Investor Reference Book 2020
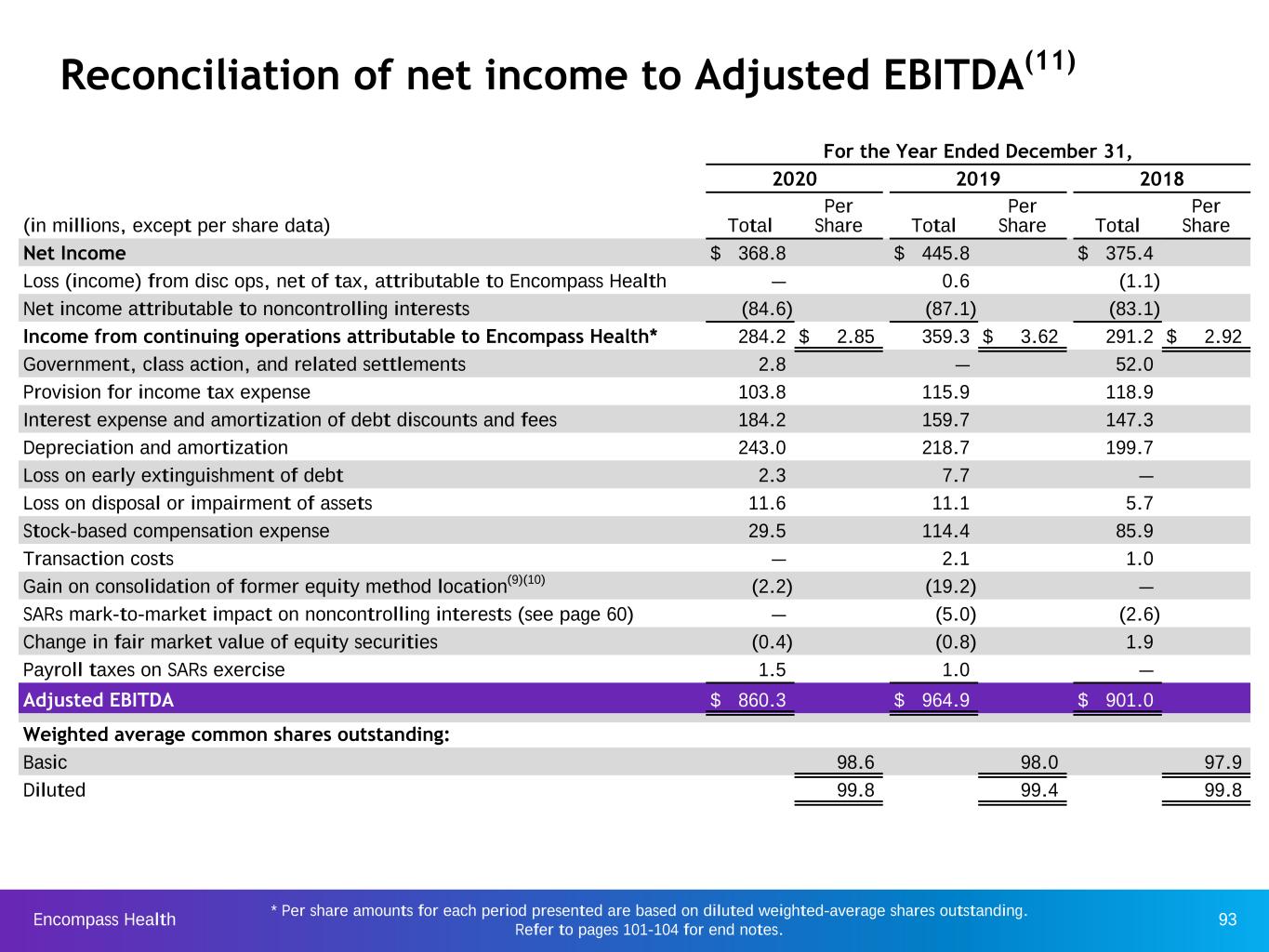
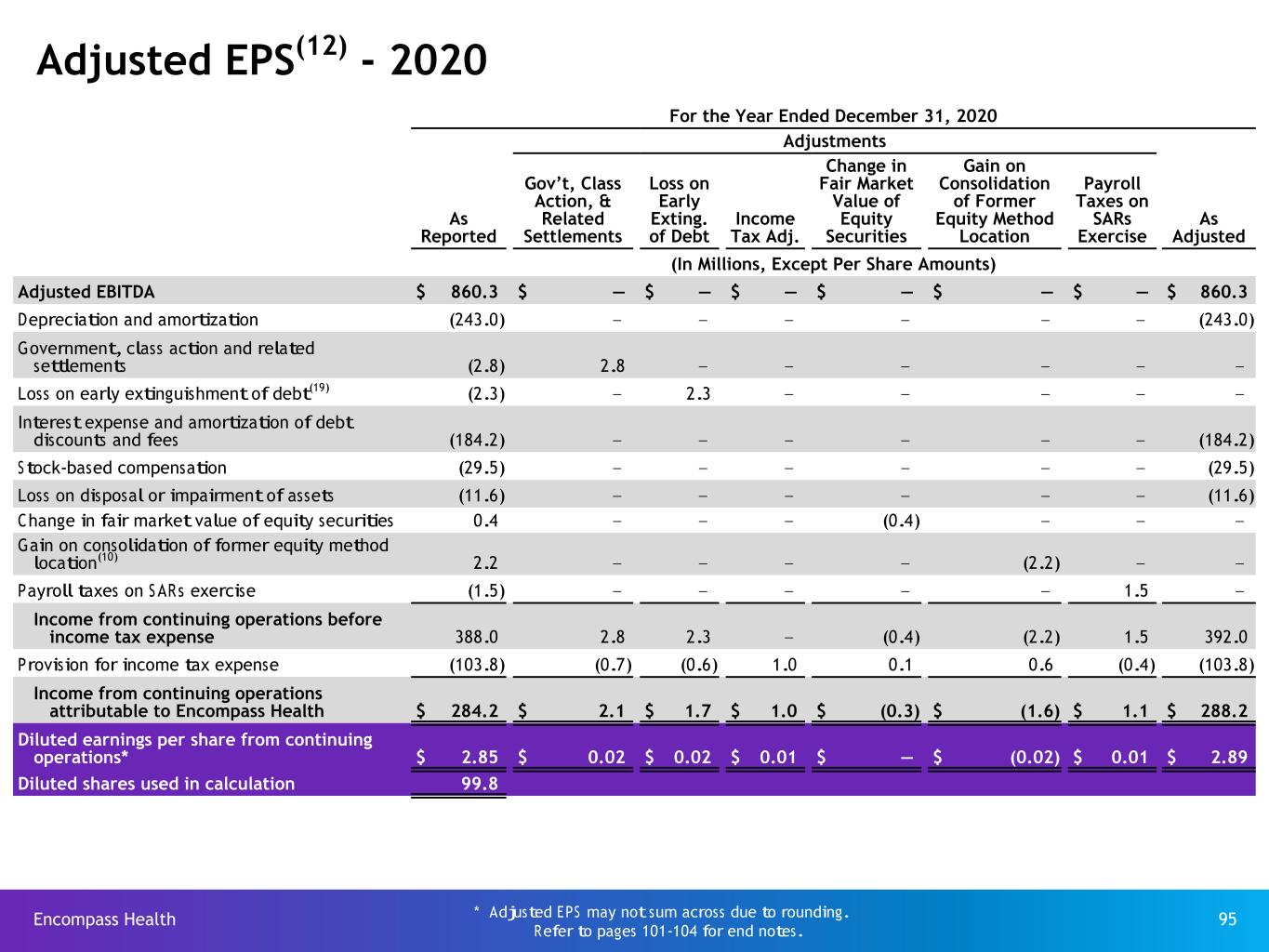
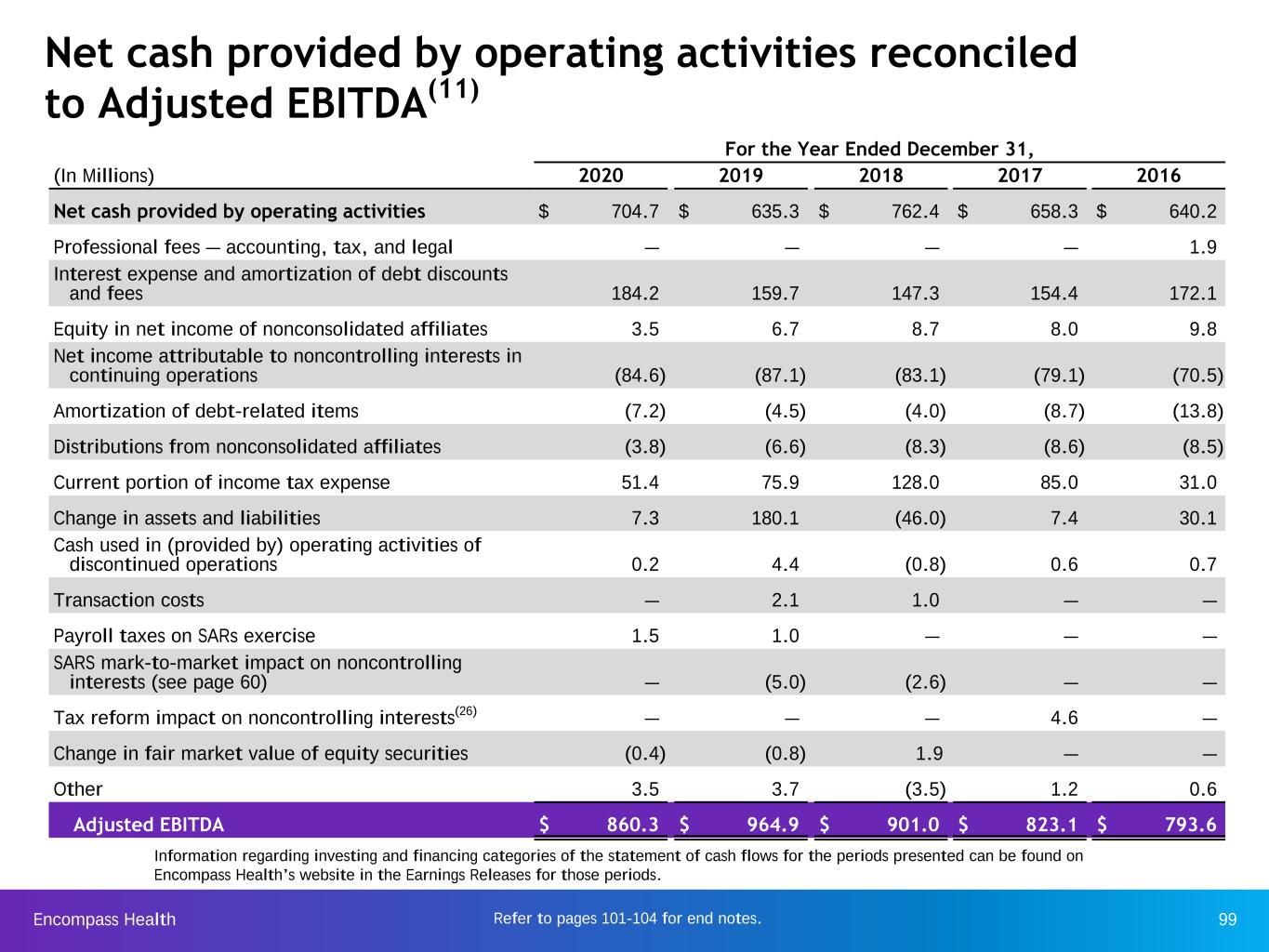
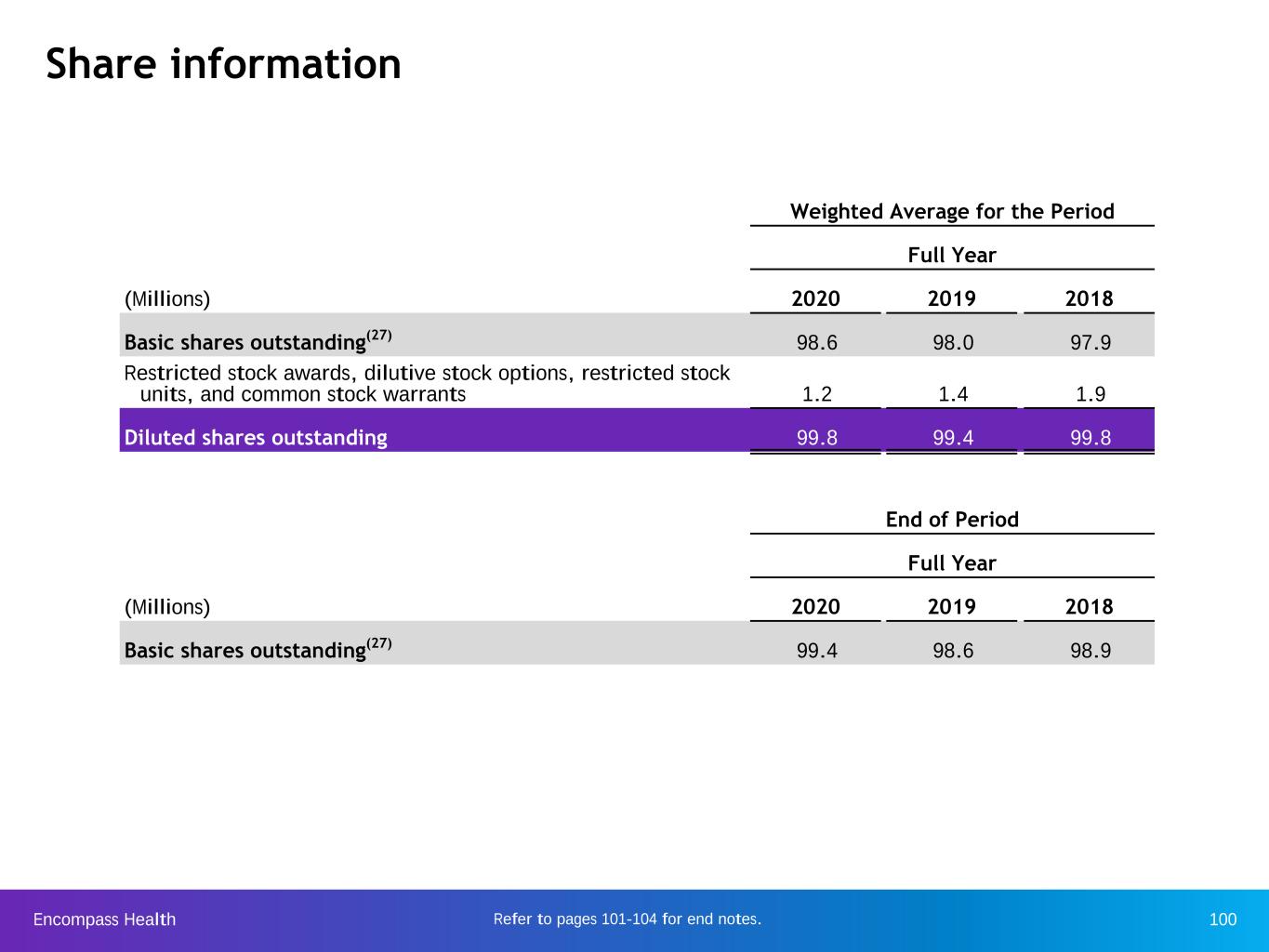
Encompass Health 2 Forward-looking statements The information contained in this Investor Reference Book includes certain estimates, projections and other forward- looking information that reflect Encompass Health’s current outlook, views and plans with respect to future events, including the ongoing strategic review and its impact on the business model, outlook and guidance, the COVID-19 pandemic and its effects, legislative and regulatory developments, strategy, capital expenditures, acquisition and other development activities, cyber security, dividend strategies, repurchases of securities, effective tax rates, financial performance, financial assumptions, business model, balance sheet and cash flow plans, market share, development of new information tools and models, and shareholder value-enhancing transactions. These estimates, projections and other forward-looking information are based on assumptions the Company believes, as of the date hereof, are reasonable. Inevitably, there will be differences between such estimates and actual events or results, and those differences may be material. There can be no assurance any estimates, projections or forward-looking information will be realized. All such estimates, projections and forward-looking information speak only as of the date hereof. Encompass Health undertakes no duty to publicly update or revise the information contained herein. You are cautioned not to place undue reliance on the estimates, projections and other forward-looking information in this Investor Reference Book as they are based on current expectations and general assumptions and are subject to various risks, uncertainties and other factors, including those set forth in the Form 10-K for the year ended December 31, 2020 and in other documents Encompass Health previously filed with the SEC, many of which are beyond Encompass Health’s control, that may cause actual events or results to differ materially from the views, beliefs, and estimates expressed herein. Note regarding presentation of non-GAAP financial measures The following Investor Reference Book includes certain “non-GAAP financial measures” as defined in Regulation G under the Securities Exchange Act of 1934, including Adjusted EBITDA, leverage ratios, adjusted earnings per share, and adjusted free cash flow. Schedules are attached that reconcile the non-GAAP financial measures included in the following Investor Reference Book to the most directly comparable financial measures calculated and presented in accordance with Generally Accepted Accounting Principles in the United States. The Company’s Form 8-K, dated March 9, 2021, to which the following Investor Reference Book is attached as Exhibit 99.1, provides further explanation and disclosure regarding Encompass Health’s use of non-GAAP financial measures and should be read in conjunction with this Investor Reference Book.
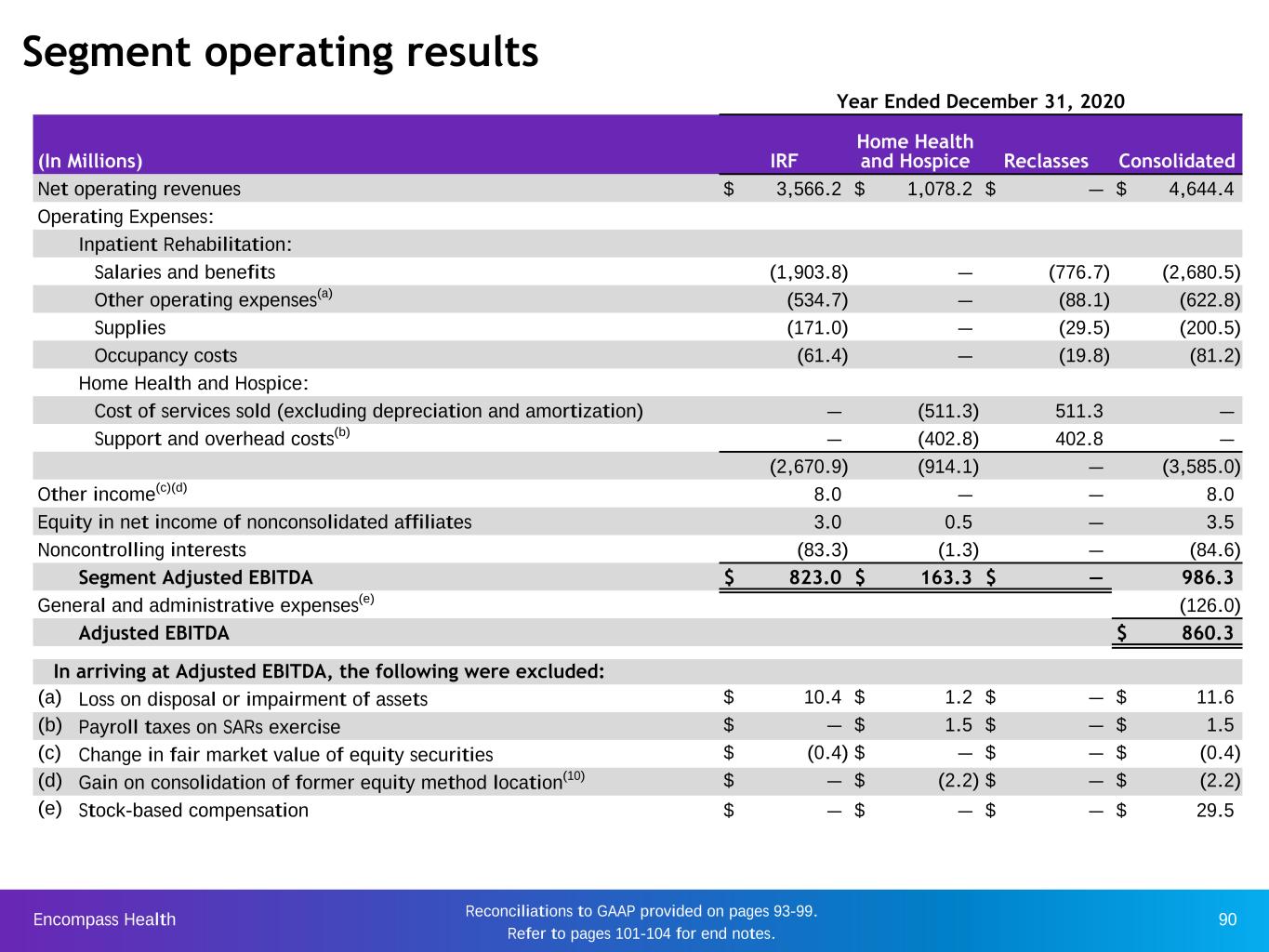
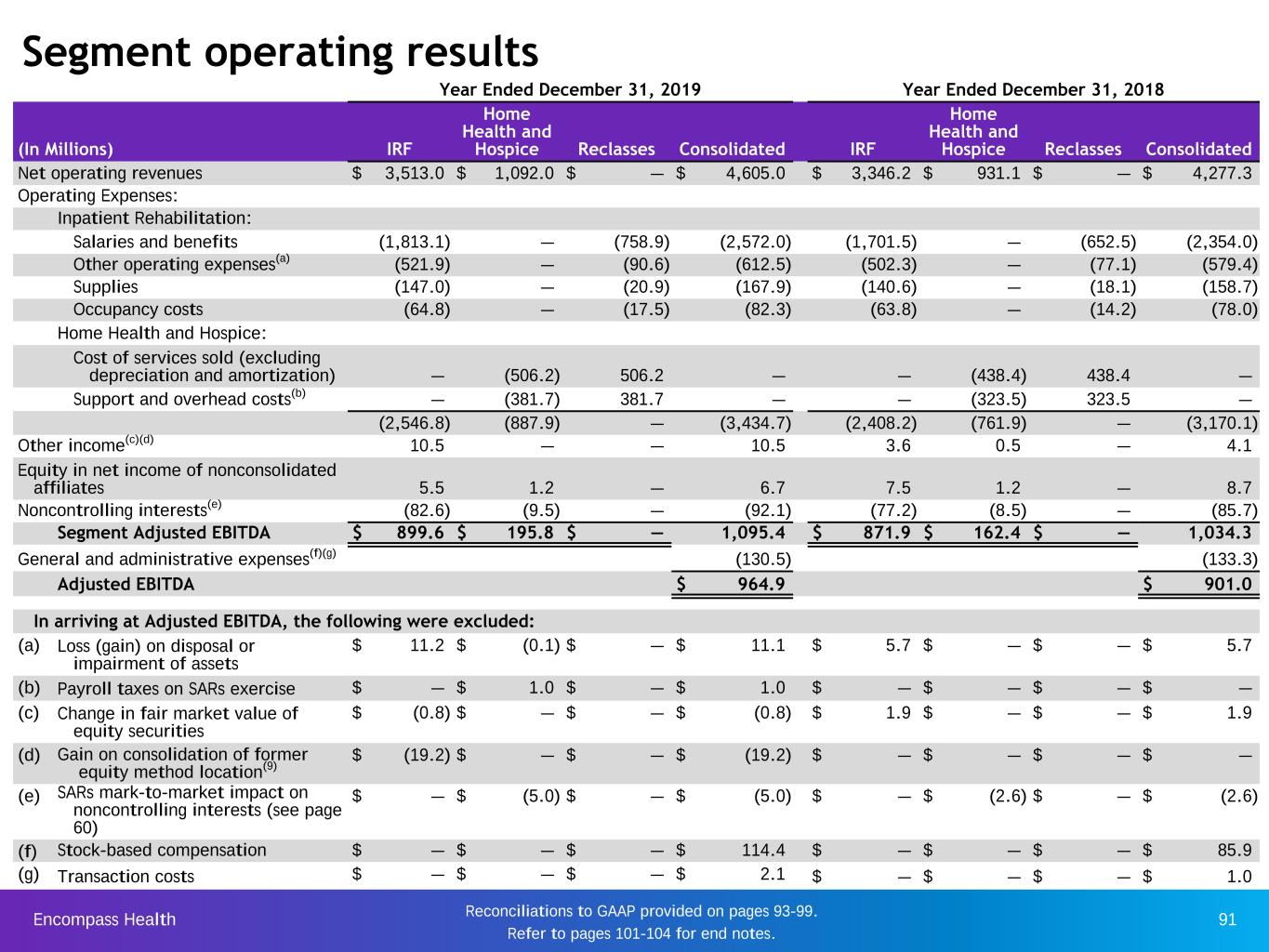
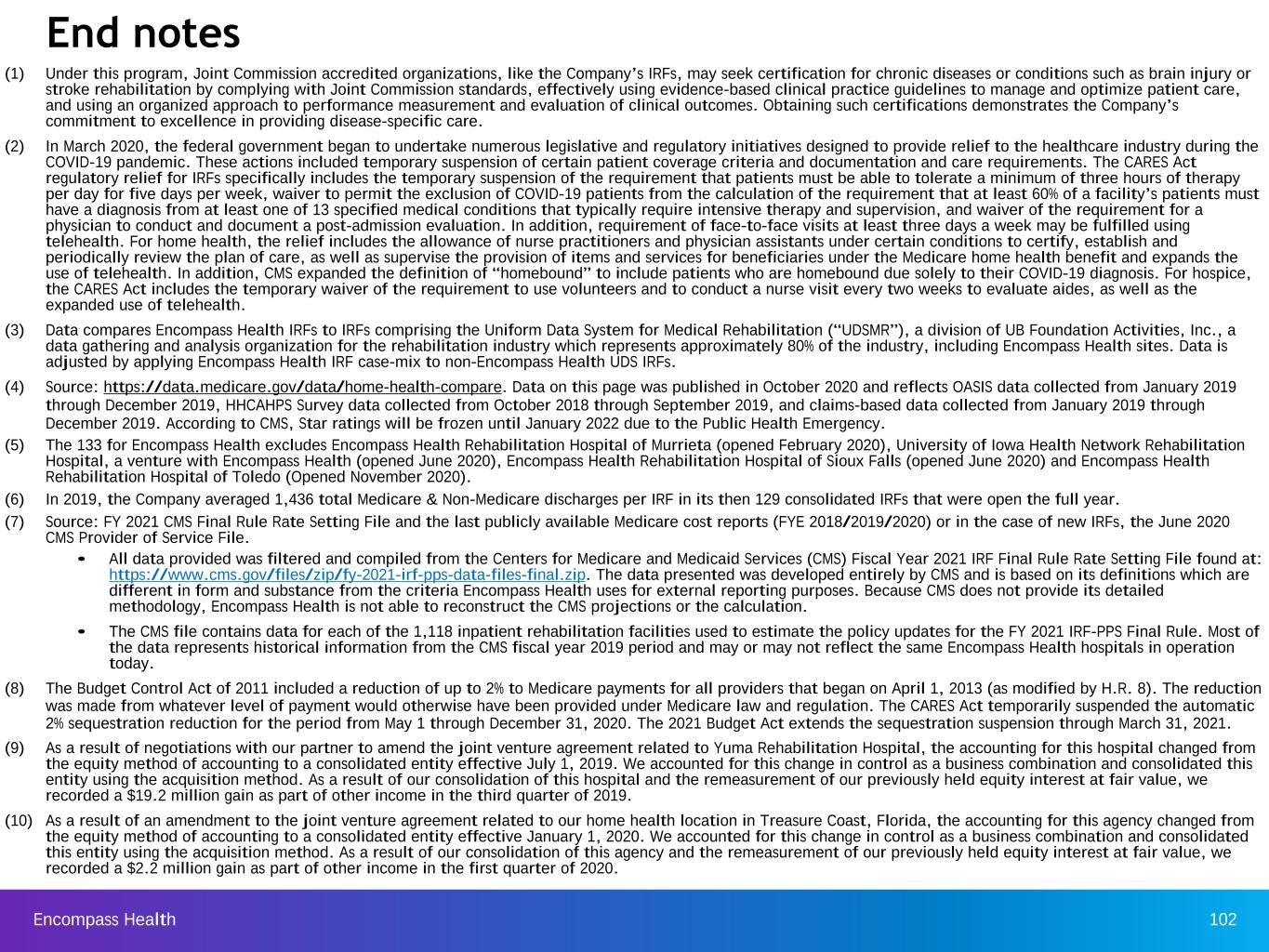
Encompass Health 3 Company overview . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4-16 Highlights from 2020 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 17-23 Business outlook, including guidance . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 24-31 Growth . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 32-42 Operational initiatives . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 43-54 Capital structure . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 55-60 Information technology . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 61-65 Operational metrics . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 66-72 Industry structure . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 73-86 Segment operating results . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 87-91 Reconciliations to GAAP and share information . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 92-100 End notes . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 101-104 Table of contents

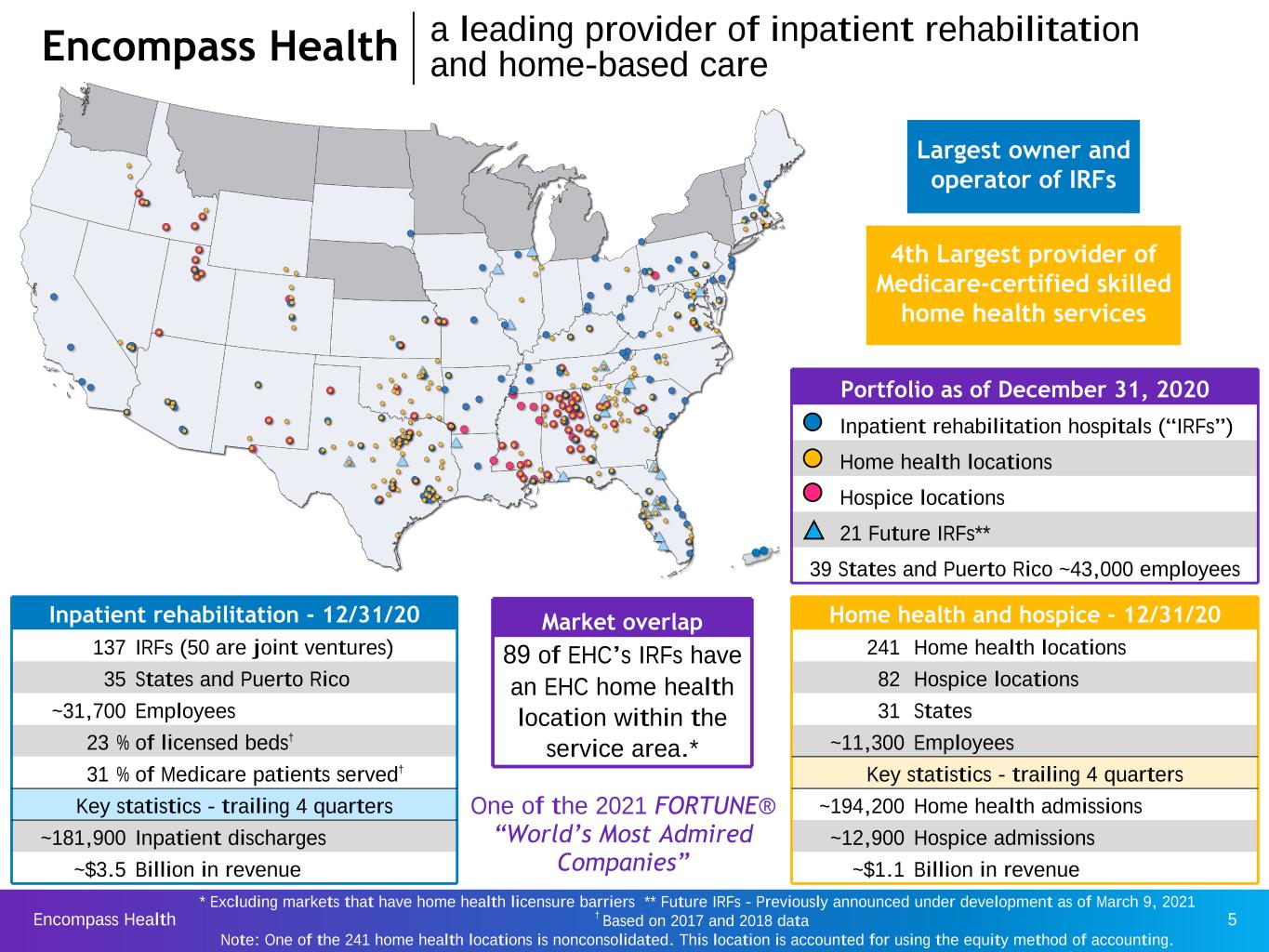
Encompass Health 4 Company overview Encompass Health is a national leader in integrated healthcare services offering both facility-based and home-based patient care through its network of inpatient rehabilitation hospitals, home health agencies, and hospice agencies. The Company is committed to delivering high-quality, cost-effective, integrated care.
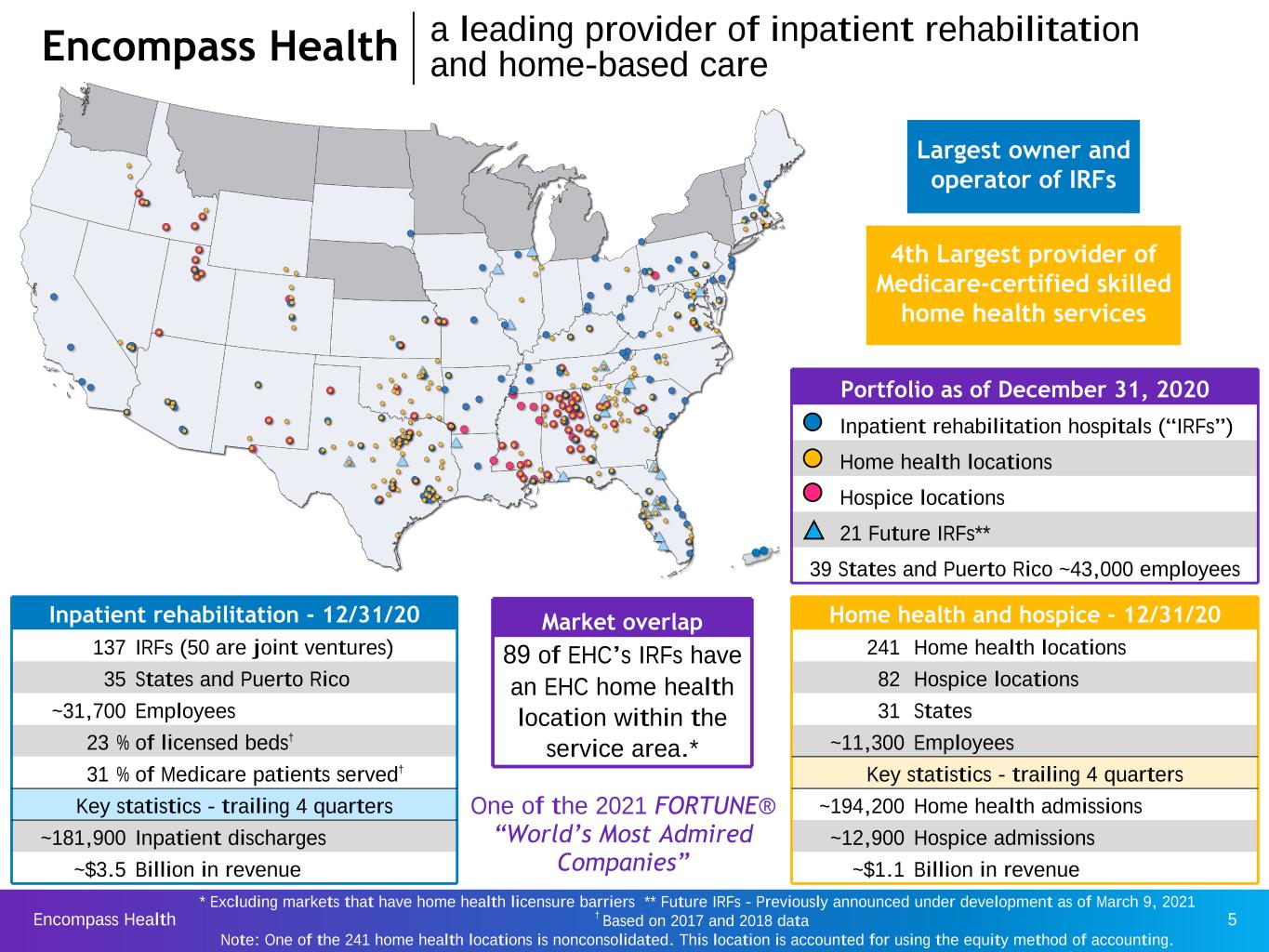
Encompass Health 5 Inpatient rehabilitation - 12/31/20 137 IRFs (50 are joint ventures) 35 States and Puerto Rico ~31,700 Employees 23 % of licensed beds† 31 % of Medicare patients served† Key statistics - trailing 4 quarters ~181,900 Inpatient discharges ~$3.5 Billion in revenue Portfolio as of December 31, 2020 Inpatient rehabilitation hospitals (“IRFs”) Home health locations Hospice locations 21 Future IRFs** 39 States and Puerto Rico ~43,000 employees Encompass Health a leading provider of inpatient rehabilitation and home-based care Market overlap 89 of EHC’s IRFs have an EHC home health location within the service area.* Home health and hospice - 12/31/20 241 Home health locations 82 Hospice locations 31 States ~11,300 Employees Key statistics - trailing 4 quarters ~194,200 Home health admissions ~12,900 Hospice admissions ~$1.1 Billion in revenue Largest owner and operator of IRFs 4th Largest provider of Medicare-certified skilled home health services * Excluding markets that have home health licensure barriers ** Future IRFs - Previously announced under development as of March 9, 2021 † Based on 2017 and 2018 data Note: One of the 241 home health locations is nonconsolidated. This location is accounted for using the equity method of accounting. One of the 2021 FORTUNE® “World’s Most Admired Companies”

Encompass Health 6 Major services • Rehabilitation physicians: manage and treat medical conditions and oversee rehabilitation program • Rehabilitation nurses: provide personal care and oversee treatment plan for patients • Physical therapists: address physical function, mobility, strength, balance, and safety • Occupational therapists: promote independence through Activities of Daily Living • Speech-language therapists: address speech/voice functions, swallowing, memory/cognition, and language/ communication • Respiratory therapists: provide assessment and treatment of patients with both acute and chronic dysfunction of the cardiopulmonary system • Case managers: coordinate care plan with physician, Care Transition Coordinators, caregivers and family • Post-discharge services: outpatient therapy and transition to home health Inpatient rehabilitation hospitals Refer to pages 101-104 for end notes. 124 of the Company’s IRFs hold one or more disease-specific certifications from The Joint Commission’s Disease-Specific Care Certification Program.(1) Company overview inpatient rehabilitation

Encompass Health 7 Major services • Skilled nurses: comprehensively assess, teach, train, and manage care related to injury or illness • Home health aides: provide personal care and assistance with Activities of Daily Living (ADLs) • Physical therapists: address physical function, mobility, strength, balance, and safety • Occupational therapists: promote independence through training on self-management of ADLs • Speech-language therapists: address speech/voice functions, swallowing, memory/cognition, and language/communication • Medical social workers: provide assessment of social and emotional factors; assist with obtaining community resources Home health agencies The Company offers evidence-based specialty programs related to: post-operative care, fall prevention, chronic disease management, and transitional care. Hospice: provides services to terminally ill patients and their families to address patients’ physical needs, including pain control and symptom management, and also provides emotional and spiritual support. Company overview home health and hospice
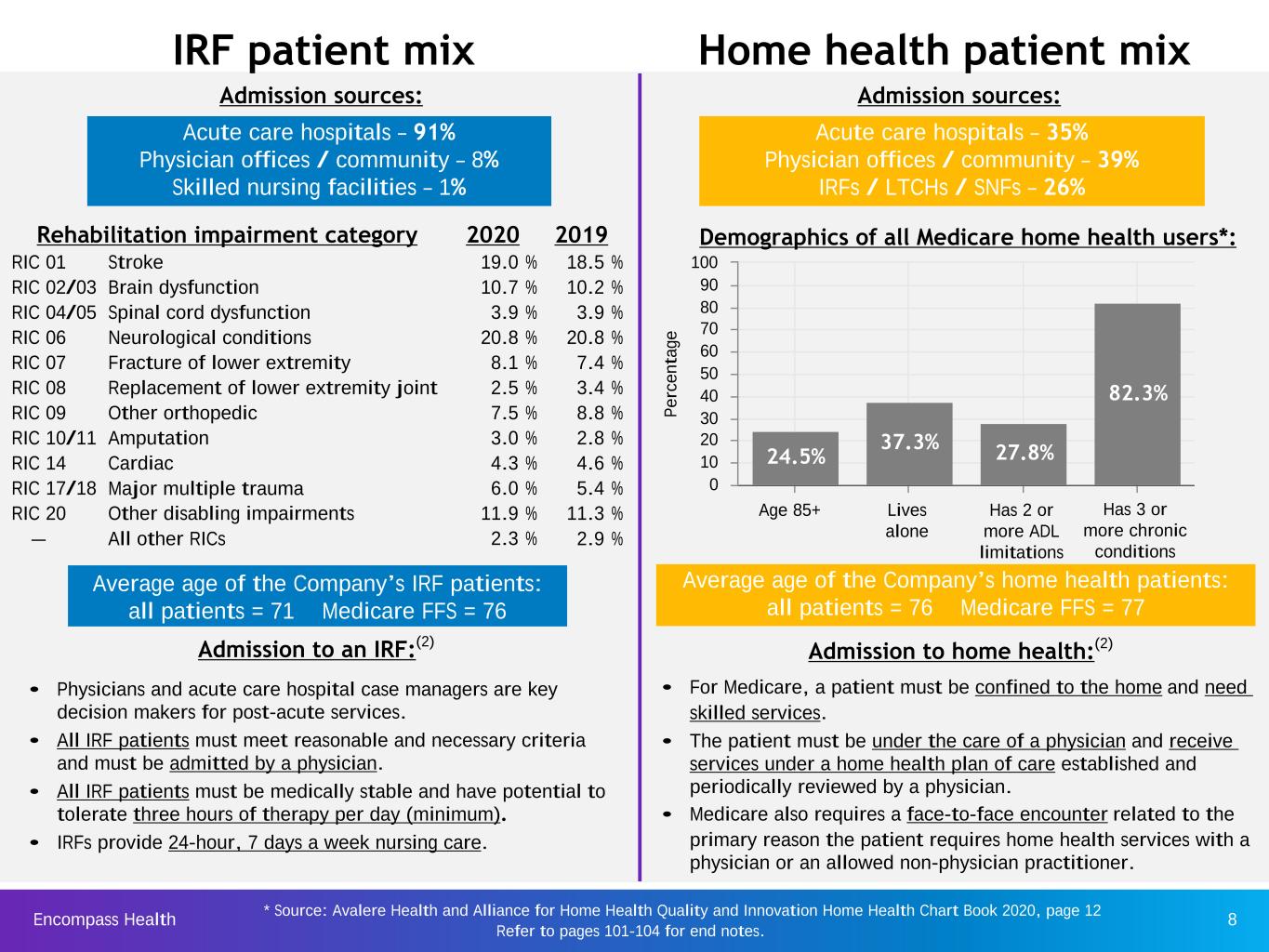
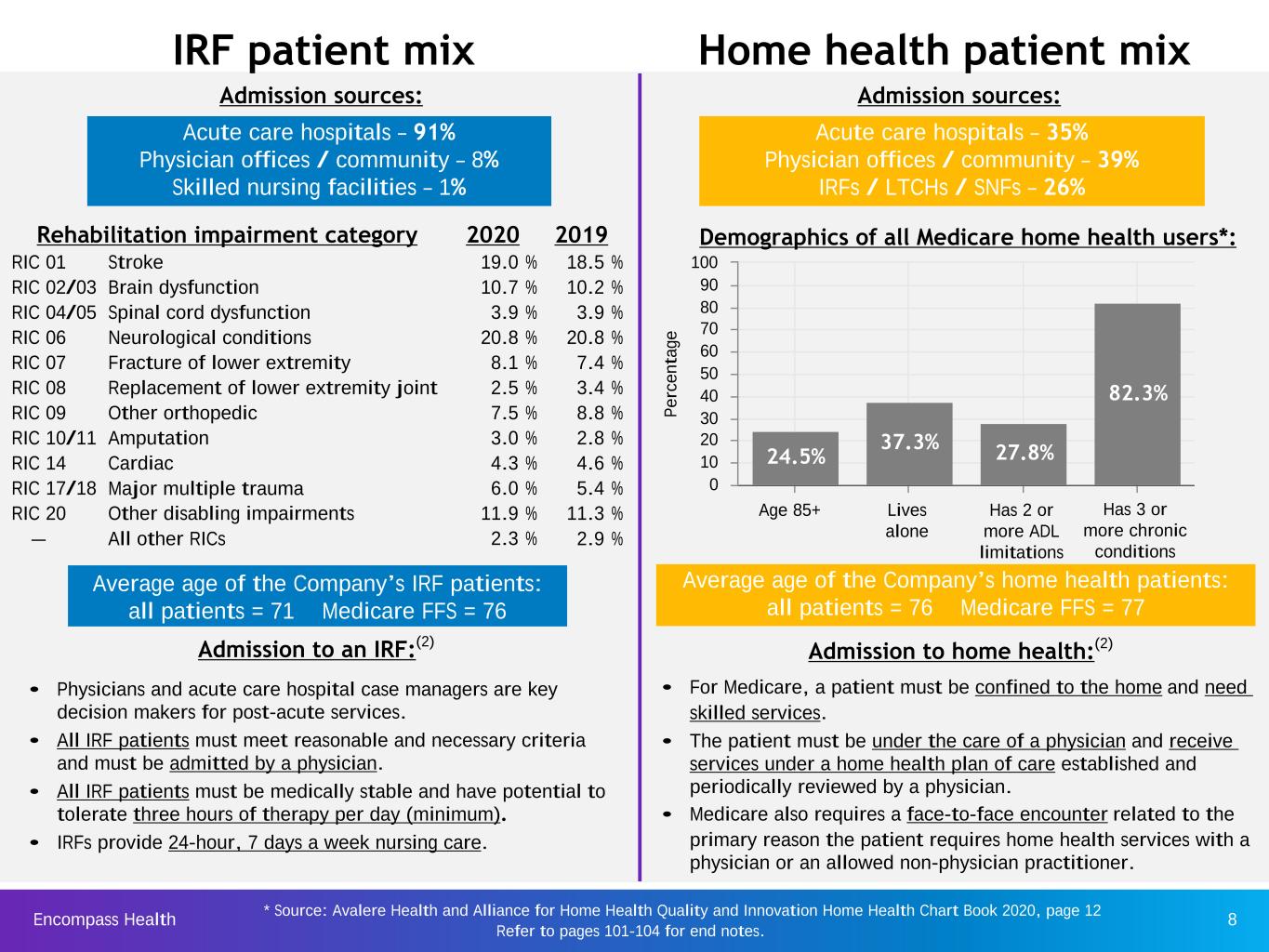
Encompass Health 8 IRF patient mix Admission sources: • Physicians and acute care hospital case managers are key decision makers for post-acute services. • All IRF patients must meet reasonable and necessary criteria and must be admitted by a physician. • All IRF patients must be medically stable and have potential to tolerate three hours of therapy per day (minimum). • IRFs provide 24-hour, 7 days a week nursing care. Admission to an IRF:(2) Average age of the Company’s IRF patients: all patients = 71 Medicare FFS = 76 Home health patient mix Acute care hospitals – 91% Physician offices / community – 8% Skilled nursing facilities – 1% Admission sources: • For Medicare, a patient must be confined to the home and need skilled services. • The patient must be under the care of a physician and receive services under a home health plan of care established and periodically reviewed by a physician. • Medicare also requires a face-to-face encounter related to the primary reason the patient requires home health services with a physician or an allowed non-physician practitioner. Admission to home health:(2) P e rc e n ta ge 24.5% 37.3% 27.8% 82.3% 0 10 20 30 40 50 60 70 80 90 100 Age 85+ Lives alone Has 2 or more ADL limitations Has 3 or more chronic conditions Demographics of all Medicare home health users*: * Source: Avalere Health and Alliance for Home Health Quality and Innovation Home Health Chart Book 2020, page 12 Rehabilitation impairment category 2020 2019 RIC 01 Stroke 19.0 % 18.5 % RIC 02/03 Brain dysfunction 10.7 % 10.2 % RIC 04/05 Spinal cord dysfunction 3.9 % 3.9 % RIC 06 Neurological conditions 20.8 % 20.8 % RIC 07 Fracture of lower extremity 8.1 % 7.4 % RIC 08 Replacement of lower extremity joint 2.5 % 3.4 % RIC 09 Other orthopedic 7.5 % 8.8 % RIC 10/11 Amputation 3.0 % 2.8 % RIC 14 Cardiac 4.3 % 4.6 % RIC 17/18 Major multiple trauma 6.0 % 5.4 % RIC 20 Other disabling impairments 11.9 % 11.3 % — All other RICs 2.3 % 2.9 % Acute care hospitals – 35% Physician offices / community – 39% IRFs / LTCHs / SNFs – 26% Average age of the Company’s home health patients: all patients = 76 Medicare FFS = 77 Refer to pages 101-104 for end notes.
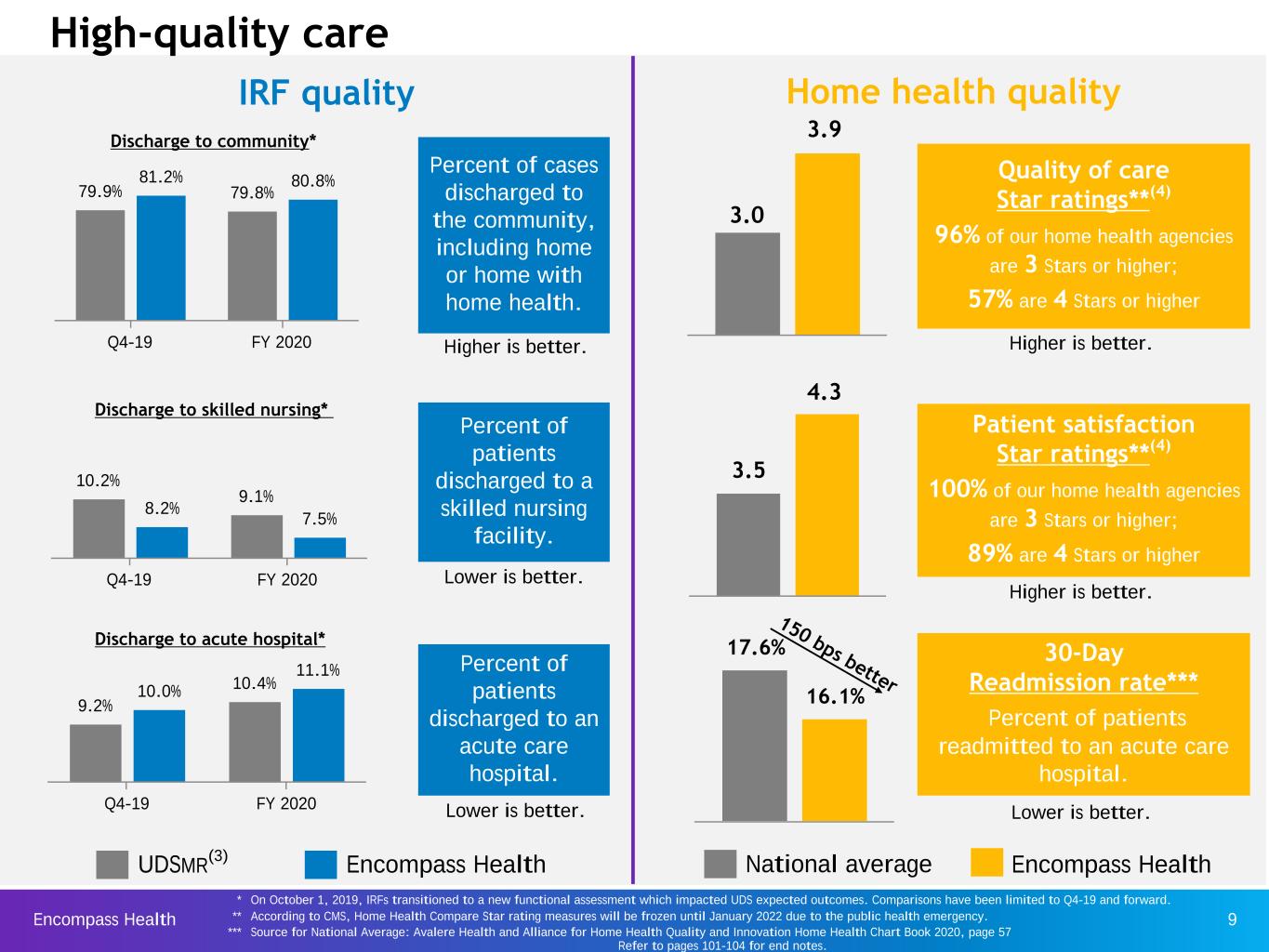
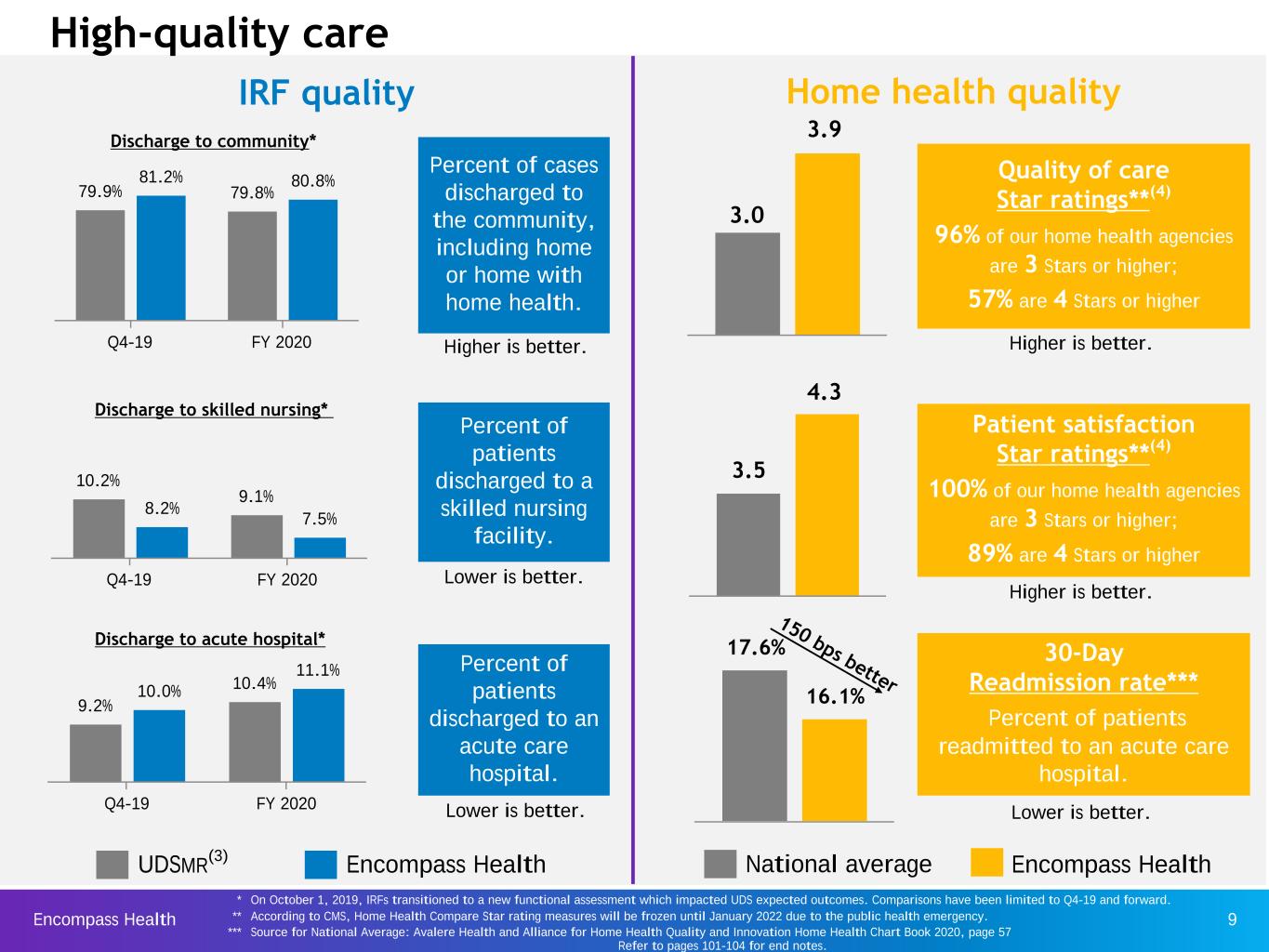
Encompass Health 9 9.2% 10.4%10.0% 11.1% Q4-19 FY 2020 10.2% 9.1% 8.2% 7.5% Q4-19 FY 2020 Home health qualityIRF quality Discharge to community* Discharge to skilled nursing* Discharge to acute hospital* Quality of care Star ratings**(4) 96% of our home health agencies are 3 Stars or higher; 57% are 4 Stars or higher Patient satisfaction Star ratings**(4) 100% of our home health agencies are 3 Stars or higher; 89% are 4 Stars or higher Encompass Health 17.6% 16.1% 30-Day Readmission rate*** Percent of patients readmitted to an acute care hospital. 150 bps better UDSMR(3) Encompass Health High-quality care National average Percent of cases discharged to the community, including home or home with home health. Percent of patients discharged to a skilled nursing facility. Percent of patients discharged to an acute care hospital. 79.9% 79.8% 81.2% 80.8% Q4-19 FY 2020 3.5 4.3 3.9 3.0 Higher is better. Lower is better. Lower is better. * On October 1, 2019, IRFs transitioned to a new functional assessment which impacted UDS expected outcomes. Comparisons have been limited to Q4-19 and forward. ** According to CMS, Home Health Compare Star rating measures will be frozen until January 2022 due to the public health emergency. *** Source for National Average: Avalere Health and Alliance for Home Health Quality and Innovation Home Health Chart Book 2020, page 57 Refer to pages 101-104 for end notes. Higher is better. Higher is better. Lower is better.
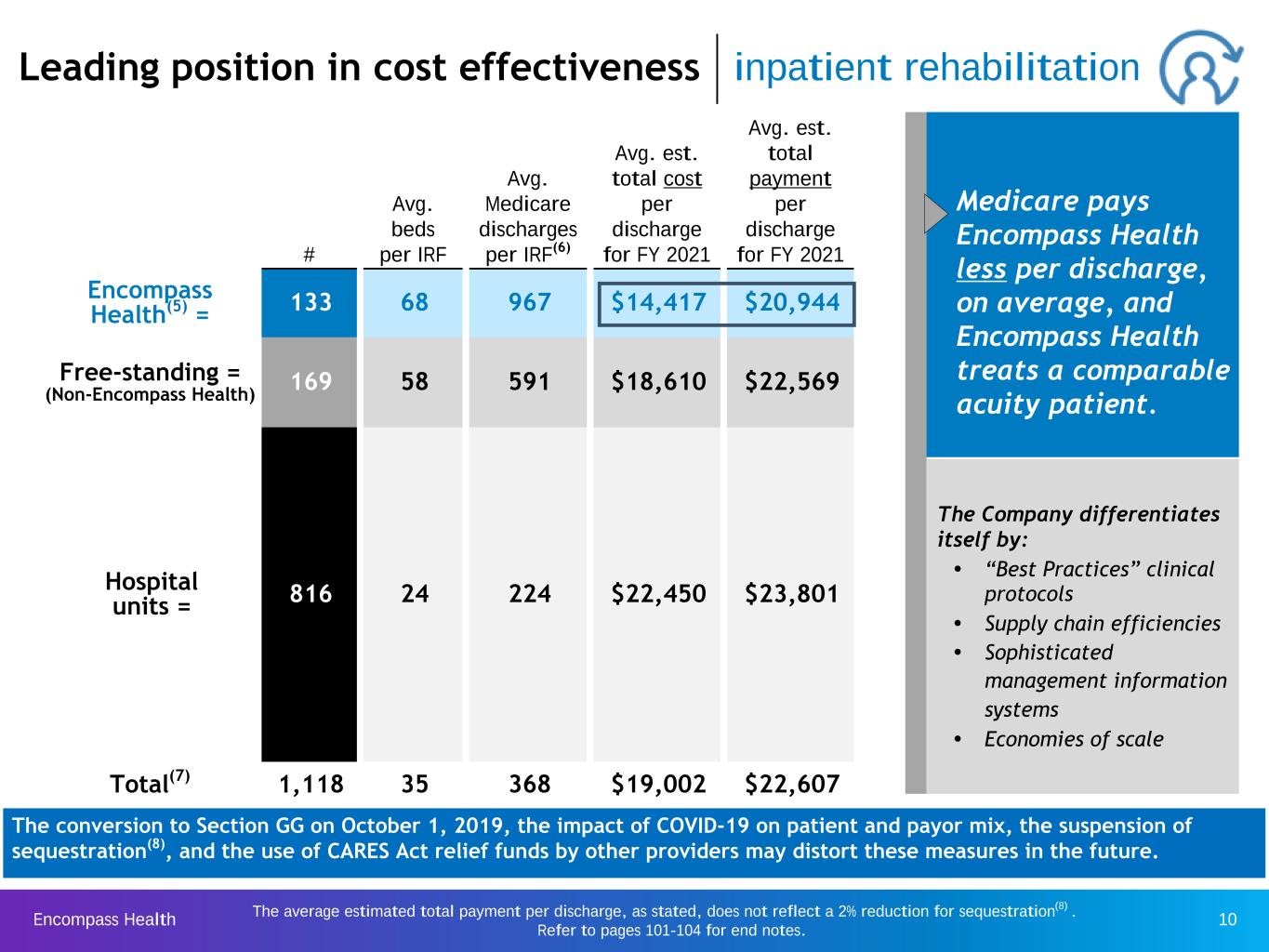
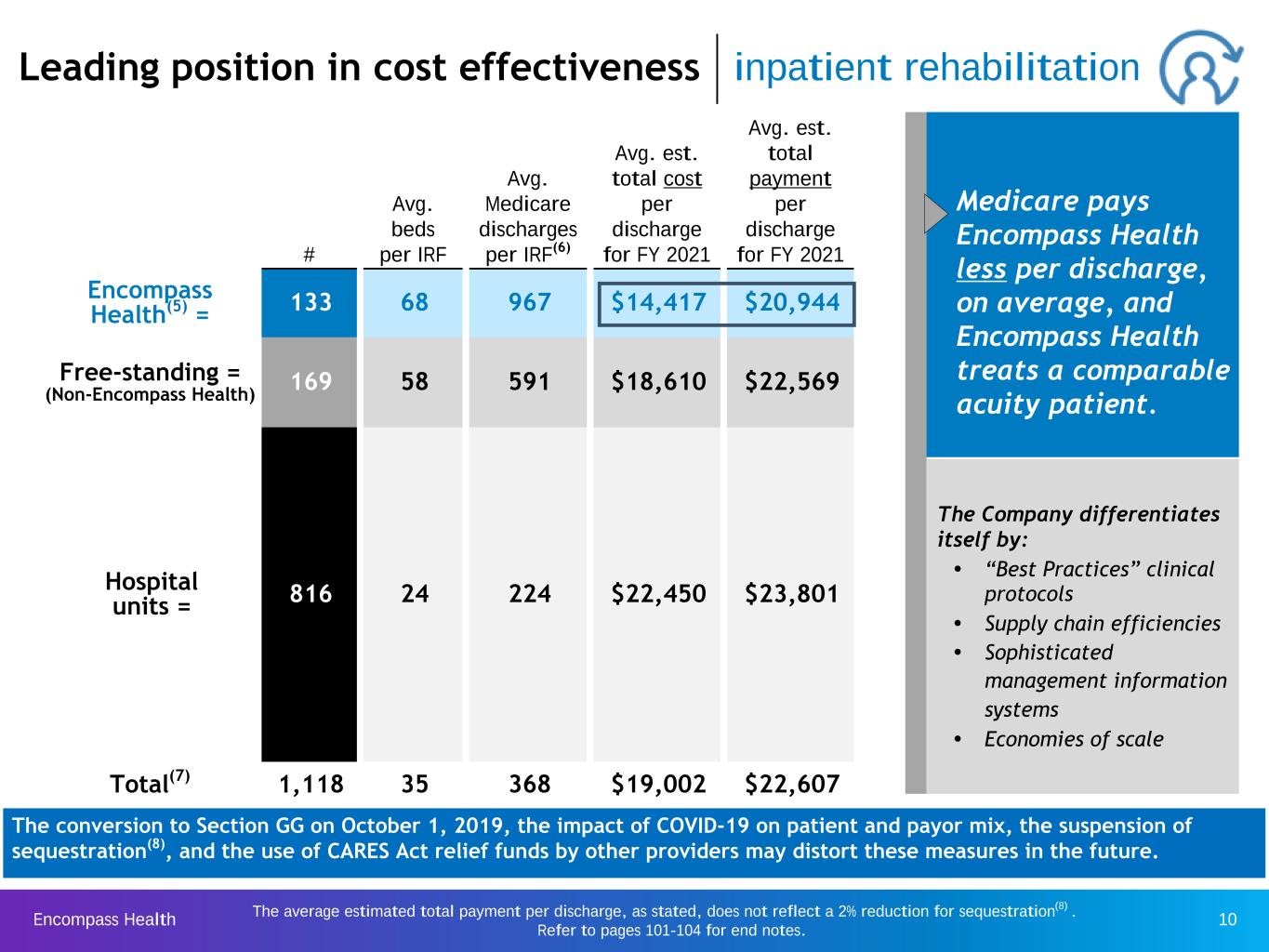
Encompass Health 10 # Avg. beds per IRF Avg. Medicare discharges per IRF(6) Avg. est. total cost per discharge for FY 2021 Avg. est. total payment per discharge for FY 2021 Encompass Health(5) = 133 68 967 $14,417 $20,944 Free-standing = (Non-Encompass Health) 169 58 591 $18,610 $22,569 Hospital units = 816 24 224 $22,450 $23,801 Total(7) 1,118 35 368 $19,002 $22,607 Leading position in cost effectiveness inpatient rehabilitation Medicare pays Encompass Health less per discharge, on average, and Encompass Health treats a comparable acuity patient. The average estimated total payment per discharge, as stated, does not reflect a 2% reduction for sequestration(8) . Refer to pages 101-104 for end notes. The Company differentiates itself by: Ÿ “Best Practices” clinical protocols Ÿ Supply chain efficiencies Ÿ Sophisticated management information systems Ÿ Economies of scale The conversion to Section GG on October 1, 2019, the impact of COVID-19 on patient and payor mix, the suspension of sequestration(8), and the use of CARES Act relief funds by other providers may distort these measures in the future.

