Exhibit 99.2 INVIVYD CANOPY DATA UPDATE August 27, 2024 © 2024 Invivyd, Inc. Invivyd , Pemgarda , and the Ribbon logos are trademarks of Invivyd, Inc. All trademarks in this presentation are the property of their respective owners.
CAUTIONARY NOTE REGARDING FORWARD-LOOKING STATEMENTS This presentation contains forward-looking statements within the meaning of the U.S. Private Securities Litigation Reform Act of 1995. Statements in this presentation that are not statements of historical fact are forward-looking statements. Words such as “may,” “will,” “should,” “expect,” “plan,” “anticipate,” “seek,” “could,” “intend,” “target,” “aim,” “project,” “designed to,” “estimate,” “believe,” “predict,” “potential” or “continue” or the negative of these terms or other similar expressions are intended to identify forward-looking statements, though not all forward-looking statements contain these identifying words. Forward-looking statements include statements concerning, among other things, the potential of pemivibart for clinical protection from symptomatic COVID-19 based on the 180-day clinical event exploratory efficacy analysis from the CANOPY clinical trial; our plans to work with the FDA to integrate clinical event findings from the CANOPY clinical trial into future mAb development work; our expectations regarding the safety profile of pemivibart; our expectations regarding the evolution of the PEMGARDA fact sheet; our belief that mAbs may be critical for managing endemic virus over the long term; our business strategies and objectives, and ability to execute on them; our future prospects; and other statements that are not historical fact. We may not actually achieve the plans, intentions or expectations disclosed in our forward-looking statements and you should not place undue reliance on our forward-looking statements. These forward-looking