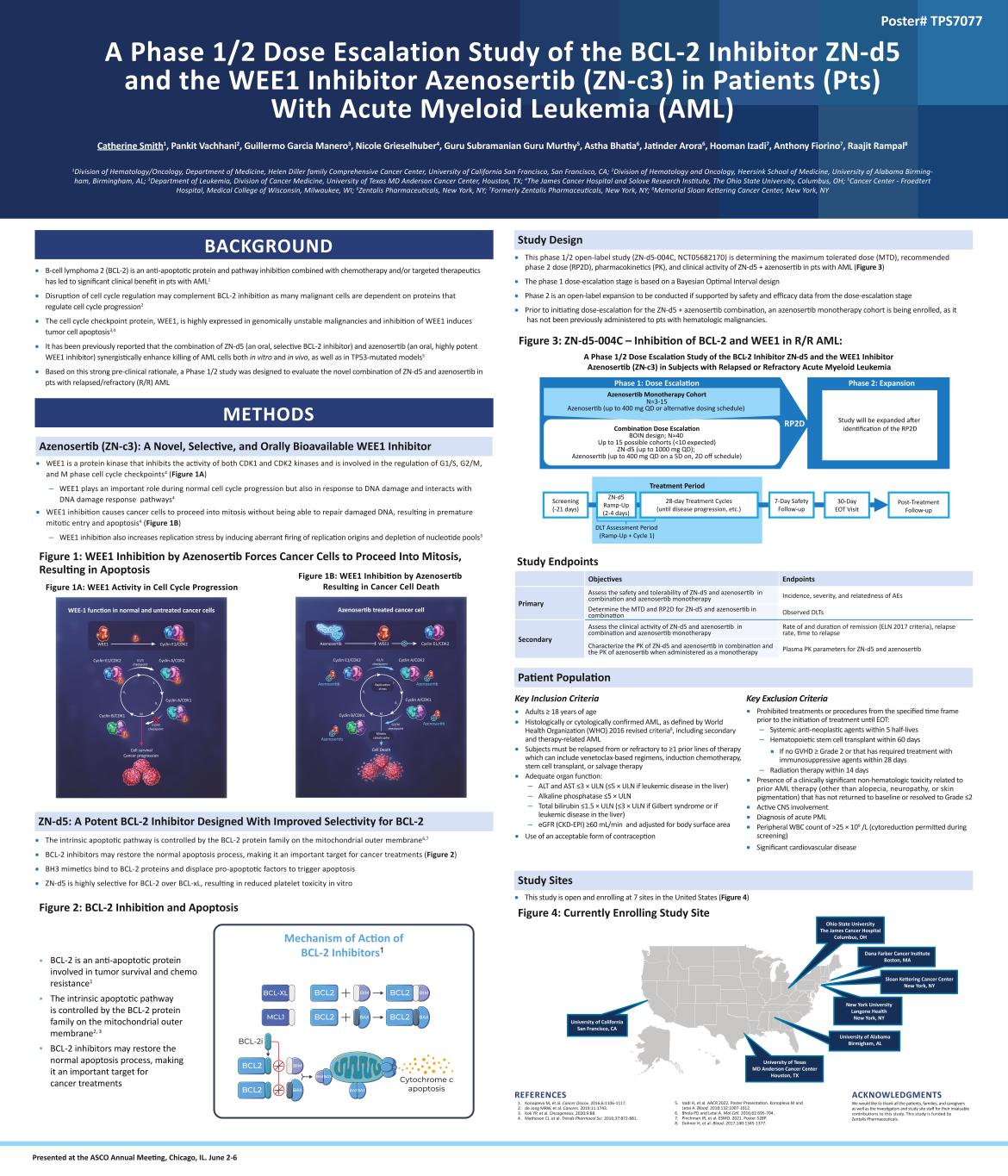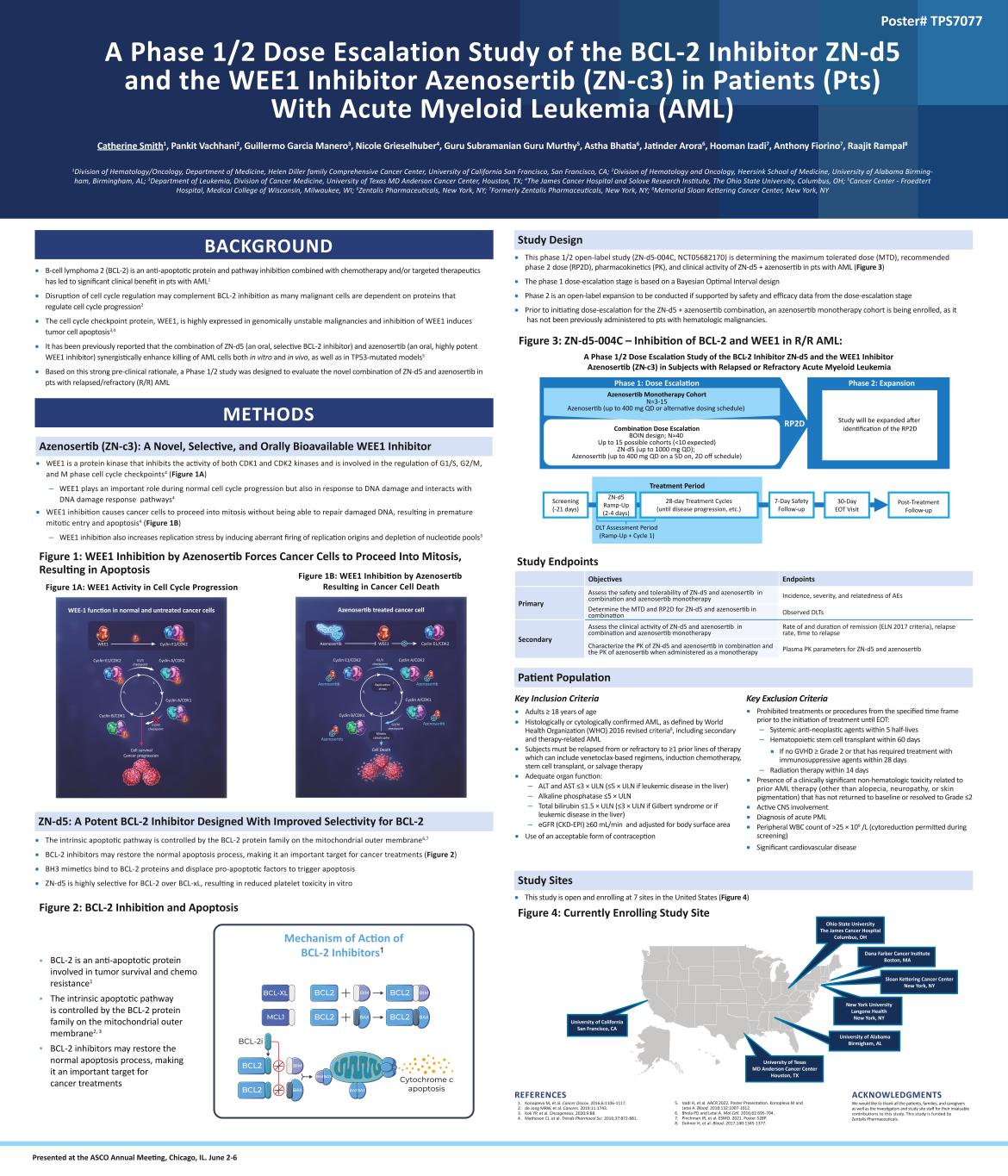
A Phase 1/2 Dose Escalation Study of the BCL-2 Inhibitor ZN-d5 and the WEE1 Inhibitor Azenosertib (ZN-c3) in Patients (Pts) With Acute Myeloid Leukemia (AML) Catherine Smith1, Pankit Vachhani2, Guillermo Garcia Manero3, Nicole Grieselhuber4, Guru Subramanian Guru Murthy5, Astha Bhatia6, Jatinder Arora6, Hooman Izadi7, Anthony Fiorino7, Raajit Rampal8 1Division of Hematology/Oncology, Department of Medicine, Helen Diller family Comprehensive Cancer Center, University of California San Francisco, San Francisco, CA; 2Division of Hematology and Oncology, Heersink School of Medicine, University of Alabama Birming- ham, Birmingham, AL; 3Department of Leukemia, Division of Cancer Medicine, University of Texas MD Anderson Cancer Center, Houston, TX; 4The James Cancer Hospital and Solove Research Institute, The Ohio State University, Columbus, OH; 5Cancer Center - Froedtert Hospital, Medical College of Wisconsin, Milwaukee, WI; 6Zentalis Pharmaceuticals, New York, NY; 7Formerly Zentalis Pharmaceuticals, New York, NY; 8Memorial Sloan Kettering Cancer Center, New York, NY BACKGROUND • B-cell lymphoma 2 (BCL-2) is an anti-apoptotic protein and pathway inhibition combined with chemotherapy and/or targeted therapeutics has led to significant clinical benefit in pts with AML1 • Disruption of cell cycle regulation may complement BCL-2 inhibition as many malignant cells are dependent on proteins that regulate cell cycle progression2 • The cell cycle checkpoint protein, WEE1, is highly expressed in genomically unstable malignancies and inhibition of WEE1 induces tumor cell apoptosis3,4 • It has been previously reported that the combination of ZN-d5 (an oral, selective BCL-2 inhibitor) and azenosertib (an oral, highly potent WEE1 inhibitor) synergistically enhance killing of AML cells both in vitro and in vivo, as well as in TP53-mutated models5 • Based on this strong pre-clinical rationale, a Phase 1/2 study was designed to evaluate the novel combination of ZN-d5 and azenosertib in pts with relapsed/refractory (R/R) AML METHODS Azenosertib (ZN-c3): A Novel, Selective, and Orally Bioavailable WEE1 Inhibitor • WEE1 is