Post Q2 2013 Earnings Release Last updated August 12, 2013 I N V E S T O R R E F E R E N C E B O O K
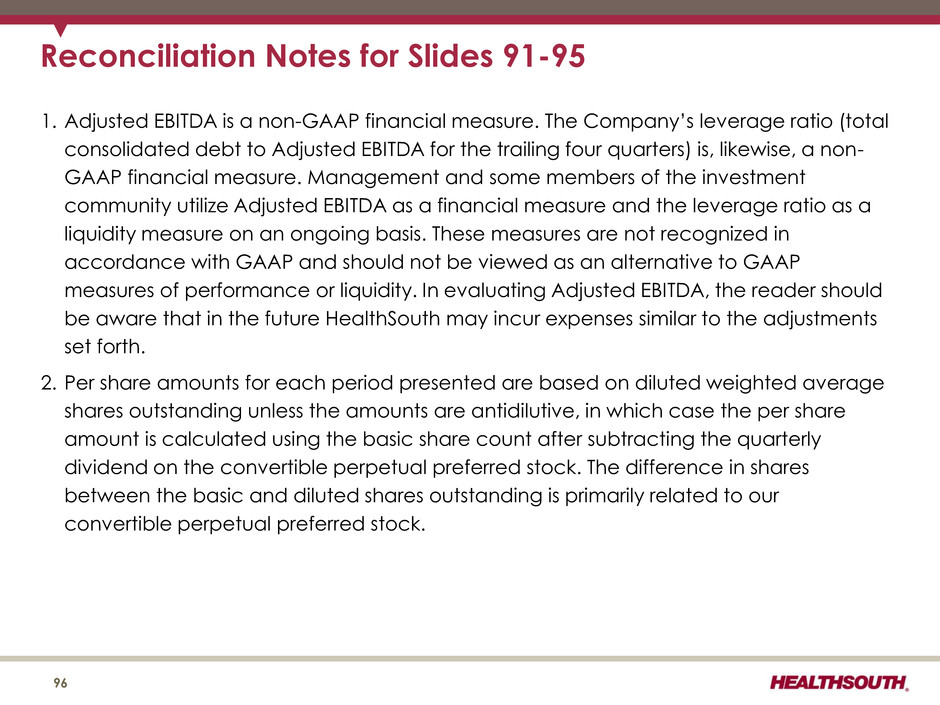
The information contained in this presentation includes certain estimates, projections and other forward- looking information that reflect our current outlook, views and plans with respect to future events, including legislative and regulatory developments, strategy, capital expenditures, development activities, dividend strategies, repurchases of securities, effective tax rates, financial performance, and business model. These estimates, projections and other forward-looking information are based on assumptions that HealthSouth believes, as of the date hereof, are reasonable. Inevitably, there will be differences between such estimates and actual events or results, and those differences may be material. There can be no assurance that any estimates, projections or forward-looking information will be realized. All such estimates, projections and forward-looking information speak only as of the date hereof. HealthSouth undertakes no duty to publicly update or revise the information contained herein. You are cautioned not to place undue reliance on the estimates, projections and other forward-looking information in this presentation as they are based on current expectations and general assumptions and are subject to various risks, uncertainties and other factors, including those set forth in the Form 10-K for the year ended December 31, 2012, the Form 10-Q for the quarters ended June 30, 2013 and March 31, 2013, and in other documents we previously filed with the SEC, many of which are beyond our control, that may cause actual results to differ materially from the views, beliefs and estimates expressed herein. Note Regarding Presentation of Non-GAAP Financial Measures The following presentation includes certain “non-GAAP financial measures” as defined in Regulation G under the Securities Exchange Act of 1934. Schedules are attached that reconcile the non-GAAP financial measures included in the following presentation to the most directly comparable financial measures calculated and presented in accordance with Generally Accepted Accounting Principles in the United States. Our Form 8-K, dated August 12, 2013 to which the following supplemental slides are attached as Exhibit 99.1, provides further explanation and disclosure regarding our use of non-GAAP financial measures and should be read in conjunction with these supplemental slides. Forward-Looking Statements 2
Table of Contents 4-17 18-34 35-44 45-48 49-53 54-57 58-62 63-73 74-85 86-89 Reconciliat ions to GAAP………………………………………………………………………………………………………………………………………………………..90-96 Growth……………………………………………………………………………………………………………………………………… Operational Init iat ives…………………………………………………………………………………………………………….. Guidance ………………………………………………………………………………………………………………………………………… Business Outlook: 2013 to 2015………………………………………………………………………………………………………………………………………… Operational Metrics……………………………………………………………………………………………………………………………………………………………. Our Company…………………………………………………………………………………………………………………………… Industry Structure………………………………………………………………………………………………………………………………………………………………. Historical Perspective…………………………………………………………………………………………………………………………………………. Free Cash Flow………………………………………………………………………………………………………………………………………. Refinancing and Delevering………………………………………………………………………………………………………………………………………… 3
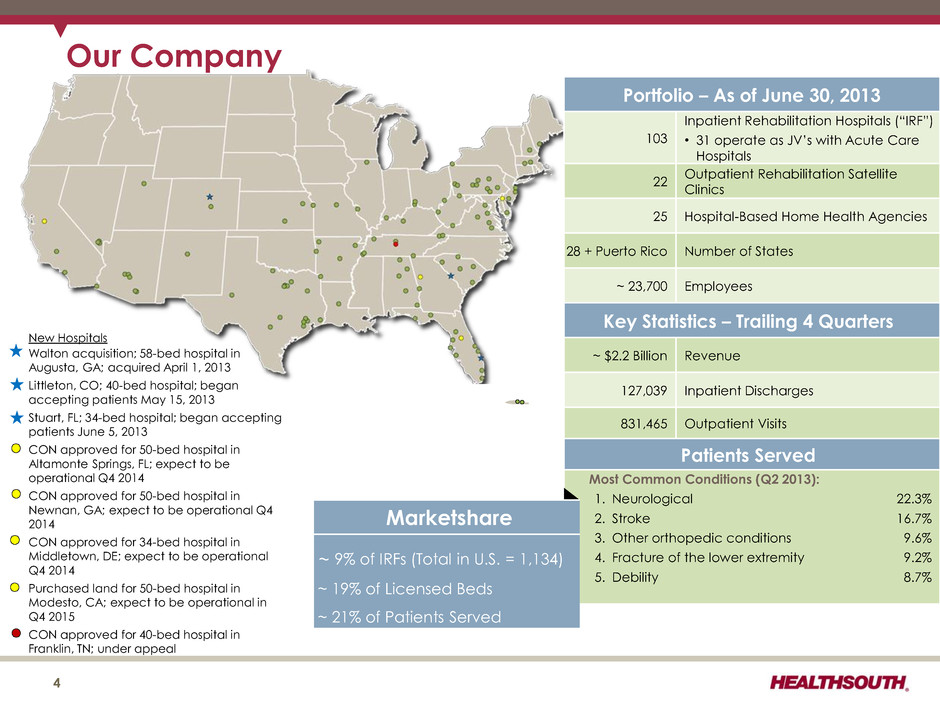
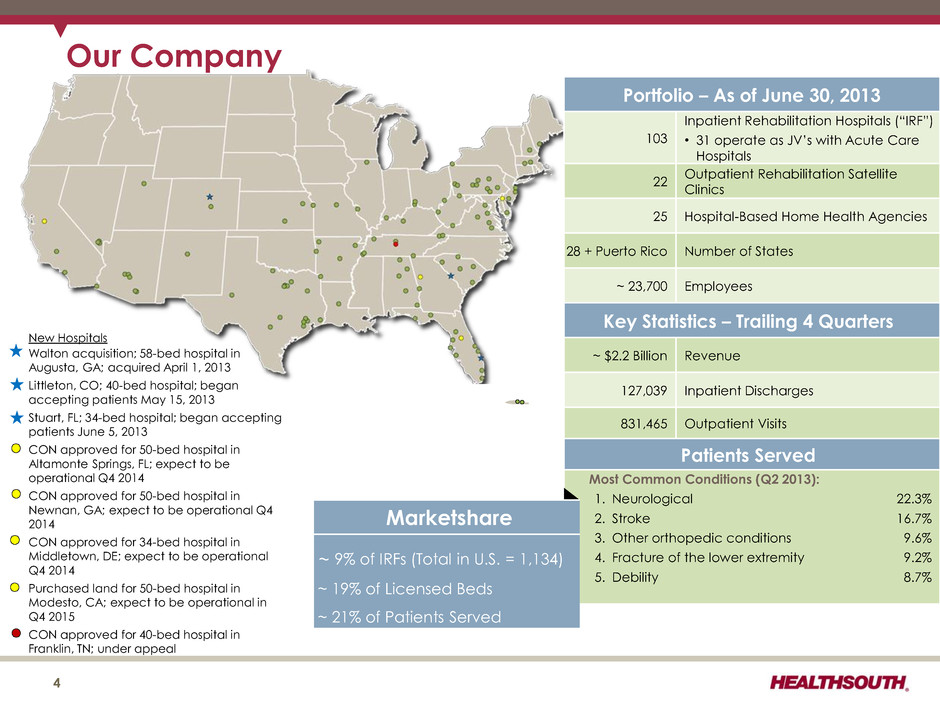
Portfolio – As of June 30, 2013 103 Inpatient Rehabilitation Hospitals (“IRF”) • 31 operate as JV’s with Acute Care Hospitals 22 Outpatient Rehabilitation Satellite Clinics 25 Hospital-Based Home Health Agencies 28 + Puerto Rico Number of States ~ 23,700 Employees Key Statistics – Trailing 4 Quarters ~ $2.2 Billion Revenue 127,039 Inpatient Discharges 831,465 Outpatient Visits Patients Served Most Common Conditions (Q2 2013): 1. Neurological 22.3% 2. Stroke 16.7% 3. Other orthopedic conditions 9.6% 4. Fracture of the lower extremity 9.2% 5. Debility 8.7% 4 Marketshare ~ 9% of IRFs (Total in U.S. = 1,134) ~ 19% of Licensed Beds ~ 21% of Patients Served Our Company New Hospitals Walton acquisition; 58-bed hospital in Augusta, GA; acquired April 1, 2013 Littleton, CO; 40-bed hospital; began accepting patients May 15, 2013 Stuart, FL; 34-bed hospital; began accepting patients June 5, 2013 CON approved for 50-bed hospital in Altamonte Springs, FL; expect to be operational Q4 2014 CON approved for 50-bed hospital in Newnan, GA; expect to be operational Q4 2014 CON approved for 34-bed hospital in Middletown, DE; expect to be operational Q4 2014 Purchased land for 50-bed hospital in Modesto, CA; expect to be operational in Q4 2015 CON approved for 40-bed hospital in Franklin, TN; under appeal

Our Hospitals Major Services • Rehabilitation Physicians: manage and treat medical needs of patients • Rehabilitation Nurses: oversee treatment programs of patients • Physical Therapists: address physical function, mobility, safety • Occupational Therapists: promote independence and re-integration • Speech-Language Therapists: treat communication and swallowing disorders • Case Managers: coordinate care plan with physician, caregivers and family • Post-discharge services: outpatient therapy and home health 5 (1) Under this program, Joint Commission accredited organizations, like our hospitals, may seek certification for chronic diseases or conditions such as brain injury or stroke rehabilitation by complying with national standards, effectively using evidence-based clinical practice guidelines to manage and optimize patient care, and using an organized approach to performance measurement and evaluation of clinical outcomes. Obtaining such certifications demonstrates our commitment to excellence in providing disease-specific care. 94 of our hospitals hold one or more disease-specific certifications from The Joint Commission’s Disease- Specific Care Certification Program. (1)
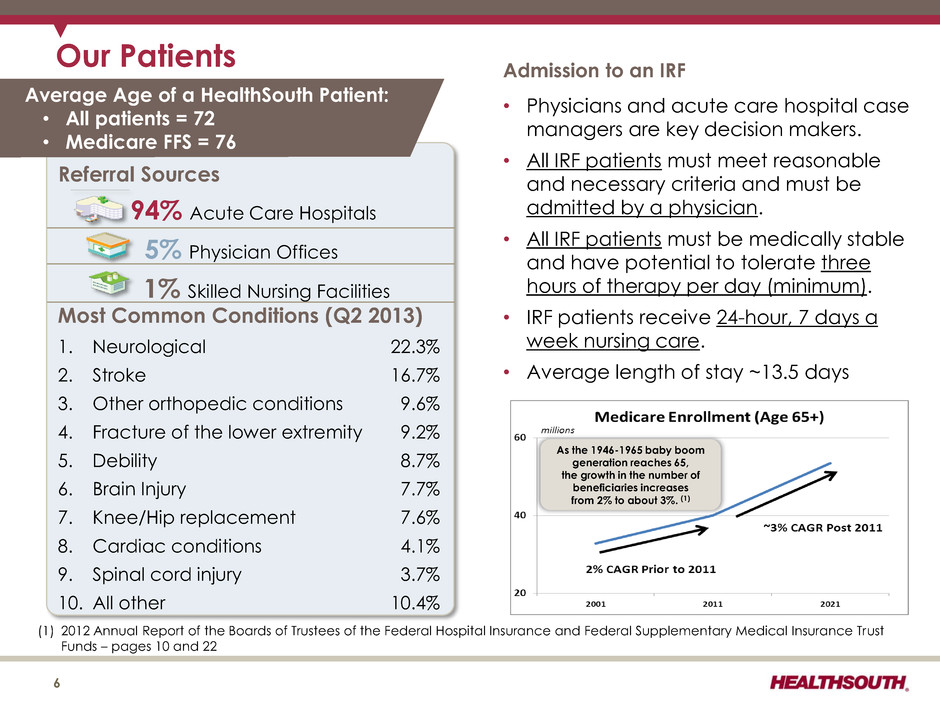
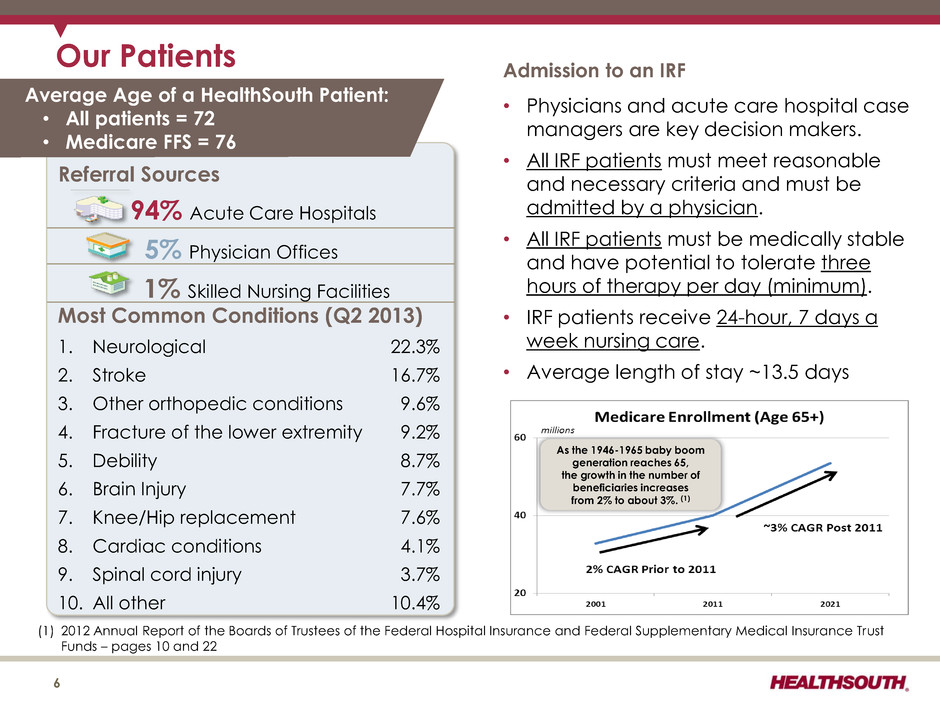
Our Patients 6 Most Common Conditions (Q2 2013) 1. Neurological 22.3% 2. Stroke 16.7% 3. Other orthopedic conditions 9.6% 4. Fracture of the lower extremity 9.2% 5. Debility 8.7% 6. Brain Injury 7.7% 7. Knee/Hip replacement 7.6% 8. Cardiac conditions 4.1% 9. Spinal cord injury 3.7% 10. All other 10.4% Referral Sources 94% Acute Care Hospitals 5% Physician Offices 1% Skilled Nursing Facilities Admission to an IRF • Physicians and acute care hospital case managers are key decision makers. • All IRF patients must meet reasonable and necessary criteria and must be admitted by a physician. • All IRF patients must be medically stable and have potential to tolerate three hours of therapy per day (minimum). • IRF patients receive 24-hour, 7 days a week nursing care. • Average length of stay ~13.5 days Average Age of a HealthSouth Patient: • All patients = 72 • Medicare FFS = 76 As the 1946-1965 baby boom generation reaches 65, the growth in the number of beneficiaries increases from 2% to about 3%. (1) (1) 2012 Annual Report of the Boards of Trustees of the Federal Hospital Insurance and Federal Supplementary Medical Insurance Trust Funds – pages 10 and 22
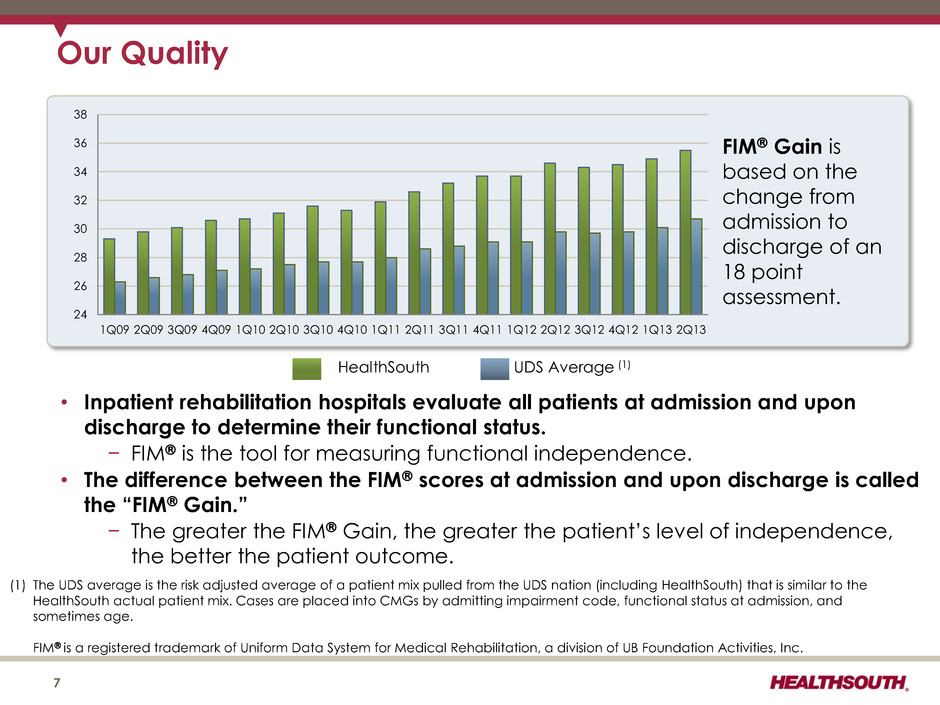
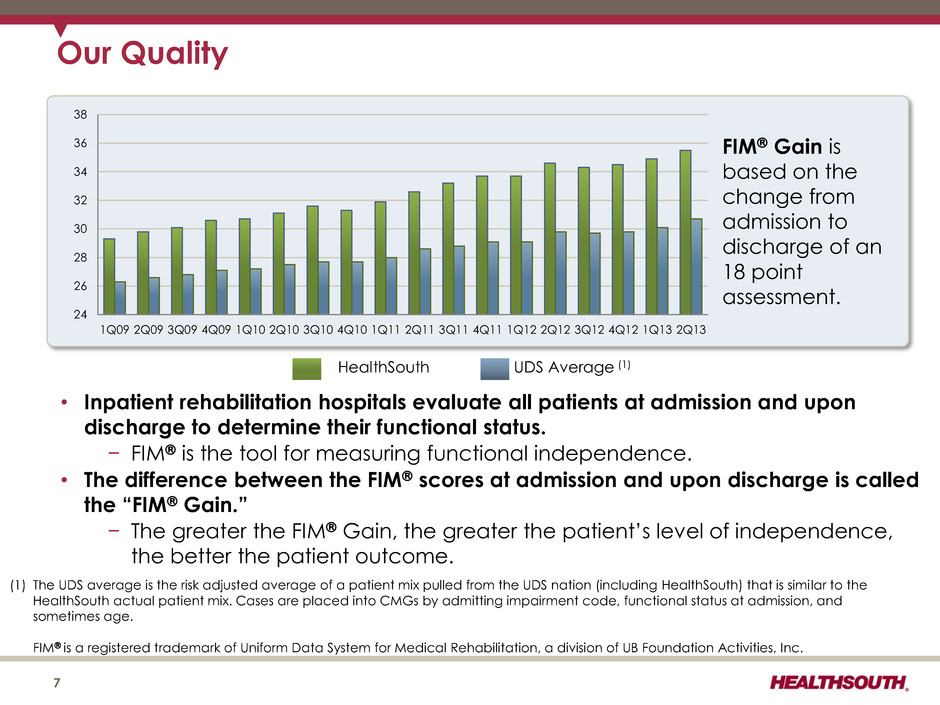
24 26 28 30 32 34 36 38 1Q09 2Q09 3Q09 4Q09 1Q10 2Q10 3Q10 4Q10 1Q11 2Q11 3Q11 4Q11 1Q12 2Q12 3Q12 4Q12 1Q13 2Q13 Our Quality FIM Gain is based on the change from admission to discharge of an 18 point assessment. HealthSouth UDS Average (1) 7 • Inpatient rehabilitation hospitals evaluate all patients at admission and upon discharge to determine their functional status. − FIM is the tool for measuring functional independence. • The difference between the FIM scores at admission and upon discharge is called the “FIM Gain.” − The greater the FIM Gain, the greater the patient’s level of independence, the better the patient outcome. (1) The UDS average is the risk adjusted average of a patient mix pulled from the UDS nation (including HealthSouth) that is similar to the HealthSouth actual patient mix. Cases are placed into CMGs by admitting impairment code, functional status at admission, and sometimes age. FIM is a registered trademark of Uniform Data System for Medical Rehabilitation, a division of UB Foundation Activities, Inc.
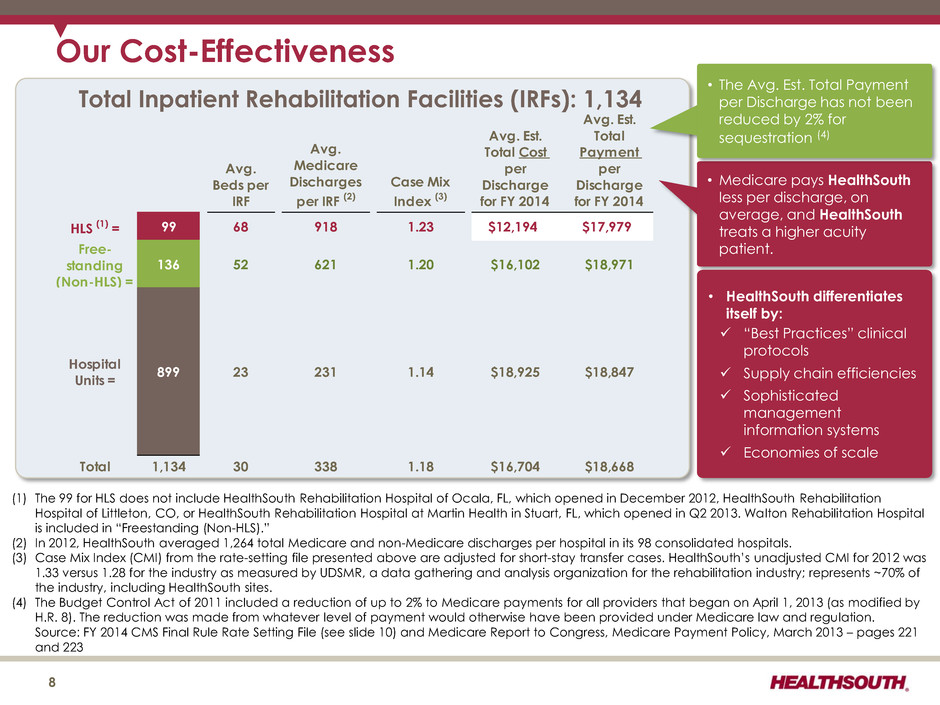
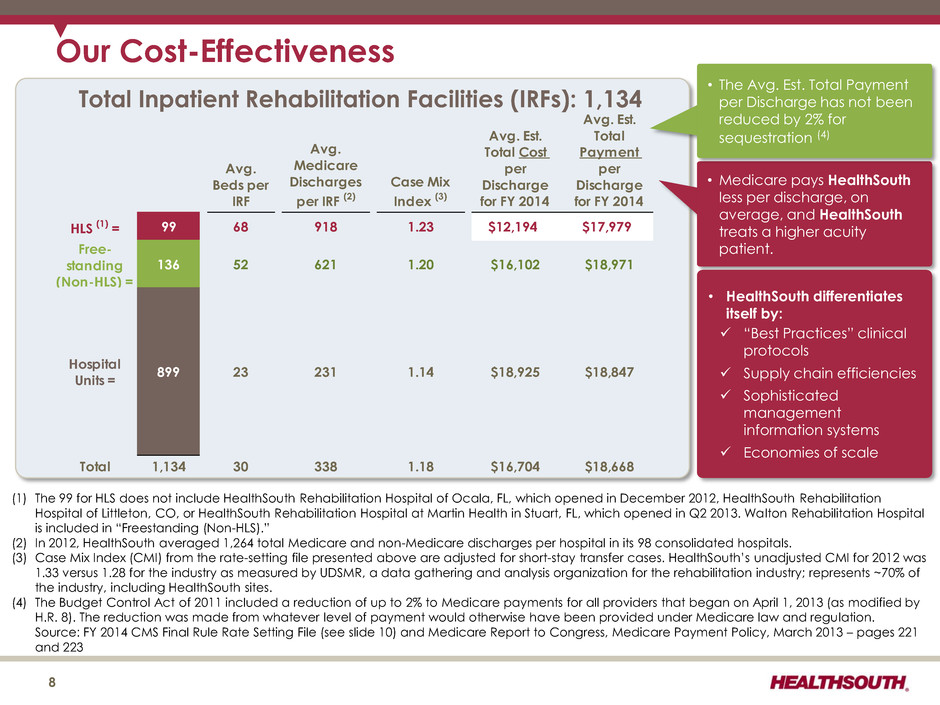
Total Inpatient Rehabilitation Facilities (IRFs): 1,134 Our Cost-Effectiveness • Medicare pays HealthSouth less per discharge, on average, and HealthSouth treats a higher acuity patient. 8 • HealthSouth differentiates itself by: “Best Practices” clinical protocols Supply chain efficiencies Sophisticated management information systems Economies of scale • The Avg. Est. Total Payment per Discharge has not been reduced by 2% for sequestration (4) (1) The 99 for HLS does not include HealthSouth Rehabilitation Hospital of Ocala, FL, which opened in December 2012, HealthSouth Rehabilitation Hospital of Littleton, CO, or HealthSouth Rehabilitation Hospital at Martin Health in Stuart, FL, which opened in Q2 2013. Walton Rehabilitation Hospital is included in “Freestanding (Non-HLS).” (2) In 2012, HealthSouth averaged 1,264 total Medicare and non-Medicare discharges per hospital in its 98 consolidated hospitals. (3) Case Mix Index (CMI) from the rate-setting file presented above are adjusted for short-stay transfer cases. HealthSouth’s unadjusted CMI for 2012 was 1.33 versus 1.28 for the industry as measured by UDSMR, a data gathering and analysis organization for the rehabilitation industry; represents ~70% of the industry, including HealthSouth sites. (4) The Budget Control Act of 2011 included a reduction of up to 2% to Medicare payments for all providers that began on April 1, 2013 (as modified by H.R. 8). The reduction was made from whatever level of payment would otherwise have been provided under Medicare law and regulation. Source: FY 2014 CMS Final Rule Rate Setting File (see slide 10) and Medicare Report to Congress, Medicare Payment Policy, March 2013 – pages 221 and 223 Avg. Beds per IRF Avg. Medicare Discharges per IRF (2) Case Mix Index (3) Avg. Est. Total Cost per Discharge for FY 2014 Avg. Est. Total Payment per Discharge for FY 2014 HLS (1) = 99 68 918 1.23 $12,194 $17,979 Free- standing (Non-HLS) = 136 52 621 1.20 $16,102 $18,971 Hospital Units = 899 23 231 1.14 $18,925 $18,847 Total 1,134 30 338 1.18 $16,704 $18,668
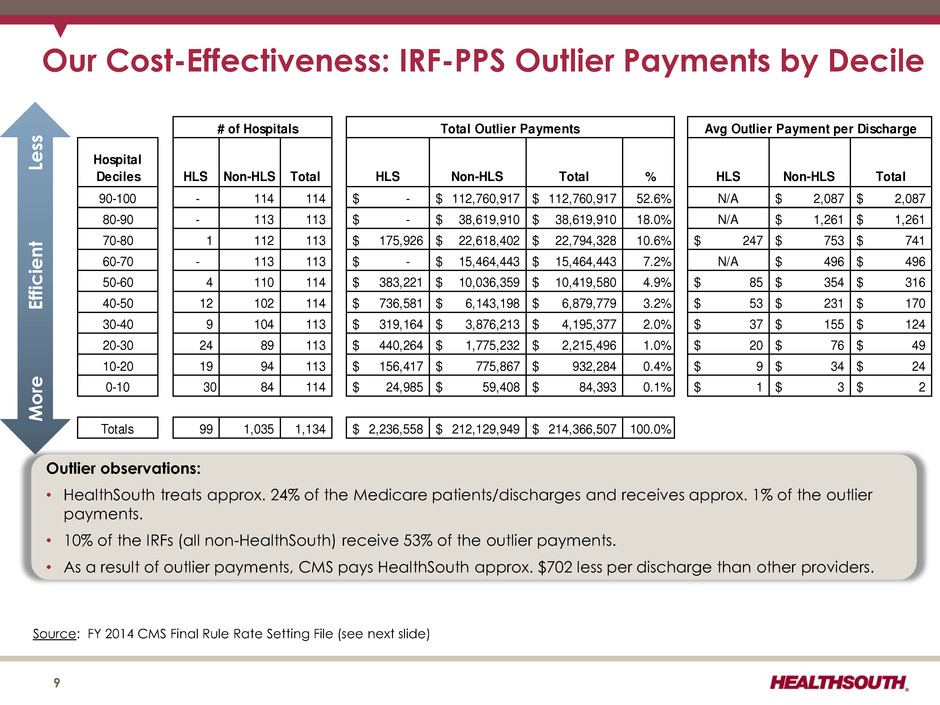
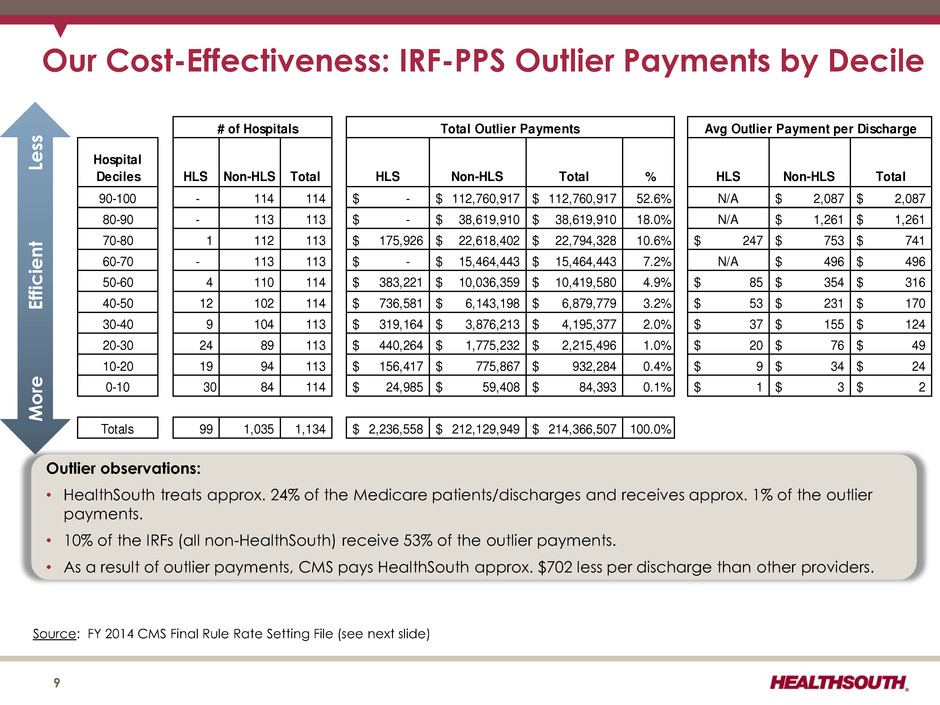
Our Cost-Effectiveness: IRF-PPS Outlier Payments by Decile 9 Hospital Deciles HLS Non-HLS Total HLS Non-HLS Total % HLS Non-HLS Total 90-100 - 114 114 -$ 112,760,917$ 112,760,917$ 52.6% N/A 2,087$ 2,087$ 80-90 - 113 113 -$ 38,619,910$ 38,619,910$ 18.0% N/A 1,261$ 1,261$ 70-80 1 112 113 175,926$ 22,618,402$ 22,794,328$ 10.6% 247$ 753$ 741$ 60-70 - 113 113 -$ 15,464,443$ 15,464,443$ 7.2% N/A 496$ 496$ 50-60 4 110 114 383,221$ 10,036,359$ 10,419,580$ 4.9% 85$ 354$ 316$ 40-50 12 102 114 736,581$ 6,143,198$ 6,879,779$ 3.2% 53$ 231$ 170$ 30 40 9 104 113 319,164$ 3,876,213$ 4,195,377$ 2.0% 37$ 155$ 124$ 20-30 24 89 113 440,264$ 1,775,232$ 2,215,496$ 1.0% 20$ 76$ 49$ 10-20 19 94 113 156,417$ 775,867$ 932,284$ 0.4% 9$ 34$ 24$ 0-10 30 84 114 24,985$ 59,408$ 84,393$ 0.1% 1$ 3$ 2$ Totals 99 1,035 1,134 2,236,558$ 212,129,949$ 214,366,507$ 100.0% # of Hospitals Total Outlier Payments Avg Outlier Payment per Discharge Outlier observations: • HealthSouth treats approx. 24% of the Medicare patients/discharges and receives approx. 1% of the outlier payments. • 10% of the IRFs (all non-HealthSouth) receive 53% of the outlier payments. • As a result of outlier payments, CMS pays HealthSouth approx. $702 less per discharge than other providers. Mo re E ff icient Le ss Source: FY 2014 CMS Final Rule Rate Setting File (see next slide)
CMS Fiscal Year 2014 IRF Final Rule Rate Setting File Analysis Notes: (1) All data provided was filtered and compiled from the Centers for Medicare and Medicaid Services (CMS) Fiscal Year 2014 IRF Final Rule rate setting file found at http://www.cms.gov/Medicare/Medicare-Fee-for-Service- Payment/InpatientRehabFacPPS/Data-Files.html . The data presented was developed entirely by CMS and is based on its definitions which are different in form and substance from the criteria HealthSouth uses for external reporting purposes. Because CMS does not provide its detailed methodology, HealthSouth is not able to reconstruct the CMS projections or the calculation. (2) The CMS file contains data for each of the 1,134 inpatient rehabilitation facilities used to estimate the policy updates for the FY 2014 IRF-PPS Final Rule. Most of the data represents historical information from the CMS fiscal year 2012 period and does not reflect the same HealthSouth hospitals in operation today. The data presented was separated into three categories: Freestanding, Units, and HealthSouth. HealthSouth is a subset of Freestanding and the Total. 10