statements involve risks and uncertainties that could cause our actual results to differ materially from the results described in or implied by the forward-looking statements, including, without limitation: the timing, progress and results of our discovery, preclinical and clinical development activities; unexpected safety or efficacy data observed during preclinical studies or clinical trials; the ability to maintain a continued acceptable safety, tolerability and efficacy profile of any product candidate following regulatory authorization or approval; the predictability of clinical success of our product candidates based on neutralizing activity in nonclinical studies; the risk that results of nonclinical studies or clinical trials may not be predictive of future results, and interim data are subject to further analysis; our reliance on third parties with respect to virus assay creation and product candidate testing and with respect to our clinical trials; potential variability in neutralizing activity of product candidates tested in different assays, such as pseudovirus assays and authentic assays; variability of results in models used to predict activity against SARS-CoV-2 variants; whether pemivibart or any other product candidate is able to demonstrate and sustain neutralizing activity against major SARS-CoV-2 variants, particularly in the face of viral evolution; the complexities of manufacturing mAb therapies; our ability to leverage our INVYMAB platform approach to facilitate the rapid, serial generation of new mAbs to address evolving viral threats; our dependence on third parties to manufacture, label, package, store and distribute clinical and commercial supplies of our product candidates; whether we can obtain and maintain third-party coverage and adequate reimbursement for pemivibart or any other product candidate; whether