points in time, and it is possible that the deferral of healthcare services could cause additional health problems in our existing members, which could increase our costs in the future. Additionally, our members’ risk adjustment factors, which are reflective of documented clinical conditions during 2020 and which impact our 2021 revenues, may be lower than would have occurred without the impact of the COVID-19 pandemic, resulting from members’ avoidance or deferral of care during 2020. We cannot accurately estimate the net ultimate impact, positive or negative, to revenue or medical services expense at this time.
Also see “Risk Factors—Risks Related to Our Business—The spread of, and response to, the novel coronavirus, or COVID-19, underscores certain risks we face and the rapid development and fluidity of this situation precludes any prediction as to the ultimate adverse impact to us of COVID-19.”
Company History
The Company is ultimately controlled by an investment fund associated with CD&R, a private equity firm headquartered in New York, NY. Our business was formed in 2016 through the completion of two acquisitions by CD&R: In July 2016, PPMC was acquired, which, together with the California IPAs, operated in Southern California. Also in July 2016, CPS was acquired, which, together with its subsidiaries and affiliates, operates a network of contracted physicians in Hawaii and provides software and medical billing solutions to independent healthcare organizations. During 2020, we implemented a plan to divest all of our California operations, which includes the entirety of our Medicaid line of business, via three separate transactions with different parties. In February 2021, we completed the divestiture of our California operations. See “Management’s Discussion and Analysis of Financial Condition and Results of Operations—California
Operations” for additional information.
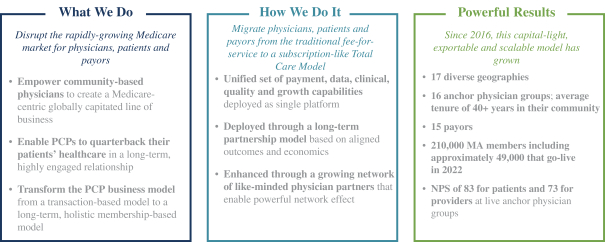
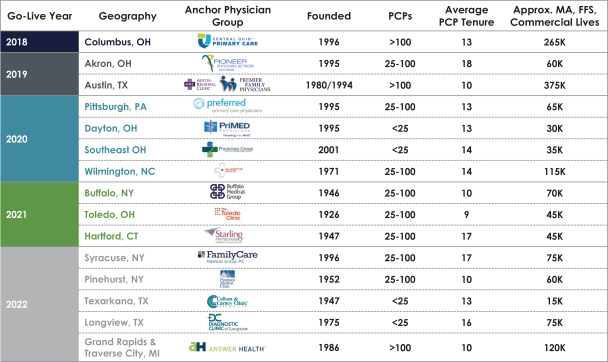
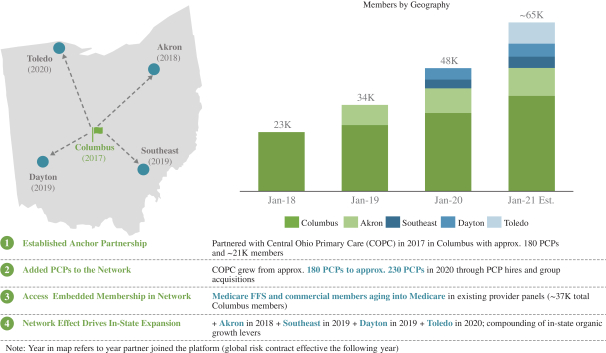
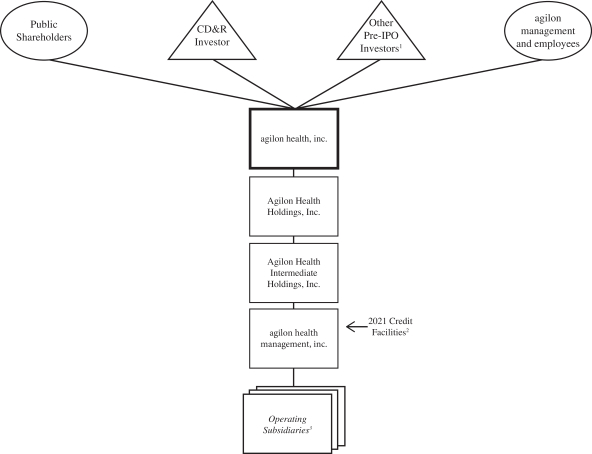
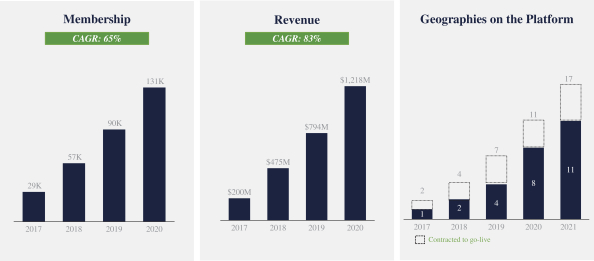
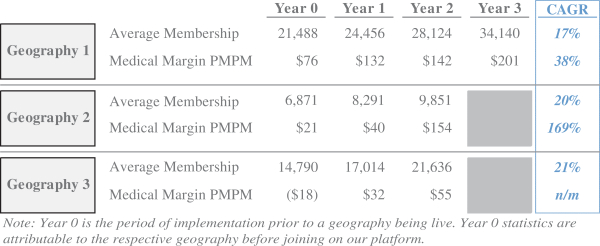
