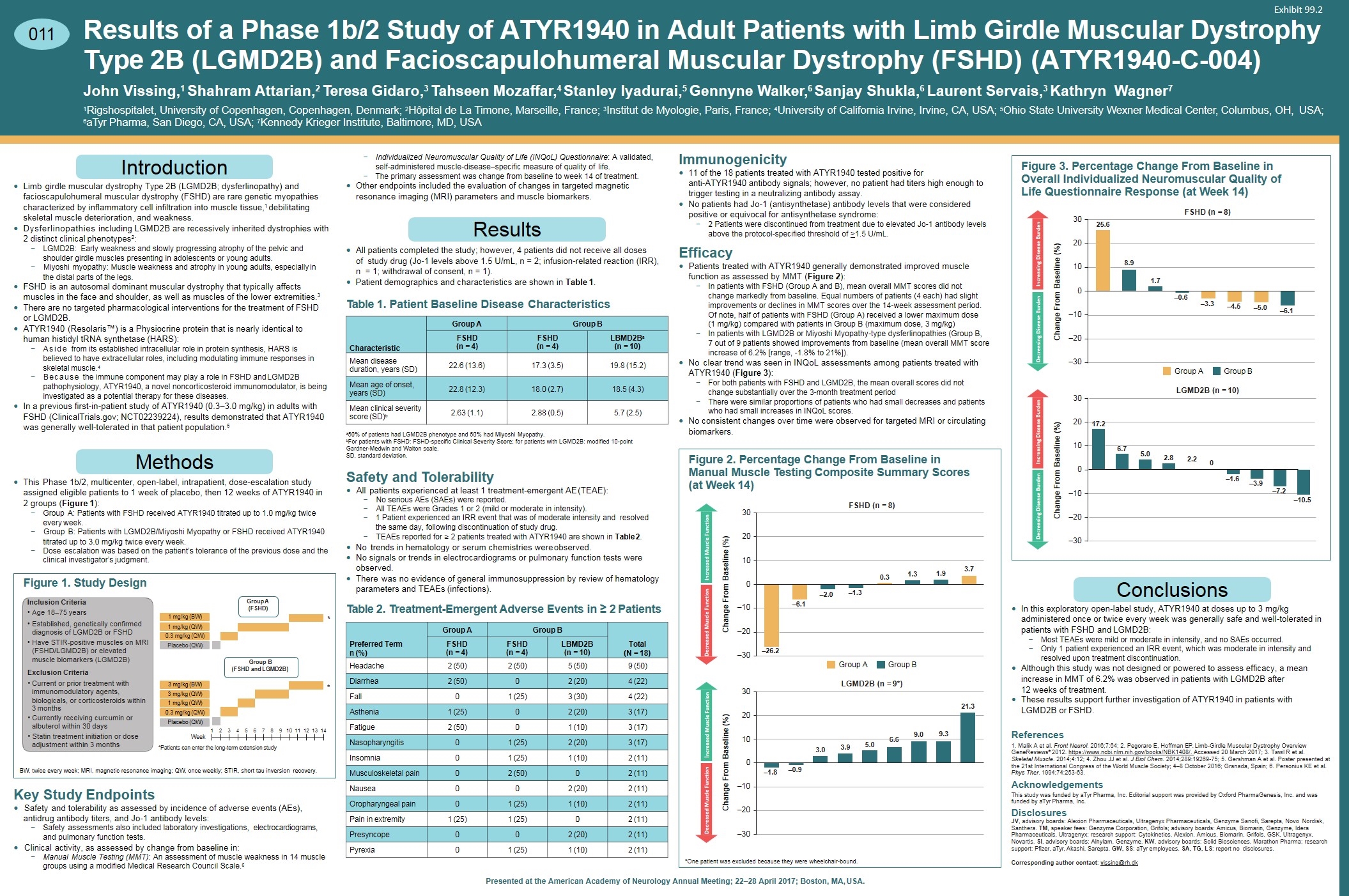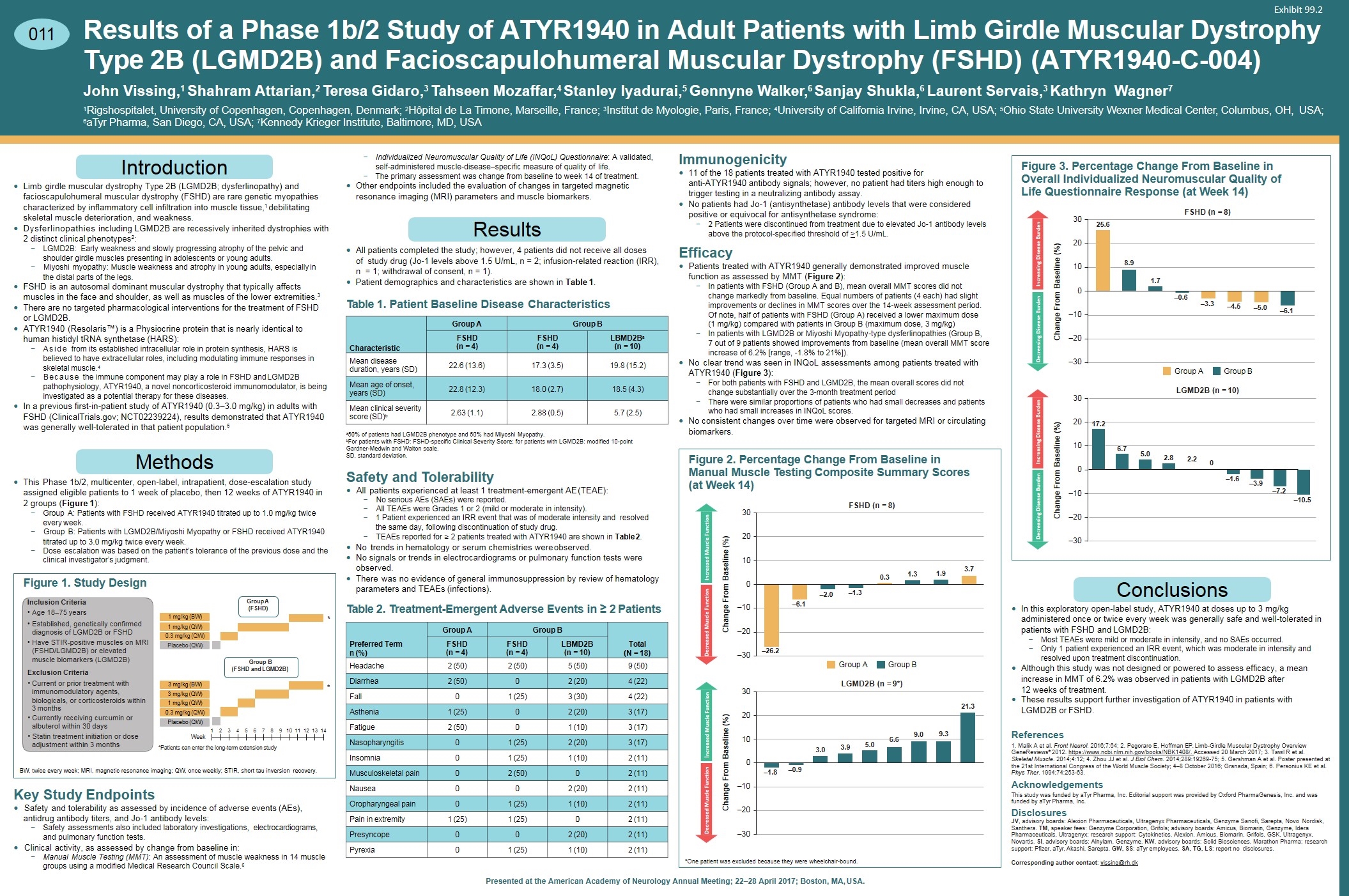
Results of a Phase 1b/2 Study of ATYR1940 in Adult Patients with Limb Girdle Muscular Dystrophy Type 2B (LGMD2B) and Facioscapulohumeral Muscular Dystrophy (FSHD) (ATYR1940-C-004) John Vissing,1 Shahram Attarian,2 Teresa Gidaro,3 Tahseen Mozaffar,4 Stanley Iyadurai,5 Gennyne Walker,6 Sanjay Shukla,6 Laurent Servais,3 Kathryn Wagner7 1Rigshospitalet, University of Copenhagen, Copenhagen, Denmark; 2Hôpital de La Timone, Marseille, France; 3Institut de Myologie, Paris, France; 4University of California Irvine, Irvine, CA, USA; 5Ohio State University Wexner Medical Center, Columbus, OH, USA; 6aTyr Pharma, San Diego, CA, USA; 7Kennedy Krieger Institute, Baltimore, MD, USA 011 Introduction —Limb girdle muscular dystrophy Type 2B (LGMD2B; dysferlinopathy) and facioscapulohumeral muscular dystrophy (FSHD) are rare genetic myopathies characterized by inflammatory cell infiltration into muscle tissue,1 debilitating skeletal muscle deterioration, and weakness. —Dysferlinopathies including LGMD2B are recessively inherited dystrophies with 2 distinct clinical phenotypes2: −LGMD2B: Early weakness and slowly progressing atrophy of the pelvic and shoulder girdle muscles presenting in adolescents or young adults. −Miyoshi myopathy: Muscle weakness and atrophy in young adults, especially in the distal parts of the legs. —FSHD is an autosomal dominant muscular dystrophy that typically affects muscles in the face and shoulder, as well as muscles of the lower extremities.3 —There are no targeted pharmacological interventions for the treatment of FSHD or LGMD2B. —ATYR1940 (Resolaris™) is a Physiocrine protein that is nearly identical to human histidyl tRNA synthetase (HARS): −Aside from its established intracellular role in protein synthesis, HARS is believed to have extracellular roles, including modulating immune responses in skeletal muscle.4 −Because the immune component may play a role in FSHD and LGMD2B pathophysiology, ATYR1940, a novel noncorticosteroid immunomodulator, is being investigated as a potential therapy for these diseases. —In a previous first-in-patient study of ATYR1940 (0.3–3.0 mg/kg) in adults with FSHD (ClinicalTrials.gov; NCT02239224), results