As filed with the U.S. Securities and Exchange Commission on September 3, 2024.
Registration No. 333-
UNITED STATES
SECURITIES AND EXCHANGE COMMISSION
Washington, D.C. 20549
FORM S-1
REGISTRATION STATEMENT
Under The Securities Act of 1933
PACS Group, Inc.
(Exact name of registrant as specified in its charter)
| Delaware | 8051 | 92-3144268 | ||||||
(State or other jurisdiction of incorporation or organization) | (Primary Standard Industrial Classification Code Number) | (I.R.S. Employer Identification No.) | ||||||
262 N. University Ave.
Farmington, Utah 84025
(801) 447-9829
(Address, including zip code, and telephone number, including area code, of registrant’s principal executive offices)
Jason Murray
Chief Executive Officer
PACS Group, Inc.
262 N. University Ave.
Farmington, Utah 84025
(801) 447-9829
(Name, address, including zip code, and telephone number, including area code, of agent for service)
Copies to:
B. Shayne Kennedy J. Ross McAloon Latham & Watkins LLP 650 Town Center Drive, 20th Floor Costa Mesa, CA 92626 (714) 540-1235 | John Mitchell Chief Legal Officer and General Counsel 262 N. University Ave. Farmington, Utah 84025 (801) 447-9829 | Benjamin K. Marsh Adam V. Johnson Goodwin Procter LLP The New York Times Building 620 Eighth Avenue New York, NY 10018 (212) 813-8800 | ||||||
Approximate date of commencement of proposed sale to the public: As soon as practicable after the effective date of this Registration Statement.
If any of the securities being registered on this Form are to be offered on a delayed or continuous basis pursuant to Rule 415 under the Securities Act of 1933, check the following box. o
If this Form is filed to register additional securities for an offering pursuant to Rule 462(b) under the Securities Act, check the following box and list the Securities Act registration statement number of the earlier effective registration statement for the same offering. o
If this Form is a post-effective amendment filed pursuant to Rule 462(c) under the Securities Act, check the following box and list the Securities Act registration statement number of the earlier effective registration statement for the same offering. o
If this Form is a post-effective amendment filed pursuant to Rule 462(d) under the Securities Act, check the following box and list the Securities Act registration statement number of the earlier effective registration statement for the same offering. o
Indicate by check mark whether the registrant is a large accelerated filer, an accelerated filer, a non-accelerated filer, a smaller reporting company or an emerging growth company. See the definitions of “large accelerated filer,” “accelerated filer,” “smaller reporting company” and “emerging growth company” in Rule 12b-2 of the Exchange Act.
| Large accelerated filer | ☐ | Accelerated filer | ☐ | |||||||||||
| Non-accelerated filer | ☒ | Smaller reporting company | ☐ | |||||||||||
| Emerging growth company | ☐ | |||||||||||||
If an emerging growth company, indicate by check mark if the registrant has elected not to use the extended transition period for complying with any new or revised financial accounting standards provided pursuant to Section 7(a)(2)(B) of the Securities Act. o
The registrant hereby amends this Registration Statement on such date or dates as may be necessary to delay its effective date until the registrant shall file a further amendment which specifically states that this Registration Statement shall thereafter become effective in accordance with Section 8(a) of the Securities Act of 1933 or until the Registration Statement shall become effective on such date as the Commission, acting pursuant to said Section 8(a), may determine.
The information in this preliminary prospectus is not complete and may be changed. We and the selling stockholders may not sell these securities until the registration statement filed with the Securities and Exchange Commission is effective. This preliminary prospectus is not an offer to sell these securities, and we are not soliciting offers to buy these securities in any jurisdiction where the offer or sale is not permitted.
Subject to Completion. Dated September 3, 2024.
PRELIMINARY PROSPECTUS
13,888,890 Shares

Common Stock
We are offering 2,777,778 shares of our common stock, and the selling stockholders identified in this prospectus are offering 11,111,112 shares of our common stock. We will not receive any proceeds from the sale of shares of our common stock by the selling stockholders. Our common stock is listed on the New York Stock Exchange under the symbol “PACS.” On August 30, 2024, the last reported sale price of our common stock as reported on the New York Stock Exchange was $39.67 per share.
The selling stockholders have granted the underwriters an option for a period of up to 30 days to purchase up to an additional 2,083,332 shares of our common stock from them at the public offering price, less the underwriting discounts and commissions.
Following this offering, our founders, Messrs. Murray and Hancock, will collectively own a significant majority of our common stock, representing approximately 73.7% of the voting power of our common stock (or approximately 72.4% if the underwriters exercise their option to purchase additional shares of our common stock from the selling stockholders in full). In addition, pursuant to the terms of our amended and restated certificate of incorporation (Amended and Restated Charter), our founders are able to control corporate matters for the foreseeable future. For example, each founder has the right to designate (i) up to two individuals for inclusion in our slate of director nominees if such founder beneficially owns at least 20% of the aggregate number of shares of common stock outstanding immediately following the completion of our initial public offering or (ii) one individual for inclusion in our slate of director nominees if such founder beneficially owns less than 20% but at least 10% of the aggregate number of shares of common stock outstanding immediately following the completion of our initial public offering. Accordingly, each founder currently has the right to designate two directors, and our founders currently collectively have the right to designate four directors, which represents four out of our five member board of directors. These rights are affirmed in the Stockholders Agreement (as defined herein). In addition, pursuant to the terms of our Amended and Restated Charter, for so long as our founders beneficially own, in the aggregate, the majority of the voting power of our outstanding shares of voting stock, our founders are able to remove any of our directors at any time with or without cause and may take action by written consent without a meeting of stockholders. If our founders beneficially own, in the aggregate, less than the majority of the voting power of our outstanding shares of voting stock, directors may be removed only for cause and only by the affirmative vote of the holders of at least 66 2/3% of the voting power of the then outstanding shares of our voting stock entitled to vote thereon and our stockholders may not take action by written consent, which has the effect of requiring all stockholder actions to be taken at a meeting of our stockholders. Our Amended and Restated Charter authorizes our board of directors to establish and determine, among others, the voting, board representation and other rights or preferences of one or more series of preferred stock, and our board of directors may determine to issue additional shares of common stock, in each case without stockholder approval. This concentrated control, due to both the provisions of the Amended and Restated Charter and the Stockholders Agreement and the voting power of our founders, will preclude your ability to influence corporate matters for the foreseeable future, including with respect to the composition of our board of directors, the election and removal of directors, the authorization and issuance of additional shares of our common stock that would be dilutive to you, the issuance of shares of preferred stock that could be dilutive to you and could have disparate voting rights, amendments to our organizational documents, and any merger, consolidation, sale of all or substantially all of our assets, or other major corporate transactions requiring stockholder approval.
We are a “controlled company” within the meaning of the corporate governance standards of the New York Stock Exchange. As a “controlled company,” we may elect to rely on exemptions from certain corporate governance standards of the New York Stock Exchange.
See the sections titled “Management—Director Independence and Controlled Company Exception,” “Certain Relationships and Related Party Transactions—Stockholders Agreement” and “Description of Capital Stock.”
Investing in our common stock involves risks. See the section titled “Risk Factors” beginning on page 21 to read about the factors you should consider before buying shares of our common stock.
Neither the Securities and Exchange Commission nor any other regulatory body has approved or disapproved of these securities or passed upon the accuracy or adequacy of this prospectus. Any representation to the contrary is a criminal offense.
| Per Share | Total | ||||||||||
| Public offering price | $ | $ | |||||||||
Underwriting discounts and commissions(1) | $ | $ | |||||||||
| Proceeds, before expenses, to us | $ | $ | |||||||||
| Proceeds, before expenses, to the selling stockholders | $ | $ | |||||||||
__________________
(1)We have agreed to reimburse the underwriters for certain expenses in connection with this offering. See the section titled “Underwriting (Conflicts of Interest)” for a description of the compensation payable to the underwriters.
The underwriters expect to deliver the shares of common stock to purchasers on or about , 2024.
| Citigroup | J.P. Morgan | Truist Securities | ||||||
| RBC Capital Markets | Goldman Sachs & Co. LLC | UBS Investment Bank | ||||||
| Stephens Inc. | Oppenheimer & Co. | |||||||
Prospectus dated , 2024.
TABLE OF CONTENTS
| Page | |||||
You should rely only on the information contained in this prospectus or contained in any free writing prospectus filed with the Securities and Exchange Commission (SEC) prepared by or on behalf of us that we have referred to you. Neither we, the selling stockholders, nor the underwriters have authorized anyone to provide you with any information other than that contained in this prospectus, any amendment or supplement to this prospectus or in any free writing prospectus we may authorize to be delivered or made available to you. Neither we, the selling stockholders, nor the underwriters take responsibility for, and can provide assurance as to the reliability of, any other information that others may give you. This prospectus is an offer to sell only the shares of our common stock offered by this prospectus, but only under circumstances and in jurisdictions where it is lawful to do so. The information contained in this prospectus is accurate only as of the date of this prospectus, regardless of the time of delivery of this prospectus or of any sale of shares of our common stock. Our business, financial condition, results of operations, and prospects may have changed since such date.
For investors outside of the United States: We have not, the selling stockholders have not, and the underwriters have not, done anything that would permit this offering or possession or distribution of this prospectus in any jurisdiction where action for that purpose is required, other than in the United States. Persons outside of the United States who come into possession of this prospectus must inform themselves about, and observe any restrictions relating to, this offering and the distribution of this prospectus outside of the United States.
i
GENERAL INFORMATION
Industry, Market and Other Data
This prospectus contains estimates, projections and information concerning our industry, our business and data regarding the market size and growth rates of the markets in which we participate. Some data and statistical and other information are based on independent reports from third parties, as well as industry and general publications and research, surveys and studies conducted by third parties. Some data and statistical and other information are based on internal estimates and calculations that are derived from publicly available information, research we conducted, internal surveys, our management’s knowledge of our industry and their assumptions based on such information and knowledge, which we believe to be reasonable.
In each case, this information and data involves a number of assumptions and limitations. Industry publications and other reports we have obtained from independent parties may state that the data contained in these publications or other reports have been obtained in good faith or from sources considered to be reliable, but they do not guarantee the accuracy or completeness of such data. In addition, projections, assumptions and estimates of the future performance of the industry in which we operate and our future performance are necessarily subject to a high degree of uncertainty and risk due to a variety of factors, including those described in “Risk Factors” and “Special Note Regarding Forward-Looking Statements.” These and other factors could cause our future performance to differ materially from the assumptions and estimates made by third parties and us.
Trademarks, Trade Names and Service Marks
PACS, our logos and our other registered or common law trade names, trademarks or service marks appearing in this prospectus are the property of PACS Group, Inc. or our subsidiaries. This prospectus contains additional trade names, trademarks and service marks of other companies that are the property of their respective owners. We do not intend our use or display of other companies’ trade names, trademarks or service marks to imply a relationship with, or endorsement or sponsorship of us by, these other companies. Solely for convenience, the trade names, trademarks and service marks referred to in this prospectus may appear without the ®, ™ or SM symbols, but the omission of such references is not intended to indicate, in any way, that we will not assert, to the fullest extent under applicable law, our rights thereto or that the applicable owner of these trade names, trademarks and service marks will not assert, to the fullest extent under applicable law, its rights thereto.
Basis of Presentation
Certain monetary amounts, percentages and other figures included elsewhere in this prospectus have been subject to rounding adjustments. Percentage amounts included in this prospectus have not in all cases been calculated on the basis of such rounded figures, but on the basis of such amounts prior to rounding. For this reason, percentage amounts in this prospectus may vary from those obtained by performing the same calculations using the figures in our combined/consolidated financial statements included elsewhere in this prospectus. Accordingly, certain other figures and amounts that appear as totals in this prospectus may not be the arithmetic aggregation of the figures or amounts that precede them, and figures or amounts expressed as a percentage may not total 100% or be the arithmetic aggregation of the percentages that precede them.
ii
PROSPECTUS SUMMARY
This summary highlights selected information contained in more detail elsewhere in this prospectus. This summary does not contain all of the information you should consider before investing in our common stock. You should carefully read this prospectus in its entirety before investing in our common stock, including the sections titled “Risk Factors,” “Management’s Discussion and Analysis of Financial Condition and Results of Operations,” and “Special Note Regarding Forward-Looking Statements,” and our audited combined/consolidated financial statements and the related notes included elsewhere in this prospectus, before making an investment decision. Unless the context otherwise requires, the terms “we,” “us,” “our,” the “Company,” “PACS” and similar references in this prospectus refer to PACS Group, Inc. together with its consolidated subsidiaries.
Business Overview
We are a leading post-acute healthcare company primarily focused on delivering high-quality skilled nursing care through a portfolio of independently operated facilities. Founded in 2013, we are one of the largest skilled nursing providers in the United States based on number of facilities, with 276 post-acute care facilities across 15 states serving over 29,000 patients daily as of September 1, 2024. We also provide senior care, assisted living, and independent living options in some of our communities. Our significant historical growth has been primarily driven by our expertise in acquiring underperforming long-term custodial care skilled nursing facilities and transforming them into higher acuity, high value-add short-term transitional care skilled nursing facilities. We believe our success is driven in significant part by our decentralized, local operating model, through which we empower local leaders at each facility to operate their facility autonomously and deliver excellence in clinical quality and a superior experience for our patients. We provide our independently operated facilities with a comprehensive suite of technology, support, and back-office services that allow local leadership teams to focus more of their time and effort on providing quality care to patients. We believe our operating model delivers value to all of our healthcare stakeholders, including patients and families, referring providers, payors, and administrators and clinicians.
The post-acute care ecosystem serves individuals who need additional help recuperating from acute conditions, illnesses, or serious medical procedures after they have been discharged from the hospital. This ecosystem ranges from higher acuity, higher-cost settings, such as long-term acute care hospitals and inpatient rehabilitation facilities, to lower acuity, lower-cost settings, such as assisted living facilities, and home health. Skilled nursing facilities (SNFs) are positioned at the center of this ecosystem and play an essential role in providing cost efficient facility-based care to patients that have been discharged from hospitals but still require 24-hour in-patient services. SNFs can provide both long-term custodial care and higher value short-term transitional care. The SNF industry is large and growing, with the Centers for Medicare & Medicaid Services (CMS) expecting total industry expenditures to increase from $209.3 billion in 2023 to $337.4 billion in 2032, representing a compound annual growth rate (CAGR) of 5.4%. Based on the number of facilities as reported by CMS, we are one of the largest SNF operators in the United States. We are primarily focused on providing higher value short-term transitional care and believe we are uniquely positioned to capitalize on the current underlying trends within the SNF industry and to capture a growing portion of the expected demand.
We believe that healthcare is local and we operate through a decentralized model, recognizing that each patient, facility, and community is unique. To that end, we believe that our local leaders and employees understand the distinct needs and priorities of their patients, staff, and facilities and are best positioned to make clinical and operational decisions in order to optimize patient outcomes and experience. To facilitate this, each of our facilities operates independently, led by a facility administrator and his or her interdisciplinary team of medical directors, nurses, therapists, specialty consultants, and operators. To assist these local teams in achieving their best clinical and operating potential, we provide each facility with access to PACS Services. PACS Services is a comprehensive suite of offerings, including accounting, finance, human resources, payroll, accounts receivable and payable, legal, and risk management services, as well as a robust suite of technology tools. We operate in a highly regulated industry with stringent regulatory compliance obligations, which requires robust regulatory compliance operations. Failure to operate in compliance with applicable laws and regulations could require significant expenditures and result in regulatory deficiencies and other regulatory penalties. PACS Services functions to support our regulatory compliance obligations across our organization, including through controlled billing and cost reporting practices and
1
legal, risk management, and compliance support. PACS Services also provides teams of regional professionals available as resources to each facility, including a regional vice president (RVP) and regional clinical and non-clinical directors and consultants. We developed PACS Services to be a resource to help reduce administrative burden so that local leadership teams can focus on making decisions that improve the care, well-being, and quality of life of their patients.
We believe that talented local leadership is critical to the success of our model of independently operated, centrally supported facilities. At the facility level, administrators are effectively the chief executive officers, and together with other local licensed professionals, are ultimately responsible for the operations of their respective facilities. We seek to recruit, train, and reward dynamic administrators for our facilities, and rely on them to work with their interdisciplinary teams to implement policies and procedures that are appropriate and effective and result in positive outcomes. We support the delivery of excellent care by building excellent teams. We believe our model attracts high caliber, entrepreneurial professionals who value having considerable autonomy, accountability, and aligned incentives. We provide these professionals with leadership and industry training, guidance, and operational support. Our model is intended to align local leaders’ incentives with facility and organizational success, encouraging them to dedicate themselves to the long-term future of their facilities. To create such alignment, we have developed an administrator compensation structure that prioritizes quality of care and operational and financial performance. Our administrators understand that a well-performing facility is the result of providing quality care in an environment of healing and caring, and one that is appropriately staffed, supplied, and equipped to meet the needs of its patients. This dedicated focus by our administrators and their local teams on patient outcomes drives demand for our services and can ultimately result in higher patient census and profitability. We also seek to provide opportunities for upward career mobility, with many of our administrators being promoted from within our company to roles of increasing levels of responsibility. Our culture of meritocracy and pride of ownership has helped us retain experienced facility administrators as well as RVPs who had average industry experience of 7.3 years, as of June 30, 2024. For the year ended December 31, 2023, we had a voluntary turnover rate of 3.1% among our facility administrators.
Excellence in clinical quality and experience for our patients is at the forefront of our mission. We believe our focus on quality is reflected in our CMS Quality Measures (QM) Star rating, occupancy rate, and skilled mix by nursing patient days (which refers to the number of days our Medicare and managed care patients receive skilled nursing services at SNFs as a percentage of the total number of days that patients from all payor sources receive skilled nursing services at SNFs for any given period). The QM Star rating is a number between 1 and 5 that is assigned to SNFs that participate in Medicare or Medicaid, and is based on an aggregate score across a range of quality reporting program requirements. As of June 30, 2024, our average QM Star rating across all our facilities was 4.3 Stars, compared to the industry average of 3.5 Stars. For the six months ended June 30, 2024 and the years ended December 31, 2023, 2022 and 2021, our average occupancy rate across our Mature facilities, which we define as facilities purchased more than 36 months prior to the measurement date, was 94%, 93%, 92% and 88% , respectively, compared to the industry average of 76%, 76%, 74% and 71%. For the six months ended June 30, 2024, our skilled mix by nursing patient days was 30%.
We have historically grown primarily through our disciplined and balanced acquisition strategy. We aim to create value by identifying and acquiring underperforming custodial care facilities and converting them into higher-value short-term transitional care facilities by investing in clinical teams and processes and upgrading technology, equipment, training, staffing, aesthetics, and other aspects of the business. The resources and guidance offered by PACS Services is key to rapid integration of new facilities and provides our local leadership teams with an effective technology infrastructure, support tools, and regional support teams that allow local leadership to focus on operational improvements. Our facilities generally undergo an up to three-year post-acquisition transition period. During this period, we seek to implement best practices designed to realize and sustain the facility’s full potential. These practices often result in significant improvements to clinical quality and other operational metrics, including skilled mix, occupancy rates and payor contracting. We believe the results of our acquisition strategy are demonstrated by our high average QM Star rating and occupancy rate for Mature facilities of 4.3 and 94%, respectively, as of June 30, 2024. As of June 30, 2024, the average QM Star rating and occupancy rate for New facilities, which we define as facilities purchased less than 18 months prior to the measurement date, was 4.1 and 84%, respectively.
2
Our portfolio of owned and leased properties is strategically located in 15 states as of September 1, 2024: Alaska, Arizona, California, Colorado, Idaho, Kansas, Kentucky, Missouri, Montana, Nevada, Ohio, Oregon, South Carolina, Texas, and Washington. We anticipate that available acquisition opportunities will enable us to further penetrate these 15 states and to enter new states in the future. We believe our current markets are attractive and that each state in which we operate have unique benefits, such as favorable reimbursement dynamics, high barriers to entry, or population growth of adults aged 65 and older, which is our primary patient demographic. We generally look for similar attributes in new markets that we enter. As of June 30, 2024, we leased 170 facilities, owned partial real estate interests in an additional 12 leased facilities through joint ventures managed by third parties, and directly owned the real estate at 38 facilities. As we continue to grow, we intend to explore additional purchases of real-estate assets, through purchase options or right-of-first refusals in existing leases, as well as acquisitions and de novo construction of purpose-built facilities.
For the six months ended June 30, 2024 and 2023, we generated total revenue of $1.9 billion and $1.5 billion, respectively. A substantial portion of our revenue is generated from payments from third-party payors, including Medicare and Medicaid, which represent our largest sources of revenue and accounted for 36.6% and 38.4% of our total revenue for the six months ended June 30, 2024, respectively, and 44.8% and 32.9% of our total revenue for the six months ended June 30, 2023, respectively. For the six months ended June 30, 2024, we generated total net income of $38.2 million, total operating expense of $1.8 billion and Adjusted EBITDA of $188.2 million. For the six months ended June 30, 2023, we generated total net income of $58.8 million, total operating expense of $1.4 billion and Adjusted EBITDA of $122.4 million. For the year ended December 31, 2023, we generated total revenue of $3.1 billion, and Medicare and Medicaid accounted for 38.6% and 37.6% of our total revenue, respectively. For the year ended December 31, 2022, we generated total revenue of $2.4 billion, and Medicare and Medicaid accounted for 47.6% and 30.2% of our total revenue, respectively. For the year ended December 31, 2023, we generated total net income of $112.9 million, total operating expense of $2.9 billion and Adjusted EBITDA of $237.5 million. For the year ended December 31, 2022, our total operating expenses were $2.2 billion, and we generated net income of $150.5 million and Adjusted EBITDA of $255.5 million. As of June 30, 2024, we had total long-term liabilities of $2.9 billion. We intend to use all of the net proceeds to us from this offering to repay a portion of the amounts outstanding under our Amended and Restated 2023 Credit Facility. See the section titled “Use of Proceeds” for additional information. Adjusted EBITDA is a non-GAAP financial measure. For a reconciliation of Adjusted EBITDA to the most directly comparable GAAP financial measure, see the section titled “Management’s Discussion and Analysis of Financial Conditions and Results of Operations—Key Skilled Services Metrics and Non-GAAP Financial Measures—Non-GAAP Financial Measures.”
Our Value Proposition
We believe that our operating model creates meaningful value for patients and their families, our referring providers, our payors, and our administrators and clinicians.
Value Proposition for Patients and Families
•Coordinated care. We empower team members at every level through skillful training, shared resources, and a collaborative spirit. We help deliver coordinated care before, during, and after a patient’s stay with us. Prior to admission, our administrators or other facility leaders meet with patients and their families, as well as hospital discharge planners, to plan for the patient’s discharge and enable a seamless transition to our facility. During a stay with us, our local facility team coordinates closely with physicians to deliver high-touch, high-quality care for patients. As care nears completion, we meet with our patients, their families, home health agencies and downstream care providers to plan for and ensure a smooth transition.
•Outstanding patient experience. Our goal is to provide each patient with superior care and an outstanding experience. When patients arrive at our facilities they are greeted by a warm, inviting, and modern environment. We often upgrade facility infrastructure shortly after acquisition and perform periodic refreshes, to ensure our facilities are comfortable and well-equipped to serve patients across a wide range of acuities with a primary focus on high acuity patients. High acuity patients generally require higher levels of medical care or monitoring due to conditions or complications that cannot be easily managed, and often
3
need more nursing resources and attention to maintain their quality of life. We believe our investment in modern equipment and technology allows our facility care teams to identify and respond to patient needs and provide them high quality care in a timely manner. Moreover, our clinicians are highly trained, have significant experience, and are able to leverage bespoke care plans to help ensure that patients receive care tailored to their particular needs.
Value Proposition for Referring Providers
•Strategic and seamless transitions. Our administrators and their interdisciplinary teams seek to become a preferred partner by developing a deep understanding of local referring providers’ and their patients’ needs. Administrators often visit with patients and their families prior to discharge to plan for and map out a smooth admission to our facility. Once a plan is set, the facility team endeavors to quickly and seamlessly transition new patients to the facility with a focus on ensuring continuity of care in the transition. We believe that hospitals and other referral sources consider our facilities to be attractive discharge options because we are able to care for a wide variety of patient needs, and are often able to accept admissions on short notice, including on nights and weekends. Our flexibility helps hospitals maintain adequate bed availability to meet their other patients' needs.
•Trusted partner with quality care. Our ability to care for higher acuity patients allows referring providers to have confidence that we will be able to adequately care for their patients and assist them in their recovery. Our facilities seek to work with patients’ doctors to create personalized care plans to help ensure that patients stay on track in their recovery and to reduce the likelihood of their readmission to the hospital. Our facility teams also seek to coordinate closely with a patient’s home health agency or other post-SNF caregivers to try to ensure the patient’s transition home or to their next care setting is successful. This close coordination allows us, where warranted, to directly readmit patients back to our facility who would have otherwise been readmitted to an acute care hospital in the event they have a change of condition after leaving our facility.
Value Proposition for Payors
•Higher value site of care. We believe we provide high acuity care in a cost-effective setting and are able to quickly transition patients from the acute care setting, reducing length of stay and delivering more overall value for payors. Moreover, we believe we provide payors with a high-quality alternative to higher cost post-acute sites of care. For example, according to MedPAC, SNFs are the lowest cost facility-based post-acute healthcare, costing an average of $550 per covered day compared to $1,850 and $1,753 per covered day for inpatient rehabilitation facilities and long-term acute care hospitals, respectively.
•Robust culture of compliance. We focus on instilling a unified, cohesive culture of innovation and compliance that we believe provides consistency in our results and confidence in our facilities as an attractive care option for patients. Our rigorous approach to billing integrity, our independent internal compliance function, and our regular facility billing audits are intended to provide a foundation of trust and collaboration that makes us a natural choice for payors.
Value Proposition for Administrators and Clinicians
•Autonomy and aligned compensation. Each facility administrator is, in effect, the local “CEO” and dedicated leader of their facility. Alongside their local interdisciplinary team, they are empowered to make real-time decisions locally around all aspects of their business and to manage their individual facility in a way that they believe is best suited to address their local market and its needs. We have designed a transparent incentive model for our administrators that is intended to align their compensation with the quality of care and operational and financial performance of their facility. We provide them the tools and the autonomy to optimize the performance of their facility, and we reward them for success in their efforts. We believe that a well-performing facility is the result of providing quality care in an environment of healing and caring and one that is appropriately staffed, supplied, and equipped to meet the needs of its
4
patients. This dedicated focus by our administrators and their local teams on patient outcomes drives demand for our services and can ultimately result in higher patient census and profitability.
•Robust technology enabled operating infrastructure. We developed PACS Services to reduce the managerial and operational burden on our administrators, allowing them to focus on leading their facilities and spending more time with patients and staff. PACS Services includes a robust suite of technology tools that provide detailed real-time data and trends that local clinicians and leadership teams can use to monitor and improve operational performance. PACS Services also includes regional support teams that leverage their deep tenure and experience across markets to provide higher-level support to local leaders on complex issues, including billing and cost reporting practices and regulatory compliance obligations. The regional teams are connected to and support the facilities within their designated region, which enables them to identify best practices and trends within the region, communicate those across their region, and provide facility-level support as needed.
•Highly entrepreneurial career development. By providing our administrators with autonomy in the operation of their facility, we believe we create a highly entrepreneurial environment that encourages and rewards leaders to optimize operational performance. We empower our clinicians to do the same and provide top performers the opportunity to progress via training for higher skill licenses and certifications. People are provided the opportunity to advance to become an administrator through our Administrator-in-Training program, and to join a regional leadership team. For example, in the year ended December 31, 2023, we promoted 26 of our administrators from within our organization after participating in our Administrator-in-Training program, and 12 of our RVPs were previously successful administrators with us.
Our Competitive Strengths
We believe our success is driven by the following competitive strengths:
Superior Overall Quality
Excellence in clinical quality and experience for our patients is at the forefront of our mission and is reflected in our above-industry average QM Star rating and occupancy rate. Our facilities employ skilled administrators and clinicians and equip them with purpose-built technology and support so they can operate at the top of their professional capacity and deliver high-quality care for patients. We continuously invest in our people, processes, and facilities to promote an excellent patient experience. We believe we deliver superior overall quality that has contributed to our reputation as a provider-of-choice in our communities, driving greater referral volumes from referring providers who value our high standards.
Decentralized Market-Driven Operating Model
Our decentralized model emphasizes local operational autonomy. We believe that placing decision-making power at the local level with teams who understand the needs of their patients and their communities facilitates responsiveness and adaptability to evolving patient needs and facility and community factors. We believe the empowerment of local leadership promotes improved quality care for patients, greater referral volumes and higher occupancy rates. Our operating model is highly transferable to new markets, and enable us to quickly integrate and enhance new facilities.
Transparent and Meritocratic Leadership Culture
We have built a transparent, competitive, and collegial culture that promotes individual growth both personally and professionally and prioritizes a deep commitment to our patients, families, and team members. We promote transparency in performance, which we believe encourages collaboration and healthy competition among local leadership that in turn drives best practices. We believe this meritocratic culture, supported by highly seasoned industry veterans, helps optimize clinical and financial outcomes at facilities and instills accountability throughout
5
the organization. This leadership mindset has empowered us to develop a deep bench of leaders capable of supporting our existing and future facilities.
Employer-of-Choice with Directly Aligned Incentive Model
We believe that we are an employer-of-choice in the post-acute care industry, which enables us to attract and retain highly motivated, entrepreneurial individuals who value operational independence and financial opportunity. This has allowed us to attract enterprising individuals from diverse backgrounds who may not have otherwise considered careers in skilled nursing. Our unique compensation model is designed to align local individual incentives with the long-term clinical quality and operational performance of the facility, which we believe fosters a shared ownership mentality. We believe this directly aligned incentive model has played a critical role in successfully attracting, incentivizing, and retaining our industry veterans.
Robust Suite of Technology-Enabled Services
Our technology focus delivers real-time data access to caregivers and administrators, facilitating delivery of the right care at the right time. Our technology tools enable our local leadership teams to focus on their first priority, providing the highest quality care possible to patients. We believe our suite of technologies helps drive decision-making and enhances operating efficiencies that can improve clinical quality, operational metrics, and the financial performance of our facilities. While other facility administrators may spend considerable time on paperwork and low-value activities, we strive to reduce the administrative burden on our facility administrators so they can walk the halls, personally meet patients, and provide a bespoke, concierge-level customer service experience. We equip our clinicians with industry-leading technology, including point-of-care and digital charting technologies, which streamlines charting and paperwork, so they can spend more time with patients and focus on providing high quality care. We believe our technology and internally developed dashboards help to facilitate better patient care, risk management, regulatory compliance, staffing, and resource allocation. We have designed our technology to be easily integrated into new facilities and allow us to scale quickly and efficiently.
Differentiated, Multi-faceted, and Disciplined Acquisition Playbook
Over the past decade, we have demonstrated the effectiveness of our disciplined, multi-faceted playbook of acquiring and improving underperforming facilities, having successfully acquired and integrated over 260 facilities to date. We believe we have established a reputation as an acquiror-of-choice, which has led to several inbound opportunities, and has helped us build an extensive opportunity pipeline. Our balanced approach to evaluation allows us to selectively pursue opportunities that meet our strategic priorities and criteria and grow in a responsible manner. Through our investment into facilities and our integration process, we are able to transition new underperforming facilities to higher-value short-term transitional care facilities. We believe our success is evidenced by our robust QM Star ratings, occupancy rates, and profitability at our Mature facilities.
Our High-Quality Facilities
We are committed to providing a high-quality experience for all of our patients, which is why we invest in capital improvements and ongoing maintenance to all of our facilities, regardless of whether we lease or own. Our investment into facilities is differentiated from traditional industry operators who we believe are often hesitant to make physical plant investments into facilities and who often seek to extract value through cost-cutting or other limitations on facility resources. Our renovations are intended to improve the look and feel of facilities in order to provide an excellent experience. Our investments into medical beds, vitals monitors, physical therapy equipment, and other improvements allows us to provide services to higher acuity patients. We believe our high-quality facilities lead to sustained referral volumes, more admissions, and high skilled mix at our facilities, ultimately leading to higher occupancy rates and revenue per patient day. We also believe our investment into leased facilities makes us a preferred tenant with our landlords and provides us leverage in negotiating favorable lease terms.
6
Our Size and Scale
We believe our market density in key regions offers strategic advantages, such as brand recognition with referring providers, including hospitals and health systems, and consistency and continuity of referrals of patients. For example, our ability to accommodate a high volume of patients within our markets allows us to accept referrals without turning patients away to competitors, and can also further our reputation as a reliable, go-to provider of care for referring providers. We also believe our size and scale has provided us with the ability to negotiate favorable contracts with managed care and other payor sources, the ability to navigate stringent regulatory compliance obligations and withstand potential reimbursement and regulatory industry dynamics, and the ability to leverage real estate value for liquidity and growth.
Industry Overview and Market Opportunity
The Post-Acute Care Continuum is Essential to the Healthcare Ecosystem
We operate in the post-acute care industry, which is an essential component of the healthcare delivery ecosystem, serving high need, medically fragile patients. Post-acute care encompasses multiple care settings outside of acute care hospitals that are differentiated by the acuity level of patients and the services they require. While services may overlap across each distinct post-acute offering, post-acute rehab or SNFs provide the most comprehensive array of services. Upstream care providers, such as acute care hospitals, generally discharge patients to post-acute facilities where patients can receive key services at lower costs.
SNFs are an Integral and Essential Part of the Post-Acute Care Continuum
SNFs play an essential role in post-acute patient care. SNFs provide higher-acuity skilled nursing care to patients that cannot be adequately treated in community-based care settings, such as assisted living or independent living facilities, and who are no longer appropriate candidates for hospital care. Patients referred to a SNF are typically recovering from surgery or non-critical conditions, such as strokes, joint replacements, and acute infections, and are admitted to a SNF within 30 days of being discharged from a hospital where they spent at least three days as an inpatient. In many instances, patients are treated at SNFs prior to receiving home health nursing care and therapy services. The majority of SNF patients are aged 65 years or older. Despite the wide array of services and variety of needs addressed, MedPAC reports that SNFs are the lowest cost facility-based post-acute healthcare, costing on average $550 per covered day compared to $1,850 and $1,753 per covered day for inpatient rehabilitation facilities and long-term acute care hospitals, respectively. According to CMS MedPAC data, SNFs accounted for approximately 44% of the total post-acute care continuum spend. According to CMS Inpatient Hospital discharge data, in 2022, approximately 22% of Medicare patients over 65 years old were discharged to SNFs, representing more than any other facility type, including inpatient rehabilitation facilities and long-term acute care hospitals (approximately 6%), and more than home health nursing care (21%) or hospice (5%). As reimbursement and coverage continues to shift toward value-based models with greater emphasis on controlling costs, SNFs are integral to post-acute care and will continue to drive high-quality outcomes in low-cost settings. Furthermore, during the COVID-19 pandemic, SNFs were widely utilized to treat medically fragile patients, reinforcing the importance of SNFs to the healthcare ecosystem.
Large, Fragmented Industry Comprised of Mostly Small and Independent Operators
According to the National Center for Health Statistics (NCHS) 2020 National Post-acute and Long-term Care Study, the SNF industry in the United States encompasses approximately 15,000 facilities and serves approximately 1.3 million patients annually. The industry is highly fragmented, with the top 10 operators, each having greater than 100 facilities, representing approximately 11% of total number of SNFs in the United States, according to CMS data as of September 2022, approximately 5,000 smaller and independent operators of less than 100 facilities making up the remainder. According to this data, of the approximately 15,000 facilities, approximately 13,200 facilities have less than 100 beds, and approximately 74% and 26% of SNFs are located in urban and rural areas, respectively. In addition, approximately 72%, 23%, and 6% of SNFs are operated as for-profit, as non-profit, and by the government, respectively, according to such data. We believe this fragmented landscape creates opportunities for
7
larger providers with greater scale to serve patients better and meet regulatory requirements nation-wide by effectively addressing staffing, quality standards, and billing processes. Moreover, many small and independent operators face pressure due to billing requirements, regulations, competition on quality of care and facilities, staffing shortages and competition, and the cessation of COVID-related provider relief funding, which has led them to pursue sales of their facilities or businesses. This provides additional opportunity for well-managed, high-quality operators to grow through acquisitions.
Growing Demand Outpacing Supply of Skilled Nursing Facilities
The demand for healthcare services in the United States has increased in recent years and is expected to continue growing, largely due to a rapidly aging population and an increasing prevalence of chronic conditions. According to the U.S. Census Bureau, the U.S. population aged 65 and older is expected to nearly double from 2020 to 2060 and reach 95 million in 2060, which exceeds the expected increase in the general population during that same period, and comprise one fifth of the total U.S. population in 2030. Moreover, according to the U.S. Census Bureau, the U.S. population aged 85 and older is expected to nearly triple from 2020 to 2060 and reach 19 million in 2060. Additionally, according to an article published in Frontiers in Public Health in 2022, the percentage of people in the United States aged 50 and older with at least one chronic condition is estimated to increase by 99.5% from 2020 to 2050. According to CMS data as of September 2022, approximately 82% of SNF patients were 65 years of age or older.
As demand has increased for SNFs, the number of SNFs has declined in recent years from approximately 15,650 in 2017 to approximately 14,900 in 2023. We believe this is due to a variety of factors, including an inability of many facilities to comply with the industry’s stringent regulatory compliance obligations and with quality standards, rigorous staffing, and billing requirements, as well as a lack of technology and sophistication at small and independent operators. Furthermore, new operators to this highly regulated industry face multiple barriers to entry, including the requirements to obtain a Certificate of Need, complex licensure and regulatory compliance requirements, lack of operating experience, and significant capital requirements. As a result, the addition of new SNFs has not kept pace with the number of SNFs exiting the market, amplifying the need for skilled nursing to serve an aging population.
Favorable Reimbursement Environment
According to CMS, approximately 72% of SNF revenue in 2022 was derived from government sources, including Medicaid and Medicare. Medicaid represents 51% of industry revenue, while Medicare represents approximately 21%. The remainder comprises managed care, private pay, and other payors. Medicare and Medicaid reimbursement has steadily increased over the past few years. Medicare reimbursement per patient day increased at a CAGR of approximately 3.6% from 2012 to 2021, while Medicaid reimbursement per patient day increased at a CAGR of approximately 1.9% from 2012 to 2021. The industry has experienced over 9 years of growth in reimbursement rates.
Regulatory Environment
The SNF industry is highly regulated with stringent regulatory compliance obligations. In the ordinary course of business, providers are subject to federal, state and local laws and regulations relating to, among other things, billing and reimbursement, relationships with vendors, business relationships with physicians and other healthcare providers and facilities, as well as licensure, accreditation, enrollment, quality, adequacy of care, physical plant, life safety, personnel, staffing and operating requirements. Changes in or new interpretations of existing laws and regulations may have a significant impact on revenue, costs and business operations of providers and other industry participants. In addition, governmental and other authorities periodically inspect the SNFs, senior living facilities and outpatient rehabilitation agencies to verify continued compliance with applicable regulations and standards, and may impose citations and other regulatory penalties for regulatory deficiencies. Such regulatory penalties include but are not limited to civil monetary penalties, temporary payment bans, suspension or revocation of a state operating license and loss of certification as a provider in the Medicare or Medicaid program, any of which may be
8
temporary or permanent in nature. This regulatory environment and related enforcement can have an adverse effect on providers and other industry participants.
Our Market Opportunity
Despite the decline in the number of SNFs, the industry is large and growing, with CMS expecting total industry expenditures to increase from $209.3 billion in 2023 to $337.4 billion in 2032, representing CAGR of 5.4%. Based on the number of facilities as reported by CMS, we are one of the largest SNF operators in the United States and believe our scale and other competitive strengths uniquely position us to capitalize on the current underlying trends within the SNF industry and capture a growing portion of this expected growth.
Our Growth Strategies
We have built a multi-faceted growth strategy with multiple organic and inorganic levers to help drive our growth and capitalize on the favorable industry dynamics. To continue our growth, we intend to:
•Expand our presence in existing and new markets. We have a robust pipeline of potential single-facility tuck-in acquisitions, larger multi-facility portfolio acquisitions and select new facility builds across existing and new markets. We have historically completed an average of approximately 20 acquisitions and one de novo, or new-build, facility per year, but have the flexibility to increase or decrease this cadence from period to period in line with our business priorities and as strategic opportunities arise. We plan to continue to strategically pursue opportunities within our pipeline to supplement our organic growth. While we expect to continue to execute on this strategy, we do not have binding agreements or commitments for any material investments at this time.
•Leverage operational upside within our existing footprint. Our portfolio has a healthy foundation for strong embedded organic growth. We are focused on driving higher occupancy and increasing skilled mix in an effort to fill unused capacity with higher acuity patients, which can improve our revenue per patient day and our profitability, which in turn drive growth. Historically, we have found that it takes up to 3 years for a New facility to scale to performance similar to that of a Mature facility. As of June 30, 2024, we had 70 New facilities and 85 Ramping facilities, which we define as facilities purchased within 18 to 36 months prior to the measurement date. We believe these facilities provide us some degree of near-term visibility into expected organic growth within our footprint.
•Continue to grow our pipeline of leaders. Our rapid growth in size and scale can be attributed to our deep bench of talented leaders. Our administrators in training provide us with leadership resources that we can use to quickly staff new facilities with qualified operators. Similarly, our RVPs enable us to scale within regions. We intend to invest heavily in training existing leaders and expanding our bench of new administrators and RVPs to support our future growth.
•Extract embedded value from real estate ownership. We plan to continue to evaluate our real estate purchase options in an effort to reduce our rent burden and grow the underlying earnings of our business. We have executed 18 purchase options since 2013 and had 13 additional options available to us as of June 30, 2024. We intend to continue to selectively exercise purchase options and continue structuring additional purchase options to provide an additional lever to grow net margins and enhance stockholder value. Moreover, we believe that our real estate ownership provides balance sheet support as an inflationary hedge, provides capital flexibility as a source of asset collateral, reduces the burden of leases and restrictive agreements, and allows us the opportunity to create additional value in improving distressed assets.
•Ancillary opportunities. We have identified and continue to evaluate multiple investment opportunities that have the potential to improve our post-acute patient experience by augmenting the services we provide. We may capitalize on these investment opportunities that are ancillary to our core business, such as pharmacy services, laboratory services, transportation, and imaging, which have the potential to be additional sources of revenue and operating income over time. We refer to these efforts to build a strategic mix of investments
9
in ancillary business lines as “PACS Ventures.” We continue to evaluate opportunities to in-source, acquire, and commercialize these ancillary opportunities. Additionally, we may choose to monetize our PACS Services by offering it to third-party SNF operators in the future.
•Expand into other post-acute sites of care. We believe that our proven operational playbook and focus on delivering high-quality care have the potential to be utilized in additional post-acute sites of care, including home health and hospice as well as within broader senior living communities. As of June 30, 2024, we had one independent living facility and five assisted living facilities which provide a foundation for further expansion.
Recent Developments
Initial Public Offering
On April 15, 2024, we closed our initial public offering (IPO), which consisted of 21,428,572 shares of common stock sold by us and 3,214,284 shares of common stock sold by selling stockholders, at a public offering price of $21.00 per share, which resulted in $423.0 million in net proceeds to us. We did not receive any of the proceeds from the sale of shares of common stock by the selling stockholders in the IPO. We used approximately $370.0 million of the net proceeds received by us in the IPO to repay amounts outstanding under our Amended and Restated 2023 Credit Facility, and the remaining amount for general corporate purposes to support the growth of our business.
Recent Acquisitions
On May 22, 2024, we announced the pending acquisition of operations of 53 skilled nursing and assisted living and independent living facilities across eight states, including Oregon (21 facilities), Washington (19 facilities), Idaho (six facilities), Nevada (three facilities), and one facility in each of Alaska, Arizona, California and Montana. The facilities were historically operated by subsidiaries of Prestige Care, Inc., a family company. Collectively, the facilities comprise 2,511 skilled nursing beds and 1,334 assisted living and independent living units. We will lease 37 of the facilities from a joint venture in which we own a 25% interest, and the remaining 16 facilities will be leased from unaffiliated third-party landlords. As of June 30, 2024, we had not finalized the acquisition of any of these operations. Since June 30, 2024, we have finalized the acquisition of operations for 53 of these facilities, representing 2,511 skilled nursing beds and 1,334 assisted living and independent living units.
On July 15, 2024, we finalized the acquisition of operations for 3 skilled nursing facilities. The operations are located in Kansas. Collectively, these facilities comprise 378 skilled nursing beds. These facilities are leased from a third-party landlord, with the option to purchase the facilities from the landlord at a later date.
Summary Risk Factors
There are a number of risks that you should understand before making an investment decision regarding this offering. You should carefully consider all of the information in this prospectus, including risks and uncertainties described in the sections titled “Management’s Discussion and Analysis of Financial Condition and Results of Operations” and “Risk Factors,” before making a decision to invest in our common stock. If any of these risks actually occur, it could have a material adverse effect on our business, financial condition, and results of operations. In such case, the trading price of our common stock would likely decline, and you could lose all or part of your investment. These risks include, but are not limited to:
•We depend upon reimbursement from third‑party payors, and our revenue, financial condition and results of operations could be negatively impacted by any changes in the acuity mix of patients in our facilities as well as changes in payor mix and payment methodologies and new cost containment initiatives by third-party payors;
10
•We may not be fully reimbursed for all services for which each facility bills through consolidated billing or bundled payments, which could have an adverse effect on our revenue, financial condition and results of operations.
•Increased competition for, or a shortage of, nurses, nurse assistants and other skilled personnel could increase our staffing and labor costs and subject us to monetary fines.
•We rely on payments from third-party payors, including Medicare, Medicaid and other governmental healthcare programs and private insurance organizations. If coverage or reimbursement for services are changed, reduced or eliminated, including through cost-containment efforts, spending requirements are changed, data reporting, measurement and evaluation standards are enhanced and changed, our operations, revenue and profitability could be materially and adversely affected.
•Reforms to the U.S. healthcare system, including new regulations under the Affordable Care Act (ACA), continue to impose new requirements upon us that could materially impact our business.
•We are subject to various government and third-party payor reviews, audits and investigations that could adversely affect our business, including an obligation to refund amounts previously paid to us, potential criminal charges, the imposition of fines, and/or the loss of our right to participate in Medicare and Medicaid programs or other third-party payor programs.
•State efforts to regulate or deregulate the healthcare services industry or the construction expansion, or acquisition of healthcare facilities could impair our ability to expand our operations, or could result in increased competition.
•We face numerous risks related to expiration of the COVID‑19 public health emergency (PHE) expiration and surrounding wind down and uncertainty, which could, individually or in the aggregate, have a material adverse effect on our business, financial condition, liquidity, results of operations and prospects.
•If we fail to attract patients and residents and to compete effectively with other healthcare providers, our revenue and profitability may decline and we may incur losses.
•We review and audit the care delivery, recordkeeping and billing processes of our operating subsidiaries. These reviews from time to time detect instances of noncompliance that we attempt to correct, which in some instances requires reduced or repayment of billed amounts or other costs.
•We are subject to litigation, which is commonplace in our industry, which could result in significant legal costs and large settlement amounts or damage awards, and our self-insurance programs may expose us to significant and unexpected costs and losses.
•We rely significantly on information technology, and any failure, inadequacy or interruption of that technology could harm our ability to effectively operate our business.
•We may be unable to complete future facility or business acquisitions at attractive prices or at all, which may adversely affect our revenue; we may also elect to dispose of underperforming or non‑strategic operating subsidiaries, which would decrease our revenue.
•In undertaking acquisitions, we may be adversely impacted by costs, liabilities and regulatory issues that may adversely affect our operations, and we may not be able to successfully integrate acquired facilities and properties into our operations, or achieve the benefits we expect from any of our facility acquisitions.
•Because we lease the majority of our facilities, we are subject to risks associated with leased real property, including risks relating to lease termination, lease extensions and special charges, any of which could have an adverse effect on our business, financial condition and results of operations.
11
•We operate in a highly regulated industry with stringent regulatory compliance obligations, and are subject to extensive and complex laws and government regulations. If we are not operating in compliance with these laws and regulations or if these laws and regulations change, we could be required to make significant expenditures or change our operations in order to bring our facilities and operations into compliance.
•We have broad discretion in how we may use the net proceeds from this offering, and we may not use them effectively. We intend to use all of the net proceeds to us from this offering to repay amounts outstanding under our Amended and Restated 2023 Credit Facility, which will reduce the extent of the net proceeds available for general corporate purposes to support the growth of our business.
•Following this offering, our founders, Jason Murray and Mark Hancock, will collectively own a significant majority of our common stock, representing approximately 73.7% of the voting power of our common stock (or approximately 72.4% if the underwriters exercise their option to purchase additional shares of our common stock from the selling stockholders in full). In addition, pursuant to the terms of our Amended and Restated Charter, our founders are able to control corporate matters for the foreseeable future. For example, each founder has the right to designate (i) up to two individuals for inclusion in our slate of director nominees if such founder beneficially owns at least 20% of the aggregate number of shares of common stock outstanding immediately following the completion of our IPO or (ii) one individual for inclusion in our slate of director nominees if such founder beneficially owns less than 20% but at least 10% of the aggregate number of shares of common stock outstanding immediately following the completion of our IPO. Accordingly, each founder has the right to designate two directors, and our founders collectively have the right to designate four directors, which represents four out of our five member board of directors. These rights are affirmed in the Stockholders Agreement. In addition, pursuant to the terms of our Amended and Restated Charter, for so long as our founders beneficially own, in the aggregate, the majority of the voting power of our outstanding shares of voting stock, our founders are able to remove any of our directors at any time with or without cause and may take action by written consent without a meeting of stockholders. Our Amended and Restated Charter authorizes our board of directors to establish and determine, among others, the voting, board representation and other rights or preferences of one or more series of preferred stock, and our board of directors may determine to issue additional shares of common stock, in each case without stockholder approval. This concentrated control, due to both the provisions of the Amended and Restated Charter and Stockholders Agreement and the voting power of our founders, will preclude your ability to influence corporate matters for the foreseeable future, including with respect to the composition of our board of directors, the election and removal of directors, the authorization and issuance of additional shares of our common stock that would be dilutive to you, the issuance of shares of preferred stock that could be dilutive to you and could have disparate voting rights, amendments to our organizational documents, and any merger, consolidation, sale of all or substantially all of our assets, or other major corporate transactions requiring stockholder approval.
•Our founders have entered into margin loans and pledged a portion of their shares of our common stock as collateral to secure such margin loans. If either Mr. Murray or Mr. Hancock default on their respective obligations under any margin loans, the lender may be entitled to foreclose on their shares pledged as collateral and sell them to the public, which could cause our stock price to decline and result in a significant change in beneficial ownership.
•We are a “controlled company” within the meaning of the corporate governance standards of the New York Stock Exchange. As a result, we may elect to rely on exemptions from certain corporate governance standards and you may not have the same protections afforded to stockholders of companies that are subject to such requirements.
•Affiliates of Citigroup Global Markets Inc., J.P. Morgan Securities LLC, Truist Securities, Inc., and RBC Capital Markets, LLC, each an underwriter in this offering, will each receive at least 5% of the net proceeds of this offering and may have an interest in this offering beyond customary underwriting discounts and commissions.
12
Corporate Information
We were initially incorporated on December 17, 2012 as Providence Group, Inc., a California corporation. On June 30, 2023, we undertook a reorganization in connection with our entry into a new credit agreement described in more detail in the section titled “Management’s Discussion and Analysis of Financial Conditions and Results of Operations—Liquidity & Capital Resources—Credit Facilities.” Pursuant to this reorganization, PACS Group, Inc., which was incorporated on March 24, 2023 as a Delaware corporation, became the parent entity for our organization. The following diagram sets forth a simplified view of our corporate structure as of June 30, 2024. This chart is for illustrative purposes only and does not represent all legal entities affiliated with the entities depicted. The operating subsidiaries that represent our various facilities are omitted.
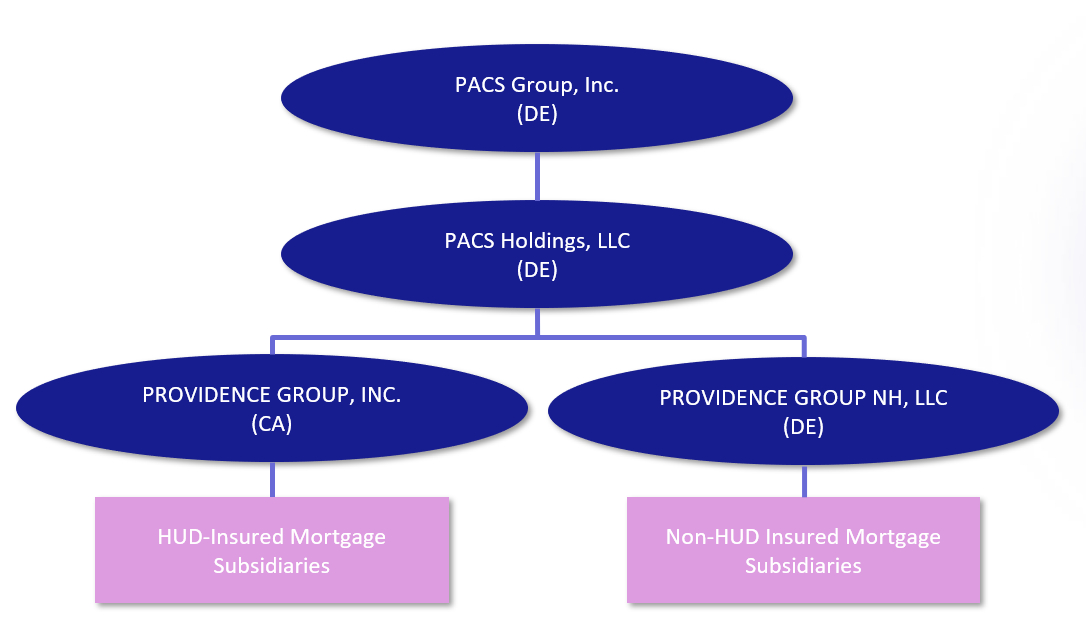
PACS Group, Inc. is a holding company with operating subsidiaries that provide skilled nursing, senior living, as well as other ancillary businesses. Each facility is structured as an operating subsidiary under one of our two subsidiary holding companies: Providence Group, Inc. and Providence Group NH, LLC. Subsidiaries of Providence Group, Inc. are currently operating subsidiaries (facilities) with mortgage loans insured by the U.S. Department of Housing and Urban Affairs. Subsidiaries of Providence Group NH, LLC are currently operating subsidiaries (facilities) without such mortgage loans.
PACS Group, Inc. and its subsidiaries that are not licensed healthcare providers do not provide healthcare services to patients, residents or any other person, and do not direct or control the provision of services provided. All healthcare services are provided solely by applicable subsidiaries that are licensed healthcare providers, under the direction and control of licensed healthcare professionals in accordance with applicable law.
Our principal executive offices are located at 262 N. University Ave, Farmington, Utah 84025, and our telephone number is (801) 447-9829. Our website address is www.pacs.com. Information contained on, or that can be accessed through, our website is deemed not to be incorporated in this prospectus and does not constitute part of this prospectus, and the inclusion of our website address in this prospectus is an inactive textual reference only. Investors should not rely on any such information in deciding whether to purchase our common stock.
13
Status as a Controlled Company
The rules of the New York Stock Exchange define a “controlled company” as a company of which more than 50% of the voting power for the election of directors is held by an individual, a group or another company. Following this offering, our founders will collectively own a significant majority of our common stock, representing approximately 73.7% of the voting power of our common stock (or approximately 72.4% if the underwriters exercise their option to purchase additional shares of our common stock from the selling stockholders in full). We are a “controlled company” under the rules of the New York Stock Exchange. As a result, we qualify for and may elect to rely on exemptions from certain corporate governance requirements under the rules.
If we cease to be a controlled company and our common stock continues to be listed on the New York Stock Exchange, we will be required to take all action necessary to comply with applicable rules. See the sections titled “Management—Director Independence and Controlled Company Exception” and “Risk Factors—We are a “controlled company” within the meaning of the corporate governance standards of the New York Stock Exchange. As a result, we may elect to rely on exemptions from certain corporate governance standards and you may not have the same protections afforded to stockholders of companies that are subject to such requirements.”
14
THE OFFERING
| Common stock offered by us | 2,777,778 shares. | |||||||
| Common stock offered by the selling stockholders | 11,111,112 shares. | |||||||
| Underwriters’ option to purchase additional shares of common stock from the selling stockholders | The selling stockholders have granted the underwriters an option for a period of 30 days from the date of this prospectus to purchase up to 2,083,332 additional shares of our common stock. | |||||||
| Common stock to be outstanding after this offering | 155,177,511 shares. | |||||||
| Use of proceeds | We estimate that we will receive net proceeds from this offering of approximately $104.8 million, based upon the assumed public offering price of $39.67 per share, which is the last reported sale price of our common stock as reported on the New York Stock Exchange on August 30, 2024 and after deducting estimated underwriting discounts and commissions and estimated offering expenses payable by us. We intend to use all of the net proceeds to us from this offering to repay amounts outstanding under our Amended and Restated 2023 Credit Facility. We will have broad discretion in the way that we use the net proceeds of this offering. We will not receive any proceeds from the sale of shares of common stock by the selling stockholders. See the section titled “Use of Proceeds” for additional information. | |||||||
| Controlled company | We are a “controlled company” within the meaning of the corporate governance rules of the New York Stock Exchange. As a “controlled company,” we may elect to rely on exemptions from certain corporate governance standards of the New York Stock Exchange. See the section titled “Management—Director Independence and Controlled Company Exception.” | |||||||
| Conflicts of interest | Because affiliates of Citigroup Global Markets Inc., J.P. Morgan Securities LLC, Truist Securities, Inc. and RBC Capital Markets, LLC are lenders under our Amended and Restated 2023 Credit Facility and will each receive at least 5% of the net proceeds to us from this offering in connection with the repayment of amounts outstanding under our Amended and Restated 2023 Credit Facility, a “conflict of interest” within the meaning of Rule 5121 of the Financial Industry Regulatory Authority, Inc. (FINRA) is deemed to exist. Accordingly, this offering is being made in compliance with the applicable requirements of FINRA Rule 5121. The appointment of a “qualified independent underwriter” is not necessary for this offering pursuant to FINRA Rule 5121(a)(1)(B) as a “bona fide public market,” as defined in FINRA Rule 5121, exists for our common stock. See the sections titled “Use of Proceeds” and “Underwriting (Conflicts of Interest)” for additional information. | |||||||
15
| Dividend policy | We have no current plans to pay dividends or other distributions on our common stock in the foreseeable future. Any decision to declare and pay dividends in the future will be made at the sole discretion of our board of directors and will depend on, among other things, our results of operations, cash requirements, financial condition, contractual restrictions and other factors that our board of directors may deem relevant. See the section titled “Dividend Policy.” | |||||||
| Risk factors | Investing in our common stock involves a high degree of risk. See the section titled “Risk Factors” and the other information included in this prospectus for a discussion of factors you should carefully consider before deciding to invest in shares of our common stock. | |||||||
| New York Stock Exchange trading symbol | Our common stock is listed and traded on the New York Stock Exchange under the symbol “PACS.” | |||||||
The number of shares of our common stock to be outstanding after this offering is based on 152,399,733 shares of our common stock outstanding as of June 30, 2024, and excludes:
•1,580,986 shares of common stock reserved for future issuance under our 2024 Incentive Award Plan (2024 Plan);
•11,561,818 shares of common stock issuable upon vesting of all restricted stock units (RSUs) awarded; and
•1,501,520 shares of common stock reserved for future issuance under our 2024 Employee Stock Purchase Plan (ESPP).
Our 2024 Plan and our ESPP provide for annual automatic increases in the number of shares reserved thereunder.
Except as otherwise indicated, all information in this prospectus, including the number of shares of our common stock that will be outstanding after this offering, reflects and assumes:
•a 1-for-6,436.1693 split of our common stock effected on April 1, 2024;
•no exercise by the underwriters of their option to purchase additional shares of our common stock from the selling stockholders; and
•the assumed public offering price of $39.67 per share, which is the last reported sale price of our common stock on the New York Stock Exchange on August 30, 2024.
16
SUMMARY COMBINED/CONSOLIDATED FINANCIAL AND OTHER DATA
The following tables summarize our combined/consolidated financial and other data for the periods and as of the dates indicated. The summary combined/consolidated statements of income for the years ended December 31, 2023, 2022 and 2021 have been derived from our audited combined/consolidated financial statements included elsewhere in this prospectus. The summary condensed combined/consolidated statements of income for the six months ended June 30, 2024 and 2023 and the condensed combined/consolidated balance sheet data as of June 30, 2024 have been derived from our unaudited interim condensed combined/consolidated financial statements included elsewhere in this prospectus. The summary combined/consolidated financial and other data set forth below should be read together with the section of this prospectus titled “Management’s Discussion and Analysis of Financial Condition and Results of Operations” and the audited combined/consolidated financial statements and the related notes included elsewhere in this prospectus. The summary combined/consolidated financial and other data in this section are not intended to replace our audited combined/consolidated financial statements and the related notes and are qualified in their entirety by our audited combined/consolidated financial statements and the related notes included elsewhere in this prospectus. Our historical results are not necessarily indicative of the results to be expected in the future.
17
Combined/Consolidated Statements of Income
| Year Ended December 31, | Six Months Ended June 30, | ||||||||||||||||||||||||||||
| 2023 | 2022 | 2021 | 2024 | 2023 | |||||||||||||||||||||||||
| (unaudited) | |||||||||||||||||||||||||||||
| (in thousands, except share and per share data) | |||||||||||||||||||||||||||||
| Revenue | |||||||||||||||||||||||||||||
| Patient and resident service revenue | $ | 3,110,114 | $ | 2,399,155 | $ | 1,135,909 | $ | 1,915,696 | $ | 1,468,250 | |||||||||||||||||||
| Additional funding | $ | 375 | $ | 21,482 | $ | 28,563 | $ | — | $ | 375 | |||||||||||||||||||
| Other revenues | $ | 1,003 | $ | 1,357 | $ | 2,091 | $ | 871 | $ | 481 | |||||||||||||||||||
| Total Revenue | $ | 3,111,492 | $ | 2,421,994 | $ | 1,166,563 | $ | 1,916,567 | $ | 1,469,106 | |||||||||||||||||||
| Expenses | |||||||||||||||||||||||||||||
| Cost of services | $ | 2,447,713 | $ | 1,861,314 | $ | 901,095 | $ | 1,498,139 | $ | 1,129,587 | |||||||||||||||||||
| Rent-cost of services | $ | 216,711 | $ | 160,003 | $ | 78,122 | $ | 129,794 | $ | 96,560 | |||||||||||||||||||
| General and administrative expense | $ | 213,664 | $ | 149,006 | $ | 96,834 | $ | 191,286 | $ | 122,137 | |||||||||||||||||||
| Depreciation and amortization | $ | 25,632 | $ | 22,311 | $ | 7,153 | $ | 16,678 | $ | 11,988 | |||||||||||||||||||
| Total Operating Expenses | $ | 2,903,720 | $ | 2,192,634 | $ | 1,083,204 | $ | 1,835,897 | $ | 1,360,272 | |||||||||||||||||||
| Operating Income | $ | 207,772 | $ | 229,360 | $ | 83,359 | $ | 80,670 | $ | 108,834 | |||||||||||||||||||
| Other (expense) income | |||||||||||||||||||||||||||||
| Interest expense | $ | (49,919) | $ | (25,538) | $ | (5,278) | $ | (24,578) | $ | (25,942) | |||||||||||||||||||
| Gain on lease termination | $ | — | $ | — | $ | — | $ | 8,046 | $ | — | |||||||||||||||||||
| Other (expense) income, net | $ | (536) | $ | 3,223 | $ | 3,345 | $ | (3,465) | $ | (2,203) | |||||||||||||||||||
| Total Other Expense, net | $ | (50,455) | $ | (22,315) | $ | (1,933) | $ | (19,997) | $ | (28,145) | |||||||||||||||||||
| Income before provision for income taxes | $ | 157,317 | $ | 207,045 | $ | 81,426 | $ | 60,673 | $ | 80,689 | |||||||||||||||||||
| Provision for income taxes | $ | (44,435) | $ | (56,549) | $ | (33,479) | $ | (22,441) | $ | (21,871) | |||||||||||||||||||
| Net income | $ | 112,882 | $ | 150,496 | $ | 47,947 | $ | 38,232 | $ | 58,818 | |||||||||||||||||||
| Less: | |||||||||||||||||||||||||||||
| Net income attributable to noncontrolling interest | $ | 8 | $ | — | $ | — | $ | 4 | $ | 3 | |||||||||||||||||||
| Net income attributable to PACS Group, Inc. | $ | 112,874 | $ | 150,496 | $ | 47,947 | $ | 38,228 | $ | 58,815 | |||||||||||||||||||
| Net income per share attributable to PACS Group, Inc. | |||||||||||||||||||||||||||||
| Basic | $ | 0.88 | $ | 1.17 | $ | 0.37 | $ | 0.27 | $ | 0.46 | |||||||||||||||||||
| Diluted | $ | 0.88 | $ | 1.17 | $ | 0.37 | $ | 0.27 | $ | 0.46 | |||||||||||||||||||
| Weighted-average common shares outstanding | |||||||||||||||||||||||||||||
| Basic | 128,723,386 | 128,723,386 | 128,723,386 | 139,093,520 | 128,723,386 | ||||||||||||||||||||||||
| Diluted | 128,723,386 | 128,723,386 | 128,723,386 | 139,684,618 | 128,723,386 | ||||||||||||||||||||||||
18
Combined/Consolidated Balance Sheet Data
| As of June 30, 2024 | |||||||||||
| Actual | As Adjusted(1)(2) | ||||||||||
| (in thousands, unaudited) | |||||||||||
| Cash and cash equivalents | $ | 73,374 | $ | 73,374 | |||||||
Working capital(3) | $ | 332,547 | $ | 332,547 | |||||||
| Total assets | $ | 3,896,348 | $ | 3,896,348 | |||||||
| Long-term liabilities | $ | 2,850,013 | $ | 2,745,213 | |||||||
| Total liabilities | $ | 3,318,114 | $ | 3,213,313 | |||||||
| Retained earnings | $ | 100,504 | $ | 100,504 | |||||||
| Total stockholders’ equity | $ | 572,128 | $ | 676,928 | |||||||
__________________
(1)The as adjusted combined/consolidated balance sheet data gives effect to the sale and issuance of 2,777,778 shares of common stock by us in this offering, based on the assumed public offering price of $39.67 per share, which is the last reported sale price of our common stock as reported on the New York Stock Exchange on August 30, 2024, after deducting the estimated underwriting discounts and commissions and estimated offering expenses payable by us, and the application of the net proceeds from this offering as described in “Use of Proceeds.”
(2)Each $1.00 increase or decrease in the assumed public offering price of $39.67 per share, which is the last reported sale price of our common stock as reported on the New York Stock Exchange on August 30, 2024, would increase or decrease, as applicable, the as adjusted amount of each of our cash and cash equivalents, working capital, total assets, and total stockholders’ equity by $2.7 million, assuming that the number of shares offered by us, as set forth on the cover page of this prospectus, remains the same, after deducting the estimated underwriting discounts and commissions and estimated offering expenses payable by us. Similarly, an increase or decrease of 1.0 million shares in the number of shares of common stock offered would increase or decrease, as applicable, each of our cash and cash equivalents, working capital, total assets, and total stockholders’ equity by $38.1 million, assuming the public offering price remains the same, after deducting the estimated underwriting discounts and commissions and estimated offering expenses payable by us. The as adjusted combined/consolidated balance sheet data discussed above is illustrative only and will depend on the actual public offering price and other terms of this offering determined at pricing.
(3)We define working capital as current assets less current liabilities. See our audited combined/consolidated financial statements and the related notes included elsewhere in this prospectus for further details regarding our current assets and current liabilities.
19
Key Skilled Services Metrics and Non-GAAP Financial Measures
We use the following key skilled services metrics and non-GAAP financial measures to help us evaluate our business, identify trends that affect our financial performance, and make strategic decisions.
| Year Ended December 31, | Six Months Ended June 30, | ||||||||||||||||||||||||||||
| 2023 | 2022 | 2021 | 2024 | 2023 | |||||||||||||||||||||||||
| (Dollars in thousands) | |||||||||||||||||||||||||||||
| Key Skilled Services Metrics | |||||||||||||||||||||||||||||
| Skilled nursing services revenue | $ | 3,092,577 | $ | 2,391,309 | $ | 1,133,103 | $ | 1,900,538 | $ | 1,461,568 | |||||||||||||||||||
| Skilled mix by revenue | 55.1 | % | 64.1 | % | 57.8 | % | 51.6 | % | 60.8 | % | |||||||||||||||||||
| Skilled mix by nursing patient days | 32.4 | % | 40.7 | % | 34.5 | % | 29.5 | % | 37.3 | % | |||||||||||||||||||
| Occupancy for skilled nursing services: | |||||||||||||||||||||||||||||
| Available patient days | 7,457,345 | 5,719,689 | 3,106,602 | 4,389,269 | 3,359,730 | ||||||||||||||||||||||||
| Actual patient days | 6,775,063 | 5,139,736 | 2,681,927 | 3,994,467 | 3,078,280 | ||||||||||||||||||||||||
| Occupancy rate (operational beds) | 90.9 | % | 89.9 | % | 86.3 | % | 91.0 | % | 91.6 | % | |||||||||||||||||||
| Number of facilities at period end | 203 | 150 | 138 | 214 | 185 | ||||||||||||||||||||||||
| Number of operational beds at period end | 22,950 | 16,345 | 14,841 | 24,483 | 20,536 | ||||||||||||||||||||||||
| Non-GAAP Financial Measures | |||||||||||||||||||||||||||||
| Performance Measures | |||||||||||||||||||||||||||||
EBITDA(1) | $ | 232,860 | $ | 254,894 | $ | 93,857 | $ | 101,925 | $ | 118,616 | |||||||||||||||||||
Adjusted EBITDA(1) | $ | 237,486 | $ | 255,516 | $ | 104,073 | $ | 188,243 | $ | 122,433 | |||||||||||||||||||
| Valuation Measure | |||||||||||||||||||||||||||||
Adjusted EBITDAR(1) | $ | 454,197 | $ | 318,037 | |||||||||||||||||||||||||
(1)EBITDA, Adjusted EBITDA and Adjusted EBITDAR are non-GAAP financial measures and should be considered in addition to, not as a substitute for or in isolation from, our financial results prepared in accordance with U.S. GAAP. EBITDA and Adjusted EBITDA are performance measures and Adjusted EBITDAR is a valuation measure therefore presented only for the current period. Other companies, including companies in our industry, may calculate these measures differently or not at all, which reduces their usefulness as comparative measures. For a reconciliation of each of EBITDA, Adjusted EBITDA, and Adjusted EBITDAR to the most directly comparable U.S. GAAP financial measure, information about why we consider these measures useful and a discussion of the material risks and limitations of these measures, please see the section titled “Management’s Discussion and Analysis of Financial Condition and Results of Operations—Key Skilled Services Metrics and Non-GAAP Financial Measures—Non-GAAP Financial Measures.”
See the section titled “Management’s Discussion and Analysis of Financial Conditions and Results of Operations—Key Skilled Services Metrics and Non-GAAP Financial Measures” included elsewhere in this prospectus for a description of, and additional information about, these key skilled services metrics and non-GAAP financial measures.
20
RISK FACTORS
Investing in our common stock involves a high degree of risk. You should carefully consider each of the following risk factors and all other information set forth in this prospectus. Based on the information currently known to us, we believe that the following information identifies the most significant risk factors affecting our company. However, the risks and uncertainties we face are not limited to those set forth in the risk factors described below. Additional risks and uncertainties not presently known to us or that we currently believe to be immaterial may also adversely affect our business. In addition, past financial performance may not be a reliable indicator of future performance and historical trends should not be used to anticipate results or trends in future periods.
If any of the following risks and uncertainties develops into actual events or circumstances, they could have a material adverse effect on our business, financial condition and results of operations. In such case, the market price of our common stock could decline. You should carefully read the following risk factors, together with our audited combined/consolidated financial statements and the related notes and all other information included in this prospectus. This prospectus contains forward-looking statements that contain risks and uncertainties. See the section titled “Cautionary Note Regarding Forward-Looking Statements” in connection with your consideration of the risk factors and other important factors that may affect future results described below.
Risks Related to Our Business and Industry
We depend upon reimbursement from third‑party payors, and our revenue, financial condition and results of operations could be negatively impacted by any changes in the acuity mix of patients in our facilities as well as changes in payor mix and payment methodologies and new cost containment initiatives by third-party payors.
Our revenue is affected by the percentage of the patients of our operating subsidiaries who require a high level of skilled nursing and rehabilitative care, whom we refer to as high acuity patients or skilled patients, and by our mix of payment sources. Changes in the acuity level of patients we attract, as well as our payor mix among Medicaid, Medicare, private payors and managed care companies, significantly affect our revenue. Because high acuity patients require more skilled nursing services and a higher level of care, we generally receive higher reimbursement rates for providing care to them. Lower acuity patients, who are typically Medicaid beneficiaries, typically require fewer skilled nursing services and thus we are typically paid lower rates by Medicaid for caring for them, sometimes at rates that do not cover our costs of providing care to the patient. Reimbursement rates provided for caring for skilled patients are more likely to meet or exceed the costs of providing care to those patients, thus allowing the facility to be fiscally sustainable. Given the generally predetermined nature of the reimbursement rates that we are paid for caring for patients, depending on their acuity level, if our labor or other operating costs increase disproportionately compared to the reimbursement rates we are paid for providing services, particularly with Medicaid patients, we will generally be unable to recover the increased costs from payors unless and until reimbursement rates are adjusted, and even then they may not be adjusted in full, in a timely manner, and are typically only adjusted on a prospective basis. Accordingly, if we fail to maintain our proportion of high acuity patients or if there is any significant increase in the percentage of the patients of our operating subsidiaries for whom we receive Medicaid reimbursement, it could have a material adverse effect on our business, financial condition, and results of operations.
Initiatives undertaken by major insurers and managed care companies, including companies who run plans commonly referred to as Managed-Medicare and Managed-Medicaid, to reduce their costs and the amounts they pay providers may adversely affect our business. These tactics include contracting with healthcare providers to obtain services on a discounted basis. We believe that this trend will continue and may limit reimbursements for healthcare services. If insurers or managed care companies from whom we receive substantial payments were to reduce the amounts they pay for services and we did not wish to accept such reductions, we may lose patients if we choose not to renew our contracts with these insurers at their lower offered rates. Additionally, some payors have used the federal “No Surprises Act” or similar state legislation as a means to initiate re‑negotiation of reimbursement rates for providers and facilities, leading to litigation between these providers and/or facilities against payors and it may adversely affect us as well. In addition, sustained unfavorable economic conditions may affect the number of
21
patients enrolled in managed care programs and the profitability of managed care companies, which could result in reduced payment rates.
We may not be fully reimbursed for all services for which each facility bills through consolidated billing or bundled payments, which could have an adverse effect on our revenue, financial condition and results of operations.
In connection with the per diem prospective payments paid to SNFs, SNFs are required to perform consolidated billing for certain items and services furnished to patients and residents. Consolidated billing generally requires the SNF to bill a single daily amount for the entire package of care that its patients receive during a SNF stay covered by Medicare Part A or Medicare Advantage plans. Given the generally predetermined nature of the reimbursement rates that SNFs are paid for caring for patients, if our operating costs increase disproportionately compared to the reimbursement rates we are paid for providing services under consolidated billing, there could be a material adverse effect on our business, financial condition, and results of operations.
In addition, CMS has implemented certain payment initiatives that bundle acute care and post-acute care reimbursement. Post‑hospitalization skilled nursing services must be “bundled” into the hospital’s diagnostic related group payment in certain limited circumstances, in which case the hospital and SNF must effectively divide the payment that otherwise would have been made to the hospital and no additional funds are paid by Medicare for the skilled nursing care of the patient. Although this practice applies to only a limited number of DRGs and is uncommon at our SNFs currently, it could adversely affect SNF utilization and payments, whether due to the practical difficulty of this apportionment or hospitals being reluctant to lose revenue by discharging patients to a SNF. If more payments are required to be bundled in the future, or if there is any significant increase in patients for whom we receive bundled payments, our SNFs may not receive full reimbursement for all the services they provide, which could have a further adverse effect on SNF utilization and our revenue, financial condition and results of operations.
Increased competition for, or a shortage of, nurses, nurse assistants and other skilled personnel could increase our staffing and labor costs and subject us to monetary fines.
Our success depends upon our ability to retain and attract nurses and other skilled personnel, such as registered nurses, licensed vocational nurses, licensed practical nurses, certified nurse assistants, social workers and speech, physical and occupational therapists, as well as skilled management personnel responsible for day‑to‑day facility operation. Each facility has a facility administrator who is ultimately responsible for the overall day‑to‑day operations of the facility, including quality of care, social services and financial performance. Each facility administrator leads a team of facility staff who are directly responsible for day‑to‑day care of the facility residents, as well as other operational functions of the facility including marketing and community outreach programs. Other key positions supporting each facility may include individuals responsible for physical, occupational and speech therapy, food service and maintenance. We compete with various healthcare service providers, including other skilled nursing providers, in retaining and attracting qualified and skilled personnel. We also compete with businesses outside of healthcare in our efforts to attract and retain talented employees.
Our subsidiaries operate SNFs in Alaska, Arizona, California, Colorado, Idaho, Kansas, Kentucky, Missouri, Montana, Nevada, Ohio, Oregon, South Carolina, Texas and Washington as of September 1, 2024. Some states have established minimum staffing requirements for facilities operating in that state, and other states may do the same in the future, or existing requirements may become more stringent. The federal government recently adopted minimum staffing requirements as well. For further discussion of federal minimum staffing requirements, see the section titled “CMS Minimum Staffing Standards Final Rule.” Failure to comply with minimum staffing requirements due to competition for, a shortage of or an inability to hire required personnel can, among other things, jeopardize a facility’s compliance with the conditions of participation under relevant state and federal healthcare programs. If a facility is determined to be out of compliance with these requirements, it may be subject to a notice of deficiency, a citation, or a significant fine or litigation risk, with penalties including the suspension of patient admissions and the termination of Medicaid participation, or the suspension, revocation or non‑renewal of the SNF’s license, and may
22
also disqualify the facility from participation in state programs that reward facilities for meeting applicable quality criteria.
If federal or state governments were to materially change the way compliance with applicable staffing standards is calculated or enforced, our labor or other operating costs could increase and the current shortage of healthcare workers could impact us more significantly. The local labor markets where we compete are sometimes in a state of disequilibrium where the needs of businesses such as ours outstrip the supply of available and willing workers, which can make it challenging to hire sufficient quantities of staff locally and may require us to use third-party staffing companies to provide healthcare workers at an even higher cost. There is additional upward pressure on wages in many of our markets from different industries and more generally due to the current rate of inflation. Some of these industries compete with us for labor, which makes it difficult to make significant hourly wage and salary increases due to the fixed nature of our reimbursement under insurance contracts as well as Medicare and Medicaid, in addition to our increasing fixed and variable costs. Due to the generally limited supply of qualified applicants who seek or are willing to accept employment in certain of our markets, these broader trends may increase our labor costs or lead to potential staffing shortages, reduced operations to comply with applicable laws and regulations, or difficulty complying with those laws and regulations at current operational levels, or limit our ability to admit all residents who would like to receive care at our facilities.
Existing or future federal, state or local laws and regulations may increase our costs of maintaining qualified nursing and skilled personnel, or make it more difficult for us to attract or retain qualified nurses and skilled staff members. For instance, the Center for Medicare and Medicaid Services (CMS) has adopted final regulations that impose minimum staffing mandates on nursing facilities nationwide, as discussed in further detail in the section titled “CMS Minimum Staffing Standards Final Rule.” The Staffing Rule is currently subject to legal challenges, and there are also congressional efforts to prevent the implementation and enforcement of the minimum staffing requirements. If the regulations are implemented in the adopted form, or even with less prescriptive requirements, many skilled nursing facilities nationwide may experience significantly increased staffing costs, even if sufficient numbers of applicants are available to meet the staffing mandate. Due to labor shortages and other opportunities available to qualified workers, there can also be no assurance that sufficient numbers of applicants will be available to fulfill any staffing requirements that may be imposed, whether at pay rates that companies can afford or otherwise. Furthermore, CMS and some states have published guidance to surveyors addressing topics that specifically include nurse staffing and collection of payroll data to evaluate staffing levels, which may lead to future regulation that increase our staffing requirements and labor costs or lower revenues.
Increased competition for, or a shortage of, nurses or other qualified personnel, or general ongoing inflationary pressures may require that we enhance our pay and benefits packages, potentially beyond what we can afford in light of applicable reimbursement rates and other cost pressures, to compete effectively for such personnel. Turnover rates and the magnitude of the shortage of nurses or other trained personnel vary substantially from market to market and facility to facility, and may adversely affect the applicable facilities’ quality and other ratings based on data reported to CMS. In addition, if we fail to attract and retain qualified and skilled personnel, our ability to conduct our business operations could be harmed.
State efforts to regulate or deregulate the healthcare services industry or the construction expansion, or acquisition of healthcare facilities could impair our ability to expand our operations, or could result in increased competition.
Some states require healthcare providers, including SNFs, to obtain prior approval, commonly known as a certificate of need, for: (1) the purchase, construction or expansion of healthcare facilities; (2) capital expenditures exceeding a prescribed amount; or (3) changes in services or bed capacity.
Other states that do not require certificates of need have effectively limited the expansion of existing facilities and the establishment of new ones by placing partial or complete moratoria on the number of new Medicaid beds those states will certify in certain areas or throughout the entire state. Still other states have established such stringent development standards and approval procedures for constructing new healthcare facilities that the construction of new facilities, or the expansion or renovation of existing facilities, may become cost‑prohibitive,
23
excessively time‑consuming or otherwise unfeasible. In addition, some states require the approval of the state Attorney General for acquisition of a facility being operated by a non‑profit organization.
Our ability to acquire or construct new facilities or expand or provide new services at existing facilities would be adversely affected if we are unable to obtain the necessary approvals, if there are changes in the standards applicable to those approvals, or if we experience delays and increased expenses associated with obtaining those approvals. We may not be able to obtain licensure, certificate of need approval, Medicaid certification, state Attorney General approval or other necessary approvals for future expansion projects or acquisitions. Conversely, the elimination or reduction of state regulations that limit the construction, expansion or renovation of new or existing facilities could result in increased competition to us or result in overbuilding of facilities in some of our markets. If overbuilding in the skilled nursing industry in the markets in which we operate were to occur, it could reduce the occupancy rates of existing facilities and, in some cases, might reduce the private rates that we charge for our services.
We face numerous risks related to expiration of the COVID‑19 public health emergency (PHE) expiration and surrounding wind‑down and uncertainty, which could, individually or in the aggregate, have a material adverse effect on our business, financial condition, liquidity, results of operations and prospects.
The extent to which the expiration and wind down of the COVID‑19 PHE will affect our operations will depend on future developments, which are highly uncertain and cannot be predicted with confidence. There remains uncertainty as to what changes will be made to the United States Department of Health and Human Services’ (HHS’s) emergency response requirements or other laws and regulations for our SNFs in order to better respond to the issues experienced during the COVID‑19 PHE or that continue to exist due to COVID-19 or other infectious diseases. Additionally, the expiration of the Emergency Waivers and other flexibilities allowed under the COVID‑19 PHE, which ended as of May 11, 2023, have required, and may continue to require, operational changes, sometimes on short notices, and these reinstatements have not occurred simultaneously, requiring heightened monitoring to ensure compliance. These reinstatements of waived state and federal regulations create the risk of non‑compliance and delays in operation as more attention is required to ensure that our operations comply with applicable laws and regulations.
To the extent COVID‑19 or other infectious diseases are endemic in nature, we and our independent operating subsidiaries may face continued challenges from ongoing infection control and emergency preparedness requirements made part of state laws or regulations. Additionally, the long‑term effects of the COVID‑19 pandemic may include long‑term decline in demand for care in SNFs, which will be borne out only through time.
The majority of our patients are older individuals and/or individuals with complex medical challenges or multiple ongoing diseases, many of whom may be more vulnerable than the general public during a pandemic or in a public health emergency. Our employees are also at greater risk of contracting contagious diseases due to their increased exposure to vulnerable individuals. Our employees could have difficulty attending to our patients if a program of social distancing or quarantine is instituted in response to a public health emergency. Healthcare providers may have heightened exposure to contagious diseases or may be impacted due to prioritization of hospital resources toward any resurgence of the COVID-19 pandemic or any future pandemic and restrictions on travel. Furthermore, as a result of supply chain, labor market and other disruptions driven by the COVID-19 pandemic and the post-COVID environment, COVID-19 or any future pandemic may further negatively affect our operations or the operations of our landlords, lenders, vendors, suppliers and other business partners that we rely upon to carry out our operations, which could have a material adverse effect on our business, financial condition, results of operations and cash flows. In addition, we may expand existing internal policies in a manner that may have a similar effect. If there is a resurgence of COVID-19, or any variants thereof, or any other pandemic contagious diseases were to occur, we could suffer significant losses to our patient population or a reduction in the availability of our employees and caregivers, and we could be required to hire replacements for affected workers at an inflated cost. Accordingly, public health emergencies could have a disproportionate material adverse effect on our financial condition and results of operations. Further, litigation and/or investigations regarding COVID-19 or similar widespread public health emergencies could materially and adversely affect our business, financial condition, results of operations, compliance with financial covenants and liquidity. Other unforeseen events, including acts of violence, war,
24
terrorism and other international, regional or local instability or conflicts (including labor issues), embargoes, natural disasters such as earthquakes, whether occurring in the United States or abroad, could restrict or disrupt our operations. We cannot presently predict the scope and severity of any potential business shutdowns or disruptions, but if we or any of the third parties with whom we engage were to experience prolonged business shutdowns or other disruptions, our ability to conduct our business in the manner and on the timelines presently planned could be materially and negatively affected, which could have a material adverse impact on our business, financial condition and results of operations.
If we fail to attract patients and residents and to compete effectively with other healthcare providers, our revenue and profitability may decline and we may incur losses.
We rely significantly on appropriate referrals from physicians, hospitals and other healthcare providers in the communities in which we deliver our services to attract appropriate residents and patients to our facilities. Our referral sources are not obligated to refer business to us and may refer business to other healthcare providers. We believe many of our referral sources refer business to us as a result of the quality of our patient care and our efforts to establish and build a relationship with our referral sources. If we lose, or fail to maintain, existing relationships with our referral resources, fail to develop new relationships, or if we are perceived by our referral sources as not providing high quality patient care, our occupancy rate and the quality of our patient mix could suffer. The establishment of joint ventures or networks between referral sources, such as acute-care hospitals, and other post-acute providers may hinder patient referrals to us. The growing emphasis on integrated care delivery across the healthcare continuum increases that risk. In addition, if any of our referral sources have a reduction in patients whom they can refer due to a decrease in their business, our occupancy rate and the quality of our patient mix could suffer.
The healthcare services industry is highly competitive. Our skilled nursing facilities compete primarily on a local and regional basis with other skilled nursing facilities and with assisted/senior living facilities, from national and regional chains to smaller providers owning as few as a single facility. Competitors include other for-profit providers as well as non-profits, religiously-affiliated facilities, and government-owned facilities. We also compete under certain circumstances with inpatient rehabilitation facilities and long-term acute care hospitals. Our ability to compete successfully varies from location to location and depends on a number of factors, including the number of competing facilities in the local market and the types of services available at those facilities, our local reputation for quality care of patients, the commitment and expertise of our caregivers, our local service offerings and treatment programs, the cost of care in each locality, and the physical appearance, location, age and condition of our facilities. If we are unable to attract patients to our facilities and agencies, particularly high-acuity patients, then our revenue and profitability will be adversely affected. Some of our competitors may have greater recognition and be more established in their respective communities than we are, and may have greater financial and other resources than we have. Competing long-term care companies may also offer newer facilities or different programs or services than we do, which, combined with the foregoing factors, may result in our competitors being more attractive to our current patients, to potential patients and to referral sources. Furthermore, while we budget for routine capital expenditures at our facilities to keep them competitive in their respective markets, to the extent that competitive forces cause those expenditures to increase in the future, our financial condition may be negatively affected.
We believe we utilize a conservative approach in complying with laws prohibiting kickbacks and referral payments to referral sources. If our competitors use more aggressive methods than we do with respect to obtaining patient referrals, our competitors may from time to time obtain patient referrals that are not otherwise available to us.
The primary competitive factors for our assisted and senior living services are similar to those for our skilled nursing businesses and include reputation, the cost of services, the quality of services, responsiveness to patient/resident needs and the ability to provide support in other areas such as third-party reimbursement, information management and patient recordkeeping. Furthermore, given the relatively low barriers to entry and continuing healthcare cost containment pressures, we expect that the markets we service will become increasingly competitive in the future. Increased competition in the future could limit our ability to attract and retain patients and residents, maintain or increase our fees, or expand our business.
25
We review and audit the care delivery, recordkeeping and billing processes of our operating subsidiaries. These reviews from time to time detect instances of noncompliance that we attempt to correct, which in some instances requires reduced or repayment of billed amounts or other costs.
We have internal compliance professionals and invest in other resources to help us comply with various requirements of federal and private healthcare programs. Our compliance program includes, among other things, (1) policies and procedures that take into account applicable laws, regulations, sub‑regulatory guidance and industry practices and customs that govern the clinical, reimbursement and operational aspects of our operating subsidiaries; (2) training about our compliance process for employees throughout our organization, our directors and officers, and training about Medicare and Medicaid laws, fraud and abuse prevention, clinical standards and practices, and claim submission and reimbursement policies and procedures for appropriate employees; and (3) internal controls that monitor, among other things, the accuracy of claims, reimbursement submissions, cost reports and source documents, provision of patient care, services, and supplies as required by applicable standards and laws, accuracy of clinical assessment and treatment documentation, and implementation of judicial and regulatory requirements (i.e., background checks, licensing and training).
While we have not experienced any material compliance issues to date, from time to time, our systems and internal controls highlight potential compliance issues, which we investigate as they arise. We similarly investigate concerns that are reported to us by employees or other persons. When errors or compliance failures are identified, we seek to rectify them as appropriate. Depending on the circumstances, in order to rectify a failure, we may be required to take certain actions, including but not limited to self-reporting them to applicable federal and state regulators, government agencies or other third parties, disgorging or paying money to the government or other third parties, and implementing changes to systems, personnel or other resources in order to mitigate the risk of recurrence, all of which could result in significant costs. Such issues, and any failure to properly remediate such issues or to timely identify and refund overpayments, for instance, could result in potential federal False Claims Act (FCA) liability and could have a material adverse effect on our business, financial condition and results of operations. Other significant compliance failures could have similar negative impacts.
We are subject to litigation, which is commonplace in our industry, which could result in significant legal costs and large settlement amounts or damage awards, and our self-insurance programs may expose us to significant and unexpected costs and losses.
The skilled nursing business involves a significant risk of liability given the age and health of the patients and residents of our operating subsidiaries and the services we provide, and malpractice and other lawsuits against providers in our industry are endemic. The industry has experienced an increased trend in the number and severity of litigation claims, particularly patient-related litigation, due in part to the number of large verdicts, including large punitive damage awards. These claims are filed based upon a wide variety of claims and theories that they allege led to patient harm, including for state healthcare survey deficiencies received, allegations of insufficient staffing, allegations of insufficient training, allegations that companies put financial considerations over patient needs, and other claims. Plaintiffs’ attorneys have become increasingly more aggressive in their pursuit of claims against healthcare providers, including skilled nursing providers, employing a wide variety of advertising and solicitation activities to generate more claims. Increased caps on damages that may be awarded in such actions has and may continue to lead to a larger frequency and severity of these lawsuits against our independent operating subsidiaries, particularly those who operate in California and other states that adopt similar legislation. We, and others in the industry, have been, and continue to be, subject to an increasing number of claims and lawsuits, including professional liability claims, alleging that services provided have resulted in personal injury, patient abuse or neglect, elder abuse, wrongful death or other related claims. For instance, in early 2023, we were subject to approximately $36 million in damages and fees awarded in a California jury verdict in a patient-care case that we inherited as part of an acquisition in 2021. While we attempt to manage our patient care risks to the extent reasonably possible, there can be no assurance that we will not be subject to similar or larger verdicts in the future, particularly in light of the fact that large tort verdicts have become somewhat common throughout the United States, particularly in comparatively litigious states such as California and Kentucky. We may in the future do business in similarly or more litigious states as well. The defense of lawsuits has in the past, and may in the future, result in significant legal costs, regardless of the outcome, particularly as we and other providers have had to take on higher
26
insurance deductibles and premiums. Additionally, increases to the frequency and/or severity of losses from such claims and suits may result in increased liability insurance premiums, increases in deductibles, a decline in available insurance coverage levels, or other negative impacts on the availability and cost of insurance, which could materially and adversely affect our business, financial condition and results of operations. In addition to carrying third-party liability insurance, starting in January 2022, we formed a wholly-owned captive insurance subsidiary, Welsch Insurance Ltd. (Welsch), that provides professional liability and general liability insurance to various consolidated operating subsidiaries. See the risk factor titled “Our self-insurance programs may expose us to significant and unexpected costs and losses.”
Furthermore, class action claims related to patient care, employment practices or other matters could be brought alleging legal violations that may materially affect our business, financial condition and results of operations. These types of claims have been filed against us and other companies in our industry in the past, and are likely to continue. For example, in recent years there has been a general increase in the number of suits filed against us and other companies in California, across industries, that purport to be wage and hour class action claims. They are typically based on alleged failures to permit or properly compensate for meal and rest periods, failure to pay for all time worked, and other alleged failures of California’s extensive wage and hour laws and regulations. While we have not had a similar experience in other states, circumstances could change in those states, or we could in the future operate in other states with litigation risks similar to California. If there were a significant increase in the number of these claims against us or an increase in amounts owing should plaintiffs be successful in their claims, this could have a material adverse effect to our business, financial condition, results of operations and cash flows.
In addition, we contract with a variety of landlords, lenders, vendors, suppliers, consultants and other individuals and businesses. These contracts typically contain covenants and default provisions. If the other party to one or more of our contracts were to allege that we have violated the contract terms, we could be subject to civil liabilities which could have a material adverse effect on our financial condition and results of operations.
If litigation is instituted against one or more of our subsidiaries, a successful plaintiff might attempt to hold us or one or more of our other subsidiaries liable for the alleged wrongdoing of the subsidiary principally targeted by the litigation. If a court in such litigation decided to disregard the corporate form and find that we or other entities are vicariously liable, the resulting judgment could increase our liability and adversely affect our financial condition and results of operations.
Our independently operating subsidiaries offer arbitration agreements to residents on admission, and require employees to enter into arbitration agreements as a condition of employment. While arbitration agreements have generally been favored by the courts, have been validated by the United States Supreme Court, and are believed to streamline the dispute resolution process and reduce the parties’ exposure to excessive legal fees and jury awards, courts in some states, as well as regulators in some states and on the federal level, have showed increasing opposition to the use and enforcement of arbitration agreements, particularly in consumer and employment contexts. Current CMS regulations prohibit nursing facility providers from requiring patients to enter into arbitration agreements as a condition of admission, and there have been prior legislative efforts on both state and federal levels to codify similar prohibitions. Furthermore, prior CMS proposals sought to prohibit any use of arbitration agreements between nursing homes and their patients. In light of its continuing negative view on arbitration, CMS has identified arbitration agreements as an area of focus and has issued guidance to state surveyors regarding federal requirements for the use of arbitration agreements in nursing home care, with non‑compliance potentially resulting in fines and other sanctions. If we are not able to secure voluntary pre‑admission arbitration agreements from our patients, our litigation exposure and costs of defense in patient liability actions could increase, our liability insurance premiums could increase, and our business may be adversely affected. We would be subject to similar risks if we are at some point prohibited from requiring employees to enter into arbitration agreements.
27
If we are unable to provide consistently high quality of care, or if our employees or staff members engage in conduct (or fail to take action) that impacts our patients’ health, safety, welfare or clinical treatment, our business will be adversely impacted and we may be subject to civil or criminal penalties, fines or other actions.
Providing quality patient care is fundamental to our business. Many of our patients have complex medical conditions or special needs, are vulnerable, and often require a substantial level of care and supervision. Our patients have in the past and could in the future be harmed by one or more of our employees or staff members, either intentionally, by accident, or through negligence, neglect, error, poor performance, mistreatment, assault, abuse, failure to provide proper care, failure to properly document or monitor or report information, failure to address risks to patients’ health or safety, failure to maintain appropriate staffing, failure to implement appropriate interventions or other actions or inaction. Employees and staff members have engaged in conduct (including failing to take action) that has impacted, and may in the future engage in conduct that impacts, our patients or their health, safety, welfare, or clinical treatment.
If one or more of our facilities experiences an adverse patient incident or is found to have failed to provide appropriate patient care (including as a result of a staffing shortages or the actions or inactions of our employees or staff members), governmental or regulatory authorities may take action against us or our employees or staff members, including an admissions ban, admissions hold, reduction in census, loss of accreditation, license revocation, administrative or other order, other adverse regulatory action, a settlement or other agreement requiring corrective actions or requiring us or a specific facility to demonstrate substantial compliance with licensure or other requirements, and the imposition of certain requirements. If such an action or a closure of a facility were to occur and result in the improper termination of patient care, we or our employees or staff members may be exposed to governmental or regulatory inquiries, investigations, liability, and litigation, including claims of patient abandonment. Certain of our independently operating subsidiaries have been, and may continue to be, subject to findings of quality of care deficiencies or practices, incidents of patient abuse or neglect, and claims regarding services rendered that do not meet the standard of care, which have resulted, and in the future may result, in civil or criminal penalties, fines and other actions.
