Pasi A. Jänne1; Igor I. Rybkin2; Alexander Spira3; Gregory J. Riely4; Kyriakos P. Papadopoulos5; Joshua Sabari6; Melissa L. Johnson7; Rebecca S. Heist8; Lyudmila Bazhenova9, Minal Barve10, Jose M. Pacheco11; Ticiana A. Leal12; Karen Velastegui13; Cornelius Cilliers13; Peter Olson13; James G. Christensen13; Thian Kheoh13; Richard C. Chao13; Sai-Hong Ignatius Ou14 KRYSTAL-1: Updated Safety and Efficacy Data With Adagrasib (MRTX849) in NSCLC With KRASG12C Mutation From a Phase 1/2 Study 1Dana-Farber Cancer Institute, Boston, Massachusetts, USA. 2Henry Ford Cancer Institute, Detroit, Michigan. 3Virginia Cancer Specialists, Fairfax, Virginia, USA; US Oncology Research, The Woodlands, Texas, USA. 4Thoracic Oncology Service, Division of Solid Tumor, Department of Medicine, Memorial Sloan Kettering Cancer Center, Weill Cornell Medical College, New York, New York, USA. 5START Center for Cancer Care, San Antonio, Texas, USA. 6Department of Medical Oncology, New York University Langone Health, New York, NY; New York University Perlmutter Cancer Center, New York, New York, USA. 7Sarah Cannon Research Institute Tennessee Oncology, Nashville, Tennessee, USA. 8Massachusetts General Hospital, Boston, Massachusetts. 9Moores Cancer Center, University of California San Diego, La Jolla, California, USA. 10Mary Crowley Cancer Center, Dallas, Texas, USA. 11Division of Medical Oncology, Department of Medicine, University of Colorado Anschutz Medical Campus, Aurora, Colorado, USA. 12University of Wisconsin Carbone Cancer Center, Madison, Wisconsin, USA. 13Mirati Therapeutics, Inc., San Diego, California. 14University of California, Irvine, Chao Family Comprehensive Cancer Center, Orange, California, USA. Exhibit 99.1
Sponsored Research: Mirati Therapeutics, Inc; Boehringer-Ingelheim; Eli Lilly and Company; Takeda Oncology; Puma Biotechnology; Astellas Pharmaceuticals; AstraZeneca; Daiichi Sankyo; Revolution Medicines Consulting Fees: Mirati Therapeutics, Inc; Boehringer-Ingelheim; Pfizer; Roche/Genentech; Chugai Pharmaceuticals; Eli Lilly and Company; Araxes Pharma; Ignyta, Takeda Oncology; Voronoi; Novartis; SFJ Pharmaceuticals; Biocartis; LOXO Oncology; Sanofi; Transcenta AstraZeneca; Daiichi Sankyo Stockholder in: Gatekeeper Pharmaceuticals; LOXO Oncology Other: Post-marketing royalties from DFCI-owned IP on EGFR mutations (licensed to LabCorp) Disclosures KRYSTAL-1: Adagrasib (MRTX849) KRASG12C Inhibitor in NSCLC Presented at the 32nd EORTC-NCI-AACR Symposium, October 24-25, 2020
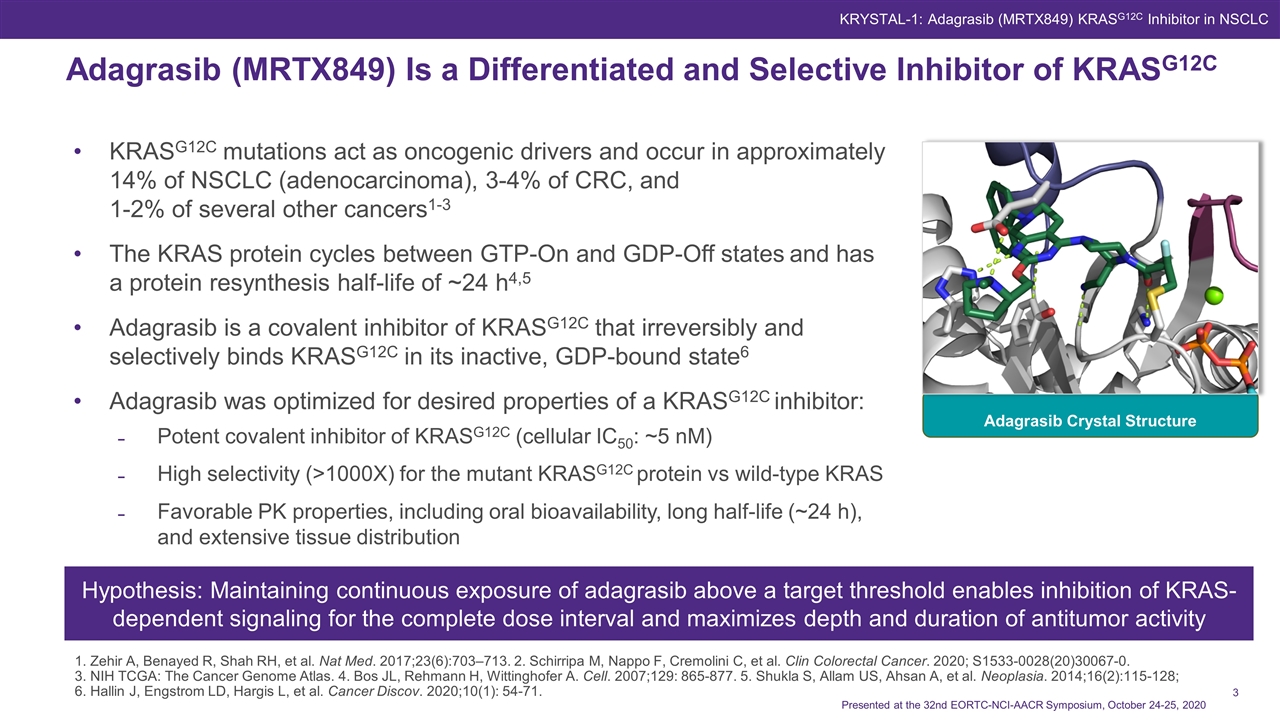
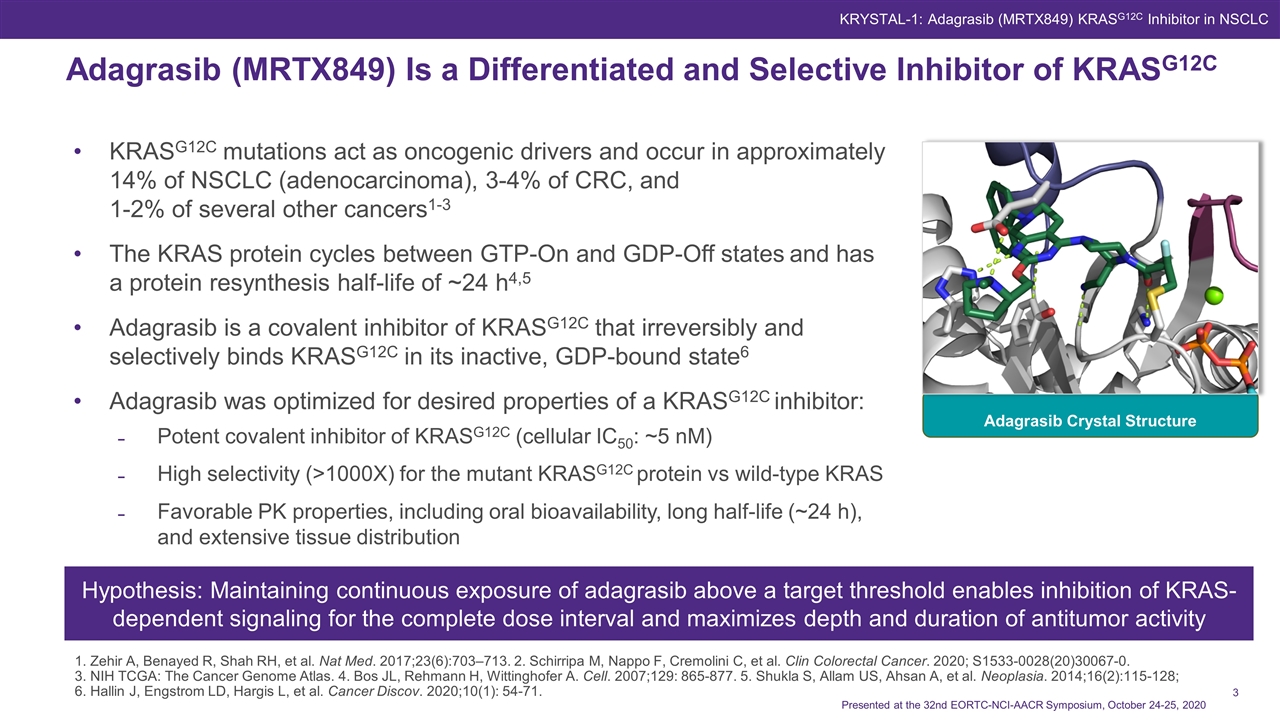