Encompass Health 11 2019 Episodes Average revenue per episode* Average visits per episode Average revenue per visit (all payors) Cost per visit** Encompass Health 275,578 $2,972 17.1 $166 $77 Public peer average 336,684 $2,995 17.6 $149 $87 Comparison to peer average (0.8)% (2.8)% 11.4% (11.5)% Public peer average represents 2019 data from publicly traded home health providers. * EHC’s average revenue per episode is 0.8% lower than the peer average due to the acquisitions of Camellia (2018) and Alacare (2019) having lower than average wage indices. ** Encompass Health Cost per Visit excludes cost of clinicians’ medical plan benefits of $4 per visit. Cost per visit is 11.5% lower due to market density and operational efficiency: Ÿ Caregiver optimization Ÿ Optimization of HCHB Ÿ Employee culture of excellence Ÿ ~80% of visits conducted by full- time staff Ÿ Daily monitoring of productivity Average revenue per visit is 11.4% higher for Encompass Health primarily due to a higher ratio of Medicare to non‑Medicare patients. Low cost leader home health The conversion to PDGM on January 1, 2020, the impact of COVID-19 on patient and payor mix, the suspension of sequestration(8), and the use of CARES Act relief funds by other providers may distort these measures in the future. Refer to pages 101-104 for end notes.
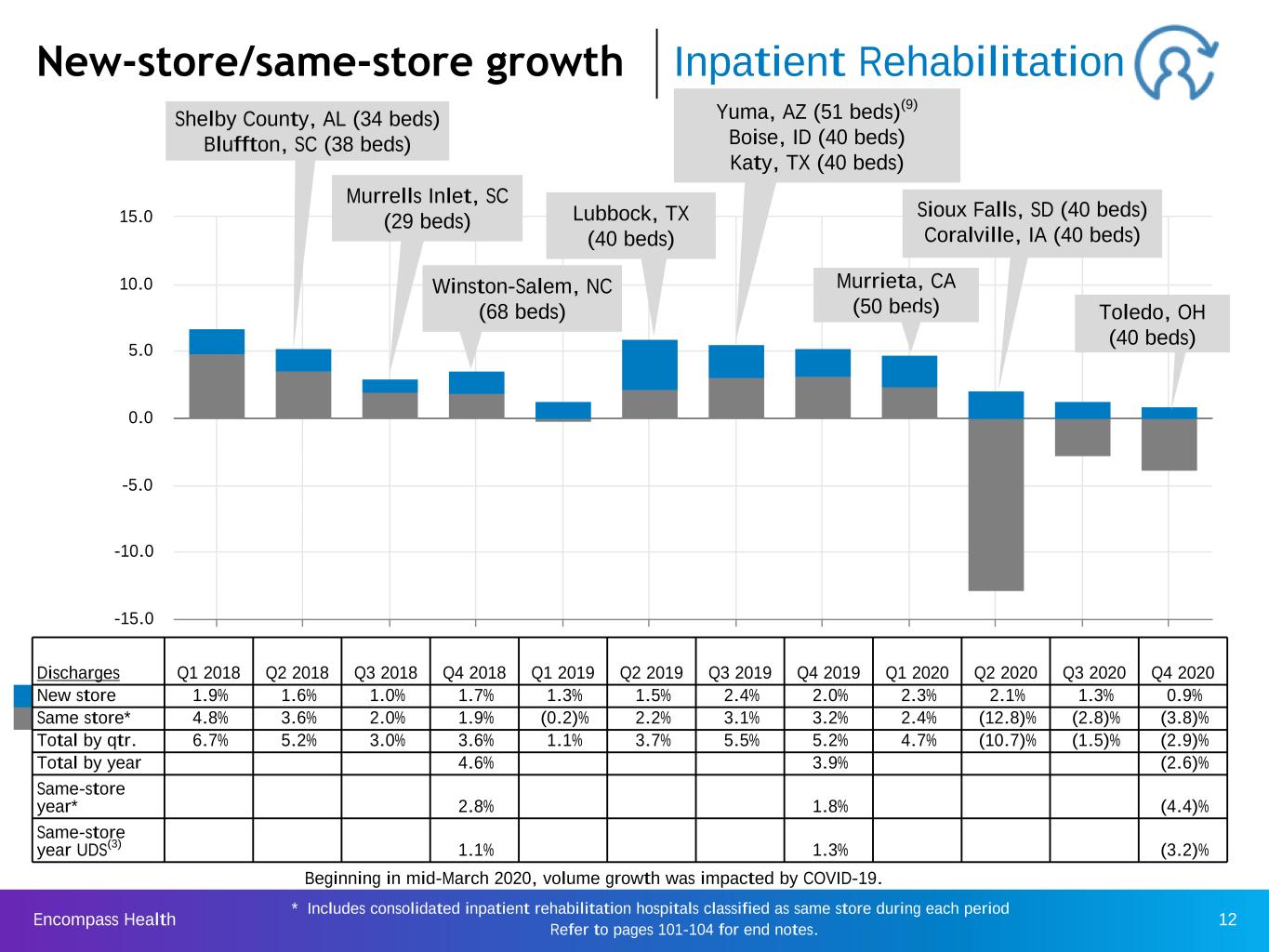
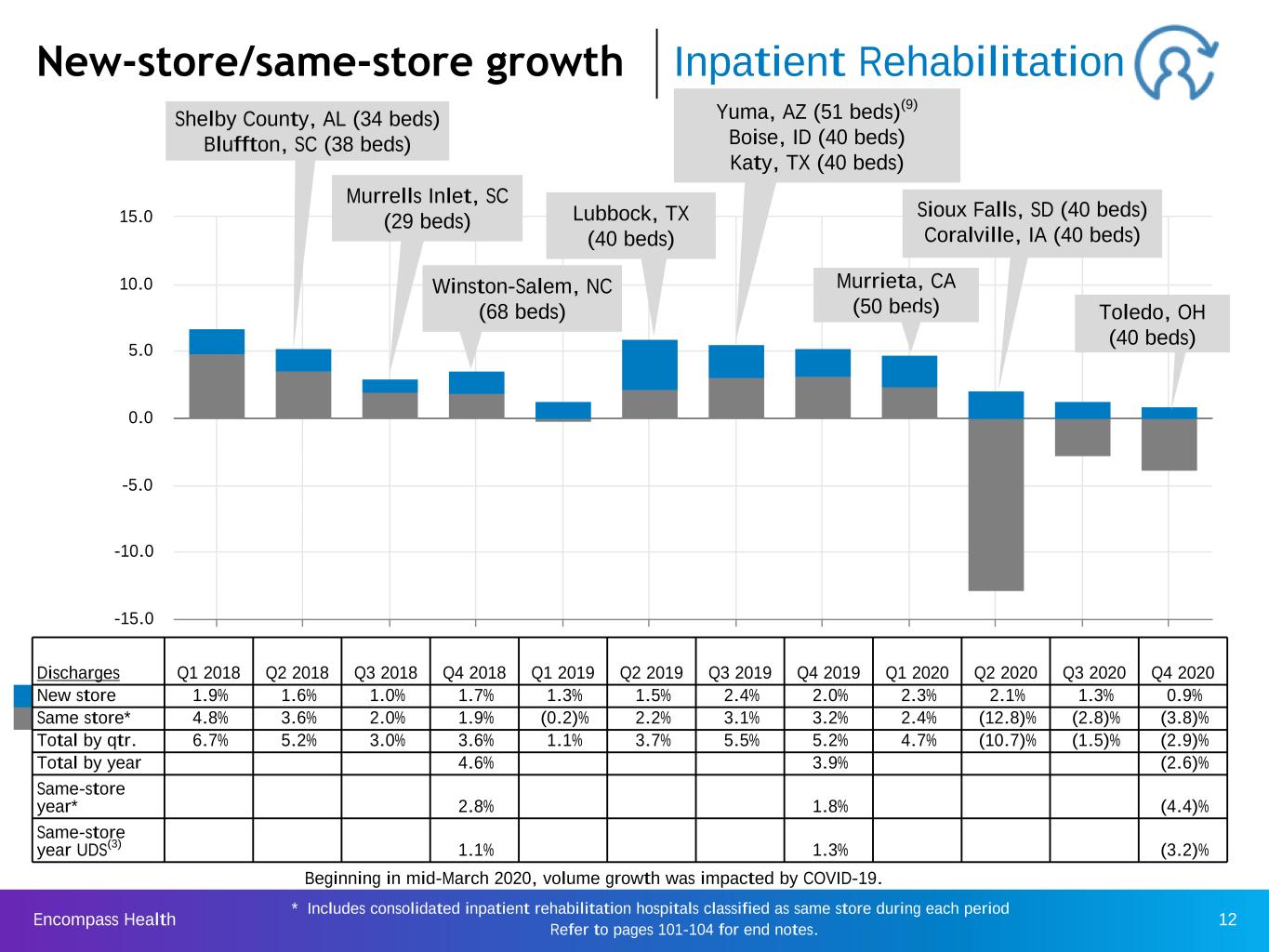
Encompass Health 12 * Includes consolidated inpatient rehabilitation hospitals classified as same store during each period Refer to pages 101-104 for end notes. Q1 2018 Q2 2018 Q3 2018 Q4 2018 Q1 2019 Q2 2019 Q3 2019 Q4 2019 Q1 2020 Q2 2020 Q3 2020 Q4 2020 -15.0 -10.0 -5.0 0.0 5.0 10.0 15.0 New-store/same-store growth Inpatient Rehabilitation Yuma, AZ (51 beds)(9) Boise, ID (40 beds) Katy, TX (40 beds) Shelby County, AL (34 beds) Bluffton, SC (38 beds) Murrells Inlet, SC (29 beds) Winston-Salem, NC (68 beds) Lubbock, TX (40 beds) Discharges Q1 2018 Q2 2018 Q3 2018 Q4 2018 Q1 2019 Q2 2019 Q3 2019 Q4 2019 Q1 2020 Q2 2020 Q3 2020 Q4 2020 New store 1.9% 1.6% 1.0% 1.7% 1.3% 1.5% 2.4% 2.0% 2.3% 2.1% 1.3% 0.9% Same store* 4.8% 3.6% 2.0% 1.9% (0.2)% 2.2% 3.1% 3.2% 2.4% (12.8)% (2.8)% (3.8)% Total by qtr. 6.7% 5.2% 3.0% 3.6% 1.1% 3.7% 5.5% 5.2% 4.7% (10.7)% (1.5)% (2.9)% Total by year 4.6% 3.9% (2.6)% Same-store year* 2.8% 1.8% (4.4)% Same-store year UDS(3) 1.1% 1.3% (3.2)% Murrieta, CA (50 beds) Sioux Falls, SD (40 beds) Coralville, IA (40 beds) Beginning in mid-March 2020, volume growth was impacted by COVID-19. Toledo, OH (40 beds)

Encompass Health 13 * Includes consolidated home health agencies classified as same store during each period Refer to pages 101-104 for end notes. Q1 2018 Q2 2018 Q3 2018 Q4 2018 Q1 2019 Q2 2019 Q3 2019 Q4 2019 Q1 2020 Q2 2020 Q3 2020 Q4 2020 -20.0 -10.0 0.0 10.0 20.0 30.0 New-store/same-store growth Home Health Episodic admissions Q1 2018 Q2 2018 Q3 2018 Q4 2018 Q1 2019 Q2 2019 Q3 2019 Q4 2019 Q1 2020 Q2 2020 Q3 2020 Q4 2020 New store 2.5% 5.3% 5.4% 5.3% 5.7% 2.9% 13.0% 12.3% 11.7% 9.4% 1.3% 1.5% Same store* 7.4% 5.1% 3.8% 5.4% 6.4% 8.3% 9.7% 6.6% 0.2% (17.3)% (4.6)% (3.8)% Total by quarter 9.9% 10.4% 9.2% 10.7% 12.1% 11.2% 22.7% 18.9% 11.9% (7.9)% (3.3)% (2.3)% Total by year 10.0% 16.3% (0.5)% Same-store year* 5.6% 7.7% (6.1)% u In 2018, the Company acquired or opened 23 home health locations. u In 2019, the Company acquired or opened 27 home health locations. u In 2020, the Company acquired or opened two home health locations and consolidated one former equity method location (10). Acquired Camellia Healthcare (14 home health locations in 3 states) in May 2018 Acquired Alacare Home Health & Hospice (23 home health locations in Alabama) in July 2019 Beginning in mid-March 2020, volume growth was impacted by COVID-19.

Encompass Health 14* Includes consolidated hospice agencies classified as same store during each period Q1 2018 Q2 2018 Q3 2018 Q4 2018 Q1 2019 Q2 2019 Q3 2019 Q4 2019 Q1 2020 Q2 2020 Q3 2020 Q4 2020 -10.0 0.0 10.0 20.0 30.0 40.0 50.0 60.0 70.0 New-store/same-store growth Hospice Admissions Q1 2018 Q2 2018 Q3 2018 Q4 2018 Q1 2019 Q2 2019 Q3 2019 Q4 2019 Q1 2020 Q2 2020 Q3 2020 Q4 2020 New store 4.4% 26.1% 40.3% 41.2% 35.5% 15.7% 34.6% 31.1% 30.9% 30.6% 0.5% 0.7% Same store* 36.8% 35.2% 21.1% 8.6% 13.7% 13.6% 5.8% 10.1% (5.3)% 6.7% 15.8% 16.1% Total by quarter 41.2% 61.3% 61.4% 49.8% 49.2% 29.3% 40.4% 41.2% 25.6% 37.3% 16.3% 16.8% Total by year 53.5% 39.8% 23.2% Same-store year* 24.6% 12.2% 8.1% u In 2018, the Company acquired or opened 22 hospice locations. u In 2019, the Company acquired or opened 25 hospice locations. u In 2020, the Company opened one hospice location. Acquired Camellia Healthcare (18 hospice locations in 3 states) in May 2018 Acquired Alacare Home Health & Hospice (23 hospice locations in Alabama) in July 2019
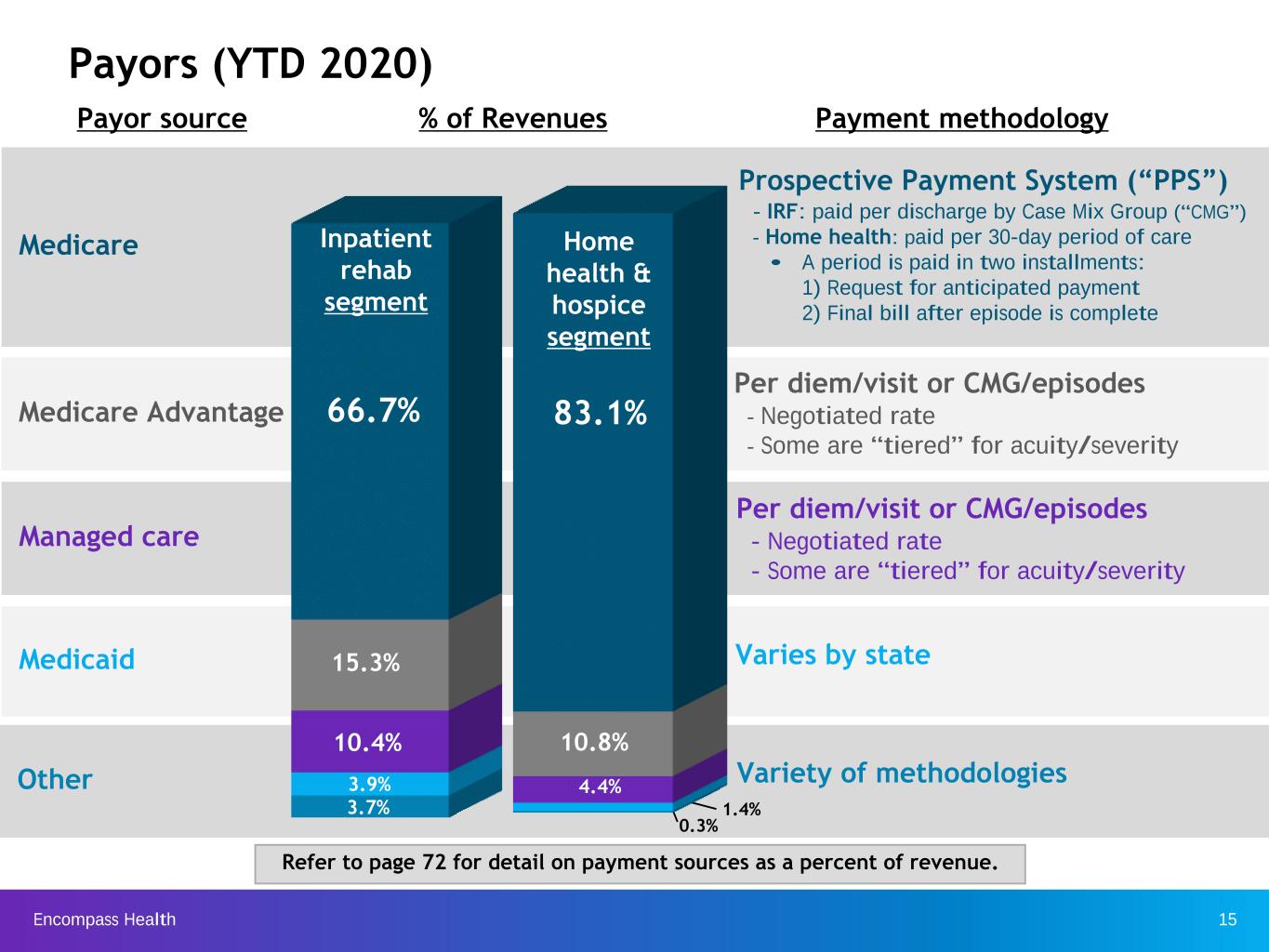
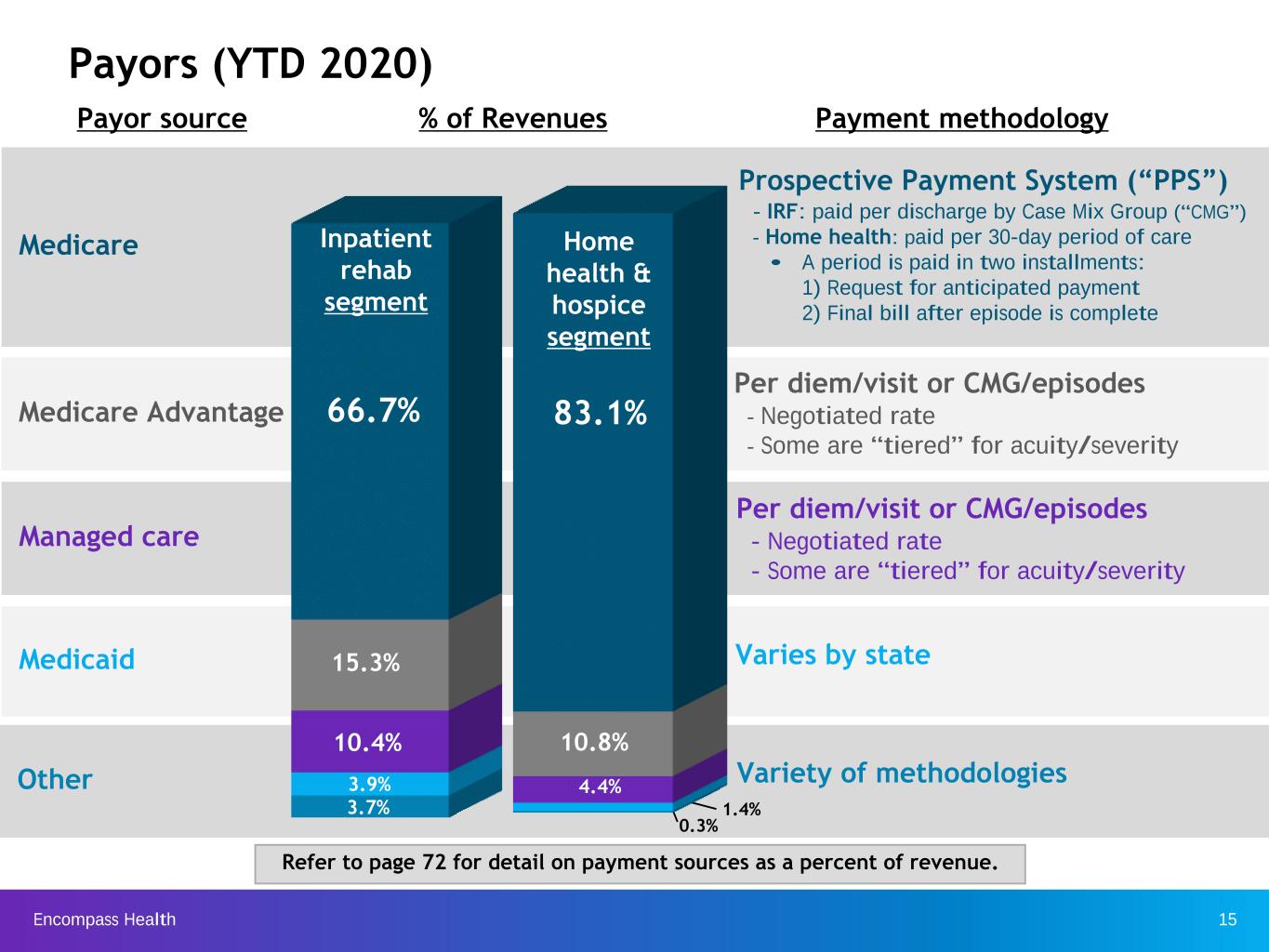
Encompass Health 15 Medicare Advantage Managed care Medicare Medicaid Other Per diem/visit or CMG/episodes - Negotiated rate - Some are “tiered” for acuity/severity Per diem/visit or CMG/episodes - Negotiated rate - Some are “tiered” for acuity/severity Varies by state Prospective Payment System (“PPS”) - IRF: paid per discharge by Case Mix Group (“CMG”) - Home health: paid per 30-day period of care • A period is paid in two installments: 1) Request for anticipated payment 2) Final bill after episode is complete Payors (YTD 2020) Payor source Payment methodology% of Revenues Variety of methodologies Refer to page 72 for detail on payment sources as a percent of revenue. 66.7% 15.3% 10.4% 3.9% 3.7% Inpatient rehab segment Home health & hospice segment 83.1% 10.8% 4.4% 1.4% 0.3%
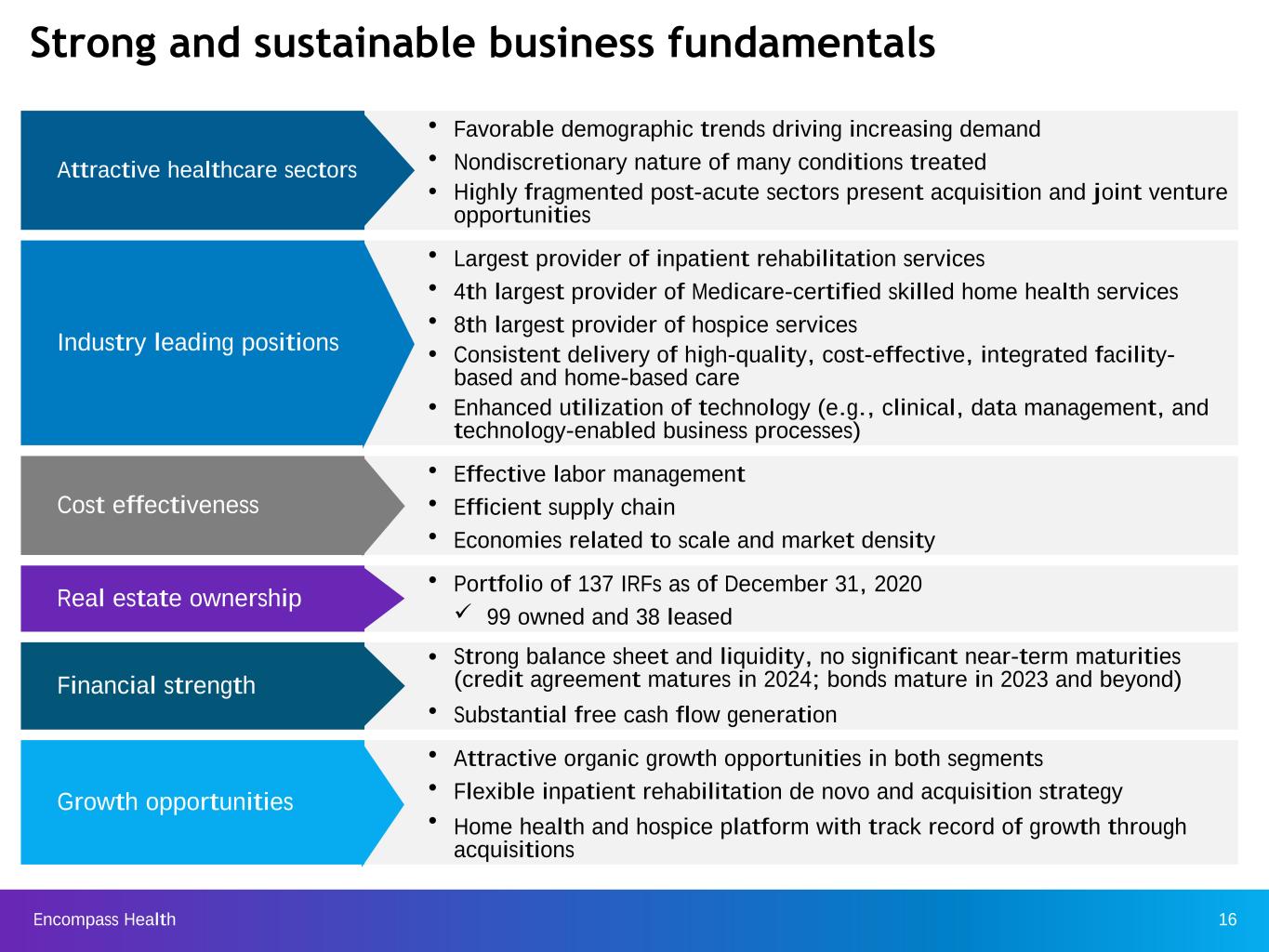
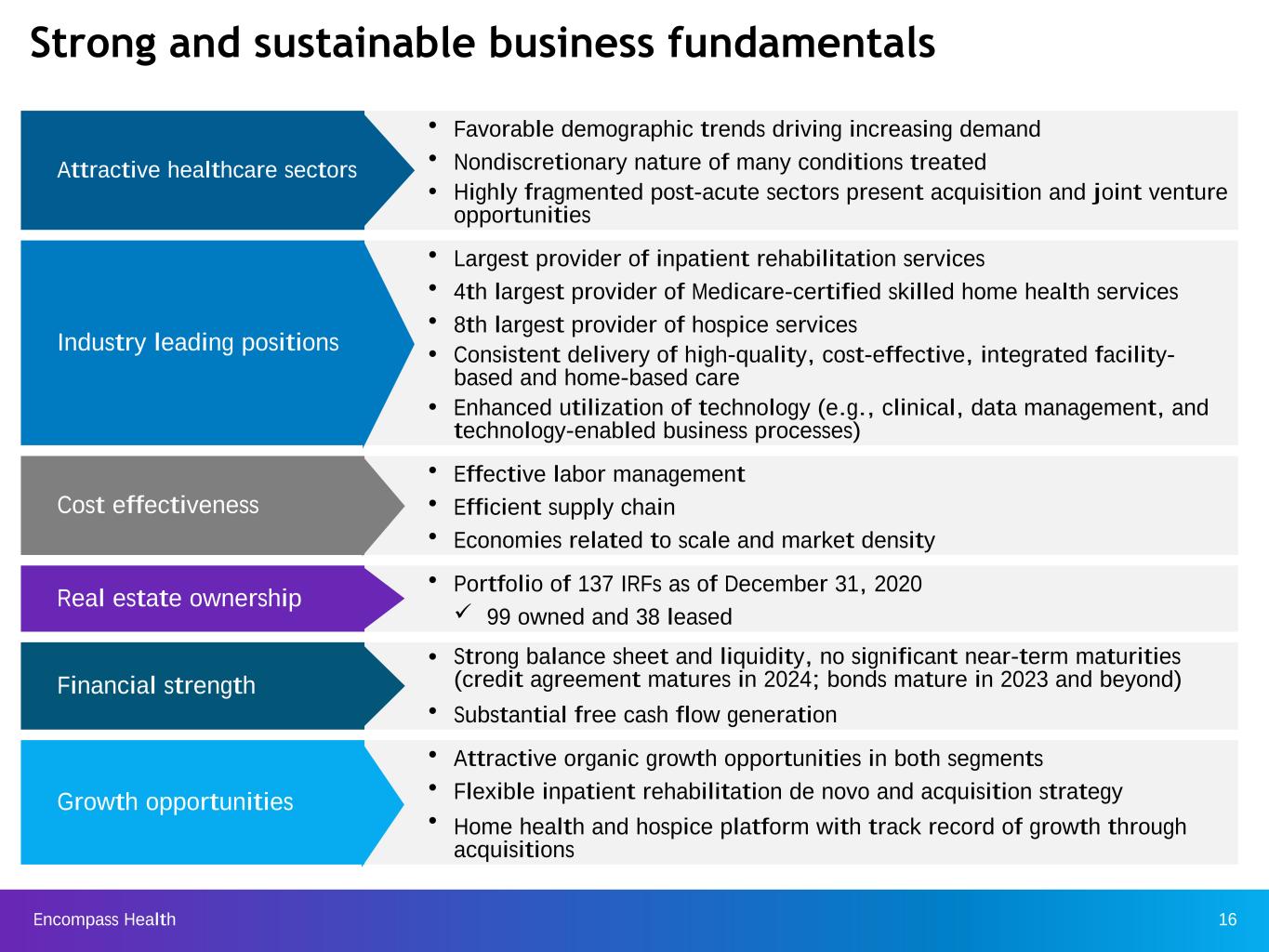
Encompass Health 16 Strong and sustainable business fundamentals Attractive healthcare sectors Ÿ Favorable demographic trends driving increasing demand Ÿ Nondiscretionary nature of many conditions treated Ÿ Highly fragmented post-acute sectors present acquisition and joint venture opportunities Industry leading positions Ÿ Largest provider of inpatient rehabilitation services Ÿ 4th largest provider of Medicare-certified skilled home health services Ÿ 8th largest provider of hospice services Ÿ Consistent delivery of high-quality, cost-effective, integrated facility- based and home-based care Ÿ Enhanced utilization of technology (e.g., clinical, data management, and technology-enabled business processes) Cost effectiveness Ÿ Effective labor management Ÿ Efficient supply chain Ÿ Economies related to scale and market density Real estate ownership Ÿ Portfolio of 137 IRFs as of December 31, 2020 ü 99 owned and 38 leased Financial strength Ÿ Strong balance sheet and liquidity, no significant near-term maturities (credit agreement matures in 2024; bonds mature in 2023 and beyond) Ÿ Substantial free cash flow generation Growth opportunities Ÿ Attractive organic growth opportunities in both segments Ÿ Flexible inpatient rehabilitation de novo and acquisition strategy Ÿ Home health and hospice platform with track record of growth through acquisitions

Encompass Health 17 Highlights from 2020

Encompass Health 18 We responded to the rapidly changing environment due to COVID-19 We remain confident in the long-term prospects of both of our business segments based on the increasing demands for the services we provide to an aging population. We believe COVID has reinforced the preferred post-acute settings of IRF and home health over SNF among referring hospitals, physicians, families, and patients Formed a multi-disciplinary task force for each segment Ÿ Developed a vaccine work group to prepare for the rollout of the vaccine Enhanced our operational and financial flexibility Ÿ Managed labor costs in response to lower patient volumes via furloughs, changes to compensation structures, and workforce reductions Ÿ Amended senior credit facility to provide additional covenant flexibility Ÿ Maintained strong liquidity with a $1 billion revolver and cash on hand Ÿ Opportunistically issued $1 billion in senior notes with maturity of 2028 and beyond COVID patients treated INPATIENT REHABILITATION HOME HEALTH & HOSPICE Over 8,000 Over 9,000 Returned all funds received under the CARES Act Focused on the safety and well-being of our patients and employees Ÿ Screened all employees daily Ÿ Limited visitors in our hospitals and reduced occupancy in our home offices Ÿ Conducted pre-visit telephone calls to assess risk factors within a home prior to home health and hospice visits Ÿ Suspended hospital-based outpatient services Ÿ Halted non-essential travel Ÿ Invested in PPE — Secured secondary domestic sources — Ensured adequate levels of inventory on hand and storage space at vendor’s warehouse — Developed a Beacon application to track PPE usage Ÿ Initiated a program for eligible frontline employees to earn additional paid-time-off in recognition of their outstanding efforts responding to COVID-19; this investment approximated $43 million
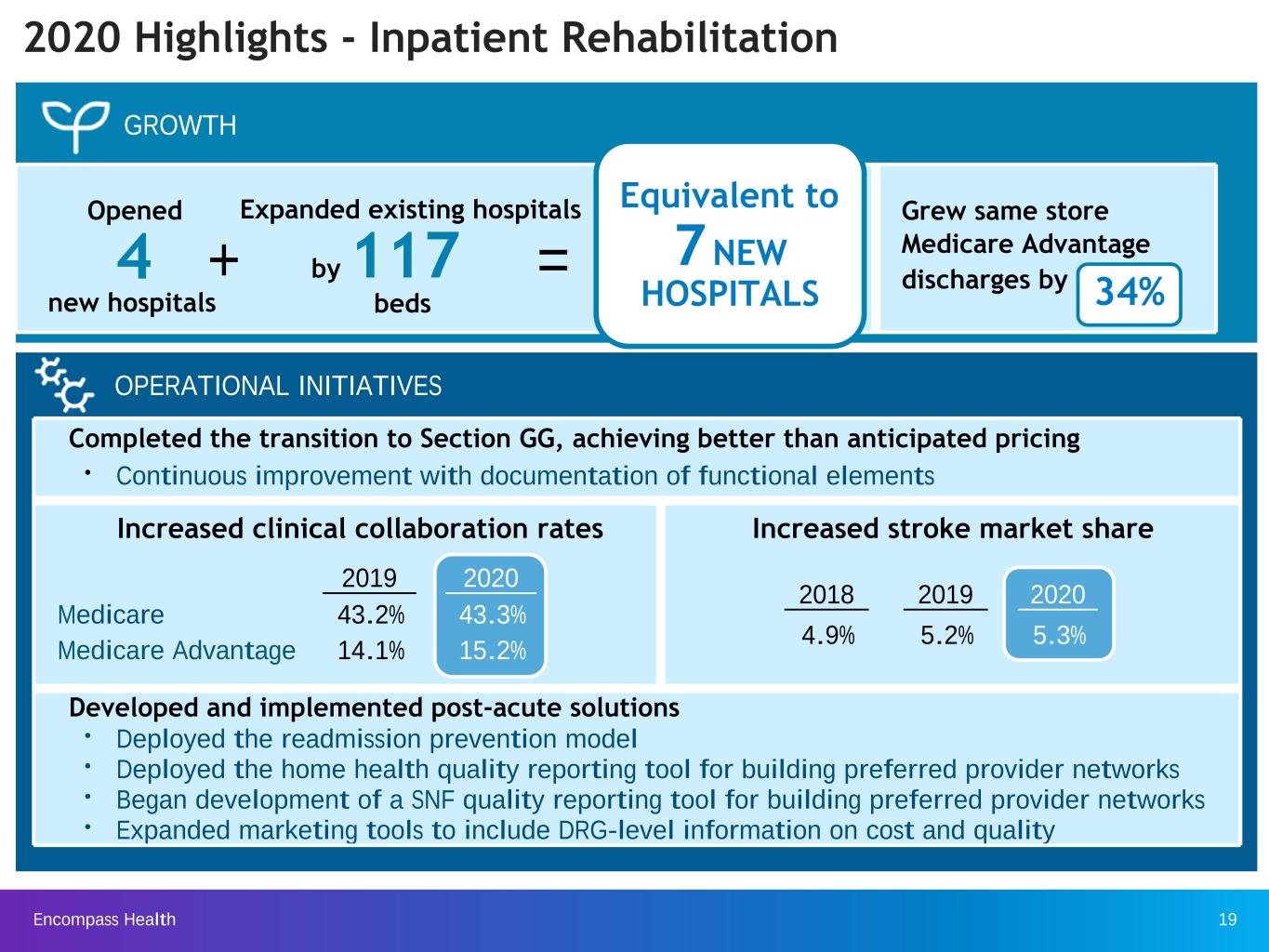
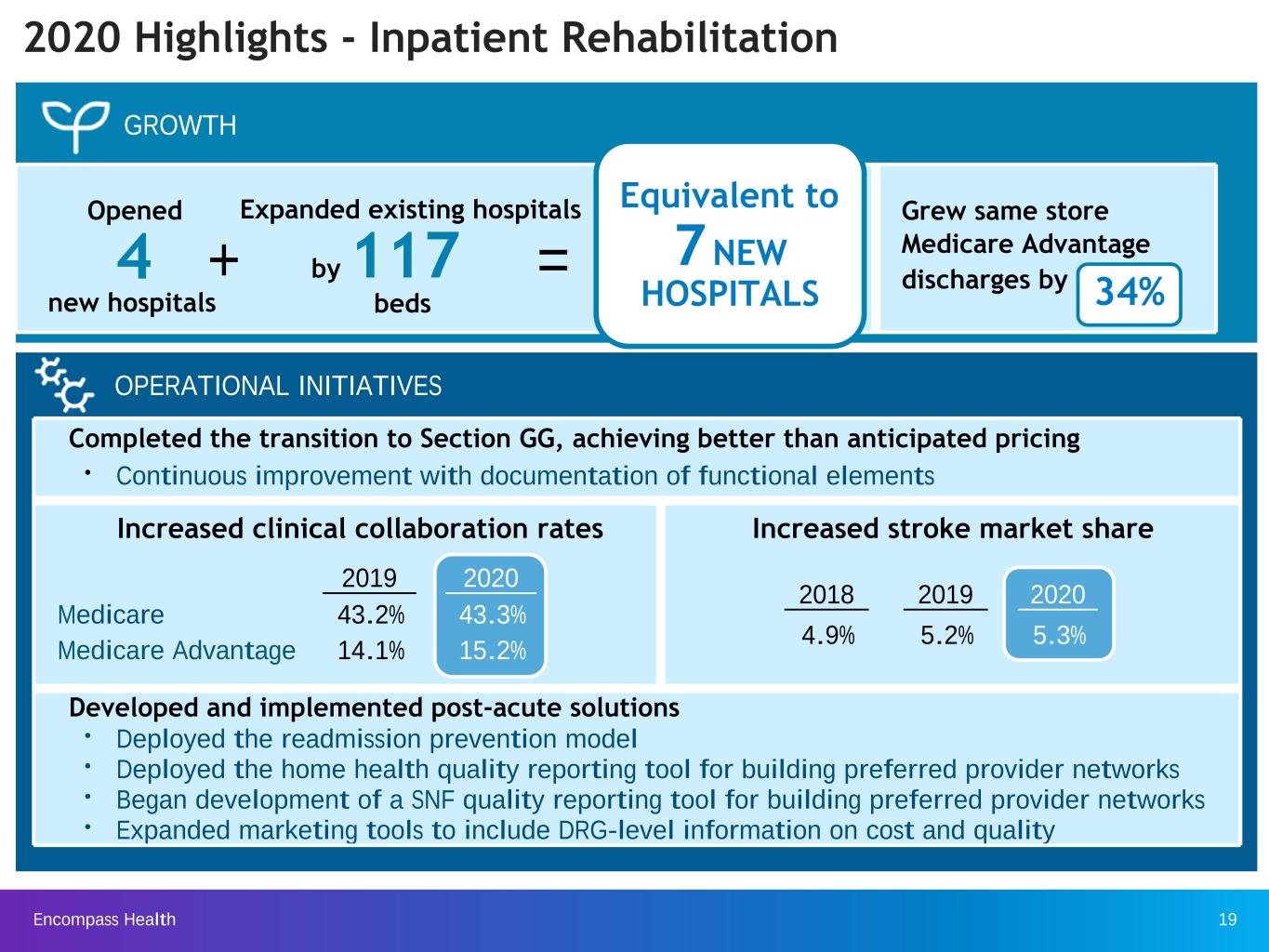
Encompass Health 19 2020 Highlights - Inpatient Rehabilitation Completed the transition to Section GG, achieving better than anticipated pricing Ÿ Continuous improvement with documentation of functional elements Increased clinical collaboration rates Increased stroke market share Developed and implemented post-acute solutions Ÿ Deployed the readmission prevention model Ÿ Deployed the home health quality reporting tool for building preferred provider networks Ÿ Began development of a SNF quality reporting tool for building preferred provider networks Ÿ Expanded marketing tools to include DRG-level information on cost and quality OPERATIONAL INITIATIVES Equivalent to Grew same store Medicare Advantage discharges by 34% GROWTH Opened 4 + = Expanded existing hospitals by 117 new hospitals beds 7 NEW HOSPITALS 2019 2020 Medicare 43.2% 43.3% Medicare Advantage 14.1% 15.2% 2018 2019 2020 4.9% 5.2% 5.3%
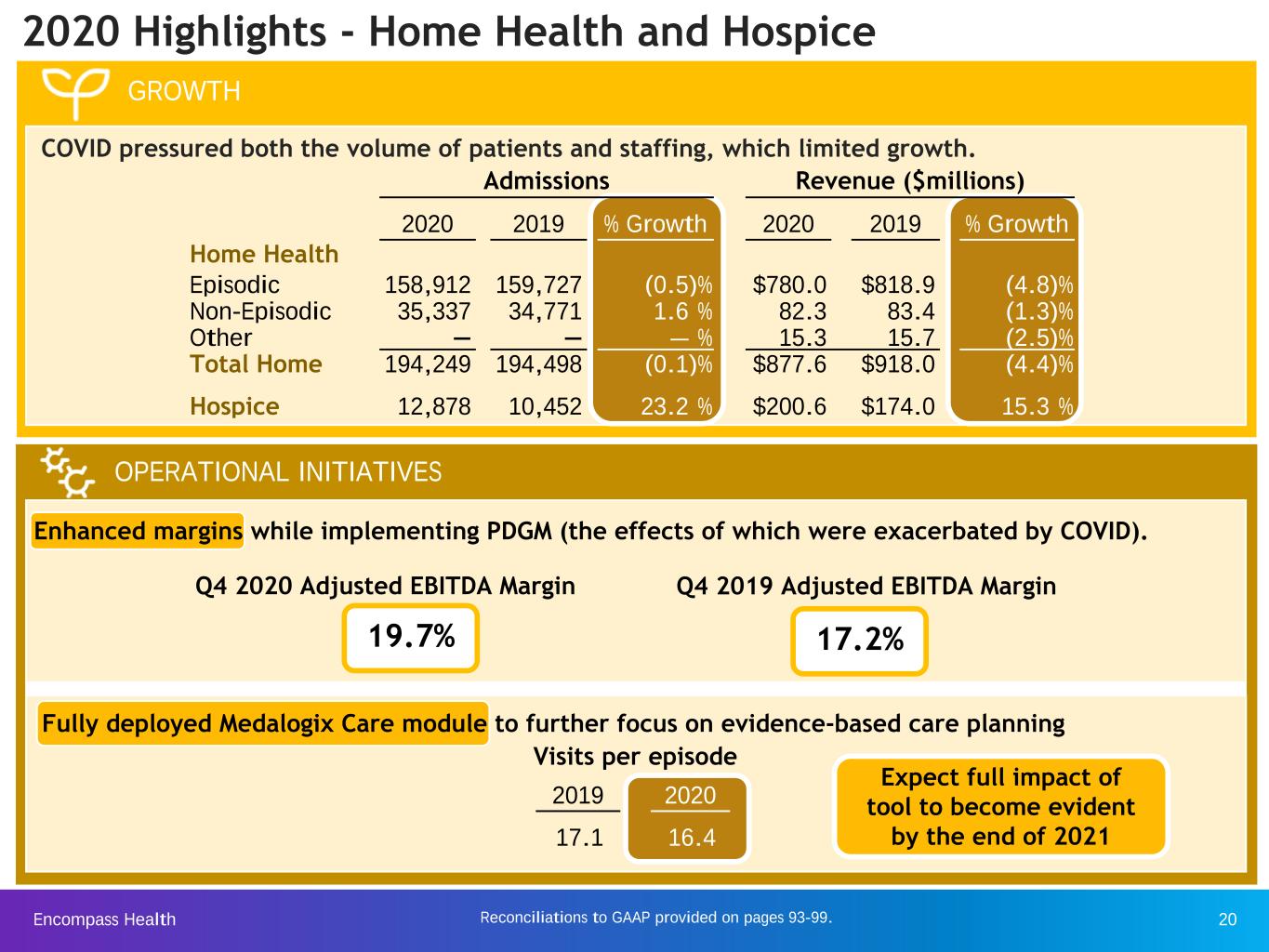
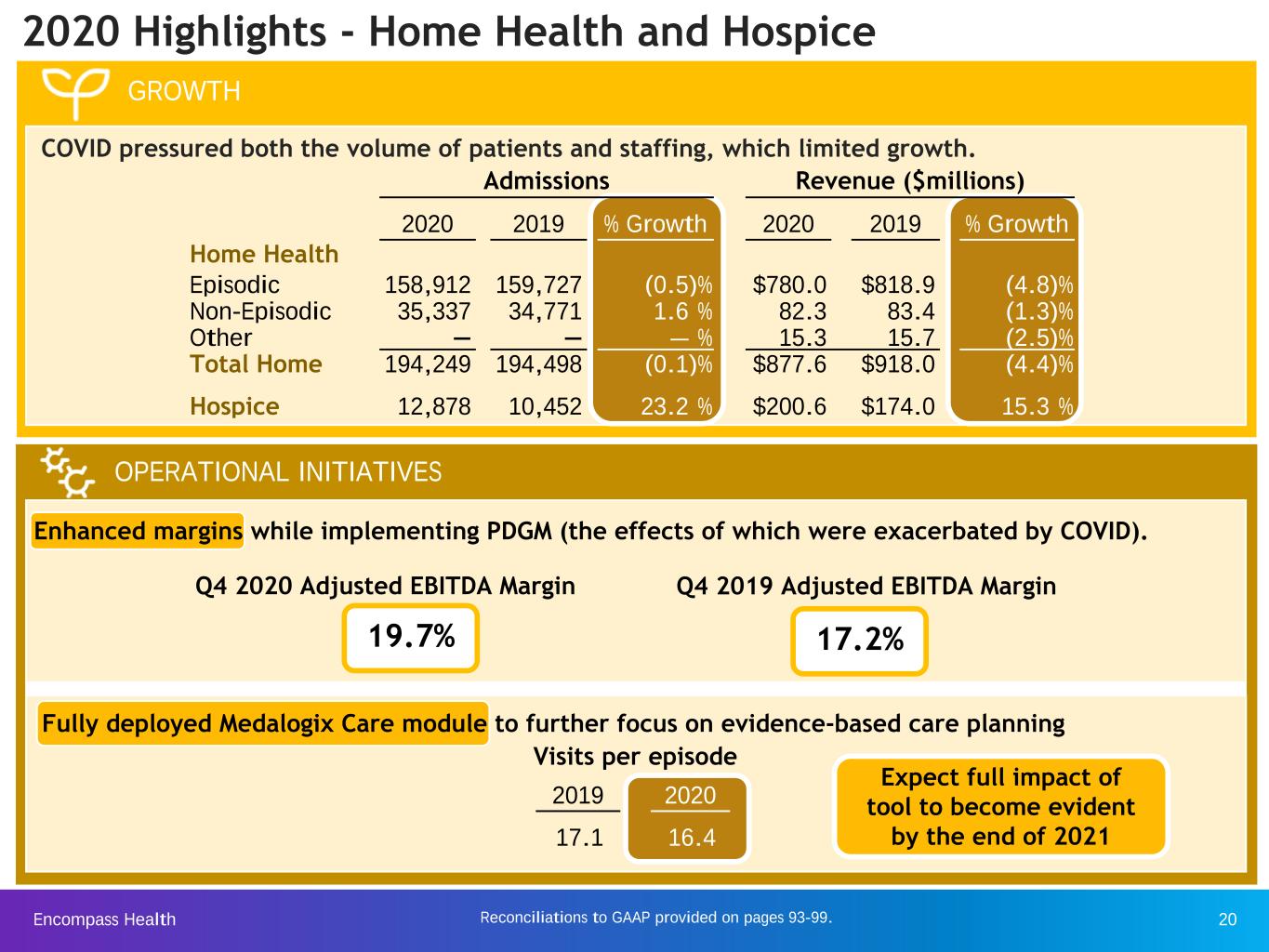
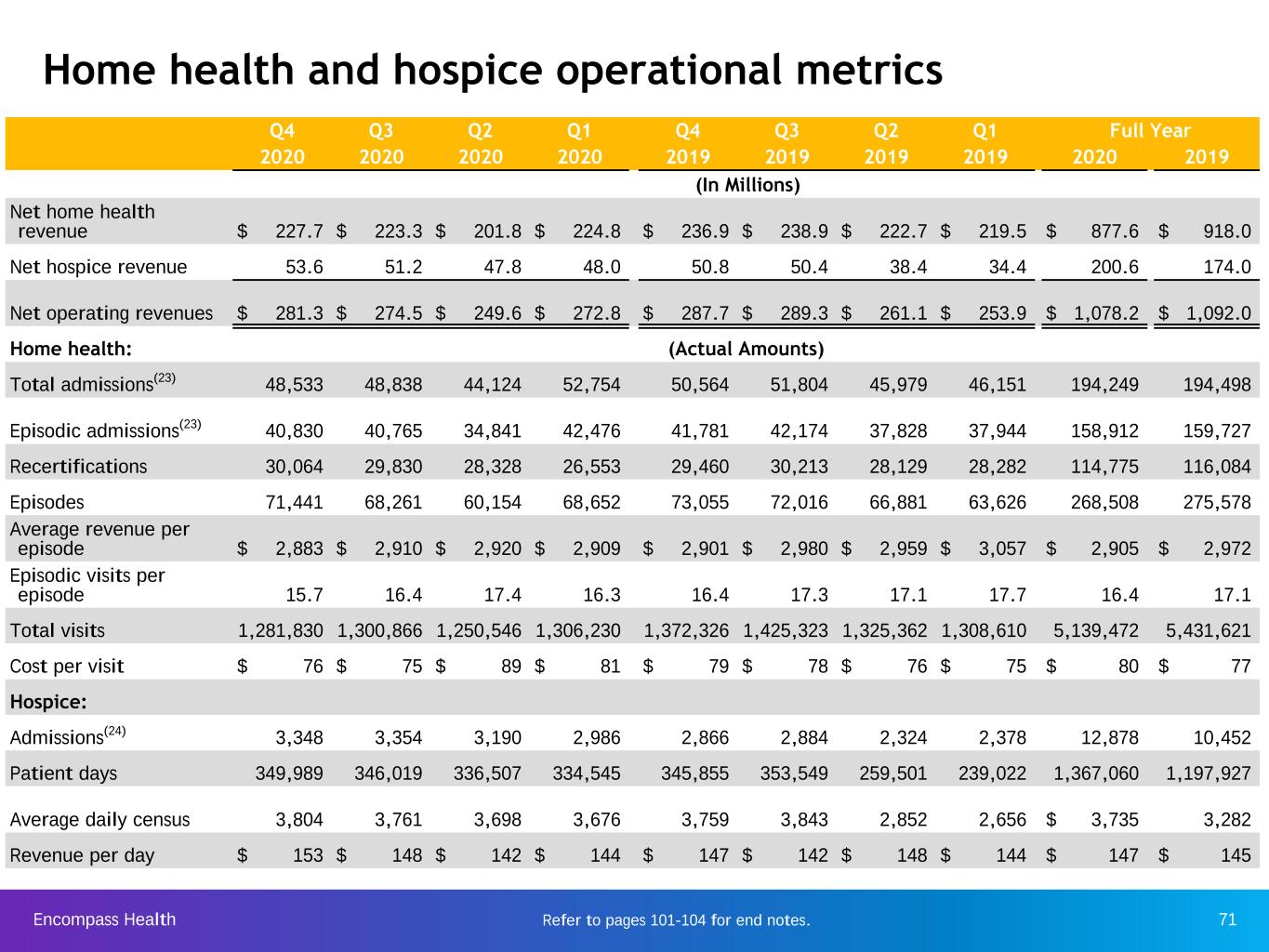
Encompass Health 20 2020 Highlights - Home Health and Hospice GROWTH COVID pressured both the volume of patients and staffing, which limited growth. OPERATIONAL INITIATIVES Q4 2020 Adjusted EBITDA Margin Q4 2019 Adjusted EBITDA Margin Expect full impact of tool to become evident by the end of 2021 19.7% Visits per episode Fully deployed Medalogix Care module to further focus on evidence-based care planning Enhanced margins while implementing PDGM (the effects of which were exacerbated by COVID). 2019 2020 17.1 16.4 Admissions Revenue ($millions) Home Health 2020 2019 % Growth 2020 2019 % Growth Episodic 158,912 159,727 (0.5) % $780.0 $818.9 (4.8) % Non-Episodic 35,337 34,771 1.6 % 82.3 83.4 (1.3) % Other — — — % 15.3 15.7 (2.5) % Total Home 194,249 194,498 (0.1) % $877.6 $918.0 (4.4) % Hospice 12,878 10,452 23.2 % $200.6 $174.0 15.3 % 17.2% Reconciliations to GAAP provided on pages 93-99.
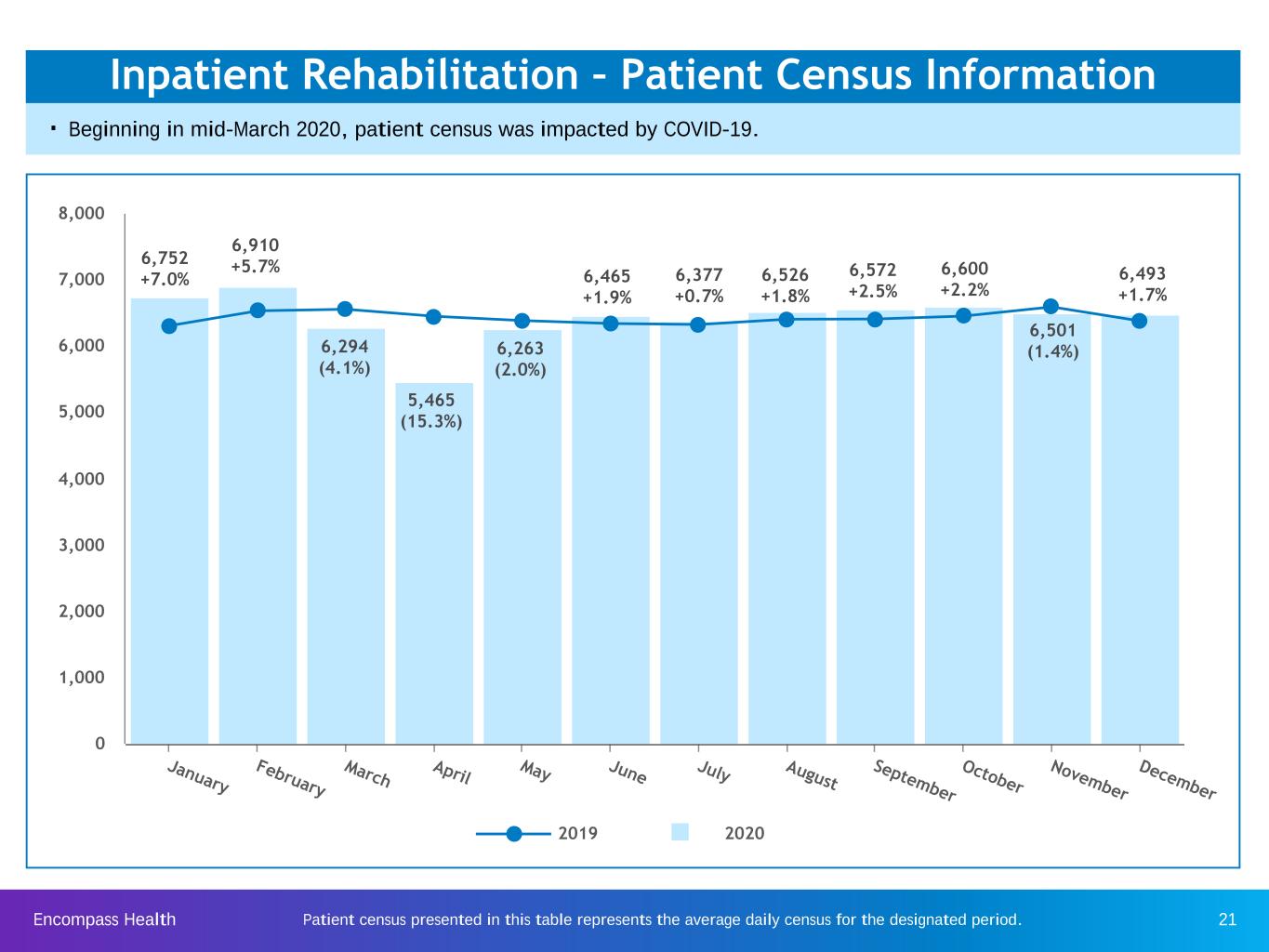
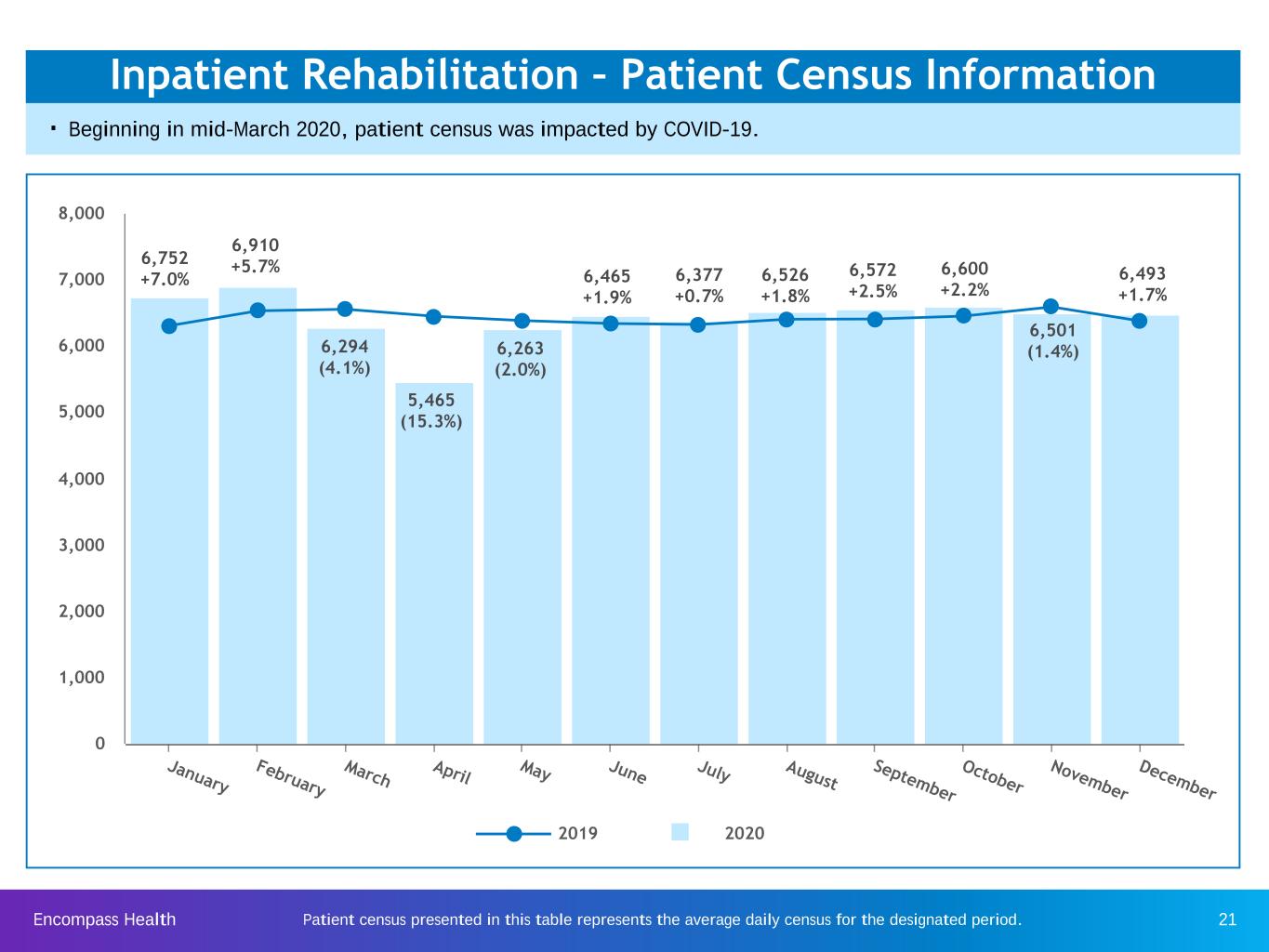
Encompass Health 21 Inpatient Rehabilitation – Patient Census Information . Beginning in mid-March 2020, patient census was impacted by COVID-19. Patient census presented in this table represents the average daily census for the designated period. 2019 2020 January February March April May June July August September October November December 0 1,000 2,000 3,000 4,000 5,000 6,000 7,000 8,000 6,752 +7.0% 6,910 +5.7% 6,294 (4.1%) 5,465 (15.3%) 6,263 (2.0%) 6,465 +1.9% 6,377 +0.7% 6,526 +1.8% 6,572 +2.5% 6,600 +2.2% 6,501 (1.4%) 6,493 +1.7%

