Table of Contents
UNITED STATES
SECURITIES AND EXCHANGE COMMISSION
WASHINGTON, DC 20549
FORM 10-K
(Mark One)
| x | ANNUAL REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 |
For the fiscal year ended December 31, 2008
| ¨ | TRANSITION REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 |
For the transition period from to
Commission File Number: 1-12718
HEALTH NET, INC.
(Exact Name of Registrant as Specified in Its Charter)
| Delaware | 95-4288333 | |
(State or Other Jurisdiction of Incorporation or Organization) | (I.R.S. Employer Identification No.) | |
| 21650 Oxnard Street, Woodland Hills, CA | 91367 | |
| (Address of Principal Executive Offices) | (Zip Code) | |
Registrant’s Telephone Number, Including Area Code: (818) 676-6000
Securities Registered Pursuant to Section 12(b) of the Act:
Title of each class | Name of each exchange on which registered | |
| Common Stock, $.001 par value | New York Stock Exchange, Inc. | |
| Rights to Purchase Series A Junior Participating Preferred Stock | New York Stock Exchange, Inc. |
Securities Registered Pursuant to Section 12(g) of the Act: None
Indicate by check mark whether the registrant is a well-known seasoned issuer, as defined in Rule 405 of the Securities Act. Yes x No ¨
Indicate by check mark whether the registrant is not required to file reports pursuant to Section 13 or Section 15(d) of the Act. Yes ¨ No x
Indicate by check mark whether the registrant: (1) has filed all reports required to be filed by Section 13 or 15(d) of the Securities Exchange Act of 1934 during the preceding 12 months (or for such shorter period that the registrant was required to file such reports), and (2) has been subject to such filing requirements for the past 90 days. Yes x No ¨
Indicate by check mark if disclosure of delinquent filers pursuant to Item 405 of Regulation S-K is not contained herein, and will not be contained, to the best of registrant’s knowledge, in definitive proxy or information statements incorporated by reference in Part III of this Form 10-K or any amendment to this Form 10-K. x
Indicate by check mark whether the registrant is a large accelerated filer, an accelerated filer, a non-accelerated filer, or a smaller reporting company. See the definitions of “large accelerated filer,” “accelerated filer” and “smaller reporting company” in Rule 12b-2 of the Exchange Act. (Check one):
x Large accelerated filer | ¨ Accelerated filer | ¨ Non-accelerated filer | ¨ Smaller reporting company | |||
| (Do not check if a smaller reporting company) |
Indicate by check mark whether the registrant is a shell company (as defined in Rule 12b-2 of the Exchange Act). Yes ¨ No x
The aggregate market value of the voting stock held by non-affiliates of the registrant at June 30, 2008 was $2,564,559,201 (which represents 106,590,158 shares of Common Stock held by such non-affiliates multiplied by $24.06, the closing sales price of such stock on the New York Stock Exchange on June 30, 2008).
The number of shares outstanding of the registrant’s Common Stock as of February 20, 2009 was 103,707,962 (excluding 40,046,152 shares held as treasury stock).
Documents Incorporated By Reference
Part III of this Form 10-K incorporates by reference certain information from the registrant’s definitive proxy statement for the 2009 Annual Meeting of Stockholders to be filed with the Securities and Exchange Commission within 120 days after the close of the year ended December 31, 2008.
Table of Contents
INDEX TO FORM 10-K
| Page | ||
| 1 | ||
| 1 | ||
| 1 | ||
| 10 | ||
| 11 | ||
| 14 | ||
| 18 | ||
| 18 | ||
| 18 | ||
| 18 | ||
| 19 | ||
| 20 | ||
| 39 | ||
| 39 | ||
| 39 | ||
| 43 | ||
| 44 | ||
| 48 | ||
Item 7—Management’s Discussion and Analysis of Financial Condition and Results of Operations | 49 | |
Item 7A—Quantitative and Qualitative Disclosures About Market Risk | 78 | |
| 79 | ||
Item 9—Changes in and Disagreements with Accountants on Accounting and Financial Disclosure | 80 | |
| 80 | ||
| 82 | ||
Item 10—Directors, Executive Officers of the Registrant and Corporate Governance | 83 | |
| 83 | ||
| 83 | ||
Item 13—Certain Relationships and Related Transactions, and Director Independence | 83 | |
| 83 | ||
| 84 | ||
| 91 | ||
| F-1 | ||
| F-2 | ||
| F-55 | ||
Table of Contents
We are an integrated managed care organization that delivers managed health care services through health plans and government sponsored managed care plans. We operate and conduct our businesses through subsidiaries of Health Net, Inc., which is among the nation’s largest publicly traded managed health care companies. In this Annual Report on Form 10-K, unless the context otherwise requires, the terms “Company,” “Health Net,” “we,” “us,” and “our” refer to Health Net, Inc. and its subsidiaries. Our health plans and government contracts subsidiaries provide health benefits through our health maintenance organizations (“HMOs”), insured preferred provider organizations (“PPOs”) and point-of-service (“POS”) plans to approximately 6.7 million individuals across the country through group, individual, Medicare, (including the Medicare prescription drug benefit commonly referred to as “Part D”), Medicaid, TRICARE and Veterans Affairs programs. Our behavioral health services subsidiary, Managed Health Network, provides behavioral health, substance abuse and employee assistance programs to approximately 6.9 million individuals, including our own health plan members. Our subsidiaries also offer managed health care products related to prescription drugs and offer managed health care product coordination for multi-region employers and administrative services for self-funded benefits programs. In addition, we own health and life insurance companies licensed to sell PPO, POS, exclusive provider organization (“EPO”) and indemnity products, as well as auxiliary non-health products such as life and accidental death and dismemberment, dental, vision, behavioral health and disability insurance, including our Medicare Part D Pharmacy coverage under Medicare.
Our executive offices are located at 21650 Oxnard Street, Woodland Hills, California 91367, and our Internet web site address iswww.healthnet.com.
We make available free of charge on or through our Internet web site,www.healthnet.com, our Annual Report on Form 10-K, quarterly reports on Form 10-Q and current reports on Form 8-K and all amendments to those reports filed or furnished pursuant to Section 13(a) or Section 15(d) of the Securities Exchange Act of 1934, as amended (the “Exchange Act”) as soon as reasonably practicable after we electronically file such material with, or furnish it to, the Securities and Exchange Commission (“SEC”). Copies of our Corporate Governance Guidelines, Code of Business Conduct and Ethics, Director Independence Standards and charters for the Audit Committee, Compensation Committee, Governance Committee and Finance Committee of our Board of Directors are also available on our Internet web site. We will provide electronic or paper copies free of charge upon request.
Our transfer agent, Wells Fargo, can help you with a variety of shareholder-related services, including change of address, lost stock certificates, transfer of stock to another person and other administrative services. You can write to our transfer agent at: Wells Fargo Shareowner Services, P.O. Box 64854, St. Paul, Minnesota 55164-0854, emailstocktransfer@wellsfargo.com, or telephone (800) 468-9716 or (651) 450-4064.
We currently operate within two reportable segments, Health Plan Services and Government Contracts, each of which is described below. For additional financial information regarding our reportable segments, see “Results of Operations” in “Item 7. Management’s Discussion and Analysis of Financial Condition and Results of Operations” and Note 16 to our consolidated financial statements included as part of this Annual Report on Form 10-K.
Health Plan Services Segment
Our Health Plan Services segment includes the operations of our commercial, Medicare (including Part D) and Medicaid health plans, the operations of our health and life insurance companies and our behavioral health and pharmaceutical services subsidiaries. As of December 31, 2008, we had approximately 3.2 million at-risk members and 0.5 million Medicare stand-alone Part D members in our Health Plan Services segment.
1
Table of Contents
Managed Health Care Operations
We offer a full spectrum of managed health care products and services. Our strategy is to offer to employers and individuals a wide range of managed health care products and services that, among other things, provide comprehensive coverage and manage health care cost increases. Our health plans offer members a wide range of health care services including ambulatory and outpatient physician care, hospital care, pharmacy services, behavioral health and ancillary diagnostic and therapeutic services. Our health plans include a matrix package, which allows members to select their desired coverage from a variety of alternatives. Our principal commercial health products are as follows:
| • | HMO Plans: Our HMO plans offer comprehensive benefits generally through contracts with participating network physicians, hospitals and other providers. When an individual enrolls in one of our HMO plans, he or she may select a primary care physician (“PCP”) from among the physicians participating in our network. PCPs generally are family practitioners, general practitioners or pediatricians who provide necessary preventive and primary medical care, and are generally responsible for coordinating other necessary health care services, including making referrals to participating network specialists. We offer HMO plans with differing benefit designs and varying levels of co-payments that result in different levels of premium rates. In California, participating providers are typically contracted through medical groups. In those cases, enrollees in HMO plans are generally required to secure specialty professional services from physicians in the group, as long as such services are available from group physicians. |
| • | PPO Plans: Our PPO plans offer coverage for services received from any health care provider, with benefits generally paid at a higher level when care is received from a participating network provider. Coverage typically is subject to deductibles and co-payments or coinsurance. |
| • | Indemnity Plans:Our indemnity plans offer the member the ability to select any health care provider for covered services. Some care management features may be included in these plans, such as inpatient precertification, disease management programs and benefits for preventive services. Coverage typically is subject to deductibles and coinsurance. |
| • | POS Plans: Our POS plans blend the characteristics of HMO and Indemnity plans. Members can have comprehensive HMO-style benefits for services received from participating network providers with lower co-payments (particularly within the medical group), but also have coverage, generally at higher co-payment or coinsurance levels, for services received outside the network. |
Over the past five years, we have expanded all of our product lines, which has enabled us to react to the changing needs of employer groups and individual insureds. As of December 31, 2008, 42% of our commercial members were covered by POS and PPO products, 54% were covered by conventional HMO products and 4% were covered by EPO and fee-for-service products, including health plans such as consumer-directed health care plans. For information on our consumer-directed health care plans see “—Additional Information Concerning Our Business—Consumer-Directed Health Care Plans; Health Savings Accounts and Health Reimbursement Accounts.”
We believe we are well positioned for further healthcare reform and a volatile economic environment. Our product portfolios include offerings such as:
| • | Flexible network options such as HMO Silver, a narrow network, in Southern California to address the need for lower cost product offerings. |
• | Salud Con Health NetSM, a family of affordable healthcare insurance products targeting the Latino community in Southern California. These products are available in Los Angeles, Orange, San Bernardino, Riverside and Ventura counties and were developed by Health Net of California to respond to the health care needs of uninsured Latino immigrants and their families. These products include group and individual coverage. The individual health care plans are the first-ever cross-border health care plans made available to individual consumers who purchase benefits directly from insurers. |
2
Table of Contents
• | Decision PowerSM, a series of programs designed to directly involve patients in their health care decisions. |
| • | Consumer Directed Health Plan products such as Health Savings Accounts and Health Reimbursement Accounts. |
| • | Community stores such as our Medicare stores in Phoenix, Arizona and Meriden, Connecticut and our community enrollment and customer service centers in East Los Angeles, California and Modesto, California. |
The pricing of our products is designed to reflect the varying costs of health care based on the benefit alternatives in our products. We provide employers and employees the ability to select and enroll in products with greater managed health care and cost containment elements. In general, our HMOs provide comprehensive health care coverage for a fixed fee or premium that does not vary with the extent or frequency of medical services actually received by the member. PPO enrollees choose their medical care from a panel of contracting providers or choose a non-contracting provider and are reimbursed on a traditional indemnity plan basis after reaching an annual deductible. POS enrollees choose, each time they receive care, from conventional HMO or indemnity-like (in-network and out-of-network) coverage, with payments and/or reimbursement depending on the coverage chosen. We assume both underwriting and administrative expense risk in return for the premium revenue we receive from our HMO, POS and PPO products. We have contractual relationships with health care providers for the delivery of health care to our enrollees in each product category.
In 2008, we continued to focus on adding more small group (generally defined as employer groups with 2 to 50 employees) members and, as of December 31, 2008, approximately 34% of our commercial risk enrollment was in small group and individual accounts. The following table contains membership information relating to our commercial large group (generally defined as an employer group with more than 50 employees) members, commercial small group and individual members, Medicare members, Medicaid members, ASO members and Part D members as of December 31, 2008 (our Medicare and Medicaid businesses are discussed below under “—Medicare Products” and “—Medicaid and Related Products”):
Commercial—Large Group | 1,341,691 | (a) | |
Commercial—Small Group & Individual | 681,852 | (b) | |
Medicare (Medicare Advantage only) | 295,344 | ||
Medicaid | 811,703 | ||
ASO | 44,034 | ||
Stand-alone PDP | 544,919 |
| (a) | Includes 852,771 HMO members, 272,467 POS members, 160,615 PPO members, 30,980 EPO members and 24,858 Fee-for-Service (“FFS”) members. |
| (b) | Includes 241,583 HMO members, 242,237 PPO members, 169,913 POS members, 28,115 EPO members and 4 FFS members. |
The following table sets forth certain information regarding our employer groups in the commercial managed care operations of our Health Plan Services segment as of December 31, 2008:
Number of Employer Groups | 57,972 | ||
Largest Employer Group as % of commercial enrollment | 6.3 | % | |
10 largest Employer Groups as % of commercial enrollment | 19.5 | % |
A general description of our health plan operations in Arizona, California, Oregon, Connecticut, New Jersey and New York is set forth below. See “Item 7. Management’s Discussion and Analysis and Results of Operations—Health Plan Services Segment Membership” for a discussion on changes in our membership levels.
Arizona.Our commercial membership in Arizona was 122,839 as of December 31, 2008, which represented a decrease of approximately 10% during 2008. This decrease was primarily due to an decrease in PPO
3
Table of Contents
membership. Our Medicare membership in Arizona was 67,152 as of December 31, 2008, which represented an increase of approximately 32% during 2008. We did not have any Medicaid members in Arizona as of December 31, 2008.
California.Health Net of California, Inc., our California HMO (“HN California”), is one of the largest HMOs in California as measured by total membership and has one of the largest provider networks in California. Our commercial membership in California as of December 31, 2008 was 1,351,511, which represented a decrease of approximately 8% during 2008. The decrease in commercial membership was primarily due to a decrease of 52,501 HMO members and 47,561 PPO members. Our Medicare membership in California as of December 31, 2008 was 132,848, which represented an increase of approximately 18% during 2008. Our Medicaid membership in California as of December 31, 2008 was 764,928 members, which represented an increase of approximately 7% during 2008.
Oregon.Our commercial membership in Oregon was 132,582 as of December 31, 2008, which represented a decrease of approximately 2% during 2008. Of these members, approximately 15,655 are covered under policies issued in Washington. Our Medicare membership in Oregon increased by 681 members to 22,427 as of December 31, 2008 from 21,746 as of December 31, 2007. We did not have any Medicaid members in Oregon as of December 31, 2008.
Northeast.Our Northeast operations are conducted in Connecticut, New Jersey and New York. For our large employer group business, we directly market commercial HMO, PPO and POS products in New Jersey, Connecticut and New York, as well as an EPO product in New York. On May 31, 2007, we completed the acquisition (the “Guardian Transaction”) of The Guardian Life Insurance Company of America’s (“The Guardian”) 50% interest in HealthCare Solutions (“HCS”). Prior to the Guardian Transaction, our small group managed care and indemnity products in Connecticut, New Jersey and New York were marketed to existing insureds of The Guardian and distributed through the brokerage community in an integrated marketing effort under the HCS trade name. As part of these arrangements, The Guardian generally had the exclusive right to market and sell our HMO, PPO and POS products to small employer groups, and we and The Guardian each retained 50% of the premiums and claims. In addition, we recovered from The Guardian a specified portion of the administrative expenses and the direct marketing costs, which were shared equally. As a result of the Guardian Transaction, we terminated all pre-existing marketing and risk sharing arrangements and acquired certain intangible rights from The Guardian. As a result, we recognize 100% of the HCS revenues, claims and administrative and marketing expenses.
Our commercial membership in Connecticut was 138,520 as of December 31, 2008, which represented a decrease of approximately 14% since December 31, 2007. Our Medicare membership in Connecticut was 57,510 as of December 31, 2008, which represented an increase of approximately 28% during 2008. We did not have any Medicaid members in Connecticut as of December 31, 2008.
Our commercial membership in New Jersey was 73,172 as of December 31, 2008, which represented a decrease of approximately 19% during 2008. Our Medicaid membership in New Jersey was 46,775 as of December 31, 2008, which represented an increase of approximately 6% during 2007. We did not have any Medicare members in New Jersey as of December 31, 2008.
In New York, we had 204,915 commercial members as of December 31, 2008, which represented a decrease of approximately 12% during 2008. Our Medicare membership in New York was 5,840 and 2,819 as of December 31, 2008 and 2007, respectively. We did not have any Medicaid members in New York as of December 31, 2008.
Medicare Products
We offer our Medicare products directly to individuals and through employer/union groups. To enroll in one of our Medicare plans, covered persons must be entitled to both Parts A and B of Medicare. We provide or
4
Table of Contents
arrange health care services normally covered by Medicare, plus a broad range of health care services not covered by traditional Medicare. Any additional benefits in our plans are covered by a monthly premium charged to the enrollee or through portions of payments received from the Centers for Medicare & Medicaid Services (“CMS”) that may be allocated, per CMS regulations and guidance, for these purposes.
We were one of the nation’s largest Medicare Advantage contractors based on membership of 295,344 members as of December 31, 2008 compared to membership of 236,301 as of December 31, 2007. We were also a major participant in the “Part D” stand-alone drug benefit with 544,919 members in all 50 states and the District of Columbia as of December 31, 2008. Our portfolio of Medicare plans focuses on simplicity so that members can sign up and use benefits with minimal paperwork and coverage that starts immediately upon enrollment. We also provide Medicare supplemental coverage to 33,651 members through either individual Medicare supplement policies or employer group sponsored coverage.
In 2008, we offered Medicare Advantage plans in select counties in thirteen states (Arizona, California, Connecticut, Georgia, Hawaii, Massachusetts, New Mexico, New York, North Carolina, Oregon, Texas, Virginia and Washington). For Georgia, Hawaii, Massachusetts, New Mexico, New York, North Carolina, Texas and Virginia, the Medicare Advantage plan offerings are our Private Fee For Service (“PFFS”) plans. PFFS plans are non-network based Medicare Advantage plans that allow Medicare-eligible consumers to participate in a private Medicare health insurance plan with the flexibility of provider choice that original Medicare provides and better benefits than the standard Medicare Part A/Part B coverage.
In 2008, Health Net offered multiple types of Medicare Advantage Special Needs Plans in several states where we offer Medicare Advantage Plans. Dual Eligible Special Needs Plans designed for low income Medicare beneficiaries were offered in Arizona, California and Connecticut. Chronic Condition Special Needs Plans, designed for beneficiaries with chronic obstructive pulmonary disease, congestive heart failure, and hypercholesterolemia were offered in Arizona, California, Connecticut and Oregon. These plans offer access to additional health care and prescription drug coverage. See “—Government Regulation—Federal Legislation and Regulation—Medicare Legislation” and “Item 1A. Risk Factors—Our efforts to capitalize on Medicare business opportunities could prove to be unsuccessful” for additional information regarding our Medicare program.
In 2008, we experienced significant growth in several of our plans. The Healthy Heart plans in Southern California were particularly successful, combining a strong marketing effort with the American Heart Association’s approach to a healthy lifestyle. The plans include benefits to help enrollees avoid tobacco use; manage stress, blood pressure and high cholesterol; and promote nutrition, weight management and physical activity. The plans also include access to Decision PowerSM, Health Net’s program of online and on-call support and resources to directly involve members with their doctors in making health care and healthy lifestyle decisions. For 2009, the Healthy Heart concept is being expanded to select counties in Northern California.
Health Net is maintaining its coverage area for 2009; however, some products are no longer being offered in select counties. Specifically, the PFFS and Dual Eligible Special Needs Plans are not being offered in Connecticut. Health Net also adjusted benefits on most plans to address higher than expected health care costs in 2008.
Medicaid and Related Products
We are one of the top ten largest Medicaid HMOs in the United States based on membership. As of December 31, 2008, we had an aggregate of 811,703 Medicaid members compared to 845,753 members as of December 31, 2007, principally in California. Of the 811,703 Medicaid members, we had 46,775 Medicaid members in New Jersey, as of December 31, 2008. We withdrew from the Connecticut Medicaid program effective April 2008 which was the primary reason for the year-over-year decrease in our 2008 Medicaid membership. See “Item 7. Management’s Discussion and Analysis of Financial Condition and Results of Operations—Results of Operations—Health Plan Services Segment Membership” for detailed information
5
Table of Contents
regarding our Medicaid enrollment by state. To enroll in our Medicaid products, an individual must be eligible for Medicaid benefits under the appropriate state regulatory requirements. The applicable state agency pays us a monthly fee for the coverage of our Medicaid members.
As of December 31, 2008, we had Medicaid operations in ten of California’s largest counties: Los Angeles, Fresno, Kern, Orange, Stanislaus, Riverside, Sacramento, San Bernardino, San Diego and Tulare. Effective February 2009, we withdrew from several counties in California, including Stanislaus. We are the sole commercial plan contractor with the State of California’s Department of Health Care Services (“DHCS”) to provide Medicaid service in Los Angeles County, California. As of December 31, 2008, 484,913 of our Medicaid members resided in Los Angeles County, California. This represents approximately 63% of our California Medicaid membership, and 60% of our total Medicaid membership. In May 2005, we renewed our contract with DHCS to provide Medicaid service in Los Angeles County. The renewed contract was effective April 1, 2006 and had an initial term of two years with three 24-month extension periods. On February 14, 2008, DHCS extended our contract for an initial 24-month extension period ending March 31, 2010.
Our California HMO, HN California, participates in the Children’s Health Insurance Program (“CHIP”), which, in California, is known as the Healthy Families program. As of December 31, 2008, there were 133,936 members (excluding 5,136 Healthy Kids members) in our Healthy Families program. CHIP was designed as a federal/state partnership, similar to Medicaid, with the goal of extending health insurance to children whose families earn too much money to be eligible for Medicaid, but not enough money to purchase private insurance. Monthly premiums are subsidized by the State of California and, as of February 1, 2009, range between $4 and $17 per child, up to a maximum of $51 for all children in a family enrolled in the Healthy Families Program. California receives two-thirds of the funding for the program from the federal government. In New Jersey, we participate in the New Jersey Medicaid program, as well as the New Jersey CHIP program, which is known as New Jersey FamilyCare. These programs provide comprehensive health care coverage for children and families as well as members who are aged, blind and disabled. We operate in 14 of 21 counties in New Jersey under a contract with the Division of Medical Assistance and Health Services. The current contract is scheduled to expire on June 30, 2009. We currently anticipate negotiating an extension of the contract to be effective July 1, 2009.
Administrative Services Only Business
We provide ASO products to large employer groups in Connecticut, New Jersey, New York and, to a more limited extent, California. Under these arrangements, we provide claims processing, customer service, medical management, provider network access and other administrative services without assuming the risk for medical costs. We are generally compensated for these services on a fixed per member per month basis. Our largest concentration of ASO business is in the Northeast, principally Connecticut. As of December 31, 2008, we had 44,034 members through our ASO business. Of those members, 38,837 were located in the Northeast.
Indemnity Insurance Products
We offer insured PPO, POS, EPO and indemnity products as “stand-alone” products and as part of multiple option products in various markets. These products are offered by our health and life insurance subsidiaries, which are licensed to sell insurance in 50 states and the District of Columbia. Through these subsidiaries, we also offer auxiliary non-health products such as life, accidental death and dismemberment, dental, vision and behavioral health insurance. Our health and life insurance products are provided throughout most of our service areas.
Other Specialty Services and Products
We offer pharmacy benefits, behavioral health, dental and vision products and services (sometimes through strategic relationships with third parties), as well as managed care products related to cost containment for hospitals, health plans and other entities as part of our Health Plan Services segment.
6
Table of Contents
Pharmacy Benefit Management. We provide pharmacy benefit management (“PBM”) services to Health Net members through our subsidiary, Health Net Pharmaceutical Services (“HNPS”). HNPS provides integrated PBM services to approximately 3.3 million Health Net members who have pharmacy benefits, including approximately 795,000 Medicare members. HNPS manages these benefits in an effort to achieve the highest quality outcomes at the lowest cost for its members. HNPS contracts with national health care providers, vendors, drug manufacturers and pharmacy distribution networks (directly and indirectly through a third party vendor), oversees pharmacy claims and administration, reviews and evaluates new FDA-approved drugs for safety and efficacy and manages data collection efforts to facilitate our health plans’ disease management programs.
HNPS focuses its effort on encouraging appropriate use of medications to enhance the overall member outcome while controlling overall cost to the health plan, member and employer. A committee of internal and external physicians and pharmacists select medications by therapeutic class that offer demonstrable clinical value. A cost effective option is then selected from equivalently effective options.
HNPS provides affiliated health plans various services including development of benefit designs, cost and trend management, sales and marketing support, and management delivery systems. HNPS outsources certain capital and labor-intensive functions of pharmacy benefit management, such as claims processing, mail order services and pharmacy network services.
Behavioral Health.We administer and arrange for behavioral health benefits and services through our subsidiary, Managed Health Network, Inc., and its subsidiaries (collectively “MHN”). MHN offers behavioral health, substance abuse and employee assistance programs (“EAPs”) on an insured and self-funded basis to groups in various states and is included as a standard part of most of our commercial health plans. They are also sold in conjunction with other commercial and Medicare products and on a stand-alone basis to unaffiliated health plans and employer groups. During 2008, MHN continued to expand its product portfolio services and client base through enhanced product wellness and behavioral change programs, and workplace and work life services, as part of its EAP solutions.
In 2008, MHN continued to implement, administer and monitor the non-medical counseling program for the U.S. Department of Defense under the Military Family Counseling Services program. See “—Government Contracts Segment—Other Department of Defense Contracts” for a description of this contract. MHN also holds contracts with the U.S. Department of State and the U.S. Agency for International Development (“USAID”) to provide EAP counseling services tailored for State Department and USAID employees and family members while posted overseas.
MHN’s products and services were provided to over 6.9 million individuals as of December 31, 2008, with approximately 1.5 million individuals under risk-based programs, approximately 1.7 million individuals under self-funded programs and approximately 3.7 million individuals under EAPs, including those who are also covered under other MHN programs. In 2008, MHN’s total revenues were $217 million. Of that amount, $145 million represented revenues from business with MHN affiliates and $72 million represented revenues from non-affiliate business.
Dental and Vision. In 2003, we sold our dental and vision subsidiaries and, as a result, we no longer underwrite or administer stand-alone dental and vision products. During 2008, we made available to our current and prospective members in Arizona and California private label dental products through a strategic relationship with SafeGuard Health Enterprises, Inc. (“SafeGuard”) and private label vision products through a strategic relationship with EyeMed Vision Care LLC (“EyeMed”). The stand-alone dental products were underwritten and administered by SafeGuard companies and the stand-alone vision products were underwritten by Fidelity Security Life Insurance Company and administered by EyeMed affiliated companies. Effective December 31, 2008, we terminated our relationship with SafeGuard. Beginning January 1, 2009, we entered into a strategic relationship with Dental Benefit Providers, Inc. (“DBP”) to provide the same services as were previously
7
Table of Contents
provided by Safeguard. The stand-alone dental products that were formerly underwritten and administered by SafeGuard companies are now underwritten and administered by DBP companies. DBP also administers dental products and coverage we provide to our members in Oregon. Liberty Dental Plans of California, Inc. serves as the administrator for the dental services we provide to our Medi-Cal and Healthy Families program enrollees and Doral Dental Services of New Jersey, LLC serves as the administrator for the dental services we provide to our New Jersey Medicaid members.
Government Contracts Segment
Our Government Contracts segment includes our TRICARE contract for the North Region and other health care related government contracts that we administer for the U.S. Department of Defense (the “Department of Defense”) and the U.S. Department of Veterans Affairs. Certain components of these contracts are subcontracted to unrelated third parties.
Under government-funded health programs, the government payor typically determines premium and reimbursement levels. Contracts under these programs are generally subject to frequent change, including changes that may reduce the number of persons enrolled or eligible, reduce the revenue received by us or increase our administrative or health care costs under such programs. The amount of government receivables set forth in our consolidated financial statements represents our best estimate of the government’s liability to us under TRICARE and other federal government contracts. In general, government receivables are estimates and are subject to government audit and negotiation. See “Item 1A. Risk Factors—A significant reduction in revenues from the government programs in which we participate could have an adverse effect on our business, financial condition or results of operations.”
TRICARE
Our wholly-owned subsidiary, Health Net Federal Services, LLC (“HNFS”), administers a large managed care federal contract with the Department of Defense under the TRICARE program in the North Region. We have been serving the Department of Defense since 1988 under the TRICARE program and its predecessor programs. We believe we have established a solid history of operating performance under our contracts with the Department of Defense. We believe there will be further opportunities to serve the Department of Defense and other governmental organizations in the future.
Our TRICARE contract for the North Region is one of three regional contracts awarded by the Department of Defense in August 2003 under the TRICARE Program. The North Region contract is a five-year contract and covers Connecticut, Delaware, Illinois, Indiana, Kentucky, Maine, Maryland, Massachusetts, Michigan, New Hampshire, New Jersey, New York, North Carolina, Ohio, Pennsylvania, Rhode Island, Vermont, Virginia, West Virginia, Wisconsin and the District of Columbia. In addition, the contract covers a small portion of Tennessee, Missouri and Iowa.
The five-year North Region contract is subject to annual renewals on April 1 of each year at the option of the Department of Defense. We are currently in the fifth option period of health care operations under our TRICARE contract for the North Region, which is scheduled to conclude on March 31, 2009 unless extended by the Department of Defense. Health Net and the Department of Defense are currently negotiating an extension of the TRICARE North contract for an additional one-year option period, which, if exercised, would extend the TRICARE North contract to March 31, 2010. Health Net and the Department of Defense are also negotiating two subsequent six-month option periods, which, if exercised, would extend the TRICARE North contract to March 31, 2011. On March 24, 2008, the government issued a Request for Proposal for the third generation of TRICARE Managed Care Support contracts (referred to as “T3”). Health Net submitted its proposal to the government on June 30, 2008. The government held discussions with Health Net regarding its proposal in December 2008 and Health Net submitted its final proposal revision on January 2, 2009. The T3 contract is scheduled to be awarded by June 1, 2009 and, if awarded, health care delivery would commence on April 1,
8
Table of Contents
2010. Health Net anticipates that the current TRICARE North contract will be extended for one year through March 31, 2010 and the additional two six-month option periods will not be exercised.
Under the TRICARE contract for the North Region, we provide health care services to approximately 3.0 million Military Health System (“MHS”) eligible beneficiaries, including 1.8 million TRICARE eligibles for whom we provide health care and administrative services and 1.2 million other MHS-eligible beneficiaries for whom we provide administrative services only. Eligible beneficiaries in the TRICARE program are able to choose from a variety of program options. They can choose to enroll in TRICARE Prime, which is similar to a conventional HMO plan, or they can select, on a case-by-case basis, to utilize TRICARE Extra, which is similar to a conventional PPO plan, or TRICARE Standard, which is similar to a conventional indemnity plan.
Under TRICARE Prime, enrollees pay an enrollment fee (which is zero for active duty participants and their dependents) and select a primary care physician from a designated provider panel. The primary care physicians are responsible for making referrals to specialists and hospitals. Except for active duty family members, who have no co-payment charges, TRICARE Prime enrollees pay co-payments each time they receive medical services from a civilian provider. TRICARE Prime enrollees may opt, on a case-by-case basis, for a point-of-service option in which they are allowed to self-refer but incur a deductible and a co-payment.
Under TRICARE Extra, eligible beneficiaries may utilize a TRICARE network provider but incur a deductible and co-payment which is greater than the TRICARE Prime co-payment. Under TRICARE Standard, eligible beneficiaries may utilize a TRICARE authorized provider who is not a network provider but pay a higher co-payment than under TRICARE Prime or TRICARE Extra. As of December 31, 2008, there were approximately 1.5 million TRICARE eligibles enrolled in TRICARE Prime under our North Region contract.
The TRICARE contract for the North Region includes a target cost and price for reimbursed health care costs which is negotiated annually during the term of the contract, with underruns and overruns of our target cost borne 80% by the government and 20% by us. In the normal course of contracting with the federal government, we recognize changes in our estimate for the target cost underruns and overruns when the amounts become determinable, supportable and the collectibility is reasonably assured. As a result of changes in the estimate, during the year ended December 31, 2008, we recognized an increase in revenue of $17 million and an increase in cost of $22 million. As a result of changes in the estimate, during the year ended December 31, 2007, we recognized a decrease in revenue of $58 million, and a decrease in cost of $75 million. The administrative price is paid on a monthly basis, one month in arrears and certain components of the administrative price are subject to volume-based adjustments.
We are paid within five business days for each health care claim run under the North Region contract based on paid claims with an annual reconciliation of the risk sharing provision. We are not responsible for providing most pharmaceutical benefits, claims processing for TRICARE and Medicare dual eligibles and certain marketing and education services. For additional information regarding our TRICARE contract for the North Region, see “Item 7. Management’s Discussion and Analysis of Financial Condition and Results of Operations.”
Other Department of Defense Contracts
In 2007, MHN was awarded a five-year contract, the Military Family & Life Consultant Program (“MFLC”), to develop, administer and monitor the non-medical counseling program for service members. Services under the MFLC began on April 1, 2007 and will end in 2012, subject to an early termination provision which is based on a funding ceiling of $300 million. The program is designed to deliver short-term situational problem solving counseling, primarily with regard to stress factors inherent in the military lifestyle.
The services provided under these subcontracts are not TRICARE benefits and are provided independently from the services provided under our TRICARE contract for the North Region. Revenues for the MFLC subcontract for the year ended December 31, 2008 were $106 million and were $143 million since the contract’s inception.
9
Table of Contents
Veterans Affairs
During 2008, HNFS administered 9 contracts with the U.S. Department of Veterans Affairs to manage community-based outpatient clinics in 9 states. HNFS also supported 23 other contracts with the U.S. Department of Veterans Affairs supporting 152 Veterans Affairs medical centers for claims repricing and audit services and one contract with the U.S. Marshals Service for claims re-pricing services. Total revenues for our Veterans Affairs business were approximately $30 million for the year ended December 31, 2008, representing a 6.3% decrease over 2007 primarily due to loss of outpatient clinic contracts. These revenues are derived from service fees received and have no insurance risk associated with them. MHN is a subcontractor in a program under the U.S. Department of Veterans Affairs, requiring MHN to make proactive outbound calls to returning veterans, perform assessments and make referrals to Veterans Affairs facilities.
We maintain a network of qualified physicians, hospitals and other health care providers in each of the states in which we offer network based managed care products and services.
Physician Relationships
The following table sets forth the number of primary care and specialist physicians contracted either directly with our HMOs or through our contracted participating physician groups (“PPGs”) as of December 31, 2008:
Primary Care Physicians (includes both HMO and PPO physicians) | 70,265 | |
Specialist Physicians (includes both HMO and PPO physicians) | 238,371 | |
Total | 308,636 |
Under our California HMO and POS plans, all members are required to select a PPG and generally also a primary care physician from within that group. In our other plans, including all of our plans outside of California, members may be required to select a primary care physician from the broader HMO network panel of primary care physicians. The primary care physicians and PPGs assume overall responsibility for the care of members. Medical care provided directly by such physicians includes the treatment of illnesses not requiring referral, and may include physical examinations, routine immunizations, maternity and childcare, and other preventive health services. The primary care physicians and PPGs are responsible for making referrals (approved by the HMO’s or PPG’s medical director as required under the terms of our various plans) to specialists and hospitals. Certain of our HMOs offer enrollees “open access” plans under which members are not required to secure prior authorization for access to network physicians in certain specialty areas, or “open panels” under which members may access any physician in the network, or network physicians in certain specialties, without first consulting their primary care physician. PPO plans generally do not require prior authorization for specialty care.
PPG and physician contracts are generally for a period of at least one year and are automatically renewable unless terminated, with certain requirements for maintenance of good professional standing and compliance with our quality, utilization and administrative procedures. In California, PPGs generally receive a monthly “capitation” fee for every member assigned to it. Under a capitation fee arrangement, we pay a provider group a fixed amount per member on a regular basis and the provider group accepts the risk of the frequency and cost of member utilization of professional services. The capitation fee represents payment in full for all medical and ancillary services specified in the provider agreements. In these capitation fee arrangements, in cases where the capitated PPG cannot provide the health care services needed, such PPGs generally contract with specialists and other ancillary service providers to furnish the requisite services under capitation agreements or negotiated fee schedules with specialists. Outside of California, most of our HMOs reimburse physicians according to a discounted fee-for-service schedule, although several have capitation arrangements with certain providers and provider groups in their market areas. For services provided under our PPO products and the out-of-network benefits of our POS products, we ordinarily reimburse physicians pursuant to discounted fee-for-service arrangements. A provider group’s financial instability or failure to pay secondary providers for services rendered
10
Table of Contents
could lead secondary providers to demand payment from us, even though we have made our regular capitated payments to the provider group. Depending on state law, we could be liable for such claims.
Health Net of Connecticut Inc, our Connecticut HMO (“HNCT”), has a contract with the Connecticut State Medical Society IPA (“CSMS-IPA”). This contract includes an agreed upon compensation budget with negotiated reimbursement rates for providers and has gain share and pay-for-performance features. Referral authorization and claims administration are performed by HNCT. This contract is scheduled to expire on March 24, 2010.
HNFS maintains a network of qualified physicians, facilities, and ancillary providers in the prime service areas of our TRICARE contract for the North Region. Services are provided on a fee-for-service basis. As of December 31, 2008, HNFS had 114,751 physicians, 2,393 facilities, and 11,695 ancillary providers in its TRICARE network.
Our behavioral health subsidiary, MHN, maintains a provider network comprised of approximately 44,839 psychiatrists, psychologists and other clinical categories of providers nationwide. Substantially all of these providers are contracted with MHN on an individual or small practice group basis and are paid on a discounted fee-for-service basis. Members who wish to access certain behavioral health services contact MHN and are referred to contracted providers for evaluation or treatment services. Generally, authorization for such services is for a limited number of appointments and must be renewed by MHN based on medical necessity. If a member needs inpatient services, MHN maintains a network of approximately 1,197 facilities.
In addition to the physicians that are in our networks, we have also entered into agreements with various third parties that have networks of physicians contracted to them (“Third Party Networks”). In general, under a Third Party Network arrangement, Health Net is licensed by the third party to access its network providers and pay the claims of these physicians pursuant to the pricing terms of their contracts with the Third Party Network.
Hospital Relationships
Our health plan subsidiaries arrange for hospital care primarily through contracts with selected hospitals in their service areas. These hospital contracts generally have multi-year terms or annual terms with automatic renewals and provide for payments on a variety of bases, including capitation, per diem rates, case rates and discounted fee-for-service schedules.
Covered inpatient hospital care for our HMO members is comprehensive. It includes the services of hospital-based physicians, nurses and other hospital personnel, room and board, intensive care, laboratory and x-ray services, diagnostic imaging and generally all other services normally provided by acute-care hospitals. HMO or PPG nurses and medical directors are actively involved in discharge planning and case management, which often involves the coordination of community support services, including visiting nurses, physical therapy, durable medical equipment and home intravenous therapy.
Ancillary and Other Provider Relationships
Our health plan subsidiaries arrange for ancillary and other provider services, such as ambulance, laboratory, radiology and home health, primarily through contracts with selected providers in their service areas. These contracts generally have multi-year terms or annual terms with automatic renewals and provide for payments on a variety of bases, including capitation, per diem rates, case rates and discounted fee-for-service schedules. In certain cases, these provider services are included in contracts our health plan subsidiaries have with PPGs and hospitals.
Additional Information Concerning Our Business
Competition
We operate in a highly competitive environment in an industry currently subject to significant changes from business consolidations, new strategic alliances, legislative reform and market pressures brought about by a
11
Table of Contents
better informed and better organized customer base. Our health plans face substantial competition from for-profit and nonprofit HMOs, PPOs, self-funded plans (including self-insured employers and union trust funds), Blue Cross/Blue Shield plans, and traditional indemnity insurance carriers, some of which have substantially larger enrollments and greater financial resources than we do. The development and growth of companies offering Internet-based connections between health care professionals, employers and members, along with a variety of services, could also create additional competitors. We believe that the principal competitive features affecting our ability to retain and increase membership include the range and prices of benefit plans offered, size and quality of provider network, quality of service, responsiveness to user demands, financial stability, comprehensiveness of coverage, diversity of product offerings, and market presence and reputation. The relative importance of each of these factors and the identity of our key competitors vary by market. Over the past several years, a health plan’s ability to interact with employers, members and other third parties (including health care professionals) via the Internet has become a more important competitive factor. To that end, we have made technology investments to enhance our electronic interactions with third parties. We believe that we compete effectively against other health care industry participants in the states in which we operate.
Our primary competitors in California are Kaiser Permanente, Anthem Blue Cross of California, UnitedHealth Group, Inc. and Blue Shield of California. Together, these four plans and Health Net account for a majority of the insured market in California. Kaiser is the largest HMO in California based on number of enrollees and Anthem Blue Cross of California is the largest PPO provider in California based on number of enrollees. There are also a number of small, regional-based health plans that compete with Health Net in California, mainly in the small business group market segment. In addition, two of the major national managed care companies, Aetna, Inc. and CIGNA Corp., are active in California. Their respective commercial full-risk market share is not as significant as our primary competitors in California and we believe that each remains in California primarily to serve their national, self-funded accounts’ California employees.
Our largest competitor in Arizona is UnitedHealth Group. Our Arizona HMO also competes with Blue Cross Blue Shield of Arizona, CIGNA, Aetna and Humana Inc. Our Oregon health plan competes primarily against Kaiser, UnitedHealth Group, Providence, Regence Blue Cross/Blue Shield, PacificSource, Lifewise and ODS Health Plans, Inc.
In the Northeast, our Connecticut health plan competes for business with Aetna, WellPoint, Inc. (Anthem BCBS), ConnectiCare, Inc., UnitedHealth Group (UnitedHealthcare/Oxford Health Plans), and CIGNA. Our main competitors in New York are UnitedHealth Group (UnitedHealthcare/Oxford Health Plans), WellPoint (Empire Blue Cross Blue Shield), Aetna, HIP/GHI and CIGNA. Our main competitors in New Jersey are UnitedHealth Group (UnitedHealthcare/Oxford Health Plans), Horizon Blue Cross Blue Shield, Aetna and CIGNA.
Marketing and Sales
We market our products and services to individuals and employer groups through inside sales staff, independent brokers, agents and consultants and through the Internet. For our group health business, we market our products and services utilizing a three-step process. We first market to potential employer groups, group insurance brokers and consultants. We then provide information directly to employees once the employer has selected our health coverage. Finally, we engage members and employers in marketing for member and group retention. For our small group business, members are enrolled by their employer based on the plan chosen by the employer. In general, once selected by a large employer group, we solicit enrollees from the employee base directly. During “open enrollment” periods when employees are permitted to change health care programs, we use a variety of techniques to attract new enrollees, including, without limitation, direct mail, work day and health fair presentations and telemarketing. Our sales efforts are supported by our marketing division, which engages in product research and development, multicultural marketing, advertising and communications, and member education and retention programs.
12
Table of Contents
Premiums for each employer group are generally contracted on a yearly basis and are payable monthly. We consider numerous factors in setting our monthly premiums, including employer group needs and anticipated health care utilization rates as forecasted by us based on the demographic composition of, and our prior experience in, our service areas. Premiums are also affected by applicable regulations that in certain circumstances prohibit experience rating of group accounts (i.e., setting the premium for the group based on its past use of health care services) and by state regulations governing the manner in which premiums are structured.
In some of our markets we sell individual policies, which are generally sold through independent brokers and agents. In some states, carriers are allowed to individually underwrite these policies (i.e.select applicants to whom coverage will be provided and others who are denied), although in other states there may be a requirement of guaranteed issue that restricts the carrier’s discretion. In guaranteed issue states, exclusions for preexisting conditions are generally permitted. Where individual underwriting is permitted, the carrier may, in certain circumstances, rescind the policy coverage if the individual misrepresents his or her medical history in the application process. See “Item 1A. Risk Factors—Proposed federal and state legislation affecting the managed health care industry could adversely affect us” and “—Regulatory activities and litigation relating to the rescission of coverage, if resolved unfavorably, could adversely affect us” for additional information on health plans’ right to rescind coverage.
We believe that the importance of the ultimate health care consumer (or member) in the health care product purchasing process is likely to increase in the future, particularly in light of advances in technology and online resources. Accordingly, we are focusing our marketing strategies on the development of distinct brand identities and innovative product service offerings that will appeal to potential health plan members. For example, Decision PowerSM is a series of programs designed to more directly involve patients in their health care decisions. These programs allow our members to access information and consult with health coaches as they are making decisions regarding health care issues. As more employers begin to offer consumer directed health plans such as Health Savings Accounts (“HSAs”) and Health Reimbursement Accounts (“HRAs”), we believe consumers need to be able to learn, plan and make complex decisions regarding their health care. Our website combines access to current Health Net and vendor content and tools.
Consumer-Directed Health Care Plans; Health Savings Accounts and Health Reimbursement Accounts
Health Savings Accounts were created in 2003 as part of the Medicare Prescription Drug Improvement and Modernization Act of 2003 (the “MMA”). HSAs are individually owned accounts, similar to an IRA or a 401(k) retirement plan, that generally allow employees or individuals to make contributions to the account on a pretax basis. Funds in HSAs can be used to pay for certain qualified medical expenses such as plan deductibles, co-payments and coinsurance on a tax-free basis. HSA funds can be invested and earnings on the investments are generally tax-free. HSAs must be used in conjunction with high-deductible health plans. High-deductible health plans provide in-and out-of-network benefits and cover a wide range of health care services.
Our HSA programs and other consumer-driven health care products provide our members with tools to determine what health care services they may need and to estimate how much those services would cost. We support our consumer-directed programs with web-based services that assist members in educating themselves about health care. The web-based program includes WebMD’s Subimo estimator tools, Decision PowerSM, prescription drug and hospital comparison tools.
Our California health plan also offers a Health Net Health Reimbursement Account. An HRA is a health reimbursement arrangement funded solely by an employer where the employer reimburses an employee for health expenses not covered by the group health insurance plan (such as deductibles and coinsurance amounts). Employees are reimbursed tax-free for qualified medical expenses that the employer agrees to reimburse, up to a maximum dollar amount for a coverage period. Subject to the employer’s discretion, up to 100% of any unused amounts in the HRA at the end of a plan year can be carried forward for reimbursement in subsequent years.
13
Table of Contents
Health Net Systems Consolidation Project
We continue to work on a number of systems and operational initiatives designed to improve our customer service, realize operational cost efficiencies and improve our decision making capability. In 2007, we completed our migration to a single medical management platform. This platform provides operational efficiency in clinical operating units, allows for better multi-disciplinary communication amongst our clinicians, and delivers our clinicians improved decision making and patient support tools.
In the third quarter of 2007, we also announced the next stage of our operational strategy. This stage is a three-year effort to consolidate claim platforms across the enterprise and to consolidate service centers and associated staff. We made significant progress in this arena in 2008, including addressing many of the manual processes and workarounds of having multiple systems. Our progress in IT applications and infrastructure outsourcing has been significant, and we continue to make progress on making it easier to do business with Health Net through the use of more sophisticated electronic channels. See “Item 1A. Risk Factors—We are subject to risks associated with outsourcing services and functions to third parties” for risks associated with our outsourcing arrangements. In addition, we have prioritized projects for 2009 with an eye to focusing on those that will bring the greatest immediate benefit. Examples of these projects include an electronic document distribution and print consolidation project, membership and accounting enrollment projects, a claims auto adjudication project and contact center technology and process improvements. Consolidating operations management and continuing to develop more consistent metrics and analytics will greatly increase our efficiency going forward and help us to deliver better service at a lower cost. The completion of the projects will enable us to improve claim turnaround times, auto adjudication rates, electronic data interchange, and internet capabilities. However, there are risks associated with these systems efforts. See “Item 1A. Risk Factors—If we fail to effectively maintain our management information systems, it could adversely affect our business.”
Medical Management
We believe that managing health care costs is an essential function for a managed care company. Among the medical management techniques we utilize to contain the growth of health care costs are pre-authorization or certification for outpatient and inpatient hospitalizations and a concurrent review of active inpatient hospital stays and discharge planning. We believe that this authorization process reduces inappropriate use of medical resources and achieves efficiencies in referring cases to the most appropriate providers. We also contract with third parties to manage certain conditions such as neonatal intensive care unit admissions and stays, as well as chronic conditions such as asthma, diabetes and congestive heart failure. These techniques are widely used in the managed care industry and are accepted practices in the medical profession.
Accreditation
We pursue accreditation for certain of our health plans from the National Committee for Quality Assurance (“NCQA”) and the Utilization Review Accreditation Commission (“URAC”). NCQA and URAC are independent, non-profit organizations that review and accredit HMOs and other healthcare organizations. HMOs that comply with review requirements and quality standards receive accreditation. The commercial line of business of our Arizona, California, Connecticut, New Jersey and New York HMO subsidiaries have all received NCQA accreditation with a score of “excellent,” which is the highest score NCQA awards. HN California’s Medicare line of business also received NCQA accreditation with a score of “excellent.” In addition, HN California’s Medicaid line of business received NCQA accreditation with a score of “Commendable,” which is customary for first-time accreditation. Our MHN subsidiary has received URAC accreditation.
Our business is subject to comprehensive federal regulation and state regulation in the jurisdictions in which we do business. These laws and regulations govern how we conduct our businesses and result in additional
14
Table of Contents
requirements, restrictions and costs to us. We believe we are in compliance in all material respects with all current state and federal laws and regulations applicable to our businesses. Certain of these laws and regulations are discussed below.
Federal Legislation and Regulation
Medicare Legislation.On December 8, 2003, the Medicare Prescription Drug Improvement and Modernization Act of 2003 (“MMA”) was signed into law. This complex legislation made many significant structural changes to the federal Medicare program and added a voluntary prescription drug benefit, called a “Part D” benefit, which was made available to Medicare beneficiaries starting January 1, 2006.
The MMA changed the methodology for payment to private plans to a competitive bidding process beginning in 2006. For the Medicare Advantage plans, the federal CMS calculates county-specific payment rates based on fee-for-service costs in the county and a legislated formula. These rates then serve as a benchmark against which we must bid for providing the Medicare package of services. The projected savings from the benchmark rate is used 75% to fund additional benefits to members. The remaining 25% is retained by CMS. CMS then pays us a monthly rate for each enrollee, which is the bid amount, with risk adjustment for that member, plus the 75% of savings (if any) in the bid. The risk adjustment factor reflects the member’s age, gender and health status. The MMA also authorized regional PPOs to serve 26 regions covering the U.S. and its territories, and authorized other products designed to provide a private market option on a broader scale.
Our Medicare contracts are subject to regulation by CMS. CMS has the right to audit HMOs and PPOs operating under Medicare contracts to determine the quality of care being rendered and the degree of compliance with CMS’ contracts and regulations. In January 2008, we were notified by the CMS that we were deficient in certain administrative procedures with respect to our stand-alone PDP products, and were directed to cease the sale of such products until resumption of sale was approved by CMS. In March 2008, CMS authorized Health Net to resume sales of its stand-alone PDP products.
In late 2008, CMS performed a routine audit of Health Net’s Medicare Advantage operations. CMS found deficiencies in many of the business areas included in the audit. Health Net received CMS’ report and corrective action request on February 2, 2009. Health Net’s corrective action plan must be submitted within 45 days of receipt of the corrective action request for review and approval. See “Item 1A. Risk Factors—Federal and state audits, review and investigations of us and our subsidiaries could have a material adverse effect on our operations” for a description of the risks associated with this audit.
In September 2008, in part to implement provisions of the Medicare Improvements for Patients and Providers Act of 2008 (“MIPPA”), CMS released final regulations regarding marketing practices of Medicare Advantage organizations (“MAO”) and PDP sponsors. The regulations prohibit certain marketing activities (including telemarketing and other unsolicited sales contacts) and require that agents and brokers selling Medicare Advantage and PDP products be state licensed and appointed in accordance with state laws. Health Net was required to be in compliance with these provisions when it began marketing activities on October 1, 2008 for 2009 plan year enrollments. CMS also released an interim final rule implementing other MIPPA provisions, including specifying restrictions on compensation to MAO and PDP sponsor contracted brokers. In November 2008, CMS released a revised interim final rule on the compensation restrictions. Health Net has implemented the requirements of the final regulations and interim final rule. Health Net could be subject to monetary and other sanctions from CMS in the event of non-compliance by Health Net or its contracted or in-house sales producers.
Medicaid and Related Legislation. Federal law has also implemented other health programs that are partially funded by the federal government, such as the Medicaid program (known as Medi-Cal in California) and CHIP (known as Healthy Families in California). They are largely regulated and administered by state agencies and thus there are variations in these programs from state to state. Federal funding remains critical to the viability of these programs. Federal law permits the federal government to oversee and, in some cases, to enact,
15
Table of Contents
regulations and other requirements that must be followed by the states. Medicaid is administered at the federal level by CMS; CHIP is administered by the Health Resources and Services Administration, another arm of the Department of Health and Human Services.
Privacy Regulations.The use and maintenance of individually identifiable health information and other data by our businesses is regulated by various laws at the federal, state and local level. These laws and regulations are changed frequently by legislation or administrative interpretation. Most of those laws are derived from Health Insurance Portability and Accountability Act of 1996 (“HIPAA”) and the privacy provisions in the federal Gramm-Leach-Bliley Financial Modernization Act of 1999 (the “Gramm-Leach-Bliley Act”).
HIPAA and the implementing regulations that have been adopted in connection therewith impose obligations for issuers of health insurance coverage and health benefit plan sponsors relating to the privacy and security of electronically transmitted protected health information (“PHI”). The regulations, which relate to privacy, electronic transactions and codesets and security regulations, require health plans, clearinghouses and providers to:
| • | comply with various requirements and restrictions related to the use, storage and disclosure of PHI, |
| • | adopt rigorous internal procedures to protect PHI, |
| • | create policies related to the privacy of PHI and |
| • | enter into specific written agreements with business associates to whom PHI is disclosed. |
The regulations also establish significant criminal penalties and civil sanctions for non-compliance. We believe we are in compliance with the HIPAA privacy regulations, the requirements relating to transactions and codesets and the security regulations.
The Gramm-Leach-Bliley Act generally requires insurers to provide customers with notice regarding how their personal health and financial information is used and the opportunity to “opt out” of certain disclosures before the insurer shares non-public personal information with a non-affiliated third party. Like HIPAA, this law sets a “floor” standard, allowing states to adopt more stringent requirements governing privacy protection.
ERISA.Most employee benefit plans are regulated by the federal government under the Employee Retirement Income Security Act of 1974, as amended (“ERISA”). Employment-based health coverage is such an employee benefit plan. ERISA is administered, in large part, by the U.S. Department of Labor (“DOL”). ERISA contains disclosure requirements for documents that define the benefits and coverage. It also contains a provision that causes federal law to preempt state law in the regulation and governance of certain benefit plans and employer groups, including the availability of legal remedies under state law.
Other Federal Regulations. We must comply with, and are affected by, laws and regulations relating to the award, administration and performance of U.S. Government contracts. Government contract laws and regulations affect how we do business with our customers and, in some instances, impose added costs on our business. A violation of specific laws and regulations could result in the imposition of fines and penalties or the termination of our contracts or debarment from bidding on contracts.
16
Table of Contents
State Laws and Regulations
Our HMOs, insurance companies and behavioral health plan are subject to extensive state regulation. Set forth below are the principal regulatory agencies that govern our health plans and insurance companies.
Company | Regulatory Agency | |
| Arizona HMO | Arizona Department of Insurance | |
| California HMO | California Department of Managed Health Care | |
| Connecticut HMO | Connecticut Department of Insurance | |
| New Jersey HMO | New Jersey Department of Banking and Insurance, New Jersey Department of Human Services and Division of Medical Assistance and Health Services (for Medicard only) | |
| New York HMO | New York Department of Insurance, New York Department of Health | |
| Oregon HMO | Oregon Department of Consumer and Business Services | |
| Health Net Life Insurance Company (Arizona, California, Connecticut and New Jersey PPO) | California Department of Insurance generally, and the Department of Insurance of each state in which it does business | |
Health Net Insurance of New York, Inc. (New York PPO) | New York Department of Insurance | |
| MHN | California Department of Managed Health Care, New York Department of Insurance, New Jersey Department of Banking and Insurance, Connecticut Department of Insurance | |
Insurance and HMO laws impose a number of financial requirements and restrictions on our regulated subsidiaries, which vary from state to state. They generally include certain minimum capital and deposit and/or reserve requirements, restrictions on dividends and other distributions to the parent corporations and affiliated corporations. See “Item 7. Management’s Discussion and Analysis of Financial Condition and Results of Operations—Liquidity and Capital Resources—Statutory Capital Requirements.” These financial requirements are subject to change, which may require us to commit additional capital to certain regulated subsidiaries or may limit our ability to move capital through dividends and other distributions.
While there are state-by-state variations, HMO regulation generally is extremely comprehensive. Among the areas regulated by these HMO regulatory agencies are:
| • | Adequacy of financial resources, network of health care providers and administrative operations; |
| • | Sales and enrollment requirements, disclosure documents and notice requirements; |
| • | Product offerings, including the scope of mandatory benefits and required offerings of benefits that are optional coverages; |
| • | Procedures for member grievance resolution and medical necessity determinations; |
| • | Accessibility of providers, handling of provider claims (including out-of-network claims) and adherence to timely and accurate payment and appeal rules; and |
| • | Linguistic and cultural accessibility standards, governance requirements and reporting requirements. |
Variations in state regulation also arise in connection with the intensity of government oversight. Variations include: the need to file or have affirmatively approved certain proposals before use or implementation by the health plan; the degree of review and comment by the regulatory agency; the amount and type of reporting by the
17
Table of Contents
health plan to the regulatory agency; the extent and frequency of audit or other examination; and the authority and extent of investigative activity, enforcement action, corrective action authority, and penalties and fines.
Our regulated subsidiaries are also subject to legal restrictions on our ability to price some of our products. Some products may be subject to regulatory approval of premium levels. Generally, insurance and HMO laws require premiums to be established at amounts reasonably related to our costs.
Pending Federal and State Legislation
There are a number of other legislative initiatives and proposed regulations currently pending or previously proposed at the federal and state levels which could increase regulation of, and costs incurred by, the health care industry. These measures and other initiatives, if enacted, could have significant adverse effects on our operations. See “Item 1A. Risk Factors—Proposed federal and state legislation and regulations affecting the managed health care industry could adversely affect us.” We cannot predict the outcome of any of the pending legislative or regulatory proposals, nor the extent to which we may be affected by the enactment of any such legislation or regulation.
We have registered and maintain various service marks, trademarks and trade names that we use in our businesses, including marks and names incorporating the “Health Net” phrase, and from time to time we apply for additional registrations of such marks. We utilize these and other marks and names in connection with the marketing and identification of products and services. We believe such marks and names are valuable and material to our marketing efforts.
As of December 31, 2008, Health Net, Inc. and its subsidiaries employed 9,396 persons on a full-time basis and 250 persons on a part-time or temporary basis. These employees perform a variety of functions, including, among other things, provision of administrative services for employers, providers and members; negotiation of agreements with physician groups, hospitals, pharmacies and other health care providers; handling of claims for payment of hospital and other services; and provision of data processing services. Our employees are not unionized and we have not experienced any work stoppages since our inception. We consider our relations with our employees to be very good.
The federal government is the only customer of the Company’s Government Contracts segment, with premiums and fees accounting for 100% of our Government Contracts revenue. In addition, the federal government is a significant customer of the Company’s Health Plan Services segment as a result of its contract with CMS for coverage of Medicare-eligible individuals, including Part D prescription plans, state agencies for federally-subsidized Medicaid and CHIP programs, and coverage of federal employees under the Federal Employees Health Benefits Program. Medicare premiums accounted for 28% of our total premium revenue in 2008.