we are able to achieve improved clinical and commercial profiles with our product pipeline; any legal proceedings or investigations relating to the company; our ability to continue as a going concern; and whether we have adequate funding to meet future operating expenses and capital expenditure requirements. Other factors that may cause our actual results to differ materially from those expressed or implied in the forward-looking statements in this presentation are described under the heading “Risk Factors” in our Annual Report on Form 10-K for the year ended December 31, 2023 and our Quarterly Report on Form 10-Q for the quarter ended June 30, 2024, each filed with the Securities and Exchange Commission (SEC), and in our other filings with the SEC, and in our future reports to be filed with the SEC and available at www.sec.gov. Forward-looking statements contained in this presentation are made as of this date, and we undertake no duty to update such information whether as a result of new information, future events or otherwise, except as required under applicable law. 2
COVID-19 PROPHYLAXIS VIA MONOCLONAL ANTIBODY: A STEP FORWARD • CANOPY exploratory clinical efficacy data demonstrated a substantial change - 84% Relative Risk Reduction (RRR) – in experiencing symptomatic COVID-19 disease with pemivibart 1 prophylaxis versus placebo (TM) • PEMGARDA (pemivibart) Fact Sheet for Healthcare Providers updated to include exploratory 2 clinical efficacy data • Safety profile of pemivibart consistent with previously reported CANOPY clinical trial data • Today’s CANOPY data represent the first look at the major medical role mAbs can play in an endemic SARS-CoV-2 environment and provide a striking contrast to estimated vaccine 3 effectiveness (VE) • We hope to work with FDA to integrate clinical event findings from CANOPY into future