Developing Next Generation Programmed T Cell Therapies February 2024 Exhibit 99.1
Disclaimer Developing Next Generation Programmed T Cell Therapies These slides contain forward-looking statements within the meaning of the "safe harbor" provisions of the Private Securities Litigation Reform Act of 1995. Forward-looking statements are statements that are not historical facts, and in some cases can be identified by terms such as "may," "will," "could," "expects," "plans," "anticipates," and "believes." These statements include, but are not limited to, statements regarding Autolus’ development of its product candidates, including the obe-cel program; the profile and potential application of obe-cel in additional disease settings; the future clinical development, efficacy, safety and therapeutic potential of the Company's product candidates, including progress, expectations as to the reporting of data, conduct and timing and potential future clinical and preclinical activity and milestones; expectations regarding the initiation, design and reporting of data from clinical trials and preclinical studies; the extension of the pipeline beyond obe-cel; expectations regarding the regulatory approval process for any product candidates; the benefits of the collaboration between Autolus and BioNTech, including the potential and timing to receive milestone payments and royalties under the terms of the strategic collaboration; the Company’s current and future manufacturing capabilities; and the Company’s anticipated cash runway. Any forward-looking statements are based on management's current views and assumptions and involve risks and uncertainties that could cause actual results, performance, or events to differ materially from those expressed or implied in such statements. These risks and uncertainties include, but are not limited to, the risks that Autolus’ preclinical or clinical programs do not advance or result in approved products on a timely or cost effective basis or at all; the results of early clinical trials are not always being predictive of future results; the cost, timing and results of clinical trials; that many product candidates do not become approved drugs on a timely or cost effective basis or at all; the ability to enroll patients in clinical trials; and possible safety and efficacy concerns. For a discussion of other risks and uncertainties, and other important factors, any of which could cause Autolus’ actual results to differ from those contained in the forward-looking statements, see the section titled "Risk Factors" in Autolus' Annual Report on Form 20-F filed with the Securities and Exchange Commission, or the SEC, on March 7, 2023 and in Autolus' Quarterly Report on Form 10-Q filed with the Securities and Exchange Commission on November 9, 2023, as well as discussions of potential risks, uncertainties, and other important factors in Autolus' subsequent filings with the Securities and Exchange Commission. All information in this presentation is as of the date of the presentation, and Autolus undertakes no obligation to publicly update any forward-looking statement, whether as a result of new information, future events, or otherwise, except as required by law. You should, therefore, not rely on these forward-looking statements as representing the Company’s views as of any date subsequent to the date of this presentation.
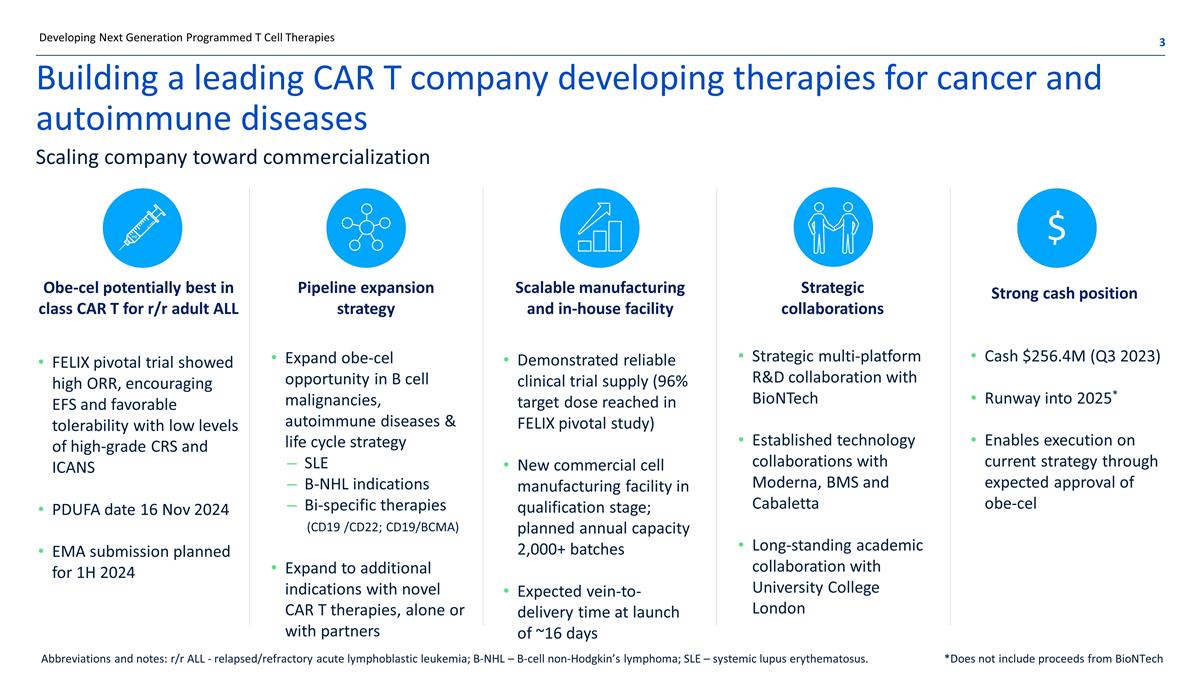
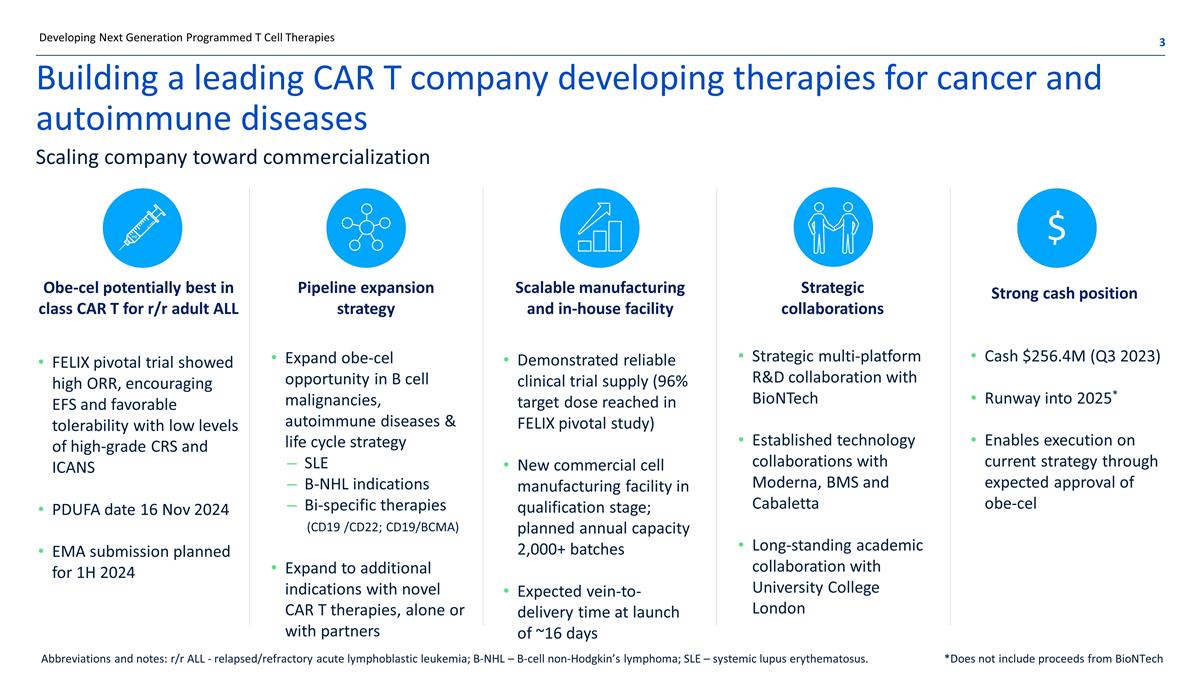