On July 27, 2006, our Board of Directors approved the extension of the benefits afforded by our former shareholder rights plan, which expired at the close of business on July 31, 2006, by adopting a new shareholder rights plan pursuant to a Rights Agreement with Wells Fargo Bank, N.A. (the “Rights Agent”), dated as of July 27, 2006 (the “Rights Agreement”).
In connection with the Rights Agreement, on July 27, 2006, our Board of Directors declared a dividend distribution of one right (a “Right”) for each outstanding share of Common Stock to stockholders of record at the
18
Table of Contents
close of business on August 7, 2006 (the “Record Date”). Our Board of Directors also authorized the issuance of one Right for each share of Common Stock issued after the Record Date and prior to the earliest of the Distribution Date (as defined below) the redemption of the Rights and the expiration of the Rights and, in certain circumstances, after the Distribution Date. Subject to certain exceptions and adjustment as provided in the Rights Agreement, each Right entitles the registered holder to purchase from us one one-thousandth (1/1000th) of a share of Series A Junior Participating Preferred Stock, par value of $0.001 per share, at a purchase price of $170.00 per Right (the “Purchase Price”). The terms of the Rights are set forth in the Rights Agreement.
Rights will attach to all common stock certificates representing shares then outstanding and no separate Rights certificates will be distributed. Subject to certain exceptions contained in the Rights Agreement, the Rights will separate from the Common Stock on the date that is 10 business days following (i) any person, together with its affiliates and associates (an Acquiring Person), becoming the beneficial owner of 15% or more of the outstanding common stock, (ii) the commencement of a tender or exchange offer that would result in any person, together with its affiliates and associates, becoming the beneficial owner of 15% or more of the outstanding common stock or (iii) the determination by the Board of Directors that a person, together with its affiliates and associates, has become the beneficial owner of 10% or more of the common stock and that such person is an “Adverse Person,” as defined in the Rights Agreement (the earliest of such dates being called the “Distribution Date”). The Rights Agreement provides that certain passive institutional investors that beneficially own less than 20% of the outstanding shares of our common stock shall not be deemed to be Acquiring Persons.
The Rights will first become exercisable on the Distribution Date and will expire at the close of business on July 31, 2016 unless such date is extended or the Rights are earlier redeemed by us as described below.
Subject to certain exceptions contained in the Rights Agreement, in the event that any person shall become an Acquiring Person or be declared to be an Adverse Person, then the Rights will “flip-in” and entitle each holder of a Right, other than any Acquiring Person or Adverse Person and such person’s affiliates and associates, to purchase, upon exercise at the then-current exercise price of such Right, that number of shares of common stock having a market value of two times such exercise price.
In addition, and subject to certain exceptions contained in the Rights Agreement, in the event that we are acquired in a merger or other business combination in which the common stock does not remain outstanding or is changed or 50% of the assets, cash flow or earning power of the Company is sold or otherwise transferred to any other person, the Rights will “flip-over” and entitle each holder of a Right, other than an Acquiring Person or an Adverse Person and such person’s affiliates and associates, to purchase, upon exercise at the then current exercise price of such Right, such number of shares of common stock of the acquiring company which at the time of such transaction would have a market value of two times such exercise price.
We may redeem the Rights at any time until the earlier of (i) 10 days following the date that any Acquiring Person becomes the beneficial owner of 15% or more of the outstanding common stock and (ii) the date the Rights expire at a price of $.01 per Right. In addition, at any time after a person becomes an Acquiring Person or is determined to be and Adverse Person and prior to such person becoming (together with such person’s affiliates and associates) the beneficial owner of 50% or more of the outstanding Common Stock, at the election of our Board of Directors, the outstanding Rights (other than those beneficially owned by an Acquiring Person, Adverse Person or an affiliate or associate of an Acquiring Person or Adverse Person) may be exchanged, in whole or in part, for shares of Common Stock, or shares of preferred stock of the Company having essentially the same value or economic rights as such shares.
Potential Acquisitions and Divestitures
We continue to evaluate the profitability realized or likely to be realized by our existing businesses and operations. From time to time we review, from a strategic standpoint, potential acquisitions and divestitures in light of our core businesses and growth strategies. In November 2008, we announced that, among other strategic
19
Table of Contents
alternatives, we are considering a divestiture of our Northeast and Arizona businesses. See “Item 1A. Risk Factors—Acquisitions, divestitures and other significant transactions may adversely affect our business.”
Cautionary Statements
The following discussion, as well as other portions of this Annual Report on Form 10-K, contain “forward-looking statements” within the meaning of Section 21E of the Exchange Act, and Section 27A of the Securities Act of 1933, as amended, regarding our business, financial condition and results of operations. We intend such forward-looking statements to be covered by the safe harbor provisions for forward-looking statements contained in the Private Securities Litigation Reform Act of 1995, and we are including this statement for purposes of complying with these safe harbor provisions. These forward-looking statements involve a number of risks and uncertainties. All statements, other than statements of historical information provided or incorporated by reference herein, may be deemed to be forward-looking statements. Without limiting the foregoing, the words “believes,” “anticipates,” “plans,” “expects,” “may,” “should,” “could,” “estimate” and “intend” and other similar expressions are intended to identify forward-looking statements. Actual results could differ materially due to, among other things, rising health care costs, negative prior period claims reserve developments, changes in the economy, volatility in the financial markets, trends in medical care ratios, unexpected utilization patterns or unexpectedly severe or widespread illnesses, membership declines, rate cuts affecting our Medicare or Medicaid businesses, issues relating to provider contracts, litigation costs, regulatory issues, operational issues, health care reform and general business and market conditions. Additional factors that could cause our actual results to differ materially from those reflected in forward-looking statements include, but are not limited to, the factors set forth below and the risks discussed in our other filings from time to time with the SEC.
Any or all forward-looking statements in this Annual Report on Form 10-K and in any other public filings or statements we make may turn out to be wrong. They can be affected by inaccurate assumptions we might make or by known or unknown risks and uncertainties. Many of the factors discussed below will be important in determining future results. These factors should be considered in conjunction with any discussion of operations or results by us or our representatives, including any forward-looking discussion, as well as comments contained in press releases, presentations to securities analysts or investors or other communications by us. You should not place undue reliance on any forward-looking statements, which reflect management’s analysis, judgment, belief or expectation only as of the date thereof. Except as may be required by law, we do not undertake to address or update forward-looking statements in future filings or communications regarding our business or operating results, and do not undertake to address how any of these factors may have caused results to differ from discussions or information contained in previous filings or communications.
Our profitability will depend, in part, on our ability to accurately predict and control health care costs.
A substantial majority of the revenue we receive is used to pay the costs of health care services or supplies delivered to our members. The total health care costs we incur are affected by the number and type of individual services provided and the cost of each service. Our future profitability will depend, in part, on our ability to accurately predict health care costs and to manage future health care utilization and costs through underwriting criteria, utilization management, product design and negotiation of favorable professional and hospital contracts. Periodic renegotiations of hospital and other provider contracts, coupled with continued consolidation of physician, hospital and other provider groups, may result in increased health care costs or limit our ability to negotiate favorable rates. Changes in utilization rates, demographic characteristics, the regulatory environment, health care practices, inflation, new technologies, clusters of high-cost cases, continued consolidation of physician, hospital and other provider groups and numerous other factors affecting health care costs may adversely affect our ability to predict and control health care costs as well as our financial condition, results of operations and cash flows. In addition, a large scale public health epidemic could affect our ability to control health care costs. See “—Large-scale public health epidemics and/or terrorist activity could cause us to incur unexpected health care and other costs and could materially and adversely affect our business, financial condition and results of operations.”
20
Table of Contents
For several years, one of the fastest increasing categories of our health care costs has been the cost of hospital-based products and services. Factors underlying the increase in hospital costs include, but are not limited to, the underfunding of public programs, such as Medicaid and Medicare and the constant pressure that places on rates from commercial health plans, growing rates of uninsured individuals, new technology, state initiated mandates, alleged abuse of hospital chargemasters, an aging population and, under certain circumstances, relatively low levels of hospital competition caused by market concentration. Another significant category of our health care costs is costs of pharmaceutical products and services. Factors affecting our pharmaceutical costs include, but are not limited to, the price of drugs, utilization of new and existing drugs and changes in discounts.
As a measure of the impact of medical cost on our financial results, relatively small differences between predicted and actual medical costs as a percentage of premium revenues can result in significant changes in our financial results. For example, if medical costs increased by 1% without a proportional change in related revenues for our health plan products, our annual net earnings for 2008 would have been reduced by approximately $107 million. The inability to forecast and manage our health care costs could have a material adverse effect on our business, financial condition or results of operations.
We face competitive pressure to contain premium prices.
In addition to the challenge of controlling health care costs, we face competitive pressure to contain premium prices. While health plans compete on the basis of many factors, including service and the quality and depth of provider networks, price will continue to be a significant basis of competition. Our premium revenue is set in advance of the actual delivery of services, and, in certain circumstances, before contracting with providers. While we attempt to take into account our estimate of expected health care costs over the premium period in setting the premiums we charge or bid, factors such as competition, regulations and other circumstances may limit our ability to fully base premiums on estimated costs. In addition, many factors may, and often do, cause actual health care costs to exceed those costs estimated and reflected in premiums or bids. These factors may include increased utilization of services, increased cost of individual services, catastrophes, epidemics, seasonality, new mandated benefits or other regulatory changes, and insured population characteristics. Our financial condition or results of operations could be adversely affected by significant disparities between the premium increases of our health plans and those of our major competitors or by limitations on our ability to increase or maintain our premium levels.
In 2008, our pricing was, we believe, generally consistent with that of our competitors but there can be no assurance that we will not institute higher premiums in the future. In addition, we continue to see decreases in our total commercial membership as we seek to improve margins. Any future increase in premiums could result in the loss of members. Additionally, there is always the possibility that adverse risk selection could occur when members who utilize higher levels of health care services compared with the insured population as a whole choose to remain with our health plans rather than risk moving to another plan. This could cause health care costs to be higher than anticipated and therefore cause our financial results to fall short of expectations.
In the various states in which we do business, premium prices are also constrained by state laws and regulations which restrict the spread between premiums and benefits, such as laws and regulations that require a minimum loss ratio of a certain percentage. These laws and regulations not only restrict our ability to raise our premiums but also create competitive pressure from some of our competitors who may have lower health care costs than we have and therefore price their premiums at relatively low levels in relation to our cost of care.
Our inability to estimate and maintain appropriate levels of reserves for claims may adversely affect our business, financial condition or results of operations.
Our reserves for claims are estimates of incurred costs based on various assumptions. The accuracy of these estimates may be affected by external forces such as changes in the rate of inflation, the regulatory environment, the judicious administration of claims, medical costs and other factors. Included in the reserves for claims are estimates for the costs of services that have been incurred but not reported and for claims received but not
21
Table of Contents
processed. These estimates are continually monitored and reviewed and, as settlements are made or estimates adjusted, differences are reflected in current operations. Given the uncertainties inherent in such estimates, the actual liability could differ significantly from the amounts reserved. If our actual liability is lower than estimated, it could mean that we set premium prices too high, which could result in a loss of membership. If our actual liability for claims payments is higher than estimated, it could have a negative impact on our profitability per enrolled member and, subsequently, our earnings per share in any particular quarter or annual period. For example, in the first quarter of 2008, we announced that our actual liability for claims incurred during the second half of 2007 was significantly higher than what we had estimated, primarily as a result of unusual seasonal physician and hospital utilization patterns that emerged as fourth quarter claims from 2007 were paid in the first quarter of 2008, and an unusually active flu season. This development was a contributing factor to the company’s first quarter 2008 profitability being lower than previous guidance and its decision to lower its full-year 2008 earnings per diluted share guidance.
Our businesses are subject to significant government regulation, which increases our cost of doing business and could adversely affect our ability to grow our businesses.
Our businesses are subject to extensive federal and state laws and regulations, including, but not limited to, financial requirements, licensing requirements, enrollment requirements and periodic examinations by governmental agencies. These laws and regulations are generally intended to benefit and protect providers and health plan members rather than stockholders of managed health care companies such as Health Net. The laws and rules governing our business and interpretations of those laws and rules are subject to frequent change, and may be interpreted in ways that differ from our understanding retroactively based upon the decisions of regulators or courts. Broad latitude is given to the agencies administering these regulations to interpret them and to impose substantial fines when they believe violations have occurred. Regulatory agencies have imposed substantial fines against us in the past, and may impose substantial fines against us in the future if they determine that we have not complied with applicable laws and regulations. See “Item 3. Legal Proceedings” for additional information. Existing or future laws and rules could force us to change how we do business and may restrict our revenue and/or enrollment growth, and/or increase our health care and administrative costs, and/or increase our exposure to liability with respect to members, providers or others. Further, individual associates may violate these laws and rules, notwithstanding our internal policies and compliance programs.
Our HMO and insurance subsidiaries are subject to regulations relating to cash reserves, minimum net worth, premium rates, approval of policy language and benefits, appeals and grievances with respect to benefit determinations, provider contracting, utilization management, issuance and termination of policies, claims payment practices and a wide variety of other regulations relating to the development and operation of health plans. There can be no assurance that we will be able to continue to obtain or maintain required governmental approvals or licenses or that regulatory changes will not have a material adverse effect on us. See “Item 7. Management’s Discussion and Analysis of Financial Condition and Results of Operations—Statutory Capital Requirements” for additional information.
As a government contractor, we are subject to U.S. government oversight. The government may ask about and investigate our business practices and audit our compliance with applicable rules and regulations. Depending on the results of those audits and investigations, the government could make claims against us. Under government procurement regulations and practices, a negative determination resulting from such claims could result in a contractor being fined, debarred and/or suspended from being able to bid on, or be awarded, new government contracts for a period of time. In addition, we are subject to state and federal false claims laws that generally prohibit the submission of false claims for reimbursement or payment to government agencies. Courts have imposed substantial fines and penalties against companies found to have violated these laws. We are also exposed to other risks associated with U.S. government contracting, including dependence upon Congressional appropriation and allotment of funds.
In addition, laws or regulations adopted in the future could adversely affect our business. See “—Proposed federal and state legislation and regulations affecting the managed care industry could adversely affect us.”
22
Table of Contents
Delays in obtaining or failure to obtain or maintain governmental approvals, or moratoria imposed by regulatory authorities, could adversely affect our revenue or the number of our members, increase costs or adversely affect our ability to bring new products to market as forecasted.
Our efforts to capitalize on Medicare business opportunities could prove to be unsuccessful.
Medicare programs represent a significant portion of our business, accounting for approximately 28% of our total premium revenue in 2008 and an expected 29% in 2009. Over the last several years we have significantly expanded our Medicare health plans and restructured our Medicare program management team and operations to enhance our ability to pursue business opportunities presented by the MMA and the Medicare program generally. For example, in 2008 we consolidated overall Medicare Program management under a single executive with responsibility for Medicare plan performance and compliance company-wide. All field-based sales and servicing operations remain in the local markets close to their customers and distribution channels.
Particular risks associated with our provision of Medicare Part D prescription drug benefits under the MMA include potential uncollectibility of receivables, inadequacy of pricing assumptions, inability to receive and process information and increased pharmaceutical costs, as well as the underlying seasonality of this business, and extended settlement periods for claims submissions. In addition, in connection with our participation in the Medicare Advantage and Part D programs, we regularly record revenues associated with the risk adjustment reimbursement mechanism employed by CMS. This mechanism is designed to appropriately reimburse health plans for the relative health care cost risk of its Medicare enrollees. While we have historically recorded revenue and received payment for risk adjustment reimbursement settlements, there can be no assurance that we will receive payment from CMS for the levels of the risk adjustment premium revenue recorded in any given quarter.
On July 15, 2008, the Medicare Improvement for Patients and Providers Act of 2008 (“MIPPA”) became law. Beginning in 2010, MIPPA may, among other things, significantly reduce funding for Medicare Advantage programs. In response to MIPPA, CMS promulgated interim final regulations governing the marketing and sale of Medicare Advantage and PDP products. These regulations prohibit certain marketing activities by contracted and in-house sales producers, including outbound calling, and place new requirements on amounts and duration of compensation payable to contracted producers. We could be subject to monetary and other sanctions by CMS for a contracted or in-house sales producer’s violation of these regulations. In addition, the new presidential administration has made it clear that health reform, including the reduction of Medicare expenditures, is an important priority.
If the cost and complexity of any changes to the Medicare program exceed our expectations or prevent effective program implementation; if the government alters or further reduces funding of Medicare programs; if we fail to design and maintain programs that are attractive to Medicare participants; if CMS suspended our ability to market, or enroll members in, our Medicare products; or if we are not successful in winning contract renewals or new contracts under the MMA’s competitive bidding process, our current Medicare business and our ability to expand our Medicare operations could be materially and adversely affected, and we may not be able to realize any return on our investments in Medicare initiatives. See “—Federal and state audits, review and investigations of us and our subsidiaries could have a material adverse effect on our operations” for information on the results of our recent CMS audit.
A significant reduction in revenues from the government programs in which we participate could have an adverse effect on our business, financial condition or results of operations.
Approximately 49% of our annual revenues relate to federal, state and local government health care coverage programs, such as Medicare, Medicaid and TRICARE. All of the revenues in our Government Contracts segment come from the federal government. Under government-funded health programs, the government payor typically determines premium and reimbursement levels. If the government payor reduces premium or reimbursement levels or increases them by less than our costs increase, and we are unable to make offsetting adjustments through supplemental premiums and changes in benefit plans, we could be adversely
23
Table of Contents
affected. Contracts under these programs are generally subject to frequent change, including changes that may reduce the number of persons enrolled or eligible, reduce the revenue received by us or increase our administrative or health care costs under such programs. Changes of this nature could have a material adverse effect on our business, financial condition or results of operations. Changes to government health care coverage programs in the future may also affect our willingness to participate in these programs.
States periodically consider reducing or reallocating the amount of money they spend for Medicaid. Currently, many states are experiencing budget deficits, and some states have reduced or have begun to reduce, or have proposed reductions in, payments to Medicaid managed care providers. For example, in July 2008, the State of California implemented a 10% reduction in the state’s Medi-Cal reimbursement rates. This rate reduction had an adverse impact on our pretax income for 2008 and was one of the factors contributing to our lowered full-year earnings per share guidance for 2008. Any additional significant reduction in payments received in connection with Medicaid could adversely affect our business, financial condition or results of operations.
In addition, states can impose requirements on Medicaid programs that make continued operations not feasible. For example, in early 2008 we completed our transition out of the Medicaid program in Connecticut due to the state requiring Medicaid contractors to publicly disclose certain proprietary and trade secret information and persistent underfunding of the program.
The amount of government receivables set forth in our consolidated financial statements represents our best estimate of the government’s liability to us under TRICARE and other federal government contracts. In general, government receivables are estimates and subject to government audit and negotiation. In addition, inherent in government contracts are an uncertainty of and vulnerability to disagreements with the government. Final amounts we ultimately receive under government contracts may be significantly greater or less than the amounts we initially recognize on our financial statements.
Health care operations under our TRICARE North contract are scheduled to conclude on March 31, 2009 unless extended by the Department of Defense. We are currently negotiating an extension of the TRICARE North contract with the Department of Defense for an additional one-year option period, which, if exercised would extend the contract until March 31, 2010. On June 30, 2008, we submitted our proposal to the Department of Defense for the third generation of TRICARE Managed Care Support contracts (referred to as “T3”) and, following discussions with the government regarding our proposal, we submitted our final proposal on January 2, 2009. The T3 contract is scheduled to be awarded on or before June 1, 2009, with implementation of the new contracts scheduled to begin on April 1, 2010. Given the effective date of the new contracts, we currently believe that the Department of Defense will extend our current TRICARE North contract for one year. There are competitive proposals from other companies for the T3 contract. If the contract is not extended, and we are not awarded a new TRICARE contract, or if the terms and conditions of a new contract were significantly changed, it could have a material adverse effect on our business, results of operation and financial condition.
Proposed federal and state legislation and regulations affecting the managed health care industry could adversely affect us.
The United States Congress and federal and state regulatory agencies frequently consider legislative proposals and regulatory initiatives which, if enacted, could materially affect the managed health care industry and the regulatory environment. These proposals have included initiatives which, if enacted, could have material adverse effects on our operations, including subjecting us to additional litigation risk, regulatory compliance costs and restrictions on our business operations. Such measures have proposed, among other things, to:
| • | Restrict or eliminate health insurers and health plans in the marketplace; |
| • | Restrict a health insurer or health plan’s profitability or regulate the medical cost ratio; |
| • | Require health plans to pay significantly higher taxes, or reduce government funding of government-sponsored health programs in which we participate; |
24
Table of Contents
| • | Mandate certain benefits and administrative or other services that could increase the cost of healthcare or administrative services, or restrict our right to manage the member’s care through authorization requirements, requirements of medical necessity, or formularies for covered pharmaceuticals; |
| • | Restrict our ability to contract with and manage access to providers and provider groups, enhance certain provider payments or appeal rights, or restrict our ability to select and terminate providers; |
| • | Mandate certain grievance and appeal rights for our members or providers, including establishment of third-party reviews of certain care decisions; and |
| • | Regulate the individual coverage market by restricting or mandating premium levels, restrict our underwriting discretion, or restrict our ability to rescind coverage based on a member’s misrepresentations and omissions. |
Recently, the issue of affordable health insurance and the challenge of insuring the uninsured have generated much public attention. In states where we conduct business, governors and state legislatures are considering various proposals to cover the uninsured. In addition, the new President and his administration, as well as members of Congress, have indicated that they intend to enact federal health reform measures in the near future. Proposals under consideration at both the state and federal levels include, but are not limited to, restructuring the health insurance market to mandate coverage, guaranteeing insurance in the individual market, merging individual and small group markets, placing a cap on loss ratios or premiums or otherwise taking steps to expand access to health insurance in a manner that does not allow for management of risk, and taking steps to limit insurance company profitability.
We cannot predict the outcome of the legislative and regulatory proposals described above or any other such legislative or regulatory proposals, nor the extent to which we may be affected by the enactment of any such legislation or regulations. Such legislation or regulation, including measures that would cause us to change our current manner of operation or increase our exposure to liability, could have a material adverse effect on our results of operations, financial condition and ability to compete in our industry.
We may experience losses as a result of the regional concentration of our business.
Our business operations are concentrated in the Northeast (in the states of Connecticut, New York and New Jersey) and in the states of California, Arizona and Oregon. Our California operations represented approximately 60% of our total revenue in 2008. In late 2008, we announced that, among other strategic alternatives, we are considering a divestiture of our Northeast and Arizona businesses. If we divest our Northeast and Arizona businesses, the geographic concentration of our remaining business operations will increase. Due to this concentration in a small number of states, and, in particular, California, we are exposed to the risk of a deterioration in our financial results arising from a significant economic downturn in one or more of these states. The state of California is experiencing a significant budget shortfall, which may lead to cuts in spending for services and the significant deterioration of economic conditions in California. If economic conditions in any of these states significantly worsen, we may experience a reduction in existing and new business, which may have a material adverse effect on our business, financial condition and results of operations. In addition, if any one of our health plans experiences significant losses, our consolidated results of operations may be materially and adversely affected. Losses of accounts or deterioration in margins in any one of the states in which we operate could have an adverse effect on our financial condition or results of operations.
Federal and state audits, review and investigations of us and our subsidiaries could have a material adverse effect on our operations.
We have been and, in some cases, currently are, involved in various federal and state governmental audits, reviews and investigations. These include routine, regular and special investigations, audits and reviews by CMS, state insurance and health and welfare departments and others pertaining to financial performance, market conduct and regulatory compliance issues. Such audits, reviews and investigations could result in the loss of
25
Table of Contents
licensure or the right to participate in certain programs, or the imposition of civil or criminal fines, penalties and other sanctions. In addition, disclosure of any adverse investigation or audit results or sanctions could negatively affect our reputation in various markets and make it more difficult for us to sell our products and services. We have entered into consent agreements relating to, and in some instances have agreed to pay fines in connection with, several recent audits and investigations.
Many regulatory audits, reviews and investigations in recent years have focused on the timeliness and accuracy of claims payments by managed care companies and health insurers. Our subsidiaries have been the subject of audits, reviews and investigations of this nature. Depending on the circumstances and the specific matters reviewed, regulatory findings could require remediation of claims payment errors and payment of penalties of material amounts that could have a material adverse effect on our results of operations.
Beginning in November, 2008, CMS performed routine audits of certain of our Medicare Advantage, PFFS and PDP products, and found deficiencies in many of the business areas included in the review. On February 2, 2009, we received the audit report and corrective action request from CMS, and we have 45 days to submit our corrective action plan to CMS for review and approval. If CMS is not satisfied with our corrective action plan, or if it believes that the deficiencies are substantial and/or repeat deficiencies, it could levy enforcement actions, including financial penalties and/or the suspension of marketing and enrollment into our Medicare products. If CMS were to impose substantial financial penalties and/or suspend the marketing of and enrollment into our Medicare products for a significant period of time in the future, it could have a material adverse effect on our Medicare business.
On February 13, 2008, the New York Attorney General (NYAG) announced that his office was conducting an industry-wide investigation into the manner in which health insurers calculate “usual, customary and reasonable” charges for purposes of reimbursing members for out-of-network medical services. The NYAG’s office issued subpoenas to 16 health insurance companies, including us, in connection with this investigation. See “Item 3. Legal Proceedings” for additional detail regarding the NYAG’s investigation. On January 13, 2009, the NYAG announced that, as a result of his investigation, his office had entered into a settlement agreement with United HealthGroup, Inc., which owns and operates the Ingenix database used by most health plans, including us, to price out-of-network claims. At the time of the announcement of the settlement with United, the NYAG indicated his intent to continue his investigation with respect to other health insurers. In the meantime, the Connecticut Attorney General has also been investigating health plans’ reimbursement of out-of-network services. On March 28, 2008, we received a request for voluntary production from the Connecticut Attorney General that seeks information similar to that subpoenaed by the NYAG. We are in the process of responding to the request and are cooperating with the Connecticut Attorney General as appropriate in his investigation. There can be no assurance that other state attorneys’ general will not take actions similar to those taken by the NYAG and the Connecticut Attorney General.
In addition, from time to time, agencies of the U.S. government investigate whether our operations are being conducted in accordance with regulations applicable to government contractors. Government investigations of us, whether relating to government contracts or conducted for other reasons, could result in administrative, civil or criminal liabilities, including repayments, fines or penalties being imposed upon us, or could lead to suspension or debarment from future U.S. government contracting, which could have a material adverse effect on our financial condition and results of operations.
Regulatory activities and litigation relating to the rescission of coverage, if resolved unfavorably, could adversely affect us.
In our individual business in certain states, persons applying for insurance policies are required to provide information about their medical history as well as that of family members for whom they are seeking coverage. These applications are subjected to a formal underwriting process to determine whether the applicants present an acceptable risk. If coverage is issued and the health plan or insurer subsequently discovers that the applicant
26
Table of Contents
materially misrepresented their or their family members’ medical history, the health plan or insurer has the legal right to rescind the policy in accordance with applicable legal standards. Although rescission has long been a legally authorized practice, the decisions of health plans to rescind coverage and decline payment to treating providers, as well as the procedures used to do so, have recently generated public attention, particularly in California. As a result, there have been both legislative and regulatory actions, as well as significant litigation, in connection with this issue.
On October 23, 2007, the California Department of Managed Health Care (DMHC) and the California Department of Insurance (DOI) announced that they would be issuing joint regulations that would restrict the ability of health plans and insurers to rescind a member’s coverage and deny payment to treating providers. The DMHC has issued draft proposed regulations but has not formally promulgated any regulations to date. The DOI has not issued any proposed regulations and at this time it is not known whether or when either agency will issue regulations. As of January 1, 2008, health plans and insurers in California, under certain defined circumstances, are obligated to pay providers for services they have rendered despite the rescission of a member’s policy.
In October, 2007, the DMHC initiated a survey of Health Net of California’s activities regarding the rescission of policies for the period January 1, 2004 through June 30, 2006. Following completion of the survey, on May 15, 2008, Health Net of California entered into a settlement agreement with the DMHC. See “Item 3. Legal Proceedings—Litigation Relating to Rescission of Policies” for information regarding the details of the settlement agreement. Failure to substantially implement the actions set forth in the corrective action plan will subject Health Net of California to a potential additional penalty of up to $3 million.
In April, 2008, the DOI commenced an audit of Health Net Life Insurance Company’s rescission practices and related claims settlement practices for the period January 1, 2004 through February 29, 2008. On September 12, 2008, Health Net Life entered into a settlement agreement with the DOI which resolves all DOI matters regarding Health Net Life’s rescission practices from January 2004 to date. See “Item 3. Legal Proceedings—Litigation Relating to Rescission of Policies” for information regarding the details of the settlement agreement. Failure to substantially comply with the settlement agreement subjects Health Net Life to a potential additional monetary penalty of up to $3.6 million.
We are also party to arbitrations and litigation, including a putative class action, in which rescinded members allege that we unlawfully rescinded their coverage. The lawsuits generally seek reimbursement for the cost of medical services that were not paid as a result of the rescission, and also seek to recover for emotional distress, attorneys’ fees and punitive damages. One of these arbitrations was decided in 2008 and resulted in an award paid to the claimant of approximately $9.4 million. Recent court of appeal decisions in California adverse to health plans and insurers have increased the risks associated with rescissions of policies based on applications containing material misrepresentations of medical history, and may make it more difficult to rescind policies in the future. On February 20, 2008, the Los Angeles City Attorney filed a complaint against us relating to our underwriting practices and rescission of certain individual policies. The complaint sought equitable relief and civil penalties for, among other things, alleged false advertising, violations of unfair competition laws and violations of the California Penal Code. On February 10, 2009, Health Net entered into settlement agreements resolving both the putative class action and the action filed by the Los Angeles City Attorney. See “Item 3. Legal Proceedings—Litigation Relating to Rescission of Policies” for additional information regarding these settlement agreements. Other government agencies, including the Attorney General of California, have indicated that they are investigating, or may be interested in investigating, rescissions and related activities.
We cannot predict the outcome of the anticipated regulatory proposals described above, nor the extent to which we may be affected by the enactment of those or other regulatory or legislative activities relating to rescissions. Such legislation or regulation, including measures that would cause us to change our current manner of operation or increase our exposure to liability, could have a material adverse effect on our results of operations, financial condition and ability to compete in our industry. Similarly, given the complexity and scope
27
Table of Contents
of rescission lawsuits, their final outcome cannot be predicted with any certainty. It is possible that in a particular quarter or annual period our results of operations could be adversely affected by an ultimate unfavorable resolution of these cases.
We face risks related to litigation, which, if resolved unfavorably, could result in substantial penalties and/or monetary damages, including punitive damages. In addition, we incur material expenses in the defense of litigation and our results of operations or financial condition could be adversely affected if we fail to accurately project litigation expenses.
We are subject to a variety of legal actions to which any corporation may be subject, including employment and employment discrimination-related suits, employee benefit claims, wage and hour claims, breach of contract actions, tort claims, fraud and misrepresentation claims, shareholder suits, including suits for securities fraud, and intellectual property and real estate related disputes. In addition, we incur and likely will continue to incur potential liability for claims related to the insurance industry in general and our business in particular, such as claims by members alleging failure to pay for or provide health care, poor outcomes for care delivered or arranged, improper rescission, termination or non-renewal of coverage and insufficient payments for out-of-network services; claims by employer groups for return of premiums; and claims by providers, including claims for withheld or otherwise insufficient compensation or reimbursement, claims related to self-funded business, and claims related to reinsurance matters. Such actions can also include allegations of fraud, misrepresentation, and unfair or improper business practices and can include claims for punitive damages. Also, there are currently, and may be in the future, attempts to bring class action lawsuits against various managed care organizations, including us. In some of the cases pending against us, substantial non-economic or punitive damages are also being sought.
Recent court decisions and legislative activity may increase our exposure for any of the types of claims we face. There is a risk that we could incur substantial legal fees and expenses, including discovery expenses, in any of the actions we defend in excess of amounts budgeted for defense. Plaintiffs’ attorneys have increasingly used expansive electronic discovery requests as a litigation tactic. Responding to these requests, the scope of which may exceed the normal capacity of our historical systems for archiving and organizing electronic documents, may require application of significant resources and impose significant costs on us. In certain cases, we could also be subject to awards of substantial legal fees and costs to plaintiffs’ counsel.
We cannot predict the outcome of any lawsuit with certainty, and we are incurring material expenses in the defense of litigation matters, including without limitation, substantial discovery costs. While we currently have insurance policies that may provide coverage for some of the potential liabilities relating to litigation matters, there can be no assurance that coverage will be available for any particular case or liability. Insurers could dispute coverage or the amount of insurance could not be sufficient to cover the damages awarded or settlement amounts. In addition, certain liabilities such as punitive damages, may not be covered by insurance. Insurance coverage for all or certain types of liability may become unavailable or prohibitively expensive in the future or the deductible on any such insurance coverage could be set at a level that would result in us effectively self-insuring cases against us. The deductible on our errors and omissions (“E&O”) insurance has reached such a level. Given the amount of the deductible, the only cases which would be covered by our E&O insurance are those involving claims that substantially exceed our average claim values and otherwise qualify for coverage under the terms of the insurance policy.
We regularly evaluate litigation matters pending against us, including those described in Note 13 to our consolidated financial statements, to determine if settlement of such matters would be in the best interests of the Company and its stockholders. The costs associated with any such settlement could be substantial and, in certain cases, such as with the McCoy case, could result in an earnings charge in any particular quarter in which we enter into a settlement agreement. Although we have recorded litigation reserves which represent our best estimate on probable losses, both known and incurred but not reported, our recorded reserves might prove to be inadequate to cover an adverse result or settlement for extraordinary matters, such as the matters described in Note 13.
28
Table of Contents
Therefore, costs associated with the various litigation matters to which we are subject and any earnings charge recorded in connection with a settlement agreement could have a material adverse effect on our financial condition or results of operations.
If we are unable to maintain good relations with the physicians, hospitals and other providers that we contract with, our profitability could be adversely affected.
We contract with physicians, hospitals and other providers as a means to assure access to health care services for our members, to manage health care costs and utilization and to better monitor the quality of care being delivered. In any particular market, providers could refuse to contract with us, demand higher payments or take other actions, including litigation, which could result in higher health care costs, less desirable products for customers and members, disruption to provider access for current members or to support growth, or difficulty in meeting regulatory or accreditation requirements. In some markets, certain providers, particularly hospitals, physician/hospital organizations and multi-specialty physician groups, may have significant market positions or even monopolies. Some of these providers may compete directly with us. If these providers refuse to contract with us or utilize their market position to negotiate favorable contracts or place us at a competitive disadvantage, our ability to market our products or to be profitable in those areas could be adversely affected.
We contract with professional providers in California primarily through capitation fee arrangements. Under a capitation fee arrangement, we pay a provider group a fixed amount per member on a regular basis and the provider group accepts the risk of the frequency and cost of member utilization of professional services. Provider groups that enter into capitation fee arrangements generally contract with specialists and other secondary providers, and may contract with primary care physicians, to provide services. The inability of provider groups to properly manage costs under capitation arrangements can result in their financial instability and the termination of their relationship with us. A provider group’s financial instability or failure to pay secondary providers for services rendered could lead secondary providers to demand payment from us, even though we have made our regular capitated payments to the provider group. Depending on state law, we could be liable for such claims. In California, the liability of our HMO subsidiaries for unpaid provider claims has not been definitively settled. There can be no assurance that we will not be liable for unpaid provider claims. There can also be no assurance that providers with whom we contract will properly manage the costs of services, maintain financial solvency or avoid disputes with secondary providers, the failure of any of which could have an adverse effect on the provision of services to members and our operations.
Some providers that render services to our members and insureds that have coverage for out-of-network services are not contracted with our plans and insurance companies. In those cases, there is no pre-established understanding between the provider and the plan about the amount of compensation that is due to the provider; rather, the plan’s obligation is to reimburse the member based upon the terms of the member’s plan. In some states and product lines, the amount of reimbursement is defined by law or regulation, but in most instances it is established by a standard set forth in the plan that is not clearly translated into dollar terms, such as “usual, customary and reasonable.” In such instances providers may believe they are underpaid for their services and may either litigate or arbitrate their dispute with the plan or balance bill our member. Regulatory authorities in various states may also challenge the manner in which we reimburse members for services performed by non-contracted providers. For example, as described in more detail in “Item 3. Legal Proceedings—Proceedings Relating to Claims Payment Practices,” the NYAG announced in February 2008 that his office is in the process of conducting such an investigation, and settlements entered into by other health plans with the NYAG in the wake of this investigation have involved certain payments by those plans. As a result of litigation or regulatory activity, we may have to pay providers additional amounts or reimburse members for their out-of-pocket payments. The uncertainty about our financial obligations for such services and the possibility of subsequent adjustment of our original payments could have a material adverse effect on our financial position or results of operations.
In addition, provider groups and hospitals that do contract with us have in certain situations commenced litigation and/or arbitration proceedings against us to recover amounts they allege to be underpayments due to
29
Table of Contents
them under their contracts with us. We believe that provider groups and hospitals have become increasingly sophisticated in their review of claim payments and contractual terms in an effort to maximize their payments from us and have increased their use of outside professionals, including accounting firms and attorneys, in these efforts. These efforts and the litigation and arbitration that result from them could have a material adverse effect on our results of operations and financial condition.
If the current unfavorable economic conditions continue or further deteriorate, it could adversely affect our revenues and results of operations.
Recent market and economic conditions in the United States have been challenging and unprecedented. Continued concerns about the systemic impact of inflation, energy costs, rising unemployment rates, geopolitical issues, the availability and cost of credit and other capital, the U.S. mortgage market, consumer spending and a declining real estate market have contributed to increased market volatility and diminished expectations for the U.S. economy and this is expected to continue going forward. These extreme events could adversely affect our revenues and results of operations.
These market conditions expose us to a number of risks, including risks associated with the potential financial instability of our customers. If our customer base experiences cash flow problems or other financial difficulties, it could, in turn, adversely impact membership in our plans. For example, our customers may modify, delay or cancel plans to purchase our products, or may make changes in the mix of products purchased from us. If our customers experience financial issues, they may not be able to pay, or may delay payment of, accounts receivable that are owed to us, or may reduce their workforce, resulting in a decline in membership in our products. Further, our customers or potential customers may force us to compete more vigorously on factors such as price and service to retain or obtain their business. The adverse economic conditions could also cause employers to stop offering certain health care coverage as an employee benefit or elect to offer this coverage on a voluntary, employee-funded basis as a means to reduce their operating costs. A significant decline in membership in our plans and the inability of current and/or potential customers to pay their premiums as a result of unfavorable economic conditions may adversely affect our business, including our revenues, profitability and cash flow.
Higher unemployment rates and significant employment layoffs and downsizings may also impact the number of enrollees in managed care programs and the profitability of our operations. If economic conditions significantly deteriorate and unemployment rates continue to rise, we may experience a reduction in existing and new business, which may have a material adverse effect on our business, financial condition and results of operations.
An extended economic downturn could adversely affect state and federal budgets, resulting in reduced reimbursements or payments in our federal and state government health care coverage programs, including Medicare, Medicaid and CHIP. A reduction in state Medicaid reimbursement rates could be implemented retrospectively to payments already negotiated and/or received from the government and could adversely affect our revenues and financial results. In addition, state and federal budgetary pressures could cause new or a higher levels of assessments or taxes for our commercial programs, such as surcharges on select fee-for-service and capitated medical claims or premium taxes on health maintenance organizations, and could adversely affect our results of operations.
Our forecasts and other forward-looking statements are based on a variety of assumptions that are subject to significant uncertainties. Our performance may not be consistent with these forecasts and forward-looking statements.
From time to time in press releases and otherwise, we publish forecasts or other forward-looking statements regarding our future results, including estimated revenues, net earnings and other operating and financial metrics. Any forecast of our future performance reflects various assumptions. These assumptions are subject to significant
30
Table of Contents
uncertainties, and, as a matter of course, any number of them may prove to be incorrect. For example, in 2008, we lowered our full-year 2008 earnings per share guidance in the first, second and third quarter, which had a significant negative impact on our full year results.
The achievement of any forecast depends on numerous risks and other factors, including those described in this Annual Report, many of which are beyond our control. In addition, the volatility in the financial markets and challenging economic conditions may make it particularly difficult to forecast our future performance. As a result, we cannot assure that our performance will meet any management forecasts or that the variation from such forecasts will not be material and adverse. You are cautioned not to base your entire analysis of our business and prospects upon isolated predictions, but instead are encouraged to utilize the entire mix of publicly available historical and forward-looking information, as well as other available information affecting us, our services, and our industry when evaluating our forecasts and other forward-looking statements relating to our operations and financial performance.
We have a material amount of indebtedness and may incur additional indebtedness, or need to refinance existing indebtedness, in the future, which may adversely affect our operations.
Our indebtedness includes $400 million in aggregate principal amount of 6.375% Senior Notes due 2017 and $175 million in borrowings under a financing facility which will amortize over a period ending December 2012. For a description of our Senior Notes and our financing facility, see “Item 7. Management’s Discussion and Analysis of Financial Condition and Results of Operations—Liquidity and Capital Resources—Capital Structure.” In addition, to provide liquidity, we have a $900 million five-year revolving credit facility that expires in June 2012. As of December 31, 2008, $150 million was outstanding under our revolving credit facility. We may incur additional debt in the future. Our existing indebtedness, and any additional debt we incur in the future through drawings on our revolving credit facility or otherwise could have an adverse effect on our business and future operations. For example, it could:
| • | require us to dedicate a substantial portion of cash flow from operations to pay principal and interest on our debt, which would reduce funds available to fund future working capital, capital expenditures and other general operating requirements; |
| • | increase our vulnerability to general adverse economic and industry conditions or a downturn in our business; and |
| • | place us at a competitive disadvantage compared to our competitors that have less debt. |
We continually evaluate options to refinance our outstanding indebtedness. Our ability to obtain any financing, whether through the issuance of new debt securities or otherwise, and the terms of any such financing are dependent on, among other things, our financial condition, financial market conditions within our industry and generally, credit ratings and numerous other factors. Recently, credit markets have experienced unusual uncertainty, and liquidity and access to capital markets have tightened. See “—Adverse conditions in the credit markets may materially affect our ability to obtain credit.” Consequently, in the event we need to access the credit markets to refinance our debt, there can be no assurance that we will be able to obtain financing on acceptable terms or within an acceptable time, if at all. If we are unable to obtain financing on terms and within a time acceptable to us it could, in addition to other negative effects, have a material adverse effect on our operations, financial condition, ability to compete or ability to comply with regulatory requirements.
Adverse conditions in the credit markets may materially affect our ability to obtain credit.
The U.S. and global capital and credit markets have been experiencing extreme volatility and disruption. Concern about the stability of the markets generally has lead many lenders to reduce and in some cases cease to provide funding to borrowers. If current levels of market disruption and volatility continue or worsen, they may materially and adversely affect our ability to access additional capital to meet liquidity needs, which could have an adverse effect on our financial condition and results of operations.
31
Table of Contents
The current economic environment and volatility in the financial markets could have an adverse impact on the value of our investment portfolio and our goodwill which could, in turn, have a negative effect on our results of operations and stockholders’ equity.
Our investment portfolio is comprised primarily of available-for-sale investment securities such as interest-yielding debt securities of varying maturities. As of December 31, 2008, our available-for-sale investment securities were $1.5 billion. The value of fixed-income securities is highly sensitive to fluctuations in short-and long-term interest rates, with the value decreasing as such rates increase and increasing as such rates decrease. These securities may also be negatively impacted by illiquidity in the market. We closely monitor the fair values of our investment securities and regularly evaluate them for any other-than-temporary impairments. We have the intent and ability to hold our investments for a sufficient period of time to allow for recovery of the principal amount invested.
The current economic environment and recent volatility of the U.S. and global capital markets have negatively impacted the liquidity of investments, such as our debt securities, and a worsening of credit market disruptions or sustained market downturns could have additional negative effects on the liquidity and value of our investment assets. In addition, such volatility has increased the difficulty of assessing investment impairment and the same influences tend to increase the risk of potential impairment of these assets.
In the third quarter of 2008, we recognized a $14.6 million loss from other-than-temporary impairments in our available-for-sale investments and money market fund. Over time, the economic and capital market environment may further deteriorate or provide additional insight regarding the fair value of certain securities, which could change our judgment regarding the impairment of certain investments. This could result in realized losses relating to other-than-temporary declines being charged against future income. Given the current market conditions and the significant judgments involved, there is continuing risk that further declines in fair value may occur and material other-than-temporary impairments may result in realized losses in future periods, which could have an adverse effect on our results of operations, liquidity and financial condition. See “Item 7. Management’s Discussion and Analysis of Financial Condition and Results of Operations—Liquidity and Capital Resources” for additional information regarding our investment portfolio.
In addition, our regulated subsidiaries are also subject to state laws and regulations that govern the types of investments that are allowable and admissible in those subsidiaries’ portfolios. There can be no assurance that our investment assets will produce total positive returns or that we will not sell investments at prices that are less than the carrying value of these investments. Changes in the value of our investment assets, as a result of interest rate fluctuations, illiquidity or otherwise, could have a negative affect on our stockholders’ equity. In addition, if it became necessary for us to liquidate our investment portfolio on an accelerated basis, it could have an adverse effect on our results of operations.
The economic environment and crisis in the financial markets also resulted in significant fluctuations in our market capitalization during 2008. As a result of the decline in our market capitalization, we updated our annual goodwill impairment test as of December 31, 2008. No impairment was found but if our stock price does not stabilize or if our market capitalization continues to decline, we could be required to update our goodwill impairment test in future quarters. Depending on the results of any such impairment test, we could be required to take an impairment charge to reduce the carrying amount of our goodwill. If we were required to take such a charge, it would be non-cash and would not affect our liquidity, tangible equity or regulatory capital levels but could have a significant adverse effect on our results of operations.
Downgrades in our debt ratings, should they occur, may adversely affect our business, financial condition and results of operations.
Claims paying ability, financial strength, and debt ratings by nationally recognized rating agencies are increasingly important factors in establishing the competitive position of insurance companies and health benefits companies. Ratings information by nationally recognized rating agencies is broadly disseminated and generally used throughout the industry. We believe our claims paying ability and financial strength ratings are important
32
Table of Contents
factors in marketing our products to certain of our customers. In addition, our debt ratings impact both the cost and availability of future borrowings and accordingly, our cost of capital, and our amortizing financing facility contains covenants requiring that we maintain certain public debt ratings. See “Item 7. Management’s Discussion and Analysis of Financial Condition and Results of Operations—Liquidity and Capital Resources—Capital Structure—Amortizing Financing Facility” for additional information on our amortizing financing facility. Each of the rating agencies reviews our ratings periodically and there can be no assurance that current ratings will be maintained in the future. Our ratings reflect each rating agency’s independent opinion of our financial strength, operating performance, ability to meet our debt obligations or obligations to policyholders and other factors. Downgrades in our ratings, should they occur, may adversely affect our business, financial condition and results of operations.
We are a holding company and a substantial amount of our cash flow is generated by our subsidiaries. Our regulated subsidiaries are subject to restrictions on the payment of dividends and maintenance of minimum levels of capital.
As a holding company, our subsidiaries conduct substantially all of our consolidated operations and own substantially all of our consolidated assets. Consequently, our cash flow and our ability to pay our debt depends, in part, on the amount of cash that we receive from our subsidiaries. Our subsidiaries’ ability to make any payments to us will depend on their earnings, business and tax considerations, legal and regulatory restrictions and economic conditions. In addition, in certain states our regulated subsidiaries are subject to risk-based capital requirements, known as RBC. These laws require our regulated subsidiaries to report their results of risk-based capital calculations to the departments of insurance in their state of domicile and the National Association of Insurance Commissioners. Failure to maintain the minimum RBC standards could subject certain of our regulated subsidiaries to corrective action, including increased reporting and/or state supervision. In addition, in most states, we are required to seek prior approval before we transfer money or pay dividends from our regulated subsidiaries that exceed specified amounts. If our regulated subsidiaries are restricted from paying us dividends or otherwise making cash transfers to us, it could have material adverse effect on our results of operations and Health Net, Inc.’s free cash flow. For additional information regarding our regulated subsidiaries’ statutory capital requirements, see “Item 7. Management’s Discussion and Analysis of Financial Condition and Results of Operations—Liquidity and Capital Resources—Statutory Capital Requirements.”
Our revolving credit facility and our financing facility contain restrictive covenants that could limit our ability to pursue our business strategies.
On June 25, 2007, we entered into a $900 million five-year revolving credit facility. On December 19, 2007, we entered into a $175 million financing facility. See “Item 7. Management’s Discussion and Analysis of Financial Condition and Results of Operations—Liquidity and Capital Resources—Capital Structure” for additional information regarding our revolving credit facility and our financing facility. Our revolving credit facility and our financing facility require us to comply with various covenants that impose restrictions on our operations, including our ability to incur additional indebtedness, pay dividends, make investments or other restricted payments, sell or otherwise dispose of assets and engage in other activities. Our revolving credit facility and our financing facility also require us to comply with certain financial covenants, including a maximum leverage ratio and a minimum fixed charge coverage ratio. Our financing facility has a covenant requiring us to maintain certain minimum public debt ratings. See “Item 7. Management’s Discussion and Analysis of Financial Condition and Results of Operations—Liquidity and Capital Resources—Capital Structure Amortizing Financing Facility” for details regarding the threshold ratings we are required to maintain under the financing facility.
The restrictive covenants under our revolving credit facility and our financing facility could limit our ability to pursue our business strategies. In addition, any failure by us to comply with these restrictive covenants could result in an event of default under the revolving credit facility, our financing facility, and, in some circumstances, under the indenture governing our Senior Notes, which, in any case, could have a material adverse effect on our financial condition.
33
Table of Contents
The markets in which we do business are highly competitive. If we do not design and price our products competitively, our membership and profitability could decline.
We are in a highly competitive industry. Many of our competitors may have certain characteristics, capabilities or resources, such as greater market share, superior provider and supplier arrangements and existing business relationships, that give them an advantage in competing with us. These competitors include HMOs, PPOs, self-funded employers, insurance companies, hospitals, health care facilities and other health care providers. In addition, other companies may enter our markets in the future.
In addition, financial services or other technology-based companies could enter the market and compete with us on the basis of their streamlined administrative functions. The addition of new competitors can occur relatively easily and customers enjoy significant flexibility in moving between competitors. There is a risk that our customers may decide to perform for themselves functions or services currently provided by us, which could result in a decrease in our revenues. In addition, our providers and suppliers may decide to market products and services to our customers in competition with us.
In recent years, there has been significant merger and acquisition activity in our industry and in industries that act as our suppliers, such as the hospital, physician, pharmaceutical and medical device industries. This activity may create stronger competitors and/or result in higher health care costs. In addition, our contracts with government agencies, such as our TRICARE North contract, are frequently up for re-bid and the loss of any significant government contract to a competitor could have an adverse effect on our financial condition and results of operations. To the extent that there is strong competition or that competition intensifies in any market, our ability to retain or increase customers, our revenue growth, our pricing flexibility, our control over medical cost trends and our marketing expenses may all be adversely affected.
Nearly every major managed care organization has launched, announced or is developing HSA-compatible high-deductible health plans. We have launched HSA programs in our Northeast, Arizona, California and Oregon health plans. Our HSA programs represented a very small percentage of our total revenue in 2008. Some of our large competitors, such as Aetna and Blue Cross Blue Shield plans, have made large investments in, and heavily marketed, their consumer-directed health plans and have gained more enrollment in many markets across the country. If their enrollment trend continues, it may widen the competitive gap between us over the next several years. If we fail to design, maintain and effectively market consumer-directed health care programs that are attractive to consumers and, as a result, are unable to achieve a competitive market share in the consumer-directed care category, it could have a material adverse effect on our business, financial condition or results of operations.
We have historically experienced significant turnover in senior management and recently reorganized our management structure. If we are unable to manage the succession of our key executives, it could adversely affect our business.
We have experienced a high turnover in our senior management team in recent years and in late 2008 reorganized our management structure. Although we have succession plans in place and have employment arrangements with our key executives, these do not guarantee that the services of these key executives will continue to be available to us. We would be adversely affected if we fail to adequately plan for future turnover of our senior management team.
If we fail to effectively maintain our management information systems, it could adversely affect our business.
Our business depends significantly on effective information systems. The information gathered and processed by our management information systems assists us in, among other things, pricing our services, monitoring utilization and other cost factors, processing provider claims, billing our customers on a timely basis
34
Table of Contents
and identifying accounts for collection. Our customers and providers also depend upon our information systems for membership verification, claims status and other information. We have many different information systems for our various businesses and these systems require continual maintenance, upgrading and enhancement to meet our operational needs. Moreover, our merger, acquisition and divestiture activity requires transitions to or from, and the integration of, various information management systems.
Health Net’s operations strategy team is currently reviewing options for transitioning to a single technology platform companywide to gain operational and cost efficiencies. We believe that by consolidating our current systems, we will gain operational and cost efficiencies. Transitioning to a single in-house system and utilizing varying levels of system outsourcing are options currently under consideration by management. See “Item 1. Business—Additional Information Concerning Our Business—Health Net Systems Consolidation Project” for additional information regarding this consolidation project.
Any difficulty or unexpected delay associated with the transition to or from information systems, any inability or failure to properly maintain management information systems, or any inability or failure to successfully update or expand processing capability or develop new capabilities to meet our business needs, could result in operational disruptions, loss of existing customers, difficulty in attracting new customers, disputes with customers and providers, regulatory problems, significant increases in administrative expenses and/or other adverse consequences. In addition, we may, from time-to-time, obtain significant portions of our systems-related or other services or facilities from independent third parties, which may make our operations vulnerable to adverse effects if such third parties fail to perform adequately. See “—We are subject to risks associated with outsourcing services and functions to third parties.”
We are subject to risks associated with outsourcing services and functions to third parties.
We contract with independent third party vendors who provide services to us and our subsidiaries or to whom we delegate selected functions. These third party vendors include, but are not limited to, information technology system providers, medical management providers, claims administration providers, billing and enrollment providers, call center providers and specialty service providers. Our arrangements with third party vendors may make our operations vulnerable if those third parties fail to satisfy their obligations to us, including their obligations to maintain and protect the security and confidentiality of our information and data, as a result of our failure to adequately monitor and regulate their performance, changes in the vendors’ operations or financial condition or other matters outside of our control. Violations of laws or regulations governing our business by third party vendors could increase our exposure to liability or otherwise increase the costs associated with the operation of our business. In addition, to the extent we outsource selected services or selected functions to third parties in foreign jurisdictions, we could be exposed to risks inherent in conducting business outside of the United States, including international economic and political conditions, additional costs associated with complying with foreign laws and fluctuations in currency values.
In 2008, we entered into an outsourcing agreement (the “IT Outsourcing Agreement”) with International Business Machines Corporation (“IBM”) and two separate outsourcing agreements (collectively, the “Applications and Claims Outsourcing Agreements”) with Cognizant Technology Solutions U.S. Corporation (“Cognizant”). Under the terms of the IT Outsourcing Agreement, IBM will, among other things, provide us with data center services, IT security management services, technical support services, administrative support services and, via an IBM partner, voice and data network services. Under the terms of the Applications and Claims Outsourcing Agreements, Cognizant will, among other things, provide application development, testing and monitoring services, application maintenance and support services, project management services, claims adjudication, adjustment, audit and process improvement services. We will retain responsibility for the payment of claims and the development of claims processing policies.
The IT Outsourcing Agreement and the Applications and Claims Outsourcing Agreements, as well as any of our other outsourcing arrangements, could increase our exposure to the risks outlined above. In addition, we may not fully realize the anticipated economic and other benefits from our outsourcing projects or other relationships
35
Table of Contents
we enter into with third party vendors, as a result of regulatory restrictions on outsourcing or otherwise. This could result in substantial costs or other operational or financial problems that could adversely impact our results of operations.
Acquisitions, divestitures and other significant transactions may adversely affect our business.
We continue to evaluate the profitability realized or likely to be realized by our existing businesses and operations. From time to time we review, from a strategic standpoint, potential acquisitions and divestitures in light of our core businesses and growth strategies. The success of any such acquisition or divestiture depends, in part, upon our ability to identify suitable buyers or sellers, negotiate favorable contractual terms and, in many cases, obtain governmental approval. For acquisitions, success is also dependent upon efficiently integrating the acquired business into the Company’s existing operations. If we are unable to consummate, successfully integrate and grow these acquisitions and to realize contemplated revenue synergies and cost savings, our financial results could be adversely affected. In addition, we may, from time to time, divest businesses that are less of a strategic fit for the company or do not produce an adequate return. In November 2008, we announced that, among other strategic alternatives, we are considering a divestiture of our Northeast and Arizona businesses. We may not be able to divest our Northeast and Arizona businesses or may not be able to do so on terms that are favorable to us. Failure to divest or execute another strategic alternative following such an announcement could adversely impact our ability to operate those businesses profitably. Should a divestiture of the Northeast and Arizona businesses occur, our profitability may be impacted by either gains or losses on the sales of those businesses or lost operating income or cash flows from those businesses. Further, in the event the structure of the transaction results in continuing obligations by the buyer to us or our customers, a buyer’s inability to fulfill these obligations could lead to future financial loss on our part. In addition, any divestiture could result in significant asset impairment charges, including those related to goodwill and other intangible assets, which could have a material adverse effect on our financial condition and results of operations. These potential acquisitions or divestitures present financial, managerial and operational challenges, including diversion of management attention from existing businesses, difficulty with integrating or separating personnel and financial and other systems, increased expenses, assumption of unknown liabilities, indemnities and potential disputes with the buyers or sellers.
We must comply with restrictions on patient privacy and information security, including taking steps to ensure compliance by our business associates with HIPAA.
In December 2000, the Department of Health and Human Services promulgated regulations under HIPAA related to the privacy and security of electronically transmitted protected health information (“PHI”). The regulations require health plans, clearinghouses and providers to: comply with various requirements and restrictions related to the use, storage, transmission and disclosure of PHI; adopt rigorous internal procedures to safeguard PHI; and enter into specific written agreements with business associates to whom PHI is disclosed. The regulations also establish significant criminal penalties and civil sanctions for non-compliance. In addition, the regulations could expose us to additional liability for, among other things, violations of the regulations by our business associates, including the third party vendors involved in our outsourcing projects. Although our contracts with business associates provide for appropriate protections of PHI, we may have limited control over the actions and practices of our business associates. Compliance with HIPAA and other state and federal privacy and security regulations may result in cost increases due to necessary systems changes, the development of new administrative processes and the effects of potential noncompliance by our business associates.
Negative publicity regarding the managed health care industry could adversely affect our ability to market and sell our products and services.
Managed health care companies have received and continue to receive negative publicity reflecting the public perception of the industry. For example, the Company and the managed health care industry have been subject to negative publicity surrounding practices in connection with the rescission of individual health insurance policies. In addition, health care and related health care reform proposals have been and are expected
36
Table of Contents
to continue to be the subject of intense media attention, especially since the new presidential administration has announced that federal health reform is one of its top priorities. Such political discourse can often generate publicity that portrays managed care in a negative light. Our marketing efforts may be affected by the amount of negative publicity to which the industry has been subject, as well as by speculation and uncertainty relating to merger and acquisition activity among companies in our industry, including speculation about a possible divestiture of our Northeast and Arizona businesses. Speculation, uncertainty or negative publicity about us, our industry or our lines of business could adversely affect our ability to market and sell our products or services, require changes to our products or services, or stimulate additional legislation, regulation, review of industry practices or litigation that could adversely affect us.
If we are unable to manage our general and administrative expenses, our business, financial condition or results of operations could be harmed.
