UNITED STATES |
SECURITIES AND EXCHANGE COMMISSION |
WASHINGTON, D.C. 20549 |
FORM 10-K |
ANNUAL REPORT PURSUANT TO SECTION 13 OR 15(d) |
OF THE SECURITIES EXCHANGE ACT OF 1934 |
FOR THE FISCAL YEAR ENDED December 31, 2017 COMMISSION FILE NUMBER 001-32244 |
INDEPENDENCE HOLDING COMPANY
(Exact name of registrant as specified in its charter)
DELAWARE |
| 58-1407235 |
(State of Incorporation) |
| (I.R.S. Employer Identification No.) |
96 CUMMINGS POINT ROAD, STAMFORD, CONNECTICUT | 06902 |
(Address of Principal Executive Offices) | (Zip Code) |
(203) 358-8000 | ||
(Registrant's telephone number, including area code) | ||
| ||
Securities registered pursuant to Section 12(b) of the Act: | ||
COMMON STOCK, $1.00 PAR VALUE PER SHARE |
| NEW YORK STOCK EXCHANGE |
(Title of each class) |
| (Name of each exchange on which registered) |
| ||
Securities registered pursuant to Section 12(g) of the Act: NONE | ||
| ||
Indicate by check mark if the registrant is a well-known seasoned issuer, as defined in Rule 405 of the Securities Act.
Yes ___ No X
Indicate by check mark if the registrant is not required to file reports pursuant to Section 13 or Section 15(d) of the Act.
Yes ___ No X
Indicate by check mark whether the registrant (1) has filed all reports required to be filed by Section 13 or 15(d) of the Securities Exchange Act of 1934 during the preceding 12 months (or for such shorter period that the registrant was required to file such reports) and (2) has been subject to such filing requirements for the past 90 days. Yes _X_ No __
Indicate by check mark whether the registrant has submitted electronically and posted on its corporate Web site, if any, every Interactive Data File required to be submitted and posted pursuant to Rule 405 of Regulation S-T (§232.405 of this chapter) during the preceding 12 months (or for such shorter period that the registrant was required to submit and post such files). Yes X No ___
Indicate by check mark if disclosure of delinquent filers pursuant to Item 405 of Regulation S-K is not contained herein, and will not be contained, to the best of the registrant's knowledge, in definitive proxy or information statements incorporated by reference in Part III of this Form 10-K or any amendment to this Form 10-K. [ X ]
Indicate by check mark whether registrant is a large accelerated filer, an accelerated filer, a non-accelerated filer or a smaller reporting company in Rule 12b-2 of the Exchange Act.
Large accelerated filer __ Accelerated filer X Non-accelerated filer Smaller reporting company __
Indicate by check mark whether the registrant is a shell company (as defined in Rule 12b-2 of the Act). Yes ___ No X
The aggregate market value of the voting and non-voting common equity held by non-affiliates computed by reference to the price at which the common equity was last sold, as of June 30, 2017 was $104,174,000.
14,803,468 shares of common stock were outstanding as of March 9, 2018.
FORM 10-K CROSS REFERENCE INDEX
PART I |
|
| PAGE | |
|
|
|
| |
| Business | 4 | ||
| Risk Factors | 14 | ||
| Unresolved Staff Comments | 28 | ||
| Properties | 28 | ||
| Legal Proceedings | 28 | ||
| Mine Safety Disclosures | 29 | ||
|
|
|
| |
PART II |
|
|
| |
| Market for Registrant's Common Equity, Related Stockholder | 29 | ||
|
|
| Matters and Issuer Purchases of Equity Securities |
|
| Selected Financial Data | 32 | ||
| Management's Discussion and Analysis of Financial Condition | 32 | ||
|
|
| and Results of Operations |
|
| Quantitative and Qualitative Disclosures about Market Risk | 56 | ||
| Financial Statements and Supplementary Data | 57 | ||
| Changes in and Disagreements with Accountants on Accounting | 57 | ||
|
|
| and Financial Disclosure |
|
| Controls and Procedures | 57 | ||
| Other Information | 58 | ||
|
|
|
| |
PART III |
|
|
| |
| Directors, Executive Officers and Corporate Governance | 58 | ||
| Executive Compensation | 58 | ||
| Security Ownership of Certain Beneficial Owners and Management | 59 | ||
|
|
| and Related Stockholder Matters |
|
| Certain Relationships, Related Transactions and Director | 59 | ||
|
|
| Independence |
|
| Principal Accounting Fees and Services | 59 | ||
|
|
|
| |
PART IV |
|
|
| |
| Exhibits and Financial Statement Schedules | 59 | ||
Forward-Looking Statements
This report on Form 10−K contains certain “forward-looking statements” within the meaning of Section 27A of the Securities Act of 1933 and Section 21E of the Securities Exchange Act of 1934, which are intended to be covered by the safe harbors created by those laws. We have based our forward-looking statements on our current expectations and projections about future events. Our forward-looking statements include information about possible or assumed future results of our operations. All statements, other than statements of historical facts, included or incorporated by reference in this report that address activities, events or developments that we expect or anticipate may occur in the future, including such things as the growth of our business and operations, our business strategy, competitive strengths, goals, plans, future capital expenditures and references to future successes may be considered forward-looking statements. Also, when we use words such as “anticipate,” “believe,” “estimate,” “expect,” “intend,” “plan,” “probably” or similar expressions, we are making forward-looking statements.
Numerous risks and uncertainties may impact the matters addressed by our forward-looking statements, any of which could negatively and materially affect our future financial results and performance. We describe some of these risks and uncertainties in greater detail in Item 1A-Risk Factors of this report.
Although we believe that the assumptions underlying our forward-looking statements are reasonable, any of these assumptions, and, therefore, the forward-looking statements based on these assumptions, could themselves prove to be inaccurate. In light of the significant uncertainties inherent in the forward-looking statements that are included in this report, our inclusion of this information is not a representation by us or any other person that our objectives and plans will be achieved. In light of these risks, uncertainties and assumptions, any forward-looking event discussed in this report may not occur. Our forward-looking statements speak only as of the date made, and we undertake no obligation to update or review any forward-looking statement, whether as a result of new information, future events or other developments, unless the securities laws require us to do so.
PART I |
ITEM 1. BUSINESS
Business Overview
Independence Holding Company is a Delaware corporation (NYSE: IHC) that was formed in 1980. We are a holding company principally engaged in the life and health insurance business with principal executive offices located at 96 Cummings Point Road, Stamford, Connecticut 06902.
Our website is located at www.ihcgroup.com. Detailed information about IHC, its corporate affiliates and insurance products and services can be found on our website. In addition, we make our Annual Reports on Form 10-K, Quarterly Reports on Form 10-Q, Current Reports on Form 8-K and all amendments to such reports available, free of charge, through our website, as soon as reasonably practicable after they are filed with or furnished to the Securities and Exchange Commission. The information on our website, however, is not incorporated by reference in, and does not form part of, this Annual Report on Form 10-K.
IHC primarily provides specialized disability and health coverages and related services to commercial customers and individuals. We focus on niche products and/or narrowly defined distribution channels primarily in the United States. Our wholly owned insurance company subsidiaries, Standard Security Life Insurance Company of New York ("Standard Security Life"), Madison National Life Insurance Company, Inc. ("Madison National Life") and Independence American Insurance Company (“Independence American”) market their products through independent and affiliated brokers, producers and agents. Independence American also distributes to consumers through dedicated controlled distribution companies and through company-owned websites.
Madison National Life, Standard Security Life and Independence American are sometimes collectively referred to as the "Insurance Group." IHC and its subsidiaries (including the Insurance Group) are sometimes collectively referred to as the "Company", or "IHC", or are implicit in the terms "we", "us" and "our".
In 2018, IHC will retain the vast majority of the risk that it underwrites, and will focus on the following lines of business:
Multiple specialty health lines
Group disability, life and New York short-term disability (“DBL”)
Pet insurance
Standard Security Life, Madison National Life and Independence American are each rated A- (Excellent) by A.M. Best Company, Inc. ("Best"). Standard Security Life is domiciled in New York and licensed as an insurance company in all 50 states, the District of Columbia, the Virgin Islands and Puerto Rico. Madison National Life is domiciled in Wisconsin, licensed to sell insurance products in 49 states, the District of Columbia, the Virgin Islands and American Samoa. Independence American is domiciled in Delaware and licensed to sell insurance products in all 50 states and the District of Columbia. We have been informed by Best that a Best rating is assigned after an extensive quantitative and qualitative evaluation of a company's financial condition and operating performance and is also based upon factors relevant to policyholders, agents, and intermediaries, and is not directed toward protection of investors. Best ratings are not recommendations to buy, sell or hold any of our securities.
Our administrative companies underwrite, market, administer and/or price life and health insurance business for our owned and affiliated carriers, and, to a lesser extent, for non-affiliated insurance companies. They receive fees for these services and do not bear any of the insurance risk of the companies to which they provide services, other than through profit commissions. During 2017, our principal administrative companies were: (i) Specialty Benefits, a technology-driven full-service marketing and distribution
company that focuses on small employer and individual consumer products through general agents, tele-brokerages, advisor centers, private label arrangements, and through the following brands: www.HealtheDeals.com; Health eDeals Advisors; Aspira A Mas; www.PetPartners.com; and www.PetPlace.com; and (ii) IHC Carrier Solutions LLC (“Carrier Solutions”), a program management, actuarial and regulatory compliance company providing product development and valuation services for IHC’s specialty health segment. IHC owns controlling interests in Global Accident Facilities, LLC (“GAF”), Healthinsurance.org LLC (“HIO”) and PetPartners, Inc. (“PetPartners”). GAF is a holding company for an agency that produces injured on duty business. HIO is an online marketing company that owns www.healthinsurance.org, a lead generation site for individual health insurance. PetPartners is the exclusive provider of pet insurance to the American Kennel Club and the Cat Fanciers Association. Specialty Benefits, GAF, HIO and PetPartners are collectively referred to as our “Agencies.” Our Agencies earn commissions for selling life and health insurance products underwritten by IHC’s owned and affiliated insurance companies and also by unaffiliated carriers. IHC also owns a significant equity interest in Ebix Health Exchange Holdings, LLC (“Ebix Health Exchange”), an administration exchange for health and pet insurance. Ebix Health Exchange administers various lines of health insurance for IHC and non-affiliated carriers through Ebix Health Administration Exchange, Inc. (“EHAE”).
On March 31, 2016, the Company sold IHC Risk Solutions, LLC (“Risk Solutions”), its managing general underwriter of excess or stop-loss insurance for self-insured employer groups that desire to manage the risk of large medical claims (“Medical Stop-Loss”) to Swiss Re Corporate Solutions, a division of Swiss Re (“Swiss Re”). In addition, under the purchase and sale agreement, all of the in-force stop-loss business of Standard Security Life and Independence American produced by Risk Solutions was co-insured by Westport Insurance Corporation (“Westport”), Swiss Re’s largest US carrier, as of January 1, 2016. The aggregate purchase price was $152,500,000 in cash, subject to adjustments and settlements. Approximately 89% of the purchase price was allocated to American Independence Corp. (“AMIC”). At the time of the transaction, IHC owned approximately 92% of AMIC. The balance of the purchase price was paid to Standard Security Life and other IHC subsidiaries. The aforementioned transaction is collectively referred to as the “Risk Solutions Sale and Coinsurance Transaction”. The Risk Solutions Sale and Coinsurance Transaction resulted in a gain on the sale estimated at approximately $100 million. IHC’s block of Medical Stop-Loss business is in run-off. The sale of Risk Solutions and exit from the medical stop-loss business represents a strategic shift that has had a major effect on the Company’s operations and financial results. The disposal transaction is reported as discontinued operations.
For information pertaining to the Company's business segments, reference is made to Note 18 of the Notes to Consolidated Financial Statements included in Item 8 of this report.
Our Philosophy
Our business strategy consists of maximizing underwriting profits through a variety of niche specialty health insurance, pet, and group disability and life products and through distribution channels that enable us to access specialized or underserved markets in which we believe we have a competitive advantage. Historically, our carriers have focused on establishing preferred relationships with producers who seek an alternative to larger, more bureaucratic health insurers, and on providing these producers with personalized service, competitive compensation and a broad array of products. In 2017, larger health insurers marketed a significant amount of our ancillary health products to supplement or in lieu of their major medical products. A growing portion of our business comes from direct-to-consumer initiatives. While our management considers a wide range of factors in its strategic planning and decision-making, underwriting profit is consistently emphasized as the primary goal in all decisions.
As a result of our increased control of distribution through corporate acquisitions, we have strengthened our ability to respond to market cycles in the health insurance sector by deploying our insurance underwriting activity across a larger number of business lines.
IHC’s greater emphasis on higher-margin specialty health products, increased distribution (including as a result of equity investments) and greater market demand have helped to increase our earnings despite having exited medical stop-loss in 2016 and, prior to that, exiting the individual and small group major medical markets as a result of the Affordable Care Act (“ACA”).
DISTRIBUTION |
Specialty Health
The Specialty Health Segment is comprised of the following categories: (i) ancillary benefits including dental, vision, short-term medical (“STM”), supplemental products (including fixed indemnity limited benefit, critical illness, and hospital indemnity); (ii) pet insurance; and (iii) non-subscriber occupational accident and injured on duty. The segment had some run-off of discontinued major medical coverage and occupational accident from one producer. Carrier Solutions and our Agencies collectively perform marketing, sales, underwriting and certain administrative functions on the majority of our Specialty Health business. EHAE and other third party administrators perform claims and other administrative functions. Prior to 2017, our pet insurance was marketed and administered by one independent agency, but IHC has expanded its distribution and administration of this product. In 2016, we reinsured expatriate health business, however, this business is now in run-off. Our non-subscriber occupational accident coverage was largely marketed and administered by a subsidiary of GAF. This subsidiary was sold in 2016 and its business is in run-off.