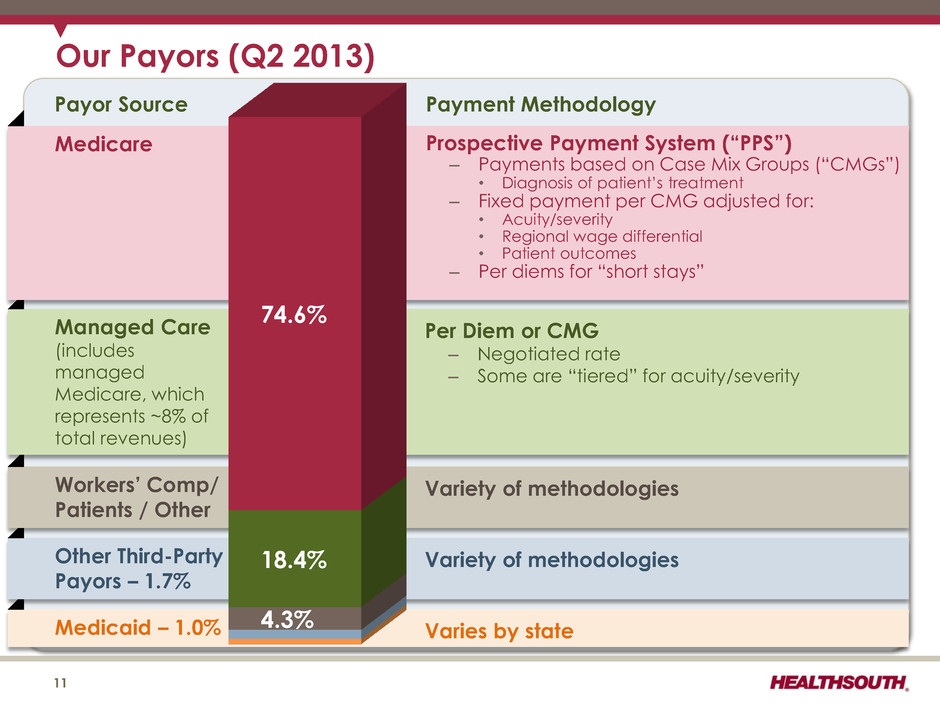
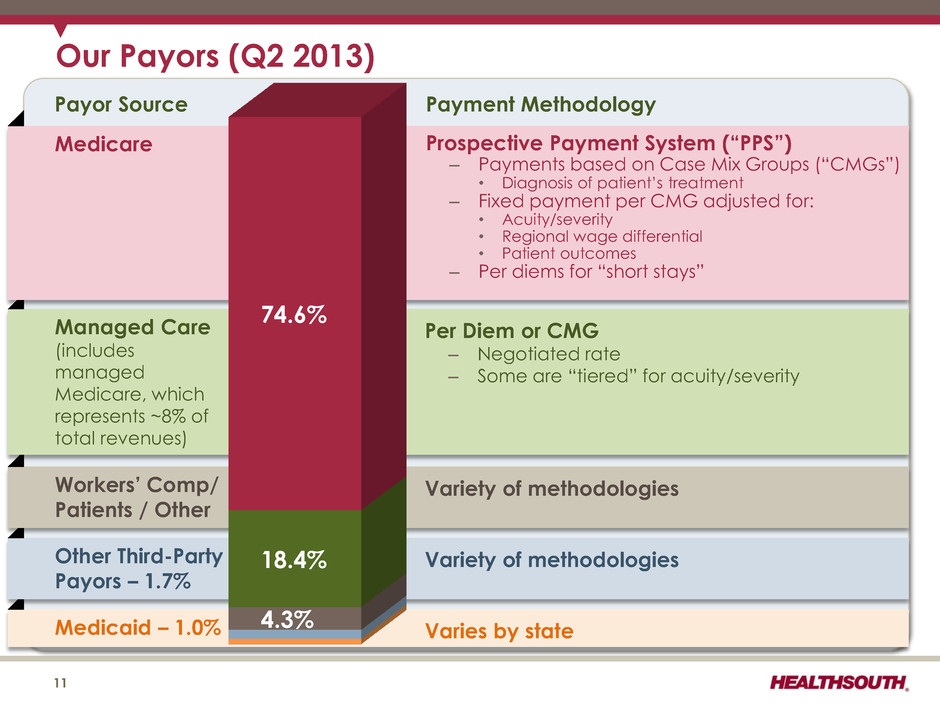
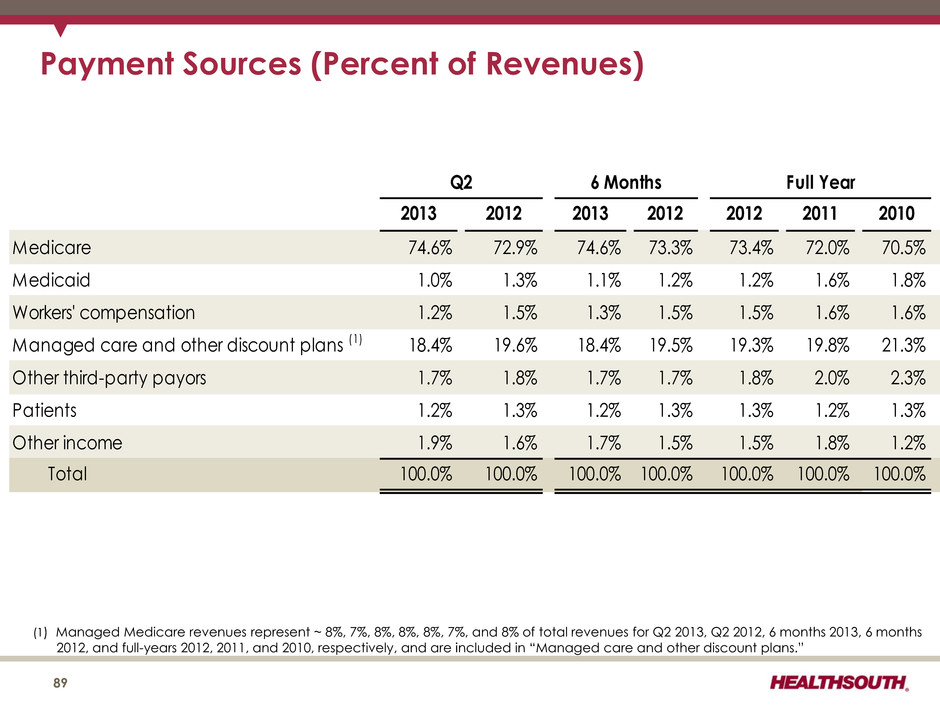
Medicaid – 1.0% Varies by state Other Third-Party Payors – 1.7% Variety of methodologies Workers’ Comp/ Patients / Other Variety of methodologies Managed Care (includes managed Medicare, which represents ~8% of total revenues) Medicare Payment Methodology Payor Source 11 Prospective Payment System (“PPS”) – Payments based on Case Mix Groups (“CMGs”) • Diagnosis of patient’s treatment – Fixed payment per CMG adjusted for: • Acuity/severity • Regional wage differential • Patient outcomes – Per diems for “short stays” Per Diem or CMG – Negotiated rate – Some are “tiered” for acuity/severity 4.3% 18.4% 74.6% Our Payors (Q2 2013)
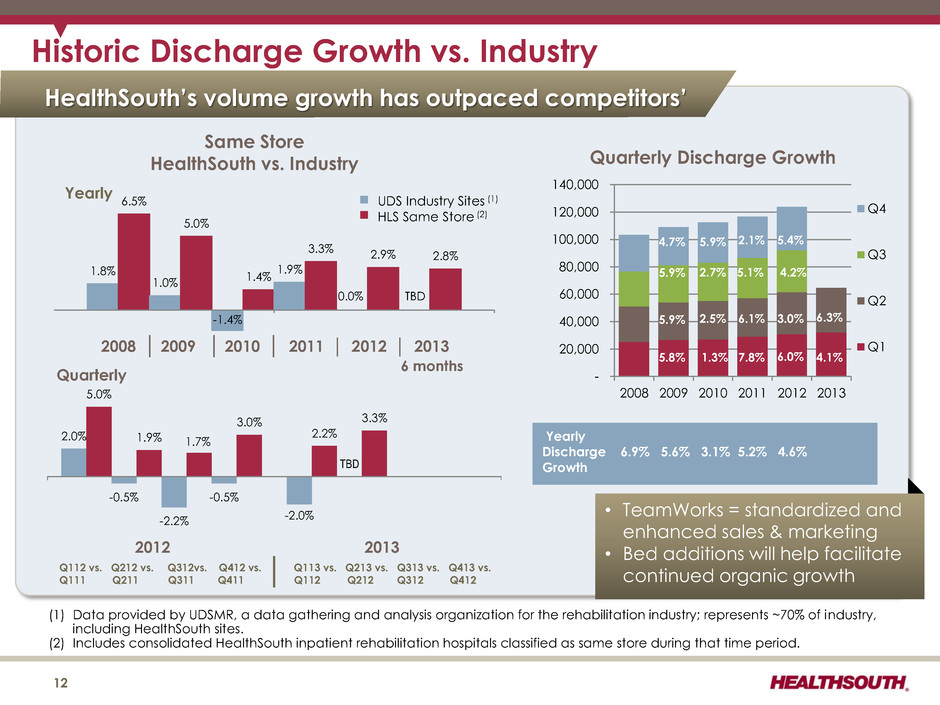
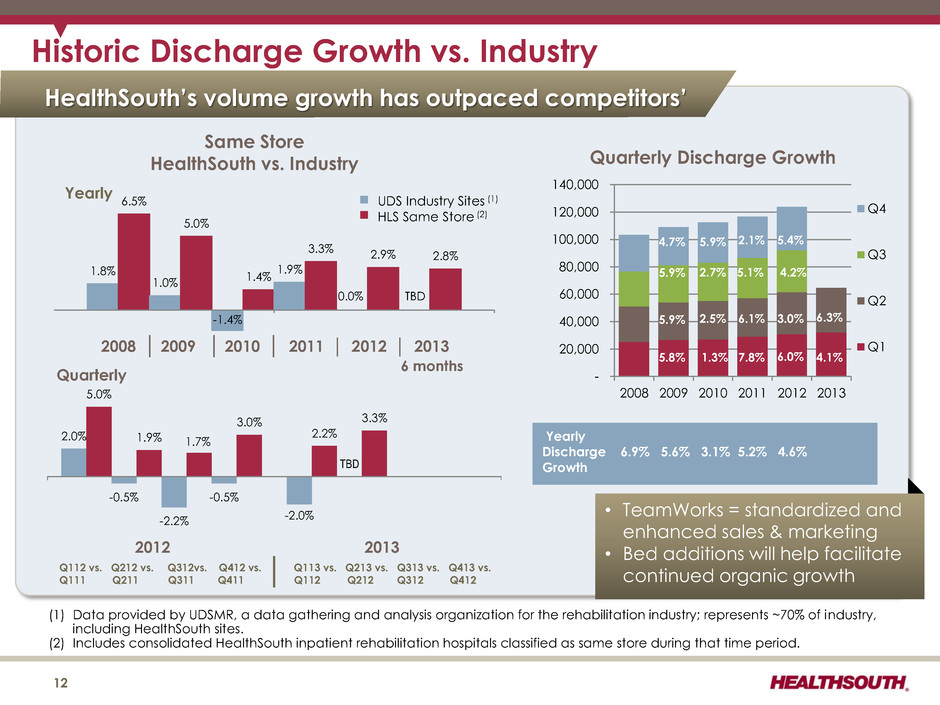
HealthSouth’s volume growth has outpaced competitors’ (1) Data provided by UDSMR, a data gathering and analysis organization for the rehabilitation industry; represents ~70% of industry, including HealthSouth sites. (2) Includes consolidated HealthSouth inpatient rehabilitation hospitals classified as same store during that time period. Historic Discharge Growth vs. Industry - 20,000 40,000 60,000 80,000 100,000 120,000 140,000 2008 2009 2010 2011 2012 2013 Q4 Q3 Q2 Q1 12 2.0% 5.0% -0.5% 1.9% -2.2% 1.7% -0.5% 3.0% -2.0% 2.2% TBD 3.3% Quarterly • TeamWorks = standardized and enhanced sales & marketing • Bed additions will help facilitate continued organic growth Yearly Discharge 6.9% 5.6% 3.1% 5.2% 4.6% Growth Q112 vs. Q212 vs. Q312vs. Q412 vs. Q113 vs. Q213 vs. Q313 vs. Q413 vs. Q111 Q211 Q311 Q411 Q112 Q212 Q312 Q412 Quarterly Discharge Growth Same Store HealthSouth vs. Industry UDS Industry Sites (1) HLS Same Store (2) 1.8% 6.5% 1.0% 5.0% 1.4% 1.9% 3.3% 0.0% 2.9% 2.8% Yearly 2012 2013 2008 │ 2009 │ 2010 │ 2011 │ 2012 │ 2013 6 months -1.4% 4.1% TBD 6.3% 6.0% 7.8% 1.3% 5.8% 3.0% 6.1% 2.5% 5.9% 4.2% 5.1% 2.7% 5.9% 5.4% 2.1% 5.9% 4.7%
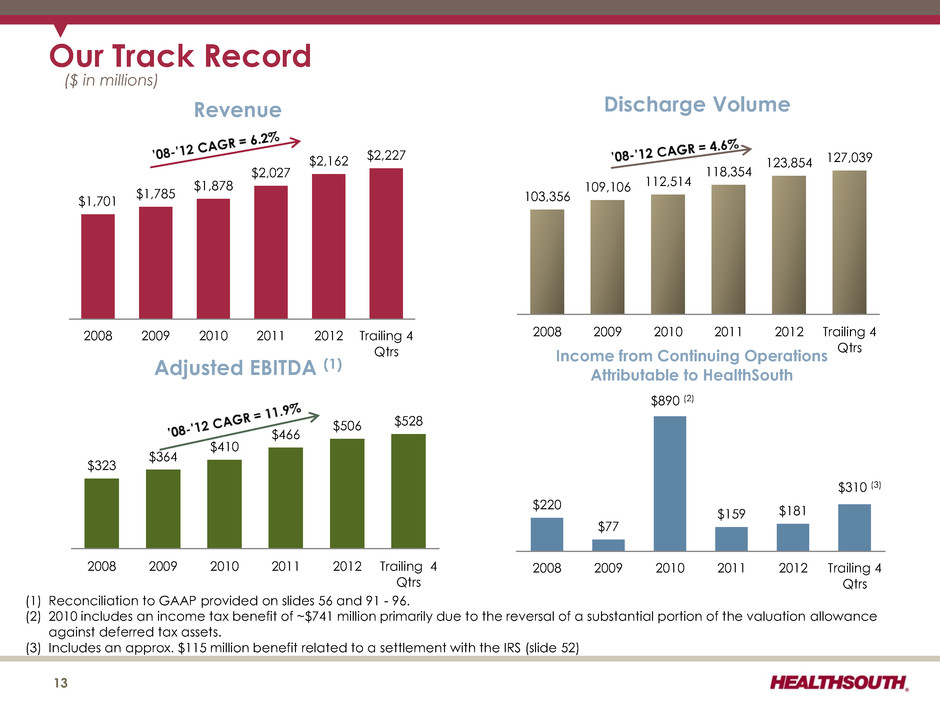
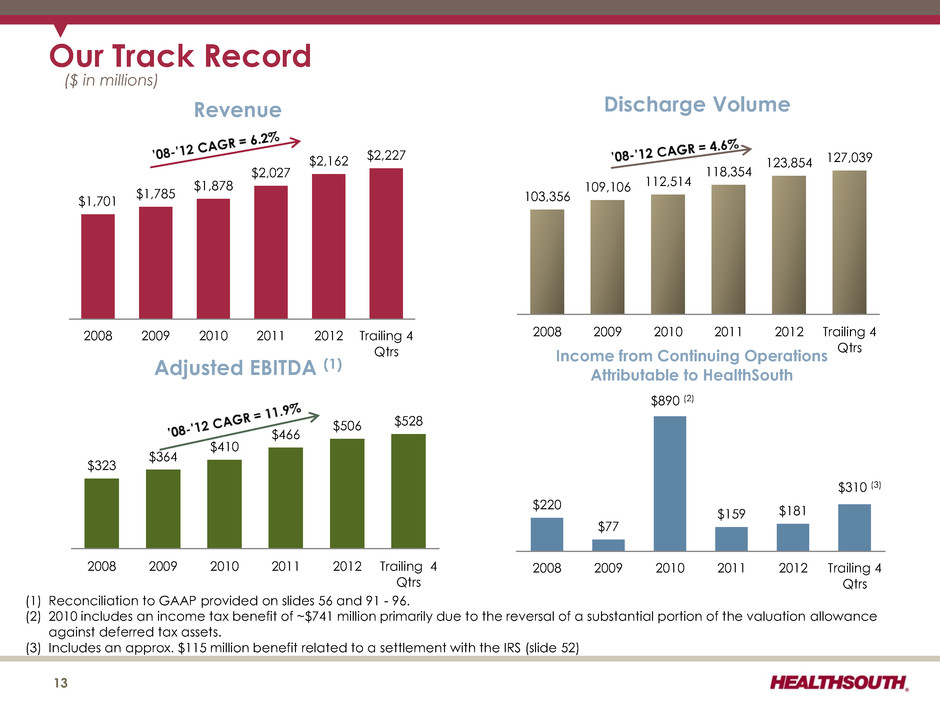
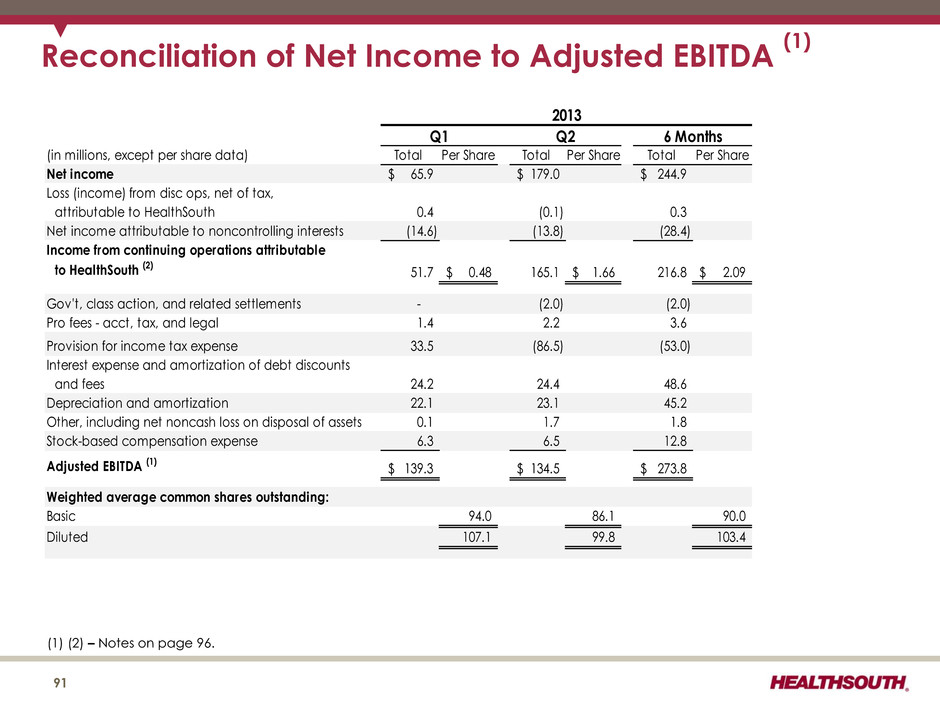
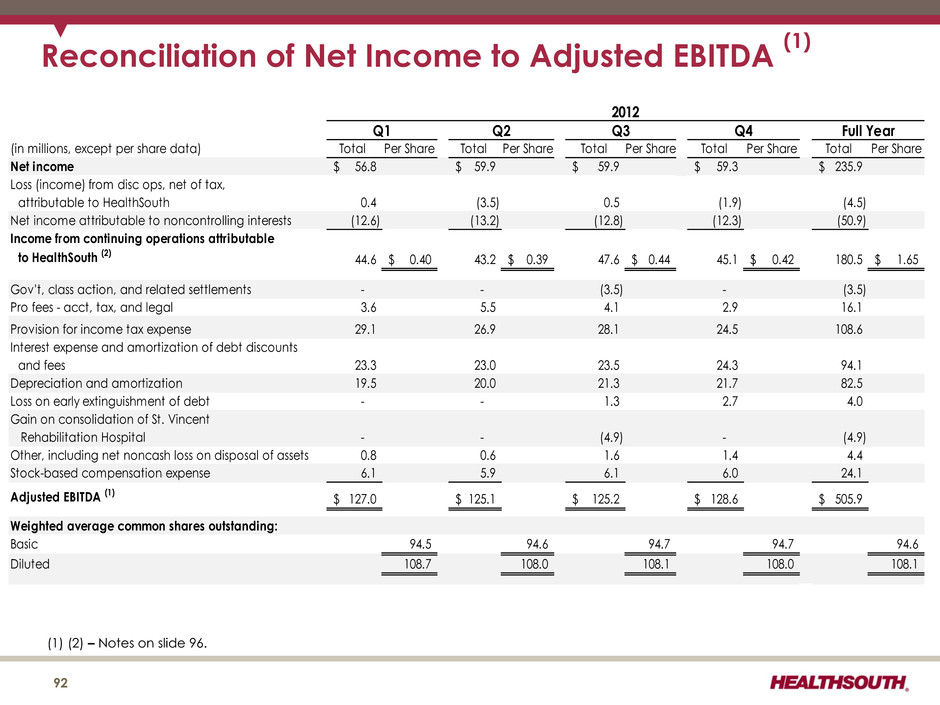
$1,701 $1,785 $1,878 $2,027 $2,162 $2,227 2008 2009 2010 2011 2012 Trailing 4 Qtrs Revenue Our Track Record ($ in millions) (1) Reconciliation to GAAP provided on slides 56 and 91 - 96. (2) 2010 includes an income tax benefit of ~$741 million primarily due to the reversal of a substantial portion of the valuation allowance against deferred tax assets. (3) Includes an approx. $115 million benefit related to a settlement with the IRS (slide 52) $323 $364 $410 $466 $506 $528 2008 2009 2010 2011 2012 Trailing 4 Qtrs Adjusted EBITDA (1) 103,356 109,106 112,514 118,354 123,854 127,039 2008 2009 2010 2011 2012 Trailing 4 Qtrs Discharge Volume 13 $220 $77 $890 (2) $159 $181 $310 (3) 2008 2009 2010 2011 2012 Trailing 4 Qtrs Income from Continuing Operations Attributable to HealthSouth
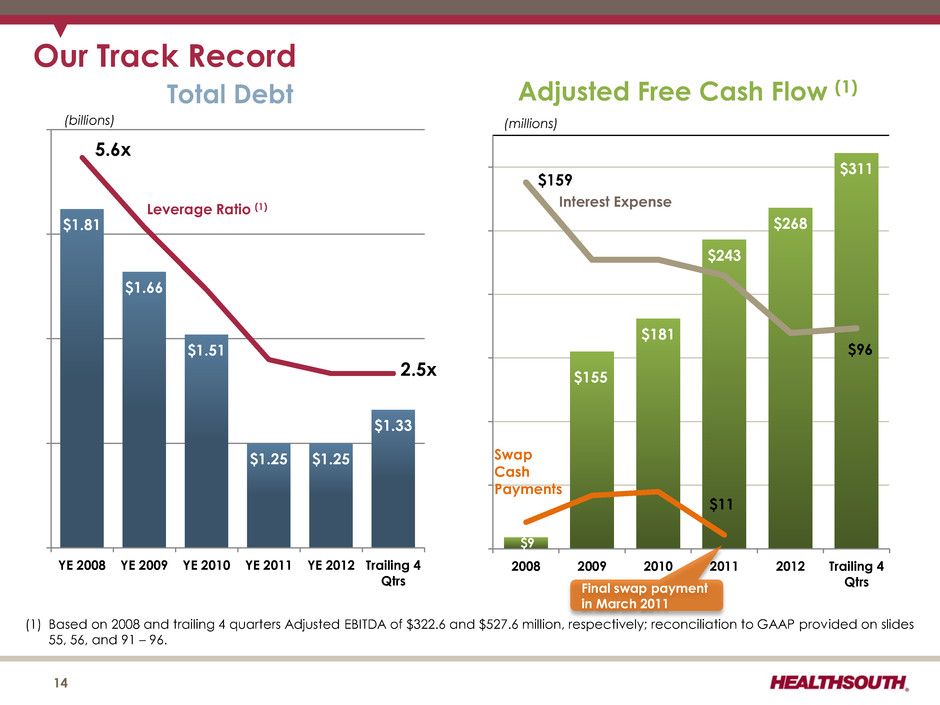
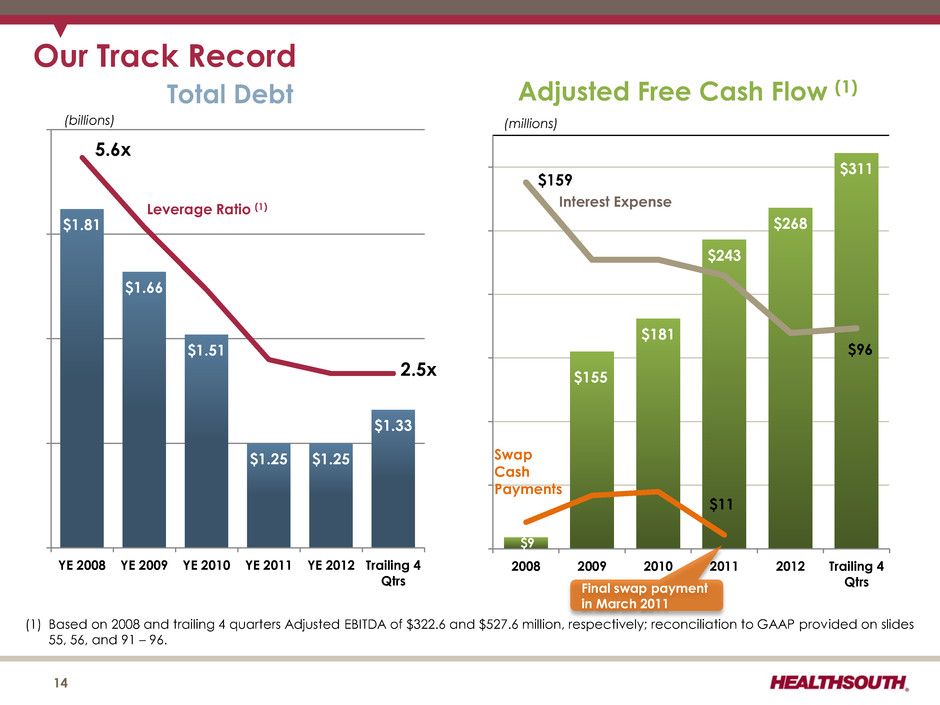
$1.81 $1.66 $1.51 $1.25 $1.25 $1.33 0 1 2 3 4 5 6 $1.00 $1.25 $1.50 $1.75 $2.00 YE 2008 YE 2009 YE 2010 YE 2011 YE 2012 Trailing 4 Qtrs Total Debt 5.6x 2.5x Our Track Record 14 Leverage Ratio (1) (billions) $9 $155 $181 $243 $268 $311 $0 $20 $40 $60 $80 $100 $120 $140 $160 $180 2008 2009 2010 2011 2012 Trailing 4 Qtrs Adjusted Free Cash Flow (1) (millions) Swap Cash Payments (1) Based on 2008 and trailing 4 quarters Adjusted EBITDA of $322.6 and $527.6 million, respectively; reconciliation to GAAP provided on slides 55, 56, and 91 – 96. Interest Expense $159 $96 $11 Final swap payment in March 2011
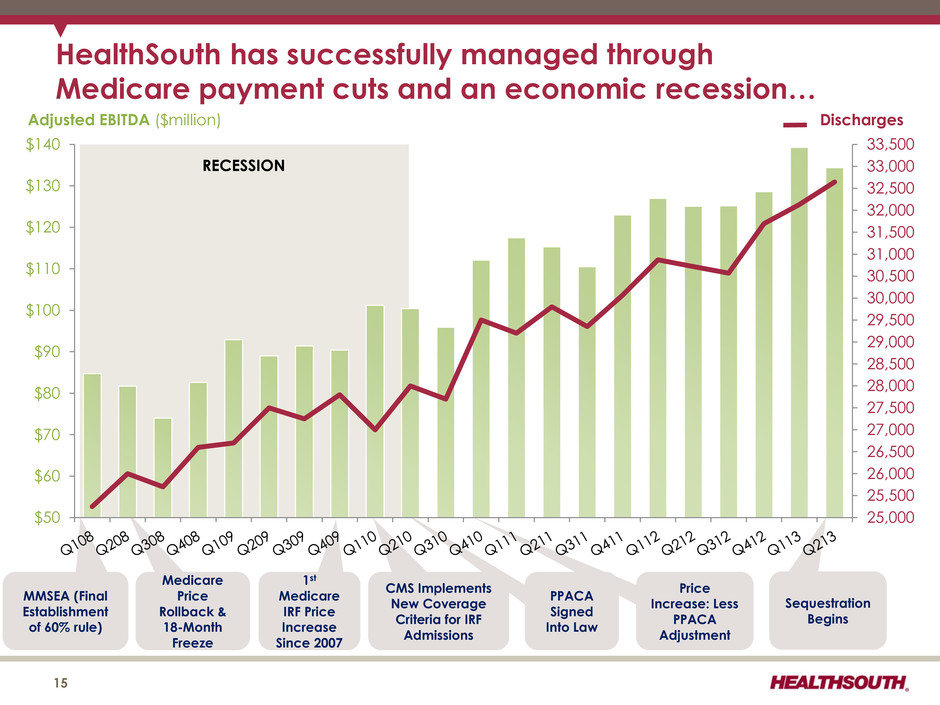
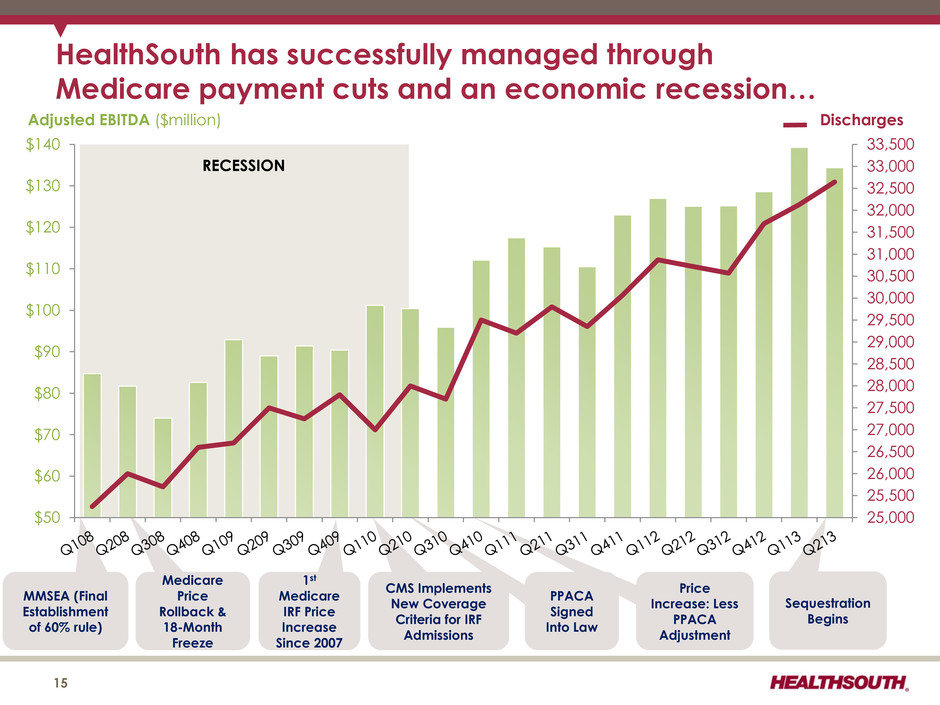
Sequestration Begins PPACA Signed Into Law MMSEA (Final Establishment of 60% rule) Medicare Price Rollback & 18-Month Freeze 1st Medicare IRF Price Increase Since 2007 CMS Implements New Coverage Criteria for IRF Admissions Price Increase: Less PPACA Adjustment RECESSION 25,000 25,500 26,000 26,500 27,000 27,500 28,000 28,500 29,000 29,500 30,000 30,500 31,000 31,500 32,000 32,500 33,000 33,500 $50 $60 $70 $80 $90 $100 $110 $120 $130 $140 HealthSouth has successfully managed through Medicare payment cuts and an economic recession… 15 Adjusted EBITDA ($million) Discharges
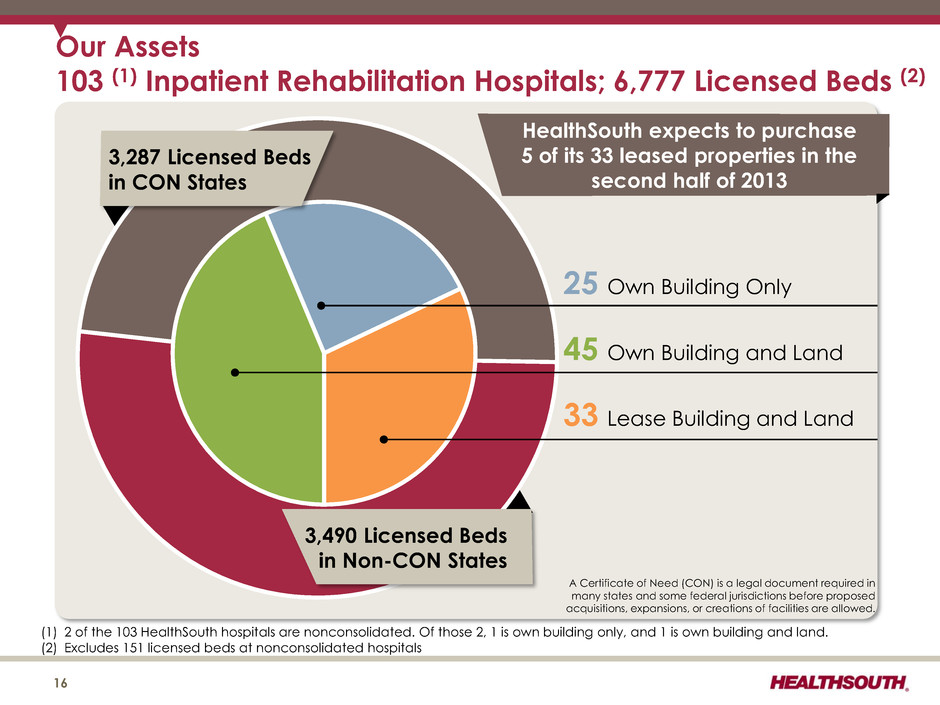
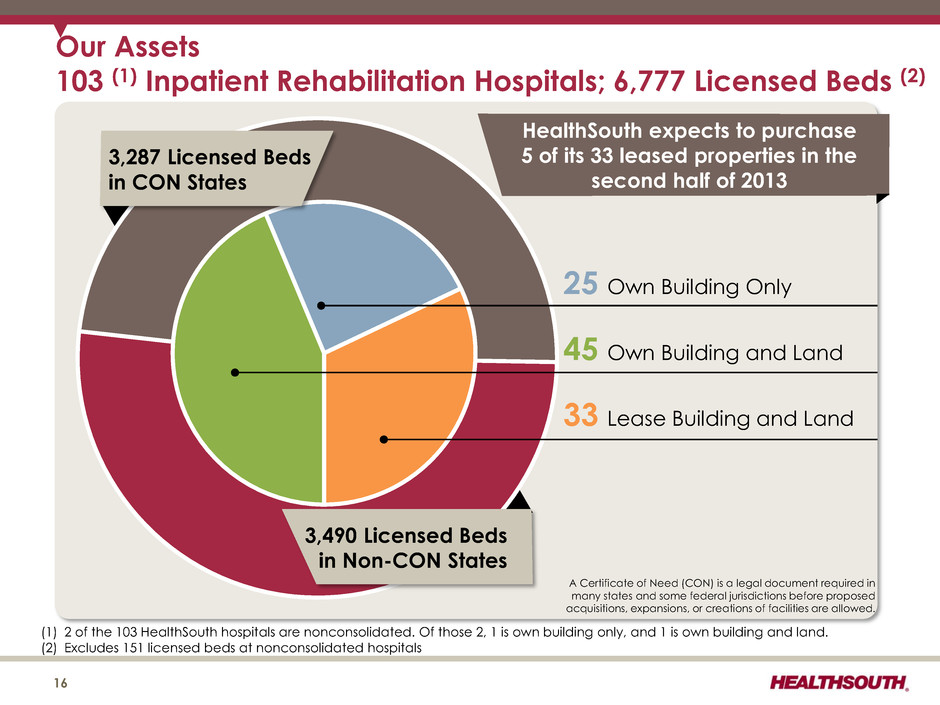
16 3,287 Licensed Beds in CON States Our Assets 103 (1) Inpatient Rehabilitation Hospitals; 6,777 Licensed Beds (2) 3,490 Licensed Beds in Non-CON States 25 Own Building Only 45 Own Building and Land 33 Lease Building and Land A Certificate of Need (CON) is a legal document required in many states and some federal jurisdictions before proposed acquisitions, expansions, or creations of facilities are allowed. (1) 2 of the 103 HealthSouth hospitals are nonconsolidated. Of those 2, 1 is own building only, and 1 is own building and land. (2) Excludes 151 licensed beds at nonconsolidated hospitals HealthSouth expects to purchase 5 of its 33 leased properties in the second half of 2013
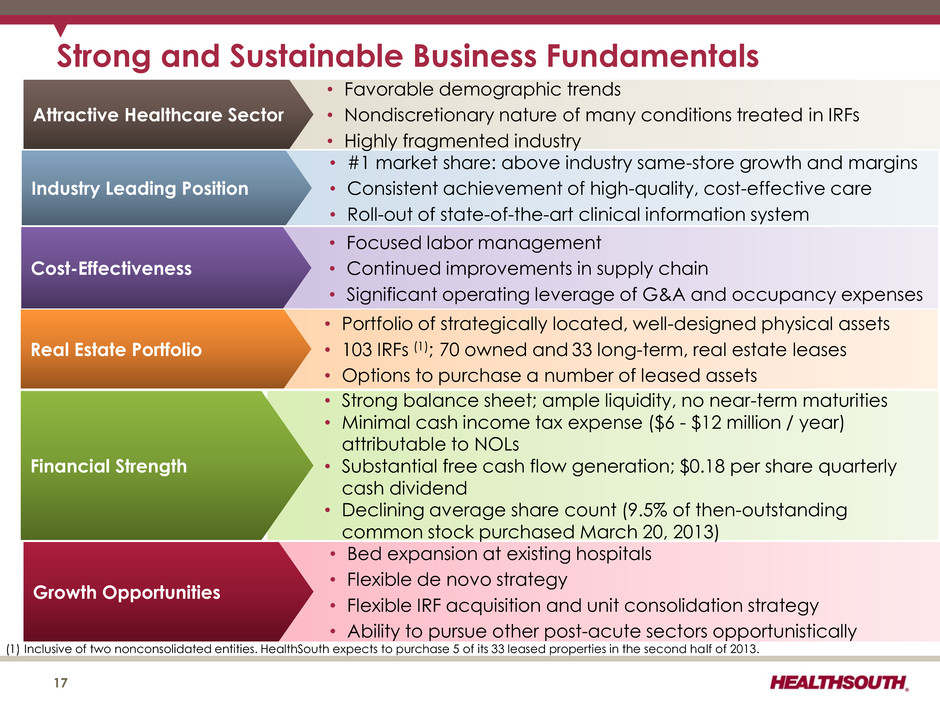
Strong and Sustainable Business Fundamentals • Bed expansion at existing hospitals • Flexible de novo strategy • Flexible IRF acquisition and unit consolidation strategy • Ability to pursue other post-acute sectors opportunistically Growth Opportunities • Strong balance sheet; ample liquidity, no near-term maturities • Minimal cash income tax expense ($6 - $12 million / year) attributable to NOLs • Substantial free cash flow generation; $0.18 per share quarterly cash dividend • Declining average share count (9.5% of then-outstanding common stock purchased March 20, 2013) Financial Strength • #1 market share: above industry same-store growth and margins • Consistent achievement of high-quality, cost-effective care • Roll-out of state-of-the-art clinical information system Industry Leading Position • Favorable demographic trends • Nondiscretionary nature of many conditions treated in IRFs • Highly fragmented industry Attractive Healthcare Sector 17 • Focused labor management • Continued improvements in supply chain • Significant operating leverage of G&A and occupancy expenses Cost-Effectiveness • Portfolio of strategically located, well-designed physical assets • 103 IRFs (1); 70 owned and 33 long-term, real estate leases • Options to purchase a number of leased assets Real Estate Portfolio (1) Inclusive of two nonconsolidated entities. HealthSouth expects to purchase 5 of its 33 leased properties in the second half of 2013.
Industry Structure 18
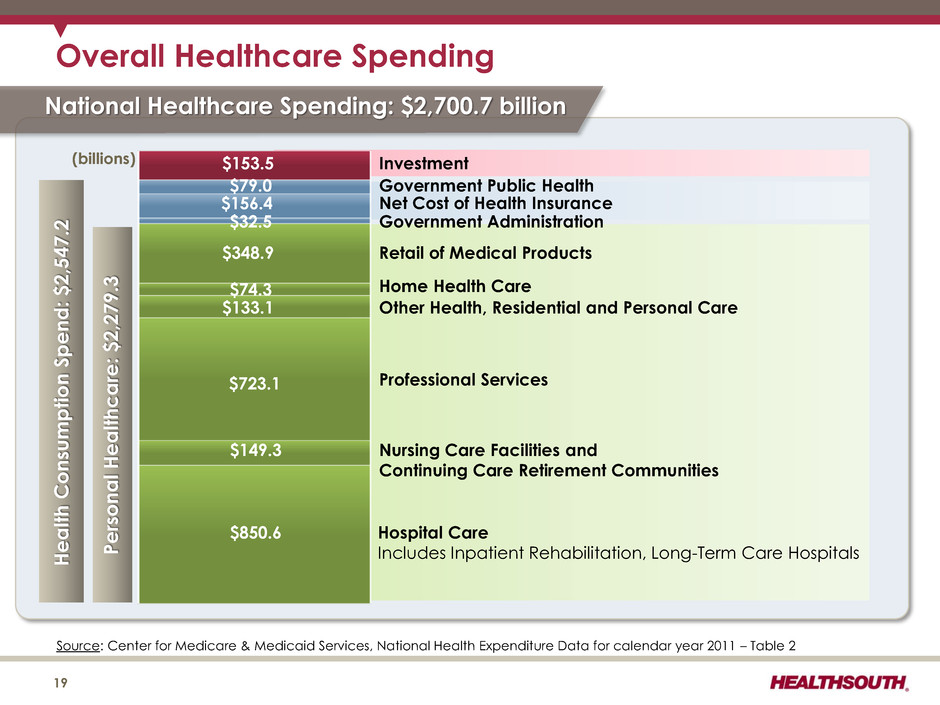
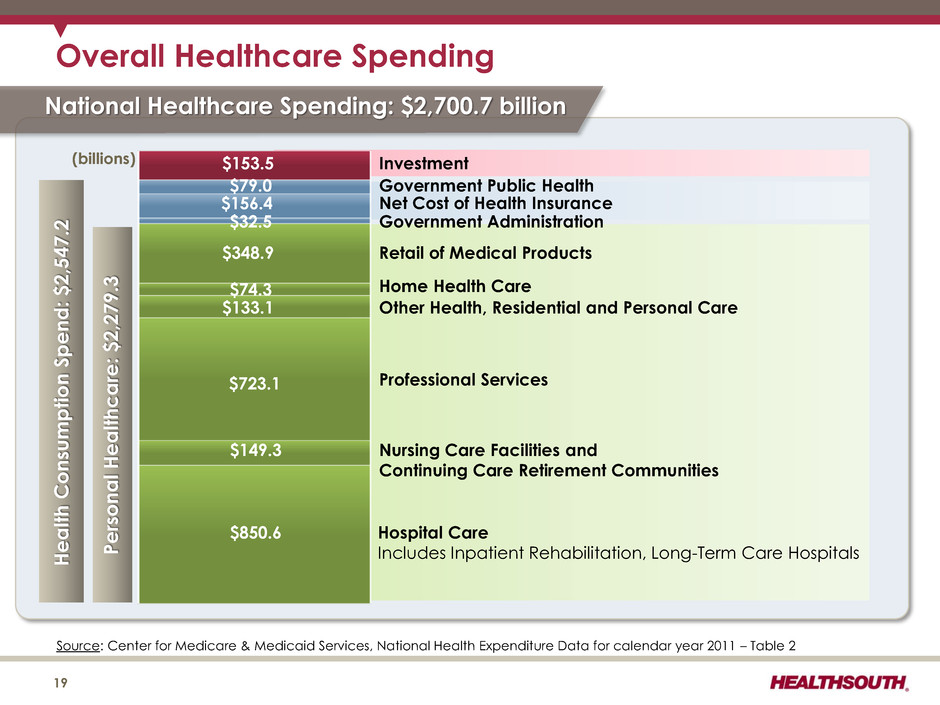
Person a l He a lt hc a re: $2,279. 3 Source: Center for Medicare & Medicaid Services, National Health Expenditure Data for calendar year 2011 – Table 2 Overall Healthcare Spending Hospital Care Includes Inpatient Rehabilitation, Long-Term Care Hospitals $850.6 $149.3 $723.1 $133.1 $74.3 $348.9 Nursing Care Facilities and Continuing Care Retirement Communities He a lt h C onsu m p tion S p en d : $2,547.2 Professional Services Other Health, Residential and Personal Care Home Health Care Retail of Medical Products $32.5 Government Administration $156.4 Net Cost of Health Insurance $79.0 Government Public Health $153.5 Investment National Healthcare Spending: $2,700.7 billion 19 (billions)
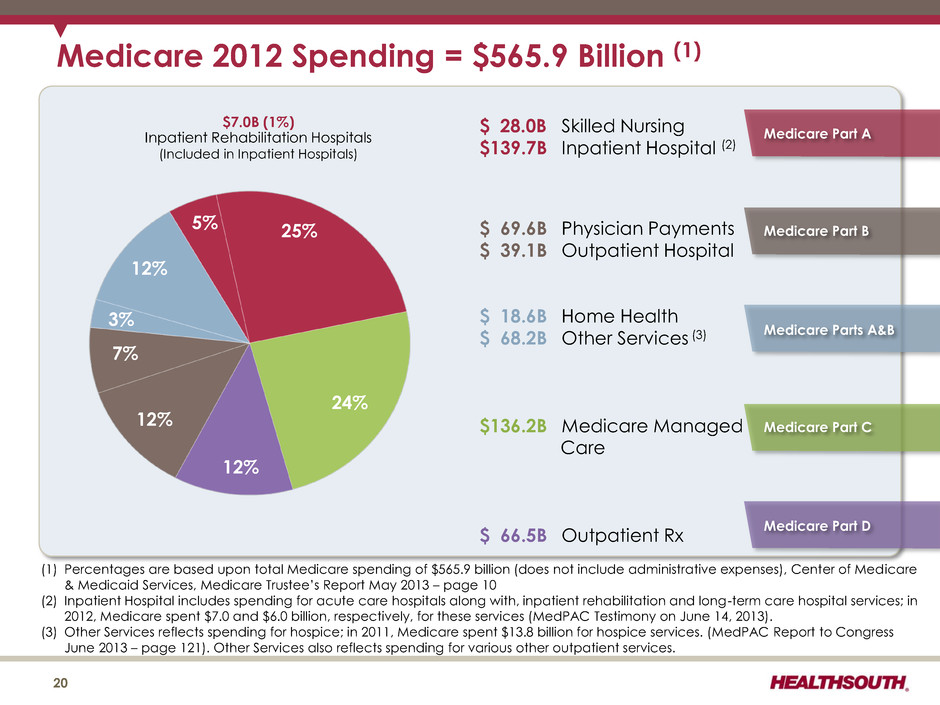
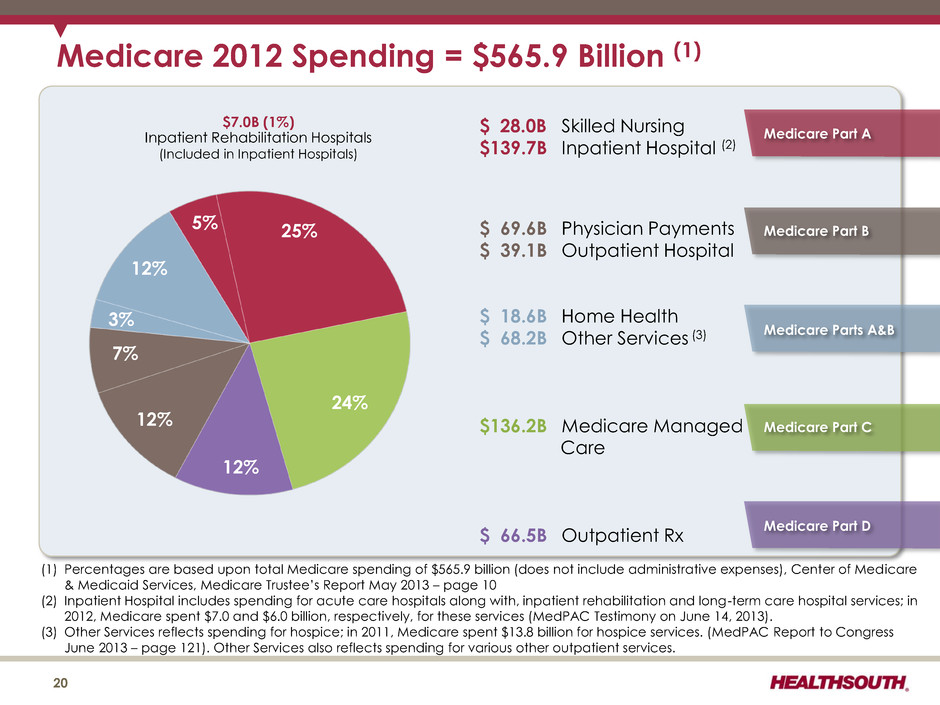
Medicare 2012 Spending = $565.9 Billion (1) (1) Percentages are based upon total Medicare spending of $565.9 billion (does not include administrative expenses), Center of Medicare & Medicaid Services, Medicare Trustee’s Report May 2013 – page 10 (2) Inpatient Hospital includes spending for acute care hospitals along with, inpatient rehabilitation and long-term care hospital services; in 2012, Medicare spent $7.0 and $6.0 billion, respectively, for these services (MedPAC Testimony on June 14, 2013). (3) Other Services reflects spending for hospice; in 2011, Medicare spent $13.8 billion for hospice services. (MedPAC Report to Congress June 2013 – page 121). Other Services also reflects spending for various other outpatient services. $ 28.0B Skilled Nursing $ 139.7B Inpatient Hospital (2) $ 69.6B Physician Payments $ 39.1B Outpatient Hospital $ 18.6B Home Health $ 68.2B Other Services (3) $ 136.2B Medicare Managed Care $ 66.5B Outpatient Rx 5% 25% 24% 12% 12% 7% 3% 12% $7.0B (1%) Inpatient Rehabilitation Hospitals (Included in Inpatient Hospitals) Medicare Part B Medicare Part C Medicare Parts A&B Medicare Part D Medicare Part A 20
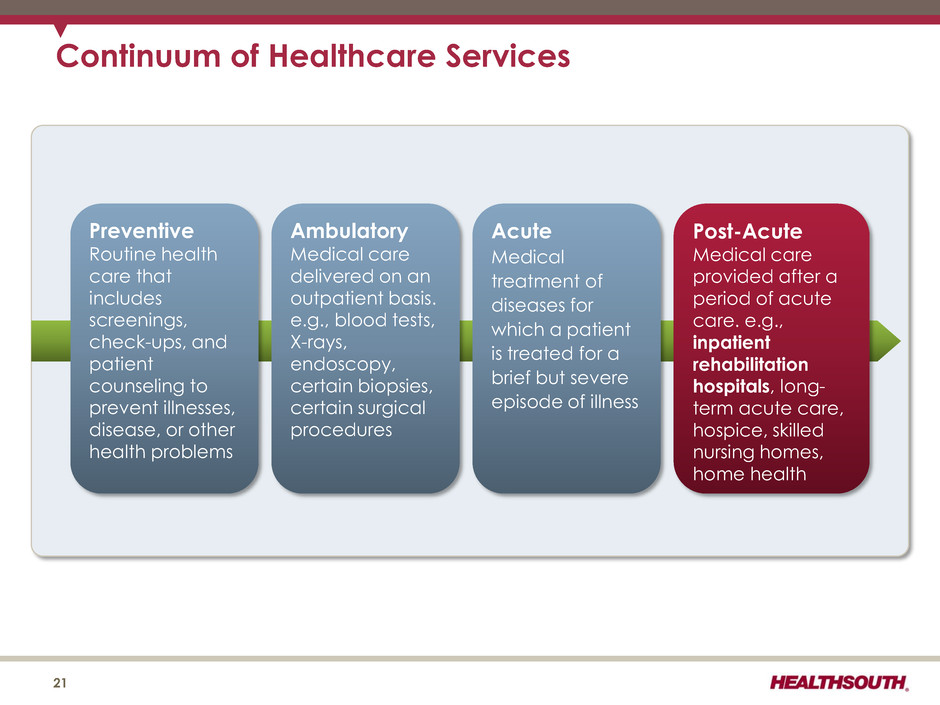
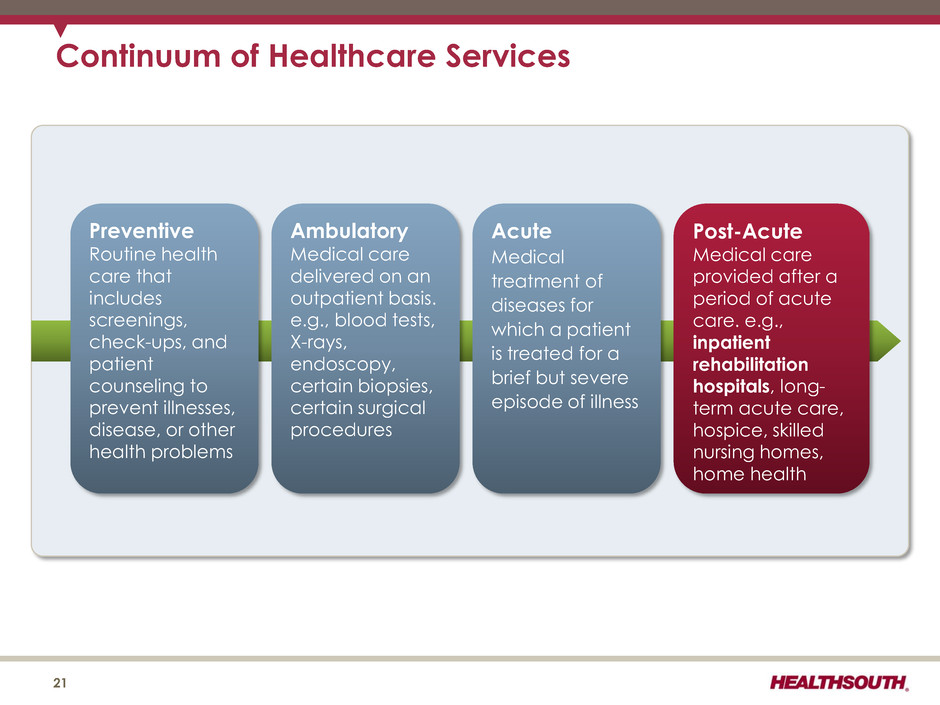
Preventive Routine health care that includes screenings, check-ups, and patient counseling to prevent illnesses, disease, or other health problems Acute Medical treatment of diseases for which a patient is treated for a brief but severe episode of illness Ambulatory Medical care delivered on an outpatient basis. e.g., blood tests, X-rays, endoscopy, certain biopsies, certain surgical procedures Post-Acute Medical care provided after a period of acute care. e.g., inpatient rehabilitation hospitals, long- term acute care, hospice, skilled nursing homes, home health Continuum of Healthcare Services 21
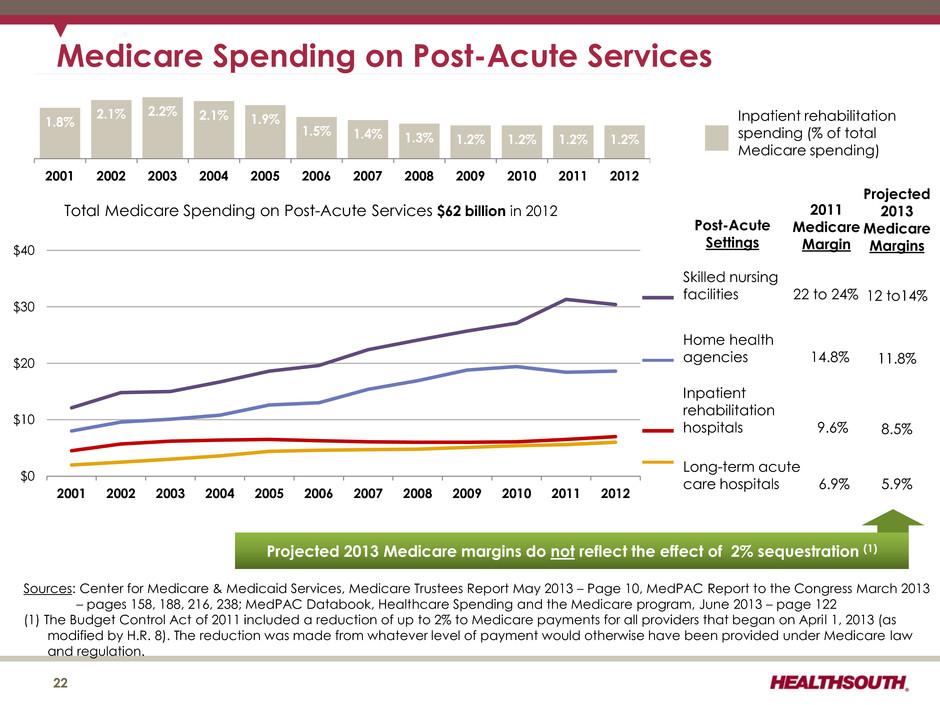
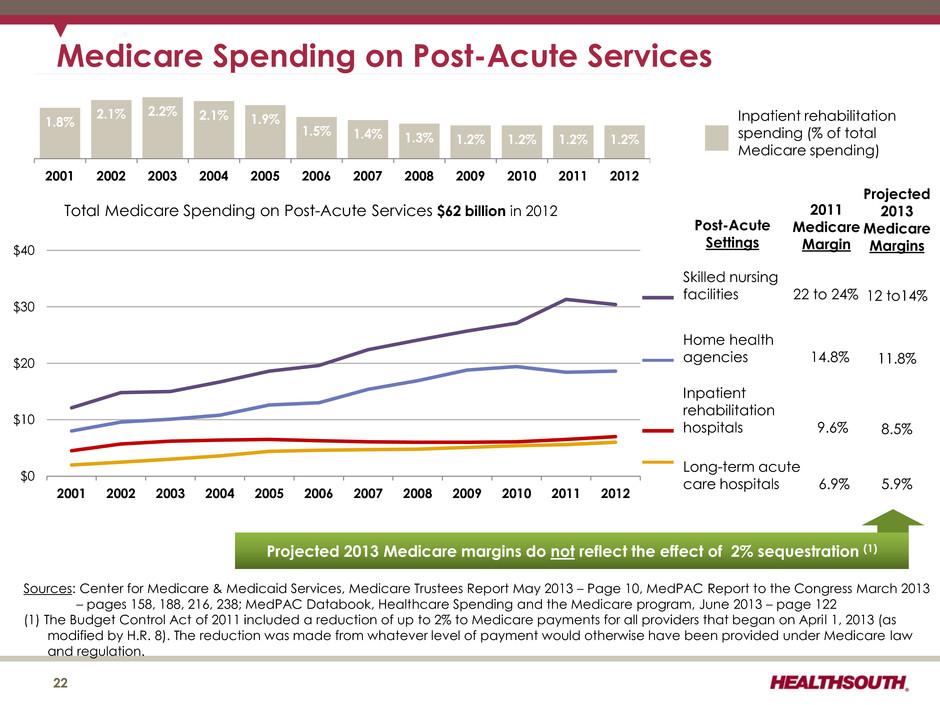
$0 $10 $20 $30 $40 2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012 Total Medicare Spending on Post-Acute Services $62 billion in 2012 Sources: Center for Medicare & Medicaid Services, Medicare Trustees Report May 2013 – Page 10, MedPAC Report to the Congress March 2013 – pages 158, 188, 216, 238; MedPAC Databook, Healthcare Spending and the Medicare program, June 2013 – page 122 (1) The Budget Control Act of 2011 included a reduction of up to 2% to Medicare payments for all providers that began on April 1, 2013 (as modified by H.R. 8). The reduction was made from whatever level of payment would otherwise have been provided under Medicare law and regulation. Medicare Spending on Post-Acute Services Skilled nursing facilities 22 to 24% Home health agencies 14.8% Inpatient rehabilitation hospitals 9.6% Long-term acute care hospitals 6.9% 22 2011 Medicare Margin Post-Acute Settings Inpatient rehabilitation spending (% of total Medicare spending) 1.8% 2.1% 2.2% 2.1% 1.9% 1.5% 1.4% 1.3% 1.2% 1.2% 1.2% 1.2% 2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012 Projected 2013 Medicare Margins 12 to14% 11.8% 8.5% 5.9% Projected 2013 Medicare margins do not reflect the effect of 2% sequestration (1)
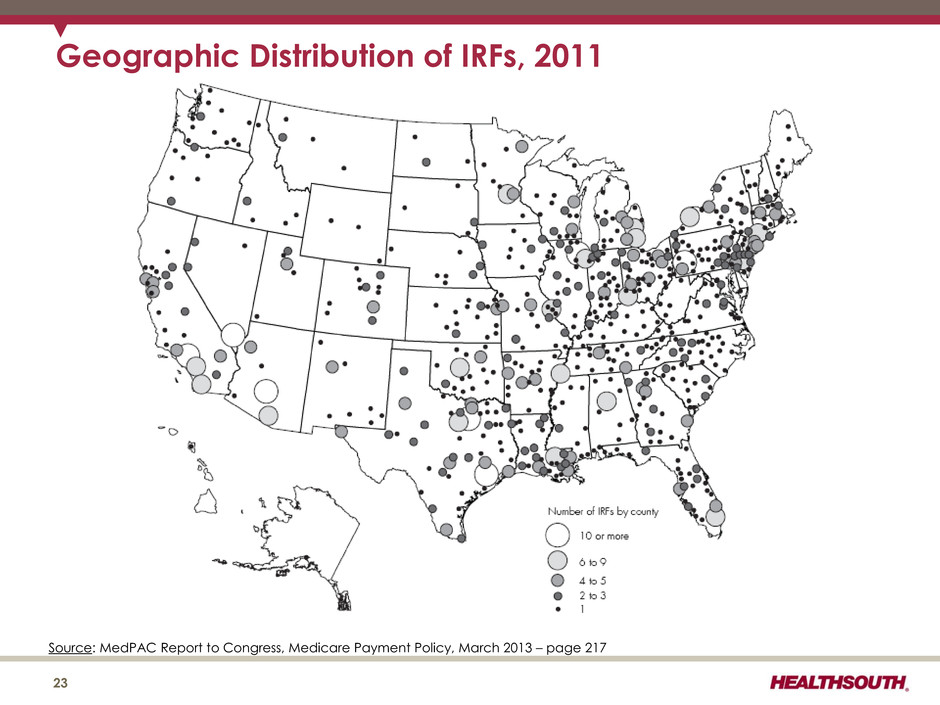
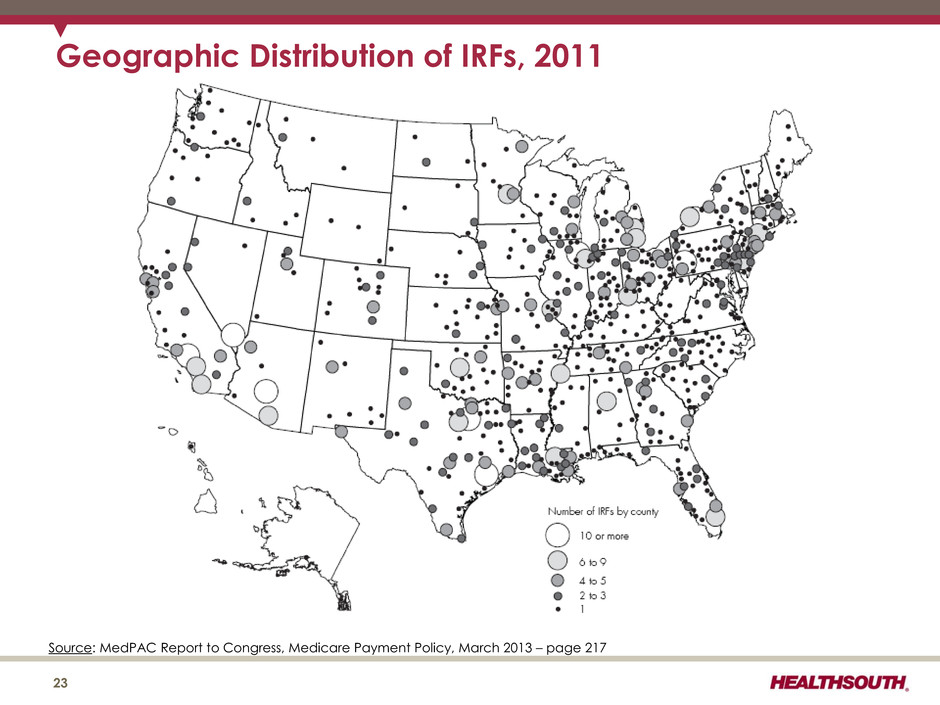
Geographic Distribution of IRFs, 2011 23 Source: MedPAC Report to Congress, Medicare Payment Policy, March 2013 – page 217
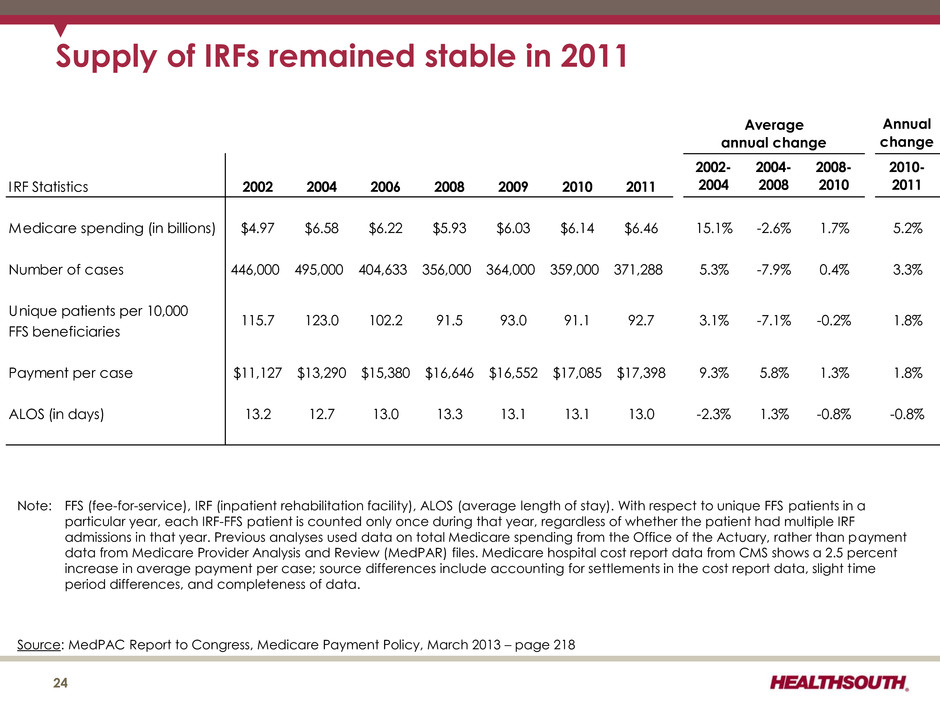
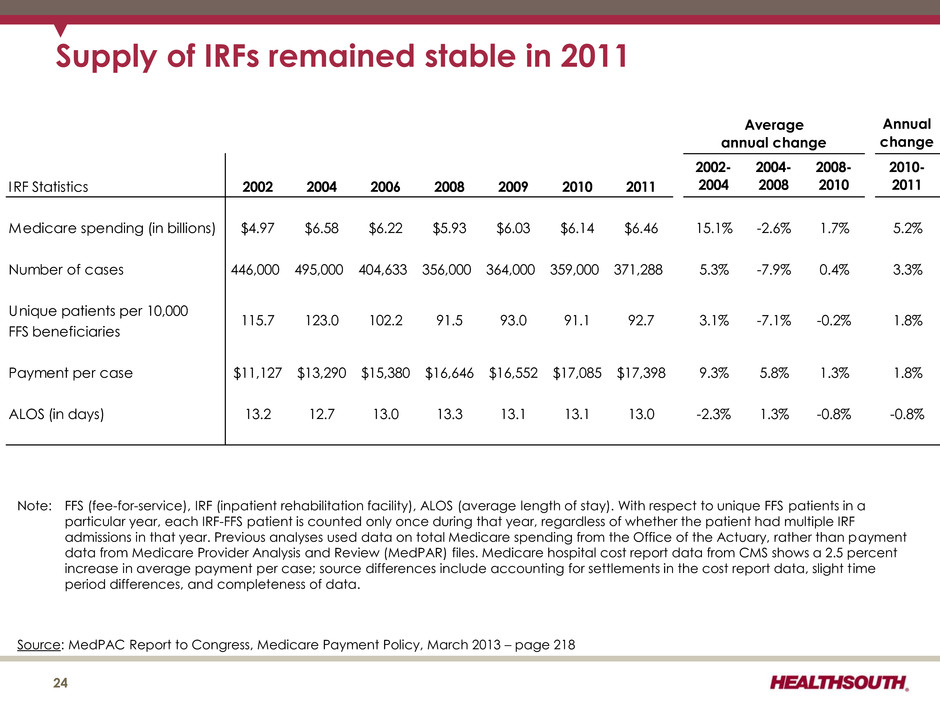
Supply of IRFs remained stable in 2011 24 Source: MedPAC Report to Congress, Medicare Payment Policy, March 2013 – page 218 Annual change IRF Statistics 2002 2004 2006 2008 2009 2010 2011 2002- 2004 2004- 2008 2008- 2010 2010- 2011 Medicare spending (in billions) $4.97 $6.58 $6.22 $5.93 $6.03 $6.14 $6.46 15.1% -2.6% 1.7% 5.2% Number of cases 446,000 495,000 404,633 356,000 364,000 359,000 371,288 5.3% -7.9% 0.4% 3.3% Unique patients per 10,000 FFS beneficiaries Payment per case $11,127 $13,290 $15,380 $16,646 $16,552 $17,085 $17,398 9.3% 5.8% 1.3% 1.8% ALOS (in days) 13.2 12.7 13.0 13.3 13.1 13.1 13.0 -2.3% 1.3% -0.8% -0.8% Average annual change 91.1102.2 1.8%115.7 123.0 91.5 93.0 92.7 3.1% -7.1% -0.2% Note: FFS (fee-for-service), IRF (inpatient rehabilitation facility), ALOS (average length of stay). With respect to unique FFS patients in a particular year, each IRF-FFS patient is counted only once during that year, regardless of whether the patient had multiple IRF admissions in that year. Previous analyses used data on total Medicare spending from the Office of the Actuary, rather than payment data from Medicare Provider Analysis and Review (MedPAR) files. Medicare hospital cost report data from CMS shows a 2.5 percent increase in average payment per case; source differences include accounting for settlements in the cost report data, slight time period differences, and completeness of data.