KRASG12C mutations act as oncogenic drivers and occur in approximately 14% of NSCLC (adenocarcinoma), 3-4% of CRC, and 1-2% of several other cancers1-3 The KRAS protein cycles between GTP-On and GDP-Off states and has a protein resynthesis half-life of ~24 h4,5 Adagrasib is a covalent inhibitor of KRASG12C that irreversibly and selectively binds KRASG12C in its inactive, GDP-bound state6 Adagrasib was optimized for desired properties of a KRASG12C inhibitor: Potent covalent inhibitor of KRASG12C (cellular IC50: ~5 nM) High selectivity (>1000X) for the mutant KRASG12C protein vs wild-type KRAS Favorable PK properties, including oral bioavailability, long half-life (~24 h), and extensive tissue distribution Adagrasib (MRTX849) Is a Differentiated and Selective Inhibitor of KRASG12C Presented at the 32nd EORTC-NCI-AACR Symposium, October 24-25, 2020 1. Zehir A, Benayed R, Shah RH, et al. Nat Med. 2017;23(6):703–713. 2. Schirripa M, Nappo F, Cremolini C, et al. Clin Colorectal Cancer. 2020; S1533-0028(20)30067-0. 3. NIH TCGA: The Cancer Genome Atlas. 4. Bos JL, Rehmann H, Wittinghofer A. Cell. 2007;129: 865-877. 5. Shukla S, Allam US, Ahsan A, et al. Neoplasia. 2014;16(2):115-128; 6. Hallin J, Engstrom LD, Hargis L, et al. Cancer Discov. 2020;10(1): 54-71. Adagrasib Crystal Structure Hypothesis: Maintaining continuous exposure of adagrasib above a target threshold enables inhibition of KRAS-dependent signaling for the complete dose interval and maximizes depth and duration of antitumor activity KRYSTAL-1: Adagrasib (MRTX849) KRASG12C Inhibitor in NSCLC
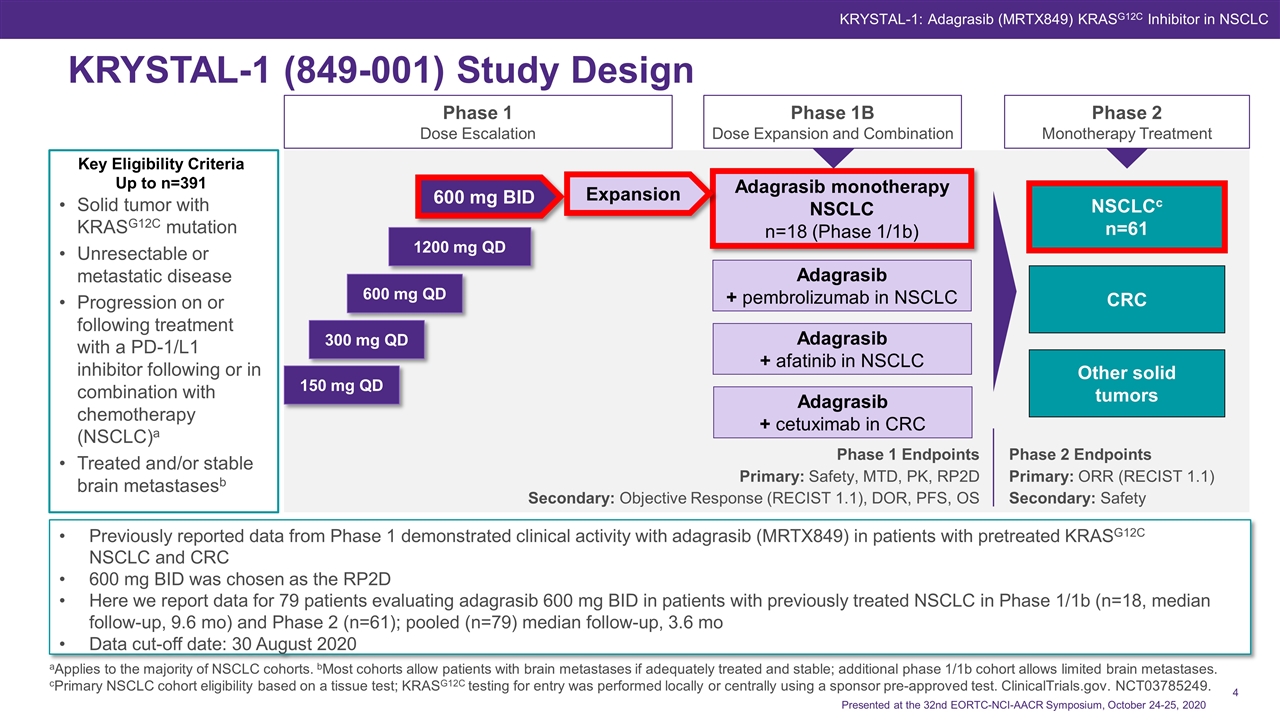
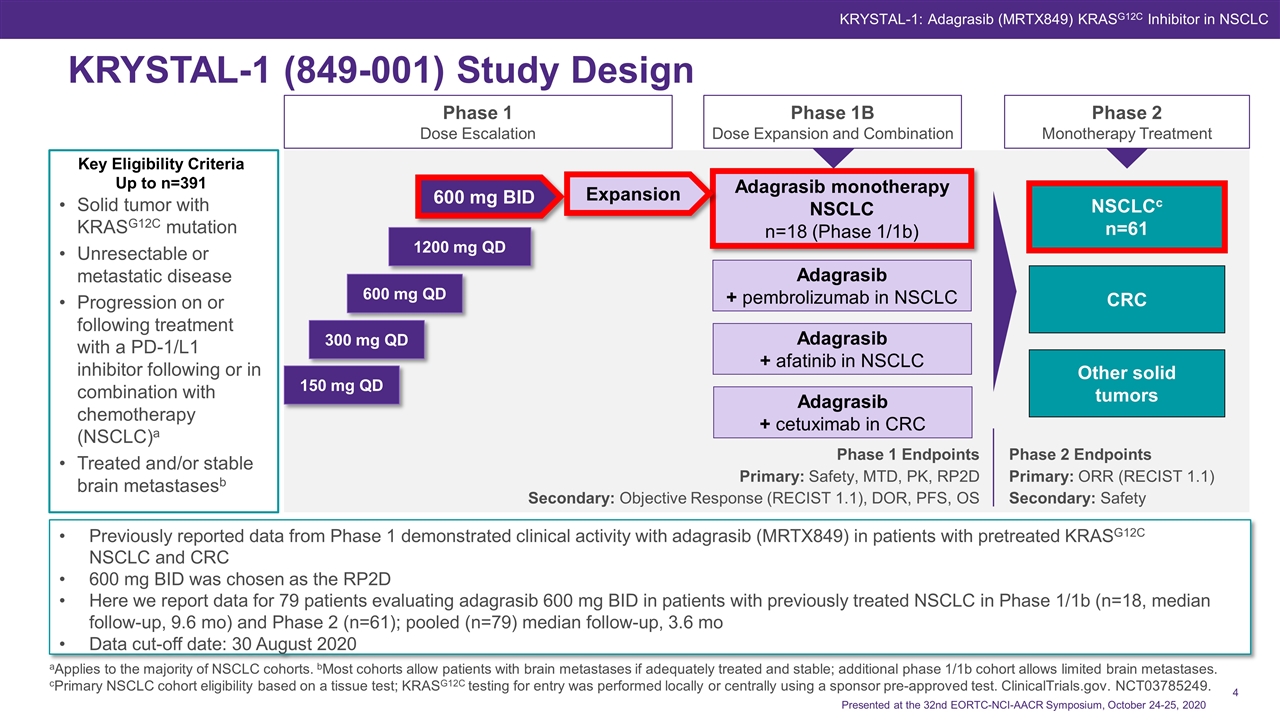
Phase 1 Endpoints Primary: Safety, MTD, PK, RP2D Secondary: Objective Response (RECIST 1.1), DOR, PFS, OS Phase 2 Endpoints Primary: ORR (RECIST 1.1) Secondary: Safety Solid tumor with KRASG12C mutation Unresectable or metastatic disease Progression on or following treatment with a PD-1/L1 inhibitor following or in combination with chemotherapy (NSCLC)a Treated and/or stable brain metastasesb Phase 1 Dose Escalation Phase 1B Dose Expansion and Combination Phase 2 Monotherapy Treatment 150 mg QD 300 mg QD 600 mg QD 1200 mg QD 600 mg BID Adagrasib + pembrolizumab in NSCLC Adagrasib + afatinib in NSCLC Adagrasib monotherapy NSCLC n=18 (Phase 1/1b) Adagrasib + cetuximab in CRC KRYSTAL-1 (849-001) Study Design Key Eligibility Criteria Up to n=391 Expansion NSCLCc n=61 CRC Other solid tumors KRYSTAL-1: Adagrasib (MRTX849) KRASG12C Inhibitor in NSCLC aApplies to the majority of NSCLC cohorts. bMost cohorts allow patients with brain metastases if adequately treated and stable; additional phase 1/1b cohort allows limited brain metastases. cPrimary NSCLC cohort eligibility based on a tissue test; KRASG12C testing for entry was performed locally or centrally using a sponsor pre-approved test. ClinicalTrials.gov. NCT03785249. Previously reported data from Phase 1 demonstrated clinical activity with adagrasib (MRTX849) in patients with pretreated KRASG12C NSCLC and CRC 600 mg BID was chosen as the RP2D Here we report data for 79 patients evaluating adagrasib 600 mg BID in patients with previously treated NSCLC in Phase 1/1b (n=18, median follow-up, 9.6 mo) and Phase 2 (n=61); pooled (n=79) median follow-up, 3.6 mo Data cut-off date: 30 August 2020 Presented at the 32nd EORTC-NCI-AACR Symposium, October 24-25, 2020