IHC has made the following investments that have increased the distribution of our specialty health products: (1) 20% of the equity of American Insurance Agencies Direct Holding, Inc., which is a call center that is one of the leading producers of hospital indemnity (“HIP”) on Independence American’s paper; (2) 10% of the equity of The iCan Group LLC, which is a call center that is also a significant producer of HIP on Independence American’s paper; (3) a 44% interest in The Abacus Group LLC (“Abacus”), which is a managing general underwriter specializing in worksite marketing of voluntary benefits that is producing life and disability business for Madison National Life and began selling group limited medical, STM, Group Gap and other ancillary products for that carrier; (4) the domain name and assets of www.petplace.com (“PetPlace”), which attracted over 15 million visitors in 2017 with more than 10,000 veterinarian-approved articles; and (5) 85% of the stock of PetPartners, a pet insurance marketing and administration company.
The Specialty Health Segment performs underwriting, risk selection and pricing, policy administration and management of the majority of our specialty health business, which totaled approximately $187.8 million of gross individual and group health premiums in 2017. In addition, our Agencies produce other coverages for multiple insurers including producing small group stop-loss for Westport. Gross earned premiums produced by our Agencies was approximately $182.4 million in 2017.
Except for a small number of licensed agents who are employed in IHC's call center, most agents and brokers who produce the Specialty Health business are non-salaried contractors who receive commissions.
Disability and Life Products
Our disability and life products are primarily distributed by general agents, agents and brokers. The short-term statutory disability benefit product in New York State is marketed primarily through independent general agents who are paid commissions based upon the amount of premiums produced. Madison National Life's disability and group life products are primarily sold in the Midwest to school districts, municipalities and hospital employer groups through a managing general agent that specializes in these target markets. Independence American also reinsured health products serving the needs of expatriates, third-party nationals and high net-worth local nationals, which is now in run out. Abacus specializes in worksite marketing of voluntary benefits and is producing life and disability business for Madison National Life.
Medical Stop-Loss
Standard Security Life was the primary carrier for our employer medical stop-loss products although, in 2016, we also wrote business for Madison National Life, Independence American and unaffiliated carriers. IHC’s carriers wrote the vast majority of their medical stop-loss business through Risk Solutions, which was sold on March 31, 2016, and TRU Services, LLC. IHC owned two managing general underwriters (“MGUs”), Majestic Underwriters, LLC and Alliance Underwriters, LLC, which transferred their stop-loss blocks and employees to Risk Solutions as of January 1, 2012 in exchange for fee income based on the business transferred. These two MGUs were liquidated in 2016 as a result of the Risk Solutions Sale and Coinsurance Transaction. Risk Solutions was responsible for underwriting accounts in accordance with guidelines formulated and approved by its carriers, billing and collecting premiums, paying commissions to agents, third party administrators and/or brokers, and processing claims. With respect to the MGUs with which we did business, we established underwriting guidelines, maintained approved policy forms and oversaw claims for reimbursement, as well as appropriate accounting procedures and reserves. In order to accomplish this, we audited their underwriting, claims and policy issuance practices to assure compliance with our guidelines, provided them with access to our medical management and cost containment expertise, and reviewed cases that required referral based on our underwriting guidelines. MGUs are non-salaried contractors that receive fee income, generally a percentage of gross premiums produced by them on behalf of the insurance carriers they represent, and typically are entitled to additional income based on underwriting results. Standard Security Life and Independence American have now ceased writing medical stop-loss business.
The agents and brokers that produce this business are non-salaried contractors that receive commissions.
PRINCIPAL PRODUCTS
Specialty Health Products
In 2017, this line of business had the following categories: (i) ancillary benefits, including dental, vision, STM, and supplemental products (including fixed indemnity limited benefit, critical illness, and hospital indemnity); (ii) pet insurance; and (iii) non-subscriber occupational accident. This category also includes reinsured international health plans sold to expatriates in 2016. In 2015, IHC exited the major medical business as a result of ACA which caused adverse underwriting results in 2013 and 2014. As a result of exiting this line of business, we focused our attention on increasing our specialty health lines of business and significantly improved our bottom line performance. Sales of specialty health products nearly doubled in 2017, and earned premiums (which will typically lag behind sales) increased by 17.8% in 2017. We expect continued growth in the specialty health lines of business in 2018.
Ancillary Products
This category is primarily comprised of dental, vision, STM, supplemental products (including fixed indemnity limited benefit, critical illness, and hospital indemnity). These are sold through multiple distribution strategies.
IHC sells group and individual dental products in all 50 states. EHAE administers the majority of IHC's dental business and IHC’s own distribution is the primary source of this line of business. The dental portfolio includes indemnity and PPO plans for employer groups of two or more lives and for individuals within affinity groups. Employer plans are offered on both employer paid and voluntary basis. As part of the distribution of our dental products, we also offer vision benefits. Vision plans will offer a flat reimbursement amount for exams and materials. We expect the dental/vision business to be relatively flat in 2018.
IHC sells STM products in the majority of states. STM is designed specifically for people with temporary needs for health coverage. Typically, STM products are written for a defined duration of at least 30 days and less than twelve months. Among the typical purchasers of STM products are people who are in between open enrollment periods or need coverage for a limited duration until their ACA-compliant plan becomes effective, and others who need insurance for a specified period of time. Our STM plans continue many, but not all, of the essential health benefit (“EHB”) found in ACA-compliant plans. In addition, our STM plans often have lower deductibles and broader networks than many ACA-compliant policies, and are almost always more affordable for qualified purchasers. IHC’s gross premium increased in this line of business in 2017, despite the Obama Administration’s executive order, which was effective April 1, 2017, that limited the duration of an STM policy to less than 90 days. Prior to the effectiveness of this executive order, the ACA and many states permitted STM to last for up to 364 days. The Trump Administration recently released for comment a rule that would reverse the executive order and restore the decision on the duration of STM to the states. Comments on this proposed rule are due April 23, 2018 and it would go into effect 60 days after a final rule is issued. Assuming adoption of a final rule similar to what has been proposed, we anticipate material growth in this line of business (and other products sold with it) in 2018 and beyond.
The Company markets supplemental products to individuals and families. These lines of business are generally used as either a supplement or in lieu of an ACA-compliant plan. The main driver for growth in this line is that consumers are moving to higher-cost sharing on their individual major medical plans, and are looking for products to help them offset the additional risk of higher deductibles and out of pocket limits. The product lines included in this supplemental grouping are hospital indemnity plans, fixed indemnity limited benefit plans, critical illness and bundled packages of accident medical coverage, critical illness and life insurance. These products, which are available in most states, are available through multiple distribution sources including Company owned direct-to-consumer websites, call center and career agents, general agents and on-line agencies. In 2017, we introduced a bundled benefit package including STM, HIP, dental and a tele-med and Rx benefit. This is being sold by Company owned direct-to-consumer websites, call center and career agents, e-Health and Anthem. We anticipate material growth in these lines of business in 2018 as a result of increased distribution and demand for these products, and additional growth in 2019 due to elimination of the individual mandate.
IHC has medical benefit plans for employers that choose to offer non-EHB coverage to their employees. We offer a fixed indemnity limited benefit policy that offers affordable health coverage to hourly, part-time and/or seasonal employees, which is approved in a majority of states. Fixed indemnity limited benefit plans are a low cost alternative to EHB plans that permit employees who do not otherwise have health insurance to begin to participate in the healthcare system. The Company anticipates meaningful growth in this line of business in 2018 due to increased consumer demand and increased distribution channels.
Prior to 2016, IHC reinsured its expatriate business which provides employee benefit insurance, including medical, life, and disability, to expatriate employees of companies based in the United States. This line of business is in run out.
Pet Insurance
In 2017, we acquired 85% of the equity of PetPartners, which is a pet insurance producer that has an exclusive distribution relationship with The American Kennel Club (“AKC”), and has a strong IT platform. Using this as our administrative platform, we are actively seeking new distribution opportunities particularly in the employer, affinity and worksite space because of our ability to deduct pet insurance premiums directly from payroll. We are also exploring opportunities with new distribution partners where Independence American would be the carrier and PetPartners would be the back-end claims payer. Also in 2017, we rebuilt the website for PetPlace.com, which we acquired in 2016, and we expect to improve lead generation from this domain. PetPlace.com attracted over 15 million visitors in 2017 with more than 10,000
veterinarian-approved articles. During 2017, we filed a new pet policy for PetPartners and have begun marketing it in states where it has been approved; we believe that this new policy will increase sales.
We entered into an agreement with an independent pet insurance distributor/administrator that has a significant block of premiums. We are in the process of filing a new pet policy for this company and expect to begin to receive approvals in the second quarter of 2018. Once this company begins writing new business on Independence American’s paper, we expect that we will receive a significant portion of their new and renewal business.
Substantially all of our pet premiums in 2017 were produced by a pet insurance distributor/administrator which was our first pet administrator, and in which we have a small equity position.
Occupational Accident
In 2017, most of IHC’s occupational accident insurance had been written by Independence American through marketing and administrative companies previously owned by GAF, and other exclusive arrangements with independent entities. This occupational accident product provides accidental death, accident disability and accident medical benefits for occupational injuries to employees of companies that have elected to not participate in the Texas Worker’s Compensation system (non-subscribers). The product also gives the employer the option to purchase coverage for employer’s liability, which protects the employer from an action brought by an injured worker. The employer is covered for damages and costs arising from the settlement of such action, subject to the terms and limits of the policy. In 2016, GAF sold the entity that provided administrative services for occupational accident insurance. Independence American still offers Injured on Duty coverage through another subsidiary of GAF and IHC continues to write a smaller block of occupational accident coverage through unaffiliated entities. As a result of the aforementioned sale, total premiums are expected to continue to decrease in 2018.
Major Medical Health Benefit Coverages
This category is primarily comprised of group major medical insurance and individual major medical policies, both of which are in run-off as we have exited that market. We were not able to earn an acceptable profit margin on ACA-compliant products. The Company will monitor proposals from the Trump Administration regarding association health plans and STM lasting longer than 12 months to see if these would be of interest to us given our continuing expertise in individual major medical business.
Group Disability; Life and DBL
Group Long-Term and Short-Term Disability
The Company sells group long-term disability ("LTD") products to employers that wish to provide this benefit to their employees. Depending on an employer's requirements, LTD policies (i) cover between 40% and 90% of insurable salary; (ii) have elimination periods (i.e., the period between the commencement of the disability and the start of benefit payments) of between 30 and 730 days; and (iii) terminate after two, five, or ten years, or extend to age 65 or the employee's Social Security normal retirement date. Benefit payments are reduced by social security, workers compensation, pension benefits and other income replacement payments. Optional benefits are available to employees, including coverage for partial or residual disabilities, survivor benefits and cost of living adjustments. The Company also markets short-term disability ("STD") policies that provide a weekly benefit to disabled employees until the earlier of: recovery from disability, eligibility for long-term disability benefits or the end of the STD benefit period. We continue our efforts to expand our position in the worksite market with new product filings and administration/distribution partners to position us for growth in 2018 and beyond. We have developed relationships with large health carriers to provide our life and disability programs. We are also negotiating with union-based entities to continue to leverage our strengths, namely overall risk management for
disability programs in a benefit-rich and complex environment. The Company anticipates moderate growth in 2018.
New York Short-Term Disability and Paid Family Leave (“PFL”)
Standard Security Life markets DBL. All companies with more than one employee in New York State are required to provide DBL insurance for their employees. DBL coverage provides temporary cash payments to replace wages lost as a result of disability due to non-occupational injury or illness. The DBL policy provides for (i) payment of 50% of salary to a maximum of $170 per week; (ii) a maximum of 26 weeks in a consecutive 52 week period; and (iii) benefit commencement on the eighth consecutive day of disability. Policies covering fewer than 50 employees have fixed rates approved by the New York State Insurance Department. Policies covering 50 or more employees are individually underwritten.
Starting January 1, 2018 the DBL policy will be amended to include PFL. The PFL benefit allows for parent bonding with a newborn or an adopted child, caring for a seriously ill family members and will help military families during times of need. Beginning January 1, 2018, with incremental changes until 2021, the benefit will be phased in. The maximum benefit (once completely phased in starting January 1, 2021) will be for 12 weeks at 67% of an employees’ weekly wage up to a maximum benefit of $869 per week. Based on our current DBL block, we anticipate DBL premiums will increase by approximately $50 million in 2018.
Group Term Life
The Company sells group term life products, including group term life, accidental death and dismemberment ("AD&D"), supplemental life and supplemental AD&D and dependent life. As with its group disability business, IHC anticipates modest growth in this line of business through expansion of its sales of these group term life products through existing distribution sources.
Medical Stop-Loss
The Company was a leading writer nationally of excess or stop-loss insurance for self-insured employer groups that desire to manage the risk of large medical claims. Medical Stop-Loss insurance provides coverage to public and private entities that elect to self-insure their employees' medical coverage for losses within specified ranges, which permits such groups to manage the risk of excessive health insurance costs by limiting specific and aggregate losses to predetermined amounts. This coverage is available on either a specific or a specific and aggregate basis, although the majority of the Insurance Group's policies covered both specific and aggregate claims. Plans were designed to fit the identified needs of the self-insured employer by offering a variety of deductibles (i.e., the level of claims after which the medical stop-loss benefits become payable).