The level of our administrative expenses can affect our profitability, and administrative expense increases are difficult to predict. While we attempt to effectively manage such expenses, including through the development of online functionalities and other projects designed to create administrative efficiencies, increases in staff-related and other administrative expenses may occur from time to time due to business or product start-ups or expansions, growth, membership declines or changes in business, difficulties or delays in projects designed to create administrative efficiencies, acquisitions, reliance on outsourced services, regulatory requirements, including compliance with HIPAA regulations, or other reasons. For example, in 2007, our administrative expenses increased as we continued to support expected commercial growth. In addition, in November 2007, we announced a reorganization plan to enhance efficiency and achieve general and administrative cost savings. The reorganization is ongoing and is intended to enable us to streamline our operations, including consolidating technology platforms, combining duplicative administrative and operational functions and outsourcing certain operations where appropriate. We are targeting annual savings of $100 million in general and administrative expenses by 2010 in connection with the reorganization. However, there can be no assurance that the reorganization will produce the anticipated savings or that the reorganization will not significantly disrupt operations thereby negatively impacting our financial performance. In addition, there can be no assurance that we will be able to successfully manage our administrative expenses, which could have an adverse effect on our business, financial condition or results of operations.
We depend, in part, on independent brokers and sales agents to market our products and services, and recent regulatory investigations have focused on certain brokerage practices, including broker compensation arrangements and bid quoting practices.
We market our products and services both through sales people employed by us and through independent sales agents. Independent sales agents typically do not work with us on an exclusive basis and may market health care products and services of our competitors. We face intense competition for the services and allegiance of independent sales agents and we cannot assure you that these agents will continue to market our products at a reasonable cost. Although we have a number of sales employees and agents, if key sales employees or agents or a large subset of these individuals were to leave us, our ability to retain existing customers and members could be impaired.
There have been a number of investigations and enforcement actions against insurance brokers and insurers over the last several years regarding allegedly inappropriate or undisclosed payments made by insurers to brokers for the placement of insurance business. For example, CMS has increased its scrutiny of insurance brokers and insurers regarding allegedly improper sales and marketing practices in connection with the sale of Medicare products. While we are not aware of any unlawful practices by the Company or any of our agents or brokers in connection with the marketing and sales of our products and services, investigations by the New York Attorney General, New York Department of Insurance, CMS and other regulators, as well as regulatory changes initiated in several states in response to allegedly inappropriate broker conduct and broker payment practices, could result in changes in industry practices that could have an adverse effect on our ability to market our products.
37
Table of Contents
The market price of our common stock is volatile.
The market price of our common stock is subject to volatility. In 2008, the Morgan Stanley Healthcare Payor Index (the “HMO Index”), an index comprised of 11 managed care organizations, including Health Net, recorded an approximate 54.8% decrease in its value, while the per-share value of our common stock decreased by 77.5%. There can be no assurance that the trading price of our common stock will vary in a manner consistent with the variation in the HMO Index or the Standard & Poor’s 400 Mid-Cap Index of which our common stock is also a component. The market prices of our common stock and the securities of certain other publicly-traded companies in our industry have shown significant volatility and sensitivity in response to many factors, including public communications regarding managed care, legislative or regulatory actions, health care reform litigation or threatened litigation, health care cost trends, pricing trends, competition, earnings, receivable collections or membership reports of particular industry participants, and market speculation about or actual acquisition activity. Additionally, adverse developments affecting any one of the companies in our sector could cause the price of our common stock to weaken, even if those adverse developments do not otherwise affect us. There can be no assurances regarding the level or stability of our share price at any time or the impact of these or any other factors on our stock price.
If we are required to publicly disclose information regarding our provider reimbursement rates and preferred drug list or other trade secret information for our programs, it could have a material adverse effect on our business.
In 2008, following a determination that the Connecticut Freedom of Information Act was applicable to managed care organizations participating in the Connecticut Medicaid Program, the State of Connecticut announced that it was considering making the state’s Freedom of Information Act applicable to other state programs, such as programs for the uninsured and the State employee health benefits program. If we are required to publicly disclose information regarding our provider reimbursement rates, preferred drug lists or other trade secret information, it could have a material adverse effect on our ability to contract with providers and compete effectively in the marketplace.
Large-scale public health epidemics and/or terrorist activity could cause us to incur unexpected health care and other costs and could materially and adversely affect our business, financial condition and results of operations.
An outbreak of a pandemic disease and/or future terrorist activities, including bio-terrorism, could materially and adversely affect the U.S. economy in general and the health care industry specifically. Depending on the government’s actions and the responsiveness of public health agencies and insurance companies, a large-scale public health epidemic or future acts of bio-terrorism could lead to, among other things, increased use of health care services, disruption of information and payment systems, increased health care costs due to increased in-patient and out-patient hospital costs and the cost of any anti-viral medication used to treat affected people.
Natural disasters, including earthquakes, fires and floods, could severely damage or interrupt our systems and operations and result in an adverse effect on our business, financial condition or results of operations.
Natural disasters such as fire, flood, earthquake, tornado, power loss, virus, telecommunications failure, break-in or similar event could severely damage or interrupt our systems and operations, result in loss of data, and/or delay or impair our ability to service our members and providers. We have in place a disaster recovery plan which is intended to provide us with the ability to maintain fully redundant systems for our operations in the event of a natural disaster utilizing various alternate sites provided by a national disaster recovery vendor. However, there can be no assurance that such adverse effects will not occur in the event of a disaster. Any such disaster or similar event could have a material adverse effect on our business, financial condition and results of operations.
38
Table of Contents
Item 1B. Unresolved Staff Comments.
None.
We lease office space for our principal executive offices in Woodland Hills, California. Our executive offices, comprising approximately 176,490 square feet, are occupied under two separate leases, one of which expired on December 31, 2008 (with respect to 51,175 square feet of space) and the other will expire on December 31, 2014 (with respect to 125,315 square feet of space). We have vacated the office space that was covered by the lease that expired on December 31, 2008. A significant portion of our California HMO operations are also housed in Woodland Hills, in a separate 333,954 square foot leased facility. The lease for this two-building facility expires December 31, 2011. Combined rent and rent-related obligations for our Woodland Hills facilities were approximately $16.2 million in 2008.
We also lease an aggregate of approximately 548,807 square feet of office space in Rancho Cordova, California for certain Health Plan Services and Government Contract operations. Our aggregate rent and rent-related obligations under these leases were approximately $11.1 million in 2008. These leases expire at various dates ranging from 2009 to 2013. We also lease a total of approximately 59,750 square feet of office space in San Rafael California for certain specialty services operations.
On March 29, 2007 we sold our 68-acre commercial campus in Shelton, Connecticut (the Shelton Property) to The Dacourt Group, Inc. (Dacourt), dba HN Property Owner, LLC, and leased it back from the Buyer under an operating lease agreement for an initial term of ten years with an option to extend for two additional terms of ten years each. We received net cash proceeds of $83.9 million and recorded a deferred gain of $60.9 million, which is amortized into income as contra-G&A expense over the lease term. Under the Shelton Property lease agreement and other lease agreements, we lease an aggregate of approximately 492,673 square feet of office space in Shelton, Connecticut for certain Health Plan Services for our Northeast Division. Our aggregate rent and rent-related obligations under these leases was approximately $9.0 million in 2008. These leases expire at various dates ranging from 2016 to 2017.
In addition to the office space referenced above, we lease approximately 76 sites in 24 states, totaling approximately 811,426 square feet of space. We also own a data center facility in Rancho Cordova, California comprising approximately 82,000 square feet of space.
We believe that our ownership and rental costs are consistent with those associated with similar space in the applicable local areas. Our properties are well maintained, adequately meet our needs and are being utilized for their intended purposes.
Litigation Related to the Sale of Businesses
AmCareco Litigation
We are a defendant in two related litigation matters pending in Louisiana and Texas state courts, both of which relate to claims asserted by three separate state receivers overseeing the liquidation of three health plans in Louisiana, Texas and Oklahoma that were previously owned by our former subsidiary, Foundation Health Corporation (FHC), which merged into Health Net, Inc. in January 2001. In 1999, FHC sold its interest in these plans to AmCareco, Inc. (AmCareco). We retained a minority interest in the three plans after the sale. Thereafter, the three plans became known as AmCare of Louisiana (AmCare-LA), AmCare of Oklahoma (AmCare-OK) and AmCare of Texas (AmCare-TX). In 2002, three years after the sale of the plans to AmCareco, each of the AmCare plans was placed under state oversight and ultimately into receivership. The receivers for each of the AmCare plans filed suit against us contending that, among other things, we were responsible as a “controlling
39
Table of Contents
shareholder” of AmCareco following the sale of the plans for post-acquisition misconduct by AmCareco and others that caused the three health plans to fail and ultimately be placed into receivership.
On June 16, 2005, a consolidated trial of the claims asserted against us by the three receivers commenced in state court in Baton Rouge, Louisiana. The claims of the receiver for AmCare-TX were tried before a jury and the claims of the receivers for the AmCare-LA and AmCare-OK were tried before the judge in the same proceeding. On June 30, 2005, the jury considering the claims of the receiver for AmCare-TX returned a verdict against us in the amount of $117.4 million, consisting of $52.4 million in compensatory damages and $65 million in punitive damages. The Court later reduced the compensatory and punitive damages awards to $36.7 million and $45.5 million, respectively, and entered judgments against us in those amounts.
The proceedings regarding the claims of the receivers for AmCare-LA and AmCare-OK concluded on July 8, 2005. On November 4, 2005, the Court issued separate judgments on those claims that awarded $9.5 million in compensatory damages to AmCare-LA and $17 million in compensatory damages to AmCare-OK, respectively. The Court later denied requests by AmCare-LA and AmCare-OK for attorneys’ fees and punitive damages. We thereafter appealed both judgments, and the receivers for AmCare-LA and AmCare-OK each appealed the orders denying them attorneys’ fees and punitive damages.
On December 30, 2008, the Court of Appeal issued its judgment on each of the appeals. It reversed in their entirety the trial court’s judgments in favor of the AmCare-TX and AmCare-OK receivers, and entered judgment in our favor against those receivers, finding that the receivers’ claims failed as a matter of law. As a result, those receivers’ cross appeals were rendered moot. The Court of Appeal also reversed the trial court judgment in favor of the AmCare-LA receiver, with the exception of a single breach of contract claim, on which it entered judgment in favor of the AmCare-LA receiver in the amount of $2 million. On January 14, 2009, the three receivers filed a request for rehearing by the Court of Appeal. On February 13, 2009, the Court of Appeal denied the request for a rehearing. The receivers have 30 days from that date to file an application for a writ with the Louisiana Supreme Court.
In light of the original trial court judgments against us, on November 3, 2006, we filed a complaint in the U.S. District Court for the Middle District of Louisiana and simultaneously filed an identical suit in the 19th Judicial District Court in East Baton Rouge Parish seeking to nullify the three judgments that were rendered against us on the grounds of ill practice which resulted in the judgments entered. We have alleged that the judgments and other prejudicial rulings rendered in these cases were the result of impermissible ex parté contacts between the receivers, their counsel and the trial court during the course of the litigation. Preliminary motions and exceptions have been filed by the receivers for AmCare-TX, AmCare-OK and AmCare-LA seeking dismissal of our claim for nullification on various grounds. The federal judge dismissed Health Net’s federal complaint and Health Net appealed to the U.S. Fifth Circuit Court of Appeals. On July 8, 2008, the Fifth Circuit issued an opinion affirming the district court’s dismissal of the federal complaint, albeit on different legal grounds from those relied upon by the district court. The state court nullity action has been stayed pending the resolution of Health Net’s jurisdictional appeal in the federal action and has remained stayed during the pendency of the appeal of the underlying judgments.
These proceedings are subject to many uncertainties, and, given their complexity and scope, their outcome, including the outcome of any appeal, cannot be predicted at this time. It is possible that in a particular quarter or annual period our results of operations, cash flow and/or liquidity could be materially affected by an ultimate unfavorable resolution of these proceedings depending, in part, upon the results of operations or cash flow for such period. However, at this time, management believes that the ultimate outcome of these proceedings should not have a material adverse effect on our financial condition.
Litigation Relating to Rescission of Policies
In recent years, there has been growing public attention, especially in California, to the practices of health plans and health insurers involving the rescission of members’ policies for misrepresenting their health status on
40
Table of Contents
applications for coverage. On October 23, 2007, the California Department of Managed Health Care (DMHC) and the California Department of Insurance (DOI) announced their intention to issue joint regulations limiting the rights of health plans and insurers to rescind coverage. The DMHC has issued draft proposed regulations but has not formally promulgated any regulations to date. The DOI has not issued any proposed regulations. In addition, effective January 1, 2008, newly enacted legislation in California requires health plans and insurers to pay health care providers who, under certain circumstances, have rendered services to members whose policies are subsequently rescinded. The issue of rescissions has also attracted increasing media attention, and both the DMHC and the DOI have been conducting surveys of the rescission practices of health plans, including ours. Other government agencies, including the Attorney General of California, are investigating, or have indicated that they may be interested in investigating, rescissions and related activities.
On October 16, 2007, the DMHC initiated a survey of Health Net of California’s activities regarding the rescission of policies for the period January 1, 2004 through June 30, 2006. Following completion of the survey, on May 15, 2008, Health Net of California entered into a settlement agreement with the DMHC. The settlement agreement requires Health Net of California to (1) pay a $300,000 administrative fine, (2) offer future coverage to all 85 HMO enrollees who had coverage rescinded from January 1, 2004 through May 15, 2008, (3) offer those enrollees an opportunity to participate in an expedited review process where the enrollee could seek to resolve claims for out-of-pocket medical expenses and other damages incurred as a result of the rescission, and (4) file a corrective action plan for various internal procedural changes by June 30, 2008. Health Net of California filed the corrective action plan by the due date and has commenced implementation of the corrective action plan. Failure to substantially implement the actions set forth in the corrective action plan will subject Health Net of California to a potential penalty of up to $3 million.
On April 7, 2008, the DOI commenced an audit of Health Net Life Insurance Company’s rescission practices and related claims settlement practices for the period January 1, 2004 through February 29, 2008. On September 12, 2008, Health Net Life entered into a settlement agreement with the DOI, which resolves all DOI matters regarding Health Net Life’s rescission practices from January 2004 to date. Under the settlement agreement, Health Net Life paid a $3.6 million penalty in and agreed to certain corrective actions, including offering future coverage to all 926 rescinded PPO insureds and offering an opportunity to participate in an expedited review process that allows former insureds to seek to resolve their claims for damages incurred as a result of their rescission. On October 7, 2008, Health Net Life filed a corrective action proposal for various procedure changes. Failure to substantially comply with the settlement agreement subjects Health Net Life to a potential additional monetary penalty of up to $3.6 million.
We are also party to arbitrations and litigation, including a putative class action lawsuit filed in April 2008 in Los Angeles Superior Court, in which rescinded members allege that we unlawfully rescinded their coverage. The lawsuits generally seek to recover the cost of medical services that were not paid for as a result of the rescission, and in some cases they also seek damages for emotional distress, attorney fees and punitive damages. On February 20, 2008, the Los Angeles City Attorney filed a complaint against Health Net in the Los Angeles Superior Court relating to our underwriting practices and rescission of certain individual policies. The complaint sought equitable relief and civil penalties for, among other things, alleged false advertising, violations of unfair competition laws and violations of the California Penal Code. On February 10, 2009, we entered into settlement agreements that resolved both the putative class action and the Los Angeles City Attorney’s lawsuit. Under the terms of the settlement agreements, we agreed to pay a total of $6.3 million to class members (individuals rescinded between February 20, 2004 and February 10, 2009), in accordance with an agreed upon distribution formula. The class action settlement agreement also provides that we will reimburse class members for certain out-of-pocket expenses related to covered medical services that occurred between the time of their original enrollment and the date of their rescission, and we will also hold them harmless for certain unpaid bills for such services. Under the agreement, our reimbursement and hold harmless obligations are capped at a total of $3 million in the aggregate. We will also pay attorney fees of approximately $2 million. Under the terms of the two agreements, we also agreed that we would not engage in any rescissions in California until January 31, 2010, unless legislation or regulations governing the process for rescissions is enacted, or we implement a third party
41
Table of Contents
independent review process that is not objected to by the DMHC or the DOI. The agreement with the City Attorney also provides that we will pay a $2 million civil penalty, as well as contribute $500,000 ascy prespayments to specified non-profit organizations that support childrens’ healthcare. We also agreed as part of the settlements to offer coverage to class members on a going forward basis without medical underwriting, similar to the offer we agreed to make as part of our settlements with the DMHC and DOI. On February 11, 2009, the court gave preliminary approval of the settlements and scheduled a final approval hearing for May 26, 2009. Class members will be given notice of the settlement, and an opportunity to opt out of the agreement, or to file objections to the settlement, which will be considered by the court at the final approval hearing. All of the settlement amounts have been fully accrued for as of December 31, 2008.
We cannot predict the outcome of the anticipated regulatory proposals described above, nor the extent to which we may be affected by the enactment of those or other regulatory or legislative activities relating to rescissions. Such legislation or regulation, including measures that would cause us to change our current manner of operation or increase our exposure to liability, could have a material adverse effect on our results of operations, financial condition and ability to compete in our industry. Similarly, given the complexity and scope of rescission lawsuits, their final outcome cannot be predicted with any certainty. It is possible that in a particular quarter or annual period our results of operations could be adversely affected by an ultimate unfavorable resolution of these cases.
Proceedings Relating to Claims Payment Practices
On March 13, 2008, we entered into a final settlement agreement with the plaintiffs in theMcCoy,Wachtel andScharfman lawsuits, which were nationwide class actions principally relating to our out-of-network claims payment practices. We are currently in the process of implementing the terms of the settlement agreement. We were also the subject of a regulatory investigation conducted by the New Jersey Department of Banking and Insurance (“DOBI”) related principally to the timeliness and accuracy of our claims payment practices for services rendered by out-of-network providers in New Jersey. On August 26, 2008, we entered into a consent order with DOBI and agreed to remediate certain claims and pay a $13 million fine. We completed the remediation of the claims as of August 1, 2008. In the third quarter of 2007, we recorded a $296.8 million charge relating to the settlement of theMcCoy,Wachtel andScharfman cases, including the $13 million fine arising from the consent order with DOBI.
On February 13, 2008, the New York Attorney General (NYAG) announced that his office was conducting an industry-wide investigation into the manner in which health insurers calculate “usual, customary and reasonable” charges for purposes of reimbursing members for out-of-network medical services. The NYAG’s office issued subpoenas to 16 health insurance companies, including us, in connection with this investigation. As described by the NYAG in a press conference on February 13, 2008, the threatened claims appear to be similar in part to those asserted by the plaintiffs in theMcCoy, Wachtel andScharfman cases described above. We are in the process of responding to the subpoena and are cooperating with the NYAG as appropriate in his investigation. On January 13, 2009, the NYAG announced that, as a result of his investigation, his office had entered into a settlement agreement with UnitedHealth Group, Inc., which owns and operates Ingenix, the company that supplied the database used by many health insurers, including us, to determine certain out-of-network reimbursements. Under the terms of the settlement, United will discontinue its ownership and operation of those databases, and will pay $50 million towards creation of a new database to be owned and operated by a non-profit organization in New York. Since the announcement of the agreement with United, the NYAG has reached agreements with some other health plans, under which they agreed to make payments towards the creation of the database and, in some instances, agree to utilize the database if certain conditions are satisfied. At the time of the announcement of the settlement, the NYAG indicated his intent to continue his investigation with respect to other health insurers. In the meantime, the Connecticut Attorney General has also been investigating health plans’ reimbursement of out-of-network services. On March 28, 2008, we received a request for voluntary production from the Connecticut Attorney General that sought information similar to that subpoenaed by the NYAG. We are in the process of responding to the request and are cooperating with the Connecticut Attorney General as appropriate in his investigation.
42
Table of Contents
Miscellaneous Proceedings
In the ordinary course of our business operations, we are also subject to periodic reviews by various regulatory agencies with respect to our compliance with a wide variety of rules and regulations applicable to our business, including, without limitation, rules relating to pre-authorization penalties, payment of out-of-network claims and timely review of grievances and appeals, which may result in remediation of certain claims and the assessment of regulatory fines or penalties.
In addition, in the ordinary course of our business operations, we are also party to various other legal proceedings, including, without limitation, litigation arising out of our general business activities, such as contract disputes, employment litigation, wage and hour claims, real estate and intellectual property claims, claims brought by members seeking coverage or additional reimbursement for services allegedly rendered to our members, but which allegedly were either denied, underpaid or not paid, and claims arising out of the acquisition or divestiture of various business units or other assets. We are also subject to claims relating to the performance of contractual obligations to providers, members, employer groups and others, including the alleged failure to properly pay claims and challenges to the manner in which we process claims. In addition, we are subject to claims relating to the insurance industry in general, such as claims relating to reinsurance agreements and rescission of coverage and other types of insurance coverage obligations.
These other regulatory and legal proceedings are subject to many uncertainties, and, given their complexity and scope, their final outcome cannot be predicted at this time. It is possible that in a particular quarter or annual period our results of operations and cash flow could be materially affected by an ultimate unfavorable resolution of any or all of these other regulatory and legal proceedings depending, in part, upon the results of operations or cash flow for such period. However, at this time, management believes that the ultimate outcome of all of these other regulatory and legal proceedings that are pending, after consideration of applicable reserves and potentially available insurance coverage benefits, should not have a material adverse effect on our financial condition and liquidity.
Potential Settlements
We regularly evaluate litigation matters pending against us, including those described above, to determine if settlement of such matters would be in the best interests of the Company and its stockholders. The costs associated with any such settlement could be substantial and, in certain cases, could result in a significant earnings charge in any particular quarter in which we enter into a settlement agreement. We have recorded reserves and accrued costs for future legal costs for certain significant matters described above. These reserves and accrued costs represent our best estimate of probable loss, including related future legal costs for such matters, both known and incurred but not reported, although our recorded amounts might ultimately be inadequate to cover such costs. Therefore, the costs associated with the various litigation matters to which we are subject and any earnings charge recorded in connection with a settlement agreement could have a material adverse effect on our financial condition or results of operations.
Item 4. Submission of Matters to a Vote of Security Holders.
There were no matters submitted to a vote of the security holders of the Company, either through solicitation of proxies or otherwise, during the fourth quarter of the year ended December 31, 2008.
43
Table of Contents
Item 5. Market For Registrant’s Common Equity, Related Stockholder Matters and Issuer Purchases of Equity Securities.
The following table sets forth the high and low sales prices of the Company’s common stock, par value $.001 per share, on The New York Stock Exchange, Inc. (“NYSE”) since January 2007.
| High | Low | |||||
Calendar Quarter—2007 | ||||||
First Quarter | $ | 56.43 | $ | 45.76 | ||
Second Quarter | $ | 59.25 | $ | 52.08 | ||
Third Quarter | $ | 56.00 | $ | 46.74 | ||
Fourth Quarter | $ | 54.66 | $ | 45.85 | ||
Calendar Quarter—2008 | ||||||
First Quarter | $ | 52.96 | $ | 27.83 | ||
Second Quarter | $ | 32.39 | $ | 24.01 | ||
Third Quarter | $ | 28.93 | $ | 20.75 | ||
Fourth Quarter | $ | 29.87 | $ | 7.38 | ||
On February 20, 2009, the last reported sales price per share of our common stock was $16.74 per share.
Securities Authorized for Issuance Under Equity Compensation Plans
Information regarding the Company’s equity compensation plans is contained in Part III of this Annual Report on Form 10-K under “Item 12. Security Ownership of Certain Beneficial Owners and Management and Related Stockholder Matters.”
Holders of Common Stock
As of February 20, 2009, there were 1,771 holders of record of our common stock.
Dividends
We have not paid any dividends on our common stock during the preceding two fiscal years. We have no present intention of paying any dividends on our common stock, although the matter will be periodically reviewed by our Board of Directors.
We are a holding company and, therefore, our ability to pay dividends depends on distributions received from our subsidiaries, which are subject to regulatory net worth requirements and additional state regulations which may restrict the declaration of dividends by HMOs, insurance companies and licensed managed health care plans. The payment of any dividend is at the discretion of our Board of Directors and depends upon our earnings, financial position (including cash position), capital requirements and such other factors as our Board of Directors deems relevant.
Under our revolving credit facility and our financing facility, we cannot declare or pay cash dividends to our stockholders or purchase, redeem or otherwise acquire shares of our capital stock or warrants, rights or options to acquire such shares for cash except to the extent permitted under the revolving credit facility and the financing facility, which are described in “Item 7. Management’s Discussion and Analysis of Financial Condition and Results of Operations—Liquidity and Capital Resources—Capital Structure.”
44
Table of Contents
Stock Repurchase Program
We have a $700 million stock repurchase program authorized by our Board of Directors. Subject to Board approval, additional amounts are added to the repurchase program from time to time based on exercise proceeds and tax benefits the Company receives from the employee stock options. We repurchased 6,851,595 shares of our common stock during the year ended December 31, 2008, for aggregate consideration of approximately $242.8 million.
We used net free cash available to fund the share repurchases. As of December 31, 2008, the remaining authorization under our stock repurchase program was $103.3 million and we had repurchased an aggregate of 36,623,347 shares of our common stock under our repurchase program at an average price of $34.40 for aggregate consideration of approximately $1,259.8 million (which amount includes exercise proceeds and tax benefits the Company had received from the exercise of employee stock options).
We may repurchase shares of our common stock under the stock repurchase program from time to time in open market transactions, privately negotiated transactions, through accelerated share repurchase programs, or by any combination of such methods. The timing of any repurchases and the actual number of shares repurchased will depend on a variety of factors, including our stock price, corporate and regulatory requirements, restrictions under our debt obligations, and other market and economic conditions.
Our stock repurchase program does not have an expiration date. The stock purchase program may be suspended or discontinued at any time.
On November 4, 2008, we announced that our stock repurchase program is on hold as a consequence of the uncertain financial environment and the announcement by Health Net’s Board of Directors that Jay Gellert, our President and Chief Executive Officer, will be undertaking a review of the Company’s strategic direction.
Under the Company’s various stock option and long term incentive plans, employees and non-employee directors may elect for the Company to withhold shares to satisfy minimum statutory federal, state and local tax withholding and exercise price obligations arising from the vesting and/or exercise of stock options and other equity awards. These repurchases are not part of our stock repurchase program.
The following table presents monthly information related to repurchases of our common stock, including shares withheld by the Company to satisfy tax withholdings and exercise price obligations in 2008, as of December 31, 2008:
Period | Total Number of Shares Purchased (a) | Average Price Paid per Share | Total Average Price Paid | Total Number of Shares Purchased as Part of Publicly Announced Programs (b) (c) | Maximum Number (or Approximate Dollar Value) of Shares (or Units) that May Yet Be Purchased Under the Programs (c) (d) | |||||||||
January 1—January 31 | — | — | — | — | $ | 346,159,116 | ||||||||
February 1—February 29 (e) | 1,904,010 | $ | 46.78 | $ | 89,064,600 | 1,895,300 | $ | 257,491,899 | ||||||
March 1—March 31 (e) | 1,306,123 | 41.51 | 54,214,053 | 1,303,800 | $ | 203,349,454 | ||||||||
April 1—April 30 | — | — | — | — | $ | 203,349,454 | ||||||||
May 1—May 31 | — | — | — | — | $ | 203,349,454 | ||||||||
June 1—June 30 (e) | 2,236 | 30.21 | 67,550 | — | $ | 203,349,454 | ||||||||
July 1—July 31 | — | — | — | — | $ | 203,349,454 | ||||||||
August 1—August 31 | 2,450,000 | 27.56 | 67,526,830 | 2,450,000 | $ | 135,822,624 | ||||||||
September 1—September 30 | 1,202,495 | 27.00 | 32,473,146 | 1,202,495 | $ | 103,349,478 | ||||||||
October 1—October 31 | — | — | — | — | $ | 103,349,478 | ||||||||
November 1—November 30 | — | — | — | — | $ | 103,349,478 | ||||||||
December 1—December 31 (e) | 1,788 | 9.65 | 17,254 | — | $ | 103,349,478 | ||||||||
| 6,866,652 | (e) | $ | 35.44 | $ | 243,363,433 | 6,851,595 | ||||||||
45
Table of Contents
| (a) | We did not repurchase any shares of our common stock during the twelve months ended December 31, 2008 outside our publicly announced stock repurchase program, except shares withheld in connection with our various stock option and long-term incentive plans. |
| (b) | Our stock repurchase program was announced in April 2002. We announced additional repurchase authorization in August 2003, October 2006 and October 2007. |
| (c) | A total of $700 million of our common stock may be repurchased under our stock repurchase program. Additional amounts may be added to the program based on exercise proceeds and tax benefits the Company receives from the exercise of employee stock options, but only upon further approval by the Board of Directors. The remaining authority under our repurchase program includes proceeds received from option exercises and tax benefits the Company received from exercise of employee stock options which have been approved for inclusion in the program by the Board. |
| (d) | Our stock repurchase program does not have an expiration date. During the twelve months ended December 31, 2008, we did not have any repurchase program that expired, and we did not terminate any repurchase program prior to its expiration date. |
| (e) | Includes 8,710, 2,323, 2,236, and 1,788 shares withheld by the Company to satisfy tax withholdings and exercise price obligations arising from the vesting and/or exercise of stock options and other equity awards in February, March, June, and December, 2008, respectively. |
46
Table of Contents
Performance Graph
The following graph compares the performance of the Company’s Common Stock with the performance of the Standard & Poor’s 500 Composite Stock Price Index (the “S&P 500 Index”) and our Industry Peer Group Index from December 31, 2003 (the last trading day of 2003) to December 31, 2004, 2005, 2006, 2007 and 2008. The graph assumes that $100 was invested on December 31, 2003 in each of the Common Stock, the S&P 500 Index, and the Industry Peer Group Index, and that all dividends were reinvested. The Industry Peer Group Index weights the constituent companies’ stock performance on the basis of market capitalization at the beginning of each annual period.
The Company’s Industry Peer Group Index includes the following companies: Aetna, Inc., Cigna Corporation, Coventry Health Care, Humana, Inc., UnitedHealth Group, Inc. and WellPoint, Inc.Sierra Health Services was removed from the Company’s Industry Peer Group Index due to UnitedHealth Group’s acquisition of Sierra in 2008.
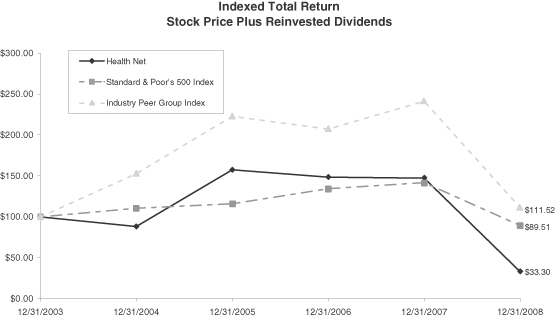
Indexed Total Return (Stock Price Plus Reinvested Dividends)
Name | 12/31/2003 | 12/31/2004 | 12/31/2005 | 12/31/2006 | 12/31/2007 | 12/31/2008 | ||||||||||||
Health Net | $ | 100.00 | $ | 88.29 | $ | 157.65 | $ | 148.81 | $ | 147.71 | $ | 33.30 | ||||||
Standard & Poor’s 500 Index | $ | 100.00 | $ | 110.87 | $ | 116.31 | $ | 134.67 | $ | 142.06 | $ | 89.51 | ||||||
Industry Peer Group Index | $ | 100.00 | $ | 152.90 | $ | 222.99 | $ | 207.45 | $ | 241.71 | $ | 111.52 | ||||||
All historical performance data reflects the performance of each Company’s own stocks only and does not include the historical performance data of acquired companies.
The preceding graph and related information are being furnished solely to accompany this Annual Report on Form 10-K pursuant to Item 201(e) of Regulation S-K and shall not be deemed “soliciting materials” or to be “filed” with the Securities and Exchange Commission (other than as provided in Item 201). Such information shall not be incorporated by reference into any filing under the Securities Act of 1933, as amended, or the Securities Exchange Act of 1934, as amended, whether made before or after the date hereof and irrespective of any general incorporation language contained therein, except to the extent that we specifically incorporate it by reference into such filing.
47
Table of Contents
Item 6. Selected Financial Data.
The following selected financial and operating data are derived from our audited consolidated financial statements. The selected financial and operating data should be read in conjunction with “Item 7. Management’s Discussion and Analysis of Financial Condition and Results of Operations” and the consolidated financial statements and notes thereto contained elsewhere in this Annual Report on Form 10-K.
| Year Ended December 31, | ||||||||||||||||||||
| 2008 | 2007 | 2006 | 2005 | 2004 | ||||||||||||||||
| (Dollars in thousands, except per share and PMPM data) | ||||||||||||||||||||
REVENUES: | ||||||||||||||||||||
Health plan services premiums | $ | 12,392,006 | $ | 11,435,314 | $ | 10,364,740 | $ | 9,506,865 | $ | 9,517,530 | ||||||||||
Government contracts | 2,835,261 | 2,501,677 | 2,376,014 | 2,307,483 | 2,021,871 | |||||||||||||||
Net investment income | 91,042 | 120,176 | 111,042 | 72,751 | 58,147 | |||||||||||||||
Administrative services fees and other income | 48,280 | 51,104 | 56,554 | 53,434 | 48,845 | |||||||||||||||
Total revenues | $ | 15,366,589 | $ | 14,108,271 | $ | 12,908,350 | $ | 11,940,533 | $ | 11,646,393 | ||||||||||
INCOME SUMMARY (1): | ||||||||||||||||||||
Income from continuing operations | $ | 95,003 | $ | 193,697 | $ | 329,313 | $ | 229,785 | $ | 42,604 | ||||||||||
Net income | $ | 95,003 | $ | 193,697 | $ | 329,313 | $ | 229,785 | $ | 42,604 | ||||||||||
NET INCOME PER SHARE—DILUTED (1): | ||||||||||||||||||||
Income from continuing operations | $ | 0.88 | $ | 1.70 | $ | 2.78 | $ | 1.99 | $ | 0.38 | ||||||||||
Net income | $ | 0.88 | $ | 1.70 | $ | 2.78 | $ | 1.99 | $ | 0.38 | ||||||||||
Weighted average shares outstanding: | ||||||||||||||||||||
Diluted | 107,610 | 113,829 | 118,310 | 115,641 | 113,038 | |||||||||||||||
BALANCE SHEET DATA: | ||||||||||||||||||||
Cash and cash equivalents and investments available for sale | $ | 2,172,859 | $ | 2,564,295 | $ | 2,120,844 | $ | 2,106,303 | $ | 1,782,102 | ||||||||||
Total assets | 4,816,350 | 4,933,055 | 4,297,022 | 3,940,722 | 3,653,194 | |||||||||||||||
Loans payable—Current | 27,335 | 35,000 | 200,000 | — | — | |||||||||||||||
Loans payable—Long term | 253,992 | 112,363 | 300,000 | — | — | |||||||||||||||
Senior notes payable | 398,276 | 398,071 | — | 387,954 | 397,760 | |||||||||||||||
Total stockholders’ equity (2) | 1,752,126 | 1,875,582 | 1,778,965 | 1,589,075 | 1,272,880 | |||||||||||||||
OPERATING DATA: | ||||||||||||||||||||
Pretax margin | 1.0 | % | 2.5 | % | 3.7 | % | 3.2 | % | 0.6 | % | ||||||||||
Health plan services medical care ratio (MCR) | 86.9 | % | 85.4 | % | 83.0 | % | 84.3 | % | 88.4 | % | ||||||||||
Government contracts cost ratio | 95.3 | % | 92.2 | % | 94.0 | % | 95.8 | % | 95.3 | % | ||||||||||
G&A expense ratio | 10.4 | % | 11.1 | % | 11.2 | % | 10.0 | % | 9.3 | % | ||||||||||
Selling costs ratio | 2.9 | % | 2.9 | % | 2.4 | % | 2.3 | % | 2.5 | % | ||||||||||
Health plan services premiums per member per month (PMPM) | $ | 277.79 | $ | 263.54 | $ | 243.70 | $ | 235.80 | $ | 216.34 | ||||||||||
Health plan services costs PMPM | $ | 241.27 | $ | 225.00 | $ | 202.22 | $ | 198.75 | $ | 191.24 | ||||||||||
Net cash (used in) provided by operating activities | $ | (158,962 | ) | $ | 605,482 | $ | 277,937 | $ | 191,394 | $ | (54,912 | ) | ||||||||
Net cash (used in) investing activities | $ | (67,871 | ) | $ | (230,195 | ) | $ | (184,879 | ) | $ | (244,046 | ) | $ | (14,242 | ) | |||||
Net cash (used in) provided by financing activities | $ | (111,983 | ) | $ | (73,076 | ) | $ | (130,737 | ) | $ | 73,035 | $ | (69,615 | ) | ||||||
| (1) | Includes a $175.1 million pretax charge in total of which $119.6 million was primarily related to severance and other expenses associated with the company’s operations strategy and included in G&A expenses, $37.5 million was included in health plan services expenses for estimated litigation liability and regulatory actions, $14.6 million investment impairment charge included in net investment income, and $3.4 million related to an impairment of the assets of a subsidiary included in other income for 2008; $306.8 million pretax litigation and regulatory-related charge for 2007; $107.2 million pretax debt refinancing and litigation charge for 2006; $83.3 million pretax litigation and severance charge for 2005; and $31.7 million pretax severance, asset impairment and other charge and $169 million pretax charge associated with provider settlements for 2004. |
| (2) | No cash dividends were declared in each of the years presented. |
48
Table of Contents
Item 7. Management’s Discussion and Analysis of Financial Condition and Results of Operations.
OVERVIEW
General
We are an integrated managed care organization that delivers managed health care services through health plans and government sponsored managed care plans. We are among the nation’s largest publicly traded managed health care companies. Our mission is to help people be healthy, secure and comfortable. We provide health benefits to approximately 6.7 million individuals across the country through group, individual, Medicare (including the Medicare prescription drug benefit commonly referred to as “Part D”), Medicaid, TRICARE and Veterans Affairs programs. Our behavioral health services subsidiary, Managed Health Network (MHN), provides behavioral health, substance abuse and employee assistance programs to approximately 6.9 million individuals, including our own health plan members. Our subsidiaries also offer managed health care products related to prescription drugs, and offer managed health care product coordination for multi-region employers and administrative services for medical groups and self-funded benefits programs.
How We Report Our Results
We currently operate within two reportable segments, Health Plan Services and Government Contracts, each of which is described below.
Our Health Plan Services reportable segment includes the operations of our commercial, Medicare (including the Medicare prescription drug benefit commonly referred to as “Part D”) and Medicaid health plans, the operations of our health and life insurance companies, and our behavioral health and pharmaceutical services subsidiaries. We have approximately 3.7 million members, including Medicare Part D members and administrative services only (ASO) members in our Health Plan Services segment.
Our Government Contracts segment includes our government-sponsored managed care federal contract with the U.S. Department of Defense (the Department of Defense) under the TRICARE program in the North Region and other health care related government contracts. Under the TRICARE contract for the North Region, we provide health care services to approximately 3.0 million Military Health System (MHS) eligible beneficiaries (active duty personnel and TRICARE/Medicare dual eligible beneficiaries), including 1.8 million TRICARE eligibles for whom we provide health care and administrative services and 1.2 million other MHS-eligible beneficiaries for whom we provide ASO. We also provide behavioral health services to military families under the Department of Defense Military Family Life Counseling contract.
How We Measure Our Profitability
Our profitability depends in large part on our ability to, among other things, effectively price our health care products; manage health care costs, including reserve estimates and pharmacy costs; contract with health care providers; attract and retain members; and manage our general and administrative (G&A) and selling expenses. In addition, factors such as regulation, competition and general economic conditions affect our operations and profitability. The effect of escalating health care costs, as well as any changes in our ability to negotiate competitive rates with our providers, may impose further risks to our ability to profitably underwrite our business, and may have a material impact on our business, financial condition or results of operations.
We measure our Health Plan Services segment profitability based on medical care ratio (MCR) and pretax income. The MCR is calculated as health plan services expense (excluding depreciation and amortization) divided by health plan services premiums. The pretax income is calculated as health plan services premiums and administrative services fees and other income less health plan services expense and G&A and other net expenses. See “—Results of Operations—Table of Summary Financial Information” for a calculation of our MCR and “—Results of Operations—Health Plan Services Segment Results” for a calculation of our pretax income.
49
Table of Contents
Health plan services premiums include health maintenance organization (HMO), point of service (POS) and preferred provider organization (PPO) premiums from employer groups and individuals and from Medicare recipients who have purchased supplemental benefit coverage (which premiums are based on a predetermined prepaid fee), Medicaid revenues based on multi-year contracts to provide care to Medicaid recipients, and revenue under Medicare risk contracts, including Medicare Part D, to provide care to enrolled Medicare recipients. Medicare revenue can also include amounts for risk factor adjustments and additional premiums that we charge in some places to members who purchase our Medicare risk plans (see Note 2 to our consolidated financial statements). The amount of premiums we earn in a given year is driven by the rates we charge and enrollment levels. Administrative services fees and other income primarily include revenue for administrative services such as claims processing, customer service, medical management, provider network access and other administrative services. Health plan services expense includes medical and related costs for health services provided to our members, including physician services, hospital and related professional services, outpatient care, and pharmacy benefit costs. These expenses are impacted by unit costs and utilization rates. Unit costs represent the health care cost per visit, and the utilization rates represent the volume of health care consumption by our members.
G&A expenses include those costs related to employees and benefits, consulting and professional fees, marketing, premium taxes and assessments, occupancy costs and litigation and regulatory-related costs. Such costs are driven by membership levels, introduction of new products, system consolidations, outsourcing activities and compliance requirements for changing regulations. These expenses also include expenses associated with corporate shared services and other costs to reflect the fact that such expenses are incurred primarily to support the Health Plan Services segment. Selling expenses consist of external broker commission expenses and generally vary with premium volume.
We measure our Government Contracts segment profitability based on government contracts cost ratio and pretax income. The government contracts cost ratio is calculated as government contracts cost divided by government contracts revenue. The pretax income is calculated as government contracts revenue less government contracts cost. See “—Results of Operations—Table of Summary Financial Information” for a calculation of our government contracts cost ratio and “—Results of Operations—Government Contracts Segment Results” for a calculation of our pretax income.
Government Contracts revenue is made up of two major components: health care and administrative services. The health care component includes revenue recorded for health care costs for the provision of services to our members, including paid claims and estimated incurred but not reported claims (IBNR) expenses for which we are at risk, and underwriting fees earned for providing the health care and assuming underwriting risk in the delivery of care. The administrative services component encompasses fees received for all other services provided to both the government customer and to beneficiaries, including services such as medical management, claims processing, enrollment, customer services and other services unique to the managed care support contract with the government. Government Contracts revenue and expenses include the impact from underruns and overruns relative to our target cost under the applicable contracts (see Note 2 to our consolidated financial statements).
Recent Developments
During the fourth quarter of 2008, we announced that the Company’s board of directors directed our Chief Operating Officer to assume responsibility for all operational matters of the Company, and our President and Chief Executive Officer to focus his efforts on the Company’s strategy, with particular emphasis on how best to deploy the Company’s assets in the current competitive and economic environment. This process includes reviewing our health plans in Arizona, Connecticut, New Jersey and New York to determine their long-term strategic position in the Company as well as a possible divestiture among other strategic alternatives. We are continuing with this process and no definitive decisions have been made at this time.
50
Table of Contents
During 2008, we have been actively engaged in the reprocurement process of the TRICARE North contract. In late December 2008, the government requested final proposal revisions from companies bidding on the TRICARE contracts. We submitted our response in early January 2009. We currently expect an award to occur during the first half of 2009.
2008 Financial Performance Summary
Health Net’s financial performance in 2008 is summarized as follows:
| • | Net income for the year ended December 31, 2008 decreased to $95.0 million, or $0.88 per diluted share, from $193.7 million, or $1.70 per diluted share, for the same period in 2007, and was impacted by after tax expenses of $104.1 million, or $0.97 per diluted share, and after-tax charges of $222.4 million, or $1.96 per diluted share, related to our operations strategy, litigation and regulatory matters, and other-than-temporary impairment of investment securities (collectively referred to as Charges) for the year ended December 31, 2008 and 2007, respectively; |
| • | Total health plan enrollment was 3,720,000 as of December 31, 2008, a decrease of 34,000 members, or approximately 1.0%, compared to December 31, 2007; |
| • | Total revenues for the year ended December 31, 2008 increased by approximately 9% to $15.4 billion from the same period in 2007; |
| • | Health plan services segment pretax income was $14.4 million, including $175.1 million of Charges, for the year ended December 31, 2008 and was $164.8 million, including $306.8 million of Charges, for the same period in 2007; |
| • | Government contracts segment pretax income was $132.7 million and $194.1 million for the years ended December 31, 2008 and 2007, respectively; and |
| • | Net cash used in operating activities totaled $159.0 million for the year ended December 31, 2008 compared to net cash provided by operating activities of $605.5 million for the same period in 2007. |
51
Table of Contents
RESULTS OF OPERATIONS
Table of Summary Financial Information
The table below and the discussion that follows summarize our results of operations for the last three fiscal years:
| Year Ended December 31, | ||||||||||||
| 2008 | 2007 | 2006 | ||||||||||
| (Dollars in thousands, except per share and PMPM data) | ||||||||||||
Revenues | ||||||||||||
Health plan services premiums | $ | 12,392,006 | $ | 11,435,314 | $ | 10,364,740 | ||||||
Government contracts | 2,835,261 | 2,501,677 | 2,376,014 | |||||||||
Net investment income | 91,042 | 120,176 | 111,042 | |||||||||
Administrative services fees and other income | 48,280 | 51,104 | 56,554 | |||||||||
Total revenues | 15,366,589 | 14,108,271 | 12,908,350 | |||||||||
Expenses | ||||||||||||
Health plan services (excluding depreciation and amortization) | 10,762,657 | 9,762,896 | 8,600,443 | |||||||||
Government contracts | 2,702,573 | 2,307,610 | 2,234,535 | |||||||||
General and administrative | 1,291,059 | 1,275,555 | 1,165,313 | |||||||||
Selling | 360,381 | 327,827 | 245,304 | |||||||||
Depreciation and amortization | 59,878 | 42,982 | 25,591 | |||||||||
Interest | 42,909 | 32,497 | 51,179 | |||||||||
Debt refinancing charge | — | — | 70,095 | |||||||||
Litigation, severance and related benefit costs | — | — | 37,093 | |||||||||
Total expenses | 15,219,457 | 13,749,367 | 12,429,553 | |||||||||
Income from operations before income taxes | 147,132 | 358,904 | 478,797 | |||||||||
Income tax provision | 52,129 | 165,207 | 149,484 | |||||||||
Net income | $ | 95,003 | $ | 193,697 | $ | 329,313 | ||||||
Net income per share: | ||||||||||||
Basic | $ | 0.89 | $ | 1.74 | $ | 2.86 | ||||||
Diluted | $ | 0.88 | $ | 1.70 | $ | 2.78 | ||||||
Pretax margin | 1.0 | % | 2.5 | % | 3.7 | % | ||||||
Health plan services medical care ratio (MCR) (a) | 86.9 | % | 85.4 | % | 83.0 | % | ||||||
Government contracts cost ratio (b) | 95.3 | % | 92.2 | % | 94.0 | % | ||||||
G&A expense ratio (c) | 10.4 | % | 11.1 | % | 11.2 | % | ||||||
Selling costs ratio (d) | 2.9 | % | 2.9 | % | 2.4 | % | ||||||
Health plan services premiums per member per month (PMPM) (e) | $ | 277.79 | $ | 263.54 | $ | 243.70 | ||||||
Health plan services costs PMPM (e) | $ | 241.27 | $ | 225.00 | $ | 202.22 | ||||||
| (a) | MCR is calculated as health plan services cost divided by health plan services premiums revenue. |
| (b) | Government contracts cost ratio is calculated as government contracts cost divided by government contracts revenue. |
| (c) | The G&A expense ratio is computed as G&A expenses divided by the sum of health plan services premium revenues and administrative services fees and other income. |
| (d) | The selling costs ratio is computed as selling expenses divided by health plan services premium revenues. |
| (e) | PMPM is calculated based on total at-risk member months and excludes ASO member months. |
52
Table of Contents
Summary of Operating Results
Year Ended December 31, 2008 compared to Year Ended December 31, 2007
Net income for 2008 decreased to $95.0 million from $193.7 million in 2007. Earnings per share fell to $0.89 per basic share and $0.88 per diluted share for 2008 compared with $1.74 per basic share and $1.70 per diluted share for 2007. Pretax margin was 1.0% for 2008 compared to 2.5% for 2007. Included in the 2008 operating results are $175.1 million in Charges including the following:
| • | $119.6 million recorded as part of G&A expenses primarily for severance and other costs associated with Health Net’s operations strategy which is aimed at achieving substantial reductions in G&A by 2010. This amount also includes attorney’s fees and regulatory fines associated with our rescission practices and in connection with the settlement agreement for theMcCoy, Wachtel andScharfman lawsuits. See “Item 3. Legal Proceedings” for additional information regarding these matters; |
| • | $37.5 million recorded as part of health plan services expenses for estimated litigation and regulatory actions related to the Company’s rescission practices in Arizona and California and claim-related matters in connection with the settlement agreement for theMcCoy, Wachteland Scharfman lawsuits; |
| • | $14.6 million loss recorded as part of net investment income from other-than-temporary impairments in our available-for-sale investments and money market funds; and |
| • | $3.4 million recorded as part of administrative services fees and other income for an impairment of assets of a small, non-core subsidiary. |
Total health plan enrollment, including Medicare Part D, decreased to 3,720,000 members at December 31, 2008 from 3,754,000 members at December 31, 2007, primarily due to a decline of 225,000 commercial and ASO members and 34,000 Medicaid members, partially offset by an increase of 166,000 Medicare Part D members and 59,000 Medicare Advantage members. Our TRICARE membership increased to approximately 3.0 million beneficiaries at December 31, 2008 from 2.9 million beneficiaries at December 31, 2007.
Health Net’s total revenues increased 9% in 2008 to $15.4 billion from $14.1 billion in 2007. Health plan services premium revenues increased 8% to $12.4 billion in 2008 compared to $11.4 billion in 2007. Our total premium revenue yield on a PMPM basis was 5% in 2008 compared to 8% in 2007. The health plan services medical care ratio (MCR) was 86.9% in 2008 compared to 85.4% in 2007. The MCR for 2008 and 2007 included 40 and 180 basis points, respectively, impact from the Charges.
Our Government contracts revenues increased 13% in 2008 to $2.8 billion from $2.5 billion in 2007. The Government contracts cost ratio increased to 95.3% in 2008 compared to 92.2% in 2007.
Our G&A expense ratio improved by 70 basis points to 10.4% in 2008 compared to 11.1% in 2007. The G&A expense ratio for 2008 and 2007 included the impact of 100 basis points and 90 basis points, respectively, of G&A expenses related to the operations strategy and litigation and regulatory-related charges. Our selling costs ratio remained stable at 2.9% in 2008 and in 2007.
Net cash used in operating activities totaled $159.0 million for the year ended December 31, 2008 compared to net cash provided by operating activities of $605.5 million for the same period in 2007. This decrease in cash was driven by payments made in 2008 related to operations strategy and regulatory related matters and an increase in our CMS receivables relating to catastrophic and low-income subsidies.
Year Ended December 31, 2007 compared to Year Ended December 31, 2006
Net income for 2007 decreased to $193.7 million from $329.3 million in 2006. Earnings per share fell to $1.74 per basic share and $1.70 per diluted share for 2007 compared with $2.86 per basic share and $2.78 per diluted share for 2006. Pretax margin was 2.5% for 2007 compared to 3.7% for 2006. The primary drivers of these declines were charges incurred related to litigation and regulatory matters and debt refinancing activities.
53
Table of Contents
In 2007, we recorded a $306.8 million pre-tax, or $222.4 million after-tax, charge incurred as a result of us reaching an agreement in principle to settle theMcCoy, Wachtel andScharfman class action lawsuits; the proposed resolution of regulatory issues with the New Jersey Department of Banking and Insurance; arbitration settlement; and other immaterial litigation matters. See “Item 3. Legal Proceedings” for additional information regarding these matters. The charge amount was comprised of the following:
| • | $201.5 million recorded as part of health plan services expenses during the year ended December 31, 2007 for claim-related matters, class disbursements and remediations; and |
| • | $105.3 million recorded as part of G&A expenses during the year ended December 31, 2007 for attorney’s fees, regulatory fines, arbitration settlement and estimated liability for litigation unrelated to the class action lawsuits. |
Results in 2006 reflect the impact of a $37.1 million litigation charge related to estimated legal defense costs for theMcCoy, Wachtel andScharfman litigation and $70.1 million of expenses related to the refinancing of our senior notes. See “Item 3. Legal Proceedings” for additional information on these litigation matters. See “Liquidity and Capital Resources—Capital Structure” for additional information on the refinancing of our senior notes.
Total health plan enrollment, including Medicare Part D, increased to 3,754,000 members at December 31, 2007 from 3,699,000 members at December 31, 2006, primarily due to a 73,000-member increase in our commercial small group/individual membership and a 116,000-member increase in our Medicare membership, partially offset by 140,000-member decrease in our commercial large group and ASO membership. Our strategy of targeting the small group and individual market resulted in changing the mix of our membership: approximately 35% of our commercial risk enrollment was in the small group and individual market at the end of 2007, up from 31% at the end of 2006. We continued to expand our Medicare membership, which increased by 116,000 members in 2007. On January 1, 2007, we began offering Medicare Advantage Private-Fee-For Service plans, and we began marketing our Medicare Part D plans in all 50 states and the District of Columbia. We also increased the number of Part D plan choices that we offer seniors from two in 2006 to three in 2007, one of which provides beneficiaries with coverage of generic drug expenses through the coverage gap, or “donut hole.” Our TRICARE membership was stable at 2.9 million beneficiaries, and we expanded our relationship with the Department of Defense by providing behavioral health counseling services starting in 2006. In addition, our behavioral health care business unit was awarded a five-year contract in 2007 to develop, administer and monitor the non-medical counseling program for military service members known as Military Family and Life Consultant Program (MFLC). The total contract is valued at approximately $250 million.
Health Net’s total revenues increased 9% in 2007 to $14.1 billion from $12.9 billion in 2006. Health plan services premium revenues increased 10% to $11.4 billion in 2007 compared to $10.4 billion in 2006. Our commercial revenue yield was 9.2% in 2007 compared to 7.6% in 2006. The health plan services MCR was 85.4% in 2007 compared to 83.0% in 2006. The MCR for 2007 included the impact of the $201.5 million, or 180 basis points, of health plan services expenses related to the litigation and regulatory-related charge noted above.
Our Government contracts revenues increased 5% in 2007 to $2.5 billion from $2.4 billion in 2006. The Government contracts cost ratio improved to 92.2% in 2007 compared to 94.0% in 2006.
Our G&A expense ratio improved by 10 basis points to 11.1% in 2007 compared to 11.2% in 2006. The G&A expense ratio for 2007 included the impact of $105.3 million, or 90 basis points, of G&A expenses related to the litigation and regulatory-related charge. Our selling costs ratio increased by 50 basis points to 2.9% in 2007 compared to 2.4% in 2006.
Net cash provided by operating activities increased to $605.5 million in 2007 compared to $277.9 million for 2006, reflecting TRICARE payment for Option 3 Period underwriting fee and the growth in our Medicare Part D business.
54
Table of Contents
Consolidated Segment Results
The following table summarizes the operating results of our reportable segments for the last three fiscal years:
| Year Ended December 31, | ||||||||||
| 2008 | 2007 | 2006 | ||||||||
| (Dollars in millions) | ||||||||||
Pretax income: | ||||||||||
Health plan services segment | $ | 14.4 | $ | 164.8 | $ | 444.5 | ||||
Government contracts segment | 132.7 | 194.1 | 141.5 | |||||||
Total segment pretax income | $ | 147.1 | $ | 358.9 | $ | 586.0 | ||||
Debt refinancing charge | — | — | (70.1 | ) | ||||||
Litigation, severance and related benefit costs | — | — | (37.1 | ) | ||||||
Income from operations before income taxes as reported | $ | 147.1 | $ | 358.9 | $ | 478.8 | ||||
Health Plan Services Segment Membership
The following table below summarizes our health plan membership information by program and by state:
| Commercial | ASO | Medicare | Medicaid | Health Plan Total | ||||||||||||||||||||||||||
| 2008 | 2007 | 2006 | 2008 | 2007 | 2006 | 2008 | 2007 | 2006 | 2008 | 2007 | 2006 | 2008 | 2007 | 2006 | ||||||||||||||||
| (Membership in thousands) | ||||||||||||||||||||||||||||||
Arizona | 123 | 137 | 125 | — | — | — | 67 | 51 | 35 | — | — | — | 190 | 188 | 160 | |||||||||||||||
California | 1,352 | 1,468 | 1,483 | 5 | 6 | 6 | 133 | 112 | 104 | 765 | 712 | 710 | 2,255 | 2,298 | 2,303 | |||||||||||||||
Connecticut | 139 | 161 | 183 | 25 | 32 | 67 | 57 | 45 | 34 | — | 90 | 84 | 221 | 328 | 368 | |||||||||||||||
New Jersey | 73 | 90 | 103 | 3 | 17 | 19 | — | — | — | 47 | 44 | 46 | 123 | 151 | 168 | |||||||||||||||
New York | 204 | 234 | 224 | 11 | 13 | 17 | 6 | 3 | 6 | — | — | — | 221 | 250 | 247 | |||||||||||||||
Oregon | 133 | 135 | 133 | — | — | — | 22 | 21 | 20 | — | — | — | 155 | 156 | 153 | |||||||||||||||
Other States | — | — | — | — | — | — | 10 | 4 | — | — | — | — | 10 | 4 | — | |||||||||||||||
| 2,024 | 2,225 | 2,251 | 44 | 68 | 109 | 295 | 236 | 199 | 812 | 846 | 840 | 3,175 | 3,375 | 3,399 | ||||||||||||||||
Medicare Part D | — | — | — | — | — | — | 545 | 379 | 300 | — | — | — | 545 | 379 | 300 | |||||||||||||||
Total | 2,024 | 2,225 | 2,251 | 44 | 68 | 109 | 840 | 615 | 499 | 812 | 846 | 840 | 3,720 | 3,754 | 3,699 | |||||||||||||||
December 31, 2008 Compared to December 31, 2007
Our total health plan membership decreased by 34,000 members, or 1%, to 3.7 million members at December 31, 2008 when compared to December 31, 2007. The decrease was driven by a decline of 225,000 commercial and ASO members and 34,000 Medicaid members, partially offset by an increase of 166,000 Medicare Part D members, and 59,000 Medicare Advantage members.
Membership in our commercial health plans decreased by 201,000 members, or 9%, at December 31, 2008 compared to December 31, 2007. This decrease was primarily attributable to our California plan, which experienced declines of 63,000 small group/individual members and 53,000 large group members, and our Northeast plans, which experienced declines of 48,000 large group members and 21,000 small group/individual members. Our Arizona and Oregon plans experienced declines of 14,000 and 2,000 members, respectively. Our ASO enrollment declined by 24,000 members, or 35%, at December 31, 2008 compared to December 31, 2007, due to membership losses in our Northeast plans.
Membership in our Medicare Advantage program increased by 59,000 members at December 31, 2008 compared to December 31, 2007, due to membership growth primarily in California, Arizona and Connecticut. Medicare Part D membership increased by 166,000 members at December 31, 2008 compared to December 31, 2007.
55
Table of Contents
In January 2008, we were directed by CMS to temporarily cease the sale of our stand-alone PDP products due to certain administrative deficiencies relating to our ability to timely process stand-alone PDP enrollment applications. On March 18, 2008, CMS lifted this suspension based on its acceptance of our Corrective Action Plan and our demonstrated correction of the deficiencies. This temporary suspension did not have a material adverse effect on our Medicare business.
