Exhibit 99.2 Building The Future of Immune Therapeutics Company Overview December 2024
Forward Looking Statements This presentation has been prepared by Q32 Bio Inc. (“we”, “us,” “our,” “Q32” or the “Company”) and is made for informational purposes only. The information set forth herein does not purport to be complete or contain all of the information you may desire. Statements contained herein are made as of the date of this presentation unless stated otherwise, and this presentation shall not under any circumstances create an implication that the information contained herein is correct as of any time after such date or that information will be updated or revised to reflect information that subsequently becomes available or changes occurring after the date hereof. This presentation contains forward-looking statements within the meaning of the U.S. Private Securities Litigation Reform Act of 1995. Forward-looking statements can be identified by words such as “may,” “will,” “should,” “would,” “expect,” “anticipate,” “plan,” “likely,” “believe,” “estimate,” “project,” “intend,” “potential,” and similar expressions regarding future periods. These forward-looking statements include, but are not limited to, our beliefs, observations, expectations and assumptions regarding the topline data from the SIGNAL-AA Phase 2a and the safety, tolerability, clinical activity including biomarker data, potential efficacy and potential benefits of bempikibart, plans and expectations for Part B of the SIGNAL-AA Phase 2a clinical trial statements regarding expected cash and the sufficiency of the Company’s cash to fund operations into mid- 2026, the expectations surrounding the potential, safety, efficacy, and regulatory and clinical progress of Q32’s product candidates, including bempikibart and ADX-097, and anticipated milestones, data readouts and timing, among others. Statements that are not historical facts are forward-looking statements. Forward-looking statements are based on current beliefs and assumptions that are subject to risks and uncertainties and are not guarantees of future performance. Actual results could differ materially from those contained in any forward-looking statement as a result of various factors, including, without limitation: the Company’s need for additional funding, which may not be available; failure to identify additional product candidates and develop or commercialize marketable products; the early stage of the Company’s development efforts; potential unforeseen events during clinical trials could cause delays or other adverse consequences; risks relating to the regulatory approval process; interim, topline and preliminary data may change as more patient data become available, and are subject to audit and verification procedures that could result in material changes in the final data; Q32’s product candidates may cause serious adverse side effects; inability to maintain our collaborations, or the failure of these collaborations; our reliance on third parties, including for the manufacture of materials for our research programs, preclinical and clinical studies; failure to obtain U.S. or international marketing approval; ongoing regulatory obligations; effects of significant competition; unfavorable pricing regulations, third-party reimbursement practices or healthcare reform initiatives; product liability lawsuits; securities class action litigation; the impact of the COVID-19 pandemic and general economic conditions on our business and operations, including our preclinical studies and clinical trials; the possibility of system failures or security breaches; risks relating to intellectual property and our ability to protect our patents and other proprietary rights; significant costs incurred as a result of operating as a public company; as well as those risk and uncertainties set forth more fully under the caption “Risk Factors” in our Quarterly Report on Form 10-Q for the quarter ended September 30, 2024, as well as other risks detailed in our subsequent filings with the United States Securities and Exchange Commission. Any forward-looking statement made by us is based only on information currently available to us and speaks only as of the date on which it is made. We undertake no obligation to publicly update any forward-looking statement, whether written or oral, that may be made from time to time, whether as a result of new information, future developments or otherwise. Certain information contained in this presentation relates to or is based on