a protein kinase that inhibits the activity of both CDK1 and CDK2 kinases and is involved in the regulation of G1/S, G2/M, and M phase cell cycle checkpoints4 (Figure 1A) – WEE1 plays an important role during normal cell cycle progression but also in response to DNA damage and interacts with DNA damage response pathways4 • WEE1 inhibition causes cancer cells to proceed into mitosis without being able to repair damaged DNA, resulting in premature mitotic entry and apoptosis4 (Figure 1B) – WEE1 inhibition also increases replication stress by inducing aberrant firing of replication origins and depletion of nucleotide pools3 Figure 1: WEE1 Inhibition by Azenosertib Forces Cancer Cells to Proceed Into Mitosis, Resulting in Apoptosis ZN-d5: A Potent BCL-2 Inhibitor Designed With Improved Selectivity for BCL-2 • The intrinsic apoptotic pathway is controlled by the BCL-2 protein family on the mitochondrial outer membrane6,7 • BCL-2 inhibitors may restore the normal apoptosis process, making it an important target for cancer treatments (Figure 2) • BH3 mimetics bind to BCL-2 proteins and displace pro-apoptotic factors to trigger apoptosis • ZN-d5 is highly selective for BCL-2 over BCL-xL, resulting in reduced platelet toxicity in vitro Figure 2: BCL-2 Inhibition and Apoptosis Figure 1A: WEE1 Activity in Cell Cycle Progression Figure 1B: WEE1 Inhibition by Azenosertib Resulting in Cancer Cell Death Poster# TPS7077 ACKNOWLEDGMENTS We would like to thank all the patients, families, and caregivers as well as the investigators and study site staff for their invaluable contributions to this study. This study is funded by Zentalis Pharmaceuticals. Study Design • This phase 1/2 open-label study (ZN-d5-004C, NCT05682170) is determining the maximum tolerated dose (MTD), recommended phase 2 dose (RP2D), pharmacokinetics (PK), and clinical activity of ZN-d5 + azenosertib in pts with AML (Figure 3) • The phase 1 dose-escalation stage is based on a Bayesian Optimal Interval design • Phase 2 is an open-label expansion to be conducted if supported by safety and efficacy data from the dose-escalation stage • Prior to initiating dose-escalation for the ZN-d5 + azenosertib combination, an azenosertib