We participate in state Medicaid programs in California and New Jersey. California membership, where the program is known as Medi-Cal, comprised 94% and 84% of our Medicaid membership at December 31, 2008 and 2007, respectively. Membership in our Medicaid programs decreased by 34,000 members at December 31, 2008 compared to December 31, 2007 primarily due to our withdrawal from the Connecticut Medicaid Program in April 2008, partially offset by a gain of 53,000 members in California due to higher enrollment in the Fresno and San Diego counties and in the Healthy Families program. We provided administrative services only to Connecticut Medicaid members during the first quarter of 2008 and completed our exit from the Connecticut Medicaid programs as of April 1, 2008.
December 31, 2007 Compared to December 31, 2006
Total health plan membership increased by 2% to 3.8 million members at December 31, 2007 from 3.7 million members at December 31, 2006. The increase was primarily driven by the addition of 79,000 stand-alone PDP members and 37,000 Medicare Advantage members, partially offset by a decrease of 67,000 commercial and ASO members.
Membership in our commercial health plans decreased by 67,000 members, or 3%, at December 31, 2007 compared to December 31, 2006. This decrease was primarily attributable to the mix shift from large group to small group/individual enrollment resulting in a net loss of 26,000 commercial risk members and a 41,000 ASO member loss. This mix shift was predominantly seen in our California plan, which experienced a decline of 73,000 large group members primarily from a loss of two large accounts, partially offset by a net gain of 58,000 small group and individual members. Our Northeast plans experienced a decline of 37,000 members in the large group market, which was partially offset by a net gain of 16,000 members in our New York small group market. As a result of our targeted mix shift, our small group and individual enrollment comprised approximately 35% of our commercial risk enrollment, excluding ASO, at December 31, 2007, up from 31% at December 31, 2006.
Membership in our Medicare Advantage program increased by 37,000 members at December 31, 2007 compared to December 31, 2006, due to membership growth primarily in Arizona and Connecticut. Our stand-alone Medicare PDP membership increased by 79,000 members at December 31, 2007 compared to December 31, 2006.
Membership in our Medicaid programs increased by 6,000 members at December 31, 2007 compared to December 31, 2006, primarily due to enrollment increases in Connecticut.
56
Table of Contents
Health Plan Services Segment Results
The following table summarizes the operating results for the Health Plan Services segment for the last three fiscal years:
| Year Ended December 31, | ||||||||||||
| 2008 | 2007 | 2006 | ||||||||||
| (Dollars in millions, except PMPM data) | ||||||||||||
Health plan services segment: | ||||||||||||
Commercial premium revenue | $ | 7,797.5 | $ | 7,468.0 | $ | 6,903.5 | ||||||
Medicare premium revenue | 3,521.5 | 2,778.9 | 2,304.4 | |||||||||
Medicaid premium revenue | 1,073.0 | 1,188.4 | 1,156.8 | |||||||||
Health plan services premium revenues | $ | 12,392.0 | $ | 11,435.3 | $ | 10,364.7 | ||||||
Health plan services costs | (10,762.7 | ) | (9,762.9 | ) | (8,600.4 | ) | ||||||
Net investment income | 91.0 | 120.2 | 111.0 | |||||||||
Administrative services fees and other income | 48.3 | 51.1 | 56.6 | |||||||||
G&A | (1,291.0 | ) | (1,275.6 | ) | (1,165.3 | ) | ||||||
Selling | (360.4 | ) | (327.8 | ) | (245.3 | ) | ||||||
Depreciation and amortization | (59.9 | ) | (43.0 | ) | (25.6 | ) | ||||||
Interest | (42.9 | ) | (32.5 | ) | (51.2 | ) | ||||||
Pretax income | $ | 14.4 | $ | 164.8 | $ | 444.5 | ||||||
MCR: | 86.9 | % | 85.4 | % | 83.0 | % | ||||||
Commercial | 85.9 | % | 85.7 | % | 83.2 | % | ||||||
Medicare | 89.9 | % | 85.4 | % | 83.3 | % | ||||||
Medicaid | 83.7 | % | 83.1 | % | 80.9 | % | ||||||
Health plan services premium PMPM | $ | 277.79 | $ | 263.54 | $ | 243.70 | ||||||
Health plan services costs PMPM | $ | 241.27 | $ | 225.00 | $ | 202.22 | ||||||
G&A expense ratio | 10.4 | % | 11.1 | % | 11.2 | % | ||||||
Selling costs ratio | 2.9 | % | 2.9 | % | 2.4 | % | ||||||
Health Plan Services Premiums
Total health plan services premiums increased by $956.7 million, or 8%, for the year ended December 31, 2008 as compared to the same period in 2007, and increased by $1,070.6 million, or 10%, for the year ended December 31, 2007 as compared to the same period in 2006. On a PMPM basis, premium yields increased by 5% for the year ended December 31, 2008 as compared to the same period in 2007, and increased by 8% for the year ended December 31, 2007 as compared to the same period in 2006.
Year Ended December 31, 2008 Compared to Year Ended December 31, 2007
Commercial premium revenues increased by $329.5 million, or 4%, for the year ended December 31, 2008 as compared to the same period in 2007. These increases were primarily attributable to our ongoing pricing discipline and premium rate increases, partially offset by membership declines.
Medicare premiums increased by $742.6 million, or 27%, for the year ended December 31, 2008 as compared to the same period in 2007. This increase was primarily due to an increase in members participating in the Medicare Advantage and Medicare Part D prescription drug program. In addition, we recognized $137.7 million in Medicare risk factor estimates for the 2008 payment year in our health plan services premium revenues in the year ended December 31, 2008. See “—Health Plan Services Costs” for detail regarding the increase in capitation expense related to the Medicare rate adjustment.
Medicaid premiums decreased by $115.4 million, or 10%, for the year ended December 31, 2008 as compared to the same period in 2007 primarily due to a decrease in Connecticut Medicaid membership. We
57
Table of Contents
served the Connecticut Medicaid members on an ASO basis through the end of the first quarter of 2008, and we completed our exit from the Connecticut Medicaid program in April 2008. We recognized $0 and $185 million of premium revenue from our Connecticut Medicaid program during the years ended December 31, 2008 and 2007, respectively. Partially offsetting the decrease in Medicaid premiums from the cessation of the Connecticut program was a $19 million increase from a change in estimate due to revised application of California Medi-Cal program premium rates for 2001 and 2002 plan years.
Year Ended December 31, 2007 Compared to Year Ended December 31, 2006
Commercial premium revenues increased by $564.5 million, or 8%, for the year ended December 31, 2007 as compared to the same period in 2006. The Guardian Transaction (see Note 3—Purchases, Acquisitions and Sales to our consolidated financial statements for information regarding the Guardian Transaction) added approximately $266 million of premium revenue in 2007. The commercial premium PMPM increased by an average of 9% in the year ended December 31, 2007 compared to the same period in 2006. These increases were primarily attributable to the impact of the Guardian Transaction and our ongoing pricing discipline.
Medicare premiums increased by $474.5 million, or 21%, for the year ended December 31, 2007 as compared to the same period in 2006. This increase was primarily due to an increase in members participating in the Medicare Advantage and Medicare Part D prescription drug program and Medicare risk factor adjustments totaling $95.1 million in the year ended December 31, 2007. See “—Health Plan Services Costs” for detail regarding the increase in capitation expense related to the Medicare rate adjustment. Of this amount, $80.3 million, $13.2 million and $1.6 million were for the 2007, 2006 and 2003 payment years, respectively. The premium yields were essentially flat in 2007 compared to 2006.
Medicaid premiums increased by $31.6 million, or 3%, for the year ended December 31, 2007 as compared to the same period in 2006 primarily due to an increase in Medicaid premium PMPM, which was 5% for the year ended December 31, 2007 over the same period in 2006. In the Connecticut Medicaid program, we came to an agreement with the State of Connecticut where we continued to serve approximately 90,000 members on an ASO basis through the first quarter of 2008. We completed our exit from the Connecticut Medicaid Program in April 2008. We recognized approximately $185 million of premium revenue from our Connecticut Medicaid program during 2007.
Health Plan Services Costs
Health plan services costs increased by $999.8 million, or 10%, for the year ended December 31, 2008 as compared to the same period in 2007, and increased by $1,162.5 million, or 14%, for the year ended December 31, 2007 as compared to the same period in 2006. Health plan MCR was 86.9% at December 31, 2008 compared to 85.4% at December 31, 2007 and 83.0% at December 31, 2006.
Year Ended December 31, 2008 Compared to Year Ended December 31, 2007
Commercial health care costs increased by $296.0 million, or 5%, for the year ended December 31, 2008 as compared to the same period in 2007. The increase in the commercial health care cost trend on a PMPM basis was 9% for the year ended December 31, 2008 over the same period in 2007. Commercial MCR increased to 85.9% for the year ended December 31, 2008 from 85.7% for the year ended December 31, 2007. Physician and hospital costs on a PMPM basis rose about 9% and 13% from higher paid claims costs, respectively, while the utilization was relatively flat with commercial bed days increasing by less than one-half of a percent in 2008 over 2007. Pharmacy costs rose approximately 12% due to higher utilization on a PMPM basis for the year ended December 31, 2008 over the same period in 2007. The litigation and regulatory-related charge recorded in 2008 impacted the commercial MCR by 50 basis points and commercial health care cost trend on a PMPM basis by 290 basis points. The litigation and regulatory-related charge recorded in 2007 impacted the commercial MCR by 270 basis points and commercial health care cost trend on a PMPM basis by 360 basis points.
58
Table of Contents
Medicare health care costs increased by $793.1 million, or 33%, for the year ended December 31, 2008 as compared to the same period in 2007, and Medicare MCR, including Medicare Advantage and Part D, increased by 450 basis points for the same comparative periods. These increases were primarily driven by a 37% enrollment growth and were primarily comprised of higher inpatient and outpatient hospital and pharmacy costs and utilization. Medicare Advantage health care cost PMPM increased by 6% for the year ended December 31, 2008, as compared to the same period in 2007. Part D health care cost PMPM increased by 20 basis points for the year ended December 31, 2008, as compared to the same period in 2007. Also contributing to the Medicare health care cost increase is $32.9 million of capitation expense related to the Medicare risk factor estimates for the 2008 plan year. See “—Health Plan Services Premiums” for detail regarding the increase in premium revenue related to the Medicare rate adjustment.
Medicaid health care costs decreased by $89.3 million, or 9%, for the year ended December 31, 2008 as compared to the same period in 2007. The decrease in the Medicaid health care cost PMPM was 4% for the year ended December 31, 2008 over the same period in 2007. These decreases were primarily driven by lower outpatient hospital and pharmacy costs and utilization. Medicaid MCR increased by 60 basis points for the year ended December 31, 2008.
Year Ended December 31, 2007 Compared to Year Ended December 31, 2006
Commercial health care costs increased by $657.6 million, or 11%, for the year ended December 31, 2007 as compared to the same period in 2006. The increase in the commercial health care cost trend on a PMPM basis was 12.5% for the year ended December 31, 2007 over the same period in 2006. Commercial MCR increased to 85.7% for the year ended December 31, 2007 from 83.2% for the year ended December 31, 2006. These increases were primarily due to a $201.5 million charge recorded the third quarter of 2007 in health care costs for proposed remediation claim settlements related to litigation and regulatory-related matters. See “Item 3. Legal Proceedings” for additional information on these litigation matters. The charge recorded in 2007 impacted the commercial MCR by 270 basis points and commercial health care cost trend on a PMPM basis by 360 basis points. Physician and hospital costs rose about 9% and 10% from higher paid claims, respectively. Commercial bed days rose by less than 1% in 2007 over 2006. Pharmacy costs rose about 6% due to higher utilization on a PMPM basis for the year ended December 31, 2007 over the same period in 2006.
Medicare health care costs increased by $453.5 million, or 24%, for the year ended December 31, 2007 as compared to the same period in 2006. Medicare health care costs increased as a result of higher hospital costs and higher pharmacy costs mainly in Arizona and the Northeast and increased capitation expense from Medicare risk factor adjustments totaling $27.2 million, which was recognized in the year ended December 31, 2007. Of this amount, $22.5 million, $3.9 million and $0.8 million were for the 2007, 2006, and 2003 payment years, respectively. See “—Health Plan Services Premiums” for detail regarding the increase in premium revenue related to the Medicare rate adjustment. Medicare MCR, including Medicare Advantage and Part D, increased by 210 basis points for the year ended December 31, 2007.
Medicaid health care costs increased by $51.4 million, or 5%, for the year ended December 31, 2007 as compared to the same period in 2006. The increase in the Medicaid health care cost PMPM was 8% for the year ended December 31, 2007 over the same period in 2006. These increases were primarily driven by higher hospital and pharmacy costs. Medicaid MCR increased by 220 basis points at December 31, 2007 compared to December 31, 2006.
Administrative Services Fees and Other Income
Year Ended December 31, 2008 Compared to Year Ended December 31, 2007
Administrative services fees and other income decreased by $2.8 million, or 6%, for the year ended December 31, 2008 as compared to the same period in 2007. The decrease was primarily due to a decline in ASO fees primarily due to membership losses in our Northeast plans.
59
Table of Contents
Year Ended December 31, 2007 Compared to Year Ended December 31, 2006
Administrative services fees and other income decreased by $5.5 million, or 10%, for the year ended December 31, 2007 as compared to the same period in 2006. The decrease was primarily due to loss of ASO membership in our Connecticut health plan.
Net Investment Income
Year Ended December 31, 2008 Compared to Year Ended December 31, 2007
Net investment income decreased by $29.1 million, or 24%, for the year ended December 31, 2008 as compared to the same period in 2007. This decrease was primarily due to lower short-term interest rates along with a slight decrease in cash balances and a $14.6 million recognized loss from other-than temporary impairments in our available-for-sale investments and money market funds. This decrease was partially offset by a $7 million increase in our interest rate swap value (see Note 2—Summary of Significant Accounting Policies to our consolidated financial statements).
Year Ended December 31, 2007 Compared to Year Ended December 31, 2006
Net investment income increased by $9.2 million, or 8%, for the year ended December 31, 2007 as compared to the same period in 2006. The increase was primarily from income on higher cash balances in 2007 than in 2006.
General, Administrative and Other Costs
Year Ended December 31, 2008 Compared to Year Ended December 31, 2007
G&A costs increased by $15.5 million, or 1%, for the year ended December 31, 2008 as compared to the same period in 2007. The increase in costs was primarily driven by operations strategy related charges and a $7.3 million increase in the allowance related to Medicare receivable. Our G&A expense ratio decreased to 10.4% for the year ended December 31, 2008, compared to 11.1% for the same period in 2007. The Charges recorded in 2008 and 2007 impacted the G&A expense ratio by 100 basis points and 90 basis points, respectively.
The selling costs ratio was 2.9% for the years ended December 31, 2008 and 2007. The selling costs ratio is a function of changes in our membership mix between large group and small and individual group members, and the growth of our Medicare Advantage business.
Amortization and depreciation expense increased by $16.9 million for the year ended December 31, 2008 as compared to the same period in 2007 primarily due to property and equipment purchased during the year, the addition of new assets placed in production related to various information technology system projects and the amortization of intangible assets from the Guardian Transaction. See Note 2—Summary of Significant Accounting Policies to the consolidated financial statements.
Interest expense increased by $10.4 million, or 32%, for the year ended December 31, 2008 as compared to the same period in 2007. The increase was primarily due to increased borrowings on our revolving credit facility and amortization of the discount on our amortizing financing facility completed in December 2007, partially offset by interest on our bridge loan paid off in March 2007 and term loan paid off in May 2007.
Year Ended December 31, 2007 Compared to Year Ended December 31, 2006
G&A costs increased by $110.2 million, or 9%, for the year ended December 31, 2007 as compared to the same period in 2006. The increase in costs was primarily driven by a $105.3 million charge for attorney’s fees and regulatory fines related to the litigation and regulatory-related matters and arbitration settlement. See “Item 3. Legal Proceedings” for additional information on these litigation matters. Our G&A expense ratio decreased to 11.1% for the year ended December 31, 2007 from 11.2% for the same period in 2006. The charge recorded in 2007 impacted the ratio by 90 basis points.
60
Table of Contents
The selling costs ratio increased to 2.9% for the year ended December 31, 2007 from 2.4% when compared to the same period in 2006. These increases are consistent with an increase in commercial new sales and higher rate of broker commissions for our small group and individual membership.
Amortization and depreciation expense increased by $17.4 million for the year ended December 31, 2007 as compared to the same period in 2006 primarily due to the addition of new assets placed in production related to various information technology system projects and the amortization of intangible assets from the Guardian Transaction.
Interest expense decreased by $18.7 million, or 37%, for the year ended December 31, 2007 as compared to the same period in 2006. The decreases were primarily due to lower interest rates on our Senior Notes in 2007 compared with the senior notes we redeemed in the third quarter of 2006, and lower interest on our term and bridge loans and revolver borrowings as a result of lower outstanding balances and early termination of the debt.
Government Contracts Segment Membership
| 2008 | 2007 | 2006 | ||||
| (Membership in thousands) | ||||||
Membership under North Region TRICARE contract | 3,004 | 2,895 | 2,930 | |||
Under our TRICARE contract for the North Region, we provided health care services to approximately 3.0 million eligible beneficiaries in MHS as of December 31, 2008. Included in the 3.0 million MHS-eligible beneficiaries as of December 31, 2008 were 1.8 million TRICARE eligibles for whom we provide health care and administrative services and 1.2 million other MHS-eligible beneficiaries for whom we provide administrative services only. As of December 31, 2008 and 2007, there were approximately 1.5 million and 1.4 million TRICARE eligibles, respectively, enrolled in TRICARE Prime under our North Region contract.
In addition to the 3.0 million eligible beneficiaries that we service under the TRICARE contract for the North Region, we administer contracts with the U.S. Department of Veterans Affairs to manage community based outpatient clinics in 9 states covering approximately 24,000 enrollees.
Government Contracts Segment Results
The following table summarizes the operating results for Government Contracts for the last three fiscal years:
| Year Ended December 31, | ||||||||||||
| 2008 | 2007 | 2006 | ||||||||||
| (Dollars in millions) | ||||||||||||
Government contracts segment: | ||||||||||||
Revenues | $ | 2,835.3 | $ | 2,501.7 | $ | 2,376.0 | ||||||
Costs | 2,702.6 | 2,307.6 | 2,234.5 | |||||||||
Pretax income | $ | 132.7 | $ | 194.1 | $ | 141.5 | ||||||
Government contracts ratio | 95.3 | % | 92.2 | % | 94.0 | % | ||||||
Year Ended December 31, 2008 Compared to Year Ended December 31, 2007
Government contracts revenues increased by $333.6 million, or 13%, for the year ended December 31, 2008 as compared to the same period in 2007. Government contracts costs increased by $395.0 million or 17% for the year ended December 31, 2008 as compared to the same period in 2007. The increases were primarily due to an increase in health care services provided under a new option year in the TRICARE contract, Option Period 5, which began April 1, 2008, and growth in the family counseling business with the Department of Defense.
61
Table of Contents
Our TRICARE contract for the North Region includes a target cost and price for reimbursed health care costs, which is negotiated annually during the term of the contract with underruns and overruns of our target cost borne 80% by the government and 20% by us. In the normal course of contracting with the federal government, we recognize changes in our estimate for the target cost underruns and overruns when the amounts become determinable, supportable, and the collectibility is reasonably assured. As a result of changes in the estimate during the year ended December 31, 2008, we recognized an increase in revenue of $17 million compared to a decrease in revenue of $58 million in the year ended December 31, 2007. As a result of changes in the estimate during the year ended December 31, 2008, we recognized an increase in cost of $22 million compared to a decrease in cost of $75 million in the year ended December 31, 2007. The administrative price is paid on a monthly basis, one month in arrears and certain components of the administrative price are subject to volume-based adjustments.
The Government contracts ratio increased by 310 basis points for the year ended December 31, 2008 as compared to the same period in 2007 primarily due to increased costs of health care services provided under Option Period 5 in the TRICARE contract.
Year Ended December 31, 2007 Compared to Year Ended December 31, 2006
Government contracts revenues increased by $125.7 million, or 5%, for the year ended December 31, 2007 as compared to the same period in 2006. Government contracts costs increased by $73.1 million or 3% for the year ended December 31, 2007 as compared to the same period in 2006. The increase was primarily due to an increase in health care services provided under a new option year in the TRICARE contract, Option Period 4, which began April 1, 2007 and growing family counseling business with the Department of Defense. In addition, 2007 includes a $36.5 million favorable settlement with the Federal Government regarding prior Option Period 1 health care cost targets.
During the years ended December 31, 2007 and 2006, we recognized a decrease in the revenue estimate of $58 million and $104 million, respectively, and a decrease in the cost estimate of $75 million and $128 million, respectively, related to the change in our estimate for the target cost underruns and overruns.
The Government contracts ratio decreased by 180 basis points for the year ended December 31, 2007 as compared to the same period in 2006 primarily due to the favorable settlement with the Government regarding prior Option 1 healthcare cost targets and ongoing expansion of our behavioral health services provided to our military men and women and their families.
Debt Refinancing
In 2006, we refinanced our 8.375% Senior Notes due 2011 and incurred $70.1 million in costs, including a $51.0 million redemption premium with respect to our senior notes and $11.1 million for the settlement of four interest rate swap contracts (Swap Contracts). We also paid $3.0 million for professional fees and incurred $5.0 million of other non-cash expenses related to such refinancing. The senior notes were redeemed on August 14, 2006.
Litigation, Severance and Related Benefit Costs
2008 Charges
We recorded the following $175.1 million pretax, or $104.1 million after tax, charges during the year ended December 31, 2008:
| • | $119.6 million recorded as part of G&A expenses primarily for severance and other costs associated with Health Net’s operations strategy which is aimed at achieving substantial reductions in G&A by 2010. This amount also includes attorney’s fees and regulatory fines associated with our rescission practices and in connection with the settlement agreement for theMcCoy, Wachteland Scharfman lawsuits. See “Item 3. Legal Proceedings” for additional information regarding these matters; |
62
Table of Contents
| • | $37.5 million recorded as part of health plan services expenses for estimated litigation and regulatory actions related to the Company’s rescission practices in Arizona and California and claim-related matters in connection with the settlement agreement for theMcCoy, Wachteland Scharfman lawsuits; |
| • | $14.6 million loss recorded as part of net investment income from other-than-temporary impairments in our available-for-sale investments and money market funds; and |
| • | $3.4 million recorded as part of administrative services fees and other income for an impairment of assets of a small, non-core subsidiary. |
2007 Charges
In 2007, we recorded a $306.8 million pretax, or $222.4 million after-tax, charge incurred as a result of us reaching an agreement in principle to settle theMcCoy, Wachtel andScharfmanclass action lawsuits; the proposed resolution of regulatory issues with the New Jersey Department of Banking and Insurance; arbitration settlement; and other immaterial litigation matters. See “Item 3. Legal Proceedings” for additional information regarding these matters. The charge amount was comprised of the following:
| • | $201.5 million recorded as part of health plan services expenses during the year ended December 31, 2007 for claim-related matters, class disbursements and remediations; and |
| • | $105.3 million recorded as part of G&A expenses during the year ended December 31, 2007 for attorney’s fees, regulatory fines, arbitration settlement and estimated liability for litigation unrelated to the class action lawsuits. |
2006 Charges
During the three months ended December 31, 2006, we recorded a pretax charge of approximately $37.1 million in connection with theMcCoy, Wachtel andScharfmanclass action lawsuits.
Income Tax Provision
Our income tax expense and the effective income tax rate for the years ended December 31, 2008, 2007 and 2006 are as follows:
2008 | 2007 | 2006 | ||||||||||
| (Dollars in millions) | ||||||||||||
Income tax expense | $ | 52.1 | $ | 165.2 | $ | 149.5 | ||||||
Effective tax rate | 35.4 | % | 46.0 | % | 31.2 | % | ||||||
The effective income tax rate differs from the statutory federal tax rate of 35% for the year ended December 31, 2008 due primarily to state income taxes, tax-exempt investment income, and favorable outcome related to the prior year nondeductible class action lawsuit expenses.
The effective income tax rate differs from the statutory federal tax rate of 35% for the year ended December 31, 2007 due primarily to state income taxes, tax-exempt investment income, the establishment of a valuation allowance against certain deferred tax assets, and nondeductible class action lawsuit expenses. The effective income tax rate differs from the statutory tax rate of 35% for the year ended December 31, 2006 due primarily to state income taxes, tax-exempt investment income, and business divestitures.
The effective income tax rate decreased from 2007 to 2008 primarily due to the favorable outcome related to the prior year nondeductible class action lawsuit expenses. The effective income tax rate increased from 2006 to 2007 primarily due to the establishment of a valuation allowance in 2007 against deferred tax assets for net operating loss carryforwards and tax credits of a particular business unit potentially impacted by theMcCoy class action lawsuit, and nondeductible class action lawsuit expenses incurred in 2007.
63
Table of Contents
LIQUIDITY AND CAPITAL RESOURCES
Market and Economic Conditions
In the U.S., recent market and economic conditions have been unprecedented in recent history and challenging with tighter credit conditions and slower growth through the third and fourth quarters of 2008. Continued concerns about the U.S. mortgage market, declining real estate market, and the availability of credit have contributed to increased market volatility and diminished expectations for the U.S. economy. In September 2008, added concerns fueled by the federal government conservatorship of the Federal Home Loan Mortgage Corporation (Freddie Mac) and the Federal National Mortgage Association (Fannie Mae), the declared bankruptcy of Lehman Brothers Holdings Inc., the U.S. government provided loan to American International Group Inc. and other federal government interventions in the U.S. credit markets led to increased market uncertainty and instability in both U.S. and international capital and credit markets. These conditions, combined with volatile oil prices, declining business and consumer confidence and increased unemployment have contributed to volatility of unprecedented levels.
As a result of these market conditions, the cost and availability of credit has been and may continue to be adversely affected by illiquid credit markets and wider credit spreads. Concern about the stability of the markets generally and the strength of counterparties specifically has caused many lenders and institutional investors to reduce, and in some cases, cease to provide funding to borrowers. While we have not experienced a reduction in the capital and funding available to us at this time, continued turbulence in the U.S. and international markets and economies may adversely affect our liquidity and financial condition. If these market conditions continue, they may limit our ability to timely replace maturing liabilities and access the capital markets to meet liquidity needs, which could adversely affect our financial condition and results of operations. Furthermore, if our customer base experiences cash flow problems and other financial difficulties, it could, in turn, adversely impact membership in our plans. For example, our customers may modify, delay or cancel plans to purchase our products, may reduce the number of individuals to whom they provide coverage, or may make changes in the mix or products purchased from us. In addition, if our customers experience financial issues, they may not be able to pay, or may delay payment of, accounts receivable that are owed to us. Further, our customers or potential customers may force us to compete more vigorously on factors such as price and service to retain or obtain their business. A significant decline in membership in our plans and the inability of current and/or potential customers to pay their premiums as a result of unfavorable conditions may adversely affect our business, including our revenues, profitability and cash flow.
Cash and Investments
As of December 31, 2008, we valued investment securities available-for-sale at $1.5 billion. Approximately 67% of our portfolio holdings is in agency mortgage-backed bonds and municipal bonds. We also hold high-quality corporate bonds. We evaluate and determine the classification of our investments based on management’s intent; currently, we have classified our investments as available-for-sale. We also closely monitor the fair values of our investment holdings and regularly evaluate them for any other-than-temporary impairments.
Our cash flow from investing activities is primarily impacted by the sales, maturities and purchases of our available-for-sale investment securities and restricted investments. Our investment objective is to maintain safety and preservation of principal by investing in a diversified mix of high-quality, investment grade securities while maintaining liquidity in each portfolio sufficient to meet our cash flow requirements and attaining the highest total return on invested funds. We do not own any investments that have direct subprime mortgage exposure.
Our investment portfolio includes $520.0 million, or 34.6% of our portfolio holdings, of mortgage-backed and asset-backed securities. The majority of our mortgage-backed securities are Fannie Mae, Freddie Mac and Ginnie Mae issues, and the average rating of our asset-backed securities is AA+/Aa1. As of December 31, 2008 and December 31, 2007, our asset-backed and mortgage-backed securities had gross unrealized holding losses of $17.2 million and $3.1 million, respectively. We have the intent and ability to hold our debt investments for a sufficient
64
Table of Contents
period of time to allow for recovery of the principal amounts invested. However, any failure by Fannie Mae or Freddie Mac to honor the obligations under the securities they have issued or guaranteed could cause a significant decline in the value or cash flow of our mortgage-backed securities. Our investment portfolio also includes $10.2 million, or less than 1% of our portfolio holdings, of auction rate securities (ARS). These ARS have long-term nominal maturities for which the interest rates are reset through a dutch auction process every 7, 28 or 35 days. At December 31, 2008, these ARS had at one point or are continuing to experience “failed” auctions. These securities are entirely municipal issues and rates are set at the maximum allowable rate as stipulated in the applicable bond indentures. We continue to receive income on all ARS. If all or any portion of the ARS continue to experience failed auctions, it could take an extended amount of time for us to realize our investments’ recorded value.
As discussed in Note 4 to our consolidated financial statements, we recognized a $14.6 million loss from other-than-temporary impairments of investment securities and money market funds in the third quarter of 2008. After this write-down, we had gross unrealized losses of $32.8 million as of December 31, 2008, compared to $7.0 million as of December 31, 2007. While we believe that these impairments are temporary and that we have the intent and ability to hold such securities until maturity or recovery, given the current market conditions, there is a continuing risk that further declines in fair value may occur and additional material other-than-temporary impairments may be recorded in future periods.
In September 2008, The Reserve announced its intention to liquidate all of its money market funds and froze all redemptions until an orderly liquidation process could be implemented. As a result, we reclassified $372 million in estimated net asset value we had invested in The Reserve money market funds from cash equivalents to investments available for sale as of September 30, 2008. As of December 31, 2008, we held $50.4 million of their Primary Fund and $69.2 million of their U.S. Government Fund due to redemptions during the fourth quarter of 2008. On January 16, 2009, The Reserve paid out in full the balance in the U.S. Government Fund and on February 20, 2009, we received $17.1 million of the Primary Fund from the Reserve. The Reserve expects to distribute the remaining amounts in the Primary Fund by the end of 2009.
Liquidity
We believe that cash flow from operating activities, existing working capital, lines of credit and cash reserves are adequate to allow us to fund existing obligations, repurchase shares under our stock repurchase program, introduce new products and services, and continue to develop health care-related businesses. We regularly evaluate cash requirements for current operations and commitments, and for capital acquisitions and other strategic transactions. We may elect to raise additional funds for these purposes, either through issuance of debt or equity, the sale of investment securities or otherwise, as appropriate. Based on the composition and quality of our investment portfolio, our expected ability to liquidate our investment portfolio as needed, and our expected operating and financing cash flows, we do not anticipate any liquidity constraints as a result of the current credit environment. However, continued turbulence in U.S. and international markets could adversely affect our liquidity.
Our cash flow from operating activities is impacted by, among other things, the timing of collections on our amounts receivable from our TRICARE contract for the North Region. Health care receivables related to TRICARE are best estimates of payments that are ultimately collectible or payable. The timing of collection of such receivables is impacted by government audit and negotiation and can extend for periods beyond a year. Amounts receivable under government contracts were $241.3 million and $190.0 million as of December 31, 2008 and December 31, 2007, respectively. Our cash flow from operating activities is also impacted by the timing of collections on our amounts receivable from CMS. Our receivable related to our Medicare business was $315.5 million, including about $150 million expected to be settled in the fourth quarter of 2009, as of December 31, 2008 and $107.2 million as of December 31, 2007.
During 2008, we recognized $175.1 million in pretax charges related to our operations strategy and litigation and regulatory related matters. The majority of these charges were settled in cash and were funded by cash flow from operating and financing activities. For additional information regarding these charges, see “—Summary of Operating Results” above.
65
Table of Contents
Our total cash and cash equivalents as of December 31, 2008 and 2007 were $668.2 million and $1,007.0 million, respectively. The changes in cash and cash equivalents are summarized as follows:
| 2008 | 2007 | 2006 | ||||||||||
| (Dollars in millions) | ||||||||||||
Net cash (used in) provided by operating activities | $ | (159.0 | ) | $ | 605.5 | $ | 277.9 | |||||
Net cash (used in) investing activities | (67.8 | ) | (230.2 | ) | (184.9 | ) | ||||||
Net cash (used in) financing activities | (112.0 | ) | (73.1 | ) | (130.7 | ) | ||||||
Net (decrease) increase in cash and cash equivalents | $ | (338.8 | ) | $ | 302.2 | $ | (37.7 | ) | ||||
Operating Cash Flows
Year Ended December 31, 2008 Compared to Year Ended December 31, 2007
Net cash from operating activities decreased by $764.5 million for the year ended December 31, 2008 compared to the same period in 2007. This decrease was primarily due to the $283 million paid in 2008 related to operations strategy and litigation and regulatory related matters, a $218 million increase in our net CMS catastrophic and low-income subsidies receivables, and approximately $83 million Medicare Part D payments received in 2007 for the final settlement of the 2006 plan year.
Year Ended December 31, 2007 Compared to Year Ended December 31, 2006
Net cash from operating activities increased by $327.6 million for the year ended December 31, 2007 compared to the same period in 2006. This increase was primarily due to increase in cash flows from a TRICARE payment for Option 3 period underwriting fees of $100 million and the growth in our Medicare business, including approximately $83 million Medicare Part D payments received for the final settlement of the 2006 plan year.
Investing Activities
Our cash flow from investing activities is primarily impacted by the sales, maturities and purchases of our available-for-sale investment securities and restricted investments. Our investment objective is to maintain safety and preservation of principal by investing in high-quality, investment grade securities while maintaining liquidity in each portfolio sufficient to meet our cash flow requirements and attaining the highest total return on invested funds.
Year Ended December 31, 2008 Compared to Year Ended December 31, 2007
Net cash used in investing activities decreased by $162.4 million compared to the year ended December 31, 2007 primarily due to the $252 million redemption from The Reserve Funds, partially offset by $97 million decrease in net proceeds from property and equipment sale.
Year Ended December 31, 2007 Compared to Year Ended December 31, 2006
Net cash used in investing activities increased by $45.3 million compared to the year ended December 31, 2006 primarily due to a net increase in purchases of investments available-for-sale portfolio of $140 million, partially offset by an increase in net proceeds of $93 million from the sales of property and equipment, including our Shelton, CT and Tucson, AZ facilities.
66
Table of Contents
Financing Activities
Year Ended December 31, 2008 Compared to Year Ended December 31, 2007
Net cash used in financing activities increased by $38.9 million primarily due to a decrease in stock option exercise proceeds of $66 million, decrease in excess tax benefits from share based compensation of $17 million and a net increase in share repurchases of $11 million, partially offset by an increase in net borrowings of $55 million.
Year Ended December 31, 2007 Compared to Year Ended December 31, 2006
Net cash used in financing activities decreased by $57.6 million primarily due to an increase in net borrowings of $36 million and decrease in share repurchases of $21 million. See “—Capital Structure” below on more information regarding these transactions.
Capital Structure
Stock Repurchase Program
We have a $700 million stock repurchase program authorized by our Board of Directors. Subject to Board approval, additional amounts are added to the repurchase program from time to time based on exercise proceeds and tax benefits the Company receives from the employee stock options. We repurchased 6,851,595 shares of our common stock during the year ended December 31, 2008, for aggregate consideration of approximately $242.8 million. We used net free cash available to fund the share repurchases. As of December 31, 2008, the remaining authorization under our stock repurchase program was $103.3 million and, since its inception, we had repurchased an aggregate of 36,623,347 shares of our common stock at an average price of $34.40 for aggregate consideration of approximately $1,259.8 million (which amount includes exercise proceeds and tax benefits the Company had received from the exercise of employee stock options).
On November 4, 2008, we announced that our stock repurchase program is on hold as a consequence of the uncertain financial environment and the announcement by Health Net’s Board of Directors that Jay Gellert, our President and Chief Executive Officer, will be undertaking a review of the Company’s strategic direction.
Amortizing Financing Facility
On December 19, 2007, we entered into a five-year, non-interest bearing, $175 million amortizing financing facility with a non-U.S. lender and we entered into amendments to the financing facility on April 29, 2008 and November 10, 2008, which were administrative in nature. The proceeds from the financing facility were used for general corporate purposes.
The financing facility requires one of our subsidiaries to pay semi-annual distributions, in the amount of $17.5 million, to a participant in the financing facility. Unless terminated earlier, the final payment under the facility is scheduled to be made on December 19, 2012.
The financing facility includes limitations (subject to specified exclusions) on our and certain of our subsidiaries’ ability to incur debt; create liens; engage in certain mergers, consolidations and acquisitions; engage in transactions with affiliates; enter into agreements which will restrict the ability to pay dividends or other distributions with respect to any shares of capital stock or the ability to make or repay loans or advances; make dividends; and alter the character of ours or their business conducted on the closing date of the financing facility. In addition, the financing facility also requires that we maintain a specified consolidated leverage ratio and consolidated fixed charge coverage ratio and maintain certain minimum public debt ratings throughout the term of the financing facility. As of December 31, 2008, we were in compliance with all of the covenants under the financing facility.
67
Table of Contents
The financing facility provides that it may be terminated through a series of put and call transactions (1) at the option of one of our wholly-owned subsidiaries at any time after December 20, 2009, or (2) upon the occurrence of certain defined early termination events. These early termination events, include, but are not limited to:
| • | nonpayment of certain amounts due by us or certain of our subsidiaries under the financing facility (if not cured within the related time period set forth therein); |
| • | a change of control (as defined in the financing facility); |
| • | our failure to maintain the following ratings on our senior indebtedness by any two of the following three rating agencies: (1) a rating of at least BB by Standard & Poor’s Ratings Services (S&P), (2) a rating of at least BB by Fitch, Inc. (Fitch), and (3) a rating of at least Ba2 by Moody’s Investors Service, Inc. (Moody’s). As of December 31, 2008 and February 12, 2009, the ratings with S&P, Fitch and Moody’s on our senior indebtedness were BB, BB+ and Ba3, respectively; |
| • | cross-acceleration to other indebtedness of our Company in excess of $50 million, including our revolving credit facility; |
| • | certain ERISA-related events; |
| • | noncompliance by Health Net with any material term or provision of the HMO Regulations or Insurance Regulations (as each such term is defined in the financing facility); |
| • | events in bankruptcy, insolvency or reorganization of our Company; |
| • | undischarged, uninsured judgments in the amount of $50 million or more against our Company; or |
| • | certain changes in law that could adversely affect a participant in the financing facility. |
In addition, in connection with the financing facility, we entered into a guaranty which will require us to guarantee the payment of the semi-annual distributions and any other amounts payable by one of our subsidiaries to the financing facility participants under certain circumstances provided under the financing facility. Also in connection with the financing facility, we entered into an interest rate swap agreement with a non-U.S. bank affiliated with one of the financing facility participants. Under the interest rate swap agreement, we pay a floating payment in an amount equal to LIBOR times a notional principal amount and receive a fixed payment in an amount equal to 4.3% times the same notional principal amount from the non-U.S. bank counterparty in return in accordance with a schedule set forth in the interest rate swap agreement.
Senior Notes
On May 18, 2007, we issued $300 million in aggregate principal amount of 6.375% Senior Notes due 2017. On May 31, 2007, we issued an additional $100 million of 6.375% Senior Notes due 2017 which were consolidated with, and constitute the same series as, the Senior Notes issued on May 18, 2007 (collectively, the “Senior Notes”). The aggregate net proceeds from the issuance of the Senior Notes were $393.5 million and were used to repay outstanding debt.
The indenture governing the Senior Notes limits our ability to incur certain liens, or consolidate, merge or sell all or substantially all of our assets. In the event of the occurrence of both (1) a change of control of Health Net, Inc. and (2) a below investment grade rating by any two of Fitch, Inc., Moody’s Investors Service, Inc. and Standard & Poor’s Ratings Services, within a specified period, we will be required to make an offer to purchase the Senior Notes at a price equal to 101% of the principal amount of the Senior Notes plus accrued and unpaid interest to the date of repurchase. As of December 31, 2008, we were in compliance with all of the covenants under the indenture governing the Senior Notes.
The Senior Notes may be redeemed in whole at any time or in part from time to time, prior to maturity at our option, at a redemption price equal to the greater of:
| • | 100% of the principal amount of the Senior Notes then outstanding to be redeemed; or |
68
Table of Contents
| • | the sum of the present values of the remaining scheduled payments of principal and interest on the Senior Notes to be redeemed (not including any portion of such payments of interest accrued to the date of redemption) discounted to the date of redemption on a semiannual basis (assuming a 360-day year consisting of twelve 30-day months) at the applicable treasury rate plus 30 basis points |
plus, in each case, accrued and unpaid interest on the principal amount being redeemed to the redemption date.
Each of the following will be an Event of Default under the indenture governing the Senior Notes:
| • | failure to pay interest for 30 days after the date payment is due and payable; provided that an extension of an interest payment period by us in accordance with the terms of the Senior Notes shall not constitute a failure to pay interest; |
| • | failure to pay principal or premium, if any, on any note when due, either at maturity, upon any redemption, by declaration or otherwise; |
| • | failure to perform any other covenant or agreement in the notes or indenture for a period of 60 days after notice that performance was required; |
| • | (A) our failure or the failure of any of our subsidiaries to pay indebtedness for money we borrowed or any of our subsidiaries borrowed in an aggregate principal amount of at least $50,000,000, at the later of final maturity and the expiration of any related applicable grace period and such defaulted payment shall not have been made, waived or extended within 30 days after notice or (B) acceleration of the maturity of indebtedness for money we borrowed or any of our subsidiaries borrowed in an aggregate principal amount of at least $50,000,000, if that acceleration results from a default under the instrument giving rise to or securing such indebtedness for money borrowed and such indebtedness has not been discharged in full or such acceleration has not been rescinded or annulled within 30 days after notice; or |
| • | events in bankruptcy, insolvency or reorganization of our Company. |
Revolving Credit Facility
On June 25, 2007, we entered into a $900 million five-year revolving credit facility with Bank of America, N.A. as Administrative Agent, Swingline Lender, and L/C Issuer, and the other lenders party thereto. We entered into an amendment to the credit facility on April 29, 2008, which was administrative in nature. Our revolving credit facility provides for aggregate borrowings in the amount of $900 million, which includes a $400 million sub-limit for the issuance of standby letters of credit and a $50 million sub-limit for swing line loans. In addition, we have the ability from time to time to increase the facility by up to an additional $250 million in the aggregate, subject to the receipt of additional commitments. The revolving credit facility matures on June 25, 2012.
Amounts outstanding under the new revolving credit facility will bear interest, at our option, at (a) the base rate, which is a rate per annum equal to the greater of (i) the federal funds rate plus one-half of one percent and (ii) Bank of America’s prime rate (as such term is defined in the facility), (b) a competitive bid rate solicited from the syndicate of banks, or (c) the British Bankers Association LIBOR rate (as such term is defined in the facility), plus an applicable margin, which is initially 70 basis points per annum and is subject to adjustment according to our credit ratings, as specified in the facility.
Our revolving credit facility includes, among other customary terms and conditions, limitations (subject to specified exclusions) on our and our subsidiaries’ ability to incur debt; create liens; engage in certain mergers, consolidations and acquisitions; sell or transfer assets; enter into agreements which restrict the ability to pay dividends or make or repay loans or advances; make investments, loans, and advances; engage in transactions with affiliates; and make dividends. In addition, we are required to maintain a specified consolidated leverage ratio and consolidated fixed charge coverage ratio throughout the term of the revolving credit facility.
69
Table of Contents
Our revolving credit facility contains customary events of default, including nonpayment of principal or other amounts when due; breach of covenants; inaccuracy of representations and warranties; cross-default and/or cross-acceleration to other indebtedness of the Company or our subsidiaries in excess of $50 million; certain ERISA-related events; noncompliance by us or any of our subsidiaries with any material term or provision of the HMO Regulations or Insurance Regulations (as each such term is defined in the facility); certain voluntary and involuntary bankruptcy events; inability to pay debts; undischarged, uninsured judgments greater than $50 million against us and/or our subsidiaries; actual or asserted invalidity of any loan document; and a change of control. If an event of default occurs and is continuing under the facility, the lenders thereunder may, among other things, terminate their obligations under the facility and require us to repay all amounts owed thereunder.
As of December 31, 2008, we were in compliance with all covenants under our revolving credit facility.
We can obtain letters of credit in an aggregate amount of $400 million under our revolving credit facility. The maximum amount available for borrowing under our revolving credit facility is reduced by the dollar amount of any outstanding letters of credit. As of December 31, 2008, we had outstanding an aggregate of $322.9 million in letters of credit and outstanding borrowings under the revolving credit facility of $150 million. As a result, the maximum amount available for borrowing under the revolving credit facility was $427.1 million as of December 31, 2008, and no amount had been drawn on the letters of credit. As of February 12, 2009, we had $115 million of outstanding borrowings under the revolving credit facility.
Statutory Capital Requirements
Certain of our subsidiaries must comply with minimum capital and surplus requirements under applicable state laws and regulations, and must have adequate reserves for claims. Management believes that as of December 31, 2008, all of our active health plans and insurance subsidiaries met their respective regulatory requirements, in all material respects.
By law, regulation and governmental policy, our health plan and insurance subsidiaries, which we refer to as our regulated subsidiaries, are required to maintain minimum levels of statutory net worth. The minimum statutory net worth requirements differ by state and are generally based on balances established by statute, a percentage of annualized premium revenue, a percentage of annualized health care costs, or risk-based capital (RBC) requirements. The RBC requirements are based on guidelines established by the National Association of Insurance Commissioners. The RBC formula, which calculates asset risk, underwriting risk, credit risk, business risk and other factors, generates the authorized control level (ACL), which represents the minimum amount of net worth believed to be required to support the regulated entity’s business. For states in which the RBC requirements have been adopted, the regulated entity typically must maintain the greater of the Company Action Level RBC, calculated as 200% of the ACL, or the minimum statutory net worth requirement calculated pursuant to pre-RBC guidelines. Because our regulated subsidiaries are also subject to their state regulators’ overall oversight authority, some of our subsidiaries are required to maintain minimum capital and surplus in excess of the RBC requirement, even though RBC has been adopted in their states of domicile. We generally manage our aggregate regulated subsidiary capital above 300% of ACL, although RBC standards are not yet applicable to all of our regulated subsidiaries. At December 31, 2008, we had sufficient capital to exceed this level.
As necessary, we make contributions to and issue standby letters of credit on behalf of our subsidiaries to meet RBC or other statutory capital requirements under state laws and regulations. During the year ended December 31, 2008, we made capital contributions of $240.6 million to various subsidiaries to maintain RBC or other statutory capital requirements. Health Net, Inc. made a capital contribution in the amount of $3.0 million to one of its subsidiaries to meet RBC or other statutory capital requirements under state laws and regulations thereafter through February 20, 2009.
70
Table of Contents
Legislation has been or may be enacted in certain states in which our subsidiaries operate imposing substantially increased minimum capital and/or statutory deposit requirements for HMOs in such states. Such statutory deposits may only be drawn upon under limited circumstances relating to the protection of policyholders.
As a result of the above requirements and other regulatory requirements, certain subsidiaries are subject to restrictions on their ability to make dividend payments, loans or other transfers of cash to their parent companies. Such restrictions, unless amended or waived or unless regulatory approval is granted, limit the use of any cash generated by these subsidiaries to pay our obligations. The maximum amount of dividends that can be paid by our insurance company subsidiaries without prior approval of the applicable state insurance departments is subject to restrictions relating to statutory surplus, statutory income and unassigned surplus.
Contractual Obligations
Our significant contractual obligations as of December 31, 2008 are summarized below for the years ending December 31:
| Total | 2009 | 2010 | 2011 | 2012 | 2013 | Thereafter | |||||||||||||||||||||
| (Dollars in Millions) | |||||||||||||||||||||||||||
Long-term debt principal | $ | 547.8 | $ | 35.0 | $ | 35.0 | $ | 35.0 | $ | 35.0 | $ | 7.8 | $ | 400.0 | |||||||||||||
Long-term debt interest | 213.7 | 25.5 | 25.5 | 25.5 | 25.5 | 25.5 | 86.2 | ||||||||||||||||||||
Floating-rate borrowings principal | 150.0 | 35.0 | — | — | 115.0 | — | — | ||||||||||||||||||||
Floating-rate borrowings interest | 9.9 | 2.5 | 2.2 | 2.9 | 2.3 | — | — | ||||||||||||||||||||
Valuation of interest rate swap contracts | (8.9 | ) | (3.0 | ) | (3.5 | ) | (1.7 | ) | (0.7 | ) | — | — | |||||||||||||||
Operating leases | 301.8 | 64.9 | 59.4 | 52.3 | 35.2 | 29.3 | 60.7 | ||||||||||||||||||||
Long-term purchase obligations | 562.0 | 140.8 | 133.4 | 126.4 | 85.4 | 70.5 | 5.5 | ||||||||||||||||||||
FIN 48 liabilities, including interest and penalties (b) | 2.2 | 2.2 | — | — | — | — | — | ||||||||||||||||||||
Deferred compensation | 41.5 | 4.9 | 3.2 | 2.0 | 2.3 | 1.8 | 27.3 | (a) | |||||||||||||||||||
Estimated future payments for pension and other benefits | 25.4 | 1.6 | 1.7 | 1.9 | 2.1 | 2.3 | 15.8 | (a) | |||||||||||||||||||
| (a) | Represents estimated future payments from 2014 through 2018. |
| (b) | The FIN 48 obligations shown above represent uncertain tax positions expected to be paid within the reporting periods presented. In addition to the obligations shown above, approximately $55.9 million of unrecognized tax benefits have been recorded as a liability in accordance with FIN 48, and we are uncertain as to if or when such amounts may be settled or paid. |
Operating Leases
We lease office space under various operating leases. Certain leases are cancelable with substantial penalties. See “Item 2. Properties” for additional information regarding our leases.
On March 29, 2007, we sold our 68-acre commercial campus in Shelton, Connecticut (the “Shelton Property”) to The Dacourt Group, Inc. (“Dacourt”) and leased it back from Dacourt under an operating lease agreement for an initial term of ten years with an option to extend for two additional terms of ten years each. The total future minimum lease commitments under the lease are approximately $70.1 million.
Effective January 1, 2005, we entered into an operating lease agreement to renew our leased office space in Woodland Hills, California for our corporate headquarters. The new lease is for a term of 10 years and has provisions for space reduction at specific times over the term of the lease, but it does not provide for complete cancellation rights. The total future minimum lease commitments under the lease are approximately $19.2 million.
71
Table of Contents
Long-Term Purchase Obligations
We have entered into long-term agreements to purchase various services, which may contain certain termination provisions and have remaining terms in excess of one year as of December 31, 2008.
We have entered into long-term agreements to receive services related to pharmacy benefit management, pharmacy claims processing services and health quality/risk scoring enhancement services with external third-party service providers. The remaining terms are approximately three years for each of these contracts. Termination of these agreements is subject to certain termination provisions. The total future minimum commitments under these agreements are $122.0 million and are included in the table above.
On August 19, 2008, we entered into a five and one-half year agreement with International Business Machines Corporation (IBM) to outsource our IT infrastructure management services including data center services, IT security management and help desk support. The total future minimum commitments under the agreement are $295.0 million.
On September 30, 2008, we entered into a five year and three month agreement with Cognizant Technology Solutions U.S. Corporation (Cognizant) to outsource our software applications development and management activities to Cognizant. Under the terms of the agreement, Cognizant will, among other things, provide us with services including the following: application development, testing and monitoring services, application maintenance and support services, project management services and cross functional services. The total future commitments under the agreement are $107.8 million.
We have excluded from the table above amounts already recorded in our current liabilities on our consolidated balance sheet as of December 31, 2008. We have also excluded from the table above various contracts we have entered into with our health care providers, health care facilities, the federal government and other contracts that we have entered into for the purpose of providing health care services. We have excluded those contracts that allow for cancellation without significant penalty, obligations that are contingent upon achieving certain goals and contracts for goods and services that are fulfilled by vendors within a short time horizon and within the normal course of business.
On January 23, 2009, we also entered into a five year and two months agreement with Cognizant to outsource a substantial portion of our claims processing activities to Cognizant. Under the terms of the agreement, Cognizant will, among other things, provide us with claims adjudication, adjustment, audit and process improvement services. The total future commitments under the agreement are $13.3 million.
The future contractual obligations in the contractual obligations table are estimated based on information currently available. The timing of and the actual payment amounts may differ based on actual events.
Surety Bonds
In order to secure judgment pending our appeal in the AmCareco litigation, we obtained surety bonds totaling $114.7 million, which are further secured by letters of credit issued in December 2005 in the amounts of $90.1 million. See Notes 6 and 13 to the consolidated financial statements for additional information.
Off-Balance Sheet Arrangements
As of December 31, 2008, we had no off-balance sheet arrangements as defined under Regulation S-K 303(a)(4) and the instructions thereto.
72
Table of Contents
Critical Accounting Estimates
The preparation of financial statements in conformity with accounting principles generally accepted in the United States of America (GAAP) requires management to make estimates and assumptions that affect the reported amounts of assets and liabilities and disclosures of contingent assets and liabilities at the date of the financial statements, and the reported amounts of revenues and expenses during the reporting period. Actual results could differ from those estimates. Principal areas requiring the use of estimates include revenue recognition, health care costs, reserves for contingent liabilities, amounts receivable or payable under government contracts, goodwill and recoverability of long-lived assets and investments and income taxes. Accordingly, we consider accounting policies on these areas to be critical in preparing our consolidated financial statements. A significant change in any one of these amounts may have a significant impact on our consolidated results of operations and financial condition. A more detailed description of the significant accounting policies that we use in preparing our financial statements is included in the notes to our consolidated financial statements, which are included elsewhere in this Annual Report on Form 10-K.
Health Plan Services
Health plan services premium revenues include HMO, POS and PPO premiums from employer groups and individuals and from Medicare recipients who have purchased supplemental benefit coverage (for which premiums are based on a predetermined prepaid fee), Medicaid revenues based on multi-year contracts to provide care to Medicaid recipients, and revenue under Medicare risk contracts (including Part D) to provide care and services to enrolled Medicare recipients. Revenue is recognized in the month in which the related enrollees are entitled to health care services. Premiums collected in advance of the month in which enrollees are entitled to health care services are recorded as unearned premiums.
Approximately 37%, 35%, and 33% in 2008, 2007 and 2006, respectively, of our health plan services premium revenues were generated under Medicare and Medicaid/Medi-Cal contracts. These revenues are subject to audit and retroactive adjustment by the respective fiscal intermediaries. Laws and regulations governing these programs are extremely complex and subject to interpretation. As a result, there is at least a reasonable possibility that recorded estimates will change by a material amount.
Our Medicare contracts are with CMS. CMS deploys a risk adjustment model which apportions premiums paid to all health plans according to health severity and certain demographic factors. The CMS risk adjustment model pays more for members whose medical history would indicate that they are expected to have higher medical costs. Under this risk adjustment methodology, CMS calculates the risk adjusted premium payment using diagnosis data from hospital inpatient, hospital outpatient and physician treatment settings. We and the health care providers collect, compile and submit the necessary and available diagnosis data to CMS within prescribed deadlines. We estimate risk adjustment revenues based upon the diagnosis data submitted and expected to be submitted to CMS.
From time to time, we make adjustments to our revenues based on retroactivity. These retroactivity adjustments reflect changes in the number of enrollees subsequent to when the revenue is billed. We estimate the amount of future retroactivity each period and accordingly adjust the billed revenue. The estimated adjustments are based on historical trends, premiums billed, the volume of contract renewal activity during the period and other information. We refine our estimates and methodologies as information on actual retroactivity becomes available.
On a monthly basis, we estimate the amount of uncollectible receivables to reflect allowances for doubtful accounts. The allowances for doubtful accounts are estimated based on the creditworthiness of our customers, our historical collection rates and the age of our unpaid balances. During this process, we also assess the recoverability of the receivables, and an allowance is recorded based upon their net realizable value. Those receivables that are deemed to be uncollectible, such as receivables from bankrupt employer groups, are fully written off against their corresponding asset account, with a debit to the allowance to the extent such an allowance was previously recorded.
73
Table of Contents
Reserves for claims and other settlements include reserves for claims (incurred but not reported claims (IBNR) and received but unprocessed claims), and other liabilities including capitation payable, shared risk settlements, provider disputes, provider incentives and other reserves for our Health Plan Services reporting segment. As of December 31, 2008, 72% of reserves for claims and other settlements were attributed to claims reserves. See Note 17 to our consolidated financial statements for a reconciliation of changes in the reserve for claims.
We estimate the amount of our reserves for claims primarily by using standard actuarial developmental methodologies. This method is also known as the chain-ladder or completion factor method. The developmental method estimates reserves for claims based upon the historical lag between the month when services are rendered and the month claims are paid while taking into consideration, among other things, expected medical cost inflation, seasonal patterns, product mix, benefit plan changes and changes in membership. A key component of the developmental method is the completion factor which is a measure of how complete the claims paid to date are relative to the estimate of the claims for services rendered for a given period. While the completion factors are reliable and robust for older service periods, they are more volatile and less reliable for more recent periods since a large portion of health care claims are not submitted to us until several months after services have been rendered. Accordingly, for the most recent months, the incurred claims are estimated from a trend analysis based on per member per month claims trends developed from the experience in preceding months. This method is applied consistently year over year while assumptions may be adjusted to reflect changes in medical cost inflation, seasonal patterns, product mix, benefit plan changes and changes in membership.
An extensive degree of actuarial judgment is used in this estimation process, considerable variability is inherent in such estimates, and the estimates are highly sensitive to changes in medical claims submission and payment patterns and medical cost trends. As such, the completion factors and the claims per member per month trend factor are the most significant factors used in estimating our reserves for claims. Since a large portion of the reserves for claims is attributed to the most recent months, the estimated reserves for claims are highly sensitive to these factors. The following table illustrates the sensitivity of these factors and the estimated potential impact on our operating results caused by these factors:
Completion Factor (a) Percentage-point Increase (Decrease) in Factor | Health Plan Services Increase (Decrease) in Reserves for Claims | ||
2% | $ | (59.8) million | |
1% | $ | (30.4) million | |
(1)% | $ | 31.6 million | |
(2)% | $ | 64.4 million | |
Medical Cost Trend (b) Percentage-point Increase (Decrease) in Factor | Health Plan Services Increase (Decrease) in Reserves for Claims | ||
2% | $ | 28.6 million | |
1% | $ | 14.3 million | |
(1)% | $ | (14.3) million | |
(2)% | $ | (28.6) million | |
| (a) | Impact due to change in completion factor for the most recent three months. Completion factors indicate how complete claims paid to date are in relation to the estimate of total claims for a given period. Therefore, an increase in completion factor percent results in a decrease in the remaining estimated reserves for claims. |
| (b) | Impact due to change in annualized medical cost trend used to estimate the per member per month cost for the most recent three months. |
Other relevant factors include exceptional situations that might require judgmental adjustments in setting the reserves for claims, such as system conversions, processing interruptions or changes, environmental changes or other factors. All of these factors are used in estimating reserves for claims and are important to our reserve
74
Table of Contents
methodology in trending the claims per member per month for purposes of estimating the reserves for the most recent months. In developing our best estimate of reserves for claims, we consistently apply the principles and methodology described above from year to year, while also giving due consideration to the potential variability of these factors. Because reserves for claims include various actuarially developed estimates, our actual health care services expense may be more or less than our previously developed estimates. Claims processing expenses are also accrued based on an estimate of expenses necessary to process such claims. Such reserves are continually monitored and reviewed, with any adjustments reflected in current operations.
HN of California, our California HMO, generally contracts with various medical groups to provide professional care to certain of its members on a capitated, or fixed per member per month fee basis. Capitation contracts generally include a provision for stop-loss and non-capitated services for which we are liable. Professional capitated contracts also generally contain provisions for shared risk. We have risk-sharing arrangements with certain of our providers related to approximately 1,167,000 members, primarily in the California commercial market. Shared-risk arrangements provide for us to share with our providers the variance between actual costs and predetermined goals.