mAb development work 1 180-day exploratory clinical event data assessment of immunocompetent participants in CANOPY clinical trial for pre-exposure prophylaxis (PrEP) of COVID-19 2 Fact Sheet also updated to reflect certain risks related to variant susceptibility to PEMGARDA 3 FDA presentation to ACIP June 28, 2024 3 mAb = monoclonal antibody
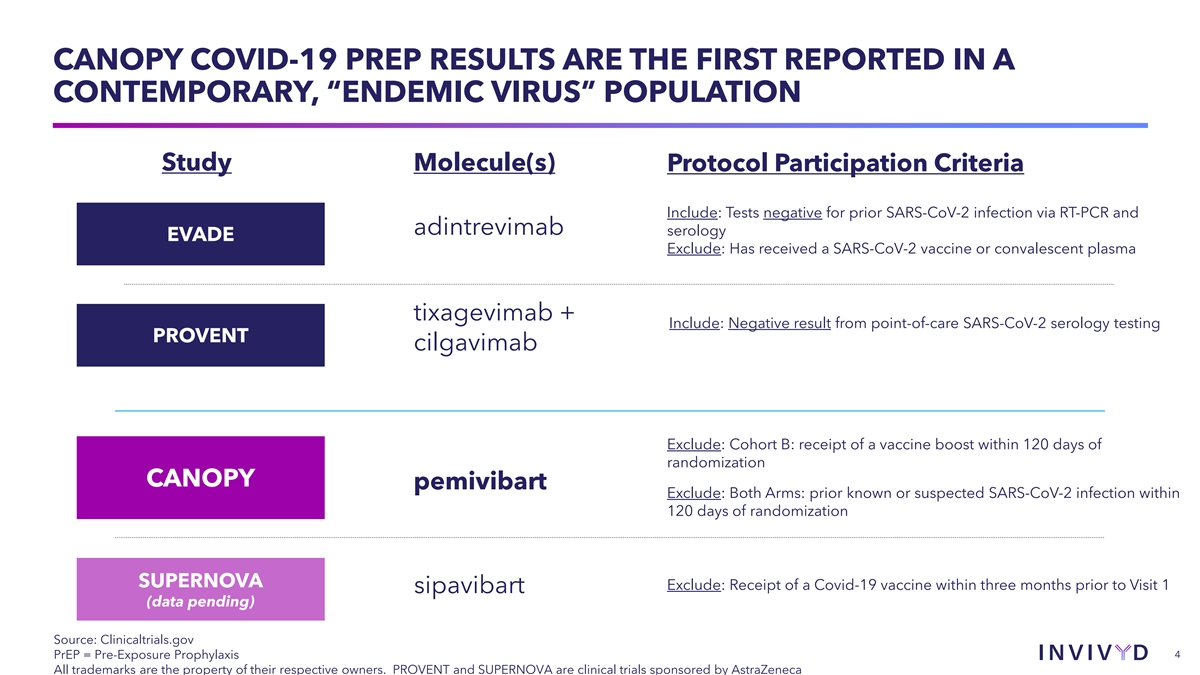
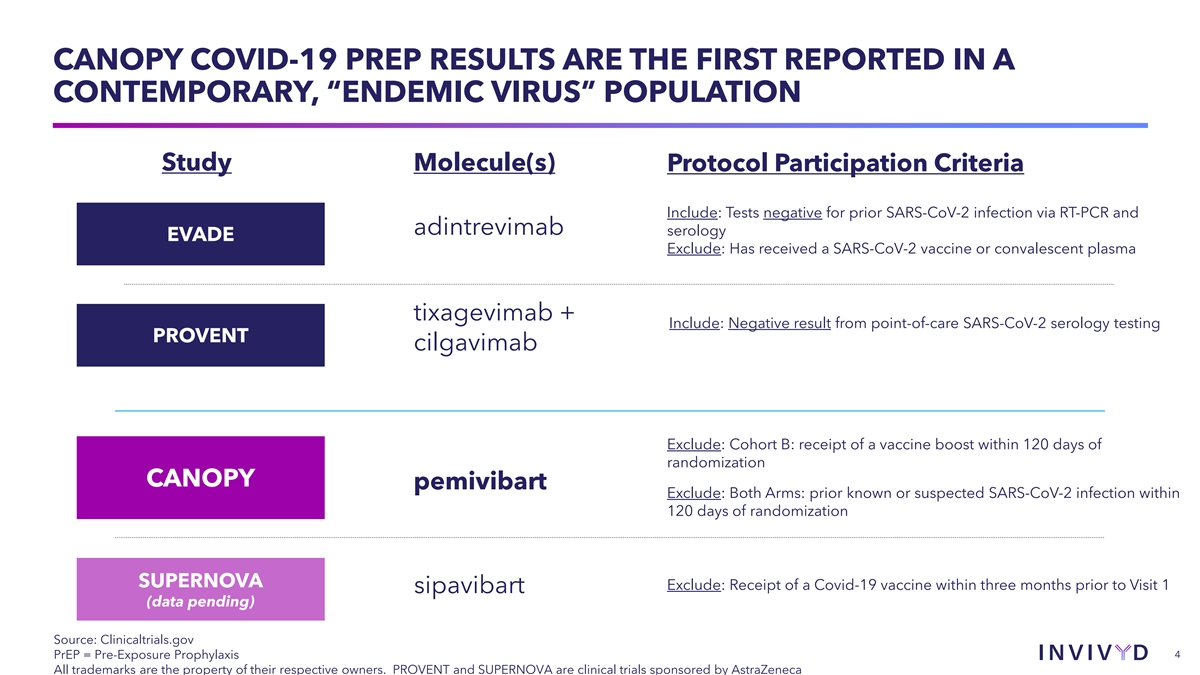
CANOPY COVID-19 PREP RESULTS ARE THE FIRST REPORTED IN A CONTEMPORARY, “ENDEMIC VIRUS” POPULATION Study Molecule(s) Protocol Participation Criteria Include: Tests negative for prior SARS-CoV-2 infection via RT-PCR and adintrevimab serology EVADE Exclude: Has received a SARS-CoV-2 vaccine or convalescent plasma tixagevimab + Include: Negative result from point-of-care SARS-CoV-2 serology testing PROVENT cilgavimab Exclude: Cohort B: receipt of a vaccine boost within 120 days of randomization CANOPY pemivibart Exclude: Both Arms: prior known or suspected SARS-CoV-2 infection within 120 days of randomization SUPERNOVA Exclude: Receipt of a Covid-19 vaccine within three months prior to Visit 1 sipavibart (data pending) Source: Clinicaltrials.gov PrEP = Pre-Exposure Prophylaxis 4 All trademarks are the property of their respective owners. PROVENT and SUPERNOVA are clinical trials sponsored by AstraZeneca
AGENDA u CANOPY Clinical Trial Results Q&A 5
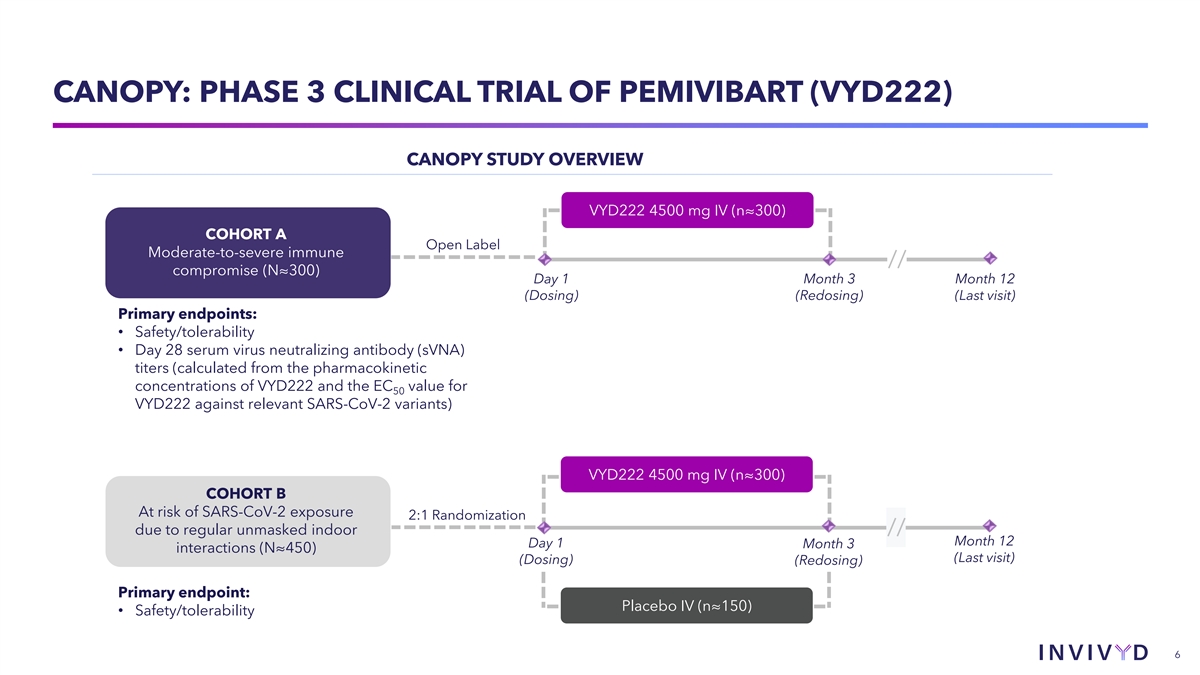
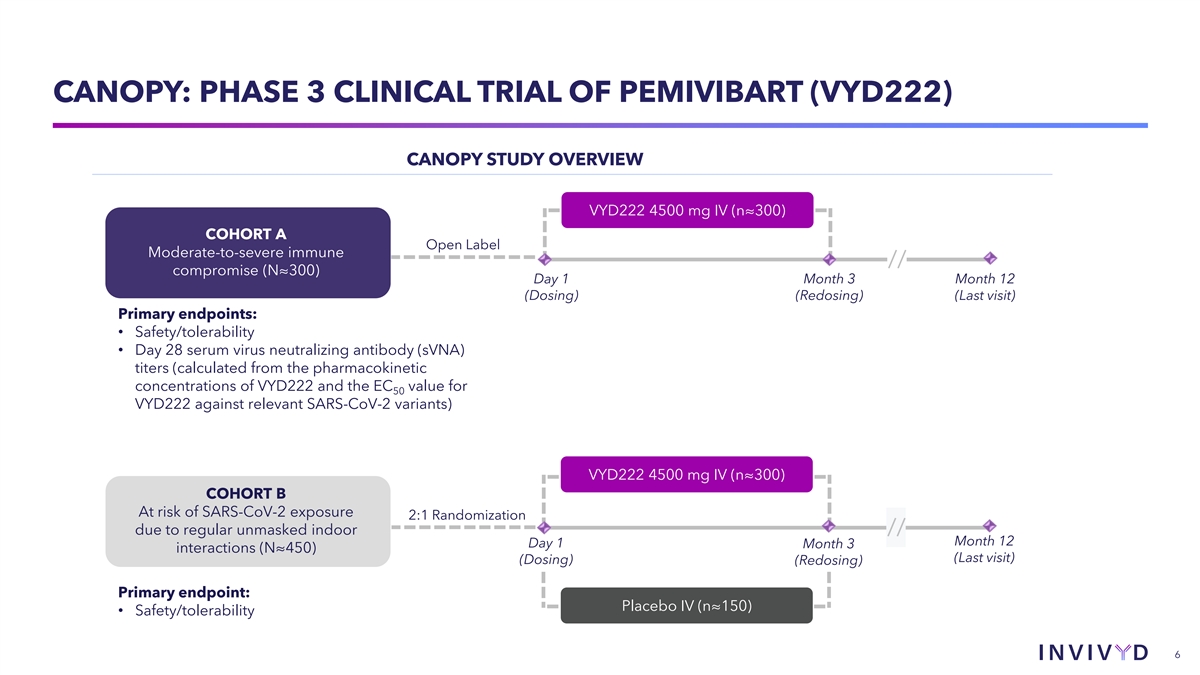
CANOPY: PHASE 3 CLINICAL TRIAL OF PEMIVIBART (VYD222) CANOPY STUDY OVERVIEW VYD222 4500 mg IV (n≈300) COHORT A Open Label Moderate-to-severe immune // compromise (N≈300) Day 1 Month 3 Month 12 (Dosing) (Redosing) (Last visit) Primary endpoints: • Safety/tolerability • Day 28 serum virus neutralizing antibody (sVNA) titers (calculated from the pharmacokinetic concentrations of VYD222 and the EC