UNITED STATES
SECURITIES AND EXCHANGE COMMISSION
Washington, D.C. 20549
FORM 10-K
(MARK ONE)
| | |
☒ | | ANNUAL REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 |
For the fiscal year ended December 31, 2024
OR
| | |
☐ | | TRANSITION REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 |
For the transition period from to
Commission File No. 1-10765
UNIVERSAL HEALTH SERVICES, INC.
(Exact name of registrant as specified in its charter)
| | |
Delaware |
| 23-2077891 |
(State or other jurisdiction of incorporation or organization) |
| (I.R.S. Employer Identification Number) |
| |
UNIVERSAL CORPORATE CENTER |
| |
367 South Gulph Road P.O. Box 61558 King of Prussia, Pennsylvania |
| 19406-0958 |
(Address of principal executive offices) |
| (Zip Code) |
Registrant’s telephone number, including area code: (610) 768-3300
Securities registered pursuant to Section 12(b) of the Act:
| | |
Title of each class | Trading Symbol(s) | Name of each exchange on which registered |
Class B Common Stock, $0.01 par value | UHS | New York Stock Exchange |
Securities registered pursuant to Section 12(g) of the Act:
Class D Common Stock, $.01 par value
(Title of each Class)
Indicate by check mark if the registrant is a well-known seasoned issuer, as defined in Rule 405 of the Securities Act. Yes ☒ No ☐
Indicate by check mark if the registrant is not required to file reports pursuant to Section 13 or Section 15(d) of the Exchange Act. Yes ☐ No ☒
Indicate by check mark whether the registrant (1) has filed all reports required to be filed by Section 13 or 15(d) of the Securities Exchange Act of 1934 during the preceding 12 months (or for such shorter period that the registrant was required to file such reports), and (2) has been subject to such filing requirements for the past 90 days. Yes ☒ No ☐
Indicate by check mark whether the registrant has submitted electronically every Interactive Data File required to be submitted pursuant to Rule 405 of Regulation S-T during the preceding 12 months (or for such shorter period that the registrant was required to submit such files). Yes ☒ No ☐
Indicate by check mark whether the registrant is a large accelerated filer, an accelerated filer, a non-accelerated filer, a smaller reporting company or an emerging growth company. See the definitions of “large accelerated filer,” “accelerated filer”, “smaller reporting company” and “emerging growth company” in Rule 12b-2 of the Exchange Act.
| | | | | | |
| | | | | | |
Large accelerated filer |
| ☒ |
| Accelerated filer |
| ☐ |
| | | |
Non-accelerated filer |
| ☐ |
| Smaller reporting company |
| ☐ |
| | | |
| | |
| Emerging growth company |
| ☐ |
If an emerging growth company, indicate by check mark if the registrant has elected not to use the extended transition period for complying with any new or revised financial accounting standards provided pursuant to Section 13(a) of the Exchange Act. ☐
Indicate by check mark whether the registrant has filed a report on and attestation to its management’s assessment of the effectiveness of its internal control over financial reporting under Section 404(b) of the Sarbanes-Oxley Act (15 U.S.C. 7262(b)) by the registered public accounting firm that prepared or issued its audit report. ☒
If securities are registered pursuant to Section 12(b) of the Act, indicate by check mark whether the financial statements of the registrant included in the filing reflect the correction of an error to previously issued financial statements. ☐
Indicate by check mark whether any of those error corrections are restatements that required a recovery analysis of incentive-based compensation received by any of the registrant’s executive officers during the relevant recovery period pursuant to §240.10D-1(b). ☐
Indicate by check mark whether the registrant is a shell company (as defined in Rule 12b-2 of the Exchange Act). Yes ☐ No ☒
The aggregate market value of voting stock held by non-affiliates at June 30, 2024 was $10.6 billion. (For the purpose of this calculation, it was assumed that Class A, Class C, and Class D Common Stock, which are not traded but are convertible share-for-share into Class B Common Stock, have the same market value as Class B Common Stock. Also, for purposes of this calculation only, all directors are deemed to be affiliates.)
The number of shares of the registrant’s Class A Common Stock, $.01 par value, Class B Common Stock, $.01 par value, Class C Common Stock, $.01 par value, and Class D Common Stock, $.01 par value, outstanding as of January 31, 2025, were 6,576,475; 57,751,199; 661,688 and 12,614, respectively.
DOCUMENTS INCORPORATED BY REFERENCE:
Portions of the registrant’s definitive proxy statement for our 2025 Annual Meeting of Stockholders, which will be filed with the Securities and Exchange Commission within 120 days after December 31, 2024 (incorporated by reference under Part III).
UNIVERSAL HEALTH SERVICES, INC.
2024 FORM 10-K ANNUAL REPORT
TABLE OF CONTENTS
This Annual Report on Form 10-K is for the year ended December 31, 2024. This Annual Report modifies and supersedes documents filed prior to this Annual Report. Information that we file with the Securities and Exchange Commission (the “SEC”) in the future will automatically update and supersede information contained in this Annual Report.
In this Annual Report, “we,” “us,” “our” “UHS” and the “Company” refer to Universal Health Services, Inc. and its subsidiaries. UHS is a registered trademark of UHS of Delaware, Inc., the management company for, and a wholly-owned subsidiary of Universal Health Services, Inc. Universal Health Services, Inc. is a holding company and operates through its subsidiaries including its management company, UHS of Delaware, Inc. All healthcare and management operations are conducted by subsidiaries of Universal Health Services, Inc. To the extent any reference to “UHS” or “UHS facilities” in this report including letters, narratives or other forms contained herein relates to our healthcare or management operations it is referring to Universal Health Services, Inc.’s subsidiaries including UHS of Delaware, Inc. Further, the terms “we,” “us,” “our” or the “Company” in such context similarly refer to the operations of Universal Health Services Inc.’s subsidiaries including UHS of Delaware, Inc. Any reference to employees or employment contained herein refers to employment with or employees of the subsidiaries of Universal Health Services, Inc. including UHS of Delaware, Inc.
PART I
ITEM 1. Business
Our principal business is owning and operating, through our subsidiaries, acute care hospitals and outpatient facilities and behavioral health care facilities.
As of February 26, 2025, we owned and/or operated 359 inpatient facilities and 60 outpatient and other facilities, including the following, located in 39 states, Washington, D.C., the United Kingdom and Puerto Rico:
Acute care facilities located in the U.S.:
•28 inpatient acute care hospitals;
•33 free-standing emergency departments, and;
•10 outpatient centers & 1 surgical hospital.
Behavioral health care facilities (331 inpatient facilities and 16 outpatient facilities):
Located in the U.S.:
•181 inpatient behavioral health care facilities, and;
•14 outpatient behavioral health care facilities.
Located in the U.K.:
•147 inpatient behavioral health care facilities, and;
•2 outpatient behavioral health care facilities.
Located in Puerto Rico:
•3 inpatient behavioral health care facilities.
Net revenues from our acute care hospitals, outpatient facilities and commercial health insurer accounted for 56% of our consolidated net revenues during 2024 and 57% during 2023. Net revenues from our behavioral health care facilities and commercial health insurer accounted for 44% of our consolidated net revenues during 2024 and 43% during 2023.
Our behavioral health care facilities located in the U.K. generated net revenues of approximately $880 million in 2024 and $761 million in 2023. Total assets at our U.K. behavioral health care facilities were approximately $1.358 billion as of December 31, 2024 and $1.327 billion as of December 31, 2023.
Services provided by our hospitals include general and specialty surgery, internal medicine, obstetrics, emergency room care, radiology, oncology, diagnostic care, coronary care, pediatric services, pharmacy services and/or behavioral health services. We provide capital resources as well as a variety of management services to our facilities, including central purchasing, information services, finance and control systems, facilities planning, physician recruitment services, administrative personnel management, marketing and public relations.
Available Information
We are a Delaware corporation that was organized in 1979. Our principal executive offices are located at Universal Corporate Center, 367 South Gulph Road, P.O. Box 61558, King of Prussia, PA 19406. Our telephone number is (610) 768-3300.
Our website is located at www.uhs.com. Copies of our annual, quarterly and current reports that we file with the SEC, and any amendments to those reports, are available free of charge on our website. Our filings are also available to the public at the website maintained by the SEC, www.sec.gov. The information posted on our website is not incorporated into this Annual Report. Our Board of Directors’ committee charters (Audit Committee, Compensation Committee, Nominating & Governance Committee and Quality and Compliance Committee), Code of Business Conduct and Corporate Standards applicable to all employees, Code of Ethics for Senior Financial Officers, Corporate Governance Guidelines and our Code of Conduct, Corporate Compliance Manual and Compliance Policies and Procedures are available free of charge on our website. Copies of such reports and charters are available in print to any stockholder who makes a request. Such requests should be made to our Secretary at our King of Prussia, PA corporate headquarters. We intend to satisfy the disclosure requirement under Item 5.05 of Form 8-K relating to amendments to or waivers of any provision of our Code of Ethics for Senior Financial Officers by promptly posting this information on our website.
In accordance with Section 303A.12(a) of the New York Stock Exchange Listed Company Manual, we submitted our CEO’s certification to the New York Stock Exchange in 2024. Additionally, contained in Exhibits 31.1 and 31.2 of this Annual Report on Form 10-K, are our CEO’s and CFO’s certifications regarding the quality of our public disclosures under Section 302 of the Sarbanes-Oxley Act of 2002.
Our Mission
Our company mission is:
To provide superior quality healthcare services that
PATIENTS recommend to families and friends,
PHYSICIANS prefer for their patients,
PURCHASERS select for their clients,
EMPLOYEES are proud of, and
INVESTORS seek for long-term returns.
To achieve this, we have a commitment to:
•continuous improvement in measurable ways
•ethical and fair treatment of all
•innovation in service delivery
Business Strategy
We believe community-based hospitals will remain the focal point of the healthcare delivery network and we are committed to a philosophy of self-determination for both the company and our hospitals.
Acquisition of Additional Hospitals. We selectively seek opportunities to expand our base of operations by acquiring, constructing or leasing additional hospital facilities. We are committed to a program of rational growth around our core businesses, while retaining the missions of the hospitals we manage and the communities we serve. Such expansion may provide us with access to new markets and new healthcare delivery capabilities. We also continue to examine our facilities and consider divestiture of those facilities that we believe do not have the potential to contribute to our growth or operating strategy. In recent years our behavioral health services segment has been focused on efforts to partner with non-UHS acute care hospitals to help operate their behavioral health services. These arrangements include hospital purchases, leased beds and joint venture operating agreements.
Improvement of Operations of Existing Hospitals and Services. We also seek to increase the operating revenues and profitability of owned hospitals by the introduction of new services, improvement of existing services, physician recruitment and the application of financial and operational controls.
We are involved in continual development activities for the benefit of our existing facilities. From time-to-time applications are filed with state health planning agencies to add new services in existing hospitals in states which require certificates of need, or CONs. Although we expect that some of these applications will result in the addition of new facilities or services to our operations, no assurances can be made for ultimate success by us in these efforts.
Quality and Efficiency of Services. Pressures to contain healthcare costs and technological developments allowing more procedures to be performed on an outpatient basis have led payers to demand a shift to ambulatory or outpatient care wherever possible. We are responding to this trend by emphasizing the expansion of outpatient services. In addition, in response to cost containment pressures, we continue to implement programs at our facilities designed to improve financial performance and efficiency while continuing to provide quality care, including more efficient use of professional and paraprofessional staff, monitoring and adjusting staffing levels and equipment usage, improving patient management and reporting procedures and implementing more efficient billing and collection procedures. In addition, we will continue to emphasize innovation in our response to the rapid changes in regulatory trends and market conditions while fulfilling our commitment to patients, physicians, employees, communities and our stockholders.
In addition, our aggressive recruiting of highly qualified physicians and developing provider networks help to establish our facilities as an important source of quality healthcare in their respective communities.
Hospital Utilization
We believe that the most important factors relating to the overall utilization of a hospital include the quality and market position of the hospital and the number, quality and specialties of physicians providing patient care within the facility. Generally, we believe that the ability of a hospital to meet the health care needs of its community is determined by its breadth of services, level of technology, emphasis on quality of care and convenience for patients and physicians. Other factors that affect utilization include
general and local economic conditions, market penetration of managed care programs, the degree of outpatient use, the availability of reimbursement programs such as Medicare and Medicaid, and demographic changes such as the growth in local populations. Utilization across the industry also is being affected by improvements in clinical practice, medical technology and pharmacology. Current industry trends in utilization and occupancy have been significantly affected by changes in reimbursement policies of third party payers. We are also unable to predict the extent to which these industry trends will continue or accelerate. In addition, our acute care services business is typically subject to certain seasonal fluctuations, such as higher patient volumes and net patient service revenues in the first and fourth quarters of the year.
Sources of Revenue
We receive payments for services rendered from private insurers, including managed care plans, the federal government under the Medicare program, state governments under their respective Medicaid programs and directly from patients. See Item 7. Management’s Discussion and Analysis of Financial Condition and Results of Operations—Sources of Revenue for additional disclosure. Other information related to our revenues, income and other operating information for each reporting segment of our business is provided in Note 12 to our Consolidated Financial Statements, Segment Reporting.
Regulation and Other Factors
Overview: The healthcare industry is subject to numerous laws, regulations and rules including, among others, those related to government healthcare participation requirements, various licensure and accreditations, reimbursement for patient services, health information privacy and security rules, and Medicare and Medicaid fraud and abuse provisions (including, but not limited to, federal statutes and regulations prohibiting kickbacks and other illegal inducements to potential referral sources, false claims submitted to federal or state health care programs and self-referrals by physicians). Providers that are found to have violated any of these laws and regulations may be excluded from participating in government healthcare programs, subjected to significant fines or penalties and/or required to repay amounts received from the government for previously billed patient services. Although we believe our policies, procedures and practices comply with governmental regulations, no assurance can be given that we will not be subjected to additional governmental inquiries or actions, or that we would not be faced with sanctions, fines or penalties if so subjected. Even if we were to ultimately prevail, a significant governmental inquiry or action under one of the above laws, regulations or rules could have a material adverse impact on us.
Licensing, Certification and Accreditation: All of our U.S. hospitals are subject to compliance with various federal, state and local statutes and regulations in the U.S. and receive periodic inspection by state licensing agencies to review standards of medical care, equipment and cleanliness. Our hospitals must also comply with the conditions of participation and licensing requirements of federal, state and local health agencies, as well as the requirements of municipal building codes, health codes and local fire departments. Various other licenses and permits are also required in order to dispense narcotics, operate pharmacies, handle radioactive materials and operate certain equipment. Our facilities in the United Kingdom are also subject to various laws and regulations.
All of our eligible hospitals have been accredited by The Joint Commission. All of our acute care hospitals and most of our behavioral health centers in the U.S. are certified as providers of Medicare and Medicaid services by the appropriate governmental authorities.
If any of our facilities were to lose its Joint Commission accreditation or otherwise lose its certification under the Medicare and Medicaid programs, the facility may be unable to receive reimbursement from the Medicare and Medicaid programs and other payers. We believe our facilities are in substantial compliance with current applicable federal, state, local and independent review body regulations and standards. The requirements for licensure, certification and accreditation are subject to change and, in order to remain qualified, it may become necessary for us to make changes in our facilities, equipment, personnel and services in the future, which could have a material adverse impact on operations.
Certificates of Need: Certain of the states in which we operate hospitals have certificates of need (“CON”) laws as a condition prior to hospital capital expenditures, construction, expansion, modernization or initiation of major new services. Failure to obtain necessary state approval can result in our inability to complete an acquisition, expansion or replacement, the imposition of civil or, in some cases, criminal sanctions, the inability to receive Medicare or Medicaid reimbursement or the revocation of a facility’s license, which could harm our business. In addition, significant CON reforms have been proposed in a number of states that would increase the capital spending thresholds and provide exemptions of various services from review requirements. In the past, we have not experienced any material adverse effects from those requirements, but we cannot predict the impact of these changes upon our operations.
Conversion Legislation: Many states have enacted or are considering enacting laws affecting the conversion or sale of not-for-profit hospitals to for-profit entities. These laws generally require prior approval from the attorney general, advance notification and community involvement. In addition, attorneys general in states without specific conversion legislation may exercise discretionary authority over these transactions. Although the level of government involvement varies from state to state, the trend is to provide for increased governmental review and, in some cases, approval of a transaction in which a not-for-profit entity sells a health care facility
to a for-profit entity. The adoption of new or expanded conversion legislation and the increased review of not-for-profit hospital conversions may limit our ability to grow through acquisitions of not-for-profit hospitals.
Utilization Review: Federal regulations require that admissions and utilization of facilities by Medicare and Medicaid patients must be reviewed in order to ensure efficient utilization of facilities and services. The law and regulations require Quality Improvement Organizations (“QIOs”) to review the appropriateness of Medicare and Medicaid patient admissions and discharges, the quality of care provided, the validity of diagnosis related group (“DRG”) classifications and the appropriateness of cases of extraordinary length of stay. QIOs may deny payment for services provided, assess fines and also have the authority to recommend to the Department of Health and Human Services (“HHS”) that a provider that is in substantial non-compliance with the standards of the QIO be excluded from participating in the Medicare program. We have contracted with QIOs in each state where we do business to perform the required reviews.
Audits: Most hospitals are subject to federal audits to validate the accuracy of Medicare and Medicaid program submitted claims. If these audits identify overpayments, we could be required to pay a substantial rebate of prior years’ payments subject to various administrative appeal rights. The federal government contracts with third-party “recovery audit contractors” (“RACs”) and “Medicaid integrity contractors” (“MICs”), on a contingent fee basis, to audit the propriety of payments to Medicare and Medicaid providers. Similarly, Medicare zone program integrity contractors (“ZPICs”) target claims for potential fraud and abuse. Additionally, Medicare administrative contractors (“MACs”) must ensure they pay the right amount for covered and correctly coded services rendered to eligible beneficiaries by legitimate providers. The Centers for Medicare and Medicaid Services (“CMS”) consolidated many of these Medicare and Medicaid program integrity functions into new unified program integrity contractors (“UPICs”), though it remains unclear what effect, if any, this consolidation may have. We have undergone claims audits related to our receipt of federal healthcare payments during the last three years, the results of which have not required material adjustments to our consolidated results of operations. However, potential liability from future federal or state audits could ultimately exceed established reserves, and any excess could potentially be substantial. Further, Medicare and Medicaid regulations also provide for withholding Medicare and Medicaid overpayments in certain circumstances, which could adversely affect our cash flow.
Self-Referral and Anti-Kickback Legislation
The Stark Law: The Social Security Act includes a provision commonly known as the “Stark Law.” This law prohibits physicians from referring Medicare and Medicaid patients to entities with which they or any of their immediate family members have a financial relationship, unless an exception is met. These types of referrals are known as “self-referrals.” Medicare may deny payment for all services related to a prohibited referral and a hospital that has billed for prohibited services may be obligated to refund the amounts collected. In addition, sanctions for violation of the Stark Law may include civil penalties or exclusion from the Medicare and Medicaid programs. There are a number of exceptions to the self-referral prohibition, including an exception for a physician’s ownership interest in an entire hospital as opposed to an ownership interest in a hospital department unit, service or subpart. However, federal laws and regulations now limit the ability of hospitals relying on this exception to expand aggregate physician ownership interest or to expand certain hospital facilities. This regulation also places a number of compliance requirements on physician-owned hospitals related to reporting of ownership interest. There are also exceptions for many of the customary financial arrangements between physicians and providers, including employment contracts, leases and recruitment agreements that adhere to certain enumerated requirements. CMS issued a final rule in 2020 that created a new Stark exception for value-based models. Although the final regulations provide exceptions to the Stark Law, there may remain regulatory risks for participating hospitals, as well as financial and operational risks.
We monitor all aspects of our business and have developed a comprehensive ethics and compliance program that is designed to meet or exceed applicable federal guidelines and industry standards. Nonetheless, because the law in this area is complex and constantly evolving, there can be no assurance that federal regulatory authorities will not determine that any of our arrangements with physicians violate the Stark Law.
Anti-kickback Statute: A provision of the Social Security Act known as the “anti-kickback statute” prohibits healthcare providers and others from directly or indirectly soliciting, receiving, offering or paying money or other remuneration to other individuals and entities in return for using, referring, ordering, recommending or arranging for such referrals or orders of services or other items covered by a federal or state health care program. However, changes to the anti-kickback statute have reduced the intent required for violation; one is no longer required to have actual knowledge or specific intent to commit a violation of the anti-kickback statute in order to be found in violation of such law.
The anti-kickback statute contains certain exceptions, and the Office of the Inspector General of the Department of Health and Human Services (“OIG”) has issued regulations that provide for “safe harbors,” from the federal anti-kickback statute for various activities. These activities, which must meet certain requirements, include (but are not limited to) the following: investment interests, space rental, equipment rental, practitioner recruitment, personnel services and management contracts, sale of practice, referral services, warranties, discounts, employees, group purchasing organizations, waiver of beneficiary coinsurance and deductible amounts, managed care arrangements, obstetrical malpractice insurance subsidies, investments in group practices, freestanding surgery centers, donation of technology for electronic health records and referral agreements for specialty services. In 2020, the OIG
issued a final rule that established an anti-kickback statute safe harbor for value based models. Although the final regulations provide safe harbors, there may remain regulatory risks for participating hospitals, as well as financial and operational risks. The fact that conduct or a business arrangement does not fall within a safe harbor or exception does not automatically render the conduct or business arrangement illegal under the anti-kickback statute. However, such conduct and business arrangements may lead to increased scrutiny by government enforcement authorities.
Although we believe that our arrangements with physicians and other referral sources have been structured to comply with current law and available interpretations, there can be no assurance that all arrangements comply with an available safe harbor or that regulatory authorities enforcing these laws will determine these financial arrangements do not violate the anti-kickback statute or other applicable laws. Violations of the anti-kickback statute may be punished by a criminal fine of up to $100,000 for each violation or imprisonment, however, under 18 U.S.C. Section 3571, this fine may be increased to $250,000 for individuals and $500,000 for organizations. Civil money penalties may include fines and damages of up to three times the total amount of the remuneration and/or exclusion from participation in Medicare and Medicaid.
Similar State Laws: Many of the states in which we operate have adopted laws that prohibit payments to physicians in exchange for referrals similar to the anti-kickback statute and the Stark Law, some of which apply regardless of the source of payment for care. These statutes typically provide criminal and civil penalties as well as loss of licensure. In many instances, the state statutes provide that any arrangement falling in a federal safe harbor will be immune from scrutiny under the state statutes. However, in most cases, little precedent exists for the interpretation or enforcement of these state laws.
These laws and regulations are extremely complex and, in many cases, we don’t have the benefit of regulatory or judicial interpretation. It is possible that different interpretations or enforcement of these laws and regulations could subject our current or past practices to allegations of impropriety or illegality or could require us to make changes in our facilities, equipment, personnel, services, capital expenditure programs and operating expenses. A determination that we have violated one or more of these laws, or the public announcement that we are being investigated for possible violations of one or more of these laws (see Item 3. Legal Proceedings), could have a material adverse effect on our business, financial condition or results of operations and our business reputation could suffer significantly. In addition, we cannot predict whether other legislation or regulations at the federal or state level will be adopted, what form such legislation or regulations may take or what their impact on us may be.
If we are deemed to have failed to comply with the anti-kickback statute, the Stark Law or other applicable laws and regulations, we could be subjected to liabilities, including criminal penalties, civil penalties (including the loss of our licenses to operate one or more facilities), and exclusion of one or more facilities from participation in the Medicare, Medicaid and other federal and state health care programs. The imposition of such penalties could have a material adverse effect on our business, financial condition or results of operations.
Federal False Claims Act and Similar State Regulations: A current trend affecting the health care industry is the increased use of the federal False Claims Act, and, in particular, actions being brought by individuals on the government’s behalf under the False Claims Act’s qui tam, or whistleblower, provisions. Whistleblower provisions allow private individuals to bring actions on behalf of the government by alleging that the defendant has defrauded the Federal government.
When a defendant is determined by a court of law to have violated the False Claims Act, the defendant may be liable for up to three times the actual damages sustained by the government, plus mandatory civil penalties for each separate false claim. There are many potential bases for liability under the False Claims Act. Liability often arises when an entity knowingly submits a false claim for reimbursement to the federal government. The Fraud Enforcement and Recovery Act of 2009 (“FERA”) amended and expanded the number of actions for which liability may attach under the False Claims Act, eliminating requirements that false claims be presented to federal officials or directly involve federal funds. FERA also clarifies that a false claim violation occurs upon the knowing retention, as well as the receipt, of overpayments. In addition, recent changes to the anti-kickback statute have made violations of that law punishable under the civil False Claims Act. Further, a number of states have adopted their own false claims provisions as well as their own whistleblower provisions whereby a private party may file a civil lawsuit on behalf of the state in state court. The False Claims Act require that federal healthcare program overpayments be returned within 60 days from the date the overpayment was identified, or by the date any corresponding cost report was due, whichever is later. Failure to return an overpayment within this period may result in additional civil False Claims Act liability.
Other Fraud and Abuse Provisions: The Social Security Act also imposes criminal and civil penalties for submitting false claims to Medicare and Medicaid. False claims include, but are not limited to, billing for services not rendered, billing for services without prescribed documentation, misrepresenting actual services rendered in order to obtain higher reimbursement and cost report fraud. Like the anti-kickback statute, these provisions are very broad.
Further, the Health Insurance Portability and Accountability Act of 1996 (“HIPAA”) broadened the scope of the fraud and abuse laws by adding several criminal provisions for health care fraud offenses that apply to all health benefit programs, whether or not payments under such programs are paid pursuant to federal programs. HIPAA also introduced enforcement mechanisms to prevent fraud and abuse in Medicare. There are civil penalties for prohibited conduct, including, but not limited to billing for medically unnecessary products or services.
HIPAA Administrative Simplification and Privacy Requirements: The administrative simplification provisions of HIPAA, as amended by the Health Information Technology for Economic and Clinical Health Act (“HITECH”), require the use of uniform electronic data transmission standards for health care claims and payment transactions submitted or received electronically. These provisions are intended to encourage electronic commerce in the health care industry. HIPAA also established federal rules protecting the privacy and security of personal health information, including recently proposed updates to HIPAA security rule requirements. The privacy and security regulations address the use and disclosure of individual health care information and the rights of patients to understand and control how such information is used and disclosed. Violations of HIPAA can result in both criminal and civil fines and penalties.
We believe that we are in material compliance with the privacy regulations of HIPAA, as we continue to develop training and revise procedures to address ongoing compliance. The HIPAA security regulations require health care providers to implement administrative, physical and technical safeguards to protect the confidentiality, integrity and availability of patient information. HITECH has since strengthened certain HIPAA rules regarding the use and disclosure of protected health information, extended certain HIPAA provisions to business associates, and created new security breach notification requirements. HITECH has also extended the ability to impose civil money penalties on providers not knowing that a HIPAA violation has occurred. We believe that we have been in substantial compliance with HIPAA and HITECH requirements to date. HIPAA regulations may result in greater compliance requirements for healthcare providers, including obligations to report breaches of unsecured patient data, as well as potential liabilities resulting from the actions of parties acting as business associates on our behalf.
Red Flags Rule: In addition, the Federal Trade Commission (“FTC”) Red Flags Rule requires financial institutions and businesses maintaining accounts to address the risk of identity theft. The Red Flag Program Clarification Act of 2010, signed on December 18, 2010, appears to exclude certain healthcare providers from the Red Flags Rule, but permits the FTC or relevant agencies to designate additional creditors subject to the Red Flags Rule through future rulemaking if the agencies determine that the person in question maintains accounts subject to foreseeable risk of identity theft. Compliance with any such future rulemaking may require additional expenditures in the future.
Patient Safety and Quality Improvement Act of 2005: On July 29, 2005, the Patient Safety and Quality Improvement Act of 2005 was enacted, which has the goal of reducing medical errors and increasing patient safety. This legislation establishes a confidential reporting structure in which providers can voluntarily report “Patient Safety Work Product” (“PSWP”) to “Patient Safety Organizations” (“PSOs”). Under the system, PSWP is made privileged, confidential and legally protected from disclosure. PSWP does not include medical, discharge or billing records or any other original patient or provider records but does include information gathered specifically in connection with the reporting of medical errors and improving patient safety. This legislation does not preempt state or federal mandatory disclosure laws concerning information that does not constitute PSWP. PSOs are certified by the Secretary of the HHS for three-year periods and analyze PSWP, provide feedback to providers and may report non-identifiable PSWP to a database. In addition, PSOs are expected to generate patient safety improvement strategies.
Environmental Regulations: Our healthcare operations generate medical waste that must be disposed of in compliance with federal, state and local environmental laws, rules and regulations. Infectious waste generators, including hospitals, face substantial penalties for improper disposal of medical waste, including civil penalties of up to $25,000 per day of noncompliance, criminal penalties of up to $50,000 per day, imprisonment, and remedial costs. In addition, our operations, as well as our purchases and sales of facilities are subject to various other environmental laws, rules and regulations. We believe that our disposal of such wastes is in material compliance with all state and federal laws.
Corporate Practice of Medicine: Several states, including Florida, Nevada, California and Texas, have laws and/or regulations that prohibit corporations and other entities from employing physicians and practicing medicine for a profit or that prohibit certain direct and indirect payments or fee-splitting arrangements between health care providers that are designed to induce or encourage the referral of patients to, or the recommendation of, particular providers for medical products and services. Possible sanctions for violation of these restrictions include loss of license and civil and criminal penalties. In addition, agreements between the corporation and the physician may be considered void and unenforceable. These statutes and/or regulations vary from state to state, are often vague and have seldom been interpreted by the courts or regulatory agencies. We do not expect these state corporate practice of medicine proscriptions to significantly affect our operations. Many states have laws and regulations which prohibit payments for referral of patients and fee-splitting with physicians. We do not make any such payments or have any such arrangements.
EMTALA: All of our hospitals are subject to the Emergency Medical Treatment and Active Labor Act (“EMTALA”). This federal law generally requires hospitals with an emergency department that are certified providers under Medicare to conduct a medical screening examination of every person who visits the hospital’s emergency room for treatment and, if the patient is suffering from a medical emergency, to either stabilize the patient’s condition or transfer the patient to a facility that can better handle the condition. Our obligation to screen and stabilize emergency medical conditions exists regardless of a patient’s ability to pay for treatment. There are severe penalties under EMTALA if a hospital fails to screen or appropriately stabilize or transfer a patient or if the hospital delays appropriate treatment in order to first inquire about the patient’s ability to pay. Penalties for violations of EMTALA include civil monetary penalties and exclusion from participation in the Medicare program. In addition to any liabilities that a hospital may incur under EMTALA, an injured patient, the patient’s family or a medical facility that suffers a financial loss as a
direct result of another hospital’s violation of the law can bring a civil suit against the hospital unrelated to the rights granted under that statute.
The federal government broadly interprets EMTALA to cover situations in which patients do not actually present to a hospital’s emergency room, but present for emergency examination or treatment to the hospital’s campus, generally, or to a hospital-based clinic that treats emergency medical conditions or are transported in a hospital-owned ambulance, subject to certain exceptions. EMTALA does not generally apply to patients admitted for inpatient services; however, CMS has sought industry comments on the potential applicability of EMTALA to hospital inpatients and the responsibilities of hospitals with specialized capabilities, respectively. CMS has not yet issued regulations or guidance in response to that request for comments. The government also has expressed its intent to investigate and enforce EMTALA violations actively in the future. We believe that we operate in substantial compliance with EMTALA.
Health Care Industry Investigations: We are subject to claims and suits in the ordinary course of business, including those arising from care and treatment afforded by our hospitals and are party to various government investigations and litigation. Please see Item 3. Legal Proceedings included herein for additional disclosure. In addition, currently, and from time to time, some of our facilities are subjected to inquiries and/or actions and receive notices of potential non-compliance of laws and regulations from various federal and state agencies. Providers that are found to have violated these laws and regulations may be excluded from participating in government healthcare programs, subjected to potential licensure, certification, and/or accreditation revocation, subjected to fines or penalties or required to repay amounts received from the government for previously billed patient services.
We monitor all aspects of our business and have developed a comprehensive ethics and compliance program that is designed to meet or exceed applicable federal guidelines and industry standards. Because the law in this area is complex and constantly evolving, governmental investigation or litigation may result in interpretations that are inconsistent with industry practices, including ours. Although we believe our policies, procedures and practices comply with governmental regulations, no assurance can be given that we will not be subjected to inquiries or actions, or that we will not be faced with sanctions, fines or penalties in connection with the investigations. Even if we were to ultimately prevail, the government’s inquiry and/or action in connection with these matters could have a material adverse effect on our future operating results.
Our substantial Medicare, Medicaid and other governmental billings may result in heightened scrutiny of our operations. It is possible that governmental entities could initiate additional investigations or litigation in the future and that such matters could result in significant penalties as well as adverse publicity. It is also possible that our executives and/or managers could be included as targets or witnesses in governmental investigations or litigation and/or named as defendants in private litigation.
Revenue Rulings 98-15 and 2004-51: In March 1998 and May 2004, the IRS issued guidance regarding the tax consequences of joint ventures between for-profit and not-for-profit hospitals. As a result of the tax rulings, the IRS has proposed, and may in the future propose, to revoke the tax-exempt or public charity status of certain not-for-profit entities which participate in such joint ventures or to treat joint venture income as unrelated business taxable income to them. The tax rulings have limited development of joint ventures and any adverse determination by the IRS or the courts regarding the tax-exempt or public charity status of a not-for-profit partner or the characterization of joint venture income as unrelated business taxable income could further limit joint venture development with not-for-profit hospitals, and/or require the restructuring of certain existing joint ventures with not-for-profits.
State Rate Review: Some states where we operate hospitals have adopted legislation mandating rate or budget review for hospitals or have adopted taxes on hospital revenues, assessments or licensure fees to fund indigent health care within the state. In the aggregate, state rate reviews and indigent tax provisions have not materially, adversely affected our results of operations.
Medical Malpractice Tort Law Reform: Medical malpractice tort law has historically been maintained at the state level. All states have laws governing medical liability lawsuits. Over half of the states have limits on damages awards. Almost all states have eliminated joint and several liability in malpractice lawsuits, and many states have established limits on attorney fees. Many states had bills introduced in their legislative sessions to address medical malpractice tort reform. Proposed solutions include enacting limits on non-economic damages, malpractice insurance reform, and gathering lawsuit claims data from malpractice insurance companies and the courts for the purpose of assessing the connection between malpractice settlements and premium rates. Reform legislation has also been proposed, but not adopted, at the federal level that could preempt additional state legislation in this area.
Compliance Program: Our company-wide compliance program has been in place since 1998. Currently, the program’s elements include a Code of Conduct, risk area specific policies and procedures, employee education and training, an internal system for reporting concerns, auditing and monitoring programs, and a means for enforcing the program’s policies.
Since its initial adoption, the compliance program continues to be expanded and developed to meet the industry’s expectations and our needs. Specific written policies, procedures, training and educational materials and programs, as well as auditing and monitoring activities have been prepared and implemented to address the functional and operational aspects of our business. Specific areas identified through regulatory interpretation and enforcement activities have also been addressed in our program. Claims preparation and submission, including coding, billing, and cost reports, comprise the bulk of these areas. Financial arrangements with physicians and other referral sources, including compliance with anti-kickback and Stark laws and emergency department treatment and transfer requirements are also the focus of policy and training, standardized documentation requirements, and review and audit.
United Kingdom Regulation: Our operations in the United Kingdom are also subject to a high level of regulation relating to registration and licensing requirements, employee regulation, clinical standards, environmental rules as well as other areas. We are also subject to a highly regulated business environment, and failure to comply with the various laws and regulations applicable to us could lead to substantial penalties and other adverse effects on our business.
Human Capital Management
Employees and Medical Staff
As of December 31, 2024, we had approximately 99,000 total employees consisting of: (i) approximately 86,000 employees located in the U.S., of which approximately 63,000 were employed full-time, and; (ii) approximately 13,000 employees located in the U.K. Our hospitals are staffed by licensed physicians who have been admitted to the medical staff of individual hospitals. In a number of our markets, physicians may have admitting privileges at other hospitals in addition to ours. Within our acute care division, approximately 370 physicians are employed by physician practice management subsidiaries of ours either directly or through contracts with affiliated group practices structured as 501A corporations. Members of the medical staffs of our hospitals also serve on the medical staffs of hospitals not owned by us and may terminate their affiliation with our hospitals at any time. In addition, within our behavioral health division, approximately 510 physicians are employed by subsidiaries of ours either directly or through contracts with affiliated group practices structured as 501A corporations. Each of our hospitals is managed on a day-to-day basis by a chief executive officer employed by a subsidiary of ours. In addition, a Board of Governors, including members of the hospital’s medical staff, governs the medical, professional and ethical practices at each hospital. We believe that our relations with our employees are satisfactory.
Labor Relations
Approximately 970 of our employees at three of our hospitals are unionized. At Valley Hospital Medical Center, housekeeping and dietary employees are represented by the Culinary Workers Union, Local 226, and engineers are represented by the International Union of Operating Engineers. At Brooke Glen Behavioral Hospital, unionized employees are represented by the Teamsters, and registered nurses are represented by the Northwestern Nurses Association/Pennsylvania Association of Staff Nurses and Allied Professionals. At the George Washington University Hospital, registered nurses are represented by the District of Columbia Nurses Association.
Culture and Work Environment
During orientation, newly hired employees learn our mission, vision, principles and values, key policies and procedures, a summary of the various benefits and resources available, and perhaps most notably, an overview of our founding principle, Service Excellence. Learning key attributes of our Service Excellence standards, which include continuous improvement, employee development, ethical and fair treatment of all, teamwork, quality, compassion and innovation in service delivery, provides newly hired employees a thorough understanding of our company culture. Other components of our Service Excellence standards, which include treating everyone as a guest, demonstrating professionalism and excellence and practicing teamwork, are shared to help guide the desired approach to day-to-day activities.
Service Excellence Facilitator Certification Workshops are available for facility employees identified by their leadership for consistently upholding and demonstrating our Service Excellence standards. Certified facilitators foster the Service Excellence culture and deliver training at their facilities. In 2024, we held 12 workshops with 137 individuals certified as Service Excellence Facilitators.
During 2024, we strengthened our recruitment efforts, improved the overall hiring and onboarding experience (89% very satisfied/satisfied with overall recruitment process), expanded the training resources employees need to do their jobs effectively and safely, facilitated more teamwork and collaboration, addressed burnout, expanded mentorship and increased employee engagement.
We conducted an Employee Engagement Survey and had an overall participation rate of 72% across the organization. 83% of staff indicated “I feel included on my team/work unit.” Engagement efforts such as services awards, safety programs and employee-led service excellence/culture committees has assisted with increased employee retention.
Ethical Standards
Each member of our Board of Directors and senior management is committed to healthcare operations that are ethical and in compliance with all applicable laws and regulations.
We are committed to fostering a culture of accountability at all levels and encourage our employees to report anything they believe could be noncompliant with our values. We prohibit retaliation for the good faith reporting of compliance concerns and offer the ability for individuals to anonymously elevate any concerns. Our commitment to fairness and integrity extends to everyone with whom we interact and do business.
Health and Safety
Policies and training programs to encourage work safety are a major focus in our organization. We continue to promote the employee assistance program which has provided a superior level of service to all our employees and members of their households.
We have continuous training on workplace safety and launched a “We Care” program guide to ensure our hospitals support employees in a detailed way in the event of an employee injury.
Employee Development
In keeping with our culture of continuous improvement, training opportunities are available for all employees, regardless of level or status. These include formal instructor-led, in-person or virtual training, informal mentoring or networking opportunities, or self-administered online courses.
Training programs are designed to assist with personal and skill development, career advancement and succession planning. In addition to mandatory training that focus on keeping employees mindful and informed of key policies and skill sets, many are voluntary. All training is tailored to include potential Americans with Disabilities Act accommodations.
Across the company, we offer educational and work opportunities, including internships, externships and clinical field placement opportunities. We have partnered with Chamberlin University and Drexel University to provide their students with opportunities to earn clinical experience at our healthcare facilities. In 2024, Chamberlin University students participated in more than 1,000 clinical rotations at various acute care and behavioral health care facilities of ours nationwide.
We also offer financial assistance programs, such as educational reimbursement, to support employees participating in degree, certification and continuing education programs.
Equal Employment Opportunity
We are committed to the principle of Equal Employment Opportunity ("EEO") for all employees and applicants. As an EEO Employer we support, and are fully committed, to recruitment, selection, placement, promotion and compensation of all individuals without regard to race, color, religion, age (40 and over or as otherwise defined by applicable law), sex (including pregnancy, gender identity, and sexual orientation), genetic information (including family medical history), national origin, disability status, protected veteran status or any other characteristic protected by federal, state or local laws.
We value each member of our team and are committed to treating everyone with dignity and respect. Our commitment to diversity, equity, and inclusion includes regularly monitoring employment practices to ensure inclusivity regardless of an employee’s gender, race or ethnicity and championing for inclusive behaviors through leadership example, policies and procedures, training and special events.
Employee Assistance
We continue to support the overall health and financial well-being of our employees across the extensive programs and benefit plans that we offer. Employees can access the UHS Resource Guide which provides details on access to the benefits, resources and support tools available to employees throughout our organization.
In 2024, the UHS Foundation continued to support employees and their families who suffered losses due to natural disasters across the country, including tornados in Arkansas and Tennessee, Hurricane Beryl (in Texas) and Hurricanes Debby, Milton and Helene (in Florida).
Environmental
We have implemented environmentally sustainable practices and we comply with applicable legal and regulatory environmental standards to protect our patients, visitors, staff and local communities. Our environmental stewardship includes following best practices when managing energy usage, constructing and designing new builds and/or major renovations and protecting the local environment.
•Smart building technology and automation are used across our enterprise to monitor and inform energy management decisions. Centralized Utility Billing Management System effectively monitors energy usage across our U.S. facilities, signaling significant deviations from normal usage consumption patterns. Automatic fault detection and diagnostics software is implemented in approximately 75% of our acute care hospitals to monitor the efficiencies of the heating, ventilation and air conditioning operations. Most of these facilities also utilize retro-commissioning and monitoring-based commissioning.
•All of our newly built facilities, or those undergoing major renovation, are required to meet, or exceed, all federal, state and local energy efficient codes, use mechanical-electrical-plumbing systems to optimize energy efficiencies and water conservation and be equipped with 100% emergency back-up generators, with 96 hours of fuel.
New construction or major renovation projects costing at least $20 million are required to be assessed for Green Globes® and/or U.S. Green Building Council’s Leadership in Energy and Environmental Design certifications. All newly constructed acute care facilities are also expected to achieve an ENERGY STAR® Portfolio Manager Score of 90 or higher.
•Our facilities have policies and procedures that are compliant with the applicable laws from the Environmental Protection Agency, local departments of health and other regulators who oversee the responsible disposal of pollution and waste.
Our Water Management Program (“WMP”), which is co-managed jointly by a third-party company specializing in water safety, oversees programs for potable and process water (e.g., surgical instrument processing) as well as utility water (e.g., cooling tower, boilers) through active management and hazard control validation. The WPM is designed to ensure safe water throughout our buildings and meets ANSI/ASHRAE Standard 188 (Legionellosis: Risk Management for Building Water Systems). The WPM recently incorporated current ANSI/AAMI ST108: 2023 Water standards for the processing of medical devices and standardized ”flushing protocols” for facilities to use during terminal cleaning process.
•Our facilities located in the U.K. advanced several environmentally friendly initiatives in 2024 and continued to procure 100% of their electricity from renewable sources. To date, the emission reduction targets for these facilities include:
oNet zero carbon for direct (Scope 1) and indirect (Scope 2) emissions by 2035.
oNet zero carbon emissions in supply chain (Scope 3) by 2040.
•By January 2024, a vehicle tracking and driver training device program, Lightfoot, was installed on all company-owned vehicles utilized in the U.K. Collectively, the program has reduced CO2 emissions by 236 metric tons across the vehicle fleet since it was introduced in 2020.
Our leadership teams actively manage opportunities and risks related to our facilities, including those related to climate change and other environmental risks.
Revenue and volume trends may be affected by seasonal and severe weather conditions, including the effects of extreme low temperatures, hurricanes and tornadoes, earthquakes, climate change, current local economic and demographic changes. We have a high concentration of facilities in various geographic areas, including states that have a potentially higher risk of experiencing events such as severe weather conditions and earthquakes. Given the location of our facilities, we are particularly susceptible to revenue loss, cost increase, or damage caused by severe weather conditions or natural disasters such as hurricanes, wildfires, earthquakes, or tornadoes. Any significant loss due to a natural disaster may not be covered by insurance and may lead to an increase in the cost of insurance or unavailability on acceptable terms. Climate change may also have effects on our business by increasing the cost of property insurance or making coverage unavailable on acceptable terms. To the extent that significant changes in the climate occur in areas where our facilities are located, we may experience increased frequency of severe weather conditions or natural disasters or other changes to weather patterns, all of which may result in physical damage to or a decrease in demand for properties affected by these conditions. Should the impact of climate change be material in nature or occur for lengthy periods of time, our financial condition, revenues, results of operations, or cash flow may be adversely affected.
In addition, operations may be subject to increases in energy prices as well as increased government regulation, such as the limiting of greenhouse gas emissions, intended to mitigate the impact of climate change, severe weather patterns, or natural disasters. These could result in additional required capital and/or operational expenditures to comply with such regulation without a corresponding increase in our revenues.
Competition
The health care industry is highly competitive. In recent years, competition among healthcare providers for patients has intensified in the United States due to, among other things, regulatory and technological changes, increasing use of managed care payment systems, cost containment pressures and a shift toward outpatient treatment. In all of the geographical areas in which we operate, there are other facilities that provide services comparable to those offered by our facilities. In addition, some of our competitors include hospitals that are owned by tax-supported governmental agencies or by nonprofit corporations and may be supported by endowments and charitable contributions and exempt from property, sale and income taxes. Such exemptions and support are not available to us.
In some markets, certain of our competitors may have greater financial resources, be better equipped and offer a broader range of services than us. Certain hospitals that are located in the areas served by our facilities are specialty or large hospitals that provide medical, surgical and behavioral health services, facilities and equipment that are not available at our hospitals. The increase in outpatient treatment and diagnostic facilities, including outpatient surgical centers and addiction treatment centers offering medically assisted treatments, also increases competition for us. In addition, some of our hospitals face competition from hospitals or surgery centers that are physician owned.
The number and quality of the physicians on a hospital’s staff are important factors in determining a hospital’s success and competitive advantage. Typically, physicians are responsible for making hospital admissions decisions and for directing the course of patient treatment. We believe that physicians refer patients to a hospital primarily on the basis of the patient’s needs and insurance coverage, the quality of other physicians on the medical staff, the location of the hospital and the breadth and scope of services offered at the hospital’s facilities. We strive to retain and attract qualified doctors by maintaining high ethical and professional standards and providing adequate support personnel, technologically advanced equipment and facilities that meet the needs of those physicians.
In addition, we depend on the efforts, abilities, and experience of our medical support personnel, including our nurses and other health care professionals, as well as non-professionals such as mental health technicians. We compete with other health care providers in recruiting and retaining qualified hospital management, nurses and other medical personnel.
Certain states in which we operate hospitals have CON laws. The application process for approval of additional covered services, new facilities, changes in operations and capital expenditures is, therefore, highly competitive in these states. In those states that do not have CON laws or which set relatively high levels of expenditures before they become reviewable by state authorities, competition in the form of new services, facilities and capital spending is more prevalent. See “Regulation and Other Factors.”
Our ability to negotiate favorable service contracts with purchasers of group health care services also affects our competitive position and significantly affects the revenues and operating results of our hospitals. Managed care plans, including managed Medicare and Medicaid plans, attempt to direct and control the use of hospital services and to demand that we accept lower rates of payment. In addition, employers and traditional health insurers are increasingly interested in containing costs through negotiations with hospitals for managed care programs and discounts from established charges. In return, hospitals secure commitments for a larger number of potential patients. Generally, hospitals compete for service contracts with group health care service purchasers on the basis of price, market reputation, geographic location, quality and range of services, quality of the medical staff and convenience. The importance of obtaining contracts with managed care organizations varies from market to market depending on the market strength of such organizations.
An element of our growth strategy is expansion through the acquisition of additional hospitals in select markets. The competition to acquire hospitals is significant. We compete for acquisitions with other for-profit health care companies, private equity and venture capital firms, as well as not-for-profit entities. Some of our competitors have greater resources than we do. We intend to selectively seek opportunities to expand our base of operations by adhering to our disciplined program of rational growth, but may not be successful in accomplishing acquisitions on favorable terms.
Relationship with Universal Health Realty Income Trust
At December 31, 2024, we held approximately 5.7% of the outstanding shares of Universal Health Realty Income Trust (the “Trust”). We serve as Advisor to the Trust under an annually renewable advisory agreement, which is scheduled to expire on December 31st of each year, pursuant to the terms of which we conduct the Trust’s day-to-day affairs, provide administrative services and present investment opportunities. The advisory agreement was renewed by the Trust for 2025 at the same rate in place for 2024, 2023 and 2022, providing for an advisory computation at 0.70% of the Trust’s average invested real estate assets. We earned an advisory fee from the Trust, which is included in net revenues in the accompanying consolidated statements of income, of approximately $5.5 million during 2024, approximately $5.3 million during 2023 and $5.1 million during 2022.
In addition, certain of our officers and directors are also officers and/or directors of the Trust. Management believes that it has the ability to exercise significant influence over the Trust, therefore we account for our investment in the Trust using the equity method of accounting.
Our pre-tax share of income from the Trust was $1.1 million during 2024, $874,000 during 2023 and $1.2 million during 2022, which are included in other income (expense), net, on the accompanying consolidated statements of income for each year. We received dividends from the Trust amounting to $2.3 million during each of 2024 and 2023 and $2.2 million during 2022. The carrying value of our investment in the Trust was $5.8 million and $7.0 million at December 31, 2024 and 2023, respectively, and is included in other assets in the accompanying consolidated balance sheets. The market value of our investment in the Trust was $29.3 million at December 31, 2024 and $34.1 million at December 31, 2023, based on the closing price of the Trust’s stock on the respective dates.
The Trust commenced operations in 1986 by purchasing certain hospital properties from us and immediately leasing the properties back to our respective subsidiaries. The base rents are paid monthly and the bonus rents, which effective as of January 1, 2022 are applicable only to McAllen Medical Center, are computed and paid on a quarterly basis, based upon a computation that compares current quarter revenue to a corresponding quarter in the base year. The leases with those subsidiaries are unconditionally guaranteed by us and are cross-defaulted with one another.
On December 31, 2021, we entered into an asset purchase and sale agreement with the Trust, which was amended during the first quarter of 2022, pursuant to the terms of which: (i) a wholly-owned subsidiary of ours purchased from the Trust the real estate assets of the Inland Valley Campus of Southwest Healthcare System located in Wildomar, California, at its fair market value; (ii) two wholly-owned subsidiaries of ours transferred to the Trust, at their respective fair-market values, the real estate assets of Aiken Regional Medical Center (“Aiken”), located in Aiken, South Carolina (which includes a 211-bed acute care hospital and a 62-bed behavioral health facility), and Canyon Creek Behavioral Health (“Canyon Creek”), located in Temple, Texas, and; (iii) we received approximately $4.1 million in cash from the Trust.
As a result of the purchase options within the lease agreements for Aiken and Canyon Creek, the asset purchase and sale transaction is accounted for as a failed sale leaseback in accordance with U.S. GAAP. We have accounted for the asset exchange and substitution transaction with the Trust as a financing arrangement and, since we did not derecognize the real property related to Aiken
and Canyon Creek, we will continue to depreciate the assets. Our consolidated balance sheets as of December 31, 2024 and December 31, 2023 reflects a financial liability of $73.8 million and $77.5 million, respectively, which is included in debt, for the fair value of real estate assets that we exchanged as part of the transaction. Our monthly lease payments payable to the Trust will be recorded to interest expense and as a reduction to the outstanding financial liability. The amount allocated to interest expense is determined using our incremental borrowing rate and is based on the outstanding financial liability.
The aggregate rent payable to the Trust in connection with the leases on McAllen Medical Center, Wellington Regional Medical Center, Aiken Regional Medical Center and Canyon Creek Behavioral Health was approximately $21.2 million during 2024 and $20.6 million during 2023.
Pursuant to the Master Leases by certain subsidiaries of ours and the Trust as described in the table below, dated 1986 and 2021 (“the Master Leases”) which govern the leases of McAllen Medical Center and Wellington Regional Medical Center (each of which is governed by the Master Lease dated 1986), and Aiken Regional Medical Center and Canyon Creek Behavioral Health (each of which is governed by the Master Lease dated 2021), we have the option to renew the leases at the lease terms described above and below by providing notice to the Trust at least 90 days prior to the termination of the then current term. We also have the right to purchase the respective leased hospitals at their appraised fair market value upon any of the following: (i) at the end of the lease terms or any renewal terms; (ii) upon one month’s notice should a change of control of the Trust occur, or; (iii) within the time period as specified in the lease in the event that we provide notice to the Trust of our intent to offer a substitution property/properties in exchange for one (or more) of the hospital properties leased from the Trust should we be unable to reach an agreement with the Trust on the properties to be substituted. In addition, we have rights of first refusal to: (i) purchase the respective leased facilities during and for a specified period after the lease terms at the same price, terms and conditions of any third-party offer, or; (ii) renew the lease on the respective leased facility at the end of, and for a specified period after, the lease term at the same terms and conditions pursuant to any third-party offer.
In addition, we are the managing, majority member in a joint venture with an unrelated third-party that operates Clive Behavioral Health, a 100-bed behavioral health care facility located in Clive, Iowa. The real property of this facility, which was completed and opened in late 2020, is also leased from the Trust (annual rental of approximately $2.8 million, $2.7 million and $2.6 million during 2024, 2023 and 2022, respectively) pursuant to the lease terms as provided in the table below. In connection with the lease on this facility, the joint venture has the right to purchase the leased facility from the Trust at its appraised fair market value upon either of the following: (i) by providing notice at least 270 days prior to the end of the lease terms or any renewal terms, or; (ii) upon 30 days' notice anytime within 12 months of a change of control of the Trust (UHS also has this right should the joint venture decline to exercise its purchase right). Additionally, the joint venture has rights of first offer to purchase the facility prior to any third-party sale.
The table below provides certain details for each of the hospitals leased from the Trust as of January 1, 2025:
| | | | | | | | | | | | |
Hospital Name | | | Annual
Minimum
Rent | | | End of Lease Term | | Renewal
Term
(years) | | |
McAllen Medical Center | | | $ | 5,485,000 | | | December, 2026 | | | 5 | | (a) |
Wellington Regional Medical Center | | | $ | 6,805,000 | | | December, 2026 | | | 5 | | (b) |
Aiken Regional Medical Center/Aurora Pavilion Behavioral Health Services | | | $ | 4,164,000 | | | December, 2033 | | | 35 | | (c) |
Canyon Creek Behavioral Health | | | $ | 1,882,000 | | | December, 2033 | | | 35 | | (c) |
Clive Behavioral Health | | | $ | 2,851,000 | | | December, 2040 | | | 50 | | (d) |
(a)We have one 5-year renewal option at existing lease rates (through 2031).
(b)We have one 5-year renewal option at fair market value lease rates (through 2031). On each January 1st through 2026, the annual rent will increase by 2.50% on a cumulative and compounded basis.
(c)We have seven 5-year renewal options at fair market value lease rates (2034 through 2068). On each January 1st through 2033, the annual rent will increase by 2.25% on a cumulative and compounded basis.
(d)This facility is operated by a joint venture in which we are the managing, majority member and an unrelated third-party holds a minority ownership interest. The joint venture has three, 10-year renewal options at computed lease rates as stipulated in the lease (2041 through 2070) and two additional, 10-year renewal options at fair market values lease rates (2071 through 2090). In each January through 2040 (and potentially through 2070 if three, 10-year renewal options are exercised), the annual rental will increase by 2.75% on a cumulative and compounded basis.
In addition, certain of our subsidiaries are tenants in several medical office buildings (“MOBs”) and two free-standing emergency departments ("FED") owned by the Trust or by limited liability companies in which the Trust holds 95% to 100% of the ownership interest. In connection with these two FEDs, in October, 2024, our subsidiaries exercised their 5-year renewal options on the facilities which are located in Weslaco and Mission, Texas. Each renewal option covers the period of February 1, 2025 through January 31, 2030 (the current lease terms were scheduled to expire on January 31, 2025; with aggregate annual lease rates of
approximately $979,000). Pursuant to terms of the leases, and consistent with the terms of the leases currently in effect for each property, the lease rates are scheduled to increase 2% per year through the end of the renewed lease terms. Our subsidiaries have five, 5-year renewal options remaining on each of these FEDs, with the first three renewal options (covering the years 2030 through 2044) providing for 2% annual increases to the lease rates, and the remaining two, 5-year renewal options (covering the years 2045 through 2054) providing for lease rates at the then fair market value. These leases are cross-defaulted with one another and our subsidiaries have the option to purchase the leased properties upon the expiration of each five-year extended term at the fair market value at that time.
During the third quarter of 2023, the Trust acquired the McAllen Doctor's Center, a 79,500 rentable square feet medical office building located in McAllen, Texas. A master lease was executed between a wholly-owned subsidiary of ours and the Trust, pursuant to the terms of which our subsidiary will master lease 100% of the rentable square feet of the MOB at an initial minimum rent of $624,000 annually. The master lease commenced during August, 2023 and is scheduled to expire in twelve years from that date.
During the first quarter of 2023, the Trust substantially completed construction on a new 86,000 rentable square foot multi-tenant MOB that is located on the campus of Northern Nevada Sierra Medical Center in Reno, Nevada. Northern Nevada Sierra Medical Center, a 170-bed newly constructed acute care hospital owned and operated by a wholly-owned subsidiary of ours, was completed and opened in April, 2022. In connection with this MOB, a ten-year master flex lease was executed between a wholly-owned subsidiary of ours and the Trust (scheduled to expire in March, 2033), pursuant to the terms of which our subsidiary initially agreed to master lease up to approximately 68% of the rentable square feet of the MOB. The master flex lease has been reduced since inception as certain conditions have been met. A ground lease for this facility commenced during 2023 and is scheduled to expire in 2098.
Executive Officers of the Registrant
The executive officers, whose terms will expire at such time as their successors are elected, are as follows:
| | |
Name and Age | | Present Position with the Company |
Marc D. Miller (54) | | Chief Executive Officer, President and Director |
Alan B. Miller (87) | | Executive Chairman of the Board |
Steve G. Filton (67) | | Executive Vice President, Chief Financial Officer and Secretary |
Matthew J. Peterson (55) | | Executive Vice President, President of Behavioral Health Division |
Edward H. Sim (53) | | Executive Vice President, President of Acute Care Division |
Mr. Marc D. Miller was appointed Chief Executive Officer and President effective January 1, 2021. He has served as President since May, 2009 and prior thereto served as Senior Vice President and co-head of our Acute Care Hospitals since 2007. He was elected a Director in May, 2006 and Vice President in 2005. He has served in various capacities related to our acute care division since 2000. He was elected to the Board of Trustees of Universal Health Realty Income Trust in December, 2008. In August, 2015, he was appointed to the Board of Directors of Premier, Inc., a publicly traded healthcare performance improvement alliance. See Note 9 to the Consolidated Financial Statements-Relationship with Universal Health Realty Income Trust and Other Related Party Transactions for additional disclosure regarding the Company’s group purchasing organization agreement with Premier, Inc. Marc D. Miller is the son of Alan B. Miller, our Executive Chairman of the Board.
Mr. Alan B. Miller was appointed Executive Chairman of the Board effective January 1, 2021. He had been Chairman of the Board and Chief Executive Officer since the Company’s inception and also served as President from inception until May, 2009. Prior thereto, he was President, Chairman of the Board and Chief Executive Officer of American Medicorp, Inc. He currently serves as Chairman of the Board, Chief Executive Officer and President of Universal Health Realty Income Trust. He is the father of Marc D. Miller, our Chief Executive Officer, President and Director.
Mr. Filton was elected Executive Vice President in 2017 and continues to serve as Chief Financial Officer since his appointment in 2003. He has also served as Secretary since 1999. He had served as Senior Vice President since 2003, as Vice President and Controller since 1991, and as Director of Corporate Accounting since 1985.
Mr. Peterson’s employment with us commenced in September, 2019 as Executive Vice President and President of our Behavioral Health Division. He was formerly employed at UnitedHealth Group for 11 years serving in various capacities including Chief Operating Officer for OptumGovernment, a health services and technology company, as well as various other Senior Vice President/Vice President roles. In addition to his civilian business career, Mr. Peterson served in the Air National Guard ("ANG"), U.S. Airforce, and was promoted to Brigadier General prior to his retirement from the ANG in August, 2024.
Mr. Sim's employment with us commenced in December, 2022 as Executive Vice President and President of our Acute Care Division. He was formerly employed as Chief Operating Officer at Centura Health, since 2017. Prior to joining Centura Health, Mr. Sim served in senior leadership roles of increasing responsibility for 11 years at Baptist Health.
ITEM 1A. Risk Factors
We are subject to numerous known and unknown risks, many of which are described below and elsewhere in this Annual Report. Any of the events described below could have a material adverse effect on our business, financial condition and results of operations. Additional risks and uncertainties that we are not aware of, or that we currently deem to be immaterial, could also impact our business and results of operations.
Risks Related to Business Operations
A significant portion of our revenue is produced by facilities located in Texas, Nevada and California.
Texas: We own 7 inpatient acute care hospitals, 13 free-standing emergency departments, 1 acute outpatient center and 20 inpatient behavioral healthcare facilities as listed in Item 2. Properties. On a combined basis, these facilities contributed 16% and 17% of our consolidated net revenues during 2024 and 2023, respectively. On a combined basis, after deducting an allocation for corporate overhead expense, these facilities generated 21% in 2024 and 26% in 2023, of our income from operations after net income attributable to noncontrolling interest.
Nevada: We own 10 inpatient acute care hospitals, 11 free-standing emergency departments, 3 acute outpatient centers and 4 inpatient behavioral healthcare facilities as listed in Item 2. Properties. On a combined basis, these facilities contributed 18% and 16% of our consolidated net revenues during 2024 and 2023, respectively. On a combined basis, after deducting an allocation for corporate overhead expense, these facilities generated 27% in 2024 and 16% in 2023, of our income from operations after net income attributable to noncontrolling interest.
California: We own 5 inpatient acute care hospitals, 2 acute outpatient centers, 9 inpatient behavioral healthcare facilities and 3 behavioral healthcare outpatient facilities as listed in Item 2. Properties. On a combined basis, these facilities contributed 11% of our consolidated net revenues during both 2024 and 2023, respectively. On a combined basis, after deducting an allocation for corporate overhead expense, these facilities generated 12% in both 2024 and 2023, of our income from operations after net income attributable to noncontrolling interest.
This geographic concentration makes us particularly sensitive to regulatory, economic, public health, environmental and competitive conditions in those states. Any material change in the current payment programs or regulatory, economic, public health, environmental or competitive conditions in those states could have a disproportionate effect on our overall business results. In addition, certain of our facilities and our operations in those states may be adversely impacted by wildfires (most particularly in California), winter storms, and other severe weather conditions, which adverse weather conditions may be more frequent and/or severe as the result of climate change. Such wildfires, storms or other severe weather conditions may cause considerable disruptions in our operations due to property damage or electrical outages experienced in affected areas by our personnel, payers, vendors and others, and may cause our commercial property insurance premiums and/or self-insured retentions to increase significantly.
Our revenues and results of operations are significantly affected by payments received from the government and other third party payers.
We derive a significant portion of our revenue from third-party payers, including the Medicare and Medicaid programs. Changes in these government programs in recent years have resulted in limitations on reimbursement and, in some cases, reduced levels of reimbursement for healthcare services. Payments from federal and state government programs are subject to statutory and regulatory changes, administrative rulings, interpretations and determinations, requirements for utilization review, and federal and state funding restrictions, all of which could materially increase or decrease program payments, as well as affect the cost of providing service to patients and the timing of payments to facilities. Changes resulting from the outcome of the 2024 elections may include increased reliance on Medicare Advantage programs, work requirements for Medicaid waiver program eligibility, increased focus on hospital outpatient site neutral payment policies, and similar initiatives that may reduce the availability of funding for federal healthcare programs or make eligibility for benefits more difficult. There have been proposals to substantially decrease federal funding for state Medicaid Programs. Any significant reduction in federal Medicaid funding to states would likely result in states reducing Medicaid payments to us which would have a material adverse effect on us. We are unable to predict the effect of recent and future policy changes on our operations. In addition, the uncertainty and fiscal pressures placed upon federal and state governments as a result of, among other things, deterioration in general economic conditions and the funding requirements from the federal healthcare reform legislation, may affect the availability of taxpayer funds for Medicare and Medicaid programs. In addition, the vast majority of the net revenues generated at our behavioral health facilities located in the United Kingdom are derived from governmental payers. If the rates paid or the scope of services covered by governmental payers in the United States or United Kingdom are reduced, there could be a material adverse effect on our business, financial position and results of operations.
As discussed in Item 7. Management’s Discussion and Analysis of Financial Condition and Results of Operations-Summary of Various State Medicaid Supplemental Payment Programs, we receive revenues from various state and county-based programs, including Medicaid in all states in which we operate. We receive annual Medicaid revenues of approximately $100 million, or greater, from each of Texas, Nevada, California, Illinois, Pennsylvania, Washington, D.C., Kentucky, Florida, Virginia, Massachusetts and Mississippi. We also receive Medicaid disproportionate share hospital payments from certain states including, most significantly,
Texas. Most of these programs are approved on a year-to-year basis and there is no assurance that these revenues will continue at their current rates or at all. We are therefore particularly sensitive to potential reductions in Medicaid and other state-based revenue programs as well as regulatory, economic, environmental and competitive changes in those states.
In addition to changes in government reimbursement programs, our ability to negotiate favorable contracts with private payers, including managed care organizations, significantly affects the revenues and operating results of our hospitals. Private payers, including managed care organizations, increasingly are demanding that we accept lower rates of payment.
We expect continued third-party efforts to aggressively manage reimbursement levels and cost controls. Reductions in reimbursement amounts received from third-party payers could have a material adverse effect on our financial position and our results of operations.