Building a leading CAR T company developing therapies for cancer and autoimmune diseases FELIX pivotal trial showed high ORR, encouraging EFS and favorable tolerability with low levels of high-grade CRS and ICANS PDUFA date 16 Nov 2024 EMA submission planned for 1H 2024 Strategic multi-platform R&D collaboration with BioNTech Established technology collaborations with Moderna, BMS and Cabaletta Long-standing academic collaboration with University College London Expand obe-cel opportunity in B cell malignancies, autoimmune diseases & life cycle strategy SLE B-NHL indications Bi-specific therapies (CD19 /CD22; CD19/BCMA) Expand to additional indications with novel CAR T therapies, alone or with partners Demonstrated reliable clinical trial supply (96% target dose reached in FELIX pivotal study) New commercial cell manufacturing facility in qualification stage; planned annual capacity 2,000+ batches Expected vein-to-delivery time at launch of ~16 days Obe-cel potentially best in class CAR T for r/r adult ALL Strategic collaborations Pipeline expansion strategy Scalable manufacturing and in-house facility Cash $256.4M (Q3 2023) Runway into 2025* Enables execution on current strategy through expected approval of obe-cel Strong cash position Scaling company toward commercialization $ Developing Next Generation Programmed T Cell Therapies Abbreviations and notes: r/r ALL - relapsed/refractory acute lymphoblastic leukemia; B-NHL – B-cell non-Hodgkin’s lymphoma; SLE – systemic lupus erythematosus. *Does not include proceeds from BioNTech
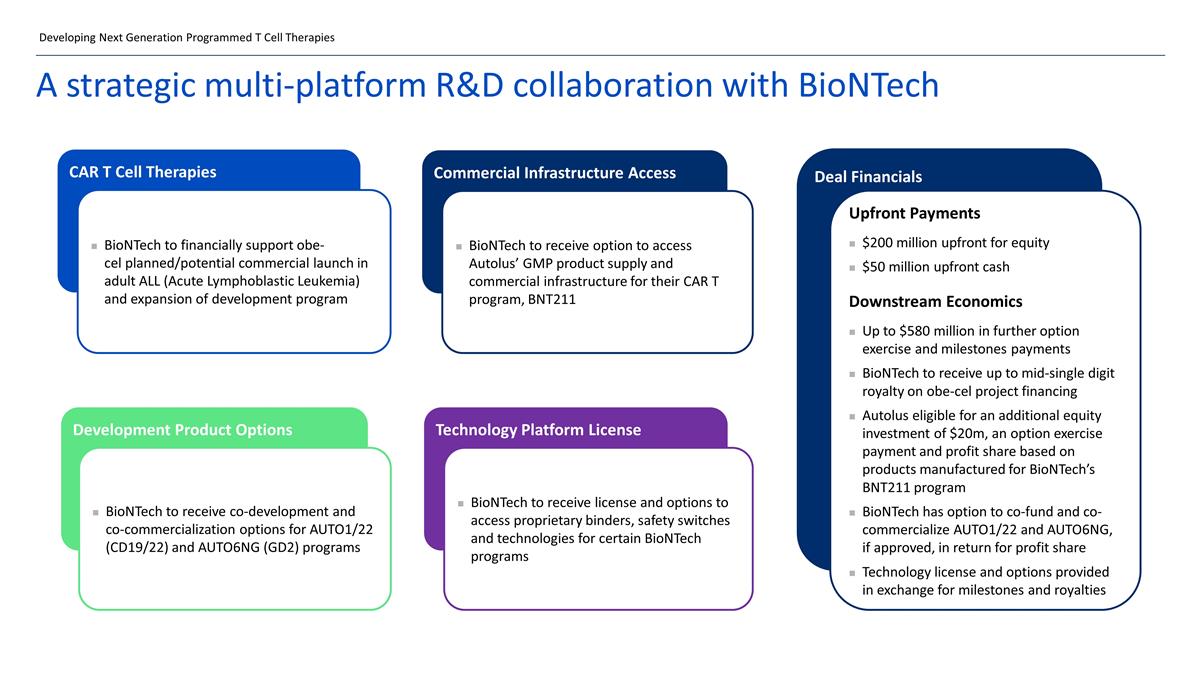
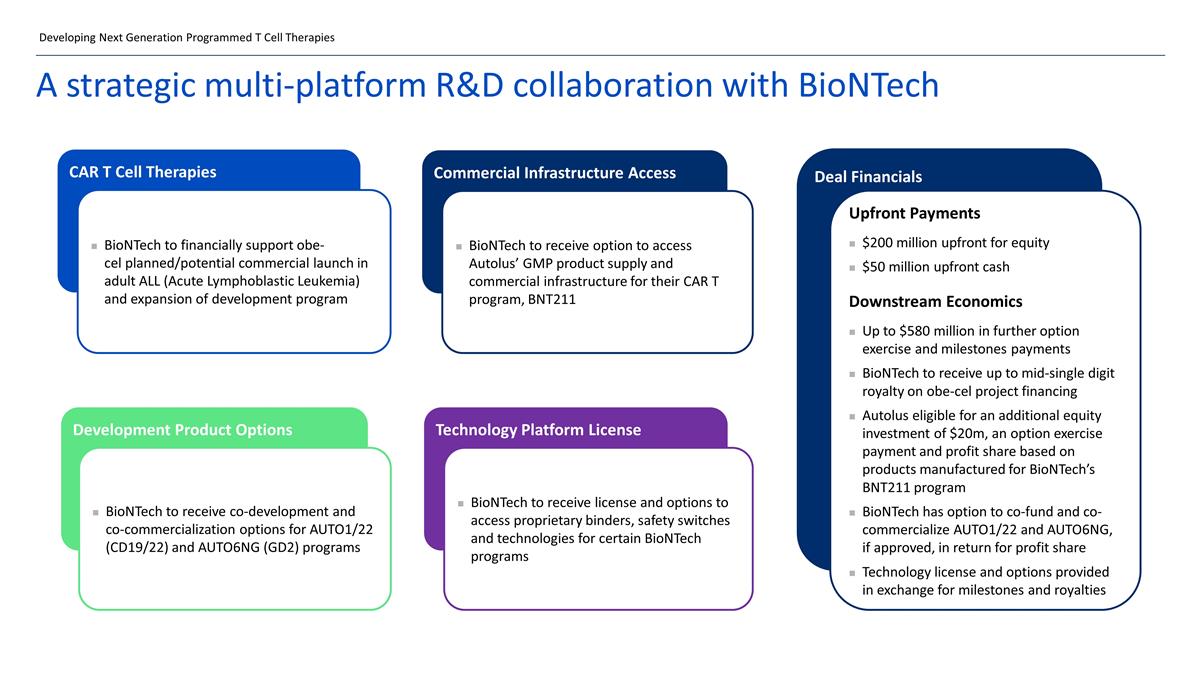
A strategic multi-platform R&D collaboration with BioNTech CAR T Cell Therapies BioNTech to financially support obe-cel planned/potential commercial launch in adult ALL (Acute Lymphoblastic Leukemia) and expansion of development program Commercial Infrastructure Access BioNTech to receive option to access Autolus’ GMP product supply and commercial infrastructure for their CAR T program, BNT211 Development Product Options BioNTech to receive co-development and co-commercialization options for AUTO1/22 (CD19/22) and AUTO6NG (GD2) programs Technology Platform License BioNTech to receive license and options to access proprietary binders, safety switches and technologies for certain BioNTech programs Deal Financials Upfront Payments $200 million upfront for equity $50 million upfront cash Downstream Economics Up to $580 million in further option exercise and milestones payments BioNTech to receive up to mid-single digit royalty on obe-cel project financing Autolus eligible for an additional equity investment of $20m, an option exercise payment and profit share based on products manufactured for BioNTech’s BNT211 program BioNTech has option to co-fund and co-commercialize AUTO1/22 and AUTO6NG, if approved, in return for profit share Technology license and options provided in exchange for milestones and royalties Developing Next Generation Programmed T Cell Therapies
Obe-cel Lead Clinical Program A standalone, potentially best-in-class CD19 CAR T cell therapy candidate
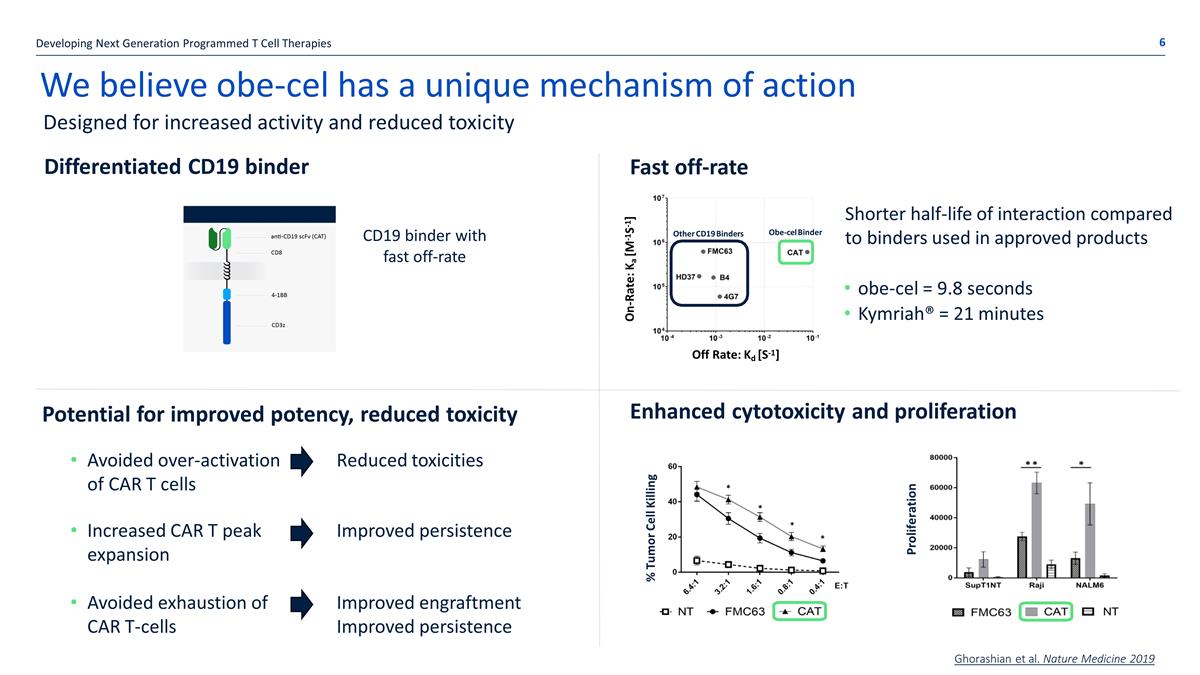
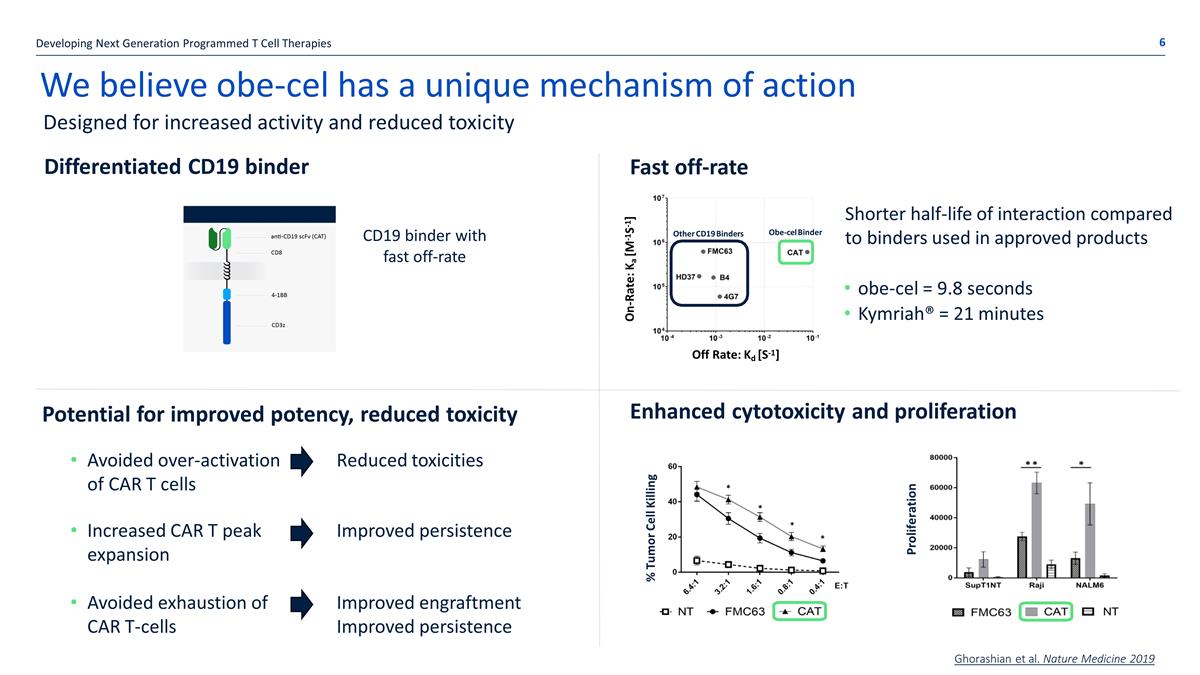
We believe obe-cel has a unique mechanism of action Avoided over-activation of CAR T cells Increased CAR T peak expansion Avoided exhaustion of CAR T-cells Enhanced cytotoxicity and proliferation Off Rate: Kd [S-1] ] 1 - S 1 - [M a K : e Rat - On Other CD19 Binders Obe-cel Binder Off Rate: Kd [S-1] On-Rate: Ka [M-1S-1] Shorter half-life of interaction compared to binders used in approved products obe-cel = 9.8 seconds Kymriah® = 21 minutes % Tumor Cell Killing Proliferation Ghorashian et al. Nature Medicine 2019 Fast off-rate CD19 binder with fast off-rate Designed for increased activity and reduced toxicity Developing Next Generation Programmed T Cell Therapies Differentiated CD19 binder Potential for improved potency, reduced toxicity Reduced toxicities Improved persistence Improved engraftment Improved persistence
Obe-cel pooled analysis ASH 2023 FELIX Phase 1b/2 trial
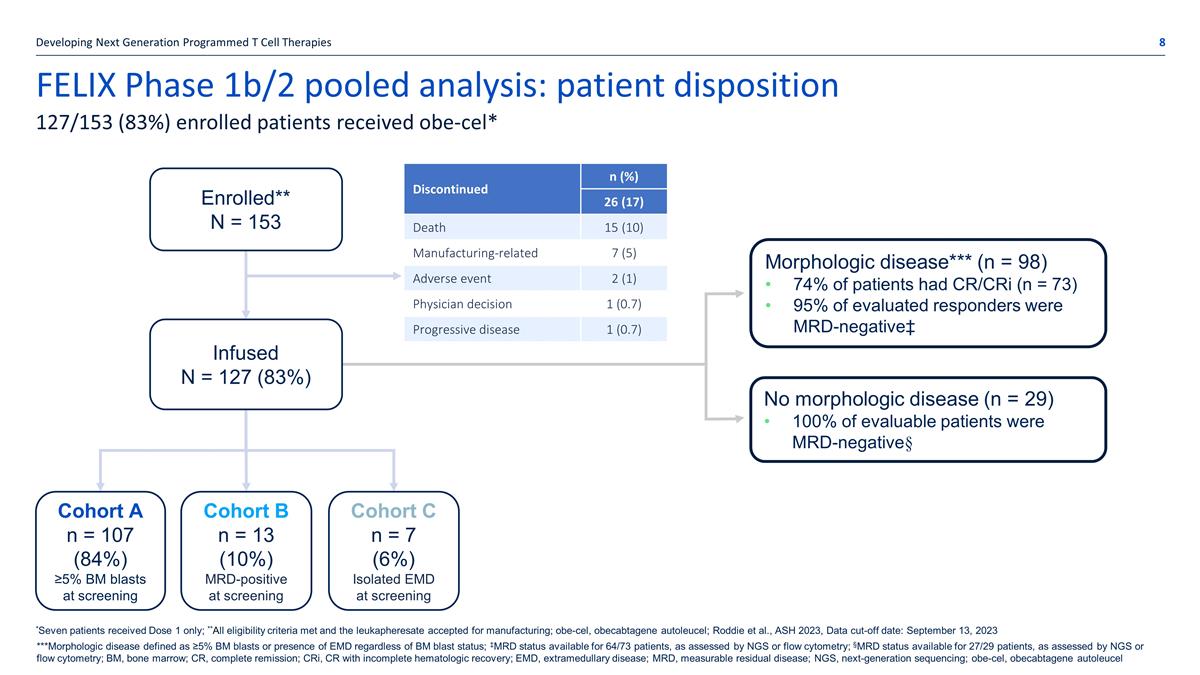
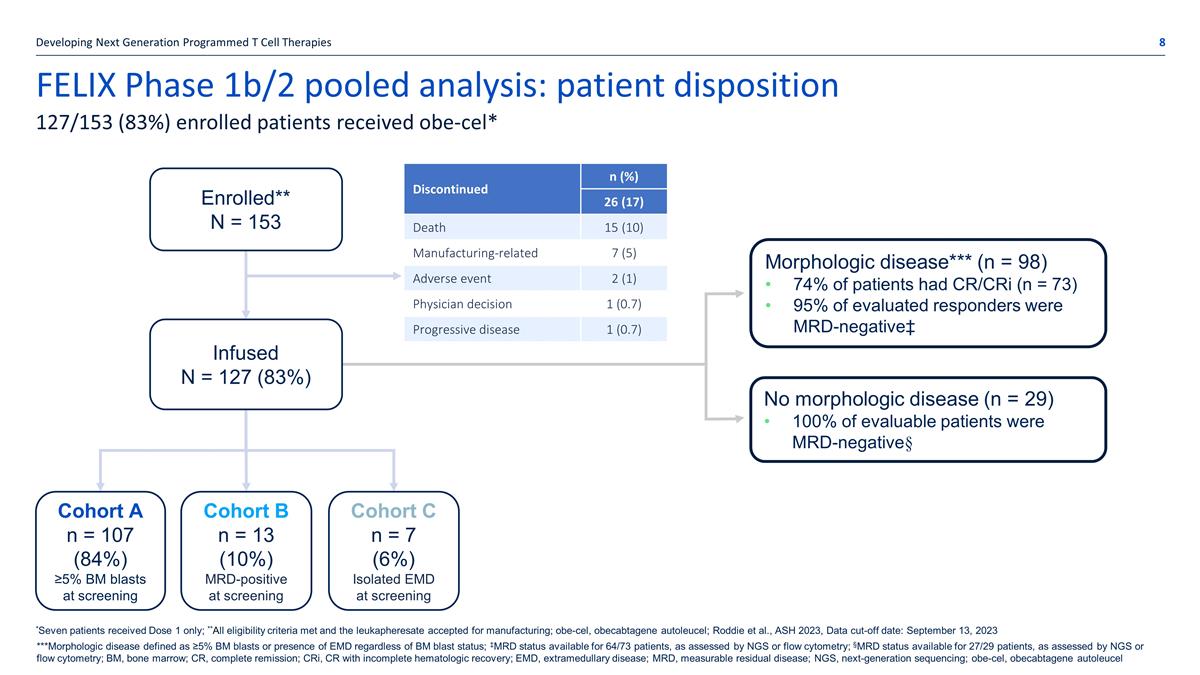