studies, publications, analyses, surveys and other data obtained from third-party sources and the Company’s own internal estimates and research. While the Company believes these third-party sources to be reliable as of the date of this presentation, it has not independently verified, and makes no representation as to the adequacy, fairness, accuracy or completeness of, any information obtained from third-party sources. In addition, all of the market data included in this presentation involves a number of assumptions and limitations, and there can be no guarantee as to the accuracy or reliability of such assumptions. Finally, while we believe our own internal research is reliable, such research may not have been verified by any independent source. 2
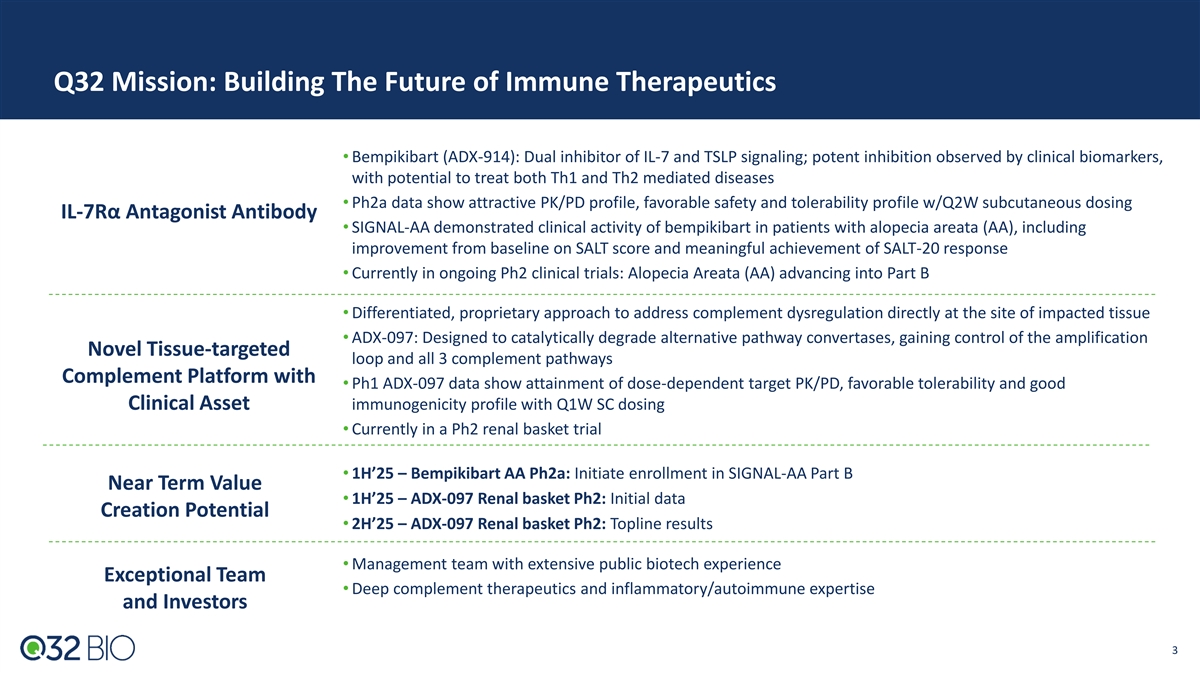
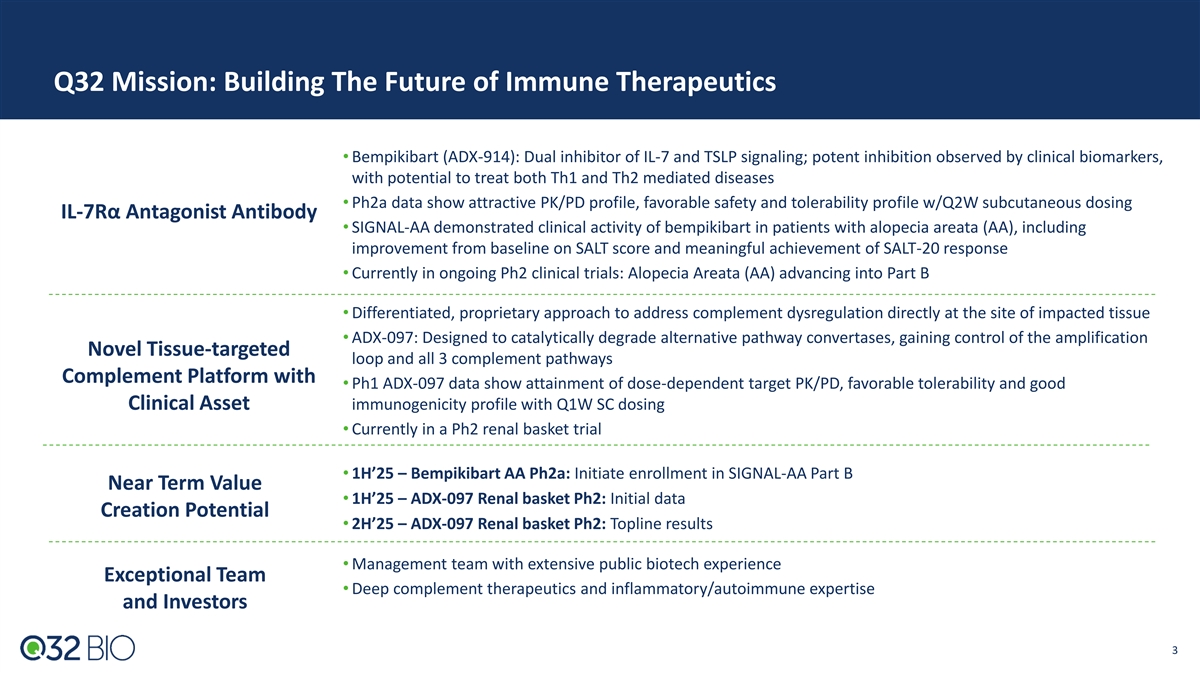
Q32 Mission: Building The Future of Immune Therapeutics • Bempikibart (ADX-914): Dual inhibitor of IL-7 and TSLP signaling; potent inhibition observed by clinical biomarkers, with potential to treat both Th1 and Th2 mediated diseases • Ph2a data show attractive PK/PD profile, favorable safety and tolerability profile w/Q2W subcutaneous dosing IL-7Rα Antagonist Antibody • SIGNAL-AA demonstrated clinical activity of bempikibart in patients with alopecia areata (AA), including improvement from baseline on SALT score and meaningful achievement of SALT-20 response • Currently in ongoing Ph2 clinical trials: Alopecia Areata (AA) advancing into Part B • Differentiated, proprietary approach to address complement dysregulation directly at the site of impacted tissue • ADX-097: Designed to catalytically degrade alternative pathway convertases, gaining control of the amplification Novel Tissue-targeted loop and all 3 complement pathways Complement Platform with • Ph1 ADX-097 data show attainment of dose-dependent target PK/PD, favorable tolerability and good Clinical Asset immunogenicity profile with Q1W SC dosing • Currently in a Ph2 renal basket trial • 1H’25 – Bempikibart AA Ph2a: Initiate enrollment in SIGNAL-AA Part B Near Term Value • 1H’25 – ADX-097 Renal basket Ph2: Initial data Creation Potential • 2H’25 – ADX-097 Renal basket Ph2: Topline results • Management team with extensive public biotech experience Exceptional Team • Deep complement therapeutics and inflammatory/autoimmune expertise and Investors 3
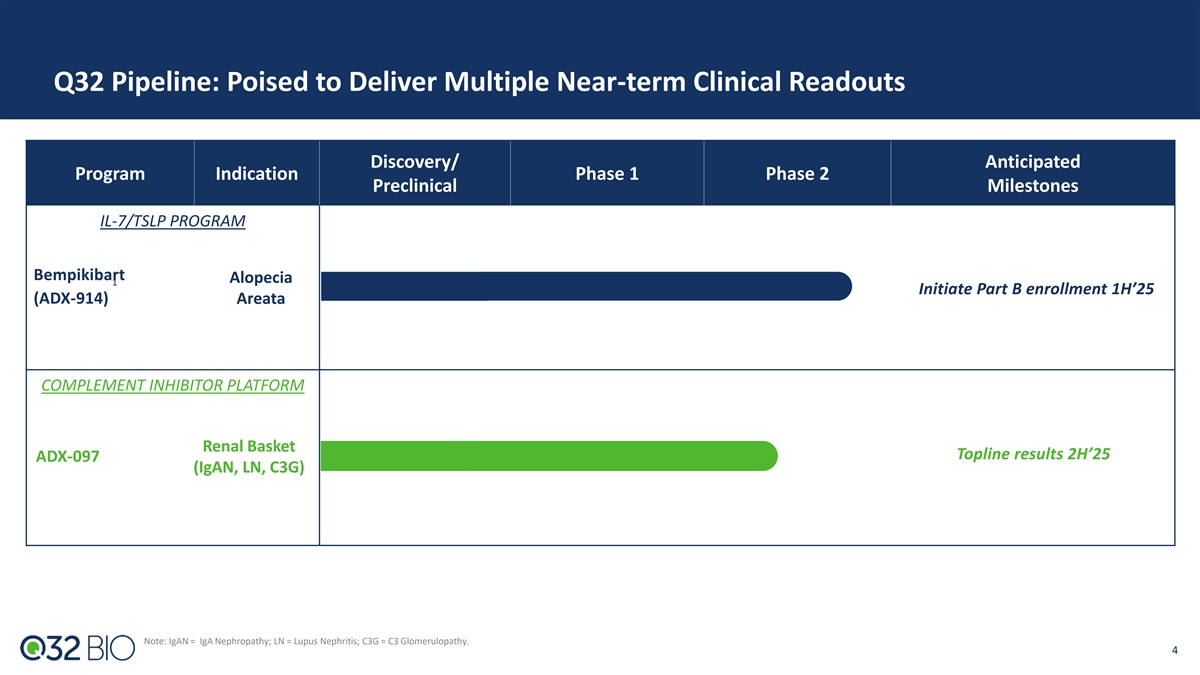
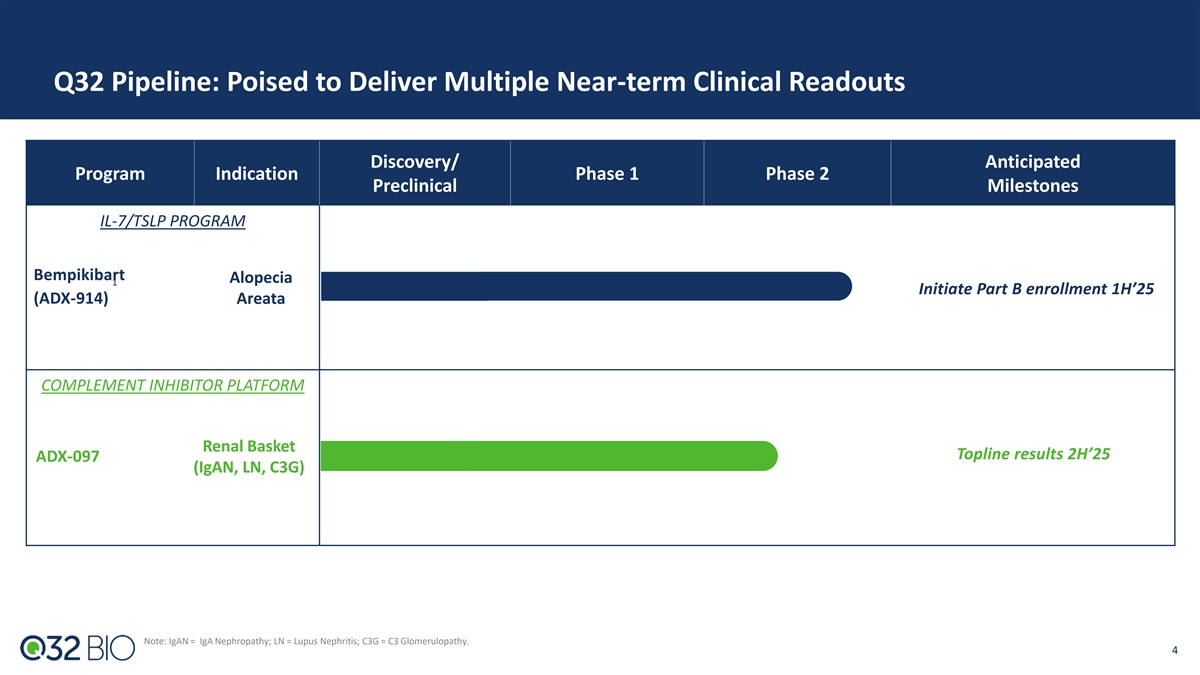
Q32 Pipeline: Poised to Deliver Multiple Near-term Clinical Readouts Discovery/ Anticipated Program Indication Phase 1 Phase 2 Preclinical Milestones IL-7/TSLP PROGRAM Bempikibart Alopecia 1 Initiate Part B enrollment 1H’25 (ADX-914) Areata COMPLEMENT INHIBITOR PLATFORM Renal Basket Topline results 2H’25 ADX-097 (IgAN, LN, C3G) Note: IgAN = IgA Nephropathy; LN = Lupus Nephritis; C3G = C3 Glomerulopathy. 4
Bempikibart (ADX-914) (IL-7 / TSLP Receptor Inhibitor)
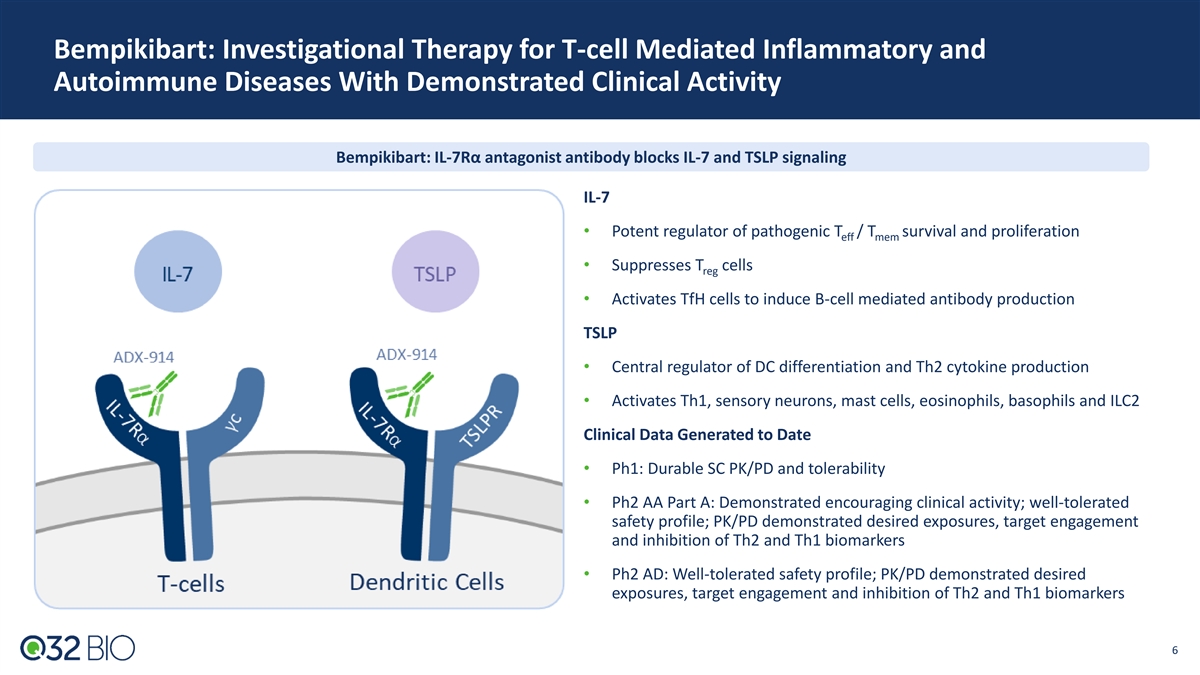
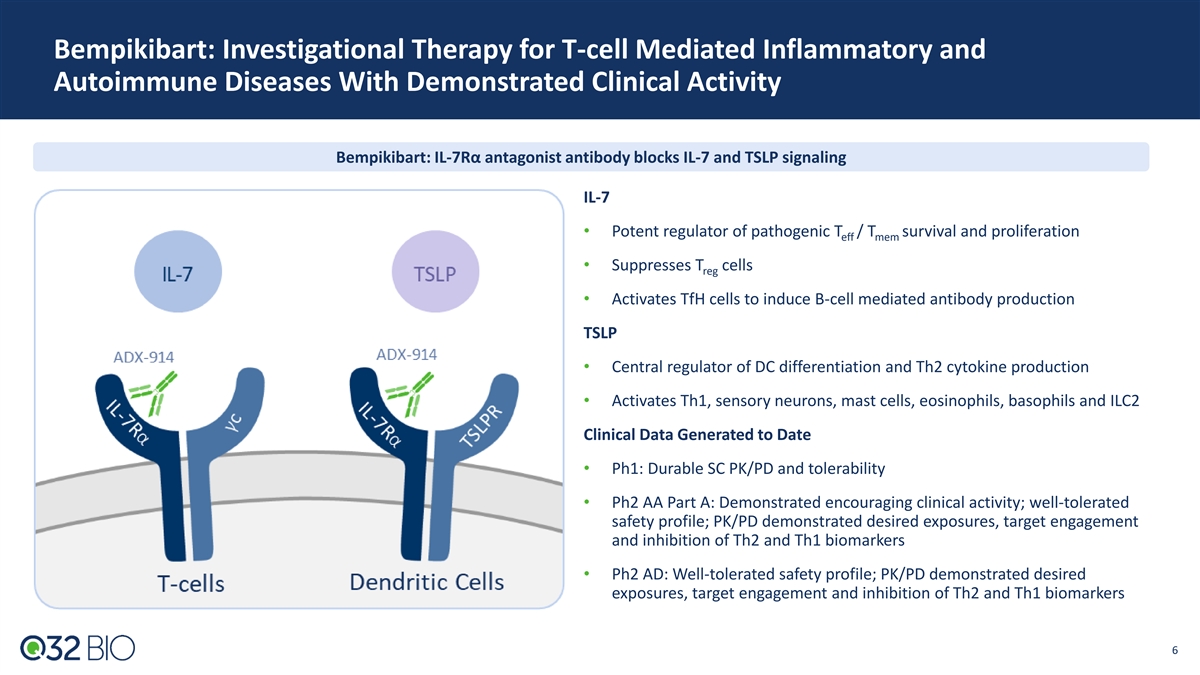
Bempikibart: Investigational Therapy for T-cell Mediated Inflammatory and Autoimmune Diseases With Demonstrated Clinical Activity Bempikibart: IL-7Rα antagonist antibody blocks IL-7 and TSLP signaling IL-7 • Potent regulator of pathogenic T / T survival and proliferation eff mem • Suppresses T cells reg • Activates TfH cells to induce B-cell mediated antibody production TSLP • Central regulator of DC differentiation and Th2 cytokine production • Activates Th1, sensory neurons, mast cells, eosinophils, basophils and ILC2 Clinical Data Generated to Date • Ph1: Durable SC PK/PD and tolerability • Ph2 AA Part A: Demonstrated encouraging clinical activity; well-tolerated safety profile; PK/PD demonstrated desired exposures, target engagement and inhibition of Th2 and Th1 biomarkers • Ph2 AD: Well-tolerated safety profile; PK/PD demonstrated desired exposures, target engagement and inhibition of Th2 and Th1 biomarkers 6 6
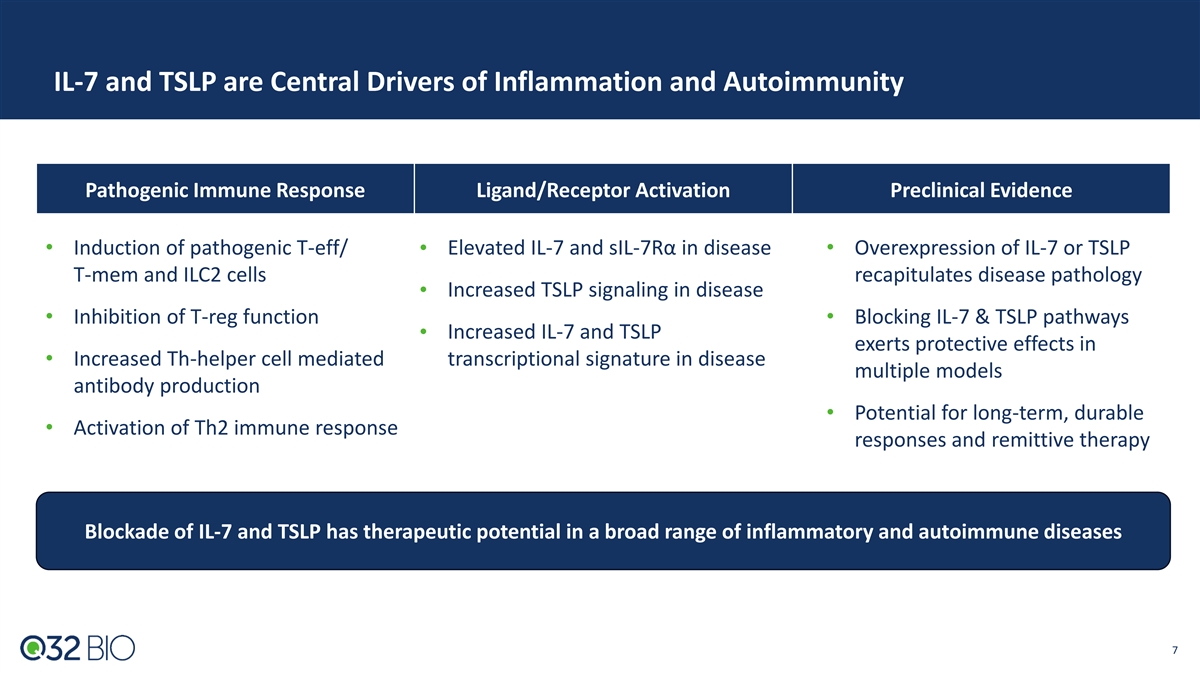
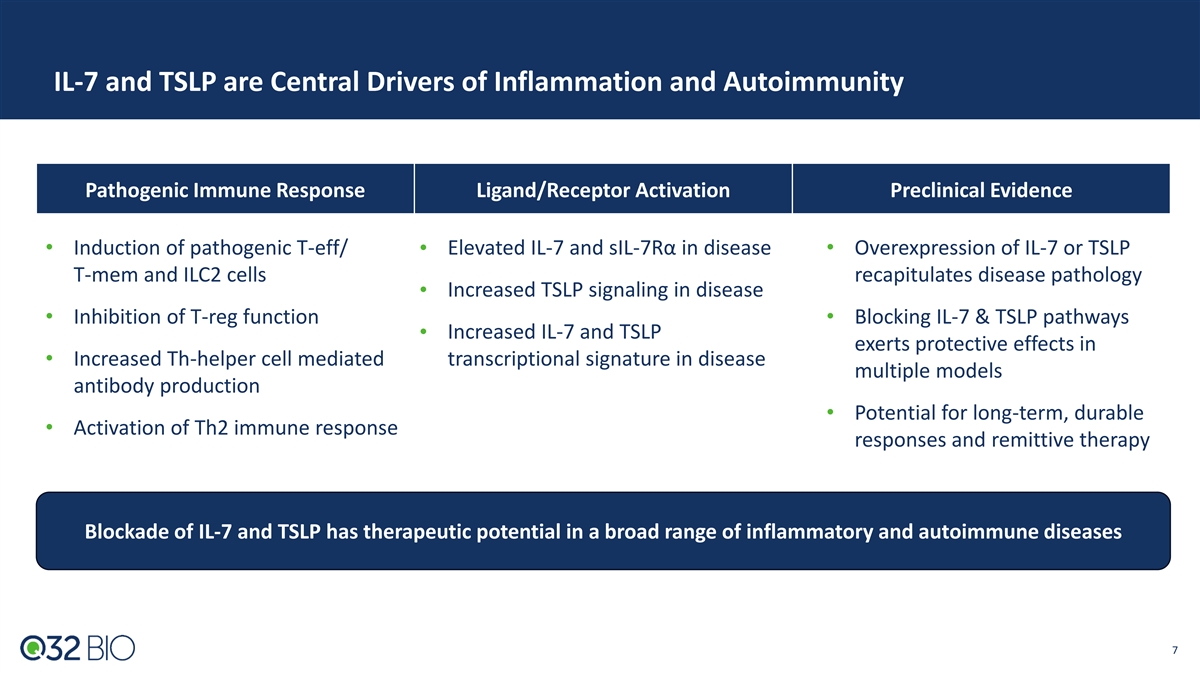
IL-7 and TSLP are Central Drivers of Inflammation and Autoimmunity Pathogenic Immune Response Ligand/Receptor Activation Preclinical Evidence • Induction of pathogenic T-eff/ • Elevated IL-7 and sIL-7Rα in disease• Overexpression of IL-7 or TSLP T-mem and ILC2 cells recapitulates disease pathology Increased TSLP signaling in disease • • Inhibition of T-reg function• Blocking IL-7 & TSLP pathways Increased IL-7 and TSLP • exerts protective effects in • Increased Th-helper cell mediated transcriptional signature in disease multiple models antibody production • Potential for long-term, durable • Activation of Th2 immune response responses and remittive therapy Blockade of IL-7 and TSLP has therapeutic potential in a broad range of inflammatory and autoimmune diseases 7