If we are not able to provide high quality medical care at a reasonable price, patients may choose to receive their health care from our competitors.
In recent years, the number of quality measures that hospitals are required to report publicly has increased. Centers for Medicare and Medicaid Services (“CMS”) publishes performance data related to quality measures and data on patient satisfaction surveys that hospitals submit in connection with the Medicare program. Federal law provides for the future expansion of the number of quality measures that must be reported. Additionally, the Patient Protection and Affordable Care Act (the “Legislation”) requires all hospitals to annually establish, update and make public a list of their standard charges for products and services. Also, the No Surprises Act, adopted as part of the Consolidated Appropriations Act, 2021 (“CAA”), creates additional price transparency requirements beginning January 1, 2022, including requiring providers to send health plans of insured patients and uninsured patients a good faith estimate of the expected charges and diagnostic codes prior to the scheduled date of the service or item. If any of our hospitals achieve poor results on the quality measures or patient satisfaction surveys (or results that are lower than our competitors) or if our standard charges are higher than our competitors, our patient volume could decline because patients may elect to use competing hospitals or other health care providers that have better metrics and pricing. This circumstance could harm our business and results of operations.
An increase in uninsured and underinsured patients in our acute care facilities or the deterioration in the collectability of the accounts of such patients could harm our results of operations.
Collection of receivables from third-party payers and patients is our primary source of cash and is critical to our operating performance. Our primary collection risks relate to uninsured patients and the portion of the bill that is the patient’s responsibility, which primarily includes co-payments and deductibles. However, we also have substantial receivables due to us from certain state-based funding programs. We estimate our provisions for doubtful accounts based on general factors such as payer mix, the agings of the receivables, historical collection experience and assessment of probability of future collections. We routinely review accounts receivable balances in conjunction with these factors and other economic conditions that might ultimately affect the collectability of the patient accounts and make adjustments to our allowances as warranted. Significant changes in business office operations, payer mix, economic conditions or trends in federal and state governmental health coverage could affect our collection of accounts receivable, cash flow and results of operations. If we experience unexpected increases in the growth of uninsured and underinsured patients or in bad debt expenses, our results of operations will be harmed.
Our hospitals face competition for patients from other hospitals and health care providers.
The healthcare industry is highly competitive, and competition among hospitals, and other healthcare providers for patients and physicians has intensified in recent years. In all of the geographical areas in which we operate, there are other facilities that provide services comparable to those offered by our facilities. Some of our competitors include hospitals that are owned by tax-supported governmental agencies or by nonprofit corporations and may be supported by endowments and charitable contributions and exempt from property, sales and income taxes. Such exemptions and support are not available to us.
In some markets, certain of our competitors may have greater financial resources, be better equipped and offer a broader range of services than we offer. The number of inpatient facilities, as well as outpatient surgical and diagnostic centers, many of which are fully or partially owned by physicians, in the geographic areas in which we operate has increased significantly. As a result, most of our hospitals operate in an increasingly competitive environment.
We also operate health care facilities in the United Kingdom where the National Health Service (the “NHS”) is the principal provider of healthcare services. In addition to the NHS, we face competition in the United Kingdom from independent sector providers and other publicly funded entities for patients.
If our competitors are better able to attract patients, recruit physicians and other healthcare professionals, expand services or obtain favorable managed care contracts at their facilities, we may experience a decline in patient volume and our business may be harmed.
Our performance depends on our ability to recruit and retain quality physicians.
Typically, physicians are responsible for making hospital admissions decisions and for directing the course of patient treatment. As a result, the success and competitive advantage of our hospitals depends, in part, on the number and quality of the physicians on
the medical staffs of our hospitals, the admitting practices of those physicians and our maintenance of good relations with those physicians. Physicians generally are not employees of our hospitals, and, in a number of our markets, physicians have admitting privileges at other hospitals in addition to our hospitals. They may terminate their affiliation with us at any time. If we are unable to maintain high ethical and professional standards, adequate support personnel and technologically advanced equipment and facilities that meet the needs of those physicians, they may be discouraged from referring patients to our facilities and our results of operations may decline.
It may become difficult for us to attract and retain an adequate number of physicians to practice in certain communities in which our hospitals are located. Our failure to recruit physicians to these communities or the loss of physicians in these communities could make it more difficult to attract patients to our hospitals and thereby may have a material adverse effect on our business, financial condition and results of operations. The loss of one or more of these physicians, even if temporary, could cause a material reduction in our revenues, which could take significant time to replace given the difficulty and cost associated with recruiting and retaining physicians.
Continued increase in hospital based physician expenses will materially affect our costs and results of operations.
In our acute care segment, during the past few years we experienced significant increases in hospital-based physician related expenses, especially in the areas of emergency room care and anesthesiology. We have implemented various initiatives to mitigate the increased expense, to the degree possible, which has moderated the rate of increase experienced during 2024 and 2023. However, significant increases in these physician related expenses could have a material unfavorable impact on our future results of operations.
If we do not continually enhance our hospitals with the most recent technological advances in diagnostic and surgical equipment, our ability to maintain and expand our markets will be adversely affected.
The technology used in medical equipment and related devices is constantly evolving and, as a result, manufacturers and distributors continue to offer new and upgraded products to health care providers. To compete effectively, we must continually assess our equipment needs and upgrade when significant technological advances occur. If our facilities do not stay current with technological advances in the health care industry, patients may seek treatment from other providers and/or physicians may refer their patients to alternate sources, which could adversely affect our results of operations and harm our business.
Our performance depends on our ability to attract and retain qualified nurses and medical support staff and we face competition for staffing that may increase our labor costs and harm our results of operations.
We depend on the efforts, abilities, and experience of our medical support personnel, including our nurses, pharmacists and lab technicians and other healthcare professionals. We compete with other healthcare providers in recruiting and retaining qualified hospital management, nurses and other medical personnel.
The nationwide shortage of nurses and other clinical staff and support personnel has been a significant operating issue facing us and other healthcare providers. In particular, like others in the healthcare industry, we experienced a shortage of nurses and other clinical staff and support personnel at our acute care and behavioral health care hospitals in many geographic areas which was exacerbated by the COVID‑19 pandemic. In some areas, the increased demand for care during the COVID-19 pandemic put a strain on our resources and staff, which required us to utilize higher‑cost temporary labor and pay premiums above standard compensation for essential workers. Personnel shortages may require us to further enhance wages and benefits to recruit and retain nurses and other clinical staff and support personnel or require us to hire expensive temporary personnel. To the extent we cannot maintain sufficient staffing levels at our hospitals, we may be required to limit the acute and behavioral health care services provided at certain of our hospitals which would have a corresponding adverse effect on our net revenues. In addition, in some markets such as California, there are requirements to maintain specified nurse-staffing levels which could adversely affect our net revenues to the extent we cannot meet those levels. If these states increase mandatory nurse-staffing ratios or additional states in which we operate adopt mandatory nurse-staffing ratios, such changes could significantly affect labor costs and have an adverse impact on revenues if we are required to limit admissions in order to meet the required ratios.
We cannot predict the degree to which we will be affected by the future availability or cost of attracting and retaining talented medical support staff. If our general labor and related expenses increase, we may not be able to raise our rates correspondingly. Our failure to either recruit and retain qualified hospital management, nurses and other medical support personnel or control our labor costs could harm our results of operations.
Increased labor union activity is another factor that could adversely affect our labor costs. Union organizing activities and certain potential changes in federal labor laws and regulations could increase the likelihood of employee unionization in the future, to the extent a greater portion of our employee base unionized, it is possible our labor costs could increase materially.
The failure of certain employers, or the closure of certain facilities, could have a disproportionate impact on our hospitals.
The economies in the communities in which our hospitals operate are often dependent on a small number of large employers. Those employers often provide income and health insurance for a disproportionately large number of community residents who may depend on our hospitals and other health care facilities for their care. The failure of one or more large employer or the closure or
substantial reduction in the number of individuals employed at facilities located in or near the communities where our hospitals operate, could cause affected employees to move elsewhere to seek employment or lose insurance coverage that was otherwise available to them. The occurrence of these events could adversely affect our revenue and results of operations, thereby harming our business.
The trend toward value-based purchasing may negatively impact our revenues.
We believe that value-based purchasing initiatives of both governmental and private payers tying financial incentives to quality and efficiency of care will increasingly affect the results of operations of our hospitals and other healthcare facilities and may negatively impact our revenues if we are unable to meet expected quality standards. The Legislation contains a number of provisions intended to promote value-based purchasing in federal healthcare programs. Medicare now requires providers to report certain quality measures in order to receive full reimbursement increases for inpatient and outpatient procedures that were previously awarded automatically. In addition, hospitals that meet or exceed certain quality performance standards will receive increased reimbursement payments, and hospitals that have “excess readmissions” for specified conditions will receive reduced reimbursement. Furthermore, Medicare no longer pays hospitals additional amounts for the treatment of certain hospital-acquired conditions unless the conditions were present at admission. Beginning in federal fiscal year 2015, hospitals that rank in the worst 25% of all hospitals nationally for hospital acquired conditions in the previous year were subject to reduced Medicare reimbursements. The Legislation also prohibits the use of federal funds under the Medicaid program to reimburse providers for treating certain provider-preventable conditions.
There is a trend among private payers toward value-based purchasing of healthcare services, as well. Many large commercial payers require hospitals to report quality data, and several of these payers will not reimburse hospitals for certain preventable adverse events. We expect value-based purchasing programs, including programs that condition reimbursement on patient outcome measures, to become more common and to involve a higher percentage of reimbursement amounts. We are unable at this time to predict how this trend will affect our results of operations, but it could negatively impact our revenues if we are unable to meet or maintain high quality standards established by both governmental and private payers.
Controls designed to reduce inpatient services and increasing rates of “denials” may reduce our revenues.
Controls imposed by third-party payers designed to reduce admissions and lengths of stay, commonly referred to as “utilization review,” have affected and are expected to continue to affect our facilities. Utilization review entails the review of the admission and course of treatment of a patient by managed care plans. Inpatient utilization, average lengths of stay and occupancy rates continue to be negatively affected by payer-required preadmission authorization and utilization review and by payer pressure to maximize outpatient and alternative healthcare delivery services for less acutely ill patients. Efforts to impose more stringent cost controls are expected to continue. In addition, we have been experiencing increasing rates of denied claims (“denials”) from managed care payers, including managed Medicare, which have reduced our net revenues and increased our operating costs as we devote additional resources to enhanced documentation and collection efforts. Although we cannot predict the effect these factors will have on our operations, significant limits on the scope of services reimbursed, and reimbursements withheld due to denials, could have a material adverse effect on our business, financial position and results of operations.
We depend heavily on key management personnel and the departure of one or more of our key executives or a significant portion of our local hospital management personnel could harm our business.
The expertise and efforts of our senior executives and key members of our local hospital management personnel are critical to the success of our business. The loss of the services of one or more of our senior executives or of a significant portion of our local hospital management personnel could significantly undermine our management expertise and our ability to provide efficient, quality healthcare services at our facilities, which could harm our business.
Risks Related to the Regulatory Environment
Reductions or changes in Medicare and Medicaid funding could have a material adverse effect on our future results of operations.
The Budget Control Act of 2011 (the “Budget Control Act”) mandated significant reductions in federal spending for fiscal years 2012-2021, including a reduction of 2% on all Medicare payments during this period. The most recent legislation extended these reductions through 2032. Please see Item 7. Management’s Discussion and Analysis of Financial Condition and Results of Operations, Sources of Revenue-Medicare, for additional disclosure.
Beginning in 2025 and continuing through 2027, the Medicaid disproportionate share hospital (“DSH”) allotment to the states from federal funds will be reduced. Such reductions have been delayed several times, most recently under the American Relief Act 2025, which delayed the DSH reductions through March 31, 2025. During the reduction period, state Medicaid DSH allotments from federal funds will be reduced by $8 billion annually. Reductions are imposed on states based on percentage of uninsured individuals, Medicaid utilization and uncompensated care. We receive Medicaid DSH payments in certain states including, most significantly, Texas. We are therefore particularly sensitive to potential reductions in Medicaid and other state-based revenue programs as well as regulatory, economic, environmental and competitive changes in those states. We can provide no assurance that reductions to revenues earned pursuant to these programs, particularly in the above-mentioned states, will not have a material adverse effect on our future results of operations.
We are subject to uncertainties regarding health care reform.
On March 23, 2010, President Obama signed into law the Legislation. Two primary goals of the Legislation are to provide for increased access to coverage for healthcare and to reduce healthcare-related expenses.
Although it was expected that as a result of the Legislation there would be a reduction in uninsured patients, which would reduce our expense from uncollectible accounts receivable, the Legislation makes a number of other changes to Medicare and Medicaid which we believe may have an adverse impact on us. The Legislation revises reimbursement under the Medicare and Medicaid programs to emphasize the efficient delivery of high quality care and contains a number of incentives and penalties under these programs to achieve these goals. The Legislation implements a value-based purchasing program, which will reward the delivery of efficient care. Conversely, certain facilities will receive reduced reimbursement for failing to meet quality parameters; such hospitals will include those with excessive readmission or hospital-acquired condition rates. As a result of the 2024 federal elections and the Braidwood Management v. Becerra litigation currently before the U.S. Supreme Court, it remains unclear what portions of that legislation may remain, or what any replacement or alternative programs may be created by future legislation.
A 2012 U.S. Supreme Court ruling limited the federal government’s ability to expand health insurance coverage by holding unconstitutional sections of the Legislation that sought to withdraw federal funding for state noncompliance with certain Medicaid coverage requirements. Pursuant to that decision, the federal government may not penalize states that choose not to participate in the Medicaid expansion program by reducing their existing Medicaid funding. Therefore, states can choose to accept or not to participate without risking the loss of federal Medicaid funding. As a result, many states, including Texas, have not expanded their Medicaid programs without the threat of loss of federal funding. In the past, CMS has granted section 1115 demonstration waivers providing for work and community engagement requirements for certain Medicaid eligible individuals. The previous Trump administration's section 1115 waiver policy emphasized work requirements, eligibility restrictions on Medicaid, and capped funding. The second Trump administration may, again, take a similar approach.
The Legislation also contained provisions aimed at reducing fraud and abuse in healthcare. The Legislation amended several existing laws, including the federal Anti-Kickback Statute and the False Claims Act, making it easier for government agencies and private plaintiffs to prevail in lawsuits brought against healthcare providers. While Congress had previously revised the intent requirement of the Anti-Kickback Statute to provide that a person is not required to “have actual knowledge or specific intent to commit a violation of” the Anti-Kickback Statute in order to be found in violation of such law, the Legislation also provides that any claims for items or services that violate the Anti-Kickback Statute are also considered false claims for purposes of the federal civil False Claims Act. The Legislation provides that a healthcare provider that retains an overpayment in excess of 60 days is subject to the federal civil False Claims Act. The Legislation also expanded the Recovery Audit Contractor program to Medicaid. These amendments also make it easier for severe fines and penalties to be imposed on healthcare providers that violate applicable laws and regulations.
We have partnered with local physicians in the ownership of certain of our facilities. These investments have been permitted under an exception to the physician self-referral law. The Legislation permits existing physician investments in a hospital to continue under a “grandfather” clause if the arrangement satisfies certain requirements and restrictions, but physicians are prohibited from increasing the aggregate percentage of their ownership in the hospital. The Legislation also imposes certain compliance and disclosure requirements upon existing physician-owned hospitals and restricts the ability of physician-owned hospitals to expand the capacity of their facilities. A repeal of the Legislation, in whole or in relevant part, may result in physicians being able to expand ownership interest in hospitals.
Initiatives to repeal or modify the Legislation, in whole or in part, have been persistent. While President Trump did not campaign on repeal of the Legislation, executive and legislative efforts to eliminate or reduce the effect of certain Legislation provisions may yet occur. The ultimate outcomes of legislative attempts to repeal or amend the Legislation and legal challenges to the Legislation are unknown. Legislation has already been enacted that has eliminated the penalty for failing to maintain health coverage that was an integral part of the original Legislation.
It remains unclear what portions of the Legislation may remain, or whether any replacement or alternative programs may be created by any future legislation. Any such future repeal or replacement may have significant impact on the reimbursement for healthcare services generally, and may create reimbursement for services competing with the services offered by our hospitals. Accordingly, there can be no assurance that the adoption of any future federal or state healthcare reform legislation will not have a negative financial impact on our hospitals, including their ability to compete with alternative healthcare services funded by such potential legislation, or for our hospitals to receive payment for services.
The Legislation and its implementation have been, and remain, politically controversial. While attempts to repeal the entirety of the Legislation have not been successful to date, a key provision of the Legislation was repealed as part of the Tax Cuts and Jobs Act and on December 14, 2018, a Texas Federal District Court Judge declared the Legislation unconstitutional, reasoning that the individual mandate tax penalty was essential to and not severable from the remainder of the Legislation. The case was appealed to the U.S. Supreme Court which ultimately held in California v. Texas that the plaintiffs lacked standing to challenge the Legislation’s requirement to obtain minimum essential health insurance coverage, or the individual mandate. The Court dismissed the case without
specifically ruling on the constitutionality of the Legislation. On September 7, 2022, the same Texas Federal District Court judge, in the case of Braidwood Management v. Becerra, ruled that the requirement that certain health plans cover services with an “A” or “B” recommendation from the U.S. Preventive Services Task Force without cost sharing violates the Appointments Clause of the U.S. Constitution and that the coverage of certain HIV prevention medication violates the Religious Freedom Restoration Act. The government has appealed the decision to the U.S. Supreme Court. We are unable to predict the outcome of this litigation or its potential impact at this time.
The Inflation Reduction Act of 2022 (“IRA”) was passed on August 16, 2022, which among other things, allows for CMS to negotiate prices for certain single-source drugs and biologics reimbursed under Medicare Part B and Part D, beginning with 10 high-cost drugs paid for by Medicare Part D starting in 2026, followed by 15 Part D drugs in 2027, 15 Part B or Part D drugs in 2028, and 20 Part B or Part D drugs in 2029 and beyond. The IRA also continued certain subsidies for individuals to obtain private health insurance under the Legislation through 2025. The effect of the 2024 federal elections on IRA price negotiation provisions or on the likelihood of extended health insurance enrollment subsidies beyond 2025 is not yet known. The Trump administration has already taken steps to undo certain Biden-era executive orders, including those intended to lower drug costs for beneficiaries, and to freeze funding for federal programs. While the administration’s initial freeze has since been rescinded, the administration is likely to make other attempts to reduce federal program expenditures and can generally be expected to oppose increases in ACA and Medicaid enrollment.
Under the Legislation, hospitals are required to make public a list of their standard charges, and effective January 1, 2019, CMS has required that this disclosure be in machine-readable format and include charges for all hospital items and services and average charges for diagnosis-related groups. On November 27, 2019, CMS published a final rule on “Price Transparency Requirements for Hospitals to Make Standard Charges Public.” This rule took effect on January 1, 2021 and requires all hospitals to also make public their payer-specific negotiated rates, minimum negotiated rates, maximum negotiated rates and cash for all items and services, including individual items and services and service packages, that could be provided by a hospital to a patient. On April 26, 2023, CMS announced updated enforcement processes that requires a shortened timeline for coming into compliance when a violation has been identified and the automatic imposition of a civil monetary penalties in certain circumstances of noncompliance. Failure to comply with these requirements may result in daily monetary penalties.
As part of the CAA, Congress passed legislation aimed at preventing or limiting patient balance billing in certain circumstances. The CAA addresses surprise medical bills stemming from emergency services, out-of-network ancillary providers at in-network facilities, and air ambulance carriers. The legislation prohibits surprise billing when out-of-network emergency services or out-of-network services at an in-network facility are provided, unless informed consent is received. The law provides for a 30-day negotiation period for providers and payers to settle out-of-network claims. If no agreement is reached after this period, either party may opt for a binding independent dispute resolution (“IDR”) process. CMS regulations and guidance implementing the IDR process has been subject to a significant amount of provider-initiated litigation. As a result, portions of those regulations and guidance materials have been vacated by a federal district court, causing CMS to, on several occasions, pause and resume IDR process operations, causing significant delay in the processing of claims. Additionally, arguments made by the plaintiffs in such litigation have included allegations that CMS’s regulations and guidance materials are favorable to payers. For these reasons, there can be no assurances that we will receive timely payments in connection with this process.
We are required to treat patients with emergency medical conditions regardless of ability to pay.
In accordance with our internal policies and procedures, as well as the Emergency Medical Treatment and Active Labor Act, or EMTALA, we provide a medical screening examination to any individual who comes to one of our hospitals while in active labor and/or seeking medical treatment (whether or not such individual is eligible for insurance benefits and regardless of ability to pay) to determine if such individual has an emergency medical condition. If it is determined that such person has an emergency medical condition, we provide such further medical examination and treatment as is required to stabilize the patient’s medical condition, within the facility’s capability, or arrange for transfer of such individual to another medical facility in accordance with applicable law and the treating hospital’s written procedures. Our obligations under EMTALA may increase substantially going forward. If the number of indigent and charity care patients with emergency medical conditions we treat increases significantly, or if regulations expanding our obligations to inpatients under EMTALA is proposed and adopted, our results of operations will be harmed.
If we fail to continue to meet the promoting interoperability criteria related to electronic health record systems (“EHR”), our operations could be harmed.
Pursuant to Health Information Technology for Economic and Clinical Health (“HITECH”) regulations, hospitals that did not qualify as a meaningful user of EHR by 2015 were subject to a reduced market basket update to the inpatient prospective payment system (“IPPS”) standardized amount in 2015 and each subsequent fiscal year. In the 2019 IPPS final rule, CMS re-named the meaningful use program to “promoting interoperability”. We believe that all of our acute care hospitals have met the applicable promoting interoperability criteria and therefore are not subject to a reduced market basked update to the IPPS standardized amount. However, under the HITECH Act, hospitals must continue to meet the applicable criteria in each fiscal year or they will be subject to a market basket update reduction in a subsequent fiscal year. Failure of our acute care hospitals to continue to meet the applicable criteria would have an adverse effect on our future net revenues and results of operations.
If we fail to comply with extensive laws and government regulations, we could suffer civil or criminal penalties or be required to make significant changes to our operations that could reduce our revenue and profitability.
The healthcare industry is required to comply with extensive and complex laws and regulations at the federal, state and local government levels relating to, among other things: hospital billing practices and prices for services; relationships with physicians and other referral sources; adequacy of medical care and quality of medical equipment and services; ownership of facilities; qualifications of medical and support personnel; confidentiality, maintenance, privacy and security issues associated with health-related information and patient medical records; the screening, stabilization and transfer of patients who have emergency medical conditions; certification, licensure and accreditation of our facilities; operating policies and procedures, and; construction or expansion of facilities and services.
Among these laws are the federal False Claims Act, the Health Insurance Portability and Accountability Act of 1996, (“HIPAA”), the federal anti-kickback statute and the provision of the Social Security Act commonly known as the “Stark Law.” These laws, and particularly the anti-kickback statute and the Stark Law, impact the relationships that we may have with physicians and other referral sources. We have a variety of financial relationships with physicians who refer patients to our facilities, including employment contracts, leases and professional service agreements. We also provide financial incentives, including minimum revenue guarantees, to recruit physicians into communities served by our hospitals. The Office of the Inspector General of the Department of Health and Human Services, or OIG, has enacted safe harbor regulations that outline practices that are deemed protected from prosecution under the anti-kickback statute. A number of our current arrangements, including financial relationships with physicians and other referral sources, may not qualify for safe harbor protection under the anti-kickback statute. Failure to meet a safe harbor does not mean that the arrangement necessarily violates the anti-kickback statute, but may subject the arrangement to greater scrutiny. We cannot assure that practices that are outside of a safe harbor will not be found to violate the anti-kickback statute. CMS published a Medicare self-referral disclosure protocol, which is intended to allow providers to self-disclose actual or potential violations of the Stark law. Because there are only a few judicial decisions interpreting the Stark law, there can be no assurance that our hospitals will not be found in violation of the Stark Law or that self-disclosure of a potential violation would result in reduced penalties.
Federal regulations issued under HIPAA contain provisions that require us to implement and, in the future, may require us to implement additional costly electronic media security systems and to adopt new business practices designed to protect the privacy and security of each of our patient’s health and related financial information. Such privacy and security regulations impose extensive administrative, physical and technical requirements on us, restrict our use and disclosure of certain patient health and financial information, provide patients with rights with respect to their health information and require us to enter into contracts extending many of the privacy and security regulatory requirements to third parties that perform duties on our behalf. Additionally, recent changes to HIPAA regulations may result in greater compliance requirements, including obligations to report breaches of unsecured patient data, as well as create new liabilities for the actions of parties acting as business associates on our behalf.
These laws and regulations are extremely complex, and, in many cases, we do not have the benefit of regulatory or judicial interpretation. In the future, it is possible that different interpretations or enforcement of these laws and regulations could subject our current or past practices to allegations of impropriety or illegality or could require us to make changes in our facilities, equipment, personnel, services, capital expenditure programs and operating expenses. A determination that we have violated one or more of these laws (see Note 8 to the Consolidated Financial Statements - Commitments and Contingencies, as included this Form 10-K), or the public announcement that we are being investigated for possible violations of one or more of these laws, could have a material adverse effect on our business, financial condition or results of operations and our business reputation could suffer significantly. In addition, we cannot predict whether other legislation or regulations at the federal or state level will be adopted, what form such legislation or regulations may take or what their impact on us may be. See Item 1 Business—Self-Referral and Anti-Kickback Legislation.
If we are deemed to have failed to comply with the anti-kickback statute, the Stark Law or other applicable laws and regulations, we could be subjected to liabilities, including criminal penalties, civil penalties (including the loss of our licenses to operate one or more facilities), and exclusion of one or more facilities from participation in the Medicare, Medicaid and other federal and state healthcare programs. The imposition of such penalties could have a material adverse effect on our business, financial condition or results of operations.
We also operate health care facilities in the United Kingdom and have operations and commercial relationships with companies in other foreign jurisdictions and, as a result, are subject to certain U.S. and foreign laws applicable to businesses generally, including anti-corruption laws. The Foreign Corrupt Practices Act regulates U.S. companies in their dealings with foreign officials, prohibiting bribes and similar practices, and requires that they maintain records that fairly and accurately reflect transactions and appropriate internal accounting controls. In addition, the United Kingdom Bribery Act has wide jurisdiction over certain activities that affect the United Kingdom.
Our operations in the United Kingdom are also subject to a high level of regulation relating to registration and licensing requirements employee regulation, clinical standards, environmental rules, data protection as well as other areas. We are also subject to a highly regulated business environment, and failure to comply with the various laws and regulations, applicable to us could lead to substantial penalties, and other adverse effects on our business. United Kingdom data protection laws, including the UK Data Protection Act and legislation commonly referred to as the UK GDPR, has required us to implement, and in the future may require us
to implement, additional costly, technical and organizational measures designed to protect the privacy and security of each of our patient’s health and related financial information, and other personal information.
We are subject to occupational health, safety and other similar regulations and failure to comply with such regulations could harm our business and results of operations.
We are subject to a wide variety of federal, state and local occupational health and safety laws and regulations. Regulatory requirements affecting us include, but are not limited to, those covering: (i) air and water quality control; (ii) occupational health and safety (e.g., standards regarding blood-borne pathogens and ergonomics, etc.); (iii) waste management; (iv) the handling of asbestos, polychlorinated biphenyls and radioactive substances; and (v) other hazardous materials. If we fail to comply with those standards, we may be subject to sanctions and penalties that could harm our business and results of operations.
We are subject to pending legal actions, purported stockholder class actions, governmental investigations and regulatory actions.
We and our subsidiaries are subject to pending legal actions, governmental investigations and regulatory actions (see Note 8 to the Consolidated Financial Statements - Commitments and Contingencies, as included this Form 10-K). We may become subject to additional medical malpractice lawsuits, product liability lawsuits, class action lawsuits and other legal actions in the ordinary course of business.
Defending ourselves against the allegations in the lawsuits and governmental investigations, or similar matters and any related publicity, could potentially entail significant costs and could require significant attention from our management and our reputation could suffer significantly.
For example, as discussed elsewhere herein:
•On March 28, 2024, a jury returned a verdict for compensatory damages of $60 million and punitive damages of $475 million and a related judgment was entered against The Pavilion Behavioral Health System (the “Pavilion”), an indirect subsidiary of the Company. In an order dated October 10, 2024, the trial court ordered a remittitur of punitive damages from $475 million to $120 million. The court denied the Pavilion’s request for reduction of compensatory damages. The Pavilion has filed an appeal of the remaining judgment and the Plaintiff filed a cross appeal of the remittitur of punitive damages. Plaintiff has filed and served a Citation to Discover Assets ("Citation") on the Pavilion as well as Universal Health Services, Inc., and UHS of Delaware, Inc. ("UHS Entities") for the purported purpose of executing on the judgment during the pendency of the appeal. We are currently contesting the Citation as to the UHS Entities who were not parties to the litigation as well as the breadth and scope of the Citation issued to the Pavilion.
•Cumberland Hospital for Children and Adolescents (“Cumberland”), an indirect subsidiary of the Company, is a defendant in multi-plaintiff lawsuits filed in the Circuit Court for Richmond, Virginia (the “Cumberland Litigation”), relating to allegations of inappropriate sexual contact during medical examinations by Dr. Daniel Davidow, an independent contractor and the former medical director for Cumberland. The Company and UHS of Delaware, Inc., our administrative services subsidiary (“UHS Delaware”), were also named as co-defendants in the Cumberland Litigation. Plaintiffs have asserted claims of negligence, assault and battery (against Dr. Davidow), false imprisonment, violations of the Virginia Consumer Protection Act (“VCPA”), and vicarious liability for Dr. Davidow’s conduct against Cumberland, the Company, and UHS Delaware. The Company and UHS Delaware were dismissed from the action during the trial, which occurred in September, 2024. On September 27, 2024, a jury entered a verdict finding Dr. Davidow and Cumberland liable and awarded these three plaintiffs combined compensatory damages of $60 million for all liability theories, an additional combined $180 million in trebled damages for violation of the VCPA, and an additional combined $120 million in punitive damages. Cumberland is evaluating all legal options and intends to challenge this verdict, including the amounts awarded in the verdict, in post-trial proceedings and on appeal. Based upon Virginia law, we expect that the punitive damage amount should be reduced to a combined maximum of $1.05 million as a matter of law. There are approximately 40 additional plaintiffs making similar allegations with claims pending in the Cumberland Litigation. We expect that the trials for the remaining plaintiffs, as well as any additional plaintiffs, will be scheduled at various times over the next several years and will continue to be tried in small groups.
We are uncertain as to the ultimate financial exposure related to the Pavilion and Cumberland matters (which relate to occurrences in the 2020 policy year) and we can make no assurances regarding timing or substance of their outcome, or the amount of damages that may be ultimately held recoverable after post-judgment proceedings and appeals. As of December 31, 2024, without reduction for any potential amounts related to the Pavilion and Cumberland matters, the Company and its subsidiaries have aggregate insurance coverage of approximately $221 million remaining under commercial policies for matters applicable to the 2020 policy year (in excess of the applicable self-insured retention amounts of $10 million per single occurrence/$25 million for multi-plaintiff matters for professional liability claims and $3 million per occurrence for general liability claims). In the event the resolution of the Pavilion and/or Cumberland matters exhausts all or a significant portion of the remaining commercial insurance coverage available to the Company and its subsidiaries related to other matters that occurred in 2020, or the Pavilion and Cumberland matters cause the posting of large bonds or other collateral during the appeal processes, our future results of operations and capital resources would be materially adversely impacted.
We are unable to predict the outcome of these matters or to reasonably estimate the amount or range of any such loss; however, these lawsuits and the related publicity and news articles that have been published concerning these matters could have a material adverse effect on our business, financial condition, results of operations and/or cash flows which in turn could cause a decline in our stock price. In an effort to resolve one or more of these matters, we may choose to negotiate a settlement. Amounts we pay to settle any of these matters may be material.
All professional and general liability insurance we purchase is subject to policy limitations. Our estimated liability for self-insured professional and general liability claims is based on a number of factors including, among other things, the number of asserted claims and reported incidents, estimates of losses for these claims based on recent and historical settlement amounts and jury verdicts, estimates of incurred but not reported claims based on historical experience, and estimates of amounts recoverable under our commercial insurance policies. All relevant information, including our own historical experience, applicable per occurrence and aggregate self-insured retentions, and limitations and exclusions pursuant to our commercial insurance policies, is used in estimating our expected liability for self-insured claims. While we continuously monitor these factors, our ultimate liability for professional and general liability claims could change materially from our current estimates due to inherent uncertainties involved in making this estimate. Given our significant exposure to professional and general liability claims, there can be no assurance that a sharp increase in the number and/or severity of claims asserted against us, and/or reductions in the amount of commercial coverage available to us, will not have a material adverse effect on our future results of operations. In addition, our commercial insurance coverage for the period commencing in March, 2025, contains less favorable terms than previous years including coverage exclusions for incidents involving sexual molestation or abuse, higher premiums and potentially lower aggregate limitations.
We are and may become subject to other loss contingencies, both known and unknown, which may relate to past, present and future facts, events, circumstances and occurrences. Should an unfavorable outcome occur in some or all of our legal proceedings or other loss contingencies, or if successful claims and other actions are brought against us in the future, there could be a material adverse impact on our financial position, results of operations and liquidity.
In particular, government investigations, as well as qui tam and stockholder lawsuits, may lead to material fines, penalties, damages payments or other sanctions, including exclusion from government healthcare programs. The federal False Claims Act permits private parties to bring qui tam, or whistleblower, lawsuits on behalf of the government against companies alleging that the defendant has defrauded the federal government. These private parties are entitled to share in any amounts recovered by the government, and, as a result, the number of whistleblower lawsuits that have been filed against providers has increased significantly in recent years. Because qui tam lawsuits are filed under seal, we could be named in one or more such lawsuits of which we are not aware. Settlements of lawsuits involving Medicare and Medicaid issues routinely require both monetary payments and corporate integrity agreements, each of which could have a material adverse effect on our business, financial condition, results of operations and/or cash flows.
If any of our existing health care facilities lose their accreditation or any of our new facilities fail to receive accreditation, such facilities could become ineligible to receive reimbursement under Medicare or Medicaid.
The construction and operation of healthcare facilities are subject to extensive federal, state and local regulation relating to, among other things, the adequacy of medical care, equipment, personnel, operating policies and procedures, fire prevention, rate-setting and compliance with building codes and environmental protection. Additionally, such facilities are subject to periodic inspection by government authorities to assure their continued compliance with these various standards.
All of our hospitals are deemed certified, meaning that they are accredited, properly licensed under the relevant state laws and regulations and certified under the Medicare program. The effect of maintaining certified facilities is to allow such facilities to participate in the Medicare and Medicaid programs. We believe that all of our healthcare facilities are in material compliance with applicable federal, state, local and other relevant regulations and standards. However, should any of our healthcare facilities lose their deemed certified status and thereby lose certification under the Medicare or Medicaid programs, such facilities would be unable to receive reimbursement from either of those programs and our business could be materially adversely effected.
State efforts to regulate the construction or expansion of health care facilities could impair our ability to expand.
Certain states in which we operate hospitals have certificates of need (“CON”) laws as a condition prior to hospital capital expenditures, construction, expansion, modernization or initiation of major new services. Our failure to obtain necessary state approval could result in our inability to complete a particular hospital acquisition, expansion or replacement, make a facility ineligible to receive reimbursement under the Medicare or Medicaid programs, result in the revocation of a facility’s license or impose civil or criminal penalties on us, any of which could harm our business.
In addition, significant CON reforms have been proposed in a number of states that would increase the capital spending thresholds and provide exemptions of various services from review requirements. In the past, we have not experienced any material adverse effects from those requirements, but we cannot predict the impact of these changes upon our operations.
Changes U.S. and other countries’ trade policies and other factors beyond our control may adversely impact our business and operating results.
Changes in laws or policies governing the terms of foreign trade, and in particular increased trade restrictions, tariffs or taxes on imports from where our import products or materials (either directly or through our suppliers) could have an impact on our competitive position, business operations and financial results. In February 2025, the U.S. government imposed or threatened to impose new tariffs, including on imported products from Mexico, Canada and China. The impact of these tariffs is subject to a number of factors, including the effective date and duration of such tariffs, changes in the amount, scope and nature of the tariffs in the future, any retaliatory responses to such actions that the target countries may take and any mitigating actions that may become available. If significant tariffs or other restrictions are imposed on our imported pharmaceutical ingredients, medical devices, medical equipment and their ingredients and components, there could be significant strain on our supply chains, causing major disruptions in procurement processes and contract negotiations with suppliers due to increased costs, pricing volatility, longer procurement lead times and supply shortages stemming from increased production costs and import restrictions. As a result, we have to attempt to shift increased costs onto insurers and patients (in the form of higher service charges), reduce procurement volumes and delay equipment upgrades to mitigate financial strain. While we continue to evaluate the potential impact of the new tariffs on our business, given the uncertainty regarding the scope and duration of any new tariffs, as well as the potential for additional tariffs or trade barriers by the U.S., Mexico, Canada, China or other countries, we can provide no assurance that any strategies we implement to mitigate the impact of such tariffs or other trade actions will be successful.
Risks Related to Information Technology
A cyber security incident could cause a violation of HIPAA, breach of patient or other persons privacy, or other negative impacts.
We rely extensively on our information technology (“IT”) systems to manage clinical and financial data, communicate with our patients, payers, vendors and other third parties and summarize and analyze operating results. In addition, we have made significant investments in technology to adopt and utilize electronic health records and to become meaningful users of health information technology pursuant to the American Recovery and Reinvestment Act of 2009. Our IT systems, and the networks and information systems of third parties that we rely on, are subject to damage or interruption from power outages, facility damage, computer and telecommunications failures, computer viruses, security breaches including credit card or personally identifiable information breaches, vandalism, theft, natural disasters, catastrophic events, human error and potential cyber threats, including malicious codes, worms, phishing attacks, denial of service attacks, ransomware and other sophisticated cyber-attacks, and our disaster recovery planning cannot account for all eventualities. Our systems, in turn, interface with and rely on third-party systems that we do not control, including medical devices and other processes supporting the interoperability of healthcare infrastructures. Third parties to whom we outsource certain of our functions, or with whom our systems interface and who may, in some instances, store our sensitive and confidential data, are also subject to the risks outlined above and may not have or use controls effective to protect such information. An attack, breach or other system disruption affecting any of these third parties could similarly harm our business.
As cyber criminals continue to become more sophisticated through evolution of their tactics, techniques and procedures, we have taken, and will continue to take, additional preventive measures to strengthen the cyber defenses of our networks and data. Although we continue to regularly review and enhance our IT systems and cybersecurity controls, we and our third-party provider have experienced, and may experience in the future, cybersecurity incidents. See “Item 1A. Risk Factors” of our Annual Report on Form 10-K for the year ended December 31, 2023 (as filed on February 27, 2024) for information regarding the 2024 cyber incident at UnitedHealth Group Incorporated and the cyber incident we experienced in 2020. While to date no incident had a material impact on our operations or financial results, we cannot guarantee that material incidents will not occur in the future. If any of our or our third-party service providers’ systems are damaged, fail to function properly or otherwise become unavailable, we may incur substantial costs to repair or replace them, and may experience loss or corruption of critical data such as protected health information or other data subject to privacy laws and proprietary business information and interruptions or disruptions and delays in our ability to perform critical functions, which could materially and adversely affect our businesses and results of operations and could result in significant penalties or fines, litigation, loss of customers, significant damage to our reputation and business, and other losses. In the event of a material breach or cyber-attack, the associated expenses and losses may exceed our current insurance coverage for such events. In addition, some adverse consequences are not insurable, such as reputational harm and third-party business interruption. In addition, our future results of operations, as well as our reputation, could be adversely impacted by theft, destruction, loss, or misappropriation of public health information, other confidential data or proprietary business information. Further, consumer confidence in the integrity, availability and confidentiality of information systems and information, including patient personal information and critical operations data, in the healthcare industry generally could be impacted to the extent there are successful cyberattacks at other healthcare services companies, which could have a material adverse effect on our business, financial position or results of operations.
Risks Related to the Market Conditions and Liquidity
Our revenues and volume trends may be adversely affected by certain factors over which we have no control.
Our revenues and volume trends are dependent on many factors, including physicians’ clinical decisions and availability, payer programs shifting to a more outpatient-based environment, whether or not certain services are offered, seasonal and severe weather conditions, including the effects of extreme low temperatures, hurricanes and tornadoes, earthquakes, climate change, current local economic and demographic changes. We have a high concentration of facilities in various geographic areas, including states that have
a potentially higher risk of experiencing events such as severe weather conditions and earthquakes. Given the location of our facilities, we are particularly susceptible to revenue loss, cost increase, or damage caused by severe weather conditions or natural disasters such as hurricanes, wildfires, earthquakes, or tornadoes. Any significant loss due to a natural disaster may not be covered by insurance and may lead to an increase in the cost of insurance or unavailability on acceptable terms. Climate change may also have effects on our business by increasing the cost of property insurance or making coverage unavailable on acceptable terms. To the extent that significant changes in the climate occur in areas where our facilities are located, we may experience increased frequency of severe weather conditions or natural disasters or other changes to weather patterns, all of which may result in physical damage to or a decrease in demand for properties affected by these conditions. Should the impact of climate change be material in nature or occur for lengthy periods of time, our financial condition, revenues, results of operations, or cash flow may be adversely affected. In addition, government regulation intended to mitigate the impact of climate change, severe weather patterns, or natural disasters could result in additional required capital expenditures to comply with such regulation without a corresponding increase in our revenues. In addition, technological developments and pharmaceutical improvements may reduce the demand for healthcare services or the profitability of the services we offer.
A worsening of economic and employment conditions in the United States could materially affect our business and future results of operations.
Our patient volumes, revenues and financial results depend significantly on the universe of patients with health insurance, which to a large extent is dependent on the employment status of individuals in our markets. Worsening of economic conditions, including inflation and rising interest rates, may result in a higher unemployment rate which may increase the number of individuals without health insurance. As a result, our facilities may experience a decrease in patient volumes, particularly in less intense, more elective service lines, or an increase in services provided to uninsured patients. These factors could have a material unfavorable impact on our future patient volumes, revenues and operating results.
In addition, as of December 31, 2024, we had approximately $3.9 billion of goodwill recorded on our consolidated balance sheets. Should the revenues and financial results of our acute care and/or behavioral health care facilities be materially, unfavorably impacted due to, among other things, a worsening of the economic and employment conditions in the United States that could negatively impact our patient volumes and reimbursement rates, a continued rise in the unemployment rate and increases in the number of uninsured patients treated at our facilities, we may incur future charges to recognize impairment in the carrying value of our goodwill and other intangible assets, which could have a material adverse effect on our financial results.
Continuing Inflationary Pressures continue to increase our operating costs and we may not be able to pass on increases in costs commensurate with these increases in costs.
We are experiencing inflationary pressures, primarily in personnel costs, and we anticipate continuing impacts on other cost areas within the next twelve months. The extent of any future impacts from inflation on our business and our results of operations will be dependent upon how long the elevated inflation levels persist and the extent to which the rate of inflation further increases, if at all, neither of which we are able to predict. If elevated levels of inflation were to persist or if the rate of inflation were to accelerate, our expenses could increase faster than anticipated and we may utilize our capital resources sooner than expected. Further, given the complexities of the reimbursement landscape in which we operate, our ability to pass on increased costs associated with providing healthcare to Medicare and Medicaid patients is limited due to various federal, state and local laws, which in certain circumstances, limit our ability to increase prices, commercial payers may be unwilling or unable to increase reimbursement rates commensurate with the inflationary impacts on our costs.
We continue to see rising costs in construction materials and labor. Such increased costs could have an adverse effect on the cash flow return on investment relating to our capital projects.
The cost of construction materials and labor has significantly increased. As we continue to invest in modern technologies, emergency rooms and operating room expansions, the construction of medical office buildings for physician expansion and reconfiguring the flow of patient care, we spend large amounts of money generated from our operating cash flow or borrowed funds. Although we evaluate the financial feasibility of such projects by determining whether the projected cash flow return on investment exceeds our cost of capital, such returns may not be achieved if the cost of construction continues to rise significantly or the expected patient volumes are not attained.
The deterioration of credit and capital markets may adversely affect our access to sources of funding and we cannot be certain of the availability and terms of capital to fund the growth of our business when needed.
We require substantial capital resources to fund our acquisition growth strategy and our ongoing capital expenditure programs for renovation, expansion, construction and addition of medical equipment and technology. We believe that our capital expenditure program is adequate to expand, improve and equip our existing hospitals. We cannot predict, however, whether financing for our growth plans and capital expenditure programs will be available to us on satisfactory terms when needed, which could harm our business.
To fund all or a portion of our future financing needs, we rely on borrowings from various sources including fixed rate, long-term debt as well as borrowings pursuant to our revolving credit facility. If any of the lenders were unable to fulfill their future commitments, our liquidity could be impacted, which could have a material unfavorable impact our results of operations and financial condition. The increase in interest rates has substantially increased our borrowing costs and reduced our ability to access the capital markets on favorable terms. Additional increases in interest rates and the effect on capital markets could adversely affect our ability to carry out our strategy.
Risks Related to Our Common Stock
The number of outstanding shares of our Class B Common Stock is subject to potential increases or decreases.
At December 31, 2024, 24.4 million shares of Class B Common Stock were reserved for issuance upon conversion of shares of Class A, C and D Common Stock outstanding, for issuance upon exercise of options to purchase Class B Common Stock and for issuance of stock under other incentive plans. Class A, C and D Common Stock are convertible on a share for share basis into Class B Common Stock. To the extent that these shares were converted into or exercised for shares of Class B Common Stock, the number of shares of Class B Common Stock available for trading in the public market place would increase substantially and the current holders of Class B Common Stock would own a smaller percentage of that class.
In addition, from time-to-time, our Board of Directors approve stock repurchase programs authorizing us to purchase shares of our Class B Common Stock on the open market at prevailing market prices or in negotiated transactions off the market. Such repurchases decrease the number of outstanding shares of our Class B Common Stock. Pursuant to our stock repurchase program, shares of our Class B Common Stock may be repurchased, from time to time as conditions allow, on the open market or in negotiated private transactions. There is no expiration date for our stock repurchase programs.
In July 2024, our Board of Directors authorized a $1.0 billion increase to our stock repurchase program. During 2024, in conjunction with this program, we have repurchased approximately 3.0 million shares at an aggregate cost of approximately $599 million. As of December 31, 2024, we had an aggregate available repurchase authorization of approximately $824 million.
Our ability to repurchase shares will depend upon, among other factors, our cash flows from operations, our available capital and potential future capital requirements for strategic transactions, including acquisitions, debt service requirements, and investing in our existing markets as well as our results of operations, financial condition, interest rates, our access to the capital markets and other factors beyond our control that our Board of Directors may deem relevant. A suspension or elimination of our share repurchase could have a negative effect on our stock price.
Conversely, as a potential means of generating additional funds to operate and expand our business, we may from time-to-time issue equity through the sale of stock which would increase the number of outstanding shares of our Class B Common Stock. Based upon factors such as, but not limited to, the market price of our stock, interest rate on borrowings and uses or potential uses for cash, repurchase or issuance of our stock could have a dilutive effect on our future basic and diluted earnings per share.
The right to elect the majority of our Board of Directors and the majority of the general shareholder voting power resides with the holders of Class A and C Common Stock, the majority of which is owned by Alan B. Miller, Executive Chairman of our Board of Directors.
Our Restated Certificate of Incorporation provides that, with respect to the election of directors, holders of Class A Common Stock vote as a class with the holders of Class C Common Stock, and holders of Class B Common Stock vote as a class with holders of Class D Common Stock, with holders of all classes of our Common Stock entitled to one vote per share.
As of March 18, 2024, the shares of Class A and Class C Common Stock, which constituted 10.8% of the aggregate outstanding shares of our Common Stock, had the right to elect five members of the Board of Directors and constituted 90.5% of our general voting power as of that date. Also as of that date, the shares of Class B and Class D Common Stock (excluding shares issuable upon exercise of options), which constituted 89.2% of the outstanding shares of our Common Stock, had the right to elect two members of the Board of Directors and constituted 9.5% of our general voting power as of that date.
As to matters other than the election of directors, our Restated Certificate of Incorporation provides that holders of Class A, Class B, Class C and Class D Common Stock all vote together as a single class, except as otherwise provided by law.
Each share of Class A Common Stock entitles the holder thereof to one vote; each share of Class B Common Stock entitles the holder thereof to one-tenth of a vote; each share of Class C Common Stock entitles the holder thereof to 100 votes (provided the holder of Class C Common Stock holds a number of shares of Class A Common Stock equal to ten times the number of shares of Class C Common Stock that holder holds); and each share of Class D Common Stock entitles the holder thereof to ten votes (provided the holder of Class D Common Stock holds a number of shares of Class B Common Stock equal to ten times the number of shares of Class D Common Stock that holder holds).
In the event a holder of Class C or Class D Common Stock holds a number of shares of Class A or Class B Common Stock, respectively, less than ten times the number of shares of Class C or Class D Common Stock that holder holds, then that holder will be entitled to only one vote for every share of Class C Common Stock, or one-tenth of a vote for every share of Class D Common Stock,
which that holder holds in excess of one-tenth the number of shares of Class A or Class B Common Stock, respectively, held by that holder. The Board of Directors, in its discretion, may require beneficial owners to provide satisfactory evidence that such owner holds ten times as many shares of Class A or Class B Common Stock as Class C or Class D Common Stock, respectively, if such facts are not apparent from our stock records.
Since a substantial majority of the Class A shares and Class C shares are controlled by Mr. Alan B. Miller and members of his family, one of whom is Marc D. Miller, our Chief Executive Officer, President and a director, and they can elect a majority of our company’s directors and effect or reject most actions requiring approval by stockholders without the vote of any other stockholders, there are potential conflicts of interest in overseeing the management of our company.
In addition, because this concentrated control could discourage others from initiating any potential merger, takeover or other change of control transaction that may otherwise be beneficial to our businesses, our business and prospects and the trading price of our securities could be adversely affected.
None.
ITEM 1C. Cybersecurity
Cybersecurity risk management and strategy
Protecting our data, which includes information related to our patients, members, and customers, is a primary area of our focus. Given the critical nature of this information, we have developed and implemented a robust cybersecurity risk management program to assess, identify, and manage risks associated with cybersecurity threats as identified in Item 106(a) of Regulation S-K. Cybersecurity is an important and integrated part of our risk management program that identifies, monitors and mitigates business, operational and legal risks.
This program has a multi-tier risk management structure that includes regular reviews of laws, policies, vulnerabilities, and resource levels to address risks facing our organization. Such risks include operational, intellectual property theft, fraud, risks that have potential unfavorable impacts on our employees and/or patients, and violation of data privacy or security laws.
To address cybersecurity risks facing our organization, we have adopted a “continuous risk assessment” process. We engage a third party to conduct a bi-annual National Institute of Technology-Cyber Security Framework assessment to determine the effectiveness of our program and related controls. The results of that assessment are shared with management, which drives prioritization and investment in resources to address those risks. Likewise, annual penetration tests occur to review the efficacy of our technical controls, results which are reviewed by management and resolved in a timely manner. Other factors that feed into our risk management practices are also operational events and incidents, which can lead to controls being reviewed and enhanced.
We also have a mature incident response process in place in the event a cybersecurity incident occurs. This process defines roles, responsibilities and action plans designed to contain and eradicate the issue and then restore systems in the event of a major disruption. Regularly, we conduct tabletop exercises to simulate responses to an incident and implement any insight gained from those exercises to improve our recovery practices. As part of these processes, we regularly engage with assessors, consultants, auditors, and other third parties to review our cybersecurity program to help identify areas for continued focus, improvement, and compliance.
We have a commercial cybersecurity insurance policy that provides for coverage for losses sustained from cybersecurity incidents, subject to certain deductibles and limitations. However, costs and damages associated with cybersecurity incidents could exceed our commercial insurance coverage which could have a material adverse effect on our business, financial position and results of operations.
Third parties who provide services and solutions to our organization are also a source of cyber risk. Through a third-party risk management program, we review risks associated with these third parties through contractual reviews, vendor risk assessments, and continual risk reviews by monitoring the cybersecurity risk exposure these third parties pose and implementing remediation where necessary.
Based on the information available as of the date of this Form 10-K, during our fiscal year 2024 and through the date of this filing, we did not identify any risks from cybersecurity threats, including as a result of any previous cybersecurity incidents (as such terms are defined in Item 106(a) of Regulation S-K), that have materially affected or are reasonably likely to materially affect us, including our business strategy, results of operations or financial condition. For more information on risks to us from cybersecurity threats, see “Risks Related to Information Technology - A cyber security incident could cause a violation of HIPAA, breach of patient or other persons privacy, or other negative impacts.” under “Item 1A. Risk Factors.”
Governance of Cybersecurity
Cybersecurity is an integral part of our risk management program and is an area of focus for our Board of Directors and management. The Audit Committee of our Board of Directors is responsible for the oversight of risks from cybersecurity threats. Members of the Audit Committee receive updates, as warranted, including quarterly updates from our Chief Information Security Officer (“CISO”) regarding matters of cybersecurity, such as key risks facing the healthcare industry and our company, core topics, review of incidents, as well as progress against key information security initiatives. Senior executive leadership also engage in ad-hoc discussions with management on cybersecurity topics. In addition, our Board of Directors are provided with an annual report regarding cybersecurity information and related topics.
Our cybersecurity risk management and strategy processes are overseen by our CISO along with leaders from our Information Security, Compliance, Legal and Internal Auditing teams. Such individuals have an average of over 20 years of prior work experience in various roles involving information technology, including security, auditing, compliance, systems and programming. These individuals monitor the prevention, mitigation, detection and remediation of cybersecurity incidents through their management of, and participation in, the cybersecurity risk management and strategy processes described above, including the operation of our incident response plan.
ITEM 2. Properties
Executive and Administrative Offices and Commercial Health Insurer
We own various office buildings in King of Prussia and Wayne, Pennsylvania, Brentwood, Tennessee, Denton, Texas and Reno, Nevada.