FELIX Phase 1b/2 pooled analysis: patient disposition Developing Next Generation Programmed T Cell Therapies 127/153 (83%) enrolled patients received obe-cel* Discontinued n (%) 26 (17) Death 15 (10) Manufacturing-related 7 (5) Adverse event 2 (1) Physician decision 1 (0.7) Progressive disease 1 (0.7) *Seven patients received Dose 1 only; **All eligibility criteria met and the leukapheresate accepted for manufacturing; obe-cel, obecabtagene autoleucel; Roddie et al., ASH 2023, Data cut-off date: September 13, 2023 Infused N = 127 (83%) Enrolled** N = 153 Cohort A n = 107 (84%) ≥5% BM blasts at screening Cohort B n = 13 (10%) MRD-positive at screening Cohort C n = 7 (6%) Isolated EMD at screening Morphologic disease*** (n = 98) 74% of patients had CR/CRi (n = 73) 95% of evaluated responders were MRD-negative‡ No morphologic disease (n = 29) 100% of evaluable patients were MRD-negative§ ***Morphologic disease defined as ≥5% BM blasts or presence of EMD regardless of BM blast status; ‡MRD status available for 64/73 patients, as assessed by NGS or flow cytometry; §MRD status available for 27/29 patients, as assessed by NGS or flow cytometry; BM, bone marrow; CR, complete remission; CRi, CR with incomplete hematologic recovery; EMD, extramedullary disease; MRD, measurable residual disease; NGS, next-generation sequencing; obe-cel, obecabtagene autoleucel
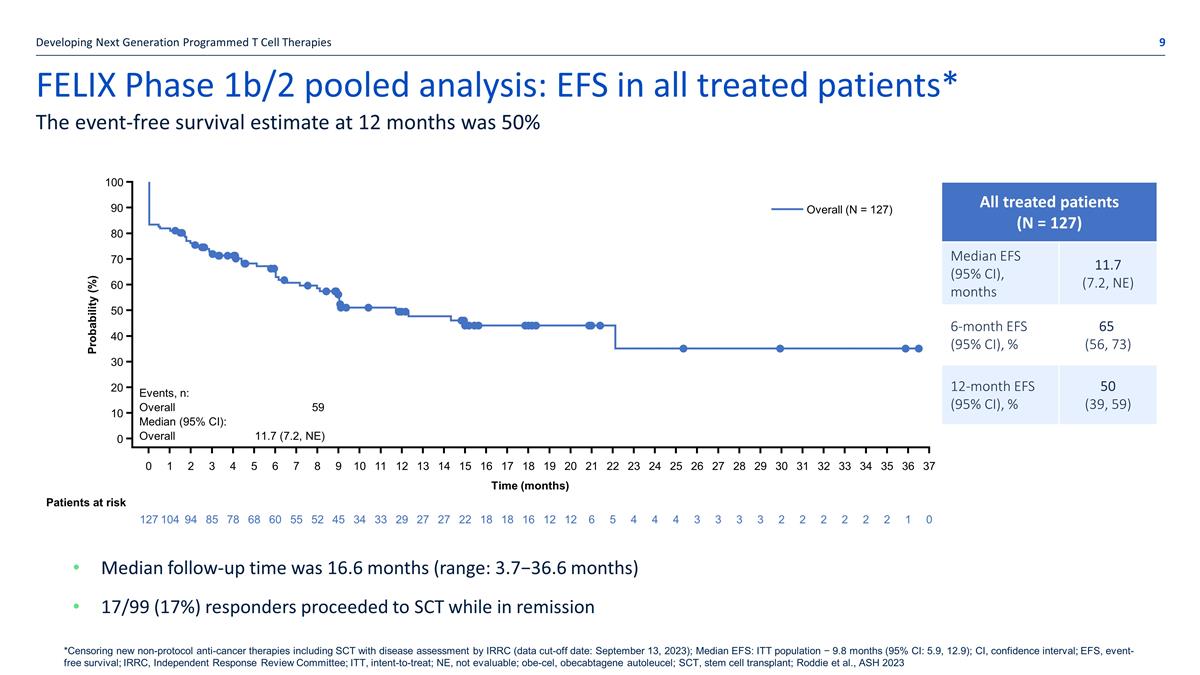
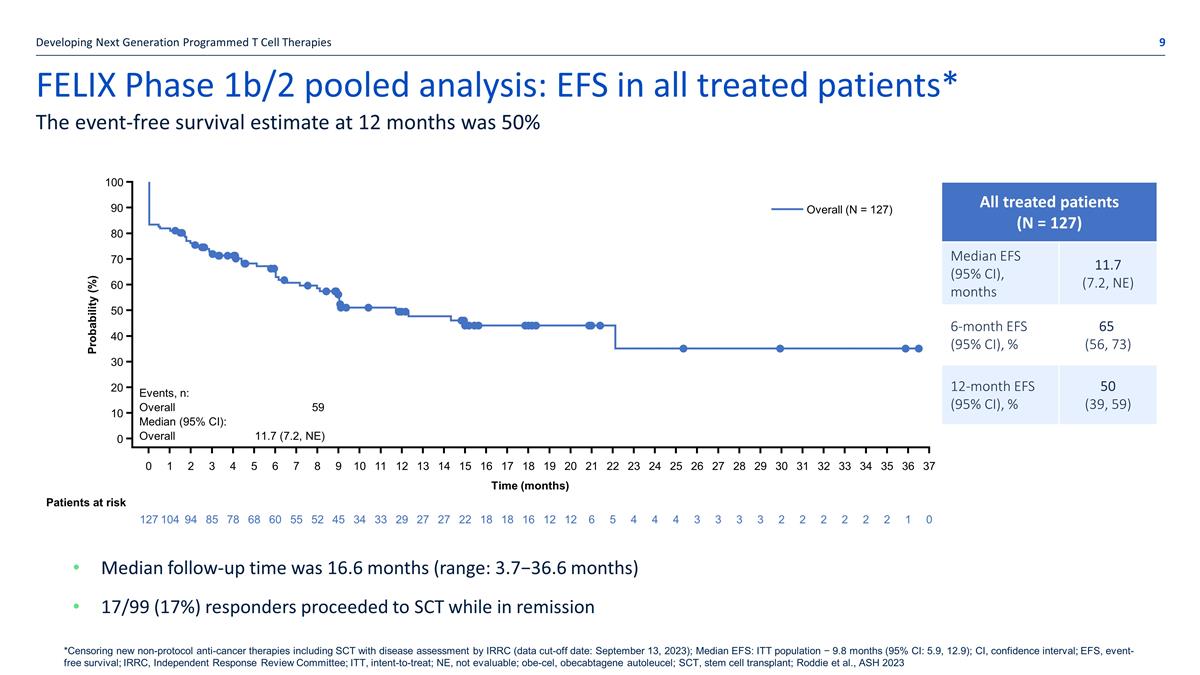
FELIX Phase 1b/2 pooled analysis: EFS in all treated patients* Developing Next Generation Programmed T Cell Therapies The event-free survival estimate at 12 months was 50% Median follow-up time was 16.6 months (range: 3.7−36.6 months) 17/99 (17%) responders proceeded to SCT while in remission *Censoring new non-protocol anti-cancer therapies including SCT with disease assessment by IRRC (data cut-off date: September 13, 2023); Median EFS: ITT population − 9.8 months (95% CI: 5.9, 12.9); CI, confidence interval; EFS, event-free survival; IRRC, Independent Response Review Committee; ITT, intent-to-treat; NE, not evaluable; obe-cel, obecabtagene autoleucel; SCT, stem cell transplant; Roddie et al., ASH 2023 All treated patients (N = 127) Total infused (N = 126) Median EFS (95% CI), months 11.7 (7.2, NE) 6-month EFS (95% CI), % 65 (56, 73) 12-month EFS (95% CI), % 50 (39, 59) Events, n: Overall Median (95% CI): Overall 59 11.7 (7.2, NE) Probability (%) 0 10 20 30 40 50 60 70 80 90 100 Time (months) 0 1 2 3 4 5 6 7 8 9 10 1 1 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 Overall (N = 127) Patients at risk 127 104 94 85 78 68 60 55 52 45 34 33 29 27 27 22 18 18 16 12 12 6 5 4 4 4 3 3 3 3 2 2 2 2 2 2 1 0
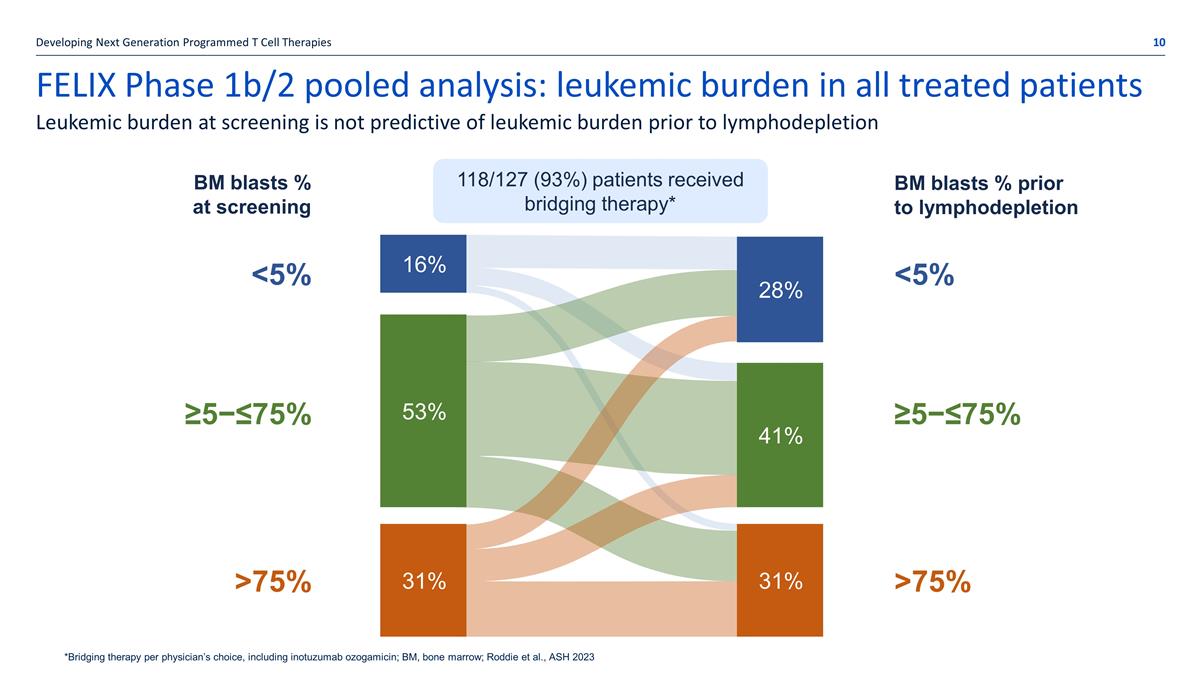
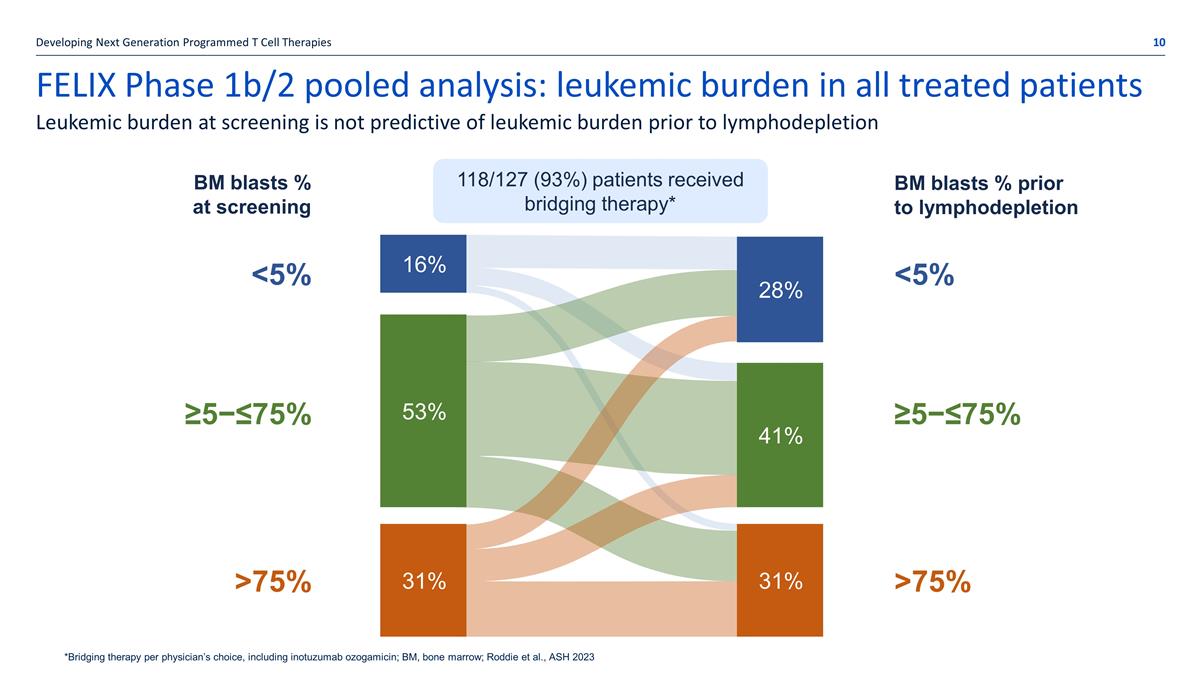
FELIX Phase 1b/2 pooled analysis: leukemic burden in all treated patients Developing Next Generation Programmed T Cell Therapies Leukemic burden at screening is not predictive of leukemic burden prior to lymphodepletion *Bridging therapy per physician’s choice, including inotuzumab ozogamicin; BM, bone marrow; Roddie et al., ASH 2023 16% 28% 53% 40% 31% 31% BM blasts % at screening BM blasts % prior to lymphodepletion 118/127 (93%) patients received bridging therapy* <5% ≥5−≤75% >75% 53% 31% 31% <5% ≥5−≤75% >75% 28% 41% 16%
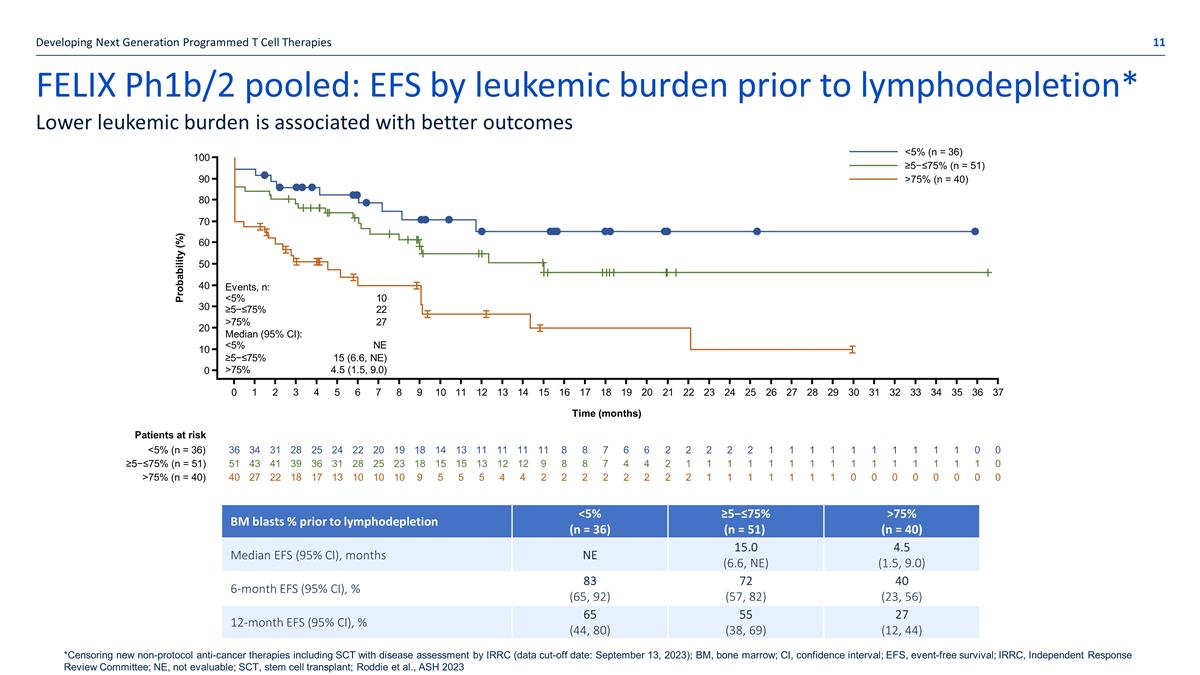
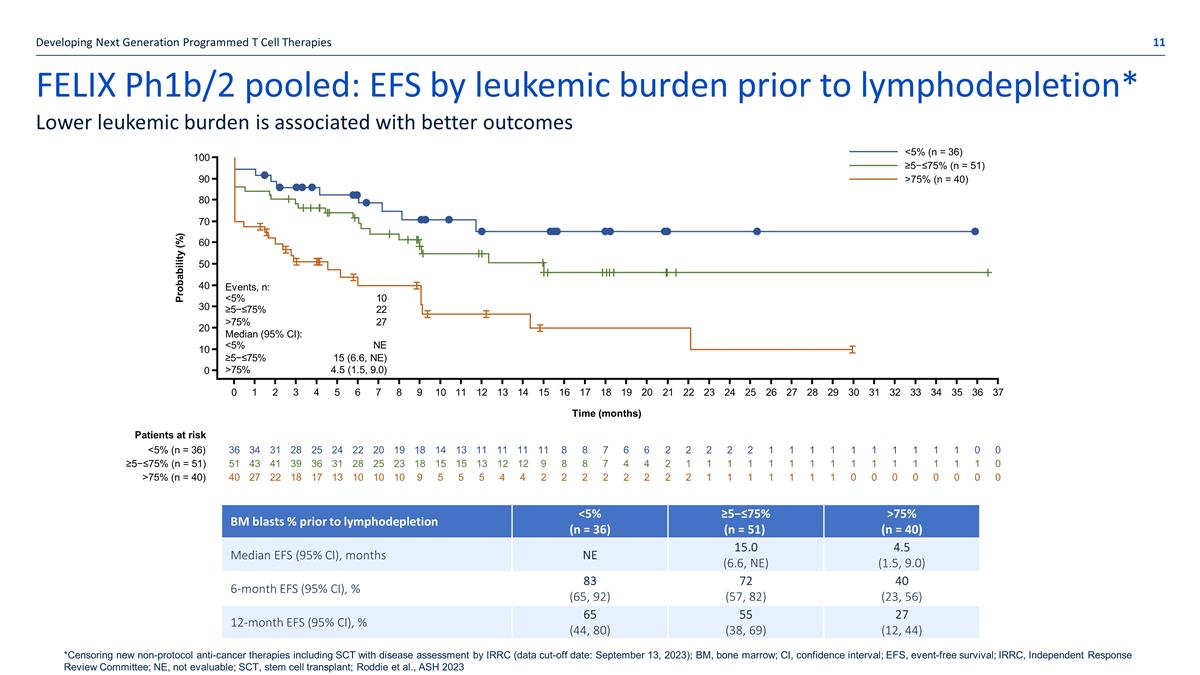
FELIX Ph1b/2 pooled: EFS by leukemic burden prior to lymphodepletion* Developing Next Generation Programmed T Cell Therapies Lower leukemic burden is associated with better outcomes BM blasts % prior to lymphodepletion <5% (n = 36) ≥5−≤75% (n = 51) >75% (n = 40) Median EFS (95% CI), months NE 15.0 (6.6, NE) 4.5 (1.5, 9.0) 6-month EFS (95% CI), % 83 (65, 92) 72 (57, 82) 40 (23, 56) 12-month EFS (95% CI), % 65 (44, 80) 55 (38, 69) 27 (12, 44) Events, n: <5% 10 ≥5−≤75% 22 >75% 27 Median (95% CI): <5% NE ≥5−≤75% 15 (6.6, NE) >75% 4.5 (1.5, 9.0) Patients at risk <5% (n = 36) ≥5−≤75% (n = 51) >75% (n = 40) <5% (n = 36) ≥5−≤75% (n = 51) >75% (n = 40) 0 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 36 34 31 28 25 24 22 20 19 18 14 13 11 11 11 11 8 8 7 6 6 2 2 2 2 2 1 1 1 1 1 1 1 1 1 1 0 0 51 43 41 39 36 31 28 25 23 18 15 15 13 12 12 9 8 8 7 4 4 2 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 0 40 27 22 18 17 13 10 10 10 9 5 5 5 4 4 2 2 2 2 2 2 2 2 1 1 1 1 1 1 1 0 0 0 0 0 0 0 0 Time (months) 0 10 20 30 40 50 60 70 80 90 100 Probability (%) *Censoring new non-protocol anti-cancer therapies including SCT with disease assessment by IRRC (data cut-off date: September 13, 2023); BM, bone marrow; CI, confidence interval; EFS, event-free survival; IRRC, Independent Response Review Committee; NE, not evaluable; SCT, stem cell transplant; Roddie et al., ASH 2023