Encompass Health 22 Home Health - Starts of Episodes (Includes Starts of Care and Recertifications) . Beginning in mid-March 2020, starts of episodes were impacted by COVID-19. . The acquisition of Alacare anniversaried on July 1, 2020. . Sequential decreases in a month were primarily related to COVID surges and corresponding limitations on elective procedures in certain states. ü Florida and Texas represent approximately 40% of our home health revenue. 2019 2020 January February March April May June July August September October November December 0 3,000 6,000 9,000 12,000 15,000 18,000 21,000 24,000 27,000 24,471 +8.5% 22,445 +8.5% 22,113 (3.8%) 22,223 (0.8%) 22,630 +5.6% 23,654 (2.2%) 23,466 (6.5%) 23,475 +1.6% 24,708 (1.3%) 22,884 (2.3%) 23,302 +2.2% 18,316 (17.2%)
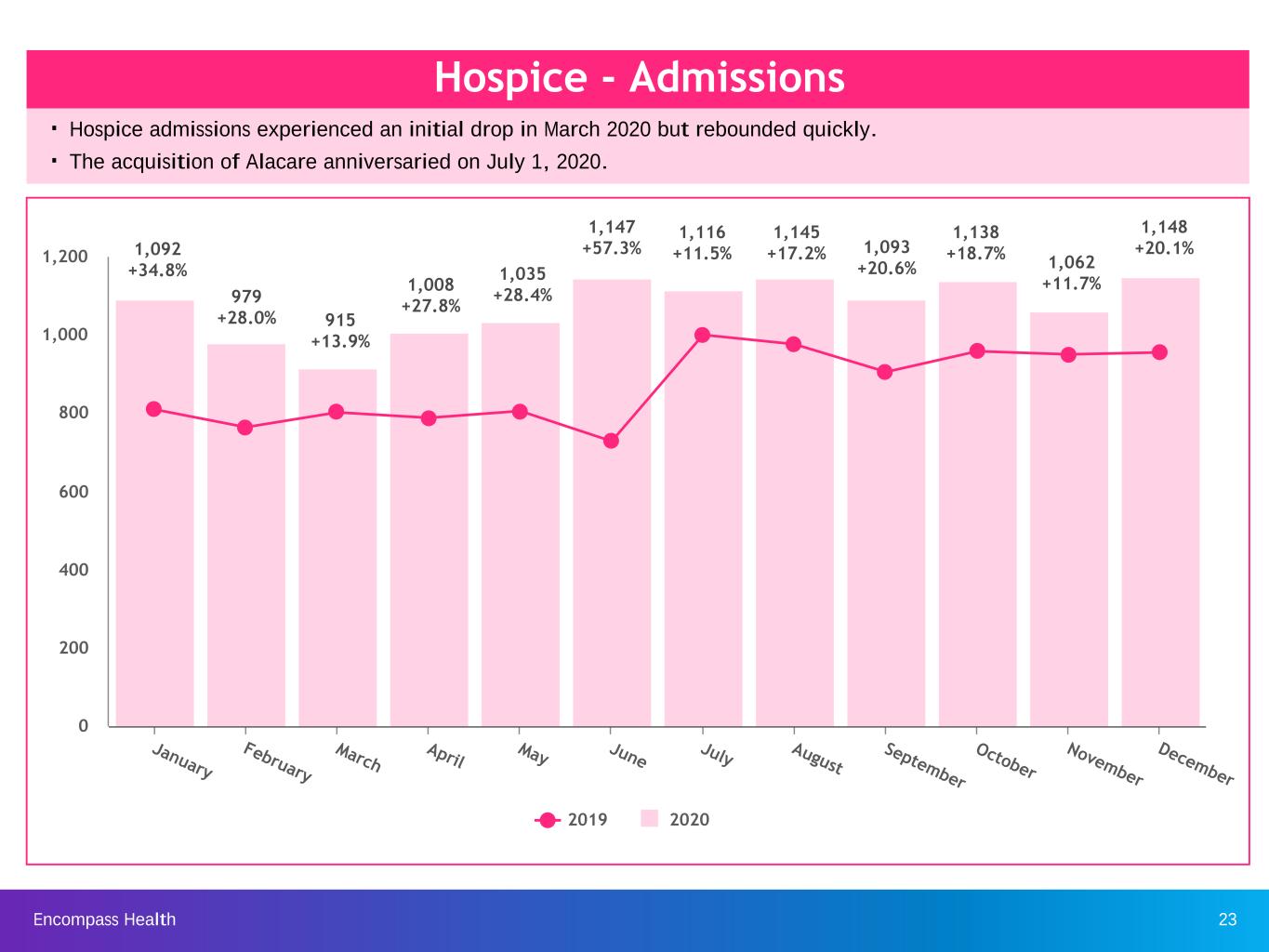
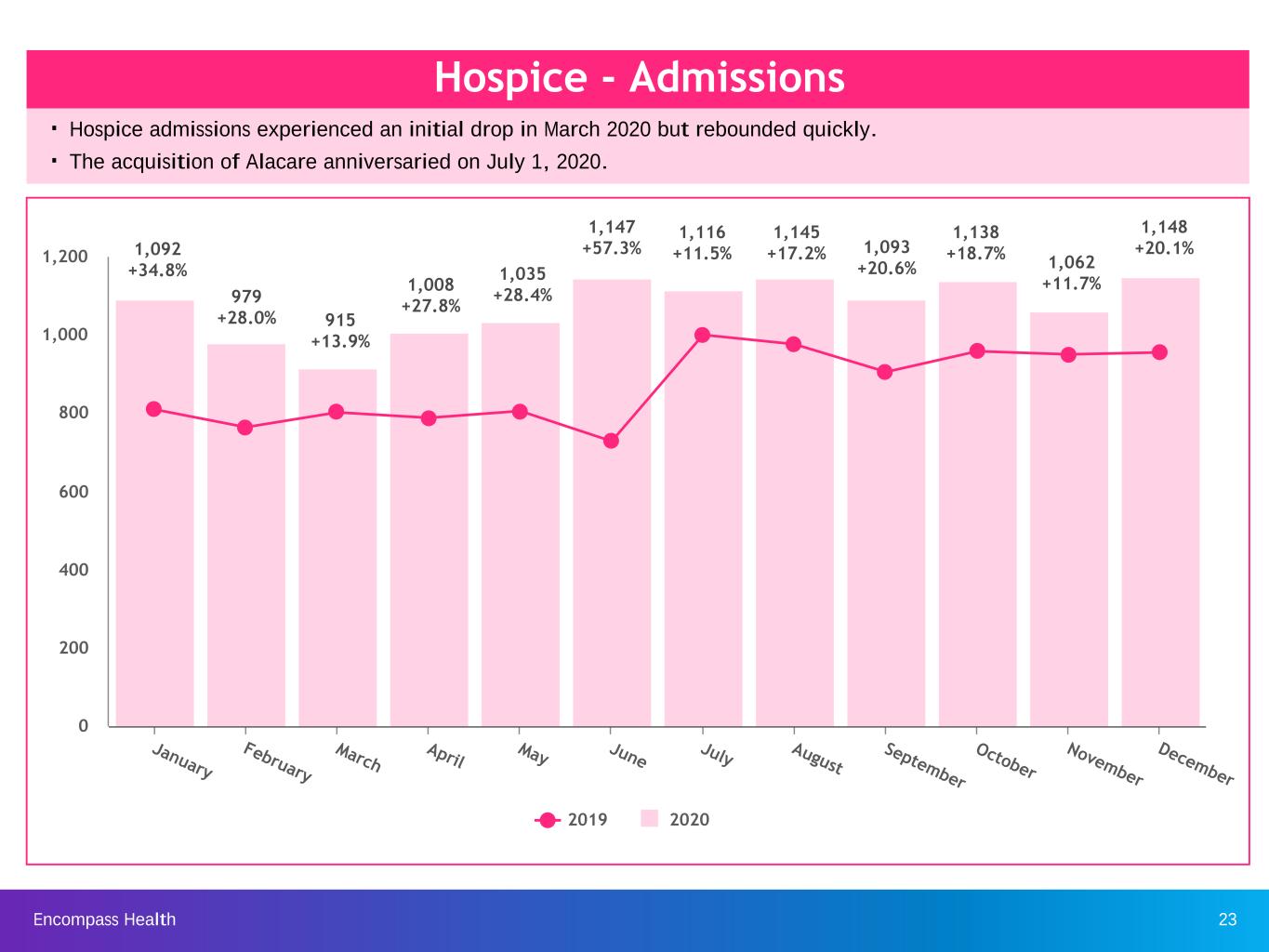
Encompass Health 23 Hospice - Admissions . Hospice admissions experienced an initial drop in March 2020 but rebounded quickly. . The acquisition of Alacare anniversaried on July 1, 2020. 2019 2020 January February March April May June July August September October November December 0 200 400 600 800 1,000 1,200 979 +28.0% 1,092 +34.8% 915 +13.9% 1,008 +27.8% 1,035 +28.4% 1,147 +57.3% 1,116 +11.5% 1,145 +17.2% 1,093 +20.6% 1,138 +18.7% 1,062 +11.7% 1,148 +20.1%
Encompass Health 24 Business outlook, including guidance (as of March 9, 2021)
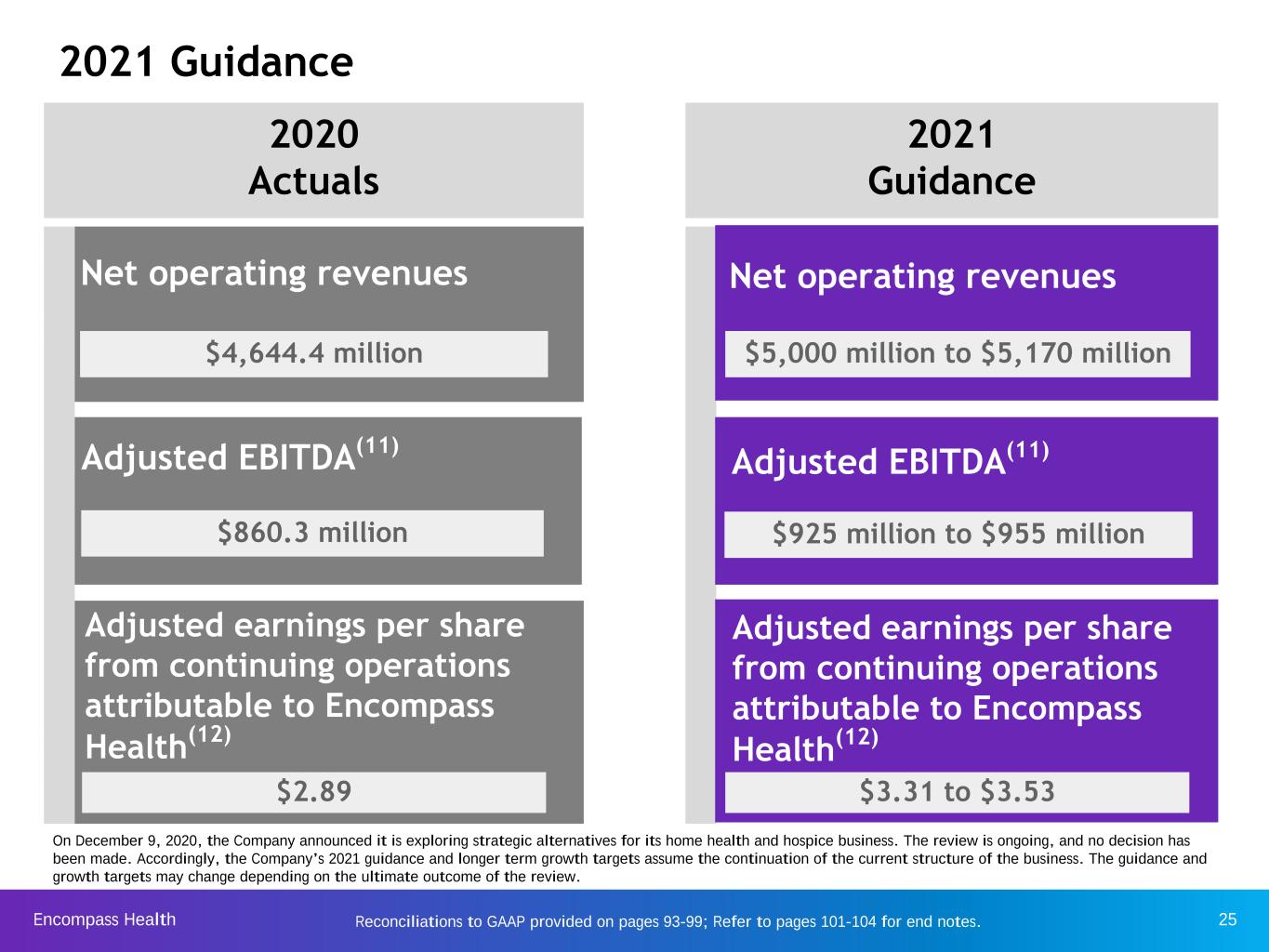
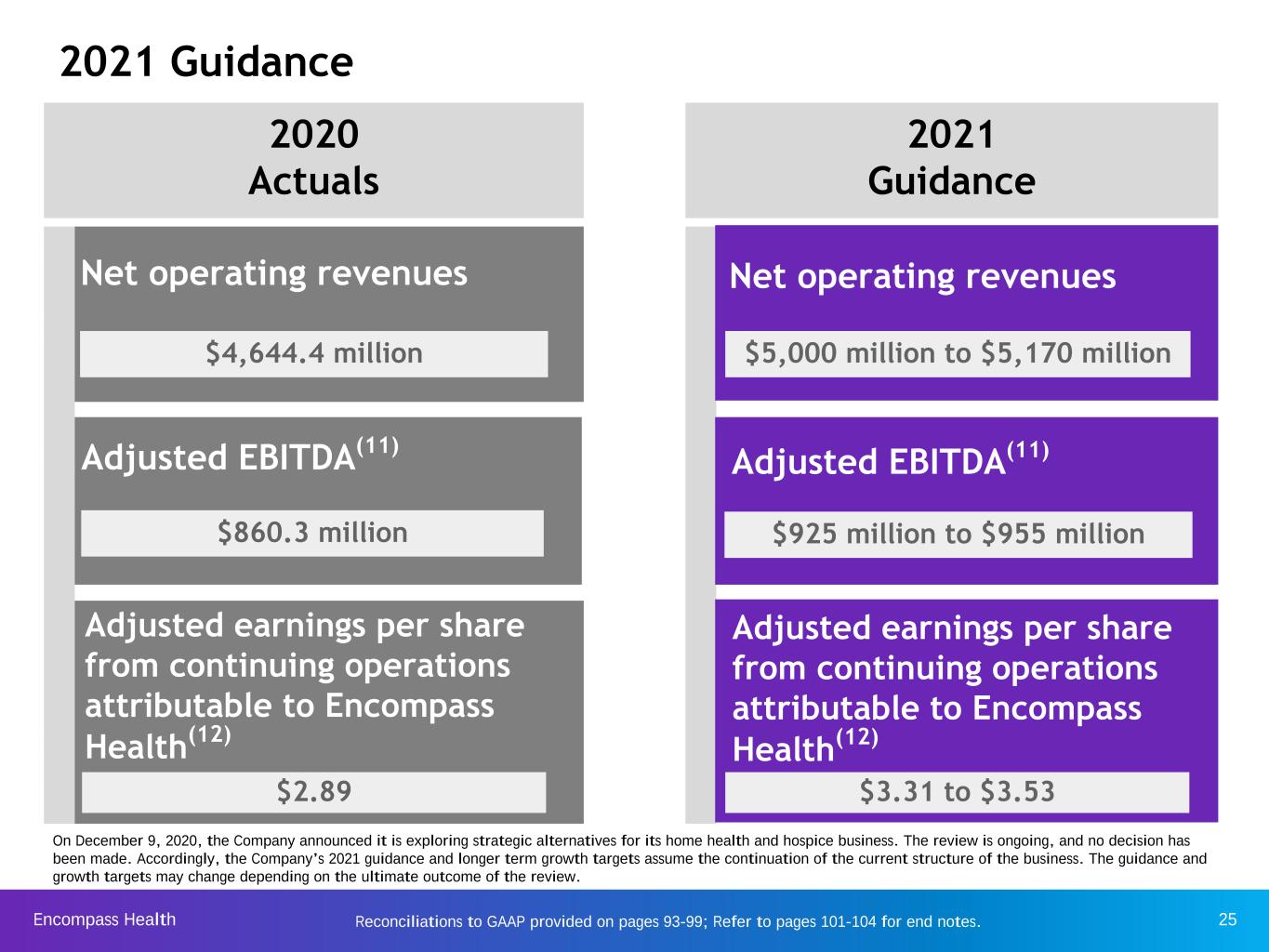
Encompass Health 25Reconciliations to GAAP provided on pages 93-99; Refer to pages 101-104 for end notes. 2021 Guidance Adjusted EBITDA(11) Adjusted earnings per share from continuing operations attributable to Encompass Health(12) Net operating revenues 2020 Actuals 2021 Guidance Net operating revenues Adjusted EBITDA(11) $925 million to $955 million Adjusted earnings per share from continuing operations attributable to Encompass Health(12) $3.31 to $3.53 $4,644.4 million $860.3 million $2.89 $5,000 million to $5,170 million On December 9, 2020, the Company announced it is exploring strategic alternatives for its home health and hospice business. The review is ongoing, and no decision has been made. Accordingly, the Company’s 2021 guidance and longer term growth targets assume the continuation of the current structure of the business. The guidance and growth targets may change depending on the ultimate outcome of the review.

Encompass Health 26 2021 Guidance considerations Inpatient Rehabilitation u Estimated 2.3% increase in Medicare pricing u Revenue reserve related to bad debt of 1.4% to 1.6% of net operating revenues u Pre-opening and new store ramp up costs of $15 million to $20 million Home Health and Hospice u Estimated 1.9% increase in Medicare pricing for home health; estimated 2.4% pricing increase for hospice u Inclusive of $50 million to $100 million of home health and hospice acquisitions Both Segments u Salary increase of approx. 3%; benefits increase of approx. 5% to 8% u Suspension of sequestration through March 31, 2021 u Continued higher utilization and costs of personal protective equipment

Encompass Health 27 2020-2025 Growth Targets 2020 through 2025 INPATIENT REHABILITATION HOME HEALTH AND HOSPICE CONSOLIDATED CAGR TARGETS Not inclusive of larger scale acquisitions 6 to 10 De Novos per year 100 to 150 bed additions per year 6% to 8% Discharge CAGR 10%+ Home Health admissions CAGR 10% to 15% Hospice admissions CAGR $50 million to $100 million Acquisitions per year 8% to 10% Consolidated net operating revenues 8% to 10% Consolidated adjusted EBITDA 5% to 7% Adjusted free cash flow* On December 9, 2020, the Company announced it is exploring strategic alternatives for its home health and hospice business. The review is ongoing, and no decision has been made. Accordingly, the Company’s 2021 guidance and longer term growth targets assume the continuation of the current structure of the business. The guidance and growth targets may change depending on the ultimate outcome of the review. * Base year 2020 adjusted free cash flow benefited from a temporary payroll tax holiday. Exclusive of this item, the adjusted free cash flow CAGR target would be 8% to 10%. Reconciliations to GAAP provided on pages 93-99
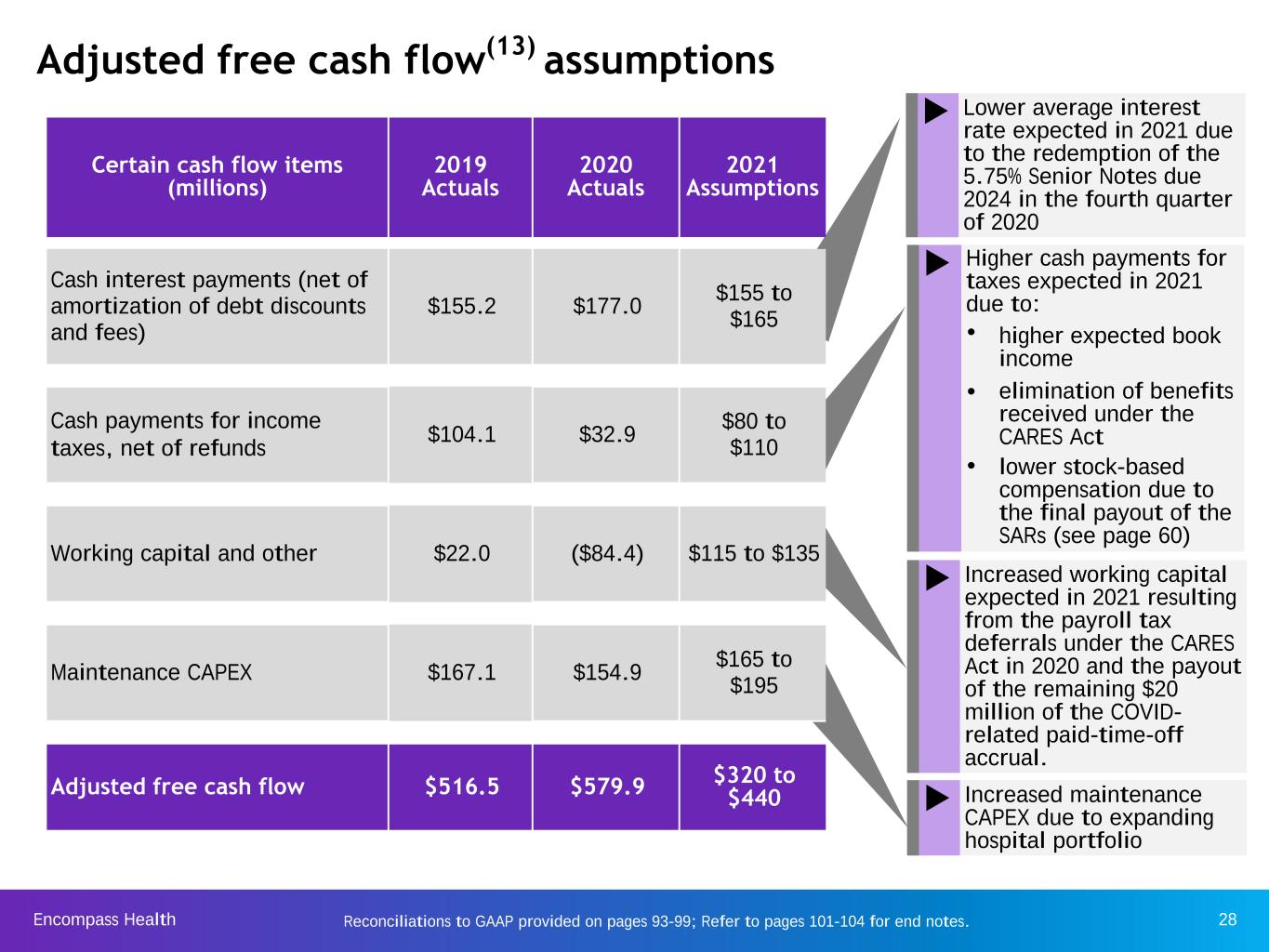
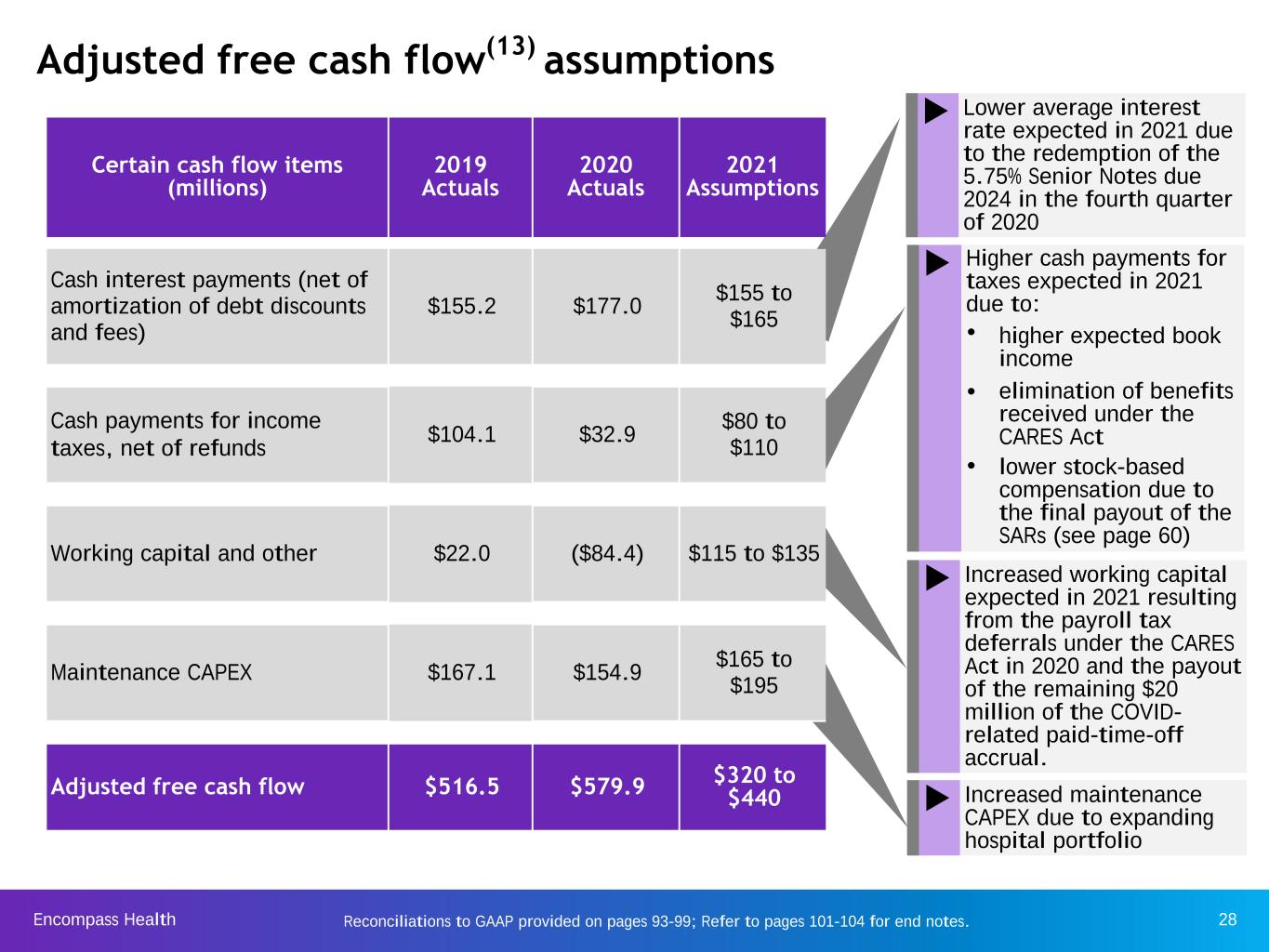
Encompass Health 28Reconciliations to GAAP provided on pages 93-99; Refer to pages 101-104 for end notes. Adjusted free cash flow(13) assumptions Certain cash flow items (millions) 2019 Actuals 2020 Actuals 2021 Assumptions Cash interest payments (net of amortization of debt discounts and fees) $155.2 $177.0 $155 to $165 Cash payments for income taxes, net of refunds $104.1 $32.9 $80 to $110 Working capital and other $22.0 ($84.4) $115 to $135 Maintenance CAPEX $167.1 $154.9 $165 to $195 Adjusted free cash flow $516.5 $579.9 $320 to $440 u Lower average interest rate expected in 2021 due to the redemption of the 5.75% Senior Notes due 2024 in the fourth quarter of 2020 u Higher cash payments for taxes expected in 2021 due to: Ÿ higher expected book income Ÿ elimination of benefits received under the CARES Act Ÿ lower stock-based compensation due to the final payout of the SARs (see page 60) u Increased working capital expected in 2021 resulting from the payroll tax deferrals under the CARES Act in 2020 and the payout of the remaining $20 million of the COVID- related paid-time-off accrual. u Increased maintenance CAPEX due to expanding hospital portfolio
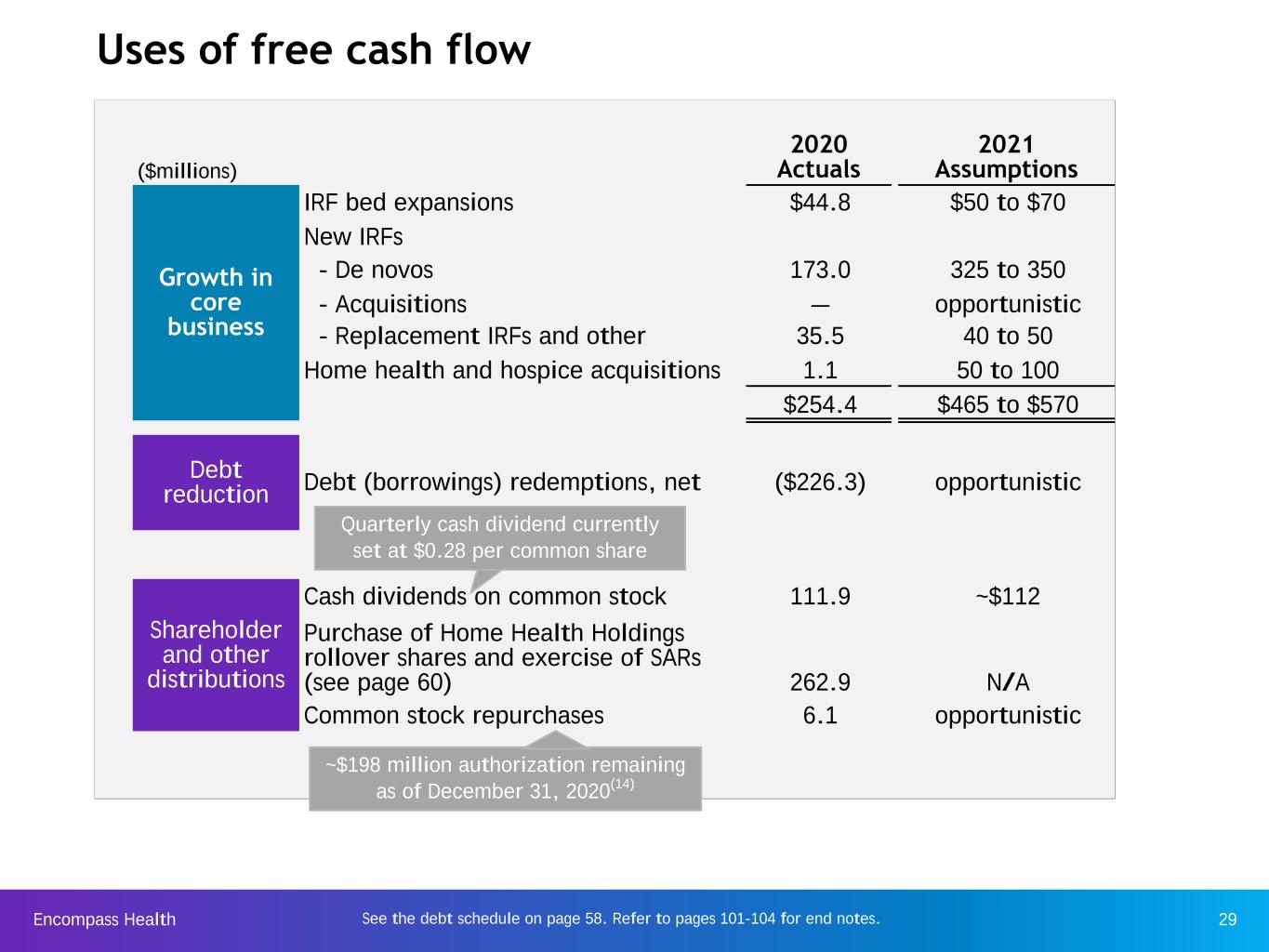
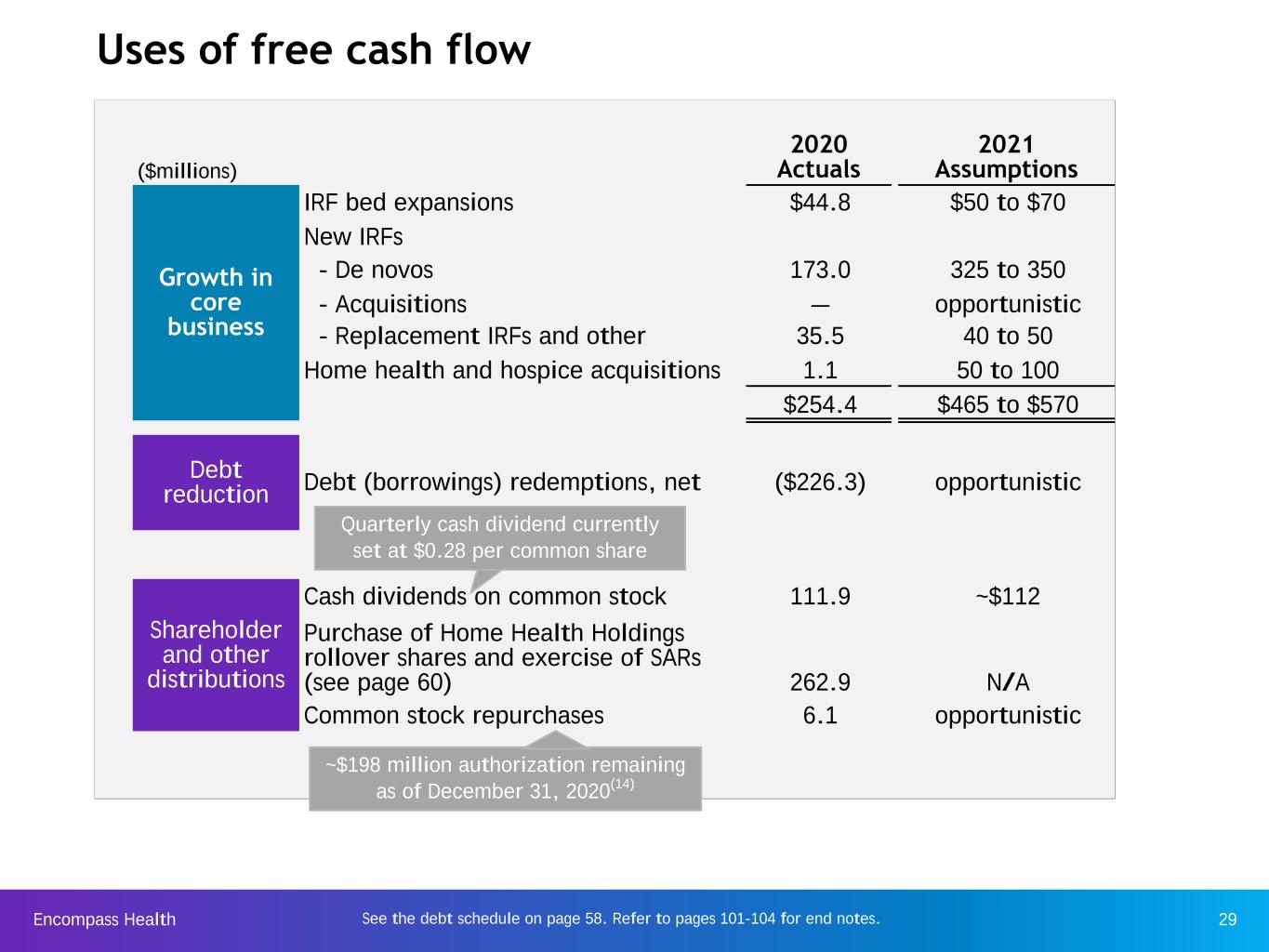
Encompass Health 29See the debt schedule on page 58. Refer to pages 101-104 for end notes. Uses of free cash flow ($millions) 2020 Actuals 2021 Assumptions Growth in core business IRF bed expansions $44.8 $50 to $70 New IRFs - De novos 173.0 325 to 350 - Acquisitions — opportunistic - Replacement IRFs and other 35.5 40 to 50 Home health and hospice acquisitions 1.1 50 to 100 $254.4 $465 to $570 Debt reduction Debt (borrowings) redemptions, net ($226.3) opportunistic Shareholder and other distributions Cash dividends on common stock 111.9 ~$112 Purchase of Home Health Holdings rollover shares and exercise of SARs (see page 60) 262.9 N/A Common stock repurchases 6.1 opportunistic ~$198 million authorization remaining as of December 31, 2020(14) Quarterly cash dividend currently set at $0.28 per common share

Encompass Health 30 IRF-PPS fiscal year 2021 final rule: key provisions Company observations Source: https://www.cms.gov/medicaremedicare-fee-service-paymentinpatientrehabfacppsirf-rules-and-related-files/cms-1729-f Update to payment rates The final rule: • implemented a net 2.4% market basket increase; • updated case mix group relative weights and average length of stay values; • decreased the outlier fixed loss threshold; and • revised the wage index and labor-related share values. ◦ CMS will apply a one year 5% cap on any FY 2021 decrease in a geographic area’s wage index value from the wage index value from the prior FY. Other provisions Pricing: • Net pricing impact to the Company expected to be approx. 2.3% for FY 2021 due to the change in wage index and other labor adjustments, based off the acuity of patients over a twelve-month period ended September 30, 2020. ◦ COVID-19 has significantly impacted our patient mix, and we expect this to continue in 2021. As such, the ability to accurately estimate the impact of the 2021 Final IRF Rule is limited.(15) • CMS: ◦ Removed the post-admission physician evaluation requirement for all IRF discharges beginning on or after October 1, 2020. ◦ Revised certain IRF coverage documentation requirements. Specifically, CMS: – Codified longstanding instructions and guidance to ensure uniformity between the Medicare Benefit Policy Manual and applicable regulations, – Finalized certain elements of the preadmission screening while not finalizing other elements, and – Clarified that, for the purposes of the intensity of therapy requirement, a “week” is defined as “a seven consecutive calendar day period beginning with the date of admission to the IRF” for purposes of the IRF coverage requirements. ◦ Allowed the use of non-physician practitioners to perform the IRF services and documentation requirements for one of the three required physician visits in a patient’s second and subsequent weeks in an IRF stay, provided that the duties are within the non‑physician practitioner’s scope of practice under applicable state law. Refer to pages 101-104 for end notes.

Encompass Health 31 The final rule: • implemented a net 2.0% market basket increase (2.3% market basket update reduced by a 0.3% productivity adjustment); • implemented a 0.1% reduction related to the rural add-on modifications as required by the Bipartisan Budget Act (BBA) of 2018; and • revised the wage index. ◦ CMS will apply a one year 5% cap on any FY 2021 decrease in a geographic area’s wage index value from the wage index value from the prior CY. CMS did not implement any additional payment changes as behavioral adjustments for CY 2021 due to lack of data and COVID-19. Quality reporting Final rule updates to 2021 payment rates Company observations CMS did not finalize any changes to the Home Health Quality Reporting Program or the Home Health Value-Based Purchasing (HHVBP) Model beyond codifying certain regulations set forth in the May 2020 COVID Interim Final Rule. The Use of Technology under the Medicare HH Benefit Pricing: • Net pricing impact to the Company expected to be an increase of 1.9% for CY 2021(16) HH-PPS calendar year 2021 final rule: key provisions CMS finalized the use of telecommunications technologies in providing care to beneficiaries under the Medicare home health benefit, as long as the telecommunications technology meets certain criteria and does not replace ordered in-person visits. These visits are not reimbursable by Medicare. Source: https://www.cms.gov/medicaremedicare-fee-service-paymenthomehealthppshome-health-prospective-payment-system- regulations/cms-1730-f Refer to pages 101-104 for end notes.
Encompass Health 32 Growth Encompass Health is a leader in serving the post-acute patient population and has multiple avenues available for sustained growth in both segments. Favorable demographic trends are driving increasing demand.
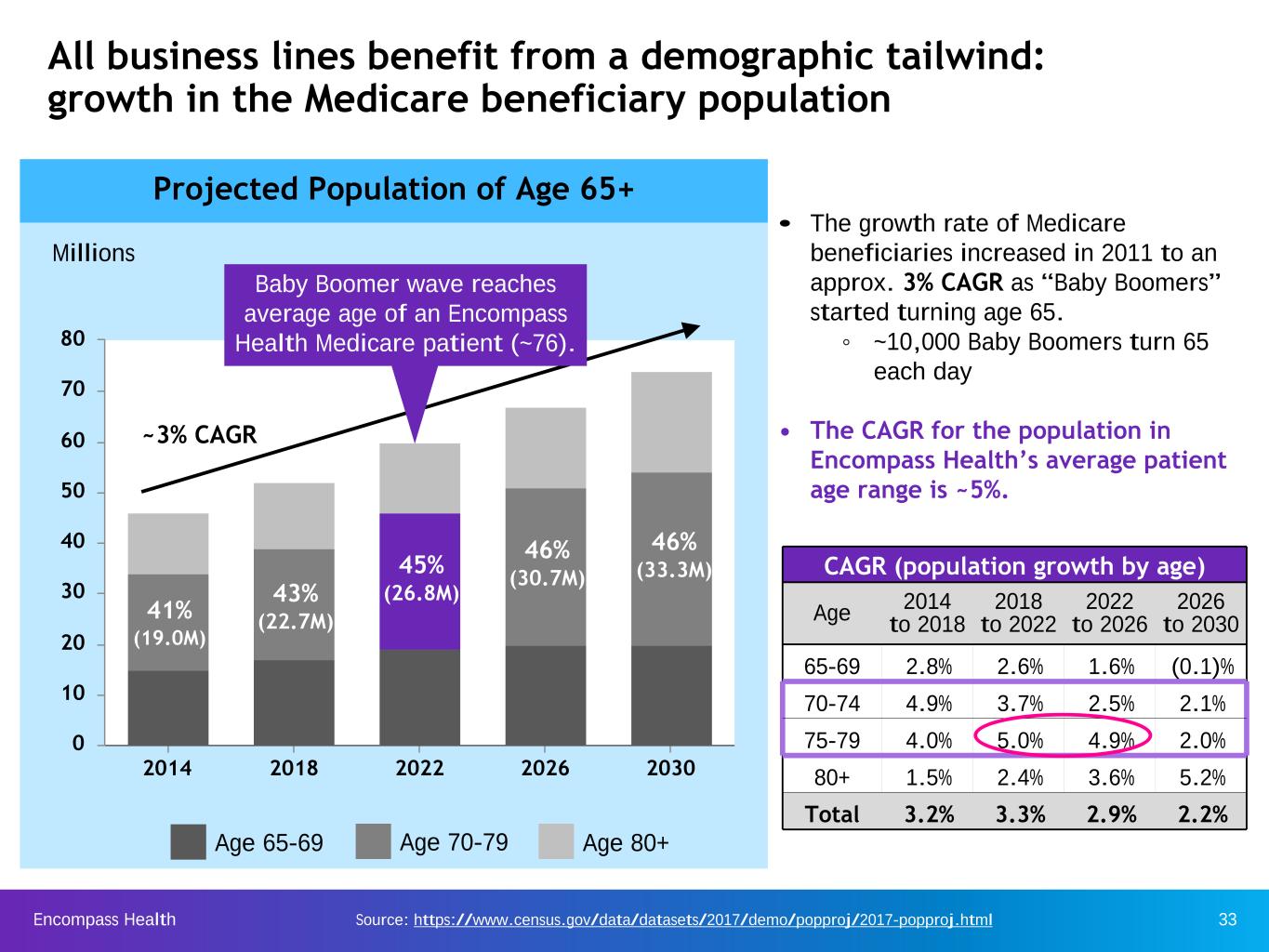
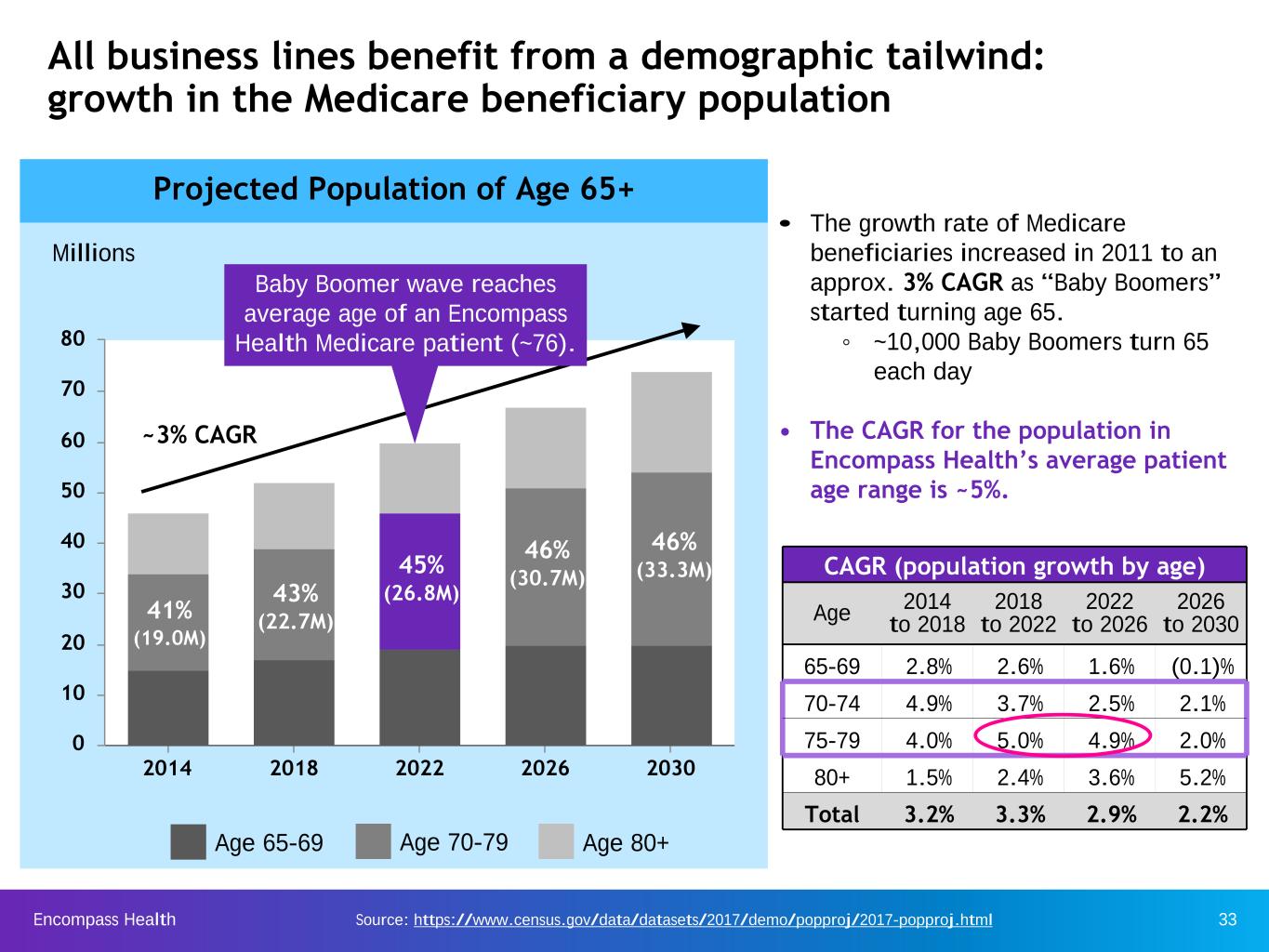
Encompass Health 33 All business lines benefit from a demographic tailwind: growth in the Medicare beneficiary population Age 80+Age 70-79Age 65-69 • The growth rate of Medicare beneficiaries increased in 2011 to an approx. 3% CAGR as “Baby Boomers” started turning age 65. ◦ ~10,000 Baby Boomers turn 65 each day • The CAGR for the population in Encompass Health’s average patient age range is ~5%. CAGR (population growth by age) Age 2014to 2018 2018 to 2022 2022 to 2026 2026 to 2030 65-69 2.8% 2.6% 1.6% (0.1)% 70-74 4.9% 3.7% 2.5% 2.1% 75-79 4.0% 5.0% 4.9% 2.0% 80+ 1.5% 2.4% 3.6% 5.2% Total 3.2% 3.3% 2.9% 2.2% Source: https://www.census.gov/data/datasets/2017/demo/popproj/2017-popproj.html 2014 2018 2022 2026 2030 0 10 20 30 40 50 60 70 80 Projected Population of Age 65+ Millions 41% (19.0M) 43% (22.7M) 45% (26.8M) 46% (30.7M) 46% (33.3M) ~3% CAGR Baby Boomer wave reaches average age of an Encompass Health Medicare patient (~76).
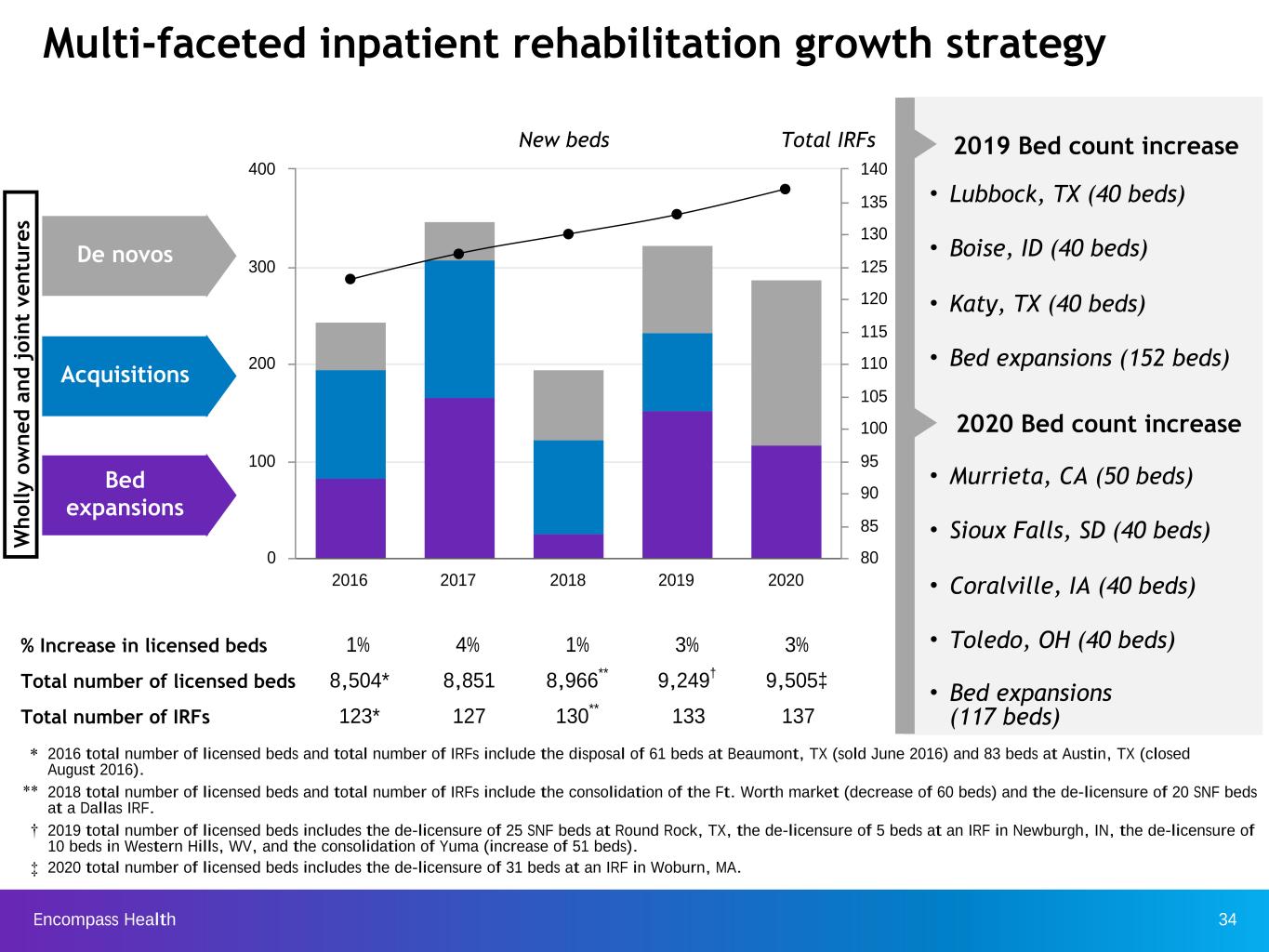
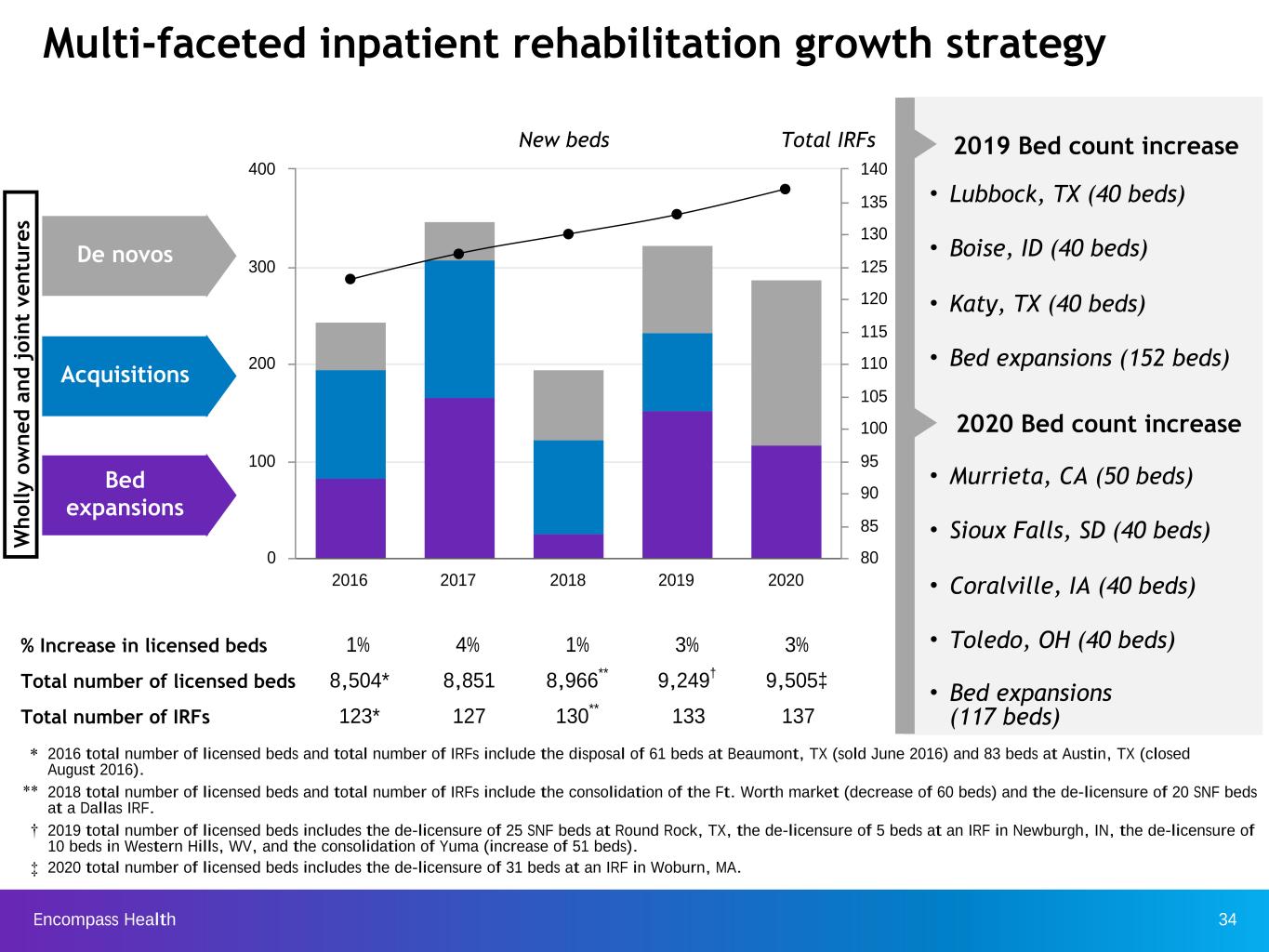
Encompass Health 34 2016 2017 2018 2019 2020 0 100 200 300 400 80 85 90 95 100 105 110 115 120 125 130 135 140 % Increase in licensed beds 1% 4% 1% 3% 3% Total number of licensed beds 8,504* 8,851 8,966** 9,249† 9,505‡ Total number of IRFs 123* 127 130** 133 137 Multi-faceted inpatient rehabilitation growth strategy Total IRFsNew beds W h o ll y o w n e d a n d j o in t ve n tu re s Bed expansions De novos Acquisitions * 2016 total number of licensed beds and total number of IRFs include the disposal of 61 beds at Beaumont, TX (sold June 2016) and 83 beds at Austin, TX (closed August 2016). ** 2018 total number of licensed beds and total number of IRFs include the consolidation of the Ft. Worth market (decrease of 60 beds) and the de-licensure of 20 SNF beds at a Dallas IRF. † 2019 total number of licensed beds includes the de-licensure of 25 SNF beds at Round Rock, TX, the de-licensure of 5 beds at an IRF in Newburgh, IN, the de-licensure of 10 beds in Western Hills, WV, and the consolidation of Yuma (increase of 51 beds). ‡ 2020 total number of licensed beds includes the de-licensure of 31 beds at an IRF in Woburn, MA. • Murrieta, CA (50 beds) • Sioux Falls, SD (40 beds) • Coralville, IA (40 beds) • Toledo, OH (40 beds) • Bed expansions (117 beds) 2019 Bed count increase • Lubbock, TX (40 beds) • Boise, ID (40 beds) • Katy, TX (40 beds) • Bed expansions (152 beds) 2020 Bed count increase
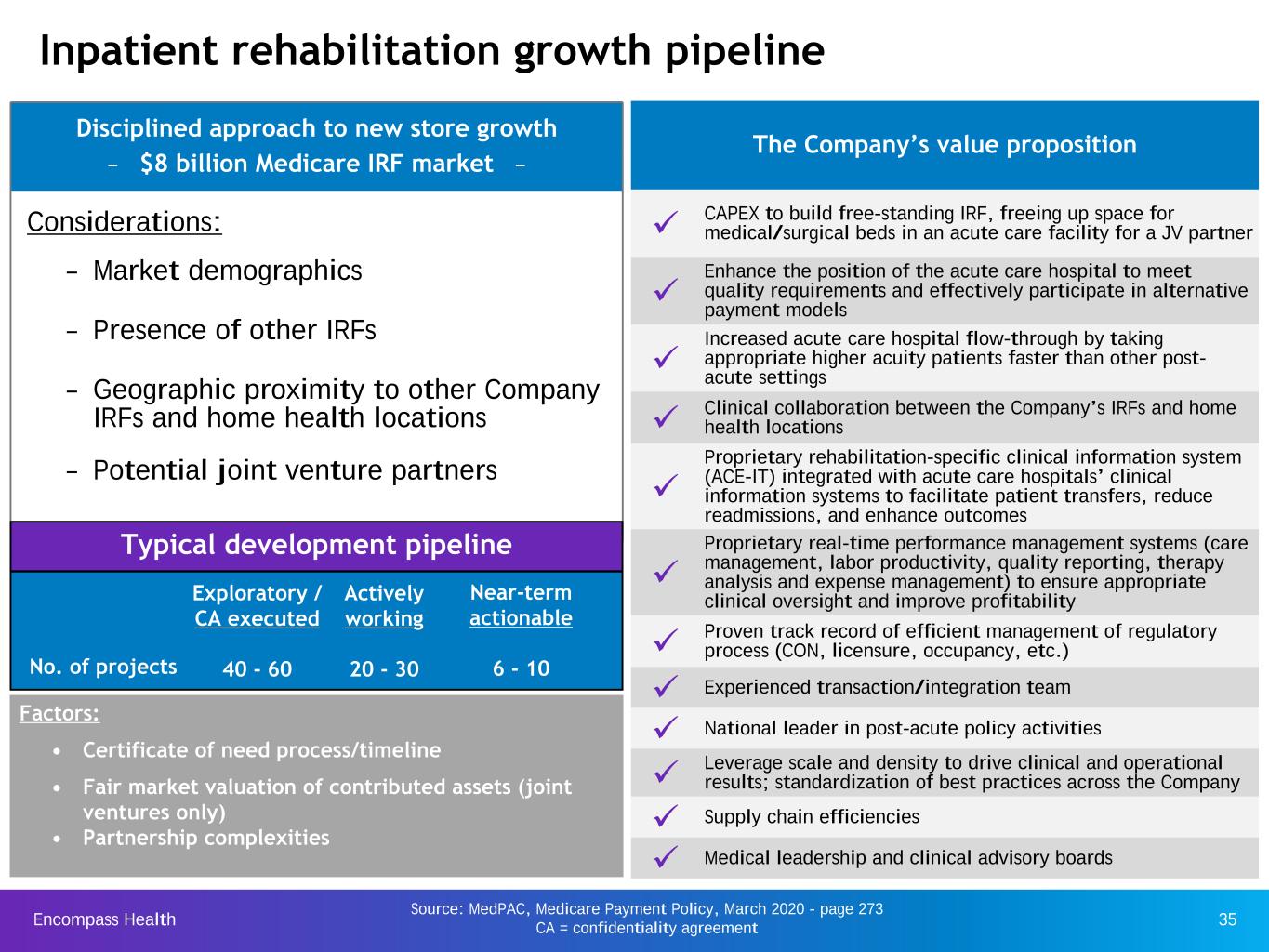
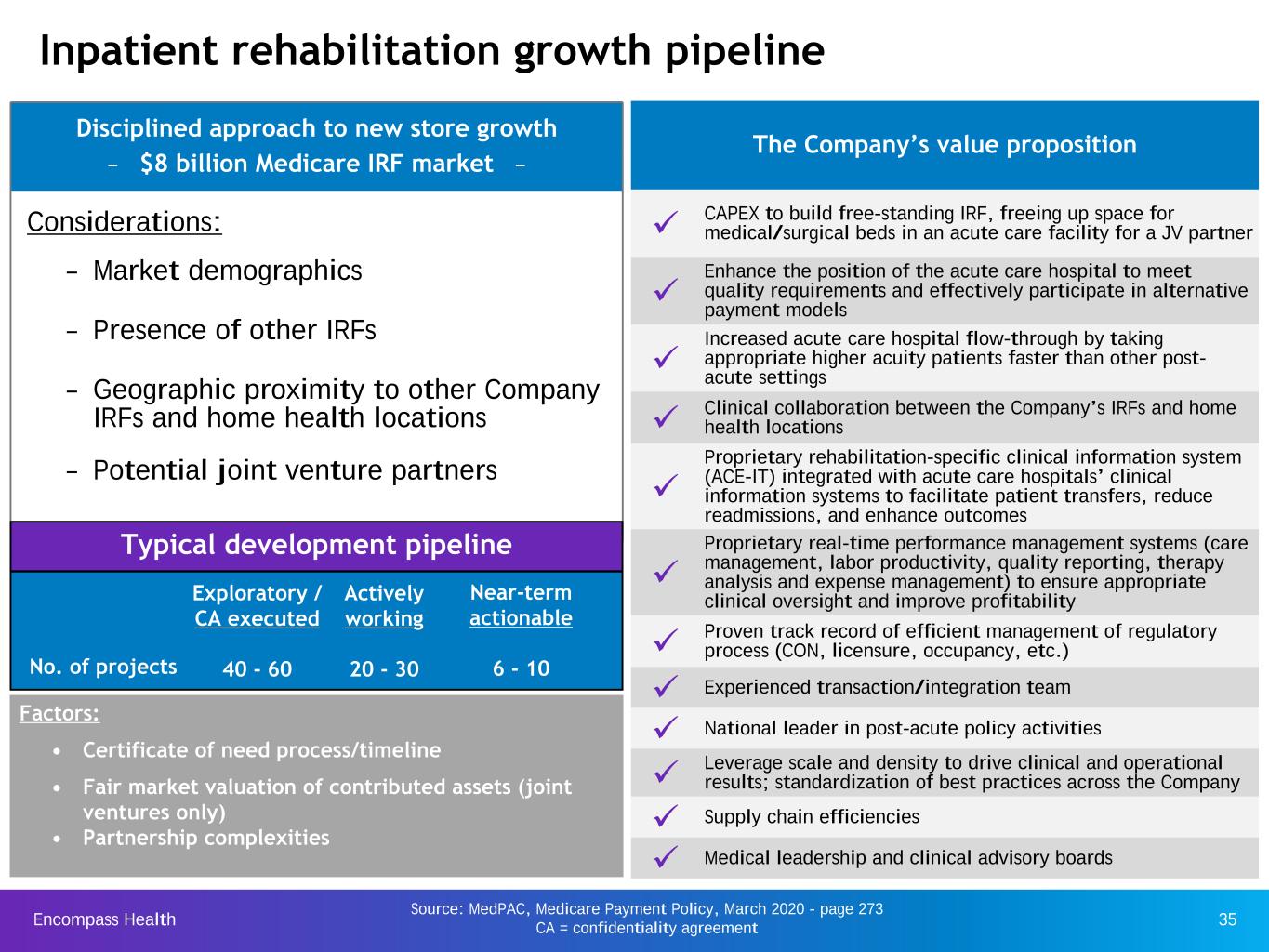
Encompass Health 35 Disciplined approach to new store growth – $8 billion Medicare IRF market – Considerations: – Market demographics – Presence of other IRFs – Geographic proximity to other Company IRFs and home health locations – Potential joint venture partners Source: MedPAC, Medicare Payment Policy, March 2020 - page 273 CA = confidentiality agreement Inpatient rehabilitation growth pipeline Typical development pipeline Factors: • Certificate of need process/timeline • Fair market valuation of contributed assets (joint ventures only) • Partnership complexities The Company’s value proposition ü CAPEX to build free-standing IRF, freeing up space for medical/surgical beds in an acute care facility for a JV partner ü Enhance the position of the acute care hospital to meet quality requirements and effectively participate in alternative payment models ü Increased acute care hospital flow-through by taking appropriate higher acuity patients faster than other post- acute settings ü Clinical collaboration between the Company’s IRFs and home health locations ü Proprietary rehabilitation-specific clinical information system (ACE-IT) integrated with acute care hospitals’ clinical information systems to facilitate patient transfers, reduce readmissions, and enhance outcomes ü Proprietary real-time performance management systems (care management, labor productivity, quality reporting, therapy analysis and expense management) to ensure appropriate clinical oversight and improve profitability ü Proven track record of efficient management of regulatory process (CON, licensure, occupancy, etc.) ü Experienced transaction/integration team ü National leader in post-acute policy activities ü Leverage scale and density to drive clinical and operational results; standardization of best practices across the Company ü Supply chain efficiencies ü Medical leadership and clinical advisory boards No. of projects Exploratory / CA executed 40 - 60 Actively working 20 - 30 Near-term actionable 6 - 10
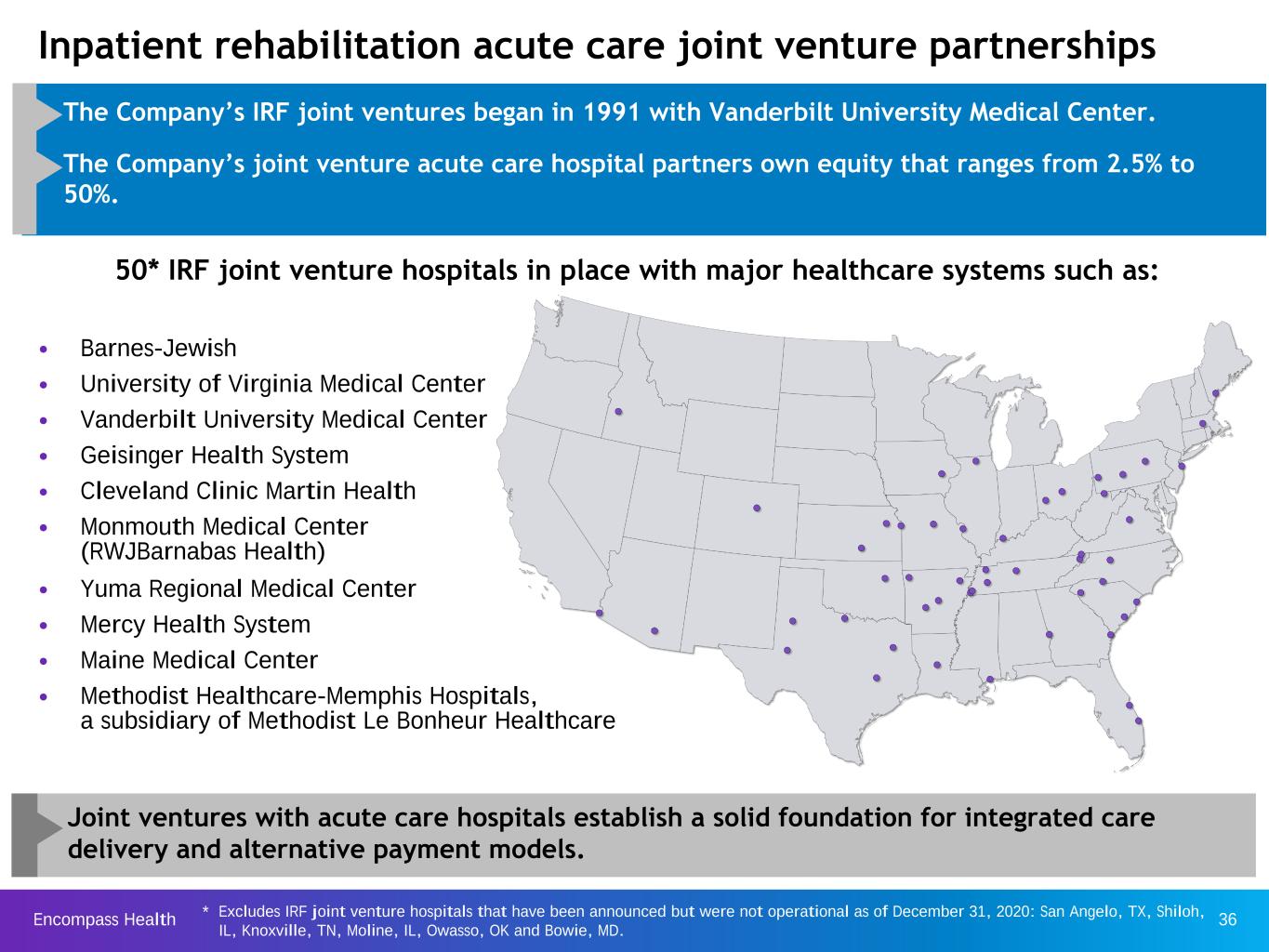
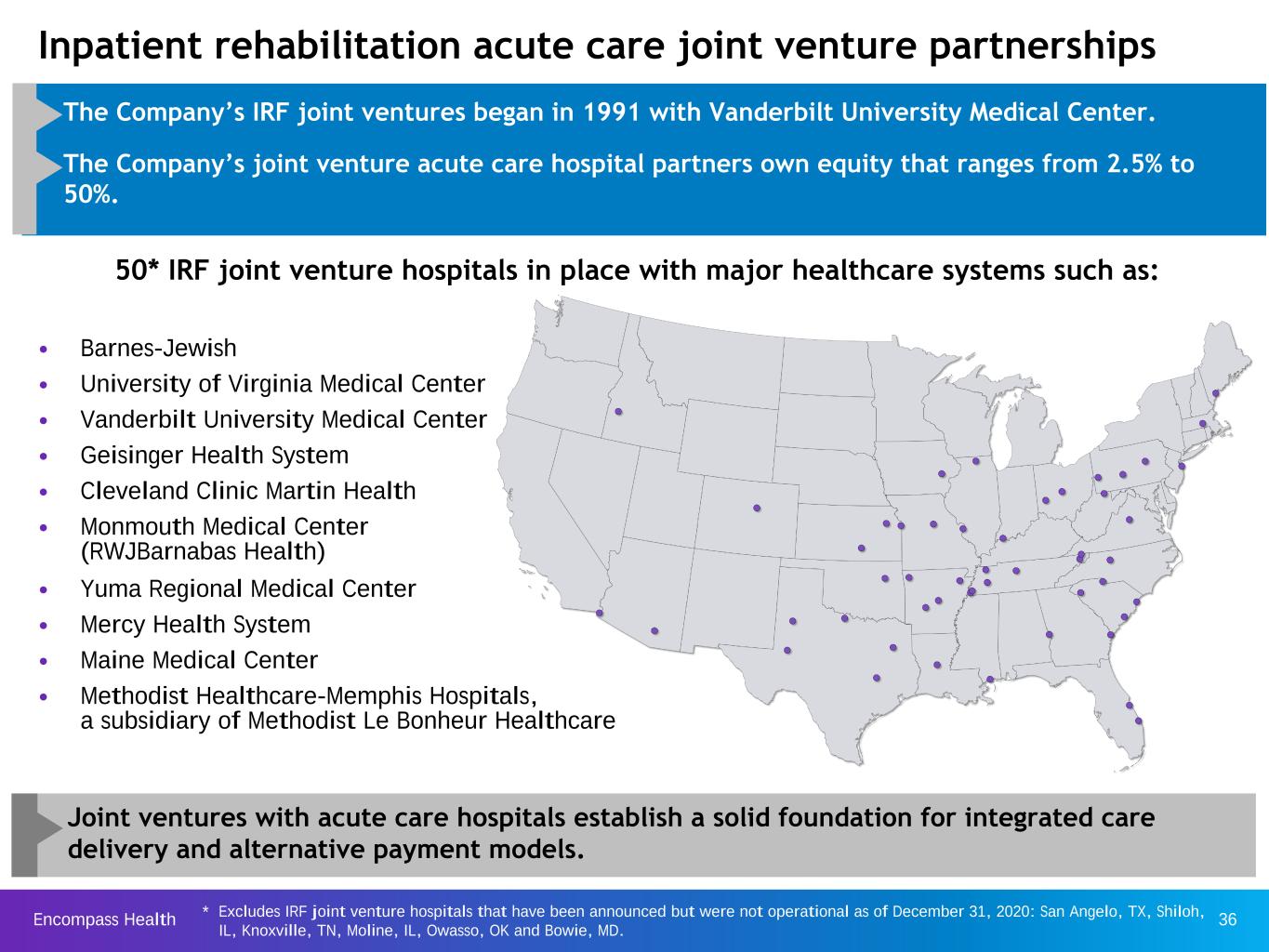
Encompass Health 36 Inpatient rehabilitation acute care joint venture partnerships • The Company’s IRF joint ventures began in 1991 with Vanderbilt University Medical Center. • The Company’s joint venture acute care hospital partners own equity that ranges from 2.5% to 50%. 50* IRF joint venture hospitals in place with major healthcare systems such as: Joint ventures with acute care hospitals establish a solid foundation for integrated care delivery and alternative payment models. • Barnes-Jewish • University of Virginia Medical Center • Vanderbilt University Medical Center • Geisinger Health System • Cleveland Clinic Martin Health • Monmouth Medical Center (RWJBarnabas Health) • Yuma Regional Medical Center • Mercy Health System • Maine Medical Center • Methodist Healthcare-Memphis Hospitals, a subsidiary of Methodist Le Bonheur Healthcare Excludes IRF joint venture hospitals that have been announced but were not operational as of December 31, 2020: San Angelo, TX, Shiloh, IL, Knoxville, TN, Moline, IL, Owasso, OK and Bowie, MD. *