Facilities
The following tables set forth the name, location, type of facility and, for acute care hospitals and behavioral health care facilities, the number of licensed beds:
Acute Care Hospitals
| | | | |
Name of Facility
|
| Location
| Number of
Beds
| Real
Property
Ownership
Interest
|
Aiken Regional Medical Centers (1) |
| Aiken, South Carolina | 211 | Leased |
Aurora Pavilion Behavioral Health Services (1) |
| Aiken, South Carolina | 62 | Leased |
ER at Sweetwater |
| North Augusta, South Carolina | — | Owned |
Centennial Hills Hospital Medical Center |
| Las Vegas, Nevada | 339 | Owned |
ER at Valley Vista |
| North Las Vegas, Nevada | — | Owned |
ER at West Craig |
| Las Vegas, Nevada | — | Owned |
Corona Regional Medical Center |
| Corona, California | 259 | Owned |
Desert View Hospital |
| Pahrump, Nevada | 25 | Owned |
Doctors Hospital of Laredo (6) |
| Laredo, Texas | 183 | Owned |
Doctors Hospital Emergency Room Saunders |
| Laredo, Texas | — | Owned |
Doctors Hospital Emergency Room South |
| Laredo, Texas | — | Leased |
Doctors Hospital Emergency Room Wright Ranch | | Laredo, Texas | — | Owned |
Fort Duncan Regional Medical Center |
| Eagle Pass, Texas | 101 | Owned |
The George Washington University Hospital (17) |
| Washington, D.C. | 395 | Leased |
Henderson Hospital |
| Henderson, Nevada | 303 | Owned |
ER at Cadence | | Henderson, Nevada | — | Owned |
ER at Green Valley Ranch |
| Henderson, Nevada | — | Owned |
Lakewood Ranch Medical Center |
| Lakewood Ranch, Florida | 120 | Owned |
ER at Fruitville |
| Sarasota, Florida | — | Owned |
Manatee Memorial Hospital |
| Bradenton, Florida | 295 | Owned |
ER at Palma Sola |
| Bradenton, Florida | — | Owned |
ER at Sun City Center |
| Wimauma, Florida | — | Owned |
Manatee ER at Bayshore Gardens |
| Bradenton, Florida | — | Owned |
Northern Nevada Medical Center |
| Sparks, Nevada | 124 | Owned |
| | | | |
Name of Facility
|
| Location
| Number of
Beds
| Real
Property
Ownership
Interest
|
Northwest Specialty Hospital (Behavioral Health) |
| Reno, Nevada | 70 | Owned |
Sierra Medical Center | | Reno, Nevada | 158 | Owned |
ER at Damonte Ranch |
| Reno, Nevada | — | Owned |
ER at McCarran NW |
| Reno, Nevada | — | Owned |
ER at Spanish Springs |
| Sparks, Nevada | — | Owned |
Northwest Texas Healthcare System |
| Amarillo, Texas | 405 | Owned |
Northwest Texas Healthcare System Behavioral Health |
| Amarillo, Texas | 90 | Owned |
Northwest Emergency at Tascosa | | Amarillo, Texas | — | Owned |
Northwest Emergency at Town Square |
| Amarillo, Texas | — | Owned |
Northwest Emergency on Georgia |
| Amarillo, Texas | — | Owned |
Palmdale Regional Medical Center |
| Palmdale, California | 184 | Owned |
South Texas Health System (2) |
|
|
|
|
South Texas Health System Edinburg/South Texas Health System Children’s (2) |
| Edinburg, Texas | 294 | Owned |
South Texas Health System Behavioral (2) |
| Edinburg, Texas | 134 | Owned |
South Texas Health System Heart (2) |
| McAllen, Texas | 60 | Owned |
South Texas Health System McAllen (1) (2) |
| McAllen, Texas | 431 | Leased |
South Texas Health System ER Alamo (2) |
| Alamo, Texas | — | Owned |
South Texas Health System ER McColl (2) |
| Edinburg, Texas | — | Owned |
South Texas Health System ER Mission (1) (2) |
| Mission, Texas | — | Leased |
South Texas Health System ER Monte Cristo (2) |
| Edinburg, Texas | — | Owned |
South Texas Health System ER Pharr (2) |
| Pharr, Texas | — | Owned |
South Texas Health System ER Ware Road (2) |
| McAllen, Texas | — | Owned |
South Texas Health System ER Weslaco (1) (2) |
| Weslaco, Texas | — | Leased |
Southwest Healthcare System |
|
|
|
|
Southwest Healthcare Inland Valley Hospital |
| Wildomar, California | 120 | Owned |
Southwest Healthcare Rancho Springs Hospital |
| Murrieta, California | 120 | Owned |
Spring Valley Hospital Medical Center |
| Las Vegas, Nevada | 364 | Owned |
ER at Blue Diamond |
| Las Vegas, Nevada | — | Owned |
Valley Health Specialty Hospital |
| Las Vegas, Nevada | 66 | Owned |
St. Mary’s Regional Medical Center |
| Enid, Oklahoma | 229 | Owned |
Summerlin Hospital Medical Center |
| Las Vegas, Nevada | 490 | Owned |
ER at South Summerlin | | Las Vegas, Nevada | — | Owned |
Temecula Valley Hospital |
| Temecula, California | 140 | Owned |
Texoma Medical Center |
| Denison, Texas | 354 | Owned |
TMC Behavioral Health Center |
| Sherman, Texas | 60 | Owned |
ER at Anna |
| Anna, Texas | — | Owned |
ER at Sherman |
| Sherman, Texas | — | Owned |
Valley Hospital Medical Center |
| Las Vegas, Nevada | 306 | Owned |
Elite Medical Center (ER) |
| Las Vegas, Nevada | — | Owned |
ER at Desert Springs |
| Las Vegas, Nevada | — | Owned |
ER at North Las Vegas |
| North Las Vegas, Nevada | — | Owned |
Wellington Regional Medical Center (1) |
| Wellington, Florida | 235 | Leased |
ER at Westlake |
| Westlake, Florida | — | Leased |
West Henderson Hospital………………………………….. |
| Henderson, Nevada | 150 | Owned |
Inpatient Behavioral Health Care Facilities
| | | | |
United States: |
|
|
|
|
Name of Facility
|
| Location
| Number of
Beds
| Real
Property
Ownership
Interest
|
Alabama Clinical Schools |
| Birmingham, Alabama | 80 | Owned |
Alliance Health Center |
| Meridian, Mississippi | 214 | Owned |
Anchor Hospital |
| Atlanta, Georgia | 122 | Owned |
Arbour Hospital |
| Jamaica Plain, Massachusetts | 142 | Owned |
Arrowhead Behavioral Health (14) |
| Maumee, Ohio | 48 | Owned |
Aspen Grove Behavioral Hospital |
| Orem, Utah | 80 | Owned |
Austin Oaks Hospital |
| Austin, Texas | 80 | Owned |
Beaumont Behavioral Health (16) |
| Dearborn, Michigan | 144 | Leased |
Behavioral Hospital of Bellaire |
| Houston, Texas | 124 | Leased |
Belmont Pines Hospital |
| Youngstown, Ohio | 127 | Owned |
Benchmark Behavioral Health Systems |
| Woods Cross, Utah | 94 | Owned |
BHC Alhambra Hospital |
| Rosemead, California | 115 | Owned |
Black Bear Lodge |
| Sautee Nacoochee, Georgia | 115 | Owned |
Bloomington Meadows Hospital |
| Bloomington, Indiana | 78 | Owned |
Brentwood Behavioral Healthcare |
| Flowood, Mississippi | 133 | Owned |
Brentwood Hospital |
| Shreveport, Louisiana | 260 | Owned |
The Bridgeway |
| North Little Rock, Arkansas | 127 | Owned |
The Brook Hospital—Dupont |
| Louisville, Kentucky | 88 | Owned |
The Brook Hospital—KMI |
| Louisville, Kentucky | 110 | Owned |
Brooke Glen Behavioral Hospital |
| Fort Washington, Pennsylvania | 146 | Owned |
Brynn Marr Hospital |
| Jacksonville, North Carolina | 102 | Owned |
Calvary Healing Center |
| Phoenix, Arizona | 68 | Owned |
Canyon Creek Behavioral Health (1) |
| Temple, Texas | 102 | Leased |
Canyon Ridge Hospital |
| Chino, California | 157 | Owned |
The Carolina Center for Behavioral Health |
| Greer, South Carolina | 156 | Owned |
Cedar Creek Hospital |
| St. Johns, Michigan | 69 | Owned |
Cedar Hills Hospital (7) |
| Portland, Oregon | 98 | Owned |
Cedar Ridge Behavioral Hospital |
| Oklahoma City, Oklahoma | 60 | Owned |
Cedar Ridge Behavioral Hospital at Bethany |
| Bethany, Oklahoma | 56 | Owned |
Cedar Ridge Residential Treatment Center |
| Oklahoma City, Oklahoma | 56 | Owned |
Cedar Springs Hospital |
| Colorado Springs, Colorado | 110 | Owned |
Centennial Peaks Hospital |
| Louisville, Colorado | 104 | Owned |
Center for Change |
| Orem, Utah | 66 | Owned |
Central Florida Behavioral Hospital |
| Orlando, Florida | 174 | Owned |
Clarion Psychiatric Center |
| Clarion, Pennsylvania | 112 | Owned |
Clive Behavioral Health (1) (11) |
| Clive, Iowa | 100 | Leased |
Coastal Behavioral Health |
| Savannah, Georgia | 50 | Owned |
Coastal Harbor Treatment Center |
| Savannah, Georgia | 145 | Owned |
Columbus Behavioral Center for Children and Adolescents |
| Columbus, Indiana | 57 | Owned |
Compass Intervention Center |
| Memphis, Tennessee | 148 | Owned |
Copper Hills Youth Center |
| West Jordan, Utah | 164 | Owned |
Coral Shores Behavioral Health |
| Stuart, Florida | 80 | Owned |
Cumberland Hall Hospital |
| Hopkinsville, Kentucky | 97 | Owned |
Cumberland Hospital for Children and Adolescents |
| New Kent, Virginia | 108 | Owned |
Cypress Creek Hospital |
| Houston, Texas | 128 | Owned |
Del Amo Behavioral Health System |
| Torrance, California | 166 | Owned |
Diamond Grove Center |
| Louisville, Mississippi | 61 | Owned |
Dover Behavioral Health System |
| Dover, Delaware | 104 | Owned |
El Paso Behavioral Health System |
| El Paso, Texas | 166 | Owned |
Emerald Coast Behavioral Hospital |
| Panama City, Florida | 86 | Owned |
Fairfax |
|
|
|
|
Fairfax Behavioral Health |
| Kirkland, Washington | 157 | Owned |
Fairfax Behavioral Health—Everett |
| Everett, Washington | 30 | Leased |
Fairfax Behavioral Health—Monroe |
| Monroe, Washington | 34 | Leased |
Fairmount Behavioral Health System |
| Philadelphia, Pennsylvania | 239 | Owned |
| | | | |
United States: |
|
|
|
|
Name of Facility
|
| Location
| Number of
Beds
| Real
Property
Ownership
Interest
|
Forest View Hospital |
| Grand Rapids, Michigan | 108 | Owned |
Fort Lauderdale Behavioral Health Center |
| Fort Lauderdale, Florida | 182 | Owned |
Foundations Behavioral Health |
| Doylestown, Pennsylvania | 122 | Leased |
Foundations for Living |
| Mansfield, Ohio | 84 | Owned |
Fox Run Center |
| St. Clairsville, Ohio | 100 | Owned |
Fremont Hospital |
| Fremont, California | 148 | Owned |
Friends Hospital (13) |
| Philadelphia, Pennsylvania | 219 | Owned |
Fuller Hospital |
| Attleboro, Massachusetts | 109 | Owned |
Garfield Park Behavioral Hospital |
| Chicago, Illinois | 88 | Owned |
Glen Oaks Hospital |
| Greenville, Texas | 54 | Owned |
Granite Hills Hospital |
| West Allis, Wisconsin | 120 | Leased |
Gulf Coast Treatment Center |
| Fort Walton Beach, Florida | 28 | Owned |
Gulfport Behavioral Health System |
| Gulfport, Mississippi | 109 | Owned |
Hampton Behavioral Health Center |
| Westampton, New Jersey | 120 | Owned |
Harbor Point Behavioral Health Center |
| Portsmouth, Virginia | 186 | Owned |
Hartgrove Behavioral Health System |
| Chicago, Illinois | 160 | Owned |
Havenwyck Hospital |
| Auburn Hills, Michigan | 253 | Owned |
Heartland Behavioral Health Services |
| Nevada, Missouri | 137 | Owned |
Heritage Oaks Hospital |
| Sacramento, California | 125 | Owned |
Heritage Oaks Patient Enrichment Center |
| Sacramento, California | 16 | Owned |
Hermitage Hall |
| Nashville, Tennessee | 111 | Owned |
Hickory Trail Hospital |
| DeSoto, Texas | 86 | Owned |
Highlands Behavioral Health System |
| Littleton, Colorado | 86 | Owned |
Hill Crest Behavioral Health Services |
| Birmingham, Alabama | 221 | Owned |
Holly Hill Hospital |
| Raleigh, North Carolina | 296 | Owned |
The Horsham Clinic |
| Ambler, Pennsylvania | 206 | Owned |
HRI Hospital |
| Brookline, Massachusetts | 66 | Owned |
The Hughes Center |
| Danville, Virginia | 96 | Owned |
Inland Northwest Behavioral Health (9) |
| Spokane, Washington | 100 | Owned |
Intermountain Hospital |
| Boise, Idaho | 155 | Owned |
Kempsville Center for Behavioral Health |
| Norfolk, Virginia | 106 | Owned |
KeyStone Center |
| Chester, Pennsylvania | 153 | Owned |
Kingwood Pines Hospital |
| Kingwood, Texas | 116 | Owned |
La Amistad Behavioral Health Services |
| Maitland, Florida | 85 | Owned |
Lakeside Behavioral Health System |
| Memphis, Tennessee | 373 | Owned |
Lancaster Behavioral Health Hospital (8) |
| Lancaster, Pennsylvania | 126 | Owned |
Laurel Heights Hospital |
| Atlanta, Georgia | 132 | Owned |
Laurel Oaks Behavioral Health Center |
| Dothan, Alabama | 118 | Owned |
Laurel Ridge Treatment Center |
| San Antonio, Texas | 330 | Owned |
Liberty Point Behavioral Healthcare |
| Stauton, Virginia | 42 | Owned |
Lighthouse Behavioral Health Hospital |
| Conway, South Carolina | 105 | Owned |
Lighthouse Care Center of Augusta |
| Augusta, Georgia | 82 | Owned |
Lincoln Prairie Behavioral Health Center |
| Springfield, Illinois | 97 | Owned |
Lincoln Trail Behavioral Health System |
| Radcliff, Kentucky | 140 | Owned |
Mayhill Hospital |
| Denton, Texas | 59 | Leased |
McDowell Center for Children |
| Dyersburg, Tennessee | 32 | Owned |
The Meadows Psychiatric Center |
| Centre Hall, Pennsylvania | 119 | Owned |
Meridell Achievement Center |
| Liberty Hill, Texas | 134 | Owned |
Mesilla Valley Hospital |
| Las Cruces, New Mexico | 120 | Owned |
Michael’s House |
| Palm Springs, California | 60 | Owned |
Michiana Behavioral Health |
| Plymouth, Indiana | 83 | Owned |
Midwest Center for Youth and Families |
| Kouts, Indiana | 75 | Owned |
Millwood Hospital |
| Arlington, Texas | 134 | Leased |
Mountain Youth Academy |
| Mountain City, Tennessee | 122 | Owned |
Newport News Behavioral Health Center |
| Newport News, Virginia | 132 | Owned |
| | | | |
United States: |
|
|
|
|
Name of Facility
|
| Location
| Number of
Beds
| Real
Property
Ownership
Interest
|
North Spring Behavioral Healthcare |
| Leesburg, Virginia | 127 | Leased |
North Star Hospital |
| Anchorage, Alaska | 74 | Owned |
Chris Kyle Patriots Hospital |
| Anchorage, Alaska | 66 | Owned |
North Star DeBarr Residential Treatment Center |
| Anchorage, Alaska | 30 | Owned |
North Star Palmer Residential Treatment Center |
| Palmer, Alaska | 30 | Owned |
Oak Plains Academy |
| Ashland City, Tennessee | 60 | Owned |
Okaloosa Youth Academy |
| Crestview, Florida | 72 | Leased |
Old Vineyard Behavioral Health Services |
| Winston-Salem, North Carolina | 164 | Owned |
Palm Point Behavioral Health |
| Titusville, FL | 74 | Owned |
Palm Shores Behavioral Health Center |
| Bradenton, Florida | 65 | Owned |
Palmetto Lowcountry Behavioral Health |
| North Charleston, South Carolina | 108 | Owned |
Palo Verde Behavioral Health |
| Tucson, Arizona | 84 | Owned |
Parkwood Behavioral Health System |
| Olive Branch, Mississippi | 148 | Owned |
The Pavilion Behavioral Health System |
| Champaign, Illinois | 122 | Owned |
Peachford Hospital |
| Atlanta, Georgia | 246 | Owned |
Pembroke Hospital |
| Pembroke, Massachusetts | 120 | Owned |
Pinnacle Pointe Behavioral Healthcare System |
| Little Rock, Arkansas | 127 | Owned |
Poplar Springs Hospital |
| Petersburg, Virginia | 208 | Owned |
Prairie St John’s |
| Fargo, North Dakota | 132 | Owned |
PRIDE Institute |
| Eden Prairie, Minnesota | 42 | Owned |
Provo Canyon School |
| Provo, Utah | 250 | Owned |
Psychiatric Institute of Washington |
| Washington, D.C. | 130 | Owned |
Quail Run Behavioral Health |
| Phoenix, Arizona | 116 | Owned |
The Ridge Behavioral Health System |
| Lexington, Kentucky | 110 | Owned |
Rivendell Behavioral Health Hospital |
| Bowling Green, Kentucky | 125 | Owned |
Rivendell Behavioral Health Services of Arkansas |
| Benton, Arkansas | 80 | Owned |
River Oaks Hospital |
| Harahan, Louisiana | 126 | Owned |
River Park Hospital |
| Huntington, West Virginia | 187 | Owned |
River Point Behavioral Health |
| Jacksonville, Florida | 84 | Owned |
River Vista Behavioral Health |
| Madera, California | 128 | Owned |
Riveredge Hospital |
| Forest Park, Illinois | 210 | Owned |
Rockford Center |
| Newark, Delaware | 148 | Owned |
Rolling Hills Hospital |
| Franklin, Tennessee | 130 | Owned |
Roxbury Treatment Center |
| Shippensburg, Pennsylvania | 112 | Owned |
Saint Simons By-The-Sea |
| Saint Simons Island, Georgia | 101 | Owned |
Salt Lake Behavioral Health |
| Salt Lake City, Utah | 118 | Leased |
San Marcos Treatment Center |
| San Marcos, Texas | 265 | Owned |
SandyPines Residential Treatment Center |
| Jupiter, Florida | 149 | Owned |
Sierra Vista Hospital |
| Sacramento, California | 171 | Owned |
Skywood Recovery |
| Augusta, Michigan | 100 | Owned |
Southeast Behavioral Health (15) |
| Cape Girardeau, Missouri | 102 | Owned |
Spring Mountain Sahara |
| Las Vegas, Nevada | 30 | Owned |
Spring Mountain Treatment Center |
| Las Vegas, Nevada | 110 | Owned |
Springwoods Behavioral Health |
| Fayetteville, Arkansas | 80 | Owned |
Stonington Institute |
| North Stonington, Connecticut | 64 | Owned |
Streamwood Behavioral Healthcare System |
| Streamwood, Illinois | 178 | Owned |
Summit Oaks Hospital |
| Summit, New Jersey | 126 | Owned |
SummitRidge Hospital |
| Lawrenceville, Georgia | 106 | Owned |
Suncoast Behavioral Health Center |
| Bradenton, Florida | 60 | Owned |
Texas NeuroRehab Center |
| Austin, Texas | 137 | Owned |
Three Rivers Behavioral Health |
| West Columbia, South Carolina | 129 | Owned |
Three Rivers Midlands |
| West Columbia, South Carolina | 64 | Owned |
Turning Point Care Center |
| Moultrie, Georgia | 79 | Owned |
University Behavioral Center |
| Orlando, Florida | 112 | Owned |
University Behavioral Health of Denton |
| Denton, Texas | 104 | Owned |
| | | | |
United States: |
|
|
|
|
Name of Facility
|
| Location
| Number of
Beds
| Real
Property
Ownership
Interest
|
Valle Vista Health System |
| Greenwood, Indiana | 140 | Owned |
Valley Hospital |
| Phoenix, Arizona | 122 | Owned |
Via Linda Behavioral Hospital (12) |
| Scottsdale, Arizona | 120 | Leased |
The Vines Hospital |
| Ocala, Florida | 98 | Owned |
Virginia Beach Psychiatric Center |
| Virginia Beach, Virginia | 100 | Owned |
Wekiva Springs Center |
| Jacksonville, Florida | 120 | Owned |
Wellstone Regional Hospital |
| Jeffersonville, Indiana | 100 | Owned |
West Oaks Hospital |
| Houston, Texas | 176 | Owned |
Willow Springs Center |
| Reno, Nevada | 116 | Owned |
Windmoor Healthcare of Clearwater |
| Clearwater, Florida | 144 | Owned |
Windsor Laurelwood Center for Behavioral Medicine |
| Willoughby, Ohio | 160 | Leased |
Wyoming Behavioral Institute |
| Casper, Wyoming | 137 | Owned |
| | | | |
United Kingdom: |
|
|
|
|
Name of Facility
|
| Location
| Number of
Beds
| Real
Property
Ownership
Interest
|
Adarna House |
| Bradford, UK | 9 | Owned |
Adele Cottages |
| Rainworth, UK | 4 | Owned |
Amberwood Lodge |
| Dorset, UK | 9 | Owned |
Ashbrook |
| Birmingham, UK | 16 | Owned |
Ashfield House |
| Huddersfield, UK | 6 | Owned |
Beacon House Lower |
| Bradford, UK | 8 | Owned |
Beacon House Upper |
| Bradford, UK | 8 | Owned |
Beckly |
| Halifax, UK | 12 | Owned |
Beeches |
| Retford, UK | 12 | Owned |
Birches |
| Newark, UK | 6 | Owned |
Broughton House |
| Lincolnshire, UK | 34 | Owned |
Broughton Lodge |
| Macclesfield, UK | 20 | Owned |
Chaseways |
| Sawbridgeworth, UK | 6 | Owned |
Cherry Tree House |
| Mansfield Woodhouse, UK | 6 | Owned |
Colchester – Chestnut Court | | Essex, UK | 8 | Owned |
Conifers |
| Derby, UK | 7 | Owned |
Cygnet Acer |
| Chesterfield, UK | 14 | Owned |
Cygnet Acer 2 |
| Chesterfield, UK | 14 | Owned |
Cygnet Alders Clinic |
| Gloucester, UK | 20 | Owned |
Cygnet Appletree |
| Meadowfield, UK | 26 | Owned |
Cygnet Aspen Clinic |
| Doncaster, UK | 16 | Owned |
Cygnet Aspen House |
| Doncaster, UK | 20 | Owned |
Cygnet Bostall House |
| Abbey Wood, UK | 6 | Owned |
Cygnet Brunel |
| Bristol, UK | 32 | Owned |
Cygnet Cedar Vale |
| East Bridgeford, UK | 16 | Owned |
Cygnet Cedars |
| Birmingham, UK | 24 | Owned |
Cygnet Churchill |
| London, UK | 57 | Owned |
Cygnet Delfryn House |
| Flintshire, UK | 28 | Owned |
Cygnet Delfryn Lodge |
| Flintshire, UK | 24 | Owned |
Cygnet Elms |
| Birmingham, UK | 10 | Owned |
Cygnet Fountains |
| Blackburn, UK | 34 | Owned |
Cygnet Grange |
| Sutton-in-Ashfield, UK | 8 | Owned |
Cygnet Heathers |
| West Bromwich, UK | 20 | Owned |
Cygnet Hospital—Beckton |
| London, UK | 62 | Owned |
Cygnet Hospital—Bierley |
| Bradford, UK | 63 | Owned |
Cygnet Hospital—Blackheath |
| London, UK | 32 | Leased |
| | | | | |
United Kingdom: |
|
|
|
|
Name of Facility
|
| Location
| Number of
Beds
| Real
Property
Ownership
Interest
|
Cygnet Hospital—Bury |
| Bury, UK | 187 | Owned |
Cygnet Hospital—Clifton |
| Nottingham, UK | 25 | Owned |
Cygnet Hospital—Derby |
| Derby, UK | 50 | Owned |
Cygnet Hospital—Ealing |
| Ealing, UK | 26 | Owned |
Cygnet Hospital—Godden Green |
| Sevenoaks, UK | 39 | Owned |
Cygnet Hospital—Harrogate |
| Harrogate, UK | 36 | Owned |
Cygnet Hospital—Harrow |
| Harrow, UK | 64 | Owned |
Cygnet Hospital—Hexham |
| Hexham, UK | 27 | Owned |
Cygnet Hospital—Kewstoke |
| Kewstoke, UK | 72 | Owned |
Cygnet Hospital—Maidstone |
| Maidstone, UK | 65 | Owned |
Cygnet Hospital—Oldbury | . | Oldbury, UK | 27 | Owned |
Cygnet Hospital—Sheffield |
| Sheffield, UK | 57 | Owned |
Cygnet Hospital—Sherwood |
| Mansfield, UK | 44 | Owned |
Cygnet Hospital—Stevenage |
| Stevenage, UK | 88 | Owned |
Cygnet Hospital—Taunton |
| Taunton, UK | 57 | Owned |
Cygnet Hospital—Woking |
| Woking, UK | 62 | Owned |
Cygnet Hospital—Wolverhampton |
| Wolverhampton, UK | 29 | Owned |
Cygnet Hospital—Wyke |
| Bradford, UK | 52 | Owned |
Cygnet Hospital Colchester - Highwoods |
| Colchester, UK | 20 | Owned |
Cygnet Hospital Colchester - Larch Court |
| Essex, UK | 4 | Owned |
Cygnet Hospital Colchester - Oak Court |
| Essex, UK | 12 | Owned |
Cygnet Hospital Colchester - Ramsey |
| Colchester, UK | 21 | Owned |
Cygnet Joyce Parker Hospital |
| Coventry, UK | 57 | Owned |
Cygnet Lodge |
| Sutton-in-Ashfield, UK | 8 | Owned |
Cygnet Lodge—Brighouse |
| Brighouse, UK | 25 | Owned |
Cygnet Lodge—Kenton |
| Middlesex, UK | 15 | Owned |
Cygnet Lodge—Lewisham |
| London, UK | 17 | Owned |
Cygnet Lodge—Salford |
| Manchester, UK | 24 | Owned |
Cygnet Lodge—Woking |
| Woking, UK | 32 | Owned |
Cygnet Manor |
| Shirebrook, UK | 20 | Owned |
Cygnet Newham House |
| Middlesbrough, UK | 20 | Owned |
Cygnet Nield House |
| Crewe, UK | 30 | Owned |
Cygnet Oaks |
| Barnsley, UK | 35 | Owned |
Cygnet Paddocks |
| Widnes, UK | 30 | Owned |
Cygnet Pindar House |
| Barnsley, UK | 22 | Owned |
Cygnet Raglan House |
| West Midlands, UK | 25 | Owned |
Cygnet Sedgley House |
| Wolverhampton, UK | 20 | Owned |
Cygnet Sedgley Lodge |
| Wolverhampton, UK | 14 | Owned |
Cygnet Sherwood House |
| Mansfield, UK | 30 | Owned |
Cygnet Sherwood Lodge |
| Mansfield, UK | 17 | Owned |
Cygnet St. Augustine’s |
| Stoke on Trent, UK | 32 | Owned |
Cygnet St. Teilo House |
| Gwent, UK | 23 | Owned |
Cygnet St. Williams |
| Darlington, UK | 12 | Owned |
Cygnet Storthfield House |
| Derbyshire, UK | 22 | Owned |
Cygnet Victoria House |
| Darlington, UK | 26 | Owned |
Cygnet Views |
| Matlock, UK | 10 | Owned |
Cygnet Wallace Hospital |
| Dundee, UK | 10 | Owned |
Cygnet Wast Hills |
| Birmingham, UK | 26 | Owned |
Dene Brook |
| Rotherham, UK | 13 | Owned |
Devon Lodge |
| Southampton, UK | 12 | Owned |
Dove Valley Mews |
| Barnsley, UK | 10 | Owned |
Ducks Halt |
| Essex, UK | 5 | Owned |
Ellen Mhor |
| Dundee, UK | 12 | Owned |
Elston House |
| Newark, UK | 8 | Owned |
Fairways |
| Ipswich, UK | 8 | Owned |
| | | | |
United Kingdom: |
|
|
|
|
Name of Facility
|
| Location
| Number of
Beds
| Real
Property
Ownership
Interest
|
The Fields |
| Sheffield, UK | 54 | Owned |
Gables |
| Essex, UK | 7 | Owned |
Gledcliffe Road |
| Huddersfield, UK | 6 | Owned |
Gledholt |
| Huddersfield, UK | 9 | Owned |
Gledholt Mews |
| Huddersfield, UK | 21 | Owned |
Glyn House |
| Stoke on Trent, UK | 5 | Owned |
Hansa Lodge |
| Rainham, UK | 5 | Owned |
Hawkstone |
| Keighley, UK | 10 | Owned |
Hollyhurst |
| Darlington, UK | 19 | Owned |
Hope House |
| Hartlepool, UK | 11 | Owned |
Kirkside House |
| Leeds, UK | 7 | Owned |
Kirkside Lodge |
| Leeds, UK | 8 | Owned |
Langdale Coach House |
| Huddersfield, UK | 3 | Owned |
Langdale House |
| Huddersfield, UK | 8 | Owned |
Lindsay House |
| Dundee, UK | 2 | Owned |
Longfield House |
| Bradford, UK | 9 | Owned |
Lowry House |
| Hyde, UK | 12 | Owned |
Malborn & Teroan |
| Mansfield, UK | 6 | Owned |
Marion House |
| Derby, UK | 5 | Owned |
Meadows Mews |
| Tipton, UK | 10 | Owned |
Morgan House |
| Stoke on Trent, UK | 5 | Owned |
Nightingale |
| Dorset, UK | 10 | Owned |
Norcott House |
| Liversedge, UK | 11 | Owned |
Norcott Lodge |
| Liversedge, UK | 9 | Owned |
Oakhurst Lodge |
| Hampshire, UK | 8 | Owned |
Oaklands |
| Northumberland, UK | 19 | Owned |
Old Leigh House |
| Essex, UK | 7 | Leased |
The Orchards |
| Essex, UK | 5 | Owned |
Outwood |
| Leeds, UK | 10 | Owned |
Oxley Lodge |
| Huddersfield, UK | 4 | Owned |
Oxley Woodhouse |
| Huddersfield, UK | 13 | Owned |
Pines |
| Mansfield Woodhouse, UK | 7 | Owned |
Ranaich House |
| Dunblane, UK | 14 | Owned |
Redlands |
| Darlington, UK | 5 | Owned |
Rhyd Alyn |
| Flintshire, UK | 6 | Owned |
River View |
| Darlington, UK | 4 | Owned |
Shear Meadow |
| Hemel Hempstead, UK | 4 | Owned |
Sherwood Lodge Step Down |
| Mansfield, UK | 9 | Owned |
The Squirrels |
| Hampshire, UK | 9 | Owned |
4, 5, 7 The Sycamores |
| South Normanton, UK | 6 | Owned |
15 The Sycamores |
| South Normanton, UK | 4 | Owned |
Tabley House Nursing Home |
| Knutsford, UK | 51 | Leased |
Thistle House |
| Dundee, UK | 10 | Owned |
Thornfield Grange |
| Bishop Auckland, UK | 9 | Owned |
Thornfield House |
| Bradford, UK | 7 | Owned |
Thors Park |
| Essex, UK | 14 | Owned |
Toller Road |
| Leicestershire, UK | 8 | Owned |
Trinity House |
| Lockerbie, UK | 13 | Owned |
Trinity Lodge |
| Lockerbie, UK | 6 | Owned |
Tupwood Gate Nursing Home |
| Caterham, UK | 33 | Owned |
Ty Alarch |
| Merthyr Tydfil | 6 | Owned |
1Vincent Court |
| Lancashire, UK | 5 | Owned |
Walkern Lodge |
| Stevenage, UK | 4 | Owned |
Willow House |
| Birmingham, UK | 8 | Owned |
Woodcross & Turls Hill |
| Wolverhampton, UK | 8 | Owned |
| | | | |
United Kingdom: |
|
|
|
|
Name of Facility
|
| Location
| Number of
Beds
| Real
Property
Ownership
Interest
|
Woodrow House |
| Stockport, UK | 9 | Owned |
| | | | |
Puerto Rico: | |
|
|
|
Name of Facility
| | Location
| Number of
Beds
| Real
Property
Ownership
Interest
|
First Hospital Panamericano—Cidra | | Cidra, Puerto Rico | 165 | Owned |
First Hospital Panamericano—Ponce | | Ponce, Puerto Rico | 30 | Owned |
First Hospital Panamericano—San Juan | | San Juan, Puerto Rico | 45 | Owned |
| |
|
|
|
Outpatient Behavioral Health Care Facilities
| | | |
United States: |
|
|
|
Name of Facility
|
| Location
| Real
Property
Ownership
Interest
|
Arbour Counseling Services |
| Rockland, Massachusetts | Owned |
The Canyon at Santa Monica |
| Los Angeles, California | Leased |
Foundations Health High Point | | High Point, North Carolina | Leased |
Foundations San Francisco |
| San Francisco, California | Leased |
Michael’s House Outpatient |
| Palm Springs, California | Leased |
The Pointe Outpatient Behavioral Health Services |
| Little Rock, Arkansas | Leased |
The Recovery Center | | Wichita Falls, Texas | Leased |
Saint Louis Behavioral Medicine Institute |
| St. Louis, Missouri | Owned |
Skywood Outpatient |
| Royal Oak, Michigan | Leased |
Talbott Recovery |
| Atlanta, Georgia | Owned |
Thousand Branches Wellness, Arden Hills | | Arden Hills, Minnesota | Leased |
Thousand Branches Wellness, Chicago Loop | | Chicago, Illinois | Leased |
Thousand Branches Wellness, Houston | | Houston, Texas | Leased |
Thousand Branches Wellness, Mission Valley | | San Diego, California | Leased |
| | | |
United Kingdom: | | | |
Name of Facility
| | Location
| Real
Property
Ownership
Interest
|
Long Eaton Day Services | | Nottingham, UK | Owned |
Sheffield Day Services | | Sheffield, UK | Owned |
| | | |
|
|
|
|
Outpatient Centers and Surgical Hospital |
Name of Facility
|
| Location
| Real
Property
Ownership Interest
|
|
|
|
|
Cancer Care Institute of Carolina |
| Aiken, South Carolina | Owned |
Cardiovascular Institute of Amarillo (19) | | Amarillo, TX | Leased |
Cornerstone Regional Hospital (3) |
| Edinburg, Texas | Leased |
Las Vegas Institute for Advanced Surgery (19) |
| Las Vegas, NV | Leased |
| | | |
|
|
|
|
Outpatient Centers and Surgical Hospital |
Name of Facility
|
| Location
| Real
Property
Ownership Interest
|
|
|
|
|
Manatee Diagnostic Center |
| Bradenton, Florida | Leased |
Palms Wellington Surgical Center (5) |
| Royal Palm Beach, Florida | Leased |
Personalized Radiation Oncology (18) |
| Reno, Nevada | Leased |
Quail Surgical and Pain Management Center (10) |
| Reno, Nevada | Leased |
Riverside Medical Clinic Surgery Center |
| Riverside, California | Leased |
The Surgery Center of Aiken |
| Aiken, South Carolina | Owned |
Temecula Valley Day Surgery (4) |
| Murrieta, California | Leased |
(1)Real property leased from Universal Health Realty Income Trust.
(2)These entities are consolidated under one license operating as the South Texas Health System.
(3)We manage and own a noncontrolling interest of approximately 50% in the entity that operates this facility.
(4)We manage and own a majority interest in an LLC that owns and operates this center.
(5)We own a noncontrolling ownership interest of approximately 50% in the entity that operates this facility that is managed by a third-party.
(6)We hold a 93% ownership interest in this facility through both general and limited partnership interests. The remaining 7% ownership interest is held by unaffiliated third parties.
(7)Land of this facility is leased.
(8)We manage and own a noncontrolling interest of 50% in this facility. The remaining 50% ownership interest is held by an unaffiliated third party. Land of this facility is leased from the unaffiliated third party member.
(9)We manage and hold an 80% ownership interest in this facility. The remaining 20% ownership interest is held by an unaffiliated third party.
(10)We hold a 51% ownership interest in this facility. The remaining 49% ownership interest is held by unaffiliated third parties.
(11)We manage and hold a 52% ownership interest in this facility. The remaining 48% ownership interest is held by an unaffiliated third party.
(12)We manage and hold a 51% ownership interest in this facility. The remaining 49% ownership interest is held by an unaffiliated third party.
(13)We manage and hold an 80% ownership interest in this facility. The remaining 20% ownership interest is held by an unaffiliated third party.
(14)We manage and hold a 70% ownership interest in this facility. The remaining 30% ownership interest is held by an unaffiliated third party.
(15)We manage and hold a 75% ownership interest in this facility. The remaining 25% ownership interest is held by an unaffiliated third party.
(16)We manage and hold a 75% ownership interest in this facility. The remaining 25% ownership interest is held by an unaffiliated third party.
(17)The land of this facility is leased pursuant to the terms of a lease that is scheduled to expire in August, 2082. The lease contains one, twenty-five year renewal option.
(18)We own a noncontrolling ownership interest of 30% in the entity that operates this facility that is managed by a third-party.
(19)We hold a 51% ownership interest in this facility. The remaining 49% ownership interest is held by unaffiliated third parties.
We own or lease medical office buildings adjoining some of our hospitals. We believe that the leases on the facilities, medical office buildings and other real estate leased or owned by us do not impose any material limitation on our operations. The aggregate lease payments on facilities leased by us were $110 million in 2024, $107 million in 2023 and $104 million in 2022.
ITEM 3. Legal Proceedings
The information regarding our legal proceedings is contained in Note 8 to the Consolidated Financial Statements - Commitments and Contingencies, as included this Form 10-K, is incorporated herein by reference.
ITEM 4. Mine Safety Disclosures
Not applicable.
PART II
ITEM 5. Market for Registrant’s Common Equity, Related Stockholder Matters and Issuer Purchases of Equity Securities
Our Class B Common Stock is traded on the New York Stock Exchange under the symbol UHS. Shares of our Class A, Class C and Class D Common Stock are not traded in any public market, but are each convertible into shares of our Class B Common Stock on a share-for-share basis.
The number of stockholders of record as of January 31, 2025, were as follows:
| | | | |
Class A Common | | | 17 | |
Class B Common | | | 230 | |
Class C Common | | | 1 | |
Class D Common | | | 80 | |
Stock Repurchase Programs
As of January 1, 2024, we had an aggregate available repurchase authorization of $422.9 million under our stock repurchase program. In July, 2024, our Board of Directors authorized a $1.0 billion increase in our stock repurchase program. Pursuant to this program, shares of our Class B Common Stock may be repurchased, from time to time as conditions allow, on the open market or in negotiated private transactions. There is no expiration date for our stock repurchase programs.
As reflected below, during the fourth quarter of 2024, we have repurchased approximately 1.25 million shares at an aggregate cost of approximately $249.6 million (average price of $199.42 per share) pursuant to the terms of our stock repurchase program. In addition, during the three-month period ended December 31, 2024, 2,653 shares were repurchased in connection with income tax withholding obligations resulting from stock-based compensation programs. For the year ended December 31, 2024, we have repurchased approximately 2.98 million shares at an aggregate cost of approximately $598.5 million (average price of $200.65 per share). In addition, for the year ended December 31, 2024, 375,248 shares were repurchased in connection with income tax withholding obligations resulting from stock-based compensation programs.
As of December 31, 2024, we had an aggregate available repurchase authorization of $824.4 million pursuant to our stock repurchase program.
During the period of October 1, 2024 through December 31, 2024, we repurchased the following shares:
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
| | Additional
Dollars
Authorized
For
Repurchase
(in
thousands) | | | Total
number of
shares
purchased (1) | | | Total
number of
shares
cancelled | | | Average
price paid
per share
for forfeited
restricted
shares | | | Total
Number
of shares
purchased
as part of
publicly
announced
programs (2) | | | Average
price paid
per share
for shares
purchased
as part of
publicly
announced
program | | | Aggregate
purchase
price paid
(in thousands) | | | Maximum
number of
dollars that
may yet be
purchased
under the
program
(in
thousands) | |
October, 2024 | | | — | | | | 255,848 | | | | — | | | $ | 0.01 | | | | 255,000 | | | $ | 205.85 | | | $ | 52,491 | | | $ | 1,021,490 | |
November, 2024 | | | — | | | | 747,874 | | | | — | | | $ | 0.01 | | | | 746,745 | | | $ | 203.71 | | | $ | 152,121 | | | $ | 869,369 | |
December, 2024 | | | — | | | | 250,676 | | | | — | | | $ | 0.01 | | | | 250,000 | | | $ | 180.03 | | | $ | 45,008 | | | $ | 824,361 | |
Total October through
December | | $ | — | | | | 1,254,398 | | | | — | | | $ | 0.01 | | | | 1,251,745 | | | $ | 199.42 | | | $ | 249,620 | | | | |
(1)Includes shares that were repurchased in connection with income tax withholding obligations resulting from the exercise of stock options and the vesting of restricted stock grants.
(2)The only publicly announced program pursuant to which the shares were repurchased was the share repurchase program described above. There is no other plan or program that has expired during this time period. Also, there is no other plan or program that we have determined to terminate prior to expiration, or under which we do not intend to make further purchases.
Dividends
During the year ended December 31, 2024 we paid dividends of $0.80 per share. Dividend equivalents are accrued on unvested restricted stock units and are paid upon vesting of the restricted stock unit.
Our Credit Agreement contains covenants that include limitations on, among other things, dividends and stock repurchases (see below in Capital Resources-Credit Facilities and Outstanding Debt Securities).
Equity Compensation
Refer to Item 12. Security Ownership of Certain Beneficial Owners and Management and Related Stockholder Matters, of this report for information regarding securities authorized for issuance under our equity compensation plans.
Stock Price Performance Graph
The following graph compares the cumulative total stockholder return on our common stock with the cumulative total return on the stock included in the Standard & Poor’s 500 Index and a Peer Group Index during the five-year period ended December 31, 2024. The graph assumes an investment of $100 made in our common stock and each Index as of January 1, 2020 and has been weighted based on market capitalization. Note that our common stock price performance shown below should not be viewed as being indicative of future performance.
Companies in the peer group, which consist of companies in the S&P 500 Index or S&P MidCap 400 Index are as follows: Acadia Healthcare Company, Inc., Community Health Systems, Inc., HCA Healthcare, Inc., and Tenet Healthcare Corporation.
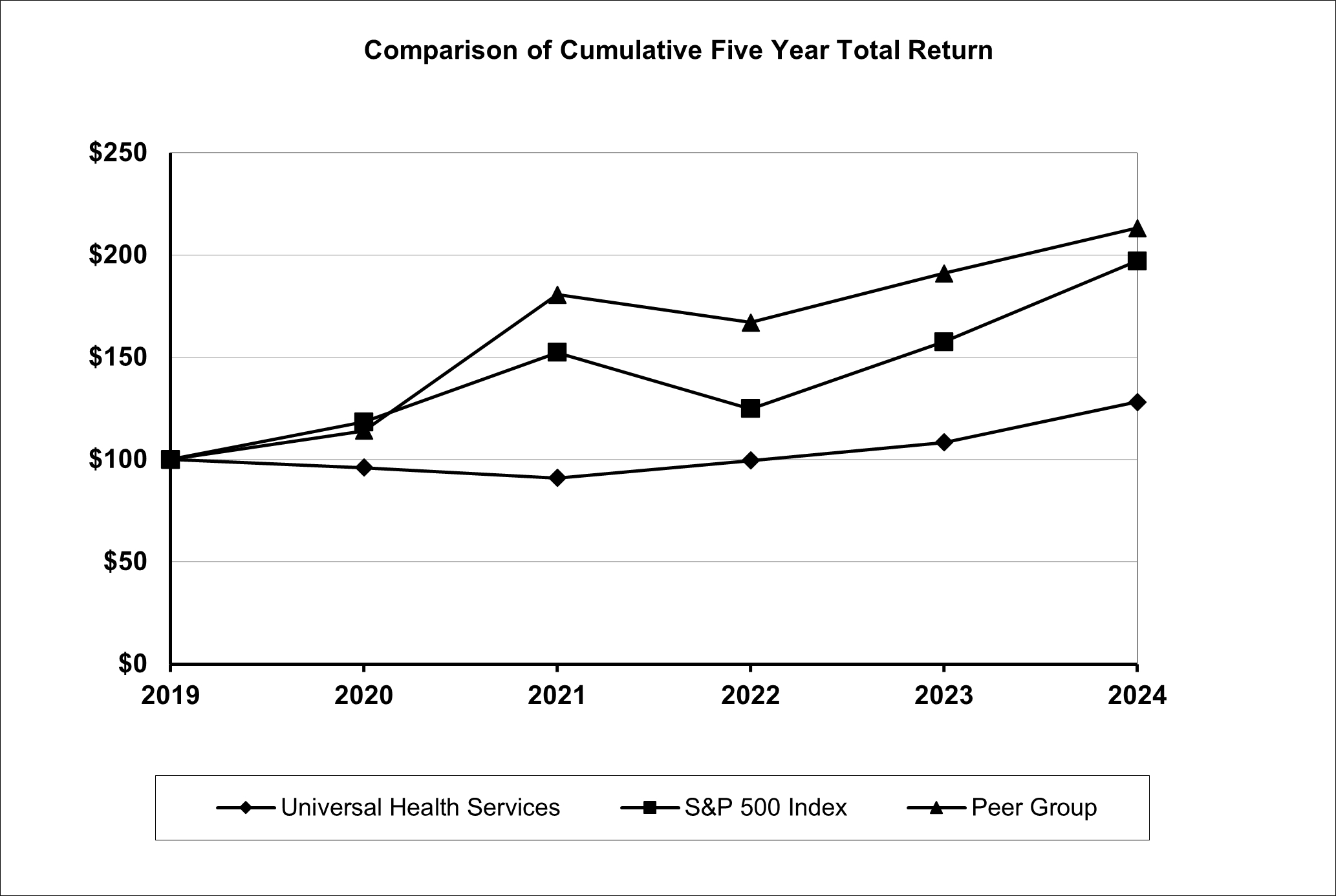
| | | | | | | | | | | | | | | | | | | | | | | | |
Company Name / Index |
| 2019 Base |
|
| 2020 | |
| 2021 |
|
| 2022 |
|
| 2023 |
|
| 2024 |
|
Universal Health Services, Inc. |
| $ | 100.00 |
|
| $ | 96.00 |
|
| $ | 91.04 |
|
| $ | 99.57 |
|
| $ | 108.37 |
|
| $ | 128.07 |
|
S&P 500 Index |
| $ | 100.00 |
|
| $ | 118.40 |
|
| $ | 152.39 |
|
| $ | 124.79 |
|
| $ | 157.59 |
|
| $ | 197.02 |
|
Peer Group |
| $ | 100.00 |
|
| $ | 114.05 |
|
| $ | 180.63 |
|
| $ | 167.00 |
|
| $ | 191.10 |
|
| $ | 213.16 |
|
ITEM 6. [RESERVED]
ITEM 7. Management’s Discussion and Analysis of Financial Condition and Results of Operations
The following Management’s Discussion and Analysis of Financial Condition and Results of Operations (“MD&A”) is intended to promote an understanding of our operating results and financial condition. The MD&A is provided as a supplement to, and should be read in conjunction with, our consolidated financial statements and the accompanying notes to the Consolidated Financial Statements, as included in this Annual Report on Form 10-K. The MD&A contains forward-looking statements that involve risks, uncertainties, and assumptions. Actual results may differ materially from those anticipated in these forward-looking statements as a result of various factors, including, but not limited to, those presented under Item 1A. Risk Factors, and below in Forward-Looking Statements and Risk Factors and as included elsewhere in this Annual Report on Form 10-K. This section generally discusses our results of operations for the year ended December 31, 2024, as compared to the year ended December 31, 2023. For discussion of our result of operations and changes in our financial condition for the year ended December 31, 2023 as compared to the year ended December 31, 2022, please refer to Part II, Item 7. Management’s Discussion and Analysis of Financial Condition and Results of Operations in our Annual Report on Form 10-K for the year ended December 31, 2023, as filed with the Securities and Exchange Commission on February 27, 2024.
Overview
Our principal business is owning and operating, through our subsidiaries, acute care hospitals and outpatient facilities and behavioral health care facilities.
As of February 26, 2025, we owned and/or operated 359 inpatient facilities and 60 outpatient and other facilities, including the following, located in 39 states, Washington, D.C., the United Kingdom and Puerto Rico:
Acute care facilities located in the U.S.:
•28 inpatient acute care hospitals;
•33 free-standing emergency departments, and;
•10 outpatient centers & 1 surgical hospital.
Behavioral health care facilities (331 inpatient facilities and 16 outpatient facilities):
Located in the U.S.:
•181 inpatient behavioral health care facilities, and;
•14 outpatient behavioral health care facilities.
Located in the U.K.:
•147 inpatient behavioral health care facilities, and;
•2 outpatient behavioral health care facilities.
Located in Puerto Rico:
•3 inpatient behavioral health care facilities.
Net revenues from our acute care hospitals, outpatient facilities and commercial health insurer accounted for 56% of our consolidated net revenues during 2024 and 57% during 2023. Net revenues from our behavioral health care facilities and commercial health insurer accounted for 44% of our consolidated net revenues during 2024 and 43% during 2023.
Our behavioral health care facilities located in the U.K. generated net revenues of approximately $880 million in 2024 and $761 million in 2023. Total assets at our U.K. behavioral health care facilities were approximately $1.358 billion as of December 31, 2024 and $1.327 billion as of December 31, 2023.
Services provided by our hospitals include general and specialty surgery, internal medicine, obstetrics, emergency room care, radiology, oncology, diagnostic care, coronary care, pediatric services, pharmacy services and/or behavioral health services. We provide capital resources as well as a variety of management services to our facilities, including central purchasing, information services, finance and control systems, facilities planning, physician recruitment services, administrative personnel management, marketing and public relations.
Forward-Looking Statements and Risk Factors
You should carefully review the information contained in this Annual Report, and should particularly consider any risk factors that we set forth in this Annual Report on Form 10-K for the year ended December 31, 2024, and in other reports or documents that we file from time to time with the Securities and Exchange Commission (the “SEC”). In this Annual Report, we state our beliefs of future events and of our future financial performance. This Annual Report contains “forward-looking statements” that reflect our current estimates, expectations and projections about our future results, performance, prospects and opportunities. Forward-looking statements include, among other things, the information concerning our possible future results of operations, business and growth
strategies, financing plans, expectations that regulatory developments or other matters will or will not have a material adverse effect on our business or financial condition, our competitive position and the effects of competition, the projected growth of the industry in which we operate, and the benefits and synergies to be obtained from our completed and any future acquisitions, and statements of our goals and objectives, and other similar expressions concerning matters that are not historical facts. Words such as “may,” “will,” “should,” “could,” “would,” “predicts,” “potential,” “continue,” “expects,” “anticipates,” “future,” “intends,” “plans,” “believes,” “estimates,” “appears,” “projects” and similar expressions, or the negative of those words and expressions, as well as statements in future tense, identify forward-looking statements. In evaluating those statements, you should specifically consider various factors, including the risks related to healthcare industry trends and those set forth herein in Item 1A. Risk Factors. Those factors may cause our actual results to differ materially from any of our forward-looking statements.
Forward-looking statements should not be read as a guarantee of future performance or results, and will not necessarily be accurate indications of the times at, or by which, such performance or results will be achieved. Forward-looking information is based on information available at the time and/or our good faith belief with respect to future events, and is subject to risks and uncertainties that are difficult to predict and many of which are outside of our control. Many factors, including those set forth herein in Item 1A. Risk Factors, and other important factors disclosed in this report, and from time to time in our other filings with the SEC, could cause actual performance or results to differ materially from those expressed in the statements. Such factors include, among other things, the following:
•the healthcare industry is labor intensive and salaries, wages and benefits are subject to inflationary pressures, as are supplies expense and other operating expenses. In the past, staffing shortages have, at times, required us to hire expensive temporary personnel and/or enhance wages and benefits to recruit and retain nurses and other clinical staff and support personnel. At certain facilities, particularly within our behavioral health care segment, there have been occasions when we were unable to fill all vacant positions and, consequently, we were required to limit patient volumes. We have also experienced general inflationary cost increases related to certain of our other operating expenses. Many of these factors, which had a material unfavorable impact on our results of operations in prior years, have moderated more recently. However, we cannot predict future inflationary increases, which if significant, could have a material unfavorable impact on our future results of operations. We have experienced inflationary pressures, primarily in personnel costs, although those pressures have moderated more recently. The extent of any future impacts from inflation on our business and our results of operations will be dependent upon how long the elevated inflation levels persist and the extent to which the rate of inflation further increases, if at all, neither of which we are able to predict. If elevated levels of inflation were to persist or if the rate of inflation were to accelerate, our expenses could increase faster than anticipated and we may utilize our capital resources sooner than expected. Further, given the complexities of the reimbursement landscape in which we operate, our ability to pass on increased costs associated with providing healthcare to Medicare and Medicaid patients is limited due to various federal, state and local laws, which in certain circumstances, limit our ability to increase prices;
•in our acute care segment, we have experienced a significant increase in hospital based physician related expenses, especially in the areas of emergency room care and anesthesiology. We have implemented various initiatives to mitigate the increased expense, to the degree possible, which has moderated the rate of increase. However, significant increases in these physician related expenses could have a material unfavorable impact on our future results of operations;
•the increase in interest rates during the past few years has increased our interest expense significantly thereby reducing our free cash flow. As such, although interest rates have moderated more recently, the effects of increased borrowing rates have adversely impacted our results of operations, financial condition and cash flows. We cannot predict future changes to interest rates, however, significant increases in our borrowing rates could have a material unfavorable impact on our future results of operations and our ability to access the capital markets on favorable terms;
•President Biden signed into law fiscal year 2025 appropriations to federal agencies for continuing projects and activities through March 14, 2025. We cannot predict whether or not there will be future legislation averting a federal government shutdown, however, our operating cash flows and results of operations could be materially unfavorably impacted by a federal government shutdown;
•on December 29, 2022, the Consolidated Appropriations Act, 2023, was signed into law phasing out the enhanced federal medical assistance percentage rate that states received during the COVID-19 public health emergency and fully eliminated the increase on December 31, 2023. States were also permitted to begin Medicaid eligibility redeterminations on March 31, 2023, which has resulted in a decrease in Medicaid enrollment;
•our ability to comply with the existing laws and government regulations, and/or changes in laws and government regulations, including the recently enacted and proposed significant new tariffs. Significant tariffs or other restrictions, if imposed on our imported pharmaceutical ingredients, medical devices, medical equipment and their ingredients and components, could escalate costs of medications, medical devices and medical equipment and disrupt our supply chains. While we continue to evaluate the potential impact of the new tariffs on our business, given the uncertainty regarding the scope and duration of any new tariffs, as well as the potential for additional tariffs or trade barriers by the U.S. and the
impacted foreign countries, we can provide no assurance that any strategies we implement to mitigate the impact of such tariffs or other trade actions will be successful;
•an increasing number of legislative initiatives have been passed into law that may result in major changes in the health care delivery system on a national or state level. For example, Congress has reduced to $0 the penalty for failing to maintain health coverage that was part of the original Patient Protection and Affordable Care Act, as amended by the Health and Education Reconciliation Act (collectively, the "Legislation") as part of the Tax Cuts and Jobs Act. To date, the Biden administration has issued executive orders implementing a special enrollment period permitting individuals to enroll in health plans outside of the annual open enrollment period and reexamining policies that may undermine the Legislation or the Medicaid program. The Inflation Reduction Act of 2022 (“IRA”) was passed on August 16, 2022, which among other things, allows for the Centers for Medicare and Medicaid Services ("CMS") to negotiate prices for certain single-source drugs reimbursed under Medicare Part B and Part D. The American Rescue Plan Act’s expansion of subsidies to purchase coverage through a Legislation exchange, which the IRA continued through 2025, has increased exchange enrollment. However, the Trump administration has already taken steps to undo certain Biden-era executive orders, including those intended to lower drug costs for beneficiaries, and to freeze funding for federal programs. While the administration’s initial freeze has since been rescinded, the administration is likely to make other attempts to reduce federal program expenditures and can generally be expected to oppose increases in ACA and Medicaid enrollment. If the subsidies are not extended beyond 2025, exchange enrollment may be adversely impacted;
•there have been numerous political and legal efforts to expand, repeal, replace or modify the Legislation, since its enactment, some of which have been successful, in part, in modifying the Legislation, as well as court challenges to the constitutionality of the Legislation. The U.S. Supreme Court held in California v. Texas that the plaintiffs lacked standing to challenge the Legislation’s requirement to obtain minimum essential health insurance coverage, or the individual mandate. The Court dismissed the case without specifically ruling on the constitutionality of the Legislation. As a result, the Legislation continued to remain law, in its entirety. On September 7, 2022, the Legislation faced its most recent challenge when a Texas Federal District Court judge, in the case of Braidwood Management v. Becerra, ruled that a requirement that certain health plans cover services without cost sharing violates the Appointments Clause of the U.S. Constitution and that the coverage of certain HIV prevention medication violates the Religious Freedom Restoration Act. The decision was appealed to the U.S. Court of Appeals for the Fifth Circuit, which on June 21, 2024, affirmed the District Court’s ruling regarding preventive services recommended by United States Preventive Services Task Force being unconstitutional. However, the Fifth Circuit overturned the nationwide injunction imposed by the District Court, preserving access to the majority of preventive services in dispute for now. The U.S. Government appealed and on January 10, 2025, the U.S. Supreme Court agreed to hear the matter. The outcome and impacts of this litigation cannot be predicted. Any future efforts to challenge, replace or replace the Legislation or expand or substantially amend its provision is unknown. See below in Sources of Revenues and Health Care Reform for additional disclosure;
•as part of the Consolidated Appropriations Act of 2021 (the "CAA"), Congress passed legislation aimed at preventing or limiting patient balance billing in certain circumstances. The CAA addresses surprise medical bills stemming from emergency services, out-of-network ancillary providers at in-network facilities, and air ambulance carriers. The CAA prohibits surprise billing when out-of-network emergency services or out-of-network services at an in-network facility are provided, unless informed consent is received. In these circumstances providers are prohibited from billing the patient for any amounts that exceed in-network cost-sharing requirements. HHS, the Department of Labor and the Department of the Treasury have issued rules to implement the legislation. The rules have limited the ability of our hospital-based physicians to receive payments for services at usually higher out-of-network rates in certain circumstances, and, as a result, have caused us to increase subsidies to these physicians or to replace their services at a higher cost level;
•in June 2024, the U.S. Supreme Court issued its decision in Loper Bright Enters. v. Raimondo and Relentless, Inc. v. Department of Commerce, which modified the regulatory interpretation standard established 40 years ago by Chevron v. National Resources Defense Council. Chevron doctrine generally required courts to defer to federal agencies in their interpretation of federal statutes when a statute was silent or ambiguous with respect to a specific issue. In Loper Bright, the Supreme Court held that courts are no longer required to grant such deference, though they may consider an agency’s statutory interpretation. As it is highly regulated, the health care industry could be significantly impacted by the Loper Bright decision, particularly in the areas of Medicare reimbursement, decision making by the Food & Drug
Administration and health care fraud and abuse compliance, where parties may no longer be able to rely on federal agencies’ policies, rules and guidance;
•possible unfavorable changes in the levels and terms of reimbursement for our charges by third party payers or government based payers, including Medicare or Medicaid in the United States, and government based payers in the United Kingdom;
•our ability to enter into managed care provider agreements on acceptable terms and the ability of our competitors to do the same;
•the outcome of known and unknown litigation, government investigations, inquiries, false claims act allegations, and liabilities and other claims asserted against us and other matters, and the effects of adverse publicity relating to such matters, including, but not limited to, the jury verdicts returned against The Pavilion Behavioral Health System (the "Pavilion") and Cumberland Hospital for Children and Adolescents ("Cumberland"), two of our indirect subsidiaries, as disclosed in Note 8 to the Consolidated Financial Statements - Commitments and Contingencies, Legal Proceedings. We are uncertain as to the ultimate financial exposure related to the Pavilion and Cumberland matters (which relate to occurrences in the 2020 policy year) and we can make no assurances regarding timing or substance of their outcome, or the amount of damages that may be ultimately held recoverable after post-judgment proceedings and appeals. As of December 31, 2024, without reduction for any potential amounts related to the Pavilion and Cumberland matters, the Company and its subsidiaries have aggregate insurance coverage of approximately $221 million remaining under commercial policies for matters applicable to the 2020 policy year (in excess of the applicable self-insured retention amounts of $10 million per single occurrence/$25 million for multi-plaintiff matters for professional liability claims and $3 million per occurrence for general liability claims). In the event the resolution of the Pavilion and/or Cumberland matters exhausts all or a significant portion of the remaining commercial insurance coverage available to the Company and its subsidiaries related to other matters that occurred in 2020, or the Pavilion and Cumberland matters cause the posting of large bonds or other collateral during the appeal processes, our future results of operations and capital resources would be materially adversely impacted;
•competition from other healthcare providers (including physician owned facilities) in certain markets;
•technological and pharmaceutical improvements that increase the cost of providing, or reduce the demand for healthcare;
•our ability to attract and retain qualified personnel, nurses, physicians and other healthcare professionals and the impact on our labor and related expenses resulting from a shortage of nurses, physicians and other healthcare professionals;
•there is a heightened risk of future cybersecurity threats, including ransomware attacks targeting healthcare providers. If successful, future cyberattacks could have a material adverse effect on our business. Any costs that we incur as a result of a data security incident or breach, including costs to update our security protocols to mitigate such an incident or breach could be significant. Any breach or failure in our operational security systems, or any third-party security systems that we rely on, can result in loss of data or an unauthorized disclosure of or access to sensitive or confidential member or protected personal or health information and could result in violations of applicable privacy and other laws, significant penalties or fines, litigation, loss of customers, significant damage to our reputation and business, and other liability or losses. We may also incur additional costs related to cybersecurity risk management and remediation. There can be no assurance that we or our service providers, if applicable, will not suffer losses relating to cyber-attacks or other information security breaches in the future or that our insurance coverage will be adequate to cover all the costs resulting from such events;
•the availability of suitable acquisition and divestiture opportunities and our ability to successfully integrate and improve our acquisitions since failure to achieve expected acquisition benefits from certain of our prior or future acquisitions could result in impairment charges for goodwill and purchased intangibles;
•the impact of severe weather conditions, including the effects of hurricanes and climate change;
•our business, results of operations, financial condition, or stock price may be adversely affected if we are not able to achieve our environmental, social and governance (“ESG”) goals or comply with emerging ESG regulations, or otherwise meet the expectations of our stakeholders with respect to ESG matters;
•as discussed below in Sources of Revenue, we receive revenues from various state and county-based programs, including Medicaid in all the states in which we operate. We receive annual Medicaid revenues of approximately $100 million, or greater, from each of Texas, Nevada, California, Illinois, Pennsylvania, Washington, D.C., Kentucky, Florida, Virginia, Massachusetts and Mississippi. Most of these programs are approved on a year-to-year basis and there is no assurance that these revenues will continue at their current rates or at all. The prior President Trump administration had attempted to limit Medicaid expenditures by, for example, attaching work requirements to eligibility for Medicaid waiver benefits. The
second Trump administration is likely to explore similar solutions to limit Medicaid enrollment or expenditure. The Trump administration has already taken steps to undo Biden-era executive orders and to freeze funding for federal programs. While the administration’s initial freeze has since been rescinded, the administration is likely to make other attempts to reduce federal program expenditures and can generally be expected to oppose increases in ACA and Medicaid enrollment. We also receive Medicaid DSH payments in certain states including, most significantly, Texas. We are therefore particularly sensitive to potential reductions in Medicaid and other state-based revenue programs as well as regulatory, economic, environmental and competitive changes in those states;
•our ability to continue to obtain capital on acceptable terms, including borrowed funds, to fund the future growth of our business;
•our inpatient acute care and behavioral health care facilities may experience decreasing admission and length of stay trends;
•our financial statements reflect large amounts due from various commercial and private payers and there can be no assurance that failure of the payers to remit amounts due to us will not have a material adverse effect on our future results of operations;
•the Budget Control Act of 2011 (the “2011 Act”) imposed annual spending limits for most federal agencies and programs aimed at reducing budget deficits by $917 billion between 2012 and 2021, according to a report released by the Congressional Budget Office. Among its other provisions, the law established a bipartisan Congressional committee, known as the Joint Select Committee on Deficit Reduction (the “Joint Committee”), which was tasked with making recommendations aimed at reducing future federal budget deficits by an additional $1.5 trillion over 10 years. The Joint Committee was unable to reach an agreement by the November 23, 2011 deadline and, as a result, across-the-board cuts to discretionary, national defense and Medicare spending were implemented on March 1, 2013 resulting in Medicare payment reductions of up to 2% per fiscal year with a uniform percentage reduction across all Medicare programs. Current legislation has extended these reductions through 2032. We cannot predict whether Congress will restructure the implemented Medicare payment reductions or what other federal budget deficit reduction initiatives may be proposed by Congress going forward;
•uninsured and self-pay patients treated at our acute care facilities unfavorably impact our ability to satisfactorily and timely collect our self-pay patient accounts;
•changes in our business strategies or development plans;
•we have exposure to fluctuations in foreign currency exchange rates, primarily the pound sterling. We have international subsidiaries that operate in the United Kingdom. We routinely hedge our exposures to foreign currencies with certain financial institutions in an effort to minimize the impact of certain currency exchange rate fluctuations, but these hedges may be inadequate to protect us from currency exchange rate fluctuations. To the extent that these hedges are inadequate, our reported financial results or the way we conduct our business could be adversely affected. Furthermore, if a financial counterparty to our hedges experiences financial difficulties or is otherwise unable to honor the terms of the foreign currency hedge, we may experience material financial losses;
•the impact of a shift of care from inpatient to lower cost outpatient settings and controls designed to reduce inpatient services on our revenue, and;
•other factors referenced herein or in our other filings with the Securities and Exchange Commission.
Given these uncertainties, risks and assumptions, as outlined above, you are cautioned not to place undue reliance on such forward-looking statements. Our actual results and financial condition could differ materially from those expressed in, or implied by, the forward-looking statements. Forward-looking statements speak only as of the date the statements are made. We assume no obligation to publicly update any forward-looking statements to reflect actual results, changes in assumptions or changes in other factors affecting forward-looking information, except as may be required by law. All forward-looking statements attributable to us or persons acting on our behalf are expressly qualified in their entirety by this cautionary statement.
Critical Accounting Policies and Estimates
The preparation of financial statements in conformity with accounting principles generally accepted in the United States requires us to make estimates and assumptions that affect the amounts reported in our consolidated financial statements and accompanying notes.
A summary of our significant accounting policies is outlined in Note 1 to the Consolidated Financial Statements. We consider our critical accounting policies to be those that require us to make significant judgments and estimates when we prepare our financial statements, including the following:
Revenue Recognition: We report net patient service revenue at the estimated net realizable amounts from patients and third-party payers and others for services rendered. We have agreements with third-party payers that provide for payments to us at amounts different from our established rates. Payment arrangements include rates per discharge, reimbursed costs, discounted charges and per diem payments. Estimates of contractual allowances under managed care plans, which represent explicit price concessions, are based upon the payment terms specified in the related contractual agreements. We closely monitor our historical collection rates, as well as changes in applicable laws, rules and regulations and contract terms, to assure that provisions are made using the most accurate information available. However, due to the complexities involved in these estimations, actual payments from payers may be different from the amounts we estimate and record.
See Note 10 to the Consolidated Financial Statements-Revenue Recognition, for additional disclosure related to our revenues including a disaggregation of our consolidated net revenues by major source for each of the periods presented herein.
We estimate our Medicare and Medicaid revenues using the latest available financial information, patient utilization data, government provided data and in accordance with applicable Medicare and Medicaid payment rules and regulations. The laws and regulations governing the Medicare and Medicaid programs are extremely complex and subject to interpretation and as a result, there is at least a reasonable possibility that recorded estimates will change by material amounts in the near term. Certain types of payments by the Medicare program and state Medicaid programs (e.g. Medicare Disproportionate Share Hospital, Medicare Allowable Bad Debts and Inpatient Psychiatric Services) are subject to retroactive adjustment in future periods as a result of administrative review and audit and our estimates may vary from the final settlements. Such amounts are included in accounts receivable, net, on our consolidated balance sheets. The funding of both federal Medicare and state Medicaid programs are subject to legislative and regulatory changes. As such, we cannot provide any assurance that future legislation and regulations, if enacted, will not have a material impact on our future Medicare and Medicaid reimbursements. Adjustments related to the final settlement of these retrospectively determined amounts did not materially impact our results in 2024, 2023 or 2022. If it were to occur, each 1% adjustment to our estimated net Medicare revenues that are subject to retrospective review and settlement as of December 31, 2024, would change our after-tax net income by approximately $2 million.
Charity Care, Uninsured Discounts and Other Adjustments to Revenue: Collection of receivables from third-party payers and patients is our primary source of cash and is critical to our operating performance. Our primary collection risks relate to uninsured patients and the portion of the bill which is the patient’s responsibility, primarily co-payments and deductibles. We estimate our revenue adjustments for implicit price concessions based on general factors such as payer mix, the aging of the receivables and historical collection experience. We routinely review accounts receivable balances in conjunction with these factors and other economic conditions which might ultimately affect the collectability of the patient accounts and make adjustments to our allowances as warranted. At our acute care hospitals, third party liability accounts are pursued until all payment and adjustments are posted to the patient account. For those accounts with a patient balance after third party liability is finalized or accounts for uninsured patients, the patient receives statements and collection letters.
Historically, a significant portion of the patients treated throughout our portfolio of acute care hospitals are uninsured patients which, in part, has resulted from patients who are employed but do not have health insurance or who have policies with relatively high deductibles. Patients treated at our hospitals for non-elective services, who have gross income of various amounts, dependent upon the state, ranging from 200% to 400% of the federal poverty guidelines, are deemed eligible for charity care. The federal poverty guidelines are established by the federal government and are based on income and family size. Because we do not pursue collection of amounts that qualify as charity care, the transaction price is fully adjusted and there is no impact in our net revenues or in our accounts receivable, net.
A portion of the accounts receivable at our acute care facilities are comprised of Medicaid accounts that are pending approval from third-party payers but we also have smaller amounts due from other miscellaneous payers such as county indigent programs in certain states. Our patient registration process includes an interview of the patient or the patient’s responsible party at the time of registration. At that time, an insurance eligibility determination is made and an insurance plan code is assigned. There are various pre-established insurance profiles in our patient accounting system which determine the expected insurance reimbursement for each patient based on the insurance plan code assigned and the services rendered. Certain patients may be classified as Medicaid pending at registration based upon a screening evaluation if we are unable to definitively determine if they are currently Medicaid eligible. When a patient is registered as Medicaid eligible or Medicaid pending, our patient accounting system records net revenues for services provided to that patient based upon the established Medicaid reimbursement rates, subject to the ultimate disposition of the patient’s Medicaid eligibility. When the patient’s ultimate eligibility is determined, reclassifications may occur which impacts net revenues in future periods. Although the patient’s ultimate eligibility determination may result in adjustments to net revenues, these adjustments did not have a material impact on our results of operations in 2024 or 2023 since our facilities make estimates at each financial reporting period to adjust revenue based on historical collections.
We also provide discounts to uninsured patients (included in “uninsured discounts” amounts below) who do not qualify for Medicaid or charity care. Because we do not pursue collection of amounts classified as uninsured discounts, the transaction price is fully adjusted and there is no impact in our net revenues or in our net accounts receivable. In implementing the discount policy, we
first attempt to qualify uninsured patients for governmental programs, charity care or any other discount program. If an uninsured patient does not qualify for these programs, the uninsured discount is applied.
Uncompensated care (charity care and uninsured discounts):
The following table shows the amounts recorded at our acute care hospitals for charity care and uninsured discounts, based on charges at established rates, for the years ended December 31, 2024 and 2023:
| | | | | | | | | | | | | | | | | |
| | (dollar amounts in thousands) |
| | 2024 | | | 2023 | | |
| | Amount | | | % | | | Amount | | | % | | |
Charity care | | $ | 819,681 | | | | 23 | % | | $ | 843,449 | | | | 32 | % | |
Uninsured discounts | | | 2,677,026 | | | | 77 | % | | | 1,792,493 | | | | 68 | % | |
Total uncompensated care | | $ | 3,496,707 | | | | 100 | % | | $ | 2,635,942 | | | | 100 | % | |
The estimated cost of providing uncompensated care:
The estimated cost of providing uncompensated care, as reflected below, were based on a calculation which multiplied the percentage of operating expenses for our acute care hospitals to gross charges for those hospitals by the above-mentioned total uncompensated care amounts. The percentage of cost to gross charges is calculated based on the total operating expenses for our acute care facilities divided by gross patient service revenue for those facilities. An increase in the level of uninsured patients to our facilities and the resulting adverse trends in the adjustments to net revenues and uncompensated care provided could have a material unfavorable impact on our future operating results.
| | | | | | | | |
| | (amounts in thousands) | |
| | 2024 | | | 2023 | |
Estimated cost of providing charity care | | $ | 75,227 | | | $ | 83,383 | |
Estimated cost of providing uninsured discounts | | | 245,687 | | | | 177,206 | |
Estimated cost of providing uncompensated care | | $ | 320,914 | | | $ | 260,589 | |
Self-Insured/Other Insurance Risks: We provide for self-insured risks, primarily general and professional liability claims, workers’ compensation claims and healthcare and dental claims. Our estimated liability for self-insured professional and general liability claims is based on a number of factors including, among other things, the number of asserted claims and reported incidents, estimates of losses for these claims based on recent and historical settlement amounts and jury verdicts, estimates of incurred but not reported claims based on historical experience, and estimates of amounts recoverable under our commercial insurance policies. All relevant information, including our own historical experience is used in estimating the expected amount of claims. While we continuously monitor these factors, our ultimate liability for professional and general liability claims could change materially from our current estimates due to inherent uncertainties involved in making this estimate. Our estimated self-insured reserves are reviewed and changed, if necessary, at each reporting date and changes are recognized currently as additional expense or as a reduction of expense.
In addition, we also: (i) own commercial health insurers headquartered in Nevada and Puerto Rico, and; (ii) maintain self-insured employee benefits programs for employee healthcare and dental claims. The ultimate costs related to these programs/operations include expenses for claims incurred and paid in addition to an accrual for the estimated expenses incurred in connection with claims incurred but not yet reported. Given our significant insurance-related exposure, there can be no assurance that a sharp increase in the number and/or severity of claims asserted against us will not have a material adverse effect on our future results of operations.
See Note 8 to the Consolidated Financial Statements-Commitments and Contingencies for additional disclosure related to our self-insured general and professional liability and workers’ compensation liability.
Long-Lived Assets: We review our long-lived assets for impairment whenever events or circumstances indicate that the carrying value of these assets may not be recoverable. The assessment of possible impairment is based on our ability to recover the carrying value of our asset based on our estimate of its undiscounted future cash flow. If the analysis indicates that the carrying value is not recoverable from future cash flows, the asset is written down to its estimated fair value and an impairment loss is recognized. Fair values are determined based on estimated future cash flows using appropriate discount rates. Please see additional disclosure below in Provision for Asset Impairments, for disclosure regarding a provision for asset impairment recorded during 2022.
Goodwill and Intangible Assets: Goodwill and indefinite-lived intangible assets are reviewed for impairment at the reporting unit level on an annual basis or more often if indicators of impairment arise. Our judgments regarding the existence of impairment indicators are based on market conditions and operational performance of each reporting unit. We have designated October 1st as our annual impairment assessment date for our goodwill and indefinite-lived intangible assets.
We performed an impairment assessment as of October 1, 2024 which indicated no impairment of goodwill. There was no goodwill impairment during 2023.
Future changes in the estimates used to conduct the impairment review, including profitability and market value projections, could indicate impairment in future periods potentially resulting in a write-off of a portion or all of our goodwill or indefinite-lived intangible assets.
Income Taxes: Deferred tax assets and liabilities are recognized for the amount of taxes payable or deductible in future years as a result of differences between the tax bases of assets and liabilities and their reported amounts in the financial statements. We believe that future income will enable us to realize our deferred tax assets net of recorded valuation allowances relating to state and foreign net operating loss carry-forwards, tax credits, and interest deduction limitations.
Due to recent guidance and enacted laws surrounding the global 15% minimum tax rate that will be effective after 2024 from the Organization for Economic Co-operation and Development ("OECD") as well as jurisdictions that we operate in, we anticipate adverse effects to our provision for income taxes as well as cash taxes. We do not expect these adverse effects to be material and will continue to monitor changes in tax policies and laws issued by the OECD and jurisdictions that we operate in.
We operate in multiple jurisdictions with varying tax laws. We are subject to audits by any of these taxing authorities. We believe that adequate accruals have been provided for federal, foreign and state taxes.
See Note 6 to the Consolidated Financial Statements-Income Taxes for additional disclosure of our effective tax rates.
Recent Accounting Pronouncements: For a summary of recent accounting pronouncements, please see Note 1 to the Consolidated Financial Statements-Business and Summary of Significant Accounting Standards as included in this Report on Form 10-K for the year ended December 31, 2024.
Results of Operations
Clinical Staffing, Physician Related Expenses and Effects of Inflation:
The healthcare industry is labor intensive and salaries, wages and benefits are subject to inflationary pressures, as are supplies expense and other operating expenses. In the past, staffing shortages have, at times, required us to hire expensive temporary personnel and/or enhance wages and benefits to recruit and retain nurses and other clinical staff and support personnel. At certain facilities, particularly within our behavioral health care segment, there have been occasions when we were unable to fill all vacant positions and, consequently, we were required to limit patient volumes. We have also experienced general inflationary cost increases related to certain of our other operating expenses. Many of these factors, which had a material unfavorable impact on our results of operations in prior years, have moderated more recently. However, we cannot predict future inflationary increases, which if significant, could have a material unfavorable impact on our future results of operations.