demonstrated that ATYR1940 was generally well-tolerated in that patient population.5 Methods —This Phase 1b/2, multicenter, open-label, intrapatient, dose-escalation study assigned eligible patients to 1 week of placebo, then 12 weeks of ATYR1940 in 2 groups (Figure 1): −Group A: Patients with FSHD received ATYR1940 titrated up to 1.0 mg/kg twice every week. −Group B: Patients with LGMD2B/Miyoshi Myopathy or FSHD received ATYR1940 titrated up to 3.0 mg/kg twice every week. −Dose escalation was based on the patient’s tolerance of the previous dose and the clinical investigator’s judgment. Figure 1. Study Design Inclusion Criteria Age 18–75 years Established, genetically confirmed diagnosis of LGMD2B or FSHD Have STIR-positive muscles on MRI (FSHD/LGMD2B) or elevated muscle biomarkers (LGMD2B) Exclusion Criteria Current or prior treatment with immunomodulatory agents, biologicals, or corticosteroids within 3 months Currently receiving curcumin or albuterol within 30 days Statin treatment initiation or dose adjustment within 3 months Group A (FSHD) Group B (FSHD and LGMD2B) 3 mg/kg (BW) 3 mg/kg (QW) 1 mg/kg (QW) 0.3 mg/kg (QW) 1 mg/kg (BW) 1 mg/kg (QW) 0.3 mg/kg (QW) Placebo (QW) Placebo (QW) 1 * * *Patients can enter the long-term extension study BW, twice every week; MRI, magnetic resonance imaging; QW, once weekly; STIR, short tau inversion recovery. Key Study Endpoints —Safety and tolerability as assessed by incidence of adverse events (AEs), antidrug antibody titers, and Jo-1 antibody levels: −Safety assessments also included laboratory investigations, electrocardiograms, and pulmonary function tests. —Clinical activity, as assessed by change from baseline in: −Manual Muscle Testing (MMT): An assessment of muscle weakness in 14 muscle groups using a modified Medical Research Council Scale.6 −Individualized Neuromuscular Quality of Life (INQoL) Questionnaire: A validated, self-administered muscle-disease–specific measure of quality of life. −The primary assessment was change from baseline to week 14 of treatment. —Other endpoints included the evaluation of changes in targeted magnetic resonance imaging (MRI) parameters and muscle biomarkers. Results —All patients completed the study; however, 4 patients did not receive all doses of study