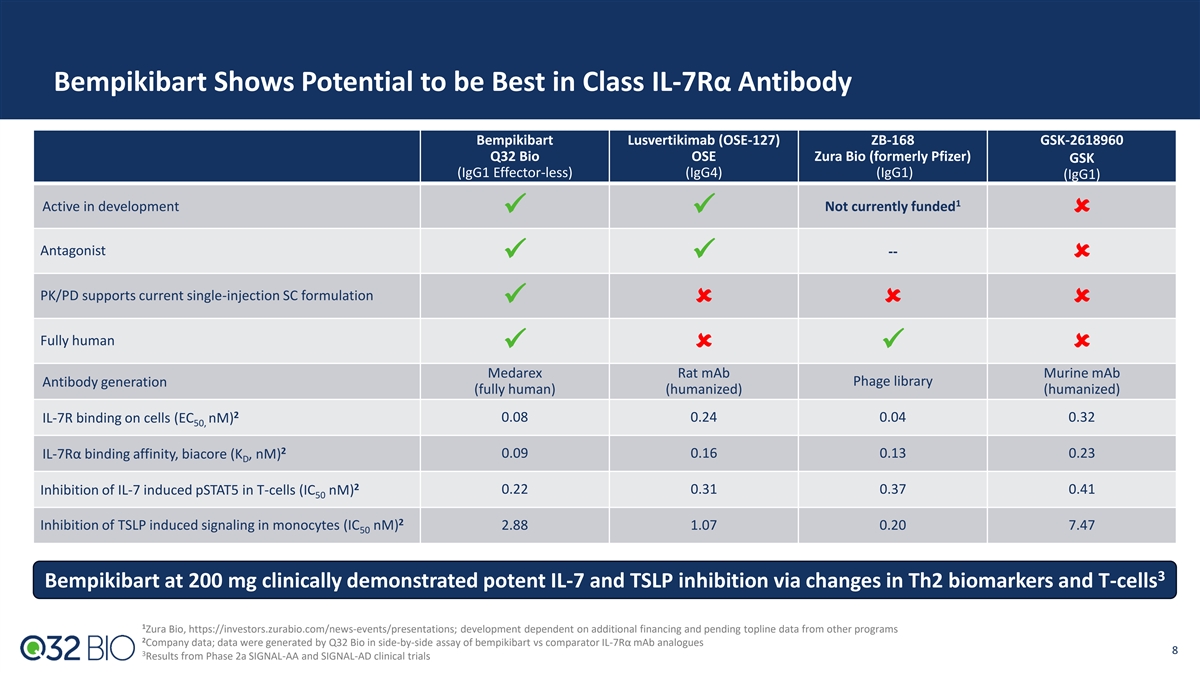
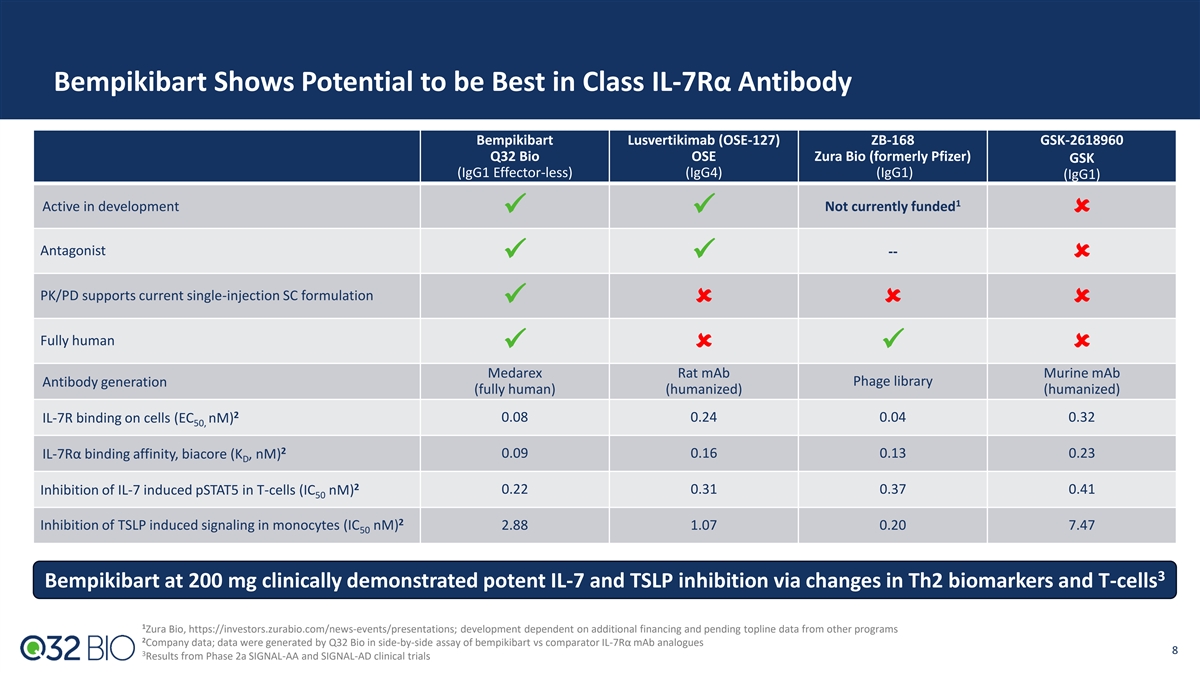
Bempikibart Shows Potential to be Best in Class IL-7Rα Antibody Bempikibart Lusvertikimab (OSE-127) ZB-168 GSK-2618960 Q32 Bio OSE Zura Bio (formerly Pfizer) GSK (IgG1 Effector-less) (IgG4) (IgG1) (IgG1) 1 Active in development Not currently funded ✓✓û Antagonist -- ✓✓û PK/PD supports current single-injection SC formulation ✓ûûû Fully human ✓û✓û Medarex Rat mAb Murine mAb Antibody generation Phage library (fully human) (humanized) (humanized) 2 IL-7R binding on cells (EC nM) 0.08 0.24 0.04 0.32 50, 2 0.09 0.16 0.13 0.23 IL-7Rα binding affinity, biacore (K , nM) D 2 0.22 0.31 0.37 0.41 Inhibition of IL-7 induced pSTAT5 in T-cells (IC nM) 50 2 Inhibition of TSLP induced signaling in monocytes (IC nM) 2.88 1.07 0.20 7.47 50 3 Bempikibart at 200 mg clinically demonstrated potent IL-7 and TSLP inhibition via changes in Th2 biomarkers and T-cells 1 Zura Bio, https://investors.zurabio.com/news-events/presentations; development dependent on additional financing and pending topline data from other programs 2 Company data; data were generated by Q32 Bio in side-by-side assay of bempikibart vs comparator IL-7Rα mAb analogues 8 3 Results from Phase 2a SIGNAL-AA and SIGNAL-AD clinical trials
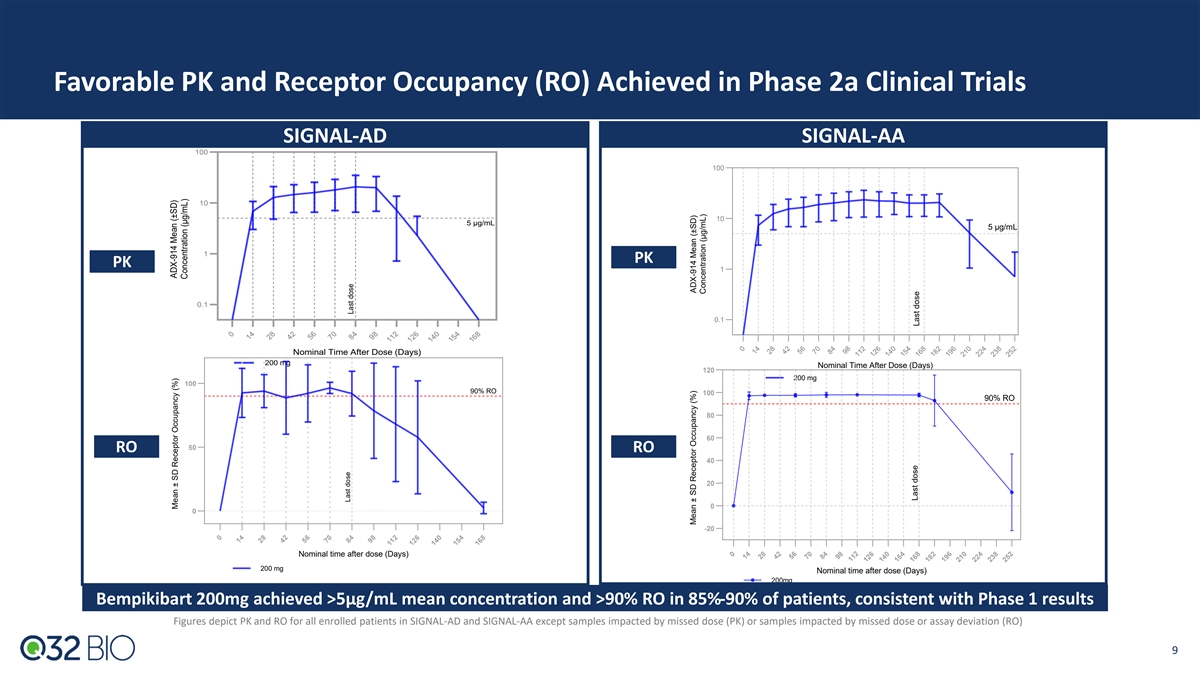
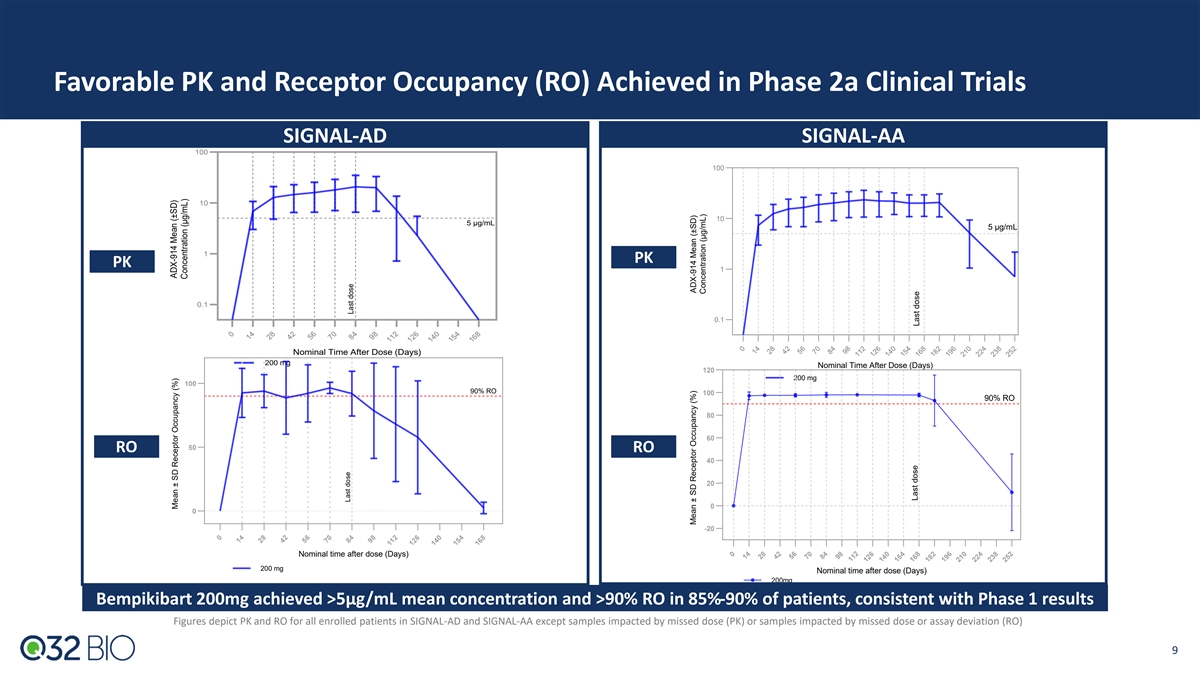
Favorable PK and Receptor Occupancy (RO) Achieved in Phase 2a Clinical Trials SIGNAL-AD SIGNAL-AA 100 100 10 10 5 μg/mL 5 μg/mL 1 PK PK 1 0.1 0.1 Nominal Time After Dose (Days) 200 mg Nominal Time After Dose (Days) 120 200 mg 100 90% RO 100 90% RO 80 60 50 RO RO 40 20 0 0 -20 Nominal time after dose (Days) 200 mg Nominal time after dose (Days) 200mg Bempikibart 200mg achieved >5µg/mL mean concentration and >90% RO in 85%-90% of patients, consistent with Phase 1 results Figures depict PK and RO for all enrolled patients in SIGNAL-AD and SIGNAL-AA except samples impacted by missed dose (PK) or samples impacted by missed dose or assay deviation (RO) 9 0 14 28 42 56 70 84 98 112 126 140 154 168 0 14 28 42 56 70 84 98 112 126 140 154 168 182 196 210 224 238 252 0 14 28 42 56 70 84 98 112 126 140 154 168 0 14 28 42 56 70 84 98 112 126 140 154 168 182 196 210 224 238 252 Mean ± SD Receptor Occupancy (%) ADX-914 Mean (±SD) Concentration (μg/mL) Last dose Last dose Mean ± SD Receptor Occupancy (%) ADX-914 Mean (±SD) Concentration (μg/mL) Last dose Last dose
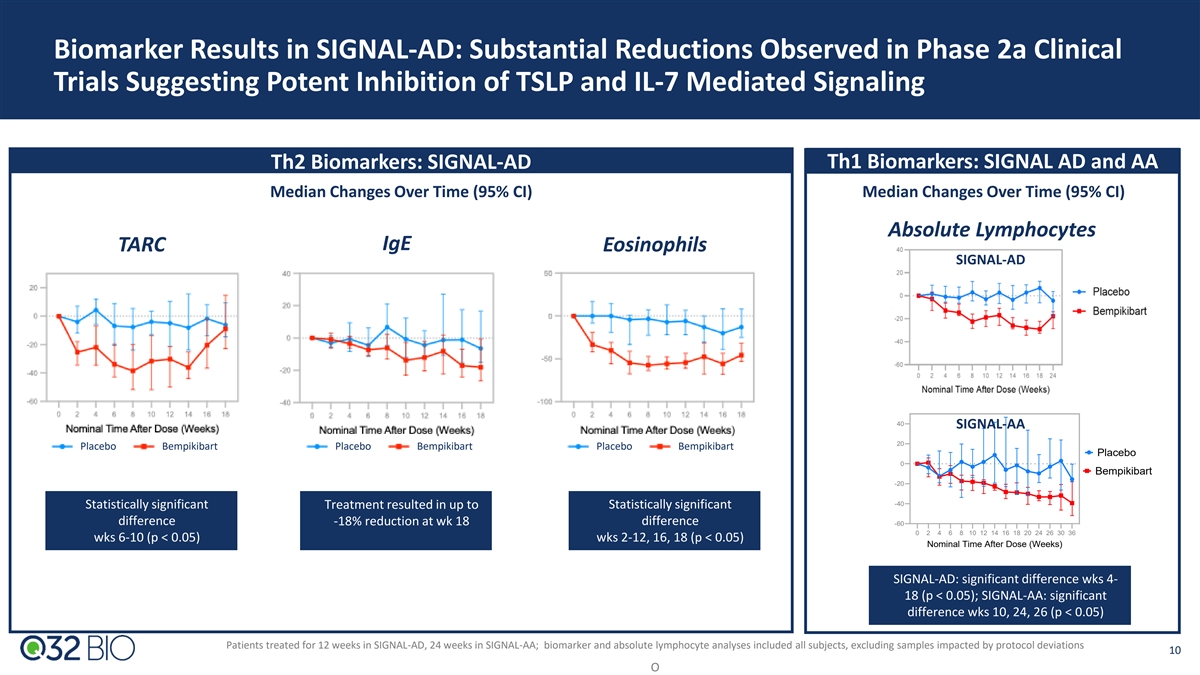
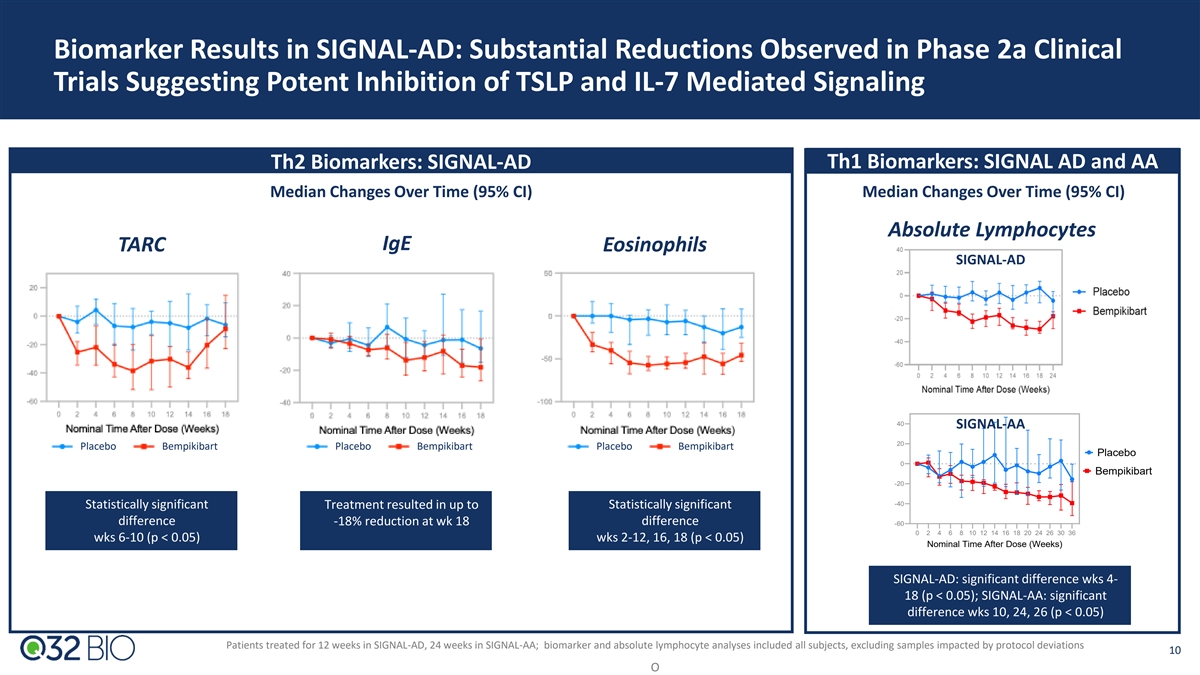
Biomarker Results in SIGNAL-AD: Substantial Reductions Observed in Phase 2a Clinical Trials Suggesting Potent Inhibition of TSLP and IL-7 Mediated Signaling Th2 Biomarkers: SIGNAL-AD Th1 Biomarkers: SIGNAL AD and AA Median Changes Over Time (95% CI) Median Changes Over Time (95% CI) Absolute Lymphocytes IgE TARC Eosinophils SIGNAL-AD 40 SIGNAL-AA 20 Placebo Bempikibart Placebo Bempikibart Placebo Bempikibart Placebo 0 Bempikibart -20 -40 Statistically significant Treatment resulted in up to Statistically significant difference -18% reduction at wk 18 difference -60 0 2 4 6 8 10 12 14 16 18 20 24 26 30 36 wks 6-10 (p < 0.05) wks 2-12, 16, 18 (p < 0.05) Nominal Time After Dose (Weeks) SIGNAL-AD: significant difference wks 4- 18 (p < 0.05); SIGNAL-AA: significant difference wks 10, 24, 26 (p < 0.05) Patients treated for 12 weeks in SIGNAL-AD, 24 weeks in SIGNAL-AA; biomarker and absolute lymphocyte analyses included all subjects, excluding samples impacted by protocol deviations 10 O % change from baseline Lymphocytes Median (95% CI)
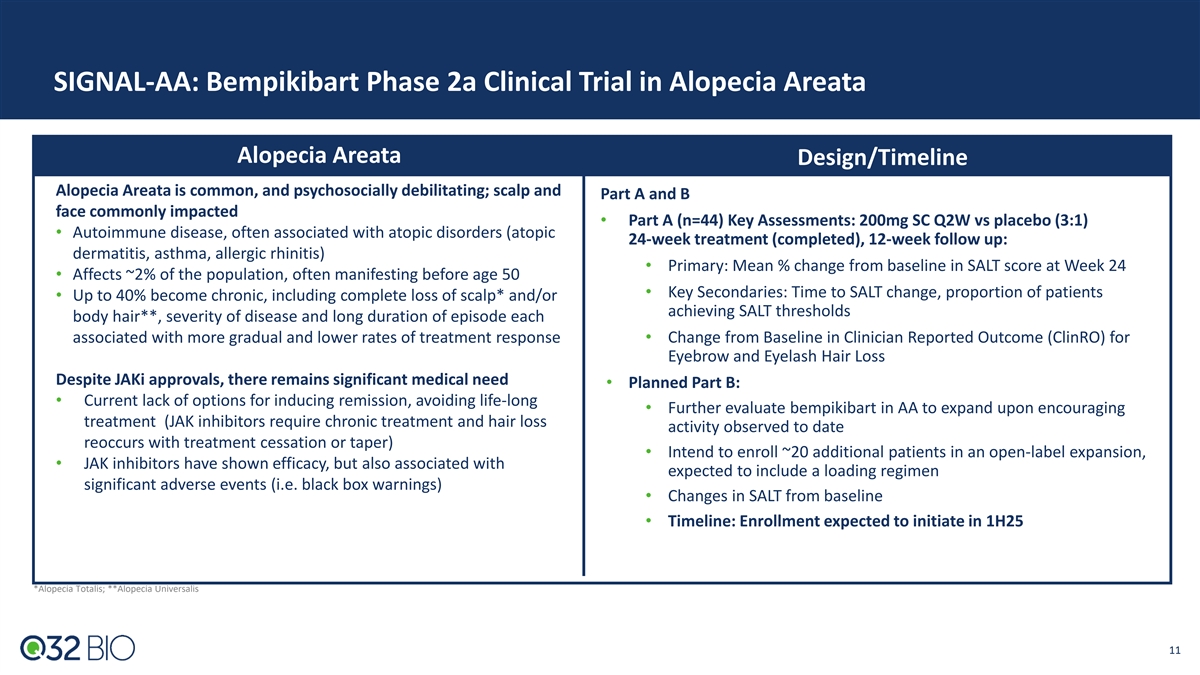
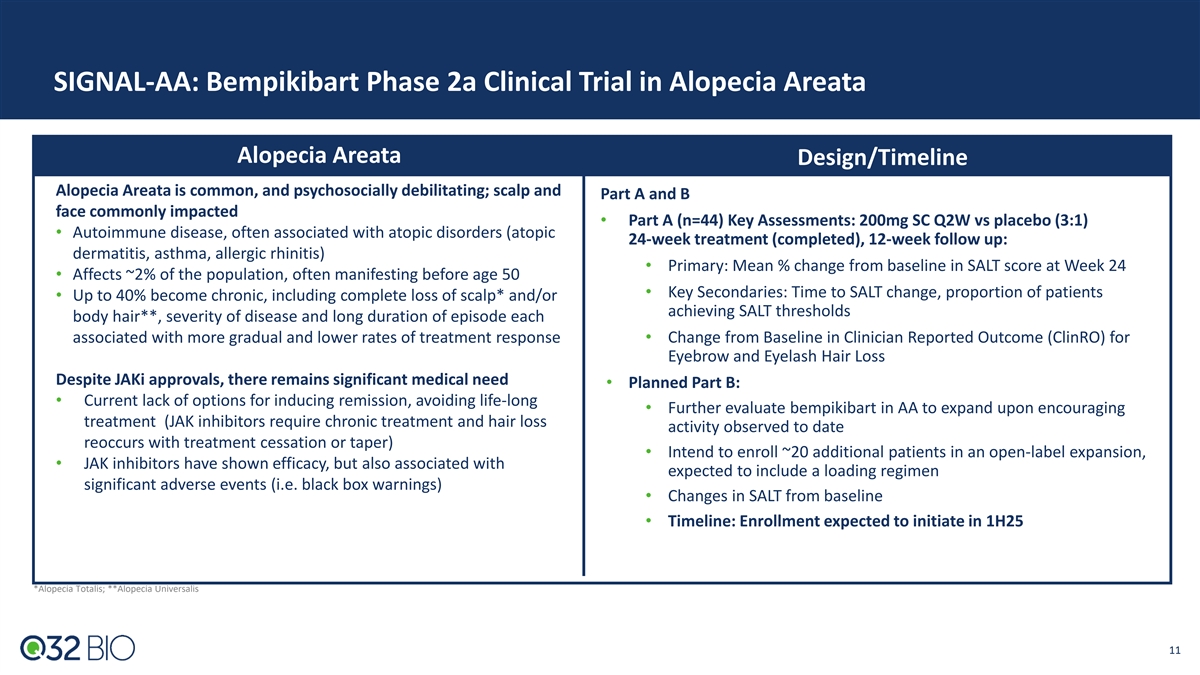
SIGNAL-AA: Bempikibart Phase 2a Clinical Trial in Alopecia Areata Alopecia Areata Design/Timeline Alopecia Areata is common, and psychosocially debilitating; scalp and Part A and B face commonly impacted • Part A (n=44) Key Assessments: 200mg SC Q2W vs placebo (3:1) • Autoimmune disease, often associated with atopic disorders (atopic 24-week treatment (completed), 12-week follow up: dermatitis, asthma, allergic rhinitis) • Primary: Mean % change from baseline in SALT score at Week 24 • Affects ~2% of the population, often manifesting before age 50 • Key Secondaries: Time to SALT change, proportion of patients • Up to 40% become chronic, including complete loss of scalp* and/or achieving SALT thresholds body