We have experienced inflationary pressures, primarily in personnel costs, although those pressures have moderated more recently. The extent of any future impacts from inflation on our business and our results of operations will be dependent upon how long the elevated inflation levels persist and the extent to which the rate of inflation further increases, if at all, neither of which we are able to predict. If elevated levels of inflation were to persist or if the rate of inflation were to accelerate, our expenses could increase faster than anticipated and we may utilize our capital resources sooner than expected. Further, given the complexities of the reimbursement landscape in which we operate, our ability to pass on increased costs associated with providing healthcare to Medicare and Medicaid patients is limited due to various federal, state and local laws, which in certain circumstances, limit our ability to increase prices.
In our acute care segment, during the past few years we experienced significant increases in hospital-based physician related expenses, especially in the areas of emergency room care and anesthesiology. We have implemented various initiatives to mitigate the increased expense, to the degree possible, which has moderated the rate of increase experienced during 2024. However, significant increases in these physician related expenses could have a material unfavorable impact on our future results of operations.
Although our ability to pass on increased costs associated with providing healthcare to Medicare and Medicaid patients is limited, as discussed above, we have been requesting and negotiating increased rates from commercial insurers to defray our increased cost of providing patient care. In addition, we have implemented various productivity enhancement programs and cost reduction initiatives including, but not limited to, the following: team-based patient care initiatives designed to optimize the level of patient care services provided by our licensed nurses/clinicians; efforts to reduce utilization of, and rates paid for, premium pay labor; consolidation of medical supply vendors to increase purchasing discounts; review and reduction of clinical variation in connection with the utilization of medical supplies, and; various other efforts to increase productivity and/or reduce costs including investments in new information technology applications.
The following table summarizes our results of operations, and is used in the discussion below, for the years ended December 31, 2024 and 2023 (dollar amounts in thousands):
| | | | | | | | | | | | | | | | | |
| | Year Ended December 31, |
| | 2024 | | | 2023 | | |
| | | | | % of Net | | | | | | % of Net | | |
| | Amount | | | Revenues | | | Amount | | | Revenues | | |
Net revenues | | $ | 15,827,935 | | | | 100.0 | % | | $ | 14,281,976 | | | | 100.0 | % | |
Operating charges: | | | | | | | | | | | | | |
Salaries, wages and benefits | | | 7,518,687 | | | | 47.5 | % | | | 7,107,484 | | | | 49.8 | % | |
Other operating expenses | | | 4,308,384 | | | | 27.2 | % | | | 3,757,216 | | | | 26.3 | % | |
Supplies expense | | | 1,587,786 | | | | 10.0 | % | | | 1,532,828 | | | | 10.7 | % | |
Depreciation and amortization | | | 584,831 | | | | 3.7 | % | | | 568,041 | | | | 4.0 | % | |
Lease and rental expense | | | 146,433 | | | | 0.9 | % | | | 141,026 | | | | 1.0 | % | |
Subtotal-operating expenses | | | 14,146,121 | | | | 89.4 | % | | | 13,106,595 | | | | 91.8 | % | |
Income from operations | | | 1,681,814 | | | | 10.6 | % | | | 1,175,381 | | | | 8.2 | % | |
Interest expense, net | | | 186,109 | | | | 1.2 | % | | | 206,674 | | | | 1.4 | % | |
Other (income) expense, net | | | (2,231 | ) | | | 0.0 | % | | | 28,281 | | | | 0.2 | % | |
Income before income taxes | | | 1,497,936 | | | | 9.5 | % | | | 940,426 | | | | 6.6 | % | |
Provision for income taxes | | | 334,827 | | | | 2.1 | % | | | 221,119 | | | | 1.5 | % | |
Net income | | | 1,163,109 | | | | 7.3 | % | | | 719,307 | | | | 5.0 | % | |
Less: Net income (loss) attributable
to noncontrolling interests | | | 21,012 | | | | 0.1 | % | | | 1,512 | | | | 0.0 | % | |
Net income attributable to UHS | | $ | 1,142,097 | | | | 7.2 | % | | $ | 717,795 | | | | 5.0 | % | |
Net revenues increased by 10.8%, or $1.55 billion, to $15.83 billion during 2024 as compared to $14.28 billion during 2023. The increase in net revenues was primarily attributable to:
•a $1.32 billion or 9.5% increase in net revenues generated from our acute care and behavioral health care operations owned during both periods (which we refer to as “same facility”), and;
•$222 million of other combined net increases consisting primarily of a $239 million increase in provider tax assessments which had no impact on income before income taxes since amounts offset between net revenues and other operating expenses.
Income before income taxes increased by $558 million, or 59%, to $1.50 billion during 2024 as compared to $940 million during 2023. The increase was attributable to:
•an increase of $295 million at our acute care facilities, as discussed below in Acute Care Hospital Services;
•an increase of $277 million at our behavioral health care facilities, as discussed below in Behavioral Health Services, and;
•$14 million of other combined net decreases.
Net income attributable to UHS increased by $424 million, or 59%, to $1.14 billion during 2024 as compared to $718 million during 2023. This increase was attributable to:
•a $558 million in income before income taxes, as discussed above;
•a decrease of $20 million due to an increase in the net income/loss attributable to noncontrolling interests, and;
•a decrease of $114 million resulting from an increase in the provision for income taxes resulting primarily from: (i) the increase in the provision for income taxes resulting from the $538 million increase in pre-tax income (consisting of $558 million increase in income before income taxes minus a $20 million increase in the income/loss attributable to noncontrolling interests), partially offset by; (ii) a $16 million decrease in the provision for income taxes during 2024, as compared to 2023, from the net tax benefit recorded pursuant to ASU 2016-09, net of the impact of executive compensation limitations pursuant to IRC section 162(m).
Adjustments to Self-Insured Professional and General Liability Reserves:
Our estimated liability for self-insured professional and general liability claims is based on a number of factors including, among other things, the number of asserted claims and reported incidents, estimates of losses for these claims based on recent and historical settlement amounts and jury verdicts, estimates of incurred but not reported claims based on historical experience, and estimates of amounts recoverable under our commercial insurance policies.
As a result of unfavorable trends experienced during 2024 and 2023, our results of operations included pre-tax increases to our reserves for self-insured professional and general liability claims amounting to approximately $79 million during 2024 and $25
million during 2023. During 2024, approximately $54 million of the reserves increase is included in our Same Facility basis acute care hospitals services’ results, and approximately $25 million is included in our behavioral health services’ results. During 2023, approximately $18 million of the reserves increase is included in our Same Facility basis acute care hospitals services’ results, and approximately $7 million is included in our behavioral health services’ results.
Acute Care Hospital Services
The following table sets forth certain operating statistics for our acute care hospital services for the years ended December 31, 2024 and 2023.
| | | | | | | | | | | | | | | | | |
| | | Same Facility Basis | | | All | |
| | | 2024 | | | 2023 | | | 2024 | | | 2023 | |
Average licensed beds | | 6,657 | | | | 6,644 | | | | 6,670 | | | | 6,691 | |
Average available beds | | 6,485 | | | | 6,472 | | | | 6,498 | | | | 6,519 | |
Patient days | | 1,600,445 | | | | 1,569,792 | | | | 1,601,579 | | | | 1,576,074 | |
Average daily census | | 4,372.8 | | | | 4,300.8 | | | | 4,375.9 | | | | 4,318.0 | |
Occupancy-licensed beds | | 65.7 | % | | | 64.7 | % | | | 65.6 | % | | | 64.5 | % |
Occupancy-available beds | | 67.4 | % | | | 66.5 | % | | | 67.3 | % | | | 66.2 | % |
Admissions | | 331,113 | | | | 321,155 | | | | 331,415 | | | | 322,218 | |
Length of stay | | 4.8 | | | | 4.9 | | | | 4.8 | | | | 4.9 | |
Acute Care Hospital Services-Same Facility Basis
We believe that providing our results on a “Same Facility” basis (which is a non-GAAP measure), which includes the operating results for facilities and businesses operated in both the current year and prior year periods, is helpful to our investors as a measure of our operating performance. Our Same Facility results also neutralize (if applicable) the effect of items that are non-operational in nature including items such as, but not limited to, gains/losses on sales of assets and businesses, impacts of settlements, legal judgments and lawsuits, impairments of long-lived and intangible assets and other amounts that may be reflected in the current or prior year financial statements that relate to prior periods.
Our Same Facility basis results reflected on the tables below also exclude from net revenues and other operating expenses, provider tax assessments incurred in each period as discussed below Sources of Revenue-Summary of Various State Medicaid Supplemental Payment Programs. However, these provider tax assessments are included in net revenues and other operating expenses as reflected in the table below under All Acute Care Hospital Services. The provider tax assessments had no impact on the income before income taxes as reflected on the tables below since the amounts offset between net revenues and other operating expenses. To obtain a complete understanding of our financial performance, the Same Facility results should be examined in connection with our net income as determined in accordance with U.S. GAAP and as presented in the consolidated financial statements and notes thereto as contained in this Annual Report on Form 10-K.
The following table summarizes the results of operations for our acute care hospital services on a Same Facility basis and is used in the discussions below for the years ended December 31, 2024 and 2023 (dollar amounts in thousands):
| | | | | | | | | | | | | | | | |
| | Year Ended | | | Year Ended | |
| | December 31, 2024 | | | December 31, 2023 | |
| | | | | % of Net | | | | | | % of Net | |
| | Amount | | | Revenues | | | Amount | | | Revenues | |
Net revenues | | $ | 8,565,845 | | | | 100.0 | % | | $ | 7,892,167 | | | | 100.0 | % |
Operating charges: | | | | | | | | | | | | |
Salaries, wages and benefits | | | 3,502,645 | | | | 40.9 | % | | | 3,387,843 | | | | 42.9 | % |
Other operating expenses | | | 2,378,512 | | | | 27.8 | % | | | 2,164,069 | | | | 27.4 | % |
Supplies expense | | | 1,358,636 | | | | 15.9 | % | | | 1,315,527 | | | | 16.7 | % |
Depreciation and amortization | | | 364,907 | | | | 4.3 | % | | | 367,067 | | | | 4.7 | % |
Lease and rental expense | | | 98,730 | | | | 1.2 | % | | | 96,429 | | | | 1.2 | % |
Subtotal-operating expenses | | | 7,703,430 | | | | 89.9 | % | | | 7,330,935 | | | | 92.9 | % |
Income from operations | | | 862,415 | | | | 10.1 | % | | | 561,232 | | | | 7.1 | % |
Interest (income) expense, net | | | 6,339 | | | | 0.1 | % | | | (2,501 | ) | | | 0.0 | % |
Other (income) expense, net | | | (2,123 | ) | | | 0.0 | % | | | 7,000 | | | | 0.1 | % |
Income before income taxes | | $ | 858,199 | | | | 10.0 | % | | $ | 556,733 | | | | 7.1 | % |
During 2024, as compared to 2023, net revenues from our acute care hospital services, on a Same Facility basis, increased by $674 million or 8.5%. Income before income taxes (and before income attributable to noncontrolling interests) increased by $301 million, or 54%, amounting to $858 million, or 10.0% of net revenues during 2024, as compared to $557 million, or 7.1% of net
revenues during 2023. Included in our Same Facility basis' net revenues and income before income taxes, during 2024, was approximately $186 million of net reimbursements (net of related provider taxes) recorded in connection with the Nevada state directed payment program which was approved by the Centers for Medicare and Medicaid Services in December, 2023. Please see additional disclosure below in Sources of Revenue-Nevada State Directed Payment Program ("SDP").
During 2024, net revenue per adjusted admission increased by 5.1% while net revenue per adjusted patient day increased by 6.3%, as compared to 2023. During 2024, as compared to 2023, inpatient admissions to our acute care hospitals increased by 3.1% while adjusted admissions increased by 2.9%. Patient days and adjusted patient days at these facilities increased by 2.0% and 1.8%, respectively, during 2024, as compared to 2023. The average length of inpatient stay at these facilities was 4.8 days and 4.9 days during 2024 and 2023, respectively. The occupancy rate, based on the average available beds at these facilities, was approximately 67% during each of 2024 and 2023.
On a Same Facility basis during 2024, as compared to 2023, salaries, wages and benefits expense increased by $115 million, or 3.4%. Although our acute care facilities experienced an increase in patient volumes during 2024, as compared to the 2023, the related incremental staffing cost increase was offset by the following: (i) a reduction in premium pay (overtime paid to employees and external temporary resources' expense) which decreased by approximately $48 million during 2024, as compared to 2023, and; (ii) a restructuring, that occurred in early 2024, at certain of our acute care hospitals that reduced the number of employees in positions that were not directly related to the delivery of patient care. As a percentage of net revenues, salaries, wages and benefits expense decreased to 40.9% during 2024 as compared to 42.9% during 2023.
Other operating expenses increased by $214 million, or 9.9%, during 2024, as compared to 2023. Operating expenses incurred by our commercial health insurer, consisting primarily of medical costs, increased by $69 million during 2024, as compared to 2023. In addition, as discussed above in Results of Operations-Adjustments to Self-Insured Professional and General Liability Reserves, included in the other operating expenses of our acute care hospital services during 2024, as compared to 2023, was a $36 million increase in the adjustments made to our self-insured professional and general liability reserves that was applicable to our acute care facilities. Excluding these expense items from each year, other operating expenses increased by $109 million, or 6.3%. Contributing to the increase during 2024, as compared to 2023, were the expenses incurred in connection with the increase in patient volumes. As a percentage of net revenues, other operating expenses increased to 27.8% during 2024, as compared to 27.4% during 2023.
Supplies expense increased by $43 million, or 3.3%, during 2024, as compared to 2023. As a percentage of net revenues, supplies expense decreased to 15.9% during 2024, as compared to 16.7% during 2023.
All Acute Care Hospital Services
The following table summarizes the results of operations for all our acute care operations during 2024 and 2023. These amounts include: (i) our acute care results on a same facility basis, as indicated above; (ii) the impact of provider tax assessments which increased net revenues and other operating expenses but had no impact on income before income taxes, and; (iii) certain other amounts including, if applicable, the operating results of recently acquired/opened facilities, or divested/closed facilities, including the operating results for Desert Springs Hospital which discontinued all inpatient operations during the first quarter of 2023. Dollar amounts below are reflected in thousands.
| | | | | | | | | | | | | | | | |
| | Year Ended | | | Year Ended | |
| | December 31, 2024 | | | December 31, 2023 | |
| | | | | % of Net | | | | | | % of Net | |
| | Amount | | | Revenues | | | Amount | | | Revenues | |
Net revenues | | $ | 8,922,327 | | | | 100.0 | % | | $ | 8,081,402 | | | | 100.0 | % |
Operating charges: | | | | | | | | | | | | |
Salaries, wages and benefits | | | 3,511,359 | | | | 39.4 | % | | | 3,406,060 | | | | 42.1 | % |
Other operating expenses | | | 2,743,420 | | | | 30.7 | % | | | 2,347,560 | | | | 29.0 | % |
Supplies expense | | | 1,360,011 | | | | 15.2 | % | | | 1,317,917 | | | | 16.3 | % |
Depreciation and amortization | | | 368,096 | | | | 4.1 | % | | | 367,644 | | | | 4.5 | % |
Lease and rental expense | | | 99,060 | | | | 1.1 | % | | | 96,589 | | | | 1.2 | % |
Subtotal-operating expenses | | | 8,081,946 | | | | 90.6 | % | | | 7,535,770 | | | | 93.2 | % |
Income from operations | | | 840,381 | | | | 9.4 | % | | | 545,632 | | | | 6.8 | % |
Interest (income) expense, net | | | 6,339 | | | | 0.1 | % | | | (2,501 | ) | | | 0.0 | % |
Other (income) expense, net | | | (1,305 | ) | | | 0.0 | % | | | 7,788 | | | | 0.1 | % |
Income before income taxes | | $ | 835,347 | | | | 9.4 | % | | $ | 540,345 | | | | 6.7 | % |
During 2024, as compared to 2023, net revenues from our acute care hospital services increased by $841 million, or 10.4%, due to: (i) the $674 million, or 8.5% increase in Same Facility revenues, as discussed above; (ii) a $187 million increase in provider tax assessments (which had no impact on income before income taxes since the amounts offset between net revenues and other operating
expenses), and; (iii) $20 million of other combined net decreases consisting primarily of decreased revenues at Desert Springs Hospital.
Income before income taxes increased by $295 million, or 54.6%, to $835 million, or 9.4% of net revenues during 2024, as compared to $540 million, or 6.7% of net revenues during 2023. The increase resulted from the $301 million, or 54%, increase in income before income taxes at our acute care hospital services, on a Same Facility basis, as discussed above, and $6 million of other combined net decreases resulting primarily from the losses incurred at the newly constructed 150-bed West Henderson Hospital located in Las Vegas, Nevada, that was completed and opened during the fourth quarter of 2024.
During 2024, as compared to 2023, salaries, wages and benefits expense increased by $105 million, or 3.1%. The increase was due primarily to the above-mentioned $115 million increase related to our acute care hospital services, on a Same Facility basis, partially offset by a combined other net decrease of $10 million (consisting primarily of a decrease related to Desert Springs Hospital, partially offset by an increase related to West Henderson Hospital).
Other operating expenses increased $396 million, or 16.9%, during 2024 as compared to 2023. The increase was due primarily to the $214 million above-mentioned increase related to our acute care hospital services, on a Same Facility basis, as well as the above-mentioned $187 million increase in provider tax assessments.
Supplies expense increased by $42 million, or 3.2%, during 2024 as compared to 2023. The increase was due primarily to the above-mentioned $43 million increase related to our acute care hospital services, on a Same Facility basis.
Please see Results of Operations - Clinical Staffing, Physician Related Expenses and Effects of Inflation above for additional disclosure regarding the factors impacting our operating costs.
Behavioral Health Care Services
The following table sets forth certain operating statistics for our behavioral health care services for the years ended December 31, 2024 and 2023.
| | | | | | | | | | | | | | | | | |
| | | Same Facility Basis | | | All | |
| | | 2024 | | | 2023 | | | 2024 | | | 2023 | |
Average licensed beds | | 24,165 | | | | 24,000 | | | | 24,367 | | | | 24,224 | |
Average available beds | | 24,065 | | | | 23,900 | | | | 24,280 | | | | 24,124 | |
Patient days | | 6,397,790 | | | | 6,277,015 | | | | 6,446,651 | | | | 6,336,927 | |
Average daily census | | 17,480.3 | | | | 17,197.3 | | | | 17,613.8 | | | | 17,361.4 | |
Occupancy-licensed beds | | 72.3 | % | | | 71.7 | % | | | 72.3 | % | | | 71.7 | % |
Occupancy-available beds | | 72.6 | % | | | 72.0 | % | | | 72.5 | % | | | 72.0 | % |
Admissions | | 472,798 | | | | 468,260 | | | | 476,584 | | | | 472,307 | |
Length of stay | | 13.5 | | | | 13.4 | | | | 13.5 | | | | 13.4 | |
Behavioral Health Care Services-Same Facility Basis
We believe that providing our results on a “Same Facility” basis (which is a non-GAAP measure), which includes the operating results for facilities and businesses operated in both the current year and prior year periods, is helpful to our investors as a measure of our operating performance. Our Same Facility results also neutralize (if applicable) the effect of items that are non-operational in nature including items such as, but not limited to, gains/losses on sales of assets and businesses, impacts of settlements, legal judgments and lawsuits, impairments of long-lived and intangible assets and other amounts that may be reflected in the current or prior year financial statements that relate to prior periods.
Our Same Facility basis results reflected on the table below also excludes from net revenues and other operating expenses, provider tax assessments incurred in each period as discussed below Sources of Revenue-Summary of Various State Medicaid Supplemental Payment Programs. However, these provider tax assessments are included in net revenues and other operating expenses as reflected in the table below under All Behavioral Health Care Services. The provider tax assessments had no impact on the income before income taxes as reflected on the tables below since the amounts offset between net revenues and other operating expenses. To obtain a complete understanding of our financial performance, the Same Facility results should be examined in connection with our net income as determined in accordance with U.S. GAAP and as presented in the consolidated financial statements and notes thereto as contained in this Annual Report on Form 10-K.
The following table summarizes the results of operations for our behavioral health care services, on a same facility basis, and is used in the discussions below for the years ended December 31, 2024 and 2023 (dollar amounts in thousands):
| | | | | | | | | | | | | | | | |
| | Year Ended | | | Year Ended | |
| | December 31, 2024 | | | December 31, 2023 | |
| | | | | % of Net | | | | | | % of Net | |
| | Amount | | | Revenues | | | Amount | | | Revenues | |
Net revenues | | $ | 6,700,469 | | | | 100.0 | % | | $ | 6,050,491 | | | | 100.0 | % |
Operating charges: | | | | | | | | | | | | |
Salaries, wages and benefits | | | 3,590,985 | | | | 53.6 | % | | | 3,346,357 | | | | 55.3 | % |
Other operating expenses | | | 1,262,446 | | | | 18.8 | % | | | 1,168,806 | | | | 19.3 | % |
Supplies expense | | | 229,795 | | | | 3.4 | % | | | 216,880 | | | | 3.6 | % |
Depreciation and amortization | | | 204,144 | | | | 3.0 | % | | | 188,237 | | | | 3.1 | % |
Lease and rental expense | | | 46,468 | | | | 0.7 | % | | | 43,819 | | | | 0.7 | % |
Subtotal-operating expenses | | | 5,333,838 | | | | 79.6 | % | | | 4,964,099 | | | | 82.0 | % |
Income from operations | | | 1,366,631 | | | | 20.4 | % | | | 1,086,392 | | | | 18.0 | % |
Interest expense, net | | | 4,027 | | | | 0.1 | % | | | 4,557 | | | | 0.1 | % |
Other (income) expense, net | | | (3,480 | ) | | | -0.1 | % | | | (3,426 | ) | | | -0.1 | % |
Income before income taxes | | $ | 1,366,084 | | | | 20.4 | % | | $ | 1,085,261 | | | | 17.9 | % |
During 2024, as compared to 2023, net revenues from our behavioral health services, on a Same Facility basis, increased by $650 million or 10.7%. Income before income taxes increased by $281 million, or 25.9%, amounting to $1.366 billion or 20.4% of net revenues during 2024, as compared to $1.085 billion or 17.9% of net revenues during 2023.
During 2024, net revenue per adjusted admission increased by 9.8% while net revenue per adjusted patient day increased by 8.8%, as compared to 2023. During 2024, as compared to 2023, inpatient admissions and adjusted admissions to our behavioral health care hospitals increased by 1.0% and 0.7%, respectively. Patient days at these facilities increased by 1.9% and adjusted patient days increased by 1.7% during 2024, as compared to 2023. The average length of inpatient stay at these facilities was 13.5 days and 13.4 days during 2024 and 2023, respectively. The occupancy rate, based on the average available beds at these facilities, was 73% and 72% during 2024 and 2023, respectively.
On a Same Facility basis during 2024, as compared to 2023, salaries, wages and benefits expense increased $245 million or 7.3%. The increase during 2024, as compared to 2023, was due to a 3.2% increase in salaries, wages and benefits expense per average full-time equivalent employee, as well as a 4.0% increase in the average number of full time equivalent employees. The increased staffing was due, in part, to increased patient volumes. As a percentage of net revenues during each year, salaries, wages and benefits expense decreased to 53.6% during 2024 as compared to 55.3% during 2023.
Other operating expenses increased $94 million, or 8.0%, during 2024, as compared to 2023. Included in the increase, as discussed above in Results of Operations-Adjustments to Self-Insured Professional and General Liability Reserves, included in the other operating expenses of our behavioral health care services during 2024, as compared to 2023, was an $18 million increase in the adjustments made to our self-insured professional and general liability reserves that was applicable to our behavioral health facilities. As a percentage of net revenues during each year, other operating expenses decreased to 18.8% during 2024 as compared to 19.3% during 2023.
Supplies expense increased $13 million, or 6.0%, during 2024, as compared to 2023. As a percentage of net revenues during each year, supplies expense decreased to 3.4% during 2024 as compared to 3.6% during 2023.
All Behavioral Health Care Services
The following table summarizes the results of operations for all our behavioral health care services during 2024 and 2023. These amounts include: (i) our behavioral health care results on a same facility basis, as indicated above; (ii) the impact of provider tax assessments which increased net revenues and other operating expenses but had no impact on income before income taxes, and; (iii) certain other amounts, if applicable, including the results of facilities acquired or opened during the past year as well as the results of facilities that were opened or closed during the past year. Dollar amounts below are reflected in thousands.
| | | | | | | | | | | | | | | | |
| | Year Ended | | | Year Ended | |
| | December 31, 2024 | | | December 31, 2023 | |
| | | | | % of Net | | | | | | % of Net | |
| | Amount | | | Revenues | | | Amount | | | Revenues | |
Net revenues | | $ | 6,895,051 | | | | 100.0 | % | | $ | 6,190,921 | | | | 100.0 | % |
Operating charges: | | | | | | | | | | | | |
Salaries, wages and benefits | | | 3,603,123 | | | | 52.3 | % | | | 3,353,008 | | | | 54.2 | % |
Other operating expenses | | | 1,447,503 | | | | 21.0 | % | | | 1,303,311 | | | | 21.1 | % |
Supplies expense | | | 230,274 | | | | 3.3 | % | | | 217,310 | | | | 3.5 | % |
Depreciation and amortization | | | 206,362 | | | | 3.0 | % | | | 189,297 | | | | 3.1 | % |
Lease and rental expense | | | 46,986 | | | | 0.7 | % | | | 44,028 | | | | 0.7 | % |
Subtotal-operating expenses | | | 5,534,248 | | | | 80.3 | % | | | 5,106,954 | | | | 82.5 | % |
Income from operations | | | 1,360,803 | | | | 19.7 | % | | | 1,083,967 | | | | 17.5 | % |
Interest expense, net | | | 4,027 | | | | 0.1 | % | | | 4,558 | | | | 0.1 | % |
Other (income) expense, net | | | (3,547 | ) | | | -0.1 | % | | | (4,271 | ) | | | -0.1 | % |
Income before income taxes | | $ | 1,360,323 | | | | 19.7 | % | | $ | 1,083,680 | | | | 17.5 | % |
During 2024, as compared to 2023, net revenues generated from our behavioral health services increased by $704 million, or 11.4%. The increase was primarily attributable to the $650 million, or 10.7%, increase in net revenues at our behavioral health facilities, on a Same Facility basis, as discussed above, as well as a $51 million increase in provider tax assessments.
Income before income taxes increased by $277 million, or 26%, to $1.360 billion or 19.7% of net revenues during 2024, as compared to $1.084 billion or 17.5% of net revenues during 2023. The increase in income before income taxes at our behavioral health facilities during 2024, as compared to 2023, was primarily attributable to the $281 million, or 26%, increase in income before income taxes generated at our behavioral health facilities, on a Same Facility basis, as discussed above.
During 2024, as compared to 2023, salaries, wages and benefits expense increased by $250 million or 7.5%. The increase was due primarily to the above-mentioned $245 million, or 7.3%, increase related to our behavioral health facilities, on a Same Facility basis.
Other operating expenses increased by $144 million, or 11.1%, during 2024, as compared to 2023. The increase was due primarily to the above-mentioned $94 million, or 8.0%, increase related to our behavioral health facilities, on a Same Facility basis, as well as a $51 million increase in provider tax assessments.
Supplies expense increased $13 million, or 6.0%, during 2024, as compared to 2023, due primarily to the above-mentioned increase related to our behavioral health facilities, on a Same Facility basis.
Please see Results of Operations - Clinical Staffing, Physician Related Expenses and Effects of Inflation above for additional disclosure regarding the factors impacting our operating costs.
Sources of Revenue
Overview: We receive payments for services rendered from private insurers, including managed care plans, the federal government under the Medicare program, state governments under their respective Medicaid programs and directly from patients.
Hospital revenues depend upon inpatient occupancy levels, the medical and ancillary services and therapy programs ordered by physicians and provided to patients, the volume of outpatient procedures and the charges or negotiated payment rates for such services. Charges and reimbursement rates for inpatient routine services vary depending on the type of services provided (e.g., medical/surgical, intensive care or behavioral health) and the geographic location of the hospital. Inpatient occupancy levels fluctuate for various reasons, many of which are beyond our control. The percentage of patient service revenue attributable to outpatient services has generally increased in recent years, primarily as a result of advances in medical technology that allow more services to be provided on an outpatient basis, as well as increased pressure from Medicare, Medicaid and private insurers to reduce hospital stays and provide services, where possible, on a less expensive outpatient basis. We believe that our experience with respect to our increased outpatient levels mirrors the general trend occurring in the health care industry and we are unable to predict the rate of growth and resulting impact on our future revenues.
Patients are generally not responsible for any difference between customary hospital charges and amounts reimbursed for such services under Medicare, Medicaid, some private insurance plans, and managed care plans, but are responsible for services not covered by such plans, exclusions, deductibles or co-insurance features of their coverage. The amount of such exclusions, deductibles and co-insurance has generally been increasing each year. Indications from recent federal and state legislation are that this trend will continue. Collection of amounts due from individuals is typically more difficult than from governmental or business payers which unfavorably impacts the collectability of our patient accounts.
Sources of Revenues and Health Care Reform: Given increasing budget deficits, the federal government and many states are currently considering additional ways to limit increases in levels of Medicare and Medicaid funding, which could also adversely affect future payments received by our hospitals. In addition, the uncertainty and fiscal pressures placed upon the federal government as a result of, among other things, economic recovery stimulus packages, responses to natural disasters, and the federal and state budget deficits in general may affect the availability of government funds to provide additional relief in the future. Changes resulting from the outcome of the 2024 elections may include increased reliance on Medicare Advantage programs, work requirements for Medicaid waiver program eligibility, increased focus on hospital outpatient site neutral payment policies, and similar initiatives that may reduce the availability of funding for federal healthcare programs or make eligibility for benefits more difficult. There have been proposals to substantially decrease federal funding for state Medicaid Programs. Any significant reduction in federal Medicaid funding to states would likely result in states reducing Medicaid payments to us which would have a material adverse effect on us. We are unable to predict the effect of future policy changes on our operations.
In 2010, the Patient Protection and Affordable Care Act, as amended by the Health and Education Reconciliation Act (collectively, the “Legislation”) was enacted and its two primary goals were to provide for increased access to coverage for healthcare and to reduce healthcare-related expenses. The Legislation revised reimbursement under the Medicare and Medicaid programs to emphasize the efficient delivery of high-quality care and contains a number of incentives and penalties under these programs to achieve these goals. The Legislation provides for reductions to Medicaid DSH payments which are scheduled to begin in 2025.
A 2012 U.S. Supreme Court ruling limited the federal government’s ability to expand health insurance coverage by holding unconstitutional sections of the Legislation that sought to withdraw federal funding for state noncompliance with certain Medicaid coverage requirements. Pursuant to that decision, the federal government may not penalize states that choose not to participate in the Medicaid expansion by reducing their existing Medicaid funding. Therefore, states can choose to expand or not to expand their Medicaid program without risking the loss of federal Medicaid funding. As a result, many states, including Texas, have not expanded their Medicaid programs without the threat of loss of federal funding. CMS has previously granted section 1115 demonstration waivers providing for work and community engagement requirements for certain Medicaid eligible individuals. CMS has also released guidance to states interested in receiving their Medicaid funding through a block grant mechanism. The Biden administration withdrew certain previously issued section 1115 demonstrations aligned with these policies, but Georgia has imposed work and community engagement requirements under a Medicaid demonstration program that launched July 1, 2023. President Trump, more favorable to work and community engagement requirements in his first administration, is more likely to again seek these obligations for Medicaid demonstration programs. If additional section 1115 demonstrations that include work and community requirements are implemented, we anticipate that they would lead to reductions in coverage and likely increases in uncompensated care in those states where these demonstration waivers are granted.
On December 14, 2018, a Texas Federal District Court deemed the Legislation to be unconstitutional in its entirety. The Court concluded that the Individual Mandate is no longer permissible under Congress’s taxing power as a result of the Tax Cut and Jobs Act of 2017 reducing the individual mandate’s tax to $0 (i.e., it no longer produces revenue, which is an essential feature of a tax), rendering the Legislation unconstitutional. The Court also held that because the individual mandate is “essential” to the Legislation and is inseverable from the rest of the law, the entire Legislation is unconstitutional. That ruling was ultimately appealed to the United States Supreme Court, which decided in California v. Texas that the plaintiffs in the matter lacked standing to bring their constitutionality claims. The Court did not reach the plaintiffs’ merits arguments, which specifically challenged the constitutionality of the Legislation’s individual mandate and the entirety of the Legislation itself. As a result, the Legislation will continue to be law, and the Department of Health and Human Services ("HHS") and its respective agencies will continue to enforce regulations implementing the law. However, on September 7, 2022, the Legislation faced its most recent challenge when a Texas Federal District Court judge, in the case of Braidwood Management v. Becerra, ruled that a requirement that certain health plans cover services without cost sharing violates the Appointments Clause of the U.S. Constitution and that the coverage of certain HIV prevention medication violates the Religious Freedom Restoration Act. The decision was appealed to the U.S. Court of Appeals for the Fifth Circuit, which on June 21, 2024 affirmed the District Court’s ruling regarding preventive services recommended by United States Preventive Services Task Force being unconstitutional. However, the Fifth Circuit overturned the nationwide injunction imposed by the District Court, preserving access to the majority of preventive services in dispute for now. The government has appealed the matter to the U.S. Supreme Court. The outcome and impacts of this litigation cannot be predicted.
The Legislation also contained provisions aimed at reducing fraud and abuse in healthcare. The Legislation amends several existing laws, including the federal Anti-Kickback Statute and the False Claims Act, making it easier for government agencies and private plaintiffs to prevail in lawsuits brought against healthcare providers. While Congress had previously revised the intent requirement of the Anti-Kickback Statute to provide that a person is not required to “have actual knowledge or specific intent to
commit a violation of” the Anti-Kickback Statute in order to be found in violation of such law, the Legislation also provides that any claims for items or services that violate the Anti-Kickback Statute are also considered false claims for purposes of the federal civil False Claims Act. The Legislation provides that a healthcare provider that retains an overpayment in excess of 60 days is subject to the federal civil False Claims Act. In December, 2024, CMS changed the standard for identification of an overpayment and now requires the report and return of an overpayment if a provider or supplier has actual knowledge of the existence of an overpayment or acts in reckless disregard or deliberate ignorance of an overpayment. The Legislation also expanded the Recovery Audit Contractor program to Medicaid. These amendments also make it easier for severe fines and penalties to be imposed on healthcare providers that violate applicable laws and regulations.
We have partnered with local physicians in the ownership of certain of our facilities. These investments have been permitted under an exception to the physician self-referral law. The Legislation permits existing physician investments in a hospital to continue under a “grandfather” clause if the arrangement satisfies certain requirements and restrictions, but physicians are prohibited from increasing the aggregate percentage of their ownership in the hospital. The Legislation also imposes certain compliance and disclosure requirements upon existing physician-owned hospitals and restricts the ability of physician-owned hospitals to expand the capacity of their facilities. A repeal of the Legislation, in whole or in relevant part, may result in physicians being able to expand ownership interest in hospitals.
In addition to legislative changes, the Legislation can be significantly impacted by executive branch actions. The Biden administration had issued executive orders implementing a special enrollment period permitting individuals to enroll in health plans outside of the annual open enrollment period and reexamining policies that may undermine the ACA or the Medicaid program. The American Rescue Plan Act of 2021's expansion of subsidies to purchase coverage through an exchange contributed to increased exchange enrollment in 2021. The IRA’s extension of subsidies through 2025 was expected to increase exchange enrollment in future years. However, the Trump administration has already taken steps to undo certain Biden-era executive orders, including those intended to lower drug costs for beneficiaries, and to freeze funding for federal programs. While the administration’s initial freeze has since been rescinded, the administration is likely to make other attempts to reduce federal program expenditures and can generally be expected to oppose increases in ACA and Medicaid enrollment.
It remains unclear what portions of the Legislation may remain, or whether any replacement or alternative programs may be created by any future legislation. Any such future repeal or replacement may have significant impact on the reimbursement for healthcare services generally, and may create reimbursement for services competing with the services offered by our hospitals. Accordingly, there can be no assurance that the adoption of any future federal or state healthcare reform legislation will not have a negative financial impact on our hospitals, including their ability to compete with alternative healthcare services funded by such potential legislation, or for our hospitals to receive payment for services.
For additional disclosure related to our revenues including a disaggregation of our consolidated net revenues by major source for each of the periods presented herein, please see Note 10 to the Consolidated Financial Statements-Revenue Recognition.
Medicare: Medicare is a federal program that provides certain hospital and medical insurance benefits to persons aged 65 and over, some disabled persons and persons with end-stage renal disease. All of our acute care hospitals and many of our behavioral health centers are certified as providers of Medicare services by the appropriate governmental authorities. Amounts received under the Medicare program are generally significantly less than a hospital’s customary charges for services provided. Since a substantial portion of our revenues will come from patients under the Medicare program, our ability to operate our business successfully in the future will depend in large measure on our ability to adapt to changes in this program.
Under the Medicare program, for inpatient services, our general acute care hospitals receive reimbursement under the inpatient prospective payment system (“IPPS”). Under the IPPS, hospitals are paid a predetermined fixed payment amount for each hospital discharge. The fixed payment amount is based upon each patient’s Medicare severity diagnosis related group (“MS-DRG”). Every MS-DRG is assigned a payment rate based upon the estimated intensity of hospital resources necessary to treat the average patient with that particular diagnosis. The MS-DRG payment rates are based upon historical national average costs and do not consider the actual costs incurred by a hospital in providing care. This MS-DRG assignment also affects the predetermined capital rate paid with each MS-DRG. The MS-DRG and capital payment rates are adjusted annually by the predetermined geographic adjustment factor for the geographic region in which a particular hospital is located and are weighted based upon a statistically normal distribution of severity. While we generally will not receive payment from Medicare for inpatient services, other than the MS-DRG payment, a hospital may qualify for an “outlier” payment if a particular patient’s treatment costs are extraordinarily high and exceed a specified threshold. MS-DRG rates are adjusted by an update factor each federal fiscal year, which begins on October 1. The index used to adjust the MS-DRG rates, known as the “hospital market basket index,” gives consideration to the inflation experienced by hospitals in purchasing goods and services. Generally, however, the percentage increases in the MS-DRG payments have been lower than the projected increase in the cost of goods and services purchased by hospitals.
In August, 2024, CMS published its IPPS 2025 final payment rule which provides for a 2.9% market basket increase to the base Medicare MS-DRG blended rate. When statutorily mandated budget neutrality factors, annual geographic wage index updates, documenting and coding adjustments, and adjustments mandated by the Legislation are considered, without consideration for the required Medicare DSH payments changes and increase to the Medicare Outlier threshold, the overall increase in IPPS payments is
approximately 1.8%. Including DSH payments, an increase to the Medicare Outlier threshold and certain other adjustments, we estimate our overall increase from the final IPPS 2025 rule (covering the period of October 1, 2024 through September 30, 2025) will approximate 1.2%.
In August, 2023, CMS published its IPPS 2024 final payment rule which provides for a 3.1% market basket increase to the base Medicare MS-DRG blended rate. When statutorily mandated budget neutrality factors, annual geographic wage index updates (including a change in the Medicare Rural Floor calculation), documenting and coding adjustments, and adjustments mandated by the Legislation are considered, without consideration for the required Medicare DSH payments changes and increase to the Medicare Outlier threshold, the overall increase in IPPS payments is approximately 6.6%. Including DSH payments, an increase to the Medicare Outlier threshold and certain other adjustments, we estimate our overall increase from the final IPPS 2024 rule (covering the period of October 1, 2023 through September 30, 2024) will approximate 5.4%.
In August, 2022, CMS published its IPPS 2023 final payment rule which provides for a 4.1% market basket increase to the base Medicare MS-DRG blended rate. When statutorily mandated budget neutrality factors, annual geographic wage index updates, documenting and coding adjustments, and adjustments mandated by the Legislation are considered, without consideration for the required Medicare DSH payments changes and increase to the Medicare Outlier threshold, the overall increase in IPPS payments is approximately 4.6.%. Including DSH payments, an increase to the Medicare Outlier threshold and certain other adjustments, we estimate our overall increase from the final IPPS 2023 rule (covering the period of October 1, 2022 through September 30, 2023) will approximate 4.4%. This projected impact from the IPPS 2023 final rule includes an increase of approximately 0.5% to partially restore cuts made as a result of the American Taxpayer Relief Act of 2012, as required by the 21st Century Cures Act, but excludes the impact of the sequestration reductions related to the 2011 Act, Bipartisan Budget Act of 2015, and Bipartisan Budget Act of 2018.
In June, 2019, the Supreme Court of the United States issued a decision favorable to hospitals impacting prior year Medicare DSH payments (Azar v. Allina Health Services, No. 17-1484 (U.S. Jun. 3, 2019)). In Allina, the hospitals challenged the Medicare DSH adjustments for federal fiscal year 2012, specifically challenging CMS’s decision to include inpatient hospital days attributable to Medicare Part C enrollee patients in the numerator and denominator of the Medicare/SSI fraction used to calculate a hospital’s DSH payments. This ruling addresses CMS’s attempts to impose the policy espoused in its vacated 2004 rulemaking to a fiscal year in the 2004–2013 time period without using notice-and-comment rulemaking. This decision should require CMS to recalculate hospitals’ DSH Medicare/SSI fractions, with Medicare Part C days excluded, for at least federal fiscal year 2012, but likely federal fiscal years 2005 through 2013. In August, 2020, CMS issued a rule that proposed to retroactively negate the effects of the aforementioned Supreme Court decision, which rule has yet to be finalized. Although we can provide no assurance that we will ultimately receive additional funds, we estimate that the favorable impact of this court ruling on certain prior year hospital Medicare DSH payments could range between $18 million to $28 million in the aggregate.
The 2011 Act included the imposition of annual spending limits for most federal agencies and programs aimed at reducing budget deficits by $917 billion between 2012 and 2021, according to a report released by the Congressional Budget Office. Among its other provisions, the law established a bipartisan Congressional committee, known as the Joint Committee, which was responsible for developing recommendations aimed at reducing future federal budget deficits by an additional $1.5 trillion over 10 years. The Joint Committee was unable to reach an agreement by the November 23, 2011 deadline and, as a result, across-the-board cuts to discretionary, national defense and Medicare spending were implemented on March 1, 2013 resulting in Medicare payment reductions of up to 2% per fiscal year. Subsequent legislation has extended this sequestration through 2032. The CARES Act, as amended, temporarily suspended or limited the application of this sequestration from May 1, 2020 through June 30, 2022, with a return to the full 2% Medicare payment reduction thereafter.
Inpatient services furnished by psychiatric hospitals under the Medicare program are paid under a Psychiatric Prospective Payment System (“Psych PPS”). Medicare payments to psychiatric hospitals are based on a prospective per diem rate with adjustments to account for certain facility and patient characteristics. The Psych PPS also contains provisions for outlier payments and an adjustment to a psychiatric hospital’s base payment if it maintains a full-service emergency department.
In July, 2024, CMS published its Psych PPS final rule for the federal fiscal year 2025. Under this final rule, payments to our behavioral health care hospitals and units from the market basket update are estimated to increase by 2.8% compared to federal fiscal year 2024. This amount includes the effect of the 3.3% net market basket update which reflects the offset of a 0.5% productivity adjustment. When all of the final patient level adjustments described below as well as proposed wage index values are considered, we estimate that Psych PPS payments will increase by 2.1% in FFY 2025.
In addition to the market basket update noted above, CMS will make the following changes:
•Revisions to the methodology for determining the payment rates under the Inpatient Psychiatric Facility ("IPF") PPS for psychiatric hospitals and psychiatric units based on a review of the data and information collected in prior years in accordance with section 1886(s)(5)(A) of the Social Security Act, as added by the Consolidated Appropriations Act of 2023 ("CAA of 2023"). CMS finalized revisions to the IPF patient-level adjustment factors. The patient-level adjustments include Medicare Severity Diagnosis Related Groups (MS–DRGs) assignment of the patient’s principal diagnosis, selected comorbidities, patient age, and the variable per diem adjustments;
•Implement these revisions in a budget-neutral manner (that is, estimated payments to IPFs for FFY 2025 would be the same with or without the final revisions), and;
•Clarified the criteria regarding all-inclusive cost reporting. This clarification requires our behavioral health care hospitals, which are currently utilizing an all-inclusive charging practice, to modify both their billing practices and information technology applications by June 1, 2025 to ensure compliance with future regulations. We intend to be in compliance with this CMS billing requirement.
This final rule also includes two requests for information on future revisions to the IPF PPS facility-level adjustment factors and development of the new standardized IPF Patient Assessment Instrument, required by the CAA of 2023, which IPFs participating in the IPF Quality Reporting Program will be required to report for Rate Year 2028.
In July, 2023, CMS published its Psych PPS final rule for the federal fiscal year 2024. Under this final rule, payments to our behavioral health care hospitals and units are estimated to increase by 3.3% compared to federal fiscal year 2023. This amount includes the effect of the 3.5% net market basket update which reflects the offset of a 0.2% productivity adjustment.
In July, 2022, CMS published its Psych PPS final rule for the federal fiscal year 2023. Under this final rule, payments to our behavioral health care hospitals and units are estimated to increase by 3.8% compared to federal fiscal year 2022. This amount includes the effect of the 4.1% net market basket update which reflects the offset of a 0.3% productivity adjustment.
On November 2, 2023, in light of the Supreme Court’s decision in American Hospital Association v. Becerra (142 S. Ct. 1896 (2022)) and the district court’s remand to the agency, CMS issued a final rule outlining the remedy for the 340B-acquired drug payment policy for calendar years 2018-2022. CMS published the final rule to remedy the payment rates the Court held were invalid aspects of their past policy and will affect nearly all hospitals paid under the OPPS. As part of the final remedy, CMS will make an adjustment to the update factor to maintain budget neutrality as required by statute. CMS finalized the 340B policy for calendar year 2018 in 2017 in a budget neutral manner that included increasing payments for non-drug items and services; this payment increase was in effect from calendar years 2018 through 2022. CMS estimates that hospitals were paid $7.8 billion more for non-drug items and services during this time period than they would have been paid in the absence of the 340B payment policy. Because CMS is now making additional payments to affected 340B covered entity hospitals to pay them what they would have been paid had the 340B policy never been implemented, CMS will make a corresponding offset to maintain budget neutrality as if the 340B payment policy had never been in effect. To carry out this required $7.8 billion budget neutrality adjustment, CMS will reduce future non-drug item and service payments by adjusting the OPPS conversion factor by minus 0.5% starting in calendar year 2026 and continuing for 16 years. The impact of this 0.5% reduction on our 2026 results of operations is approximately $4 million.
In November, 2024, CMS issued its OPPS final rule for 2025. The hospital market basket increase is 3.4% and the productivity adjustment reduction is 0.5% for a net market basket increase of 2.9%. When other statutorily required adjustments and hospital patient service mix are considered, including a 14.2% increase to the partial hospitalization rate, we estimate that our overall Medicare OPPS update for 2025 will aggregate to a net increase of 3.6%.
In November, 2023, CMS issued its OPPS final rule for 2024. The hospital market basket increase is 3.3% and the productivity adjustment reduction is 0.2% for a net market basket increase of 3.1%. When other statutorily required adjustments and hospital patient service mix are considered, we estimate that our overall Medicare OPPS update for 2024 will aggregate to a net increase of 9.7%. This percentage reflects the impact resulting from rural floor changes to the Medicare wage index adjustment factor where certain states, such as California and Nevada, will materially benefit from this change.
In November, 2022, CMS issued its OPPS final rule for 2023. The hospital market basket increase is 4.1% and the productivity adjustment reduction is -0.3% for a net market basket increase of 3.8%. The final rule provides that in light of the Supreme Court decision in American Hospital Association v. Becerra, CMS is applying the default rate, generally average sales price plus 6%, to 340B acquired drugs and biologicals for 2023. During the 2018-2022 time period, we recorded an aggregate of approximately $45 million to $50 million of Medicare revenues related to the prior 340B payment policy. When other statutorily required adjustments and hospital patient service mix are considered, as well as impact of the aforementioned 340B Program policy change, our overall Medicare OPPS update for 2023 aggregated to a net increase of approximately 0.9% which includes a 0.3% increase to behavioral health division partial hospitalization rates.
On November 2, 2021, CMS issued its OPPS final rule for 2022. The hospital market basket increase is 2.7% and the productivity adjustment reduction is -0.7% for a net market basket increase of 2.0%. When other statutorily required adjustments and hospital patient service mix are considered, our overall Medicare OPPS update for 2022 aggregated to a net increase of approximately 2.4% which includes a 3.0% increase to behavioral health division partial hospitalization rates.
In November, 2019, CMS finalized its Hospital Price Transparency rule that implements certain requirements under the June 24, 2019 Presidential Executive Order related to Improving Price and Quality Transparency in American Healthcare to Put Patients First. Under this final rule, effective January 1, 2021, CMS will require: hospitals to make public: (1) their standard changes (both gross charges and payer-specific negotiated charges) for all items and services online in a machine-readable format, and; (2) standard charge data for a limited set of “shoppable services” the hospital provides in a form and manner that is more consumer friendly. On
November 2, 2021, CMS released a final rule increasing the monetary penalty that CMS can impose on hospitals that fail to comply with the price transparency requirements. We believe that our hospitals are in full compliance with the applicable federal regulations. In November, 2023, CMS finalized multiple provisions, effective as of January 1, 2024, focused on increasing hospital price transparency and compliance enforcement including but not limited to: (1) standard charges data would be posted online using a CMS template, instead of using the hospital’s own form/format; (2) all standard charge information would be encoded with a specified set of data elements (e.g., hospital name; license number; payer/plan name; description of service; billing codes, among others); (3) other technical changes related to increasing consumers’ automated accessibility to hospital standard charges, and; (4) certifications regarding accuracy of standard charge data and related compliance warning notices from CMS and requiring accessibility to health system leadership regarding transparency noncompliance.
In September, 2024, the Departments of Labor, Health and Human Services and the Treasury published final rules that:
•Mandate that insurers analyze the outcomes of their coverage to ensure there's equivalent access to mental health care, including provider networks, prior authorization rates and payment for out-of-network providers, and take action to get in compliance;
•Establish when health plans can’t use prior authorization or other tactics to make it more difficult to access mental health and substance use treatment, and;
•Require additional insurers to comply with the 2008 Mental Health Parity and Addiction Equity Act.
While these rules will likely improve patient access to inpatient and outpatient mental health services, we are unable to estimate the related potential impact on our results of operations.
Medicaid: Medicaid is a joint federal-state funded health care benefit program that is administered by the states to provide benefits to qualifying individuals. Most state Medicaid payments are made under a PPS-like system, or under programs that negotiate payment levels with individual hospitals. Amounts received under the Medicaid program are generally significantly less than a hospital’s customary charges for services provided. In addition to revenues received pursuant to the Medicare program, we receive a large portion of our revenues either directly from Medicaid programs or from managed care companies managing Medicaid. All of our acute care hospitals and most of our behavioral health centers are certified as providers of Medicaid services by the appropriate governmental authorities.
We receive revenues from various state and county-based programs, including Medicaid in all the states in which we operate. We receive annual Medicaid revenues of approximately $100 million, or greater, from each of Texas, Nevada, California, Illinois, Pennsylvania, Washington, D.C., Kentucky, Florida, Virginia, Massachusetts and Mississippi. We also receive Medicaid disproportionate share hospital payments in certain states including, most significantly, Texas. Many of these programs have a Medicaid supplemental payment component that are subject to approval on a year-to-year basis and there is no assurance that these supplemental payment revenues will continue at their current rates or at all. We are therefore particularly sensitive to potential reductions in Medicaid and other state-based revenue programs as well as regulatory, economic, environmental and competitive changes in those states. We can provide no assurance that reductions to revenues earned pursuant to these programs, particularly in the above-mentioned states, will not have a material adverse effect on our future results of operations.
The Legislation substantially increases the federally and state-funded Medicaid insurance program, and authorizes states to establish federally subsidized non-Medicaid health plans for low-income residents not eligible for Medicaid starting in 2014. However, the Supreme Court has struck down portions of the Legislation requiring states to expand their Medicaid programs in exchange for increased federal funding. Accordingly, many states in which we operate have not expanded Medicaid coverage to individuals at 133% of the federal poverty level. Facilities in states not opting to expand Medicaid coverage under the Legislation may be additionally penalized by corresponding reductions to Medicaid disproportionate share hospital payments beginning in fiscal year 2024, as discussed below. We can provide no assurance that further reductions to Medicaid revenues, particularly in the above-mentioned states, will not have a material adverse effect on our future results of operations.
Summary of Various State Medicaid Supplemental Payment Programs:
The following table summarizes the revenues, healthcare provider taxes (“Provider Taxes”) and net benefit related to each of the below-mentioned Medicaid supplemental programs for the years ended December 31, 2024 and 2023. The Provider Taxes are recorded in other operating expenses on the consolidated statements of income, as included herein. The "Estimated 2025" amounts reflected on the table below are, in many cases, subject to federal and potentially state approval and may be affected by any reductions or other changes in federal funding for these programs.
| | | | | | | | | |
| (amounts in millions) | |
| Estimated 2025 | | 2024 | | 2023 | |
Texas Supplemental Payment Programs: | | | | | | |
Revenues | $ | 308 | | $ | 336 | | $ | 247 | |
Provider Taxes | | (127 | ) | | (131 | ) | | (82 | ) |
Net benefit | $ | 181 | | $ | 205 | | $ | 165 | |
| | | | | | |
Nevada SDP: | | | | | | |
Revenues | $ | 347 | | $ | 310 | | $ | 13 | |
Provider Taxes | | (125 | ) | | (116 | ) | | (4 | ) |
Net benefit | $ | 222 | | $ | 194 | | $ | 9 | |
| | | | | | |
Various Other State Programs: | | | | | | |
Revenues | $ | 836 | | $ | 853 | | $ | 593 | |
Provider Taxes | | (290 | ) | | (289 | ) | | (211 | ) |
Net benefit | $ | 546 | | $ | 564 | | $ | 382 | |
| | | | | | |
Subtotal-Provider Tax Programs: | | | | | | |
Revenues | $ | 1,491 | | $ | 1,499 | | $ | 853 | |
Provider Taxes | | (542 | ) | | (536 | ) | | (297 | ) |
Aggregate net benefit from Provider Tax Programs | $ | 949 | | $ | 963 | | $ | 556 | |
| | | | | | |
Texas, Nevada and South Carolina DSH/SPA Programs: | | | | | | |
Revenues | $ | 48 | | $ | 53 | | $ | 73 | |
Provider Taxes | | 0 | | | 0 | | | 0 | |
Net benefit | $ | 48 | | $ | 53 | | $ | 73 | |
| | | | | | |
Total Supplemental Medicaid Programs: | | | | | | |
Revenues | $ | 1,539 | | $ | 1,552 | | $ | 926 | |
Provider Taxes | | (542 | ) | | (536 | ) | | (297 | ) |
Aggregate net benefit from all Supplemental Programs | $ | 997 | | $ | 1,016 | | $ | 629 | |
Texas Supplemental Payment Programs:
Certain of our acute care hospitals located in various counties of Texas participate in Medicaid supplemental payment Section 1115 Waiver indigent care programs. The 1115 Waiver has been approved by CMS through September 30, 2030. These hospitals also have affiliation agreements with third-party hospitals to provide free hospital and physician care to qualifying indigent residents of these counties. Our hospitals receive both supplemental payments from the Medicaid program and indigent care payments from third-party, affiliated hospitals. The supplemental payments are contingent on the county or hospital district making an Inter-Governmental Transfer (“IGT”) to the state Medicaid program while the indigent care payment is contingent on a transfer of funds from the applicable affiliated hospitals. However, the county or hospital district is prohibited from entering into an agreement to condition any IGT on the amount of any private hospital’s indigent care obligation.
CHIRP (including QIF)
On August 1, 2022, CMS approved the Comprehensive Hospital Increase Reimbursement Program ("CHIRP"), with a pool of $5.2 billion, for the rate period effective September 1, 2022 to August 31, 2023. On July 31, 2023, CMS approved the CHIRP program, with a pool of $6.5 billion, for the rate period of September 1, 2023 to August 31, 2024. On September 13, 2024, CMS approved the CHIRP program with a pool of $6.5 billion for the rate period September 1, 2024 to August 31, 2025 (with an amended CMS approval on October 1, 2024).
On January 26, 2024, the Texas Health and Human Services Commission ("THHSC") issued a final rule that will modify the CHIRP payments beginning with the State Fiscal Year (SFY) 2025 rate period to promote the advancement of the quality goals and strategies the program is designed to advance.
The final modifications include:
•Creation of a new pay-for-performance incentive payment through a third component in CHIRP, the Alternate Participating Hospital Reimbursement for Improving Quality Award ("APHRIQA"). For state fiscal years beginning with SFY 2025, behavioral health hospitals and rural hospitals will not be included in the pay-for-performance program, and;
•The funds for payment of the APHRIQA component will be transitioned from the existing uniform rate increase components of the Uniform Hospital Rate Increase Percentage and the Average Commercial Incentive Award and will be paid using a scorecard that directs managed care organizations to pay providers for performance achievements on quality outcome measures. Payments will be distributed under APHRIQA on a semi-annual basis that aligns with the measurement period determined for quality metrics reporting.
CHIRP payment levels could be reduced materially if our hospitals are not able meet the required APHRIQA pay-for-performance metrics.
In connection with the Quality Incentive Fund (“QIF”), the results of operations of certain of our acute care hospitals located in Texas included aggregate revenues of $50 million and $33 million during the years ended December 31, 2024 and 2023, respectively. These amounts were earned pursuant to contract terms with various Medicaid managed care plans which requires the annual payout of QIF funds when a managed care service delivery area’s actual claims-based CHIRP payments are less than targeted CHIRP payments for a specific rate year.
We estimate that these hospitals will be entitled to approximately $29 million of aggregate QIF revenues during the year ended December 31, 2025.
UC
Included in these provider tax programs are reimbursements received in connection with the Texas Uncompensated Care program ("UC"). The size and distribution of the UC pool are determined based on charity care costs reported to THHSC in accordance with Medicare cost report Worksheet S-10 principles.
HARP
On September 24, 2021, THHSC finalized New Fee-for-Service Supplemental Payment Program: Hospital Augmented Reimbursement Program (“HARP”) to be effective October 1, 2021. The HARP program continues the financial transition for providers who have historically participated in the Delivery System Reform Incentive Payment program described below. The program, which was approved by CMS on August 15, 2023, will provide additional funding to hospitals to help offset the cost hospitals incur while providing Medicaid services. HARP is technically a Medicaid Upper Payment Limit as payment under this program is based on a reasonable estimate of the amount that would be paid for the services under Medicare payment principles but is referred to as HARP by THHSC.
In connection with this program, included in our results of operations was approximately $43 million and $20 million during the years ended December 31, 2024 and 2023, respectively. Approximately $16 million of the amount recorded during 2024 was applicable to the period of October 1, 2022 through September 30, 2023. Approximately $13 million of the amount recorded during 2023 was applicable to the period of October 1, 2021 through September 30, 2022.
We expect our net reimbursements pursuant to HARP to approximate $24 million during the year ended December 31, 2025.
Nevada State Directed Payment Program ("SDP"):
As previously reported, in February, 2023, the Nevada Division of Health Care Financing and Policy (“DHCFP”) outlined a new provider fee on private hospitals located in Nevada that would effectively capture new Medicaid federal share for certain categories of services eligible for the new payment program. In late December, 2023, CMS approved the Medicaid managed care component of the Nevada SDP program, with an effective date of January 1, 2024. In November 2024, CMS approved an increased assessment rate which funded an increase in the SDP pool size covering the period of July 1, 2024 through December 31, 2024. Payments made pursuant to this component of the Nevada SDP program, which requires annual approval by CMS, are subject to reconciliation by DHCFP based on actual Medicaid managed care utilization during 2024. There can be no assurance that the Medicaid managed care component of the Nevada SDP will continue for any period after December 31, 2024, or that it will not be modified.
In connection with this program, included in our results of operations was approximately $194 million and $9 million recorded during the years ended December 31, 2024 and 2023, respectively.
We estimate that our aggregate net reimbursements pursuant to both components of the Nevada SDP program (net of related provider taxes) will approximate $222 million during the year ended December 31, 2025. The Nevada SDP for the period of January 1, 2025 through December 31, 2025 is under CMS' review for approval.
Various Other State Programs:
We receive substantial reimbursement from multiple states in connection with various supplemental Medicaid payment programs. The states include, but are not limited to, the state programs listed below from which we receive significant reimbursements.
Kentucky Hospital Rate Increase Program (“HRIP”)
In early 2021, CMS approved the Kentucky Medicaid Managed Care Hospital Rate Increase Program. In connection with this program, included in our results of operations was approximately $88 million and $73 million during the years ended December 31, 2024 and 2023, respectively. In December, 2024, CMS approved the program for the period of January 1, 2025 through December 31, 2025 at rates comparable to the prior year.
We estimate that our net reimbursements pursuant to HRIP will approximate $84 million during the year ended December 31, 2025.
California Supplemental Payments
In California, the state continues to operate Medicaid supplemental payment programs consisting of three components: Fee For Service Payment, Managed Care-Pass-Through Payment and Managed Care-Directed Payment. The non-federal share for these programs are financed by a statewide provider tax. The Directed Payment method will be based on actual concurrent hospital Medicaid managed care in-network patient volume whereas the other programs are based on prior year Medicaid utilization. The CMS program approval status is outlined in the table below.
California Hospital Fee Program CMS Approval Status:
| | |
Hospital Fee Program Component | CMS Methodology Approval Status | CMS Rate Setting Approval Status |
Fee For Service Payment | Approved through December 31, 2024 | Approved through December 31, 2024; Paid through September 30, 2024 |
Managed Care-Pass-Through Payment | Approved through December 31, 2024 | Approved through December 31, 2022 and paid in advance through December 31, 2023 |
Managed Care-Directed Payment | Approved through December 31, 2024 | Approved through December 31, 2022 and paid in advance through June 30, 2023 |
In connection with this program, included in our results of operations was $47 million and $46 million during the years ended December 31, 2024 and 2023, respectively.
We estimate that our net reimbursements pursuant to this program will approximate $63 million during the year ended December 31, 2025.
Mississippi Hospital Access Program
In September, 2023, subject to CMS approval, Mississippi announced a $689 million, two-part Medicaid payment proposal, effective retroactively to July 1, 2023, that would be funded by annual hospital assessments to the state's Medicaid program. These hospital assessments are calculated using a formula provided under state law. The first part of the program, known as the Mississippi Hospital Access Program (“MHAP”), provides direct payments for hospitals that serve patients in the state's Medicaid managed care delivery system. Hospitals are reimbursed near the average commercial rate, which is the upper limit ("UPL") for Medicaid managed care reimbursements. The second part of the program supplements traditional Medicaid payment rates for hospitals providing inpatient and outpatient services up to Medicaid's regulated UPL. In June 2024, CMS approved the MHAP program component for the period July 1, 2024 to June 30, 2025. The UPL component was approved in April, 2024.
In connection with this program, included in our results of operations was approximately $48 million and $33 million recorded during the years ended December 31, 2024 and 2023, respectively.
We estimate that our net reimbursements pursuant to these supplemental payment programs will approximate $44 million during the year ended December 31, 2025.
Florida Medicaid Managed Care Directed Payment Program (“DPP”)
The Florida DPP provides for an additional payment for Medicaid managed care contracted services. For the years ended December 31, 2024 and 2023, our results of operations included approximately $46 million and $43 million recorded in connection with this program (substantially all of which was recorded during the fourth quarters of each year).
We estimate that our reimbursements pursuant to this DPP will approximate $37 million during the year ended December 31, 2025. The Florida DPP for the period of October 1, 2024 to September 30, 2025 is under CMS' review for approval.
Illinois Medicaid Supplemental Payment Programs
The Illinois Medicaid Supplemental Payment Programs are comprised of three components: (1) Medicaid managed care directed payment program; (2) Medicaid managed care pass-through program, and; (3) Medicaid fee for service supplemental payment program. These programs require various related legislative and regulatory approvals each year.
In connection with this program, included in our results of operations was approximately $39 million and $36 million during the years ended December 31, 2024 and 2023, respectively.
We estimate that our net reimbursements pursuant to these supplemental payment programs will approximate $36 million during the year ended December 31, 2025. Approval of these programs for the period of January 1, 2025 to December 31, 2025 is under CMS' review.
Indiana Medicaid Managed Care DPP
The Indiana DPP provides for an additional payment for Medicaid managed care contracted services. In connection with this program, included in our results of operations was approximately $31 million recorded during each of the years ended December 31, 2024 and 2023.
We estimate that our net reimbursements pursuant to this program will approximate $33 million during the year ended December 31, 2025.
Oklahoma (Transition to Managed Care and Implementation of a Medicaid Managed Care DPP)
The current Oklahoma Medicaid supplemental payment program in effect, prior to the planned implementation of the new DPP in 2024, is the Supplemental Hospital Offset Payment Program (“SHOPP”). The SHOPP component will remain in place for certain categories of Medicaid patients that will continue to be enrolled in the traditional Medicaid Fee for Service program.
In May, 2022, Oklahoma enacted legislation that directs the Oklahoma Health Care Authority ("OHCA") to: (i) transition its Medicaid program from a fee for service payment model to a managed care payment model by no later than October 1, 2023, and: (ii) concurrently implement a Medicaid managed care DPP using a managed care gap of 90% of average commercial rates. In December, 2022, the OHCA delayed the implementation date of the Medicaid managed care change and related DPP until April 1, 2024. In September, 2023, CMS approved the DPP program for the 15-momth period effective as of April 1, 2024 through June 30, 2025.
In connection with this program, included in our results of operations was approximately $20 million and $12 million recorded during the years ended December 31, 2024 and 2023, respectively.
We estimate that our net reimbursements pursuant to these two supplemental payment programs (i.e. SHOPP and DPP) will approximate $22 million during the year ended December 31, 2025.
