Fantom Encore case review and introduction to the REVA Technique Dr. med Matthias Lutz Universitätsklinikum Schleswig-Holstein Kiel, Germany Exhibit 99.4
Potential conflicts of interest Speaker's name : Matthias, Lutz, Kiel ☑ I have the following potential conflicts of interest to report: Receipt of honoraria or consultation fees: Abbott, REVA Medical
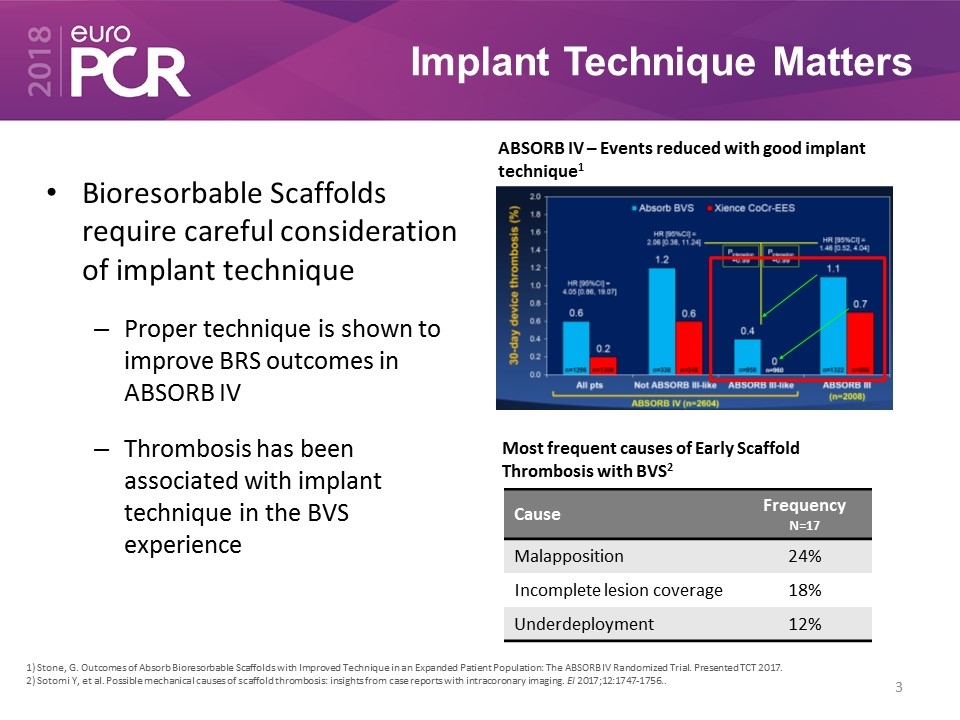
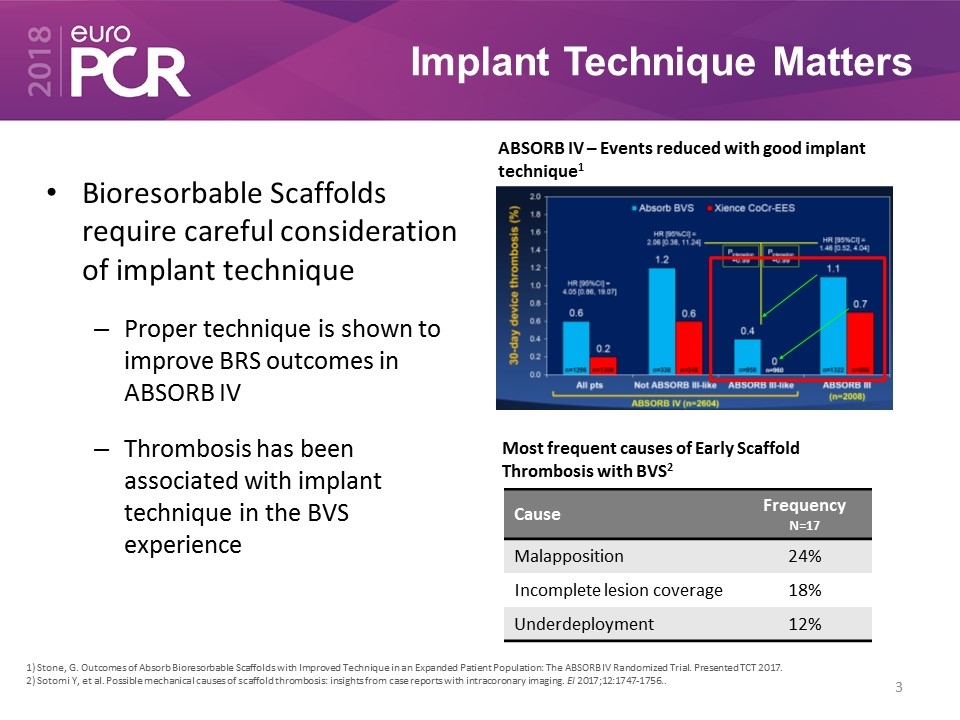
Implant Technique Matters Bioresorbable Scaffolds require careful consideration of implant technique Proper technique is shown to improve BRS outcomes in ABSORB IV Thrombosis has been associated with implant technique in the BVS experience ABSORB IV – Events reduced with good implant technique1 Cause Frequency N=17 Malapposition 24% Incomplete lesion coverage 18% Underdeployment 12% Most frequent causes of Early Scaffold Thrombosis with BVS2 1) Stone, G. Outcomes of Absorb Bioresorbable Scaffolds with Improved Technique in an Expanded Patient Population: The ABSORB IV Randomized Trial. Presented TCT 2017. 2) Sotomi Y, et al. Possible mechanical causes of scaffold thrombosis: insights from case reports with intracoronary imaging. EI 2017;12:1747-1756..