Our HMOs in other states also contract with hospitals, physicians and other providers of health care, pursuant to discounted fee-for-service arrangements, hospital per diems, and case rates under which providers bill the HMOs for each individual service provided to enrollees. Additionally, we contract with certain hospitals to provide hospital care to enrolled members on a capitation basis.
We assess the profitability of contracts for providing health care services when operating results or forecasts indicate probable future losses. Significant factors that can lead to a change in our profitability estimates include premium yield and health care cost trend assumptions, risk share terms and non-performance of a provider under a capitated agreement resulting in membership reverting to fee-for-service arrangements with other providers. Contracts are grouped in a manner consistent with the method of determining premium rates. Losses are determined by comparing anticipated premiums to estimates for the total of health care related costs less reinsurance recoveries, if any, and the cost of maintaining the contracts. Losses, if any, are recognized in the period the losses are determined and are classified as Health Plan Services. We held no premium deficiency reserves as of December 31, 2008.
Government Contracts
The TRICARE North Region contract is made up of two major revenue components, health care and administrative services. Health care services revenue includes health care costs, including paid claims and estimated IBNR expenses, for care provided for which we are at risk and underwriting fees earned for providing the health care and assuming underwriting risk in the delivery of care. Administrative services revenue encompasses all other services provided to both the government customer and to beneficiaries, including services such as medical management, claims processing, enrollment, customer services and other services unique to the managed care support contracts with the government. Health care costs and associated revenues are recognized as the costs are incurred and the associated revenue is earned. Revenue related to administrative services is recognized as the services are provided and earned. Revenues associated with the transition to the TRICARE contract for the North Region are recognized over the entire term of the contract.
There are different variables that impact the estimate of the IBNR reserves for our TRICARE business than those that impact our managed care businesses. These variables consist of changes in the level of our nation’s military activity, including the call-up of reservists in support of heightened military activity, continual changes in the number of eligible beneficiaries, changes in the health care facilities in which the eligible beneficiaries seek treatment, and revisions to the provisions of the contract in the form of change orders. Each of these factors is subject to significant judgment, and we have incorporated our best estimate of these factors in estimating the reserve for IBNR claims.
75
Table of Contents
As part of our TRICARE contract for the North Region, we have a risk-sharing arrangement with the federal government whereby variances in actual claim experience from the targeted medical claim amount negotiated in our annual bid are shared. Due to this risk-sharing arrangement provided for in the TRICARE contract for the North Region, the changes in the estimate of the IBNR reserves are not expected to have a material effect on the favorable or adverse development of our liability under the TRICARE contract.
Other government contracts revenues are recognized in the month in which the eligible beneficiaries are entitled to health care services or in the month in which the administrative services are performed or the period that coverage for services is provided. Under our TRICARE contract for the North Region we recognize amounts receivable and payable under the government contracts related to estimated health care IBNR expenses which are reported separately on the accompanying consolidated balance sheet as of December 31, 2008. These amounts are the same since all of the estimated health care IBNR expenses incurred are offset by an equal amount of revenues earned.
Some of the amounts receivable under government contracts are comprised primarily of contractually defined billings, deferred underwriting fees under the terms of the contract and change orders for services not originally specified in the contracts. Change orders arise because the government often directs us to implement changes to our contracts before the scope and/or value is defined or negotiated. We start to incur costs immediately, before we have proposed a price to the government. In these situations, we make no attempt to estimate and record revenue. Our policy is to defer the costs as incurred until we have submitted a cost proposal to the government, at which time we will record the costs and the appropriate value for revenue, using our best estimate of what will ultimately be negotiated. In the normal course of contracting with the federal government, we may make claims for contract and price adjustments arising from cost overruns against the government. We recognize such claims when the amounts become determinable, supportable and the collectibility is reasonably assured.
Reserves For Contingent Liabilities
In the course of our operations, we are involved on a routine basis in various disputes with members, health care providers, and other entities, as well as audits by government agencies that relate to our services and/or business practices that expose us to potential losses.
We recognize an estimated loss, which may represent damages, settlement costs, future legal expenses or a combination of the foregoing, as appropriate, from such loss contingencies when it is both probable that a loss will be incurred and that the amount of the loss can be reasonably estimated. Our loss estimates are based in part on an analysis of potential results, the stage of the proceedings, consultation with outside counsel and any other relevant information available.
Goodwill
Goodwill and other intangible assets arise primarily as a result of various business acquisitions and consist of identifiable intangible assets acquired and the excess of the cost of the acquisitions over the tangible and intangible assets acquired and liabilities assumed (goodwill). Identifiable intangible assets primarily consist of the value of employer group contracts, provider networks and customer relationships, which are all subject to amortization.
We perform our annual impairment test on our recorded goodwill as of June 30 or more frequently if events or changes in circumstances indicate that we might not recover the carrying value of these assets for each of our reporting units. Health Plans Services is our only reporting unit with goodwill as of December 31, 2008 and 2007. We test goodwill for impairment annually based on the estimated fair value of our Health Plan Services reporting unit. We test for impairment on a more frequent basis in cases where events and changes in circumstances would indicate that we might not recover the carrying value of goodwill. Our measurement of fair
76
Table of Contents
value is primarily based on the income approach to fair value determination. The income approach is based on a discounted cash flow methodology. The discounted cash flow methodology is based upon converting expected cash flows to present value. Annual cash flows are estimated for each year of a defined multi-year period until the growth pattern becomes stable. The interim cash flows expected after the growth pattern becomes stable are calculated using an appropriate capitalization technique and then discounted. There are numerous assumptions and estimates underlying the determination of the estimated fair value of our reporting units, including certain assumptions and estimates related to future earnings and membership levels based on current and future plans and initiatives, long-term strategies and our annual planning and forecasting process as well as the weighted average cost of capital used in the discounting process. If these planned initiatives do not accomplish their targeted objectives, the assumptions and estimates underlying the goodwill impairment tests could be adversely affected and have a material effect upon our financial condition, results of operations or liquidity.
During the year ended December 31, 2008, we recorded higher than expected health care costs and lowered our earnings guidance. The reduction in guidance was primarily driven by lower than expected commercial enrollment, higher than expected commercial health care cost trends, and the volatile economic environment. As a result of this revised outlook combined with a decline in our market capitalization, we updated our annual impairment test on our goodwill asset as of September 30, 2008 and as of December 31, 2008, which indicated that there was no impairment.
Recoverability of Long-Lived Assets and Investments
We periodically assess the recoverability of our long-lived assets including property and equipment and other long-term assets and investments where events and changes in circumstances would indicate that we might not recover the carrying value as follows:
Long-lived Assets Held and Used
We test long-lived assets or asset groups for recoverability when events or changes in circumstances indicate that their carrying amount may not be recoverable. Circumstances which could trigger a review include, but are not limited to: significant decreases in the market price of the asset, significant adverse changes in the business climate or legal factors, current period cash flow or operating losses combined with a history of losses or a forecast of continuing losses associated with the use of the asset and current expectation that the asset will more likely than not be sold or disposed of significantly before the end of its estimated useful life.
If we identify an indicator of impairment, we assess recoverability by comparing the carrying amount of the asset to the sum of the undiscounted cash flows expected to result from the use and the eventual disposal of the asset. An impairment loss is recognized when the carrying amount is not recoverable and is measured as the excess of carrying value over fair value. We recognized such an impairment of $47.9 million in 2008 representing impairments of investment securities and long-lived assets, including property and equipment.
Income Taxes
We record deferred tax assets and liabilities based on differences between the book and tax bases of assets and liabilities. The deferred tax assets and liabilities are calculated by applying enacted tax rates and laws to taxable years in which such differences are expected to reverse. We establish a valuation allowance in accordance with the provisions of Statement of Financial Accounting Standards (SFAS) No. 109,Accounting for Income Taxes (SFAS No. 109). We continually review the adequacy of the valuation allowance and recognize the benefits from our deferred tax assets only when an analysis of both positive and negative factors indicate that it is more likely than not that the benefits will be realized.
We file tax returns in many tax jurisdictions. Often, application of tax rules within the various jurisdictions is subject to differing interpretation. Despite our belief that our tax return positions are fully supportable, we believe that it is probable certain positions will be challenged by taxing authorities, and we may not prevail on
77
Table of Contents
the positions as filed. Accordingly, we maintain a liability for the estimated amount of contingent tax challenges by taxing authorities upon examination, in accordance with Financial Accounting Standards Board Interpretation No. 48,Accounting for Uncertainty in Income Taxes (FIN 48), which we adopted as of January 1, 2007. Prior to 2007, we maintained a liability pursuant to SFAS No. 5,Accounting for Contingencies. FIN 48 clarifies the accounting for uncertain taxes recognized in a company’s financial statements in accordance with SFAS No. 109. The interpretation requires us to analyze the amount at which each tax position meets a “more likely than not” standard for sustainability upon examination by taxing authorities. Only tax benefit amounts meeting or exceeding this standard will be reflected in tax provision expense and deferred tax asset balances. The interpretation also requires that any differences between the amounts of tax benefits reported on tax returns and tax benefits reported in the financial statements be recorded in a liability for unrecognized tax benefits. The liability for unrecognized tax benefits is reported separately from deferred tax assets and liabilities and classified as current or noncurrent based upon the expected period of payment. See Note 11 to the consolidated financial statements for additional disclosures related to FIN 48 policies and the impact of adoption.
Item 7A. Quantitative and Qualitative Disclosures About Market Risk.
We are exposed to interest rate and market risk primarily due to our investing and borrowing activities. Market risk generally represents the risk of loss that may result from the potential change in the value of a financial instrument as a result of fluctuations in interest rates and in equity prices. Interest rate risk is a consequence of maintaining variable interest rate earning investments and fixed rate liabilities or fixed income investments and variable rate liabilities. We are exposed to interest rate risks arising from changes in the level or volatility of interest rates, prepayment speeds and/or the shape and slope of the yield curve. In addition, we are exposed to the risk of loss related to changes in credit spreads. Credit spread risk arises from the potential changes in an issuer’s credit rating or credit perception that will affect the value of financial instruments.
We attempt to manage the interest rate risks related to our investment portfolios by actively managing the asset duration of our investment portfolios. The overall goal for the investment portfolios is to provide a source of liquidity and support the ongoing operations of our business units. Our philosophy is to actively manage assets to maximize total return over a multiple-year time horizon, subject to appropriate levels of risk. Each business unit has additional requirements with respect to liquidity, current income and contribution to surplus. We manage these risks by setting risk tolerances, targeting asset-class allocations, diversifying among assets and asset characteristics, and using performance measurement and reporting.
We use a value-at-risk (VAR) model, which follows a variance/co-variance methodology, to assess the market risk for our investment portfolio. VAR is a method of assessing investment risk that uses standard statistical techniques to measure the worst expected loss in the portfolio over an assumed portfolio disposition period under normal market conditions. The determination is made at a given statistical confidence level.
We assumed a portfolio disposition period of 30 days with a confidence level of 95% for the computation of VAR for 2008. The computation further assumes that the distribution of returns is normal. Based on such methodology and assumptions, the computed VAR was approximately $16.8 million as of December 31, 2008.
Our calculated VAR exposure represents an estimate of reasonably possible net losses that could be recognized on our investment portfolios assuming hypothetical movements in future market rates and are not necessarily indicative of actual results which may occur. It does not represent the maximum possible loss nor any expected loss that may occur, since actual future gains and losses will differ from those estimated, based upon actual fluctuations in market rates, operating exposures, and the timing thereof, and changes in our investment portfolios during the year.
Except for those securities held by trustees or regulatory agencies (see Note 2 to our consolidated financial statements), all of our investment securities are designated as “available-for-sale” assets. As such, they are reflected at their estimated fair value, with the difference between amortized cost and estimated fair value
78
Table of Contents
reflected in accumulated other comprehensive income, a component of Stockholders’ Equity (see Note 4 to the consolidated financial statements). Virtually, all of our investment securities are fixed income securities. Approximately 35% of our available-for-sale investment securities are mortgage-backed securities (MBS) and asset-backed securities (ABS). Approximately 98% of the MBS are backed by federal agencies. Therefore, we believe that our exposure to credit-related market value risk for our MBS is limited. Generally, in a rising interest rate environment, the estimated fair value of fixed income securities would be expected to decrease; conversely, in a decreasing interest rate environment, the estimated fair value of fixed income securities would be expected to increase. However, these securities may be negatively impacted by illiquidity in the market. The recent disruptions in the credit markets have negatively impacted the liquidity of investments. However, such disruptions did not have a material impact to the liquidity of our investments. A worsening of credit market disruptions or sustained market downturns could have negative effects on the liquidity and value of our investment assets.
Borrowings under our revolving credit facility, which totaled $150.0 million as of December 31, 2008, are subject to variable interest rates. For additional information regarding our revolving credit facility, see “Management’s Discussion and Analysis of Financial Condition and Results of Operations—Liquidity and Capital Resources.” Our floating rate borrowings, if any, are presumed to have equal book and fair values because the interest rates paid on these borrowings, if any, are based on prevailing market rates.
The fair value of our fixed rate borrowings, including our Senior Notes and financing facility as of December 31, 2008, was approximately $291.3 million, which was based on quoted market prices. Where quoted market prices were not readily available, fair values were estimated using valuation methodologies based on available and observable market information. Such valuation methodologies include reviewing the value ascribed to the most recent financing, comparing the security with securities of publicly traded companies in a similar line of business, and reviewing the underlying financial performance including estimating discounted cash flows. The following table presents the expected cash outflows relating to market risk sensitive debt obligations as of December 31, 2008. These cash outflows include expected principal and interest payments consistent with the terms of the outstanding debt as of December 31, 2008.
| 2009 | 2010 | 2011 | 2012 | 2013 | Thereafter | Total | ||||||||||||||||||||
| (Amounts in millions) | ||||||||||||||||||||||||||
Fixed-rate borrowings: | ||||||||||||||||||||||||||
Principal | $ | 35.0 | $ | 35.0 | $ | 35.0 | $ | 35.0 | $ | 7.8 | $ | 400.0 | $ | 547.8 | ||||||||||||
Interest | 25.5 | 25.5 | 25.5 | 25.5 | 25.5 | 86.2 | 213.7 | |||||||||||||||||||
Valuation of interest rate swap contracts | (3.0 | ) | (3.5 | ) | (1.7 | ) | (0.7 | ) | — | — | (8.9 | ) | ||||||||||||||
Cash outflow on fixed-rate borrowings | $ | 57.5 | $ | 57.0 | $ | 58.8 | $ | 59.8 | $ | 33.3 | $ | 486.2 | $ | 752.6 | ||||||||||||
| 2009 | 2010 | 2011 | 2012 | 2013 | Thereafter | Total | ||||||||||||||||||||
| (Amounts in millions) | ||||||||||||||||||||||||||
Floating-rate borrowings: | ||||||||||||||||||||||||||
Principal | $ | 35.0 | $ | — | $ | — | $ | 115.0 | $ | — | $ | — | $ | 150.0 | ||||||||||||
Interest | 2.5 | 2.2 | 2.9 | 2.3 | — | — | 9.9 | |||||||||||||||||||
Cash outflow on fixed-rate borrowings | $ | 37.5 | $ | 2.2 | $ | 2.9 | $ | 117.3 | $ | — | $ | — | $ | 159.9 | ||||||||||||
Total Cash outflow on borrowings | $ | 95.0 | $ | 59.2 | $ | 61.7 | $ | 177.1 | $ | 33.3 | $ | 486.2 | $ | 912.5 | ||||||||||||
Item 8. Financial Statements and Supplementary Data.
The financial statements listed on the accompanying Index to Consolidated Financial Statements set forth on page F-1 and covered by the Report of Independent Registered Public Accounting Firm are incorporated in this Item 8 by reference and filed as part of this Annual Report on Form 10-K.
79
Table of Contents
Item 9. Changes in and Disagreements with Accountants on Accounting and Financial Disclosure.
Not applicable.
Item 9A. Controls and Procedures.
Evaluation of Disclosure Controls and Procedures
We maintain disclosure controls and procedures (as such term is defined in Rules 13a-15(e) and 15d-15(e) under the Exchange Act) that are designed to ensure that information required to be disclosed in the reports we file or submit under the Exchange Act is recorded, processed, summarized and reported within the time periods specified in the SEC’s rules and forms, and that such information is accumulated and communicated to our management, including our Chief Executive Officer and our Chief Financial Officer, as appropriate, to allow timely decisions regarding required disclosure. In designing and evaluating the disclosure controls and procedures, management recognized that any controls and procedures, no matter how well designed and operated, can provide only reasonable assurance of achieving the desired control objectives, and management necessarily was required to apply its judgment in evaluating the cost-benefit relationship of possible controls and procedures.
As required by Rule 13a-15(b) under the Exchange Act, we carried out an evaluation, under the supervision and with the participation of our management, including our Chief Executive Officer and our Chief Financial Officer, of the effectiveness of the design and operation of our disclosure controls and procedures as of the end of the period covered by this report. Based upon the evaluation of the effectiveness of the design and operation of our disclosure controls and procedures as of the end of the period covered by this report, our Chief Executive Officer and Chief Financial Officer concluded that our disclosure controls and procedures were effective at the reasonable assurance level as of the end of such period.
Management’s Report on Internal Control Over Financial Reporting
Our management is responsible for establishing and maintaining adequate internal control over financial reporting, as such term is defined in Rules 13a-15(f) and 15d-15(f) under the Exchange Act. Our management, under the supervision and with the participation of our principal executive officer and principal financial officer, conducted an evaluation of the effectiveness of our internal control over financial reporting based on the framework inInternal Control—Integrated Framework issued by the Committee of Sponsoring Organizations of the Treadway Commission. Based on its evaluation, management concluded that our internal control over financial reporting was effective as of December 31, 2008.
Because of its inherent limitations, internal control over financial reporting may not prevent or detect misstatements. Projections of any evaluation of effectiveness to future periods are subject to the risks that controls may become inadequate because of changes in conditions, or that the degree of compliance with the policies or procedures may deteriorate.
Deloitte & Touche LLP, the independent registered public accounting firm that audited the financial statements included in this 2008 Annual Report on Form 10-K, has issued an attestation report on our internal control over financial reporting as of December 31, 2008, which is included herein.
Changes in Internal Control Over Financial Reporting
There have not been any changes in the Company’s internal control over financial reporting (as such term is defined in Rules 13a-15(f) and 15d-15(f) under the Exchange Act) during the fourth quarter ended December 31, 2008 that have materially affected, or are reasonably likely to materially affect, the Company’s internal control over financial reporting.
80
Table of Contents
REPORT OF INDEPENDENT REGISTERED PUBLIC ACCOUNTING FIRM
To the Board of Directors and Stockholders of
Health Net, Inc.
Woodland Hills, California
We have audited the internal control over financial reporting of Health Net, Inc., and subsidiaries (“the Company”) as of December 31, 2008, based on criteria established in Internal Control—Integrated Framework issued by the Committee of Sponsoring Organizations of the Treadway Commission. The Company’s management is responsible for maintaining effective internal control over financial reporting and for its assessment of the effectiveness of internal control over financial reporting included in the accompanying Management’s Report on Internal Control Over Financial Reporting. Our responsibility is to express an opinion on the Company’s internal control over financial reporting based on our audit.
We conducted our audit in accordance with the standards of the Public Company Accounting Oversight Board (United States). Those standards require that we plan and perform the audit to obtain reasonable assurance about whether effective internal control over financial reporting was maintained in all material respects. Our audit included obtaining an understanding of internal control over financial reporting, assessing the risk that a material weakness exists, testing and evaluating the design and operating effectiveness of internal control based on the assessed risk, and performing such other procedures as we considered necessary in the circumstances. We believe that our audit provides a reasonable basis for our opinion.
A company’s internal control over financial reporting is a process designed by, or under the supervision of, the company’s principal executive and principal financial officers, or persons performing similar functions, and effected by the company’s board of directors, management, and other personnel to provide reasonable assurance regarding the reliability of financial reporting and the preparation of financial statements for external purposes in accordance with generally accepted accounting principles. A company’s internal control over financial reporting includes those policies and procedures that (1) pertain to the maintenance of records that, in reasonable detail, accurately and fairly reflect the transactions and dispositions of the assets of the company; (2) provide reasonable assurance that transactions are recorded as necessary to permit preparation of financial statements in accordance with generally accepted accounting principles, and that receipts and expenditures of the company are being made only in accordance with authorizations of management and directors of the company; and (3) provide reasonable assurance regarding prevention or timely detection of unauthorized acquisition, use, or disposition of the company’s assets that could have a material effect on the financial statements.
Because of the inherent limitations of internal control over financial reporting, including the possibility of collusion or improper management override of controls, material misstatements due to error or fraud may not be prevented or detected on a timely basis. Also, projections of any evaluation of the effectiveness of the internal control over financial reporting to future periods are subject to the risk that the controls may become inadequate because of changes in conditions, or that the degree of compliance with the policies or procedures may deteriorate.
In our opinion, the Company maintained, in all material respects, effective internal control over financial reporting as of December 31, 2008, based on the criteria established in Internal Control—Integrated Framework issued by the Committee of Sponsoring Organizations of the Treadway Commission.
We have also audited, in accordance with the standards of the Public Company Accounting Oversight Board (United States), the consolidated financial statements and financial statement schedules as of and for the year ended December 31, 2008 of the Company and our report dated February 26, 2009 expressed an unqualified opinion on those financial statements and financial statement schedules.
/s/ DELOITTE & TOUCHE, LLP
Los Angeles, California
February 26, 2009
81
Table of Contents
None.
82
Table of Contents
Item 10. Directors, Executive Officers of the Registrant and Corporate Governance.
The information required by this Item as to (1) directors and executive officers of the Company and (2) compliance with Section 16(a) of the Securities Exchange Act of 1934 is set forth in the Company’s definitive proxy statement, which will be filed with the SEC within 120 days of December 31, 2008, under the captions “Director Nominees,” “Information Concerning Current Members of the Board of Directors and Nominees,” “Executive Officers,” “Corporate Governance” and “Section 16(a) Beneficial Ownership Reporting Compliance.” Such information is incorporated herein by reference and made a part hereof.
On May 30, 2008, the Company submitted to the New York Stock Exchange the Annual CEO Certification required pursuant to Section 303A.12(a) of the New York Stock Exchange Listed Company Manual.
We have adopted a Code of Business Conduct and Ethics that applies to our employees, directors and officers, including our principal executive officer, principal financial officer and principal accounting officer. The Code of Business Conduct and Ethics is posted on our Internet web site,www.healthnet.com. We intend to post on our Internet web site any amendment to or waiver from the Code of Business Conduct and Ethics that applies to our principal executive officer, principal financial officer or principal accounting officer and that is required to be disclosed under applicable rules and regulations of the SEC.
Item 11. Executive Compensation.
The information required by this Item is set forth in the Company’s definitive proxy statement, which will be filed with the SEC within 120 days of December 31, 2008, under the captions “Compensation Discussion & Analysis,” “Executive Compensation,” “Directors’ Compensation” and “Report of the Compensation Committee of the Board of Directors.” Such information is incorporated herein by reference and made a part hereof.
Item 12. Security Ownership of Certain Beneficial Owners and Management and Related Stockholder Matters.
The information required by this Item is set forth in the Company’s definitive proxy statement, which will be filed with the SEC within 120 days of December 31, 2008, under the captions “Security Ownership of Certain Beneficial Owners and Management” and “Equity Compensation Plan Information.” Such information is incorporated herein by reference and made a part hereof.
Item 13. Certain Relationships and Related Transactions, and Director Independence.
The information required by this Item is set forth in the Company’s definitive proxy statement, which will be filed with the SEC within 120 days of December 31, 2008, under the caption “Certain Relationships and Related Party Transactions” and “Corporate Governance—Director Independence.” Such information is incorporated herein by reference and made a part hereof.
Item 14. Principal Accountant Fees and Services.
The information required by this Item is set forth in the Company’s definitive proxy statement, which will be filed with the SEC within 120 days of December 31, 2008, under the caption “Principal Independent Registered Accounting Firm Fees and Services.” Such information is incorporated herein by reference and made a part hereof.
83
Table of Contents
Item 15. Exhibits and Financial Statement Schedules.
(a) Financial Statements, Schedules and Exhibits
1. Financial Statements
The financial statements listed on the accompanying Index to Consolidated Financial Statements set forth on page F-1 and covered by the Report of Independent Registered Public Accounting Firm are incorporated into this Item 15(a) by reference and filed as part of this Annual Report on Form 10-K.
2. Financial Statement Schedules
The financial statement schedules listed on the accompanying Index to Consolidated Financial Statements set forth on page F-1 and covered by the Report of Independent Registered Public Accounting Firm are incorporated into this Item 15(a) by reference and filed as part of this Annual Report on Form 10-K.
3. Exhibits
The following exhibits are filed as part of this Annual Report on Form 10-K or are incorporated herein by reference:
EXHIBIT INDEX
Exhibit Number | Description | |
| 3.1 | Sixth Amended and Restated Certificate of Incorporation of Health Net, Inc. (filed as Exhibit 3.1 to the Company’s Current Report on Form 8-K filed with the Commission on July 28, 2006 and incorporated herein by reference). | |
| 3.2 | Ninth Amended and Restated Bylaws of Health Net, Inc. (filed as Exhibit 3.2 to the Company’s Annual Report on Form 10-K for the year ended December 31, 2003 and incorporated herein by reference). | |
| 3.3 | Amendment Number One to Ninth Amended and Restated Bylaws of Health Net, Inc. (filed as Exhibit 3.1 to the Company’s Current Report on Form 8-K filed with the Commission on March 7, 2005 (File No. 1-12718) and incorporated herein by reference). | |
| 4.1 | Specimen Common Stock Certificate (filed as Exhibit 8 to the Company’s Registration Statement on Form 8-A/A (Amendment No. 3) (File No. 1-12718) on July 26, 2004 and incorporated herein by reference). | |
| 4.2 | Rights Agreement dated as of July 27, 2006, by and between Heath Net, Inc. and Wells Fargo Bank, N.A., as Rights Agent (filed as Exhibit 4.1 to the Company’s Current Report on Form 8-K filed with the Commission on July 28, 2006 (File No. 1-12718) and incorporated herein by reference). | |
| 4.3 | Indenture, dated as of May 18, 2007, by and between Health Net, Inc. as issuer, and The Bank of New York Trust Company, N.A., as trustee (filed as Exhibit 4.1 to the Company’s Current Report on Form 8-K filed with the SEC on May 18, 2007 (File No. 1-12718) and incorporated herein by reference). | |
| 4.4 | Officer’s Certificate, dated May 18, 2007, establishing the terms and form of the Company’s $300,000,000 aggregate principal amount of its 6.375% Senior Notes due 2017 (the “Notes”) (filed as Exhibit 4.2 to the Company’s Current Report on Form 8-K filed with the SEC on May 18, 2007 (File No. 1-12718) and incorporated herein by reference). | |
84
Table of Contents
Exhibit Number | Description | |
| 4.5 | Officer’s Certificate, dated May 31, 2007, establishing the terms and form of the Company’s $100,000,000 aggregate principal amount of its 6.375% Senior Notes due 2017 (the “Additional Notes”) (filed as Exhibit 4.1 to the Company’s Current Report on Form 8-K filed with the SEC on May 31, 2007 (File No. 1-12718) and incorporated herein by reference). | |
| †*10.1 | Amended and Restated Employment Agreement, dated as of December 3, 2008, by and between Health Net, Inc. and Karin Mayhew, a copy of which is filed herewith. | |
| †*10.2 | Amended and Restated Employment Agreement, dated as of December 3, 2008, by and between Health Net, Inc. and Patricia T. Clarey, a copy of which is filed herewith. | |
| †*10.3 | Amended and Restated Employment Agreement, dated as of December 3, 2008, by and between Health Net, Inc. and Jay M. Gellert, a copy of which is filed herewith. | |
| †*10.4 | Amended and Restated Employment Agreement, dated as of December 3, 2008, by and between James E. Woys and Health Net, Inc., a copy of which is filed herewith. | |
| †*10.5 | Amended and Restated Employment Agreement, dated as of December 3, 2008, by and between Joseph C. Capezza and Health Net, Inc., a copy of which is filed herewith. | |
| †*10.6 | Amended and Restated Employment Letter Agreement, dated as of December 3, 2008, by and between Health Net, Inc. and Stephen D. Lynch, a copy of which is filed herewith. | |
| †*10.7 | Amended and Restated Employment Agreement, dated as of December 3, 2008, by and between Health Net, Inc. and Linda Tiano, a copy of which is filed herewith. | |
| †*10.8 | Amended and Restated Employment Agreement, dated as of February 17, 2009, by and between Health Net, Inc. and John Sivori, a copy of which is filed herewith. | |
| †*10.9 | Amended and Restated Employment Agreement, dated as of February 17, 2009, by and between Health Net, Inc. and Steve Tough, a copy of which is filed herewith. | |
| *10.10 | Certain Compensation Arrangements With Respect to the Company’s Non-Employee Directors, as amended and restated on February 18, 2008 (filed as Exhibit 10.13 to the Company’s Annual Report on Form 10-K for the year ended December 31, 2007 (File No. 1-12718) and incorporated herein by reference). | |
| *10.11 | Form of Nonqualified Stock Option Agreement utilized for eligible employees of Health Net, Inc. (filed as Exhibit 10.4 to the Company’s Current Report on Form 8-K filed with the Commission on January 21, 2009 (File No. 1-12718) and incorporated herein by reference). | |
| *10.12 | Form of Restricted Stock Agreement utilized for eligible employees of Health Net, Inc. (filed as Exhibit 10.3 to the Company’s Current Report on Form 8-K filed with the Commission on January 21, 2009 (File No. 1-12718) and incorporated herein by reference). | |
| *10.13 | Form of Restricted Stock Unit Award Agreement utilized for eligible employees of Health Net, Inc. (filed as Exhibit 10.2 to the Company’s Current Report on Form 8-K filed with the Commission on January 21, 2009 (File No. 1-12718) and incorporated herein by reference). | |
| *10.14 | Form of Performance Share Award Agreement utilized for eligible employees of Health Net, Inc. (filed as Exhibit 10.1 to the Company’s Current Report on Form 8-K filed with the Commission on January 21, 2009 (File No. 1-12718) and incorporated herein by reference). | |
| *10.15 | Form of 2007 Performance Award Agreement for CEO of Health Net, Inc. (filed as Exhibit 10.2 to the Company’s Current Report on Form 8-K filed with the Commission on February 28, 2007 (File No. 1-12718) and incorporated herein by reference). | |
85
Table of Contents
Exhibit Number | Description | |
| *10.16 | Form of Nonqualified Stock Option Agreement utilized for non-employee directors under the 2006 Long-Term Incentive Plan (filed as Exhibit 10.5 to the Company’s Current Report on Form 8-K filed with the Commission on January 21, 2009 (File No. 1-12718) and incorporated herein by reference). | |
| *10.17 | Form of Nonqualified Stock Option Agreement utilized for non-employee directors under the Third Amended and Restated Non-Employee Director Stock Option Plan (filed as Exhibit 10.22 to the Company’s Annual Report on Form 10-K for the year ended December 31, 2004 (File No. 1-12718) and incorporated herein by reference). | |
| *10.18 | Form of Nonqualified Stock Option Agreement utilized for non-employee directors under the Health Net, Inc. Amended and Restated 1998 Stock Option Plan (filed as Exhibit 10.6 to the Company’s Current Report on Form 8-K filed with the Commission on January 21, 2009 (File No. 1-12718) and incorporated herein by reference). | |
| †*10.19 | Health Net, Inc. Deferred Compensation Plan, as amended and restated effective November 12, 2007, a copy of which is filed herewith. | |
| *10.20 | Amendment No. 1 to the Health Net, Inc. Deferred Compensation Plan dated December 3, 2008 (filed as Exhibit 10.4 to the Company’s Current Report on Form 8-K filed with the Commission on December 9, 2008 (File No. 1-12718) and incorporated herein by reference). | |
| †*10.21 | Health Net, Inc. Deferred Compensation Plan for Directors, as amended and restated effective November 12, 2007, a copy of which is filed herewith. | |
| *10.22 | Amendment No. 1 to the Health Net, Inc. Deferred Compensation Plan for Directors dated December 3, 2008 (filed as Exhibit 10.5 to the Company’s Current Report on Form 8-K filed with the Commission on December 9, 2008 (File No. 1-12718) and incorporated herein by reference). | |
| *10.23 | Health Net, Inc. (formerly Foundation Health Systems, Inc.) Deferred Compensation Plan Trust Agreement effective September 1, 1998 between Foundation Health Systems, Inc. and Union Bank of California (filed as Exhibit 10.31 to the Company’s Annual Report on Form 10-K for the year ended December 31, 1998 (File No. 1-12718) and incorporated herein by reference). | |
| *10.24 | Amendment Number One to the Health Net, Inc. (formerly Foundation Health Systems, Inc.) Deferred Compensation Plan Trust Agreement between Health Net, Inc. and Union Bank of California, adopted January 1, 2001 (filed as Exhibit 10.27 to the Company’s Annual Report on Form 10-K for the year ended December 31, 2004 (File No. 1-12718) and incorporated herein by reference). | |
| *10.25 | Foundation Health Systems, Inc. Second Amended and Restated 1991 Stock Option Plan (filed as Exhibit 10.16 to the Company’s Quarterly Report on Form 10-Q for the quarter ended September 30, 2000 (File No. 1-12718) and incorporated herein by reference). | |
| *10.26 | Amendment to Second Amended and Restated 1991 Stock Option Plan (filed as Exhibit 10.15 to the Company’s Annual Report on Form 10-K for the year ended December 31, 2000 (File No. 1-12718) and incorporated herein by reference). | |
| *10.27 | Foundation Health Systems, Inc. 1997 Stock Option Plan (as amended and restated on May 4, 2000) (filed as Exhibit 10.45 to the Company’s Quarterly Report on Form 10-Q for the quarter ended June 30, 1997 (File No. 1-12718) and incorporated herein by reference). | |
| *10.28 | Amendment to 1997 Stock Option Plan (filed as Exhibit 10.17 to the Company’s Annual Report on Form 10-K for the year ended December 31, 2000 (File No. 1-12718) and incorporated herein by reference). | |
86
Table of Contents
Exhibit Number | Description | |
| *10.29 | Second Amendment to 1997 Stock Option Plan (filed as Exhibit 10.25 to the Company’s Quarterly Report on Form 10-Q for the quarter ended June 30, 2002 (file No. 1-12718) and incorporated herein by reference). | |
| *10.30 | Foundation Health Systems, Inc. Amended and Restated 1998 Stock Option Plan (filed as Exhibit 10.1 to the Company’s Current Report on Form 8-K filed with the Commission on August 16, 2004 (File No. 1-12718) and incorporated herein by reference). | |
| *10.31 | Amendment No. 1 to Foundation Health Systems, Inc. Amended and Restated 1998 Stock Option Plan (filed as Exhibit 10.1 to the Company’s Current Report on Form 8-K filed with the Commission on March 6, 2006 (File No. 1-12718) and incorporated herein by reference). | |
| †*10.32 | Amendment No. 2 to Foundation Health Systems, Inc. Amended and Restated 1998 Stock Option Plan dated January 14, 2009, a copy of which is filed herewith. | |
| *10.33 | Health Net, Inc. 2002 Stock Option Plan (filed as Exhibit 10.29 to the Company’s Quarterly Report on Form 10-Q for the quarter ended June 30, 2002 (file No. 1-12718) and incorporated herein by reference). | |
| *10.34 | Health Net, Inc. 2005 Long-Term Incentive Plan (filed as Exhibit 10.3 to the Company’s Current Report on Form 8-K filed with the Commission on May 13, 2005 (File No. 1-12718) and incorporated herein by reference). | |
| †*10.35 | Amendment No. 1 to Health Net, Inc. 2005 Long-Term Incentive Plan dated December 4, 2008, a copy of which is filed herewith. | |
| †*10.36 | Amendment No. 2 to Health Net, Inc. 2005 Long-Term Incentive Plan dated January 14, 2009, a copy of which is filed herewith. | |
| *10.37 | Health Net, Inc. 2006 Long-Term Incentive Plan (as filed as Exhibit 10.1 to the Company’s Current Report on Form 8-K filed with the Commission on May 15, 2006 and incorporated herein by reference). | |
| †*10.38 | Amendment No. 1 to Health Net, Inc. 2006 Long-Term Incentive Plan dated January 14, 2009, a copy of which is filed herewith. | |
| *10.39 | Health Net, Inc. 2006 Executive Officer Incentive Plan (filed as Exhibit 10.1 to the Company’s Current Report on Form 8-K filed with the Commission on May 13, 2005 (File No. 1-12718) and incorporated herein by reference). | |
| *10.40 | Amendment One to the Health Net, Inc. 2006 Executive Officer Incentive Plan (filed as Exhibit 10.2 to the Company’s Current Report on Form 8-K filed with the Commission on May 13, 2005 (File No. 1-12718 and incorporated herein by reference). | |
| †*10.41 | Amendment No. 2 to the Health Net, Inc. 2006 Executive Officer Incentive Plan dated November 12, 2008, a copy of which is filed herewith. | |
| *10.42 | Health Systems International, Inc. Second Amended and Restated Non-Employee Director Stock Option Plan (filed as Exhibit 10.31 to Registration Statement on Form S-4 (File No. 33-86524) on November 18, 1994 and incorporated herein by reference). | |
| *10.43 | Foundation Health Systems, Inc. Third Amended and Restated Non-Employee Director Stock Option Plan (filed as Exhibit 10.46 to the Company’s Quarterly Report on Form 10-Q for the quarter ended June 30, 1997 (File No. 1-12718) and incorporated herein by reference). | |
| *10.44 | Health Net, Inc. Management Incentive Plan adopted December 2004 (filed as Exhibit 10.40 to the Company’s Annual Report on Form 10-K for the year ended December 31, 2004 (File No. 1-12718) and incorporated herein by reference). | |
87
Table of Contents
Exhibit Number | Description | |
| †*10.45 | Amendment No. 1 to Health Net, Inc. Management Incentive Plan dated November 12, 2008, a copy of which is filed herewith. | |
| †*10.46 | Health Net, Inc. 401(k) Savings Plan as amended and restated effective January 1, 2008, a copy of which is filed herewith. | |
| *10.47 | Amended and Restated Health Net, Inc. Supplemental Executive Retirement Plan effective as of January 1, 2008 (filed as Exhibit 10.1 to the Company’s Current Report on Form 8-K filed December 9, 2008 (File No. 1-12718) and incorporated herein by reference). | |
| *10.48 | Amended and Restated Deferred Compensation Plan of Foundation Health Corporation (filed as Exhibit 10.99 to Foundation Health Corporation’s Annual Report on Form 10-K for the year ended June 30, 1995 (File No. 1-10540) and incorporated herein by reference). | |
| *10.49 | Amendment Number One Through Three to the Amended and Restated Deferred Compensation Plan of Foundation Health Corporation (filed as Exhibit 10.49 to the Company’s Annual Report on Form 10-K for the year ended December 31, 2004 (File No. 1-12718) and incorporated herein by reference). | |
| *10.50 | Foundation Health Corporation Executive Retiree Medical Plan (as amended and restated effective April 25, 1995) (filed as Exhibit 10.101 to Foundation Health Corporation’s Annual Report on Form 10-K for the year ended June 30, 1995 (File No. 1-10540) and incorporated herein by reference). | |
| 10.51 | Participation Agreement dated as of December 19, 2007, by and among Health Net Funding, Inc., Health Net, Inc., Lodgemore Holdings, Inc. ING Bank, N.V. and Health Net Financing, L.P. (filed as Exhibit 10.1 to the Company’s Current Report on Form 8-K filed with the SEC on December 20, 2007 (File No. 1-12718) and incorporated herein by reference). | |
| 10.52 | First Amendment to Participation Agreement, dated as of April 29, 2008, by and among Health Net, Inc., Health Net Funding, Inc., Lodgemore Holdings, Inc., ING Bank, N.V. and Health Net Financing, LP (filed as Exhibit 10.1 to the Company’s Quarterly Report on Form 10-Q for the quarter ended March 31, 2008 (File No. 1-12718) and incorporated herein by reference). | |
| †10.53 | Omnibus Amendment to Participation Agreement and Put Option Agreement dated as of November 10, 2008 by and among Health Net Funding, Inc., Health Net, Inc., Lodgemore Holdings Inc., ING Bank N.V. and Health Net Financing, L.P., a copy of which is filed herewith. | |
| 10.54 | Credit Agreement, dated as of June 25, 2007, by and among Health Net, Inc., Bank of America, N.A., as Administrative Agent, Swing Line Lender and L/C Issuer, JP Morgan Chase Bank, N.A., as Syndication Agent, Citicorp USA, Inc., as Documentation Agent, the other lenders party thereto and Banc of America Securities LLC and J.P. Morgan Securities Inc., as Joint Lead Arrangers and as Co-Book Managers (filed as Exhibit 10 to the Company’s Current Report on Form 8-K filed with the SEC on June 27, 2007 (File No. 1-12718) and incorporated herein by reference). | |
| 10.55 | First Amendment to Credit Agreement, dated as of April 29, 2008, by and among Health Net, Inc., Bank of America, N.A., as Administrative Agent and the other lenders party thereto (filed as Exhibit 10.1 to the Company’s Quarterly Report on Form 10-Q for the quarter ended March 31, 2008 (File No. 1-12718) and incorporated herein by reference). | |
| ^10.56 | Master Agreement, dated August 19, 2008, between Health Net, Inc. and International Business Machines Corporation (filed as Exhibit 10.1 to the Company’s Quarterly Report on Form 10-Q for the quarter ended September 30, 2008 (File No. 1-12718) and incorporated herein by reference). | |
88
Table of Contents
Exhibit Number | Description | |
| ^10.57 | Master Services Agreement, dated September 30, 2008, between Health Net, Inc. and Cognizant Technology Solutions U.S. Corporation (filed as Exhibit 10.2 to the Company’s Quarterly Report on Form 10-Q for the quarter ended September 30, 2008 (File No. 1-12718) and incorporated herein by reference). | |
| *10.58 | Form of Amended and Restated Indemnification Agreement for directors and executive officers of Health Net, Inc. (filed as Exhibit 10.3 to the Company’s Current Report on Form 8-K filed with the Commission on December 9, 2008 (File No. 1-12718) and incorporated herein by reference). | |
| 10.59 | First Amendment to Office Lease, dated May 14, 2001, by and between Health Net (a California corporation) and LNR Warner Center, LLC (filed as Exhibit 10.38 to the Company’s Annual Report on Form 10-K for the year ended December 31, 2001 (File No. 1-12718) and incorporated herein by reference). | |
| 10.60 | Lease Agreements, dated as of March 5, 2001, by and between Health Net, Inc. and Landhold, Inc. (filed as Exhibit 10.44 to the Company’s Annual Report on Form 10-K for the year ended December 31, 2003 (File No. 1-12718) and incorporated herein by reference). | |
| †10.61 | Amendment No. 1 to Lease Agreement, dated as of November 22, 2002, by and between Gold Pointe C, LLC, as successor-in-interest to Landhold, Inc., and Health Net, Inc., a copy of which is filed herewith. | |
| †10.62 | Amendment No. 2 to Lease Agreement, dated as of April 28, 2006, by and between McMorgan Institutional Real Estate Fund I, LLC, as successor-in-interest to Landhold, Inc., and Health Net, Inc., a copy of which is filed herewith. | |
| †10.63 | Amendment No. 1 to Lease Agreement, dated as of November 22, 2002, by and between Gold Pointe D, LLC, as successor-in-interest to Landhold, Inc., and Health Net, Inc., a copy of which is filed herewith. | |
| †10.64 | Standard Lease Agreement, dated as of July 24, 2006, by and between Panattoni Development Company and Health Net, Inc., a copy of which is filed herewith. | |
| †10.65 | First Amendment to Lease and Acknowledgment, dated as of February 8, 2007, by and between Panattoni Development Company and Health Net of California, Inc., a copy of which is filed herewith. | |
| †10.66 | Office Building Lease, dated as of July 13, 1995, by and between Aerojet-General Corporation and Foundation Health, a copy of which is filed herewith. | |
| †10.67 | Addendums 1-12 to Office Building Lease, by and between Aerojet-General Corporation and Health Net Federal Services, LLC, a copy of which is filed herewith. | |
| 10.68 | Office Lease Agreement, dated as of December 22, 2003, by and between Health Net, Inc. and Douglas Emmett Realty Fund 2000 L.P. (filed as Exhibit 10.46 to the Company’s Annual Report on Form 10-K for the year ended December 31, 2003 (File No. 1-12718) and incorporated herein by reference). | |
| 10.69 | Office Lease, dated September 20, 2000, by and among Health Net of California, Inc., DCA Homes, Inc. and Lennar Rolling Ridge, Inc. (filed as Exhibit 10.46 to the Company’s Quarterly Report on Form 10-Q for the quarter ended September 30, 2000 (File No. 1-12718) and incorporated herein by reference). | |
| 10.70 | Office Lease Agreement, dated August 18, 2000, by and between Physicians Health Services of Connecticut, Inc. (predecessor to Health Net of Connecticut, Inc.) and Beard Sawmill, LLC (filed as Exhibit 10.68 to the Company’s Annual Report on Form 10-K for the year ended December 31, 2005 (File No. 1-12718) and incorporated herein by reference). | |
89
Table of Contents
Exhibit Number | Description | |
| 10.71 | First Amendment to Office Lease Agreement, dated December 23, 2002, by and between Health Net of Connecticut, Inc. and Beard Sawmill, LLC (filed as Exhibit 10.67 to the Company’s Annual Report on Form 10-K for the year ended December 31, 2005 (File No. 1-12718) and incorporated herein by reference). | |
| 10.72 | Second Amendment to Office Lease Agreement, dated June 14, 2004, by and between Health Net of Connecticut, Inc. and Beard Sawmill, LLC (filed as Exhibit 10.66 to the Company’s Annual Report on Form 10-K for the year ended December 31, 2005 (File No. 1-12718) and incorporated herein by reference). | |
| 10.73 | Absolute Net Lease, dated as of March 29, 2007, by and between HN Property Owner LLC and Health Net of the Northeast (filed as Exhibit 10.1 to the Company’s Quarterly Report on Form 10-Q for the quarter ended March 31, 2007 (File No. 1-12718) and incorporated herein by reference). | |
| †11 | Statement relative to computation of per share earnings of the Company (included in Note 2 to the consolidated financial statements included as part of this Annual Report on Form 10-K). | |
| †21 | Subsidiaries of Health Net, Inc., a copy of which is filed herewith. | |
| †23 | Consent of Deloitte & Touche LLP, Independent Registered Public Accounting Firm, a copy of which is filed herewith. | |
| †31.1 | Certification of Chief Executive Officer pursuant to Section 302 of the Sarbanes-Oxley Act of 2002, a copy of which is filed herewith. | |
| †31.2 | Certification of Chief Financial Officer pursuant to Section 302 of the Sarbanes-Oxley Act of 2002, a copy of which is filed herewith. | |
| †32 | Certification of Chief Executive Officer and Chief Financial Officer pursuant to 18 U.S.C. Section 1350, as adopted pursuant to Section 906 of the Sarbanes-Oxley Act of 2002, a copy of which is filed herewith. | |
| * | Management contract or compensatory plan or arrangement required to be filed (and/or incorporated by reference) as an exhibit to this Annual Report on Form 10-K pursuant to Item 15(c) of Form 10-K. |
| † | A copy of the exhibit is being filed with this Annual Report on Form 10-K. |
| ^ | This exhibit has been redacted pursuant to a request for confidential treatment under Rule 24b-2 of the Securities Exchange Act of 1934, as amended. |
90
Table of Contents
Pursuant to the requirements of Section 13 or 15(d) of the Securities Exchange Act of 1934, the registrant has duly caused this report to be signed on its behalf by the undersigned thereunto duly authorized.
| HEALTH NET, INC. | ||
| By: | /s/ JOSEPH C. CAPEZZA | |
| Joseph C. Capezza | ||
| Chief Financial Officer | ||
Pursuant to the requirements of the Securities Exchange Act of 1934, this report has been signed below by the following persons on behalf of the registrant and in the capacities and on the dates indicated.
Signature | Title | Date | ||
/s/ JAY M. GELLERT Jay M. Gellert | President and Chief Executive Officer and Director (Principal Executive Officer) | February 17, 2009 | ||
/s/ JOSEPH C. CAPEZZA Joseph C. Capezza | Chief Financial Officer (Principal Financial Officer) | February 17, 2009 | ||
/s/ BRET A. MORRIS Bret A. Morris | Senior Vice President and Corporate Controller (Principal Accounting Officer) | February 17, 2009 | ||
/s/ THEODORE F. CRAVER, JR. Theodore F. Craver, Jr. | Director | February 17, 2009 | ||
/s/ VICKI B. ESCARRA Vicki B. Escarra | Director | February 17, 2009 | ||
/s/ THOMAS T. FARLEY Thomas T. Farley | Director | February 17, 2009 | ||
/s/ GALE S. FITZGERALD Gale S. Fitzgerald | Director | February 17, 2009 | ||
/s/ PATRICK FOLEY Patrick Foley | Director | February 17, 2009 | ||
/s/ ROGER F. GREAVES Roger F. Greaves | Director | February 17, 2009 | ||
/s/ BRUCE G. WILLISON Bruce G. Willison | Director | February 17, 2009 | ||
/s/ FREDERICK C. YEAGER Frederick C. Yeager | Director | February 17, 2009 | ||
91
Table of Contents
INDEX TO CONSOLIDATED FINANCIAL STATEMENTS
The following consolidated financial statements and financial statement schedules are filed as part of this Annual Report on Form 10-K:
Consolidated Financial Statements | ||
| F-2 | ||
F-3 | ||
Consolidated Balance Sheets as of December 31, 2008 and 2007 | F-4 | |
F-5 | ||
F-6 | ||
| F-7 | ||
Financial Statement Schedules | ||
Schedule I—Condensed Financial Information of Registrant (Parent Company Only) | F-55 | |
| F-59 | ||
F-1
Table of Contents
REPORT OF INDEPENDENT REGISTERED PUBLIC ACCOUNTING FIRM
To the Board of Directors and Stockholders of
Health Net, Inc.
Woodland Hills, California
We have audited the accompanying consolidated balance sheets of Health Net, Inc. and subsidiaries (the “Company”) as of December 31, 2008 and 2007, and the related consolidated statements of operations, stockholders’ equity, and cash flows for each of the three years in the period ended December 31, 2008. Our audits also included the financial statement schedules listed in the Index at Page F-1. These financial statements and financial statement schedules are the responsibility of the Company’s management. Our responsibility is to express an opinion on the financial statements and financial statement schedules based on our audits.
We conducted our audits in accordance with the standards of the Public Company Accounting Oversight Board (United States). Those standards require that we plan and perform the audit to obtain reasonable assurance about whether the financial statements are free of material misstatement. An audit includes examining, on a test basis, evidence supporting the amounts and disclosures in the financial statements. An audit also includes assessing the accounting principles used and significant estimates made by management, as well as evaluating the overall financial statement presentation. We believe that our audits provide a reasonable basis for our opinion.
In our opinion, such consolidated financial statements present fairly, in all material respects, the financial position of Health Net, Inc. and subsidiaries at December 31, 2008 and 2007, and the results of their operations and their cash flows for each of the three years in the period ended December 31, 2008, in conformity with accounting principles generally accepted in the United States of America. Also, in our opinion, such financial statement schedules, when considered in relation to the basic consolidated financial statements taken as a whole, present fairly, in all material respects, the information set forth therein.
As discussed in Note 11 to the consolidated financial statements, on January 1, 2007, the Company adopted Financial Accounting Standards Board (“FASB”) Interpretation No. 48, “Accounting for Uncertainty in Income Taxes”. Also, as discussed in Note 2 to the consolidated financial statements, the Company changed its method of accounting for share-based compensation in 2006 upon adoption of FASB Statement No. 123(R), “Share-Based Payment.”
We have also audited, in accordance with the standards of the Public Company Accounting Oversight Board (United States), the Company’s internal control over financial reporting as of December 31, 2008, based on the criteria established inInternal Control—Integrated Framework issued by the Committee of Sponsoring Organizations of the Treadway Commission and our report dated February 26, 2009 expressed an unqualified opinion on the Company’s internal control over financial reporting.
/s/ DELOITTE & TOUCHE LLP
Los Angeles, California
February 26, 2009
F-2
Table of Contents
CONSOLIDATED STATEMENTS OF OPERATIONS
(Amounts in thousands, except per share data)
| Year Ended December 31, | |||||||||
| 2008 | 2007 | 2006 | |||||||
Revenues | |||||||||
Health plan services premiums | $ | 12,392,006 | $ | 11,435,314 | $ | 10,364,740 | |||
Government contracts | 2,835,261 | 2,501,677 | 2,376,014 | ||||||
Net investment income | 91,042 | 120,176 | 111,042 | ||||||
Administrative services fees and other income | 48,280 | 51,104 | 56,554 | ||||||
Total revenues | 15,366,589 | 14,108,271 | 12,908,350 | ||||||
Expenses | |||||||||
Health plan services (excluding depreciation and amortization) | 10,762,657 | 9,762,896 | 8,600,443 | ||||||
Government contracts | 2,702,573 | 2,307,610 | 2,234,535 | ||||||
General and administrative | 1,291,059 | 1,275,555 | 1,165,313 | ||||||
Selling | 360,381 | 327,827 | 245,304 | ||||||
Depreciation and amortization | 59,878 | 42,982 | 25,591 | ||||||
Interest | 42,909 | 32,497 | 51,179 | ||||||
Debt refinancing charge | — | — | 70,095 | ||||||
Litigation | — | — | 37,093 | ||||||
Total expenses | 15,219,457 | 13,749,367 | 12,429,553 | ||||||
Income from operations before income taxes | 147,132 | 358,904 | 478,797 | ||||||
Income tax provision | 52,129 | 165,207 | 149,484 | ||||||
Net income | $ | 95,003 | $ | 193,697 | $ | 329,313 | |||
Net income per share: | |||||||||
Basic | $ | 0.89 | $ | 1.74 | $ | 2.86 | |||
Diluted | $ | 0.88 | $ | 1.70 | $ | 2.78 | |||
Weighted average shares outstanding: | |||||||||
Basic | 106,532 | 111,316 | 115,128 | ||||||
Diluted | 107,610 | 113,829 | 118,310 | ||||||
See accompanying notes to consolidated financial statements.
F-3
Table of Contents
CONSOLIDATED BALANCE SHEETS
(Amounts in thousands, except per share data)
| December 31, | ||||||||
| 2008 | 2007 | |||||||
ASSETS | ||||||||
Current Assets: | ||||||||
Cash and cash equivalents | $ | 668,201 | $ | 1,007,017 | ||||
Investments—available for sale (amortized cost: 2008—$1,516,316, 2007—$1,557,411) | 1,504,658 | 1,557,278 | ||||||
Premiums receivable, net of allowance for doubtful accounts (2008—$13,567, 2007—$6,724) | 307,529 | 264,691 | ||||||
Amounts receivable under government contracts | 241,269 | 189,976 | ||||||
Incurred but not reported (IBNR) health care costs receivable under TRICARE North contract | 302,022 | 266,767 | ||||||
Other receivables | 254,026 | 72,518 | ||||||
Deferred taxes | 87,712 | 132,818 | ||||||
Other assets | 179,649 | 210,039 | ||||||
Total current assets | 3,545,066 | 3,701,104 | ||||||
Property and equipment, net | 202,356 | 178,758 | ||||||
Goodwill | 751,949 | 751,949 | ||||||
Other intangible assets, net | 91,289 | 109,386 | ||||||
Deferred taxes | 81,771 | 47,765 | ||||||
Other noncurrent assets | 143,919 | 144,093 | ||||||
Total Assets | $ | 4,816,350 | $ | 4,933,055 | ||||
LIABILITIES AND STOCKHOLDERS’ EQUITY | ||||||||
Current Liabilities: | ||||||||
Reserves for claims and other settlements | $ | 1,338,149 | $ | 1,300,432 | ||||
Health care and other costs payable under government contracts | 69,876 | 69,014 | ||||||
IBNR health care costs payable under TRICARE North contract | 302,022 | 266,767 | ||||||
Unearned premiums | 180,548 | 176,981 | ||||||
Loans payable and other financing arrangement | 27,335 | 35,000 | ||||||
Accounts payable and other liabilities | 294,840 | 463,823 | ||||||
Total current liabilities | 2,212,770 | 2,312,017 | ||||||
Senior notes payable | 398,276 | 398,071 | ||||||
Borrowings under amortizing financing facility | 103,992 | 112,363 | ||||||
Borrowings under revolving credit facility | 150,000 | — | ||||||
Other noncurrent liabilities | 199,186 | 235,022 | ||||||
Total Liabilities | 3,064,224 | 3,057,473 | ||||||
Commitments and contingencies | ||||||||
Stockholders’ Equity: | ||||||||
Preferred stock ($0.001 par value, 10,000 shares authorized, none issued and outstanding) | — | — | ||||||
Common stock ($0.001 par value, 350,000 shares authorized; issued 2008—143,753 shares; 2007—143,477) | 144 | 144 | ||||||
Additional paid-in capital | 1,182,067 | 1,151,251 | ||||||
Treasury common stock, at cost (2008—40,045 shares of common stock; 2007—33,178 shares of common stock) | (1,367,319 | ) | (1,123,750 | ) | ||||
Retained earnings | 1,944,100 | 1,849,097 | ||||||
Accumulated other comprehensive loss | (6,866 | ) | (1,160 | ) | ||||
Total Stockholders’ Equity | 1,752,126 | 1,875,582 | ||||||
Total Liabilities and Stockholders’ Equity | $ | 4,816,350 | $ | 4,933,055 | ||||
See accompanying notes to consolidated financial statements.