The Risk Solutions Sale and Coinsurance Transaction closed on March 31, 2016 and as a result, this line is in run-off and had substantially reduced premiums in 2017.
Individual Life, Annuities and Other
Madison National Life ceded 100% of its remaining runoff life and annuity policies to National Guardian Life Insurance Company in 2015. In addition, Madison National Life ceased writing any life or annuity policies in the summer of 2015.
The following lines of Standard Security Life's in-force business are in runoff: individual accident and health, individual life (of which a significant portion was 100% ceded to National Guardian Life Insurance Company in 2015), single premium immediate annuities, disability income and miscellaneous insurance business.
ACQUISITIONS OF POLICY BLOCKS |
Prior to reinsuring the life and annuity business in 2015 IHC’s acquisition group acquired blocks of existing life insurance, annuity and disability policies from other insurance companies, guaranty associations and liquidators. Now the acquisition group’s focus is on existing blocks of long-term and short-term disability policies, group life policies, and specialty health policies.
REINSURANCE AND POLICY RETENTIONS |
IHC retained approximately 97%, 94%, and 92%, of gross and assumed Specialty Health exposure in 2017, 2016 and 2015. The Company's average retention of gross and assumed Medical Stop-Loss exposure was 2% in 2017, 5% in 2016, and 69% in 2015. The reduction in 2016 and 2017 was a result of closing the Risk Solutions Sale and Coinsurance Transaction, pursuant to which all of the in-force stop-loss business of Security Life and Independence American produced by Risk Solutions was co-insured as of January 1, 2016.
The Company purchases quota share reinsurance and excess reinsurance in amounts deemed appropriate by its risk committee. The Company monitors its retention amounts by product line, and has the ability to adjust its retention as appropriate.
Reinsurance is used to reduce the potentially adverse financial impact of large individual or group risks, and to reduce the strain on statutory income and surplus related to new business. By using reinsurance, the Insurance Group is able to write policies in amounts larger than it could otherwise accept. The amount reinsured is the portion of each policy in excess of the retention limit on a particular policy.
In 2015, Madison National Life and Standard Security Life together entered into a coinsurance and sale agreement with an unaffiliated reinsurer to cede substantially all of their individual life and annuity policy blocks, which are currently in run-off.
The following reinsurers represent approximately 86% of the total ceded premium for the year ended December 31, 2017:
RGA Reinsurance Company |
| 41% |
National Guardian Life Insurance Company |
| 31% |
Westport Insurance Corporation |
| 9% |
GBG Insurance Ltd. |
| 5% |
|
|
|
|
| 86% |
The Insurance Group remains liable with respect to the insurance in-force, which has been reinsured in the unlikely event that the assuming reinsurers are unable to satisfy their obligations. The Insurance Group cedes business (i) to individual reinsurance companies that are rated "A-" or better by Best or (ii) upon provision of adequate security. The ceding of reinsurance does not discharge the primary liability of the original insurer to the insured. At December 31, 2017 and 2016, the Insurance Group's ceded reinsurance in-force was $6.9 billion and $6.3 billion, respectively.
For further information pertaining to reinsurance, reference is made to Note 9 of Notes to Consolidated Financial Statements included in Item 8.
INVESTMENTS AND RESERVES |
The Company's cash, cash equivalents and securities portfolio are managed by employees of IHC and its affiliates, and ultimate investment authority rests with IHC's in-house investment group. As a result of the nature of IHC's insurance liabilities, IHC endeavors to maintain a significant percentage of its assets in investment grade securities, cash and cash equivalents. At December 31, 2017, 100% of the fixed maturities were investment grade and continue to be rated on average AA. The internal investment group provides a summary of the investment portfolio and the performance thereof at the meetings of the Company's board of directors.
As required by insurance laws and regulations, the Insurance Group establishes reserves to meet obligations on policies in-force. These reserves are amounts that, with additions from premiums expected to be received and with interest on such reserves at certain assumed rates, are calculated to be sufficient to meet anticipated future policy obligations. Premiums and reserves are based upon certain assumptions with respect to mortality, morbidity on health insurance, lapses and interest rates effective at the time the polices are issued. The Insurance Group also establishes appropriate reserves for substandard business, annuities and additional policy benefits, such as waiver of premium and accidental death. Standard Security Life and Madison National Life are also required by law to have an annual asset adequacy analysis, which, in general, projects the amount and timing of cash flows to the estimated maturity date of liabilities, prepared by the certifying actuary for each insurance company. The Insurance Group invests their respective assets, which support the reserves and other funds in accordance with applicable insurance law, under the supervision of their respective board of directors. The Company manages interest rate risk seeking to maintain a portfolio with a duration and average life that falls within the band of the duration and average life of the applicable liabilities. The Company occasionally utilizes options to modify the duration and average life of the assets.
Under Wisconsin insurance law, there are restrictions relating to the percentage of an insurer's admitted assets that may be invested in a specific issuer or in the aggregate in a particular type of investment. With respect to the portion of an insurer's assets equal to its liabilities plus a statutorily-determined security surplus amount, a Wisconsin insurer cannot, for example, invest more than a certain percentage of its assets in non-amortizable evidences of indebtedness, securities of any issuer and its affiliates (other than a subsidiary and the United States government), or common stock of any corporation and its affiliates (other than a subsidiary or mutual funds).
Under New York insurance law, there are restrictions relating to the percentage of an insurer's admitted assets that may be invested in a specific issuer or in the aggregate in a particular type of investment. For example, a New York life insurer cannot invest more than a certain percentage of its admitted assets in common or preferred shares of any one institution, obligations secured by any one property (other than those issued, guaranteed or insured by the United States or any state government or agency thereof), or medium and lower grade obligations. In addition, there are certain qualitative investment restrictions.
Under Delaware insurance law, there are restrictions relating to the percentage of an insurer's admitted assets that may be invested in a specific issuer or in the aggregate in a particular type of investment. In addition, there are qualitative investment restrictions.
The Company's total pre-tax investment performance for each of the last three years is summarized below, including amounts recognized in net income and unrealized gains and losses recognized in other comprehensive income or loss (in thousands):
|
| 2017 |
| 2016 |
| 2015 |
|
|
|
|
|
|
|
Consolidated Statements of Income: |
|
|
|
|
|
|
Net investment income | $ | 16,276 | $ | 16,570 | $ | 17,237 |
Net realized investment gains |
| 2,539 |
| 4,502 |
| 3,094 |
Other-than-temporary impairments |
| - |
| (1,475) |
| (228) |
|
|
|
|
|
|
|
Consolidated Statements of Comprehensive Income (Loss): |
|
|
|
|
|
|
Net unrealized gains (losses) on available-for-sale securities |
| 4,996 |
| (5,424) |
| (5,475) |
|
|
|
|
|
|
|
Total pre-tax investment performance | $ | 23,811 | $ | 14,173 | $ | 14,628 |
Net unrealized gains (losses) on available-for-sale securities recognized through other comprehensive income (loss) represents the pre-tax change in unrealized gains and losses on available-for-sale securities arising during the year net of reclassification adjustments and includes the portion attributable to noncontrolling interests. The Company does not have any non-performing fixed maturity investments at December 31, 2017.
COMPETITION AND REGULATION |
We compete with many large mutual and stock insurance companies, small regional health insurers and managed care organizations. Mutual companies may have certain competitive advantages since profits inure directly to the benefit of the policyholders.
The health insurance industry tends to be cyclical, and excess products, such as medical stop-loss, tend to be more volatile than specialty health products. During a “soft” market cycle, a larger number of companies offer insurance on a certain line of business, which causes premiums in that line to trend downward. In a “hard” market cycle, insurance companies limit their writings in certain lines of business following periods of excessive losses and insurance and reinsurance companies redeploy their capital to lines that they believe will achieve higher margins.
IHC is an insurance holding company; and as such, IHC and its subsidiary carriers and administrative companies are subject to regulation and supervision by multiple state insurance regulators, including the New York State Insurance Department (Standard Security Life's domestic regulator), the Wisconsin Office of the Commissioner of Insurance (Madison National Life's domestic regulator) and the Office of the Insurance Commissioner of the State of Delaware (Independence American’s domestic regulator). Each of Standard Security Life, Madison National Life and Independence American is subject to regulation and supervision in every state in which it is licensed to transact business. These supervisory agencies have broad administrative powers with respect to the granting and revocation of licenses to transact business, the licensing of agents, the approval of policy forms, the approval of commission rates, the form and content of mandatory financial statements, reserve requirements and the types and maximum amounts of investments which may be made. Such regulation is primarily designed for the benefit of policyholders rather than the stockholders of an insurance company or insurance holding company.
Certain transactions within the IHC holding company system are also subject to regulation and supervision by such regulatory agencies. All such transactions must be fair and equitable. Notice to or prior approval by the applicable insurance department is required with respect to transactions affecting the ownership or control of an insurer and of certain material transactions, including dividend declarations, between an insurer and any person in its holding company system. Under New York, Wisconsin and Delaware insurance laws, "control" is defined as the possession, directly or indirectly, of the power to direct or cause the direction of the management and policies of a person. Under New York law, control is
presumed to exist if any person, directly or indirectly, owns, controls or holds, with the power to vote ten percent or more of the voting securities of any other person. In Wisconsin, control is presumed if any person, directly or indirectly, owns, controls or holds with the power to vote more than ten percent of the voting securities of another person. In Delaware, control is presumed if any person, directly or indirectly, owns, controls or holds with the power to vote ten percent or more of the voting securities of any other person. In all three states, the acquisition of control of a domestic insurer needs to be approved in advance by the Commissioner of Insurance. See Note 17 of Notes to Consolidated Financial Statements included in Item 8 for information as to restrictions on the ability of the Company's insurance subsidiaries to pay dividends.
Risk-based capital requirements are imposed on life and property and casualty insurance companies. The risk-based capital ratio is determined by dividing an insurance company's total adjusted capital, as defined, by its authorized control level risk-based capital. Companies that do not meet certain minimum standards require specified corrective action. The risk-based capital ratios for each of Standard Security Life, Madison National Life and Independence American exceed such minimum ratios.
EMPLOYEES |
At December 31, 2017, the Company, including its direct and indirect majority or wholly owned subsidiaries, collectively had approximately 350 employees.
ITEM 1A.RISK FACTORS
Investors should carefully consider the risks set forth below and all other information contained in this report and other documents we file with the SEC. Many of the factors that affect our business and operations involve risk and uncertainty. The risks and uncertainties described below are not the only ones that we face, but are those that we have identified as being the most significant factors. Our business is also subject to general risk and uncertainties that affect many other companies, such as market conditions, geopolitical events, changes in laws or accounting rules, fluctuations in interest rates, terrorism, wars or conflicts, major health concerns, natural disasters or other disruptions of expected economic or business conditions. Additional risks and uncertainties that we do not know about, or that we deem less significant than those identified below, may also materially and adversely affect our business, financial condition or results of operations and the trading price of our common stock.
Risks related to our Business
Our investment portfolio is subject to various risks that may result in realized investment losses. In particular, decreases in the fair value of fixed maturities may greatly reduce the value of our investments, and as a result, our financial condition may suffer.
We are subject to credit risk in our investment portfolio. Defaults by third parties in the payment or performance of their obligations under these securities could reduce our investment income and realized investment gains or result in the continued recognition of investment losses. The value of our investments may be materially adversely affected by increases in interest rates, downgrades in the preferred stocks and bonds included in our portfolio and by other factors that may result in the continued recognition of other-than-temporary impairments. Each of these events may cause us to reduce the carrying value of our investment portfolio.
In particular, at December 31, 2017, fixed maturities represented $441.9 million or 92.7% of our total investments of $476.9 million. The fair value of fixed maturities and the related investment income fluctuates depending on general economic and market conditions. The fair value of these investments generally increases or decreases in an inverse relationship with fluctuations in interest rates, while net investment income realized by us will generally increase or decrease in line with changes in market interest rates. In addition, actual net investment income and/or cash flows from investments that carry prepayment risk, such as mortgage-backed and other asset-backed securities, may differ from those anticipated at the
time of investment as a result of interest rate fluctuations. An investment has prepayment risk when there is a risk that the timing of cash flows that result from the repayment of principal might occur earlier than anticipated because of declining interest rates or later than anticipated because of rising interest rates. The impact of value fluctuations affects our Consolidated Financial Statements. Because all of our fixed maturities are classified as available for sale, changes in the fair value of our securities are reflected in our stockholders' equity (accumulated other comprehensive income or loss). No similar adjustment is made for liabilities to reflect a change in interest rates. Therefore, interest rate fluctuations and economic conditions could adversely affect our stockholders' equity, total comprehensive income (loss) and/or cash flows. For mortgage-backed securities, credit risk exists if mortgagees default on the underlying mortgages. Although, at December 31, 2017, 100% of the fixed maturities were investment grade and continue to be rated on average AA, all of our fixed maturities are subject to credit risk. If any of the issuers of our fixed maturities suffer financial setbacks, the ratings on the fixed maturities could fall (with a concurrent fall in fair value) and, in a worst-case scenario, the issuer could default on its financial obligations. If the issuer defaults, we could have realized losses associated with the impairment of the securities.
We regularly monitor our investment portfolio to ensure that investments that are other-than-temporarily impaired are identified in a timely fashion, properly valued and any impairment is charged against earnings in the proper period. Assessment factors include, but are not limited to, the length of time and the extent to which the market value has been less than cost, the financial condition and rating of the issuer, whether any collateral is held and the Company's intent to sell, or be required to sell, debt securities before the anticipated recovery of its remaining amortized cost basis. However, the determination that a security has incurred an other-than-temporary decline in value requires the judgment of management. Inherently, there are risks and uncertainties involved in making these judgments. Therefore, changes in facts and circumstances and critical assumptions could result in management’s decision that further impairments have occurred. This could lead to additional losses on investments, particularly those that management has the intent and ability to hold until recovery in value occurs.