Any such patient incident, adverse regulatory action, self-disclosure, self-report, claim or other event, action or inaction has in the past, and could in the future, result in governmental investigations, judgments, or fines and have a material adverse effect on our business, financial condition, and results of operations. While such enforcement actions are typically taken against individuals, we cannot predict how law enforcement or governmental or regulatory authorities will enforce the laws or whether governmental or regulatory authorities will assert that we or any of our employees or staff members are responsible for such actions, or should have known about such actions. In addition, we have been and could become the subject of negative publicity or unfavorable media attention or governmental or regulatory scrutiny, regardless of whether the allegations are substantiated, that could have a significant, adverse effect on the trading price of our common stock or adversely impact our reputation, our relationships with referral sources and payors, whether patients and their family members choose us, and whether our referral sources choose other providers.
We rely significantly on information technology, and any failure, inadequacy or interruption of that technology could harm our ability to effectively operate our business.
Our business relies on information technology. Our ability to effectively manage our business depends significantly information systems, including those operated by certain of our third-party partners. We also heavily rely on information systems to process financial and accounting information for financial reporting purposes. Any of these information systems could fail or experience a service interruption for a number of reasons, including computer viruses, programming errors, hacking or other unlawful activities, disasters or our failure to properly maintain system redundancy or protect, repair, maintain or upgrade our systems. The failure of our third-party partners’ information systems to operate effectively or to integrate with other systems, or a breach in security of these systems, could negatively impact our financial results. If we experience any significant disruption to our financial information systems that we are unable to mitigate, our ability to timely report our financial results could be impacted, which could negatively impact our stock price. We also communicate electronically throughout the United States with our employees and with third parties, such as patients. A service interruption or shutdown could
28
have a materially adverse impact on our operating activities and could result in reputational, competitive, and business harm. Furthermore, remediation and repair of any failure, problem or breach of our key information systems could require significant capital investments.
We calculate certain operational metrics using internal systems and tools and do not independently verify such metrics. Certain metrics are subject to inherent challenges in measurement, and real or perceived inaccuracies in such metrics may harm our reputation and negatively affect our business.
We refer to a number of operational metrics herein, including, but not limited to, skilled mix, average daily rates, occupancy percentage, and other metrics. We use these metrics to monitor and evaluate our business as well as the various facilities that we own and operate, and these metrics have an influence on our strategy, operational decision-making, budgeting, and planning. We calculate these metrics using internal systems and tools that are not independently verified by any third-party. These metrics may differ from estimates or similar metrics published by third parties or other companies due to differences in sources, methodologies or the assumptions on which we rely. Our internal systems and tools have a number of limitations, and our methodologies for tracking these metrics may change over time, which could result in unexpected changes to our metrics, including the metrics we publicly disclose on an ongoing basis. If the internal systems and tools we use to track these metrics under count or over count performance or contain algorithmic or other technical errors, the data we present may not be accurate. While these numbers are based on what we believe to be reasonable estimates of our metrics for the applicable period of measurement, there are inherent challenges in measuring savings, the use of our solutions, services and offerings and other metrics. In addition, limitations or errors with respect to how we measure data or with respect to the data that we measure may affect our understanding of certain details of our business, which would affect our long-term strategies. If our operating metrics or our estimates are not accurate representations of our business, or if investors do not perceive our operating metrics to be accurate, or if we discover material inaccuracies with respect to these figures, our reputation may be significantly harmed, and our operating and financial results could be adversely affected.
We may be unable to complete future facility or business acquisitions at attractive prices or at all, which may adversely affect our revenue; we may also elect to dispose of underperforming or non‑strategic operating subsidiaries, which would decrease our revenue.
To date, our revenue growth has been significantly impacted by our acquisition of new facilities and properties. Subject to general market conditions and the availability of essential resources and leadership within our company, we continue to seek both single‑and multi‑facility acquisition and property acquisition opportunities that are consistent with our strategic objectives.
We face competition for the acquisition of facilities and properties and expect this competition to continue and potentially increase. Based upon factors such as our ability to identify suitable acquisition candidates, future regulations affecting our ability to acquire new facility operations and related real estate, the purchase or lease price of the facilities, increasing interest rates for debt‑financed purchases, prevailing market conditions, the availability of leadership to manage new facilities and our own willingness to take on new operations, the rate at which we have historically acquired facilities has fluctuated significantly. In the future, we anticipate the rate at which we may acquire facilities will continue to fluctuate, which may affect our revenue and profitability.
We have also previously acquired facilities, which over time became non‑strategic or less desirable, and have divested them. In the future we may consider divesting similar facilities that we determine at that time to be non-strategic or less desirable. Divesting facilities will typically negatively impact our revenue, may divert management and other resources from acquisitions or other efforts, and may have other adverse effects on our business, financial condition and results of operation.
29
We may not be able to successfully integrate acquired facilities and properties into our operations, and we may not achieve the benefits we expect from any of our facility acquisitions.
We may not be able to successfully or efficiently integrate new acquisitions with our existing operating subsidiaries, culture and systems. The process of integrating acquisitions into our existing operations may result in unforeseen operating difficulties, divert management’s attention from existing operations, or require an unexpected commitment of staff and financial resources, and may ultimately be unsuccessful. Integrating larger portfolios of acquired facilities concurrently may present similar but more acute challenges than integrating fewer facilities. Existing operations available for acquisition frequently serve or target different markets than those that we currently serve. We also may determine that renovations of acquired facilities and changes in staff and operating management personnel are necessary to successfully integrate those acquisitions into our existing operations. We may not be able to recover the costs incurred to reposition or renovate newly operating subsidiaries. The financial benefits we expect to realize from many of our acquisitions are largely dependent upon our ability to improve clinical performance, overcome regulatory deficiencies, rehabilitate or improve the reputation of the operations in the community, increase and maintain occupancy, control costs, and in some cases change the patient acuity mix. If we are unable to accomplish any of these objectives at the operating subsidiaries we acquire, we will not realize the anticipated benefits and we may experience lower than anticipated profits, or even losses.
During the six months ended June 30, 2024, and during the years ended December 31, 2023 and 2022, we added 12, 58 and nine stand-alone skilled nursing, assisted living, and subacute facilities, respectively. In addition, on May 22, 2024, we announced the pending acquisition of operations of 53 skilled nursing and assisted living and independent living facilities across eight states, which facilities were historically operated by subsidiaries of Prestige Care, Inc., a family company. As of June 30, 2024, we had not finalized the acquisition of any of these operations. Since June 30, 2024, we have finalized the acquisition of operations for 53 of these facilities, representing 2,511 skilled nursing beds and 1,334 assisted living and independent living units. In addition, on July 15, 2024, we finalized the acquisition of operations for 3 skilled nursing facilities located in Kansas. This growth, as well as growth in the current year and future years, has placed and will continue to place significant demands on our current management resources. Our ability to manage our growth effectively and to successfully integrate new acquisitions into our existing business will require us to continue to expand our operational, financial and management information systems and to continue to retain, attract, train, motivate and manage key employees, including facility‑level leaders and our local directors of nursing. We may not be successful in attracting qualified individuals necessary for future acquisitions to be successful, and our management team may expend significant time and energy working to attract qualified personnel to manage facilities we may acquire in the future. Also, the newly acquired facilities may require us to spend significant time improving services at the facilities, and if we are unable to improve them quickly enough, we may be subject to litigation and/or loss of licensure or certification. If we are not able to successfully overcome these and other integration challenges, we may not achieve the benefits we expect from any of our acquisitions, which could have an adverse effect on our business, financial condition and results of operation.
In undertaking acquisitions, we may be adversely impacted by costs, liabilities and regulatory issues that may adversely affect our operations, and we may not be able to successfully integrate acquired facilities and properties into our operations, or achieve the benefits we expect from any of our facility acquisitions.
In undertaking acquisitions, we also may be adversely impacted by unforeseen liabilities attributable to the prior providers who operated those facilities, against whom we may have little or no recourse. Many facilities we have historically acquired were underperforming financially and had issues, including but not limited to, clinical, regulatory and litigation, prior to and at the time of acquisition. Even where we have improved patient care and operations at facilities that we have acquired, we still may face post‑acquisition regulatory issues related to pre‑acquisition events. These may include, without limitation, payment recoupment related to our predecessors’ prior noncompliance, the imposition of fines, penalties, operational restrictions or special regulatory status. Further, we may incur post‑acquisition compliance risk due to the difficulty or impossibility of immediately or quickly bringing non‑compliant facilities into substantial compliance with applicable healthcare regulations. Diligence materials pertaining to acquisition targets, especially the underperforming facilities that often represent the greatest opportunity for operational and financial improvement, are often inadequate, inaccurate or impossible to obtain,
30
sometimes requiring us to make acquisition decisions with incomplete information. Despite our due diligence procedures, facilities that we have acquired or may acquire in the future may generate unexpectedly low returns, may cause us to incur substantial losses, may require unexpected expenditures or other resources, or may otherwise not meet a risk profile that our investors find acceptable.
In addition, we might encounter unanticipated difficulties and expenditures relating to any of the acquired facilities, including contingent liabilities. For example, when we acquire a facility, we generally assume the facility’s existing Medicare provider number for purposes of billing Medicare for services. If CMS later determines that the prior owner of the facility had received overpayments from Medicare for the period of time during which it operated the facility, or had incurred fines in connection with the operation of the facility, CMS could hold us liable for repayment of the overpayments or fines. We may be unable to improve every facility that we acquire.
We also incur regulatory risk in acquiring certain facilities due to the licensing, certification and other regulatory requirements affecting our right to operate the acquired facilities. For example, in order to acquire facilities on a predictable schedule, or to acquire declining operations quickly to prevent further pre‑acquisition declines, we frequently acquire such facilities prior to receiving license approval or provider certification. We operate such facilities as the interim manager for the outgoing licensee, assuming financial responsibility and other obligations for the facility. To the extent that we may be unable or delayed in obtaining a license, we may need to operate the facility under a management agreement from the prior operator. If we were subsequently denied licensure or certification for any reason, we might not realize the expected benefits of the acquisition and would likely incur unanticipated costs and other challenges which could cause our business to suffer.
We may have difficulty completing joint ventures that increase our capacity consistent with our growth strategy.
We selectively pursue strategic acquisitions of, and we frequently pursue joint ventures with, other healthcare providers. We may face limitations on our ability to identify sufficient joint venture, acquisition or other development targets and to complete those transactions to meet goals. These joint ventures may not be profitable or may not achieve the profitability that justifies the investments made. Furthermore, the nature of a joint venture requires us to consult with and share certain decision-making powers with unaffiliated third parties, some of which may be not-for-profit health systems. We do not manage any of the joint ventures in which we invest, and operational and strategic decision making power is held by entities that we do not control. If our joint venture partners do not fulfill their obligations, the affected joint venture may not be able to operate according to its business or strategic plans, which could have a material adverse effect on our results of operations, or require us to increase our level of financial commitment to the joint venture. Moreover, differences in economic or business interests or goals among joint venture participants could result in delayed decisions, failures to agree on major issues and even litigation. If these differences cause the joint ventures to deviate from their business or strategic plans, or if our joint venture partners take actions contrary to our policies, objectives or the best interests of the joint venture, it could have a material adverse effect on our business, financial condition and results of operations.
If we do not achieve or maintain competitive quality of care ratings from CMS or private organizations engaged in similar rating activities, our business may be negatively affected.
CMS provides comparative public data, rating every SNF operating in each state based upon quality‑of‑care indicators. Certain private organizations engage in similar monitoring and ranking activities. CMS’s system is commonly known as the Five‑Star Quality Rating System. It gives each nursing home a rating of between one and five stars in various categories, with five‑star ratings harder to obtain over time. The ratings are available on a publicly available website maintained by CMS currently called Care Compare. In cases of acquisitions, the previous operator’s clinical ratings are included in our overall Five‑Star Quality Rating and the rating may not reflect the improvements we were able to make until it is recalculated. Some of the ratings include a multi-year lookback period, which causes the prior operator’s data to be factored into our ratings for some period of time. Based on CMS’s guidance and regulations, we expect more data to be collected by CMS and reported on their website in the future.
31
CMS continues to increase quality measure thresholds, making it more difficult to achieve upward and five‑star ratings. For instance, CMS increased its quality measure thresholds in October of 2022, making it more difficult for facilities to obtain or maintain four‑ and five‑star ratings, allowing only 10% of nursing facilities within a state to receive a five‑star rating. CMS discloses the increasing standards for four‑ and five‑star ratings in its star rating cut point table, which discloses the points needed for each star rating within every state. CMS has indicated that it will increase these quality measure thresholds every six months. Some facilities may see a decline in their overall five‑star rating absent any new inspection information, and as a result the five‑star ratings of affected facilities may decline even as their quality measures remain unchanged or improve. Additionally, CMS displays on the Care Compare website a consumer alert icon for nursing homes that have been cited on inspection reports for incidents of abuse, neglect, or exploitation. If our facilities fail to have attractive or otherwise acceptable ratings on the Care Compare website it could negatively impact their operations, including their ability to attract or retain patients and an increase in expenses to improve such ratings.
Providing quality patient care is the cornerstone of our business. We believe that patients and their families choose our facilities, and hospitals, physicians and other referral sources refer patients to us, in large part because of our facilities’ reputation for delivering quality care. If our facilities fail to achieve their rating goals or otherwise maintain positive reputations in their local communities, due to nursing and administrative staffing and turnover or otherwise, or if they receive a consumer alert icon for incidents of abuse, neglect, or exploitation or other negative ratings on Care Compare, it may affect our ability to attract patients, which could have a material adverse effect upon our business and consolidated financial condition, results of operations and cash flows. See the section titled “Business—Regulatory Matters.”
If we are unable to obtain insurance, or if insurance becomes more costly for us to obtain, our business may be adversely affected.
It may become more difficult and costly for us to obtain coverage for resident care liabilities and other risks, including property, automobile and casualty insurance. For example, the following circumstances may adversely affect our ability to obtain insurance at favorable rates:
•we experience higher‑than‑expected professional liability, property and casualty, or other types of claims or losses;
•we receive survey deficiencies or citations of higher‑than‑normal scope or severity or experience higher-than-expected number of deficiencies or citations;
•we acquire especially troubled operations or facilities that present unattractive risks to current or prospective insurers;
•insurers tighten underwriting standards applicable to us or our industry; or
•insurers or reinsurers are unable or unwilling to insure us or the industry at historical premiums and coverage levels.
If any of these potential circumstances were to occur, our insurance carriers may require us to significantly increase our self‑insured retention or deductible levels or pay substantially higher premiums for the same or reduced coverage for insurance, including workers compensation, property and casualty, automobile, employment practices liability, directors and officers liability, employee healthcare and general and professional liability coverages.
In some states, the law prohibits or limits insurance coverage for the risk of punitive damages arising from professional liability and general liability claims or litigation. Coverage for punitive damages is also excluded under some insurance policies. As a result, we may be liable for punitive damage awards in these states that either are not covered or are in excess of our insurance policy limits. Claims against us, regardless of their merit or eventual outcome, could also inhibit our ability to attract patients or expand our business and could require our management to devote time to matters unrelated to the day‑to‑day operation of our business.
32
With few exceptions, workers compensation and employee health insurance costs have also increased markedly in recent years. Due to the nature of our business and the residents we serve, including the risk of claims from residents as well as potential governmental action, it may be difficult to complete the underwriting process and obtain insurance at commercially reasonable rates. If we are unable to obtain insurance, or if insurance becomes more costly for us to obtain, or if the coverage levels we can economically obtain decline, our business may be adversely affected.
We do not carry insurance for all categories of risk that our business may encounter. Some of the policies we currently maintain include property, general liability, employment benefits liability, business automobile, workers’ compensation, and directors’ and officers’, employment practices and fiduciary liability insurance. We do not know, however, if we will be able to maintain insurance with adequate levels of coverage. Any significant uninsured liability may require us to pay substantial amounts, which would have an adverse effect on our financial condition and results of operations.
Our self-insurance programs may expose us to significant and unexpected costs and losses.
We are self-insured up to certain limits for workers compensation, property and casualty, automobile, employment practices liability, directors and officers liability, employee healthcare and general and professional liability coverages. The types and amounts of self-insurance may vary from time to time based on our decisions with respect to risk retention and regulatory requirements. We establish the insurance loss reserves based on an estimation process that uses information obtained from both company-specific and industry data. Estimated costs are subject to a variety of assumptions and other factors including the severity, duration and frequency of claims, legal costs associated with claims, healthcare trends and projected inflation of related factors. Material increases in the number of insurance claims, changes to healthcare costs, accident frequency and severity, legal expenses and other factors could result in unfavorable difference between actual self-insurance costs and our reserve estimates. As a result, our self-insurance costs could increase which may have a material adverse effect upon our business and consolidated financial condition, results of operations and cash flows.
The geographic concentration of our facilities could leave us vulnerable to an economic downturn, regulatory changes or acts of nature in those areas.
Our facilities located in California account for a significant majority of our total revenue. As a result of this concentration, the conditions of local economies, changes in governmental rules, regulations and reimbursement rates or criteria, changes in demographics, state funding, acts of nature and other factors that may result in a decrease in demand and/or reimbursement for skilled nursing services in these states could have a disproportionately adverse effect on our revenue, costs and results of operations. Moreover, since approximately 64% of our skilled nursing beds are located in California as of June 30, 2024, we are particularly susceptible to revenue loss, cost increase or damage caused by natural disasters such as electrical power shortages, fires, earthquakes or mudslides, or increased liabilities that may arise from regulations. See the section titled “Business—Regulatory Matters.”
In addition, our facilities in certain states, such as Kansas, Kentucky, South Carolina, Missouri, Ohio and Texas, are more susceptible to revenue loss, cost increases or damage caused by natural disasters including hurricanes, tornadoes and flooding. These acts of nature may cause disruption to us, the employees of our operating subsidiaries and our facilities, which could have an adverse impact on the patients of our operating subsidiaries and our business. In order to provide care for the patients of our operating subsidiaries, we are dependent on consistent and reliable delivery of food, pharmaceuticals, utilities and other goods to our facilities, and the availability of qualified employees to provide services at our facilities. If the delivery of goods or the ability of employees to reach our facilities were interrupted in any material respect due to a natural disaster or other reasons, it would have a significant impact on our facilities and our business. Furthermore, the impact, or impending threat, of a natural disaster may require that we evacuate one or more facilities, which would be costly and would involve risks, including potentially fatal risks, for the patients. The impact of disasters and similar events is inherently uncertain. Furthermore, due to the concentration of our operations in these states, our business may be adversely affected by economic conditions, contagious disease outbreaks, including COVID-19, political unrest, and other conditions over which we have no control that disproportionately affect these states as compared to other states. Such events could
33
harm the patients and employees of our operating subsidiaries, severely damage or destroy one or more of our facilities, adversely affect our business, reputation and financial condition, or otherwise cause our business to suffer in ways that we currently cannot predict.
The actions of national labor unions may adversely affect our revenue and our profitability.
Some of our facilities are parties to collective bargaining agreements with labor unions, and we anticipate that additional facilities will enter into collective bargaining agreements in the future. Forthcoming proposed rules from CMS, which, based on the Biden Administration’s executive orders, as well as potential legislation such as the HCBS Access Act aimed toward providing more resources to those considering care‑based careers, may increase the likelihood of employee unionization due to increased emphasis on care‑based careers in SNF facilities. If employees decide to unionize, our cost of doing business could increase, and we could experience contract delays, difficulty in adapting to a changing regulatory and economic environment, cultural conflicts between unionized and non‑unionized employees, strikes and work stoppages, and we may conclude that affected facilities or operations would be uneconomical to continue operating. See the section titled “Business—Regulatory Matters.”
Because we lease the majority of our facilities, we are subject to risks associated with leased real property, including risks relating to lease termination, lease extensions and special charges, any of which could have an adverse effect on our business, financial condition and results of operations.
As of June 30, 2024, we leased 182 facilities (including 12 leased facilities partially owned through our joint ventures managed by third parties), or 83% of our facilities. Most of our leases are triple‑net leases, which means that, in addition to rent, we are required to pay for the costs related to the property (including property taxes, insurance, and maintenance and repair costs). Some of our leases cover more than one facility, including some leases that cover 25 or more facilities on a single master lease. We are responsible for paying these costs notwithstanding the fact that some of the benefits associated with paying these costs accrue to the landlords as owners of the associated facilities.
Each lease provides that the landlord may terminate the lease for a variety of reasons, including the default in any payment of rent, taxes or other payment obligations or the breach of any other covenant or agreement in the lease. Termination of a lease could result in a default under our debt agreements and could have an adverse effect on our business, financial condition and results of operations. There can be no assurance that we will be able to comply with all of our obligations under the leases in the future. Furthermore, there may be disputes with landlords regarding the obligations under such lease, or the ability of the landlord to terminate the lease, which could disrupt our business operations and increase expenses.
Failure to generate sufficient cash flow to cover required payments or meet operating covenants under our long‑term debt, mortgages and long‑term operating leases could result in defaults under those agreements and cross‑defaults under other debt, mortgage or operating lease arrangements, which could harm our operating subsidiaries and cause us to lose facilities or experience foreclosures.
We may not generate sufficient cash flow from operations to cover interest, principal and lease payments. Additionally, under the terms of our amended and restated credit agreement with Truist Bank and a syndicate of lenders (Amended and Restated 2023 Credit Facility), we are subject to certain affirmative and negative covenants customary for credit facilities of this type as well as two financial covenants, a total leverage financial covenant and a fixed charge coverage ratio financial covenant. These restrictions may interfere with our ability to obtain additional advances under our Amended and Restated 2023 Credit Facility or to obtain new financing or to engage in other business activities, which may inhibit our ability to grow our business and increase revenue. See the section titled “Management’s Discussion and Analysis of Financial Condition and Results of Operations—Liquidity & Capital Resources—Credit Facilities.”
From time to time, the financial performance of one or more of our mortgaged facilities may not comply with the required operating covenants under the terms of the mortgage. Any non‑payment, noncompliance or other default under our financing arrangements could, subject to cure provisions, cause the lender to foreclose upon the
34
facility or facilities securing such indebtedness or, in the case of a lease, cause the lessor to terminate the lease, each with a consequent loss of revenue and asset value to us or a loss of property. Furthermore, in many cases, indebtedness is secured by both a mortgage on one or more facilities, and a guaranty by us. In the event of a default under one of these scenarios, the lender could avoid judicial procedures required to foreclose on real property by declaring all amounts outstanding under the guaranty immediately due and payable, and requiring us to fulfill our obligations to make such payments. If any of these scenarios were to occur, our financial condition would be adversely affected. For tax purposes, a foreclosure on any of our properties would be treated as a sale of the property for a price equal to the outstanding balance of the debt secured by the mortgage. If the outstanding balance of the debt secured by the mortgage exceeds our tax basis in the property, we would recognize taxable income on foreclosure, but would not receive any cash proceeds, which would negatively impact our earnings and cash position. Further, because our mortgages and operating leases generally contain cross‑default and cross‑collateralization provisions, a default by us related to one facility could affect a significant number of other facilities and their corresponding financing arrangements and operating leases.
Because our Amended and Restated 2023 Credit Facility, mortgages and lease obligations are fixed expenses and secured by specific assets, and because our revolving loan obligations are secured by virtually all of our assets, if reimbursement rates, patient acuity mix or occupancy levels decline, or if for any reason we are unable to meet our loan or lease obligations, we may not be able to cover our costs and some or all of our assets may become at risk. Our ability to make payments of principal and interest on our indebtedness and to make lease payments on our operating leases depends upon our future performance, which will be subject to general economic conditions, industry cycles and financial, business and other factors affecting our operating subsidiaries, many of which are beyond our control. If we are unable to generate sufficient cash flow from operations in the future to service our debt or to make lease payments on our operating leases, we may be required, among other things, to seek additional financing in the debt or equity markets, refinance or restructure all or a portion of our indebtedness, sell selected assets, reduce or delay planned capital expenditures or delay or abandon desirable acquisitions. Such measures might not be sufficient to enable us to service our debt or to make lease payments on our operating leases. The failure to make required payments on our debt or operating leases or the delay or abandonment of our planned growth strategy could result in an adverse effect on our future ability to generate revenue and sustain profitability. In addition, any such financing, refinancing or sale of assets might not be available on terms that are economically favorable to us, or at all.
Our founders have personal guarantees under certain of our leases, which subjects them to increased risk of default.
Our founders have provided personal guarantees under certain of our leases using their personal property. Under the personal guarantees provided by our founders, our founders have agreed to satisfy our obligations under the leases in the event that we are unable to perform our obligations thereunder. In the event that the guarantee is enforced against either or both of our founders, they could be obliged to use their personal property to fulfill their obligations under the leases. If our founders are subject to personal bankruptcy or refute the guarantees, we may be subject to an increased risk of default under our leases. Our founders owe a fiduciary duty of loyalty to us. However, there is potential for conflicts of interest between each of their personal interests and ours whether their respective guaranty is called upon or not. No assurance can be given that material conflicts will not arise that could be detrimental to our operations and financial prospects.
We may need additional capital to fund our operating subsidiaries and finance our growth, and we may not be able to obtain it on terms acceptable to us, or at all, which may limit our ability to grow.
Our ability to maintain and enhance our operating subsidiaries and facilities in a suitable condition to meet regulatory standards, operate efficiently and remain competitive in our markets requires us to commit substantial resources to continued investment in our facilities and equipment. We are sometimes more aggressive than our competitors in capital spending to address issues that arise in connection with aging and obsolete facilities and equipment, and to otherwise make our facilities more attractive in their local markets. In addition, continued expansion of our business through the acquisition of existing facilities, expansion of our existing facilities and construction of new facilities may require additional capital, particularly if we were to accelerate our acquisition and
35
expansion plans. Financing may not be available to us or may be available to us only on terms that are not favorable, including being subject to interest rates that are higher than those incurred in the past. In addition, some of our outstanding indebtedness and long‑term leases restrict, among other things, our ability to incur additional debt. If we are unable to raise additional funds or obtain additional funds on terms acceptable to us, we may have to delay or abandon some or all of our growth strategies. Further, if additional funds are raised through the issuance of additional equity securities, the percentage ownership of our stockholders would be diluted. Any newly issued equity securities may have rights, preferences or privileges senior to those of our common stock.
Adverse market or macroeconomic conditions or market volatility resulting from global economic developments, political elections or political unrest, high inflation, rising or consistently high interest rates, the post-COVID environment or other factors, could materially and adversely affect our business operations.
Adverse market or macroeconomic conditions or market volatility resulting from global economic developments, political elections or political unrest, high inflation, rising or consistently high interest rates, the post-COVID environment or other factors, could materially and adversely affect our business operations. For instance, actual events involving limited liquidity, defaults, non-performance or other adverse developments that affect financial institutions, transactional counterparties or other companies in the financial services industry or the financial services industry generally, or concerns or rumors about any events of these kinds or other similar risks, have in the past and may in the future lead to market-wide liquidity problems. For example, on March 10, 2023, Silicon Valley Bank was closed by the California Department of Financial Protection and Innovation, which appointed the Federal Deposit Insurance Corporation (FDIC), as receiver. Similarly, on March 12, 2023, Signature Bank Corp. and Silvergate Capital Corp. were each swept into receivership, and uncertainty remains over liquidity concerns in the broader financial services industry. We may maintain cash balances at third-party financial institutions in excess of the FDIC standard insurance limit. Although the U.S. Department of Treasury, FDIC and Federal Reserve Board announced a program to provide up to $25.0 billion of loans to financial institutions secured by certain of such government securities held by financial institutions, widespread demands for customer withdrawals or other liquidity needs of financial institutions may exceed the capacity of such program, and there is no guarantee that the U.S. Department of Treasury, FDIC and Federal Reserve Board will provide access to uninsured funds in the future in the event of the closure of such banks or financial institutions, or that they would do so in a timely fashion. These events could result in a variety of material and adverse impacts on our current and projected business operations and our financial condition and results of operations, including, but not limited to, the following:
•delayed access to deposits or other financial assets or the uninsured loss of deposits or other financial assets;
•potential or actual breach of statutory, regulatory or contractual obligations, including obligations that require us to maintain letters of credit or other credit support arrangements; or
•termination of cash management arrangements and/or delays in accessing or actual loss of funds subject to cash management arrangements.
In addition, any further deterioration in the macroeconomic economy or financial services industry could lead to losses or defaults by our partners, vendors or suppliers, which in turn, could have a material adverse effect on our current and/or projected business operations and results of operations and financial condition. For example, a partner may fail to make payments when due, default under their agreements with us, become insolvent or declare bankruptcy, or a supplier may determine that it will no longer deal with us as a customer. In addition, a vendor or supplier could be adversely affected by any of the liquidity or other risks that are described above as factors that could result in material adverse impacts on us, including but not limited to delayed access or loss of access to uninsured deposits or loss of the ability to draw on existing credit facilities involving a troubled or failed financial institution. The bankruptcy or insolvency of any partner, vendor or supplier, or the failure of any partner to make payments when due, or any breach or default by a partner, vendor or supplier, or the loss of any significant supplier relationships, could cause us to suffer material losses and may have a material adverse impact on our business.
36
The condition of the financial markets, including volatility and deterioration in the capital and credit markets, could limit the availability of debt and equity financing sources to fund the capital and liquidity requirements of our business, as well as negatively impact or impair the value of our current portfolio of cash, cash equivalents and investments, including U.S.‑backed investments.
Our cash and cash equivalents are held in a mixture of bank accounts, overnight investments, and other interest-bearing accounts. As a result of the uncertain domestic and global political, economic, credit and financial market conditions, including the significant increases in interest rates and inflation in 2023 as compared to 2022 and prior years, investments in these types of financial instruments pose risks arising from liquidity and credit concerns. Given that future deterioration in the U.S. and global credit and financial markets is a possibility, no assurance can be made that losses or significant deterioration in the fair value of our cash, cash equivalents, or investments will not occur. Uncertainty surrounding the trading market for U.S. government securities or impairment of the U.S. government’s ability to satisfy its obligations under such treasury securities could impact the liquidity or valuation of our current portfolio of cash, cash equivalents, and investments. Further, continued domestic and international political uncertainty, along with credit, and financial market uncertainty, may make it difficult for us to liquidate our investments prior to their maturity without incurring a loss, which could have a material adverse effect on our business financial condition, results of operations and cash flows.
We may need additional capital if a substantial acquisition or other growth opportunity becomes available, or if other unexpected challenges or opportunities arise. U.S. capital markets can be volatile. We cannot assure you that additional capital will be available or available on terms acceptable to us. If capital is not available, we may not be able to fund internal or external business expansion or respond to competitive pressures or other market conditions.
Delays in reimbursement may cause liquidity problems.
If we experience problems with our billing information systems or if issues arise with Medicare, Medicaid or other payors, we may encounter delays in our payment cycle. In addition, third-party payors may not make timely payment to us. From time to time, we have experienced such delays as a result of government payors instituting planned reimbursement delays for budget balancing purposes or as a result of prepayment reviews. Delays also happen from time to time with managed care organizations and other insurance companies who are payors for our patients.
Some states in which we operate are operating with budget deficits or could have budget deficit in the future, which may delay reimbursement in a manner that would adversely affect our liquidity. In addition, from time to time, procedural issues require us to resubmit or appeal claims before payment is remitted, which contributes to our aged receivables. Unanticipated delays in receiving reimbursement from state programs or commercial payors due to changes in their policies or billing or audit procedures may adversely impact our liquidity and working capital.
The continued use and growth of managed care organizations (MCOs) may contribute to delays or reductions in our reimbursement, including Managed Medicaid.
In many states, including some of the largest where we operate, including California, state Medicaid benefits are administered through MCOs. Typically, these MCOs manage commercial health and federal Medicare Advantage benefits under a managed care contract.
MCOs and other third-party payors have continued to consolidate in order to enhance their ability to influence the delivery and cost structure of healthcare services. Consequently, the healthcare needs of a large percentage of the U.S. population are increasingly served by a smaller number of managed care organizations. These organizations generally enter into service agreements with a limited number of providers for needed services. In addition, third-party payors, including managed care payors, increasingly are demanding discounted fee structures.
Nationally, MCOs cover increasingly large numbers of Medicaid and Medicare Advantage beneficiaries. MCOs may be more aggressive than state Medicaid and federal Medicare agencies in denying claims or seeking recoupment of payments so that their services under these managed contracts are profitable. The additional steps
37
created by the use of MCOs in disbursement of funds creates more risk of delayed, reduced, or recouped payments for our independent operating subsidiaries, and additional avenues for risks that include fines and other sanctions, including suspension or exclusion from participation in various governmental programs. To the extent that these organizations terminate us as a preferred provider, engage our competitors as a preferred or exclusive provider, demand discounted fee structures, limit the patients eligible for our services, or seek our assumption of all or a portion of the financial risk through a prepaid capitation arrangement, it could have a material adverse effect on our business, financial condition, results of operations and liquidity.
Compliance with the regulations of the Department of Housing and Urban Development (HUD) may require us to make unanticipated expenditures which could increase our costs.
Certain of our facilities are currently subject to regulatory agreements with HUD that give the Commissioner of HUD broad authority to require us to be replaced as the operator of those facilities in the event that the Commissioner determines there are operational deficiencies at such facilities under HUD regulations. Compliance with HUD’s requirements can often be difficult because these requirements are not always consistent with the requirements of other federal and state agencies. Appealing a failed inspection can be costly and time‑consuming and, if we do not successfully remediate the failed inspection, we could be precluded from obtaining HUD financing in the future or we may encounter limitations or prohibitions on our operation of HUD‑insured facilities.
If we fail to safeguard the monies held in our patient trust funds, we will be required to reimburse those monies, and we may be subject to citations, fines and penalties.
Each of our facilities is required by federal law to maintain a patient trust fund to safeguard certain assets of their residents and patients. If any money held in a patient trust fund is misappropriated, we are required to reimburse the patient trust fund for the misappropriated money. If any monies held in our patient trust funds are misappropriated in the future and are unrecoverable, we will be required to reimburse those monies, and we may also be subject to citations, fines and penalties pursuant to federal and state laws.
Security breaches, cyber‑security incidents, or our inability to effectively integrate, manage and keep our information systems secure and operational could violate security laws, disrupt our operations, and subject us to significant liability.
Healthcare businesses are increasingly the target of cyberattacks whereby hackers disrupt business operations or obtain protected health information, often demanding large ransoms. Our business is dependent on the proper functioning and availability of our computer systems and networks. While we have taken steps to protect the safety and security of our information systems and the patient health information and other data maintained within those systems, we cannot assure you that our safety and security measures and disaster recovery plan will prevent damage, interruption or breach of our information systems and operations. Additionally, we cannot control the safety and security of our information held by third‑party vendors with whom we contract. The techniques used to obtain unauthorized access, disable or degrade service, or sabotage systems change frequently and may be difficult to detect, and as such we (or third‑party vendors) may be unable to anticipate these techniques or implement adequate preventive measures. In addition, hardware, software or applications we (or third‑party vendors) develop or procure from third parties may contain defects in design or manufacture or other problems that could unexpectedly compromise the security of information systems. Unauthorized parties may attempt to gain access to our systems or facilities, or those of third parties with whom we do business, through fraud or other forms of deception.
On occasion, we have acquired additional information systems through our business acquisitions, and these acquired systems may expose us to risk. We also license certain third‑party software to support our operations and information systems. Our inability, or the inability of third‑party vendors, to continue to maintain and upgrade information systems and software could disrupt or reduce the efficiency of our operations. In addition, costs and potential problems and interruptions associated with the implementation of new or upgraded systems and technology or with maintenance or adequate support of existing systems also could disrupt or reduce the efficiency of our operations.
38
A cyber‑attack or other incident that bypasses the security measures of our information systems could cause a security breach, which may lead to a material disruption to our information systems infrastructure or business, significant costs to remediate (e.g., data recovery) and may involve a significant loss of business or patient health information. If a cyber‑attack or other unauthorized attempt to access our systems or facilities were successful, it could also result in the theft, destruction, loss, misappropriation or release of confidential information or intellectual property, could cause operational or business delays that may materially impact our ability to provide various healthcare services and otherwise conduct our business operations, and could require us to expend significant costs to remediate the breach and retrieve our data or access to our systems. Any successful cyber‑attack or other unauthorized attempt to access our systems or facilities also could result in negative publicity which could damage our reputation or brand with our patients, referral sources, payors or other third parties and could subject us to a number of adverse consequences, the vast majority of which are not insurable, including but not limited to, disruptions in our operations, regulatory and other civil and criminal penalties, fines, investigations and enforcement actions (including, but not limited to, those arising from the SEC, Federal Trade Commission, Office of Civil Rights, the Office of the Inspector General (OIG) or state attorneys general), fines, private litigation with those affected by the data breach (including class action litigation), loss of customers, disputes with payors and increased operating expense, which either individually or in the aggregate could have a material adverse effect on our business, financial condition, results of operations and liquidity.
If we are unable to obtain, maintain and enforce intellectual property protection for our technology or if the scope of our intellectual property protection is not sufficiently broad, our ability to successfully compete and utilize our technology may be adversely affected.
Our business depends, in part, on internally developed technology and content, including software and know-how, the protection of which is important to the success of our business and strategy. We rely on a combination of trademark, trade-secret, and copyright laws and confidentiality procedures and contractual provisions to protect our intellectual property rights. We may, over time, increase our investment in protecting our intellectual property through additional trademark, patent and other intellectual property filings. These measures, however, may not be sufficient to offer us meaningful protection. If we are unable to establish or protect our intellectual property and other rights, our competitive position and our business could be harmed, as third parties may be able to develop technologies that are substantially the same as ours or challenge our ability to use our existing technologies.
Also, some of our services rely on technologies and software developed by or licensed from third parties, and we may not be able to maintain our relationships with such third parties or enter into similar relationships in the future on reasonable terms or at all. Our failure to obtain, maintain and enforce our intellectual property rights could have a material adverse effect on our business, financial condition and results of operations.
We are a holding company with no operations and rely upon our multiple independent operating subsidiaries to provide us with the funds necessary to meet our financial obligations. Liabilities of any one or more of our subsidiaries could be imposed upon us or our other subsidiaries.
We are a holding company with no direct operating assets, employees or revenue. Each of our facilities is operated through a separate, wholly owned, independent subsidiary, which has its own local management, employees and assets. Our principal assets are the equity interests we directly or indirectly hold in our multiple operating and real estate holding subsidiaries. As a result, we are dependent upon distributions from our subsidiaries to generate the funds necessary to meet our financial obligations and pay dividends. Our subsidiaries are legally distinct from us and have no obligation to make funds available to us. The ability of our subsidiaries to make distributions to us will depend substantially on their respective operating results and will be subject to restrictions under, among other things, the laws of their jurisdiction of organization, which may limit the amount of funds available for distribution to investors or stockholders, agreements of those subsidiaries, the terms of our financing arrangements and the terms of any future financing arrangements of our subsidiaries. If the cash distributions we receive from our subsidiaries are insufficient for us to fund our financial obligations, we may be required to raise cash through the incurrence of debt, the issuance of equity or the sale of assets to fund. However, there is no assurance that we would be able to raise cash by these means. If the ability of any of our subsidiaries to pay dividends or make distributions or payments to us is materially restricted by regulatory or legal requirements,
39
bankruptcy or insolvency, or our need to maintain our financial strength ratings, or is limited due to operating results or other factors, it could adversely affect our ability to meet our financial obligations and to pay dividends or make distributions to our stockholders.
Our future success depends on the continuing efforts of our management and key employees, and on our ability to attract and retain highly skilled personnel and senior management.
We depend on the talents and continued efforts of our senior management and key employees. The loss of members of our management or key employees may disrupt our business and harm our results of operations. Furthermore, our ability to manage further expansion will require us to continue to attract, motivate, and retain additional qualified personnel. Competition for this type of personnel is intense, and we may not be successful in attracting, integrating, and retaining the personnel required to grow and operate our business effectively. There can be no assurance that our current management team or any new members of our management team will be able to successfully execute our business and operating strategies.
Risks Related to Government Regulation
We rely on payments from third-party payors, including Medicare, Medicaid and other governmental healthcare programs and private insurance organizations. If coverage or reimbursement for services are changed, reduced or eliminated, including through cost-containment efforts, spending requirements are changed, data reporting, measurement and evaluation standards are enhanced and changed, our operations, revenue and profitability could be materially and adversely affected.
We derive substantial revenue from government healthcare programs, primarily Medicare and state Medicaid programs. Medicare is our largest source of total revenue, accounting for 38.6% and 47.6% of total revenue for the years ended December 31, 2023 and 2022, respectively, and 36.6% and 44.8% of total revenue for the six months ended June 30, 2024 and 2023, respectively. Additionally, we derived 37.6% and 30.2% of our total revenue from the Medicaid program for the years ended December 31, 2023 and 2022, respectively, and 38.4% and 32.9% of our total revenue from the Medicaid program for the six months ended June 30, 2024 and 2023, respectively. Many other payors may use published Medicare rates as a basis for reimbursements. Accordingly, if Medicare reimbursement rates are reduced or fail to increase as quickly as our costs, if there are changes in the rules governing the Medicare program that are disadvantageous to our business or industry, or if there are delays in Medicare, Medicaid and other third-party payors payments, it could have a material adverse effect on our business, financial condition and results of operations.
Congress and the CMS often change the rules governing the Medicare program, including those governing reimbursement. Payments received from state Medicaid programs vary from state to state. These payments and programs are subject to statutory and regulatory changes, administrative rulings, interpretations, budgetary and funding constraints, and changes to the methods of calculating payments and reimbursements and requirements to participate in the programs. When these changes are implemented, we must also modify our operations and internal billing processes and procedures accordingly, which can require significant time and expense. As federal healthcare expenditures continue to increase and state governments may face budgetary shortfalls, federal and state governments have made, and may continue to make, significant changes to the Medicare and Medicaid programs and reimbursement received for services rendered to beneficiaries of such programs. The U.S. federal budget is subject to change, including reductions in federal spending, and the Medicare program is frequently mentioned as a target for spending cuts. The full impact on our business of any changes is uncertain. Changes to the Medicare program, state Medicaid programs and other third-party payor program that could adversely affect our business include:
•statutory and regulatory changes, including policy interpretations and changes that impact state reimbursement programs, particularly Medicaid reimbursement and managed care payments;
•administrative or legislative changes to base rates or the bases for payment;
40
•the reduction or elimination of annual rate increases, or the end of the reduced payments deferment;
•limits on the services or types of providers for which Medicare will provide reimbursement;
•changes in methodology for patient assessment and/or determination of payment levels;
•payment or other delays by fiscal intermediaries, carriers or payors;
•redefining enrollment standards and participation in government healthcare programs;
•changes in staff requirements (i.e., requiring all workers to be vaccinated against COVID‑19 and receive booster injections for those vaccinations) as a condition of payment or eligibility for Medicare reimbursement;
•reduced reimbursement rates and changes in coverage under commercial and managed care contracts;
•changes in reimbursement rates, methods, or timing under governmental reimbursement programs, including reductions in annual reimbursement updates due to budgetary or other pressures;
•interruption or delays in payments due to any ongoing governmental investigations and audits or due to a partial or total federal or state government shutdown for a prolonged period of time;
•an increase in co‑payments or deductibles payable by beneficiaries;
•recoupment efforts and recovery of overpayments;
•federal, state, and local litigation, administrative proceedings, and enforcement actions, including those relating to false claims, COVID-19 or future pandemics and the failure to satisfy the terms and conditions of financial relief; and
•reputational harm of publicly disclosed enforcement actions, audits, or investigations related to quality of care, patient harm and abuse, billing and reimbursement.
The healthcare industry broadly, including government and commercial payors, is initiating cost containment efforts. The Medicare program and its reimbursement rates and rules are subject to frequent change, including statutory and regulatory changes, rate adjustments (including retroactive adjustments), annual caps that limit the amount that can be paid (including deductible and coinsurance amounts), administrative or executive orders and government funding restrictions, all of which may materially adversely affect the rates at which Medicare reimburses us for our services. Additionally, payments can be delayed or declined due to determinations that certain costs are not reimbursable or reasonable because either adequate or additional documentation was not provided or because certain services were not covered or considered medically necessary. Revenue from these payors can be retroactively adjusted after a new examination during the claims settlement process or as a result of post‑payment audits. Additionally, both government and private payors are increasingly looking to value-based purchasing to contain costs. Value-based purchasing focuses on quality of outcomes and efficiency of care, rather than quantity of care. Reductions in reimbursement rates or the scope of services being reimbursed could have a material, adverse effect on our business, financial condition and results of operations or even result in reimbursement rates that are insufficient to cover our operating costs.
For the fiscal year 2024, SNF prospective payment system (PPS) rule issued on July 31, 2023, Medicare Part A reimbursement for SNFs increased by 4%. CMS also added new quality measures to take effect in fiscal years 2024 through 2027 that assess staff turnover, discharge success, re‑hospitalization, and resident falls with injuries, which may adversely affect revenues obtained through the Medicare program. CMS’s changes to the SNF Value-Based Purchasing (VBP) program, such as the SNF healthcare‑associated infections measure, total nursing hours per resident day measures, discharge to community – post acute care measure, and replacement of the SNF 30‑day
41
All‑Cause Readmission Measure with the SNF Within-Stay Potentially Preventable Readmission Measure beginning in fiscal year 2028, may reduce the compensation our independent operating subsidiaries may receive under the SNF VBP program. Under the final fiscal year 2025 SNF PPS rule, CMS will increase Medicare Part A reimbursement for SNFs by 4.2% in fiscal year 2025. The rate increase will take effect on October 1, 2024.
CMS implemented a final rule in October 2019 implementing a new case‑mix classification system, PDPM (patient-driven payment model), that focuses on the clinical condition of the patient. CMS may make future adjustments to reimbursement levels and underlying reimbursement formulae as it continues to monitor the impact of PDPM on patient outcomes and budget neutrality. The Biden Administration continues to study the nursing home industry and to call for HHS to issue proposed rules based on those studies.
Loss of Medicare reimbursement, or a delay or default by the government in making Medicare payments, would also have a material adverse effect on our revenue. Non‑compliance with Medicare regulations exist, and any penalty, suspension, termination, or other sanction under any state’s Medicaid program could lead to reciprocal and commensurate penalties being imposed under the Medicare program, up to termination or rescission of our Medicare participation and payor agreements as noted above.
A significant portion of reimbursement for skilled nursing services comes from Medicaid. Medicaid is a state‑administered program financed by both state funds and matching federal funds. Medicaid spending has increased rapidly in recent years, becoming a significant component of state budgets, which has led both the federal government and many states to institute measures aimed at controlling the growth of Medicaid spending, and in some instances reducing aggregate Medicaid spending. Since a significant majority of our total revenue is generated from our skilled nursing operating subsidiaries in California, any budget reductions or delays in California could adversely affect our net patient service revenue and profitability. Despite present state budget surpluses in many of the states in which we operate, we can expect continuing cost containment pressures on Medicaid outlays for SNFs, and any such decline could have an adverse effect on our business financial condition and results of operations.
The Medicaid program and its reimbursement rates and rules are subject to frequent change at both the federal and state level, including through changes in laws, regulations, rate adjustments (including retroactive adjustments), administrative or executive orders and government funding restrictions, all of which may materially adversely affect the rates at which our services are reimbursed by state Medicaid plans or the amount of expense we incur.
To generate funds to pay for the increasing costs of the Medicaid program, many states utilize financial arrangements commonly referred to as provider taxes. Under provider tax arrangements, states collect taxes from healthcare providers and then use the revenue to pay the providers as a Medicaid expenditure, which allows the states to then claim additional federal matching funds on the additional reimbursements. Current federal law provides for a cap on the maximum allowable provider tax as a percentage of the providers’ net patient revenue. There can be no assurance that federal law will continue to provide matching federal funds on state Medicaid expenditures funded through provider taxes, or that the current caps on provider taxes will not be reduced. Any discontinuance or reduction in federal matching of provider tax‑related Medicaid expenditures could have a significant and adverse effect on states’ Medicaid expenditures, and as a result could have a material adverse effect on our business, financial condition or results of operations.
The CAA 2023 provided for the wind‑down and termination of increased Federal Medicaid Assistance Percentage (FMAP) payments under the Families First Coronavirus Relief Act (FFCRA), and also provided for the disenrollment of Medicaid beneficiaries who have participated in the program since early in the COVID‑19 pandemic. CMS’s increased FMAP payments declined from 5% in the second quarter of 2023 to 2.5% in the third quarter, and to 1.5% in the fourth quarter. The increased FMAP payments will be discontinued in 2024. The CAA 2023 granted CMS the authority to impose fines, penalties, and other sanctions upon states that did not comply with this law’s requirements for the unwinding of increased FMAP payments. As a result, these reductions may impose further burdens on the Medicaid programs in states where we operate in the form of fines and penalties, which may result in reduced payments.
42
Beginning on April 1, 2023, states were allowed to begin disenrolling Medicaid beneficiaries. CMS guidance allowing for a return to Medicaid’s historical renewal, enrollment, and eligibility determination practices permits states up to 14 months to initiate and process traditional Medicaid renewals. The CAA 2023’s allowance of disenrollment and return to traditional Medicaid renewal processes, which includes pre‑COVID eligibility determinations, may result in a reduction of the number of Medicaid beneficiaries and may result in a reduction of our current and potential patient population. As a result, there may be fewer current or potential patients able to pay for our operating subsidiaries’ services, and increased competition for Medicaid beneficiaries able to provide reimbursement for those services.
CMS is monitoring the disenrollment process in an effort to protect eligible beneficiaries from inappropriate coverage losses during the return to Medicaid’s historical renewal, enrollment and eligibility determination practices, and has required certain states to pause disenrollments unless they could ensure all eligible people are not improperly disenrolled. CMS is continuing to monitor states’ compliance with federal requirements and is working with the affected states to address issues related to renewal requirements. States risk losing federal Medicaid matching funds for non‑compliance with CMS’s instructions, which could result in reduced Medicaid funds available for timely reimbursement of our operating subsidiaries for their operations.
Effective January 16, 2024, with disclosure requirements taking effect once CMS develops and publishes the required forms, Medicare and Medicaid nursing facilities are required to disclose new data about the facility’s ownership, management and the owners of real property lessors upon initial enrollment and revalidation. In addition, the nursing facilities are required to timely report any changes, including in connection with any change of ownership. CMS defines the new disclosable parties to include members of the facility’s governing body, persons or entities who are an officer, director, member, partner, trustee or managing employee of the facility, persons or entities that exercise operational, financial or managerial control, lease or sublease real property to the facility, own a direct or indirect interest of five percent or greater of the real property or provide management or administrative services to the facility. Additionally, for any disclosable party that is a corporation, the disclosure must include the stockholders who have a five percent or greater direct or indirect ownership interest. Additionally, facilities will be required to disclose whether any entity on the form is a private equity company or real estate investment trust (REIT). CMS will make the information that is provided publicly available. This new disclosure requirement involves reporting extensive information and may complicate our efforts to comply with Medicare and Medicaid requirements. Failure to comply with the new disclosure requirements could affect our participation in Medicare and state Medicaid programs and adversely impact our business and financial condition.
Medicaid is an important source of funding for our independent operating subsidiaries. We may be adversely affected by the disenrollment of Medicaid beneficiaries, which may lead to a reduction in reimbursement that may adversely impact our revenue and profit. The temporary restoration of Medicaid benefits in states where redetermination has been paused can help relieve some of these economic concerns. The disruption caused by the temporary pauses and restoration of Medicaid coverage for beneficiaries can also create operational challenges for our independent operating subsidiaries, including adverse effects on cash flow, available funds to pay wages for staffing, and overall financial stability. The ultimate impact of Medicaid disenrollment on our finances and operations will depend on individual states’ specific circumstances and actions. See the section titled “Business—Regulatory Matters.”
Reforms to the U.S. healthcare system, including new regulations under the Affordable Care Act (ACA), continue to impose new requirements upon us that could materially impact our business.
The ACA has resulted in significant changes to our operations and reimbursement models for services we provide. CMS continues to issue rules to implement the ACA, including most recently, new rules regarding the implementation of the anti‑discrimination provisions and new rules requiring the disclosure of SNF ownership, organization, management and the identity of the real property owners from which the SNF leases or subleases its operating space. With the passage of the Inflation Reduction Act of 2022 (IRA) in August of 2022, Congress continues to expand and supplement the ACA, including through the continuation of federally funded insurance premium subsidies. This modification of the ACA by the IRA indicates that Congress may continue to change and expand the ACA in the future.
43
The efficacy of the ACA is the subject of much debate among members of Congress and the public and it has been the subject of extensive litigation before numerous courts, including the United States Supreme Court, with varying outcomes ‑ some expanding and others limiting the ACA. In the event that the ACA is repealed or any elements of the ACA that are beneficial to our business are materially amended or changed, such as provisions regarding the health insurance industry, reimbursement and insurance coverage by payers, our business, operating results and financial condition could be harmed. Thus, the future impact of the ACA on our business is difficult to predict and its continued uncertain future may negatively impact our business. However, any material changes to the ACA or its implementing regulations may negatively impact our operations.
While it is not possible to predict whether and when any such changes will occur, specific proposals discussed during and after the election, including a repeal or material amendment of the ACA, could harm our business, operating results and financial condition. In addition, even if the ACA is not amended or repealed, the President and the executive branch of the federal government, as well as CMS and HHS have a significant impact on the implementation of the provisions of the ACA, and a new administration could make changes impacting the implementation and enforcement of the ACA, which could harm our business, operating results and financial condition. We have already seen this with regulatory activity promulgating rules regarding anti‑discrimination under Section 1557 of the ACA and the disclosure of SNF ownership and service providers under Section 6101 of the ACA. If we are slow or unable to adapt to any such changes, our business, operating results and financial condition could be adversely affected.
Since the ACA, there have been healthcare reform proposals and we expect that other healthcare reform legislative and regulatory changes will be proposed and enacted, including reductions in payments to SNFs and impose the staffing and reporting requirements. We cannot predict what effect future reforms to the U.S. healthcare system will have on our business, including the demand for our services, the cost of our operations, or the amount of reimbursement available for those services. However, it is possible these new laws may lower reimbursement or increase the cost of doing business and adversely affect our business. See the section titled “Business—Regulatory Matters.”
We are subject to various government and third-party payor reviews, audits and investigations that could adversely affect our business, including an obligation to refund amounts previously paid to us, potential criminal charges, the imposition of fines, and/or the loss of our right to participate in Medicare and Medicaid programs or other third-party payor programs.
Regulators and third-party payors are increasing scrutiny of claims, which may require additional resources to response to audits and may cause additional delays or denials in receiving payment. As a result of our participation in the Medicaid and Medicare programs, we and other program participants are subject to various governmental reviews, audits and investigations to verify compliance with the rules associated with these programs and related applicable laws and regulations, including claims for payments submitted to those programs, which are subject to reviews by Recovery Audit Contractors, Zone Program Integrity Contractors, Program Safeguard Contractors, Unified Program Integrity Contractors, Supplemental Medical Review Contractors and Medicaid Integrity Contractors programs (collectively referred to as Reviews). In these Reviews, third-party firms engaged by CMS conduct extensive analysis of claims data and medical and other records to identify potential improper payments under the Federal and State programs. Although we have always been subject to post‑payment audits and Reviews, more intensive “probe reviews” performed by Medicare administrative contractors in recent years appear to be a regular procedure with our fiscal intermediaries. Managed care and other third-party payors also often reserve the right to conduct audits and do on a regular basis.
We believe that billing and reimbursement errors and disagreements are common in our industry, and thus we are regularly engaged in reviews, audits and appeals of our claims for reimbursement due to the subjectivities inherent in the process related to patient diagnosis and care, record keeping, claims processing and other aspects of
44
the patient service and reimbursement processes, and the errors and disagreements those subjectivities can produce. An adverse review, audit or investigation could result in:
•an obligation to refund amounts previously paid to us pursuant to the Medicare or Medicaid programs or from private payors, in amounts that could be material to our business;
•state or federal agencies imposing fines, penalties or other sanctions on us;
•temporary or permanent loss of our right to participate in the Medicare or Medicaid programs or one or more private payor networks or admission bans or moratoriums;
•protracted regulatory oversight, including education and sampling of claims, extended pre‑payment review, referral of the operating business to recovery audit or integrity contractors, or extrapolation of an error rate to other reimbursement made outside of specifically reviewed claims;
•an increase in private litigation against us; and
•damage to our reputation in the geographies served by our independent operating subsidiaries.
Both federal and state government continue to pursue intensive enforcement polices resulting in a significant number of investigations, audits, citations or regulatory deficiencies and other regulatory actions. Federal and state agencies have heightened and coordinated civil and criminal enforcement efforts as part of numerous ongoing audits, inquiries and investigations of healthcare companies and, in particular, SNFs. The focus of these investigations includes, among other things, billing and cost reporting practices; quality of care provided; and the medical necessity of rendered services. CMS announced a new nationwide audit, the “SNF 5‑Claim Probe & Educate Review,” in which the Medicare Administrative Contractors will review five claims from each of the facilities to check for compliance with PDPM billings, which could result in individual claim payment denials if errors are identified. All facilities that are not undergoing Targeted Probe and Educate (TPE) reviews, or have not recently passed a TPE review, will be subject to the nationwide audit.
If we fail to comply with these extensive laws, regulations and prohibitions to our business, we and certain officers could become subject to demands for refund of alleged overpayments, civil and criminal penalties, termination, exclusion or payment suspensions from the Medicare and Medicaid program, loss of Medicare or Medicaid certification, bans on Medicare and Medicaid payments for new admissions, admission moratoriums. We may also become subject to corporate integrity agreements or extensive monitoring by regulatory agencies. We could be forced to expend considerable resources responding to investigations, audits and other enforcement actions diverting material time, resources and attention away from our management team and our staff, and could have a materially detrimental impact on our results of operations during and after any such investigation or proceedings, regardless of whether we prevail on the underlying claim.
We are subject to extensive and complex laws and government regulations. If we are not operating in compliance with these laws and regulations or if these laws and regulations change, we could be required to make significant expenditures or change our operations in order to bring our facilities and operations into compliance.
The laws and regulations governing our operations, along with the terms of participation in various government programs, regulate how we conduct our business, the services we offer, the manner in which we provide and bill for services and collect reimbursement from governmental programs and private payors, and our interactions with patients, healthcare providers and referral sources, our marketing activities, and other aspects of our operations. These laws and regulations are subject to frequent change. We, along with other companies in the healthcare industry, are required to comply with extensive and complex laws and regulations at the federal, state and local
45
government levels. Restrictions under applicable federal and state laws and regulations that may affect our ability to operate include the following:
•the federal Anti-Kickback Statute (AKS) that prohibits the knowing and willful offer, payment, solicitation or receipt of any bribe, kickback, rebate or other remuneration for referring an individual, in return for ordering, leasing, purchasing or recommending or arranging for or to induce the referral of an individual or the ordering, purchasing or leasing of items or services covered, in whole or in part, by any federal healthcare program, such as Medicare and Medicaid. “Remuneration” includes the transfer of anything of value, in cash or in kind and directly or indirectly. A person or entity does not need to have actual knowledge of the statute or specific intent to violate it to have committed a violation;
•the federal physician self-referral law (Stark Law), that, subject to limited exceptions, prohibits physicians, which includes a doctor of medicine, from referring Medicare or Medicaid patients to an entity for the provision of certain designated health services if the physician or a member of such physician’s immediate family has a direct or indirect financial relationship (including an ownership interest or a compensation arrangement) with the entity, and prohibit the entity from billing Medicare or Medicaid for such designated health services. Unlike the AKS, the Stark Law is violated if the financial arrangement does not meet an applicable exception, regardless of any intent by the parties to induce or reward referrals or the reasons for the financial relationship and the referral;
•the federal False Claims Act (FCA), that imposes civil and criminal liability on individuals or entities that knowingly submit false or fraudulent claims for payment to the government or knowingly making, or causing to be made, a false statement in order to have a false claim paid. There are many potential bases for liability under the FCA. The government has used the FCA to prosecute Medicare and other government healthcare program fraud such as coding errors, billing for services not provided, and providing care that is not medically necessary or that is substandard in quality. In addition, the government may assert that a claim including items or services resulting from a violation of the federal AKS or Stark Law constitutes a false or fraudulent claim for purposes of the FCA. Actions under the FCA may be brought by the Attorney General, the U.S. Department of Justice (DOJ), the United States Attorney Offices, or as a qui tam action by a private individual in the name of the government. These private parties, often referred to as relators or whistleblowers, are entitled to share in any amounts recovered by the government through trial or settlement, and these qui tam cases are sealed by the court at the time of filing;
•the criminal healthcare fraud provisions of HIPAA and related rules that prohibit knowingly and willfully executing a scheme or artifice to defraud any healthcare benefit program or falsifying, concealing or covering up a material fact or making any materially false, fictitious or fraudulent statement in connection with the delivery of or payment for healthcare benefits, items or services. Similar to the AKS, a person or entity does not need to have actual knowledge of the statute or specific intent to violate it to have committed a violation; and
•similar state law provisions pertaining to anti-kickback, self-referral and false claims issues, some of which may apply to items or services reimbursed by any payor, including patients and commercial insurers;
•state corporate practice and fee-splitting laws that prohibit general business corporations such as us, from practicing medicine or other healthcare professionals, controlling licensed healthcare professionals’ medical decisions or engaging in some practices, such as spitting fees with licensed healthcare professionals;
•laws that regulate debt collection practices;
•federal and state antitrust laws that prohibit or limit exclusive contracting relationships with healthcare providers, prohibit or limit the sharing of cost and pricing data, prohibit competitors from taking collective action to set commercial payer reimbursement rates, and determine when a joint venture or healthcare network is sufficiently integrated, by either sharing substantial financial risk or substantial clinical integration, to jointly contract with commercial payers;
46
•laws that impose criminal penalties on healthcare providers who fail to disclose or refund known overpayments;
•laws that require maintenance of licensure, certification and accreditation;
•laws relating to adequacy and quality of healthcare services, quality and maintenance of medical equipment and facilities;
•laws that impose reporting, transparency and disclosure requirements of the ownership, management. managing employees and the owners of real property lessors or sublessors, including any private equity companies or REITs;
•laws relating to staffing levels and qualifications and vaccination (including boosting) of healthcare and support personnel;
•confidentiality, maintenance and security issues associated with medical records and claims processing; and
•constraints on protective contractual provisions with patients and third‑party payors.
These laws and regulations are complex, and we do not always have the benefit of significant regulatory or judicial interpretation of these laws and regulations. We are unable to predict the future course of federal, state and local regulation or legislation, including as it pertains to Medicare, Medicaid, or fraud and abuse laws, and how they are enforced. Additionally, in the future, different interpretations or enforcement of these laws and regulations could subject our current or past practices to allegations of impropriety or illegality or could require us to make changes in our facilities, equipment, personnel, services, operations, capital expenditure programs and operating expenses. Our efforts to comply with these laws and regulations could be costly and result in diversion of management time and effort and may still not guarantee compliance. Regulators continue to increase their scrutiny of compliance with these obligations, which may require us to further revise or expand our compliance program. While we do not believe we are in violation of these laws, we cannot assure you that governmental officials charged with the responsibility for enforcing these prohibitions will not assert that we are violating the provisions of such laws and regulations.
If we fail to comply with these applicable laws and regulations, or their interpretations as determined by courts or enforced by regulators, we could suffer civil or criminal penalties, sanctions, remedial measures and other detrimental consequences, including denial of reimbursement, imposition of fines, temporary suspension of admission of new patients, suspension or decertification from the Medicaid and Medicare programs, restrictions on our ability to acquire new facilities or expand or operate existing facilities, the loss of our licenses to operate and the loss of our ability to participate in federal and state reimbursement programs. In addition, if we fail to comply, even inadvertently, with any of these requirements, we could be required to alter our operations and enter into a corporate integrity agreement, deferred prosecution or similar agreements with state or federal government agencies. Furthermore, should we lose licenses or certifications for a number of our facilities or other businesses as a result of regulatory action or legal proceedings, we could be deemed to be in default under some of our agreements, including agreements governing outstanding indebtedness. See the section titled “Business—Regulatory Matters.”
We face and are currently subject to surveys, investigations, and other proceedings relating to our licenses and certification and potential sanctions and remedies based upon alleged regulatory deficiencies could negatively affect our financial condition and results of operations. Public and government calls for increased survey and enforcement efforts toward SNFs, and potential rulemaking that may result in enhanced enforcement and penalties, could result in increased scrutiny by state and federal survey agencies.
Our facilities must comply with required conditions of participation in the Medicare program and state Medicaid programs and state licensure requirements. We are subject to surveys and investigations from federal and state agencies as well as accreditation organizations. We receive deficiency reports from state and federal regulatory bodies resulting from such inspections or surveys. If we fail to meet the conditions of participation or licensure
47
standards, we may receive a notice of deficiency from the applicable surveyor. Although most inspection deficiencies are resolved through an agreed‑upon plan of corrective action, the reviewing agency typically has the authority to take further action against a licensed or certified facility.
We have received notices of potential sanctions and remedies based upon alleged regulatory deficiencies from time to time, and such sanctions have been imposed on some of our facilities. No material remedial actions have been taken against us to date, however, we have had facilities placed on special focus facility status in the past, continue to have some facilities on this status currently and other operating subsidiaries may be identified for such status in the future. In particular, as our strategy includes the targeted acquisition of underperforming SNFs, we from time to time acquire facilities with special focus facility status. As of September 1, 2024, we had three facilities with special focus facility status. Two such facilities were acquired with this status and one was placed on such status following our acquisition of the facility. These facilities received such status as a result of accumulating an above average number survey deficiency points over the course of multiple surveys, some of which occurred prior to their acquisition. Survey deficiency points are issued by the government survey agency when inspecting a nursing facility to reflect the deficiencies that the facility is cited for in the survey, which include, but are not limited to, quality of life and care, freedom from abuse, neglect and exploitation deficiencies.
If a facility then fails to institute an acceptable plan of correction to remediate the deficiency within the correction period provided by the state surveyor, that facility could be subject to remedial action. These actions include the imposition of fines, imposition of a license to a conditional or provisional status, admission holds, suspension or revocation of a license, payment suspension, loss of certification as a provider under state or federal healthcare programs, or imposition of other sanctions, including civil monetary penalties and criminal penalties. Termination of one or more of our facilities from the Medicare or state Medicaid programs for failure to satisfy conditions of participation, or the imposition of alternative sanctions, could disrupt operations, require significant attention by management or have a material adverse effect on our business and reputation and consolidated financial condition, results of operations and cash flows.
From time to time, we have opted to voluntarily stop accepting new patients pending completion of a new state survey, in order to avoid possible denial of payment for new admissions during the deficiency cure period, or simply to avoid straining staff and other resources while retraining staff, upgrading operating systems or making other operational improvements. If we elect to voluntary close any operations in the future or to opt to stop accepting new patients pending completion of a state or federal survey, it could negatively impact our financial condition and results of operation.
Furthermore, in some states, citation of one affiliated facility could negatively impact other facilities in the same state. Revocation of a license at a given facility could therefore impair our ability to obtain new licenses or to renew, or maintain, existing licenses at other facilities, which may also trigger defaults or cross‑defaults under our leases and our credit arrangements, or adversely affect our ability to operate or obtain financing in the future. CMS’s rules requiring disclosure of ownership, management and the owners of real property lessors or sublessors, heighten this risk. Our failure to comply with applicable legal and regulatory requirements in any single facility could negatively impact our financial condition and results of operations.
As CMS turns its attention to enhancing enforcement activities towards SNFs, state survey agencies will have more accountability for their survey and enforcement efforts. In addition, the Biden Administration has called for HHS and CMS to increase the level of scrutiny of SNF facilities and requested those agencies to adopt rules that would impose greater penalties upon non‑compliant SNF operators. The Biden Administration’s fact sheet regarding enhanced penalties against special focus facilities (SFFs) represents further federal calls for oversight and penalties for low‑ranked and underperforming SNFs. This fact sheet precedes greater focus by CMS in obtaining oversight over SFFs, and continuing that oversight even after those SFFs improve, and subjecting them to more exacting and routine oversight. In addition, effective October 1, 2024, CMS finalized expanded authority to impose multiple per-day and per-instance civil monetary penalties (CMPs) on facilities for non-compliance identified in surveys, with a look-back period of three standard surveys. The likely result may be more frequent surveys of our facilities, with more substantial penalties, fines and consequences if they do not perform well. For low‑performing facilities in the SFF program, the standards for successfully emerging from that program and not being subject to ongoing and
48
enhanced government oversight will be higher and measured over a longer period of time, prolonging the risks of monetary penalties, fines and potential suspension or exclusion from the Medicare and Medicaid programs. Additionally, CMS recently updated the survey resources that CMS and state surveyors use in evaluating our SNFs’ compliance with federal Requirements for Participation. The application of CMS’s new guidance could result in more aggressive and stringent surveys, and potential fines, penalties, sanctions, or administrative actions taken against our independent operating subsidiaries.
Federal minimum staffing mandates may adversely affect our labor costs, ability to maintain desired levels of patient or resident capacity, and profitability.
In April 2024, the Biden Administration adopted a minimum staffing standard through CMS. The Staffing Rule is currently subject to legal challenges, and there are also congressional efforts to prevent the implementation and enforcement of the minimum staffing requirements. For further discussion, see the section titled “CMS Minimum Staffing Standards Final Rule.” While the full effect of federal staff level minimums, if they are ultimately implemented in the adopted or another form, is not fully known at this time, we expect that the mandate could have adverse financial consequences upon our business. We may be required to hire substantially more staff members, particularly nurse practitioners, registered nurses, licensed practical nurses and nursing aides than currently staffed. Additionally, the federal mandate would place similar pressure on our competitors and result in sudden, expanded demand for nursing staff across the SNF industry. This added demand across the SNF industry may exacerbate an already difficult labor market, with demand for nursing staff far outstripping the supply of qualified individuals, and the compensation requirements of both current and prospective staff increasing markedly to increase the likelihood of recruiting and retaining skilled caregivers. Changes in Medicare reimbursements for physician and non‑physician services could impact reimbursement for medical professionals.
The Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) revised the payment system for physician and non‑physician services. The changes to the therapy caps imposed on Medicare Part B outpatient therapy from this law have been changed by the Bipartisan Budget Act of 2018 (BBA), and are subject to future budgetary changes through rulemaking and legislation, resulting in ongoing uncertainty regarding payment for these Medicare Part B services. Under the proposed Current Year (CY) 2024 Physician Fee Schedule (PFS) Final Rule, reductions in payment and conditions imposed in exchange for higher payments may impose operational requirements and working conditions that further detract from and reduce our financial performance. Similarly, new final rules concerning the Programs of All-Inclusive Care for the Elderly (PACE) program and the information it will collect may adversely affect the risk‑adjusted reimbursement.
We may be subject to increased investigation and enforcement activities related to the Health Insurance Portability and Accountability Act of 1996 (HIPAA) violations.
HIPAA, as amended by the Health Information Technology for Economic and Clinical Health (HITECH) Act, requires us to adopt and maintain business procedures and systems designed to protect the privacy, security and integrity of patients’ individual health information, in addition to state laws governing the privacy of patient information. We must comply with these state privacy laws to the extent that they are more protective of healthcare information or provide additional protections not afforded by HIPAA. HIPAA and other comparable state and federal laws and regulations change periodically. If we fail to comply with these state and federal laws and regulations, we could be subject to criminal penalties, civil sanctions, litigation, and be forced to modify our policies and procedures, in addition to undertaking costly breach notification and remediation efforts, as well as sustaining reputational harm.
In addition to breaches of protected patient information, under HIPAA and other federal and state laws and regulations, healthcare entities are also required to afford patients with certain rights of access to their health information and to promote sharing of patient data between and among healthcare providers involved in the same patient’s course of care. Recently, the Office for Civil Rights, the agency responsible for HIPAA enforcement, has targeted investigative and enforcement efforts on violations of patients’ rights of access, imposing significant fines for violations largely initiated from patient complaints. If we fail to comply with our obligations under HIPAA or other comparable federal or state laws and regulations, we could face significant fines and penalties.
49
Annual caps and other cost‑reductions for outpatient therapy services may reduce our future revenue and profitability or cause us to incur losses.
Several government actions have been taken in recent years to try and contain the costs of rehabilitation therapy services provided under Medicare Part B, including the Multiple Procedure Payment Reduction (MPPR), institution of annual caps, mandatory medical reviews for annual claims beyond a certain monetary threshold, and a reduction in reimbursement rates for therapy assistant claim modifiers. Of specific concern has been CMS’s efforts to lower Medicare Part B reimbursement rates for outpatient therapy services in 2021, 2022, and 2023. Such cost‑containment measures and ongoing payment changes could have an adverse effect on our revenue. The Office of the Inspector General (OIG) or other regulatory authorities may choose to more closely scrutinize billing practices in areas where we operate or propose to expand, which could result in an increase in regulatory monitoring and oversight, decreased reimbursement rates, or otherwise adversely affect our business, financial condition and results of operations.
The OIG regularly conducts investigations regarding certain payment or compliance issues within the healthcare industry. The OIG identified SNF compliance as an issue of concern in its 2021 and 2022 semi‑annual reports to Congress, and its January 2023 study regarding SNF emergency preparedness identified the need for further oversight and addition of SNF emergency readiness to the OIG’s 2023 work plan. Nursing homes were also a topic of discussion in the OIG’s 2023 semi-annual report to Congress, which emphasized the continued protection and oversight of care that nursing facilities provide to residents. Among other things, the OIG recommended a reduction in the use of psychotropic drugs in nursing homes and urged CMS to evaluate the appropriateness of psychotropic drug use among residents, including the use of data to identify nursing homes with higher rates of use for potential further scrutiny and action. Based on this information, SNFs in particular are potential targets for more robust scrutiny and examination by regulators. Recent publications and statements by the Biden Administration have also called for greater scrutiny of SNF facilities.
Our business model, like those of some other for‑profit operators, is based in part on attracting higher‑acuity patients whom we believe provide us more opportunity to be profitable due to the higher level of services they need and accordingly higher reimbursement rates, and over time our overall patient mix has consistently shifted to higher‑acuity and higher‑resource utilization patients in most facilities we operate. These efforts may place us under greater scrutiny with the OIG, CMS, our fiscal intermediaries, recovery audit contractors and others. See the section titled “Business—Regulatory Matters.”
Newly enacted and proposed legislation in the states where our independently operating entities are located may affect our operations in terms of individual litigation and the broader regulatory environment.
A bill in the State of California, where a significant majority of our facilities are located, was recently signed into law which increases the cap of non‑economic damages awarded to plaintiffs who are successful in medical malpractice litigation. The cap increased from $250,000 to $350,000 beginning on January 1, 2023, then increases over the following 10 years until the cap reaches a maximum of $750,000, with further adjustments for inflation. In wrongful death cases, the cap increased from $250,000 to $500,000 on January 1, 2023, with incremental increases over the following 10 years until the cap reaches a maximum of $1,000,000, with adjustments for inflation. Due to California’s influence on other states, other jurisdictions where we operate may enact similar laws. Similar to the potential incentive of increased damages caps, the Supreme Court’s recent decision in Health and Hospital Corporation of Marion City v. Talevskimay increase public interest in potential claims against SNFs, particularly pertaining to specific civil rights claims against governmental actors rather than general liability claims against privately owned SNFs such as those operated by our independent operating subsidiaries.
As another example, California’s adoption of the Skilled Nursing Facility Ownership and Management Reform Act of 2022 imposes new requirements for obtaining licenses to operate SNFs. These new requirements may delay or limit the ability to obtain new SNF licenses within that state, whether through acquisition of existing facilities or opening a new facility. This new law’s obligations may increase the costs of obtaining licensure, make applications more time‑consuming and complex, and may result in civil penalties and other sanctions against our facilities in the event they are not compliant with these new licensure application requirements. As a result, this new law may delay
50
or impede growth within California. As with the bill that increases the cap of non‑economic damages for medical malpractice litigation, California’s influence on other states may result in this legislation becoming a model for other states and having similar, potentially adverse effects within those jurisdictions as well.
More recently, California’s legislature has proposed, among other things, bills related to increasing the minimum wage for workers, spending requirements and increased disclosure. These and other bills would create new and costly obligations on our independent operating subsidiaries if they became law and if enacted, would adversely affect our business, operations, and profitability. In October 2023, California adopted legislation that requires, if and when a minimum spending bill is later enacted with respect to skilled nursing facilities, workers at skilled nursing facilities, as well as most other healthcare facilities throughout the state, be paid a minimum wage that begins at $21 per hour beginning June 1, 2024, increasing to $23 per hour beginning June 1, 2026, and then increasing to $25 per hour beginning June 1, 2028. While California’s state Medicaid reimbursement program will, barring intervening changes to the program, reimburse providers for some of the increased operating costs, there can be no assurance that they will be reimbursed for the full increase, or that they will be reimbursed in a timely manner.
As another example, Texas passed a bill which partially restored Medicaid state relief funding for SNFs through August 31, 2023; it also considered regulation, which contained direct care spending requirements and ownership. While this bill provides financial relief to our independent operating subsidiaries in Texas, other proposed bills may impose the same regulatory requirements and limitations inherent in both the proposed legislation in other states and the federal rule requiring disclosure of such information in applications and change‑of‑ownership disclosures, which may adversely affect our business, operations, and profitability. See the section titled “Business—Regulatory Matters.”
Changes to federal and state employment‑related laws and regulations could increase our cost of doing business.
Our operating subsidiaries are subject to a variety of federal and state employment‑related laws and regulations, including, but not limited to, the U.S. Fair Labor Standards Act that governs such matters as minimum wages, overtime and other working conditions, the Americans with Disabilities Act (ADA) and similar state laws that provide civil rights protections to individuals with disabilities in the context of employment, public accommodations and other areas, the National Labor Relations Act, regulations of the U.S. Equal Employment Opportunity Commission (EEOC), regulations of the Office of Civil Rights, regulations of state attorney generals, family leave mandates and a variety of similar laws enacted by the federal and state governments that govern these and other employment law matters.
On June 5, 2023, CMS published the Omnibus Final Rule, withdrawing the COVID‑19 vaccination IFR 60 days after the rule’s publication. At present, there is no nationally significant litigation concerning such mandates. The effects of the COVID‑19 vaccination IFR’s withdrawal on our operations and the labor pool for nursing and administrative staff is unknown, but may have an impact on our business, operations, and profitability.
Furthermore, the Biden Administration has requested HHS and CMS study and issue proposed rules regarding care‑based careers, including improving access to training, increasing the attractiveness of compensation in care‑based positions, and improving the retention and career progression of care workers. The Biden Administration has sought proposed rules that tie some of these issues, such as wages and retention, to Medicare reimbursement for facilities. Other pending legislation, such as the HCBS Access Act, indicate a legislative priority of providing funding for care‑based careers that may affect our pool of desired workers. Rising operating costs due to labor shortages, greater compensation and incentives required to attract and retain qualified personnel and higher‑than‑usual inflation on items including energy, utilities, food and other goods used in our facilities and the costs for transporting these items could increase our cost and decrease our profits.
The compliance costs associated with these laws and evolving regulations could be substantial. By way of example, all of our facilities are required to comply with the ADA, which has separate compliance requirements for “public accommodations” and “commercial properties,” but generally requires that buildings be made accessible to people with disabilities. Compliance with ADA requirements could require removal of access barriers and
51
non‑compliance could result in imposition of government fines or an award of damages to private litigants. Further legislation may impose additional burdens or restrictions with respect to access by disabled persons. In addition, federal proposals to introduce a system of mandated health insurance and flexible work time and other similar initiatives could, if implemented, adversely affect our operations. We also may be subject to employee‑related claims such as wrongful discharge, discrimination or violation of equal employment law. While we are insured for these types of claims, we could be subject to damages that are not covered by our insurance policies or that exceed our insurance limits, and we may be required to pay such damages directly, which would negatively impact our cash flow from operations.
In addition, there currently is pending legislation in California to raise the minimum wage to $25 per hour for all healthcare workers and require SNFs to maintain a minimum spend of 85% of revenue on direct care costs. As of June 30, 2024, approximately 64% of our skilled nursing beds are located in California. Although there currently is no similar proposed legislation in the other states in which we operate, if we expand to other states, we may be subject to similar legislation.
Required regulatory approvals could delay or prohibit transfers of our healthcare operations, which could result in periods in which we are unable to receive reimbursement for such properties.
The operations of our operating subsidiaries must be licensed under applicable state law and, depending upon the type of operation, certified or approved as providers under the Medicare and/or Medicaid programs. In the process of acquiring or transferring operating assets, our operations must receive change of ownership approvals from state certificate of need boards, licensing agencies, Medicare and Medicaid as well as third-party payors. Rules regarding the disclosure of SNF facility ownership may increase the scrutiny placed on companies that operate, directly or indirectly, multiple SNFs, and may subject our licensing and approval process to additional scrutiny or delays.
In recent years, states including California, Connecticut, Illinois, Massachusetts, Minnesota, Nevada, New York, Oregon, Rhode Island and Washington have become increasingly interested in the review of healthcare transactions for impacts on costs, access to care and quality, and certain states are particularly focused on transactions involving private equity investments. Transactions involving single multi-state organizations with hundreds of healthcare providers and facilities across the country are and may be in the future subject to state reviews because one or more providers or facilities derive revenue from patients within the state. Certain state review processes can involve lengthy review and approval periods, require enhanced disclosure obligations and impact analysis, public notices and hearings, and approval conditions and post-closing oversight, including ongoing reporting obligations. Overall, these state laws regulating costs, access to care and quality, in effect and those that may go into effect in the future, may delay or burden our transactions, including future add-on acquisitions, increase costs associated with expansion, require intrusive disclosures, and impose onerous, ongoing reporting obligations.
If there are any delays in receiving regulatory approvals from the applicable federal, state or local government agencies, or the inability to receive such approvals, such delays or denials could result in delayed or lost reimbursement related to periods of service prior to the receipt of such approvals, which could negatively impact our cash position.
Compliance with federal and state fair housing, fire, safety and other regulations may require us to make unanticipated expenditures, which could be costly to us.
We must comply with the federal Fair Housing Act and similar state laws, which prohibit us from discriminating against individuals if it would cause such individuals to face barriers in gaining residency in any of our facilities. Additionally, the Fair Housing Act and other similar state laws require that we advertise our services in such a way that we promote diversity and not limit it. We may be required, among other things, to change our marketing techniques to comply with these requirements.
In addition, we are required to operate our facilities in compliance with applicable fire and safety regulations, building codes and other land use regulations and food licensing or certification requirements as they may be
52
adopted by governmental agencies and bodies from time to time. Like other healthcare facilities, our affiliated SNFs are subject to periodic surveys or inspections by governmental authorities to assess and assure compliance with regulatory requirements. Surveys occur on a regular (often annual or biannual) schedule, and special surveys may result from a specific complaint filed by a patient, a family member or one of our competitors. We may be required to make substantial capital expenditures to comply with these requirements.
Our operations are subject to environmental and occupational health and safety regulations, which could subject us to fines, penalties and increased operational costs.
We are subject to a wide variety of federal, state and local environmental and occupational health and safety laws and regulations. Regulatory requirements faced by healthcare providers such as us include those relating to air emissions, wastewater discharges, air and water quality control, occupational health and safety (such as standards regarding blood-borne pathogens and ergonomics), management and disposal of low-level radioactive medical waste, biohazards and other wastes, management of explosive or combustible gases, such as oxygen, specific regulatory requirements applicable to asbestos, lead-based paints, polychlorinated biphenyls and mold, other occupational hazards associated with our workplaces, and providing notice to employees and members of the public about our use and storage of regulated or hazardous materials and wastes. Failure to comply with these requirements could subject us to fines, penalties and increased operational costs. Moreover, changes in existing requirements or more stringent enforcement of them, as well as discovery of currently unknown conditions at our owned or leased facilities, could result in additional cost and potential liabilities, including liability for conducting cleanup, and there can be no guarantee that such increased expenditures would not be significant.
Risks Related to This Offering and Ownership of Our Common Stock
The market price of our common stock may be volatile or may decline steeply or suddenly regardless of our operating performance, which could result in substantial losses for purchasers of our common stock in this offering, and we may not be able to meet investor or analyst expectations.
The market price of our common stock may be highly volatile and fluctuate or decline significantly in response to numerous factors, many of which are beyond our control, including:
•variations between our actual operating results, or those of companies that are perceived to be similar to us, and the expectations of securities analysts, investors and the financial community;
•any forward-looking financial or operating information we may provide to the public or securities analysts, any changes in this information or our failure to meet expectations based on this information;
•actions of securities analysts who initiate or maintain coverage of us, changes in financial estimates by any securities analysts who follow our Company or our failure to meet these estimates or the expectations of investors;
•additional shares of our common stock being sold into the market by us or our existing stockholders, or the anticipation of such sales, including if existing stockholders sell shares into the market when applicable “lock-up” period ends;
•hedging activities by market participants;
•announcements by us or our competitors of significant features, technical innovations in facilities, acquisitions, strategic partnerships, joint ventures or capital commitments;
•changes in operating performance and stock market valuations of companies in our industry, including our competitors;
•changes in third-party payor reimbursement policies;
53
•an inability to obtain additional funding;
•general economic, political, industry and market conditions, including rising inflation, high interest rates, capital market disruptions, and price and volume fluctuations in the overall stock market;
•expiration of market stand-off or lock-up agreements;
•lawsuits threatened or filed against us;
•developments in new legislation and pending lawsuits or regulatory actions, including interim or final rulings by judicial or regulatory bodies; and
•other events or factors, including those resulting from political conditions, election cycles, pandemics, war or incidents of terrorism, or responses to these events, many of which are outside of our control.
In addition, extreme price and volume fluctuations in the stock markets have affected and continue to affect many healthcare companies’ stock prices. Stock prices often fluctuate in ways unrelated or disproportionate to the companies’ operating performance. In the past, stockholders have filed securities class action litigation following periods of market volatility. This risk is especially relevant for us because companies in the healthcare industry have experienced significant stock price volatility in recent years. If we were to become involved in securities litigation, it could subject us to substantial costs, divert resources and the attention of management from our business and seriously harm our business.
Moreover, because of these fluctuations, comparing our operating results on a period-to-period basis may not be meaningful. You should not rely on our past results as an indication of our future performance. This variability and unpredictability could also result in our failure to meet the expectations of industry or financial analysts or investors for any period. If our revenues or operating results fall below the expectations of analysts or investors or below any forecasts we may provide to the market, or if the forecasts we provide to the market are below the expectations of analysts or investors, the price of our common stock could decline substantially. Such a stock price decline could occur even when we have met any previously publicly stated revenue or earnings forecasts that we may provide.
An active trading market for our common stock may not be sustainable, and you may not be able to resell your shares at or above the offering price.
Although our common stock is listed on the New York Stock Exchange under the symbol “PACS,” an active trading market for our common stock may not be sustained. In the absence of an active trading market for our common stock, you may not be able to sell your shares of our common stock when desired or at or above the public offering price. An inactive market may also impair our ability to raise capital by selling shares and may impair our ability to acquire other businesses or properties using our shares as consideration, which, in turn, could materially and adversely affect our business.
Our founders, Jason Murray and Mark Hancock, will continue to have substantial control over us and will hold a substantial portion of our outstanding common stock, and their interests may conflict, or appear to conflict, with our interests and the interests of other stockholders.
Following the completion of this offering, and without giving effect to any purchases that may be made otherwise in this offering, our founders, Jason Murray and Mark Hancock, will collectively beneficially own approximately 73.7% of the voting power of our common stock (or 72.4% if the underwriters exercise their option to purchase additional shares from the selling stockholders in full). In addition, pursuant to the terms of our Amended and Restated Charter, our founders are able to control corporate matters for the foreseeable future. For example, each founder has the right to designate (i) up to two individuals for inclusion in our slate of director nominees if such founder beneficially owns at least 20% of the aggregate number of shares of common stock outstanding immediately following the completion of our IPO or (ii) one individual for inclusion in our slate of director nominees if such founder beneficially owns less than 20% but at least 10% of the aggregate number of shares of
54
common stock outstanding immediately following the completion of our IPO. Accordingly, each founder has the right to designate two directors, and our founders collectively have the right to designate four directors, which represents four out of our five member board of directors. These rights are affirmed in the Stockholders Agreement. See the section titled “Certain Relationships and Related Party Transactions—Stockholders Agreement.”
In addition, pursuant to the terms of our Amended and Restated Charter, for so long as Messrs. Murray and Hancock beneficially own, in the aggregate, the majority of the voting power of our outstanding shares of voting stock, they will be able to remove any of our directors at any time with or without cause and may take action by written consent without a meeting of stockholders. As a result, Messrs. Murray and Hancock are able to determine or significantly influence our management, business plans, policies, and governance for the foreseeable future. This concentrated control of the composition of the board of directors and voting power of our common stock will preclude your ability to influence corporate matters for the foreseeable future, including with respect to the composition of our board of directors, the election and removal of directors, the authorization and issuance of additional shares of our common stock that would be dilutive to you, the issuance of shares of preferred stock that could be dilutive to you and could have disparate voting rights, amendments to our organizational documents, and any merger, consolidation, sale of all or substantially all of our assets, or other major corporate transaction requiring stockholder approval. In addition, this may prevent or discourage unsolicited acquisition proposals or offers for our capital stock that you may feel are in your best interests as one of our stockholders, and may deprive us of what we perceive as an attractive business combination opportunity. These limitations could deprive you of an opportunity to receive a premium for your shares of common stock as part of a sale of our company and ultimately might affect the market price of our common stock.
Even when the parties to our Stockholders Agreement cease to own shares of our stock representing a majority of the total voting power, for so long as such parties continue to own a significant percentage of our stock, they will still be able to significantly influence or effectively control the composition of our board of directors and the approval of actions requiring stockholder approval through their voting power. Accordingly, for such period of time, the parties to our Stockholders Agreement will have significant influence with respect to our management, business plans, policies, and governance.
Our founders, Jason Murray and Mark Hancock, have entered into margin loans and pledged a portion of their shares of our common stock as collateral to secure such margin loans. If either Mr. Murray or Mr. Hancock defaults on their respective obligations under any margin loans, the lender may be entitled to foreclose on their shares pledged as collateral and sell them to the public, which could cause our stock price to decline and result in a significant change in beneficial ownership.
Each of Mr. Murray and Mr. Hancock has entered into a margin loan and each has pledged 9,500,000 of their respective shares of our common stock as collateral to secure such margin loan. The underwriters in our IPO and in this offering have provided Messrs. Murray and Hancock an exception under their respective lock-up agreements that permits each of them to pledge a portion of their shares of our common stock as collateral to secure one or more margin loans with one or more nationally or internationally recognized financial institutions, subject to certain exceptions and specified conditions, including that the aggregate number of shares of our common stock pledged as collateral pursuant to any such margin loans by Messrs. Murray and Hancock during the respective lock-up periods shall not, for each of Messrs. Murray and Hancock, exceed 7.5% of the total number of shares of our common stock issued and outstanding in the aggregate on the closing date of this offering. As a result, the lock-up agreements permit an aggregate of up to 15% of the total number of shares of our common stock outstanding to be pledged as collateral pursuant to margin loans during the 180 day period covered by the lock-up agreements entered into in connection with the IPO and the 90 day period covered by the lock-up agreements entered into in connection with this offering. It is possible that margin loan lenders under any such margin loans, who could potentially benefit from a greater percentage of shares of common stock being pledged as collateral, and with the consent of the representatives of the underwriters under the respective lock-up agreements, agree to permit a greater percentage of shares of common stock to be pledged. With respect to margin loans, Messrs. Murray and/or Hancock retain their ability to vote the shares of our common stock pledged as collateral and pledged shares shall not impact their beneficial ownership for purposes of the rights under the Stockholders Agreement or otherwise in connection with matters to be voted on by stockholders. Pursuant to Rule 13d-3(d)(3) under the Exchange Act, a margin loan lender
55
would not beneficially own the pledged shares unless and until such lender has taken all formal steps necessary which are required to declare a default and determines that the power to vote or to direct the vote or to dispose or to direct the disposition of pledged securities will be exercised. However, if either of Mr. Murray or Mr. Hancock were to default on their respective obligations under any margin loan (including but not limited to the borrower’s inability to satisfy certain payments required under such margin loan) and fail to cure such default, the margin loan lender may be entitled to exercise its right under such margin loan to foreclose on the pledged interests and, subject to the recipients agreeing to be bound by lock-up agreements, sell the pledged shares of our common stock in order to satisfy the borrower’s obligations. Such an event could cause our stock price to decline and result in a change in beneficial ownership of our existing stockholders in the event that the margin loan lender determines to exercise voting or dispositive power over the shares.
Depending upon the beneficial ownership of Messrs. Murray and Mr. Hancock at the time of any such event, it is possible that the resulting change in beneficial ownership could result in changes to the rights of the holders of our common stock under our Amended and Restated Charter. For example, if, following such an event, Messrs. Murray and Hancock beneficially own, in the aggregate, less than a majority of the voting power of our outstanding shares of voting stock, they would no longer be able to remove any of our directors at any time with or without cause or take action by written consent without a meeting of stockholders. In such event, pursuant to the terms of our Amended and Restated Charter, directors could only be removed for cause and only by the affirmative vote of the holders of at least two-thirds of the voting power of all then outstanding shares of our voting stock and our stockholders would not be able to take action by written consent, which would have the effect of requiring all stockholder actions to be taken at a meeting of our stockholders. In addition, any such changes in the beneficial ownership of Messrs. Murray and Mr. Hancock may result in the reduction or loss of their respective rights to designate individuals for inclusion in our slate of director nominees, and may result in the loss of our ability to qualify as a controlled company.
Except as may be limited by any lock-up agreement Messrs. Murray and Hancock are a party to, they may pledge additional shares of our common stock to secure additional margin loans.
Future sales, or the perception of future sales, of shares of common stock by existing stockholders could cause the market price of our common stock to decline.
If our existing stockholders sell, or indicate an intention to sell, substantial amounts of our common stock in the public market after the lock-up and legal restrictions on resale discussed in this prospectus lapse, the trading price of our common stock could decline.
Upon consummation of this offering, based on the number of shares of our common stock outstanding on June 30, 2024, we will have outstanding a total of 155,177,511 shares of our common stock. Of these shares, 115,615,378 shares (assuming no exercise of the underwriters’ option to purchase additional shares from the selling stockholders) are held by our directors and officers and are subject to lock-up and market stand-off agreements that restrict their ability to, among other things and subject to certain exceptions, sell or transfer their shares for a period of 90 days after the date of this prospectus. However, Citigroup Global Markets Inc., J.P. Morgan Securities LLC and Truist Securities, Inc. may, in their sole discretion as representatives of the underwriters in this offering, waive the contractual lock-up before the lock-up agreements expire. The representatives have granted our executive officers, other than Messrs. Murray and Hancock, an exception under their respective lock-up agreements that permits them collectively to sell up to 400,000 shares in the aggregate during such 90 day period. Additionally, the representatives have granted each of Messrs. Murray and Hancock an exception under their respective lock-up agreements that permits each of them to pledge a portion of their shares of our common stock to secure one or more margin loans. See “—Our founders, Jason Murray and Mark Hancock, have entered into margin loans and pledged a portion of their shares of our common stock as collateral to secure such margin loans. If either Mr. Murray or Mr. Hancock default on their respective obligations under any margin loans, the lender may be entitled to foreclose on their shares pledged as collateral and sell them to the public, which could cause our stock price to decline and result in a significant change in beneficial ownership.”
56
After the lock-up agreements expire, all shares of our common stock outstanding as of June 30, 2024 (assuming the closing of this offering) will be eligible for sale in the public market, of which shares held by directors, executive officers and other affiliates will be subject to volume limitations under Rule 144 of the Securities Act (Rule 144), and various vesting agreements. Sales of a substantial number of such shares upon expiration of the lock-up and market stand-off agreements, the perception that such sales may occur or early release of these agreements, could cause our market price to fall or make it more difficult for you to sell your common stock at a time and price that you deem appropriate. Messrs. Murray and Hancock are additionally entitled to rights with respect to the registration of all of their shares following this offering and if they were to exercise those rights they may be able to sell their shares outside of the volume limitations imposed by Rule 144. See the section titled “Description of Capital Stock—Registration Rights” for a description of these registration rights.
Additionally, the shares of our common stock registered on our registration statement on Form S-8 under the Securities Act and issuable or reserved for issuance under our 2024 Plan and our ESPP are eligible for sale in the public market, subject to Rule 144 limitations applicable to affiliates and the lock-up agreements described above. If these additional shares are sold, or if it is perceived that they will be sold in the public market, the trading price of our common stock could decline.
If you purchase our common stock in this offering, you will incur immediate and substantial dilution.
The offering price is substantially higher than the as adjusted net tangible book value per share of our common stock of $3.36 per share as of June 30, 2024. Investors purchasing common stock in this offering will pay a price per share that substantially exceeds the book value of our tangible assets after subtracting our liabilities. As a result, investors purchasing common stock in this offering will incur immediate dilution of $35.69 per share, based on the assumed public offering price of $39.67 per share, which is the last reported sale price of our common stock as reported on the New York Stock Exchange on August 30, 2024. This dilution is due to the substantially lower price paid by our investors who purchased shares of common stock prior to this offering as compared to the price offered to the public in this offering.
Future issuances of shares of our common stock, or the perception that these sales may occur, could depress the market price of our common stock and result in dilution to existing holders of our common stock. Our authorized capital stock consists of 1,250,000,000 shares of common stock. The authorized but unissued shares of our common stock are available for future issuance by our board of directors without stockholder approval, subject to any limitations imposed by the listing standards of the New York Stock Exchange. These additional shares may be utilized for a variety of corporate purposes, including future public offerings to raise additional capital, acquisitions and employee benefit plans. Also, to the extent outstanding options, restricted stock units or other stock-based awards are issued or become vested, there will be further dilution. The amount of dilution could be substantial depending upon the size of the issuances or exercises. Furthermore, we may issue additional equity securities that could have rights senior to those of our common stock. For example, our Amended and Restated Charter will also authorize our board of directors to establish and determine, among others, the voting, board representation and other rights or preferences of one or more series of preferred stock, and our board of directors may determine to issue additional shares of common stock, in each case without stockholder approval. As a result, purchasers of our common stock in this offering bear the risk that future issuances of debt or equity securities may reduce the value of our common stock and further dilute their ownership interest.