F-4
Table of Contents
CONSOLIDATED STATEMENTS OF STOCKHOLDERS’ EQUITY
(Amounts in thousands)
| Common Stock | Restricted Common Stock | Unearned Compensation | Additional Paid-In Capital | Common Stock Held in Treasury | Retained Earnings | Accumulated Other Comprehensive (Loss) Income | Total | |||||||||||||||||||||||||||||
| Shares | Amount | Shares | Amount | |||||||||||||||||||||||||||||||||
Balance as of January 1, 2006 | 137,898 | $ | 137 | $ | 6,883 | $ | (2,137 | ) | $ | 906,789 | (23,182 | ) | $ | (633,375 | ) | $ | 1,324,165 | $ | (13,387 | ) | $ | 1,589,075 | ||||||||||||||
Comprehensive income: | ||||||||||||||||||||||||||||||||||||
Net income | 329,313 | 329,313 | ||||||||||||||||||||||||||||||||||
Minimum pension liability adjustment (pre-SFAS No. 158) | 39 | 39 | ||||||||||||||||||||||||||||||||||
Change in unrealized loss on investments, net of tax impact of $2,585 | 4,111 | 4,111 | ||||||||||||||||||||||||||||||||||
Total comprehensive income | 333,463 | |||||||||||||||||||||||||||||||||||
Exercise of stock options | 2,852 | 3 | 74,968 | 74,971 | ||||||||||||||||||||||||||||||||
Share-based compensation expense | 21,074 | 21,074 | ||||||||||||||||||||||||||||||||||
Tax benefit related to equity compensation plans | 19,803 | 19,803 | ||||||||||||||||||||||||||||||||||
Defined benefit pension plans adjustment (adoption of SFAS No. 158) | (2,000 | ) | (2,000 | ) | ||||||||||||||||||||||||||||||||
Repurchases of common stock | (5,633 | ) | (257,919 | ) | (257,919 | ) | ||||||||||||||||||||||||||||||
Forfeiture of restricted stock | (60 | ) | (1,113 | ) | (1,113 | ) | ||||||||||||||||||||||||||||||
Amortization of restricted stock grants | 1,611 | 1,611 | ||||||||||||||||||||||||||||||||||
Reclassification in connection with adopting SFAS No. 123(R) | (6,883 | ) | 2,137 | 4,746 | — | |||||||||||||||||||||||||||||||
Balance as of December 31, 2006 | 140,690 | $ | 140 | $ | — | $ | — | $ | 1,027,878 | (28,815 | ) | $ | (891,294 | ) | $ | 1,653,478 | $ | (11,237 | ) | $ | 1,778,965 | |||||||||||||||
Implementation of FIN 48 | 1,922 | 1,922 | ||||||||||||||||||||||||||||||||||
Adjusted balance as of January 1, 2007 | 140,690 | $ | 140 | $ | — | $ | — | $ | 1,027,878 | (28,815 | ) | $ | (891,294 | ) | $ | 1,655,400 | $ | (11,237 | ) | $ | 1,780,887 | |||||||||||||||
Comprehensive income: | ||||||||||||||||||||||||||||||||||||
Net income | 193,697 | 193,697 | ||||||||||||||||||||||||||||||||||
Change in unrealized loss on investments, net of tax impact of $5,738 | 8,885 | 8,885 | ||||||||||||||||||||||||||||||||||
Defined benefit pension plans: | ||||||||||||||||||||||||||||||||||||
Prior service cost and net loss | 1,192 | 1,192 | ||||||||||||||||||||||||||||||||||
Total comprehensive income | 203,774 | |||||||||||||||||||||||||||||||||||
Exercise of stock options | 2,657 | 4 | 73,005 | 73,009 | ||||||||||||||||||||||||||||||||
Share-based compensation expense | 24,294 | 24,294 | ||||||||||||||||||||||||||||||||||
Tax benefit related to equity compensation plans | 26,197 | 26,197 | ||||||||||||||||||||||||||||||||||
Repurchases of common stock and accelerated stock repurchase settlement | 133 | (125 | ) | (4,363 | ) | (232,456 | ) | (232,581 | ) | |||||||||||||||||||||||||||
Forfeiture of restricted stock | (3 | ) | (94 | ) | (94 | ) | ||||||||||||||||||||||||||||||
Amortization of restricted stock grants | 96 | 96 | ||||||||||||||||||||||||||||||||||
Balance as of January 1, 2008 | 143,477 | $ | 144 | $ | — | $ | — | $ | 1,151,251 | (33,178 | ) | $ | (1,123,750 | ) | $ | 1,849,097 | $ | (1,160 | ) | $ | 1,875,582 | |||||||||||||||
Comprehensive income: | ||||||||||||||||||||||||||||||||||||
Net income | 95,003 | 95,003 | ||||||||||||||||||||||||||||||||||
Change in unrealized loss on investments, net of tax impact of $4,319 | (7,207 | ) | (7,207 | ) | ||||||||||||||||||||||||||||||||
Defined benefit pension plans: | ||||||||||||||||||||||||||||||||||||
Prior service cost and net loss | 1,501 | 1,501 | ||||||||||||||||||||||||||||||||||
Total comprehensive income | 89,297 | |||||||||||||||||||||||||||||||||||
Exercise of stock options and vesting of restricted stock units | 276 | 6,679 | 6,679 | |||||||||||||||||||||||||||||||||
Share-based compensation expense | 24,065 | 24,065 | ||||||||||||||||||||||||||||||||||
Tax benefit related to equity compensation plans | 72 | 72 | ||||||||||||||||||||||||||||||||||
Repurchases of common stock and accelerated stock repurchase agreement | (6,867 | ) | (243,569 | ) | (243,569 | ) | ||||||||||||||||||||||||||||||
Balance as of December 31, 2008 | 143,753 | $ | 144 | $ | — | $ | — | $ | 1,182,067 | (40,045 | ) | $ | (1,367,319 | ) | $ | 1,944,100 | $ | (6,866 | ) | $ | 1,752,126 | |||||||||||||||
See accompanying notes to consolidated financial statements.
F-5
Table of Contents
CONSOLIDATED STATEMENTS OF CASH FLOWS
(Amounts in thousands)
| Year Ended December 31, | ||||||||||||
| 2008 | 2007 | 2006 | ||||||||||
CASH FLOWS FROM OPERATING ACTIVITIES: | ||||||||||||
Net income | $ | 95,003 | $ | 193,697 | $ | 329,313 | ||||||
Adjustments to reconcile net income to net cash (used in) provided by operating activities: | ||||||||||||
Amortization and depreciation | 59,878 | 42,982 | 25,591 | |||||||||
Asset and investment impairment charges | 47,869 | — | — | |||||||||
Debt refinancing charge | — | — | 70,095 | |||||||||
Share-based compensation expense | 24,065 | 24,298 | 20,115 | |||||||||
Deferred income taxes | 15,420 | (98,629 | ) | 51,271 | ||||||||
Excess tax benefit on share-based compensation | (815 | ) | (17,987 | ) | (11,889 | ) | ||||||
Other changes | (5,976 | ) | (7,955 | ) | 13,624 | |||||||
Changes in assets and liabilities, net of effects of acquisitions and dispositions: | ||||||||||||
Premiums receivable and unearned premiums | (39,271 | ) | (74,184 | ) | 11,907 | |||||||
Other current assets, receivables and noncurrent assets | (153,310 | ) | 143,783 | (178,337 | ) | |||||||
Amounts receivable/payable under government contracts | (50,431 | ) | 26,223 | (86,925 | ) | |||||||
Reserves for claims and other settlements | 37,717 | 251,636 | 8,624 | |||||||||
Accounts payable and other liabilities | (189,111 | ) | 121,618 | 24,548 | ||||||||
Net cash (used in) provided by operating activities | (158,962 | ) | 605,482 | 277,937 | ||||||||
CASH FLOWS FROM INVESTING ACTIVITIES: | ||||||||||||
Sales of investments | 1,219,291 | 807,649 | 464,787 | |||||||||
Maturities of investments | 257,149 | 213,833 | 113,125 | |||||||||
Purchases of investments | (1,473,664 | ) | (1,180,854 | ) | (635,611 | ) | ||||||
Sales of property and equipment | 4 | 96,748 | 4,242 | |||||||||
Purchases of property and equipment | (95,641 | ) | (64,850 | ) | (72,807 | ) | ||||||
Cash paid related to the acquisition of businesses | — | (80,277 | ) | (73,999 | ) | |||||||
Sales (purchases) of restricted investments and other | 24,990 | (22,444 | ) | 15,384 | ||||||||
Net cash used in investing activities | (67,871 | ) | (230,195 | ) | (184,879 | ) | ||||||
CASH FLOWS FROM FINANCING ACTIVITIES: | ||||||||||||
Proceeds from exercise of stock options and employee stock purchases | 6,636 | 72,622 | 70,294 | |||||||||
Excess tax benefit on share-based compensation | 815 | 17,987 | 11,889 | |||||||||
Repurchases of common stock | (243,172 | ) | (232,220 | ) | (253,502 | ) | ||||||
Borrowings under financing arrangements | 520,000 | 668,535 | 497,334 | |||||||||
Repayment of borrowings under financing arrangements | (396,262 | ) | (600,000 | ) | (465,045 | ) | ||||||
Other | — | — | 8,293 | |||||||||
Net cash used in financing activities | (111,983 | ) | (73,076 | ) | (130,737 | ) | ||||||
Net (decrease) increase in cash and cash equivalents | (338,816 | ) | 302,211 | (37,679 | ) | |||||||
Cash and cash equivalents, beginning of year | 1,007,017 | 704,806 | 742,485 | |||||||||
Cash and cash equivalents, end of year | $ | 668,201 | $ | 1,007,017 | $ | 704,806 | ||||||
SUPPLEMENTAL CASH FLOWS DISCLOSURE: | ||||||||||||
Interest paid | $ | 31,330 | $ | 42,495 | $ | 51,994 | ||||||
Income taxes paid | 97,715 | 183,843 | 74,003 | |||||||||
SUPPLEMENTAL SCHEDULE OF NON-CASH INVESTING AND FINANCING ACTIVITIES: | ||||||||||||
Imputed interest discount and deferred revenue | $ | 9,745 | $ | 27,637 | — | |||||||
Reclassification of certain properties held for sale | — | — | $ | 21,772 | ||||||||
See accompanying notes to consolidated financial statements.
F-6
Table of Contents
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS
Note 1—Description of Business
Health Net, Inc. (referred to herein as the Company, we, us, our or HNT) is an integrated managed care organization that delivers managed health care services. We are among the nation’s largest publicly traded managed health care companies. Our health plans and government contracts subsidiaries provide health benefits through our health maintenance organizations (HMOs), insured preferred provider organizations (PPOs) and point of service (POS) plans to approximately 6.7 million individuals across the country through group, individual, Medicare (including the Medicare prescription drug benefit commonly referred to as “Part D”), Medicaid and TRICARE programs. Our subsidiaries also offer managed health care products related to behavioral health and prescription drugs. We also own health and life insurance companies licensed to sell exclusive provider organization (EPO), PPO, POS and indemnity products as well as auxiliary non-health products such as life and accidental death and dismemberment, dental, vision, behavioral health and disability insurance. These products are offered by our health and life insurance subsidiaries, which are licensed to sell insurance in 50 states and the District of Columbia.
We currently operate within two reportable segments: Health Plan Services and Government Contracts. Our Health Plan Services reportable segment includes the operations of our commercial, Medicare (including Part D) and Medicaid health plans, the operations of our health and life insurance companies and our behavioral health and pharmaceutical services subsidiaries.
Our Government Contracts reportable segment includes government-sponsored managed care plans through the TRICARE program and other health care-related government contracts, including our behavioral health contracts with the Department of Defense. The Government Contracts reportable segment administers a large managed care contract with the U.S. Department of Defense under the TRICARE program in the North Region. The North Region covers Connecticut, Delaware, Illinois, Indiana, Kentucky, Maine, Maryland, Massachusetts, Michigan, New Hampshire, New Jersey, New York, North Carolina, Ohio, Pennsylvania, Rhode Island, Vermont, Virginia, West Virginia, Wisconsin and the District of Columbia and a small portion of Tennessee, Missouri and Iowa. The Company administers health care programs covering approximately 3.0 million eligible individuals in the Military Health System under the TRICARE contract.
Our current TRICARE contract for the North Region is scheduled to conclude on March 31, 2009 unless extended by the Department of Defense. Health Net and the Department of Defense are currently negotiating an extension of the TRICARE North contract for an additional one-year option period, which, if exercised, would extend the TRICARE North contract to March 31, 2010. Health Net and the Department of Defense are also negotiating two subsequent six-month option periods, which, if exercised, would extend the TRICARE North contract to March 31, 2011.
Note 2—Summary of Significant Accounting Policies
Consolidation and Basis of Presentation
The consolidated financial statements include the accounts of the Company and its wholly-owned subsidiaries. All intercompany transactions have been eliminated in consolidation.
Use of Estimates
The preparation of financial statements in conformity with accounting principles generally accepted in the United States of America (GAAP) requires management to make estimates and assumptions that affect the reported amounts of assets and liabilities and disclosures of contingent assets and liabilities at the date of the
F-7
Table of Contents
HEALTH NET, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
financial statements, and the reported amounts of revenues and expenses during the reporting period. These estimates require the Company to apply complex assumptions and judgments, and often the Company must make estimates about effects of matters that are inherently uncertain and will likely change in subsequent periods. Actual results could differ from those estimates. Principal areas requiring the use of estimates include the determination of Medicare risk factor adjustments, risk sharing revenues, allowances for doubtful accounts, reserves for claims and other settlements, reserves for contingent liabilities (including litigation and workers’ compensation reserves), amounts receivable or payable under government contracts, income taxes and assumptions when determining net realizable values on long-lived assets.
Revenue Recognition
Health plan services premium revenues include HMO, POS and PPO premiums from employer groups and individuals and from Medicare recipients who have purchased supplemental benefit coverage, for which premiums are based on a predetermined prepaid fee, Medicaid revenues based on multi-year contracts to provide care to Medicaid recipients, and revenue under Medicare risk contracts to provide care to enrolled Medicare recipients, and revenues from behavioral health services. Revenue is recognized in the month in which the related enrollees are entitled to health care services. Premiums collected in advance are recorded as unearned premiums.
The TRICARE contract for the North Region is made up of two major revenue components, health care services and administrative services. Health care services revenue includes health care costs, including paid claims and estimated incurred but not reported (IBNR) expenses, for care provided for which we are at risk and underwriting fees earned for providing the health care and assuming underwriting risk in the delivery of care. Administrative services revenue encompasses all other services provided to both the government customer and to beneficiaries, including services such as medical management, claims processing, enrollment, customer services and other services unique to the managed care support contracts with the government. Revenue is recognized as earned when the services are provided.
Other government contracts revenues are recognized in the month in which the eligible beneficiaries are entitled to health care services or in the month in which the administrative services are performed or the period that coverage for services is provided.
Amounts receivable under government contracts are comprised primarily of contractually defined billings, deferred underwriting fees under the terms of the contract and change orders for services not originally specified in the contracts. Change orders arise because the government often directs us to implement changes to our contracts before the scope and/or value is defined or negotiated. We start to incur costs immediately, before we have proposed a price to the government. In these situations, we make no attempt to estimate and record revenue. Our policy is to defer the costs as incurred until we have submitted a cost proposal to the government, at which time we will record the costs and the appropriate value for revenue, using our best estimate of what will ultimately be negotiated.
We provide administrative services only (ASO) products to large employer groups in California, Connecticut, New Jersey and New York. Under these arrangements, we provide claims processing, customer services, medical management, provider network access and other administrative services. Administrative services fees are recognized as revenue in the period services are provided.
Health Care Services and Government Contract Expenses
The cost of health care services is recognized in the period in which services are provided and includes an estimate of the cost of services that have been incurred but not yet reported. Such costs include payments to
F-8
Table of Contents
HEALTH NET, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
primary care physicians, specialists, hospitals, outpatient care facilities and the costs associated with managing the extent of such care. Our health care cost can also include from time to time remediation of certain claims as a result of periodic reviews by various regulatory agencies. We estimate the amount of the provision for service costs incurred but not reported using standard actuarial methodologies based upon historical data including the period between the date services are rendered and the date claims are received and paid, denied claim activity, expected medical cost inflation, seasonality patterns and changes in membership. The estimates for service costs incurred but not reported are made on an accrual basis and adjusted in future periods as required. Any adjustments to the prior period estimates are included in the current period. Such estimates are subject to the impact of changes in the regulatory environment and economic conditions. Given the inherent variability of such estimates, the actual liability could differ significantly from the amounts provided. While the ultimate amount of claims and losses paid are dependent on future developments, management is of the opinion that the recorded reserves are adequate to cover such costs. These estimated liabilities are reduced by estimated amounts recoverable from third parties for subrogation.
Our HMOs, primarily in California, generally contract with various medical groups to provide professional care to certain of their members on a capitated, or fixed per member per month fee basis. Capitation contracts generally include a provision for stop-loss and non-capitated services for which we are liable. Professional capitated contracts also generally contain provisions for shared risk, whereby the Company and the medical groups share in the variance between actual costs and predetermined goals. Additionally, we contract with certain hospitals to provide hospital care to enrolled members on a capitation basis. Our HMOs also contract with hospitals, physicians and other providers of health care, pursuant to discounted fee-for-service arrangements, hospital per diems, and case rates under which providers bill the HMOs for each individual service provided to enrollees.
Approximately 37%, 35%, and 33% in 2008, 2007 and 2006, respectively, of our health plan services premium revenues were generated under Medicare and Medicaid/Medi-Cal contracts. These revenues are subject to audit and retroactive adjustment by the respective fiscal intermediaries. Laws and regulations governing these programs are extremely complex and subject to interpretation. As a result, there is at least a reasonable possibility that recorded estimates will change by a material amount.
We assess the profitability of contracts for providing health care services when operating results or forecasts indicate probable future losses. Contracts are grouped in a manner consistent with the method of determining premium rates. Losses are determined by comparing anticipated premiums to estimates for the total of health care related costs less reinsurance recoveries, if any, and the cost of maintaining the contracts. Losses, if any, are recognized in the period the loss is determined and are classified as Health Plan Services cost. We had no premium deficiency reserves as of December 31, 2008 and 2007.
Under the TRICARE contract for the North Region, we record amounts receivable and payable for estimated health care IBNR expenses and report such amounts separately on the accompanying consolidated balance sheet. These amounts are equal since the estimated health care IBNR expenses incurred are offset by an equal amount of revenues earned.
Medicare Part D
Effective January 1, 2006, Health Net began offering the Medicare Part D benefit as a fully insured product to our existing and new members. The Part D benefit consists of pharmacy benefits for Medicare beneficiaries. Part D renewal occurs annually, but it is not a guaranteed renewable product. We report Part D as part of our health plan services reportable segment. The majority of our Part D members in the Prescription Drug Plan (PDP) fall into the low-income category.
F-9
Table of Contents
HEALTH NET, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
Health Net has two primary contracts under Part D, one with the Centers for Medicare and Medicaid Services (CMS) and one with the Part D enrollees. The CMS contract covers the portions of the revenue and expenses that will be paid for by CMS. The enrollee contract covers the services to be performed by Health Net for the premiums paid by the enrollees. The insurance contracts are directly underwritten with the enrollees, not CMS, and therefore there is a direct insurance relationship with the enrollees. The premiums are received directly from the enrollees and from CMS for low-income subsidy members.
Part D offers two types of plans: Prescription Drug Plan (PDP) and Medicare Advantage Plus Prescription Drug (MAPD). PDP covers only prescription drugs and can be combined with traditional Medicare, certain Medicare Advantage Plans or Medicare supplemental plans. MAPD covers both prescription drugs and medical care.
The revenue recognition of the revenue and cost reimbursement components under Part D is described below:
CMS Premium Direct Subsidy—Health Net receives a monthly premium from CMS based on an original bid amount. This payment for each individual is a fixed amount per member for the entire plan year and is based upon that individual’s risk score status. The CMS premium is recognized evenly over the contract period and reported as part of health plan services premium revenue.
Member Premium—Health Net receives a monthly premium from members based on the original bid submitted to CMS. The member premium, which is fixed for the entire plan year is recognized evenly over the contract period and reported as part of health plan services premium revenue.
Low-Income Premium Subsidy—For qualifying low-income members, CMS will reimburse Health Net, on the member’s behalf, some or all of the monthly member premium depending on the member’s income level in relation to the Federal Poverty Level. The low-income premium subsidy is recognized evenly over the contract period and reported as part of health plan services premium revenue.
Catastrophic Reinsurance Subsidy—CMS will reimburse Health Net for 80% of the drug costs after a member reaches his or her out of pocket catastrophic threshold of $4,050, $3,850 and $3,600 for the years ended December 31, 2008, 2007 and 2006, respectively. The CMS prospective payment (a flat PMPM cost reimbursement estimate) is received monthly based on the original CMS bid. After the year is complete, a settlement is made based on actual experience. Catastrophic reinsurance subsidy is accounted for as deposit accounting.
Low-Income Member Cost Sharing Subsidy—For qualifying low-income members, CMS will reimburse Health Net, on the member’s behalf, some or all of a member’s cost sharing amounts (e.g. deductible, co-pay/coinsurance). The amount paid for the member by CMS is dependent on the member’s income level in relation to the Federal Poverty Level. Health Net receives prospective payments on a monthly basis, and they represent a cost reimbursement that is finalized and settled after the end of the year. Low-income member cost sharing subsidy is accounted for as deposit accounting.
CMS Risk Share—Premiums from CMS are subject to risk corridor provisions which compare costs targeted in our annual bids to actual prescription drug costs, limited to actual costs that would have been incurred under the standard coverage as defined by CMS. Variances of more than 5% above or below the original bid submitted by us may result in CMS making additional payments to us or require us to refund to CMS a portion of the premiums we received. We estimate and recognize an adjustment to premium revenues related to the risk corridor payment settlement based upon pharmacy claims experience. The estimate of the settlement associated with these risk corridor provisions requires us to consider factors that may not be certain including member
F-10
Table of Contents
HEALTH NET, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
eligibility status differences with CMS. The risk-share adjustment, if any, is recorded as an adjustment to premium revenues and premiums receivable.
Health care costs and general and administrative expenses associated with Part D are recognized as the costs and expenses are incurred.
CMS Risk Factor Adjustments
We have an arrangement with CMS for certain of our Medicare products whereby periodic changes in our risk factor adjustment scores for certain diagnostic codes result in changes to our health plan services premium revenues. We recognize such changes when the amounts become determinable, supportable and the collectibility is reasonably assured.
We recognized $137.7 million of Medicare risk factor estimates, which were for the 2008 payment year in our health plan services premium revenues in the year ended December 31, 2008. We also recognized $32.9 million of capitation expense related to the Medicare risk factor estimates, which were for the 2008 payment year in our health plan services costs in the year ended December 31, 2008.
We recognized $95.1 million of Medicare risk factor estimates in our health plan services premium revenues in the year ended December 31, 2007. Of this amount, $80.3 million, $13.2 million and $1.6 million were for the 2007, 2006 and 2003 payment years, respectively. We also recognized $27.2 million of capitation expense related to the Medicare risk factor estimates in our health plan services costs in the year ended December 31, 2007. Of this amount, $22.5 million, $3.9 million and $ 0.8 million were for the 2007, 2006, and 2003 payment years, respectively.
We recognized $92.0 million of Medicare risk factor estimates in our health plan services premium revenues in the year ended December 31, 2006. Of this amount, $51.9 million, $37.0 million and $3.1 million were for the 2006, 2005 and 2004 payment years, respectively. We also recognized $29.1 million of capitation expense related to the Medicare risk factor estimates in our health plan services costs in the year ended December 31, 2006. Of this amount, $14.9 million, $13.2 million and $1.0 million were for the 2006, 2005, and 2004 payment years, respectively.
TRICARE Contract Target Costs
Our TRICARE contract for the North Region includes a target cost and price for reimbursed health care costs, which is negotiated annually during the term of the contract with underruns and overruns of our target cost borne 80% by the government and 20% by us. In the normal course of contracting with the federal government, we recognize changes in our estimate for the target cost underruns and overruns when the amounts become determinable, supportable, and the collectibility is reasonably assured. As a result of changes in the estimate during the year ended December 31, 2008, we recognized an increase in revenue of $17 million and an increase in cost of $22 million. As a result of changes in the estimate during the years ended December 31, 2007 and 2006, we recognized decreases in revenue of $58 million and $104 million, respectively, and decreases in costs of $75 million and $128 million, respectively. In addition, 2007 includes a $36.5 million favorable settlement with the Federal Government regarding prior Option Period 1 health care cost targets. The administrative price is paid on a monthly basis, one month in arrears and certain components of the administrative price are subject to volume-based adjustments.
Share-Based Compensation Expense
As of December 31, 2008, we had various long-term incentive plans that permit the grant of stock options and other equity awards to certain employees, officers and non-employee directors, which are described more
F-11
Table of Contents
HEALTH NET, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
fully in Note 8. Prior to January 1, 2006, we accounted for stock-based compensation under the intrinsic value method prescribed in Accounting Principles Board Opinion No. 25, “Accounting for Stock Issued to Employees” (APB Opinion No. 25), and related Interpretations, as permitted under Statement of Financial Accounting Standards (SFAS) No. 123, “Accounting for Stock-Based Compensation” (SFAS No. 123).
Effective January 1, 2006, we adopted the fair value recognition provisions of SFAS No. 123(R), “Share-Based Payment,” (SFAS No. 123(R)) using the modified—prospective transition method. Under such transition method, compensation cost recognized in the year ended December 31, 2006 includes: (a) compensation cost for all stock options granted prior to, but not yet vested as of January 1, 2006, based on the grant date fair value estimated in accordance with the original provisions of SFAS No. 123, and (b) compensation cost for all share-based payments granted on or after January 1, 2006, based on the grant-date fair value estimated in accordance with the provisions of SFAS No. 123(R). Results for prior periods have not been restated. The compensation cost that has been charged against income under our various long-term incentive plans was $24.1 million, $24.3 million and $20.1 million during the years ended December 31, 2008, 2007 and 2006, respectively. The total income tax benefit recognized in the income statement for share-based compensation arrangements was $9.3 million, $9.4 million and $7.8 million for the years ended December 31, 2008, 2007 and 2006, respectively.
Cash flows resulting from the tax deductions in excess of the compensation cost recognized for those options (excess tax benefits) are classified as financing cash flows and such amounts are approximately $0.8 million, $18.0 million and $11.9 million for the years ended December 31, 2008, 2007 and 2006, respectively. Prior to the adoption of SFAS No. 123(R) and upon issuance of the restricted shares pursuant to the restricted stock agreements, an unamortized compensation expense equivalent to the market value of the shares on the date of grant was charged to stockholders’ equity as unearned compensation and amortized over the applicable restricted periods. As a result of adopting SFAS No. 123(R) on January 1, 2006, we transferred the remaining unearned compensation balance in our stockholders’ equity to additional paid in capital. Prior to the adoption of SFAS No. 123(R), we recorded forfeitures of restricted stock, if any, and any compensation cost previously recognized for unvested awards was reversed in the period of forfeiture.
Forfeiture rates for share based awards are estimated upfront and true-up adjustments are recorded for the actual forfeitures.
Cash and Cash Equivalents
Cash equivalents include all highly liquid investments with maturity of three months or less when purchased.
Investments
Investments classified as available-for-sale, which consist primarily of debt securities, are stated at fair value. Unrealized gains and losses are excluded from earnings and reported as other comprehensive income, net of income tax effects. The cost of investments sold is determined in accordance with the specific identification method and realized gains and losses are included in net investment income. We periodically assess our available-for-sale investments for other-than-temporary impairment. Any such other-than-temporary impairment loss is recognized as a realized loss and measured as the excess of carrying value over fair value at the time the assessment is made. During the year ended December 31, 2008, we recognized a $14.6 million loss from other-than-temporary impairments. During the years ended December 31, 2007 and 2006, we had no other-than-temporary impairment loss (see Note 4 for additional information regarding our loss from other-than-temporary impairments).
F-12
Table of Contents
HEALTH NET, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
Fair Value of Financial Instruments
The estimated fair value amounts of cash equivalents, investments available for sale, trade accounts and notes receivable and notes payable have been determined by us using available market information and appropriate valuation methodologies. The carrying amounts of cash equivalents approximate fair value due to the short maturity of those instruments. Fair values for debt and equity securities are generally based upon quoted market prices. Where quoted market prices were not readily available, fair values were estimated using valuation methodologies based on available and observable market information. Such valuation methodologies include reviewing the value ascribed to the most recent financing, comparing the security with securities of publicly traded companies in a similar line of business, and reviewing the underlying financial performance including estimating discounted cash flows. The carrying value of trade receivables, long-term notes receivable and nonmarketable securities approximate the fair value of such financial instruments. The fair value of notes payable is estimated based on the quoted market prices for the same or similar issues or on the current rates offered to us for debt with the same remaining maturities. The fair value of our fixed rate borrowings, including our Senior Notes and financing facility was $291.3 million as of December 31, 2008. The fair value of our fixed rate borrowings, including our Senior Notes and financing facility was $541.4 million as of December 31, 2007. The fair value of our variable rate borrowings, from our revolving credit facility, as of December 31, 2008 was $150 million, which was equal to the carrying value because the interest rates paid on these borrowings were based on prevailing market rates. See Note 6 for our financing arrangements.
Restricted Assets
We and our consolidated subsidiaries are required to set aside certain funds which may only be used for certain purposes pursuant to state regulatory requirements. We have discretion as to whether we invest such funds in cash and cash equivalents or other investments. As of December 31, 2008 and December 31, 2007, the restricted cash and cash equivalents balances totaled $63.5 million and $30.5 million, respectively, and are included in other noncurrent assets. Investment securities held by trustees or agencies were $55.3 million and $79.3 million as of December 31, 2008 and 2007, respectively, and are included in investments available-for-sale.
In connection with our purchase of The Guardian Life Insurance Company of America’s interest in the HealthCare Solutions business in 2007 (see Note 3), we established escrowed funds to secure the payment of projected run-out claims for the purchased block of business. As of December 31, 2008 and December 31, 2007, this restricted cash balance amounted to $5.9 million and $37.0 million, respectively, and is included in other noncurrent assets on the accompanying consolidated balance sheets.
Interest Rate Swap Contracts
On December 19, 2007, we entered into a five-year, $175 million amortizing financing facility with a non-U.S. lender (see Note 6). In connection with the financing facility, we entered into an interest rate swap agreement under which we pay an amount equal to LIBOR times a notional principal amount and receive in return an amount equal to 4.3% times the same notional principal amount. The interest rate swap does not qualify for hedge accounting. Accordingly, the interest rate swap is reflected at positive fair value of $8.0 million and $1.1 million in our consolidated balance sheet with an offset to net investment income in our consolidated statement of operations for the change in fair value during the years ended December 31, 2008 and 2007, respectively.
F-13
Table of Contents
HEALTH NET, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
Property and Equipment
Property and equipment are stated at historical cost less accumulated depreciation. Property and equipment that are held for sale are reported as part of current assets. Depreciation is computed using the straight-line method over the lesser of estimated useful lives of the various classes of assets or the remaining lease term, in the case of leasehold improvements. The useful life for buildings and improvements is estimated at 35 to 40 years, and the useful lives for furniture, equipment and software range from three to ten years (see Note 5).
We capitalize certain consulting costs, payroll and payroll-related costs for employees related to computer software developed for internal use. We generally amortize such costs over a three to five-year period. Expenditures for maintenance and repairs are expensed as incurred. Major improvements, which increase the estimated useful life of an asset, are capitalized. Upon the sale or retirement of assets, the recorded cost and the related accumulated depreciation are removed from the accounts, and any gain or loss on disposal is reflected in operations.
We periodically assess long-lived assets or asset groups including property and equipment for recoverability when events or changes in circumstances indicate that their carrying amount may not be recoverable. If we identify an indicator of impairment, we assess recoverability by comparing the carrying amount of the asset to the sum of the undiscounted cash flows expected to result from the use and the eventual disposal of the asset. An impairment loss is recognized when the carrying amount is not recoverable and is measured as the excess of carrying value over fair value. Long-lived assets are classified as held for sale and included as part of current assets when certain criteria are met. We measure long-lived assets to be disposed of by sale at the lower of carrying amount or fair value less cost to sell. Fair value is determined using quoted market prices or the anticipated cash flows discounted at a rate commensurate with the risk involved. During the year ended December 31, 2008, we recorded $26.9 million in impairment charges in general and administrative expenses for software internally developed and under development, information technology equipment, furniture and other equipment in connection with our operations strategy. During the years ended December 31, 2007 and 2006, we recorded no impairment charges.
Goodwill and Other Intangible Assets
Goodwill and other intangible assets arise primarily as a result of various business acquisitions and consist of identifiable intangible assets acquired and the excess of the cost of the acquisitions over the tangible and intangible assets acquired and liabilities assumed (goodwill). Identifiable intangible assets primarily consist of the value of employer group contracts, provider networks and customer relationships, which are all subject to amortization.
We perform our annual impairment test on our recorded goodwill as of June 30 or more frequently if events or changes in circumstances indicate that we might not recover the carrying value of these assets for each of our reporting units. Health Plans Services is our only reporting unit with goodwill as of December 31, 2008 and 2007. We test goodwill for impairment annually based on the estimated fair value of our Health Plan Services reporting unit. We test for impairment on a more frequent basis in cases where events and changes in circumstances would indicate that we might not recover the carrying value of goodwill. Our measurement of fair value is primarily based on the income approach to fair value determination. The income approach is based on a discounted cash flow methodology. The discounted cash flow methodology is based upon converting expected cash flows to present value. Annual cash flows are estimated for each year of a defined multi-year period until the growth pattern becomes stable. The interim cash flows expected after the growth pattern becomes stable are calculated using an appropriate capitalization technique and then discounted. There are numerous assumptions and estimates underlying the determination of the estimated fair value of our reporting units, including certain assumptions and estimates related to future earnings and membership levels based on current and future plans
F-14
Table of Contents
HEALTH NET, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
and initiatives, long-term strategies and our annual planning and forecasting process as well as the weighted average cost of capital used in the discounting process. If these planned initiatives do not accomplish their targeted objectives, the assumptions and estimates underlying the goodwill impairment tests could be adversely affected and have a material effect upon our financial condition, results of operations or liquidity.
During the year ended December 31, 2008, we recorded higher than expected health care costs and lowered our earnings guidance. The reduction in guidance was primarily driven by lower than expected commercial enrollment, higher than expected commercial health care cost trends, and the volatile economic environment. As a result of this revised outlook combined with a decline in our market capitalization, we updated our annual impairment test on our goodwill asset as of September 30, 2008 and as of December 31, 2008, which indicated that there was no impairment.
The changes in the carrying amount of goodwill by reporting unit are as follows:
| Health Plan Services | Total | |||||
| (Dollars in millions) | ||||||
Balance as of December 31, 2008 and 2007 | $ | 752.0 | $ | 752.0 | ||
The intangible assets that continue to be subject to amortization using the straight-line method over their estimated lives are as follows:
| Gross Carrying Amount | Accumulated Amortization | Net Balance | Weighted Average Life (in years) | |||||||||
| (Dollars in millions) | ||||||||||||
As of December 31, 2007: | ||||||||||||
Provider networks | $ | 40.5 | $ | (27.7 | ) | $ | 12.8 | 19.4 | ||||
Employer groups (Note 3) | 75.0 | (6.5 | ) | 68.5 | 6.5 | |||||||
Customer relationships and other (Note 3) | 29.5 | (4.9 | ) | 24.6 | 11.1 | |||||||
Trade name (Note 3) | 3.1 | (1.2 | ) | 1.9 | 1.5 | |||||||
Covenant not–to-compete (Note 3) | 2.2 | (0.6 | ) | 1.6 | 2.0 | |||||||
| $ | 150.3 | $ | (40.9 | ) | $ | 109.4 | ||||||
As of December 31, 2008: | ||||||||||||
Provider networks | $ | 40.5 | $ | (30.1 | ) | $ | 10.4 | 19.4 | ||||
Employer groups (Note 3) | 76.8 | (18.3 | ) | 58.5 | 6.5 | |||||||
Customer relationships and other (Note 3) | 29.5 | (7.6 | ) | 21.9 | 11.1 | |||||||
Trade name (Note 3) | 3.2 | (3.2 | ) | — | 1.5 | |||||||
Covenant not–to-compete (Note 3) | 2.2 | (1.7 | ) | 0.5 | 2.0 | |||||||
| $ | 152.2 | $ | (60.9 | ) | $ | 91.3 | ||||||
The amortization expense was $20.0 million, $12.7 million and $4.1 million for the years ended December 31, 2008, 2007 and 2006, respectively.
F-15
Table of Contents
HEALTH NET, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
Estimated annual pretax amortization expense for other intangible assets for each of the next five years ending December 31 is as follows (dollars in millions):
Year | Amount | ||
2009 | $ | 16.3 | |
2010 | 15.8 | ||
2011 | 15.5 | ||
2012 | 15.4 | ||
2013 | 14.0 | ||
Policy Acquisition Costs
Policy acquisition costs are those costs that vary directly with and related to the acquisition of new and renewal commercial health insurance business. Such costs include broker commissions, costs of policy issuance and underwriting, and other costs we incur to acquire new commercial business or renew existing business. Our commercial health insurance business typically has a one-year term and may be canceled upon a 30-day notice. We expense these costs as incurred in accordance with theHealth Care Organization Audit and Accounting Guide and report them as selling expenses in our consolidated statements of operations.
Reserves for Contingent Liabilities
In the course of our operations, we are involved on a routine basis in various disputes with members, health care providers, and other entities, as well as audits by government agencies that relate to our services and/or business practices that expose us to potential losses.
We recognize an estimated loss, which may represent damages, assessment of regulatory fines or penalties, settlement costs, future legal expenses or a combination of the foregoing, as appropriate, from such loss contingencies when it is both probable that a loss will be incurred and that the amount of the loss can be reasonably estimated. Our loss estimates are based in part on an analysis of potential results, the stage of the proceedings, consultation with outside counsel and any other relevant information available.
Insurance Programs
The Company is insured for various errors and omissions, property, casualty and other risks. The Company maintains various self-insured retention amounts, or “deductibles,” on such insurance coverage. The Company also maintains litigation reserves to cover those self-insured retention amounts for errors and omissions claims based on historical claims filed, as well as estimates of claims incurred but not reported.
Concentrations of Credit Risk
Financial instruments that potentially subject us to concentrations of credit risk consist primarily of cash equivalents, investments and premiums receivable. All cash equivalents and investments are managed within established guidelines, which provide us diversity among issuers. Concentrations of credit risk with respect to premiums receivable are limited due to the large number of payers comprising our customer base. Our 10 largest employer group premiums receivable balances within each of our plans accounted for 48% and 27% of our total premiums receivable as of December 31, 2008 and 2007, respectively. Our Medicare receivable from CMS represented 56% of total receivables as of December 31, 2008, compared with 32% as of December 31, 2007. Our 10 largest employer group premiums within each of our plans accounted for 18%, 18% and 20% of our health plan services premiums for the years then ended December 31, 2008, 2007 and 2006, respectively. The
F-16
Table of Contents
HEALTH NET, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
federal government is the only customer of our Government Contracts segment, with premiums and fees accounting for 100% of our Government Contracts revenue. In addition, the federal government is a significant customer of the Company’s Health Plan Services segment as a result of its contract with CMS for coverage of Medicare-eligible individuals. Medicare revenues accounted for 28%, 24% and 22% of our health plan premiums in 2008, 2007 and 2006, respectively.
Earnings Per Share
Basic earnings per share excludes dilution and reflects net income divided by the weighted average shares of common stock outstanding during the periods presented. Diluted earnings per share is based upon the weighted average shares of common stock and dilutive common stock equivalents (this reflects the potential dilution that could occur if stock options were exercised and restricted stock units (RSUs) and restricted shares were vested) outstanding during the periods presented.
Common stock equivalents arising from dilutive stock options, restricted common stock and RSUs are computed using the treasury stock method; for the years ended December 31, 2008, 2007 and 2006, this amounted to 1,078,000, 2,513,000 and 3,182,000 shares, respectively, which include 299,000, 239,000 and 145,000 aggregate common stock equivalents from dilutive RSUs and restricted common stock, respectively.
Options to purchase an aggregate of 3,051,000, 1,256,000 and 1,258,000 shares of common stock were considered anti-dilutive during 2008, 2007 and 2006, respectively, and were not included in the computation of diluted earnings per share because the options’ exercise price was greater than the average market price of the common stock for each respective period. These options expire at various times through November 2018 (see Note 8).
We have a $700 million stock repurchase program authorized by our Board of Directors. The remaining authorization under our stock repurchase program as of December 31, 2008 was $103.3 million (see Note 9). On November 4, 2008, we announced that our stock repurchase program is on hold as a consequence of the uncertain financial environment and the announcement by Health Net’s Board of Directors that Jay Gellert, our President and Chief Executive Officer, will be undertaking a review of the Company’s strategic direction.
Comprehensive Income
Comprehensive income includes all changes in stockholders’ equity (except those arising from transactions with stockholders) and includes net income, net unrealized appreciation (depreciation), after tax, on investments available-for-sale and prior service cost and net loss related to our defined benefit pension plan (see Note 10).
F-17
Table of Contents
HEALTH NET, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
Our accumulated other comprehensive income (loss) are as follows:
| For the Years Ended December 31, | ||||||||
| 2008 | 2007 | |||||||
| (Dollars in millions) | ||||||||
Investments: | ||||||||
Unrealized losses on investments available for sale as of January 1 | $ | (0.1 | ) | $ | (8.9 | ) | ||
Net change in unrealized (losses) gains on investments available for sale | (10.1 | ) | 12.0 | |||||
Reclassification of unrealized losses (gains) to earnings | 2.9 | (3.2 | ) | |||||
Unrealized losses on investments available for sale as of December 31 | (7.3 | ) | (0.1 | ) | ||||
Defined benefit pension plans: | ||||||||
Prior service cost and net loss amortization as of January 1 | (1.1 | ) | (2.3 | ) | ||||
Net change in prior service cost and net loss amortization | 1.5 | 1.2 | ||||||
Prior service cost and net loss amortization as of December 31 | 0.4 | (1.1 | ) | |||||
Accumulated other comprehensive income (loss) | $ | (6.9 | ) | $ | (1.2 | ) | ||
Taxes Based on Premiums
We provide services in certain states, which require premium taxes to be paid by us based on membership or billed premiums. These taxes are paid in lieu of or in addition to state income taxes and totaled $48.0 million in 2008, $43.6 million in 2007 and $36.2 million in 2006. These amounts are recorded in general and administrative expenses on our consolidated statements of operations.
Income Taxes
We record deferred tax assets and liabilities based on differences between the book and tax bases of assets and liabilities. The deferred tax assets and liabilities are calculated by applying enacted tax rates and laws to taxable years in which such differences are expected to reverse. We establish a valuation allowance in accordance with the provisions of Statement of Financial Accounting Standards (SFAS) No. 109,Accounting for Income Taxes (SFAS No. 109). We continually review the adequacy of the valuation allowance and recognize the benefits from our deferred tax assets only when an analysis of both positive and negative factors indicate that it is more likely than not that the benefits will be realized.
We file tax returns in many tax jurisdictions. Often, application of tax rules within the various jurisdictions is subject to differing interpretation. Despite our belief that our tax return positions are fully supportable, we believe that it is probable certain positions will be challenged by taxing authorities, and we may not prevail on the positions as filed. Accordingly, we maintain a liability for the estimated amount of contingent tax challenges by taxing authorities upon examination, in accordance with Financial Accounting Standards Board Interpretation No. 48,Accounting for Uncertainty in Income Taxes (FIN 48), which we adopted as of January 1, 2007. Prior to 2007, we maintained a liability pursuant to SFAS No. 5,Accounting for Contingencies. FIN 48 clarifies the accounting for uncertain taxes recognized in a company’s financial statements in accordance with SFAS No. 109. The interpretation requires us to analyze the amount at which each tax position meets a “more likely than not” standard for sustainability upon examination by taxing authorities. Only tax benefit amounts meeting or exceeding this standard will be reflected in tax provision expense and deferred tax asset balances. The interpretation also requires that any differences between the amounts of tax benefits reported on tax returns and tax benefits reported in the financial statements be recorded in a liability for unrecognized tax benefits. The
F-18
Table of Contents
HEALTH NET, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
liability for unrecognized tax benefits is reported separately from deferred tax assets and liabilities and classified as current or noncurrent based upon the expected period of payment. See Note 11 to the consolidated financial statements for additional disclosures related to FIN 48 policies and the impact of adoption.
Recently Issued Accounting Pronouncements
In October 2008, the Financial Accounting Standards Board (FASB) issued FASB Staff Position (FSP) No. FAS 157-3,Determining the Fair Value of a Financial Asset When the Market for That Asset Is Not Active (FSP FAS 157-3). This FSP clarifies the application of SFAS No. 157,Fair Value Measurements, in a market that is not active and provides an example to illustrate key considerations in determining the fair value of a financial asset when the market for that financial asset is not active. FSP FAS 157-3 is effective upon issuance, including prior periods for which financial statements have not been issued. Revisions resulting from a change in the valuation technique or its application shall be accounted for as a change in accounting estimate. The adoption of FSP FAS 157-3 did not have a material impact on our financial statements or require a change in accounting estimate.
In April 2008, the FASB issued FSP No. FAS 142-3,Determination of the Useful Life of Intangible Assets (FSP FAS 142-3). FSP 142-3 amends the factors to be considered in developing renewal and extension assumptions used to determine the useful life of a recognized intangible asset accounted for under SFAS No. 142,Goodwill and Other Intangible Assets. FSP FAS 142-3 is effective prospectively to intangible assets acquired after January 1, 2009. We do not expect the adoption of FSP FAS 142-3 to have a material impact on our consolidated financial statements.
In March 2008, the FASB issued SFAS No. 161,Disclosures about Derivative Instruments and Hedging Activities-an amendment of SFAS No. 133 (SFAS No. 161). This statement changes the disclosure requirements for derivative instruments and hedging activities. Entities are required to provide enhanced disclosures about how and why an entity uses derivative instruments, how derivative instruments and related hedged items are accounted for under SFAS No. 133,Accounting for Derivative Instruments and Hedging Activities,and how derivative instruments and related hedged items affect an entity’s financial position, financial performance and cash flows. This statement requires that objectives for using derivative instruments be disclosed in terms of underlying risks and accounting designation. Fair values of derivatives and their gains and losses are required to be disclosed in a tabular format. SFAS No. 161 is effective for financial statements issued for fiscal years and interim periods beginning after November 15, 2008. We do not expect the adoption of SFAS No. 161 as of January 1, 2009 to have a material impact on our financial statements.
In December 2007, the FASB issued SFAS No. 141(R),Business Combinations (SFAS No. 141(R)).This statement replaces SFAS No. 141,Business Combinations.While retaining the fundamental requirements in SFAS No. 141 that the acquisition method of accounting be used for all business combinations, SFAS No. 141 (R) establishes principles and requirements for how the acquirer recognizes and measures in its financial statements the identifiable assets acquired, the liabilities assumed, and any noncontrolling interest in the acquiree. The standard also provides requirements for recognition and measurement of the goodwill acquired in the business combination or gain from a bargain purchase and establishes disclosure requirements to enable users of the financial statements to evaluate the nature and financial effects of the business combination. SFAS No. 141(R) is effective for business combinations for which the acquisition date is in the fiscal year beginning on or after December 15, 2008. We do not expect the adoption of SFAS No. 141 (R) to have a material impact on our consolidated financial statements.
In December 2007, the FASB issued SFAS No. 160,Noncontrolling Interests in Consolidated Financial Statements- an amendment of ARB No. 51 (SFAS No. 160).SFAS No. 160 establishes accounting and reporting
F-19
Table of Contents
HEALTH NET, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
standards for the noncontrolling interest in a subsidiary and for the deconsolidation of a subsidiary. It clarifies that a noncontrolling interest in a subsidiary is an ownership interest in the consolidated entity that should be reported as equity in the consolidated financials statements. Under the new standard, noncontrolling interests no longer will be classified within a mezzanine section of the balance sheet but will be reported as a part of equity. The standard also changes a way the consolidated income statement is presented. It requires consolidated net income to be reported at amounts that include the amounts attributable to both the parent and the noncontrolling interest. SFAS No. 160 is effective for fiscal years, and interim periods within those fiscal years, beginning on or after December 15, 2008. We do not expect the adoption of SFAS No. 160 to have a material impact on our consolidated financial statements.
Note 3—Purchases, Acquisitions and Sales
Purchase of The Guardian Life Insurance Company of America’s (The Guardian) Interest in HealthCare Solutions
In 1995, we entered into marketing and risk sharing arrangements with The Guardian covering primarily small group membership in the States of Connecticut, New York and New Jersey. Under these arrangements, our managed care and indemnity products were marketed to existing insureds of The Guardian. In addition, these products were distributed through the brokerage community in an integrated marketing effort under the trade name HealthCare Solutions (HCS). As part of these arrangements, we and The Guardian each retained 50% of the premiums and claims. In addition, we recovered from The Guardian a specified portion of the administrative expenses and the direct marketing costs, which were shared equally.
On February 27, 2007, we announced that we entered into an agreement with The Guardian to, in substance, purchase The Guardian’s 50% interest in HCS (the “Guardian Transaction”). On May 31, 2007, we completed the Guardian Transaction, which included terminating all pre-existing marketing and risk sharing arrangements and acquiring certain intangible rights from The Guardian. As a result, we recognize 100% of the HCS revenues, claims and administrative and marketing expenses. In connection with the Guardian Transaction, we paid The Guardian $80.3 million in cash, which was all allocated to acquired intangibles and was based on the future profits we expect to generate by owning 100% of the employer group contract relationships associated with the HCS business.
In accordance with SFAS No. 142,Goodwill and Other Intangible Assets, goodwill and other intangible assets with indefinite useful lives are not amortized, but instead are subject to impairment tests. Identified intangible assets with definite useful lives are amortized on a straight-line basis over their estimated remaining lives. We have allocated the entire purchase price of $80.3 million to intangible assets with definite useful lives (see Note 2). All of the assets acquired were assigned to our Health Plan Services reportable segment.
The on-going financial results of the HCS business since May 31, 2007 are included in our Health Plan Services reportable segment for the year ended December 31, 2007 and are not material to our consolidated results of operations.
Sale-Leaseback of Shelton, Connecticut Property
On March 29, 2007, we sold our 68-acre commercial campus in Shelton, Connecticut (the Shelton Property) to The Dacourt Group, Inc. (Dacourt) and leased it back from Dacourt under an operating lease agreement for an initial term of ten years with an option to extend for two additional terms of ten years each. We received net cash proceeds of $83.9 million and recorded a deferred gain of $60.9 million, which is amortized into income as contra-G&A expense over the lease term.
F-20
Table of Contents
HEALTH NET, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
Sale-Leaseback of Tucson, Arizona Property
On June 29, 2007, we sold our commercial campus in Tucson, Arizona (the Tucson Property) to West Coast Capital Partners, LLC (West Coast) and leased it back from West Coast under an operating lease agreement for an initial term of one year, with an option to extend for two additional one-year terms, which we exercised. We received net cash proceeds of $12.7 million and recorded a gain of $6.1 million as contra-G&A expense in the statement of operations in the three months ended June 30, 2007.
Sale of Pennsylvania Subsidiaries
On July 31, 2006, we completed the sale of the subsidiary that formerly held our Pennsylvania health plan and certain of its affiliates (Pennsylvania Subsidiaries). We recognized an estimated $32 million tax benefit and a $0.4 million pretax loss related to this sale in the year ended December 31, 2006. See Note 11 for further information regarding our tax accounting policies related to sales of subsidiaries.
The Pennsylvania Subsidiaries were historically reported as part of our Health Plan Services reportable segment. The revenues and expenses of the Pennsylvania Subsidiaries were negligible for the year ended December 31, 2006.
Acquisition of Universal Care Business
On March 31, 2006, we completed the acquisition of certain health plan businesses of Universal Care, Inc. (Universal Care), a California-based health care company, and paid $74.0 million, including transaction-related costs. The purchase price was allocated to goodwill and intangibles (see Note 2). With this acquisition, we added 83,000 members as of December 31, 2006.
Note 4—Investments
Investments classified as available-for-sale, which consist primarily of debt securities, are stated at fair value. Unrealized gains and losses are excluded from earnings and reported as other comprehensive income, net of income tax effects. The cost of investments sold is determined in accordance with the specific identification method and realized gains and losses are included in net investment income. We periodically assess our available-for-sale investments for other-than-temporary impairment. Any such other-than-temporary impairment loss is recognized as a realized loss and measured as the excess of amortized cost over fair value at the time the assessment is made.
During the year ended December 31, 2008, we recognized a $14.6 million loss from other-than-temporary impairments of our cash equivalents and available-for-sale investments. Such other-than-temporary impairments primarily were as a result of investments in corporate debt from Lehman Brothers, money market funds from The Reserve Primary Institutional Fund and preferred stock from Federal National Mortgage Association (Fannie Mae) and Federal Home Loan Mortgage Corporation (Freddie Mac). Included in the $14.6 million loss is $8.3 million of our investments in Lehman Brothers corporate debt, which were written down to a cost basis of zero. In September 2008, Lehman Brothers Holdings Inc. filed for bankruptcy protection under Chapter 11 of the U.S. Bankruptcy Code. Accordingly, we deemed the recovery of our investments in Lehman Brothers bonds as remote and recognized a loss from other-than-temporary impairment of $8.3 million during the year ended December 31, 2008.
Due to the Lehman bankruptcy, our investment in The Reserve Primary Institutional Fund fell below a net asset value of $1 per share. Lehman short-term debt is one of the underlying investments in this fund. Consistent
F-21
Table of Contents
HEALTH NET, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
with our treatment of our Lehman Brothers investments, we recognized a loss from other-than-temporary impairment of $4.1 million (included in the $14.6 million loss) during the year ended December 31, 2008, in connection with our investments in The Reserve Primary Institutional Fund.
In September 2008, The Reserve announced its intention to liquidate all of its money market funds and froze all redemptions until an orderly liquidation process could be implemented. As a result, we reclassified $372 million in estimated net asset value we had invested in The Reserve money market funds from cash equivalents to investments available for sale as of September 30, 2008. As of December 31, 2008, we held $50.4 million of their Primary Institutional Fund and $69.2 million of their U.S. Government Fund. On January 16, 2009, The Reserve paid out in full the balance in the U.S. Government Fund and on February 20, 2009, we received $17.1 million of the Primary Fund from The Reserve. The Reserve expects to distribute the remaining amounts in the Primary Institutional Fund by the end of 2009.
Actions taken by the U.S. government to seize control of Fannie Mae and Freddie Mac due to the financial condition and liquidity issues of these government-sponsored entities coupled with weakness in the banking and financial services sectors led us to conclude that the recovery of our investments in these securities is not expected in the near term. In the year ended December 31, 2008, we recognized a loss from other-than-temporary impairments of Fannie Mae and Freddie Mac preferred stock totaling $1.2 million, and our investments in those securities were written down to a cost basis of zero.
In addition, we recognized $1 million in losses from other-than-temporary impairments of other corporate debt and preferred stock primarily issued by financial institutions or banks. Due to credit downgrades and declines in fair values in light of current market conditions, we deemed such impairments to be other-than-temporary.
As of December 31, 2008 and 2007, the amortized cost, gross unrealized holding gains and losses, and fair value of our available-for-sale investments after giving effect to other-than-temporary impairments were as follows:
| 2008 | |||||||||||||
| Amortized Cost | Gross Unrealized Holding Gains | Gross Unrealized Holding Losses | Carrying Value | ||||||||||
| (Dollars in millions) | |||||||||||||
Asset-backed securities | $ | 527.4 | $ | 9.8 | $ | (17.2 | ) | $ | 520.0 | ||||
U.S. government and agencies | 69.5 | 0.5 | — | 70.0 | |||||||||
Obligations of states and other political subdivisions | 577.9 | 7.3 | (9.8 | ) | 575.4 | ||||||||
Corporate debt securities | 341.1 | 3.4 | (5.8 | ) | 338.7 | ||||||||
Other securities | 0.4 | 0.2 | — | 0.6 | |||||||||
| $ | 1,516.3 | $ | 21.2 | $ | (32.8 | ) | $ | 1,504.7 | |||||
F-22
Table of Contents
HEALTH NET, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
| 2007 | |||||||||||||
| Amortized Cost | Gross Unrealized Holding Gains | Gross Unrealized Holding Losses | Carrying Value | ||||||||||
| (Dollars in millions) | |||||||||||||
Asset-backed securities | $ | 504.9 | $ | 2.5 | $ | (3.1 | ) | $ | 504.3 | ||||
U.S. government and agencies | 197.7 | 0.4 | (0.5 | ) | 197.6 | ||||||||
Obligations of states and other political subdivisions | 563.0 | 2.8 | (1.4 | ) | 564.4 | ||||||||
Corporate debt securities | 290.0 | 1.0 | (2.0 | ) | 289.0 | ||||||||
Other securities | 1.8 | 0.1 | — | 1.9 | |||||||||
| $ | 1,557.4 | $ | 6.8 | $ | (7.0 | ) | $ | 1,557.2 | |||||
As of December 31, 2008, the contractual maturities of our available-for-sale investments were as follows:
| Amortized Cost | Estimated Fair Value | |||||
| (Dollars in millions) | ||||||
Due in one year or less | $ | 227.2 | $ | 227.2 | ||
Due after one year through five years | 169.2 | 169.3 | ||||
Due after five years through ten years | 316.4 | 314.1 | ||||
Due after ten years | 275.7 | 273.5 | ||||
Asset-backed securities | 527.4 | 520.0 | ||||
Other securities | 0 .4 | 0.6 | ||||
Total available for sale | $ | 1,516.3 | $ | 1,504.7 | ||
Proceeds from sales of investments available for sale during 2008 were $1,219.3 million, resulting in gross realized gains and losses of $10.5 million and $14.9 million, respectively. Included in the 2008 gross realized losses of $14.9 million is an other-than-temporary impairment write-down of $14.6 million. Proceeds from sales of investments available for sale during 2007 were $807.6 million, resulting in gross realized gains and losses of $6.2 million and $1.2 million, respectively. Proceeds from sales of investments available for sale during 2006 were $464.8 million, resulting in gross realized gains and losses of $6.5 million and $3.4 million, respectively.
The following table shows our investments’ gross unrealized losses and fair value for individual securities that have been in a continuous loss position through December 31, 2008:
| Less than 12 Months | 12 Months or More | Total | |||||||||||||||||||
| Fair Value | Unrealized Losses | Fair Value | Unrealized Losses | Fair Value | Unrealized Losses | ||||||||||||||||
| (Dollars in millions) | |||||||||||||||||||||
Asset-backed | $ | 91.4 | $ | (10.7 | ) | $ | 40.7 | $ | (6.5 | ) | $ | 132.1 | $ | (17.2 | ) | ||||||
Obligation of states and other political subdivisions | 141.4 | (4.9 | ) | 52.3 | (4.9 | ) | 193.7 | (9.8 | ) | ||||||||||||
Corporate debt | 111.0 | (4.7 | ) | 16.0 | (1.1 | ) | 127.0 | (5.8 | ) | ||||||||||||
Other securities | 0.4 | — | — | — | 0.4 | — | |||||||||||||||
| $ | 344.2 | $ | (20.3 | ) | $ | 109.0 | $ | (12.5 | ) | $ | 453.2 | $ | (32.8 | ) | |||||||
F-23
Table of Contents
HEALTH NET, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
The following table shows the number of our individual securities that have been in a continuous loss position at December 31, 2008:
| Less than 12 Months | 12 Months or More | Total | ||||
Asset-backed | 48 | 20 | 68 | |||
Obligation of states and other political subdivisions | 61 | 15 | 76 | |||
Corporate debt | 55 | 8 | 63 | |||
Other securities | 1 | — | 1 | |||
| 165 | 43 | 208 | ||||
The following table shows our investments’ gross unrealized losses and fair value for individual securities that have been in a continuous loss position through December 31, 2007:
| Less than 12 Months | 12 Months or More | Total | |||||||||||||||||||
| Fair Value | Unrealized Losses | Fair Value | Unrealized Losses | Fair Value | Unrealized Losses | ||||||||||||||||
| (Dollars in millions) | |||||||||||||||||||||
Asset-backed | $ | 23.1 | $ | (0.2 | ) | $ | 188.7 | $ | (2.9 | ) | $ | 211.8 | $ | (3.1 | ) | ||||||
U.S. government and agencies | 3.7 | — | 100.3 | (0.5 | ) | 104.0 | (0.5 | ) | |||||||||||||
Obligation of states and other political subdivisions | 110.8 | (1.0 | ) | 69.7 | (0.4 | ) | 180.5 | (1.4 | ) | ||||||||||||
Corporate debt | 26.5 | (0.4 | ) | 111.3 | (1.6 | ) | 137.8 | (2.0 | ) | ||||||||||||
| $ | 164.1 | $ | (1.6 | ) | $ | 470.0 | $ | (5.4 | ) | $ | 634.1 | $ | (7.0 | ) | |||||||
The above referenced investments are interest-yielding debt securities of varying maturities. The unrealized loss position for these securities is due to market volatility. Generally, in a rising interest rate environment, the estimated fair value of fixed income securities would be expected to decrease; conversely, in a decreasing interest rate environment, the estimated fair value of fixed income securities would be expected to increase. However, these securities may be negatively impacted by illiquidity in the market.
The investments listed above are investment grade securities with an average rating of “AA” and “Aa1” as rated by S&P and/or Moody’s, respectively. At this time, there is no indication of default on interest and/or principal payments. We have the ability and current intent to hold to recovery all securities with an unrealized loss position.