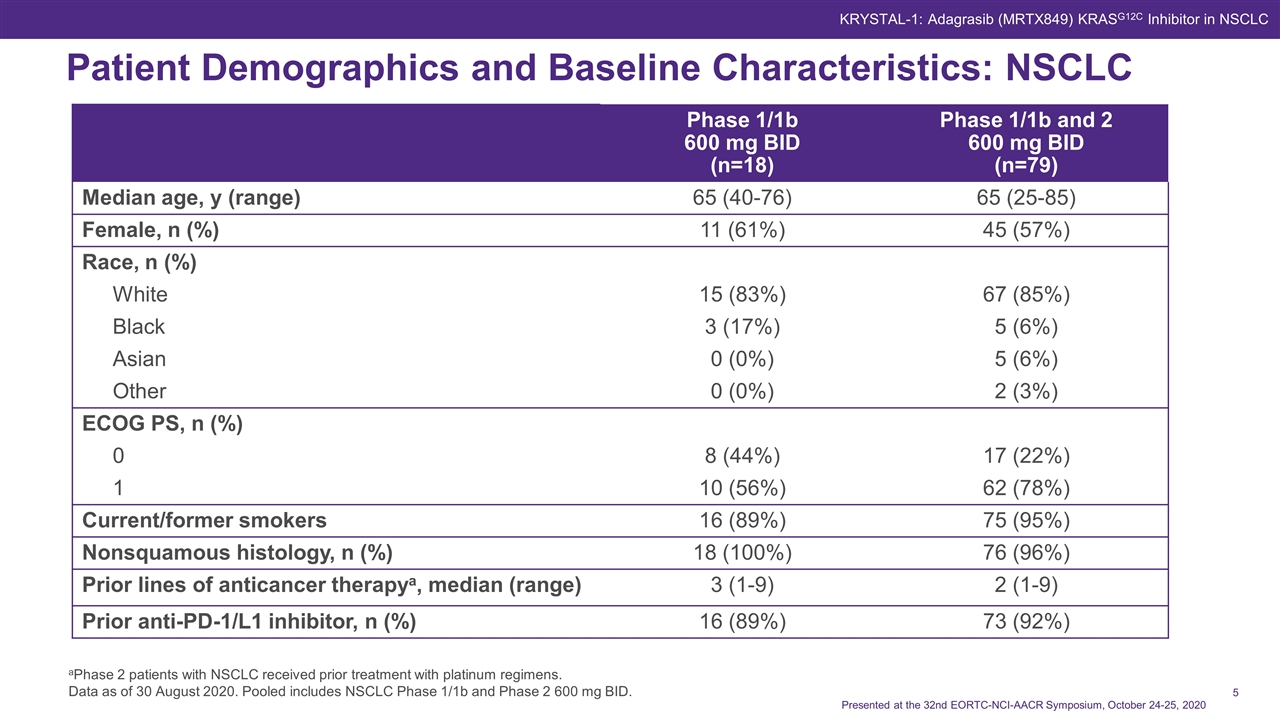
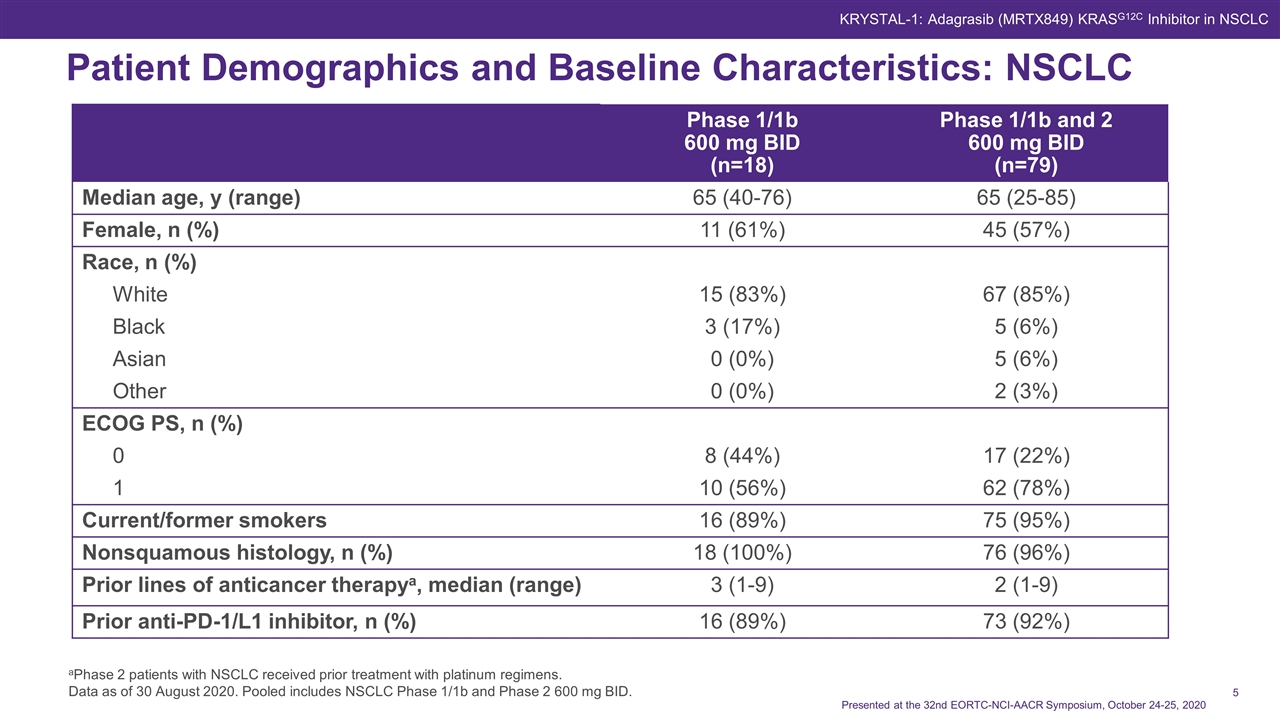
Patient Demographics and Baseline Characteristics: NSCLC Phase 1/1b 600 mg BID (n=18) Phase 1/1b and 2 600 mg BID (n=79) Median age, y (range) 65 (40-76) 65 (25-85) Female, n (%) 11 (61%) 45 (57%) Race, n (%) White 15 (83%) 67 (85%) Black 3 (17%) 5 (6%) Asian 0 (0%) 5 (6%) Other 0 (0%) 2 (3%) ECOG PS, n (%) 0 8 (44%) 17 (22%) 1 10 (56%) 62 (78%) Current/former smokers 16 (89%) 75 (95%) Nonsquamous histology, n (%) 18 (100%) 76 (96%) Prior lines of anticancer therapya, median (range) 3 (1-9) 2 (1-9) Prior anti-PD-1/L1 inhibitor, n (%) 16 (89%) 73 (92%) aPhase 2 patients with NSCLC received prior treatment with platinum regimens. Data as of 30 August 2020. Pooled includes NSCLC Phase 1/1b and Phase 2 600 mg BID. KRYSTAL-1: Adagrasib (MRTX849) KRASG12C Inhibitor in NSCLC Presented at the 32nd EORTC-NCI-AACR Symposium, October 24-25, 2020
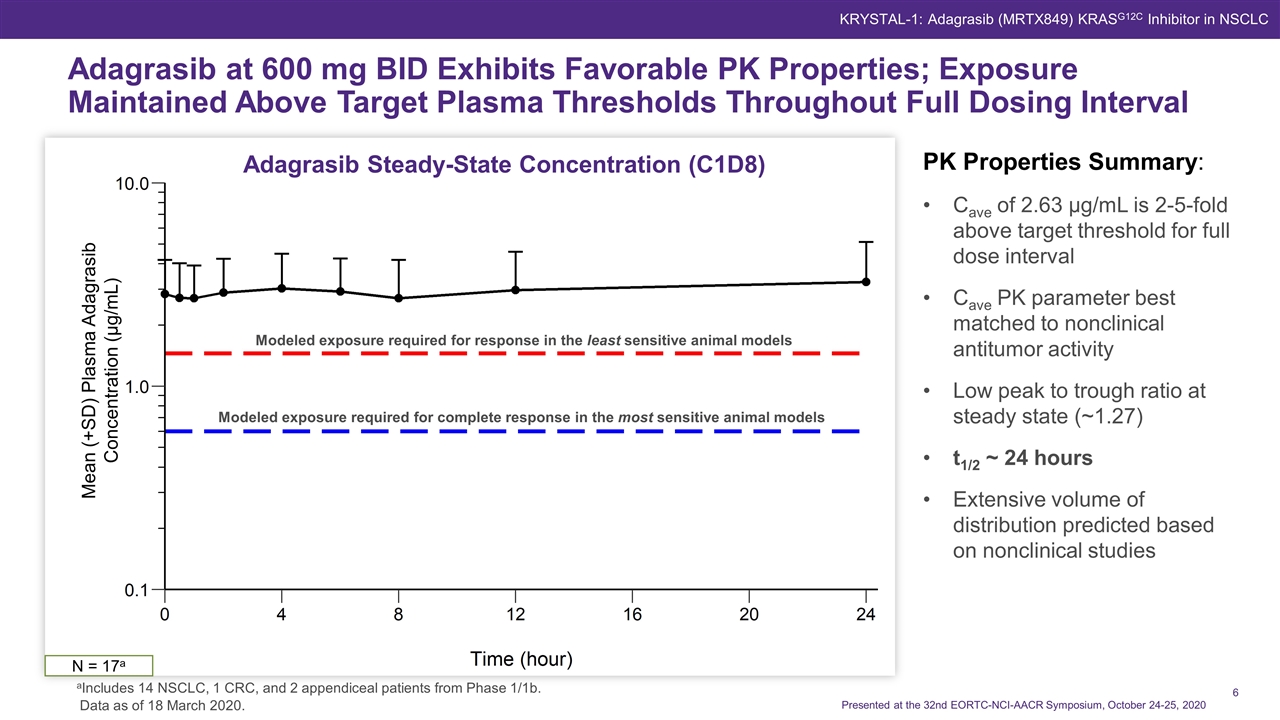
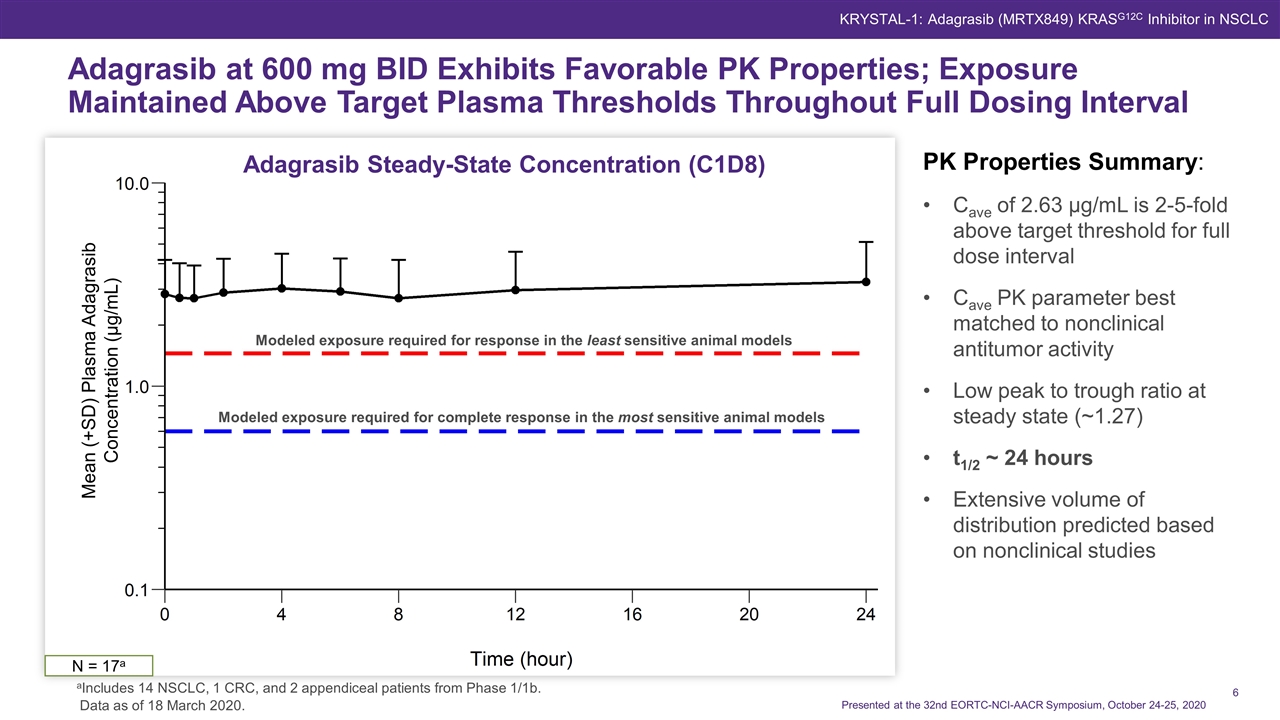
: January 30, 2020. Adagrasib at 600 mg BID Exhibits Favorable PK Properties; Exposure Maintained Above Target Plasma Thresholds Throughout Full Dosing Interval Modeled exposure required for response in the least sensitive animal models Modeled exposure required for complete response in the most sensitive animal models N = 17a Adagrasib Steady-State Concentration (C1D8) PK Properties Summary: Cave of 2.63 μg/mL is 2-5-fold above target threshold for full dose interval Cave PK parameter best matched to nonclinical antitumor activity Low peak to trough ratio at steady state (~1.27) t1/2 ~ 24 hours Extensive volume of distribution predicted based on nonclinical studies Data as of 18 March 2020. aIncludes 14 NSCLC, 1 CRC, and 2 appendiceal patients from Phase 1/1b. Presented at the 32nd EORTC-NCI-AACR Symposium, October 24-25, 2020 KRYSTAL-1: Adagrasib (MRTX849) KRASG12C Inhibitor in NSCLC Mean (+SD) Plasma Adagrasib Concentration (μg/mL)
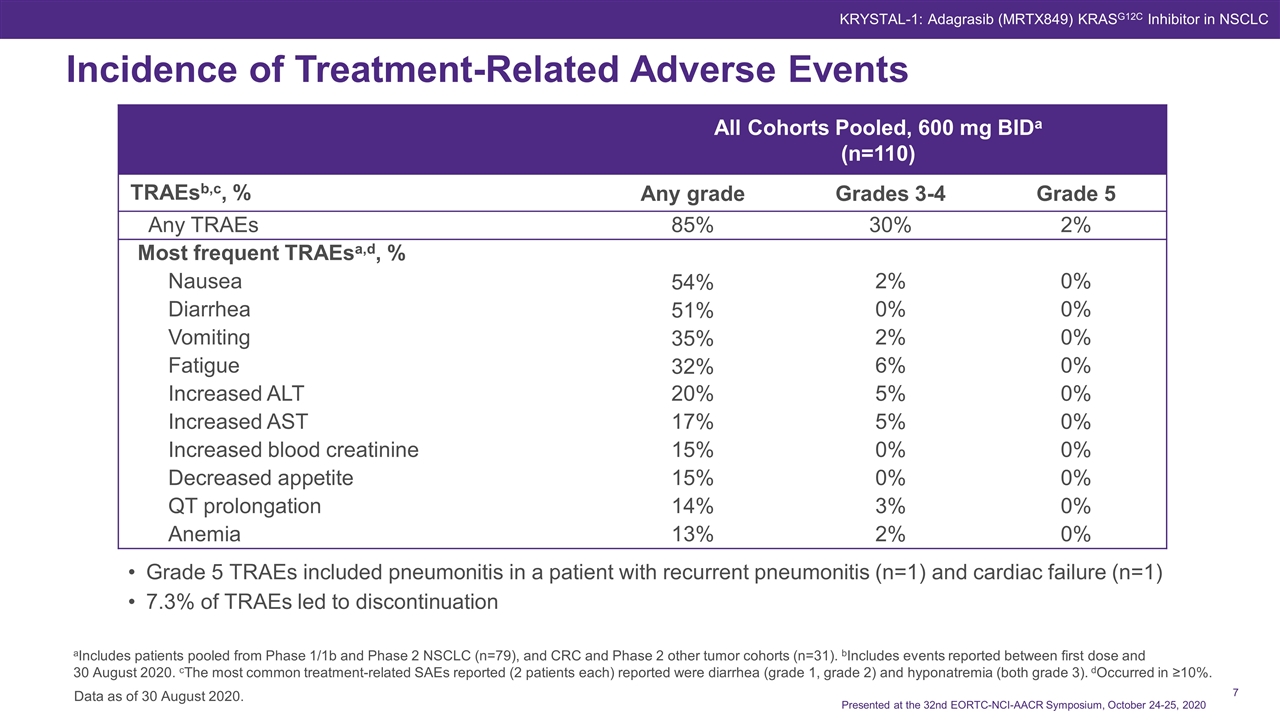
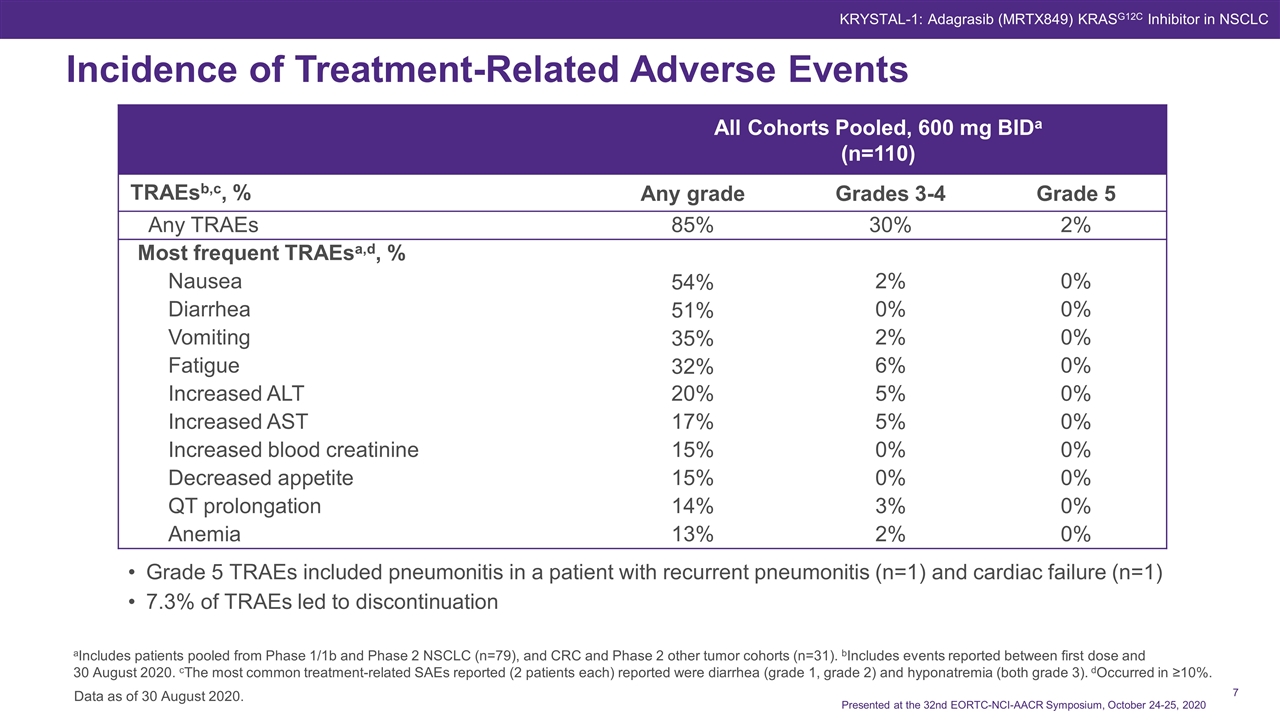
Data as of 30 August 2020. Incidence of Treatment-Related Adverse Events KRYSTAL-1: Adagrasib (MRTX849) KRASG12C Inhibitor in NSCLC Presented at the 32nd EORTC-NCI-AACR Symposium, October 24-25, 2020 Grade 5 TRAEs included pneumonitis in a patient with recurrent pneumonitis (n=1) and cardiac failure (n=1) 7.3% of TRAEs led to discontinuation All Cohorts Pooled, 600 mg BIDa (n=110) TRAEsb,c, % Any grade Grades 3-4 Grade 5 Any TRAEs 85% 30% 2% Most