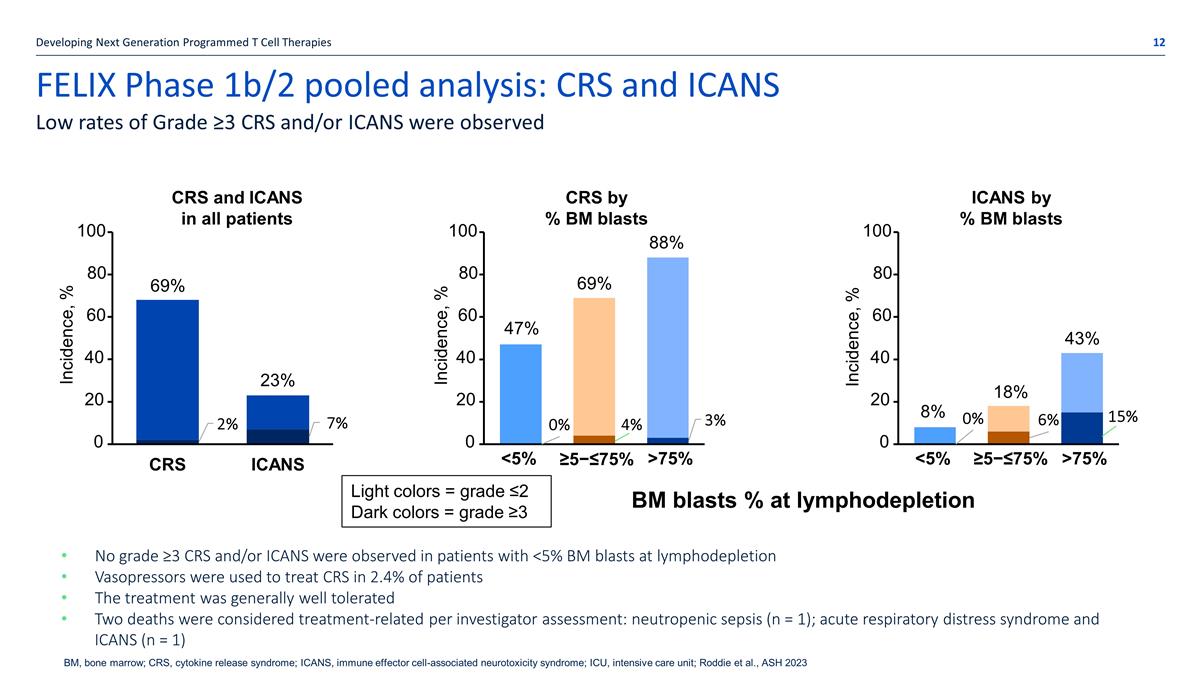
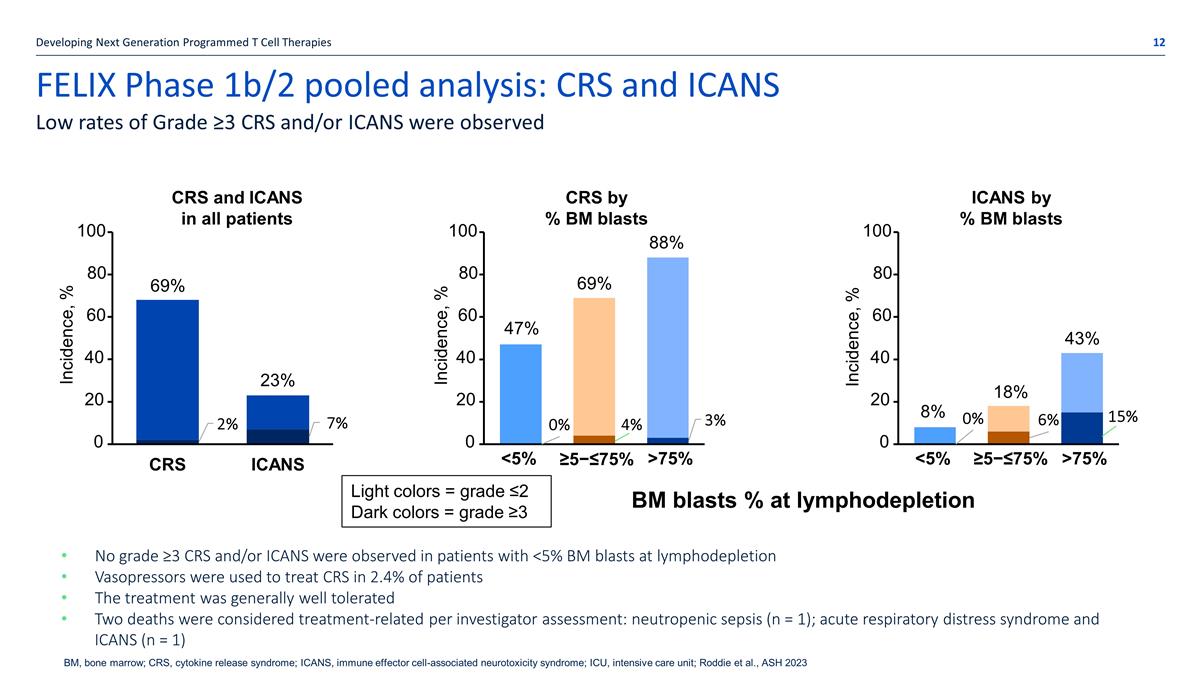
FELIX Phase 1b/2 pooled analysis: CRS and ICANS Developing Next Generation Programmed T Cell Therapies Low rates of Grade ≥3 CRS and/or ICANS were observed BM blasts % at lymphodepletion 20 0 40 60 80 100 Incidence, % CRS ICANS 20 0 40 60 80 100 Incidence, % <5% ≥5−≤75% >75% 20 0 40 60 80 100 Incidence, % <5% ≥5−≤75% >75% CRS and ICANS in all patients CRS by % BM blasts ICANS by % BM blasts Light colors = grade ≤2 Dark colors = grade ≥3 69% 23% 47% 69% 88% 8% 18% 43% No grade ≥3 CRS and/or ICANS were observed in patients with <5% BM blasts at lymphodepletion Vasopressors were used to treat CRS in 2.4% of patients The treatment was generally well tolerated Two deaths were considered treatment-related per investigator assessment: neutropenic sepsis (n = 1); acute respiratory distress syndrome and ICANS (n = 1) BM, bone marrow; CRS, cytokine release syndrome; ICANS, immune effector cell-associated neurotoxicity syndrome; ICU, intensive care unit; Roddie et al., ASH 2023
Obe-cel pooled analysis ASH 2023 ALLCAR19 Phase 1b /FELIX Ph 1b
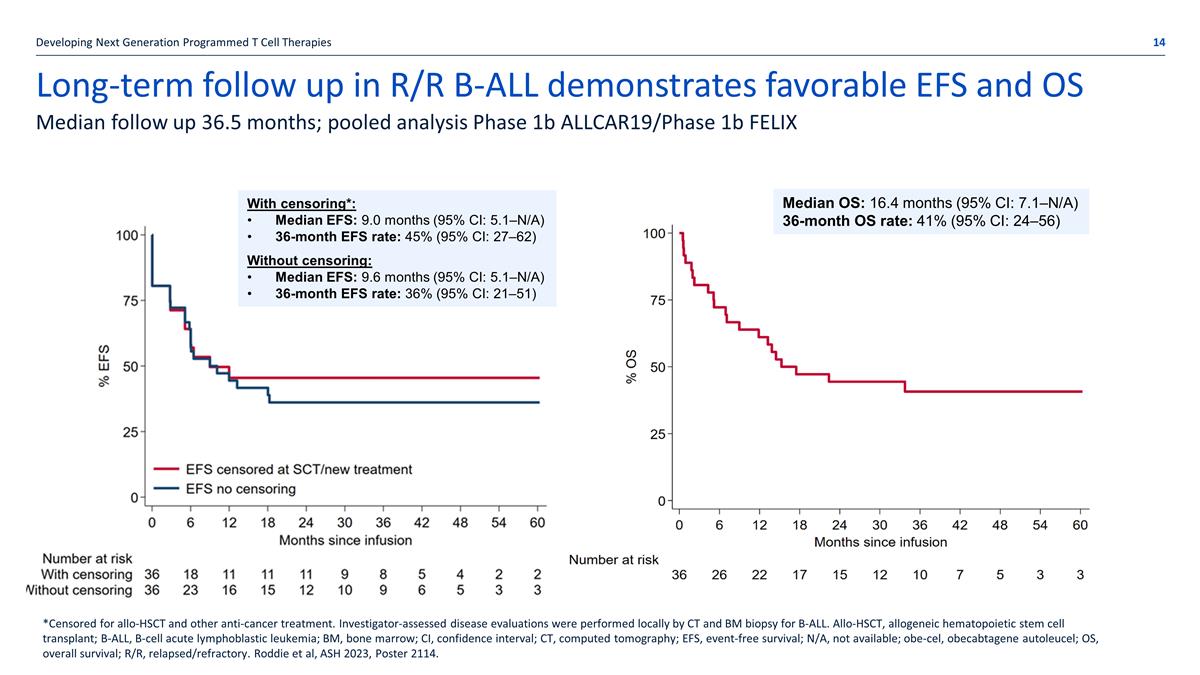
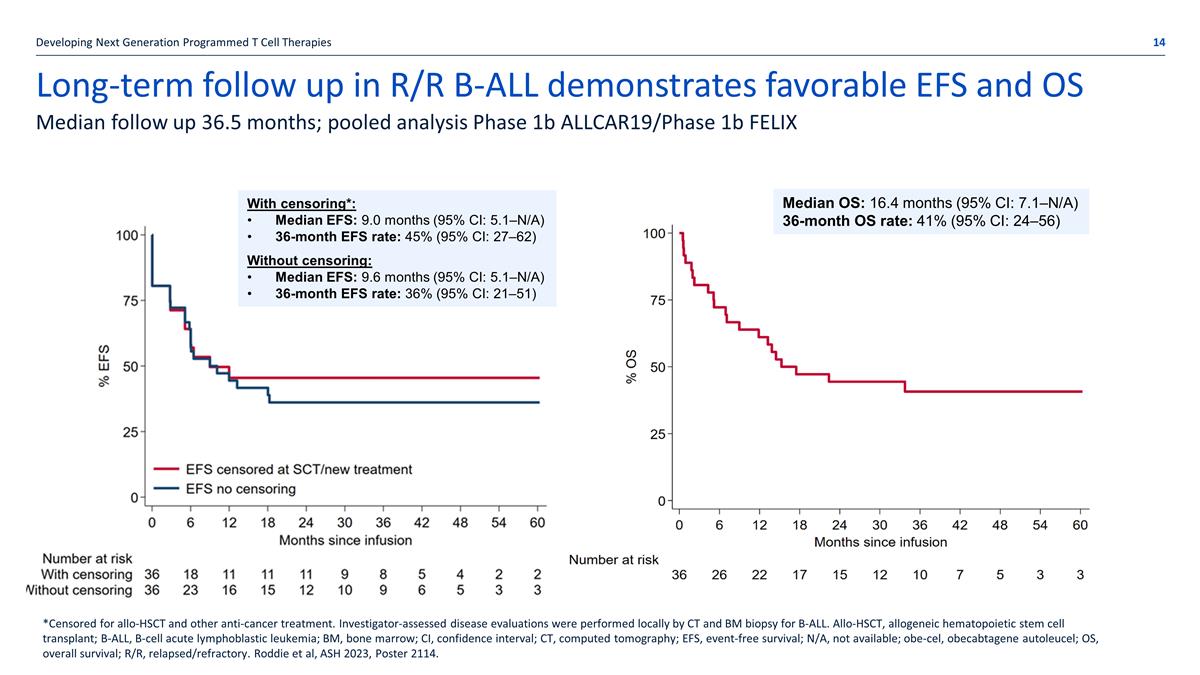
Long-term follow up in R/R B-ALL demonstrates favorable EFS and OS Developing Next Generation Programmed T Cell Therapies Median follow up 36.5 months; pooled analysis Phase 1b ALLCAR19/Phase 1b FELIX *Censored for allo-HSCT and other anti-cancer treatment. Investigator-assessed disease evaluations were performed locally by CT and BM biopsy for B-ALL. Allo-HSCT, allogeneic hematopoietic stem cell transplant; B-ALL, B-cell acute lymphoblastic leukemia; BM, bone marrow; CI, confidence interval; CT, computed tomography; EFS, event-free survival; N/A, not available; obe-cel, obecabtagene autoleucel; OS, overall survival; R/R, relapsed/refractory. Roddie et al, ASH 2023, Poster 2114. Median OS: 16.4 months (95% CI: 7.1–N/A) 36-month OS rate: 41% (95% CI: 24–56) With censoring*: Median EFS: 9.0 months (95% CI: 5.1–N/A) 36-month EFS rate: 45% (95% CI: 27–62) Without censoring: Median EFS: 9.6 months (95% CI: 5.1–N/A) 36-month EFS rate: 36% (95% CI: 21–51)
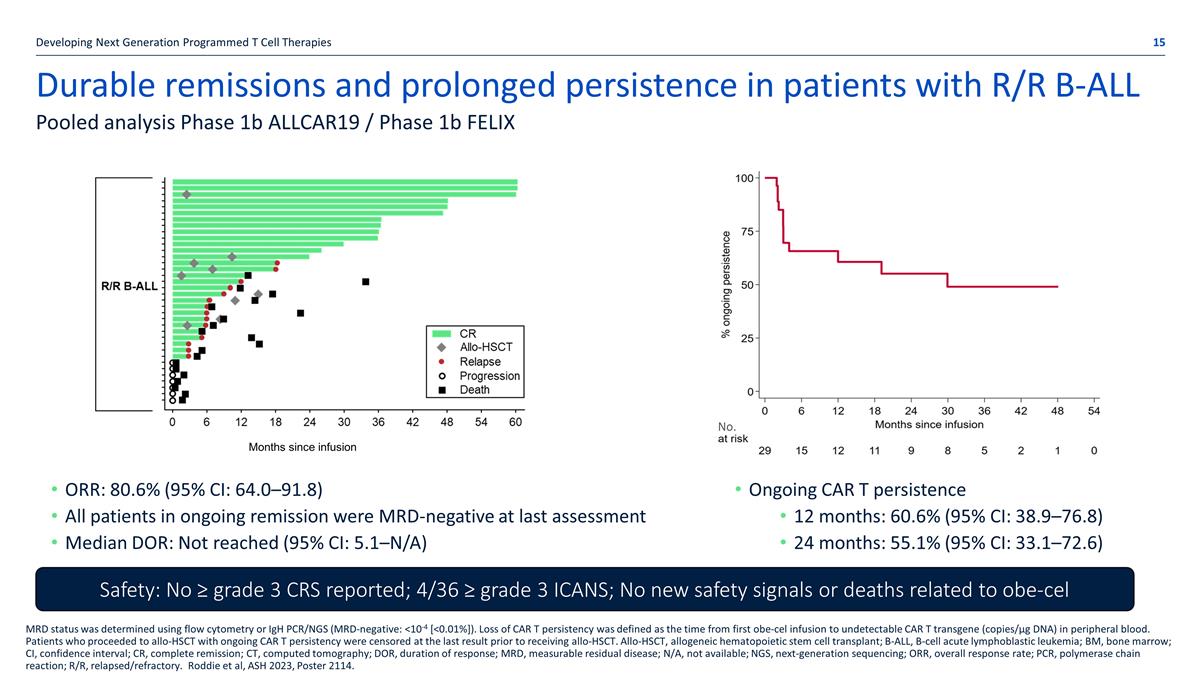
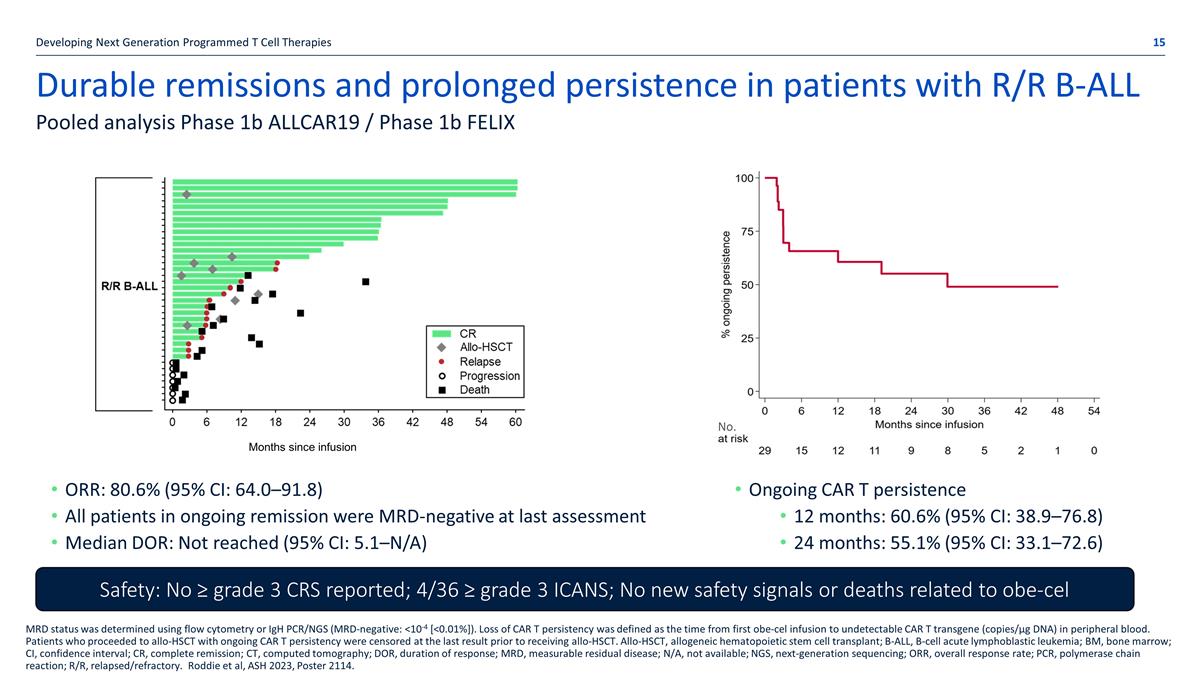
Durable remissions and prolonged persistence in patients with R/R B-ALL Developing Next Generation Programmed T Cell Therapies Pooled analysis Phase 1b ALLCAR19 / Phase 1b FELIX MRD status was determined using flow cytometry or IgH PCR/NGS (MRD-negative: <10-4 [<0.01%]). Loss of CAR T persistency was defined as the time from first obe-cel infusion to undetectable CAR T transgene (copies/µg DNA) in peripheral blood. Patients who proceeded to allo-HSCT with ongoing CAR T persistency were censored at the last result prior to receiving allo-HSCT. Allo-HSCT, allogeneic hematopoietic stem cell transplant; B-ALL, B-cell acute lymphoblastic leukemia; BM, bone marrow; CI, confidence interval; CR, complete remission; CT, computed tomography; DOR, duration of response; MRD, measurable residual disease; N/A, not available; NGS, next-generation sequencing; ORR, overall response rate; PCR, polymerase chain reaction; R/R, relapsed/refractory. Roddie et al, ASH 2023, Poster 2114. Months since infusion ORR: 80.6% (95% CI: 64.0–91.8) All patients in ongoing remission were MRD-negative at last assessment Median DOR: Not reached (95% CI: 5.1–N/A) Safety: No ≥ grade 3 CRS reported; 4/36 ≥ grade 3 ICANS; No new safety signals or deaths related to obe-cel Ongoing CAR T persistence 12 months: 60.6% (95% CI: 38.9–76.8) 24 months: 55.1% (95% CI: 33.1–72.6) No.