Our earnings could be materially affected by an impairment of goodwill.
Goodwill represented $50.7 million of our $1.0 billion in total assets as of December 31, 2017. We review our goodwill annually for impairment or more frequently if indicators of impairment exist. We regularly assess whether any indicators of impairment exist, which requires a significant amount of judgment. Such indicators may include: a sustained significant decline in our share price and market capitalization; a decline in our expected future cash flows; a significant adverse change in the business climate; and/or slower growth rates, among others. Any adverse change in one of these factors could have a significant impact on the recoverability of these assets and could have a material impact on our consolidated financial statements. If we experience a sustained decline in our results of operations and cash flows, or other indicators of impairment exist, we may incur a material non-cash charge to earnings relating to impairment of our goodwill, which could have a material adverse effect on our results.
Our loss reserves are based on an estimate of our future liability, and if actual claims prove to be greater than our reserves, our results of operations and financial condition may be adversely affected.
We maintain loss reserves to cover our estimated liability for unpaid losses and loss adjustment expenses, where material, including legal and other fees, and costs not associated with specific claims but related to the claims payment functions for reported and unreported claims incurred as of the end of each accounting period. Because setting reserves is inherently uncertain, we cannot be sure that current reserves will prove adequate. If our reserves are insufficient to cover our actual losses and loss adjustment expenses, we would have to augment our reserves and incur a charge to our earnings, and these charges could be material. Reserves do not represent an exact calculation of liability. Rather, reserves represent an estimate of what we expect the ultimate settlement and administration of claims will cost. These estimates, which generally involve actuarial projections, are based on our assessment of known facts and circumstances. Many factors could affect these reserves, including economic and social conditions, frequency and severity of claims, medical trends resulting from the influences of underlying cost inflation, changes in utilization
and demand for medical services, and changes in doctrines of legal liability and damage awards in litigation. Many of these items are not directly quantifiable in advance. Additionally, there may be a significant reporting lag between the occurrence of the insured event and the time it is reported to us. The inherent uncertainties of estimating reserves are greater for certain types of liabilities, particularly those in which the various considerations affecting the type of claim are subject to change and in which long periods of time may elapse before a definitive determination of liability is made. Reserve estimates are continually refined in a regular and ongoing process as experience develops and further claims are reported and settled and are reflected in the results of the periods in which such estimates are changed.
Our inability to assess underwriting risk accurately could reduce our net income.
Our success is dependent on our ability to assess accurately the risks associated with the businesses on which we retain risk. If we fail to assess accurately the risks we retain, we may fail to establish the appropriate premium rates and our reserves may be inadequate to cover our losses, requiring augmentation of the reserves, which in turn would reduce our net income.
Our agreements with our producers that underwrite on our behalf require that each such producer follow underwriting guidelines published by us and amended from time to time. Failure to follow these guidelines may result in termination or modification of the agreement. We perform periodic audits to confirm adherence to the guidelines, but it is possible that we would not detect a breach in the guidelines for some time after the infraction, which could result in a material impact on the Net Loss Ratio (defined as insurance benefits, claims and reserves divided by the difference between premiums earned and underwriting expenses) for that producer and could have an adverse impact on our operating results.
The results of operations of our insurance business will decline if our premium rates are not adequate or if we are unable to increase rates.
We set the premium rates on our health insurance policies based on facts and circumstances known at the time we issue the policies and on assumptions about numerous variables, including the actuarial probability of a policyholder incurring a claim, the probable size of the claim, maintenance costs to administer the policies and the interest rate earned on our investment of premiums. In setting premium rates, we consider historical claims information, industry statistics, the rates of our competitors and other factors, but we cannot predict with certainty the future actual claims on our products. If our actual claims experience proves to be less favorable than we assumed and we are unable to raise our premium rates to the extent necessary to offset the unfavorable claims experience, our financial results will be adversely affected.
Retentions in various lines of business expose us to potential losses.
We retain most of the risk for our own account on some business underwritten by our insurance companies. The determination to not purchase reinsurance, or to reduce the amount of reinsurance we purchase, for a particular risk or line of business is based on a variety of factors including market conditions, pricing, availability of reinsurance, the level of our capital and our loss history. Such determinations have the effect of increasing our financial exposure to losses associated with such risks or in such lines of business and, in the event of significant losses associated with such risks or lines of business, could have a material adverse effect on our financial position, results of operations and cash flows.
If rating agencies downgrade our insurance companies, our results of operations and competitive position in the industry may suffer.
Ratings have become an increasingly important factor in establishing the competitive position of insurance companies and are important to maintaining public confidence in our company and our products, and our ability to market our products. Standard Security Life, Madison National Life and Independence American are all rated “A-” (Excellent) by A.M. Best Company, Inc. A.M. Best's ratings reflect its opinions
of an insurance company's financial strength, operating performance, strategic position, and ability to meet its obligations to policyholders and are not evaluations directed to investors. The ratings of our carriers are subject to periodic review by A.M. Best, and we cannot assure the continued maintenance of our current ratings. Because these ratings have become an increasingly important factor in establishing the competitive position of insurance companies, a downgrade in our financial strength ratings, or the announced potential for a downgrade, could have an adverse effect on our financial condition, results of operations and cash flows in several ways, including: (i) materially increasing the number or amount of policy surrenders and withdrawals by contract holders and policyholders, as policyholders might move to other companies with higher claims-paying and financial strength ratings; (ii) reducing new sales of insurance products; (iii) increasing our cost of capital; (iv) adversely affecting our relationships with distribution partners; (v) requiring us to reduce prices or increase crediting rates for many of our products and services to remain competitive; and (vi) adversely affecting our ability to obtain reinsurance or obtain reasonable pricing on reinsurance.
Changes in accounting and reporting standards issued by the Financial Accounting Standards Board or other standard-setting bodies and insurance regulators could materially adversely affect our financial condition and results of operations.
Our financial statements are subject to the application of U.S. generally accepted accounting principles (“GAAP”), which is periodically revised and/or expanded. Accordingly, from time to time, we are required to adopt new or revised accounting standards issued by recognized authoritative bodies, including the Financial Accounting Standards Board. It is possible that future accounting and reporting standards we are required to adopt could change the current accounting treatment that we apply to our financial statements and that such changes could have a material adverse effect on our financial condition and results of operations. In addition, the required adoption of future accounting and reporting standards may result in significant costs to implement. For example, current proposals may change the accounting for insurance contracts and financial instruments and could result in increased volatility of net income as well as other comprehensive income. In addition, these proposals could require us to make significant changes to systems and use additional resources, resulting in significant incremental costs to implement the proposals.
The Trump Administration made substantial changes to fiscal and tax policies that may adversely affect our business.
The Trump Administration has called for substantial changes to fiscal and tax policies, which included comprehensive tax reform. On December 22, 2017, President Trump enacted tax legislation commonly referred to as the Tax Cuts and Jobs Act (the “Tax Act”). The Tax Act makes broad and complex changes to the U.S. tax code, including, but not limited to reducing the Federal corporate income tax rate from 35% to 21%. Notwithstanding the reduction in the corporate income tax rate as well as other significant changes to the U.S. tax code, the overall impact of the Tax Act is uncertain and our business and financial condition could be adversely affected. In addition, the impact of current and future fiscal policy changes are unknown and could, likewise, affect our business and financial condition adversely.
The impact of this tax reform on holders of our common stock is also uncertain and could be adverse. We urge our stockholders to consult with their legal and tax advisors with respect to this legislation and the potential tax consequences of investing in or holding our common stock.
Increases in insurance claim costs will negatively impact the revenues and profitability of our insurance business.
The major component of insurance cost represents the cost of claims, which are not within our control. While we seek to limit our exposure on any single insured, significant unfavorable claims experience will reduce our revenues and profitability. Increases in insurance claim costs will negatively impact the revenues and profitability of our insurance business.
Legal and regulatory investigations and actions are increasingly common in the insurance business and may result in financial losses and harm our reputation.
We face a risk of litigation and regulatory investigations and actions in the ordinary course of operating our business, including the risk of class actions, regulatory actions and individual lawsuits relating, among other things, to sales or underwriting practices, payment of contingent or other sales commissions, claims payments and procedures, product design, disclosure, administration, additional premium charges for premiums paid on a periodic basis, interest crediting practices, denial or delay of benefits and breaches of fiduciary or other duties to customers. Adverse judgments in one or more of such lawsuits could require us to pay significant damage amounts or to change aspects of our operations. Plaintiffs in class action and other lawsuits against us may seek very large or indeterminate amounts, including punitive and treble damages, which may remain unknown for substantial periods of time. Further, industry trends, such as increased litigation against the insurance industry and individual insurers, the willingness of courts to expand covered causes of loss and the size of awards, rising jury awards, escalating medical costs, and increasing loss severity may render the loss reserves of our insurance subsidiaries inadequate for current and future losses. The unpredictability of court decisions in the insurance business could have a material adverse effect on our financial position, results of operation and cash flows. In addition, the political divisiveness leading, in some cases, to the stalling of the legislative process, may cause judicial activism and result in rulings concerning our products, the way we sell our products, and the profitability of our products, which may result in the states being divided in their approach to insurance.
We are also subject to various regulatory inquiries, such as information requests, subpoenas, market conduct exams and books and record examinations, from state and federal regulators and other authorities, which may find that our policies, procedures, practices or contracts are not compliant with or in violation of applicable healthcare regulations, which may result in fines, recommendations for corrective action, or other regulatory actions. Increased regulatory scrutiny and any resulting investigations or proceedings could result in new legal actions or precedents and industry-wide regulations or practices that could adversely affect our business. Even if we ultimately prevail in the litigation, regulatory action or investigation, we could suffer significant reputational harm, which could have an adverse effect on our business.
Our reliance upon third party administrators and other outsourcing arrangements may disrupt or adversely affect our operations.
We depend, and may in the future increase our dependence, on third parties for significant portions of our operations, including claims processing, premium billing, claims management, claims payment and voice communication services, and other systems-related support. This dependence makes our operations vulnerable to the third parties' failure to perform adequately under the contract due to internal or external factors. In the future, this dependence may increase as we may outsource additional areas of our business operations to additional vendors. There can be no assurance that any conversion or transition of business process functions from the Company to a vendor or between vendors will be seamless and these projects could result in significant operational challenges that cause financial difficulties. In addition, if our relationships with our outsourcing partners are significantly disrupted or terminated for any reason or if the financial terms of such outsourcing partners changes materially, we may not be able to find an alternative partner in a timely manner or on acceptable financial terms. As a result, we may not be able to meet the demands of our customers and, in turn, our business, cash flows, financial condition and results of operations may be harmed.
Our dependence on third parties makes our operations vulnerable to such parties’ failure to perform as agreed. Incorrect information from these entities could cause us to incur additional expense to utilize additional resources to validate, reconcile and correct the information. We have not been able to independently test and verify some of these third party systems and data. Any failure to recommend payment on claims fairly could lead to material litigation, undermine our reputation in the marketplace, impair our image and adversely affect our financial results. There can be no assurance that future third
party data will not disrupt or adversely affect our results of operations. A change in service providers, or a move of services from a third party to internal operations, could result in significant operational challenges, a decline in service quality and effectiveness, increased cost or less favorable contract terms, which could adversely affect our operating results. Some of our outsourced services are being performed offshore. Prevailing economic conditions and other circumstances could prevent our offshore vendors' ability to adequately perform as agreed, which could have a material adverse effect on our results of operations and financial condition
Our financial condition and results of operations could be materially adversely affected if our third party administrators, managing general agents, general agents or other producers exceed their authorities, otherwise breach obligations owed to us or commit fraud.
In connection with certain lines of business and insurance programs, we authorize third party administrators, managing general agents, general agents and other producers to write business and/or settle claims on our behalf within underwriting and claims settlement authorities prescribed by us. We have less control and supervision over these underwriters and claims staff than our own employees and rely on the controls of our agents to write business within the underwriting authorities and settle claims within guidelines provided by us. Although we monitor our business on an ongoing basis, our monitoring efforts may not be adequate and our agents may exceed their underwriting authorities or otherwise breach their obligations owed to us. To the extent that our agents exceed their authorities, otherwise breach their obligations owed to us or commit fraud, this may result in a material adverse effect upon our financial condition and results of operations.
We utilize reinsurance arrangements to help manage our business risks, and failure to perform by the counterparties to our reinsurance arrangements may expose us to risks we had sought to mitigate.
We utilize reinsurance to mitigate our risks in various circumstances. Through reinsurance, we have the contractual right to collect the amount reinsured from our reinsurers. Although reinsurance makes the reinsurer liable to us to the extent the risk is transferred or ceded to the reinsurer, reinsurance does not relieve us of our direct liability to our policyholders. Accordingly, we bear credit risk with respect to our reinsurers. We cannot assure that our reinsurers will pay all of our reinsurance claims, or that they will pay our claims on a timely basis. Additionally, catastrophic losses from multiple direct insurers may accumulate within the more concentrated reinsurance market and result in claims that adversely impact the financial condition of such reinsurers and thus their ability to pay such claims. Further, additional adverse developments in the capital markets could affect our reinsurers’ ability to meet their obligations to us. If we become liable for risks we have ceded to reinsurers or if our reinsurers cease to meet their obligations to us because they are insolvent or in a weakened financial position as a result of incurred losses or otherwise, our financial position, results of operations and cash flows could be materially adversely affected.