frequent TRAEsa,d, % Nausea 54% 2% 0% Diarrhea 51% 0% 0% Vomiting 35% 2% 0% Fatigue 32% 6% 0% Increased ALT 20% 5% 0% Increased AST 17% 5% 0% Increased blood creatinine 15% 0% 0% Decreased appetite 15% 0% 0% QT prolongation 14% 3% 0% Anemia 13% 2% 0% aIncludes patients pooled from Phase 1/1b and Phase 2 NSCLC (n=79), and CRC and Phase 2 other tumor cohorts (n=31). bIncludes events reported between first dose and 30 August 2020. cThe most common treatment-related SAEs reported (2 patients each) reported were diarrhea (grade 1, grade 2) and hyponatremia (both grade 3). dOccurred in ≥10%.

Adagrasib in Patients With NSCLC: ORR in Pooled Dataset Efficacy Outcomea, n (%) Phase 1/1b, NSCLC 600 mg BID (n=14) Phase 1/1b and 2, NSCLC 600 mg BID (n=51) Objective Response Rate 6 (43%) 23 (45%)b Best Overall Response Complete Response (CR) 0 (0%) 0 (0%) Partial Response (PR) 6 (43%) 23 (45%) Stable Disease (SD) 8 (57%) 26 (51%) Progressive Disease (PD) 0 (0%) 1 (2%) Not Evaluable (NE) 0 (0%) 1 (2%)c Disease control 14 (100%) 49 (96%) aBased on investigator assessment of the clinically evaluable patients (measurable disease with ≥1 on-study scan); 14/18 patients (Phase 1/1b) and 51/79 patients (Phase 1/1b and 2 pooled) met these criteria. bAt the time of the 30 August 2020 data cut off, 5 patients had unconfirmed PRs. All 5 were confirmed by scans that were performed after the 30 August 2020 data cut off. cOne patient had tumor reimaging too early for response assessment. Data as of 30 August 2020. Pooled includes NSCLC Phase 1/1b and Phase 2 600 mg BID. Presented at the 32nd EORTC-NCI-AACR Symposium, October 24-25, 2020 KRYSTAL-1: Adagrasib (MRTX849) KRASG12C Inhibitor in NSCLC
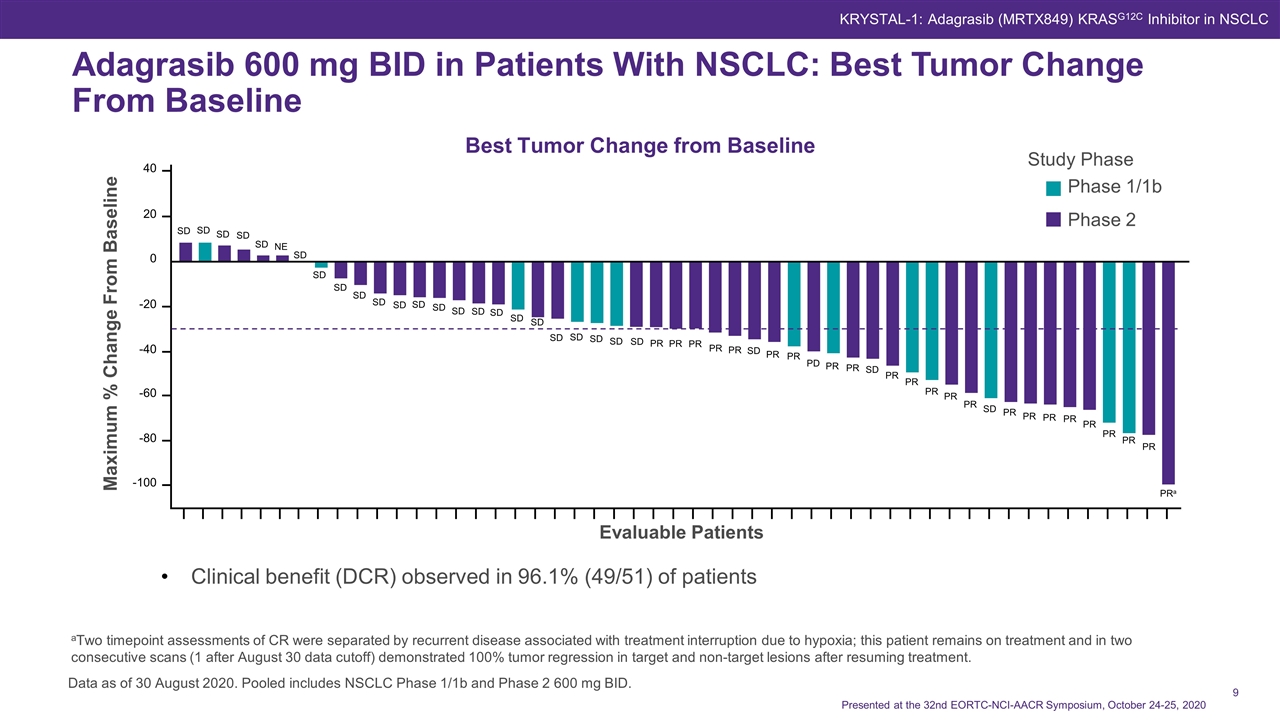
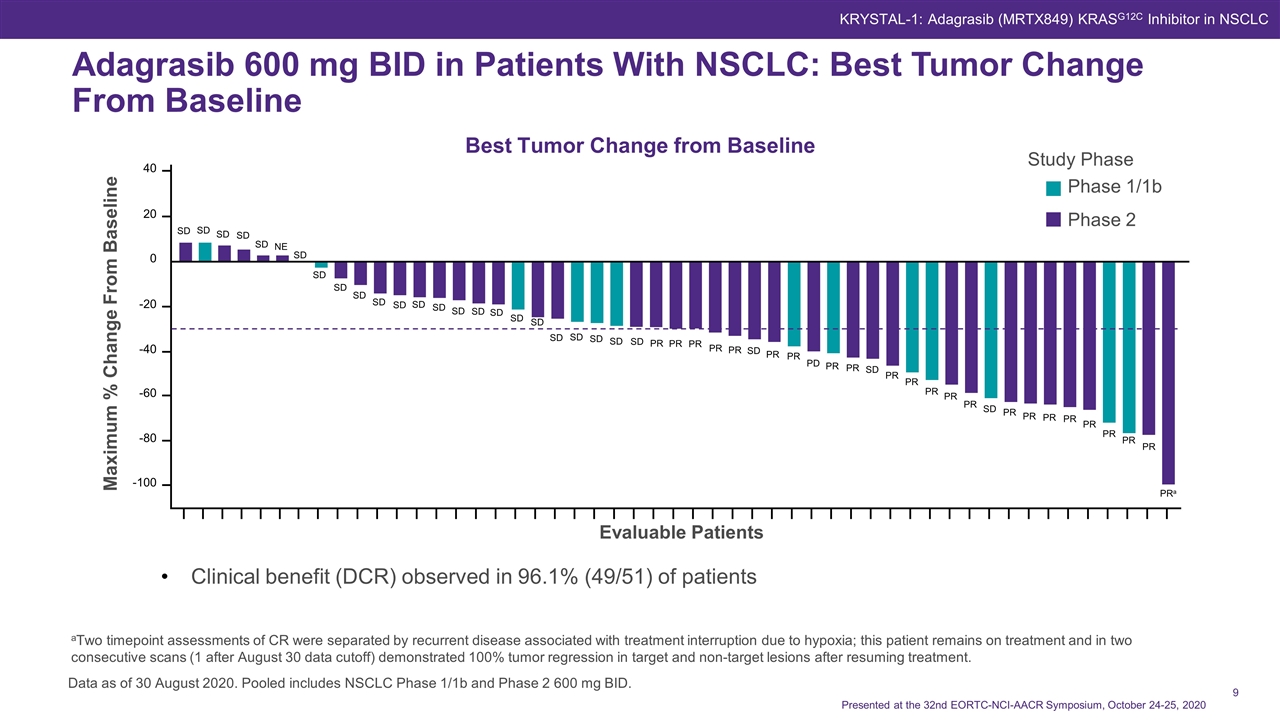
Adagrasib 600 mg BID in Patients With NSCLC: Best Tumor Change From Baseline Clinical benefit (DCR) observed in 96.1% (49/51) of patients Data as of 30 August 2020. Pooled includes NSCLC Phase 1/1b and Phase 2 600 mg BID. Presented at the 32nd EORTC-NCI-AACR Symposium, October 24-25, 2020 KRYSTAL-1: Adagrasib (MRTX849) KRASG12C Inhibitor in NSCLC aTwo timepoint assessments of CR were separated by recurrent disease associated with treatment interruption due to hypoxia; this patient remains on treatment and in two consecutive scans (1 after August 30 data cutoff) demonstrated 100% tumor regression in target and non-target lesions after resuming treatment. Best Tumor Change from Baseline Study Phase Phase 1/1b Phase 2 Maximum % Change From Baseline Evaluable Patients 40 20 0 -20 -40 -60 -80 -100 SD SD SD SD SD NE SD SD SD SD SD SD SD SD SD SD SD SD SD SD SD SD SD PR PR PR PR PR SD PR PR PD PR PR SD PR PR PR PR PR SD PR PR PR PR PR PR PR PR PRa SD
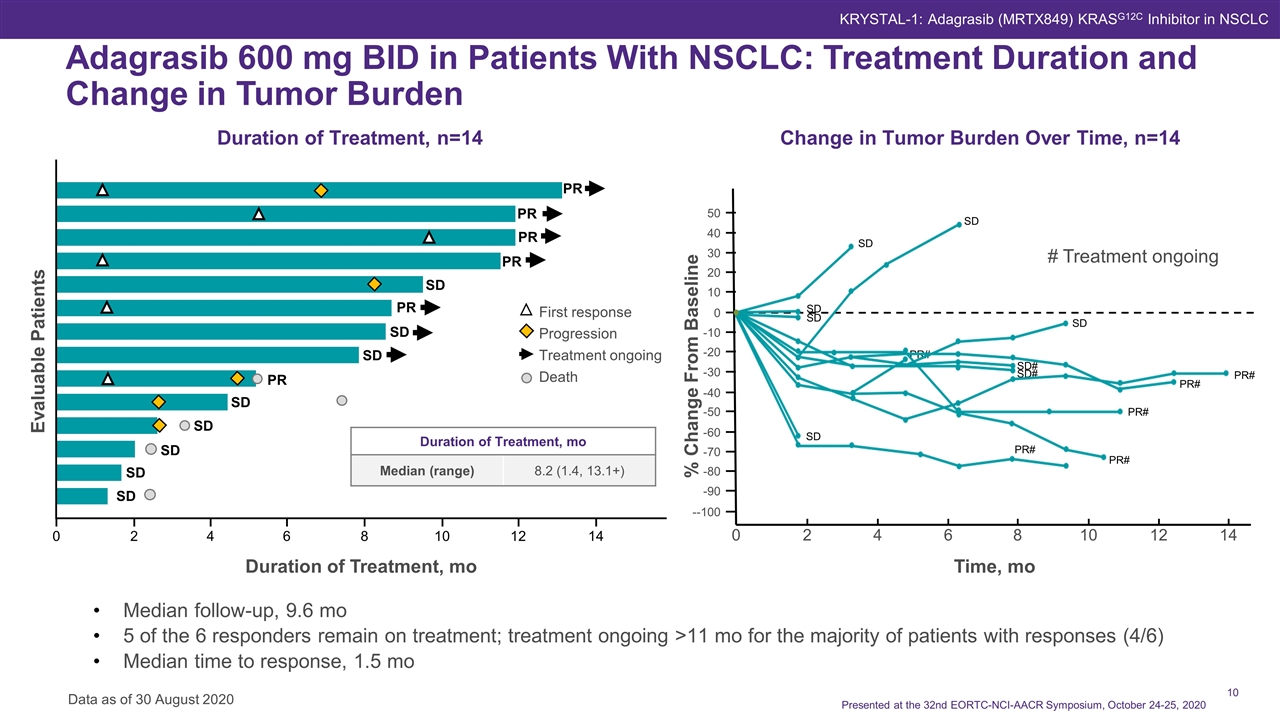
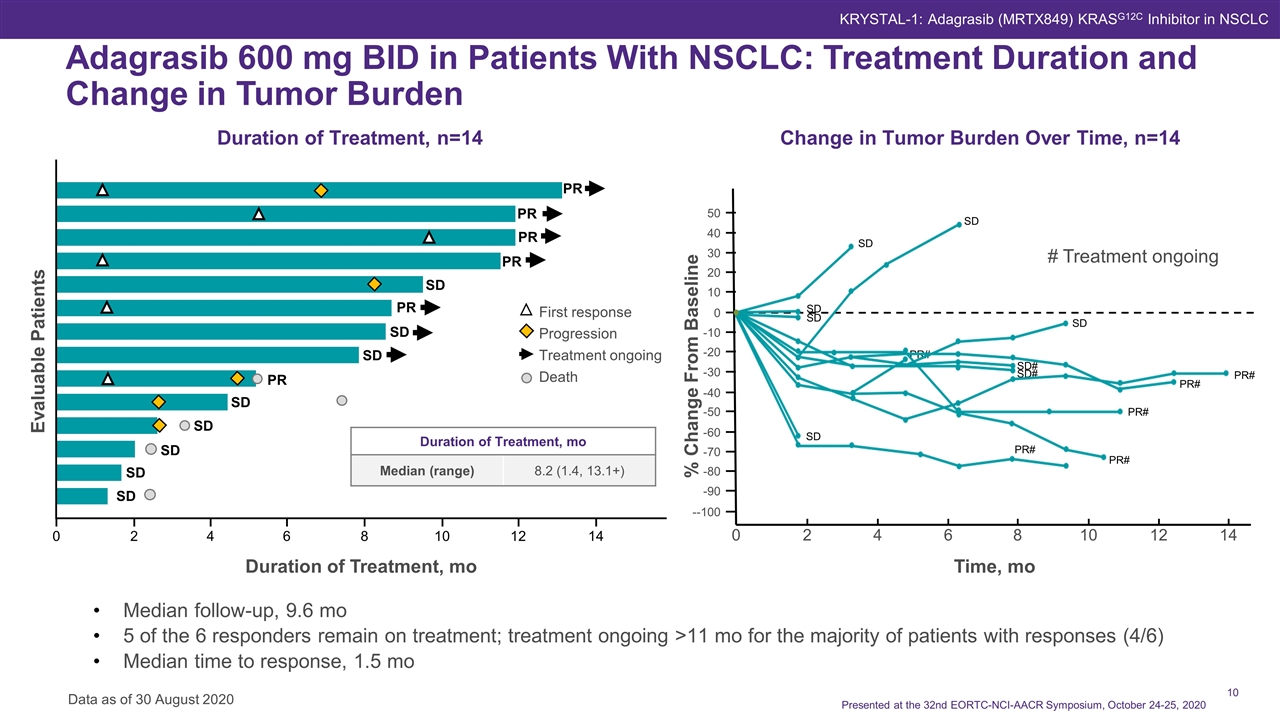