drug (Jo-1 levels above 1.5 U/mL, n = 2; infusion-related reaction (IRR), n = 1; withdrawal of consent, n = 1). —Patient demographics and characteristics are shown in Table 1. Table 1. Patient Baseline Disease Characteristics a 50% of patients had LGMD2B phenotype and 50% had Miyoshi Myopathy. bFor patients with FSHD: FSHD-specific Clinical Severity Score; for patients with LGMD2B: modified 10-point Gardner-Medwin and Walton scale. SD, standard deviation. Safety and Tolerability —All patients experienced at least 1 treatment-emergent AE (TEAE): −No serious AEs (SAEs) were reported. −All TEAEs were Grades 1 or 2 (mild or moderate in intensity). −1 Patient experienced an IRR event that was of moderate intensity and resolved the same day, following discontinuation of study drug. −TEAEs reported for ≥ 2 patients treated with ATYR1940 are shown in Table 2. —No trends in hematology or serum chemistries were observed. —No signals or trends in electrocardiograms or pulmonary function tests were observed. —There was no evidence of general immunosuppression by review of hematology parameters and TEAEs (infections). Table 2. Treatment-Emergent Adverse Events in ≥ 2 Patients Preferred Term n (%) Group A Group B Total (N = 18) FSHD (n = 4) FSHD (n = 4) LBMD2B (n = 10) Headache 2 (50) 2 (50) 5 (50) 9 (50) Diarrhea 2 (50) 0 2 (20) 4 (22) Fall 0 1 (25) 3 (30) 4 (22) Asthenia 1 (25) 0 2 (20) 3 (17) Fatigue 2 (50) 0 1 (10) 3 (17) Nasopharyngitis 0 1 (25) 2 (20) 3 (17) Insomnia 0 1 (25) 1 (10) 2 (11) Musculoskeletal pain 0 2 (50) 0 2 (11) Nausea 0 0 2 (20) 2 (11) Oropharyngeal pain 0 1 (25) 1 (10) 2 (11) Pain in extremity 1 (25) 1 (25) 0 2 (11) Presyncope 0 0 2 (20) 2 (11) Pyrexia 0 1 (25) 1 (10) 2 (11) Immunogenicity —11 of the 18 patients treated with ATYR1940 tested positive for anti-ATYR1940 antibody signals; however, no patient had titers high enough to trigger testing in a neutralizing antibody assay. —No patients had Jo-1 (antisynthetase) antibody levels that were considered positive or equivocal for antisynthetase syndrome: −2 Patients were discontinued from treatment due to elevated Jo-1 antibody levels above the protocol-specified threshold of >1.5 U/mL. Efficacy —Patients treated with ATYR1940 generally demonstrated improved muscle function