monotherapy cohort is being enrolled, as it has not been previously administered to pts with hematologic malignancies. Figure 3: ZN-d5-004C – Inhibition of BCL-2 and WEE1 in R/R AML: Study Endpoints Objectives Endpoints Primary Assess the safety and tolerability of ZN-d5 and azenosertib in combination and azenosertib monotherapy Incidence, severity, and relatedness of AEs Determine the MTD and RP2D for ZN-d5 and azenosertib in combination Observed DLTs Secondary Assess the clinical activity of ZN-d5 and azenosertib in combination and azenosertib monotherapy Rate of and duration of remission (ELN 2017 criteria), relapse rate, time to relapse Characterize the PK of ZN-d5 and azenosertib in combination and the PK of azenosertib when administered as a monotherapy Plasma PK parameters for ZN-d5 and azenosertib Patient Population Study Sites • This study is open and enrolling at 7 sites in the United States (Figure 4) Figure 4: Currently Enrolling Study Site Treatment Period ZN-d5 Ramp-Up (2-4 days) Combination Dose Escalation BOIN design; N≈40 Up to 15 possible cohorts (<10 expected) ZN-d5 (up to 1000 mg QD); Azenosertib (up to 400 mg QD on a 5D on, 2D off schedule) Phase 1: Dose Escalation Phase 2: Expansion RP2D Screening (-21 days) 28-day Treatment Cycles (until disease progression, etc.) DLT Assessment Period (Ramp-Up + Cycle 1) Post-Treatment Follow-up 7-Day Safety Follow-up 30-Day EOT Visit A Phase 1/2 Dose Escalation Study of the BCL-2 Inhibitor ZN-d5 and the WEE1 Inhibitor Azenosertib (ZN-c3) in Subjects with Relapsed or Refractory Acute Myeloid Leukemia Azenosertib Monotherapy Cohort N=3-15 Azenosertib (up to 400 mg QD or alternative dosing schedule) Study will be expanded after identification of the RP2D REFERENCES 1. Konopleva M, et al. Cancer Discov. 2016;6:1106-1117. 2. de Jong MRW, et al. Cancers. 2019;11:1743. 3. Kok YP, et al. Oncogenesis. 2020;9:88. 4. Matheson CJ, et al. Trends Pharmacol Sci. 2016;37:872-881. 5. Izadi H, et al. AACR 2022. Poster Presentation. Konopleva M and Letai A. Blood. 2018;132:1007-1012. 6. Bhola PD and Letai A. Mol Cell. 2016;61:695-704. 7. Pinchman JR, et al. ESMO. 2021. Poster 528P. 8. Dohner H, et al. Blood. 