Our reliance on brokers, program administrators and third-party claims adjusters subjects us to risk.
We transact business through intermediaries, frequently paying insured claims through brokers, program administrators or third-party claims adjustment services, and these parties, in turn, pay these amounts to the clients that have purchased insurance from us. If such an intermediary were to fail to pass such a payment through to the claimant or policyholder, we may remain liable for the deficiency because of applicable local laws or contractual obligations. Likewise, when a customer pays its policy premium to a broker or program administrator for further remittance to us, that premium is generally considered to have been paid and the client is no longer liable for such amount even if we do not actually receive the premium. Consequently, we assume a degree of credit risk associated with the intermediaries we use with respect to our insurance and reinsurance business.
The success of our business strategy depends on the continuing service of key executives, the members of our senior management team and other highly-skilled personnel.
We rely on the continued service of key executives, members of our senior management team and highly skilled personnel throughout all levels of our business. Our business could be harmed if we are unable to retain or motivate key personnel or hire qualified personnel. We believe that our future success depends in substantial part on our ability to recruit, hire, motivate, develop, and retain talented and highly skilled personnel who are knowledgeable about our business. Doing so may be difficult due to many factors, including fluctuations in economic and industry conditions and the effectiveness of our compensation programs and competition. If we do not succeed in retaining and motivating our existing key employees and in attracting new key personnel, our revenue growth and profitability may be materially adversely affected.
We may be unsuccessful in competing against larger or better-established business rivals.
We compete with a large number of other companies in our selected lines of business. We face competition from specialty insurance companies, and from diversified financial services companies and insurance companies that are much larger than we are and that have far greater financial, marketing and other resources. Some of these competitors also have greater experience and more market recognition than we do in certain lines of business. In addition to competition in the operation of our business, we face competition from a variety of sources in attracting and retaining qualified employees. There can be no assurance that we will maintain our current competitive position in the markets in which we operate, or that we will be able to expand operations into new markets. If we fail to do so, our results of operations and cash flows could be materially adversely affected.
Also, insurance companies may seek to consolidate through mergers and acquisitions. Continued consolidation within the insurance industry will further enhance the already competitive underwriting environment as we would likely experience more robust competition from larger competitors. These consolidated entities may use their enhanced market power and broader capital base to take business from us or to drive down pricing, which could adversely affect the results of our operations.
We may be unsuccessful in our continued efforts to execute on our strategies to diversify sources of income.
We have devoted significant effort and financial resources to build new products, distribution and service capabilities to diversify our product portfolio. We aim to continue implementing our strategies while maintaining current positions of strength in our existing businesses, as well as maintaining the strength of our balance sheet. Our success will depend on a number of factors, including our ability to achieve customer name recognition, accurately predict market trends, differentiate our product offerings from our competitors’ products, provide excellent customer service, attract and retain skilled employees, maintain comprehensive focus on all company priorities, develop new products in a timely manner and achieve market acceptance, effectively implement new technology and operational platforms, deepen our existing distribution relationships and add new distribution partners, and set appropriate prices for our products. We may incur higher-than-expected costs or fail to generate expected levels of revenue and profitability associated with this strategy. Further, if we fail to accomplish all or a combination of these strategies, our ability to profitably grow our business could be materially and adversely affected.
The failure to maintain effective and efficient information systems and to safeguard the security of our data could adversely affect our business.
Our business is highly dependent upon the successful and uninterrupted functioning of our computer systems, and we have different information systems for our various businesses. We rely on these systems to perform actuarial and other modeling functions necessary for writing business, to provide insurance quotes, to process our premiums and policies, to administer our products, to process and make
claims payments, to establish our loss reserves, and to prepare our management and external financial statements and information. The failure of these systems could interrupt our operation and we could experience adverse consequences, including: (i) inadequate information on which to base pricing, underwriting and reserving decisions; (ii) inadequate information for accurate financial reporting; (iii) increases in administrative expenses; (iv) the loss of existing customers or key distributors; (v) difficulty in attracting new customers or distributors; (vi) an inability to comply with regulations or customer or vendor expectations, such as failure to meet prompt payment obligations; (vii) customer, provider and agent disputes; and (viii) litigation or regulatory enforcement exposure. We have committed and will continue to commit significant resources to develop, maintain and enhance our existing information systems, transition existing systems to upgraded systems, and develop new information systems in order to keep pace with continuing changes in information processing technology, evolving industry and regulatory standards, and changing customer preferences.
Moreover, our computer systems have been, and will continue to be, subject to computer viruses or other malicious codes, unauthorized access, acts of vandalism, theft, cyber-attacks, hackers or other computer-related penetrations. Such threats require additional layers of security, which may disrupt or impact efficiency of operations. To date, we are not aware of a material breach of cyber-security. We commit significant resources to administrative and technical controls to prevent cyber incidents and protect our information technology, but our preventative actions to reduce the risk of cyber threats may be insufficient to prevent physical and electronic break-ins, denial of service and other cyber-attacks or security breaches. Such an event could compromise our confidential information as well as that of our clients and third parties, with whom we interact, impede or interrupt business operations and may result in other negative consequences, including remediation costs, loss of revenue, disruption of our operations, additional regulatory scrutiny, sanctions (such as penalties, fines and loss of license) and litigation, and reputational damage.
Our database and systems are also vulnerable to damage or interruption from system outages, disasters such as earthquakes, fires, floods, acts of terrorism, blackouts, power loss, telecommunications failures, and similar events, which would compromise our ability to conduct business. In the event of such failures, we may be unable to perform critical functions in a timely manner, and our systems may not be available to our employees, customers or business partners for an extended period of time. Any such interruptions may reduce our revenues or increase our expenses, and may also have an adverse impact upon our reputation, distribution partnerships, or our customer or vendor relationships. Such an occurrence may also impair our ability to timely and accurately complete our financial reporting and other regulatory obligations and may impact the effectiveness of our internal control over financial reporting. We also utilize and/or rely on computer systems developed and maintained by outsourcing relationships and key vendors. Their systems could experience the same risks, which could result in a material adverse effect on our business results.
Our failure to maintain effective and efficient information systems and protect the security of such systems could have a material adverse effect on our financial condition and results of operations.
Additionally, past or future negligence or misconduct by our employees or employees of our vendors or suppliers could result in misplaced or lost data, programming and/or human errors, violations of laws by us, regulatory sanctions against us and/or serious reputational, legal or financial harm to our business, and the precautions we employ to prevent and detect this activity may not be effective in all cases. Although we employ controls and procedures designed to monitor the business decisions and activities of these individuals to prevent us from engaging in inappropriate activities, excessive risk taking, fraud or security breaches, these individuals may take such risks regardless of such controls and procedures and such controls and procedures may fail to detect all such decisions and activities. We review our compensation policies and procedures as part of our overall risk management program, but it is possible that such compensation policies and practices could inadvertently incentivize excessive or inappropriate risk taking. If these individuals take excessive or inappropriate risks, those risks could harm our reputation and have a material adverse effect on our business, results of operations and financial condition.
If we fail to comply with applicable privacy and security laws and emerging security threats and potential security incidents, our business, reputation, results of operations, financial positions and cash flows could be materially affect.
In the conduct of our business, we are subject to privacy regulations and to confidentiality obligations. The collection, maintenance, protection, use, transmission, disclosure and disposal of sensitive personal information are regulated at the federal, state and industry levels and requirements are imposed on us by contracts with customers. For example, the collection and use of patient data in our health insurance operations is regulated by the Health Insurance Portability and Accountability Act of 1996, or HIPAA, and certain other activities we conduct, are subject to the privacy regulations of the Gramm-Leach-Bliley Act. HIPAA also requires business associates as well as covered entities to comply with certain privacy and security requirements. In addition, we also have contractual obligations to protect certain confidential information we obtain from our existing vendors, partners and policyholders. These obligations generally include protecting such confidential information in the same manner and to the same extent as we protect our own confidential information. If we do not properly comply with privacy regulations and protect confidential information, we could experience adverse consequences, including regulatory sanctions, such as penalties, fines and loss of license, as well as loss of reputation and possible litigation.
Our business depends on the uninterrupted operation of our information technology systems.
We rely on various information technology systems and computer and telecommunications equipment in the normal course of business. The maintenance and security of our information systems are important to our operations. Our ability to effectively run our business depends on the reliability and capacity of our information technology systems, including technology services and systems for which we contract from third parties. Advances in technology may render our current information technology systems obsolete and require upgrading and maintenance over time, which may require significant future commitments of resources and capital. If we upgrade or change systems, we may suffer interruptions in service, loss of data or reduced functionality. Despite any precautions we may take, such problems could result in, among other consequences, interruptions in our services, which could harm our reputation and financial results. If there is a material failure in our information technology systems, our business operations and profits could be negatively affected, and our systems may be inadequate to support our future growth strategies.
We may be unable to renew our existing licenses when they expire and may not be able to obtain new licenses on favorable terms.
We may be unable to renew expiring licenses on terms favorable to us or at all, and we may have difficulties obtaining new licenses needed for our business on terms acceptable to us, if at all. In addition, these licensors could decide to license to our competitors. Failure to maintain or renew our existing licenses or to obtain additional licenses necessary for our business could harm our operating results and financial condition.
We have risks from exiting the individual life and annuities business.
We exited the individual life and annuities business in July 2015 when our subsidiaries, Madison National Life and Standard Security Life, closed on an agreement to coinsure substantially all of their run-off blocks of individual life and annuities and sold Madison National Life's infrastructure related to those blocks, to National Guardian Life Insurance Company (“NGL”). If NGL defaults on its reinsurance commitments and/or its administration commitments, then the policies may come back to us. Since we have sold our infrastructure, we would not have the ability to administer the business because we no longer have the IT systems or staff to support the business. We may have to incur expenses to rebuild our capabilities and for regulatory and other legal actions, which could have an adverse effect on our financial condition, results of operations and cash flows.
Our risk management policies and procedures may prove to be ineffective and leave us exposed to unidentified or unanticipated risk, which could adversely affect our businesses or result in losses.
We have developed an enterprise-wide risk management and governance framework to mitigate risk and loss to the Company. We maintain policies, procedures and controls intended to identify, measure, monitor, report and analyze the risks to which we are exposed. However, there are inherent limitations to risk management strategies because there may exist, or develop in the future, risks that we have not appropriately anticipated or identified. If our risk management framework proves ineffective, we may suffer unexpected losses and could be materially adversely affected. As our business changes and the markets in which we operate evolve, our risk management framework may not evolve at the same pace as those changes. As a result, there is a risk that new products or new business strategies may present risks that are not appropriately identified, monitored or managed. In times of market stress, unanticipated market movements or unanticipated claims experience, the effectiveness of our risk management strategies may be limited, resulting in losses to the Company.
Many of our risk management strategies or techniques are based upon historical customer and market behavior and all such strategies and techniques are based to some degree on management’s subjective judgment. We cannot provide assurance that our risk management framework, including the underlying assumptions or strategies, will be accurate and effective.
Risks related to our Industry
Our industry is highly regulated and we are subject to extensive governmental regulation, which may adversely affect our ability to achieve our business objectives. Also, changes in regulations may affect our businesses and reduce our profitability and limit our growth. Moreover, if we fail to comply with these regulations, we may be subject to penalties, including fines and suspensions, which may adversely affect our financial condition and results of operations.
Our insurance subsidiaries are subject to state insurance laws and regulated by the insurance departments of the various states in which they are domiciled and licensed, which, among other things, conduct periodic examination of insurance companies. State laws grant insurance regulatory authorities broad administrative powers with respect to various aspects of our insurance businesses, including:
olicensing companies and agents to transact business and regulating their respective conduct in the market;
orestricting agreements with large revenue-producing agents;
oapproving policy forms and premium rates;
ocancelling and non-renewal of policies;
orequiring certain methods of accounting and prescribing the form and content of records of financial condition required to be filed;
ocalculating the value of assets to determine compliance with statutory requirements;
oestablishing statutory capital and reserve requirements, such as for unearned premiums and losses;
oregulating certain premium rates and requiring deposits for the benefit of policyholders;
oestablishing maximum interest rates on insurance policy loans and minimum rates for guaranteed crediting rates on life insurance policies;
oestablishing standards of solvency, including risk-based capital measurements, which are a measure developed by the National Association of Insurance Commissioners (NAIC) and used by state insurance regulators to identify insurance companies that potentially are inadequately capitalized;
omandating certain insurance benefits and restricting the size of risks insurable under a single policy;
oregulating unfair trade and claims practices, including the imposition of restrictions on marketing and sales practices, distribution arrangements and payment of inducements;
orequiring the filing of annual and other reports relating to the financial condition of insurance companies, holding company issues and other matters;
oapproving changes in control of insurance companies;
orestricting transactions between insurance companies and their affiliates, including the payment of dividends to affiliates; and
oregulating the nature or types, concentration or amounts, quality and valuation of investments.
Currently, the U.S. federal government does not directly regulate the business of insurance. However, the Dodd-Frank Wall Street Reform and Consumer Protection Act (the “Dodd-Frank Act”), which was signed into law in July 2010 by President Obama, expanded the U.S. federal government’s presence in insurance oversight, streamlined state-based regulation of reinsurance and non-admitted insurance and established a new Federal Insurance Office with powers over most lines of insurance other than health insurance. The Federal Insurance Office is authorized to gather data and information to monitor aspects of the insurance industry, identify issues in the regulation of insurers about insurance matters, and preempt state insurance measures under certain circumstances. As the Dodd-Frank Act calls for numerous studies and contemplates further regulation, its future impact on our results of operations or financial position cannot be determined at this time.