as assessed by MMT (Figure 2): −In patients with FSHD (Group A and B), mean overall MMT scores did not change markedly from baseline. Equal numbers of patients (4 each) had slight improvements or declines in MMT scores over the 14-week assessment period. Of note, half of patients with FSHD (Group A) received a lower maximum dose (1 mg/kg) compared with patients in Group B (maximum dose, 3 mg/kg) −In patients with LGMD2B or Miyoshi Myopathy-type dysferlinopathies (Group B, 7 out of 9 patients showed improvements from baseline (mean overall MMT score increase of 6.2% [range, -1.8% to 21%]). —No clear trend was seen in INQoL assessments among patients treated with ATYR1940 (Figure 3): −For both patients with FSHD and LGMD2B, the mean overall scores did not change substantially over the 3-month treatment period −There were similar proportions of patients who had small decreases and patients who had small increases in INQoL scores. —No consistent changes over time were observed for targeted MRI or circulating biomarkers. Figure 2. Percentage Change From Baseline in Manual Muscle Testing Composite Summary Scores (at Week 14) FSHD (n = 8) Group AGroup B LGMD2B (n = 9*) 0.3 1.3 –1.3 –6.1 –2.0 –26.2 1.9 3.7 –1.8 –0.9 3.0 3.9 5.0 6.69.0 9.3 21.3 Change From Baseline (%) Change From Baseline (%) 30 20 10 0 –10 –20 –30 30 20 10 0 Decreased Muscle Function Increased Muscle Function Decreased Muscle FunctionIncreased Muscle Function –10 –20 –30 *One patient was excluded because they were wheelchair-bound. Figure 3. Percentage Change From Baseline in Overall Individualized Neuromuscular Quality of Life Questionnaire Response (at Week 14) Change From Baseline (%) Change From Baseline (%) 30 20 10 0 –10 –20 –30 30 20 10 0 –10 –20 –30 FSHD (n = 8) Group AGroup B LGMD2B (n = 10) 25.6 8.9 1.7 –0.6 –3.3 –4.5 –5.0 –6.1 17.2 6.7 5.0 2.8 –1.6 –3.9 –7.2 –10.5 Decreasing Disease Burden Increasing Disease Burden Decreasing Disease Burden Increasing Disease Burden 2.20 Conclusions —In this exploratory open-label study, ATYR1940 at doses up to 3 mg/kg administered once or twice every week was generally safe and well-tolerated in patients with FSHD and LGMD2B: −Most TEAEs were mild or moderate in intensity, and no SAEs occurred. −Only 1 patient experienced