Adagrasib 600 mg BID in Patients With NSCLC: Treatment Duration and Change in Tumor Burden Data as of 30 August 2020 KRYSTAL-1: Adagrasib (MRTX849) KRASG12C Inhibitor in NSCLC Change in Tumor Burden Over Time, n=14 # Treatment ongoing Time, mo 0 2 4 6 8 10 12 14 40 20 50 -10 0 -50 -60 -90 --100 -80 -20 -70 -40 -30 10 30 SD SD SD SD SD PR# SD SD# SD# PR# PR# PR# PR# PR# Duration of Treatment, mo Duration of Treatment, n=14 Evaluable Patients 4 2 0 6 8 10 12 14 PR PR PR PR SD PR SD SD PR SD SD SD SD SD First response Progression Treatment ongoing Death Duration of Treatment, mo Median (range) 8.2 (1.4, 13.1+) Median follow-up, 9.6 mo 5 of the 6 responders remain on treatment; treatment ongoing >11 mo for the majority of patients with responses (4/6) Median time to response, 1.5 mo % Change From Baseline Presented at the 32nd EORTC-NCI-AACR Symposium, October 24-25, 2020
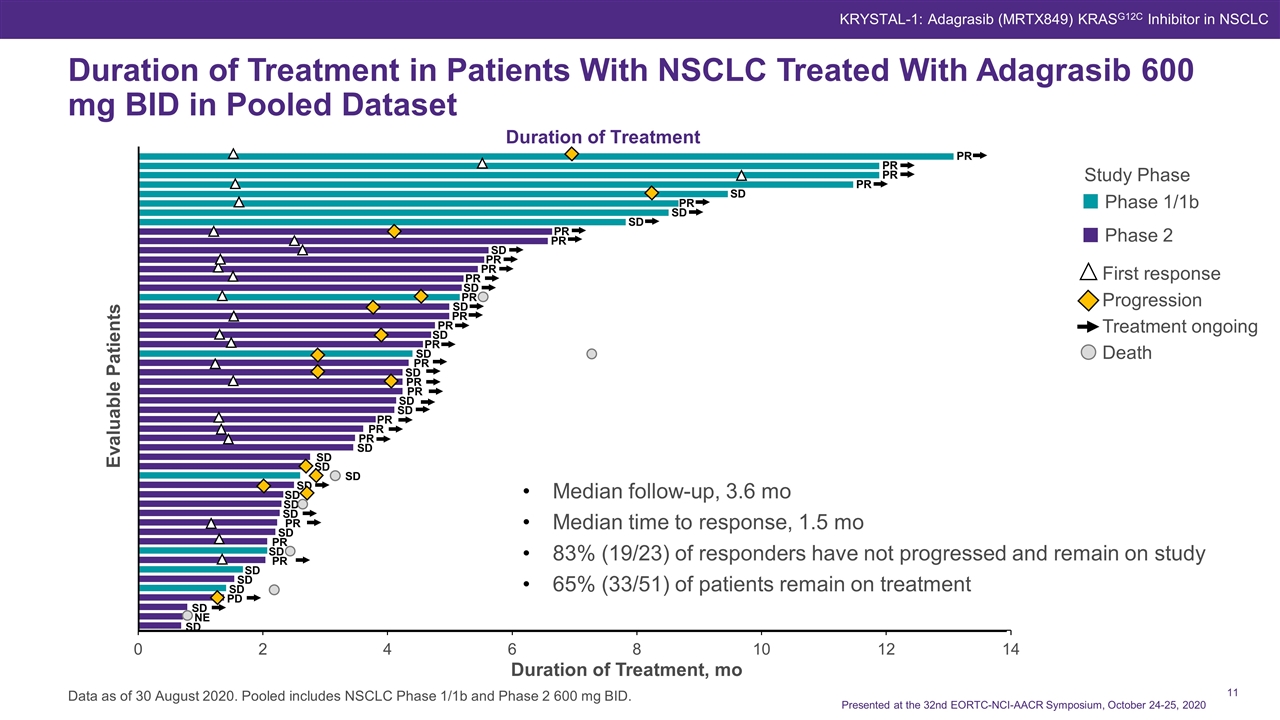
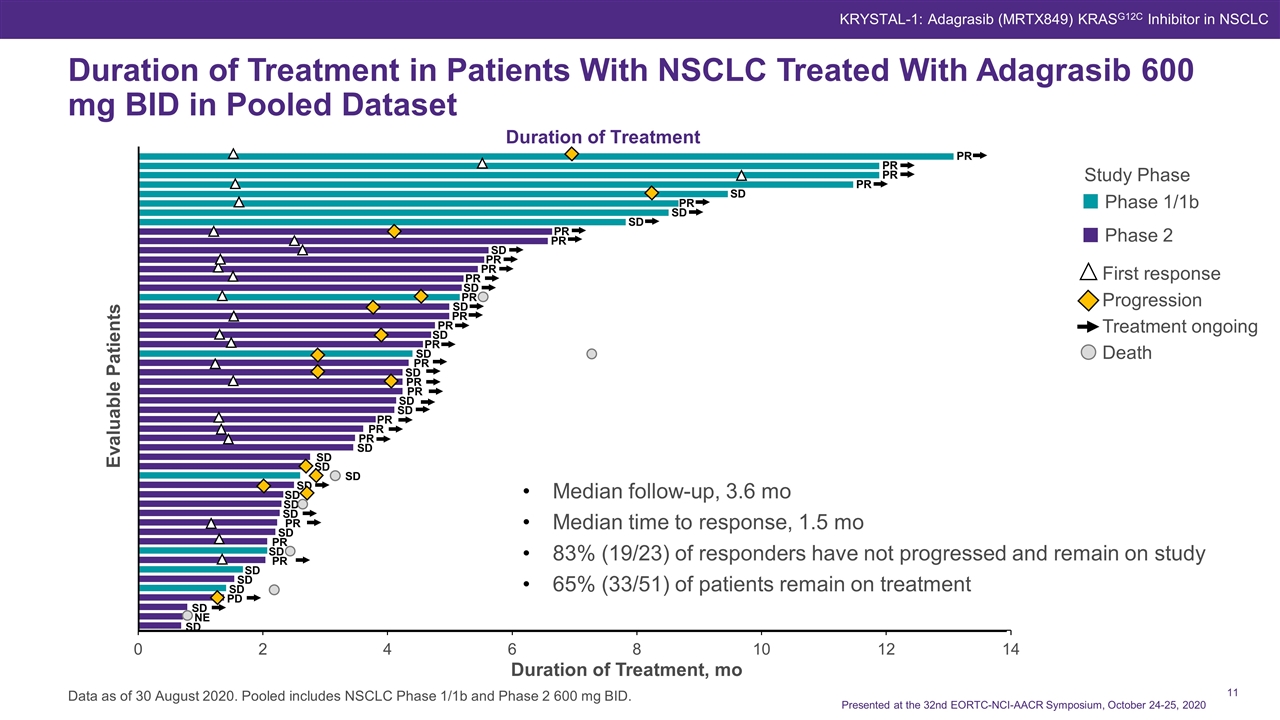
Duration of Treatment Duration of Treatment in Patients With NSCLC Treated With Adagrasib 600 mg BID in Pooled Dataset Data as of 30 August 2020. Pooled includes NSCLC Phase 1/1b and Phase 2 600 mg BID. Study Phase Phase 1/1b Phase 2 First response Progression Treatment ongoing Death Presented at the 32nd EORTC-NCI-AACR Symposium, October 24-25, 2020 KRYSTAL-1: Adagrasib (MRTX849) KRASG12C Inhibitor in NSCLC Evaluable Patients Duration of Treatment, mo Median follow-up, 3.6 mo Median time to response, 1.5 mo 83% (19/23) of responders have not progressed and remain on study 65% (33/51) of patients remain on treatment PR PR PR PR SD PR SD SD PR PR SD PR PR PR SD PR SD PR SD PR PR SD PR SD PR PR SD SD PR PR SD SD SD SD SD SD NE SD PD SD SD SD PR SD PR SD PR SD SD SD PR
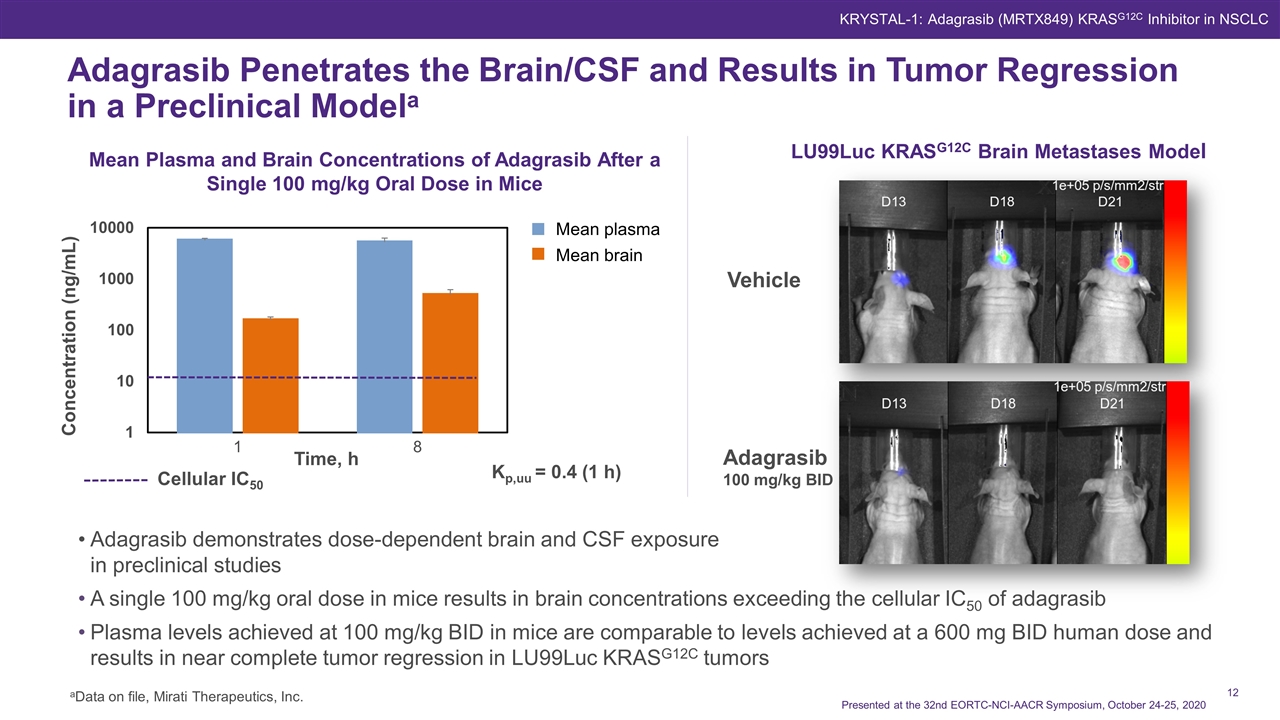
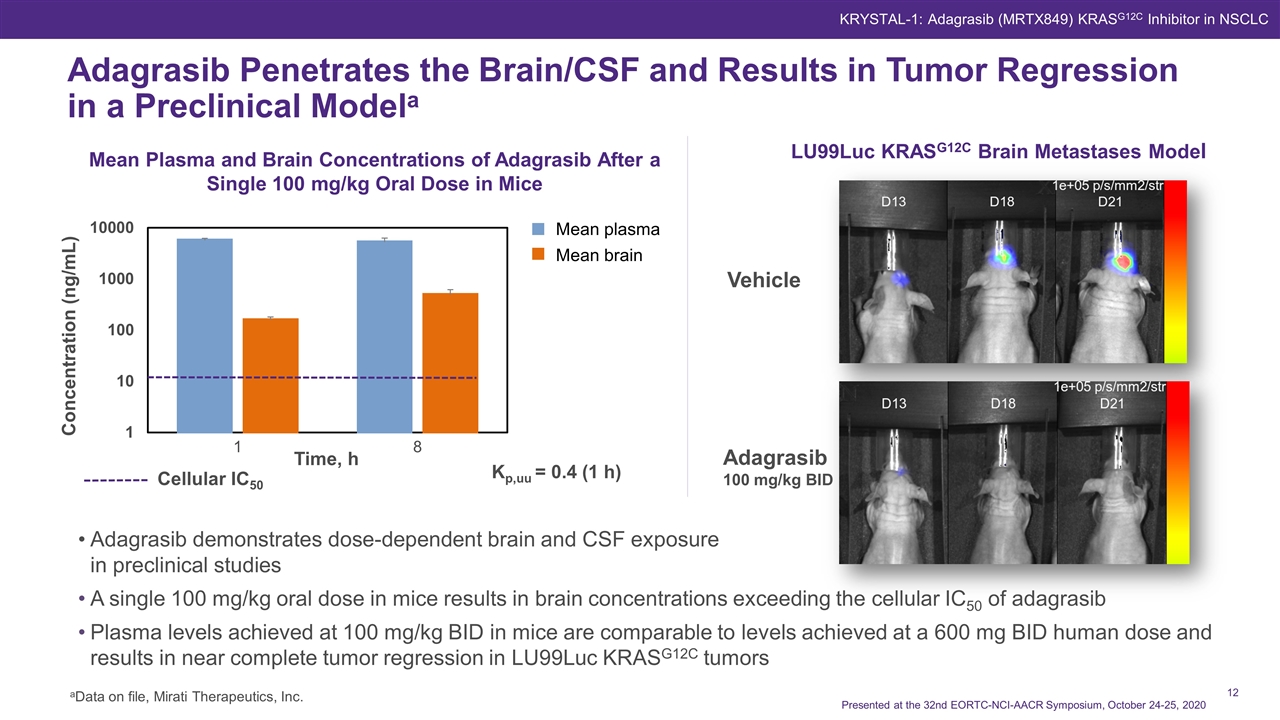
Adagrasib Penetrates the Brain/CSF and Results in Tumor Regression in a Preclinical Modela KRYSTAL-1: Adagrasib (MRTX849) KRASG12C Inhibitor in NSCLC Vehicle Adagrasib 100 mg/kg BID LU99Luc KRASG12C Brain Metastases Model Adagrasib demonstrates dose-dependent brain and CSF exposure in preclinical studies A single 100 mg/kg oral dose in mice results in brain concentrations exceeding the cellular IC50 of adagrasib Plasma levels achieved at 100 mg/kg BID in mice are comparable to levels achieved at a 600 mg BID human dose and results in near complete tumor regression in LU99Luc KRASG12C tumors aData on file, Mirati Therapeutics, Inc. Cellular IC50 Presented at the 32nd EORTC-NCI-AACR Symposium, October 24-25, 2020 Mean plasma Mean brain Mean Plasma and Brain Concentrations of Adagrasib After a Single 100 mg/kg Oral Dose in Mice
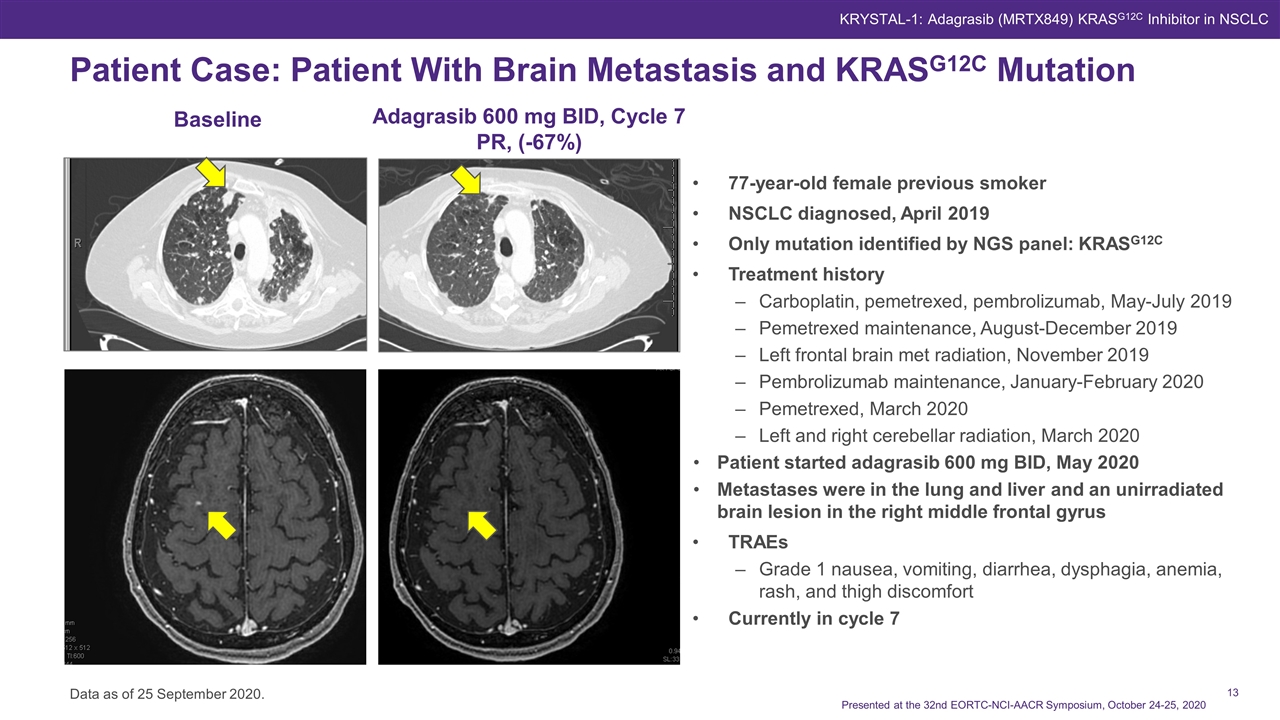
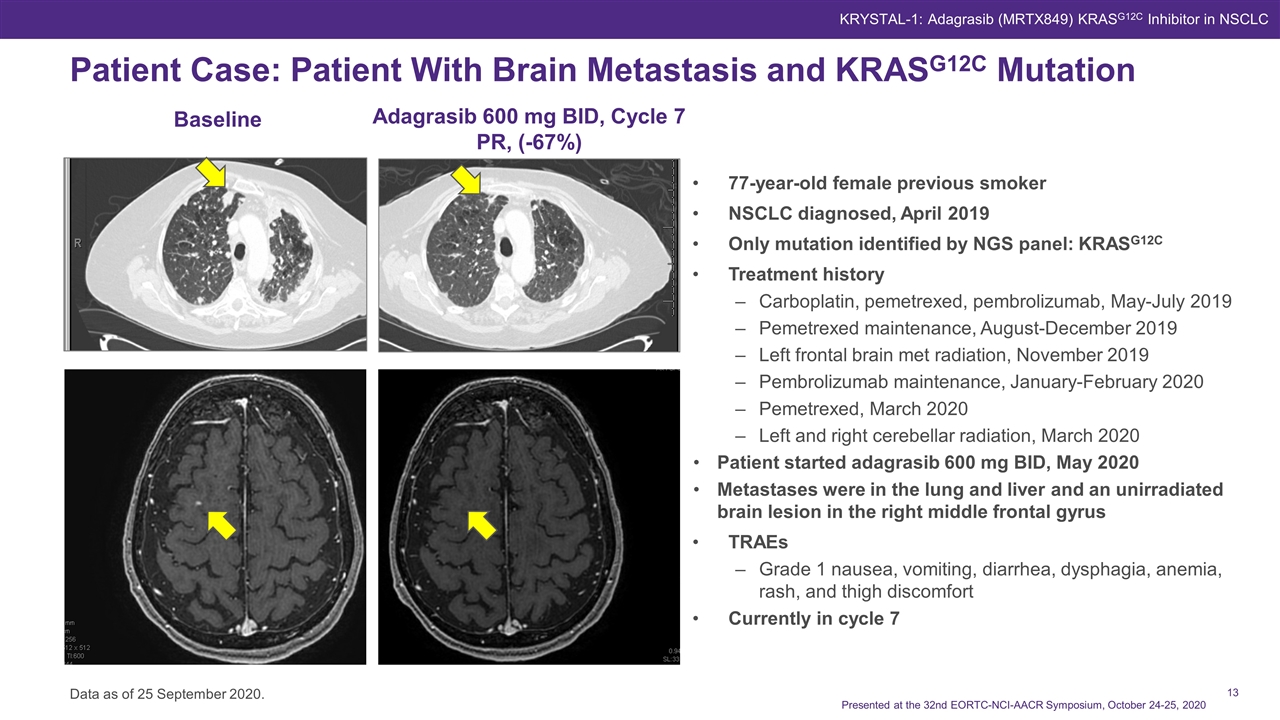