In addition, the Dodd-Frank Act, along with the Sarbanes-Oxley Act of 2002, regulates corporate governance, executive compensation and other areas, as well as laws relating to federal trade restrictions, privacy/data security, crop insurance and terrorism risk insurance laws. Additionally, federal legislation and administrative policies in other areas can significantly and adversely affect insurance companies, including general financial services regulation, securities regulation, privacy regulation, tort reform legislation, and taxation.
We are uncertain as to the impact that this new legislation and regulatory guidance will have on the Company and cannot assure that it will not adversely affect our financial condition and results of operations. In addition, compliance with applicable laws and regulations is time consuming and personnel-intensive, and changes in these laws and regulations may materially increase our direct and indirect compliance efforts and other expenses of doing business.
Changes in regulation, or the application thereof, may reduce our profitability and limit our growth.
Legislation or other regulatory reform that increases the regulatory requirements imposed on us or that changes the way we are able to do business may significantly harm our business or results of operations in the future. Further, state insurance regulators and the NAIC regularly re-examine existing laws and regulations applicable to insurance companies and their products. Changes in these laws and regulations or in interpretations or enforcement thereof, enactment of new laws or regulations, or new judicial decisions affecting the insurance industry, are often made for the benefit of the consumer at the expense of the insurer and thus could have an adverse effect on our business. We cannot predict what impact, if any, the results of these studies or other such proposals, if enacted, may have on our financial condition, results of operations and cash flows. If we were unable for any reason to comply with these requirements, it could result in substantial costs to us and may materially adversely affect our results of operations and financial condition.
Several proposals have been adopted or are currently pending to amend state insurance holding company laws to increase the scope of insurance holding company regulation. The timing of their adoption and content will vary by state. These proposals include the NAIC “Solvency Modernization Initiative,” which focuses on capital requirements, as well as the Own Risk Solvency Assessment (“ORSA”), which requires large- and medium-sized U.S. insurers and insurance groups to regularly perform an ORSA and
file a confidential ORSA Summary Report of the assessment with the regulator of each insurance company upon request.
We cannot predict the full effect of these or any other regulatory initiatives on the Company at this time, but they could have a material adverse effect on the Company’s results of operations, cash flows and financial condition.
Changes to health insurance laws may adversely affect our business, cash flows, financial condition and results of operations.
Although health insurance is generally regulated at the state level, actions at the federal level have affected and will likely continue to affect our business. Since the ACA became law in March 2010, it has caused sweeping and fundamental changes to the U.S. health care and health insurance industries. The effects on our business include our decisions to exit the major medical business, which is directly affected by the ACA, and to focus on ancillary health insurance products that are only indirectly affected by the ACA.
The ACA also affects us as an employer because it significantly affects the provision of both health care services and benefits in the United States. The ACA may impact our cost of providing our employees with health insurance and/or benefits, and may also impact various other aspects of our business. We are continually assessing the impact of the ACA on our health care benefit costs.
The Trump Administration has and will undoubtedly continue to have an impact on the ACA. On October 12, 2017, President Trump signed an Executive Order that ordered the Secretaries of the Treasury, Labor, and Health and Human Services to consider proposing regulations or revising guidance to (i) allow more employers to form association health plans, (ii) expand the availability of short-term limited duration insurance and allow longer coverage periods and (iii) increase the usability of health reimbursement arrangements. While we are unable to predict what additional legislation or regulation, if any, relating to the health insurance industry may be enacted in the future or what effect such legislation or regulation would have on our business, it is clear that the Trump Administration is taking concrete steps to provided more healthcare options to consumers. The unsettled nature of reforms, the numerous steps required to implement them, and the potential repeal makes us unable to predict what additional health insurance requirements will be implemented at the federal or state level, or the effect that any future legislation or regulation will have on our business or our growth opportunities.
We will continue to monitor efforts to amend or impact the ACA and reassess our business strategies accordingly. We have made, and are continuing to make, significant changes to our operations, products and strategy to adapt to the new environment. However, if our plans for operating in the new environment are unsuccessful or are less successful than our competitors, or if there is less demand than we expect for our products in the new environment, our results could be adversely affected.
If we fail to comply with extensive state and federal regulations, we will be subject to penalties, which may include fines and suspension and which may adversely affect our results of operations and financial condition.
Some states have imposed time limits for the payment of uncontested covered claims and require health care and dental service plans to pay interest on uncontested claims not paid promptly within the required time period. Some states have also granted their insurance regulatory agencies additional authority to impose monetary penalties and other sanctions on health and dental plans engaging in certain unfair payment practices. If we were unable, for any reason, to comply with these requirements, it could result in substantial costs to us and could materially adversely affect our results of operations and financial condition.
A large portion of our business depends on our compliance with applicable laws and regulations and our ability to maintain valid licenses and approvals for our operations. Regulatory authorities have
broad discretion to grant, renew, revoke or deny licenses and approvals. In some instances, we follow practices based on our interpretations of regulations, or interpretations that we believe to be generally followed by the industry, which may be different from the requirements or interpretations of regulatory authorities. If we do not have the requisite licenses and approvals and do not comply with applicable regulatory requirements, the insurance regulatory authorities could preclude or temporarily suspend us from carrying on some or all of our insurance-related activities or otherwise penalize us. That type of action could have a material adverse effect on our business. Also, changes in the level of regulation of the insurance industry (whether federal, state or foreign), or changes in laws or regulations themselves or interpretations by regulatory authorities, could have a material adverse effect on our business.
Our results may fluctuate as a result of factors generally affecting the insurance and reinsurance industry.
The results of companies in the insurance and reinsurance industry historically have been subject to significant fluctuations and uncertainties. The industry and our financial condition and results of operations may be affected significantly by:
oFluctuations in interest rates, inflationary pressures and other changes in the investment environment, which affect returns on invested capital;
oRising levels of actual costs that are not known by companies at the time they price their products;
oLosses related to epidemics, terrorist activities, random acts of violence or declared or undeclared war;
oDevelopment of judicial interpretations relating to the scope of insurers' liability;
oThe overall level of economic activity and the competitive environment in the industry;
oGreater than expected use of health care services by members;
oNew mandated benefits or other regulatory changes that change the scope of business or increase our costs; and
oFailure of managing general underwriters, agents, third-party administrators and producers to adhere to the underwriting guidelines, market-conduct practices and other requirements (as applicable) under their agreements with us.
The occurrence of any or a combination of these factors, which is beyond our control, could have a material adverse effect on our results.
We may experience periods with excess underwriting capacity and unfavorable premium rates because the insurance and reinsurance business is historically cyclical, which could cause our results to fluctuate.
The insurance and reinsurance business historically has been a cyclical industry characterized by periods of intense price competition due to excessive underwriting capacity, as well as periods when shortages of capacity permitted an increase in pricing and, thus, more favorable premium levels. An increase in premium levels is often, over time, offset by an increasing supply of insurance and reinsurance capacity, either by capital provided by new entrants or by the commitment of additional capital by existing insurers or reinsurers, which may cause prices to decrease. Any of these factors could lead to a significant reduction in premium rates, less favorable policy terms and fewer opportunities to underwrite insurance risks, which could have a material adverse effect on our results of operations and cash flows.
Failures elsewhere in the insurance industry could obligate us to pay assessments through guaranty associations.
Virtually all states require insurers licensed to do business in that state to bear a portion of the loss suffered by some insureds as the result of impaired or insolvent insurance companies or to bear a portion of the cost of insurance for high-risk or uninsured individuals. When an insurance company becomes
insolvent, state insurance guaranty associations have the right to assess other insurance companies doing business in their state for funds to pay obligations to policyholders of the insolvent company, up to the state-specific limit of coverage. Depending on state law, insurers can be assessed up to 2% of premium written for the relevant line of insurance in that state. The total amount of the assessment is based on the number of insured residents in each state, and each company’s portion is based on its proportionate share of premium volume in the relevant lines of business. The future failure of a large life, health or annuity insurer could trigger assessments that we would be obligated to pay. Further, amounts for historical insolvencies may be assessed over many years, and there can be significant uncertainty around the total obligation for a given insolvency. Existing liabilities may not be sufficient to fund the ultimate obligations of a historical insolvency, and we may be required to increase our liability, which could have an adverse effect on our results of operations.
Economic, governmental and competitive factors, and changes in societal attitudes such as work ethic, motivation or stability, can significantly affect the demand for and underwriting results from disability products.
Both economic and societal factors can affect claim incidence and recoveries for disability insurance. Claim incidence and claim recovery rates may be influenced by, among other factors, the rate of unemployment and consumer confidence and the emergence of new infectious diseases or illnesses. Claim durations may be extended by medical improvements that could extend life expectancies. These factors and overall incidence rates affect pricing, underwriting and adjudication of claims.
Group life insurance may be affected by the characteristics of the employees insured, the amount of insurance employees may elect voluntarily, our risk selection process, our ability to retain employer groups with favorable risk characteristics, the geographical concentration of employees, and mortality rates. Claim incidence may also be influenced by unexpected catastrophic events such as terrorist attacks, natural disasters, and pandemic health events, which may also affect the cost of and availability of reinsurance coverage. Although pricing and renewal actions can be taken in reaction to higher claim rates, these actions take time to implement, and there is a risk that the market will not sustain increased prices. In addition, changes in economic and external conditions may not manifest themselves in claims experience for an extended period of time. It is difficult to predict how the above factors will affect our business, financial condition or results of operations.
ITEM 1B. UNRESOLVED STAFF COMMENTS
None.
ITEM 2. PROPERTIES
IHC
IHC has entered into a renewable short-term arrangement with Geneve Corporation, an affiliate, for the use of 6,750 square feet of office space as its corporate headquarters in Stamford, Connecticut.
Standard Security Life
Standard Security Life leases 13,000 square feet of office space in New York, New York as its corporate headquarters.
Madison National Life
Madison National Life leases 15,357 square feet of space in Madison, Wisconsin as its corporate headquarters.
IHC Carrier Solutions
IHC Carrier Solutions leases 11,297 square feet of office space in Phoenix, Arizona as its corporate headquarters.
IHC Specialty Benefits
IHC Specialty Benefits leases 6,391 square feet of office space in Minneapolis, Minnesota as its corporate headquarters.
PetPartners
PetPartners leases 5,963 square feet of office space in Raleigh, North Carolina as its corporate headquarters.
ITEM 3.LEGAL PROCEEDINGS
We are involved in legal proceedings and claims that arise in the ordinary course of our businesses. We have established reserves that we believe are sufficient given information presently available relating to our outstanding legal proceedings and claims. We do not anticipate that the result of any pending legal proceeding or claim will have a material adverse effect on our financial condition or cash flows, although there could be such an effect on our results of operations for any particular period.
A third party administrator with whom we formerly did business (“Plaintiff”) filed a Complaint dated May 17, 2017 in the United States District Court, Northern District of Texas, Dallas Division, naming IHC, Madison National Life, Standard Security Life, and IHC Carrier Solutions, Inc. (collectively referred to as “Defendants”). The Complaint concerns agreements entered into by Standard Security Life and Madison National Life with Plaintiff, as well as other allegations made by Plaintiff against the Defendants. The Complaint seeks injunctive relief and damages in an amount exceeding $50,000,000, profit share payments allegedly owed to Plaintiff under the agreements totaling at least $3,082,000 through 2014, plus additional amounts for 2015 and 2016, and exemplary and punitive damages as allowed by law and fees and costs. The Defendants believe these claims to be without merit. The Defendants moved to Compel Arbitration and Dismiss or Stay the original Complaint. The Plaintiff filed an Amended Complaint on
August 18, 2017. The Defendants filed a Motion to Compel Arbitration or Stay the Amended Complaint, which is still pending. Madison National Life and Standard Security Life have demanded arbitration against this third party administrator. In the fourth quarter of 2017, Madison National Life paid fines in the state of Texas primarily related to the claims payment practices of the Plaintiff.
ITEM 4. MINE SAFETY DISCLOSURES
Not applicable.
PART II
ITEM 5.MARKET FOR REGISTRANT'S COMMON EQUITY, RELATED
STOCKHOLDER MATTERS AND ISSUER PURCHASES OF EQUITY SECURITIES
Market Information
The Company's common stock trades under the symbol IHC on the New York Stock Exchange. The following table shows for the periods indicated the high and low sales prices for IHC's common stock as reported by the New York Stock Exchange.
|
|
| HIGH |
|
| LOW | |
QUARTER ENDED: |
|
|
|
|
|
| |
| December 31, 2017 |
| $ | 30.00 |
| $ | 24.85 |
| September 30, 2017 |
|
| 25.95 |
|
| 20.52 |
| June 30, 2017 |
|
| 20.95 |
|
| 17.25 |
| March 31, 2017 |
|
| 20.68 |
|
| 16.55 |
|
|
|
|
|
|
| |
QUARTER ENDED: |
|
|
|
|
|
| |
| December 31, 2016 |
| $ | 21.23 |
| $ | 17.03 |
| September 30, 2016 |
|
| 19.15 |
|
| 16.20 |
| June 30, 2016 |
|
| 17.97 |
|
| 15.05 |
| March 31, 2016 |
|
| 16.91 |
|
| 13.16 |
IHC's stock price closed at $27.45 on December 31, 2017.
Holders of Record
At March 09, 2018, the number of record holders of IHC's common stock was 1,598. The number of record owners was determined from the Company’s stockholder records maintained by the Company’s transfer agent.
Dividends
IHC declared a cash dividend of $.06 per share on its common stock on July 5, 2017 and declared a cash dividend of $.10 per share on its common stock on December 20, 2017, for a total annual dividend of $.16 per share.