If our estimates or judgments relating to our critical accounting policies are based on assumptions that change or prove to be incorrect, our operating results could fall below our publicly announced guidance or the expectations of securities analysts and investors, resulting in a decline in the market price of our common stock.
The preparation of financial statements in conformity with GAAP requires management to make estimates and assumptions that affect the amounts reported in our combined/consolidated financial statements and the accompanying notes thereto. We base our estimates on historical experience and on various other assumptions that we believe to be reasonable under the circumstances, the results of which form the basis for making judgments about the carrying values of assets, liabilities, equity, revenue and expenses that are not readily apparent from other sources. It is possible that interpretation, industry practice and guidance involving estimates and assumptions may
57
evolve or change over time. If our assumptions change or if actual circumstances differ from our assumptions, our operating results may be adversely affected and could fall below our publicly announced guidance or the expectations of securities analysts and investors, resulting in a decline in the market price of our common stock.
We have broad discretion in how we may use the net proceeds from this offering, and we may not use them effectively. We intend to use all of the net proceeds to us from this offering to repay amounts outstanding under our Amended and Restated 2023 Credit Facility, which will reduce the extent of the net proceeds available for general corporate purposes to support the growth of our business.
Our management will have broad discretion in applying the net proceeds we receive from this offering, and accordingly, investors in this offering will need to rely upon the judgment of our management with respect to the use of proceeds with only limited information concerning management’s specific intentions. We currently intend to use all of the net proceeds to us from this offering to repay a portion of amounts outstanding under our Amended and Restated 2023 Credit Facility. The amount of net proceeds we use to repay amounts outstanding under our Amended and Restated 2023 Credit Facility will reduce the extent of the net proceeds available for general corporate purposes to support the growth of our business. While we may borrow amounts under our Amended and Restated 2023 Credit Facility for general corporate purposes, such amounts are subject to the terms of our Amended and Restated 2023 Credit Facility, must be repaid and will accrue interest obligations. See the sections titled “Use of Proceeds” and “Management’s Discussion and Analysis of Financial Condition and Results of Operations—Liquidity & Capital Resources—Credit Facilities.” If our management fails to use these funds effectively, our business could be seriously harmed.
We are a “controlled company” within the meaning of the corporate governance standards of the New York Stock Exchange. As a result, we may elect to rely on exemptions from certain corporate governance standards and you may not have the same protections afforded to stockholders of companies that are subject to such requirements.
Jason Murray and Mark Hancock collectively control a majority of the voting power of shares eligible to vote in the election of our directors. Because more than 50% of the voting power in the election of our directors is held by an individual, group, or another company, we are a “controlled company” within the meaning of the corporate governance standards of the New York Stock Exchange. As a controlled company, we may elect not to comply with certain corporate governance requirements, including the requirements that, within one year of the date of the listing of our common stock:
•a majority of our board of directors consists of “independent directors,” as defined under the rules of the New York Stock Exchange;
•our board of directors has a compensation committee that is composed entirely of independent directors with a written charter addressing the committee’s purpose and responsibilities;
•our board of directors has a nominating and corporate governance committee that is composed entirely of independent directors with a written charter addressing the committee’s purpose and responsibilities; and
•there will be an annual performance evaluation of the nominating and corporate governance and compensation committees.
For so long as we remain a “controlled company,” we may elect to rely on these exemptions. Accordingly, you may not have the same protections afforded to stockholders of companies that are subject to all of the corporate governance requirements of the New York Stock Exchange rules.
58
After this offering, our principal stockholders and management will own a significant percentage of our stock and will be able to exercise significant influence over matters subject to stockholder approval.
As of June 30, 2024, our executive officers, directors and 5% or greater stockholders beneficially owned 83.2% of the outstanding shares of our capital stock, and, upon the closing of this offering, that same group will hold approximately 74.5% of our outstanding shares of common stock (assuming no exercise of the underwriters’ option to purchase additional shares from the selling stockholders). Therefore, even after this offering, these stockholders (in particular, Messrs. Murray and Hancock) will have the ability to influence us through this ownership position. The interests of these stockholders may not be the same as or may even conflict, or appear to conflict, with your interests. For example, these stockholders could attempt to delay or prevent a change in control of us, even if such change in control would benefit our other stockholders, which could deprive our stockholders of an opportunity to receive a premium for their common stock as part of a sale of us or our assets, and might affect the prevailing market price of our common stock due to investors’ perceptions that conflicts of interest may exist or arise. In addition, these stockholders, acting together, will be able to significantly influence all matters requiring stockholder approval, including the election and removal of directors and any merger or other significant corporate transactions after the completion of this offering. As a result, this concentration of ownership may not be in the best interests of our other stockholders.
Participation in this offering by our directors, officers, existing stockholders and their affiliated entities may reduce the public float for our common stock.
To the extent our directors, officers or certain of our existing stockholders and their affiliated entities participate in this offering, such purchases would reduce the non-affiliate public float of our shares, meaning the number of shares of our common stock that are not held by officers, directors and principal stockholders. A reduction in the public float could reduce the number of shares that are available to be traded at any given time, thereby adversely impacting the liquidity of our common stock and depressing the price at which you may be able to sell shares of common stock purchased in this offering.
Delaware law and provisions in our Amended and Restated Charter and Amended and Restated Bylaws could make a merger, tender offer or proxy contest difficult, thereby depressing the trading price of our common stock.
Our Amended and Restated Charter and Amended and Restated Bylaws contain provisions that could depress the trading price of our common stock by acting to discourage, delay or prevent a change of control of our company or changes in our management that the stockholders of our company may deem advantageous. These provisions include the following:
•establishing a classified board of directors so that not all members of our board of directors are elected at one time;
•permitting our board of directors to establish the number of directors and fill any vacancies and newly-created directorships, subject to rights granted to Messrs. Murray and Hancock pursuant to our Amended and Restated Charter and the Stockholders Agreement;
•providing that directors may be removed at any time with or without cause by the affirmative vote of the holders of a majority of the voting power of the then outstanding shares of our voting stock; provided, however, that at any time when Messrs. Murray and Hancock beneficially own, in the aggregate, less than the majority of the voting power of our outstanding shares of voting stock, directors may only be removed for cause and only by the affirmative vote of the holders of at least two-thirds of the voting power of all then outstanding shares of our voting stock;
•requiring the approval of holders of two-thirds of the total voting power of all then outstanding shares of our capital stock to amend certain provisions in our Amended and Restated Charter and our Amended and Restated Bylaws;
59
•authorizing the issuance of “blank check” preferred stock that our board of directors could use to implement a stockholder rights plan;
•prohibiting stockholders from calling special meetings of stockholders;
•providing that, at any time when Messrs. Murray and Hancock beneficially own, in the aggregate, at least a majority of the voting power of our outstanding shares of voting stock, our stockholders may take action by written consent without a meeting, and at any time when Messrs. Murray and Hancock beneficially own, in the aggregate, less than a majority of the voting power of our outstanding shares of voting stock, our stockholders may not take action by written consent, which has the effect of requiring all stockholder actions to be taken at a meeting of our stockholders;
•providing that the board of directors is expressly authorized to make, alter or repeal our Amended and Restated Bylaws;
•restricting the forum for certain litigation involving us to Delaware or federal courts, as applicable; and
•establishing advance notice requirements for nominations for election to our board of directors or for proposing matters that can be acted upon by stockholders at annual stockholder meetings.
Any provision of our Amended and Restated Charter or Amended and Restated Bylaws or Delaware law that has the effect of delaying or deterring a change in control could limit the opportunity for our stockholders to receive a premium for their shares of our common stock, and could also affect the price that some investors are willing to pay for our common stock. See the section titled “Description of Capital Stock—Anti-Takeover Effects of Provisions of the General Corporation Law of the State of Delaware and our Amended and Restated Charter and Amended and Restated Bylaws.”
The provisions of our Amended and Restated Charter requiring exclusive forum in the Court of Chancery of the State of Delaware and the federal district courts of the United States for certain types of lawsuits may have the effect of discouraging lawsuits against our directors and officers.
Our Amended and Restated Charter provides that, unless we otherwise consent in writing, (A) (i) any derivative action or proceeding brought on our behalf, (ii) any action asserting a claim of breach of a fiduciary duty owed by any current or former director, officer, other employee or stockholder of us to the us or the our stockholders, (iii) any action asserting a claim arising pursuant to any provision of the Delaware General Corporation Law, our Amended and Restated Charter or our Amended and Restated Bylaws (as either may be amended or restated) or as to which the Delaware General Corporation Law confers exclusive jurisdiction on the Court of Chancery of the State of Delaware or (iv) any action asserting a claim governed by the internal affairs doctrine of the law of the State of Delaware shall, to the fullest extent permitted by law, be exclusively brought in the Court of Chancery of the State of Delaware or, if such court does not have subject matter jurisdiction thereof, the federal district court of the State of Delaware; and (B) the federal district courts of the United States shall be the exclusive forum for the resolution of any complaint asserting a cause of action arising under the Securities Act; however, there is uncertainty as to whether a court would enforce such provision, and investors cannot waive compliance with federal securities laws and the rules and regulations thereunder. Notwithstanding the foregoing, the exclusive forum provision shall not apply to claims seeking to enforce any liability or duty created by the Exchange Act or any other claim for which the federal courts of the United States have exclusive jurisdiction. The choice of forum provision may limit a stockholder’s ability to bring a claim in a judicial forum that it finds favorable for disputes with us or our directors, officers or other employees and may also result in increased costs for stockholders to bring any such claim, which may discourage such lawsuits against us and our directors, officers, and other employees, although our stockholders will not be deemed to have waived our compliance with federal securities laws and the rules and regulations thereunder. Alternatively, if a court were to find the choice of forum provision contained in our Amended and Restated Charter to be inapplicable or unenforceable in an action, we may incur additional costs associated with resolving such action in other jurisdictions, which could have an adverse effect on our business, financial condition and results of operations. Any person or entity purchasing or otherwise acquiring or holding any interest in shares of
60
our capital stock shall be deemed to have notice of and consented to the forum provisions in our Amended and Restated Charter (as may be amended or restated).
Non-U.S. Holders who own more than 5% of our common stock may be subject to U.S. federal income tax on gain realized on the sale or other taxable disposition of such common stock.
Because the determination of whether we are a “U.S. real property holding corporation” (USRPHC) for U.S. federal income tax purposes depends on the fair market value of our “U.S. real property interests” (USRPIs) relative to the fair market value of our non-U.S. real property interests and our other business assets, and because we have significant interests in real property located in the U.S., we may currently be, or may become in the future, a USRPHC. There can be no assurance that we do not currently constitute, or will not become, a USRPHC. As a result, a “Non-U.S. Holder” (as defined below under “Material U.S. Federal Income Tax Consequences to Non-U.S. Holders”) may be subject to U.S. federal income tax on gain realized on a sale or other taxable disposition of our common stock if such Non-U.S. Holder has owned, actually or constructively, more than 5% of our common stock at any time during the shorter of the five-year period ending on the date of the sale or other taxable disposition or the Non-U.S. Holder’s holding period in such stock.
Affiliates of Citigroup Global Markets Inc., J.P. Morgan Securities LLC, Truist Securities, Inc. and RBC Capital Markets, LLC, underwriters in this offering, will each receive at least 5% of the net proceeds of this offering and may have an interest in this offering beyond customary underwriting discounts and commissions.
Because affiliates of Citigroup Global Markets Inc., J.P. Morgan Securities LLC, Truist Securities, Inc. and RBC Capital Markets, LLC are lenders under our Amended and Restated 2023 Credit Facility and will each receive at least 5% of the net proceeds from this offering in connection with the repayment of amounts outstanding under our Amended and Restated 2023 Credit Facility, a “conflict of interest” within the meaning of FINRA Rule 5121 is deemed to exist. Accordingly, this offering is being made in compliance with the applicable requirements of FINRA Rule 5121. The appointment of a “qualified independent underwriter” is not necessary for this offering pursuant to FINRA Rule 5121(a)(1)(B) as a “bona fide public market,” as defined in FINRA Rule 5121, exists for our common stock. See the sections titled “Use of Proceeds,” “Management’s Discussion and Analysis of Financial Conditions and Results of Operations—Liquidity & Capital Resources—Credit Facilities,” and “Underwriting (Conflicts of Interest)” for additional information.
Risks Related to Being a Public Company
We continue to incur increased costs as a result of operating as a public company, and our management is required to devote substantial time to new compliance initiatives and corporate governance practices. Additionally, if we fail to maintain proper and effective internal controls, our ability to produce accurate financial statements on a timely basis could be impaired.
As a public company, we continue to incur significant legal, accounting, and other expenses that we did not incur as a private company. We are subject to the reporting requirements of the Exchange Act, the Sarbanes-Oxley Act, the Dodd-Frank Wall Street Reform and Protection Act, as well as rules adopted, and to be adopted, by the Securities and Exchange Commission (SEC), and the New York Stock Exchange. Our management and other personnel devote a substantial amount of time to these compliance initiatives. Moreover, these rules and regulations to substantially increase our legal and financial compliance costs and to make some activities more time-consuming and costly, which increases our operating expenses. For example, these rules and regulations to make it more difficult and more expensive for us to obtain director and officer liability insurance and are required to incur substantial costs to maintain sufficient coverage. We cannot accurately predict or estimate the amount or timing of additional costs we may incur to respond to these requirements. The impact of these requirements could also make it more difficult for us to attract and retain qualified persons to serve on our board of directors, our board committees, or as executive officers.
In addition, as a public company we are required to incur additional costs and obligations in order to comply with SEC rules that implement Section 404 of the Sarbanes-Oxley Act. Under these rules, beginning with our
61
second annual report on Form 10-K, we will be required to make a formal assessment of the effectiveness of our internal control over financial reporting, and we will be required to include an attestation report on internal control over financial reporting issued by our independent registered public accounting firm. To achieve compliance with Section 404 within the prescribed period, we will be engaging in a process to document and evaluate our internal control over financial reporting, which is both costly and challenging. In this regard, we will need to continue to dedicate internal resources, potentially engage outside consultants and adopt a detailed work plan to assess and document the adequacy of our internal control over financial reporting, continue steps to improve control processes as appropriate, validate through testing that controls are designed and operating effectively, and implement a continuous reporting and improvement process for internal control over financial reporting.
The rules governing the standards that must be met for management to assess our internal control over financial reporting are complex and require significant documentation, testing, and possible remediation to meet the detailed standards under the rules. During the course of its testing, our management may identify material weaknesses which may not be remedied in time to meet the deadline imposed by the Sarbanes-Oxley Act. Our internal control over financial reporting will not prevent or detect all errors and all fraud. A control system, no matter how well designed and operated, can provide only reasonable, not absolute, assurance that the control system’s objectives will be met. Because of the inherent limitations in all control systems, no evaluation of controls can provide absolute assurance that misstatements due to error or fraud will not occur or that all control issues and instances of fraud will be detected.
If we are not able to comply with the requirements of Section 404 of the Sarbanes-Oxley Act in a timely manner, if we identify or fail to remediate material weaknesses in our internal controls, or if we are unable to maintain proper and effective internal controls, we may not be able to produce timely and accurate financial statements. If that were to happen, the market price of our stock could decline and we could be subject to sanctions or investigations by the stock exchange on which our common stock is listed, the SEC or other regulatory authorities.
We previously identified a material weakness in our internal controls. During 2021 and 2020, we recorded tax credits as calculated by a third-party consulting firm. A subsequent review of those calculations, when also considering additional guidance issued by the Internal Revenue Service, caused management to conclude that the claimed credits may not be fully supportable and, accordingly, no tax benefits should have been recognized for those periods. While we remediated this material weakness as of December 31, 2023 by implementing specific review procedures for tax credit calculations performed by a third-party and ensuring we have personnel with the technical expertise to perform timely review of such calculations to properly conclude on their accounting treatment, we cannot assure you that additional material weaknesses will not be identified in the future. A material weakness is a deficiency, or a combination of deficiencies, in internal control over financial reporting, such that there is a reasonable possibility that a material misstatement of our financial statements will not be prevented or detected on a timely basis. We cannot assure you that the measures we have taken to date, and actions we may take in the future, will be sufficient to prevent or avoid potential future material weaknesses. A material weakness in our internal control over financial reporting could result in an increased probability of fraud, litigation from our stockholders, reduction in our ability to obtain financing, and require additional expenditures to remediate. Our failure to implement and maintain effective internal control over financial reporting could result in errors in our financial statements that could result in loss of investor confidence in the accuracy and completeness of our financial reports and a decline in our stock price, and we could be subject to sanctions or investigations by the SEC or other regulatory authorities.
Our management team has limited experience managing a public company.
Most members of our management team have limited experience managing a publicly traded company, interacting with public company investors and complying with the increasingly complex laws pertaining to public companies. Our management team may not successfully or efficiently manage us as a public company that is subject to significant regulatory oversight and reporting obligations under the federal securities laws and the continuous scrutiny of securities analysts and investors. These new obligations and constituents require significant attention
62
from our senior management and could divert their attention away from the day-to-day management of our business, which could have an adverse effect on our business, financial condition and results of operations.
Our disclosure controls and procedures may not prevent or detect all errors or acts of fraud.
As a public company, we are subject to the periodic reporting requirements of the Exchange Act. We must design our disclosure controls and procedures to reasonably assure that information we must disclose in reports we file or submit under the Exchange Act is accumulated and communicated to management, and recorded, processed, summarized, and reported within the time periods specified in the rules and forms of the SEC. Any disclosure controls and procedures or internal controls and procedures, no matter how well-conceived and operated, can provide only reasonable, not absolute, assurance that the objectives of the control system are met. These inherent limitations include the realities that judgments in decision-making can be faulty, and that breakdowns can occur because of simple error or mistake. For example, our directors or executive officers could inadvertently fail to disclose a new relationship or arrangement causing us to fail to make a required related party transaction disclosure. Additionally, controls can be circumvented by the individual acts of some persons, by collusion of two or more people or by an unauthorized override of the controls. Accordingly, because of the inherent limitations in our control system, misstatements due to error or fraud may occur and not be detected.
We could be subject to securities class action litigation.
In the past, securities class action litigation has often been brought against companies following a decline in the market price of its securities. This risk is especially relevant for us because companies in the healthcare industry have experienced significant stock price volatility in recent years. If we face such litigation, it could result in substantial costs and a diversion of management’s attention and resources, which could harm our business.
Our failure to meet the New York Stock Exchange’s continued listing requirements could result in a delisting of our common stock.
If we fail to satisfy the continued listing requirements of the New York Stock Exchange, such as the corporate governance requirements or the minimum closing bid price requirement, the New York Stock Exchange may take steps to delist our common stock. Such a delisting would likely have a negative effect on the price of our common stock and would impair your ability to sell or purchase our common stock when you wish to do so. In the event of a delisting, we can provide no assurance that any action taken by us to restore compliance with listing requirements would allow our common stock to become listed again, stabilize the market price or improve the liquidity of our common stock, or prevent future non-compliance with the listing requirements of the New York Stock Exchange.
If securities or industry analysts either do not publish research about us or publish inaccurate or unfavorable research about us, our business or our market, or if they change their recommendations regarding our common stock adversely, the trading price or trading volume of our common stock could decline.
The trading market for our common stock is influenced in part by the research and reports that securities or industry analysts may publish about us, our business, our market or our competitors. If one or more analysts initiate research with an unfavorable rating or downgrade our common stock, provide a more favorable recommendation about our competitors or publish inaccurate or unfavorable research about our business, our common stock price would likely decline. If any analyst who may cover us were to cease coverage of us or fail to regularly publish reports on us, we could lose visibility in the financial markets, which in turn could cause the trading price or trading volume of our common stock to decline.
Regardless of accuracy, unfavorable interpretations of our financial information and other public disclosures could have a negative impact on our stock price. If our financial performance fails to meet analyst estimates, for any of the reasons discussed above or otherwise, or one or more of the analysts who cover us downgrade our common stock or change their opinion of our common stock, our stock price would likely decline.
63
Even if our common stock is actively covered by analysts, we do not have any control over the analysts or the measures that analysts or investors may rely upon to forecast our future results. Overreliance by analysts or investors on any particular metric to forecast our future results may lead to forecasts that differ significantly from our own.
General Risks
Global economic and financial market conditions, including severe market disruptions and the potential for a significant and prolonged global economic downturn, could impact our business operations in a number of ways, including, but not limited to, reduced demand in key customer end-markets.
The global economy can be negatively impacted by a variety of factors such as the spread or fear of spread of contagious diseases, man-made or natural disasters, actual or threatened war, terrorist activity, political unrest, civil strife and other geopolitical uncertainty. Such adverse and uncertain economic conditions may impact the post-acute services industry and consumer demand for our services. Decreases in demand for our services without a corresponding decrease in our costs would put downward pressure on margins and would negatively impact our financial results. Prolonged unfavorable economic conditions or uncertainty may have an adverse effect on our sales and profitability.
Changes in the U.S. and global social, political, regulatory and economic conditions or in laws and policies governing foreign trade, manufacturing, development and investment could also adversely affect our business. If global economic conditions remain volatile for a prolonged period or experience further disruptions, it could have a material adverse effect on our business, financial condition and results of operations.
Increased attention to, and evolving expectations for, environmental, social, and governance (ESG) initiatives could increase our costs, harm our reputation, or otherwise adversely impact our business.
Companies across industries are facing increasing scrutiny from a variety of stakeholders related to their ESG and sustainability practices. Expectations regarding voluntary ESG initiatives and disclosures may result in increased costs (including but not limited to increased costs related to compliance, stakeholder engagement, contracting and insurance), enhanced compliance or disclosure obligations, or other adverse effects on to our business, financial condition and results of operations.
While we may at times engage in voluntary initiatives (such as voluntary disclosures, certifications, or goals, among others) to improve our ESG profile, such initiatives may be costly and may not have the desired effect. Moreover, we may not be able to successfully complete such initiatives due to factors that are within or outside of our control. Even if this is not the case, our actions may subsequently be determined to be insufficient by various stakeholders, and we may be subject to investor or regulator engagement on our ESG efforts, even if such initiatives are currently voluntary.
Certain market participants, including major institutional investors and capital providers, use third-party benchmarks and scores to assess companies’ ESG profiles in making investment or voting decisions. Unfavorable ESG ratings could lead to increased negative investor sentiment towards us, which could negatively impact our share price as well as our access to and cost of capital. To the extent ESG matters negatively impact our reputation, it may also impede our ability to compete as effectively to attract and retain employees, which may adversely impact our operations.
In addition, we expect there will likely be increasing levels of regulation, disclosure-related and otherwise, with respect to ESG matters. For example, the SEC has published propose rules that would require companies to provide significantly expanded climate-related disclosures in their periodic reporting, which may require us to incur significant additional costs to comply, including the implementation of significant additional internal controls processes and procedures regarding matters that have not been subject to such controls in the past, and impose increased oversight obligations on our management and board of directors. These and other changes in stakeholder expectations will likely lead to increased costs as well as scrutiny that could heighten all of the risks identified in this
64
risk factor. Additionally, our business partners may be subject to similar expectations, which may augment or create additional risks, including risks that may not be known to us.
We may acquire or invest in companies, which may divert our management’s attention and result in additional dilution to our stockholders. We may be unable to integrate acquired businesses and technologies successfully or achieve the expected benefits of such acquisitions.
We may evaluate and consider potential strategic transactions, including acquisitions of, or investments in, businesses, technologies, services, products, and other assets in the future. An acquisition, investment or business relationship may result in unforeseen operating difficulties and expenditures. In particular, we may encounter difficulties assimilating or integrating the businesses, technologies, products, personnel, or operations of the acquired companies. Key personnel of the acquired companies may choose not to work for us, their software may not be easily adapted to work with ours, or we may have difficulty retaining the customers of any acquired business due to changes in ownership, management, or otherwise. We may also experience difficulties integrating personnel of the acquired company into our business and culture. Acquisitions may also disrupt our business, divert our resources and require significant management attention that would otherwise be available for development of our existing business. The anticipated benefits of any acquisition, investment, or business relationship may not be realized or we may be exposed to unknown risks or liabilities.
Negotiating these transactions can be time-consuming, difficult, and expensive, and our ability to close these transactions may often be subject to approvals that are beyond our control. Consequently, these transactions, even if undertaken and announced, may not close. For one or more of those transactions, we may:
•issue additional equity securities that would dilute our stockholders;
•use cash that we may need in the future to operate our business;
•incur debt on terms unfavorable to us or that we are unable to repay;
•incur large charges or substantial liabilities;
•encounter difficulties retaining key employees of the acquired company or integrating diverse software codes or business cultures; and
•become subject to adverse tax consequences, substantial depreciation, or deferred compensation charges.
We may not be able to pay or maintain dividends and the failure to do so would adversely affect our stock price.
For the years ended December 31, 2023, 2022 and 2021, and during the six months ended June 30, 2024, we paid $80.4 million, $60.3 million, $53.8 million, and $33.7 million, respectively, in cash dividends to holders of our common stock. We currently anticipate that we will retain future earnings for the development, operation and expansion of our business and do not anticipate declaring or paying any cash dividends for the foreseeable future. Any return to stockholders will therefore be limited to any appreciation in the value of their stock. Our ability to pay and maintain cash dividends is based on many factors, including our ability to make and finance acquisitions, our ability to negotiate favorable lease and other contractual terms, anticipated operating cost levels, the level of demand for occupancy at our facilities, the rates we charge and actual results that may vary substantially from estimates. Some of the factors are beyond our control and a change in any such factor could affect our ability to pay or maintain dividends. The Amended and Restated 2023 Credit Facility restricts our ability to pay dividends to stockholders if we receive notice that we are in default under the agreement. The failure to pay or maintain dividends could adversely affect the market price of our common stock.
65
SPECIAL NOTE REGARDING FORWARD-LOOKING STATEMENTS
This prospectus contains forward-looking statements that involve substantial risks and uncertainties. All statements contained in this prospectus other than statements of historical facts, including, but not limited to, statements regarding our business strategy, plans, market growth and our objectives for future operations, are forward-looking statements. The words “may,” “will,” “should,” “expect,” “plan,” “anticipate,” “could,” “intend,” “target,” “project,” “contemplate,” “believe,” “estimate,” “forecast,” “predict,” “potential” or “continue” or the negative of these terms and other similar expressions are intended to identify forward-looking statements, although not all forward-looking statements contain these identifying words.
Forward-looking statements contained in this prospectus include, but are not limited to, statements about:
•our future financial performance, including our expectations regarding our revenue, operating expenses, and our ability to achieve and maintain future profitability;
•the demand for our services in general;
•our ability and the ability of local leaders and others to transform SNFs and other acquired facilities into higher acuity, high value-add short-term transitional care SNFs, including through the implementation of PACS Services;
•our expectations regarding improvement in clinical quality, patient experience, and operating metrics over time as facilities mature over a transition period, and our ability to maintain standards in our Mature facilities;
•our ability to successfully execute upon our strategy to deploy our decentralized, local operating model in acquired SNFs and in existing and new markets;
•our ability to successfully execute upon our acquisition strategy, including with respect to SNFs, and our ability to successfully identify, acquire and integrate facilities, businesses and operations;
•the scalability of PACS Services and our operating model;
•our ability to successfully compete with existing and new competitors generally and in specific existing and new geographical markets;
•the size of our market and market trends, including with respect to SNFs, expected growth rates of the market and our ability to grow within and further penetrate our market;
•our ability to attract, train, and retain motivated, entrepreneurial individuals, including local leaders. administrators, clinicians, and other important employees and personnel;
•our expectations regarding the effects of existing and developing laws and regulations;
•our ability to comply with regulations applicable to our business;
•our ability to develop and protect our brand;
•our expectations regarding, and management of, future growth;
•our ability to maintain, protect and enhance our technology and intellectual property;
•our ability to implement, maintain and improve effective internal controls and remediate material weaknesses;
66
•the sufficiency of our cash to meet our liquidity needs; and
•our anticipated uses of the net proceeds from this offering.
We caution you that the foregoing list may not contain all of the forward-looking statements made in this prospectus.
You should not rely upon forward-looking statements as predictions of future events. We have based the forward-looking statements contained in this prospectus primarily on our current expectations, estimates, forecasts, and projections about future events and trends that we believe may affect our business, financial condition, results of operations, and prospects. Although we believe that we have a reasonable basis for each forward-looking statement contained in this prospectus, we cannot guarantee that the future results, levels of activity, performance, or events and circumstances reflected in the forward-looking statements will be achieved or occur at all. Forward-looking statements involve known and unknown risks, uncertainties and other important factors that may cause our actual results, performance, or achievements to be materially different from any future results, performance, or achievements expressed or implied by the forward-looking statements. The outcome of the events described in these forward-looking statements is subject to risks, uncertainties, and other factors described in the section titled “Risk Factors,” “Management’s Discussion and Analysis of Financial Condition” and elsewhere in this prospectus. Because forward-looking statements are inherently subject to risks and uncertainties, some of which cannot be predicted or quantified, you should not rely on these forward-looking statements as predictions of future events. Moreover, we operate in a very competitive and rapidly changing environment. New risks and uncertainties emerge from time to time, and it is not possible for us to predict all risks and uncertainties that could have an impact on the forward-looking statements contained in this prospectus. The results, events, and circumstances reflected in the forward-looking statements may not be achieved or occur, and actual results, events, or circumstances could differ materially from those described in the forward-looking statements.
The forward-looking statements made in this prospectus relate only to events as of the date on which the statements are made. We undertake no obligation to update any forward-looking statements made in this prospectus to reflect events or circumstances after the date of this prospectus or to reflect new information or the occurrence of unanticipated events, except as required by applicable law. We may not actually achieve the plans, intentions, or expectations disclosed in our forward-looking statements, and you should not place undue reliance on our forward-looking statements. Our forward-looking statements do not reflect the potential impact of any future acquisitions, mergers, dispositions, joint ventures, or investments we may make.
In addition, statements that “we believe” and similar statements reflect our beliefs and opinions on the relevant subject. These statements are based upon information available to us as of the date of this prospectus, and while we believe such information forms a reasonable basis for such statements, such information may be limited or incomplete, and our statements should not be read to indicate that we have conducted an exhaustive inquiry into, or review of, all potentially available relevant information. These statements are inherently uncertain and you are cautioned not to unduly rely upon these statements.
You should read this prospectus and the documents that we reference in this prospectus and have filed with the SEC as exhibits to the registration statement of which this prospectus is a part with the understanding that our actual future results, performance, and events and circumstances may be materially different from what we expect. We qualify all of the forward-looking statements in this prospectus by these cautionary statements.
67
USE OF PROCEEDS
We estimate that the net proceeds to us from the sale of shares of our common stock in this offering will be approximately $104.8 million, after deducting the underwriting discounts and commissions and estimated offering expenses payable by us. We will not receive any proceeds from the sale of common stock by the selling stockholders in this offering.
Each $1.00 increase or decrease in the assumed public offering price per share of $39.67, which is the last reported sale price of our common stock as reported on the New York Stock Exchange on August 30, 2024, would increase or decrease the net proceeds to us from this offering by approximately $2.7 million, assuming that the number of shares of common stock offered by us, as set forth on the cover page of this prospectus, remains the same, and after deducting estimated underwriting discounts and commissions and estimated offering expenses payable by us. Similarly, each 1,000,000 share increase or decrease in the number of shares of common stock offered by us in this offering would increase or decrease the net proceeds to us from this offering by approximately $38.1 million, assuming that the public offering price per share remains the same, and after deducting estimated underwriting discounts and commissions and estimated offering expenses payable by us.
We intend to use all of the net proceeds to us from this offering to repay amounts outstanding under our Amended and Restated 2023 Credit Facility.
Our Amended and Restated 2023 Credit Facility provides for total commitments in an aggregate principal amount of $600.0 million. As of the date of this prospectus, the total principal amount outstanding under our Amended and Restated 2023 Credit Facility was $160.0 million, resulting in available cash of $426.7 million, net of letter of credit usage. Our Amended and Restated 2023 Credit Facility matures on December 7, 2028. Amounts outstanding under our Amended and Restated 2023 Credit Facility currently bear interest based on the Secured Overnight Financing Rate (plus a 0.10% credit spread adjustment) plus a margin ranging from 2.25% to 3.25% per annum, resulting in a current effective interest rate of 8.14% as of the date of this prospectus. The proceeds under our Amended and Restated 2023 Credit Facility were used to repay and refinance all term loans and revolving loans under our previous credit facility, to repay certain other outstanding indebtedness, and to pay transaction costs in connection with our Amended and Restated 2023 Credit Facility, as well as for working capital. For further information on our Amended and Restated 2023 Credit Facility, see “Management’s Discussion and Analysis of Financial Condition and Results of Operations—Liquidity & Capital Resources.”
The expected use of net proceeds from this offering represents our intentions based upon our present plans and business conditions. We cannot predict with certainty all of the particular uses for the proceeds of this offering or the amounts that we will actually spend on the uses set forth above. Accordingly, our management will have broad discretion in applying the net proceeds of this offering. The timing and amount of our actual expenditures will be based on many factors, including cash flows from operations and the anticipated growth of our business. Pending their use, we intend to invest the net proceeds of this offering in one or more capital-preservation investments, which may include short- and intermediate-term investments, interest-bearing investments, investment-grade securities, U.S. government securities, certificates of deposit and money market funds.
We will not receive any proceeds from the sale of shares of our common stock by selling stockholders. We will, however, bear the costs, other than the underwriting discounts and commissions, associated with the sale of these shares.
68
DIVIDEND POLICY
For the years ended December 31, 2023, 2022 and 2021, and during the six months ended June 30, 2024, we paid $80.4 million, $60.3 million, $53.8 million, and $33.7 million, respectively, in cash dividends to holders of our common stock. We have no current plans to pay dividends or other distributions on our common stock in the foreseeable future following this offering. Any decision to declare and pay dividends in the future will be made at the sole discretion of our board of directors and will depend on, among other things, our results of operations, cash requirements, financial condition, contractual restrictions and other factors that our board of directors may deem relevant, and subject to the restrictions contained in any future financing instruments and applicable law.
69
CAPITALIZATION
The following table sets forth our cash, cash equivalents and capitalization as of June 30, 2024 as follows:
(1)on an actual basis;
(2)on an as adjusted basis, giving effect to the issuance and sale by us of 2,777,778 shares of our common stock in this offering at the assumed public offering price of $39.67 per share, which is the last reported sale price of our common stock as reported on the New York Stock Exchange on August 30, 2024, and after deducting the estimated underwriting discounts and commissions and estimated offering expenses payable by us, and the application of the net proceeds from this offering as described in “Use of Proceeds.”
The information below is illustrative only. Our capitalization following the closing of this offering will be adjusted based on the actual public offering price and other terms of this offering determined at the pricing of this offering. You should read this table together with the sections titled “Use of Proceeds” and “Management’s Discussion and Analysis of Financial Condition and Results of Operations” and our audited combined/consolidated financial statements and the related notes included elsewhere in this prospectus.
| As of June 30, 2024 | |||||||||||
| Actual | As Adjusted | ||||||||||
| (in thousands, except share and per share data) | |||||||||||
| Cash and cash equivalents | $ | 73,374 | $ | 73,374 | |||||||
| Debt (including current portion of long-term debt) | 490,852 | 386,052 | |||||||||
| PACS Group, Inc. stockholders' equity | |||||||||||
| Common stock, par value $0.001 per share; 1,250,000,000 shares authorized, 152,399,733 shares issued and outstanding, actual; and 1,250,000,000 shares authorized, 155,177,511 shares issued and outstanding, as adjusted | 152 | 155 | |||||||||
| Preferred stock | — | — | |||||||||
| Additional paid-in capital | 471,472 | 576,269 | |||||||||
| Retained earnings | 100,504 | 100,504 | |||||||||
| Total PACS Group, Inc. stockholders' equity | $ | 572,128 | $ | 676,928 | |||||||
| Total capitalization | $ | 1,062,980 | $ | 1,062,980 | |||||||
Each $1.00 increase (decrease) in the assumed public offering of $39.67 per share, which is the last reported sale price of our common stock as reported on the New York Stock Exchange on August 30, 2024, would increase (decrease) the as adjusted amount of cash and cash equivalents, additional paid-in capital, total stockholders’ equity and total capitalization by approximately $2.7 million, assuming that the number of shares offered by us, as set forth on the cover page of this prospectus, remains the same, and after deducting the estimated underwriting discounts and commissions and estimated offering expenses payable by us. We may also increase or decrease the number of shares we are offering. Each increase (decrease) of 1,000,000 shares in the number of shares offered by us would increase (decrease) the as adjusted amount of each of cash and cash equivalents, additional paid-in capital, total stockholders’ equity and total capitalization by approximately $38.1 million, assuming that the price to the public remains the same, and after deducting the estimated underwriting discounts and commissions and estimated offering expenses payable by us.
The number of shares of our common stock to be outstanding after this offering is based on 152,399,733 shares of our common stock outstanding as of June 30, 2024, and excludes:
•1,580,986 shares of common stock reserved for future issuance under our 2024 Plan;
•11,561,818 shares of common stock issuable upon vesting of all RSUs awarded; and
70
•1,501,520 shares of common stock reserved for future issuance under our ESPP.
Our 2024 Plan and our ESPP provide for annual automatic increases in the number of shares reserved thereunder.
71
DILUTION
If you invest in our common stock in this offering, your ownership interest will be immediately diluted to the extent of the difference between the offering price per share and the as adjusted net tangible book value per share of our common stock immediately after this offering. Dilution in the as adjusted net tangible book value per share to new investors represents the difference between the amount per share paid by purchasers of shares of our common stock in this offering and the as adjusted net tangible book value per share of our common stock immediately after the completion of this offering.
As of June 30, 2024, we had a net tangible book value of $512.7 million, or $3.36 per share of common stock. Our historical net tangible book value represents our total tangible assets excluding deferred offering costs, less our total liabilities, divided by the total number of shares of our common stock outstanding as of June 30, 2024.
After giving effect to receipt of the net proceeds from our sale of 2,777,778 shares of common stock at the assumed public offering price of $39.67 per share, which is the last reported sale price of our common stock as reported on the New York Stock Exchange on August 30, 2024, after deducting the estimated underwriting discounts and commissions and estimated offering expenses payable by us, and the application of the net proceeds from this offering as described in “Use of Proceeds,” our as adjusted net tangible book value as of June 30, 2024 would have been approximately $617.4 million , or $3.98 per share. This represents an immediate increase in net tangible book value of $0.62 per share to our existing stockholders and an immediate dilution of $35.69 per share to new investors participating in this offering.
The following table illustrates this dilution on a per share basis to new investors:
| Assumed public offering price per share | $ | 39.67 | |||||||||
| Net tangible book value per share as of June 30, 2024 | $ | 3.36 | |||||||||
| Increase in net tangible book value per share attributable to new investors participating in this offering | $ | 0.62 | |||||||||
| As adjusted net tangible book value per share after this offering | $ | 3.98 | |||||||||
| Dilution per share to new investors in this offering | $ | 35.69 | |||||||||
Each $1.00 increase or decrease in the assumed public offering price per share of $39.67, which is the last reported sale price of our common stock as reported on the New York Stock Exchange on August 30, 2024, would increase or decrease, as applicable, our as adjusted net tangible book value after this offering by approximately $2.7 million, or $0.02 per share, and would increase or decrease, as applicable, the dilution per share to new investors purchasing our common stock in this offering by $0.98 per share, assuming that the number of shares offered by us in this offering, as set forth on the cover page of this prospectus, remains the same, and after deducting estimated underwriting discounts and commissions, and estimated offering expenses payable by us. Similarly, each 1,000,000 share increase in the number of shares of common stock offered by us would increase the as adjusted net tangible book value after this offering by $0.22 per share and decrease the dilution per share to new investors participating in this offering by $0.22 per share, and each 1,000,000 share decrease in the number of shares of common stock offered by us in this offering would decrease the as adjusted net tangible book value by $0.22 per share, and increase the dilution per share to new investors in this offering by $0.22 per share, assuming that the assumed public offering price per share of $39.67, which is the last reported sale price of our common stock as reported on the New York Stock Exchange on August 30, 2024, remains the same and after deducting estimated underwriting discounts and commissions and estimated offering expenses payable by us.
The foregoing discussion and table are based on 152,399,733 shares of our common stock outstanding as of June 30, 2024, and excludes:
•1,580,986 shares of common stock reserved for future issuance under our 2024 Plan;
•11,561,818 shares of common stock issuable upon vesting of all RSUs awarded; and
72
•1,501,520 shares of common stock reserved for future issuance under our ESPP.
Our 2024 Plan and our ESPP provide for annual automatic increases in the number of shares reserved thereunder.
The dilution information discussed above is illustrative only and may change based on the actual public offering price and other terms of this offering. To the extent any options are granted and exercised in the future, there may be additional economic dilution to new investors. In addition, we may choose to raise additional capital due to market conditions or strategic considerations, even if we believe we have sufficient funds for our current or future operating plans. To the extent that we raise additional capital through the sale of equity or convertible debt securities, the issuance of these securities could result in further dilution to our stockholders.
73
MANAGEMENT’S DISCUSSION AND ANALYSIS OF FINANCIAL CONDITION AND RESULTS OF OPERATIONS
You should read the following discussion and analysis of our financial condition and results of operations together with our audited combined/consolidated financial statements and the related notes included elsewhere in this prospectus. Some of the information contained in this discussion and analysis or set forth elsewhere in this prospectus, including information with respect to our plans and strategy for our business, includes forward-looking statements that involve risks and uncertainties. You should read the sections titled “Risk Factors” and “Special Note Regarding Forward-Looking Statements” for a discussion of important factors that could cause actual results to differ materially from the results described in or implied by the forward-looking statements contained in the following discussion and analysis. Our historical results are not necessarily indicative of the results to be expected in the future.
Overview
We are a leading post-acute healthcare company primarily focused on delivering high-quality skilled nursing care through a portfolio of independently operated facilities. Founded in 2013, we are one of the largest skilled nursing providers in the United States based on number of facilities, with 276 post-acute care facilities across 15 states serving over 29,000 patients daily as of September 1, 2024. We also provide senior care, assisted living, and independent living options in some of our communities. Our significant historical growth has been primarily driven by our expertise in acquiring underperforming long-term custodial care skilled nursing facilities and transforming them into higher acuity, high value-add short-term transitional care skilled nursing facilities. We believe our success is driven in significant part by our decentralized, local operating model, through which we empower local leaders at each facility to operate their facility autonomously and deliver excellence in clinical quality and a superior experience for our patients. We provide our independently operated facilities with a comprehensive suite of technology, support, and back-office services that allow local leadership teams to focus more of their time and effort on providing quality care to patients. We believe our operating model delivers value to all of our healthcare stakeholders, including patients and families, referring providers, payors, and administrators and clinicians.
We were founded in 2013 with two skilled nursing facilities located in San Diego and a mission to improve the delivery, leadership and quality of post-acute care. By implementing our operating model across our SNFs, we quickly expanded using a disciplined and balanced acquisition strategy. A significant amount of our early expansion was in California, where we were able to leverage our experience from our initial facilities as we expanded our footprint across the state by acquiring select SNFs that fit our acquisition strategy. Over time, we expanded into additional states, such as Texas, Missouri, South Carolina, and Nevada, among others. In 2021, we acquired the operating assets of Plum Healthcare Group (Plum), then one of the largest operators of SNFs in California, which significantly increased our number of SNF facilities and operational beds. Since 2021, we have remained disciplined but opportunistic in our acquisition strategy, having acquired or opened 12 facilities in 2022, 58 in 2023 and 12 in the first half of 2024. The graphic below provides an overview of our corporate history and sets forth our acquisitions per year for the periods indicated, as well as our number of post-acute facilities, inclusive of skilled nursing facilities and assisted living facilities, and SNF operational beds as of the end of the periods indicated.
74
Number of Post-Acute Care Facilities Operated
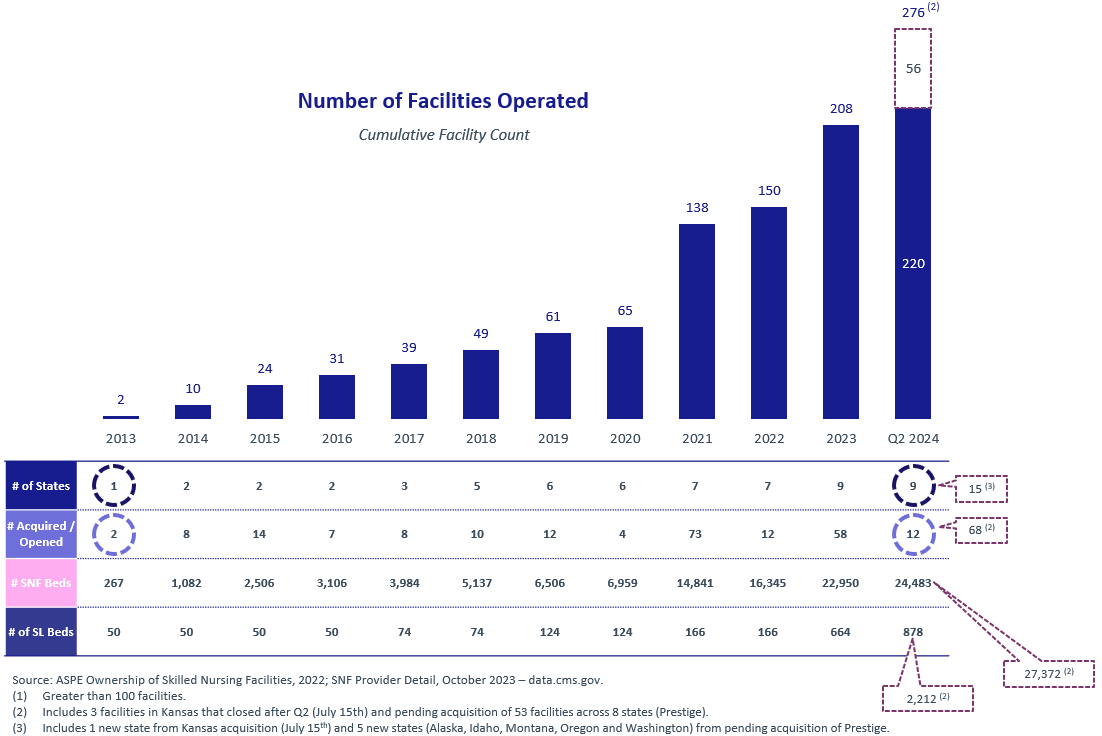
We aim to create value by identifying and acquiring underperforming custodial care facilities and converting them into higher-value short-term transitional care facilities by investing in clinical teams and processes and upgrading technology, equipment, training, staffing, aesthetics, and other aspects of the business. The resources and guidance offered by PACS Services is key to rapid integration of new facilities and provides our local leadership teams with an effective technology infrastructure, support tools, and regional support teams that allow local leadership to focus on operational improvements. Our facilities generally undergo an up to three-year post-acquisition transition period. During this period, we seek to implement best practices designed to realize and sustain the facility’s full potential. These practices often result in significant improvements to clinical quality and other operational metrics, including skilled mix, occupancy rates and payor contracting. We believe the results of our acquisition strategy are demonstrated by our high average QM Star rating and occupancy rate for Mature facilities of 4.3 and 94%, respectively, as of June 30, 2024. As of June 30, 2024, the average QM Star rating and occupancy rate for New facilities, which we define as facilities purchased less than 18 months prior to the measurement date, was 4.1 and 84%, respectively.
Our portfolio of owned and leased properties is strategically located in 15 states as of September 1, 2024: Alaska, Arizona, California, Colorado, Idaho, Kansas, Kentucky, Missouri, Montana, Nevada, Ohio, Oregon, South Carolina, Texas and Washington. We anticipate that available acquisition opportunities will enable us to further penetrate these 15 states and to enter new states in the future. We believe our current markets are attractive and that the states in which we operate each has unique benefits, such as favorable reimbursement dynamics, high barriers to entry, or population growth of adults aged 65 and older, which is our primary patient demographic. We generally look for similar attributes in new markets that we enter. As of June 30, 2024, we leased 170 facilities, owned partial real estate interests in an additional 12 leased facilities through joint ventures, and directly owned the real estate at 38 facilities. The joint venture operations were formed to develop, own, and lease health care facilities to our operational subsidiaries, and our investment in these joint ventures is accounted for under the equity method because
75
we do not have a controlling financial interest in such ventures. Each joint venture is governed by a managing member that makes significant decisions that impact the performance of the joint venture. We are not the managing member for any of the joint ventures in which we invest and operational and strategic decision making power is held by entities that we do not control. However, certain of our joint venture agreements provide for specified consent rights to the members regarding, among others, the ability of the joint venture to enter into a material contract, engage in new business outside the specified business purpose of the joint venture, enter into leases, incur capital expenses above specified thresholds, and file for bankruptcy or similar acts. Pursuant to the respective agreements, some of the joint ventures hold options to purchase the related real estate property holdings. As we continue to grow, we intend to explore additional purchases of real-estate assets, through purchase options or right-of-first refusals in existing leases, as well as acquisitions and de novo construction of purpose-built facilities.
Industry Trends
We operate in the post-acute care industry, which is an essential component of the healthcare delivery ecosystem, serving high need, medically fragile patients. The post-acute care industry has evolved to meet the growing demand for post-acute and custodial healthcare services generated by an aging population, increasing life expectancies and the trend toward shifting patient care to lower cost settings. The industry continues to evolve, driven by several trends, including the following:
SNFs are an Integral and Essential Part of the Post-Acute Care Continuum. SNFs play an essential role in post-acute patient care. SNFs provide higher-acuity skilled nursing care to patients that cannot be adequately treated in community-based care settings, such as assisted living or independent living facilities, and who are no longer appropriate candidates for hospital care. Despite the wide array of services and variety of needs addressed, SNFs are the lowest cost facility-based post-acute healthcare. As reimbursement and coverage continues to shift toward value-based models with greater emphasis on controlling costs, SNFs are integral to post-acute care and will continue to drive high-quality outcomes in low-cost settings.
Large, Fragmented Industry Comprised of Mostly Small and Independent Operators. According to the National Center for Health Statistics (NCHS) 2020 National Post-acute and Long-term Care Study, the SNF industry in the United States encompasses approximately 15,000 facilities and serves approximately 1.3 million patients annually. The industry is highly fragmented, with the top 10 operators, each having greater than 100 facilities, representing approximately 11% of total number of SNFs in the United States, according to CMS data as of September 2022, approximately 5,000 smaller and independent operators of less than 100 facilities making up the remainder. According to this data, of the approximately 15,000 facilities, approximately 13,200 facilities have less than 100 beds, and approximately 74% and 26% of SNFs are located in urban and rural areas, respectively. In addition, approximately 72%, 23%, and 6% of SNFs are operated as for-profit, non-profit, and by the government, respectively, according to such data. We believe this fragmented landscape creates opportunities for larger providers with greater scale to serve patients better and meet regulatory requirements nation-wide by effectively addressing staffing, quality standards, and billing processes. In addition, due to the increasing demands from hospitals and insurance carriers to implement sophisticated and expensive reporting systems, we believe this fragmentation provides us with significant acquisition and consolidation opportunities.
Growing Demand Outpacing Supply of Skilled Nursing Facilities. The demand for healthcare services in the United States has increased in recent years and is expected to continue growing, largely due to a rapidly aging population and an increasing prevalence of chronic conditions. While demand has increased for SNFs, the number of SNFs has declined in recent years from approximately 15,650 in 2017 to approximately 14,900 in 2023. We believe this is due to a variety of factors, including an inability of many facilities to comply with the industry’s stringent regulatory compliance obligations and with quality standards, rigorous staffing, and billing requirements, as well as a lack of technology and sophistication at small and independent operators. Furthermore, new operators to this highly regulated industry face multiple barriers to entry, including the requirements to obtain a Certificate of Need, complex licensure and regulatory compliance requirements, lack of operating experience, and significant capital requirements. As a result, the addition of new SNFs has not kept pace with the number of SNFs exiting the market, amplifying the need for skilled nursing to serve an aging population.
76
Favorable Reimbursement Environment. According to CMS, approximately 72% of SNF revenue in 2022 was derived from government sources, including Medicaid and Medicare. Medicaid represents 51% of industry revenue, while Medicare represents approximately 21%. The remainder comprises managed care, private pay, and other payors. Medicare and Medicaid reimbursement has steadily increased over the past few years. Medicare reimbursement per patient day increased at a CAGR of approximately 3.6% from 2012 to 2021, while Medicaid reimbursement per patient day increased at a CAGR of approximately 1.9% from 2012 to 2021. The industry has experienced over 9 years of growth in reimbursement rates.
Regulatory Environment. The SNF industry is highly regulated with stringent regulatory compliance obligations. In the ordinary course of business, providers are subject to federal, state and local laws and regulations relating to, among other things, billing and reimbursement, relationships with vendors, business relationships with physicians and other healthcare providers and facilities, as well as licensure, accreditation, enrollment, quality, adequacy of care, physical plant, life safety, personnel, staffing and operating requirements. Changes in law or new interpretations of existing laws and regulations may have a significant impact on revenue, costs and business operations of providers and other industry participants. In addition, governmental and other authorities periodically inspect the SNFs, senior living facilities and outpatient rehabilitation agencies to verify continued compliance with applicable regulations and standards and may impose citations and other regulatory penalties for regulatory deficiencies. Such regulatory penalties include but are not limited to civil monetary penalties, temporary payment bans, suspension or revocation of a state operating license and loss of certification as a provider in the Medicare or Medicaid program, which may be temporary or permanent in nature. This regulatory environment and related enforcement can have an adverse effect on providers and other industry participants. See the section titled “Business—Regulatory Matters.”
Key Skilled Services Metrics and Non-GAAP Financial Measures
We use the following key skilled services metrics and non-GAAP financial measures to help us evaluate our business, identify trends that affect our financial performance, and make strategic decisions.
Key Skilled Services Metrics
We monitor the below key skilled services metrics across all of our facilities and by Mature facilities, Ramping facilities, and New facilities. Mature facilities are defined as facilities purchased more than 36 months prior to a respective measurement date. Ramping facilities are defined as facilities purchased within 18 to 36 months prior to a respective measurement date. New facilities are defined as facilities purchased less than 18 months prior to a respective measurement date.
•Skilled nursing services revenue — Skilled nursing services revenue reflects the portion of patient and resident service revenue generated from all patients in skilled nursing facilities, excluding revenue generated from our assisted and independent living services.
•Skilled mix — We measure both revenue and nursing patient days by payor. Medicare and managed care patients, whom we refer to as high acuity patients, typically require a higher level of skilled nursing care. As a result, Medicare and managed care reimbursement rates are typically higher than those from other payors. In most states, Medicaid reimbursement rates are generally the lowest of all payor types. Changes in the payor mix can significantly affect our revenue and profitability. To monitor this performance, we evaluate two different measures of skilled mix:
◦Skilled mix by revenue — Skilled mix by revenue represents the portion of routine revenue generated from treating high acuity Medicare and managed care patients. Routine revenue refers to skilled nursing services revenue generated by contracted daily rates charged for skilled nursing services. Services provided outside of routine contractual agreements are recorded separately as ancillary revenue, including Medicare Part B therapy services, and are not routine revenue. The inclusion of therapy and other ancillary treatments in the contracted daily rate varies by payor source and by contract. Revenue associated with calculating skilled mix is based on contractually agreed-upon
77
amounts or rates, excluding the estimates of variable consideration under the revenue recognition standard, Financial Accounting Standards Board (FASB) Accounting Standards Codification (ASC) Topic 606.
◦Skilled mix by nursing patient days — Skilled mix by nursing patient days represents the number of days our high acuity Medicare and managed care patients receive skilled nursing services at skilled nursing facilities as a percentage of the total number of days that patients from all payor sources receive skilled nursing services at skilled nursing facilities for any given period.
•Occupancy — The total number of patients occupying a bed in a skilled nursing facility as a percentage of the beds in such facility that are available for occupancy during the period.
•Number of facilities — The total number of skilled nursing facilities that we operate. Excludes five and one assisted living facilities for the years ended December 31, 2023 and 2022, respectively, and six and three assisted living and independent living facilities for the six months ended June 30, 2024 and 2023, respectively.
•Number of operational beds — The total number of operational beds associated with the skilled nursing facilities that we own.
The following tables present the above key skilled services metrics by category for all facilities, Mature facilities, Ramping facilities and New facilities as of and for the years ended December 31, 2023, 2022 and 2021:
| Year ended December 31, | Growth Rate for the year ended December 31, | ||||||||||||||||||||||||||||
| 2023 | 2022 | 2021 | 2023 | 2022 | |||||||||||||||||||||||||
| (dollars in thousands) | |||||||||||||||||||||||||||||
| Total facility results: | |||||||||||||||||||||||||||||
| Skilled nursing services revenue | $ | 3,092,577 | $ | 2,391,309 | $ | 1,133,103 | 29.3 | % | 111.0 | % | |||||||||||||||||||
| Skilled mix by revenue | 55.1 | % | 64.1 | % | 57.8 | % | (9.0) | % | 6.3 | % | |||||||||||||||||||
| Skilled mix by nursing patient days | 32.4 | % | 40.7 | % | 34.5 | % | (8.3) | % | 6.2 | % | |||||||||||||||||||
| Occupancy for skilled nursing services: | |||||||||||||||||||||||||||||
| Available patient days | 7,457,345 | 5,719,689 | 3,106,602 | 30.4 | % | 84.1 | % | ||||||||||||||||||||||
| Actual patient days | 6,775,063 | 5,139,736 | 2,681,927 | 31.8 | % | 91.6 | % | ||||||||||||||||||||||
| Occupancy rate (operational beds) | 90.9 | % | 89.9 | % | 86.3 | % | 1.0 | % | 3.6 | % | |||||||||||||||||||
| Number of facilities at period end | 203 | 150 | 138 | 35.3 | % | 8.7 | % | ||||||||||||||||||||||
| Number of operational beds at period end | 22,950 | 16,345 | 14,841 | 40.4 | % | 10.1 | % | ||||||||||||||||||||||
78
| Year ended December 31, | Growth Rate for the year ended December 31, | ||||||||||||||||||||||||||||
| 2023 | 2022 | 2021 | 2023 | 2022 | |||||||||||||||||||||||||
| (dollars in thousands) | |||||||||||||||||||||||||||||
Mature facility(1) results: | |||||||||||||||||||||||||||||
| Skilled nursing services revenue | $ | 1,095,106 | $ | 951,936 | $ | 653,871 | 15.0 | % | 45.6 | % | |||||||||||||||||||
| Skilled mix by revenue | 58.8 | % | 66.1 | % | 59.6 | % | (7.3) | % | 6.5 | % | |||||||||||||||||||
| Skilled mix by nursing patient days | 35.6 | % | 43.1 | % | 36.2 | % | (7.5) | % | 6.9 | % | |||||||||||||||||||
| Occupancy for skilled nursing services: | |||||||||||||||||||||||||||||
| Available patient days | 2,497,872 | 2,175,718 | 1,637,371 | 14.8 | % | 32.9 | % | ||||||||||||||||||||||
| Actual patient days | 2,333,584 | 1,995,321 | 1,441,566 | 17.0 | % | 38.4 | % | ||||||||||||||||||||||
| Occupancy rate (operational beds) | 93.4 | % | 91.7 | % | 88.0 | % | 1.7 | % | 3.7 | % | |||||||||||||||||||
| Number of facilities at period end | 65 | 62 | 49 | 4.8 | % | 26.5 | % | ||||||||||||||||||||||
| Number of operational beds at period end | 6,959 | 6,525 | 5,137 | 6.7 | % | 27.0 | % | ||||||||||||||||||||||
__________________
(1)Mature facilities represent facilities purchased more than 36 months before the date presented.
| Year ended December 31, | Growth Rate for the year ended December 31, | ||||||||||||||||||||||||||||
| 2023 | 2022 | 2021 | 2023 | 2022 | |||||||||||||||||||||||||
| (dollars in thousands) | |||||||||||||||||||||||||||||
Ramping facility(1) results: | |||||||||||||||||||||||||||||
| Skilled nursing services revenue | $ | 924,697 | $ | 141,542 | $ | 240,631 | 553.3 | % | (41.2) | % | |||||||||||||||||||
| Skilled mix by revenue | 55.3 | % | 64.3 | % | 55.4 | % | (9.0) | % | 8.9 | % | |||||||||||||||||||
| Skilled mix by nursing patient days | 32.5 | % | 38.4 | % | 31.6 | % | (5.9) | % | 6.8 | % | |||||||||||||||||||
| Occupancy for skilled nursing services: | |||||||||||||||||||||||||||||
| Available patient days | 2,135,644 | 365,702 | 765,547 | 484.0 | % | (52.2) | % | ||||||||||||||||||||||
| Actual patient days | 1,994,742 | 330,306 | 652,272 | 503.9 | % | (49.4) | % | ||||||||||||||||||||||
| Occupancy rate (operational beds) | 93.4 | % | 90.3 | % | 85.2 | % | 3.1 | % | 5.1 | % | |||||||||||||||||||
| Number of facilities at period end | 76 | 4 | 17 | 1800.0 | % | (76.5) | % | ||||||||||||||||||||||
| Number of operational beds at period end | 8,330 | 453 | 1,822 | 1738.9 | % | (75.1) | % | ||||||||||||||||||||||
__________________
(1)Ramping facilities represent facilities purchased within 18-36 months of the date presented.
79
| Year ended December 31, | Growth Rate for the year ended December 31, | ||||||||||||||||||||||||||||
| 2023 | 2022 | 2021 | 2023 | 2022 | |||||||||||||||||||||||||
| (dollars in thousands) | |||||||||||||||||||||||||||||
New facility(1) results: | |||||||||||||||||||||||||||||
| Skilled nursing services revenue | $ | 1,072,774 | $ | 1,297,831 | $ | 238,601 | (17.3) | % | 443.9 | % | |||||||||||||||||||
| Skilled mix by revenue | 51.1 | % | 62.5 | % | 55.4 | % | (11.4) | % | 7.1 | % | |||||||||||||||||||
| Skilled mix by nursing patient days | 29.2 | % | 39.4 | % | 33.5 | % | (10.2) | % | 5.9 | % | |||||||||||||||||||
| Occupancy for skilled nursing services: | |||||||||||||||||||||||||||||
| Available patient days | 2,823,829 | 3,178,269 | 703,684 | (11.2) | % | 351.7 | % | ||||||||||||||||||||||
| Actual patient days | 2,446,737 | 2,814,109 | 588,089 | (13.1) | % | 378.5 | % | ||||||||||||||||||||||
| Occupancy rate (operational beds) | 86.6 | % | 88.5 | % | 83.6 | % | (1.9) | % | 4.9 | % | |||||||||||||||||||
| Number of facilities at period end | 62 | 84 | 72 | (26.2) | % | 16.7 | % | ||||||||||||||||||||||
| Number of operational beds at period end | 7,661 | 9,367 | 7,882 | (18.2) | % | 18.8 | % | ||||||||||||||||||||||
__________________
(1)New facilities represent facilities purchased less than 18 months from the date presented.
The following tables present the above key skilled services metrics by category for all facilities, Mature facilities, Ramping facilities and New facilities as of and for the six months ended June 30, 2024 and 2023:
| Six Months Ended June 30, | |||||||||||||||||||||||
| 2024 | 2023 | Change | % Change | ||||||||||||||||||||
| (dollars in thousands) | |||||||||||||||||||||||
| Total facility results: | |||||||||||||||||||||||
| Skilled nursing services revenue | $ | 1,900,538 | $ | 1,461,568 | $ | 438,970 | 30.0 | % | |||||||||||||||
| Skilled mix by revenue | 51.6 | % | 60.8 | % | (9.2) | % | |||||||||||||||||
| Skilled mix by nursing patient days | 29.5 | % | 37.3 | % | (7.8) | % | |||||||||||||||||
| Occupancy for skilled nursing services: | |||||||||||||||||||||||
| Available patient days | 4,389,269 | 3,359,730 | 1,029,539 | 30.6 | % | ||||||||||||||||||
| Actual patient days | 3,994,467 | 3,078,280 | 916,187 | 29.8 | % | ||||||||||||||||||
| Occupancy rate (operational beds) | 91.0 | % | 91.6 | % | (0.6) | % | |||||||||||||||||
| Number of facilities at period end | 214 | 185 | 29 | 15.7 | % | ||||||||||||||||||
| Number of operational beds at period end | 24,483 | 20,536 | 3,947 | 19.2 | % | ||||||||||||||||||
80
| Six Months Ended June 30, | |||||||||||||||||||||||
| 2024 | 2023 | Change | % Change | ||||||||||||||||||||
| (dollars in thousands) | |||||||||||||||||||||||
Mature facility(1) results: | |||||||||||||||||||||||
| Skilled nursing services revenue | $ | 584,618 | $ | 544,170 | $ | 40,448 | 7.4 | % | |||||||||||||||
| Skilled mix by revenue | 55.4 | % | 63.0 | % | (7.6) | % | |||||||||||||||||
| Skilled mix by nursing patient days | 32.3 | % | 39.4 | % | (7.1) | % | |||||||||||||||||
| Occupancy for skilled nursing services: | |||||||||||||||||||||||
| Available patient days | 1,268,904 | 1,217,416 | 51,488 | 4.2 | % | ||||||||||||||||||
| Actual patient days | 1,197,660 | 1,134,502 | 63,158 | 5.6 | % | ||||||||||||||||||
| Occupancy rate (operational beds) | 94.4 | % | 93.2 | % | 1.2 | % | |||||||||||||||||
| Number of facilities at period end | 65 | 65 | — | — | % | ||||||||||||||||||
| Number of operational beds at period end | 6,971 | 6,959 | 12 | 0.2 | % | ||||||||||||||||||
__________________
(1)Mature facilities represent facilities purchased more than 36 months before the date presented.
| Six Months Ended June 30, | |||||||||||||||||||||||
| 2024 | 2023 | Change | % Change | ||||||||||||||||||||
| (dollars in thousands) | |||||||||||||||||||||||
Ramping facility(1) results: | |||||||||||||||||||||||
| Skilled nursing services revenue | $ | 817,146 | $ | 271,152 | $ | 545,994 | 201.4 | % | |||||||||||||||
| Skilled mix by revenue | 56.8 | % | 59.1 | % | (2.3) | % | |||||||||||||||||
| Skilled mix by nursing patient days | 33.6 | % | 35.9 | % | (2.3) | % | |||||||||||||||||
| Occupancy for skilled nursing services: | |||||||||||||||||||||||
| Available patient days | 1,679,388 | 627,582 | 1,051,806 | 167.6 | % | ||||||||||||||||||
| Actual patient days | 1,590,306 | 583,678 | 1,006,628 | 172.5 | % | ||||||||||||||||||
| Occupancy rate (operational beds) | 94.7 | % | 93.0 | % | 1.7 | % | |||||||||||||||||
| Number of facilities at period end | 84 | 72 | 12 | 16.7 | % | ||||||||||||||||||
| Number of operational beds at period end | 9,378 | 7,882 | 1,496 | 19.0 | % | ||||||||||||||||||
__________________
(1)Ramping facilities represent facilities purchased within 18-36 months of the date presented.
| Six Months Ended June 30, | |||||||||||||||||||||||
| 2024 | 2023 | Change | % Change | ||||||||||||||||||||
| (dollars in thousands) | |||||||||||||||||||||||
New facility(1) results: | |||||||||||||||||||||||
| Skilled nursing services revenue | $ | 498,774 | $ | 646,246 | $ | (147,472) | (22.8) | % | |||||||||||||||
| Skilled mix by revenue | 38.7 | % | 59.7 | % | (21.0) | % | |||||||||||||||||
| Skilled mix by nursing patient days | 21.3 | % | 36.2 | % | (14.9) | % | |||||||||||||||||
| Occupancy for skilled nursing services: | |||||||||||||||||||||||
| Available patient days | 1,440,977 | 1,514,732 | (73,755) | (4.9) | % | ||||||||||||||||||
| Actual patient days | 1,206,501 | 1,360,100 | (153,599) | (11.3) | % | ||||||||||||||||||
| Occupancy rate (operational beds) | 83.7 | % | 89.8 | % | (6.1) | % | |||||||||||||||||
| Number of facilities at period end | 65 | 48 | 17 | 35.4 | % | ||||||||||||||||||
| Number of operational beds at period end | 8,134 | 5,695 | 2,439 | 42.8 | % | ||||||||||||||||||
__________________
(1)New facilities represent facilities purchased less than 18 months from the date presented.
81
The following tables present additional detail regarding our skilled mix, including our percentage of nursing patient days and revenue by payor source for all facilities, Mature facilities, Ramping facilities and New facilities for the years ended December 31, 2023, 2022 and 2021:
| Year ended December 31, | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Skilled mix by revenue | Mature | Ramping | New | Total | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 2023 | 2022 | 2021 | 2023 | 2022 | 2021 | 2023 | 2022 | 2021 | 2023 | 2022 | 2021 | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Medicare | 41.5 | % | 51.5 | % | 45.7 | % | 35.7 | % | 49.8 | % | 43.6 | % | 36.1 | % | 44.9 | % | 36.7 | % | 37.9 | % | 47.8 | % | 43.3 | % | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Managed care | 17.3 | 14.6 | 13.9 | 19.6 | 14.5 | 11.8 | 15.0 | 17.6 | 18.7 | 17.2 | 16.3 | 14.5 | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Skilled mix | 58.8 | 66.1 | 59.6 | 55.3 | 64.3 | 55.4 | 51.1 | 62.5 | 55.4 | 55.1 | 64.1 | 57.8 | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Medicaid | 35.2 | 29.0 | 35.5 | 37.7 | 30.8 | 38.3 | 41.9 | 31.8 | 37.2 | 38.3 | 30.6 | 36.4 | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Private and other | 6.0 | 4.9 | 4.9 | 7.0 | 4.9 | 6.3 | 7.0 | 5.7 | 7.4 | 6.6 | 5.3 | 5.8 | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Total | 100.0 | % | 100.0 | % | 100.0 | % | 100.0 | % | 100.0 | % | 100.0 | % | 100.0 | % | 100.0 | % | 100.0 | % | 100.0 | % | 100.0 | % | 100.0 | % | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Year ended December 31, | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Skilled mix by nursing patient days | Mature | Ramping | New | Total | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 2023 | 2022 | 2021 | 2023 | 2022 | 2021 | 2023 | 2022 | 2021 | 2023 | 2022 | 2021 | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Medicare | 21.7 | % | 30.3 | % | 25.5 | % | 18.3 | % | 27.8 | % | 23.0 | % | 18.2 | % | 25.5 | % | 19.5 | % | 19.4 | % | 27.5 | % | 23.6 | % | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Managed care | 13.9 | 12.8 | 10.7 | 14.2 | 10.6 | 8.6 | 11.0 | 13.9 | 14.0 | 13.0 | 13.2 | 10.9 | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Skilled mix | 35.6 | 43.1 | 36.2 | 32.5 | 38.4 | 31.6 | 29.2 | 39.4 | 33.5 | 32.4 | 40.7 | 34.5 | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Medicaid | 55.8 | 49.4 | 56.7 | 58.0 | 53.6 | 59.4 | 62.0 | 52.1 | 57.8 | 58.7 | 51.2 | 57.6 | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Private and other | 8.6 | 7.5 | 7.1 | 9.5 | 8.0 | 9.0 | 8.8 | 8.5 | 8.7 | 8.9 | 8.1 | 7.9 | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Total | 100.0 | % | 100.0 | % | 100.0 | % | 100.0 | % | 100.0 | % | 100.0 | % | 100.0 | % | 100.0 | % | 100.0 | % | 100.0 | % | 100.0 | % | 100.0 | % | ||||||||||||||||||||||||||||||||||||||||||||||||||
The following tables present additional detail regarding our skilled mix, including our percentage of nursing patient days and revenue by payor source for all facilities, Mature facilities, Ramping facilities and New facilities for the six months ended June 30, 2024 and 2023:
| Six Months Ended June 30, | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Skilled mix by revenue | Mature | Ramping | New | Total | ||||||||||||||||||||||||||||||||||||||||||||||
| 2024 | 2023 | 2024 | 2023 | 2024 | 2023 | 2024 | 2023 | |||||||||||||||||||||||||||||||||||||||||||
| Medicare | 37.5 | % | 46.7 | % | 38.2 | % | 39.9 | % | 22.4 | % | 44.2 | % | 33.8 | % | 44.3 | % | ||||||||||||||||||||||||||||||||||
| Managed care | 17.9 | 16.3 | 18.6 | 19.2 | 16.3 | 15.5 | 17.8 | 16.5 | ||||||||||||||||||||||||||||||||||||||||||
| Skilled mix | 55.4 | 63.0 | 56.8 | 59.1 | 38.7 | 59.7 | 51.6 | 60.8 | ||||||||||||||||||||||||||||||||||||||||||
| Medicaid | 37.9 | 31.8 | 35.6 | 34.1 | 52.1 | 34.6 | 40.7 | 33.5 | ||||||||||||||||||||||||||||||||||||||||||
| Private and other | 6.7 | 5.2 | 7.6 | 6.8 | 9.2 | 5.7 | 7.7 | 5.7 | ||||||||||||||||||||||||||||||||||||||||||
| Total | 100.0 | % | 100.0 | % | 100.0 | % | 100.0 | % | 100.0 | % | 100.0 | % | 100.0 | % | 100.0 | % | ||||||||||||||||||||||||||||||||||
| Six Months Ended June 30, | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Skilled mix by nursing patient days | Mature | Ramping | New | Total | ||||||||||||||||||||||||||||||||||||||||||||||
| 2024 | 2023 | 2024 | 2023 | 2024 | 2023 | 2024 | 2023 | |||||||||||||||||||||||||||||||||||||||||||
| Medicare | 18.5 | % | 25.9 | % | 19.7 | % | 21.4 | % | 9.7 | % | 24.3 | % | 16.3 | % | 24.3 | % | ||||||||||||||||||||||||||||||||||
| Managed care | 13.8 | 13.5 | 13.9 | 14.5 | 11.6 | 11.9 | 13.2 | 13.0 | ||||||||||||||||||||||||||||||||||||||||||
| Skilled mix | 32.3 | 39.4 | 33.6 | 35.9 | 21.3 | 36.2 | 29.5 | 37.3 | ||||||||||||||||||||||||||||||||||||||||||
| Medicaid | 59.6 | 52.6 | 57.5 | 54.3 | 68.1 | 55.9 | 61.3 | 54.4 | ||||||||||||||||||||||||||||||||||||||||||
| Private and other | 8.1 | 8.0 | 8.9 | 9.8 | 10.6 | 7.9 | 9.2 | 8.3 | ||||||||||||||||||||||||||||||||||||||||||
| Total | 100.0 | % | 100.0 | % | 100.0 | % | 100.0 | % | 100.0 | % | 100.0 | % | 100.0 | % | 100.0 | % | ||||||||||||||||||||||||||||||||||
•Average daily rates — The routine revenue by payor source for a period at the skilled nursing facilities divided by actual patient days for that revenue source for that given period. These rates exclude additional state relief funding, which includes payments we recognized as part of The Families First Coronavirus Response Act (FFCRA). Revenue associated with calculating average daily rates is based on contractually agreed-upon amounts or rates, excluding the estimates of variable consideration under the revenue
82
recognition standard, Financial Accounting Standards Board (FASB) Accounting Standards Codification (ASC) Topic 606.
The following table presents average daily rates by payor source, excluding services that are not covered by the daily rate, for the years ended December 31, 2023, 2022 and 2021:
| Year ended December 31, | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Average daily rate | Mature | Ramping | New | Total | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 2023 | 2022 | 2021 | 2023 | 2022 | 2021 | 2023 | 2022 | 2021 | 2023 | 2022 | 2021 | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Medicare | 885.18 | $ | 802.83 | $ | 795.90 | $ | 905.90 | $ | 773.15 | $ | 695.43 | $ | 874.32 | $ | 817.51 | $ | 765.33 | $ | 887.27 | $ | 808.35 | $ | 766.53 | ||||||||||||||||||||||||||||||||||||||||||||||||
| Managed care | 572.65 | 544.92 | 575.73 | 643.35 | 590.76 | 501.86 | 597.86 | 588.94 | 540.78 | 603.18 | 572.60 | 551.72 | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Total for skilled patient payors (1) | 762.84 | 726.56 | 730.92 | 791.41 | 722.75 | 642.79 | 769.97 | 736.89 | 671.08 | 773.61 | 731.80 | 698.54 | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Medicaid | 291.86 | 278.25 | 277.94 | 303.14 | 248.66 | 236.02 | 296.81 | 283.38 | 261.73 | 297.03 | 279.12 | 263.85 | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Private and other | 328.1 | 301.46 | 311.66 | 346.80 | 261.47 | 258.02 | 351.42 | 313.43 | 343.94 | 342.27 | 305.76 | 304.62 | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Total (2) | 462.8 | $ | 473.09 | $ | 444.38 | $ | 466.11 | $ | 431.75 | $ | 366.52 | $ | 439.66 | $ | 464.75 | $ | 406.17 | $ | 455.42 | $ | 465.87 | $ | 417.06 | ||||||||||||||||||||||||||||||||||||||||||||||||
__________________
(1)Represents weighted average of revenue generated by Medicare and managed care payor sources.
(2)Represents weighted average.
The following table presents average daily rates by payor source, excluding services that are not covered by the daily rate, for the six months ended June 30, 2024 and 2023:
| Six Months Ended June 30, | |||||||||||||||||||||||||||||||||||||||||||||||
| Average daily rate | Mature | Ramping | New | Total | |||||||||||||||||||||||||||||||||||||||||||
| 2024 | 2023 | 2024 | 2023 | 2024 | 2023 | 2024 | 2023 | ||||||||||||||||||||||||||||||||||||||||
| Medicare | $ | 939.91 | $ | 852.46 | $ | 966.33 | $ | 869.07 | $ | 930.02 | $ | 868.65 | $ | 950.80 | $ | 862.37 | |||||||||||||||||||||||||||||||
| Managed care | 604.43 | 573.93 | 664.97 | 617.61 | 567.60 | 623.11 | 620.08 | 603.11 | |||||||||||||||||||||||||||||||||||||||
Total for skilled patient payors (1) | 796.73 | 757.22 | 841.57 | 767.70 | 733.14 | 787.99 | 803.17 | 772.32 | |||||||||||||||||||||||||||||||||||||||
| Medicaid | 295.48 | 286.70 | 308.29 | 292.51 | 308.72 | 296.20 | 304.70 | 292.11 | |||||||||||||||||||||||||||||||||||||||
| Private and other | 385.84 | 310.77 | 417.29 | 328.06 | 349.97 | 346.82 | 385.59 | 329.83 | |||||||||||||||||||||||||||||||||||||||
Total (2) | $ | 464.80 | $ | 474.14 | $ | 497.10 | $ | 466.65 | $ | 403.58 | $ | 478.36 | $ | 459.17 | $ | 474.58 | |||||||||||||||||||||||||||||||
__________________
(1)Represents weighted average of revenue generated by Medicare and managed care payor sources.
(2)Represents weighted average.
Non-GAAP Financial Measures
In addition to our results provided throughout that are determined in accordance with GAAP, we also present the following non-GAAP financial measures: EBITDA, Adjusted EBITDA and Adjusted EBITDAR (collectively, Non-GAAP Financial Measures). EBITDA and Adjusted EBITDA are performance measures. Adjusted EBITDAR is a valuation measure. These Non-GAAP Financial Measures have no standardized meaning defined by GAAP, and therefore have limitations as analytical tools, and they should not be considered in isolation, or as a substitute for analysis of our results as reported in accordance with GAAP. You should review the reconciliation of net (loss) income to the Non-GAAP Financial Measures in the table below, together with our audited combined/consolidated financial statements and the related notes in their entirety, and should not rely on any single financial measure. Additionally, other companies may define these or similar Non-GAAP Financial Measures with the same or similar names differently, and because these Non-GAAP Financial Measures are not standardized, it may not be possible to compare these financial measures to those of other companies.
Performance Measures
We use EBITDA and Adjusted EBITDA to facilitate internal comparisons of our historical operating performance on a more consistent basis, as well as for business planning and forecasting purposes. In addition, we believe the presentation of EBITDA and Adjusted EBITDA is useful to investors, analysts and other interested
83
parties in comparing our operating performance across reporting periods on a consistent basis by excluding items that we do not believe are indicative of our ongoing operating performance.
EBITDA – We calculate EBITDA as net income, adjusted for net losses attributable to noncontrolling interest, before: other expense, net; provision for income taxes; and depreciation and amortization.
Adjusted EBITDA – We calculate Adjusted EBITDA as EBITDA further adjusted for non-core business items, which for the reported periods includes, to the extent applicable, costs incurred to acquire operations that are not capitalizable, costs related to the integration of acquired companies, lease termination fees, losses incurred from debt restructuring, gains on lease termination, stock-based compensation expense, loss from equity method investment in joint venture and certain one-time expenses that are not representative of our underlying operating performance. Costs related to acquisitions include costs related to our acquisition of SNF facilities and providers, including related costs such as legal fees, financial and tax due diligence, consulting and escrow fees. Costs associated with acquisition integration include legal settlements paid following acquisitions made in prior periods. The loss related to our equity method investment in joint venture is a loss allocated to us from a discrete disposal recognized by one of our joint ventures.
Valuation Measure
We use Adjusted EBITDAR as a measure to determine the value of prospective acquisitions and to assess the enterprise value of our business without regard to differences in capital structures and leasing arrangements. In addition, we believe that Adjusted EBITDAR is also a commonly used measure by investors, analysts and other interested parties to compare the enterprise value of different companies in the healthcare industry without regard to differences in capital structures and leasing arrangements, particularly for companies with operating and finance leases. For example, finance lease expenditures are recorded in depreciation and interest and are therefore removed from Adjusted EBITDA, whereas operating lease expenditures are recorded in rent expense and are therefore retained in Adjusted EBITDA. Adjusted EBITDAR is a financial valuation measure that is not specified in GAAP, and is not displayed as a performance measure as it excludes rent expense, which is a normal and recurring cash operating expense, and is therefore presented only for the current period. While we believe that Adjusted EBITDAR provides useful insight regarding our underlying operations, excluding the impact of our operating leases, we must still incur cash operating expenses related to our operating leases and rent and such expenses are necessary to operate our leased operations. As a result, Adjusted EBITDAR may understate the extent of our cash operating expenses for the respective period relative to our actual cash needs to operate our leased operations and business.
Adjusted EBITDAR – We calculate Adjusted EBITDAR as Adjusted EBITDA less rent-cost of services.
84
The tables below present a reconciliation of EBITDA, Adjusted EBITDA and Adjusted EBITDAR to net income, the most directly comparable financial measure calculated in accordance with GAAP, on a combined/consolidated basis for the periods presented:
| Year Ended December 31, | |||||||||||||||||
| 2023 | 2022 | 2021 | |||||||||||||||
| (in thousands) | |||||||||||||||||
| Net income | $ | 112,882 | $ | 150,496 | $ | 47,947 | |||||||||||
| Less: Net income attributable to noncontrolling interest | 8 | — | — | ||||||||||||||
| Add: Interest expense | 49,919 | 25,538 | 5,278 | ||||||||||||||
| Provision for income taxes | 44,435 | 56,549 | 33,479 | ||||||||||||||
| Depreciation and amortization | 25,632 | 22,311 | 7,153 | ||||||||||||||
| EBITDA | $ | 232,860 | $ | 254,894 | $ | 93,857 | |||||||||||
| Adjustments to EBITDA: | |||||||||||||||||
| Acquisition related costs | 998 | 201 | 3,216 | ||||||||||||||
| Acquisition - integration related costs | — | — | 7,000 | ||||||||||||||
| Lease termination fees | — | 421 | — | ||||||||||||||
| Loss resulting from debt restructuring | 3,628 | — | — | ||||||||||||||
| Adjusted EBITDA | $ | 237,486 | $ | 255,516 | $ | 104,073 | |||||||||||
| Rent - cost of services | 216,711 | 160,003 | 78,122 | ||||||||||||||
| Adjusted EBITDAR | $ | 454,197 | |||||||||||||||
| Six Months Ended June 30, | |||||||||||
| 2024 | 2023 | ||||||||||
| (in thousands) | |||||||||||
| Net income | $ | 38,232 | $ | 58,818 | |||||||
| Less: Net income attributable to noncontrolling interest | 4 | 3 | |||||||||
| Add: Interest expense | 24,578 | 25,942 | |||||||||
| Provision for income taxes | 22,441 | 21,871 | |||||||||
| Depreciation and amortization | 16,678 | 11,988 | |||||||||
EBITDA | $ | 101,925 | $ | 118,616 | |||||||
| Adjustments to EBITDA: | |||||||||||
| Acquisition related costs | 692 | 708 | |||||||||
| Loss resulting from debt restructuring | — | 3,109 | |||||||||
| Gain on lease termination | (8,046) | — | |||||||||
| Stock-based compensation expense | 90,936 | — | |||||||||
| Loss from equity method investment in joint venture | 2,736 | — | |||||||||
Adjusted EBITDA | $ | 188,243 | $ | 122,433 | |||||||
| Rent - cost of services | 129,794 | 96,560 | |||||||||
Adjusted EBITDAR | $ | 318,037 | |||||||||
85
Components of Results of Operations
Revenue
Patient and Resident Service Revenue
Patient and resident service revenue typically represents over 99% our total revenue. Patient and resident service revenue comprises skilled nursing services revenue, revenue generated from our senior assisted living services and revenue generated from certain ancillary services provided outside of routine contractual agreements. For each of the years ended December 31, 2023, 2022, and 2021, and for the six months ended June 30, 2024 and 2023, skilled nursing services revenue represented over 99% of patient and resident service revenue.
We derive patient and resident service revenue from services rendered, under short-term contracts, to patients for skilled and intermediate nursing, rehabilitation therapy, assisted living and hospice services. This revenue is reported at the amount that reflects the consideration to which we expect to be entitled in exchange for providing patient services. These amounts are due from patients, governmental programs, and other third-party payors, and include variable consideration for retroactive revenue adjustments due to settlement of audits, reviews, and investigations. Within our skilled nursing operations, we generate revenue from Medicaid, Medicare and other payors such as commercial insurance companies, health maintenance organizations, and preferred provider organizations.
We expect patient and resident service revenue to continue to represent the vast majority of our total revenue and that such revenue will continue to increase to the extent we successfully execute on our acquisition strategy.
Additional Funding
We received funding from the U.S. Department of Health and Human Services (HHS) through the Provider Relief Fund (PRF) as we are the healthcare providers who diagnose, test, or care for individuals with cases of COVID-19 and have health care related expenses and lost revenues attributable to COVID-19. In 2023, this program ended and we do not expect to recognize any revenue based on funding through the PRF in the future.
Other Revenue
Other revenue relates to ancillary revenue generating activities and primarily consists of revenue associated with arrangements in which we are a lessor of certain facilities. Other revenue typically represents an immaterial portion of our total revenue and we expect this to continue for the foreseeable future.
Cost of Services (exclusive of rent and depreciation and amortization shown separately)
Our cost of services represents the costs of operating our operating subsidiaries, which primarily consist of payroll and related benefits, supplies, purchased services, and ancillary expenses such as the cost of pharmacy and therapy services provided to patients. Cost of services also includes the cost of general and professional liability insurance, rent expenses related to leasing our operational facilities (such as taxes, insurance, impounds, capital reserves or other charges payable under the applicable lease agreements), dietary services, contracted services and other general cost of services with respect to our operations. As we continue to execute on our acquisitions strategy and grow our business, we expect that our cost of services will continue to increase.
Rent - Cost of Services
Rent - cost of services consists solely of base minimum rent amounts payable under lease agreements to third-party real estate owners. Our operating subsidiaries lease and operate but do not own the underlying real estate and these amounts do not include taxes, insurance, impounds, capital reserves or other charges payable under the applicable lease agreements. As we continue to execute on our acquisitions strategy and expand our network of facilities, we expect that our rent - cost of services will continue to increase.
86
General and Administrative Expense
General and administrative expense consists primarily of payroll and related benefits and travel expenses for our PACS Services personnel, including training and other operational support. General and administrative expense also includes professional fees (including accounting and legal fees) and costs relating to our information systems. Historically, our general and administrative expense has not included any stock-based compensation. In connection with our IPO in April 2024, we adopted the 2024 Plan and ESPP. From this point forward, our general and administrative expense includes stock-based compensation.
We expect general and administrative expense to increase on an absolute dollar basis for the foreseeable future as we continue to increase investments to support our growth. As a public company, our costs related to legal, audit, accounting, regulatory and tax-related services associated with maintaining compliance with exchange listing and SEC requirements, director and officer insurance costs, investor and public relations costs, and other expenses that we did not incur as a private company are higher than when we were a private company. We anticipate that general and administrative expense as a percentage of revenue will vary from period to period, but we expect to leverage these expenses over time as we grow our revenue.
Depreciation and Amortization
Property and equipment are recorded at their original historical cost. Depreciation is computed using the straight-line method over the estimated useful lives of the depreciable assets. The following is a summary of the depreciable lives of our depreciable assets:
•Buildings and improvements - minimum of 5 years to a maximum of 40 years, but generally 30 years
•Leasehold improvements - shorter of the lease term or the estimated useful life, generally 5 to 15 years
•Furniture and equipment - minimum of 3 to a maximum of 15 years
Other (Expense) Income, net
Other expense, net consists primarily of interest expense related to our debt, as well as income from gains and losses from investments in partnerships, including joint ventures.
Provision for Income Taxes
Provision for income taxes consists primarily of income taxes in certain jurisdictions in which we conduct business.
87
Results of Operations
Year Ended December 31, 2023 Compared to the Year Ended December 31, 2022
| Year ended December 31, | Change | ||||||||||||||||||||||
| 2023 | 2022 | $ | % | ||||||||||||||||||||
| (in thousands) | |||||||||||||||||||||||
| Revenue | |||||||||||||||||||||||
| Patient and resident service revenue | $ | 3,110,114 | $ | 2,399,155 | $ | 710,959 | 29.6 | % | |||||||||||||||
| Additional funding | $ | 375 | 21,482 | $ | (21,107) | (98.3) | % | ||||||||||||||||
| Other revenue | $ | 1,003 | 1,357 | $ | (354) | (26.1) | % | ||||||||||||||||
Total revenue | $ | 3,111,492 | $ | 2,421,994 | $ | 689,498 | 28.5 | % | |||||||||||||||
| Operating expenses | |||||||||||||||||||||||
| Cost of services | $ | 2,447,713 | 1,861,314 | $ | 586,399 | 31.5 | % | ||||||||||||||||
| Rent - cost of services | $ | 216,711 | 160,003 | $ | 56,708 | 35.4 | % | ||||||||||||||||
| General and administrative expense | $ | 213,664 | 149,006 | $ | 64,658 | 43.4 | % | ||||||||||||||||
| Depreciation and amortization | $ | 25,632 | 22,311 | $ | 3,321 | 14.9 | % | ||||||||||||||||
Total operating expenses | $ | 2,903,720 | $ | 2,192,634 | $ | 711,086 | 32.4 | % | |||||||||||||||
| Operating income | $ | 207,772 | $ | 229,360 | $ | (21,588) | (9.4) | % | |||||||||||||||
| Other (expense) income | |||||||||||||||||||||||
| Interest expense | $ | (49,919) | (25,538) | $ | (24,381) | 95.5 | % | ||||||||||||||||
| Other (expense) income, net | $ | (536) | 3,223 | $ | (3,759) | (116.6) | % | ||||||||||||||||
Total other expense, net | $ | (50,455) | $ | (22,315) | $ | (28,140) | 126.1 | % | |||||||||||||||
| Income before provision for income taxes | $ | 157,317 | 207,045 | $ | (49,728) | (24.0) | % | ||||||||||||||||
| Provision for income taxes | $ | (44,435) | (56,549) | $ | 12,114 | (21.4) | % | ||||||||||||||||
Net income | $ | 112,882 | $ | 150,496 | $ | (37,614) | (25.0) | % | |||||||||||||||
Revenue
Patient and resident service revenue - Patient and resident service revenue increased by $711 million or 29.6% to $3,110.1 million, for the year ended December 31, 2023, compared to the year ended December 31, 2022. For each of the years ended December 31, 2023 and 2022, skilled nursing services revenue represented more than 99.0% of patient and resident service revenue.
Skilled nursing services revenue increased by $701.3 million, or 29.3%, to $3,092.6 million for the year ended December 31, 2023, compared to the year ended December 31, 2022. This change was driven by an increase in operational beds of 6,605 from December 31, 2023 to December 31, 2022 leading to a 31.8% increase in patient days across the year. Additionally we experienced a higher occupancy rate across all facilities of 90.9% for the year ended December 31, 2023, compared to 89.9% for the year ended December 31, 2022, due to increased demand as a result of continued execution on our business model. The increases were offset by a decrease in revenue from New facilities of $225.1 million driven in part by many New facilities being acquired part way through the year and therefore having less than a full year of results.
Our skilled nursing services revenue was impacted by developments in our average daily rates and fluctuations in our payor sources. Our Medicare daily rates at Mature and Ramping facilities increased by 10.3% and 17.2%, respectively, for the year ended December 31, 2023, compared to the year ended December 31, 2022. This increase was primarily due to the 5.1% net market basket update that became effective in October 2022, offset by the removal of the temporary sequestration suspension. In 2022, Medicare daily rates included nine months of sequestration suspension with three months of sequestration suspension of 1% and six months of sequestration suspension of 2%, whereas there was no sequestration suspension in 2023.
88
Our average Medicaid rates increased 6.4% due to state reimbursement increases and our participation in supplemental Medicaid payment programs and quality improvement programs in various states. Medicaid rates exclude the amount of state relief revenue we recorded.
Additional funding - Additional funding revenue decreased by $21.1 million, or 98.3% to $0.4 million for the year ended December 31, 2023, compared to the year ended December 31, 2022. The decrease was primarily attributable to a reduced amount of funding from the HHS.
Other revenue - Other revenue decreased by $0.4 million, or 26.1%, to $1.0 million for the year ended December 31, 2023, compared to $1.4 million for the year ended December 31, 2022.
Cost of services
Cost of services increased by $586.4 million, or 31.5% to $2,447.7 million, for the year ended December 31, 2023, compared to the year ended December 31, 2022. The increase was primarily driven by an increase of $360.8 million in salaries and wages. Of the salaries and wages increase, those attributable to New and Ramping facilities accounted for $303.9 million or 84% of the increase. Our total number of post-acute care facilities, inclusive of skilled nursing facilities and assisted living facilities, increased from 151 as of December 31, 2022 to 208 as of December 31, 2023, an increase of 37.7%. This increase in operations and employees led to the increase in labor cost for New facilities as they were acquired throughout the year. Further, as a large number of acquisitions from 2021 moved from New to Ramping, costs shifted to the Ramping cohort. Changes attributable to Mature facilities accounted for the remaining change. Aside from labor costs, the increase in cost of services was due to increases of $95.0 million in administrative expenses for facilities increases, $62.0 million in contracted services, and $20.0 million in nursing expenses with the remainder spread out across various expense types. Of these non-labor costs, increases in New and Ramping facilities accounted for 83% of the change with Mature facilities accounting for the remaining 17%.
Rent - cost of services
Rent - cost of services increased by $56.7 million, or 35.4% to $216.7 million, for the year ended December 31, 2023, compared to the year ended December 31, 2022. The increase was primarily attributable to the addition of New facilities, which accounted for approximately 71% of the increase, with the remainder attributable to annual escalators on Mature and Ramping facilities’ rent.
General and administrative expense
General and administrative expense increased by $64.7 million, or 43.4% to $213.7 million, for the year ended December 31, 2023, compared to the year ended December 31, 2022. This increase was primarily due to the continued expansion of the company and an increase in acquisitions as compared to the prior year. Of the $64.7 million increase, $53.6 million was in administrative costs, driven by $39.1 million of costs associated with litigation settlements and an increase in liabilities for professional and general liability claims. Of this $39.1 million, $21.7 million in costs were due to claims experience primarily related to the entities that were acquired from Plum. As part of the Plum acquisition, Plum’s professional and general liability claims, both asserted and unasserted, remained with the acquired businesses post-acquisition, and are thus included in our results of operations subsequent to finalizing the accounting for the business combination. The Company typically acquires assets of other businesses, and the acquisition of Plum represents the only material instance in which the Company structured the related acquisition transaction as a business combination. Additionally, we had an increase of $10.6 million in salaries and wages.
Depreciation and amortization
Depreciation and amortization increased by $3.3 million, or 14.9% to $25.6 million, for the year ended December 31, 2023, compared to $22.3 million for the year ended December 31, 2022. This increase is directly attributable to new facilities acquired during the year. On a cohort basis, there was an $11.8 million increase in
89
expense from Ramping facilities offset by a corresponding decrease to New facilities as a large number of facilities acquired in 2021 changed from New to Ramping. The decrease to New facilities was offset by an increase of $2.6 million from newly acquired facilities throughout the year.
Other expense, net
Other expense, net increased by $28.1 million, or 126.1% to $50.5 million, for the year ended December 31, 2023, compared to the year ended December 31, 2022. Other expense, net primarily consists of interest expense related to our debt, which increased by $24.4 million, to $49.9 million for the year ended December 31, 2023, compared to the year ended December 31, 2022, due to an increase in lines of credit and long-term debt of $232.8 million during the year. In the year ended December 31, 2023, Other expense, net also includes losses on extinguishment of existing debt of $3.6 million.
Provision for income taxes
Provision for income taxes totaled $44.4 million for the year ended December 31, 2023, representing an effective tax rate of 28.1%, compared to a provision for income tax of $56.5 million and an effective tax rate of 27.3% for the year ended December 31, 2022. The difference in the effective tax rate from the statutory rate is mainly due to state taxes, permanent book-tax differences, establishment of a deferred tax asset valuation allowance, and other adjustments. The decrease in provision for income taxes in 2023 compared to 2022 was primarily due to lower pre-tax book income in 2023. The effective tax rate for the year ended December 31, 2023 was higher than that for the year ended December 31, 2022, which was primarily attributable to a valuation allowance for the Captive Insurance Dual Consolidated Loss deferred tax asset. See Note 10, “Provision for Income Taxes”, to our audited combined/consolidated financial statements for more information.