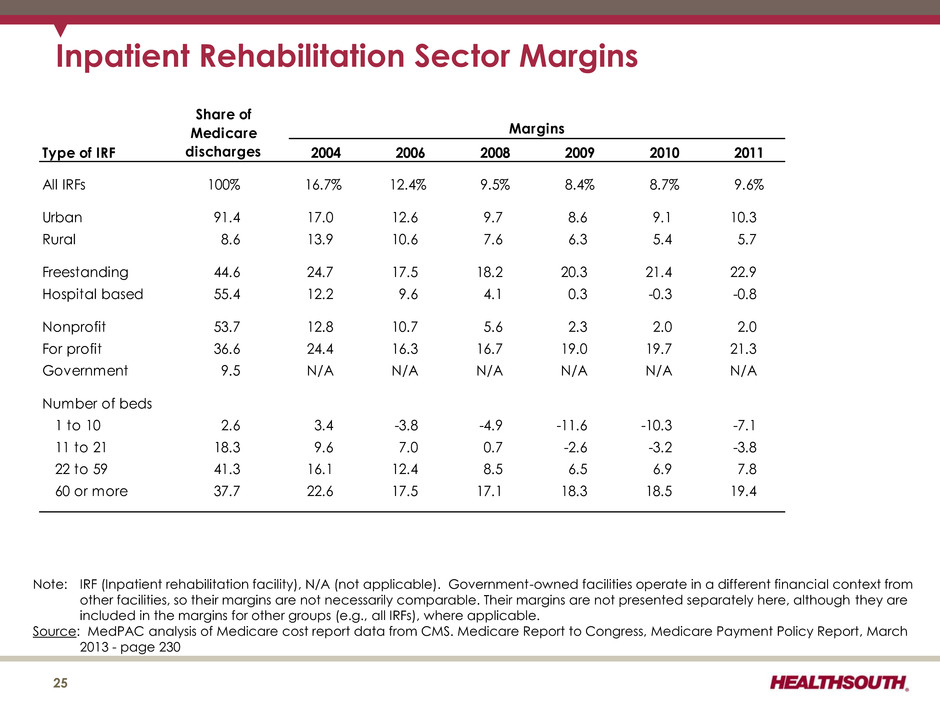
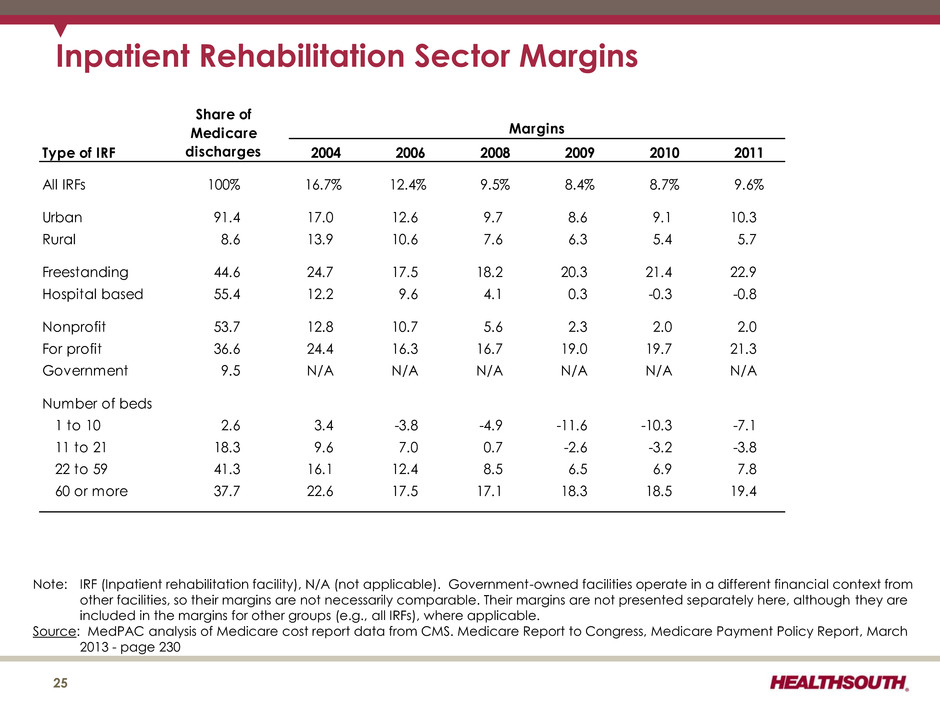
25 Inpatient Rehabilitation Sector Margins Type of IRF 2004 2006 2008 2009 2010 2011 All IRFs 100% 16.7% 12.4% 9.5% 8.4% 8.7% 9.6% Urban 91.4 17.0 12.6 9.7 8.6 9.1 10.3 Rural 8.6 13.9 10.6 7.6 6.3 5.4 5.7 Freestanding 44.6 24.7 17.5 18.2 20.3 21.4 22.9 Hospital based 55.4 12.2 9.6 4.1 0.3 -0.3 -0.8 Nonprofit 53.7 12.8 10.7 5.6 2.3 2.0 2.0 For profit 36.6 24.4 16.3 16.7 19.0 19.7 21.3 Government 9.5 N/A N/A N/A N/A N/A N/A Number of beds 1 to 10 2.6 3.4 -3.8 -4.9 -11.6 -10.3 -7.1 11 to 21 18.3 9.6 7.0 0.7 -2.6 -3.2 -3.8 22 to 59 41.3 16.1 12.4 8.5 6.5 6.9 7.8 60 or more 37.7 22.6 17.5 17.1 18.3 18.5 19.4 Share of Medicare discharges Margins Note: IRF (Inpatient rehabilitation facility), N/A (not applicable). Government-owned facilities operate in a different financial context from other facilities, so their margins are not necessarily comparable. Their margins are not presented separately here, although they are included in the margins for other groups (e.g., all IRFs), where applicable. Source: MedPAC analysis of Medicare cost report data from CMS. Medicare Report to Congress, Medicare Payment Policy Report, March 2013 - page 230
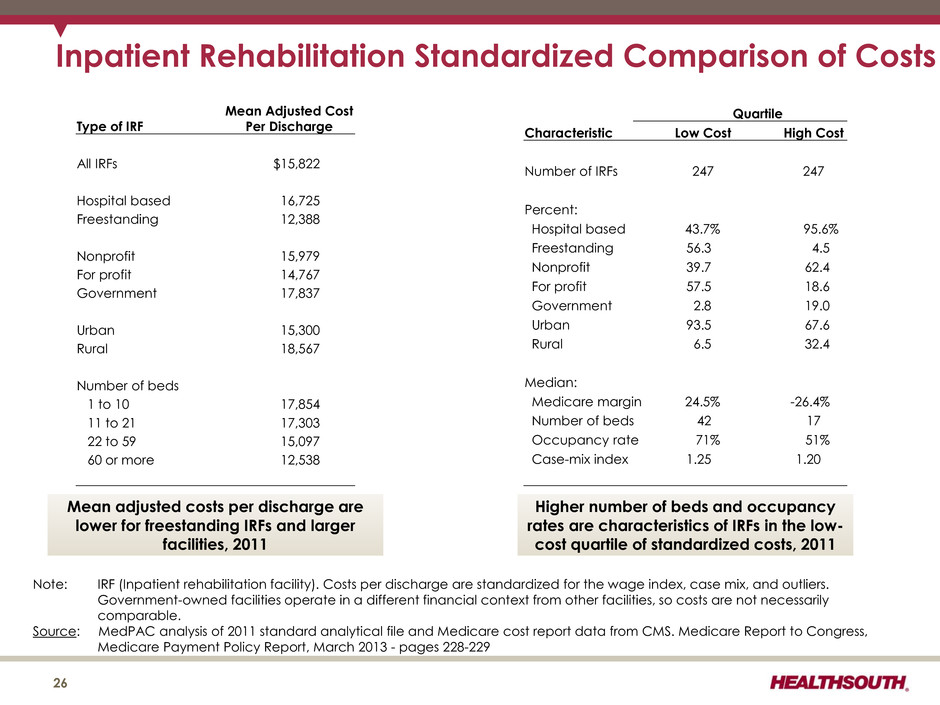
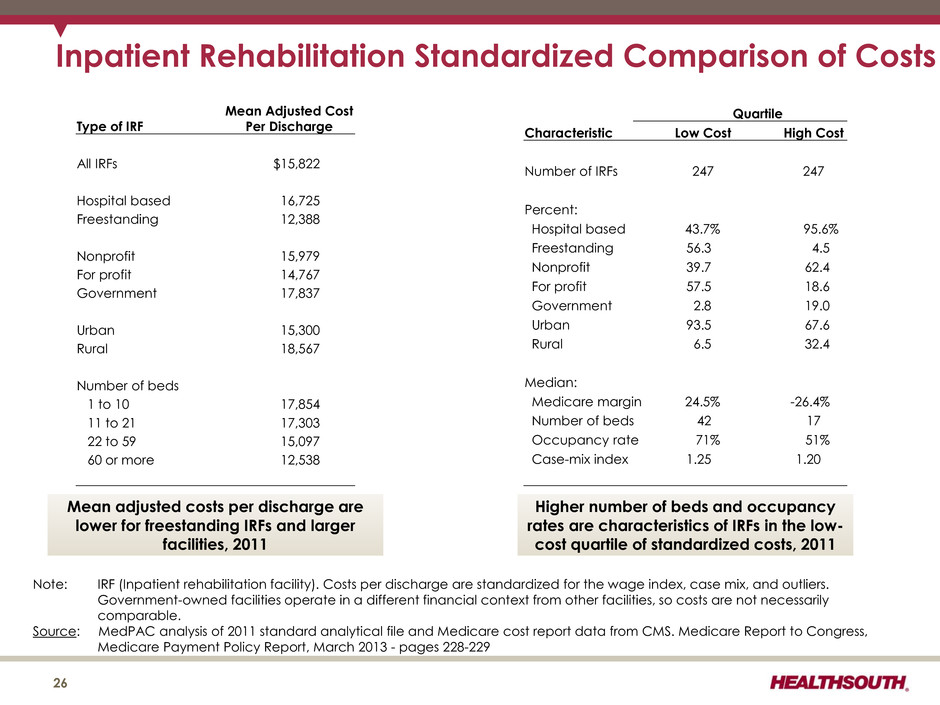
26 Inpatient Rehabilitation Standardized Comparison of Costs Note: IRF (Inpatient rehabilitation facility). Costs per discharge are standardized for the wage index, case mix, and outliers. Government-owned facilities operate in a different financial context from other facilities, so costs are not necessarily comparable. Source: MedPAC analysis of 2011 standard analytical file and Medicare cost report data from CMS. Medicare Report to Congress, Medicare Payment Policy Report, March 2013 - pages 228-229 Mean adjusted costs per discharge are lower for freestanding IRFs and larger facilities, 2011 Higher number of beds and occupancy rates are characteristics of IRFs in the low- cost quartile of standardized costs, 2011 Mean Adjusted Cost Per Discharge Type of IRF All IRFs $15,822 Hospital based 16,725 Freestanding 12,388 Nonprofit 15,979 For profit 14,767 Government 17,837 Urban 15,300 Rural 18,567 Number of beds 1 to 10 17,854 11 to 21 17,303 22 to 59 15,097 60 or more 12,538 Quartile Characteristic Low Cost High Cost Number of IRFs 247 247 Percent: Hospital based 43.7% 95.6% Freestanding 56.3 4.5 Nonprofit 39.7 62.4 For profit 57.5 18.6 Government 2.8 19.0 Urban 93.5 67.6 Rural 6.5 32.4 Median: Medicare margin 24.5% -26.4% Number of beds 42 17 Occupancy rate 71% 51% Case-mix index 1.25 1.20
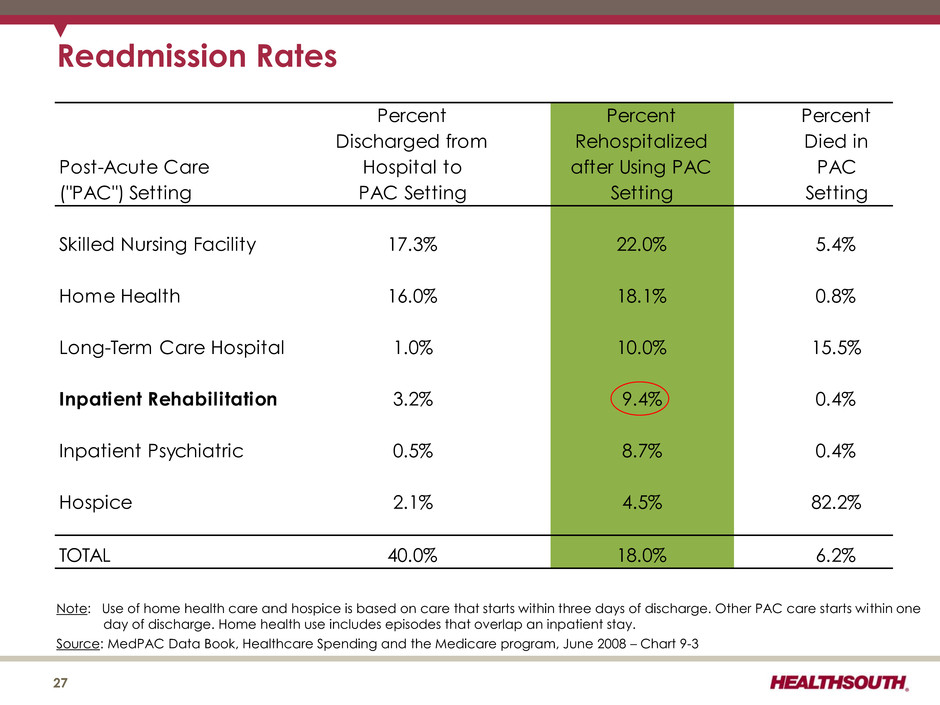
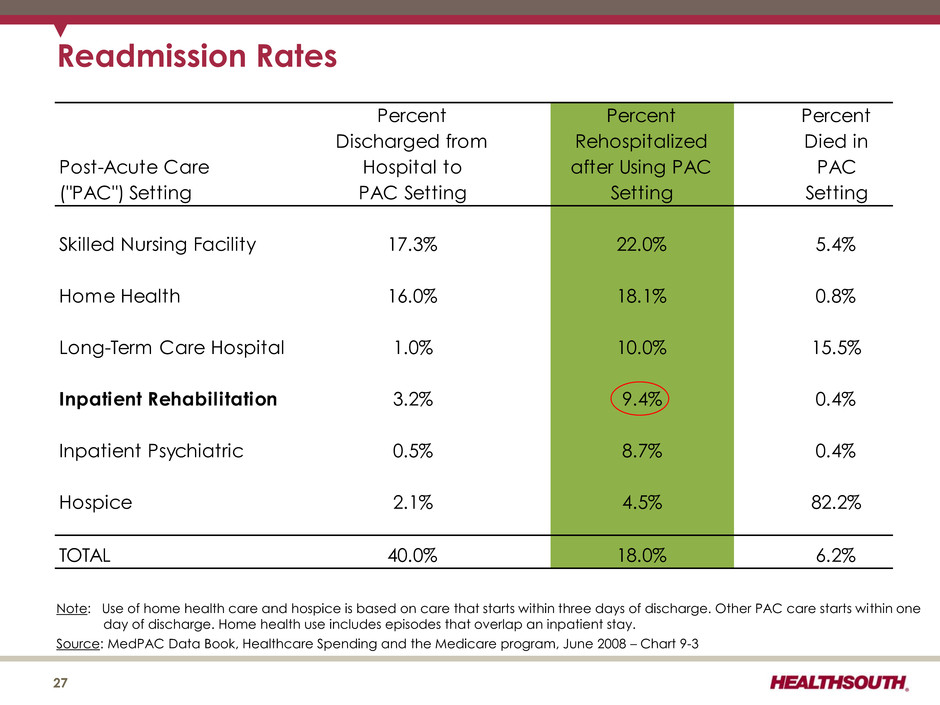
Post-Acute Care ("PAC") Setting Percent Discharged from Hospital to PAC Setting Percent Rehospitalized after Using PAC Setting Percent Died in PAC Setting Skilled Nursing Facility 17.3% 22.0% 5.4% Home Health 16.0% 18.1% 0.8% Long-Term Care Hospital 1.0% 10.0% 15.5% Inpatient Rehabilitation 3.2% 9.4% 0.4% Inpatient Psychiatric 0.5% 8.7% 0.4% Hospice 2.1% 4.5% 82.2% TOTAL 40.0% 18.0% 6.2% Readmission Rates Note: Use of home health care and hospice is based on care that starts within three days of discharge. Other PAC care starts within one day of discharge. Home health use includes episodes that overlap an inpatient stay. Source: MedPAC Data Book, Healthcare Spending and the Medicare program, June 2008 – Chart 9-3 27
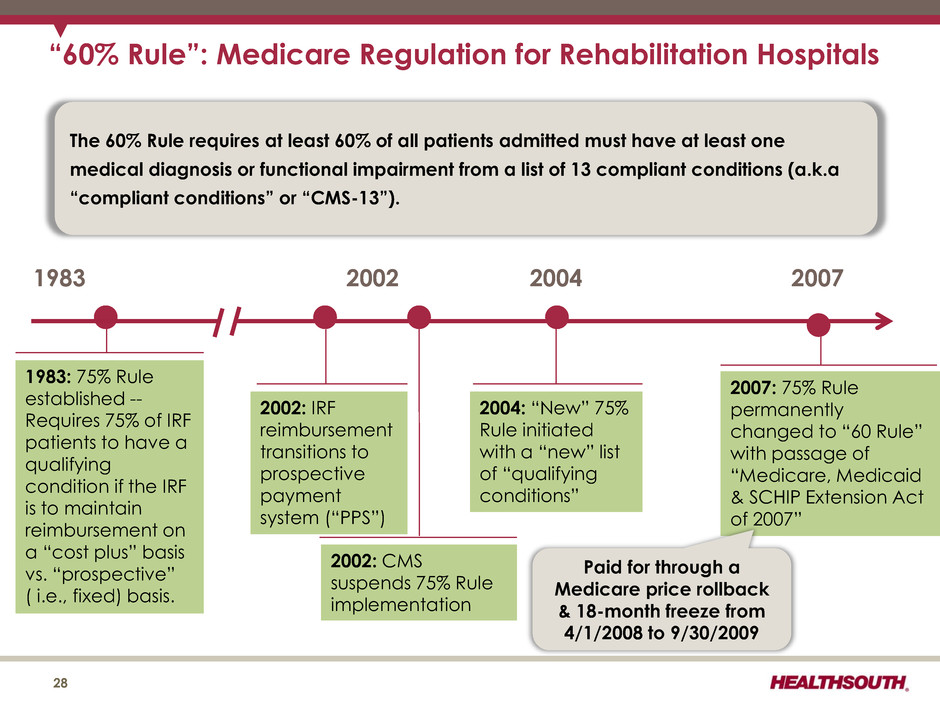
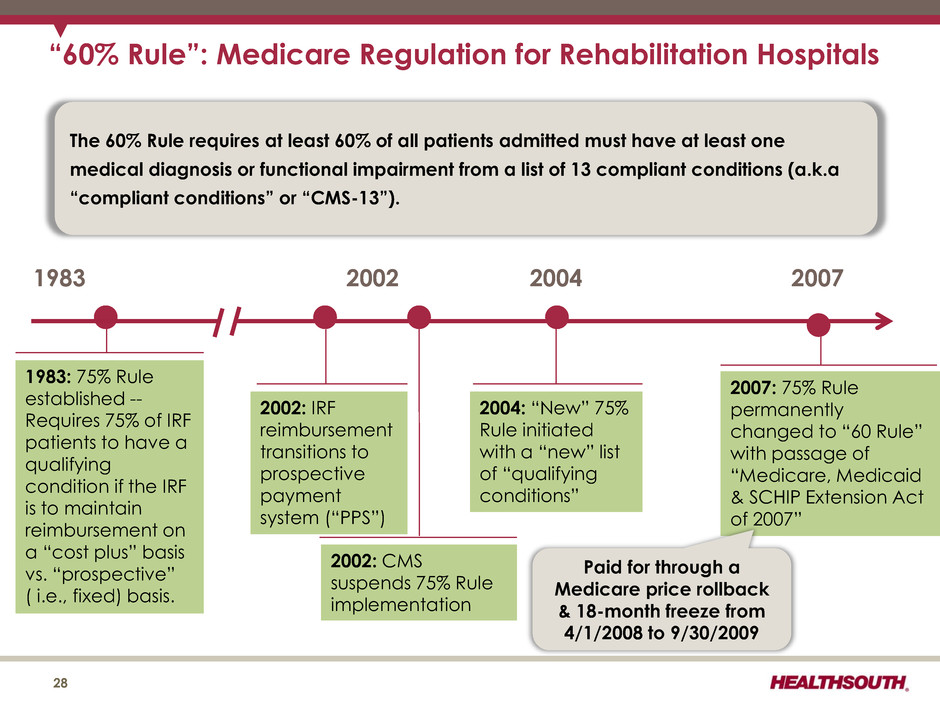
“60% Rule”: Medicare Regulation for Rehabilitation Hospitals 28 1983 1983: 75% Rule established -- Requires 75% of IRF patients to have a qualifying condition if the IRF is to maintain reimbursement on a “cost plus” basis vs. “prospective” ( i.e., fixed) basis. The 60% Rule requires at least 60% of all patients admitted must have at least one medical diagnosis or functional impairment from a list of 13 compliant conditions (a.k.a “compliant conditions” or “CMS-13”). 2002 2004 2007 2002: IRF reimbursement transitions to prospective payment system (“PPS”) 2002: CMS suspends 75% Rule implementation 2004: “New” 75% Rule initiated with a “new” list of “qualifying conditions” 2007: 75% Rule permanently changed to “60 Rule” with passage of “Medicare, Medicaid & SCHIP Extension Act of 2007” Paid for through a Medicare price rollback & 18-month freeze from 4/1/2008 to 9/30/2009
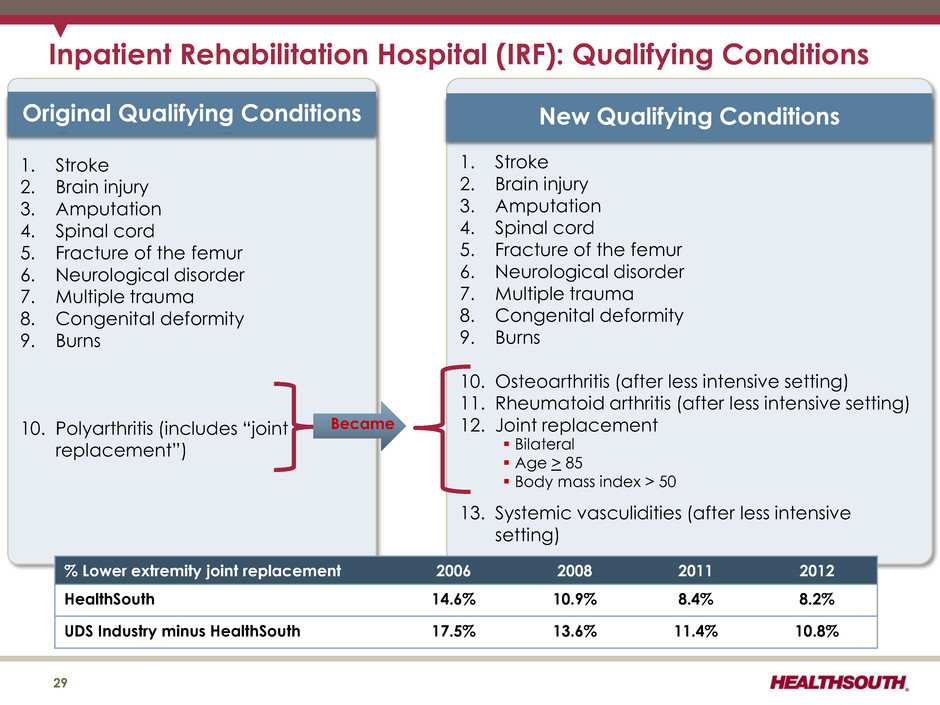
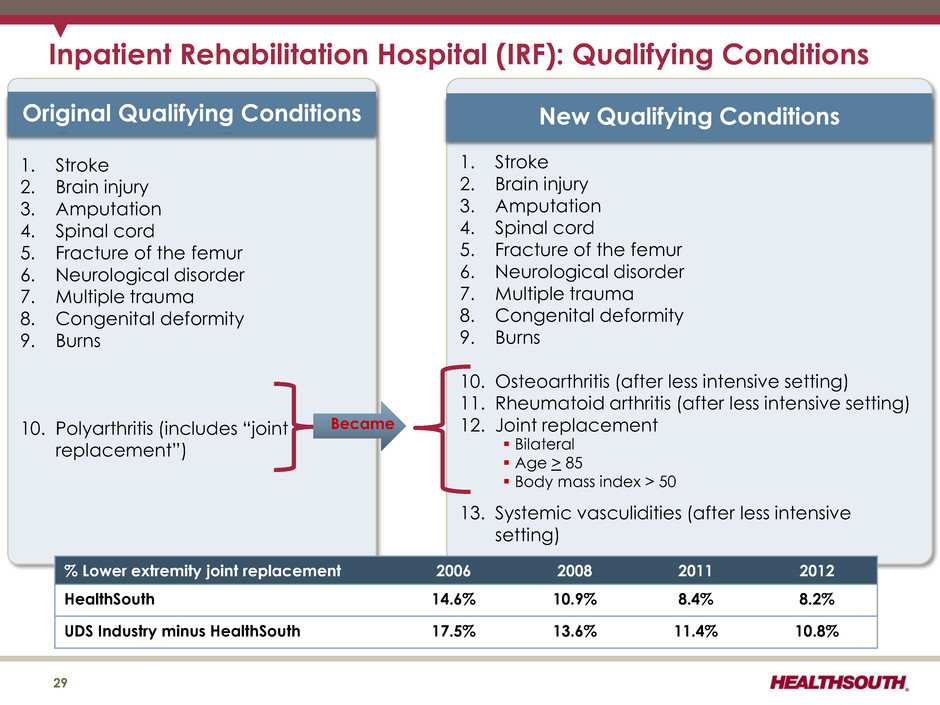
Inpatient Rehabilitation Hospital (IRF): Qualifying Conditions 29 1. Stroke 2. Brain injury 3. Amputation 4. Spinal cord 5. Fracture of the femur 6. Neurological disorder 7. Multiple trauma 8. Congenital deformity 9. Burns 10. Polyarthritis (includes “joint replacement”) Original Qualifying Conditions 1. Stroke 2. Brain injury 3. Amputation 4. Spinal cord 5. Fracture of the femur 6. Neurological disorder 7. Multiple trauma 8. Congenital deformity 9. Burns 10. Osteoarthritis (after less intensive setting) 11. Rheumatoid arthritis (after less intensive setting) 12. Joint replacement 13. Systemic vasculidities (after less intensive setting) New Qualifying Conditions Became Bilateral Age > 85 Body mass index > 50 % Lower extremity joint replacement 2006 2008 2011 2012 HealthSouth 14.6% 10.9% 8.4% 8.2% UDS Industry minus HealthSouth 17.5% 13.6% 11.4% 10.8%

30 • The final rule would implement a net 1.8% market basket increase. ― 2.6% market basket increase ― (30 bps) Affordable Care Act reduction ― (50 bps) Affordable Care Act productivity reduction • Final rule includes updates to the IRF facility-level rural, low-income patient and teaching status adjustments. Also includes update to the outlier threshold. IRF-PPS Fiscal Year 2014 Final Rule: Key Provisions Pricing: • Net pricing impact to HealthSouth expected to be approx. +1.95% for FY 2014 before sequestration (1) • Because of its low cost structure, HealthSouth receives very few outlier payments despite higher acuity patients (see slide 9). Update to Payment Rates • CMS finalized revisions to the list of codes it uses to presumptively test compliance with the 60% Rule. ― The final rule eliminates 259 ICD-9-CM codes used for presumptive testing starting October 1, 2014. ― CMS indicates that the vast majority of these eliminated codes are non-specific codes that can be substituted with a more specific code. ― The remaining eliminated codes are primarily arthritis-related codes. 60 Percent Rule – Presumptive Methodology Code List Update Coding: • HealthSouth expects no material financial impact. • These 259 codes will be cross walked to applicable ICD-10-CM codes effective October 1, 2014, which could result in further refinement. • Some arthritis patients may be denied access to inpatient rehabilitative care. • Final changes to IRF patient assessment instrument (“PAI”) • FY 2016 new quality measure: influenza vaccines for IRF employees • FY 2017 two new quality measures: all-cause unplanned readmission and influenza vaccines for residents or patients New Quality Reporting Quality: • PAI changes are straightforward and will be implemented by HealthSouth hospitals. • HealthSouth will continue to comply with all quality reporting requirements. 1) Because sequestration began in Q2 2013 and does not anniversary until Q2 2014, HealthSouth expects Medicare pricing after sequestration to be approx. flat for Q4 2013 and Q1 2014. Source: https://www.federalregister.gov/articles/2013/08/06/2013-18770/medicare-program-inpatient-rehabilitation-facility-prospective- payment-system-for-federal-fiscal HealthSouth Observations
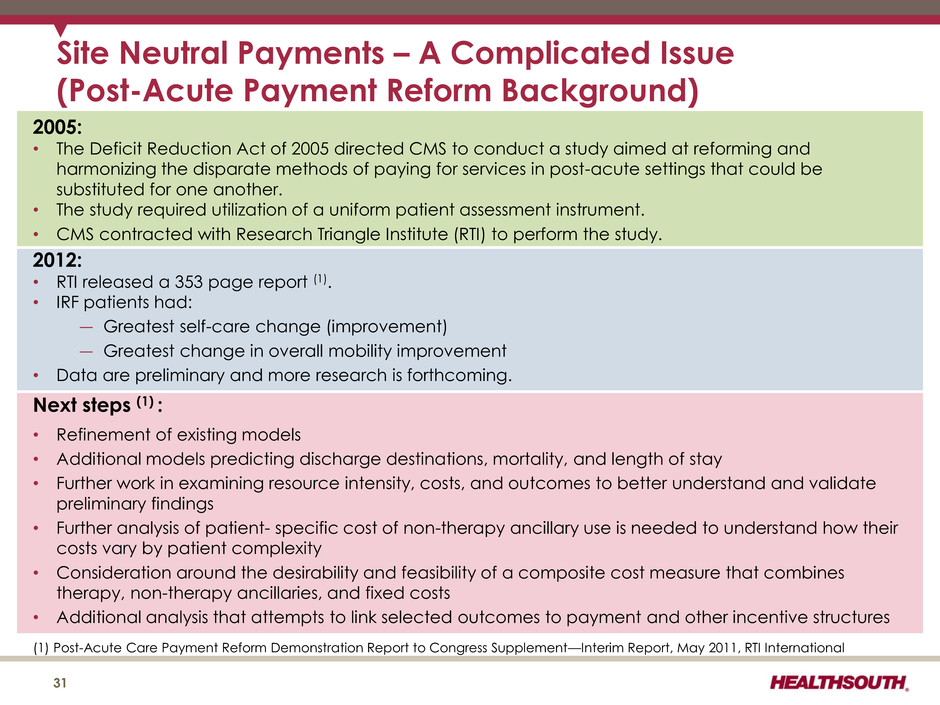
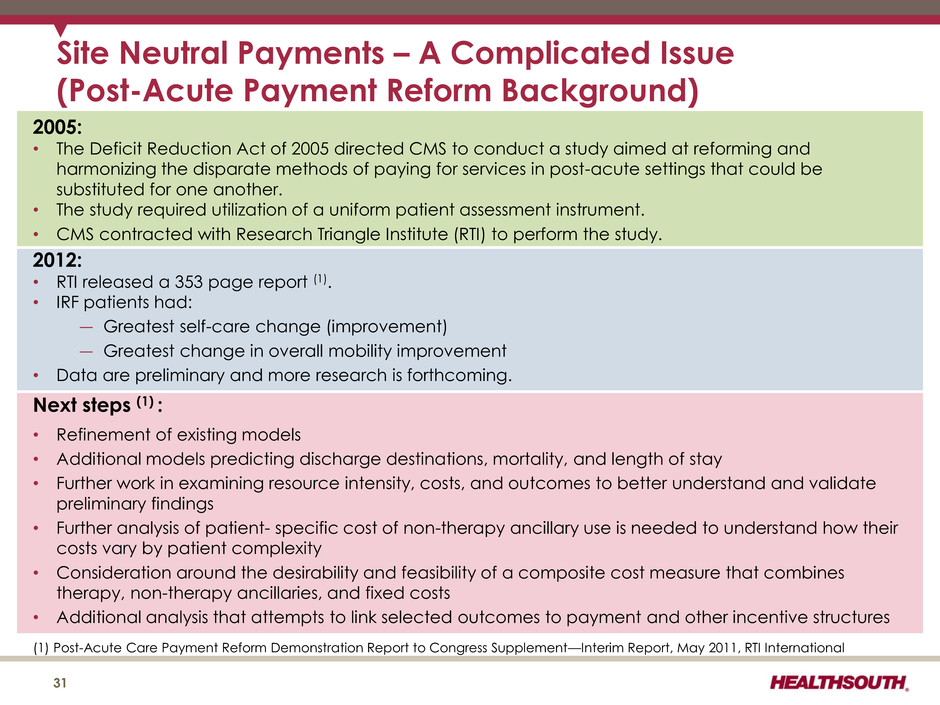
Site Neutral Payments – A Complicated Issue (Post-Acute Payment Reform Background) 31 (1) Post-Acute Care Payment Reform Demonstration Report to Congress Supplement—Interim Report, May 2011, RTI International 2005: • The Deficit Reduction Act of 2005 directed CMS to conduct a study aimed at reforming and harmonizing the disparate methods of paying for services in post-acute settings that could be substituted for one another. • The study required utilization of a uniform patient assessment instrument. • CMS contracted with Research Triangle Institute (RTI) to perform the study. 2012: • RTI released a 353 page report (1). • IRF patients had: ― Greatest self-care change (improvement) ― Greatest change in overall mobility improvement • Data are preliminary and more research is forthcoming. Next steps (1) : • Refinement of existing models • Additional models predicting discharge destinations, mortality, and length of stay • Further work in examining resource intensity, costs, and outcomes to better understand and validate preliminary findings • Further analysis of patient- specific cost of non-therapy ancillary use is needed to understand how their costs vary by patient complexity • Consideration around the desirability and feasibility of a composite cost measure that combines therapy, non-therapy ancillaries, and fixed costs • Additional analysis that attempts to link selected outcomes to payment and other incentive structures
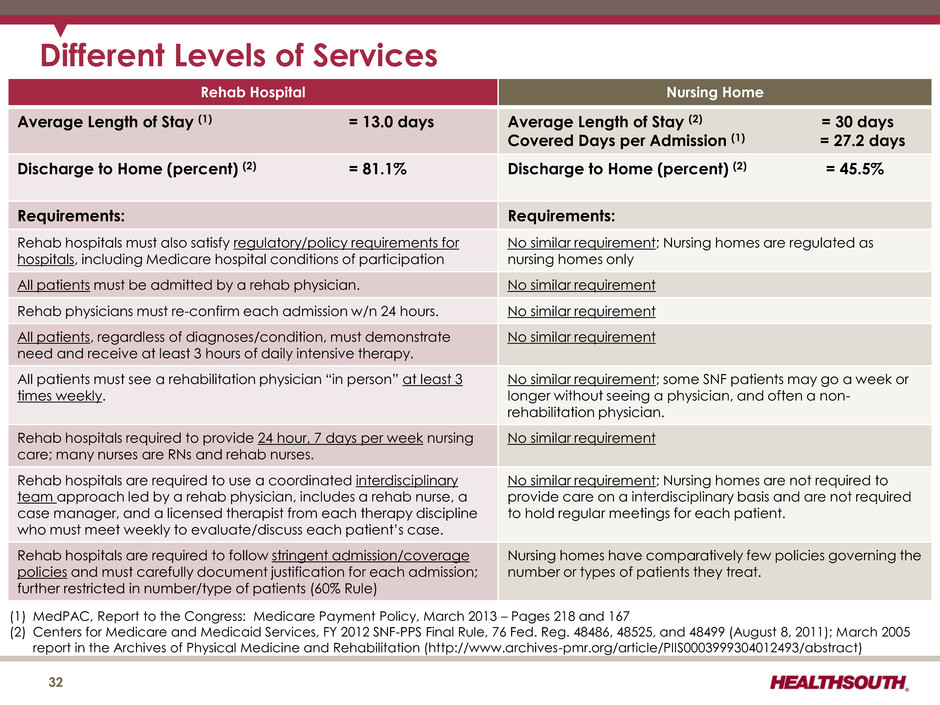
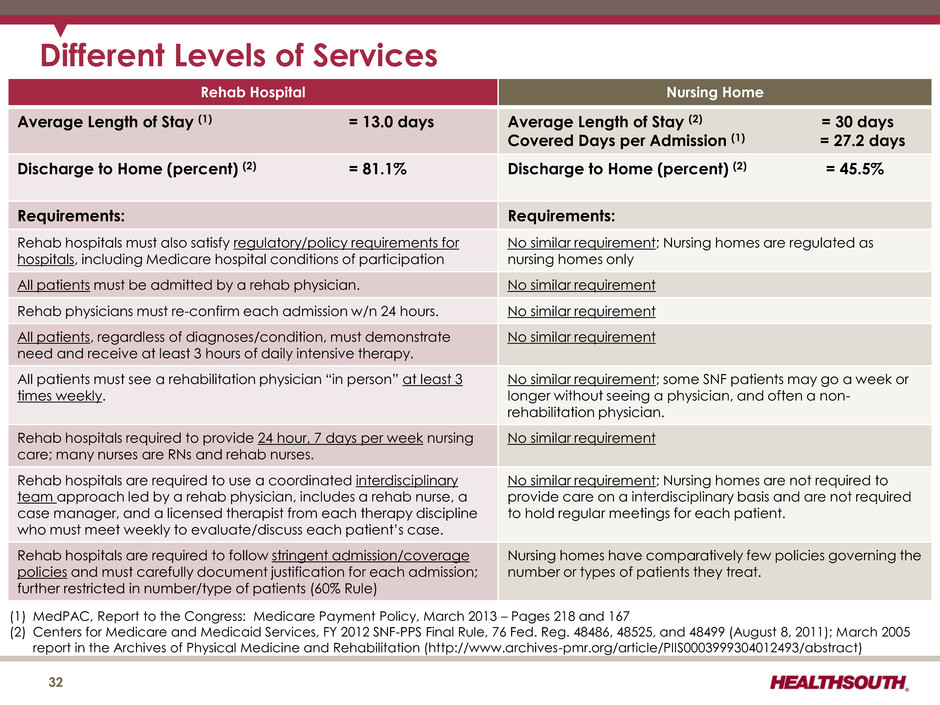
Different Levels of Services Rehab Hospital Nursing Home Average Length of Stay (1) = 13.0 days Average Length of Stay (2) = 30 days Covered Days per Admission (1) = 27.2 days Discharge to Home (percent) (2) = 81.1% Discharge to Home (percent) (2) = 45.5% Requirements: Requirements: Rehab hospitals must also satisfy regulatory/policy requirements for hospitals, including Medicare hospital conditions of participation No similar requirement; Nursing homes are regulated as nursing homes only All patients must be admitted by a rehab physician. No similar requirement Rehab physicians must re-confirm each admission w/n 24 hours. No similar requirement All patients, regardless of diagnoses/condition, must demonstrate need and receive at least 3 hours of daily intensive therapy. No similar requirement All patients must see a rehabilitation physician “in person” at least 3 times weekly. No similar requirement; some SNF patients may go a week or longer without seeing a physician, and often a non- rehabilitation physician. Rehab hospitals required to provide 24 hour, 7 days per week nursing care; many nurses are RNs and rehab nurses. No similar requirement Rehab hospitals are required to use a coordinated interdisciplinary team approach led by a rehab physician, includes a rehab nurse, a case manager, and a licensed therapist from each therapy discipline who must meet weekly to evaluate/discuss each patient’s case. No similar requirement; Nursing homes are not required to provide care on a interdisciplinary basis and are not required to hold regular meetings for each patient. Rehab hospitals are required to follow stringent admission/coverage policies and must carefully document justification for each admission; further restricted in number/type of patients (60% Rule) Nursing homes have comparatively few policies governing the number or types of patients they treat. (1) MedPAC, Report to the Congress: Medicare Payment Policy, March 2013 – Pages 218 and 167 (2) Centers for Medicare and Medicaid Services, FY 2012 SNF-PPS Final Rule, 76 Fed. Reg. 48486, 48525, and 48499 (August 8, 2011); March 2005 report in the Archives of Physical Medicine and Rehabilitation (http://www.archives-pmr.org/article/PIIS0003999304012493/abstract) 32
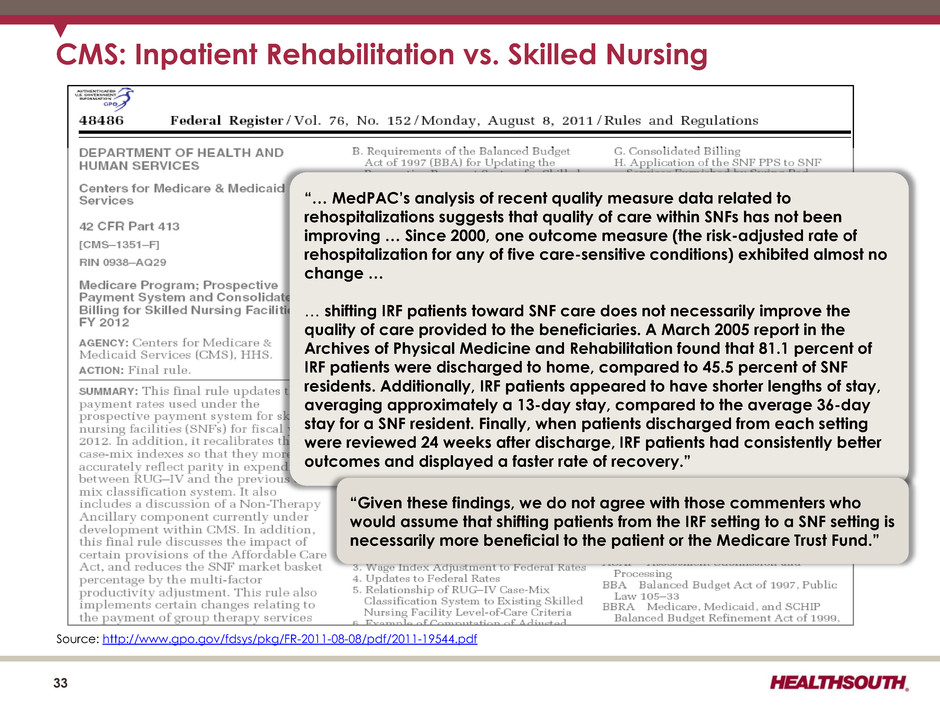
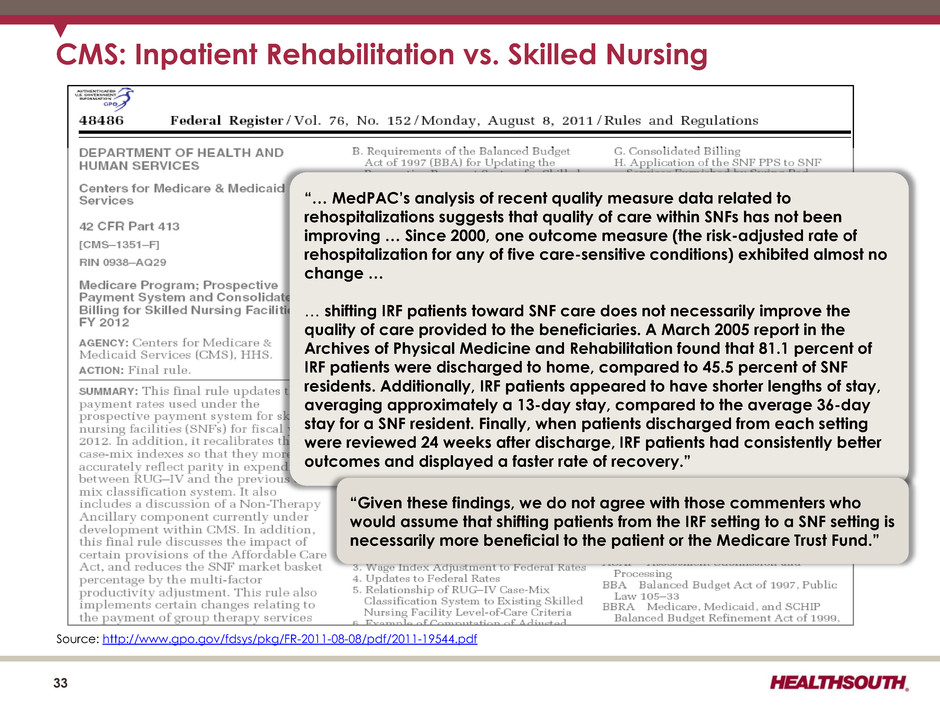