hair**, severity of disease and long duration of episode each associated with more gradual and lower rates of treatment response• Change from Baseline in Clinician Reported Outcome (ClinRO) for Eyebrow and Eyelash Hair Loss Despite JAKi approvals, there remains significant medical need • Planned Part B: • Current lack of options for inducing remission, avoiding life-long • Further evaluate bempikibart in AA to expand upon encouraging treatment (JAK inhibitors require chronic treatment and hair loss activity observed to date reoccurs with treatment cessation or taper) • Intend to enroll ~20 additional patients in an open-label expansion, • JAK inhibitors have shown efficacy, but also associated with expected to include a loading regimen significant adverse events (i.e. black box warnings) • Changes in SALT from baseline • Timeline: Enrollment expected to initiate in 1H25 *Alopecia Totalis; **Alopecia Universalis 11
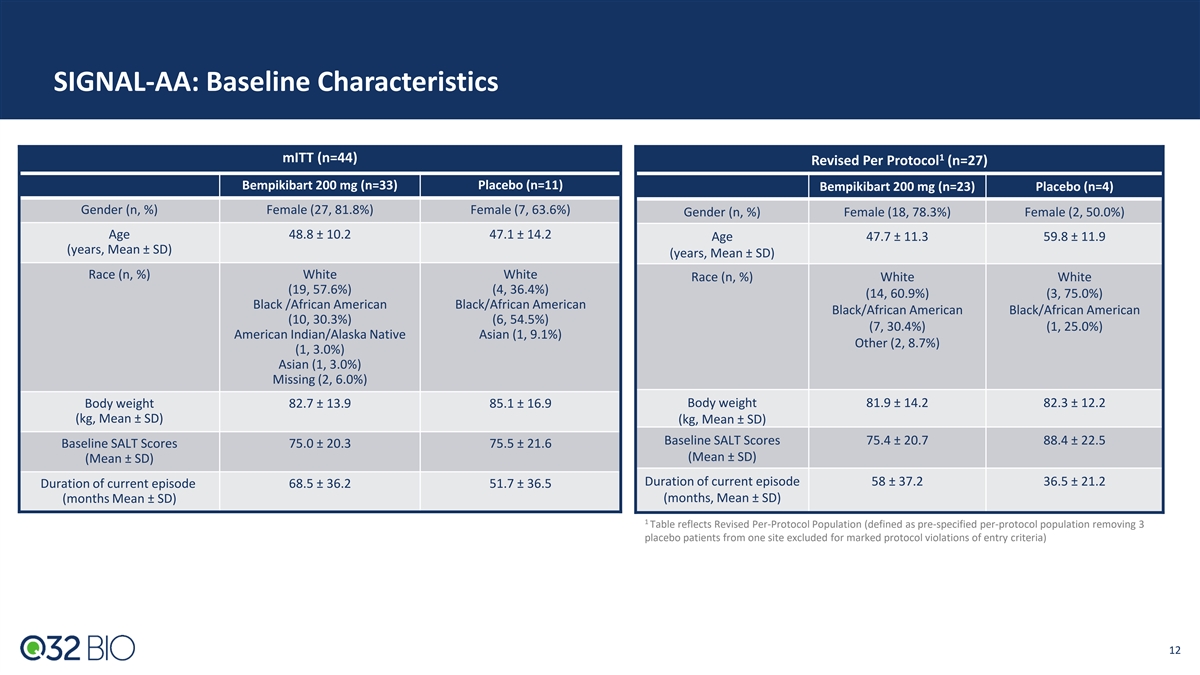
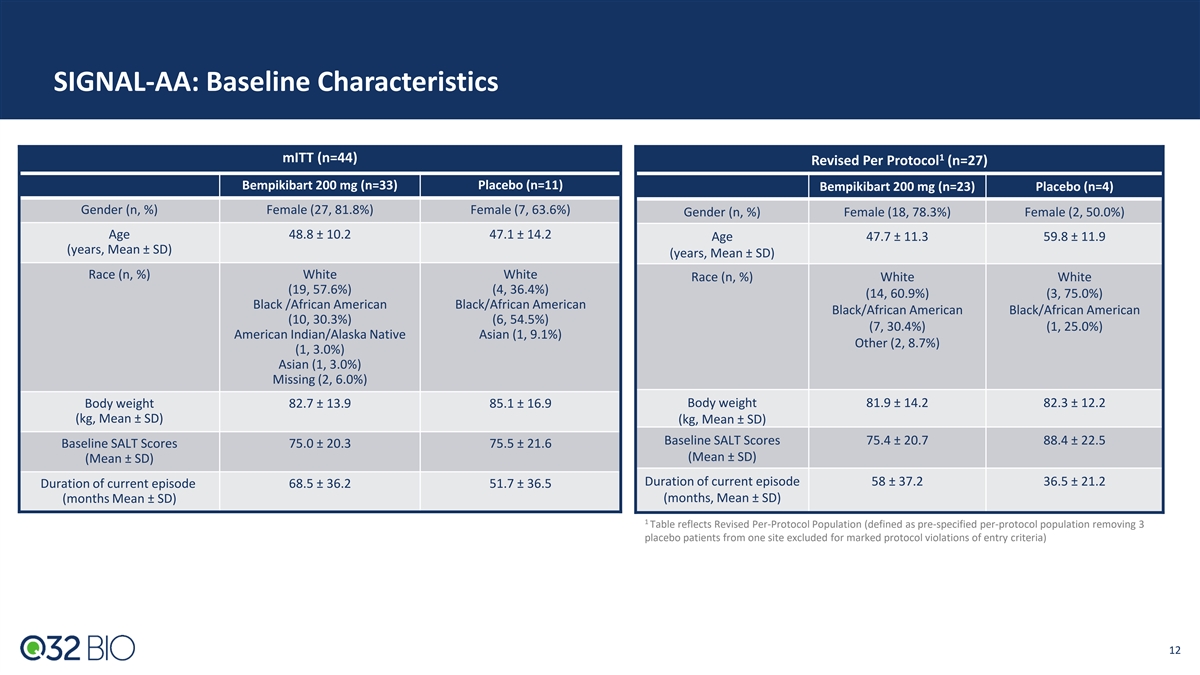
SIGNAL-AA: Baseline Characteristics 1 mITT (n=44) Revised Per Protocol (n=27) Bempikibart 200 mg (n=33) Placebo (n=11) Bempikibart 200 mg (n=23) Placebo (n=4) Gender (n, %) Female (27, 81.8%) Female (7, 63.6%) Gender (n, %) Female (18, 78.3%) Female (2, 50.0%) Age 48.8 ± 10.2 47.1 ± 14.2 Age 47.7 ± 11.3 59.8 ± 11.9 (years, Mean ± SD) (years, Mean ± SD) Race (n, %) White White Race (n, %) White White (19, 57.6%) (4, 36.4%) (14, 60.9%) (3, 75.0%) Black /African American Black/African American Black/African American Black/African American (10, 30.3%) (6, 54.5%) (7, 30.4%) (1, 25.0%) American Indian/Alaska Native Asian (1, 9.1%) Other (2, 8.7%) (1, 3.0%) Asian (1, 3.0%) Missing (2, 6.0%) Body weight 82.7 ± 13.9 85.1 ± 16.9 Body weight 81.9 ± 14.2 82.3 ± 12.2 (kg, Mean ± SD) (kg, Mean ± SD) Baseline SALT Scores 75.4 ± 20.7 88.4 ± 22.5 Baseline SALT Scores 75.0 ± 20.3 75.5 ± 21.6 (Mean ± SD) (Mean ± SD) Duration of current episode 58 ± 37.2 36.5 ± 21.2 Duration of current episode 68.5 ± 36.2 51.7 ± 36.5 (months Mean ± SD) (months, Mean ± SD) 1 Table reflects Revised Per-Protocol Population (defined as pre-specified per-protocol population removing 3 placebo patients from one site excluded for marked protocol violations of entry criteria) 12 12
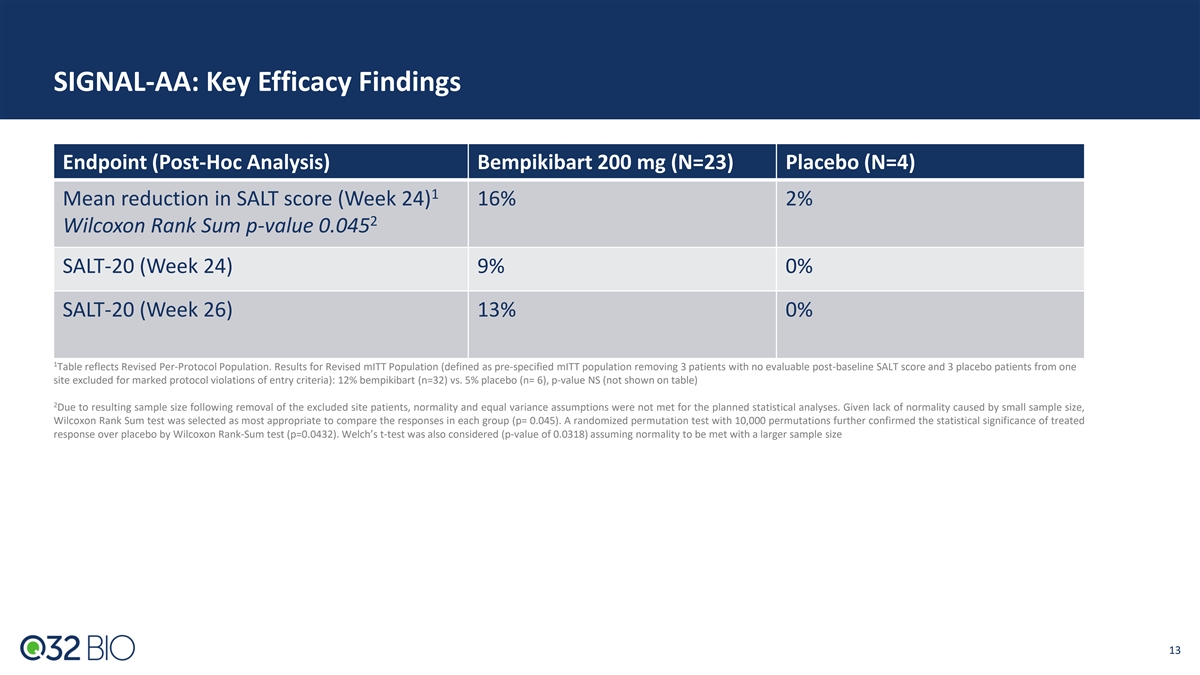
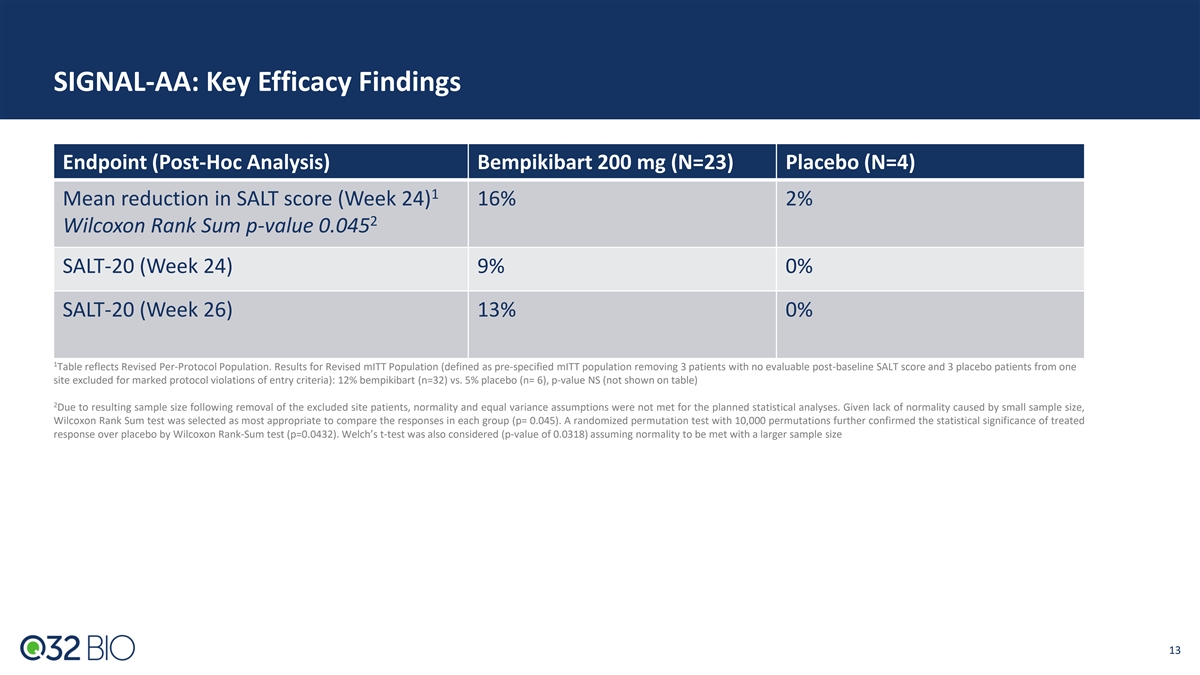
SIGNAL-AA: Key Efficacy Findings Endpoint (Post-Hoc Analysis) Bempikibart 200 mg (N=23) Placebo (N=4) 1 Mean reduction in SALT score (Week 24) 16% 2% 2 Wilcoxon Rank Sum p-value 0.045 SALT-20 (Week 24) 9% 0% SALT-20 (Week 26) 13% 0% 1 Table reflects Revised Per-Protocol Population. Results for Revised mITT Population (defined as pre-specified mITT population removing 3 patients with no evaluable post-baseline SALT score and 3 placebo patients from one site excluded for marked protocol violations of entry criteria): 12% bempikibart (n=32) vs. 5% placebo (n= 6), p-value NS (not shown on table) 2 Due to resulting sample size following removal of the excluded site patients, normality and equal variance assumptions were not met for the planned statistical analyses. Given lack of normality caused by small sample size, Wilcoxon Rank Sum test was selected as most appropriate to compare the responses in each group (p= 0.045). A randomized permutation test with 10,000 permutations further confirmed the statistical significance of treated response over placebo by Wilcoxon Rank-Sum test (p=0.0432). Welch’s t-test was also considered (p-value of 0.0318) assuming normality to be met with a larger sample size 13 13
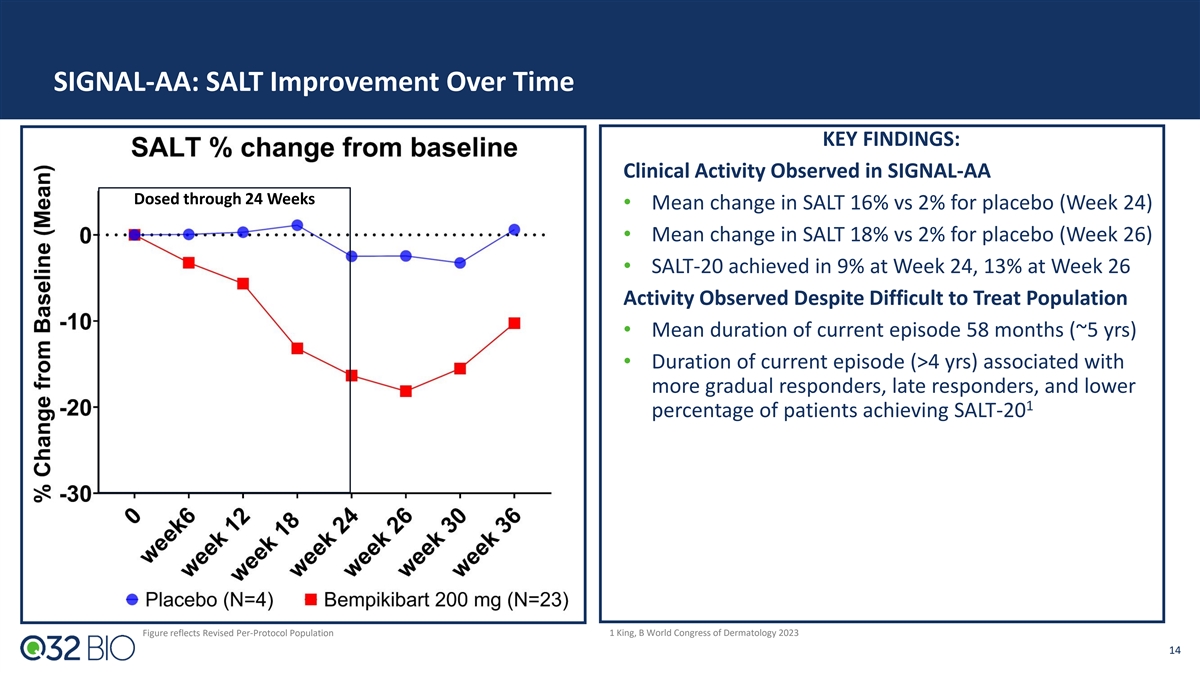
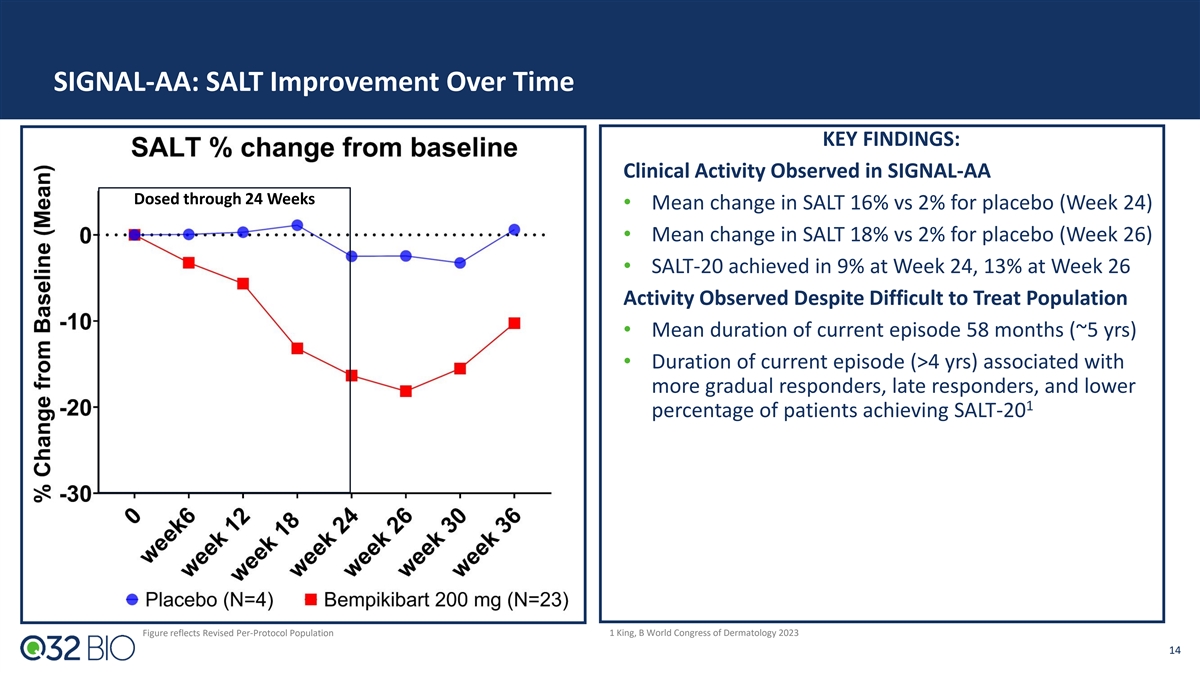
SIGNAL-AA: SALT Improvement Over Time KEY FINDINGS: Clinical Activity Observed in SIGNAL-AA Dosed through 24 Weeks • Mean change in SALT 16% vs 2% for placebo (Week 24) • Mean change in SALT 18% vs 2% for placebo (Week 26) • SALT-20 achieved in 9% at Week 24, 13% at Week 26 Activity Observed Despite Difficult to Treat Population • Mean duration of current episode 58 months (~5 yrs) • Duration of current episode (>4 yrs) associated with more gradual responders, late responders, and lower 1 percentage of patients achieving SALT-20 Figure reflects Revised Per-Protocol Population 1 King, B World Congress of Dermatology 2023 14
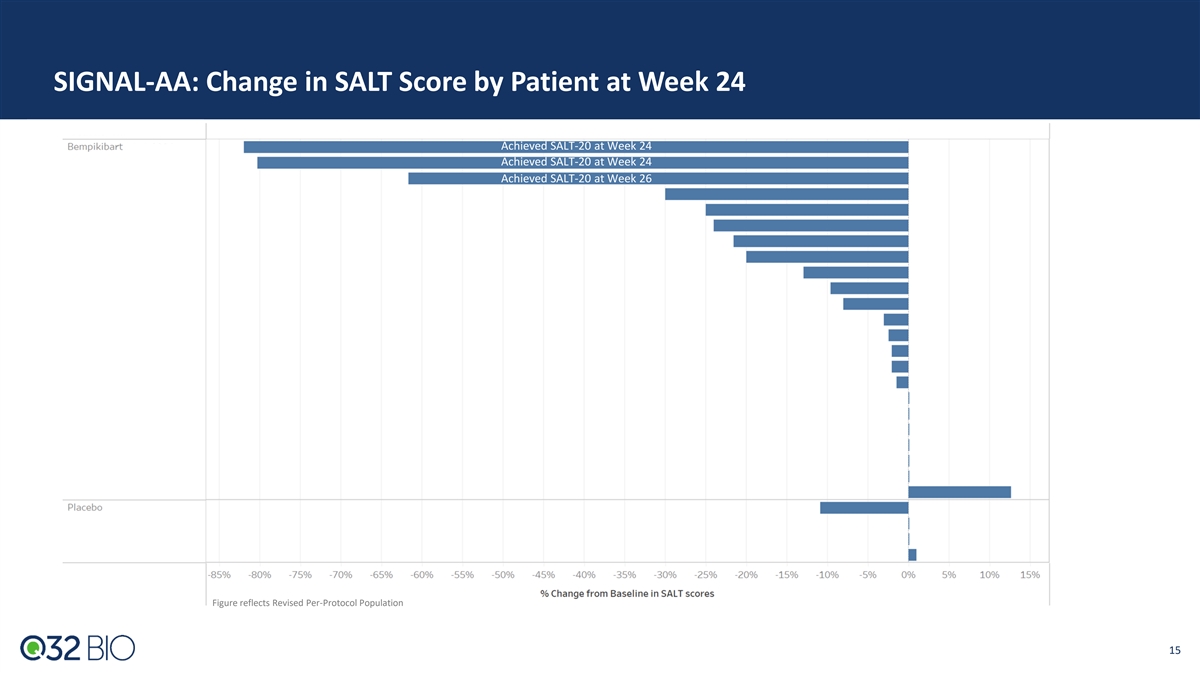
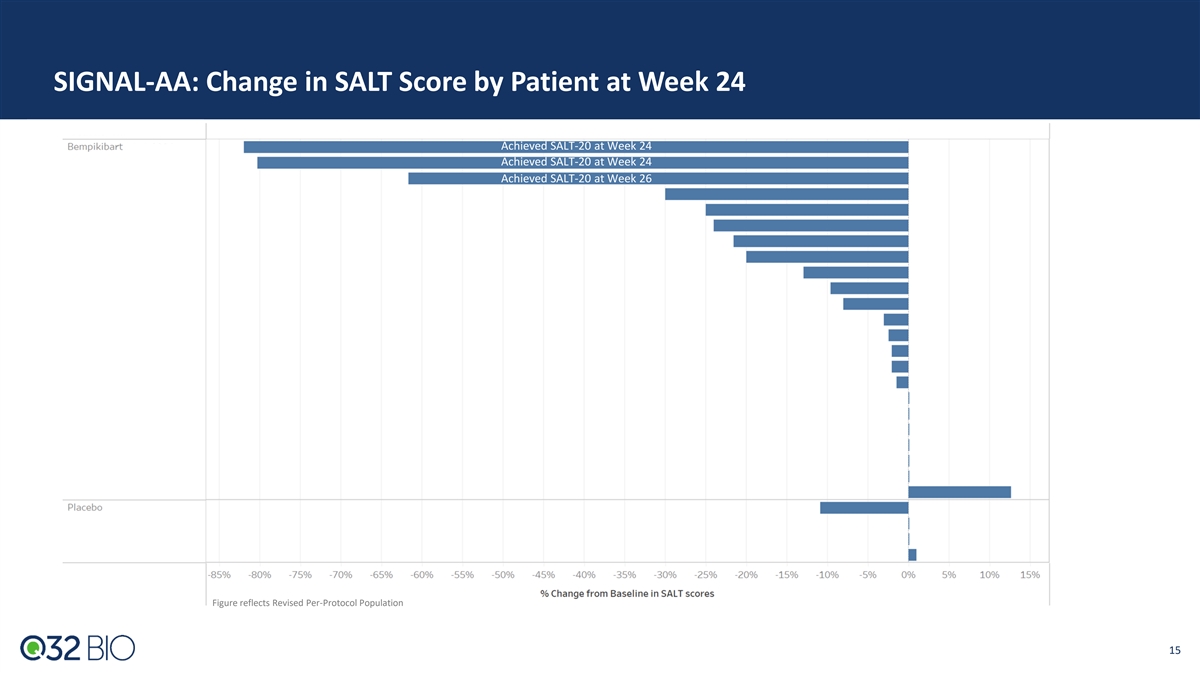
SIGNAL-AA: Change in SALT Score by Patient at Week 24 Achieved SALT-20 at Week 24 Achieved SALT-20 at Week 24 Achieved SALT-20 at Week 26 Figure reflects Revised Per-Protocol Population 15