IHC declared a cash dividend of $.045 per share on its common stock on June 20, 2016 and declared a cash dividend of $.06 per share on its common stock on November 29, 2016, for a total annual dividend of $.105 per share.
IHC declared a cash dividend of $.045 per share on its common stock on each of June 22, 2015 and December 23, 2015 for a total annual dividend of $.09 per share.
Tender Offer
On May 26, 2017, IHC commenced a tender offer to purchase up to 2,000,000 shares of its common stock at a price per share of $20.00, net, to the seller in cash. On June 26, 2017, at the close of business, the offer expired and the Company accepted for purchase 1,385,118 shares of its common stock at $20.00 per share, for an aggregate purchase price of $27.7 million.
Share Repurchase Program
IHC has a program, initiated in 1991, under which it repurchases shares of its common stock. In August 2016, the Board of Directors increased the number of shares that can be repurchased to 3,000,000 shares of IHC common stock, excluding the shares under the aforementioned tender offer. As of December 31, 2017, 1,991,058 shares were still authorized to be repurchased.
Share repurchases during the fourth quarter of 2017 are summarized as follows:
2017 | |||||
|
|
| Maximum Number | ||
|
| Average Price | of Shares which | ||
Month of | Shares | of Repurchased | can be | ||
Repurchase | Repurchased | Shares | Repurchased | ||
|
|
|
| ||
October | 46,171 | $ | 26.15 | 2,022,760 | |
November | 25,043 | $ | 27.65 | 1,997,717 | |
December | 6,659 | $ | 27.88 | 1,991,058 | |
Performance Graph
Set forth below is a line graph comparing the five year cumulative total return of IHC’s common stock with that of the Russell 2000 Index and the S & P 500 Life & Health Insurance index. The graph assumes that dividends were reinvested and is based on a $100 investment on December 31, 2012. Indices data was obtained from Research Data Group, Inc. The performance graph represents past performance and should not be considered to be an indication of future performance.
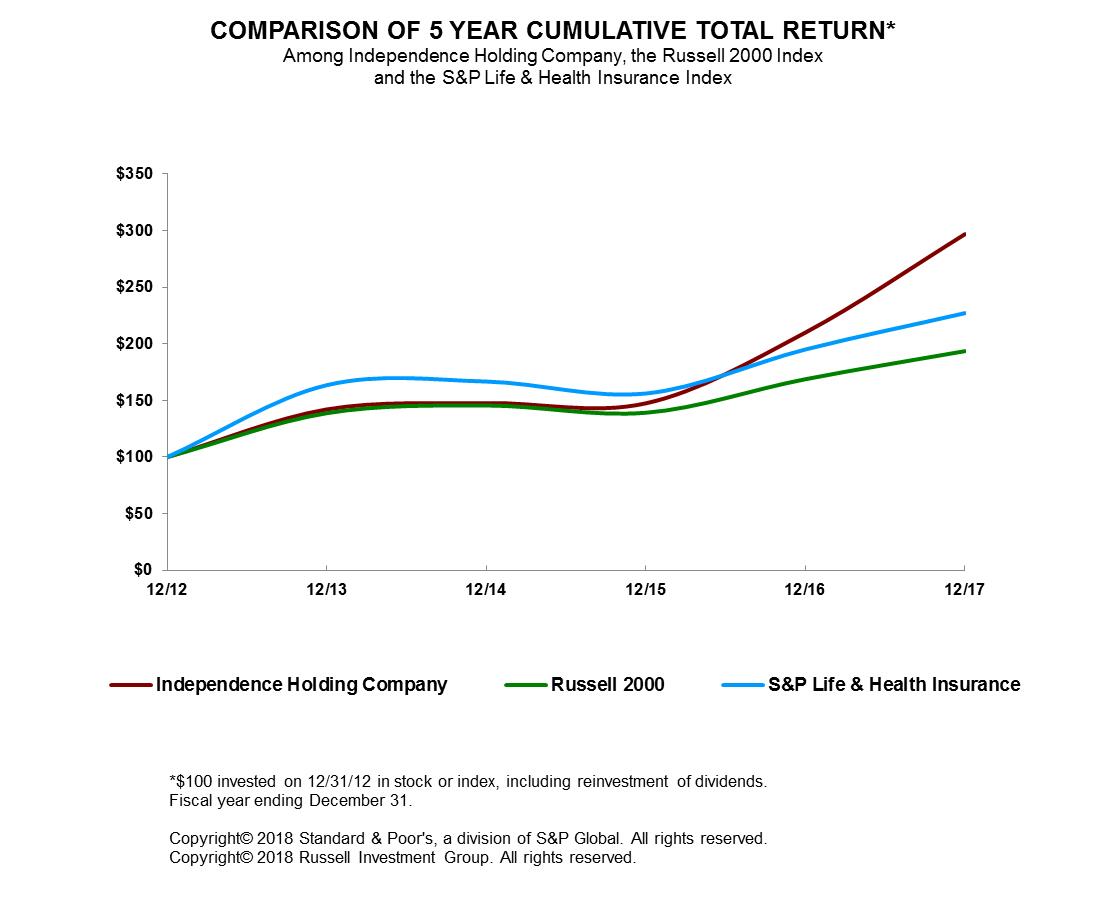
ITEM 6. SELECTED FINANCIAL DATA
The following is a summary of selected consolidated financial data of the Company for each of the last five years.
|
|
| |||||||||
|
| Year Ended December 31, | |||||||||
|
|
|
|
|
|
|
|
|
|
| |
|
| 2017 |
| 2016 |
| 2015 |
| 2014 |
| 2013 | |
Income Data: |
|
|
|
|
|
|
|
|
|
| |
| Total revenues | $ | 320,494 | $ | 311,004 | $ | 530,495 | $ | 530,348 | $ | 574,445 |
| Income from continuing operations |
| 42,130 |
| 22,510 |
| 27,974 |
| 15,021 |
| 15,472 |
Balance Sheet Data: |
|
|
|
|
|
|
|
|
|
| |
| Total investments |
| 476,898 |
| 514,820 |
| 488,159 |
| 650,961 |
| 608,982 |
| Total assets |
| 1,040,623 |
| 1,134,464 |
| 1,197,963 |
| 1,196,227 |
| 1,277,545 |
| Insurance liabilities |
| 544,054 |
| 603,867 |
| 711,475 |
| 728,883 |
| 837,581 |
| Debt and junior subordinated |
|
|
|
|
|
|
|
|
|
|
| debt securities |
| - |
| - |
| 43,335 |
| 42,146 |
| 44,146 |
| IHC stockholders' equity |
| 431,544 |
| 436,559 |
| 323,351 |
| 299,687 |
| 277,301 |
Per Share Data: |
|
|
|
|
|
|
|
|
|
| |
| Cash dividends declared per |
|
|
|
|
|
|
|
|
|
|
| common share |
| .16 |
| .105 |
| .09 |
| .07 |
| .07 |
| Basic income (loss) per common share |
|
|
|
|
|
|
|
|
|
|
| from continuing operations |
| 2.67 |
| 1.28 |
| 1.59 |
| .83 |
| .79 |
| Diluted income (loss) per common |
|
|
|
|
|
|
|
|
|
|
| share from continuing operations |
| 2.63 |
| 1.27 |
| 1.58 |
| .82 |
| .78 |
| Book value per common share |
| 28.98 |
| 25.53 |
| 18.73 |
| 17.25 |
| 15.70 |
|
|
|
|
|
|
|
|
|
|
| |
The Selected Financial Data should be read in conjunction with the accompanying Consolidated Financial Statements and Notes thereto included in Item 8 of this report.
ITEM 7. MANAGEMENT'S DISCUSSION AND ANALYSIS OF FINANCIAL CONDITION AND RESULTS OF OPERATIONS
OVERVIEW |
Independence Holding Company, a Delaware corporation (NYSE: IHC), is a holding company principally engaged in the life and health insurance business through: (i) its insurance companies, Standard Security Life Insurance Company of New York ("Standard Security Life"), Madison National Life Insurance Company, Inc. ("Madison National Life"), and Independence American Insurance Company (“Independence American”); and (ii) its marketing and administrative companies, including IHC Specialty Benefits Inc. IHC Carrier Solutions, Inc. and a majority interest in PetPartners, Inc. (“PetPartners”). IHC also owns a significant equity interest in Ebix Health Exchange Holdings, LLC (“Ebix Health Exchange”), an administration exchange for health insurance. Standard Security Life, Madison National Life and Independence American are sometimes collectively referred to as the “Insurance Group”. IHC and its subsidiaries (including the Insurance Group) are sometimes collectively referred to as the "Company", or “IHC”, or are implicit in the terms “we”, “us” and “our”.
IHC’s health insurance products serve niche sectors of the commercial market through multiple classes of business and varied distribution channels. With regard to those persons in the growing individual market, IHC’s products offer coverage for individuals and families with short-term needs, and fixed indemnity limited benefit and scheduled benefit plans through multiple distribution partners. We offer pet insurance for dogs and cats in all 50 states through select distributors. Our fixed indemnity limited benefit product is primarily purchased by hourly workers and others who are generally not eligible for coverage
under their employer’s group medical plan. The dental and vision products are marketed to large and small groups as well as individuals. With respect to IHC’s life and disability business, Madison National Life has historically sold almost all of this business through one distribution source specializing in serving school districts and municipalities.
Medical stop-loss was marketed to employer groups that self-insure their medical risks. On March 31, 2016, the Company sold IHC Risk Solutions, LLC (“Risk Solutions”), a managing general underwriter that was its principal source of medical stop-loss business. In addition, all of the in-force medical stop-loss business of Standard Security Life and Independence American produced by Risk Solutions was 100% co-insured as of January 1, 2016 and IHC’s block of medical stop-loss business is in run-off.
On December 22, 2017, President Trump signed tax legislation commonly referred to as the Tax Cuts and Jobs Act (the “Tax Act”). The Tax Act makes broad and complex changes to the U.S. tax code, including, but not limited to reducing the federal corporate income tax rate from 35% to 21%.The Company has completed its accounting for the income tax effects under the Tax Act that are relevant to the Company using best estimates based on reasonable and supportable assumptions and available inputs and underlying information. We believe that our accounting is final relative to the Tax Act. The Consolidated Financial Statements reflect all such adjustments and disclosures related to the Tax Act. Refer to Note 12 of the Consolidated Financial Statements for more information regarding the impacts of the Tax Act.
While management considers a wide range of factors in its strategic planning and decision-making, underwriting profit is consistently emphasized as the primary goal in all decisions as to whether or not to increase our retention in a core line, expand into new products, acquire an entity or a block of business, or otherwise change our business model. Management's assessment of trends in healthcare and morbidity, with respect to specialty medical, disability and New York short-term disability (“DBL”); mortality rates with respect to life insurance; and changes in market conditions in general play a significant role in determining the rates charged, deductibles and attachment points quoted, and the percentage of business retained. IHC also seeks transactions that permit it to leverage its vertically integrated organizational structure by generating fee income from production and administrative operating companies as well as risk income for its carriers. Management has always focused on managing the costs of its operations.
The following is a summary of key performance information and events:
Results of operations are summarized as follows for the periods indicated (in thousands):
|
| 2017 |
|
| 2016 |
|
| 2015 |
|
|
|
|
|
|
|
|
|
Revenues | $ | 320,494 |
| $ | 311,004 |
| $ | 530,495 |
Expenses |
| 292,158 |
|
| 278,939 |
|
| 486,617 |
|
|
|
|
|
|
|
|
|
Income from continuing operations before income taxes |
| 28,336 |
|
| 32,065 |
|
| 43,878 |
Income taxes |
| (13,794) |
|
| 9,555 |
|
| 15,904 |
|
|
|
|
|
|
|
|
|
Income from continuing operations, net of tax |
| 42,130 |
|
| 22,510 |
|
| 27,974 |
Income from discontinued operations, net of tax |
| - |
|
| 110,804 |
|
| 2,548 |
|
|
|
|
|
|
|
|
|
Net income |
| 42,130 |
|
| 133,314 |
|
| 30,522 |
Less: Income from noncontrolling interest in subsidiaries |
| (88) |
|
| (10,016) |
|
| (578) |
|
|
|
|
|
|
|
|
|
Net income attributable to IHC | $ | 42,042 |
| $ | 123,298 |
| $ | 29,944 |
|
|
|
|
|
|
|
|
|
Income from continuing operations of $2.63 per share, diluted, for the year ended December 31, 2017 compared to $1.27 per share, diluted, for the same period in 2016.
oThe Company reduced AMIC’s deferred tax asset valuation allowance by $20.3 million at December 31, 2017 primarily due to an increase in projected future income and associated utilization of Federal net operating losses. No such adjustment was recorded for the years ended December 31, 2016 or 2015.
oIncome taxes for the years ended December 31, 2017 and 2016, include income tax benefits of $11.6 million and $3.9 million, respectively, on worthless stock deductions representing the Company’s tax basis on its unrecovered investments in those subsidiaries.
oAs a result of the Tax Act, the Company recorded a deferred income tax expense of $9.4 million due to the re-measurement of deferred tax assets, liabilities and related valuation allowance.
Consolidated investment yields (on an annualized basis) of 3.2% in 2017 compared to 2.7% in 2016; and
Book value of $28.98 per common share at December 31, 2017 compared to $25.53 at December 31, 2016.