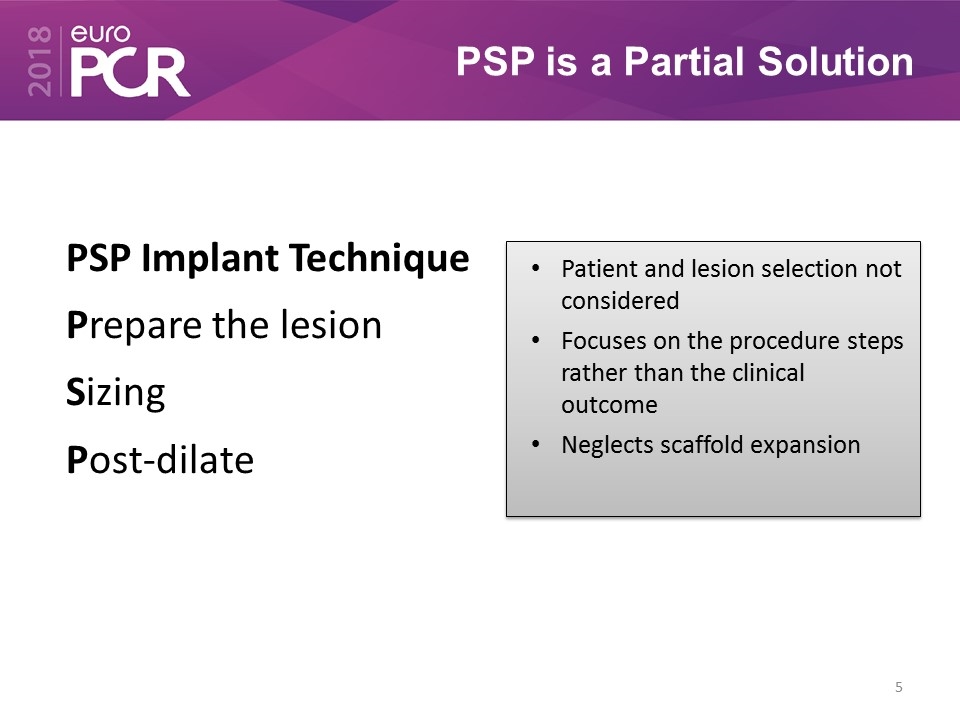
PSP is a Partial Solution PSP Implant Technique Prepare the lesion Sizing Post-dilate
PSP is a Partial Solution PSP Implant Technique Prepare the lesion Sizing Post-dilate Patient and lesion selection not considered Focuses on the procedure steps rather than the clinical outcome Neglects scaffold expansion
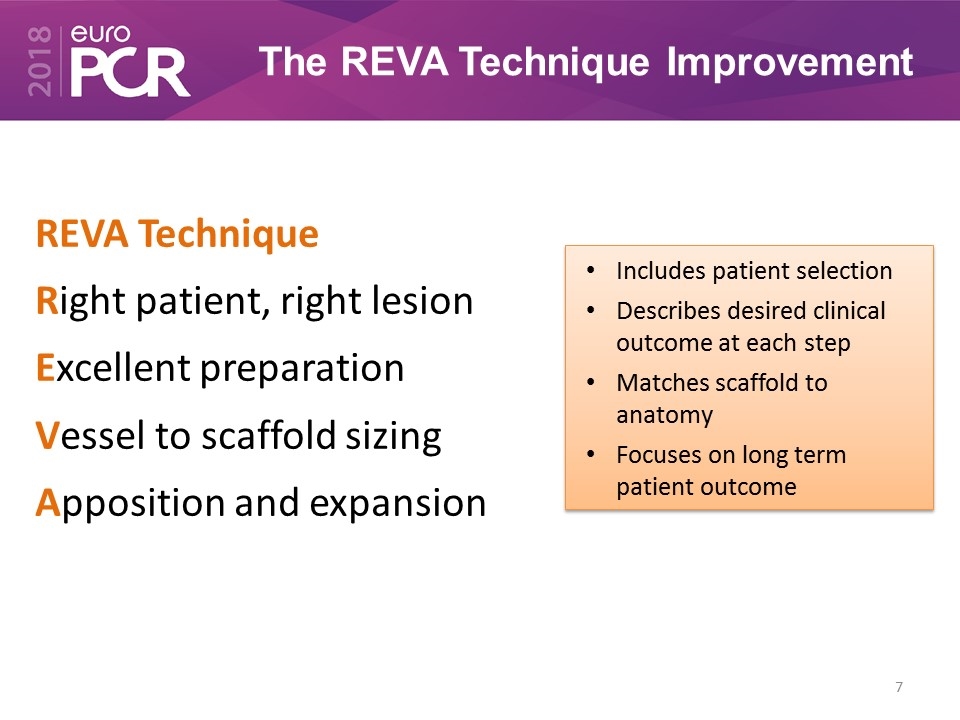
The REVA Technique Improvement REVA Technique Right patient, right lesion Excellent preparation Vessel to scaffold sizing Apposition and expansion
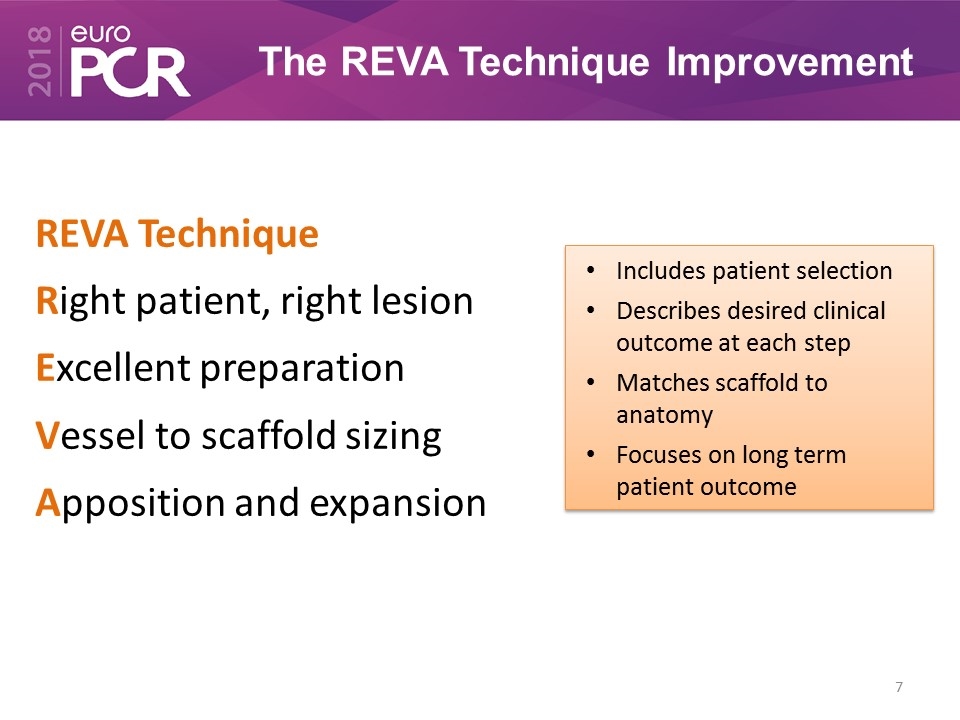