Encompass Health 37 Location Operations date Joint venture? # of New Beds 2021 2022 2023 De novo IRFs: San Angelo, TX Q1 2021 Yes 40 Cumming, GA Q2 2021 50 North Tampa, FL Q2 2021 50 Greenville, SC Q3 2021 40 Shreveport, LA Q3 2021 40 Waco, TX Q3 2021 40 Pensacola, FL Q3 2021 40 Stockbridge, GA Q4 2021 50 Libertyville, IL Q1 2022 60 St. Augustine, FL Q1 2022 40 Lakeland, FL Q1 2022 50 Shiloh, IL Q1 2022 Yes 40 Knoxville, TN Q2 2022 Yes 73 Clermont, FL TBD 2022 50 Naples, FL TBD 2022 50 Cape Coral, FL TBD 2022 40 Jacksonville, FL TBD 2022 50 Moline, IL TBD 2022 Yes 40 Owasso, OK TBD 2022 Yes 40 Bowie, MD TBD 2022 Yes 60 Kissimmee, FL TBD 50 Bed expansions, net* ~100 ~100 ~100 ~450 ~690 ~150 De novo IRFs and acquisitions Investment considerations • IRR objective of 13% (after tax) • Joint venture capitalization • Certificate of need (“CON”) costs, where applicable • Clinical information system (“CIS”) installation costs • Medicare certification for de novo hospitals (minimum of 20 patients treated for zero revenue) 21 IRF development projects announced and underway Net bed expansions in each year may change due to the timing of certain regulatory approvals and/or construction delays. For 2021 and 2022, the currently expected range for bed expansions is 100 to 150. *
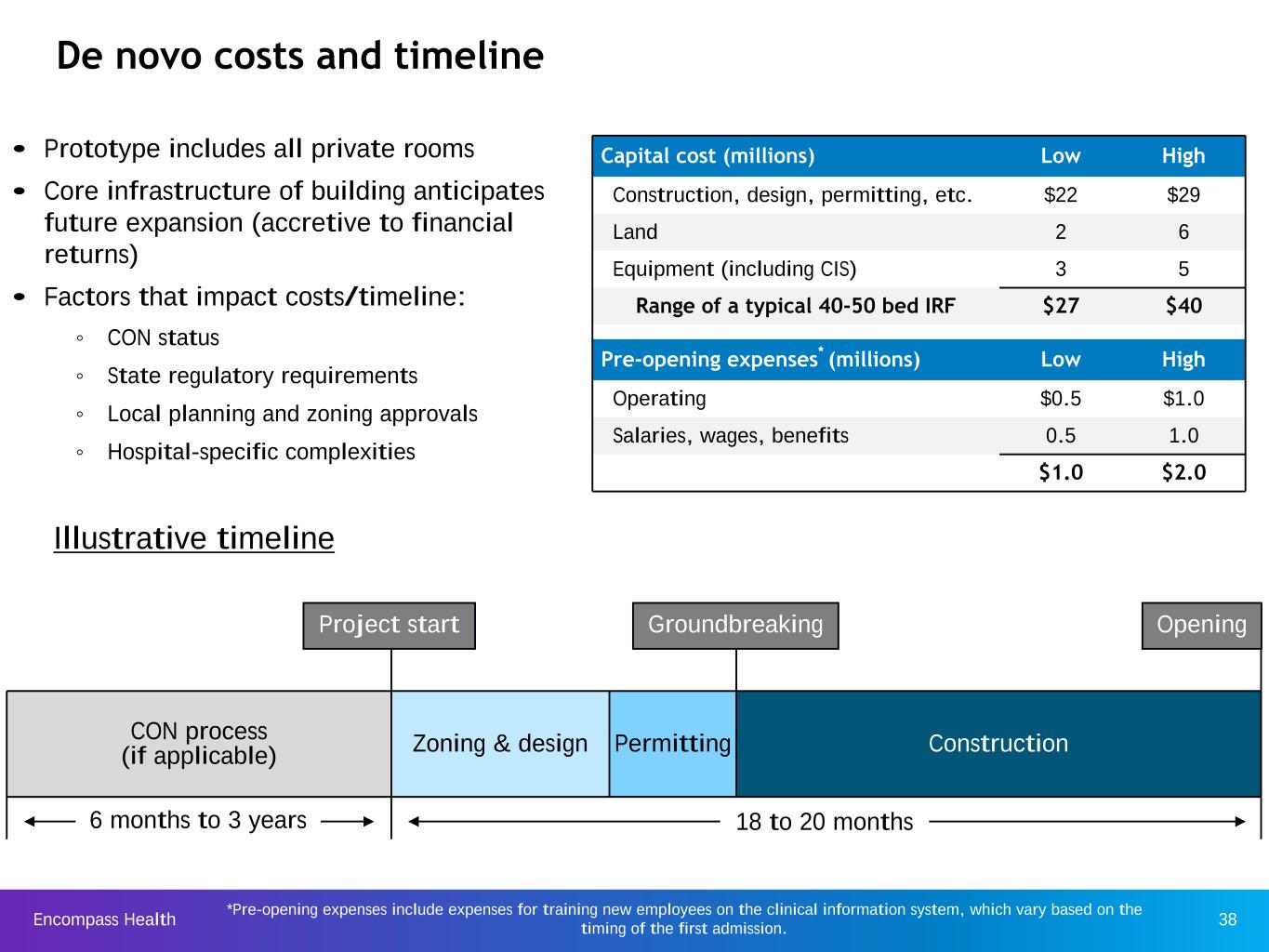
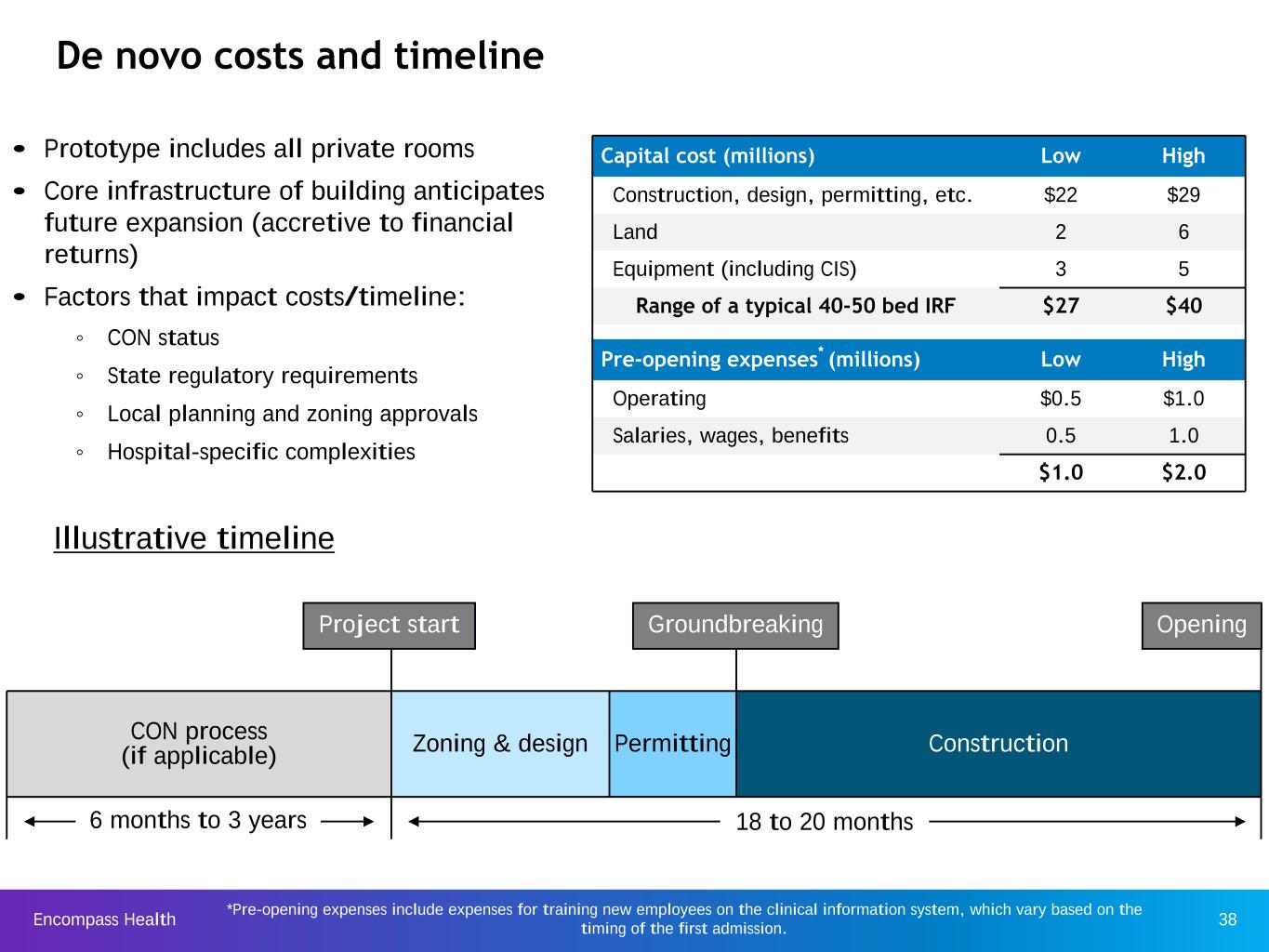
Encompass Health 38 CON process (if applicable) Zoning & design Permitting Construction OpeningGroundbreaking De novo costs and timeline Capital cost (millions) Low High Construction, design, permitting, etc. $22 $29 Land 2 6 Equipment (including CIS) 3 5 Range of a typical 40-50 bed IRF $27 $40 Pre-opening expenses* (millions) Low High Operating $0.5 $1.0 Salaries, wages, benefits 0.5 1.0 $1.0 $2.0 • Prototype includes all private rooms • Core infrastructure of building anticipates future expansion (accretive to financial returns) • Factors that impact costs/timeline: ◦ CON status ◦ State regulatory requirements ◦ Local planning and zoning approvals ◦ Hospital-specific complexities Project start 18 to 20 months6 months to 3 years Illustrative timeline *Pre-opening expenses include expenses for training new employees on the clinical information system, which vary based on the timing of the first admission.
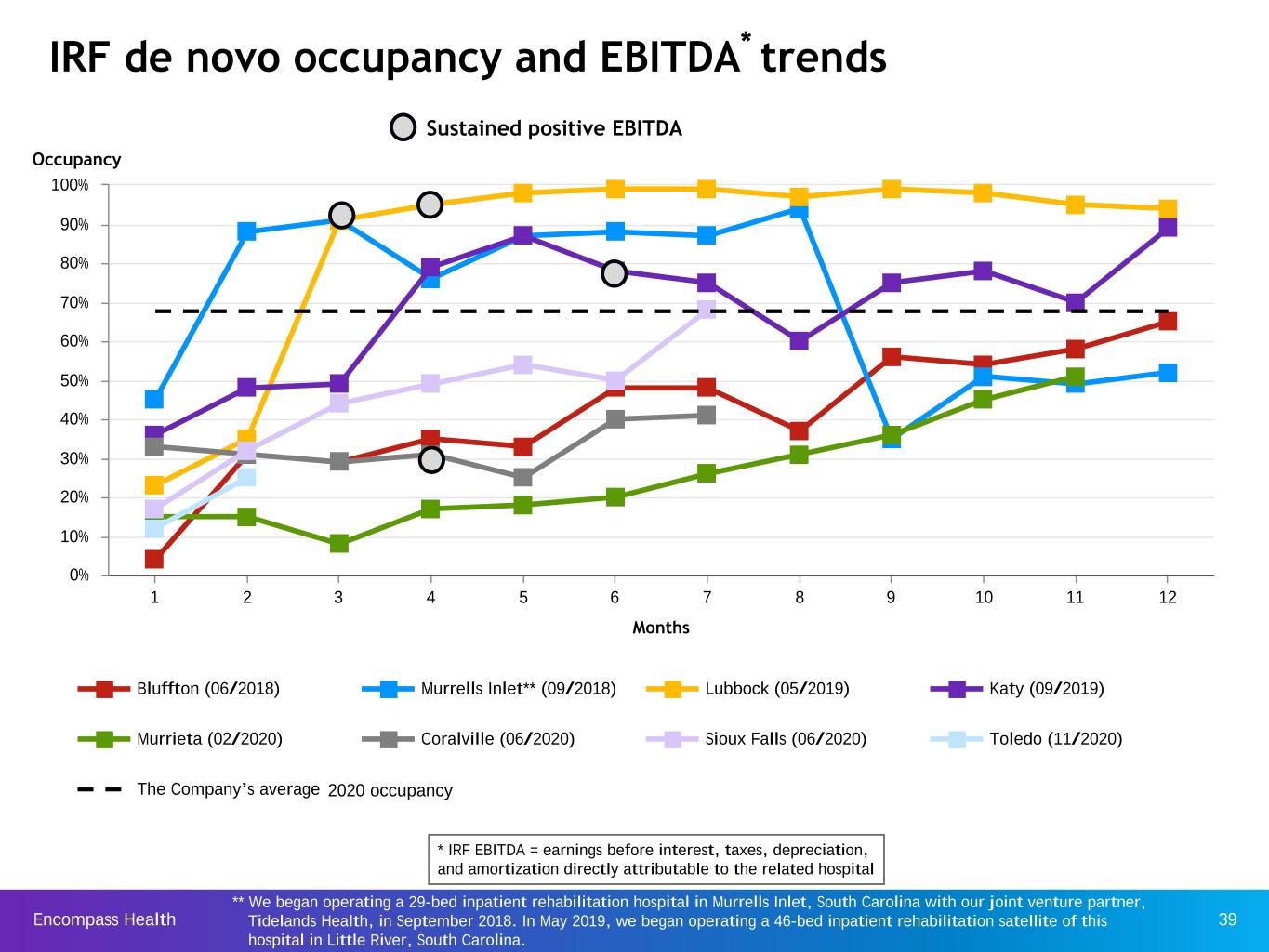
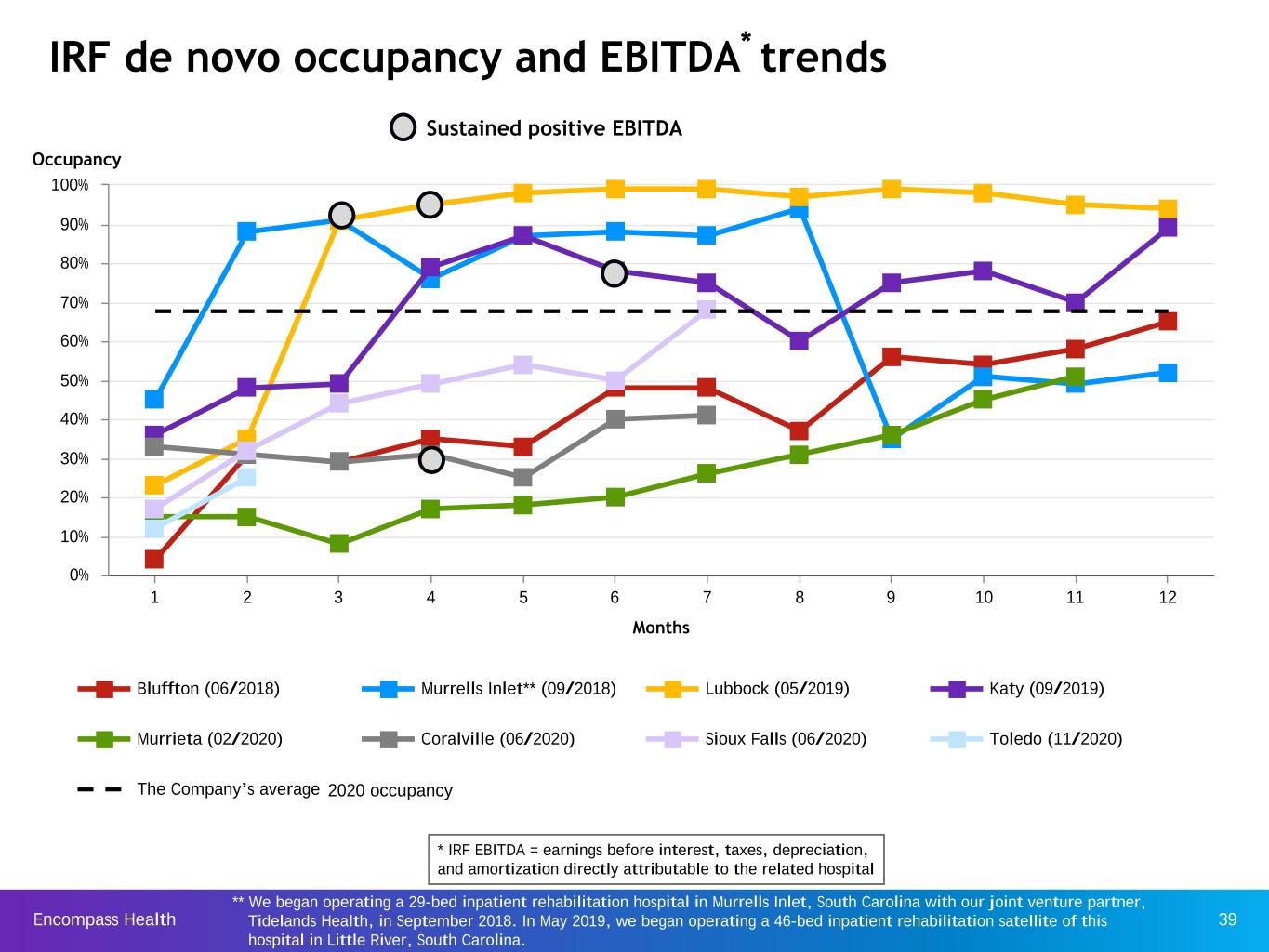
Encompass Health 39 Months Bluffton (06/2018) Murrells Inlet** (09/2018) Lubbock (05/2019) Katy (09/2019) Murrieta (02/2020) Coralville (06/2020) Sioux Falls (06/2020) Toledo (11/2020) The Company’s average 1 2 3 4 5 6 7 8 9 10 11 12 0% 10% 20% 30% 40% 50% 60% 70% 80% 90% 100% IRF de novo occupancy and EBITDA* trends Occupancy Sustained positive EBITDA ** We began operating a 29-bed inpatient rehabilitation hospital in Murrells Inlet, South Carolina with our joint venture partner, Tidelands Health, in September 2018. In May 2019, we began operating a 46-bed inpatient rehabilitation satellite of this hospital in Little River, South Carolina. 2020 occupancy * IRF EBITDA = earnings before interest, taxes, depreciation, and amortization directly attributable to the related hospital
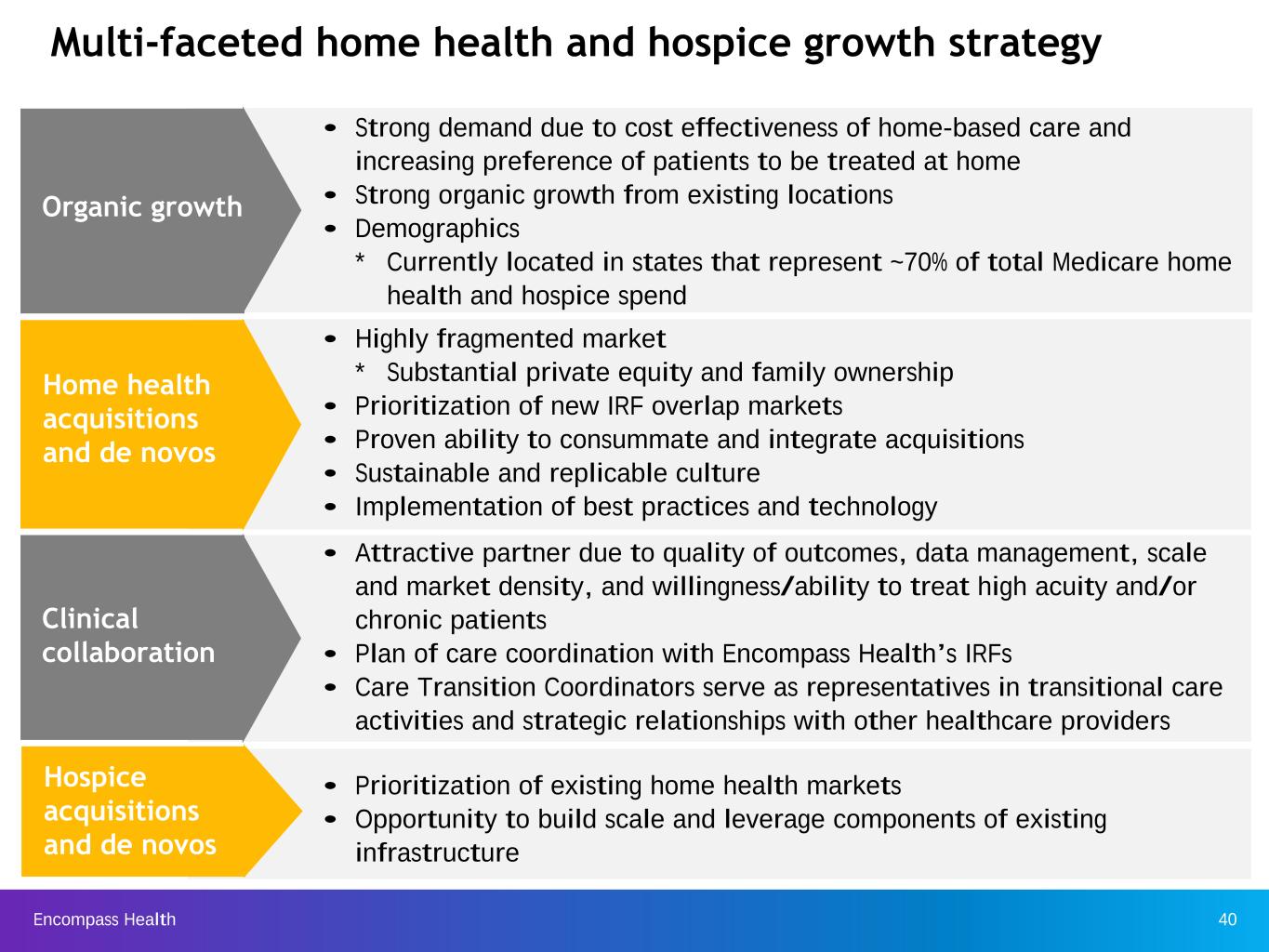
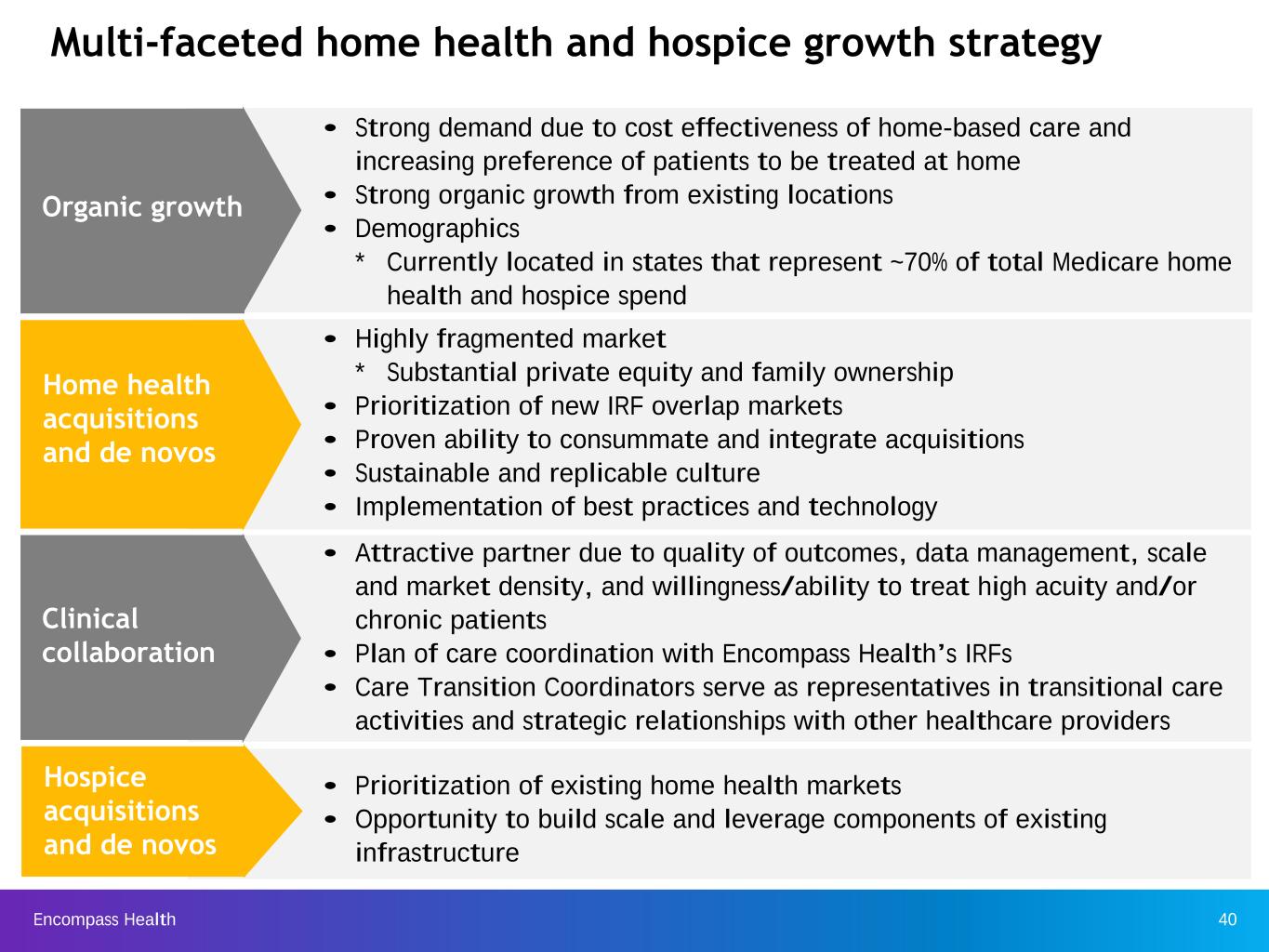
Encompass Health 40 • Strong demand due to cost effectiveness of home-based care and increasing preference of patients to be treated at home • Strong organic growth from existing locations • Demographics * Currently located in states that represent ~70% of total Medicare home health and hospice spend • Prioritization of existing home health markets • Opportunity to build scale and leverage components of existing infrastructure • Attractive partner due to quality of outcomes, data management, scale and market density, and willingness/ability to treat high acuity and/or chronic patients • Plan of care coordination with Encompass Health’s IRFs • Care Transition Coordinators serve as representatives in transitional care activities and strategic relationships with other healthcare providers • Highly fragmented market * Substantial private equity and family ownership • Prioritization of new IRF overlap markets • Proven ability to consummate and integrate acquisitions • Sustainable and replicable culture • Implementation of best practices and technology Organic growth Home health acquisitions and de novos Hospice acquisitions and de novos Clinical collaboration Multi-faceted home health and hospice growth strategy

Encompass Health 41 # of A ge n ci e s 1998 2000 2002 2004 2006 2008 2010 2012 2014 2016 2018 4,000 5,000 6,000 7,000 8,000 9,000 10,000 11,000 12,000 13,000 Home health growth pipeline • $17.9 billion Medicare home health market is highly fragmented with over 11,500 home health agencies. • Approx. 92% of these have annual revenue of less than $5 million. • Top four public companies represent approx. 22% of the Medicare market. • The Company represents 4.4% of the Medicare home health market. Number of home health agencies over time Cost- based Interim payment systems (IPS) Prospective Payment System (PPS) The number of home health agencies is near an all-time high and presents significant consolidation opportunities. Source: MedPAC, Medicare Payment Policy - March 2020, pages 252 and 259; March 2019, page 234; March 2018, page 246; March 2017, page 231; March 2016, page 214; March 2015, page 218; March 2014, page 221; March 2013, page 194; and March 2003, page 112; MedPAC - Healthcare spending and the Medicare program, June 2006, page 131; Medicare Claims Data
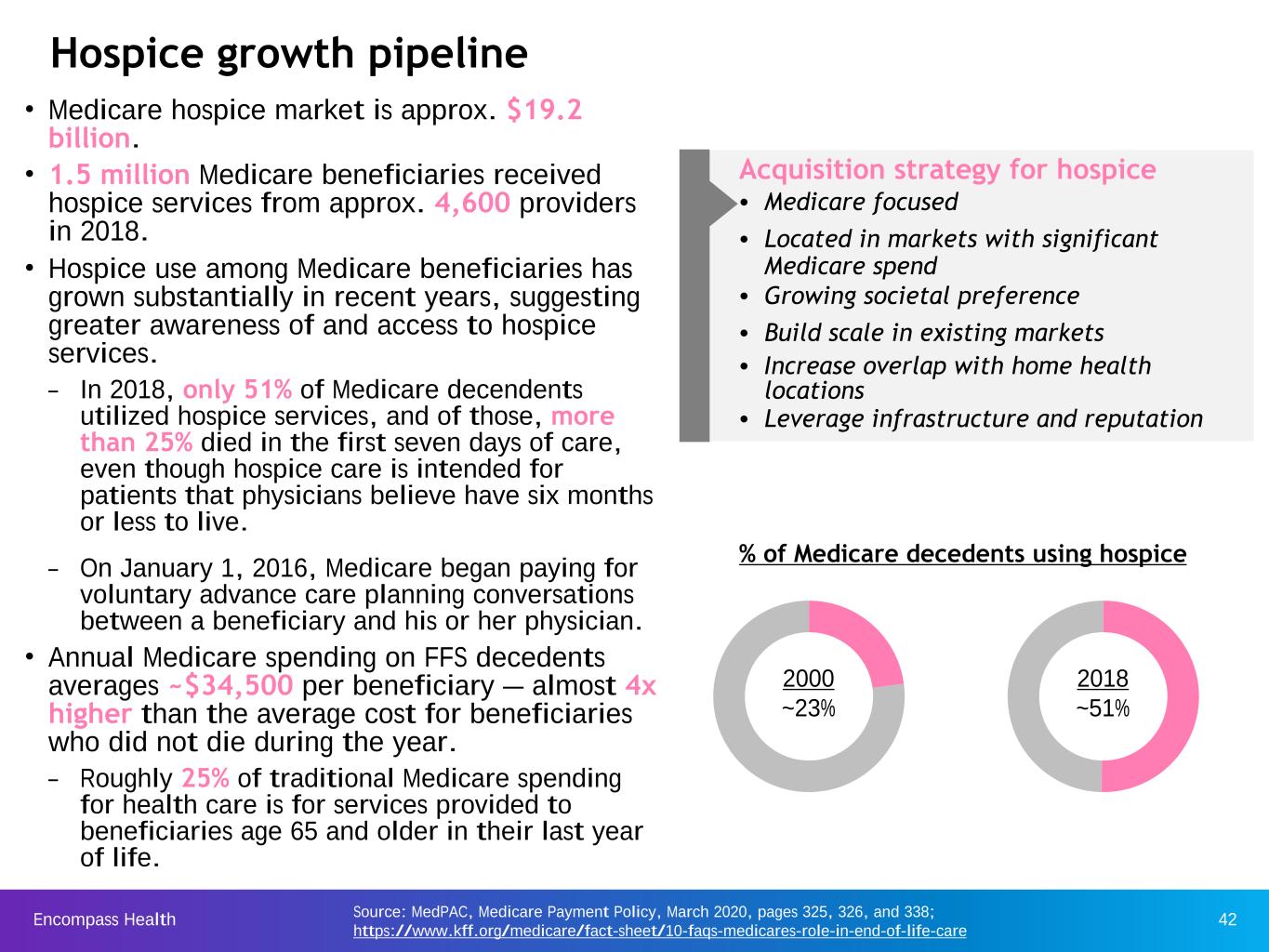
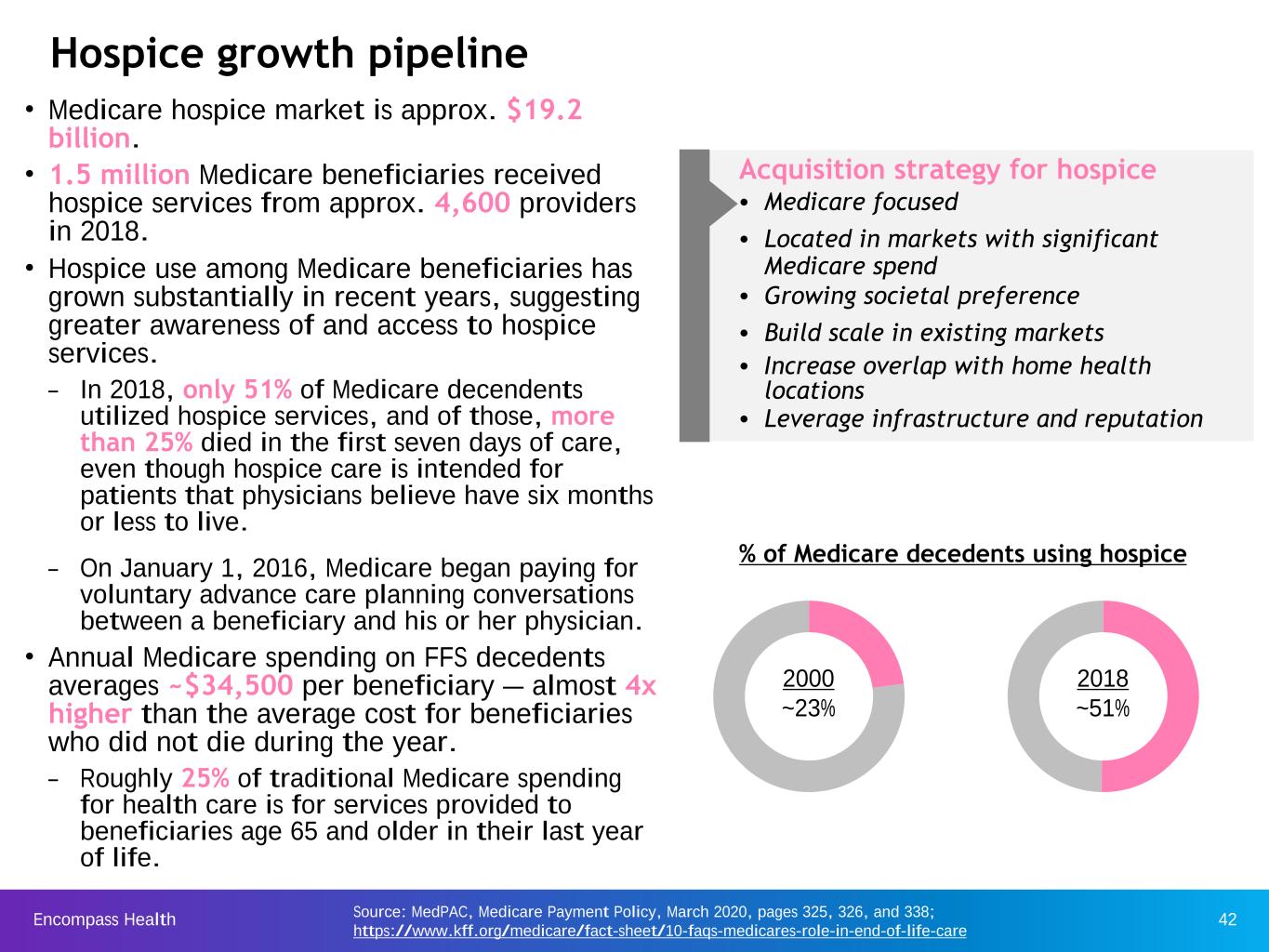
Encompass Health 42 Hospice growth pipeline Source: MedPAC, Medicare Payment Policy, March 2020, pages 325, 326, and 338; https://www.kff.org/medicare/fact-sheet/10-faqs-medicares-role-in-end-of-life-care • Medicare hospice market is approx. $19.2 billion. • 1.5 million Medicare beneficiaries received hospice services from approx. 4,600 providers in 2018. • Hospice use among Medicare beneficiaries has grown substantially in recent years, suggesting greater awareness of and access to hospice services. – In 2018, only 51% of Medicare decendents utilized hospice services, and of those, more than 25% died in the first seven days of care, even though hospice care is intended for patients that physicians believe have six months or less to live. – On January 1, 2016, Medicare began paying for voluntary advance care planning conversations between a beneficiary and his or her physician. • Annual Medicare spending on FFS decedents averages ~$34,500 per beneficiary — almost 4x higher than the average cost for beneficiaries who did not die during the year. – Roughly 25% of traditional Medicare spending for health care is for services provided to beneficiaries age 65 and older in their last year of life. 2000 ~23% 2018 ~51% % of Medicare decedents using hospice Acquisition strategy for hospice • Medicare focused • Located in markets with significant Medicare spend • Growing societal preference • Build scale in existing markets • Increase overlap with home health locations • Leverage infrastructure and reputation
Encompass Health 43 Operational Initiatives Our operational initiatives are designed to respond to regulatory changes, expand our services to more patients in need of our higher level of care, enhance our clinical expertise, and ensure the delivery of high-quality outcomes.
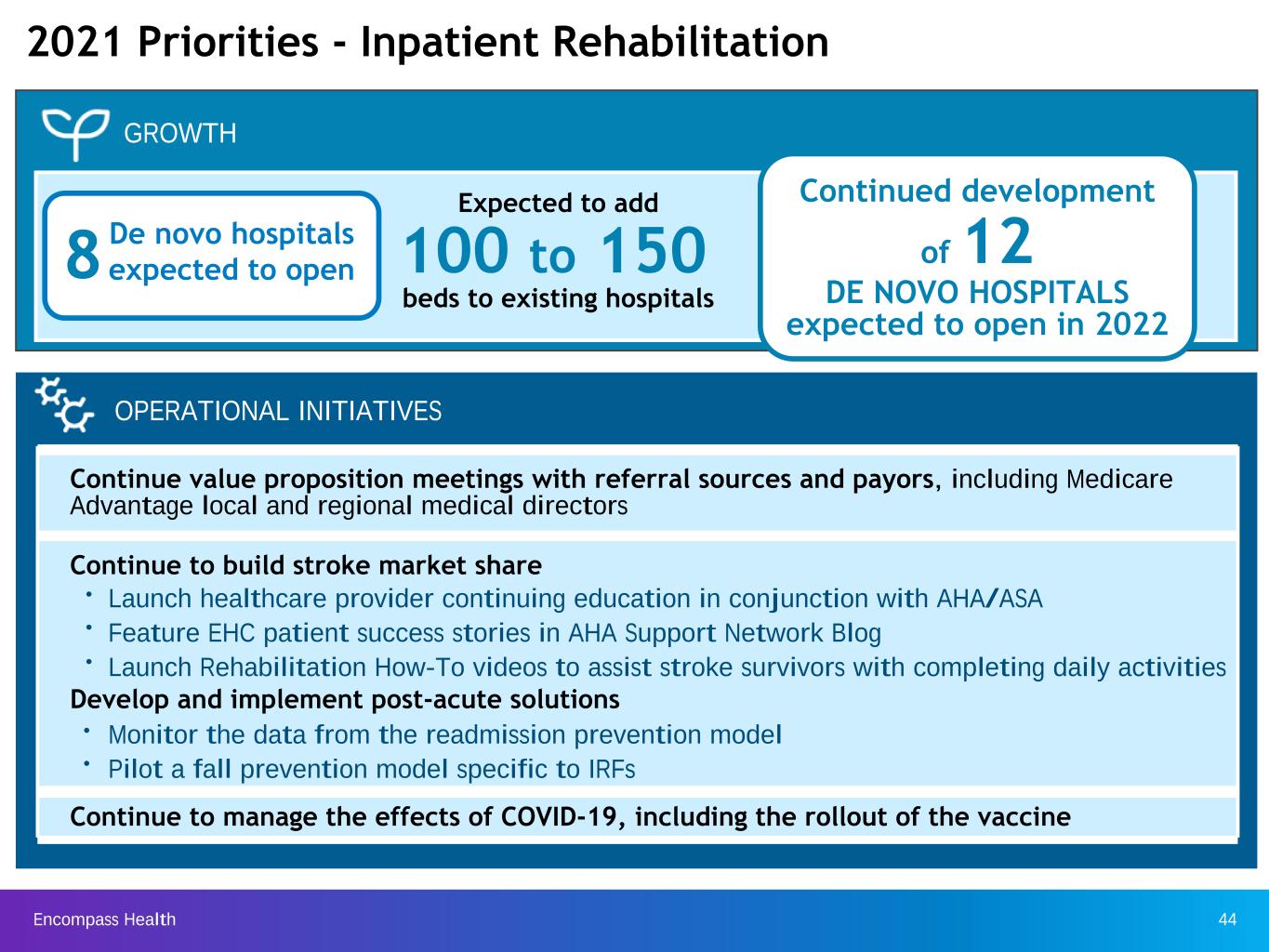
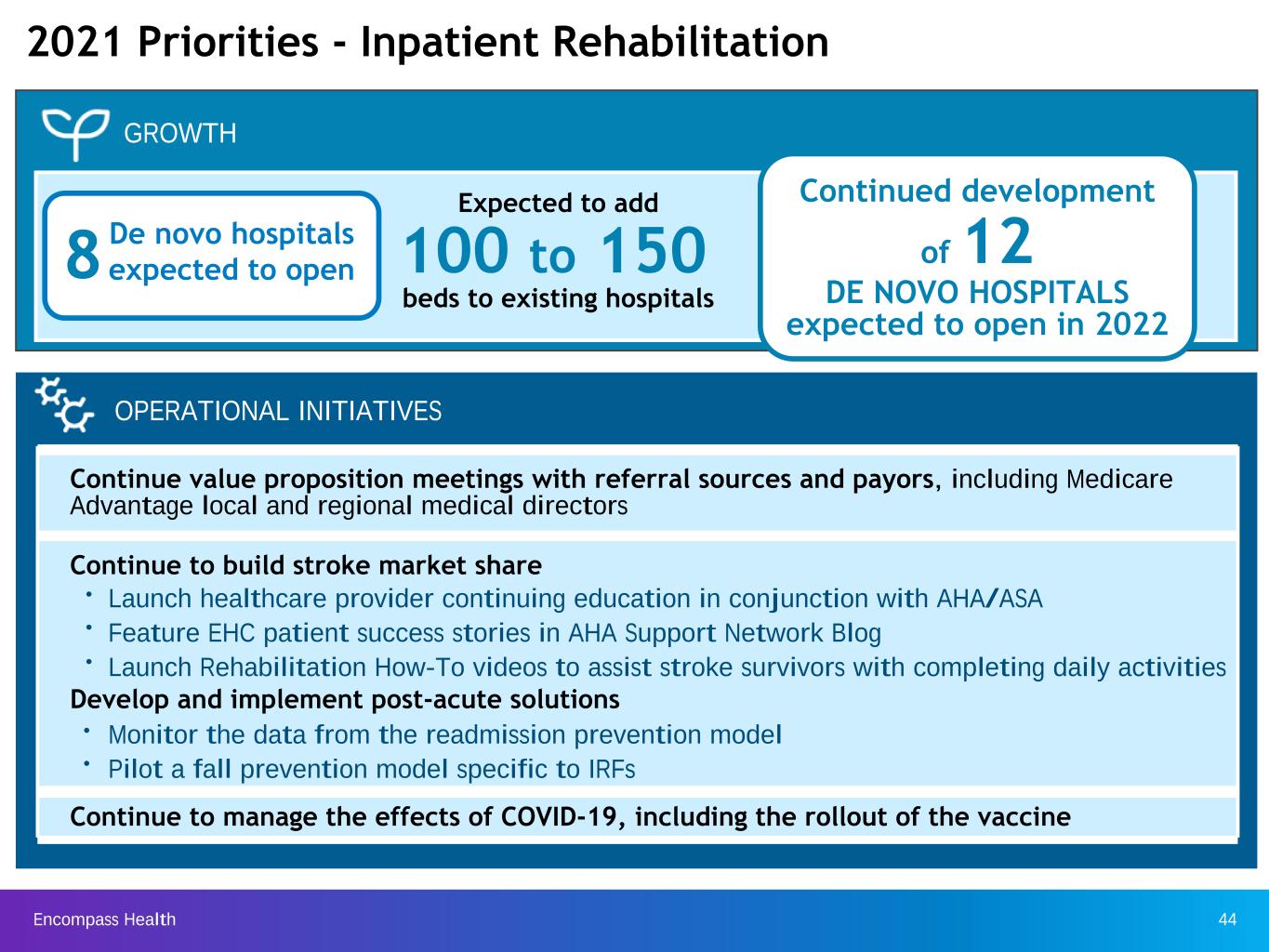
Encompass Health 44 2021 Priorities - Inpatient Rehabilitation Continue value proposition meetings with referral sources and payors, including Medicare Advantage local and regional medical directors Continue to build stroke market share Ÿ Launch healthcare provider continuing education in conjunction with AHA/ASA Ÿ Feature EHC patient success stories in AHA Support Network Blog Ÿ Launch Rehabilitation How-To videos to assist stroke survivors with completing daily activities Develop and implement post-acute solutions Ÿ Monitor the data from the readmission prevention model Ÿ Pilot a fall prevention model specific to IRFs Continue to manage the effects of COVID-19, including the rollout of the vaccine OPERATIONAL INITIATIVES Continued development of 12 DE NOVO HOSPITALS expected to open in 2022 GROWTH Expected to add beds to existing hospitals 100 to 150De novo hospitals expected to open8