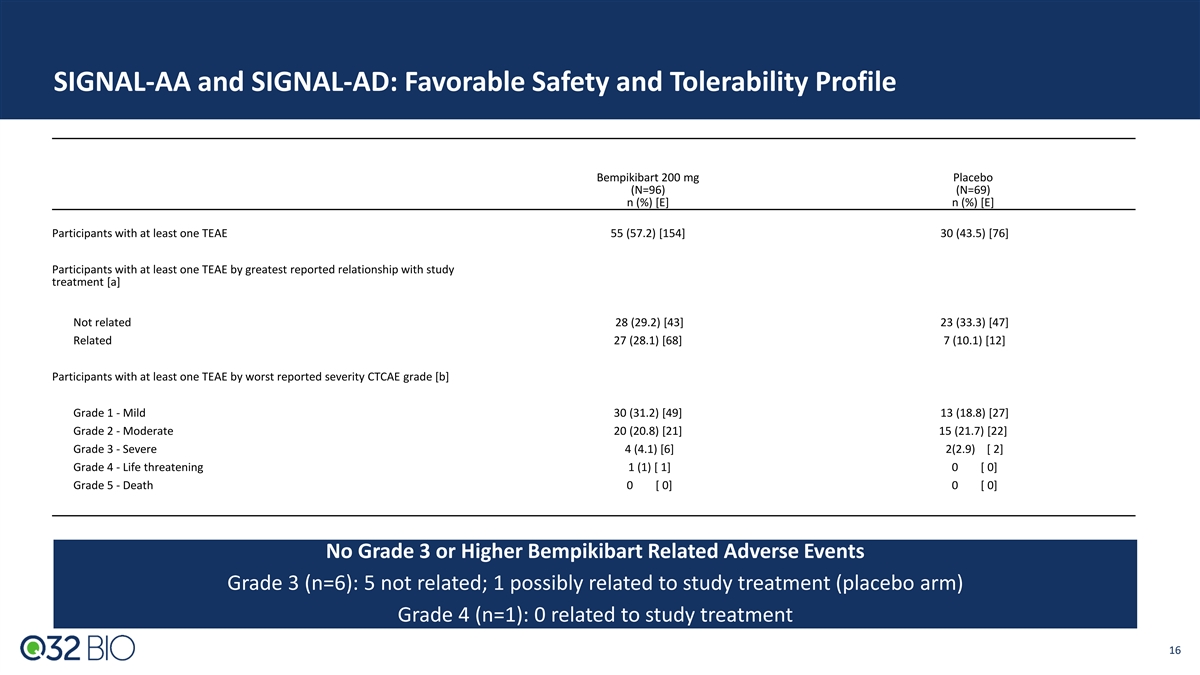
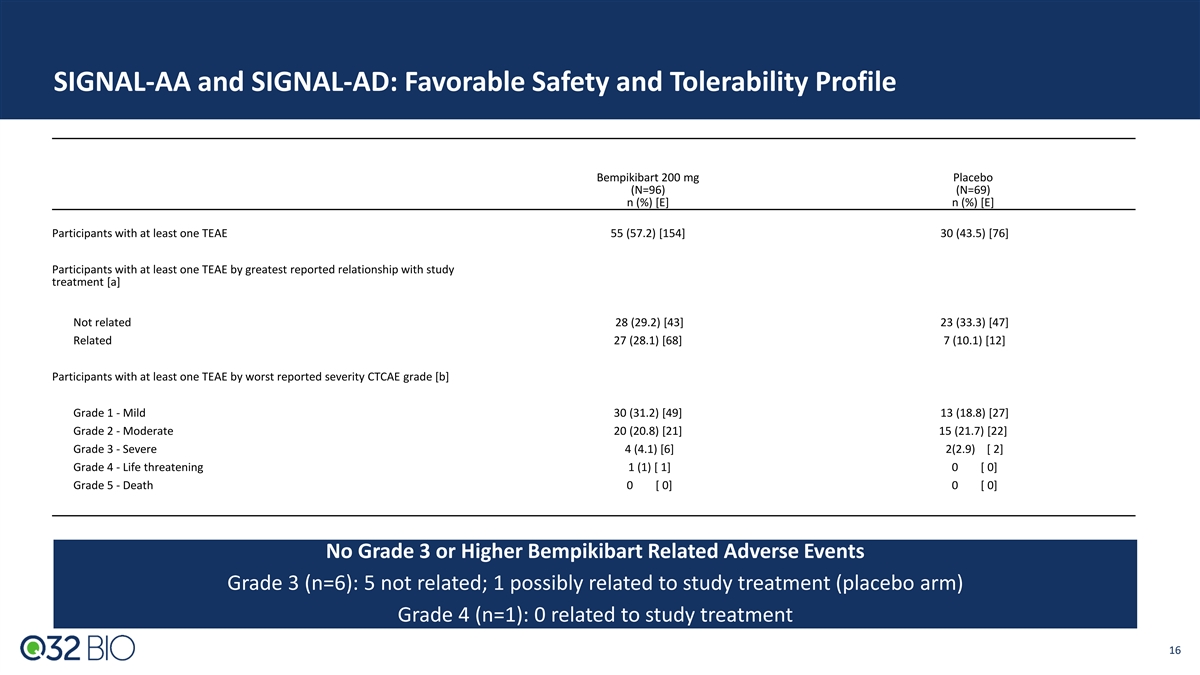
SIGNAL-AA and SIGNAL-AD: Favorable Safety and Tolerability Profile Bempikibart 200 mg Placebo (N=96) (N=69) n (%) [E] n (%) [E] Participants with at least one TEAE 55 (57.2) [154] 30 (43.5) [76] Participants with at least one TEAE by greatest reported relationship with study treatment [a] Not related 28 (29.2) [43] 23 (33.3) [47] Related 27 (28.1) [68] 7 (10.1) [12] Participants with at least one TEAE by worst reported severity CTCAE grade [b] Grade 1 - Mild 30 (31.2) [49] 13 (18.8) [27] Grade 2 - Moderate 20 (20.8) [21] 15 (21.7) [22] Grade 3 - Severe 4 (4.1) [6] 2(2.9) [ 2] Grade 4 - Life threatening 1 (1) [ 1] 0 [ 0] Grade 5 - Death 0 [ 0] 0 [ 0] No Grade 3 or Higher Bempikibart Related Adverse Events Grade 3 (n=6): 5 not related; 1 possibly related to study treatment (placebo arm) Grade 4 (n=1): 0 related to study treatment 16
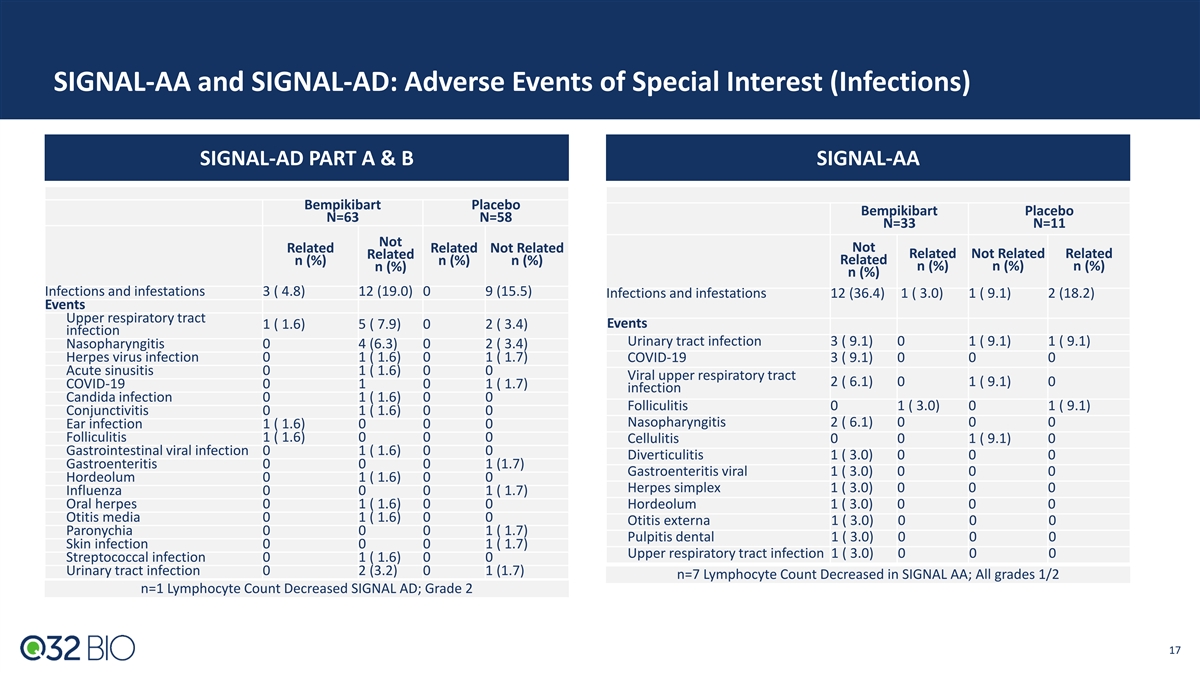
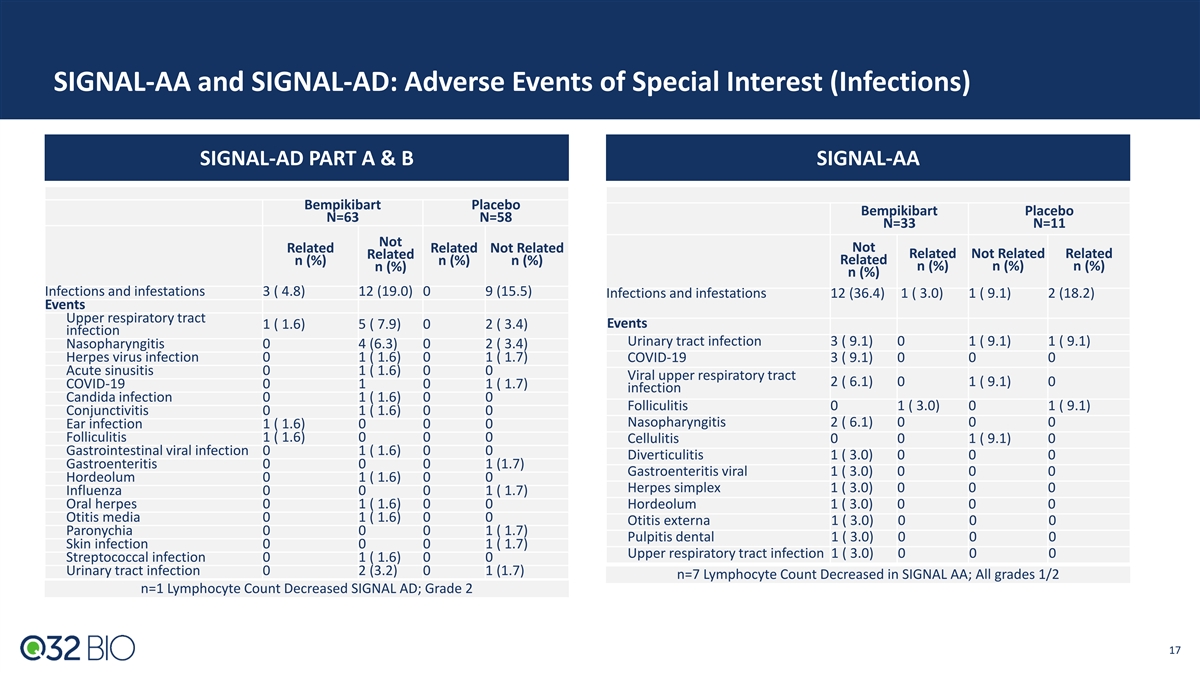
SIGNAL-AA and SIGNAL-AD: Adverse Events of Special Interest (Infections) SIGNAL-AD PART A & B SIGNAL-AA Bempikibart Placebo Bempikibart Placebo N=63 N=58 N=33 N=11 Not Related Related Not Related Not Related Related Not Related Related n (%) n (%) n (%) Related n (%) n (%) n (%) n (%) n (%) Infections and infestations 3 ( 4.8) 12 (19.0) 0 9 (15.5) Infections and infestations 12 (36.4) 1 ( 3.0) 1 ( 9.1) 2 (18.2) Events Upper respiratory tract Events 1 ( 1.6) 5 ( 7.9) 0 2 ( 3.4) infection Urinary tract infection 3 ( 9.1) 0 1 ( 9.1) 1 ( 9.1) Nasopharyngitis 0 4 (6.3) 0 2 ( 3.4) Herpes virus infection 0 1 ( 1.6) 0 1 ( 1.7) COVID-19 3 ( 9.1) 0 0 0 Acute sinusitis 0 1 ( 1.6) 0 0 Viral upper respiratory tract 2 ( 6.1) 0 1 ( 9.1) 0 COVID-19 0 1 0 1 ( 1.7) infection Candida infection 0 1 ( 1.6) 0 0 Folliculitis 0 1 ( 3.0) 0 1 ( 9.1) Conjunctivitis 0 1 ( 1.6) 0 0 Nasopharyngitis 2 ( 6.1) 0 0 0 Ear infection 1 ( 1.6) 0 0 0 Folliculitis 1 ( 1.6) 0 0 0 Cellulitis 0 0 1 ( 9.1) 0 Gastrointestinal viral infection 0 1 ( 1.6) 0 0 Diverticulitis 1 ( 3.0) 0 0 0 Gastroenteritis 0 0 0 1 (1.7) Gastroenteritis viral 1 ( 3.0) 0 0 0 Hordeolum 0 1 ( 1.6) 0 0 Herpes simplex 1 ( 3.0) 0 0 0 Influenza 0 0 0 1 ( 1.7) Oral herpes 0 1 ( 1.6) 0 0 Hordeolum 1 ( 3.0) 0 0 0 Otitis media 0 1 ( 1.6) 0 0 Otitis externa 1 ( 3.0) 0 0 0 Paronychia 0 0 0 1 ( 1.7) Pulpitis dental 1 ( 3.0) 0 0 0 Skin infection 0 0 0 1 ( 1.7) Upper respiratory tract infection 1 ( 3.0) 0 0 0 Streptococcal infection 0 1 ( 1.6) 0 0 Urinary tract infection 0 2 (3.2) 0 1 (1.7) n=7 Lymphocyte Count Decreased in SIGNAL AA; All grades 1/2 n=1 Lymphocyte Count Decreased SIGNAL AD; Grade 2 17
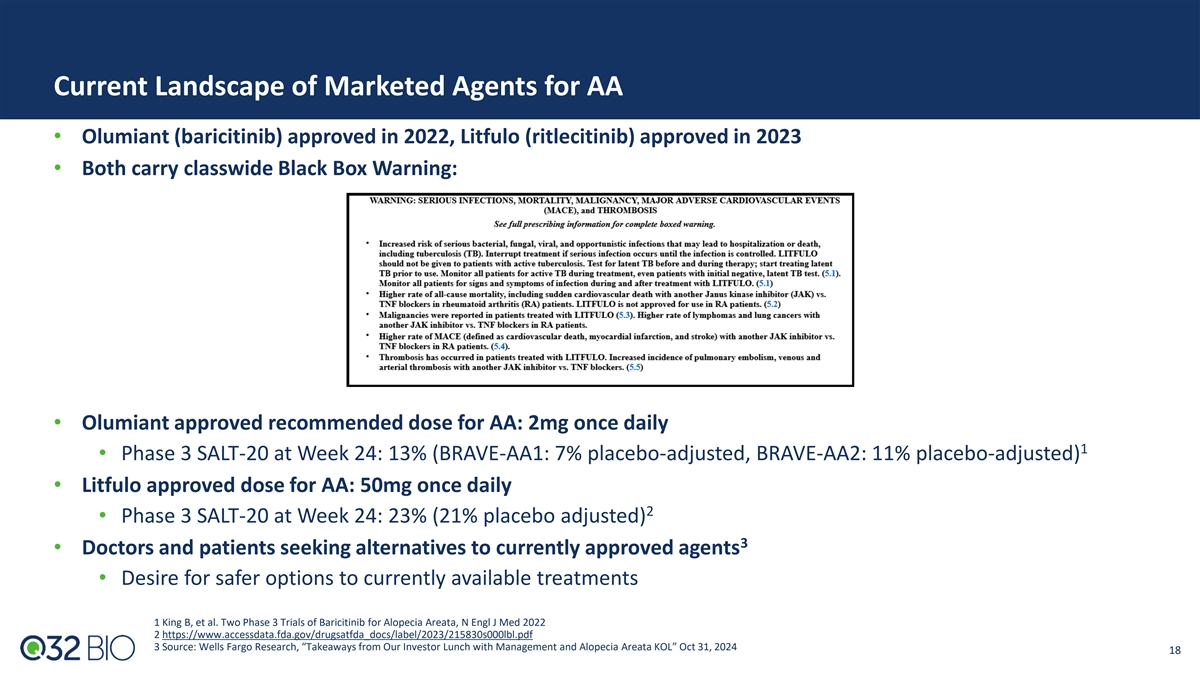
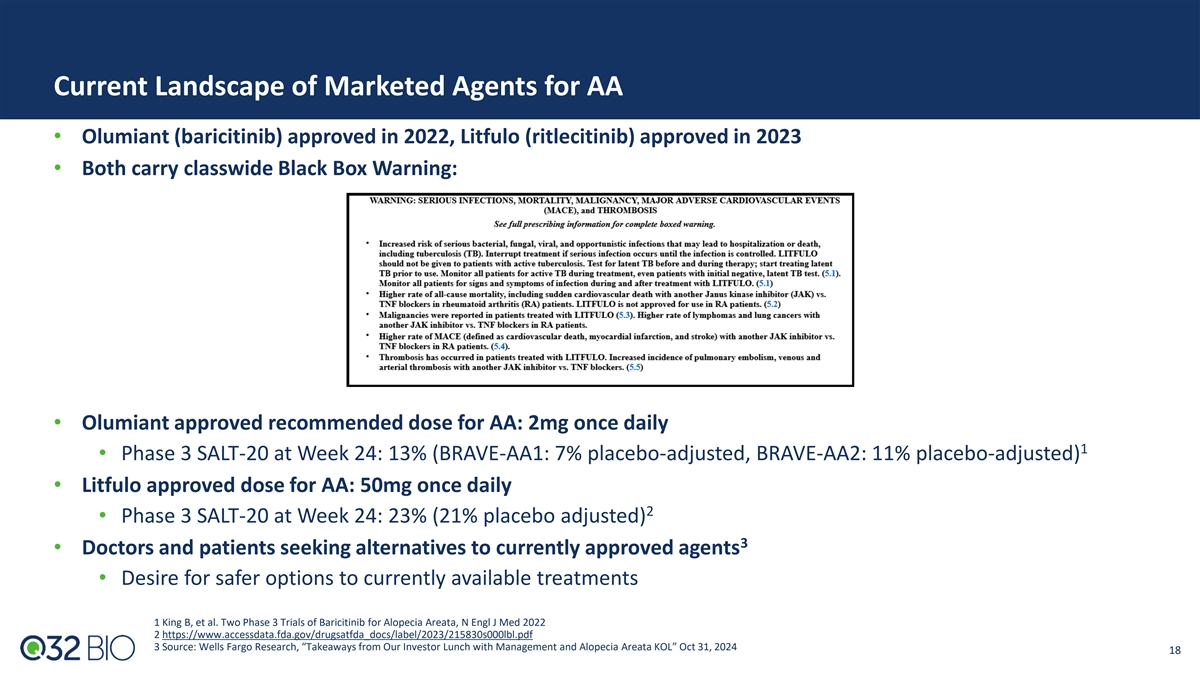
Current Landscape of Marketed Agents for AA • Olumiant (baricitinib) approved in 2022, Litfulo (ritlecitinib) approved in 2023 • Both carry classwide Black Box Warning: • Olumiant approved recommended dose for AA: 2mg once daily 1 • Phase 3 SALT-20 at Week 24: 13% (BRAVE-AA1: 7% placebo-adjusted, BRAVE-AA2: 11% placebo-adjusted) • Litfulo approved dose for AA: 50mg once daily 2 • Phase 3 SALT-20 at Week 24: 23% (21% placebo adjusted) 3 • Doctors and patients seeking alternatives to currently approved agents • Desire for safer options to currently available treatments 1 King B, et al. Two Phase 3 Trials of Baricitinib for Alopecia Areata, N Engl J Med 2022 2 https://www.accessdata.fda.gov/drugsatfda_docs/label/2023/215830s000lbl.pdf 3 Source: Wells Fargo Research, “Takeaways from Our Investor Lunch with Management and Alopecia Areata KOL” Oct 31, 2024 18

Tissue Targeted Platform: Building The Future of Complement Therapeutics
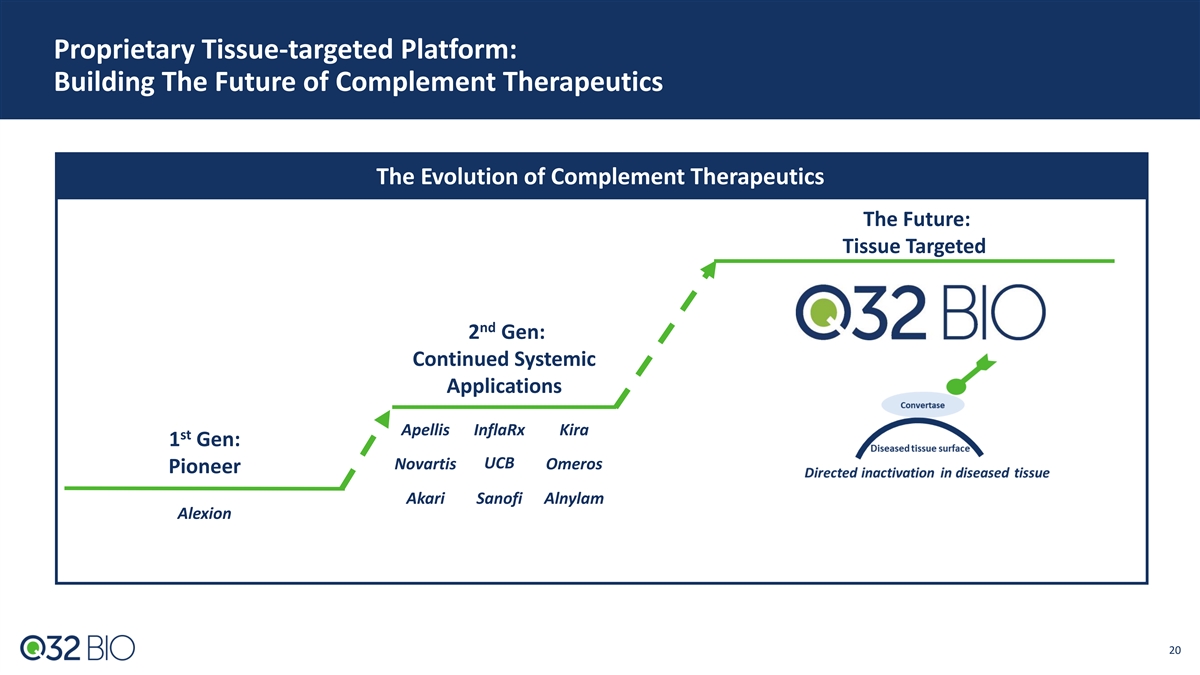
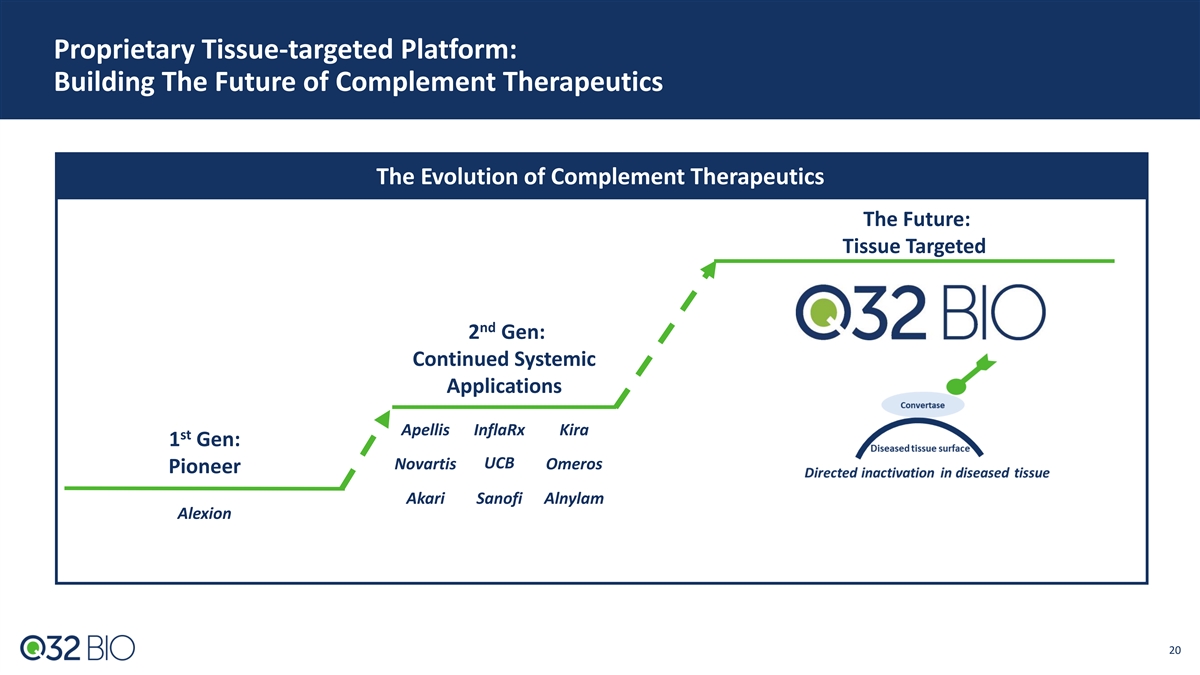
Proprietary Tissue-targeted Platform: Building The Future of Complement Therapeutics The Evolution of Complement Therapeutics The Future: Tissue Targeted nd 2 Gen: Continued Systemic Applications Apellis InflaRx Kira st 1 Gen: UCB Novartis Omeros Pioneer Akari Sanofi Alnylam Alexion 20

Q32 Tissue-targeted Platform Value Proposition: Designed to Enable Clinical Profile Superior to Systemic Complement Inhibitors The Unmet Need The Opportunity • Limited activity: • Enhanced activity through tissue targeting: Reliant on systemic blockade for impact on Differentiated approach to driving efficacy by affected organ inactivating convertases directly at site of destruction • High doses, frequent administration required: • R ed u ced tr e a tme nt burden: High abundance, rapid turnover of most target SC route with QW dosing; potential for Q2W complement proteins • Infection risk: • Improved risk/benefit profile: Complement plays critical role in combating Designed to maximize therapeutic index while infection; systemic blockade increases risk maintaining intact immune surveillance; broader indication potential 21