Note 5—Property and Equipment
Property and equipment is comprised of the following as of December 31:
| 2008 | 2007 | |||||||
| (Dollars in millions) | ||||||||
Land | $ | 1.7 | $ | 1.7 | ||||
Leasehold improvements under development | 4.6 | 2.6 | ||||||
Buildings and improvements | 49.4 | 43.4 | ||||||
Furniture, equipment and software | 304.1 | 247.6 | ||||||
| 359.8 | 295.3 | |||||||
Less accumulated depreciation | (157.4 | ) | (116.5 | ) | ||||
Property and equipment, net | $ | 202.4 | $ | 178.8 | ||||
F-24
Table of Contents
HEALTH NET, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
Our depreciation expense was $40.8 million, $30.3 million and $21.5 million for the years ended December 31, 2008, 2007 and 2006, respectively.
Note 6—Financing Arrangements
Amortizing Financing Facility
On December 19, 2007, we entered into a five-year, non-interest bearing, $175 million amortizing financing facility with a non-U.S. lender, and on April 29, 2008, and November 10, 2008, we entered into amendments to the financing facility, which were administrative in nature. In connection with the financing facility, we entered into an interest rate swap agreement (see Note 2). Under the interest rate swap agreement, we pay an amount equal to LIBOR times a notional principal amount and receive in return an amount equal to 4.3% times the same notional principal amount. The financing facility requires one of our subsidiaries to pay semi-annual distributions, in the amount of $17.5 million, to a participant in the financing facility. Unless terminated earlier, the final payment under the facility is scheduled to be made on December 19, 2012.
The financing facility includes limitations (subject to specified exclusions) on our and certain of our subsidiaries’ ability to incur debt; create liens; engage in certain mergers, consolidations and acquisitions; engage in transactions with affiliates; enter into agreements which will restrict the ability to pay dividends or other distributions with respect to any shares of capital stock or the ability to make or repay loans or advances; make dividends; and alter the character of the business we and our subsidiaries conducted on the closing date of the financing facility. In addition, the financing facility also requires that we maintain a specified consolidated leverage ratio and consolidated fixed charge coverage ratio and maintain certain minimum public debt ratings throughout the term of the financing facility. As of December 31, 2008, we were in compliance with all of the covenants under the financing facility.
The financing facility provides that it may be terminated through a series of put and call transactions (1) at the option of one of our wholly-owned subsidiaries at any time after December 20, 2009, or (2) upon the occurrence of certain defined early termination events. These early termination events, include, but are not limited to:
| • | nonpayment of certain amounts due by us or certain of our subsidiaries under the financing facility (if not cured within the related time period set forth therein); |
| • | a change of control (as defined in the financing facility); |
| • | our failure to maintain the following ratings on our senior indebtedness by any two of the following three rating agencies: (1) a rating of at least BB by Standard & Poor’s Ratings Services (S&P), (2) a rating of at least BB by Fitch, Inc. (Fitch), and (3) a rating of at least Ba2 by Moody’s Investors Service, Inc. (Moody’s). As of December 31, 2008, the ratings with S&P, Fitch and Moody’s on our senior indebtedness were BB, BB+ and Ba3, respectively; |
| • | cross-acceleration to other indebtedness of our Company in excess of $50 million, including our revolving credit facility; |
| • | certain ERISA-related events; |
| • | noncompliance by Health Net with any material term or provision of the HMO Regulations or Insurance Regulations (as each such term is defined in the financing facility); |
| • | events in bankruptcy, insolvency or reorganization of our Company; |
F-25
Table of Contents
HEALTH NET, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
| • | undischarged, uninsured judgments in the amount of $50 million or more against our Company; or |
| • | certain changes in law that could adversely affect a participant in the financing facility. |
In addition, in connection with the financing facility, we entered into a guaranty which will require us to guarantee the payment of the semi-annual distributions and any other amounts payable by one of our subsidiaries to the financing facility participants under certain circumstances provided under the financing facility. Also in connection with the financing facility, we entered into an interest rate swap agreement with a non-U.S. bank affiliated with one of the financing facility participants. Under the interest rate swap agreement, we pay a floating payment in an amount equal to LIBOR times a notional principal amount and receive a fixed payment in an amount equal to 4.3% times the same notional principal amount from the non-U.S. bank counterparty in return in accordance with a schedule set forth in the interest rate swap agreement.
As of December 31, 2008, our current and noncurrent amortizing financing facility payables were $27.3 million and $104.0 million, respectively. As of December 31, 2007, our current and noncurrent amortizing financing facility payables were $35.0 million and $112.4 million, respectively.
Senior Notes
On May 18, 2007 we issued $300 million in aggregate principal amount of 6.375% Senior Notes due 2017. On May 31, 2007, we issued an additional $100 million of 6.375% Senior Notes due 2017 which were consolidated with, and constitute the same series as, the Senior Notes issued on May 18, 2007 (collectively, Senior Notes). The aggregate net proceeds from the issuance of the Senior Notes were $393.5 million and were used to repay outstanding debt.
The indenture governing the Senior Notes limits our ability to incur certain liens, or consolidate, merge or sell all or substantially all of our assets. In the event of the occurrence of both (1) a change of control of Health Net, Inc. and (2) a below investment grade rating by any two of Fitch, Inc., Moody’s Investors Service, Inc. and Standard & Poor’s Ratings Services within a specified period, we will be required to make an offer to purchase the Senior Notes at a price equal to 101% of the principal amount of the Senior Notes plus accrued and unpaid interest to the date of repurchase. As of December 31, 2008, no default or event of default had occurred under the indenture governing the Senior Notes.
The Senior Notes may be redeemed in whole at any time or in part from time to time, prior to maturity at our option, at a redemption price equal to the greater of:
| • | 100% of the principal amount of the Senior Notes then outstanding to be redeemed; or |
| • | the sum of the present values of the remaining scheduled payments of principal and interest on the Senior Notes to be redeemed (not including any portion of such payments of interest accrued to the date of redemption) discounted to the date of redemption on a semiannual basis (assuming a 360-day year consisting of twelve 30-day months) at the applicable treasury rate plus 30 basis points |
plus, in each case, accrued and unpaid interest on the principal amount being redeemed to the redemption date.
Each of the following will be an Event of Default under the indenture governing the Senior Notes:
| • | failure to pay interest for 30 days after the date payment is due and payable; provided that an extension of an interest payment period by us in accordance with the terms of the Senior Notes shall not constitute a failure to pay interest; |
F-26
Table of Contents
HEALTH NET, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
| • | failure to pay principal or premium, if any, on any note when due, either at maturity, upon any redemption, by declaration or otherwise; |
| • | failure to perform any other covenant or agreement in the notes or indenture for a period of 60 days after notice that performance was required; |
| • | (A) our failure or the failure of any of our subsidiaries to pay indebtedness for money we borrowed or any of our subsidiaries borrowed in an aggregate principal amount of at least $50,000,000, at the later of final maturity and the expiration of any related applicable grace period and such defaulted payment shall not have been made, waived or extended within 30 days after notice or (B) acceleration of the maturity of indebtedness for money we borrowed or any of our subsidiaries borrowed in an aggregate principal amount of at least $50,000,000, if that acceleration results from a default under the instrument giving rise to or securing such indebtedness for money borrowed and such indebtedness has not been discharged in full or such acceleration has not been rescinded or annulled within 30 days after notice; or |
| • | events in bankruptcy, insolvency or reorganization of our Company. |
Our Senior Notes payable balance was $398.3 million and $398.1 million as of December 31, 2008 and 2007, respectively.
Revolving Credit Facility
On June 25, 2007, we entered into a $900 million five-year revolving credit facility with Bank of America, N.A. as Administrative Agent, Swingline Lender, and L/C Issuer, and the other lenders party thereto. We entered into an amendment to the credit facility on April 29, 2008, which was administrative in nature. As of December 31, 2008, $150 million was outstanding under our revolving credit facility and the maximum amount available for borrowing under the revolving credit facility was $427.1 million (see “—Letters of Credit” below).
Amounts outstanding under our revolving credit facility will bear interest, at our option, at (a) the base rate, which is a rate per annum equal to the greater of (i) the federal funds rate plus one-half of one percent and (ii) Bank of America’s prime rate (as such term is defined in the facility), (b) a competitive bid rate solicited from the syndicate of banks, or (c) the British Bankers Association LIBOR rate (as such term is defined in the facility), plus an applicable margin, which is initially 70 basis points per annum and is subject to adjustment according to our credit ratings, as specified in the facility.
Our revolving credit facility includes, among other customary terms and conditions, limitations (subject to specified exclusions) on our and our subsidiaries’ ability to incur debt; create liens; engage in certain mergers, consolidations and acquisitions; sell or transfer assets; enter into agreements which restrict the ability to pay dividends or make or repay loans or advances; make investments, loans, and advances; engage in transactions with affiliates; and make dividends. In addition, we are required to maintain a specified consolidated leverage ratio and consolidated fixed charge coverage ratio throughout the term of the revolving credit facility.
Our revolving credit facility contains customary events of default, including nonpayment of principal or other amounts when due; breach of covenants; inaccuracy of representations and warranties; cross-default and/or cross-acceleration to other indebtedness of the Company or our subsidiaries in excess of $50 million; certain ERISA-related events; noncompliance by us or any of our subsidiaries with any material term or provision of the HMO Regulations or Insurance Regulations (as each such term is defined in the facility); certain voluntary and involuntary bankruptcy events; inability to pay debts; undischarged, uninsured judgments greater than $50 million against us and/or our subsidiaries; actual or asserted invalidity of any loan document; and a change of
F-27
Table of Contents
HEALTH NET, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
control. If an event of default occurs and is continuing under the credit facility, the lenders thereunder may, among other things, terminate their obligations under the facility and require us to repay all amounts owed thereunder.
Redemption of 8.375% Senior Notes
On August 14, 2006, we redeemed $400 million in aggregate principal amount of 8.375% senior notes, which were scheduled to mature in April 2011 and refinanced the 8.375% senior notes with $500 million of bridge and term loans. In connection with this refinancing, we incurred $70.1 million in costs, including $51.0 million in redemption premiums with respect to these senior notes, $11.1 million for the termination and settlement of our interest rate swap agreements and $8.0 million for professional fees and other expenses.
Letters of Credit
We can obtain letters of credit in an aggregate amount of $400 million under our revolving credit facility. The maximum amount available for borrowing under our revolving credit facility is reduced by the dollar amount of any outstanding letters of credit. As of December 31, 2008 and 2007, we had outstanding letters of credit for $322.9 million and $120.8 million, respectively, resulting in the maximum amount available for borrowing under the revolving credit facility of $427.1 million and $779.2 million, respectively. As of December 31, 2008 and 2007, no amounts have been drawn on any of these letters of credit.
The weighted average annual interest rate on our financing arrangements was approximately 5.7%, 6.5% and 8.9% for the years ended December 31, 2008, 2007 and 2006, respectively.
Note 7—Fair Value Measurements
In September 2006, the FASB issued SFAS No. 157,Fair Value Measurements, which we adopted on January 1, 2008. SFAS No. 157 does not require any new fair value measurements, but it defines fair value, establishes a framework for measuring fair value in accordance with existing GAAP, and expands disclosures about fair value measurements. Assets and liabilities recorded at fair value in the consolidated balance sheets are categorized based upon the level of judgment associated with the inputs used to measure their fair value and the level of market price observability.
Investments measured and reported at fair value using Level inputs, as defined by SFAS No. 157, are classified and disclosed in one of the following categories:
Level 1—Quoted prices are available in active markets for identical investments as of the reporting date. The type of investments included in Level I include U.S. treasury securities and listed equities. As required by SFAS No. 157, we do not adjust the quoted price for these investments, even in situations where we hold a large position and a sale could reasonably impact the quoted price.
Level 2—Pricing inputs are other than quoted prices in active markets, which are either directly or indirectly observable as of the reporting date, and fair value is determined through the use of models or other valuation methodologies. Investments that are generally included in this category include asset-backed securities, corporate bonds and loans, municipal bonds, auction rate securities and interest rate swap asset.
Level 3—Pricing inputs are unobservable for the investment and include situations where there is little, if any, market activity for the investment. The inputs into the determination of fair value require significant management judgment or estimation.
F-28
Table of Contents
HEALTH NET, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
In certain cases, the inputs used to measure fair value may fall into different levels of the fair value hierarchy. In such cases, an investment’s level within the fair value hierarchy is based on the lowest level of input that is significant to the fair value measurement. Our assessment of the significance of a particular input to the fair value measurement in its entirety requires judgment and considers factors specific to the investment.
The following table presents information about our assets measured at fair value on a recurring basis at December 31, 2008, and indicate the fair value hierarchy of the valuation techniques utilized by us to determine such fair value.
| Level 1 | Level 2 | Level 3 | Total | |||||||||
| (Dollars in millions) | ||||||||||||
Assets: | ||||||||||||
Investments—available for sale | ||||||||||||
Asset-backed securities | $ | — | $ | 520.0 | $ | — | $ | 520.0 | ||||
U.S. government and agencies | 36.9 | 33.1 | — | 70.0 | ||||||||
Obligations of states and other political subdivisions | — | 565.2 | 10.2 | 575.4 | ||||||||
Corporate debt securities | — | 338.7 | — | 338.7 | ||||||||
Other securities | 0.6 | — | — | 0.6 | ||||||||
| $ | 37.5 | $ | 1,457.0 | $ | 10.2 | $ | 1,504.7 | |||||
Interest rate swap asset | — | 8.0 | — | 8.0 | ||||||||
Total assets at fair value | $ | 37.5 | $ | 1,465.0 | $ | 10.2 | $ | 1,512.7 | ||||
The changes in the balances of Level 3 financial assets for the year ended December 31, 2008 were as follows (dollars in millions):
| 2008 | ||||
| (Dollars in millions) | ||||
Beginning balance | $ | — | ||
Total gains and losses | ||||
Realized in net income | — | |||
Unrealized in accumulated other comprehensive income | — | |||
Purchases, sales, issuances and settlements | (11.6 | ) | ||
Transfers into Level 3 | 21.8 | |||
Ending balance at December 31, 2008 | $ | 10.2 | ||
Change in unrealized gains (losses) included in net income related to assets still held | $ | — | ||
During the year ended December 31, 2008, certain auction rate securities experienced “failed” auctions. As a result, these securities’ fair values were determined to be equal to their par values due to the short time periods between coupon resets and the issuers’ credit worthiness.
Note 8—Long-Term Equity Compensation
For the year ended December 31, 2008, the compensation cost that has been charged against income under our long-term incentive plans (the Plans) was $24.1 million. The total income tax benefit recognized in the income statement for share-based compensation arrangements was $9.3 million (See Note 2).
F-29
Table of Contents
HEALTH NET, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
The Plans permit the grant of stock options and other equity awards, including but not limited to restricted stock, restricted stock units (RSUs) and performance share awards to certain employees, officers and non-employee directors. The grant of any award other than an option reduces the number of shares of common stock available for issuance under the 2006 Long-Term Incentive Plan by two shares of common stock for each award and is deemed to be an award of two shares of common stock for each share subject to the award. Stock options are granted with an exercise price at or above the fair market value of the Company’s common stock on the date of grant. Stock options carry a maximum term of ten years, and, in general, stock options and other equity awards vest based on one to five years of continuous service, except for certain awards where vesting may be accelerated by virtue of attaining certain performance targets. As of December 31, 2008, there were no outstanding options or awards that had market or performance condition accelerated vesting provisions. Certain stock options and other equity awards also provide for accelerated vesting under the circumstances set forth in the Plans and equity award agreements upon the occurrence of a change in control (as defined in the Plans). At the end of the ten-year term, unexercised stock options are set to expire.
Performance share awards were granted in 2007 and 2008 with 100% cliff vesting at the end of a three-year performance period and provide for vesting in 0% to 200% of shares granted. Shares delivered pursuant to each performance share award will take into account the Company’s attainment of specific performance conditions as outlined in each performance share award agreement.
As of December 31, 2008, we have reserved up to an aggregate of 10.8 million shares of our common stock for issuance under the Plans.
The fair value of each option award is estimated on the date of grant using a closed-form option valuation model (Black-Scholes) based on the assumptions noted in the following table. Expected volatilities are based on implied volatilities from traded options on our stock and historical volatility of our stock. We estimated the expected term of options by using historical data to estimate option exercise and employee termination within a lattice-based valuation model; separate groups of employees that have similar historical exercise behavior are considered separately for valuation purposes. The expected term of options granted is derived from a lattice-based option valuation model and represents the period of time that options granted are expected to be outstanding. The risk-free rate for periods within the contractual life of the option is based on the U.S. Treasury Strip yields in effect at the time of grant with maturity dates approximately equal to the expected life of the option at the grant date.
The following table provides the weighted-average values of assumptions used in the calculation of grant-date fair values during the years ended December 31:
| 2008 | 2007 | 2006 | |||||||
Risk-free interest rate | 2.96 | % | 4.53 | % | 4.83 | % | |||
Expected option lives (in years) | 5.3 | 4.8 | 4.4 | ||||||
Expected volatility for options | 34.2 | % | 27.3 | % | 27.7 | % | |||
Expected dividend yield | None | None | None |
The weighted-average grant-date fair values for options granted during 2008, 2007 and 2006 were $8.56, $16.91 and $14.52, respectively. The total intrinsic value of options exercised was $3.9 million, $69.4 million and $52.6 million during the years ended December 31, 2008, 2007 and 2006, respectively.
F-30
Table of Contents
HEALTH NET, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
A summary of option activity under our various plans as of December 31, 2008, and changes during the year then ended is presented below:
| Number of Options | Weighted Average Exercise Price | Weighted Average Remaining Contractual Term (Years) | Aggregate Intrinsic Value | ||||||||
Outstanding at January 1, 2008 | 6,542,016 | $ | 30.38 | ||||||||
Granted | 325,047 | 24.00 | |||||||||
Exercised | (244,984 | ) | 27.23 | ||||||||
Forfeited or expired | (491,566 | ) | 35.33 | ||||||||
Outstanding at December 31, 2008 | 6,130,513 | $ | 29.77 | 5.05 | $ | 251,535 | |||||
Vested or expected to vest at December 31, 2008 (reflecting estimated forfeiture rates effective January 1, 2008) | 5,992,632 | $ | 29.57 | 4.98 | $ | 251,535 | |||||
Exercisable at December 31, 2008 | 4,882,717 | $ | 27.58 | 4.34 | $ | 242,205 | |||||
| Options Outstanding | Options Exercisable | |||||||||||
Range of Exercise Prices | Number of Options | Weighted Average Remaining Contractual Life (Years) | Weighted Average Exercise Price | Number of Options | Weighted Average Exercise Price | |||||||
$ 7.63 – 20.00 | 291,172 | 4.07 | $ | 11.43 | 192,672 | $ | 10.95 | |||||
20.01 – 25.00 | 2,695,245 | 3.52 | 23.24 | 2,657,245 | 23.23 | |||||||
25.01 – 30.00 | 1,471,848 | 5.84 | 28.67 | 1,109,722 | 28.67 | |||||||
30.01 – 40.00 | 440,259 | 5.91 | 33.67 | 353,050 | 33.44 | |||||||
40.01 – 50.00 | 1,014,776 | 7.18 | 47.00 | 504,648 | 46.88 | |||||||
50.01 – 58.07 | 217,213 | 8.18 | 54.30 | 65,380 | 54.09 | |||||||
$ 7.63 – 58.07 | 6,130,513 | 5.05 | $ | 29.77 | 4,882,717 | $ | 27.58 | |||||
We have entered into restricted stock and RSU agreements with certain employees. We have awarded shares of restricted common stock under the restricted stock agreements and rights to receive common stock under the RSU agreements to certain employees. Each RSU represents the right to receive, upon vesting, one share of common stock. Awards of restricted stock and RSUs are subject to restrictions on transfer and forfeiture prior to vesting. During the years ended December 31, 2008, 2007 and 2006, we did not award any restricted stock. During the years ended December 31, 2008, 2007 and 2006, we awarded 1,000,699, 945,479 and 607,379 RSUs, respectively.
F-31
Table of Contents
HEALTH NET, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
A summary of the status of the Company’s restricted common stock as of December 31, 2008, and changes during the year then ended is presented below:
| Restricted Shares | Weighted Average Grant-Date Fair Value | |||||
Balance at January 1, 2008 | 1,250 | $ | 23.64 | |||
Granted | — | — | ||||
Vested | (1,250 | ) | 23.64 | |||
Forfeited | — | — | ||||
Balance at December 31, 2008 | — | $ | — | |||
Expected to vest at December 31, 2008 | — | $ | — | |||
A summary of RSU activity under our various plans as of December 31, 2008, and changes during the year then ended is presented below:
| Number of Restricted Stock Units | Weighted Average Grant-Date Fair Value | Weighted Average Purchase Price | Weighted Average Remaining Contractual Term (Years) | Aggregate Intrinsic Value | ||||||||||
Outstanding at January 1, 2008 | 1,338,330 | $ | 48.30 | $ | 0.001 | |||||||||
Granted | 1,000,699 | 47.47 | 0.001 | |||||||||||
Vested | (31,250 | ) | 46.76 | 0.001 | ||||||||||
Forfeited | (338,700 | ) | 51.02 | 0.001 | ||||||||||
Outstanding at December 31, 2008 | 1,969,079 | $ | 49.59 | $ | 0.001 | 8.46 | $ | 21,441,301 | ||||||
Expected to vest at December 31, 2008 (reflecting estimated forfeiture rates effective January 1, 2008) | 1,349,228 | $ | 49.61 | $ | 0.001 | 8.37 | $ | 14,691,744 | ||||||
The fair value of restricted common stock and RSUs is determined based on the market value of the shares on the date of grant. We did not grant any restricted common stock during the years ended December 31, 2008, 2007 and 2006. The aggregate intrinsic values of restricted shares vested during the years ended December 31, 2008, 2007 and 2006, were $40 thousand, $4.6 million and $6.0 million, respectively. The weighted-average grant-date fair values of RSUs granted during the years ended December 31, 2008, 2007 and 2006 were $47.47, $54.13 and $47.16, respectively. The aggregate intrinsic values of RSUs vested during the years ended December 31, 2008, 2007 and 2006, were $0.5 million, $10 thousand and $0, respectively. Compensation expense recorded for the restricted common stock was $2,000, $2,000 and $498,000 during the years ended December 31, 2008, 2007 and 2006, respectively. Compensation expense recorded for the RSUs was $19,274,000, $14,973,000 and $4,049,000 during the years ended December 31, 2008, 2007 and 2006, respectively.
As of December 31, 2008, the total remaining unrecognized compensation cost related to non-vested stock options, RSUs and restricted stock was $10.0 million, $48.9 million and $0, respectively, which is expected to be recognized over a weighted-average period of 1.05 years, 1.44 years and 0 years, respectively.
Under the Company’s various stock option and long-term incentive plans, employees and non-employee directors may elect for the Company to withhold shares to satisfy minimum statutory federal, state and local tax withholding and exercise price obligations arising from the vesting of stock options and other equity awards made there-under. During the year ended December 31, 2008, we withheld 15,057 shares of common stock at the
F-32
Table of Contents
HEALTH NET, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
election of employees and non-employee directors to satisfy their tax withholding and exercise price obligations arising from the vesting of stock options and restricted stock awards.
We become entitled to an income tax deduction in an amount equal to the taxable income reported by the holders of the stock options, restricted shares and RSUs when vesting occurs, the restrictions are released and the shares are issued. Stock options, restricted common stock and RSUs are forfeited if the employees terminate their employment prior to vesting.
Note 9—Capital Stock
As of December 31, 2008, there were 143,753,000 shares of our Common Stock issued and 40,045,000 shares of Common Stock held in treasury, resulting in 103,708,000 shares of our Common Stock outstanding.
Shareholder Rights Plan
On July 27, 2006, our Board of Directors approved the extension of the benefits afforded by our former shareholder rights plan, which expired at the close of business on July 31, 2006, by adopting a new shareholder rights plan pursuant to a Rights Agreement with Wells Fargo Bank, N.A. (the “Rights Agent”), dated as of July 27, 2006 (the “Rights Agreement”).
In connection with the Rights Agreement, on July 27, 2006, our Board of Directors declared a dividend distribution of one right (a “Right”) for each outstanding share of Common Stock to stockholders of record at the close of business on August 7, 2006 (the “Record Date”). Our Board of Directors also authorized the issuance of one Right for each share of Common Stock issued after the Record Date and prior to the earliest of the Distribution Date (as defined below) the redemption of the Rights and the expiration of the Rights and, in certain circumstances, after the Distribution Date. Subject to certain exceptions and adjustment as provided in the Rights Agreement, each Right entitles the registered holder to purchase from us one one-thousandth (1/1000th) of a share of Series A Junior Participating Preferred Stock, par value of $0.001 per share, at a purchase price of $170.00 per Right (the “Purchase Price”). The terms of the Rights are set forth in the Rights Agreement.
Rights will attach to all common stock certificates representing shares then outstanding and no separate Rights certificates will be distributed. Subject to certain exceptions contained in the Rights Agreement, the Rights will separate from the Common Stock on the date that is 10 business days following (i) any person, together with its affiliates and associates (an Acquiring Person), becoming the beneficial owner of 15% or more of the outstanding common stock, (ii) the commencement of a tender or exchange offer that would result in any person, together with its affiliates and associates, becoming the beneficial owner of 15% or more of the outstanding common stock or (iii) the determination by the Board of Directors that a person, together with its affiliates and associates, has become the beneficial owner of 10% or more of the common stock and that such person is an “Adverse Person,” as defined in the Rights Agreement (the earliest of such dates being called the “Distribution Date”). The Rights Agreement provides that certain passive institutional investors that beneficially own less than 20% of the outstanding shares of our common stock shall not be deemed to be Acquiring Persons.
The Rights will first become exercisable on the Distribution Date and will expire at the close of business on July 31, 2016 unless such date is extended or the Rights are earlier redeemed by us as described below.
Subject to certain exceptions contained in the Rights Agreement, in the event that any person shall become an Acquiring Person or be declared to be an Adverse Person, then the Rights will “flip-in” and entitle each holder of a Right, other than any Acquiring Person or Adverse Person and such person’s affiliates and associates, to
F-33
Table of Contents
HEALTH NET, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
purchase, upon exercise at the then-current exercise price of such Right, that number of shares of common stock having a market value of two times such exercise price.
In addition, and subject to certain exceptions contained in the Rights Agreement, in the event that we are acquired in a merger or other business combination in which the common stock does not remain outstanding or is changed or 50% of the assets, cash flow or earning power of the Company is sold or otherwise transferred to any other person, the Rights will “flip-over” and entitle each holder of a Right, other than an Acquiring Person or an Adverse Person and such person’s affiliates and associates, to purchase, upon exercise at the then current exercise price of such Right, such number of shares of common stock of the acquiring company which at the time of such transaction would have a market value of two times such exercise price.
We may redeem the Rights at any time until the earlier of (i) 10 days following the date that any Acquiring Person becomes the beneficial owner of 15% or more of the outstanding common stock and (ii) the date the Rights expire at a price of $.01 per Right. In addition, at any time after a person becomes an Acquiring Person or is determined to be and Adverse Person and prior to such person becoming (together with such person’s affiliates and associates) the beneficial owner of 50% or more of the outstanding Common Stock, at the election of our Board of Directors, the outstanding Rights (other than those beneficially owned by an Acquiring Person, Adverse Person or an affiliate or associate of an Acquiring Person or Adverse Person) may be exchanged, in whole or in part, for shares of Common Stock, or shares of preferred stock of the Company having essentially the same value or economic rights as such shares.
Stock Repurchase Program
We have a $700 million stock repurchase program authorized by our Board of Directors. Subject to Board approval, additional amounts are added to the repurchase program from time to time based on exercise proceeds and tax benefits the Company receives from employee stock options. We repurchased 6,851,595 shares of our common stock during the year ended December 31, 2008, for aggregate consideration of approximately $242.8 million.
The remaining authorization under our stock repurchase program as of December 31, 2008 was $103.3 million. As of December 31, 2008, we had repurchased a cumulative aggregate of 36,623,347 shares of our common stock under our stock repurchase program at an average price of $34.40 per share for aggregate consideration of $1,259.8 million (which amount includes exercise proceeds and tax benefits the Company had received from the exercise of employee stock options). We used net free cash available to fund the share repurchases.
On December 14, 2006, we entered into an accelerated share repurchase (ASR) agreement with JP Morgan and repurchased 2,689,538 shares at an initial purchase price of $47.22 per share, or $127 million. Under the ASR agreement, JP Morgan purchased an equivalent number of shares in the open market. The repurchased shares were subject to a price adjustment based on JP Morgan’s volume-weighted average purchase price for the shares. If JP Morgan’s volume-weighted average purchase price for the shares was greater than $47.22 per share, we were required to pay JP Morgan an amount equal to the difference between the volume-weighted average purchase price and $47.22 (True-Up). Under the ASR agreement, we could elect to settle the True-Up in shares of Health Net common stock or cash. On March 15, 2007, we settled the True-Up of approximately $7.1 million by delivering 132,806 shares of our common stock to JP Morgan. The settlement is recorded in our statement of stockholders’ equity.
We may repurchase shares of our common stock under the stock repurchase program from time to time in open market transactions, privately negotiated transactions, or through accelerated share repurchase programs, or
F-34
Table of Contents
HEALTH NET, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
by any combination of such methods. The timing of any repurchases and the actual number of shares repurchased will depend on a variety of factors, including our stock price, corporate and regulatory requirements, restrictions under our debt obligations, and other market and economic conditions.
Our stock repurchase program does not have an expiration date. The stock purchase program may be suspended or discontinued at any time.
On November 4, 2008, we announced that our stock repurchase program is on hold as a consequence of the uncertain financial environment and the announcement by Health Net’s Board of Directors that Jay Gellert, our President and Chief Executive Officer, will be undertaking a review of the Company’s strategic direction.
Note 10—Employee Benefit Plans
Defined Contribution Retirement Plans
We and certain of our subsidiaries sponsor defined contribution retirement plans intended to qualify under Sections 401(a) and 401(k) of the Internal Revenue Code of 1986, as amended (the Code). The plans were amended in December 2008 to comply with, among other things, Section 415 of the Code. Participation in the plans is available to substantially all employees who meet certain eligibility requirements and elect to participate. Employees may contribute up to the maximum limits allowed by Sections 401(k) and 415 of the Code, with Company contributions based on matching or other formulas. Our expense under these plans totaled $19.8 million, $20.6 million and $16.0 million for the years ended December 31, 2008, 2007 and 2006, respectively, and is included in general and administrative expense in our consolidated statements of operations.
Deferred Compensation Plans
We have a voluntary deferred compensation plan pursuant to which certain management and highly compensated employees are eligible to defer a certain portion of their regular compensation and bonuses. The compensation deferred under this plan is credited with earnings or losses measured by the mirrored rate of return on investments elected by plan participants. This plan is unfunded. Each plan participant is fully vested in all deferred compensation and earnings credited to his or her account. In December 2008, the plan was amended to comply with, among other things, Section 409A of the Code.
As of December 31, 2008 and 2007, the liability under these plans amounted to $41.5 million and $48.6 million, respectively. These liabilities are included in other noncurrent liabilities on our consolidated balance sheets. Deferred compensation expense is recognized for the amount of earnings or losses credited to participant accounts. Our expense under these plans totaled $5.7 million, $3.3 million and $4.6 million for the years ended December 31, 2008, 2007 and 2006, respectively, and is included in general and administrative expense in our consolidated statements of operations.
Pension and Other Postretirement Benefit Plans
In 2006, the FASB issued SFAS No. 158, “Employers’ Accounting for Defined Benefit Pension and Other Postretirement Plans, an amendment of FASB Statements No. 87, 88, 106 and 132 (R)” (SFAS No. 158). SFAS No. 158 requires an entity to recognize in its statement of financial position an asset for a defined benefit postretirement plan’s overfunded status or a liability for a plan’s underfunded status, measure a defined benefit postretirement plan’s assets and obligations that determine its funded status as of the employer’s fiscal year end, and recognize changes in the funded status of a defined benefit postretirement plan in comprehensive income in the year in which the changes occur. SFAS No. 158 does not change the amount of net periodic benefit cost included in net income or address the various measurements issues associated with postretirement benefit plan
F-35
Table of Contents
HEALTH NET, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
accounting. SFAS No. 158 also requires an employer to measure the funded status of a plan as of the date of its year-end statement of financial position. The requirement to recognize the funded status of a defined benefit postretirement plan and the disclosure requirements are effective for fiscal years ending after December 15, 2006 for public entities. The requirement to measure the funded status of a plan as of the date of its year-end statement of financial position is effective for fiscal years ending after December 15, 2008. We adopted the provisions of SFAS No. 158 at December 31, 2006, which resulted in an increase in pension obligation of $2.0 million and a decrease in accumulated other comprehensive income for the same amount.
Pension Plans—We have an unfunded non-qualified defined benefit pension plan, the Supplemental Executive Retirement Plan. The plan was amended and restated effective in January 2008 to comply with Section 409A of the Code. This plan is noncontributory and covers key executives as selected by the Board of Directors. Benefits under the plan are based on years of service and level of compensation during the final five years of service.
Postretirement Health and Life Plans—Certain of our subsidiaries sponsor postretirement defined benefit health care and life insurance plans that provide postretirement medical and life insurance benefits to directors, key executives, employees and dependents who meet certain eligibility requirements. The Health Net health care plan is non-contributory for employees retired prior to December 1, 1995 who have attained the age of 62; employees retiring after December 1, 1995 who have attained age 62 contribute from 25% to 100% of the cost of coverage depending upon years of service. The plan was amended in 2008 to vest benefits for eligible associates who were terminated in connection with the Company’s operations strategy. We have two other benefit plans that we have acquired as part of the acquisitions made in 1997. One of the plans is frozen and non-contributory, whereas the other plan is contributory by certain participants. Under these plans, we pay a percentage of the costs of medical, dental and vision benefits during retirement. The plans include certain cost-sharing features such as deductibles, co-insurance and maximum annual benefit amounts that vary based principally on years of credited service.
The following table sets forth the plans’ obligations and funded status at December 31:
| Pension Benefits | Other Benefits | |||||||||||||||
| 2008 | 2007 | 2008 | 2007 | |||||||||||||
| (Dollars in millions) | ||||||||||||||||
Change in benefit obligation: | ||||||||||||||||
Benefit obligation, beginning of year | $ | 26.2 | $ | 25.2 | $ | 9.5 | $ | 9.7 | ||||||||
Service cost | 1.2 | 1.3 | 0.2 | 0.3 | ||||||||||||
Interest cost | 1.6 | 1.4 | 0.6 | 0.5 | ||||||||||||
Benefits paid | (1.0 | ) | (0.9 | ) | (0.5 | ) | (0.4 | ) | ||||||||
Actuarial (gain) loss | (2.3 | ) | (0.8 | ) | 0.3 | (0.6 | ) | |||||||||
Benefit obligation, end of year | $ | 25.7 | $ | 26.2 | $ | 10.1 | $ | 9.5 | ||||||||
Change in fair value of plan assets: | ||||||||||||||||
Plan assets, beginning of year | $ | — | $ | — | $ | — | $ | — | ||||||||
Employer contribution | 1.0 | 0.9 | 0.5 | 0.4 | ||||||||||||
Benefits paid | (1.0 | ) | (0.9 | ) | (0.5 | ) | (0.4 | ) | ||||||||
Plan assets, end of year | $ | — | $ | — | $ | — | $ | — | ||||||||
Underfunded status, end of year | $ | (25.7 | ) | $ | (26.2 | ) | $ | (10.1 | ) | $ | (9.5 | ) | ||||
F-36
Table of Contents
HEALTH NET, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
Amounts recognized in our consolidated balance sheet as of December 31 consist of:
| Pension Benefits | Other Benefits | |||||||||||||||
| 2008 | 2007 | 2008 | 2007 | |||||||||||||
| (Dollars in millions) | ||||||||||||||||
Noncurrent assets | — | — | — | — | ||||||||||||
Current liabilities | $ | (1.0 | ) | $ | (1.0 | ) | $ | (0.6 | ) | $ | (0.5 | ) | ||||
Noncurrent liabilities | (24.7 | ) | (25.2 | ) | (9.5 | ) | (9.0 | ) | ||||||||
Net amount recognized | $ | (25.7 | ) | $ | (26.2 | ) | $ | (10.1 | ) | $ | (9.5 | ) | ||||
Amounts recognized in accumulated other comprehensive income as of December 31 consist of:
| Pension Benefits | Other Benefits | |||||||||||||
| 2008 | 2007 | 2008 | 2007 | |||||||||||
| (Dollars in millions) | ||||||||||||||
Prior service cost | $ | 0.5 | $ | 0.8 | $ | 0.1 | $ | 0.1 | ||||||
Net loss (gain) | (1.0 | ) | 0.4 | 0.1 | (0.2 | ) | ||||||||
| $ | (0.5 | ) | $ | 1.2 | $ | 0.2 | $ | (0.1 | ) | |||||
The following table sets forth our plans with an accumulated benefit obligation in excess of plan assets at December 31:
| Pension Benefits | Other Benefits | |||||||||||
| 2008 | 2007 | 2008 | 2007 | |||||||||
| (Dollars in millions) | ||||||||||||
Projected benefit obligation | $ | 25.7 | $ | 26.2 | $ | 10.1 | $ | 9.5 | ||||
Accumulated benefit obligation | 18.4 | 17.7 | 10.1 | 9.5 | ||||||||
Fair value of plan assets | $ | — | $ | — | $ | — | $ | — | ||||
Components of net periodic benefit cost recognized in our consolidated statements of operations as general and administrative expense for years ended December 31:
| Pension Benefits | Other Benefits | |||||||||||||||||
| 2008 | 2007 | 2006 | 2008 | 2007 | 2006 | |||||||||||||
| (Dollars in millions) | ||||||||||||||||||
Service Cost | $ | 1.2 | $ | 1.3 | $ | 1.1 | $ | 0.2 | $ | 0.3 | $ | 0.4 | ||||||
Interest Cost | 1.6 | 1.4 | 1.2 | 0.6 | 0.5 | 0.6 | ||||||||||||
Amortization of prior service cost | 0.5 | 0.5 | 0.5 | — | — | — | ||||||||||||
Amortization of net (gain) loss | — | — | 0.1 | — | 0.1 | 0.1 | ||||||||||||
Net periodic benefit cost | $ | 3.3 | $ | 3.2 | $ | 2.9 | $ | 0.8 | $ | 0.9 | $ | 1.1 | ||||||
The estimated net (gain) loss and prior service cost for the defined benefit pension plans that will be amortized from accumulated other comprehensive income into net periodic benefit cost over the next fiscal year are $49,000 and $0.5 million, respectively.
All of our pension and other postretirement benefit plans are unfunded. Employer contributions equal benefits paid during the year. Therefore, no return on assets is expected.
F-37
Table of Contents
HEALTH NET, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
Additional Information
| Pension Benefits | Other Benefits | |||||||||||
| 2008 | 2007 | 2008 | 2007 | |||||||||
Assumptions | ||||||||||||
Weighted average assumptions used to determine benefit obligations at | ||||||||||||
Discount rate | 6.6 | % | 6.5 | % | 6.6 | % | 6.5 | % | ||||
Rate of compensation increase | 5.9 | % | 5.9 | % | N/A | N/A | ||||||
| Pension Benefits | Other Benefits | |||||||||||||||||
| 2008 | 2007 | 2006 | 2008 | 2007 | 2006 | |||||||||||||
Weighted average assumptions used to determine net cost for years ended December 31: | ||||||||||||||||||
Discount rate | 6.5 | % | 5.8 | % | 5.5 | % | 6.5 | % | 5.8 | % | 5.5 | % | ||||||
Rate of compensation increase | 5.9 | % | 5.9 | % | 5.8 | % | N/A | N/A | N/A | |||||||||
The discount rates we used to measure our obligations under our pension and other post-retirement plans at December 31, 2008 and 2007 mirror the rate of return expected from high-quality fixed income investments.
| 2008 | 2007 | |||||
Assumed Health Care Cost Trend Rates at December 31: | ||||||
Health care cost trend rate assumed for next year | 10.0 | % | 10.2 | % | ||
Rate to which the cost trend rate is assumed to decline (the ultimate trend rate) | 5.0 | % | 5.0 | % | ||
Year that the rate reaches the ultimate trend rate | 2016 | 2013 |
Assumed health care cost trend rates have a significant effect on the amounts reported for the health care plans. A one-percentage-point change in assumed health care cost trend rates would have the following effects for the year ended December 31, 2008:
| 1-Percentage Point Increase | 1-Percentage Point Decrease | ||||||
| (Dollars in millions) | |||||||
Effect on total of service and interest cost | $ | 0.1 | $ | (0.1 | ) | ||
Effect on postretirement benefit obligation | $ | 1.0 | $ | (0.9 | ) | ||
Contributions
We expect to contribute $1,010,000 to our pension plan and $575,000 to our postretirement health and life plans throughout 2009. The entire amount expected to be contributed, in the form of cash, to the defined benefit pension and postretirement health and life plans during 2009 is expected to be paid out as benefits during the same year.
F-38
Table of Contents
HEALTH NET, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
Estimated Future Benefit Payments
We estimate that benefit payments related to our pension and postretirement health and life plans over the next ten years will be as follows:
| Pension Benefits | Other Benefits | |||||
| (Dollars in millions) | ||||||
2009 | $ | 1.0 | $ | 0.6 | ||
2010 | 1.0 | 0.7 | ||||
2011 | 1.1 | 0.8 | ||||
2012 | 1.2 | 0.9 | ||||
2013 | 1.4 | 0.9 | ||||
Years 2014 – 2018 | 11.9 | 3.9 | ||||
Note 11—Income Taxes
We have restated the current and deferred tax expense amounts for the year ended December 31, 2007 from amounts previously reported due to an offsetting clerical error discovered subsequent to the issuance of our consolidated financial statements and notes thereto for the year ended December 31, 2007. This restatement has no impact to the total income tax provision for the year ended December 31, 2007. This restatement also has no impact to the 2007 consolidated balance sheet and statement of operations as previously reported.
The following table summarizes the restatement adjustments and their impact on the components of our income tax expense as previously reported for the year ended December 31, 2007.
| As Previously Reported | Adjustment | As Restated | |||||||||
(In millions) | |||||||||||
Current tax expense: Federal | $ | 50.8 | $ | 172.8 | $ | 223.6 | |||||
Current tax expense: State | 15.9 | 24.4 | 40.3 | ||||||||
Current tax expense | 66.7 | 197.2 | 263.9 | ||||||||
Deferred income taxes | 98.6 | (197.2 | ) | $ | (98.6 | ) | |||||
The income tax expense restatement also had the following impact to the Deferred income taxes and Other current assets, receivables and noncurrent assets reported in the Cash flows from operating activities section of the Statement of Cash Flows for the year ended December 31, 2007. This restatement has no impact to the Net cash provided by operating activities as previously reported.
| As Previously Reported | Adjustment | As Restated | ||||||||||
(In millions) | ||||||||||||
Deferred income taxes | $ | 98.6 | $ | (197.2 | ) | $ | (98.6 | ) | ||||
Other current assets, receivables and noncurrent assets | (53.5 | ) | 197.2 | 143.7 | ||||||||
Net cash provided by operating activities | 605.5 | — | 605.5 | |||||||||
F-39
Table of Contents
HEALTH NET, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
Significant components of the provision for income taxes are as follows for the years ended December 31:
| 2008 | 2007 As Restated | 2006 | ||||||||||
| (Dollars in millions) | ||||||||||||
Current tax expense: | ||||||||||||
Federal | $ | 37.2 | $ | 223.6 | $ | 79.7 | ||||||
State | (0.1 | ) | 40.3 | 19.1 | ||||||||
Total current tax expense | 37.1 | 263.9 | 98.8 | |||||||||
Deferred tax expense (benefit) | 15.4 | (98.6 | ) | 51.3 | ||||||||
Interest expense, gross of related tax effects | (0.4 | ) | (0.1 | ) | (0.6 | ) | ||||||
Total income tax provision | $ | 52.1 | $ | 165.2 | $ | 149.5 | ||||||
A reconciliation of the statutory federal income tax rate and the effective income tax rate on income is as follows for the years ended December 31:
| 2008 | 2007 | 2006 | |||||||
Statutory federal income tax rate | 35.0 | % | 35.0 | % | 35.0 | % | |||
State and local taxes, net of federal income tax effect | 4.8 | 5.1 | 2.9 | ||||||
Tax exempt interest income | (4.1 | ) | (1.4 | ) | (0.9 | ) | |||
Fines and penalties | 1.1 | 0.2 | — | ||||||
Class action lawsuit expenses | (3.0 | ) | 2.4 | — | |||||
Valuation allowance against net operating losses and tax credits | — | 5.3 | — | ||||||
Sale of subsidiaries | — | — | (6.2 | ) | |||||
Other, net | 1.6 | (0.6 | ) | 0.4 | |||||
Effective income tax rate | 35.4 | % | 46.0 | % | 31.2 | % | |||
Significant components of our deferred tax assets and liabilities as of December 31 are as follows:
| 2008 | 2007 | |||||||
| (Dollars in millions) | ||||||||
DEFERRED TAX ASSETS: | ||||||||
Accrued liabilities | $ | 138.0 | $ | 173.1 | ||||
Insurance loss reserves and unearned premiums | 22.5 | 20.4 | ||||||
Tax credit carryforwards | 4.4 | 7.2 | ||||||
Accrued compensation and benefits | 72.0 | 63.4 | ||||||
Deferred gain and revenues | 31.3 | 33.3 | ||||||
Net operating and capital loss carryforwards | 57.6 | 59.7 | ||||||
Other | 5.4 | 0.9 | ||||||
Deferred tax assets before valuation allowance | 331.2 | 358.0 | ||||||
Valuation allowance | (50.4 | ) | (51.5 | ) | ||||
Net deferred tax assets | $ | 280.8 | $ | 306.5 | ||||
DEFERRED TAX LIABILITIES: | ||||||||
Depreciable and amortizable property | $ | 27.2 | $ | 55.4 | ||||
Deferred revenue | 45.1 | 34.7 | ||||||
Discount on notes | 6.9 | 10.9 | ||||||
Other | 32.1 | 24.9 | ||||||
Deferred tax liabilities | $ | 111.3 | $ | 125.9 | ||||
F-40
Table of Contents
HEALTH NET, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
In 2008, 2007 and 2006, income tax benefits attributable to employee stock option and restricted stock transactions of $0.1 million, $26.2 million and $21.3 million, respectively, were allocated to stockholders’ equity.
As of December 31, 2008, we had federal and state net operating loss carryforwards of approximately $117.8 million and $234.9 million, respectively. The net operating loss carryforwards expire at various dates through 2028.
Limitations on utilization may apply to approximately $92 million and $179.1 million of the federal and state net operating loss carryforwards, respectively. Accordingly, valuation allowances have been provided to account for the potential limitations on utilization of these tax benefits. Of the $50.4 million total valuation allowance, $13.1 million will be allocated to reduce goodwill in the event the deferred tax assets for the net operating loss carry-forwards from a prior acquisition are realized.
Our tax provision for 2008 includes the impact of a $1.1 million decrease to valuation allowances as a result of the utilization of previously unrecognized deferred tax assets.
Our tax provision for 2007 includes the impact of a $30.3 million increase to valuation allowances established against deferred tax assets for primarily net operating loss carryforwards and tax credits of a particular subsidiary. The Company weighed both positive and negative evidence in evaluating the realizability of the tax benefits relating to the net operating loss and credit carryforwards and believes, due to a sharp decline in 2007 profit and future profit forecasts of the subsidiary, that it is unlikely any tax benefits relating to these loss and credit carry-forwards will be realized.
Included in our tax provision for 2006 is a $31.8 million tax benefit from the sale of a subsidiary primarily due to the difference in the amount of goodwill included in the carrying value of the stock prior to sale. The difference in carrying value and resulting loss on sale has been reported as a permanent difference in accordance with SFAS No. 109,Accounting for Income Taxes. This practice has been consistently applied with respect to prior, substantially similar transactions.
We adopted the provisions of FIN 48 on January 1, 2007. As a result of the implementation of FIN 48, we increased the liability for unrecognized tax benefits by $77.2 million. Approximately $65.7 million of this increase also increased deferred tax assets, as the amount relates to tax benefits that we expect will be recognized but for which there exists uncertainty as to the timing of the benefits. Also included in the $77.2 million increase is a reclassification of $13.4 million from federal and state taxes payable to the liability for unrecognized benefits. The reclassification was necessary to properly encompass the potential impact of all uncertain tax positions within the liability for unrecognized tax benefits. The remaining impact of adopting FIN 48 was $1.9 million increase to retained earnings, recorded as a cumulative-effect adjustment as of January 1, 2007.
A reconciliation of the beginning and ending amount of unrecognized tax benefits, exclusive of related interest, is as follows:
| 2008 | 2007 | |||||||
| (Dollars in millions) | ||||||||
Gross unrecognized tax benefits at beginning of year | $ | 55.1 | $ | 105.5 | ||||
Decreases in unrecognized tax benefits related to a prior year | (0.5 | ) | (38.4 | ) | ||||
Increases in unrecognized tax benefits related to the current year | 3.2 | 7.9 | ||||||
Settlements with taxing authorities | — | (16.2 | ) | |||||
Lapse in statute of limitations for assessment | (4.6 | ) | (3.7 | ) | ||||
Gross unrecognized tax benefits at end of year | $ | 53.2 | $ | 55.1 | ||||
F-41
Table of Contents
HEALTH NET, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
Of the $58.1 million total liability at December 31, 2008 for unrecognized tax benefits, approximately $18.4 million would, if recognized, impact the company’s effective tax rate. The remaining $39.7 million would impact deferred tax assets. Of the $59.8 million total liability at December 31, 2007 for unrecognized tax benefits, approximately $20.5 million would, if recognized, impact the company’s effective tax rate. The remaining $39.3 million would impact deferred tax assets.
We recognized interest and any applicable penalties, which could be assessed related to unrecognized tax benefits in income tax provision expense. Accrued interest and penalties are included within the related tax liability in the consolidated balance sheet. During 2008, 2007 and 2006, $(0.4) million, $(0.1) million and $(0.4) million of interest was recorded as income tax provision benefit, respectively. We reported interest accruals of $4.8 million and $4.4 million at December 31, 2008 and 2007, respectively. Provision expense and accruals for penalties were immaterial in all reporting periods.
We file tax returns in the federal as well as several state tax jurisdictions. As of December 31, 2008, tax years subject to examination in the federal jurisdiction are 2006 and forward. The most significant state tax jurisdiction for the company is California, and tax years subject to examination by that jurisdiction are 2003 and forward. Presently we are under examination as a large taxpayer by the Internal Revenue Service covering tax year 2006, and in addition, we are in the process of examination by various state taxing authorities. We do not believe that any ongoing examination will have a material impact on our consolidated balance sheet. In addition, we do not anticipate any significant changes to our liability for unrecognized tax benefits within the next 12 months.
During the year ended December 31, 2007, an examination was closed by the Internal Revenue Service of tax years 2003 through 2005. As a result, we paid approximately $17.0 million to resolve issues relating to the timing of deductions for certain items of deferred revenue, bad debts and a reserve for workers’ compensation. These issues had previously been included as uncertain tax positions in our liability for unrecognized tax benefits and as such, the settlement did not have a material impact on our consolidated statement of operations.
Note 12—Regulatory Requirements
All of our health plans as well as our insurance subsidiaries are required to periodically file financial statements with regulatory agencies in accordance with statutory accounting and reporting practices. Under the Knox-Keene Health Care Service Plan Act of 1975, as amended, California plans must comply with certain minimum capital or tangible net equity requirements. Our non-California health plans, as well as our health and life insurance companies, must comply with their respective state’s minimum regulatory capital requirements and, in certain cases, maintain minimum investment amounts for the restricted use of the regulators in certain limited circumstances. Within the scope of state statutes and/or other parameters established by the regulators, we have discretion as to whether we invest such funds in cash and cash equivalents or other investments. Restricted cash and cash equivalents, as of December 31, 2008 and 2007, totaled $63.5 million and $30.5 million, respectively. Investment securities held by trustees or agencies pursuant to state regulatory requirements were $55.3 million and $79.3 million as of December 31, 2008 and 2007, respectively. See the “Restricted Assets” section in Note 2 for additional information.
As necessary, we make contributions to and issue standby letters of credit on behalf of our subsidiaries to meet risk based capital (RBC) or other statutory capital requirements under various state laws and regulations. During the year ended December 31, 2008, we made capital contributions of $240.6 million to various subsidiaries to meet RBC or other statutory capital requirements. As a result of the above requirements and other regulatory requirements, certain subsidiaries are subject to restrictions on their ability to make dividend payments, loans or other transfers of cash to us. Such restrictions, unless amended or waived, limit the use of any
F-42
Table of Contents
HEALTH NET, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
cash generated by these subsidiaries to pay our obligations. The maximum amount of dividends which can be paid by the insurance company subsidiaries to us without prior approval of the insurance departments is subject to restrictions relating to statutory surplus, statutory income and unassigned surplus. Management believes that as of December 31, 2008 all of our active health plans and insurance subsidiaries met their respective regulatory requirements in all material respects.
Note 13—Commitments and Contingencies
Legal Proceedings
Litigation Related to the Sale of Businesses
AmCareco Litigation
We are a defendant in two related litigation matters pending in Louisiana and Texas state courts, both of which relate to claims asserted by three separate state receivers overseeing the liquidation of three health plans in Louisiana, Texas and Oklahoma that were previously owned by our former subsidiary, Foundation Health Corporation (FHC), which merged into Health Net, Inc. in January 2001. In 1999, FHC sold its interest in these plans to AmCareco, Inc. (AmCareco). We retained a minority interest in the three plans after the sale. Thereafter, the three plans became known as AmCare of Louisiana (AmCare-LA), AmCare of Oklahoma (AmCare-OK) and AmCare of Texas (AmCare-TX). In 2002, three years after the sale of the plans to AmCareco, each of the AmCare plans was placed under state oversight and ultimately into receivership. The receivers for each of the AmCare plans filed suit against us contending that, among other things, we were responsible as a “controlling shareholder” of AmCareco following the sale of the plans for post-acquisition misconduct by AmCareco and others that caused the three health plans to fail and ultimately be placed into receivership.
On June 16, 2005, a consolidated trial of the claims asserted against us by the three receivers commenced in state court in Baton Rouge, Louisiana. The claims of the receiver for AmCare-TX were tried before a jury and the claims of the receivers for the AmCare-LA and AmCare-OK were tried before the judge in the same proceeding. On June 30, 2005, the jury considering the claims of the receiver for AmCare-TX returned a verdict against us in the amount of $117.4 million, consisting of $52.4 million in compensatory damages and $65 million in punitive damages. The Court later reduced the compensatory and punitive damages awards to $36.7 million and $45.5 million, respectively, and entered judgments against us in those amounts.
The proceedings regarding the claims of the receivers for AmCare-LA and AmCare-OK concluded on July 8, 2005. On November 4, 2005, the Court issued separate judgments on those claims that awarded $9.5 million in compensatory damages to AmCare-LA and $17 million in compensatory damages to AmCare-OK, respectively. The Court later denied requests by AmCare-LA and AmCare-OK for attorneys’ fees and punitive damages. We thereafter appealed both judgments, and the receivers for AmCare-LA and AmCare-OK each appealed the orders denying them attorneys’ fees and punitive damages.
On December 30, 2008, the Court of Appeal issued its judgment on each of the appeals. It reversed in their entirety the trial court’s judgments in favor of the AmCare-TX and AmCare-OK receivers, and entered judgment in our favor against those receivers, finding that the receivers’ claims failed as a matter of law. As a result, those receivers’ cross appeals were rendered moot. The Court of Appeal also reversed the trial court judgment in favor of the AmCare-LA receiver, with the exception of a single breach of contract claim, on which it entered judgment in favor of the AmCare-LA receiver in the amount of $2 million. On January 14, 2009, the three receivers filed a request for rehearing by the Court of Appeal. On February 13, 2009, the Court of Appeal denied the request for a rehearing. The receivers have 30 days from that date to file an application for a writ with the Louisiana Supreme Court.
F-43
Table of Contents
HEALTH NET, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
In light of the original trial court judgments against us, on November 3, 2006, we filed a complaint in the U.S. District Court for the Middle District of Louisiana and simultaneously filed an identical suit in the 19th Judicial District Court in East Baton Rouge Parish seeking to nullify the three judgments that were rendered against us on the grounds of ill practice which resulted in the judgments entered. We have alleged that the judgments and other prejudicial rulings rendered in these cases were the result of impermissible ex parté contacts between the receivers, their counsel and the trial court during the course of the litigation. Preliminary motions and exceptions have been filed by the receivers for AmCare-TX, AmCare-OK and AmCare-LA seeking dismissal of our claim for nullification on various grounds. The federal judge dismissed Health Net’s federal complaint and Health Net appealed to the U.S. Fifth Circuit Court of Appeals. On July 8, 2008, the Fifth Circuit issued an opinion affirming the district court’s dismissal of the federal complaint, albeit on different legal grounds from those relied upon by the district court. The state court nullity action has been stayed pending the resolution of Health Net’s jurisdictional appeal in the federal action and has remained stayed during the pendency of the appeal of the underlying judgments.
These proceedings are subject to many uncertainties, and, given their complexity and scope, their outcome, including the outcome of any appeal, cannot be predicted at this time. It is possible that in a particular quarter or annual period our results of operations, cash flow and/or liquidity could be materially affected by an ultimate unfavorable resolution of these proceedings depending, in part, upon the results of operations or cash flow for such period. However, at this time, management believes that the ultimate outcome of these proceedings should not have a material adverse effect on our financial condition.
Litigation Relating to Rescission of Policies
In recent years, there has been growing public attention, especially in California to the practices of health plans and health insurers involving the rescission of members’ policies for misrepresenting their health status on applications for coverage. On October 23, 2007, the California Department of Managed Health Care (DMHC) and the California Department of Insurance (DOI) announced their intention to issue joint regulations limiting the rights of health plans and insurers to rescind coverage. The DMHC has issued draft proposed regulations but has not formally promulgated any regulations to date. The DOI has not issued any proposed regulations. In addition, effective January 1, 2008, newly enacted legislation in California requires health plans and insurers to pay health care providers who, under certain circumstances, have rendered services to members whose policies are subsequently rescinded. The issue of rescissions has also attracted increasing media attention, and both the DMHC and the DOI have been conducting surveys of the rescission practices of health plans, including ours. Other government agencies, including the Attorney General of California, are investigating, or have indicated that they may be interested in investigating, rescissions and related activities.
On October 16, 2007, the DMHC initiated a survey of Health Net of California’s activities regarding the rescission of policies for the period January 1, 2004 through June 30, 2006. Following completion of the survey, on May 15, 2008, Health Net of California entered into a settlement agreement with the DMHC. The settlement agreement requires Health Net of California to (1) pay a $300,000 administrative fine, (2) offer future coverage to all 85 HMO enrollees who had coverage rescinded from January 1, 2004 through May 15, 2008, (3) offer those enrollees an opportunity to participate in an expedited review process where the enrollee could seek to resolve claims for out-of-pocket medical expenses and other damages incurred as a result of the rescission, and (4) file a corrective action plan for various internal procedural changes by June 30, 2008. Health Net of California filed the corrective action plan by the due date and has commenced implementation of the corrective action plan. Failure to substantially implement the actions set forth in the corrective action plan will subject Health Net of California to a potential penalty of up to $3 million.
On April 7, 2008, the DOI commenced an audit of Health Net Life Insurance Company’s rescission practices and related claims settlement practices for the period January 1, 2004 through February 29, 2008. On
F-44
Table of Contents
HEALTH NET, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
September 12, 2008, Health Net Life entered into a settlement agreement with the DOI, which resolves all DOI matters regarding Health Net Life’s rescission practices from January 2004 to date. Under the settlement agreement, Health Net Life paid a $3.6 million penalty in and agreed to certain corrective actions, including offering future coverage to all 926 rescinded PPO insureds and offering an opportunity to participate in an expedited review process that allows former insureds to seek to resolve their claims for damages incurred as a result of their rescission. On October 7, 2008, Health Net Life filed a corrective action proposal for various procedure changes. Failure to substantially comply with the settlement agreement subjects Health Net Life to a potential additional monetary penalty of up to $3.6 million.