33 CMS: Inpatient Rehabilitation vs. Skilled Nursing “… MedPAC’s analysis of recent quality measure data related to rehospitalizations suggests that quality of care within SNFs has not been improving … Since 2000, one outcome measure (the risk-adjusted rate of rehospitalization for any of five care-sensitive conditions) exhibited almost no change … … shifting IRF patients toward SNF care does not necessarily improve the quality of care provided to the beneficiaries. A March 2005 report in the Archives of Physical Medicine and Rehabilitation found that 81.1 percent of IRF patients were discharged to home, compared to 45.5 percent of SNF residents. Additionally, IRF patients appeared to have shorter lengths of stay, averaging approximately a 13-day stay, compared to the average 36-day stay for a SNF resident. Finally, when patients discharged from each setting were reviewed 24 weeks after discharge, IRF patients had consistently better outcomes and displayed a faster rate of recovery.” “Given these findings, we do not agree with those commenters who would assume that shifting patients from the IRF setting to a SNF setting is necessarily more beneficial to the patient or the Medicare Trust Fund.” Source: http://www.gpo.gov/fdsys/pkg/FR-2011-08-08/pdf/2011-19544.pdf
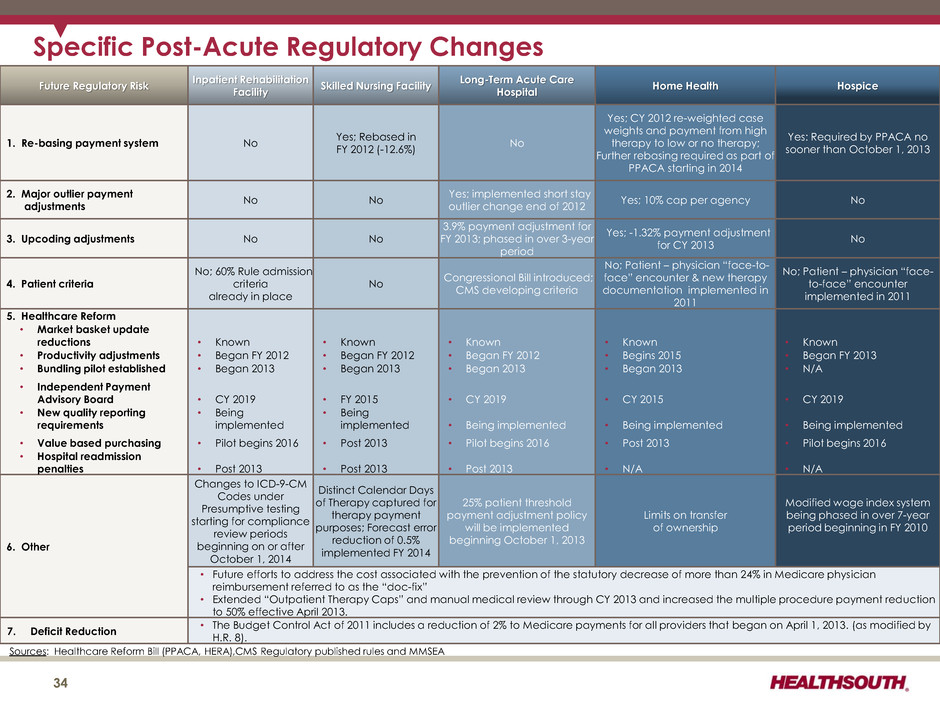
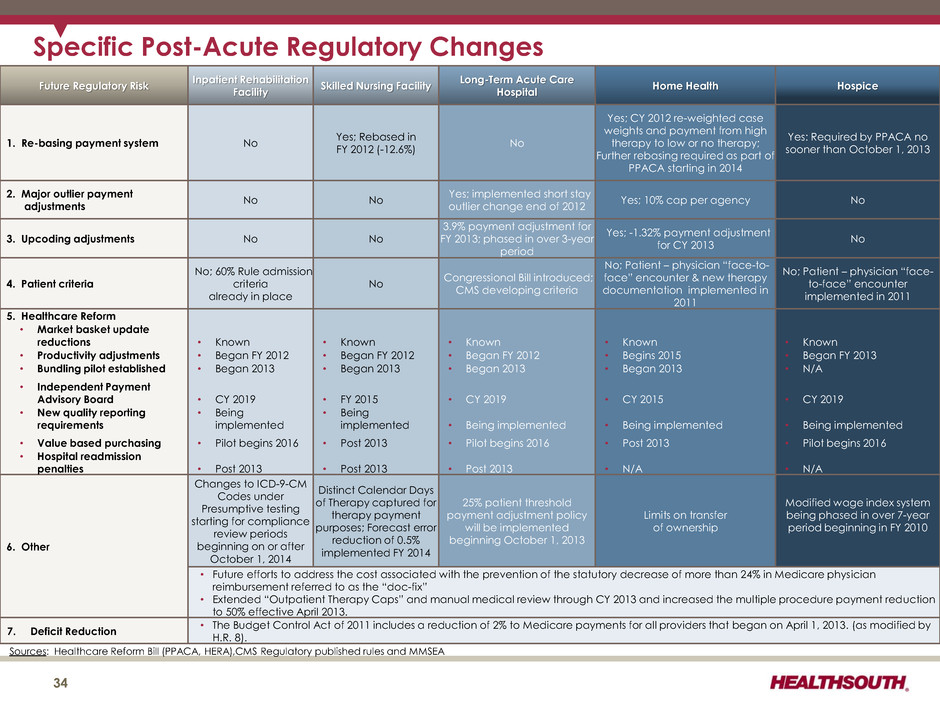
Future Regulatory Risk Inpatient Rehabilitation Facility Skilled Nursing Facility Long-Term Acute Care Hospital Home Health Hospice 1. Re-basing payment system No Yes; Rebased in FY 2012 (-12.6%) No Yes; CY 2012 re-weighted case weights and payment from high therapy to low or no therapy; Further rebasing required as part of PPACA starting in 2014 Yes: Required by PPACA no sooner than October 1, 2013 2. Major outlier payment adjustments No No Yes; implemented short stay outlier change end of 2012 Yes; 10% cap per agency No 3. Upcoding adjustments No No 3.9% payment adjustment for FY 2013; phased in over 3-year period Yes; -1.32% payment adjustment for CY 2013 No 4. Patient criteria No; 60% Rule admission criteria already in place No Congressional Bill introduced; CMS developing criteria No; Patient – physician “face-to- face” encounter & new therapy documentation implemented in 2011 No; Patient – physician “face- to-face” encounter implemented in 2011 5. Healthcare Reform • Market basket update reductions • Known • Known • Known • Known • Known • Productivity adjustments • Began FY 2012 • Began FY 2012 • Began FY 2012 • Begins 2015 • Began FY 2013 • Bundling pilot established • Began 2013 • Began 2013 • Began 2013 • Began 2013 • N/A • Independent Payment Advisory Board • CY 2019 • FY 2015 • CY 2019 • CY 2015 • CY 2019 • New quality reporting requirements • Being implemented • Being implemented • Being implemented • Being implemented • Being implemented • Value based purchasing • Pilot begins 2016 • Post 2013 • Pilot begins 2016 • Post 2013 • Pilot begins 2016 • Hospital readmission penalties • Post 2013 • Post 2013 • Post 2013 • N/A • N/A 6. Other Changes to ICD-9-CM Codes under Presumptive testing starting for compliance review periods beginning on or after October 1, 2014 Distinct Calendar Days of Therapy captured for therapy payment purposes; Forecast error reduction of 0.5% implemented FY 2014 25% patient threshold payment adjustment policy will be implemented beginning October 1, 2013 Limits on transfer of ownership Modified wage index system being phased in over 7-year period beginning in FY 2010 • Future efforts to address the cost associated with the prevention of the statutory decrease of more than 24% in Medicare physician reimbursement referred to as the “doc-fix” • Extended “Outpatient Therapy Caps” and manual medical review through CY 2013 and increased the multiple procedure payment reduction to 50% effective April 2013. 7. Deficit Reduction • The Budget Control Act of 2011 includes a reduction of 2% to Medicare payments for all providers that began on April 1, 2013. (as modified by H.R. 8). Specific Post-Acute Regulatory Changes Sources: Healthcare Reform Bill (PPACA, HERA),CMS Regulatory published rules and MMSEA 34
Historical Perspective 35
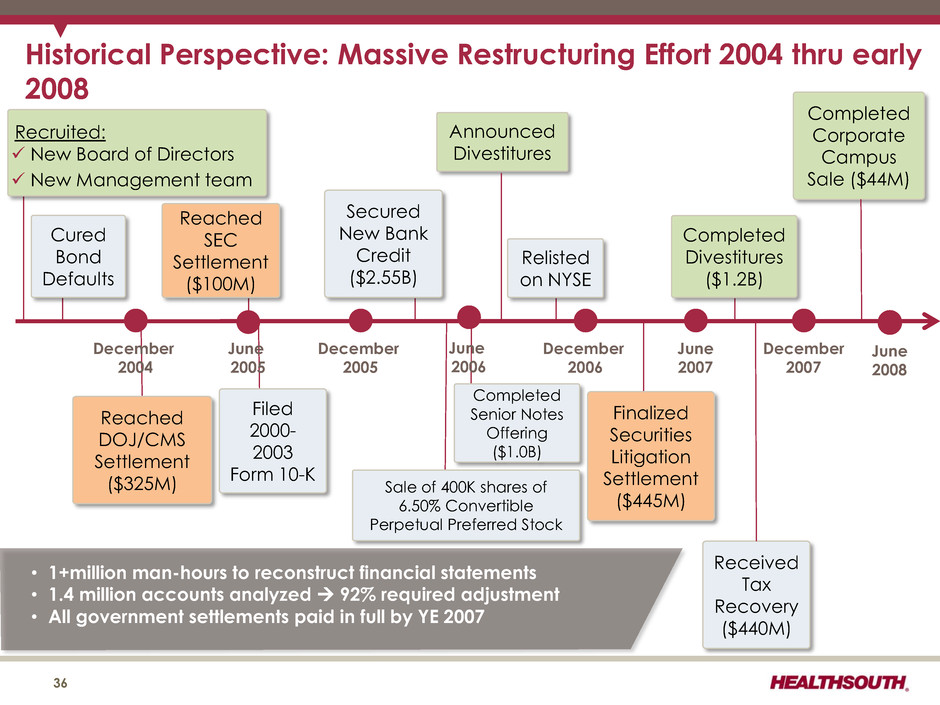
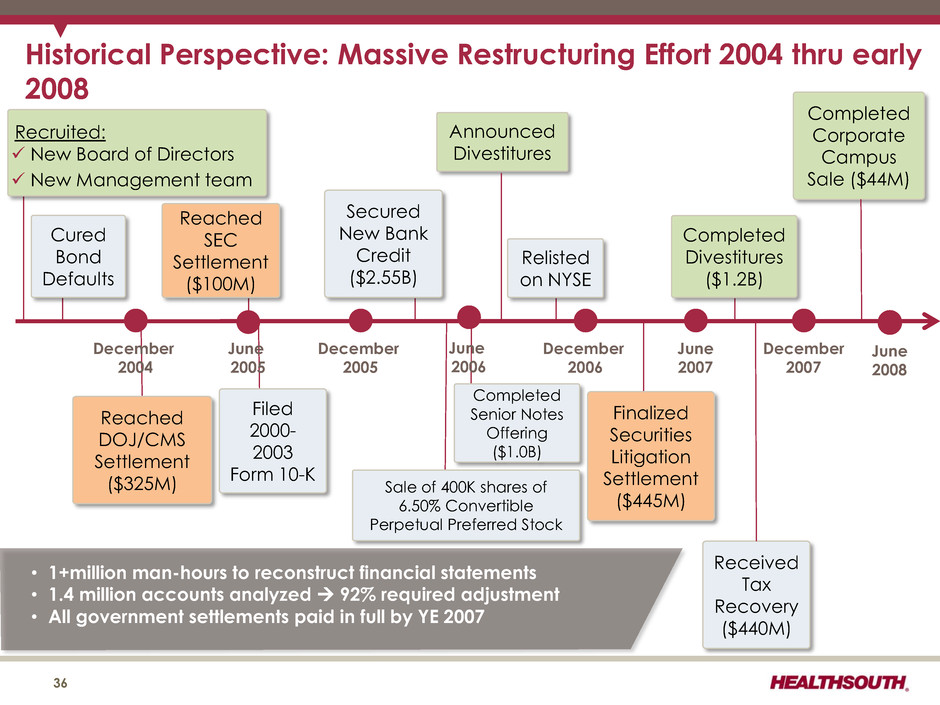
Historical Perspective: Massive Restructuring Effort 2004 thru early 2008 December 2004 June 2005 December 2005 June 2006 December 2006 June 2007 December 2007 Reached DOJ/CMS Settlement ($325M) Filed 2000- 2003 Form 10-K Completed Senior Notes Offering ($1.0B) Announced Divestitures Finalized Securities Litigation Settlement ($445M) Received Tax Recovery ($440M) Completed Corporate Campus Sale ($44M) Cured Bond Defaults Secured New Bank Credit ($2.55B) Reached SEC Settlement ($100M) Relisted on NYSE Completed Divestitures ($1.2B) • 1+million man-hours to reconstruct financial statements • 1.4 million accounts analyzed 92% required adjustment • All government settlements paid in full by YE 2007 36 Recruited: New Board of Directors New Management team Sale of 400K shares of 6.50% Convertible Perpetual Preferred Stock June 2008

Historical Perspective 37 $323 $364 $410 $466 $506 2008 2009 2010 2011 2012 Adjusted EBITDA (1) (1) Reconciliation to GAAP provided on slides 56 and 92 - 96. 2008: Focused on Achieving Balance between Debt Reduction and Organic Growth • Established 2008-2010 business model ― 4% discharge growth; 5-8% Adjusted EBITDA growth; 15-20% adjusted EPS growth • Balanced delevering and growth/development strategies • Completed TeamWorks sales and marketing roll-out • Absorbed Medicare reimbursement rollback (Q2) • Repaid $228 million of long-term debt (8.8 million share equity issuance and prior period tax refunds) • Financial market turmoil (Q3) ― HealthSouth suspended development and increased focus on delevering 2009: Focused on Debt Reduction with Increased Emphasis on Organic Growth • Continued focus on delevering (approx. $151 million in debt repaid) • Focused on organic growth; TeamWorks sustainability module rolled out • Issued 5 million shares for securities litigation settlement (Q3) • Received first Medicare market basket update in 18 months (Q4) • Reinvigorated development efforts (Q4)
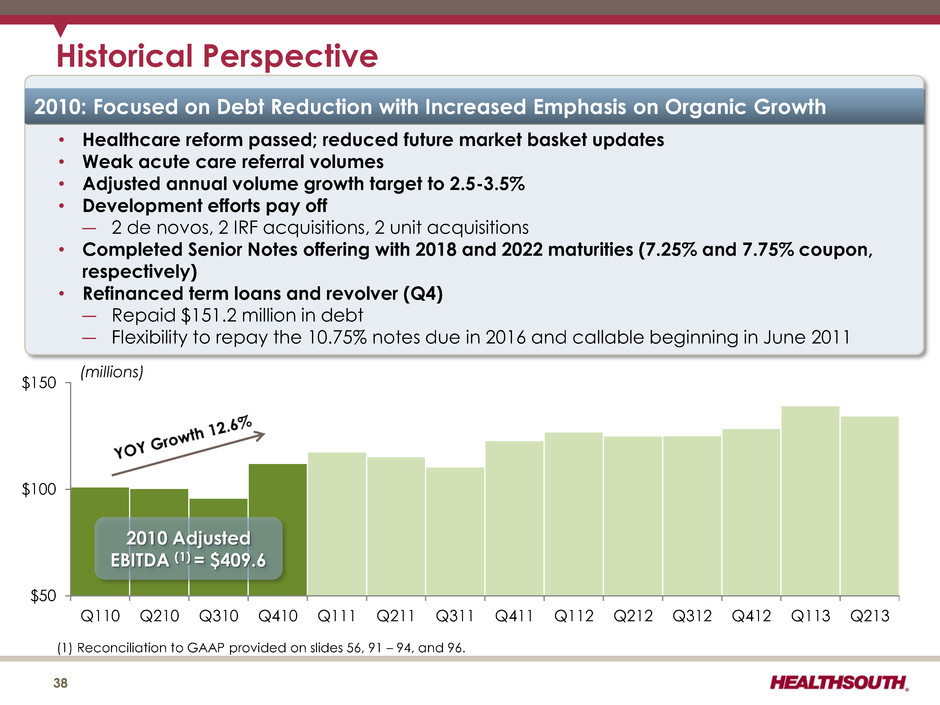
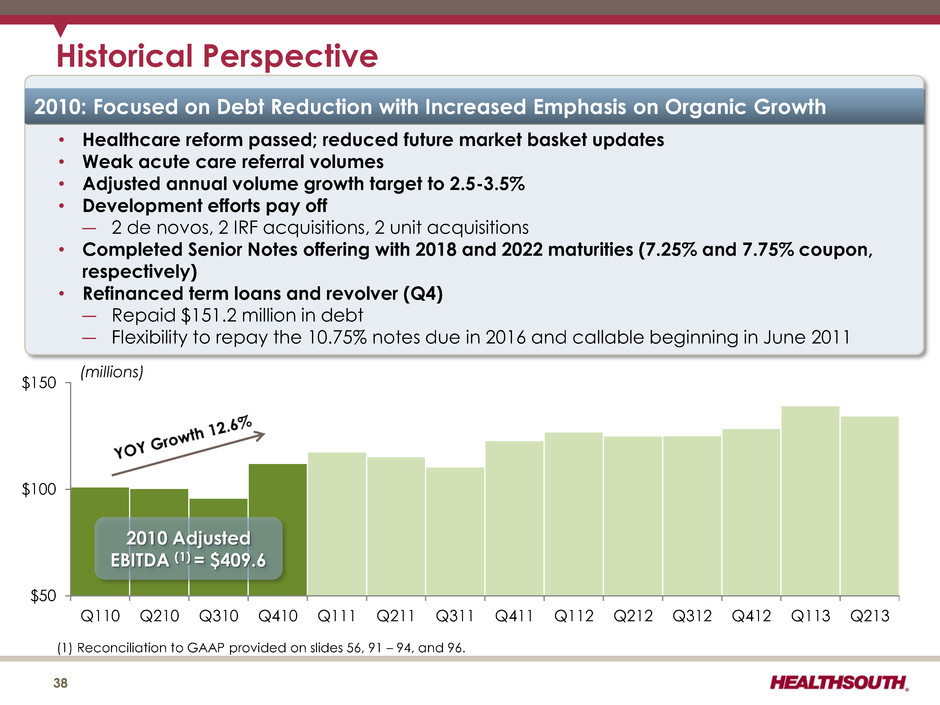
$50 $100 $150 Q110 Q210 Q310 Q410 Q111 Q211 Q311 Q411 Q112 Q212 Q312 Q412 Q113 Q213 Historical Perspective 38 2010 Adjusted EBITDA (1) = $409.6 (1) Reconciliation to GAAP provided on slides 56, 91 – 94, and 96. (millions) 2010: Focused on Debt Reduction with Increased Emphasis on Organic Growth • Healthcare reform passed; reduced future market basket updates • Weak acute care referral volumes • Adjusted annual volume growth target to 2.5-3.5% • Development efforts pay off ― 2 de novos, 2 IRF acquisitions, 2 unit acquisitions • Completed Senior Notes offering with 2018 and 2022 maturities (7.25% and 7.75% coupon, respectively) • Refinanced term loans and revolver (Q4) ― Repaid $151.2 million in debt ― Flexibility to repay the 10.75% notes due in 2016 and callable beginning in June 2011
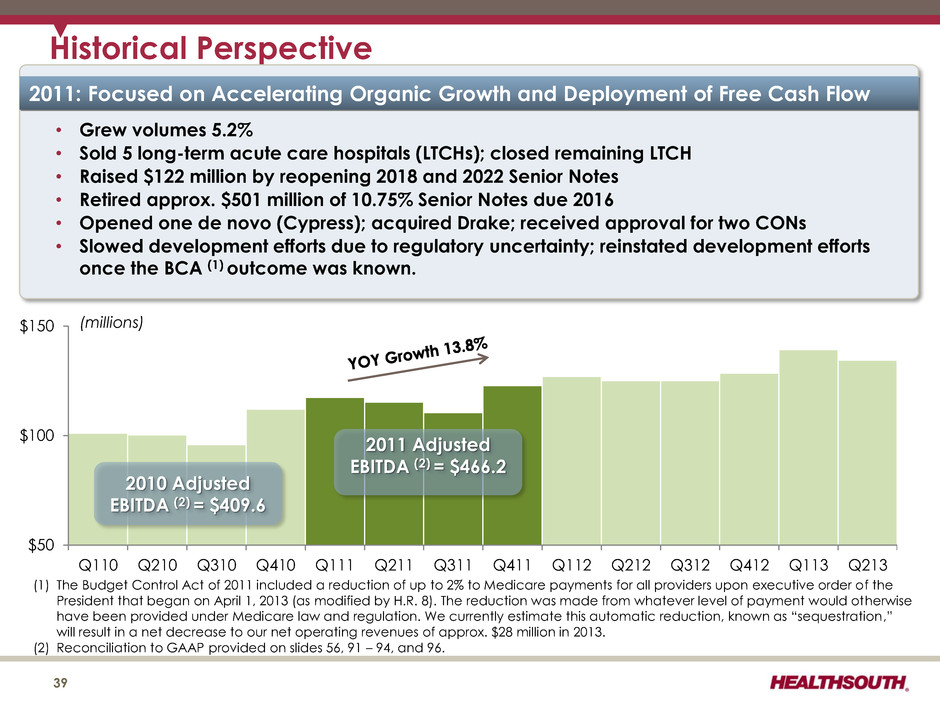
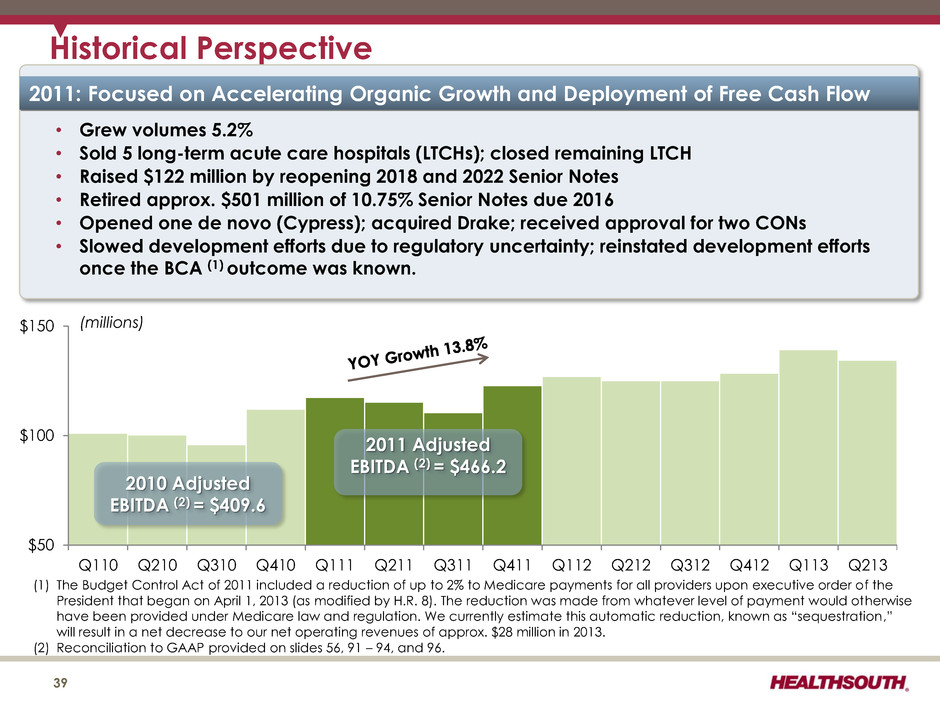
$50 $100 $150 Q110 Q210 Q310 Q410 Q111 Q211 Q311 Q411 Q112 Q212 Q312 Q412 Q113 Q213 2011 Adjusted EBITDA (2) = $466.2 Historical Perspective 39 2010 Adjusted EBITDA (2) = $409.6 (1) The Budget Control Act of 2011 included a reduction of up to 2% to Medicare payments for all providers upon executive order of the President that began on April 1, 2013 (as modified by H.R. 8). The reduction was made from whatever level of payment would otherwise have been provided under Medicare law and regulation. We currently estimate this automatic reduction, known as “sequestration,” will result in a net decrease to our net operating revenues of approx. $28 million in 2013. (2) Reconciliation to GAAP provided on slides 56, 91 – 94, and 96. (millions) 2011: Focused on Accelerating Organic Growth and Deployment of Free Cash Flow • Grew volumes 5.2% • Sold 5 long-term acute care hospitals (LTCHs); closed remaining LTCH • Raised $122 million by reopening 2018 and 2022 Senior Notes • Retired approx. $501 million of 10.75% Senior Notes due 2016 • Opened one de novo (Cypress); acquired Drake; received approval for two CONs • Slowed development efforts due to regulatory uncertainty; reinstated development efforts once the BCA (1) outcome was known.
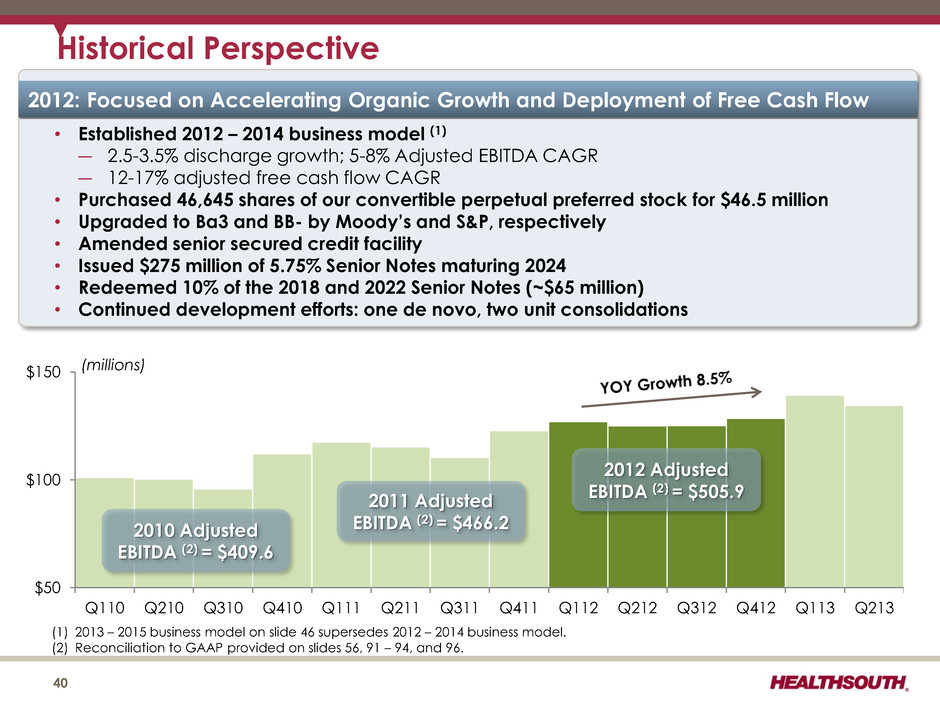
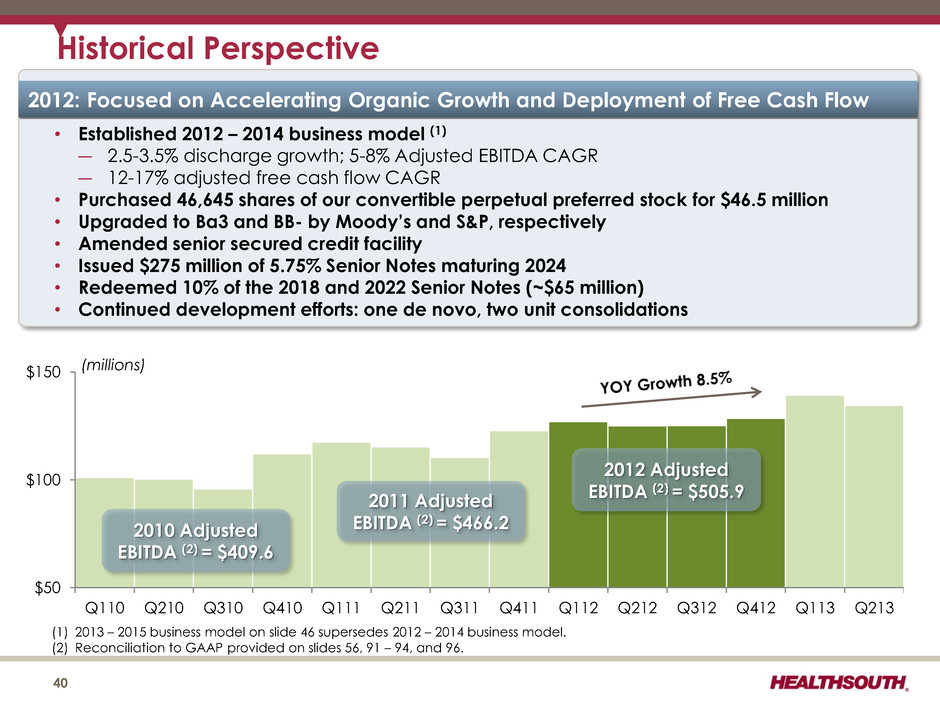
$50 $100 $150 Q110 Q210 Q310 Q410 Q111 Q211 Q311 Q411 Q112 Q212 Q312 Q412 Q113 Q213 2011 Adjusted EBITDA (2) = $466.2 Historical Perspective 40 2010 Adjusted EBITDA (2) = $409.6 (1) 2013 – 2015 business model on slide 46 supersedes 2012 – 2014 business model. (2) Reconciliation to GAAP provided on slides 56, 91 – 94, and 96. (millions) 2012 Adjusted EBITDA (2) = $505.9 2012: Focused on Accelerating Organic Growth and Deployment of Free Cash Flow • Established 2012 – 2014 business model (1) ― 2.5-3.5% discharge growth; 5-8% Adjusted EBITDA CAGR ― 12-17% adjusted free cash flow CAGR • Purchased 46,645 shares of our convertible perpetual preferred stock for $46.5 million • Upgraded to Ba3 and BB- by Moody’s and S&P, respectively • Amended senior secured credit facility • Issued $275 million of 5.75% Senior Notes maturing 2024 • Redeemed 10% of the 2018 and 2022 Senior Notes (~$65 million) • Continued development efforts: one de novo, two unit consolidations
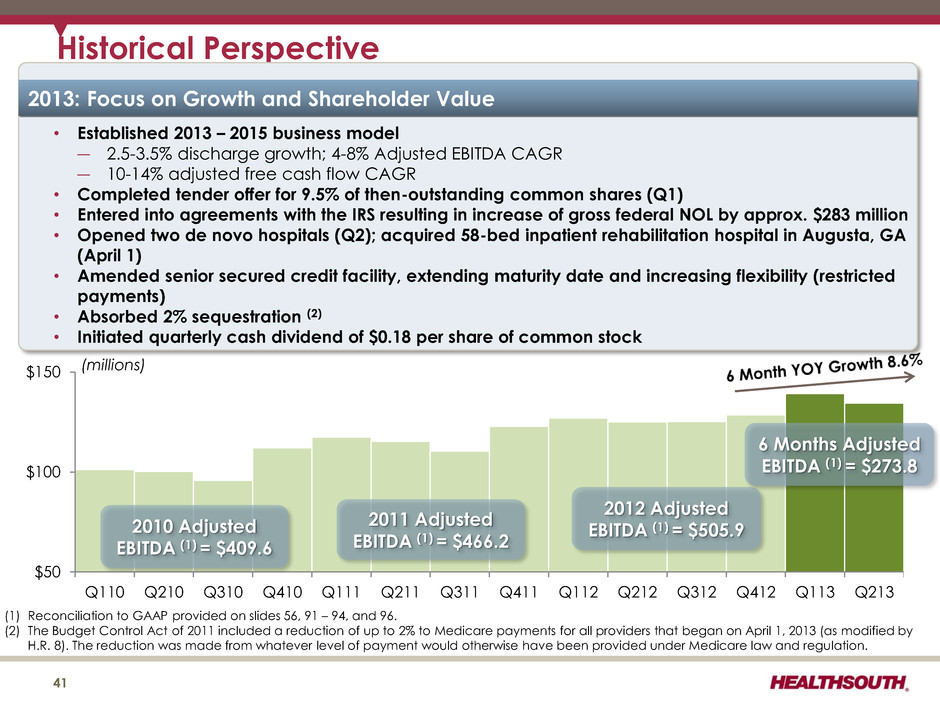
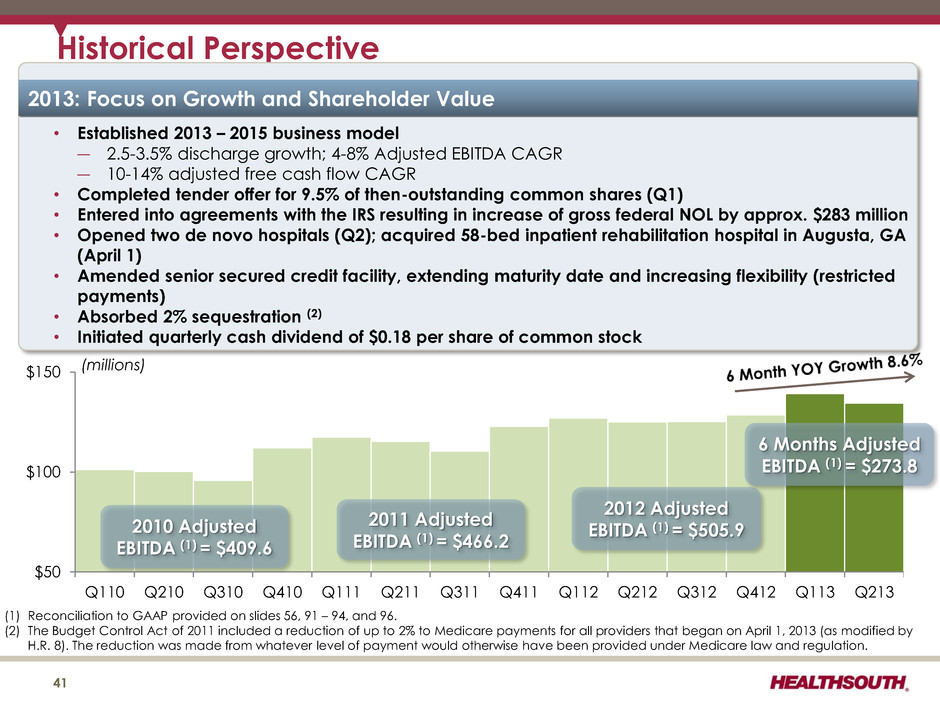
$50 $100 $150 Q110 Q210 Q310 Q410 Q111 Q211 Q311 Q411 Q112 Q212 Q312 Q412 Q113 Q213 2011 Adjusted EBITDA (1) = $466.2 Historical Perspective 41 2010 Adjusted EBITDA (1) = $409.6 (1) Reconciliation to GAAP provided on slides 56, 91 – 94, and 96. (2) The Budget Control Act of 2011 included a reduction of up to 2% to Medicare payments for all providers that began on April 1, 2013 (as modified by H.R. 8). The reduction was made from whatever level of payment would otherwise have been provided under Medicare law and regulation. (millions) 2012 Adjusted EBITDA (1) = $505.9 2013: Focus on Growth and Shareholder Value • Established 2013 – 2015 business model ― 2.5-3.5% discharge growth; 4-8% Adjusted EBITDA CAGR ― 10-14% adjusted free cash flow CAGR • Completed tender offer for 9.5% of then-outstanding common shares (Q1) • Entered into agreements with the IRS resulting in increase of gross federal NOL by approx. $283 million • Opened two de novo hospitals (Q2); acquired 58-bed inpatient rehabilitation hospital in Augusta, GA (April 1) • Amended senior secured credit facility, extending maturity date and increasing flexibility (restricted payments) • Absorbed 2% sequestration (2) • Initiated quarterly cash dividend of $0.18 per share of common stock 6 Months Adjusted EBITDA (1) = $273.8
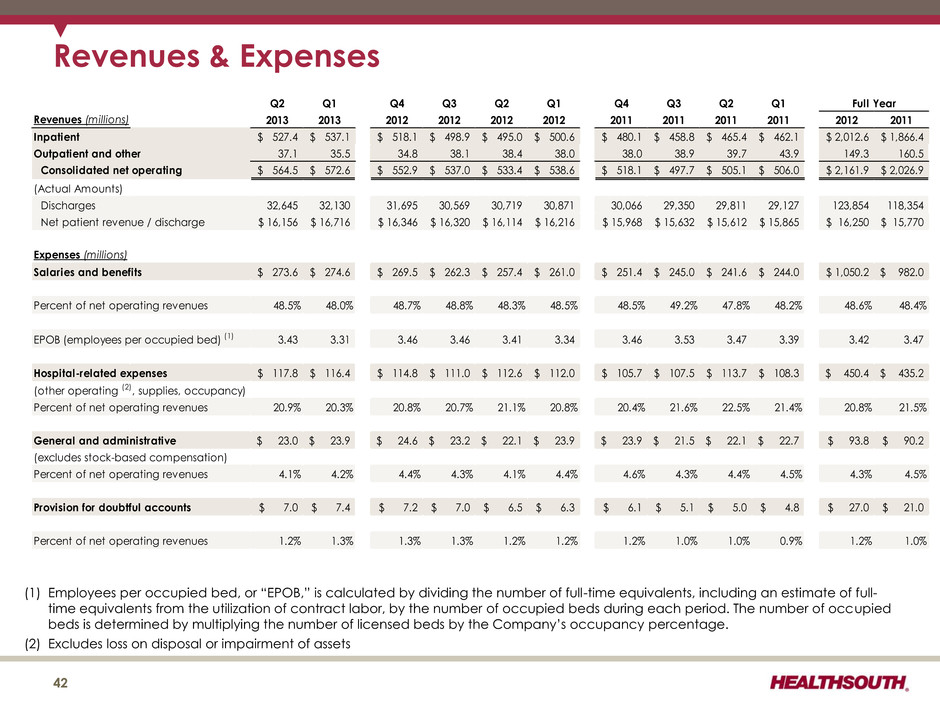
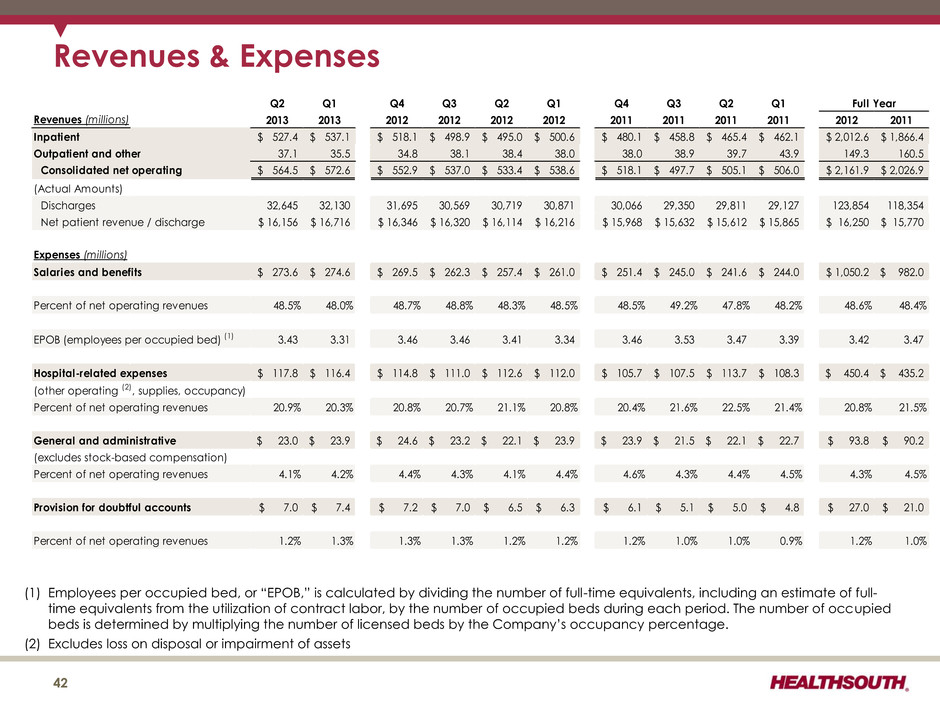
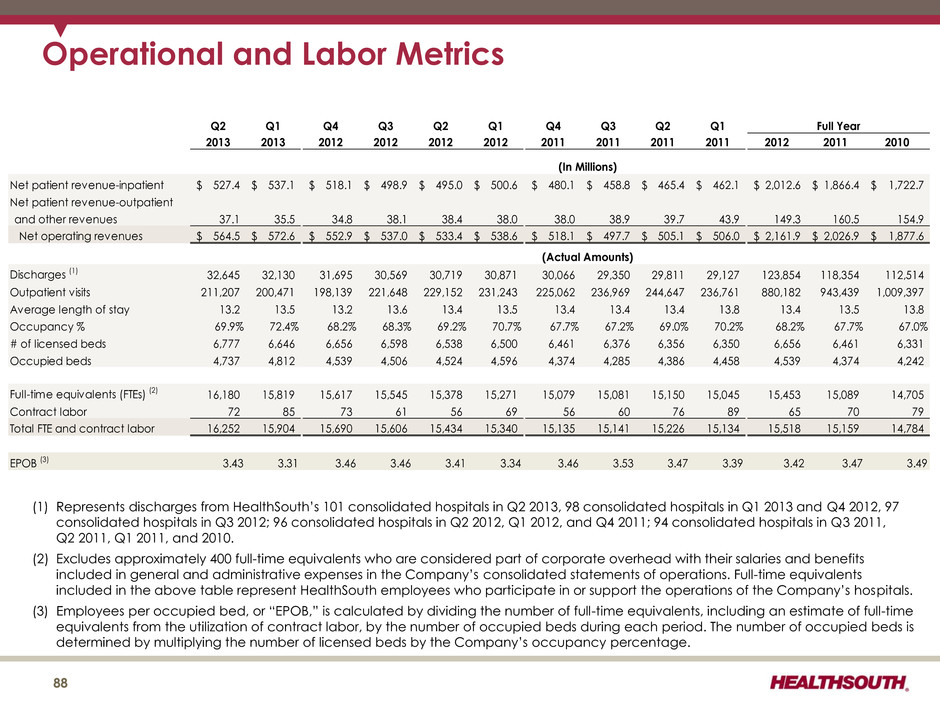
Revenues & Expenses 42 (1) Employees per occupied bed, or “EPOB,” is calculated by dividing the number of full-time equivalents, including an estimate of full- time equivalents from the utilization of contract labor, by the number of occupied beds during each period. The number of occupied beds is determined by multiplying the number of licensed beds by the Company’s occupancy percentage. (2) Excludes loss on disposal or impairment of assets Q2 Q1 Q4 Q3 Q2 Q1 Q4 Q3 Q2 Q1 Revenues (millions) 2013 2013 2012 2012 2012 2012 2011 2011 2011 2011 2012 2011 Inpatient 527.4$ 537.1$ 518.1$ 498.9$ 495.0$ 500.6$ 480.1$ 458.8$ 465.4$ 462.1$ 2,012.6$ 1,866.4$ Outpatient and other 37.1 35.5 34.8 38.1 38.4 38.0 38.0 38.9 39.7 43.9 149.3 160.5 Consolidated net operating 564.5$ 572.6$ 552.9$ 537.0$ 533.4$ 538.6$ 518.1$ 497.7$ 505.1$ 506.0$ 2,161.9$ 2,026.9$ (Actual Amounts) Discharges 32,645 32,130 31,695 30,569 30,719 30,871 30,066 29,350 29,811 29,127 123,854 118,354 Net patient revenue / discharge 16,156$ 16,716$ 16,346$ 16,320$ 16,114$ 16,216$ 15,968$ 15,632$ 15,612$ 15,865$ 16,250$ 15,770$ Expenses (millions) Salaries and benefits 273.6$ 274.6$ 269.5$ 262.3$ 257.4$ 261.0$ 251.4$ 245.0$ 241.6$ 244.0$ 1,050.2$ 982.0$ Percent of net operating revenues 48.5% 48.0% 48.7% 48.8% 48.3% 48.5% 48.5% 49.2% 47.8% 48.2% 48.6% 48.4% EPOB (employees per occupied bed) (1) 3.43 3.31 3.46 3.46 3.41 3.34 3.46 3.53 3.47 3.39 3.42 3.47 Hospital-related expenses 117.8$ 116.4$ 114.8$ 111.0$ 112.6$ 112.0$ 105.7$ 107.5$ 113.7$ 108.3$ 450.4$ 435.2$ (other operating (2), supplies, occupancy) Percent of net operating revenues 20.9% 20.3% 20.8% 20.7% 21.1% 20.8% 20.4% 21.6% 22.5% 21.4% 20.8% 21.5% General and administrative 23.0$ 23.9$ 24.6$ 23.2$ 22.1$ 23.9$ 23.9$ 21.5$ 22.1$ 22.7$ 93.8$ 90.2$ (excludes stock-based compensation) Percent of net operating revenues 4.1% 4.2% 4.4% 4.3% 4.1% 4.4% 4.6% 4.3% 4.4% 4.5% 4.3% 4.5% Provision for doubtful accounts 7.0$ 7.4$ 7.2$ 7.0$ 6.5$ 6.3$ 6.1$ 5.1$ 5.0$ 4.8$ 27.0$ 21.0$ Percent of net operating revenues 1.2% 1.3% 1.3% 1.3% 1.2% 1.2% 1.2% 1.0% 1.0% 0.9% 1.2% 1.0% Full Year