South Carolina Health Access, Workforce and Quality (“HAWQ”) Program
In September 2023, CMS approved the South Carolina HAWQ Program retroactive to July 1, 2023 and subsequently approved by CMS in July, 2024 for the period of July 1, 2024 to June 30, 2025. This program is a Medicaid managed care directed payment program that provides for a rate enhancement to Medicaid managed care encounters. In connection with this program, included in our results of operations was approximately $28 million and $11 million recorded during the years ended December 31, 2024 and 2023, respectively.
We estimate that our net reimbursements pursuant to this program will approximate $26 million during the year ended December 31, 2025.
Michigan Directed Payment Program (“DPP”)
In March 2024, CMS approved the Michigan Medicaid DPP retroactive to October 1, 2023 based on average commercial rates. The Michigan DPP provides for an additional payment for Medicaid managed care contracted services. In connection with this program, included in our results of operations was approximately $37 million and $17 million recorded during the years ended December 31, 2024 and 2023, respectively.
We estimate that our net reimbursements pursuant to this program will approximate $31 million during the year ended December 31, 2025. The Michigan DPP for the period of October 1, 2024 to September 30, 2025 is under CMS' review for approval.
Idaho Upper Payment Limit (“UPL”)
In April 2024, the Idaho Department of Health and Welfare (“IDHW”) released its updated Medicaid UPL calculation for SFY 2024 (July 1, 2023 to June 30, 2024) and revised its SFY 2023 (July 1, 2022 to June 30, 2023) UPL calculation. Subject to CMS approval, the IDHW plans to continue this UPL program through SFY 2025 (July 1, 2024 to June 30, 2025) at payment levels comparable to SFY 2024. In SFY 2026, the IDHW intends to replace the UPL program with a Medicaid managed care state directed payment program. We are unable to predict whether payments levels under the planned new state directed payment program will be comparable to the SFY 2024 UPL payment levels.
In connection with this program, included in our results of operations was approximately $31 million and $22 million recorded during the years ended December 31, 2024 and 2023, respectively.
We estimate that our net reimbursements pursuant to this program will approximate $19 million during the year ended December 31, 2025.
Washington Safety Net Assessment Program
On April 2, 2024, CMS approved an expanded state directed payment program in Washington whereby payments will now be based on the average commercial rates. The program was approved retroactively for the period January 1, 2024 to December 31, 2024.
In connection with this program, included in our results of operations was approximately $46 million and $3 million recorded during the years ended December 31, 2024 and 2023, respectively.
We estimate that our net reimbursements pursuant to this expanded program will approximate $48 million during the year ended December 31, 2025. Approval of this program for the period of January 1, 2025 to December 31, 2025 is under CMS' review.
New Mexico State Directed Payment Program (“SDP”)
In November, 2024, CMS approved the New Mexico Medicaid SDP, retroactive to July 1, 2024, based on average commercial rates. The New Mexico SDP provides for an additional payment for Medicaid managed care contracted services. In connection with this program, included in our results of operations was approximately $8 million in the year ended December 31, 2024. There was no impact from this program included in our results of operations for the year ended December 31, 2023. The program requires the submission of an annual report that demonstrates that 75% of the incremental net funds were used for the delivery of and access to healthcare services in the state.
The state agency intends to renew the program for calendar year 2025 at payments level consistent with the 2024 annualized payment level. The New Mexico SDP for the period of January 1, 2025 to December 31, 2025 is under CMS' review. We estimate that our net reimbursements pursuant to this program will approximate $16 million during the year ended December 31, 2025.
Tennessee Directed Payment Program (“DPP”)
Tennessee SB1740, enacted in May, 2024, imposes an annual coverage assessment on covered hospitals for fiscal year 2024-2025. The total assessment on all covered hospitals in the aggregate will be equal to 6% of the federally recognized annual coverage assessment base. The assessment proceeds will be used to fund an increase to the state’s DPP payment pool to be based on average commercial rates. In January, 2025, CMS approved the DPP payment increase for the period July 1, 2024 to December 31, 2024, contingent upon CMS' approval of the state's 1115 Medicaid Waiver amendment . The DPP preprint for calendar year (January 1, 2025 to December 31, 2025) is pending CMS approval.
We estimate that our net reimbursements pursuant to this program will approximate $28 million during the year ended December 31, 2025 (related to the six-month period July 1, 2024 to December 31, 2024), if CMS' approval of the state's 1115 Medicaid Waiver amendment occurs during 2025. In addition, although we are unable to predict whether the DPP program for calendar year 2025 will be approved by CMS, or the timing of such approval, TennCare's financial models indicate that our annual DPP reimbursements could range from $40 million to $56 million. The "Estimated 2025" amounts reflected on the table above do not include any net reimbursements in connection with the Tennessee DPP.
Washington, D.C. State Directed Payment program (“SDP”)
In July, 2024, the Budget Support Act (B24-0784) was approved by the mayor of Washington, D.C. This legislation includes a new Medicaid managed care directed payment program that, if ultimately approved, could become effective for the period of October 1, 2024 through September 30, 2025, with potential subsequent annual programs. Finalization of this program remains contingent upon U.S. Congressional and CMS approval. Estimated amounts related to this program are subject to change for various reasons including modifications based upon CMS' review of the preprint payment methodology terms, as well as actual Medicaid managed care utilization for hospitals that operate in the District of Columbia, including ours. If ultimately approved, there can be no assurance that this program will continue for any period after September 30, 2025, or that it will not be modified. The Washington, D.C., Medicaid agency submitted the SDP preprint to CMS in July 2024, for review and approval.
Although we cannot predict if this new SDP program will be ultimately approved, or the timing of such approval should it occur, if approved in its current form, we estimate that our aggregate net benefit from this program for the period of October 1, 2024 through September 30, 2025, related to our two existing hospitals in the market, will approximate $85 million. The "Estimated 2025" amounts reflected on the table above do not include any net reimbursements in connection with the Washington, D.C. SDP program.
Texas DSH and Nevada SPA Programs:
Texas DSH
Upon meeting certain conditions and serving a disproportionately high share of Texas’ low income patients, our qualifying facilities located in Texas receive additional reimbursement from the state’s DSH fund. The Texas DSH program was renewed for the state’s 2025 DSH fiscal year (covering the period of October 1, 2024 through September 30, 2025).
In connection with this program, included in our results of operations was approximately $36 million and $47 million recorded during the years ended December 31, 2024 and 2023, respectively.
We estimate that our aggregate net reimbursements earned pursuant to the Texas DSH program will approximate $30 million during the year ended December 31, 2025.
The Legislation and subsequent federal legislation provides for a significant reduction in Medicaid disproportionate share payments beginning in federal fiscal year 2025 (see above in Sources of Revenues and Health Care Reform-Medicaid for additional disclosure related to the delay of these DSH reductions). HHS is to determine the amount of Medicaid DSH payment cuts imposed on each state based on a defined methodology. As Medicaid DSH payments to states will be cut, consequently, payments to Medicaid-participating providers, including our hospitals in Texas, will be reduced in the coming years. Based on the CMS final rule published in September, 2019 (as amended by the CARES Act and the CAA), beginning in fiscal year 2025, annual Medicaid DSH payments in Texas could be reduced by approximately 41% from current DSH payment levels. A series of federal continuing resolutions were passed by the federal government which provided for ongoing federal funding.
In connection with certain previous DSH and UC adverse federal court decisions, including the Children’s Hospital Association of Texas v. Azar, we continue to maintain reserves in the financial statements for cumulative Medicaid DSH and UC reimbursements related to our behavioral health hospitals located in Texas that amounted to $34 million as of December 31, 2024 and $31 million as of December 31, 2023.
Nevada State Plan Amendment ("SPA")
CMS initially approved an SPA in Nevada in August, 2014 and this SPA has been approved for additional state fiscal years, including the 2024 fiscal year covering the period of July 1, 2023 through June 30, 2024. CMS approval for the 2025 fiscal year, which is still pending, is expected to occur.
In connection with this program, included in our results of operations was approximately $17 million and $25 million recorded during the years ended December 31, 2024 and 2023, respectively.
We estimate that our net reimbursements pursuant to this program will approximate $18 million during the year ended December 31, 2025.
Risk Factors Related To State Supplemental Medicaid Payments:
As outlined above, we receive substantial reimbursement from multiple states in connection with various supplemental Medicaid payment programs. Failure to renew these programs beyond their scheduled termination dates, failure of the public hospitals to provide the necessary IGTs for the states’ share of the DSH programs, failure of our hospitals that currently receive supplemental Medicaid revenues to qualify for future funds under these programs, or reductions in reimbursements, could cause our estimates to differ by material amounts which could have a material adverse effect on our future results of operations.
In April, 2016, CMS published its final Medicaid Managed Care Rule which explicitly permits but phases out the use of pass-through payments (including supplemental payments) by Medicaid Managed Care Organizations (“MCO”) to hospitals over ten years but allows for a transition of the pass-through payments into value-based payment structures, delivery system reform initiatives or payments tied to services under a MCO contract. Since we are unable to determine the financial impact of this aspect of the final rule, we can provide no assurance that the final rule will not have a material adverse effect on our future results of operations. In November, 2020, CMS issued a final rule permitting pass-through supplemental provider payments during a time-limited period when states transition populations or services from fee-for-service Medicaid to managed care.
We receive Medicaid SDP payments from MCOs authorized by CMS under 42 CFR § 438.6(c). Consistent with capitated rates paid by Medicaid state agencies to MCO’s for managing Medicaid beneficiary lives under a risk-based arrangement, SDP program related capitated rates must also be developed by the state in accordance with actuarial soundness standards noted at 42 CFR § 438.4 and non-compliance could result in a reduction to SDP payment levels. In general, Medicaid SDP payments under 42 CFR § 438.6(c) are subject to annual CMS approval via the submission of a preprint application by a state agency which provides details of the SDP payment methodology and conformity with the applicable federal regulations. CMS SDP preprint approval, and the timing of such approval, if it occurs, are not certain which can affect the both the SDP payment level and timing of SDP revenue recorded by us.
We incur Provider Taxes imposed by states in the form of a licensing fee, assessment or other mandatory payment which are related to: (i) healthcare items or services; (ii) the provision of, or the authority to provide, the health care items or services, or; (iii) the payment for the health care items or services that are used by respective states to finance the non-federal share of SDP’s (or other Medicaid supplemental payment programs). Such Provider Taxes are subject to various federal regulations that limit the scope and amount of the taxes that can be levied by states in order to secure federal matching funds as part of their respective state Medicaid supplemental payment programs. States are subject to CMS both concurrent and retrospective review for their compliance with the applicable Provider Tax regulations and related federal statute. If CMS determines Provider Taxes used by a state Medicaid program to finance the non-federal share of a SDP (or other Medicaid supplemental payment programs) are not in compliance with the
applicable Provider Tax regulations and related federal statute, Company SDP payments (and other Medicaid supplemental payments) could be subject to recoupment by the respective state agency when non-compliance is determined by CMS to exist.
We believe that the SDP (and other state supplemental payment) programs are designed by each state to be in full compliance with the applicable federal regulations and federal statutes. However, we are unable to provide assurance CMS will determine on a retroactive basis that a state’s SDP (or other Medicaid supplemental payment program) design and Medicaid financing structures is in full compliance with the applicable federal regulations and federal statute(s).
On April 22, 2024, CMS issued Medicaid and Children’s Health Insurance Program ("CHIP") Managed Care Access, Finance, and Quality Final Rule (“Managed Care Rule”). CMS intends for the Managed Care Rule to:
•Strengthen standard for timely access to care and states’ monitoring and enforcement efforts;
•Enhance quality and fiscal and program integrity standards for state directed payments (“SDPs”);
•Specify the scope of in lieu of services and settings to better address health-related social needs;
•Further specify medical loss ratio requirements, and;
•Establish a quality rating system for Medicaid and CHIP managed care plans.
The SDP provisions included in the Managed Care Rule:
•Requires that provider payment levels for state directed payments for inpatient and outpatient hospital services, nursing facility services, and the professional services at an academic medical center not exceed the average commercial rate;
•Prohibits the use of post-payment reconciliation processes for state directed payments that are based on fee schedules;
•Makes explicit in regulation the existing requirement that state directed payments must comply with all federal laws concerning funding sources of the non-federal share, and;
•Requires that states ensure each provider receiving a state directed payment attest that it does not participate in any arrangement that holds taxpayers harmless for the cost of a tax. CMS concurrently released an informational bulletin regarding CMS’ exercise of enforcement discretion until calendar year 2028 for existing health-care related tax programs with certain hold-harmless arrangements involving the redistribution of Medicaid payments.
As disclosed herein, we receive a significant amount of Medicaid and Medicaid managed care revenue from both base payments and supplemental payments. Although we are unable to estimate the impact of the Managed Care Rule on our future results of operations, if implemented as proposed, Managed Care Rule related changes could have a material adverse impact on our future results of operations.
Future changes to the terms and conditions of the various programs outlined above could materially reduce our net benefit derived from the programs which could have a material adverse impact on our future results of operations. In addition, Provider Taxes are governed by both federal and state laws and are subject to future legislative changes that, if reduced from current rates in several states, could have a material adverse impact on our future results of operations.
A 6.2% increase to the Medicaid Federal Matching Assistance Percentage (“FMAP”) was included in the Families First Coronavirus Response Act. The CAA of 2023 provided for the transitional reduction of the 6.2% enhanced FMAP during 2023 to 5.0% during the second quarter, 2.5% during the third quarter and 1.5% during the fourth quarter of 2023. The impact of the enhanced FMAP Medicaid supplemental and DSH payments are reflected in our financial results for the three and nine-month periods ended September 30, 2024 and 2023.
HITECH Act: In July 2010, HHS published final regulations implementing the health information technology provisions of the American Recovery and Reinvestment Act (referred to as the “HITECH Act”). The final regulation defines the “meaningful use” of Electronic Health Records (“EHR”) and establishes the requirements for the Medicare and Medicaid EHR payment incentive programs. The final rule established an initial set of standards and certification criteria. The implementation period for these Medicare and Medicaid incentive payments started in federal fiscal year 2011 and can end as late as 2016 for Medicare and 2021 for the state Medicaid programs. State Medicaid program participation in this federally funded incentive program is voluntary but all of the states in which our eligible hospitals operate have chosen to participate. Our acute care hospitals qualified for these EHR incentive payments upon implementation of the EHR application assuming they meet the “meaningful use” criteria. The government’s ultimate goal is to promote more effective (quality) and efficient healthcare delivery through the use of technology to reduce the total cost of healthcare for all Americans and utilizing the cost savings to expand access to the healthcare system.
All of our acute care hospitals have met the applicable meaningful use criteria. However, under the HITECH Act, hospitals must continue to meet the applicable meaningful use criteria in each fiscal year or they will be subject to a market basket update reduction in a subsequent fiscal year. Failure of our acute care hospitals to continue to meet the applicable meaningful use criteria would have an adverse effect on our future net revenues and results of operations.
In the 2019 IPPS final rule, CMS overhauled the Medicare and Medicaid EHR Incentive Program to focus on interoperability, improve flexibility, relieve burden and place emphasis on measures that require the electronic exchange of health information between providers and patients. We can provide no assurance that the changes will not have a material adverse effect on our future results of operations.
Managed Care: A significant portion of our net patient revenues are generated from managed care companies, which include health maintenance organizations, preferred provider organizations and managed Medicare (referred to as Medicare Part C or Medicare Advantage) and Medicaid programs. In general, we expect the percentage of our business from managed care programs to continue to grow. The consequent growth in managed care networks and the resulting impact of these networks on the operating results of our facilities vary among the markets in which we operate. Typically, we receive lower payments per patient from managed care payers than we do from traditional indemnity insurers, however, during the past few years we have secured price increases from many of our commercial payers including managed care companies.
Commercial Insurance: Our hospitals also provide services to individuals covered by private health care insurance. Private insurance carriers typically make direct payments to hospitals or, in some cases, reimburse their policy holders, based upon the particular hospital’s established charges and the particular coverage provided in the insurance policy. Private insurance reimbursement varies among payers and states and is generally based on contracts negotiated between the hospital and the payer.
Commercial insurers are continuing efforts to limit the payments for hospital services by adopting discounted payment mechanisms, including predetermined payment or DRG-based payment systems, for more inpatient and outpatient services. To the extent that such efforts are successful and reduce the insurers’ reimbursement to hospitals and the costs of providing services to their beneficiaries, such reduced levels of reimbursement may have a negative impact on the operating results of our hospitals.
Surprise Billing Interim Final Rule: On September 30, 2021, the Department of Labor, and the Department of the Treasury, along with the Office of Personnel Management (“OPM”), released an interim final rule with comment period, entitled “Requirements Related to Surprise Billing; Part II.” This rule is related to Title I (the “No Surprises Act”) of Division BB of the Consolidated Appropriations Act, 2021, and establishes new protections from surprise billing and excessive cost sharing for consumers receiving health care items/services. It implements additional protections against surprise medical bills under the No Surprises Act, including provisions related to the independent dispute resolution ("IDR") process, good faith estimates for uninsured (or self-pay) individuals, the patient-provider dispute resolution process, and expanded rights to external review. On February 28, 2022, a district judge in the Eastern District of Texas invalidated portions of the rule governing aspects of the IDR process. In light of this decision, the government issued a final rule on August 19, 2022 eliminating the rebuttable presumption in favor of the qualifying payment amount by the IDR entity and providing additional factors the IDR entity should consider when choosing between two competing offers. CMS regulations and guidance implementing the IDR process has been subject to a significant amount of provider-initiated litigation. As a result, portions of those regulations and guidance materials have been vacated by a federal district court, causing CMS to, on several occasions, pause and resume IDR process operations, causing significant delay in the processing of claims. On October 27, 2023, HHS, the Department of Labor, the Department of the Treasury, and OPM issued a proposed rule intended to improve the functioning of the federal IDR process. Additionally, arguments made by the plaintiffs in such litigation have included allegations that CMS’s regulations and guidance materials are favorable to payers. We cannot predict the impact of the proposed rule on our operations at this time.
Other Sources: Our hospitals provide services to individuals that do not have any form of health care coverage. Such patients are evaluated, at the time of service or shortly thereafter, for their ability to pay based upon federal and state poverty guidelines, qualifications for Medicaid or other state assistance programs, as well as our local hospitals’ indigent and charity care policy. Patients without health care coverage who do not qualify for Medicaid or indigent care write-offs are offered substantial discounts in an effort to settle their outstanding account balances.
Health Care Reform: Listed below are the Medicare, Medicaid and other health care industry changes which have been, or are scheduled to be, implemented as a result of the Legislation.
Medicaid Federal DSH Allotment
Although the implementation has been delayed several times, the Legislation (as amended by subsequent federal legislation) requires annual aggregate reductions in federal Medicaid DSH allotment from FFY 2025 through FFY 2027. Commencing in federal fiscal year 2025, and continuing through 2027, DSH payments are scheduled to be reduced by $8 billion annually. The American Relief Act, 2025 (HR 10545, Public Law No. 118-158) enacted into law on December 21, 2024 postponed the scheduled ACA Medicaid DSH cuts that were to take effect January 1, 2025 to April 1, 2025. The $8 billion DSH reduction for FFY 2025 will be implemented over six months rather than twelve months if not delayed further by Congressional action.
Value-Based Purchasing
There is a trend in the healthcare industry toward value-based purchasing of healthcare services. These value-based purchasing programs include both public reporting of quality data and preventable adverse events tied to the quality and efficiency of care provided by facilities. Governmental programs including Medicare and Medicaid currently require hospitals to report certain quality
data to receive full reimbursement updates. In addition, Medicare does not reimburse for care related to certain preventable adverse events. Many large commercial payers currently require hospitals to report quality data, and several commercial payers do not reimburse hospitals for certain preventable adverse events.
The Legislation required HHS to implement a value-based purchasing program for inpatient hospital services which became effective on October 1, 2012. The Legislation requires HHS to reduce inpatient hospital payments for all discharges by 2% in FFY 2017 and subsequent years. HHS will pool the amount collected from these reductions to fund payments to reward hospitals that meet or exceed certain quality performance standards established by HHS. HHS will determine the amount each hospital that meets or exceeds the quality performance standards will receive from the pool of dollars created by these payment reductions. As part of the FFY 2022 IPPS final rule and FFY 2023 final rule, as discussed above, and as a result of the COVID-19 pandemic, CMS has implemented a budget neutral payment policy to fully offset the 2% VBP withhold during each of FFY 2022 and FFY 2023. In FFY 2024, as part of the FFY 2024 IPPS final rule, CMS removed the budget neutral policy that was in place in FFY 2022 and FFY 2023.
Hospital Acquired Conditions
The Legislation prohibits the use of federal funds under the Medicaid program to reimburse providers for medical assistance provided to treat hospital acquired conditions (“HAC”). Beginning in FFY 2015, hospitals that fall into the top 25% of national risk-adjusted HAC rates for all hospitals in the previous year will receive a 1% reduction in their total Medicare payments. As part of the FFY 2023 final rule discussed above, and as a result of the on-going COVID-19 pandemic, CMS suppressed all nine measures in the HAC Reduction Program for the FY 2023 program year and eliminated the HAC reduction program’s one percent payment penalty. In FFY 2024, as part of the FFY 2024 IPPS final rule, CMS eliminated the suppression of the applicable HAC measures and as a result reinstated the HAC reduction program.
Readmission Reduction Program
In the Legislation, Congress also mandated implementation of the hospital readmission reduction program (“HRRP”). Hospitals with excessive readmissions for conditions designated by HHS will receive reduced payments for all inpatient discharges, not just discharges relating to the conditions subject to the excessive readmission standard. The HRRP currently assesses penalties on hospitals having excess readmission rates for heart failure, myocardial infarction, pneumonia, acute exacerbation of chronic obstructive pulmonary disease ("COPD") and elective total hip arthroplasty ("THA") and/or total knee arthroplasty ("TKA"), excluding planned readmissions, when compared to expected rates. In the fiscal year 2015 IPPS final rule, CMS added readmissions for coronary artery bypass graft ("CABG") surgical procedures beginning in fiscal year 2017. To account for excess readmissions, an applicable hospital's base operating DRG payment amount is adjusted for each discharge occurring during the fiscal year. Readmissions payment adjustment factors can be no more than a 3% reduction. As part of the FFY 2023 IPPS final rule discussed above, CMS modified all of the condition-specific readmission measures to include an adjustment for patient history of COVID-19 for FFY 2024.
Accountable Care Organizations
The Legislation requires HHS to establish a Medicare Shared Savings Program that promotes accountability and coordination of care through the creation of accountable care organizations (“ACOs”). The ACO program allows providers (including hospitals), physicians and other designated professionals and suppliers to voluntarily work together to invest in infrastructure and redesign delivery processes to achieve high quality and efficient delivery of services. The program is intended to produce savings as a result of improved quality and operational efficiency. ACOs that achieve quality performance standards established by HHS will be eligible to share in a portion of the amounts saved by the Medicare program. CMS also developed and implemented more advanced ACO payment models that require ACOs to assume greater risk for attributed beneficiaries. Through various subsidiaries, we participate in ACOs in many of our acute care hospital markets.
Infectious Disease Outbreaks, Pandemics, or Other Public Health Emergencies or Crisis
Our business and financial results may be harmed by an international, national or localized outbreak of a highly contagious or epidemic disease, including but not limited to, COVID-19 or similar corona viruses, Ebola or Zika, may put stress on the capacity of all or a part of our health care facilities, could result in an abnormally high demand for health care services, require that resources be diverted from one part of operations to another part, or disrupt the supply chain for equipment and supplies necessary for operations. In addition, unaffected individuals may decide to defer elective procedures or otherwise avoid medical treatment, resulting in reduced patient volumes and operating revenues.
In addition to statutory and regulatory changes to the Medicare program and each of the state Medicaid programs, our operations and reimbursement may be affected by administrative rulings, new or novel interpretations and determinations of existing laws and regulations, post-payment audits, requirements for utilization review and new governmental funding restrictions, all of which may materially increase or decrease program payments as well as affect the cost of providing services and the timing of payments to our facilities. The final determination of amounts we receive under the Medicare and Medicaid programs often takes many years, because of audits by the program representatives, providers’ rights of appeal and the application of numerous technical reimbursement provisions. We believe that we have made adequate provisions for such potential adjustments. Nevertheless, until final adjustments are
made, certain issues remain unresolved and previously determined allowances could become either inadequate or more than ultimately required.
Finally, we expect continued third-party efforts to aggressively manage reimbursement levels and cost controls. Reductions in reimbursement amounts received from third-party payers could have a material adverse effect on our financial position and our results.
Other Operating Results
Interest Expense
As reflected on the schedule below, interest expense was $186 million during 2024 and $207 million during 2023 (amounts in thousands):
| | | | | | | | |
| | 2024 | | | 2023 | |
Revolving credit & demand notes (a.) | | $ | 18,770 | | | $ | 23,139 | |
Tranche A term loan, extinguished (a.) | | | 113,934 | | | | 155,673 | |
Tranche A term loan, 2029 (a.) | | | 20,001 | | | | — | |
$800 million, 2.65% Senior Notes due 2030 (b.) | | | 21,426 | | | | 21,426 | |
$700 million, 1.65% Senior Notes due 2026 (c.) | | | 11,725 | | | | 11,725 | |
$500 million, 2.65% Senior Notes due 2032 (d.) | | | 13,380 | | | | 13,380 | |
$500 million, 4.625% Senior Notes due 2029 (e.) | | | 6,113 | | | | — | |
$500 million, 5.05% Senior Notes due 2034 (f.) | | | 6,705 | | | | — | |
Subtotal - revolving credit, term loan A and Senior Notes | | | 212,054 | | | | 225,343 | |
Amortization of financing fees | | | 5,021 | | | | 5,035 | |
Other combined interest expense | | | 9,381 | | | | 1,290 | |
Capitalized interest on major projects | | | (38,922 | ) | | | (24,422 | ) |
Interest income | | | (1,425 | ) | | | (572 | ) |
Interest expense, net | | $ | 186,109 | | | $ | 206,674 | |
(a.)On September 26, 2024, we entered into the tenth amendment to our credit agreement dated November 15, 2010, as amended and restated at various times from March, 2011 to June, 2022 (the "Credit Agreement"). The tenth amendment provides for, among other things, the following: (i) an extension of the maturity date to September 26, 2029; (ii) a $100 million increase in the revolving credit facility to $1.3 billion of aggregate borrowing capacity (which as of December 31, 2024, had $1.17 billion of aggregate available borrowing capacity, net of $130 million of borrowings outstanding and $3 million of letters of credit), and; (iii) a $1.0 billion reduction in the outstanding borrowings pursuant to the tranche A term loan facility, to $1.2 billion from $2.2 billion previously, utilizing the proceeds generated from the September, 2024, issuance of the below-mentioned senior notes due in 2029 and 2034.
(b.)In September, 2020, we completed the offering of $800 million aggregate principal amount of 2.65% Senior Notes due in 2030.
(c.)In August, 2021, we completed the offering of $700 million aggregate principal amount of 1.65% Senior Notes due in 2026.
(d.)In August, 2021, we completed the offering of $500 million aggregate principal amount of 2.65% Senior Notes due in 2032.
(e.)On September 26, 2024, we completed the offering of $500 million aggregate principal amount of 4.625% Senior Notes due in 2029.
(f.)On September 26, 2024, we completed the offering of $500 million aggregate principal amount of 5.050% Senior Notes due in 2034.
Interest expense decreased by $21 million during 2024 to $186 million as compared to $207 million during 2023. The decrease was primarily due to: (i) a net $13 million decrease in aggregate interest expense on our revolving credit, term loan A and senior notes, resulting from a decrease in our aggregate average cost of borrowings pursuant to these facilities (4.65% during 2024 as compared to 4.8% during 2023), as well as a decrease in the aggregate average outstanding borrowings ($4.47 billion during 2024 as compared to $4.63 billion during 2023); (ii) a $15 million decrease resulting from an increase in capitalized interest on major projects, partially offset by; (iii) a net $7 million increase in other combined interest expenses.
The average effective interest rate, including amortization of deferred financing costs, on borrowings outstanding under our revolving credit, term loan A and senior notes, which amounted to approximately $4.47 billion as of 2024 and $4.63 billion as of 2023, were 4.8% during 2024 and 4.9% during 2023.
Provision for Asset Impairments
Our financial statements for the year ended December 31, 2022, include a pre-tax provision for asset impairment of approximately $58 million, which is included in other operating expenses on the accompanying consolidated statements of income, to write-down the asset value of Desert Springs Hospital Medical Center, a 282-bed acute care hospital located in Las Vegas, Nevada. In early 2023, as a result of various competitive pressures and operational challenges experienced in the market, which had a significant unfavorable impact on the hospital's results of operations during the past year, as well as physical plant constraints and limitations resulting from the advanced age of the facility (which opened in 1971), we announced plans to discontinue all inpatient operations by March of 2023. For a period of time, we plan to continue providing emergency department services within a portion of the existing facility while we construct a new free-standing emergency department on the hospital's campus. The provision for asset impairment reduced the asset values of the facility's real estate and equipment to their estimated fair values.
Provision for Income Taxes and Effective Tax Rates
The effective tax rates, as calculated by dividing the provision for income taxes by income before income taxes, were as follows for each of the years ended December 31, 2024 and 2023 (dollar amounts in thousands):
| | | | | | | | | |
| | 2024 | | | 2023 | | |
Provision for income taxes | | $ | 334,827 | | | $ | 221,119 | | |
Income before income taxes | | | 1,497,936 | | | | 940,426 | | |
Effective tax rate | | | 22.4 | % | | | 23.5 | % | |
The provision for income taxes increased $114 million during 2024, as compared to 2023, due primarily to: (i) the increase in the provision for income taxes resulting from the $538 million increase in pre-tax income (consisting of $558 million increase in income before income taxes minus a $20 million increase in the income/loss attributable to noncontrolling interests), partially offset by; (ii) a $16 million decrease in the provision for income taxes during 2024, as compared to 2023, from the net tax benefit recorded pursuant to ASU 2016-09, net of the impact of executive compensation limitations pursuant to IRC section 162(m).
Due to recent guidance and enacted laws surrounding the global 15% minimum tax rate that will be effective after 2024 from the Organization for Economic Co-operation and Development ("OECD"), as well as jurisdictions that we operate in, we anticipate adverse effects to our provision for income taxes as well as cash taxes. Currently, the United States has not enacted legislation that aligns with the OECD global minimum tax rate. We do not expect these effects to be material and will continue to monitor changes in tax policies and laws issued by the OECD and jurisdictions in which we operate.
Effects of Inflation and Seasonality
Seasonality —Our acute care services business is typically seasonal, with higher patient volumes and net patient service revenue in the first and fourth quarters of the year. This seasonality occurs because, generally, more people become ill during the winter months, which results in significant increases in the number of patients treated in our hospitals during those months.
Inflation — See disclosure above in Results of Operations-Clinical Staffing, Physician Related Expenses and Effects of Inflation.
Liquidity
Year ended December 31, 2024 as compared to December 31, 2023:
Net cash provided by operating activities
Net cash provided by operating activities was $2.067 billion during 2024 as compared to $1.268 million during 2023. The net increase of $799 million was primarily attributable to the following:
•a favorable change of $472 million resulting from an increase in net income plus/minus depreciation and amortization expense, stock-based compensation expense, gains on sales of assets and businesses and costs related to the extinguishment of debt;
•a favorable change of $250 million in accounts receivable due, in part, to a decrease in our days sales outstanding as of December 31, 2024, as compared to December 31, 2023, as discussed below;
•a favorable change of $94 million from other working capital accounts due primarily to the timing of disbursements for certain accrued liabilities;
•an unfavorable change of $61 million in other assets and deferred charges;
•a favorable change of $56 million in accrued and deferred income taxes, and;
•$12 million of other combined net unfavorable changes.
Days sales outstanding (“DSO”): Our DSO are calculated by dividing our net revenue by the number of days in the year. The result is divided into the accounts receivable balance at the end of the year. Our DSO were 50 days at December 31, 2024 and 57 days at December 31, 2023.
Net cash used in investing activities
Net cash used in investing activities was $911 million during 2024 and $763 million during 2023.
2024:
The $911 million of net cash used in investing activities during 2024 consisted of:
•$944 million spent on capital expenditures including capital expenditures for equipment, renovations and new projects at various existing facilities;
•$39 million of proceeds received from sales of assets and businesses;
•$19 million spent on the acquisition of businesses and property, and;
•$13 million received in connection with net cash inflows from forward exchange contracts that hedge our investment in the U.K. against movements in exchange rates;
2023:
The $763 million of net cash used in investing activities during 2023 consisted of:
•$743 million spent on capital expenditures including capital expenditures for equipment, renovations and new projects at various existing facilities;
•$41 million paid in connection with net cash outflows from forward exchange contracts that hedge our investment in the U.K. against movements in exchange rates;
•$24 million of proceeds received from sales of assets and businesses, and;
•$4 million spent on the acquisition of businesses and property.
Net cash used in financing activities
Net cash used in financing activities was $1.145 billion during 2024 and $494 million during 2023.
2024:
The $1.145 billion of net cash used in financing activities during 2024 consisted of the following:
•spent $2.640 billion on net repayments of debt as follows: (i) $2.259 billion related to our previous tranche A term loan facility which was extinguished in September, 2024, and replaced with a new $1.2 billion tranche A term loan facility; (ii) $366 million related to our revolving credit facility, and; (iii) $15 million related to other debt facilities;
•generated $2.210 billion of proceeds from additional borrowings as follows: (i) $1.200 billion related to our new tranche A term loan facility, as mentioned above; (ii) generated approximately $500 million of net proceeds (before expenses) related to the public offering, in September, 2024, of 4.625% senior secured notes due in 2029; (iii) generated approximately $498 million of net proceeds (before expenses) related to the public offering, in September, 2024, of 5.050% senior secured notes due in 2034, and; (iv) $12 million of proceeds related to other debt facilities;
•spent $671 million to repurchase shares of our Class B Common Stock in connection with: (i) open market purchases pursuant to our stock repurchase program ($599 million), and; (ii) income tax withholding obligations related to stock-based compensation programs ($72 million);
•spent $53 million to pay quarterly cash dividends of $.20 per share;
•generated $15 million from the issuance of shares of our Class B Common Stock pursuant to the terms of employee stock purchase plans;
•received $13 million from the sale of ownership interests to minority members;
•spent $13 million to pay financing costs, and;
•spent $7 million to pay profit distributions related to noncontrolling interests in majority owned businesses.
2023:
The $494 million of net cash used in financing activities during 2023 consisted of the following:
•generated $185 million of proceeds from additional borrowings pursuant to our revolving credit facility;
•spent $547 million to repurchase shares of our Class B Common Stock in connection with: (i) open market purchases pursuant to our stock repurchase program ($524 million), and; (ii) income tax withholding obligations related to stock-based compensation programs ($23 million);
•spent $85 million on net repayment of debt as follows: (i) $79 million related to our tranche A term loan facility, and; (ii) $6 million related to other debt facilities;
•spent $55 million to pay quarterly cash dividends of $.20 per share;
•generated $14 million from the issuance of shares of our Class B Common Stock pursuant to the terms of employee stock purchase plans;
•spent $7 million to pay profit distributions related to noncontrolling interests in majority owned businesses, and;
•received $3 million for the purchase of minority ownership interests in majority owned businesses.
2025 Expected Capital Expenditures:
During 2025, we expect to spend approximately $850 million to $1.000 billion on capital expenditures which includes expenditures for capital equipment, construction of new facilities, and renovations and expansions at existing hospitals. We believe that our capital expenditure program is adequate to expand, improve and equip our existing hospitals. We expect to finance all capital expenditures and acquisitions with internally generated funds and/or additional funds, as discussed below.
Capital Resources:
Credit Facilities and Outstanding Debt Securities
In September, 2024, we completed the following financing transactions:
•The public offering of $500 million of aggregate principal amount of 4.625% senior secured notes due on October 15, 2029 ("2029 Notes");
•The public offering of $500 million of aggregate principal amount of 5.050% senior secured notes due on October 15, 2034 ("2034 Notes");
•Amended our credit agreement to:
oExtend the maturity date to September, 2029 (from August, 2026 previously);
oIncrease the revolving credit facility to $1.3 billion (from $1.2 billion previously), and;
oreduce the outstanding borrowings pursuant to the tranche term loan A facility by approximately $1.0 billion, to $1.2 billion, utilizing the proceeds generated from the issuance of the above-mentioned 2029 Notes and 2034 Notes.
On September 26, 2024, we entered into a tenth amendment ("Tenth Amendment") to our credit agreement ("Credit Agreement"), dated as of November 15, 2010, as amended and restated at various times from March, 2011 to June, 2022, among UHS, as borrower, the several banks and other financial institutions or entities from time to time parties thereto, as lenders, and JPMorgan Chase Bank, N.A., as administrative agent. The Tenth Amendment provided for: (i) an extension of the maturity date to September 26, 2029; (ii) a new revolving credit facility of up to $1.3 billion (which as of December 31, 2024, had $1.17 billion of aggregate available borrowing capacity, net of $130 million of outstanding borrowings and $3 million of letters of credit), and; (iii) a new replacement tranche A term loan facility ("Tranche A Term Loan") of up to $1.2 billion (which had $1.19 billion of outstanding borrowings as of December 31, 2024).
Pursuant to the terms of the Tenth Amendment, the Tranche A Term Loan provides for installment payments of $7.5 million per quarter commencing on December 31, 2024 through September 30, 2026, and $15.0 million per quarter commencing on December 31, 2026 through June 30, 2029. The unpaid principal balance at June 30, 2029 (scheduled to be $975.0 million) is payable on the September 26, 2029 scheduled maturity date of the Credit Agreement.
Revolving credit and Tranche A Term Loan borrowings under the Credit Agreement bear interest at our election at either (1) the ABR rate which is defined as the rate per annum equal to the greatest of (a) the lender’s prime rate, (b) the greater of the federal funds effective rate and the overnight bank funding rate, plus 0.5% and (c) one month term SOFR rate plus 1.1%, in each case, plus an applicable margin based upon our consolidated leverage ratio at the end of each quarter ranging from 0.25% to 0.625%, or (2) the one, three or six month term SOFR rate plus 0.1% (at our election), plus an applicable margin based upon our consolidated leverage ratio at the end of each quarter ranging from 1.25% to 1.625%. As of December 31, 2024, the applicable margins were 0.375% for ABR-based loans and 1.375% for SOFR-based loans under the revolving credit and term loan A facilities. The revolving credit facility includes a $125 million sub-limit for letters of credit. The Credit Agreement is secured by certain assets of the Company and our material subsidiaries (which generally excludes asset classes such as substantially all of the patient-related accounts receivable of our acute care hospitals, if sold to a receivables facility pursuant to the Credit Agreement, and certain real estate assets and assets held in joint-ventures with third parties) and is guaranteed by our material subsidiaries.
The Credit Agreement includes a material adverse change clause that must be represented at each draw. The Credit Agreement also contains covenants that include a limitation on sales of assets, mergers, change of ownership, liens, indebtedness, transactions with affiliates, dividends and stock repurchases; and requires compliance with financial covenants including maximum leverage. We were in compliance with all required covenants as of December 31, 2024 (pursuant to the terms of the Credit Agreement, as amended on September 26, 2024) and as of December 31, 2023 (pursuant to the terms of the previous credit agreement).
As mentioned above, on September 26, 2024, we completed the public offering of: (i) $500,000,000 aggregate principal amount of the 4.625%, 2029 Notes, and; (ii) $500,000,000 aggregate principal amount of the 5.050%, 2034 Notes (and together with the 2029 Notes, the "2029 and 2034 Notes"), each guaranteed on a senior secured basis by all of our existing and future direct and indirect subsidiaries that guarantee our senior secured credit facility or our other first lien obligations or any junior lien obligations (the “Subsidiary Guarantors”). The 2029 and 2034 Notes have been registered under the Securities Act of 1933, as amended (the “Securities Act”), pursuant to the Issuer’s and the Subsidiary Guarantors’ registration statement on Form S-3 (File No. 333-282135), including the prospectus dated September 16, 2024, and a related prospectus supplement dated September 17, 2024, as filed with the Securities and Exchange Commission on September 19, 2024.
As of December 31, 2024, including the above-mentioned newly issued Notes, we had combined aggregate principal of $3.0 billion from the following senior secured notes:
•$700 million aggregate principal amount of 1.65% senior secured notes due in September, 2026 ("2026 Notes") which were issued on August 24, 2021. Interest on the 2026 Notes is payable on March 1st and September 1st until the maturity date of September 1, 2026.
•$500 million of aggregate principal amount of 4.625% senior secured notes due in October, 2029 ("2029 Notes") which were issued on September 26, 2024. Interest on the 2029 Notes is payable on April 15th and October 15th, commencing April 15, 2025 until the maturity date of October 15, 2029.
•$800 million aggregate principal amount of 2.65% senior secured notes due in October, 2030 ("2030 Notes") which were issued on September 21, 2020. Interest on the 2030 Notes is payable on April 15th and October 15th, until the maturity date of October 15, 2030.
•$500 million of aggregate principal amount of 2.65% senior secured notes due in January, 2032 ("2032 Notes") which were issued on August 24, 2021. Interest on the 2032 Notes is payable on January 15th and July 15th until the maturity date of January 15, 2032.
•$500 million of aggregate principal amount of 5.050% senior secured notes due in October, 2034 ("2034 Notes") which were issued on September 26, 2024. Interest on the 2034 Notes is payable on April 15th and October 15th, commencing on April 15, 2025 until the maturity date of October 15, 2034.
The 2026 Notes, 2030 Notes and 2032 Notes (collectively the "2026, 2030 and 2032 Notes") were initially issued only to qualified institutional buyers under Rule 144A and to non-U.S. persons outside the United States in reliance on Regulation S under the Securities Act. In December, 2022, we completed a registered exchange offer in which virtually all previously outstanding 2026, 2030 and 2032 Notes were exchanged for identical 2026, 2030 and 2032 Notes that were registered under the Securities Act, and thereby became freely transferable (subject to certain restrictions applicable to affiliates and broker dealers). 2026, 2030 and 2032 Notes originally issued under Rule 144A or Regulation S that were not exchanged remain outstanding and may not be offered or sold in the United States absent registration under the Securities Act or an applicable exemption from registration requirements thereunder.
The 2026, 2030 and 2032 Notes, and the 2029 and 2034 Notes (collectively "All the Notes") are guaranteed (the “Guarantees”) on a senior secured basis by our Subsidiary Guarantors that guarantee our Credit Agreement, or other first lien obligations or any junior lien obligations. All the Notes and the Guarantees are secured by first-priority liens, subject to permitted liens, on certain of the Company’s and the Subsidiary Guarantors’ assets now owned or acquired in the future by the Company or the Subsidiary Guarantors (other than real property, accounts receivable sold pursuant to a Company-related receivables facility (as defined in the Indenture pursuant to which All the Notes were issued (the “Indentures”), and certain other excluded assets). The Company’s obligations with respect to All the Notes, the obligations of the Subsidiary Guarantors under the Guarantees, and the performance of all of the Company’s and the Subsidiary Guarantors’ other obligations under the Indentures, are secured equally and ratably with the Company’s and the Subsidiary Guarantors’ obligations under the Credit Agreement. However, the liens on the collateral securing All the Notes and the Guarantees will be released if: (i) All the Notes have investment grade ratings; (ii) no default has occurred and is continuing, and; (iii) the liens on the collateral securing all first lien obligations (including the Credit Agreement and All the Notes) and any junior lien obligations are released or the collateral under the Credit Agreement, any other first lien obligations and any junior lien obligations is released or no longer required to be pledged. The liens on any collateral securing All the Notes and the Guarantees will also be released if the liens on that collateral securing the Credit Agreement, other first lien obligations and any junior lien obligations are released.
As discussed in Note 9 to the Consolidated Financial Statements-Relationship with Universal Health Realty Income Trust and Other Related Party Transactions, on December 31, 2021, we (through wholly-owned subsidiaries of ours) entered into an asset purchase and sale agreement with Universal Health Realty Income Trust (the “Trust”). Pursuant to the terms of the agreement, as amended, we, among other things, transferred to the Trust, the real estate assets of Aiken Regional Medical Center (“Aiken”) and Canyon Creek Behavioral Health (“Canyon Creek”). In connection with this transaction, Aiken and Canyon Creek (as lessees), entered into a master lease and individual property leases, as amended, (with the Trust as lessor), for initial lease terms on each property of approximately twelve years, ending on December 31, 2033. As a result of our purchase option within the Aiken and Canyon Creek lease agreements, this asset purchase and sale transaction is accounted for as a failed sale leaseback in accordance with
U.S. GAAP and we have accounted for the transaction as a financing arrangement. Our lease payments payable to the Trust are recorded to interest expense and as a reduction of the outstanding financial liability, and the amount allocated to interest expense is determined based upon our incremental borrowing rate and the outstanding financial liability. In connection with this transaction, our consolidated balance sheets at December 31, 2024 and December 31, 2023 reflect financial liabilities, which are included in debt, of approximately $74 million and $77 million, respectively.
At December 31, 2024, the carrying value and fair value of our debt were approximately $4.5 billion and $4.2 billion, respectively. At December 31, 2023, the carrying value and fair value of our debt were approximately $4.9 billion and $4.6 billion, respectively. The fair value of our debt was computed based upon quotes received from financial institutions. We consider these to be “level 2” in the fair value hierarchy as outlined in the authoritative guidance for disclosures in connection with debt instruments.
Our total debt as a percentage of total capitalization was approximately 40% at December 31, 2024 and 44% at December 31, 2023.
We expect to finance all capital expenditures and acquisitions and pay dividends and potentially repurchase shares of our common stock utilizing internally generated and additional funds. Additional funds may be obtained through: (i) borrowings under our existing revolving credit facility, which had $1.17 billion of available borrowing capacity as of December 31, 2024, or through refinancing the existing Credit Agreement; (ii) the issuance of other short-term and/or long-term debt, and/or; (iii) the issuance of equity. We believe that our operating cash flows, cash and cash equivalents, available commitments under existing agreements, as well as access to the capital markets, provide us with sufficient capital resources to fund our operating, investing and financing requirements for the next twelve months. However, in the event we need to access the capital markets or other sources of financing, there can be no assurance that we will be able to obtain financing on acceptable terms or within an acceptable time. Our inability to obtain financing on terms acceptable to us could have a material unfavorable impact on our results of operations, financial condition and liquidity.
Supplemental Guarantor Financial Information
As of December 31, 2024, we had combined aggregate principal of $3.0 billion from All the Notes:
•$700 million aggregate principal amount of the 2026 Notes;
•$500 million aggregate principal amount of the 2029 Notes;
•$800 million aggregate principal amount of the 2030 Notes;
•$500 million of aggregate principal amount of the 2032 Notes, and;
•$500 million of aggregate principal amount of the 2034 Notes.
All the Notes are fully and unconditionally guaranteed pursuant to the Guarantees on a senior secured basis by the Subsidiary Guarantors. All the Notes and the Guarantees are secured by first-priority liens, subject to permitted liens, on certain of the Company’s and the Subsidiary Guarantors’ assets now owned or acquired in the future by the Company or the Subsidiary Guarantors (other than real property, accounts receivable sold pursuant to the Company’s existing receivables facility (as defined in the Indentures pursuant to which All the Notes were issued), and certain other excluded assets). The Company’s obligations with respect to All the Notes, the obligations of the Subsidiary Guarantors under the Guarantees, and the performance of all of the Company’s and the Subsidiary Guarantors’ other obligations under the Indentures, are secured equally and ratably with the Company’s and the Subsidiary Guarantors’ obligations under the Credit Agreement and All the Notes by a perfected first-priority security interest, subject to permitted liens, in the collateral owned by the Company and its Subsidiary Guarantors, whether now owned or hereafter acquired. However, the liens on the collateral securing All the Notes and the Guarantees will be released if: (i) All the Notes have investment grade ratings; (ii) no default has occurred and is continuing, and; (iii) the liens on the collateral securing all first lien obligations (including the Credit Agreement and All the Notes) and any junior lien obligations are released or the collateral under the Credit Agreement, any other first lien obligations and any junior lien obligations is released or no longer required to be pledged. The liens on any collateral securing All the Notes and the Guarantees will also be released if the liens on that collateral securing the Credit Agreement, other first lien obligations and any junior lien obligations are released.
All the Notes will be structurally subordinated to all obligations of our existing and future subsidiaries that are not and do not become Subsidiary Guarantors of All the Notes. No appraisal of the value of the collateral has been made, and the value of the collateral in the event of liquidation will depend on market and economic conditions, the availability of buyers and other factors. Consequently, liquidating the collateral securing All the Notes may not produce proceeds in an amount sufficient to pay any amounts due on All the Notes.
We and our subsidiaries may be able to incur significant additional indebtedness in the future. Although our Credit Agreement contains restrictions on the incurrence of additional indebtedness and our Credit Agreement and All the Notes contain restrictions on our ability to incur liens to secure additional indebtedness, these restrictions are subject to a number of qualifications and exceptions, and the additional indebtedness incurred in compliance with these restrictions could be substantial. These restrictions also will not prevent us from incurring obligations that do not constitute indebtedness. In addition, if we incur any additional indebtedness secured by liens that rank equally with All the Notes, subject to collateral arrangements, the holders of that debt will be entitled to share
ratably with holders of All the Notes in any proceeds distributed in connection with any insolvency, liquidation, reorganization, dissolution or other winding up of our company. This may have the effect of reducing the amount of proceeds paid to holders of All the Notes.
Federal and state fraudulent transfer and conveyance statutes may apply to the issuance of All the Notes and the incurrence of the Guarantees. Under federal bankruptcy law and comparable provisions of state fraudulent transfer or conveyance laws, which may vary from state to state, All the Notes or the Guarantees (or the grant of collateral securing any such obligations) could be voided as a fraudulent transfer or conveyance if we or any of the Subsidiary Guarantors, as applicable, (a) issued All the Notes or incurred the Guarantees with the intent of hindering, delaying or defrauding creditors or (b) under certain circumstances received less than reasonably equivalent value or fair consideration in return for either issuing All the Notes or incurring the Guarantees.
Basis of Presentation
The following tables include summarized financial information of Universal Health Services, Inc. and the other obligors in respect of debt issued by Universal Health Services, Inc. The summarized financial information of each obligor group is presented on a combined basis with balances and transactions within the obligor group eliminated. Investments in and the equity in earnings of non-guarantor subsidiaries, which would otherwise be consolidated in accordance with GAAP, are excluded from the below summarized financial information pursuant to SEC Regulation S-X Rule 13-01.
The summarized balance sheet information for the consolidated obligor group of debt issued by Universal Health Services, Inc. is presented in the table below:
| | | | | | | |
| | | | | |
(in thousands) | December 31, 2024 | | | December 31, 2023 | |
Current assets | $ | 2,279,988 | | | $ | 2,292,716 | |
Noncurrent assets (1) | $ | 9,214,924 | | | $ | 8,876,623 | |
Current liabilities | $ | 1,870,563 | | | $ | 1,786,642 | |
Noncurrent liabilities | $ | 5,451,167 | | | $ | 5,728,371 | |
Due to non-guarantors | $ | 912,958 | | | $ | 913,481 | |
(1) Includes goodwill of $3,262 million and $3,267 million as of December 31, 2024 and 2023, respectively. | |
The summarized results of operations information for the consolidated obligor group of debt issued by Universal Health Services, Inc. is presented in the table below:
| | | | | | | |
| Twelve Months Ended | | | Twelve Months Ended | |
(in thousands) | December 31, 2024 | | | December 31, 2023 | |
Net revenues | $ | 12,642,381 | | | $ | 11,454,260 | |
Operating charges | | 11,200,769 | | | | 10,416,176 | |
Interest expense, net | | 248,568 | | | | 277,521 | |
Other (income) expense, net | | (3,186 | ) | | | 24,996 | |
Net income | $ | 920,944 | | | $ | 556,423 | |
Affiliates Whose Securities Collateralize the Senior Secured Notes
All the Notes and the Guarantees are secured by, among other things, pledges of the capital stock of our subsidiaries held by us or by our secured Guarantors, in each case other than certain excluded assets and subject to permitted liens. Such collateral securities are secured equally and ratably with our and the Guarantors’ obligations under our Credit Agreement. For a list of our subsidiaries the capital stock of which has been pledged to secure All the Notes, see Exhibit 22.1 to this Report.
Upon the occurrence and during the continuance of an event of default under the indentures governing All the Notes, subject to the terms of the Security Agreement relating to All the Notes provide for (among other available remedies) the foreclosure upon and sale of the Collateral (including the pledged stock) and the distribution of the net proceeds of any such sale to the holders of All the Notes, the lenders under the Credit Agreement and the holders of any other permitted first priority secured obligations on a pro rata basis, subject to any prior liens on the collateral.
No appraisal of the value of the collateral securities has been made, and the value of the collateral securities in the event of liquidation will depend on market and economic conditions, the availability of buyers and other factors. Consequently, liquidating the collateral securities securing All the Notes may not produce proceeds in an amount sufficient to pay any amounts due on All the Notes.
The security agreement relating to All the Notes provides that the representative of the lenders under our Credit Agreement will initially control actions with respect to that collateral and, consequently, exercise of any right, remedy or power with respect to enforcing interests in or realizing upon such collateral will initially be at the direction of the representative of the lenders.
No trading market exists for the capital stock pledged as collateral.
The assets, liabilities and results of operations of the combined affiliates whose securities are pledged as collateral are not materially different than the corresponding amounts presented in the consolidated financial information of Universal Health Services, Inc.
Contractual Obligations and Off-Balance Sheet Arrangements
As of December 31, 2024 we were party to certain off balance sheet arrangements consisting of standby letters of credit and surety bonds which totaled $154 million consisting of: (i) $130 million related to our self-insurance programs, and; (ii) $24 million of other debt and public utility guarantees.
Obligations under operating leases for real property, real property master leases and equipment amount to $919 million as of December 31, 2024. The real property master leases are leases for buildings on or near hospital property for which we guarantee a certain level of rental income. We sublease space in these buildings and any amounts received from these subleases are offset against the expense. In addition, we lease certain hospital facilities from Universal Health Realty Income Trust (the “Trust”) with terms scheduled to expire in 2026, 2033 and 2040. These leases contain various renewal options, as disclosed in Note 9 to the Consolidated Financial Statements-Relationship with Universal Health Realty Income Trust and Other Related Party Transactions. We also lease two free-standing emergency departments and space in certain medical office buildings which are owned by the Trust. In addition, we lease the real property of certain other facilities from non-related parties as indicated in Item 2. Properties, as included herein.
The following represents the scheduled maturities of our contractual obligations as of December 31, 2024:
| | | | | | | | | | | | | | | | | | | | |
| | Payments Due by Period (dollars in thousands) | |
| | | | | Less than | | | 2-3 | | | 4-5 | | | After | |
| | Total | | | 1 year | | | years | | | years | | | 5 years | |
Long-term debt obligations (a) | | $ | 4,524,366 | | | $ | 40,059 | | | $ | 811,903 | | | $ | 1,728,010 | | | $ | 1,944,394 | |
Estimated future interest payments on debt
outstanding as of December 31, 2024 (b) | | | 1,075,408 | | | | 179,726 | | | | 344,051 | | | | 311,132 | | | | 240,499 | |
Construction commitments (c) | | | 31,568 | | | | 31,568 | | | | 0 | | | | 0 | | | | 0 | |
Purchase and other obligations (d) | | | 435,845 | | | | 95,840 | | | | 162,684 | | | | 95,553 | | | | 81,768 | |
Operating leases (e) | | | 918,880 | | | | 88,488 | | | | 141,183 | | | | 90,757 | | | | 598,452 | |
Estimated future payments for defined benefit
pension plan, and other retirement plan (f) | | | 159,299 | | | | 22,253 | | | | 14,659 | | | | 14,656 | | | | 107,731 | |
Health and dental unpaid claims (g) | | | 117,829 | | | | 117,829 | | | | 0 | | | | 0 | | | | 0 | |
Total contractual cash obligations | | $ | 7,263,195 | | | $ | 575,763 | | | $ | 1,474,480 | | | $ | 2,240,108 | | | $ | 2,972,844 | |
(a)Reflects debt outstanding, after unamortized financing costs, as of December 31, 2024 as discussed in Note 4 to the Consolidated Financial Statements.
(b)Assumes that all debt outstanding as of December 31, 2024, including borrowings under our Credit Agreement, remain outstanding until the final maturity of the debt agreements at the same interest rates (some of which are floating) which were in effect as of December 31, 2024. We have the right to repay borrowings upon short notice and without penalty, pursuant to the terms of the Credit Agreement.
(c)Our share of the estimated construction cost of two behavioral health care facilities scheduled to be completed in 2025 that, subject to approval of certain regulatory conditions, we are required to build pursuant to joint-venture agreements with third parties. In addition, we had various other projects under construction as of December 31, 2024. Because we can terminate substantially all of the construction contracts related to the various other projects at any time without paying a termination fee, these costs are excluded from the table above.
(d)Consists of: (i) $183 million related to the ongoing operation of an electronic health records application and purchase and implementation of a revenue cycle and other applications for our facilities; (ii) $85 million related to the development, implementation and operation of an enterprise resource planning application; (iii) $61 million in healthcare infrastructure in Washington D.C. in connection with various agreements with the District of Columbia, as discussed below; (iv) $52 million related to long-term contracts with third-parties consisting primarily of certain revenue cycle data processing services for our acute care facilities; (v) $43 million for administrative software applications, and; (vi) $12 million for other software applications.
(e)Reflects our future minimum operating lease payment obligations related to our operating lease agreements outstanding as of December 31, 2024 as discussed in Note 7 to the Consolidated Financial Statements. Some of the lease agreements provide us with the option to renew the lease and our future lease obligations would change if we exercised these renewal options. In connection with these operating lease commitments, our consolidated balance sheet as of December 31, 2024 includes right of use assets amounting to $419 million and aggregate operating lease liabilities of $451 million ($75 million included in current liabilities and $376 million included in noncurrent liabilities).
(f)Consists of $133 million of estimated future payments related to our non-contributory, defined benefit pension plan (estimated through 2080), as disclosed in Note 8 to the Consolidated Financial Statements, and $26 million of estimated future payments related to other retirement plan liabilities ($23 million of liabilities recorded in other non-current liabilities as of December 31, 2024 in connection with these retirement plans).
(g)Consists of accrued and unpaid estimated claims expense incurred in connection with our commercial health insurers and self-insured employee benefit plans.
As of December 31, 2024, the total net accrual for our self-insured professional and general liability claims was $487 million, of which $85 million is included in other current liabilities and $402 million is included in other non-current liabilities. We exclude the $487 million for professional and general liability claims from the contractual obligations table because there are no significant contractual obligations associated with these liabilities and because of the uncertainty of the dollar amounts to be ultimately paid as well as the timing of such payments. Please see Self-Insured/Other Insurance Risks above for additional disclosure related to our professional and general liability claims and reserves.
During 2020, we entered into various agreements with the District of Columbia (the “District”) related to the development, leasing and operation of an acute care hospital (that is expected to be completed and opened in the Spring of 2025) and certain other facilities/structures on land owned by the District (“District Facilities”). The agreements contemplate that we will serve as manager for development and construction of the District Facilities on behalf of the District, with a projected aggregate cost of approximately $439 million, approximately $344 million of which was incurred as of December 31, 2024, which is being entirely funded by the District. Upon completion of the District Facilities, we will lease the District Facilities for a nominal rental amount for a period of 75 years and are obligated to operate the District Facilities during the lease term. We have certain lease termination rights in connection with the District Facilities beginning on the tenth anniversary of the lease commencement date for various and decreasing amounts as provided for in the agreements. Additionally, any time after the 10th anniversary of the lease term, we have a right to purchase the District Facilities for a price equal to the greater of fair market value of the District Facilities or the amount necessary to defease the bonds issued by the District to fund the construction of the District Facilities. The lease agreement also entitles the District to participation rent should certain specified earnings before interest, taxes, depreciation and amortization thresholds be achieved by the acute care hospital. Additionally, we have committed to expend no less than $75 million, over a projected 12-year period, in healthcare infrastructure including expenditures related to the District Facilities as well as other healthcare related expenditures in certain specified areas of Washington, D.C. This financial commitment is included in “Purchase and other obligations” as reflected on the contractual obligations table above. Pursuant to the agreements, the District is entitled to certain termination fees and other amounts as specified in the agreements in the event we, within certain specified periods of time, cease to operate the acute care hospital or there is a transfer of control of us or our subsidiary operating the hospital.
ITEM 7A. Quantitative and Qualitative Disclosures About Market Risk
We manage our ratio of fixed and floating rate debt with the objective of achieving a mix that management believes is appropriate. To manage this risk in a cost-effective manner, we, from time to time, enter into interest rate swap agreements in which we agree to exchange various combinations of fixed and/or variable interest rates based on agreed upon notional amounts. We account for our derivative and hedging activities using the Financial Accounting Standard Board’s guidance which requires all derivative instruments, including certain derivative instruments embedded in other contracts, to be carried at fair value on the balance sheet. For derivative transactions designated as hedges, we formally document all relationships between the hedging instrument and the related hedged item, as well as its risk-management objective and strategy for undertaking each hedge transaction.
Derivative instruments designated in a hedge relationship to mitigate exposure to variability in expected future cash flows, or other types of forecasted transactions, are considered cash flow hedges. Cash flow hedges are accounted for by recording the fair value of the derivative instrument on the balance sheet as either an asset or liability, with a corresponding amount recorded in accumulated other comprehensive income (“AOCI”) within shareholders’ equity. Amounts are reclassified from AOCI to the income statement in the period or periods the hedged transaction affects earnings. From time to time, we use interest rate derivatives in our cash flow hedge transactions. Such derivatives are designed to be highly effective in offsetting changes in the cash flows related to the hedged liability.
For hedge transactions that do not qualify for the short-cut method, at the hedge’s inception and on a regular basis thereafter, a formal assessment is performed to determine whether changes in the fair values or cash flows of the derivative instruments have been highly effective in offsetting changes in cash flows of the hedged items and whether they are expected to be highly effective in the future.
The fair value of interest rate swap agreements approximates the amount at which they could be settled, based on estimates obtained from the counterparties. When applicable, we assess the effectiveness of our hedge instruments on a quarterly basis. Although we do not anticipate nonperformance by our counterparties to interest rate swap agreements, the counterparties expose us to credit risk in the event of nonperformance. We do not hold or issue derivative financial instruments for trading purposes.
When applicable, we measure our interest rate swaps at fair value on a recurring basis. The fair value of our interest rate swaps is based on quotes from our counterparties. We consider those inputs to be “level 2” in the fair value hierarchy as outlined in the authoritative guidance for disclosures in connection with derivative instruments and hedging activities.
The table below presents information about our long-term financial instruments that are sensitive to changes in interest rates as of December 31, 2024. For debt obligations, the table presents principal cash flows and related weighted-average interest rates by contractual maturity dates.
Maturity Date, Fiscal Year Ending December 31
(dollar amounts in thousands)
| | | | | | | | | | | | | | | | | | | | | | | | | | | | |
| | 2025 | | | 2026 | | | 2027 | | | 2028 | | | 2029 | | | Thereafter | | | Total | |
Long-term debt: | | | | | | | | | | | | | | | | | | | | | |
Fixed rate: | | | | | | | | | | | | | | | | | | | | | |
Debt | | $ | 10,059 | | | $ | 708,317 | | | $ | 11,501 | | | $ | 12,402 | | | $ | 508,665 | | | $ | 1,931,356 | | | $ | 3,182,300 | |
Average interest rates | | | 3.2 | % | | | 3.2 | % | | | 3.7 | % | | | 3.6 | % | | | 3.6 | % | | | 3.8 | % | | | 3.5 | % |
Variable rate: | | | | | | | | | | | | | | | | | | | | | |
Debt | | $ | 30,000 | | | $ | 30,000 | | | | 60,000 | | | | 60,000 | | | | 1,142,241 | | | | 0 | | | $ | 1,322,241 | |
Average interest rates | | | 5.8 | % | | | 5.8 | % | | | 5.8 | % | | | 5.8 | % | | | 5.8 | % | | | 0.0 | % | | | 5.8 | % |
Interest rate swaps: | | | | | | | | | | | | | | | | | | | | | |
Notional amount | |
| | | | | | | | | | | | | | | | | | | |
Average interest rates | |
| | | | | | | | | | | | | | | | | | | |
As calculated based upon our variable rate debt outstanding as of December 31, 2024 that is subject to interest rate fluctuations, each 1% change in interest rates would impact our pre-tax income by approximately $13 million.
ITEM 8. Financial Statements and Supplementary Data
Our Consolidated Balance Sheets, Consolidated Statements of Income, Consolidated Statements of Changes in Equity, Consolidated Statements of Cash Flows and Consolidated Statements of Comprehensive Income, together with the reports of PricewaterhouseCoopers LLP, independent registered public accounting firm, are included elsewhere herein. Reference is made to the “Index to Financial Statements and Financial Statement Schedule.”
ITEM 9. Changes in and Disagreements with Accountants on Accounting and Financial Disclosure
None.
ITEM 9A. Controls and Procedures.
As of December 31, 2024, under the supervision and with the participation of our management, including our Chief Executive Officer (“CEO”) and Chief Financial Officer (“CFO”), we performed an evaluation of the effectiveness of our disclosure controls and procedures as defined in Rule 13a-15(e) or Rule 15d-15(e) of the Securities Exchange Act of 1934, as amended. Based on this evaluation, the CEO and CFO have concluded that our disclosure controls and procedures are effective to ensure that material information is recorded, processed, summarized and reported by management on a timely basis in order to comply with our disclosure obligations under the Securities Exchange Act of 1934, as amended, and the SEC rules thereunder.
Changes in Internal Control Over Financial Reporting
There have been no changes in our internal control over financial reporting or in other factors during the fourth quarter of 2024 that have materially affected, or are reasonably likely to materially affect, our internal control over financial reporting.
Management’s Report on Internal Control Over Financial Reporting
Management is responsible for establishing and maintaining an adequate system of internal control over our financial reporting. In order to evaluate the effectiveness of internal control over financial reporting, as required by Section 404 of the Sarbanes-Oxley Act, management has conducted an assessment, including testing, using the criteria on Internal Control—Integrated Framework (2013), issued by the Committee of Sponsoring Organizations of the Treadway Commission (COSO). Our system of internal control over financial reporting is designed to provide reasonable assurance regarding the reliability of financial reporting and the preparation and fair presentation of financial statements for external purposes in accordance with U.S. generally accepted accounting principles.