an IRR event, which was moderate in intensity and resolved upon treatment discontinuation. —Although this study was not designed or powered to assess efficacy, a mean increase in MMT of 6.2% was observed in patients with LGMD2B after 12 weeks of treatment. —These results support further investigation of ATYR1940 in patients with LGMD2B or FSHD. References 1. Malik A et al. Front Neurol. 2016;7:64; 2. Pegoraro E, Hoffman EP. Limb-Girdle Muscular Dystrophy Overview GeneReviews® 2012. https://www.ncbi.nlm.nih.gov/books/NBK1408/. Accessed 20 March 2017; 3. Tawil R et al. Skeletal Muscle. 2014;4:12; 4. Zhou JJ et al. J Biol Chem. 2014;289:19269-75; 5. Gershman A et al. Poster presented at the 21st International Congress of the World Muscle Society; 4–8 October 2016; Granada, Spain; 6. Personius KE et al. Phys Ther. 1994;74:253-63. Acknowledgements This study was funded by aTyr Pharma, Inc. Editorial support was provided by Oxford PharmaGenesis, Inc. and was funded by aTyr Pharma, Inc. Disclosures JV, advisory boards: Alexion Pharmaceuticals, Ultragenyx Pharmaceuticals, Genzyme Sanofi, Sarepta, Novo Nordisk, Santhera. TM, speaker fees: Genzyme Corporation, Grifols; advisory boards: Amicus, Biomarin, Genzyme, Idera Pharmaceuticals, Ultragenyx; research support: Cytokinetics, Alexion, Amicus, Biomarin, Grifols, GSK, Ultragenyx, Novartis. SI, advisory boards: Alnylam, Genzyme. KW, advisory boards: Solid Biosciences, Marathon Pharma; research support: Pfizer, aTyr, Akashi, Sarepta. GW, SS: aTyr employees. SA, TG, LS: report no disclosures. Corresponding author contact: vissing@rh.dk Presented at the American Academy of Neurology Annual Meeting; 22–28 April 2017; Boston, MA, USA. 011 Introduction Methods Results Characteristic Group A Group B FSHD (n = 4) FSHD (n = 4) LBMD2Ba (n = 10) Mean disease duration, years (SD) 22.6 (13.6) 17.3 (3.5) 19.8 (15.2) Mean age of onset, years (SD) 22.8 (12.3) 18.0 (2.7) 18.5 (4.3) Mean clinical severity score (SD)b 2.63 (1.1) 2.88 (0.5) 5.7 (2.5) Decreased Muscle Function Increased Muscle Function Decreased Muscle Function Increased Muscle Function Decreasing Disease Burden Increasing Disease Burden Decreasing Disease Burden Increasing Disease Burden Conclusions Week 2 3 4 5 6 7 8 9 10 11 12 13 14 Exhibit 99.2