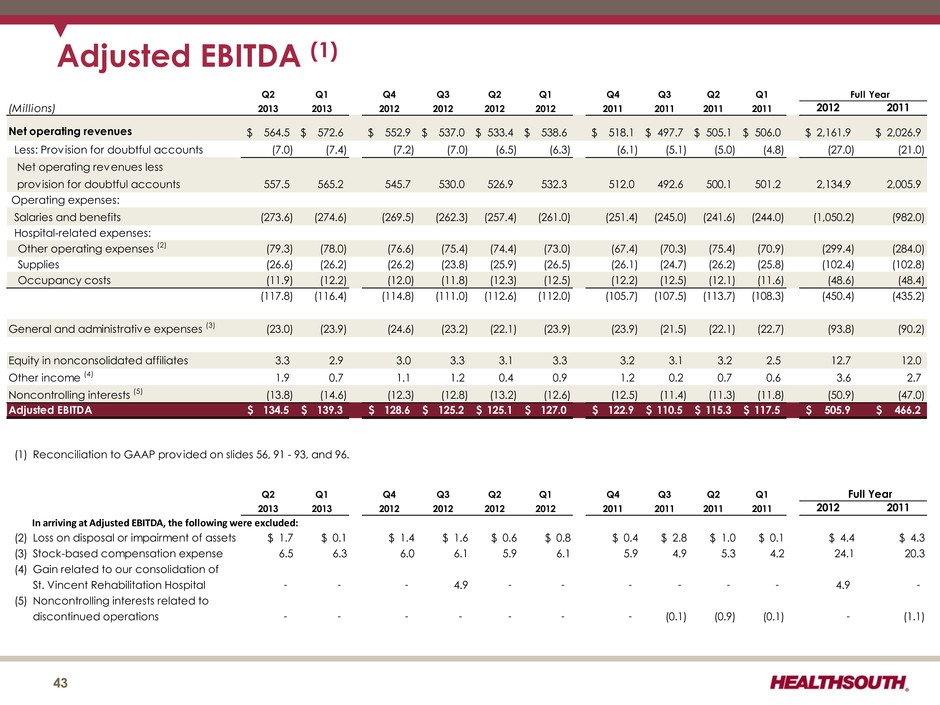
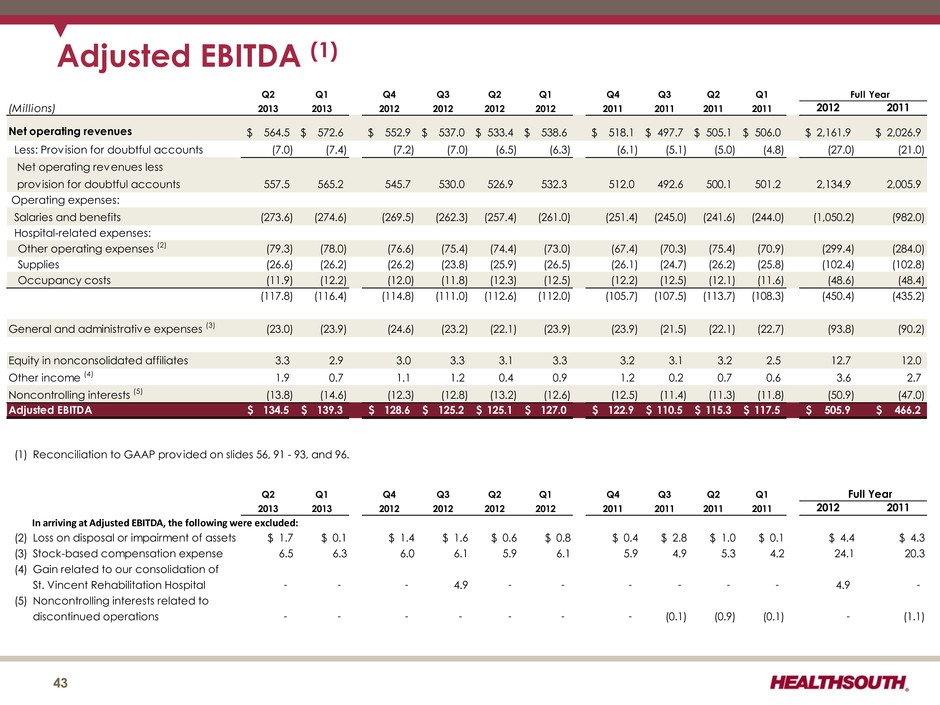
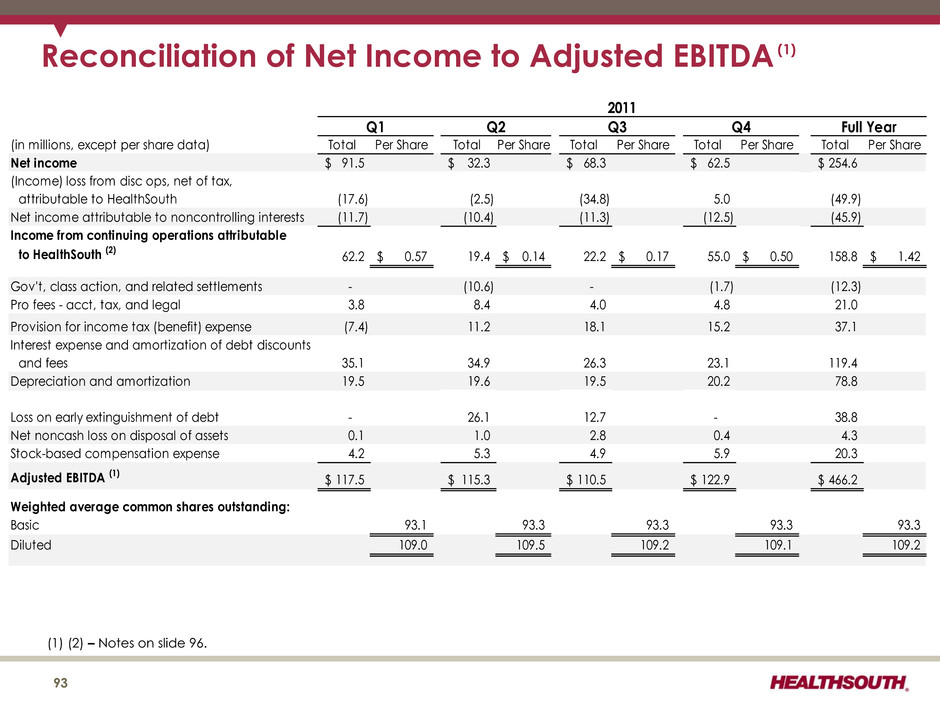
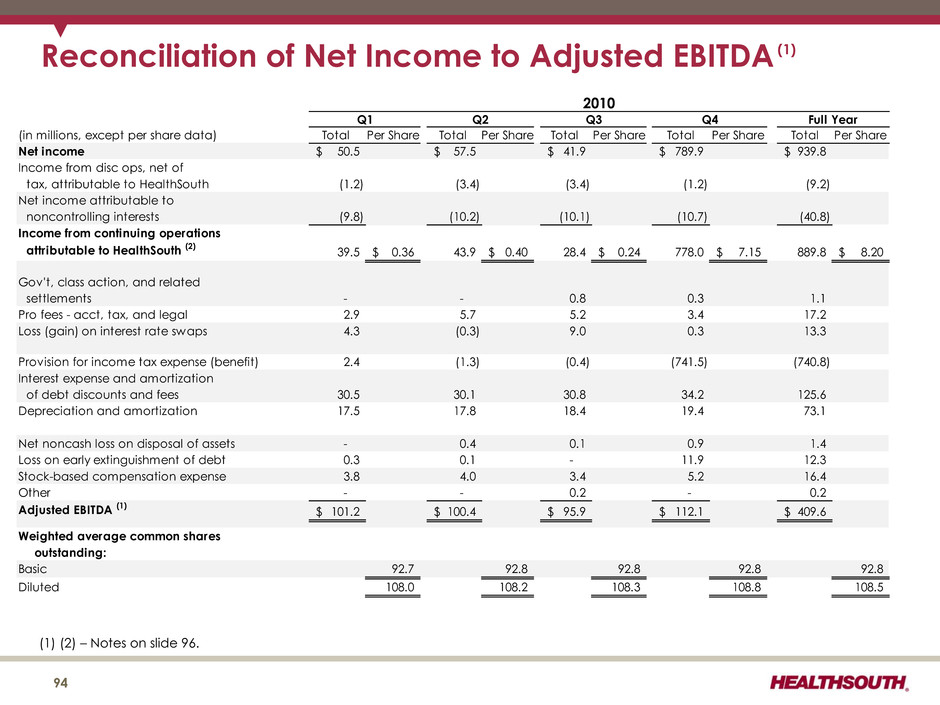
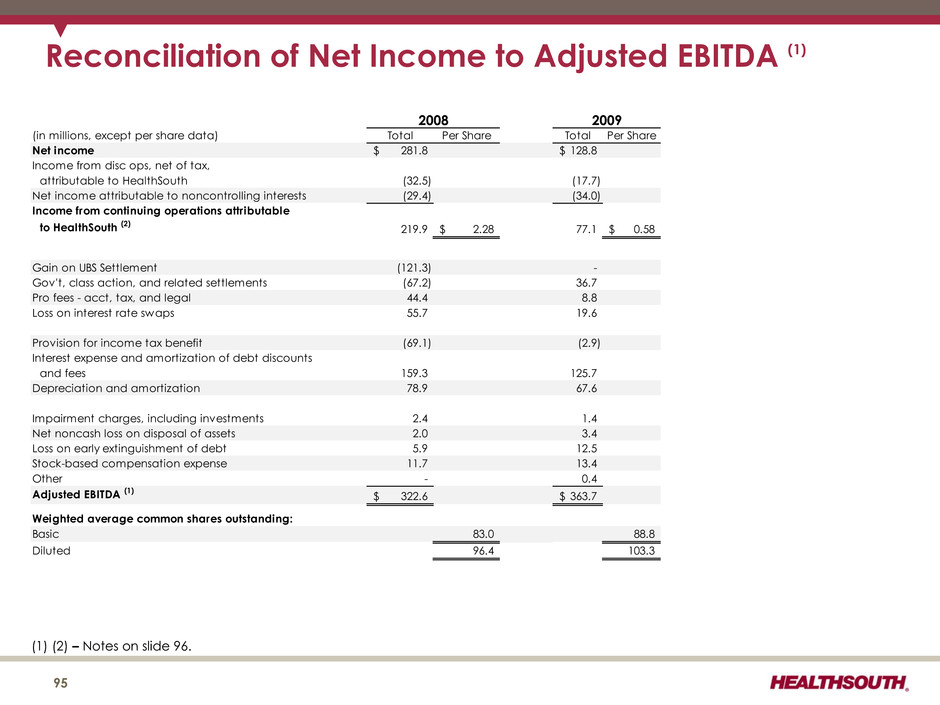
Adjusted EBITDA (1) 43 Q2 Q1 Q4 Q3 Q2 Q1 Q4 Q3 Q2 Q1 (Millions) 2013 2013 2012 2012 2012 2012 2011 2011 2011 2011 2012 2011 Net operating revenues 564.5$ 572.6$ 552.9$ 537.0$ 533.4$ 538.6$ 518.1$ 497.7$ 505.1$ 506.0$ 2,161.9$ 2,026.9$ Less: Provision for doubtful accounts (7.0) (7.4) (7.2) (7.0) (6.5) (6.3) (6.1) (5.1) (5.0) (4.8) (27.0) (21.0) Net operating revenues less provision for doubtful accounts 557.5 565.2 545.7 530.0 526.9 532.3 512.0 492.6 500.1 501.2 2,134.9 2,005.9 Operating expenses: Salaries and benefits (273.6) (274.6) (269.5) (262.3) (257.4) (261.0) (251.4) (245.0) (241.6) (244.0) (1,050.2) (982.0) Hospital-related expenses: Other operating expenses (2) (79.3) (78.0) (76.6) (75.4) (74.4) (73.0) (67.4) (70.3) (75.4) (70.9) (299.4) (284.0) Supplies (26.6) (26.2) (26.2) (23.8) (25.9) (26.5) (26.1) (24.7) (26.2) (25.8) (102.4) (102.8) Occupancy costs (11.9) (12.2) (12.0) (11.8) (12.3) (12.5) (12.2) (12.5) (12.1) (11.6) (48.6) (48.4) (117.8) (116.4) (114.8) (111.0) (112.6) (112.0) (105.7) (107.5) (113.7) (108.3) (450.4) (435.2) General and administrative expenses (3) (23.0) (23.9) (24.6) (23.2) (22.1) (23.9) (23.9) (21.5) (22.1) (22.7) (93.8) (90.2) Equity in nonconsolidated affiliates 3.3 2.9 3.0 3.3 3.1 3.3 3.2 3.1 3.2 2.5 12.7 12.0 Other income (4) 1.9 0.7 1.1 1.2 0.4 0.9 1.2 0.2 0.7 0.6 3.6 2.7 Noncontrolling interests (5) (13.8) (14.6) (12.3) (12.8) (13.2) (12.6) (12.5) (11.4) (11.3) (11.8) (50.9) (47.0) Adjusted EBITDA 134.5$ 139.3$ 128.6$ 125.2$ 125.1$ 127.0$ 122.9$ 110.5$ 115.3$ 117.5$ 505.9$ 466.2$ (1) Reconciliation to GAAP provided on slides 56, 91 - 93, and 96. Q2 Q1 Q4 Q3 Q2 Q1 Q4 Q3 Q2 Q1 2013 2013 2012 2012 2012 2012 2011 2011 2011 2011 2012 2011 In arriving at Adjusted EBITDA, the following were excluded: (2) Loss on disposal or impairment of assets $ 1.7 $ 0.1 $ 1.4 $ 1.6 $ 0.6 $ 0.8 $ 0.4 $ 2.8 $ 1.0 $ 0.1 $ 4.4 $ 4.3 (3) Stock-based compensation expense 6.5 6.3 6.0 6.1 5.9 6.1 5.9 4.9 5.3 4.2 24.1 20.3 (4) Gain related to our consolidation of St. Vincent Rehabilitation Hospital - - - 4.9 - - - - - - 4.9 - (5) Noncontrolling interests related to discontinued operations - - - - - - - (0.1) (0.9) (0.1) - (1.1) Full Year Full Year
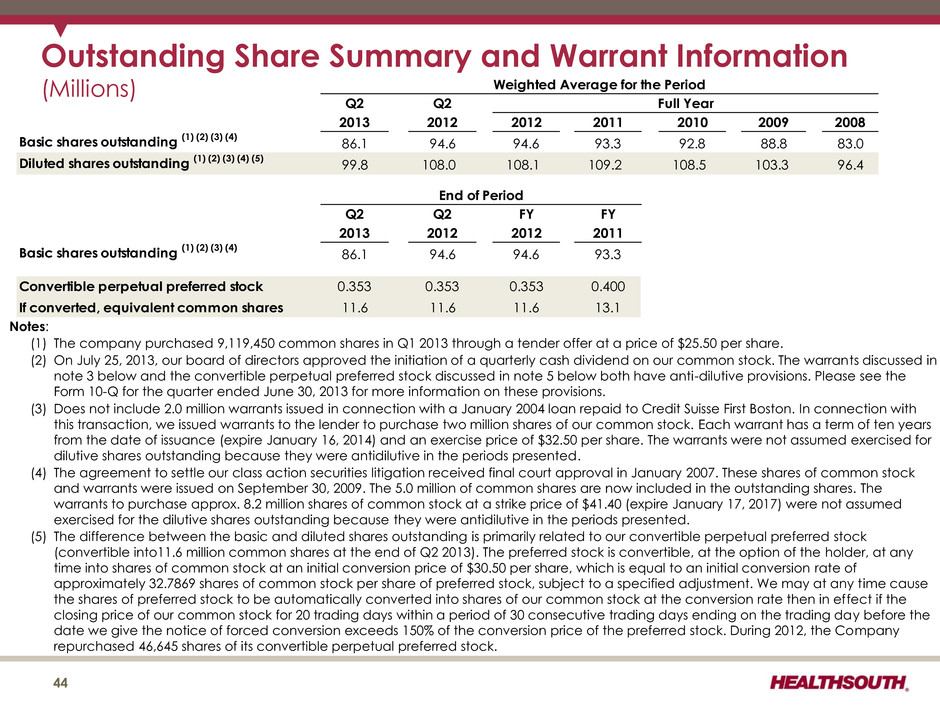
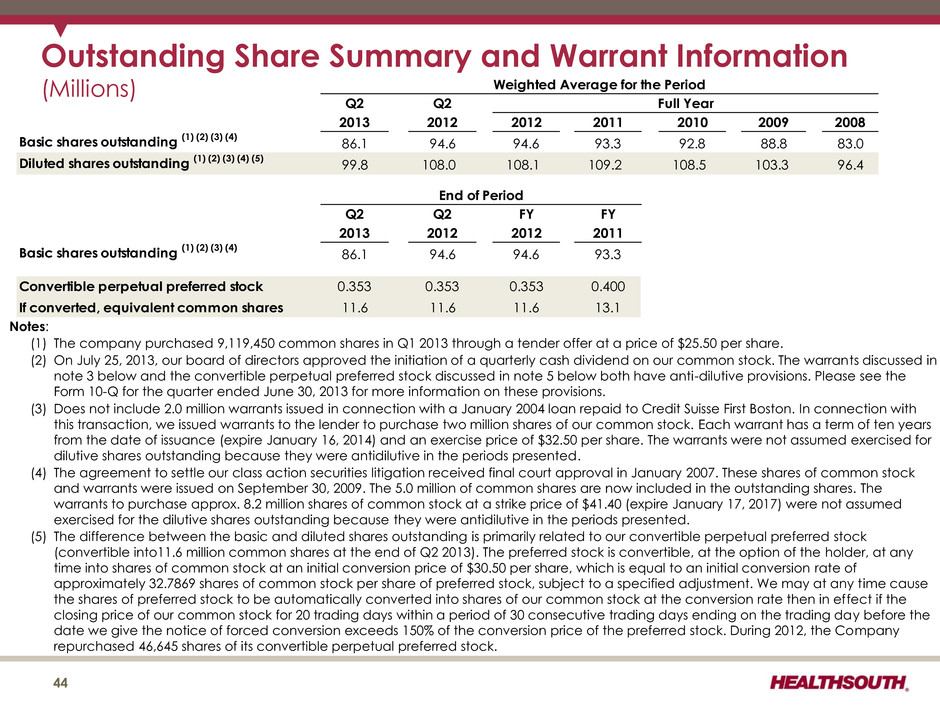
Outstanding Share Summary and Warrant Information (Millions) Q2 Q2 2013 2012 2012 2011 2010 2009 2008 Basic shares outstanding (1) (2) (3) (4) 86.1 94.6 94.6 93.3 92.8 88.8 83.0 Diluted shares outstanding (1) (2) (3) (4) (5) 99.8 108.0 108.1 109.2 108.5 103.3 96.4 Q2 Q2 FY FY 2013 2012 2012 2011 Basic shares outstanding (1) (2) (3) (4) 86.1 94.6 94.6 93.3 Convertible perpetual preferred stock 0.353 0.353 0.353 0.400 If converted, equivalent common shares 11.6 11.6 11.6 13.1 Weighted Average for the Period Full Year End of Period 44 Notes: (1) The company purchased 9,119,450 common shares in Q1 2013 through a tender offer at a price of $25.50 per share. (2) On July 25, 2013, our board of directors approved the initiation of a quarterly cash dividend on our common stock. The warrants discussed in note 3 below and the convertible perpetual preferred stock discussed in note 5 below both have anti-dilutive provisions. Please see the Form 10-Q for the quarter ended June 30, 2013 for more information on these provisions. (3) Does not include 2.0 million warrants issued in connection with a January 2004 loan repaid to Credit Suisse First Boston. In connection with this transaction, we issued warrants to the lender to purchase two million shares of our common stock. Each warrant has a term of ten years from the date of issuance (expire January 16, 2014) and an exercise price of $32.50 per share. The warrants were not assumed exercised for dilutive shares outstanding because they were antidilutive in the periods presented. (4) The agreement to settle our class action securities litigation received final court approval in January 2007. These shares of common stock and warrants were issued on September 30, 2009. The 5.0 million of common shares are now included in the outstanding shares. The warrants to purchase approx. 8.2 million shares of common stock at a strike price of $41.40 (expire January 17, 2017) were not assumed exercised for the dilutive shares outstanding because they were antidilutive in the periods presented. (5) The difference between the basic and diluted shares outstanding is primarily related to our convertible perpetual preferred stock (convertible into11.6 million common shares at the end of Q2 2013). The preferred stock is convertible, at the option of the holder, at any time into shares of common stock at an initial conversion price of $30.50 per share, which is equal to an initial conversion rate of approximately 32.7869 shares of common stock per share of preferred stock, subject to a specified adjustment. We may at any time cause the shares of preferred stock to be automatically converted into shares of our common stock at the conversion rate then in effect if the closing price of our common stock for 20 trading days within a period of 30 consecutive trading days ending on the trading day before the date we give the notice of forced conversion exceeds 150% of the conversion price of the preferred stock. During 2012, the Company repurchased 46,645 shares of its convertible perpetual preferred stock.
Business Outlook 2013 to 2015 (as of August 12, 2013) 45
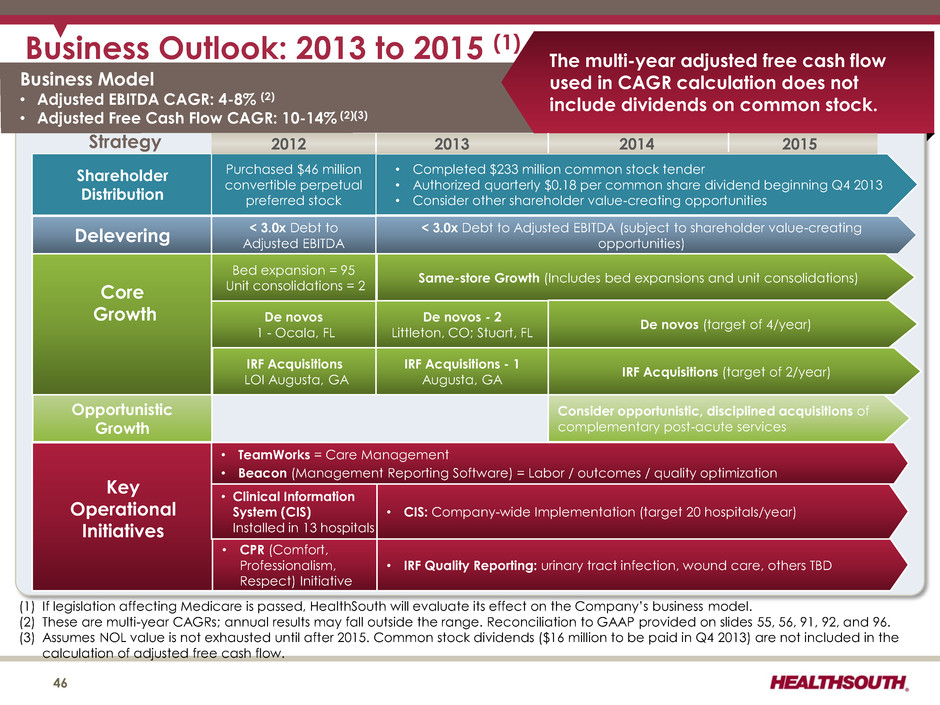
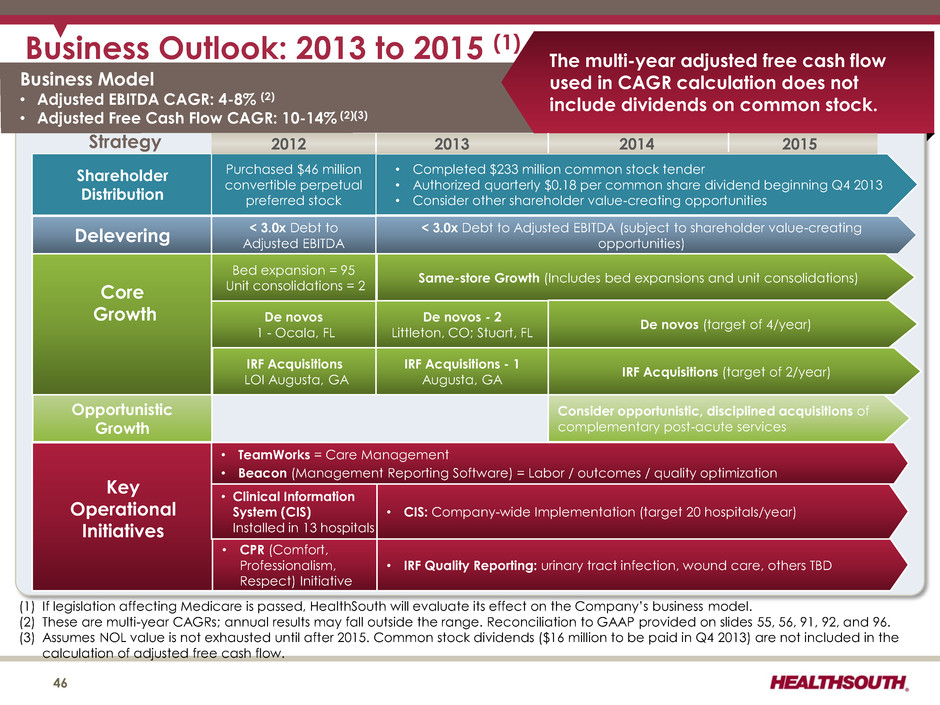
Business Outlook: 2013 to 2015 (1) Business Model • Adjusted EBITDA CAGR: 4-8% (2) • Adjusted Free Cash Flow CAGR: 10-14% (2)(3) Strategy Delevering < 3.0x Debt to Adjusted EBITDA < 3.0x Debt to Adjusted EBITDA (subject to shareholder value-creating opportunities) Core Growth Same-store Growth (Includes bed expansions and unit consolidations) De novos (target of 4/year) IRF Acquisitions (target of 2/year) Consider opportunistic, disciplined acquisitions of complementary post-acute services (1) If legislation affecting Medicare is passed, HealthSouth will evaluate its effect on the Company’s business model. (2) These are multi-year CAGRs; annual results may fall outside the range. Reconciliation to GAAP provided on slides 55, 56, 91, 92, and 96. (3) Assumes NOL value is not exhausted until after 2015. Common stock dividends ($16 million to be paid in Q4 2013) are not included in the calculation of adjusted free cash flow. 46 De novos 1 - Ocala, FL • Clinical Information System (CIS) Installed in 13 hospitals Key Operational Initiatives • TeamWorks = Care Management • Beacon (Management Reporting Software) = Labor / outcomes / quality optimization • CIS: Company-wide Implementation (target 20 hospitals/year) IRF Acquisitions LOI Augusta, GA De novos - 2 Littleton, CO; Stuart, FL Opportunistic Growth The multi-year adjusted free cash flow used in CAGR calculation does not include dividends on common stock. Bed expansion = 95 Unit consolidations = 2 • CPR (Comfort, Professionalism, Respect) Initiative • IRF Quality Reporting: urinary tract infection, wound care, others TBD IRF Acquisitions - 1 Augusta, GA Shareholder Distribution • Completed $233 million common stock tender • Authorized quarterly $0.18 per common share dividend beginning Q4 2013 • Consider other shareholder value-creating opportunities Purchased $46 million convertible perpetual preferred stock 2012 2013 2014 2015
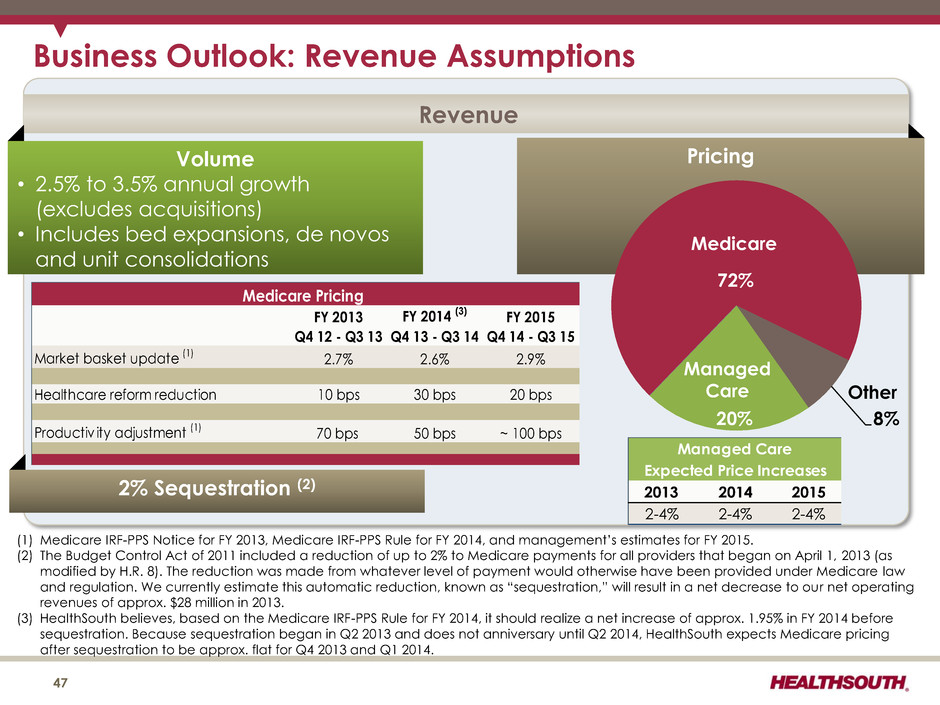
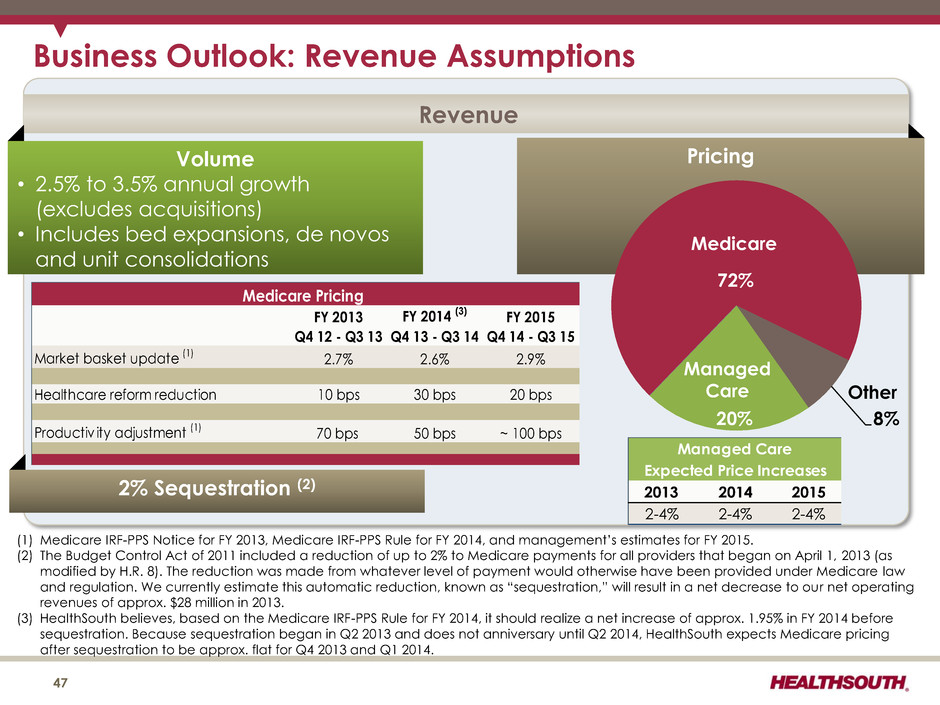
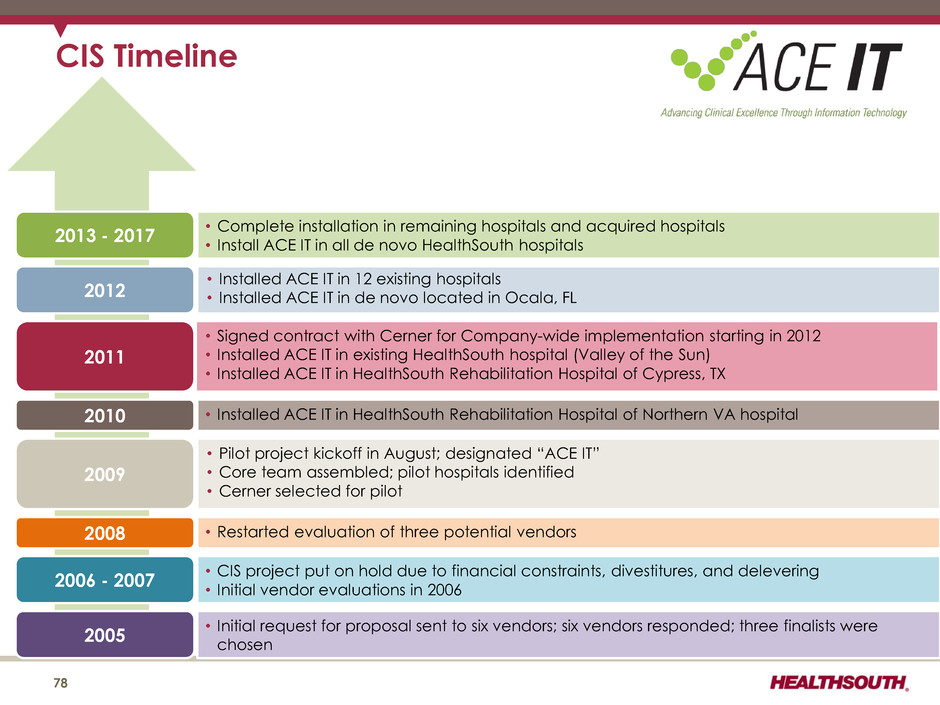
Business Outlook: Revenue Assumptions Revenue Volume • 2.5% to 3.5% annual growth (excludes acquisitions) • Includes bed expansions, de novos and unit consolidations Pricing 72% 8% 20% FY 2013 FY 2014 (3) FY 2015 Q4 12 - Q3 13 Q4 13 - Q3 14 Q4 14 - Q3 15 Market basket update (1) 2.7% 2.6% 2.9% Healthcare reform reduction 10 bps 30 bps 20 bps Productiv ity adjustment (1) 70 bps 50 bps ~ 100 bps Medicare Pricing 2013 2014 2015 2-4% 2-4% 2-4% Expected Price Increases Managed Care Medicare Managed Care Other (1) Medicare IRF-PPS Notice for FY 2013, Medicare IRF-PPS Rule for FY 2014, and management’s estimates for FY 2015. (2) The Budget Control Act of 2011 included a reduction of up to 2% to Medicare payments for all providers that began on April 1, 2013 (as modified by H.R. 8). The reduction was made from whatever level of payment would otherwise have been provided under Medicare law and regulation. We currently estimate this automatic reduction, known as “sequestration,” will result in a net decrease to our net operating revenues of approx. $28 million in 2013. (3) HealthSouth believes, based on the Medicare IRF-PPS Rule for FY 2014, it should realize a net increase of approx. 1.95% in FY 2014 before sequestration. Because sequestration began in Q2 2013 and does not anniversary until Q2 2014, HealthSouth expects Medicare pricing after sequestration to be approx. flat for Q4 2013 and Q1 2014. 47 2% Sequestration (2)
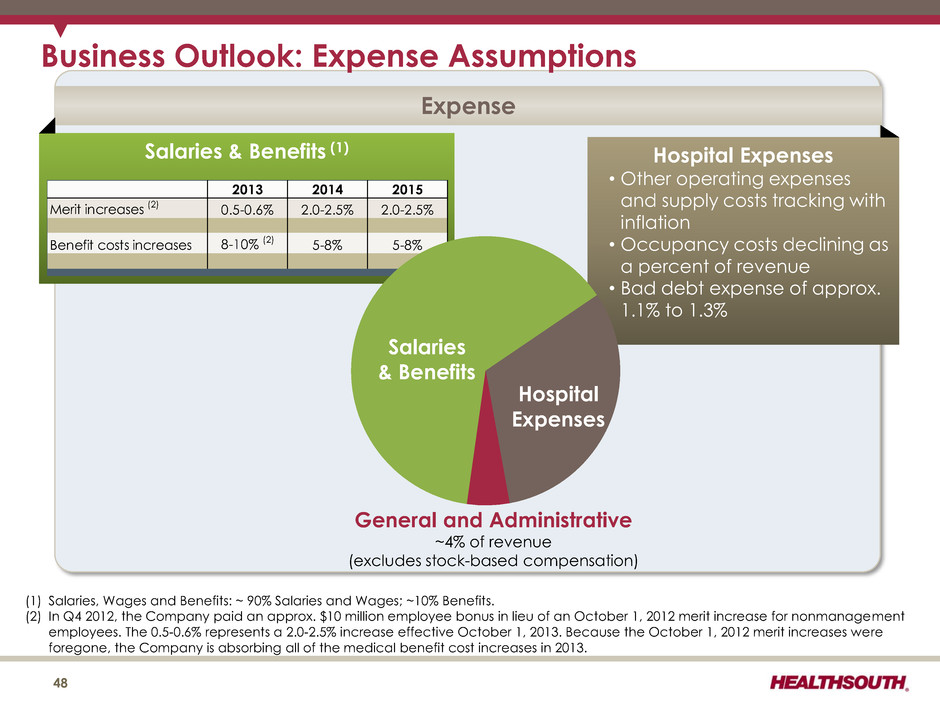
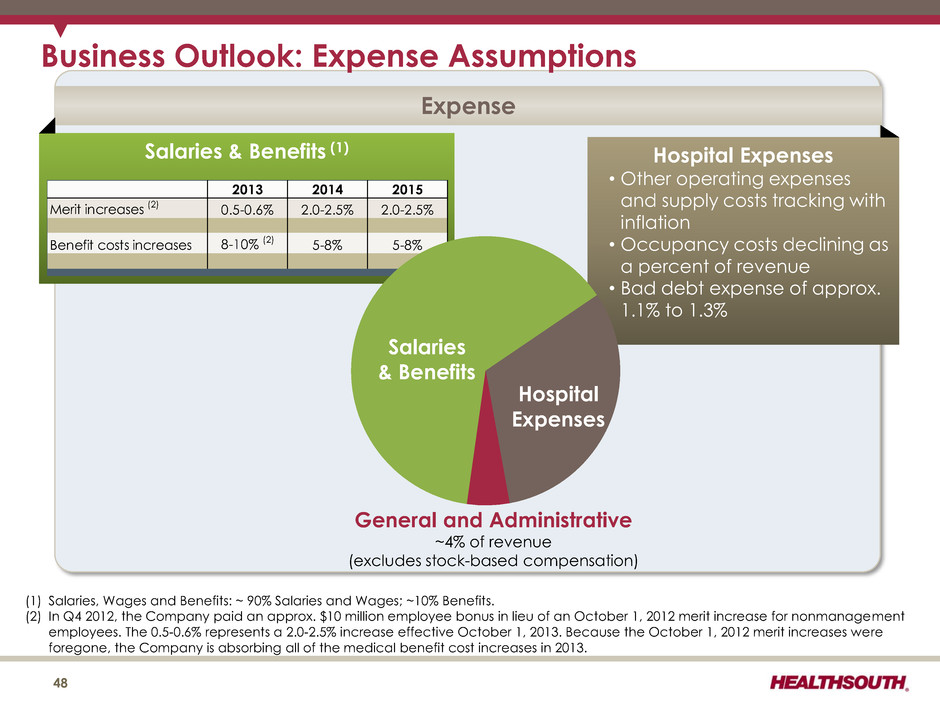
Business Outlook: Expense Assumptions Expense Salaries & Benefits (1) Hospital Expenses • Other operating expenses and supply costs tracking with inflation • Occupancy costs declining as a percent of revenue • Bad debt expense of approx. 1.1% to 1.3% 2013 2014 2015 Merit increases (2) 0.5-0.6% 2.0-2.5% 2.0-2.5% Benefit costs in reases 8-10% (2) 5-8% 5-8% General and Administrative ~4% of revenue (excludes stock-based compensation) Salaries & Benefits Hospital Expenses (1) Salaries, Wages and Benefits: ~ 90% Salaries and Wages; ~10% Benefits. (2) In Q4 2012, the Company paid an approx. $10 million employee bonus in lieu of an October 1, 2012 merit increase for nonmanagement employees. The 0.5-0.6% represents a 2.0-2.5% increase effective October 1, 2013. Because the October 1, 2012 merit increases were foregone, the Company is absorbing all of the medical benefit cost increases in 2013. 48
Guidance (as of August 12, 2013) 49

2013 Revised Guidance – Adjusted EBITDA (1) 2013 Adjusted EBITDA $520 million to $530 million (previous guidance $506 million to $516 million) (1) Reconciliation to GAAP provided on slides 56, 91, 92, and 96. Considerations for July through December: Revenue growth of 5.0% to 6.0% before sequestration ― Discharge growth between 3.0% and 4.0% ― Revenue per discharge growth between 2.3% and 2.6% before sequestration Adjusted EBITDA reduction of approx. $16 million (net of noncontrolling interests) for sequestration Q4 2013 will include a planned merit increase Installation of new clinical information system is expected to increase operating expenses by approx. $2 million Higher noncontrolling interests expense of $3 million due to changes at two joint ventures (Jonesboro, Memphis) Based on results for the first 6 months of 2013, HealthSouth raised its expectations for full- year 2013 results. 50