The REVA Technique Improvement Includes patient selection Describes desired clinical outcome at each step Matches scaffold to anatomy Focuses on long term patient outcome REVA Technique Right patient, right lesion Excellent preparation Vessel to scaffold sizing Apposition and expansion
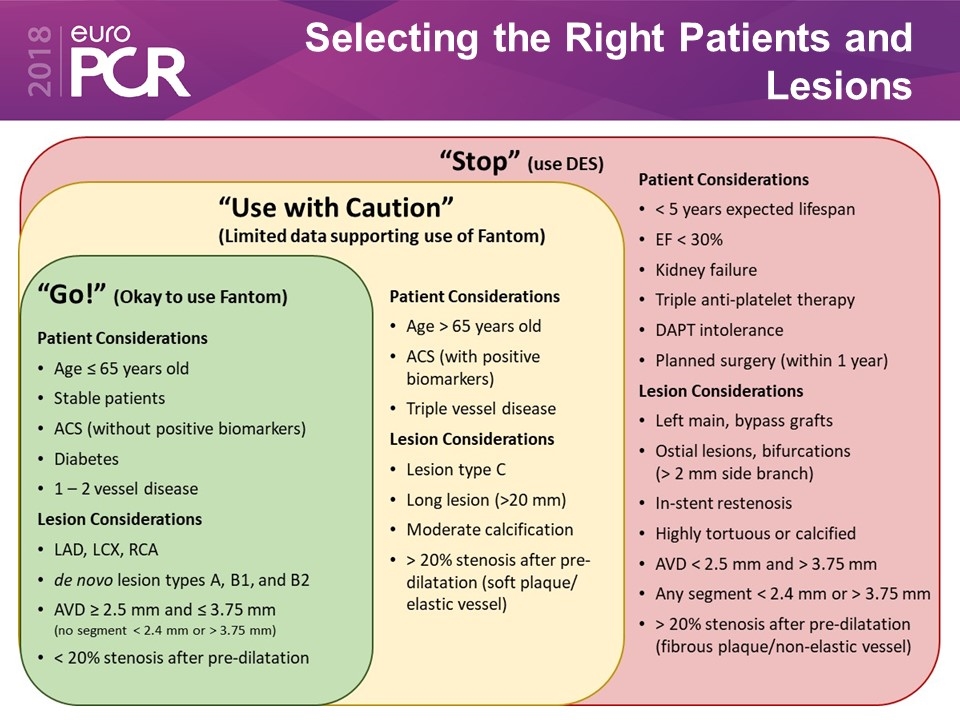
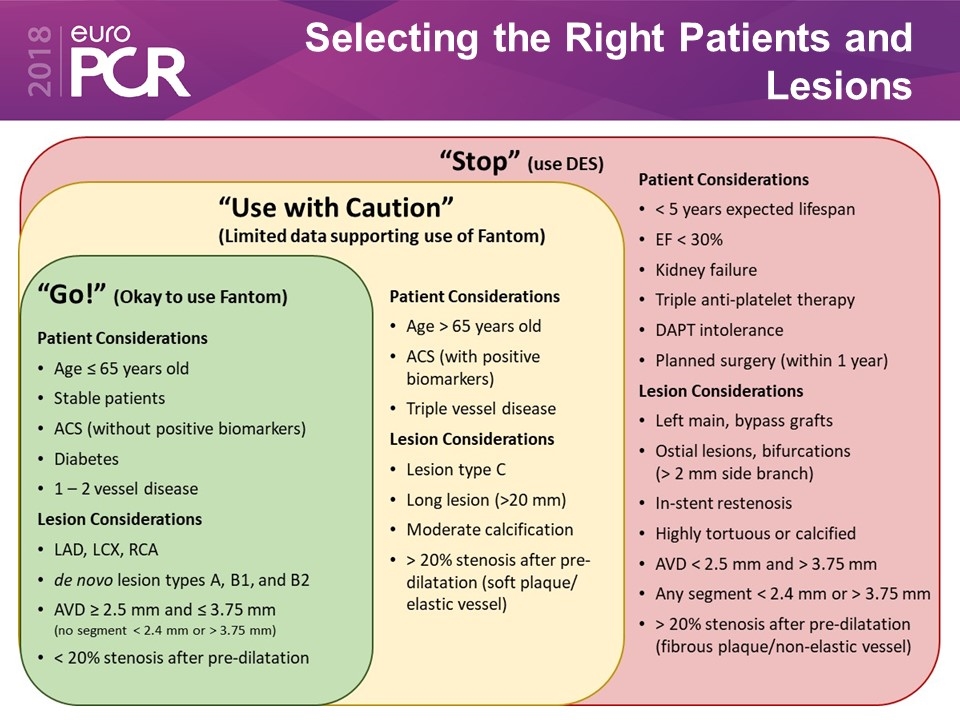
Selecting the Right Patients and Lesions
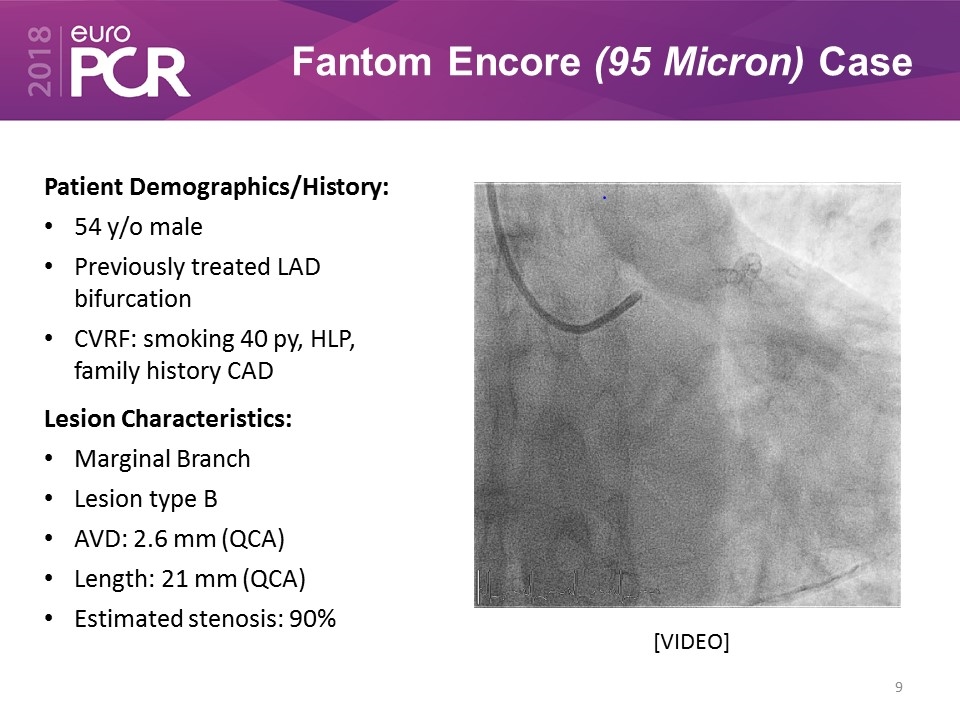
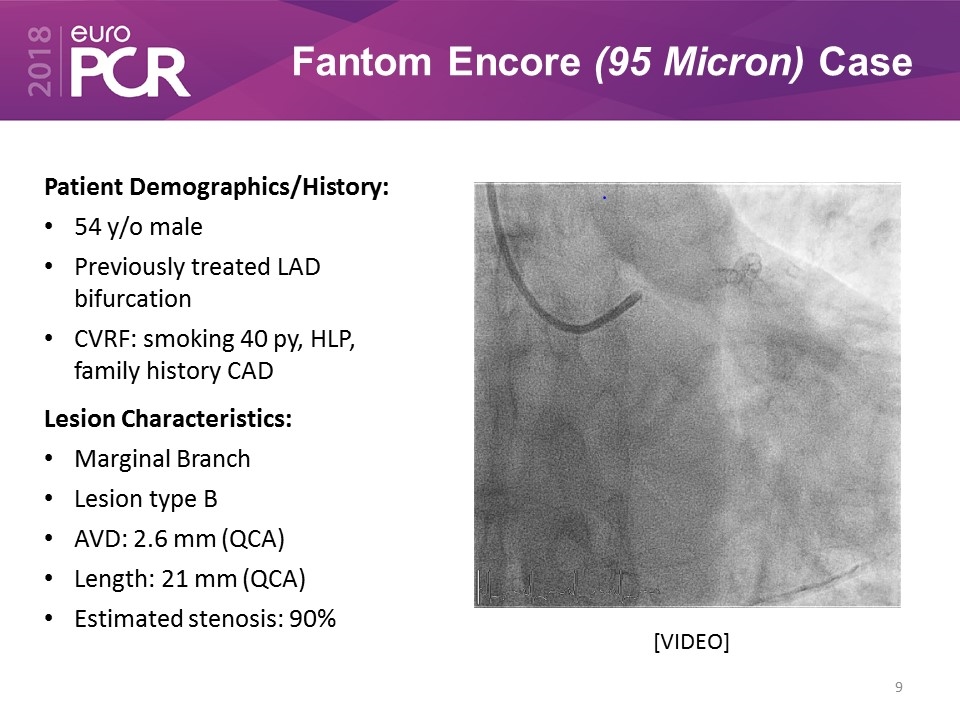
Fantom Encore (95 Micron) Case Patient Demographics/History: 54 y/o male Previously treated LAD bifurcation CVRF: smoking 40 py, HLP, family history CAD Lesion Characteristics: Marginal Branch Lesion type B AVD: 2.6 mm (QCA) Length: 21 mm (QCA) Estimated stenosis: 90% [VIDEO]