ALL: unmet need and market overview
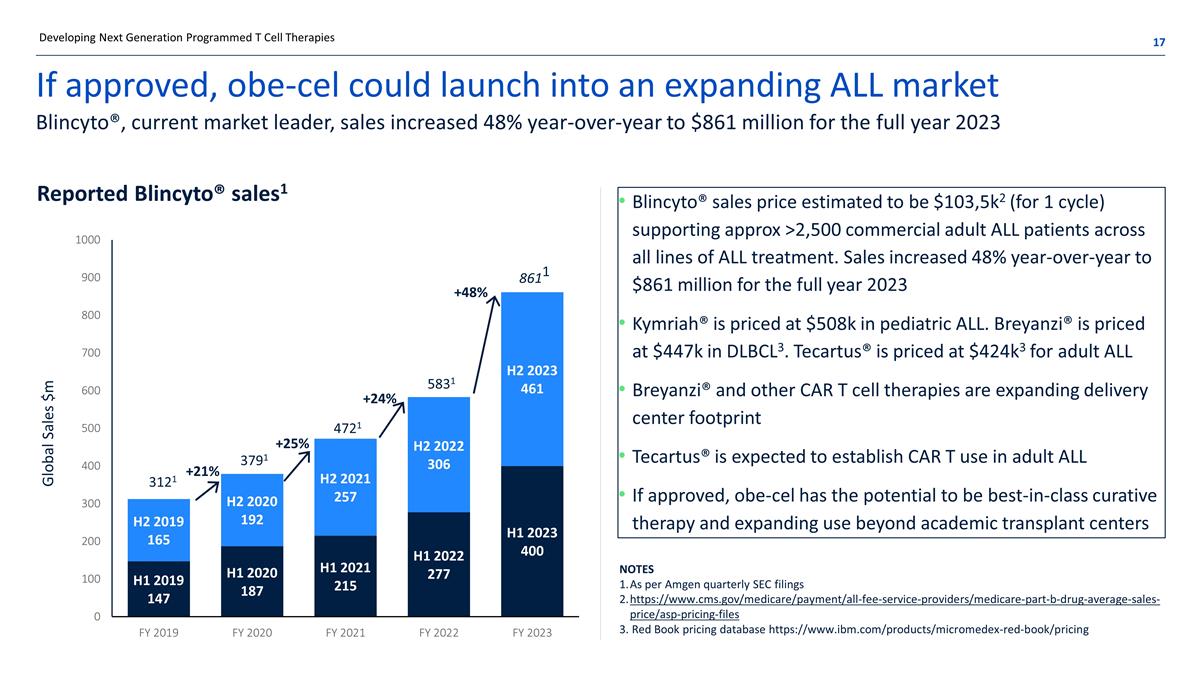
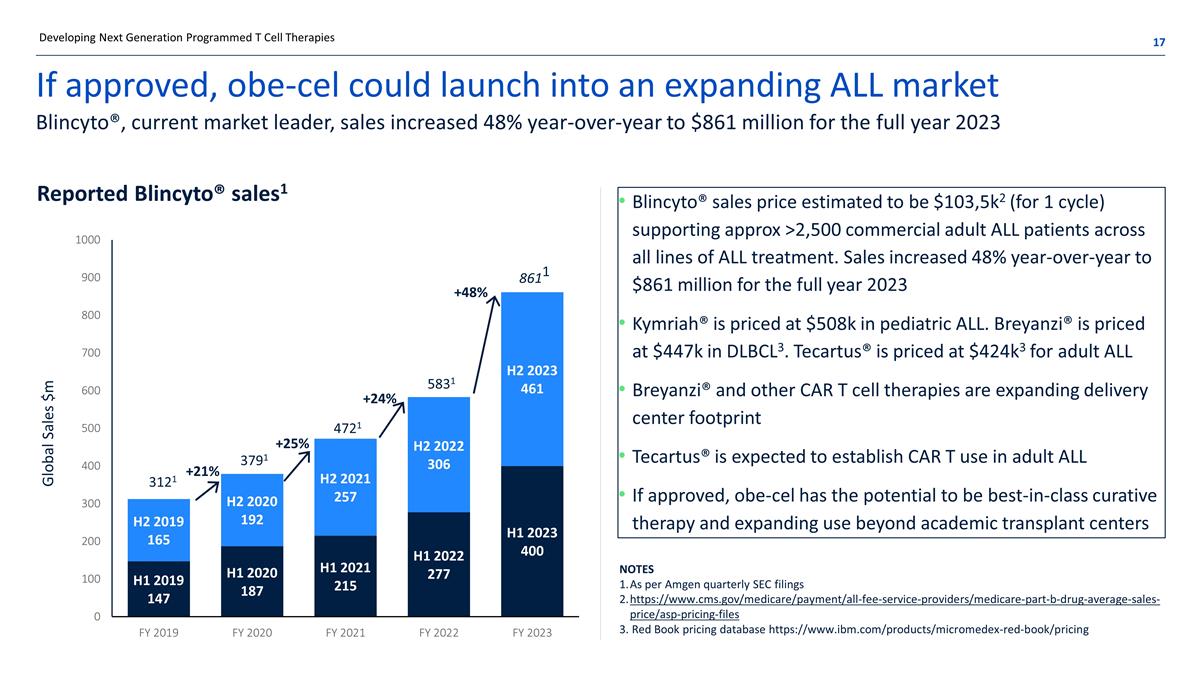
If approved, obe-cel could launch into an expanding ALL market Blincyto®, current market leader, sales increased 48% year-over-year to $861 million for the full year 2023 Blincyto® sales price estimated to be $103,5k2 (for 1 cycle) supporting approx >2,500 commercial adult ALL patients across all lines of ALL treatment. Sales increased 48% year-over-year to $861 million for the full year 2023 Kymriah® is priced at $508k in pediatric ALL. Breyanzi® is priced at $447k in DLBCL3. Tecartus® is priced at $424k3 for adult ALL Breyanzi® and other CAR T cell therapies are expanding delivery center footprint Tecartus® is expected to establish CAR T use in adult ALL If approved, obe-cel has the potential to be best-in-class curative therapy and expanding use beyond academic transplant centers 3121 3791 4721 +21% Reported Blincyto® sales1 Notes As per Amgen quarterly SEC filings https://www.cms.gov/medicare/payment/all-fee-service-providers/medicare-part-b-drug-average-sales-price/asp-pricing-files 3. Red Book pricing database https://www.ibm.com/products/micromedex-red-book/pricing +25% +24% Developing Next Generation Programmed T Cell Therapies 5831 8611 +48%

Over 8,000 new cases of adult ALL annually worldwide Successful therapy requires high level of activity and sustained persistence paired with good tolerability Median overall survival is < 1 year in r/r adult ALL Combination chemotherapy enables 90% of adult ALL patients to experience Complete Response (CR) Only 30% to 40% achieve long-term remission Current T cell therapies for adult patients are Blincyto® and Tecartus® Both therapies are highly active, but frequently followed by subsequent treatments (e.g. alloSCT) Blincyto®: favorable safety profile, few patients experiencing severe CRS and ICANS, but limitations on convenience - continuous i.v. infusion during 4-week treatment cycles Tecartus® more challenging to manage - induces elevated levels of severe CRS, a high levels of severe ICANS, and requires vasopressors for many patients Opportunity to expand the addressable patient population in earlier lines of therapy Notes SEER and EUCAN estimates (respectively) for US and EU 8,4001 New cases of adult ALL diagnosed yearly 3,000 Addressable patient population Developing Next Generation Programmed T Cell Therapies
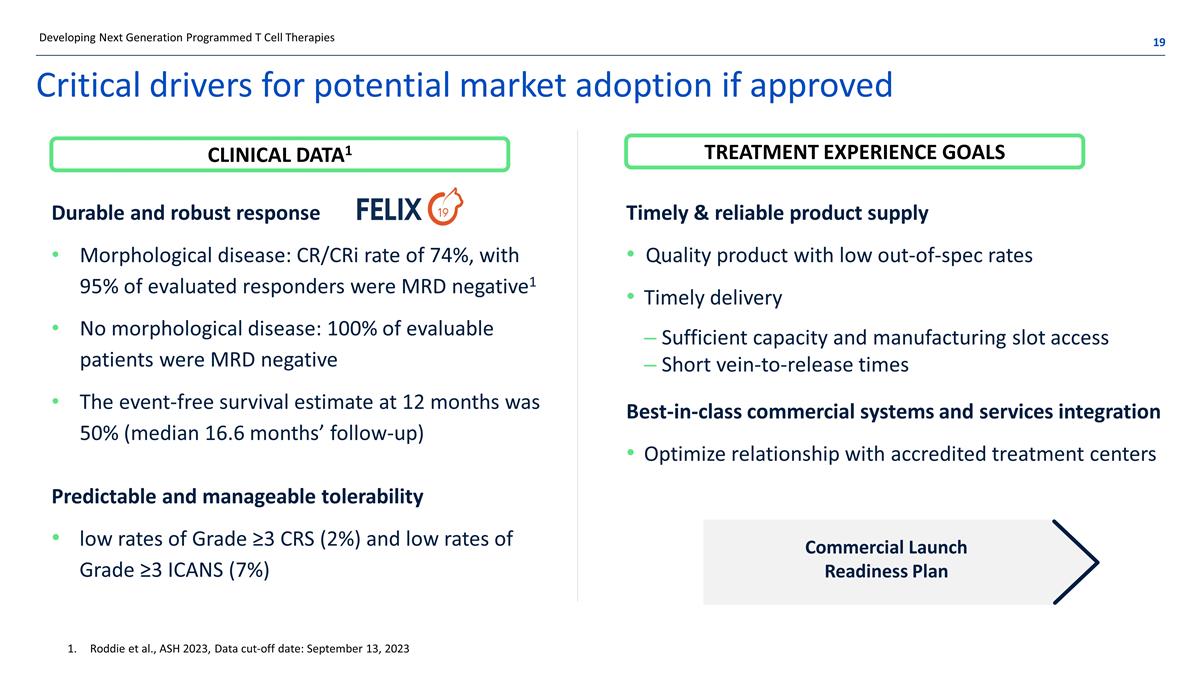
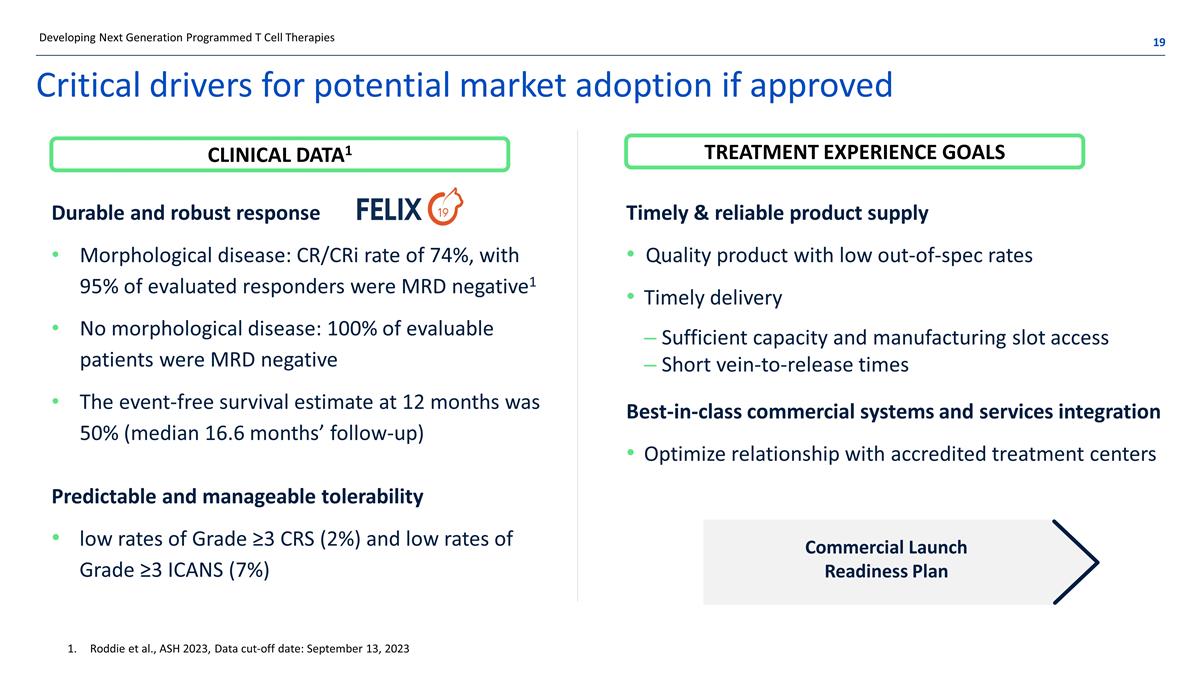
Critical drivers for potential market adoption if approved Best-in-class commercial systems and services integration Optimize relationship with accredited treatment centers Developing Next Generation Programmed T Cell Therapies Durable and robust response Morphological disease: CR/CRi rate of 74%, with 95% of evaluated responders were MRD negative1 No morphological disease: 100% of evaluable patients were MRD negative The event-free survival estimate at 12 months was 50% (median 16.6 months’ follow-up) Timely & reliable product supply Quality product with low out-of-spec rates Timely delivery Sufficient capacity and manufacturing slot access Short vein-to-release times Predictable and manageable tolerability low rates of Grade ≥3 CRS (2%) and low rates of Grade ≥3 ICANS (7%) Roddie et al., ASH 2023, Data cut-off date: September 13, 2023 Commercial Launch Readiness Plan CLINICAL DATA1 TREATMENT EXPERIENCE GOALS

Commercial Launch Readiness
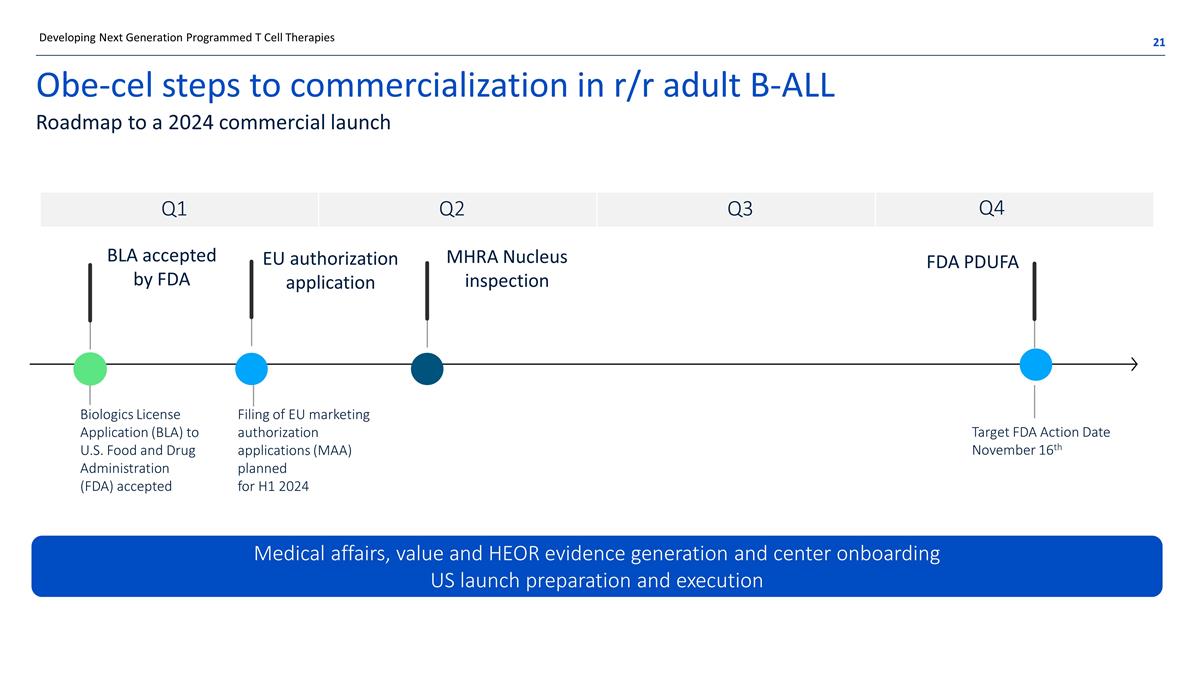
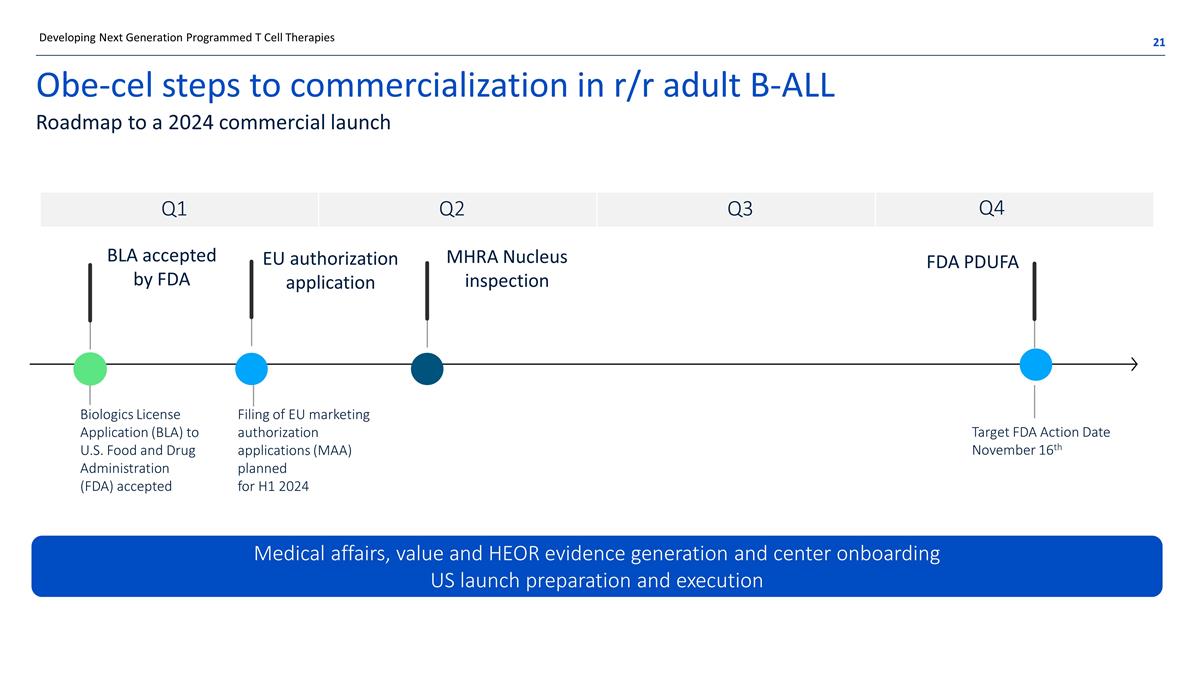
Obe-cel steps to commercialization in r/r adult B-ALL Roadmap to a 2024 commercial launch BLA accepted by FDA EU authorization application MHRA Nucleus inspection Medical affairs, value and HEOR evidence generation and center onboarding US launch preparation and execution Developing Next Generation Programmed T Cell Therapies FDA PDUFA Filing of EU marketing authorization applications (MAA) planned for H1 2024 Q1 Q2 Q3 Q4 Target FDA Action Date November 16th Biologics License Application (BLA) to U.S. Food and Drug Administration (FDA) accepted