Patient Case: Patient With Brain Metastasis and KRASG12C Mutation Presented at the 32nd EORTC-NCI-AACR Symposium, October 24-25, 2020 Cycle 3, D1 KRYSTAL-1: Adagrasib (MRTX849) KRASG12C Inhibitor in NSCLC C3D1 C1D1 Baseline Adagrasib 600 mg BID, Cycle 7 PR, (-67%) 77-year-old female previous smoker NSCLC diagnosed, April 2019 Only mutation identified by NGS panel: KRASG12C Treatment history Carboplatin, pemetrexed, pembrolizumab, May-July 2019 Pemetrexed maintenance, August-December 2019 Left frontal brain met radiation, November 2019 Pembrolizumab maintenance, January-February 2020 Pemetrexed, March 2020 Left and right cerebellar radiation, March 2020 Patient started adagrasib 600 mg BID, May 2020 Metastases were in the lung and liver and an unirradiated brain lesion in the right middle frontal gyrus TRAEs Grade 1 nausea, vomiting, diarrhea, dysphagia, anemia, rash, and thigh discomfort Currently in cycle 7 Data as of 25 September 2020.
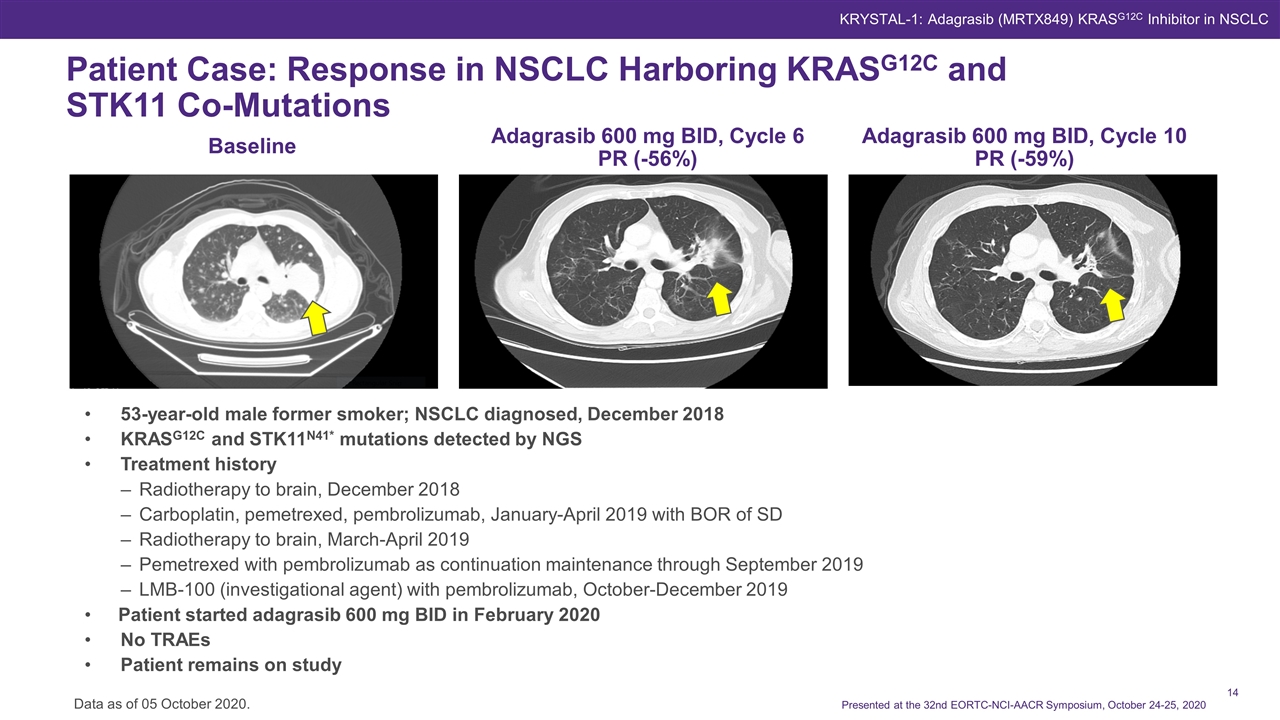
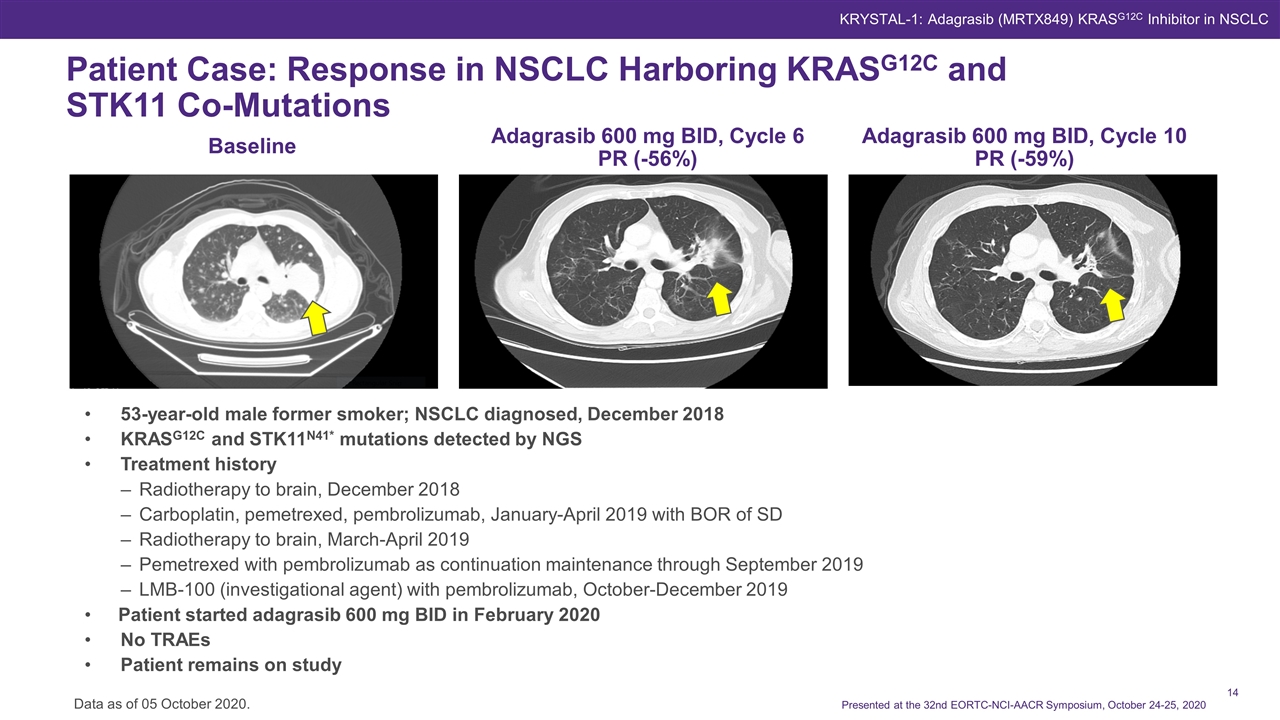
Patient Case: Response in NSCLC Harboring KRASG12C and STK11 Co-Mutations KRYSTAL-1: Adagrasib (MRTX849) KRASG12C Inhibitor in NSCLC Presented at the 32nd EORTC-NCI-AACR Symposium, October 24-25, 2020 Baseline Adagrasib 600 mg BID, Cycle 6 PR (-56%) Adagrasib 600 mg BID, Cycle 10 PR (-59%) Data as of 05 October 2020. 53-year-old male former smoker; NSCLC diagnosed, December 2018 KRASG12C and STK11N41* mutations detected by NGS Treatment history Radiotherapy to brain, December 2018 Carboplatin, pemetrexed, pembrolizumab, January-April 2019 with BOR of SD Radiotherapy to brain, March-April 2019 Pemetrexed with pembrolizumab as continuation maintenance through September 2019 LMB-100 (investigational agent) with pembrolizumab, October-December 2019 Patient started adagrasib 600 mg BID in February 2020 No TRAEs Patient remains on study
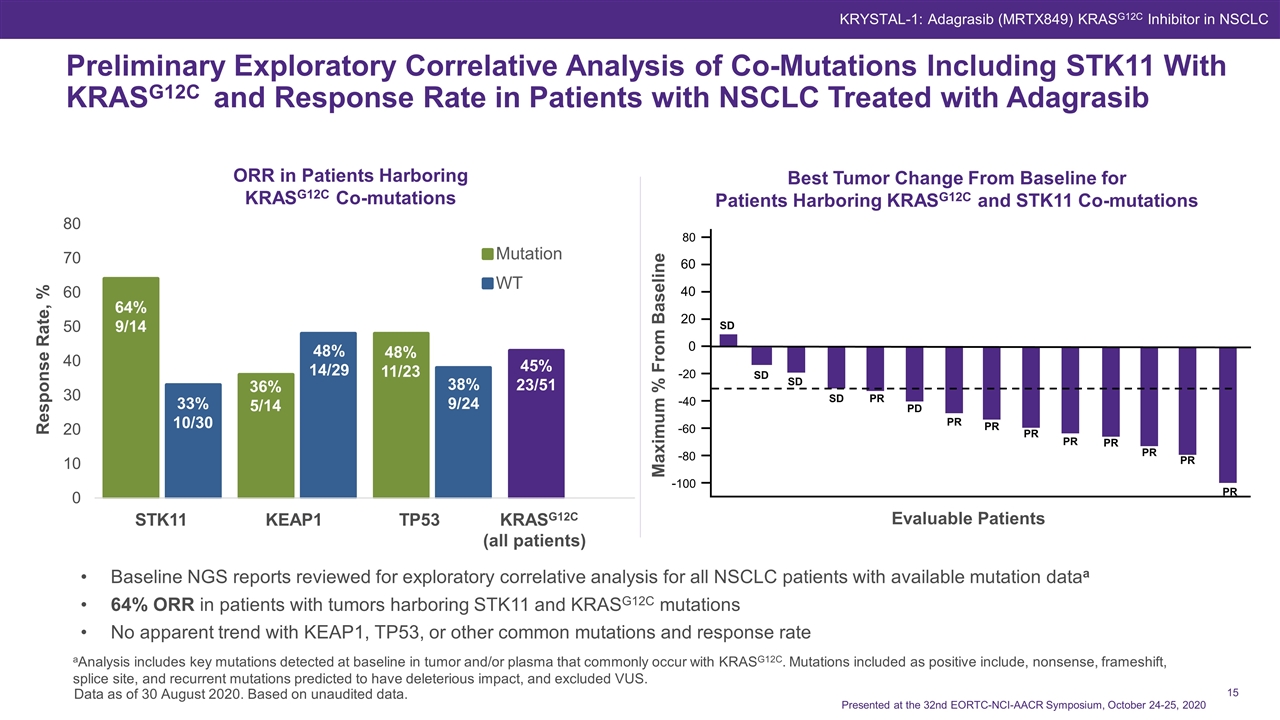
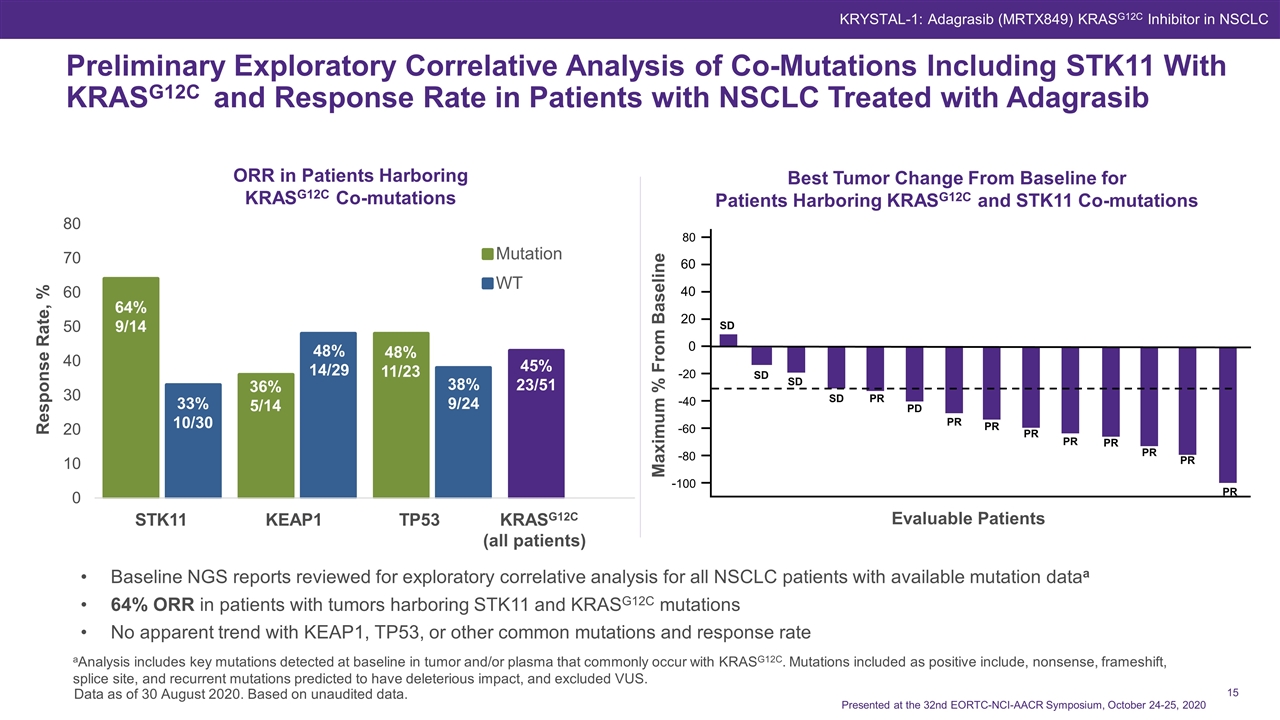
Response Rate, % 64% 9/14 33% 10/30 36% 5/14 48% 14/29 48% 11/23 38% 9/24 45% 23/51 Preliminary Exploratory Correlative Analysis of Co-Mutations Including STK11 With KRASG12C and Response Rate in Patients with NSCLC Treated with Adagrasib Baseline NGS reports reviewed for exploratory correlative analysis for all NSCLC patients with available mutation dataa 64% ORR in patients with tumors harboring STK11 and KRASG12C mutations No apparent trend with KEAP1, TP53, or other common mutations and response rate aAnalysis includes key mutations detected at baseline in tumor and/or plasma that commonly occur with KRASG12C. Mutations included as positive include, nonsense, frameshift, splice site, and recurrent mutations predicted to have deleterious impact, and excluded VUS. Data as of 30 August 2020. Based on unaudited data. Best Tumor Change From Baseline for Patients Harboring KRASG12C and STK11 Co-mutations ORR in Patients Harboring KRASG12C Co-mutations Presented at the 32nd EORTC-NCI-AACR Symposium, October 24-25, 2020 KRYSTAL-1: Adagrasib (MRTX849) KRASG12C Inhibitor in NSCLC Evaluable Patients STK11 KEAP1 TP53 KRASG12C (all patients) Maximum % From Baseline -100 -80 -60 -40 -20 0 20 40 60 80 SD SD SD PR PD PR PR PR PR PR PR PR PR SD