Because of its inherent limitations, internal control over financial reporting may not prevent or detect misstatements. Also, projections of any evaluation of effectiveness of internal control over financial reporting to future periods are subject to the risk that controls may become inadequate because of changes in conditions, or that the degree of compliance with the policies or procedures may deteriorate.
Based on its assessment, management has concluded that we maintained effective internal control over financial reporting as of December 31, 2024, based on criteria in Internal Control—Integrated Framework (2013), issued by the COSO. The effectiveness of the Company’s internal control over financial reporting as of December 31, 2024 has been audited by PricewaterhouseCoopers LLP, an independent registered public accounting firm as stated in its report which appears herein.
ITEM 9B Other Information
None of the Company’s directors or officers adopted, modified or terminated a Rule 10b5-1 trading arrangement or a non-Rule 10b5-1 trading arrangement during the Company’s quarter ended December 31, 2024, as such terms are defined under Item 408(a) of Regulation S-K.
ITEM 9C Disclosure Regarding Foreign Jurisdictions that Prevent Inspections. Other Information
Not applicable.
PART III
ITEM 10. Directors, Executive Officers and Corporate Governance
There is hereby incorporated by reference the information to appear under the captions “Election of Directors”, “Section 16(a) Beneficial Ownership Reporting Compliance” and “Corporate Governance” in our Proxy Statement, to be filed with the Securities and Exchange Commission within 120 days after December 31, 2024. See also “Executive Officers of the Registrant” appearing in Item 1 hereof.
ITEM 11. Executive Compensation
There is hereby incorporated by reference the information to appear under the caption “Executive Compensation” in our Proxy Statement to be filed with the Securities and Exchange Commission within 120 days after December 31, 2024.
ITEM 12. Security Ownership of Certain Beneficial Owners and Management and Related Stockholder Matters
There is hereby incorporated by reference the information to appear under the caption “Security Ownership of Certain Beneficial Owners and Management” and “Executive Compensation” in our Proxy Statement, to be filed with the Securities and Exchange Commission within 120 days after December 31, 2024.
ITEM 13. Certain Relationships and Related Transactions, and Director Independence
There is hereby incorporated by reference the information to appear under the captions “Certain Relationships and Related Transactions” and “Corporate Governance” in our Proxy Statement, to be filed with the Securities and Exchange Commission within 120 days after December 31, 2024.
ITEM 14. Principal Accountant Fees and Services.
There is hereby incorporated by reference the information to appear under the caption “Relationship with Independent Auditors” in our Proxy Statement, to be filed with the Securities and Exchange Commission within 120 days after December 31, 2024.
PART IV
ITEM 15. Exhibits and Financial Statement Schedules
(a) Documents filed as part of this report:
(1) Financial Statements:
See “Index to Financial Statements and Financial Statement Schedule.”
(2) Financial Statement Schedules:
See “Index to Financial Statements and Financial Statement Schedule.”
(3) Exhibits:
| | |
No. | | Description |
3.1 | | Registrant’s Restated Certificate of Incorporation, and Amendments thereto, previously filed as Exhibit 3.1 to the Company’s Quarterly Report on Form 10-Q for the quarter ended June 30, 1997, are incorporated herein by reference. |
| | |
3.2 | | Amended and Restated Bylaws of Registrant, previously filed as Exhibit 3.1 to the Company’s Current Report on Form 8-K dated September 21, 2022, is incorporated herein by reference. |
| | |
3.3 | | Amendment to the Registrant’s Restated Certificate of Incorporation previously filed as Exhibit 3.1 to the Company’s Current Report on Form 8-K dated July 3, 2001 is incorporated herein by reference. |
| | |
4.1 | | Description of Securities of the Registrant previously filed as Exhibit 4.5 to the Company’s Annual Report on Form 10-K for the year ended December 31, 2019, is incorporated herein by reference. |
| | |
4.2 | | Indenture, dated as of September 21, 2020, by and among the Company, the Subsidiary Guarantors party thereto, MUFG Union Bank, N.A., as trustee, and JPMorgan Chase Bank, N.A., as collateral agent., previously filed as Exhibit 4.1 to the Company’s Current Report on Form 8-K dated September 21, 2020, is incorporated herein by reference. |
| | |
4.3 | | Additional Authorized Representative Joinder Agreement, dated as of September 21, 2020, among the Company, the Subsidiary Guarantors party thereto, JPMorgan Chase Bank, N.A., as collateral agent, the Authorized Representatives specified therein and MUFG Union Bank, N.A., as trustee, as an Additional Authorized Representative, previously filed as Exhibit 4.2 to the Company’s Current Report on Form 8-K dated September 21, 2020, is incorporated herein by reference. |
| | |
4.4 | | Indenture, dated as of August 24, 2021, by and among the Company, the Subsidiary Guarantors party thereto, U.S. Bank National Association, as Trustee, and JPMorgan Chase Bank, N.A., as collateral agent, previously filed as Exhibit 4.1 to the Company’s Current Report on Form 8-K dated August 24, 2021, is incorporated herein by reference. |
| | |
4.5 | | Additional Authorized Representative Joinder Agreement, dated as of August 24, 2021, among U.S. Bank National Association, as Trustee and Additional Authorized Representative, the Company, the Subsidiary Guarantors party thereto, and JPMorgan Chase Bank, N.A., as collateral agent and administrative agent, previously filed as Exhibit 4.2 to the Company’s Current Report on Form 8-K dated August 24, 2021, is incorporated herein by reference. |
| | |
4.6 | | Supplemental Indenture, dated as of August 24, 2021, among the Company, the Subsidiary Guarantors party thereto, U.S. Bank National Association (as successor to MUFG Union Bank, N.A.), as trustee, and JPMorgan Chase Bank, N.A., as collateral agent, to the indenture, dated as of September 21, 2020, governing the Existing 2030 Notes, previously filed as Exhibit 4.3 to the Company’s Current Report on Form 8-K dated August 24, 2021, is incorporated herein by reference. |
| | |
4.7 | | Second Supplemental Indenture, dated as of June 23, 2022, among the Company, the Subsidiary Guarantors party thereto, U.S. Bank Trust Company and National Association (as successor to U.S. Bank National Association), as trustee to the indenture, dated as of September 21, 2020, previously filed as Exhibit 4.1 to the Company’s Current Report on Form 8-K dated June 27, 2022, is incorporated herein by reference. |
| | |
4.8 | | First Supplemental Indenture, dated as of June 23, 2022, among the Company, the Subsidiary Guarantors party thereto, and U.S. Bank Trust Company, National Association (as successor to U.S. Bank National Association), as trustee, to the indenture, dated as of August 24, 2021, previously filed as Exhibit 4.2 to the Company’s Current Report on Form 8-K dated June 27, 2022, is incorporated herein by reference. |
| | |
| | |
No. | | Description |
4.9 | | Third Supplemental Indenture, dated as of November 4, 2022, among the Company, the Subsidiary Guarantors party thereto and U.S. Bank Trust Company, National Association (as successor to U.S. Bank National Association), as trustee, to the indenture, dated as of September 21, 2020, previously filed as Exhibit 4.1 to the Company’s Quarterly Report on Form 10-Q dated November 8, 2022, is incorporated herein by reference. |
| | |
4.10 | | Second Supplemental Indenture, dated as of November 4, 2022, among the Company, the Subsidiary Guarantors party thereto and U.S. Bank Trust Company, National Association (as successor to U.S. Bank National Association), as trustee, to the indenture, dated as of August 24, 2021, previously filed as Exhibit 4.2 to the Company’s Quarterly Report on Form 10-Q dated November 8, 2022, is incorporated herein by reference. |
| | |
4.11 | | Indenture, dated as of September 26, 2024, among the Company, the Subsidiary Guarantors party thereto, U.S. Bank Trust Company, National Association, as trustee, and JPMorgan Chase Bank, N.A., as collateral agent, previously filed as Exhibit 4.1 to the Company’s Current Report on Form 8-K dated October 1, 2024, is incorporated herein by reference. |
| | |
4.12 | | First Supplemental Indenture, dated as of September 26, 2024, among the Company, the Subsidiary Guarantors party thereto, U.S. Bank Trust Company, National Association, as trustee, and JPMorgan Chase Bank, N.A., as collateral agent, to the indenture, dated as of September 26, 2024, governing the Issuer’s 4.625% Senior Secured Notes due 2029 and the Issuer’s 5.050% Senior Secured Notes due 2034, previously filed as Exhibit 4.2 to the Company’s Current Report on Form 8-K dated October 1, 2024, is incorporated herein by reference. |
| | |
4.13 | | Additional Authorized Representative Joinder Agreement, dated as of September 26, 2024, among U.S. Bank Trust Company, National Association, as trustee and additional authorized representative for the holders of the Notes, the Issuer, the Subsidiary Guarantors party thereto, and JPMorgan Chase Bank, N.A., as collateral agent and administrative agent, previously filed as Exhibit 4.5 to the Company’s Current Report on Form 8-K dated October 1, 2024, is incorporated herein by reference. |
| | |
10.1 | | Agreement, dated December 7, 2023, to renew Advisory Agreement dated as of December 24, 1986, and amended and restated effective as of January 1, 2019 between Universal Health Realty Income Trust and UHS of Delaware, Inc. |
| | |
10.2 | | Agreement, dated as of December 4, 2019, to renew Advisory Agreement, dated as of December 24, 1986, and amended and restated effective as of January 1, 2019 between Universal Health Realty Income Trust and UHS of Delaware, Inc., previously filed as Exhibit 10.3 to the Company’s Annual Report on Form 10-K for the year ended December 31, 2018, is incorporated herein by reference. |
| | |
10.3 | | Form of Leases, including Form of Master Lease Document for Leases, between certain subsidiaries of the Company and Universal Health Realty Income Trust, filed as Exhibit 10.3 to Amendment No. 3 of the Registration Statement on Form S-11 and Form S-2 of Registrant and Universal Health Realty Income Trust (Registration No. 33-7872), is incorporated herein by reference (P). |
| | |
10.4 | | Corporate Guaranty of Obligations of Subsidiaries Pursuant to Leases and Contract of Acquisition, dated December 24, 1986, issued by the Company in favor of Universal Health Realty Income Trust, previously filed as Exhibit 10.5 to the Company’s Current Report on Form 8-K dated December 24, 1986, is incorporated herein by reference (P). |
| | |
10.5 | | Universal Health Services, Inc. Executive Retirement Income Plan dated January 1, 1993, previously filed as Exhibit 10.7 to the Company’s Annual Report on Form 10-K for the year ended December 31, 2002, is incorporated herein by reference. |
| | |
10.6 | | Universal Health Services, Inc. Supplemental Executive Retirement Income Plan effective as of June 1, 2018, dated as of June 18, 2018, previously filed as Exhibit 10.1 to the Company’s Quarterly Report on Form 10-Q for the quarterly period ended March 31, 2019, is incorporated herein by reference. |
| | |
10.7 | | Asset Purchase Agreement dated as of February 6, 1996, among Amarillo Hospital District, UHS of Amarillo, Inc. and Universal Health Services, Inc., previously filed as Exhibit 10.28 to the Company’s Annual Report on Form 10-K for the year ended December 31, 1995, is incorporated herein by reference (P). |
| | |
10.8* | | Amended and Restated Universal Health Services, Inc. Supplemental Deferred Compensation Plan dated as of January 1, 2002, previously filed as Exhibit 10.29 to the Company’s Annual Report on Form 10-K for the year ended December 31, 2002, is incorporated herein by reference. |
| | |
| | |
No. | | Description |
10.9 | | Amendment No. 1 to the Master Lease Document, between certain subsidiaries of Universal Health Services, Inc. and Universal Health Realty Income Trust, dated April 24, 2006, previously filed as Exhibit 10.29 to the Company’s Annual Report on Form 10-K for the year ended December 31, 2006, is incorporated herein by reference. |
| | |
10.10 | | Credit Agreement, dated as of November 15, 2010, by and among Universal Health Services, Inc., JPMorgan Chase Bank, N.A. and the various financial institutions as are or may become parties thereto, as Lenders, SunTrust Bank, The Royal Bank of Scotland, Plc, Bank of Tokyo-Mitsubishi UFJ Trust Company and Credit Agricole Corporate and Investment Bank, as co-documentation agents, Deutsche Bank Securities Inc. and Bank of America N.A. as co-syndication agents, and JPMorgan Chase Bank, N.A., as administrative agent for the Lenders and as collateral agent for the secured parties, previously filed as Exhibit 10.1 to the Company’s Current Report on Form 8-K dated November 17, 2010, is incorporated herein by reference. |
| | |
10.11 | | First Amendment, dated as of March 15, 2011, to the Credit Agreement, dated as of November 15, 2010, by and among Universal Health Services, Inc., JPMorgan Chase Bank, N.A. and the various financial institutions as are or may become parties thereto, as Lenders, certain banks as co-documentation agents, and as co-syndication agents, and JPMorgan Chase Bank, N.A., as administrative agent for the Lenders and as collateral agent for the secured parties, previously filed as Exhibit 10.1 to the Company’s Current Report on Form 8-K dated March 15, 2011, is incorporated herein by reference. |
| | |
10.12 | | Credit Agreement, dated as of November 15, 2010 and amended and restated as of September 21, 2012, by and among Universal Health Services, Inc. (the borrower), the several lenders from time to time parties thereto, Credit Agricole Corporate and Investment Bank, Mizuho Corporate Bank LTD., Royal Bank of Canada and The Royal Bank of Scotland PLC (as co-documentation agents), Bank of Tokyo-Mitsubishi UFJ Trust Company, Bank of America N.A. and SunTrust Bank (as co-syndication agents), and JPMorgan Chase Bank, N.A. (as administrative agent), previously filed as Exhibit 10.1 to the Company’s Current Report on Form 8-K dated September 26, 2012, is incorporated herein by reference. |
| | |
10.13 | | Second Amendment, dated as of September 21, 2012, to the Credit Agreement, dated as of November 15, 2010 (as amended from time to time), among Universal Health Services, Inc., a Delaware corporation, the several banks and other financial institutions from time to time parties thereto, JPMorgan Chase Bank, N.A., as administrative agent and the other agents party thereto, previously filed as Exhibit 10.2 to the Company’s Current Report on Form 8-K dated September 26, 2012, is incorporated herein by reference. |
| | |
10.14 | | Third Amendment, dated as of May 16, 2013, to the Credit Agreement, dated as of November 15, 2010, as amended from time to time, among Universal Health Services, Inc., a Delaware corporation, the several banks and other financial institutions from time to time parties thereto, JPMorgan Chase Bank, N.A., as administrative agent and the other agents party thereto, previously filed as Exhibit 10.1 to the Company’s Current Report on Form 8-K dated May 17, 2013, is incorporated herein by reference. |
| | |
10.15 | | Fourth Amendment, dated as of August 7, 2014, to the Credit Agreement, dated as of November 15, 2010, as previously amended from time to time, by and among Universal Health Services, Inc., the several banks and other financial institutions from time to time parties thereto, JPMorgan Chase Bank, N.A., as administrative agent and the other agents party thereto, previously filed as Exhibit 10.1 to the Company’s Current Report on Form 8-K dated August 12, 2014, is incorporated herein by reference. |
10.16 | | Credit Agreement, dated as of November 15, 2010 and amended and restated as of August 7, 2014, by and among Universal Health Services, Inc., the several banks and other financial institutions from time to time parties thereto, JPMorgan Chase Bank, N.A., as administrative agent and the other agents party thereto, previously filed as Exhibit 10.2 to the Company’s Current Report on Form 8-K dated August 12, 2014, is incorporated herein by reference. |
| | |
10.17 | | Fifth Amendment, dated as of November 7, 2016, to the Credit Agreement, dated as of November 15, 2010, as amended on March 15, 2011, September 21, 2012, May 16, 2013 and August 7, 2014, among the Company, as borrower, the several banks and other financial institutions from time to time parties thereto, as lenders, JPMorgan Chase Bank, N.A., as administrative agent, and the other agents party thereto, previously filed as Exhibit 10.1 to the Company’s Current Report on Form 8-K dated June 8, 2016, is incorporated herein by reference. |
10.18 | | Sixth Amendment, dated as of October 23, 2018, to the Credit Agreement, dated as of November 15, 2010, as amended on March 15, 2011, September 21, 2012, May 16, 2013, August 7, 2014 and June 7, 2016, among the Company, as borrower, the several banks and other financial institutions from time to time parties thereto, as lenders, JPMorgan Chase Bank, N.A., as administrative agent, and the other agents party thereto, previously filed as Exhibit 10.1 to the Company’s Current Report on Form 8-K dated October 24, 2018, is incorporated herein by reference. |
| | |
No. | | Description |
| | |
10.19 | | Increased Facility Activation Notice – Incremental Term Loans, dated as of October 31, 2018, to the Credit Agreement, dated as of November 15, 2010, as amended on March 15, 2011, September 21, 2012, May 16, 2013, August 7, 2014, June 7, 2016 and October 23, 2018, among the Company, as borrower, the several banks and other financial institutions from time to time parties thereto, as lenders, JPMorgan Chase Bank, N.A., as administrative agent, and the other agents party thereto, previously filed as Exhibit 10.1 to the Company’s Current Report on Form 8-K dated November 2, 2018, is incorporated herein by reference. |
| | |
10.20 | | Seventh Amendment, dated as of August 24, 2021, to the Credit Agreement, dated as of November 15, 2010, as amended on March 15, 2011, September 21, 2012, May 16, 2013, August 7, 2014, June 7, 2016 and October 23, 2018, among the Company, as borrower, the several banks and other financial institutions from time to time parties thereto, as lenders, JPMorgan Chase Bank, N.A., as administrative agent, and the other agents party thereto, previously filed as Exhibit 10.2 to the Company’s Current Report on Form 8-K dated August 24, 2021, is incorporated herein by reference. |
| | |
10.21 | | Eighth Amendment, dated as of September 10, 2021, to the Credit Agreement, dated as of November 15, 2010, as amended on March 15, 2011, September 21, 2012, May 16, 2013, August 7, 2014, June 7, 2016, October 23, 2018 and August 24, 2021, among the Company, as borrower, the several banks and other financial institutions from time to time parties thereto, as lenders, JPMorgan Chase Bank, N.A., as administrative agent, and the other agents party thereto, previously filed as Exhibit 10.3 to the Company’s Quarterly Report on Form 10-Q dated November 8, 2021, is incorporated herein by reference. |
| | |
10.22 | | Ninth Amendment and Increased Facility Activation Notice dated as of June 23, 2022, to Credit Agreement, dated as of November 15, 2010 and as amended and restated as of March 15, 2011, September 21, 2012, May 16, 2013, August 7, 2014, June 7, 2016, October 23, 2018, August 24, 2021 and September 10, 2021, among the Company, JP Morgan Chase Bank, N.A., as administrative agent and other financial institutions or entities from time to time parties thereto, previously filed as Exhibit 10.1 to the Company’s Current Report on Form 8-K dated June 27, 2022, is incorporated herein by reference. |
| | |
10.23* | | Form of Supplemental Life Insurance Plan and Agreement Part A: Alan B. Miller 1998 Dual Life Insurance Trust (effective December 9, 2010, by and between Universal Health Services, Inc., a Delaware corporation (the “Company”), and Anthony Pantaleoni as Trustee), previously filed as Exhibit 10.1 to the Company’s Current Report on Form 8-K dated December 10, 2010, is incorporated herein by reference. |
| | |
10.24* | | Form of Supplemental Life Insurance Plan and Agreement Part B: Alan B. Miller 2002 Trust (effective December 9, 2010, by and between Universal Health Services, Inc., a Delaware corporation (the “Company”), and Anthony Pantaleoni as Trustee), previously filed as Exhibit 10.2 to the Company’s Current Report on Form 8-K dated December 10, 2010, is incorporated herein by reference. |
| | |
10.25* | | Universal Health Services, Inc. Termination, Assignment and Release Agreement (effective December 9, 2010, by and between Universal Health Services, Inc., a Delaware corporation (the “Company”), Anthony Pantaleoni as Trustee of the Alan B. Miller 1998 Dual Life Insurance Trust, and Alan B. Miller, Executive), previously filed as Exhibit 10.3 to the Company’s Current Report on Form 8-K dated December 10, 2010, is incorporated herein by reference. |
| | |
10.26* | | Universal Health Services, Inc. Termination, Assignment and Release Agreement (effective December 9, 2010, by and between Universal Health Services, Inc., a Delaware corporation (the “Company”), Anthony Pantaleoni as Trustee of the Alan B. Miller 2002 Trust, and Alan B. Miller, Executive), previously filed as Exhibit 10.4 to the Company’s Current Report on Form 8-K dated December 10, 2010, is incorporated herein by reference. |
| | |
10.27 | | Collateral Agreement, dated as of August 7, 2014, among Universal Health Services, Inc., the subsidiary guarantors party thereto, MUFG Union Bank, N.A., as 2014 Trustee, The Bank of New York Mellon Trust Company, N.A., as 2006 Trustee, and JPMorgan Chase Bank, N.A., as collateral agent, previously filed as Exhibit 10.4 to the Company’s Current Report on Form 8-K dated August 12, 2014, is incorporated herein by reference. |
| | |
10.28* | | Form of Stock Option Award Agreement under the Universal Health Services, Inc. 2020 Omnibus Stock and Incentive Plan, previously filed as Exhibit 10.5 to the Company’s Quarterly Report on Form 10-Q filed on August 7, 2020, is incorporated herein by reference. |
| | |
| | |
No. | | Description |
10.29* | | Form of Restricted Stock Award Agreement under the Universal Health Services, Inc. 2020 Omnibus Stock and Incentive Plan, previously filed as Exhibit 10.6 to the Company’s Quarterly Report on Form 10-Q filed on August 7, 2020, is incorporated herein by reference. |
| | |
10.30* | | Form of Restricted Stock Unit Award Agreement under the Universal Health Services, Inc. 2020 Omnibus Stock and Incentive Plan, previously filed as Exhibit 10.7 to the Company’s Quarterly Report on Form 10-Q filed on August 7, 2020, is incorporated herein by reference. |
| | |
10.31 | | Settlement Agreement among: (i) the United States of America, acting through the United States Department of Justice and on behalf of the Office of Inspector General (OIG-HHS) of the Department of Health and Human Services (HHS); the Defense Health Agency (DHA), acting on behalf of the TRICARE Program; the Office of Personnel Management (OPM), which administers the Federal Employees Health Benefits Program (FEHBP); and the United States Department of Veteran Affairs (VA) (collectively, the United States); (ii) Universal Health Services, Inc. (“UHS, Inc.”) and UHS of Delaware, Inc. (“UHS of Delaware, Inc.”), acting on behalf of the entities listed on Exhibits A and B, (collectively the “Defendants” or “UHS”); and (iii) various individuals (collectively, the “Relators”), previously filed as Exhibit 10.1 to the Company’s Current Report on Form 8-K dated July 10, 2020, is incorporated herein by reference. |
| | |
10.32 | | Form of Settlement Agreement between various states and Universal Health Services, Inc. and UHS of Delaware, Inc., acting on behalf of the entities listed on Exhibits A and B, previously filed as Exhibit 10.2 to the Company’s Current Report on Form 8-K dated July 10, 2020, is incorporated herein by reference. |
| | |
10.33 | | Corporate Integrity Agreement between the Office of Inspector General of the Department of Health and Human Services and Universal Health Services, Inc. and UHS of Delaware, Inc., previously filed as Exhibit 10.3 to the Company’s Current Report on Form 8-K dated July 10, 2020, is incorporated herein by reference. |
| | |
10.34* | | Employment Agreement between Universal Health Services, Inc. and Marc D. Miller dated as of December 23, 2020, previously filed as Exhibit 10.1 to the Company’s Current Report on Form 8-K dated December 23, 2020, is incorporated herein by reference. |
| | |
10.35* | | Amendment, dated as of March 23, 2022, to Employment Agreement, dated as of December 23, 2020, between Universal Health Services, Inc. and Marc D. Miller, previously filed as Exhibit 10.2 to the Company’s Current Report on Form 8-K dated March 23, 2022, is incorporated herein by reference. |
| | |
10.36* | | Employment Agreement between Universal Health Services, Inc. and Alan B. Miller dated as of December 23, 2020, previously filed as Exhibit 10.2 to the Company’s Current Report on Form 8-K dated December 23, 2020, is incorporated herein by reference. |
10.37* | | Amendment, dated as of March 23, 2022, to Employment Agreement, dated as of December 23, 2020, between Universal Health Services, Inc. and Alan B. Miller, previously filed as Exhibit 10.3 to the Company’s Current Report on Form 8-K dated March 23, 2022, is incorporated herein by reference. |
| | |
10.38 | | Master Lease Document between certain subsidiaries of Universal Health Services, Inc. and Universal Health Realty Income Trust, dated December 31, 2021 previously filed as Exhibit 10.54 to the Company’s Annual Report on Form 10-K dated February 24, 2022, is incorporated herein by reference. |
| | |
10.39* | | Universal Health Services, Inc. 2022 Executive Incentive Plan, previously filed as Exhibit 10.1 to the Company’s Current Report on Form 8-K dated March 23, 2022, is incorporated herein by reference. |
| | |
10.40* | | Form of Restricted Stock Unit Award Agreement under the Universal Health Services, Inc. 2020 Omnibus Stock and Incentive Plan, previously filed as Exhibit 10.4 to the Company’s Quarterly Report on Form 10-Q filed on August 8, 2022, is incorporated herein by reference. |
| | |
10.41* | | Form of Restricted Stock Units Award Agreement for Named Executive Officers with Employment Agreements, , previously filed as Exhibit 10.5 to the Company’s Quarterly Report on Form 10-Q filed on May 6, 2022, is incorporated herein by reference. |
| | |
| | |
No. | | Description |
10.42* | | Form of Restricted Stock Units Award Agreement for Named Executive Officers without Employment Agreements, previously filed as Exhibit 10.6 to the Company’s Quarterly Report on Form 10-Q filed on May 6, 2022, is incorporated herein by reference. |
| | |
10.43* | | Form of Restricted Stock Units Award Agreement for Directors, previously filed as Exhibit 10.7 to the Company’s Quarterly Report on Form 10-Q filed on May 6, 2022, is incorporated herein by reference. |
| | |
10.44* | | Separation Agreement and General Release by and between UHS of Delaware, Inc. and Marvin Pember effective as of December 31, 2022, previously filed as Exhibit 99.1 to the Company’s Current Report on Form 8-K/A dated December 7, 2022, is incorporated herein by reference. |
| | |
10.45* | | Employment Agreement between Universal Health Services, Inc. and Edward Sim dated October 18, 2022 previously filed as Exhibit 10.66 to the Company’s Annual Report on Form 10-K dated February 27, 2023, is incorporated herein by reference. |
| | |
10.46* | | Universal Health Services, Inc. Amended and Restated 2020 Omnibus Stock and Incentive Plan, as amended by the Amendment thereto, previously filed as Exhibit A to the Company’s Proxy Statement filed on April 4, 2024, is incorporated herein by reference. |
| | |
10.47* | | Universal Health Services, Inc. Amended and Restated Employee Stock Purchase Plan, previously filed as Exhibit B to the Company’s Proxy Statement filed on April 4, 2024, is incorporated herein by reference. |
| | |
10.48 | | Tenth Amendment, dated as of September 26, 2024, to Credit Agreement, dated as of November 15, 2010 and as amended and restated as of September 21, 2012, August 7, 2014, October 23, 2018, August 21, 2021, September 10, 2021, June 23, 2022 and September 26, 2024, among the Company, JP Morgan Chase Bank, N.A., as administrative agent and other financial institutions or entities from time to time parties thereto, including the amendment and restatement thereof, effective as of September 26, 2024, attached as Exhibit A thereto and referred to herein as the Senior Secured Credit Facility, previously filed as Exhibit 10.1 to the Company’s Current Report on Form 8-K dated October 1, 2024, is incorporated herein by reference. |
| | |
11 | | Statement regarding computation of per share earnings is set forth in Note 1 of the Notes to the Consolidated Financial Statements. |
| | |
19* | | Universal Health Services, Inc. Inside Information and Trading of Company Stock Policy. |
| | |
21 | | Subsidiaries of Registrant. |
| | |
22.1 | | List of Guarantor Subsidiaries and Issuers of Guaranteed Securities and Affiliates Whose Securities Collateralize Securities of the Registrant. |
| | |
23.1 | | Consent of Independent Registered Public Accounting Firm-PricewaterhouseCoopers LLP. |
| | |
31.1 | | Certification from the Company’s Chief Executive Officer Pursuant to Rule 13a-14(a)/15d-14(a) of the Securities Exchange Act of 1934. |
| | |
31.2 | | Certification from the Company’s Chief Financial Officer Pursuant to Rule 13a-14(a)/15d-14(a) of the Securities Exchange Act of 1934. |
| | |
32.1 | | Certification from the Company’s Chief Executive Officer Pursuant to 18 U.S.C. Section 1350, as Adopted Pursuant to Section 906 of the Sarbanes-Oxley Act of 2002. |
| | |
32.2 | | Certification from the Company’s Chief Financial Officer Pursuant to 18 U.S.C. Section 1350, as Adopted Pursuant to Section 906 of the Sarbanes-Oxley Act of 2002. |
| | |
97 | | Universal Health Services, Inc. Clawback Policy. |
| | |
101.INS | | Inline XBRL Instance Document - the instance document does not appear in the Interactive Data File as its XBRL tags are embedded within the Inline XBRL document |
| | |
| | |
No. | | Description |
101.SCH | | Inline XBRL Taxonomy Extension Schema With Embedded Linkbase Documents |
| | |
104 | | Cover page formatted as Inline XBRL and contained in Exhibit 101 |
* Management contract or compensatory plan or arrangement.
Exhibits, other than those incorporated by reference, have been included in copies of this Annual Report filed with the Securities and Exchange Commission. Stockholders of the Company will be provided with copies of those exhibits upon written request to the Company.
ITEM 16. Form 10-K Summary
None.
SIGNATURES
Pursuant to the requirements of Section 13 or 15(d) of the Securities Exchange Act of 1934, the Registrant has duly caused this report to be signed on its behalf by the undersigned, thereunto duly authorized.
| | |
| | |
UNIVERSAL HEALTH SERVICES, INC. |
| |
By: |
| /s/ MARC D. MILLER |
|
| Marc D. Miller Chief Executive Officer February 26, 2025 |
Pursuant to the requirements of the Securities Exchange Act of 1934, this report has been signed below by the following persons on behalf of the Registrant and in the capacities and on the dates indicated.
| | | | | | | | | | |
| | | | |
| Signatures | | | | Title | | | | Date | |
| | |
/s/ ALAN B. MILLER Alan B. Miller | | Executive Chairman of the Board |
| February 26, 2025 |
| | |
/s/ MARC D. MILLER Marc D. Miller | | Director, President and Chief Executive Officer (Principal Executive Officer) |
| February 26, 2025 |
| | |
/s/ NINA CHEN-LANGENMAYR | | Director | | February 26, 2025 |
Nina Chen-Langenmayr | | | | |
| | | | |
/s/ EILEEN C. MCDONNELL Eileen C. McDonnell | | Director |
| February 26, 2025 |
| | |
/s/ WARREN J. NIMETZ Warren J. Nimetz | | Director |
| February 26, 2025 |
| | |
/s/ MARIA SINGER Maria Singer | | Director |
| February 26, 2025 |
| | |
/s/ ELLIOTT J. SUSSMAN M.D. Elliot J. Sussman M.D. | | Director |
| February 26, 2025 |
| | |
/s/ STEVE FILTON Steve Filton | | Executive Vice President, Chief Financial Officer and Secretary (Principal Financial and Accounting Officer) |
| February 26, 2025 |
UNIVERSAL HEALTH SERVICES, INC.
INDEX TO FINANCIAL STATEMENTS
AND FINANCIAL STATEMENT SCHEDULE
| |
Consolidated Financial Statements: | |
Report of Independent Registered Public Accounting Firm (PCAOB ID: 238) | 88 |
Consolidated Statements of Income for December 31, 2024, 2023 and 2022 | 90 |
Consolidated Statements of Comprehensive Income for December 31, 2024, 2023 and 2022 | 91 |
Consolidated Balance Sheets as of December 31, 2024 and 2023 | 92 |
Consolidated Statements of Changes in Equity for December 31, 2024, 2023 and 2022 | 93 |
Consolidated Statements of Cash Flows for December 31, 2024, 2023 and 2022 | 96 |
Notes to Consolidated Financial Statements | 97 |
Supplemental Financial Statement Schedule II: Valuation and Qualifying Accounts as of and for December 31, 2024, 2023, and 2022 | 130 |
Report of Independent Registered Public Accounting Firm
To the Board of Directors and Stockholders of Universal Health Services, Inc.
Opinions on the Financial Statements and Internal Control over Financial Reporting
We have audited the accompanying consolidated balance sheets of Universal Health Services, Inc. and its subsidiaries (the "Company") as of December 31, 2024 and 2023, and the related consolidated statements of income, of comprehensive income, of changes in equity and of cash flows for each of the three years in the period ended December 31, 2024, including the related notes and financial statement schedule listed in the accompanying index (collectively referred to as the "consolidated financial statements"). We also have audited the Company's internal control over financial reporting as of December 31, 2024, based on criteria established in Internal Control - Integrated Framework (2013) issued by the Committee of Sponsoring Organizations of the Treadway Commission (COSO).
In our opinion, the consolidated financial statements referred to above present fairly, in all material respects, the financial position of the Company as of December 31, 2024 and 2023, and the results of its operations and its cash flows for each of the three years in the period ended December 31, 2024 in conformity with accounting principles generally accepted in the United States of America. Also in our opinion, the Company maintained, in all material respects, effective internal control over financial reporting as of December 31, 2024, based on criteria established in Internal Control - Integrated Framework (2013) issued by the COSO.
Basis for Opinions
The Company's management is responsible for these consolidated financial statements, for maintaining effective internal control over financial reporting, and for its assessment of the effectiveness of internal control over financial reporting, included in Management’s Report on Internal Control over Financial Reporting appearing under Item 9A. Our responsibility is to express opinions on the Company’s consolidated financial statements and on the Company's internal control over financial reporting based on our audits. We are a public accounting firm registered with the Public Company Accounting Oversight Board (United States) (PCAOB) and are required to be independent with respect to the Company in accordance with the U.S. federal securities laws and the applicable rules and regulations of the Securities and Exchange Commission and the PCAOB.
We conducted our audits in accordance with the standards of the PCAOB. Those standards require that we plan and perform the audits to obtain reasonable assurance about whether the consolidated financial statements are free of material misstatement, whether due to error or fraud, and whether effective internal control over financial reporting was maintained in all material respects.
Our audits of the consolidated financial statements included performing procedures to assess the risks of material misstatement of the consolidated financial statements, whether due to error or fraud, and performing procedures that respond to those risks. Such procedures included examining, on a test basis, evidence regarding the amounts and disclosures in the consolidated financial statements. Our audits also included evaluating the accounting principles used and significant estimates made by management, as well as evaluating the overall presentation of the consolidated financial statements. Our audit of internal control over financial reporting included obtaining an understanding of internal control over financial reporting, assessing the risk that a material weakness exists, and testing and evaluating the design and operating effectiveness of internal control based on the assessed risk. Our audits also included performing such other procedures as we considered necessary in the circumstances. We believe that our audits provide a reasonable basis for our opinions.
Definition and Limitations of Internal Control over Financial Reporting
A company’s internal control over financial reporting is a process designed to provide reasonable assurance regarding the reliability of financial reporting and the preparation of financial statements for external purposes in accordance with generally accepted accounting principles. A company’s internal control over financial reporting includes those policies and procedures that (i) pertain to the maintenance of records that, in reasonable detail, accurately and fairly reflect the transactions and dispositions of the assets of the company; (ii) provide reasonable assurance that transactions are recorded as necessary to permit preparation of financial statements in accordance with generally accepted accounting principles, and that receipts and expenditures of the company are being made only in accordance with authorizations of management and directors of the company; and (iii) provide reasonable assurance regarding prevention or timely detection of unauthorized acquisition, use, or disposition of the company’s assets that could have a material effect on the financial statements.
Because of its inherent limitations, internal control over financial reporting may not prevent or detect misstatements. Also, projections of any evaluation of effectiveness to future periods are subject to the risk that controls may become inadequate because of changes in conditions, or that the degree of compliance with the policies or procedures may deteriorate.
Critical Audit Matters
The critical audit matter communicated below is a matter arising from the current period audit of the consolidated financial statements that was communicated or required to be communicated to the audit committee and that (i) relates to accounts or disclosures that are material to the consolidated financial statements and (ii) involved our especially challenging, subjective, or complex judgments. The communication of critical audit matters does not alter in any way our opinion on the consolidated financial statements, taken as a whole, and we are not, by communicating the critical audit matter below, providing a separate opinion on the critical audit matter or on the accounts or disclosures to which it relates.
Valuation of accounts receivable
As described in Notes 1 and 10 to the consolidated financial statements, the Company reports net patient service revenue at the estimated net realizable amounts from patients and third-party payers and others for services rendered. The Company has agreements with third-party payers that provide for payments to the Company at amounts different from established rates. Payment arrangements include rates per discharge, reimbursed costs, discounted charges and per diem payments. Estimates of contractual allowances, which represent explicit price concessions, under managed care plans are based upon the payment terms specified in the related contractual agreements. Management estimates Medicare and Medicaid revenues using the latest available financial information, patient utilization data, government provided data and in accordance with applicable Medicare and Medicaid payment rules and regulations. Management monitors the historical collection rates, as well as changes in applicable laws, rules and regulations and contract terms, to assure that provisions are made using the most accurate information available. In addition to explicit price concessions, management estimates revenue adjustments for implicit price concessions based on general factors such as payer mix, the aging of the receivables and historical collection experience. Management routinely reviews accounts receivable balances in conjunction with these factors and other economic conditions which might ultimately affect the collectability of the patient accounts and make adjustments to the allowances as warranted. As of December 31, 2024, the net accounts receivable balance was $2.2 billion.
The principal considerations for our determination that performing procedures relating to the valuation of accounts receivable is a critical audit matter are the significant judgment by management in estimating net accounts receivable, specifically as it relates to developing the estimate for explicit and implicit price concessions, which in turn led to significant auditor judgment, subjectivity and effort in performing procedures and evaluating audit evidence obtained related to the estimation of price concessions.
Addressing the matter involved performing procedures and evaluating audit evidence in connection with forming our overall opinion on the consolidated financial statements. These procedures included testing the effectiveness of controls relating to the valuation of accounts receivable, including controls over management’s valuation approach, assumptions and data used to estimate the explicit and implicit price concessions. These procedures also included, among others, (i) testing management’s process for developing the estimate for price concessions, as well as the relevance of the historical billing and collection data as an input to the valuation approach; (ii) testing the accuracy of a sample of revenue transactions and a sample of cash collections from the historical billing data and historical collection data used in management’s estimation of price concessions; (iii) evaluating the historical accuracy of management’s process for developing the estimate of the amount which will ultimately be collected by comparing actual cash collections to the previously recorded net accounts receivable balance; and (iv) developing an independent expectation of the net accounts receivable balance. Developing an independent expectation involved calculating the percentage of cash collections as compared to the recorded net accounts receivable balance as of the end of the prior year, applying those calculated percentages to the recorded accounts receivable balance as of December 31, 2024, and comparing the calculated balance to management’s estimate of the net accounts receivable balance.
/s/ PricewaterhouseCoopers LLP
Philadelphia, Pennsylvania
February 26, 2025
We have served as the Company’s auditor since 2007.
UNIVERSAL HEALTH SERVICES, INC. AND SUBSIDIARIES
CONSOLIDATED STATEMENTS OF INCOME
| | | | | | | | | | | | |
| | Year Ended December 31, | |
| | 2024 | | | 2023 | | | 2022 | |
| | (in thousands, except per share data) | |
Net revenues | | $ | 15,827,935 | | | $ | 14,281,976 | | | $ | 13,399,370 | |
Operating charges: | | | | | | | | | |
Salaries, wages and benefits | | | 7,518,687 | | | | 7,107,484 | | | | 6,762,256 | |
Other operating expenses | | | 4,308,384 | | | | 3,757,216 | | | | 3,445,733 | |
Supplies expense | | | 1,587,786 | | | | 1,532,828 | | | | 1,474,339 | |
Depreciation and amortization | | | 584,831 | | | | 568,041 | | | | 581,861 | |
Lease and rental expense | | | 146,433 | | | | 141,026 | | | | 131,626 | |
| | | 14,146,121 | | | | 13,106,595 | | | | 12,395,815 | |
Income from operations | | | 1,681,814 | | | | 1,175,381 | | | | 1,003,555 | |
Interest expense, net | | | 186,109 | | | | 206,674 | | | | 126,889 | |
Other (income) expense, net | | | (2,231 | ) | | | 28,281 | | | | 10,406 | |
Income before income taxes | | | 1,497,936 | | | | 940,426 | | | | 866,260 | |
Provision for income taxes | | | 334,827 | | | | 221,119 | | | | 209,278 | |
Net income | | | 1,163,109 | | | | 719,307 | | | | 656,982 | |
Less: Net income (loss) attributable to noncontrolling interests | | | 21,012 | | | | 1,512 | | | | (18,627 | ) |
Net income attributable to UHS | | $ | 1,142,097 | | | $ | 717,795 | | | $ | 675,609 | |
Basic earnings per share attributable to UHS | | $ | 17.16 | | | $ | 10.35 | | | $ | 9.23 | |
Diluted earnings per share attributable to UHS | | $ | 16.82 | | | $ | 10.23 | | | $ | 9.14 | |
Weighted average number of common shares—basic | | | 66,554 | | | | 69,321 | | | | 73,118 | |
Add: Other share equivalents | | | 1,342 | | | | 804 | | | | 714 | |
Weighted average number of common shares and equivalents—diluted | | | 67,896 | | | | 70,125 | | | | 73,832 | |
The accompanying notes are an integral part of these consolidated financial statements.
UNIVERSAL HEALTH SERVICES, INC. AND SUBSIDIARIES
CONSOLIDATED STATEMENTS OF COMPREHENSIVE INCOME
| | | | | | | | | | | | |
| | Year Ended December 31, | |
| | 2024 | | | 2023 | | | 2022 | |
| | (Dollar amounts in thousands) | |
Net income | | $ | 1,163,109 | | | $ | 719,307 | | | $ | 656,982 | |
Other comprehensive income (loss): | | | | | | | | | |
Minimum pension liability | | | 2,416 | | | | 4,166 | | | | (2,869 | ) |
Foreign currency translation adjustment | | | (3,237 | ) | | | 15,271 | | | | (37,310 | ) |
Other | | | 17 | | | | 0 | | | | 0 | |
Other comprehensive income before tax | | | (804 | ) | | | 19,437 | | | | (40,179 | ) |
Income tax expense related to items of other
comprehensive income | | | 1,284 | | | | 480 | | | | (220 | ) |
Total other comprehensive income (loss), net of tax | | | (2,088 | ) | | | 18,957 | | | | (39,959 | ) |
Comprehensive income | | | 1,161,021 | | | | 738,264 | | | | 617,023 | |
Less: Comprehensive loss (income) attributable to noncontrolling
interests | | | 21,012 | | | | 1,512 | | | | (18,627 | ) |
Comprehensive income attributable to UHS | | $ | 1,140,009 | | | $ | 736,752 | | | $ | 635,650 | |
The accompanying notes are an integral part of these consolidated financial statements.
UNIVERSAL HEALTH SERVICES, INC. AND SUBSIDIARIES
CONSOLIDATED BALANCE SHEETS
| | | | | | | | |
| | December 31, | |
| | 2024 | | | 2023 | |
| | (Dollar amounts in thousands) | |
Assets | | | | | | |
Current assets: | | | | | | |
Cash and cash equivalents | | $ | 125,983 | | | $ | 119,439 | |
Accounts receivable, net | | | 2,177,751 | | | | 2,238,265 | |
Supplies | | | 220,940 | | | | 216,988 | |
Other current assets | | | 291,614 | | | | 236,658 | |
Total current assets | | | 2,816,288 | | | | 2,811,350 | |
Property and Equipment | | | | | | |
Land | | | 745,706 | | | | 737,226 | |
Buildings and improvements | | | 7,671,206 | | | | 7,139,980 | |
Equipment | | | 3,260,350 | | | | 3,066,339 | |
Property under finance lease | | | 125,018 | | | | 101,318 | |
| | | 11,802,280 | | | | 11,044,863 | |
Accumulated depreciation | | | (6,071,058 | ) | | | (5,652,518 | ) |
| | | 5,731,222 | | | | 5,392,345 | |
Construction-in-progress | | | 841,003 | | | | 732,184 | |
| | | 6,572,225 | | | | 6,124,529 | |
Other assets: | | | | | | |
Goodwill | | | 3,932,879 | | | | 3,932,407 | |
Deferred income taxes | | | 118,449 | | | | 85,626 | |
Right of use assets-operating leases | | | 418,719 | | | | 433,962 | |
Deferred charges | | | 9,404 | | | | 6,974 | |
Other | | | 601,785 | | | | 572,754 | |
| | | 5,081,236 | | | | 5,031,723 | |
Total Assets | | $ | 14,469,749 | | | $ | 13,967,602 | |
Liabilities and Stockholders’ Equity | | | | | | |
Current liabilities: | | | | | | |
Current maturities of long-term debt | | $ | 40,059 | | | $ | 126,686 | |
Accounts payable | | | 632,001 | | | | 613,974 | |
Accrued liabilities | | | | | | |
Compensation and related benefits | | | 622,625 | | | | 549,470 | |
Interest | | | 30,250 | | | | 17,436 | |
Taxes other than income | | | 161,683 | | | | 154,186 | |
Operating lease liabilities | | | 74,649 | | | | 71,600 | |
Deferred grant revenue | | | 0 | | | | 5,375 | |
Other | | | 634,920 | | | | 472,574 | |
Current federal and state income taxes | | | 14,219 | | | | 2,046 | |
Total current liabilities | | | 2,210,406 | | | | 2,013,347 | |
| | | | | | |
Other noncurrent liabilities | | | 655,806 | | | | 584,007 | |
Operating lease liabilities noncurrent | | | 376,239 | | | | 382,559 | |
Long-term debt | | | 4,464,482 | | | | 4,785,783 | |
Commitments and contingencies (Note 8) | | | | | | |
Redeemable noncontrolling interest | | | 13,293 | | | | 5,191 | |
Equity: | | | | | | |
Class A Common Stock, voting, $.01 par value; authorized 12,000,000 shares: issued
and outstanding 6,576,475 shares in 2024 and 6,577,100 shares in 2023 | | | 66 | | | | 66 | |
Class B Common Stock, limited voting, $.01 par value; authorized 150,000,000
shares: issued and outstanding 57,726,557 shares in 2024 and 59,930,083 shares in 2023 | | | 577 | | | | 599 | |
Class C Common Stock, voting, $.01 par value; authorized 1,200,000 shares: issued
and outstanding 661,688 shares in 2023 and 661,688 shares in 2022 | | | 7 | | | | 7 | |
Class D Common Stock, limited voting, $.01 par value; authorized 5,000,000 shares:
issued and outstanding 12,614 shares in 2024 and 12,962 shares in 2023 | | | 0 | | | | 0 | |
Cumulative dividends | | | (713,705 | ) | | | (659,890 | ) |
Retained earnings | | | 7,372,061 | | | | 6,798,930 | |
Accumulated other comprehensive income | | | 7,201 | | | | 9,289 | |
Universal Health Services, Inc. common stockholders’ equity | | | 6,666,207 | | | | 6,149,001 | |
Noncontrolling interest | | | 83,316 | | | | 47,714 | |
Total Equity | | | 6,749,523 | | | | 6,196,715 | |
Total Liabilities and Stockholders’ Equity | | $ | 14,469,749 | | | $ | 13,967,602 | |
The accompanying notes are an integral part of these consolidated financial statements.
UNIVERSAL HEALTH SERVICES, INC. AND SUBSIDIARIES
CONSOLIDATED STATEMENTS OF CHANGES IN EQUITY
FOR THE TWELVE MONTHS ENDED DECEMBER 31, 2024
(in thousands)
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
| | | | | | | | | | | | | | | | | | | | | | | Accumulated | | | UHS | | | | | | | |
| | Redeemable | | | | | | | | | | | | | | | | | | | | | Other | | | Common | | | | | | | |
| | Noncontrolling | | | Class A | | | Class B | | | Class C | | | Class D | | | Cumulative | | | Retained | | | Comprehensive | | | Stockholders' | | | Noncontrolling | | | | |
| | Interest | | | Common | | | Common | | | Common | | | Common | | | Dividends | | | Earnings | | | Income (Loss) | | | Equity | | | Interest | | | Total | |
Balance, January 1, 2024 | | $ | 5,191 | | | $ | 66 | | | $ | 599 | | | $ | 7 | | | $ | — | | | $ | (659,890 | ) | | $ | 6,798,930 | | | $ | 9,289 | | | $ | 6,149,001 | | | $ | 47,714 | | | $ | 6,196,715 | |
Common Stock | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
Issued/(converted) including tax benefits from
exercise of stock options | | | — | | | | — | | | | 12 | | | | — | | | | — | | | | — | | | | 15,226 | | | | — | | | | 15,238 | | | | — | | | | 15,238 | |
Repurchased | | | — | | | | — | | | | (34 | ) | | | — | | | | — | | | | — | | | | (674,946 | ) | | | — | | | | (674,980 | ) | | | — | | | | (674,980 | ) |
Restricted share-based compensation expense | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | 43,626 | | | | — | | | | 43,626 | | | | — | | | | 43,626 | |
Dividends paid | | | — | | | | — | | | | — | | | | — | | | | — | | | | (53,815 | ) | | | — | | | | — | | | | (53,815 | ) | | | — | | | | (53,815 | ) |
Stock option expense | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | 54,289 | | | | — | | | | 54,289 | | | | — | | | | 54,289 | |
Change in redemption amount of redeemable noncontrolling interest | | | 7,144 | | | | — | | | | — | | | | — | | | | — | | | | — | | | | (7,144 | ) | | | — | | | | (7,144 | ) | | | — | | | | (7,144 | ) |
Distributions to noncontrolling interests | | | (650 | ) | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | (5,860 | ) | | | (5,860 | ) |
Purchase of ownership interests by minority members | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | 22,056 | | | | 22,056 | |
Comprehensive income: | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
Net income to UHS / noncontrolling interests | | | 1,608 | | | | — | | | | — | | | | — | | | | — | | | | — | | | | 1,142,097 | | | | — | | | | 1,142,097 | | | | 19,406 | | | | 1,161,503 | |
Other | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | (17 | ) | | | 17 | | | | — | | | | — | | | | — | |
Foreign currency translation adjustments (net of income tax effect of $704) | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | (3,941 | ) | | | (3,941 | ) | | | — | | | | (3,941 | ) |
Minimum pension liability (net of income tax effect of $580) | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | 1,836 | | | | 1,836 | | | | — | | | | 1,836 | |
Subtotal - comprehensive income | | | 1,608 | | | | — | | | | — | | | | — | | | | — | | | | — | | | | 1,142,080 | | | | (2,088 | ) | | | 1,139,992 | | | | 19,406 | | | | 1,159,398 | |
Balance, December 31, 2024 | | $ | 13,293 | | | $ | 66 | | | $ | 577 | | | $ | 7 | | | $ | — | | | $ | (713,705 | ) | | $ | 7,372,061 | | | $ | 7,201 | | | $ | 6,666,207 | | | $ | 83,316 | | | $ | 6,749,523 | |
The accompanying notes are an integral part of these consolidated financial statements.
UNIVERSAL HEALTH SERVICES, INC. AND SUBSIDIARIES
CONSOLIDATED STATEMENTS OF CHANGES IN EQUITY—(Continued)
FOR THE TWELVE MONTHS ENDED DECEMBER 31, 2023
(in thousands)
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
| | | | | | | | | | | | | | | | | | | | | | | Accumulated | | | UHS | | | | | | | |
| | Redeemable | | | | | | | | | | | | | | | | | | | | | Other | | | Common | | | | | | | |
| | Noncontrolling | | | Class A | | | Class B | | | Class C | | | Class D | | | Cumulative | | | Retained | | | Comprehensive | | | Stockholders' | | | Noncontrolling | | | | |
| | Interest | | | Common | | | Common | | | Common | | | Common | | | Dividends | | | Earnings | | | Income (Loss) | | | Equity | | | Interest | | | Total | |
Balance, January 1, 2023 | | $ | 4,695 | | | $ | 66 | | | $ | 637 | | | $ | 7 | | | $ | — | | | $ | (604,127 | ) | | $ | 6,533,667 | | | $ | (9,668 | ) | | $ | 5,920,582 | | | $ | 44,768 | | | $ | 5,965,350 | |
Common Stock | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
Issued/(converted) including tax benefits from
exercise of stock options | | | — | | | | — | | | | 3 | | | | — | | | | — | | | | — | | | | 13,760 | | | | — | | | | 13,763 | | | | — | | | | 13,763 | |
Repurchased | | | — | | | | — | | | | (41 | ) | | | — | | | | — | | | | — | | | | (552,567 | ) | | | — | | | | (552,608 | ) | | | — | | | | (552,608 | ) |
Restricted share-based compensation expense | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | 22,032 | | | | — | | | | 22,032 | | | | — | | | | 22,032 | |
Dividends paid | | | — | | | | — | | | | — | | | | — | | | | — | | | | (55,763 | ) | | | — | | | | — | | | | (55,763 | ) | | | — | | | | (55,763 | ) |
Stock option expense | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | 64,243 | | | | — | | | | 64,243 | | | | — | | | | 64,243 | |
Distributions to noncontrolling interests | | | (1,050 | ) | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | (5,780 | ) | | | (5,780 | ) |
Purchase of ownership interests by minority members | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | 8,760 | | | | 8,760 | |
Comprehensive income: | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
Net income to UHS / noncontrolling interests | | | 1,546 | | | | — | | | | — | | | | — | | | | — | | | | — | | | | 717,795 | | | | — | | | | 717,795 | | | | (34 | ) | | | 717,761 | |
Foreign currency translation adjustments (net of income tax effect of $520) | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | 15,791 | | | | 15,791 | | | | — | | | | 15,791 | |
Minimum pension liability (net of income tax effect of $1,000) | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | 3,166 | | | | 3,166 | | | | — | | | | 3,166 | |
Subtotal - comprehensive income | | | 1,546 | | | | — | | | | — | | | | — | | | | — | | | | — | | | | 717,795 | | | | 18,957 | | | | 736,752 | | | | (34 | ) | | | 736,718 | |
Balance, December 31, 2023 | | $ | 5,191 | | | $ | 66 | | | $ | 599 | | | $ | 7 | | | $ | — | | | $ | (659,890 | ) | | $ | 6,798,930 | | | $ | 9,289 | | | $ | 6,149,001 | | | $ | 47,714 | | | $ | 6,196,715 | |
The accompanying notes are an integral part of these consolidated financial statements.
UNIVERSAL HEALTH SERVICES, INC. AND SUBSIDIARIES
CONSOLIDATED STATEMENTS OF CHANGES IN EQUITY—(Continued)
FOR THE TWELVE MONTHS ENDED DECEMBER 31, 2022
(in thousands)
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
| | | | | | | | | | | | | | | | | | | | | | | Accumulated | | | UHS | | | | | | | |
| | Redeemable | | | | | | | | | | | | | | | | | | | | | Other | | | Common | | | | | | | |
| | Noncontrolling | | | Class A | | | Class B | | | Class C | | | Class D | | | Cumulative | | | Retained | | | Comprehensive | | | Stockholders' | | | Noncontrolling | | | | |
| | Interest | | | Common | | | Common | | | Common | | | Common | | | Dividends | | | Earnings | | | Income (Loss) | | | Equity | | | Interest | | | Total | |
Balance, January 1, 2022 | | $ | 5,119 | | | $ | 66 | | | $ | 698 | | | $ | 7 | | | $ | 0 | | | $ | (545,487 | ) | | $ | 6,604,089 | | | $ | 30,291 | | | $ | 6,089,664 | | | $ | 103,389 | | | $ | 6,193,053 | |
Common Stock | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
Issued/(converted) including tax benefits from
exercise of stock options | | | — | | | | — | | | | 11 | | | | — | | | | — | | | | — | | | | 14,196 | | | | — | | | | 14,207 | | | | — | | | | 14,207 | |
Repurchased | | | — | | | | — | | | | (72 | ) | | | — | | | | — | | | | — | | | | (832,846 | ) | | | — | | | | (832,918 | ) | | | — | | | | (832,918 | ) |
Restricted share-based compensation expense | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | 17,649 | | | | — | | | | 17,649 | | | | — | | | | 17,649 | |
Dividends paid | | | — | | | | — | | | | — | | | | — | | | | — | | | | (58,640 | ) | | | — | | | | — | | | | (58,640 | ) | | | — | | | | (58,640 | ) |
Stock option expense | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | 66,244 | | | | — | | | | 66,244 | | | | — | | | | 66,244 | |
Acquisition of noncontrolling interest in majority owned business | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | (11,274 | ) | | | — | | | | (11,274 | ) | | | (37,608 | ) | | | (48,882 | ) |
Distributions to noncontrolling interests | | | (650 | ) | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | (4,741 | ) | | | (4,741 | ) |
Purchase of ownership interests by minority members | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | 2,581 | | | | 2,581 | |
Comprehensive income: | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
Net income to UHS / noncontrolling interests | | | 226 | | | | — | | | | — | | | | — | | | | — | | | | — | | | | 675,609 | | | | — | | | | 675,609 | | | | (18,853 | ) | | | 656,756 | |
Foreign currency translation adjustments (net of income tax effect of $469) | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | (37,779 | ) | | | (37,779 | ) | | | — | | | | (37,779 | ) |
Minimum pension liability (net of income tax effect of $689) | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | — | | | | (2,180 | ) | | | (2,180 | ) | | | — | | | | (2,180 | ) |
Subtotal - comprehensive income | | | 226 | | | | — | | | | — | | | | — | | | | — | | | | — | | | | 675,609 | | | | (39,959 | ) | | | 635,650 | | | | (18,853 | ) | | | 616,797 | |
Balance, December 31, 2022 | | $ | 4,695 | | | $ | 66 | | | $ | 637 | | | $ | 7 | | | $ | — | | | $ | (604,127 | ) | | $ | 6,533,667 | | | $ | (9,668 | ) | | $ | 5,920,582 | | | $ | 44,768 | | | $ | 5,965,350 | |
The accompanying notes are an integral part of these consolidated financial statements.
UNIVERSAL HEALTH SERVICES, INC. AND SUBSIDIARIES
CONSOLIDATED STATEMENTS OF CASH FLOWS
| | | | | | | | | | | | |
| | Year Ended December 31, | |
| | 2024 | | | 2023 | | | 2022 | |
| | (Amounts in thousands) | |
Cash Flows from Operating Activities: | | | | | | | | | |
Net income | | $ | 1,163,109 | | | $ | 719,307 | | | $ | 656,982 | |
Adjustments to reconcile net income to net cash provided by operating
activities: | | | | | | | | | |
Depreciation & amortization | | | 584,831 | | | | 568,041 | | | | 581,861 | |
(Gain) loss on sales of assets and businesses | | | (9,920 | ) | | | (6,250 | ) | | | 584 | |
Stock-based compensation expense | | | 99,349 | | | | 87,720 | | | | 85,378 | |
Costs related to extinguishment of debt | | | 3,158 | | | | 0 | | | | 0 | |
Provision for asset impairment | | | 0 | | | | 0 | | | | 57,550 | |
Changes in assets & liabilities, net of effects from acquisitions and
dispositions: | | | | | | | | | |
Accounts receivable | | | 67,355 | | | | (182,444 | ) | | | (258,338 | ) |
Accrued interest | | | 12,814 | | | | 1,193 | | | | 1,835 | |
Accrued and deferred income taxes | | | 12,651 | | | | (43,450 | ) | | | (29,510 | ) |
Other working capital accounts | | | 61,897 | | | | (32,321 | ) | | | (146,692 | ) |
Deferred grant revenue | | | 0 | | | | 2,978 | | | | 2,391 | |
Other assets and deferred charges | | | (12,163 | ) | | | 48,517 | | | | 19,918 | |
Other | | | 21,811 | | | | 39,133 | | | | (8,676 | ) |
Accrued insurance expense, net of commercial premiums paid | | | 254,394 | | | | 183,462 | | | | 174,723 | |
Payments made in settlement of self-insurance claims | | | (192,185 | ) | | | (118,089 | ) | | | (141,983 | ) |
Net cash provided by operating activities | | | 2,067,101 | | | | 1,267,797 | | | | 996,023 | |
Cash Flows from Investing Activities: | | | | | | | | | |
Property and equipment additions | | | (943,810 | ) | | | (743,055 | ) | | | (734,001 | ) |
Acquisition of businesses and property | | | (18,998 | ) | | | (3,728 | ) | | | (20,309 | ) |
Inflows (outflows) from foreign exchange contracts that hedge our net U.K. investment | | | 12,860 | | | | (40,695 | ) | | | 94,913 | |
Proceeds received from sales of assets and businesses | | | 38,563 | | | | 24,187 | | | | 12,001 | |
Decrease in capital reserves of commercial insurance subsidiary | | | 276 | | | | 16 | | | | 100 | |
Net cash used in investing activities | | | (911,109 | ) | | | (763,275 | ) | | | (647,296 | ) |
Cash Flows from Financing Activities: | | | | | | | | | |
Repayments of long-term debt | | | (2,640,001 | ) | | | (85,480 | ) | | | (89,367 | ) |
Additional borrowings | | | 2,210,248 | | | | 185,100 | | | | 705,321 | |
Financing costs | | | (12,566 | ) | | | (308 | ) | | | (3,164 | ) |
Repurchase of common shares | | | (670,754 | ) | | | (547,363 | ) | | | (832,918 | ) |
Dividends paid | | | (53,346 | ) | | | (55,480 | ) | | | (58,449 | ) |
Issuance of common stock | | | 15,070 | | | | 13,654 | | | | 14,068 | |
Profit distributions to noncontrolling interests | | | (6,508 | ) | | | (6,830 | ) | | | (5,391 | ) |
Purchase (sale) of ownership interests by (from) minority member | | | 12,980 | | | | 2,762 | | | | (48,500 | ) |
Net cash used in financing activities | | | (1,144,877 | ) | | | (493,945 | ) | | | (318,400 | ) |
Effect of exchange rate changes on cash and cash equivalents | | | (833 | ) | | | 3,056 | | | | (8,424 | ) |
Increase in cash, cash equivalents and restricted cash | | | 10,282 | | | | 13,633 | | | | 21,903 | |
Cash, cash equivalents and restricted cash, beginning of period | | | 214,470 | | | | 200,837 | | | | 178,934 | |
Cash, cash equivalents and restricted cash, end of period | | $ | 224,752 | | | $ | 214,470 | | | $ | 200,837 | |
Supplemental Disclosures of Cash Flow Information: | | | | | | | | | |
Interest paid | | $ | 168,274 | | | $ | 200,446 | | | $ | 120,136 | |
Income taxes paid, net of refunds | | $ | 325,430 | | | $ | 257,896 | | | $ | 250,759 | |
Noncash purchases of property and equipment | | $ | 118,109 | | | $ | 66,899 | | | $ | 72,064 | |
The accompanying notes are an integral part of these consolidated financial statements.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS
1) BUSINESS AND SUMMARY OF SIGNIFICANT ACCOUNTING POLICIES
Services provided by our hospitals, all of which are operated by subsidiaries of ours, include general and specialty surgery, internal medicine, obstetrics, emergency room care, radiology, oncology, diagnostic care, coronary care, pediatric services, pharmacy services and/or behavioral health services. We, through our subsidiaries, provide capital resources as well as a variety of management services to our facilities, including central purchasing, information services, finance and control systems, facilities planning, physician recruitment services, administrative personnel management, marketing and public relations.
Principles of Consolidation: The consolidated financial statements include the accounts of our majority-owned subsidiaries and partnerships controlled by us or our subsidiaries as the managing general partner. All intercompany accounts and transactions have been eliminated.
Revenue Recognition: We report net patient service revenue at the estimated net realizable amounts from patients and third-party payers and others for services rendered. We have agreements with third-party payers that provide for payments to us at amounts different from our established rates. Payment arrangements include rates per discharge, reimbursed costs, discounted charges and per diem payments. Estimates of contractual allowances under managed care plans, which represent explicit price concessions, are based upon the payment terms specified in the related contractual agreements. We closely monitor our historical collection rates, as well as changes in applicable laws, rules and regulations and contract terms, to assure that provisions are made using the most accurate information available. However, due to the complexities involved in these estimations, actual payments from payers may be different from the amounts we estimate and record.
See Note 10-Revenue Recognition, for additional disclosure related to our revenues including a disaggregation of our consolidated net revenues by major source for each of the periods presented herein.
We estimate our Medicare and Medicaid revenues using the latest available financial information, patient utilization data, government provided data and in accordance with applicable Medicare and Medicaid payment rules and regulations. The laws and regulations governing the Medicare and Medicaid programs are extremely complex and subject to interpretation and as a result, there is at least a reasonable possibility that recorded estimates will change by material amounts in the near term. Certain types of payments by the Medicare program and state Medicaid programs (e.g. Medicare Disproportionate Share Hospital, Medicare Allowable Bad Debts and Inpatient Psychiatric Services) are subject to retroactive adjustment in future periods as a result of administrative review and audit and our estimates may vary from the final settlements. Such amounts are included in accounts receivable, net, on our consolidated balance sheets. The funding of both federal Medicare and state Medicaid programs are subject to legislative and regulatory changes. As such, we cannot provide any assurance that future legislation and regulations, if enacted, will not have a material impact on our future Medicare and Medicaid reimbursements. Adjustments related to the final settlement of these retrospectively determined amounts did not materially impact our results in 2024, 2023 or 2022. If it were to occur, each 1% adjustment to our estimated net Medicare revenues that are subject to retrospective review and settlement as of December 31, 2024, would change our after-tax net income by approximately $2 million.