Encompass Health 45 Expand relationships with Medicare Shared Savings Program ACOs Enter into more value-based payment arrangements with Medicare Advantage payors Collaborate with home care organizations on a SNF at home program Pilot virtual visit platform Monitor improvement resulting from full Medalogix deployment Continue to manage the effects of COVID-19, including the rollout of the vaccine GROWTH 2021 Priorities - Home Health and Hospice Pursue industry consolidation opportunities Return to organic volume growth Ÿ new national contract with United Healthcare Continued focus on home health and hospice de novos 17.5% Industry-leading hospital readmission rates make EHC the clear choice for risk- based payment models. OPERATIONAL INITIATIVES 17.6% 16.1% 30-day readmission rate* National Average EHC (lower is better) * Source for National Average: Avalere Health and Alliance for Home Health Quality and Innovation Home Health Chart Book 2020, page 57
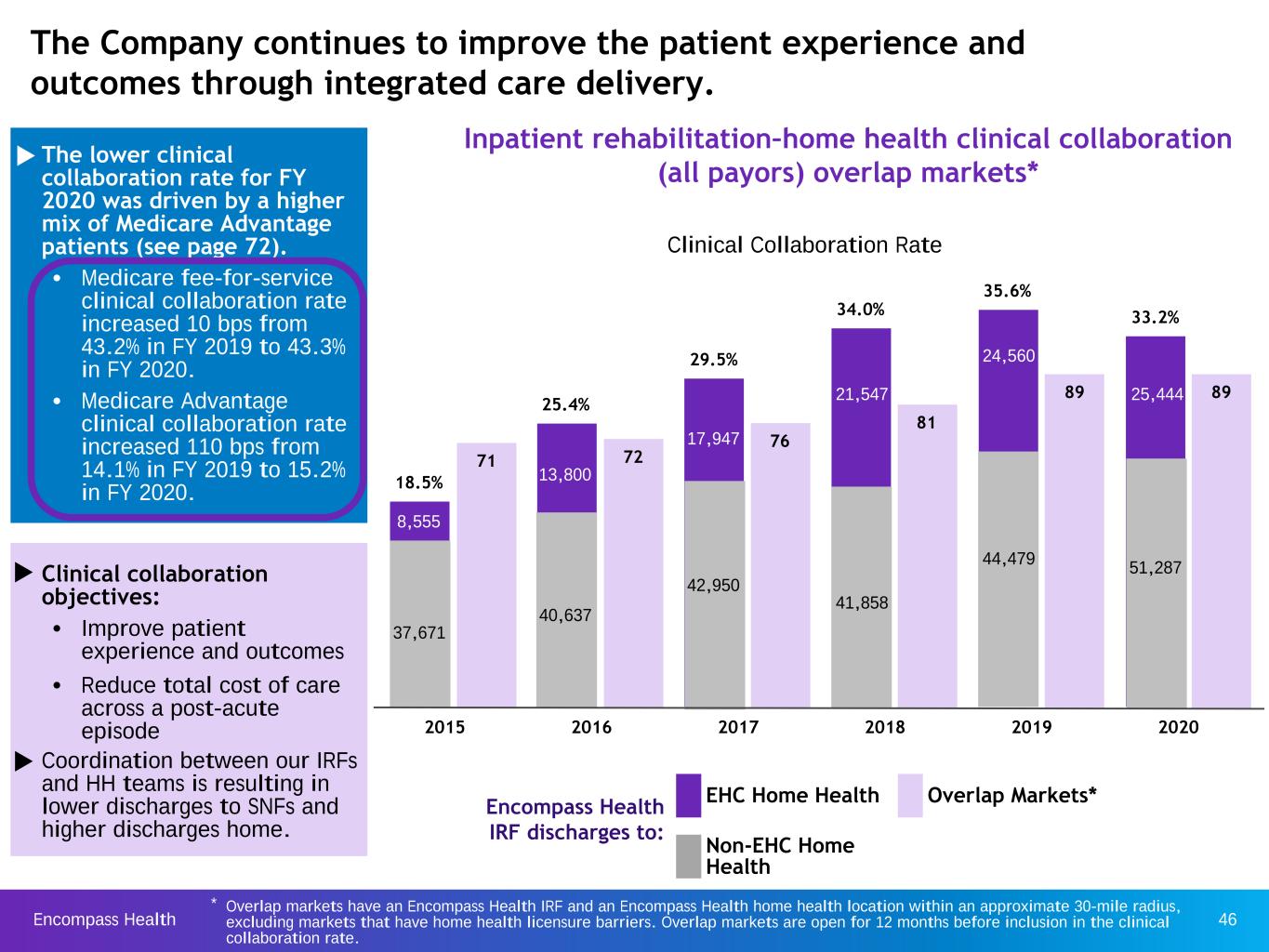
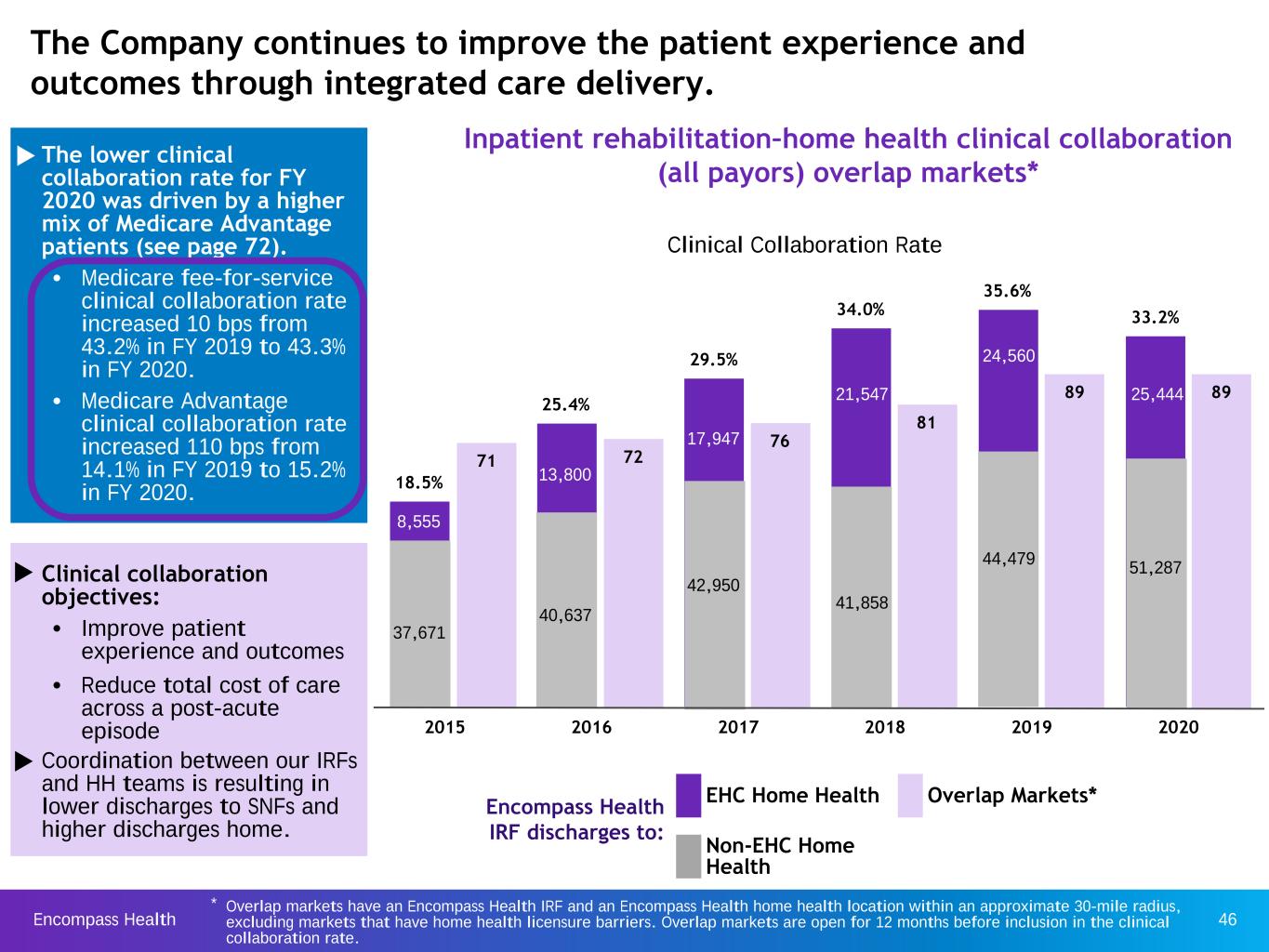
Encompass Health 46 * Overlap markets have an Encompass Health IRF and an Encompass Health home health location within an approximate 30-mile radius, excluding markets that have home health licensure barriers. Overlap markets are open for 12 months before inclusion in the clinical collaboration rate. The Company continues to improve the patient experience and outcomes through integrated care delivery. Inpatient rehabilitation–home health clinical collaboration (all payors) overlap markets* EHC Home Health Non-EHC Home Health Encompass Health IRF discharges to: Overlap Markets* 8,555 Clinical Collaboration Rate 17.260 u The lower clinical collaboration rate for FY 2020 was driven by a higher mix of Medicare Advantage patients (see page 72). Ÿ Medicare fee-for-service clinical collaboration rate increased 10 bps from 43.2% in FY 2019 to 43.3% in FY 2020. Ÿ Medicare Advantage clinical collaboration rate increased 110 bps from 14.1% in FY 2019 to 15.2% in FY 2020. u Clinical collaboration objectives: Ÿ Improve patient experience and outcomes Ÿ Reduce total cost of care across a post-acute episode u Coordination between our IRFs and HH teams is resulting in lower discharges to SNFs and higher discharges home. 71 72 76 81 89 89 18.5% 25.4% 29.5% 34.0% 35.6% 33.2% 2015 2016 2017 2018 2019 2020 37,671 40,637 42,950 41,858 44,479 51,287 8,555 13,800 17,947 21,547 24,560 25,444
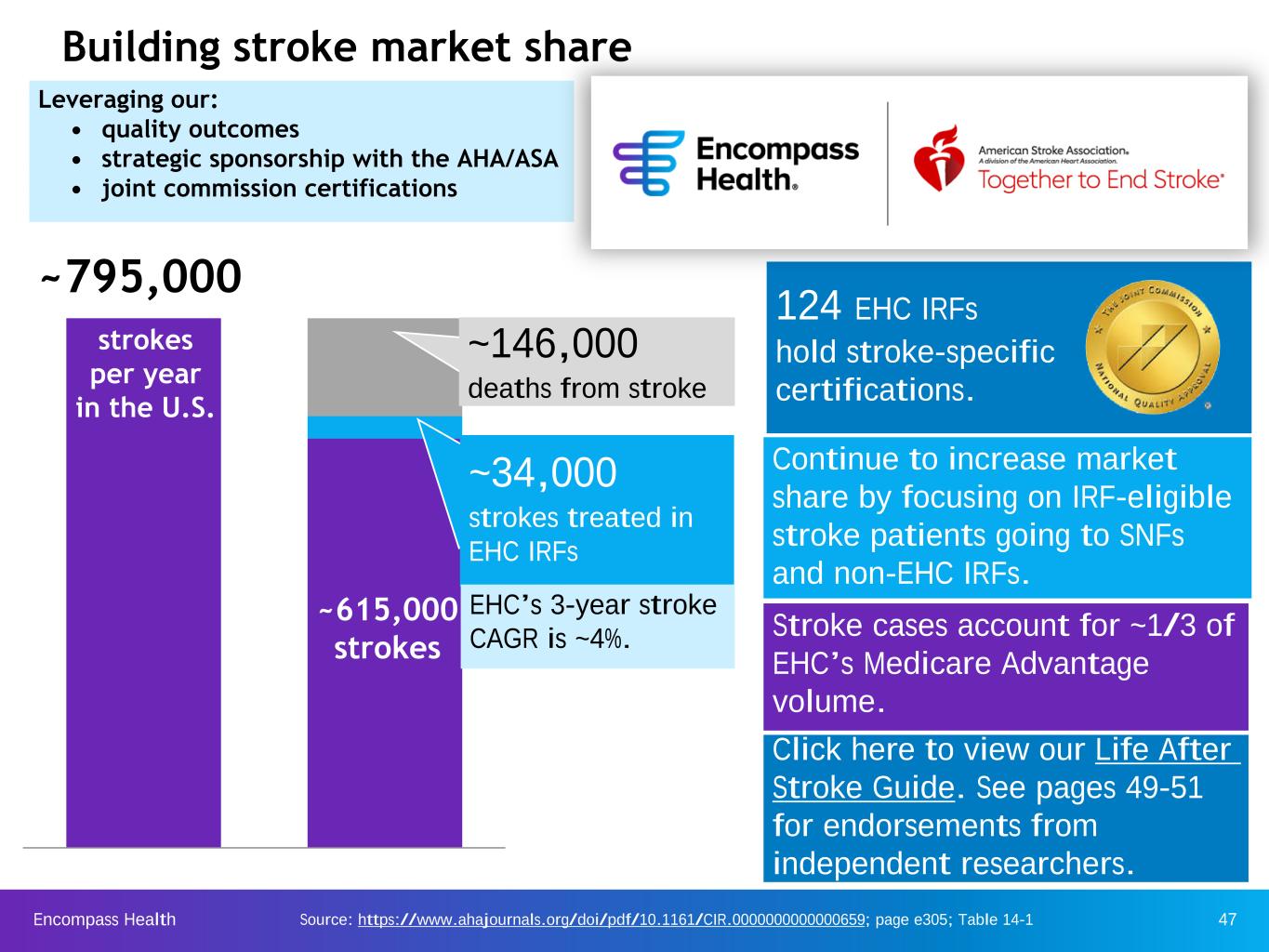
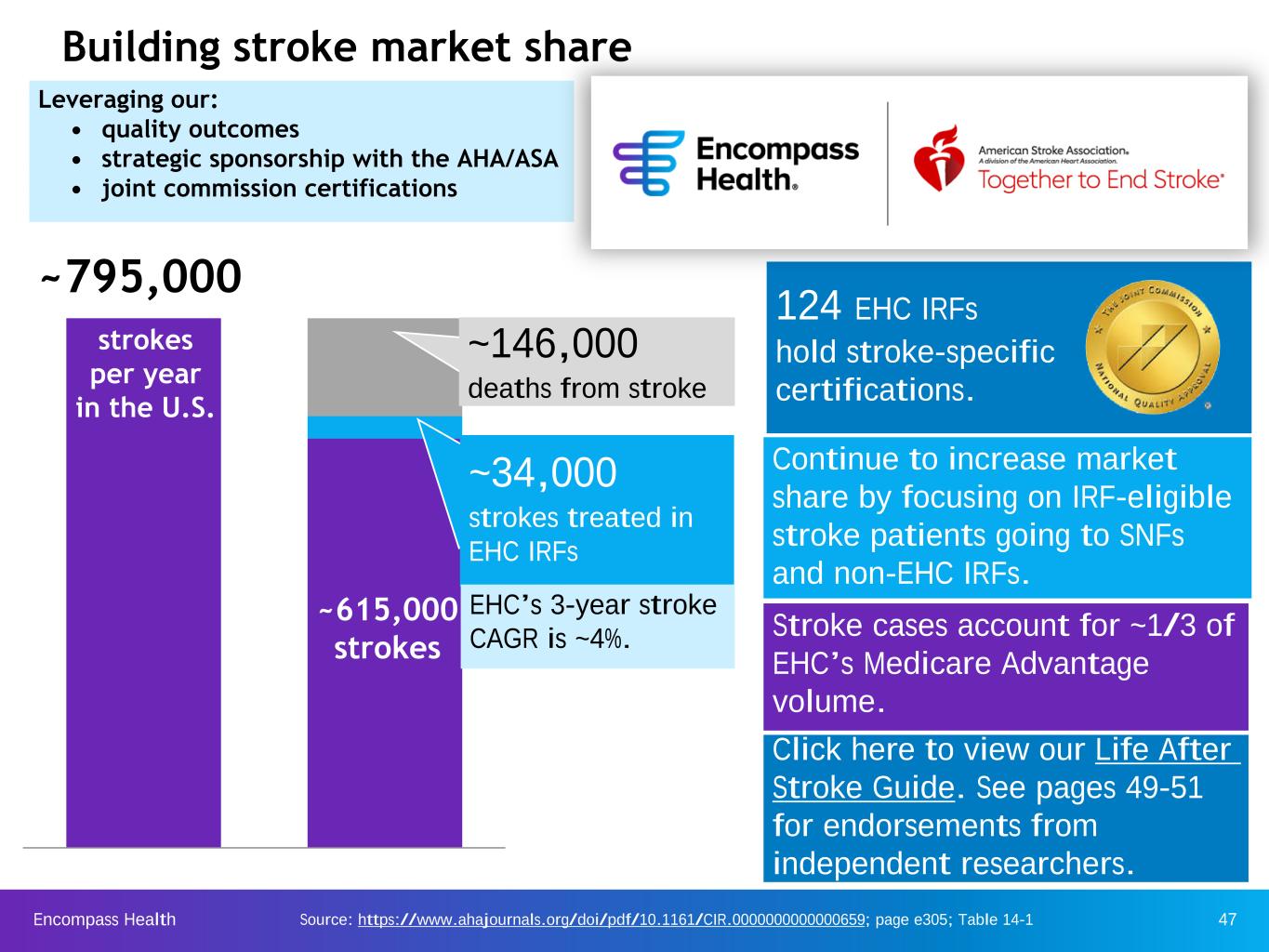
Encompass Health 47 Building stroke market share Source: https://www.ahajournals.org/doi/pdf/10.1161/CIR.0000000000000659; page e305; Table 14-1 Leveraging our: • quality outcomes • strategic sponsorship with the AHA/ASA • joint commission certifications 124 EHC IRFs hold stroke-specific certifications. Continue to increase market share by focusing on IRF-eligible stroke patients going to SNFs and non-EHC IRFs. Stroke cases account for ~1/3 of EHC’s Medicare Advantage volume. ~34,000 strokes treated in EHC IRFs EHC’s 3-year stroke CAGR is ~4%. ~795,000 strokes per year in the U.S. ~146,000 deaths from stroke ~615,000 strokes Click here to view our Life After Stroke Guide. See pages 49-51 for endorsements from independent researchers.

Encompass Health 48 • Total stroke incidence based on statistics released in annual AHA report • Mortality within stroke incidence is updated by AHA with greater frequency • EHC stroke market share defined as: Defining Stroke Market Share EHC LTM Stroke Discharges AHA Stroke Incidence Less Deaths** Medicare FFS 54.8%Medicare Adv. 19.9% Other 25.3% 2019 2020 Medicare FFS 48.8% Medicare Adv. 24.5% Other 26.7% Stroke % of Payor 2019 2020 % of total discharges 18.4% 19.0% % of Medicare FFS discharges 14.8% 14.9% % of Medicare Advantage discharges* 32.7% 29.8% 30,643 32,309 34,465 34,331 EHC Stroke Discharges 2017 2018 2019 2020 Building stroke market share Stroke market share EHC stroke payor mix 4.7% Market share 5.2% Market share 4.9% Market share 5.3% Market share * COVID-19 impacted patient mix in 2020 ** The denominator typically decreases over time as deaths resulting from stroke may lag the incidence of stroke.

Encompass Health 49 Independent research concludes IRFs are a better rehabilitation option for stroke patients than SNFs * ** AHA/ASA press release, “Inpatient rehab recommended over nursing homes for stroke rehab,” issued May 4, 2016 (newsroom.heart.org) “Guidelines for Adult Stroke Rehabilitation and Recovery,” issued May 2016 (stroke.ahajournals.org) “Whenever possible, the American Stroke Association strongly recommends that stroke patients be treated at an inpatient rehabilitation facility rather than a skilled nursing facility.” “IRF patients have higher rates of return to community living and greater functional recovery...” “If the hospital suggests sending your loved one to a skilled nursing facility after a stroke, advocate for the patient to go to an inpatient rehabilitation facility instead…”* 124 of the Company’s IRFs hold The Joint Commission’s Disease- Specific Care Certification in stroke rehabilitation.

Encompass Health 50 The Department of Veterans Affairs endorses the AHA/ASA Guidelines in their 2019 Guidelines on Stroke Rehabilitation There are ~20 million veterans and ~10 million are served by the Veterans Administration each year. “The Management of Stroke Rehabilitation” issued November 2019 (https://annals.org/aim/ fullarticle/2755728/management-stroke-rehabilitation-synopsis-2019-u-s-department-veterans-affairs)

Encompass Health 51 2019 JAMA published article comparing functional improvements of stroke patients receiving care in IRF vs SNF Conclusions This cohort study found that Medicare beneficiaries who received services at an IRF after a stroke demonstrated greater improvement in mobility and self-care compared with patients who received inpatient rehabilitation at a SNF. A significant difference in functional improvement remained after accounting for patient, clinical, and facility characteristics at admission. Our findings indicate the need to carefully manage discharge to postacute care based on the patient's needs and potential for recovery. Postacute care reform based on the IMPACT Act must avoid a payment system that shifts patients with stroke who could benefit from intensive inpatient rehabilitation to lower cost settings. “The Management of Stroke Rehabilitation” issued December 2019 (https://jamanetwork.com/journals/ jamanetworkopen/fullarticle/2756256?resultClick=1)
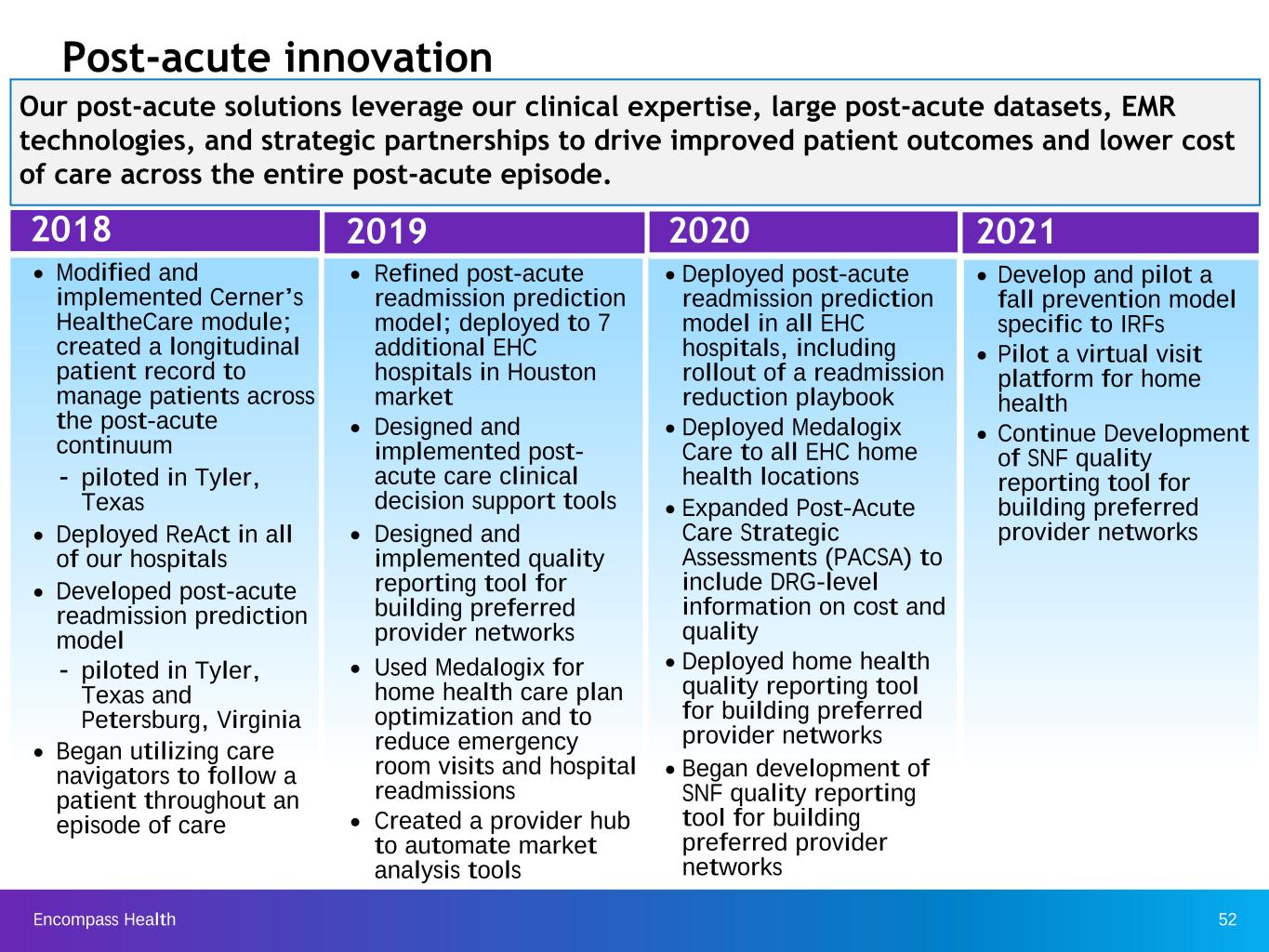
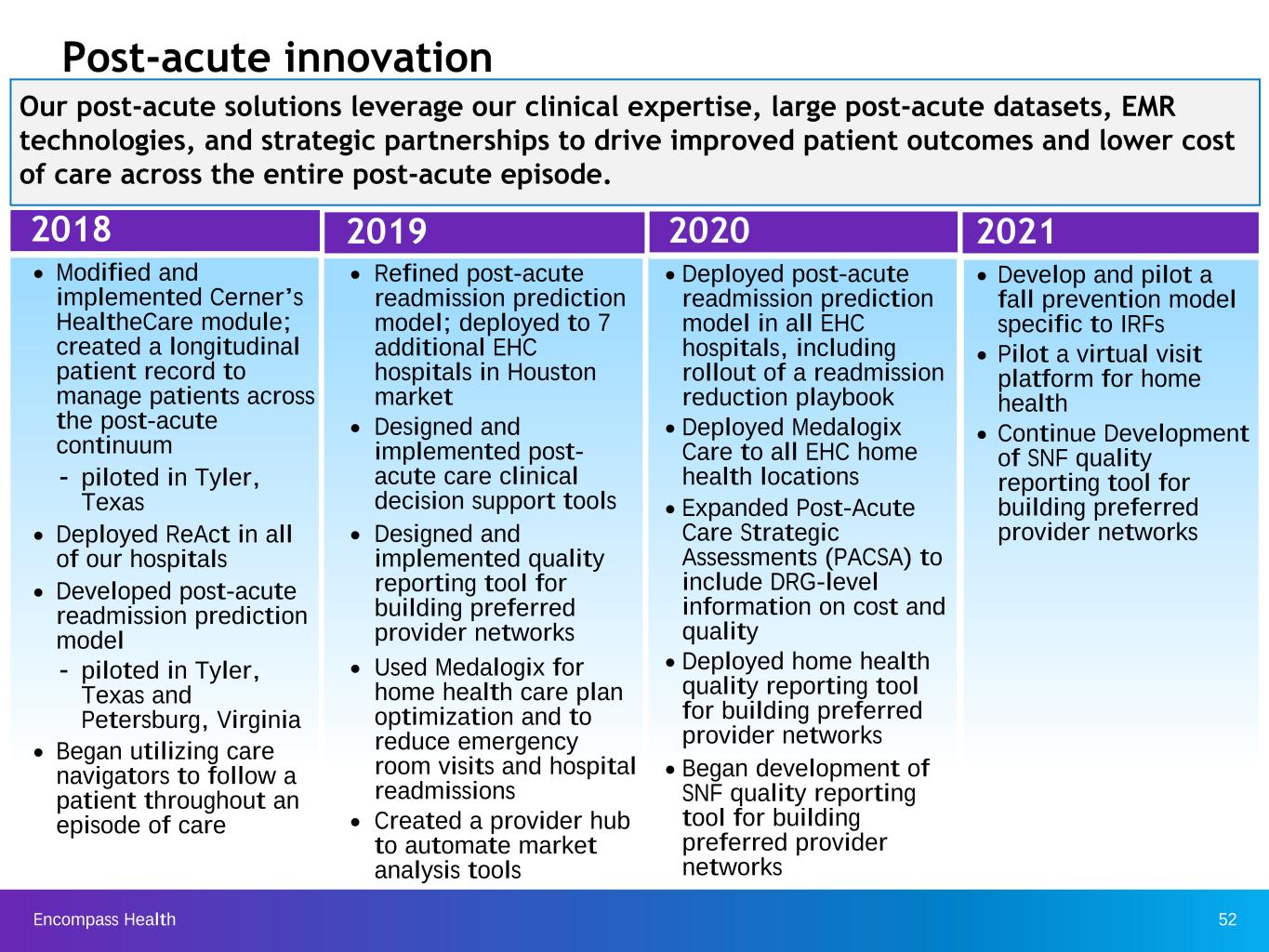
Encompass Health 52 2018 Ÿ Modified and implemented Cerner’s HealtheCare module; created a longitudinal patient record to manage patients across the post-acute continuum – piloted in Tyler, Texas Ÿ Deployed ReAct in all of our hospitals Ÿ Developed post-acute readmission prediction model – piloted in Tyler, Texas and Petersburg, Virginia Ÿ Began utilizing care navigators to follow a patient throughout an episode of care Post-acute innovation Our post-acute solutions leverage our clinical expertise, large post-acute datasets, EMR technologies, and strategic partnerships to drive improved patient outcomes and lower cost of care across the entire post-acute episode. 2019 Ÿ Refined post-acute readmission prediction model; deployed to 7 additional EHC hospitals in Houston market Ÿ Designed and implemented post- acute care clinical decision support tools Ÿ Designed and implemented quality reporting tool for building preferred provider networks Ÿ Used Medalogix for home health care plan optimization and to reduce emergency room visits and hospital readmissions Ÿ Created a provider hub to automate market analysis tools 2020 Ÿ Deployed post-acute readmission prediction model in all EHC hospitals, including rollout of a readmission reduction playbook Ÿ Deployed Medalogix Care to all EHC home health locations Ÿ Expanded Post-Acute Care Strategic Assessments (PACSA) to include DRG-level information on cost and quality Ÿ Deployed home health quality reporting tool for building preferred provider networks Ÿ Began development of SNF quality reporting tool for building preferred provider networks 2021 Ÿ Develop and pilot a fall prevention model specific to IRFs Ÿ Pilot a virtual visit platform for home health Ÿ Continue Development of SNF quality reporting tool for building preferred provider networks
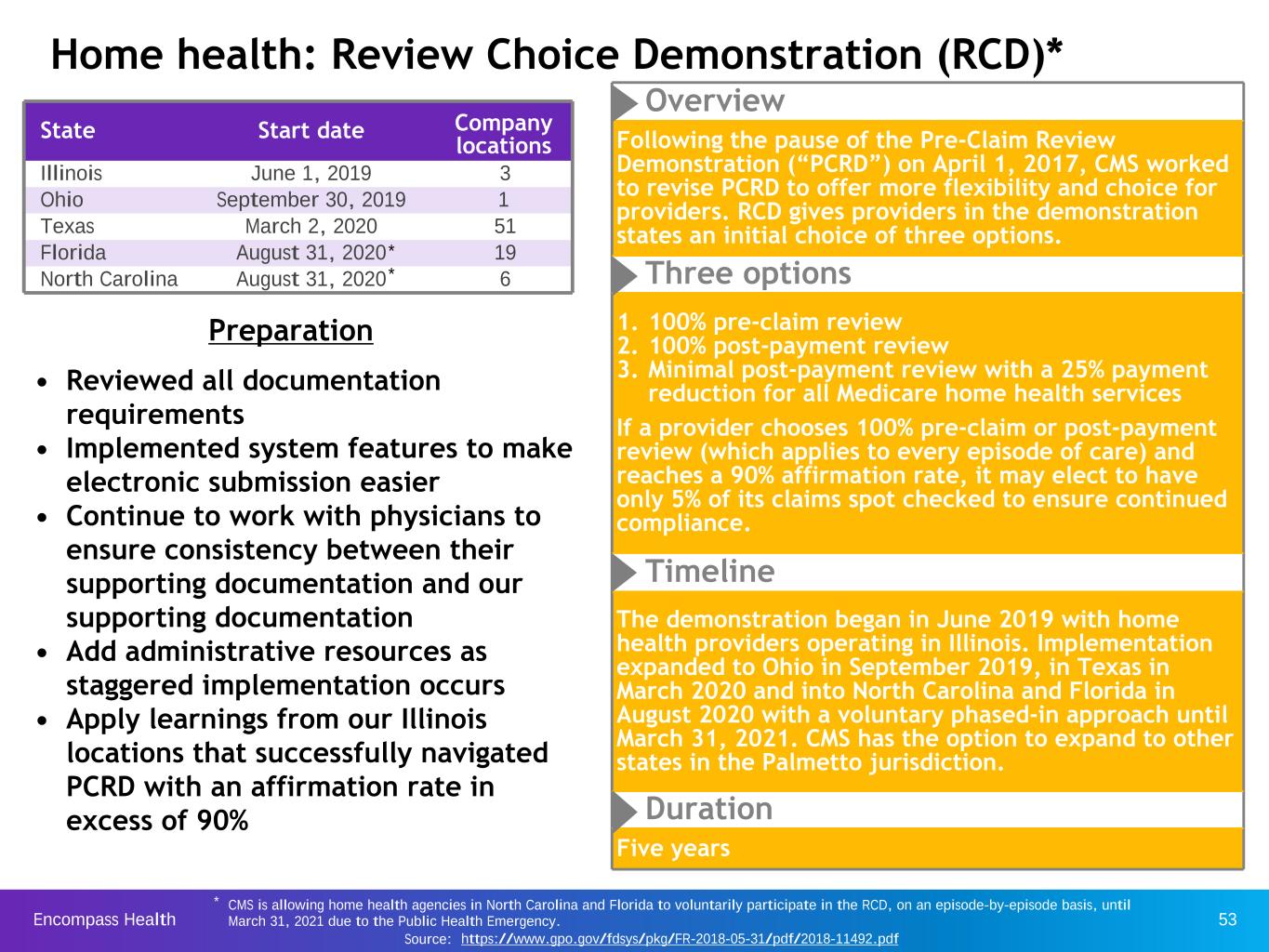
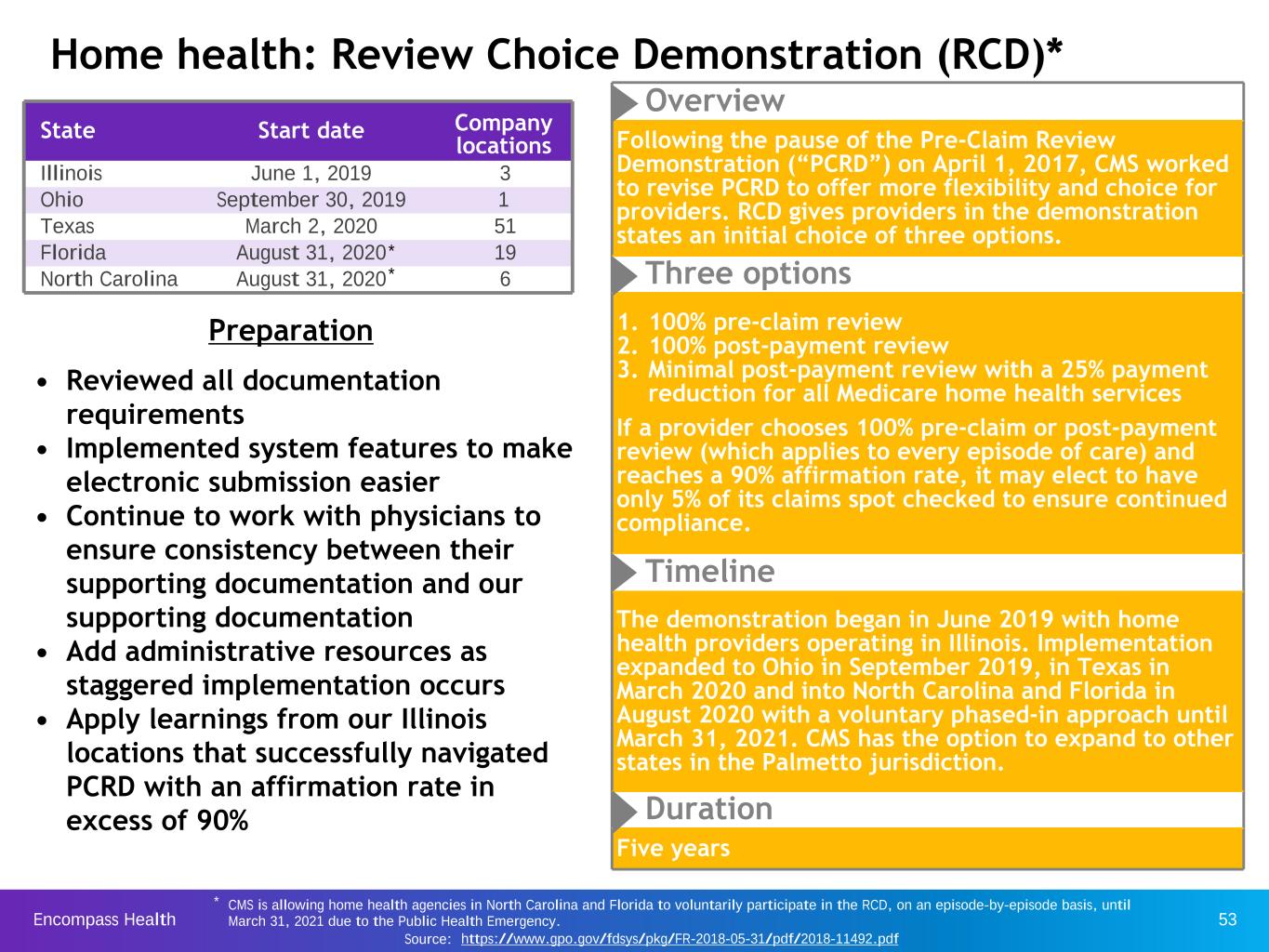
Encompass Health 53 State Start date Company locations Illinois June 1, 2019 3 Ohio September 30, 2019 1 Texas March 2, 2020 51 Florida August 31, 2020 19 North Carolina August 31, 2020 6 Preparation • Reviewed all documentation requirements • Implemented system features to make electronic submission easier • Continue to work with physicians to ensure consistency between their supporting documentation and our supporting documentation • Add administrative resources as staggered implementation occurs • Apply learnings from our Illinois locations that successfully navigated PCRD with an affirmation rate in excess of 90% Overview Following the pause of the Pre-Claim Review Demonstration (“PCRD”) on April 1, 2017, CMS worked to revise PCRD to offer more flexibility and choice for providers. RCD gives providers in the demonstration states an initial choice of three options. Three options 1. 100% pre-claim review 2. 100% post-payment review 3. Minimal post-payment review with a 25% payment reduction for all Medicare home health services If a provider chooses 100% pre-claim or post-payment review (which applies to every episode of care) and reaches a 90% affirmation rate, it may elect to have only 5% of its claims spot checked to ensure continued compliance. Timeline The demonstration began in June 2019 with home health providers operating in Illinois. Implementation expanded to Ohio in September 2019, in Texas in March 2020 and into North Carolina and Florida in August 2020 with a voluntary phased-in approach until March 31, 2021. CMS has the option to expand to other states in the Palmetto jurisdiction. Duration Five years Home health: Review Choice Demonstration (RCD)* * CMS is allowing home health agencies in North Carolina and Florida to voluntarily participate in the RCD, on an episode-by-episode basis, until March 31, 2021 due to the Public Health Emergency. Source: https://www.gpo.gov/fdsys/pkg/FR-2018-05-31/pdf/2018-11492.pdf * *

Encompass Health 54 Evidence-based clinical initiatives to reduce readmissions and improve patient outcomes "ReACT" and Readmission prevention • Standardized and improved infection control practices across the company. These practices and oversight provide the clinicians with tools to successfully navigate the COVID-19 pandemic. • Applied evidence- based decision making Sepsis/SIRS alert Infection control • Developed predictive models to identify patients at risk for transfer and readmission to acute-care hospitals • Implemented intervention strategies as part of the plan of care and notify home health provider of risk prior to discharge • Implemented an evidenced-based predictive model to identify patients at-risk for sepsis or SIRS • Applied intervention strategies as part of the plan of care Medication reconciliation • Implemented a multidisciplinary reconciliation process using the Company's EMR upon admission and discharge Reduce opioid use • Implemented a multidisciplinary approach to improve pain management, including non- pharmacologic treatment of pain and vigilant opioid stewardship Reduce readmissions & improve outcomes
Encompass Health 55 Capital structure Encompass Health is positioned with a cost-efficient, flexible capital structure.
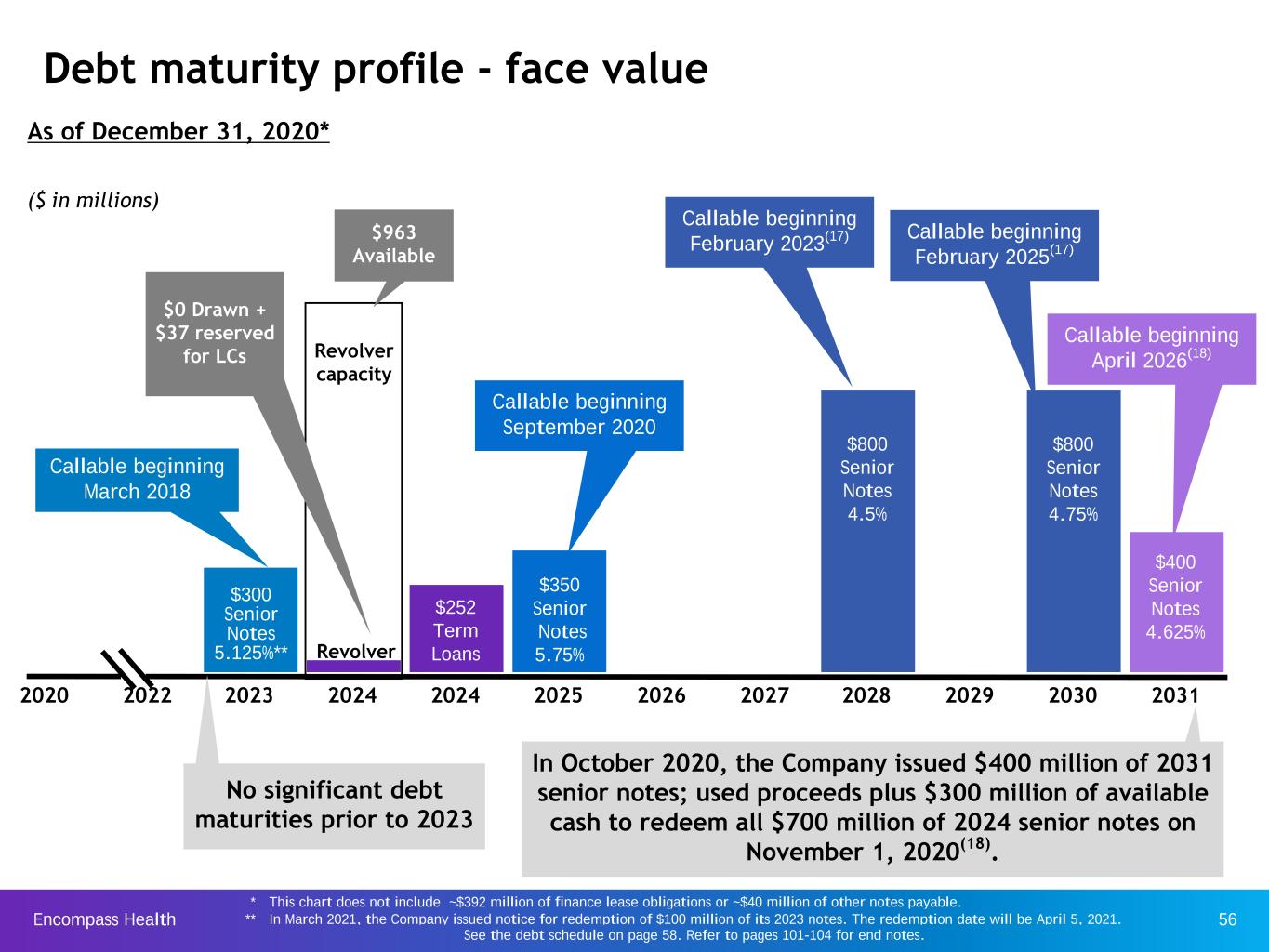
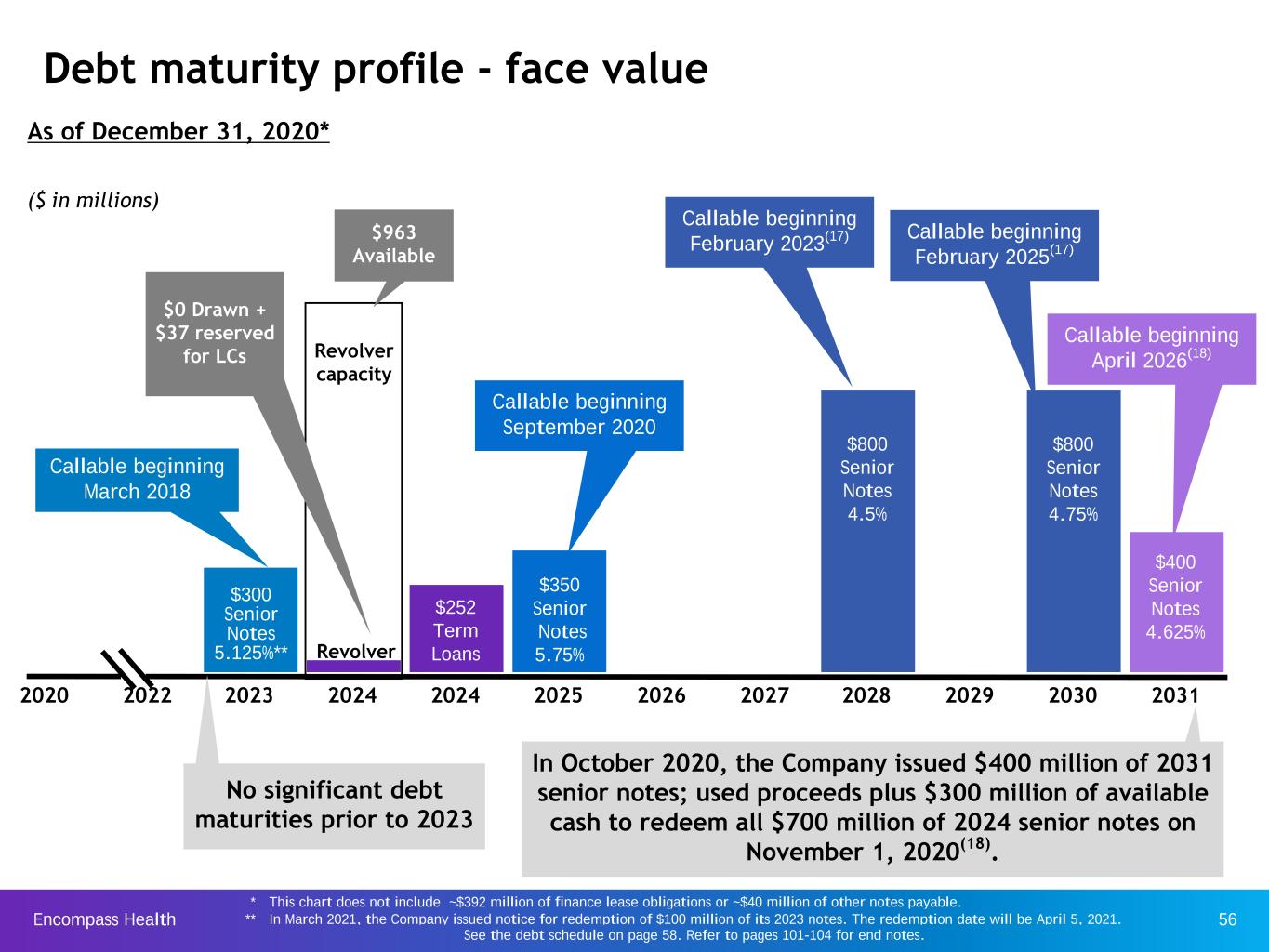
Encompass Health 56 Debt maturity profile - face value 2020 2022 2023 2024 2024 2025 2026 2027 2028 2029 2030 2031 $350 Senior Notes 5.75% $300 Senior Notes 5.125%** ($ in millions) Revolver capacity $252 Term Loans No significant debt maturities prior to 2023 Callable beginning March 2018 $800 Senior Notes 4.75% $800 Senior Notes 4.5% Revolver As of December 31, 2020* $963 Available $0 Drawn + $37 reserved for LCs Callable beginning September 2020 Callable beginning February 2025(17) Callable beginning February 2023(17) $400 Senior Notes 4.625% Callable beginning April 2026(18) In October 2020, the Company issued $400 million of 2031 senior notes; used proceeds plus $300 million of available cash to redeem all $700 million of 2024 senior notes on November 1, 2020(18). * This chart does not include ~$392 million of finance lease obligations or ~$40 million of other notes payable. ** In March 2021, the Company issued notice for redemption of $100 million of its 2023 notes. The redemption date will be April 5, 2021. See the debt schedule on page 58. Refer to pages 101-104 for end notes.

Encompass Health 57 3.02 2.58 2.51 3.06 3.29 S&P Moody’s Corporate rating BB- Ba3 Outlook Stable Stable Revolver rating BB+ Baa3 Senior notes rating B+ B1 Financial leverage and liquidity (1) Liquidity Credit ratings (Billions) Leverage ratio* Total debt 3.8x*** December 31, 2020 December 31, 2019 Cash available $ 224.0 $ 94.8 Revolver 1,000.0 1,000.0 Less: - Draws — (45.0) - Letters of credit (36.7) (38.9) Available $ 963.3 $ 916.1 Total liquidity $ 1,187.3 $ 1,010.9 Reconciliations to GAAP provided on pages 93-99. See debt schedule on page 58. 3.8x** * The leverage ratio is based on trailing four quarters of Adjusted EBITDA. ** Increase in financial leverage due to the acquisition of Encompass Home Health and Hospice (Dec. 2014), Reliant Hospital Partners (Oct. 2015), and CareSouth Health System, Inc. (Nov. 2015). *** Increase in financial leverage due to funding of final put of Home Health Holdings rollover shares and exercise of SARs (see page 60) as well as the impact of COVID-19 on Adjusted EBITDA. 20202016 2017 2018 2019 The leverage ratio net of cash on the balance sheet was 3.6x as of December 31, 2020.
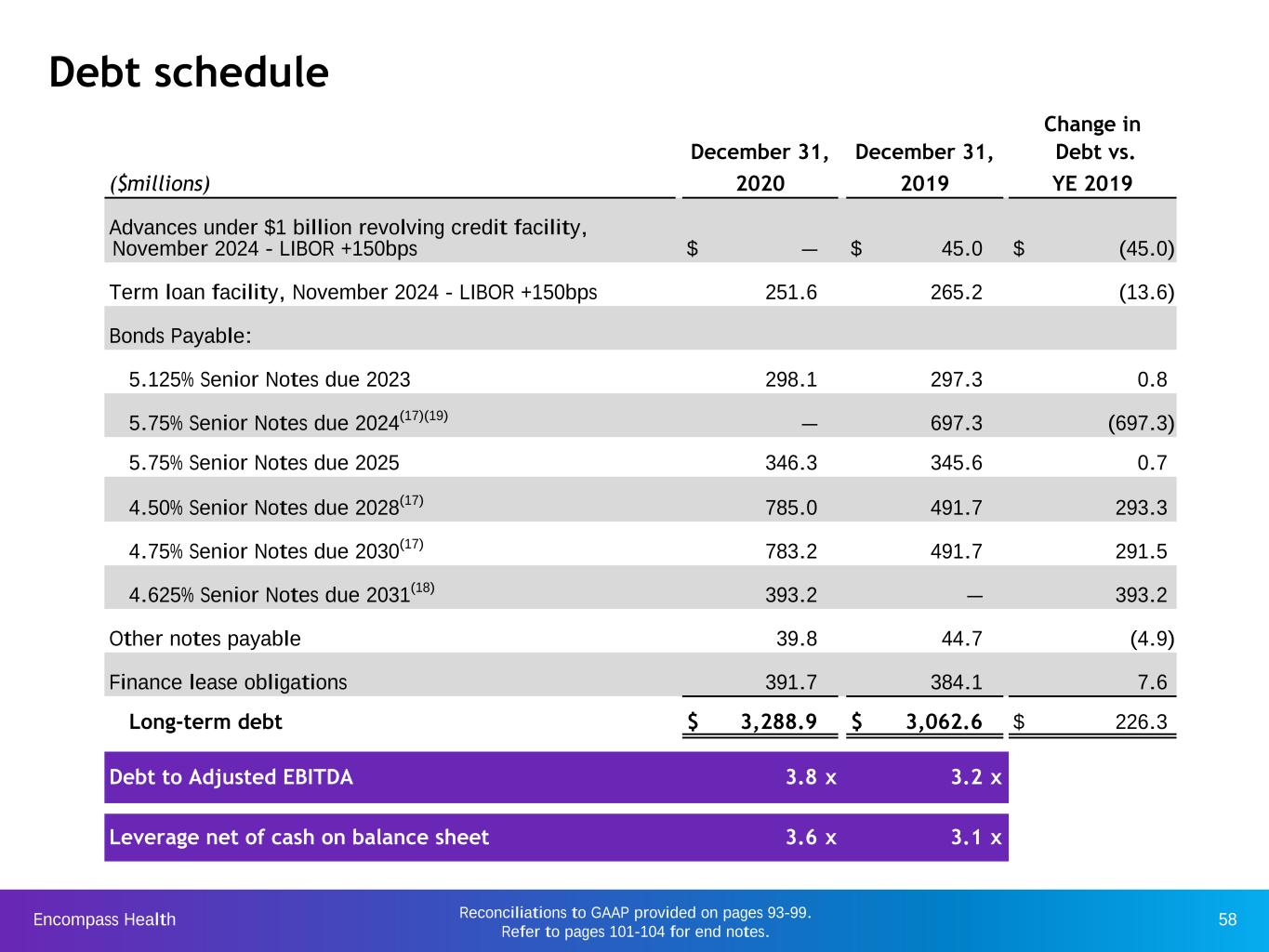
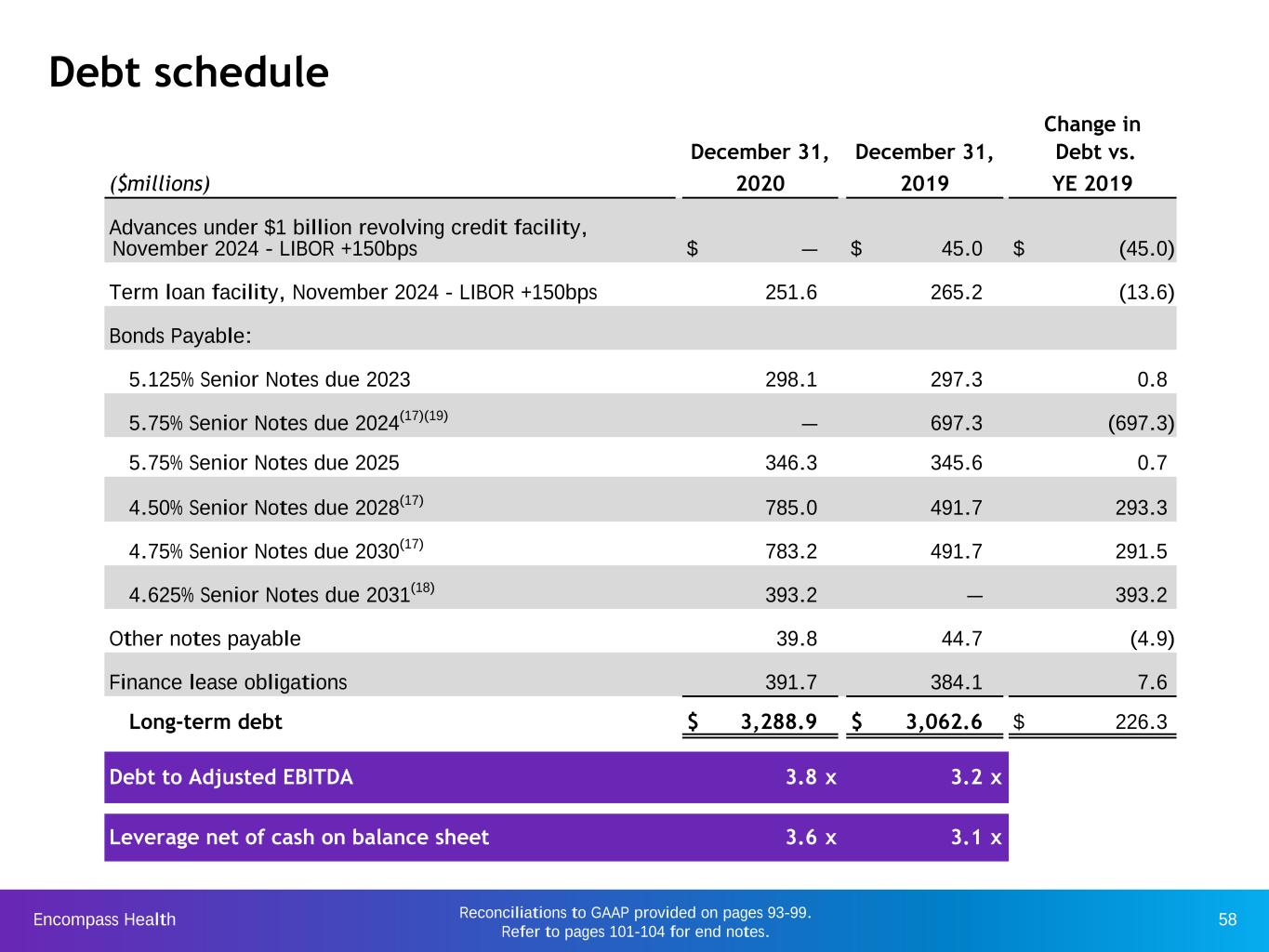
Encompass Health 58Reconciliations to GAAP provided on pages 93-99. Refer to pages 101-104 for end notes. Debt schedule Change in December 31, December 31, Debt vs. ($millions) 2020 2019 YE 2019 Advances under $1 billion revolving credit facility, November 2024 - LIBOR +150bps $ — $ 45.0 $ (45.0) Term loan facility, November 2024 - LIBOR +150bps 251.6 265.2 (13.6) Bonds Payable: 5.125% Senior Notes due 2023 298.1 297.3 0.8 5.75% Senior Notes due 2024(17)(19) — 697.3 (697.3) 5.75% Senior Notes due 2025 346.3 345.6 0.7 4.50% Senior Notes due 2028(17) 785.0 491.7 293.3 4.75% Senior Notes due 2030(17) 783.2 491.7 291.5 4.625% Senior Notes due 2031(18) 393.2 — 393.2 Other notes payable 39.8 44.7 (4.9) Finance lease obligations 391.7 384.1 7.6 Long-term debt $ 3,288.9 $ 3,062.6 $ 226.3 Debt to Adjusted EBITDA 3.8 x 3.2 x Leverage net of cash on balance sheet 3.6 x 3.1 x
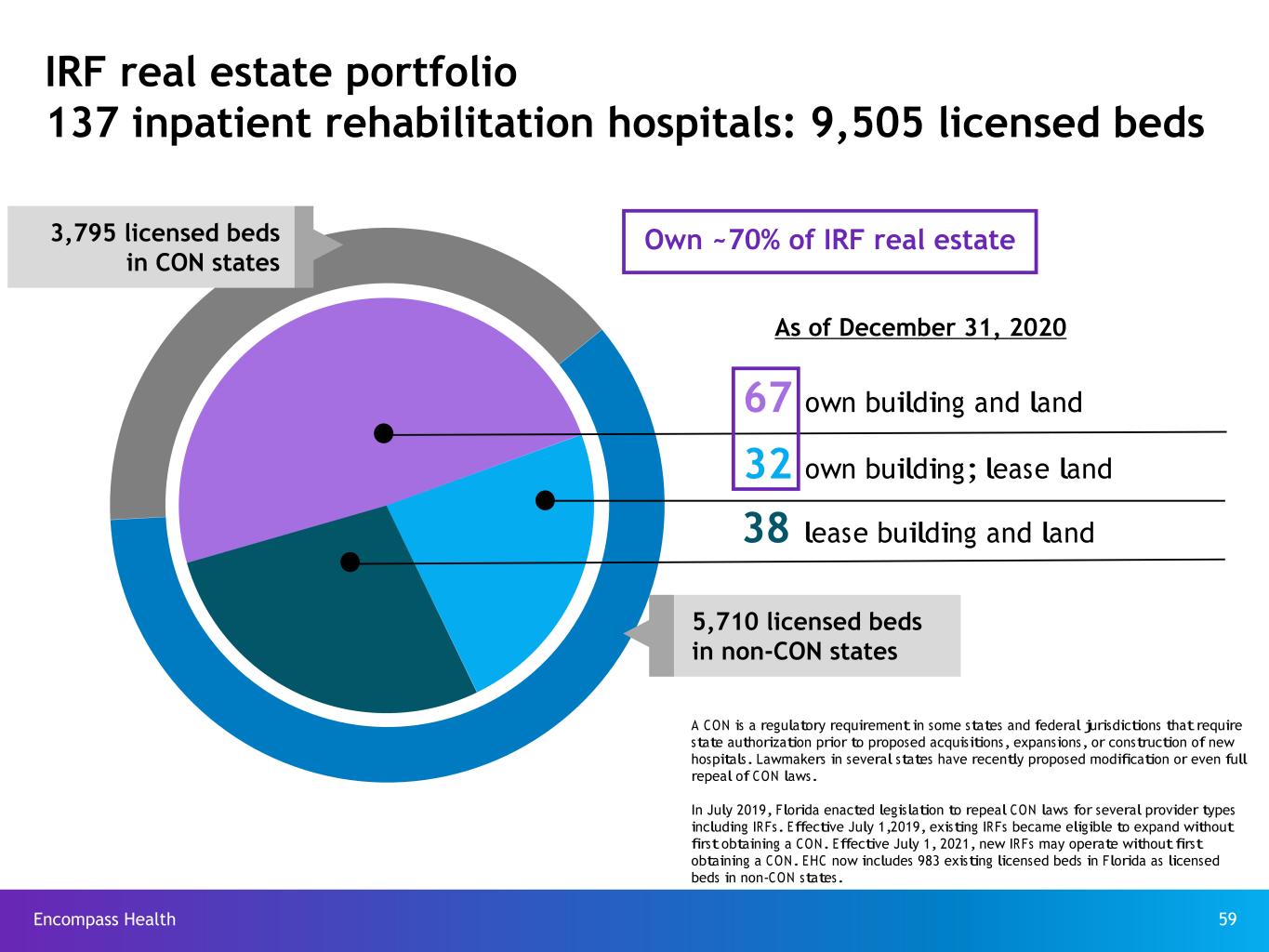
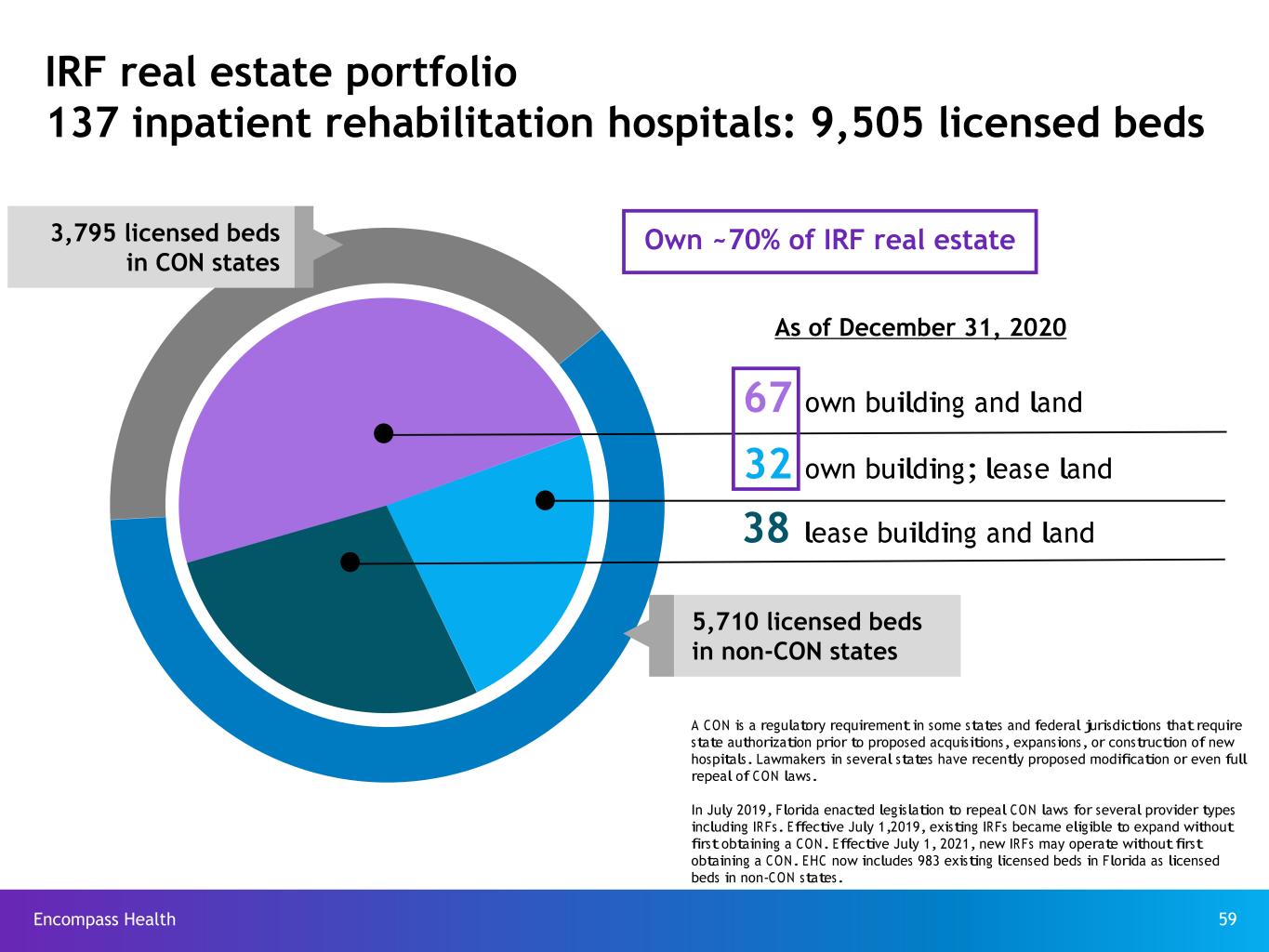
Encompass Health 59 38 lease building and land A CON is a regulatory requirement in some states and federal jurisdictions that require state authorization prior to proposed acquisitions, expansions, or construction of new hospitals. Lawmakers in several states have recently proposed modification or even full repeal of CON laws. In July 2019, Florida enacted legislation to repeal CON laws for several provider types including IRFs. Effective July 1,2019, existing IRFs became eligible to expand without first obtaining a CON. Effective July 1, 2021, new IRFs may operate without first obtaining a CON. EHC now includes 983 existing licensed beds in Florida as licensed beds in non-CON states. 67 own building and land 32 own building; lease land IRF real estate portfolio 137 inpatient rehabilitation hospitals: 9,505 licensed beds 3,795 licensed beds in CON states 5,710 licensed beds in non-CON states As of December 31, 2020 Own ~70% of IRF real estate
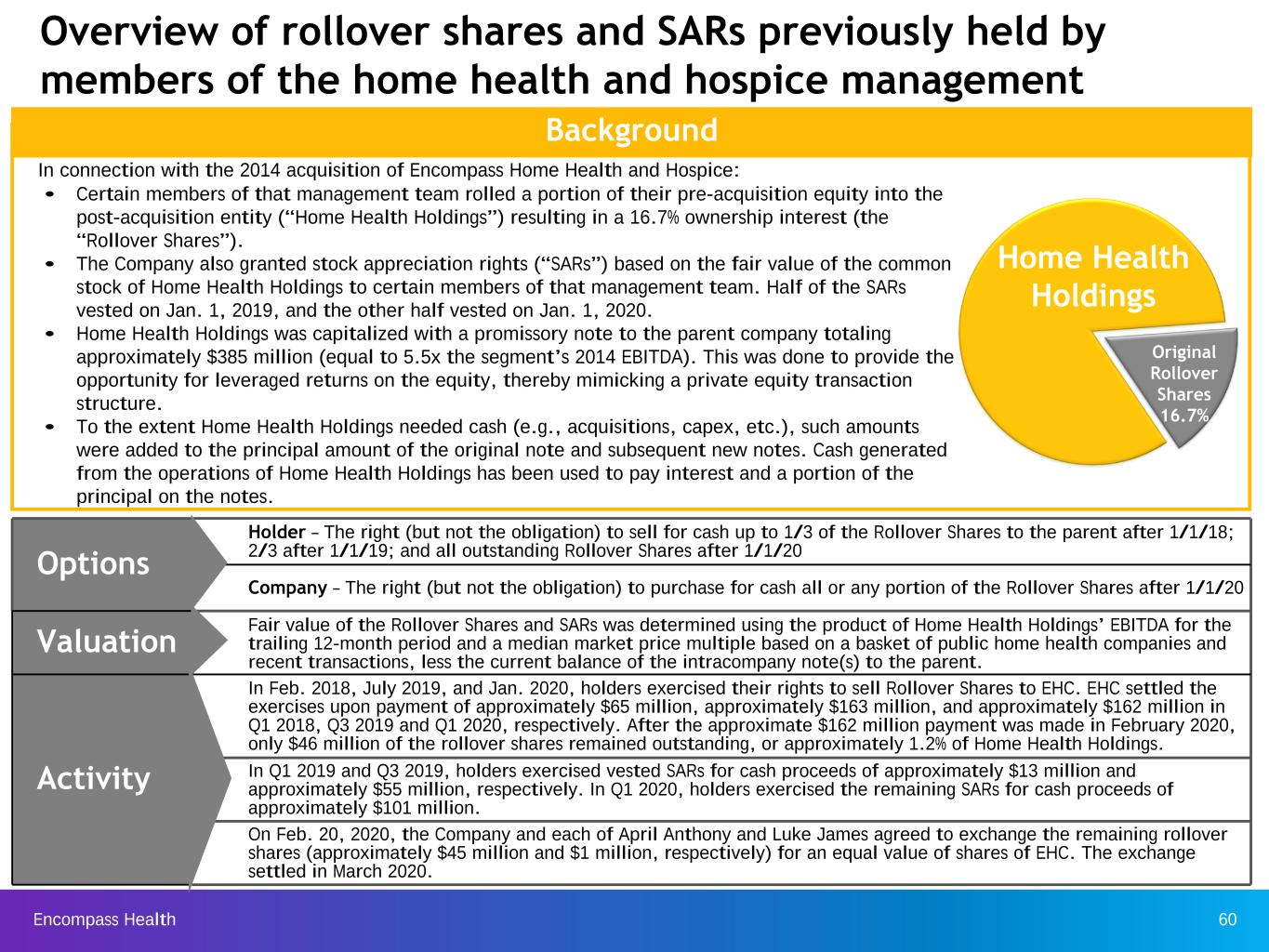
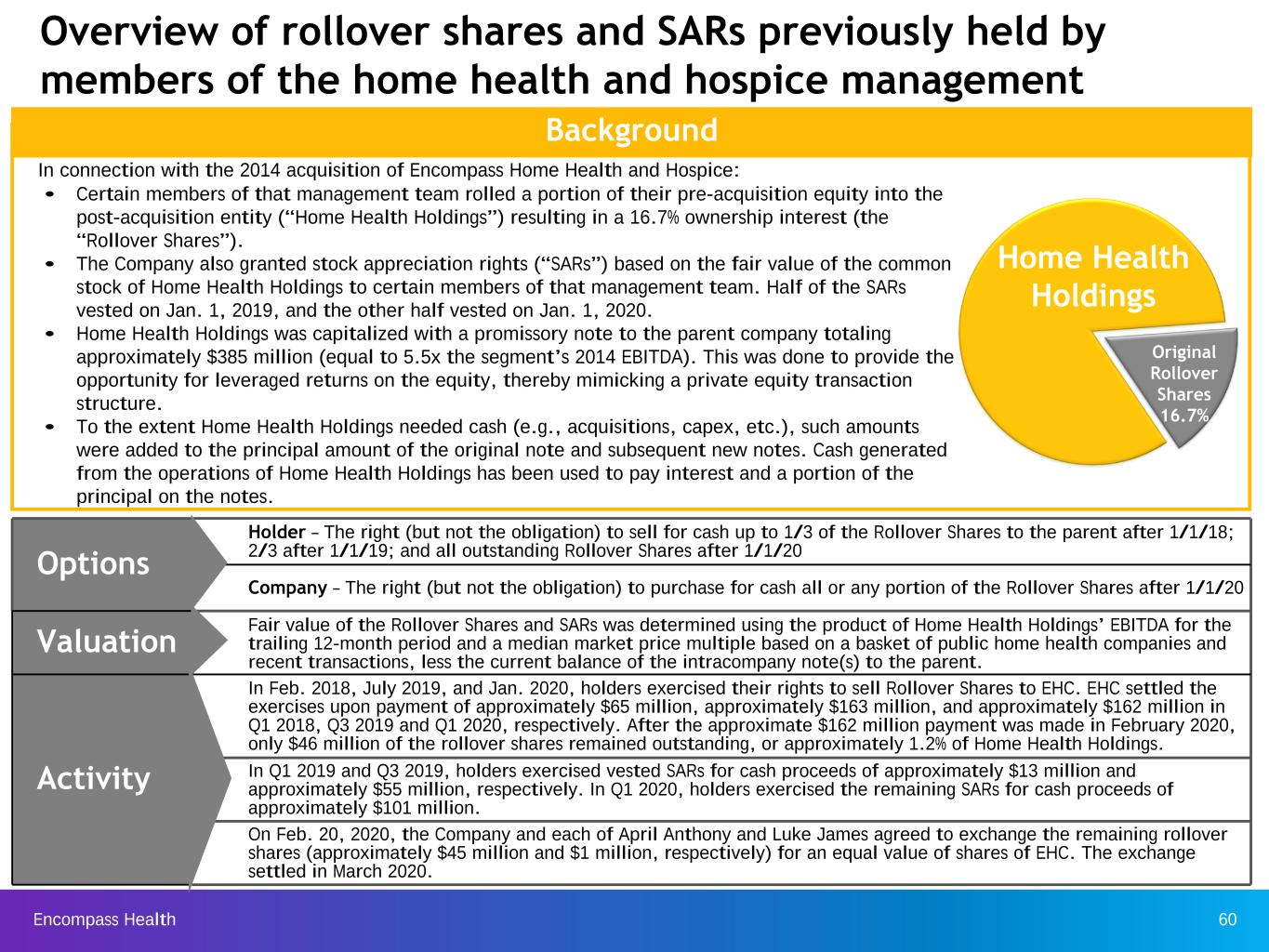
Encompass Health 60 Options Holder – The right (but not the obligation) to sell for cash up to 1/3 of the Rollover Shares to the parent after 1/1/18; 2/3 after 1/1/19; and all outstanding Rollover Shares after 1/1/20 Company – The right (but not the obligation) to purchase for cash all or any portion of the Rollover Shares after 1/1/20 Valuation Fair value of the Rollover Shares and SARs was determined using the product of Home Health Holdings’ EBITDA for the trailing 12-month period and a median market price multiple based on a basket of public home health companies and recent transactions, less the current balance of the intracompany note(s) to the parent. Activity In Feb. 2018, July 2019, and Jan. 2020, holders exercised their rights to sell Rollover Shares to EHC. EHC settled the exercises upon payment of approximately $65 million, approximately $163 million, and approximately $162 million in Q1 2018, Q3 2019 and Q1 2020, respectively. After the approximate $162 million payment was made in February 2020, only $46 million of the rollover shares remained outstanding, or approximately 1.2% of Home Health Holdings. In Q1 2019 and Q3 2019, holders exercised vested SARs for cash proceeds of approximately $13 million and approximately $55 million, respectively. In Q1 2020, holders exercised the remaining SARs for cash proceeds of approximately $101 million. On Feb. 20, 2020, the Company and each of April Anthony and Luke James agreed to exchange the remaining rollover shares (approximately $45 million and $1 million, respectively) for an equal value of shares of EHC. The exchange settled in March 2020. In connection with the 2014 acquisition of Encompass Home Health and Hospice: • Certain members of that management team rolled a portion of their pre-acquisition equity into the post-acquisition entity (“Home Health Holdings”) resulting in a 16.7% ownership interest (the “Rollover Shares”). • The Company also granted stock appreciation rights (“SARs”) based on the fair value of the common stock of Home Health Holdings to certain members of that management team. Half of the SARs vested on Jan. 1, 2019, and the other half vested on Jan. 1, 2020. • Home Health Holdings was capitalized with a promissory note to the parent company totaling approximately $385 million (equal to 5.5x the segment’s 2014 EBITDA). This was done to provide the opportunity for leveraged returns on the equity, thereby mimicking a private equity transaction structure. • To the extent Home Health Holdings needed cash (e.g., acquisitions, capex, etc.), such amounts were added to the principal amount of the original note and subsequent new notes. Cash generated from the operations of Home Health Holdings has been used to pay interest and a portion of the principal on the notes. Overview of rollover shares and SARs previously held by members of the home health and hospice management team Background Home Health Holdings Original Rollover Shares 16.7%