We are also party to arbitrations and litigation, including a putative class action lawsuit filed in April 2008 in Los Angeles Superior Court, in which rescinded members allege that we unlawfully rescinded their coverage. The lawsuits generally seek to recover the cost of medical services that were not paid for as a result of the rescission, and in some cases they also seek damages for emotional distress, attorney fees and punitive damages. On February 20, 2008, the Los Angeles City Attorney filed a complaint against Health Net in the Los Angeles Superior Court relating to our underwriting practices and rescission of certain individual policies. The complaint sought equitable relief and civil penalties for, among other things, alleged false advertising, violations of unfair competition laws and violations of the California Penal Code. On February 10, 2009, we entered into settlement agreements that resolved both the putative class action and the Los Angeles City Attorney’s lawsuit. Under the terms of the settlement agreements, we agreed to pay a total of $6.3 million to class members (individuals rescinded between February 20, 2004 and February 10, 2009), in accordance with an agreed upon distribution formula. The class action settlement agreement also provides that we will reimburse class members for certain out-of-pocket expenses related to covered medical services that occurred between the time of their original enrollment and the date of their rescission, and we will also hold them harmless for certain unpaid bills for such services. Under the agreement, our reimbursement and hold harmless obligations are capped at a total of $3 million in the aggregate. We will also pay attorney fees of approximately $2 million. Under the terms of the two agreements, we also agreed that we would not engage in any rescissions in California until January 31, 2010, unless legislation or regulations governing the process for rescissions is enacted, or we implement a third party independent review process that is not objected to by the DMHC or the DOI. The agreement with the City Attorney also provides that we will pay a $2 million civil penalty, as well as contribute $500,000 ascy prespayments to specified non-profit organizations that support childrens’ healthcare. We also agreed as part of the settlements to offer coverage to class members on a going forward basis without medical underwriting, similar to the offer we agreed to make as part of our settlements with the DMHC and DOI. On February 11, 2009, the court gave preliminary approval of the settlements and scheduled a final approval hearing for May 26, 2009. Class members will be given notice of the settlement, and an opportunity to opt out of the agreement, or to file objections to the settlement, which will be considered by the court at the final approval hearing. All of the settlement amounts have been fully accrued for as of December 31, 2008.
We cannot predict the outcome of the anticipated regulatory proposals described above, nor the extent to which we may be affected by the enactment of those or other regulatory or legislative activities relating to rescissions. Such legislation or regulation, including measures that would cause us to change our current manner of operation or increase our exposure to liability, could have a material adverse effect on our results of operations, financial condition and ability to compete in our industry. Similarly, given the complexity and scope of rescission lawsuits, their final outcome cannot be predicted with any certainty. It is possible that in a particular quarter or annual period our results of operations could be adversely affected by an ultimate unfavorable resolution of these cases.
Proceedings Relating to Claims Payment Practices
On March 13, 2008, we entered into a final settlement agreement with the plaintiffs in theMcCoy,Wachtel andScharfman lawsuits, which were nationwide class actions principally relating to our out-of-network claims
F-45
Table of Contents
HEALTH NET, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
payment practices. We are currently in the process of implementing the terms of the settlement agreement. We were also the subject of a regulatory investigation conducted by the New Jersey Department of Banking and Insurance (“DOBI”) related principally to the timeliness and accuracy of our claims payment practices for services rendered by out-of-network providers in New Jersey. On August 26, 2008, we entered into a consent order with DOBI and agreed to remediate certain claims and pay a $13 million fine. We completed the remediation of the claims as of August 1, 2008. In the third quarter of 2007, we recorded a $296.8 million charge relating to the settlement of theMcCoy,Wachtel andScharfman cases, including the $13 million fine arising from the consent order with DOBI.
On February 13, 2008, the New York Attorney General (NYAG) announced that his office was conducting an industry-wide investigation into the manner in which health insurers calculate “usual, customary and reasonable” charges for purposes of reimbursing members for out-of-network medical services. The NYAG’s office issued subpoenas to 16 health insurance companies, including us, in connection with this investigation. As described by the NYAG in a press conference on February 13, 2008, the threatened claims appear to be similar in part to those asserted by the plaintiffs in theMcCoy, Wachtel andScharfman cases described above. We are in the process of responding to the subpoena and are cooperating with the NYAG as appropriate in his investigation. On January 13, 2009, the NYAG announced that, as a result of his investigation, his office had entered into a settlement agreement with UnitedHealth Group, Inc., which owns and operates Ingenix, the company that supplied the database used by many health insurers, including us, to determine certain out-of-network reimbursements. Under the terms of the settlement, United will discontinue its ownership and operation of those databases, and will pay $50 million towards creation of a new database to be owned and operated by a non-profit organization in New York. Since the announcement of the agreement with United, the NYAG has reached agreements with some other health plans, under which they agreed to make payments towards the creation of the database and, in some instances, agree to utilize the database if certain conditions are satisfied. At the time of the announcement of the settlement, the NYAG indicated his intent to continue his investigation with respect to other health insurers. In the meantime, the Connecticut Attorney General has also been investigating health plans’ reimbursement of out-of-network services. On March 28, 2008, we received a request for voluntary production from the Connecticut Attorney General that sought information similar to that subpoenaed by the NYAG. We are in the process of responding to the request and are cooperating with the Connecticut Attorney General as appropriate in his investigation.
Miscellaneous Proceedings
In the ordinary course of our business operations, we are also subject to periodic reviews by various regulatory agencies with respect to our compliance with a wide variety of rules and regulations applicable to our business, including, without limitation, rules relating to pre-authorization penalties, payment of out-of-network claims and timely review of grievances and appeals, which may result in remediation of certain claims and the assessment of regulatory fines or penalties.
In addition, in the ordinary course of our business operations, we are also party to various other legal proceedings, including, without limitation, litigation arising out of our general business activities, such as contract disputes, employment litigation, wage and hour claims, real estate and intellectual property claims, claims brought by members seeking coverage or additional reimbursement for services allegedly rendered to our members, but which allegedly were either denied, underpaid or not paid, and claims arising out of the acquisition or divestiture of various business units or other assets. We are also subject to claims relating to the performance of contractual obligations to providers, members, employer groups and others, including the alleged failure to properly pay claims and challenges to the manner in which we process claims. In addition, we are subject to claims relating to the insurance industry in general, such as claims relating to reinsurance agreements and rescission of coverage and other types of insurance coverage obligations.
F-46
Table of Contents
HEALTH NET, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
These other regulatory and legal proceedings are subject to many uncertainties, and, given their complexity and scope, their final outcome cannot be predicted at this time. It is possible that in a particular quarter or annual period our results of operations and cash flow could be materially affected by an ultimate unfavorable resolution of any or all of these other regulatory and legal proceedings depending, in part, upon the results of operations or cash flow for such period. However, at this time, management believes that the ultimate outcome of all of these other regulatory and legal proceedings that are pending, after consideration of applicable reserves and potentially available insurance coverage benefits, should not have a material adverse effect on our financial condition and liquidity.
Potential Settlements
We regularly evaluate litigation matters pending against us, including those described above, to determine if settlement of such matters would be in the best interests of the Company and its stockholders. The costs associated with any such settlement could be substantial and, in certain cases, could result in a significant earnings charge in any particular quarter in which we enter into a settlement agreement. We have recorded reserves and accrued costs for future legal costs for certain significant matters described above. These reserves and accrued costs represent our best estimate of probable loss, including related future legal costs for such matters, both known and incurred but not reported, although our recorded amounts might ultimately be inadequate to cover such costs. Therefore, the costs associated with the various litigation matters to which we are subject and any earnings charge recorded in connection with a settlement agreement could have a material adverse effect on our financial condition or results of operations.
Operating Leases and Long-Term Purchase Obligations
Operating Leases
We lease administrative office space throughout the country under various operating leases. Certain leases contain renewal options and rent escalation clauses. Certain leases are cancelable with substantial penalties.
On March 29, 2007, we sold our 68-acre commercial campus in Shelton, Connecticut (the “Shelton Property”) to The Dacourt Group, Inc. (“Dacourt”) and leased it back from Dacourt under an operating lease agreement for an initial term of ten years with an option to extend for two additional terms of ten years each. The total future minimum lease commitments under the lease are approximately $70.1 million.
Effective January 1, 2005, we entered into an operating lease agreement to renew our leased office space in Woodland Hills, California for our corporate headquarters. The new lease is for a term of 10 years and has provisions for space reduction at specific times over the term of the lease, but it does not provide for complete cancellation rights. The total future minimum lease commitments under the lease are approximately $19.2 million.
Long-Term Purchase Obligations
We have entered into long-term agreements to purchase various services, which may contain certain termination provisions and have remaining terms in excess of one year as of December 31, 2008.
We have entered into long-term agreements to receive services related to pharmacy benefit management, pharmacy claims processing services and health quality/risk scoring enhancement services with external third-party service providers. The remaining terms are approximately three years for each of these contracts. Termination of these agreements is subject to certain termination provisions. The total future minimum commitments under these agreements are $122.0 million and are included in the table below.
F-47
Table of Contents
HEALTH NET, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
On August 19, 2008, we entered into a five and one-half year agreement with International Business Machines Corporation (IBM) to outsource our IT infrastructure management services including data center services, IT security management and help desk support. The total future minimum commitments under the agreement are $295.0 million.
On September 30, 2008, we entered into a five year and three month agreement with Cognizant Technology Solutions U.S. Corporation (Cognizant) to outsource our software applications development and management activities to Cognizant. Under the terms of the agreement, Cognizant will, among other things, provide us with services including the following: application development, testing and monitoring services, application maintenance and support services, project management services and cross functional services. The total future commitments under the agreement are $107.8 million.
On January 23, 2009, we also entered into a five year and two months agreement with Cognizant to outsource a substantial portion of our claims processing activities to Cognizant. Under the terms of the agreement, Cognizant will, among other things, provide us with claims adjudication, adjustment, audit and process improvement services. The total future commitments under the agreement are $13.3 million.
We have also entered into contracts with our health care providers and facilities, the federal government, other IT service companies and other parties within the normal course of our business for the purpose of providing health care services. Certain of these contracts are cancelable with substantial penalties.
As of December 31, 2008, future minimum commitments for operating leases and long-term purchase obligations for the years ending December 31 are as follows:
| Operating Leases | Long-Term Purchase Obligations | |||||
| (Dollars in millions) | ||||||
2009 | $ | 64.9 | $ | 140.8 | ||
2010 | 59.4 | 133.4 | ||||
2011 | 52.3 | 126.4 | ||||
2012 | 35.2 | 85.4 | ||||
2013 | 29.3 | 70.5 | ||||
Thereafter | 60.7 | 5.5 | ||||
Total minimum commitments | $ | 301.8 | $ | 562.0 | ||
Lease expense totaled $71.1 million, $70.7 million and $69.3 million for the years ended December 31, 2008, 2007 and 2006, respectively. Long-term purchase obligation expenses totaled $33.9 million, $39.3 million and $33.8 million for the years ended December 31, 2008, 2007 and 2006, respectively.
Surety Bonds
During December 2005, the Company elected to post $114.7 million of surety bonds to suspend the effect, and secure appeal, of the final judgment entered against the Company in connection with the AmCareco litigation. The surety bonds are secured by $90.1 million of irrevocable standby letters of credit (the “LC”) issued under the Company’s revolving credit facility in favor of the issuers of the surety bonds.
Under the surety bond and LC arrangement, if the Company were to fail to pay the amount, if any, of a final judgment in connection with the AmCareco litigation following appeal, the issuers of the surety bonds would
F-48
Table of Contents
HEALTH NET, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
make payment in satisfaction of the judgment. The Company would, in turn, be responsible for reimbursing the issuing bank under the LC to the extent that the issuers of the surety bonds were to draw on the LC. To the extent the Company incurs liabilities as a result of the arrangements under the surety bonds or the LC, such liabilities would be included on the Company’s consolidated balance sheet.
We will recognize a liability for any amounts actually, or expected to be, funded to these surety bonds or drawn down from the letters of credit. At this time, the Company does not believe it will be required to fund or draw down any amounts related to the surety bonds or the LC. Accordingly, no liability related to the surety bonds or the LC has been recognized in the Company’s financial statements as of December 31, 2008 and 2007.
Note 14—Related Parties
One current executive officer of the Company is a director of an industry-related association, of which the Company is a member and we paid dues of $1.0 million, $1.1 million and $1.1 million in 2008, 2007 and 2006, respectively.
As of December 31, 2008, there were no employee loans outstanding.
Note 15—2006 Litigation Charges
We recorded a $37.1 million litigation charge in the fourth quarter of 2006 in connection with recent developments in theWachtel v. Health Net, Inc. et al. andMcCoy v. Health Net, Inc. et al. cases. These two lawsuits are styled as nationwide class actions and are pending in the United States District Court for the District of New Jersey on behalf of a class of subscribers in a number of our large and small employer group plans. The litigation charge was recorded in anticipation of the Company’s on-going litigation defense expenses in these matters. These lawsuits were preliminarily settled in the third quarter of 2007. See Note 13 for additional information on this litigation matter.
Note 16—Segment Information
We currently operate within two reportable segments: Health Plan Services and Government Contracts. Our Health Plan Services reportable segment includes the operations of our commercial, Medicare (including Part D) and Medicaid health plans, the operations of our health and life insurance companies and our behavioral health and pharmaceutical services subsidiaries. Our Government Contracts reportable segment includes government-sponsored managed care plans through the TRICARE program and other health care-related government contracts. Our Government Contracts segment administers one large, multi-year managed health care government contract and other health care related government contracts.
Our two reportable segments are determined by applying the aggregation criteria in SFAS No. 131, “Disclosures About Segments of An Enterprise and Related Information.” The financial results of our two reportable segments are reviewed on a monthly basis by our executive operating team which comprises the chief operating decision maker (CODM). We continuously monitor our reportable segments to ensure that they reflect how our CODM manages our company. The operating segments within our Health Plan Services reportable segment all have similar economic characteristics and they meet the additional following five aggregation criteria:
| • | Similar managed health care products and services including HMO, PPO and POS, |
| • | Similar production process as they support similar customer groups and products, |
F-49
Table of Contents
HEALTH NET, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
| • | Same type of customers, individuals within large and small employer groups and senior and commercial individuals, |
| • | Similar distribution channels primarily consisting of insurance brokers, and |
| • | Similar regulatory environment in that the health care industry is highly regulated at both the federal and state levels. |
We evaluate performance and allocate resources based on segment pretax income. The accounting policies of the reportable segments are the same as those described in the summary of significant accounting policies (see Note 2), except that intersegment transactions are not eliminated. We include investment income, administrative services fees and other income and expenses associated with our corporate shared services and other costs in determining Health Plan Services segment’s pretax income to reflect the fact that these revenues and expenses are primarily used to support Health Plan Services reportable segment. We currently manage our assets on consolidated basis. Accordingly, asset information by reportable segments have not been disclosed.
The debt refinancing charge and litigation, severance and related benefit costs are excluded from our measurement of segment performance since they are not managed within either of our reportable segments.
Presented below are segment data for the three years ended December 31.
2008
| Health Plan Services | Government Contracts | Eliminations | Total | ||||||||||
| (Dollars in millions) | |||||||||||||
Revenues from external sources | $ | 12,392.0 | $ | 2,835.3 | $ | — | $ | 15,227.3 | |||||
Intersegment revenues | 55.1 | 0.2 | (55.3 | ) | — | ||||||||
Net investment income | 91.0 | — | — | 91.0 | |||||||||
Administrative services fees and other income | 48.3 | — | — | 48.3 | |||||||||
Interest expense | 42.9 | — | — | 42.9 | |||||||||
Depreciation and amortization | 59.9 | — | — | 59.9 | |||||||||
Share-based compensation expense | 21.9 | 2.2 | — | 24.1 | |||||||||
Segment pretax income | $ | 14.4 | $ | 132.7 | — | $ | 147.1 | ||||||
2007
| Health Plan Services | Government Contracts | Eliminations | Total | ||||||||||
| (Dollars in millions) | |||||||||||||
Revenues from external sources | $ | 11,435.3 | $ | 2,501.7 | $ | — | $ | 13,937.0 | |||||
Intersegment revenues | 9.6 | — | (9.6 | ) | — | ||||||||
Net investment income | 120.2 | — | — | 120.2 | |||||||||
Administrative services fees and other income | 51.1 | — | — | 51.1 | |||||||||
Interest expense | 32.5 | — | — | 32.5 | |||||||||
Depreciation and amortization | 43.0 | — | — | 43.0 | |||||||||
Share-based compensation expense | 22.7 | 1.6 | — | 24.3 | |||||||||
Segment pretax income | $ | 164.8 | $ | 194.1 | $ | — | $ | 358.9 | |||||
F-50
Table of Contents
HEALTH NET, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
2006
| Health Plan Services | Government Contracts | Eliminations | Total | ||||||||||
| (Dollars in millions) | |||||||||||||
Revenues from external sources | $ | 10,364.7 | $ | 2,376.0 | $ | — | $ | 12,740.7 | |||||
Intersegment revenues | 10.1 | — | (10.1 | ) | — | ||||||||
Net investment income | 111.0 | — | — | 111.0 | |||||||||
Administrative services fees and other income | 56.6 | — | — | 56.6 | |||||||||
Interest expense | 51.2 | — | — | 51.2 | |||||||||
Depreciation and amortization | 25.6 | — | — | 25.6 | |||||||||
Share-based compensation expense | 18.0 | 2.1 | — | 20.1 | |||||||||
Segment pretax income | $ | 444.5 | $ | 141.5 | $ | — | $ | 586.0 | |||||
Our health plan services premium revenue by line of business is as follows:
| Year Ended December 31, | |||||||||
| 2008 | 2007 | 2006 | |||||||
| (Dollars in millions) | |||||||||
Commercial premium revenue | $ | 7,797.5 | $ | 7,468.0 | $ | 6,903.5 | |||
Medicare Risk premium revenue | 3,521.5 | 2,778.9 | 2,304.4 | ||||||
Medicaid premium revenue | 1,073.0 | 1,188.4 | 1,156.8 | ||||||
Total Health Plan Services premiums | $ | 12,392.0 | $ | 11,435.3 | $ | 10,364.7 | |||
A reconciliation of the total reportable segments’ measures of profit to the Company’s consolidated income from continuing operations before income taxes and cumulative effect of a change in accounting principle for the years ended December 31, 2008, 2007 and 2006 is as follows:
| 2008 | 2007 | 2006 | ||||||||
| (Dollars in millions) | ||||||||||
Total reportable segment pretax income | $ | 147.1 | $ | 358.9 | $ | 586.0 | ||||
Debt refinancing charge | — | — | (70.1 | ) | ||||||
Litigation, severance and related benefit costs | — | — | (37.1 | ) | ||||||
Income from continuing operations before income taxes | $ | 147.1 | $ | 358.9 | $ | 478.8 | ||||
F-51
Table of Contents
HEALTH NET, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
Note 17—Reserves for Claims and Other Settlements
Reserves for claims and other settlements include reserves for claims (incurred but not reported (IBNR) claims and received but unprocessed claims), and other liabilities including capitation payable, shared risk settlements, provider disputes, provider incentives and other reserves for our Health Plan Services reporting segment. The table below provides a reconciliation of changes in reserve for claims for the years ended December 31, 2008, 2007 and 2006.
| Health Plan Services Year Ended December 31, | |||||||||||
| 2008 | 2007 | 2006 | |||||||||
| (Dollars in millions) | |||||||||||
Reserve for claims (a), beginning of period | $ | 838.7 | $ | 754.2 | $ | 768.7 | |||||
Incurred claims related to: | |||||||||||
Current year | 6,372.2 | 5,790.7 | 5,222.0 | ||||||||
Prior years (c) | (8.3 | ) | 0.6 | (77.3 | ) | ||||||
Total incurred (b) | 6,363.9 | 5,791.3 | 5,144.7 | ||||||||
Paid claims related to: | |||||||||||
Current year | 5,443.2 | 4,972.3 | 4,485.7 | ||||||||
Prior years | 802.3 | 734.5 | 673.5 | ||||||||
Total paid (b) | 6,245.5 | 5,706.8 | 5,159.2 | ||||||||
Reserve for claims (a), end of period | 957.1 | 838.7 | 754.2 | ||||||||
Add: | |||||||||||
Claims payable | 187.8 | 161.9 | 195.6 | ||||||||
Claims-related remediations (e) | 93.1 | 201.5 | — | ||||||||
Reserve for provider disputes | 3.9 | 2.2 | 8.3 | ||||||||
Other (d) | 96.2 | 96.1 | 90.7 | ||||||||
Reserves for claims and other settlements, end of period | $ | 1,338.1 | $ | 1,300.4 | $ | 1,048.8 | |||||
| (a) | Consists of incurred but not reported claims and received but unprocessed claims and reserves for loss adjustment expenses. |
| (b) | Includes medical claims only. Capitation, pharmacy and other payments including provider settlements are not included. |
| (c) | This line represents the change in reserves attributable to the difference between the original estimate of incurred claims for prior years and the revised estimate. In developing the revised estimate, there have been no changes in the approach used to determine the key actuarial assumptions, which are the completion factor and medical cost trend. Claims liabilities are estimated under actuarial standards of practice and generally accepted accounting principles. The majority of the reserve balance held at each quarter-end is associated with the most recent months’ incurred services because these are the services for which the fewest claims have been paid. The majority of the adjustments to reserves relate to variables and uncertainties associated with actuarial assumptions. The degree of uncertainty in the estimates of incurred claims is greater for the most recent months’ incurred services. Revised estimates for prior years are determined in each quarter based on the most recent updates of paid claims for prior years. As of December 31, 2008, incurred claims related to prior years were estimated to be $8.3 million lower than originally estimated at December 31, 2007. The majority of this amount was due to adjustments to our reserves that related to variables and uncertainties associated with our assumptions. In 2008, as our reserve balance for older months of service decreased, and estimates of our incurred costs for older dates of service became more certain and predictable, our estimates of incurred claims related to prior periods were adjusted accordingly. |
F-52
Table of Contents
HEALTH NET, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
As of December 31, 2007, incurred claims related to prior years were estimated to be $0.6 million higher than originally estimated at December 31, 2006.
As of December 31, 2006, incurred claims related to prior years were estimated to be $77.3 million lower than originally estimated at December 31, 2005.
| (d) | Includes accrued capitation, shared risk settlements, provider incentives and other reserve items. |
| (e) | Includes charges for claims-related matters, class disbursements and remediations recognized during 2007 and 2008. See Note 13 for further information on this class action litigation. |
The following table shows the Company’s health plan services capitated and non-capitated expenses for the years ended December 31:
| Health Plan Services | |||||||||
| 2008 | 2007 | 2006 | |||||||
| (Dollars in millions) | |||||||||
Total incurred claims | $ | 6,363.9 | $ | 5,791.3 | $ | 5,144.7 | |||
Capitated expenses and shared risk | 2,644.5 | 2,398.5 | 2,396.8 | ||||||
Pharmacy and other | 1,754.3 | 1,573.1 | 1,058.9 | ||||||
Health plan services | $ | 10,762.7 | $ | 9,762.9 | $ | 8,600.4 | |||
For the years ended December 31, 2008, 2007 and 2006, the Company’s capitated, shared risk, pharmacy and other expenses represented 41%, 41% and 40%, respectively, of the Company’s total health plan services.
Note 18—Quarterly Information (Unaudited)
The following interim financial information presents the 2008 and 2007 results of operations on a quarterly basis:
2008
| March 31 | June 30 | September 30 | December 31 | |||||||||||||
| (Dollars in millions, except per share data) | ||||||||||||||||
Total revenues (6), (7), (9) | $ | 3,836.8 | $ | 3,841.5 | $ | 3,818.9 | $ | 3,869.4 | (8) | |||||||
Health plan services costs (6) | 2,788.4 | 2,655.1 | 2,689.8 | 2,629.4 | ||||||||||||
Government contracts costs (7) | 637.6 | 658.3 | 687.8 | 718.9 | ||||||||||||
(Loss) income from operations before income taxes | (51.0 | ) | 118.1 | 26.1 | 54.0 | |||||||||||
Net (loss) income | (35.7 | )(1) | 76.7 | (2) | 18.5 | (3) | 35.5 | (4) | ||||||||
Basic (loss) earnings per share | $ | (0.33 | ) | $ | 0.71 | $ | 0.17 | $ | 0.34 | |||||||
Diluted (loss) earnings per share (5) | $ | (0.33 | ) | $ | 0.71 | $ | 0.17 | $ | 0.34 | |||||||
| (1) | Includes $82.4 million charge related to litigation and regulatory-related matters and operations strategy which is aimed at achieving substantial reductions in G&A. |
| (2) | Includes $13.0 million charge related to litigation and regulatory-related matters and operations strategy. |
| (3) | Includes $17.2 million charge related to operations strategy and $14.6 million charge related to other-than-temporary impairment of investment securities. |
| (4) | Includes $47.9 million charge related to litigation and regulatory-related matters and operations strategy. |
| (5) | The sum of the quarterly amounts may not equal the year-to-date amounts due to rounding. |
| (6) | Includes $41 million, $48 million, $20 million, and $29 million of health plan services premium revenues and $13 million, $11 million, $4 million, and $5 million of health plan services costs due to CMS Medicare risk factor adjustments for the quarters ended March 31, June 30, September 30, and December 31, 2008, respectively. |
F-53
Table of Contents
HEALTH NET, INC.
NOTES TO CONSOLIDATED FINANCIAL STATEMENTS—(Continued)
| (7) | Includes $(4) million, $4 million, $48 million, and $(31) million of government contracts revenue and $(6) million, $5 million, $62 million, and $(39) million of government contracts cost due to TRICARE estimated health care cost adjustments for the quarters ended March 31, June 30, September 30, and December 31, 2008, respectively. |
| (8) | Includes $19 million of 2001-2002 California Medi-Cal premium rate adjustment in the quarter ended December 31, 2008. |
| (9) | Includes $4.1 million, $(3.6) million, $1.0 million, and $5.4 million of changes in the interest rate swap valuations for the quarters ended March 31, June 30, September 30, and December 31, 2008, respectively. |
2007
| March 31 | June 30(1) | September 30 | December 31 | |||||||||||
| (Dollars in millions, except per share data) | ||||||||||||||
Total revenues (5), (6) | $ | 3,428.9 | $ | 3,464.2 | $ | 3,631.9 | $ | 3,583.3 | ||||||
Health plan services costs (5) | 2,341.1 | 2,381.3 | 2,631.2 | 2,409.3 | ||||||||||
Government contracts costs (6) | 567.1 | 570.5 | 613.3 | 556.7 | ||||||||||
Income (loss) from operations before income taxes | 143.1 | 148.7 | (121.5 | )(2) | 188.6 | (3) | ||||||||
Net income (loss) | 88.6 | 92.0 | (103.8 | ) | 116.9 | |||||||||
Basic earnings per share | $ | 0.79 | $ | 0.82 | $ | (0.93 | ) | $ | 1.06 | |||||
Diluted earnings per share (4) | $ | 0.77 | $ | 0.80 | $ | (0.93 | ) | $ | 1.04 | |||||
| (1) | Includes the impact of Guardian Transaction (see Note 3) effective May 31, 2007. |
| (2) | Includes $296.8 million litigation and regulatory-related charge. |
| (3) | Includes $10.0 million arbitration award. |
| (4) | The sum of the quarterly amounts may not equal the year-to-date amounts due to rounding. |
| (5) | Includes $27 million, $23 million, $27 million, and $18 million of health plan services premium revenues and $9 million, $6 million, $7 million, and $5 million of health plan services costs due to CMS Medicare risk factor adjustments for the quarters ended March 31, June 30, September 30, and December 31, 2007, respectively. |
| (6) | Includes $(44) million, $(19) million, $10 million, and $(5) million of government contracts revenue and $(54) million, $(24) million, $(7) million, and $10 million of government contracts cost due to TRICARE estimated health care cost adjustments for the quarters ended March 31, June 30, September 30, and December 31, 2007, respectively. |
F-54
Table of Contents
CONDENSED FINANCIAL INFORMATION OF REGISTRANT
(PARENT COMPANY ONLY)
HEALTH NET, INC.
CONDENSED STATEMENTS OF OPERATIONS
(Amounts in thousands)
| Year Ended December 31, | ||||||||||||
| 2008 | 2007 | 2006 | ||||||||||
REVENUES: | ||||||||||||
Net investment income | $ | 10,359 | $ | 8,294 | $ | 15,269 | ||||||
Other income | 2,117 | 2,641 | 2,902 | |||||||||
Administrative service fees | 430,499 | 411,232 | 376,562 | |||||||||
Total revenues | 442,975 | 422,167 | 394,733 | |||||||||
EXPENSES: | ||||||||||||
General and administrative | 493,330 | 643,971 | 392,594 | |||||||||
Depreciation and amortization | 36,661 | 21,263 | 14,280 | |||||||||
Interest | 37,620 | 32,005 | 51,149 | |||||||||
Debt refinancing charge | — | — | 70,095 | |||||||||
Litigation, severance and related benefit costs | — | — | 37,093 | |||||||||
Total expenses | 567,611 | 697,239 | 565,211 | |||||||||
Loss from operations before income taxes and equity in net income of subsidiaries | (124,636 | ) | (275,072 | ) | (170,478 | ) | ||||||
Income tax benefit | 44,159 | 126,615 | 53,221 | |||||||||
Equity in net income of subsidiaries | 175,480 | 342,154 | 446,570 | |||||||||
Net income | $ | 95,003 | $ | 193,697 | $ | 329,313 | ||||||
See accompanying notes to condensed financial statements.
F-55
Table of Contents
SUPPLEMENTAL SCHEDULE I
CONDENSED FINANCIAL INFORMATION OF REGISTRANT
(PARENT COMPANY ONLY)
HEALTH NET, INC.
CONDENSED BALANCE SHEETS
(Amounts in thousands)
| December 31, 2008 | December 31, 2007 | |||||||
ASSETS | ||||||||
Current Assets: | ||||||||
Cash and cash equivalents | $ | 82,238 | $ | 271,012 | ||||
Investment—available for sale | 69,806 | — | ||||||
Other assets | 22,162 | 30,772 | ||||||
Deferred taxes | 39,444 | 90,737 | ||||||
Due from subsidiaries | 70,117 | 84,254 | ||||||
Total current assets | 283,767 | 476,775 | ||||||
Property and equipment, net | 151,760 | 125,598 | ||||||
Goodwill | 394,783 | 394,784 | ||||||
Other intangible assets, net | 4,323 | 4,948 | ||||||
Investment in subsidiaries | 3,692,590 | 3,758,637 | ||||||
Other deferred taxes | 26,253 | — | ||||||
Notes receivable due from subsidiaries | 10,000 | 10,000 | ||||||
Other assets | 69,732 | 67,734 | ||||||
Total Assets | $ | 4,633,208 | $ | 4,838,476 | ||||
LIABILITIES AND STOCKHOLDERS’ EQUITY | ||||||||
Current Liabilities: | ||||||||
Due to subsidiaries | $ | 229,936 | $ | 203,195 | ||||
Other liabilities | 118,871 | 338,179 | ||||||
Total current liabilities | 348,807 | 541,374 | ||||||
Intercompany notes payable—long term | 1,856,443 | 1,876,936 | ||||||
Long term debt | 548,276 | 398,071 | ||||||
Long term deferred taxes | — | 8,271 | ||||||
Other liabilities | 127,556 | 138,242 | ||||||
Total Liabilities | 2,881,082 | 2,962,894 | ||||||
Commitments and contingencies | ||||||||
Stockholders’ Equity: | ||||||||
Common stock | 144 | 144 | ||||||
Additional paid-in capital | 1,182,067 | 1,151,251 | ||||||
Treasury common stock, at cost | (1,367,319 | ) | (1,123,750 | ) | ||||
Retained earnings | 1,944,100 | 1,849,097 | ||||||
Accumulated other comprehensive loss | (6,866 | ) | (1,160 | ) | ||||
Total Stockholders’ Equity | 1,752,126 | 1,875,582 | ||||||
Total Liabilities and Stockholders’ Equity | $ | 4,633,208 | $ | 4,838,476 | ||||
See accompanying notes to condensed financial statements.
F-56
Table of Contents
SUPPLEMENTAL SCHEDULE I
CONDENSED FINANCIAL INFORMATION OF REGISTRANT
(PARENT COMPANY ONLY)
HEALTH NET, INC.
CONDENSED STATEMENTS OF CASH FLOWS
(Amounts in thousands)
| Year Ended December 31, | ||||||||||||
| 2008 | 2007 | 2006 | ||||||||||
NET CASH FLOWS (USED IN) PROVIDED BY OPERATING ACTIVITIES | $ | (11,656 | ) | $ | 216,043 | $ | 183,188 | |||||
CASH FLOWS FROM INVESTING ACTIVITIES: | ||||||||||||
Maturities of investments | 124,825 | — | — | |||||||||
Purchases of investments | (194,631 | ) | — | — | ||||||||
Sales of property and equipment | — | 34 | 393 | |||||||||
Purchases of property and equipment | (62,198 | ) | (52,198 | ) | (55,033 | ) | ||||||
Notes receivable due from subsidiaries | — | — | (10,000 | ) | ||||||||
Cash (paid) received related to the (acquisition) sale of businesses | — | (79,484 | ) | (70,394 | ) | |||||||
Capital contributions returned to Parent | 304,543 | — | — | |||||||||
Capital contributions to subsidiaries | (240,630 | ) | (1,002,273 | ) | — | |||||||
Sales (purchases) of restricted investments and other | — | (5,915 | ) | 12,456 | ||||||||
Net cash (used in) provided by investing activities | (68,091 | ) | (1,139,836 | ) | (122,578 | ) | ||||||
CASH FLOWS FROM FINANCING ACTIVITIES: | ||||||||||||
Net increase (decrease) in checks outstanding, net of deposits | (2,240 | ) | 2,240 | (12,650 | ) | |||||||
Excess tax benefit on share-based compensation | 242 | 10,912 | 8,083 | |||||||||
Net borrowings from subsidiaries | (20,493 | ) | 1,241,551 | 105,299 | ||||||||
Proceeds from exercise of stock options and employee stock purchases | 6,636 | 72,622 | 70,294 | |||||||||
Proceeds from issuance of notes and other financing arrangements | 520,000 | 493,535 | 497,334 | |||||||||
Repayment of debt under financing arrangements | (370,000 | ) | (600,000 | ) | (465,045 | ) | ||||||
Repurchase of common stock | (243,172 | ) | (232,220 | ) | (253,502 | ) | ||||||
Net cash (used in) provided by financing activities | (109,027 | ) | 988,640 | (50,187 | ) | |||||||
Net (decrease) increase in cash and cash equivalents | (188,774 | ) | 64,847 | 10,423 | ||||||||
Cash and cash equivalents, beginning of period | 271,012 | 206,165 | 195,742 | |||||||||
Cash and cash equivalents, end of period | $ | 82,238 | $ | 271,012 | $ | 206,165 | ||||||
SUPPLEMENTAL CASH FLOWS DISCLOSURE: | ||||||||||||
Interest paid | $ | 31,330 | $ | 42,495 | $ | 51,994 | ||||||
Income taxes paid | 97,715 | 183,843 | 74,003 | |||||||||
See accompanying notes to condensed financial statements.
F-57
Table of Contents
SUPPLEMENTAL SCHEDULE I
CONDENSED FINANCIAL INFORMATION OF REGISTRANT
(PARENT COMPANY ONLY)
HEALTH NET, INC.
NOTE TO CONDENSED FINANCIAL STATEMENTS
Note 1—Basis of Presentation
Health Net, Inc.’s (HNT) investment in subsidiaries is stated at cost plus equity in undistributed earnings (losses) of subsidiaries. HNT’s share of net income (loss) of its unconsolidated subsidiaries is included in consolidated income using the equity method.
This condensed financial information of registrant (parent company only) should be read in conjunction with the consolidated financial statements of Health Net, Inc. and subsidiaries.
F-58
Table of Contents
VALUATION AND QUALIFYING ACCOUNTS AND RESERVES
HEALTH NET, INC.
(Amounts in thousands)
| Balance at Beginning of Period | Charged to Costs and Expenses | Credited to Other Accounts (1) | Deductions | Balance at End of Period | ||||||||||||
2008: | ||||||||||||||||
Allowance for doubtful accounts: | ||||||||||||||||
Premiums receivable | $ | 6,724 | $ | 20,332 | $ | (13,489 | ) | $ | — | $ | 13,567 | |||||
2007: | ||||||||||||||||
Allowance for doubtful accounts: | ||||||||||||||||
Premiums receivable | $ | 7,526 | $ | 10,102 | $ | (10,904 | ) | $ | — | $ | 6,724 | |||||
2006: | ||||||||||||||||
Allowance for doubtful accounts: | ||||||||||||||||
Premiums receivable | $ | 7,204 | $ | 6,512 | $ | (6,190 | ) | $ | — | $ | 7,526 | |||||
| (1) | Credited to premiums receivable on the Consolidated Balance Sheets. |
F-59
Table of Contents
EXHIBIT INDEX
Exhibit Number | Description | |
| 3.1 | Sixth Amended and Restated Certificate of Incorporation of Health Net, Inc. (filed as Exhibit 3.1 to the Company’s Current Report on Form 8-K filed with the Commission on July 28, 2006 and incorporated herein by reference). | |
| 3.2 | Ninth Amended and Restated Bylaws of Health Net, Inc. (filed as Exhibit 3.2 to the Company’s Annual Report on Form 10-K for the year ended December 31, 2003 and incorporated herein by reference). | |
| 3.3 | Amendment Number One to Ninth Amended and Restated Bylaws of Health Net, Inc. (filed as Exhibit 3.1 to the Company’s Current Report on Form 8-K filed with the Commission on March 7, 2005 (File No. 1-12718) and incorporated herein by reference). | |
| 4.1 | Specimen Common Stock Certificate (filed as Exhibit 8 to the Company’s Registration Statement on Form 8-A/A (Amendment No. 3) (File No. 1-12718) on July 26, 2004 and incorporated herein by reference). | |
| 4.2 | Rights Agreement dated as of July 27, 2006, by and between Heath Net, Inc. and Wells Fargo Bank, N.A., as Rights Agent (filed as Exhibit 4.1 to the Company’s Current Report on Form 8-K filed with the Commission on July 28, 2006 (File No. 1-12718) and incorporated herein by reference). | |
| 4.3 | Indenture, dated as of May 18, 2007, by and between Health Net, Inc. as issuer, and The Bank of New York Trust Company, N.A., as trustee (filed as Exhibit 4.1 to the Company’s Current Report on Form 8-K filed with the SEC on May 18, 2007 (File No. 1-12718) and incorporated herein by reference). | |
| 4.4 | Officer’s Certificate, dated May 18, 2007, establishing the terms and form of the Company’s $300,000,000 aggregate principal amount of its 6.375% Senior Notes due 2017 (the “Notes”) (filed as Exhibit 4.2 to the Company’s Current Report on Form 8-K filed with the SEC on May 18, 2007 (File No. 1-12718) and incorporated herein by reference). | |
| 4.5 | Officer’s Certificate, dated May 31, 2007, establishing the terms and form of the Company’s $100,000,000 aggregate principal amount of its 6.375% Senior Notes due 2017 (the “Additional Notes”) (filed as Exhibit 4.1 to the Company’s Current Report on Form 8-K filed with the SEC on May 31, 2007 (File No. 1-12718) and incorporated herein by reference). | |
| †*10.1 | Amended and Restated Employment Agreement, dated as of December 3, 2008, by and between Health Net, Inc. and Karin Mayhew, a copy of which is filed herewith. | |
| †*10.2 | Amended and Restated Employment Agreement, dated as of December 3, 2008, by and between Health Net, Inc. and Patricia T. Clarey, a copy of which is filed herewith. | |
| †*10.3 | Amended and Restated Employment Agreement, dated as of December 3, 2008, by and between Health Net, Inc. and Jay M. Gellert, a copy of which is filed herewith. | |
| †*10.4 | Amended and Restated Employment Agreement, dated as of December 3, 2008, by and between James E. Woys and Health Net, Inc., a copy of which is filed herewith. | |
| †*10.5 | Amended and Restated Employment Agreement, dated as of December 3, 2008, by and between Joseph C. Capezza and Health Net, Inc., a copy of which is filed herewith. | |
| †*10.6 | Amended and Restated Employment Letter Agreement, dated as of December 3, 2008, by and between Health Net, Inc. and Stephen D. Lynch, a copy of which is filed herewith. | |
| †*10.7 | Amended and Restated Employment Agreement, dated as of December 3, 2008, by and between Health Net, Inc. and Linda Tiano, a copy of which is filed herewith. | |
Table of Contents
Exhibit Number | Description | |
| †*10.8 | Amended and Restated Employment Agreement, dated as of February 17, 2009, by and between Health Net, Inc. and John Sivori, a copy of which is filed herewith. | |
| †*10.9 | Amended and Restated Employment Agreement, dated as of February 17, 2009, by and between Health Net, Inc. and Steve Tough, a copy of which is filed herewith. | |
| *10.10 | Certain Compensation Arrangements With Respect to the Company’s Non-Employee Directors, as amended and restated on February 18, 2008 (filed as Exhibit 10.13 to the Company’s Annual Report on Form 10-K for the year ended December 31, 2007 (File No. 1-12718) and incorporated herein by reference). | |
| *10.11 | Form of Nonqualified Stock Option Agreement utilized for eligible employees of Health Net, Inc. (filed as Exhibit 10.4 to the Company’s Current Report on Form 8-K filed with the Commission on January 21, 2009 (File No. 1-12718) and incorporated herein by reference). | |
| *10.12 | Form of Restricted Stock Agreement utilized for eligible employees of Health Net, Inc. (filed as Exhibit 10.3 to the Company’s Current Report on Form 8-K filed with the Commission on January 21, 2009 (File No. 1-12718) and incorporated herein by reference). | |
| *10.13 | Form of Restricted Stock Unit Award Agreement utilized for eligible employees of Health Net, Inc. (filed as Exhibit 10.2 to the Company’s Current Report on Form 8-K filed with the Commission on January 21, 2009 (File No. 1-12718) and incorporated herein by reference). | |
| *10.14 | Form of Performance Share Award Agreement utilized for eligible employees of Health Net, Inc. (filed as Exhibit 10.1 to the Company’s Current Report on Form 8-K filed with the Commission on January 21, 2009 (File No. 1-12718) and incorporated herein by reference). | |
| *10.15 | Form of 2007 Performance Award Agreement for CEO of Health Net, Inc. (filed as Exhibit 10.2 to the Company’s Current Report on Form 8-K filed with the Commission on February 28, 2007 (File No. 1-12718) and incorporated herein by reference). | |
| *10.16 | Form of Nonqualified Stock Option Agreement utilized for non-employee directors under the 2006 Long-Term Incentive Plan (filed as Exhibit 10.5 to the Company’s Current Report on Form 8-K filed with the Commission on January 21, 2009 (File No. 1-12718) and incorporated herein by reference). | |
| *10.17 | Form of Nonqualified Stock Option Agreement utilized for non-employee directors under the Third Amended and Restated Non-Employee Director Stock Option Plan (filed as Exhibit 10.22 to the Company’s Annual Report on Form 10-K for the year ended December 31, 2004 (File No. 1-12718) and incorporated herein by reference). | |
| *10.18 | Form of Nonqualified Stock Option Agreement utilized for non-employee directors under the Health Net, Inc. Amended and Restated 1998 Stock Option Plan (filed as Exhibit 10.6 to the Company’s Current Report on Form 8-K filed with the Commission on January 21, 2009 (File No. 1-12718) and incorporated herein by reference). | |
| †*10.19 | Health Net, Inc. Deferred Compensation Plan, as amended and restated effective November 12, 2007, a copy of which is filed herewith. | |
| *10.20 | Amendment No. 1 to the Health Net, Inc. Deferred Compensation Plan dated December 3, 2008 (filed as Exhibit 10.4 to the Company’s Current Report on Form 8-K filed with the Commission on December 9, 2008 (File No. 1-12718) and incorporated herein by reference). | |
| †*10.21 | Health Net, Inc. Deferred Compensation Plan for Directors, as amended and restated effective November 12, 2007, a copy of which is filed herewith. | |
| *10.22 | Amendment No. 1 to the Health Net, Inc. Deferred Compensation Plan for Directors dated December 3, 2008 (filed as Exhibit 10.5 to the Company’s Current Report on Form 8-K filed with the Commission on December 9, 2008 (File No. 1-12718) and incorporated herein by reference). | |
Table of Contents
Exhibit Number | Description | |
| *10.23 | Health Net, Inc. (formerly Foundation Health Systems, Inc.) Deferred Compensation Plan Trust Agreement effective September 1, 1998 between Foundation Health Systems, Inc. and Union Bank of California (filed as Exhibit 10.31 to the Company’s Annual Report on Form 10-K for the year ended December 31, 1998 (File No. 1-12718) and incorporated herein by reference). | |
| *10.24 | Amendment Number One to the Health Net, Inc. (formerly Foundation Health Systems, Inc.) Deferred Compensation Plan Trust Agreement between Health Net, Inc. and Union Bank of California, adopted January 1, 2001 (filed as Exhibit 10.27 to the Company’s Annual Report on Form 10-K for the year ended December 31, 2004 (File No. 1-12718) and incorporated herein by reference). | |
| *10.25 | Foundation Health Systems, Inc. Second Amended and Restated 1991 Stock Option Plan (filed as Exhibit 10.16 to the Company’s Quarterly Report on Form 10-Q for the quarter ended September 30, 2000 (File No. 1-12718) and incorporated herein by reference). | |
| *10.26 | Amendment to Second Amended and Restated 1991 Stock Option Plan (filed as Exhibit 10.15 to the Company’s Annual Report on Form 10-K for the year ended December 31, 2000 (File No. 1-12718) and incorporated herein by reference). | |
| *10.27 | Foundation Health Systems, Inc. 1997 Stock Option Plan (as amended and restated on May 4, 2000) (filed as Exhibit 10.45 to the Company’s Quarterly Report on Form 10-Q for the quarter ended June 30, 1997 (File No. 1-12718) and incorporated herein by reference). | |
| *10.28 | Amendment to 1997 Stock Option Plan (filed as Exhibit 10.17 to the Company’s Annual Report on Form 10-K for the year ended December 31, 2000 (File No. 1-12718) and incorporated herein by reference). | |
| *10.29 | Second Amendment to 1997 Stock Option Plan (filed as Exhibit 10.25 to the Company’s Quarterly Report on Form 10-Q for the quarter ended June 30, 2002 (file No. 1-12718) and incorporated herein by reference). | |
| *10.30 | Foundation Health Systems, Inc. Amended and Restated 1998 Stock Option Plan (filed as Exhibit 10.1 to the Company’s Current Report on Form 8-K filed with the Commission on August 16, 2004 (File No. 1-12718) and incorporated herein by reference). | |
| *10.31 | Amendment No. 1 to Foundation Health Systems, Inc. Amended and Restated 1998 Stock Option Plan (filed as Exhibit 10.1 to the Company’s Current Report on Form 8-K filed with the Commission on March 6, 2006 (File No. 1-12718) and incorporated herein by reference). | |
| †*10.32 | Amendment No. 2 to Foundation Health Systems, Inc. Amended and Restated 1998 Stock Option Plan dated January 14, 2009, a copy of which is filed herewith. | |
| *10.33 | Health Net, Inc. 2002 Stock Option Plan (filed as Exhibit 10.29 to the Company’s Quarterly Report on Form 10-Q for the quarter ended June 30, 2002 (file No. 1-12718) and incorporated herein by reference). | |
| *10.34 | Health Net, Inc. 2005 Long-Term Incentive Plan (filed as Exhibit 10.3 to the Company’s Current Report on Form 8-K filed with the Commission on May 13, 2005 (File No. 1-12718) and incorporated herein by reference). | |
| †*10.35 | Amendment No. 1 to Health Net, Inc. 2005 Long-Term Incentive Plan dated December 4, 2008, a copy of which is filed herewith. | |
| †*10.36 | Amendment No. 2 to Health Net, Inc. 2005 Long-Term Incentive Plan dated January 14, 2009, a copy of which is filed herewith. | |
Table of Contents
Exhibit Number | Description | |
| *10.37 | Health Net, Inc. 2006 Long-Term Incentive Plan (as filed as Exhibit 10.1 to the Company’s Current Report on Form 8-K filed with the Commission on May 15, 2006 and incorporated herein by reference). | |
| †*10.38 | Amendment No. 1 to Health Net, Inc. 2006 Long-Term Incentive Plan dated January 14, 2009, a copy of which is filed herewith. | |
| *10.39 | Health Net, Inc. 2006 Executive Officer Incentive Plan (filed as Exhibit 10.1 to the Company’s Current Report on Form 8-K filed with the Commission on May 13, 2005 (File No. 1-12718) and incorporated herein by reference). | |
| *10.40 | Amendment One to the Health Net, Inc. 2006 Executive Officer Incentive Plan (filed as Exhibit 10.2 to the Company’s Current Report on Form 8-K filed with the Commission on May 13, 2005 (File No. 1-12718 and incorporated herein by reference). | |
| †*10.41 | Amendment No. 2 to the Health Net, Inc. 2006 Executive Officer Incentive Plan dated November 12, 2008, a copy of which is filed herewith. | |
| *10.42 | Health Systems International, Inc. Second Amended and Restated Non-Employee Director Stock Option Plan (filed as Exhibit 10.31 to Registration Statement on Form S-4 (File No. 33-86524) on November 18, 1994 and incorporated herein by reference). | |
| *10.43 | Foundation Health Systems, Inc. Third Amended and Restated Non-Employee Director Stock Option Plan (filed as Exhibit 10.46 to the Company’s Quarterly Report on Form 10-Q for the quarter ended June 30, 1997 (File No. 1-12718) and incorporated herein by reference). | |
| *10.44 | Health Net, Inc. Management Incentive Plan adopted December 2004 (filed as Exhibit 10.40 to the Company’s Annual Report on Form 10-K for the year ended December 31, 2004 (File No. 1-12718) and incorporated herein by reference). | |
| †*10.45 | Amendment No. 1 to Health Net, Inc. Management Incentive Plan dated November 12, 2008, a copy of which is filed herewith. | |
| †*10.46 | Health Net, Inc. 401(k) Savings Plan as amended and restated effective January 1, 2008, a copy of which is filed herewith. | |
| *10.47 | Amended and Restated Health Net, Inc. Supplemental Executive Retirement Plan effective as of January 1, 2008 (filed as Exhibit 10.1 to the Company’s Current Report on Form 8-K filed December 9, 2008 (File No. 1-12718) and incorporated herein by reference). | |
| *10.48 | Amended and Restated Deferred Compensation Plan of Foundation Health Corporation (filed as Exhibit 10.99 to Foundation Health Corporation’s Annual Report on Form 10-K for the year ended June 30, 1995 (File No. 1-10540) and incorporated herein by reference). | |
| *10.49 | Amendment Number One Through Three to the Amended and Restated Deferred Compensation Plan of Foundation Health Corporation (filed as Exhibit 10.49 to the Company’s Annual Report on Form 10-K for the year ended December 31, 2004 (File No. 1-12718) and incorporated herein by reference). | |
| *10.50 | Foundation Health Corporation Executive Retiree Medical Plan (as amended and restated effective April 25, 1995) (filed as Exhibit 10.101 to Foundation Health Corporation’s Annual Report on Form 10-K for the year ended June 30, 1995 (File No. 1-10540) and incorporated herein by reference). | |
| 10.51 | Participation Agreement dated as of December 19, 2007, by and among Health Net Funding, Inc., Health Net, Inc., Lodgemore Holdings, Inc. ING Bank, N.V. and Health Net Financing, L.P. (filed as Exhibit 10.1 to the Company’s Current Report on Form 8-K filed with the SEC on December 20, 2007 (File No. 1-12718) and incorporated herein by reference). | |
Table of Contents
Exhibit Number | Description | |
| 10.52 | First Amendment to Participation Agreement, dated as of April 29, 2008, by and among Health Net, Inc., Health Net Funding, Inc., Lodgemore Holdings, Inc., ING Bank, N.V. and Health Net Financing, LP (filed as Exhibit 10.1 to the Company’s Quarterly Report on Form 10-Q for the quarter ended March 31, 2008 (File No. 1-12718) and incorporated herein by reference). | |
| †10.53 | Omnibus Amendment to Participation Agreement and Put Option Agreement dated as of November 10, 2008 by and among Health Net Funding, Inc., Health Net, Inc., Lodgemore Holdings Inc., ING Bank N.V. and Health Net Financing, L.P., a copy of which is filed herewith. | |
| 10.54 | Credit Agreement, dated as of June 25, 2007, by and among Health Net, Inc., Bank of America, N.A., as Administrative Agent, Swing Line Lender and L/C Issuer, JP Morgan Chase Bank, N.A., as Syndication Agent, Citicorp USA, Inc., as Documentation Agent, the other lenders party thereto and Banc of America Securities LLC and J.P. Morgan Securities Inc., as Joint Lead Arrangers and as Co-Book Managers (filed as Exhibit 10 to the Company’s Current Report on Form 8-K filed with the SEC on June 27, 2007 (File No. 1-12718) and incorporated herein by reference). | |
| 10.55 | First Amendment to Credit Agreement, dated as of April 29, 2008, by and among Health Net, Inc., Bank of America, N.A., as Administrative Agent and the other lenders party thereto (filed as Exhibit 10.1 to the Company’s Quarterly Report on Form 10-Q for the quarter ended March 31, 2008 (File No. 1-12718) and incorporated herein by reference). | |
| ^10.56 | Master Agreement, dated August 19, 2008, between Health Net, Inc. and International Business Machines Corporation (filed as Exhibit 10.1 to the Company’s Quarterly Report on Form 10-Q for the quarter ended September 30, 2008 (File No. 1-12718) and incorporated herein by reference). | |
| ^10.57 | Master Services Agreement, dated September 30, 2008, between Health Net, Inc. and Cognizant Technology Solutions U.S. Corporation (filed as Exhibit 10.2 to the Company’s Quarterly Report on Form 10-Q for the quarter ended September 30, 2008 (File No. 1-12718) and incorporated herein by reference). | |
| *10.58 | Form of Amended and Restated Indemnification Agreement for directors and executive officers of Health Net, Inc. (filed as Exhibit 10.3 to the Company’s Current Report on Form 8-K filed with the Commission on December 9, 2008 (File No. 1-12718) and incorporated herein by reference). | |
| 10.59 | First Amendment to Office Lease, dated May 14, 2001, by and between Health Net (a California corporation) and LNR Warner Center, LLC (filed as Exhibit 10.38 to the Company’s Annual Report on Form 10-K for the year ended December 31, 2001 (File No. 1-12718) and incorporated herein by reference). | |
| 10.60 | Lease Agreements, dated as of March 5, 2001, by and between Health Net, Inc. and Landhold, Inc. (filed as Exhibit 10.44 to the Company’s Annual Report on Form 10-K for the year ended December 31, 2003 (File No. 1-12718) and incorporated herein by reference). | |
| †10.61 | Amendment No. 1 to Lease Agreement, dated as of November 22, 2002, by and between Gold Pointe C, LLC, as successor-in-interest to Landhold, Inc., and Health Net, Inc., a copy of which is filed herewith. | |
| †10.62 | Amendment No. 2 to Lease Agreement, dated as of April 28, 2006, by and between McMorgan Institutional Real Estate Fund I, LLC, as successor-in-interest to Landhold, Inc., and Health Net, Inc., a copy of which is filed herewith. | |
| †10.63 | Amendment No. 1 to Lease Agreement, dated as of November 22, 2002, by and between Gold Pointe D, LLC, as successor-in-interest to Landhold, Inc., and Health Net, Inc., a copy of which is filed herewith. | |
| †10.64 | Standard Lease Agreement, dated as of July 24, 2006, by and between Panattoni Development Company and Health Net, Inc., a copy of which is filed herewith. | |
| †10.65 | First Amendment to Lease and Acknowledgment, dated as of February 8, 2007, by and between Panattoni Development Company and Health Net of California, Inc., a copy of which is filed herewith. | |
Table of Contents
Exhibit Number | Description | |
| †10.66 | Office Building Lease, dated as of July 13, 1995, by and between Aerojet-General Corporation and Foundation Health, a copy of which is filed herewith. | |
| †10.67 | Addendums 1-12 to Office Building Lease, by and between Aerojet-General Corporation and Health Net Federal Services, LLC, a copy of which is filed herewith. | |
| 10.68 | Office Lease Agreement, dated as of December 22, 2003, by and between Health Net, Inc. and Douglas Emmett Realty Fund 2000 L.P. (filed as Exhibit 10.46 to the Company’s Annual Report on Form 10-K for the year ended December 31, 2003 (File No. 1-12718) and incorporated herein by reference). | |
| 10.69 | Office Lease, dated September 20, 2000, by and among Health Net of California, Inc., DCA Homes, Inc. and Lennar Rolling Ridge, Inc. (filed as Exhibit 10.46 to the Company’s Quarterly Report on Form 10-Q for the quarter ended September 30, 2000 (File No. 1-12718) and incorporated herein by reference). | |
| 10.70 | Office Lease Agreement, dated August 18, 2000, by and between Physicians Health Services of Connecticut, Inc. (predecessor to Health Net of Connecticut, Inc.) and Beard Sawmill, LLC (filed as Exhibit 10.68 to the Company’s Annual Report on Form 10-K for the year ended December 31, 2005 (File No. 1-12718) and incorporated herein by reference). | |
| 10.71 | First Amendment to Office Lease Agreement, dated December 23, 2002, by and between Health Net of Connecticut, Inc. and Beard Sawmill, LLC (filed as Exhibit 10.67 to the Company’s Annual Report on Form 10-K for the year ended December 31, 2005 (File No. 1-12718) and incorporated herein by reference). | |
| 10.72 | Second Amendment to Office Lease Agreement, dated June 14, 2004, by and between Health Net of Connecticut, Inc. and Beard Sawmill, LLC (filed as Exhibit 10.66 to the Company’s Annual Report on Form 10-K for the year ended December 31, 2005 (File No. 1-12718) and incorporated herein by reference). | |
| 10.73 | Absolute Net Lease, dated as of March 29, 2007, by and between HN Property Owner LLC and Health Net of the Northeast (filed as Exhibit 10.1 to the Company’s Quarterly Report on Form 10-Q for the quarter ended March 31, 2007 (File No. 1-12718) and incorporated herein by reference). | |
| †11 | Statement relative to computation of per share earnings of the Company (included in Note 2 to the consolidated financial statements included as part of this Annual Report on Form 10-K). | |
| †21 | Subsidiaries of Health Net, Inc., a copy of which is filed herewith. | |
| †23 | Consent of Deloitte & Touche LLP, Independent Registered Public Accounting Firm, a copy of which is filed herewith. | |
| †31.1 | Certification of Chief Executive Officer pursuant to Section 302 of the Sarbanes-Oxley Act of 2002, a copy of which is filed herewith. | |
| †31.2 | Certification of Chief Financial Officer pursuant to Section 302 of the Sarbanes-Oxley Act of 2002, a copy of which is filed herewith. | |
| †32 | Certification of Chief Executive Officer and Chief Financial Officer pursuant to 18 U.S.C. Section 1350, as adopted pursuant to Section 906 of the Sarbanes-Oxley Act of 2002, a copy of which is filed herewith. | |
| * | Management contract or compensatory plan or arrangement required to be filed (and/or incorporated by reference) as an exhibit to this Annual Report on Form 10-K pursuant to Item 15(c) of Form 10-K. |
| † | A copy of the exhibit is being filed with this Annual Report on Form 10-K. |
| ^ | This exhibit has been redacted pursuant to a request for confidential treatment under Rule 24b-2 of the Securities Exchange Act of 1934, as amended. |