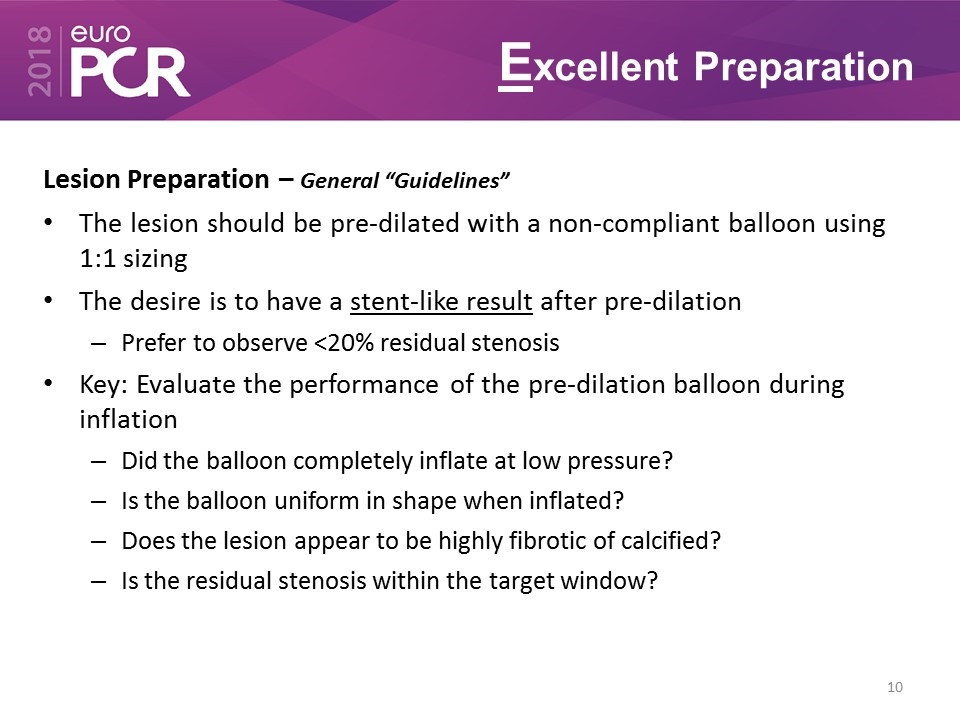
Excellent Preparation Lesion Preparation – General “Guidelines” The lesion should be pre-dilated with a non-compliant balloon using 1:1 sizing The desire is to have a stent-like result after pre-dilation Prefer to observe <20% residual stenosis Key: Evaluate the performance of the pre-dilation balloon during inflation Did the balloon completely inflate at low pressure? Is the balloon uniform in shape when inflated? Does the lesion appear to be highly fibrotic of calcified? Is the residual stenosis within the target window?