ADX-097 (C3d targeted antibody – fH 1-5 fusion protein)
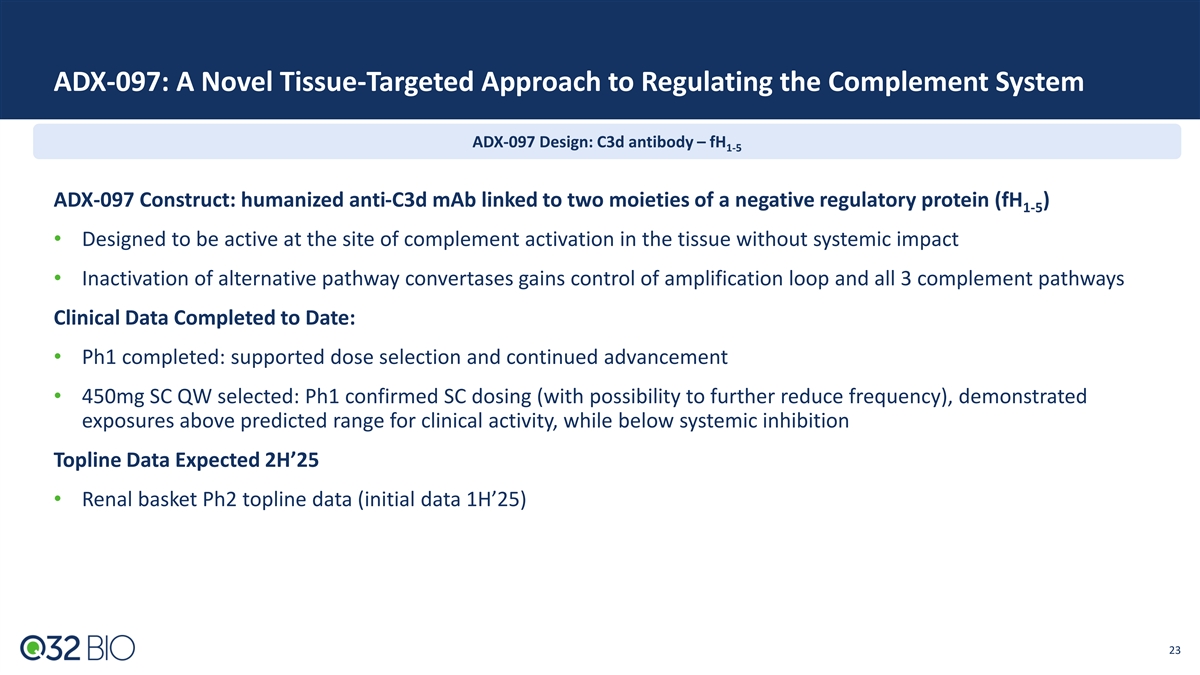
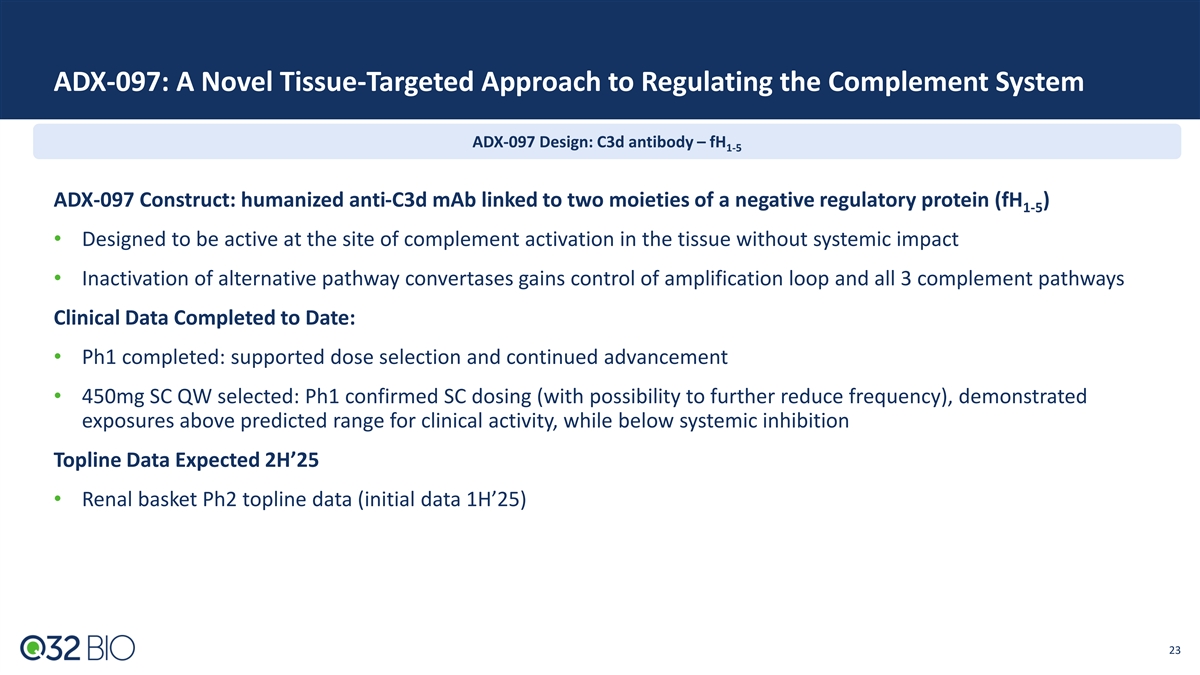
ADX-097: A Novel Tissue-Targeted Approach to Regulating the Complement System ADX-097 Design: C3d antibody – fH 1-5 ADX-097 Construct: humanized anti-C3d mAb linked to two moieties of a negative regulatory protein (fH ) 1-5 • Designed to be active at the site of complement activation in the tissue without systemic impact • Inactivation of alternative pathway convertases gains control of amplification loop and all 3 complement pathways Clinical Data Completed to Date: • Ph1 completed: supported dose selection and continued advancement • 450mg SC QW selected: Ph1 confirmed SC dosing (with possibility to further reduce frequency), demonstrated exposures above predicted range for clinical activity, while below systemic inhibition Topline Data Expected 2H’25 • Renal basket Ph2 topline data (initial data 1H’25) 23 23
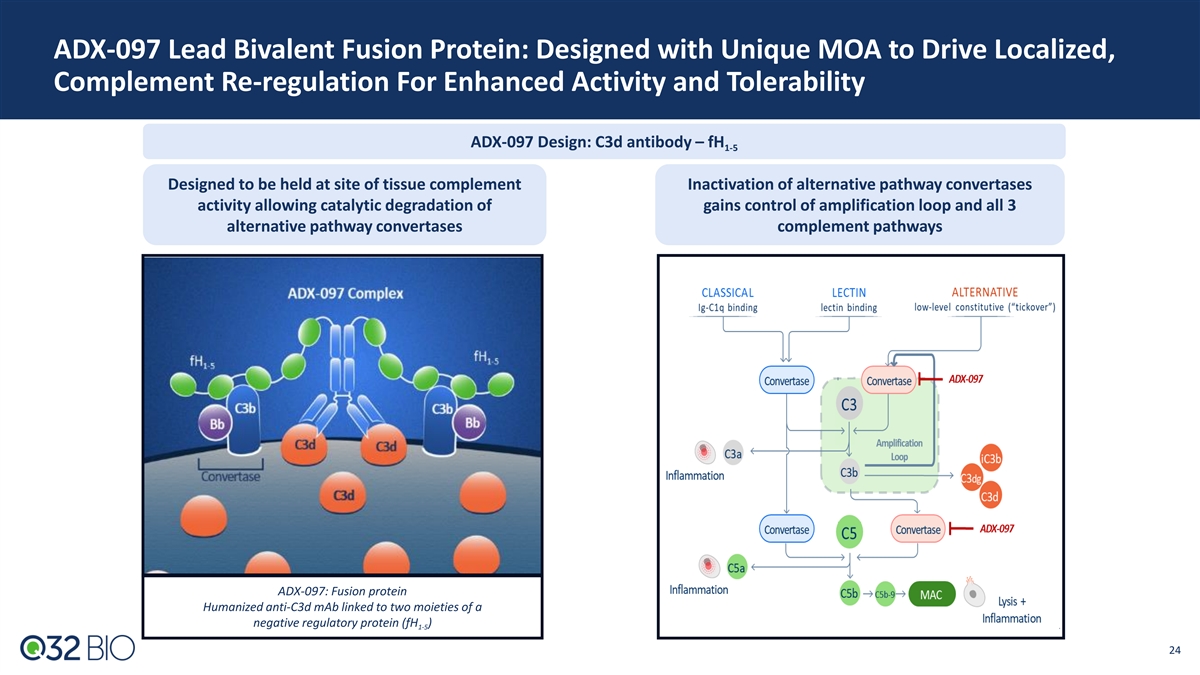
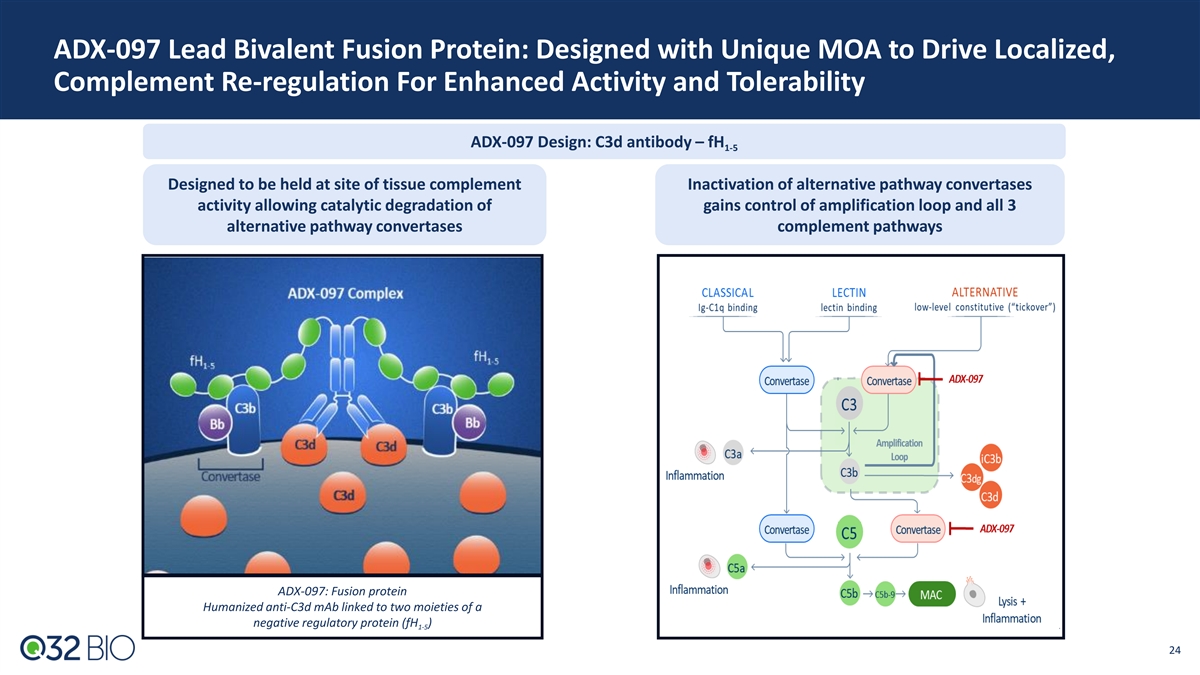
ADX-097 Lead Bivalent Fusion Protein: Designed with Unique MOA to Drive Localized, Complement Re-regulation For Enhanced Activity and Tolerability ADX-097 Design: C3d antibody – fH 1-5 Designed to be held at site of tissue complement Inactivation of alternative pathway convertases activity allowing catalytic degradation of gains control of amplification loop and all 3 alternative pathway convertases complement pathways ADX-097: Fusion protein Humanized anti-C3d mAb linked to two moieties of a negative regulatory protein (fH ) 1-5 24 24
ADX-097 Preclinical and Ph1 Data: Robust Data Package Supports Desired PK and PD with Favorable Tolerability and Immunogenicity Profile Preclinical Data • Tissue distribution and target binding • Durable (>7 days) tissue PK/PD after SC dosing • Reduction in key proof of mechanism (POM)/proof of concept (POC) biomarkers including proteinuria and albuminuria • >40X safety margin for planned Ph2 clinical dosing Ph1 Clinical Data • Favorable tolerability and good immunogenicity profile across all SAD/MAD doses • Weekly SC dosing met desired exposures for predicted complete tissue inhibition (based on preclinical modeling) with no systemic inhibition • Proximal POM supports in-vivo ADX-097 integrity 25 25
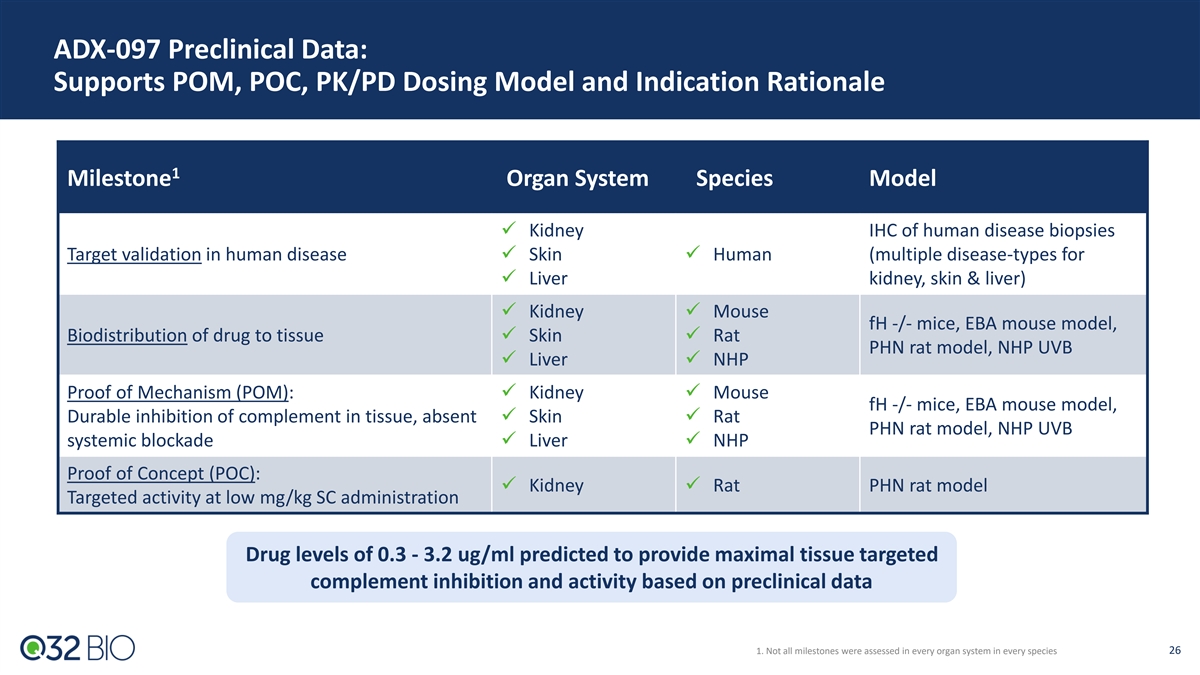
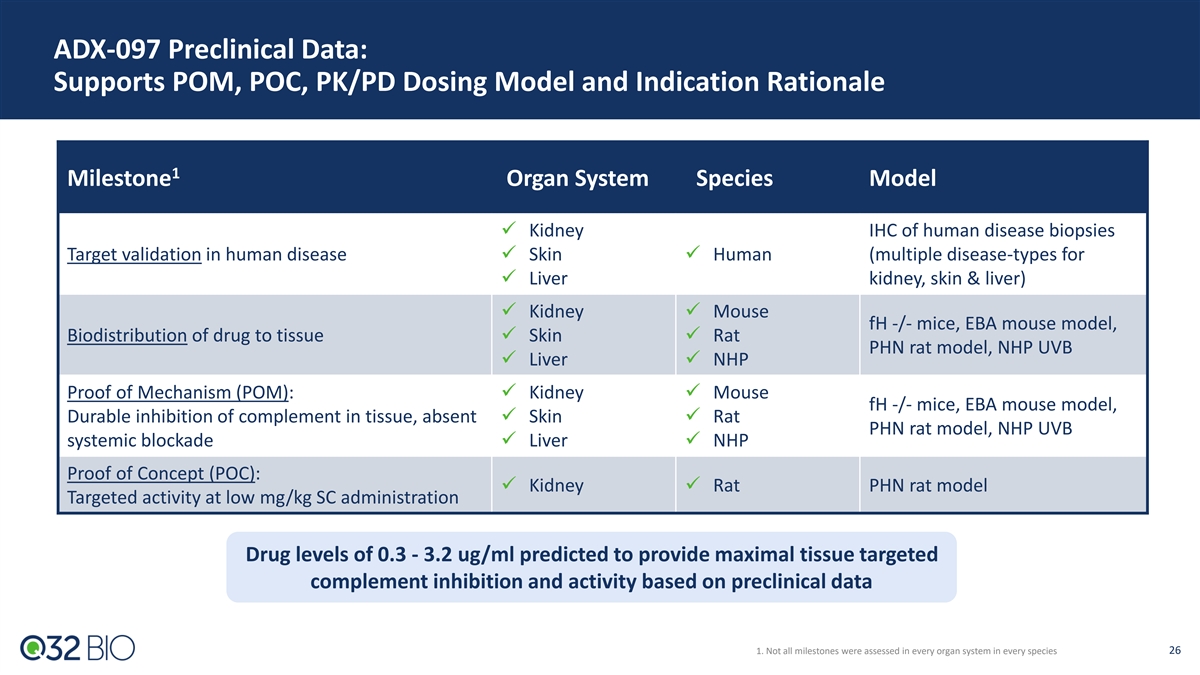
ADX-097 Preclinical Data: Supports POM, POC, PK/PD Dosing Model and Indication Rationale 1 Milestone Organ System Species Model ✓ Kidney IHC of human disease biopsies Target validation in human disease✓ Skin✓ Human (multiple disease-types for ✓ Liver kidney, skin & liver) ✓ Kidney✓ Mouse fH -/- mice, EBA mouse model, Biodistribution of drug to tissue✓ Skin✓ Rat PHN rat model, NHP UVB ✓ Liver✓ NHP Proof of Mechanism (POM): ✓ Kidney✓ Mouse fH -/- mice, EBA mouse model, Durable inhibition of complement in tissue, absent ✓ Skin✓ Rat PHN rat model, NHP UVB systemic blockade✓ Liver✓ NHP Proof of Concept (POC): ✓ Kidney✓ Rat PHN rat model Targeted activity at low mg/kg SC administration Drug levels of 0.3 - 3.2 ug/ml predicted to provide maximal tissue targeted complement inhibition and activity based on preclinical data 1. Not all milestones were assessed in every organ system in every species 26
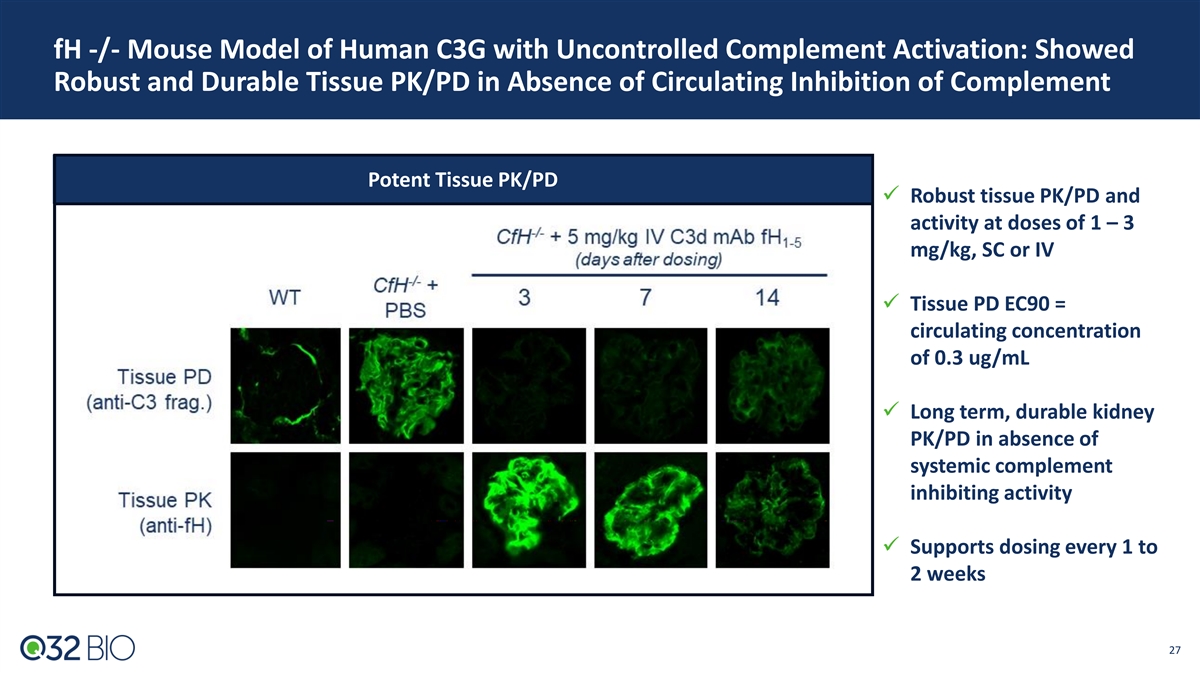
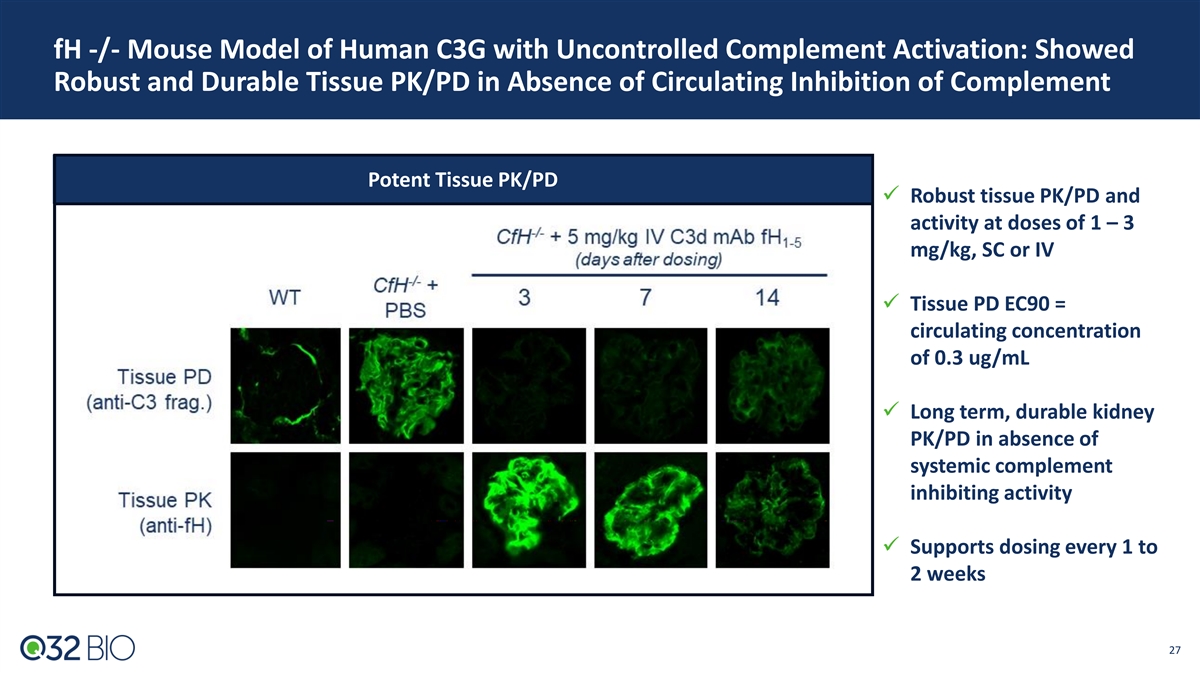
fH -/- Mouse Model of Human C3G with Uncontrolled Complement Activation: Showed Robust and Durable Tissue PK/PD in Absence of Circulating Inhibition of Complement Potent Tissue PK/PD ✓ Robust tissue PK/PD and activity at doses of 1 – 3 mg/kg, SC or IV ✓ Tissue PD EC90 = circulating concentration of 0.3 ug/mL ✓ Long term, durable kidney PK/PD in absence of systemic complement inhibiting activity ✓ Supports dosing every 1 to 2 weeks 27
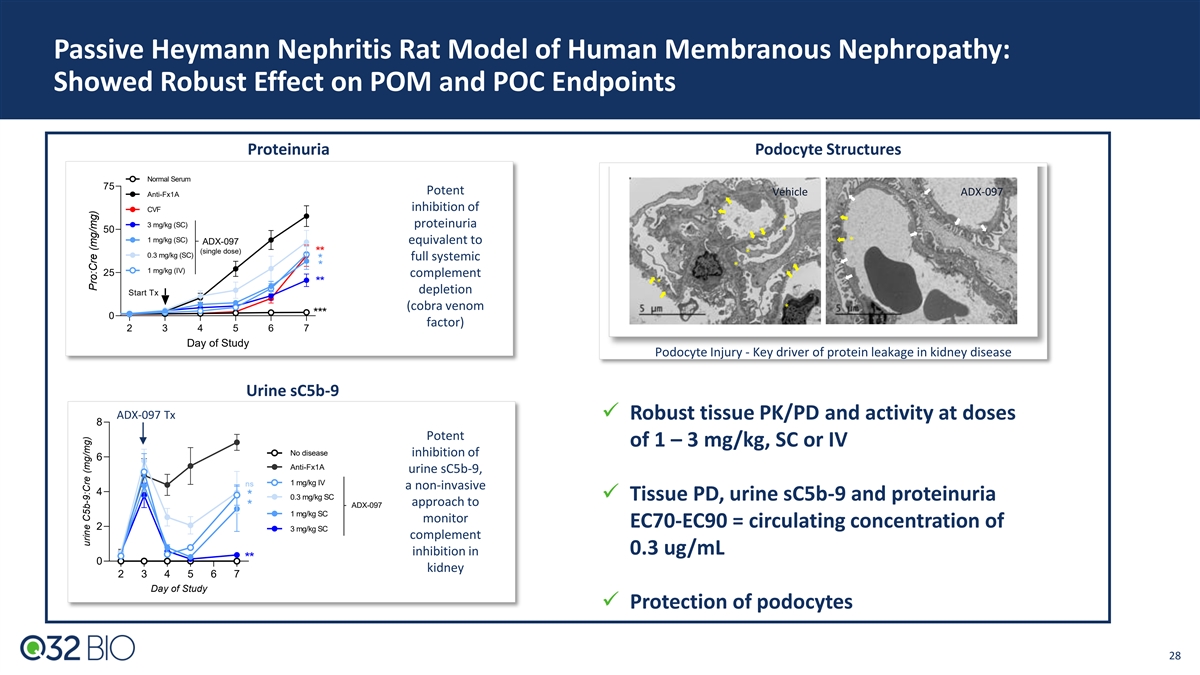
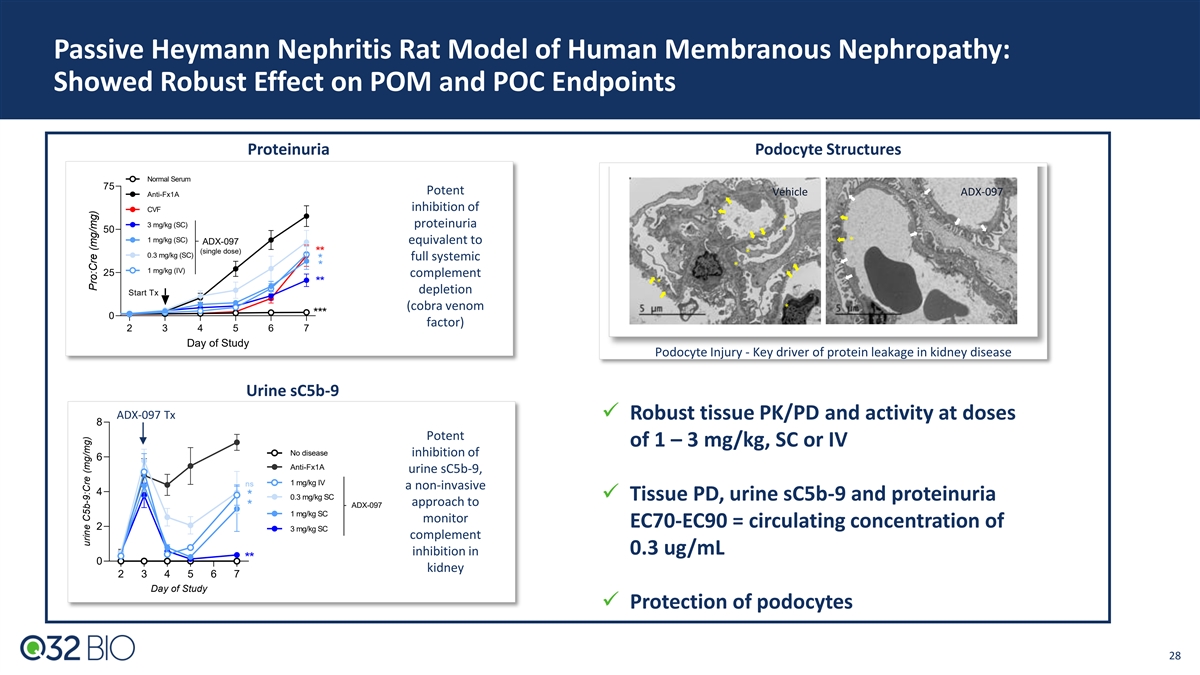