The Nucleus State of the art design and operations established – groundbreaking to complete validation in 2 years Developing Next Generation Programmed T Cell Therapies Design Build Operations ~70,000 sq ft facility Modular build using PAMs 70% built off-site 60% reduced build time BREEAM Excellent rating for sustainability Designed for 2,000+ batches per year Target vein to delivery time 16 days at launch Nov 8, 2021 Groundbreaking Nov 25, 2022 First clean room operational May 2023 Capacity challenge 2021 2022 2023 2024 Dec 14, 2022 First prodigy operational 2H 2023 Facility validation complete
Expanding the obe-cel opportunity Deep value program with potentially broad applicability
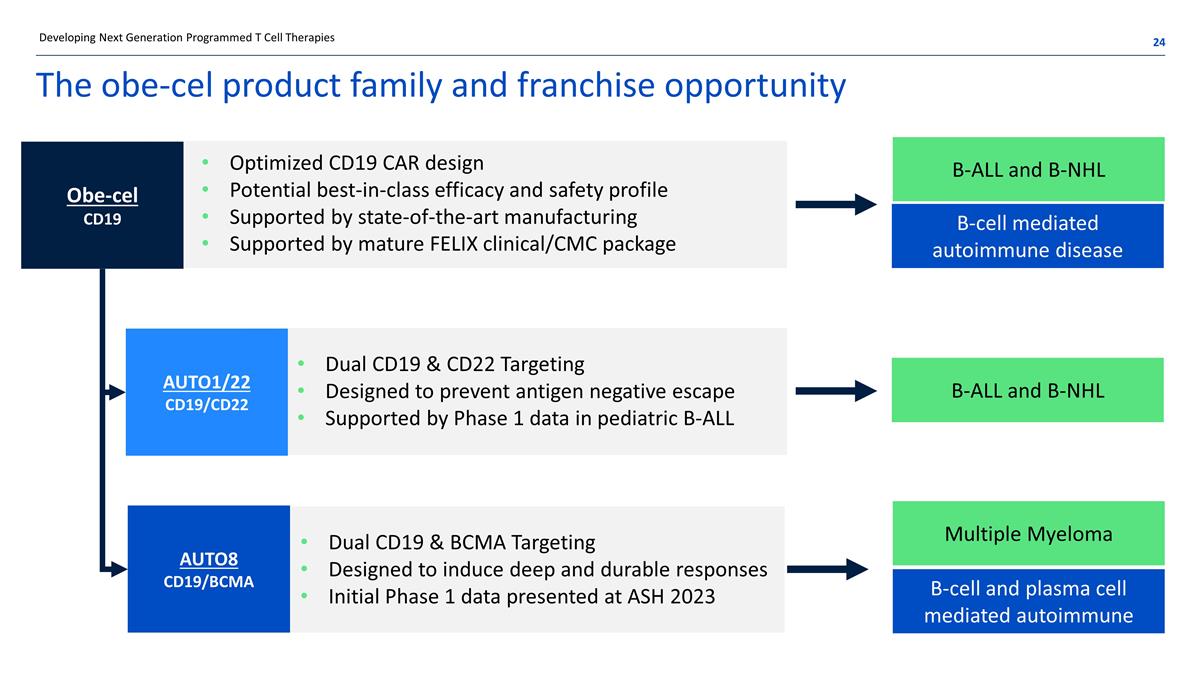
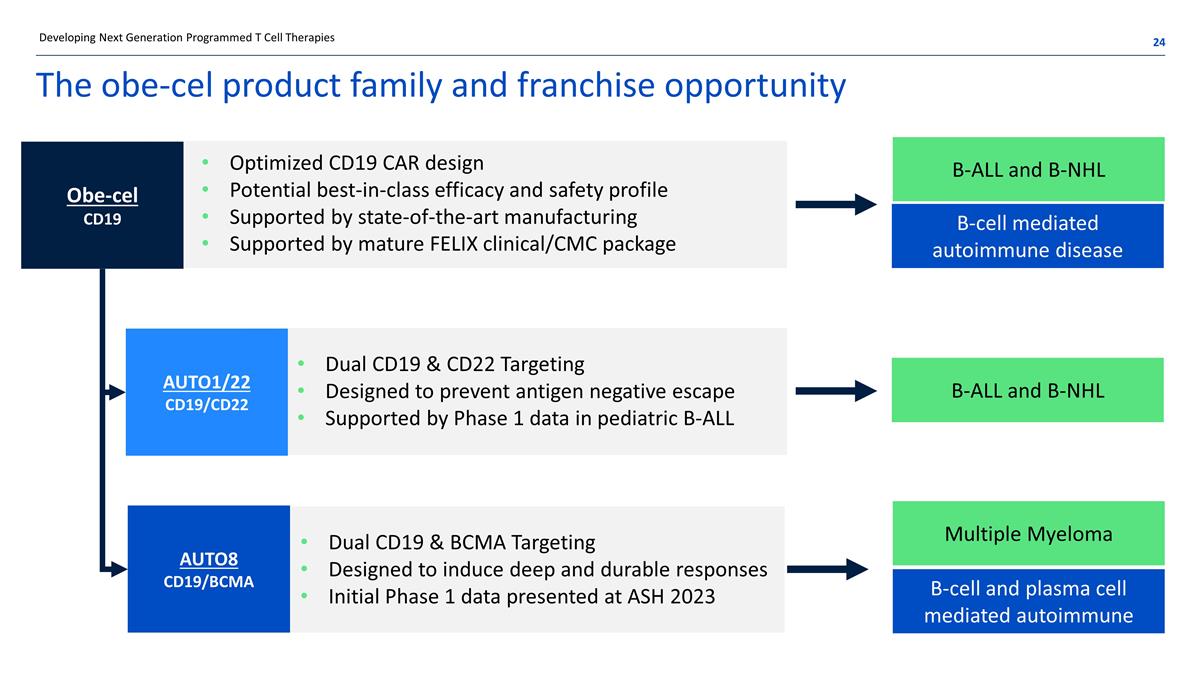
The obe-cel product family and franchise opportunity Optimized CD19 CAR design Potential best-in-class efficacy and safety profile Supported by state-of-the-art manufacturing Supported by mature FELIX clinical/CMC package Dual CD19 & CD22 Targeting Designed to prevent antigen negative escape Supported by Phase 1 data in pediatric B-ALL Dual CD19 & BCMA Targeting Designed to induce deep and durable responses Initial Phase 1 data presented at ASH 2023 B-ALL and B-NHL B-cell mediated autoimmune disease B-ALL and B-NHL Multiple Myeloma B-cell and plasma cell mediated autoimmune Developing Next Generation Programmed T Cell Therapies Obe-cel CD19 AUTO1/22 CD19/CD22 AUTO8 CD19/BCMA
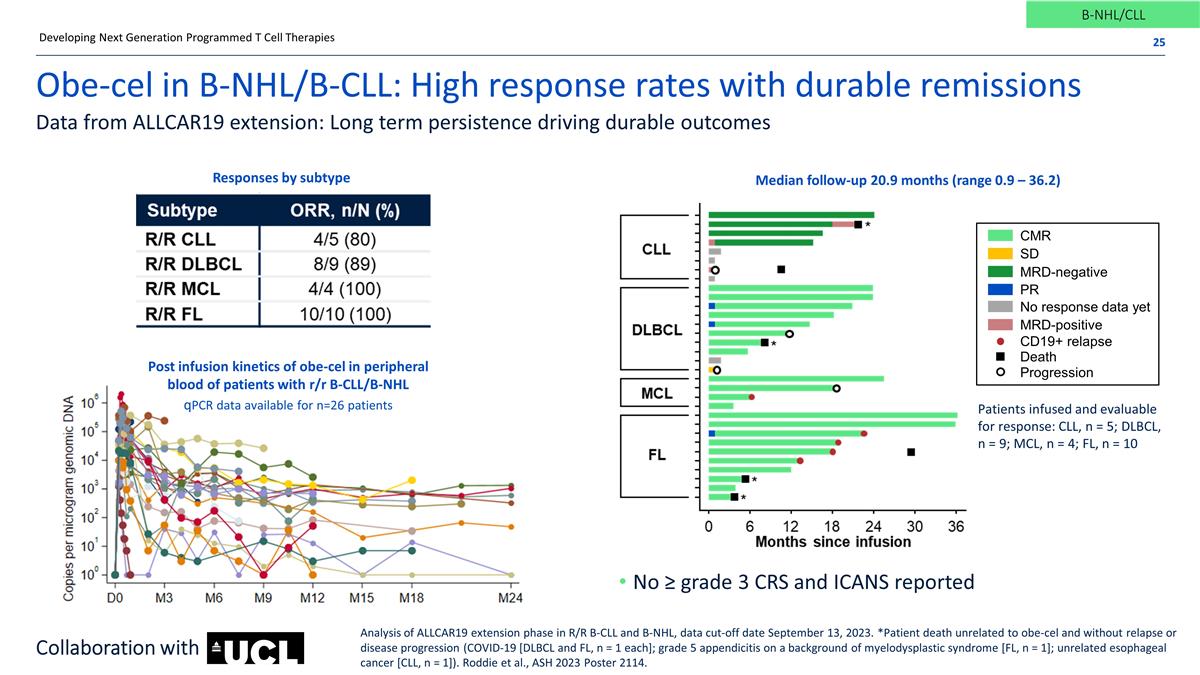
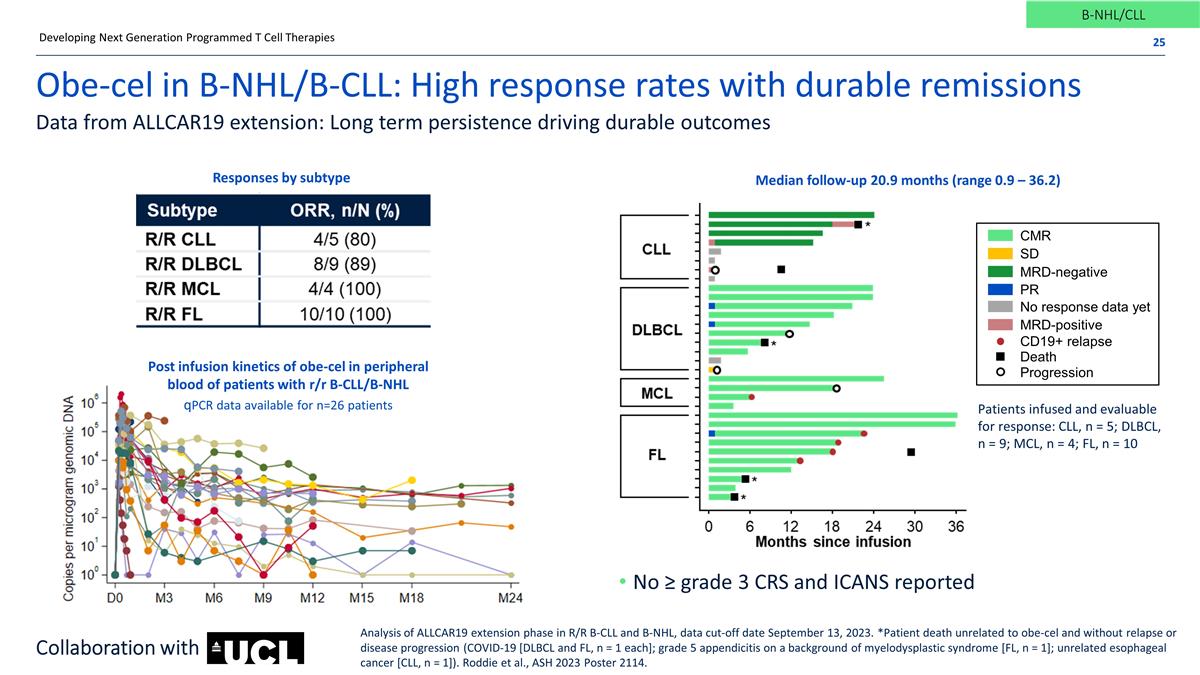
Obe-cel in B-NHL/B-CLL: High response rates with durable remissions Data from ALLCAR19 extension: Long term persistence driving durable outcomes No ≥ grade 3 CRS and ICANS reported Developing Next Generation Programmed T Cell Therapies Median follow-up 20.9 months (range 0.9 – 36.2) B-NHL/CLL Analysis of ALLCAR19 extension phase in R/R B-CLL and B-NHL, data cut-off date September 13, 2023. *Patient death unrelated to obe-cel and without relapse or disease progression (COVID-19 [DLBCL and FL, n = 1 each]; grade 5 appendicitis on a background of myelodysplastic syndrome [FL, n = 1]; unrelated esophageal cancer [CLL, n = 1]). Roddie et al., ASH 2023 Poster 2114. Collaboration with Post infusion kinetics of obe-cel in peripheral blood of patients with r/r B-CLL/B-NHL qPCR data available for n=26 patients Responses by subtype CMR SD MRD-negative MRD-positive CD19+ relapse Death Progression PR No response data yet Patients infused and evaluable for response: CLL, n = 5; DLBCL, n = 9; MCL, n = 4; FL, n = 10
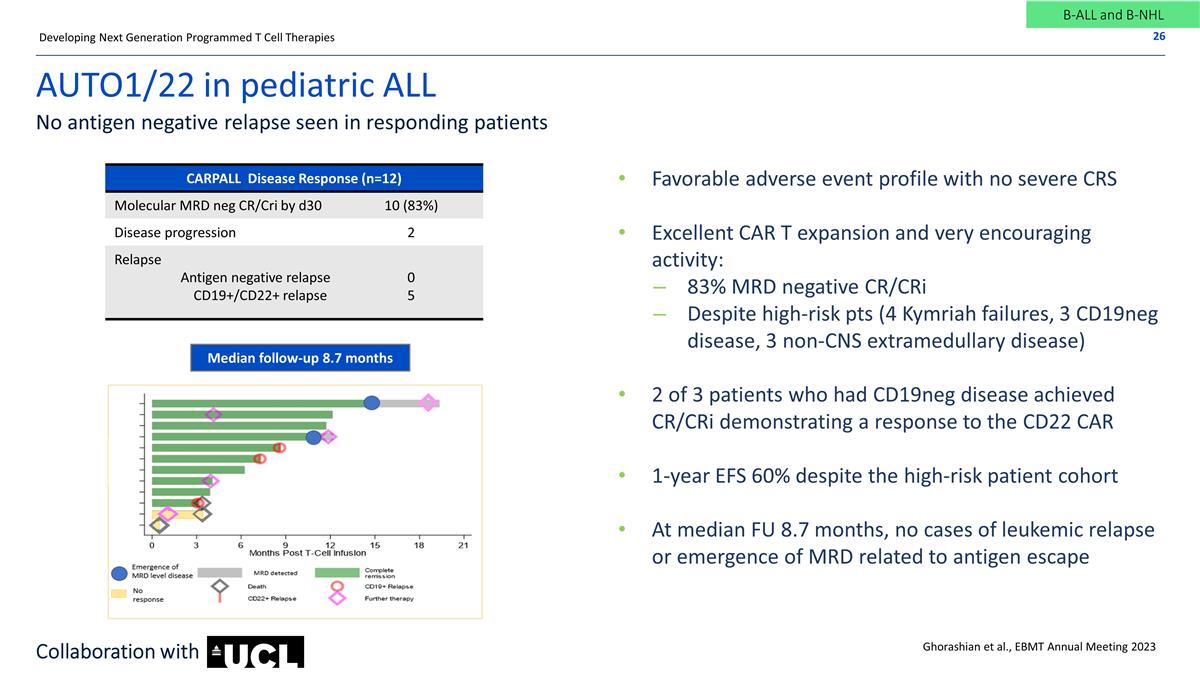
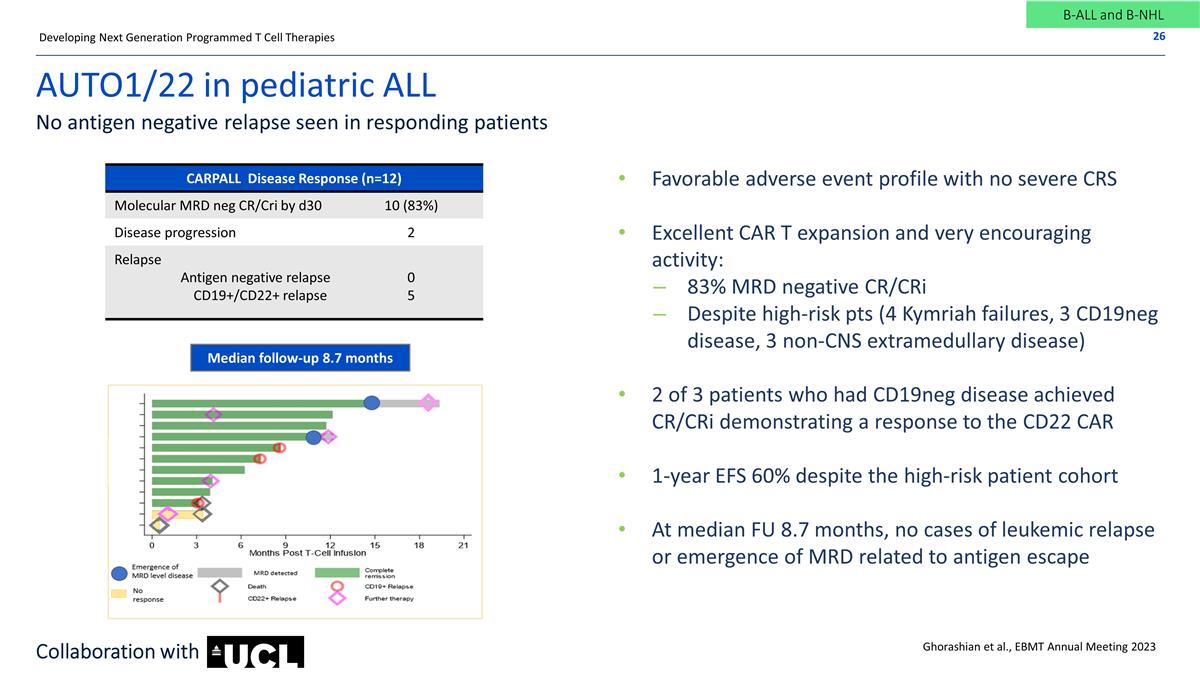
AUTO1/22 in pediatric ALL No antigen negative relapse seen in responding patients Favorable adverse event profile with no severe CRS Excellent CAR T expansion and very encouraging activity: 83% MRD negative CR/CRi Despite high-risk pts (4 Kymriah failures, 3 CD19neg disease, 3 non-CNS extramedullary disease) 2 of 3 patients who had CD19neg disease achieved CR/CRi demonstrating a response to the CD22 CAR 1-year EFS 60% despite the high-risk patient cohort At median FU 8.7 months, no cases of leukemic relapse or emergence of MRD related to antigen escape Ghorashian et al., EBMT Annual Meeting 2023 CARPALL Disease Response (n=12) ALLCAR19 Adult ALL Molecular MRD neg CR/Cri by d30 10 (83%) Disease progression 2 Relapse Antigen negative relapse CD19+/CD22+ relapse 0 5 Developing Next Generation Programmed T Cell Therapies Median follow-up 8.7 months B-ALL and B-NHL Collaboration with
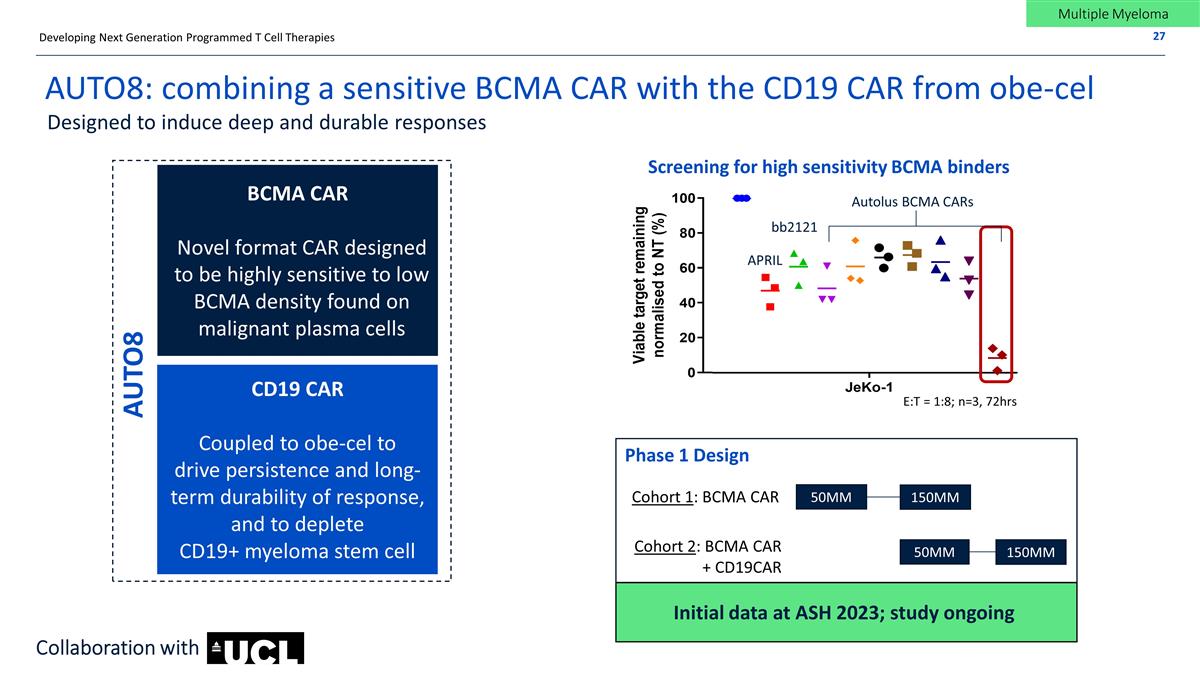
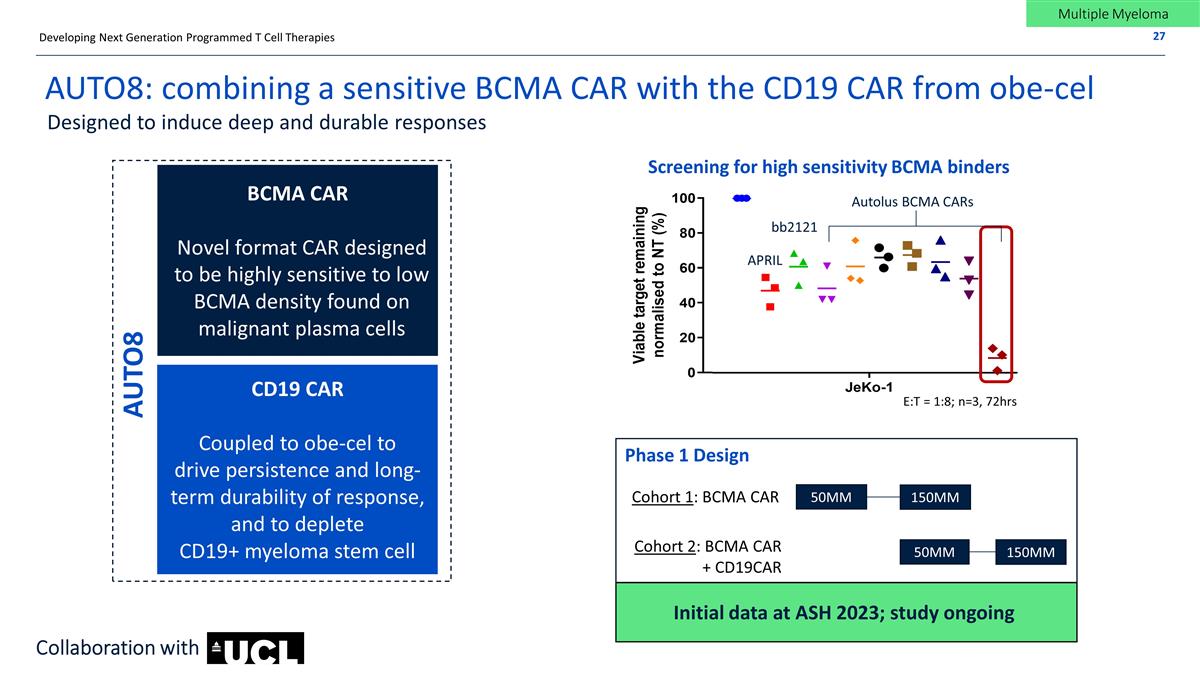
AUTO8: combining a sensitive BCMA CAR with the CD19 CAR from obe-cel Designed to induce deep and durable responses Confidential BCMA CAR Novel format CAR designed to be highly sensitive to low BCMA density found on malignant plasma cells CD19 CAR Coupled to obe-cel to drive persistence and long-term durability of response, and to deplete CD19+ myeloma stem cell AUTO8 50MM Cohort 1: BCMA CAR Cohort 2: BCMA CAR + CD19CAR Developing Next Generation Programmed T Cell Therapies Screening for high sensitivity BCMA binders APRIL bb2121 Autolus BCMA CARs E:T = 1:8; n=3, 72hrs Phase 1 Design Initial data at ASH 2023; study ongoing 150MM 50MM 150MM Collaboration with Multiple Myeloma