value for 50 VYD222 against relevant SARS-CoV-2 variants) VYD222 4500 mg IV (n≈300) COHORT B At risk of SARS-CoV-2 exposure 2:1 Randomization due to regular unmasked indoor // Month 12 Day 1 Month 3 interactions (N≈450) (Last visit) (Dosing) (Redosing) Primary endpoint: Placebo IV (n≈150) • Safety/tolerability 6
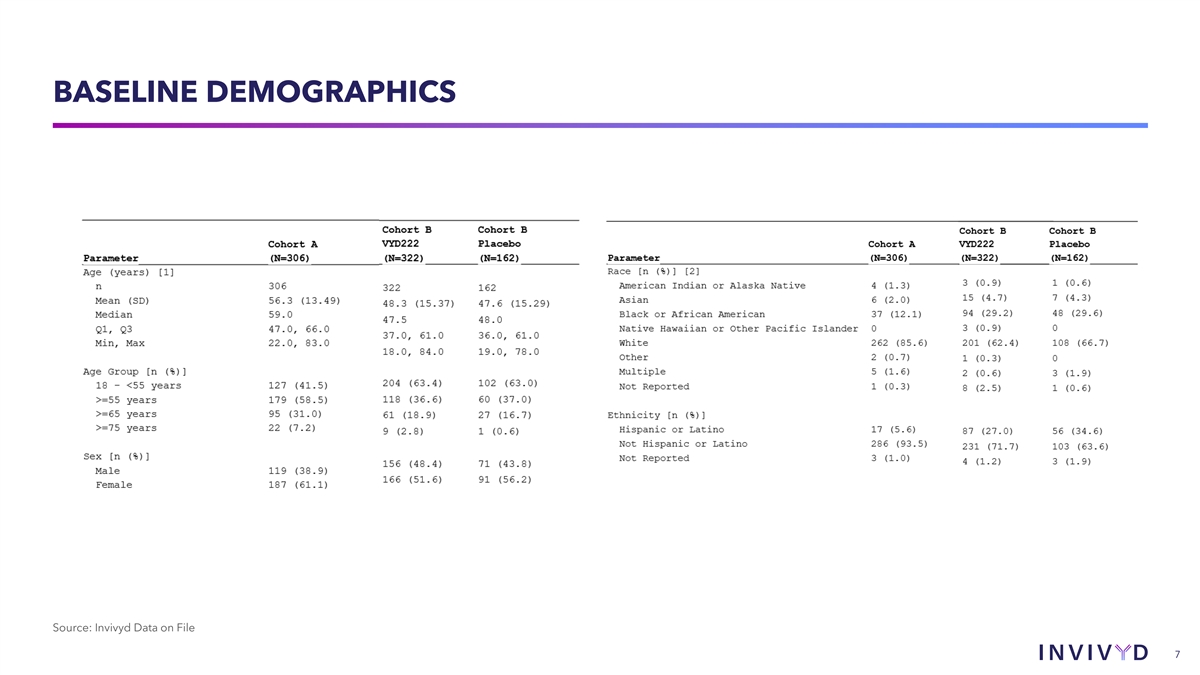
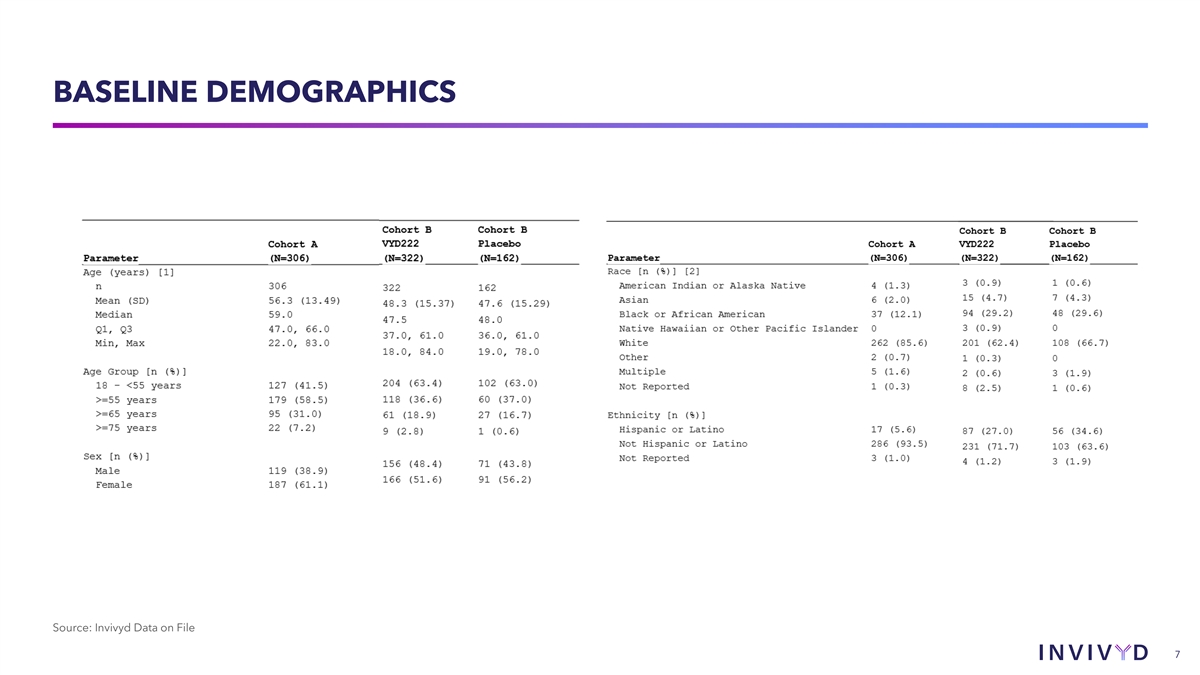
BASELINE DEMOGRAPHICS Source: Invivyd Data on File 7
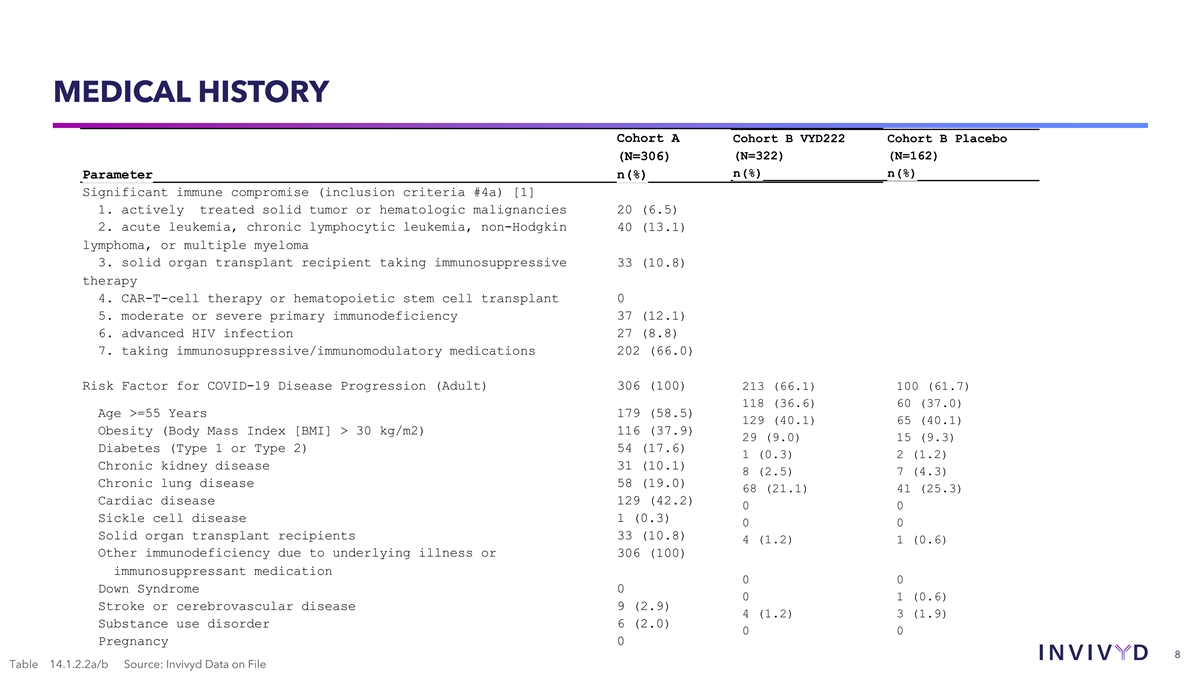
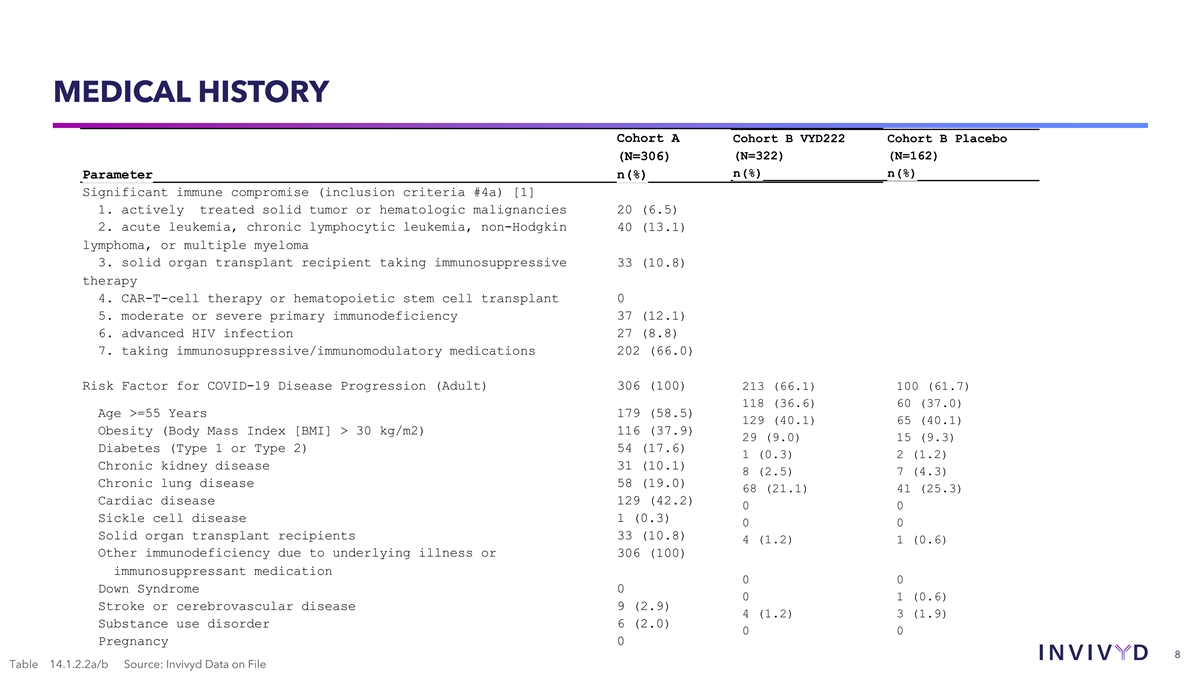
MEDICAL HISTORY Cohort A Cohort B VYD222 Cohort B Placebo (N=306) (N=322) (N=162) n(%) n(%) Parameter n(%) Significant immune compromise (inclusion criteria #4a) [1] 1. actively treated solid tumor or hematologic malignancies 20 (6.5) 2. acute leukemia, chronic lymphocytic leukemia, non-Hodgkin 40 (13.1) lymphoma, or multiple myeloma 3. solid organ transplant recipient taking immunosuppressive 33 (10.8) therapy 4. CAR-T-cell therapy or hematopoietic stem cell transplant 0 5. moderate or severe primary immunodeficiency 37 (12.1) 6. advanced HIV infection 27 (8.8) 7. taking immunosuppressive/immunomodulatory medications 202 (66.0) Risk Factor for COVID-19 Disease Progression (Adult) 306 (100) 213 (66.1) 100 (61.7) 118 (36.6) 60 (37.0) Age >=55 Years 179 (58.5) 129 (40.1) 65 (40.1) Obesity (Body Mass Index [BMI] > 30 kg/m2) 116 (37.9) 29 (9.0) 15 (9.3) Diabetes (Type 1 or Type 2) 54 (17.6) 1 (0.3) 2 (1.2) Chronic kidney disease 31 (10.1) 8 (2.5) 7 (4.3) Chronic lung disease 58 (19.0) 68 (21.1) 41 (25.3) Cardiac disease 129 (42.2) 0 0 Sickle cell disease 1 (0.3) 0 0 Solid organ transplant recipients 33 (10.8) 4 (1.2) 1 (0.6) Other immunodeficiency due to underlying illness or 306 (100) immunosuppressant medication 0 0 Down Syndrome 0 0 1 (0.6) Stroke or cerebrovascular disease 9 (2.9) 4 (1.2) 3 (1.9) Substance use disorder 6 (2.0) 0 0 Pregnancy 0 8 Table 14.1.2.2a/b Source: Invivyd Data on File