Year Ended December 31, 2022 Compared to the Year Ended December 31, 2021
| Year ended December 31, | Change | ||||||||||||||||||||||
| 2022 | 2021 | $ | % | ||||||||||||||||||||
| (in thousands) | |||||||||||||||||||||||
| Revenue | |||||||||||||||||||||||
| Patient and resident service revenue | $ | 2,399,155 | $ | 1,135,909 | $ | 1,263,246 | 111.2 | % | |||||||||||||||
| Additional funding | 21,482 | 28,563 | (7,081) | (24.8) | % | ||||||||||||||||||
| Other revenue | 1,357 | 2,091 | (734) | (35.1) | % | ||||||||||||||||||
Total revenue | $ | 2,421,994 | $ | 1,166,563 | $ | 1,255,431 | 107.6 | % | |||||||||||||||
| Operating expenses | |||||||||||||||||||||||
| Cost of services | 1,861,314 | 901,095 | 960,219 | 106.6 | % | ||||||||||||||||||
| Rent - cost of services | 160,003 | 78,122 | 81,881 | 104.8 | % | ||||||||||||||||||
| General and administrative expense | 149,006 | 96,834 | 52,172 | 53.9 | % | ||||||||||||||||||
| Depreciation and amortization | 22,311 | 7,153 | 15,158 | 211.9 | % | ||||||||||||||||||
Total operating expenses | $ | 2,192,634 | $ | 1,083,204 | $ | 1,109,430 | 102.4 | % | |||||||||||||||
| Operating income | 229,360 | 83,359 | 146,001 | 175.1 | % | ||||||||||||||||||
| Other (expense) income | |||||||||||||||||||||||
| Interest expense | (25,538) | (5,278) | (20,260) | 383.9 | % | ||||||||||||||||||
| Other (expense) income, net | 3,223 | 3,345 | (122) | (3.6) | % | ||||||||||||||||||
Total other expense, net | $ | (22,315) | $ | (1,933) | $ | (20,382) | 1054.4 | % | |||||||||||||||
| Income before provision for income taxes | 207,045 | 81,426 | 125,619 | 154.3 | % | ||||||||||||||||||
| Provision for income taxes | (56,549) | (33,479) | (23,070) | 68.9 | % | ||||||||||||||||||
Net income | $ | 150,496 | $ | 47,947 | $ | 102,549 | 213.9 | % | |||||||||||||||
90
Revenue
Patient and resident service revenue - Patient and resident service revenue increased by $1,263.2 million, or 111.2%, to $2,399.2 million for the year ended December 31, 2022, compared to the year ended December 31, 2021. For each of the years ended December 31, 2022 and 2021, skilled nursing services revenue represented over 99% of patient and resident service revenue.
Skilled nursing services revenue increased by $1,258.2 million, or 111.0%, to $2,391.3 million for the year ended December 31, 2022, compared to the year ended December 31, 2021, which increase was primarily driven by an increase in revenue from New facilities of $1,059.2 million resulting from the acquisitions. Skilled nursing services revenue also increased due to increases in skilled mix by revenue and skilled mix by nursing patient days across Mature, Ramping and New facilities due to the application of Emergency Waivers under the COVID-19 PHE to skilled nursing patients and resumption of elective procedures resulting in increased demand for skilled nursing services. In addition, skilled nursing services revenue was positively impacted by a higher occupancy rate across all facilities of 89.9% for the year ended December 31, 2022, compared to 86.3% for the year ended December 31, 2021, due to increased demand as a result of continued execution on our business model.
Our skilled nursing services revenue was impacted by developments in our average daily rates and fluctuations in our payor sources. Our Medicare daily rates at Mature and Ramping facilities increased by 0.9% and 11.2%, respectively, compared to the year ended December 31, 2021. This increase was primarily due to the 1.2% net market basket update that became effective in October 2021, offset by the removal of the temporary sequestration suspension. In 2022, Medicare daily rates includes three months of sequestration suspension of 0%, three months of sequestration suspension of 1% and six months of sequestration suspension of 2% in comparison to what was in place for the entire year of 2021.
Our average Medicaid rates increased 5.8% due to state reimbursement increases and our participation in supplemental Medicaid payment programs and quality improvement programs in various states. Medicaid rates exclude the amount of state relief revenue we recorded.
Additional funding - Additional funding revenue decreased by $7.1 million, or 24.8%, to $21.5 million for the year ended December 31, 2022, compared to the year ended December 31, 2021. The decrease was primarily attributable to a reduced amount of funding from the HHS.
Other revenue - Other revenue decreased by $0.7 million, or 35.1%, to $1.4 million for the year ended December 31, 2022, compared to the year ended December 31, 2021. The decrease was primarily attributable to a reduction of fees from an external management contract in 2021 related to a facility that we acquired in 2022. Following this acquisition, the facility generated patient and resident services revenue.
Cost of services
Cost of services increased by $960.2 million, or 106.6%, to $1,861.3 million for the year ended December 31, 2022, compared to the year ended December 31, 2021. The increase was primarily driven by an increase of $612.7 million in salaries and wages. Of the salaries and wages increase, those attributable to New facilities accounted for 88% of the increase and those attributable to Ramping and Mature facilities accounted for the remaining 12%. Aside from labor costs, the increase in cost of services was due to increases of $120.5 million in contracted services, $91.4 million in administrative expenses for facilities, $40.7 million in nursing expenses, and $37.1 million in dietary expenses with the remainder spread out across various expense types. Of these non-labor costs, increases in New facilities accounted for 93% of the change with Ramping and Mature facilities accounting for the remaining 7%.
Rent - cost of services
Rent - cost of services increased $81.9 million, or 104.8%, to $160.0 million for the year ended December 31, 2022, compared to the year ended December 31, 2021. The increase was primarily attributable to the addition of
91
New facilities, which accounted for approximately 98% of the increase, with the remainder attributable to annual escalators on Mature and Ramping facilities' rent.
General and administrative expense
General and administrative expense increased $52.2 million, or 53.9%, to $149.0 million for the year ended December 31, 2022, compared to the year ended December 31, 2021. This increase was primarily due to a $48.0 million increase in salaries and wages of which 92% was attributable to New facilities with 8% attributable to Ramping and Mature facilities.
Depreciation and amortization
Depreciation and amortization increased by $15.2 million, or 211.9%, to $22.3 million for the year ended December 31, 2022, compared to the year ended December 31, 2021. This increase was primarily attributable to a $10.5 million increase in expense from New facilities. Additionally, there was an increase in expense of $4.7 million from Mature and Ramping facilities.
Other expense, net
Other expense, net increased by $20.4 million to $22.3 million for the year ended December 31, 2022, compared to the year ended December 31, 2021. Other expense, net primarily consists of interest expense related to our debt, which increased by $20.3 million, to $25.5 million for the year ended December 31, 2022, compared to the year ended December 31, 2021, due to an increase in lines of credit and long-term debt of $80.3 million during the year. Other expense, net also includes other income and expenses from gains and losses from investments in partnerships, including joint ventures, which decreased by $0.1 million, or 4%, to $3.2 million, for the year ended December 31, 2022, compared to the year ended December 31, 2021.
Provision for income taxes
Provision for income taxes totaled $56.5 million for the year ended December 31, 2022, representing an effective tax rate of 27.3%, compared to a provision for income tax of $33.5 million and an effective tax rate of 41.0% for the year ended December 31, 2021. The difference of the effective tax rate from the statutory rate is mainly due to state taxes, permanent book-tax difference, and other adjustments. The increase of provision for income taxes in 2022 compared to 2021 was primarily due to much higher pre-tax book income in 2022. The effective tax rate for the year ended December 31, 2022 was lower than that for the year ended December 31, 2021, which was primarily attributable to our transition from an S-Corporation to a C-Corporation during 2021 and the associated increase to the 2021 effective tax rate of 10.2% due to the recognition of prior period deferred tax liabilities. See Note 10, “Provision for Income Taxes”, to our audited combined/consolidated financial statements for more information.
92
Six Months Ended June 30, 2024 Compared to the Six Months Ended June 30, 2023 (Unaudited)
| Six Months Ended June 30, | Change | ||||||||||||||||||||||
| 2024 | 2023 | $ | % | ||||||||||||||||||||
| ( in thousands) | |||||||||||||||||||||||
| Revenue | |||||||||||||||||||||||
| Patient and resident service revenue | $ | 1,915,696 | $ | 1,468,250 | $ | 447,446 | 30.5 | % | |||||||||||||||
| Additional funding | — | 375 | (375) | (100.0) | % | ||||||||||||||||||
| Other revenue | 871 | 481 | 390 | 81.1 | % | ||||||||||||||||||
Total revenue | $ | 1,916,567 | $ | 1,469,106 | $ | 447,461 | 30.5 | % | |||||||||||||||
| Operating expenses | |||||||||||||||||||||||
| Cost of services | 1,498,139 | 1,129,587 | 368,552 | 32.6 | % | ||||||||||||||||||
| Rent - cost of services | 129,794 | 96,560 | 33,234 | 34.4 | % | ||||||||||||||||||
| General and administrative expense | 191,286 | 122,137 | 69,149 | 56.6 | % | ||||||||||||||||||
| Depreciation and amortization | 16,678 | 11,988 | 4,690 | 39.1 | % | ||||||||||||||||||
Total operating expenses | $ | 1,835,897 | $ | 1,360,272 | $ | 475,625 | 35.0 | % | |||||||||||||||
| Operating income | 80,670 | 108,834 | (28,164) | (25.9) | % | ||||||||||||||||||
| Other (expense) income | |||||||||||||||||||||||
| Interest expense | (24,578) | (25,942) | 1,364 | (5.3) | % | ||||||||||||||||||
| Gain on lease termination | 8,046 | — | 8,046 | 100.0 | % | ||||||||||||||||||
| Other expense, net | (3,465) | (2,203) | (1,262) | 57.3 | % | ||||||||||||||||||
Total other expense, net | $ | (19,997) | $ | (28,145) | $ | 8,148 | (29.0) | % | |||||||||||||||
| Income before provision for income taxes | 60,673 | 80,689 | (20,016) | (24.8) | % | ||||||||||||||||||
| Provision for income taxes | (22,441) | (21,871) | (570) | 2.6 | % | ||||||||||||||||||
Net income | $ | 38,232 | $ | 58,818 | $ | (20,586) | (35.0) | % | |||||||||||||||
Revenue
Patient and resident service revenue - Patient and resident service revenue increased by $447.4 million to $1,915.7 million for the six months ended June 30, 2024, a 30.5% increase compared to the six months ended June 30, 2023. For the six months ended June 30, 2024 and 2023, skilled nursing services revenue represented more than 99.0% of patient and resident service revenue.
Skilled nursing services revenue increased by 30.0%, or $439.0 million, to $1,900.5 million for the six months ended June 30, 2024, compared to the six months ended June 30, 2023. This change was driven by an increase in operational beds of 3,947 from June 30, 2023 to June 30, 2024, leading to a 29.8% increase in patient days year-over-year. Additionally, we experienced consistent occupancy across all facilities of 91.0% for the six months ended June 30, 2024, a slight decrease as compared to 91.6% for the six months ended June 30, 2023. The decrease in occupancy across all facilities can be attributed to our New facilities only being 83.7% occupied for the six months ended June 30, 2024, compared to 89.8% for the six months ended June 30, 2023.
Our skilled nursing services revenue was impacted by developments in our average daily rates and fluctuations in our payor sources. Our average Medicare daily rates increased by 10.3% for the six months ended June 30, 2024, compared to the six months ended June 30, 2023.
Our average Medicaid rates increased 4.3% for the six months ended June 30, 2024, compared to the six months ended June 30, 2023, due to state reimbursement increases and our participation in supplemental Medicaid payment programs and quality improvement programs in various states. Medicaid rates exclude the amount of state relief revenue we recorded.
93
Additional funding - Additional funding revenue was $0 for the six months ended June 30, 2024, compared to $0.4 million for the six months ended June 30, 2023. The decrease was due to the termination of additional funding from the HHS under the Pandemic PHE in 2023.
Other revenue - Other revenue increased by 81.1% to $0.9 million for the six months ended June 30, 2024, compared to the same period in the prior year.
Cost of services
Cost of services increased by $368.6 million to $1,498.1 million, for the six months ended June 30, 2024, compared to the six months ended June 30, 2023. The 32.6% increase was primarily driven by an increase of $220.1 million in salaries and wages. Of the salaries and wages increase, those attributable to New facilities purchased after June 30, 2023 accounted for $110.2 million or 50.1% of the increase. Our total number of post-acute care facilities, inclusive of skilled nursing facilities and assisted living facilities, increased from 188 as of June 30, 2023 to 220 as of June 30, 2024, an increase of 17.0%. This increase in operations and employees led to the increase in labor cost for New facilities as they were acquired throughout the year. Headcount and operational changes attributable to Ramping and Mature facilities accounted for the remaining change in salaries and wages. Aside from labor costs, the increase in cost of services was due to increases of $74.6 million in administrative expenses for facilities driven by a $41.3 million increase in professional and general liability insurance; $38.5 million in contracted services made up of $20.9 million from New facilities, or 54.2%, and $17.6 million from Ramping and Mature facilities; and $23.0 million in nursing and dietary expenses, $16.3 million from New facilities, with the remainder spread out across various expense types.
Rent - cost of services
Rent - cost of services increased to $129.8 million for the six months ended June 30, 2024, compared to $96.6 million for the six months ended June 30, 2023. The increase was primarily attributable to the addition of new facilities throughout the year, as well as to annual escalators on existing facilities' rent.
General and administrative expense
General and administrative expense increased by $69.1 million, to $191.3 million for the six months ended June 30, 2024, compared to $122.1 million for the six months ended June 30, 2023. This increase was primarily due to the increase in stock compensation expense as a result of our IPO, which accounted for $90.9 million of the increase. The remainder was driven by an increase in salaries and wages of $15.1 million, offset by a decrease in costs associated with professional and general liability insurance within general and administrative expense in 2023 of $34.8 million. The remainder was spread out across various expense types.
Depreciation and amortization
Depreciation and amortization increased by $4.7 million to $16.7 million, for the six months ended June 30, 2024, compared to the six months ended June 30, 2023. This increase is directly attributable to new real estate obtained through acquisitions.
Other expense, net
Other expense, net was $20.0 million for the six months ended June 30, 2024, a decrease of $8.1 million compared to the six months ended June 30, 2023. Other expense, net consists of interest expense related to our debt, which decreased by $1.4 million, to $24.6 million for the six months ended June 30, 2024, driven by a decrease in lines of credit and long-term debt of $55.1 million from June 30, 2023 to June 30, 2024 Additionally, in the six months ended June 30, 2024, other expense, net included a gain of $8.0 million recognized upon the termination of a lease. These changes were offset by a loss of $2.7 million on a joint venture disposal during the six months ended June 30, 2024. The remaining changes were spread out across various other expense types.
94
Provision for income taxes
Provision for income taxes totaled $22.4 million for the six months ended June 30, 2024, representing an effective tax rate of 37.0%, compared to a provision for income tax of $21.9 million and an effective tax rate of 27.1% for the six months ended June 30, 2023. The change in effective tax rate in the six months ended June 30, 2024 compared to the six months ended June 30, 2023 was primarily due to an increase in non-deductible expenses, including non-deductible compensation in 2024. See Note 8, “Income Taxes”, in our condensed combined/consolidated financial statements for more information.
Holding Company Status
We are a holding company with no significant direct operating assets, employees or revenues. Our operating subsidiaries are operated by separate, independent entities, each of which has its own management, employees and assets. In addition, through a separate wholly-owned subsidiary, we provide centralized accounting, payroll, human resources, information technology, legal, risk management and other consulting and centralized services to the other operating subsidiaries through contractual relationships with those subsidiaries. We also have a wholly-owned captive insurance subsidiary that provides some claims-made coverage to our operating subsidiaries for professional liability and general liability insurance.
Liquidity & Capital Resources
Our primary sources of liquidity have historically been derived from our cash flows from operations, mortgage loans (including both Housing and Urban Development (HUD)-insured and non-HUD mortgage loans), and credit facilities maintained with commercial banks. Our liquidity as of December 31, 2023 is impacted by cash generated from strong operational performance that improved through a combination of long-term leases and real estate purchases and increased acquisitions. As of December 31, 2023, we had cash and cash equivalents of $73.4 million, total assets of $3,512.7 million, total liabilities of $3,411.0 million, and total equity of $101.7 million, compared to cash and cash equivalents of $58.3 million, total assets of $2,461.9 million, total liabilities of $2,393.2 million and total equity of $68.7 million as of December 31, 2022. Our liquidity as of June 30, 2024 is impacted by cash generated from strong operational performance that improved through a combination of long-term leases and real estate purchases and increased acquisitions. As of June 30, 2024, we had cash and cash equivalents of $73.4 million, total assets of $3.9 billion, total liabilities of $3.3 billion, and total equity of $578.2 million, compared to cash and cash equivalents of $38.2, total assets of $3.1 billion, total liabilities of $3.0 billion, and total equity of $83.7 million as of June 30, 2023
On April 15, 2024, we completed our IPO obtaining total net proceeds of $414.2 million, after deducting underwriting discounts and commissions and offering expenses.
Historically, we have primarily financed the majority of our property and operation acquisitions through mortgages on our properties, our credit facilities and cash generated from operations, and we expect to continue to use these sources of capital for these purposes. We currently maintain our Amended and Restated 2023 Credit Facility, which has a total commitment limit of $600.0 million, as our single line-of-credit. As of June 30, 2024, the total principal amount outstanding under our Amended and Restated 2023 Credit Facility was $248.0 million. After giving effect to the application of all of the net proceeds to us from this offering to repay a portion of the amounts outstanding under our Amended and Restated 2023 Credit Facility, the total principal amount outstanding under our Amended and Restated 2023 Credit Facility at June 30, 2024 would have been $143.2 million, resulting in available borrowing capacity of $445.2 million, net of letter of credit usage. As of the date of this prospectus, the total principal amount outstanding under our Amended and Restated 2023 Credit Facility was $160.0 million , resulting in available cash of $426.7 million, net of letter of credit usage. See the section titled “Use of Proceeds” for additional information. The terms of the Amended and Restated 2023 Credit Facility permit optional prepayments from time to time without premium or penalty. Following such repayment, we expect to continue to use the Amended and Restated 2023 Credit Facility as our single line-of-credit and to fund the potential acquisition of additional property and operation acquisitions, as well as for working capital and for general corporate purposes. Cash paid to fund acquisitions was $127.0 million, $55.4 million, and $79.7 million for the years ended
95
December 31, 2023, 2022, and 2021, respectively. Total capital expenditures for property and equipment were $45.8 million, $22.9 million, and $124.1 million for the years ended December 31, 2023, 2022, and 2021, respectively, and $26.1 million and $16.6 million for the six months ended June 30, 2024 and 2023, respectively. Cash paid to fund real estate acquisitions was $174.7 million for the six months ended June 30, 2024, compared to $52.4 million, for the six months ended June 30, 2023. This increase was driven by our continued execution of our business strategy of acquiring distressed operations in 2024. We used approximately $370.0 million of the net proceeds from our IPO to repay amounts outstanding under our Amended and Restated 2023 Credit Facility.
We believe our current cash balances, our cash flow from operations and the amounts available for borrowing under our credit facilities will be sufficient to cover our operating needs for at least the next 12 months. We may, in the future, seek to raise additional capital to fund growth, capital renovations, operations and other business activities, but such additional capital may not be available on acceptable terms, on a timely basis, or at all.
Our cash and cash equivalents as of June 30, 2024 consisted of cash and short-term investments with original maturities of three months or less at the time of purchase.
Cash Flows for the Years Ended December 31, 2023, 2022, and 2021
The following table presents selected data from our combined/consolidated statement of cash flows for the periods presented:
| Year ended December 31, | |||||||||||||||||
| 2023 | 2022 | 2021 | |||||||||||||||
| (in thousands) | |||||||||||||||||
| Net cash provided by/(used in): | |||||||||||||||||
| Operating activities | $ | 63,697 | $ | 92,615 | $ | 57,602 | |||||||||||
| Investing activities | (172,791) | (75,321) | (218,600) | ||||||||||||||
| Financing activities | 129,592 | 12,350 | 182,048 | ||||||||||||||
Net change in cash | 20,498 | 29,644 | 21,050 | ||||||||||||||
| Cash, cash equivalents, and restricted cash - beginning of period | 98,206 | 68,562 | 47,512 | ||||||||||||||
Cash, cash equivalents, and restricted cash - end of period | $ | 118,704 | $ | 98,206 | $ | 68,562 | |||||||||||
Operating activities
Cash provided by operating activities is net income adjusted for certain non-cash items and changes in operating assets and liabilities.
Net cash provided by operating activities for the year ended December 31, 2023 of $63.7 million decreased by $28.9 million as compared with the same period in 2022. The decrease to net cash provided by operating activities was primarily driven by a $28.5 million decrease to net income (inclusive of adjustments for noncash expenses) and changes in working capital. Working capital balances continued to increase in 2023, however the increases were at a smaller rate than from 2021 to 2022 resulting in a decrease year-over-year in net cash provided. The primary working capital accounts contributing to the decrease in operating cash flows include accounts receivable, prepaid expenses and other current assets, accrued self-insurance liabilities, and other accrued expenses. These decreases were offset by changes to the operating assets and liability accounts other assets, accrued payroll and benefits, and other liabilities. Changes in working capital were driven by growth of the business during the year and an increase in days sales outstanding, or time to collect accounts receivable, in days, of 3.6, from 52.0 for the year ended December 31, 2022 to 55.6 for the year ended December 31, 2023. This growth is primarily due to the increase of newly acquired facilities during the year which typically have a longer collection period due to the distressed state of many of the facilities we acquire.
96
Net cash provided by operating activities for the year ended December 31, 2022 of $92.6 million increased by $35.0 million as compared with the same period in 2021. The increase to net cash provided by operating activities was primarily driven by the $124.9 million increase to net income (inclusive of adjustments for non-cash expenses) offset by changes in working capital. Changes in working capital were driven by growth of the business during the year and timing of collections of accounts receivable, including an increase in days sales outstanding, and of accrued wages and related liabilities. Days sales outstanding was 52.0 and 48.4 for the years ended December 31, 2022 and 2021, respectively, growing primarily due to the increase of New facilities which typically have a longer collection period due to the distressed state of many of the facilities we acquire.
Investing activities
Investing cash flows consist primarily of capital expenditures, investment activities, proceeds from sale of property and equipment and cash used for acquisitions.
Net cash used in investing activities for the year ended December 31, 2023 of $172.8 million increased by $97.5 million as compared with the same period in 2022. The increase in cash used was primarily attributable to an increase of $71.6 million in cash used to acquire facilities and an increase of $22.9 million in cash used to purchase property and equipment, in excess of cash used for these purposes in 2022. Further, in 2023 we made an additional $2.6 million investment in partnerships as opposed to no cash used for this purpose in 2022.
Net cash used in investing activities for the year ended December 31, 2022 of $75.3 million decreased by $143.3 million as compared with the same period in 2021. This decrease was primarily attributable to a decrease in acquisitions in 2022 as compared to 2021, in which a large portfolio of facilities was acquired consisting of a cash outflow of $104.2 million. Additionally, in 2022 we did not make any additional investments in partnerships as compared to 2021 which had related cash outflows of $15.7 million.
Financing activities
Financing cash flows consist primarily of payment of lines of credit, distributions and repayment of short-term and long-term debt, borrowings on lines of credit and contributions from non-controlling interest.
Net cash provided by financing activities for the year ended December 31, 2023 of $129.6 million increased by $117.2 million as compared with the same period in 2022. The increase was primarily driven by a year-over-year increase of $322.3 million in net cash flow on lines of credit. This increase was offset by a year-over-year decrease of $182.3 million in net cash flow on long-term debt. This activity was due to a debt restructuring that occurred during 2023 as described in the Credit Facilities and Long-term Debt sections below. Dividends also increased $20.1 million in 2023.
Net cash provided by financing activities for the year ended December 31, 2022 of $12.3 million decreased by $169.7 million as compared with the same period in 2021. The decrease was primarily driven by a decrease of $306.4 million in borrowing on our lines-of-credit offset by a decrease of $233.0 million in payments on the lines-of-credit. Also contributing to the decrease in net cash provided by financing activities, we had a decrease of $73.6 million in borrowings of long-term debt and an increase of $19.5 million in payments on long-term debt. The high level of borrowings in 2021 was primarily related to the high acquisition activity in that year. Dividends also increased $6.5 million in 2022.
97
Cash Flows for the Six Months Ended June 30, 2024 and 2023 (Unaudited)
The following table presents selected data from our condensed combined/consolidated statement of cash flows for the periods presented:
| Six Months Ended June 30, | |||||||||||
| 2024 | 2023 | ||||||||||
| (in thousands) | |||||||||||
| Net cash provided by/(used in): | |||||||||||
| Operating activities | $ | 93,600 | $ | 58,212 | |||||||
| Investing activities | (239,634) | (67,261) | |||||||||
| Financing activities | 105,184 | (8,627) | |||||||||
| Net change in cash | (40,850) | (17,676) | |||||||||
| Cash, cash equivalents, and restricted cash - beginning of period | 118,704 | 98,206 | |||||||||
| Cash, cash equivalents, and restricted cash - end of period | $ | 77,854 | $ | 80,530 | |||||||
Operating activities
Cash provided by operating activities consists of our net (loss) income adjusted for certain non-cash items and changes in operating assets and liabilities.
Net cash provided by operating activities for the six months ended June 30, 2024 of $93.6 million increased by $35.4 million as compared with the same period in 2023. The increase to net cash provided by operating activities was driven by an increase in operational performance. This increase was offset in part by a decrease in cash flows from the change in operating assets and liabilities of $37.9 million due primarily to the timing of accounts receivable collections as well as the timing of payables and other accrued liabilities. The timing of collections and impacts to net income are driven by growth in operating facilities period-over-period and an increase in days sales outstanding of 3.4, from 54.0 as of June 30, 2023 to 57.4 as of June 30, 2024. This growth in days sales outstanding is primarily due to the increase of newly acquired facilities during the year which typically have a longer collection period during the facility ownership transition.
Investing activities
Investing cash flows consist primarily of capital expenditures, investment activities, proceeds from sale of property and equipment and cash used for acquisitions.
Net cash used in investing activities for the six months ended June 30, 2024 of $239.6 million increased by $172.4 million as compared with the same period in 2023. The increase in cash used was attributable to an increase of $122.3 million used to acquire real estate facilities and an increase of $9.5 million used to purchase property and equipment, in excess of cash used for these purposes in the six months ended June 30, 2023. In the six months ended June 30, 2024 we also purchased investments of $35.0 million through our captive insurance subsidiary using funds held as long-term restricted cash previously held in other assets and we made an additional $5.1 million investment in partnerships during the period, as opposed to no cash used for these purposes in the same period in 2023. See Note 5, "Fair Value Measurement", to our condensed combined/consolidated financial statements for more information.
Financing activities
Financing cash flows consist primarily of payment of lines of credit, distributions and repayment of short-term and long-term debt, borrowings on lines of credit and contributions from noncontrolling interest.
98
Net cash provided by financing activities for the six months ended June 30, 2024 of $105.2 million increased by $113.8 million as compared with the same period in 2023. The increase was primarily driven by a year-over-year increase of $414.2 million from net IPO proceeds. Offsetting this inflow were $228.9 million and $48.4 million decreases in net cash flows from lines of credit and long-term debt, respectively. The total long-term debt additions of $39.8 million during the six months ended June 30, 2024 had more favorable terms, as compared to our existing debt, including the additions to the HUD-insured mortgage loans of $34.7 million with interest rates ranging from 2.9% to 3.6% and remaining terms of 24 to 26 years.
Material cash requirements from known contractual and other obligations
The table below sets forth the total long-term debt obligations outstanding as of the periods presented.
| December 31, | June 30, | ||||||||||||||||||||||
| 2023 | 2022 | 2024 | 2023 | ||||||||||||||||||||
| (in thousands) | |||||||||||||||||||||||
| (unaudited) | |||||||||||||||||||||||
| Lines of credit | $ | 520,000 | $ | 146,820 | $ | 248,000 | $ | 107,118 | |||||||||||||||
| Mortgage, loan, and promissory notes | $ | 215,010 | $ | 356,232 | $ | 245,425 | $ | 445,409 | |||||||||||||||
| Total | $ | 735,010 | $ | 503,052 | $ | 493,425 | $ | 552,527 | |||||||||||||||
The table above does not reflect our intended use of proceeds from this offering. After giving effect to the application of approximately $ million of the net proceeds from this offering to repay a portion of the amounts outstanding under our Amended and Restated 2023 Credit Facility, we estimate that our total obligations outstanding would have been $ million as of June 30, 2024. See the section titled “Use of Proceeds” for additional information.
The table below sets forth the significant contractual obligations as of June 30, 2024, including the future periods in which payments are expected.
| 2024 (remainder) | 2025 | 2026 | 2027 | 2028 | Thereafter | Total | |||||||||||||||||||||||||||||||||||
| (in thousands) | |||||||||||||||||||||||||||||||||||||||||
| Operating lease obligations | $ | 116,501 | $ | 232,133 | $ | 231,843 | $ | 229,876 | $ | 231,979 | $ | 2,167,328 | $ | 3,209,660 | |||||||||||||||||||||||||||
| Finance lease obligations | $ | 1,929 | $ | 23,560 | $ | 2,241 | $ | 17,995 | $ | 782 | $ | 391 | $ | 46,898 | |||||||||||||||||||||||||||
| Long-term debt and line of credit obligations | $ | 8,213 | $ | 14,314 | $ | 4,616 | $ | 8,692 | $ | 251,821 | $ | 205,769 | $ | 493,425 | |||||||||||||||||||||||||||
| Interest payments on long-term debt | $ | 4,996 | $ | 9,494 | $ | 9,015 | $ | 8,558 | $ | 8,351 | $ | 140,381 | $ | 180,795 | |||||||||||||||||||||||||||
| Total | $ | 131,639 | $ | 279,501 | $ | 247,715 | $ | 265,121 | $ | 492,933 | $ | 2,513,869 | $ | 3,930,778 | |||||||||||||||||||||||||||
The table above does not reflect our intended use of proceeds from this offering. After giving effect to the application of approximately $ million of the net proceeds from this offering to repay a portion of the amounts outstanding under our Amended and Restated 2023 Credit Facility, we estimate that our total long-term debt and line of credit obligations and our total obligations would decrease to approximately $ million and $ million, respectively. See the section titled “Use of Proceeds” for additional information.
Credit facilities
On February 28, 2023, we entered into a working capital loan agreement (Working Capital Loan) in connection with the acquisition of various new facilities. The Working Capital Loan allowed us to borrow up to $17.5 million at
99
an annual interest rate of 9%. On May 8, 2023, we drew on the Working Capital Loan in the amount of $15.0 million. As described below, the Working Capital Loan was repaid during the year and, as such, has a zero balance as of June 30, 2024.
On June 30, 2023, PACS Group, Inc., as holdings, PACS Holdings, LLC, as borrower, and certain of their subsidiaries entered into a credit agreement with Truist Bank (Truist) and a syndicate of lenders (2023 Credit Agreement) that extended credit in the form of a revolving credit facility thereunder (2023 Revolving Credit Facility), including letter of credit and swing line sub facilities, and a term loan facility (Truist Term Loan), together referred to as the 2023 Credit Facility. The 2023 Credit Agreement provided for: (i) the 2023 Revolving Credit Facility with revolving commitments in an aggregate principal amount of $150.0 million, including a letter of credit sub facility in an amount representing that portion of the aggregate revolving commitments that may be used by the borrower for the issuance of letters of credit in an aggregate face amount not to exceed $30.0 million and a swingline loan sub facility in an aggregate principal amount at any time outstanding not to exceed $20.0 million and (ii) the Truist Term Loan in an aggregate principal amount of $275.0 million.
Outstanding borrowings under the 2023 Credit Facility accrued interest, at our option, equal to either: (a) the Secured Overnight Financing Rate (SOFR) plus a margin ranging from 2.50% to 3.50% per annum; or (b) the Base Rate (which was defined in a customary manner for credit facilities of this type) plus a margin ranging from 1.50% to 2.50% per annum. The applicable margin was based on the Total Leverage Ratio (which was defined as the ratio of (x) total indebtedness of PACS Group, Inc. and its subsidiaries less up to $50.0 million of unrestricted cash to (y) the consolidated EBITDA of PACS Group, Inc. and its subsidiaries). In addition, we agreed to pay a commitment fee on the unused portion of the 2023 Revolving Credit Facility, which ranged from 0.30% to 0.50% per annum, depending on the Total Leverage Ratio.
In connection with executing the 2023 Credit Agreement, deferred financing costs associated with both lines-of-credit and long-term debt of $3.1 million were written off, and additional deferred financing costs of $9.7 million were capitalized during the year ended December 31, 2023. In addition, on the closing date of the 2023 Credit Agreement, we drew $75.0 million on the 2023 Revolving Credit Facility and borrowed the entirety of the $275.0 million Truist Term Loan. We used approximately $142.0 million of such proceeds to repay certain outstanding indebtedness on prior lines of credit and the Working Capital Loan.
On December 7, 2023, we amended and restated the 2023 Credit Facility (Amended and Restated 2023 Credit Facility). The Amended and Restated 2023 Credit Facility provides for revolving commitments in an aggregate principal amount of $600.0 million, which revolving commitments may also be utilized for (x) the issuance of letters of credit in an aggregate face amount not to exceed $50.0 million and/or (y) the borrowing of swingline loans in aggregate principal amount not to exceed $20.0 million at any time outstanding.
Outstanding borrowings under the Amended and Restated 2023 Credit Facility bear interest, at our option, based on (a) SOFR (plus a 0.10% credit spread adjustment) or the Base Rate (which is defined consistent with the 2023 Credit Facility), in each case, plus a margin ranging from 2.25% to 3.25% for SOFR borrowings and 1.25% to 2.25% for Base Rate borrowings based upon our Total Leverage Ratio (which is defined consistent with the 2023 Credit Facility) as determined with reference to our most recently delivered financial statements. In addition to interest paid on all outstanding revolving loans, we are required to pay (i) a commitment fee on the unused portion of the revolving commitments, which ranges from 0.25% to 0.45% per annum based upon our Total Leverage Ratio as determined with reference to our most recently delivered financial statements, (ii) a letter of credit fee in respect of each revolving lender’s participation in each outstanding letter of credit, which is based on the then applicable margin for SOFR loans, and (iii) other fees customary for credit facilities of this type.
Upon the closing of the Amended and Restated 2023 Credit Facility, we borrowed $460.0 million of revolving loans, the proceeds of which were used to repay and refinance all term loans and revolving loans under the 2023 Credit Facility, to repay certain other outstanding indebtedness, and to pay transaction costs in connection with the Amended and Restated 2023 Credit Facility. Deferred financing costs associated with both lines-of-credit and long-term debt of $0.5 million were written off as part of the refinance during the year ended December 31, 2023.
100
The Amended and Restated 2023 Credit Facility contains affirmative and negative covenants customary for credit facilities of this type as well as two financial covenants, a total leverage financial covenant and a fixed charge coverage ratio financial covenant. The leverage covenant requires that we maintain a Total Leverage Ratio of not greater than 3.00:1.00 as of the end of each fiscal quarter (calculated for the four consecutive fiscal quarter period ending on the applicable date of determination), commencing with the fiscal quarter ending December 31, 2023. The fixed charge coverage ratio financial covenant requires that we maintain a Fixed Charge Coverage Ratio (as defined in the Amended and Restated 2023 Credit Facility) of not less than 1.10:1.00 as of the end of each fiscal quarter (calculated for the four consecutive fiscal quarter period ending on the applicable date of determination), commencing with the fiscal quarter ending on December 31, 2023. We were in compliance with all such covenants and restrictions as of June 30, 2024.
We maintain the Amended and Restated 2023 Credit Facility as our single line-of-credit. At June 30, 2024, the total commitment limit continues to be $600.0 million and was secured by PACS Group Inc. assets. The agreements mature on December 7, 2028. The balance outstanding on all applicable lines was $248.0 million at June 30, 2024, resulting in available cash of $340.4 million, net of letter of credit usage.
As of December 31, 2022, we maintained several other lines-of-credit with commercial banks. At December 31, 2022, the total commitment limit amounted to $176.0 million and was secured by PACS Group, Inc. assets. These agreements bear interest at rates ranging from LIBOR to LIBOR plus 3.5% and SOFR plus 3.15%. The agreements matured through November 5, 2024. The balance outstanding on these other applicable lines was $146.8 million at December 31, 2022, resulting in available cash of $29.2 million. As discussed above, these other lines-of-credit were closed in connection with executing the 2023 Credit Agreement.
Deferred financing fees on lines-of-credit were $15.1 million as of June 30, 2024 and December 31, 2023, and $4.2 million as of December 31, 2022. Amortization expense relating to deferred financing fees on lines-of-credit for the six months ended June 30, 2024 was $1.5 million, for the year ended December 31, 2023 was $889.3 thousand, and was immaterial for each of the years ended December 31, 2022 and 2021. Accumulated amortization related to deferred financing fees on lines-of-credit was $1.7 million, $192.9 thousand, and $2.8 million as of June 30, 2024, December 31, 2023 and December 31, 2022, respectively.
Long-term debt
During the six months ended June 30, 2024 and the year ended December 31, 2023, some of our subsidiaries entered into Department of Housing and Urban Development (HUD)-insured mortgage loans in the aggregate amount of $34.7 million and $88.8 million, respectively. As a result, 11 of our subsidiaries had mortgage loans insured with HUD in the aggregate amount of $199.4 million as of June 30, 2024, of which $3.3 million is classified as short-term and the remaining $196.1 million is classified as long-term. As of December 31, 2023, our subsidiaries had HUD-insured mortgage loans in the aggregate amount of $166.2 million of which $2.3 million was classified as short-term and the remaining $163.8 million was classified as long-term. These subsidiaries are subject to HUD-mortgage oversight and periodic inspections. As of June 30, 2024, our HUD-insured mortgage loans bear fixed interest rates ranging from 2.4% to 6.3% per annum and have various maturity dates through December 31, 2058. In addition to the interest rate, we incur other fees for HUD placement, including but not limited to audit fees. Amounts borrowed under the mortgage loans may be prepaid, subject to prepayment fees based on the principal balance on the date of prepayment. The original terms for all the HUD-insured mortgage loans are 24 to 35 years.
In addition to the HUD-insured mortgage loans above, we have 12 other mortgage loans or promissory notes. The non-HUD insured mortgage loans and notes bear interest rates in the range of 2.0% and 7.5% per annum with various maturity dates through June 1, 2027. The notes are secured by equipment and guarantees by the Company and certain stockholders. As of June 30, 2024 and December 31, 2023, we had $46.0 million and $48.8 million, respectively, of debt principal outstanding under the mortgage loans and promissory notes, of which $12.4 million is classified as short-term and the remaining $33.6 million is classified as long-term as of June 30, 2024, and $14.5 million is classified as short-term and the remaining $34.4 million is classified as long-term as of December 31, 2023.
101
Operating and finance leases
We lease most of our skilled nursing and assisted living facilities, as well as office space and certain vehicles and equipment, under various non-cancelable operating lease agreements. These operating leases expire at various dates throughout 2049.
Substantially all operating leases for skilled nursing and assisted living facilities are on a “triple-net” basis, which require lessees to pay for all insurance, repairs, utilities, and real property taxes assessed on the leased property, and most of the leases are guaranteed by us and/or our stockholders.
As of June 30, 2024, for 13 of the facility operating leases, we hold an option to purchase the real estate which can be exercised at varying times starting September 9, 2021 through March 31, 2038. At lease inception it was determined that the exercise of these purchase options was not reasonably assured.
At our option, the facility leases are generally renewable for additional terms ranging from 3 to 30 years. All facility leases provide for an additional percentage rent based upon specified rates per the terms of the agreements.
We also lease certain skilled nursing and assisted living facilities under finance lease agreements. The economic substance of each lease is that we are financing the facilities through the lease. The lease terms of these finance leases allow for a purchase option during a specified window. We have determined that we are reasonably certain to exercise the purchase option at the end of each purchase option window. Therefore, we have calculated the lease term through the end of the purchase option window for each lease.
Inflation
We have historically derived a substantial portion of our revenue from the Medicare program. We also derive revenue from state Medicaid and similar reimbursement programs. Payments under these programs generally provide for reimbursement levels that are adjusted for inflation annually based upon the state’s fiscal year for the Medicaid programs and in each October for the Medicare program. These adjustments may not continue in the future, and even if received, such adjustments may not reflect the actual increase in our costs for providing healthcare services.
Labor, supply expenses and capital expenditures make up a substantial portion of our cost of services. Those expenses can be subject to increase in periods of rising inflation and when labor shortages occur in the marketplace. To date, we have generally been able to implement cost control measures or obtain increases in reimbursement sufficient to offset increases in these expenses. There can be no assurance that we will be able to anticipate fully or otherwise respond to any future inflationary pressures.
Off-Balance Sheet Arrangements
We may enter into off-balance sheet arrangements and transactions that can give rise to material off-balance sheet obligations. As of June 30, 2024, we had $11.7 million of borrowing capacity under the Amended and Restated 2023 Credit Facility pledged as collateral to secure outstanding letters of credit. We may enter into further contractual arrangements in the future in order to support our business plans. There are no other transactions, arrangements or other relationships with unconsolidated entities or other persons that are reasonably likely to materially affect our liquidity or availability of our capital resources.
Critical Accounting Estimates
Our discussion and analysis of our financial condition and results of operations are based on our combined/consolidated financial statements, which have been prepared in accordance with GAAP. The preparation of these combined/consolidated financial statements and related disclosures requires us to make judgments, estimates and assumptions that affect the reported amounts of assets and liabilities and disclosure of contingent assets and liabilities at the date of the combined/consolidated financial statements and the reported amounts of revenue and
102
expenses during the reporting period. We believe that the application of the following accounting policies, which are important to our financial condition and results of operations, require significant judgments and estimates on the part of management. See Note 2, “Summary of Significant Accounting Policies,” to our audited combined/consolidated financial statements for a summary of our significant accounting policies, including the accounting policies discussed below.
Revenue Recognition- Revenue recognized from healthcare services is adjusted for estimates of variable consideration to arrive at the transaction price. We determine the transaction price based on contractually agreed-upon amounts or rates, adjusted for estimates of variable consideration. Variable consideration includes estimates of implicit price concessions so that the estimated transaction price is reflective of the amount to which we expect to be entitled in exchange for providing the healthcare services to customers. If actual amounts of consideration ultimately received differ from the estimates, we adjust these estimates, which would affect net service revenue in the period such variances become known.
Accrued Risk Reserves- We are principally self-insured for risks related to professional and general liability. Accrued risk reserves include the accrual for risks associated with professional liability claims and include a liability for unpaid reported claims and estimates for incurred but unreported claims.
We utilize a wholly owned captive insurance subsidiary to provide coverage to our various consolidated operating subsidiaries related to professional and general liability insurance. The related assets and liabilities of this consolidated subsidiary are included in the accompanying financial statements.
Our policy is to accrue amounts using the information obtained from the actuarially determined estimated costs to settle open claims of insureds, as well as an estimate of the cost of insured claims that have been incurred but not reported. We develop information about the size of the ultimate claims based on historical experience, current industry information and actuarial analysis, and evaluate the estimates for claim loss exposure on a quarterly basis. We use actuarial valuations to estimate the liability based on historical experience and industry information.
Recent Accounting Pronouncements
See Note 2, “Summary of Significant Accounting Policies”, to our audited combined/consolidated financial statements for a description of recently adopted accounting pronouncements and recently issued accounting pronouncements not yet adopted as of the date of this prospectus.
Qualitative and Quantitative Disclosure About Market Risk
We are exposed to risks associated with market changes in interest rates through our borrowing arrangements. As of June 30, 2024, we had approximately $248.0 million of variable rate debt, none of which was subject to an interest rate hedge. In particular, our credit facility exposes us to variability in interest payments due to changes in SOFR interest rates. We manage our exposure to this market risk by monitoring available financing alternatives. Our mortgages and promissory notes require principal and interest payments through maturity pursuant to amortization schedules.
Our mortgages generally contain provisions that allow us to make repayments earlier than the stated maturity date. In some cases, we are not allowed to make early repayment prior to a cutoff date. Where prepayment is permitted, we are generally allowed to make prepayments only at a premium which is often designed to preserve a stated yield to the note holder. These prepayment rights may afford us opportunities to mitigate the risk of refinancing our debts at maturity at higher rates by refinancing prior to maturity.
Our cash and cash equivalents as of June 30, 2024 consisted of cash and short-term investments with original maturities of three months or less at the time of purchase. Risks due to changing interest rates impact the return we realize related to our cash and short-term investment balances.
103
As of June 30, 2024, we had outstanding indebtedness under mortgage loans insured with HUD and two promissory notes to third parties of $213.4 million, all of which are at fixed interest rates.
The above only incorporates those exposures that exist as of June 30, 2024 and does not consider those exposures or positions which could arise after that date.
104
BUSINESS
Business Overview
We are a leading post-acute healthcare company primarily focused on delivering high-quality skilled nursing care through a portfolio of independently operated facilities. Founded in 2013, we are one of the largest skilled nursing providers in the United States based on number of facilities, with 276 post-acute care facilities across 15 states serving over 29,000 patients daily as of September 1, 2024. We also provide senior care, assisted living, and independent living options in some of our communities. Our significant historical growth has been primarily driven by our expertise in acquiring underperforming long-term custodial care skilled nursing facilities and transforming them into higher acuity, high value-add short-term transitional care skilled nursing facilities. We believe our success is driven in significant part by our decentralized, local operating model, through which we empower local leaders at each facility to operate their facility autonomously and deliver excellence in clinical quality and a superior experience for our patients. We provide our independently operated facilities with a comprehensive suite of technology, support, and back-office services that allow local leadership teams to focus more of their time and effort on providing quality care to patients. We believe our operating model delivers value to all of our healthcare stakeholders, including patients and families, referring providers, payors, and administrators and clinicians.
The post-acute care ecosystem serves individuals who need additional help recuperating from acute conditions, illnesses, or serious medical procedures after they have been discharged from the hospital. This ecosystem ranges from higher acuity, higher-cost settings, such as long-term acute care hospitals and inpatient rehabilitation facilities, to lower acuity, lower-cost settings, such as assisted living facilities, and home health. Skilled nursing facilities (SNFs) are positioned at the center of this ecosystem and play an essential role in providing cost efficient facility-based care to patients that have been discharged from hospitals but still require 24-hour in-patient services. SNFs can provide both long-term custodial care and higher value short-term transitional care. The SNF industry is large and growing, with the Centers for Medicare & Medicaid Services (CMS) expecting total industry expenditures to increase from $193.6 billion in 2022 to $283.3 billion in 2031, representing a compound annual growth rate (CAGR) of 4.3%. Based on the number of facilities as reported by CMS, we are one of the largest SNF operators in the United States. We are primarily focused on providing higher value short-term transitional care and believe we are uniquely positioned to capitalize on the current underlying trends within the SNF industry and to capture a growing portion of the expected demand.
We believe that healthcare is local and we operate through a decentralized model, recognizing that each patient, facility, and community is unique. To that end, we believe that our local leaders and employees understand the distinct needs and priorities of their patients, staff, and facilities and are best positioned to make clinical and operational decisions in order to optimize patient outcomes and experience. To facilitate this, each of our facilities operates independently, led by a facility administrator and his or her interdisciplinary team of medical directors, nurses, therapists, specialty consultants, and operators. To assist these local teams in achieving their best clinical and operating potential, we provide each facility with access to PACS Services. PACS Services is a comprehensive suite of offerings, including accounting, finance, human resources, payroll, accounts receivable and payable, legal, and risk management services, as well as a robust suite of technology tools. We operate in a highly regulated industry with stringent regulatory compliance obligations, which requires robust regulatory compliance operations. Failure to operate in compliance with applicable laws and regulations could require significant expenditures and result in regulatory deficiencies and other regulatory penalties. PACS Services functions to support our regulatory compliance obligations across our organization, including through controlled billing and cost reporting practices and legal, risk management, and compliance support. PACS Services also provides teams of regional professionals available as resources to each facility, including a regional vice president (RVP) and regional clinical and non-clinical directors and consultants. We developed PACS Services to be a resource to help reduce administrative burden so that local leadership teams can focus on making decisions that improve the care, well-being, and quality of life of their patients.
We believe that talented local leadership is critical to the success of our model of independently operated, centrally supported facilities. At the facility level, administrators are effectively the chief executive officers, and together with other local licensed professionals, are ultimately responsible for the operations of their respective
105
facilities. We seek to recruit, train, and reward dynamic administrators for our facilities, and rely on them to work with their interdisciplinary teams to implement policies and procedures that are appropriate and effective and result in positive outcomes. We support the delivery of excellent care by building excellent teams. We believe our model attracts high caliber, entrepreneurial professionals who value having considerable autonomy, accountability, and aligned incentives. We provide these professionals with leadership and industry training, guidance, and operational support. Our model is intended to align local leaders’ incentives with facility and organizational success, encouraging them to dedicate themselves to the long-term future of their facilities. To create such alignment, we have developed an administrator compensation structure that prioritizes quality of care and operational and financial performance. Our administrators understand that a well-performing facility is the result of providing quality care in an environment of healing and caring, and one that is appropriately staffed, supplied, and equipped to meet the needs of its patients. This dedicated focus by our administrators and their local teams on patient outcomes drives demand for our services and can ultimately result in higher patient census and profitability. We also seek to provide opportunities for upward career mobility, with many of our administrators being promoted from within our company to roles of increasing levels of responsibility. Our culture of meritocracy and pride of ownership has helped us retain experienced facility administrators as well as RVPs who had average industry experience of 7.3 years as of June 30, 2024. For the year ended December 31, 2023, we had a voluntary turnover rate of 3.1% among our facility administrators.
Excellence in clinical quality and experience for our patients is at the forefront of our mission. We believe our focus on quality is reflected in our CMS Quality Measures (QM) Star rating, occupancy rate, and skilled mix by nursing patient days (which refers to the number of days our Medicare and managed care patients receive skilled nursing services at SNFs as a percentage of the total number of days that patients from all payor sources receive skilled nursing services at SNFs for any given period). The QM Star rating is a number between 1 and 5 that is assigned to SNFs that participate in Medicare or Medicaid, and is based on an aggregate score across a range of quality reporting program requirements. As of June 30, 2024, our average QM Star rating across all our facilities was 4.3 Stars, compared to the industry average of 3.5 Stars. For the six months ended June 30, 2024 and the years ended December 31, 2023, 2022 and 2021, our average occupancy rate across our Mature facilities, which we define as facilities purchased more than 36 months prior to the measurement date, was 94%, 93%, 92% and 88%, respectively, compared to the industry average of 76%, 76%, 74% and 71%. For the six months ended June 30, 2024, our skilled mix by nursing patient days was 30%.
We have historically grown primarily through our disciplined and balanced acquisition strategy. We aim to create value by identifying and acquiring underperforming custodial care facilities and converting them into higher-value short-term transitional care facilities by investing in clinical teams and processes and upgrading technology, equipment, training, staffing, aesthetics, and other aspects of the business. The resources and guidance offered by PACS Services is key to rapid integration of new facilities and provides our local leadership teams with an effective technology infrastructure, support tools, and regional support teams that allow local leadership to focus on operational improvements. Our facilities generally undergo an up to three-year post-acquisition transition period. During this period, we seek to implement best practices designed to realize and sustain the facility’s full potential. These practices often result in significant improvements to clinical quality and other operational metrics, including skilled mix, occupancy rates and payor contracting. We believe the results of our acquisition strategy are demonstrated by our high average QM Star rating and occupancy rate for Mature facilities of 4.3 and 94%, respectively, as of June 30, 2024. As of June 30, 2024, the average QM Star rating and occupancy rate for New facilities, which we define as facilities purchased less than 18 months prior to the measurement date, was 4.1 and 84%, respectively.
Our portfolio of owned and leased properties is strategically located in 15 states as of September 1, 2024: Alaska, Arizona, California, Colorado, Idaho, Kansas, Kentucky, Missouri, Montana, Nevada, Ohio, Oregon, South Carolina, Texas and Washington. We anticipate that available acquisition opportunities will enable us to further penetrate these 15 states and to enter new states in the future. We believe our current markets are attractive and that the states in which we operate have unique benefits, such as favorable reimbursement dynamics, high barriers to entry, or population growth of adults aged 65 and older, which is our primary patient demographic. We generally look for similar attributes in new markets that we enter. As of June 30, 2024 we leased 170 facilities, owned partial real estate interests in an additional 12 leased facilities through joint ventures managed by third parties and directly
106
owned the real estate at 38 facilities. As we continue to grow, we intend to explore additional purchases of real-estate assets, through purchase options or right-of-first refusals in existing leases, as well as acquisitions and de novo construction of purpose-built facilities.
For the six months ended June 30, 2024 and 2023, we generated total revenue of $1.9 billion and $1.5 billion, respectively. A substantial portion of our revenue is generated from payments from third-party payors, including Medicare and Medicaid, which represent our largest sources of revenue and accounted for 36.6% and 38.4% of our total revenue for the six months ended June 30, 2024, respectively, and 44.8% and 32.9% of our total revenue for the six months ended June 30, 2023, respectively. For the six months ended June 30, 2024, we generated total net income of $38.2 million, total operating expense of $1.8 billion and Adjusted EBITDA of $188.2 million. For the six months ended June 30, 2023, we generated total net income of $58.8 million, total operating expense of $1.4 billion and Adjusted EBITDA of $122.4 million. For the year ended December 31, 2023, we generated total revenue of $3.1 billion, and Medicare and Medicaid accounted for 38.6% and 37.6% of our total revenue, respectively. For the year ended December 31, 2022, we generated total revenue of $2.4 billion, and Medicare and Medicaid accounted for 47.6% and 30.2% of our total revenue, respectively. For the year ended December 31, 2023, we generated total net income of $112.9 million, total operating expense of $2.9 billion and Adjusted EBITDA of $237.5 million. For the year ended December 31, 2022, our total operating expenses were $2.2 billion, and we generated net income of $150.5 million and Adjusted EBITDA of $255.5 million. As of June 30, 2024, we had total long-term liabilities of $2.9 billion. We intend to use all of the net proceeds to us from this offering to repay a portion of the amounts outstanding under our Amended and Restated 2023 Credit Facility. See the section titled “Use of Proceeds” for additional information. Adjusted EBITDA is a non-GAAP financial measure. For a reconciliation of Adjusted EBITDA to the most directly comparable GAAP financial measure, see the section titled “Management’s Discussion and Analysis of Financial Conditions and Results of Operations—Key Skilled Services Metrics and Non-GAAP Financial Measures—Non-GAAP Financial Measures.”
Our Operating Model
Decentralized Operations
Our decentralized model is informed by our beliefs that “healthcare is local” and that each patient, facility and community is unique. Our administrators have autonomy in the decision-making process because they know what is best for their community and their markets. As of September 1, 2024, our 276 post-acute facilities are independently operated by autonomous local teams with robust administrative and consulting support from our PACS Services.
Each of our facilities is led by an experienced and highly qualified local facility administrator, who serves in effect as a “local CEO,” alongside an interdisciplinary team of medical directors, clinicians, specialty consultants, and operators. In addition to a full clinical team of certified nursing assistants (CNAs), licensed practical nurses (LPNs), registered nurses (RNs), directors of nursing (DONs), and clinical directors, each facility has a local team of non-clinical staff including supervisors, admissions professionals, marketing professionals, and other business support personnel who have the common goal of providing excellent care and superior experiences for patients.
We provide PACS Services to each of our facilities, which includes support through a regional team of seasoned, highly qualified, cross-functional professionals, and led by an RVP. The team also includes regional clinical support personnel (such as directors of therapy, quality assurance, medical records, and clinical services personnel) as well as non-clinical personnel such as regional directors of recruitment and accounts receivable and payable, reimbursement, and risk and compliance personnel. As of December 31, 2023, we had 14 RVPs and regional teams who each cover an average of 14.9 facilities within a region and have an intimate understanding of the intricacies and challenges of the post-acute industry. We place the utmost importance on clinical quality, and as a result, many employees that provide PACS Services are clinicians by trade.
107
Technology and Services
Our technology focus delivers real-time data access to caregivers and administrators, allowing delivery of the best care at the right time. We have invested into internally developed and third-party technologies that comprise part of PACS Services. This robust suite of technologies helps support facility administrators, clinicians, and local teams by providing them with valuable tools to enable them to reduce the time and effort they spend on administrative tasks so that they can better focus on providing quality care and driving efficient business operations. PACS Services includes access to an industry-leading, third-party Electronic Health Record system, and a singular Enterprise Resource Program. In addition, we have internally developed an operational dashboard that is custom-built to provide invaluable tools and real-time data insights to our local teams in order to enhance resource management and improve the delivery of care. This app-based, mobile technology integrates facility-level detail on admissions, occupancy, revenue, staffing, collections, and other key operational data points. Our technology platform enables local leaders and regional teams to continually review and monitor this data, which allows them to be agile in assessing the ongoing needs of their facility and to more easily identify and address the unique needs and priorities.
With this readily-available, real-time data, our local leaders are able to more easily assess what works well in their facilities and can appropriately manage their operations and share best practices with their colleagues within the company. This data also facilitates greater risk management and compliance efforts, as financial and clinical information can be analyzed, which we believe helps promote accountability across the company. Across the company, we use insights from our data management tools to benchmark performance, manage expenses, monitor risk, and manage compliance.
We believe PACS Services provides technology systems and support infrastructure that can enable seamless integration of new facilities and help to reduce risk when we acquire new facilities.
Clinical and Operational Leadership
We believe we are an employer-of-choice in the SNF industry and have attracted highly qualified local leadership and clinicians. Our facility-forward model helps attract and retain motivated professionals whom we provide with extensive training, professional guidance by seasoned experts, and access to best practices. We offer challenging and fulfilling opportunities for clinicians to gain meaningful experience treating higher acuity patients. Through work-education programs, we also offer many of our clinicians the opportunity to improve or enhance their clinical licenses with sponsored certification programs. We believe we are at the forefront of enabling operators and clinicians to operate in their highest value capacity and at the best of their professional capabilities.
Our Administrator-in-Training program, geared towards recent college graduates, and our PACS Professional Program for experienced nursing home administrators, both provide valuable, intensive training and mentorship to help aspiring PACS administrators build important skills, such as operational systems management, administrative effectiveness, and leadership and people development. Our placement process assesses skill sets, qualifications, and career interests in order to pair leaders with the facilities and teams that will be a good fit.
Our frontline CNAs, LPNs, and RNs are also encouraged to participate in our internal continuing education programs, as well as outside programs, to help them continue to develop their skills and to meet any mandated continuing education requirements. We also offer our clinicians and other personnel educational assistance to enable them to sharpen their skills and enhance their capabilities.
Disciplined Acquisition Playbook
We have an established track record of successful acquisitions. Our significant historical growth has been primarily driven by implementing our expertise in acquiring underperforming long-term custodial care SNFs and converting them into higher acuity, high value-add short-term transitional care SNFs. In pursuing each acquisition opportunity, we employ a disciplined evaluation process to identify facilities that meet our acquisition criteria and
108
strategic priorities. We believe our framework and focused approach for acquisitions has contributed to our overall success. Our approach involves:
•Sourcing and evaluation. We have developed specific acquisition criteria to drive efficient sourcing and growth, and we continually monitor our pipeline of suitable acquisition targets. We believe we have a reputation as an acquiror-of-choice, which has led to regular inbound opportunities from small operators, larger platforms, and industry partners, such as landlords, brokers, and REITs.
•Integration and execution. Prior to and following closing of an acquisition, we perform a full facility evaluation focused on operational, clinical, financial, and administrative functions. Through this evaluation, we develop a detailed action plan with goals for IT integration and implementation of best practices led by facility administrators. We believe that administrators can create immediate additional value through technology integrations and then drive continued growth over time with improvements to clinical quality, operations, and financial performance. Our facilities generally undergo an up to three-year post-acquisition transition period. During this period, our integration efforts and implementation of best practices often result in significant improvements to clinical quality and other operational metrics. We believe the results of our acquisition strategy are demonstrated by our high average QM Star rating and occupancy rate for Mature facilities of 4.3 and 94%, respectively, as of June 30, 2024. As of June 30, 2024, the average QM Star rating and occupancy rate for New facilities, which we define as facilities purchased less than 18 months prior to the measurement date, was 4.1 and 84%, respectively.
Our Diversified Portfolio of Properties
We have a diverse portfolio of facilities that are located in selected attractive markets. A majority of our facilities are leased, with our remaining facilities either wholly-owned or partially-owned through joint ventures managed by third parties. Real-estate ownership is a key component of our growth strategy as it can provide balance sheet support as an inflationary hedge, provide capital flexibility as a source of asset collateral, reduce the burden of leases and restrictive agreements, and allow us the opportunity to create additional value in improving distressed assets.
The following is a summary of our leased and owned facilities:
•Leased Properties. As of June 30, 2024, we had 182 leased facilities (including 12 leased facilities partially owned through our joint ventures managed by third parties). The majority of these leased facilities are in California, with the remainder in Arizona, Colorado, Kentucky, Missouri, Nevada, Ohio, South Carolina, and Texas. We leverage our financial and operational condition to negotiate favorable lease terms, including low annual rent escalators, long expiration dates, and purchase options. As of June 30, 2024, our weighted average annual lease escalator was 2%, our average monthly lease expense per bed was $882 per bed, our average remaining lease term across our portfolio was approximately 14 years, and we had 13 total purchase options and 3 right of first refusals that we may exercise in future years.
•Owned Properties. We have historically purchased the real-estate assets for certain of the post-acute care facilities we operate. Many of our owned properties were acquired with limited cash outlay while in a distressed state, or through the exercise of a purchase option that was originally negotiated while in a distressed state. We seek to create value in our properties by purchasing these distressed facilities and making improvements under our operations and ownership. As of June 30, 2024 we owned 38 post-acute care facilities, and we have investments in joint ventures that own the underlying real estate and related improvements of 12 post-acute care facilities that are operated and leased by other PACS Group subsidiaries. The majority of our owned real-estate properties are located in California, South Carolina, Texas, and Kentucky. We have also explored facility ownership through de novo, or new-build, facilities where we construct facilities and own them. Since 2013, we have opened or are in the process of opening 8 de novo facilities.
109
We classify each of our facilities into three distinct categories based on the amount of time that has passed since acquisition: Mature, Ramping and New. Mature facilities are defined as facilities purchased more than 36 months prior to a respective measurement date. Ramping facilities are defined as facilities purchased within 18 to 36 months prior to a respective measurement date. New facilities are defined as facilities purchased less than 18 months prior to a respective measurement date. As of December 31, 2023, we operated 65 Mature facilities, 77 Ramping facilities, and 66 New facilities. For the year ended December 31, 2023, our Mature, Ramping, and New facilities generated skilled nursing services revenue of $1.1 billion, $0.9 billion, and $1.1 billion, respectively. As of June 30, 2024, we operated 65 Mature facilities, 85 Ramping facilities, and 70 New facilities. For the six months ended June 30, 2024, our Mature, Ramping, and New facilities generated skilled nursing services revenue of $584.6 million, $817.1 million, and $498.8 million, respectively.
We believe our success in improving our acquired properties is reflected in the average QM Star rating, occupancy rate, and skilled mix by revenue for each of our Mature, Ramping and New facilities, depicted in the table below for the year ended December 31, 2023 and six months ended June 30, 2024:
| Year Ended December 31, 2023 | Six Months Ended June 30, 2024 | ||||||||||||||||||||||||||||||||||
Mature facilities | Ramping facilities | New facilities | Mature facilities | Ramping facilities | New facilities | ||||||||||||||||||||||||||||||
| Average QM Star rating | 4.2 | 4.2 | 3.9 | 4.3 | 4.3 | 4.1 | |||||||||||||||||||||||||||||
| Occupancy rate (operational beds) | 93 | % | 93 | % | 87 | % | 94 | % | 95 | % | 84 | % | |||||||||||||||||||||||
| Skilled mix by revenue | 59 | % | 55 | % | 51 | % | 55 | % | 57 | % | 39 | % | |||||||||||||||||||||||
As of December 31, 2023 and June 30, 2024, our facilities had an average QM Star rating of 4.1 and 4.3 Stars, respectively, compared to the industry average of 3.6 and 3.5 Stars, respectively, and an average occupancy rate of 91%, compared to the industry average occupancy rate of 76%. See the section titled “Management’s Discussion and Analysis of Financial Condition and Results of Operations—Key Skilled Services Metrics and Non-GAAP Financial Measures.” We believe our strategy drives these results and is central to our ability to develop acquired facilities into higher performing facilities over time. For example, based on an analysis of the 24 facilities that we have acquired since 2018 and that have developed into Mature facilities as of December 31, 2023, we estimate that we were able to increase the occupancy rate and QM Star rating for acquired facilities by an average of 19% and 0.4 stars, respectively, as they progressed from New facilities to Mature facilities.
We believe the success of our strategy is further exemplified by our historical ability establish and maintain a QM Star rating for our Mature facilities that is higher than the industry average, The graphic below sets forth our QM Star rating over time for our Mature facilities, as well as the industry average QM Star rating, for the periods indicated.
110
QM Star Ratings Over Time for PACS Mature Facilities vs. Industry Average
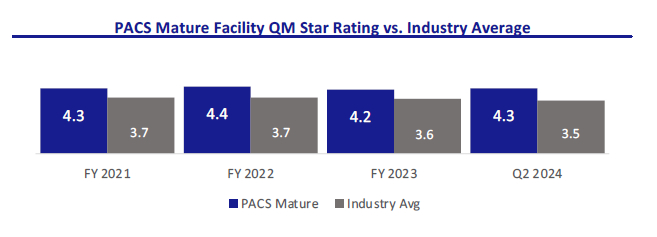
Source: CMS SNF Provider Information (Aug. 2023); PACS data for facilities with CMS certification and QM Star rating.
Execution of our strategy has also increased our number of facilities with QM Star ratings of 4 or 5 Stars over time. The graphic below sets forth our number of facilities by QM Star rating from 2015 through the first half of 2024.
QM Star Ratings Over Time for PACS Facilities
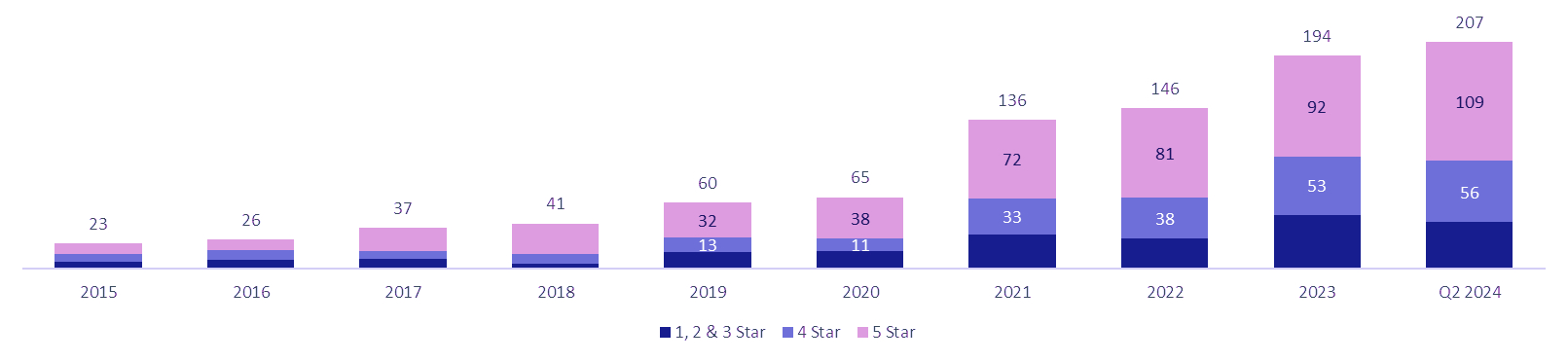
Our Value Proposition
We believe that our operating model creates meaningful value for patients and their families, our referring providers, our payors, and our administrators and clinicians.
Value Proposition for Patients and Families
•Coordinated care. We empower team members at every level through skillful training, shared resources, and a collaborative spirit. We help deliver coordinated care before, during, and after a patient’s stay with us. Prior to admission, our administrators or other facility leaders meet with patients and their families, as well as hospital discharge planners, to plan for the patient’s discharge and enable a seamless transition to our facility. During a stay with us, our local facility team coordinates closely with physicians to deliver high-touch, high-quality care for patients. As care nears completion, we meet with our patients, their families, home health agencies and downstream care providers to plan for and ensure a smooth transition.
•Outstanding patient experience. Our goal is to provide each patient with superior care and an outstanding experience. When patients arrive at our facilities they are greeted by a warm, inviting, and modern environment. We often upgrade facility infrastructure shortly after acquisition and perform periodic
111
refreshes, to ensure our facilities are comfortable and well-equipped to serve patients across a wide range of acuities with a primary focus on high acuity patients. High acuity patients generally require higher levels of medical care or monitoring due to conditions or complications that cannot be easily managed, and often need more nursing resources and attention to maintain their quality of life. We believe our investment in modern equipment and technology allows our facility care teams to identify and respond to patient needs and provide them high quality care in a timely manner. Moreover, our clinicians are highly trained, have significant experience, and are able to leverage bespoke care plans to help ensure that patients receive care tailored to their particular needs.
Value Proposition for Referring Providers
•Strategic and seamless transitions. Our administrators and their interdisciplinary teams seek to become a preferred partner by developing a deep understanding of local referring providers’ and their patients’ needs. Administrators often visit with patients and their families prior to discharge to plan for and map out a smooth admission to our facility. Once a plan is set, the facility team endeavors to quickly and seamlessly transition new patients to the facility with a focus on ensuring continuity of care in the transition. We believe that hospitals and other referral sources consider our facilities to be attractive discharge options because we are able to care for a wide variety of patient needs, and are often able to accept admissions on short notice, including on nights and weekends. Our flexibility helps hospitals maintain adequate bed availability to meet their other patients' needs.
•Trusted partner with quality care. Our ability to care for higher acuity patients allows referring providers to have confidence that we will be able to adequately care for their patients and assist them in their recovery. Our facilities seek to work with patients’ doctors to create personalized care plans to help ensure that patients stay on track in their recovery and to reduce the likelihood of their readmission to the hospital. Our facility teams also seek to coordinate closely with a patient’s home health agency or other post-SNF caregivers to try to ensure the patient’s transition home or to their next care setting is successful. This close coordination allows us, where warranted, to directly readmit patients back to our facility who would have otherwise been readmitted to an acute care hospital in the event they have a change of condition after leaving our facility.
Value Proposition for Payors
•Higher value site of care. We believe we provide high acuity care in a cost-effective setting and are able to quickly transition patients from the acute care setting, reducing length of stay and delivering more overall value for payors. Moreover, we believe we provide payors with a high-quality alternative to higher cost post-acute sites of care. For example, according to MedPAC, SNFs are the lowest cost facility-based post-acute healthcare, costing an average of $550 per covered day compared to $1,850 and $1,753 per covered day for inpatient rehabilitation facilities and long-term acute care hospitals, respectively.
•Robust culture of compliance. We focus on instilling a unified, cohesive culture of innovation and compliance that we believe provides consistency in our results and confidence in our facilities as an attractive care option for patients. Our rigorous approach to billing integrity, our independent internal compliance function, and our regular facility billing audits are intended to provide a foundation of trust and collaboration that makes us a natural choice for payors.
Value Proposition for Administrators and Clinicians
•Autonomy and aligned compensation. Each facility administrator is, in effect, the local “CEO” and dedicated leader of their facility. Alongside their local interdisciplinary team, they are empowered to make real-time decisions locally around all aspects of their business and to manage their individual facility in a way that they believe is best suited to address their local market and its needs. We have designed a transparent incentive model for our administrators that is intended to align their compensation with the quality of care and operational and financial performance of their facility. We provide them the tools and
112
the autonomy to optimize the performance of their facility, and we reward them for success in their efforts. We believe that a well-performing facility is the result of providing quality care in an environment of healing and caring and one that is appropriately staffed, supplied, and equipped to meet the needs of its patients. This dedicated focus by our administrators and their local teams on patient outcomes drives demand for our services and can ultimately result in higher patient census and profitability.
•Robust technology enabled operating infrastructure. We developed PACS Services to reduce the managerial and operational burden on our administrators, allowing them to focus on leading their facilities and spending more time with patients and staff. PACS Services includes a robust suite of technology tools that provide detailed real-time data and trends that local clinicians and leadership teams can use to monitor and improve operational performance. PACS Services also includes regional support teams that leverage their deep tenure and experience across markets to provide higher-level support to local leaders on complex issues, including billing and cost reporting practices and regulatory compliance obligations. The regional teams are connected to and support the facilities within their designated region, which enables them to identify best practices and trends within the region, communicate those across their region, and provide facility-level support as needed.
•Highly entrepreneurial career development. By providing our administrators with autonomy in the operation of their facility, we believe we create a highly entrepreneurial environment that encourages and rewards leaders to optimize operational performance. We empower our clinicians to do the same and provide top performers the opportunity to progress via training for higher skill licenses and certifications. People are provided the opportunity to advance to become an administrator through our Administrator-in-Training program, and to join a regional leadership team. For example, in the year ended December 31, 2023, we promoted 26 of our administrators from within our organization after participating in our Administrator-in-Training program, and 12 of our RVPs were previously successful administrators with us.
Our Competitive Strengths
We believe our success is driven by the following competitive strengths:
Superior Overall Quality
Excellence in clinical quality and experience for our patients is at the forefront of our mission and is reflected in our above-industry average QM Star rating and occupancy rate. Our facilities employ skilled administrators and clinicians and equip them with purpose-built technology and support so they can operate at the top of their professional capacity and deliver high-quality care for patients. We continuously invest in our people, processes, and facilities to promote an excellent patient experience. We believe we deliver superior overall quality that has contributed to our reputation as a provider-of-choice in our communities, driving greater referral volumes from referring providers who value our high standards.
Decentralized Market-Driven Operating Model
Our decentralized model emphasizes local operational autonomy. We believe that placing decision-making power at the local level with teams who understand the needs of their patients and their communities facilitates responsiveness and adaptability to evolving patient needs and facility and community factors. We believe the empowerment of local leadership promotes improved quality care for patients, greater referral volumes and higher occupancy rates. Our operating model is highly transferable to new markets, and enable us to quickly integrate and enhance new facilities.
Transparent and Meritocratic Leadership Culture
We have built a transparent, competitive, and collegial culture that promotes individual growth both personally and professionally and prioritizes a deep commitment to our patients, families, and team members. We promote transparency in performance, which we believe encourages collaboration and healthy competition among local
113
leadership that in turn drives best practices. We believe this meritocratic culture, supported by highly seasoned industry veterans, helps optimize clinical and financial outcomes at facilities and instills accountability throughout the organization. This leadership mindset has empowered us to develop a deep bench of leaders capable of supporting our existing and future facilities.
Employer-of-Choice with Directly Aligned Incentive Model
We believe that we are an employer-of-choice in the post-acute care industry, which enables us to attract and retain highly motivated, entrepreneurial individuals who value operational independence and financial opportunity. This has allowed us to attract enterprising individuals from diverse backgrounds who may not have otherwise considered careers in skilled nursing. Our unique compensation model is designed to align local individual incentives with the long-term clinical quality and operational performance of the facility, which we believe fosters a shared ownership mentality. We believe this directly aligned incentive model has played a critical role in successfully attracting, incentivizing, and retaining our industry veterans.
Robust Suite of Technology-Enabled Services
Our technology focus delivers real-time data access to caregivers and administrators, facilitating delivery of the right care at the right time. Our technology tools enable our local leadership teams to focus on their first priority, providing the highest quality care possible to patients. We believe our suite of technologies helps drive decision-making and enhances operating efficiencies that can improve clinical quality, operational metrics, and the financial performance of our facilities. While other facility administrators may spend considerable time on paperwork and low-value activities, we strive to reduce the administrative burden on our facility administrators so they can walk the halls, personally meet patients, and provide a bespoke, concierge-level customer service experience. We equip our clinicians with industry-leading technology, including point-of-care and digital charting technologies, which streamlines charting and paperwork, so they can spend more time with patients and focus on providing high quality care. We believe our technology and internally developed dashboards help to facilitate better patient care, risk management, regulatory compliance, staffing, and resource allocation. We have designed our technology to be easily integrated into new facilities and allow us to scale quickly and efficiently.
Differentiated, Multi-faceted, and Disciplined Acquisition Playbook
Over the past decade, we have demonstrated the effectiveness of our disciplined, multi-faceted playbook of acquiring and improving underperforming facilities, having successfully acquired and integrated over 230 facilities to date. We believe we have established a reputation as an acquiror-of-choice, which has led to several inbound opportunities, and has helped us build an extensive opportunity pipeline. Our balanced approach to evaluation allows us to selectively pursue opportunities that meet our strategic priorities and criteria and grow in a responsible manner. Through our investment into facilities and our integration process, we are able to transition new underperforming facilities to higher-value short-term transitional care facilities. We believe our success is evidenced by our robust QM Star ratings, occupancy rates, and profitability at our Mature facilities.
Our High-Quality Facilities
We are committed to providing a high-quality experience for all of our patients, which is why we invest in capital improvements and ongoing maintenance to all of our facilities, regardless of whether we lease or own. Our investment into facilities is differentiated from traditional industry operators who we believe are often hesitant to make physical plant investments into facilities and who often seek to extract value through cost-cutting or other limitations on facility resources. Our renovations are intended to improve the look and feel of facilities in order to provide an excellent experience. Our investments into medical beds, vitals monitors, physical therapy equipment, and other improvements allows us to provide services to higher acuity patients. We believe our high-quality facilities lead to sustained referral volumes, more admissions, and high skilled mix at our facilities, ultimately leading to higher occupancy rates and revenue per patient day. We also believe our investment into leased facilities makes us a preferred tenant with our landlords and provides us leverage in negotiating favorable lease terms.
114
Our Size and Scale
We believe our market density in key regions offers strategic advantages, such as brand recognition with referring providers, including hospitals and health systems, and consistency and continuity of referrals of patients. For example, our ability to accommodate a high volume of patients within our markets allows us to accept referrals without turning patients away to competitors, and can also further our reputation as a reliable, go-to provider of care for referring providers. We also believe our size and scale has provided us with the ability to negotiate favorable contracts with managed care and other payor sources, the ability to navigate stringent regulatory compliance obligations and withstand potential reimbursement and regulatory industry dynamics, and the ability to leverage real estate value for liquidity and growth.
Industry Overview and Market Opportunity
The Post-Acute Care Continuum is Essential to the Healthcare Ecosystem
We operate in the post-acute care industry, which is an essential component of the healthcare delivery ecosystem, serving high need, medically fragile patients. Post-acute care encompasses multiple care settings outside of acute care hospitals that are differentiated by the acuity level of patients and the services they require. While services may overlap across each distinct post-acute offering, post-acute rehab or SNFs provide the most comprehensive array of services. Upstream care providers, such as acute care hospitals, generally discharge patients to post-acute facilities where patients can receive key services at lower costs. For example, according to MedPAC, SNFs cost an average of $550 per covered day compared to $2,914 for short-term acute care hospitals.
115
Post-Acute Care Continuum
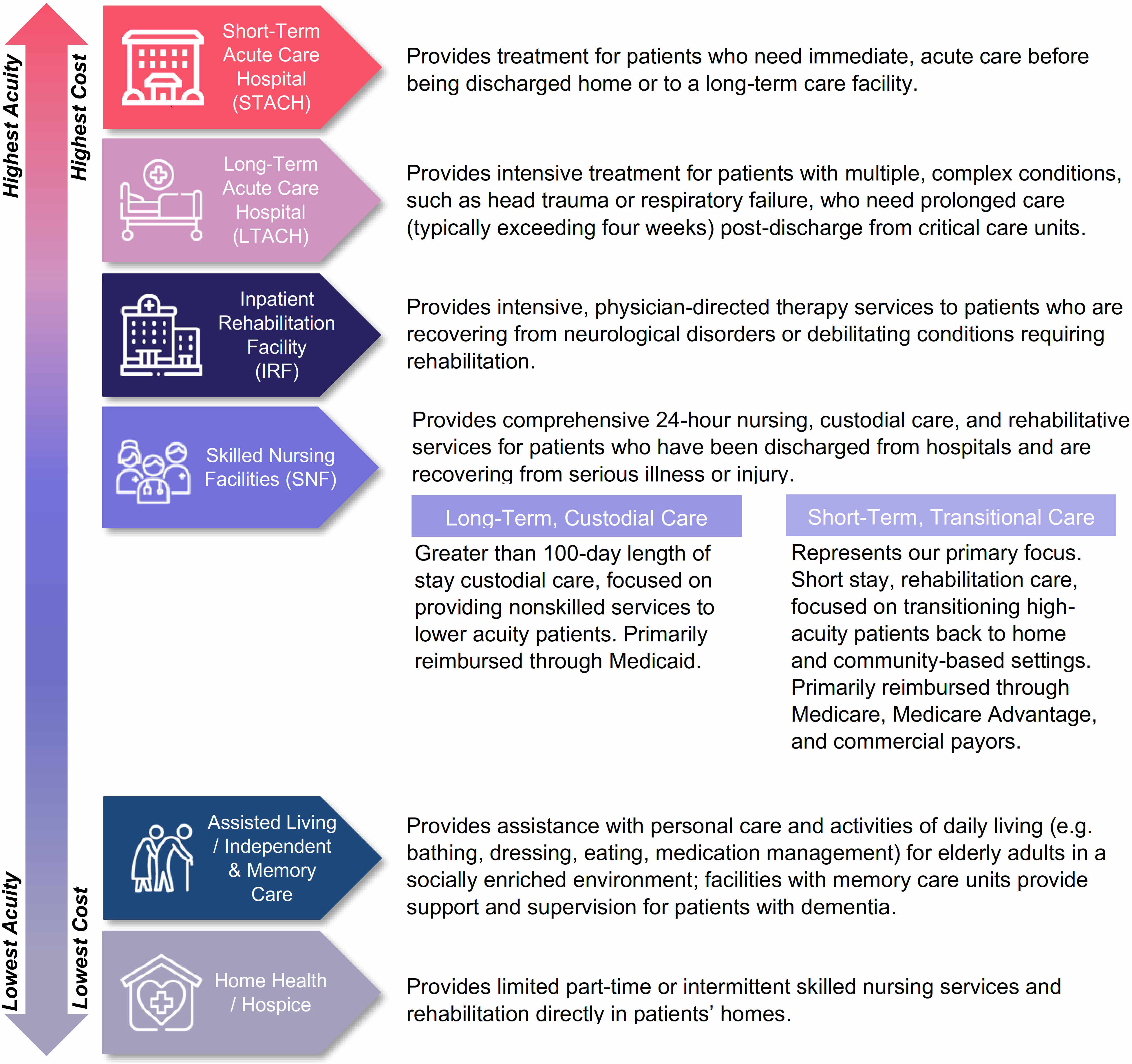
SNFs are an Integral and Essential Part of the Post-Acute Care Continuum
SNFs play an essential role in post-acute patient care. SNFs provide higher-acuity skilled nursing care to patients that cannot be adequately treated in community-based care settings, such as assisted living or independent living facilities, and who are no longer appropriate candidates for hospital care. Patients referred to a SNF are typically recovering from surgery or non-critical conditions, such as strokes, joint replacements, and acute infections, and are admitted to a SNF within 30 days of being discharged from a hospital where they spent at least three days as an inpatient. In many instances, patients are treated at SNFs prior to receiving home health nursing care and therapy services. The majority of SNF patients are aged 65 years or older. Despite the wide array of services and variety of needs addressed, MedPAC reports that SNFs are the lowest cost facility-based post-acute healthcare, costing on average $550 per covered day compared to $1,850 and $1,753 per covered day for inpatient rehabilitation facilities and long-term acute care hospitals, respectively. According to CMS MedPAC data, SNFs accounted for approximately 44% of the total post-acute care continuum spend. According to CMS Inpatient Hospital discharge data, in 2022, approximately 22% of Medicare patients over 65 years old were discharged to
116
SNFs, representing more than any other facility type, including inpatient rehabilitation facilities and long-term acute care hospitals (approximately 6%), and more than home health nursing care (21%) or hospice (5%). As reimbursement and coverage continues to shift toward value-based models with greater emphasis on controlling costs, SNFs are integral to post-acute care and will continue to drive high-quality outcomes in low-cost settings. Furthermore, during the COVID-19 pandemic, SNFs were widely utilized to treat medically fragile patients, reinforcing the importance of SNFs to the healthcare ecosystem.
The skilled nursing industry can be classified into two main sub verticals: A) long-term custodial care and B) short-term transitional care. Long-term custodial care predominantly focuses on lower acuity, Medicaid-eligible patients and provides institutional, custodial care services, including nonskilled, personal care services such as assistance with bathing, dressing, or eating. Short-term transitional care predominantly treats higher acuity, Medicare-eligible patients and primarily provides short-term inpatient-level skilled nursing care such as rehabilitation, physical therapy services, and intravenous injections.
Large, Fragmented Industry Comprised of Mostly Small and Independent Operators
According to the National Center for Health Statistics (NCHS) 2020 National Post-acute and Long-term Care Study, the SNF industry in the United States encompasses approximately 15,000 facilities and serves approximately 1.3 million patients annually. The industry is highly fragmented, with the top 10 operators, each having greater than 100 facilities, representing approximately 11% of total number of SNFs in the United States, according to CMS data as of September 2022, approximately 5,000 smaller and independent operators of less than 100 facilities making up the remainder. According to such data, of the approximately 15,000 facilities, approximately 13,200 facilities have less than 100 beds, and approximately 74% and 27% of SNFs are located in urban and rural areas, respectively. In addition, approximately 72%, 23%, and 6% of SNFs are operated as for-profit, non-profit, and by the government, respectively, according to such data. We believe this fragmented landscape creates opportunities for larger providers with greater scale to serve patients better and meet regulatory requirements nation-wide by effectively addressing staffing, quality standards, and billing processes. Moreover, many small and independent operators face pressure due to billing requirements, regulations, competition on quality of care and facilities, staffing shortages and competition, and the cessation of COVID-related provider relief funding, which has led them to pursue sales of their facilities or businesses. This provides additional opportunity for well-managed, high-quality operators to grow through acquisitions.
Growing Demand Outpacing Supply of Skilled Nursing Facilities
The demand for healthcare services in the United States has increased in recent years and is expected to continue growing, largely due to a rapidly aging population and an increasing prevalence of chronic conditions. According to the U.S. Census Bureau, the U.S. population aged 65 and older is expected to nearly double from 2020 to 2060 and reach 95 million in 2060, which exceeds the expected increase in the general population during that same period, and comprise one fifth of the total U.S. population in 2030. Moreover, according to the U.S. Census Bureau, the U.S. population aged 85 and older is expected to nearly triple from 2020 to 2060 and reach 19 million in 2060. Additionally, according to an article published in Frontiers in Public Health in 2022, the percentage of people in the United States aged 50 and older with at least one chronic condition is estimated to increase by 99.5% from 2020 to 2050. According to CMS data as of September 2022, approximately 82% of SNF patients were 65 years of age or older.
As demand has increased for SNFs, the number of SNFs has declined in recent years from approximately 15,650 in 2017 to approximately 14,900 in 2023. We believe this is due to a variety of factors, including an inability of many facilities to comply with quality standards, rigorous staffing, and billing requirements, and a lack of technology and sophistication at small and independent operators. Furthermore, new operators face multiple barriers to entry, including the requirements to obtain a Certificate of Need, complex licensure requirements, lack of operating experience, and significant capital requirements. As a result, the addition of new SNFs has not kept pace with the number of SNFs exiting the market, amplifying the need for skilled nursing to serve an aging population.
117
Favorable Reimbursement Environment
According to CMS, approximately 72% of SNF revenue in 2022 was derived from government sources, including Medicaid and Medicare. Medicaid represents 51% of industry revenue, while Medicare represents approximately 21%. The remainder comprises managed care, private pay, and other payors. Medicare and Medicaid reimbursement has steadily increased over the past few years. Medicare reimbursement per patient day increased at a CAGR of approximately 3.6% from 2012 to 2021, while Medicaid reimbursement per patient day increased at a CAGR of approximately 1.9% from 2012 to 2021. The industry has experienced over 9 years of growth in reimbursement rates.
The following charts depict the increase in Medicaid and Medicare Fee for Service reimbursement per patient day from 2015 through 2021 as reported by CMS.
Medicaid and Medicare Reimbursement Per Patient Day
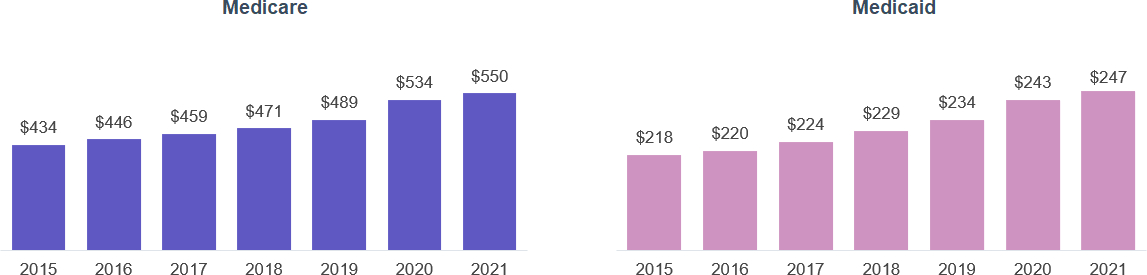
Regulatory Environment
The SNF industry is highly regulated with stringent regulatory compliance obligations. In the ordinary course of business, providers are subject to federal, state and local laws and regulations relating to, among other things, billing and reimbursement, relationships with vendors, business relationships with physicians and other healthcare providers and facilities, as well as licensure, accreditation, enrollment, quality, adequacy of care, physical plant, life safety, personnel, staffing and operating requirements. Changes in law or new interpretations of existing laws and regulations may have a significant impact on revenue, costs and business operations of providers and other industry participants. In addition, governmental and other authorities periodically inspect the SNFs, senior living facilities and outpatient rehabilitation agencies to verify continued compliance with applicable regulations and standards and may impose citations and other regulatory penalties for regulatory deficiencies. Such regulatory penalties include but are not limited to civil monetary penalties, temporary payment bans, suspension or revocation of a state operating license and loss of certification as a provider in the Medicare or Medicaid program, which may be temporary or permanent in nature. This regulatory environment and related enforcement can have an adverse effect on providers and other industry participants. See the section titled “Business—Regulatory Matters.”
Our Market Opportunity
Despite the decline in the number of SNFs, the industry is large and growing, with CMS expecting total industry expenditures to increase from $193.6 billion in 2022 to $283.3 billion in 2031, representing a CAGR of 4.3%. Based on the number of facilities as reported by CMS, we are one of the largest SNF operators in the United States and believe our scale and other competitive strengths uniquely position us to capitalize on the current underlying trends within the SNF industry and capture a growing portion of this expected growth.
118
Our Growth Strategy
We have built a multi-faceted growth strategy with multiple organic and inorganic levers to help drive our growth and capitalize on the favorable industry dynamics. To continue our growth, we intend to:
•Expand our presence in existing and new markets. We have a robust pipeline of potential single-facility tuck-in acquisitions, larger multi-facility portfolio acquisitions and select new facility builds across existing and new markets. We have historically completed an average of approximately 20 acquisitions and one de novo, or new-build, facility per year, but have the flexibility to increase or decrease this cadence from period to period in line with our business priorities and as strategic opportunities arise. We plan to continue to strategically pursue opportunities within our pipeline to supplement our organic growth. While we expect to continue to execute on this strategy, we do not have binding agreements or commitments for any material investments at this time.
•Leverage operational upside within our existing footprint. Our portfolio has a healthy foundation for strong embedded organic growth. We are focused on driving higher occupancy and increasing skilled mix in an effort to fill unused capacity with higher acuity patients, which can improve our revenue per patient day and our profitability, which in turn drive growth. Historically, we have found that it takes up to 3 years for a New facility to scale to performance similar to that of a Mature facility. As of June 30, 2024, we had 70 New facilities and 85 Ramping facilities, which we believe provides us some degree of near-term visibility into expected organic growth within our footprint.
•Continue to grow our pipeline of leaders. Our rapid growth in size and scale can be attributed to our deep bench of talented leaders. Our administrators in training provide us with leadership resources that we can use to quickly staff new facilities with qualified operators. Similarly, our RVPs enable us to scale within regions. We intend to invest heavily in training existing leaders and expanding our bench of new administrators and RVPs to support our future growth.
•Extract embedded value from real estate ownership. We plan to continue to evaluate our real estate purchase options in an effort to reduce our rent burden and grow the underlying earnings of our business. We have executed 18 purchase options since 2013 and had 13 additional options available to us as of June 30, 2024. We intend to continue to selectively exercise purchase options and continue structuring additional purchase options to provide an additional lever to grow net margins and enhance stockholder value. Moreover, we believe that our real estate ownership provides balance sheet support as an inflationary hedge, provides capital flexibility as a source of asset collateral, reduces the burden of leases and restrictive agreements, and allows us the opportunity to create additional value in improving distressed assets.
•Ancillary opportunities. We have identified and continue to evaluate multiple investment opportunities that have the potential to improve our post-acute patient experience by augmenting the services we provide. We may capitalize on these investment opportunities that are ancillary to our core business, such as pharmacy services, laboratory services, transportation, and imaging, which have the potential to be additional sources of revenue and operating income over time. We refer to these efforts to build a strategic mix of investments in ancillary business lines as “PACS Ventures.” We continue to evaluate opportunities to in-source, acquire, and commercialize these ancillary opportunities. Additionally, we may choose to monetize our PACS Services by offering it to third-party SNF operators in the future.
•Expand into other post-acute sites of care. We believe that our proven operational playbook and focus on delivering high-quality care have the potential to be utilized in additional post-acute sites of care, including home health and hospice as well as within broader senior living communities. As of June 30, 2024, we had one independent living facility and five assisted living facilities which provide a foundation for further expansion.
119
Human Capital Resources
Our Culture and Values
Our leading culture of collegiality and committed focus on quality is driven from the top with entrepreneurial, passionate leaders who are determined to deliver a superior experience for patients and staff. Our culture of transparency across our regions and facilities fosters an environment where best-practices are shared among regions which promotes healthy competitiveness and constant improvement across our facilities.
Our culture is centered on the following core values:
•Love. We recognize that love is the foundation for providing care to the vulnerable. We support our clients as they build a culture of loving care within and beyond their communities.
•Excellence. We look for and act on opportunities to improve every day.
•Trust. We act with integrity and expect the same of others.
•Accountability. We seek responsibility for our actions, attitudes, and mistakes.
•Mutual respect. We treat others the way they want to be treated.
•Fun. We create and instill fun and enjoyment in everything we do.
Our Employees
As of June 30, 2024, we had 35,582 employees working across 220 post-acute care facilities in 9 states and at our corporate headquarters in Farmington, Utah. Of our 35,582 employees, 20,946 are clinicians, including approximately 2,509 RNs including DONs, approximately 5,804 LPNs, and approximately 12,633 CNAs. Approximately 14,636 of our employees work in non-clinical functions and administrative / support functions, including 14 RVPs, and 160 facility administrators, 160 clinical and compliance support, 72 information technology support, and approximately 14,230 additional administrative and support staff. We also employ a dedicated team specifically focused on ensuring smooth functioning and support for our point-of-care including the clinical and compliance support, information technology support above. Additionally, 3,552 of our employees were represented by unions under collective bargaining agreements as of June 30, 2024. As of September 1, 2024, we had approximately 40,000 employees working across 276 post-acute care facilities in 15 states.
Our senior management team boasts extensive experience, totaling an average of over 11.4 years with us and 17.8 years within the SNF industry as of June 30, 2024. As of June 30, 2024, our RVPs had an average of 7.3 years of experience, our administrators an average of 2.6 years and our Directors of Nursing an average of 2.9 years.
Competition
The post-acute care industry is highly competitive and fragmented and we compete with numerous local and regional providers, in addition to large national providers that have achieved geographic diversity and economies of scale. We expect that the industry will become increasingly competitive in the future. Our independently operated facilities also compete with inpatient rehabilitation facilities and long-term acute care hospitals. Increasingly, we are competing with home health and community-based providers who have developed programs designed to provide services to seniors outside a facility-based setting, potentially decreasing the time they need the higher level of care provided in a SNF. Competitiveness may vary significantly from location to location, depending upon factors such as the number of competing facilities, availability of services, expertise of staff, and the physical appearance and amenities of each location. We believe that the primary competitive factors in the post-acute care industry are:
•ability to attract and to retain qualified management and clinicians;
120
•reputation and achievements of quality healthcare outcomes;
•attractiveness and location of facilities;
•ability to charge competitive prices;
•the expertise and commitment of the management team and employees; and
•community value, including amenities and ancillary services.
We seek to compete effectively in each market by establishing a reputation within the local community as a preferred provider of post-acute care services This means that the facility administrators are generally free to discern and address the unique needs and priorities of referring providers, patients, payors and other stakeholders in the local community or market, and then create a superior service offering and reputation for that particular community or market that is calculated to encourage prospective patients and referral sources to choose or recommend the facility.
Increased competition could limit our ability to attract and retain patients, qualified management and caregivers, maintain or increase rates or to expand our business. Some of our competitors have greater financial and other resources than we have, may have greater brand recognition and may be more established in their respective communities than we are. Competing companies may also offer lower costs, newer facilities or different programs or services than we offer, and may therefore attract individuals who are currently patients of our facilities, potential patients of our facilities, or who are otherwise receiving our healthcare services. Other competitors may have lower expenses or other competitive advantages than us and, therefore, provide services at lower prices than we offer.
Regulatory Matters
Healthcare
Healthcare is an area of extensive and frequent regulatory change. Changes in the law or new interpretations of existing laws may have a significant impact on revenue, costs and business operations. Our independent operating facilities that provide healthcare services are subject to federal, state and local laws relating to, among other things, licensure, accreditation, enrollment, quality, adequacy of care, physical plant, life safety, personnel, staffing and operating requirements. In addition, these facilities are subject to federal and state laws that govern billing and reimbursement, relationships with vendors, business relationships with physicians and other healthcare providers and facilities, and workplace protection for healthcare staff.