Adagrasib is a KRASG12C-selective covalent inhibitor with a long half-life, and extensive predicted target coverage throughout the dosing interval Adagrasib is well tolerated Adagrasib provides durable benefit to patients with NSCLC harboring KRASG12C mutations Durable responses were observed Broad disease control rate was observed In a preliminary exploratory genomic analysis, ORR was higher in patients with tumors harboring KRASG12C and STK11 co-mutations Pembrolizumab combination (NSCLC) arm has cleared the DLT observation period and enrollment in Phase 1b expansion at full dose of each agent is ongoinga Combination clinical trials are enrolling or planned in NSCLC with afatiniba, TNO155b (SHP2-inhibitor), and palbociclib Responses observed in CRC (n=3/18; 17%), and in patients with pancreatic, ovarian, and endometrial cancers, and cholangiocarcinoma See Johnson ML et al., abstract LBA-04. Conclusions KRYSTAL-1: Adagrasib (MRTX849) KRASG12C Inhibitor in NSCLC Presented at the 32nd EORTC-NCI-AACR Symposium, October 24-25, 2020 aClinicalTrials.gov. NCT03785249. bClinicalTrials.gov. NCT04330664.
The patients and their families who make this trial possible The clinical study teams for their work and contributions This study is supported by Mirati Therapeutics, Inc. All authors contributed to and approved this presentation; writing and editorial assistance were provided by Robin Serody of Axiom Healthcare Strategies, funded by Mirati Therapeutics, Inc. Acknowledgements Presented at the 32nd EORTC-NCI-AACR Symposium, October 24-25, 2020 KRYSTAL-1: Adagrasib (MRTX849) KRASG12C Inhibitor in NSCLC
Investigators KRYSTAL-1: Adagrasib (MRTX849) KRASG12C Inhibitor in NSCLC Presented at the 32nd EORTC-NCI-AACR Symposium, October 24-25, 2020 Harshad Amin Boca Raton Clinical Research Global USA Daniel Anderson Metro-Minnesota Community Oncology Research Consortium Minal Barve Mary Crowley Cancer Center Bruno R. Bastos Miami Cancer Institute and Baptist Health of South Florida Lyudmila Bazhenova Moores Cancer Center, University of California San Diego Tanios Bekaii-Saab Mayo Clinic David Berz Beverly Hills Cancer Center Alberto Bessudo California Cancer Associates for Research and Excellence Alejandro Calvo Kettering Cancer Center Patrick Cobb Sisters of Charity of Leavenworth Health St. Mary’s Mike Cusnir Mount Sinai Comprehensive Cancer Center Keith Eaton Seattle Cancer Care Alliance Yousuf Gaffar Maryland Oncology Hematology Navid Hafez Yale Cancer Center David Hakimian Illinois Cancer Specialists