Passive Heymann Nephritis Rat Model of Human Membranous Nephropathy: Showed Robust Effect on POM and POC Endpoints Proteinuria Podocyte Structures Normal Serum 75 Potent Vehicle ADX-097 Anti-Fx1A inhibition of CVF * 3 mg/kg (SC) proteinuria 50 * 1 mg/kg (SC) equivalent to * ADX-097 (single dose) ** * 0.3 mg/kg (SC) full systemic * * * 1 mg/kg (IV) 25 complement * ** depletion Start Tx (cobra venom * *** 0 factor) 2 3 4 5 6 7 Day of Study Podocyte Injury - Key driver of protein leakage in kidney disease Urine sC5b-9 ADX-097 Tx ✓ Robust tissue PK/PD and activity at doses 8 Potent of 1 – 3 mg/kg, SC or IV No disease inhibition of 6 Anti-Fx1A urine sC5b-9, 1 mg/kg IV ns a non-invasive 4 * 0.3 mg/kg SC ✓ Tissue PD, urine sC5b-9 and proteinuria approach to ADX-097 * 1 mg/kg SC monitor EC70-EC90 = circulating concentration of 2 3 mg/kg SC complement inhibition in 0.3 ug/mL ** 0 kidney 2 3 4 5 6 7 Day of Study ✓ Protection of podocytes 28 urine C5b-9:Cre (mg/mg) Pro:Cre (mg/mg)
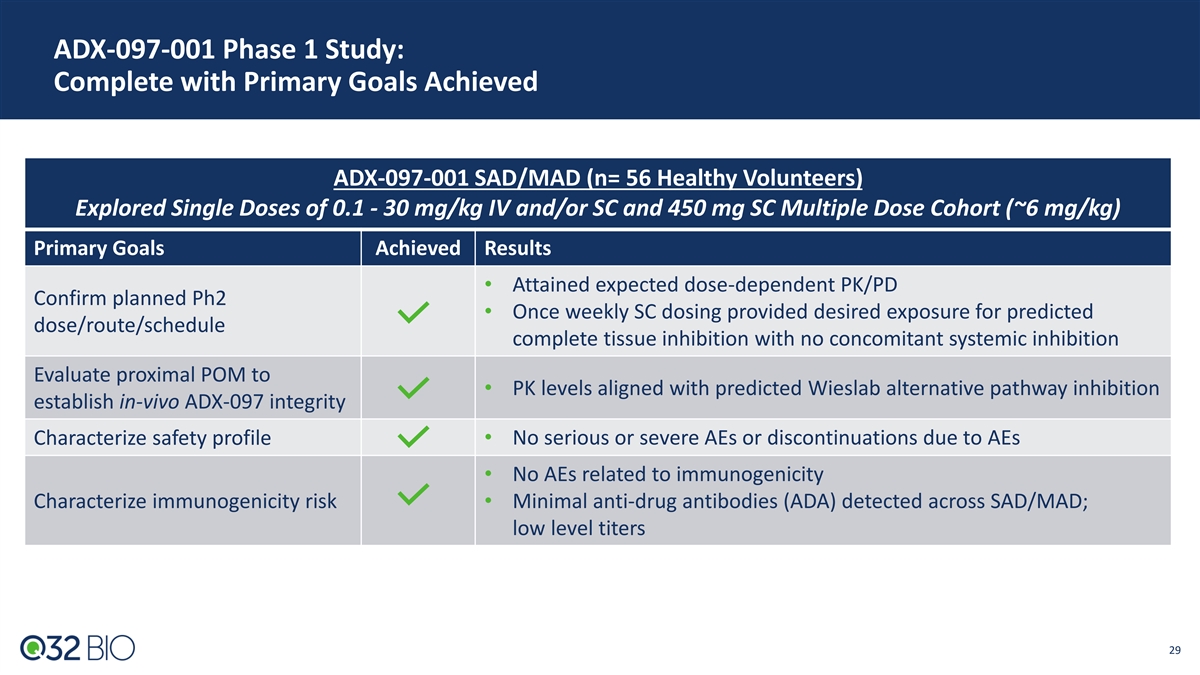
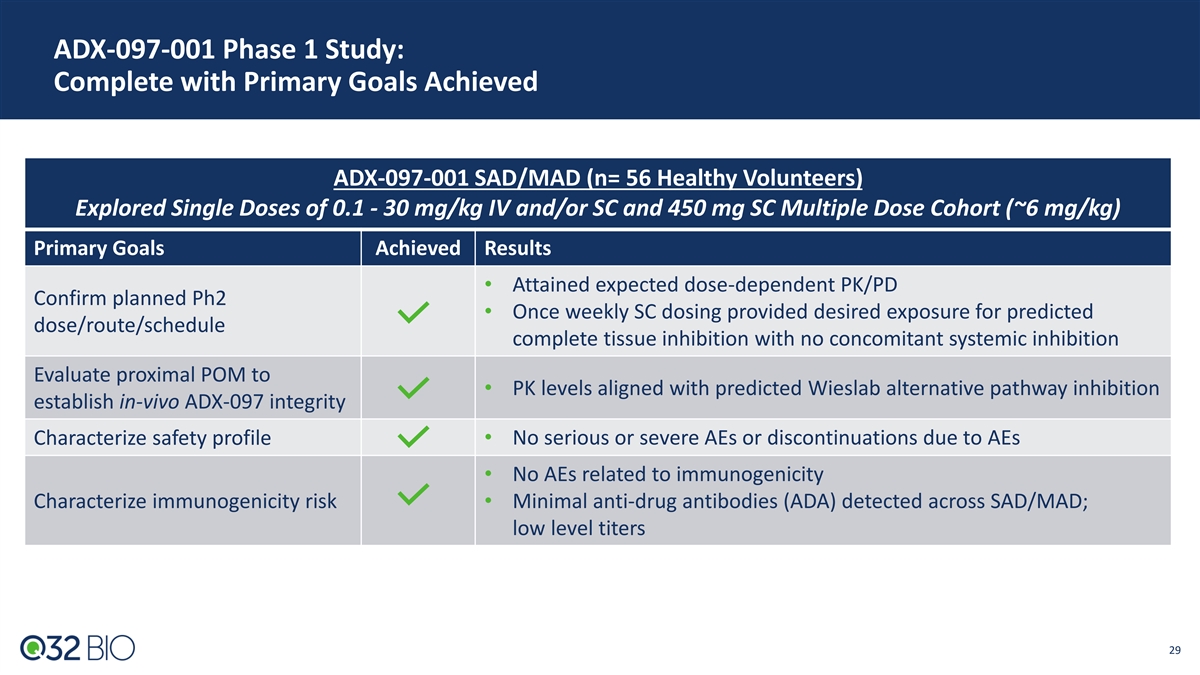
ADX-097-001 Phase 1 Study: Complete with Primary Goals Achieved ADX-097-001 SAD/MAD (n= 56 Healthy Volunteers) Explored Single Doses of 0.1 - 30 mg/kg IV and/or SC and 450 mg SC Multiple Dose Cohort (~6 mg/kg) Primary Goals Achieved Results • Attained expected dose-dependent PK/PD Confirm planned Ph2 • Once weekly SC dosing provided desired exposure for predicted dose/route/schedule complete tissue inhibition with no concomitant systemic inhibition Evaluate proximal POM to • PK levels aligned with predicted Wieslab alternative pathway inhibition establish in-vivo ADX-097 integrity Characterize safety profile• No serious or severe AEs or discontinuations due to AEs • No AEs related to immunogenicity Characterize immunogenicity risk• Minimal anti-drug antibodies (ADA) detected across SAD/MAD; low level titers 29

ADX-097 Phase 1 PK Data: Weekly SC Dosing Met Desired Exposures for Predicted Complete Tissue Inhibition With No Concomitant Systemic Inhibition Phase 2 Dose Identified: 450 mg SC Met Key Exposure Goals 50% systemic complement inhibition 450mg SC achieved exposures below systemic inhibition and above conservative end of predicted range for clinical activity Drug levels predicted to provide maximal tissue complement inhibition and activity based on mouse, rat and NHP preclinical data 30 Updated to include cohorts SAD 6b and SAD 8
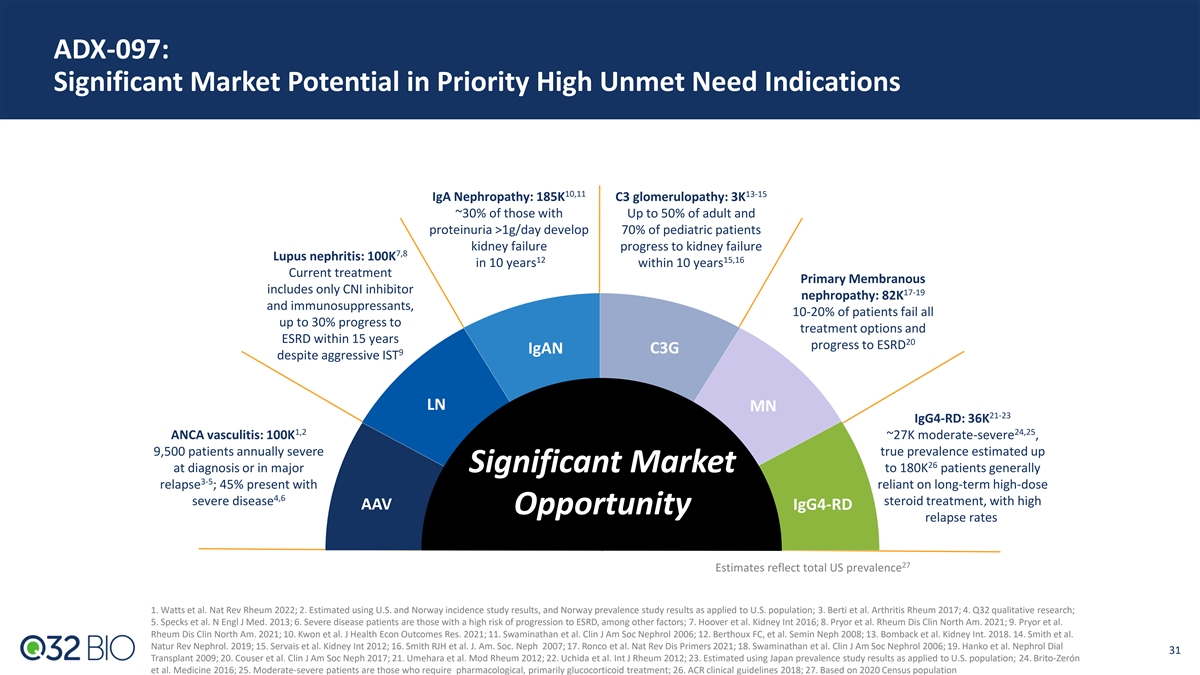
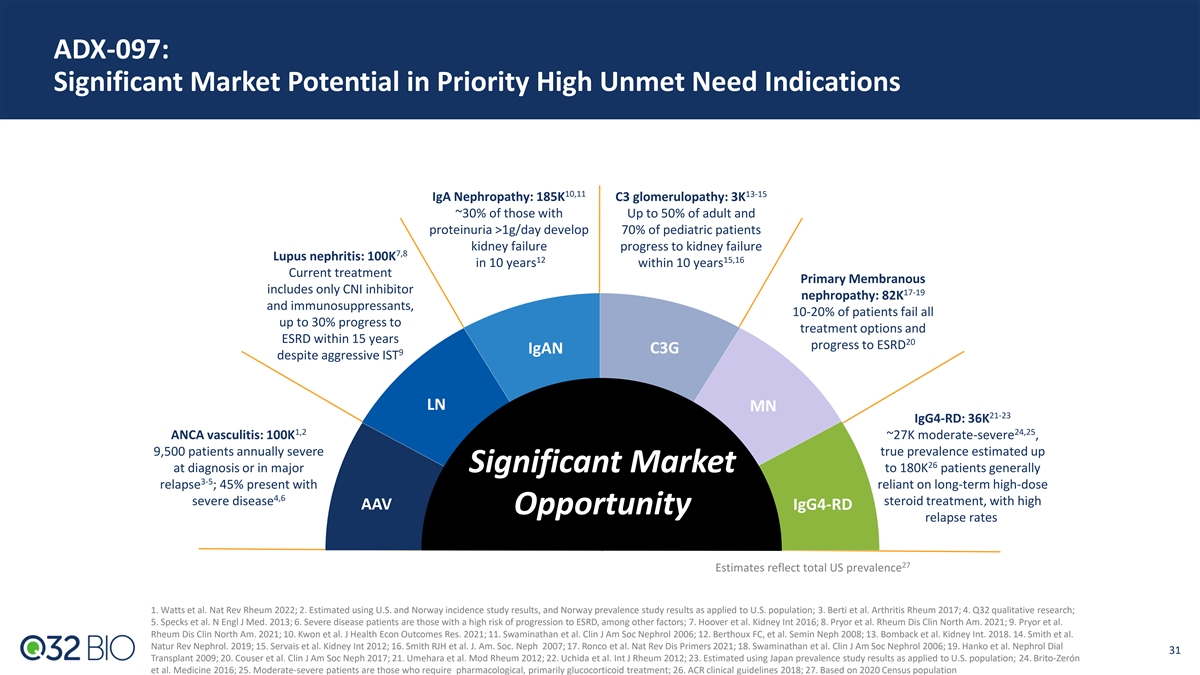
ADX-097: Significant Market Potential in Priority High Unmet Need Indications 10,11 13-15 IgA Nephropathy: 185K C3 glomerulopathy: 3K ~30% of those with Up to 50% of adult and proteinuria >1g/day develop 70% of pediatric patients kidney failure progress to kidney failure 7,8 Lupus nephritis: 100K 12 15,16 in 10 years within 10 years Current treatment Primary Membranous includes only CNI inhibitor 17-19 nephropathy: 82K and immunosuppressants, 10-20% of patients fail all up to 30% progress to treatment options and ESRD within 15 years 20 progress to ESRD IgAN C3G 9 despite aggressive IST LN MN 21-23 IgG4-RD: 36K 1,2 24,25 ANCA vasculitis: 100K ~27K moderate-severe , 9,500 patients annually severe true prevalence estimated up 26 at diagnosis or in major Significant Market to 180K patients generally 3-5 relapse ; 45% present with reliant on long-term high-dose 4,6 severe disease steroid treatment, with high AAV IgG4-RD Opportunity relapse rates 27 Estimates reflect total US prevalence 1. Watts et al. Nat Rev Rheum 2022; 2. Estimated using U.S. and Norway incidence study results, and Norway prevalence study results as applied to U.S. population; 3. Berti et al. Arthritis Rheum 2017; 4. Q32 qualitative research; 5. Specks et al. N Engl J Med. 2013; 6. Severe disease patients are those with a high risk of progression to ESRD, among other factors; 7. Hoover et al. Kidney Int 2016; 8. Pryor et al. Rheum Dis Clin North Am. 2021; 9. Pryor et al. Rheum Dis Clin North Am. 2021; 10. Kwon et al. J Health Econ Outcomes Res. 2021; 11. Swaminathan et al. Clin J Am Soc Nephrol 2006; 12. Berthoux FC, et al. Semin Neph 2008; 13. Bomback et al. Kidney Int. 2018. 14. Smith et al. Natur Rev Nephrol. 2019; 15. Servais et al. Kidney Int 2012; 16. Smith RJH et al. J. Am. Soc. Neph 2007; 17. Ronco et al. Nat Rev Dis Primers 2021; 18. Swaminathan et al. Clin J Am Soc Nephrol 2006; 19. Hanko et al. Nephrol Dial 31 Transplant 2009; 20. Couser et al. Clin J Am Soc Neph 2017; 21. Umehara et al. Mod Rheum 2012; 22. Uchida et al. Int J Rheum 2012; 23. Estimated using Japan prevalence study results as applied to U.S. population; 24. Brito-Zerón et al. Medicine 2016; 25. Moderate-severe patients are those who require pharmacological, primarily glucocorticoid treatment; 26. ACR clinical guidelines 2018; 27. Based on 2020 Census population
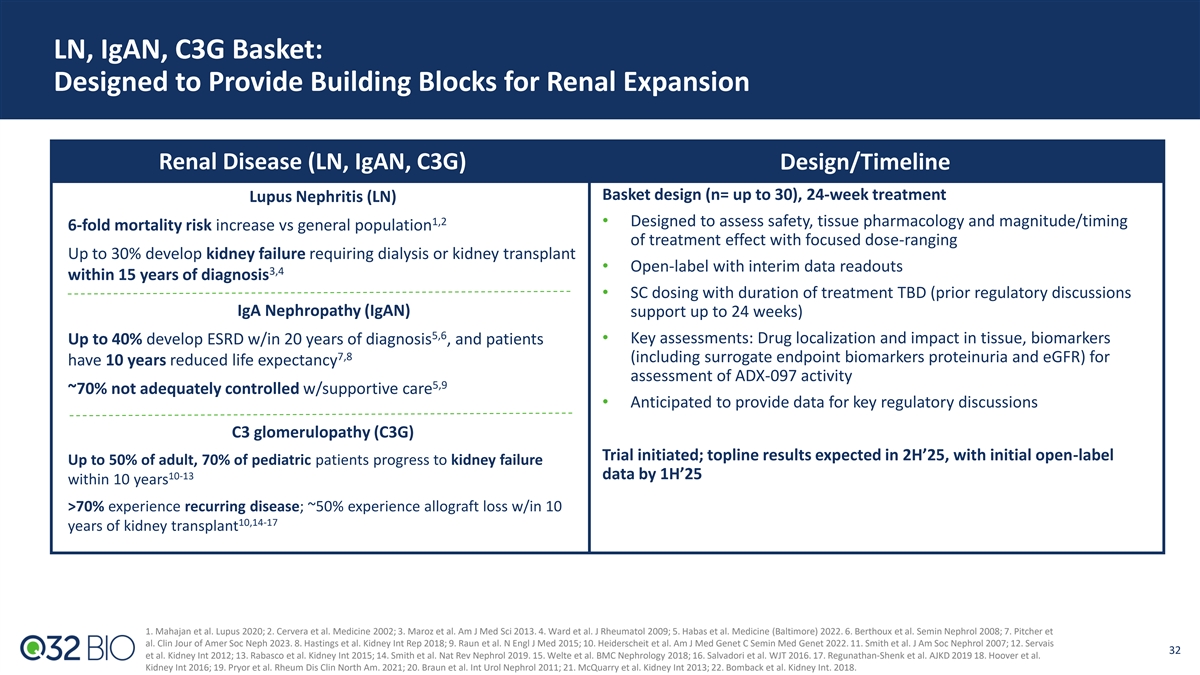
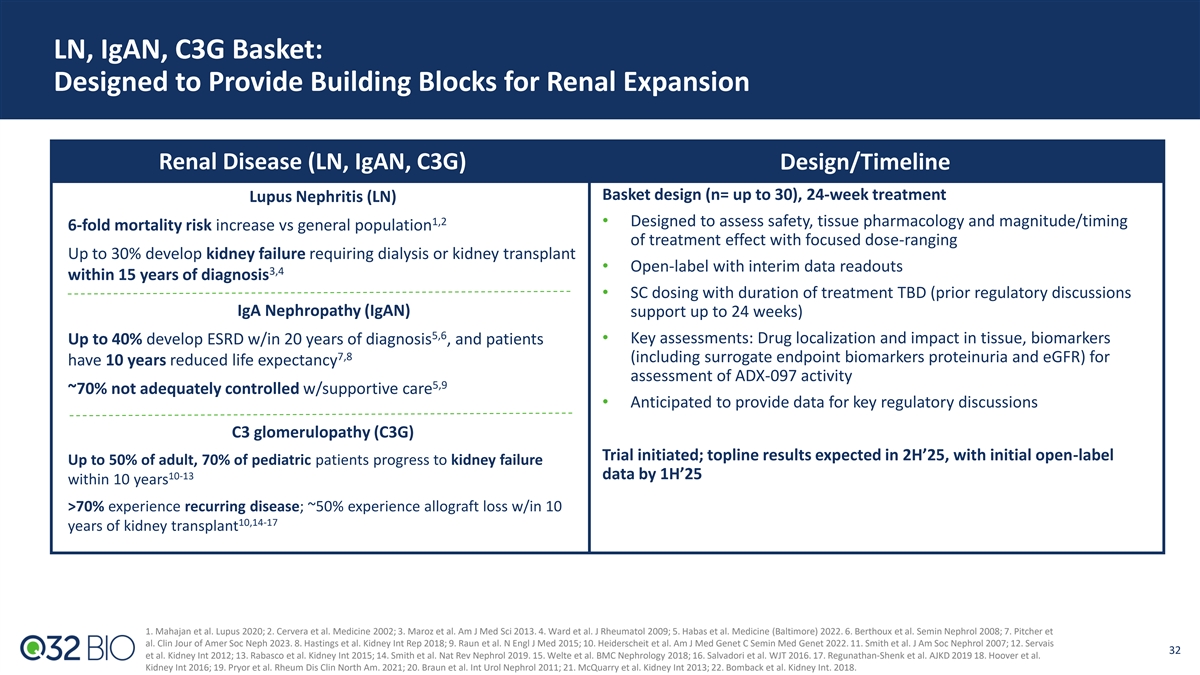