Governmental and other authorities periodically inspect the SNFs, senior living facilities and outpatient rehabilitation agencies to verify continued compliance with applicable regulations and standards. The operations must pass these inspections to remain licensed under state laws and to comply with Medicare and Medicaid provider agreements. The operations can only participate in these third-party payment programs if inspections by regulatory authorities reveal that the operations are in substantial compliance with applicable state and federal requirements. In the ordinary course of business, federal or state regulatory authorities may issue notices to the operations alleging deficiencies in certain regulatory practices. These statements of deficiency may require corrective action to regain and maintain compliance. In some cases, federal or state regulators may impose other remedies including imposition of civil monetary penalties, temporary payment bans, loss of certification as a provider in the Medicare or Medicaid program, or suspension or revocation of a state operating license.
The regulatory environment surrounding the healthcare industry subjects providers to significant scrutiny. In the ordinary course of business, providers are subject to inquiries, investigations and audits by federal and state agencies related to compliance with participation and payment rules under government payment programs. These inquiries may originate from the United States Department of Health and Human Services (HHS) Office of the Inspector General (OIG), state Medicaid agencies, state Attorney Generals, local and state ombudsman offices and CMS Recovery Audit Contractors, among other agencies. In response to the inquiries, investigations and audits, federal and state agencies continue to impose citations for regulatory deficiencies and other regulatory penalties, including
121
demands for refund of overpayments, expanded civil monetary penalties that extend over long periods of time and date back to incidents prior to surveyor visits, Medicare and Medicaid payment bans and terminations from the Medicare and Medicaid programs, which may be temporary or permanent in nature. We vigorously contest each such regulatory outcome when appropriate; however, there are significant legal and other expenses involved that consume our financial and personnel resources. Expansion of enforcement activity could have an adverse effect on our business, financial condition or results of operations.
Coronavirus
In an effort to decrease the spread of COVID-19, federal, state and local regulators have implemented new regulations and requirements on our subsidiaries.
Testing requirements - On September 23, 2022, CMS issued an interim final rule (IFR) regarding COVID-19 testing of staff, stating that individuals who show symptoms of COVID-19, regardless of vaccination status, should be tested for COVID-19 as soon as possible. Additionally, this IFR called for testing of residents and staff and investigation of an outbreak when there is a single positive COVID-19 case among residents or staff of the long term care (LTC) facility. We have implemented procedures for testing for COVID-19 that are intended to comply with federal and state mandates.
Federal and state COVID-19 vaccination requirements - CMS developed an IFR requiring all workers within Medicare and Medicaid-participating nursing homes to be vaccinated against COVID-19 as a condition of participation in the Medicare and Medicaid programs. In addition, OSHA introduced an emergency temporary standard (ETS) requiring employers with more than 100 employees to mandate that its employees be fully vaccinated against COVID-19 or submit to weekly testing for the virus. Both CMS’s IFR and OSHA’s ETS for vaccination were challenged in court and halted from enforcement in certain states, but the United States Supreme Court allowed CMS to enforce its vaccine mandate nationwide.
In addition to the IFR mandating vaccinations for health facility workers, several states where our facilities are located have issued vaccine mandates that apply to facility staff. These vaccine mandates are largely aligned with CMS's requirements. For example, California issued an order requiring adult care facilities and direct care workers to be vaccinated as well, and for all affected workers to be fully vaccinated by November 30, 2021. The order was expanded to allow workers who had completed their primary vaccination series and contracted COVID-19 since becoming fully vaccinated to defer the receipt of a vaccine booster dose by up to 90 days after infection with COVID-19; otherwise, booster vaccine doses were required to be completed by March 1, 2022. On October 23, 2022, CMS issued further guidance unifying its recommendations for all facilities under its oversight, including SNFs and LTC facilities, reaffirming CMS's activities to verify vaccination of all SNF and LTC facility staff, and where necessary, to pursue corrective action for facilities found deficient in this requirement.
Reporting requirements - In accordance with CMS reporting guidance, SNFs are required to report to the CDC National Health Safety Network certain information related to COVID-19 cases on a weekly basis. Facilities are also required to provide residents and staff with vaccine education and offer vaccines, when available, to residents and staff. The IFR published on August 23, 2021 requires facilities to develop policies and procedures to ensure the availability of the COVID-19 vaccine to residents and staff and to educate them concerning the benefits, risks and potential side effects associated with the vaccine. CMS may initiate enforcement activities and assess civil monetary penalties for not meeting any of these COVID-19 related reporting requirements under this IFR and reaffirmed its intent to seek corrective action against SNFs and LTC facilities that do not satisfy these requirements.
Medicare and Medicaid Reimbursement and Requirements
For the year ended December 31, 2023, Medicare and Medicaid represented our largest sources of revenue and accounted for 38.6% and 37.6% of our routine revenue for the year ended December 31, 2023, respectively, and 36.6% and 38.4% of our routine revenue for the six months ended June 30, 2024, respectively. The federal government and state governments continue to focus on efforts to curb spending on healthcare programs such as Medicare and Medicaid. The Medicare program and state Medicaid programs and their reimbursement rates and
122
rules are subject to frequent change. These include statutory and regulatory changes, rate adjustments (including retroactive adjustments), administrative or executive orders and government funding restrictions, all of which may materially adversely affect the rates at which Medicare and state Medicaid programs reimburse us for our services. Budget pressures often lead the federal government to reduce or place limits on reimbursement rates under Medicare and Medicaid. We cannot predict the extent to which such proposals will be adopted or, if adopted and implemented, what effect, if any, such proposals and legislation will have on us. Historically, adjustments to reimbursement under Medicare and Medicaid programs have had a significant effect on our revenue.
Medicaid - In March of 2020, the FFCRA provided a 6.2% increase to the FMAP during the PHE. In addition to this funding increase, the FFCRA imposed conditions restricting the disenrollment and standards for re-enrolling Medicaid beneficiaries to promote continuous care of beneficiaries during the PHE. The bipartisan omnibus spending plan passed by Congress and signed into law by the President on December 29, 2022, amended these Medicaid enrollment protections and increased FMAP funding provided in the FFCRA. The FMAP increase CMS provides to states was subject to reduction reductions in 2023 as noted below: for the second quarter, April through June 2023, this increase was reduced to 5.0%; in the third quarter, from July through September, the FMAP increase was reduced to 2.5%, and in October through December, the FMAP increase will be reduced to 1.5%. The ultimate amount of funding from each state will vary substantially based on that states’ policies.
CMS’s provision of these increased FMAP funds to states is conditioned upon states reporting to CMS certain Medicaid-related information, including data pertaining to Medicaid renewals, termination of Medicaid coverage, beneficiary customer service information, and other eligibility and renewal information that may be identified in regulations or by the HHS Secretary. States that do not report required data to CMS beginning in July of 2023 will be penalized 0.25% percentage points, up to a total of 1.0%, for each quarter the state does not report data to CMS. The omnibus spending plan also grants CMS authority to impose fines, penalties, and other sanctions upon states that do not comply with this law’s requirements for increased FMAP payments. These requirements and budgetary pressures can lead state governments to reduce or limit Medicaid spending.
Under the omnibus spending bill adopted in December of 2022, states began disenrolling Medicaid beneficiaries on April 1, 2023. During the PHE, funding was provided for continuous Medicaid enrollment, and the unwinding of the continuous enrollment period reduces CMS’s contribution to state-administered Medicaid programs. CMS guidance permits states up to 14 months to initiate and process traditional Medicaid renewals, including the eligibility and enrollment process.
Medicare Annual Payment Rule and Updates - The Balanced Budget Act of 1997 required the implementation of a per diem prospective payment system (PPS) for SNFs covering all costs related to the provision of services to Medicare Part A beneficiaries. The SNF PPS payment rates are adjusted for case mix and geographic variation in wages and cover all costs of furnishing covered SNF services (routine, ancillary, and capital-related costs). CMS is required to calculate an annual Medicare market-basket update to the payment rates. On July 31, 2023, CMS issued a final rule for Fiscal Year (FY) 2024 that updated Medicare payment rates for skilled nursing facilities under the SNF PPS. For FY 2024, SNF PPS rates under Medicare Part A increased by 4.0%. This estimate reflects a 6.4% net market basket update to the payment rates, which is based on a 3.0% SNF market basket increase plus a 3.6% market basket forecast error adjustment and less a 0.2% productivity adjustment and less a 2.3% adjustment as a result of the second phase of the recalibrated parity adjustment under the Patient Driven Payment Model (PDPM). Under a final rule for Fiscal Year 2025, CMS will increase Medicare Part A reimbursement for SNFs by 4.2% for FY 2025. The rate increase will take effect on October 1, 2024.
The Skilled Nursing Facility Prospective Payment System Final Rule for Fiscal Year (FY) 2025, published on August 6, 2025, also includes significant enhancements to CMS’ enforcement capabilities within nursing homes, aiming to reinforce the safety and quality of care. The final rule broadens CMS’s ability to levy financial penalties as a means to ensure sustained remediation of health and safety infractions, thereby motivating facilities to quickly comply with CMS regulations. The final rule eliminates the restrictions of per instance (PI) civil monetary penalties (CMPs) for isolated violations or per day (PD) CMPs for ongoing non‐compliance restrictions, allowing for more flexible imposition of both PD and PI penalties, which cannot exceed statutory limits. In addition, the revisions enable the imposition of CMPs for any noncompliance that was previously cited in the past three standard surveys
123
for which no CMP was yet imposed. These changes are intended to provide CMS with enhanced tools to address violations more effectively and reflect the severity of the impact on residents’ health and safety. The expanded enforcement policies become effective on October 1, 2024, and will be operationalized beginning March 3, 2025.
Sequestration of Medicare Rates - The Budget Control Act of 2011 requires a mandatory, across the board reduction in federal spending, called a sequestration. Medicare FFS claims with dates of service or dates of discharge on or after April 1, 2013 incur a 2.0% reduction in Medicare payments. Due to subsequent legislative amendments to the statute, the sequestrations will remain in effect through 2032, with the exception of a temporary suspension from May 1, 2020 through March 31, 2022.
Patient-Driven Payment Model (PDPM) - The PDPM, a case-mix classification model used in the SNF PPS for classifying SNF patients in a stay covered under Medicare Part A, became effective October 1, 2019. PDPM classifies patients into payment groups based on the patient’s condition (clinically relevant factors) and resulting care needs, rather than on the volume of services provided, to determine Medicare reimbursement. PDPM utilizes five case-mix adjusted payment components: physical therapy, occupational therapy, speech language pathology, nursing and social services and non-therapy ancillary services. It also uses a sixth non-case mix component to cover utilization of SNFs’ resources that do not vary depending on resident characteristics.
Skilled Nursing Facility Value-Based Purchasing (SNF-VBP) Program - All SNFs that receive reimbursement under the SNF PPS are also subject to the SNF Value Based Purchasing (VBP) Program. The SNF-VBP Program awards SNFs with incentive payments based on the quality of care they provide to Medicare beneficiaries. For the FY2024 Program year, performance in the SNF VBP Program is based on a single measure of all-cause hospital readmissions. Beginning in the FY 2026 program year, the measures will be expanded to include (1) Skilled Nursing Facility Healthcare Associated Infections Requiring Hospitalization (SNF HAI), and (2) Total Nursing Hours per Resident Day Staffing (Total Nurse Staffing), and beginning in the FY 2027 program year, the measures will be further expanded to include Discharge to Community—Post-Acute Care Measure for Skilled Nursing Facilities (DTC PAC SNF).
Skilled Nursing Facility – Quality Reporting Program (SNF QRP) - The Improving Medicare Post-Acute Care Transformation Act of 2014 (IMPACT Act) created data reporting requirements for certain Post-Acute-Care (PAC) providers. The IMPACT Act requires that each SNF submit its quality data and standardized patient assessment data elements in connection with the Quality Reporting Program (QRP). If a SNF does not submit required quality data, the SNF’s payment rates are reduced by 2.0% for each such fiscal year.
Medicare Part B Requirements - Some of our revenue is paid by the Medicare Part B program under a fee schedule. Medicare Part B provides reimbursement for certain physician services, limited drug coverage, and other outpatient services outside of a Medicare Part A covered patient stay. Although certain therapy services were historically subject to a payment cap, the Bipartisan Budget Act of 2018 (BBA) repealed those caps while retaining and adding additional limitations to ensure appropriate therapy services. The BBA also establishes coding modifier requirements and retains the targeted medical review process established under the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) at a threshold amount of $3,000. The Current Year (CY) 2024 Physician Fee Schedule (PFS) Final Rule reduced the conversion factor (i.e., the number by which CMS determine all current procedural terminology code payments) by 3.4% from the CY 2023 conversion factor. This changed lowered the overall payment rate under the PFS by 1.25% in CY 2024 compared to CY 2023.
Programs of All-Inclusive Care for the Elderly
Programs of All-Inclusive Care for the Elderly (PACE) provides medical and social services to elderly individuals who qualify for nursing home care but, at the time of enrollment, can still live safely in the community. CMS conducts a comprehensive annual review of the PACE organization's operation of the PACE program during a 3-year trial period to assure compliance with all significant requirements. For example, each PACE organization must establish an interdisciplinary team that, among other responsibilities, comprehensively assesses the individual needs of each participant and assigns each participant to an interdisciplinary team. On April 12, 2023, CMS
124
published updates to the PACE program, including to the determination of a contract year and the types of contracted services.
Federal Healthcare Reform
Patient Protection and Affordable Care Act - In recent years, there have been, and we expect there will continue to be, a number of legislative and regulatory changes to the U.S. healthcare system, many of which are intended to contain or reduce healthcare costs. For example, the Affordable Care Act (ACA) affects how healthcare services are covered, delivered and reimbursed, and it expanded health insurance coverage through a combination of public program expansion and private sector health insurance reforms. Several of the reforms are very significant and could ultimately change the nature of our services, the methods of payment for our services and the underlying regulatory environment. These reforms include modifications to the conditions of qualification for payment, bundling of payments to cover both acute and post-acute care and the imposition of enrollment limitations on new providers. Since its enactment, there have been judicial, executive and Congressional challenges to certain aspects of the ACA and, on June 17, 2021, the U.S. Supreme Court dismissed the most recent judicial challenge to the ACA brought by several states without specifically ruling on the constitutionality of the ACA.
In August of 2022, Congress passed and the Biden Administration signed into law the Inflation Reduction Act of 2022 (IRA), which continued and expanded certain provisions of the ACA. Among other things, the IRA extended premium subsidies paid by the federal government, which were scheduled to expire at the end of 2022, until the end of 2024, resulting in subsidies being available to offset or reduce the costs of private health insurance policies for older persons on fixed incomes or with limited savings. This may aid older patients in obtaining or keeping their health insurance in order to pay for long-term care services. Other healthcare-related provisions of the IRA include phased-in provisions for Medicare to negotiate the prices of certain prescription drugs, limiting the out-of-pocket cost of prescribed drugs to Medicare Part D recipients to $2,000 per year (in addition to a monthly cap on out-of-pocket prescription drug expenses) and limiting the monthly cost of insulin to $35.
Five-Star Quality Reporting Metrics - CMS created the Five-Star Quality Rating System, which assigns each a nursing home a rating between one and five stars, as a resource to assist consumers with comparing nursing homes. Each nursing home receives an overall rating, as well as separate ratings for health inspections, staffing and quality measures. In part due to the competitive nature of the system, achieving a four- or five-star ranking can be challenging. The results of the Five-Star Quality Rating System are published on CMS’s public website, Care Compare. CMS also displays a consumer alert icon next to nursing homes that have been cited for incidents of abuse, neglect, or exploitation, which is updated monthly with CMS’s refresh of survey inspection results on that website.
Proposed and Enacted Federal and State Legislation - The U.S. Congress has introduced various bills intended to improve quality of care and oversight in nursing homes. For example, on August 10, 2021, the Nursing Home Improvement and Accountability Act of 2021 was introduced in the U.S. Senate and proposed to reduce SNF payments for inaccurate submission of certain data, provide federal funding to carry out SNF data validation and ensure accuracy of cost report information, and mandate staffing requirements for SNFs. Although this bill was not approved by Congress, similar proposed legislation may be introduced in the future.
In addition to proposed legislation at the federal level, state legislatures have introduced and enacted legislation to address quality of care and oversight in nursing homes. For example, California enacted the Skilled Nursing Facility Ownership and Management Reform Act of 2022, which took effect on July 1, 2023, increases the oversight authority of the California Department of Public Health and changes several provisions regarding SNF licensing. We expect for states to continue to introduce and pass legislation that increases the regulation of SNFs.
Quality of Care Initiatives - The Biden Administration has published several fact sheets related to the quality of care in nursing homes. On October 21, 2022, the Biden Administration published a fact sheet calling for improvements to the quality of care in nursing homes, and on September 1, 2023, the Biden Administration published another fact sheet regarding initiatives to improve resident safety in nursing homes, such as minimum staffing requirements. Additionally, on April 22, 2024, CMS issued a final rule that creates minimum staffing
125
standards for skilled nursing facilities and nursing facilities and requirements for states to report the percent of Medicaid payments spent on compensation to direct care workers and support staff at each nursing facility and each intermediate care facility for individuals with intellectual disabilities. For further discussion, see the section titled “CMS Minimum Staffing Standards Final Rule.” We anticipate there will be continued administrative, regulatory, and legislative efforts at the federal and state level to monitor and regulate LTC facilities.
CMS Minimum Staffing Standards Final Rule — On April 22, 2024, CMS issued a final rule establishing new federal minimum staffing standards for skilled nursing facilities (SNFs) (Staffing Rule). The Staffing Rule expands upon existing facility assessment requirements. Both non-rural and rural facilities must have met the new enhanced facility assessment requirements by August 10, 2024. In addition, SNFs will be required to: (1) ensure the presence of a registered nurse (RN) on-site 24 hours per day, seven days per week and (2) provide a minimum of 3.48 hours per resident day (HPRD) of direct nursing care to residents, which must include at least 0.55 HPRD provided by RNs and 2.45 HPRD provided by nurse aides (NAs), while the remaining 0.48 HPRD may be provided by any combination of RNs, licensed practical nurses (LPNs), licensed vocational nurses (LVNs), or NAs. The Staffing Rule provides for a staggered implementation for these staffing requirements over a three-year period for non-rural facilities, with longer implementation timeframe for rural facilities.
The first phase, which took effect August 10, 2024, requires both rural and non-rural facilities to satisfy the new facility assessment requirements. Currently, all SNFs must perform and document annually and on an as-needed basis. The Staffing Rule’s imposes an enhanced self-assessment standard that requires facilities to: (1) use evidence-based methods when care planning for residents, including consideration for those residents with behavioral health needs; (2) use the facility assessment to assess the specific needs of each resident and adjust as necessary for changes in the resident population; (3) include the input of the SNF’s leadership (including a member of the governing body and the medical director), management, nurse and other direct care staff and solicit and consider input from residents and other stakeholders; and (4) develop a staffing plan to maximize recruitment and retention of staff in a manner consistent with the President’s April 2023 Executive Order on Increasing Access to High-Quality Care and Supporting Caregivers.
The second phase, effective May 2026 for non-rural facilities and May 2027 for rural facilities, requires SNFs to satisfy the two staffing requirements. First, SNFs must have a RN available to provide direct resident care onsite 24 hours per day, seven days per week (24/7). The Staffing Rule states that administrative nurses may satisfy this requirement, provided that the nurse is available to provide direct resident care. Second, SNFs must provide a minimum of 3.48 HPRD of direct nursing care to residents.
The third phase, effective May 2027 for non-rural facilities and May 2029 for rural facilities, requires that the HPRD are satisfied through RNs providing 0.55 HPRD, NAs providing 2.45 HPRD, and any combination of RNs, LPNs, LVNs, or NAs to account for the final 0.48 HPRD.
The Staffing Rule finalized the hardship exemption for the HPRD requirements. A facility can qualify for a temporary hardship exemption from the new minimum staffing ratios and 24/7 RN onsite staffing requirement (the self-assessment standards must still be satisfied) if it is located in an area where the supply of RN, NA, or total nursing staff is insufficient to meet the needs of that area. This exemption is based on the provider-to-population ratio for the nursing workforce, which must be at least 20% below the national average as calculated by CMS.
In addition, the Medicaid Institutional Payment Transparency Reporting (MIPTR) provisions of the Staffing Rule enhance transparency for the use of Medicaid payments for facility services by requiring states to report to CMS the percentage of Medicaid payments for nursing facility services spent on direct care workers and support staff, regardless of whether such payments are made under a fee-for-service or managed care model.
Congressional efforts to block the implementation and enforcement of the Staffing Rule’s requirements have been introduced in both the House and Senate, including the Protecting America’s Seniors’ Access to Care Act (H.R. 7513, introduced March 1, 2024) and the Protecting Rural Seniors’ Access to Care Act (S. 3410, introduced December 5, 2023). In addition, private parties have brought claims challenging the Staffing Rule. For example, on May 23, 2024, the American Health Care Association, along with other plaintiffs, filed a lawsuit in the Northern
126
District of Texas alleging that the Staffing Rule exceeds CMS’ statutory authority in violation of the Administrative Procedure Act and requesting that the court issue an order and judgment setting aside the Staffing Rule’s requirements. The minimum staffing standards of the Staffing Rule have been widely criticized as endangering rural nursing facilities, subjecting them to potential fines and closures for failure to comply, and might require them to discharge residents or limit the number of residents they accept in an effort to meet the new requirements. We cannot predict the outcome of any litigation involving the Staffing Rule or the extent to which legislative proposals will be adopted or, if adopted and implemented, what effect, if any, such legislation would have on the requirements under the Staffing Rule.
Medicare and Medicaid Enrollment and Participation Requirements
Healthcare providers, including SNFs and other LTC facilities, must comply with certain requirements in order to participate in the Medicare and Medicaid Programs. Examples include requirements related to resident rights, admission, transfer and discharge, resident assessments, care planning, availability of certain services, administration and governance, emergency preparedness, quality assurance and performance improvement programs, infection control, compliance and ethics programs, physical environment, and training requirements. Compliance with these requirements can be burdensome and costly.
One such requirement of participation in the Medicare and Medicaid programs involves limitations around the use of pre-dispute, binding arbitration agreements by LTC facilities. CMS has issued guidance and direction around arbitration, to include: the facility must not require signing of an arbitration agreement as a condition of admission or a requirement to continue to receive care at the facility, and the agreement must expressly contain language to this effect; the facility must inform the resident or the resident's representative of the right not to sign the agreement; the facility must confirm that the agreement is explained in a manner that can be understood and that the resident or their representative acknowledges their understanding of the agreement; the agreement must provide for the right to rescind the agreement within 30 calendar days of signing; and the agreement may not contain language that prohibits or discourages communications with federal, state, or local officials, including federal and state surveyors, other federal or state health department employees, and representatives of the Office of the State Long-Term Care Ombudsperson. Congress has routinely introduced, but not passed, legislation addressing the issue of arbitration agreements used by LTC facilities. While legislative action is possible in the future, federal regulations and state/federal laws remain our primary source of authority over the use of pre-dispute binding arbitration agreements.
The requirements of participation serve as the basis for survey activities for the purpose of determining whether a facility meets the requirements for participation in Medicare and Medicaid. CMS has updated its guidance for surveyors and state agencies in order to, among other things, enhance responses to resident complaints and reported incidents. The guidance focuses on the following topics: (1) resident abuse and neglect (including reporting of abuse); (2) admission, transfer and discharge; (3) mental health and substance abuse disorders; (4) nurse staffing and reporting of payroll to evaluate staffing sufficiency; (5) residents’ rights (including visitation); (6) potential inaccurate diagnoses or assessments; (7) prescription and use of pharmaceuticals, including psychotropics and drugs that act like psychotropics; (8) infection prevention and control; (9) arbitration of disputes between facilities and residents; (10) psychosocial outcomes and related severity; and (11) the timeliness and completion of state investigations to improve consistency in the application of standards among various states. In 2022, CMS published the survey resources CMS and state surveyors would be using to evaluate LTC facilities' compliance with vaccination and reporting requirements. These updates provided more information for state surveyors to utilize when evaluating LTC facilities’ compliance with the Medicare Requirements of Participation, as well as included guidance for facilities on operationalizing compliance with these requirements based on how surveyors would measure and evaluate facility performance. CMS has also made significant software enhancement, including those used to measure and evaluate LTC facility compliance with the Medicare Requirements of Participation.
Licensure and Certification
Our facilities and healthcare professionals are subject to various federal, state, and local licensure and certification requirements in connection with our provision of healthcare services. Certain states in which we operate have certificate of need or similar programs regulating the establishment or expansion of healthcare facilities. The
127
initial and continued licensure of our facilities and certification to participate in government healthcare programs depends upon many factors including various state licensure regulations relating to quality of care, environment of care, equipment, services, minimum staffing requirements, staff training, personnel, and the existence of adequate policies, procedures, and controls. In addition to facility licensure requirements, states also impose licensing requirements on the healthcare professionals who provide services at our facilities. States may impose restrictions on, or revoke, licenses of healthcare providers for, among other things, improper clinical conduct and delegation of such services, patient mistreatment, ethical violations and substance abuse, or aiding and abetting the unlicensed practice of medicine.
Federal, state, and local agencies survey our facilities on a regular basis to determine whether the facilities are in compliance with regulatory operating and health standards and conditions for participating in government healthcare programs. Unannounced surveys or inspections generally occur at least annually and may also follow a government agency's receipt of a complaint about a facility. Facilities must pass these inspections to maintain licensure under state law, to obtain or maintain certification under the Medicare and Medicaid programs, to continue participation in the Veterans Administration program at some facilities, and to comply with provider contracts with managed care clients at many facilities. From time to time, our facilities, like others in the healthcare industry, may receive notices from federal and state regulatory agencies of an alleged failure to substantially comply with applicable standards, rules or regulations. These notices may require corrective action, may impose civil monetary penalties for noncompliance, and may threaten or impose other operating restrictions on SNFs such as admission holds, provisional skilled nursing license, or increased staffing requirements. If our independent operating subsidiaries fail to comply with these directives or otherwise fail to comply substantially with licensure and certification laws, rules and regulations, the facility could lose its certification as a Medicare or Medicaid provider, or lose its license permitting operation in the State.
In addition, CMS has increased its focus on facilities with a history of serious or sustained quality of care problems through the special focus facility (SFF) initiative. SFFs receive heightened scrutiny and more frequent regulatory surveys. Failure to improve the quality of care can result in fines and termination from participation in Medicare and Medicaid. A facility “graduates” from the program once it demonstrates significant improvements in quality of care that are continued over a defined period of time. On October 21, 2022, CMS issued a Memorandum identifying the changes it intends to make in connection with the oversight of those facilities that fall under the SFF Program. These proposed measures included increased penalties for SFFs that fail to improve their performance upon further inspection by CMS, increasing the standards SFFs must meet to graduate from the SFF program, maintaining heightened oversight of any SFF for a period of three years after it graduates and increasing the technical assistance CMS provides to SFFs.
CMS has undertaken several initiatives to increase or intensify Medicaid and Medicare survey and enforcement activities, including federal oversight of state actions. CMS is taking steps to focus more survey and enforcement efforts on facilities with findings of substandard care or repeat violations of Medicaid and Medicare standards and to identify multi-facility providers with patterns of noncompliance. CMS is also increasing its oversight of state survey agencies and requiring state agencies to use enforcement sanctions and remedies more promptly when substandard care or repeat violations are identified, to investigate complaints more promptly, and to survey facilities more consistently.
Civil and Criminal Fraud and Abuse Laws and Enforcement
The U.S. healthcare industry is heavily regulated by federal, state and local governments. We are subject to federal and state laws that regulate our relationships with physicians and other healthcare providers, the manner in which our facilities provide and bill for services and collect reimbursement from governmental programs and private payors, our marketing activities, and other aspects of our operations.
The federal Anti-Kickback statute (AKS) prohibits, among other things, knowingly and willfully offering, paying, soliciting or receiving remuneration, directly or indirectly, in cash or kind, to induce or reward either the referral of an individual for, or the purchase, order or recommendation of, any good or service, for which payment may be made under federal and state healthcare programs such as Medicare and Medicaid. A person or entity does
128
not need to have actual knowledge of the statute or specific intent to violate it in order to have committed a violation. The AKS includes statutory exceptions and regulatory safe harbors that protect certain arrangements. Failure to meet the requirements of the safe harbor, however, does not render an arrangement illegal. Rather, the government may evaluate such arrangements on a case-by-case basis, taking into account all facts and circumstances, including the parties’ intent and the arrangement’s potential for abuse, and may be subject to greater scrutiny by enforcement agencies.
Additionally, the Stark Law prohibits a physician from referring a Medicare or Medicaid patient for a “designated health service” to an entity with which the physician or an immediate family member has a financial relationship, unless an exception applies. Designated health services include inpatient and outpatient hospital services, physical therapy, occupational therapy, speech language pathology services, durable medical equipment, prosthetics, orthotics and supplies, diagnostic imaging, and enteral and parenteral feeding and supplies and home health services. Under the Stark Law, a “financial relationship” is defined as an ownership or investment interest or a compensation arrangement. If such a financial relationship exists and does not meet a Stark Law exception, the entity is prohibited from submitting or claiming payment under the Medicare or Medicaid programs or from collecting from the patient or other payor.
The federal False Claims Act (FCA) prohibits a person from knowingly presenting, or caused to be presented, a false or fraudulent request for payment from the federal government, or from making a false statement or using a false record to have a claim approved. The FCA further provides that a lawsuit thereunder may be initiated in the name of the government by an individual referred to as a “whistleblower.” Moreover, the government may assert that a claim including items and services resulting from a violation of the AKS or the Stark Law constitutes a false or fraudulent claim for purposes of the civil FCA. Penalties for a violation of the FCA include fines for each false claim, plus up to three times the amount of damages caused by each false claim.
Further, the Civil Monetary Penalties Statute authorizes the imposition of civil monetary penalties, assessments and exclusion against an individual or entity based on a variety of prohibited conduct, including, but not limited to offering remuneration to a federal healthcare program beneficiary that the individual or entity knows or should know is likely to influence the beneficiary to order or receive healthcare items or services from a particular provider.
Many states have also adopted or may adopt similar anti-kickback, self-referral, false claim, and fraud and abuse laws as described above. The scope of these laws and the interpretations of them vary by jurisdiction and are enforced by local courts and regulatory authorities, each with broad discretion. Some state fraud and abuse laws apply to items or services reimbursed by any third-party payor, including commercial insurers, and to funds paid out of pocket by a patient.
Violation of any of these laws or any other governmental regulations that apply may result in significant penalties, including, without limitation, administrative civil and criminal penalties, damages, fines, additional reporting requirements and compliance oversight obligations, contractual damages, the curtailment or restructuring of operations, exclusion from participation in governmental healthcare programs and/ or imprisonment.
In the ordinary course of business, providers are subject to inquiries, investigations and audits by federal and state agencies related to compliance with participation and payment rules under government payment programs, as well commercial payors. These inquiries may originate from the United States Department of Health and Human Services (HHS) Office of the Inspector General (OIG), state Medicaid agencies, state Attorney Generals, local and state ombudsman offices and CMS Recovery Audit Contractors, among other agencies and commercial payors. In response to the inquiries, investigations and audits, federal and state agencies and other payors may impose citations for regulatory deficiencies and other regulatory penalties, including demands for refund of overpayments, civil monetary penalties, payment bans and terminations from the Medicare and Medicaid programs, which may be temporary or permanent in nature.
In recent years, there has been increased regulatory scrutiny into post-hospital SNF care. For example, in November 2019, the OIG released a report of its investigation into overpayments to hospitals that did not comply with Medicare’s post-acute-care transfer policy. Hospitals violating this policy transferred patients to certain post-
129
acute-care settings, such as SNFs, but claimed the higher reimbursements associated with discharges to homes. A similar OIG audit report, released in February 2019, focused on improper payments for SNF services when the Medicare three-day inpatient hospital stay requirement was not met. In 2021, the OIG released the result of an audit finding that Medicare overpaid millions of dollars of chronic care management (CCM) services. The OIG's 2021 report found that in calendar years 2017 and 2018, Medicare overpaid millions of dollars in CCM claims. In 2022, the OIG released an audit revealing that CMS had not collected $226 million, or 45%, of identified overpayments within that period, potentially affecting SNFs. These investigatory actions by OIG demonstrate its increased scrutiny into post-hospital SNF care provided to beneficiaries and may encourage additional oversight or stricter compliance standards.
On numerous occasions, CMS has indicated its intent to vigilantly monitor overall payments to SNFs, paying particular attention to facilities that have high reimbursements for ultra-high therapy, therapy resource utilization groups with higher activities of daily living scores and long average lengths of stay. The OIG recognizes that there is a strong financial incentive for facilities to bill for higher levels of therapies, even when not needed by patients. We cannot predict the extent to which the OIG's recommendations to CMS will be implemented and, what effect, if any, such proposals would have on us. We expect for regulators to continue to focus on post-hospital SNF care, which may result in additional oversight or stricter compliance standards.
Facilities
PACS Services. Our PACS Services’ main office is located in Farmington, Utah. The property consists of approximately 35,000 square feet of usable office space.
Operating Facilities. As of June 30, 2024, we operated 220 post-acute care facilities in Arizona, California, Colorado, Kentucky, Missouri, Nevada, Ohio, South Carolina and Texas, with the operational capacity to serve approximately 25,361 patients with 24,483 skilled nursing beds and 878 assisted living beds. Of these post-acute care facilities, we leased 170 facilities, owned partial real estate interests in an additional 12 leased facilities through joint ventures managed by third parties and directly owned the real estate at 38 facilities. Of our total bed count as of June 30, 2024, approximately 62.3% of beds were at leased facilities, 15.3% of beds were at leased facilities with real estate purchase options, and approximately 22.4% of beds were at directly owned or joint venture facilities.
The following table provides summary information regarding the location of our post-acute care facilities and operational beds by property type as of June 30, 2024:
| Leased | Owned | Total | |||||||||||||||||||||||||||||||||
| Facilities | Beds | Facilities | Beds | Facilities | Beds | ||||||||||||||||||||||||||||||
| Arizona | 9 | 1,219 | — | — | 9 | 1,219 | |||||||||||||||||||||||||||||
| California | 114 | 13,144 | 24 | 2,587 | 138 | 15,731 | |||||||||||||||||||||||||||||
| Colorado | 19 | 2,226 | 1 | 242 | 20 | 2,468 | |||||||||||||||||||||||||||||
| Kentucky | 5 | 596 | 2 | 340 | 7 | 936 | |||||||||||||||||||||||||||||
| Missouri | 2 | 190 | 3 | 424 | 5 | 614 | |||||||||||||||||||||||||||||
| Nevada | 3 | 215 | 2 | 165 | 5 | 380 | |||||||||||||||||||||||||||||
| Ohio | 6 | 637 | — | — | 6 | 637 | |||||||||||||||||||||||||||||
| South Carolina | 21 | 2,352 | 4 | 488 | 25 | 2,840 | |||||||||||||||||||||||||||||
| Texas | 3 | 290 | 2 | 246 | 5 | 536 | |||||||||||||||||||||||||||||
On July 15, 2024, we finalized the acquisition of operations for 3 skilled nursing facilities. The operations are located in Kansas. Collectively, these facilities comprise 378 skilled nursing beds. These facilities are leased from a third-party landlord, with the option to purchase the facilities from the landlord at a later date.
On August 1, 2024, we finalized the acquisition of operations for 12 skilled nursing and 13 assisted living and independent living facilities. The operations are located across six states, including 19 facilities in Washington, two
130
in Nevada, and one facility each in Alaska, Arizona, California, and Montana. Collectively, these facilities comprise 1,072 skilled nursing beds and 831 assisted living and independent living units. Of these facilities, 21 are leased from a new joint venture we entered into on the same date in which it owns a 25.8% interest. The remaining four facilities are leased from unaffiliated third-party landlords.
On September 1, 2024, we finalized the acquisition of an additional 20 skilled nursing and eight assisted living and independent living facilities. The operations are located across three states, including 21 in Oregon, six in Idaho and one in Nevada. These facilities comprise 1,439 skilled nursing beds and 503 assisted living and independent living units with 16 facilities leased from our new joint venture and 12 leased from unaffiliated third-party landlords.
As a result of the foregoing acquisitions, as of September 1, 2024, we operated 276 post-acute care facilities in 15 states, with operational capacity to serve approximately 29,584 patients with 27,372 skilled nursing beds and 2,212 assisted living beds. Of these post-acute care facilities, we leased 188 facilities, owned partial interests in an additional 49 leased facilities and directly owned the real estate at 39 facilities. Of our total bed count, approximately 58.2% of beds were at leased facilities, approximately 13.0% of beds were at leased facilities with real estate purchase options, and approximately 28.8% of beds were at directly owned or joint venture facilities.
Legal Proceedings
We are subject to various legal proceedings, claims, and governmental inspections, audits, and investigations that arise in the ordinary course of our business. Although the results of these legal proceedings, claims, and investigations cannot be predicted with certainty, we do not believe that the final outcome of any matters that we are currently involved in are reasonably likely to have a material adverse effect on our business, financial condition or results of operations. Regardless of final outcomes, however, any such proceedings, claims, and investigations may nonetheless impose a significant burden on management and employees and be costly to defend, with unfavorable preliminary or interim rulings.
131
MANAGEMENT
Directors and Executive Officers
The following table sets forth information regarding our directors and executive officers as of the date hereof.
| Name | Age | Position | ||||||||||||
| Executive Officers | ||||||||||||||
| Jason Murray | 45 | Director, Co-Founder, Chief Executive Officer and Chairman | ||||||||||||
| Mark Hancock | 49 | Director, Co-Founder and Executive Vice Chairman | ||||||||||||
| Joshua Jergensen | 39 | President and Chief Operating Officer | ||||||||||||
| Derick Apt | 41 | Chief Financial Officer | ||||||||||||
| John Mitchell | 49 | Chief Legal Officer and Secretary | ||||||||||||
| Peter (P.J.) Sanford | 39 | President, Providence Administrative Consulting Services, Inc. | ||||||||||||
| Michelle Lewis | 48 | Chief Accounting Officer | ||||||||||||
| Joseph Lee | 46 | Chief Compliance Officer | ||||||||||||
| Non-Employee Directors | ||||||||||||||
Jacqueline Millard(1)(2)(3) | 63 | Director | ||||||||||||
Taylor Leavitt(1)(2)(3) | 46 | Director | ||||||||||||
Evelyn Dilsaver(1)(2)(3) | 69 | Director | ||||||||||||
__________________
(1)Member of the Nominating and Corporate Governance Committee.
(2)Member of the Audit Committee.
(3)Member of the Compensation Committee.
Executive Officers
Jason Murray has served as our Chief Executive Officer and a member of our board of directors since January 2013 and has served as Chairman since January 2024. Mr. Murray co-founded our company and has worked in the post-acute sector for 23 years. Prior to our founding, Mr. Murray was an Operations Officer for Intermountain Healthcare, Inc. a non-profit healthcare system, from June 2011 to January 2013 where he was the interim Chief Executive Officer of Park City Medical Center from June 2012 to October 2012. From February 2009 to June 2011, Mr. Murray served as a nursing home administrator with Plum Healthcare Group, a skilled nursing facility operator. Mr. Murray received a B.A. in Healthcare Administration and a Master of Healthcare Administration from Weber State University. We believe Mr. Murray is qualified to serve on our board of directors because of his business acumen, executive leadership and extensive knowledge of our business.
Mark Hancock has served as our Executive Vice Chairman since January 2024 and a member of our board of directors since January 2013 and previously served as our Chief Financial Officer and Secretary from January 2013 to January 2024. Mr. Hancock is also a co-founder of our company. Prior to our founding, Mr. Hancock was Vice President of Finance and Treasurer of Farm Credit Mid-America, a financial services provider, from 2010 to 2013 and served as a nursing home administrator at a facility affiliated with Plum Healthcare Group, a skilled nursing facility operator, from 2009 to 2010. From 2007 to 2009, Mr. Hancock was the Director of Corporate Finance for Steel Technologies Inc., a publicly traded steel processor, and served as a Finance Manager for Ford Motor Company, a publicly traded multinational automobile manufacturer, from 2000 to 2007. Mr. Hancock received a B.S. in Civil Engineering and a Master of Business Administration with a focus in Finance from Brigham Young University. We believe Mr. Hancock is qualified to serve on our board of directors because of his extensive leadership experience, financial expertise and strong understanding of our business.
132
Joshua Jergensen has served as our President and Chief Operating Officer since January 2023. Prior to that, Mr. Jergensen served as our Executive Vice President of Operations from July 2014 to January 2023. From October 2009 to July 2014, Mr. Jergensen was a nursing home administrator at Balboa Nursing and Rehabilitation Center, one of our affiliated skilled nursing facilities. Mr. Jergensen received a B.S. in Business Management with an emphasis in Finance from Brigham Young University and a Master of Healthcare Administration from the University of Southern California.
Derick Apt has served as our Chief Financial Officer since January 2024 and previously served as our Executive Vice President, Chief Investment Officer and Treasurer from January 2023 to January 2024. Prior to that, Mr. Apt served as our Executive Vice President of Corporate Finance and Treasurer since joining our company in April 2018. From February 2015 to April 2018, Mr. Apt was Manager of Treasury and Finance for Vivint, Inc., a smart home platform company. Prior to Vivint, Mr. Apt worked at Intermountain Healthcare’s Treasury department and began his finance career at Goldman Sachs. Mr. Apt received a B.S. in Biological Engineering from the University of Missouri and a Master of Business Administration from the George Washington University School of Business.
John Mitchell has served as our Chief Legal Officer since January 2023. Prior to that, Mr. Mitchell served as our Executive Vice President and General Counsel since joining our company in January 2017. From April 2016 to November 2016, Mr. Mitchell served as Vice President, Legal at HCP, a publicly traded REIT. Prior to that, Mr. Mitchell was Senior Vice President of Legal Affairs and Chief Compliance Officer of Skilled Healthcare Group, Inc., a publicly traded provider of post-acute healthcare services, from January 2011 to May 2015. Mr. Mitchell received a B.A. in History and a J.D. from Brigham Young University.
Peter (P.J.) Sanford has served as President of Providence Administrative Consulting Services, Inc., which provides PACS Services, since January 2024. Prior to that, Mr. Sanford served as our Chief Administrative Officer from January 2023 to December 2023 and as our Executive Vice President of Operations and Finance from October 2015 to January 2023. From December 2012 to October 2015, Mr. Sanford served as a nursing home administrator at Paradise Valley Health Care Center, one of our affiliated skilled nursing facilities. Mr. Sanford received a B.A. in English with a minor in Business from Brigham Young University and received a Master of Business Administration from the University of Michigan.
Michelle Lewis has served as our Chief Accounting Officer since January 2023. Prior to that, Ms. Lewis served in various roles of increasing responsibility, including as our Controller, since joining our company in July 2018. Prior to that, Ms. Lewis owned and operated Michelle Lewis Accounting Services, PLLC, a certified public accounting firm, and also provided controller functions at a privately held healthcare organization, from January 2008 to May 2015. Ms. Lewis received a B.S. in Business Administration from the California State University, East Bay.
Joseph Lee has served as our Chief Compliance Officer since February 2024. Prior to that, Mr. Lee served in various senior leadership positions, including as our Senior Vice President of Support Services, since joining our company in June 2017. From January 2016 to May 2017, Mr. Lee served as a branch president of operations for Plum Healthcare Group, a skilled nursing facility operator. Prior to that, Mr. Lee served as an executive director and administrator at facilities affiliated with Plum Healthcare Group from February 2010 to December 2015. Mr. Lee received a B.S. in Sociology from Brigham Young University and a J.D. from Gonzaga University School of Law.
Non-Employee Directors
Jacqueline Millard has served as a member of our board of directors since July 2023. Since January 2021, Ms. Millard has owned and operated a private investment advisory firm. Previously, Ms. Millard was the Vice President and Chief Investment Officer of Intermountain Healthcare, Inc., a non-profit healthcare system, from June 1993 to January 2021. Ms. Millard received a B.S. in Finance from Weber State University and a Master of Business Administration from Westminster College. We believe Ms. Millard is qualified to serve on our board of directors because of her extensive financial and leadership experience.
133
Taylor Leavitt has served as a member of our board of directors since July 2023. Mr. Leavitt owns and has served as the Chief Executive Officer and Managing Partner of Leavitt Equity Partners, a healthcare-focused private equity firm, since August 2014. Mr. Leavitt currently serves on the board of directors of several private entities that provide healthcare services. Previously, Mr. Leavitt was a co-founder and Partner of Leavitt Partners, a healthcare strategy consulting firm, from June 2009 to December 2020. Mr. Leavitt received a B.S. in Finance and Economics from Utah State University and a Master of Business Administration from the UCLA Anderson School of Management. We believe Mr. Leavitt is qualified to serve on our board of directors because of his strong business acumen and extensive experience in finance and investing.
Evelyn Dilsaver has served as a member of our board of directors since May 2024. Ms. Dilsaver has served on the board of directors of Tempur Sealy International, Inc., since 2014, QuidelOrtho Corporation, since 2022, and HealthEquity, Inc. since 2014. In the past five years, Ms. Dilsaver has also served as a director of Aéropostale Inc., HighMark Funds, Russell Exchange Traded Funds, Longs Drug Stores Corp. and Tamalpais Bancorp. She is also a member of the board of directors of a privately held corporation and real estate investment trust. Ms. Dilsaver was formerly a member of The Charles Schwab Corporation from 1991 until her retirement in 2007. During her tenure at The Charles Schwab Corporation, Ms. Dilsaver held various senior management positions within the organization, including Executive Vice President (The Charles Schwab Corporation) and President and Chief Executive Officer (Charles Schwab Investment Management). Prior to becoming President and Chief Executive Officer of Charles Schwab Investment Management, a position she held from 2003 to 2007, Ms. Dilsaver held the position of Senior Vice President, Asset Management Products and Services. Ms. Dilsaver holds a B.S. in Accounting from California State University, East Bay, and is a Certified Public Accountant. We believe that Ms. Dilsaver’s extensive financial industry experience and public company board experience qualifies her to serve as a member of our board of directors.
Family Relationships
There are no family relationships among any of our directors or executive officers.
Board Composition
Our board of directors currently consists of five directors. When considering whether directors have the experience, qualifications, attributes, or skills, taken as a whole, to enable our board of directors to satisfy its oversight responsibilities effectively in light of our business and structure, the board of directors focuses primarily on each person’s background and experience as reflected in the information discussed in each of the directors’ individual biographies set forth above. We believe that our directors provide an appropriate mix of experience and skills relevant to the size and nature of our business.
Board Leadership Structure
Mr. Murray is chairman of our board of directors. As Mr. Murray is not an “independent director,” our board of directors has appointed Taylor Leavitt to serve as our lead independent director. The lead independent director’s responsibilities include, but are not limited to: presiding over all meetings of the board of directors at which the chairman of our board of directors is not present, including any executive sessions of the independent directors; approving board meeting schedules and agendas; and acting as the liaison between the independent directors on the one hand and the chief executive officer, chairman of our board of directors and executive chairman on the other. Our corporate governance guidelines provide the flexibility for our board of directors to modify our leadership structure in the future as it deems appropriate.
Classified Board
Our Amended and Restated Charter provides that our board of directors will be divided into three classes with staggered three-year terms. Upon expiration of the term of a class of directors, directors for that class will be elected for three-year terms at the annual meeting of stockholders in the year in which that term expires. As a result, only
134
one class of directors will be elected at each annual meeting of our stockholders, with the other classes continuing for the remainder of their respective three-year terms. Our directors are divided among the three classes as follows:
•Class I directors, whose initial term will expire at our 2025 annual meeting of stockholders consists of Jacqueline Millard and Taylor Leavitt;
•Class II directors, whose initial term will expire at our 2026 annual meeting of stockholders consists of Mark Hancock and Evelyn Dilsaver; and
•Class III directors, whose initial term will expire at our 2027 annual meeting of stockholders consists of Jason Murray.
We expect that any additional directorships resulting from an increase in the number of directors will be distributed among the three classes so that, as nearly as possible, each class will consist of one-third of the total number of directors.
The classification of our board of directors may have the effect of delaying or preventing changes in our control or management. See the section titled “Description of Capital Stock—Description of Capital Stock—Anti-Takeover Effects of Provisions of the General Corporation Law of the State of Delaware and our Amended and Restated Charter and Amended and Restated Bylaws” for additional information.
Amended and Restated Charter and Stockholders Agreement
Our Amended and Restated Charter provides that the authorized number of directors may be changed exclusively by one or more resolution adopted from time to time by our board of directors, and that each director shall hold office until his or her successor is duly elected and qualified or until his or her earlier death, resignation, disqualification or removal.
Our Amended and Restated Charter grants Messrs. Murray and Hancock board designation rights. Mr. Murray has the right, but not the obligation, to designate (i) up to two individuals for inclusion in our slate of director nominees if he beneficially owns at least 20% of the aggregate number of shares of common stock outstanding immediately following the completion of our IPO or (ii) one individual for inclusion in our slate of director nominees if he beneficially owns less than 20% but at least 10% of the aggregate number of shares of common stock outstanding immediately following the completion of our IPO. Mr. Hancock has the right, but not the obligation, to designate (i) up to two individuals for inclusion in our slate of director nominees if he beneficially owns at least 20% of the aggregate number of shares of common stock outstanding immediately following the completion of our IPO or (ii) one individual for inclusion in our slate of director nominees if he beneficially owns less than 20% but at least 10% of the aggregate number of shares of common stock outstanding immediately following the completion of our IPO.
Each of Messrs. Murray and Hancock also have the right to fill any vacancies created by reason of death, resignation, disqualification or removal of their respective designees. These rights are also affirmed in the Stockholders Agreement that we entered into with Messrs. Murray and Hancock, and these rights will terminate upon the termination of the Stockholders Agreement. See “Certain Relationships and Related Party Transactions—Stockholders Agreement” for more information. If the number of individuals that Messrs. Murray and Hancock have the right to designate is decreased because of a decrease in their respective ownership or upon termination of the Stockholders Agreement, then the corresponding designee (if such designee is serving on our board of directors) may remain on our board of directors through the end of his or her then current term; provided, that a director may resign at any time regardless of the period of time left in his or her then current term.
As a result, Messrs. Murray and Hancock will each have the right to designate two directors for nomination to our board of directors, and will collectively have the right to designate four directors, which represents the four out of our current five member board of directors.
135
In addition, our Amended and Restated Charter provides for the removal of any of our directors at any time with or without cause by the affirmative vote of the holders of a majority of the voting power of the then outstanding shares of our voting stock entitled to vote thereon; provided, however, that at any time when Messrs. Murray and Hancock beneficially own, in the aggregate, less than the majority of the voting power of our outstanding shares of voting stock, directors may be removed only for cause and only by the affirmative vote of the holders of at least 66 2/3% of the voting power of the then outstanding shares of our voting stock entitled to vote thereon. As a result, for so long as Messrs. Murray and Hancock own, in the aggregate, more than a majority of the voting power of our outstanding shares of our voting stock, they will be able to remove any of our directors at any time with or without cause.
Furthermore, our Amended and Restated Charter provides that, at any time when Messrs. Murray and Hancock beneficially own, in the aggregate, at least a majority of the voting power of our outstanding shares of voting stock, our stockholders may take action by written consent without a meeting, and at any time when Messrs. Murray and Hancock beneficially own, in the aggregate, less than the majority of the voting power of our outstanding shares of voting stock, our stockholders may not take action by written consent and may only take action at a meeting of stockholders. As a result, for so long as Messrs. Murray and Hancock own, in the aggregate, more than a majority of the voting power of our outstanding shares of our voting stock, they may take action by written consent without a meeting of stockholders.
See the section titled “Description of Capital Stock—Designation Rights” and “Description of Capital Stock—Anti-Takeover Effects of Provisions of the General Corporation Law of the State of Delaware and our Amended and Restated Charter and Amended and Restated Bylaws” for additional information.
Director Independence and Controlled Company Exception
The rules of the New York Stock Exchange define a “controlled company” as a company of which more than 50% of the voting power for the election of directors is held by an individual, a group or another company. Following this offering, Messrs. Murray and Hancock will collectively own approximately 73.7% of the voting power of our common stock (or approximately 72.4% if the underwriters exercise their option to purchase additional shares of our common stock from the selling stockholders in full). As such, we are a “controlled company” under the rules of the New York Stock Exchange. As a result, we qualify for exemptions from certain corporate governance requirements under the rules.
If we cease to be a controlled company and our common stock continues to be listed on the New York Stock Exchange, we will be required to take all action necessary to comply with applicable rules, subject to specified transition periods applicable to certain requirements, as the case may be. See the section “Risk Factors—We are a “controlled company” within the meaning of the corporate governance standards of the New York Stock Exchange. As a result, we may elect to rely on exemptions from certain corporate governance standards and you may not have the same protections afforded to stockholders of companies that are subject to such requirements.”
Our board of directors has affirmatively determined that Jacqueline Millard, Taylor Leavitt and Evelyn Dilsaver are each an “independent director,” as defined under the Exchange Act and the rules of the New York Stock Exchange.
Risk Oversight
Our board of directors is responsible for overseeing our risk management process. Our board of directors focuses on our general risk management strategy, the most significant risks facing us, and oversees the implementation of risk mitigation strategies by management. Our board of directors is also apprised of particular risk management matters in connection with its general oversight and approval of corporate matters and significant transactions.
136
Board Committees
Our board of directors has established an audit committee, a compensation committee, and nominating and corporate governance committee, each of which has the composition and the responsibilities described below. In addition, from time to time, special committees may be established under the direction of our board of directors when necessary to address specific issues.
Each of the audit committee, the compensation committee, and nominating and corporate governance committee operates under a written charter that was approved by our board of directors in connection with our initial public offering. A current copy of each of the audit committee, compensation committee, and nominating and corporate governance committee charters are available on our corporate website at www.pacs.com. The reference to our website address in this prospectus does not include or incorporate by reference the information on our website into this prospectus. We have included our website address in this prospectus solely as an inactive textual reference.
Our board of directors directs the management of our business and affairs, as provided by Delaware law, and conducts its business through meetings of the board of directors and standing committees. We will have a standing audit committee, compensation committee, and nominating and corporate governance committee. In addition, from time to time, special committees may be established under the direction of the board of directors when necessary to address specific issues.
Audit Committee
Our audit committee is responsible for, among other things:
•appointing, compensating, retaining, evaluating, terminating, and overseeing our independent registered public accounting firm;
•discussing with our independent registered public accounting firm their independence from management;
•reviewing with our independent registered public accounting firm the scope and results of their audit;
•approving all audit and permissible non-audit services to be performed by our independent registered public accounting firm;
•overseeing the financial reporting process and discussing with management and our independent registered public accounting firm the interim and annual financial statements that we file with the SEC;
•reviewing and monitoring our accounting principles, accounting policies, financial and accounting controls, and compliance with legal and regulatory requirements;
•reviewing our policies on risk assessment and risk strategy and management, including risk policies and risk mitigation strategies by management;
•reviewing related party transactions; and
•establishing procedures for the confidential anonymous submission of concerns regarding questionable accounting, internal controls, or auditing matters.
Our audit committee consists of Jacqueline Millard, Taylor Leavitt, and Evelyn Dilsaver with Ms. Millard serving as chair. Our board of directors has affirmatively determined that Ms. Millard, Mr. Leavitt and Ms. Dilsaver each meet the definition of “independent director” for purposes of serving on the audit committee under Rule 10A-3 and the New York Stock Exchange rules. Each member of our audit committee meets the financial literacy requirements of the New York Stock Exchange listing standards. In addition, our board of directors has determined that Ms. Millard will qualify as an “audit committee financial expert,” as such term is defined in Item 407(d)(5) of
137
Regulation S-K. Our board of directors adopted a new written charter for the audit committee, which is available on our website at www.pacs.com. The information on, or that can be accessed through, our website is deemed not to be incorporated in this prospectus or to be part of this prospectus.
Compensation Committee
Our compensation committee is responsible for, among other things:
•reviewing and approving, or recommending that our board of directors approve, the compensation of our Chief Executive Officer, Executive Vice Chairman and other executive officers;
•appointing and overseeing any compensation consultants;
•reviewing and approving or making recommendations to our board of directors regarding our incentive compensation and equity-based plans;
•reviewing and making recommendations to our board of directors with respect to director compensation;
•reviewing and discussing annually with management our “Compensation Discussion and Analysis” disclosure if and to the extent then required by SEC rules; and
•preparing the compensation committee report if and to the extent then required by SEC rules.
Our compensation committee consists of Jacqueline Millard, Taylor Leavitt, and Evelyn Dilsaver, with Mr. Leavitt serving as chair. Our board has determined that Mr. Leavitt, Ms. Millard and Ms. Dilsaver are “non-employee directors” as defined in Section 16b-3 of the Exchange Act. Our board of directors has adopted a new written charter for the compensation committee, which is available on our website at www.pacs.com. The information on, or that can be accessed through, our website is deemed not to be incorporated in this prospectus or to be part of this prospectus. The composition of our compensation committee meets the New York Stock Exchange requirements for independence under the current listing standards and SEC rules and regulations.
Nominating and Corporate Governance Committee
Our nominating and corporate governance committee is responsible for, among other things:
•identifying individuals qualified to become members of our board of directors, consistent with criteria approved by our board of directors;
•reviewing and making recommendations to our board with respect to management succession planning;
•evaluating the overall effectiveness of our board of directors and its committees; and
•reviewing developments in corporate governance compliance and developing and recommending to our board of directors a set of corporate governance guidelines and principles.
Our nominating and corporate governance committee consists of Jacqueline Millard, Taylor Leavitt, and Evelyn Dilsaver, with Ms. Dilsaver serving as chair. Our board of directors adopted a new written charter for the nominating and corporate governance committee, which is available on our website at www.pacs.com. The information on, or that can be accessed through, our website is deemed not to be incorporated in this prospectus or to be part of this prospectus. The composition of our nominating and corporate governance committee meets the New York Stock Exchange requirements for independence under the current listing standards and SEC rules and regulations.
138
Compensation Committee Interlocks and Insider Participation
None of the members of the compensation committee is currently, or has been at any time, one of our executive officers or employees. None of our executive officers serves as a member of the board of directors or compensation committee (or other committee performing equivalent functions) of any entity that has one or more executive officers serving on our board of directors or compensation committee.
Board Diversity
Our nominating and corporate governance committee is responsible for reviewing with the board of directors, on an annual basis, the appropriate characteristics, skills and experience required for the board of directors as a whole and its individual members. Although our board of directors does not have a formal written diversity policy with respect to the evaluation of director candidates, in its evaluation of director candidates, our nominating and corporate governance committee considers factors including, without limitation, issues of character, integrity, judgment, potential conflicts of interest, other commitments, and diversity, and with respect to diversity, such factors as gender, race, ethnicity, experience, and area of expertise, as well as other individual qualities and attributes that contribute to the total diversity of viewpoints and experience represented on the board of directors.
Code of Ethics and Code of Conduct
We have adopted a written code of business conduct and ethics that applies to our directors, officers, and employees, including our principal executive officer, principal financial officer, principal accounting officer or controller, or persons performing similar functions. A copy of the code is available on our website, www.pacs.com. In addition, we have posted and intend to continue to post on our website all disclosures that are required by law or the New York Stock Exchange listing standards concerning any amendments to, or waivers from, any provision of the code. The information on, or that can be accessed through, our website is deemed not to be incorporated in this prospectus or to be part of this prospectus.
139
COMPENSATION DISCUSSION AND ANALYSIS
This section provides an overview and analysis of the compensation awarded to or earned by our “named executive officers,” including the elements of our compensation program for our named executive officers, material compensation decisions made under that program for fiscal 2023 and the material factors considered in making those decisions. Where relevant, the discussion below also reflects certain contemplated changes to our compensation programs that we intend to implement following the effectiveness of the registration statement of which this prospectus forms a part. Our named executive officers for 2023 (and their current positions) are:
•Jason Murray, Director, Co-Founder, Chief Executive Officer and Chairman;
•Mark Hancock, Director, Co-Founder and Executive Vice Chairman;
•Josh Jergensen, President and Chief Operating Officer;
•Peter (P.J.) Sanford, President of Providence Administrative Consulting Services, Inc.; and
•Derick Apt, Chief Financial Officer.
Effective January 1, 2024, Mark Hancock resigned as our Chief Financial Officer and Secretary and was appointed as our Executive Vice Chairman. In connection with Mr. Hancock’s resignation as Chief Financial Officer, Derick Apt, previously our EVP, Chief Investment Officer and Treasurer, was appointed as our Chief Financial Officer.
This discussion may contain forward-looking statements that are based on our current plans, considerations, expectations and determinations regarding future compensation programs.
Executive Compensation Philosophy and Objectives
We believe that for us to be successful we must hire and retain people who can continue to develop our strategy and innovate our services. To achieve these objectives, our executive compensation program has been designed to motivate, reward, attract and retain high caliber management and to align compensation with our short- and long-term business objectives, business strategy and financial performance.
Our compensation programs for our named executive officers are built to support the following objectives:
•attract the top talent in our leadership positions and motivate our executives to deliver the highest level of individual and team impact and results; and
•reward high levels of performance with commensurate levels of compensation.
Determination of Compensation
Our board of directors is responsible for overseeing all aspects of our executive compensation programs, including executive salaries, performance-based incentives and any executive perquisites for our named executive officers. Our board of directors has the authority to engage its own advisors to assist in carrying out its responsibilities. For fiscal 2023, in preparation for our IPO, we engaged Pearl Meyer, an outside compensation advisor, for purposes of setting executive or director compensation.
With respect to 2023, Messrs. Murray and Hancock were the sole members of our board of directors at the time our 2023 compensation program was established. No other executive officer participated directly in the final deliberations or determinations regarding his own compensation package. We expect that our board of directors or its compensation committee will review and establish our executive compensation programs.
140
Elements of Our Executive Compensation Program
The primary elements of our named executive officers’ compensation and the main objectives of each are:
•Base Salary. Base salary attracts and retains talented executives, recognizes individual roles and responsibilities and provides stable income;
•Performance-Based Bonuses: Performance-based bonuses promote short-term performance objectives and reward executives for their contributions toward achieving those objectives; and
•Other Benefits and Perquisites: In addition, our named executive officers are eligible to participate in our health and welfare programs and our retirement programs. We also provide certain perquisites, which aid in attracting and retaining executive talent.
Each of these elements of compensation is described further below.
Base Salaries
The base salary of each named executive officer is an important part of the officer’s total compensation package, and is intended to reflect the officer’s respective position, duties and responsibilities. Base salaries provide our named executive officers with a reasonable degree of financial certainty and stability. For fiscal year 2023, the base salaries of our named executive officers were $3,000,000 for each of Messrs. Murray and Hancock and $200,000 for each of Messrs. Jergensen, Sanford and Apt. Our named executive officers’ base salaries were not increased from fiscal year 2022.
On December 31, 2023, we terminated the consulting and strategic advisory services agreement between us and Helios Consulting, LLC (Helios), an entity jointly owned and operated by Messrs. Murray and Hancock (the Helios Consulting Agreement), pursuant to which we paid Helios consulting fees for services provided by Messrs. Murray and Hancock. In connection with the termination of the Helios Consulting Agreement, and the reduction in payments made to Messrs. Murray and Hancock, the base salaries for each of Messrs. Murray and Hancock were increased to $5,000,000, effective as of January 1, 2024. See the section titled “Related Party Agreement in Effect Prior to our IPO—Helios Consulting Agreement” below for additional information about the Helios Consulting Agreement.
Additionally, in connection with Mr. Apt’s appointment as our Chief Financial Officer, his base salary was increased to $400,000, effective January 1, 2024.
Following our IPO, the base salaries for our named executive officers are $500,000 for Messrs. Murray, Hancock, Jergensen and $400,000 for Messrs. Sanford and Apt.
2023 Bonuses
In addition to base salaries, certain named executive officers are eligible to receive performance-based cash bonuses, which are designed to provide appropriate incentives to our executives to increase our operating subsidiaries’ net income, and to reward our executives for achievements towards this goal. The performance-based bonus each named executive officer is eligible to receive is equal to a percentage of the monthly net income of our operating subsidiaries.
For 2023, Messrs. Jergensen, Sanford and Apt were each eligible to receive a performance-based bonus equal to 3.0%, 2.0% and 0.75% of the monthly net income of our operating subsidiaries, respectively. For Messrs. Jergensen and Sanford, 0.25% of each earned monthly bonus will be earned and paid only if we achieve certain clinical criteria for the year. For 2023, Messrs. Jergensen, Sanford, and Apt’s aggregate performance-based bonuses earned based on net income of our operating subsidiaries was $7,482,275, $4,796,975, and $2,408,635, respectively. In addition,
141
Messrs. Jergensen and Sanford’s aggregate performance-based bonuses earned based on achievement of certain clinical criteria in 2023 was $581,538.
Additionally, in connection with Mr. Apt’s appointment as our Chief Financial Officer, his bonus opportunity was increased to 2.0% of the monthly net income of our operating subsidiaries, effective January 1, 2024.
For 2023, Mr. Apt also was eligible to receive performance-based bonus(es) based on the net operating income (NOI) of our acquisitions. Specifically, he was eligible to receive bonus(es) equal to 3.0% of the applicable entity’s NOI in the first year after the acquisition, 2.0% of the applicable entity’s NOI in the second year after the acquisition and 1.0% of the applicable entity’s NOI for each year thereafter. Bonuses are payable on the closing anniversary of the applicable acquisition. For 2023, Mr. Apt’s aggregate performance-based bonus under this program was $3,216,945.
Equity Compensation
Historically, we have not granted equity awards to our employees and executives, including our named executive officers. However, we view equity-based compensation as a critical component of our balanced total compensation program going forward as a public company. Equity-based compensation creates an ownership culture among our employees that provides an incentive to contribute to the continued growth and development of our business and aligns interest of executives with those of our stockholders.
Accordingly, we adopted a 2024 Incentive Award Plan (2024 Plan), in order to facilitate the grant of cash and equity incentives to directors, employees (including our named executive officers), and consultants of our Company and certain of its affiliates and to enable our Company and certain of its affiliates to obtain and retain the services of these individuals, which is essential to our long-term success. The 2024 Plan became effective in connection with our IPO. See the section titled “Equity Incentive Award Plans—2024 Incentive Award Plan” below for additional information about the 2024 Plan.
IPO Equity Awards
In connection with our IPO, we granted restricted stock unit awards pursuant to the 2024 Plan to certain of our employees, including Messrs. Jergensen, Sanford, and Apt, which grants became effective prior to the completion of our IPO (IPO Equity Awards). The aggregate number of restricted stock units underlying the IPO Equity Awards was 15,390,579 shares. Of this amount, the awards granted to each of Messrs. Jergensen, Sanford, and Apt were 3,003,039, 1,501,520, and 1,313,830 shares, respectively, which represents approximately 2.00%, 1.00% , and 0.875%, respectively, of the number of shares of our common stock outstanding as of the closing of our IPO (disregarding the shares issuable under the 2024 Plan).
Each IPO Equity Award will vest as follows: (i) 25% of the restricted stock units underlying the IPO Equity Award vested on the grant date, and (ii) 75% of the restricted stock units underlying the IPO Equity Award will vest in substantially equal annual installments on each of the first, second, third, fourth, and fifth anniversaries of the closing of our IPO, subject to the executive’s continued service with us through the applicable vesting date.
If the executive experiences a termination of service by us without cause, by the executive for good reason, or due to death or disability, a portion of the restricted stock units subject to the IPO Equity Awards will vest in the amount that would have vested during the 12-month period following the date of termination (had the executive remained in continued service with us during such period and assuming that the shares vest in equal monthly installments, rather than annual installments, over the vesting period). If such termination occurs on or within 24 months after a change in control, then all of the executive’s remaining unvested restricted stock units subject to the IPO Equity Award will vest. This accelerated vesting treatment will be subject to the executive’s execution and, as applicable, non-revocation of a general release of claims in our favor, and continued compliance with any applicable restrictive covenants.
142
Deferred Compensation Plan
We currently maintain the Providence Administrative Consulting Services, Inc. Nonqualified Deferred Compensation Plan (Deferred Compensation Plan), as may be amended from time to time, for certain of our employees, including our named executive officers. Participating employees may defer up to 100% of their bonus compensation per plan year.
The Deferred Compensation Plan provides our employees an opportunity to elect to defer a portion of their bonus compensation and to provide a deferred compensation vehicle to which we may credit discretionary contributions and matching contributions pursuant to the terms of the plan. Discretionary and matching contributions, if any, are 100% vested after participants complete three years and five years of service as our full-time employee, respectively. We have not historically made any matching or discretionary contributions under the Deferred Compensation Plan. Participants have an opportunity to earn returns (positive or negative) based on investment options as determined by us. Typically, participants elect a level of risk tolerance for their deferred compensation at the beginning of each fiscal year and the plan administrator invests and manages the asset mix accordingly. In the event of a “separation from service” (as defined in the Deferred Compensation Plan and determined pursuant to Section 409A of the Code), a participant will be paid his or her account balance in two annual installments.
In 2023, Messrs. Jergensen, Sanford and Apt were the only named executive officers to participate in our Deferred Compensation Plan and each elected to defer up to $180,000, $120,000, and $200,000, respectively, of their aggregate 2023 bonus compensation. The “Executive Contributions in Last FY” column of the Non-Qualified Deferred Compensation for 2023 table below shows the actual amounts deferred pursuant to the Deferred Compensation Plan for Messrs. Jergensen, Sanford and Apt in 2023.
Executive Severance Plan
We have an Executive Severance Plan (Executive Severance Plan) pursuant to which our named executive officers are eligible to receive severance payments upon a qualifying involuntary termination of employment, including in connection with a change in control of our company. These severance arrangements are designed to retain certain of our executives in these key positions as we compete for talented executives in the marketplace where such protections are commonly offered. For a detailed description of the severance provisions contained in our Executive Severance Plan, see the section titled “Potential Payments Upon Termination or Change in Control” below.
Employee Benefits and Perquisites
All of our full-time employees are eligible to participate in our health and welfare plans, including medical, dental and vision benefits, medical and dependent care flexible spending accounts, short-term and long-term disability insurance, and life and accidental death and disability insurance. Our named executive officers are eligible to participate in health and welfare plans on the same basis as other similarly-situated executive officers.
Other Benefits. Certain of our named executive officers participate in a 401(k) retirement savings plan. The Internal Revenue Code allows eligible employees to defer a portion of their compensation, within prescribed limits, on a pre-tax basis through contributions to the 401(k) plan. In 2023, we matched a portion of the contributions to the 401(k) plan on behalf of eligible employees. The discretionary employer match for 2023 was 25% of the participant’s contribution to the plan up to a max of 4% of their eligible compensation. We believe that providing a vehicle for tax-deferred retirement savings though our 401(k) plan adds to the overall desirability of our executive compensation package and further incentivizes our employees, including our named executive officers, in accordance with our compensation policies. In addition, we maintain a non-qualified deferred compensation plan for the benefit of certain officers and employees who qualify for participation in the plan, including our named executive officers. See the section titled “—Compensation Discussion and Analysis—Deferred Compensation Plan” for a description of the Deferred Compensation Plan.
143
Clawback Policy
We have a compensation recovery policy that is compliant with the listing rules of the national securities exchange or association on which our securities are listed, as required by the Dodd-Frank Act.
Accounting for Share-Based Compensation
In connection with our IPO, we issued stock-based compensation awards and followed the Financial Accounting Standard Board Accounting Standards Codification Topic 718, Compensation — Stock Compensation (ASC Topic 718). ASC Topic 718 requires companies to measure the compensation expense for all share-based awards made to employees and directors, including stock options and RSUs, based on the grant-date fair value of these awards.
144
EXECUTIVE COMPENSATION TABLES
2023 Summary Compensation Table
The following table contains information about the compensation earned by each of our named executive officers during our most recently completed fiscal year ended December 31, 2023.
| Name and Principal Position | Year | Salary ($) | Non-Equity Incentive Plan Compensation ($) | Change in Pension Value and Nonqualified Deferred Compensation Earnings ($) (1) | All Other Compensation ($)(2) | Total ($) | |||||||||||||||||||||||||||||||||||
| Jason Murray | 2023 | 3,000,000 | — | — | 2,056,976 | 5,056,976 | |||||||||||||||||||||||||||||||||||
| Co-Founder, Chief Executive Officer and Chairman | |||||||||||||||||||||||||||||||||||||||||
| Mark Hancock | 2023 | 3,000,000 | — | — | 2,056,976 | 5,056,976 | |||||||||||||||||||||||||||||||||||
| Co-Founder, Executive Vice Chairman and former Chief Financial Officer and Secretary | |||||||||||||||||||||||||||||||||||||||||
| Josh Jergensen | 2023 | 200,000 | 8,063,813 | (3) | 61,808 | 31,208 | 8,356,829 | ||||||||||||||||||||||||||||||||||
| President and Chief Operating Officer | |||||||||||||||||||||||||||||||||||||||||
| PJ Sanford | 2023 | 200,000 | 5,378,513 | (3) | 18,917 | 32,299 | 5,629,729 | ||||||||||||||||||||||||||||||||||
| President of Providence Administrative Consulting Services, Inc. and former Chief Administrative Officer | |||||||||||||||||||||||||||||||||||||||||
| Derick Apt | 2023 | 200,000 | 5,625,580 | (3) | 23,314 | 47,722 | 5,896,616 | ||||||||||||||||||||||||||||||||||
| Chief Financial Officer and former Chief Investment Officer and Treasurer | |||||||||||||||||||||||||||||||||||||||||
__________________
(1)Represents the above-market earnings on deferred compensation that is not tax-qualified, which is calculated as the excess of the earnings credited on deferred amounts under our Deferred Compensation Plan that were deemed invested in the investment vehicles under such plan over the amount that would have been earned had the deferred amounts been credited with a return equal to 120% of the applicable federal rate in effect for 2023. For more information, see “Nonqualified Deferred Compensation for 2023” table below.
(2)Amounts reported in this column represent our contributions towards our named executive officers’ medical insurance premiums ($31,208 for Messrs. Murray, Hancock, Jergensen, and Sanford and $35,021 for Mr. Apt), life insurance premiums ($25,770 for Messrs. Murray and Hancock), life and disability insurance premiums ($1,091 for Mr. Sanford and $10,778 for Mr. Apt) and for Mr. Apt $1,923 for our 401(k) match. In addition, $1,999,998 represents amounts paid by us to each of Messrs. Murray and Hancock pursuant to the Helios Consulting Agreement, which was terminated effective December 31, 2023, as further described in detail under “Certain Relationships and Related Party Transactions.”
(3)Amounts reflect cumulative payouts earned pursuant to our performance-based bonus programs maintained in 2023, including amounts that were earned but deferred pursuant to our Deferred Compensation Plan, as described below. For Messrs. Jergensen and Sanford, amounts represent aggregate bonus amounts earned in 2023 based on the monthly net income of our operating subsidiaries ($7,482,275 for Mr. Jergensen and $4,796,975 for Mr. Sanford) and achievement of certain clinical criteria ($581,538 for Messrs. Jergensen and Sanford). For Mr. Apt, amount represents aggregate bonus amounts earned in 2023 based on the monthly net income of our operating subsidiaries ($2,408,635) and the NOI of our acquisitions ($3,216,945). Please see the description of such awards under “Elements of Our Executive Officer Compensation program—2023 Bonuses” above.
145
Grants of Plan-Based Awards in 2023
The following table provides information relating to grants of plan-based awards made to our named executive officers during fiscal 2023.
| Name | Estimated Possible Payouts Under Non-Equity Incentive Plan Awards(1) | |||||||||||||||||||
| Threshold ($) | Target ($) | Maximum ($) | ||||||||||||||||||
| Jason Murray | — | — | — | |||||||||||||||||
| Mark Hancock | — | — | — | |||||||||||||||||
| Josh Jergensen | — | — | — | |||||||||||||||||
| PJ Sanford | — | — | — | |||||||||||||||||
| Derick Apt | — | — | — | |||||||||||||||||
______________
(1)Amounts shown in these columns represent each named executive officer’s annual cash bonus opportunity under our 2023 performance-based bonus program and Mr. Apt’s annual cash bonus opportunity related to the NOI of our acquisitions. There are no threshold, target or maximum payouts under these bonus programs given the final payments in respect of such awards are based on a percentage of net income and NOI, as applicable. For additional detail on these awards, please see the description of such awards under “Elements of Our Executive Officer Compensation program—2023 Bonuses” above. The amounts earned by our named executive officers under our bonus programs are reflected in the Summary Compensation Table above.
Employment Arrangements with Our Executive Officers
On December 19, 2023, we entered into an employment offer letter with Mr. Apt in connection with his appointment as our Chief Financial Officer, effective January 1, 2024 (Apt Offer Letter).The Apt Offer Letter provides for an annual base salary of $400,000 and an annual cash bonus opportunity equal to 2% of our monthly net operating income, which is expected to be adjusted to a target amount between 5x – 10x his annual base salary, which amount will be approved by our compensation committee.
We do not have any other existing employment arrangements with our executive officers.
Outstanding Equity Awards at Year-End
Our named executive officer did not hold any unvested equity awards as of December 31, 2023.
Option Exercises and Stock Vested in 2023
None of our named executive officers exercised any stock options or vested in any stock awards during 2023.
Non-Qualified Deferred Compensation for 2023
The following table sets forth information regarding our Deferred Compensation Plan that provides for the deferral of bonus compensation for certain of our employees, including our named executive officers, on a basis that is not tax-qualified, as described further under “Compensation Discussion and Analysis—Deferred Compensation Plan” above.
| Name | Executive Contributions in Last FY ($)(1) | Registrant Contributions in Last FY ($) | Aggregate Earnings in Last FY ($)(2) | Aggregate Withdrawals / Distributions ($) | Aggregate Balance at Last FYE ($) | |||||||||||||||||||||||||||
| Jason Murray | — | — | — | — | — | |||||||||||||||||||||||||||
| Mark Hancock | — | — | — | — | — | |||||||||||||||||||||||||||
| Josh Jergensen | 166,667 | — | 88,197 | — | 614,285 | |||||||||||||||||||||||||||
146
| Name | Executive Contributions in Last FY ($)(1) | Registrant Contributions in Last FY ($) | Aggregate Earnings in Last FY ($)(2) | Aggregate Withdrawals / Distributions ($) | Aggregate Balance at Last FYE ($) | |||||||||||||||||||||||||||
| PJ Sanford | 108,000 | — | 32,806 | — | 321,576 | |||||||||||||||||||||||||||
| Derick Apt | 183,333 | — | 33,303 | — | 298,156 | |||||||||||||||||||||||||||
__________________
(1)Represents amounts the named executive officer elected to defer in 2023, which are deferred from bonus compensation earned in 2023 and therefore reported in the appropriate column in the Summary Compensation Table.
(2)Represents net amounts credited to the named executive officers’ accounts as a result of performance of the investment vehicle in which their accounts were deemed invested. These amounts include above-market earnings, which are reported in the appropriate column in the Summary Compensation Table.
Potential Payments Upon Termination or Change in Control
Prior to our initial public offering, we maintained a long-term incentive compensation program (LTIP) that was intended to provide cash payments to certain of our executives, including Messrs. Jergensen, Sanford and Apt, in connection with a “qualifying sale” of our Company. A “qualifying sale” included a sale, whether through merger, consolidation, combination, the sale of all or substantially all of the Company’s assets, or otherwise, of the Company to a third party such that the then-current shareholders of the Company, as measured immediately prior to the closing of the transaction, sold at least 50% of the Company. Any cash payments that could have become payable pursuant to the LTIP would have been based on the participant’s individual participation percentage multiplied by the total net cash proceeds that we received in the qualifying sale. Because any potential payments under the LTIP to the participating executives in connection with a qualifying sale presumed to occur on December 31, 2023 would have been based on the total net cash proceeds received in the qualifying sale, such amounts are not quantifiable. We terminated the LTIP in connection with our IPO.
Other than as described above with respect to our LTIP, upon a termination of employment or a change in control, prior to the closing of our IPO, our named executive officers would not have been entitled to any payments or benefits other than those required by applicable law.
Executive Severance Plan
In connection with our IPO, we adopted the Executive Severance Plan. The Executive Severance Plan became effective upon the completion of our IPO, and will provide for the payment of certain cash severance and other benefits to participants, including each of our named executive officers, in the event of a qualifying termination of employment with us.
Under the Executive Severance Plan, in the event of a termination of the executive’s employment by us without cause or by the executive for good reason, in either case, outside of the 24-month period commencing on a change in control, the executive will be eligible to receive the following payments and benefits:
•cash payments equal to 100% of the executive’s then-current annual base salary, paid in substantially equal installments over the 12-month period following the termination date; and
•company-paid COBRA premium payments for the executive and the executive’s eligible dependents for up to 12 months.
In the event of a termination of the executive’s employment by us without cause or by the executive for good reason, in either case, within the 24-month period commencing on a change in control, the executive will be eligible to receive the following payments and benefits:
•cash payments equal to 200% of the executive’s then-current annual base salary, paid in substantially equal installments over the 24-month period following the termination date; and
147
•company-paid COBRA premium payments for the executive and the executive’s eligible dependents for up to 24 months.
An executive’s right to receive the severance payments and benefits described above is subject to the execution and, as applicable, non-revocation of a general release of claims in our favor, and continued compliance with any applicable restrictive covenants.
In addition, in the event that any payment under the Executive Severance Plan, together with any other amounts paid to the executive by us, would subject such executive to an excise tax under Section 4999 of the Internal Revenue Code, such payments will be reduced to the extent that such reduction would produce a better net after-tax result for the executive.
Equity Incentive Award Plans
The principal features of our 2024 Plan and ESPP are summarized below.
2024 Incentive Award Plan
In connection with our IPO, our board of directors adopted, and our stockholders approved, the 2024 Plan, under which we may grant cash and equity incentive awards to eligible service providers in order to attract, motivate and retain the talent for which we compete, subject to stockholder approval. The 2024 Plan became effective on the day prior to the Public Trading Date (as defined in the 2024 Plan). The material terms of the 2024 Plan are summarized below.
Eligibility and Administration. Our employees, consultants and directors and employees and consultants of our subsidiaries are eligible to receive awards under the 2024 Plan. The 2024 Plan is administered by our board of directors with respect to awards to non-employee directors and by our compensation committee with respect to other participants, each of which may delegate its duties and responsibilities to one or more committees of its directors and/or officers (referred to collectively as the plan administrator), subject to the limitations imposed under the 2024 Plan, Section 16 of the Exchange Act, and/or stock exchange rules and other applicable laws. The plan administrator has the authority to take all actions and make all determinations under the 2024 Plan, to interpret the 2024 Plan and award agreements and to adopt, amend and repeal rules for the administration of the 2024 Plan as it deems advisable. The plan administrator also has the authority to determine which eligible service providers receive awards, grant awards, and set the terms and conditions of all awards under the 2024 Plan, including any vesting and vesting acceleration provisions, subject to the conditions and limitations in the 2024 Plan.
Limitation on Awards and Shares Available. The initial aggregate number of shares of our common stock that was available for issuance under the 2024 Plan is equal to 15,391,579 shares. We believe the size of the initial share reserve was appropriate because historically we had not granted equity-based compensation and therefore granted sizable equity awards to certain of our employees in connection with our IPO. The size of those awards was intended, in part, to take into account the impact of the termination of the LTIP, and cancellation of each participant’s LTIP award, in connection with our IPO.
In addition, the number of shares of our common stock available for issuance under the 2024 Plan will be subject to an annual increase on the first day of each calendar year beginning on and including January 1, 2025 and ending on and including January 1, 2034, equal to (A) 2% of the aggregate number of shares of our common stock outstanding on the final day of the immediately preceding calendar year or (B) such smaller number of shares as is determined by our board of directors. The maximum number of shares that may be issued pursuant to the exercise of incentive stock options (ISOs) granted under the 2024 Plan is 50,000,000. Any shares issued pursuant to the 2024 Plan may consist, in whole or in part, of authorized and unissued common stock, treasury common stock or common stock purchased on the open market.
If an award under the 2024 Plan expires, lapses or is terminated, exchanged for, or settled in cash, any shares subject to such award (or portion thereof) may, to the extent of such expiration, lapse, termination, or cash
148
settlement, be used again for new grants under the 2024 Plan. Prior to the tenth anniversary of the effective date of the 2024 Plan, shares tendered or withheld to satisfy the exercise price or tax withholding obligation for any award will not reduce the shares available for grant under the 2024 Plan. Further, the payment of dividend equivalents in cash in conjunction with any awards under the 2024 Plan will not reduce the shares available for grant under the 2024 Plan. However, the following shares may not be used again for grant under the 2024 Plan: (i) shares subject to stock appreciation rights (SARs) that are not issued in connection with the stock settlement of the SAR on exercise, and (ii) shares purchased on the open market with the cash proceeds from the exercise of options.
Awards granted under the 2024 Plan upon the assumption of, or in substitution for, awards authorized or outstanding under a qualifying equity plan maintained by an entity with which we enter into a merger or similar corporate transaction will not reduce the shares available for grant under the 2024 Plan but will count against the maximum number of shares that may be issued upon the exercise of ISOs.
The 2024 Plan provides that the sum of any cash compensation and the aggregate grant date fair value (determined as of the date of the grant under Financial Accounting Standards Board Accounting Standards Codification Topic 718, or any successor thereto) of all awards granted to a non-employee director as compensation for services as a non-employee director during any fiscal year, or director limit, may not exceed an amount equal to $750,000 (increased to $1,000,000 in the calendar year of a non-employee director’s initial service as a non-employee director or any calendar year during which a non-employee director serves as lead independent director), which limits shall not apply to the compensation for any non-employee director who serves in any capacity in addition to that of a non-employee director for which he or she receives additional compensation or any compensation paid prior to the calendar year following the calendar year in which the 2024 Plan becomes effective.
Awards. The 2024 Plan provides for the grant of stock options, including ISOs and nonqualified stock options (NSOs), SARs, restricted stock, dividend equivalents, restricted stock units (RSUs), and other stock or cash based awards. Certain awards under the 2024 Plan may constitute or provide for payment of “nonqualified deferred compensation” under Section 409A of the Code, which may impose additional requirements on the terms and conditions of such awards. All awards under the 2024 Plan will be evidenced by award agreements, which will detail the terms and conditions of awards, including any applicable vesting and payment terms and post-termination exercise limitations. Awards other than cash awards generally will be settled in shares of our common stock, but the applicable award agreement may provide for cash settlement of any award. A brief description of each award type follows.
•Stock Options and SARs. Stock options provide for the purchase of shares of our common stock in the future at an exercise price set on the grant date. ISOs, in contrast to NSOs, may provide tax deferral beyond exercise and favorable capital gains tax treatment to their holders if certain holding period and other requirements of the Code are satisfied. SARs entitle their holder, upon exercise, to receive from us an amount equal to the appreciation of the shares subject to the award between the grant date and the exercise date. Unless otherwise determined by our board of directors, the exercise price of a stock option or SAR may not be less than 100% of the fair market value of the underlying share on the grant date (or 110% in the case of ISOs granted to certain significant stockholders), except with respect to certain substitute awards granted in connection with a corporate transaction. The term of a stock option or SAR may not be longer than ten years (or five years in the case of ISOs granted to certain significant stockholders). Conditions applicable to stock options and/or SARs may be based on continuing service, the attainment of performance goals and/or such other conditions as the plan administrator may determine.
•Restricted Stock and RSUs. Restricted stock is an award of nontransferable shares of our common stock that are subject to certain vesting conditions and other restrictions. RSUs are contractual promises to deliver shares of our common stock in the future, which may also remain forfeitable unless and until specified conditions are met and may be accompanied by the right to receive the equivalent value of dividends paid on shares of our common stock prior to the delivery of the underlying shares (i.e., dividend equivalent rights). The plan administrator may provide that the delivery of the shares underlying RSUs will be deferred on a mandatory basis or at the election of the participant. The terms and conditions applicable to RSUs will be determined by the plan administrator, subject to the conditions and limitations contained in
149
the 2024 Plan. Conditions applicable to restricted stock and RSUs may be based on continuing service, the attainment of performance goals and/or such other conditions as the plan administrator may determine.
•Other Stock or Cash Based Awards. Other stock or cash based awards are awards of cash, fully vested shares of our common stock and other awards valued wholly or partially by referring to, or otherwise based on, shares of our common stock. Other stock or cash based awards may be granted to participants and may also be available as a payment form in the settlement of other awards, as standalone payments and as payment in lieu of compensation to which a participant is otherwise entitled.
•Dividend Equivalents. Dividend equivalents represent the right to receive the equivalent value of dividends paid on shares of our common stock and may be granted alone or in tandem with awards other than stock options or SARs. Dividend equivalents are credited as of the dividend record dates during the period between the date an award is granted and the date such award vests, is exercised, is distributed, or expires, as determined by the plan administrator. Dividend equivalents payable with respect to an award prior to the vesting of such award instead will be paid out to the participant only to the extent that the vesting conditions are subsequently satisfied and the award vests.
Certain transactions. The plan administrator has broad discretion to act under the 2024 Plan, as well as make adjustments to the terms and conditions of existing and future awards, to prevent the dilution or enlargement of intended benefits and facilitate necessary or desirable changes in the event of certain transactions and events affecting our common stock, such as stock dividends, stock splits, mergers, acquisitions, consolidations and other corporate transactions. In addition, in the event of certain non-reciprocal transactions with our stockholders known as “equity restructurings,” the plan administrator will make equitable adjustments to the 2024 Plan and outstanding awards. In the event of a change in control (as defined in the 2024 Plan), to the extent that the surviving entity declines to continue, convert, assume, or replace outstanding awards, then all such awards will become fully vested and exercisable in connection with the transaction. Upon or in anticipation of a change in control, the plan administrator may cause any outstanding awards to terminate at a specified time in the future and give the participant the right to exercise such awards during a period of time determined by the plan administrator in its sole discretion. Individual award agreements may provide for additional accelerated vesting and payment provisions.
Repricing. Our board of directors may, without approval of the stockholders, reduce the exercise price of any stock option or SAR, or cancel any stock option or SAR in exchange for cash, other awards or stock options or SARs with an exercise price per share that is less than the exercise price per share of the original stock options or SARs.
Plan Amendment and Termination. Our board of directors may amend or terminate the 2024 Plan at any time; however, no amendment, other than an amendment that increases the number of shares available under the 2024 Plan, may materially and adversely affect an award outstanding under the 2024 Plan without the consent of the affected participant, and stockholder approval will be obtained for any amendment to the extent necessary to comply with applicable laws. Unless earlier terminated by our board of directors, the 2024 Plan will remain in effect until the tenth anniversary of the Public Trading Date. No awards may be granted under the 2024 Plan after its termination.
Foreign Participants, Claw-back Provisions, Transferability and Participant Payments. The plan administrator may modify award terms, establish subplans and/or adjust other terms and conditions of awards, subject to the share limits described above, in order to facilitate grants of awards subject to the laws and/or stock exchange rules of countries outside of the United States. All awards will be subject to any Company clawback policy as set forth in such clawback policy or the applicable award agreement. Awards under the 2024 Plan are generally non-transferrable, except by will or the laws of descent and distribution, or, subject to the plan administrator’s consent, pursuant to a domestic relations order, and are generally exercisable only by the participant. With regard to tax withholding, exercise price and purchase price obligations arising in connection with awards under the 2024 Plan, the plan administrator may, in its discretion, accept cash or check, shares of our common stock that meet specified conditions, a “market sell order” or such other consideration as it deems suitable.
150
2024 Employee Stock Purchase Plan
In connection with our IPO, our board of directors adopted, and our stockholders approved, the 2024 Employee Stock Purchase Plan (ESPP). The ESPP authorizes the grant of options to U.S. employees that are intended to qualify for favorable U.S. federal tax treatment under Section 423 of the Code. The material terms of the ESPP are summarized below.
Purpose of the ESPP. The purpose of the ESPP is to assist eligible employees of the Company and its participating subsidiaries in acquiring a stock ownership interest in the Company pursuant to a plan which is intended to qualify as an “employee stock purchase plan” within the meaning of Section 423(b) of the Code.
Eligibility and Administration. Unless otherwise determined by our board of directors, the compensation committee will administer and will have authority to interpret the terms of the ESPP and determine eligibility of participants. The plan administrator may designate certain of our subsidiaries as participating “designated subsidiaries” in the ESPP and may change these designations from time to time. Employees of the Company and its participating designated subsidiaries are eligible to participate in the ESPP if they meet the eligibility requirements under the ESPP established from time to time by the plan administrator. However, an employee may not be granted rights to purchase shares under the ESPP if such employee, immediately after the grant, would own (directly or through attribution) shares possessing 5% or more of the total combined voting power or value of all classes of common stock or other classes of shares.
If the grant of a purchase right under the ESPP to any eligible employee who is a citizen or resident of a foreign jurisdiction would be prohibited under the laws of such foreign jurisdiction or the grant of a purchase right to such employee in compliance with the laws of such foreign jurisdiction would cause the ESPP to violate the requirements of Section 423 of the Code, as determined by the plan administrator in its sole discretion, such employee will not be permitted to participate in the ESPP.
Eligible employees become participants in the ESPP by enrolling and authorizing payroll deductions by the deadline established by the plan administrator prior to the first day of the applicable offering period. Non-employee directors, as well as consultants, are not eligible to participate in the ESPP. Employees who choose not to participate, or are not eligible to participate at the start of an offering period but who become eligible thereafter, may enroll in any subsequent offering period.
Shares Available for Awards. The initial aggregate number of shares of our common stock that is available for issuance under the ESPP is equal to 1,501,520 shares. In addition, the number of shares of our common stock available for issuance under the ESPP will be annually increased on January 1 of each calendar year beginning in 2025 and ending in and including 2034 by an amount equal to (a) 1% of the shares outstanding on the final day of the immediately preceding calendar year or (b) such smaller number of shares as is determined by our board of directors. The maximum number of shares that may be issued pursuant to the ESPP is 20,000,000.
Any shares issued pursuant to the ESPP may consist, in whole or in part, of authorized and unissued common stock, treasury common stock or common stock purchased on the open market.
Participating in an Offering
Offering Periods and Purchase Periods. We intend for the ESPP to qualify under Section 423 of the Code and stock will be offered under the ESPP during offering periods. The length of the offering periods under the ESPP will be determined by the plan administrator and may be up to 27 months long. Employee payroll deductions will be used to purchase shares on each purchase date during an offering period. The number of purchase periods within, and purchase dates during, each offering period will be established by the plan administrator. Offering periods under the ESPP will commence when determined by the plan administrator. The plan administrator may, in its discretion, modify the terms of future offering periods.
151
Enrollment and Contributions. The ESPP permits participants to purchase shares through payroll deductions of up to a specified percentage of their eligible compensation (which, in the absence of a contrary designation, shall be 15% of eligible compensation), which will include a participant’s gross base compensation for services to us, including overtime payments, periodic bonuses and commissions, and excluding one-time bonuses, expense reimbursements, fringe benefits and other special payments. The plan administrator will establish a maximum number of shares that may be purchased by a participant during any offering period or purchase period, which, in the absence of a contrary designation, will be 5,000 shares for an offering period and/or a purchase period. In addition, no employee will be permitted to accrue the right to purchase stock under the ESPP at a rate in excess of $25,000 worth of shares during any calendar year during which such a purchase right is outstanding (based on the fair market value per share of common stock as of the first day of the offering period).
Purchase Rights. On the first trading day of each offering period, each participant will automatically be granted an option to purchase shares of common stock. The option will be exercised on the applicable purchase date(s) during the offering period to the extent of the payroll deductions accumulated during the offering period. Any remaining balance shall be carried forward to the next offering period unless the participant has elected to withdraw from the plan, as described below, or has ceased to be an eligible employee.
Purchase Price. The purchase price of the shares, in the absence of a contrary designation by the plan administrator, will be 85% of the lower of the fair market value of common stock on the first trading day of the offering period or the applicable purchase date, which will be the final trading day of the applicable purchase period.
Withdrawal and Termination of Employment. Participants may voluntarily end their participation in the ESPP at any time during an offering period by giving written notice to the Company no later than one week prior to the end of the offering period (or such longer or shorter period specified by the plan administrator), and will be paid their accrued payroll deductions that have not yet been used to purchase shares of common stock. Participation in the ESPP ends automatically upon a participant’s termination of employment.
Certain Transactions. In the event of certain transactions or events affecting common stock, such as any stock dividend or other distribution, change in control, reorganization, merger, consolidation or other corporate transaction, the ESPP plan administrator will make equitable adjustments to the ESPP and outstanding rights. In addition, in the event of the foregoing transactions or events or certain significant transactions, including a change in control, the plan administrator may provide for (i) either the replacement of outstanding rights with other rights or property or termination of outstanding rights in exchange for cash, (ii) the assumption or substitution of outstanding rights by the successor or survivor corporation or parent or subsidiary thereof, (iii) the adjustment in the number and type of shares of stock subject to outstanding rights, (iv) the use of participants’ accumulated payroll deductions to purchase stock on a new purchase date prior to the next scheduled purchase date and termination of any rights under ongoing offering periods or (v) the termination of all outstanding rights. Under the ESPP, a change in control has the same definition as given to such term in the 2024 Plan.
Foreign Participants. The plan administrator may provide special terms, establish supplements to, or amendments, restatements or alternative versions of the ESPP, subject to the share limits described above, in order to facilitate grants of awards subject to the laws and/or stock exchange rules of countries outside of the United States.
Transferability. A participant may not transfer rights granted under the ESPP other than by will or the laws of descent and distribution, and such rights are generally exercisable only by the participant.
Plan Amendment and Termination. The plan administrator may amend, suspend or terminate the ESPP at any time. However, stockholder approval will be obtained for any amendment that increases the aggregate number or changes the type of shares that may be sold pursuant to rights under the ESPP or changes the ESPP in any way that would be considered to be the adoption of a new plan within the meaning of Treasury Regulation Section 1.423-2(c)(4) or cause the ESPP to no longer be an employee stock purchase plan within the meaning of Section 423(b) of the Code.