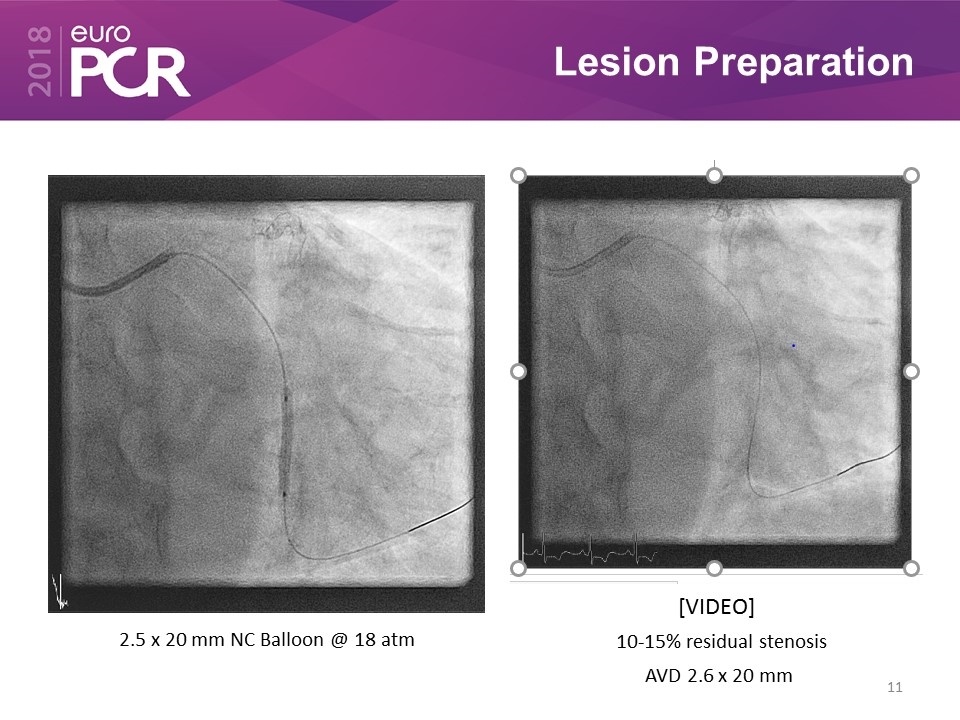
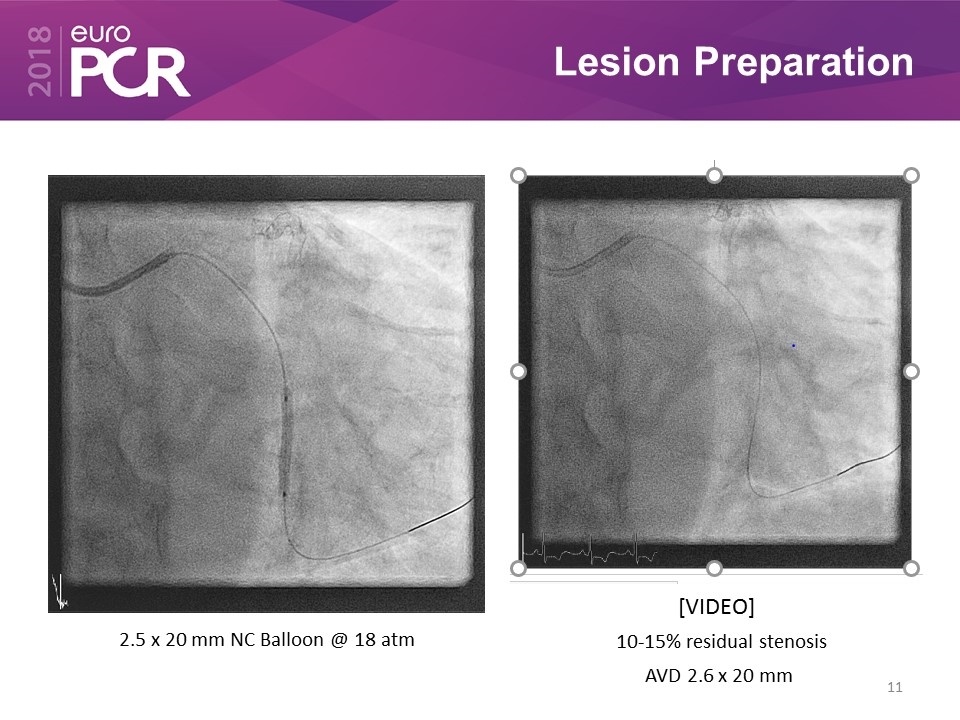
Lesion Preparation 2.5 x 20 mm NC Balloon @ 18 atm 10-15% residual stenosis AVD 2.6 x 20 mm [VIDEO]
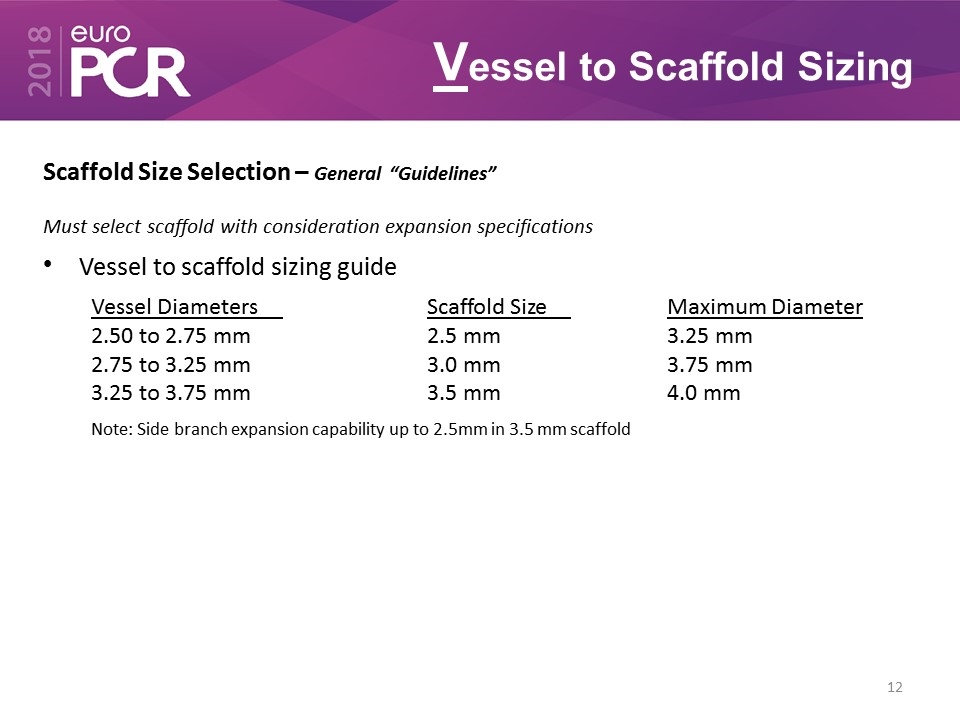
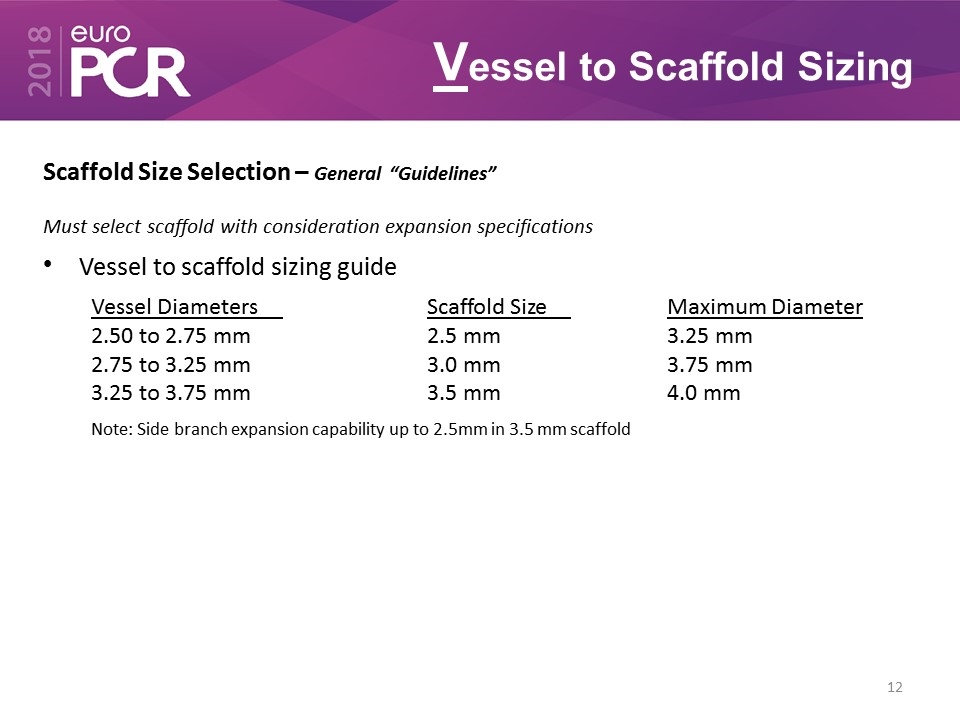
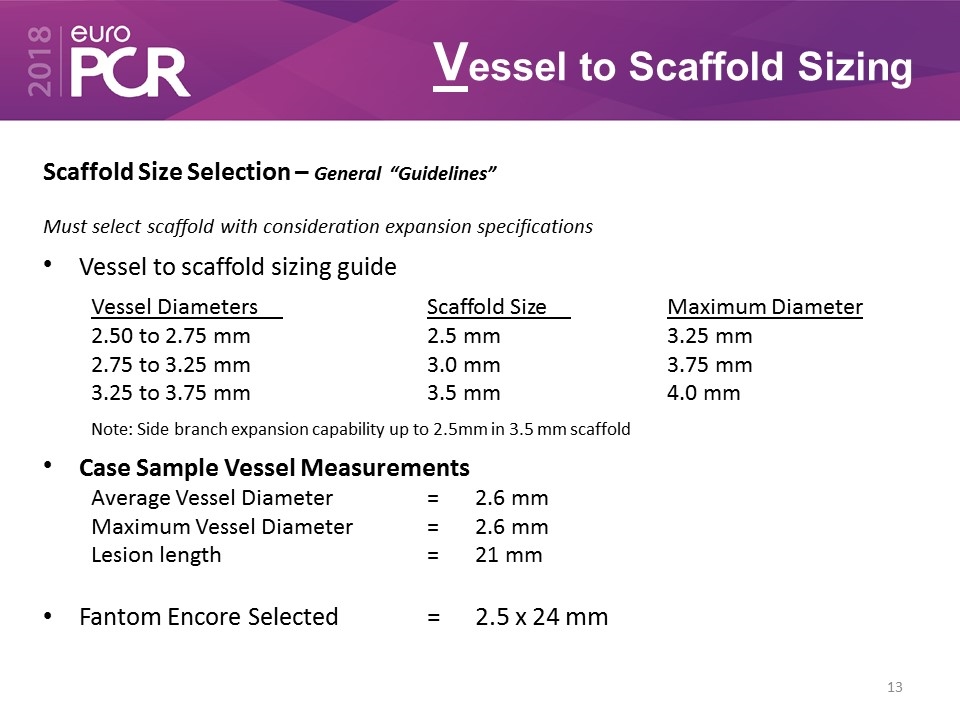
Vessel to Scaffold Sizing Scaffold Size Selection – General “Guidelines” Must select scaffold with consideration expansion specifications Vessel to scaffold sizing guide Vessel DiametersScaffold SizeMaximum Diameter 2.50 to 2.75 mm2.5 mm3.25 mm 2.75 to 3.25 mm3.0 mm3.75 mm 3.25 to 3.75 mm3.5 mm4.0 mm Note: Side branch expansion capability up to 2.5mm in 3.5 mm scaffold