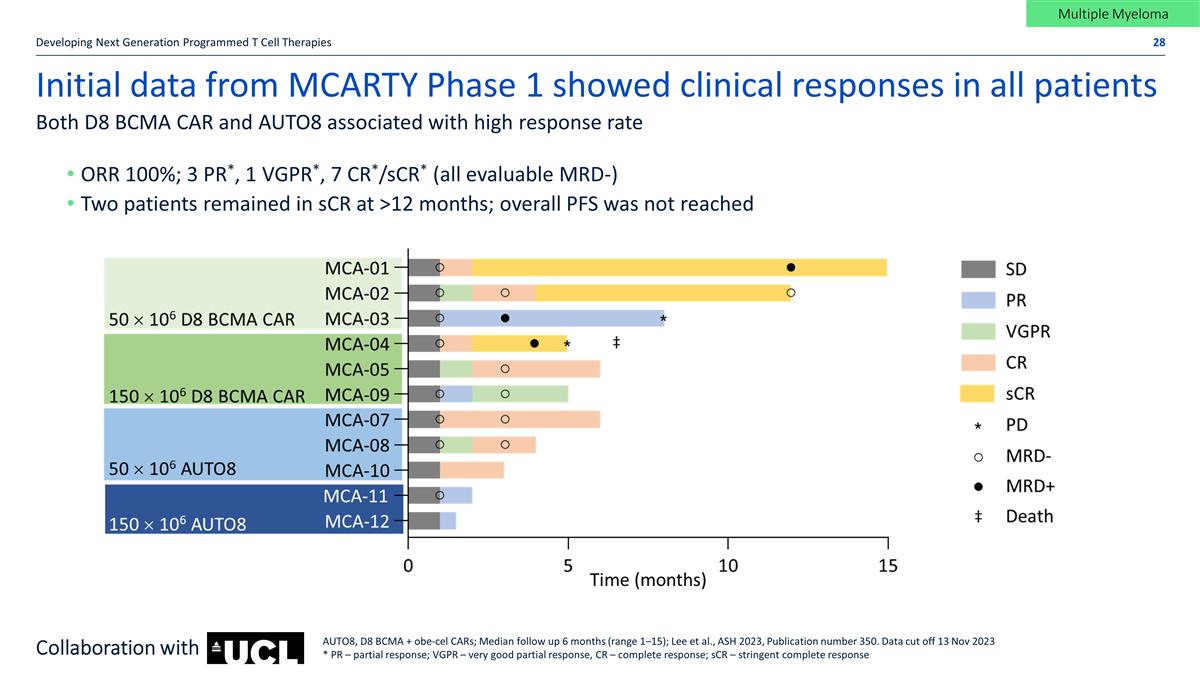
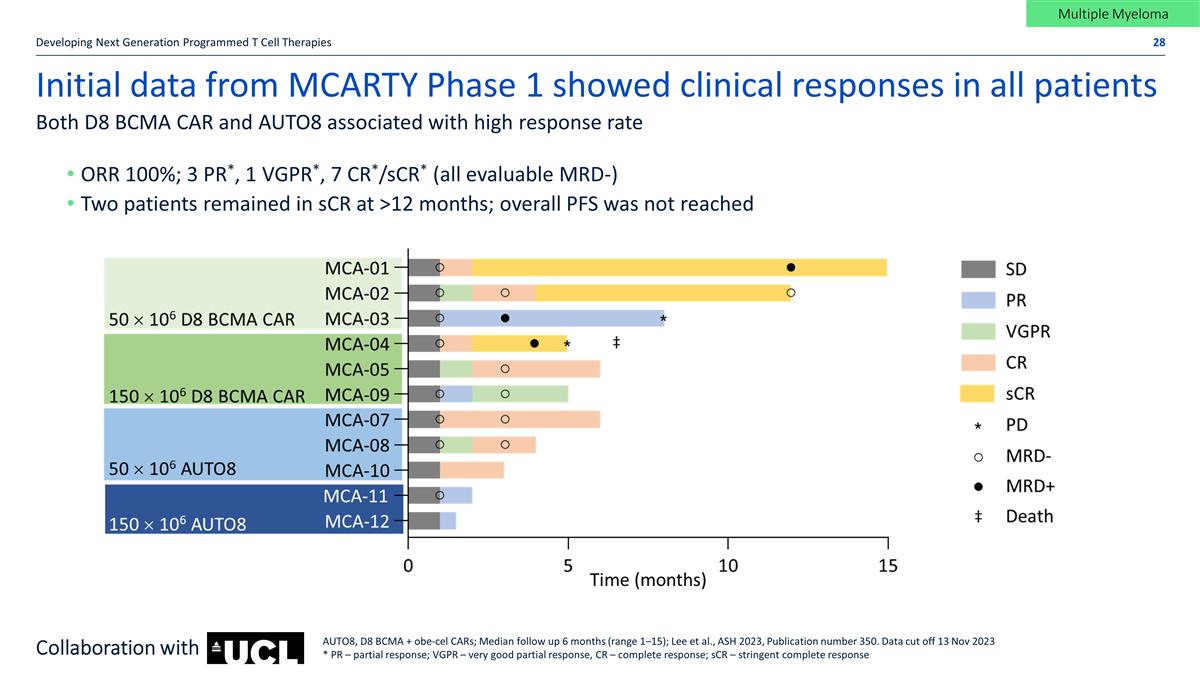
Initial data from MCARTY Phase 1 showed clinical responses in all patients Developing Next Generation Programmed T Cell Therapies Both D8 BCMA CAR and AUTO8 associated with high response rate AUTO8, D8 BCMA + obe-cel CARs; Median follow up 6 months (range 1–15); Lee et al., ASH 2023, Publication number 350. Data cut off 13 Nov 2023 * PR – partial response; VGPR – very good partial response, CR – complete response; sCR – stringent complete response ORR 100%; 3 PR*, 1 VGPR*, 7 CR*/sCR* (all evaluable MRD-) Two patients remained in sCR at >12 months; overall PFS was not reached Collaboration with Multiple Myeloma
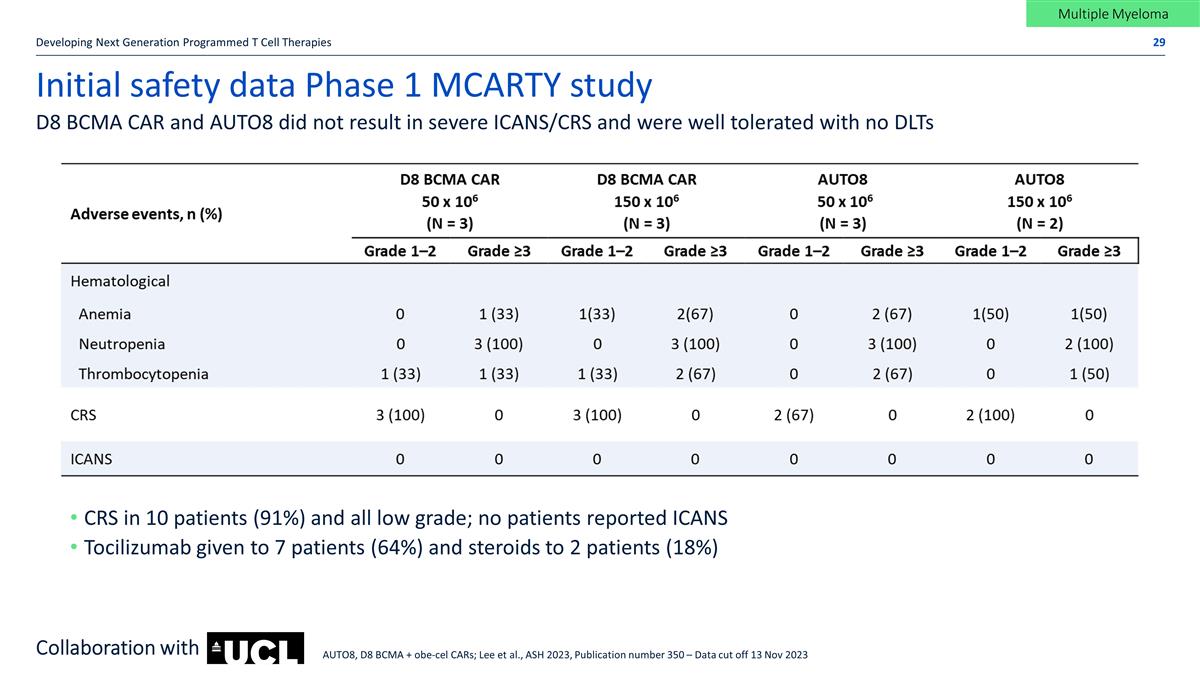
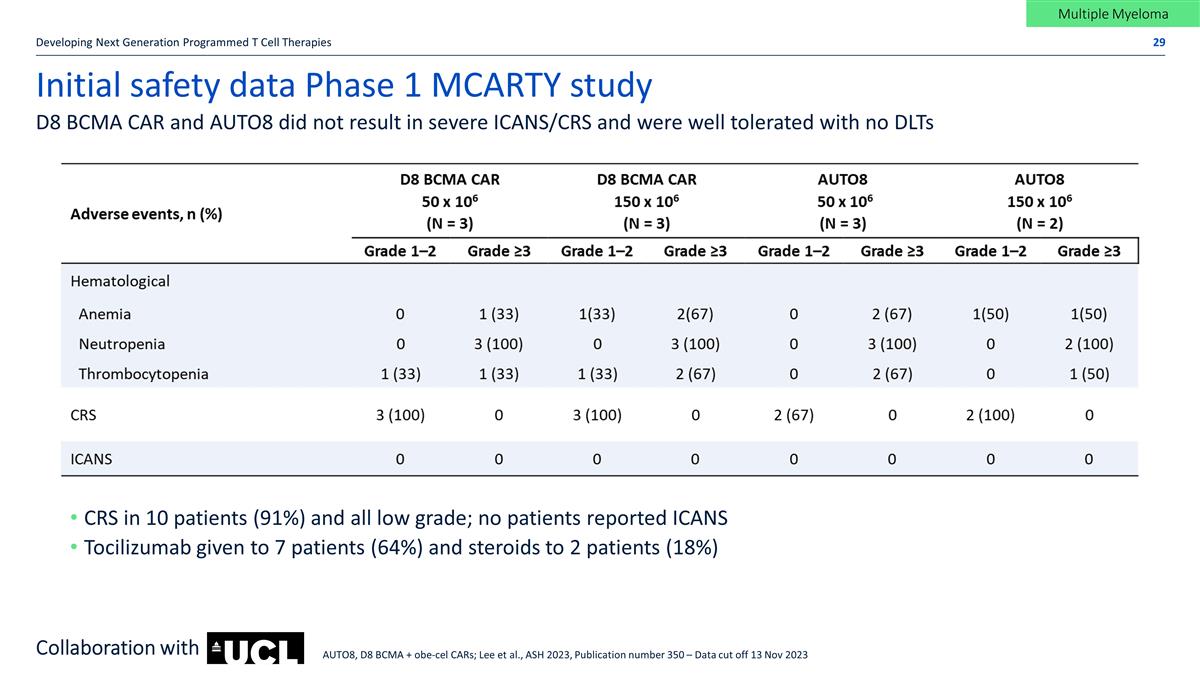
Initial safety data Phase 1 MCARTY study Developing Next Generation Programmed T Cell Therapies D8 BCMA CAR and AUTO8 did not result in severe ICANS/CRS and were well tolerated with no DLTs CRS in 10 patients (91%) and all low grade; no patients reported ICANS Tocilizumab given to 7 patients (64%) and steroids to 2 patients (18%) Collaboration with Multiple Myeloma AUTO8, D8 BCMA + obe-cel CARs; Lee et al., ASH 2023, Publication number 350 – Data cut off 13 Nov 2023
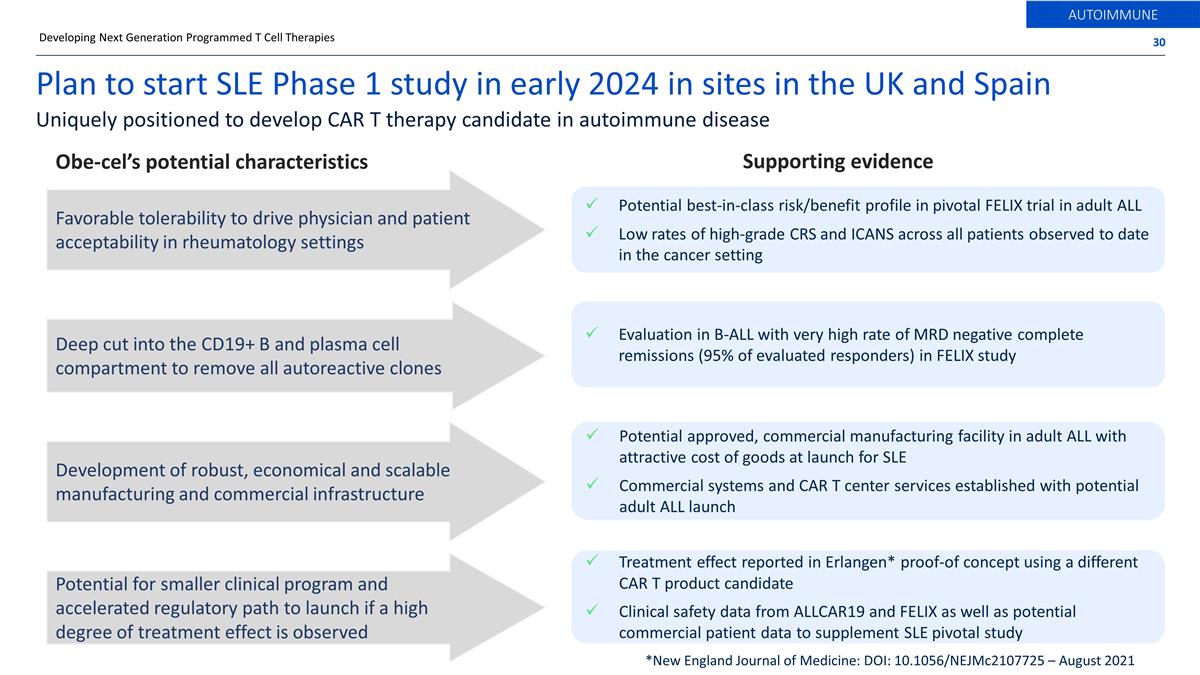
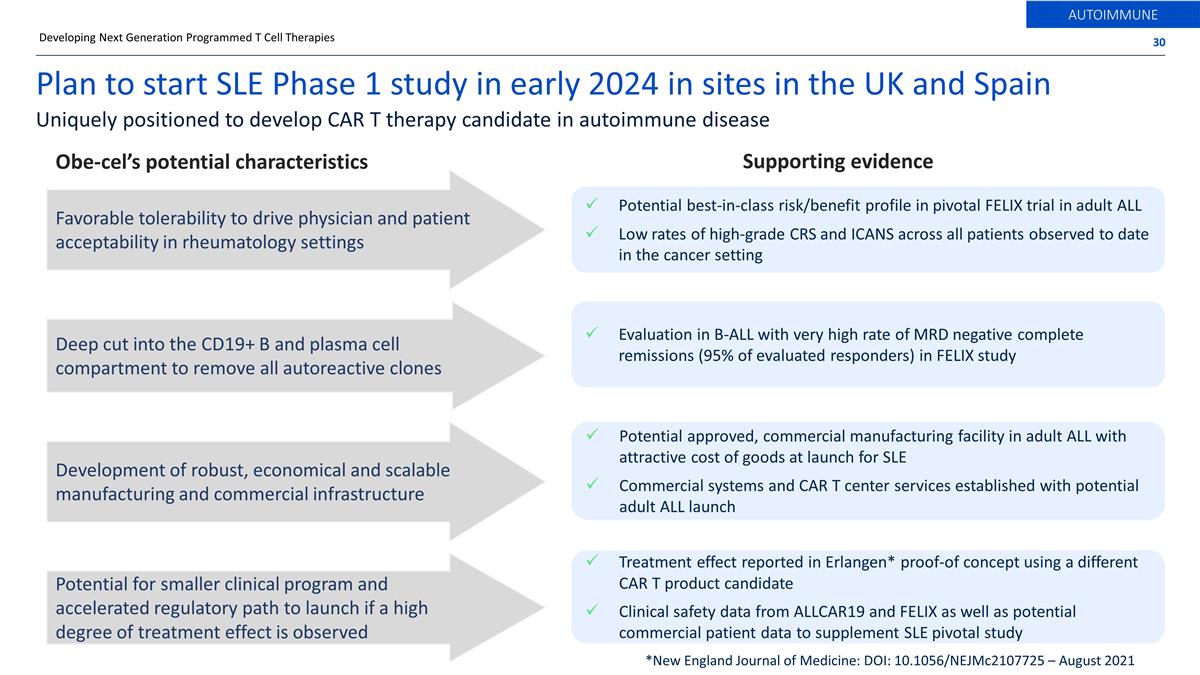
Potential best-in-class risk/benefit profile in pivotal FELIX trial in adult ALL Low rates of high-grade CRS and ICANS across all patients observed to date in the cancer setting Obe-cel’s potential characteristics Deep cut into the CD19+ B and plasma cell compartment to remove all autoreactive clones Potential for smaller clinical program and accelerated regulatory path to launch if a high degree of treatment effect is observed Development of robust, economical and scalable manufacturing and commercial infrastructure Plan to start SLE Phase 1 study in early 2024 in sites in the UK and Spain Supporting evidence Treatment effect reported in Erlangen* proof-of concept using a different CAR T product candidate Clinical safety data from ALLCAR19 and FELIX as well as potential commercial patient data to supplement SLE pivotal study Potential approved, commercial manufacturing facility in adult ALL with attractive cost of goods at launch for SLE Commercial systems and CAR T center services established with potential adult ALL launch Favorable tolerability to drive physician and patient acceptability in rheumatology settings Evaluation in B-ALL with very high rate of MRD negative complete remissions (95% of evaluated responders) in FELIX study Developing Next Generation Programmed T Cell Therapies AUTOIMMUNE Uniquely positioned to develop CAR T therapy candidate in autoimmune disease *New England Journal of Medicine: DOI: 10.1056/NEJMc2107725 – August 2021

Other pipeline programs and technologies A broad portfolio of potential next generation modular T cell therapies

PRODUCT INDICATION TARGET STUDY NAME PARTNER PHASE STATUS/EXPECTED MILESTONES Obe-cel Adult B-ALL CD19 FELIX Pivotal H1 2024: MAA Application to EMA November 16, 2024: PDUFA date Obe-cel Systemic Lupus Erythematosus CD19 CARLYSLE Preclinical Early 2024: Phase 1 initiation in UK Obe-cel B-NHL and CLL CD19 ALLCAR19 Phase 1 Data in peer reviewed journal Obe-cel PCNSL CD19 CAROUSEL Phase 1 Data in peer reviewed journal AUTO1/22 Pediatric ALL CD19 & CD22 CARPALL Phase1 Data in BLOOD August 2023 AUTO8 Multiple Myeloma CD19 & BCMA MCARTY Phase 1 Updated clinical data in 2024 Autolus pipeline Developing Next Generation Programmed T Cell Therapies AUTO4 TRBC1+ Peripheral TCL TRBC1 LibrA T1 Phase 1 Data in peer reviewed journal AUTO5 TRBC2+ Peripheral TCL TRBC2 - Preclinical Preclinical data in peer reviewed journal AUTO6NG Neuroblastoma GD2 MAGNETO Phase 1 Study open for enrollment AUTO9 Acute Myeloid Leukemia CD33, CD123 & CLL1 TBD Preclinical Estimated Phase 1 start 2025 Oncology Autoimmune Obe-cel product family Additional pipeline programs * BioNTech holds an option to co-fund and co-commercialize * *