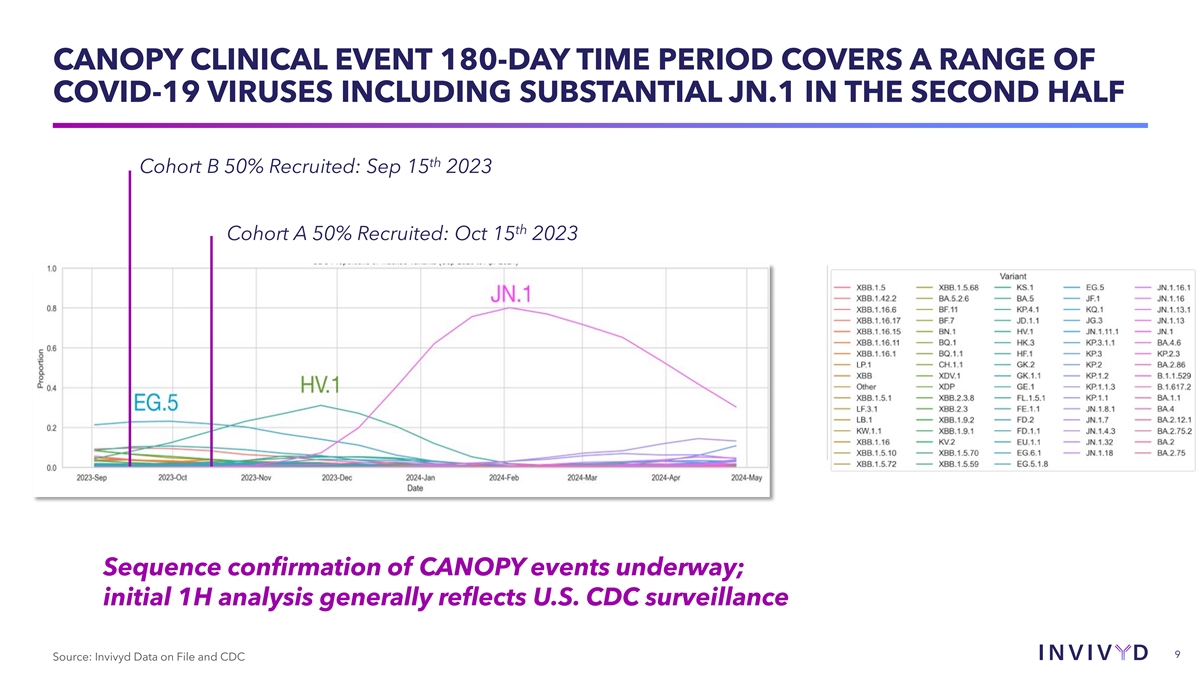
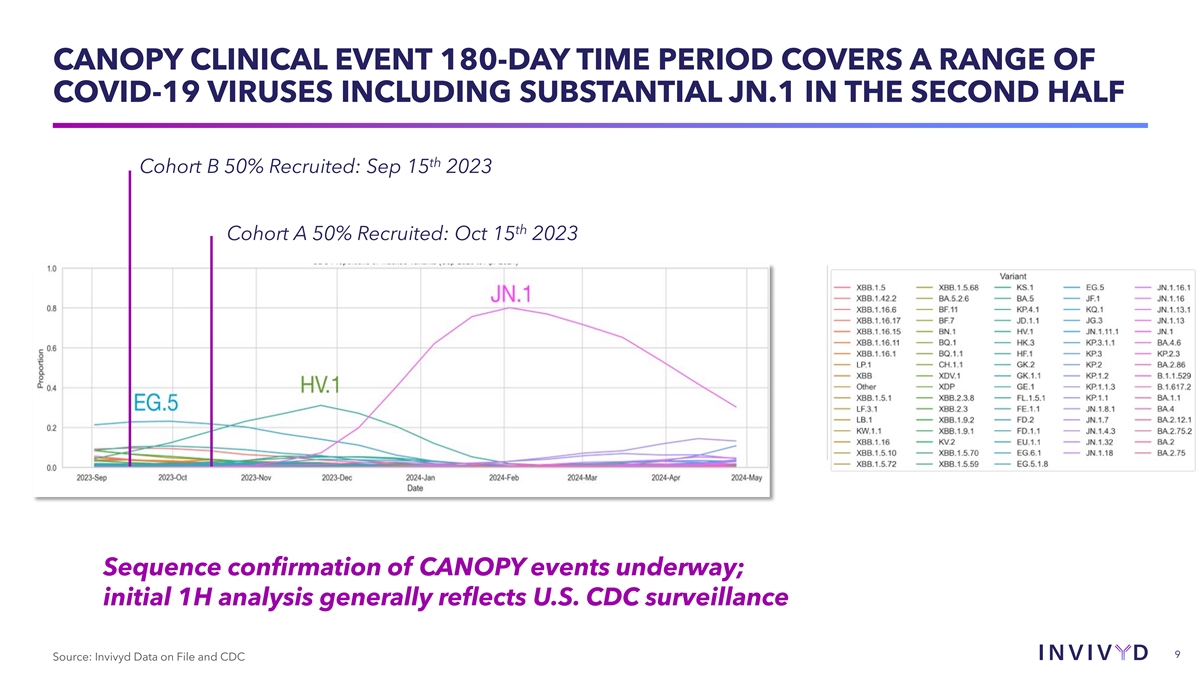
CANOPY CLINICAL EVENT 180-DAY TIME PERIOD COVERS A RANGE OF COVID-19 VIRUSES INCLUDING SUBSTANTIAL JN.1 IN THE SECOND HALF th Cohort B 50% Recruited: Sep 15 2023 th Cohort A 50% Recruited: Oct 15 2023 Sequence confirmation of CANOPY events underway; initial 1H analysis generally reflects U.S. CDC surveillance 9 Source: Invivyd Data on File and CDC
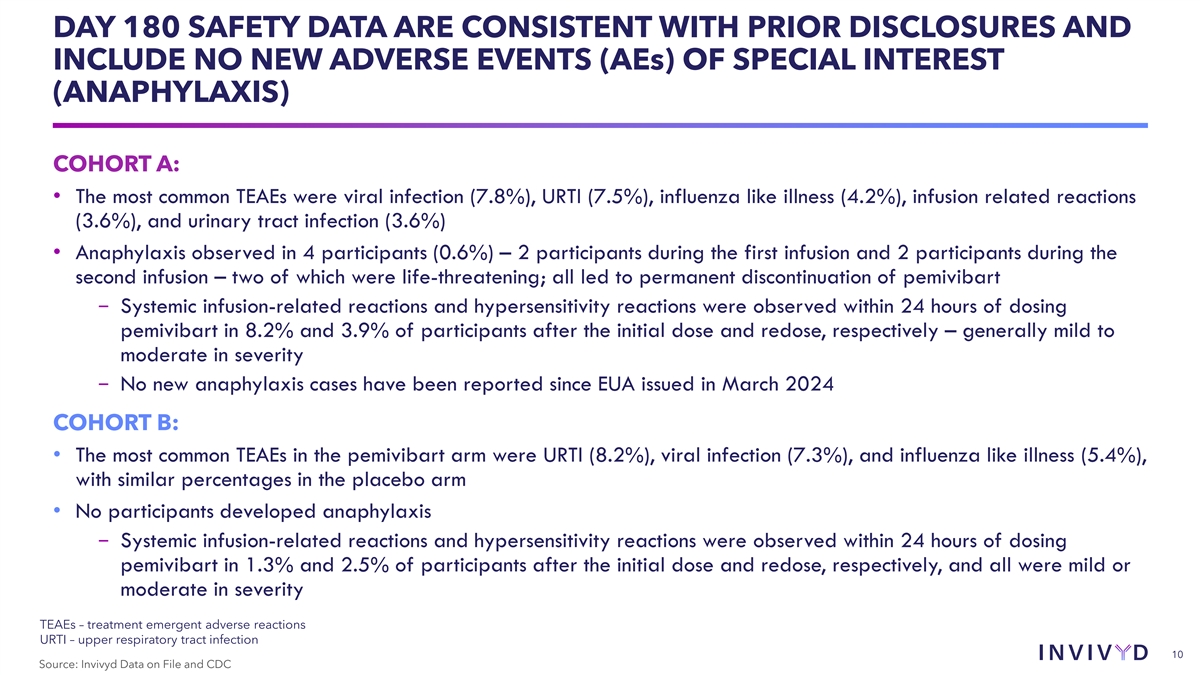
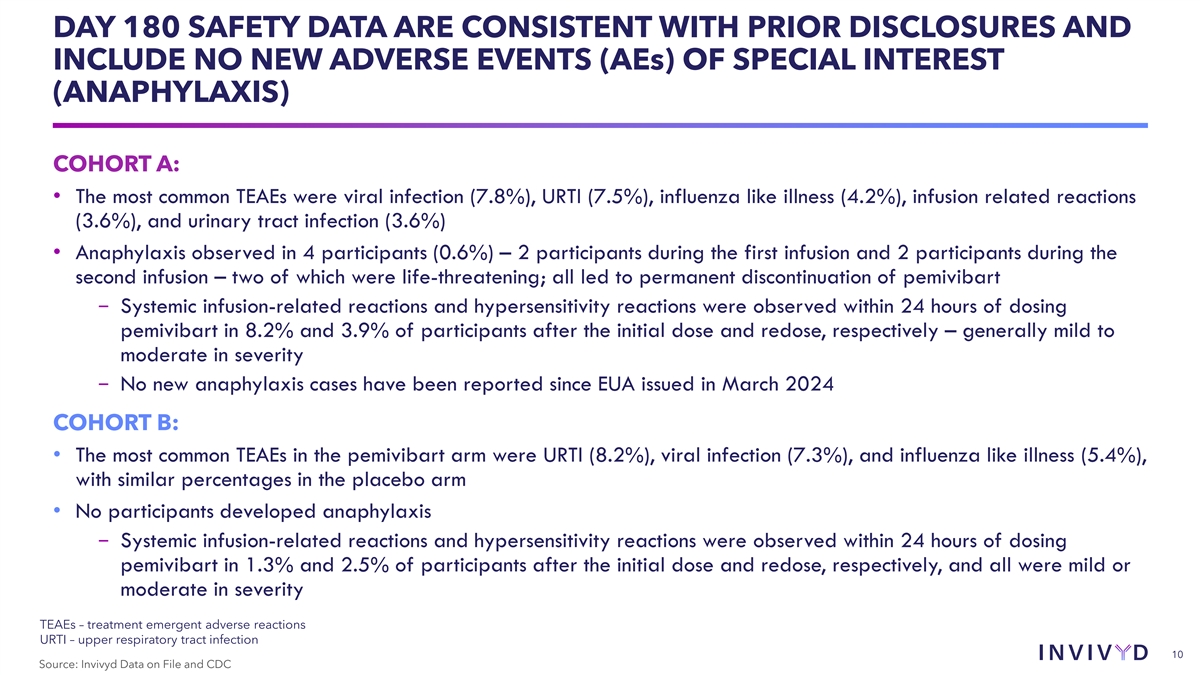
DAY 180 SAFETY DATA ARE CONSISTENT WITH PRIOR DISCLOSURES AND INCLUDE NO NEW ADVERSE EVENTS (AEs) OF SPECIAL INTEREST (ANAPHYLAXIS) COHORT A: • The most common TEAEs were viral infection (7.8%), URTI (7.5%), influenza like illness (4.2%), infusion related reactions (3.6%), and urinary tract infection (3.6%) • Anaphylaxis observed in 4 participants (0.6%) – 2 participants during the first infusion and 2 participants during the second infusion – two of which were life-threatening; all led to permanent discontinuation of pemivibart − Systemic infusion-related reactions and hypersensitivity reactions were observed within 24 hours of dosing pemivibart in 8.2% and 3.9% of participants after the initial dose and redose, respectively – generally mild to moderate in severity − No new anaphylaxis cases have been reported since EUA issued in March 2024 COHORT B: • The most common TEAEs in the pemivibart arm were URTI (8.2%), viral infection (7.3%), and influenza like illness (5.4%), with similar percentages in the placebo arm • No participants developed anaphylaxis − Systemic infusion-related reactions and hypersensitivity reactions were observed within 24 hours of dosing pemivibart in 1.3% and 2.5% of participants after the initial dose and redose, respectively, and all were mild or moderate in severity TEAEs – treatment emergent adverse reactions URTI – upper respiratory tract infection 10 Source: Invivyd Data on File and CDC