Encompass Health 61 Information technology Encompass Health utilizes information technology to improve patient care and generate operating efficiencies.

Encompass Health 62 IRF clinical information system: improved patient outcomes and streamlined operational efficiencies Discharge planning and patient education •Patient history •Problems and diagnoses •Orders and results •Plan of care •Workflow alerts and reminders •Treatment and interventions Document imaging Charge and registration services •Registration •Census •Coding •Billing Quality reporting •Uniform data systems •Clinical data warehouse •Clinical intelligence Referral hospitals Ancillary services Clinical notes • Physician • Nursing • Therapy • Care mgmt. Integrated and bar-coded point of care medication administration Treatment plan • Computerized Physician Order Entry ("CPOE") • Clinical Decision Support ("CDS") • Predictive algorithm and clinical protocols to identify and reduce the risk of acute care transfer Coordinate care and engage patients Pre-admission assessment & approval Integrated electronic medical record
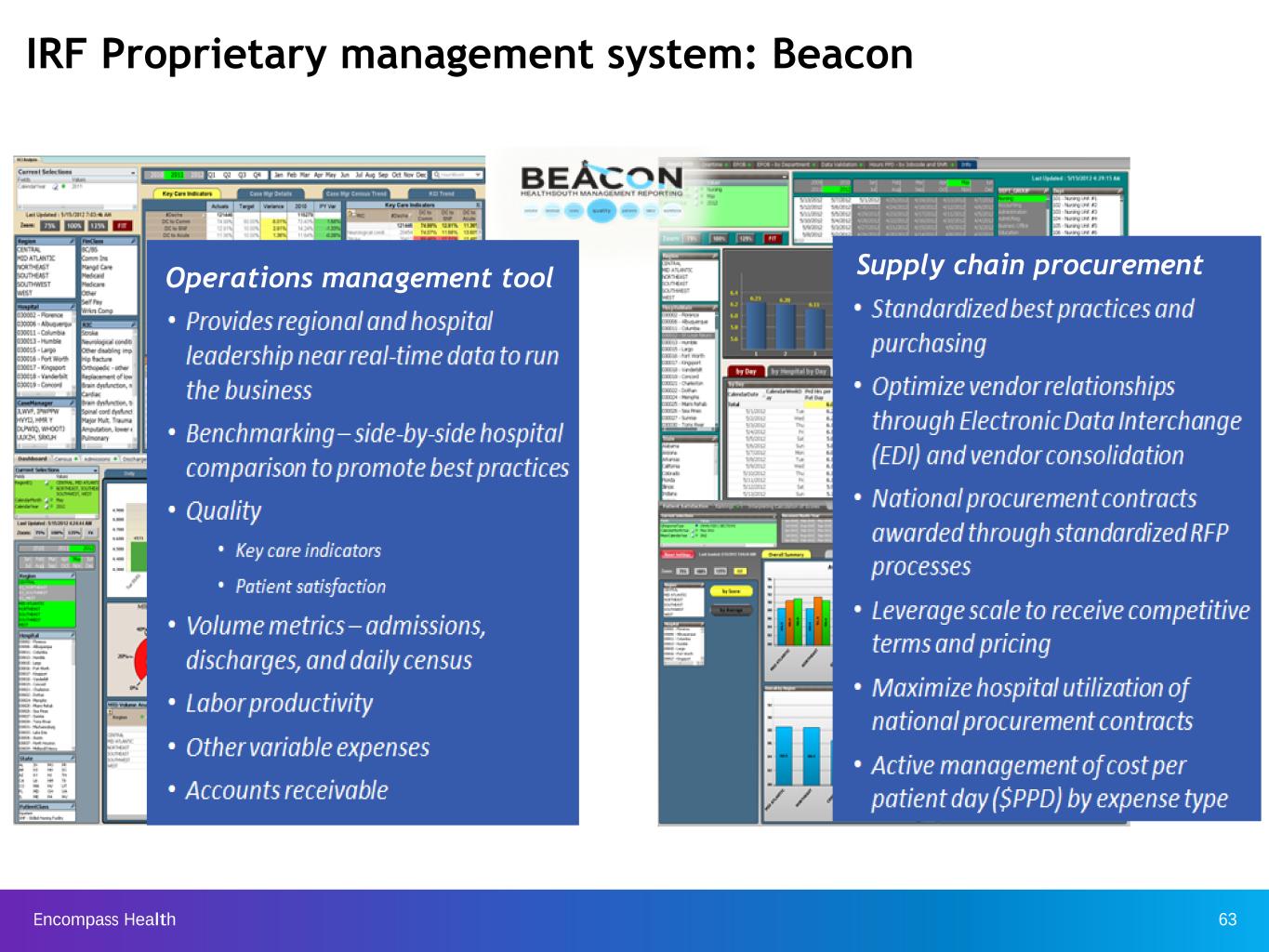
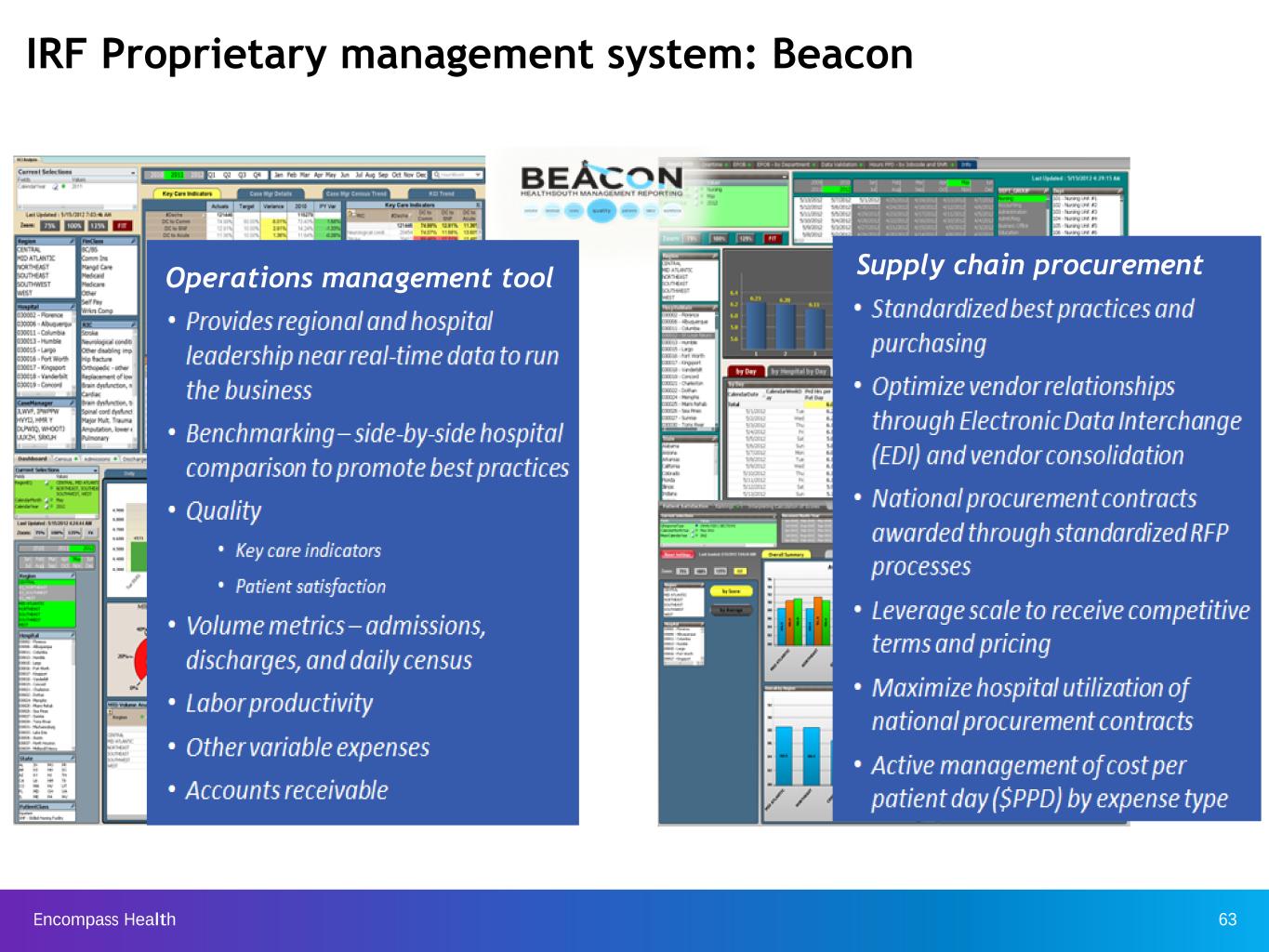
Encompass Health 63 IRF Proprietary management system: Beacon Operations management tool Supply chain procurement
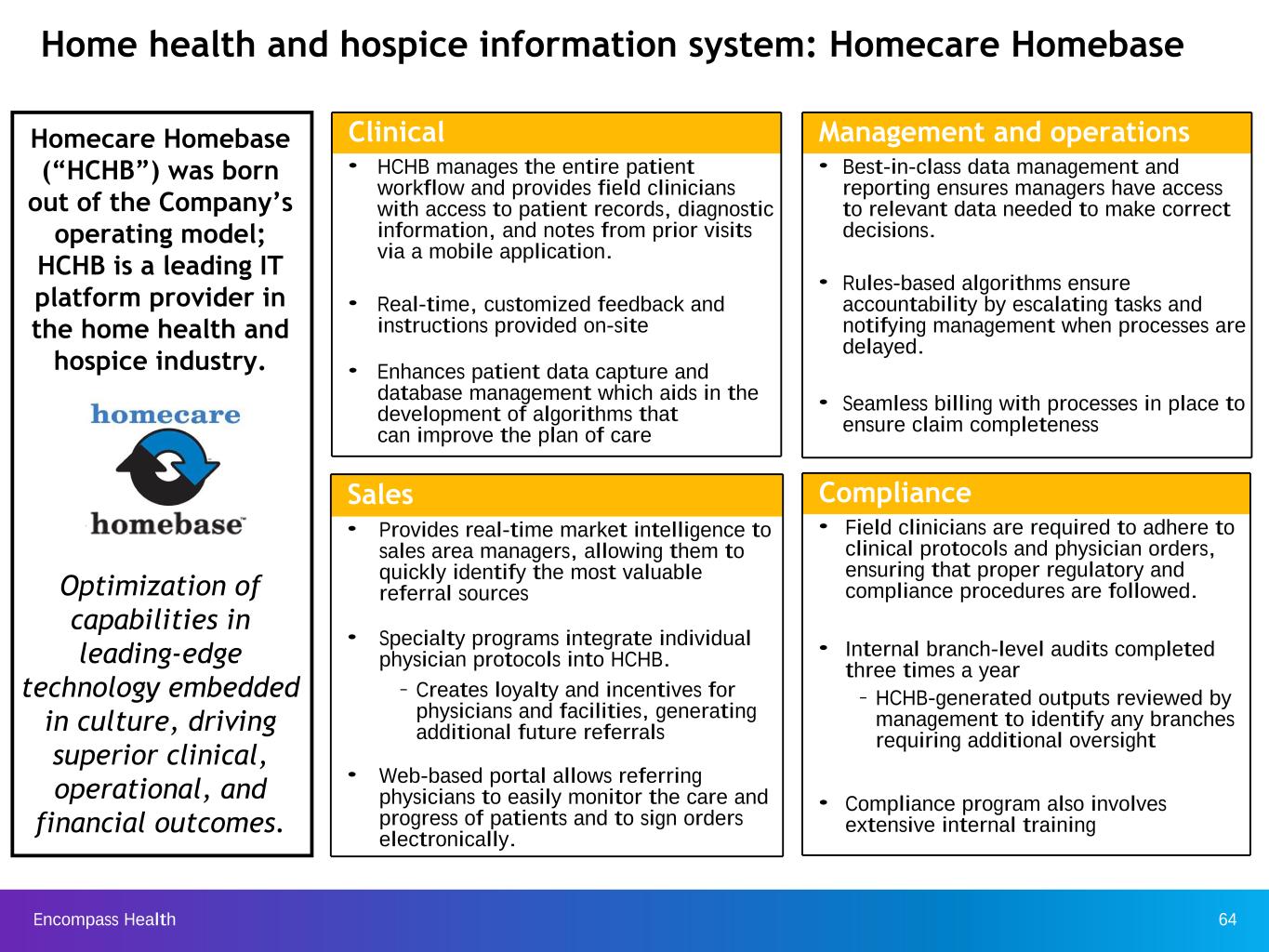
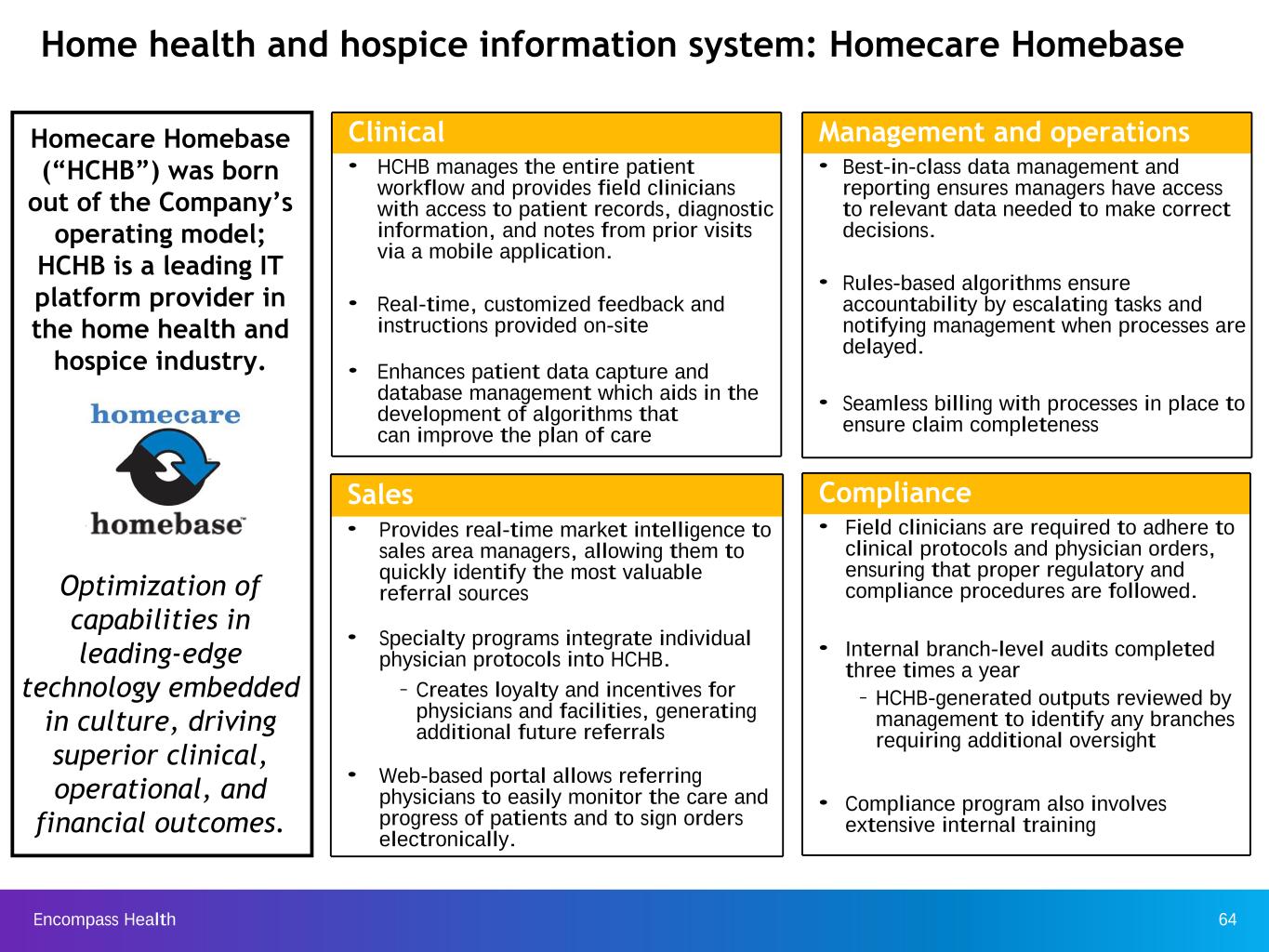
Encompass Health 64 Homecare Homebase (“HCHB”) was born out of the Company’s operating model; HCHB is a leading IT platform provider in the home health and hospice industry. Optimization of capabilities in leading-edge technology embedded in culture, driving superior clinical, operational, and financial outcomes. Home health and hospice information system: Homecare Homebase Clinical • HCHB manages the entire patient workflow and provides field clinicians with access to patient records, diagnostic information, and notes from prior visits via a mobile application. • Real-time, customized feedback and instructions provided on-site • Enhances patient data capture and database management which aids in the development of algorithms that can improve the plan of care Sales • Provides real-time market intelligence to sales area managers, allowing them to quickly identify the most valuable referral sources • Specialty programs integrate individual physician protocols into HCHB. – Creates loyalty and incentives for physicians and facilities, generating additional future referrals • Web-based portal allows referring physicians to easily monitor the care and progress of patients and to sign orders electronically. Compliance • Field clinicians are required to adhere to clinical protocols and physician orders, ensuring that proper regulatory and compliance procedures are followed. • Internal branch-level audits completed three times a year – HCHB-generated outputs reviewed by management to identify any branches requiring additional oversight • Compliance program also involves extensive internal training Management and operations • Best-in-class data management and reporting ensures managers have access to relevant data needed to make correct decisions. • Rules-based algorithms ensure accountability by escalating tasks and notifying management when processes are delayed. • Seamless billing with processes in place to ensure claim completeness

Encompass Health 65 Medalogix’s predictive models for home health care help identify patients at risk for unplanned rehospitalization. Medalogix Modules Proactively identifies home health patients who are potentially better suited and eligible for the hospice benefit. Recommends a patient-centered visit utilization plan that optimizes care to promote discharge to community without hospitalization Prompts continued touch points with discharged patients to identify and prevent post-discharge hospitalizations Risk stratifies the patient population based on hospitalization risk and utilizes interactive voice response to increase touch points with high risk patients
Encompass Health 66 Operational metrics
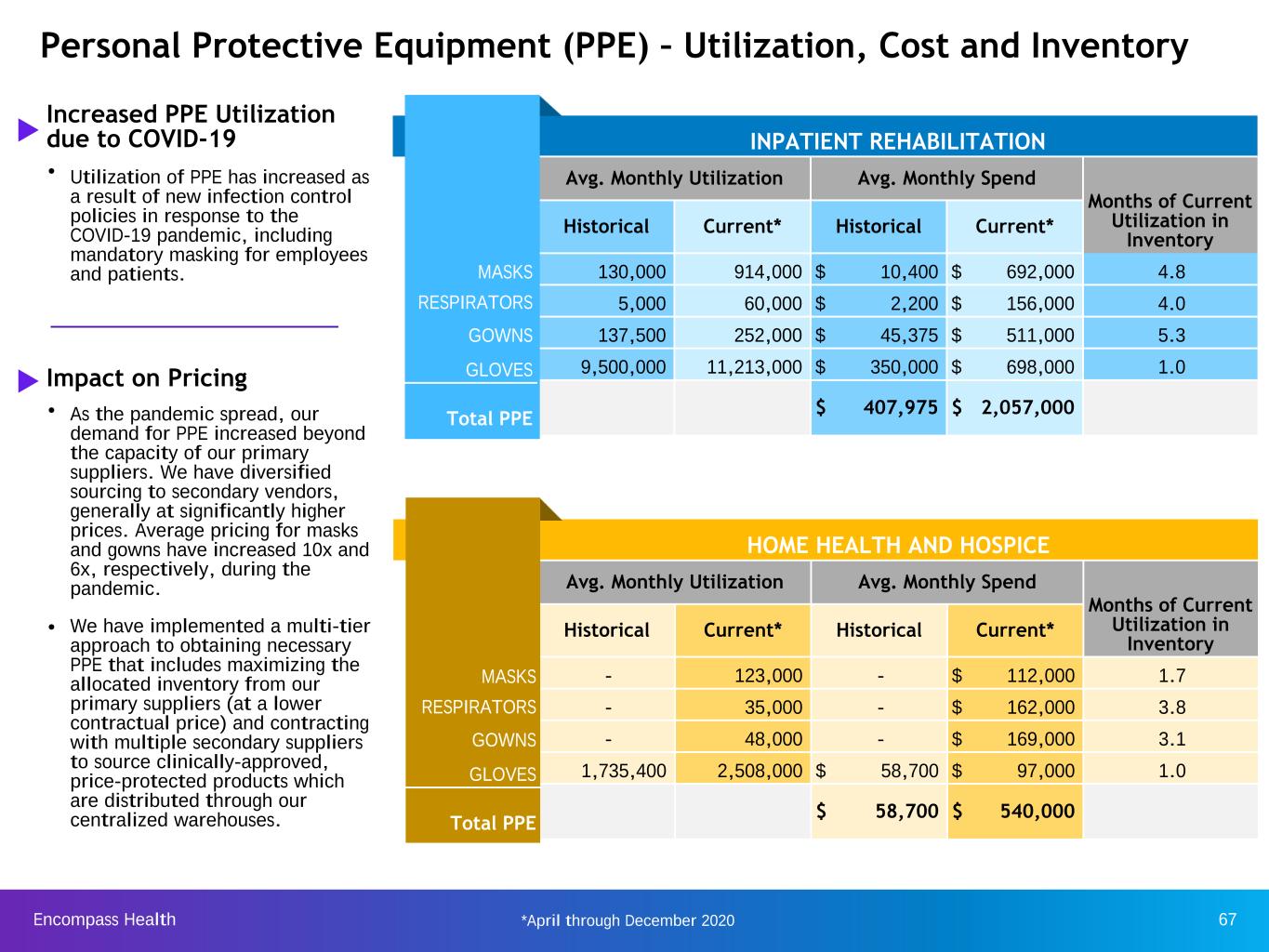
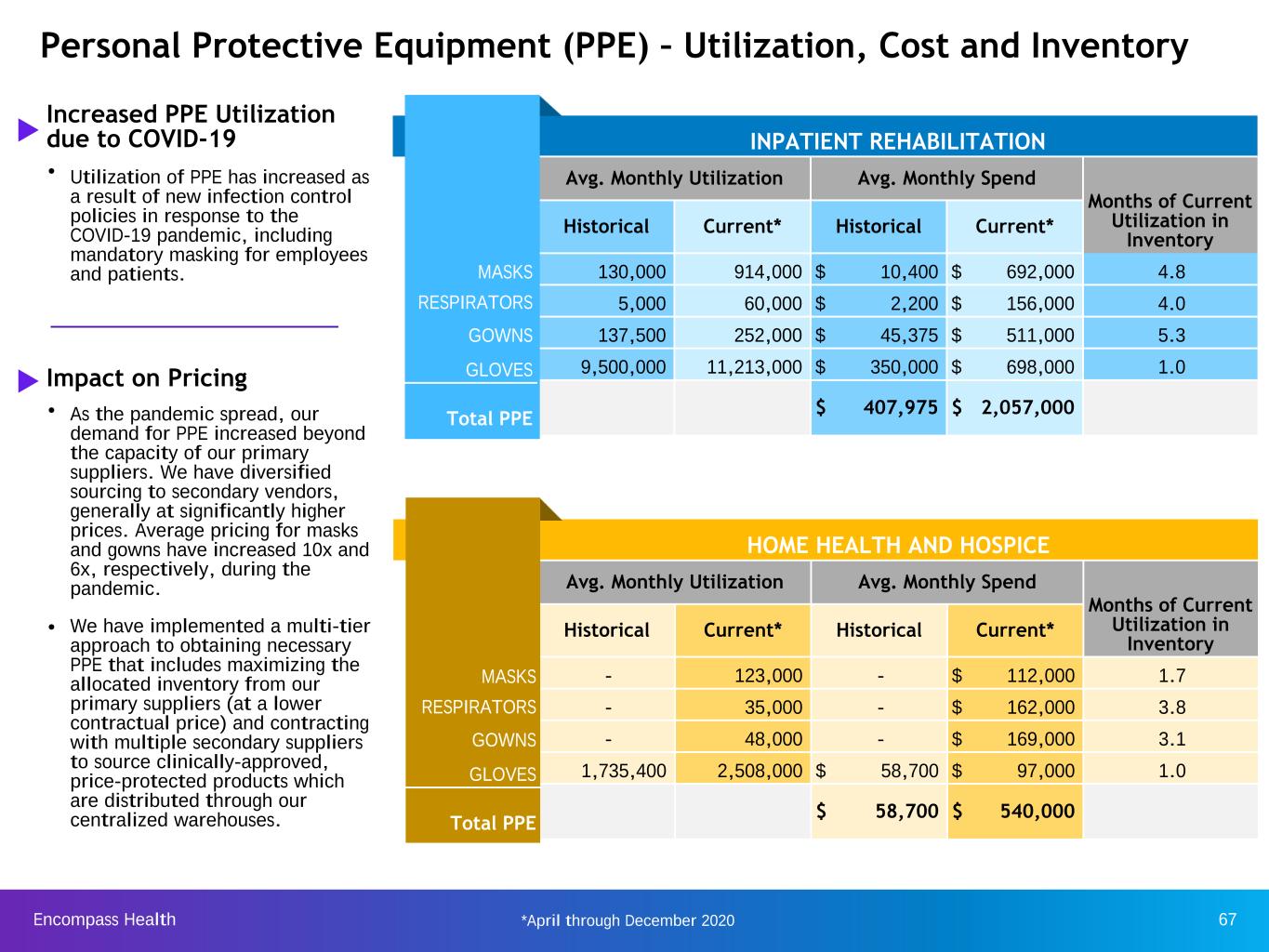
Encompass Health 67 INPATIENT REHABILITATION Avg. Monthly Utilization Avg. Monthly Spend Months of Current Utilization in Inventory Historical Current* Historical Current* MASKS 130,000 914,000 $ 10,400 $ 692,000 4.8 RESPIRATORS 5,000 60,000 $ 2,200 $ 156,000 4.0 GOWNS 137,500 252,000 $ 45,375 $ 511,000 5.3 **GLOVES 9,500,000 11,213,000 $ 350,000 $ 698,000 1.0 Total PPE $ 407,975 $ 2,057,000 u Increased PPE Utilization due to COVID-19 ñ Utilization of PPE has increased as a result of new infection control policies in response to the COVID-19 pandemic, including mandatory masking for employees and patients. u Impact on Pricing ñ As the pandemic spread, our demand for PPE increased beyond the capacity of our primary suppliers. We have diversified sourcing to secondary vendors, generally at significantly higher prices. Average pricing for masks and gowns have increased 10x and 6x, respectively, during the pandemic. ñ We have implemented a multi-tier approach to obtaining necessary PPE that includes maximizing the allocated inventory from our primary suppliers (at a lower contractual price) and contracting with multiple secondary suppliers to source clinically-approved, price-protected products which are distributed through our centralized warehouses. Personal Protective Equipment (PPE) – Utilization, Cost and Inventory MAS RESPIRAT GO GLO Total PPE HOME HEALTH AND HOSPICE Avg. Monthly Utilization Avg. Monthly Spend Months of Current Utilization in Inventory Historical Current* Historical Current* MASKS - 123,000 - $ 112,000 1.7 RESPIRATORS - 35,000 - $ 162,000 3.8 GOWNS - 48,000 - $ 169,000 3.1 **GLOVES 1,735,400 2,508,000 $ 58,700 $ 97,000 1.0 Total PPE $ 58,700 $ 540,000 RESPIR S Total PPE *April through December 2020

Encompass Health 68* For more information regarding TPE, see https://www.cms.gov/Research-Statistics-Data-and-Systems/Monitoring-Programs/Medicare-FFS-Compliance-Programs/Medical-Review/Targeted-Probe-and-EducateTPE.html Pre-payment claims denials - inpatient rehabilitation segment Impact to Income Statement Period New Denials Collections of Previously Denied Claims Revenue Reserve for New Denials Update of Reserve for Prior Denials (In Millions) Q4 2020 $(0.4) $(7.2) $— $4.5 Q3 2020 (0.6) (6.3) — — Q2 2020 (1.5) (3.5) — — Q1 2020 4.2 (5.0) 1.3 — Q4 2019 3.8 (4.6) 1.1 — Q3 2019 11.3 (6.1) 3.4 — Q2 2019 3.5 (1.7) 1.1 — Q1 2019 1.6 (2.5) 0.5 — Q4 2018 4.6 (3.2) 1.4 — Q3 2018 0.7 (1.3) 0.2 — Q2 2018 1.8 (2.8) 0.5 — Q1 2018 3.1 (6.8) 0.9 — Impact to Balance Sheet Dec. 31, 2020 Dec. 31, 2019 Dec. 31, 2018 (In Millions) Pre-payment claims denials $ 122.8 $ 155.3 $ 158.1 Recorded reserves (41.3) (46.6) (47.4) Net accounts receivable from pre-payment claims denials $ 81.5 $ 108.7 $ 110.7 Background • For several years prior to 2018, under programs designated as “widespread probes,” certain Medicare Administrative Contractors (“MACs”) conducted pre-payment claim reviews and denied payment for certain diagnosis codes. • Encompass Health appeals most denials. – MACs identify medical documentation issues as a leading basis for denials. – Encompass Health’s investment in clinical information systems and its medical services department has further improved its documentation and reduced technical denials. • By statute, ALJ decisions are due within 90 days of a request for hearing, but appeals are taking years. HHS has implemented rule changes to address the backlog of appeals, but their effect is uncertain. • In November 2018, a federal court ordered HHS to reduce the backlog in the following increments: a 19% reduction by the end of FY 2019; a 49% reduction by the end of FY 2020; a 75% reduction by the end of FY 2021; and elimination of the backlog by the end of FY 2022. • After years of delay in processing appeals, ALJs recently increased the frequency of hearings and the number of claims set at each hearing. Notwithstanding the recent acceleration, Encompass Health still has over 7,500 claims in the backlog, including claims from up to 10 years ago. • Since 2018, CMS has replaced the “widespread probes” with the Targeted Probe and Educate (“TPE”) initiative.* • Effective March 2020, CMS suspended most Medicare fee-for-service medical reviews during the public health emergency, including TPE and current post-payment reviews, allowing reviews for potential fraud. CMS authorized its contractors to resume reviews as of Aug. 3, 2020. Encompass Health reserves pre-payment claim denials as a reduction of net operating revenues upon notice from a MAC a claim is under review.
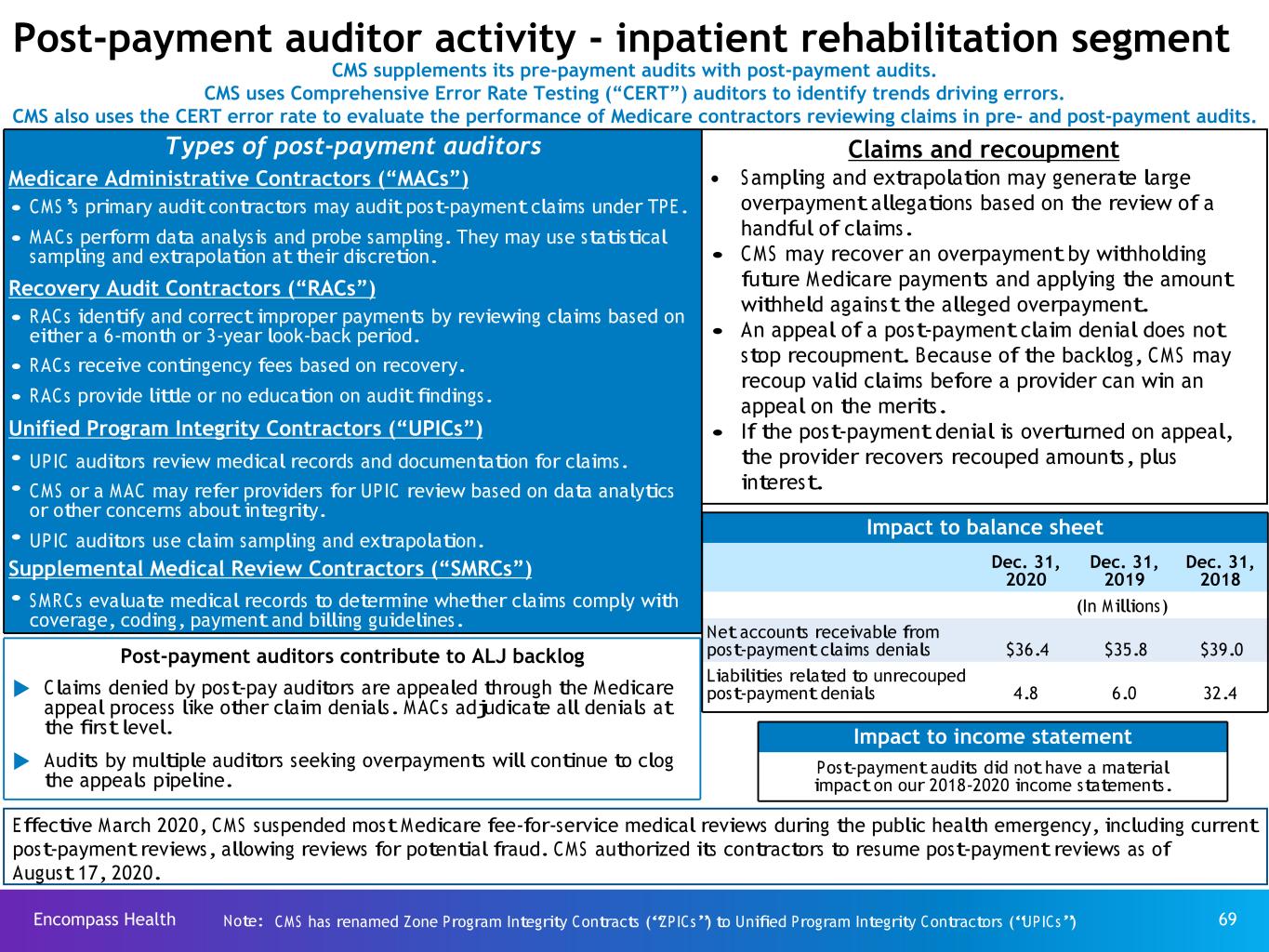
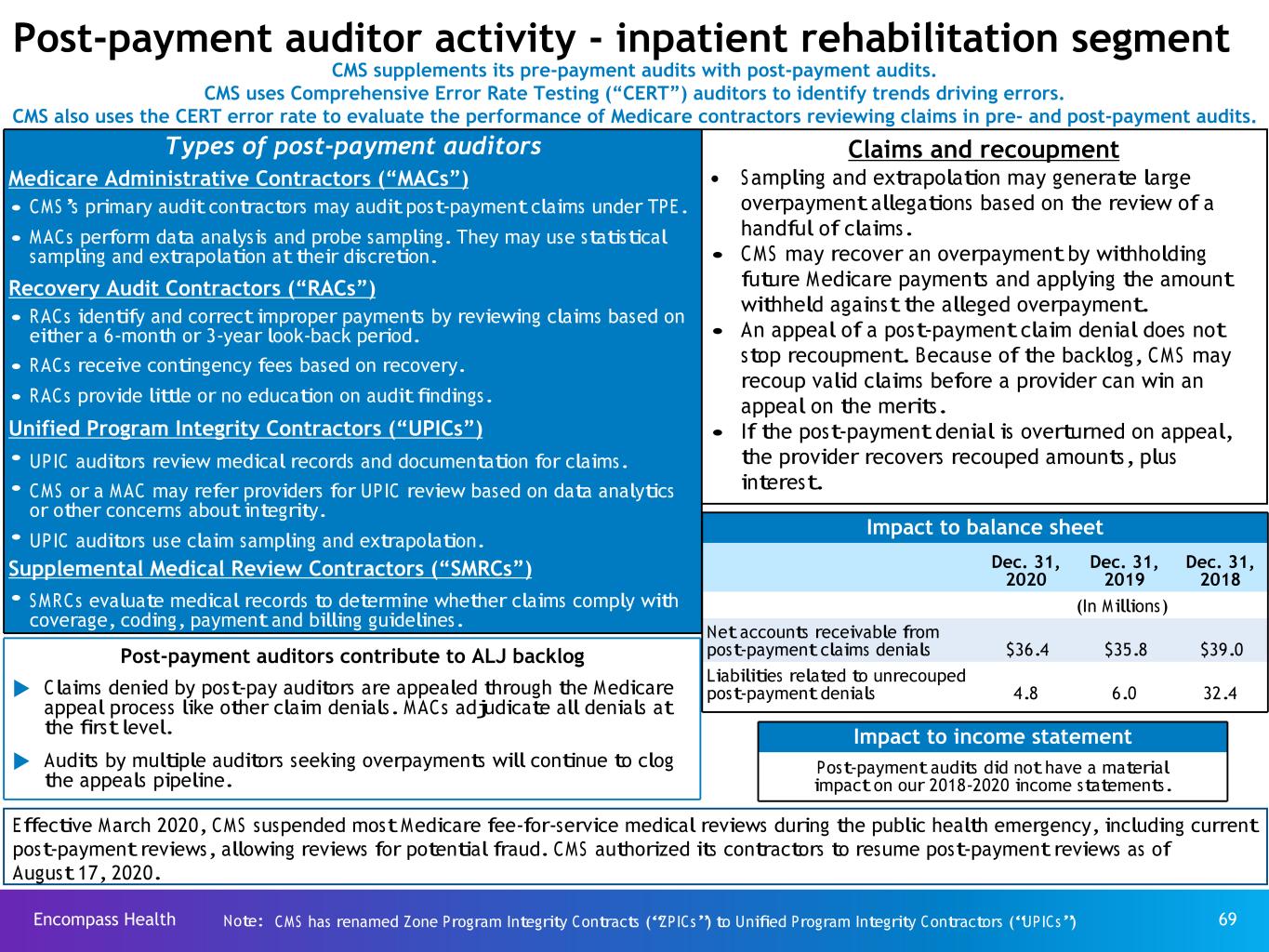
Encompass Health 69 Post-payment auditor activity - inpatient rehabilitation segment CMS supplements its pre-payment audits with post-payment audits. CMS uses Comprehensive Error Rate Testing (“CERT”) auditors to identify trends driving errors. CMS also uses the CERT error rate to evaluate the performance of Medicare contractors reviewing claims in pre- and post-payment audits. Claims and recoupment • Sampling and extrapolation may generate large overpayment allegations based on the review of a handful of claims. • CMS may recover an overpayment by withholding future Medicare payments and applying the amount withheld against the alleged overpayment. • An appeal of a post-payment claim denial does not stop recoupment. Because of the backlog, CMS may recoup valid claims before a provider can win an appeal on the merits. • If the post-payment denial is overturned on appeal, the provider recovers recouped amounts, plus interest. Types of post-payment auditors Medicare Administrative Contractors (“MACs”) • CMS’s primary audit contractors may audit post-payment claims under TPE. • MACs perform data analysis and probe sampling. They may use statistical sampling and extrapolation at their discretion. Recovery Audit Contractors (“RACs”) • RACs identify and correct improper payments by reviewing claims based on either a 6-month or 3-year look-back period. • RACs receive contingency fees based on recovery. • RACs provide little or no education on audit findings. Unified Program Integrity Contractors (“UPICs”) • UPIC auditors review medical records and documentation for claims. • CMS or a MAC may refer providers for UPIC review based on data analytics or other concerns about integrity. • UPIC auditors use claim sampling and extrapolation. Supplemental Medical Review Contractors (“SMRCs”) • SMRCs evaluate medical records to determine whether claims comply with coverage, coding, payment and billing guidelines. Post-payment auditors contribute to ALJ backlog u Claims denied by post-pay auditors are appealed through the Medicare appeal process like other claim denials. MACs adjudicate all denials at the first level. u Audits by multiple auditors seeking overpayments will continue to clog the appeals pipeline. Impact to balance sheet Dec. 31, 2020 Dec. 31, 2019 Dec. 31, 2018 (In Millions) Net accounts receivable from post-payment claims denials $36.4 $35.8 $39.0 Liabilities related to unrecouped post-payment denials 4.8 6.0 32.4 Impact to income statement Post-payment audits did not have a material impact on our 2018-2020 income statements. Effective March 2020, CMS suspended most Medicare fee-for-service medical reviews during the public health emergency, including current post-payment reviews, allowing reviews for potential fraud. CMS authorized its contractors to resume post-payment reviews as of August �� 17, 2020. Note: CMS has renamed Zone Program Integrity Contracts (“ZPICs”) to Unified Program Integrity Contractors (“UPICs”)
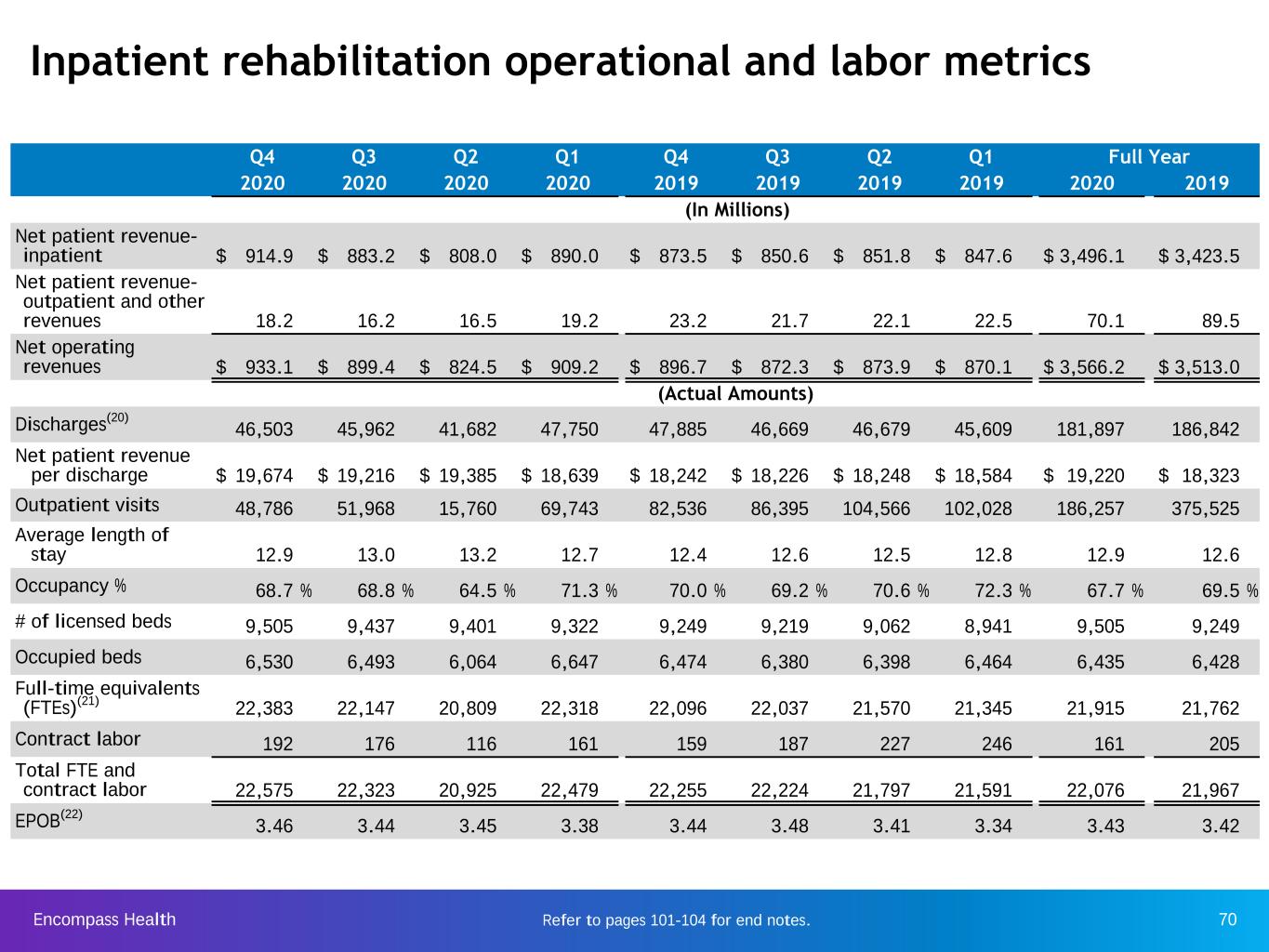
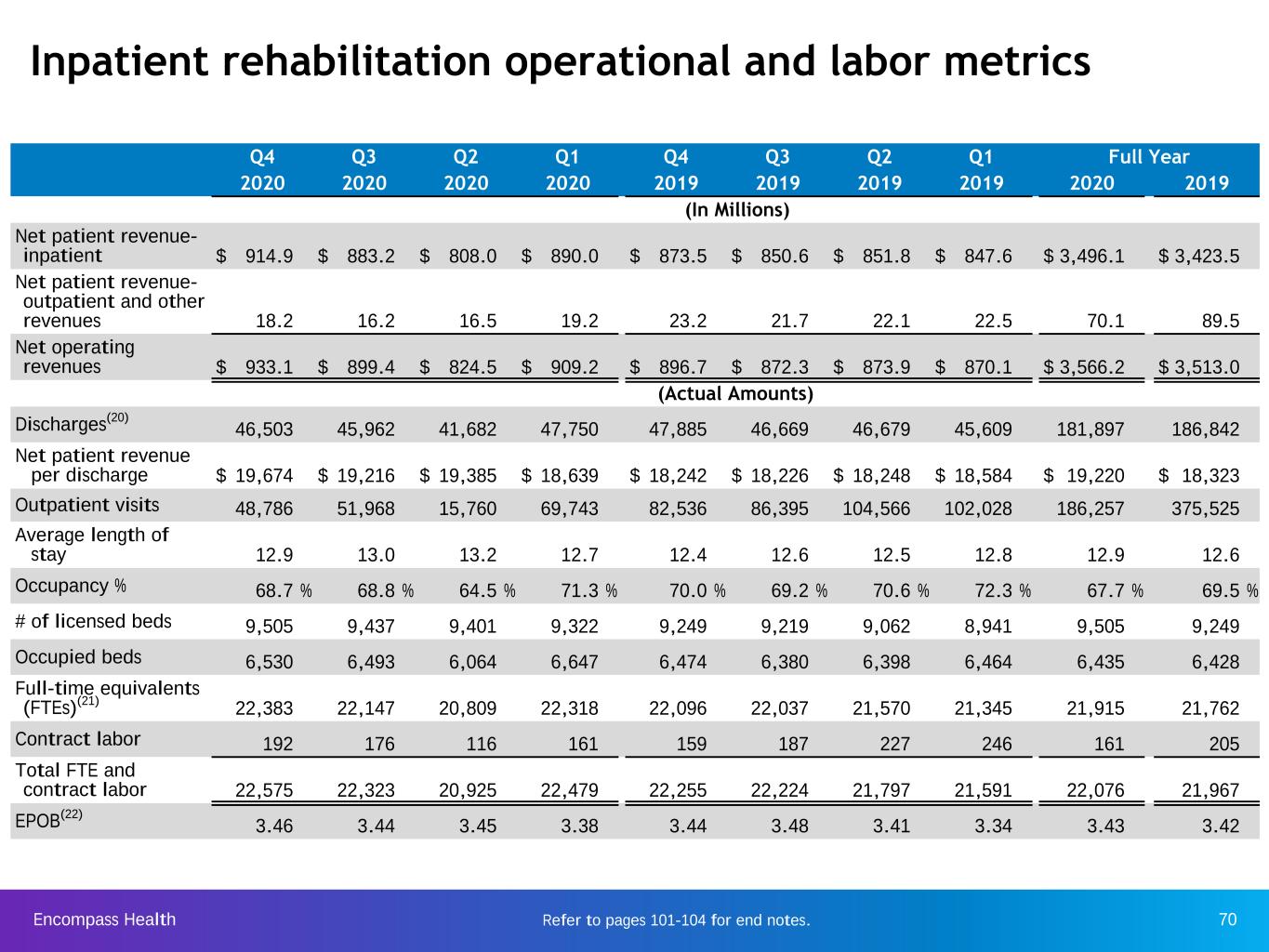
Encompass Health 70 Inpatient rehabilitation operational and labor metrics xxx-xxx Q4 Q3 Q2 Q1 Q4 Q3 Q2 Q1 Full Year 2020 2020 2020 2020 2019 2019 2019 2019 2020 2019 (In Millions) Net patient revenue- inpatient $ 914.9 $ 883.2 $ 808.0 $ 890.0 $ 873.5 $ 850.6 $ 851.8 $ 847.6 $ 3,496.1 $ 3,423.5 Net patient revenue- outpatient and other revenues 18.2 16.2 16.5 19.2 23.2 21.7 22.1 22.5 70.1 89.5 Net operating revenues $ 933.1 $ 899.4 $ 824.5 $ 909.2 $ 896.7 $ 872.3 $ 873.9 $ 870.1 $ 3,566.2 $ 3,513.0 (Actual Amounts) Discharges(20) 46,503 45,962 41,682 47,750 47,885 46,669 46,679 45,609 181,897 186,842 Net patient revenue per discharge $ 19,674 $ 19,216 $ 19,385 $ 18,639 $ 18,242 $ 18,226 $ 18,248 $ 18,584 $ 19,220 $ 18,323 Outpatient visits 48,786 51,968 15,760 69,743 82,536 86,395 104,566 102,028 186,257 375,525 Average length of stay 12.9 13.0 13.2 12.7 12.4 12.6 12.5 12.8 12.9 12.6 Occupancy % 68.7 % 68.8 % 64.5 % 71.3 % 70.0 % 69.2 % 70.6 % 72.3 % 67.7 % 69.5 % # of licensed beds 9,505 9,437 9,401 9,322 9,249 9,219 9,062 8,941 9,505 9,249 Occupied beds 6,530 6,493 6,064 6,647 6,474 6,380 6,398 6,464 6,435 6,428 Full-time equivalents (FTEs)(21) 22,383 22,147 20,809 22,318 22,096 22,037 21,570 21,345 21,915 21,762 Contract labor 192 176 116 161 159 187 227 246 161 205 Total FTE and contract labor 22,575 22,323 20,925 22,479 22,255 22,224 21,797 21,591 22,076 21,967 EPOB(22) 3.46 3.44 3.45 3.38 3.44 3.48 3.41 3.34 3.43 3.42 Refer to pages 101-104 for end notes.
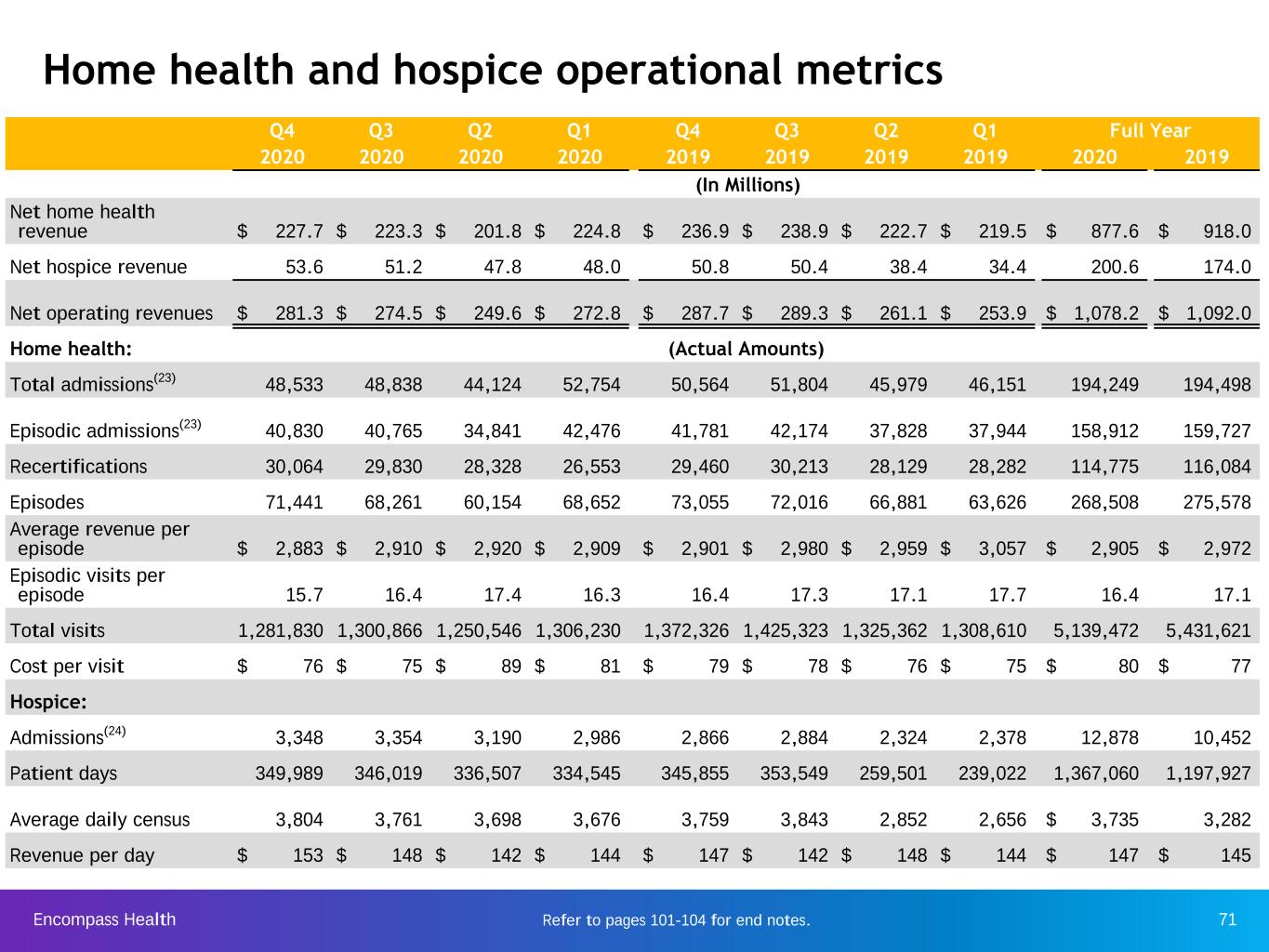
Encompass Health 71 Home health and hospice operational metrics Q4 Q3 Q2 Q1 Q4 Q3 Q2 Q1 Full Year 2020 2020 2020 2020 2019 2019 2019 2019 2020 2019 (In Millions) Net home health revenue $ 227.7 $ 223.3 $ 201.8 $ 224.8 $ 236.9 $ 238.9 $ 222.7 $ 219.5 $ 877.6 $ 918.0 Net hospice revenue 53.6 51.2 47.8 48.0 50.8 50.4 38.4 34.4 200.6 174.0 Net operating revenues $ 281.3 $ 274.5 $ 249.6 $ 272.8 $ 287.7 $ 289.3 $ 261.1 $ 253.9 $ 1,078.2 $ 1,092.0 Home health: (Actual Amounts) Total admissions(23) 48,533 48,838 44,124 52,754 50,564 51,804 45,979 46,151 194,249 194,498 Episodic admissions(23) 40,830 40,765 34,841 42,476 41,781 42,174 37,828 37,944 158,912 159,727 Recertifications 30,064 29,830 28,328 26,553 29,460 30,213 28,129 28,282 114,775 116,084 Episodes 71,441 68,261 60,154 68,652 73,055 72,016 66,881 63,626 268,508 275,578 Average revenue per episode $ 2,883 $ 2,910 $ 2,920 $ 2,909 $ 2,901 $ 2,980 $ 2,959 $ 3,057 $ 2,905 $ 2,972 Episodic visits per episode 15.7 16.4 17.4 16.3 16.4 17.3 17.1 17.7 16.4 17.1 Total visits 1,281,830 1,300,866 1,250,546 1,306,230 1,372,326 1,425,323 1,325,362 1,308,610 5,139,472 5,431,621 Cost per visit $ 76 $ 75 $ 89 $ 81 $ 79 $ 78 $ 76 $ 75 $ 80 $ 77 Hospice: Admissions(24) 3,348 3,354 3,190 2,986 2,866 2,884 2,324 2,378 12,878 10,452 Patient days 349,989 346,019 336,507 334,545 345,855 353,549 259,501 239,022 1,367,060 1,197,927 Average daily census 3,804 3,761 3,698 3,676 3,759 3,843 2,852 2,656 $ 3,735 3,282 Revenue per day $ 153 $ 148 $ 142 $ 144 $ 147 $ 142 $ 148 $ 144 $ 147 $ 145 Refer to pages 101-104 for end notes.