Charity Care, Uninsured Discounts and Other Adjustments to Revenue: Collection of receivables from third-party payers and patients is our primary source of cash and is critical to our operating performance. Our primary collection risks relate to uninsured patients and the portion of the bill which is the patient’s responsibility, primarily co-payments and deductibles. We estimate our revenue adjustments for implicit price concessions based on general factors such as payer mix, the aging of the receivables and historical collection experience. We routinely review accounts receivable balances in conjunction with these factors and other economic conditions which might ultimately affect the collectability of the patient accounts and make adjustments to our allowances as warranted. At our acute care hospitals, third party liability accounts are pursued until all payment and adjustments are posted to the patient account. For those accounts with a patient balance after third party liability is finalized or accounts for uninsured patients, the patient receives statements and collection letters.
Historically, a significant portion of the patients treated throughout our portfolio of acute care hospitals are uninsured patients which, in part, has resulted from patients who are employed but do not have health insurance or who have policies with relatively high deductibles. Patients treated at our hospitals for non-elective services, who have gross income of various amounts, dependent upon the state, ranging from 200% to 400% of the federal poverty guidelines, are deemed eligible for charity care. The federal poverty guidelines are established by the federal government and are based on income and family size. Because we do not pursue collection of amounts that qualify as charity care, the transaction price is fully adjusted and there is no impact in our net revenues or in our accounts receivable, net.
A portion of the accounts receivable at our acute care facilities are comprised of Medicaid accounts that are pending approval from third-party payers but we also have smaller amounts due from other miscellaneous payers such as county indigent programs in certain states. Our patient registration process includes an interview of the patient or the patient’s responsible party at the time of registration. At that time, an insurance eligibility determination is made and an insurance plan code is assigned. There are various
pre-established insurance profiles in our patient accounting system which determine the expected insurance reimbursement for each patient based on the insurance plan code assigned and the services rendered. Certain patients may be classified as Medicaid pending at registration based upon a screening evaluation if we are unable to definitively determine if they are currently Medicaid eligible. When a patient is registered as Medicaid eligible or Medicaid pending, our patient accounting system records net revenues for services provided to that patient based upon the established Medicaid reimbursement rates, subject to the ultimate disposition of the patient’s Medicaid eligibility. When the patient’s ultimate eligibility is determined, reclassifications may occur which impacts net revenues in future periods. Although the patient’s ultimate eligibility determination may result in adjustments to net revenues, these adjustments do not have a material impact on our results of operations in 2024, 2023 or 2022 since our facilities make estimates at each financial reporting period to adjust revenue based on historical collections.
We also provide discounts to uninsured patients (included in “uninsured discounts” amounts below) who do not qualify for Medicaid or charity care. Because we do not pursue collection of amounts classified as uninsured discounts, the transaction price is fully adjusted and there is no impact in our net revenues or in our net accounts receivable. In implementing the discount policy, we first attempt to qualify uninsured patients for governmental programs, charity care or any other discount program. If an uninsured patient does not qualify for these programs, the uninsured discount is applied.
Uncompensated care (charity care and uninsured discounts):
The following table shows the amounts recorded at our acute care hospitals for charity care and uninsured discounts, based on charges at established rates, for the years ended December 31, 2024, 2023 and 2022:
| | | | | | | | | | | | | | | | | | | | | | | | |
| | (dollar amounts in thousands) | |
| | 2024 | | | 2023 | | | 2022 | |
| | Amount | | | % | | | Amount | | | % | | | Amount | | | % | |
Charity care | | $ | 819,681 | | | | 23 | % | | $ | 843,449 | | | | 32 | % | | $ | 786,962 | | | | 35 | % |
Uninsured discounts | | | 2,677,026 | | | | 77 | % | | | 1,792,493 | | | | 68 | % | | | 1,474,933 | | | | 65 | % |
Total uncompensated care | | $ | 3,496,707 | | | | 100 | % | | $ | 2,635,942 | | | | 100 | % | | $ | 2,261,895 | | | | 100 | % |
The estimated cost of providing uncompensated care:
The estimated cost of providing uncompensated care, as reflected below, were based on a calculation which multiplied the percentage of operating expenses for our acute care hospitals to gross charges for those hospitals by the above-mentioned total uncompensated care amounts. The percentage of cost to gross charges is calculated based on the total operating expenses for our acute care facilities divided by gross patient service revenue for those facilities. An increase in the level of uninsured patients to our facilities and the resulting adverse trends in the adjustments to net revenues and uncompensated care provided could have a material unfavorable impact on our future operating results.
| | | | | | | | | | | | |
| | (amounts in thousands) | |
| | 2024 | | | 2023 | | | 2022 | |
Estimated cost of providing charity care | | $ | 75,227 | | | $ | 83,383 | | | $ | 85,434 | |
Estimated cost of providing uninsured discounts | | | 245,687 | | | | 177,206 | | | | 160,122 | |
Estimated cost of providing uncompensated care | | $ | 320,914 | | | $ | 260,589 | | | $ | 245,556 | |
Concentration of Revenues: Our seven acute care hospitals and seven free-standing emergency departments in the Las Vegas, Nevada, market contributed, on a combined basis, 15% in 2024, 14% in 2023 and 15% in 2022 of our consolidated net revenues.
Cash, Cash Equivalents and Restricted Cash: We consider all highly liquid investments purchased with maturities of three months or less to be cash equivalents.
Cash, cash equivalents, and restricted cash as reported in the consolidated statements of cash flows are presented separately on our consolidated balance sheets as follow:
| | | | | | | | | | | | |
| | (amounts in thousands) | |
| | 2024 | | | 2023 | | | 2022 | |
Cash and cash equivalents | | $ | 125,983 | | | $ | 119,439 | | | $ | 102,818 | |
Restricted cash (a) | | | 98,769 | | | | 95,031 | | | | 98,019 | |
Total cash, cash equivalents and restricted cash | | $ | 224,752 | | | $ | 214,470 | | | $ | 200,837 | |
| |
(a)Restricted cash is included in other assets on the accompanying consolidated balance sheets and consists of statutorily required capital reserves related to our commercial insurance subsidiary. The fair value of our restricted cash was computed based upon quotes received from financial institutions. We consider these to be “level 1” in the fair value hierarchy as outlined in the authoritative guidance for disclosures in connection with financial securities. |
|
Property and Equipment: Property and equipment are stated at cost. Expenditures for renewals and improvements are charged to the property accounts. Replacements, maintenance and repairs which do not improve or extend the life of the respective asset are expensed as incurred. We remove the cost and the related accumulated depreciation from the accounts for assets sold or retired and the resulting gains or losses are included in the results of operations. Construction-in-progress includes both construction projects and equipment not yet placed into service.
Our financial statements for the year ended December 31, 2022, include a pre-tax provision for asset impairment of approximately $58 million, which is included in other operating expenses on the accompanying consolidated statements of income, to write-down the asset value of Desert Springs Hospital Medical Center, a 282-bed acute care hospital located in Las Vegas, Nevada. In early 2023, as a result of various competitive pressures and operational challenges experienced in the market, which had a significant unfavorable impact on the hospital's results of operations during the past year, as well as physical plant constraints and limitations resulting from the advanced age of the facility (which opened in 1971), we announced plans to discontinue all inpatient operations by March of 2023. For a period of time, we plan to continue providing emergency department services within a portion of the existing facility while we construct a new free-standing emergency department on the hospital's campus. The provision for asset impairment reduced the asset values of the facility's real estate and equipment to their estimated fair values.
We capitalized interest during the construction period of major construction projects and during the development and implementation of information technology applications amounting to $38.9 million during 2024, $24.4 million during 2023 and $8.6 million during 2022.
Depreciation is provided on the straight-line method over the estimated useful lives of buildings and improvements (twenty to forty years) and equipment (three to fifteen years). Depreciation expense was $559.6 million during 2024, $535.6 million during 2023 and $544.0 million during 2022.
Long-Lived Assets: We review our long-lived assets, including intangible assets, for impairment whenever events or circumstances indicate that the carrying value of these assets may not be recoverable. The assessment of possible impairment is based on our ability to recover the carrying value of our asset based on our estimate of its undiscounted future cash flows. If the analysis indicates that the carrying value is not recoverable from future cash flows, the asset is written down to its estimated fair value and an impairment loss is recognized. Fair values are determined based on estimated future cash flows using appropriate discount rates.
Goodwill: Goodwill is reviewed for impairment at the reporting unit level on an annual basis or sooner if the indicators of impairment arise. Our judgments regarding the existence of impairment indicators are based on market conditions and operational performance of each reporting unit. We have designated October 1st as our annual impairment assessment date and performed quantitative impairment assessments as of October 1, 2024 which indicated no impairment of goodwill. There were also no goodwill impairments during 2023 or 2022. Future changes in the estimates used to conduct the impairment reviews, including profitability and market value projections, could indicate impairment in future periods potentially resulting in a write-off of a portion or all of our goodwill.
Changes in the carrying amount of goodwill for the two years ended December 31, 2024 were as follows (in thousands):
| | | | | | | | | | | | |
| | Acute Care
Services | | | Behavioral
Health
Services | | | Total
Consolidated | |
Balance, January 1, 2023 | | $ | 516,626 | | | $ | 3,392,830 | | | $ | 3,909,456 | |
Goodwill acquired during the period | | | 0 | | | | 4,598 | | | | 4,598 | |
Goodwill divested during the period | | | 0 | | | | (6,062 | ) | | | (6,062 | ) |
Adjustments to goodwill (a) | | | 2 | | | | 24,413 | | | | 24,415 | |
Balance, December 31, 2023 | | | 516,628 | | | | 3,415,779 | | | | 3,932,407 | |
Goodwill acquired during the period | | | 13,252 | | | | 0 | | | | 13,252 | |
Goodwill divested during the period | | | 0 | | | | (5,298 | ) | | | (5,298 | ) |
Adjustments to goodwill (a) | | | 0 | | | | (7,482 | ) | | | (7,482 | ) |
Balance, December 31, 2024 | | $ | 529,880 | | | $ | 3,402,999 | | | $ | 3,932,879 | |
(a)The changes in the Behavioral Health Services’ goodwill consist of foreign currency translation adjustments.
Other Assets and Intangible Assets: Other assets consist primarily of amounts related to: (i) intangible assets acquired in connection with our acquisitions of Cambian Group, PLC’s adult services’ division during 2015, Ascend Health Corporation during 2012 and Psychiatric Solutions, Inc. during 2010; (ii) prepaid fees for various software and other applications used by our hospitals; (iii) costs incurred in connection with the purchase and implementation of an electronic health records application for each of our acute care facilities; (iv) statutorily required capital reserves related to our commercial insurance subsidiary ($118 million and $113 million as of December 31, 2024 and 2023, respectively); (v) deposits; (vi) investments in various businesses, including Universal Health Realty Income Trust ($6 million and $7 million as of as of December 31, 2024 and 2023, respectively) and Premier, Inc. ($47 million and $50 million as of December 31, 2024 and 2023, respectively); (vii) the invested assets related to a deferred compensation
plan that is held by an independent trustee in a rabbi-trust and that has a related payable included in other noncurrent liabilities, and; (viii) other miscellaneous assets.
Intangible assets are reviewed for impairment on an annual basis or more often if indicators of impairment arise. Our judgments regarding the existence of impairment indicators are based on market conditions and operational performance of each asset. We have designated October 1st as our annual impairment assessment date and performed impairment assessments as of October 1, 2024 which indicated no impairment. There were also no intangible asset impairments during 2023 or 2022.
The following table shows the amounts recorded as net intangible assets for the years ended December 31, 2024 and 2023:
| | | | | | | | |
| | (amounts in thousands) | |
| | 2024 | | | 2023 | |
Medicare licenses (a) | | $ | 57,226 | | | $ | 57,226 | |
Certificates of need | | | 7,987 | | | | 7,501 | |
Contract relationships and other (net of $57,236 and $56,288 of accumulated amortization for 2024 and 2023, respectively) | | | 11,060 | | | | 12,291 | |
Net Intangible Assets | | $ | 76,273 | | | $ | 77,018 | |
(a) Indefinite lives.
Supplies: Supplies, which consist primarily of medical supplies, are stated at the lower of cost (first-in, first-out basis) or market.
Self-Insured/Other Insurance Risks: We provide for self-insured risks, primarily general and professional liability claims, workers’ compensation claims and healthcare and dental claims. Our estimated liability for self-insured professional and general liability claims is based on a number of factors including, among other things, the number of asserted claims and reported incidents, estimates of losses for these claims based on recent and historical settlement amounts and jury verdicts, estimates of incurred but not reported claims based on historical experience, and estimates of amounts recoverable under our commercial insurance policies. All relevant information, including our own historical experience, applicable per occurrence and aggregate self-insured retentions, and limitations and exclusions pursuant to our commercial insurance policies, is used in estimating our expected liability for self-insured claims. While we continuously monitor these factors, our ultimate liability for professional and general liability claims could change materially from our current estimates due to inherent uncertainties involved in making this estimate. Our estimated self-insured reserves are reviewed and changed, if necessary, at each reporting date and changes are recognized currently as additional expense or as a reduction of expense. Given our significant exposure to professional and general liability claims, there can be no assurance that a sharp increase in the number and/or severity of claims asserted against us, and/or reductions in the amount of commercial coverage available to us, will not have a material adverse effect on our future results of operations.
In addition, we also: (i) own commercial health insurers headquartered in Nevada and Puerto Rico, and; (ii) maintain self-insured employee benefits programs for employee healthcare and dental claims. The ultimate costs related to these programs/operations include expenses for claims incurred and paid in addition to an accrual for the estimated expenses incurred in connection with claims incurred but not yet reported. See Note 8 - Commitments and Contingencies for additional disclosure related to our self-insured general and professional liability and workers’ compensation liability.
Income Taxes: Deferred tax assets and liabilities are recognized for the amount of taxes payable or deductible in future years as a result of differences between the tax bases of assets and liabilities and their reported amounts in the financial statements. We believe that future income will enable us to realize our deferred tax assets net of recorded valuation allowances relating to state and foreign net operating loss carry-forwards, tax credits, and interest deduction limitations.
Due to recent guidance and enacted laws surrounding the global 15% minimum tax rate that will be effective after 2024 from the Organization for Economic Co-operation and Development ("OECD"), as well as jurisdictions that we operate in, we anticipate adverse effects to our provision for income taxes as well as cash taxes. Currently, the United States has not enacted legislation that aligns with the OECD global minimum tax rate. We do not expect these effects to be material and will continue to monitor changes in tax policies and laws issued by the OECD and jurisdictions in which we operate.
We operate in multiple jurisdictions with varying tax laws. We are subject to audits by any of these taxing authorities. We believe that adequate accruals have been provided for federal, foreign and state taxes.
See Note 6-Income Taxes for additional disclosure.
Other Noncurrent Liabilities: Other noncurrent liabilities include the long-term portion of our professional and general liability, workers’ compensation reserves, pension and deferred compensation liabilities, and liabilities incurred in connection with split-dollar life insurance agreements on the lives of our executive chairman of the board and his wife.
Redeemable Noncontrolling Interests and Noncontrolling Interest: As of December 31, 2024, outside owners held noncontrolling, minority ownership interests of: (i) approximately 7% in an acute care facility located in Texas; (ii) 49%, 20%, 30%,
20%, 25%, and 48% in six behavioral health care facilities located in Arizona, Pennsylvania, Ohio, Washington, Missouri, and Iowa, respectively, (iii) 26% and 49% in two behavioral health care facilities located in Michigan (one currently under construction with an expected opening in the second quarter of 2025) and; (iv) approximately 5% in an acute care facility and 49% in a surgery center, located in Nevada. The noncontrolling interest and redeemable noncontrolling interest balances of $83 million and $13 million, respectively, as of December 31, 2024, consist primarily of the third-party ownership interests in these hospitals.
In August, 2022, we purchased the 20% noncontrolling ownership interest in a hospital majority owned by us, located in Washington D.C. for $51 million. We now have 100% ownership interest in the hospital. The noncontrolling interest balance was reclassified to retained earnings and is included in common stockholders’ equity in the accompanying consolidated balance sheets and in retained earnings in the accompanying consolidated statements of changes in equity.
In connection with the two behavioral health care facilities located in Pennsylvania and Ohio, the minority ownership interests of which are reflected as redeemable noncontrolling interests on our consolidated balance sheets, the outside owners have “put options” to put their entire ownership interest to us at any time. If exercised, the put option requires us to purchase the minority member’s interest at fair market value. Accordingly, the amounts recorded as redeemable noncontrolling interests on our consolidated balance sheets reflect the estimated fair market value of these ownership interests.
Accumulated Other Comprehensive Income: The accumulated other comprehensive income (“AOCI”) component of stockholders’ equity includes: net unrealized gains and losses on effective cash flow hedges, foreign currency translation adjustments and the net minimum pension liability of a non-contributory defined benefit pension plan which covers employees at one of our subsidiaries. See Note 11 - Pension Plan for additional disclosure regarding the defined benefit pension plan.
The amounts recognized in AOCI for the three years ended December 31, 2024 were as follows (in thousands):
| | | | | | | | | | | | | | | | |
| | Net Unrealized
Gains (Losses) on
Effective Cash
Flow Hedges | | | Foreign
Currency
Translation
Adjustment | | | Minimum
Pension
Liability | | | Total
AOCI | |
Balance, January 1, 2022, net of income tax | | $ | (17 | ) | | $ | 33,524 | | | $ | (3,216 | ) | | $ | 30,291 | |
2022 activity: | | | | | | | | | | | | |
Pretax amount | | | 0 | | | | (37,310 | ) | | | (2,869 | ) | | | (40,179 | ) |
Income tax effect | | | 0 | | | | (469 | ) | | | 689 | | | | 220 | |
Change, net of income tax | | | 0 | | | | (37,779 | ) | | | (2,180 | ) | | | (39,959 | ) |
Balance, January 1, 2023, net of income tax | | $ | (17 | ) | | $ | (4,255 | ) | | $ | (5,396 | ) | | $ | (9,668 | ) |
2023 activity: | | | | | | | | | | | | |
Pretax amount | | | 0 | | | | 15,271 | | | | 4,166 | | | | 19,437 | |
Income tax effect | | | 0 | | | | 520 | | | | (1,000 | ) | | | (480 | ) |
Change, net of income tax | | | 0 | | | | 15,791 | | | | 3,166 | | | | 18,957 | |
Balance, January 1, 2024, net of income tax | | | (17 | ) | | | 11,536 | | | | (2,230 | ) | | | 9,289 | |
2024 activity: | | | | | | | | | | | | |
Pretax amount | | | 17 | | | | (3,237 | ) | | | 2,416 | | | | (804 | ) |
Income tax effect | | | 0 | | | | (704 | ) | | | (580 | ) | | | (1,284 | ) |
Change, net of income tax | | | 17 | | | | (3,941 | ) | | | 1,836 | | | | (2,088 | ) |
Balance, December 31, 2024, net of income tax | | $ | — | | | $ | 7,595 | | | $ | (394 | ) | | $ | 7,201 | |
Accounting for Derivative Financial Investments and Hedging Activities and Foreign Currency Forward Exchange Contracts: We manage our ratio of fixed and floating rate debt with the objective of achieving a mix that management believes is appropriate. To manage this risk in a cost-effective manner, we, from time to time, enter into interest rate swap agreements in which we agree to exchange various combinations of fixed and/or variable interest rates based on agreed upon notional amounts. We account for our derivative and hedging activities using the Financial Accounting Standard Board’s (“FASB”) guidance which requires all derivative instruments, including certain derivative instruments embedded in other contracts, to be carried at fair value on the balance sheet. For derivative transactions designated as hedges, we formally document all relationships between the hedging instrument and the related hedged item, as well as its risk-management objective and strategy for undertaking each hedge transaction.
Derivative instruments designated in a hedge relationship to mitigate exposure to variability in expected future cash flows, or other types of forecasted transactions, are considered cash flow hedges. Cash flow hedges are accounted for by recording the fair value of the derivative instrument on the balance sheets as either an asset or liability, with a corresponding amount recorded in accumulated other comprehensive income (“AOCI”) within statements of changes in equity. Amounts are reclassified from AOCI to the income statement in the period or periods the hedged transaction affects earnings. From time to time, we use interest rate derivatives in our cash flow hedge transactions. Such derivatives are designed to be highly effective in offsetting changes in the cash flows related to the hedged liability.
For hedge transactions that do not qualify for the short-cut method, at the hedge’s inception and on a regular basis thereafter, a formal assessment is performed to determine whether changes in the fair values or cash flows of the derivative instruments have been highly effective in offsetting changes in cash flows of the hedged items and whether they are expected to be highly effective in the future.
We use forward exchange contracts to hedge our net investment in foreign operations against movements in exchange rates. The effective portion of the unrealized gains or losses on these contracts is recorded in foreign currency translation adjustment within accumulated other comprehensive income and remains there until either the sale or liquidation of the subsidiary.
Stock-Based Compensation: We have a number of stock-based employee compensation plans. Pursuant to the FASB’s guidance, we expense the grant-date fair value of stock options and other equity-based compensation pursuant to the straight-line method over the stated vesting period of the award using the Black-Scholes option-pricing model. The expense associated with share-based compensation arrangements is a non-cash charge. In the consolidated statements of cash flows, share-based compensation expense is an adjustment to reconcile net income to cash provided by operating activities.
Earnings per Share: Basic earnings per share are based on the weighted average number of common shares outstanding during the year. Diluted earnings per share are based on the weighted average number of common shares outstanding during the year adjusted to give effect to common stock equivalents.
The following table sets forth the computation of basic and diluted earnings per share, for the periods indicated (in thousands, except per share data):
| | | | | | | | | | | | |
| | Twelve Months Ended December 31, | |
| | 2024 | | | 2023 | | | 2022 | |
Basic and diluted: | | | | | | | | | |
Net Income | | $ | 1,163,109 | | | $ | 719,307 | | | $ | 656,982 | |
Less: Net (income) loss attributable to noncontrolling
interest ("NCI") | | | (21,012 | ) | | | (1,512 | ) | | | 18,627 | |
Less: Net income attributable to unvested restricted share
grants | | | (50 | ) | | | (308 | ) | | | (748 | ) |
Net income attributable to UHS—basic and diluted | | $ | 1,142,047 | | | $ | 717,487 | | | $ | 674,861 | |
Basic earnings per share attributable to UHS: | | | | | | | | | |
Weighted average number of common shares—basic | | | 66,554 | | | | 69,321 | | | | 73,118 | |
Total basic earnings per share | | $ | 17.16 | | | $ | 10.35 | | | $ | 9.23 | |
Diluted earnings per share attributable to UHS: | | | | | | | | | |
Weighted average number of common shares | | | 66,554 | | | | 69,321 | | | | 73,118 | |
Net effect of dilutive stock options and grants based
on the treasury stock method | | | 1,342 | | | | 804 | | | | 714 | |
Weighted average number of common shares and
equivalents—diluted | | | 67,896 | | | | 70,125 | | | | 73,832 | |
Total diluted earnings per share | | $ | 16.82 | | | $ | 10.23 | | | $ | 9.14 | |
The “Net effect of dilutive stock options and grants based on the treasury stock method”, for all years presented above, excludes certain outstanding stock options applicable to each year since the effect would have been anti-dilutive. The excluded weighted-average stock options totaled approximately 600,000 during 2024, 5.1 million during 2023 and 6.0 million during 2022.
Fair Value of Financial Instruments: The fair values of our debt and investments are based on quoted market prices. The fair values of other long-term debt, including capital lease obligations, are estimated by discounting cash flows using period-end interest rates and market conditions for instruments with similar maturities and credit quality. The carrying amounts reported in the balance sheets for cash, accounts receivable, accounts payable, and short-term borrowings approximates their fair values due to the short-term nature of these instruments. Accordingly, these items have been excluded from the fair value disclosures included elsewhere in these notes to consolidated financial statements.
Use of Estimates: The preparation of financial statements in conformity with U.S. generally accepted accounting principles requires us to make estimates and assumptions that affect the reported amounts of assets and liabilities and disclosure of contingent assets and liabilities at the date of the financial statements and the reported amounts of revenues and expenses during the reporting period. Actual results could differ from those estimates.
Mergers and Acquisitions: The acquisition method of accounting for business combinations requires that the assets acquired and liabilities assumed be recorded at the date of acquisition at their respective fair values with limited exceptions. Fair value is defined as the exchange price that would be received for an asset or paid to transfer a liability (an exit price) in the principal or most advantageous market for the asset or liability in an orderly transaction between market participants on the measurement date. Any
excess of the purchase price (consideration transferred) over the estimated fair values of net assets acquired is recorded as goodwill. Transaction costs and costs to restructure the acquired company are expensed as incurred. The fair value of intangible assets, including Medicare licenses, certificates of need, tradenames and certain contracts, is based on significant judgments made by our management, and accordingly, for significant items we typically obtain assistance from third party valuation specialists.
GPO Agreement/Minority Ownership Interest: During 2013, we entered into a new group purchasing organization agreement (“GPO”) with Premier, Inc. (“Premier"), a healthcare performance improvement alliance, and acquired a minority interest in the GPO for a nominal amount. During the fourth quarter of 2013, in connection with the completion of an initial public offering of the stock of Premier, we received cash proceeds for the sale of a portion of our ownership interest in the GPO, which were recorded as deferred income, on a pro rata basis, as a reduction to our supplies expense over the initial expected life of the GPO agreement. Also in connection with this GPO agreement, we received shares of restricted stock in Premier which vest ratably over a seven-year period (2014 through 2020), contingent upon our continued participation and minority ownership interest in the GPO. We recognized the fair value of this restricted stock, as a reduction to our supplies expense, in our consolidated statements of income, on a pro rata basis, over the vesting period. During the third quarter of 2020, we entered into an agreement with Premier pursuant to the terms of which, among other things, our ownership interest in Premier was converted into shares of Class A Common Stock of Premier. We have elected to retain a portion of the previously vested shares of Premier, the value of which is included in other assets on our consolidated balance sheets. Based upon the closing price of Premier’s stock on each respective date, the market value of our shares of Premier was $47 million and $50 million as of December 31, 2024 and 2023, respectively. The change in market value of these shares is recorded as an unrealized gain/loss and included in “Other (income) expense, net” on our consolidated statements of income. Additionally, Premier paid cash dividends of $1.9 million during both 2024 and 2023 and $1.8 million during 2022, which are included in “Other (income) expense, net” in our consolidated statements of income.
Provider Taxes: We incur health-care related taxes (“Provider Taxes”) imposed by states in the form of a licensing fee, assessment or other mandatory payment which are related to: (i) healthcare items or services; (ii) the provision of, or the authority to provide, the health care items or services, or; (iii) the payment for the health care items or services. Such Provider Taxes are subject to various federal regulations that limit the scope and amount of the taxes that can be levied by states in order to secure federal matching funds as part of their respective state Medicaid programs. We derive a related Medicaid reimbursement benefit from assessed Provider Taxes in the form of Medicaid claims based payment increases and/or lump sum Medicaid supplemental payments.
Under these programs, including the impact of the Texas Uncompensated Care and Upper Payment Limit program, the Texas Delivery System Reform Incentive program, and various other state programs, we earned revenues (before Provider Taxes) of approximately $1.499 billion during 2024, $853 million during 2023 and $784 million during 2022. These revenues were offset by Provider Taxes of approximately $536 million during 2024, $297 million during 2023 and $287 million during 2022, which are recorded in other operating expenses on the consolidated statements of income as included herein. The aggregate net benefit from these programs was $963 million during 2024, $556 million during 2023 and $497 million during 2022. The aggregate net benefit pursuant to these programs is earned from multiple states and therefore no particular state’s portion is individually material to our consolidated financial statements. In addition, under various disproportionate share hospital payment programs and state plan amendment programs, we earned revenues of $53 million in 2024, $73 million in 2023 and $75 million in 2022.
Recent Accounting Standards: During 2024, we adopted ASU 2023-07, “Improvements to Reportable Segment Disclosures (Topic 280)”. ASU 2023-07 modifies reportable segment disclosure requirements, primarily through enhanced disclosures about segment expenses categorized as significant or regularly provided to the Chief Operating Decision Maker (CODM). The standard was applied retrospectively to all periods presented in the financial statements. See Note 12 - Segment Reporting for the required disclosures.
In November 2024, the FASB issued ASU 2024-03, “Income Statement-Reporting Comprehensive Income-Expense Disaggregation Disclosures (subtopic 220-40)". ASU 2024-03 requires disclosures, in the notes to financial statements, of specified information about certain costs and expenses. This ASU is effective for fiscal years beginning after December 15, 2026, and interim periods within fiscal years beginning after December 15, 2027. We are currently evaluating the impact this new standard will have on the related disclosures in the consolidated financial statements.
In December 2023, the FASB issued ASU 2023-09, “Improvements to Income Tax Disclosures (Topic 740)”. ASU 2023-09 requires enhanced disclosures on income taxes paid, adds disaggregation of continuing operations before income taxes between foreign and domestic earnings and defines specific categories for the reconciliation of jurisdictional tax rate to effective tax rate. This ASU is effective for fiscal years beginning after December 15, 2024, and can be applied on a prospective basis. We are currently evaluating the impact this new standard will have on the related disclosures in the consolidated financial statements.
From time to time, new accounting guidance is issued by the FASB or other standard setting bodies that is adopted by us as of the effective date or, in some cases where early adoption is permitted, in advance of the effective date. We have assessed the recently
issued guidance that are not yet effective and, unless otherwise indicated above, we believe the new guidance will not have a material impact on our results of operations, cash flows or financial position.
Foreign Currency Translation: Assets and liabilities of our U.K. subsidiaries are denominated in pound sterling and translated into U.S. dollars at: (i) the rates of exchange at the balance sheet date, and; (ii) average rates of exchange prevailing during the year for revenues and expenses. The currency translation adjustments are reported as a component of accumulated other comprehensive income. See Note 3 - Financial Instruments and Fair Value Measurement for additional disclosure.
2) ACQUISITIONS AND DIVESTITURES
Years ended December 31, 2024:
2024 Acquisitions of Assets and Businesses:
During 2024, we spent $19 million on the acquisition of businesses and properties.
2024 Divestiture of Assets and Businesses:
During 2024, we received $39 million from the sale of assets and businesses.
Year ended December 31, 2023:
2023 Acquisitions of Assets and Businesses:
During 2023, we spent $4 million on the acquisition of businesses and properties.
2023 Divestiture of Assets and Businesses:
During 2023, we received $24 million from the sale of assets and businesses.
Year ended December 31, 2022:
2022 Acquisitions of Assets and Businesses:
During 2022, we spent $20 million to acquire various businesses and properties.
2022 Divestiture of Assets:
During 2022, we received $12 million from the sales of various assets
3) FINANCIAL INSTRUMENTS AND FAIR VALUE MEASUREMENT
Cash Flow Hedges:
When applicable, we measure our interest rate swaps at fair value on a recurring basis. The fair value of our interest rate swaps is based on quotes from our counterparties. We consider those inputs to be “level 2” in the fair value hierarchy as outlined in the authoritative guidance for disclosures in connection with derivative instruments and hedging activities. During the years ended December 31, 2024, 2023 and 2022, we had no cash flow hedges outstanding.
Foreign Currency Forward Exchange Contracts:
We use forward exchange contracts to hedge our net investment in foreign operations against movements in exchange rates. The effective portion of the unrealized gains or losses on these contracts is recorded in foreign currency translation adjustment within accumulated other comprehensive income and remains there until either the sale or liquidation of the subsidiary. In connection with these forward exchange contracts, we recorded net cash inflows of approximately $13 million during 2024, net cash outflows of approximately $41 million during 2023 and net cash inflows of approximately $95 million during 2022.
Derivatives Hedging Relationships:
The following table presents the effects of our foreign currency foreign exchange contracts on our results of operations for the three years ended December 31 (in thousands):
| | | | | | | | | | | | |
| | | | | | | | | |
| Gain/(Loss) recognized in AOCI | | |
| | | |
| December 31, | | | December 31, | | | December 31, | | |
| 2024 | | | 2023 | | | 2022 | | |
| | | | | | | | | |
Net Investment Hedge relationships | | | | | | | | | |
Foreign currency foreign exchange contracts | $ | 15,344 | | | $ | (45,748 | ) | | $ | 96,698 | | |
No other gains or losses were recognized in income related to derivatives in Subtopic 815-20.
Fair Value Measurement
Fair value is defined as the price that would be received to sell an asset or paid to transfer a liability (an exit price) in the principal or most advantageous market for the asset or liability in an orderly transaction between market participants on the measurement date. The following fair value hierarchy classifies the inputs to valuation techniques used to measure fair value into one of three levels:
•Level 1: Unadjusted quoted prices in active markets for identical assets or liabilities.
•Level 2: Inputs other than quoted prices that are observable for the asset or liability, either directly or indirectly. These included quoted prices for similar assets or liabilities in active markets and quoted prices for identical or similar assets or liabilities in markets that are not active.
•Level 3: Unobservable inputs that reflect the reporting entity’s own assumptions.
The following tables present the assets and liabilities recorded at fair value on a recurring basis:
| | | | | | | | | | | | | |
| Balance at | | Balance Sheet | Basis of Fair Value Measurement | |
(in thousands) | December 31, 2024 | | Location | Level 1 | | Level 2 | | Level 3 | |
Assets: | | | | | | | | | |
Money market mutual funds | $ | 115,399 | | Other noncurrent assets | $ | 115,399 | | | | | |
Certificates of deposit | | 2,206 | | Other noncurrent assets | | | | 2,206 | | | |
Equity securities | | 47,333 | | Other noncurrent assets | | 47,333 | | | | | |
Deferred compensation assets | | 49,222 | | Other noncurrent assets | | 49,222 | | | | | |
Foreign currency forward exchange contracts | | 572 | | Other current assets | | | | 572 | | | |
| $ | 214,732 | | | $ | 211,954 | | $ | 2,778 | | | - | |
Liabilities: | | | | | | | | | |
Deferred compensation liability | | 49,222 | | Other noncurrent liabilities | | 49,222 | | | | | |
| $ | 49,222 | | | $ | 49,222 | | $ | - | | | - | |
| | | | | | | | | |
| Balance at | | Balance Sheet | Basis of Fair Value Measurement | |
(in thousands) | December 31, 2023 | | Location | Level 1 | | Level 2 | | Level 3 | |
Assets: | | | | | | | | | |
Money market mutual funds | $ | 111,129 | | Other noncurrent assets | $ | 111,129 | | | | | |
Certificates of deposit | | 2,300 | | Other noncurrent assets | | | | 2,300 | | | |
Equity securities | | 49,923 | | Other noncurrent assets | | 49,923 | | | | | |
Deferred compensation assets | | 43,060 | | Other noncurrent assets | | 43,060 | | | | | |
| $ | 206,412 | | | $ | 204,112 | | $ | 2,300 | | | - | |
Liabilities: | | | | | | | | | |
Foreign currency forward exchange contracts | $ | 1,911 | | Accrued liabilities other | | | $ | 1,911 | | | |
Deferred compensation liability | | 43,060 | | Other noncurrent liabilities | | 43,060 | | | | | |
| $ | 44,971 | | | $ | 43,060 | | $ | 1,911 | | | - | |
The fair value of our money market mutual funds, certificates of deposit and equity securities with a readily determinable fair value are computed based upon quoted market prices in an active market. The fair value of deferred compensation assets and the
offsetting liability are computed based on market prices in an active market held in a rabbi trust. The fair value of our foreign currency exchange contracts is valued using quoted forward exchange rates and spot rates at the reporting date.
4) LONG-TERM DEBT
A summary of long-term debt follows:
| | | | | | | | |
| | December 31, | |
| | 2024 | | | 2023 | |
| | (amounts in thousands) | |
Long-term debt: | | | | | | |
Notes and Mortgages payable (including obligations under finance leases of $92,530 in 2024 and $72,693 in 2023) and term loans with varying maturities through 2099; weighted average interest rates of 3.8% in 2024 and 3.5% in 2023 (see Note 7 regarding finance leases) | | $ | 206,046 | | | $ | 178,511 | |
Tranche A term loan | | | 1,192,500 | | | | 2,258,750 | |
Revolving credit facility | | | 130,000 | | | | 495,500 | |
2.65% Senior Secured Notes due 2030, net of unamortized discount of $1,291 in 2024 and $1,517 in 2023 | | | 798,709 | | | | 798,483 | |
1.65% Senior Secured Notes due 2026, net of unamortized discount of $288 in 2024 and $463 in 2023 | | | 699,712 | | | | 699,537 | |
2.65% Senior Secured Notes due 2032, net of unamortized discount of $864 in 2024 and $994 in 2023 | | | 499,136 | | | | 499,006 | |
4.625% Senior Secured Notes due 2029, net of unamortized discount of $204 in 2024 | | | 499,796 | | | | — | |
5.050% Senior Secured Notes due 2034, net of unamortized discount of $1,533 in 2024 | | | 498,467 | | | | — | |
Total debt before unamortized financing costs | | | 4,524,366 | | | | 4,929,787 | |
Less-Unamortized financing costs | | | (19,825 | ) | | | (17,318 | ) |
Total debt after unamortized financing costs | | | 4,504,541 | | | | 4,912,469 | |
Less-Amounts due within one year | | | (40,059 | ) | | | (126,686 | ) |
Long-term debt | | $ | 4,464,482 | | | $ | 4,785,783 | |
Credit Facilities and Outstanding Debt Securities
In September, 2024, we completed the following financing transactions:
•The public offering of $500 million of aggregate principal amount of 4.625% senior secured notes due on October 15, 2029 ("2029 Notes");
•The public offering of $500 million of aggregate principal amount of 5.050% senior secured notes due on October 15, 2034 ("2034 Notes");
•Amended our credit agreement to:
oExtend the maturity date to September, 2029 (from August, 2026 previously);
oIncrease the revolving credit facility to $1.3 billion (from $1.2 billion previously), and;
oreduce the outstanding borrowings pursuant to the tranche term loan A facility by approximately $1.0 billion, to $1.2 billion, utilizing the proceeds generated from the issuance of the above-mentioned 2029 Notes and 2034 Notes.
On September 26, 2024, we entered into a tenth amendment ("Tenth Amendment") to our credit agreement ("Credit Agreement"), dated as of November 15, 2010, as amended and restated at various times from March, 2011 to June, 2022, among UHS, as borrower, the several banks and other financial institutions or entities from time to time parties thereto, as lenders, and JPMorgan Chase Bank, N.A., as administrative agent. The Tenth Amendment provided for: (i) an extension of the maturity date to September 26, 2029; (ii) a new revolving credit facility of up to $1.3 billion (which as of December 31, 2024, had $1.17 billion of aggregate available borrowing capacity, net of $130 million of outstanding borrowings and $3 million of letters of credit), and; (iii) a new replacement tranche A term loan facility ("Tranche A Term Loan") of up to $1.2 billion (which had $1.19 billion of outstanding borrowings as of December 31, 2024).
Pursuant to the terms of the Tenth Amendment, the Tranche A Term Loan provides for installment payments of $7.5 million per quarter commencing on December 31, 2024 through September 30, 2026, and $15.0 million per quarter commencing on December 31, 2026 through June 30, 2029. The unpaid principal balance at June 30, 2029 (scheduled to be $975.0 million) is payable on the September 26, 2029 scheduled maturity date of the Credit Agreement.
Revolving credit and Tranche A Term Loan borrowings under the Credit Agreement bear interest at our election at either (1) the ABR rate which is defined as the rate per annum equal to the greatest of (a) the lender’s prime rate, (b) the greater of the federal funds effective rate and the overnight bank funding rate, plus 0.5% and (c) one month term SOFR rate plus 1.1%, in each case, plus an applicable margin based upon our consolidated leverage ratio at the end of each quarter ranging from 0.25% to 0.625%, or (2) the one, three or six month term SOFR rate plus 0.1% (at our election), plus an applicable margin based upon our consolidated leverage ratio at the end of each quarter ranging from 1.25% to 1.625%. As of December 31, 2024, the applicable margins were 0.375% for ABR-based loans and 1.375% for SOFR-based loans under the revolving credit and term loan A facilities. The revolving credit facility includes a $125 million sub-limit for letters of credit. The Credit Agreement is secured by certain assets of the Company and our material subsidiaries (which generally excludes asset classes such as substantially all of the patient-related accounts receivable of our acute care hospitals, if sold to a receivables facility pursuant to the Credit Agreement, and certain real estate assets and assets held in joint-ventures with third parties) and is guaranteed by our material subsidiaries.
The Credit Agreement includes a material adverse change clause that must be represented at each draw. The Credit Agreement also contains covenants that include a limitation on sales of assets, mergers, change of ownership, liens, indebtedness, transactions with affiliates, dividends and stock repurchases; and requires compliance with financial covenants including maximum leverage. We were in compliance with all required covenants as of December 31, 2024 (pursuant to the terms of the Credit Agreement, as amended on September 26, 2024) and as of December 31, 2023 (pursuant to the terms of the previous credit agreement).
As mentioned above, on September 26, 2024, we completed the public offering of: (i) $500,000,000 aggregate principal amount of the 4.625%, 2029 Notes, and; (ii) $500,000,000 aggregate principal amount of the 5.050%, 2034 Notes (and together with the 2029 Notes, the "2029 and 2034 Notes"), each guaranteed on a senior secured basis by all of our existing and future direct and indirect subsidiaries that guarantee our senior secured credit facility or our other first lien obligations or any junior lien obligations (the “Subsidiary Guarantors”). The 2029 and 2034 Notes have been registered under the Securities Act of 1933, as amended (the “Securities Act”), pursuant to the Issuer’s and the Subsidiary Guarantors’ registration statement on Form S-3 (File No. 333-282135), including the prospectus dated September 16, 2024, and a related prospectus supplement dated September 17, 2024, as filed with the Securities and Exchange Commission on September 19, 2024.
As of December 31, 2024, including the above-mentioned newly issued Notes, we had combined aggregate principal of $3.0 billion from the following senior secured notes:
•$700 million aggregate principal amount of 1.65% senior secured notes due in September, 2026 ("2026 Notes") which were issued on August 24, 2021. Interest on the 2026 Notes is payable on March 1st and September 1st until the maturity date of September 1, 2026.
•$500 million of aggregate principal amount of 4.625% senior secured notes due in October, 2029 ("2029 Notes") which were issued on September 26, 2024. Interest on the 2029 Notes is payable on April 15th and October 15th, commencing April 15, 2025 until the maturity date of October 15, 2029.
•$800 million aggregate principal amount of 2.65% senior secured notes due in October, 2030 ("2030 Notes") which were issued on September 21, 2020. Interest on the 2030 Notes is payable on April 15th and October 15th, until the maturity date of October 15, 2030.
•$500 million of aggregate principal amount of 2.65% senior secured notes due in January, 2032 ("2032 Notes") which were issued on August 24, 2021. Interest on the 2032 Notes is payable on January 15th and July 15th until the maturity date of January 15, 2032.
•$500 million of aggregate principal amount of 5.050% senior secured notes due in October, 2034 ("2034 Notes") which were issued on September 26, 2024. Interest on the 2034 Notes is payable on April 15th and October 15th, commencing on April 15, 2025 until the maturity date of October 15, 2034.
The 2026 Notes, 2030 Notes and 2032 Notes (collectively the "2026, 2030 and 2032 Notes") were initially issued only to qualified institutional buyers under Rule 144A and to non-U.S. persons outside the United States in reliance on Regulation S under the Securities Act. In December, 2022, we completed a registered exchange offer in which virtually all previously outstanding 2026, 2030 and 2032 Notes were exchanged for identical 2026, 2030 and 2032 Notes that were registered under the Securities Act, and thereby became freely transferable (subject to certain restrictions applicable to affiliates and broker dealers). 2026, 2030 and 2032 Notes originally issued under Rule 144A or Regulation S that were not exchanged remain outstanding and may not be offered or sold in the United States absent registration under the Securities Act or an applicable exemption from registration requirements thereunder.
The 2026, 2030 and 2032 Notes, and the 2029 and 2034 Notes (collectively "All the Notes") are guaranteed (the “Guarantees”) on a senior secured basis by our Subsidiary Guarantors that guarantee our Credit Agreement, or other first lien obligations or any junior lien obligations. All the Notes and the Guarantees are secured by first-priority liens, subject to permitted liens, on certain of the Company’s and the Subsidiary Guarantors’ assets now owned or acquired in the future by the Company or the Subsidiary Guarantors (other than real property, accounts receivable sold pursuant to a Company-related receivables facility (as defined in the Indenture pursuant to which All the Notes were issued (the “Indentures”), and certain other excluded assets). The Company’s obligations with
respect to All the Notes, the obligations of the Subsidiary Guarantors under the Guarantees, and the performance of all of the Company’s and the Subsidiary Guarantors’ other obligations under the Indentures, are secured equally and ratably with the Company’s and the Subsidiary Guarantors’ obligations under the Credit Agreement. However, the liens on the collateral securing All the Notes and the Guarantees will be released if: (i) All the Notes have investment grade ratings; (ii) no default has occurred and is continuing, and; (iii) the liens on the collateral securing all first lien obligations (including the Credit Agreement and All the Notes) and any junior lien obligations are released or the collateral under the Credit Agreement, any other first lien obligations and any junior lien obligations is released or no longer required to be pledged. The liens on any collateral securing All the Notes and the Guarantees will also be released if the liens on that collateral securing the Credit Agreement, other first lien obligations and any junior lien obligations are released.
As discussed in Note 9 to the Consolidated Financial Statements-Relationship with Universal Health Realty Income Trust and Other Related Party Transactions, on December 31, 2021, we (through wholly-owned subsidiaries of ours) entered into an asset purchase and sale agreement with Universal Health Realty Income Trust (the “Trust”). Pursuant to the terms of the agreement, as amended, we, among other things, transferred to the Trust, the real estate assets of Aiken Regional Medical Center (“Aiken”) and Canyon Creek Behavioral Health (“Canyon Creek”). In connection with this transaction, Aiken and Canyon Creek (as lessees), entered into a master lease and individual property leases, as amended, (with the Trust as lessor), for initial lease terms on each property of approximately twelve years, ending on December 31, 2033. As a result of our purchase option within the Aiken and Canyon Creek lease agreements, this asset purchase and sale transaction is accounted for as a failed sale leaseback in accordance with U.S. GAAP and we have accounted for the transaction as a financing arrangement. Our lease payments payable to the Trust are recorded to interest expense and as a reduction of the outstanding financial liability, and the amount allocated to interest expense is determined based upon our incremental borrowing rate and the outstanding financial liability. In connection with this transaction, our consolidated balance sheets at December 31, 2024 and December 31, 2023 reflect financial liabilities, which are included in debt, of approximately $74 million and $77 million, respectively.
At December 31, 2024, the carrying value and fair value of our debt were approximately $4.5 billion and $4.2 billion, respectively. At December 31, 2023, the carrying value and fair value of our debt were approximately $4.9 billion and $4.6 billion, respectively. The fair value of our debt was computed based upon quotes received from financial institutions. We consider these to be “level 2” in the fair value hierarchy as outlined in the authoritative guidance for disclosures in connection with debt instruments.
The aggregate scheduled maturities of our total debt outstanding as of December 31, 2024 are as follows:
| | | | |
| | (000s) | |
2025 | | $ | 40,059 | |
2026 | | | 740,402 | |
2027 | | | 71,501 | |
2028 | | | 72,402 | |
2029 | | | 1,655,608 | |
Later | | | 1,944,394 | |
Total maturities before unamortized financing costs | | | 4,524,366 | |
Less-Unamortized financing costs | | | (19,825 | ) |
Total | | $ | 4,504,541 | |
5) COMMON STOCK
Dividends
We declared and paid cash dividends of $.80 per share during each of the last three years amounting to, in the aggregate, $53.3 million during 2024, $55.5 million during 2023 and $58.4 million during 2022. All classes of our common stock have similar economic rights.
Stock Repurchase Programs
As of January 1, 2024, we had an aggregate available repurchase authorization of $422.88 million under our stock repurchase program. In July, 2024, our Board of Directors authorized a $1.0 billion increase in our stock repurchase program. As of December 31, 2024, we had an aggregate available repurchase authorization of $824.36 million. Pursuant to this program, shares of our Class B Common Stock may be repurchased, from time to time as conditions allow, on the open market or in negotiated private transactions. There is no expiration date for our stock repurchase programs.
The following schedule provides information related to our stock repurchase program for each of the three years ended December 31, 2024. During 2024, 2,982,906 shares ($598.5 million in the aggregate) were repurchased pursuant to the terms of the stock repurchase program and 375,248 shares ($72.2 million in the aggregate) were repurchased in connection with the income tax withholding obligations resulting from stock-based compensation programs. During 2023, 3,855,046 shares ($524.5 million in the aggregate) were repurchased pursuant to the terms of the stock repurchase program and 164,649 shares ($22.9 million in the aggregate) were repurchased in connection with the income tax withholding obligations resulting from stock-based compensation
programs. During 2022, 6,666,547 shares ($810.9 million in the aggregate) were repurchased pursuant to the terms of the stock repurchase program and 153,305 shares ($22.0 million in the aggregate) were repurchased in connection with the income tax withholding obligations resulting from stock-based compensation programs.
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | |
| | Additional
dollars
authorized
for
repurchase
(in
thousands) | | | Total
number of
shares
purchased (a.) | | | Total
number
of shares
cancelled | | | Average
price
paid per
share for
forfeited
restricted
shares | | | Total
number of
shares
purchased
as part of
publicly
announced
programs | | | Average
price paid
per share
for shares
purchased
as part of
publicly
announced
program | | | Aggregate
purchase
price paid
(in
thousands) | | | Aggregate
purchase
price paid
for shares
purchased
as part of
publicly
announced
program | | | Maximum
number of
dollars
that may
yet be
purchased
under the
program
(in
thousands) | |
Balance as of
January 1, 2022 | | | | | | | | | | | | | | | | | | | | | | | | | | $ | 358,233 | |
2022 | | $ | 1,400,000 | | | | 6,828,319 | | | | 8,467 | | | $ | 0.01 | | | | 6,666,547 | | | $ | 121.63 | | | $ | 832,915 | | | $ | 810,865 | | | $ | 947,368 | |
2023 | | $ | — | | | | 4,022,051 | | | | 2,356 | | | $ | 0.01 | | | | 3,855,046 | | | $ | 136.05 | | | $ | 547,362 | | | $ | 524,485 | | | $ | 422,883 | |
2024 | | $ | 1,000,000 | | | | 3,358,261 | | | | 107 | | | $ | 0.01 | | | | 2,982,906 | | | $ | 200.65 | | | $ | 670,753 | | | $ | 598,522 | | | $ | 824,361 | |
Total for three year
period ended
December 31, 2024 | | $ | 2,400,000 | | | | 14,208,631 | | | | 10,930 | | | $ | 0.01 | | | | 13,504,499 | | | $ | 143.20 | | | $ | 2,051,030 | | | $ | 1,933,872 | | | | |
(a.)Includes 107, 2,356, and 8,467 of restricted shares that were forfeited by former employees pursuant to the terms of our restricted stock purchase plan during 2024, 2023 and 2022, respectively.
Stock-based Compensation Plans
At December 31, 2024, we have a number of stock-based employee compensation plans. Pursuant to the FASB’s guidance, we expense the grant-date fair value of stock options (computed utilizing the Black-Scholes option-pricing model) and other equity-based compensation pursuant to the straight-line method over the stated vesting period of the awards.
Pre-tax share-based compensation costs of $54.3 million during 2024, $64.2 million during 2023 and $66.2 million during 2022 were recognized related to outstanding stock options. In addition, pre-tax compensation costs of $45.1 million during 2024, $23.5 million during 2023 and $19.1 million during 2022 were recognized related to amortization of restricted stock and units as well as discounts provided in connection with shares purchased pursuant to our 2005 Employee Stock Purchase Plan. As of December 31, 2024, there was approximately $149.4 million of unrecognized compensation cost related to unvested stock options and restricted stock which is expected to be recognized over the remaining average vesting period of 2.3 years.
The expense associated with stock-based compensation arrangements is a non-cash charge. In the consolidated statements of cash flows, stock-based compensation expense is an adjustment to reconcile net income to cash provided by operating activities and aggregated to $99.3 million in 2024, $87.7 million in 2023 and $85.4 million in 2022. In connection with our January 1, 2017 adoption of ASU 2016-09, “Compensation-Stock Compensation (Topic 718): Improvements to Employee Share-Based Payment Accounting”, our provision for income taxes and our net income attributable to UHS were favorably impacted by $15.9 million during 2024 (net of a $10.2 million unfavorable impact resulting from executive compensation limitations pursuant to IRC section 162(m)), unfavorably impacted by $4.7 million during 2023, and unfavorably impacted by $636,000 during 2022.
In 2005, we adopted the 2005 Stock Incentive Plan (the “Stock Incentive Plan”) which was amended in 2008, 2010, 2015 and 2017 and was canceled in 2020, as discussed below. An aggregate of 35.6 million shares of Class B Common Stock had been reserved under the Stock Incentive Plan, the remaining balance of which was canceled in 2020. During 2020, stock options, net of cancellations of approximately 2.2 million were granted under the Stock Incentive Plan. Stock options to purchase Class B Common Stock have been granted to our officers, key employees and members of our Board of Directors. Commencing in 2018, our key employees and non-executive officers began receiving a portion of their stock-based compensation in the form of restricted stock or restricted stock units (as discussed below) in addition to receiving options to purchase Class B Common Stock. Commencing in 2024 our key employees and non-executive officers began receiving their stock-based compensation in the form of restricted stock units only.
In 2020, we adopted the 2020 Omnibus Stock and Incentive Plan (the “2020 Stock Incentive Plan”) which was amended in 2022 and 2024. An aggregate of 18.1 million shares of Class B Common Stock has been reserved for issuance under the 2020 Stock Incentive Plan. As of December 31, 2024, approximately 8.62 million shares of Class B Common Stock remain available for issuance pursuant to the 2020 Stock Incentive Plan. Under the 2020 Stock Incentive Plan, shares that are subject to stock options shall be counted as one share per stock option, and every share that is subject to restricted stock awards or restricted stock units shall be counted as four shares. Various other types of equity awards are also permitted under the 2020 Stock Incentive Plan.
During each of the last three years, the following were granted pursuant to the 2020 Stock Incentive Plan (net of cancellations):
•2024: 3,000 stock options and 514,765 restricted stock units (including 63,362 performance based restricted stock units).
•2023: 1.6 million stock options and 255,085 restricted stock units (including 93,606 performance based restricted stock units).
•2022: 1.5 million stock options and 207,253 restricted stock units (including 65,768 performance based restricted stock units, net of cancellations).
Prior to 2024, our annual stock-based compensation awards were generally issued as a blend restricted stock units and stock options. Commencing in 2024, our annual stock-based compensation awards were issued fully in restricted stock units and are expected to remain so in future years. Restricted stock and restricted stock units issued under the 2020 Stock Incentive Plan do not have rights to receive dividends on unvested restricted awards, however, the accrual of dividend equivalents on unvested restricted awards may be permitted. Upon adoption of the 2020 Stock Incentive Plan, no additional awards were granted under the 2005 Stock Incentive Plan or the 2010 Employees’ Restricted Stock Purchase Plan (discussed below), and reserves for future issuance pursuant to each plan were canceled.
The weighted average grant-date fair values of the restricted stock units issued under the 2020 Stock Incentive Plan during each of the last three years, as reflected above, were $181.05 during 2024, $118.14 during 2023 and $142.70 during 2022. The fair value of each restricted stock unit was determined as the closing UHS market price on the date of grant. Restricted shares and/or units of Class B Common Stock have been granted to our officers, key employees and members of our Board of Directors.
The per option weighted-average grant-date fair values for options granted under the 2020 Stock Incentive Plan were $44.58 during 2024, $41.88 during 2023 and $45.63 during 2022. All stock options issued in 2024, 2023 and 2022 were granted with an exercise price equal to the fair market value on the date of the grant. The majority of options are exercisable ratably over a four-year period beginning one year after the date of the grant. All outstanding options expire five years after the date of the grant.
The fair value of each option grant was estimated on the date of grant using the Black-Scholes option-pricing model. The following weighted average assumptions were derived from averaging the number of options granted during the most recent five-year period. The weighted-average assumptions reflected below were based upon twenty-two option grants for the five-year period ending December 31, 2024, thirty option grants for the five-year period ending December 31, 2023 and twenty-nine option grants for the five-year period ending December 31, 2022.
| | | | | | | | | | | | |
Year Ended December 31, | | 2024 | | | 2023 | | | 2022 | |
Expected volatility | | | 39 | % | | | 36 | % | | | 33 | % |
Risk free Interest rate | | | 2 | % | | | 2 | % | | | 2 | % |
Expected life (years) | | | 3.5 | | | | 3.5 | | | | 3.6 | |
Forfeiture rate | | | 7 | % | | | 7 | % | | | 7 | % |
Dividend yield | | | 0.8 | % | | | 0.7 | % | | | 0.6 | % |
The risk-free rate is based on the U.S. Treasury zero coupon four year yield curve in effect at the time of grant. The expected life of the stock options granted was estimated using the historical behavior of employees. Expected volatility was based on historical volatility for a period equal to the stock option’s expected life. Expected dividend yield is based on our dividend yield at the time of grant. The forfeiture rate is based upon the actual historical forfeitures utilizing the 5-year term of the option.
The table below summarizes our stock option activity during the year ended December 31, 2024:
| | | | | | | | | |
Outstanding Options | | Number
of Shares | | | Weighted Average
Exercise
Price | | |
Balance, January 1, 2024 | | | 6,794,794 | | | $ | 121.13 | | |
Granted | | | 3,000 | | | $ | 154.71 | | |
Exercised | | | (2,628,331 | ) | | $ | 114.80 | | |
Cancelled | | | (260,215 | ) | | $ | 128.59 | | |
Balance, December 31, 2024 | | | 3,909,248 | | | $ | 124.91 | | |
Outstanding options vested and exercisable as of
December 31, 2024 | | | 1,603,412 | | | $ | 116.94 | | |
The following table provides information about unvested options for the year ended December 31, 2024:
| | | | | | | | |
| | Shares | | | Weighted
Average
Grant Date
Fair Value | |
Unvested options as of January 1, 2024 | | | 4,344,181 | | | $ | 39.22 | |
Granted | | | 3,000 | | | $ | 44.58 | |
Vested | | | (1,783,851 | ) | | $ | 34.43 | |
Cancelled | | | (257,494 | ) | | $ | 42.53 | |
Unvested options as of December 31, 2024 | | | 2,305,836 | | | $ | 42.56 | |
The following table provides information regarding all options outstanding at December 31, 2024:
| | | | | | | | |
| | Options
Outstanding | | | Options
Exercisable | |
Number of options outstanding | | | 3,909,248 | | | | 1,603,412 | |
Weighted average exercise price | | $ | 124.91 | | | $ | 116.94 | |
Aggregate intrinsic value as of December 31, 2024 | | $ | 213,073,701 | | | $ | 100,184,865 | |
Weighted average remaining contractual life (years) | | | 2.0 | | | | 1.2 | |
The total in-the-money value of all stock options exercised during the years ended December 31, 2024, 2023 and 2022 were $185.3 million, $57.1 million and $49.4 million, respectively.
The weighted average remaining contractual life for options outstanding and weighted average exercise price per share for exercisable options at December 31, 2022, 2023 and 2024 were as follows:
| | | | | | | | | | | | | | | | | | | | | | | | | | | | |
Year Ended: | | Options
Outstanding | | | Weighted
Average
Exercise Price
Per Share | | | Weighted
Average
Remaining
Contractual Life
(in Years) | | | Exercisable
Options | | | Weighted
Average
Exercise Price
Per Share | | | Expected to
Vest
Options | | | Weighted
Average
Exercise Price
Per Share | |
| | Shares | | | | | | | | | Shares | | | | | | Shares | | | | |
2022 | | | 7,875,667 | | | $ | 122.04 | | | | 2.5 | | | | 3,073,714 | | | $ | 116.89 | | | | 4,508,480 | | | $ | 121.89 | |
2023 | | | 6,794,794 | | | | 121.13 | | | | 2.6 | | | | 2,450,613 | | | | 114.96 | | | | 4,178,237 | | | | 124.86 | |
2024 | | | 3,909,248 | | | | 124.91 | | | | 2.0 | | | | 1,603,412 | | | | 116.94 | | | | 1,838,407 | | | | 130.20 | |
In addition to the 2020 Stock Incentive Plan, we have our 2005 Employee Stock Purchase Plan (the “Employee Stock Plan”), as amended during 2024, which allows eligible employees to purchase shares of Class B Common Stock at a 10% discount. There were 81,146, 100,507 and 127,538 shares issued pursuant to the Employee Stock Purchase Plan during 2024, 2023 and 2022, respectively. In connection with the Employee Stock Plan, we have reserved 3.0 million shares of Class B Common Stock for issuance and have issued approximately 1.9 million shares as of December 31, 2024. As of December 31, 2024, approximately 1.1 million shares of Class B Common Stock remain available for issuance pursuant to this plan.
At December 31, 2024, 24,386,891 shares of Class B Common Stock were reserved for issuance upon conversion of shares of Class A, C and D Common Stock outstanding, for issuance upon exercise of options to purchase Class B Common Stock and for issuance of stock under other incentive plans. Class A, C and D Common Stock are convertible on a share for share basis into Class B Common Stock.
6) INCOME TAXES
Components of income tax expense/(benefit) are as follows (amounts in thousands):
| | | | | | | | | | | | |
| | Year Ended December 31, | |
| | 2024 | | | 2023 | | | 2022 | |
Current | | | | | | | | | |
Federal | | $ | 311,545 | | | $ | 202,895 | | | $ | 178,666 | |
Foreign | | | 10,962 | | | | 6,505 | | | | 14,740 | |
State | | | 45,780 | | | | 29,677 | | | | 33,423 | |
| | | 368,287 | | | | 239,077 | | | | 226,829 | |
Deferred | | | | | | | | | |
Federal | | | (28,499 | ) | | | (19,716 | ) | | | (9,935 | ) |
Foreign | | | (1,318 | ) | | | 3,367 | | | | (1,509 | ) |
State | | | (3,643 | ) | | | (1,609 | ) | | | (6,107 | ) |
| | | (33,460 | ) | | | (17,958 | ) | | | (17,551 | ) |
Total | | $ | 334,827 | | | $ | 221,119 | | | $ | 209,278 | |
Our provision for income taxes for the years ended December 31, 2024, 2023 and 2022 included tax benefits of $13 million and tax expenses of $5 million and $1 million, respectively, related to employee share-based payments. Excess tax benefits (when the deductible amount related to the settlement of employee equity awards for tax purposes exceeds the cumulative compensation cost recognized for financial reporting purposes) and deficiencies, if applicable, are recorded as a component of our tax provision.
The foreign provision for income taxes is based on foreign pre-tax earnings of $80 million during each of 2024 and 2023 and $76 million in 2022. In the future, we anticipate repatriating only previously taxed foreign earnings subjected as well as any future earnings that would qualify for a full dividend received deduction for distributions post-December 31, 2017. As of December 31, 2024, the amount of previously taxed earnings and earnings that would qualify for a full dividend received deduction total $79 million. At this time, there are no material tax effects related to future cash repatriation of undistributed foreign earnings. As such, we have not recognized a deferred tax liability related to existing undistributed earnings.
A reconciliation between the federal statutory rate and the effective tax rate is as follows:
| | | | | | | | | | | | |
| | Year Ended December 31, | |
| | 2024 | | | 2023 | | | 2022 | |
Federal statutory rate | | | 21.0 | % | | | 21.0 | % | | | 21.0 | % |
State taxes, net of federal income tax benefit | | | 2.3 | % | | | 2.4 | % | | | 2.4 | % |
Tax effects of foreign operations | | | -0.5 | % | | | -0.7 | % | | | -0.3 | % |
Tax benefit from settlement of employee equity awards | | | -0.8 | % | | | 0.4 | % | | | 0.1 | % |
Other items | | | 0.7 | % | | | 0.4 | % | | | 0.5 | % |
Impact of income attributable to noncontrolling interests | | | -0.3 | % | | | 0.0 | % | | | 0.5 | % |
Effective tax rate | | | 22.4 | % | | | 23.5 | % | | | 24.2 | % |
Our effective tax rates were 22.4%, 23.5% and 24.2% for the years ended December 31, 2024, 2023 and 2022, respectively. The decrease in our effective tax rate for the year ended December 31, 2024, as compared to 2023, is due primarily to a $16 million decrease in the provision for income taxes during 2024, as compared to 2023, from the net tax benefit recorded pursuant to ASU 2016-09, net of the impact of executive compensation limitations pursuant to IRC section 162(m). The decrease in our effective tax rate for the year ended December 31, 2023, as compared to 2022, is due primarily to the increase in net income attributable to noncontrolling interests during 2023, as compared to 2022.
Included in “Other current assets” on our consolidated balance sheets are prepaid federal, state and foreign income taxes amounting to approximately $3 million and $37 million as of December 31, 2024 and 2023, respectively.
The components of deferred taxes are as follows (amounts in thousands):
| | | | | | | | | | | | | | | | | | | |
| | Year Ended December 31, | |
| | 2024 | | | | 2023 | |
| | Assets | | | | Liabilities | | | | Assets | | | | Liabilities | |
Self-insurance reserves | $ | | 131,945 | | | $ | | |
| $ | | 118,824 | | | $ | | |
Compensation accruals | | | 80,673 | | | | | |
| | | 81,747 | | | | | |
Doubtful accounts and other reserves | | | 136,067 | | | | | |
| | | 123,634 | | | | | |
Other currently non-deductible accrued liabilities | | | 19,492 | | | | | |
| | | 19,926 | | | | | |
Depreciable and amortizable assets | | | | | | | 278,412 | |
| | | | | | | 280,678 | |
Operating lease liabilities | | | 105,444 | | | | | | | | | 106,590 | | | | | |
Right of use assets-operating leases | | | | | | | 97,925 | | | | | | | | | 101,853 | |
State and foreign net operating loss carryforwards and other state and foreign deferred tax assets | | | 111,388 | | | | | |
| | | 96,117 | | | | | |
Net pension liabilities – OCI only | | | 121 | | | | | |
| | | 701 | | | | | |
Other liabilities | | | | | | | 7,654 | | | | | | | | | 6,715 | |
| $ | | 585,130 | | | $ | | 383,991 | |
| $ | | 547,539 | | | $ | | 389,246 | |
Valuation allowance | | | (82,690 | ) | | | | 0 | |
| | | (72,667 | ) | | | | 0 | |
Total deferred income taxes | $ | | 502,440 | | | $ | | 383,991 | |
| $ | | 474,872 | | | $ | | 389,246 | |
At December 31, 2024, state net operating loss carryforwards (losses originating in tax years beginning prior to January 1, 2024, expiring in years 2025 through 2043), and credit carryforwards available to offset future taxable income approximated $1.1 billion representing approximately $76 million in deferred state tax benefit (net of the federal benefit); and state related interest expense carryforwards approximated $129 million representing approximately $9 million in deferred state tax benefit (net of the federal benefit). At December 31, 2024, there were foreign net operating losses and interest expense carryforwards of approximately $101 million, most of which are carried forward indefinitely, representing approximately $25 million in deferred foreign tax benefit. At December 31, 2024, related to a prior year stock acquisition, there were federal net operating losses of approximately $6 million carried forward indefinitely for federal purposes representing approximately $1 million in deferred federal tax benefits.