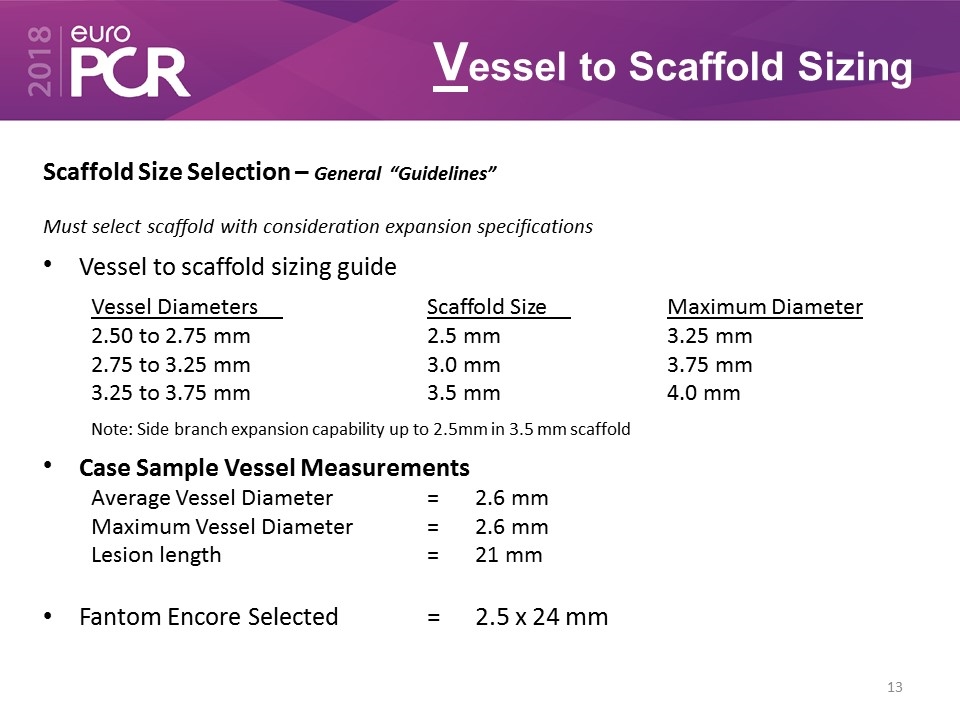
Vessel to Scaffold Sizing Scaffold Size Selection – General “Guidelines” Must select scaffold with consideration expansion specifications Vessel to scaffold sizing guide Vessel DiametersScaffold SizeMaximum Diameter 2.50 to 2.75 mm2.5 mm3.25 mm 2.75 to 3.25 mm3.0 mm3.75 mm 3.25 to 3.75 mm3.5 mm4.0 mm Note: Side branch expansion capability up to 2.5mm in 3.5 mm scaffold Case Sample Vessel Measurements Average Vessel Diameter=2.6 mm Maximum Vessel Diameter=2.6 mm Lesion length=21 mm Fantom Encore Selected =2.5 x 24 mm
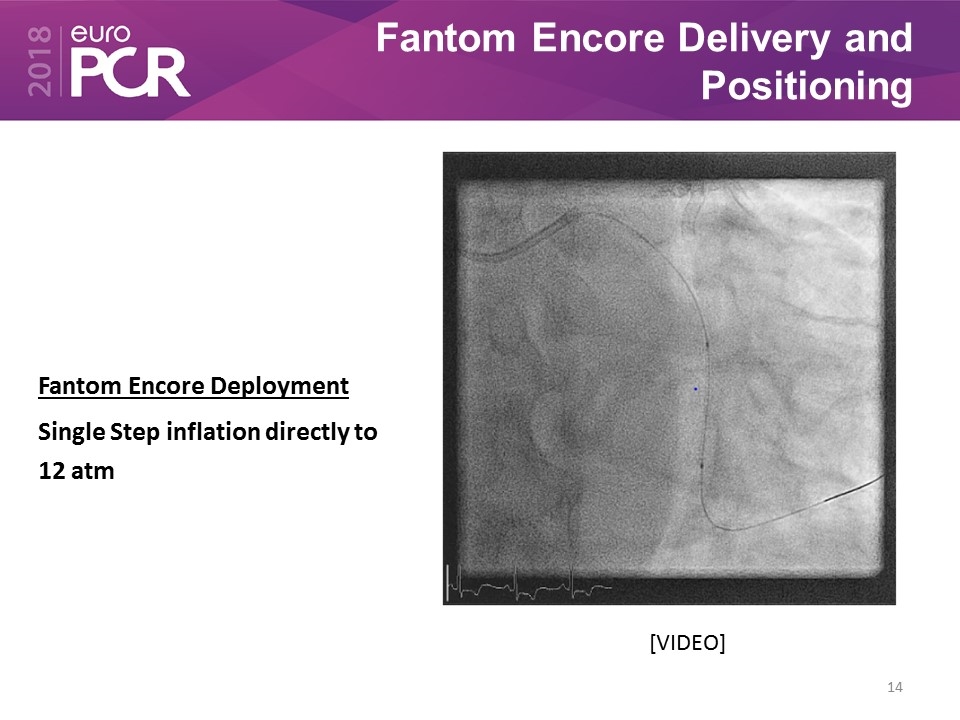