2013 Revised Guidance - EPS Earnings per Share from Continuing Operations Attributable to HealthSouth (1) $2.87 to $2.93 (Previous guidance $1.61 to $1.68) Considerations: Higher depreciation and amortization related to recent capital expenditures Assumes provision for income tax of approx. 40% in 2nd half of 2013 (cash taxes expected to be $6 to $12 million for full year 2013) Basic share count reflects the purchase of approx. 9.1 million shares in Q1 2013 through a tender offer Based on results for the first 6 months of 2013 which includes the $1.15 per share tax benefit related to the IRS settlement (slide 52), HealthSouth raised its expectations for full-year 2013 results. (1) Income from continuing operations attributable to HealthSouth (2) The dividends related to our convertible perpetual preferred stock in 2012 must be subtracted from income from continuing operations when calculating basic earnings per share. 51 Actual Low High (In Millions, Except Per Share Data) 2012 Adjusted EBITDA 505.9$ 520$ 530$ Interest expense and amortization of debt discounts and fees (94.1) Depreciation and amortization (82.5) Stock-based compensation expense (24.1) Other, including non-cash loss on disposal of assets (4.4) 300.8 293 303 Certain Nonrecurring Expenses: Government, class action and related settlements 3.5 Professional fees - accounting, tax and legal (16.1) Loss on early extinguishment of debt (4.0) Gain on consolidation of St. Vincent Rehabilitation Hospital 4.9 Pre-tax income 289.1 290 300 Income tax (108.6) 2 (2) Income from continuing operations (1) 180.5$ 292$ 298$ Basic shares 94.6 88.0 88.0 Diluted shares 108.1 101.8 101.8 Earnings per share (1)(2) 1.65$ 2.87$ 2.93$ EPS Guidance 2013 (100) (95) (25) - - 2 (5) (7)
Income Tax Considerations GAAP Considerations: •As of 6/30/13, the Company’s federal NOL had a gross balance of approx. $1.1 billion. ― As a result of the April 25, 2013 agreements with the IRS, the Company increased its federal NOL (on a gross basis) by approx. $283 million in Q2 2013. • The Company has a remaining valuation allowance of approx. $37 million, primarily related to state NOLs. Cash Tax Payments: • The Company expects to pay approx. $6 million to $12 million per year of income tax. •HealthSouth is not currently subject to an annual use limitation (“AUL”) under Internal Revenue Code Section 382 (“Section 382”). An “ownership change,” as defined by Section 382, could subject the Company to an AUL, which would approximate the value of the Company at the time of the “ownership change” multiplied by the long- term tax exempt rate. 52
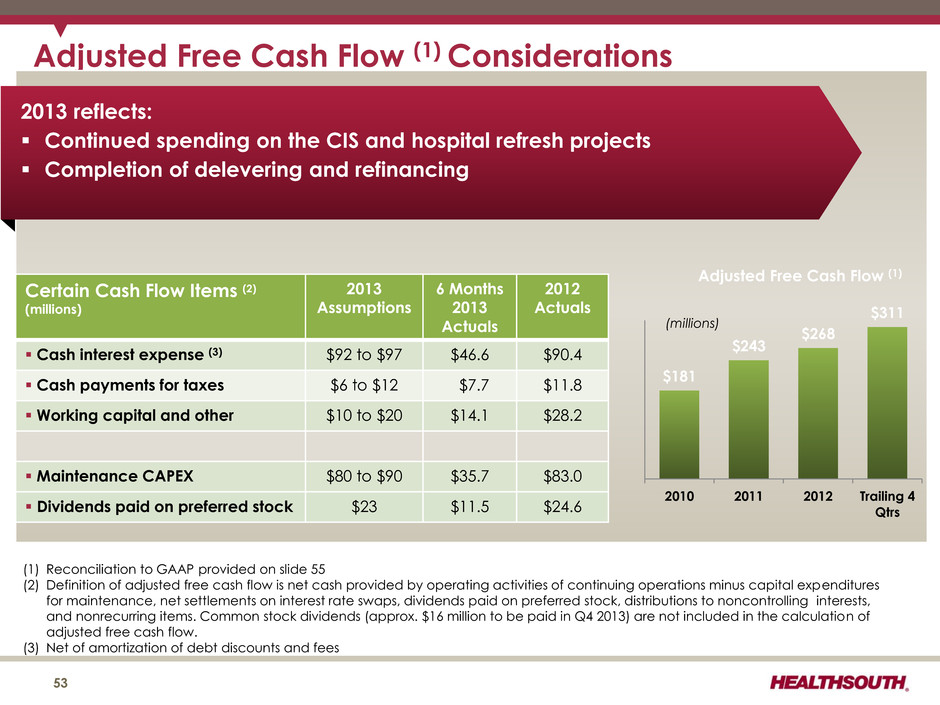
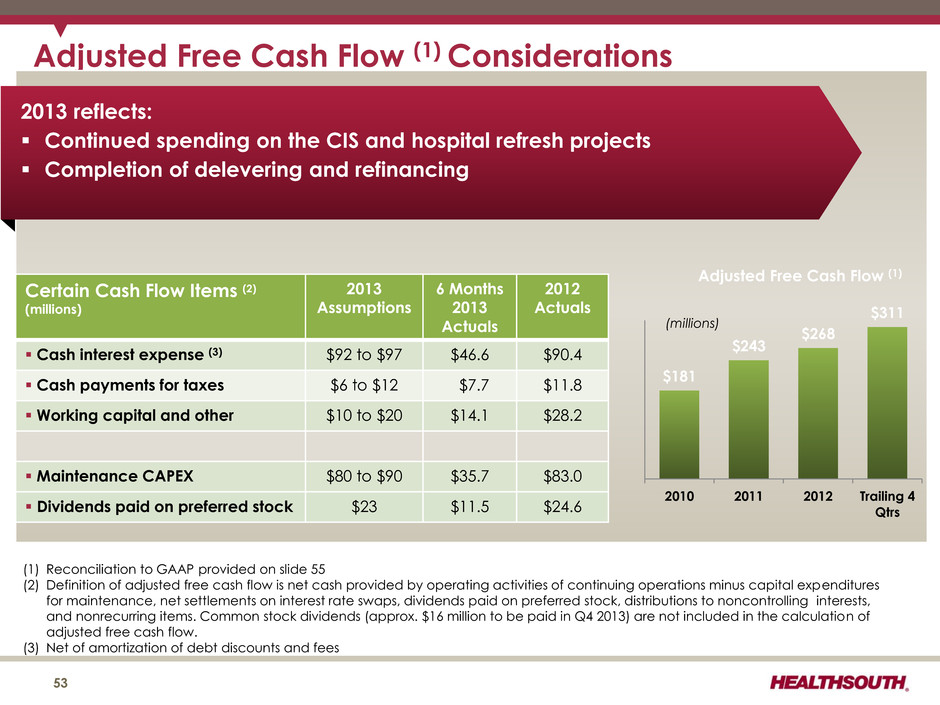
Adjusted Free Cash Flow (1) Considerations (1) Reconciliation to GAAP provided on slide 55 (2) Definition of adjusted free cash flow is net cash provided by operating activities of continuing operations minus capital expenditures for maintenance, net settlements on interest rate swaps, dividends paid on preferred stock, distributions to noncontrolling interests, and nonrecurring items. Common stock dividends (approx. $16 million to be paid in Q4 2013) are not included in the calculation of adjusted free cash flow. (3) Net of amortization of debt discounts and fees 53 Certain Cash Flow Items (2) (millions) 2013 Assumptions 6 Months 2013 Actuals 2012 Actuals Cash interest expense (3) $92 to $97 $46.6 $90.4 Cash payments for taxes $6 to $12 $7.7 $11.8 Working capital and other $10 to $20 $14.1 $28.2 Maintenance CAPEX $80 to $90 $35.7 $83.0 Dividends paid on preferred stock $23 $11.5 $24.6 2013 reflects: Continued spending on the CIS and hospital refresh projects Completion of delevering and refinancing $181 $243 $268 $311 2010 2011 2012 Trailing 4 Qtrs Adjusted Free Cash Flow (1) (millions)
Free Cash Flow 54
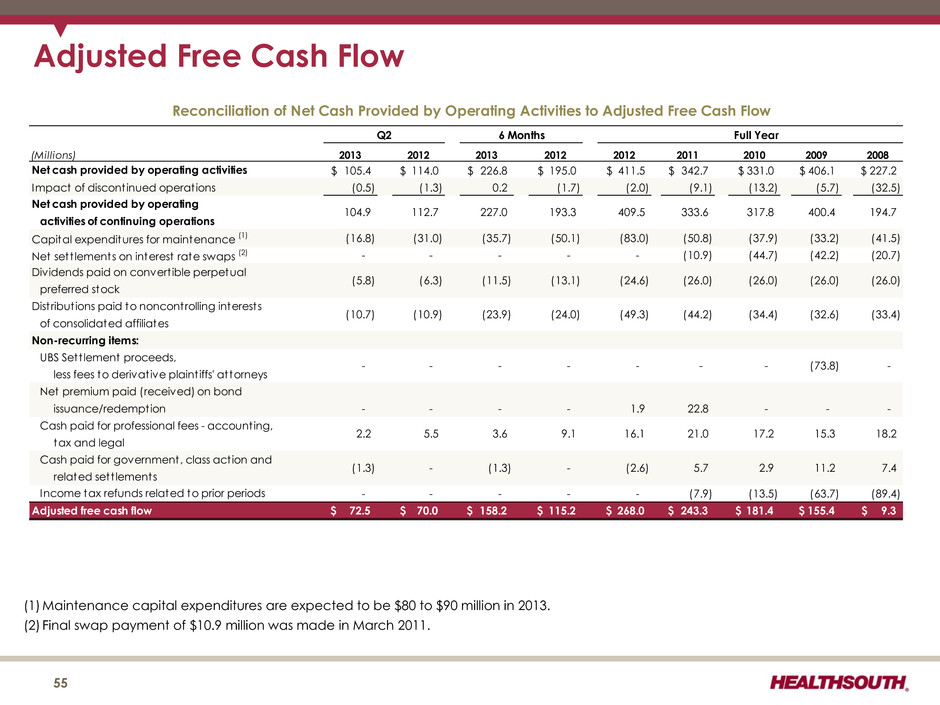
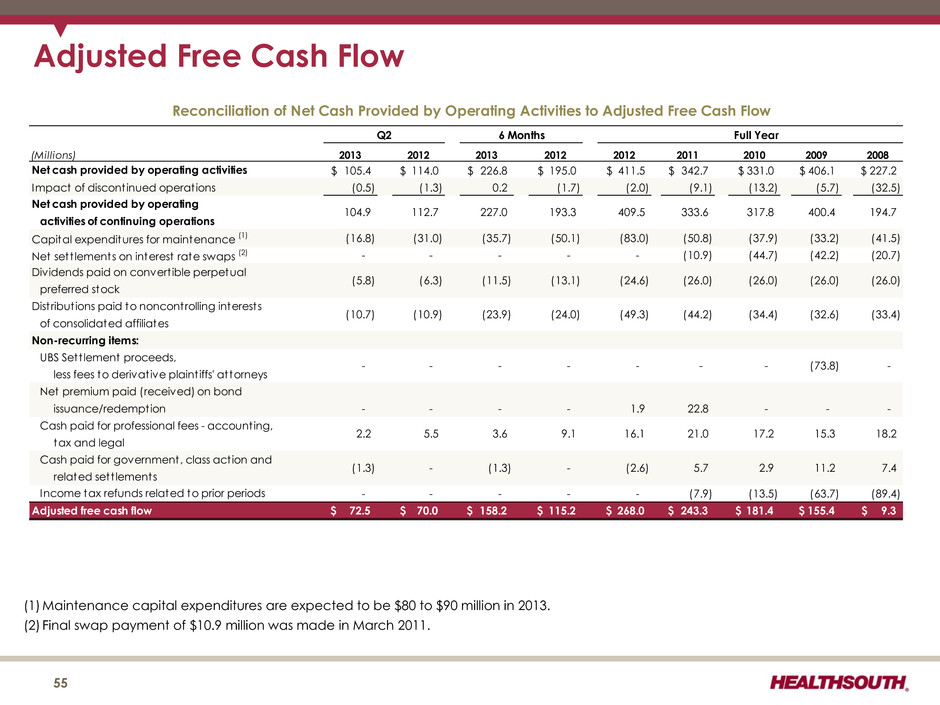
Adjusted Free Cash Flow (Millions) 2013 2012 2013 2012 2012 2011 2010 2009 2008 105.4$ 114.0$ 226.8$ 195.0$ 411.5$ 342.7$ 331.0$ 406.1$ 227.2$ (0.5) (1.3) 0.2 (1.7) (2.0) (9.1) (13.2) (5.7) (32.5) Capital expenditures for maintenance (1) (16.8) (31.0) (35.7) (50.1) (83.0) (50.8) (37.9) (33.2) (41.5) Net sett lements on interest rate swaps (2) - - - - - (10.9) (44.7) (42.2) (20.7) Dividends paid on convert ible perpetual preferred stock Distribut ions paid to noncontrolling interests of consolidated affiliates Non-recurring items: UBS Sett lement proceeds, less fees to derivative plaint iffs' attorneys Net premium paid (received) on bond issuance/redemption - - - - 1.9 22.8 - - - Cash paid for professional fees - accounting, tax and legal Cash paid for government, class action and related sett lements - - - - - (7.9) (13.5) (63.7) (89.4) Adjusted free cash flow 72.5$ 70.0$ 158.2$ 115.2$ 268.0$ 243.3$ 181.4$ 155.4$ 9.3$ (1.3) - 194.7 (26.0) (33.4) - 18.2 104.9 112.7 - - 400.4 (34.4) (26.0) (26.0) activities of continuing operations Net cash provided by operating Impact of discontinued operations - (73.8) (32.6) Q2 Full Year 317.8 5.7 2.9 2.2 5.5 21.0 7.4 15.3 333.6 (26.0) Net cash provided by operating activities Income tax refunds related to prior periods (5.8) (6.3) (10.7) (10.9) 409.5 - (44.2) (24.6) (49.3) Reconciliation of Net Cash Provided by Operating Activities to Adjusted Free Cash Flow - 6 Months 227.0 193.3 (11.5) (13.1) (23.9) (24.0) - 3.6 9.1 (1.3) - 11.2 17.2 - (2.6) 16.1 (1) Maintenance capital expenditures are expected to be $80 to $90 million in 2013. (2) Final swap payment of $10.9 million was made in March 2011. 55
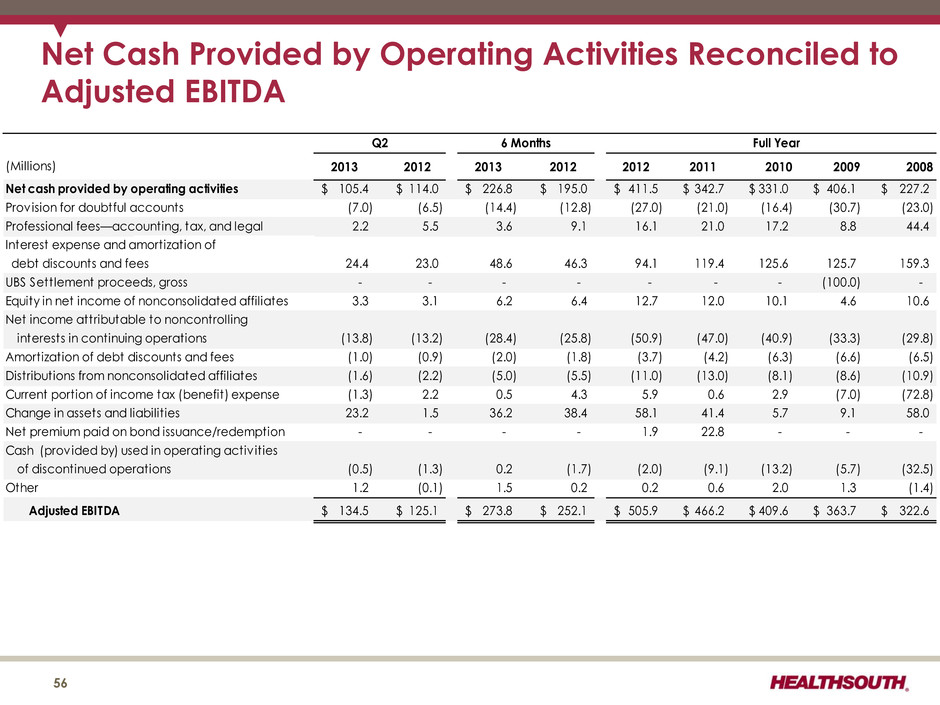
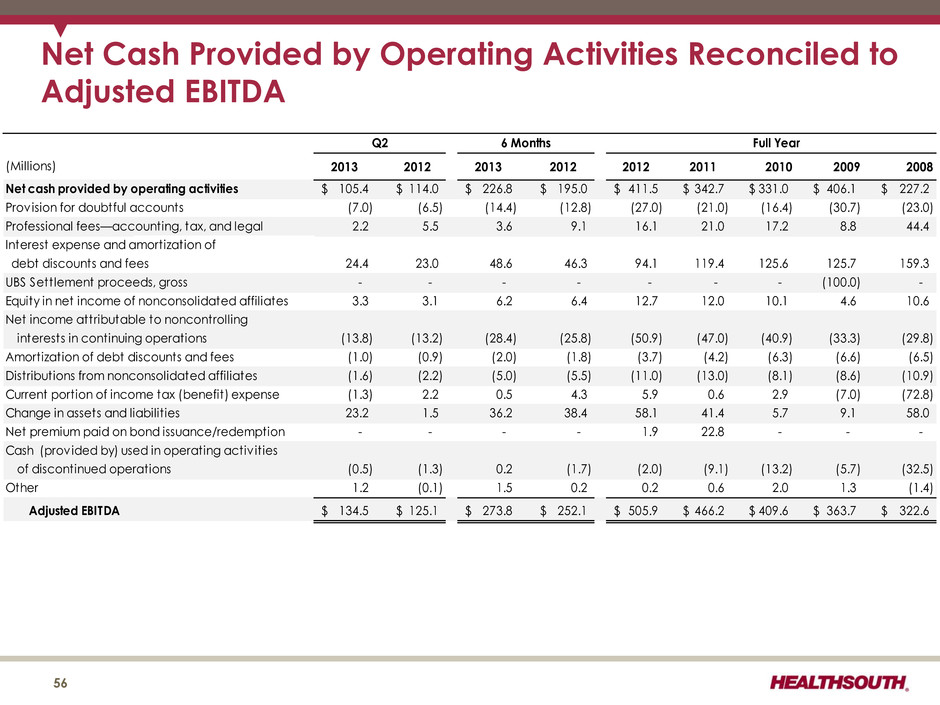
(Millions) 2013 2012 2013 2012 2012 2011 2010 2009 2008 Net cash provided by operating activities 105.4$ 114.0$ 226.8$ 195.0$ 411.5$ 342.7$ 331.0$ 406.1$ 227.2$ Prov ision for doubtful accounts (7.0) (6.5) (14.4) (12.8) (27.0) (21.0) (16.4) (30.7) (23.0) Professional fees—accounting, tax, and legal 2.2 5.5 3.6 9.1 16.1 21.0 17.2 8.8 44.4 Interest expense and amortization of debt discounts and fees 24.4 23.0 48.6 46.3 94.1 119.4 125.6 125.7 159.3 UBS Settlement proceeds, gross - - - - - - - (100.0) - Equity in net income of nonconsolidated affiliates 3.3 3.1 6.2 6.4 12.7 12.0 10.1 4.6 10.6 Net income attributable to noncontrolling interests in continuing operations (13.8) (13.2) (28.4) (25.8) (50.9) (47.0) (40.9) (33.3) (29.8) Amortization of debt discounts and fees (1.0) (0.9) (2.0) (1.8) (3.7) (4.2) (6.3) (6.6) (6.5) Distributions from nonconsolidated affiliates (1.6) (2.2) (5.0) (5.5) (11.0) (13.0) (8.1) (8.6) (10.9) Current portion of income tax (benefit) expense (1.3) 2.2 0.5 4.3 5.9 0.6 2.9 (7.0) (72.8) Change in assets and liabilit ies 23.2 1.5 36.2 38.4 58.1 41.4 5.7 9.1 58.0 Net premium paid on bond issuance/redemption - - - - 1.9 22.8 - - - Cash (provided by) used in operating activ ities of discontinued operations (0.5) (1.3) 0.2 (1.7) (2.0) (9.1) (13.2) (5.7) (32.5) Other 1.2 (0.1) 1.5 0.2 0.2 0.6 2.0 1.3 (1.4) Adjusted EBITDA 134.5$ 125.1$ 273.8$ 252.1$ 505.9$ 466.2$ 409.6$ 363.7$ 322.6$ Q2 Full Year6 Months Net Cash Provided by Operating Activities Reconciled to Adjusted EBITDA 56
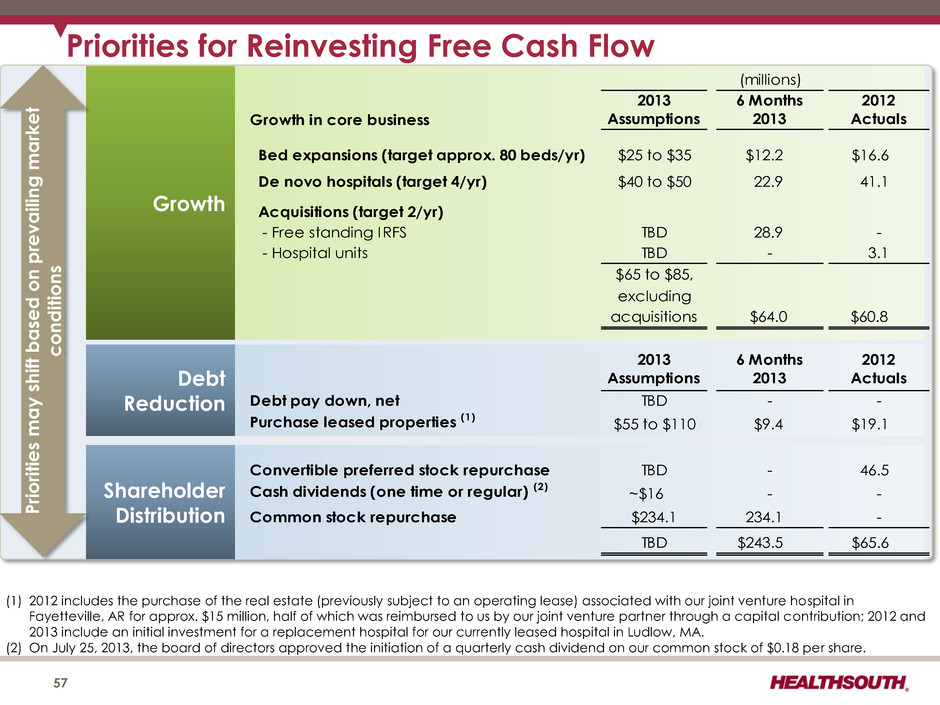
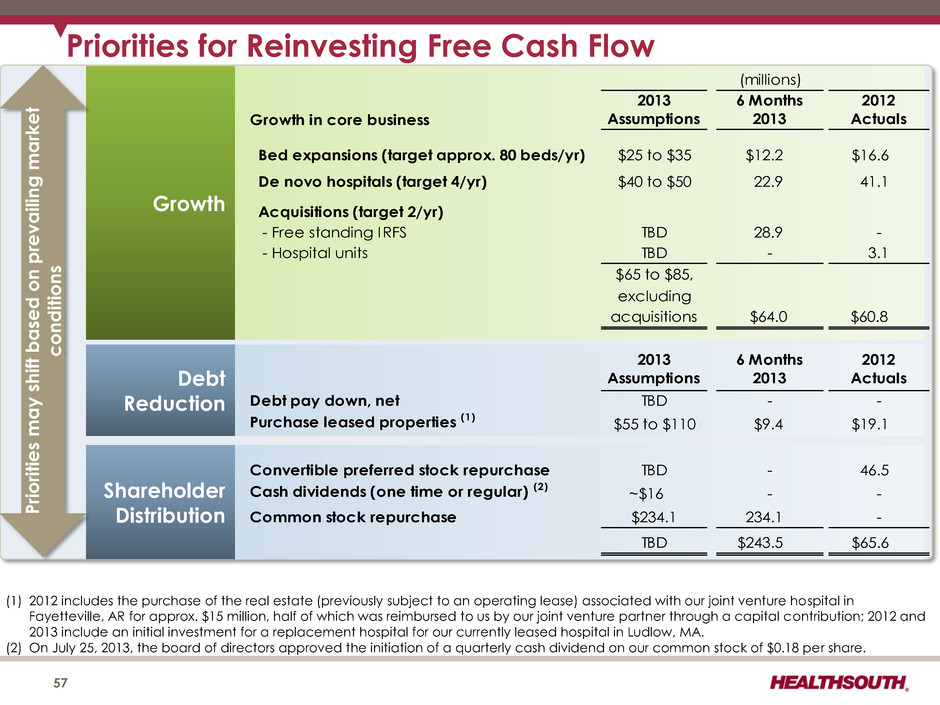
Priorities for Reinvesting Free Cash Flow 57 Growth Debt Reduction Shareholder Distribution (1) 2012 includes the purchase of the real estate (previously subject to an operating lease) associated with our joint venture hospital in Fayetteville, AR for approx. $15 million, half of which was reimbursed to us by our joint venture partner through a capital contribution; 2012 and 2013 include an initial investment for a replacement hospital for our currently leased hospital in Ludlow, MA. (2) On July 25, 2013, the board of directors approved the initiation of a quarterly cash dividend on our common stock of $0.18 per share. (millions) Growth in core business 2013 Assumptions 6 Months 2013 2012 Actuals Bed expansions (target approx. 80 beds/yr) $25 to $35 $12.2 $16.6 De novo hospitals (target 4/yr) $40 to $50 22.9 41.1 Acquisitions (target 2/yr) - Free standing IRFS TBD 28.9 - - Hospital units TBD - 3.1 $65 to $85, excluding acquisitions $64.0 $60.8 2013 Assumptions 6 Months 2013 2012 Actuals Debt pay down, net TBD - - Purchase leased properties (1) $55 to $110 $9.4 $19.1 Convertible preferred stock repurchase TBD - 46.5 Cash dividends (one time or regular) (2) ~$16 - - Common stock repurchase $234.1 234.1 - TBD $243.5 $65.6 P riori ties ma y s hift ba sed on p re v ailing mark e t c o ndition s
Refinancing and Delevering 58
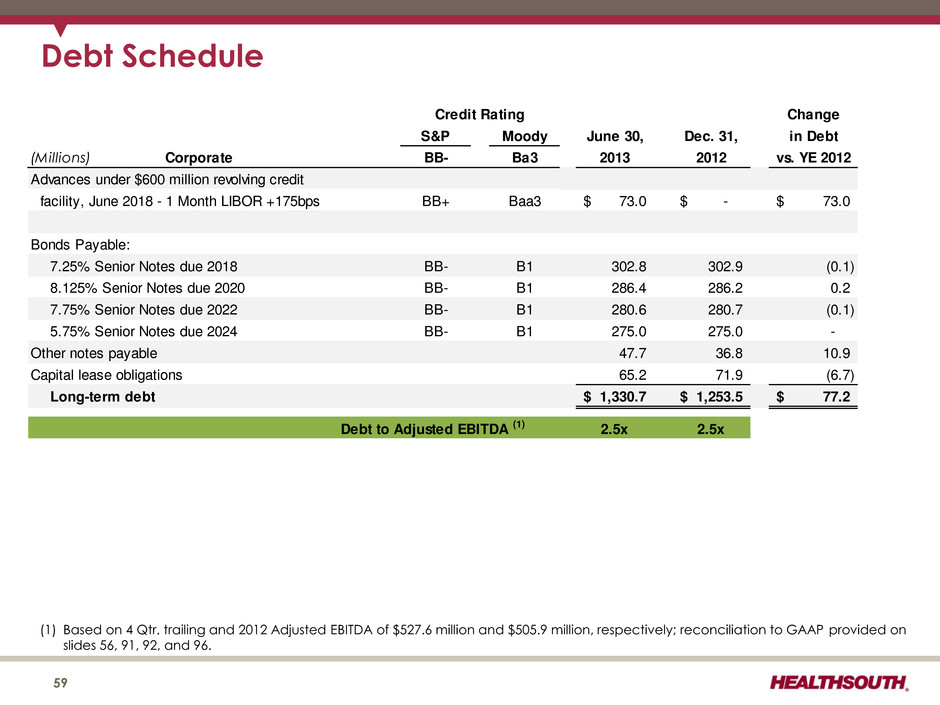
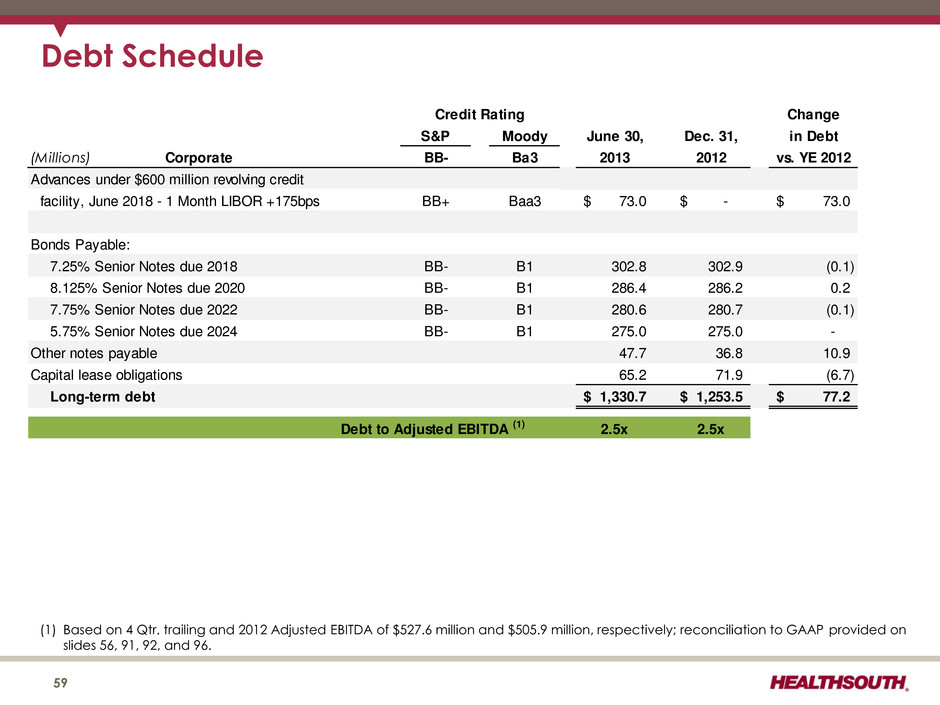
Debt Schedule (1) Based on 4 Qtr. trailing and 2012 Adjusted EBITDA of $527.6 million and $505.9 million, respectively; reconciliation to GAAP provided on slides 56, 91, 92, and 96. 59 Change S&P Moody June 30, Dec. 31, in Debt (Millions) Corporate BB- Ba3 2013 2012 vs. YE 2012 Advances under $600 million revolving credit facility, June 2018 - 1 Month LIBOR +175bps BB+ Baa3 73.0$ -$ 73.0$ Bonds Payable: 7.25% Senior Notes due 2018 BB- B1 302.8 302.9 (0.1) 8.125% Senior Notes due 2020 BB- B1 286.4 286.2 0.2 7.75% Senior Notes due 2022 BB- B1 280.6 280.7 (0.1) 5.75% Senior Notes due 2024 BB- B1 275.0 275.0 - Other notes payable 47.7 36.8 10.9 Capital lease obligations 65.2 71.9 (6.7) Long-term debt 1,330.7$ 1,253.5$ 77.2$ 2.5x 2.5x Credit Rating Debt to Adjusted EBITDA (1)
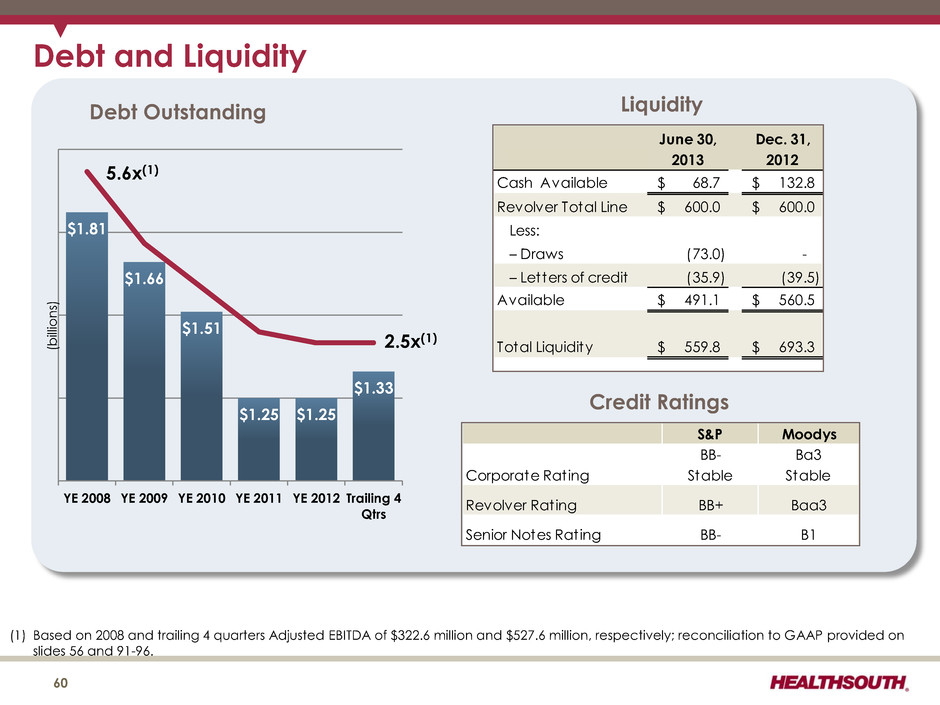
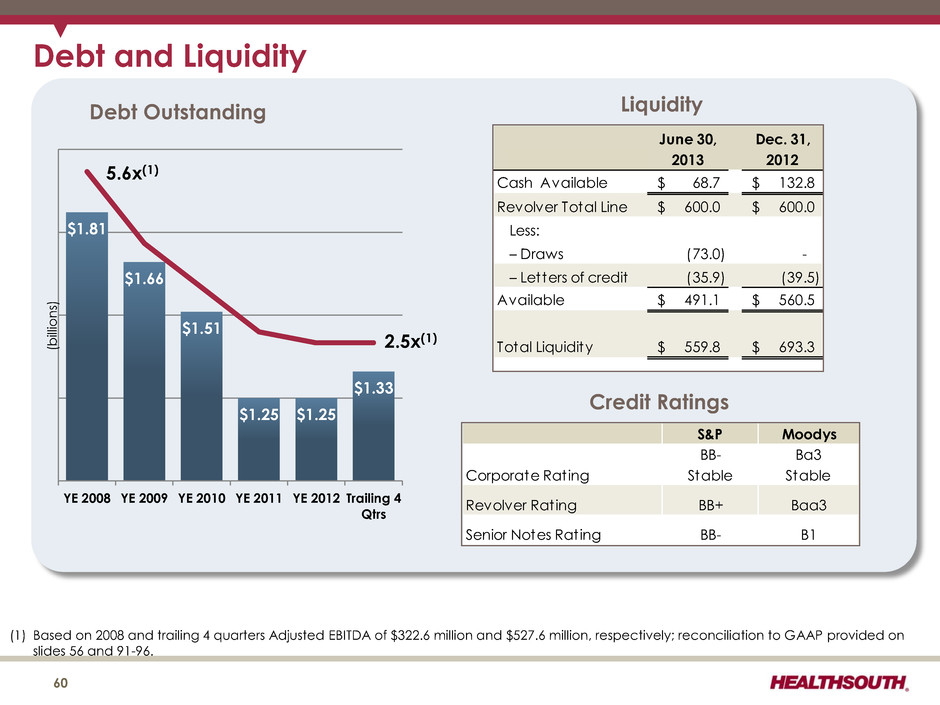
($ Billions) Year-End 2010 Goal: 3.75x to 4.00x (1) Based on 2008 and trailing 4 quarters Adjusted EBITDA of $322.6 million and $527.6 million, respectively; reconciliation to GAAP provided on slides 56 and 91-96. Debt and Liquidity June 30, Dec. 31, 2013 2012 Cash Available 68.7$ 132.8$ Revolver Total Line 600.0$ 600.0$ Less: – Draws (73.0) - – Letters of credit (35.9) (39.5) 491.1$ 560.5$ Total Liquidity 559.8$ 693.3$ Available Liquidity 60 $1.81 $1.66 $1.51 $1.25 $1.25 $1.33 YE 2008 YE 2009 YE 2010 YE 2011 YE 2012 Trailing 4 Qtrs 5.6x(1) 2.5x(1) Debt Outstanding Credit Ratings S&P Moodys Corporate Rating BB- Stable Ba3 Stable Revolver Rating BB+ Baa3 Senior Notes Rating BB- B1 (b ill io n s)
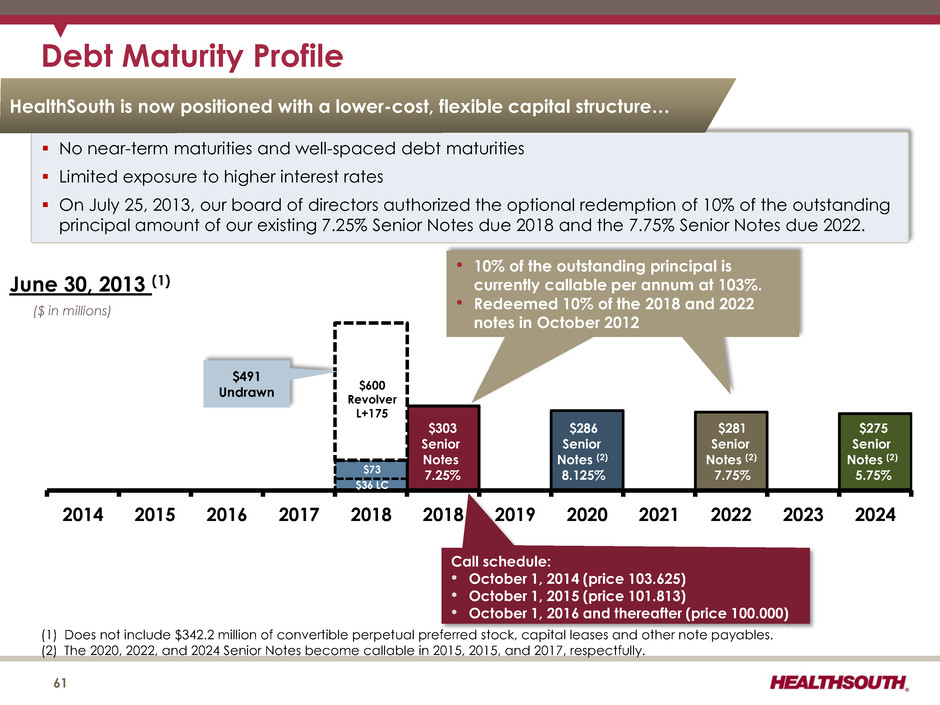
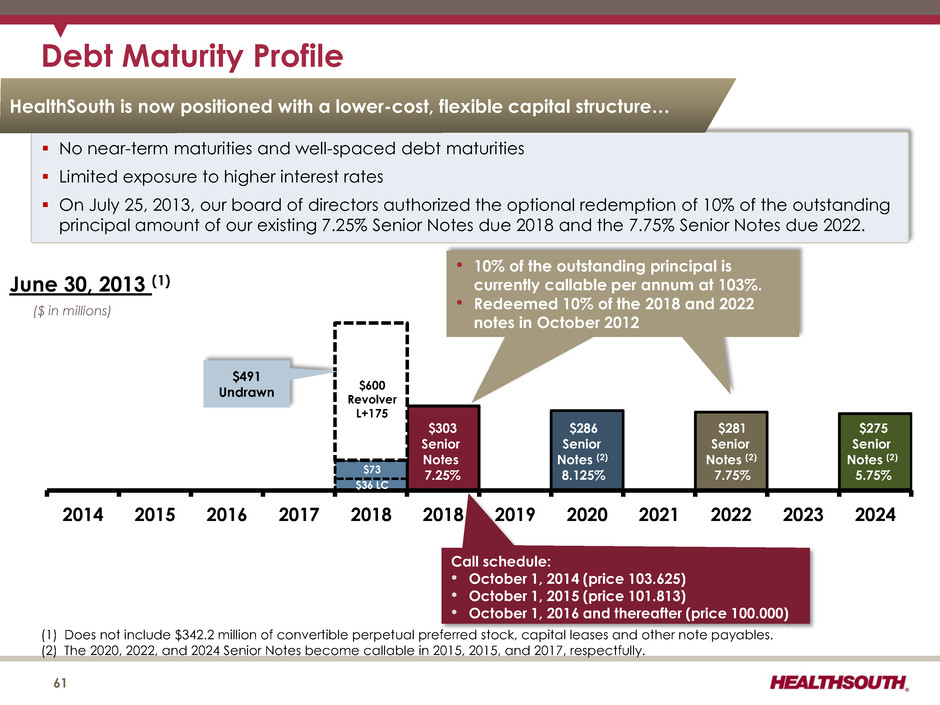
Call schedule: • October 1, 2014 (price 103.625) • October 1, 2015 (price 101.813) • October 1, 2016 and thereafter (price 100.000) Debt Maturity Profile 2014 2015 2016 2017 2018 2018 2019 2020 2021 2022 2023 2024 $303 Senior Notes 7.25% $286 Senior Notes (2) 8.125% $281 Senior Notes (2) 7.75% ($ in millions) $36 LC $600 Revolver L+175 June 30, 2013 (1) $491 Undrawn • 10% of the outstanding principal is currently callable per annum at 103%. • Redeemed 10% of the 2018 and 2022 notes in October 2012 (1) Does not include $342.2 million of convertible perpetual preferred stock, capital leases and other note payables. (2) The 2020, 2022, and 2024 Senior Notes become callable in 2015, 2015, and 2017, respectfully. No near-term maturities and well-spaced debt maturities Limited exposure to higher interest rates On July 25, 2013, our board of directors authorized the optional redemption of 10% of the outstanding principal amount of our existing 7.25% Senior Notes due 2018 and the 7.75% Senior Notes due 2022. $275 Senior Notes (2) 5.75% HealthSouth is now positioned with a lower-cost, flexible capital structure… 61 $73
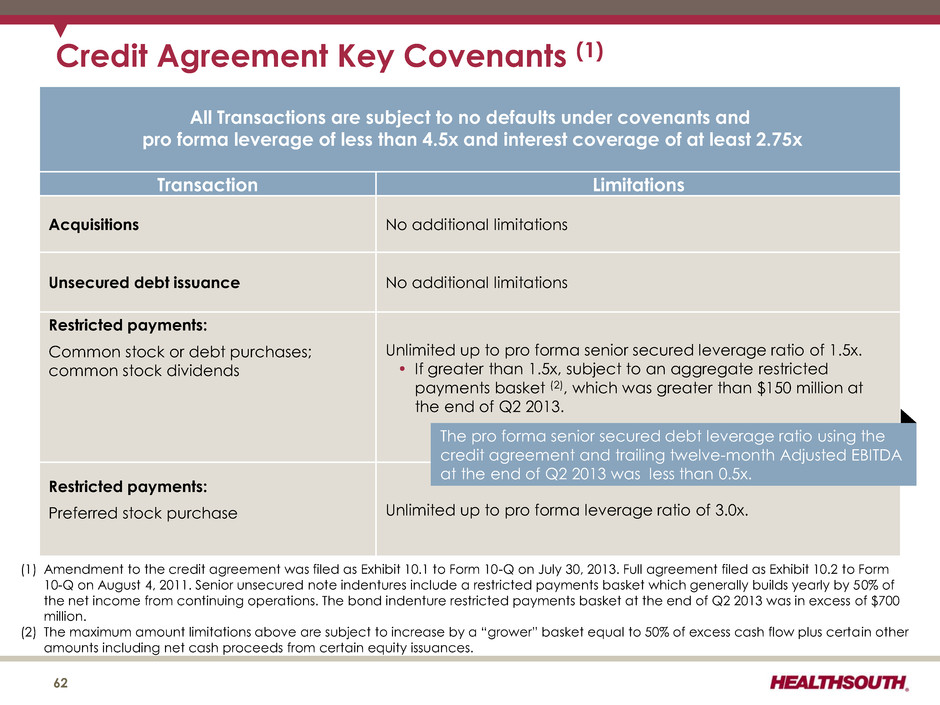
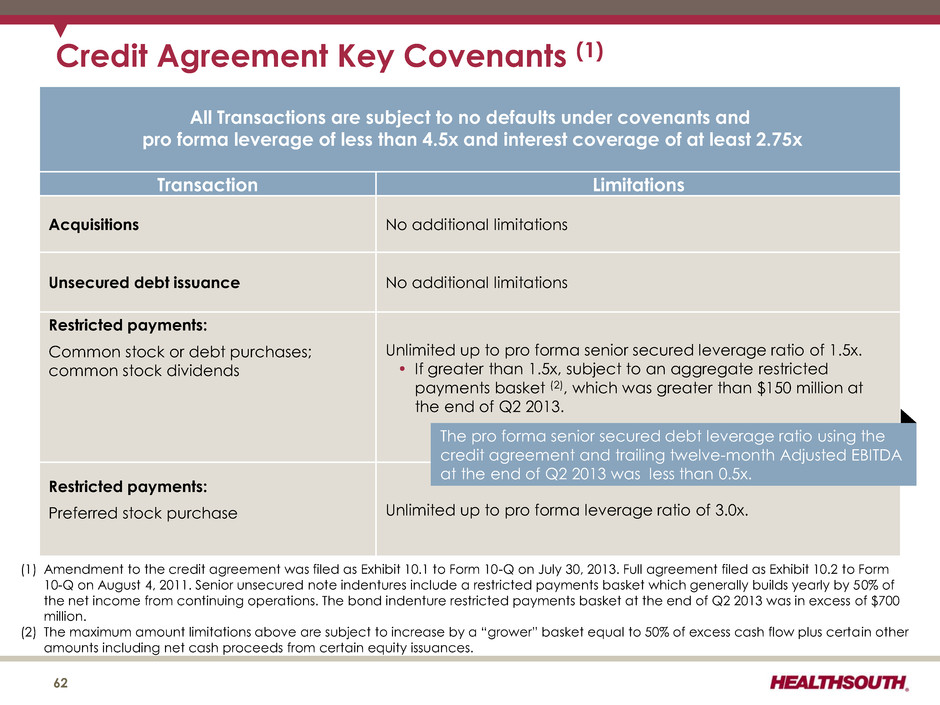
Credit Agreement Key Covenants (1) All Transactions are subject to no defaults under covenants and pro forma leverage of less than 4.5x and interest coverage of at least 2.75x Transaction Limitations Acquisitions No additional limitations Unsecured debt issuance No additional limitations Restricted payments: Common stock or debt purchases; common stock dividends Unlimited up to pro forma senior secured leverage ratio of 1.5x. • If greater than 1.5x, subject to an aggregate restricted payments basket (2), which was greater than $150 million at the end of Q2 2013. Restricted payments: Preferred stock purchase Unlimited up to pro forma leverage ratio of 3.0x. 62 (1) Amendment to the credit agreement was filed as Exhibit 10.1 to Form 10-Q on July 30, 2013. Full agreement filed as Exhibit 10.2 to Form 10-Q on August 4, 2011. Senior unsecured note indentures include a restricted payments basket which generally builds yearly by 50% of the net income from continuing operations. The bond indenture restricted payments basket at the end of Q2 2013 was in excess of $700 million. (2) The maximum amount limitations above are subject to increase by a “grower” basket equal to 50% of excess cash flow plus certa in other amounts including net cash proceeds from certain equity issuances. The pro forma senior secured debt leverage ratio using the credit agreement and trailing twelve-month Adjusted EBITDA at the end of Q2 2013 was less than 0.5x.