A valuation allowance is required when it is more likely than not that some portion of the deferred tax assets will not be realized. Based on available evidence, it is more likely than not that certain of our state tax benefits will not be realized. Therefore, valuation allowances of approximately $78 million and $68 million have been reflected as of December 31, 2024 and 2023, respectively. During 2024, the valuation allowance on these state tax benefits increased by $10 million primarily due to additional net operating losses incurred. In addition, valuation allowances of approximately $4 million have been reflected as of December 31, 2024 and 2023, related to foreign net operating losses and credit carryforwards.
During 2024 and 2023, the estimated liabilities for uncertain tax positions (including accrued interest and penalties) were increased less than $1 million due to tax positions taken in the current and prior years. The balance at each of the years ended December 31, 2024 and 2023, if subsequently recognized, that would favorably affect the effective tax rate and the provision for income taxes is approximately $2 million as of each date.
We recognize accrued interest and penalties associated with uncertain tax positions as part of the tax provision. As of December 31, 2024 and 2023, we have accrued interest and penalties of less than $1 million as of each date. The U.S. federal statute of limitations remains open for the 2021 and subsequent years. Foreign and U.S. state and local jurisdictions have statutes of limitations generally ranging for 3 to 4 years. The statute of limitations on certain jurisdictions could expire within the next twelve months. It is reasonably possible that the amount of unrecognized tax benefits will change during the next 12 months, however, it is anticipated that any such change, if it were to occur, would not have a material impact on our results of operations.
The tabular reconciliation of unrecognized tax benefits for the years ended December 31, 2024, 2023 and 2022 is as follows (amounts in thousands):
| | | | | | | | | | | | |
| | As of December 31, | |
| | 2024 | | | 2023 | | | 2022 | |
Balance at January 1, | | $ | 2,850 | | | $ | 2,727 | | | $ | 2,544 | |
Additions based on tax positions related to the current year | | | 500 | | | | 500 | | | | 500 | |
Additions for tax positions of prior years | | | 189 | | | | 180 | | | | 159 | |
Reductions for tax positions of prior years | | | (677 | ) | | | (557 | ) | | | (461 | ) |
Settlements | | | 0 | | | | 0 | | | | (15 | ) |
Balance at December 31, | | $ | 2,862 | | | $ | 2,850 | | | $ | 2,727 | |
7) LEASE COMMITMENTS
We follow FASB ASU 2016-02 ("Topic 842") "Leases." Under Topic 842, lessees are required to recognize assets and liabilities on the balance sheets for most leases and provide enhanced disclosures. Leases will be classified as either finance or operating.
We have elected the policy exemption that allows lessees to choose to not separate lease and non-lease components by class of underlying asset and are applying this expedient to all relevant asset classes.
We determine if an arrangement is or contains a lease at inception of the contract. Our right-of-use assets represent our right to use the underlying assets for the lease term and our lease liabilities represent our obligation to make lease payments arising from the leases. Right-of-use assets and lease liabilities are recognized at commencement date based on the present value of lease payments over the lease term. We use the implicit rate noted within the contract if known or determinable. If the implicit rate is not readily available, we use our estimated incremental borrowing rate, which is derived using a collateralized borrowing rate for the same currency and term as the associated lease. A right-of-use asset and lease liability is not recognized for leases with an initial term of 12 months or less and we recognize lease expense for these leases on a straight-line basis over the lease term within lease and rental expense.
Our operating leases are primarily for real estate, including certain acute care facilities, off-campus outpatient facilities, medical office buildings, and corporate and other administrative offices. Our real estate lease agreements typically have initial terms of five to ten years. These real estate leases may include one or more options to renew, with renewals that can extend the lease term from five to ten years. The exercise of lease renewal options is at our sole discretion. When determining the lease term, we included options to extend or terminate the lease when it is reasonably certain that we will exercise that option.
Five of our hospital facilities are held under operating leases with Universal Health Realty Income Trust with two hospital terms expiring in 2026, two expiring in 2033, and one expiring in 2040 (see Note 9 for additional disclosure). We also lease the real property of certain facilities (see Item 2. Properties for additional disclosure).
The components of lease expense for the years ended December 31, 2024, 2023 and 2022 are as follows (in thousands):
| | | | | | | | | | | |
| Twelve months ended
December 31, | |
| 2024 | | | 2023 | | | 2022 | |
| | | | | | | | |
Operating lease cost | $ | 101,915 | | | $ | 99,812 | | | $ | 90,326 | |
Variable and short term lease cost (a) | | 44,518 | | | | 41,214 | | | | 41,300 | |
Total lease and rental expense | $ | 146,433 | | | $ | 141,026 | | | $ | 131,626 | |
| | | | | | | | |
Finance lease cost: | | | | | | | | |
Amortization of property under capital lease | $ | 5,923 | | | $ | 4,998 | | | $ | 5,110 | |
Interest on debt of property under capital lease | | 2,006 | | | | 3,771 | | | | 3,903 | |
Total finance lease cost | $ | 7,929 | | | $ | 8,769 | | | $ | 9,013 | |
(a)Includes equipment, month-to-month and leases with a maturity of less than 12 months.
Supplemental cash flow information related to leases for the years ended December 31, 2024, 2023 and 2022 are as follows (in thousands):
| | | | | | | | | | | |
| Twelve months ended
December 31, | |
| 2024 | | | 2023 | | | 2022 | |
| | | | | | | | |
Cash paid for amounts included in the measurement of lease liabilities: | | | | | | | | |
Operating cash flows from operating leases | $ | 134,543 | | | $ | 129,299 | | | $ | 124,704 | |
Operating cash flows from finance leases | $ | 3,652 | | | $ | 3,832 | | | $ | 3,963 | |
Financing cash flows from finance leases | $ | 3,973 | | | $ | 3,817 | | | $ | 3,454 | |
| | | | | | | | |
Right-of-use assets obtained in exchange for lease obligations: | | | | | | | | |
Operating leases | $ | 68,029 | | | $ | 62,223 | | | $ | 163,679 | |
Finance leases | $ | 23,700 | | | $ | 452 | | | $ | 1,066 | |
Supplemental balance sheets information related to leases as of December 31, 2024 and 2023 are as follows (in thousands):
| | | | | | | |
| December 31, | | | December 31, | |
| 2024 | | | 2023 | |
| | | | | |
Operating Leases | | | | | |
Right of use assets-operating leases | $ | 418,719 | | | $ | 433,962 | |
| | | | | |
Operating lease liabilities | $ | 74,649 | | | $ | 71,600 | |
Operating lease liabilities noncurrent | | 376,239 | | | | 382,559 | |
Total operating lease liabilities | $ | 450,888 | | | $ | 454,159 | |
| | | | | |
Finance Leases | | | | | |
Property and equipment | $ | 125,018 | | | $ | 101,318 | |
Accumulated depreciation | | (44,346 | ) | | | (38,423 | ) |
Property and equipment, net | $ | 80,672 | | | $ | 62,895 | |
| | | | | |
Current maturities of long-term debt | $ | 5,282 | | | $ | 3,050 | |
Long-term debt | | 87,248 | | | | 69,643 | |
Total finance lease liabilities | $ | 92,530 | | | $ | 72,693 | |
| | | | | |
Weighted Average remaining lease term, years | | | | | |
Operating leases | | 17.1 | | | | 16.5 | |
Finance leases | | 19.6 | | | | 20.0 | |
| | | | | |
Weighted Average discount rate | | | | | |
Operating leases | | 5.4 | % | | | 5.2 | % |
Finance leases | | 5.5 | % | | | 5.5 | % |
Future maturities of lease liabilities as of December 31, 2024 are as follows (in thousands):
| | | | | | | |
| Operating Leases | | | Finance Leases | |
Year ending December 31, | | | | | |
2025 | $ | 88,488 | | | $ | 10,069 | |
2026 | | 79,309 | | | | 10,074 | |
2027 | | 61,874 | | | | 10,231 | |
2028 | | 50,009 | | | | 10,391 | |
2029 | | 40,748 | | | | 10,556 | |
Later years | | 598,452 | | | | 95,795 | |
Total lease payments | | 918,880 | | | | 147,116 | |
less imputed interest | | (467,992 | ) | | | (54,586 | ) |
Total | $ | 450,888 | | | $ | 92,530 | |
We assumed approximately $24 million in finance lease obligations during 2024 and $1 million during each of 2023 and 2022. In the ordinary course of business, our facilities routinely lease equipment pursuant to new lease arrangements that will likely result in future lease and rental expense in excess of amounts indicated above.
8) COMMITMENTS AND CONTINGENCIES
Professional and General Liability, Workers’ Compensation Liability
The vast majority of our subsidiaries are self-insured for professional and general liability exposure up to: (i) $20 million for professional liability and $3 million for general liability per occurrence in 2024, 2023, 2022 and 2021; (ii) $10 million and $3 million per occurrence, respectively, in 2020; (iii) $5 million and $3 million per occurrence, respectively, during 2019, 2018 and 2017, and; (iv) $10 million and $3 million per occurrence, respectively, prior to 2017. For each of the years indicated above, for claims involving multiple plaintiffs, a single self-insured retention may apply, as stipulated in and subject to the terms and conditions of the applicable commercial policies, for claims qualifying as group related integrated occurrences and/or medical incidents.
These subsidiaries are provided with several excess policies through commercial insurance carriers which provide for coverage in excess of the applicable per occurrence and aggregate self-insured retention or underlying policy limits up to approximately $175 million in 2024; $165 million in 2023; $162 million in 2022; $155 million in 2021 and $250 million during each of 2014 through 2020. In addition, from time to time based upon marketplace conditions, we may elect to purchase additional commercial coverage for certain of our facilities or businesses. Our behavioral health care facilities located in the U.K. have policies through a commercial insurance carrier located in the U.K. that provides for £20 million of professional liability coverage and £25 million of general liability coverage. The commercial insurance limits indicated above for each policy year may have been reduced due to payment of covered claims or suits, subject to the policy terms and conditions.
As of December 31, 2024, the total net accrual for our self-insured professional and general liability claims was $487 million, of which $85 million was included in current liabilities. As of December 31, 2023, the total net accrual for our self-insured professional and general liability claims was $431 million, of which $70 million was included in current liabilities.
As a result of unfavorable trends experienced during the last three years, our results of operations included pre-tax increases to our reserves for self-insured professional and general liability claims amounting to approximately $79 million during 2024, $25 million during 2023 and $16 million during 2022. All professional and general liability insurance we purchase is subject to policy limitations. Our estimated liability for self-insured professional and general liability claims is based on a number of factors including, among other things, the number of asserted claims and reported incidents, estimates of losses for these claims based on recent and historical settlement amounts and jury verdicts, estimates of incurred but not reported claims based on historical experience, and estimates of amounts recoverable under our commercial insurance policies. All relevant information, including our own historical experience, applicable per occurrence and aggregate self-insured retentions, and limitations and exclusions pursuant to our commercial insurance policies, is used in estimating our expected liability for self-insured claims. While we continuously monitor these factors, our ultimate liability for professional and general liability claims could change materially from our current estimates due to inherent uncertainties involved in making this estimate. Given our significant exposure to professional and general liability claims, there can be no assurance that a sharp increase in the number and/or severity of claims asserted against us, and/or reductions in the amount of commercial coverage available to us, will not have a material adverse effect on our future results of operations. In addition, our commercial insurance coverage for the period commencing in March, 2025, contains less favorable terms than previous years including coverage exclusions for incidents involving sexual molestation or abuse, higher premiums and potentially lower aggregate limitations.
As of December 31, 2024, the total accrual for our workers’ compensation liability claims was $137 million, $58 million of which was included in current liabilities. As of December 31, 2023, the total accrual for our workers’ compensation liability claims was $130 million, $55 million of which was included in current liabilities. As a result of favorable trends experienced during 2023, included in our results of operations during 2023 was a pre-tax decrease to our reserves for self-insured workers' compensation liability claims of approximately $10 million.
Although we are unable to predict whether or not our future financial statements will require updates to estimates for our prior year reserves for self-insured general and professional and workers’ compensation claims, given the relatively unpredictable nature of these potential liabilities and the factors impacting these reserves, as discussed above, it is reasonably likely that our future financial results may include material adjustments to prior period reserves.
As disclosed below in Legal Proceedings:
•On March 28, 2024, a jury returned a verdict for compensatory damages of $60 million and punitive damages of $475 million and a related judgment was entered against The Pavilion Behavioral Health System (the “Pavilion”), an indirect subsidiary of the Company. In an order dated October 10, 2024, the trial court ordered a remittitur of punitive damages from $475 million to $120 million. The court denied the Pavilion’s request for reduction of compensatory damages. The Pavilion has filed an appeal of the remaining judgment and the Plaintiff has filed a cross appeal of the remittitur of punitive damages. Plaintiff has filed and served a Citation to Discover Assets ("Citation") on the Pavilion as well as Universal Health Services, Inc., and UHS of Delaware, Inc. ("UHS Entities") for the purported purpose of executing on the judgment during the pendency of the appeal. We are currently contesting the Citation as to the UHS Entities who were not parties to the litigation as well as the breadth and scope of the Citation issued to the Pavilion.
•Cumberland Hospital for Children and Adolescents (“Cumberland”), an indirect subsidiary of the Company, is a defendant in multi-plaintiff lawsuits filed in the Circuit Court for Richmond, Virginia (the “Cumberland Litigation”), relating to allegations of inappropriate sexual contact during medical examinations by Dr. Daniel Davidow, an independent contractor and the former medical director for Cumberland. The Company and UHS of Delaware, Inc., our administrative services subsidiary (“UHS Delaware”), were also named as co-defendants in the Cumberland Litigation. Plaintiffs have asserted claims of negligence, assault and battery (against Dr. Davidow), false imprisonment, violations of the Virginia Consumer Protection Act (“VCPA”), and vicarious liability for Dr. Davidow’s conduct against Cumberland, the Company, and UHS Delaware. The Company and UHS Delaware were dismissed from the action during the trial, which occurred in September, 2024. On September 27, 2024, a jury entered a verdict finding Dr. Davidow and Cumberland liable and awarded these three plaintiffs combined compensatory damages of $60 million for all liability theories, an additional combined $180 million in trebled
damages for violation of the VCPA, and an additional combined $120 million in punitive damages. Cumberland is evaluating all legal options and intends to challenge this verdict, including the amounts awarded in the verdict, in post-trial proceedings and on appeal. Based upon Virginia law, we expect that the punitive damage amount should be reduced to a combined maximum of $1.05 million as a matter of law. There are approximately 40 additional plaintiffs making similar allegations with claims pending in the Cumberland Litigation. We expect that the trials for the remaining plaintiffs, as well as any additional plaintiffs, will be scheduled at various times over the next several years and will continue to be tried in small groups.
We are uncertain as to the ultimate financial exposure related to the Pavilion and Cumberland matters (which relate to occurrences in the 2020 policy year) and we can make no assurances regarding timing or substance of their outcome, or the amount of damages that may be ultimately held recoverable after post-judgment proceedings and appeals. As of December 31, 2024, without reduction for any potential amounts related to the Pavilion and Cumberland matters, the Company and its subsidiaries have aggregate insurance coverage of approximately $221 million remaining under commercial policies for matters applicable to the 2020 policy year (in excess of the applicable self-insured retention amounts of $10 million per single occurrence/$25 million for multi-plaintiff matters for professional liability claims and $3 million per occurrence for general liability claims). In the event the resolution of the Pavilion and/or Cumberland matters exhausts all or a significant portion of the remaining commercial insurance coverage available to the Company and its subsidiaries related to other matters that occurred in 2020, or the Pavilion and Cumberland matters cause the posting of large bonds or other collateral during the appeal processes, our future results of operations and capital resources would be materially adversely impacted.
Below is a schedule showing the changes in our general and professional liability and workers’ compensation reserves during the three years ended December 31, 2024 (amount in thousands):
| | | | | | | | | | | | |
| | General and | | | | | | | |
| | Professional | | | Workers’ | | | | |
| | Liability | | | Compensation | | | Total | |
Balance at January 1, 2022 | | $ | 348,693 | | | $ | 114,985 | | | $ | 463,678 | |
Plus: Accrued insurance expense, net of commercial
premiums paid | | | 111,763 | | | | 62,960 | | | | 174,723 | |
Less: Payments made in settlement of self-insured claims | | | (88,556 | ) | | | (53,429 | ) | | | (141,985 | ) |
Balance at January 1, 2023 | | | 371,900 | | | | 124,516 | | | | 496,416 | |
Plus: Accrued insurance expense, net of commercial
premiums paid | | | 127,445 | | | | 56,017 | | | | 183,462 | |
Less: Payments made in settlement of self-insured claims | | | (67,860 | ) | | | (50,229 | ) | | | (118,089 | ) |
Balance at January 1, 2024 | | | 431,485 | | | | 130,304 | | | | 561,789 | |
Plus: Accrued insurance expense, net of commercial
premiums paid | | | 184,110 | | | | 70,284 | | | | 254,394 | |
Less: Payments made in settlement of self-insured claims | | | (128,707 | ) | | | (63,478 | ) | | | (192,185 | ) |
Balance at December 31, 2024 | | $ | 486,888 | | | $ | 137,110 | | | $ | 623,998 | |
Property Insurance
We have commercial property insurance policies for our properties, covering the period of June 1, 2024 to June 1, 2025, providing property and business interruption coverage for losses in excess of $15 million per occurrence or per location (as applicable based upon the event) up to a $1 billion annual policy limitation for certain catastrophic events or perils. These commercial policies provide for coverage of up to $250 million of annual aggregate coverage for losses resulting from windstorm damage. Losses resulting from named windstorms are subject to deductibles between 3% and 5% of the total insurable value of the property. In addition, we have commercial property insurance policies covering catastrophic losses resulting from earthquake and flood damage, each subject to aggregated loss limits (as opposed to per occurrence losses). Commercially insured earthquake coverage for our facilities is subject to various deductibles and limitations including: (i) $100 million limitation for our facilities located in California, New Madrid Seismic Zone, Pacific Northwest Seismic Zone, Alaska and certain counties in Nevada; (ii) $100 million limitation for our facilities located in fault zones within the United States; (iii) $40 million limitation for our facilities located in Puerto Rico, and; (iv) $250 million limitation for many of our facilities located in other states. Our commercially insured flood coverage has a limit of $100 million annually. There is also a $10 million sublimit for one of our facilities located in Houston, Texas, and a $1 million sublimit for our facilities located in Puerto Rico. In addition, subject to the underlying policies' deductible provisions, our facilities located in California, New Madrid Seismic Zone, Pacific Northwest Seismic Zone, Alaska and certain counties in Nevada, have $50 million of excess commercial property insurance coverage for earthquake losses in excess of $100 million. Property insurance for our behavioral health facilities located in the U.K. are provided on an all risk basis up to a £1.5 billion policy limit, with coverage caps per location, that includes coverage for real and personal property as well as business interruption losses.
These commercial policies are subject to a deductible of: (i) $5 million per location for damage resulting from earthquake, wind, hail and flood, and; (ii) $5 million per occurrence for all other events. For per location or per occurrence losses in excess of the applicable deductible, we are self-insured, through our wholly-owned captive insurance company, for up to $10 million of annual
aggregate losses. Should the $10 million self-insured annual aggregate limitation be exhausted during the policy year, we have commercial insurance coverage for the next $30 million of annual aggregate losses in excess of the applicable deductible. In the event the $30 million of commercial coverage is also exhausted, we are self-insured for all per location or per occurrence losses up to $25 million, including the $5 million deductible.
Commitment to Develop, Lease and Operate an Acute Care Hospital in Washington, D.C.
During 2020, we entered into various agreements with the District of Columbia (the “District”) related to the development, leasing and operation of an acute care hospital and certain other facilities/structures on land owned by the District (“District Facilities”). The agreements contemplate that we will serve as manager for development and construction of the District Facilities on behalf of the District, with a projected aggregate cost of approximately $439 million, approximately $344 million of which was incurred as of December 31, 2024, which will be entirely funded by the District. Construction of the District Facilities is expected to be completed in the Spring of 2025.
Upon completion of the District Facilities, we will lease the District Facilities for a nominal rental amount for a period of 75 years and are obligated to operate the District Facilities during the lease term. We have certain lease termination rights in connection with the District Facilities beginning on the tenth anniversary of the lease commencement date for various and decreasing amounts as provided for in the agreements. Additionally, any time after the 10th anniversary of the lease term, we have a right to purchase the District Facilities for a price equal to the greater of fair market value of the District Facilities or the amount necessary to defease the bonds issued by the District to fund the construction of the District Facilities. The lease agreement also entitles the District to participation rent should certain specified earnings before interest, taxes, depreciation and amortization thresholds be achieved by the acute care hospital.
Additionally, we have committed to expend no less than $75 million (approximately $14 million of which has been incurred as of December 31, 2024), over a projected 12-year period, in healthcare infrastructure including expenditures related to the District Facilities as well as other healthcare related expenditures in certain specified areas of Washington, D.C. Pursuant to the agreements, the District is entitled to certain termination fees and other amounts as specified in the agreements in the event we, within certain specified periods of time, cease to operate the acute care hospital or there is a transfer of control of us or our subsidiary operating the hospital.
Information Technology Incident
In connection with an information technology security incident in late September, 2020, our results of operations for the year ended December 31, 2022 were favorably impacted by approximately $13 million resulting from receipt of commercial cyber insurance proceeds.
Other Contractual Commitments:
In addition to our long-term debt obligations as discussed in Note 4 - Long-Term Debt and our operating lease obligations as discussed in Note 7 - Lease Commitments, we have various other contractual commitments outstanding as of December 31, 2024 as follows: (i) other combined estimated future purchase obligations of $436 million related to a long-term contract with third-parties consisting primarily of certain revenue cycle data processing services for our acute care facilities ($52 million), expected future costs to be paid to a third-party vendor in connection with the ongoing operation of an electronic health records application and purchase implementation of a revenue cycle and other applications for our acute care facilities ($183 million), healthcare infrastructure in Washington D.C. in connection with various agreements with the District of Columbia ($61 million), development, implementation and operation of an enterprise resource planning application ($85 million), administrative software applications ($43 million) and other software applications ($12 million); (ii) estimated construction commitment of $32 million representing our share of the construction cost of two behavioral health care facilities scheduled to be completed in 2025 that, subject to approval of certain regulatory conditions, we are required to build pursuant to joint-venture agreements with a third-party; (iii) combined estimated future payments of $159 million related to our non-contributory, defined benefit pension plan ($133 million consisting of estimated payments through 2080) and other retirement plan liabilities ($26 million), and; (iv) accrued and unpaid estimated claims expense incurred in connection with our commercial health insurers and self-insured employee benefit plans ($118 million).
Legal Proceedings
We operate in a highly regulated and litigious industry which subjects us to various claims and lawsuits in the ordinary course of business as well as regulatory proceedings and government investigations. These claims or suits include claims for damages for personal injuries, medical malpractice, commercial/contractual disputes, wrongful restriction of, or interference with, physicians’ staff privileges, and employment related claims. In addition, health care companies are subject to investigations and/or actions by various state and federal governmental agencies or those bringing claims on their behalf. Government action has increased with respect to investigations and/or allegations against healthcare providers concerning possible violations of fraud and abuse and false claims statutes as well as compliance with clinical and operational regulations. Currently, and from time to time, we and some of our facilities are subjected to inquiries in the form of subpoenas, Civil Investigative Demands, audits and other document requests from various federal and state agencies. These inquiries can lead to notices and/or actions including repayment obligations from state and federal
government agencies associated with potential non-compliance with laws and regulations. Further, the federal False Claims Act allows private individuals to bring lawsuits (qui tam actions) against healthcare providers that submit claims for payments to the government. Various states have also adopted similar statutes. When such a claim is filed, the government will investigate the matter and decide if they are going to intervene in the pending case. These qui tam lawsuits are placed under seal by the court to comply with the False Claims Act’s requirements. If the government chooses not to intervene, the private individual(s) can proceed independently on behalf of the government. Health care providers that are found to violate the False Claims Act may be subject to substantial monetary fines/penalties as well as face potential exclusion from participating in government health care programs or be required to comply with Corporate Integrity Agreements as a condition of a settlement of a False Claims Act matter. In September 2014, the Criminal Division of the Department of Justice (“DOJ”) announced that all qui tam cases will be shared with their Division to determine if a parallel criminal investigation should be opened. The DOJ has also announced an intention to pursue civil and criminal actions against individuals within a company as well as the corporate entity or entities. In addition, health care facilities are subject to monitoring by state and federal surveyors to ensure compliance with program Conditions of Participation. In the event a facility is found to be out of compliance with a Condition of Participation and unable to remedy the alleged deficiency(s), the facility faces termination from the Medicare and Medicaid programs or compliance with a System Improvement Agreement to remedy deficiencies and ensure compliance.
The laws and regulations governing the healthcare industry are complex covering, among other things, government healthcare participation requirements, licensure, certification and accreditation, privacy of patient information, reimbursement for patient services as well as fraud and abuse compliance. These laws and regulations are constantly evolving and expanding. Further, the original Patient Protection and Affordable Care Act, as amended by the Health and Education Reconciliation Act, has added additional obligations on healthcare providers to report and refund overpayments by government healthcare programs and authorizes the suspension of Medicare and Medicaid payments “pending an investigation of a credible allegation of fraud.” We monitor our business and have developed an ethics and compliance program with respect to these complex laws, rules and regulations. Although we believe our policies, procedures and practices comply with government regulations, there is no assurance that we will not be faced with the sanctions referenced above which include fines, penalties and/or substantial damages, repayment obligations, payment suspensions, licensure revocation, and expulsion from government healthcare programs. Even if we were to ultimately prevail in any action brought against us or our facilities or in responding to any inquiry, such action or inquiry could have a material adverse effect on us.
Certain legal matters are described below:
Disproportionate Share Hospital Payment Matter
In late September, 2015, many hospitals in Pennsylvania, including certain of our behavioral health care hospitals located in the state, received letters from the Pennsylvania Department of Human Services (the “Department”) demanding repayment of allegedly excess Medicaid Disproportionate Share Hospital payments (“DSH”), primarily consisting of managed care payments characterized as DSH payments, for the federal fiscal year (“FFY”) 2011 amounting to approximately $4 million in the aggregate. Since that time, certain of our behavioral health care hospitals in Pennsylvania have received similar requests for repayment for alleged DSH overpayments for FFYs 2012 through 2015. For FFY 2012, the claimed overpayment amounts to approximately $4 million. For FY 2013, FY 2014 and FY 2015 the initial claimed overpayments and attempted recoupment by the Department were approximately $7 million, $8 million and $7 million, respectively. The Department has agreed to a change in methodology which, upon confirmation of the underlying data being accepted by the Department, could reduce the initial claimed overpayments for FY 2013, FY 2014 and FY 2015 to approximately $2 million, $2 million and $3 million, respectively. We filed administrative appeals for all of our facilities contesting the recoupment efforts for FFYs 2011 through 2015 as we believe the Department’s calculation methodology is inaccurate and conflicts with applicable federal and state laws and regulations. The Department agreed to postpone the recoupment of the state’s share for FFY 2011 to 2013 until all hospital appeals are resolved but recouped the federal share. For FFY 2014 and FFY 2015, the Department initiated the recoupment of the alleged overpayments (both federal and state shares). Starting in FY 2016, the first full fiscal year after the January 1, 2015 effective date of Medicaid expansion in Pennsylvania, the Department no longer characterized managed care payments received by the hospitals as DSH payments. While the administrative appeals on the disputed DSH payments were pending, we were in settlement discussions with the Department. As a part of these discussions, we presented certain calculation errors that we believed, if corrected, could materially reduce the alleged overpayments. Recently, we finalized a settlement agreement with the Department, received the funds representing the agreed upon portion of amounts previously recouped, and the matter has been concluded.
Rachel Capriglione, as natural mother and Next Friend of A.T., a minor, Plaintiff, v. The Pavilion Foundation d/b/a The Pavilion Behavioral Health System
The Pavilion Behavioral Health System (the “Pavilion”), an indirect subsidiary of the Company, is the sole defendant in a lawsuit filed in Champaign County, Illinois, relating to the sexual assault of one minor patient by another minor patient in 2020. Plaintiff asserted claims of negligence and misrepresentation. The Pavilion denied any liability.
The case went to trial in March of 2024. On March 28, 2024, a jury rejected the misrepresentation claim, returned a verdict for ordinary negligence, and awarded compensatory damages of $60 million and punitive damages of $475 million. Based on a search of verdicts in comparable cases, the magnitude of this verdict was unexpected and is unprecedented for a single-plaintiff injury case of
this type in Champaign County, Illinois. The Pavilion filed post-trial motions, among other items, contesting the excessiveness of the damage awards.
In an order dated October 10, 2024, the trial court ordered a remittitur of punitive damages from $475 million to $120 million. The court denied the Pavilion’s request for reduction of compensatory damages. The Pavilion has filed an appeal of the remaining judgment and the Plaintiff has filed a cross appeal of the remittitur of punitive damages. Plaintiff has filed and served a Citation to Discover Assets ("Citation") on the Pavilion as well as Universal Health Services, Inc., and UHS of Delaware, Inc. ("UHS Entities") for the purported purpose of executing on the judgment during the pendency of the appeal. We are currently contesting the Citation as to the UHS Entities who were not parties to the litigation as well as the breadth and scope of the Citation issued to the Pavilion.
Although we can make no assurances regarding the ultimate outcome of this matter, or what damages will ultimately be awarded, its final resolution could have a material adverse effect on the Company.
K.E.E., et al., Plaintiffs v. Cumberland Hospital, LLC d/b/a Cumberland Hospital for Children and Adolescents, et al. (and related lawsuits)
Cumberland Hospital for Children and Adolescents (“Cumberland”), an indirect subsidiary of the Company, is a defendant in multi-plaintiff lawsuits filed in the Circuit Court for Richmond, Virginia (the “Cumberland Litigation”), relating to allegations of inappropriate sexual contact during medical examinations by Dr. Daniel Davidow, an independent contractor and the former medical director for Cumberland. The Company and UHS of Delaware, Inc., our administrative services subsidiary (“UHS Delaware”), were also named as co-defendants in the Cumberland Litigation. Plaintiffs have asserted claims of negligence, assault and battery (against Dr. Davidow), false imprisonment, violations of the Virginia Consumer Protection Act (“VCPA”), and vicarious liability for Dr. Davidow’s conduct against Cumberland, the Company, and UHS Delaware. All defendants have denied liability.
The claims asserted by three of the plaintiffs in the Cumberland Litigation were consolidated for trial in September of 2024. The Company and UHS Delaware were dismissed from the action during trial. On September 27, 2024, a jury entered a verdict finding Dr. Davidow and Cumberland liable and awarded these three plaintiffs combined compensatory damages of $60 million for all liability theories, an additional combined $180 million in trebled damages for violation of the VCPA, and an additional combined $120 million in punitive damages. Cumberland filed post-trial motions challenging this verdict and briefing is currently underway. Based upon Virginia law, we expect that the punitive damage amount should be reduced to a combined maximum of $1.05 million as a matter of law.
There are approximately 40 additional plaintiffs making similar allegations with claims pending in the Cumberland Litigation. We expect that the trials for the remaining plaintiffs, as well as any additional plaintiffs, will be scheduled at various times over the next several years and will continue to be tried in small groups.
Although we can make no assurances regarding the ultimate outcomes of the various claims made in connection with the Cumberland Litigation, or what damages will ultimately be awarded, the final resolution of these matters could have a material adverse effect on the Company.
Other Matters
Various other suits, claims and investigations, including government subpoenas, arising against, or issued to, us are pending and additional such matters may arise in the future. Management will consider additional disclosure from time to time to the extent it believes such matters may be or become material. The outcome of any current or future litigation or governmental or internal investigations, including the matters described above, cannot be accurately predicted, nor can we predict any resulting penalties, fines or other sanctions that may be imposed at the discretion of federal or state regulatory authorities. We record accruals for such contingencies to the extent that we conclude it is probable that a liability has been incurred and the amount of the loss can be reasonably estimated. No estimate of the possible loss or range of loss in excess of amounts accrued, if any, can be made at this time regarding the matters described above or that are otherwise pending because the inherently unpredictable nature of legal proceedings may be exacerbated by various factors, including, but not limited to: (i) the damages sought in the proceedings are unsubstantiated or indeterminate; (ii) discovery is not complete; (iii) the matter is in its early stages; (iv) the matters present legal uncertainties; (v) there are significant facts in dispute; (vi) there are a large number of parties, or; (vii) there is a wide range of potential outcomes. It is possible that the outcome of these matters could have a material adverse impact on our future results of operations, financial position, cash flows and, potentially, our reputation.
9) RELATIONSHIP WITH UNIVERSAL HEALTH REALTY INCOME TRUST AND OTHER RELATED PARTY TRANSACTIONS
Relationship with Universal Health Realty Income Trust:
At December 31, 2024, we held approximately 5.7% of the outstanding shares of Universal Health Realty Income Trust (the “Trust”). We serve as Advisor to the Trust under an annually renewable advisory agreement, which is scheduled to expire on December 31st of each year, pursuant to the terms of which we conduct the Trust’s day-to-day affairs, provide administrative services
and present investment opportunities. The advisory agreement was renewed by the Trust for 2025 at the same rate in place for 2024, 2023 and 2022, providing for an advisory computation at 0.70% of the Trust’s average invested real estate assets. We earned an advisory fee from the Trust, which is included in net revenues in the accompanying consolidated statements of income, of approximately $5.5 million during 2024, $5.3 million during 2023 and $5.1 million during 2022.
In addition, certain of our officers and directors are also officers and/or directors of the Trust. Management believes that it has the ability to exercise significant influence over the Trust, therefore we account for our investment in the Trust using the equity method of accounting.
Our pre-tax share of income from the Trust was $1.1 million during 2024, $874,000 during 2023 and $1.2 million during 2022, which are included in other income (expense), net, on the accompanying consolidated statements of income for each year. We received dividends from the Trust amounting to $2.3 million during each of 2024 and 2023 and $2.2 million during 2022. The carrying value of our investment in the Trust was $5.8 million and $7.0 million at December 31, 2024 and 2023, respectively, and is included in other assets in the accompanying consolidated balance sheets. The market value of our investment in the Trust was $29.3 million at December 31, 2024 and $34.1 million at December 31, 2023, based on the closing price of the Trust’s stock on the respective dates.
The Trust commenced operations in 1986 by purchasing certain hospital properties from us and immediately leasing the properties back to our respective subsidiaries. The base rents are paid monthly and the bonus rents, which effective as of January 1, 2022 are applicable only to McAllen Medical Center, are computed and paid on a quarterly basis, based upon a computation that compares current quarter revenue to a corresponding quarter in the base year. The leases with those subsidiaries are unconditionally guaranteed by us and are cross-defaulted with one another.
On December 31, 2021, we entered into an asset purchase and sale agreement with the Trust, which was amended during the first quarter of 2022, pursuant to the terms of which: (i) a wholly-owned subsidiary of ours purchased from the Trust the real estate assets of the Inland Valley Campus of Southwest Healthcare System located in Wildomar, California, at its fair market value; (ii) two wholly-owned subsidiaries of ours transferred to the Trust, at their respective fair-market values, the real estate assets of Aiken Regional Medical Center (“Aiken”), located in Aiken, South Carolina (which includes a 211-bed acute care hospital and a 62-bed behavioral health facility), and Canyon Creek Behavioral Health (“Canyon Creek”), located in Temple, Texas, and; (iii) we received approximately $4.1 million in cash from the Trust.
As a result of the purchase options within the lease agreements for Aiken and Canyon Creek, the asset purchase and sale transaction is accounted for as a failed sale leaseback in accordance with U.S. GAAP. We have accounted for the asset exchange and substitution transaction with the Trust as a financing arrangement and, since we did not derecognize the real property related to Aiken and Canyon Creek, we will continue to depreciate the assets. Our consolidated balance sheets as of December 31, 2024 and December 31, 2023 reflects a financial liability of $73.8 million and $77.5 million, respectively, which is included in debt, for the fair value of real estate assets that we exchanged as part of the transaction. Our monthly lease payments payable to the Trust will be recorded to interest expense and as a reduction to the outstanding financial liability. The amount allocated to interest expense is determined using our incremental borrowing rate and is based on the outstanding financial liability.
The aggregate rent payable to the Trust in connection with the leases on McAllen Medical Center, Wellington Regional Medical Center, Aiken Regional Medical Center and Canyon Creek Behavioral Health was approximately $21.2 million during 2024 and $20.6 million during 2023.
Pursuant to the Master Leases by certain subsidiaries of ours and the Trust as described in the table below, dated 1986 and 2021 (“the Master Leases”) which govern the leases of McAllen Medical Center and Wellington Regional Medical Center (each of which is governed by the Master Lease dated 1986), and Aiken Regional Medical Center and Canyon Creek Behavioral Health (each of which is governed by the Master Lease dated 2021), we have the option to renew the leases at the lease terms described above and below by providing notice to the Trust at least 90 days prior to the termination of the then current term. We also have the right to purchase the respective leased hospitals at their appraised fair market value upon any of the following: (i) at the end of the lease terms or any renewal terms; (ii) upon one month’s notice should a change of control of the Trust occur, or; (iii) within the time period as specified in the lease in the event that we provide notice to the Trust of our intent to offer a substitution property/properties in exchange for one (or more) of the hospital properties leased from the Trust should we be unable to reach an agreement with the Trust on the properties to be substituted. In addition, we have rights of first refusal to: (i) purchase the respective leased facilities during and for a specified period after the lease terms at the same price, terms and conditions of any third-party offer, or; (ii) renew the lease on the respective leased facility at the end of, and for a specified period after, the lease term at the same terms and conditions pursuant to any third-party offer.
In addition, we are the managing, majority member in a joint venture with an unrelated third-party that operates Clive Behavioral Health, a 100-bed behavioral health care facility located in Clive, Iowa. The real property of this facility, which was completed and opened in late 2020, is also leased from the Trust (annual rental of approximately $2.8 million, $2.7 million and $2.6 million during 2024, 2023 and 2022, respectively) pursuant to the lease terms as provided in the table below. In connection with the lease on this facility, the joint venture has the right to purchase the leased facility from the Trust at its appraised fair market value
upon either of the following: (i) by providing notice at least 270 days prior to the end of the lease terms or any renewal terms, or; (ii) upon 30 days' notice anytime within 12 months of a change of control of the Trust (UHS also has this right should the joint venture decline to exercise its purchase right). Additionally, the joint venture has rights of first offer to purchase the facility prior to any third-party sale.
The table below provides certain details for each of the hospitals leased from the Trust as of January 1, 2025:
| | | | | | | | | | | | |
Hospital Name | | | Annual
Minimum
Rent | | | End of Lease Term | | Renewal
Term
(years) | | |
McAllen Medical Center | | | $ | 5,485,000 | | | December, 2026 | | | 5 | | (a) |
Wellington Regional Medical Center | | | $ | 6,805,000 | | | December, 2026 | | | 5 | | (b) |
Aiken Regional Medical Center/Aurora Pavilion Behavioral Health Services | | | $ | 4,164,000 | | | December, 2033 | | | 35 | | (c) |
Canyon Creek Behavioral Health | | | $ | 1,882,000 | | | December, 2033 | | | 35 | | (c) |
Clive Behavioral Health | | | $ | 2,851,000 | | | December, 2040 | | | 50 | | (d) |
(a)We have one 5-year renewal option at existing lease rates (through 2031).
(b)We have one 5-year renewal option at fair market value lease rates (through 2031). On each January 1st through 2026, the annual rent will increase by 2.50% on a cumulative and compounded basis.
(c)We have seven 5-year renewal options at fair market value lease rates (2034 through 2068). On each January 1st through 2033, the annual rent will increase by 2.25% on a cumulative and compounded basis.
(d)This facility is operated by a joint venture in which we are the managing, majority member and an unrelated third-party holds a minority ownership interest. The joint venture has three, 10-year renewal options at computed lease rates as stipulated in the lease (2041 through 2070) and two additional, 10-year renewal options at fair market value lease rates (2071 through 2090). In each January through 2040 (and potentially through 2070 if three, 10-year renewal options are exercised), the annual rental will increase by 2.75% on a cumulative and compounded basis.
In addition, certain of our subsidiaries are tenants in several medical office buildings (“MOBs”) and two free-standing emergency departments ("FED") owned by the Trust or by limited liability companies in which the Trust holds 95% to 100% of the ownership interest. In connection with these two FEDs, in October, 2024, our subsidiaries exercised their 5-year renewal options on the facilities which are located in Weslaco and Mission, Texas. The renewal option covers the period of February 1, 2025 through January 31, 2030 (the current lease terms were scheduled to expire on January 31, 2025; with aggregate annual lease rates of approximately $1.07 million). Pursuant to terms of the leases, and consistent with the terms of the leases currently in effect for each property, the lease rates are scheduled to increase 2% per year through the end of the renewed lease terms. Our subsidiaries have four, 5-year renewal options remaining on each of these FEDs, with the first three renewal options (covering the years 2030 through 2044) providing for 2% annual increases to the lease rates, and the remaining two, 5-year renewal options (covering the years 2045 through 2054) providing for lease rates at the then fair market value. These leases are cross-defaulted with one another and our subsidiaries have the option to purchase the leased properties upon the expiration of each five-year extended term at the fair market value at that time.
During the third quarter of 2023, the Trust acquired the McAllen Doctor's Center, a 79,500 rentable square feet medical office building located in McAllen, Texas. A master lease was executed between a wholly-owned subsidiary of ours and the Trust, pursuant to the terms of which our subsidiary will master lease 100% of the rentable square feet of the MOB at an initial minimum rent of $624,000 annually. The master lease commenced during August, 2023 and is scheduled to expire in twelve years from that date.
During the first quarter of 2023, the Trust substantially completed construction on a new 86,000 rentable square foot multi-tenant MOB that is located on the campus of Northern Nevada Sierra Medical Center in Reno, Nevada. Northern Nevada Sierra Medical Center, a 170-bed newly constructed acute care hospital owned and operated by a wholly-owned subsidiary of ours, was completed and opened in April, 2022. In connection with this MOB, a ten-year master flex lease was executed between a wholly-owned subsidiary of ours and the Trust (scheduled to expire in March, 2033), pursuant to the terms of which our subsidiary initially agreed to master lease up to approximately 68% of the rentable square feet of the MOB. The master flex lease has been reduced since inception as certain conditions have been met. A ground lease for this facility commenced during 2023 and is scheduled to expire in 2098.
Other Related Party Transactions:
In December, 2010, our Board of Directors approved the Company’s entering into supplemental life insurance plans and agreements on the lives of Alan B. Miller (our Executive Chairman of the Board) and his wife. As a result of these agreements, as amended in October, 2016, based on actuarial tables and other assumptions, during the life expectancies of the insureds, we would pay approximately $28 million in premiums, and certain trusts owned by our Executive Chairman of the Board, would pay approximately $9 million in premiums. Based on the projected premiums mentioned above, and assuming the policies remain in effect until the death of the insureds, we will be entitled to receive death benefit proceeds of no less than approximately $37 million representing the $28
million of aggregate premiums paid by us as well as the $9 million of aggregate premiums paid by the trusts. In connection with these policies, we paid approximately $1.0 million, net, in premium payments during 2024, 2023 and 2022.
In August, 2015, Marc D. Miller, our President and Chief Executive Officer and member of our Board of Directors, was appointed to the Board of Directors of Premier, Inc. (“Premier”), a healthcare performance improvement alliance. During 2013, we entered into a new group purchasing organization agreement (“GPO”) with Premier. In conjunction with the GPO agreement, we acquired a minority interest in Premier for a nominal amount. During the fourth quarter of 2013, in connection with the completion of an initial public offering of the stock of Premier, we received cash proceeds for the sale of a portion of our ownership interest in the GPO. Also in connection with this GPO agreement, we received shares of restricted stock of Premier which vested ratably over a seven-year period (2014 through 2020), contingent upon our continued participation and minority ownership interest in the GPO. During the third quarter of 2020, we entered into an agreement with Premier pursuant to the terms of which, among other things, our ownership interest in Premier was converted into shares of Class A Common Stock of Premier. We have elected to retain a portion of the previously vested shares of Premier, the market value of which is included in other assets on our consolidated balance sheets. Based upon the closing price of Premier’s stock on each respective date, the market value of our shares of Premier was $47 million as of December 31, 2024 and $50 million as of December 31, 2023. The $3 million decrease in market value of our vested Premier shares since December 31, 2023 was recorded as an unrealized loss and included in “Other (income) expense, net” in our consolidated statements of income for the year ended December 31, 2024. A $28 million decrease in the market value of our vested Premier shares during 2023 was recorded as an unrealized loss and included in “Other (income) expense, net” in our consolidated statements of income for the year ended December 31, 2023. A $14 million decrease in the market value of our vested Premier shares during 2022 was recorded as an unrealized loss and included in “Other (income) expense, net” in our consolidated statements of income for the year ended December 31, 2022.
Additionally, we received cash dividends from Premier amounting to $1.9 million during each of 2024 and 2023 and $1.8 million during 2022, which are included in “Other (income) expense, net” in our consolidated statements of income.
A member of our Board of Directors and member of the Executive Committee and Finance Committee is Of Counsel for Norton Rose Fulbright US LLP, a law firm engaged by us for a variety of legal services. The Board member and his law firm also provide personal legal services to our Executive Chairman and he acts as trustee of certain trusts for the benefit of our Executive Chairman and his family.
10) REVENUE RECOGNITION
We recognize revenue when it transfers promised goods or services to customers in an amount that reflects the consideration to which we expect to be entitled in exchange for those goods or services. Our estimate for amounts not expected to be collected based on historical experience will continue to be recognized as a reduction to net revenue. However, subsequent changes in estimate of collectability due to a change in the financial status of a payer, for example a bankruptcy, will be recognized as bad debt expense in operating charges.
The performance obligation is separately identifiable from other promises in the customer contract. As the performance obligations are met (i.e.: room, board, ancillary services, level of care), revenue is recognized based upon allocated transaction price. The transaction price is allocated to separate performance obligations based upon the relative standalone selling price. In instances where we determine there are multiple performance obligations across multiple months, the transaction price will be allocated by applying an estimated implicit and explicit rate to gross charges based on the separate performance obligations.
In assessing collectability, we have elected the portfolio approach. This portfolio approach is being used as we have large volume of similar contracts with similar classes of customers. We reasonably expect that the effect of applying a portfolio approach to a group of contracts would not differ materially from considering each contract separately. Management’s judgment to group the contracts by portfolio is based on the payment behavior expected in each portfolio category. As a result, aggregating all of the contracts (which are at the patient level) by the particular payer or group of payers, will result in the recognition of the same amount of revenue as applying the analysis at the individual patient level.
We group our revenues into categories based on payment behaviors. Each component has its own reimbursement structure which allows us to disaggregate the revenue into categories that share the nature and timing of payments. The other patient revenue consists primarily of self-pay, government-funded non-Medicaid, and other.
The following table disaggregates our revenue by major source for the years ended December 31, 2024, 2023 and 2022 (in thousands):
| | | | | | | | | | | | | | | | | | | | | | | | |
| For the year ended December 31, 2024 | |
| Acute Care | | | Behavioral Health | | | Other | | | Total | |
Medicare | $ | 1,361,167 | | | 15 | % | | $ | 307,958 | | | 4 | % | | | | | $ | 1,669,125 | | | 11 | % |
Managed Medicare | | 1,478,331 | | | 17 | % | | | 405,574 | | | 6 | % | | | | | | 1,883,905 | | | 12 | % |
Medicaid | | 1,106,728 | | | 12 | % | | | 1,145,302 | | | 17 | % | | | | | | 2,252,030 | | | 14 | % |
Managed Medicaid | | 619,262 | | | 7 | % | | | 1,684,676 | | | 24 | % | | | | | | 2,303,938 | | | 15 | % |
Managed Care (HMO and PPOs) | | 2,861,956 | | | 32 | % | | | 1,634,446 | | | 24 | % | | | | | | 4,496,402 | | | 28 | % |
UK Revenue | | 0 | | | 0 | % | | | 880,148 | | | 13 | % | | | | | | 880,148 | | | 6 | % |
Other patient revenue and adjustments, net | | 498,749 | | | 6 | % | | | 614,059 | | | 9 | % | | | | | | 1,112,808 | | | 7 | % |
Other non-patient revenue | | 996,134 | | | 11 | % | | | 222,888 | | | 3 | % | | | 10,557 | | | | 1,229,579 | | | 8 | % |
Total Net Revenue | $ | 8,922,327 | | | 100 | % | | $ | 6,895,051 | | | 100 | % | | $ | 10,557 | | | $ | 15,827,935 | | | 100 | % |
| | | | | | | | | | | | | | | | | |
| For the year ended December 31, 2023 | |
| Acute Care | | | Behavioral Health | | | Other | | | Total | |
Medicare | $ | 1,297,084 | | | 16 | % | | $ | 310,321 | | | 5 | % | | | | | $ | 1,607,405 | | | 11 | % |
Managed Medicare | | 1,368,284 | | | 17 | % | | | 345,771 | | | 6 | % | | | | | | 1,714,055 | | | 12 | % |
Medicaid | | 638,986 | | | 8 | % | | | 893,918 | | | 14 | % | | | | | | 1,532,904 | | | 11 | % |
Managed Medicaid | | 716,380 | | | 9 | % | | | 1,574,281 | | | 25 | % | | | | | | 2,290,661 | | | 16 | % |
Managed Care (HMO and PPOs) | | 2,658,890 | | | 33 | % | | | 1,552,304 | | | 25 | % | | | | | | 4,211,194 | | | 29 | % |
UK Revenue | | 0 | | | 0 | % | | | 761,124 | | | 12 | % | | | | | | 761,124 | | | 5 | % |
Other patient revenue and adjustments, net | | 452,781 | | | 6 | % | | | 528,422 | | | 9 | % | | | | | | 981,203 | | | 7 | % |
Other non-patient revenue | | 948,997 | | | 12 | % | | | 224,780 | | | 4 | % | | | 9,653 | | | | 1,183,430 | | | 8 | % |
Total Net Revenue | $ | 8,081,402 | | | 100 | % | | $ | 6,190,921 | | | 100 | % | | $ | 9,653 | | | $ | 14,281,976 | | | 100 | % |
| | | | | | | | | | | | | | | | | |
| For the year ended December 31, 2022 | |
| Acute Care | | | Behavioral Health | | | Other | | | Total | |
Medicare | $ | 1,289,425 | | | 17 | % | | $ | 326,337 | | | 6 | % | | | | | $ | 1,615,762 | | | 12 | % |
Managed Medicare | | 1,274,719 | | | 17 | % | | | 285,870 | | | 5 | % | | | | | | 1,560,589 | | | 12 | % |
Medicaid | | 719,870 | | | 9 | % | | | 792,526 | | | 14 | % | | | | | | 1,512,396 | | | 11 | % |
Managed Medicaid | | 757,488 | | | 10 | % | | | 1,449,367 | | | 25 | % | | | | | | 2,206,855 | | | 16 | % |
Managed Care (HMO and PPOs) | | 2,536,818 | | | 33 | % | | | 1,476,136 | | | 26 | % | | | | | | 4,012,954 | | | 30 | % |
UK Revenue | | 0 | | | 0 | % | | | 684,594 | | | 12 | % | | | | | | 684,594 | | | 5 | % |
Other patient revenue and adjustments, net | | 261,879 | | | 3 | % | | | 483,763 | | | 8 | % | | | | | | 745,642 | | | 6 | % |
Other non-patient revenue | | 806,550 | | | 11 | % | | | 231,165 | | | 4 | % | | | 22,863 | | | | 1,060,578 | | | 8 | % |
Total Net Revenue | $ | 7,646,749 | | | 100 | % | | $ | 5,729,758 | | | 100 | % | | $ | 22,863 | | | $ | 13,399,370 | | | 100 | % |
11) PENSION PLAN
We maintain contributory and non-contributory retirement plans for eligible employees. Our contributions to the contributory plan amounted to $82.1 million, $73.9 million and $72.0 million in 2024, 2023 and 2022, respectively. The non-contributory plan is a defined benefit pension plan which covers employees of one of our subsidiaries. The benefits are based on years of service and the employee’s highest compensation for any five years of employment. Our funding policy is to contribute annually at least the minimum amount that should be funded in accordance with the provisions of ERISA.
For defined benefit pension plans, the benefit obligation is the “projected benefit obligation”, the actuarial present value, as of December 31 measurement date, of all benefits attributed by the pension benefit formula to employee service rendered to that date. The amount of benefit to be paid depends on a number of future events incorporated into the pension benefit formula, including estimates of the average life of employees/survivors and average years of service rendered. It is measured based on assumptions
concerning future interest rates and future compensation levels. The following table shows the reconciliation of the defined benefit pension plan as of December 31, 2024 and 2023:
| | | | | | | | |
| | 2024 | | | 2023 | |
| | (000s) | |
Change in plan assets: | | | | | | |
Fair value of plan assets at beginning of year | | $ | 98,415 | | | $ | 96,627 | |
Actual return (loss) on plan assets | | | 1,865 | | | | 8,779 | |
Benefits paid | | | (6,289 | ) | | | (6,417 | ) |
Administrative expenses | | | (576 | ) | | | (574 | ) |
Fair value of plan assets at end of year | | $ | 93,415 | | | $ | 98,415 | |
Change in benefit obligation: | | | | | | |
Benefit obligation at beginning of year | | $ | 85,625 | | | $ | 87,277 | |
Service cost | | | 616 | | | | 803 | |
Interest cost | | | 3,874 | | | | 4,118 | |
Benefits paid | | | (6,289 | ) | | | (6,417 | ) |
Actuarial (gain) loss | | | (5,404 | ) | | | (156 | ) |
Benefit obligation at end of year | | $ | 78,422 | | | $ | 85,625 | |
Amounts recognized in the Consolidated Balance Sheet: | | | | | | |
Other noncurrent assets | | $ | 14,993 | | | $ | 12,790 | |
Total amounts recognized at end of year | | $ | 14,993 | | | $ | 12,790 | |
| | | | | | | | | | | | |
| | 2024 | | | 2023 | | | 2022 | |
| | (000s) | |
Components of net periodic cost (benefit) | | | | | | | | | |
Service cost | | $ | 616 | | | $ | 803 | | | $ | 607 | |
Interest cost | | | 3,874 | | | | 4,118 | | | | 2,836 | |
Expected return on plan assets | | | (4,277 | ) | | | (4,195 | ) | | | (4,335 | ) |
Net periodic cost | | $ | 213 | | | $ | 726 | | | $ | (892 | ) |
| | | | |
| | 2024 | | 2023 |
Measurement Dates | | | | |
Benefit obligations | | 12/31/2024 | | 12/31/2023 |
Fair value of plan assets | | 12/31/2024 | | 12/31/2023 |
| | | | | | | | |
| | 2024 | | | 2023 | |
Weighted average assumptions as of December 31 | | | | | | |
Discount rate | | | 5.36 | % | | | 4.71 | % |
Rate of compensation increase | | | 4.00 | % | | | 4.00 | % |
| | | | | | | | | | | | |
| | 2024 | | | 2023 | | | 2022 | |
Weighted-average assumptions for net periodic benefit
cost calculations | | | | | | | | | |
Discount rate | | | 4.71 | % | | | 4.91 | % | | | 2.52 | % |
Expected long-term rate of return on plan assets | | | 4.50 | % | | | 4.50 | % | | | 3.50 | % |
Rate of compensation increase | | | 4.00 | % | | | 4.00 | % | | | 4.00 | % |
The “accumulated benefit obligation” for our pension plan represents the actuarial present value of benefits based on employee service and compensation as of a certain date and does not include an assumption about future compensation levels. The accumulated benefit obligation for our plan was $78.4 million and $85.6 million as of December 31, 2024 and 2023, respectively. The fair value of plan assets exceeded the accumulated benefit obligation by $15.0 million and $12.8 million as of December 31, 2024 and 2023, respectively.
We estimate that there will be no net loss or prior service cost amortized from accumulated other comprehensive income during 2025.
The market values of our pension plan assets at December 31, 2024 and 2023, reported using net asset value as a practical expedient, by asset category are as follows (in thousands):
| | | | | | | | |
| | 2024 | | | 2023 | |
Equities: | | | | | | |
U.S. Large Cap | | $ | 5,131 | | | $ | 5,423 | |
U.S. Mid Cap | | | 1,351 | | | | 1,480 | |
U.S. Small Cap | | | 1,259 | | | | 1,491 | |
International Developed | | | 3,746 | | | | 3,943 | |
Emerging Markets | | | 2,291 | | | | 2,540 | |
Fixed income: | | | | | | |
Core Fixed Income | | | 28,175 | | | | 17,492 | |
Long Duration Fixed Income | | | 50,674 | | | | 65,289 | |
Cash/Currency: | | | | | | |
Cash Equivalents | | | 788 | | | | 757 | |
Total market value | | $ | 93,415 | | | $ | 98,415 | |
To develop the expected long-term rate of return on plan assets assumption, we considered the historical returns and the future expectations for returns for each asset class, as well as the target asset allocation of the pension portfolio.
The following table shows expected benefit payments for the years 2025 through 2034 for our defined pension plan. There will be benefit payments under this plan beyond 2034.
| | | | |
Estimated Future Benefit Payments (000s) | | | |
2025 | | $ | 6,675 | |
2026 | | | 6,664 | |
2027 | | | 6,635 | |
2028 | | | 6,575 | |
2029 | | | 6,492 | |
2030-2034 | | | 30,648 | |
Total | | $ | 63,689 | |
| | | | | | | | |
| | 2024 | | | 2023 | |
Plan Assets | | | | | | |
Asset Category | | | | | | |
Equity securities | | | 15 | % | | | 15 | % |
Fixed income securities | | | 84 | % | | | 84 | % |
Other | | | 1 | % | | | 1 | % |
Total | | | 100 | % | | | 100 | % |
Investment Policy, Guidelines and Objectives have been established for the defined benefit pension plan. The investment policy is in keeping with the fiduciary requirements under existing federal laws and managed in accordance with the Prudent Investor Rule. Total portfolio risk is regularly evaluated and compared to that of the plan’s policy target allocation and judged on a relative basis over a market cycle. The following asset allocation policy and ranges have been established in accordance with the overall risk and return objectives of the portfolio:
| | | | | | |
| | As of 12/31/2024 | | | Permitted
Range |
Total Equity | | | 15 | % | | 10-30% |
Total Fixed Income | | | 84 | % | | 70-90% |
Other | | | 1 | % | | 0-10% |
In accordance with the investment policy, the portfolio will invest in high quality, large and small capitalization companies traded on national exchanges, and investment grade securities. The investment managers will not write or buy options for speculative purposes; securities may not be margined or sold short. The manager may employ futures or options for the purpose of hedging exposure, and will not purchase unregistered sectors, private placements, partnerships or commodities.
12) SEGMENT REPORTING
We operate in two reportable segments: Acute Care Hospital Services and Behavioral Health Care Services. Our chief operating decision making (“CODM”) group is comprised of our President and Chief Executive Officer and each of our respective division Presidents for our Acute Care Hospital Services and Behavioral Health Care Services. The operating segments are managed separately because each operating segment represents a business unit that offers different types of healthcare services or operates in different healthcare environments. The primary profitability measurement utilized by the President and Chief Executive Officer as
well as the Presidents of each operating segment is segment income before income taxes. Segment income before income taxes is utilized by the CODM group during the annual budgeting process and during their reviews of our monthly operating results to monitor each segment’s operating results as compared to prior periods, and the respective operating budgets.
The expenses included in our non-segment operating expenses below include centralized services including, but not limited to, information technology, purchasing, reimbursement, accounting and finance, taxation, legal, advertising and design and construction. The accounting policies of the operating segments are the same as those described in the summary of significant accounting policies included in Note 1-Business and Summary of Significant Accounting Policies. We do not present asset information for our segments as this information is not used to allocate resources.
| | | | | | | | | | | | |
2024 | | Acute Care
Hospital
Services | | | Behavioral
Health Care
Services (c) | | | Total | |
| | (amounts in thousands) | |
Net revenue from reportable segments | | $ | 8,922,327 | | | $ | 6,895,051 | | | $ | 15,817,378 | |
| | | | | | | | | |
Reconciliation of Net Revenue | | | | | | | | | |
Non-segment revenue | | | | | | | | | 10,557 | |
Total Net Revenue | | | | | | | | $ | 15,827,935 | |
| | | | | | | | | |
Salaries, wages and benefits | | $ | 3,511,359 | | | $ | 3,603,123 | | | | |
Other segment item operating expenses (a) | | | 4,202,491 | | | | 1,724,763 | | | | |
Depreciation and amortization expense | | | 368,096 | | | | 206,362 | | | | |
Interest (income) expense, net | | | 6,339 | | | | 4,027 | | | | |
Other (income) expense, net | | | (1,305 | ) | | | (3,547 | ) | | | |
Reportable segment income before income taxes | | $ | 835,347 | | | $ | 1,360,323 | | | $ | 2,195,670 | |
| | | | | | | | | |
Reconciliation of non-segment revenue/expenses to consolidated income before income taxes | | | | | | | | | |
Non-segment revenue | | | | | | | | | 10,557 | |
Non-segment operating expenses (b) | | | | | | | | | 529,927 | |
Non-segment interest expense, net | | | | | | | | | 175,743 | |
Non-segment other (income) expense, net | | | | | | | | | 2,621 | |
Income before income taxes | | | | | | | | $ | 1,497,936 | |
| | | | | | | | | | | | |
2023 | | Acute Care
Hospital
Services | | | Behavioral
Health Care
Services (c) | | | Total | |
| | (amounts in thousands) | |
Net revenue from reportable segments | | $ | 8,081,402 | | | $ | 6,190,921 | | | $ | 14,272,323 | |
| | | | | | | | | |
Reconciliation of Net Revenue | | | | | | | | | |
Non-segment revenue | | | | | | | | | 9,653 | |
Total Net Revenue | | | | | | | | $ | 14,281,976 | |
| | | | | | | | | |
Salaries, wages and benefits | | $ | 3,406,060 | | | $ | 3,353,008 | | | | |
Other segment item operating expenses (a) | | | 3,762,066 | | | | 1,564,649 | | | | |
Depreciation and amortization expense | | | 367,644 | | | | 189,297 | | | | |
Interest (income) expense, net | | | (2,501 | ) | | | 4,558 | | | | |
Other (income) expense, net | | | 7,788 | | | | (4,271 | ) | | | |
Reportable segment income before income taxes | | $ | 540,345 | | | $ | 1,083,680 | | | $ | 1,624,025 | |
| | | | | | | | | |
Reconciliation of non-segment revenue/expenses to consolidated income before income taxes | | | | | | | | | |
Non-segment revenue | | | | | | | | | 9,653 | |
Non-segment operating expenses (b) | | | | | | | | | 463,871 | |
Non-segment interest expense, net | | | | | | | | | 204,617 | |
Non-segment other (income) expense, net | | | | | | | | | 24,764 | |
Income before income taxes | | | | | | | | $ | 940,426 | |
| | | | | | | | | | | | |
2022 | | Acute Care
Hospital
Services (d) | | | Behavioral
Health Care
Services (c) | | | Total | |
| | (amounts in thousands) | |
Net revenue from reportable segments | | $ | 7,646,749 | | | $ | 5,729,758 | | | $ | 13,376,507 | |
| | | | | | | | | |
Reconciliation of Net Revenue | | | | | | | | | |
Non-segment revenue | | | | | | | | | 22,863 | |
Total Net Revenue | | | | | | | | $ | 13,399,370 | |
| | | | | | | | | |
Salaries, wages and benefits | | $ | 3,332,535 | | | $ | 3,107,216 | | | | |
Other segment item operating expenses (a) | | | 3,497,538 | | | | 1,457,217 | | | | |
Depreciation and amortization expense | | | 383,115 | | | | 186,555 | | | | |
Interest (income) expense, net | | | 1,109 | | | | 5,323 | | | | |
Other (income) expense, net | | | 2,788 | | | | (6,843 | ) | | | |
Reportable segment income before income taxes | | $ | 429,664 | | | $ | 980,290 | | | $ | 1,409,954 | |
| | | | | | | | | |
Reconciliation of non-segment revenue/expenses to consolidated income before income taxes | | | | | | | | | |
Non-segment revenue | | | | | | | | | 22,863 | |
Non-segment operating expenses (b) | | | | | | | | | 431,639 | |
Non-segment interest expense, net | | | | | | | | | 120,457 | |
Non-segment other (income) expense, net | | | | | | | | | 14,461 | |
Income before income taxes | | | | | | | | $ | 866,260 | |
(a)Other segment operating expenses for each period includes other operating expenses, supplies expense and lease and rental expense.
(b)Non-segment operating expenses for each period includes salaries, wages and benefits, other operating expenses, supplies expense and lease and rental expense.
(c)Includes net revenues generated from our behavioral health care facilities located in the U.K. amounting to approximately $880 million in 2024, $761 million in 2023 and $685 million in 2022.
(d)Included in our 2022 acute care hospital services reportable segment income before income taxes is a pre-tax $58 million provision for asset impairment charge to reduce the carrying value of real property assets.
SCHEDULE II—VALUATION AND QUALIFYING ACCOUNTS
(amounts in thousands)
| | | | | | | | | | | | |
| | Balance at | | | Charges to | | | Balance | |
| | beginning | | | costs and | | | at end | |
Valuation Allowance for Deferred Tax Assets: | | of period | | | expenses | | | of period | |
Year ended December 31, 2024 | | $ | 72,667 | | | $ | 10,023 | | | $ | 82,690 | |
Year ended December 31, 2023 | | $ | 63,325 | | | $ | 9,342 | | | $ | 72,667 | |
Year ended December 31, 2022 | | $ | 62,356 | | | $ | 969 | | | $ | 63,325 | |