Amended and Restated Guaranty and Security Agreement, dated April 1, 2015, by Diplomat and each other grantor party thereto in favor of General Electric Capital Corporation, as agent |
|
|
| 8-K |
|
|
| 10.2 |
| 04/06/15 |
|
|
|
|
|
|
|
|
|
|
|
|
|
10.15 |
| Consent to Acquisition, dated June 19, 2015, by and among Diplomat, the other credit parties party thereto, General Electric Capital Corporation, as agent and as lender, and the other lenders party thereto |
|
|
| 8-K |
|
|
| 10.1 |
| 06/22/15 |
|
|
|
|
|
|
|
|
|
|
|
|
|
10.16 |
| Joinder Agreement to Guaranty and Security Agreement and Credit Agreement, dated June 19, 2015, by and among Burman’s Apothecary, L.L.C. and its wholly owned subsidiaries and accepted and agreed by Diplomat and General Electric Capital Corporation, as agent |
|
|
| 8-K |
|
|
| 10.2 |
| 06/22/15 |
|
|
|
|
|
|
|
|
|
|
|
|
|
10.17 |
| Consent to Loan and Agency Transfer, dated as of September 22, 2015, by and among Diplomat, General Electric Capital Corporation, in its capacity as Agent, and the other Credit Parties thereto |
|
|
| 10-K |
| 12/31/15 |
| 10.17 |
| 02/29/16 |
|
|
|
|
|
|
|
|
|
|
|
|
|
10.18 |
| Letter Agreement dated as of October 29, 2015, by and among Diplomat, BioRx, LLC and Healthcare Financial Solutions, LLC, as Agent |
|
|
| 10-K |
| 12/31/15 |
| 10.19 |
| 02/29/16 |
|
|
|
|
|
|
|
|
|
|
|
|
|
10.19* |
| Diplomat Pharmacy, Inc. Annual Performance Bonus Plan |
|
|
| 8-K |
|
|
| 10.2 |
| 06/09/15 |
|
|
|
|
|
|
|
|
|
|
|
|
|
10.20 |
| Consent to Sale of Compounding Business, dated August 27, 2015, by and among Diplomat, General Electric Capital Corporation, and the other lender parties thereto |
|
|
| 10-Q |
| 9/30/16 |
| 10.2 |
| 11/04/15 |
|
|
|
|
|
|
|
|
|
|
|
|
|
10.21* |
| Diplomat Non-Employee Director Compensation Program (February 2016) |
| X |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
10.22* |
| Permanent Release and Settlement Agreement, dated October 25, 2016, by and between the Company and Sean Whelan |
|
|
| 8-K |
|
|
| 10.2 |
| 10/26/16 |
|
|
|
|
|
| Incorporated by reference | ||||||
Exhibit |
| Exhibit description |
| Filed/Furnished |
| Form |
| Period |
| Exhibit |
| Filing |
10.23* |
| Employment Agreement, dated October 25, 2016, by and between the Company and Paul Urick |
|
|
| 8-K |
|
|
| 10.1 |
| 10/26/16 |
|
|
|
|
|
|
|
|
|
|
|
|
|
10.24† |
| Distribution and Services Agreement dated August 7, 2013 by and between Pharmacyclics, Inc. and Diplomat |
| X |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
10.25† |
| Amendment No. 1 to Distribution and Services Agreement by and between Pharmacyclics, Inc. and Diplomat, dated March 3, 2014 |
| X |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
21 |
| List of subsidiaries of Diplomat |
| X |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
23 |
| Consent of BDO USA, LLP |
| X |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
31.1 |
| Section 302 Certification—CEO |
| X |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
31.2 |
| Section 302 Certification—PFO |
| X |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
32.1 |
| Section 906 Certification—CEO |
| X |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
32.2 |
| Section 906 Certification—PFO |
| X |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
101.INS |
| XBRL Instance Document |
| X |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
101.SCH |
| XBRL Taxonomy Extension Schema Document |
| X |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
101.CAL |
| XBRL Taxonomy Extension Calculation Linkbase Document |
| X |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
101.DEF |
| XBRL Taxonomy Extension Definition Linkbase Document |
| X |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
101.LAB |
| XBRL Taxonomy Extension Label Linkbase Document |
| X |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
101.PRE |
| XBRL Taxonomy Extension Presentation Linkbase Document |
| X |
|
|
|
|
|
|
|
|
* Indicates a management contract or compensatory plan or arrangement.
** Exhibits and schedules have been omitted in accordance with Item 601(b)(2) of Regulation S-K. A copy of omitted exhibits and schedules will be furnished to the Commission upon request.
† Confidential treatment has been requested for portions of this exhibit. These portions have been omitted from these exhibits to this Annual Report on Form 10-K and submitted separately to the Securities and Exchange Commission.