EXPLORATORY CLINICAL EFFICACY ENDPOINTS Incidence of RT-PCR confirmed symptomatic COVID-19, Key Exploratory Endpoint COVID-19 related hospitalizations, and all-cause mortality as Measured through 3, 6 and 12 months Incidence of RT-PCR confirmed symptomatic COVID-19 Post-hoc COVID-19-Related Analysis 11 Source: Invivyd Data on File
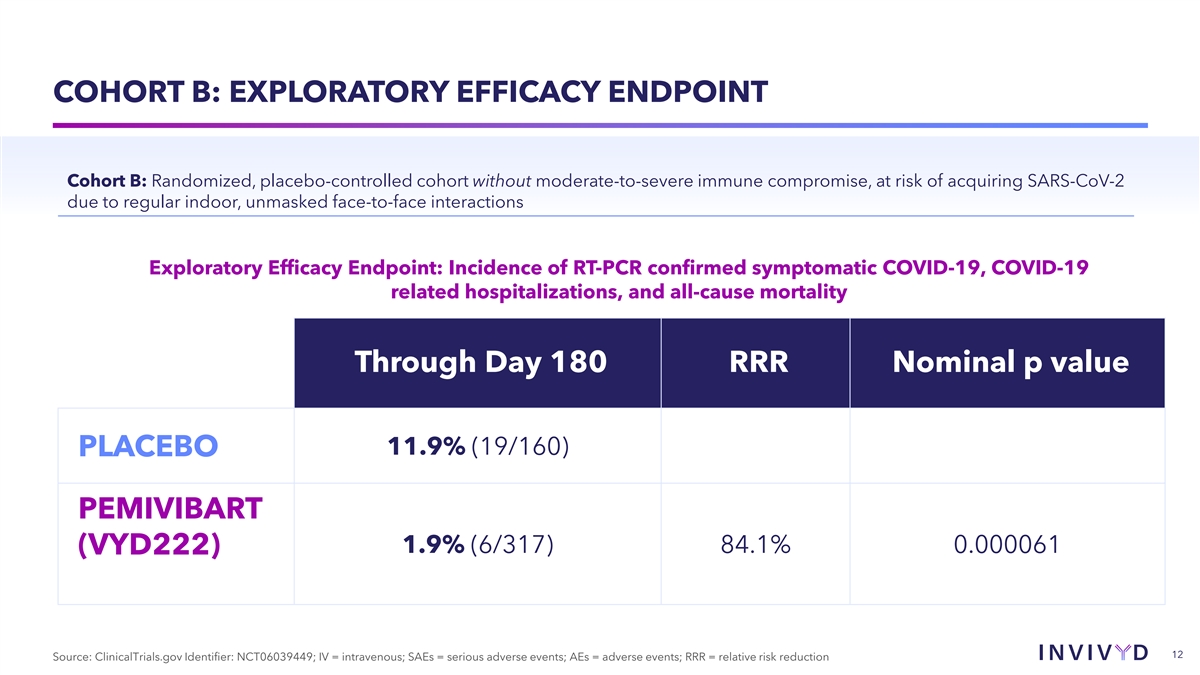
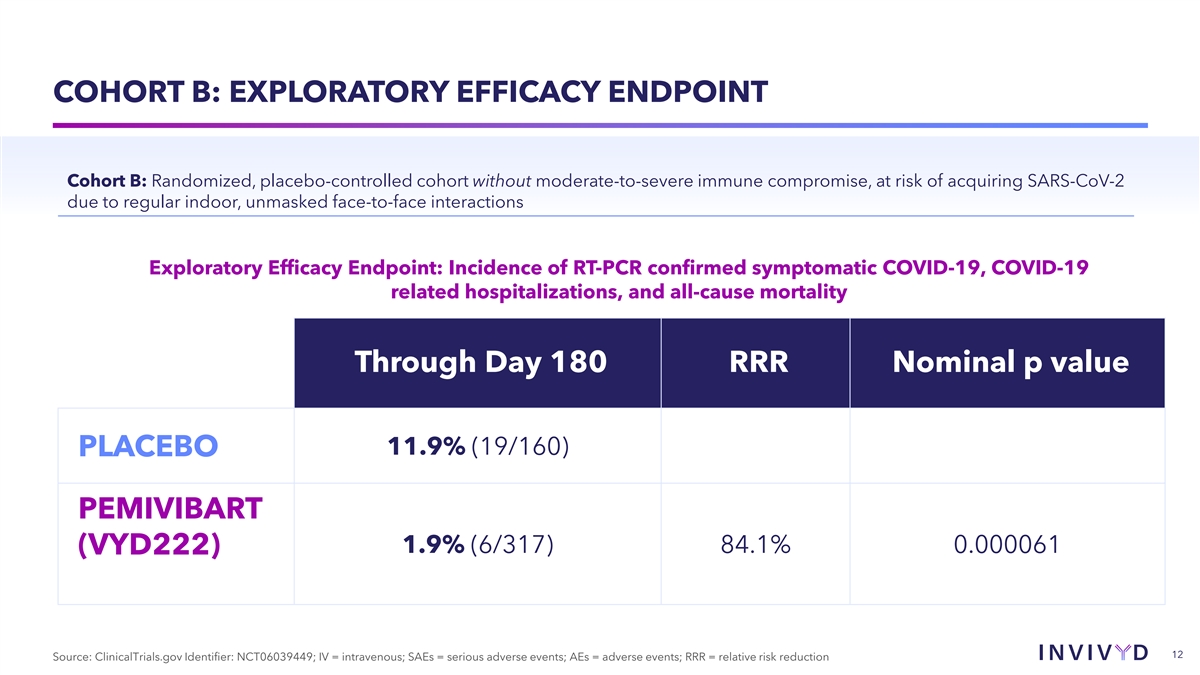
COHORT B: EXPLORATORY EFFICACY ENDPOINT Cohort B: Randomized, placebo-controlled cohort without moderate-to-severe immune compromise, at risk of acquiring SARS-CoV-2 due to regular indoor, unmasked face-to-face interactions Exploratory Efficacy Endpoint: Incidence of RT-PCR confirmed symptomatic COVID-19, COVID-19 related hospitalizations, and all-cause mortality Through Day 180 RRR Nominal p value 11.9% (19/160) PLACEBO PEMIVIBART 1.9% (6/317) 84.1% 0.000061 (VYD222) 12 Source: ClinicalTrials.gov Identifier: NCT06039449; IV = intravenous; SAEs = serious adverse events; AEs = adverse events; RRR = relative risk reduction
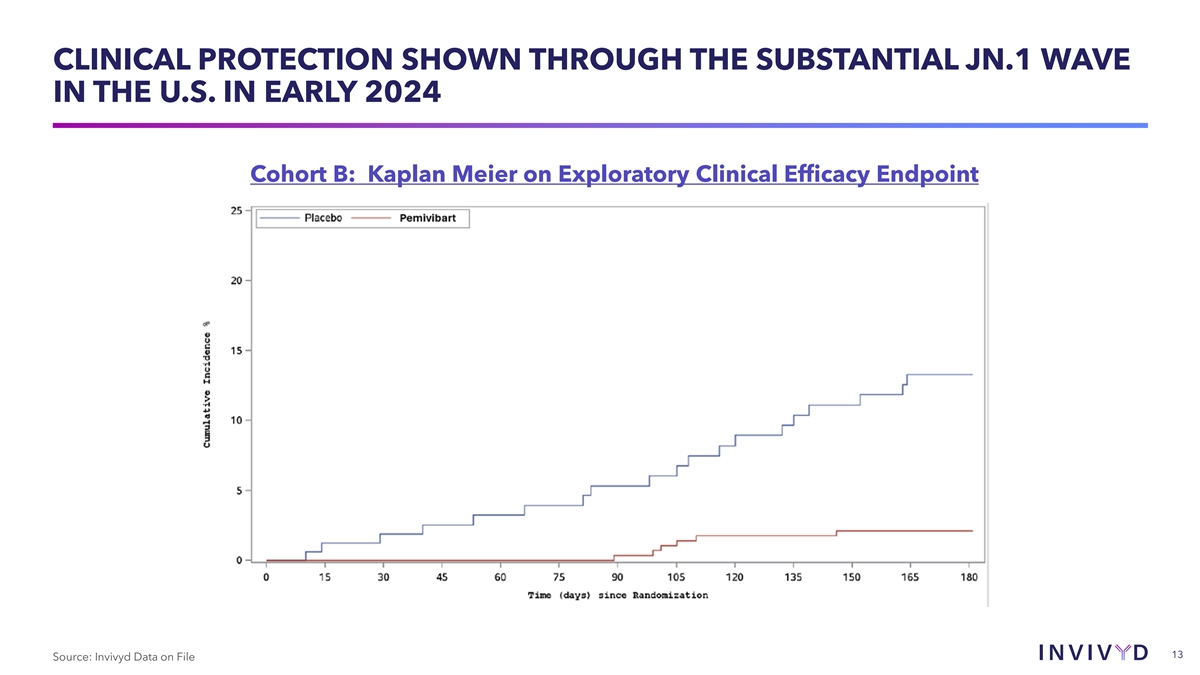
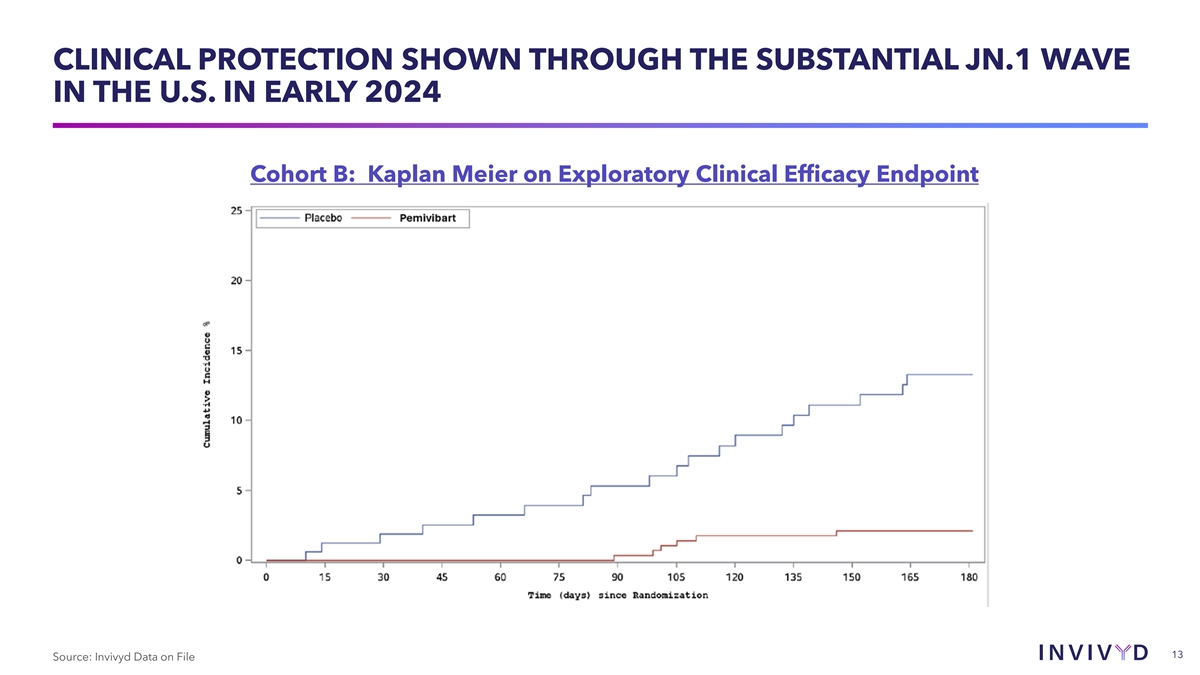
CLINICAL PROTECTION SHOWN THROUGH THE SUBSTANTIAL JN.1 WAVE IN THE U.S. IN EARLY 2024 Cohort B: Kaplan Meier on Exploratory Clinical Efficacy Endpoint 13 Source: Invivyd Data on File
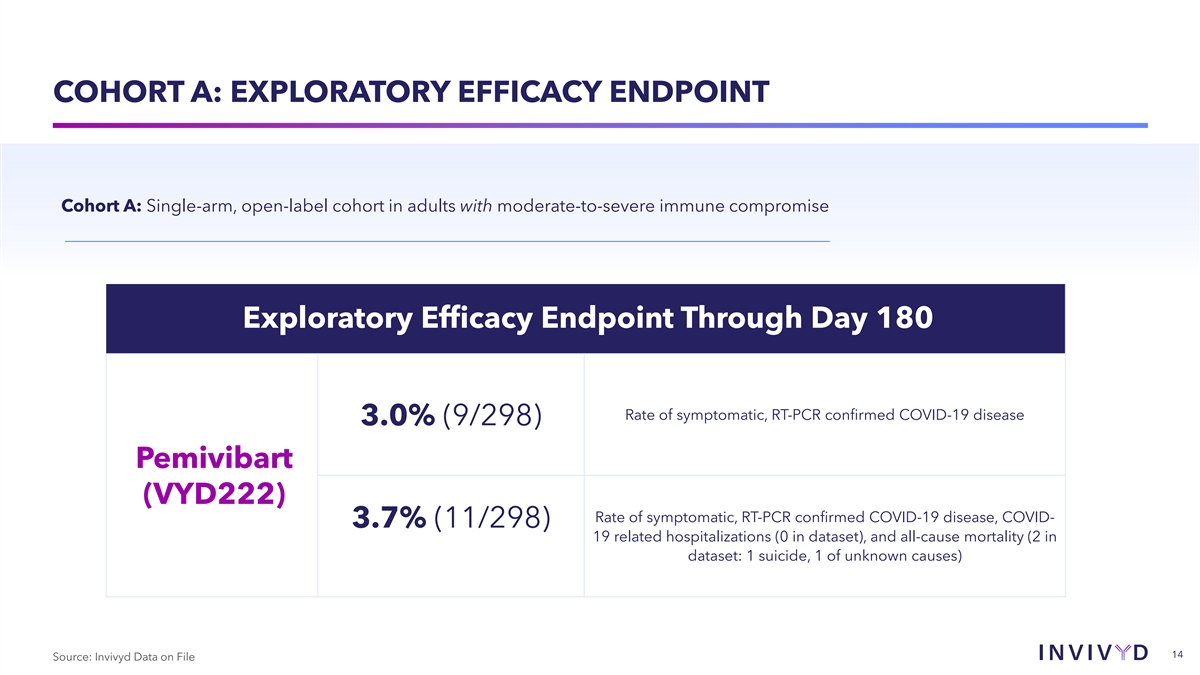
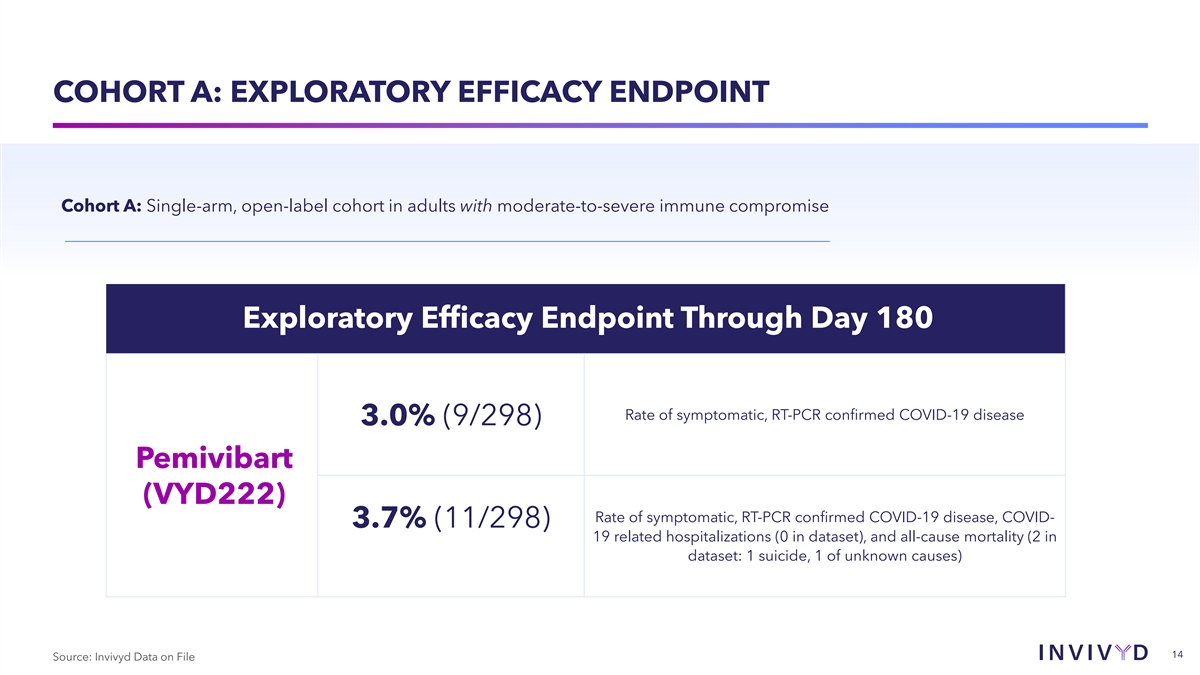
COHORT A: EXPLORATORY EFFICACY ENDPOINT Cohort A: Single-arm, open-label cohort in adults with moderate-to-severe immune compromise Exploratory Efficacy Endpoint Through Day 180 Rate of symptomatic, RT-PCR confirmed COVID-19 disease 3.0% (9/298) Pemivibart (VYD222) Rate of symptomatic, RT-PCR confirmed COVID-19 disease, COVID- 3.7% (11/298) 19 related hospitalizations (0 in dataset), and all-cause mortality (2 in dataset: 1 suicide, 1 of unknown causes) 14 Source: Invivyd Data on File