152
DIRECTOR COMPENSATION
The following table sets forth information for the year ended December 31, 2023 regarding the compensation awarded to, earned by or paid to our non-employee directors who served on our board of directors during 2023. Ms. Millard and Mr. Leavitt joined our board of directors on July 1, 2023; prior to that time, our board of directors consisted only of Messrs. Murray and Hancock. Messrs. Murray and Hancock do not receive any additional compensation for their board service and therefore are not included in the Director Compensation table below. All compensation paid to Messrs. Murray and Hancock is reported above in the “2023 Summary Compensation Table.”
| Name | Fees Earned or Paid in Cash ($)(1) | Total ($) | ||||||||||||
| Jacqueline Millard | 250,000 | 250,000 | ||||||||||||
| Taylor Leavitt | 250,000 | 250,000 | ||||||||||||
__________________
(1)Amounts reflect fees paid to each of Mses. Millard and Leavitt pursuant to an initial board retainer fee of $125,000 in connection with their appointment to our board of directors, as well as quarterly fees of $62,500. Our non-employee directors were not granted any equity awards in 2023 nor do they hold any outstanding equity awards as of December 31, 2023.
Post-IPO Director Compensation Program
In connection with our IPO, our board of directors adopted, and our stockholders approved, a compensation program (Director Compensation Program), which became effective upon the closing of our IPO. The Director Compensation Program provides for annual retainer fees and equity awards for our non-employee directors, who we refer to as eligible directors. The material terms of the Director Compensation Program are summarized below.
The Director Compensation Program consists of the following components:
Cash Compensation
•Annual Retainer: $80,000
◦Annual Committee Chair Retainers:
–Audit Chair: $25,000
–Compensation Chair: $17,500
–Nominating and Governance Chair: $15,000
◦Annual Committee Member Retainers:
–Audit Member: $12,500
–Compensation Member: $8,750
–Nominating and Governance Member: $7,500
Annual cash retainers will be paid in quarterly installments in arrears and will be pro-rated for any partial calendar quarter of service.
153
Equity Compensation
Each eligible director who is initially elected or appointed to serve on our Board automatically shall be granted, on the date on which such eligible director is appointed or elected to serve on the Board, a restricted stock unit award with an aggregate value of $160,000, pro-rated to reflect the partial period serving on our Board until the next occurring annual meeting. An eligible director who is serving on our board of directors as of the date of the annual meeting of our stockholders each calendar year (beginning with calendar year 2025) will be granted, on such annual meeting date, a restricted stock unit award with a value of approximately $160,000. Each initial grant and annual grant will vest in full on the earlier to occur of (i) the first anniversary of the applicable grant date and (ii) the date of the next annual meeting following the grant date, subject to such eligible director’s continued service through the applicable vesting date.
In addition, each initial award and annual award will vest in full upon a change in control of us (as defined in the 2024 Plan) if the eligible director will not become a member of our board or our ultimate parent as of immediately following such change in control.
154
CERTAIN RELATIONSHIPS AND RELATED PARTY TRANSACTIONS
In addition to the equity and other compensation and other arrangements discussed in the section titled “Compensation Discussion and Analysis,” the following is a description of each transaction since January 1, 2021 and each currently proposed transaction which:
•we have been or are to be a participant;
•the amount involved exceeded or will exceed $120,000; and
•any of our directors, executive officers or, to our knowledge, beneficial owners of more than 5% of our capital stock or any member of the immediate family of any of the foregoing persons had or will have a direct or indirect material interest.
Related Party Agreement in Effect Prior to our IPO
Helios Consulting Agreement
On July 1, 2021, we entered into a Consulting and Strategic Advisory Services Agreement with Helios Consulting, LLC (Helios), a limited liability company owned and operated by Jason Murray, our Co-Founder, Chief Executive Officer, Chairman and a member of our board of directors, and Mark Hancock, our Executive Vice Chairman and a member of our board of directors (Helios Consulting Agreement), pursuant to which we paid Helios consulting fees for services provided by Messrs. Murray and Hancock. The Helios Consulting Agreement provided for a cash consulting fee of approximately $4 million annually, paid in monthly installments, for consulting and strategic advisory services provided to us by Helios. For the years ended December 31, 2023, 2022 and 2021, we paid approximately $4.0 million, $4.0 million, and $2.3 million (inclusive of approximately $150,000 paid to a subsidiary of Helios), respectively. On December 31, 2023, we terminated the Helios Consulting Agreement.
Subscription Agreements
On March 24, 2023, we entered into subscription agreements with Messrs. Murray and Hancock, pursuant to which Messrs. Murray and Hancock each purchased 64,361,693 shares of our common stock for a purchase price of $10.00, or $0.001 per share, in a private placement concurrent with our incorporation in the State of Delaware and in anticipation of effecting our reorganization on June 30, 2023.
Stockholders Agreement
On April 10, 2024, we entered into a stockholders agreement (Stockholders Agreement) with Messrs. Murray and Hancock. The Stockholders Agreement affirms the board designation rights granted to each of Messrs. Murray and Hancock pursuant to our Amended and Restated Charter, subject to certain limitations and exceptions. Pursuant to the terms of our Amended and Restated Charter and the Stockholders Agreement, we agree to include in our slate of director nominees certain individuals designated by each of Messrs. Murray and Hancock:
•Mr. Murray has the right, but not the obligation, to designate (i) up to two individuals for inclusion in our slate of director nominees if he beneficially owns at least 20% of the aggregate number of shares of common stock outstanding immediately following the completion of our IPO or (ii) one individual for inclusion in our slate of director nominees if he beneficially owns less than 20% but at least 10% of the aggregate number of shares of common stock outstanding immediately following the completion of our IPO.
•Mr. Hancock has the right, but not the obligation, to designate (i) up to two individuals for inclusion in our slate of director nominees if he beneficially owns at least 20% of the aggregate number of shares of common stock outstanding immediately following the completion of our IPO or (ii) one individual for inclusion in our slate of director nominees if he beneficially owns less than 20% but at least 10% of the
155
aggregate number of shares of common stock outstanding immediately following the completion of our IPO.
Accordingly, Messrs. Murray and Hancock each have the right to designate two directors for nomination to our board of directors, and collectively have the right to designate four directors, which represents four out of our current five member board of directors. Subject to certain limitations, each of Messrs. Murray and Hancock also have the right to replace their respective designees and fill any vacancies created by reason of death, resignation, disqualification or removal of their respective designees. If the number of individuals that Messrs. Murray and Hancock have the right to designate is decreased because of a decrease in their respective ownership or upon termination of the Stockholders Agreement, then the corresponding designee (if such designee is serving on our board of directors) may remain on our board of directors through the end of his or her then current term; provided, that a director may resign at any time regardless of the period of time left in his or her then current term.
Pursuant to the Stockholders Agreement, each of Messrs. Murray and Hancock also agree to vote, or cause to vote, all of their outstanding shares of our common stock at any annual or special meeting of stockholders in which directors are elected, so as to cause the election of their respective designees, in each case to the extent that each or any of Messrs. Murray and Hancock have exercised their right to designate individuals for nomination to the board of directors.
Each of Messrs. Murray and Hancock has entered into a margin loan, pursuant to which they have pledged a portion of their respective shares of our common stock as collateral to secure such margin loan. Each of Messrs. Murray and Hancock retains their ability to vote the shares of our common stock pledged as collateral and such pledged shares do not impact their beneficial ownership for purposes of the rights under the Stockholders Agreement or otherwise in connection with matters to be voted on by stockholders. Pursuant to Rule 13d-3(d)(3) under the Exchange Act, a margin loan lender would not beneficially own the pledged shares unless and until such lender has taken all formal steps necessary which are required to declare a default and determines that the power to vote or to direct the vote or to dispose or to direct the disposition of pledged securities will be exercised.
The Stockholders Agreement will terminate upon the earlier of (i) a change in control or (ii) written agreement of each of Messrs. Murray and Hancock. Following the termination of the Stockholders Agreement, the designation rights granted to each of Messrs. Murray and Hancock pursuant to our Amended and Restated Charter will no longer be exercisable. See the sections titled “Management—Amended and Restated Charter and Stockholders Agreement,” “Description of Capital Stock—Designation Rights” and “Description of Capital Stock—Anti-Takeover Effects of Provisions of the General Corporation Law of the State of Delaware and our Amended and Restated Charter and Amended and Restated Bylaws” for additional information.
Registration Rights Agreement
On April 10, 2024, we entered into a registration rights agreement (Registration Rights Agreement) with Messrs. Murray and Hancock. The Registration Rights Agreement provides Messrs. Murray and Hancock, under certain circumstances and subject to certain restrictions, with certain rights with respect to the registration of their shares of common stock under the Securities Act, including customary demand and piggyback registration rights. For a description of these registration rights, see “Description of Capital Stock—Registration Rights.”
Lease Guarantees
Certain of our operating leases for our facilities include personal guarantees by Messrs. Murray and Hancock and their respective spouses. We will agree to indemnify Messrs. Murray and Hancock and their respective spouses on account of any damage, loss and/or expense that they may incur in connection with the obligations made by them in respect of these lease guarantees.
156
Company Pledge Acknowledgments and Consents
Mr. Murray has entered into a margin loan with UBS AG Stamford Branch (“UBS”), as agent, and certain lenders party thereto, pursuant to which he has pledged 9,500,000 shares of common stock as collateral to secure such margin loan. In connection with this margin loan, we executed a pledge acknowledgement and consent together with UBS, certain lenders party thereto and Mr. Murray, in which we, among other matters, provided for certain confirmations and agreements relating to the enforcement of the rights and remedies under the margin loan documents.
Mr. Hancock has entered into a margin loan with UBS, as agent, and certain lenders party thereto, pursuant to which he has pledged 9,500,000 shares of common stock as collateral to secure such margin loan. In connection with this margin loan, we executed a pledge acknowledgement and consent together with UBS, certain lenders party thereto and Mr. Hancock, in which we, among other matters, provided for certain confirmations and agreements relating to the enforcement of the rights and remedies under the margin loan documents.
Director and Officer Indemnification and Insurance
We entered into separate indemnification agreements with each of our directors and executive officers. We have also purchased directors’ and officers’ liability insurance. See the section titled “Description of Capital Stock—Limitations on Liability and Indemnification of Officers and Directors.”
Policies and Procedures for Related Party Transactions
Our board of directors adopted a written related party transaction policy setting forth the policies and procedures for the review and approval or ratification of related party transactions. This policy will cover, with certain exceptions set forth in Item 404 of Regulation S-K under the Securities Act, any transaction, arrangement or relationship, or any series of similar transactions, arrangements or relationships in which we were or are to be a participant, where the amount involved exceeds $120,000 and a related party had or will have a direct or indirect material interest, including without limitation purchases of goods or services by or from the related party or entities in which the related party has a material interest, indebtedness, guarantees of indebtedness and employment by us of a related party. In reviewing and approving any such transactions, our audit committee is tasked to consider all relevant facts and circumstances, including but not limited to whether the transaction is on terms comparable to those that could be obtained in an arm’s length transaction with an unrelated third-party and the extent of the related party’s interest in the transaction. All of the transactions described in this section occurred prior to the adoption of this policy.
157
PRINCIPAL AND SELLING STOCKHOLDERS
The following table sets forth information with respect to the beneficial ownership of our common stock as of August 9, 2024, and as adjusted to reflect the sale of common stock offered by us in this offering, by:
•each of our directors;
•each of our named executive officers;
•all of our directors and executive officers as a group; and
•each person or group of affiliated persons known by us to beneficially own more than 5% of our outstanding shares of common stock.
The number of shares beneficially owned by each stockholder is determined under rules issued by the SEC. Under these rules, a person is deemed to be a “beneficial” owner of a security if that person has or shares voting power or investment power, which includes the power to dispose of or to direct the disposition of such security. Except as indicated in the footnotes below, we believe, based on the information furnished to us, that the individuals and entities named in the table below have sole voting and investment power with respect to all shares beneficially owned by them, subject to any applicable community property laws.
We have based percentage ownership of our common stock before this offering on 152,399,733 shares of our common stock outstanding as of August 9, 2024. The percentage ownership of our common stock after this offering also assumes the foregoing and the issuance and sale of 2,777,778 shares of common stock by us in this offering, and is presented assuming both no exercise and full exercise of the underwriters’ option to purchase 2,083,332 additional shares from the selling stockholders.
Each of the stockholders listed has sole voting and investment power with respect to the shares beneficially owned by the stockholder unless noted otherwise, subject to community property laws where applicable. Unless otherwise indicated, the address of each beneficial owner in the table below is c/o PACS Group, Inc., 262 N. University Ave., Farmington, Utah 84025.
| Beneficial Ownership Before the Offering | Shares Being Sold in This Offering | Beneficial Ownership After the Offering Assuming no Exercise of Underwriters’ Option | Beneficial Ownership After the Offering Assuming Full Exercise of Underwriters’ Option | |||||||||||||||||||||||||||||||||||||||||||||||
| Name of Beneficial Owner | Number of Shares | Percentage of Shares | No Exercise of Underwriters’ Options | Full Exercise of Underwriters’ Options | Number of Shares | Percentage of Shares | Number of Shares | Percentage of Shares | ||||||||||||||||||||||||||||||||||||||||||
Named Executive Officers and Directors: | ||||||||||||||||||||||||||||||||||||||||||||||||||
Jason Murray(1) | 62,754,551 | 41.2 | % | 5,555,556 | 6,597,222 | 57,198,995 | 36.9 | % | 56,157,329 | 36.2 | % | |||||||||||||||||||||||||||||||||||||||
Mark Hancock(2) | 62,754,551 | 41.2 | % | 5,555,556 | 6,597,222 | 57,198,995 | 36.9 | % | 56,157,329 | 36.2 | % | |||||||||||||||||||||||||||||||||||||||
| Peter (P.J.) Sanford | 227,656 | * | — | — | 227,656 | * | 227,656 | * | ||||||||||||||||||||||||||||||||||||||||||
| Josh Jergensen | 455,319 | * | — | — | 455,319 | * | 455,319 | * | ||||||||||||||||||||||||||||||||||||||||||
| Derick Apt | 199,209 | * | — | — | 199,209 | * | 199,209 | * | ||||||||||||||||||||||||||||||||||||||||||
| Jacqueline Millard | 433 | * | — | — | 433 | * | 433 | * | ||||||||||||||||||||||||||||||||||||||||||
| Taylor Leavitt | — | * | — | — | — | * | — | * | ||||||||||||||||||||||||||||||||||||||||||
| Evelyn Dilsaver | — | * | — | — | — | * | — | * | ||||||||||||||||||||||||||||||||||||||||||
| All Executive Officers and Directors as a Group (11 individuals) | 126,726,923 | 83.2 | % | 11,111,112 | 13,194,444 | 115,615,811 | 74.5 | % | 113,532,479 | 73.2 | % | |||||||||||||||||||||||||||||||||||||||
__________________
— None
*Less than 1%.
158
(1) Mr. Murray has pledged 9,500,000 shares of common stock beneficially owned by him pursuant to a margin loan and related pledge and security agreement with customary default provisions as security in favor of UBS AG Stamford Branch and certain lenders party thereto. See “Certain Relationships and Related Party Transactions—Company Pledge Acknowledgments and Consents.”
(2) Mr. Hancock has pledged 9,500,000 shares of common stock beneficially owned by him pursuant to a margin loan and related pledge and security agreement with customary default provisions as security in favor of UBS AG Stamford Branch and certain lenders party thereto. See “Certain Relationships and Related Party Transactions—Company Pledge Acknowledgments and Consents.”
159
DESCRIPTION OF CAPITAL STOCK
The following summary describes our capital stock and the material provisions of our Amended and Restated Charter and our Amended and Restated Bylaws. The following is a summary and is qualified by reference to the Amended and Restated Charter and the Amended and Restated Bylaws currently in effect. Copies of these documents will be filed with the SEC as exhibits to our registration statement, of which this prospectus forms a part.
General
Our authorized capital stock will consist of 1,250,000,000 shares of common stock, par value $0.001 per share, and 50,000,000 shares of preferred stock, par value $0.001 per share, the rights and preferences of which our board of directors may establish from time to time. As of June 30, 2024, there were 152,399,733 shares of our common stock outstanding and no shares of our preferred stock outstanding.
Common Stock
Dividend Rights
Holders of shares of our common stock are entitled to receive dividends when, as and if declared by our board of directors out of funds legally available therefor, subject to any statutory or contractual restrictions on the payment of dividends and to any restrictions on the payment of dividends imposed by the terms of any outstanding stock. Under Delaware law, we can only pay dividends either out of “surplus” or out of the current or the immediately preceding year’s net profits. Surplus is defined as the excess, if any, at any given time, of the total assets of a corporation over its total liabilities and statutory capital. The value of a corporation’s assets can be measured in a number of ways and may not necessarily equal their book value.
See the section titled “Dividend Policy” for additional information.
Voting Rights
Holders of our common stock are entitled to one vote for each share held on all matters submitted to a vote of stockholders. The holders of our common stock vote together as a single class, unless otherwise required by law. The holders of our common stock do not have cumulative voting rights in the election of directors.
Our Amended and Restated Bylaws provides for a classified board of directors consisting of three classes of approximately equal size, each serving staggered three-year terms. If the number of directors is changed, any increase or decrease shall be apportioned among the classes by the board of directors so as to maintain the number of directors in each class as nearly equal as possible, and any additional director of any class elected to fill a vacancy resulting from an increase in such class shall hold office for a term that shall coincide with the remaining term of that class. In no case will a decrease in the number of directors shorten the term of any incumbent director.
No Preemptive or Similar Rights
Our common stock is not entitled to preemptive rights, and is not subject to conversion, redemption, or sinking fund provisions.
Right to Receive Liquidation Distributions
If we become subject to a liquidation, dissolution, or winding-up, the assets legally available for distribution to our stockholders would be distributable ratably among the holders of our common stock and any participating preferred stock outstanding at that time, subject to prior satisfaction of all outstanding debt and liabilities and the preferential rights of and the payment of liquidation preferences, if any, on any outstanding shares of preferred stock.
160
Fully Paid and Non-Assessable
All shares of our common stock that will be outstanding upon the completion of this offering will be fully paid and non-assessable.
Preferred Stock
Our Amended and Restated Charter authorizes our board of directors to establish one or more series of preferred stock. Unless required by law or any stock exchange, the authorized shares of preferred stock will be available for issuance without further action by the holders of our common stock. Our board of directors is able to determine, without stockholder approval and with respect to any series of preferred stock, the powers (including voting powers), preferences and relative, participating, optional, or other special rights, and the qualifications, limitations, or restrictions thereof, including, without limitation:
•the designation of the series;
•the number of shares of the series, which our board of directors may, except where otherwise provided in the preferred stock designation, increase (but not above the total number of authorized shares of the class) or decrease (but not below the number of shares then outstanding);
•whether dividends, if any, will be cumulative or non-cumulative and the dividend rate of the series;
•the dates at which dividends, if any, will be payable;
•the redemption or repurchase rights and price or prices, if any, for shares of the series;
•the terms and amounts of any sinking fund provided for the purchase or redemption of shares of the series;
•the amounts payable on shares of the series in the event of any voluntary or involuntary liquidation, dissolution, or winding-up of our affairs;
•whether the shares of the series will be convertible into shares of any other class or series, or any other security, of us or any other entity, and, if so, the specification of the other class or series or other security, the conversion price or prices, or rate or rates, any rate adjustments, the date or dates as of which the shares will be convertible and all other terms and conditions upon which the conversion may be made;
•restrictions on the issuance of shares of the same series or of any other class or series;
•whether the shares of the series will have board representation rights; and
•the voting rights, if any, of the holders of the series.
We could issue a series of preferred stock that could, depending on the terms of the series, impede or discourage an acquisition attempt or other transaction that some, or a majority, of the holders of our common stock might believe to be in their best interests or in which the holders of our common stock might receive a premium over the market price of the shares of our common stock. Additionally, the issuance of preferred stock may adversely affect the rights of holders of our common stock by restricting dividends on the common stock, diluting the voting power of the common stock or subordinating the liquidation rights of the common stock, or adding directors appointed by the holders of such preferred stock. As a result of these or other factors, the issuance of preferred stock could have an adverse impact on the market price of our common stock and on the rights of holders of common stock to influence corporate matters. We have no current plan for the issuance of any shares of preferred stock.
161
Registration Rights
In connection with our IPO, we, Jason Murray and Mark Hancock entered into the Registration Rights Agreement, pursuant to which Messrs. Murray and Hancock have registration rights. Registration of these shares under the Securities Act would result in these shares becoming fully tradable without restriction under the Securities Act immediately upon the effectiveness of the registration, except for shares purchased by affiliates. Shares covered by a registration statement will be eligible for sale in the public market upon the expiration or release from the terms of the lock-up agreement. Under the Registration Rights Agreement, we are generally required to pay all expenses (other than underwriting discounts and commissions and certain other expenses) related to any registration, whether or not such registration becomes effective or this offering is consummated. The Registration Rights Agreement also contains customary indemnification and procedural terms.
Demand Registration Rights
Following the completion of this offering (assuming no exercise of the underwriters’ option to purchase additional shares from the selling stockholders), Messrs. Murray and Hancock will hold an aggregate of 114,397,990 shares of our common stock, which together represents 73.7% of our outstanding shares of common stock after this offering, and will be entitled to certain demand registration rights.
The foregoing demand registration rights are subject to a number of exceptions and limitations.
Piggyback Registration Rights
In the event that we propose to register any of our securities under the Securities Act, either for our own account or for the account of other stockholders, Messrs. Murray and Hancock will be entitled to certain “piggyback” registration rights, entitling them to notice of the registration and allowing them to include their registrable securities in such registration. These rights will apply whenever we propose to file a registration statement under the Securities Act other than with respect to (1) a registration related to the sale of securities to employees pursuant to a stock option, stock purchase or similar plan or (2) a registration relating to a corporate reorganization or other transaction covered by Rule 145 promulgated under the Securities Act.
Designation Rights
Our Amended and Restated Charter grants Messrs. Murray and Hancock board designation rights. Mr. Murray has the right, but not the obligation, to designate (i) up to two individuals for inclusion in our slate of director nominees if he beneficially owns at least 20% of the aggregate number of shares of common stock outstanding immediately following the completion of our IPO or (ii) one individual for inclusion in our slate of director nominees if he beneficially owns less than 20% but at least 10% of the aggregate number of shares of common stock outstanding immediately following the completion of our IPO. Mr. Hancock has the right, but not the obligation, to designate (i) up to two individuals for inclusion in our slate of director nominees if he beneficially owns at least 20% of the aggregate number of shares of common stock outstanding immediately following the completion of our IPO or (ii) one individual for inclusion in our slate of director nominees if he beneficially owns less than 20% but at least 10% of the aggregate number of shares of common stock outstanding immediately following the completion of our IPO.
Each of Messrs. Murray and Hancock also have the right to fill any vacancies created by reason of death, resignation, disqualification or removal of their respective designees. These rights are also affirmed in the Stockholders Agreement that we entered into with Messrs. Murray and Hancock, and these rights will terminate upon the termination of the Stockholders Agreement. See “Certain Relationships and Related Party Transactions—Stockholders Agreement” for more information. If the number of individuals that Messrs. Murray and Hancock have the right to designate is decreased because of a decrease in their respective ownership or upon termination of the Stockholders Agreement, then the corresponding designee (if such designee is serving on our board of directors) may remain on our board of directors through the end of his or her then current term; provided, that a director may resign at any time regardless of the period of time left in his or her then current term.
162
As a result, Messrs. Murray and Hancock will each have the right to designate two directors for nomination to our board of directors, and will collectively have the right to designate four directors, which represents four out of our current five member board of directors.
Anti-Takeover Effects of Provisions of the General Corporation Law of the State of Delaware and our Amended and Restated Charter and Amended and Restated Bylaws
Certain provisions of the General Corporation Law of the State of Delaware (DGCL) and our Amended and Restated Charter and our Amended and Restated Bylaws contain provisions that could make the following transactions more difficult: e.g., acquisition of us by means of a tender offer; acquisition of us by means of a proxy contest or otherwise; or removal of our incumbent officers and directors. It is possible that these provisions could make it more difficult to accomplish or could deter transactions that stockholders may otherwise consider to be in their best interest or in our best interests, including transactions that might result in a premium over the market price for our shares.
These provisions, summarized below, are expected to discourage coercive takeover practices and inadequate takeover bids. These provisions are also designed to encourage persons seeking to acquire control of us to first negotiate with our board of directors. We believe that the benefits of increased protection of our potential ability to negotiate with the proponent of an unfriendly or unsolicited proposal to acquire or restructure us outweigh the disadvantages of discouraging these proposals because negotiation of these proposals could result in an improvement of their terms.
Delaware Anti-Takeover Statute
We are subject to Section 203 of the DGCL, which prohibits persons deemed “interested stockholders” from engaging in a “business combination” with a publicly held Delaware corporation for three years following the date these persons become interested stockholders unless the business combination is, or the transaction in which the person became an interested stockholder was, approved in a prescribed manner or another prescribed exception applies. Generally, an “interested stockholder” is a person who, together with affiliates and associates, owns, or within three years prior to the determination of interested stockholder status did own, 15% or more of a corporation’s voting stock. Generally, a “business combination” includes a merger, asset or stock sale, or other transaction resulting in a financial benefit to the interested stockholder. The existence of this provision may have an anti-takeover effect with respect to transactions not approved in advance by the board of directors, such as discouraging takeover attempts that might result in a premium over the market price of our common stock.
Authorized but Unissued Shares of Common Stock
The authorized but unissued shares of our common stock are available for future issuance without stockholder approval, subject to any limitations imposed by the listing standards of the New York Stock Exchange. These additional shares may be utilized for a variety of corporate purposes, including future public offerings to raise additional capital, acquisitions and employee benefit plans. The existence of authorized but unissued and unreserved common stock could make it more difficult or discourage an attempt to obtain control of us by means of a proxy contest, tender offer, merger or otherwise and may have the effect of deterring hostile takeovers or delaying changes in control or management of our company.
Undesignated Preferred Stock
The ability of our board of directors, without further action by our stockholders, to authorize undesignated preferred stock will make it possible for our board of directors to issue preferred stock with voting or other rights or preferences that could impede the success of any attempt to effect a change in control of our company. These and other provisions may have the effect of deterring hostile takeovers or delaying changes in control or management of our company.
163
Special Stockholder Meetings
Our Amended and Restated Charter provides that a special meeting of stockholders may be called at any time by our board of directors, the chairperson of our board of directors, our Chief Executive Officer or our Executive Vice Chairman, but such special meetings may not be called by the stockholders or any other person or persons.
Requirements for Advance Notification of Stockholder Nominations and Proposals
Our Amended and Restated Bylaws establishes advance notice procedures with respect to stockholder proposals and the nomination of candidates for election as directors, other than nominations made by or at the direction of the board of directors or a committee of the board of directors.
Stockholder Action by Written Consent
Our Amended and Restated Charter provides that, at any time when Messrs. Murray and Hancock beneficially own, in the aggregate, at least a majority of the voting power of our outstanding shares of voting stock, our stockholders may take action by written consent without a meeting, and at any time when Messrs. Murray and Hancock beneficially own, in the aggregate, less than the majority of the voting power of our outstanding shares of voting stock, our stockholders may not take action by written consent and may only take action at a meeting of stockholders.
Classified Board; Election and Removal of Directors; Filling Vacancies
Our board of directors is divided into three classes, divided as nearly as equal in number as possible. The directors in each class will serve for a three-year term, one class being elected each year by our stockholders, with staggered three-year terms. Only one class of directors will be elected at each annual meeting of our stockholders, with the other classes continuing for the remainder of their respective three-year terms. See the section titled “Management—Board Composition” for more information on the classified board. Our Amended and Restated Charter provides for the removal of any of our directors at any time with or without cause by the affirmative vote of the holders of a majority of the voting power of the then outstanding shares of our voting stock entitled to vote thereon; provided, however, that at any time when Messrs. Murray and Hancock beneficially own, in the aggregate, less than the majority of the voting power of our outstanding shares of voting stock, directors may be removed only for cause and only by the affirmative vote of the holders of at least 66 2/3% of the voting power of the then outstanding shares of our voting stock entitled to vote thereon. Furthermore, subject to the rights of the holders of any series of preferred stock to elect directors and rights granted to Messrs. Murray and Hancock pursuant to the Amended and Restated Charter and the Stockholders Agreement, any vacancy on our board of directors, however occurring, including a vacancy resulting from an increase in the size of the board, may only be filled by a resolution of the board of directors. This system of electing and removing directors and filling vacancies may tend to discourage a third-party from making a tender offer or otherwise attempting to obtain control of us because it generally makes it more difficult for stockholders to replace a majority of the directors.
Choice of Forum
Our Amended and Restated Charter provides that, unless we consent in writing to the selection of an alternative forum, the Court of Chancery of the State of Delaware will be the exclusive forum for the following types of actions or proceedings under Delaware statutory or common law: any derivative action or proceeding brought on our behalf; any action asserting a claim of breach of fiduciary duty owed by any of our directors, officers or stockholders to us or to our stockholders; any action asserting a claim against us arising pursuant to the DGCL, our Amended and Restated Charter or our Amended and Restated Bylaws (as either may be amended from time to time); or any action asserting a claim against us that is governed by the internal affairs doctrine. As a result, any action brought by any of our stockholders with regard to any of these matters will need to be filed in the Court of Chancery of the State of Delaware and cannot be filed in any other jurisdiction; provided that, if and only if the Court of Chancery of the State of Delaware dismisses any such action for lack of subject matter jurisdiction, such action may be brought in another state or federal court sitting in the State of Delaware.
164
Our Amended and Restated Charter also provides that the federal district courts of the United States of America is the exclusive forum for the resolution of any complaint asserting a cause or causes of action under the Securities Act, including all causes of action asserted against any defendant to such complaint. The choice of forum provisions will not apply to suits brought to enforce any liability or duty created by the Exchange Act or any other claim for which the federal courts have exclusive jurisdiction.
If any action the subject matter of which is within the scope described above is filed in a court other than a court located within the State of Delaware, or a foreign action, in the name of any stockholder, such stockholder shall be deemed to have consented to the personal jurisdiction of the state and federal courts located within the State of Delaware in connection with any action brought in any such court to enforce the applicable provisions of our Amended and Restated Charter and having service of process made upon such stockholder in any such action by service upon such stockholder’s counsel in the foreign action as agent for such stockholder. Section 22 of the Securities Act creates concurrent jurisdiction for federal and state courts over all suits brought to enforce any duty or liability created by the Securities Act or the rules and regulations thereunder. As a result, both state and federal courts have jurisdiction to entertain such Securities Act claims. To prevent having to litigate claims in multiple jurisdictions and the threat of inconsistent or contrary rulings by different courts, among other considerations, our Amended and Restated Charter will contain the choice of forum provision described above. Our decision to adopt a such a provision follows a decision by the Supreme Court of the State of Delaware holding that such provisions are facially valid under the DGCL; however, there is uncertainty as to whether a federal court or state court would enforce such a provision, and investors cannot waive compliance with federal securities laws and the rules and regulations thereunder.
Accordingly, although our Amended and Restated Charter contains the choice of forum provision described above, it is possible that a court could find that such a provision is inapplicable for a particular claim or action or that such provision is unenforceable.
This choice of forum provision may limit a stockholder’s ability to bring a claim in a judicial forum that it finds favorable for disputes with us or any of our directors, officers, other employees or stockholders, which may discourage lawsuits with respect to such claims and may result in increased costs for stockholders to bring a claim, although our stockholders will not be deemed to have waived our compliance with federal securities laws and the rules and regulations thereunder.
Amendment of Charter Provisions
The amendment of any of the above provisions in our Amended and Restated Charter requires approval by a stockholder vote by the holders of at least a 66 2/3% of the voting power of the then outstanding voting stock.
The provisions of the DGCL, our Amended and Restated Charter, and our Amended and Restated Bylaws could have the effect of discouraging others from attempting hostile takeovers and, as a consequence, they may also inhibit temporary fluctuations in the market price of our common stock that often result from actual or rumored hostile takeover attempts. These provisions may also have the effect of preventing changes in our management. It is possible that these provisions could make it more difficult to accomplish transactions that stockholders may otherwise deem to be in their best interests.
Limitations on Liability and Indemnification of Officers and Directors
The DGCL authorizes corporations to limit or eliminate the personal liability of directors and officers to corporations and their stockholders for monetary damages for breaches of directors’ or officers’ fiduciary duties, subject to certain exceptions. Our Amended and Restated Charter includes a provision that eliminates the personal liability of directors for monetary damages to the corporation or its stockholders for any breach of fiduciary duty as a director, except to the extent such exemption from liability or limitation thereof is not permitted under the DGCL. The effect of these provisions is to eliminate the rights of us and our stockholders, through stockholders’ derivative suits on our behalf, to recover monetary damages from a director for breach of fiduciary duty as a director, including breaches resulting from grossly negligent behavior. However, exculpation does not apply to any breaches of the
165
director’s duty of loyalty, any acts or omissions not in good faith or that involve intentional misconduct or knowing violation of law, any authorization of dividends or stock redemptions or repurchases paid or made in violation of the DGCL, or for any transaction from which the director derived an improper personal benefit.
Our Amended and Restated Bylaws generally provide that we must indemnify and advance expenses to our directors and officers to the fullest extent authorized by the DGCL. We also are expressly authorized to carry directors’ and officers’ liability insurance providing indemnification for our directors, officers, and certain employees for some liabilities. We believe that these indemnification and advancement provisions and insurance are useful to attract and retain qualified directors and executive officers.
The limitation of liability, indemnification, and advancement provisions in our Amended and Restated Charter and Amended and Restated Bylaws may discourage stockholders from bringing a lawsuit against directors for breach of their fiduciary duty. These provisions also may have the effect of reducing the likelihood of derivative litigation against directors and officers, even though such an action, if successful, might otherwise benefit us and our stockholders. In addition, your investment may be adversely affected to the extent we pay the costs of settlement and damage awards against directors and officers pursuant to these indemnification provisions.
There is currently no pending material litigation or proceeding involving any of our directors, officers, or employees for which indemnification is sought.
Indemnification Agreements
We entered into an indemnification agreement with each of our directors and executive officers as described in “Certain Relationships and Related Party Transactions—Director and Officer Indemnification and Insurance.” Insofar as indemnification for liabilities arising under the Securities Act may be permitted to directors or executive officers, we have been informed that in the opinion of the SEC such indemnification is against public policy and is therefore unenforceable.
Stock Exchange Listing
Our common stock is listed on the New York Stock Exchange under the symbol “PACS.”
Transfer Agent and Registrar
The transfer agent and registrar for our common stock is Broadridge Corporate Issuer Solutions, Inc.
166
SHARES ELIGIBLE FOR FUTURE SALE
Future sales of our common stock in the public market, or the perception that those sales may occur, could adversely affect the prevailing market price for our common stock from time to time or impair our ability to raise equity capital in the future. As described below, only a limited number of shares of our common stock will be available for sale in the public market for a period of several months after the completion of this offering due to contractual and legal restrictions on resale described below. Future sales of our common stock in the public market either before or after restrictions lapse, or the perception that those sales may occur, could adversely affect the prevailing market price of our common stock at such time and our ability to raise equity capital at a time and price we deem appropriate.
Sale of Restricted Shares
Based on the number of shares of our common stock outstanding as of June 30, 2024, upon the completion of this offering we will have outstanding an aggregate of 155,177,511 shares of common stock. Of these shares, all of the shares of common stock sold in our IPO and to be sold in this offering will be freely tradable in the public market without restriction or further registration under the Securities Act, unless the shares are held by any of our “affiliates” as such term is defined in Rule 144, or subject to lock-up agreements. The remaining shares of common stock held by existing stockholders will be “restricted securities,” as such term is defined in Rule 144. These restricted securities were issued and sold by us in private transactions and are eligible for public sale only if registered under the Securities Act or if they qualify for an exemption from registration under the Securities Act, including the exemptions provided by Rule 144 which rule is summarized below.
As a result of the lock-up agreements referred to below and the provisions of Rule 144, based on the number of shares of our common stock outstanding (calculated as of June 30, 2024, on the basis of the assumptions described above), the shares of our common stock (excluding the shares sold in this offering) that will be available for sale in the public market are as follows:
| Approximate Number of Shares | First Date Available For Sale Into Public Market | |||||||
| 115,615,811 shares | 91 days after the date of this prospectus, upon expiration of the lock-up agreements referred to below, subject in some cases to applicable volume, manner of sale and other limitations under Rule 144. | |||||||
We may issue shares of common stock from time to time as consideration for future acquisitions, investments or other corporate purposes. In the event that any such acquisition, investment or other transaction is significant, the number of shares of common stock that we may issue may in turn be significant. We may also grant registration rights covering those shares of common stock issued in connection with any such acquisition and investment.
In addition, the shares of common stock reserved for future issuance under our 2024 Plan will become eligible for sale in the public market to the extent permitted by the provisions of various vesting schedules, the lock-up agreements, a registration statement under the Securities Act or an exemption from registration, including Rule 144.
Rule 144
Under Rule 144, as currently in effect, once we have been subject to the public company reporting requirements of the Exchange Act for at least 90 days, and we are current in our Exchange Act reporting at the time of sale, a person (or persons whose shares are required to be aggregated) who is not deemed to have been one of our “affiliates” for purposes of Rule 144 at any time during the 90 days preceding a sale and who has beneficially owned restricted securities within the meaning of Rule 144 for at least six months, including the holding period of any prior owner other than one of our “affiliates,” is entitled to sell those shares in the public market (subject to the lock-up agreement referred to below, if applicable) without complying with the manner of sale, volume limitations or notice provisions of Rule 144, but subject to compliance with the public information requirements of Rule 144. If such a person has beneficially owned the shares proposed to be sold for at least one year, including the holding period of
167
any prior owner other than “affiliates,” then such person is entitled to sell such shares in the public market without complying with any of the requirements of Rule 144 (subject to the lock-up agreement referred to below, if applicable).
In general, under Rule 144, as currently in effect, once we have been subject to the public company reporting requirements of the Exchange Act for at least 90 days, our “affiliates,” as defined in Rule 144, who have beneficially owned the shares proposed to be sold for at least six months, are entitled to sell in the public market, upon expiration of any applicable lock-up agreements and within any three-month period, a number of those shares of our common stock that does not exceed the greater of:
•1% of the number of shares of our common stock then outstanding, which will equal approximately 1,551,785 shares of common stock immediately upon the completion of this offering (calculated as of June 30, 2024 on the basis of the assumptions described above); or
•the average weekly trading volume of our common stock on the New York Stock Exchange during the four calendar weeks preceding the filing of a notice on Form 144 with respect to such sale.
Such sales under Rule 144 by our “affiliates” or persons selling shares on behalf of our “affiliates” are also subject to certain manner of sale provisions, notice requirements and requirements related to the availability of current public information about us. Notwithstanding the availability of Rule 144, the holders of substantially all of our restricted securities have entered into lock-up agreements as referenced above and their restricted securities will become eligible for sale (subject to the above limitations under Rule 144) upon the expiration of the restrictions set forth in those agreements.
Lock-Up Agreements
In connection with our IPO, we and our officers, directors, and holders of substantially all of our common stock agreed with the underwriters, subject to certain exceptions, not to dispose of, directly or indirectly, or hedge any of our or their shares of common stock or securities convertible into or exchangeable for shares of common stock during the period from the date of our IPO prospectus continuing through October 7, 2024, which is 180 days after the date of our IPO prospectus, except with the prior written consent of Citigroup Global Markets Inc., J.P. Morgan Securities LLC and Truist Securities, Inc, as representatives of the underwriters in our IPO. This agreement does not apply to any existing employee benefit plans. For a further description of these lock-up agreements, please see the section titled “Underwriting (Conflicts of Interest).”
Pursuant to the lock-up agreements entered into in connection with our IPO (IPO lock-up agreements), the representatives granted each of Messrs. Murray and Hancock an exception under their respective IPO lock-up agreements to permit each of them to pledge a portion of their shares of our common stock owned by them to secure one or more margin loans that they may seek to obtain or enter into with one or more nationally or internationally recognized financial institutions, subject to certain exceptions and specified conditions; provided, however, that (i) Messrs. Murray and Hancock or we, as the case may be, shall provide the representatives with prior written notice informing them of any public filing, report or announcement made by or on behalf of them or us with respect thereto; and (ii) in the case of any transfer or distribution pursuant to a pledge or any other bona fide loan or pledge pursuant to this paragraph, any transferee that acquires the shares of our common stock from each such institution agrees to be bound in writing by the terms of the IPO lock-up agreement prior to such transfer; provided, further, that the aggregate number of shares of our common stock pledged as collateral pursuant to any such margin loans by Messrs. Murray and Hancock during the lock-up period shall not, for each of Messrs. Murray and Hancock, exceed 7.5% of the total number of shares of our common stock issued and outstanding in the aggregate on the closing date of this offering. As a result, the lock-up agreements permit an aggregate of up to 15% of the total number of shares of our common stock outstanding to be pledged as collateral pursuant to margin loans.
Certain of our employees, including our executive officers, and/or directors, may enter into written trading plans that are intended to comply with Rule 10b5-1 under the Exchange Act. Sales under these trading plans would not be permitted until the expiration of the lock-up agreements entered into in connection with this offering.
168
In connection with this offering, Citigroup Global Markets Inc., J.P. Morgan Securities LLC and Truist Securities, Inc. have provided a limited waiver of certain of the IPO lock-up agreements to the extent necessary to permit us and the selling stockholders to sell shares of common stock in this offering and to permit the filing of the registration statement of which this prospectus forms a part.
In connection with this offering, we and our officers and directors will agree with the underwriters, subject to certain exceptions, not to dispose of, directly or indirectly, or hedge any of our or their shares of common stock or securities convertible into or exchangeable for shares of common stock during the period from the date of this prospectus continuing through 90 days after the date of this prospectus, except with the prior written consent of Citigroup Global Markets Inc., J.P. Morgan Securities LLC and Truist Securities, Inc., as representatives of the underwriters in this offering, other than up to 400,000 shares of common stock in the aggregate that may be sold by our executive officers, other than Messrs. Murray and Hancock, during the 90 day lock-up period covered by the lock-up agreements entered into in connection with this offering. Pursuant to the lock-up agreements entered into in connection with this offering, the representatives granted each of Messrs. Murray and Hancock an exception under their respective lock-up agreements to permit each of them to pledge a portion of their shares of our common stock on the same terms as set forth in their IPO lock-up agreements, including that each of Messrs. Murray and Hancock, may not in the aggregate pledge shares of our common stock in excess of 7.5% of the total number of shares of our common stock issued and outstanding in the aggregate on the closing date of this offering. As a result, the lock-up agreements permit an aggregate of up to 15% of the total number of shares of our common stock outstanding to be pledged as collateral pursuant to margin loans during the 180 day period covered by the IPO lock-up agreements and the 90 day period covered by the lock-up agreements entered into in connection with this offering. These agreements do not apply to any existing employee benefit plans. These agreements are described in the section titled “Underwriting (Conflicts of Interest).”
Following the respective lock-up periods set forth in the agreements described above, and assuming that the representatives of the underwriters in our IPO and in this offering do not release any parties from these agreements and that there is no extension of the respective lock-up periods, all of the shares of our common stock that are restricted securities or are held by our affiliates as of the date of this prospectus will be eligible for sale in the public market, subject to the limitations discussed above.
Registration Rights
Upon the completion of this offering, the holders of up to 114,397,990 shares of our common stock will be entitled to rights with respect to the registration of their shares under the Securities Act, subject to the lock-up agreements described under “—Lock-Up Agreements” above. Registration of these shares under the Securities Act would result in the shares becoming freely tradable without restriction under the Securities Act, except for shares purchased by affiliates, immediately upon the effectiveness of the registration statement of which this prospectus is a part. Any sales of securities by these stockholders could have a material adverse effect on the trading price of our common stock. The requisite percentage of these stockholders will waive all such stockholders’ rights to notice of this offering and to include their shares of registrable securities in this offering. See the section titled “Description of Capital Stock—Registration Rights.”
Equity Incentive Plans
We have filed with the SEC a registration statement on Form S-8 under the Securities Act covering the shares of common stock issuable or reserved for issuance under our 2024 Plan and our ESPP. Such registration statement is expected to be filed and become effective as soon as practicable following the effectiveness of this registration statement.
169
MATERIAL U.S. FEDERAL INCOME TAX CONSEQUENCES TO NON-U.S. HOLDERS
The following discussion is a summary of the material U.S. federal income tax consequences to Non-U.S. Holders (as defined below) of the purchase, ownership and disposition of our common stock issued or sold pursuant to this offering, but does not purport to be a complete analysis of all potential tax effects. The effects of other U.S. federal tax laws, such as estate and gift tax laws, and any applicable state, local or non-U.S. tax laws are not discussed. This discussion is based on the U.S. Internal Revenue Code of 1986, as amended (Code), Treasury Regulations promulgated thereunder, judicial decisions, and published rulings and administrative pronouncements of the U.S. Internal Revenue Service (IRS), in each case in effect as of the date hereof.
These authorities may change or be subject to differing interpretations. Any such change or differing interpretation may be applied retroactively in a manner that could adversely affect a Non-U.S. Holder. We have not sought and will not seek any rulings from the IRS regarding the matters discussed below. There can be no assurance the IRS or a court will not take a contrary position to that discussed below regarding the tax consequences of the purchase, ownership and disposition of our common stock.
This discussion is limited to Non-U.S. Holders that hold our common stock as a “capital asset” within the meaning of Section 1221 of the Code (generally, property held for investment). This discussion does not address all U.S. federal income tax consequences relevant to a Non-U.S. Holder’s particular circumstances, including the impact of the Medicare contribution tax on net investment income and the alternative minimum tax. In addition, it does not address consequences relevant to Non-U.S. Holders subject to special rules, including, without limitation:
•U.S. expatriates and former citizens or long-term residents of the United States;
•persons holding our common stock as part of a hedge, straddle or other risk reduction strategy or as part of a conversion transaction or other integrated investment;
•banks, insurance companies and other financial institutions;
•brokers, dealers or traders in securities;
•“controlled foreign corporations,” “passive foreign investment companies” and corporations that accumulate earnings to avoid U.S. federal income tax;
•partnerships or other entities or arrangements treated as partnerships for U.S. federal income tax purposes (and investors therein);
•tax-exempt organizations or governmental organizations;
•persons deemed to sell our common stock under the constructive sale provisions of the Code;
•persons who hold or receive our common stock pursuant to the exercise of any employee stock option or otherwise as compensation;
•persons that own or have owned (directly, indirectly or constructively) more than 5% of our common stock;
•tax-qualified retirement plans; and
•“qualified foreign pension funds” as defined in Section 897(l)(2) of the Code and entities all of the interests of which are held by qualified foreign pension funds.
If an entity treated as a partnership for U.S. federal income tax purposes holds our common stock, the tax treatment of a partner in the partnership will depend on the status of the partner, the activities of the partnership and certain determinations made at the partner level. Accordingly, partnerships holding our common stock and the
170
partners in such partnerships should consult their tax advisors regarding the U.S. federal income tax consequences to them.
THIS DISCUSSION IS FOR INFORMATIONAL PURPOSES ONLY AND IS NOT TAX ADVICE. INVESTORS SHOULD CONSULT THEIR TAX ADVISORS WITH RESPECT TO THE APPLICATION OF THE U.S. FEDERAL INCOME TAX LAWS TO THEIR PARTICULAR SITUATIONS AS WELL AS ANY TAX CONSEQUENCES OF THE PURCHASE, OWNERSHIP AND DISPOSITION OF OUR COMMON STOCK ARISING UNDER THE U.S. FEDERAL ESTATE OR GIFT TAX LAWS OR UNDER THE LAWS OF ANY STATE, LOCAL OR NON-U.S. TAXING JURISDICTION OR UNDER ANY APPLICABLE INCOME TAX TREATY.
Definition of a Non-U.S. Holder
For purposes of this discussion, a “Non-U.S. Holder” is any beneficial owner of our common stock that is neither a “U.S. person” nor an entity treated as a partnership for U.S. federal income tax purposes. A U.S. person is any person that, for U.S. federal income tax purposes, is or is treated as any of the following:
•an individual who is a citizen or resident of the United States;
•a corporation created or organized under the laws of the United States, any state thereof or the District of Columbia;
•an estate, the income of which is subject to U.S. federal income tax regardless of its source; or
•a trust that (i) is subject to the primary supervision of a U.S. court and all substantial decisions of which are subject to the control of one or more “United States persons” (within the meaning of Section 7701(a)(30) of the Code) or (ii) has a valid election in effect to be treated as a United States person for U.S. federal income tax purposes.
Distributions
As described in the section titled “Dividend Policy,” we have no current plans to pay dividends or other distributions on our common stock in the foreseeable future following this offering. However, if we do make distributions of cash or property on our common stock, such distributions will constitute dividends for U.S. federal income tax purposes to the extent paid from our current or accumulated earnings and profits, as determined under U.S. federal income tax principles. Amounts not treated as dividends for U.S. federal income tax purposes will constitute a return of capital and first be applied against and reduce a Non-U.S. Holder’s adjusted tax basis in its common stock, but not below zero. Any excess will be treated as capital gain and will be treated as described below under the subsection titled “—Sale or Other Taxable Disposition.”
Subject to the discussion below regarding effectively connected income, dividends paid to a Non-U.S. Holder will be subject to U.S. federal withholding tax at a rate of 30% of the gross amount of the dividends (or such lower rate specified by an applicable income tax treaty, provided the Non-U.S. Holder furnishes a valid IRS Form W-8BEN or W-8BEN-E (or other applicable documentation) certifying qualification for the lower treaty rate). A Non-U.S. Holder that does not timely furnish the required documentation, but that qualifies for a reduced treaty rate, may obtain a refund of any excess amounts withheld by timely filing an appropriate claim for refund with the IRS. Non-U.S. Holders should consult their tax advisors regarding their entitlement to benefits under any applicable tax treaties.
If dividends paid to a Non-U.S. Holder are effectively connected with the Non-U.S. Holder’s conduct of a trade or business within the United States (and, if required by an applicable income tax treaty, the Non-U.S. Holder maintains a permanent establishment in the United States to which such dividends are attributable), the Non-U.S. Holder will be exempt from the U.S. federal withholding tax described above. To claim the exemption, the Non-U.S. Holder must furnish to the applicable withholding agent a valid IRS Form W-8ECI, certifying that the dividends are
171
effectively connected with the Non-U.S. Holder’s conduct of a trade or business within the United States. Any such effectively connected dividends will be subject to U.S. federal income tax on a net income basis at the regular rates applicable to U.S. persons. A Non-U.S. Holder that is a corporation also may be subject to a branch profits tax at a rate of 30% (or such lower rate specified by an applicable income tax treaty) on such effectively connected dividends, as adjusted for certain items. Non-U.S. Holders should consult their tax advisors regarding any applicable tax treaties that may provide for different rules.
Sale or Other Taxable Disposition
A Non-U.S. Holder will not be subject to U.S. federal income tax on any gain realized upon the sale or other taxable disposition of our common stock unless:
•the gain is effectively connected with the Non-U.S. Holder’s conduct of a trade or business within the United States (and, if required by an applicable income tax treaty, the Non-U.S. Holder maintains a permanent establishment in the United States to which such gain is attributable);
•the Non-U.S. Holder is a nonresident alien individual present in the United States for 183 days or more during the taxable year of the disposition and certain other requirements are met; or
•our common stock constitutes a U.S. real property interest (USRPI), by reason of our status as a U.S. real property holding corporation (USRPHC), for U.S. federal income tax purposes.
Gain described in the first bullet point above generally will be subject to U.S. federal income tax on a net income basis at the regular rates applicable to U.S. persons. A Non-U.S. Holder that is a corporation also may be subject to a branch profits tax at a rate of 30% (or such lower rate specified by an applicable income tax treaty) on such effectively connected gain, as adjusted for certain items.
A Non-U.S. Holder described in the second bullet point above will be subject to U.S. federal income tax at a rate of 30% (or such lower rate specified by an applicable income tax treaty) on gain realized upon the sale or other taxable disposition of our common stock, which may be offset by certain U.S.-source capital losses of the Non-U.S. Holder (even though the individual is not considered a resident of the United States), provided the Non-U.S. Holder has timely filed U.S. federal income tax returns with respect to such losses.
With respect to the third bullet point above, because the determination of whether we are a USRPHC depends on the fair market value of our USRPIs relative to the fair market value of our non-U.S. real property interests and our other business assets, and because we have significant interests in real property located in the United States, there can be no assurance that we currently are not a USRPHC or will not become one in the future. Even if we are or were to become a USRPHC, gain arising from the sale or other taxable disposition of our common stock by a Non-U.S. Holder will not be subject to U.S. federal income tax if our common stock is “regularly traded,” as defined by applicable Treasury Regulations, on an established securities market, and such Non-U.S. Holder owned, actually and constructively, 5% or less of our common stock throughout the shorter of the five-year period ending on the date of the sale or other taxable disposition or the Non-U.S. Holder’s holding period.
Non-U.S. Holders should consult their tax advisors regarding any applicable tax treaties that may provide for different rules.
Information Reporting and Backup Withholding
Payments of dividends on our common stock will not be subject to backup withholding, provided the Non-U.S. Holder certifies its non-U.S. status, such as by furnishing a valid IRS Form W-8BEN, W-8BEN-E or W-8ECI, or otherwise establishes an exemption. However, information returns are required to be filed with the IRS in connection with any distributions on our common stock paid to the Non-U.S. Holder, regardless of whether such distributions constitute dividends or whether any tax was actually withheld. In addition, proceeds of the sale or other taxable disposition of our common stock within the United States or conducted through certain U.S.-related brokers
172
generally will not be subject to backup withholding or information reporting if the applicable withholding agent receives the certification described above or the Non-U.S. Holder otherwise establishes an exemption. Proceeds of a disposition of our common stock conducted through a non-U.S. office of a non-U.S. broker that does not have certain enumerated relationships with the United States generally will not be subject to backup withholding or information reporting.
Copies of information returns that are filed with the IRS may also be made available under the provisions of an applicable treaty or agreement to the tax authorities of the country in which the Non-U.S. Holder resides or is established.
Backup withholding is not an additional tax. Any amounts withheld under the backup withholding rules may be allowed as a refund or a credit against a Non-U.S. Holder’s U.S. federal income tax liability, provided the required information is timely furnished to the IRS.
Additional Withholding Tax on Payments Made to Foreign Accounts
Withholding taxes may be imposed under Sections 1471 to 1474 of the Code (such Sections commonly referred to as the Foreign Account Tax Compliance Act (FATCA)) on certain types of payments made to non-U.S. financial institutions and certain other non-U.S. entities. Specifically, a 30% withholding tax may be imposed on dividends on, or (subject to the proposed Treasury Regulations discussed below) gross proceeds from the sale or other disposition of, our common stock paid to a “foreign financial institution” or a “non-financial foreign entity” (each as defined in the Code), unless (i) the foreign financial institution undertakes certain diligence and reporting obligations, (ii) the non-financial foreign entity either certifies it does not have any “substantial United States owners” (as defined in the Code) or furnishes identifying information regarding each substantial United States owner or (iii) the foreign financial institution or non-financial foreign entity otherwise qualifies for an exemption from these rules. If the payee is a foreign financial institution and is subject to the diligence and reporting requirements in (i) above, it must enter into an agreement with the U.S. Department of the Treasury requiring, among other things, that it undertake to identify accounts held by certain “specified United States persons” or “United States owned foreign entities” (each as defined in the Code), annually report certain information about such accounts, and withhold 30% on certain payments to non-compliant foreign financial institutions and certain other account holders. Foreign financial institutions located in jurisdictions that have an intergovernmental agreement with the United States governing FATCA may be subject to different rules.
Under applicable Treasury Regulations and administrative guidance, withholding under FATCA generally applies to payments of dividends on our common stock. While withholding under FATCA would have applied also to payments of gross proceeds from the sale or other disposition of our common stock beginning on January 1, 2019, proposed Treasury Regulations eliminate FATCA withholding on payments of gross proceeds entirely. Taxpayers generally may rely on these proposed Treasury Regulations until final Treasury Regulations are issued.
Prospective investors should consult their tax advisors regarding the potential application of withholding under FATCA to their investment in our common stock.
173
UNDERWRITING (CONFLICTS OF INTEREST)
Citigroup Global Markets Inc., J.P. Morgan Securities LLC and Truist Securities, Inc. are acting as joint book-running managers of this offering and as representatives of the underwriters named below. Subject to the terms and conditions stated in the underwriting agreement, which will be filed as an exhibit to the registration statement of which this prospectus is a part, each underwriter named below has severally agreed to purchase, and we and the selling stockholders have agreed to sell to that underwriter, the number of shares of our common stock set forth opposite the underwriter’s name in the following table:
| Underwriter | Number of Shares | |||||||
| Citigroup Global Markets Inc. | ||||||||
| J.P. Morgan Securities LLC | ||||||||
| Truist Securities, Inc. | ||||||||
| RBC Capital Markets, LLC | ||||||||
| Goldman Sachs & Co. LLC | ||||||||
| UBS Securities LLC | ||||||||
| Stephens Inc. | ||||||||
| Oppenheimer & Co. Inc. | ||||||||
| Total | 13,888,890 | |||||||
The underwriting agreement provides that the obligations of the underwriters to purchase the shares of our common stock included in this offering are subject to approval of legal matters by counsel and to other conditions. The underwriters are obligated to purchase all of the shares of our common stock (other than those covered by the option to purchase additional shares described below) if they purchase any of the shares.
Shares of our common stock sold by the underwriters to the public will initially be offered at the public offering price set forth on the cover of this prospectus. Any shares of our common stock sold by the underwriters to securities dealers may be sold at a discount from the public offering price not to exceed $ per share. After the public offering of the shares of our common stock, if all of the shares of our common stock are not sold at the public offering price, the underwriters may change the offering price and the other selling terms.
If the underwriters sell more shares of our common stock than the total number set forth in the table above, the selling stockholders have granted to the underwriters an option, exercisable for 30 days from the date of this prospectus, to purchase up to an additional 2,083,332 shares of our common stock from the selling stockholders at the public offering price less the underwriting discounts and commissions. The underwriters may exercise the option solely for the purpose of covering over-allotments, if any, in connection with this offering. To the extent the option is exercised, each underwriter must purchase a number of additional shares of our common stock approximately proportionate to that underwriter’s initial purchase commitment set forth in the table above. Any shares of our common stock issued or sold under the option will be issued and sold on the same terms and conditions as the other shares of our common stock that are the subject of this offering.
In connection with our IPO, we and our officers, directors, and holders of substantially all of our common stock agreed with the underwriters, subject to certain exceptions, not to dispose of, directly or indirectly, or hedge any of our or their shares of common stock or securities convertible into or exchangeable for shares of common stock during the period from the date of our IPO prospectus continuing through October 7, 2024, which is 180 days after the date of our IPO prospectus, except with the prior written consent of Citigroup Global Markets Inc., J.P. Morgan Securities LLC and Truist Securities, Inc., as representatives of the underwriters in our IPO. In connection with this offering, Citigroup Global Markets Inc., J.P. Morgan Securities LLC and Truist Securities, Inc. have provided a limited waiver of certain of the IPO lock-up agreements to the extent necessary to permit us and the selling stockholders to sell shares of common stock in this offering and to permit the filing of the registration statement of which this prospectus forms a part. See “Shares Eligible for Future Sale—Lock-Up Agreements” for a discussion of certain transfer restrictions.
174
In connection with this offering, we, our directors, executive officers and the selling stockholders have agreed that, subject to specified limited exceptions, for a period of 90 days from the date of this prospectus (lock-up period), we and they will not, without the prior written consent of Citigroup Global Markets Inc., J.P. Morgan Securities LLC and Truist Securities, Inc., as representatives of the underwriters in this offering, offer, sell, contract to sell, pledge or otherwise dispose of, including the filing of a registration statement in respect of, or hedge any shares of our common stock or any securities convertible into, or exercisable or exchangeable for, shares of our common stock.
In connection with this offering, Citigroup Global Markets Inc., J.P. Morgan Securities LLC and Truist Securities, Inc. have granted our directors and executive officers, other than Messrs. Murray and Hancock, an exception under their respective lock-up agreements that permits them to collectively sell up to 400,000 shares in the aggregate during the lock-up period. Additionally, the representatives have granted each of Messrs. Murray and Hancock an exception under their respective lock-up agreements that permits each of them to transfer, pledge or otherwise encumber, pursuant to the grant and maintenance of a bona fide lien, security interest, pledge or other similar encumbrance (each, a Pledge), a portion of their shares of our common stock owned by them to one or more nationally or internationally recognized financial institutions each having assets of not less than $10 billion (each, an Institution) in connection with a loan to them or pursuant to the exercise of any such Pledge by any such Institution; provided, however, that (i) Messrs. Murray and Hancock or we, as the case may be, shall provide the representatives with prior written notice informing them of any public filing, report or announcement made by or on behalf of them or us with respect thereto; and (ii) in the case of any transfer or distribution pursuant to a Pledge or any other bona fide loan or pledge pursuant to this paragraph, any transferee that acquires the shares of our common stock from each such Institution agrees to be bound in writing by the terms of the lock-up agreement prior to such transfer; provided, further, that the number of shares of our common stock pledged as collateral pursuant to the IPO lock-up agreements and the lock-up agreements entered into in connection with this offering by Messrs. Murray and Hancock during the respective lock-up periods shall not, for each of Messrs. Murray and Hancock, exceed 7.5% of the total number of shares of our common stock outstanding in the aggregate. As a result, the lock-up agreements permit an aggregate of up to 15% of the total number of shares of our common stock outstanding to be pledged as collateral pursuant to margin loans during the 180 day period covered by the IPO lock-up agreements and the 90 day period covered by the lock-up agreements entered into in connection with this offering.
The representatives, in their sole discretion, may release any of the securities subject to these lock-up agreements at any time, which, in the case of our executive officers, shall be with notice.
Our common stock is listed on the New York Stock Exchange under the symbol “PACS.”
The following table shows the per share and total public offering price, underwriting discounts and commissions that we and the selling stockholders are to pay to the underwriters and proceeds to us and the selling stockholders, before expenses, in connection with this offering. These amounts are shown assuming both no exercise and full exercise of the underwriters’ option to purchase additional shares.
| Total | |||||||||||||||||
| Per share | No exercise | Full exercise | |||||||||||||||
| Public offering price | |||||||||||||||||
| Underwriting discounts and commissions paid by us | |||||||||||||||||
| Underwriting discounts and commissions paid by the selling stockholders | |||||||||||||||||
| Proceeds to us, before expenses | |||||||||||||||||
| Proceeds to selling stockholders, before expenses | |||||||||||||||||
We estimate that expenses payable by us in connection with this offering, exclusive of underwriting discounts and commissions, will be approximately $ million. We have also agreed to reimburse the underwriters for certain of their expenses in an amount up to $35,000.
175
In connection with this offering, the underwriters may purchase and sell shares of our common stock in the open market. Purchases and sales in the open market may include short sales, purchases to cover short positions, which may include purchases pursuant to the underwriters’ option to purchase additional shares, and stabilizing purchases.
•Short sales involve secondary market sales by the underwriters of a greater number of shares of our common stock than they are required to purchase in this offering.
◦“Covered” short sales are sales of shares of our common stock in an amount up to the number of shares of our common stock represented by the underwriters’ option to purchase additional shares.
◦“Naked” short sales are sales of shares of our common stock in an amount in excess of the number of shares of our common stock represented by the underwriters’ option to purchase additional shares.
•Covering transactions involve purchases of shares, either pursuant to the underwriters’ option to purchase additional shares or in the open market.
◦To close a naked short position, the underwriters must purchase shares of our common stock in the open market. A naked short position is more likely to be created if the underwriters are concerned that there may be downward pressure on the price of the shares of our common stock in the open market after pricing that could adversely affect investors who purchase in this offering.
◦To close a covered short position, the underwriters must purchase shares of our common stock in the open market or exercise their option to purchase additional shares. In determining the source of shares of our common stock to close the covered short position, the underwriters will consider, among other things, the price of shares of our common stock available for purchase in the open market as compared to the price at which they may purchase shares of our common stock through their option to purchase additional shares.
•Stabilizing transactions involve bids to purchase shares of our common stock on the New York Stock Exchange, as long as the stabilizing bids do not exceed a specified maximum.
Purchases to cover short positions and stabilizing purchases, as well as other purchases by the underwriters for their own accounts, may have the effect of preventing or retarding a decline in the market price of the shares. They may also cause the price of the shares of our common stock to be higher than the price that would otherwise exist in the open market in the absence of these transactions. The underwriters may conduct these transactions on the New York Stock Exchange, in the over-the-counter market or otherwise. The underwriters are not required to engage in any of these transactions and, if they do commence any, they may discontinue them at any time.
A prospectus in electronic format may be made available on websites maintained by one or more of the underwriters or their respective affiliates. The representatives may agree with us to allocate a number of shares of our common stock to underwriters for sale to their online brokerage account holders. Any such allocation for online distributions will be made by the underwriters on the same basis as other allocations. Other than the prospectus in electronic format, the information on the underwriters’ or their respective affiliates’ websites and any information contained in any other website maintained by any of the underwriters or their respective affiliates is not part of this prospectus, has not been approved and/or endorsed by us or the underwriters and should not be relied upon by investors in this offering.
Other Relationships
The underwriters are full service financial institutions engaged in various activities, which may include securities trading, commercial and investment banking, financial advisory, investment management, principal investment, hedging, financing and brokerage activities. The underwriters and their respective affiliates have in the past performed commercial banking, investment banking and advisory services for us from time to time for which they have received customary fees and reimbursement of expenses and may, from time to time, engage in
176
transactions with and perform services for us in the ordinary course of their business for which they may receive customary fees and reimbursement of expenses. In the ordinary course of their various business activities, the underwriters and their respective affiliates may make or hold a broad array of investments and actively trade debt and equity securities (or related derivative securities) and financial instruments (which may include bank loans and/or credit default swaps) for their own account and for the accounts of their customers and may at any time hold long and short positions in such securities and instruments. Such investments and securities activities may involve securities and/or instruments of ours or our affiliates. Certain of the underwriters or their affiliates that have a lending relationship with us routinely hedge their credit exposure to us consistent with their customary risk management policies. A typical such hedging strategy would include these underwriters or their affiliates hedging such exposure by entering into transactions which consist of either the purchase of credit default swaps or the creation of short positions in our securities. The underwriters and their affiliates may also make investment recommendations and/or publish or express independent research views in respect of such securities or financial instruments and may hold, or recommend to clients that they acquire, long and/or short positions in such securities and instruments.
In addition, each of Messrs. Murray and Hancock may, pursuant to an exception granted by the representatives of the underwriters in our IPO and in this offering under their respective lock-up agreements, pledge a portion of their shares of our common stock owned by them to secure one or more margin loans that they may seek to obtain or enter into with one or more financial institutions, including an affiliate of Citigroup Global Markets Inc., subject to certain exceptions and specified conditions. See the sections titled “Risk Factors—Future sales, or the perception of future sales, of shares of common stock by existing stockholders could cause the market price of our common stock to decline” and “Certain Relationships and Related Party Transactions—Stockholders Agreement” for additional information.
Conflicts of Interest
Because affiliates of Citigroup Global Markets Inc., J.P. Morgan Securities LLC, Truist Securities, Inc. and RBC Capital Markets, LLC are lenders under our Amended and Restated 2023 Credit Facility and will each receive at least 5% of the net proceeds from this offering in connection with the repayment of amounts outstanding under our Amended and Restated 2023 Credit Facility, a “conflict of interest” within the meaning of FINRA Rule 5121 is deemed to exist. Therefore, this offering is being made in compliance with the applicable requirements of FINRA Rule 5121. The appointment of a “qualified independent underwriter” is not necessary for this offering pursuant to FINRA Rule 5121(a)(1)(B) as a “bona fide public market,” as defined in FINRA Rule 5121, exists for our common stock. In accordance with FINRA Rule 5121, Citigroup Global Markets Inc., J.P. Morgan Securities LLC and Truist Securities, Inc. will not confirm any sales to any account over which they exercise discretionary authority without the specific written approval of the transaction from the account holder. See the sections titled “Use of Proceeds” and “Management’s Discussion and Analysis of Financial Conditions and Results of Operations—Liquidity & Capital Resources—Credit Facilities” for additional information.
We and the selling stockholders have agreed to indemnify the underwriters against certain liabilities, including liabilities under the Securities Act, or to contribute to payments the underwriters may be required to make because of any of those liabilities.
Selling Restrictions
Notice to Prospective Investors in the European Economic Area
In relation to each Member State of the European Economic Area (each a Relevant State), no shares of common stock have been offered or will be offered pursuant to this offering to the public in that Relevant State prior to the publication of a prospectus in relation to the shares of our common stock which has been approved by the competent authority in that Relevant State or, where appropriate, approved in another Relevant State and notified to the competent authority in that Relevant State, all in accordance with the Prospectus Regulation, except that offers of
177
shares of common stock may be made to the public in that Relevant State at any time under the following exemptions under the Prospectus Regulation:
a.to any legal entity which is a qualified investor as defined under the Prospectus Regulation;
b.to fewer than 150 natural or legal persons (other than qualified investors as defined under the Prospectus Regulation), subject to obtaining the prior consent of the representatives for any such offer; or
c.in any other circumstances falling within Article 1(4) of the Prospectus Regulation,
provided that no such offer of shares of common stock shall require the Company or any underwriter to publish a prospectus pursuant to Article 3 of the Prospectus Regulation or supplement a prospectus pursuant to Article 23 of the Prospectus Regulation.
Each person in a Relevant State who initially acquires any shares of common stock or to whom any offer is made will be deemed to have represented, acknowledged and agreed to and with the Company and the underwriters that it is a qualified investor within the meaning of the Prospectus Regulation.
In the case of any shares of common stock being offered to a financial intermediary as that term is used in Article 5(1) of the Prospectus Regulation, each such financial intermediary will be deemed to have represented, acknowledged and agreed that the shares of our common stock acquired by it in the offer have not been acquired on a non-discretionary basis on behalf of, nor have they been acquired with a view to their offer or resale to, persons in circumstances which may give rise to an offer to the public other than their offer or resale in a Relevant State to qualified investors, in circumstances in which the prior consent of the representatives has been obtained to each such proposed offer or resale.
The Company, the underwriters and their respective affiliates will rely upon the truth and accuracy of the foregoing representations, acknowledgments and agreements.
For the purposes of this provision, the expression an “offer to the public” in relation to any shares of common stock in any Relevant State means the communication in any form and by any means of sufficient information on the terms of the offer and any shares of common stock to be offered so as to enable an investor to decide to purchase or subscribe for any shares of common stock, and the expression “Prospectus Regulation” means Regulation (EU) 2017/1129.
The above selling restriction is in addition to any other selling restrictions set out below.
Notice to Prospective Investors in the United Kingdom
In relation to the United Kingdom (UK), no shares of common stock have been offered or will be offered pursuant to this offering to the public in the UK prior to the publication of a prospectus in relation to the shares of our common stock which has been approved by the Financial Conduct Authority in the UK in accordance with the UK Prospectus Regulation and the FSMA, except that offers of shares of common stock may be made to the public in the UK at any time under the following exemptions under the UK Prospectus Regulation and the FSMA:
a.to any legal entity which is a qualified investor as defined under the UK Prospectus Regulation;
b.to fewer than 150 natural or legal persons (other than qualified investors as defined under the UK Prospectus Regulation), subject to obtaining the prior consent of the representatives for any such offer; or
c.at any time in other circumstances falling within section 86 of the FSMA,
178
provided that no such offer of shares of common stock shall require the Company or any underwriter to publish a prospectus pursuant to Section 85 of the FSMA or Article 3 of the UK Prospectus Regulation or supplement a prospectus pursuant to Article 23 of the UK Prospectus Regulation.
Each person in the UK who initially acquires any shares of common stock or to whom any offer is made will be deemed to have represented, acknowledged and agreed to and with the Company and the underwriters that it is a qualified investor within the meaning of the UK Prospectus Regulation.
In the case of any shares of common stock being offered to a financial intermediary as that term is used in Article 5(1) of the UK Prospectus Regulation, each such financial intermediary will be deemed to have represented, acknowledged and agreed that the shares of our common stock acquired by it in the offer have not been acquired on a non-discretionary basis on behalf of, nor have they been acquired with a view to their offer or resale to, persons in circumstances which may give rise to an offer to the public other than their offer or resale in the UK to qualified investors, in circumstances in which the prior consent of the representatives has been obtained to each such proposed offer or resale.
The Company, the underwriters and their respective affiliates will rely upon the truth and accuracy of the foregoing representations, acknowledgements and agreements.
For the purposes of this provision, the expression an “offer to the public” in relation to any shares of common stock in the UK means the communication in any form and by any means of sufficient information on the terms of the offer and any shares of common stock to be offered so as to enable an investor to decide to purchase or subscribe for any shares of common stock, and the expression “UK Prospectus Regulation” means Regulation (EU) 2017/1129 as it forms part of domestic law by virtue of the European Union (Withdrawal) Act 2018, and the expression “FSMA” means the Financial Services and Markets Act 2000.
This document is for distribution only to persons who (i) have professional experience in matters relating to investments and who qualify as investment professionals within the meaning of Article 19(5) of the FSMA Order 2005 (as amended, Financial Promotion Order), (ii) are persons falling within Article 49(2)(a) to (d) (“high net worth companies, unincorporated associations etc.”) of the Financial Promotion Order, (iii) are outside the UK, or (iv) are persons to whom an invitation or inducement to engage in investment activity (within the meaning of Section 21 of the FSMA) in connection with the issue or sale of any securities may otherwise lawfully be communicated or caused to be communicated (all such persons together being referred to as relevant persons). This document is directed only at relevant persons and must not be acted on or relied on by persons who are not relevant persons. Any investment or investment activity to which this document relates is available only to relevant persons and will be engaged in only with relevant persons.
Notice to Prospective Investors in France
Neither this prospectus nor any other offering material relating to the shares of our common stock described in this prospectus has been submitted to the clearance procedures of the Autorité des Marchés Financiers or of the competent authority of another member state of the European Economic Area and notified to the Autorité des Marchés Financiers. The shares of our common stock have not been offered or sold and will not be offered or sold, directly or indirectly, to the public in France. Neither this prospectus nor any other offering material relating to the shares of our common stock has been or will be:
a.released, issued, distributed or caused to be released, issued or distributed to the public in France; or
b.used in connection with any offer for subscription or sale of the shares of our common stock to the public in France.
179
Such offers, sales and distributions will be made in France only:
a.to qualified investors (investisseurs qualifiés) and/or to a restricted circle of investors (cercle restreint d’investisseurs), in each case investing for their own account, all as defined in, and in accordance with articles L.411-2, D.411-1, D.411-2, D.734-1, D.744-1, D.754-1 and D.764-1 of the French Code monétaire et financier;
b.to investment services providers authorized to engage in portfolio management on behalf of third parties; or
c.in a transaction that, in accordance with article L.411-2-II-1°-or-2°-or 3° of the French Code monétaire et financier and article 211-2 of the General Regulations (Règlement Général) of the Autorité des Marchés Financiers, does not constitute a public offer (appel public à l’épargne).
The shares of our common stock may be resold directly or indirectly, only in compliance with articles L.411-1, L.411-2, L.412-1 and L.621-8 through L.621-8-3 of the French Code monétaire et financier.
Notice to Prospective Investors in Hong Kong
The shares of our common stock have not been offered or sold and will not be offered or sold in Hong Kong, by means of any document, other than (a) to “professional investors” as defined in the Securities and Futures Ordinance (Cap. 571) of Hong Kong and any rules made under that Ordinance; or (b) in other circumstances which do not result in the document being a “prospectus” as defined in the Companies Ordinance (Cap. 32) of Hong Kong or which do not constitute an offer to the public within the meaning of that Ordinance. No advertisement, invitation or document relating to the shares of our common stock has been or may be issued or has been or may be in the possession of any person for the purposes of issue, whether in Hong Kong or elsewhere, which is directed at, or the contents of which are likely to be accessed or read by, the public of Hong Kong (except if permitted to do so under the securities laws of Hong Kong) other than with respect to the shares of our common stock which are or are intended to be disposed of only to persons outside Hong Kong or only to “professional investors” as defined in the Securities and Futures Ordinance and any rules made under that Ordinance.
Notice to Prospective Investors in Japan
The shares of our common stock have not been and will not be registered under the Financial Instruments and Exchange Law of Japan (Law No. 25 of 1948, as amended) and, accordingly, will not be offered or sold, directly or indirectly, in Japan, or for the benefit of any Japanese Person or to others for re-offering or resale, directly or indirectly, in Japan or to any Japanese Person, except in compliance with all applicable laws, regulations and ministerial guidelines promulgated by relevant Japanese governmental or regulatory authorities in effect at the relevant time. For the purposes of this paragraph, “Japanese Person” shall mean any person resident in Japan, including any corporation or other entity organized under the laws of Japan.
Notice to Prospective Investors in Singapore
This prospectus has not been registered as a prospectus with the Monetary Authority of Singapore. Accordingly, the shares of our common stock were not offered or sold or caused to be made the subject of an invitation for subscription or purchase and will not be offered or sold or caused to be made the subject of an invitation for subscription or purchase, and this prospectus or any other document or material in connection with the offer or sale, or invitation for subscription or purchase, of the shares of our common stock, has not been circulated or distributed, nor will it be circulated or distributed, whether directly or indirectly, to any person in Singapore other than (i) to an institutional investor (as defined in Section 4A of the Securities and Futures Act (Chapter 289) of Singapore, as modified or amended from time to time (SFA)) pursuant to Section 274 of the SFA, (ii) to a relevant person (as defined in Section 275(2) of the SFA) pursuant to Section 275(1) of the SFA, or any person pursuant to Section 275(1A) of the SFA, and in accordance with the conditions specified in Section 275 of the SFA, or (iii) otherwise pursuant to, and in accordance with the conditions of, any other applicable provision of the SFA.
180
Where the shares of our common stock are subscribed or purchased under Section 275 of the SFA by a relevant person which is:
a.a corporation (which is not an accredited investor (as defined in Section 4A of the SFA)) the sole business of which is to hold investments and the entire share capital of which is owned by one or more individuals, each of whom is an accredited investor; or
b.a trust (where the trustee is not an accredited investor) whose sole purpose is to hold investments and each beneficiary of the trust is an individual who is an accredited investor,
securities or securities-based derivatives contracts (each term as defined in Section 2(1) of the SFA) of that corporation or the beneficiaries’ rights and interest (howsoever described) in that trust shall not be transferred within six months after that corporation or that trust has acquired the shares of our common stock pursuant to an offer made under Section 275 of the SFA except:
a.to an institutional investor or to a relevant person, or to any person arising from an offer referred to in Section 275(1A) or Section 276(4)(i)(B) of the SFA;
b.where no consideration is or will be given for the transfer;
c.where the transfer is by operation of law; or
d.as specified in Section 276(7) of the SFA.
Notice to Prospective Investors in Canada
The shares of our common stock may be sold only to purchasers purchasing, or deemed to be purchasing, as principal that are accredited investors, as defined in National Instrument 45-106 Prospectus Exemptions or subsection 73.3(1) of the Securities Act (Ontario), and are permitted clients, as defined in National Instrument 31-103 Registration Requirements, Exemptions and Ongoing Registrant Obligations. Any resale of the shares of our common stock must be made in accordance with an exemption from, or in a transaction not subject to, the prospectus requirements of applicable securities laws.
Securities legislation in certain provinces or territories of Canada may provide a purchaser with remedies for rescission or damages if this prospectus (including any amendment thereto) contains a misrepresentation, provided that the remedies for rescission or damages are exercised by the purchaser within the time limit prescribed by the securities legislation of the purchaser’s province or territory. The purchaser should refer to any applicable provisions of the securities legislation of the purchaser’s province or territory for particulars of these rights or consult with a legal advisor.
Pursuant to section 3A.3 (or, in the case of securities issued or guaranteed by the government of a non-Canadian jurisdiction, section 3A.4) of National Instrument 33-105 Underwriting Conflicts (NI 33-105), the underwriters are not required to comply with the disclosure requirements of NI 33-105 regarding underwriter conflicts of interest in connection with this offering.
Notice to Prospective Investors in Australia
No placement document, prospectus, product disclosure statement or other disclosure document has been lodged with the Australian Securities and Investments Commission (ASIC) in relation to this offering. This prospectus does not constitute a prospectus, product disclosure statement or other disclosure document under the Corporations Act 2001 (Corporations Act), and does not purport to include the information required for a prospectus, product disclosure statement or other disclosure document under the Corporations Act.
181
Any offer in Australia of the shares of our common stock may only be made to persons (Exempt Investors) who are “sophisticated investors” (within the meaning of section 708(8) of the Corporations Act), “professional investors” (within the meaning of section 708(11) of the Corporations Act) or otherwise pursuant to one or more exemptions contained in section 708 of the Corporations Act so that it is lawful to offer the shares of our common stock without disclosure to investors under Chapter 6D of the Corporations Act.
The shares of our common stock applied for by Exempt Investors in Australia must not be offered for sale in Australia in the period of 12 months after the date of allotment under this offering, except in circumstances where disclosure to investors under Chapter 6D of the Corporations Act would not be required pursuant to an exemption under section 708 of the Corporations Act or otherwise or where the offer is pursuant to a disclosure document which complies with Chapter 6D of the Corporations Act. Any person acquiring shares of our common stock must observe such Australian on-sale restrictions.
This prospectus contains general information only and does not take account of the investment objectives, financial situation or particular needs of any particular person. It does not contain any securities recommendations or financial product advice. Before making an investment decision, investors need to consider whether the information in this prospectus is appropriate to their needs, objectives and circumstances, and, if necessary, seek expert advice on those matters.
Notice to Prospective Investors in Chile
The shares of our common stock are not registered in the Securities Registry (Registro de Valores) or subject to the control of the Chilean Securities and Exchange Commission (Superintendencia de Valores y Seguros de Chile). This prospectus and other offering materials relating to the offer of the shares of our common stock do not constitute a public offer of, or an invitation to subscribe for or purchase, the shares of our common stock in the Republic of Chile, other than to individually identified purchasers pursuant to a private offering within the meaning of Article 4 of the Chilean Securities Market Act (Ley de Mercado de Valores) (an offer that is not “addressed to the public at large or to a certain sector or specific group of the public”).
Notice to Prospective Investors in Switzerland
The shares of our common stock may not be publicly offered in Switzerland and will not be listed on the SIX Swiss Exchange (SIX) or on any other stock exchange or regulated trading facility in Switzerland. This document has been prepared without regard to the disclosure standards for issuance prospectuses under art. 652a or art. 1156 of the Swiss Code of Obligations or the disclosure standards for listing prospectuses under art. 27 ff. of the SIX Listing Rules or the listing rules of any other stock exchange or regulated trading facility in Switzerland. Neither this document nor any other offering or marketing material relating to the shares of our common stock or this offering may be publicly distributed or otherwise made publicly available in Switzerland.
Neither this document nor any other offering or marketing material relating to this offering, the Company, or the shares of our common stock have been or will be filed with or approved by any Swiss regulatory authority. In particular, this document will not be filed with, and the offer of shares of our common stock will not be supervised by, the Swiss Financial Market Supervisory Authority FINMA (FINMA), and the offer of shares of our common stock has not been and will not be authorized under the Swiss Federal Act on Collective Investment Schemes (CISA). The investor protection afforded to acquirers of interests in collective investment schemes under the CISA does not extend to acquirers of shares of our common stock.
Notice to Prospective Investors in the Dubai International Financial Centre
This prospectus relates to an Exempt Offer in accordance with the Offered Securities Rules of the Dubai Financial Services Authority (DFSA). This prospectus is intended for distribution only to persons of a type specified in the Offered Securities Rules of the DFSA. It must not be delivered to, or relied on by, any other person. The DFSA has no responsibility for reviewing or verifying any documents in connection with Exempt Offers. The DFSA has not approved this prospectus nor taken steps to verify the information set forth herein and has no responsibility
182
for the prospectus. The shares of our common stock to which this prospectus relates may be illiquid and/or subject to restrictions on their resale. Prospective purchasers of the shares of our common stock offered should conduct their own due diligence on the shares of our common stock. If you do not understand the contents of this prospectus you should consult an authorized financial advisor.
Notice to Prospective Investors in the United Arab Emirates
The shares of our common stock have not been, and are not being, publicly offered, sold, promoted or advertised in the United Arab Emirates (including the Dubai International Financial Centre) other than in compliance with the laws of the United Arab Emirates (and the Dubai International Financial Centre) governing the issue, offering and sale of securities. Further, this prospectus does not constitute a public offer of securities in the United Arab Emirates (including the Dubai International Financial Centre) and is not intended to be a public offer. This prospectus has not been approved by or filed with the Central Bank of the United Arab Emirates, the Securities and Commodities Authority or the Dubai Financial Services Authority.
Notice to Prospective Investors in Qatar
The shares of our common stock described in this prospectus have not been, and will not be, offered, sold or delivered, at any time, directly or indirectly in the State of Qatar in a manner that would constitute a public offering. This prospectus has not been, and will not be, registered with or approved by the Qatar Financial Markets Authority or Qatar Central Bank and may not be publicly distributed. This prospectus is intended for the original recipient only and must not be provided to any other person. It is not for general circulation in the State of Qatar and may not be reproduced or used for any other purpose.
183
LEGAL MATTERS
The validity of the shares of our common stock offered hereby will be passed upon for us by Latham & Watkins LLP, Costa Mesa, California. Goodwin Procter LLP, New York, New York, is acting as counsel for the underwriters in connection with certain legal matters related to this offering. Latham & Watkins LLP is acting as counsel for the selling stockholders in connection with this offering.
EXPERTS
Ernst & Young LLP, independent registered public accounting firm, has audited our combined/consolidated financial statements at December 31, 2023 and 2022, and for each of the three years in the period ended December 31, 2023, as set forth in their report. We’ve included our financial statements in the prospectus and elsewhere in the registration statement in reliance on Ernst & Young LLP’s report, given on their authority as experts in accounting and auditing.
WHERE YOU CAN FIND MORE INFORMATION
We have filed with the SEC a registration statement on Form S-1 under the Securities Act with respect to the shares of common stock offered hereby. This prospectus, which constitutes a part of the registration statement, does not contain all of the information set forth in the registration statement or the exhibits filed therewith. For further information about us and the shares of our common stock offered hereby, reference is made to the registration statement and the exhibits filed therewith. Statements contained in this prospectus regarding the contents of any contract or any other document that is filed as an exhibit to the registration statement are not necessarily complete, and in each instance, we refer you to the copy of such contract or other document filed as an exhibit to the registration statement. The SEC maintains a website that contains reports, proxy and information statements and other information regarding registrants that file electronically with the SEC. The address of the website is www.sec.gov.
We are subject to the information and reporting requirements of the Exchange Act and, in accordance with this law, file periodic reports, proxy and information statements and other information with the SEC. These periodic reports, proxy and information statements and other information will be available for inspection at the website of the SEC referred to above. We also maintain a website at www.pacs.com. You may access these materials free of charge as soon as reasonably practicable after they are filed electronically with, or furnished to, the SEC. The inclusion of our website address in this prospectus is an inactive textual reference only. The information contained on, or that can be accessed through, our website is not incorporated by reference into, and is not a part of, this prospectus or the registration statement of which this prospectus forms a part. Investors should not rely on any such information in deciding whether to purchase our common stock.
184
INDEX TO FINANCIAL STATEMENTS
| Page | ||||||||
| Combined/Consolidated Financial Statements as of December 31, 2023 and 2022 and for the years ended December 31, 2023, 2022, and 2021 | ||||||||
| Unaudited Interim Condensed Combined/Consolidated Financial Statements as of December 31, 2023 and June 30, 2024 and for the Three and Six Months Ended June 30, 2024 and 2023 | ||||||||
F-1
Report of Independent Registered Public Accounting Firm
To the Stockholders and the Board of Directors of PACS Group, Inc.
Opinion on the Financial Statements
We have audited the accompanying combined/consolidated balance sheets of PACS Group, Inc. and subsidiaries (the Company) as of December 31, 2023 and 2022, the related combined/consolidated statements of income, stockholders' equity/(deficit) and cash flows for each of the three years in the period ended December 31, 2023, and the related notes (collectively referred to as the “combined/consolidated financial statements”). In our opinion, the combined/consolidated financial statements present fairly, in all material respects, the financial position of the Company at December 31, 2023 and 2022, and the results of its operations and its cash flows for each of the three years in the period ended December 31, 2023, in conformity with U.S. generally accepted accounting principles.
Basis for Opinion
These financial statements are the responsibility of the Company's management. Our responsibility is to express an opinion on the Company’s financial statements based on our audits. We are a public accounting firm registered with the Public Company Accounting Oversight Board (United States) (PCAOB) and are required to be independent with respect to the Company in accordance with the U.S. federal securities laws and the applicable rules and regulations of the Securities and Exchange Commission and the PCAOB.
We conducted our audits in accordance with the standards of the PCAOB. Those standards require that we plan and perform the audit to obtain reasonable assurance about whether the financial statements are free of material misstatement, whether due to error or fraud. The Company is not required to have, nor were we engaged to perform, an audit of its internal control over financial reporting. As part of our audits we are required to obtain an understanding of internal control over financial reporting but not for the purpose of expressing an opinion on the effectiveness of the Company's internal control over financial reporting. Accordingly, we express no such opinion.
Our audits included performing procedures to assess the risks of material misstatement of the financial statements, whether due to error or fraud, and performing procedures that respond to those risks. Such procedures included examining, on a test basis, evidence regarding the amounts and disclosures in the financial statements. Our audits also included evaluating the accounting principles used and significant estimates made by management, as well as evaluating the overall presentation of the financial statements. We believe that our audits provide a reasonable basis for our opinion.
Critical Audit Matter
The critical audit matter communicated below is a matter arising from the current period audit of the financial statements that was communicated or required to be communicated to the audit committee and that: (1) relates to accounts or disclosures that are material to the financial statements and (2) involved our especially challenging, subjective or complex judgments. The communication of the critical audit matter does not alter in any way our opinion on the combined/consolidated financial statements, taken as a whole, and we are not, by communicating the critical audit matter below, providing a separate opinion on the critical audit matter or on the account or disclosure to which it relates.
F-2
| Professional liability and general liability claims reserve | ||||||||
| Description of the Matter | At December 31, 2023, the Company’s professional liability and general liability claims reserve was $163.0 million. As further described in Note 14 to the combined/consolidated financial statements, the professional liability and general liability claims reserve includes an estimate of the Company’s liability for professional and general claims that have been reported as well as claims that have been incurred but not reported. The Company utilizes an external actuary to assist management in estimating the exposure for claims obligations, both asserted and unasserted. Auditing the professional liability and general liability claims reserve is complex and highly judgmental due to the significant estimation required in determining the claims reserve, particularly the assumptions regarding the severity and frequency of claims. The Company develops information relating to the ultimate size of the claims based on historical experience and current industry information which is used in the actuarial analysis. | |||||||
| How We Addressed the Matter in Our Audit | To test the professional liability and general liability claims reserve, our audit procedures included, among others, obtaining an understanding of the factors considered and assumptions made by management and its external actuary in developing the estimate of the professional liability and general liability claims reserve, including the sources of data relevant to these factors and assumptions. We tested underlying claims data, including the completeness and accuracy of open and settled cases. We reviewed the Company’s insurance contracts to understand the policy terms and verified that the policy terms were incorporated within the actuarial report. We also involved our actuaries to assist in evaluating the methodologies and key assumptions used in the actuarial report. We compared the Company’s professional liability and general liability claims reserve to an independent range calculated by our actuaries. | |||||||
/s/ Ernst & Young LLP
We have served as the Company’s auditor since 2022.
Salt Lake City, Utah
March 13, 2024,
except for the retroactive effect of the 1-for-6,436.1693 stock split as described in the fourth paragraph of Note 17, as to which the date is
April 1, 2024
F-3
| PACS GROUP, INC. AND SUBSIDIARIES | |||||||||||||||||
| COMBINED/CONSOLIDATED BALANCE SHEETS | |||||||||||||||||
| (dollars in thousands, except for share values) | |||||||||||||||||
| December 31, | |||||||||||||||||
| 2023 | 2022 | ||||||||||||||||
| ASSETS | |||||||||||||||||
| Current Assets: | |||||||||||||||||
| Cash and cash equivalents | $ | 73,416 | $ | 58,269 | |||||||||||||
| Accounts receivable, net | 547,807 | 370,924 | |||||||||||||||
| Other receivables | 52,259 | 49,200 | |||||||||||||||
| Prepaid expenses and other current assets | 48,665 | 32,770 | |||||||||||||||
| Total Current Assets | 722,147 | 511,163 | |||||||||||||||
| Property and equipment, net | 577,528 | 430,565 | |||||||||||||||
| Operating lease right-of-use assets | 2,007,812 | 1,345,044 | |||||||||||||||
| Escrow funds | 15,649 | 16,217 | |||||||||||||||
| Goodwill and other indefinite-lived assets | 65,291 | 61,491 | |||||||||||||||
| Other assets | 124,312 | 97,411 | |||||||||||||||
Total Assets | $ | 3,512,739 | $ | 2,461,891 | |||||||||||||
| LIABILITIES AND EQUITY | |||||||||||||||||
| Current Liabilities: | |||||||||||||||||
| Accounts payable | $ | 140,947 | $ | 110,576 | |||||||||||||
| Accrued payroll and benefits | 92,234 | 77,360 | |||||||||||||||
| Current operating lease liabilities | 109,438 | 83,171 | |||||||||||||||
| Current maturities of long term debt | 16,822 | 61,363 | |||||||||||||||
| Current portion of accrued self-insurance liabilities | 27,536 | 24,233 | |||||||||||||||
| Other accrued expenses | 69,949 | 127,159 | |||||||||||||||
| Total Current Liabilities | 456,926 | 483,862 | |||||||||||||||
| Long-Term Liabilities: | |||||||||||||||||
| Long-term operating lease liabilities | 1,961,997 | 1,304,780 | |||||||||||||||
| Accrued benefits, less current portion | 6,738 | 15,287 | |||||||||||||||
| Lines of credit | 520,000 | 146,820 | |||||||||||||||
| Long-term debt, less current maturities, net of deferred financing fees | 195,708 | 291,521 | |||||||||||||||
| Accrued self-insurance liabilities, less current portion | 146,167 | 113,894 | |||||||||||||||
| Other liabilities | 123,477 | 37,076 | |||||||||||||||
| Total Long-Term Liabilities | 2,954,087 | 1,909,378 | |||||||||||||||
Total Liabilities | 3,411,013 | 2,393,240 | |||||||||||||||
| Commitments and contingencies (Note 14) | |||||||||||||||||
| Equity: | |||||||||||||||||
| Common stock - 64,361,693,000 shares authorized, $0.001 par value, 128,723,386 shares issued and outstanding | 129 | 129 | |||||||||||||||
| Retained earnings | 95,997 | 63,517 | |||||||||||||||
| Total stockholders' equity | 96,126 | 63,646 | |||||||||||||||
| Non-controlling interest in subsidiary | 5,600 | 5,005 | |||||||||||||||
| Total Equity | 101,726 | 68,651 | |||||||||||||||
| Total Liabilities and Equity | $ | 3,512,739 | $ | 2,461,891 | |||||||||||||
See accompanying notes to combined/consolidated financial statements.
F-4
| PACS GROUP, INC. AND SUBSIDIARIES | |||||||||||||||||
| COMBINED/CONSOLIDATED STATEMENTS OF INCOME | |||||||||||||||||
| (dollars in thousands, except for share and per share values) | |||||||||||||||||
| December 31, | |||||||||||||||||
| 2023 | 2022 | 2021 | |||||||||||||||
| Revenue | |||||||||||||||||
| Patient and resident service revenue | $ | 3,110,114 | $ | 2,399,155 | $ | 1,135,909 | |||||||||||
| Additional funding | 375 | 21,482 | 28,563 | ||||||||||||||
| Other revenues | 1,003 | 1,357 | 2,091 | ||||||||||||||
Total Revenue | $ | 3,111,492 | $ | 2,421,994 | $ | 1,166,563 | |||||||||||
| Operating Expenses | |||||||||||||||||
| Cost of services | 2,447,713 | 1,861,314 | 901,095 | ||||||||||||||
| Rent - cost of services | 216,711 | 160,003 | 78,122 | ||||||||||||||
| General and administrative expense | 213,664 | 149,006 | 96,834 | ||||||||||||||
| Depreciation and amortization | 25,632 | 22,311 | 7,153 | ||||||||||||||
Total Operating Expenses | $ | 2,903,720 | $ | 2,192,634 | $ | 1,083,204 | |||||||||||
| Operating Income | $ | 207,772 | $ | 229,360 | $ | 83,359 | |||||||||||
| Other (Expense) Income | |||||||||||||||||
| Interest expense | (49,919) | (25,538) | (5,278) | ||||||||||||||
| Other (expense) income, net | (536) | 3,223 | 3,345 | ||||||||||||||
Total Other Expense, net | $ | (50,455) | $ | (22,315) | $ | (1,933) | |||||||||||
| Income before provision for income taxes | 157,317 | 207,045 | 81,426 | ||||||||||||||
| Provision for income taxes | (44,435) | (56,549) | (33,479) | ||||||||||||||
| Net Income | $ | 112,882 | $ | 150,496 | $ | 47,947 | |||||||||||
| Less: | |||||||||||||||||
| Net income attributable to noncontrolling interest | $ | 8 | — | — | |||||||||||||
| Net income attributable to PACS Group, Inc. | $ | 112,874 | $ | 150,496 | $ | 47,947 | |||||||||||
| Net income per common share attributable to PACS Group, Inc. | |||||||||||||||||
| Basic and diluted | $ | 0.88 | $ | 1.17 | $ | 0.37 | |||||||||||
| Weighted-average shares outstanding | |||||||||||||||||
| Basic and diluted | 128,723,386 | 128,723,386 | 128,723,386 | ||||||||||||||
See accompanying notes to combined/consolidated financial statements.