agilon health, inc., the issuer in this offering, was incorporated in the State of Delaware in April 2017 in connection with our entry into a physician partnership with COPC, a physician-owned medical group, to establish a Medicare-centric, globally capitated line of business in the Columbus, Ohio region. Since that time, we have focused on collaborating with leading community-based physician groups to establish Medicare-centric, globally capitated lines of business for their existing practices in their local geography. The Company has expanded and entered into new partnerships in Austin, Akron, Pittsburgh, North Carolina, Hartford, Buffalo, Toledo, Dayton and Southeast Ohio. In March 2021, we changed our name from Agilon Health Topco, Inc. to agilon health, inc., and changed the name of our subsidiary, agilon health, inc., to agilon health management, inc.
Reimbursement Model and Organization
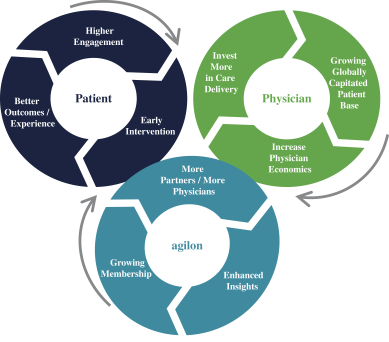
Under a traditional FFS reimbursement model, physicians are paid a fixed amount for services provided during a patient visit, regardless of a patient’s medical need or health outcome. As a result, physician reimbursement is solely related to the volume of patient visits and procedures performed, thereby offering limited financial incentive to focus on preventative care and cost containment. Value-based care models offer alternative reimbursement models, which typically incentivize physicians for improving the cost and quality of healthcare provided for an attributed patient population. Various types of value-based care reimbursement models exist, including capitation, bundled payments, or payments for attainment of improved quality metrics or medical cost efficiency.
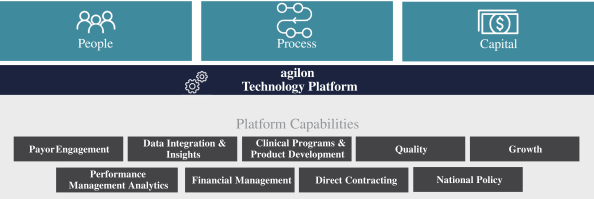
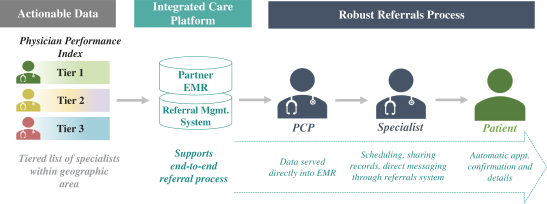
Under our Total Care Model, which is a type of value-based care reimbursement model, we are responsible for managing the medical costs associated with our attributed members. This structure empowers physicians to focus on the improvement of the quality of care provided, and to share in the financial surplus created to the extent premiums received exceed the cost of medical care. Under such a structure, physicians are incentivized to improve the quality and efficiency of care as well as health outcomes for their patients.
126