Encompass Health 72 Payment sources (percent of revenues) Inpatient Rehabilitation Segment Home Health and Hospice Segment Consolidated Q4 Q4 Q4 Full Year 2020 2019 2020 2019 2020 2019 2020 2019 Medicare 68.3 % 71.9 % 84.3 % 83.8 % 72.0 % 74.8 % 70.5 % 75.1 % Medicare Advantage 13.6 % 11.1 % 9.9 % 10.1 % 12.7 % 10.8 % 14.2 % 10.6 % Managed care 10.4 % 9.5 % 4.2 % 4.3 % 9.0 % 8.2 % 9.0 % 8.3 % Medicaid 3.9 % 3.2 % 1.4 % 1.6 % 3.3 % 2.8 % 3.4 % 2.8 % Other third-party payors 1.3 % 1.2 % — % — % 1.0 % 0.9 % 0.9 % 0.9 % Workers’ compensation 0.6 % 0.8 % 0.1 % 0.1 % 0.5 % 0.7 % 0.5 % 0.7 % Patients 0.5 % 0.6 % — % — % 0.4 % 0.5 % 0.4 % 0.5 % Other income 1.4 % 1.7 % 0.1 % 0.1 % 1.1 % 1.3 % 1.1 % 1.1 % Total 100.0 % 100.0 % 100.0 % 100.0 % 100.0 % 100.0 % 100.0 % 100.0 % Growth in Medicare Advantage as a percent of revenue within the inpatient rehabilitation segment for Q4 and year-to-date 2020 resulted in part from suspension of prior authorization requirements.
Encompass Health 73 Industry structure

Encompass Health 74 H e al th c o n su m p ti o n s p e n d in g* : $ 3 ,2 1 7 Overall healthcare spending (billions) Source: Centers for Medicare & Medicaid Services, National Health Expenditure Data (Historical), Table 2 - 2018 * Excludes Net Cost of Private Health Insurance of $258 billion. National healthcare spending: $3,649 billion in 2018 P e rs o n al h e al th ca re : $ 3 ,0 7 6 $174 Investment $48 Government administration $93 Government public health $456 Retail of medical products $102 Home health care $192 Other health, residential and personal care $965 Professional services $169 Nursing care facilities and continuing care retirement communities $1,192 Hospital careIncludes inpatient rehabilitation, long-term care hospitals
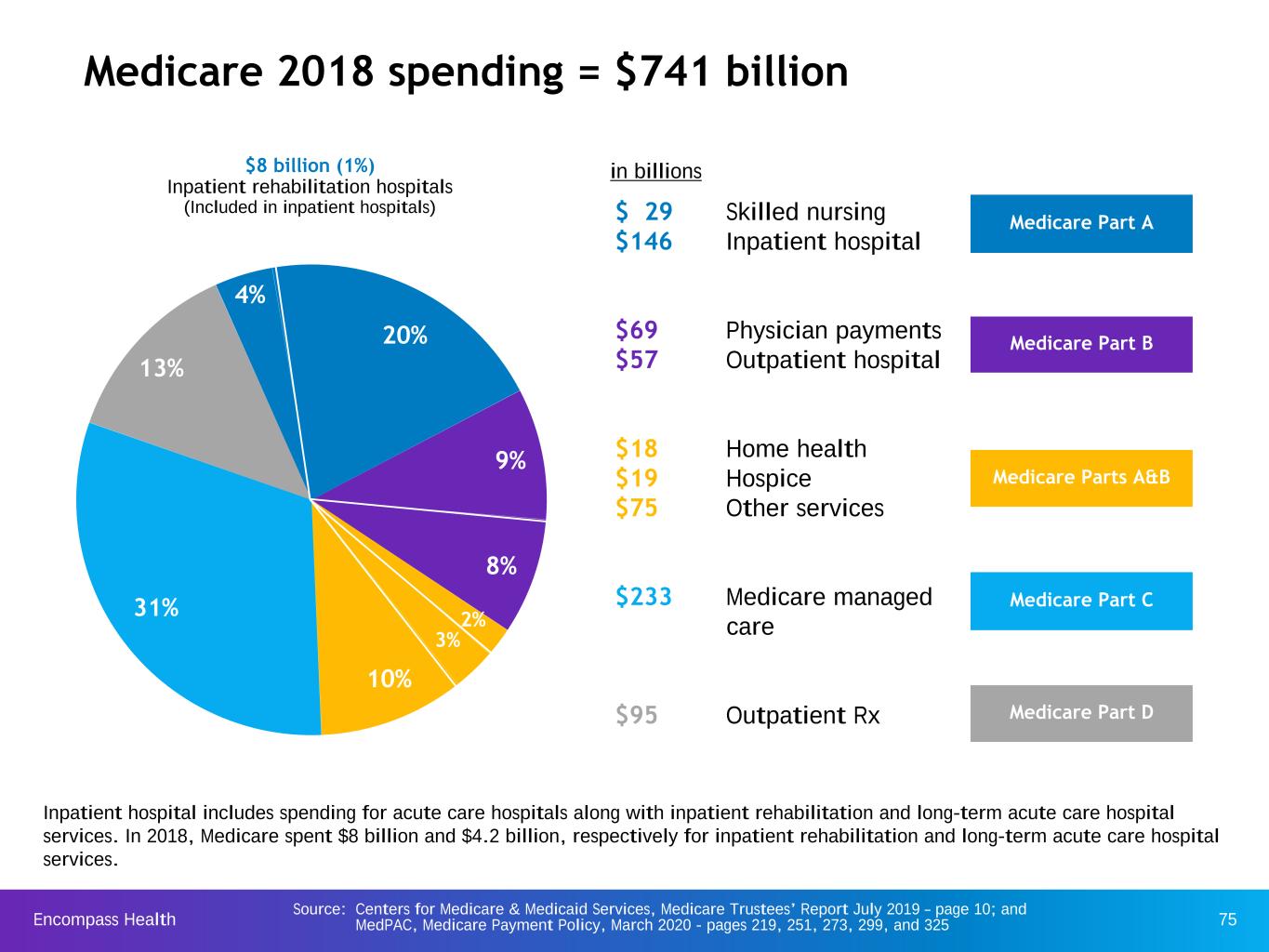
Encompass Health 75 Source: Centers for Medicare & Medicaid Services, Medicare Trustees’ Report July 2019 – page 10; and MedPAC, Medicare Payment Policy, March 2020 - pages 219, 251, 273, 299, and 325 Medicare 2018 spending = $741 billion $ 29 Skilled nursing $146 Inpatient hospital $69 Physician payments $57 Outpatient hospital $18 Home health $19 Hospice $75 Other services $233 Medicare managed care $95 Outpatient Rx $8 billion (1%) Inpatient rehabilitation hospitals (Included in inpatient hospitals) 13% 2% 8% 10% 9% 31% 20% Medicare Part A Medicare Part B Medicare Parts A&B Medicare Part C Medicare Part D 4% Inpatient hospital includes spending for acute care hospitals along with inpatient rehabilitation and long-term acute care hospital services. In 2018, Medicare spent $8 billion and $4.2 billion, respectively for inpatient rehabilitation and long-term acute care hospital services. in billions 3%
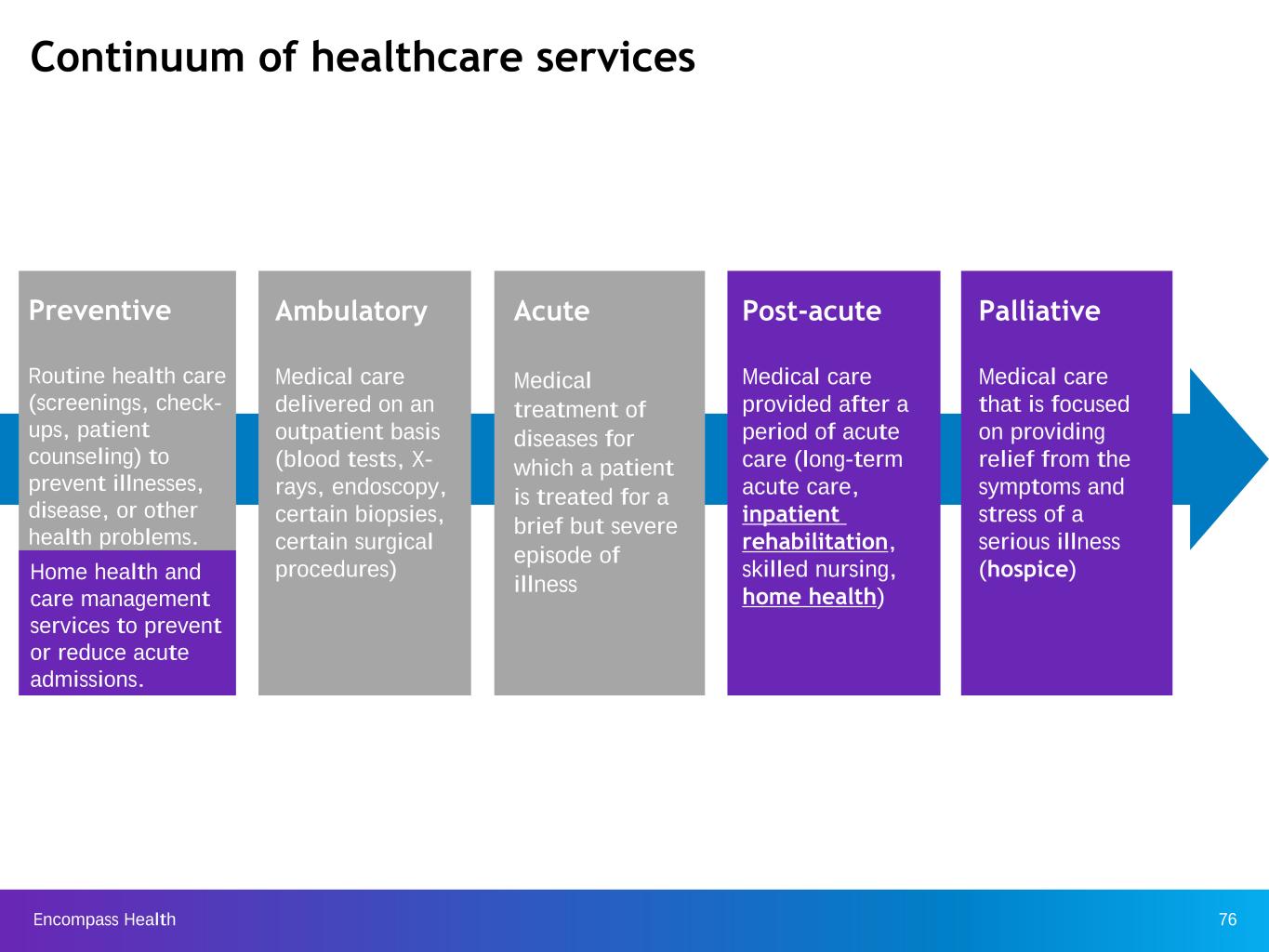
Encompass Health 76 Preventive Routine health care (screenings, check- ups, patient counseling) to prevent illnesses, disease, or other health problems. Continuum of healthcare services Acute Medical treatment of diseases for which a patient is treated for a brief but severe episode of illness Ambulatory Medical care delivered on an outpatient basis (blood tests, X- rays, endoscopy, certain biopsies, certain surgical procedures) Post-acute Medical care provided after a period of acute care (long-term acute care, inpatient rehabilitation, skilled nursing, home health) Palliative Medical care that is focused on providing relief from the symptoms and stress of a serious illness (hospice)Home health and care management services to prevent or reduce acute admissions.
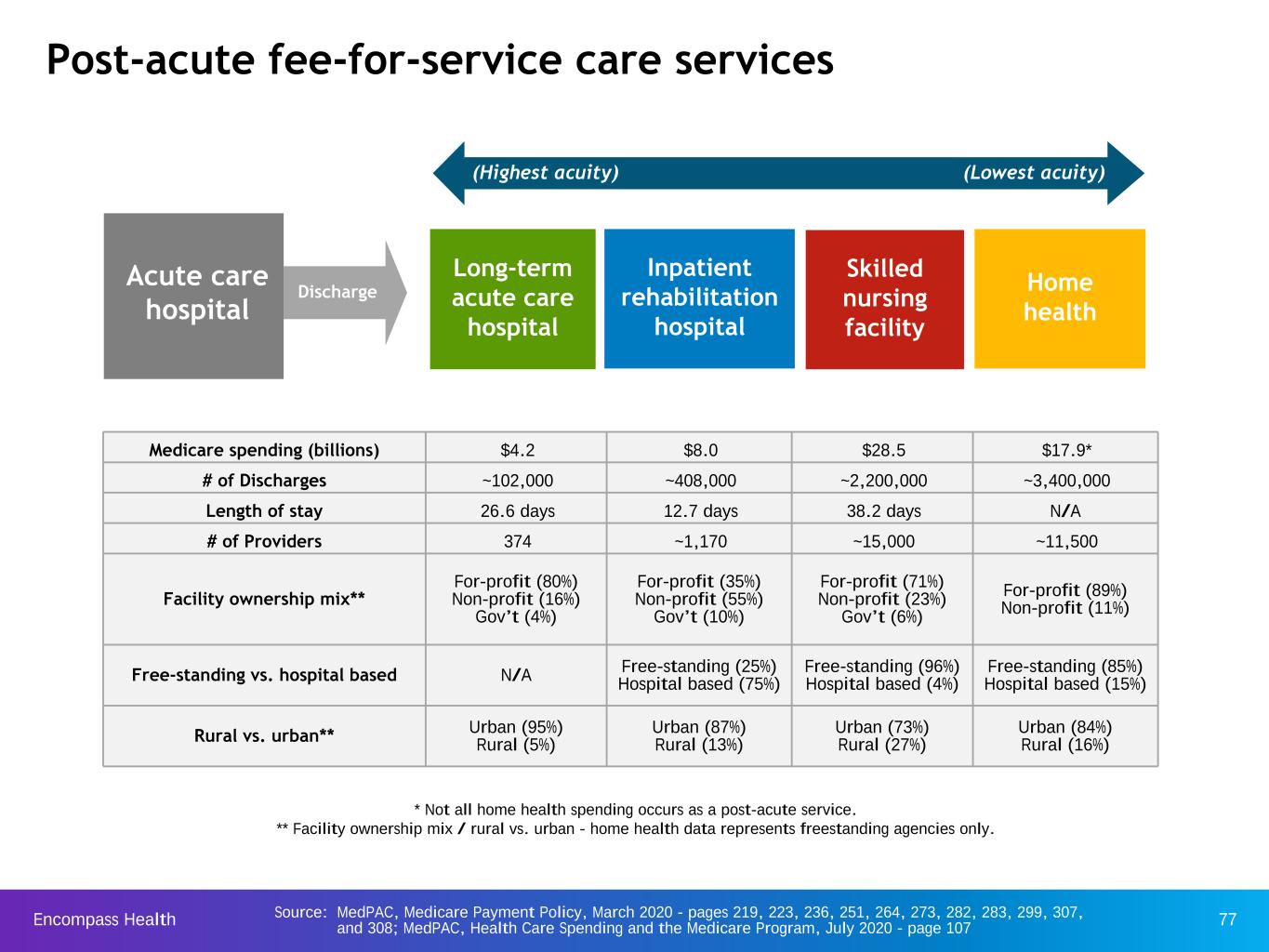
Encompass Health 77 Post-acute fee-for-service care services Acute care hospital Home health Long-term acute care hospital Inpatient rehabilitation hospital Skilled nursing facility Discharge Medicare spending (billions) $4.2 $8.0 $28.5 $17.9* # of Discharges ~102,000 ~408,000 ~2,200,000 ~3,400,000 Length of stay 26.6 days 12.7 days 38.2 days N/A # of Providers 374 ~1,170 ~15,000 ~11,500 Facility ownership mix** For-profit (80%) Non-profit (16%) Gov’t (4%) For-profit (35%) Non-profit (55%) Gov’t (10%) For-profit (71%) Non-profit (23%) Gov’t (6%) For-profit (89%) Non-profit (11%) Free-standing vs. hospital based N/A Free-standing (25%)Hospital based (75%) Free-standing (96%) Hospital based (4%) Free-standing (85%) Hospital based (15%) Rural vs. urban** Urban (95%)Rural (5%) Urban (87%) Rural (13%) Urban (73%) Rural (27%) Urban (84%) Rural (16%) (Lowest acuity)(Highest acuity) Source: MedPAC, Medicare Payment Policy, March 2020 - pages 219, 223, 236, 251, 264, 273, 282, 283, 299, 307, and 308; MedPAC, Health Care Spending and the Medicare Program, July 2020 - page 107 * Not all home health spending occurs as a post-acute service. ** Facility ownership mix / rural vs. urban - home health data represents freestanding agencies only.

Encompass Health 78 2002 2003 20042005 20062007 2008 20092010 2011 20122013 2014 20152016 2017 2018 $0 $5 $10 $15 $20 $25 $30 $35 Medicare fee-for-service spending on post-acute services Post-acute settings 2018 Medicare margin** Projected 2020 Medicare margin** 10.3% 10.0% 15.3% 17.0% 14.7% 12.7% 4.7% 3.7%*** Skilled nursing facilities Home health agencies* Inpatient rehabilitation hospitals Long-term acute care hospitals Inpatient rehabilitation fee-for-service spending (% of total Medicare spending) (P e rc e n t) 1.6 1.5 1.5 1.6 1.5 1.6 1.6 1.6 1.6 4.8 4.3 4.1 4.1 3.9 3.8 3.7 3.5 3.5 2010 2011 2012 2013 2014 2015 2016 2017 2018 0 3 6 Home health fee-for- service spending* (% of total Medicare spending) Total Medicare fee-for-service spending on post-acute services ~$59 billion in 2018 Source: MedPAC, Medicare Payment Policy, March 2020 – pages 211, 219, 234, 240, 251, 264, 266, 273, 287, 291, 299, 317 and Centers for Medicare and Medicaid Services, Medicare Trustees’ Report April 2019 - page 10 * Not all home health spending occurs as a post-acute service. ** 2018 Medicare margin / Projected 2020 Medicare margin - skilled nursing and home health data represents freestanding facilities and agencies only. *** 2020 LTCH Projected Medicare margin reflects the cohort of LTCHs with more than 85 percent of Medicare cases meeting the LTCH PPS criteria.

Encompass Health 79 Different fee-for-service levels of services Inpatient rehabilitation hospital Nursing home Industry averages: Industry averages: Average length of stay = 12.7 days Average length of stay = 38.2 days Discharge to community = 76.4% Discharge to community = 41.4% Requirements(2): Requirements: IRFs must also satisfy regulatory/policy requirements for hospitals, including Medicare hospital conditions of participation. No similar requirement; Nursing homes are regulated as nursing homes only All patients must be admitted by a rehab physician. No similar requirement Rehab physicians must re-confirm each admission within 24 hours. No similar requirement All patients, regardless of diagnoses/condition, must demonstrate need and receive at least three hours of daily intensive therapy. No similar requirement All patients must weekly see a rehabilitation physician at least two to three times “in person”. No similar requirement; some SNF patients may go a week or longer without seeing a physician, and often a non- rehabilitation physician. IRFs are required to provide 24 hour, 7 days per week nursing care; many nurses are RNs and rehab nurses. No similar requirement IRFs are required to use a coordinated interdisciplinary team approach led by a rehab physician; includes a rehab nurse, a case manager, and a licensed therapist from each therapy discipline who must meet weekly to evaluate/discuss each patient’s case. No similar requirement; Nursing homes are not required to provide care on a interdisciplinary basis and are not required to hold regular meetings for each patient. IRFs are required to follow stringent admission/coverage policies and must carefully document justification for each admission; further restricted in number/type of patients (60% Rule). Nursing homes have comparatively few policies governing the number or types of patients they treat. Source: MedPAC, Medicare Payment Policy, March 2020 - pages 231, 236, 283, and 286. Refer to pages 101-104 for end notes.
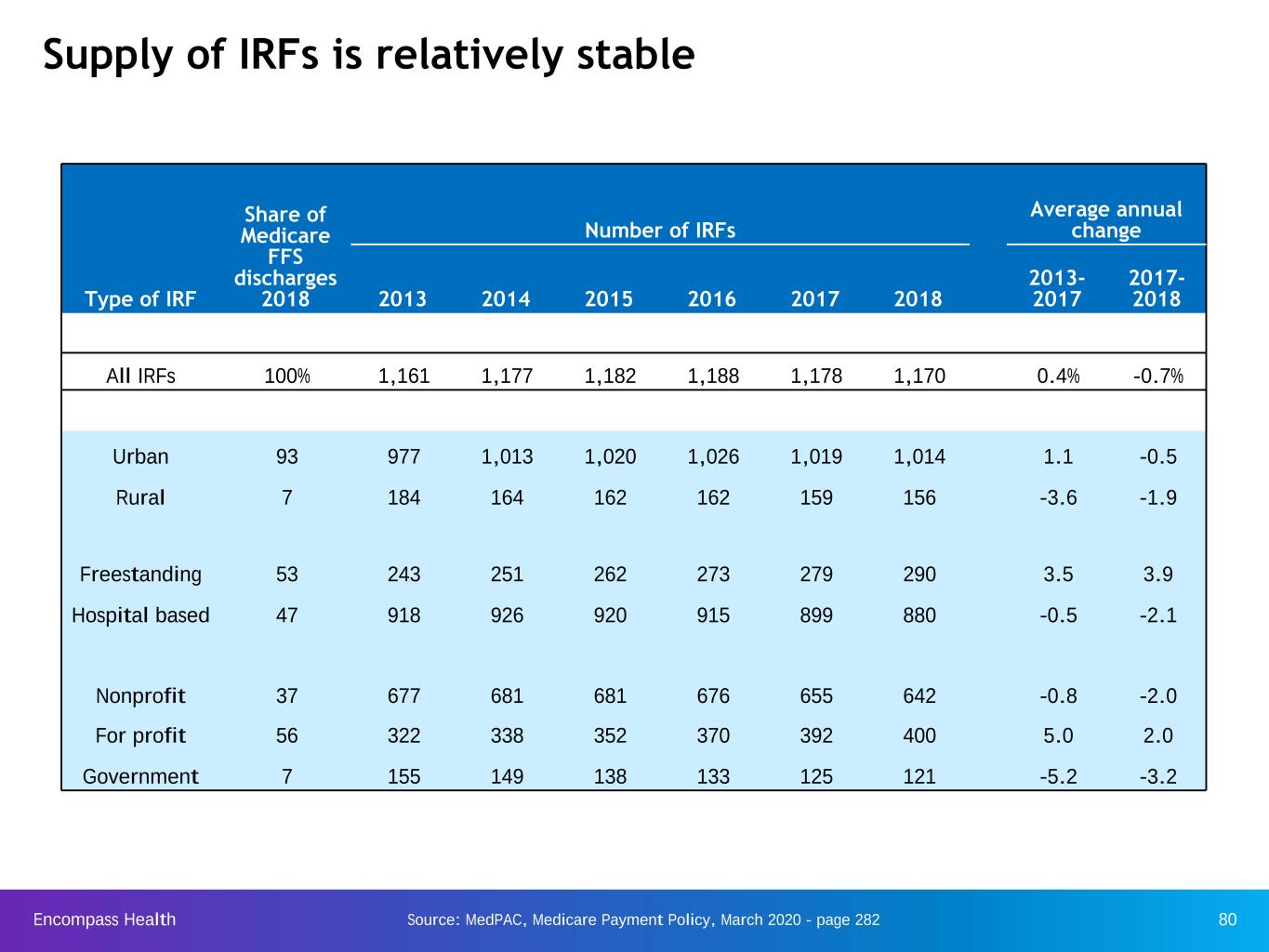
Encompass Health 80 Supply of IRFs is relatively stable Share of Medicare FFS discharges 2018 Number of IRFs Average annual change Type of IRF 2013 2014 2015 2016 2017 2018 2013- 2017 2017- 2018 All IRFs 100% 1,161 1,177 1,182 1,188 1,178 1,170 0.4% -0.7% Urban 93 977 1,013 1,020 1,026 1,019 1,014 1.1 -0.5 Rural 7 184 164 162 162 159 156 -3.6 -1.9 Freestanding 53 243 251 262 273 279 290 3.5 3.9 Hospital based 47 918 926 920 915 899 880 -0.5 -2.1 Nonprofit 37 677 681 681 676 655 642 -0.8 -2.0 For profit 56 322 338 352 370 392 400 5.0 2.0 Government 7 155 149 138 133 125 121 -5.2 -3.2 Source: MedPAC, Medicare Payment Policy, March 2020 - page 282
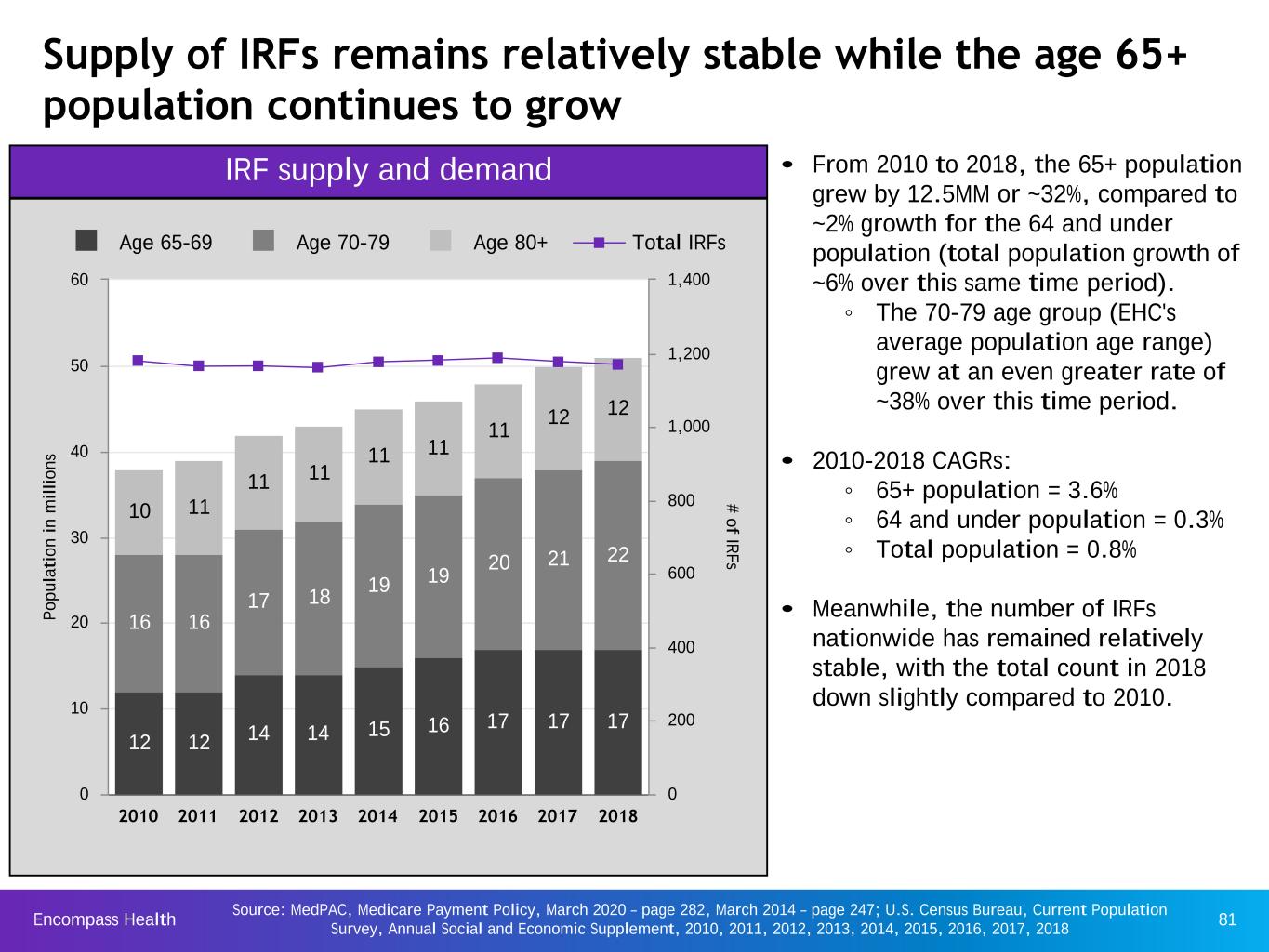
Encompass Health 81 Supply of IRFs remains relatively stable while the age 65+ population continues to grow P op u la ti on i n m il li on s # of IR Fs 12 12 14 14 15 16 17 17 17 16 16 17 18 19 19 20 21 22 10 11 11 11 11 11 11 12 12 Age 65-69 Age 70-79 Age 80+ Total IRFs 2010 2011 2012 2013 2014 2015 2016 2017 2018 0 10 20 30 40 50 60 0 200 400 600 800 1,000 1,200 1,400 IRF supply and demand • From 2010 to 2018, the 65+ population grew by 12.5MM or ~32%, compared to ~2% growth for the 64 and under population (total population growth of ~6% over this same time period). ◦ The 70-79 age group (EHC's average population age range) grew at an even greater rate of ~38% over this time period. • 2010-2018 CAGRs: ◦ 65+ population = 3.6% ◦ 64 and under population = 0.3% ◦ Total population = 0.8% • Meanwhile, the number of IRFs nationwide has remained relatively stable, with the total count in 2018 down slightly compared to 2010. Source: MedPAC, Medicare Payment Policy, March 2020 – page 282, March 2014 – page 247; U.S. Census Bureau, Current Population Survey, Annual Social and Economic Supplement, 2010, 2011, 2012, 2013, 2014, 2015, 2016, 2017, 2018
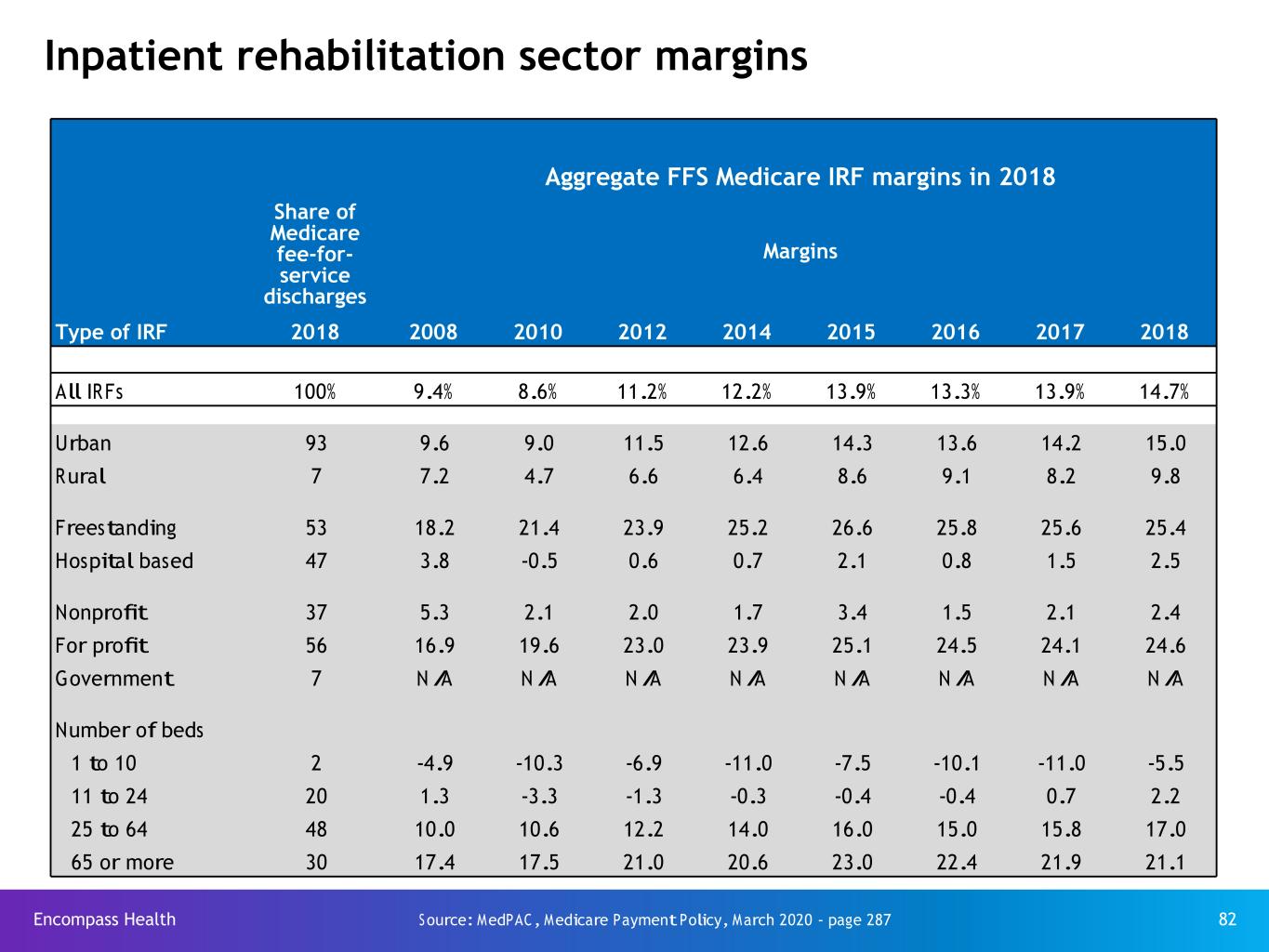
Encompass Health 82 Inpatient rehabilitation sector margins Aggregate FFS Medicare IRF margins in 2018 Share of Medicare fee-for- service discharges Margins Type of IRF 2018 2008 2010 2012 2014 2015 2016 2017 2018 All IRFs 100% 9.4% 8.6% 11.2% 12.2% 13.9% 13.3% 13.9% 14.7% Urban 93 9.6 9.0 11.5 12.6 14.3 13.6 14.2 15.0 Rural 7 7.2 4.7 6.6 6.4 8.6 9.1 8.2 9.8 Freestanding 53 18.2 21.4 23.9 25.2 26.6 25.8 25.6 25.4 Hospital based 47 3.8 -0.5 0.6 0.7 2.1 0.8 1.5 2.5 Nonprofit 37 5.3 2.1 2.0 1.7 3.4 1.5 2.1 2.4 For profit 56 16.9 19.6 23.0 23.9 25.1 24.5 24.1 24.6 Government 7 N/A N/A N/A N/A N/A N/A N/A N/A Number of beds 1 to 10 2 -4.9 -10.3 -6.9 -11.0 -7.5 -10.1 -11.0 -5.5 11 to 24 20 1.3 -3.3 -1.3 -0.3 -0.4 -0.4 0.7 2.2 25 to 64 48 10.0 10.6 12.2 14.0 16.0 15.0 15.8 17.0 65 or more 30 17.4 17.5 21.0 20.6 23.0 22.4 21.9 21.1 Source: MedPAC, Medicare Payment Policy, March 2020 - page 287
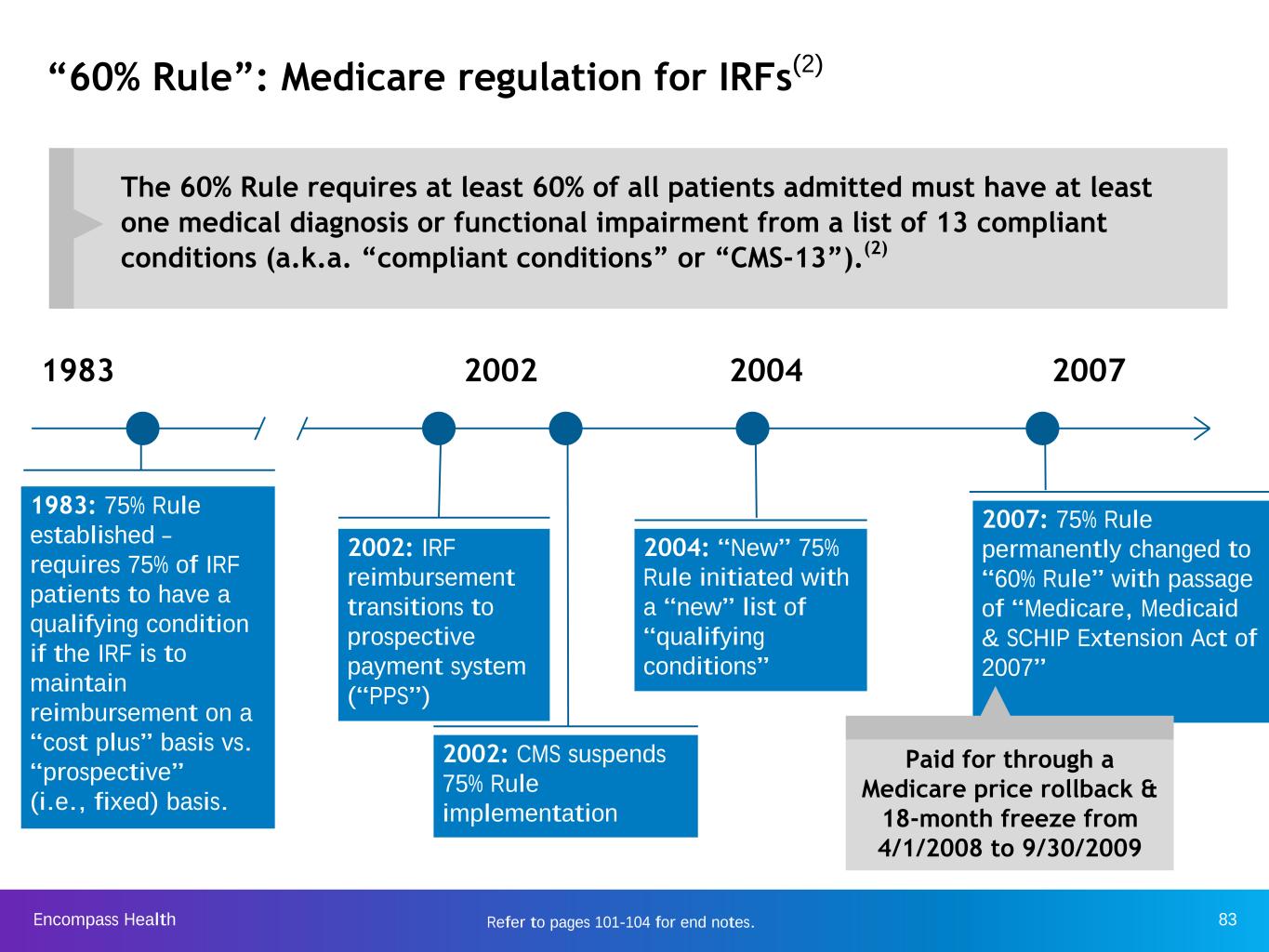
Encompass Health 83 “60% Rule”: Medicare regulation for IRFs(2) 1983 1983: 75% Rule established – requires 75% of IRF patients to have a qualifying condition if the IRF is to maintain reimbursement on a “cost plus” basis vs. “prospective” (i.e., fixed) basis. 2002 2004 2007 2002: IRF reimbursement transitions to prospective payment system (“PPS”) 2002: CMS suspends 75% Rule implementation 2004: “New” 75% Rule initiated with a “new” list of “qualifying conditions” 2007: 75% Rule permanently changed to “60% Rule” with passage of “Medicare, Medicaid & SCHIP Extension Act of 2007” Paid for through a Medicare price rollback & 18-month freeze from 4/1/2008 to 9/30/2009 The 60% Rule requires at least 60% of all patients admitted must have at least one medical diagnosis or functional impairment from a list of 13 compliant conditions (a.k.a. “compliant conditions” or “CMS-13”).(2) Refer to pages 101-104 for end notes.
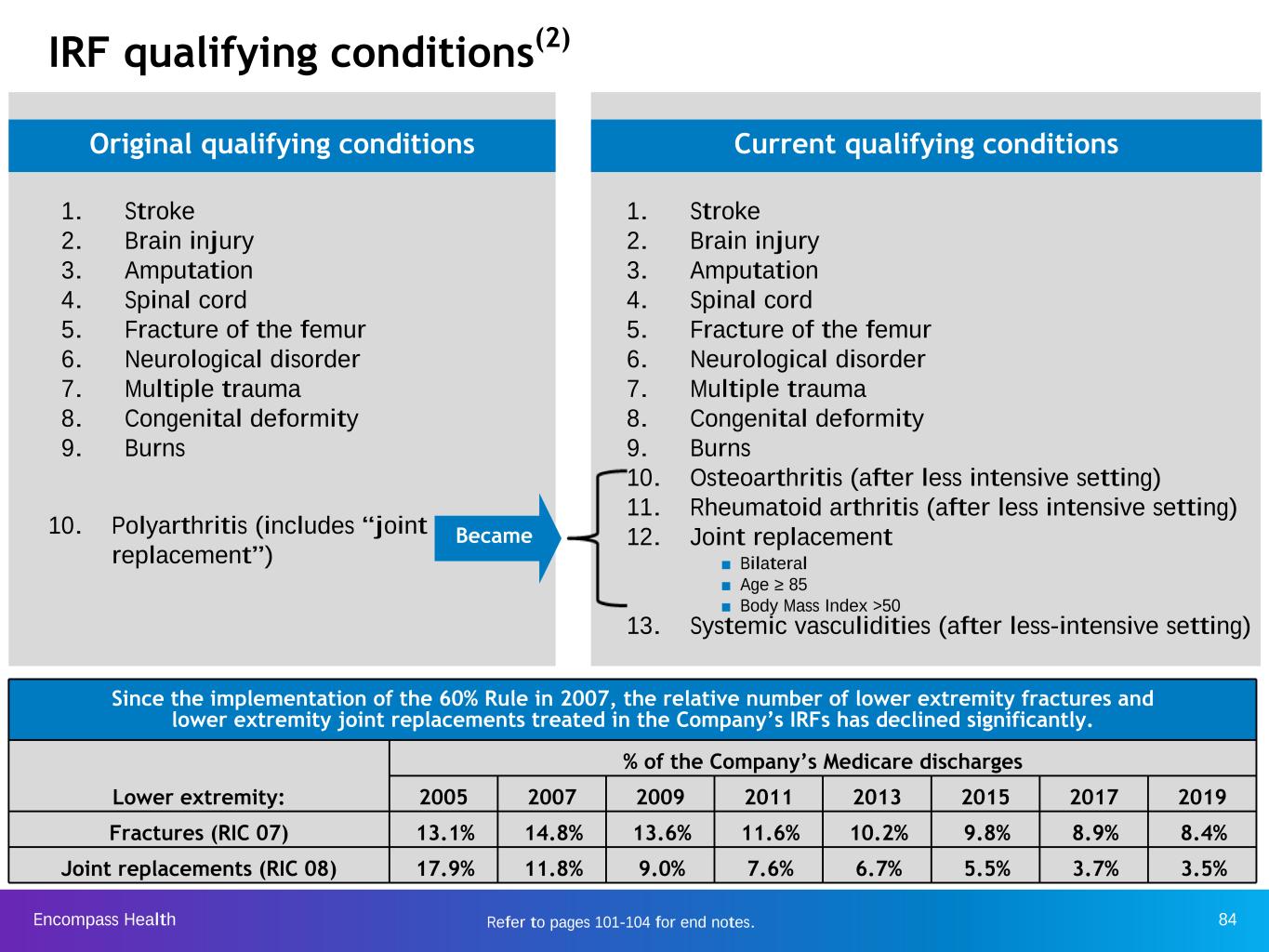
Encompass Health 84 1. Stroke 2. Brain injury 3. Amputation 4. Spinal cord 5. Fracture of the femur 6. Neurological disorder 7. Multiple trauma 8. Congenital deformity 9. Burns IRF qualifying conditions(2) 1. Stroke 2. Brain injury 3. Amputation 4. Spinal cord 5. Fracture of the femur 6. Neurological disorder 7. Multiple trauma 8. Congenital deformity 9. Burns 10. Osteoarthritis (after less intensive setting) 11. Rheumatoid arthritis (after less intensive setting) 12. Joint replacement 13. Systemic vasculidities (after less-intensive setting) Original qualifying conditions Current qualifying conditions ■ Bilateral ■ Age ≥ 85 ■ Body Mass Index >50 10. Polyarthritis (includes “joint replacement”) Became Since the implementation of the 60% Rule in 2007, the relative number of lower extremity fractures and lower extremity joint replacements treated in the Company’s IRFs has declined significantly. Lower extremity: % of the Company’s Medicare discharges 2005 2007 2009 2011 2013 2015 2017 2019 Fractures (RIC 07) 13.1% 14.8% 13.6% 11.6% 10.2% 9.8% 8.9% 8.4% Joint replacements (RIC 08) 17.9% 11.8% 9.0% 7.6% 6.7% 5.5% 3.7% 3.5% Refer to pages 101-104 for end notes.
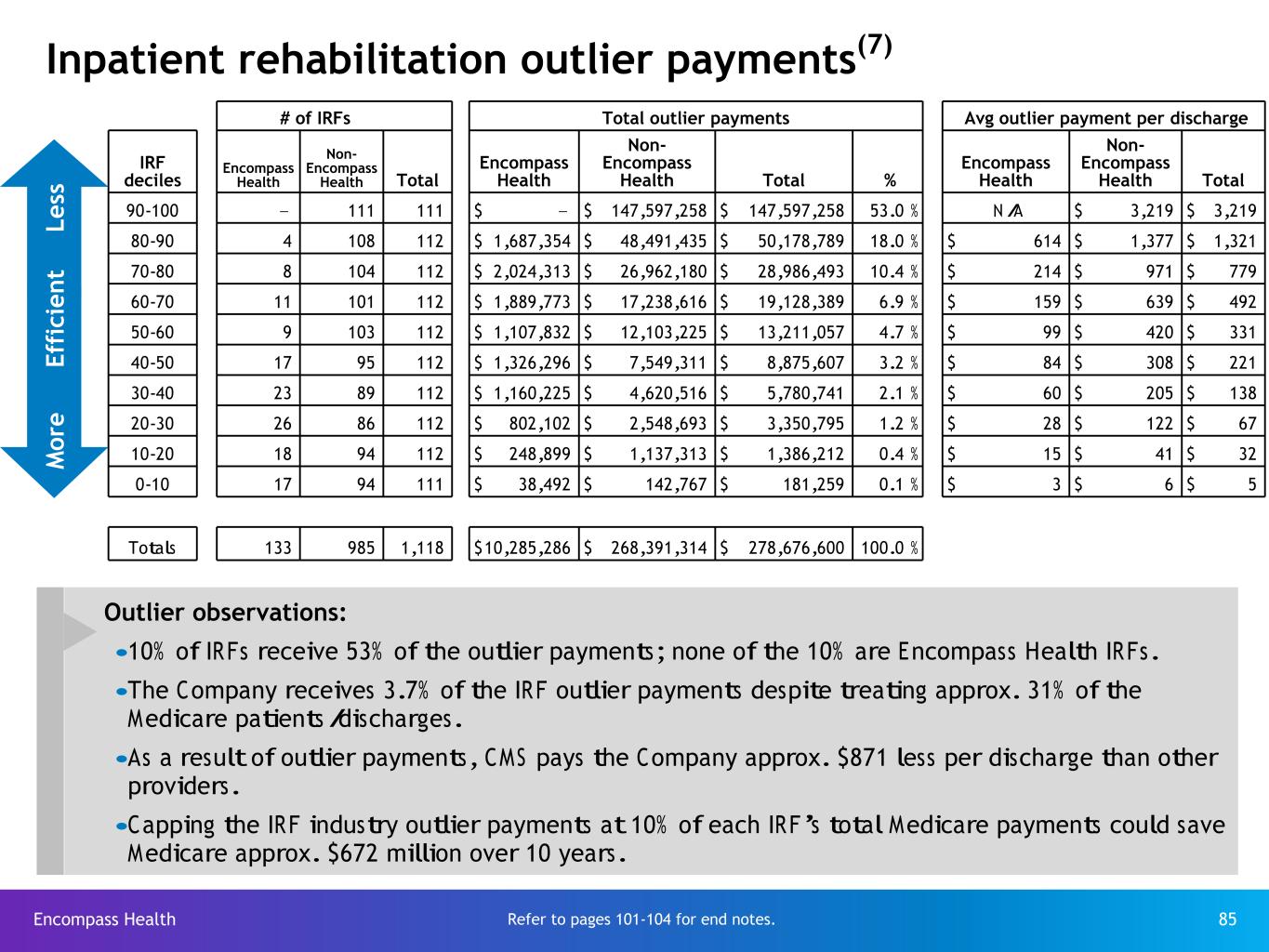
Encompass Health 85 Inpatient rehabilitation outlier payments(7) Refer to pages 101-104 for end notes. M o re E ff ic ie n t Le ss Outlier observations: •10% of IRFs receive 53% of the outlier payments; none of the 10% are Encompass Health IRFs. •The Company receives 3.7% of the IRF outlier payments despite treating approx. 31% of the Medicare patients/discharges. •As a result of outlier payments, CMS pays the Company approx. $871 less per discharge than other providers. •Capping the IRF industry outlier payments at 10% of each IRF’s total Medicare payments could save Medicare approx. $672 million over 10 years. # of IRFs Total outlier payments Avg outlier payment per discharge IRF deciles Encompass Health Non- Encompass Health Total Encompass Health Non- Encompass Health Total % Encompass Health Non- Encompass Health Total 90-100 — 111 111 $ — $ 147,597,258 $ 147,597,258 53.0 % N/A $ 3,219 $ 3,219 80-90 4 108 112 $ 1,687,354 $ 48,491,435 $ 50,178,789 18.0 % $ 614 $ 1,377 $ 1,321 70-80 8 104 112 $ 2,024,313 $ 26,962,180 $ 28,986,493 10.4 % $ 214 $ 971 $ 779 60-70 11 101 112 $ 1,889,773 $ 17,238,616 $ 19,128,389 6.9 % $ 159 $ 639 $ 492 50-60 9 103 112 $ 1,107,832 $ 12,103,225 $ 13,211,057 4.7 % $ 99 $ 420 $ 331 40-50 17 95 112 $ 1,326,296 $ 7,549,311 $ 8,875,607 3.2 % $ 84 $ 308 $ 221 30-40 23 89 112 $ 1,160,225 $ 4,620,516 $ 5,780,741 2.1 % $ 60 $ 205 $ 138 20-30 26 86 112 $ 802,102 $ 2,548,693 $ 3,350,795 1.2 % $ 28 $ 122 $ 67 10-20 18 94 112 $ 248,899 $ 1,137,313 $ 1,386,212 0.4 % $ 15 $ 41 $ 32 0-10 17 94 111 $ 38,492 $ 142,767 $ 181,259 0.1 % $ 3 $ 6 $ 5 Totals 133 985 1,118 $ 10,285,286 $ 268,391,314 $ 278,676,600 100.0 %

Encompass Health 86 IMPACT Act of 2014 - enacted Oct. 6, 2014 Source: https://www.govtrack.us/congress/bills/113/hr4994/text Company observations and considerations with respect to the IMPACT Act: ▪ It was developed on a bi-partisan basis by the House Ways and Means and Senate Finance Committees and incorporated feedback from healthcare providers and provider organizations that responded to the Committees’ solicitation of post-acute payment reform ideas and proposals. ▪ It directs the United States Department of Health and Human Services (“HHS”), in consultation with healthcare stakeholders, to implement standardized data collection processes for post-acute quality and resource use measures. On May 8, 2020, CMS issued an Interim Final Rule with comment period (85 Fed. Reg. 27,550) in which it rescheduled the timeframes during which these data collection processes will be implemented, in accordance with the timing of the conclusion of the COVID-19 public health emergency (“PHE”). ▪ Although the IMPACT Act does not specifically call for the implementation of a new post-acute payment system, the Company believes this Act will lay the foundation for possible future post-acute payment policies that would be based on patients’ medical conditions and other clinical factors rather than the setting where the care is provided. It has created additional data collection and reporting requirements for the Company’s IRFs and home health agencies. ▪ While the Company cannot quantify the potential financial effect of the IMPACT Act on Encompass Health, the Company believes any post-acute payment system that is data driven and focuses on the needs and underlying medical conditions of post-acute patients will be positive for providers who offer high-quality, cost-effective care. Encompass Health believes it is doing just that and expects this act will be positive for the Company. ▪ However, it will likely take years for the quality data to be gathered, standardized patient assessment data to be assembled and disseminated, and potential payment policies to be developed, tested and promulgated. As a national leader in integrated healthcare services, offering both facility-based and home-based patient care, the Company looks forward to working with HHS, the Medicare Payment Advisory Commission and other healthcare stakeholders on these initiatives.