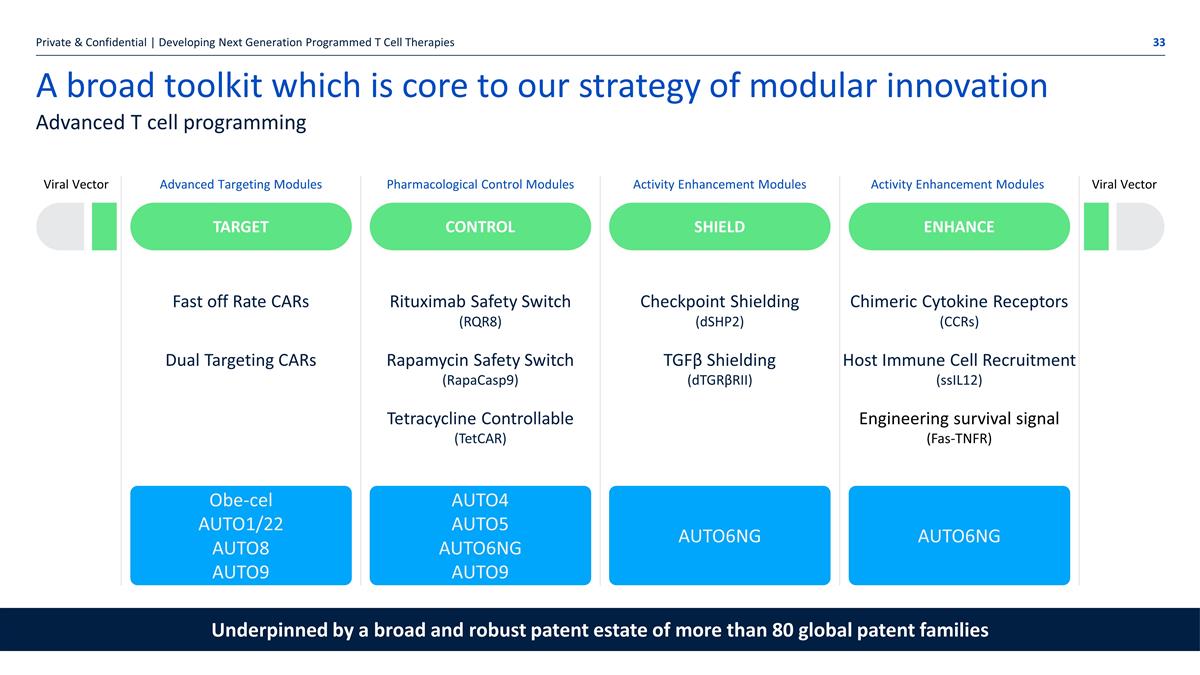
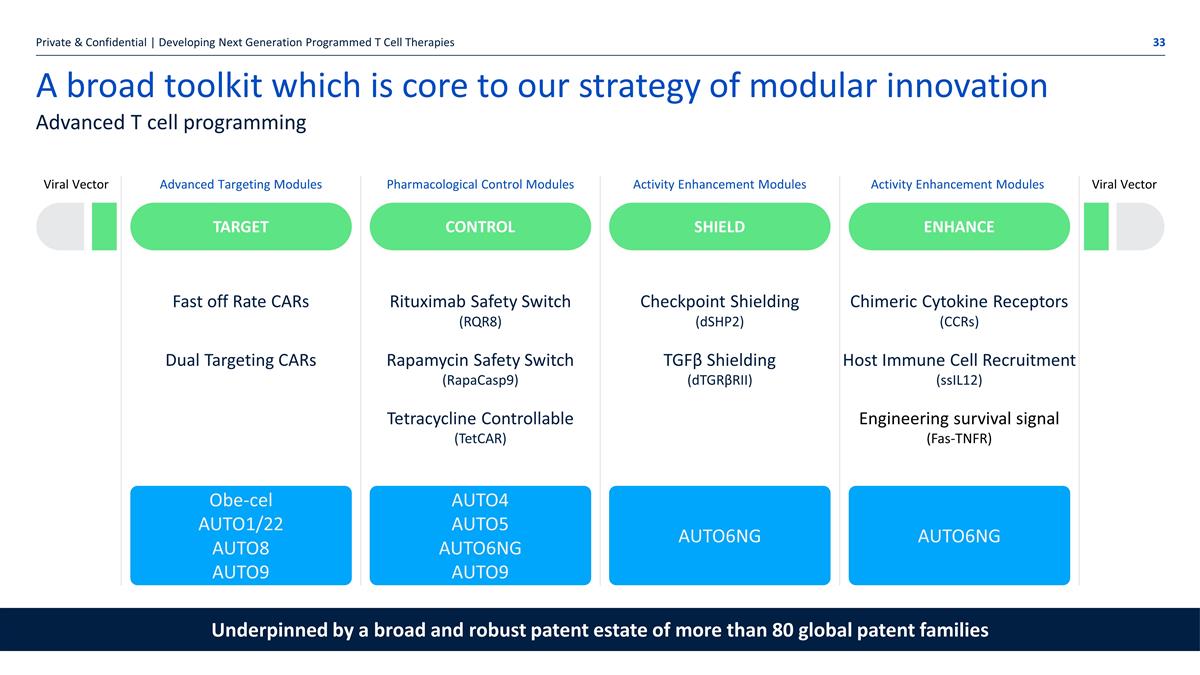
A broad toolkit which is core to our strategy of modular innovation Viral Vector Advanced T cell programming Target Fast off Rate CARs Dual Targeting CARs Advanced Targeting Modules Control Pharmacological Control Modules SHieLD Activity Enhancement Modules ENHANCE Activity Enhancement Modules Viral Vector Obe-cel AUTO1/22 AUTO8 AUTO9 Rituximab Safety Switch (RQR8) Rapamycin Safety Switch (RapaCasp9) Tetracycline Controllable (TetCAR) Checkpoint Shielding (dSHP2) TGFβ Shielding (dTGRβRII) Chimeric Cytokine Receptors (CCRs) Host Immune Cell Recruitment (ssIL12) Engineering survival signal (Fas-TNFR) AUTO4 AUTO5 AUTO6NG AUTO9 AUTO6NG AUTO6NG Private & Confidential | Developing Next Generation Programmed T Cell Therapies Underpinned by a broad and robust patent estate of more than 80 global patent families

Developing Next Generation Programmed T Cell Therapies Technology partnerships Leveraging our modular programming technology to generate safer and more effective therapies Tumor targeting, pharmacological control and activity enhancement for cellular therapies Validating collaborations with leading pharma and biotech companies Potential for value creation through near term option exercise fees, milestone payments and royalties from net sales Access to proprietary binders for the development of mRNA-based therapeutics for the treatment of cancer Access to the RQR8 safety switch for selected cell therapy programs for the treatment of cancer Leveraging our industry leading technology platform via partnerships Leveraging technology platform for BioNTech’s programs

Upcoming news flow
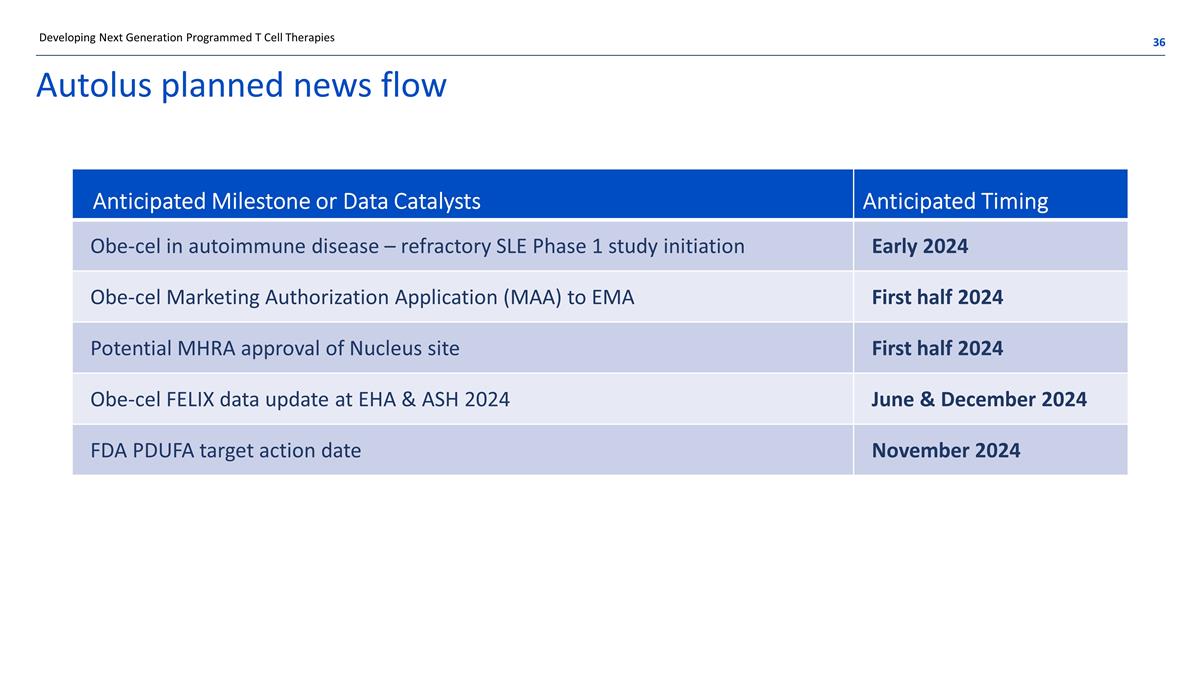
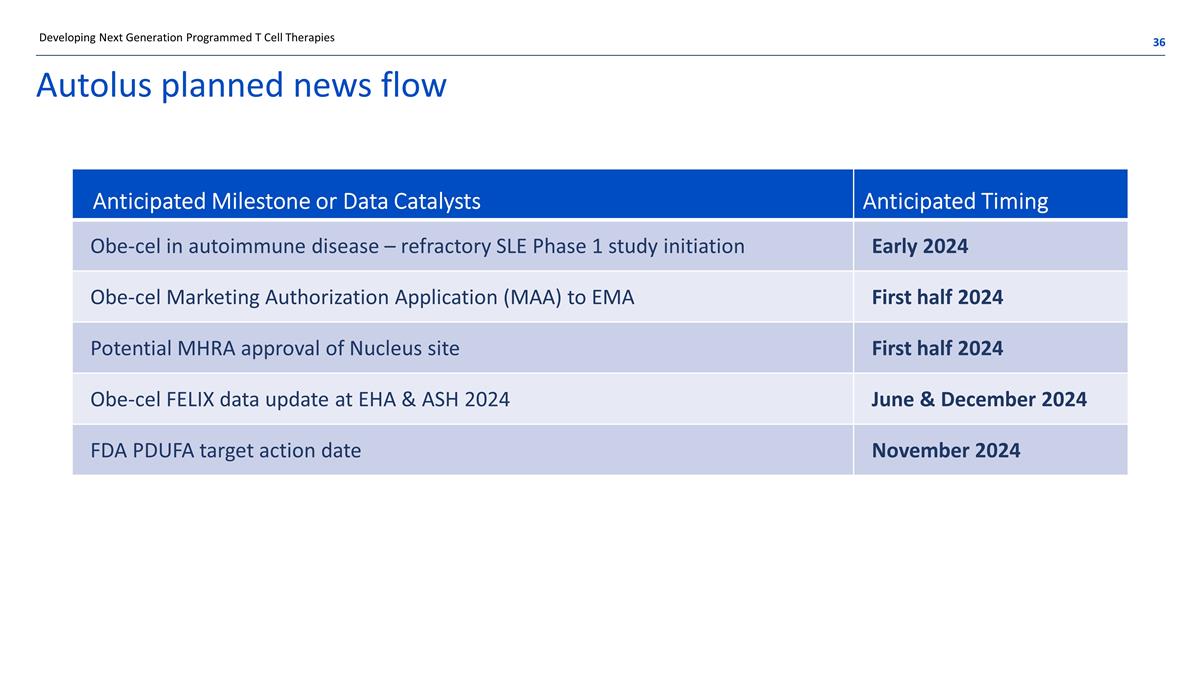
Autolus planned news flow Developing Next Generation Programmed T Cell Therapies Anticipated Milestone or Data Catalysts Anticipated Timing Obe-cel in autoimmune disease – refractory SLE Phase 1 study initiation Early 2024 Obe-cel Marketing Authorization Application (MAA) to EMA First half 2024 Potential MHRA approval of Nucleus site First half 2024 Obe-cel FELIX data update at EHA & ASH 2024 June & December 2024 FDA PDUFA target action date November 2024

Summary

Building a leading CAR T company developing therapies for cancer and autoimmune diseases FELIX pivotal trial showed high ORR, encouraging EFS and favorable tolerability with low levels of high-grade CRS and ICANS PDUFA date 16 Nov 2024 EMA submission planned for 1H 2024 Strategic multi-platform R&D collaboration with BioNTech Established technology collaborations with Moderna, BMS and Cabaletta Long-standing academic collaboration with University College London Expand obe-cel opportunity in B cell malignancies, autoimmune diseases & life cycle strategy SLE B-NHL indications Bi-specific therapies (CD19 /CD22; CD19/BCMA) Expand to additional indications with novel CAR T therapies, alone or with partners Demonstrated reliable clinical trial supply (96% target dose reached in FELIX pivotal study) New commercial cell manufacturing facility in qualification stage; planned annual capacity 2,000+ batches Expected vein-to-delivery time at launch of ~16 days Obe-cel potentially best in class CAR T for r/r adult ALL Strategic collaborations Pipeline expansion strategy Scalable manufacturing and in-house facility Cash $256.4M (Q3 2023) Runway into 2025* Enables execution on current strategy through expected approval of obe-cel Strong cash position Scaling company toward commercialization $ Developing Next Generation Programmed T Cell Therapies Abbreviations and notes: r/r ALL - relapsed/refractory acute lymphoblastic leukemia; B-NHL – B-cell non-Hodgkin’s lymphoma; SLE – systemic lupus erythematosus. *Does not include proceeds from BioNTech

autolus.com Thank you