LN, IgAN, C3G Basket: Designed to Provide Building Blocks for Renal Expansion Renal Disease (LN, IgAN, C3G) Design/Timeline Basket design (n= up to 30), 24-week treatment Lupus Nephritis (LN) 1,2 • Designed to assess safety, tissue pharmacology and magnitude/timing 6-fold mortality risk increase vs general population of treatment effect with focused dose-ranging Up to 30% develop kidney failure requiring dialysis or kidney transplant • Open-label with interim data readouts 3,4 within 15 years of diagnosis • SC dosing with duration of treatment TBD (prior regulatory discussions IgA Nephropathy (IgAN) support up to 24 weeks) 5,6 • Key assessments: Drug localization and impact in tissue, biomarkers Up to 40% develop ESRD w/in 20 years of diagnosis , and patients 7,8 (including surrogate endpoint biomarkers proteinuria and eGFR) for have 10 years reduced life expectancy assessment of ADX-097 activity 5,9 ~70% not adequately controlled w/supportive care • Anticipated to provide data for key regulatory discussions C3 glomerulopathy (C3G) Trial initiated; topline results expected in 2H’25, with initial open-label Up to 50% of adult, 70% of pediatric patients progress to kidney failure 10-13 data by 1H’25 within 10 years >70% experience recurring disease; ~50% experience allograft loss w/in 10 10,14-17 years of kidney transplant 1. Mahajan et al. Lupus 2020; 2. Cervera et al. Medicine 2002; 3. Maroz et al. Am J Med Sci 2013. 4. Ward et al. J Rheumatol 2009; 5. Habas et al. Medicine (Baltimore) 2022. 6. Berthoux et al. Semin Nephrol 2008; 7. Pitcher et al. Clin Jour of Amer Soc Neph 2023. 8. Hastings et al. Kidney Int Rep 2018; 9. Raun et al. N Engl J Med 2015; 10. Heiderscheit et al. Am J Med Genet C Semin Med Genet 2022. 11. Smith et al. J Am Soc Nephrol 2007; 12. Servais 32 et al. Kidney Int 2012; 13. Rabasco et al. Kidney Int 2015; 14. Smith et al. Nat Rev Nephrol 2019. 15. Welte et al. BMC Nephrology 2018; 16. Salvadori et al. WJT 2016. 17. Regunathan-Shenk et al. AJKD 2019 18. Hoover et al. Kidney Int 2016; 19. Pryor et al. Rheum Dis Clin North Am. 2021; 20. Braun et al. Int Urol Nephrol 2011; 21. McQuarry et al. Kidney Int 2013; 22. Bomback et al. Kidney Int. 2018.
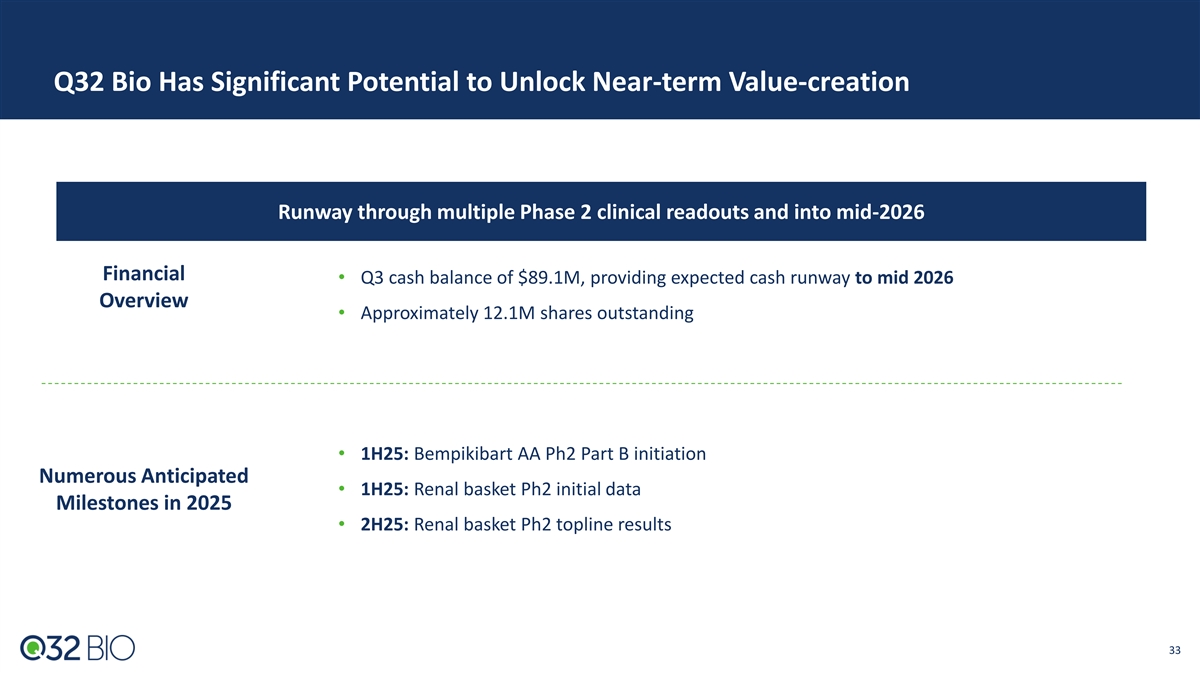
Q32 Bio Has Significant Potential to Unlock Near-term Value-creation Runway through multiple Phase 2 clinical readouts and into mid-2026 Financial • Q3 cash balance of $89.1M, providing expected cash runway to mid 2026 Overview • Approximately 12.1M shares outstanding • 1H25: Bempikibart AA Ph2 Part B initiation Numerous Anticipated • 1H25: Renal basket Ph2 initial data Milestones in 2025 • 2H25: Renal basket Ph2 topline results 33

APPENDIX
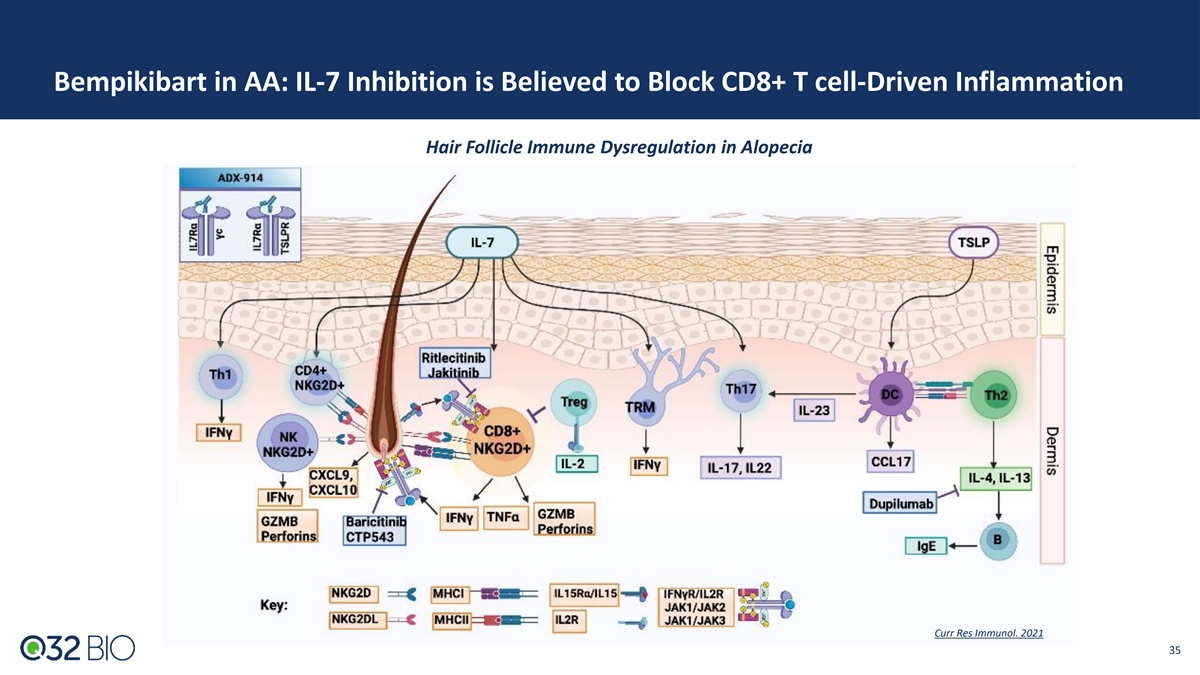
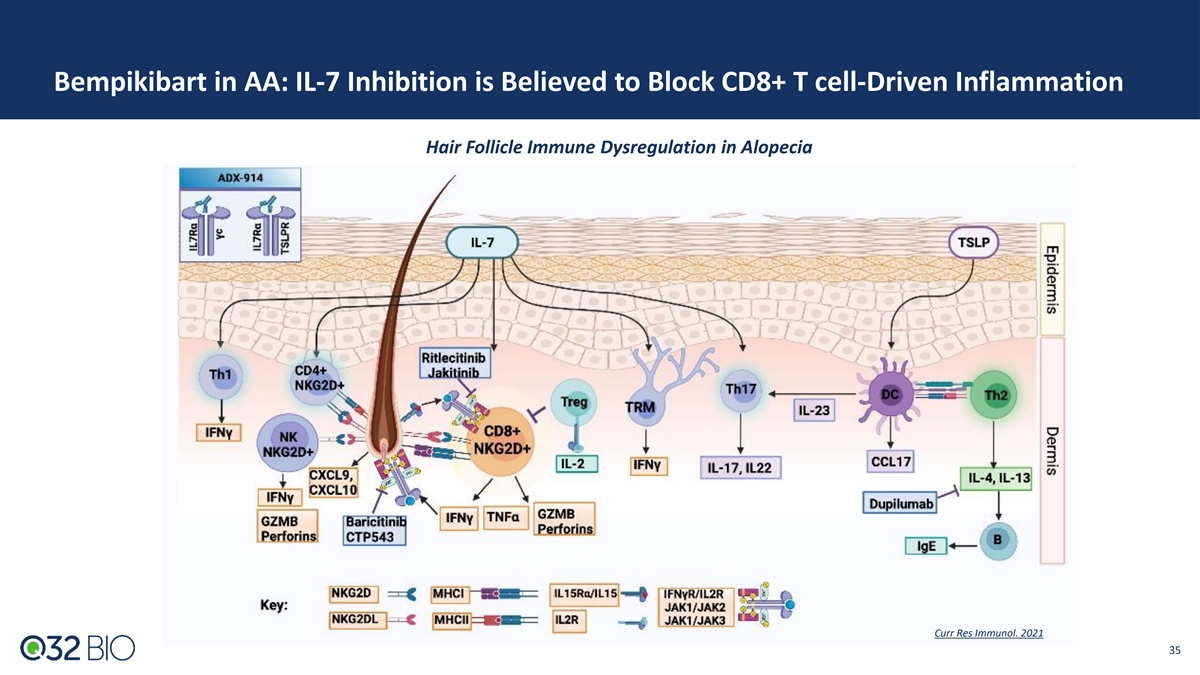
Bempikibart in AA: IL-7 Inhibition is Believed to Block CD8+ T cell-Driven Inflammation Hair Follicle Immune Dysregulation in Alopecia Curr Res Immunol. 2021 35

Bempikibart Phase 2 Clinical Trial in Atopic Dermatitis Topline Results ADX-914-202 SIGNAL-AD Part A Part B 12-week treatment (n= 15 patients in Part A), 12-week follow-up 12-week treatment (n= ~100 patients in B), 12-week follow-up • Part A Key Assessments • Part B Key assessments: 200mg SC Q2W vs placebo (1:1) • Safety and PK • Primary: Mean % change from baseline in EASI score at week 14 • Evaluated two doses: 2 mg/kg and 3 mg/kg Q2W for dose • Key Secondaries: Time to EASI change, mean % change from baseline selection in Part B and AA: 200mg SC (~2.7mg/kg) flat dose in SCORAD, proportion of patients achieving EASI thresholds, selected for Part proportion of patients achieving specified vIGA-AD improvements 1 • Proportion of patients achieving an AD-IGA of 0 or 1 with a ≥2 • Part A Topline Results at Week 14 grade improvement • At 2 mg/kg Q2W, mean % change in EASI score from baseline was 58.0%; at 3 mg/kg Q2W, mean % change in EASI score from baseline was 83.9% 2 • Part B Topline Results at Week 14 • On a pooled basis, mean % change in EASI score from baseline • Patients treated with bempikibart showed a 74.4% mean % change was 72.3% in EASI from baseline, compared to 76.2% for placebo (p= NS) • Mean % change in EASI score was 38.3% for placebo • Results of the primary endpoint were generally consistent when stratified for pre-specified baseline entry criteria • Results from analysis of key secondary endpoints were generally consistent with findings from the primary endpoint 1 Actual Percent Change from Baseline EASI (modified Full Analysis Set) 2 Least-Squares Mean Change as per pre-specified primary endpoint 36