Growth 63
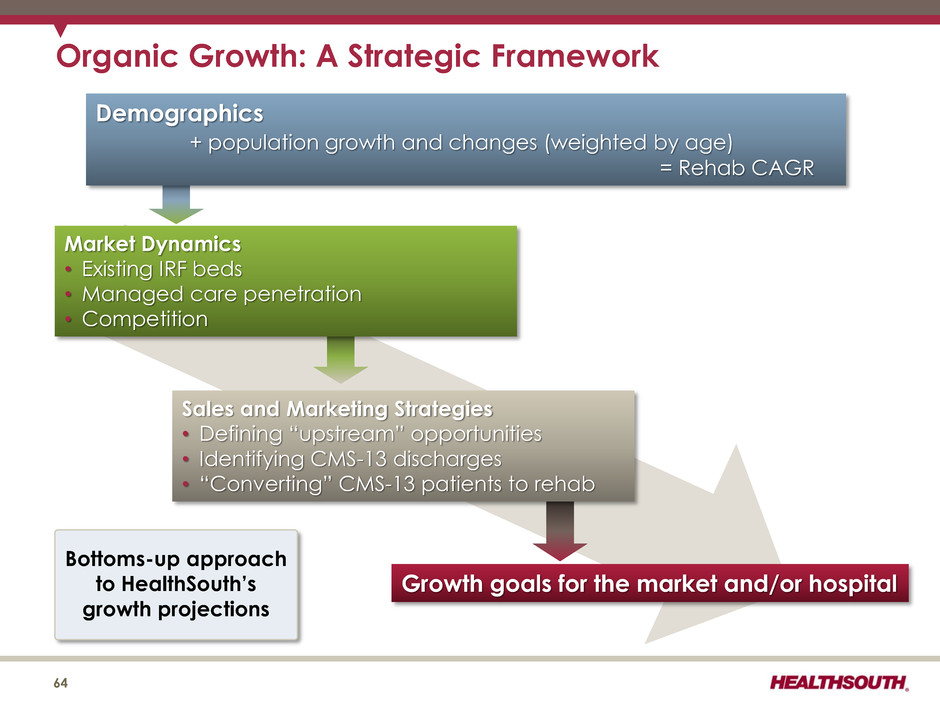
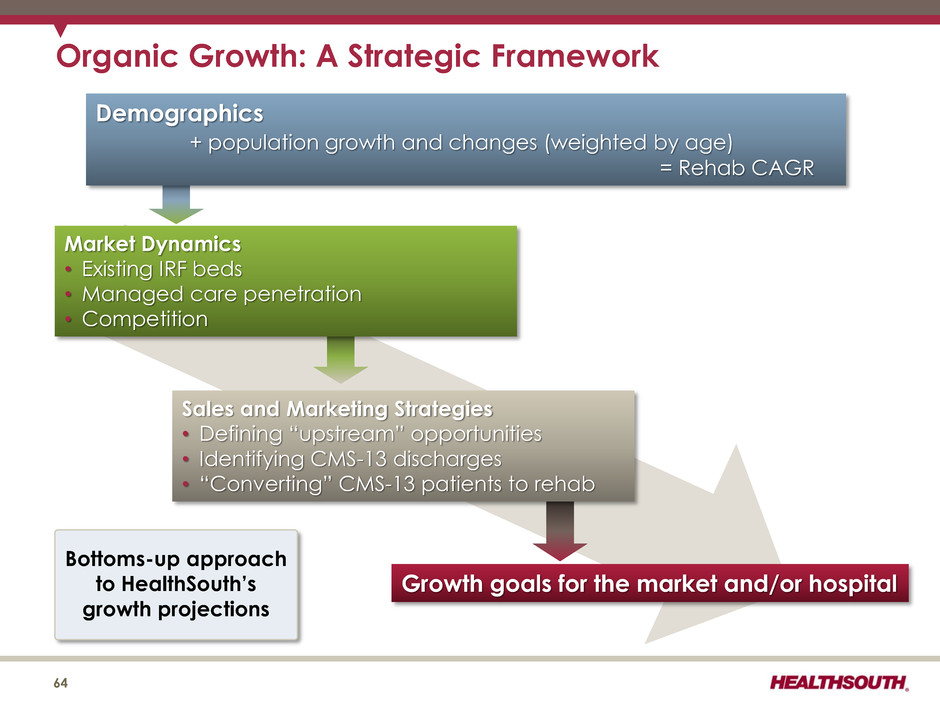
Demographics + population growth and changes (weighted by age) = Rehab CAGR Growth goals for the market and/or hospital Sales and Marketing Strategies • Defining “upstream” opportunities • Identifying CMS-13 discharges • “Converting” CMS-13 patients to rehab Market Dynamics • Existing IRF beds • Managed care penetration • Competition Organic Growth: A Strategic Framework Bottoms-up approach to HealthSouth’s growth projections 64
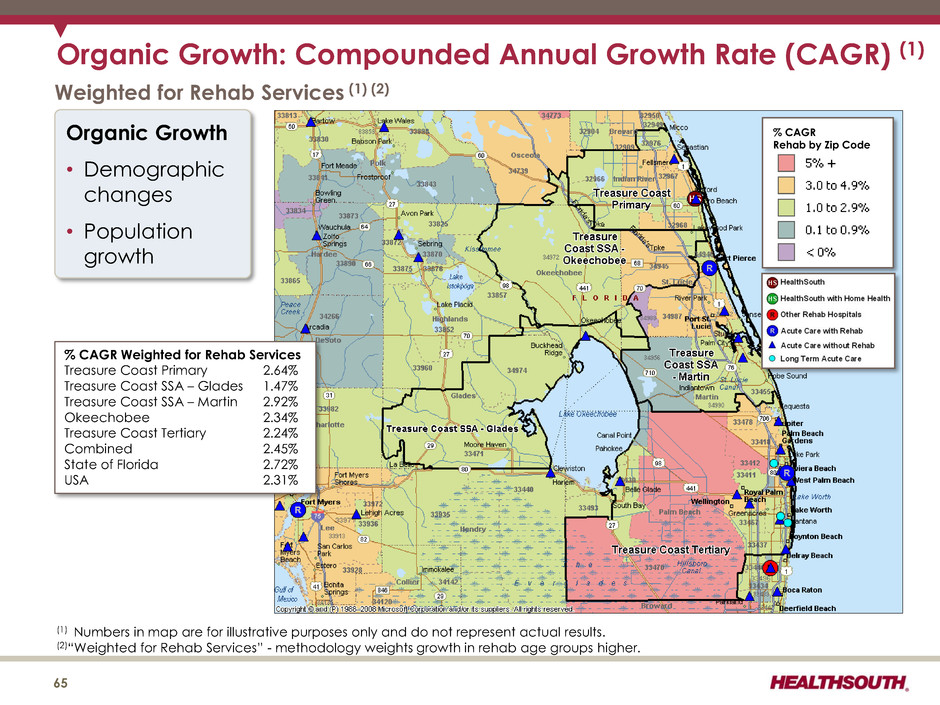
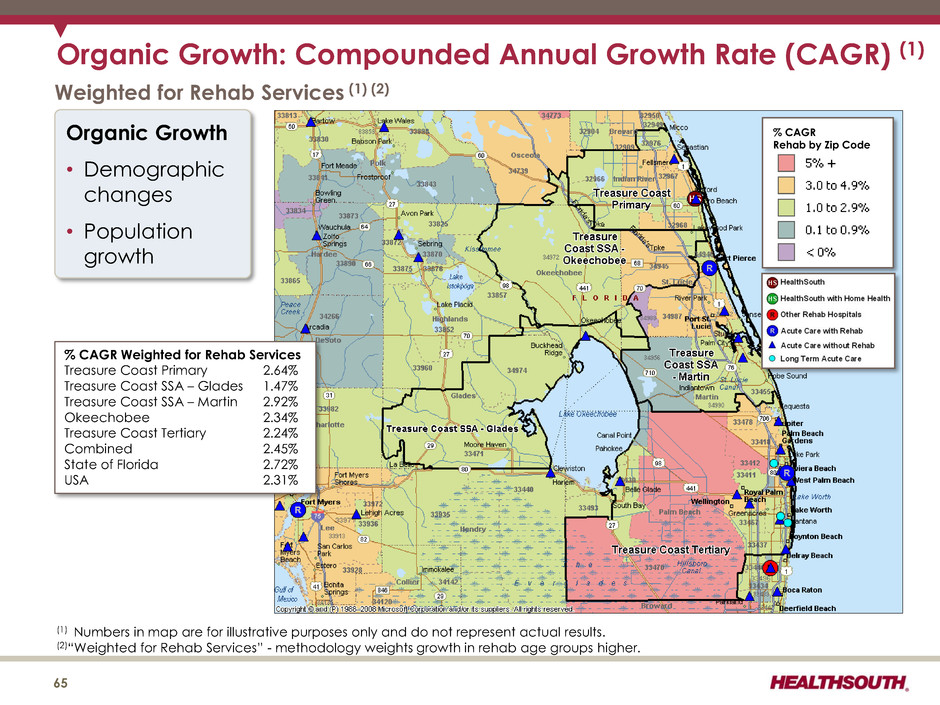
Organic Growth: Compounded Annual Growth Rate (CAGR) (1) (1) Numbers in map are for illustrative purposes only and do not represent actual results. (2)“Weighted for Rehab Services” - methodology weights growth in rehab age groups higher. % CAGR Rehab by Zip Code Weighted for Rehab Services (1) (2) Organic Growth • Demographic changes • Population growth % CAGR Weighted for Rehab Services Treasure Coast Primary 2.64% Treasure Coast SSA – Glades 1.47% Treasure Coast SSA – Martin 2.92% Okeechobee 2.34% Treasure Coast Tertiary 2.24% Combined 2.45% State of Florida 2.72% USA 2.31% 65
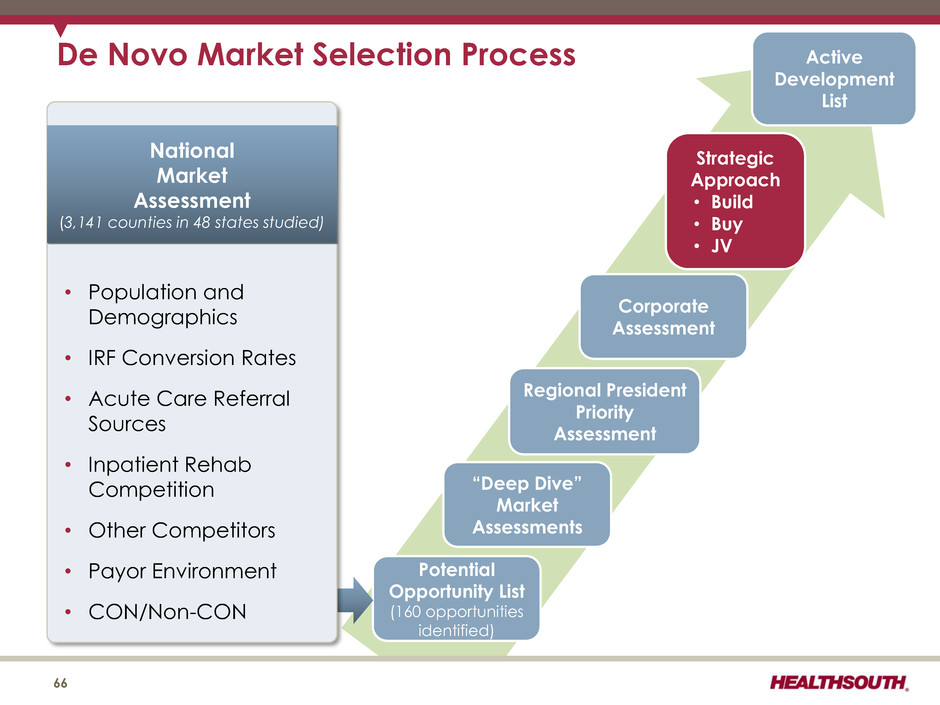
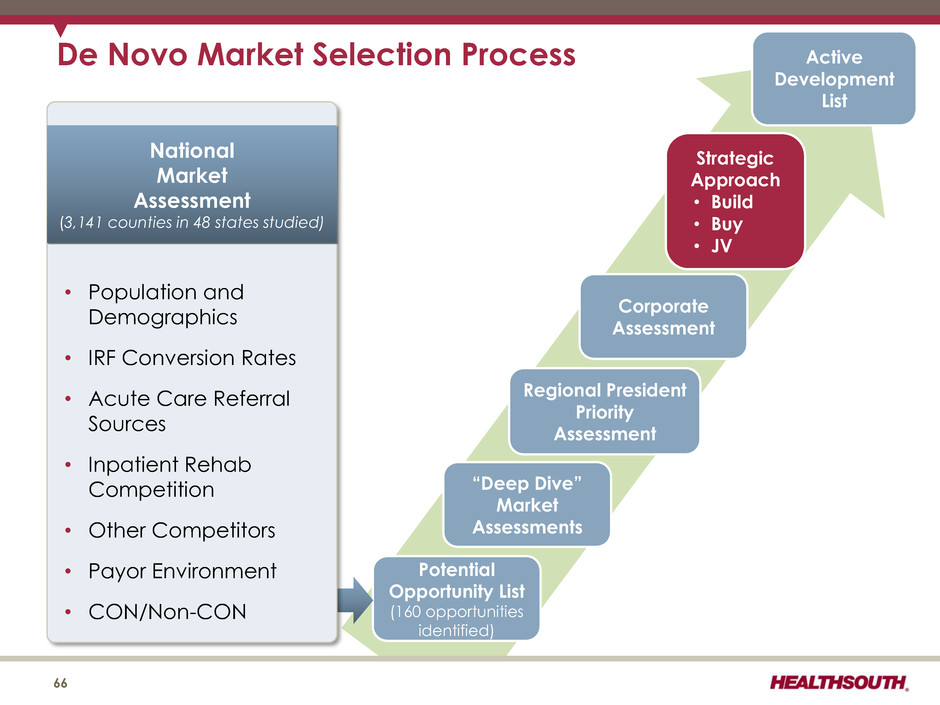
De Novo Market Selection Process 66 Active Development List Corporate Assessment Strategic Approach • Build • Buy • JV Regional President Priority Assessment “Deep Dive” Market Assessments Potential Opportunity List (160 opportunities identified) National Market Assessment (3,141 counties in 48 states studied) • Population and Demographics • IRF Conversion Rates • Acute Care Referral Sources • Inpatient Rehab Competition • Other Competitors • Payor Environment • CON/Non-CON
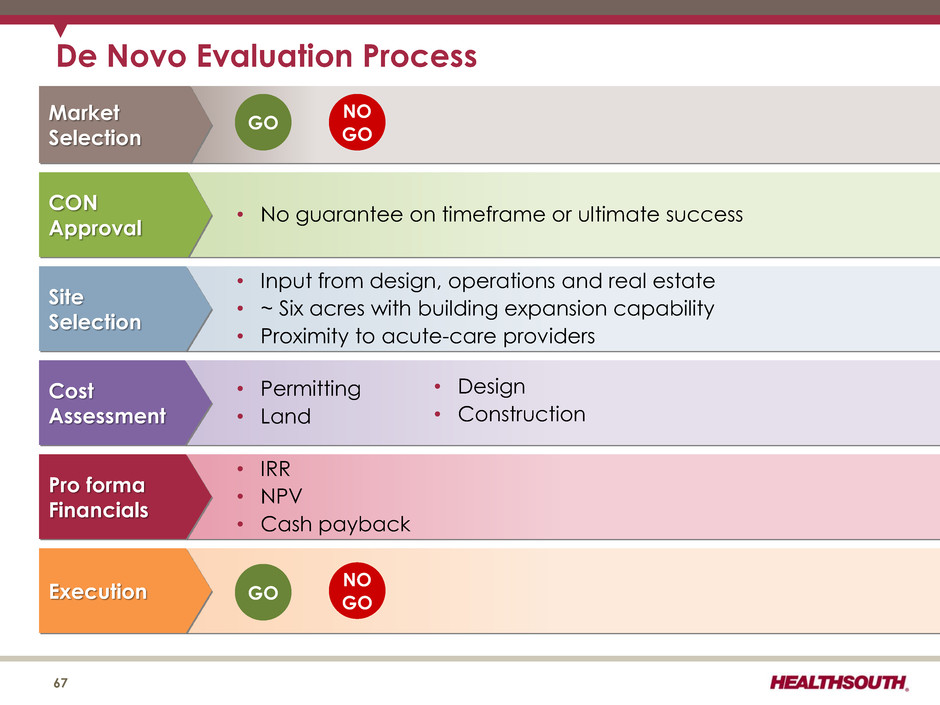
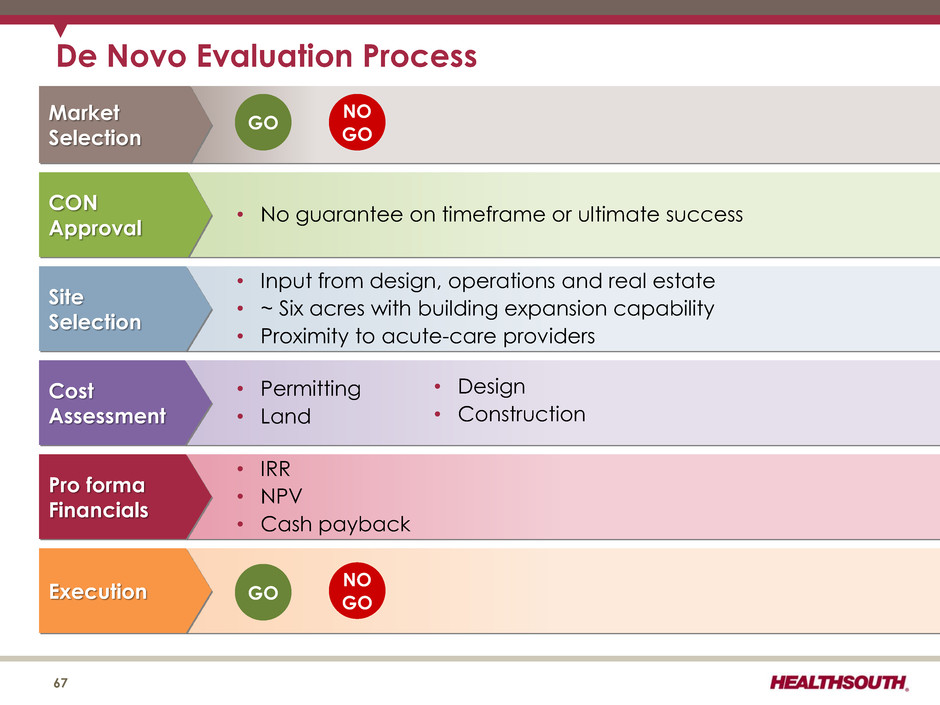
• No guarantee on timeframe or ultimate success • Input from design, operations and real estate • ~ Six acres with building expansion capability • Proximity to acute-care providers • Permitting • Land • IRR • NPV • Cash payback ..... CON Approval Site Selection Cost Assessment Pro forma Financials Execution • Design • Construction NO GO GO De Novo Evaluation Process 67 Market Selection GO NO GO
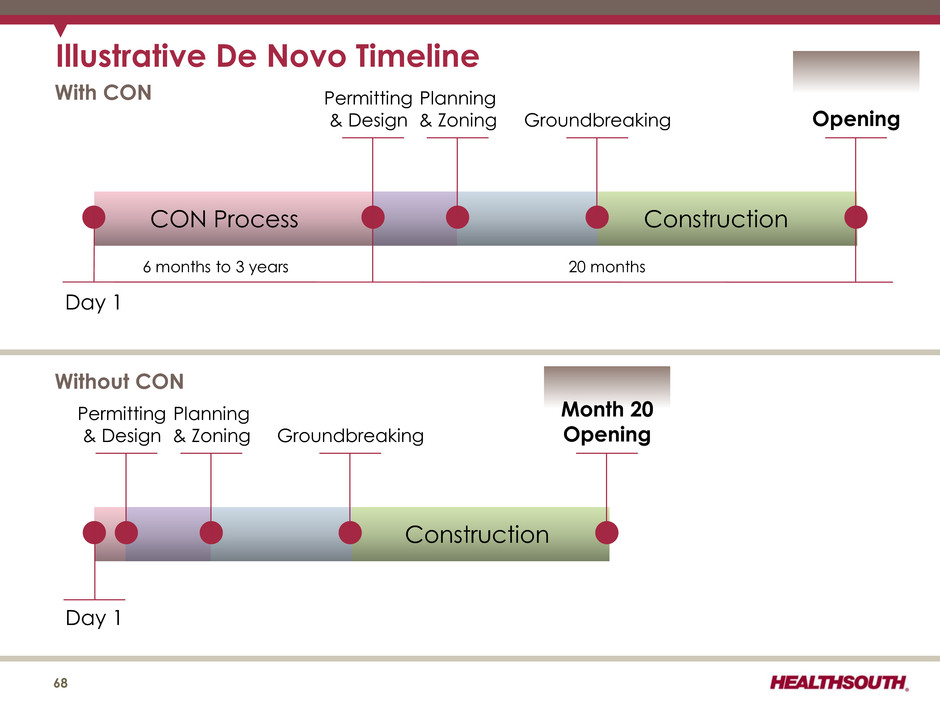
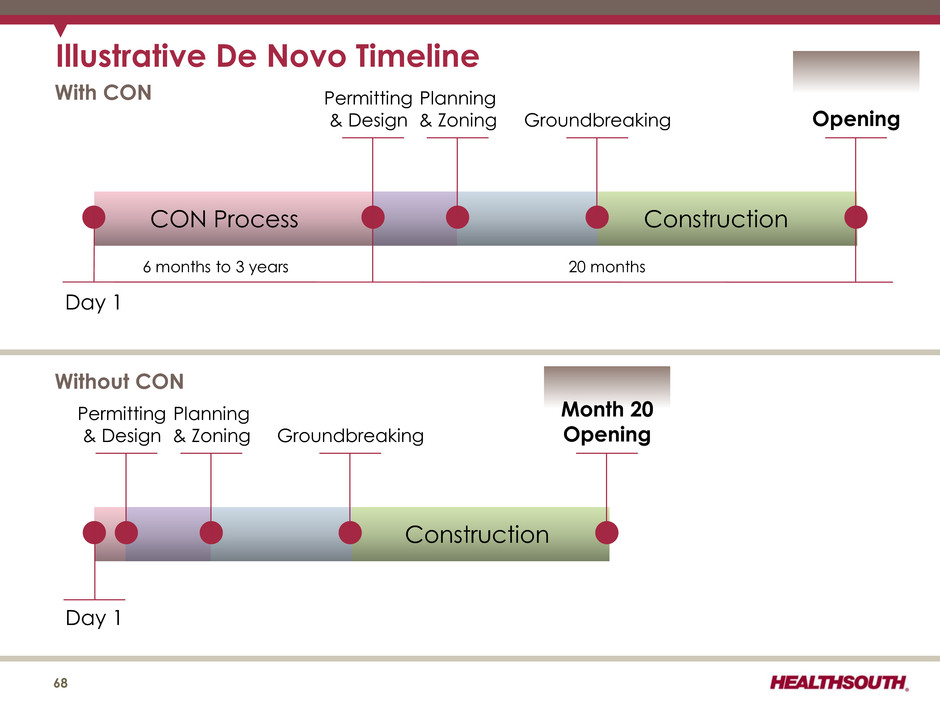
Illustrative De Novo Timeline 68 Day 1 CON Process Construction With CON Permitting & Design Planning & Zoning Groundbreaking Opening Construction Permitting & Design Planning & Zoning Groundbreaking Month 20 Opening Day 1 Without CON 6 months to 3 years 20 months
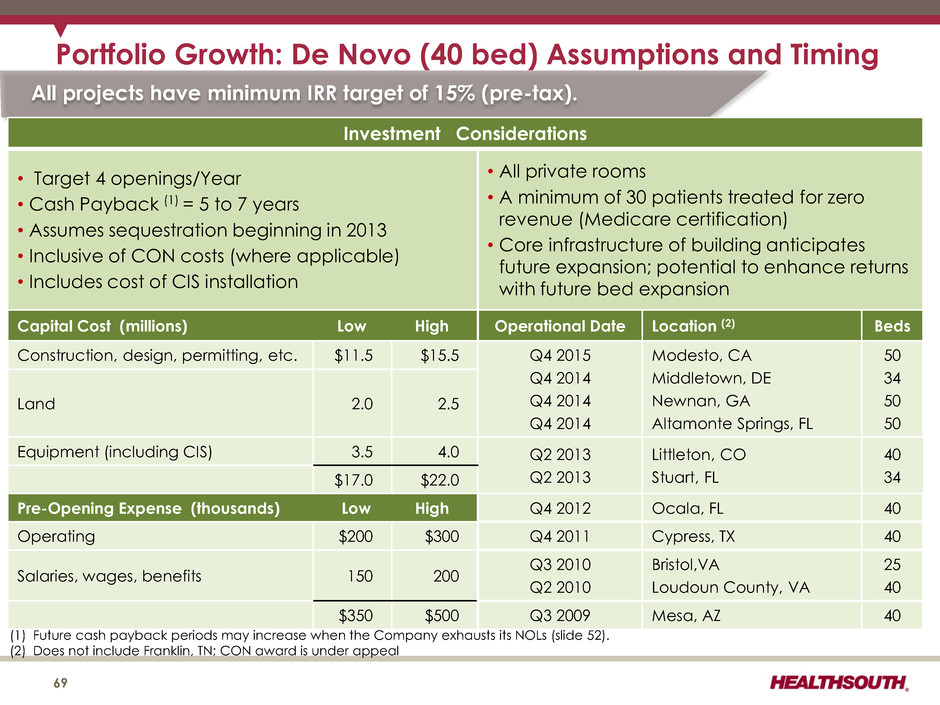
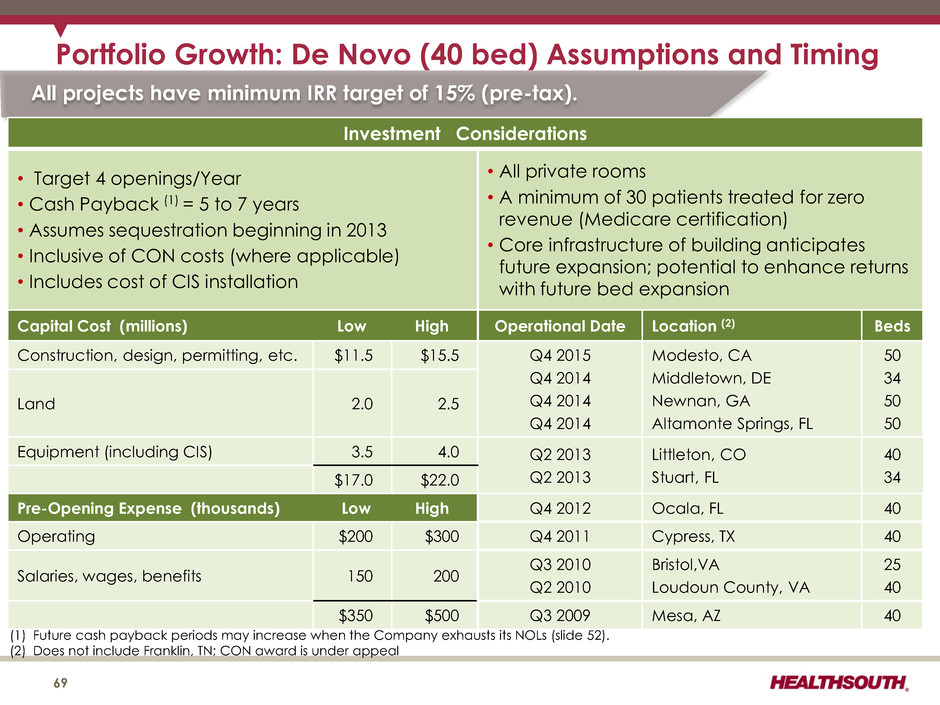
Portfolio Growth: De Novo (40 bed) Assumptions and Timing 69 (1) Future cash payback periods may increase when the Company exhausts its NOLs (slide 52). (2) Does not include Franklin, TN; CON award is under appeal All projects have minimum IRR target of 15% (pre-tax). Investment Considerations • Target 4 openings/Year • Cash Payback (1) = 5 to 7 years • Assumes sequestration beginning in 2013 • Inclusive of CON costs (where applicable) • Includes cost of CIS installation • All private rooms • A minimum of 30 patients treated for zero revenue (Medicare certification) • Core infrastructure of building anticipates future expansion; potential to enhance returns with future bed expansion Capital Cost (millions) Low High Operational Date Location (2) Beds Construction, design, permitting, etc. $11.5 $15.5 Q4 2015 Q4 2014 Q4 2014 Q4 2014 Modesto, CA Middletown, DE Newnan, GA Altamonte Springs, FL 50 34 50 50 Land 2.0 2.5 Equipment (including CIS) 3.5 4.0 Q2 2013 Q2 2013 Littleton, CO Stuart, FL 40 34 $17.0 $22.0 Pre-Opening Expense (thousands) Low High Q4 2012 Ocala, FL 40 Operating $200 $300 Q4 2011 Cypress, TX 40 Salaries, wages, benefits 150 200 Q3 2010 Q2 2010 Bristol,VA Loudoun County, VA 25 40 $350 $500 Q3 2009 Mesa, AZ 40
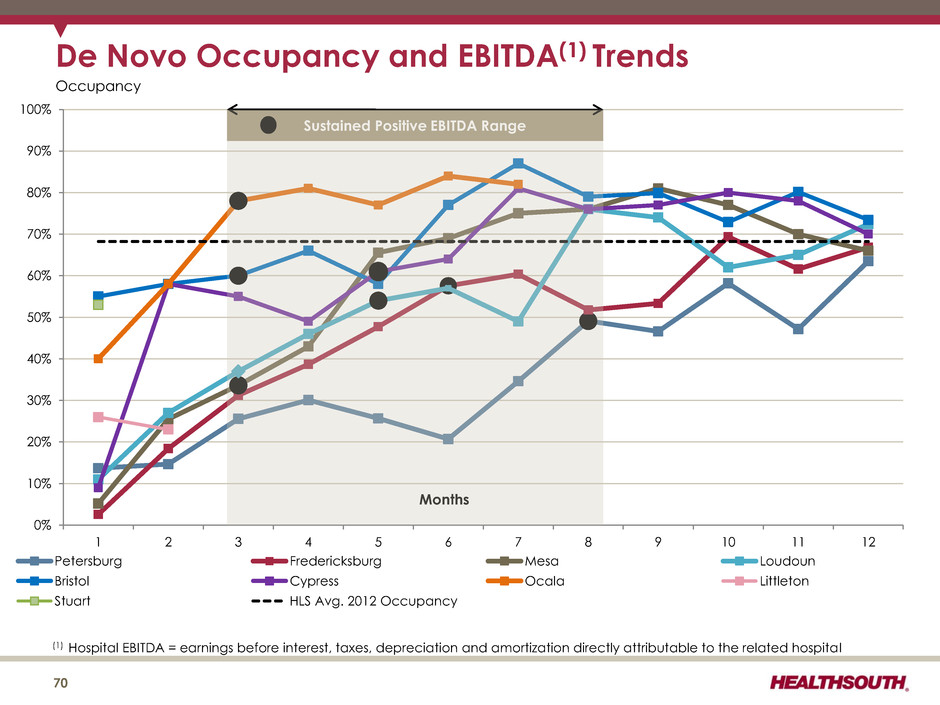
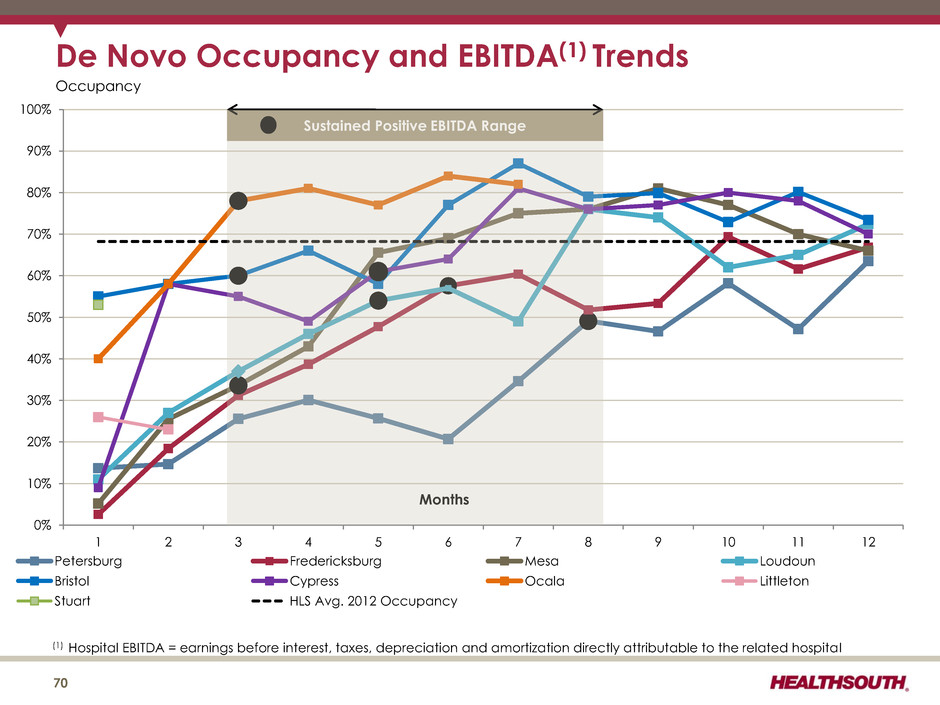
(1) Hospital EBITDA = earnings before interest, taxes, depreciation and amortization directly attributable to the related hospital De Novo Occupancy and EBITDA(1) Trends 0% 10% 20% 30% 40% 50% 60% 70% 80% 90% 100% 1 2 3 4 5 6 7 8 9 10 11 12 Petersburg Fredericksburg Mesa Loudoun Bristol Cypress Ocala Littleton Stuart HLS Avg. 2012 Occupancy Months 70 Occupancy Sustained Positive EBITDA Range
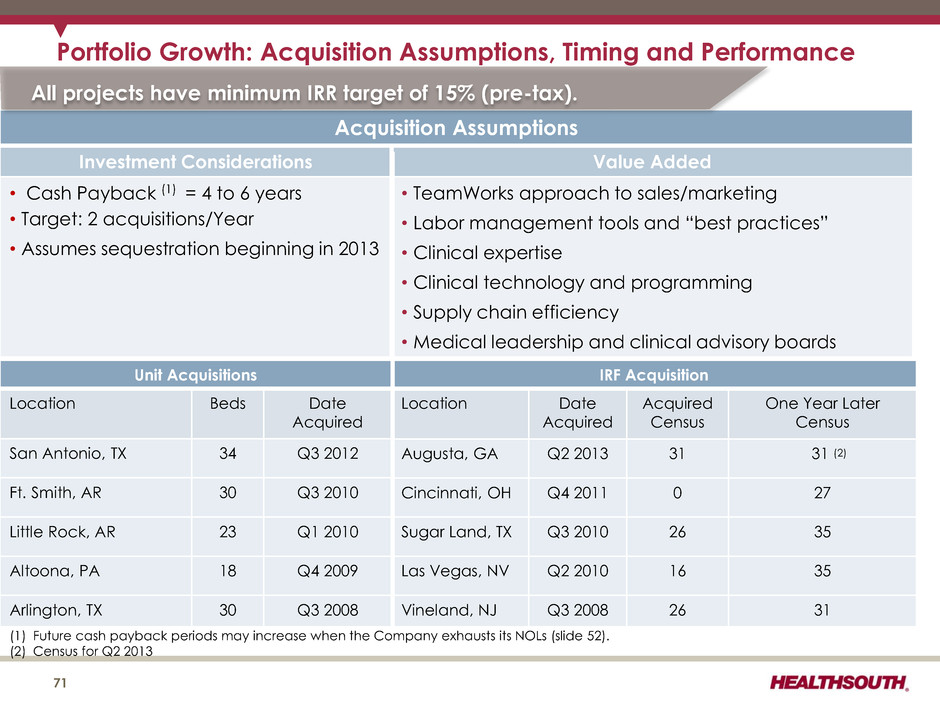
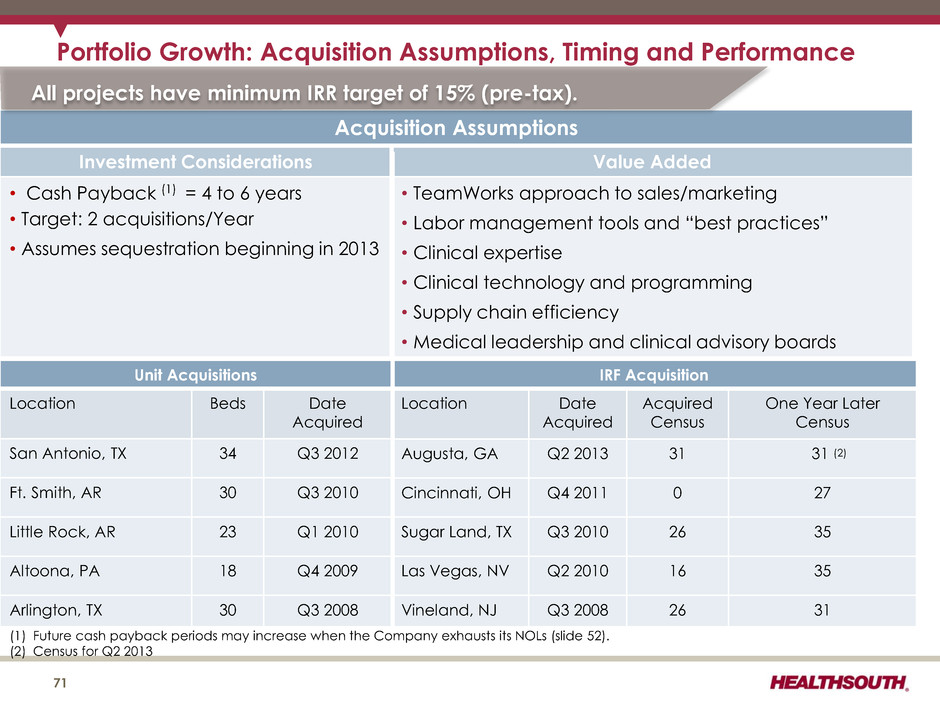
Portfolio Growth: Acquisition Assumptions, Timing and Performance 71 (1) Future cash payback periods may increase when the Company exhausts its NOLs (slide 52). (2) Census for Q2 2013 Acquisition Assumptions Investment Considerations Value Added • Cash Payback (1) = 4 to 6 years • Target: 2 acquisitions/Year • Assumes sequestration beginning in 2013 • TeamWorks approach to sales/marketing • Labor management tools and “best practices” • Clinical expertise • Clinical technology and programming • Supply chain efficiency • Medical leadership and clinical advisory boards All projects have minimum IRR target of 15% (pre-tax). Unit Acquisitions Location Beds Date Acquired San Antonio, TX 34 Q3 2012 Ft. Smith, AR 30 Q3 2010 Little Rock, AR 23 Q1 2010 Altoona, PA 18 Q4 2009 Arlington, TX 30 Q3 2008 IRF Acquisition Location Date Acquired Acquired Census One Year Later Census Augusta, GA Q2 2013 31 31 (2) Cincinnati, OH Q4 2011 0 27 Sugar Land, TX Q3 2010 26 35 Las Vegas, NV Q2 2010 16 35 Vineland, NJ Q3 2008 26 31
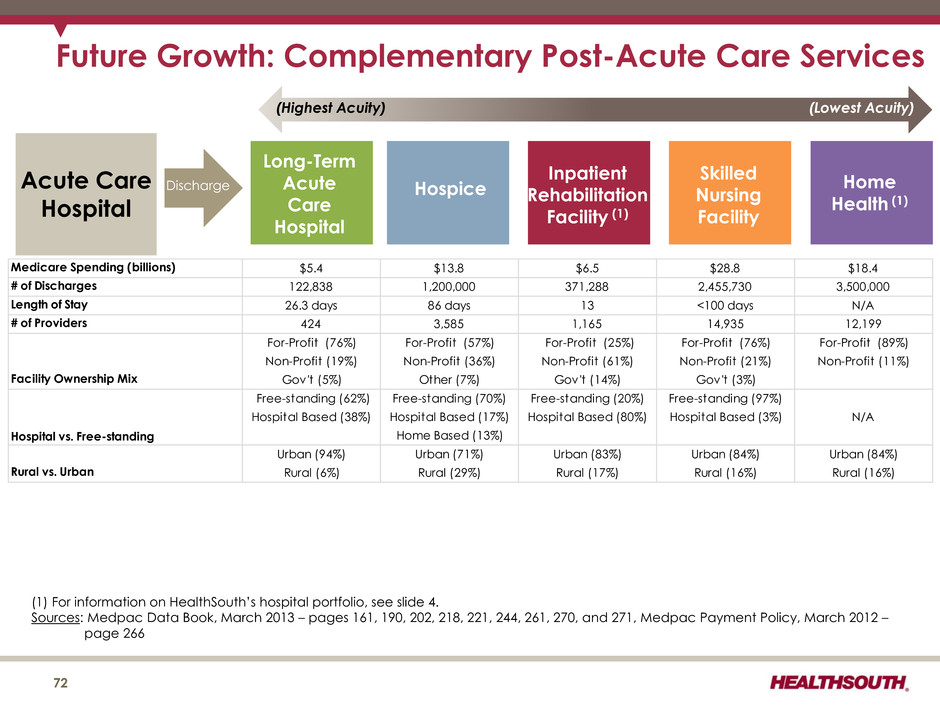
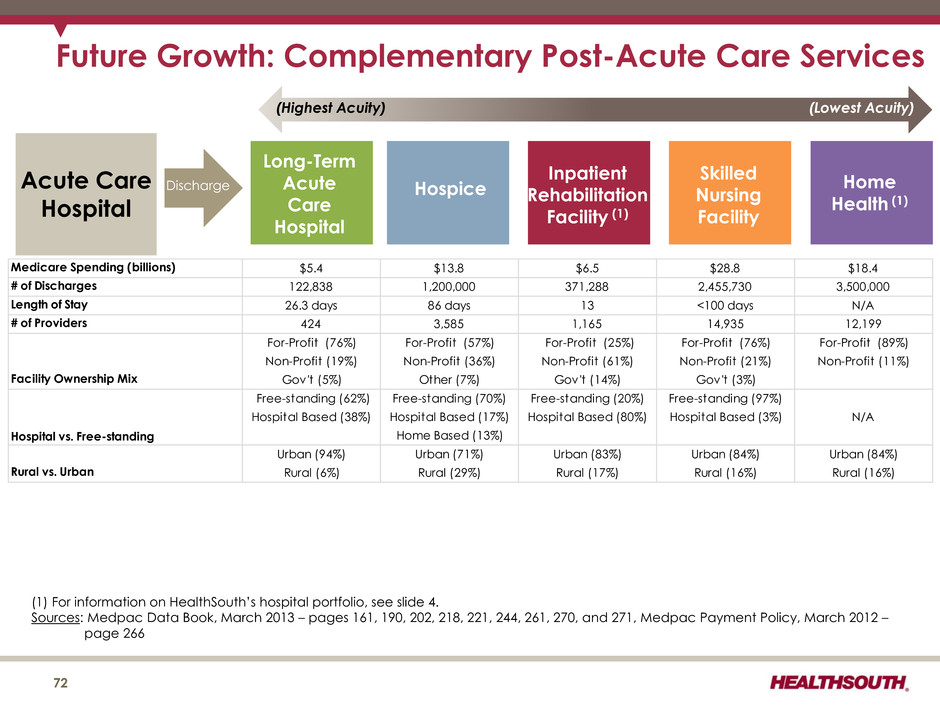
72 Acute Care Hospital Discharge Long-Term Acute Care Hospital Hospice Inpatient Rehabilitation Facility (1) Skilled Nursing Facility Home Health (1) (Highest Acuity) (Lowest Acuity) Future Growth: Complementary Post-Acute Care Services Medicare Spending (billions) $5.4 $13.8 $6.5 $28.8 $18.4 # of Discharges 122,838 1,200,000 371,288 2,455,730 3,500,000 Length of Stay 26.3 days 86 days 13 <100 days N/A # of Providers 424 3,585 1,165 14,935 12,199 Facility Ownership Mix For-Profit (76%) Non-Profit (19%) Gov't (5%) For-Profit (57%) Non-Profit (36%) Other (7%) For-Profit (25%) Non-Profit (61%) Gov't (14%) For-Profit (76%) Non-Profit (21%) Gov't (3%) For-Profit (89%) Non-Profit (11%) Hospital vs. Free-standing Free-standing (62%) Hospital Based (38%) Free-standing (70%) Hospital Based (17%) Home Based (13%) Free-standing (20%) Hospital Based (80%) Free-standing (97%) Hospital Based (3%) N/A Rural vs. Urban Urban (94%) Rural (6%) Urban (71%) Rural (29%) Urban (83%) Rural (17%) Urban (84%) Rural (16%) Urban (84%) Rural (16%) (1) For information on HealthSouth’s hospital portfolio, see slide 4. Sources: Medpac Data Book, March 2013 – pages 161, 190, 202, 218, 221, 244, 261, 270, and 271, Medpac Payment Policy, March 2012 – page 266
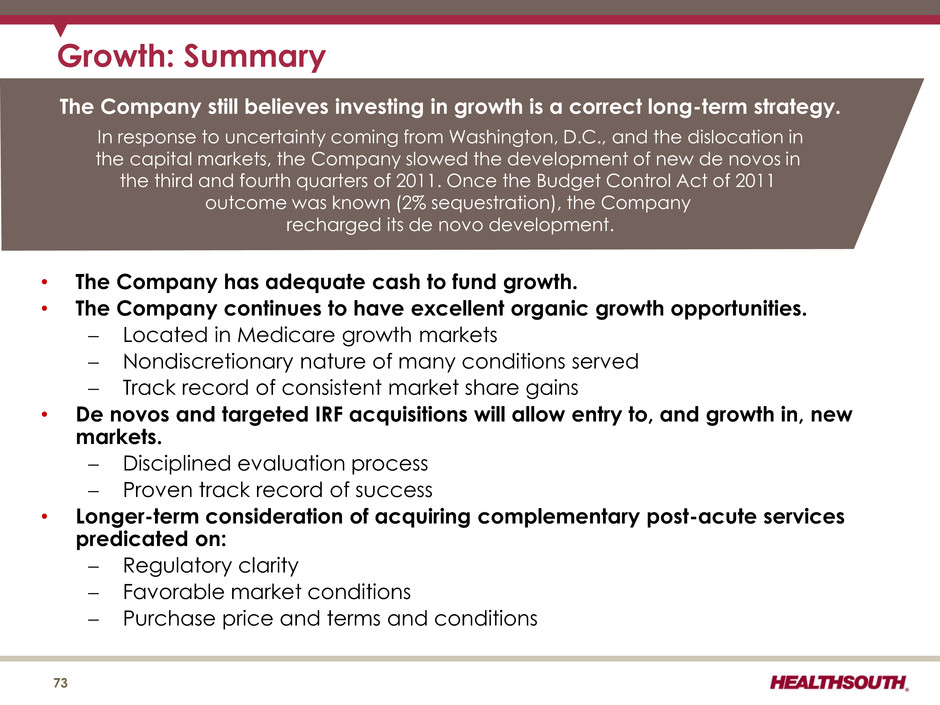
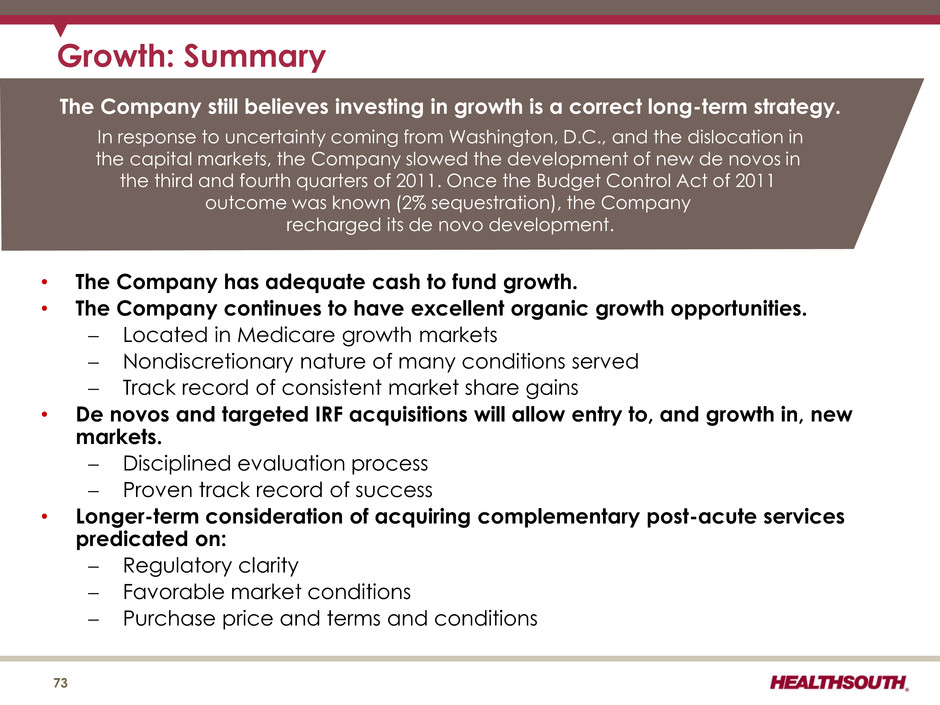
• The Company has adequate cash to fund growth. • The Company continues to have excellent organic growth opportunities. Located in Medicare growth markets Nondiscretionary nature of many conditions served Track record of consistent market share gains • De novos and targeted IRF acquisitions will allow entry to, and growth in, new markets. Disciplined evaluation process Proven track record of success • Longer-term consideration of acquiring complementary post-acute services predicated on: Regulatory clarity Favorable market conditions Purchase price and terms and conditions Growth: Summary 73 The Company still believes investing in growth is a correct long-term strategy. In response to uncertainty coming from Washington, D.C., and the dislocation in the capital markets, the Company slowed the development of new de novos in the third and fourth quarters of 2011. Once the Budget Control Act of 2011 outcome was known (2% sequestration), the Company recharged its de novo development.
Operational Initiatives 74
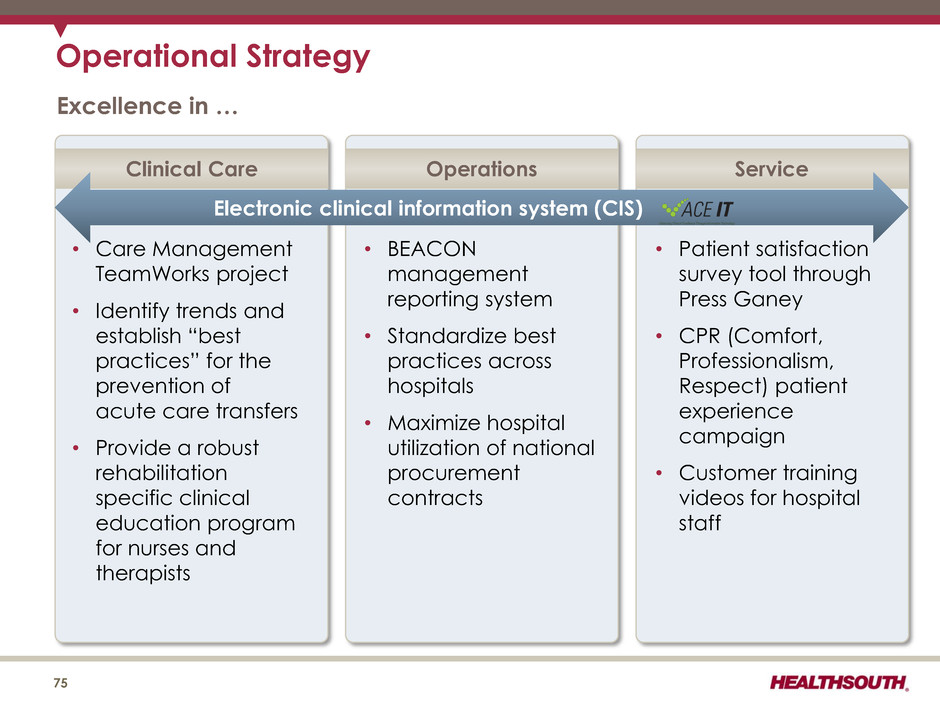
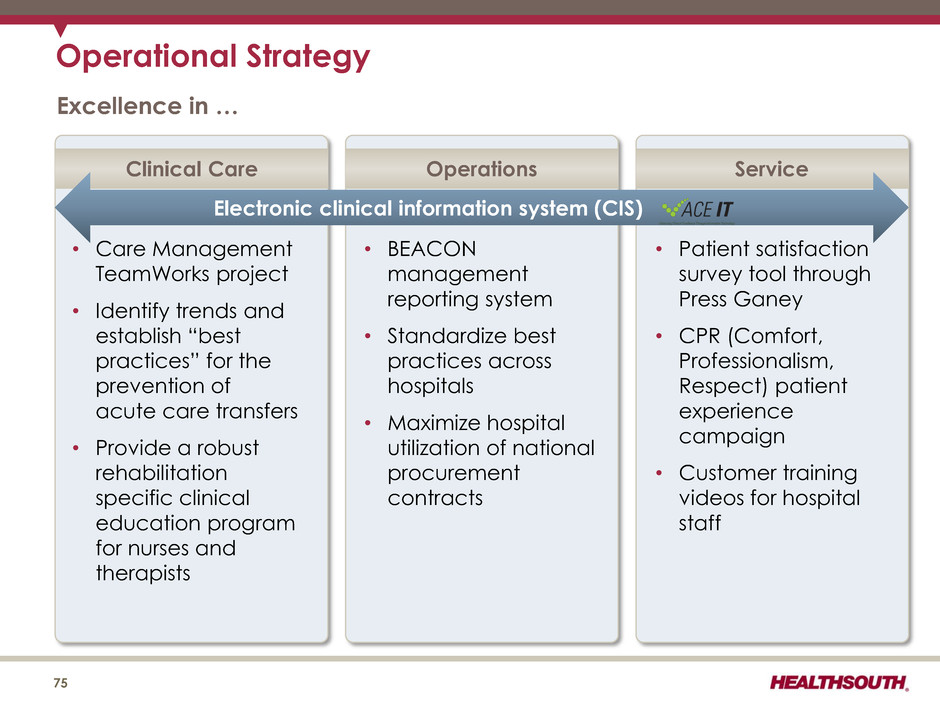
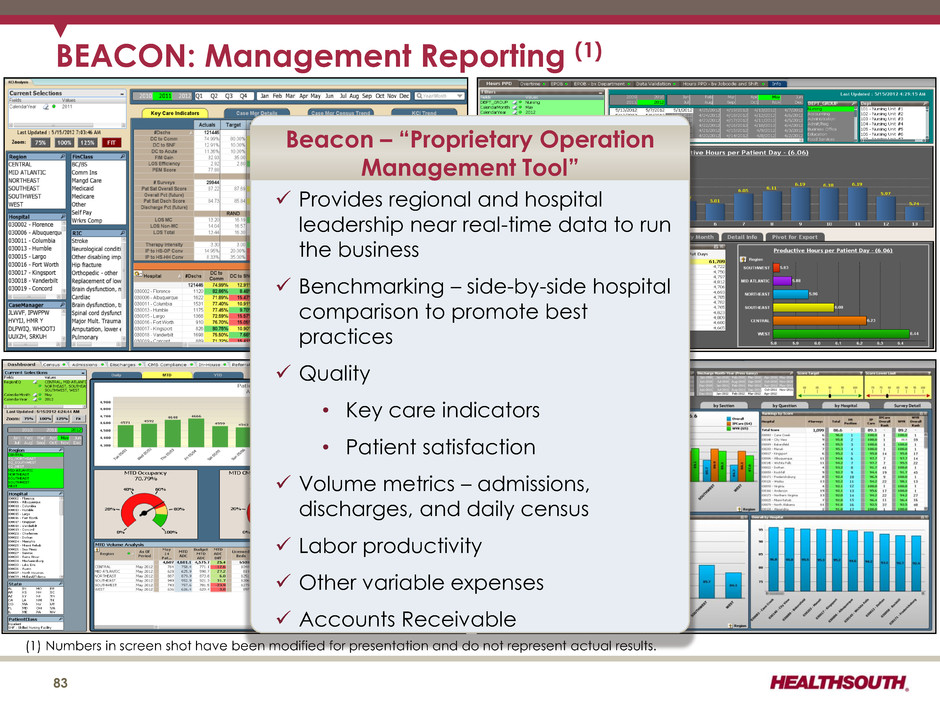
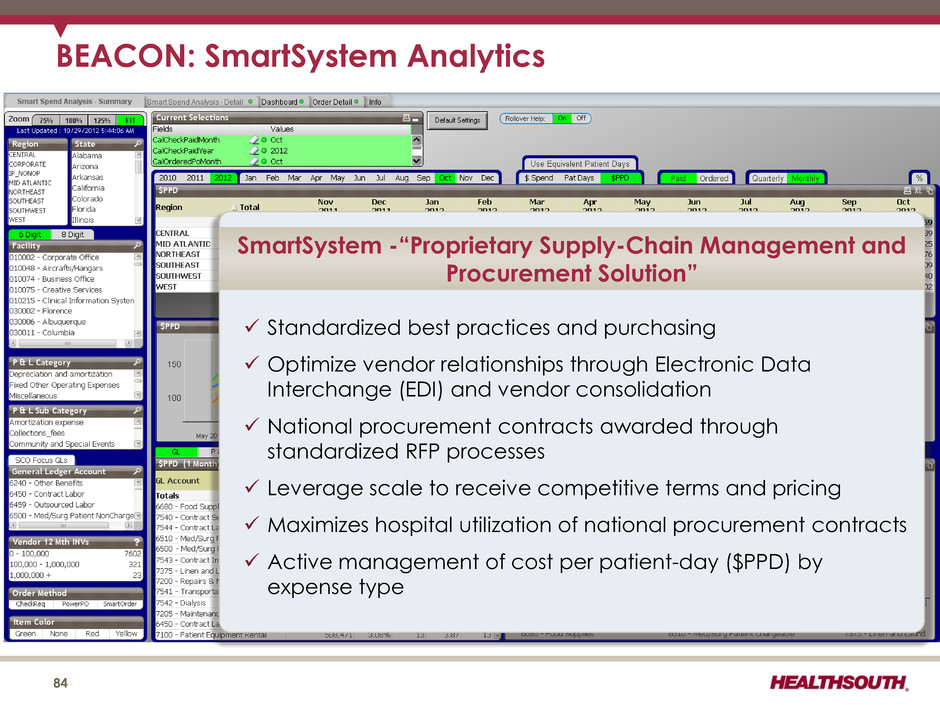
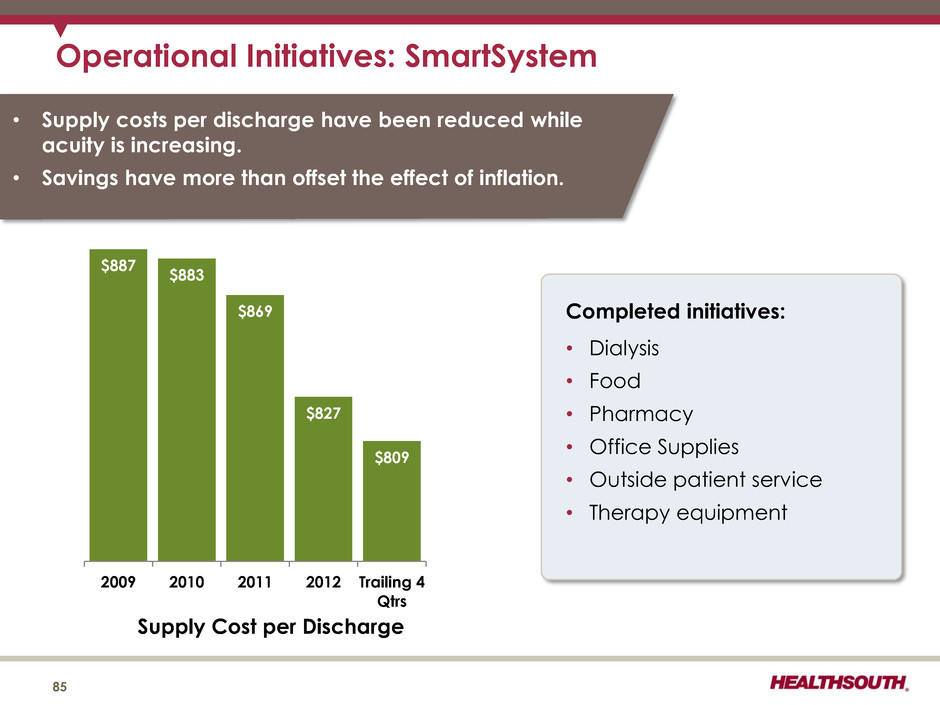
Operational Strategy Excellence in … 75 • Care Management TeamWorks project • Identify trends and establish “best practices” for the prevention of acute care transfers • Provide a robust rehabilitation specific clinical education program for nurses and therapists • BEACON management reporting system • Standardize best practices across hospitals • Maximize hospital utilization of national procurement contracts • Patient satisfaction survey tool through Press Ganey • CPR (Comfort, Professionalism, Respect) patient experience campaign • Customer training videos for hospital staff Clinical Care Operations Service Electronic clinical information system (CIS)
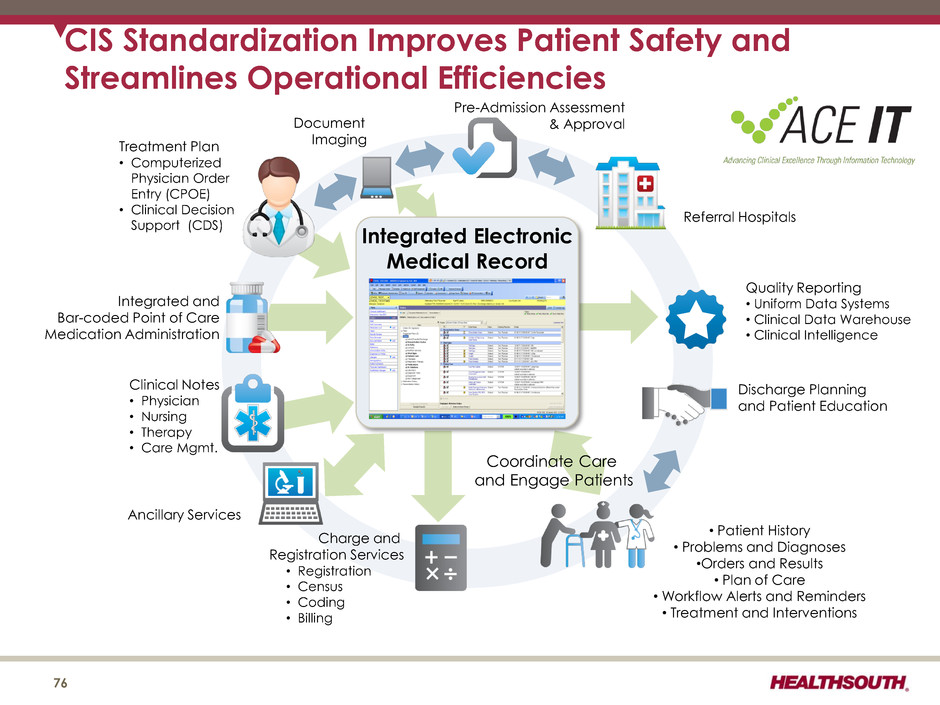
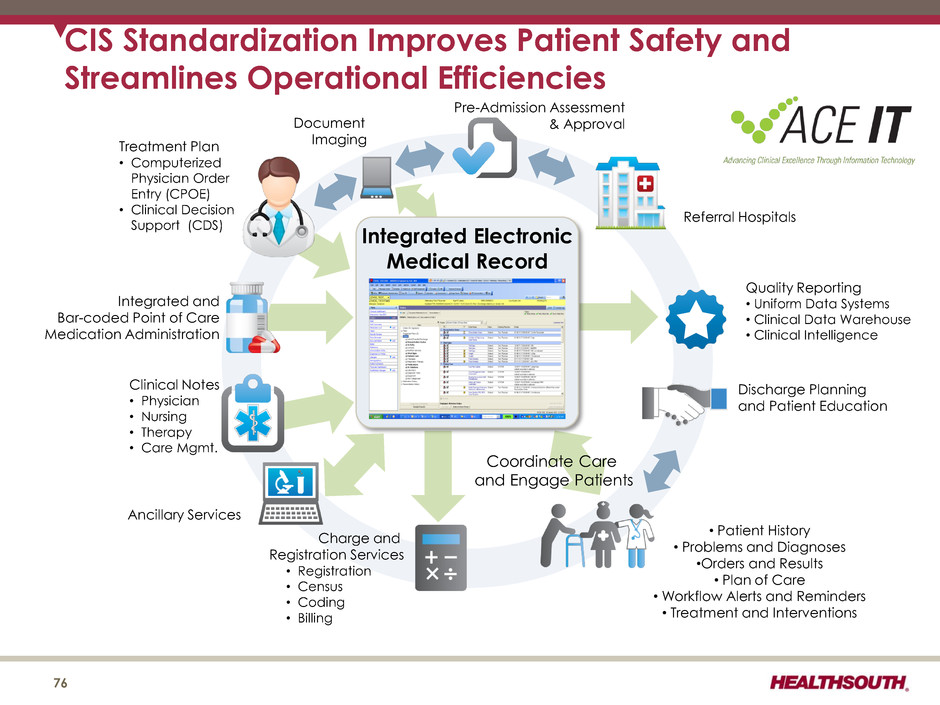
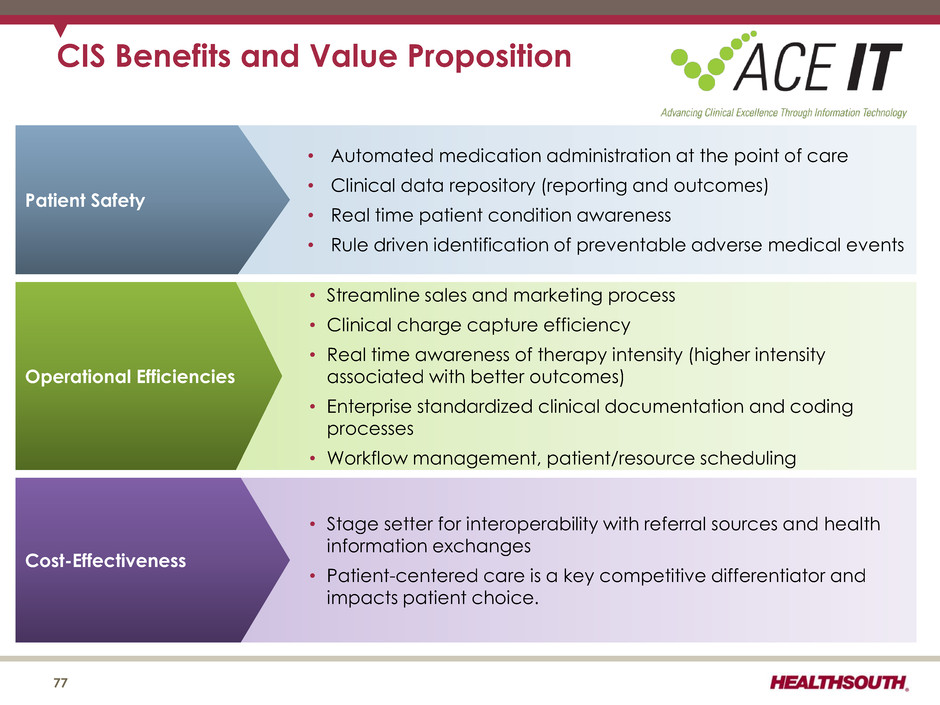
CIS Standardization Improves Patient Safety and Streamlines Operational Efficiencies Pre-Admission Assessment & Approval Discharge Planning and Patient Education • Patient History • Problems and Diagnoses •Orders and Results • Plan of Care • Workflow Alerts and Reminders • Treatment and Interventions Document Imaging Charge and Registration Services • Registration • Census • Coding • Billing Quality Reporting • Uniform Data Systems • Clinical Data Warehouse • Clinical Intelligence Integrated Electronic Medical Record Referral Hospitals Coordinate Care and Engage Patients Ancillary Services Clinical Notes • Physician • Nursing • Therapy • Care Mgmt. Integrated and Bar-coded Point of Care Medication Administration Treatment Plan • Computerized Physician Order Entry (CPOE) • Clinical Decision Support (CDS) CIS Benefits and Value Proposition • Streamline sales and marketing process • Clinical charge capture efficiency • Real time awareness of therapy intensity (higher intensity associated with better outcomes) • Enterprise standardized clinical document ion a d coding processes • Workflow management, patient/resource scheduling Operational Efficiencies • Automated medication administration at the point of care • Clinical data repository (reporting and outcomes) • Real time patient condition awareness • Rule driven identification of preventable adverse medical events Patient Safety 76 • Stage setter for interoperability with referral sources and health information exchanges • Patient-centered care is a key competitive differentiator and impacts patient choice Cost-Effectiveness 76
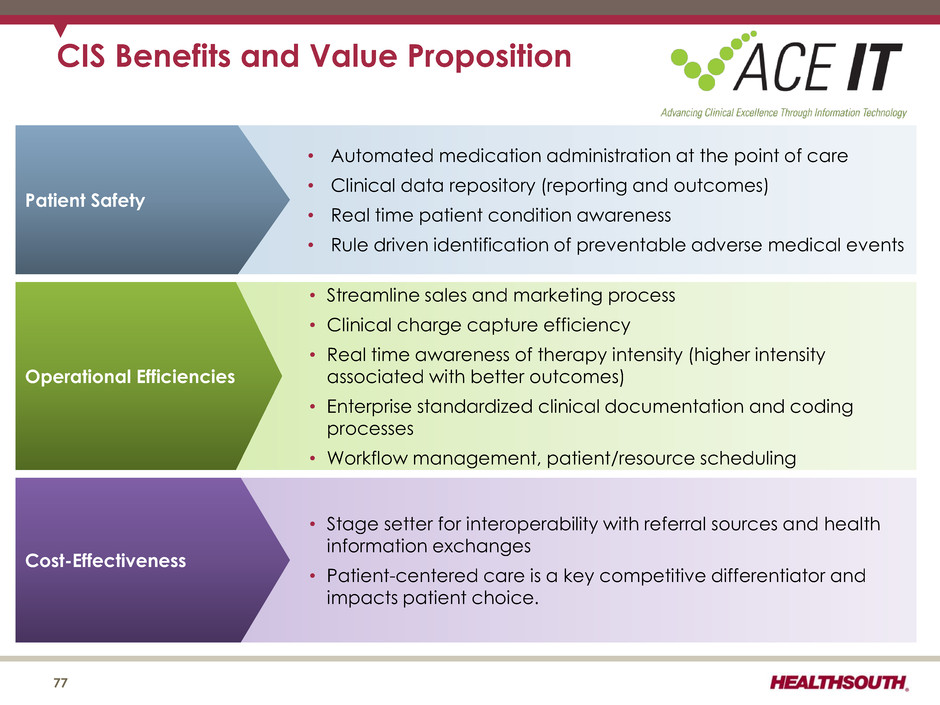
CIS Benefits and Value Proposition • Streamline sales and marketing process • Clinical charge capture efficiency • Real time awareness of therapy intensity (higher intensity associated with better outcomes) • Enterprise standardized clinical documentation and coding processes • Workflow management, patient/resource scheduling Operational Efficiencies • Automated medication administration at the point of care • Clinical data repository (reporting and outcomes) • Real time patient condition awareness • Rule driven identification of preventable adverse medical events Patient Safety 77 • Stage setter for interoperability with referral sources and health information exchanges • Patient-centered care is a key competitive differentiator and impacts patient choice. Cost-Effectiveness
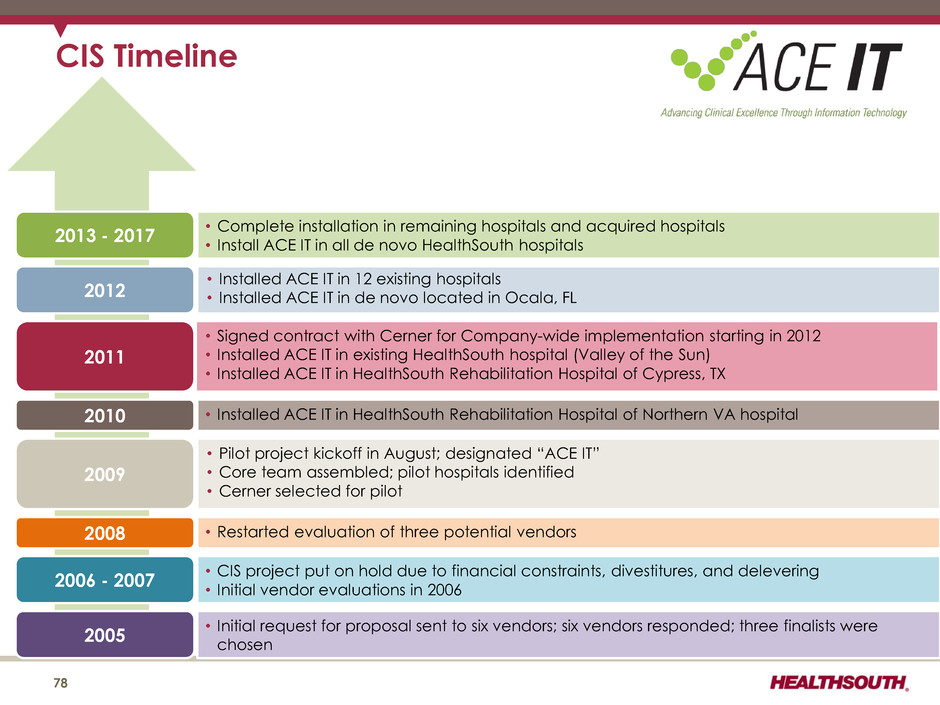
• Installed ACE IT in HealthSouth Rehabilitation Hospital of Northern VA hospital • Pilot project kickoff in August; designated “ACE IT” • Core team assembled; pilot hospitals identified • Cerner selected for pilot • Signed contract with Cerner for Company-wide implementation starting in 2012 • Installed ACE IT in existing HealthSouth hospital (Valley of the Sun) • Installed ACE IT in HealthSouth Rehabilitation Hospital of Cypress, TX • Installed ACE IT in 12 existing hospitals • Installed ACE IT in de novo located in Ocala, FL • Complete installation in remaining hospitals and acquired hospitals • Install ACE IT in all de novo HealthSouth hospitals CIS Timeline 78 2010 2011 2012 2013 - 2017 2009 2008 2006 - 2007 2005 • Restarted evaluation of three potential vendors • CIS project put on hold due to financial constraints, divestitures, and delevering • Initial vendor evaluations in 2006 • Initial request for proposal sent to six vendors; six vendors responded; three finalists were chosen

CIS Cost 79 • No incentive payments (i.e. “HITECH”) for inpatient rehabilitation hospitals (1) – Only acute care hospitals are eligible • Installation cost will vary by hospital depending on items such as size and physical plan. – Installation cost expected to be in a range of $1 million to $1.5 million per hospital. – Approx. 70% of the initial spend will be capital expense and the remainder will be operating expense. • Projected/estimated costs: (1) The American Recovery and Reinvestment Act of 2009 (Pub. L. 111–5) provides incentive payments to eligible professionals, eligible hospitals, and critical access hospitals participating in Medicare and Medicaid programs that adopt and successfully demonstrate “meaningful use” of certified electronic health record technology. ($ millions) 2012 Actual 2013 Estimate 2014 Estimate 2015 Estimate No. of hospitals installed 13 20 20 20 Operating expenses $9 ~$13 ~$15 ~$17 CAPEX $18 ~$21 ~$18 ~$24

TeamWorks: Care Management 80 Goals • Improve operational effectiveness, patient satisfaction, and quality outcomes • Engage interdisciplinary teams • Reduce: ― Complication rates ― Cost per case ― Payor denials • Increase: ― Quality outcomes ― Patient involvement in care decisions • Standardize “Care Management” staffing (added approx. one clinical resource per hospital) 2012 was the first full year of “Care Management” implementation. Referral Management Pre- authorization / Pre-certification Patient Assessment Care Delivery & Documentation Interdisciplinary Team Process Denials & Approvals Outcomes Analysis Effective & Efficient Care Management