Rebecca S. Heist Massachusetts General Hospital Pasi A Jänne Dana-Farber Cancer Institute Melissa L. Johnson Sarah Cannon Research Institute Tennessee Oncology Han Koh Kaiser Permanente Scott Kruger Virginia Oncology Associates Timothy Larson Minnesota Oncology Ticiana A. Leal University of Wisconsin Carbone Cancer Center Konstantinos Leventakos Mayo Clinic Yanyan Lou Mayo Clinic Steven McCune Northwest Georgia Oncology Centers Jamal Misleh Medical Oncology Hematology Consultants Suresh Nair Lehigh Valley Physician Group Sujatha Nallapareddy Rocky Mountain Cancer Center Marcelo Negrao MD Anderson Cancer Center Gregg Newman Ridley-Tree Cancer Center Sai-Hong Ignatius Ou University of California, Irvine, Chao Family Comprehensive Cancer Center Rami Owera Woodlands Medical Specialists Jose M. Pacheco University of Colorado Anschutz Medical Campus Kyriakos P. Papadopoulos START Center for Cancer Care David Park Virginia K. Crosson Cancer Center Scott Paulson Texas Oncology, USOR Nathan Pennell Cleveland Clinic Lerner College Of Medicine Muhammad Riaz University of Cincinnati Health Barrett Cancer Center Donald Richards Texas Oncology, USOR Gregory J. Riely MSKCC, Weill Cornell Medical College Francisco Robert University of Alabama at Birmingham School of Medicine Richard Rosenberg Arizona Oncology Peter Rubin MaineHealth Cancer Care Robert Ruxer Texas Oncology Igor I. Rybkin Henry Ford Cancer Institute Joshua Sabari New York University Langone Health, New York University Perlmutter Cancer Center Alexander I. Spira Virginia Cancer Specialists, US Oncology Research Caesar Tin-U Texas Oncology Anthony Van Ho Compass Oncology Jared Weiss Lineberger Comprehensive Cancer Center, University of North Carolina John Wrangle Medical University of South Carolina Edwin Yau Roswell Park Comprehensive Cancer Center Jeffrey Yorio Texas Oncology Jun Zhang University of Kansas Medical Center
BID = twice daily Cave = average drug plasma concentration CBR = clinical benefit rate CRC = colorectal cancer CSF = cerebrospinal fluid DCR = disease control rate DLT = dose limiting toxicity DOR = duration of response ECOG = Eastern Cooperative Oncology Group MTD = maximum tolerated dose nM = nanomolar NE = not evaluable NGS = next-generation sequencing NSCLC = non–small-cell lung cancer Abbreviations ORR = objective response rate OS = overall survival PD = progressive disease PFS = progression-free survival PK = pharmacokinetics PR = partial response PS = performance status QD = once daily RP2D = recommended Phase 2 dose SAE = serious adverse event SD = stable disease TRAE = treatment-related adverse event uPR = unconfirmed partial response VUS = variant of unknown significance Presented at the 32nd EORTC-NCI-AACR Symposium, October 24-25, 2020 KRYSTAL-1: Adagrasib (MRTX849) KRASG12C Inhibitor in NSCLC