2017;140:1345-1377. Mechanism of Action of BCL-2 Inhibitors 1 • BCL-2 is an anti-apoptotic protein involved in tumor survival and chemo resistance1 The intrinsic apoptotic pathway is controlled by the BCL-2 protein family on the mitochondrial outer membrane2, 3 BCL-2 inhibitors may restore the normal apoptosis process, making it an important target for cancer treatments • • Presented at the ASCO Annual Meeting, Chicago, IL. June 2-6 University of California San Francisco, CA Ohio State University The James Cancer Hospital Columbus, OH Dana Farber Cancer Institute Boston, MA University of Texas MD Anderson Cancer Center Houston, TX New York University Langone Health New York, NY University of Alabama Birmigham, AL Sloan Kettering Cancer Center New York, NY Key Inclusion Criteria • Adults ≥ 18 years of age • Histologically or cytologically confirmed AML, as defined by World Health Organization (WHO) 2016 revised criteria8, including secondary and therapy-related AML • Subjects must be relapsed from or refractory to ≥1 prior lines of therapy which can include venetoclax-based regimens, induction chemotherapy, stem cell transplant, or salvage therapy • Adequate organ function: – ALT and AST ≤3 × ULN (≤5 × ULN if leukemic disease in the liver) – Alkaline phosphatase ≤5 × ULN – Total bilirubin ≤1.5 × ULN (≤3 × ULN if Gilbert syndrome or if leukemic disease in the liver) – eGFR (CKD-EPI) ≥60 mL/min and adjusted for body surface area • Use of an acceptable form of contraception Key Exclusion Criteria • Prohibited treatments or procedures from the specified time frame prior to the initiation of treatment until EOT: – Systemic anti-neoplastic agents within 5 half-lives – Hematopoietic stem cell transplant within 60 days ■ If no GVHD ≥ Grade 2 or that has required treatment with immunosuppressive agents within 28 days – Radiation therapy within 14 days • Presence of a clinically significant non-hematologic toxicity related to prior AML therapy (other than alopecia, neuropathy, or skin pigmentation) that has not returned to baseline or resolved to Grade ≤2 • Active CNS involvement • Diagnosis of acute PML • Peripheral WBC count of >25 × 109 /L (cytoreduction permitted during screening) • Significant cardiovascular disease