Encompass Health 87 Segment operating results
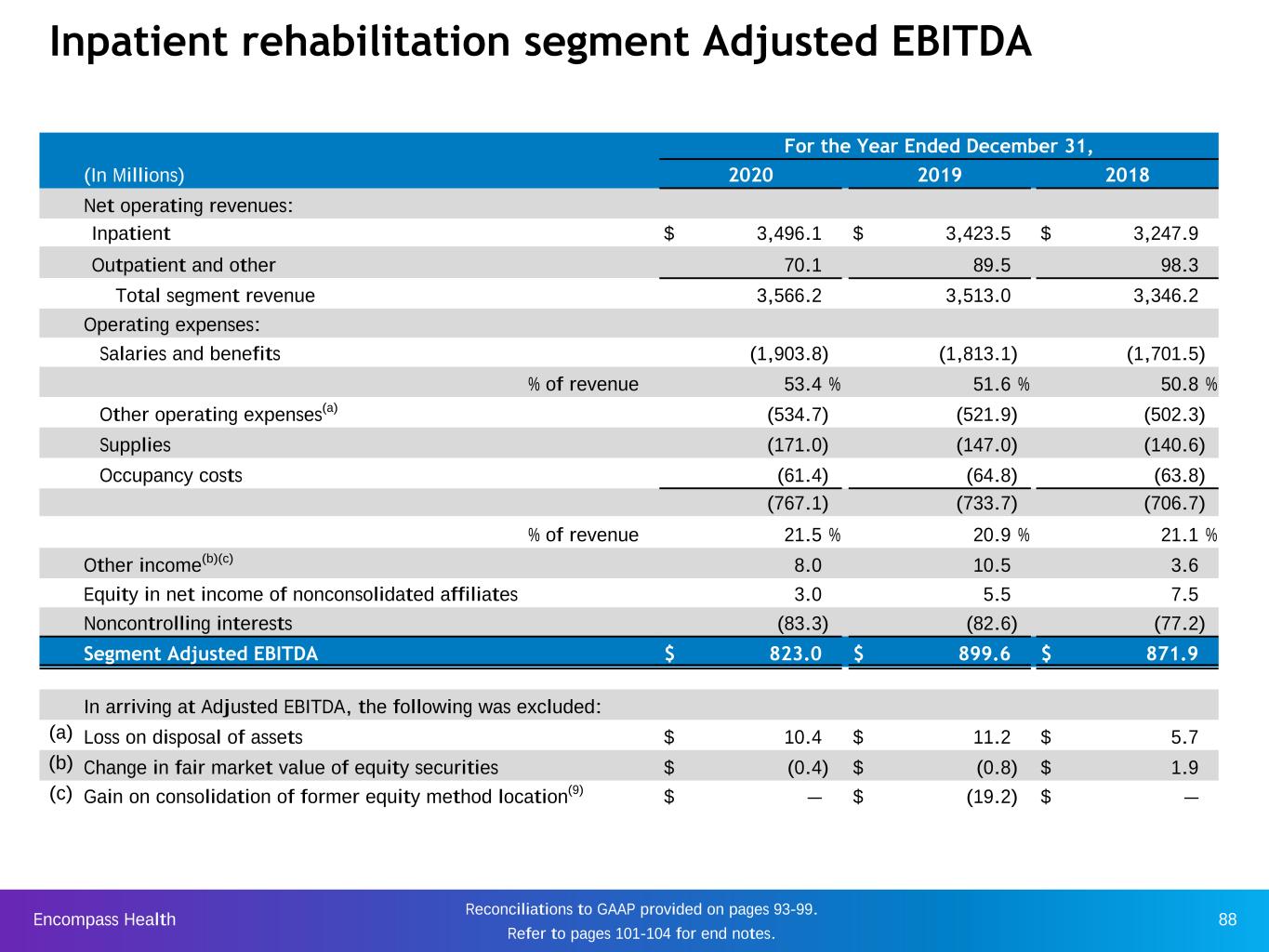
Encompass Health 88 Inpatient rehabilitation segment Adjusted EBITDA For the Year Ended December 31, (In Millions) 2020 2019 2018 Net operating revenues: Inpatient $ 3,496.1 $ 3,423.5 $ 3,247.9 Outpatient and other 70.1 89.5 98.3 Total segment revenue 3,566.2 3,513.0 3,346.2 Operating expenses: Salaries and benefits (1,903.8) (1,813.1) (1,701.5) % of revenue 53.4 % 51.6 % 50.8 % Other operating expenses(a) (534.7) (521.9) (502.3) Supplies (171.0) (147.0) (140.6) Occupancy costs (61.4) (64.8) (63.8) (767.1) (733.7) (706.7) % of revenue 21.5 % 20.9 % 21.1 % Other income(b)(c) 8.0 10.5 3.6 Equity in net income of nonconsolidated affiliates 3.0 5.5 7.5 Noncontrolling interests (83.3) (82.6) (77.2) Segment Adjusted EBITDA $ 823.0 $ 899.6 $ 871.9 In arriving at Adjusted EBITDA, the following was excluded: (a) Loss on disposal of assets $ 10.4 $ 11.2 $ 5.7 (b) Change in fair market value of equity securities $ (0.4) $ (0.8) $ 1.9 (c) Gain on consolidation of former equity method location(9) $ — $ (19.2) $ — Reconciliations to GAAP provided on pages 93-99. Refer to pages 101-104 for end notes.
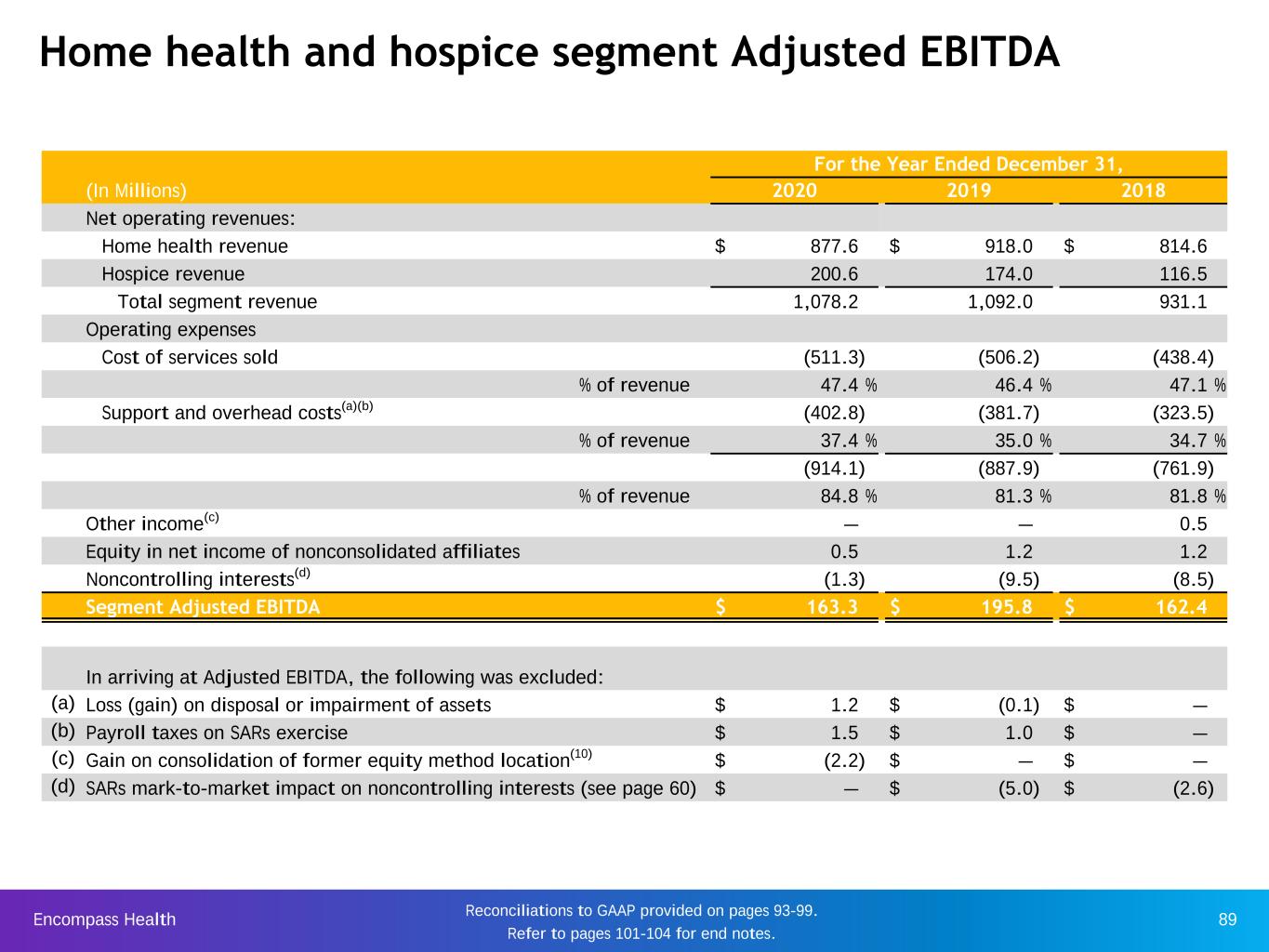
Encompass Health 89 Home health and hospice segment Adjusted EBITDA For the Year Ended December 31, (In Millions) 2020 2019 2018 Net operating revenues: Home health revenue $ 877.6 $ 918.0 $ 814.6 Hospice revenue 200.6 174.0 116.5 Total segment revenue 1,078.2 1,092.0 931.1 Operating expenses Cost of services sold (511.3) (506.2) (438.4) % of revenue 47.4 % 46.4 % 47.1 % Support and overhead costs(a)(b) (402.8) (381.7) (323.5) % of revenue 37.4 % 35.0 % 34.7 % (914.1) (887.9) (761.9) % of revenue 84.8 % 81.3 % 81.8 % Other income(c) — — 0.5 Equity in net income of nonconsolidated affiliates 0.5 1.2 1.2 Noncontrolling interests(d) (1.3) (9.5) (8.5) Segment Adjusted EBITDA $ 163.3 $ 195.8 $ 162.4 In arriving at Adjusted EBITDA, the following was excluded: (a) Loss (gain) on disposal or impairment of assets $ 1.2 $ (0.1) $ — (b) Payroll taxes on SARs exercise $ 1.5 $ 1.0 $ — (c) Gain on consolidation of former equity method location(10) $ (2.2) $ — $ — (d) SARs mark-to-market impact on noncontrolling interests (see page 60) $ — $ (5.0) $ (2.6) Reconciliations to GAAP provided on pages 93-99. Refer to pages 101-104 for end notes.
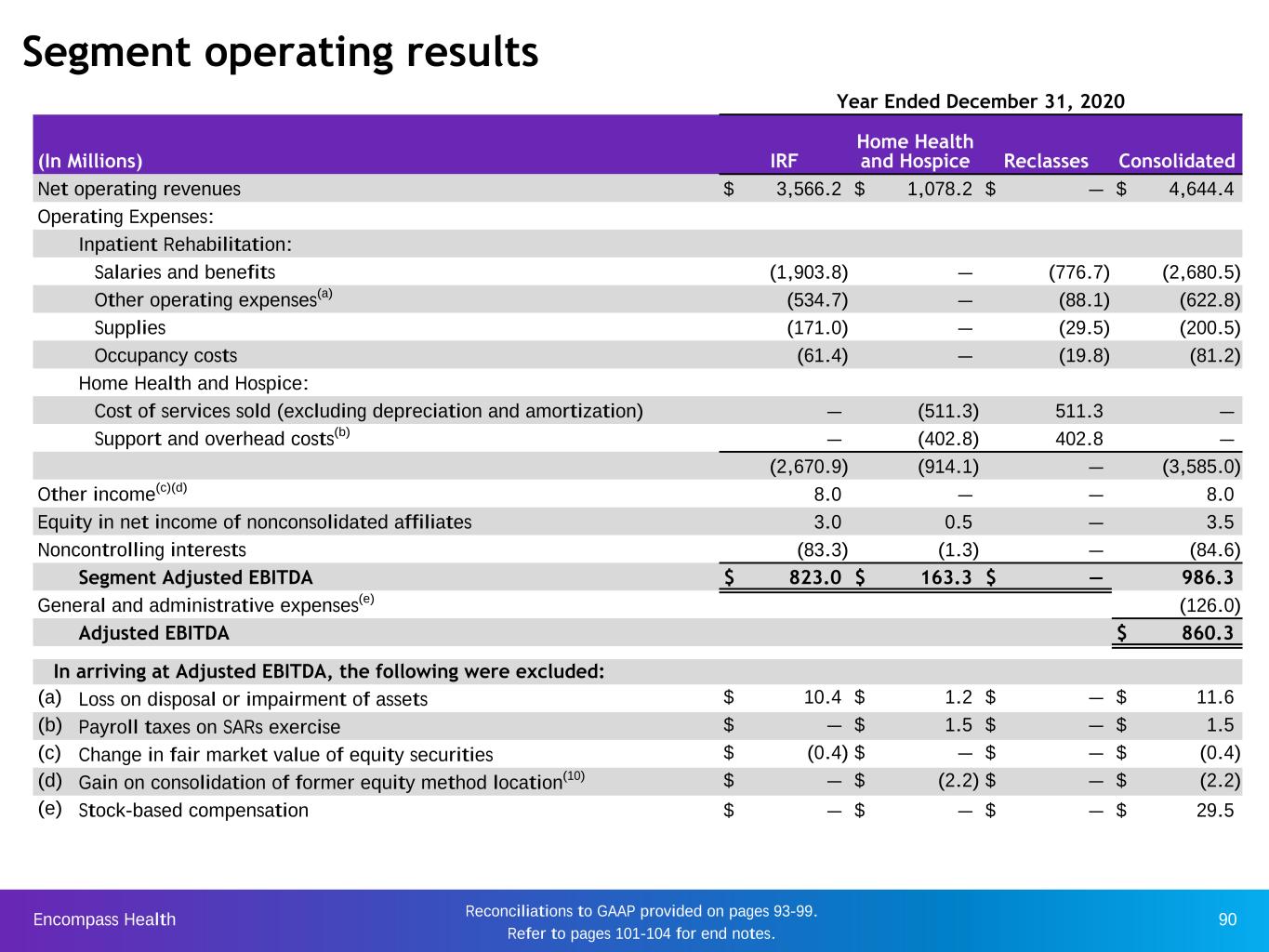
Encompass Health 90 Year Ended December 31, 2020 (In Millions) IRF Home Health and Hospice Reclasses Consolidated Net operating revenues $ 3,566.2 $ 1,078.2 $ — $ 4,644.4 Operating Expenses: Inpatient Rehabilitation: Salaries and benefits (1,903.8) — (776.7) (2,680.5) Other operating expenses(a) (534.7) — (88.1) (622.8) Supplies (171.0) — (29.5) (200.5) Occupancy costs (61.4) — (19.8) (81.2) Home Health and Hospice: Cost of services sold (excluding depreciation and amortization) — (511.3) 511.3 — Support and overhead costs(b) — (402.8) 402.8 — (2,670.9) (914.1) — (3,585.0) Other income(c)(d) 8.0 — — 8.0 Equity in net income of nonconsolidated affiliates 3.0 0.5 — 3.5 Noncontrolling interests (83.3) (1.3) — (84.6) Segment Adjusted EBITDA $ 823.0 $ 163.3 $ — 986.3 General and administrative expenses(e) (126.0) Adjusted EBITDA $ 860.3 In arriving at Adjusted EBITDA, the following were excluded: (a) Loss on disposal or impairment of assets $ 10.4 $ 1.2 $ — $ 11.6 (b) Payroll taxes on SARs exercise $ — $ 1.5 $ — $ 1.5 (c) Change in fair market value of equity securities $ (0.4) $ — $ — $ (0.4) (d) Gain on consolidation of former equity method location(10) $ — $ (2.2) $ — $ (2.2) (e) Stock-based compensation $ — $ — $ — $ 29.5 Segment operating results Reconciliations to GAAP provided on pages 93-99. Refer to pages 101-104 for end notes.
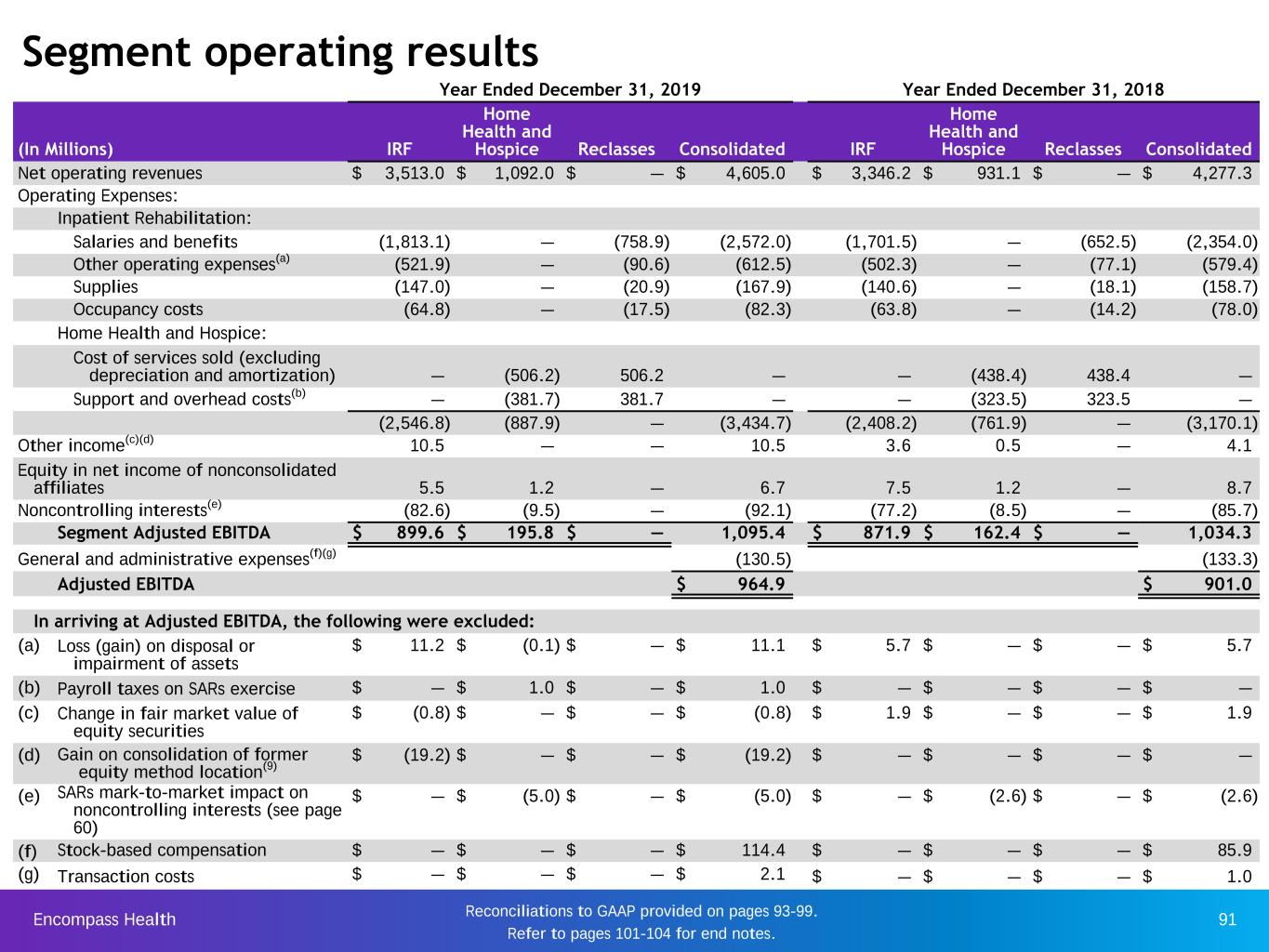
Encompass Health 91 Year Ended December 31, 2019 Year Ended December 31, 2018 (In Millions) IRF Home Health and Hospice Reclasses Consolidated IRF Home Health and Hospice Reclasses Consolidated Net operating revenues $ 3,513.0 $ 1,092.0 $ — $ 4,605.0 $ 3,346.2 $ 931.1 $ — $ 4,277.3 Operating Expenses: Inpatient Rehabilitation: Salaries and benefits (1,813.1) — (758.9) (2,572.0) (1,701.5) — (652.5) (2,354.0) Other operating expenses(a) (521.9) — (90.6) (612.5) (502.3) — (77.1) (579.4) Supplies (147.0) — (20.9) (167.9) (140.6) — (18.1) (158.7) Occupancy costs (64.8) — (17.5) (82.3) (63.8) — (14.2) (78.0) Home Health and Hospice: Cost of services sold (excluding depreciation and amortization) — (506.2) 506.2 — — (438.4) 438.4 — Support and overhead costs(b) — (381.7) 381.7 — — (323.5) 323.5 — (2,546.8) (887.9) — (3,434.7) (2,408.2) (761.9) — (3,170.1) Other income(c)(d) 10.5 — — 10.5 3.6 0.5 — 4.1 Equity in net income of nonconsolidated affiliates 5.5 1.2 — 6.7 7.5 1.2 — 8.7 Noncontrolling interests(e) (82.6) (9.5) — (92.1) (77.2) (8.5) — (85.7) Segment Adjusted EBITDA $ 899.6 $ 195.8 $ — 1,095.4 $ 871.9 $ 162.4 $ — 1,034.3 General and administrative expenses(f)(g) (130.5) (133.3) Adjusted EBITDA $ 964.9 $ 901.0 In arriving at Adjusted EBITDA, the following were excluded: (a) Loss (gain) on disposal or impairment of assets $ 11.2 $ (0.1) $ — $ 11.1 $ 5.7 $ — $ — $ 5.7 (b) Payroll taxes on SARs exercise $ — $ 1.0 $ — $ 1.0 $ — $ — $ — $ — (c) Change in fair market value of equity securities $ (0.8) $ — $ — $ (0.8) $ 1.9 $ — $ — $ 1.9 (d) Gain on consolidation of former equity method location(9) $ (19.2) $ — $ — $ (19.2) $ — $ — $ — $ — (e) SARs mark-to-market impact on noncontrolling interests (see page 60) $ — $ (5.0) $ — $ (5.0) $ — $ (2.6) $ — $ (2.6) (f) Stock-based compensation $ — $ — $ — $ 114.4 $ — $ — $ — $ 85.9 (g) Transaction costs $ — $ — $ — $ 2.1 $ — $ — $ — $ 1.0 Segment operating results Reconciliations to GAAP provided on pages 93-99. Refer to pages 101-104 for end notes.
Encompass Health 92 Reconciliations to GAAP and share information
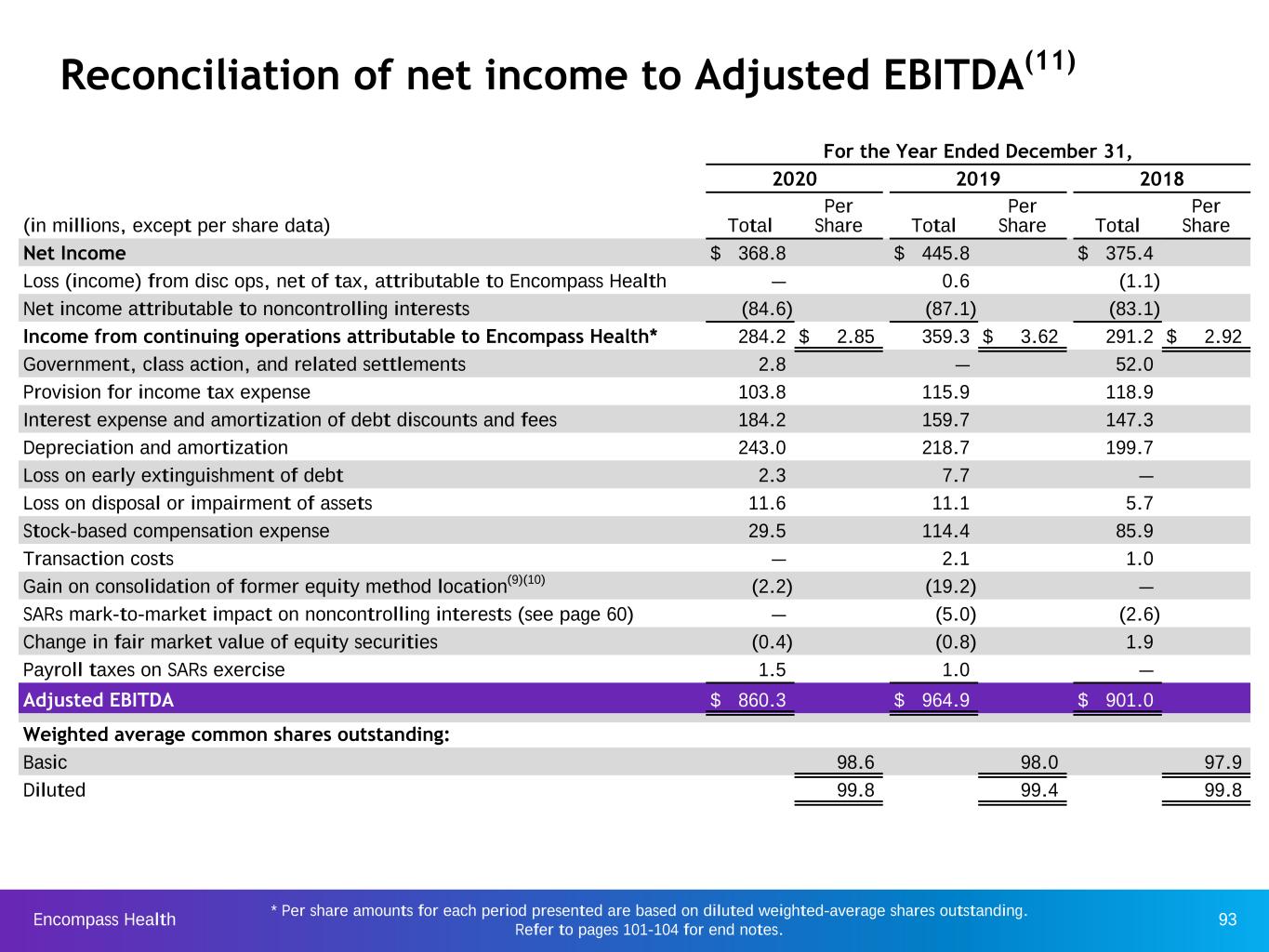
Encompass Health 93 Reconciliation of net income to Adjusted EBITDA(11) * Per share amounts for each period presented are based on diluted weighted-average shares outstanding. Refer to pages 101-104 for end notes. For the Year Ended December 31, 2020 2019 2018 (in millions, except per share data) Total Per Share Total Per Share Total Per Share Net Income $ 368.8 $ 445.8 $ 375.4 Loss (income) from disc ops, net of tax, attributable to Encompass Health — 0.6 (1.1) Net income attributable to noncontrolling interests (84.6) (87.1) (83.1) Income from continuing operations attributable to Encompass Health* 284.2 $ 2.85 359.3 $ 3.62 291.2 $ 2.92 Government, class action, and related settlements 2.8 — 52.0 Provision for income tax expense 103.8 115.9 118.9 Interest expense and amortization of debt discounts and fees 184.2 159.7 147.3 Depreciation and amortization 243.0 218.7 199.7 Loss on early extinguishment of debt 2.3 7.7 — Loss on disposal or impairment of assets 11.6 11.1 5.7 Stock-based compensation expense 29.5 114.4 85.9 Transaction costs — 2.1 1.0 Gain on consolidation of former equity method location(9)(10) (2.2) (19.2) — SARs mark-to-market impact on noncontrolling interests (see page 60) — (5.0) (2.6) Change in fair market value of equity securities (0.4) (0.8) 1.9 Payroll taxes on SARs exercise 1.5 1.0 — Adjusted EBITDA $ 860.3 $ 964.9 $ 901.0 Weighted average common shares outstanding: Basic 98.6 98.0 97.9 Diluted 99.8 99.4 99.8

Encompass Health 94 Reconciliation of segment Adjusted EBITDA to income from continuing operations before income tax expense For the Year Ended December 31, 2020 2019 2018 (in millions) Total segment Adjusted EBITDA $ 986.3 $ 1,095.4 $ 1,034.3 General and administrative expenses (155.5) (247.0) (220.2) Depreciation and amortization (243.0) (218.7) (199.7) Loss on disposal or impairment of assets (11.6) (11.1) (5.7) Government, class action, and related settlements (2.8) — (52.0) Loss on early extinguishment of debt(19) (2.3) (7.7) — Interest expense and amortization of debt discounts and fees (184.2) (159.7) (147.3) Net income attributable to noncontrolling interests 84.6 87.1 83.1 SARs mark-to-market impact on noncontrolling interests (see page 60) — 5.0 2.6 Change in fair market value of equity securities 0.4 0.8 (1.9) Gain on consolidation of former equity method location(9)(10) 2.2 19.2 — Payroll taxes on SARs exercise (1.5) (1.0) — Income from continuing operations before income tax expense $ 472.6 $ 562.3 $ 493.2 Refer to pages 101-104 for end notes.
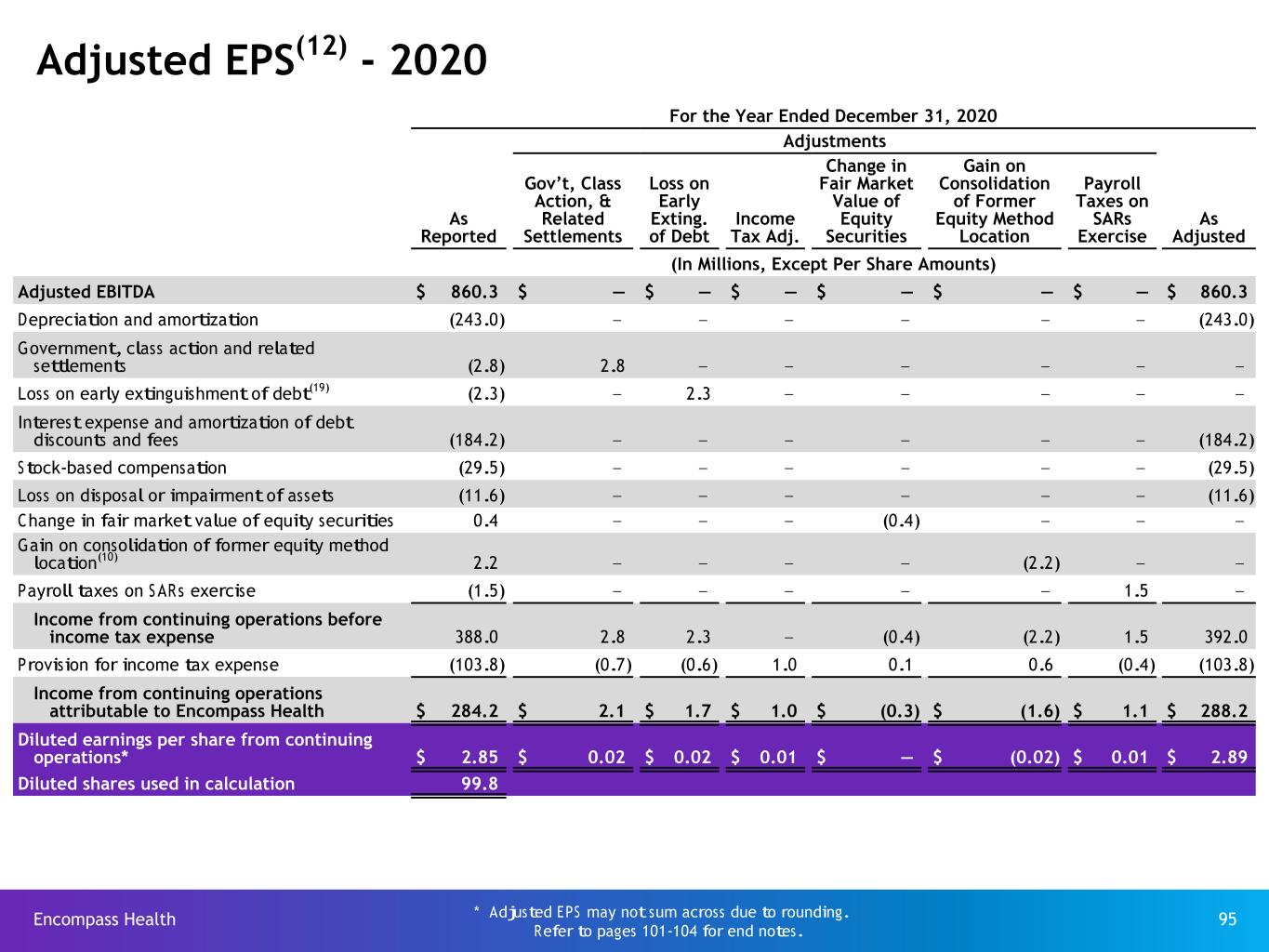
Encompass Health 95 For the Year Ended December 31, 2020 Adjustments As Reported Gov’t, Class Action, & Related Settlements Loss on Early Exting. of Debt Income Tax Adj. Change in Fair Market Value of Equity Securities Gain on Consolidation of Former Equity Method Location Payroll Taxes on SARs Exercise As Adjusted (In Millions, Except Per Share Amounts) Adjusted EBITDA $ 860.3 $ — $ — $ — $ — $ — $ — $ 860.3 Depreciation and amortization (243.0) — — — — — — (243.0) Government, class action and related settlements (2.8) 2.8 — — — — — — Loss on early extinguishment of debt(19) (2.3) — 2.3 — — — — — Interest expense and amortization of debt discounts and fees (184.2) — — — — — — (184.2) Stock-based compensation (29.5) — — — — — — (29.5) Loss on disposal or impairment of assets (11.6) — — — — — — (11.6) Change in fair market value of equity securities 0.4 — — — (0.4) — — — Gain on consolidation of former equity method location(10) 2.2 — — — — (2.2) — — Payroll taxes on SARs exercise (1.5) — — — — — 1.5 — Income from continuing operations before income tax expense 388.0 2.8 2.3 — (0.4) (2.2) 1.5 392.0 Provision for income tax expense (103.8) (0.7) (0.6) 1.0 0.1 0.6 (0.4) (103.8) Income from continuing operations attributable to Encompass Health $ 284.2 $ 2.1 $ 1.7 $ 1.0 $ (0.3) $ (1.6) $ 1.1 $ 288.2 Diluted earnings per share from continuing operations* $ 2.85 $ 0.02 $ 0.02 $ 0.01 $ — $ (0.02) $ 0.01 $ 2.89 Diluted shares used in calculation 99.8 Adjusted EPS(12) - 2020 * Adjusted EPS may not sum across due to rounding. Refer to pages 101-104 for end notes.

Encompass Health 96 Adjusted EPS(12) - 2019 For the Year Ended December 31, 2019 Adjustments As Reported Mark-to- Market Adjustment for Stock Comp. Expense Loss on Early Exting. of Debt Income Tax Adj. Transaction Costs Change in Fair Market Value of Equity Securities Gain on Consolidation of Former Equity Method Location Payroll Taxes on SARs Exercise As Adjusted (In Millions, Except Per Share Amounts) Adjusted EBITDA $ 964.9 $ — $ — $ — $ — $ — $ — $ — $ 964.9 Depreciation and amortization (218.7) — — — — — — — (218.7) Loss on early extinguishment of debt(19) (7.7) — 7.7 — — — — — — Interest expense and amortization of debt discounts and fees (159.7) — — — — — — — (159.7) Stock-based compensation (114.4) 68.5 — — — — — — (45.9) Loss on disposal of assets (11.1) — — — — — — — (11.1) Transaction costs (2.1) — — — 2.1 — — — — SARs mark-to-market impact on noncontrolling interests (see page 60) 5.0 (5.0) — — — — — — — Change in fair market value of equity securities 0.8 — — — — (0.8) — — — Gain on consolidation of former equity method location(9) 19.2 — — — — — (19.2) — — Payroll taxes on SARs exercise (1.0) — — — — — — 1.0 — Income from continuing operations before income tax expense 475.2 63.5 7.7 — 2.1 (0.8) (19.2) 1.0 529.5 Provision for income tax expense (115.9) (17.2) (2.1) (10.3) (0.6) 0.2 5.2 (0.2) (140.9) Income from continuing operations attributable to Encompass Health $ 359.3 $ 46.3 $ 5.6 $ (10.3) $ 1.5 $ (0.6) $ (14.0) $ 0.8 $ 388.6 Diluted earnings per share from continuing operations* $ 3.62 $ 0.47 $ 0.06 $ (0.10) $ 0.02 $ (0.01) $ (0.14) $ 0.01 $ 3.91 Diluted shares used in calculation 99.4 * Adjusted EPS may not sum across due to rounding. Refer to pages 101-104 for end notes.

Encompass Health 97 For the Year Ended December 31, 2018 Adjustments As Reported Gov’t, Class Action, & Related Settlements Mark-to- Market Adjustment for Stock Comp. Expense Income Tax Adj. Transaction Costs Change in Fair Market Value of Equity Securities As Adjusted (In Millions, Except Per Share Amounts) Adjusted EBITDA $ 901.0 $ — $ — $ — $ — $ — $ 901.0 Depreciation and amortization (199.7) — — — — — (199.7) Government, class action and related settlements (52.0) 52.0 — — — — — Interest expense and amortization of debt discounts and fees (147.3) — — — — — (147.3) Stock-based compensation (85.9) — 31.2 — — — (54.7) Loss on disposal of assets (5.7) — — — — — (5.7) Transaction costs (1.0) — — — 1.0 — — SARs mark-to-market impact on noncontrolling interests (see page 60) 2.6 — (2.6) — — — — Change in fair market value of equity securities (1.9) — — — — 1.9 — Income from continuing operations before income tax expense 410.1 52.0 28.6 — 1.0 1.9 493.6 Provision for income tax expense (118.9) — (8.0) (3.3) (0.3) (0.5) (131.0) Income from continuing operations attributable to Encompass Health $ 291.2 $ 52.0 $ 20.6 $ (3.3) $ 0.7 $ 1.4 $ 362.6 Diluted earnings per share from continuing operations* $ 2.92 $ 0.52 $ 0.21 $ (0.03) $ 0.01 $ 0.01 $ 3.63 Diluted shares used in calculation 99.8 Adjusted EPS(12) - 2018 * Adjusted EPS may not sum across due to rounding. Refer to pages 101-104 for end notes.

Encompass Health 98 Adjusted free cash flow history(13) For the Year Ended December 31, (In Millions) 2020 2019 2018 Net cash provided by operating activities $ 704.7 $ 635.3 $ 762.4 Impact of discontinued operations 0.2 4.4 (0.8) Net cash provided by operating activities of continuing operations 704.9 639.7 761.6 Capital expenditures for maintenance (154.9) (167.1) (152.9) Distributions paid to noncontrolling interests of consolidated affiliates (72.2) (79.8) (75.4) Items non-indicative of ongoing operating performance: Cash paid for SARs exercise (inclusive of payroll taxes) 102.1 69.6 4.3 Transaction costs and related assumed liabilities — 2.1 0.5 Cash paid for government, class action, and related settlements — 52.0 — Adjusted free cash flow $ 579.9 $ 516.5 $ 538.1 Cash dividends on common stock(25) $ 111.9 $ 108.7 $ 100.8 Refer to pages 101-104 for end notes. Information regarding investing and financing categories of the statement of cash flows for the periods presented can be found on Encompass Health’s website in the Earnings Releases for those periods.
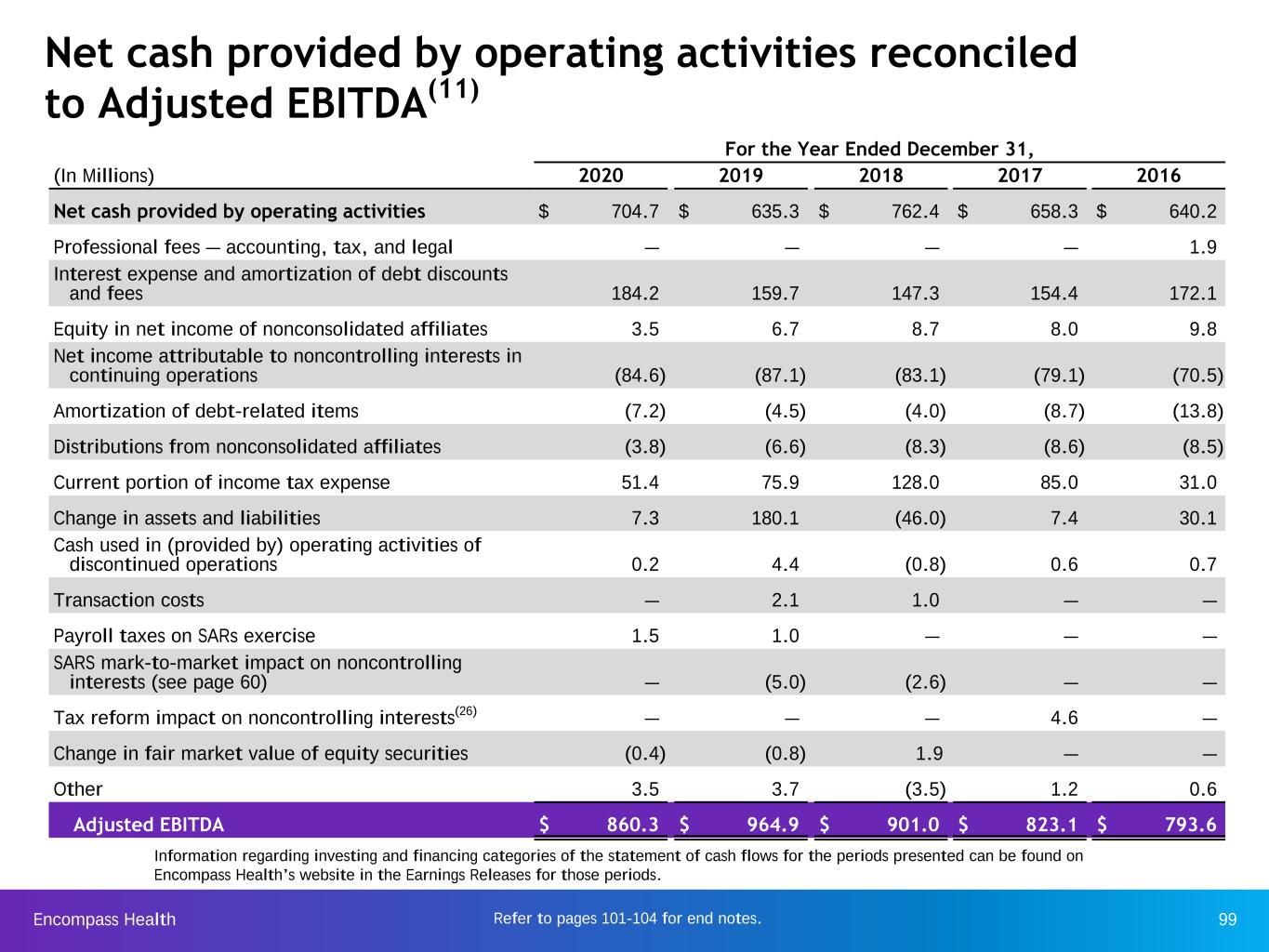
Encompass Health 99 Net cash provided by operating activities reconciled to Adjusted EBITDA(11) Information regarding investing and financing categories of the statement of cash flows for the periods presented can be found on Encompass Health’s website in the Earnings Releases for those periods. For the Year Ended December 31, (In Millions) 2020 2019 2018 2017 2016 Net cash provided by operating activities $ 704.7 $ 635.3 $ 762.4 $ 658.3 $ 640.2 Professional fees — accounting, tax, and legal — — — — 1.9 Interest expense and amortization of debt discounts and fees 184.2 159.7 147.3 154.4 172.1 Equity in net income of nonconsolidated affiliates 3.5 6.7 8.7 8.0 9.8 Net income attributable to noncontrolling interests in continuing operations (84.6) (87.1) (83.1) (79.1) (70.5) Amortization of debt-related items (7.2) (4.5) (4.0) (8.7) (13.8) Distributions from nonconsolidated affiliates (3.8) (6.6) (8.3) (8.6) (8.5) Current portion of income tax expense 51.4 75.9 128.0 85.0 31.0 Change in assets and liabilities 7.3 180.1 (46.0) 7.4 30.1 Cash used in (provided by) operating activities of discontinued operations 0.2 4.4 (0.8) 0.6 0.7 Transaction costs — 2.1 1.0 — — Payroll taxes on SARs exercise 1.5 1.0 — — — SARS mark-to-market impact on noncontrolling interests (see page 60) — (5.0) (2.6) — — Tax reform impact on noncontrolling interests(26) — — — 4.6 — Change in fair market value of equity securities (0.4) (0.8) 1.9 — — Other 3.5 3.7 (3.5) 1.2 0.6 Adjusted EBITDA $ 860.3 $ 964.9 $ 901.0 $ 823.1 $ 793.6 Refer to pages 101-104 for end notes.
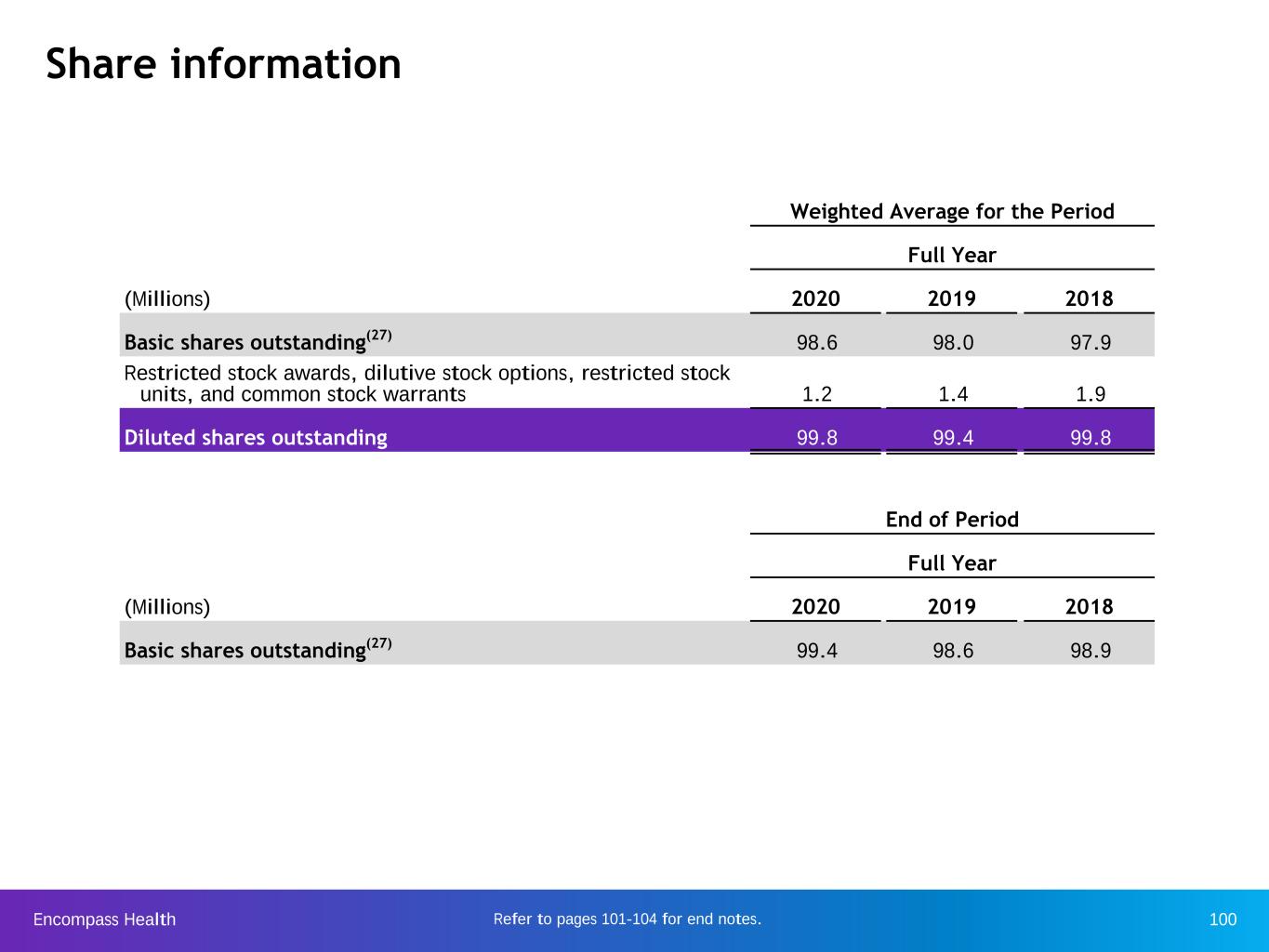
Encompass Health 100Refer to pages 101-104 for end notes. Share information Weighted Average for the Period Full Year (Millions) 2020 2019 2018 Basic shares outstanding(27) 98.6 98.0 97.9 Restricted stock awards, dilutive stock options, restricted stock units, and common stock warrants 1.2 1.4 1.9 Diluted shares outstanding 99.8 99.4 99.8 End of Period Full Year (Millions) 2020 2019 2018 Basic shares outstanding(27) 99.4 98.6 98.9
Encompass Health 101 End notes
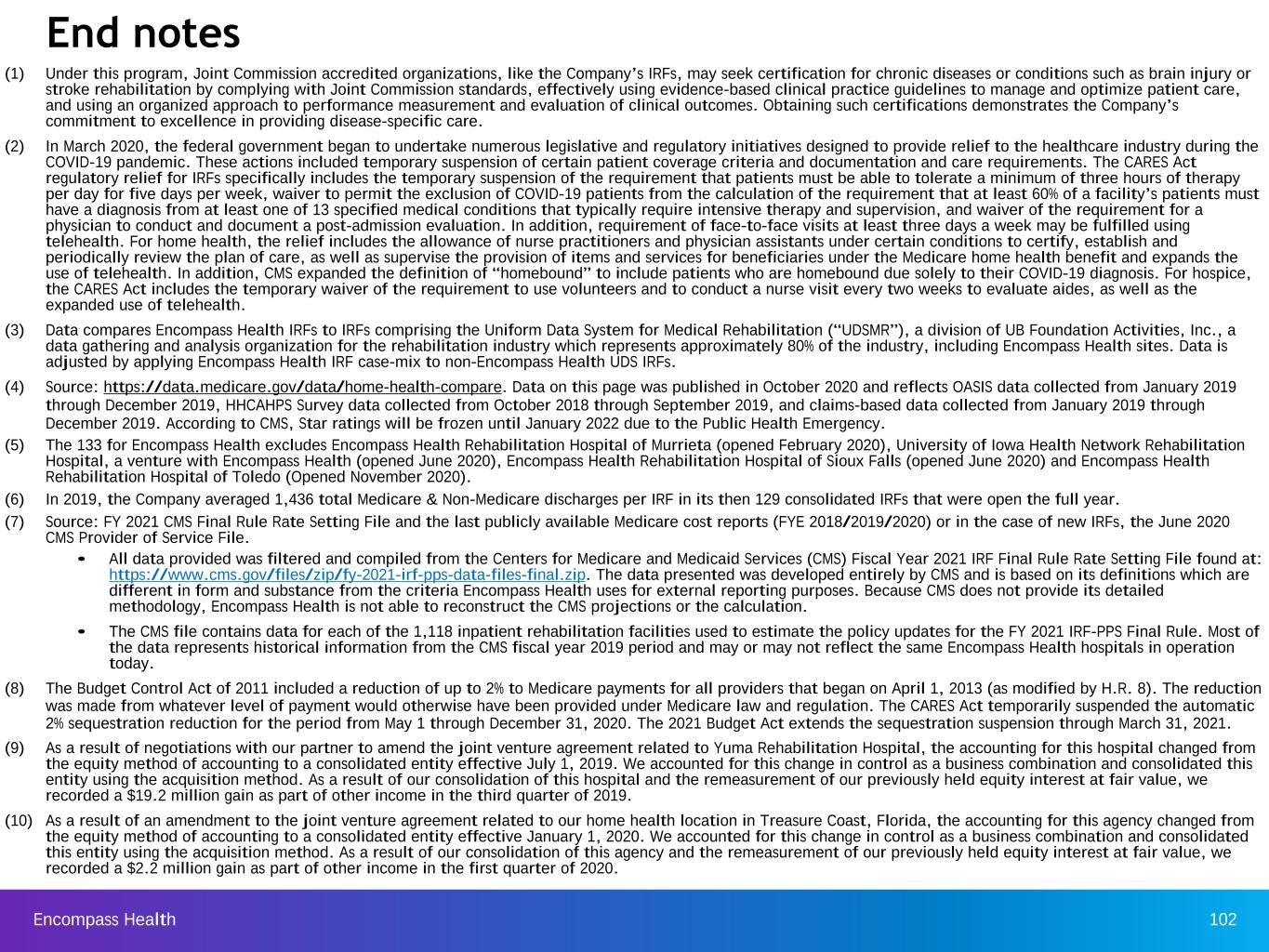
Encompass Health 102 (1) Under this program, Joint Commission accredited organizations, like the Company’s IRFs, may seek certification for chronic diseases or conditions such as brain injury or stroke rehabilitation by complying with Joint Commission standards, effectively using evidence-based clinical practice guidelines to manage and optimize patient care, and using an organized approach to performance measurement and evaluation of clinical outcomes. Obtaining such certifications demonstrates the Company’s commitment to excellence in providing disease-specific care. (2) In March 2020, the federal government began to undertake numerous legislative and regulatory initiatives designed to provide relief to the healthcare industry during the COVID-19 pandemic. These actions included temporary suspension of certain patient coverage criteria and documentation and care requirements. The CARES Act regulatory relief for IRFs specifically includes the temporary suspension of the requirement that patients must be able to tolerate a minimum of three hours of therapy per day for five days per week, waiver to permit the exclusion of COVID-19 patients from the calculation of the requirement that at least 60% of a facility’s patients must have a diagnosis from at least one of 13 specified medical conditions that typically require intensive therapy and supervision, and waiver of the requirement for a physician to conduct and document a post-admission evaluation. In addition, requirement of face-to-face visits at least three days a week may be fulfilled using telehealth. For home health, the relief includes the allowance of nurse practitioners and physician assistants under certain conditions to certify, establish and periodically review the plan of care, as well as supervise the provision of items and services for beneficiaries under the Medicare home health benefit and expands the use of telehealth. In addition, CMS expanded the definition of “homebound” to include patients who are homebound due solely to their COVID-19 diagnosis. For hospice, the CARES Act includes the temporary waiver of the requirement to use volunteers and to conduct a nurse visit every two weeks to evaluate aides, as well as the expanded use of telehealth. (3) Data compares Encompass Health IRFs to IRFs comprising the Uniform Data System for Medical Rehabilitation (“UDSMR”), a division of UB Foundation Activities, Inc., a data gathering and analysis organization for the rehabilitation industry which represents approximately 80% of the industry, including Encompass Health sites. Data is adjusted by applying Encompass Health IRF case-mix to non-Encompass Health UDS IRFs. (4) Source: https://data.medicare.gov/data/home-health-compare. Data on this page was published in October 2020 and reflects OASIS data collected from January 2019 through December 2019, HHCAHPS Survey data collected from October 2018 through September 2019, and claims-based data collected from January 2019 through December 2019. According to CMS, Star ratings will be frozen until January 2022 due to the Public Health Emergency. (5) The 133 for Encompass Health excludes Encompass Health Rehabilitation Hospital of Murrieta (opened February 2020), University of Iowa Health Network Rehabilitation Hospital, a venture with Encompass Health (opened June 2020), Encompass Health Rehabilitation Hospital of Sioux Falls (opened June 2020) and Encompass Health Rehabilitation Hospital of Toledo (Opened November 2020). (6) In 2019, the Company averaged 1,436 total Medicare & Non-Medicare discharges per IRF in its then 129 consolidated IRFs that were open the full year. (7) Source: FY 2021 CMS Final Rule Rate Setting File and the last publicly available Medicare cost reports (FYE 2018/2019/2020) or in the case of new IRFs, the June 2020 CMS Provider of Service File. • All data provided was filtered and compiled from the Centers for Medicare and Medicaid Services (CMS) Fiscal Year 2021 IRF Final Rule Rate Setting File found at: https://www.cms.gov/files/zip/fy-2021-irf-pps-data-files-final.zip. The data presented was developed entirely by CMS and is based on its definitions which are different in form and substance from the criteria Encompass Health uses for external reporting purposes. Because CMS does not provide its detailed methodology, Encompass Health is not able to reconstruct the CMS projections or the calculation. • The CMS file contains data for each of the 1,118 inpatient rehabilitation facilities used to estimate the policy updates for the FY 2021 IRF-PPS Final Rule. Most of the data represents historical information from the CMS fiscal year 2019 period and may or may not reflect the same Encompass Health hospitals in operation today. (8) The Budget Control Act of 2011 included a reduction of up to 2% to Medicare payments for all providers that began on April 1, 2013 (as modified by H.R. 8). The reduction was made from whatever level of payment would otherwise have been provided under Medicare law and regulation. The CARES Act temporarily suspended the automatic 2% sequestration reduction for the period from May 1 through December 31, 2020. The 2021 Budget Act extends the sequestration suspension through March 31, 2021. (9) As a result of negotiations with our partner to amend the joint venture agreement related to Yuma Rehabilitation Hospital, the accounting for this hospital changed from the equity method of accounting to a consolidated entity effective July 1, 2019. We accounted for this change in control as a business combination and consolidated this entity using the acquisition method. As a result of our consolidation of this hospital and the remeasurement of our previously held equity interest at fair value, we recorded a $19.2 million gain as part of other income in the third quarter of 2019. (10) As a result of an amendment to the joint venture agreement related to our home health location in Treasure Coast, Florida, the accounting for this agency changed from the equity method of accounting to a consolidated entity effective January 1, 2020. We accounted for this change in control as a business combination and consolidated this entity using the acquisition method. As a result of our consolidation of this agency and the remeasurement of our previously held equity interest at fair value, we recorded a $2.2 million gain as part of other income in the first quarter of 2020. End notes
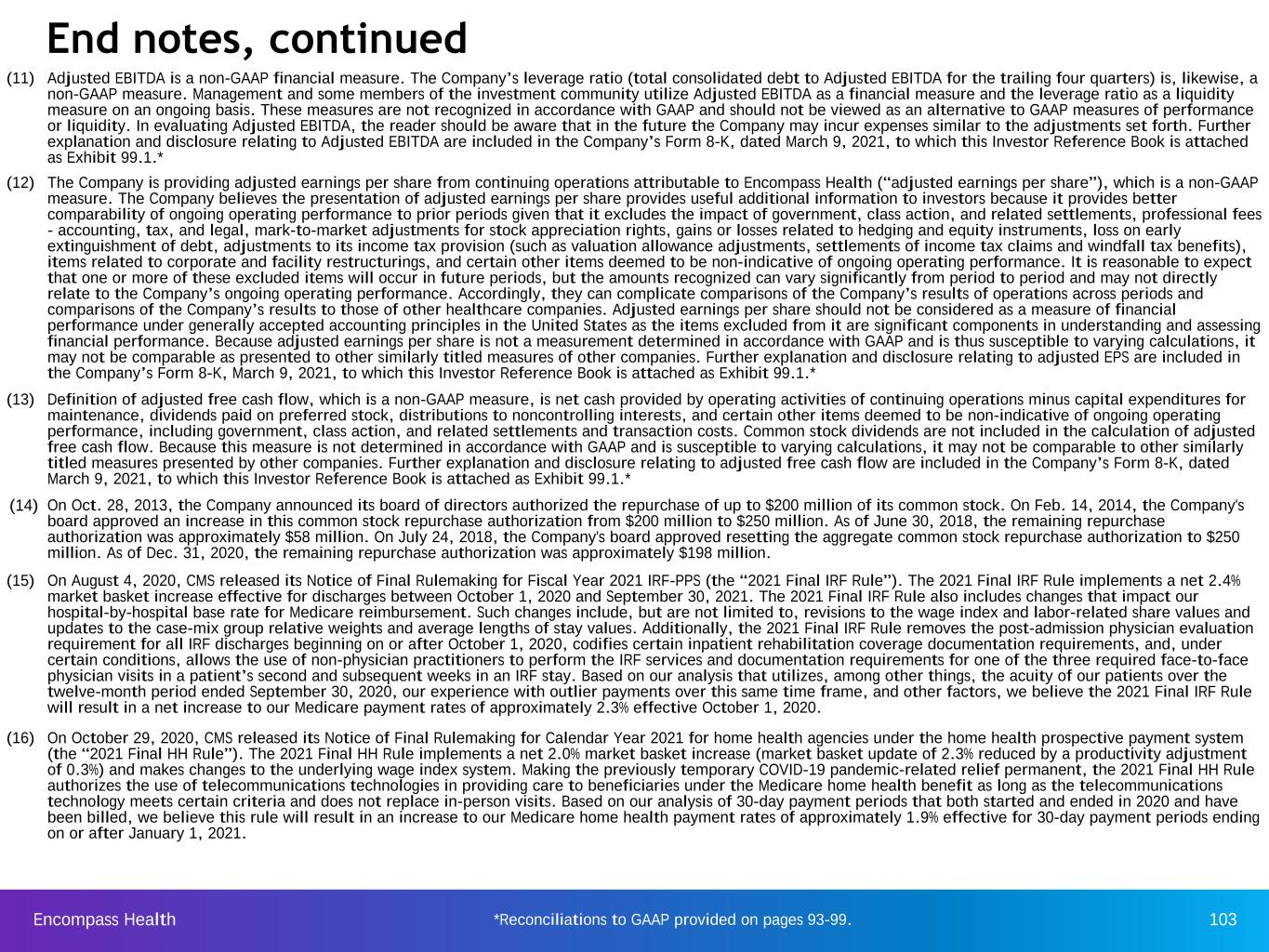
Encompass Health 103 (11) Adjusted EBITDA is a non-GAAP financial measure. The Company’s leverage ratio (total consolidated debt to Adjusted EBITDA for the trailing four quarters) is, likewise, a non-GAAP measure. Management and some members of the investment community utilize Adjusted EBITDA as a financial measure and the leverage ratio as a liquidity measure on an ongoing basis. These measures are not recognized in accordance with GAAP and should not be viewed as an alternative to GAAP measures of performance or liquidity. In evaluating Adjusted EBITDA, the reader should be aware that in the future the Company may incur expenses similar to the adjustments set forth. Further explanation and disclosure relating to Adjusted EBITDA are included in the Company’s Form 8-K, dated March 9, 2021, to which this Investor Reference Book is attached as Exhibit 99.1.* (12) The Company is providing adjusted earnings per share from continuing operations attributable to Encompass Health (“adjusted earnings per share”), which is a non-GAAP measure. The Company believes the presentation of adjusted earnings per share provides useful additional information to investors because it provides better comparability of ongoing operating performance to prior periods given that it excludes the impact of government, class action, and related settlements, professional fees - accounting, tax, and legal, mark-to-market adjustments for stock appreciation rights, gains or losses related to hedging and equity instruments, loss on early extinguishment of debt, adjustments to its income tax provision (such as valuation allowance adjustments, settlements of income tax claims and windfall tax benefits), items related to corporate and facility restructurings, and certain other items deemed to be non-indicative of ongoing operating performance. It is reasonable to expect that one or more of these excluded items will occur in future periods, but the amounts recognized can vary significantly from period to period and may not directly relate to the Company’s ongoing operating performance. Accordingly, they can complicate comparisons of the Company’s results of operations across periods and comparisons of the Company’s results to those of other healthcare companies. Adjusted earnings per share should not be considered as a measure of financial performance under generally accepted accounting principles in the United States as the items excluded from it are significant components in understanding and assessing financial performance. Because adjusted earnings per share is not a measurement determined in accordance with GAAP and is thus susceptible to varying calculations, it may not be comparable as presented to other similarly titled measures of other companies. Further explanation and disclosure relating to adjusted EPS are included in the Company’s Form 8-K, March 9, 2021, to which this Investor Reference Book is attached as Exhibit 99.1.* (13) Definition of adjusted free cash flow, which is a non-GAAP measure, is net cash provided by operating activities of continuing operations minus capital expenditures for maintenance, dividends paid on preferred stock, distributions to noncontrolling interests, and certain other items deemed to be non-indicative of ongoing operating performance, including government, class action, and related settlements and transaction costs. Common stock dividends are not included in the calculation of adjusted free cash flow. Because this measure is not determined in accordance with GAAP and is susceptible to varying calculations, it may not be comparable to other similarly titled measures presented by other companies. Further explanation and disclosure relating to adjusted free cash flow are included in the Company’s Form 8-K, dated March 9, 2021, to which this Investor Reference Book is attached as Exhibit 99.1.* (14) On Oct. 28, 2013, the Company announced its board of directors authorized the repurchase of up to $200 million of its common stock. On Feb. 14, 2014, the Company's board approved an increase in this common stock repurchase authorization from $200 million to $250 million. As of June 30, 2018, the remaining repurchase authorization was approximately $58 million. On July 24, 2018, the Company's board approved resetting the aggregate common stock repurchase authorization to $250 million. As of Dec. 31, 2020, the remaining repurchase authorization was approximately $198 million. (15) On August 4, 2020, CMS released its Notice of Final Rulemaking for Fiscal Year 2021 IRF-PPS (the “2021 Final IRF Rule”). The 2021 Final IRF Rule implements a net 2.4% market basket increase effective for discharges between October 1, 2020 and September 30, 2021. The 2021 Final IRF Rule also includes changes that impact our hospital-by-hospital base rate for Medicare reimbursement. Such changes include, but are not limited to, revisions to the wage index and labor-related share values and updates to the case-mix group relative weights and average lengths of stay values. Additionally, the 2021 Final IRF Rule removes the post-admission physician evaluation requirement for all IRF discharges beginning on or after October 1, 2020, codifies certain inpatient rehabilitation coverage documentation requirements, and, under certain conditions, allows the use of non-physician practitioners to perform the IRF services and documentation requirements for one of the three required face-to-face physician visits in a patient’s second and subsequent weeks in an IRF stay. Based on our analysis that utilizes, among other things, the acuity of our patients over the twelve-month period ended September 30, 2020, our experience with outlier payments over this same time frame, and other factors, we believe the 2021 Final IRF Rule will result in a net increase to our Medicare payment rates of approximately 2.3% effective October 1, 2020. (16) On October 29, 2020, CMS released its Notice of Final Rulemaking for Calendar Year 2021 for home health agencies under the home health prospective payment system (the “2021 Final HH Rule”). The 2021 Final HH Rule implements a net 2.0% market basket increase (market basket update of 2.3% reduced by a productivity adjustment of 0.3%) and makes changes to the underlying wage index system. Making the previously temporary COVID-19 pandemic-related relief permanent, the 2021 Final HH Rule authorizes the use of telecommunications technologies in providing care to beneficiaries under the Medicare home health benefit as long as the telecommunications technology meets certain criteria and does not replace in-person visits. Based on our analysis of 30-day payment periods that both started and ended in 2020 and have been billed, we believe this rule will result in an increase to our Medicare home health payment rates of approximately 1.9% effective for 30-day payment periods ending on or after January 1, 2021. End notes, continued *Reconciliations to GAAP provided on pages 93-99.

Encompass Health 104 (17) In September 2019, the Company issued $500 million of 4.5% Senior Notes due 2028 and $500 million of 4.75% Senior Notes due 2030. The proceeds were used to fund the purchase of the home health rollover shares and exercise of SARs in Q3 2019, fund a call of $400 million of 5.75% Senior Notes due 2024 in Q4 2019, and repay borrowings under the Company’s revolving credit facility. In May 2020, the Company re-opened these notes and issued an additional $300 million of 4.5% Senior Notes due 2028 and $300 million of 4.75% Senior Notes due 2030. The proceeds were used to repay certain borrowings under its revolving credit facility. (18) In October 2020, the Company issued $400 million of 4.625% Senior Notes due 2031. The proceeds plus approximately $300 million of cash on hand were used to fully redeem $700 million of 5.75% Senior Notes due 2024 at par on November 1, 2020. As a result of this redemption, the Company recorded an approximate $2 million loss on early extinguishment of debt in the fourth quarter of 2020. (19) In June 2019, the Company redeemed $100 million of its 5.75% Senor Notes due 2024 at a price of 101.917%, which resulted in a total cash outlay of approximately $102 million. The redemption was funded using cash on hand and funding under the Company’s revolving credit facility. As a result of the redemption, the Company recorded an approximate $2 million loss on early extinguishment of debt in the second quarter of 2019. In November 2019, the Company redeemed $400 million of its 5.75% Senior Notes due 2024 at a price of 100.958%, which resulted in a total cash outlay of approximately $404 million. The redemption was funded using a portion of the proceeds from the Company’s September 2019 public offering of $1 billion of senior unsecured notes (see end note 17). As a result of the redemption, the Company recorded an approximate $5 million loss on early extinguishment of debt in the fourth quarter of 2019. (20) Represents discharges from 137 consolidated hospitals in Q4 2020; 136 consolidated hospitals in Q3 and Q2 2020; 134 consolidated hospitals in Q1 2020; 133 consolidated hospitals in Q4 and Q3 2019; 130 consolidated hospitals in Q2 2019; and 129 consolidated hospitals in Q1 2019 (21) Full-time equivalents included in the table represent Encompass Health employees who participate in or support the operations of our hospitals and include an estimate of full-time equivalents related to contract labor. (22) Employees per occupied bed, or “EPOB,” is calculated by dividing the number of full-time equivalents, including an estimate of full-time equivalents from the utilization of contract labor, by the number of occupied beds during each period. The number of occupied beds is determined by multiplying the number of licensed beds by the Company’s occupancy percentage. (23) Represents home health admissions from 240 consolidated locations in Q4 2020; 241 consolidated locations in Q3 2020; 244 consolidated locations in Q2 2020 and Q1 2020; 243 consolidated locations in Q4 2019; 243 consolidated locations in Q3 2019; 220 consolidated locations in Q2 2019; and 219 consolidated locations in Q1 2019 (24) Represents hospice admissions from 82 locations in Q4 2020; 83 locations in Q3 and Q2 2020; Q1 2020 and Q4 2019; 82 locations in Q3 2019; and 59 locations in Q2 and Q1 2019 (25) On July 20, 2017, the board of directors approved a $0.01 per share, or 4.2%, increase to the quarterly cash dividend on the Company’s common stock, bringing the quarterly cash dividend to $0.25 per common share. On July 24, 2018, the board of directors approved a $0.02 per share, or 8.0%, increase to the quarterly cash dividend on the Company’s common stock, bringing the quarterly cash dividend to $0.27 per common share. On July 23, 2019, the board of directors approved a $0.01 per share, or 3.7%, increase to the quarterly cash dividend on the Company’s common stock, bringing the quarterly cash dividend to $0.28 per common share. (26) The application of the lower income tax rate that resulted from the Tax Cuts and Jobs Act to the Company’s net deferred tax assets resulted in a net $13.6 million decrease in tax expense in Q4 2017. Application of the new tax rate to the Company’s joint venture entities’ deferred tax liabilities resulted in a net reduction in tax expense in Q4 2017. The Company’s joint venture partners’ share of this net tax benefit was $4.6 million, which resulted in an increase in noncontrolling interest expense in Q4 2017. (27) In November 2013, the Company closed separate, privately negotiated exchanges in which it issued $320 million of 2.0% Convertible Senior Subordinated Notes due 2043 in exchange for 257,110 shares of its 6.5% Series A Convertible Perpetual Preferred Stock. The Company recorded ~$249 million as debt and ~$71 million as equity. In May 2017, the Company provided notice of its intent to redeem all $320 million of outstanding convertible notes. In lieu of receiving the redemption price, the holders had the right to convert their notes into shares of the Company’s common stock at a conversion rate of 27.2221 shares per $1,000 principal amount of Notes, which rate was increased by a make-whole premium. In the aggregate, holders of $319.4 million in principal elected to convert, which resulted in the Company issuing 8,895,483 shares of common stock (approximately 8.6 million shares were previously included in the diluted share count). The remaining $0.6 million of principal was redeemed by cash payment. End notes, continued