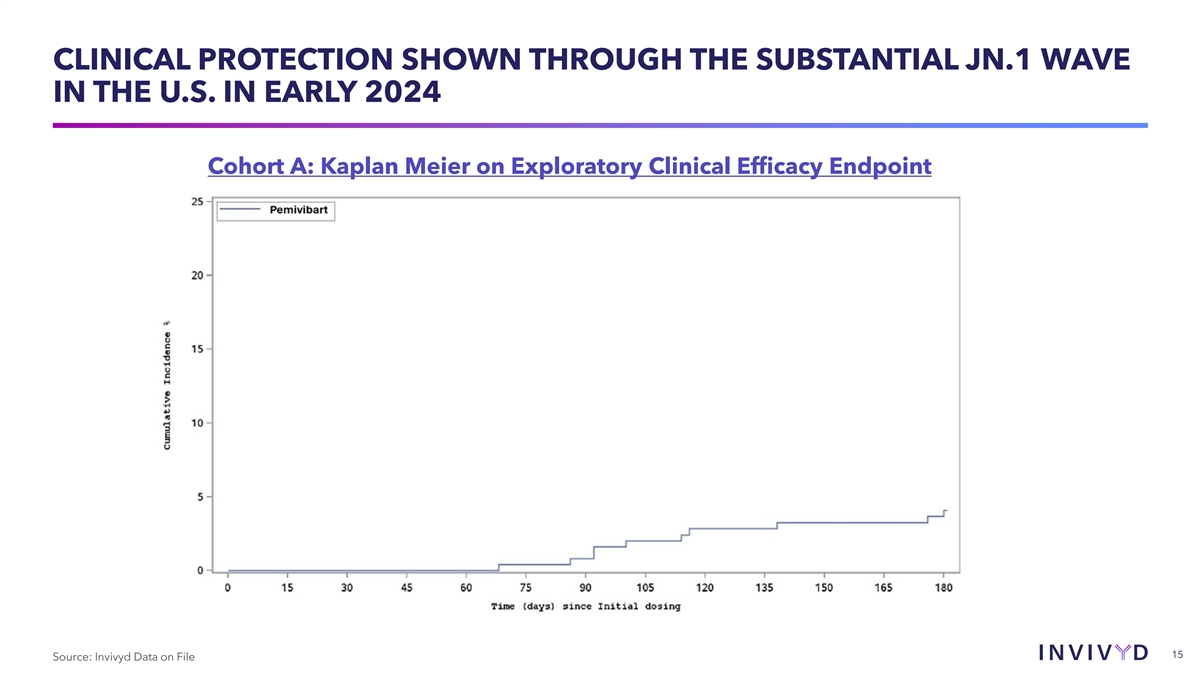
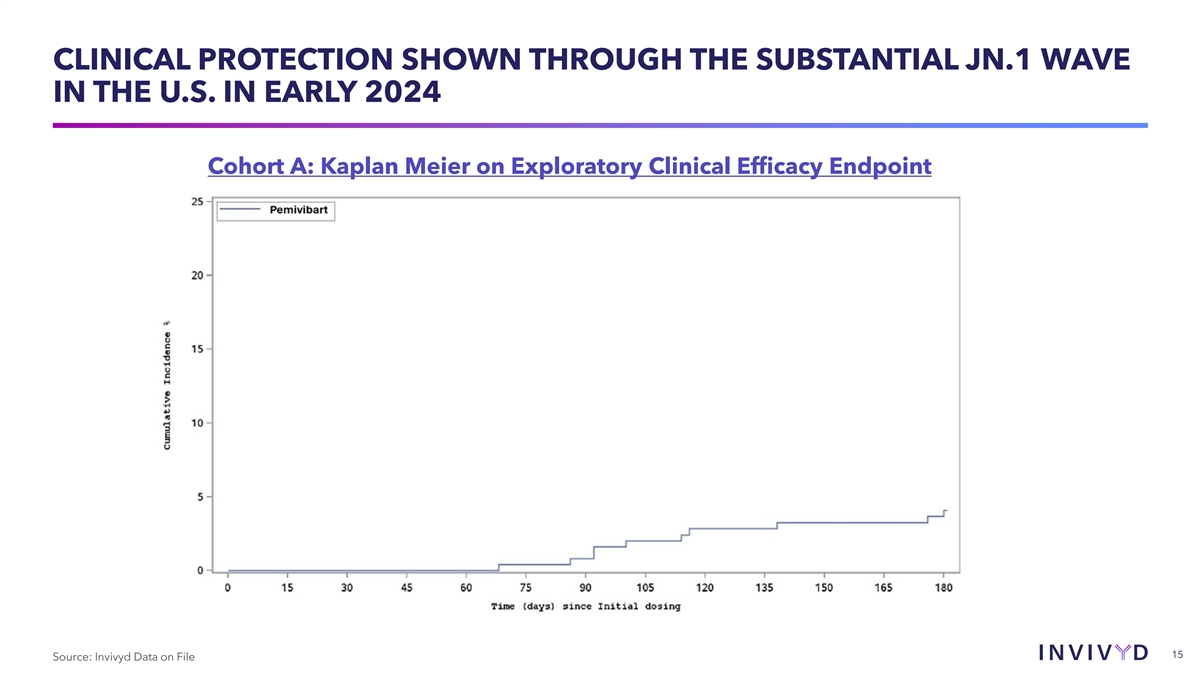
CLINICAL PROTECTION SHOWN THROUGH THE SUBSTANTIAL JN.1 WAVE IN THE U.S. IN EARLY 2024 Cohort A: Kaplan Meier on Exploratory Clinical Efficacy Endpoint 15 Source: Invivyd Data on File
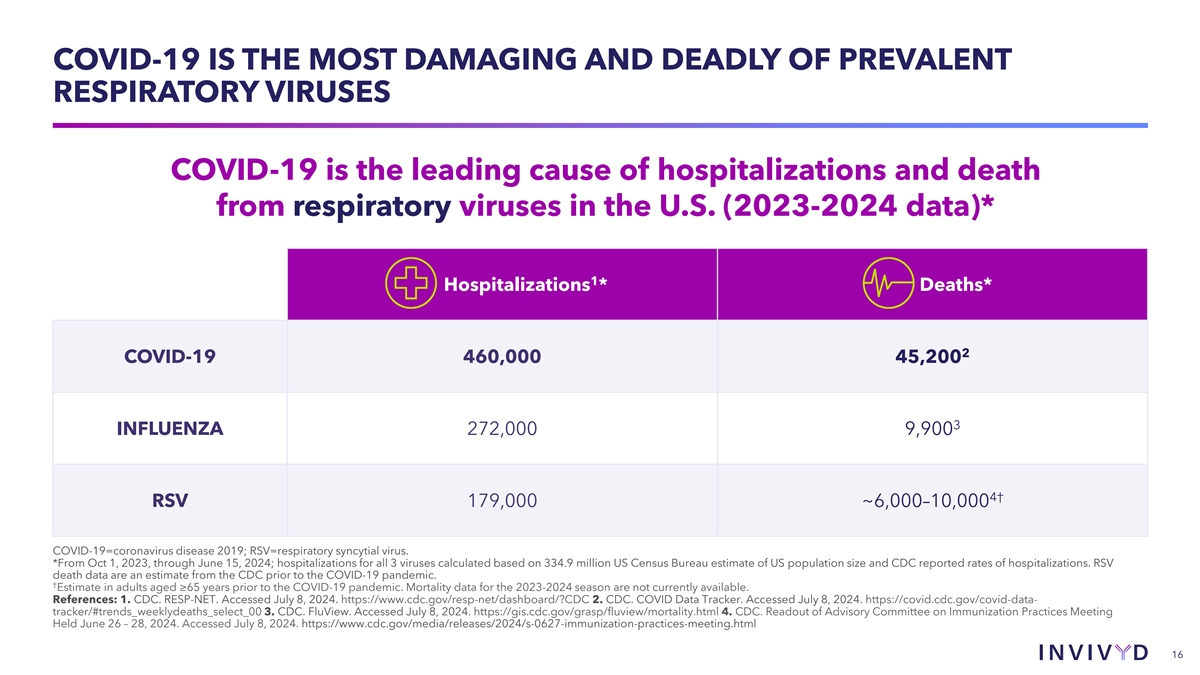
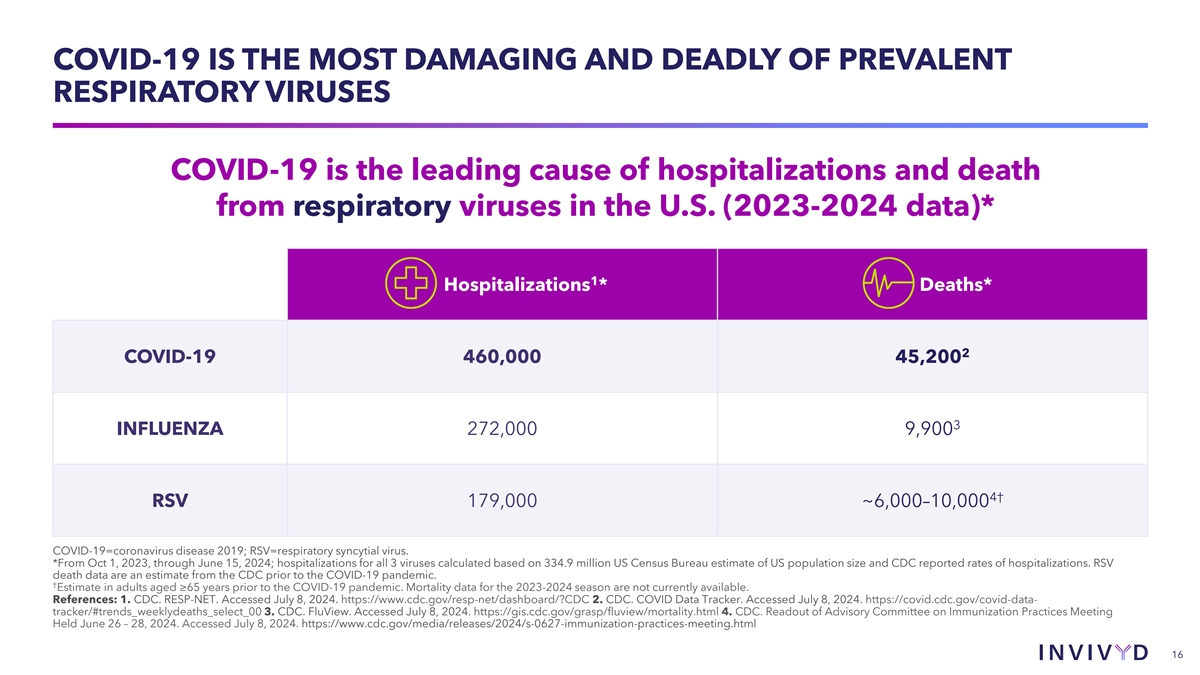
COVID-19 IS THE MOST DAMAGING AND DEADLY OF PREVALENT RESPIRATORY VIRUSES COVID-19 is the leading cause of hospitalizations and death from respiratory viruses in the U.S. (2023-2024 data)* 1 Hospitalizations * Deaths* 2 COVID-19 460,000 45,200 3 INFLUENZA 272,000 9,900 4† RSV 179,000 ~6,000–10,000 COVID-19=coronavirus disease 2019; RSV=respiratory syncytial virus. *From Oct 1, 2023, through June 15, 2024; hospitalizations for all 3 viruses calculated based on 334.9 million US Census Bureau estimate of US population size and CDC reported rates of hospitalizations. RSV death data are an estimate from the CDC prior to the COVID-19 pandemic. † Estimate in adults aged ≥65 years prior to the COVID-19 pandemic. Mortality data for the 2023-2024 season are not currently available. References: 1. CDC. RESP-NET. Accessed July 8, 2024. https://www.cdc.gov/resp-net/dashboard/?CDC 2. CDC. COVID Data Tracker. Accessed July 8, 2024. https://covid.cdc.gov/covid-data- tracker/#trends_weeklydeaths_select_00 3. CDC. FluView. Accessed July 8, 2024. https://gis.cdc.gov/grasp/fluview/mortality.html 4. CDC. Readout of Advisory Committee on Immunization Practices Meeting Held June 26 – 28, 2024. Accessed July 8, 2024. https://www.cdc.gov/media/releases/2024/s-0627-immunization-practices-meeting.html 16
AGENDA u CANOPY Results u Q&A 17