F-5
| PACS GROUP, INC. AND SUBSIDIARIES | |||||||||||||||||||||||||||||
| COMBINED/CONSOLIDATED STATEMENTS OF STOCKHOLDERS' EQUITY/(DEFICIT) | |||||||||||||||||||||||||||||
| (dollars in thousands, except for share values) | |||||||||||||||||||||||||||||
| Common Stock | Retained Earnings (Accumulated Deficit) | Non-Controlling Interest | Total Stockholders' Equity (Deficit) | ||||||||||||||||||||||||||
| Shares | Amount | ||||||||||||||||||||||||||||
| Balance January 1, 2021 | 128,723,386 | $ | 129 | $ | (40,992) | $ | 1,759 | $ | (39,104) | ||||||||||||||||||||
| Dividends on Common Stock ($0.26 per share) | — | — | (33,654) | — | (33,654) | ||||||||||||||||||||||||
| Net Income | — | — | 47,947 | — | 47,947 | ||||||||||||||||||||||||
| Balance December 31, 2021 | 128,723,386 | $ | 129 | $ | (26,699) | $ | 1,759 | $ | (24,811) | ||||||||||||||||||||
| Contributions | — | — | — | 3,246 | 3,246 | ||||||||||||||||||||||||
| Dividends on Common Stock ($0.47 per share) | — | — | (60,280) | — | (60,280) | ||||||||||||||||||||||||
| Net Income | — | — | 150,496 | — | 150,496 | ||||||||||||||||||||||||
| Balance December 31, 2022 | 128,723,386 | $ | 129 | $ | 63,517 | $ | 5,005 | $ | 68,651 | ||||||||||||||||||||
| Contributions | — | — | — | 587 | 587 | ||||||||||||||||||||||||
| Dividends on Common Stock ($0.62 per share) | — | — | (80,394) | — | (80,394) | ||||||||||||||||||||||||
| Net income attributable to noncontrolling interest | — | — | — | 8 | 8 | ||||||||||||||||||||||||
| Net income attributable to PACS Group, Inc. | — | — | 112,874 | — | 112,874 | ||||||||||||||||||||||||
| Balance December 31, 2023 | 128,723,386 | $ | 129 | $ | 95,997 | $ | 5,600 | $ | 101,726 | ||||||||||||||||||||
See accompanying notes to combined/consolidated financial statements.
F-6
| PACS GROUP, INC. AND SUBSIDIARIES | |||||||||||||||||
| COMBINED/CONSOLIDATED STATEMENTS OF CASH FLOWS | |||||||||||||||||
| (dollars in thousands) | |||||||||||||||||
| December 31, | |||||||||||||||||
| 2023 | 2022 | 2021 | |||||||||||||||
| Cash flows from operating activities: | |||||||||||||||||
| Net income | $ | 112,882 | $ | 150,496 | $ | 47,947 | |||||||||||
| Adjustments to reconcile net income to net cash provided by operating activities | |||||||||||||||||
| Depreciation and amortization | 25,632 | 22,311 | 7,153 | ||||||||||||||
| Amortization and write-off of deferred financing fees | 6,068 | 1,205 | 902 | ||||||||||||||
| Loss (gain) on disposition of property and equipment | 581 | 4 | (2,974) | ||||||||||||||
| Loss (gain) on investment in partnership | 391 | 346 | (232) | ||||||||||||||
| Deferred taxes | (9,923) | (1,921) | 7,834 | ||||||||||||||
| Noncash lease expense | 22,727 | 14,464 | 1,329 | ||||||||||||||
| Change in operating assets and liabilities | |||||||||||||||||
| Accounts receivable, net | (176,883) | (114,416) | (36,903) | ||||||||||||||
| Other receivables | (3,059) | (202) | (3,185) | ||||||||||||||
| Prepaid expenses and other current assets | (18,765) | (6,371) | 14,967 | ||||||||||||||
| Other assets | (3,338) | (39,341) | 2,193 | ||||||||||||||
| Escrow funds | 568 | (4,526) | (5,112) | ||||||||||||||
| Operating lease obligations | (2,011) | (92) | (1,091) | ||||||||||||||
| Accounts payable | 33,371 | 32,808 | 30,778 | ||||||||||||||
| Accrued payroll and benefits | 6,325 | (5,564) | 6,825 | ||||||||||||||
| Accrued self-insurance liabilities | 35,576 | 67,636 | 32,633 | ||||||||||||||
| Other accrued expenses | (55,501) | (24,390) | (25,294) | ||||||||||||||
| Other liabilities | 89,056 | 168 | (20,168) | ||||||||||||||
| NET CASH PROVIDED BY OPERATING ACTIVITIES | $ | 63,697 | $ | 92,615 | $ | 57,602 | |||||||||||
| Cash flows from investing activities | |||||||||||||||||
| Investment in partnership | $ | (2,597) | $ | — | $ | (15,714) | |||||||||||
| Non-operating distributions from investment in partnership | 1,862 | 2,905 | 877 | ||||||||||||||
| Acquisition of facilities | (127,024) | (55,374) | (79,676) | ||||||||||||||
| Purchase of property and equipment | (45,782) | (22,862) | (124,087) | ||||||||||||||
| Cash proceeds from the sale of assets | 750 | 10 | — | ||||||||||||||
| NET CASH USED IN INVESTING ACTIVITIES | $ | (172,791) | $ | (75,321) | $ | (218,600) | |||||||||||
| Cash flows from financing activities | |||||||||||||||||
| Borrowing on lines-of-credit, net of deferred financing fees | $ | 855,704 | $ | 154,528 | $ | 460,923 | |||||||||||
| Payments on lines-of-credit | (497,986) | (119,149) | (352,120) | ||||||||||||||
| Dividends on common stock | (80,394) | (60,280) | (53,797) | ||||||||||||||
| Contributions from non-controlling interest | 587 | 3,246 | — | ||||||||||||||
| Borrowings of long-term debt, net of deferred financing fees | 411,313 | 87,906 | 161,474 | ||||||||||||||
| Payments on long-term debt | (559,632) | (53,901) | (34,432) | ||||||||||||||
| NET CASH PROVIDED BY FINANCING ACTIVITIES | $ | 129,592 | $ | 12,350 | $ | 182,048 | |||||||||||
F-7
| PACS GROUP, INC. AND SUBSIDIARIES | |||||||||||||||||
| COMBINED/CONSOLIDATED STATEMENTS OF CASH FLOWS (CONTINUED) | |||||||||||||||||
| (dollars in thousands) | |||||||||||||||||
| December 31, | |||||||||||||||||
| 2023 | 2022 | 2021 | |||||||||||||||
| Net change in cash | $ | 20,498 | $ | 29,644 | $ | 21,050 | |||||||||||
| Cash, cash equivalents, and restricted cash - beginning of year | 98,206 | 68,562 | 47,512 | ||||||||||||||
| Cash, cash equivalents, and restricted cash - end of year | $ | 118,704 | $ | 98,206 | $ | 68,562 | |||||||||||
| Supplemental disclosures of cash flow information | |||||||||||||||||
| Cash paid during the period for: | |||||||||||||||||
| Interest | $ | 50,558 | $ | 25,911 | $ | 6,943 | |||||||||||
| Income taxes | 60,009 | 42,554 | 29,110 | ||||||||||||||
| Non-cash financing and investing activity | |||||||||||||||||
| Accrued capital expenditures | $ | 3,000 | $ | 717 | $ | 1,799 | |||||||||||
| Assets acquired in operation expansions in exchange for notes payable | 2,150 | 8,200 | 12,800 | ||||||||||||||
See accompanying notes to combined/consolidated financial statements.
F-8
PACS GROUP, INC. AND SUBSIDIARIES
NOTES TO COMBINED/CONSOLIDATED FINANCIAL STATEMENTS
(dollars in thousands, except for share and per share values)
NOTE 1.ORGANIZATION AND NATURE OF BUSINESS
PACS Group, Inc. (PACS Group), a Delaware corporation, was incorporated on March 24, 2023. PACS Group is a holding company which consolidates various operating and other subsidiaries. PACS Group’s applicable operating subsidiaries operate various skilled nursing facilities (SNF) and assisted living facilities (ALF). PACS Group also owns other subsidiaries that are engaged in the acquisition, ownership, and leasing of health care-related properties. As of December 31, 2023 PACS Group subsidiaries operated 208 health care facilities in the states of Arizona, California, Colorado, Kentucky, Missouri, Nevada, Ohio, South Carolina, and Texas. PACS Group subsidiaries operated approximately 22,950 skilled nursing beds and 690 assisted living beds as of that date. As of December 31, 2023, PACS Group subsidiaries operated 179 facilities under long-term lease arrangements and had options to purchase 11 of those facilities.
PACS Group subsidiaries have investments in joint ventures that own the underlying real estate and related improvements of 14 post-acute care facilities that are operated by other PACS Group subsidiaries. PACS Group also owns subsidiaries that own real estate and related improvements that are leased to applicable affiliated SNF operating entities and one non-affiliated ALF operating entity. PACS Group’s real estate portfolio includes 29 properties which are operated and managed by applicable PACS Group subsidiaries.
Providence Administrative Consulting Services, Inc. (PACS), a California corporation, is a subsidiary of PACS Group and provides administrative support services, on a consulting basis, to other subsidiaries of PACS Group.
PACS Group also has a wholly-owned captive insurance subsidiary, Welsch Insurance Ltd. (Welsch). Welsch provides coverage to various consolidated operating subsidiaries related to Professional Liability and General Liability (PLGL) insurance.
Reorganization
Prior to June 30, 2023, Providence Group, Inc. (PGI) owned the operating subsidiaries of PACS Group. On June 30, 2023, PGI and its consolidated subsidiaries reorganized (the Reorganization) to facilitate their entrance into a new credit agreement, dated June 30, 2023 (the New Credit Agreement), between certain lenders party thereto, Truist Bank, as administrative agent, PACS Group, and PACS Holdings, LLC (PACS Holdings) as borrower thereunder. PACS Group and its wholly owned subsidiary PACS Holdings were created on March 24, 2023, and April 10, 2023, respectively, in anticipation of the Reorganization. The equity interests of certain other direct or indirect wholly-owned subsidiaries of PGI at the time of the Reorganization were also contributed to other new direct or indirect wholly-owned subsidiaries of PACS Group to facilitate the New Credit Agreement. PACS Group and its consolidated subsidiaries subsequent to the Reorganization are collectively referred to herein as the Company. The New Credit Agreement is described in Note 8.
The Reorganization was effected by the two then-existing stockholders of PGI (which at the time was the direct or indirect parent company of all consolidated entities comprising the Company), contributing their respective shares in PGI to newly-formed PACS Holdings, in exchange for a proportionate interest of shares in newly-formed PACS Group (via issuance of shares of PACS Group), and thus became the sole stockholders of PACS Group.
As a result of the Reorganization, (i) for most practical purposes PACS Group in effect became the successor to the historical consolidated business of PGI, and (ii) both of the two stockholders of PGI immediately prior to the Reorganization became the sole stockholders of PACS Group, and maintained their respective pro rata ownership percentage in PACS Group that they held in PGI immediately prior to the Reorganization (which was and remained 50/50).
The Reorganization was accounted for as an equity reorganization between entities under common control. The Reorganization combined entities that historically have not been presented together resulting in financial statements that are effectively considered to be those of a different reporting entity. Accordingly, the historical financial statements for periods prior to the Reorganization represent combined financial statements and the financial statements after the Reorganization represent consolidated financial statements. The contribution of shares of PGI
F-9
PACS GROUP, INC. AND SUBSIDIARIES
NOTES TO COMBINED/CONSOLIDATED FINANCIAL STATEMENTS
(dollars in thousands, except for share and per share values)
and receipt of shares of PACS Group will be accounted on a retrospective basis. Accordingly, all share and per share amounts in these combined/consolidated financial statements and related notes have been retrospectively restated, where applicable, for all periods herein, to give effect to the current shares outstanding of PACS Group.
NOTE 2.SUMMARY OF SIGNIFICANT ACCOUNTING POLICIES
Basis of Presentation
The accompanying combined/consolidated financial statements have been prepared in accordance with accounting principles generally accepted in the United States (U.S. GAAP). The combined/consolidated financial statements include the accounts of PACS Group, and its consolidated subsidiaries, or the Company as defined above. All intercompany transactions and balances have been eliminated in consolidation. The Company presents noncontrolling interests within the equity section of its combined/consolidated balance sheets and the amount of combined/consolidated income that is attributable to the Company and the noncontrolling interest in its combined/consolidated statements of income.
Use of Estimates
The preparation of the combined/consolidated financial statements in accordance with U.S. GAAP requires management to make estimates and assumptions that affect the reported amounts of assets and liabilities and disclosure of contingent assets and liabilities at the date of the combined/consolidated financial statements and the reported amounts of revenue and expenses during the reporting period. The most significant estimates in the Company’s financial statements relate to revenue, acquired property, right-of-use assets, lease liabilities, impairment of long-lived assets, and general and professional liabilities included in accrued self-insurance liabilities. Actual results could differ from estimated amounts.
Restricted Cash, Cash and Cash Equivalents
Cash and cash equivalents consist of cash and short-term investments with original maturities of three months or less at the time of purchase and therefore approximate fair value. The Company considers highly liquid debt instruments purchased with a maturity of three months or less to be cash equivalents. The Company maintains its cash and short-term investment balances in several high-credit quality financial institutions.
Included in restricted cash are funds held for PLGL and, prior to 2023, workers’ compensation (WC) claims. Funds held in restricted cash are contractually obligated to be segregated from the Company’s other cash accounts and are legally restricted for the use of funding WC and PLGL claims.
At any point in time the Company has funds in operating accounts and restricted cash accounts that are with third-party financial institutions. While management monitors the cash balances in operating accounts, these cash and restricted cash balances could be impacted if the underlying financial institutions fail or could be subject to other adverse conditions in the financial markets.
The following is a reconciliation of cash and cash equivalents on the combined/consolidated balance sheets to total cash, cash equivalents, and restricted cash on the combined/consolidated statement of cash flows as of December 31, 2023, 2022 and 2021:
| Year Ended December 31, | |||||||||||||||||
| 2023 | 2022 | 2021 | |||||||||||||||
| Cash and cash equivalents | $ | 73,416 | $ | 58,269 | $ | 31,962 | |||||||||||
| Restricted cash (included in prepaid expenses and other current assets) | 4,977 | 7,847 | 5,700 | ||||||||||||||
| Restricted cash (included in other assets) | 40,311 | 32,090 | 30,900 | ||||||||||||||
| Total cash, cash equivalents, and restricted cash | $ | 118,704 | $ | 98,206 | $ | 68,562 | |||||||||||
F-10
PACS GROUP, INC. AND SUBSIDIARIES
NOTES TO COMBINED/CONSOLIDATED FINANCIAL STATEMENTS
(dollars in thousands, except for share and per share values)
Cash in Excess of FDIC Limits
The Company currently has bank deposits with financial institutions in the U.S. that exceed FDIC insurance limits. FDIC insurance provides protection for bank deposits up to $250,000. The Company has not experienced any losses in such amounts.
Insurance Subsidiary Deposits and Investments
The Company's captive insurance subsidiary cash and cash equivalents, deposits and investments are designated to support long-term insurance subsidiary liabilities and have been classified as short-term and long-term assets based on the timing of expected future payments of the Company's captive insurance liabilities.
Patient and Resident Service Revenue
Patient and resident service revenue is derived from services rendered, under short-term contracts, to patients for skilled and intermediate nursing, rehabilitation therapy, and assisted living services. Patient and resident service revenue is reported at the amount that reflects the consideration to which the Company expects to be entitled in exchange for providing patient services. These amounts are due from patients, governmental programs, and other third-party payors, and include variable consideration for retroactive revenue adjustments due to settlement of audits, reviews, and investigations.
The Company recognizes revenue as its performance obligations are completed. Routine services are treated as a single performance obligation satisfied over time as services are rendered. These routine services represent a bundle of services that are not capable of being distinct. The performance obligations are satisfied over time as the patient simultaneously receives and consumes the benefits of the healthcare services provided. Additionally, there may be ancillary services which are not included in the daily rates for routine services, but instead are treated as separate performance obligations satisfied at a point in time when those services are rendered.
Accounts Receivable and Allowance for Doubtful Accounts
Accounts receivable consist primarily of amounts due from Medicare and Medicaid, managed care health plans and private payor sources, net of estimates for variable consideration. At December 31, 2023 and 2022, the allowance for doubtful accounts was immaterial to the combined/consolidated financial statements.
The Company determines the transaction price based on established billing rates reduced by contractual adjustments provided to third-party payors. Contractual adjustments are based on contractual agreements and historical experience. The Company considers the patient's ability and intent to pay the amount of consideration upon admission and records an implicit price concession based on historical patient collection experience. The allowance for implicit price concession is routinely evaluated and any subsequent changes are recorded as an adjustment to patient and resident service revenue in the combined/consolidated statements of income. The implicit price concession recorded as a reduction to patient and resident service revenue was $52,078, $33,927 and $13,733 for the years ended December 31, 2023, 2022, and 2021, respectively. As of December 31, 2023 and 2022, the Company has recorded estimated implicit price concessions as a reduction to accounts receivable of $42,171, and $33,988, respectively.
Government Grants
In the absence of specific guidance to account for government grants under U.S. GAAP, the Company has concluded to account for government grants in accordance with International Accounting Standard (IAS) 20, Accounting for Government Grants and Disclosure of Government Assistance, and as such, the Company recognizes grant income on a systematic basis in line with the recognition of specific expenses and lost revenues for which the grants are intended to compensate. Additional funding presented on the combined/consolidated statements of income is associated with government grants received through the Coronavirus Aid, Relief, and Economic Security Act (CARES Act). See Note 3 for more details.
F-11
PACS GROUP, INC. AND SUBSIDIARIES
NOTES TO COMBINED/CONSOLIDATED FINANCIAL STATEMENTS
(dollars in thousands, except for share and per share values)
Property and Equipment, Net
Property and equipment are stated at historical cost less accumulated depreciation and amortization. Repair and maintenance charges which do not increase the useful lives of the assets are charged to expense as incurred. Depreciation is computed using the straight-line method over the estimated useful life of the property and equipment. The following is a summary of the depreciable lives of the Company’s depreciable assets:
Buildings and improvements - minimum of 5 years to a maximum of 40 years, but generally 30 years
Leasehold improvements - shorter of the lease term or the estimated useful life, generally 5 to 15 years
Furniture and equipment - 3 to 15 years
Leasehold improvements are amortized over the lesser of the estimated useful life of the improvement or the term of the lease. Upon sale or retirement, the cost and the related accumulated depreciation and amortization are eliminated from the respective accounts and the resulting gain or loss included in current income.
Leases
The Company leases skilled nursing facilities, assisted living facilities, and commercial office space. The Company determines if an arrangement is a lease (for accounting purposes) at the inception of each lease.
Real estate leases are generally classified as operating leases and therefore the Company records rent expense on a straight-line basis over the term of the lease. The lease term used for straight-line rent expense is calculated from the date the Company is given control of the leased premises through the end of the lease term. Renewals are not assumed in the determination of the lease term unless they are deemed to be reasonably assured at the inception of the lease. The lease term used for this evaluation also provides the basis for establishing depreciable lives for buildings subject to lease and leasehold improvements. The Company has made an accounting policy election to keep leases with an initial term of 12 months or less off of the balance sheets and recognize those lease payments in the combined/consolidated statements of income on a straight-line basis over the lease term. The Company has also elected the practical expedient to not separate lease and non-lease components for all of its leases as the non-lease components are not significant to the overall lease costs.
The Company’s real estate leases generally have initial lease terms of ten years or more and typically include one or more options to renew, with renewal terms that generally extend the lease term for an additional three to twenty years. Exercise of renewal options is generally subject to the satisfaction of certain conditions which vary by contract and generally follow payment terms that are consistent with those in place during the initial term.
Business Combinations
The Company accounts for acquisitions using the acquisition method of accounting in accordance with Financial Accounting Standards Board (FASB) Accounting Standards Codification (ASC) 805, Business Combinations (ASC 805). Acquisitions are accounted for as purchases and are included in the combined/consolidated financial statements from their respective acquisition dates. Assets acquired and liabilities assumed, if any, are measured at fair value on the acquisition date. Goodwill generated from acquisitions is recognized for the excess of the purchase price over tangible and identifiable intangible assets. In determining the fair value of identifiable assets, the Company uses various valuation techniques. These valuation methods require management to make estimates and assumptions surrounding projected revenues and costs, future growth, and discount rates.
Goodwill and Other Indefinite-Lived Intangible Assets
Goodwill represents the excess of the purchase price of acquired businesses over the estimated fair value assigned to the individual assets acquired and liabilities assumed. The Company assesses goodwill for impairment at least annually on October 1st. The Company will perform an impairment assessment at other times if facts and circumstances indicate that it is more likely than not that the fair value of a reporting unit that has goodwill is less than its carrying value.
F-12
PACS GROUP, INC. AND SUBSIDIARIES
NOTES TO COMBINED/CONSOLIDATED FINANCIAL STATEMENTS
(dollars in thousands, except for share and per share values)
When assessing goodwill for impairment the Company may elect to first perform a qualitative assessment to determine if the quantitative impairment test is necessary. If the Company does not perform a qualitative assessment, or if the qualitative assessment indicates it is more likely than not that the fair value of a reporting unit is less than its carrying amount, the Company performs a quantitative test. The Company recognizes an impairment charge for the amount by which the carrying amount exceeds the reporting unit’s fair value; however, the loss recognized would not exceed the total amount of goodwill allocated to the reporting unit.
The Company’s indefinite-lived intangible assets primarily consist of licenses. The Company reviews indefinite-lived intangible assets for impairment on an annual basis or more frequently if events or changes in circumstances indicate that the carrying amount of the intangible asset may not be recoverable.
The Company may elect to first perform a qualitative assessment to determine whether it is more likely than not that the fair value of an indefinite-lived intangible asset is less than its carrying value. If the Company does not perform the qualitative assessment, or if the qualitative assessment indicates it is more likely than not that the fair value of the indefinite-lived intangible asset is less than its carrying amount, the Company calculates the estimated fair value of the indefinite-lived intangible asset. If the estimated fair value of the indefinite-lived intangible asset is lower than its carrying amount, an impairment loss is recognized for the difference.
Fair Value Measurements
The Company’s financial instruments consist principally of cash and cash equivalents, accounts receivable, insurance subsidiary deposits, accounts payable and borrowings.
Fair value measurements are based on a three-tier hierarchy that prioritizes the inputs used to measure fair value. The three-tiers include: Level 1: observable inputs such as quoted market prices in active markets; Level 2: inputs other than quoted market prices included in Level 1 that are directly or indirectly observable for the asset or liability and Level 3: unobservable inputs for which little or no market data exists, thereby requiring management to develop their own estimates and assumptions.
Impairment of Long-Lived Assets
In accordance with ASC Topic 360, Property, Plant, and Equipment (ASC 360), long-lived assets are reviewed for impairment whenever events or changes in circumstances indicate that the carrying amount may not be recoverable. Recoverability of these assets is determined based upon expected undiscounted future net cash flows from the operating subsidiaries to which the assets relate, utilizing management’s best estimate, appropriate assumptions, and projections at the time. If the expected future cash flow from the use of the asset and its eventual disposition is less than the carrying amount of the asset, an impairment loss is recognized and measured using the fair value of the related assets. The Company did not identify any indicators of impairment of its long-lived assets during the years ended December 31, 2023, 2022, and 2021.
Accrued Risk Reserves
The Company is principally self-insured for risks related to PLGL claims. Additionally, the Company is partially self-insured for risks related to WC policies. Accrued risk reserves primarily represent the accrual for risks associated with WC and PLGL claims. The accrued risk reserves include a liability for unpaid reported claims and estimates for incurred but unreported claims. The Company’s policy with respect to a significant portion of its WC program assumed as part of the Plum acquisitions (this acquisition is discussed further in Note 15), and its PLGL claims is to use an actuary to assist management in estimating the Company’s exposure for claims obligation (for both asserted and unasserted claims). The Company’s retrospective-rated premium WC policy is subject to an annual assessment of the policy premium in relation to the payroll and losses incurred for the policy period. The Company recognizes the WC retrospective policy adjustment as the amount of settlement is determined.
F-13
PACS GROUP, INC. AND SUBSIDIARIES
NOTES TO COMBINED/CONSOLIDATED FINANCIAL STATEMENTS
(dollars in thousands, except for share and per share values)
Investments in Joint Ventures
Investments in joint ventures, in which the Company exercises significant influence over operating and financial policies, are accounted for using the equity method of accounting. Under this method, the investment is carried at cost and is adjusted to recognize the investor’s share of earnings or losses of the investee after the date of acquisition and is adjusted for impairment whenever it is determined that a decline in the fair value below the cost basis is other than temporary. The fair value of the investment then becomes the new cost basis of the investment, and it is not adjusted for subsequent recoveries in fair value. The Company evaluates its investment in joint ventures, including cost in excess of book value (equity method goodwill) for impairment whenever indicators of impairment exist. No indicators of impairment existed as of December 31, 2023, 2022 and 2021.
Noncontrolling Interest
The Company is the majority-owner in a subsidiary which was formed to develop land, a building, and other assets to be leased to a facility operated by the Company upon completion. The noncontrolling interest in subsidiary is initially recognized at estimated fair value on the contribution date and is presented within total equity in the Company’s combined/consolidated balance sheets since these interests are not redeemable.
Advertising
Advertising costs are expensed as incurred. For the years ended December 31, 2023, 2022, and 2021, advertising expenses included in the Company’s combined/consolidated statements of income were $7,127, $5,414, and $4,870, respectively.
Income Taxes
The Company utilizes ASC Topic 740, Income Taxes (ASC 740), which requires an asset and liability approach for financial accounting and reporting for income taxes. Under this guidance, deferred tax assets and liabilities are determined based upon differences between financial reporting and tax basis of assets and liabilities and are measured using the enacted tax laws that will be in effect when the differences are expected to reverse. The effect on deferred tax assets and liabilities of a change in tax rates is recognized in income in the period that includes the enactment date. See Note 10 for further discussion of the Company’s accounting for income taxes.
Under ASC 740, tax positions are evaluated for recognition using a more–likely–than–not threshold, and those tax positions requiring recognition are measured at the largest amount of tax benefit that is greater than 50 percent likely of being realized upon ultimate settlement with a taxing authority that has full knowledge of all relevant information. Liabilities for income tax matters include amounts for income taxes, applicable penalties, and interest thereon and are the result of the potential alternative interpretations of tax laws and the judgmental nature of the timing of recognition of taxable income.
The Company recognizes deferred tax assets (DTAs) to the extent that it believes that the assets are more likely than not to be realized. In making such a determination, the Company considers all available positive and negative evidence, including future reversals of existing taxable temporary differences, projected future taxable income, tax-planning strategies, carryback potential if permitted under the tax law, and results of recent operations. The Company generally expects to fully utilize its DTAs; however, when necessary, the Company records a valuation allowance to reduce its net deferred tax assets to the amount that is more likely than not to be realized.
Concentration of Credit Risks
The Company’s credit risks primarily relate to cash and cash equivalents, restricted cash, and accounts receivable. Cash and cash equivalents are primarily held in bank accounts and overnight investments. The Company holds amounts of cash in excess of the FDIC insured limits. Restricted cash is primarily invested in commercial paper and certificates of deposit with financial institutions and other interest-bearing accounts. Accounts receivable consist primarily of amounts due from patients (funded through Medicare, Medicaid, other contractual programs and
F-14
PACS GROUP, INC. AND SUBSIDIARIES
NOTES TO COMBINED/CONSOLIDATED FINANCIAL STATEMENTS
(dollars in thousands, except for share and per share values)
through private payors) and from other health care companies for management, accounting and other services. The collectability of account receivable balances is dependent on the availability of funds from certain programs that rely on governmental funding, primarily Medicare and Medicaid. The Company’s receivables from Medicare and Medicaid programs accounted for 20% and 36% of total accounts receivable, respectively, at December 31, 2023 and 32% and 21% of total accounts receivable, respectively, at December 31, 2022. These receivables represent the only significant concentration of credit risk for the Company. The Company does not believe there are significant credit risks associated with these governmental programs. The Company performs continual credit evaluations of the Company’s clients and maintains appropriate allowances for doubtful accounts on any accounts receivable proving uncollectible, and continually monitors and adjusts these allowances as necessary.
The Company’s operating subsidiaries, excluding four subsidiaries that exclusively operate assisted living facilities, have all of their skilled nursing beds designated for care of patients under federal Medicare and/or state Medicaid programs. 63% of skilled nursing beds are located in California.
Comprehensive Income
The Company does not have any components of other comprehensive income recorded within its combined/consolidated financial statements and, therefore, does not separately present a statement of comprehensive income in its combined/consolidated financial statements.
Segment Presentation
The Company’s chief operating decision maker (CODM), the Chief Operating Officer, reviews the consolidated results of operations when making decisions about allocating resources and assessing the performance of the Company as a whole and, hence, the Company has only one reportable segment. The Company does not distinguish between markets or regions for the purpose of allocating resources.
Recent Accounting Standards Issued But Not Yet Adopted by the Company
In November 2023, the FASB issued ASU 2023-07, Segment Reporting (Topic 280): Improvements to Reportable Segment Disclosures. The standard improves reportable segment disclosure requirements for public business entities primarily through enhanced disclosures about significant segment expenses that are regularly provided to the CODM and included within each reported measure of segment profit (referred to as the “significant expense principle”). The standard will become effective for the Company for the fiscal year 2024 annual financial statements and interim financial statements thereafter and will be applied retrospectively for all prior periods presented in the financial statements, with early adoption permitted. The Company is currently evaluating the impact this guidance will have on the disclosures included in the Notes to the combined/consolidated financial statements.
In December 2023, the FASB issued ASU 2023-09, Income Taxes (Topic 740): Improvements to Income Tax Disclosures, which requires the Company to disclose disaggregated jurisdictional and categorical information for the tax rate reconciliation, income taxes paid and other income tax related amounts. The standard will become effective for the Company for the fiscal year 2024 annual financial statements and may be applied prospectively or retrospectively for all prior periods presented in the financial statements, with early adoption permitted. The Company is currently evaluating the impact this guidance will have on the disclosures included in the Notes to the combined/consolidated financial statements.
NOTE 3.REVENUE AND ACCOUNTS RECEIVABLE
Patient and Resident Service Revenue
The Company’s patient and resident service revenue is derived primarily from the Company’s applicable subsidiaries providing healthcare services to their respective patients and residents. Revenue is recognized when services are provided to the patients at the amount that reflects the consideration to which the Company expects to be entitled. These amounts are due from residents, third-party payors (including health insurers and government
F-15
PACS GROUP, INC. AND SUBSIDIARIES
NOTES TO COMBINED/CONSOLIDATED FINANCIAL STATEMENTS
(dollars in thousands, except for share and per share values)
payors), and others and includes variable consideration for retroactive revenue adjustments due to settlement of audits and other reviews by the payor. Generally, the licensed healthcare provider entity providing the applicable services bills the applicable payors monthly.
The healthcare services in skilled patient contracts include routine services in exchange for a contractual agreed-upon amount or rate. Revenue is recognized as the performance obligations are satisfied.
Performance obligations are determined based on the nature of the services provided by the applicable licensed healthcare provider entity. Revenue for performance obligations satisfied over time is recognized based on actual charges incurred in relation to total expected (or actual) charges. The Company believes that this method provides a faithful depiction of the transfer of services over the term of the performance obligation based on the inputs needed to satisfy the obligation. Generally, performance obligations satisfied over time relate to residents receiving services in the facility and, when applicable, residents receiving services in their homes (independent care or assisted living). The Company measures the performance obligation from admission into the facility, or the commencement of the service, to the point when the applicable licensed healthcare provider entity is no longer required to provide services to that resident, which is generally at the time that the resident discharges from the applicable facility or passes away.
Revenue recognized from healthcare services is adjusted for estimates of variable consideration to arrive at the transaction price. The Company determines the transaction price based on contractually agreed-upon amounts or rates, adjusted for estimates of variable consideration. Variable consideration includes estimates of implicit price concessions so that the estimated transaction price is reflective of the amount to which the Company expects to be entitled in exchange for providing the healthcare services to customers. Variable consideration is estimated using the expected value method based on the Company’s historical reimbursement experience. The amount of variable consideration constrains the transaction price, such that it is probable that a significant reversal in the amount of the cumulative revenue recognized will not occur in a future period. Historically the Company has not had material differences between its estimated transaction price and actual collections from payors. If actual amounts of consideration ultimately received differ from the Company’s estimates, it adjusts these estimates, which would affect net service revenue in the period such variances become known.
Agreements with third-party payors typically provide for payments at amounts less than established charges. A summary of the payment arrangements with major third-party payors is as follows:
Medicaid: Payments for skilled nursing facility services rendered to Medicaid (including Medi-Cal, which is the name of the state Medicaid program in California) program beneficiaries are based on an annually established daily reimbursement rate for eligible stays. The rate is adjusted annually. The final settlement is determined after submission of an annual cost report and audits thereof by Medicaid. Revenue from the Medicaid program amounted to 38%, 30%, and 35% of the Company’s combined/consolidated net patient and resident revenue for the years ended December 31, 2023, 2022, and 2021, respectively.
Medicare: Payments for skilled nursing facility services rendered to Medicare program beneficiaries are based on prospectively determined daily rates which vary according to a patient diagnostic classification system. The applicable licensed healthcare provider entity is paid for certain reimbursable services at the approved rate with final settlement determined after submission of the annual cost report and audit thereof by the designated Medicare fiscal intermediary. Revenue from the Medicare program amounted to 39%, 48%, and 44% of the Company’s combined/consolidated net patient and resident revenue for the years ended December 31, 2023, 2022, and 2021, respectively.
Managed Care, Private and Other: Payments for services rendered to private payors and other primary payors included in the table below are based on established rates or on agreements with certain commercial insurance companies, health maintenance organizations, and preferred provider organizations, which provide for various discounts from the established rates. Revenue from these sources collectively amounted to 24%, 22%, and 21% of the Company’s combined/consolidated net patient and resident revenue for the years ended December 31, 2023, 2022, and 2021, respectively.
F-16
PACS GROUP, INC. AND SUBSIDIARIES
NOTES TO COMBINED/CONSOLIDATED FINANCIAL STATEMENTS
(dollars in thousands, except for share and per share values)
The Company’s contracts are short term in nature with a duration of one year or less. The Company has minimal unsatisfied performance obligations at the end of the reporting period as patients are typically under no obligation to remain admitted in the Company’s facilities or under the Company’s care. As the period between the time of service and time of payment is typically one year or less, the Company does not adjust for the effects of a significant financing component.
Included in the Company’s combined/consolidated balance sheets are contract balances, comprising of billed accounts receivable and unbilled receivables, which are the result of the timing of revenue recognition, billings and cash collections, as well as contract liabilities, which primarily represent payments the Company receives in advance of services provided. The Company has no material contract liabilities and contract assets as of December 31, 2023 and 2022.
Laws and regulations concerning government programs, including Medicare and Medicaid, are complex and subject to varying interpretation. As a result of audits and other reviews by governmental agencies or payor sources, health care providers from time to time receive requests for information and notices regarding billing audits and potential noncompliance with applicable laws and regulations, which, in some instances, can ultimately result in substantial monetary recoupments or other remedies being imposed on the healthcare provider. Compliance with such laws and regulations may also be subject to future government review and interpretation, as well as significant regulatory action, including fines, penalties, and potential exclusion from the related programs. The Company believes that it is in compliance with all applicable laws and regulations.
The contracts the Company has with commercial payors also provide for retrospective audit and review of claims.
Settlements with third-party payors for retroactive adjustments due to audits or other reviews are considered variable consideration and are included in the determination of the estimated transaction price for providing resident services. These settlements are estimated based on the terms of the payment agreement with the payor, correspondence from the payor, and the Company’s historical settlement activity, including an assessment to ensure that it is probable that a significant reversal in the amount of cumulative revenue recognized will not occur when the uncertainty associated with the retroactive adjustment is subsequently resolved. Estimated settlements are adjusted in future periods as adjustments become known (that is, new information becomes available), or as years are settled or are no longer subject to such audits or other reviews. These amounts are immaterial.
The Company disaggregates revenue from contracts with its patients by payors. The Company determines that disaggregating revenue into these categories achieves the disclosure objectives to depict how the nature, amount, timing, and uncertainty of revenue and cash flows are affected by economic factors. The composition of patient and resident service revenue by primary payors for the years ended December 31, 2023, 2022, and 2021 are as follows:
| 2023 | % of Revenue | 2022 | % of Revenue | 2021 | % of Revenue | ||||||||||||||||||||||||||||||
| Medicare | $ | 1,200,801 | 38.6 | % | $ | 1,142,863 | 47.6 | % | $ | 496,311 | 43.7 | % | |||||||||||||||||||||||
| Medicaid | 1,168,455 | 37.6 | % | 723,896 | 30.2 | % | 399,141 | 35.1 | % | ||||||||||||||||||||||||||
| Managed care | 586,850 | 18.9 | % | 416,089 | 17.3 | % | 159,541 | 14.0 | % | ||||||||||||||||||||||||||
| Private and other | 154,008 | 4.9 | % | 116,307 | 4.9 | % | 80,916 | 7.2 | % | ||||||||||||||||||||||||||
| Total patient and resident service revenue | $ | 3,110,114 | 100.0 | % | $ | 2,399,155 | 100.0 | % | $ | 1,135,909 | 100.0 | % | |||||||||||||||||||||||
Additional Funding and CARES Act
Through the CARES Act, the Company received $14,962 and $5,654 in funding from the U.S. Department of Health and Human Services (HHS) through the Provider Relief Fund (PRF) during the years ended December 31, 2022 and 2021, respectively. These funds were provided to healthcare providers who diagnose, test, or care for individuals with cases of COVID-19 and have health care related expenses and lost revenues attributable to
F-17
PACS GROUP, INC. AND SUBSIDIARIES
NOTES TO COMBINED/CONSOLIDATED FINANCIAL STATEMENTS
(dollars in thousands, except for share and per share values)
COVID-19. The Company recorded these funds as deferred revenue upon receipt and revenue is recognized only to the extent that health-care related expenses or lost revenues have been incurred and are not reimbursed from other funding sources. The company did not receive any funds related to this program during 2023.
The CARES Act also provided for refundable payroll tax credits known as the Employee Retention Tax Credit (ERTC), which allowed qualified employers to receive a credit of 70% of the employee qualified wages and related payroll costs paid after December 31, 2020 through September 30, 2021, up to a maximum credit of $7 per employee, per quarter, for a maximum of $21 per employee in 2021. The Company treated these credits under the accrual basis of accounting in conformity with U.S. GAAP. The Company interpreted the condition of partial suspension through governmental orders during all quarters of 2020 and the first three quarters of 2021, as defined by the CARES Act and to incur qualified payroll and related costs during the applicable quarters. The Company claimed a total of $32,428 under the ERTC, $18,656 related to 2021 qualified wages and $13,772 related to 2020 qualified wages. The Company utilized outside consultants to calculate the qualified wages and the ERTC amounts, and to prepare and submit the applications. Subsequently, due to uncertainty related to meeting the necessary qualifications, the Company recorded a reserve against the entire amount claimed. As of December 31, 2023 and 2022, the Company has recorded $36,477 and $17,119, respectively, in other liabilities to reflect the cash already received related to these credits which may need to be returned and potential penalties.
Additionally, under the CARES Act, employers could elect to defer the deposit and payment of the employers share of Social Security taxes through the end of 2020. One half of the deferral was required to be repaid on or before December 31, 2021 with the remaining half due on or before December 31, 2022. The deferral of social security tax payments in the amount of $7,793 was recorded as a liability at December 31, 2021. The Company paid $7,793 during the year ended December 31, 2022 and there are no remaining short-term or long-term balances as of December 31, 2022 and 2023.
NOTE 4.ESCROW FUNDS
Certain subsidiaries of the Company have obtained Department of Housing and Urban Development (HUD)-insured mortgages on properties that they lease to affiliated operating subsidiaries of the Company, while various other subsidiaries of the Company lease properties from unrelated third-party landlords that have obtained HUD-insured mortgages on the applicable properties. Under the terms of the HUD-insured mortgages, borrowers and/or their tenants are required to make certain deposits into escrow funds to be used for payment of property insurance, mortgage insurance premiums, and taxes. The deposits are generally maintained in an interest-bearing account with a federally insured financial institution.
Additionally, some HUD-insured mortgages require a reserve for replacement account and a non-critical repair reserve. Under the terms of the HUD-insured mortgages and the related regulatory agreements required by HUD, the tenants are required to make regular monthly deposits into a reserve for replacement account to assure the availability of funds to replace building components, furniture and equipment over time. All disbursements from this account require prior written approval by HUD and the mortgage lender. The non-critical repair reserve is used to cover estimated repairs on the properties typically within 12 months of closing on the HUD loans.
During 2021, the Company obtained a construction loan from an unaffiliated third-party lender that the subsidiary expects will be refinanced through a HUD-insured mortgage at a future date. At December 31, 2023 and 2022, this subsidiary had escrows related to debt service reserves, working capital escrows, and various other construction related escrows, in accordance with the terms of the loan agreement.
These reserve and escrow accounts are maintained under the control of the mortgage lender for the benefit of the applicable tenant and are generally held in an interest-bearing account with a federally insured financial institution.
F-18
PACS GROUP, INC. AND SUBSIDIARIES
NOTES TO COMBINED/CONSOLIDATED FINANCIAL STATEMENTS
(dollars in thousands, except for share and per share values)
NOTE 5.PROPERTY AND EQUIPMENT
Property and equipment consisted of the following at:
| December 31, | |||||||||||||||||
| 2023 | 2022 | ||||||||||||||||
| Buildings and improvements | $ | 372,554 | $ | 265,520 | |||||||||||||
| Leasehold improvements | 58,958 | 47,238 | |||||||||||||||
| Furniture, fixtures, and other | 64,750 | 46,842 | |||||||||||||||
| Construction in process | 50,937 | 39,813 | |||||||||||||||
| Land | 55,593 | 36,357 | |||||||||||||||
| Finance lease right-of-use assets | 40,536 | 34,960 | |||||||||||||||
| 643,328 | 470,730 | ||||||||||||||||
| Less: accumulated depreciation and amortization | (65,800) | (40,165) | |||||||||||||||
Property and equipment, net | $ | 577,528 | $ | 430,565 | |||||||||||||
The Company evaluated its long-lived assets and did not record an impairment charge for the years ended December 31, 2023, 2022, and 2021.
See Note 15 for information on expansions during the years ended December 31, 2023, 2022, and 2021.
NOTE 6.GOODWILL AND OTHER INDEFINITE-LIVED INTANGIBLE ASSETS
Goodwill consisted of the following:
| Goodwill | |||||
| Balance as of January 1, 2022 | $ | 27,882 | |||
| Acquisitions | 8,495 | ||||
| Divestitures | — | ||||
| Measurement period adjustment - Plum | 18,844 | ||||
| Balance as of December 31, 2022 | $ | 55,221 | |||
| Acquisitions | $ | 3,800 | |||
| Divestitures | $ | — | |||
| Balance as of December 31, 2023 | $ | 59,021 | |||
There are no prior period accumulated goodwill impairment losses nor any goodwill impairment losses for the years ended December 31, 2023, 2022, and 2021.
As of the year ended December 31, 2023 and 2022, the Company's indefinite-lived intangible assets consisted of the following:
| December 31, | |||||||||||||||||
| 2023 | 2022 | ||||||||||||||||
| Licenses | $ | 6,270 | $ | 6,270 | |||||||||||||
Total other indefinite-lived intangible assets | $ | 6,270 | $ | 6,270 | |||||||||||||
There are no prior period accumulated indefinite-lived intangible asset impairment losses nor any indefinite-lived intangible asset impairment losses for the years ended December 31, 2023, 2022, and 2021.
F-19
PACS GROUP, INC. AND SUBSIDIARIES
NOTES TO COMBINED/CONSOLIDATED FINANCIAL STATEMENTS
(dollars in thousands, except for share and per share values)
NOTE 7.INVESTMENT IN PARTNERSHIP
For the years ended December 31, 2023, 2022, and 2021, the Company had invested $12,362, $12,018, and $15,269, respectively, in multiple equity investments. These joint venture operations were formed to develop, own, and lease health care facilities to operational subsidiaries of the Company. Some of the joint ventures hold options to purchase the related real estate property holdings. Each of the joint ventures is governed by a managing member who makes the significant decisions that impact the economic performance of the joint venture. The Company is not the managing member of any of the joint ventures in which it is invested. All of the investments are individually immaterial with the Company’s largest equity investment of $9,481 in a joint venture representing an ownership of 27%. All investments are included in other assets in the Company’s combined/consolidated balance sheets. The Company accounts for its share in its equity method investments in the other income (expense), net line item in the Company’s combined/consolidated statements of income. (Loss) income from the investments in partnerships was $(391), $(346), and $232 for the years ended December 31, 2023, 2022, and 2021, respectively.
NOTE 8.CREDIT FACILITIES
On February 28, 2023, the Company entered into a working capital loan agreement (the Working Capital Loan) in connection with the acquisition of various new facilities. The Working Capital Loan allowed the Company to borrow up to $17,500 at an annual interest rate of 9%. On May 8, 2023, the Company drew on the Working Capital Loan in the amount of $15,000. As described below, the Working Capital Loan was repaid during the year and, as such, has a zero balance as of December 31, 2023.
On June 30, 2023, the Company and certain of its subsidiaries entered into a credit agreement with Truist Bank (Truist) and a syndicate of lenders (the 2023 Credit Agreement), that extended credit in the form of the revolving credit facility thereunder, (the 2023 Revolving Credit Facility), including letter of credit and swing line sub facilities and a term loan facility (Truist Term Loan), together referred to as the 2023 Credit Facility. The 2023 Credit Agreement provided for: (i) 2023 Revolving Credit Facility with revolving commitments in an aggregate principal amount of $150,000, including a letter of credit sub facility in an amount representing that portion of the aggregate revolving commitments that may be used by the borrower for the issuance of letters of credit in an aggregate face amount not to exceed $30,000 and a swingline loan sub facility in an aggregate principal amount at any time outstanding not to exceed $20,000 and (ii) the Truist Term Loan in an aggregate principal amount of $275,000.
Outstanding borrowings under the 2023 Credit Facility accrued interest at either: (a) the Secured Overnight Financing Rate (SOFR) (plus a 0.10% credit spread adjustment) plus a margin ranging from 2.50% to 3.50% per annum; or (b) Base Rate (which was defined in a customary manner for credit facilities of this type) plus a margin ranging from 1.50% to 2.50% per annum. The applicable margin was based on the Company’s debt to income ratio as calculated in accordance with the terms of the 2023 Credit Agreement. In addition, the Company agreed to pay a commitment fee on the unused portion of the 2023 Revolving Credit Facility, which ranged from 0.30% to 0.50% per annum, depending on the same debt to income ratio.
In connection with executing the 2023 Credit Agreement, deferred financing costs associated with both lines-of-credit and long-term debt of $3,109 were written off, and additional deferred financing costs of $9,662 were capitalized during the year ended December 31, 2023. In addition, on the closing date of the 2023 Credit Agreement, the Company drew $75,000 on the 2023 Revolving Credit Facility and borrowed the entirety of the $275,000 Truist Term Loan. See Note 9 for more details. The Company used approximately $142,000 of the net proceeds to repay certain outstanding indebtedness on prior lines of credit and the Working Capital Loan.
On December 7, 2023, the Company amended and restated the 2023 Credit Facility (Amended and Restated 2023 Credit Facility). The Amended and Restated 2023 Credit Facility provided for an increase of the 2023 Revolving Credit Facility to an aggregate principal amount of $600,000, which revolving commitments may also be utilized for (x) the issuance of letters of credit in an aggregate face amount not to exceed $50,000 and/or (y) the borrowing of swingline loans in aggregate principal amount not to exceed $20,000 at any time outstanding.
F-20
PACS GROUP, INC. AND SUBSIDIARIES
NOTES TO COMBINED/CONSOLIDATED FINANCIAL STATEMENTS
(dollars in thousands, except for share and per share values)
Outstanding borrowings under the Amended and Restated 2023 Credit Facility bear interest at the option of the Company based on: (a) SOFR (plus a 0.10% credit spread adjustment) plus a margin ranging from 2.25% to 3.25% per annum; or (b) the Base Rate (which is defined consistent with the 2023 Credit Facility) plus the applicable margin ranging from 1.25% to 2.25% per annum. The applicable margin is based on the Company’s debt to income ratio as calculated consistent with the 2023 Credit Facility. In addition, the Company will pay a commitment fee on the unused portion of the commitments, which ranges from 0.25% to 0.45% per annum, depending on the same debt to income ratio.
Upon the closing of the Amended and Restated 2023 Credit Facility, the Company borrowed $460,000 of revolving loans, the proceeds of which were used to repay and refinance all term loans and revolving loans under the 2023 Credit Facility, to repay certain other outstanding indebtedness, and to pay transaction costs in connection with the Amended and Restated 2023 Credit Facility. Deferred financing costs associated with both lines-of-credit and long-term debt of $519 were written off as part of the refinance during the year ended December 31, 2023.
The agreement above contains certain financial and non-financial covenants and restrictions. Default by the applicable credit party on any covenant or restriction could affect the lender’s commitment to lend, and, if not waived or corrected, could make the outstanding balances due on demand. Under the Amended and Restated 2023 Credit Facility, the Company must maintain a debt-to-income ratio of not greater than 3.00:1.00. The Amended and Restated 2023 Credit Facility also requires that the Company maintain a minimum interest/rent coverage ratio of not less than 1.10:1.00. The Company was in compliance with all such covenants and restrictions as of December 31, 2023.
The Company maintains the Amended and Restated 2023 Credit Facility as its single line-of-credit. At December 31, 2023, the total commitment limit continues to be $600,000 and was secured by Company assets. The agreements mature on December 7, 2028. The balance outstanding on all applicable lines was $520,000 at December 31, 2023, resulting in available cash of $80,000. The Company had no letters of credit outstanding as of December 31, 2023 and had $22,370 in letters of credit outstanding as of December 31, 2022.
As of December 31, 2022, the Company maintained several other lines-of-credit with commercial banks. At December 31, 2022, the total commitment limit amounted to $176,000 and was secured by Company assets. These agreements bear interest at rates ranging from LIBOR to LIBOR plus 3.5% and SOFR plus 3.15%. The agreements matured through November 5, 2024. The balance outstanding on these other applicable lines was $146,820 at December 31, 2022, resulting in available cash of $29,180. As discussed above, these other lines-of-credit were closed in connection with executing the 2023 Credit Agreement.
Deferred financing fees on lines-of-credit were $15,099 and $4,218 as of December 31, 2023 and 2022, respectively. Amortization expense relating to deferred financing fees on lines-of-credit for the year ended December 31, 2023 was $889 and was immaterial for the years ended December 31, 2022 and 2021, respectively. Accumulated amortization related to deferred financing fees on lines-of-credit was $193 and $2,811 for the years ended December 31, 2023 and 2022, respectively.
NOTE 9.LONG-TERM DEBT
During the years ended December 31, 2023 and 2022, some of the Company's subsidiaries entered into Department of Housing and Urban Development (HUD)-insured mortgage loans in the aggregate amount of $88,809 and $7,027, respectively. As a result, eight of the Company's subsidiaries had mortgage loans insured with HUD in the aggregate amount of $166,181 as of December 31, 2023, of which $2,346 is classified as short-term and the remaining $163,834 is classified as long-term. As of December 31, 2022, the Company’s subsidiaries had HUD-insured mortgage loans in the aggregate amount of $79,031 of which $1,509 was classified as short-term and the remaining $77,522 was classified as long-term. These subsidiaries are subject to HUD-mortgage oversight and periodic inspections. As of December 31, 2023, the Company’s HUD-insured mortgage loans bear fixed interest rates ranging from 2.4% to 6.3% per annum and have various maturity dates through December 31, 2058. In addition to the interest rate, the Company incurs other fees for HUD placement, including but not limited to audit fees. Amounts borrowed under the mortgage loans may be prepaid, subject to prepayment fees based on the
F-21
PACS GROUP, INC. AND SUBSIDIARIES
NOTES TO COMBINED/CONSOLIDATED FINANCIAL STATEMENTS
(dollars in thousands, except for share and per share values)
principal balance on the date of prepayment. The original terms for all the HUD-insured mortgage loans are 30 to 35 years.
In addition to the HUD-insured mortgage loans above, the Company has 12 other mortgage loans or promissory notes. The non-HUD insured mortgage loans and notes bear interest rates in the range of 2.0% and 8.0% per annum with various maturity dates through June 1, 2027. The notes are secured by equipment and guarantees by the Company and its stockholders. As of December 31, 2023 and 2022, the Company had $48,829 and $277,201, respectively, of debt principal outstanding under the mortgage loans and promissory notes, of which $14,476 is classified as short-term and the remaining $34,354 is classified as long-term as of December 31, 2023, and $59,854 is classified as short-term and the remaining $217,347 is classified as long-term as of December 31, 2022.
The Company was in compliance with all applicable loan covenants with respect to the foregoing as of December 31, 2023 and 2022. The loans above are guaranteed by the Company. Additionally, various loans are secured by real property with a carrying value amounting to $438,645, and $323,439 at December 31, 2023 and 2022, respectively.
Long-term debt consists of the following at:
| December 31, | |||||||||||||||||
| 2023 | 2022 | ||||||||||||||||
| HUD-insured mortgage loans | $ | 166,181 | $ | 79,031 | |||||||||||||
| Other mortgage loans and promissory notes | 48,829 | 277,201 | |||||||||||||||
| Less: current maturities | (16,822) | (61,363) | |||||||||||||||
| Less: deferred financing fees, net | (2,480) | (3,348) | |||||||||||||||
| Total | $ | 195,708 | $ | 291,521 | |||||||||||||
Long-term debt and line-of-credit maturities, excluding deferred financing fees, for the next five years and in the aggregate are as follows as of December 31, 2023:
| Amount | |||||
| 2024 | $ | 16,822 | |||
| 2025 | 13,278 | ||||
| 2026 | 3,545 | ||||
| 2027 | 2,772 | ||||
| 2028 | 522,770 | ||||
| Thereafter | 175,823 | ||||
| Total | $ | 735,010 | |||
Deferred financing fees incurred in conjunction with debt financing of $2,611 and $4,734 for the years ended December 31, 2023 and 2022, respectively, are being amortized over the life of the respective loans. Total amortization related to deferred financing fees is included in interest expense and amounted to $1,551, $978, and $462 for the years ended December 31, 2023, 2022, and 2021, respectively. Accumulated amortization related to those deferred financing fees was $131 and $1,386 for the years ended December 31, 2023 and 2022, respectively.
As discussed in Note 8, on June 30, 2023, the Company borrowed under the Truist Term Loan in connection with the execution of the 2023 Credit Agreement. Under the Truist Term Loan, the Company borrowed $275,000. The Truist Term Loan has a maturity date of June 30, 2028. Upon closing of the Truist Term Loan, the Company paid off certain other mortgage loans and promissory notes in the aggregate amount of $224,802. The Truist Term Loan was repaid on December 7, 2023 in connection with the closing of the Amended and Restated 2023 Credit Facility and as such, has a zero balance as of December 31, 2023.
F-22
PACS GROUP, INC. AND SUBSIDIARIES
NOTES TO COMBINED/CONSOLIDATED FINANCIAL STATEMENTS
(dollars in thousands, except for share and per share values)
NOTE 10.PROVISION FOR INCOME TAXES
Effective January 1, 2021, the Company elected “C” corporation status with the Internal Revenue Service.
For financial reporting purposes, income before income taxes includes the following components:
| 2023 | 2022 | 2021 | |||||||||||||||
| Income before provision for income taxes | 157,317 | 207,045 | 81,426 | ||||||||||||||
The provision for income taxes on continuing operations for the years ended December 31, 2023, 2022, and 2021, respectively, is summarized as follows:
| 2023 | 2022 | 2021 | |||||||||||||||
| Current | |||||||||||||||||
| Federal | $ | 38,242 | $ | 37,044 | $ | 16,438 | |||||||||||
| State | 16,116 | 15,932 | 9,551 | ||||||||||||||
| Total current provision | 54,358 | 52,976 | 25,989 | ||||||||||||||
| Deferred | |||||||||||||||||
| Federal | (6,641) | 3,345 | 8,700 | ||||||||||||||
| State | (3,282) | 228 | (1,210) | ||||||||||||||
| Total deferred provision | (9,923) | 3,573 | 7,490 | ||||||||||||||
| Total income tax provision | $ | 44,435 | $ | 56,549 | $ | 33,479 | |||||||||||
A reconciliation of the federal statutory rate to the effective tax rate for the years ended December 31, 2023, 2022 and 2021, respectively, is comprised as follows:
| 2023 | 2022 | 2021 | |||||||||||||||
| Income tax expense at statutory rate | 21.0 | % | 21.0 | % | 21.0 | % | |||||||||||
| State income taxes – net of federal benefit | 6.5 | 6.3 | 8.3 | ||||||||||||||
| Non-deductible expenses | 0.9 | 0.4 | 1.6 | ||||||||||||||
| Change in valuation allowance | 1.3 | — | — | ||||||||||||||
| Recognition of prior year deferred tax liability | — | — | 10.2 | ||||||||||||||
| Non-deductible transaction costs | — | — | 0.8 | ||||||||||||||
| Change to deferred taxes | (1.6) | — | — | ||||||||||||||
| Other Adjustments | — | (0.4) | (0.9) | ||||||||||||||
| Total effective tax rate | 28.1 | % | 27.3 | % | 41.0 | % | |||||||||||
F-23
PACS GROUP, INC. AND SUBSIDIARIES
NOTES TO COMBINED/CONSOLIDATED FINANCIAL STATEMENTS
(dollars in thousands, except for share and per share values)
The Company’s deferred tax assets and liabilities as of December 31, 2023 and 2022 are summarized as follows:
| 2023 | 2022 | ||||||||||
| Deferred tax assets (liabilities) | |||||||||||
| Accrued expenses | $ | 17,523 | $ | 13,740 | |||||||
| Allowance for doubtful accounts | 8,247 | 5,919 | |||||||||
| Deferred revenue | — | 910 | |||||||||
| Insurance | 15,428 | 11,131 | |||||||||
| Intangible assets | 4,073 | 4,353 | |||||||||
| Deferred compensation | 1,202 | 554 | |||||||||
| Lease liability | 573,227 | 375,669 | |||||||||
| Total deferred tax assets | 619,700 | 412,276 | |||||||||
| Valuation allowance | (2,107) | — | |||||||||
| Total net deferred tax assets | 617,593 | 412,276 | |||||||||
| Cash to accrual method change | (6,125) | (12,082) | |||||||||
| Fixed assets | (36,838) | (31,622) | |||||||||
| Prepaid expenses | (10,802) | (6,579) | |||||||||
| Investment in partnership | (4,904) | (5,252) | |||||||||
| Right of use asset | (555,766) | (364,055) | |||||||||
| Other | (1,411) | (861) | |||||||||
| Total deferred tax liabilities | (615,846) | (420,451) | |||||||||
| Net deferred tax assets (liabilities) | $ | 1,747 | $ | (8,175) | |||||||
As of December 31, 2023, the Company has recorded a valuation allowance of 2,107 against its captive insurance dual consolidated loss deferred tax asset. This valuation allowance has been established because it is more likely than not that the deferred tax asset will not be realized.
The Company is subject to U.S. federal income tax, as well as income tax in certain states in which it operates. The Company’s federal returns for tax years 2020 and forward are subject to examination, and state returns for tax years 2019 and forward are subject to examination. The Company is not, to its knowledge under examination by any federal or state income tax authority. The Company’s balance of net deferred tax assets and net deferred tax liabilities is included within other assets and other liabilities on the combined/consolidated balance sheets as of December 31, 2023 and 2022, respectively.
As of December 31, 2023 and 2022, the Company did not have any unrecognized tax benefits. The Company recognizes accrued interest and penalties related to unrecognized tax benefits in income tax expense. The Company does not anticipate the uncertain tax position to change materially within the next 12 months.
The Inflation Reduction Act 2022 (IRA), which incorporates a Corporate Alternative Minimum Tax (CAMT), was signed on August 16, 2022. The changes were effective for tax years beginning after December 31, 2022. The new tax requires companies to compute two separate calculations for federal income tax purposes and pay the greater of the new minimum tax or their regular tax liability. The IRA does not have a material impact for the Company.
F-24
PACS GROUP, INC. AND SUBSIDIARIES
NOTES TO COMBINED/CONSOLIDATED FINANCIAL STATEMENTS
(dollars in thousands, except for share and per share values)
NOTE 11.LEASES
Operating Leases
The Company leases most of its skilled nursing and assisted living facilities, as well as its office space and certain vehicles and equipment, under various non-cancelable operating lease agreements. These operating leases expire at various dates throughout 2049.
Substantially all operating leases for skilled nursing and assisted living facilities are on a “triple-net” basis, which require lessees to pay for all insurance, repairs, utilities, and real property taxes assessed on the leased property, and most of the leases are guaranteed by the Company and/or its stockholders.
For 11 of the facility operating leases, the Company holds an option to purchase the real estate which can be exercised at varying times starting September 9, 2021 through January 31, 2038. At lease inception it was determined that the exercise of these purchase options was not reasonably assured.
The facility leases are generally renewable at the Company’s option for additional terms ranging from 3 to 30 years. All facility leases provide for an additional percentage rent based upon specified rates per the terms of the agreements.
During the year ended December 31, 2021, the Company acquired facility leases and various leases for laptops, copiers, and vehicles as part of the acquisition further described in Note 15.
Real estate lease payments are deemed to constitute the right to use the underlying facilities and operate as a skilled nursing facility as permitted by the accompanying license. As the license is deemed to be inseparable from the related real estate in determining value, the payments related to these components have been combined into a single lease obligation representing the right to use the facilities and to operate under the terms of the accompanying license, respectively.
Finance Leases
The Company leases certain skilled nursing and assisted living facilities under finance lease agreements. The economic substance of each lease is that the Company is financing the facilities through the lease. The lease terms of these finance leases allow for a purchase option during a specified window. The Company has determined that it is reasonably certain to exercise the purchase option at the end of each purchase option window. Therefore the Company has calculated the lease term through the end of the purchase option window for each lease. Accordingly, such leases are recorded in the Company’s combined/consolidated financial statements as assets and liabilities.
Finance lease right-of-use assets are included in property and equipment and have a balance of $37,850 and $33,593 as of December 31, 2023 and 2022, respectively. The current portion of finance lease liabilities is included in other accrued expenses and has a balance of $942 and $37,895 as of December 31, 2023 and 2022, respectively. The long-term portion of finance lease liabilities is included in other liabilities and has a balance of $40,766 and $0 as of December 31, 2023 and 2022, respectively.
F-25
PACS GROUP, INC. AND SUBSIDIARIES
NOTES TO COMBINED/CONSOLIDATED FINANCIAL STATEMENTS
(dollars in thousands, except for share and per share values)
The components of lease expense were as follows:
| Year Ended December 31, | |||||||||||||||||
| 2023 | 2022 | 2021 | |||||||||||||||
| Operating lease expense | |||||||||||||||||
Rent - cost of services (1) | 216,711 | 160,003 | 78,122 | ||||||||||||||
| General and administrative expense | 941 | 542 | 587 | ||||||||||||||
Variable lease costs (2) | 26,399 | 21,252 | 9,337 | ||||||||||||||
| Total operating lease expense | $ | 244,051 | $ | 181,797 | $ | 88,046 | |||||||||||
| Finance lease expense | |||||||||||||||||
| Amortization of right-of-use assets | 1,264 | 1,230 | 191 | ||||||||||||||
| Interest on lease liabilities | 1,113 | 546 | 87 | ||||||||||||||
| Total financing lease expense | 2,377 | 1,776 | 278 | ||||||||||||||
Total lease expense | $ | 246,428 | $ | 183,573 | $ | 88,324 | |||||||||||
__________________
(1)Rent - cost of services includes other variable lease costs such as Consumer Price Index (CPI) increases and other rent adjustments of $2,745, $964 and $242 for the years ended December 31, 2023, 2022, and 2021, respectively.
(2)Variable lease costs, including property taxes and insurance, are classified in Cost of services in the Company’s combined/consolidated statements of income.
Operating lease expense is included in Rent - cost of services and General and administrative expense as indicated above. For finance lease expense, the amortization of right-of-use assets is included in depreciation and amortization while the interest component is included in interest expense.
The following table summarizes supplemental cash flow information related to leases:
| Year Ended December 31, | |||||||||||||||||
| 2023 | 2022 | 2021 | |||||||||||||||
| Operating cash paid for amounts included in the measurement of operating lease liabilities | $ | 194,925 | $ | 143,683 | $ | 86,717 | |||||||||||
| Operating cash paid for amounts included in the measurement of finance lease liabilities | 1,113 | 546 | 87 | ||||||||||||||
| Financing cash paid for amounts included in the measurement of finance lease liabilities | 1,708 | 2,088 | 300 | ||||||||||||||
| Operating lease right-of-use assets obtained in exchange for lease liabilities | 805,866 | 99,843 | 916,823 | ||||||||||||||
| Financing lease right-of-use assets obtained in exchange for lease liabilities | 5,521 | — | 34,960 | ||||||||||||||
Information relating to the lease term and discount rate is as follows:
| Year Ended December 31, | |||||||||||||||||
| 2023 | 2022 | 2021 | |||||||||||||||
| Weighted-average remaining lease term (years) | |||||||||||||||||
| Operating leases | 13 | 13 | 14 | ||||||||||||||
| Financing leases | 3 | 1 | 2 | ||||||||||||||
| Weighted-average discount rate | |||||||||||||||||
| Operating leases | 5.7 | % | 5.1 | % | 5.1 | % | |||||||||||
| Financing leases | 7.2 | % | 1.4 | % | 1.4 | % | |||||||||||
F-26
PACS GROUP, INC. AND SUBSIDIARIES
NOTES TO COMBINED/CONSOLIDATED FINANCIAL STATEMENTS
(dollars in thousands, except for share and per share values)
In determining the discount rate used to measure the right-of-use asset and lease liability, the Company uses rates implicit in the lease, or if not readily available, the Company will use its incremental borrowing rate. The Company’s incremental borrowing rate is based on an estimated secured rate comprised of a risk-free rate plus a credit spread as secured by its assets. Determining a credit spread as secured by the Company’s assets may require significant judgment.
Maturities of lease liabilities as of December 31, 2023 were as follows:
| Finance Leases | Operating Leases | Total | |||||||||||||||
| 2024 | $ | 3,843 | $ | 220,272 | $ | 224,115 | |||||||||||
| 2025 | 23,560 | 220,997 | 244,557 | ||||||||||||||
| 2026 | 2,241 | 220,331 | 222,572 | ||||||||||||||
| 2027 | 17,995 | 217,976 | 235,971 | ||||||||||||||
| 2028 | 782 | 219,679 | 220,461 | ||||||||||||||
| Thereafter | 390 | 1,900,357 | 1,900,747 | ||||||||||||||
| Total lease payments | $ | 48,811 | $ | 2,999,612 | $ | 3,048,423 | |||||||||||
| Less: present value discount | (7,103) | (928,177) | (935,280) | ||||||||||||||
| Present value of lease liabilities | $ | 41,708 | $ | 2,071,435 | $ | 2,113,143 | |||||||||||
In addition to its lessee activity, the Company generates an immaterial amount of revenue from arrangements where it is a lessor of certain facilities. Revenue from those arrangements is included in other revenue on the combined/consolidated statements of income.
NOTE 12.RETIREMENT PLANS
The Company has two 401(k) defined contribution plans for the benefit of all eligible union and non-union employees. Employees over the age of 21 may begin elective deferrals and become eligible for matching contributions after two months of service. Employer discretionary matching contributions may be up to 25% of the employee’s elective deferrals that do not exceed 4% of the employee’s compensation. Employees vest in matching contributions over five years in accordance with the vesting schedule set out in the plan documents.
In conjunction with the acquisition of Bay Bridge Capital Partners, LLC (see Note 15), the Company acquired another 401(k) defined contribution plan for the benefit of all eligible employees. Eligible employees may enter the plan immediately upon being hired.
Employees are eligible to receive discretionary matching contributions up to 25% of the employee’s elective deferrals that do not exceed $1,060 per participant after completing six months of service. Employees vest in matching contributions over five years in accordance with the vesting schedule set out in the plan document.
On July 19, 2019, the Company adopted a non-qualified deferred compensation plan. The deferred compensation plan allows certain employees to receive supplemental retirement income payments through the deferral of base salary and bonus compensation. Eligible employees may elect to defer receipt of no less than twenty thousand dollars of base salary and bonus compensation for any plan year. Additionally, the Company may elect to make a discretionary matching contribution on behalf of the participant. Participants become fully vested in discretionary matching contributions after five years of continued employment from the date of the applicable matching contribution. Payment of vested balances will occur at future dates, as defined by the plan documents. Deferred compensation plan balances are recorded in other long-term liabilities on the combined/consolidated balance sheets and amounted to $4,379 and $2,047 at December 31, 2023 and 2022, respectively.
F-27
PACS GROUP, INC. AND SUBSIDIARIES
NOTES TO COMBINED/CONSOLIDATED FINANCIAL STATEMENTS
(dollars in thousands, except for share and per share values)
NOTE 13.RELATED PARTY TRANSACTIONS
On July 1, 2021, the Company entered into a Consulting and Strategic Advisory Services Agreement with Helios Consulting, LLC (Helios), a limited liability company owned by Jason Murray, the Company’s Chief Executive Officer and Chairman of its board of directors, and Mark Hancock, Executive Vice Chairman of its board of directors, (Helios Consulting Agreement) which automatically renewed for successive one-year terms. The Helios Consulting Agreement provides for a cash consulting fee of approximately $4,000 annually, paid in monthly installments, for consulting and strategic advisory services provided to the Company by Helios. For the years ended December 31, 2023, 2022, and 2021, the Company paid approximately $4,000, $4,000, and 2,333 (inclusive of approximately $150 paid to a subsidiary of Helios), respectively. As of December 31, 2023, the Company terminated the Helios Consulting Agreement.
2023 Related Party Transactions
On March 24, 2023, the Company entered into subscription agreements with Mr. Murray and Mr. Hancock, pursuant to which Mr. Murray and Mr. Hancock each purchased 10,000 shares of the Company’s common stock for a purchase price of $0.001 per share, in a private placement concurrent with the Company’s incorporation in the State of Delaware and in anticipation of effecting the reorganization on June 30, 2023.
NOTE 14.COMMITMENTS AND CONTINGENCIES
Regulatory Matters
Laws and regulations governing Medicare and Medicaid programs are complex and subject to review and interpretation. Compliance with such laws and regulations is evaluated regularly, the results of which can be subject to future governmental review and interpretation, and can include significant regulatory action including fines, penalties, and exclusion from certain governmental programs. Included in these laws and regulations is monitoring performed by the Office of Civil Rights which covers the Health Insurance Portability and Accountability Act of 1996, the terms of which require healthcare providers (among other things) to safeguard the privacy and security of certain patient protected health information.
Litigation
The skilled nursing business involves a significant risk of liability given the age and health of the patients and residents served by the Company’s independent operating subsidiaries. The Company, and others in the industry are subject to an increasing number of claims and lawsuits, including professional liability claims, alleging that services provided have resulted in personal injury, elder abuse, wrongful death or other related claims. In addition, the Company, its independent operating subsidiaries, and others in the industry are subject to claims and lawsuits in connection with COVID-19 and a facility’s preparation for and/or response to COVID-19. The defense of these lawsuits may result on significant legal costs, regardless of the outcome, and can result in large settlement amounts or damage awards.
Healthcare litigation (including class action litigation) is common and is filed based upon a wide variety of claims and theories. The Company and other companies in its industry are routinely subjected to varying types of claims and suits, including class-actions. Class-action suits have the potential to result in large jury verdicts and settlements, and may result in significant legal costs. The Company expects the plaintiffs’ bar to continue to be aggressive in their pursuit of claims. The Company has been subjected to, and is currently involved in, litigation alleging violations of state and federal wage and hour laws as resulting from the alleged failure to pay wages, to timely provide and authorize meal and rest breaks, and related causes of action. While there can be no assurance, based on the Company’s evaluation of information currently available, management does not believe that the ultimate resolution of these actions will have a material adverse effect on the Company’s business, cash flows, financial condition, or results of operations.
F-28
PACS GROUP, INC. AND SUBSIDIARIES
NOTES TO COMBINED/CONSOLIDATED FINANCIAL STATEMENTS
(dollars in thousands, except for share and per share values)
The Company has been, and continues to be, subject to claims and legal actions that arise in the normal course of business, including potential claims filed by patients or others on their behalf related to patient care and treatment (professional negligence claims), as well as employment related claims filed by current or former employees. While there can be no assurance, based on the Company’s evaluation of information currently available, management does not believe the results of such litigation and investigations would have a material adverse effect on the results of operations, financial position or cash flows of the Company, taken as a whole. However, the Company’s assessment may evolve based upon further developments in the proceedings at issue. The results of legal proceedings are inherently uncertain, and material adverse outcomes are possible.
Insurance Claims
The Company purchased PLGL claims made insurance policies to cover applicable claims through an unrelated insurer. The PLGL policies are claims-made high deductible self-insured policies whereby the Company is responsible for the first layer of coverage, generally ranging from $250 to $500 per claim, as well as an aggregate one-time deductible generally ranging from $750 to $4,000 per policy, with the unrelated insurer typically covering up to $10,000 in aggregate claims paid per policy year. The Company uses its wholly-owned captive insurance company for the purpose of insuring certain portions of its risk retained under its PLGL programs. Accordingly, the Company is in essence self-insured for claims that are less than policy deductible amounts, claims not covered by such policies, and claims that exceed policy limits. It is the Company’s policy to use an actuary to assist management in recording the expense and related liability for PLGL claims, both asserted and unasserted, on an undiscounted basis. Included as part of accrued self-insurance liabilities in the accompanying combined/consolidated balance sheets are PLGL self-insurance liabilities amounting to $162,976, and $138,127 as of December 31, 2023 and 2022, respectively, which includes $34,676 and $42,549, respectively, of estimated obligations that will be covered by the unrelated insurer. PLGL self-insurance liabilities as of December 31, 2023 and 2022 include $43,083 and $38,742, respectively, that were related to unasserted claims. As of December 31, 2023, the Company recorded an asset for the estimated obligations that will be covered by the unrelated insurer amounting to $5,895 and $28,781 within other receivables and other assets, respectively, and as of December 31, 2022, the Company recorded an asset for the estimated obligations that will be covered by the unrelated insurer amounting to $7,233 and $35,316 within other receivables and other assets, respectively, as the claims related to the Company's general and professional liability and the anticipated insurance recoveries are recorded on a gross rather than net basis in accordance with U.S. GAAP.
As part of the Plum acquisition in 2021 (refer to Note 15), the Company assumed Plum’s workers’ compensation plan. Plum purchased an occurrence-based high deductible self-insured workers’ compensation policy whereby the Company is responsible for the first layer of coverage, generally ranging from $250 to $500 per claim. The estimated obligation recorded at December 31, 2023 and 2022 was $8,323, and $17,062, respectively. The Plum facilities were transferred onto the Company’s retrospective-rated premium workers’ compensation policy as of the acquisition date.
F-29
PACS GROUP, INC. AND SUBSIDIARIES
NOTES TO COMBINED/CONSOLIDATED FINANCIAL STATEMENTS
(dollars in thousands, except for share and per share values)
The following table represents activity in the Company’s PLGL self- insurance liabilities as of and for the years ended December 31, 2023 and 2022:
| Amount | |||||
Balance January 1, 2022 | $ | 70,491 | |||
| Current year expense | 40,964 | ||||
| Claims paid | (28,914) | ||||
| Change in obligations covered by unrelated insurer | 31,247 | ||||
| Remeasurement of Plum Assumed Liabilities (Note 15) | 24,339 | ||||
Balance December 31, 2022 | $ | 138,127 | |||
| Current year expense | 106,107 | ||||
| Claims paid | (73,385) | ||||
| Change in obligations covered by unrelated insurer | (7,873) | ||||
Balance December 31, 2023 | $ | 162,976 | |||
Indemnities
From time to time, the Company enters into certain types of contracts that contingently require it to indemnify parties against third-party claims. These contracts primarily include (i) certain real estate leases, under which the Company may be required to indemnify property owners or prior facility operators for post-transfer environmental or other liabilities and other claims arising from the Company use of the applicable premises, (ii) operations transfer agreements, in which the Company agrees to indemnify past operators of facilities against certain liabilities arising from the transfer of the operation and/or the operation thereof after the transfer to the Company's independent operating subsidiary, (iii) certain lending agreements, under which the Company may be required to indemnify the lender against various claims and liabilities, and (iv) certain agreements with the Company officers, directors and others, under which the Company may be required to indemnify such persons for liabilities arising out of the nature of their relationship to the Company. The terms of such obligations vary by contract and, in most instances, do not expressly state or include a specific or maximum dollar amount. Generally, amounts under these contracts cannot be reasonably estimated until a specific claim is asserted. Consequently, because no claims have been asserted, no liabilities have been recorded for these obligations on the combined/consolidated balance sheets for any of the periods presented.
NOTE 15.OPERATION EXPANSIONS
FASB ASC Topic 805, Business Combinations (ASC 805) defines the definition of a business to assist entities with evaluating when a set of transferred assets and activities is deemed to be a business. Determining whether a transferred set constitutes a business is important because the accounting for a business combination differs from that of an asset acquisition. The definition of a business also affects the accounting for dispositions. When substantially all of the fair value of assets acquired is concentrated in a single asset, or a group of similar assets, the assets acquired would not represent a business and business combination accounting would not be required.
2023 Expansions
During the year ended December 31, 2023, the Company’s consolidated operations and real estate portfolio grew through a combination of long-term leases and real estate purchases. The Company acquired operations at 58 stand-alone skilled nursing, assisted living, and subacute facilities and six real estate purchases. Of the six real estate purchases, two of the properties were acquired in conjunction with the operations of the associated facility. For the other four acquired properties, the Company previously operated the respective facilities and has now acquired the real estate associated with those operations. These new operations added 6,744 operational skilled nursing beds. The purpose of any such expansion, may include, without limitation, to expand the scope of the Company's operations, add additional team members with important skill sets, and/or realize synergies.
F-30
PACS GROUP, INC. AND SUBSIDIARIES
NOTES TO COMBINED/CONSOLIDATED FINANCIAL STATEMENTS
(dollars in thousands, except for share and per share values)
The aggregate purchase price for these expansions during the year ended December 31, 2023 was $129,174. The fair value of assets for the entities where real estate was acquired were concentrated in property and equipment amounting to $124,874. As such, these transactions were classified as asset acquisitions. The remaining aggregate purchase price for transactions during the year ended December 31, 2023 was concentrated in goodwill and other assets in the amount of $3,800 and $500, respectively. Such transactions were classified as business combinations. The Company expects 100% of the goodwill to be deductible for income tax purposes.
In connection with the new operations made through long-term leases, the Company did not acquire any material assets or assume any liabilities other than the tenant's post-assumption rights and obligations under the long-term lease. The Company entered into separate agreements with the applicable prior operators as part of each transaction.
2022 Expansions
During the year ended December 31, 2022, the Company’s consolidated operations and real estate portfolio grew through a combination of long-term leases and real estate purchases. The Company acquired operations at nine stand-alone skilled nursing, assisted living, and subacute facilities and four real estate purchases. Of the four real estate purchases, two of the properties were acquired in conjunction with the operations of the associated facility. For the other two acquired properties, the Company previously operated the respective facilities and has now acquired the real estate associated with those operations. These new operations added 1,180 operational skilled nursing beds. The purpose of any such expansion, may include, without limitation, to expand the scope of the Company's operations, add additional team members with important skill sets, and/or realize synergies.
The aggregate purchase price for these expansions during the year ended December 31, 2022 was $55,374. The fair value of assets for the entities where real estate was acquired were concentrated in property and equipment and other assets, amounting to $46,500 and $378, respectively. As such, these transactions were classified as asset acquisitions. The remaining aggregate purchase price for transactions during the year ended December 31, 2022 was concentrated in goodwill in the amount of $8,496 and as such, the transactions were classified as business combinations. The Company expects 100% of the goodwill to be deductible for income tax purposes.
In connection with the new operations made through long-term leases, the Company did not acquire any material assets or assume any liabilities other than the tenant's post-assumption rights and obligations under the long-term lease. The Company entered into separate agreements with the applicable prior operators as part of each transaction.
2021 Expansions
Plum Healthcare Group Acquisition
On November 5, 2021, the Company completed the acquisition of all of the equity interest of 58 stand-alone skilled nursing, assisted living, and subacute facilities and eight real estate entities from Bay Bridge Capital Partners, LLC d/b/a Plum Healthcare Group (Plum) for $121,000, consisting of cash of $104,200 and notes due to prior owner of $16,800, in order to grow and expand its footprint. The acquisition added 6,380 operational skilled nursing beds, 40 assisted living beds, and 190 subacute beds.
F-31
PACS GROUP, INC. AND SUBSIDIARIES
NOTES TO COMBINED/CONSOLIDATED FINANCIAL STATEMENTS
(dollars in thousands, except for share and per share values)
The table below represents the purchase price allocation to total identifiable assets acquired and net liabilities assumed using the acquisition method, based on their respective fair values as of November 5, 2021.
| Amount | |||||
| Cash and cash equivalents | $ | 7,957 | |||
| Accounts receivable | 94,555 | ||||
| Prepaid and other | 43,076 | ||||
| Restricted cash | 22,483 | ||||
| Property and equipment | 166,072 | ||||
| Operating lease right-of-use assets | 612,522 | ||||
| Other assets | 5,781 | ||||
| Goodwill and other indefinite-lived assets | 32,345 | ||||
| Current operating lease liabilities assumed | (28,324) | ||||
| Other current liabilities assumed | (134,886) | ||||
| Long-term operating lease liabilities assumed | (576,848) | ||||
| Debt and finance lease liabilities assumed | (55,095) | ||||
| Other liabilities assumed | (68,638) | ||||
| Total purchase price | $ | 121,000 | |||
The indefinite-lived intangible assets acquired include the certificates of need and licenses. Fair value of the indefinite-lived intangible assets was determined using a cost approach. The cost approach uses the replacement or reproduction cost as an indicator of fair value. The cost approach utilized assumptions for the current replacement costs of similar assets which for these indefinite-lived intangible assets included assumptions regarding estimated fees on a per unit basis in the applicable jurisdictions.
Fair value of property and equipment was determined using a combination of an income and cost approach. The income approach utilized significant assumptions including management’s best estimates of the expected future cash flows and the estimated useful life of the asset group. The cost approach utilized assumptions for the current replacement costs of similar assets adjusted for estimated depreciation and deterioration of the existing property and equipment and economic obsolescence.
Fair value of the right-of-use assets was determined under a market approach. The market approach utilized significant assumptions based on estimated market rent assessments for the acquired lease contracts.
The goodwill is primarily attributed to the workforce acquired. The Company expects 100% of the goodwill to be deductible for income tax purposes.
During the year ended December 31, 2022, the Company recorded a measurement period adjustment primarily related to the finalization of professional liability loss reserves, which increased the amount of goodwill and other liabilities assumed in the Plum acquisition by $18,844. At the time of the adjustment, the measurement period was still open as the Company was gathering further information about facts and circumstances that existed as of the acquisition date related to the legal matters that gave rise to the professional liability loss reserve adjustment.
Other 2021 Expansions
Additionally, the Company invested in two joint ventures during the year ended December 31, 2021. Information related to joint venture activity is disclosed in Note 7.
In June 2021, the Company sold one real estate entity, resulting in a gain on sale of $3,100. In conjunction with the sale, the Company entered into a note receivable agreement with the buyer in the principal amount of $5,000 with monthly interest payments accruing at 6% percent. Annual principal payments are due on each anniversary
F-32
PACS GROUP, INC. AND SUBSIDIARIES
NOTES TO COMBINED/CONSOLIDATED FINANCIAL STATEMENTS
(dollars in thousands, except for share and per share values)
date, with the remaining principal due and payable on the maturity date of June 1, 2024. At December 31, 2023, the outstanding balance of the note was $3,500 which is included in Other Assets.
During the year ended December 31, 2021, the Company’s consolidated operations grew through a combination of long-term leases and real estate purchases, with the addition of 17 stand-alone skilled nursing facilities and five real estate purchases. These new operations added approximately 1,780 operational skilled nursing beds.
The aggregate purchase price for these acquisitions during the year ended December 31, 2021 was $118,324. The fair value of assets for the real estate entities were concentrated in property and equipment amounting to $116,423. As such, these transactions were classified as asset acquisitions. The remaining aggregate purchase price for transactions during the year ended December 31, 2021 was concentrated in goodwill in the amount of $1,901 and as such, the transactions were classified as business combinations. The Company expects 100% of the goodwill to be deductible for tax purposes.
In connection with the new operations acquired for the stand-alone skilled nursing facilities, the Company did not acquire any material assets or assume any liabilities other than the tenant's post-assumption rights and obligations under the long-term lease. The Company entered into agreements with the applicable prior operators as part of each transaction.
The Company’s expansion strategy has been focused on identifying both opportunistic and strategic acquisitions within its target markets that offer strong opportunities for return. The operations added by the Company are frequently underperforming financially and can have regulatory and clinical challenges to overcome. Financial information, especially with underperforming operations, is often inadequate, inaccurate or unavailable. Consequently, the Company believes that prior operating results are not a meaningful representation of the Company’s current operating results or indicative of the integration potential of its newly acquired operating subsidiaries. The assets added during the year ended December 31, 2023, 2022 and 2021 and through the issuance of the financial statements were not material operations to the Company individually or in the aggregate. Accordingly, pro forma financial information is not presented. The additions have been included in the December 31, 2023 and 2022 combined/consolidated balance sheets of the Company, and the operating results have been included in the combined/consolidated statements of income of the Company since the date the Company gained effective control.
2024 Expansions
Subsequent to December 31, 2023, the Company’s operations and real estate portfolio grew through a combination of long-term leases and real estate purchases, with the addition of 10 stand-alone facilities and six real estate purchases. Of the six real estate purchases, three of the properties were acquired in conjunction with the operations of the associated facility. For the other three acquired properties, the Company previously operated the respective facilities and has now acquired the real estate associated with those operations. These new operations added 1,334 skilled nursing beds and 174 assisted living beds operated by the Company's affiliated operating subsidiaries. The aggregate purchase price for these acquisitions was $78,500.
NOTE 16.OTHER ACCRUED EXPENSES
Other accrued expenses consisted of the following:
| December 31, | |||||||||||
| 2023 | 2022 | ||||||||||
| Current portion of finance lease liabilities | 942 | 37,895 | |||||||||
| Amounts due to former Plum shareholders | — | 36,586 | |||||||||
| Other | 69,007 | 52,678 | |||||||||
| Total other accrued expenses | $ | 69,949 | $ | 127,159 | |||||||
F-33
PACS GROUP, INC. AND SUBSIDIARIES
NOTES TO COMBINED/CONSOLIDATED FINANCIAL STATEMENTS
(dollars in thousands, except for share and per share values)
The amounts due to former Plum shareholders is unchanged in 2023, however the Company has determined that the payment of this amount will most likely be due after 2024 and therefore the amount has been reclassified to other liabilities.
NOTE 17.EARNINGS PER SHARE
Basic net income per share is calculated by dividing net income attributable to the common stockholders by the weighted-average shares of Common Stock outstanding for the period. The computation of diluted net income per share is similar to the computation of basic net income per share, except that the denominator is increased to include the number of additional shares of common stock that would have been outstanding if the dilutive potential shares of common stock had been issued. As the Company did not have any potentially dilutive securities, basic and diluted EPS are the same.
The following table sets forth the computation of the Company’s basic and diluted net income attributable per share to common stockholders for the years ended December 31, 2023, 2022, and 2021:
| Years Ended December 31, | |||||||||||||||||
| 2023 | 2022 | 2021 | |||||||||||||||
| Basic EPS: | |||||||||||||||||
| Numerator: | |||||||||||||||||
| Net income | $ | 112,882 | $ | 150,496 | $ | 47,947 | |||||||||||
| Less: net income attributable to noncontrolling interest | $ | 8 | $ | — | $ | — | |||||||||||
| Net income attributable to PACS Group, Inc. | $ | 112,874 | $ | 150,496 | $ | 47,947 | |||||||||||
| Denominator: | |||||||||||||||||
| Basic and diluted weighted average common stock outstanding | 128,723,386 | 128,723,386 | 128,723,386 | ||||||||||||||
| Net income per common share attributable to PACS Group, Inc. | |||||||||||||||||
| Basic and diluted | $ | 0.88 | $ | 1.17 | $ | 0.37 | |||||||||||
The Reorganization referred to in Note 1 resulted in the common shares outstanding being converted from 600 shares of PGI to 20,000 shares of PACS Group (a 1 to 33.33 conversion ratio).
On March 31, 2024, the Company’s board of directors approved a 1 to 6,436.1693 stock split of its issued and outstanding common stock, which was effective by amendment to the Company’s charter on April 1, 2024. As part of the amendment, the number of authorized shares of common stock was revised to 1,250,000,000 and the par value of the common stock was not adjusted. All issued and outstanding common stock and per share amounts contained in the combined/consolidated financial statements have been retrospectively adjusted to give effect to the stock split for all periods presented.
NOTE 18.SUBSEQUENT EVENTS
2024 Equity Incentive Plans (unaudited)
On March 31, 2024, the Company’s board of directors and stockholders approved the PACS Group, Inc. 2024 Incentive Award Plan (the 2024 Plan), which will become effective on the date immediately preceding the date on which the Company’s registration statement will be declared effective by the SEC. The 2024 Plan allows the Company to make equity-based and cash-based incentive awards to its officers, employees, directors and consultants.
F-34
PACS GROUP, INC. AND SUBSIDIARIES
NOTES TO COMBINED/CONSOLIDATED FINANCIAL STATEMENTS
(dollars in thousands, except for share and per share values)
The number of shares initially available for issuance under awards granted pursuant to the 2024 Plan (which number includes 15,146,772 shares of common stock issuable upon the exercise of restricted stock unit awards, to be granted in connection with the offering) is equal to 10.25% of the number of shares of our common stock outstanding as of immediately following the completion of this offering (disregarding the shares issuable under the 2024 Plan).
2024 Employee Stock Purchase Plan (unaudited)
On March 31, 2024, the Company’s board of directors and stockholders approved the 2024 Employee Stock Purchase Plan (the 2024 ESPP), which will become effective on the date immediately preceding the date on which the Company’s registration statement will be declared effective by the SEC. The number of shares initially available for issuance pursuant to the 2024 ESPP will be equal to the number of shares equal to 1% of the number of shares of our common stock outstanding as of immediately following the completion of this offering (disregarding the shares issuable under the 2024 Plan).
F-35
| PACS GROUP, INC. AND SUBSIDIARIES | |||||||||||
| CONDENSED COMBINED/CONSOLIDATED BALANCE SHEETS | |||||||||||
| (dollars in thousands, except for share and per share values) | |||||||||||
| (unaudited) | |||||||||||
| June 30, | December 31, | ||||||||||
| 2024 | 2023 | ||||||||||
| ASSETS | |||||||||||
| Current Assets: | |||||||||||
| Cash and cash equivalents | $ | 73,374 | $ | 73,416 | |||||||
| Accounts receivable, net | 610,577 | 547,807 | |||||||||
| Other receivables | 50,396 | 52,259 | |||||||||
| Prepaid expenses and other current assets | 66,301 | 48,665 | |||||||||
| Total Current Assets | 800,648 | 722,147 | |||||||||
| Property and equipment, net | 763,904 | 577,528 | |||||||||
| Operating lease right-of-use assets | 2,112,914 | 2,007,812 | |||||||||
| Insurance subsidiary deposits and investments | 35,476 | — | |||||||||
| Escrow funds | 19,531 | 15,649 | |||||||||
| Goodwill and other indefinite-lived assets | 65,291 | 65,291 | |||||||||
| Other assets | 98,584 | 124,312 | |||||||||
| Total Assets | $ | 3,896,348 | $ | 3,512,739 | |||||||
| LIABILITIES AND EQUITY | |||||||||||
| Current Liabilities: | |||||||||||
| Accounts payable | $ | 125,746 | $ | 140,947 | |||||||
| Accrued payroll and benefits | 107,077 | 92,234 | |||||||||
| Current operating lease liabilities | 113,278 | 109,438 | |||||||||
| Current maturities of long term debt | 15,745 | 16,822 | |||||||||
| Current portion of accrued self-insurance liabilities | 31,252 | 27,536 | |||||||||
| Other accrued expenses | 75,003 | 69,949 | |||||||||
| Total Current Liabilities | 468,101 | 456,926 | |||||||||
| Long-term operating lease liabilities | 2,068,585 | 1,961,997 | |||||||||
| Accrued benefits, less current portion | 6,738 | 6,738 | |||||||||
| Lines of credit | 248,000 | 520,000 | |||||||||
| Long-term debt, less current maturities, net of deferred financing fees | 227,107 | 195,708 | |||||||||
| Accrued self-insurance liabilities, less current portion | 172,111 | 146,167 | |||||||||
| Other liabilities | 127,472 | 123,477 | |||||||||
| Total Liabilities | $ | 3,318,114 | $ | 3,411,013 | |||||||
| Commitments and contingencies (Note 11) | |||||||||||
| Equity: | |||||||||||
| PACS Group, Inc. stockholders’ equity: | |||||||||||
| Common stock: $0.001 par value; 1,250,000,000 shares authorized, 152,399,733 shares issued and outstanding as of June 30, 2024, and 64,361,693,000 shares authorized, 128,723,386 shares issued and outstanding as of December 31, 2023 | 152 | 129 | |||||||||
| Additional paid-in capital | 471,472 | — | |||||||||
| Retained earnings | 100,504 | 95,997 | |||||||||
| Total stockholders' equity | 572,128 | 96,126 | |||||||||
| Non-controlling interest in subsidiary | 6,106 | 5,600 | |||||||||
| Total Equity | $ | 578,234 | $ | 101,726 | |||||||
| Total Liabilities and Equity | $ | 3,896,348 | $ | 3,512,739 | |||||||
See accompanying notes to unaudited condensed combined/consolidated financial statements.
F-36
| PACS GROUP, INC. AND SUBSIDIARIES | |||||||||||||||||||||||
| UNAUDITED CONDENSED COMBINED/CONSOLIDATED STATEMENTS OF (LOSS) INCOME AND COMPREHENSIVE (LOSS) INCOME | |||||||||||||||||||||||
| (dollars in thousands, except for share and per share values) | |||||||||||||||||||||||
| Three Months Ended June 30, | Six Months Ended June 30, | ||||||||||||||||||||||
| 2024 | 2023 | 2024 | 2023 | ||||||||||||||||||||
| Revenue | |||||||||||||||||||||||
| Patient and resident service revenue | $ | 981,398 | $ | 760,424 | $ | 1,915,696 | $ | 1,468,250 | |||||||||||||||
| Additional funding | — | — | — | 375 | |||||||||||||||||||
| Other revenues | 448 | 240 | 871 | 481 | |||||||||||||||||||
Total Revenue | $ | 981,846 | $ | 760,664 | $ | 1,916,567 | $ | 1,469,106 | |||||||||||||||
| Operating Expenses | |||||||||||||||||||||||
| Cost of services | 762,147 | 590,815 | 1,498,139 | 1,129,587 | |||||||||||||||||||
| Rent - cost of services | 65,833 | 51,456 | 129,794 | 96,560 | |||||||||||||||||||
| General and administrative expense | 144,380 | 62,695 | 191,286 | 122,137 | |||||||||||||||||||
| Depreciation and amortization | 8,776 | 6,159 | 16,678 | 11,988 | |||||||||||||||||||
Total Operating Expenses | $ | 981,136 | $ | 711,125 | $ | 1,835,897 | $ | 1,360,272 | |||||||||||||||
| Operating Income | $ | 710 | $ | 49,539 | $ | 80,670 | $ | 108,834 | |||||||||||||||
| Other (Expense) Income | |||||||||||||||||||||||
| Interest expense | (9,187) | (15,306) | (24,578) | (25,942) | |||||||||||||||||||
| Gain on lease termination | — | — | 8,046 | — | |||||||||||||||||||
| Other expense, net | (3,905) | (2,643) | (3,465) | (2,203) | |||||||||||||||||||
Total Other Expense, net | $ | (13,092) | $ | (17,949) | $ | (19,997) | $ | (28,145) | |||||||||||||||
| (Loss) income before provision for income taxes | (12,382) | 31,590 | 60,673 | 80,689 | |||||||||||||||||||
| Benefit (provision) for income taxes | 1,474 | (10,370) | (22,441) | (21,871) | |||||||||||||||||||
| Net (Loss) Income | $ | (10,908) | $ | 21,220 | $ | 38,232 | $ | 58,818 | |||||||||||||||
| Less: | |||||||||||||||||||||||
| Net income attributable to noncontrolling interest | 2 | 2 | 4 | 3 | |||||||||||||||||||
| Net (loss) income attributable to PACS Group, Inc. | $ | (10,910) | $ | 21,218 | $ | 38,228 | $ | 58,815 | |||||||||||||||
| Net (loss) income per share attributable to PACS Group, Inc. | |||||||||||||||||||||||
| Basic | $ | (0.07) | $ | 0.16 | $ | 0.27 | $ | 0.46 | |||||||||||||||
| Diluted | $ | (0.07) | $ | 0.16 | $ | 0.27 | $ | 0.46 | |||||||||||||||
| Weighted-average common shares outstanding | |||||||||||||||||||||||
| Basic | 149,463,655 | 128,723,386 | 139,093,520 | 128,723,386 | |||||||||||||||||||
| Diluted | 149,463,655 | 128,723,386 | 139,684,618 | 128,723,386 | |||||||||||||||||||
| Other comprehensive loss, net of tax: | |||||||||||||||||||||||
| Unrealized loss on available-for-sale debt securities, net of tax | $ | (201) | $ | — | $ | — | $ | — | |||||||||||||||
| Total other comprehensive loss | (201) | — | — | — | |||||||||||||||||||
| Comprehensive (loss) income | $ | (11,109) | $ | 21,220 | $ | 38,232 | $ | 58,818 | |||||||||||||||
| Less: | |||||||||||||||||||||||
| Comprehensive income attributable to noncontrolling interest | 2 | 2 | 4 | 3 | |||||||||||||||||||
| Comprehensive (loss) income attributable to PACS Group, Inc. | $ | (11,111) | $ | 21,218 | $ | 38,228 | $ | 58,815 | |||||||||||||||
See accompanying notes to unaudited condensed combined/consolidated financial statements.