CPR: Comfort, Professionalism, Respect • All employees trained in the CPR campaign. • Hospital-based trained facilitators will work directly with employees. • A series of short videos is used to depict common scenarios of patient/staff situations. • Facilitator training is highly interactive, encouraging discussions among staff. CPR is an in-house course designed to train all employees to realize that even minor encounters between staff and patients can have a memorable impact on the patient’s entire experience. Ultimate goal is to improve employee- to-patient interactions, leading to: • Improved patient satisfaction scores • Reduced patient complaints • More satisfied employees 81
82
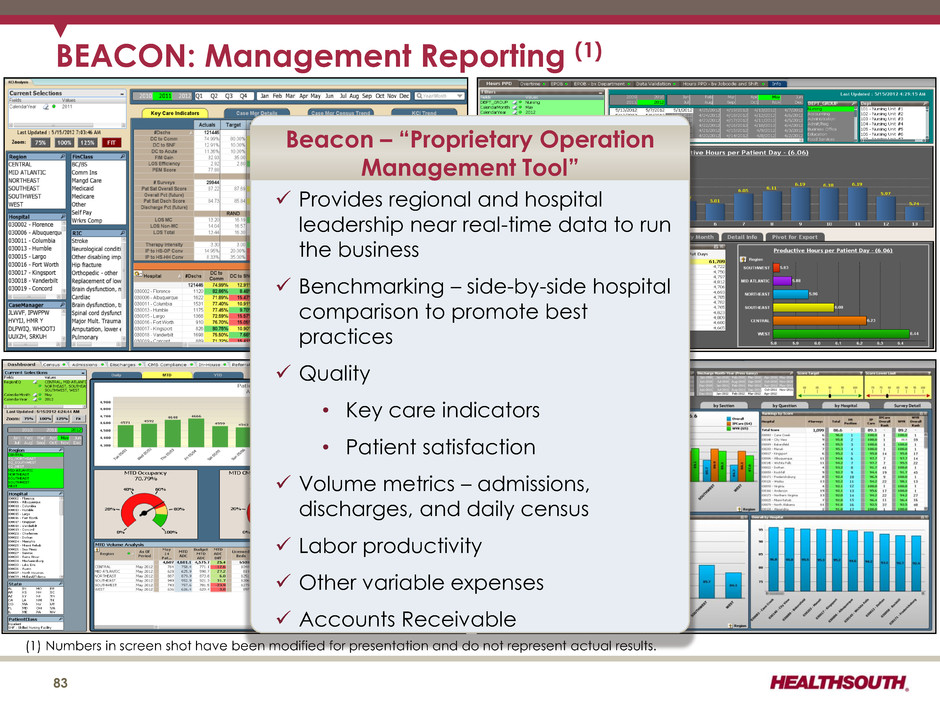
83 BEACON: Management Reporting (1) (1) Numbers in screen shot have been modified for presentation and do not represent actual results. Provides regional and hospital leadership near real-time data to run the business Benchmarking – side-by-side hospital comparison to promote best practices Quality • Key care indicators • Patient satisfaction Volume metrics – admissions, discharges, and daily census Labor productivity Other variable expenses Accounts Receivable Beacon – “Proprietary Operation Management Tool”
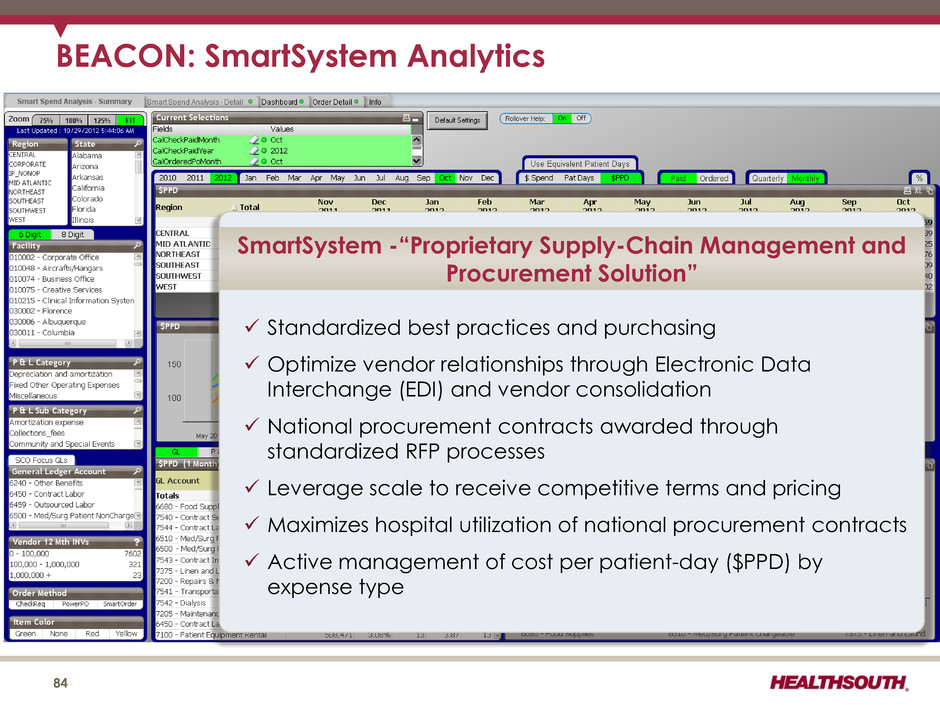
84 BEACON: SmartSystem Analytics Standardized best practices and purchasing Optimize vendor relationships through Electronic Data Interchange (EDI) and vendor consolidation National procurement contracts awarded through standardized RFP processes Leverage scale to receive competitive terms and pricing Maximizes hospital utilization of national procurement contracts Active management of cost per patient-day ($PPD) by expense type SmartSystem -“Proprietary Supply-Chain Management and Procurement Solution”
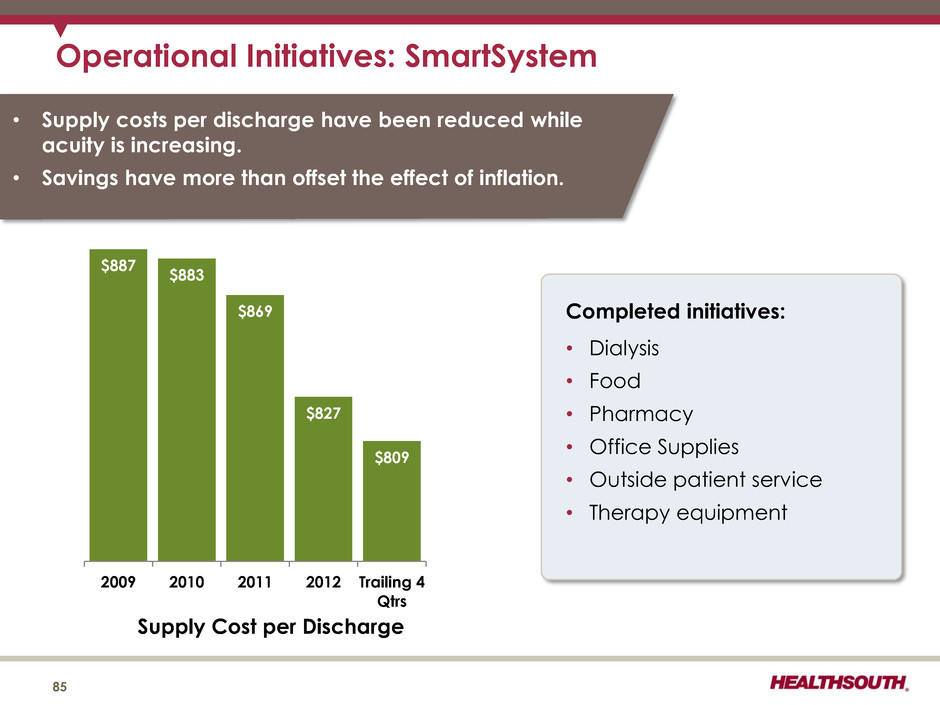
Operational Initiatives: SmartSystem 85 $887 $883 $869 $827 $809 2009 2010 2011 2012 Trailing 4 Qtrs Supply Cost per Discharge 85 Completed initiatives: • Dialysis • Food • Pharmacy • Office Supplies • Outside patient service • Therapy equipment • Supply costs per discharge have been reduced while acuity is increasing. • Savings have more than offset the effect of inflation.
Operational Metrics 86

• Salaries and Benefits reflects continued improvement from productivity gains and growing revenue base. • Hospital-related Expenses includes other operating (1), supplies, and occupancy. • General and Administrative excludes stock-based compensation. • Provision for Doubtful Accounts varies based on the level of denials by Medicare contractors. • Employees per Occupied Bed (“EPOB”) is calculated by dividing the number of full-time equivalents, including an estimate of full-time equivalents from the utilization of contract labor, by the number of occupied beds during each period. The number of occupied beds is determined by multiplying the number of licensed beds by the Company’s occupancy percentage. 50.8% 22.3% 5.5% 1.4% 49.7% 21.8% 5.1% 1.7% 49.1% 22.0% 4.8% 0.9% 48.4% 21.5% 4.5% 1.0% 48.6% 20.8% 4.3% 1.2% 48.2% 20.6% 4.1% 1.3% Salaries and Benefits Hospital-related Expenses General & Administrative Provision for Doubtful Accounts Operational Metrics: Expense Efficiencies (% of Net Operating Revenues) 2008 2009 2010 2011 2012 2013 2008 2009 2010 2011 2012 2013 2008 2009 2010 2011 2012 2013 2008 2009 2010 2011 2012 2013 (6 Months) (6 Months) (6 Months) (6 Months) 3.59 3.52 3.49 3.47 3.42 3.37 EPOB 87 (1) Excludes loss on disposal or impairment of assets
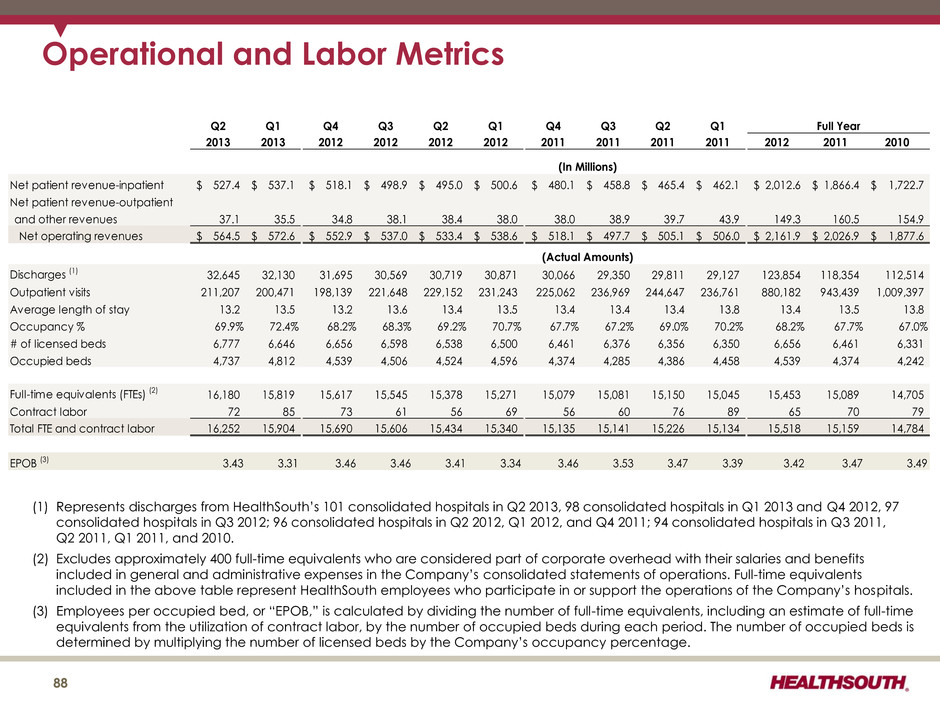
Operational and Labor Metrics (1) Represents discharges from HealthSouth’s 101 consolidated hospitals in Q2 2013, 98 consolidated hospitals in Q1 2013 and Q4 2012, 97 consolidated hospitals in Q3 2012; 96 consolidated hospitals in Q2 2012, Q1 2012, and Q4 2011; 94 consolidated hospitals in Q3 2011, Q2 2011, Q1 2011, and 2010. (2) Excludes approximately 400 full-time equivalents who are considered part of corporate overhead with their salaries and benefits included in general and administrative expenses in the Company’s consolidated statements of operations. Full-time equivalents included in the above table represent HealthSouth employees who participate in or support the operations of the Company’s hospitals. (3) Employees per occupied bed, or “EPOB,” is calculated by dividing the number of full-time equivalents, including an estimate of full-time equivalents from the utilization of contract labor, by the number of occupied beds during each period. The number of occupied beds is determined by multiplying the number of licensed beds by the Company’s occupancy percentage. 88 Q2 Q1 Q4 Q3 Q2 Q1 Q4 Q3 Q2 Q1 2013 2013 2012 2012 2012 2012 2011 2011 2011 2011 2012 2011 2010 Net patient revenue-inpatient 527.4$ 537.1$ 518.1$ 498.9$ 495.0$ 500.6$ 480.1$ 458.8$ 465.4$ 462.1$ 2,012.6$ 1,866.4$ 1,722.7$ Net patient revenue-outpatient and other revenues 37.1 35.5 34.8 38.1 38.4 38.0 38.0 38.9 39.7 43.9 149.3 160.5 154.9 Net operating revenues 564.5$ 572.6$ 552.9$ 537.0$ 533.4$ 538.6$ 518.1$ 497.7$ 505.1$ 506.0$ 2,161.9$ 2,026.9$ 1,877.6$ Discharges (1) 32,645 32,130 31,695 30,569 30,719 30,871 30,066 29,350 29,811 29,127 123,854 118,354 112,514 Outpatient visits 211,207 200,471 198,139 221,648 229,152 231,243 225,062 236,969 244,647 236,761 880,182 943,439 1,009,397 Average length of stay 13.2 13.5 13.2 13.6 13.4 13.5 13.4 13.4 13.4 13.8 13.4 13.5 13.8 Occupancy % 69.9% 72.4% 68.2% 68.3% 69.2% 70.7% 67.7% 67.2% 69.0% 70.2% 68.2% 67.7% 67.0% # of licensed beds 6,777 6,646 6,656 6,598 6,538 6,500 6,461 6,376 6,356 6,350 6,656 6,461 6,331 Occupied beds 4,737 4,812 4,539 4,506 4,524 4,596 4,374 4,285 4,386 4,458 4,539 4,374 4,242 Full-time equivalents (FTEs) (2) 16,180 15,819 15,617 15,545 15,378 15,271 15,079 15,081 15,150 15,045 15,453 15,089 14,705 Contract labor 72 85 73 61 56 69 56 60 76 89 65 70 79 Total FTE and contract labor 16,252 15,904 15,690 15,606 15,434 15,340 15,135 15,141 15,226 15,134 15,518 15,159 14,784 EPOB (3) 3.43 3.31 3.46 3.46 3.41 3.34 3.46 3.53 3.47 3.39 3.42 3.47 3.49 (In Millions) (Actual Amounts) Full Year
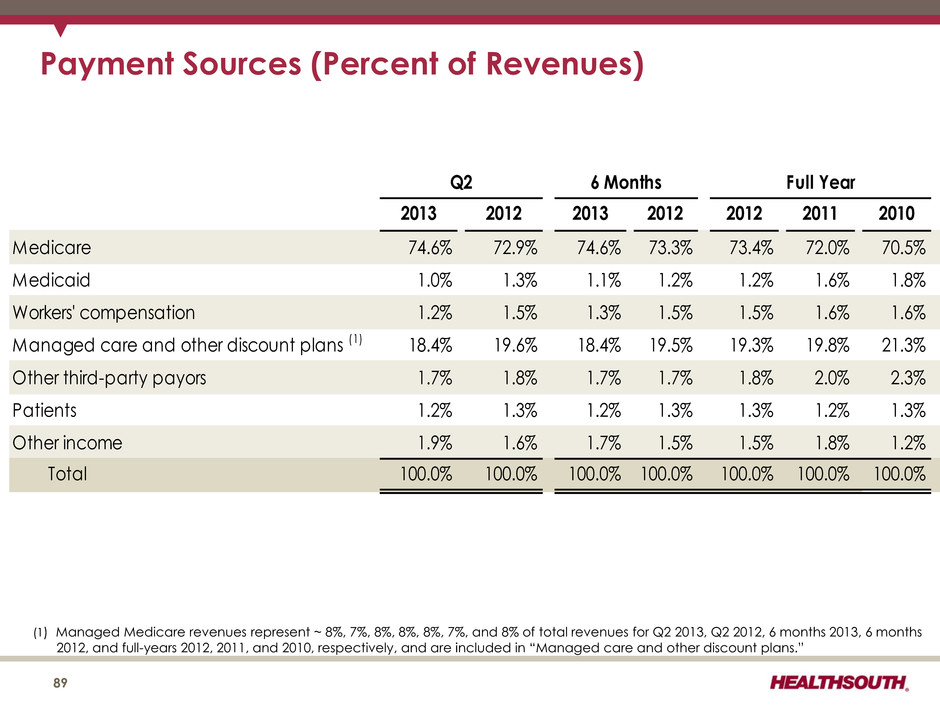
Payment Sources (Percent of Revenues) 2013 2012 2013 2012 2012 2011 2010 Medicare 74.6% 72.9% 74.6% 73.3% 73.4% 72.0% 70.5% Medicaid 1.0% 1.3% 1.1% 1.2% 1.2% 1.6% 1.8% Workers' compensation 1.2% 1.5% 1.3% 1.5% 1.5% 1.6% 1.6% Managed care and other discount plans (1) 18.4% 19.6% 18.4% 19.5% 19.3% 19.8% 21.3% Other third-party payors 1.7% 1.8% 1.7% 1.7% 1.8% 2.0% 2.3% Patients 1.2% 1.3% 1.2% 1.3% 1.3% 1.2% 1.3% Other income 1.9% 1.6% 1.7% 1.5% 1.5% 1.8% 1.2% Total 100.0% 100.0% 100.0% 100.0% 100.0% 100.0% 100.0% 6 Months Full YearQ2 (1) Managed Medicare revenues represent ~ 8%, 7%, 8%, 8%, 8%, 7%, and 8% of total revenues for Q2 2013, Q2 2012, 6 months 2013, 6 months 2012, and full-years 2012, 2011, and 2010, respectively, and are included in “Managed care and other discount plans.” 89
Reconciliations to GAAP 90
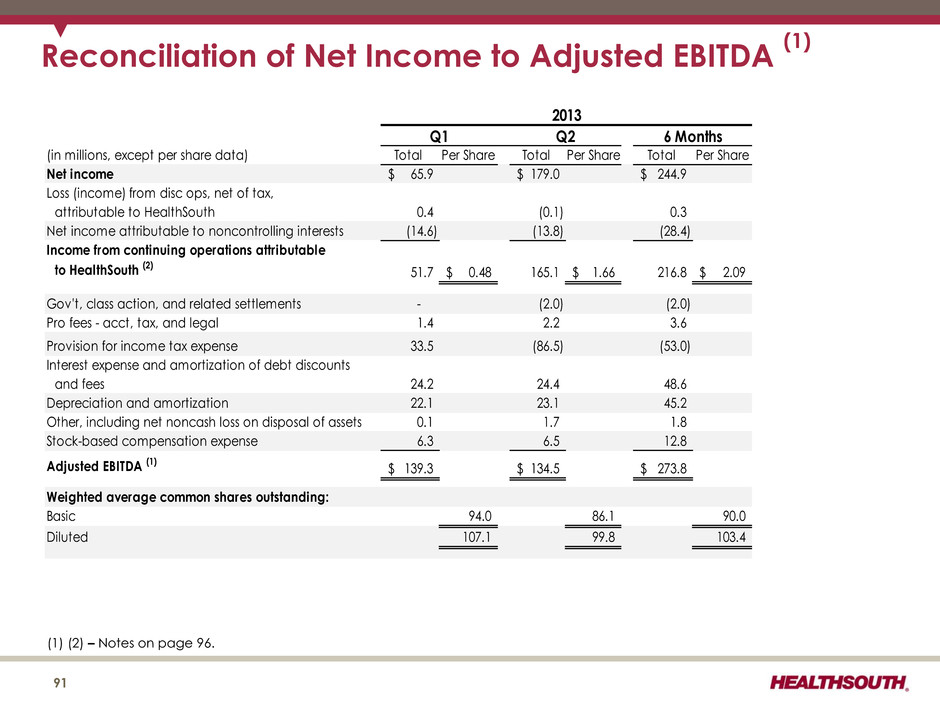
Reconciliation of Net Income to Adjusted EBITDA (1) (1) (2) – Notes on page 96. (in millions, except per share data) Total Per Share Total Per Share Total Per Share Net income 65.9$ 179.0$ 244.9$ Loss (income) from disc ops, net of tax, attributable to HealthSouth 0.4 (0.1) 0.3 Net income attributable to noncontrolling interests (14.6) (13.8) (28.4) Income from continuing operations attributable to HealthSouth (2) 51.7 0.48$ 165.1 1.66$ 216.8 2.09$ Gov't, class action, and related settlements - (2.0) (2.0) Pro fees - acct, tax, and legal 1.4 2.2 3.6 Provision for income tax expense 33.5 (86.5) (53.0) Interest expense and amortization of debt discounts and fees 24.2 24.4 48.6 Depreciation and amortization 22.1 23.1 45.2 Other, including net noncash loss on disposal of assets 0.1 1.7 1.8 Stock-based compensation expense 6.3 6.5 12.8 Adjusted EBITDA (1) 139.3$ 134.5$ 273.8$ Weighted average common shares outstanding: Basic 94.0 86.1 90.0 Diluted 107.1 99.8 103.4 2013 6 MonthsQ1 Q2 91
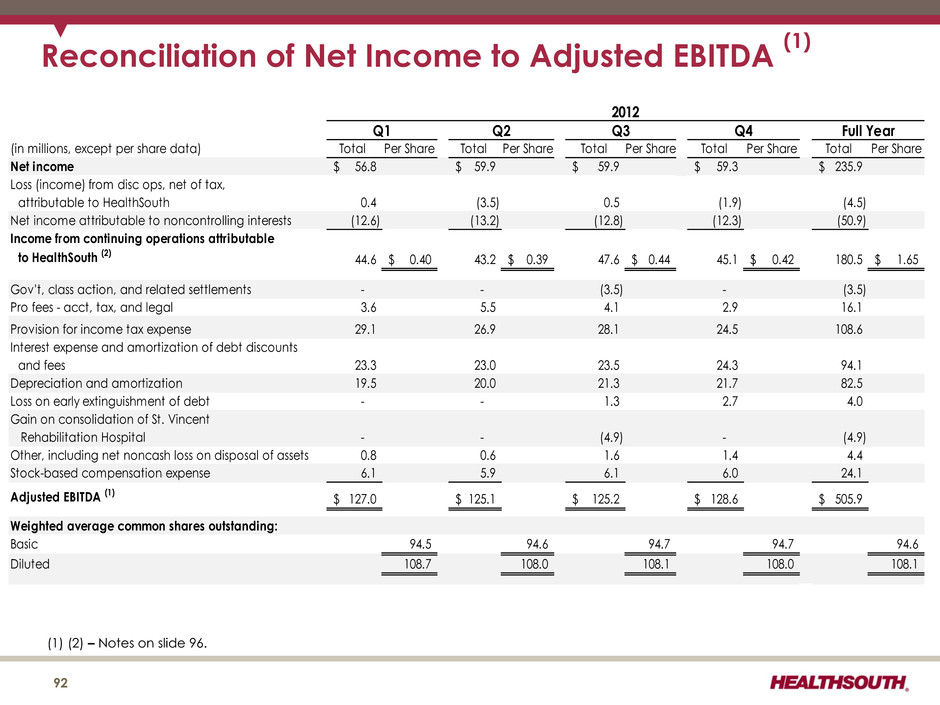
Reconciliation of Net Income to Adjusted EBITDA (1) (1) (2) – Notes on slide 96. (in millions, except per share data) Total Per Share Total Per Share Total Per Share Total Per Share Total Per Share Net income 56.8$ 59.9$ 59.9$ 59.3$ 235.9$ Loss (income) from disc ops, net of tax, attributable to HealthSouth 0.4 (3.5) 0.5 (1.9) (4.5) Net income attributable to noncontrolling interests (12.6) (13.2) (12.8) (12.3) (50.9) Income from continuing operations attributable to HealthSouth (2) 44.6 0.40$ 43.2 0.39$ 47.6 0.44$ 45.1 0.42$ 180.5 1.65$ Gov't, class action, and related settlements - - (3.5) - (3.5) Pro fees - acct, tax, and legal 3.6 5.5 4.1 2.9 16.1 Provision for income tax expense 29.1 26.9 28.1 24.5 108.6 Interest expense and amortization of debt discounts and fees 23.3 23.0 23.5 24.3 94.1 Depreciation and amortization 19.5 20.0 21.3 21.7 82.5 Loss on early extinguishment of debt - - 1.3 2.7 4.0 Gain on consolidation of St. Vincent Rehabilitation Hospital - - (4.9) - (4.9) Other, including net noncash loss on disposal of assets 0.8 0.6 1.6 1.4 4.4 Stock-based compensation expense 6.1 5.9 6.1 6.0 24.1 Adjusted EBITDA (1) 127.0$ 125.1$ 125.2$ 128.6$ 505.9$ Weighted average common shares outstanding: Basic 94.5 94.6 94.7 94.7 94.6 Diluted 108.7 108.0 108.1 108.0 108.1 Full YearQ1 Q2 Q4Q3 2012 92
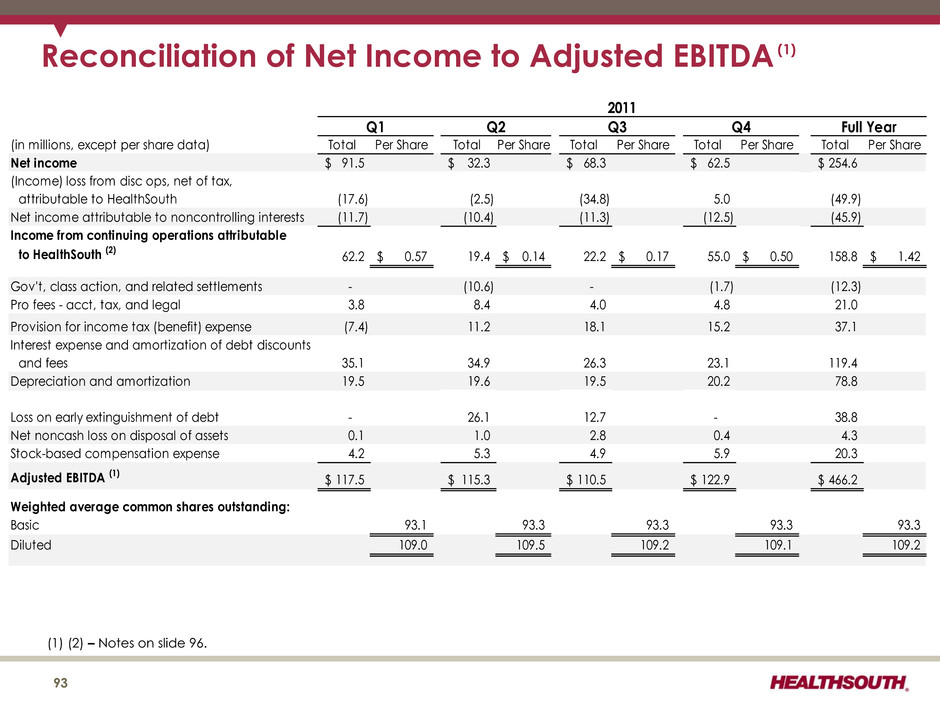
Reconciliation of Net Income to Adjusted EBITDA (1) (1) (2) – Notes on slide 96. 93 (in millions, except per share data) Total Per Share Total Per Share Total Per Share Total Per Share Total Per Share Net income 91.5$ 32.3$ 68.3$ 62.5$ 254.6$ (Income) loss from disc ops, net of tax, attributable to HealthSouth (17.6) (2.5) (34.8) 5.0 (49.9) Net income attributable to noncontrolling interests (11.7) (10.4) (11.3) (12.5) (45.9) Income from continuing operations attributable to HealthSouth (2) 62.2 0.57$ 19.4 0.14$ 22.2 0.17$ 55.0 0.50$ 158.8 1.42$ Gov't, class action, and related settlements - (10.6) - (1.7) (12.3) Pro fees - acct, tax, and legal 3.8 8.4 4.0 4.8 21.0 Provision for income tax (benefit) expense (7.4) 11.2 18.1 15.2 37.1 Interest expense and amortization of debt discounts and fees 35.1 34.9 26.3 23.1 119.4 Depreciation and amortization 19.5 19.6 19.5 20.2 78.8 Loss on early extinguishment of debt - 26.1 12.7 - 38.8 Net noncash loss on disposal of assets 0.1 1.0 2.8 0.4 4.3 Stock-based compensation expense 4.2 5.3 4.9 5.9 20.3 Adjusted EBITDA (1) 117.5$ 115.3$ 110.5$ 122.9$ 466.2$ Weighted average common shares outstanding: Basic 93.1 93.3 93.3 93.3 93.3 Diluted 109.0 109.5 109.2 109.1 109.2 2011 Q1 Q2 Full YearQ3 Q4
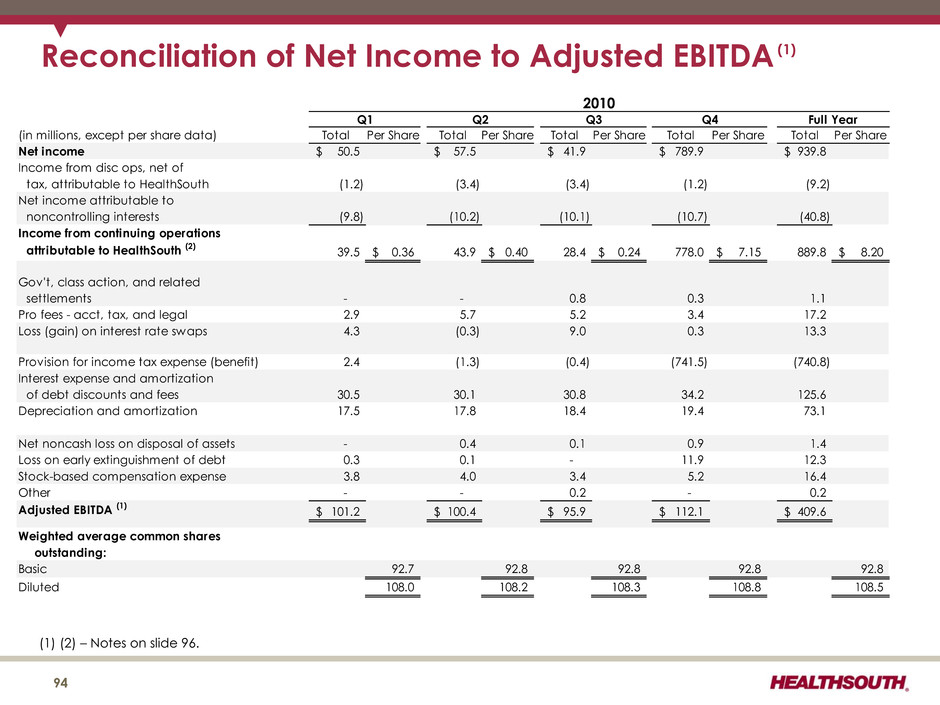
Reconciliation of Net Income to Adjusted EBITDA (1) (1) (2) – Notes on slide 96. (in millions, except per share data) Total Per Share Total Per Share Total Per Share Total Per Share Total Per Share Net income 50.5$ 57.5$ 41.9$ 789.9$ 939.8$ Income from disc ops, net of tax, attributable to HealthSouth (1.2) (3.4) (3.4) (1.2) (9.2) Net income attributable to noncontrolling interests (9.8) (10.2) (10.1) (10.7) (40.8) Income from continuing operations attributable to HealthSouth (2) 39.5 0.36$ 43.9 0.40$ 28.4 0.24$ 778.0 7.15$ 889.8 8.20$ Gov't, class action, and related settlements - - 0.8 0.3 1.1 Pro fees - acct, tax, and legal 2.9 5.7 5.2 3.4 17.2 Loss (gain) on interest rate swaps 4.3 (0.3) 9.0 0.3 13.3 Provision for income tax expense (benefit) 2.4 (1.3) (0.4) (741.5) (740.8) Interest expense and amortization of debt discounts and fees 30.5 30.1 30.8 34.2 125.6 Depreciation and amortization 17.5 17.8 18.4 19.4 73.1 Net noncash loss on disposal of assets - 0.4 0.1 0.9 1.4 Loss on early extinguishment of debt 0.3 0.1 - 11.9 12.3 Stock-based compensation expense 3.8 4.0 3.4 5.2 16.4 Other - - 0.2 - 0.2 Adjusted EBITDA (1) 101.2$ 100.4$ 95.9$ 112.1$ 409.6$ Weighted average common shares outstanding: Basic 92.7 92.8 92.8 92.8 92.8 Diluted 108.0 108.2 108.3 108.8 108.5 2010 Q1 Q2 Q3 Q4 Full Year 94
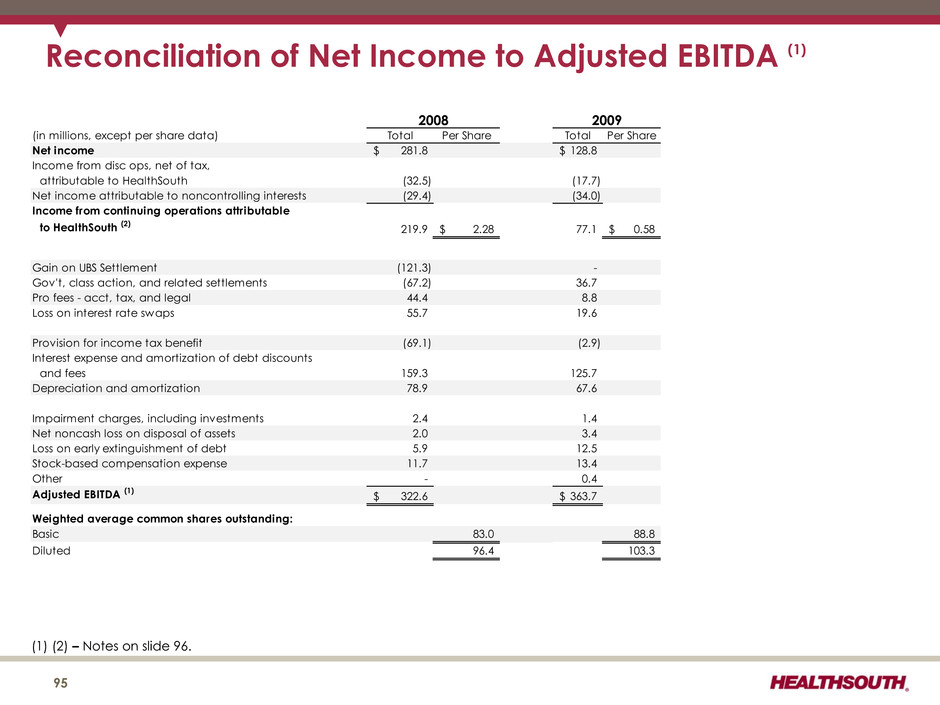
Reconciliation of Net Income to Adjusted EBITDA (1) (in millions, except per share data) Total Per Share Total Per Share Net income 281.8$ 128.8$ Income from disc ops, net of tax, attributable to HealthSouth (32.5) (17.7) Net income attributable to noncontrolling interests (29.4) (34.0) Income from continuing operations attributable to HealthSouth (2) 219.9 2.28$ 77.1 0.58$ Gain on UBS Settlement (121.3) - Gov't, class action, and related settlements (67.2) 36.7 Pro fees - acct, tax, and legal 44.4 8.8 Loss on interest rate swaps 55.7 19.6 Provision for income tax benefit (69.1) (2.9) Interest expense and amortization of debt discounts and fees 159.3 125.7 Depreciation and amortization 78.9 67.6 Impairment charges, including investments 2.4 1.4 Net noncash loss on disposal of assets 2.0 3.4 Loss on early extinguishment of debt 5.9 12.5 Stock-based compensation expense 11.7 13.4 Other - 0.4 Adjusted EBITDA (1) 322.6$ 363.7$ Weighted average common shares outstanding: Basic 83.0 88.8 Diluted 96.4 103.3 2008 2009 (1) (2) – Notes on slide 96. 95
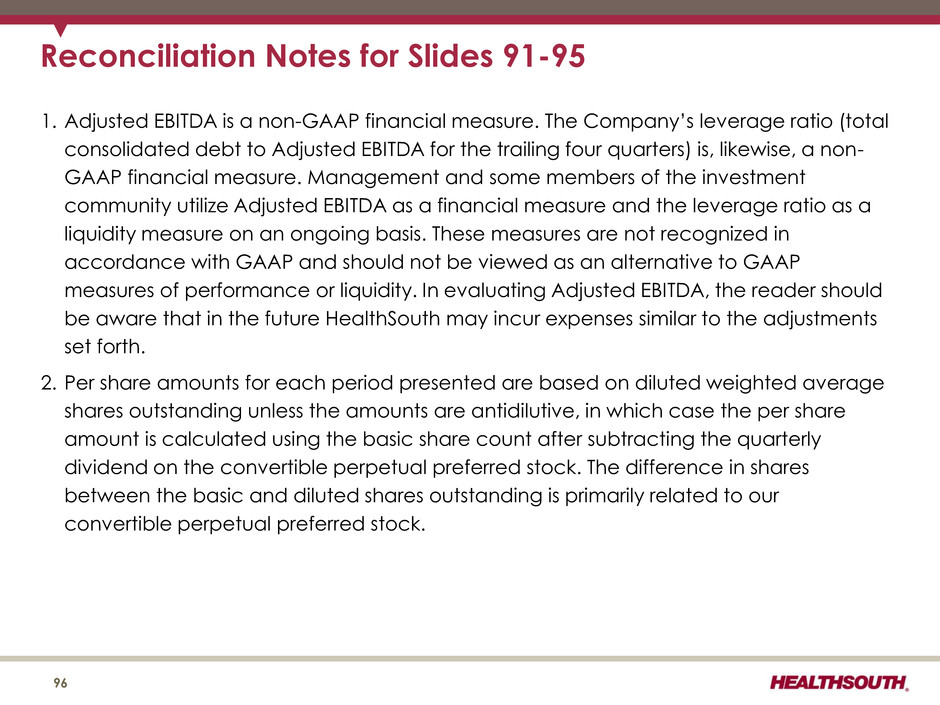
Reconciliation Notes for Slides 91-95 1. Adjusted EBITDA is a non-GAAP financial measure. The Company’s leverage ratio (total consolidated debt to Adjusted EBITDA for the trailing four quarters) is, likewise, a non- GAAP financial measure. Management and some members of the investment community utilize Adjusted EBITDA as a financial measure and the leverage ratio as a liquidity measure on an ongoing basis. These measures are not recognized in accordance with GAAP and should not be viewed as an alternative to GAAP measures of performance or liquidity. In evaluating Adjusted EBITDA, the reader should be aware that in the future HealthSouth may incur expenses similar to the adjustments set forth. 2. Per share amounts for each period presented are based on diluted weighted average shares outstanding unless the amounts are antidilutive, in which case the per share amount is calculated using the basic share count after subtracting the quarterly dividend on the convertible perpetual preferred stock. The difference in shares between the basic and diluted shares outstanding is primarily related to our convertible perpetual preferred stock. 96