Fantom Encore Delivery and Positioning Fantom Encore Deployment Single Step inflation directly to 12 atm [VIDEO]
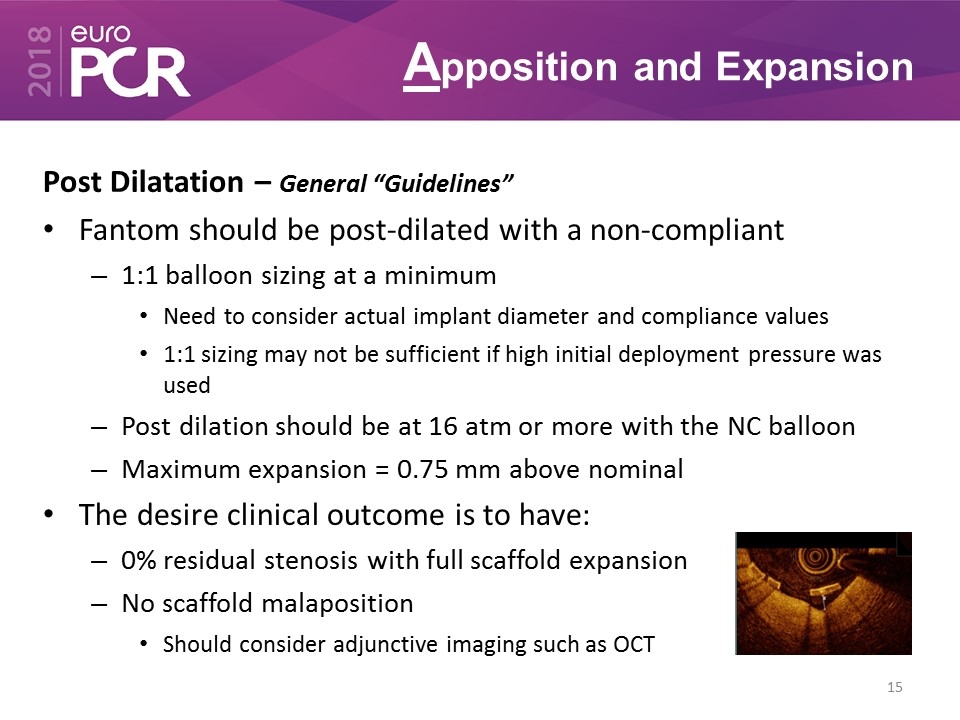
Apposition and Expansion Post Dilatation – General “Guidelines” Fantom should be post-dilated with a non-compliant 1:1 balloon sizing at a minimum Need to consider actual implant diameter and compliance values 1:1 sizing may not be sufficient if high initial deployment pressure was used Post dilation should be at 16 atm or more with the NC balloon Maximum expansion = 0.75 mm above nominal The desire clinical outcome is to have: 0% residual stenosis with full scaffold expansion No scaffold malaposition Should consider adjunctive imaging such as OCT