F-37
| PACS GROUP, INC. AND SUBSIDIARIES | |||||||||||||||||||||||||||||||||||||||||
| UNAUDITED CONDENSED COMBINED/CONSOLIDATED STATEMENTS OF STOCKHOLDERS' EQUITY | |||||||||||||||||||||||||||||||||||||||||
| (dollars in thousands, except for share and per share values) | |||||||||||||||||||||||||||||||||||||||||
| Common Stock | Additional Paid-In Capital | Retained Earnings | Non-Controlling Interest | Accumulated Other Comprehensive Income | Total | ||||||||||||||||||||||||||||||||||||
| Shares | Amount | ||||||||||||||||||||||||||||||||||||||||
| Balance January 1, 2024 | 128,723,386 | $ | 129 | $ | — | $ | 95,997 | $ | 5,600 | $ | — | $ | 101,726 | ||||||||||||||||||||||||||||
| Dividends on common stock ($0.1358 per share) | — | — | — | (17,474) | — | — | (17,474) | ||||||||||||||||||||||||||||||||||
| Other comprehensive income | — | — | — | — | — | 201 | 201 | ||||||||||||||||||||||||||||||||||
| Net income attributable to noncontrolling interest | — | — | — | — | 2 | — | 2 | ||||||||||||||||||||||||||||||||||
| Net income attributable to PACS Group, Inc. | — | — | — | 49,138 | — | — | 49,138 | ||||||||||||||||||||||||||||||||||
| Balance March 31, 2024 | 128,723,386 | $ | 129 | $ | — | $ | 127,661 | $ | 5,602 | $ | 201 | $ | 133,593 | ||||||||||||||||||||||||||||
| Contributions | — | — | — | — | 502 | — | 502 | ||||||||||||||||||||||||||||||||||
| Issuance of common stock | 21,428,572 | 21 | 414,136 | — | — | — | 414,157 | ||||||||||||||||||||||||||||||||||
| Employee stock-based compensation | 3,847,652 | 4 | 90,932 | — | — | — | 90,936 | ||||||||||||||||||||||||||||||||||
| Tax withholdings related to net share settlement of equity awards | (1,599,877) | (2) | (33,596) | — | — | — | (33,598) | ||||||||||||||||||||||||||||||||||
| Dividends on common stock ($0.1066 per share) | — | — | — | (16,247) | — | — | (16,247) | ||||||||||||||||||||||||||||||||||
| Other comprehensive loss | — | — | — | — | — | (201) | (201) | ||||||||||||||||||||||||||||||||||
| Net income attributable to noncontrolling interest | — | — | — | — | 2 | — | 2 | ||||||||||||||||||||||||||||||||||
| Net loss attributable to PACS Group, Inc. | — | — | — | (10,910) | — | — | (10,910) | ||||||||||||||||||||||||||||||||||
| Balance June 30, 2024 | 152,399,733 | $ | 152 | $ | 471,472 | $ | 100,504 | $ | 6,106 | $ | — | $ | 578,234 | ||||||||||||||||||||||||||||
| Common Stock | Additional Paid-In Capital | Retained Earnings | Non-Controlling Interest | Accumulated Other Comprehensive Income | Total | ||||||||||||||||||||||||||||||||||||
| Shares | Amount | ||||||||||||||||||||||||||||||||||||||||
| Balance January 1, 2023 | 128,723,386 | $ | 129 | — | $ | 63,517 | $ | 5,005 | $ | — | $ | 68,651 | |||||||||||||||||||||||||||||
| Dividends on common stock ($0.1438 per share) | — | — | — | (18,513) | — | — | (18,513) | ||||||||||||||||||||||||||||||||||
| Net income attributable to noncontrolling interest | — | — | — | — | 1 | — | 1 | ||||||||||||||||||||||||||||||||||
| Net income attributable to PACS Group, Inc. | — | — | — | 37,597 | — | — | 37,597 | ||||||||||||||||||||||||||||||||||
| Balance March 31, 2023 | 128,723,386 | $ | 129 | $ | — | $ | 82,601 | $ | 5,006 | $ | — | $ | 87,736 | ||||||||||||||||||||||||||||
| Dividends on common stock ($0.1959 per share) | — | — | — | (25,215) | — | — | (25,215) | ||||||||||||||||||||||||||||||||||
| Net income attributable to noncontrolling interest | — | — | — | — | 2 | — | 2 | ||||||||||||||||||||||||||||||||||
| Net income attributable to PACS Group, Inc. | — | — | — | 21,218 | — | — | 21,218 | ||||||||||||||||||||||||||||||||||
| Balance June 30, 2023 | 128,723,386 | $ | 129 | $ | — | $ | 78,604 | $ | 5,008 | $ | — | $ | 83,741 | ||||||||||||||||||||||||||||
See accompanying notes to unaudited condensed combined/consolidated financial statements.
F-38
| PACS GROUP, INC. AND SUBSIDIARIES | |||||||||||
| UNAUDITED CONDENSED COMBINED/CONSOLIDATED STATEMENTS OF CASH FLOWS | |||||||||||
| (dollars in thousands) | |||||||||||
| Six Months Ended June 30, | |||||||||||
| 2024 | 2023 | ||||||||||
| Cash flows from operating activities | |||||||||||
| Net income | $ | 38,232 | $ | 58,818 | |||||||
| Adjustments to reconcile net income to net cash provided by operating activities | |||||||||||
| Depreciation and amortization | 16,678 | 11,988 | |||||||||
| Amortization and write-off of deferred financing fees | 1,551 | 4,279 | |||||||||
| Stock-based compensation | 90,936 | — | |||||||||
| Loss on disposition of property and equipment | 343 | 516 | |||||||||
| Loss on investment in partnership | 4,288 | — | |||||||||
| Gain on other investments | (476) | — | |||||||||
| Deferred taxes | (15,969) | (7,253) | |||||||||
| Noncash lease expense | 15,185 | 9,093 | |||||||||
| Change in operating assets and liabilities | |||||||||||
| Accounts receivable, net | (62,770) | (76,563) | |||||||||
| Other receivables | 1,863 | (9,925) | |||||||||
| Prepaid expenses and other current assets | (18,286) | 378 | |||||||||
| Other assets | (1,021) | (12,009) | |||||||||
| Escrow funds | (3,882) | 2,130 | |||||||||
| Operating lease obligations | (9,859) | (1,320) | |||||||||
| Accounts payable | (17,203) | 33,467 | |||||||||
| Accrued payroll and benefits | 14,843 | 7,092 | |||||||||
| Accrued self-insurance liabilities | 29,660 | 40,413 | |||||||||
| Other accrued expenses | 5,492 | (36,367) | |||||||||
| Other liabilities | 3,995 | 33,475 | |||||||||
| NET CASH PROVIDED BY OPERATING ACTIVITIES | $ | 93,600 | $ | 58,212 | |||||||
| Cash flows from investing activities | |||||||||||
| Investment in partnership | $ | (5,081) | $ | — | |||||||
| Non-operating distributions from investment in partnership | 1,190 | 945 | |||||||||
| Purchase of investments | (35,000) | — | |||||||||
| Acquisition of facilities | (174,650) | (52,365) | |||||||||
| Purchase of property and equipment | (26,093) | (16,591) | |||||||||
| Cash proceeds from the sale of assets | — | 750 | |||||||||
| NET CASH USED IN INVESTING ACTIVITIES | $ | (239,634) | $ | (67,261) | |||||||
| Cash flows from financing activities | |||||||||||
| Borrowing on lines-of-credit, net of deferred financing fees | $ | 288,000 | $ | 178,905 | |||||||
| Payments on lines-of-credit | (560,000) | (222,002) | |||||||||
| Dividends on common stock | (33,721) | (43,728) | |||||||||
| Contributions from non-controlling interest | 502 | — | |||||||||
| Borrowings of long-term debt, net of deferred financing fees | 39,757 | 315,167 | |||||||||
| Payments on long-term debt | (9,913) | (236,969) | |||||||||
| Proceeds from initial public offering, net of issuance costs | 414,157 | — | |||||||||
| Taxes paid related to net share settlement of stock-based compensation awards | (33,598) | — | |||||||||
| NET CASH PROVIDED BY/(USED IN) FINANCING ACTIVITIES | $ | 105,184 | $ | (8,627) | |||||||
| Net change in cash | (40,850) | (17,676) | |||||||||
| Cash, cash equivalents, and restricted cash - beginning of period | 118,704 | 98,206 | |||||||||
| Cash, cash equivalents, and restricted cash - end of period | $ | 77,854 | $ | 80,530 | |||||||
| Supplemental disclosures of cash flow information | |||||||||||
| Cash paid during the period for: | |||||||||||
| Interest | $ | 25,550 | $ | 28,004 | |||||||
| Income taxes | 43,455 | 16,540 | |||||||||
| Non-cash financing and investing activity | |||||||||||
| Accrued capital expenditures | $ | 5,154 | $ | 2,552 | |||||||
| Assets acquired in operation expansions in exchange for notes payable | — | 3,635 | |||||||||
| Assets acquired in operation expansions through settlement of notes receivable | 500 | — | |||||||||
See accompanying notes to unaudited condensed combined/consolidated financial statements.
F-39
PACS GROUP, INC. AND SUBSIDIARIES
NOTES TO UNAUDITED CONDENSED COMBINED/CONSOLIDATED FINANCIAL STATEMENTS
(dollars in thousands, except for share and per share values)
NOTE 1.ORGANIZATION AND NATURE OF BUSINESS
PACS Group, Inc. (PACS Group or the Company), a Delaware corporation, was incorporated on March 24, 2023. PACS Group is a holding company which consolidates various operating and other subsidiaries. PACS Group’s applicable operating subsidiaries operate various skilled nursing facilities (SNF) and assisted living facilities (ALF). PACS Group also owns other subsidiaries that are engaged in the acquisition, ownership, and leasing of health care-related properties. As of June 30, 2024, PACS Group subsidiaries operated 220 health care facilities in the states of Arizona, California, Colorado, Kentucky, Missouri, Nevada, Ohio, South Carolina, and Texas. PACS Group subsidiaries operated approximately 24,480 skilled nursing beds and 880 assisted living beds as of that date. As of June 30, 2024, PACS Group subsidiaries operated 182 facilities under long-term lease arrangements and had options to purchase 13 of those facilities.
PACS Group subsidiaries have investments in joint ventures that own the underlying real estate and related improvements of 12 post-acute care facilities that are operated by other PACS Group subsidiaries. PACS Group also owns subsidiaries that own real estate and related improvements that are leased to applicable affiliated SNF operating entities and one non-affiliated ALF operating entity. PACS Group’s real estate portfolio includes 38 properties which are operated and managed by applicable PACS Group subsidiaries.
Providence Administrative Consulting Services, Inc., a California corporation, is a subsidiary of PACS Group and provides administrative support services, on a consulting basis, to other subsidiaries of PACS Group.
PACS Group also has a wholly-owned captive insurance subsidiary, Welsch Insurance Ltd. (Welsch). Welsch provides coverage to various consolidated operating subsidiaries related to professional liability and general liability (PLGL) insurance.
Reorganization
Prior to June 30, 2023, Providence Group, Inc. (PGI) owned the operating subsidiaries of PACS Group. On June 30, 2023, PGI and its consolidated subsidiaries reorganized (the Reorganization) to facilitate their entrance into a new credit agreement, dated June 30, 2023 (the New Credit Agreement), between certain lenders party thereto, Truist Bank (Truist), as administrative agent, PACS Group, and PACS Holdings, LLC (PACS Holdings) as borrower thereunder. PACS Group and its wholly owned subsidiary PACS Holdings were created on March 24, 2023, and April 10, 2023, respectively, in anticipation of the Reorganization. The equity interests of certain other direct or indirect wholly-owned subsidiaries of PGI at the time of the Reorganization were also contributed to other new direct or indirect wholly-owned subsidiaries of PACS Group to facilitate the New Credit Agreement. PACS Group and its consolidated subsidiaries subsequent to the Reorganization are collectively referred to herein as the Company. The New Credit Agreement is described in Note 6, “Credit Facilities”.
The Reorganization was effected by the two then-existing stockholders of PGI (which at the time was the direct or indirect parent company of all consolidated entities comprising the Company), contributing their respective shares in PGI to newly-formed PACS Holdings, in exchange for a proportionate interest of shares in newly-formed PACS Group (via issuance of shares of PACS Group), and thus became the sole stockholders of PACS Group.
As a result of the Reorganization, (i) for most practical purposes PACS Group in effect became the successor to the historical consolidated business of PGI, and (ii) both of the two stockholders of PGI immediately prior to the Reorganization became the sole stockholders of PACS Group, and maintained their respective pro rata ownership percentage in PACS Group that they held in PGI immediately prior to the Reorganization (which was and remained 50/50).
The Reorganization was accounted for as an equity reorganization between entities under common control. The Reorganization combined entities that historically have not been presented together resulting in financial statements that are effectively considered to be those of a different reporting entity. Accordingly, the historical financial statements for periods prior to the Reorganization represent combined financial statements and the financial
F-40
PACS GROUP, INC. AND SUBSIDIARIES
NOTES TO UNAUDITED CONDENSED COMBINED/CONSOLIDATED FINANCIAL STATEMENTS
(dollars in thousands, except for share and per share values)
statements after the Reorganization represent consolidated financial statements. The contribution of shares of PGI and receipt of shares of PACS Group were accounted for on a retrospective basis. Accordingly, all share and per share amounts in these condensed combined/consolidated financial statements and related notes have been retrospectively restated, where applicable, for all periods herein, to give effect to the current shares outstanding of PACS Group.
NOTE 2.SUMMARY OF SIGNIFICANT ACCOUNTING POLICIES
Basis of Presentation
The accompanying condensed combined/consolidated financial statements have been prepared in accordance with accounting principles generally accepted in the United States (U.S. GAAP). The condensed combined/consolidated financial statements include the accounts of PACS Group, and its consolidated subsidiaries, or the Company as defined above. All intercompany transactions and balances have been eliminated in consolidation. The Company presents noncontrolling interests within the equity section of its condensed combined/consolidated balance sheets and the amount of condensed combined/consolidated (loss) income that is attributable to the Company and the noncontrolling interest in its condensed combined/consolidated statements of (loss) income and comprehensive (loss) income.
The accompanying condensed combined/consolidated financial statements as of June 30, 2024 and for the three and six months ended June 30, 2024 and 2023 are unaudited. The December 31, 2023 balance sheet data was derived from audited financial statements; however, the accompanying notes to the condensed combined/consolidated financial statements do not include all of the annual disclosures required under GAAP and should be read in conjunction with the audited combined/consolidated financial statements included in the Company’s final prospectus filed with the SEC on April 12, 2024. Management believes that the condensed combined/consolidated financial statements reflect all adjustments which are of a normal and recurring nature necessary to present fairly the Company’s financial position and results of operations in all material respects. The results of operations presented in the condensed combined/consolidated financial statements are not necessarily representative of operations for the entire year.
Use of Estimates
The preparation of the condensed combined/consolidated financial statements in accordance with U.S. GAAP requires management to make estimates and assumptions that affect the reported amounts of assets and liabilities and disclosure of contingent assets and liabilities at the date of the condensed combined/consolidated financial statements and the reported amounts of revenue and expenses during the reporting period. The most significant estimates in the Company’s financial statements relate to revenue, acquired property, right-of-use assets, lease liabilities, impairment of long-lived assets, and general and professional liabilities included in accrued self-insurance liabilities. Actual results could differ from estimated amounts.
Restricted Cash, Cash and Cash Equivalents
Cash and cash equivalents consist of cash and short-term investments with original maturities of three months or less at the time of purchase and therefore approximate fair value. The Company considers highly liquid debt instruments purchased with a maturity of three months or less to be cash equivalents. The Company maintains its cash and short-term investment balances in several high-credit quality financial institutions.
Included in restricted cash are funds held for PLGL claims. Funds held in restricted cash are contractually obligated to be segregated from the Company’s other cash accounts and are legally restricted for the use of funding PLGL claims. See Note 5, “Fair Value Measurement”, for information on the use of restricted cash in other assets to purchase investments in the period.
At any point in time the Company has funds in operating accounts and restricted cash accounts that are with third-party financial institutions. While management monitors the cash balances in operating accounts, these
F-41
PACS GROUP, INC. AND SUBSIDIARIES
NOTES TO UNAUDITED CONDENSED COMBINED/CONSOLIDATED FINANCIAL STATEMENTS
(dollars in thousands, except for share and per share values)
cash and restricted cash balances could be impacted if the underlying financial institutions fail or could be subject to other adverse conditions in the financial markets.
The following presents all cash and cash equivalents and restricted cash on the condensed combined/consolidated balance sheets and reconcile to total cash included the condensed combined/consolidated statements of cash flows as of June 30, 2024, December 31, 2023, June 30, 2023:
| June 30, 2024 | December 31, 2023 | June 30, 2023 | |||||||||||||||
| Cash and cash equivalents | $ | 73,374 | $ | 73,416 | $ | 38,164 | |||||||||||
| Restricted cash (included in prepaid expenses and other current assets) | 4,480 | 4,977 | 7,907 | ||||||||||||||
| Restricted cash (included in other assets) | — | 40,311 | 34,459 | ||||||||||||||
| Total cash, cash equivalents, and restricted cash | $ | 77,854 | $ | 118,704 | $ | 80,530 | |||||||||||
Cash in Excess of FDIC Limits
The Company currently has bank deposits with financial institutions in the U.S. that exceed FDIC insurance limits. FDIC insurance provides protection for bank deposits up to $250,000. The Company has not experienced any losses in such amounts.
Insurance Subsidiary Deposits and Investments
The Company's captive insurance subsidiary cash and cash equivalents, deposits and investments are designated to support long-term insurance subsidiary liabilities and have been classified as short-term and long-term assets based on the timing of expected future payments of the Company's captive insurance liabilities.
Patient and Resident Service Revenue
Patient and resident service revenue is derived from services rendered, under short-term contracts, to patients for skilled and intermediate nursing, rehabilitation therapy, and assisted living services. Patient and resident service revenue is reported at the amount that reflects the consideration to which the Company expects to be entitled in exchange for providing patient services. These amounts are due from patients, governmental programs, and other third-party payors, and include variable consideration for retroactive revenue adjustments due to settlement of audits, reviews, and investigations.
The Company recognizes revenue as its performance obligations are completed. Routine services are treated as a single performance obligation satisfied over time as services are rendered. These routine services represent a bundle of services that are not capable of being distinct. The performance obligations are satisfied over time as the patient simultaneously receives and consumes the benefits of the healthcare services provided. Additionally, there may be ancillary services which are not included in the daily rates for routine services, but instead are treated as separate performance obligations satisfied at a point in time when those services are rendered.
Accounts Receivable and Allowance for Credit Losses
Accounts receivable consist primarily of amounts due from Medicare and Medicaid, managed care health plans and private payor sources, net of estimates for variable consideration. At June 30, 2024 and December 31, 2023, the allowance for credit losses was immaterial to the condensed combined/consolidated financial statements.
The Company determines the transaction price based on established billing rates reduced by contractual adjustments provided to third-party payors. Contractual adjustments are based on contractual agreements and historical experience. The Company considers the patient's ability and intent to pay the amount of consideration upon admission and records an implicit price concession based on historical patient collection experience. The
F-42
PACS GROUP, INC. AND SUBSIDIARIES
NOTES TO UNAUDITED CONDENSED COMBINED/CONSOLIDATED FINANCIAL STATEMENTS
(dollars in thousands, except for share and per share values)
allowance for implicit price concession is routinely evaluated and any subsequent changes are recorded as an adjustment to patient and resident service revenue in the condensed combined/consolidated statements of (loss) income and comprehensive (loss) income. The implicit price concession recorded as a reduction to patient and resident service revenue was $21,980 and $11,336 for the three months ended June 30, 2024 and 2023, respectively, and was $42,936, and $22,411 for the six months ended June 30, 2024 and 2023, respectively. As of June 30, 2024 and December 31, 2023, the Company has recorded estimated implicit price concessions as a reduction to accounts receivable of $59,201 and $42,171, respectively.
Property and Equipment, Net
Property and equipment are stated at historical cost less accumulated depreciation and amortization. Repair and maintenance charges which do not increase the useful lives of the assets are charged to expense as incurred. Depreciation is computed using the straight-line method over the estimated useful life of the property and equipment. The following is a summary of the depreciable lives of the Company’s depreciable assets:
Buildings and improvements - minimum of 5 years to a maximum of 40 years, but generally 30 years
Leasehold improvements - shorter of the lease term or the estimated useful life, generally 5 to 15 years
Furniture and equipment - minimum of 3 to a maximum of 15 years
Leasehold improvements are amortized over the lesser of the estimated useful life of the improvement or the term of the lease. Upon sale or retirement, the cost and the related accumulated depreciation and amortization are eliminated from the respective accounts and the resulting gain or loss included in current income.
Leases
The Company leases skilled nursing facilities, assisted living facilities, and commercial office space. The Company determines if an arrangement is a lease (for accounting purposes) at the inception of each lease.
Real estate leases are generally classified as operating leases and therefore the Company records rent expense on a straight-line basis over the term of the lease. The lease term used for straight-line rent expense is calculated from the date the Company is given control of the leased premises through the end of the lease term. Renewals are not assumed in the determination of the lease term unless they are deemed to be reasonably assured at the inception of the lease. The lease term used for this evaluation also provides the basis for establishing depreciable lives for buildings subject to lease and leasehold improvements. The Company has made an accounting policy election to keep leases with an initial term of 12 months or less off of the balance sheets and recognize those lease payments in the combined/consolidated statements of (loss) income and comprehensive (loss) income on a straight-line basis over the lease term. The Company has also elected the practical expedient to not separate lease and non-lease components for all of its leases as the non-lease components are not significant to the overall lease costs.
The Company’s real estate leases generally have initial lease terms of ten years or more and typically include one or more options to renew, with renewal terms that generally extend the lease term for an additional three to twenty years. Exercise of renewal options is generally subject to the satisfaction of certain conditions which vary by contract and generally follow payment terms that are consistent with those in place during the initial term.
Business Combinations
The Company accounts for acquisitions using the acquisition method of accounting in accordance with Financial Accounting Standards Board (FASB) Accounting Standards Codification (ASC) 805, Business Combinations (ASC 805). Acquisitions are accounted for as purchases and are included in the combined/consolidated financial statements from their respective acquisition dates. Assets acquired and liabilities assumed, if any, are measured at fair value on the acquisition date. Goodwill generated from acquisitions is recognized for the excess of the purchase price over tangible and identifiable intangible assets. In determining the fair value of identifiable assets, the Company uses various valuation techniques. These valuation methods require management to make estimates and assumptions surrounding projected revenues and costs, future growth, and discount rates.
F-43
PACS GROUP, INC. AND SUBSIDIARIES
NOTES TO UNAUDITED CONDENSED COMBINED/CONSOLIDATED FINANCIAL STATEMENTS
(dollars in thousands, except for share and per share values)
Goodwill and Other Indefinite-Lived Intangible Assets
Goodwill represents the excess of the purchase price of acquired businesses over the estimated fair value assigned to the individual assets acquired and liabilities assumed. The Company assesses goodwill for impairment at least annually on October 1st. The Company will perform an impairment assessment at other times if facts and circumstances indicate that it is more likely than not that the fair value of a reporting unit that has goodwill is less than its carrying value.
When assessing goodwill for impairment the Company may elect to first perform a qualitative assessment to determine if the quantitative impairment test is necessary. If the Company does not perform a qualitative assessment, or if the qualitative assessment indicates it is more likely than not that the fair value of a reporting unit is less than its carrying amount, the Company performs a quantitative test. The Company recognizes an impairment charge for the amount by which the carrying amount exceeds the reporting unit’s fair value; however, the loss recognized would not exceed the total amount of goodwill allocated to the reporting unit.
The Company’s indefinite-lived intangible assets primarily consist of licenses. The Company reviews indefinite-lived intangible assets for impairment on an annual basis or more frequently if events or changes in circumstances indicate that the carrying amount of the intangible asset may not be recoverable.
The Company may elect to first perform a qualitative assessment to determine whether it is more likely than not that the fair value of an indefinite-lived intangible asset is less than its carrying value. If the Company does not perform the qualitative assessment, or if the qualitative assessment indicates it is more likely than not that the fair value of the indefinite-lived intangible asset is less than its carrying amount, the Company calculates the estimated fair value of the indefinite-lived intangible asset. If the estimated fair value of the indefinite-lived intangible asset is lower than its carrying amount, an impairment loss is recognized for the difference.
Fair Value Measurements
The Company’s financial instruments consist principally of cash and cash equivalents, accounts receivable, insurance subsidiary deposits, accounts payable and borrowings.
Fair value measurements are based on a three-tier hierarchy that prioritizes the inputs used to measure fair value. The three-tiers include: Level 1: observable inputs such as quoted market prices in active markets; Level 2: inputs other than quoted market prices included in Level 1 that are directly or indirectly observable for the asset or liability and Level 3: unobservable inputs for which little or no market data exists, thereby requiring management to develop their own estimates and assumptions.
Impairment of Long-Lived Assets
In accordance with ASC Topic 360, Property, Plant, and Equipment (ASC 360), long-lived assets are reviewed for impairment whenever events or changes in circumstances indicate that the carrying amount may not be recoverable. Recoverability of these assets is determined based upon expected undiscounted future net cash flows from the operating subsidiaries to which the assets relate, utilizing management’s best estimate, appropriate assumptions, and projections at the time. If the expected future cash flow from the use of the asset and its eventual disposition is less than the carrying amount of the asset, an impairment loss is recognized and measured using the fair value of the related assets. The Company did not identify any indicators of impairment of its long-lived assets during the six months ended June 30, 2024 and 2023.
Accrued Risk Reserves
The Company is principally self-insured for risks related to PLGL claims. Accrued risk reserves primarily represent the accrual for risks associated with PLGL claims. The accrued risk reserves include a liability for unpaid reported claims and estimates for incurred but unreported claims. The Company’s policy with respect to its PLGL
F-44
PACS GROUP, INC. AND SUBSIDIARIES
NOTES TO UNAUDITED CONDENSED COMBINED/CONSOLIDATED FINANCIAL STATEMENTS
(dollars in thousands, except for share and per share values)
claims is to use an actuary to assist management in estimating the Company’s exposure for claims obligation (for both asserted and unasserted claims).
Investments in Joint Ventures
Investments in joint ventures, in which the Company exercises significant influence over operating and financial policies, are accounted for using the equity method of accounting. Under this method, the investment is carried at cost and is adjusted to recognize the investor’s share of earnings or losses of the investee after the date of acquisition and is adjusted for impairment whenever it is determined that a decline in the fair value below the cost basis is other than temporary. The fair value of the investment then becomes the new cost basis of the investment, and it is not adjusted for subsequent recoveries in fair value. The Company evaluates its investment in joint ventures, including cost in excess of book value (equity method goodwill) for impairment whenever indicators of impairment exist. No indicators of impairment existed during the six months ended June 30, 2024 and 2023.
Noncontrolling Interest
The Company is the majority-owner in a subsidiary which was formed to develop land, a building, and other assets to be leased to a facility operated by the Company upon completion. The noncontrolling interest in subsidiary is initially recognized at estimated fair value on the contribution date and is presented within total equity in the Company’s condensed combined/consolidated balance sheets since these interests are not redeemable.
Advertising
Advertising costs are expensed as incurred. Advertising expenses included in the Company’s condensed combined/consolidated statements of (loss) income and comprehensive (loss) income were $1,710 and $1,758 for the three months ended June 30, 2024 and 2023, respectively, and were $3,740 and $3,573 for the six months ended June 30, 2024 and 2023, respectively.
Income Taxes
The Company utilizes ASC Topic 740, Income Taxes (ASC 740), which requires an asset and liability approach for financial accounting and reporting for income taxes. Under this guidance, deferred tax assets and liabilities are determined based upon differences between financial reporting and tax basis of assets and liabilities and are measured using the enacted tax laws that will be in effect when the differences are expected to reverse. The effect on deferred tax assets and liabilities of a change in tax rates is recognized in income in the period that includes the enactment date. See Note 8, “Income Taxes”, for further discussion of the Company’s accounting for income taxes.
Under ASC 740, tax positions are evaluated for recognition using a more–likely–than–not threshold, and those tax positions requiring recognition are measured at the largest amount of tax benefit that is greater than 50 percent likely of being realized upon ultimate settlement with a taxing authority that has full knowledge of all relevant information. Liabilities for income tax matters include amounts for income taxes, applicable penalties, and interest thereon and are the result of the potential alternative interpretations of tax laws and the judgmental nature of the timing of recognition of taxable income.
The Company recognizes deferred tax assets (DTAs) to the extent that it believes that the assets are more likely than not to be realized. In making such a determination, the Company considers all available positive and negative evidence, including future reversals of existing taxable temporary differences, projected future taxable income, tax-planning strategies, carryback potential if permitted under the tax law, and results of recent operations. The Company generally expects to fully utilize its DTAs; however, when necessary, the Company records a valuation allowance to reduce its net deferred tax assets to the amount that is more likely than not to be realized.
F-45
PACS GROUP, INC. AND SUBSIDIARIES
NOTES TO UNAUDITED CONDENSED COMBINED/CONSOLIDATED FINANCIAL STATEMENTS
(dollars in thousands, except for share and per share values)
Concentration of Credit Risks
The Company’s credit risks primarily relate to cash and cash equivalents, restricted cash, and accounts receivable. Cash and cash equivalents are primarily held in bank accounts and overnight investments. Restricted cash is primarily invested in commercial paper and certificates of deposit with financial institutions and other interest-bearing accounts. Accounts receivable consist primarily of amounts due from patients (funded through Medicare, Medicaid, other contractual programs and through private payors) and from other health care companies for management, accounting and other services. The collectability of account receivable balances is dependent on the availability of funds from certain programs that rely on governmental funding, primarily Medicare and Medicaid. The Company’s receivables from Medicare and Medicaid programs accounted for 23% and 37% of total accounts receivable, respectively, at June 30, 2024 and 20% and 36% of total accounts receivable, respectively, at December 31, 2023. These receivables represent the only significant concentration of credit risk for the Company. The Company does not believe there are significant credit risks associated with these governmental programs. The Company performs continual credit evaluations of the Company’s clients and maintains appropriate allowances for credit losses on any accounts receivable proving uncollectible, and continually monitors and adjusts these allowances as necessary.
The Company’s operating subsidiaries, excluding the subsidiaries that exclusively operate assisted living and independent living facilities, have all of their skilled nursing beds designated for care of patients under federal Medicare and/or state Medicaid programs. 64% of the Company’s skilled nursing beds are located in California.
Stock-based Compensation
The Company measures and recognizes compensation expense for all stock-based payment awards made to employees and directors based on estimated fair values, ratably over the requisite service period of the award. Net (loss) income has been reduced as a result of the recognition of the fair value of all restricted stock unit awards issued, the amount of which is based upon the number of grants and other variables. The Company accounts for award forfeitures as they occur.
Comprehensive (Loss) Income
Comprehensive (loss) income consists of gains and losses affecting stockholders’ equity that, under U.S. GAAP, are excluded from net (loss) income. For the six months ended June 30, 2024 and 2023, comprehensive (loss) income includes unrealized gains and losses on the Company’s available-for-sale debt securities.
Segment Presentation
The Company’s chief operating decision maker (CODM), the Chief Operating Officer, reviews the consolidated results of operations when making decisions about allocating resources and assessing the performance of the Company as a whole and, hence, the Company has only one reportable segment. The Company does not distinguish between markets or regions for the purpose of allocating resources.
Recent Accounting Standards Issued But Not Yet Adopted by the Company
In November 2023, the FASB issued ASU 2023-07, Segment Reporting (Topic 280): Improvements to Reportable Segment Disclosures. The standard improves reportable segment disclosure requirements for public business entities primarily through enhanced disclosures about significant segment expenses that are regularly provided to the CODM and included within each reported measure of segment profit (referred to as the “significant expense principle”). The standard will become effective for the Company for the fiscal year 2024 annual financial statements and interim financial statements thereafter and will be applied retrospectively for all prior periods presented in the financial statements, with early adoption permitted. The Company is currently evaluating the impact this guidance will have on the disclosures included in the Notes to the combined/consolidated financial statements.
F-46
PACS GROUP, INC. AND SUBSIDIARIES
NOTES TO UNAUDITED CONDENSED COMBINED/CONSOLIDATED FINANCIAL STATEMENTS
(dollars in thousands, except for share and per share values)
In December 2023, the FASB issued ASU 2023-09, Income Taxes (Topic 740): Improvements to Income Tax Disclosures, which requires the Company to disclose disaggregated jurisdictional and categorical information for the tax rate reconciliation, income taxes paid and other income tax related amounts. The standard will become effective for the Company for the fiscal year 2024 annual financial statements and may be applied prospectively or retrospectively for all prior periods presented in the financial statements, with early adoption permitted. The Company is currently evaluating the impact this guidance will have on the disclosures included in the Notes to the combined/consolidated financial statements.
NOTE 3.REVENUE AND ACCOUNTS RECEIVABLE
Patient and Resident Service Revenue
The Company’s patient and resident service revenue is derived primarily from the Company’s applicable subsidiaries providing healthcare services to their respective patients and residents. Revenue is recognized when services are provided to the patients at the amount that reflects the consideration to which the Company expects to be entitled. These amounts are due from residents, third-party payors (including health insurers and government payors), and others and includes variable consideration for retroactive revenue adjustments due to settlement of audits and other reviews by the payor. Generally, the licensed healthcare provider entity providing the applicable services bills the applicable payors monthly.
The healthcare services in skilled patient contracts include routine services in exchange for a contractual agreed-upon amount or rate. Revenue is recognized as the performance obligations are satisfied.
Performance obligations are determined based on the nature of the services provided by the applicable licensed healthcare provider entity. Revenue for performance obligations satisfied over time is recognized based on actual charges incurred in relation to total expected (or actual) charges. The Company believes that this method provides a faithful depiction of the transfer of services over the term of the performance obligation based on the inputs needed to satisfy the obligation. Generally, performance obligations satisfied over time relate to residents receiving services in the facility and, when applicable, residents receiving services in their homes (independent care or assisted living). The Company measures the performance obligation from admission into the facility, or the commencement of the service, to the point when the applicable licensed healthcare provider entity is no longer required to provide services to that resident, which is generally at the time that the resident discharges from the applicable facility or passes away.
Revenue recognized from healthcare services is adjusted for estimates of variable consideration to arrive at the transaction price. The Company determines the transaction price based on contractually agreed-upon amounts or rates, adjusted for estimates of variable consideration. Variable consideration includes estimates of implicit price concessions so that the estimated transaction price is reflective of the amount to which the Company expects to be entitled in exchange for providing the healthcare services to customers. Variable consideration is estimated using the expected value method based on the Company’s historical reimbursement experience. The amount of variable consideration constrains the transaction price, such that it is probable that a significant reversal in the amount of the cumulative revenue recognized will not occur in a future period. Historically the Company has not had material differences between its estimated transaction price and actual collections from payors. If actual amounts of consideration ultimately received differ from the Company’s estimates, it adjusts these estimates, which would affect net service revenue in the period such variances become known.
Agreements with third-party payors typically provide for payments at amounts less than established charges. A summary of the payment arrangements with major third-party payors is as follows:
Medicaid: Payments for skilled nursing facility services rendered to Medicaid (including Medi-Cal, which is the name of the state Medicaid program in California) program beneficiaries are based on an annually established daily reimbursement rate for eligible stays. The rate is adjusted annually. The final settlement is determined after submission of an annual cost report and audits thereof by Medicaid. Revenue from the Medicaid program amounted to 38.1% and 35.4% of the Company’s condensed combined/consolidated net patient and resident revenue for the
F-47
PACS GROUP, INC. AND SUBSIDIARIES
NOTES TO UNAUDITED CONDENSED COMBINED/CONSOLIDATED FINANCIAL STATEMENTS
(dollars in thousands, except for share and per share values)
three months ended June 30, 2024 and 2023, respectively, and 38.4% and 32.9% of the Company’s condensed combined/consolidated net patient and resident revenue for the six months ended June 30, 2024 and 2023, respectively.
Medicare: Payments for skilled nursing facility services rendered to Medicare program beneficiaries are based on prospectively determined daily rates which vary according to a patient diagnostic classification system. The applicable licensed healthcare provider entity is paid for certain reimbursable services at the approved rate with final settlement determined after submission of the annual cost report and audit thereof by the designated Medicare fiscal intermediary. Revenue from the Medicare program amounted to 37.5% and 41.7% of the Company’s condensed combined/consolidated net patient and resident revenue for the three months ended June 30, 2024 and 2023, respectively, and 36.6% and 44.8% of the Company’s condensed combined/consolidated net patient and resident revenue for the six months ended June 30, 2024 and 2023, respectively.
Managed Care, Private and Other: Payments for services rendered to private payors and other primary payors included in the table below are based on established rates or on agreements with certain commercial insurance companies, health maintenance organizations, and preferred provider organizations, which provide for various discounts from the established rates. Revenue from these sources collectively amounted to 24.4% and 22.9% of the Company’s condensed combined/consolidated net patient and resident revenue for the three months ended June 30, 2024 and 2023, respectively, and 25.0% and 22.3% of the Company’s condensed combined/consolidated net patient and resident revenue for the six months ended June 30, 2024 and 2023, respectively.
The Company’s contracts are short term in nature with a duration of one year or less. The Company has minimal unsatisfied performance obligations at the end of the reporting period as patients are typically under no obligation to remain admitted in the Company’s facilities or under the Company’s care. As the period between the time of service and time of payment is typically one year or less, the Company does not adjust for the effects of a significant financing component.
Included in the Company’s condensed combined/consolidated balance sheets are contract balances, comprising of billed accounts receivable and unbilled receivables, which are the result of the timing of revenue recognition, billings and cash collections, as well as contract liabilities, which primarily represent payments the Company receives in advance of services provided. The Company has no material contract liabilities or contract assets as of June 30, 2024 and December 31, 2023.
Laws and regulations concerning government programs, including Medicare and Medicaid, are complex and subject to varying interpretation. As a result of audits and other reviews by governmental agencies or payor sources, health care providers from time to time receive requests for information and notices regarding billing audits and potential noncompliance with applicable laws and regulations, which, in some instances, can ultimately result in substantial monetary recoupments or other remedies being imposed on the healthcare provider. Compliance with such laws and regulations may also be subject to future government review and interpretation, as well as significant regulatory action, including fines, penalties, and potential exclusion from the related programs. The Company believes that it is in compliance with all applicable laws and regulations.
The contracts the Company has with commercial payors also provide for retrospective audits and review of claims.
Settlements with third-party payors for retroactive adjustments due to audits or other reviews are considered variable consideration and are included in the determination of the estimated transaction price for providing resident services. These settlements are estimated based on the terms of the payment agreement with the payor, correspondence from the payor, and the Company’s historical settlement activity, including an assessment to ensure that it is probable that a significant reversal in the amount of cumulative revenue recognized will not occur when the uncertainty associated with the retroactive adjustment is subsequently resolved. Estimated settlements are adjusted in future periods as adjustments become known (that is, new information becomes available), or as years are settled or are no longer subject to such audits or other reviews. These amounts are immaterial.
F-48
PACS GROUP, INC. AND SUBSIDIARIES
NOTES TO UNAUDITED CONDENSED COMBINED/CONSOLIDATED FINANCIAL STATEMENTS
(dollars in thousands, except for share and per share values)
The Company disaggregates revenue from contracts with its patients by payors. The Company determined that disaggregating revenue into these categories achieves the disclosure objectives to depict how the nature, amount, timing, and uncertainty of revenue and cash flows are affected by economic factors. The composition of patient and resident service revenue by primary payors for the three and six months ended June 30, 2024 and 2023 are as follows:
| Three Months Ended June 30, | |||||||||||||||||||||||
| 2024 | % of Revenue | 2023 | % of Revenue | ||||||||||||||||||||
| Medicare | $ | 368,044 | 37.5 | % | $ | 316,877 | 41.7 | % | |||||||||||||||
| Medicaid | 373,818 | 38.1 | % | 268,867 | 35.4 | % | |||||||||||||||||
| Managed care | 191,273 | 19.5 | % | 138,440 | 18.2 | % | |||||||||||||||||
| Private and other | 48,263 | 4.9 | % | 36,240 | 4.7 | % | |||||||||||||||||
| Total patient and resident service revenue | $ | 981,398 | 100.0 | % | $ | 760,424 | 100.0 | % | |||||||||||||||
| Six Months Ended June 30, | |||||||||||||||||||||||
| 2024 | % of Revenue | 2023 | % of Revenue | ||||||||||||||||||||
| Medicare | $ | 701,387 | 36.6 | % | $ | 657,287 | 44.8 | % | |||||||||||||||
| Medicaid | 736,170 | 38.4 | % | 483,026 | 32.9 | % | |||||||||||||||||
| Managed care | 375,553 | 19.6 | % | 261,877 | 17.8 | % | |||||||||||||||||
| Private and other | 102,586 | 5.4 | % | 66,060 | 4.5 | % | |||||||||||||||||
| Total patient and resident service revenue | $ | 1,915,696 | 100.0 | % | $ | 1,468,250 | 100.0 | % | |||||||||||||||
Additional Funding and CARES Act
Through the CARES Act, the Company received funding from the U.S. Department of Health and Human Services (HHS) through the Provider Relief Fund (PRF) during the years ended December 31, 2022 and 2021. These funds were provided to healthcare providers who diagnose, test, or care for individuals with cases of COVID-19 and have health care related expenses and lost revenues attributable to COVID-19. The Company recorded these funds as deferred revenue upon receipt and revenue was recognized only to the extent that health-care related expenses or lost revenues had been incurred and were not reimbursed from other funding sources. The Company recognized an immaterial amount of additional funding in the six months ended June 30, 2023 for funds received prior to 2023. The Company did not receive any additional funds related to this program during 2023 or 2024.
The CARES Act also provided for refundable payroll tax credits known as the Employee Retention Tax Credit, which allowed qualified employers to receive a credit of 70% of the employee qualified wages and related payroll costs paid after December 31, 2020 through September 30, 2021, up to a maximum credit of $7 per employee, per quarter, for a maximum of $21 per employee in 2021. Due to uncertainty related to meeting the necessary qualifications, the Company recorded a reserve against the entire amount claimed. As of June 30, 2024 and December 31, 2023, the Company has recorded $36,508 and $36,477, respectively, in other liabilities to reflect the cash already received related to these credits which may need to be returned and potential penalties.
F-49
PACS GROUP, INC. AND SUBSIDIARIES
NOTES TO UNAUDITED CONDENSED COMBINED/CONSOLIDATED FINANCIAL STATEMENTS
(dollars in thousands, except for share and per share values)
NOTE 4.PROPERTY AND EQUIPMENT
Property and equipment consisted of the following at:
| June 30, 2024 | December 31, 2023 | ||||||||||||||||
| Buildings and improvements | $ | 533,808 | $ | 372,554 | |||||||||||||
| Leasehold improvements | 68,298 | 58,958 | |||||||||||||||
| Furniture, fixtures, and other | 80,229 | 64,750 | |||||||||||||||
| Construction in process | 53,589 | 50,937 | |||||||||||||||
| Land | 69,678 | 55,593 | |||||||||||||||
| Finance lease right-of-use assets | 40,536 | 40,536 | |||||||||||||||
| 846,138 | 643,328 | ||||||||||||||||
| Less: accumulated depreciation and amortization | (82,234) | (65,800) | |||||||||||||||
Property and equipment, net | $ | 763,904 | $ | 577,528 | |||||||||||||
The Company did not record an impairment charge for the six months ended June 30, 2024, and 2023.
See Note 12, “Operation Expansions”, for information on expansions during the six months ended June 30, 2024.
NOTE 5.FAIR VALUE MEASUREMENT
The Company's financial assets include insurance subsidiary deposits and highly liquid investments which are held by the consolidated captive insurance entity and are designated to support long-term insurance subsidiary liabilities and are recorded at fair value of $35,476 and $0 as of June 30, 2024 and December 31, 2023, respectively. As of June 30, 2024, the components of the fair value of the insurance subsidiary deposits and investments include amortized costs of $35,000 and net unrealized gains of $476. Gains and losses on investments are recorded within other expense, net. Insurance subsidiary deposits and investments consist of holdings in investment grade bond mutual funds and are derived using Level 2 inputs. These assets are recorded in insurance subsidiary deposits and investments on our condensed combined/consolidated balance sheets and are classified as available-for-sale securities. These mutual funds are primarily valued utilizing calculations which incorporate observable inputs such as yield, maturity and credit quality.
The Company's non-financial assets, which includes goodwill, intangible assets, property and equipment and right-of-use assets, are not required to be measured at fair value on a recurring basis. However, on a periodic basis, or whenever events or changes in circumstances indicate that their carrying value may not be recoverable, the Company assesses its long-lived assets for impairment. When impairment has occurred, such long-lived assets are written down to fair value.
NOTE 6.CREDIT FACILITIES
On February 28, 2023, the Company entered into a working capital loan agreement (the Working Capital Loan) in connection with the acquisition of various new facilities. The Working Capital Loan allowed the Company to borrow up to $17,500 at an annual interest rate of 9%. On May 8, 2023, the Company drew on the Working Capital Loan in the amount of $15,000. As described below, the Working Capital Loan was repaid during 2023 and, as such, has a zero balance as of June 30, 2024.
On June 30, 2023, the Company and certain of its subsidiaries entered into a credit agreement with Truist and a syndicate of lenders (the 2023 Credit Agreement), that extended credit in the form of the revolving credit facility thereunder, (the 2023 Revolving Credit Facility), including letter of credit and swing line sub facilities and a term loan facility (Truist Term Loan), together referred to as the 2023 Credit Facility. The 2023 Credit Agreement
F-50
PACS GROUP, INC. AND SUBSIDIARIES
NOTES TO UNAUDITED CONDENSED COMBINED/CONSOLIDATED FINANCIAL STATEMENTS
(dollars in thousands, except for share and per share values)
provided for: (i) the 2023 Revolving Credit Facility with revolving commitments in an aggregate principal amount of $150,000, including a letter of credit sub facility in an amount representing that portion of the aggregate revolving commitments that may be used by the borrower for the issuance of letters of credit in an aggregate face amount not to exceed $30,000 and a swingline loan sub facility in an aggregate principal amount at any time outstanding not to exceed $20,000 and (ii) the Truist Term Loan in an aggregate principal amount of $275,000.
Outstanding borrowings under the 2023 Credit Facility accrued interest at either: (a) the Secured Overnight Financing Rate (SOFR) (plus a 0.10% credit spread adjustment) plus a margin ranging from 2.50% to 3.50% per annum; or (b) Base Rate (which was defined in a customary manner for credit facilities of this type) plus a margin ranging from 1.50% to 2.50% per annum. The applicable margin was based on the Company’s debt to income ratio as calculated in accordance with the terms of the 2023 Credit Agreement. In addition, the Company agreed to pay a commitment fee on the unused portion of the 2023 Revolving Credit Facility, which ranged from 0.30% to 0.50% per annum, depending on the same debt to income ratio.
In connection with executing the 2023 Credit Agreement, deferred financing costs associated with both lines-of-credit and long-term debt of $3,109 were written off, and additional deferred financing costs of $9,662 were capitalized during the year ended December 31, 2023. In addition, on the closing date of the 2023 Credit Agreement, the Company drew $75,000 on the 2023 Revolving Credit Facility and borrowed the entirety of the $275,000 Truist Term Loan. The Company used approximately $142,000 of the net proceeds to repay certain outstanding indebtedness on prior lines of credit and the Working Capital Loan.
On December 7, 2023, the Company amended and restated the 2023 Credit Facility (the Amended and Restated 2023 Credit Facility). The Amended and Restated 2023 Credit Facility provided for an increase of the 2023 Revolving Credit Facility to an aggregate principal amount of $600,000, which revolving commitments may also be utilized for (x) the issuance of letters of credit in an aggregate face amount not to exceed $50,000 and/or (y) the borrowing of swingline loans in aggregate principal amount not to exceed $20,000 at any time outstanding.
Outstanding borrowings under the Amended and Restated 2023 Credit Facility bear interest at the option of the Company based on: (a) SOFR (plus a 0.10% credit spread adjustment) plus a margin ranging from 2.25% to 3.25% per annum; or (b) the Base Rate (which is defined consistent with the 2023 Credit Facility) plus the applicable margin ranging from 1.25% to 2.25% per annum. The applicable margin is based on the Company’s debt to income ratio as calculated consistent with the 2023 Credit Facility. In addition, the Company will pay a commitment fee on the unused portion of the commitments, which ranges from 0.25% to 0.45% per annum, depending on the same debt to income ratio.
Upon the closing of the Amended and Restated 2023 Credit Facility, the Company borrowed $460,000 of revolving loans, the proceeds of which were used to repay and refinance all term loans and revolving loans under the 2023 Credit Facility, to repay certain other outstanding indebtedness, and to pay transaction costs in connection with the Amended and Restated 2023 Credit Facility. Deferred financing costs associated with both lines-of-credit and long-term debt of $519 were written off as part of the refinance during the year ended December 31, 2023.
The agreement above contains certain financial and non-financial covenants and restrictions. Default by the applicable credit party on any covenant or restriction could affect the lender’s commitment to lend, and, if not waived or corrected, could make the outstanding balances due on demand. Under the Amended and Restated 2023 Credit Facility, the Company must maintain a debt-to-income ratio of not greater than 3.00:1.00. The Amended and Restated 2023 Credit Facility also requires that the Company maintain a minimum interest/rent coverage ratio of not less than 1.10:1.00. The Company was in compliance with all such covenants and restrictions as of June 30, 2024.
The Company maintains the Amended and Restated 2023 Credit Facility as its single line-of-credit. At June 30, 2024, the total commitment limit continued to be $600,000 and was secured by Company assets. The agreements mature on December 7, 2028. The balance outstanding on all applicable lines was $248,000 and $520,000 at June 30, 2024 and December 31, 2023, resulting in available cash of $340,350 and $80,000, respectively, net of letter of credit usage.
F-51
PACS GROUP, INC. AND SUBSIDIARIES
NOTES TO UNAUDITED CONDENSED COMBINED/CONSOLIDATED FINANCIAL STATEMENTS
(dollars in thousands, except for share and per share values)
Deferred financing fees on lines-of-credit were $15,099 as of June 30, 2024 and December 31, 2023. Amortization expense relating to deferred financing fees on lines-of-credit for the three months ended June 30, 2024 and 2023 was $755 and $165, respectively and for the six months ended June 30, 2024 and 2023 were $1,510 and $352, respectively. Accumulated amortization related to deferred financing fees on lines-of-credit was $1,703 and $193 as of June 30, 2024 and December 31, 2023, respectively.
On April 15, 2024, the Company completed an Initial Public Offering (IPO), as described in Note 13, “Capital Stock”, receiving initial net proceeds of $423,000. The Company used $370,000 of the net proceeds from the IPO, which represented 87.5% of the net proceeds from the IPO, to repay amounts outstanding under the Amended and Restated 2023 Credit Facility, and used the remaining amount for general corporate purposes to support the growth of the business.
NOTE 7.LONG-TERM DEBT
During the six months ended June 30, 2024 and the year ended December 31, 2023, some of the Company's subsidiaries entered into Department of Housing and Urban Development (HUD)-insured mortgage loans in the aggregate amount of $34,685 and $88,809, respectively. As a result, 11 of the Company's subsidiaries had mortgage loans insured with HUD in the aggregate amount of $199,404 as of June 30, 2024, of which $3,339 is classified as short-term and the remaining $196,058 is classified as long-term. As of December 31, 2023, the Company’s subsidiaries had HUD-insured mortgage loans in the aggregate amount of $166,181 of which $2,346 was classified as short-term and the remaining $163,835 was classified as long-term. These subsidiaries are subject to HUD-mortgage oversight and periodic inspections. As of June 30, 2024, the Company’s HUD-insured mortgage loans bear fixed interest rates ranging from 2.4% to 6.3% per annum and have various maturity dates through December 31, 2058. In addition to the interest rate, the Company incurs other fees for HUD placement, including but not limited to audit fees. Amounts borrowed under the mortgage loans may be prepaid, subject to prepayment fees based on the principal balance on the date of prepayment. The original terms for all the HUD-insured mortgage loans are 24 to 35 years.
In addition to the HUD-insured mortgage loans above, the Company has 12 other mortgage loans or promissory notes. The non-HUD insured mortgage loans and notes bear interest rates in the range of 2.0% and 7.5% per annum with various maturity dates through June 1, 2027. The notes are secured by equipment and guarantees by the Company and certain stockholders. As of June 30, 2024 and December 31, 2023, the Company had $46,021 and $48,829, respectively, of debt principal outstanding under the mortgage loans and promissory notes, of which $12,407 is classified as short-term and the remaining $33,614 is classified as long-term as of June 30, 2024, and $14,476 is classified as short-term and the remaining $34,353 is classified as long-term as of December 31, 2023.
The Company was in compliance with all applicable loan covenants with respect to the foregoing as of June 30, 2024 and December 31, 2023. The loans above are guaranteed by the Company. Additionally, various loans are secured by real property with a carrying value amounting to $235,222 and $438,645 at June 30, 2024 and December 31, 2023, respectively.
Long-term debt consists of the following at:
| June 30, 2024 | December 31, 2023 | ||||||||||||||||
| HUD-insured mortgage loans | $ | 199,404 | $ | 166,181 | |||||||||||||
| Other mortgage loans and promissory notes | 46,021 | 48,829 | |||||||||||||||
| Less: current maturities | (15,745) | (16,822) | |||||||||||||||
| Less: deferred financing fees, net | (2,573) | (2,480) | |||||||||||||||
| Total | $ | 227,107 | $ | 195,708 | |||||||||||||
Deferred financing fees incurred in conjunction with debt financing of $2,745 and $2,611 as of June 30, 2024 and December 31, 2023, respectively, are being amortized over the life of the respective loans. Total amortization
F-52
PACS GROUP, INC. AND SUBSIDIARIES
NOTES TO UNAUDITED CONDENSED COMBINED/CONSOLIDATED FINANCIAL STATEMENTS
(dollars in thousands, except for share and per share values)
related to deferred financing fees is included in interest expense and amounted to $21 and $390 for the three months ended June 30, 2024 and 2023, respectively, and $41 and $818 for the six months ended June 30, 2024 and 2023, respectively. Accumulated amortization related to those deferred financing fees was $172 and $131 at June 30, 2024 and December 31, 2023, respectively.
As discussed in Note 6, “Credit Facilities”, on June 30, 2023, the Company borrowed under the Truist Term Loan in connection with the execution of the 2023 Credit Agreement. Under the Truist Term Loan, the Company borrowed $275,000. The Truist Term Loan has a maturity date of June 30, 2028. Upon closing of the Truist Term Loan, the Company paid off certain other mortgage loans and promissory notes in the aggregate amount of $224,802. The Truist Term Loan was repaid on December 7, 2023 in connection with the closing of the Amended and Restated 2023 Credit Facility and as such, has a zero balance as of June 30, 2024.
NOTE 8.INCOME TAXES
The Company recorded income tax expense of $22,441 and $21,871 during the six months ended June 30, 2024, and 2023, respectively, or 37.0% of earnings before income taxes for the six months ended June 30, 2024, compared to 27.1% for the six months ended June 30, 2023. The change in effective tax rate in the six months ended June 30, 2024, compared to the six months ended June 30, 2023, was primarily due to an increase in non-deductible expenses, including non-deductible compensation in 2024.
The Company is subject to U.S. federal income tax, as well as income tax in certain states in which it operates. The Company’s federal returns for tax years 2020 and forward are subject to examination, and state returns for tax years 2019 and forward are subject to examination. The Company’s balance of net deferred tax assets and net deferred tax liabilities are included within other assets and other liabilities on the condensed combined/consolidated balance sheets as of June 30, 2024 and 2023, respectively.
As of June 30, 2024 and 2023, the Company did not have any unrecognized tax benefits. The Company recognizes accrued interest and penalties related to unrecognized tax benefits in income tax expense. The Company does not anticipate the uncertain tax position to change materially within the next twelve months.
NOTE 9.LEASES
Operating Leases
The Company leases most of its skilled nursing and assisted living facilities, as well as its office space and certain vehicles and equipment, under various non-cancelable operating lease agreements. These operating leases expire at various dates throughout 2049.
Substantially all operating leases for skilled nursing and assisted living facilities are on a “triple-net” basis, which require lessees to pay for all insurance, repairs, utilities, and real property taxes assessed on the leased property, and most of the leases are guaranteed by the Company and/or its stockholders.
For 13 of the facility operating leases, the Company holds an option to purchase the real estate which can be exercised at varying times until March 31, 2038. At lease inception it was determined that the exercise of these purchase options was not reasonably assured.
The facility leases are generally renewable at the Company’s option for additional terms ranging from 3 to 20 years. All facility leases provide for an additional percentage rent based upon specified rates per the terms of the agreements.
Real estate lease payments are deemed to constitute the right to use the underlying facilities and operate as a skilled nursing facility as permitted by the accompanying license. As the license is deemed to be inseparable from the related real estate in determining value, the payments related to these components have been combined into a
F-53
PACS GROUP, INC. AND SUBSIDIARIES
NOTES TO UNAUDITED CONDENSED COMBINED/CONSOLIDATED FINANCIAL STATEMENTS
(dollars in thousands, except for share and per share values)
single lease obligation representing the right to use the facilities and to operate under the terms of the accompanying license, respectively.
Finance Leases
The Company leases certain skilled nursing and assisted living facilities under finance lease agreements. The economic substance of each lease is that the Company is financing the facilities through the lease. The lease terms of these finance leases allow for a purchase option during a specified window. The Company has determined that it is reasonably certain to exercise the purchase option at the end of each purchase option window. Therefore the Company has calculated the lease term through the end of the purchase option window for each lease. Accordingly, such leases are recorded in the Company’s condensed combined/consolidated financial statements as assets and liabilities.
Finance lease right-of-use assets are included in property and equipment and have a balance of $37,205 and $37,850 as of June 30, 2024 and December 31, 2023, respectively. The current portion of finance lease liabilities is included in other accrued expenses and has a balance of $991 and $942 as of June 30, 2024 and December 31, 2023, respectively. The long-term portion of finance lease liabilities is included in other liabilities and has a balance of $40,279 and $40,766 as of June 30, 2024 and December 31, 2023, respectively.
The components of lease expense were as follows:
| Three Months Ended June 30, | Six Months Ended June 30, | ||||||||||||||||||||||
| 2024 | 2023 | 2024 | 2023 | ||||||||||||||||||||
| Operating lease expense | |||||||||||||||||||||||
Rent - cost of services (1) | $ | 65,833 | $ | 51,456 | $ | 129,794 | $ | 96,560 | |||||||||||||||
| General and administrative expense | 607 | 353 | 1,417 | 708 | |||||||||||||||||||
Variable lease costs (2) | 8,119 | 6,044 | 17,033 | 11,964 | |||||||||||||||||||
| Total operating lease expense | $ | 74,559 | $ | 57,853 | $ | 148,244 | $ | 109,232 | |||||||||||||||
| Finance lease expense | |||||||||||||||||||||||
| Amortization of right-of-use assets | 322 | 313 | 645 | 620 | |||||||||||||||||||
| Interest on lease liabilities | 736 | 198 | 1,476 | 330 | |||||||||||||||||||
| Total financing lease expense | 1,058 | 511 | 2,121 | 950 | |||||||||||||||||||
| Total Lease Expense | $ | 75,617 | $ | 58,364 | $ | 150,365 | $ | 110,182 | |||||||||||||||
__________________
(1)Rent - cost of services includes other variable lease costs such as Consumer Price Index (CPI) increases and other rent adjustments of $497 and $620 for the three months ended June 30, 2024 and 2023, respectively, and $1,035 and $1,578 for the six months ended June 30, 2024 and 2023, respectively.
(2)Variable lease costs, including property taxes and insurance, are classified in Cost of services in the Company’s unaudited condensed combined/consolidated statements of (loss) income and comprehensive (loss) income.
Operating lease expense is included in Rent - cost of services and General and administrative expense as indicated above. For finance lease expense, the amortization of right-of-use assets is included in depreciation and amortization while the interest component is included in interest expense.
F-54
PACS GROUP, INC. AND SUBSIDIARIES
NOTES TO UNAUDITED CONDENSED COMBINED/CONSOLIDATED FINANCIAL STATEMENTS
(dollars in thousands, except for share and per share values)
The following table summarizes supplemental cash flow information related to leases:
| Six Months Ended June 30, | |||||||||||
| 2024 | 2023 | ||||||||||
| Operating cash paid for amounts included in the measurement of operating lease liabilities | $ | 116,026 | $ | 88,175 | |||||||
| Operating cash paid for amounts included in the measurement of finance lease liabilities | 1,476 | 330 | |||||||||
| Financing cash paid for amounts included in the measurement of finance lease liabilities | 438 | 1,065 | |||||||||
| Operating lease right-of-use assets obtained in exchange for lease liabilities | 259,201 | 557,412 | |||||||||
| Financing lease right-of-use assets obtained in exchange for lease liabilities | — | 2,028 | |||||||||
Information relating to the lease term and discount rate is as follows:
| As of June 30, 2024 | |||||
| Weighted-average remaining lease term (years) | |||||
| Operating leases | 14 | ||||
| Financing leases | 2 | ||||
| Weighted-average discount rate | |||||
| Operating leases | 5.8 | % | |||
| Financing leases | 7.2 | % | |||
In determining the discount rate used to measure the right-of-use asset and lease liability, the Company uses rates implicit in the lease, or if not readily available, the Company will use its incremental borrowing rate. The Company’s incremental borrowing rate is based on an estimated secured rate comprised of a risk-free rate plus a credit spread as secured by its assets. Determining a credit spread as secured by the Company’s assets may require significant judgment.
Maturities of lease liabilities as of June 30, 2024 were as follows:
| Finance Leases | Operating Leases | Total | |||||||||||||||
| 2024 (remainder) | $ | 1,929 | $ | 116,501 | $ | 118,430 | |||||||||||
| 2025 | 23,560 | 232,133 | 255,693 | ||||||||||||||
| 2026 | 2,241 | 231,843 | 234,084 | ||||||||||||||
| 2027 | 17,995 | 229,876 | 247,871 | ||||||||||||||
| 2028 | 782 | 231,979 | 232,761 | ||||||||||||||
| 2029 | 391 | 233,208 | 233,599 | ||||||||||||||
| Thereafter | — | 1,934,120 | 1,934,120 | ||||||||||||||
| Total lease payments | $ | 46,898 | $ | 3,209,660 | $ | 3,256,558 | |||||||||||
| Less: present value discount | (5,627) | (1,027,797) | (1,033,424) | ||||||||||||||
| Present value of lease liabilities | $ | 41,271 | $ | 2,181,863 | $ | 2,223,134 | |||||||||||
In addition to its lessee activity, the Company generates an immaterial amount of revenue from arrangements where it is a lessor of certain facilities. Revenue from those arrangements is included in other revenue on the condensed combined/consolidated statements of (loss) income and comprehensive (loss) income.
F-55
PACS GROUP, INC. AND SUBSIDIARIES
NOTES TO UNAUDITED CONDENSED COMBINED/CONSOLIDATED FINANCIAL STATEMENTS
(dollars in thousands, except for share and per share values)
NOTE 10.RELATED PARTY TRANSACTIONS
On July 1, 2021, the Company entered into a Consulting and Strategic Advisory Services Agreement with Helios Consulting, LLC (Helios), a limited liability company owned by Jason Murray, the Company’s Chief Executive Officer and Chairman of its board of directors, and Mark Hancock, Executive Vice Chairman of its board of directors, (Helios Consulting Agreement) which automatically renewed for successive one-year terms. The Helios Consulting Agreement provided for a cash consulting fee of approximately $4,000 annually, paid in monthly installments, for consulting and strategic advisory services provided to the Company by Helios. For the three months ended June 30, 2024 and 2023, the Company paid $0 and $1,000 (inclusive of $0 and $38, respectively, paid to a subsidiary of Helios), respectively. For the six months ended June 30, 2024 and 2023, the Company paid $0 and $2,000 (inclusive of $0 and $75, respectively, paid to a subsidiary of Helios), respectively. As of December 31, 2023, the Company terminated the Helios Consulting Agreement.
On March 24, 2023, the Company entered into subscription agreements with Mr. Murray and Mr. Hancock, pursuant to which Mr. Murray and Mr. Hancock each purchased 10,000 shares of the Company’s common stock for a purchase price of $0.001 per share, in a private placement concurrent with the Company’s incorporation in the State of Delaware and in anticipation of effecting the reorganization on June 30, 2023.
NOTE 11.COMMITMENTS AND CONTINGENCIES
Regulatory Matters
Laws and regulations governing Medicare and Medicaid programs are complex and subject to review and interpretation. Compliance with such laws and regulations is evaluated regularly, the results of which can be subject to future governmental review and interpretation, and can include significant regulatory action including fines, penalties, and exclusion from certain governmental programs. Included in these laws and regulations is monitoring performed by the Office of Civil Rights which covers the Health Insurance Portability and Accountability Act of 1996, the terms of which require healthcare providers (among other things) to safeguard the privacy and security of certain patient protected health information.
Litigation
The skilled nursing business involves a significant risk of liability given the age and health of the patients and residents served by the Company’s independent operating subsidiaries. The Company, and others in the industry are subject to an increasing number of claims and lawsuits, including professional liability claims, alleging that services provided have resulted in personal injury, elder abuse, wrongful death or other related claims. In addition, the Company, its independent operating subsidiaries, and others in the industry are subject to claims and lawsuits in connection with COVID-19 and a facility’s preparation for and/or response to COVID-19. The defense of these lawsuits may result on significant legal costs, regardless of the outcome, and can result in large settlement amounts or damage awards.
Healthcare litigation (including class action litigation) is common and is filed based upon a wide variety of claims and theories. The Company and other companies in its industry are routinely subjected to varying types of claims and suits, including class-actions. Class-action suits have the potential to result in large jury verdicts and settlements, and may result in significant legal costs. The Company expects the plaintiffs’ bar to continue to be aggressive in their pursuit of claims. The Company has been subjected to, and is currently involved in, litigation alleging violations of state and federal wage and hour laws as resulting from the alleged failure to pay wages, to timely provide and authorize meal and rest breaks, and related causes of action. While there can be no assurance, based on the Company’s evaluation of information currently available, management does not believe that the ultimate resolution of these actions will have a material adverse effect on the Company’s business, cash flows, financial condition, or results of operations.
The Company has been, and continues to be, subject to claims and legal actions that arise in the normal course of business, including potential claims filed by patients or others on their behalf related to patient care and treatment
F-56
PACS GROUP, INC. AND SUBSIDIARIES
NOTES TO UNAUDITED CONDENSED COMBINED/CONSOLIDATED FINANCIAL STATEMENTS
(dollars in thousands, except for share and per share values)
(professional negligence claims), as well as employment related claims filed by current or former employees. While there can be no assurance, based on the Company’s evaluation of information currently available, management does not believe the results of such litigation and investigations would have a material adverse effect on the results of operations, financial position or cash flows of the Company, taken as a whole. However, the Company’s assessment may evolve based upon further developments in the proceedings at issue. The results of legal proceedings are inherently uncertain, and material adverse outcomes are possible.
Insurance Claims
The Company purchased PLGL claims made insurance policies to cover applicable claims through an unrelated insurer. The PLGL policies are claims-made high deductible self-insured policies whereby the Company is responsible for the first layer of coverage, generally ranging from $250 to $500 per claim, as well as an additional aggregate one-time deductible generally ranging from $750 to $4,000 per policy, with the unrelated insurer typically covering up to $10,000 in aggregate claims paid per policy year. The Company uses its wholly-owned captive insurance company for the purpose of insuring certain portions of its risk retained under its PLGL programs. Accordingly, the Company is in essence self-insured for claims that are less than policy deductible amounts, claims not covered by such policies, and claims that exceed policy limits. It is the Company’s policy to use an actuary to assist management in recording the expense and related liability for PLGL claims, both asserted and unasserted, on an undiscounted basis. Included as part of accrued self-insurance liabilities in the accompanying condensed combined/consolidated balance sheets are PLGL self-insurance liabilities amounting to $183,836 and $162,976 as of June 30, 2024 and December 31, 2023, respectively, which include $31,628 and $34,676, respectively, of estimated obligations that will be covered by the unrelated insurer. PLGL self-insurance liabilities as of June 30, 2024 and December 31, 2023 include $53,673 and $43,083, respectively, that were related to unasserted claims. The Company recorded an asset for the estimated obligations that will be covered by the unrelated insurer. As of June 30, 2024 this asset amounted to $5,377 and $26,251 recorded within other receivables and other assets, respectively, and as of December 31, 2023, this asset amounted to $5,895 and $28,781 recorded within other receivables and other assets, respectively, as the claims related to the Company's general and professional liability and the anticipated insurance recoveries are recorded on a gross rather than net basis in accordance with U.S. GAAP.
Indemnities
From time to time, the Company enters into certain types of contracts that contingently require it to indemnify parties against third-party claims. These contracts primarily include (i) certain real estate leases, under which the Company may be required to indemnify property owners or prior facility operators for post-transfer environmental or other liabilities and other claims arising from the Company use of the applicable premises, (ii) operations transfer agreements, in which the Company agrees to indemnify past operators of facilities against certain liabilities arising from the transfer of the operation and/or the operation thereof after the transfer to the Company's independent operating subsidiary, (iii) certain lending agreements, under which the Company may be required to indemnify the lender against various claims and liabilities, and (iv) certain agreements with the Company officers, directors and others, under which the Company may be required to indemnify such persons for liabilities arising out of the nature of their relationship to the Company. The terms of such obligations vary by contract and, in most instances, do not expressly state or include a specific or maximum dollar amount. Generally, amounts under these contracts cannot be reasonably estimated until a specific claim is asserted. Consequently, because no claims have been asserted, no liabilities have been recorded for these obligations on the combined/consolidated balance sheets for any of the periods presented.
NOTE 12.OPERATION EXPANSIONS
FASB ASC Topic 805, Business Combinations (ASC 805) defines the definition of a business to assist entities with evaluating when a set of transferred assets and activities is deemed to be a business. Determining whether a transferred set constitutes a business is important because the accounting for a business combination differs from that of an asset acquisition. The definition of a business also affects the accounting for dispositions. When substantially all of the fair value of assets acquired is concentrated in a single asset, or a group of similar assets, the assets acquired would not represent a business and business combination accounting would not be required.
F-57
PACS GROUP, INC. AND SUBSIDIARIES
NOTES TO UNAUDITED CONDENSED COMBINED/CONSOLIDATED FINANCIAL STATEMENTS
(dollars in thousands, except for share and per share values)
2024 Expansions
During the six months ended June 30, 2024, the Company’s operations and real estate portfolio grew through a combination of long-term leases and real estate purchases, with the addition of 12 stand-alone facilities and nine real estate purchases. Of the nine real estate purchases, four of the properties were acquired in conjunction with the operations of the associated facility. For the other five acquired properties, the Company’s subsidiaries previously operated the respective facilities and have now acquired the real estate associated with those operations. The aggregate purchase price for these acquisitions was $175,150. These new operations added 1,501 skilled nursing beds and 174 assisted living beds operated by the Company's affiliated operating subsidiaries.
The Company’s expansion strategy has been focused on identifying both opportunistic and strategic acquisitions within its target markets that offer strong opportunities to improve both clinical and financial performance of the acquired facility. The operations added by the Company are underperforming financially and have regulatory and clinical challenges to overcome. Financial information, especially with underperforming operations, is often inadequate, inaccurate or unavailable. Consequently, the Company believes that prior operating results are not a meaningful representation of the Company’s current operating results or indicative of the integration potential of its newly acquired operating subsidiaries. The assets added during the six months ended June 30, 2024 and through the issuance of the financial statements were not material operations to the Company individually or in the aggregate. Accordingly, pro forma financial information is not presented. The additions have been included in the June 30, 2024 condensed combined/consolidated balance sheets of the Company, and the operating results have been included in the condensed combined/consolidated statements of (loss) income and comprehensive (loss) income of the Company since the date the Company gained effective control.
Expansions After Period End
On August 1, 2024, the Company finalized the acquisition of operations for 12 skilled nursing and 13 assisted living and independent living facilities. The operations are located across six states, including 19 facilities in Washington, two in Nevada, and one facility each in Alaska, Arizona, California, and Montana. Collectively, these facilities comprise 1,072 skilled nursing beds and 831 assisted living and independent living units. Of these facilities, 21 are leased from a new joint venture the Company entered into on the same date for $10,000 in which it owns a 25.8% interest. The remaining four facilities are leased from unaffiliated third-party landlords.
Additionally, subsequent to June 30, 2024, the Company’s operations grew with the addition of three stand-alone facilities in Kansas through a long-term lease. The new operations added 378 skilled nursing beds operated by the Company’s affiliated operating subsidiaries.
NOTE 13.CAPITAL STOCK
The Reorganization on June 30, 2023 referred to in Note 1, “Organization and Nature of Business”, resulted in the Common Shares outstanding being converted from 600 shares of PGI to 20,000 shares of PACS Group (a 1 to 33.33 conversion ratio). On March 31, 2024, the Company’s board of directors approved a 1 to 6,436.1693 stock split of its issued and outstanding common stock, which was effective by amendment to the Company’s charter on April 1, 2024. As part of the amendment, the number of authorized shares of common stock was revised to 1,250,000,000 with the par value remaining at $0.001 per share, and the number of authorized shares of preferred stock was approved to be 50,000,000 with a par value of $0.001. All issued and outstanding common stock and per share amounts contained in the condensed combined/consolidated financial statements have been retrospectively adjusted to give effect to the stock split for all periods presented.
On April 15, 2024, the Company completed an IPO in which the Company issued and sold 21,428,572 shares of common stock at a public offering price of $21.00 per share, generating aggregate gross proceeds of $450,000 before underwriter discounts and commissions, fees and other expenses of $35,843. In addition, the underwriters exercised their 30-day option to purchase an additional 3,214,284 shares of the Company’s common stock at the initial public offering price from the selling stockholders, less underwriting discounts and commissions. The
F-58
PACS GROUP, INC. AND SUBSIDIARIES
NOTES TO UNAUDITED CONDENSED COMBINED/CONSOLIDATED FINANCIAL STATEMENTS
(dollars in thousands, except for share and per share values)
Company did not receive any proceeds from any sale of shares by the selling stockholders. The Company’s common stock is traded on the New York Stock Exchange under the symbol “PACS”.
As of June 30, 2024, the amount of issued and outstanding common stock is 152,399,733. The Company has not issued any shares of preferred stock.
NOTE 14.COMPUTATION OF NET (LOSS) INCOME PER COMMON SHARE
Basic net (loss) income per share is calculated by dividing net (loss) income attributable to the common stockholders by the weighted-average shares of Common Stock outstanding for the period. The computation of diluted net (loss) income per share is similar to the computation of basic net (loss) income per share, except that the denominator is increased to include the number of additional shares of common stock that would have been outstanding if the dilutive potential shares of common stock had been issued.
A reconciliation of the numerator and denominator used in the calculation of basic net (loss) income per common share follows:
| Three Months Ended June 30, | Six Months Ended June 30, | ||||||||||||||||||||||
| 2024 | 2023 | 2024 | 2023 | ||||||||||||||||||||
| Numerator: | |||||||||||||||||||||||
| Net (loss) income | $ | (10,908) | $ | 21,220 | $ | 38,232 | $ | 58,818 | |||||||||||||||
| Less: net income attributable to noncontrolling interest | 2 | 2 | 4 | 3 | |||||||||||||||||||
| Net (loss) income attributable to PACS Group, Inc. | $ | (10,910) | $ | 21,218 | $ | 38,228 | $ | 58,815 | |||||||||||||||
| Denominator: | |||||||||||||||||||||||
| Weighted average common shares outstanding | 149,463,655 | 128,723,386 | 139,093,520 | 128,723,386 | |||||||||||||||||||
| Basic net (loss) income per common share | $ | (0.07) | $ | 0.16 | $ | 0.27 | $ | 0.46 | |||||||||||||||
A reconciliation of the numerator and denominator used in the calculation of diluted net (loss) income per common share follows:
| Three Months Ended June 30, | Six Months Ended June 30, | ||||||||||||||||||||||
| 2024 | 2023 | 2024 | 2023 | ||||||||||||||||||||
| Numerator: | |||||||||||||||||||||||
| Net (loss) income | $ | (10,908) | $ | 21,220 | $ | 38,232 | $ | 58,818 | |||||||||||||||
| Less: net income attributable to noncontrolling interest | 2 | 2 | 4 | 3 | |||||||||||||||||||
| Net (loss) income attributable to PACS Group, Inc. | $ | (10,910) | $ | 21,218 | $ | 38,228 | $ | 58,815 | |||||||||||||||
| Denominator: | |||||||||||||||||||||||
| Weighted average common shares outstanding | 149,463,655 | 128,723,386 | 139,093,520 | 128,723,386 | |||||||||||||||||||
Plus: effect of diluted shares(1) | — | — | 591,098 | — | |||||||||||||||||||
| Adjusted weighted average common shares outstanding | 149,463,655 | 128,723,386 | 139,684,618 | 128,723,386 | |||||||||||||||||||
| Diluted net (loss) income per common share | $ | (0.07) | $ | 0.16 | $ | 0.27 | $ | 0.46 | |||||||||||||||
__________________
(1)The diluted per share amounts do not reflect 1,182,196 common share equivalents from restricted stock units for the three months ended June 30, 2024 because of their anti-dilutive effect.
F-59
PACS GROUP, INC. AND SUBSIDIARIES
NOTES TO UNAUDITED CONDENSED COMBINED/CONSOLIDATED FINANCIAL STATEMENTS
(dollars in thousands, except for share and per share values)
NOTE 15.STOCK AWARDS
Stock-based compensation expense consists of stock-based payment awards made to employees and directors, comprised of restricted stock units, based on their estimated fair values. Stock-based compensation expense recognized in the Company’s condensed combined/consolidated statements of (loss) income and comprehensive (loss) income for the three and six months ended June 30, 2024 and 2023 was based on the vesting of awards granted to date.
2024 Incentive Award Plan (2024 Plan)
On March 31, 2024, the Company’s board of directors and stockholders approved the PACS Group, Inc. 2024 Incentive Award Plan (2024 Plan), which became effective on the date immediately preceding the date on which the Company’s IPO registration statement was declared effective by the Securities and Exchange Commission (SEC). The 2024 Plan allows the Company to make equity-based and cash-based incentive awards to its officers, employees, directors and consultants. The number of shares initially available for issuance under awards granted pursuant to the 2024 Plan (which number includes 15,390,579 shares of common stock issuable upon the vesting of restricted stock unit (RSU) awards granted in connection with the IPO) was equal to 10.25% of the number of shares of common stock outstanding immediately following the completion of the IPO (disregarding the shares issuable under the 2024 Plan).
2024 Employee Stock Purchase Plan (2024 ESPP)
On March 31, 2024, the Company’s board of directors and stockholders approved the 2024 Employee Stock Purchase Plan (2024 ESPP), which became effective on the date immediately preceding the date on which the Company’s registration statement was declared effective by the SEC. The number of shares initially available for issuance pursuant to the 2024 ESPP was equal to the number of shares equal to 1% of the number of shares of common stock outstanding as of immediately following the completion of the IPO (disregarding the shares issuable under the 2024 Plan). As of June 30, 2024 there have been no shares issued under this plan.
Restricted Stock Unit Awards
The Company granted RSU awards to key executives and directors of 15,409,470 and 0 shares during the six months ended June 30, 2024 and 2023, respectively. For certain awards granted to key executives, the stock price used to determine the award fair value was the initial public offering price of $21.00 per share. Subsequent grants to non-employee directors used the market price on the date of respective grant to determine the award fair value. Awards granted to key executives at the time of the IPO vested 25% upon issuance with the remaining shares scheduled to vest in equal increments on an annual basis over the next five years as the grantee meets the requisite service condition. Other awards granted vest over one year. The fair value per share of RSU awards granted during the six months ended June 30, 2024 ranged from $21.00 to $24.85. The fair value per share includes awards to non-employee directors.
A summary of the status of the Company’s non-vested RSU awards for the six months ended June 30, 2024 is presented below (there was no such activity prior to the approval of the 2024 Plan, including in 2023):
| Non-Vested Restricted Stock Unit Awards | Weighted Average Grant Date Fair Value | ||||||||||
| Non-vested at January 1, 2024 | — | $ | — | ||||||||
| Granted | 15,409,470 | 21.00 | |||||||||
| Vested | (3,847,652) | 21.00 | |||||||||
| Forfeited | — | — | |||||||||
| Non-vested at June 30, 2024 | 11,561,818 | $ | 21.01 | ||||||||
F-60
PACS GROUP, INC. AND SUBSIDIARIES
NOTES TO UNAUDITED CONDENSED COMBINED/CONSOLIDATED FINANCIAL STATEMENTS
(dollars in thousands, except for share and per share values)
During the six months ended June 30, 2024, the company granted 18,891 RSU awards to non-employee directors for their service on the Company’s board of directors from the 2024 Plan. The fair value per share of these awards were $24.85 based on the market price on the grant date.
Stock-based compensation expense
Stock-based compensation expense recognized for the Company’s equity incentive plans was as follows:
| Three Months Ended June 30, | Six Months Ended June 30, | ||||||||||||||||||||||
| 2024 | 2023 | 2024 | 2023 | ||||||||||||||||||||
| Stock-based compensation expense related to restricted stock unit awards | $ | 90,936 | $ | — | $ | 90,936 | $ | — | |||||||||||||||
| Total stock-based compensation expense | $ | 90,936 | $ | — | $ | 90,936 | $ | — | |||||||||||||||
In future periods, the Company expects to recognize approximately $232,736 in stock-based compensation expense for unvested RSU awards that were outstanding as of June 30, 2024. Future stock-based compensation expense will be recognized over 4.8 weighted average years for unvested RSU awards.
F-61
PACS GROUP, INC.
Shares

COMMON STOCK
| Citigroup | J.P. Morgan | Truist Securities | ||||||
| RBC Capital Markets | Goldman Sachs & Co. LLC | UBS Investment Bank | ||||||
| Stephens Inc. | Oppenheimer & Co. | |||||||
PART II
INFORMATION NOT REQUIRED IN PROSPECTUS
Item 13. Other expenses of issuance and distribution.
The following table indicates the expenses to be incurred in connection with the offering described in this registration statement, other than the underwriting discounts and commissions, all of which will be paid by us. All amounts are estimated except the Securities and Exchange Commission registration fee and the Financial Industry Regulatory Authority, Inc. (FINRA) filing fee.
| Amount | |||||
| Securities and Exchange Commission registration fee | $ | 92,485 | |||
| Accountants’ fees and expenses | 250,000 | ||||
| Legal fees and expenses | 450,000 | ||||
| Printing and engraving expenses | 120,000 | ||||
| Miscellaneous | 87,515 | ||||
| Total expenses | $ | 1,000,000 | |||
Item 14. Indemnification of directors and officers.
Section 102 of the General Corporation Law of the State of Delaware (DGCL) permits a corporation to eliminate the personal liability of directors or officers of a corporation to the corporation or its stockholders for monetary damages for a breach of fiduciary duty as a director or officer, except where the director or officer breached his or her duty of loyalty, failed to act in good faith, engaged in intentional misconduct or knowingly violated a law, obtained an improper personal benefit, and in the case of a director, authorized the payment of a dividend or approved a stock repurchase in violation of Delaware corporate law, and in the case of an officer, a breach of fiduciary duty in any action by or in the right of the corporation. Our Amended and Restated Charter provides that no director or officer of PACS Group, Inc. shall be personally liable to it or its stockholders for monetary damages for any breach of fiduciary duty as a director or officer, notwithstanding any provision of law imposing such liability, except to the extent that the DGCL prohibits the elimination or limitation of liability of directors or officers for breaches of fiduciary duty.
Section 145 of the DGCL provides that a corporation has the power to indemnify a director, officer, employee, or agent of the corporation, or a person serving at the request of the corporation for another corporation, partnership, joint venture, trust, or other enterprise in related capacities against expenses (including attorneys’ fees), judgments, fines, and amounts paid in settlement actually and reasonably incurred by the person in connection with an action, suit, or proceeding to which he or she was or is a party or is threatened to be made a party to any threatened, pending, or completed action, suit, or proceeding, whether civil, criminal, administrative, or investigative, by reason of such position, if such person acted in good faith and in a manner he or she reasonably believed to be in or not opposed to the best interests of the corporation, and, in any criminal action or proceeding, had no reasonable cause to believe his or her conduct was unlawful, except that, in the case of actions brought by or in the right of the corporation, no indemnification shall be made with respect to any claim, issue, or matter as to which such person shall have been adjudged to be liable to the corporation unless and only to the extent that the Court of Chancery or other adjudicating court determines that, despite the adjudication of liability but in view of all of the circumstances of the case, such person is fairly and reasonably entitled to indemnity for such expenses which the Court of Chancery or such other court shall deem proper.
Our Amended and Restated Charter and Amended and Restated Bylaws provide indemnification for our directors and officers to the fullest extent permitted by the DGCL, as it now exists or may in the future be amended. We will indemnify each person who was or is a party or threatened to be made a party to any threatened, pending, or completed action, suit or proceeding (other than an action by or in the right of us) by reason of the fact that he or she
II-2
is or was, or has agreed to become, a director, or officer, or is or was serving, or has agreed to serve, at our request as a director, officer, partner, employee, or trustee of, or in a similar capacity with, another corporation, partnership, joint venture, trust, or other enterprise (all such persons being referred to as an “Indemnitee”), or by reason of any action alleged to have been taken or omitted in such capacity, against all expenses (including attorneys’ fees), judgments, fines, and amounts paid in settlement actually and reasonably incurred in connection with such action, suit, or proceeding and any appeal therefrom, if such Indemnitee acted in good faith and in a manner he or she reasonably believed to be in, or not opposed to, our best interests, and, with respect to any criminal action or proceeding, he or she had no reasonable cause to believe his or her conduct was unlawful. Our Amended and Restated Charter and Amended and Restated Bylaws provide that we will indemnify any Indemnitee who was or is a party to an action or suit by or in the right of us to procure a judgment in our favor by reason of the fact that the Indemnitee is or was, or has agreed to become, a director or officer, or is or was serving, or has agreed to serve, at our request as a director, officer, partner, employee, or trustee of, or in a similar capacity with, another corporation, partnership, joint venture, trust, or other enterprise, or by reason of any action alleged to have been taken or omitted in such capacity, against all expenses (including attorneys’ fees) and, to the extent permitted by law, amounts paid in settlement actually and reasonably incurred in connection with such action, suit, or proceeding, and any appeal therefrom, if the Indemnitee acted in good faith and in a manner he or she reasonably believed to be in, or not opposed to, our best interests, except that no indemnification shall be made with respect to any claim, issue, or matter as to which such person shall have been adjudged to be liable to us, unless a court determines that, despite such adjudication but in view of all of the circumstances, he or she is entitled to indemnification of such expenses. Notwithstanding the foregoing, to the extent that any Indemnitee has been successful, on the merits or otherwise, he or she will be indemnified by us against all expenses (including attorneys’ fees) actually and reasonably incurred in connection therewith. Expenses must be advanced to an Indemnitee under certain circumstances.
In connection with our IPO, we entered into separate indemnification agreements with each of our directors and executive officers. Each indemnification agreement provides, among other things, for indemnification to the fullest extent permitted by law and our Amended and Restated Charter and Amended and Restated Bylaws against any and all expenses, judgments, fines, penalties, and amounts paid in settlement of any claim. The indemnification agreements provide for the advancement or payment of all expenses to the indemnitee and for the reimbursement to us if it is found that such indemnitee is not entitled to such indemnification under applicable law and our Amended and Restated Charter and Amended and Restated Bylaws.
We maintain a general liability insurance policy that covers certain liabilities of directors and officers of our corporation arising out of claims based on acts or omissions in their capacities as directors or officers.
In any underwriting agreement we enter into in connection with the sale of our common stock being registered hereby, the underwriters will agree to indemnify, under certain conditions, us, our directors, our officers, and persons who control us within the meaning of the Securities Act of 1933, as amended (Securities Act) against certain liabilities arising in connection with such offering.
Item 15. Recent sales of unregistered securities.
Set forth below is information regarding all unregistered securities sold by us since January 1, 2020. Also included is the consideration received by us for such shares and information relating to the section of the Securities Act, or rule of the Securities and Exchange Commission, under which exemption from registration was claimed.
Common Stock Issuances
(1)On March 24, 2023, and in connection with our incorporation in the State of Delaware, we issued and sold an aggregate of 128,723,386 shares of our common stock to Jason Murray and Mark Hancock for an aggregate purchase price of $20.00, or $0.001 per share.
Unless otherwise stated, the issuances of the above were deemed to be exempt from registration under the Securities Act in reliance upon Section 4(a)(2) of the Securities Act or Regulation D promulgated thereunder, or Rule 701 promulgated under the Securities Act, as transactions by an issuer not involving any public offering or
II-3
pursuant to benefit plans and contracts relating to compensation as provided under Rule 701. Individuals who purchased securities as described above represented their intentions to acquire the securities for investment purposes only and not with a view to, or for sale in connection with, any distribution thereof.
None of the foregoing transactions involved any underwriters, underwriting discounts or commissions or any public offering.
Item 16. Exhibits and financial statement schedules.
(a)Exhibits.
The following documents are filed as exhibits to this registration statement.
| Incorporated by Reference | ||||||||||||||||||||||||||||||||||||||
| Exhibit Number | Exhibit Description | Form | File No. | Exhibit | Filing Date | Filed Herewith | ||||||||||||||||||||||||||||||||
| 1.1 | X | |||||||||||||||||||||||||||||||||||||
| 3.1 | 8-K | 001-42011 | 3.1 | 4/15/2024 | ||||||||||||||||||||||||||||||||||
| 3.2 | 8-K | 001-42011 | 3.2 | 4/15/2024 | ||||||||||||||||||||||||||||||||||
| 4.1 | S‑1/A | 333-277893 | 4.1 | 4/8/2024 | ||||||||||||||||||||||||||||||||||
| 4.2 | 8-K | 001-42011 | 10.1 | 4/15/2024 | ||||||||||||||||||||||||||||||||||
| 4.3 | 8-K | 001-42011 | 10.2 | 4/15/2024 | ||||||||||||||||||||||||||||||||||
| 5.1 | X | |||||||||||||||||||||||||||||||||||||
| 10.1 | S-1 | 333-277893 | 10.2 | 3/13/2024 | ||||||||||||||||||||||||||||||||||
| 10.2# | S-1/A | 333-277893 | 10.3 | 4/1/2024 | ||||||||||||||||||||||||||||||||||
| 10.3# | S‑8 | 333-277893 | 99.1 | 4/11/2024 | ||||||||||||||||||||||||||||||||||
| 10.4# | S‑8 | 333-277893 | 99.2 | 4/11/2024 | ||||||||||||||||||||||||||||||||||
| 10.5# | S‑8 | 333-277893 | 99.3 | 4/11/2024 | ||||||||||||||||||||||||||||||||||
| 10.6# | S‑8 | 333-277893 | 99.4 | 4/11/2024 | ||||||||||||||||||||||||||||||||||
| 10.7# | S‑8 | 333-277893 | 99.5 | 4/11/2024 | ||||||||||||||||||||||||||||||||||
| 10.8# | 10-Q | 001-42011 | 10.10 | 5/13/2024 | ||||||||||||||||||||||||||||||||||
II-4
| 10.9# | S-1 | 333-277893 | 10.10 | 3/13/2024 | ||||||||||||||||||||||||||||||||||
| 10.10# | 10-Q | 001-42011 | 10.11 | 5/13/2024 | ||||||||||||||||||||||||||||||||||
| 10.11^ | S-1 | 333-277893 | 10.1 | 3/13/2024 | ||||||||||||||||||||||||||||||||||
| 21.1 | X | |||||||||||||||||||||||||||||||||||||
| 23.1 | X | |||||||||||||||||||||||||||||||||||||
| 23.2 | X | |||||||||||||||||||||||||||||||||||||
| 24.1 | X | |||||||||||||||||||||||||||||||||||||
| 101.INS | XBRL Instance Document. | X | ||||||||||||||||||||||||||||||||||||
| 101.SCH | XBRL Taxonomy Extension Schema Document. | X | ||||||||||||||||||||||||||||||||||||
| 101.CAL | XBRL Taxonomy Extension Calculation Linkbase Document. | X | ||||||||||||||||||||||||||||||||||||
| 101.DEF | XBRL Taxonomy Extension Definition Linkbase Document | X | ||||||||||||||||||||||||||||||||||||
| 101.LAB | XBRL Taxonomy Extension Label Linkbase Document | X | ||||||||||||||||||||||||||||||||||||
| 101.PRE | XBRL Taxonomy Extension Presentation Linkbase Document | X | ||||||||||||||||||||||||||||||||||||
| 107.1 | X | |||||||||||||||||||||||||||||||||||||
__________________
#Indicates management contract or compensatory plan.
^Registrant has omitted schedules and exhibits pursuant to Item 601(a)(5) of Regulation S-K. The Registrant agrees to furnish supplementally a copy of the omitted schedules and exhibits to the SEC upon request.
(b)Financial Statement Schedules. Schedules not listed above have been omitted because the information required to be set forth therein is not applicable or is shown in the financial statements or notes thereto.
II-5
Item 17. Undertakings.
The undersigned registrant hereby undertakes to provide to the underwriters, at the closing specified in the underwriting agreement, certificates in such denominations and registered in such names as required by the underwriter to permit prompt delivery to each purchaser.
Insofar as indemnification for liabilities arising under the Securities Act may be permitted to directors, officers and controlling persons of the registrant pursuant to the foregoing provisions, or otherwise, the registrant has been advised that in the opinion of the Securities and Exchange Commission such indemnification is against public policy as expressed in the Securities Act and is, therefore, unenforceable. In the event that a claim for indemnification against such liabilities (other than the payment by the registrant of expenses incurred or paid by a director, officer or controlling person of the registrant in the successful defense of any action, suit or proceeding) is asserted by such director, officer or controlling person in connection with the securities being registered, the registrant will, unless in the opinion of its counsel the matter has been settled by controlling precedent, submit to a court of appropriate jurisdiction the question whether such indemnification by it is against public policy as expressed in the Securities Act and will be governed by the final adjudication of such issue.
The undersigned hereby undertakes that:
(1)For purposes of determining any liability under the Securities Act, the information omitted from the form of prospectus filed as part of this registration statement in reliance upon Rule 430A and contained in a form of prospectus filed by the registrant pursuant to Rule 424(b)(1) or (4) or 497(h) under the Securities Act shall be deemed to be part of this registration statement as of the time it was declared effective.
(2)For the purpose of determining any liability under the Securities Act, each post-effective amendment that contains a form of prospectus shall be deemed to be a new registration statement relating to the securities offered therein, and the offering of such securities at that time shall be deemed to be the initial bona fide offering thereof.
II-6
SIGNATURES
Pursuant to the requirements of the Securities Act of 1933, as amended, the registrant has duly caused this Registration Statement on Form S-1 to be signed on its behalf by the undersigned, thereunto duly authorized, in the City of Farmington, State of Utah, on September 3, 2024.
| PACS GROUP, INC. | |||||
| By: | /s/ Jason Murray | ||||
| Jason Murray | |||||
| Chief Executive Officer | |||||
SIGNATURES AND POWER OF ATTORNEY
We, the undersigned officers and directors of PACS Group, Inc., hereby severally constitute and appoint Jason Murray, Derick Apt and John Mitchell, and each of them singly (with full power to each of them to act alone), our true and lawful attorneys-in-fact and agents, with full power of substitution and re-substitution in each of them for him or her and in his or her name, place and stead, and in any and all capacities, to sign any and all amendments (including post-effective amendments) to this registration statement (or any other registration statement for the same offering that is to be effective upon filing pursuant to Rule 462(b) under the Securities Act of 1933, as amended), and to file the same, with all exhibits thereto and other documents in connection therewith, with the Securities and Exchange Commission, granting unto said attorneys-in-fact and agents, and each of them, full power and authority to do and perform each and every act and thing requisite or necessary to be done in and about the premises, as full to all intents and purposes as he or she might or could do in person, hereby ratifying and confirming all that said attorneys-in-fact and agents or any of them, or their or his or her substitute or substitutes, may lawfully do or cause to be done by virtue hereof.
Pursuant to the requirements of the Securities Act of 1933, as amended, this registration statement on Form S-1 has been signed by the following persons in the capacities held on the dates indicated.
| Signature | Title | Date | ||||||||||||
| /s/ Jason Murray | Director, Co-Founder, Chairman and Chief Executive Officer (Principal Executive Officer) | September 3, 2024 | ||||||||||||
| Jason Murray | ||||||||||||||
| /s/ Derick Apt | Chief Financial Officer (Principal Financial Officer) | September 3, 2024 | ||||||||||||
| Derick Apt | ||||||||||||||
| /s/ Michelle Lewis | Chief Accounting Officer (Principal Accounting Officer) | September 3, 2024 | ||||||||||||
| Michelle Lewis | ||||||||||||||
| /s/ Mark Hancock | Director, Co-Founder and Executive Vice Chairman | September 3, 2024 | ||||||||||||
| Mark Hancock | ||||||||||||||
| /s/ Jacqueline Millard | Director | September 3, 2024 | ||||||||||||
| Jacqueline Millard | ||||||||||||||
| /s/ Taylor Leavitt | Director | September 3, 2024 | ||||||||||||
| Taylor Leavitt | ||||||||||||||
| /s/ Evelyn Dislaver | Director | September 3, 2024 | ||||||||||||
| Evelyn Dislaver | ||||||||||||||
II-7