Final Angiographic Result 2.5 x 24 mm Fantom Encore Post-Dilatation 2.5 x 20 mm @18 atm 2 times covering proximal and distal edge [VIDEO]
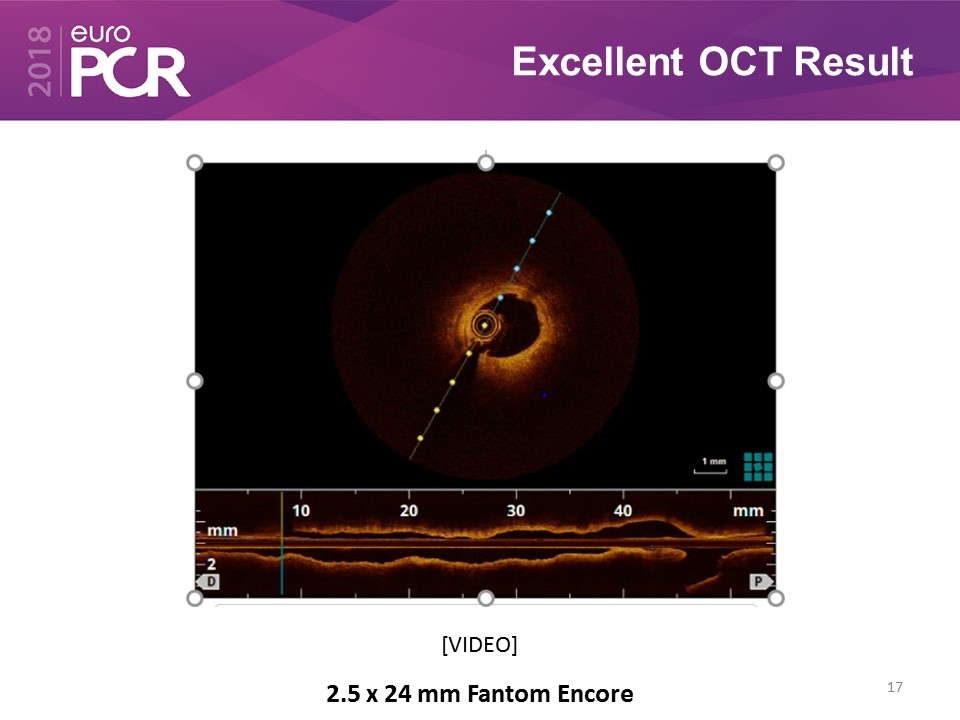
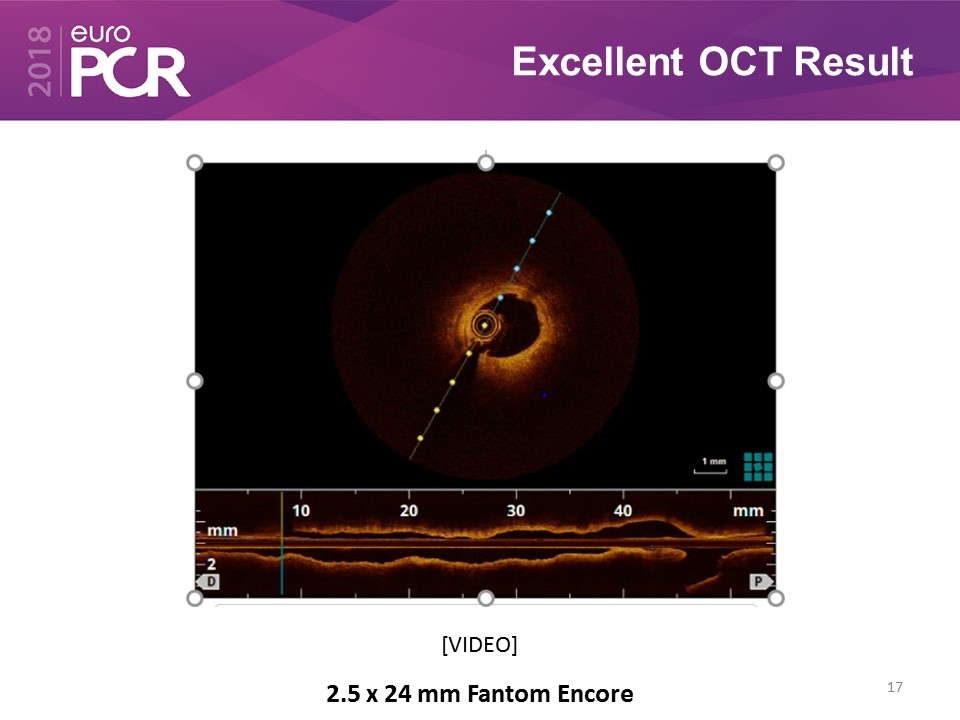
Excellent OCT Result 2.5 x 24 mm Fantom Encore [VIDEO]
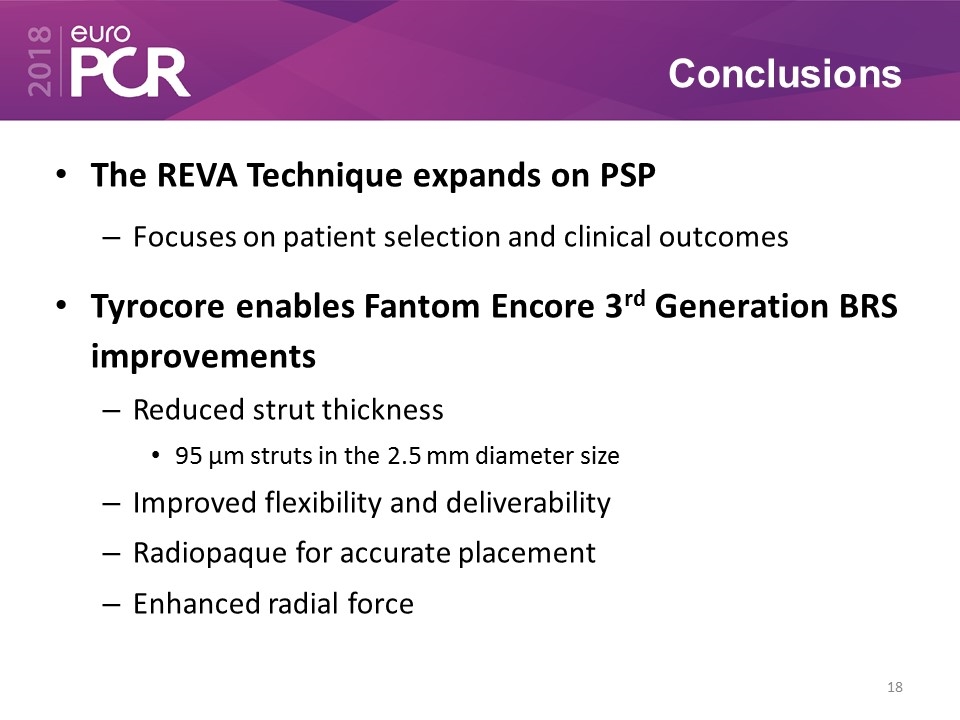
Conclusions The REVA Technique expands on PSP Focuses on patient selection and clinical outcomes Tyrocore enables Fantom Encore 3rd Generation BRS improvements Reduced strut thickness 95 µm struts in the 2.5 mm diameter size Improved flexibility and deliverability Radiopaque for accurate placement Enhanced radial force