The following is a summary of key performance information by segment:
The Specialty Health segment reported $13.2 million of income before taxes for the year ended December 31, 2017 compared to $7.2 million for the comparable period in 2016.
oPremiums earned increased 17.8% or $27.5 million for the year ended December 31, 2017 over the comparable period in 2016. Short term medical premiums increased $9.7 million, and fixed indemnity limited benefit premiums increased $36.7 million as a result of the growing demand for these products and new significant distribution relationships. Premium increases in these lines were partially offset by reduced premium volume in occupational accident business following the sale of Accident Insurance Services, Inc., our primary producer of occupational accident business, in 2016, other lines in run-off, and dental business.
oUnderwriting experience, as indicated by its U.S. GAAP Combined Ratios, for the Specialty Health segment are as follows for the years indicated (in thousands):
|
|
| 2017 |
| 2016 |
| 2015 |
|
|
|
|
|
|
|
|
Premiums Earned |
| $ | 181,851 | $ | 154,397 | $ | 171,912 |
Insurance Benefits, Claims & Reserves |
|
| 84,380 |
| 81,215 |
| 93,916 |
Expenses |
|
| 89,809 |
| 68,891 |
| 71,641 |
|
|
|
|
|
|
|
|
Loss Ratio |
|
| 46.4% |
| 52.6% |
| 54.6% |
Expense Ratio |
|
| 49.4% |
| 44.6% |
| 41.7% |
Combined Ratio |
|
| 95.8% |
| 97.2% |
| 96.3% |
(A)Loss ratio represents insurance benefits claims and reserves divided by premiums earned.
(B)Expense ratio represents net commissions, administrative fees, premium taxes and other underwriting expenses divided by premiums earned.
(C)The combined ratio is equal to the sum of the loss ratio and the expenses ratio.
oAlthough the loss ratios in 2017 are lower than in the comparable periods in 2016, the expense ratios are higher in 2017 because of changes in the mix of products within the Specialty Health segment and as a result of the reallocation of certain fixed costs from the Medical Stop-Loss segment to the Specialty Health segment as the premium volume of one segment shrinks and the other one grows.
Income before taxes from the Group disability, life and DBL segment increased $0.4 million in 2017 compared to prior year results primarily due to lower claims in the short and long term disability and group term life lines, partially offset by lower income from the international line due to run-off of that line of business;
The Individual life, annuities and other segment reported losses before income taxes of $0.5 million in 2017 compared with losses of $2.5 million in 2016. The losses in 2016 were related to the accelerated amortization of deferred costs in connection with the assumption of certain ceded life and annuity policies for which there are no minimal amounts in 2017;
The Medical Stop-Loss segment reported income before taxes of $2.8 million for the year ended December 31, 2017 as compared to income before taxes of $16.7 million for the year ended December 31, 2016. The reduction in income in 2017 in the Medical Stop-loss segment is principally due to the sale of Risk Solutions and exit from the medical stop-loss business. Premiums earned and amounts recorded for benefits, claims and reserves in the Medical Stop-Loss segment represent the activity of the medical stop-loss business in run-off;
Loss before tax from the Corporate segment for the year ended December 31, 2017 decreased $0.7 million over the same period in 2016 primarily due to changes in share-based compensation, consulting, legal and accounting expenses; and
Premiums by principal product for the years indicated are as follows (in thousands):
Gross Direct and Assumed |
|
|
|
|
|
|
|
|
|
Earned Premiums: |
|
| 2017 |
|
| 2016 |
|
| 2015 |
|
|
|
|
|
|
|
|
|
|
Specialty Health |
| $ | 187,793 |
| $ | 163,810 |
| $ | 186,716 |
Group disability; life and DBL |
|
| 129,142 |
|
| 123,245 |
|
| 116,500 |
Individual life, annuities and other |
|
| 26,053 |
|
| 30,285 |
|
| 23,552 |
Medical Stop-Loss |
|
| 10,848 |
|
| 264,101 |
|
| 302,709 |
|
|
|
|
|
|
|
|
|
|
|
| $ | 353,836 |
| $ | 581,441 |
| $ | 629,477 |
Net Premiums Earned: |
|
| 2017 |
|
| 2016 |
|
| 2015 |
|
|
|
|
|
|
|
|
|
|
Specialty Health |
| $ | 181,851 |
| $ | 154,397 |
| $ | 171,912 |
Group disability; life and DBL |
|
| 99,953 |
|
| 96,190 |
|
| 85,953 |
Individual life, annuities and other |
|
| 210 |
|
| 47 |
|
| 11,904 |
Medical Stop-Loss |
|
| 252 |
|
| 12,070 |
|
| 209,765 |
|
|
|
|
|
|
|
|
|
|
|
| $ | 282,266 |
| $ | 262,704 |
| $ | 479,534 |
Information pertaining to the Company's business segments is provided in Note 18 of Notes to Consolidated Financial Statements included in Item 8.
CRITICAL ACCOUNTING POLICIES |
The accounting and reporting policies of the Company conform to U.S. GAAP. The preparation of the Consolidated Financial Statements in conformity with U.S. GAAP requires the Company's management to make estimates and assumptions that affect the amounts reported in the financial statements and accompanying notes. Actual results could differ from those estimates. A summary of the Company's significant accounting policies and practices is provided in Note 1 of the Notes to the Consolidated Financial Statements included in Item 8 of this report. Management has identified the accounting policies described below as those that, due to the judgments, estimates and assumptions inherent in those policies, are critical to an understanding of the Company's Consolidated Financial Statements and this Management's Discussion and Analysis.
Insurance Premium Revenue Recognition and Policy Charges
Premiums for short-duration medical insurance contracts are intended to cover expected claim costs resulting from insured events that occur during a fixed period of short duration. The Company has the ability to not renew the contract or to revise the premium rates at the end of each annual contract period to cover future insured events. Insurance premiums from annual health contracts are collected monthly and are recognized as revenue evenly as insurance protection is provided.
Premiums related to long-term and short-term disability contracts are recognized on a pro rata basis over the applicable contract term.
Traditional life insurance products consist principally of products with fixed and guaranteed premiums and benefits, primarily term and whole life insurance products. Premiums from these products are recognized as revenue when due.
Annuities and interest-sensitive life contracts, such as universal life and interest-sensitive whole life, are contracts whose terms are not fixed and guaranteed. Premiums from these policies are reported as funds on deposit. Policy charges consist of fees assessed against the policyholder for cost of insurance (mortality risk), policy administration and early surrender. These revenues are recognized when assessed against the policyholder account balance.
Policies that do not subject the Company to significant risk arising from mortality or morbidity are considered investment contracts. Deposits received from such contracts are reported as other policyholder funds. Policy charges for investment contracts consist of fees assessed against the policyholder account for maintenance, administration and surrender of the policy prior to contractually specified dates, and are recognized when assessed against the policyholder account balance.
Insurance Liabilities
Policy Benefits and Claims
The Company maintains loss reserves to cover its estimated liability for unpaid losses and loss adjustment expenses, where material, (including legal, other fees, and costs not associated with specific claims but related to the claims payment function) for reported and unreported claims incurred as of the end of each accounting period. These loss reserves are based on actuarial assumptions and are maintained at levels that are in accordance with U.S. GAAP accounting principles. Many factors could affect these reserves, including economic and social conditions, frequency and severity of claims, medical trend resulting from the influences of underlying cost inflation, changes in utilization and demand for medical services, and changes in doctrines of legal liability and damage awards in litigation. Therefore, the Company’s reserves are necessarily based on estimates, assumptions and analysis of historical experience. The Company’s results depend upon the variation between actual claims experience and the assumptions used in determining reserves and pricing products. Reserve assumptions and estimates require significant judgment and, therefore, are inherently uncertain. The Company cannot determine with precision the ultimate amounts that will be paid for actual claims or the timing of those payments. The Company's estimate of loss represents management's best estimate of the Company's liability at the balance sheet date.
Loss reserves differ for short-duration and long-duration insurance policies, including annuities. Reserves are based on approved actuarial methods, but necessarily include assumptions about expenses, mortality, morbidity, lapse rates and future yield on related investments.
All of the Company’s short-duration contracts are generated from its accident, health, term life, disability and pet insurance business, and are accounted for based on actuarial estimates of the amount of loss inherent in that period’s claims, including losses incurred for which claims have not been reported. Short-duration contract loss estimates rely on actuarial observations of ultimate loss experience for similar historical events.
The Company believes that its liability for policy benefits and claims is reasonable and adequate to satisfy its ultimate liability. The Company primarily uses its own loss development experience, but will also supplement that with data from its outside actuaries, reinsurers and industry loss experience as warranted. To illustrate the impact that Loss Ratios have on the Company’s loss reserves and related expenses, each hypothetical 1% change in the Loss Ratio for the health business (i.e., the ratio of insurance benefits, claims and settlement expenses to earned health premiums) for the year ended December 31, 2017, would increase reserves (in the case of a higher ratio) or decrease reserves (in the case of a lower ratio) by approximately $2.6 million with a corresponding increase or decrease in the pre-tax expense for insurance benefits, claims and reserves in the Consolidated Statement of Income. Depending on the circumstances surrounding a change in the Loss Ratio, other pre-tax amounts reported in the Consolidated Statement of Income could also be affected, such as amortization of deferred acquisition costs and commission expense.
The liability for policy benefits and claims by segment is as follows (in thousands):
|
| December 31, 2017 | ||||
|
| Policy |
| Policy |
| Policy Benefits |
|
| Benefits |
| Claims |
| and Claims |
|
|
|
|
|
|
|
Specialty Health | $ | 53,531 | $ | - | $ | 53,531 |
Group Disability |
| 80,788 |
| 23,160 |
| 103,948 |
Individual Accident and Health |
|
|
|
|
|
|
and Other |
| 6,469 |
| 2,181 |
| 8,650 |
Medical Stop-Loss |
| 2,554 |
| - |
| 2,554 |
| $ | 143,342 | $ | 25,341 | $ | 168,683 |
|
| December 31, 2016 | ||||
|
| Policy |
| Policy |
| Policy Benefits |
|
| Benefits |
| Claims |
| and Claims |
|
|
|
|
|
|
|
Specialty Health | $ | 50,237 | $ | - | $ | 50,237 |
Group Disability |
| 83,017 |
| 21,411 |
| 104,428 |
Individual Accident and Health |
|
|
|
|
|
|
and Other |
| 6,391 |
| 3,297 |
| 9,688 |
Medical Stop-Loss |
| 54,760 |
| - |
| 54,760 |
| $ | 194,405 | $ | 24,708 | $ | 219,113 |
Specialty Health
For the Specialty Health business, incurred but not reported (“IBNR”) claims liabilities plus expected development on reported claims are calculated using standard actuarial methods and practices. The “primary” assumption in the determination of Specialty Health reserves is that historical Claim Development Patterns are representative of future Claim Development Patterns. Factors that may affect this assumption include changes in claim payment processing times and procedures, changes in time delay in submission of claims, and the incidence of unusually large claims. Liabilities for policy benefits and claims for specialty health medical and disability coverage are computed using completion factors and expected Net Loss Ratios derived from actual historical premium and claim data. The reserving analysis includes a review of claim processing statistical measures and large claim early notifications; the potential impacts of any changes in these factors are not material. The Company has business that is serviced by third-party administrators. From time to time, there are changes in the timing of claims processing due to any number of factors including, but not limited to, system conversions and staffing changes during the year. These changes are monitored by the Company and the effects of these changes are taken into consideration during the claim reserving process. Other than these considerations, there have been no significant changes to methodologies and assumptions from the prior year.
While these calculations are based on standard methodologies, they are estimates based on historical patterns. To the extent that actual claim payment patterns differ from historical patterns, such estimated reserves may be redundant or inadequate. The effects of such deviations are evaluated by considering claim backlog statistics and reviewing the reasonableness of projected claim ratios. Other factors which may affect the accuracy of policy benefits and claim estimates include the proportion of large claims which may take longer to adjudicate, changes in billing patterns by providers and changes in claim management practices such as hospital bill audits.
Since our analysis considered a variety of outcomes related to these factors, the Company does not believe that any reasonably likely change in these factors will have a Material Effect.
Disability
The Company’s disability business is comprised of group disability and DBL. The two “primary” assumptions on which disability policy benefits and claims are based are: (i) morbidity levels; and (ii) recovery rates. If morbidity levels increase, for example due to an epidemic or a recessionary environment, the Company would increase reserves because there would be more new claims than expected. In regard to the assumed recovery rate, if disabled lives recover more quickly than anticipated then the existing claims reserves would be reduced; if less quickly, the existing claims reserves would be increased. Advancements in medical treatments could affect future recovery, termination, and mortality rates.
With respect to DBL, the liability for policy benefits and claims for the most recent quarter of earned premium is established using a Net Loss Ratio methodology. The Net Loss Ratio is determined by applying the completed prior four quarters of historical Net Loss Ratios to the last quarter of earned premium. Policy benefits and claims associated with the premium earned prior to the last quarter are established using a completion factor methodology. The completion factors are developed using the historical payment patterns for DBL.
With respect to group disability, other assumptions are: (i) changes in market interest rates; (ii) changes in offsets; (iii) advancements in medical treatments; and (iv) cost of living. Changes in market interest rates could change reserve assumptions since the payout period could be as long as 40 years. Changes in offsets such as Social Security benefits, retirement plans and state disability plans also impact reserving. As a result of the forgoing assumptions, it is possible that the historical trend may not be an accurate predictor of the future development of the block. As with most long term insurance reserves that require judgment, the reserving process is subject to uncertainty and volatility and fluctuations may not be indicative of the claim development overall.
While the Company believes that larger variations are possible, the Company does not believe that reasonably likely changes in its “primary” assumptions would have a Material Effect.
Medical Stop-Loss
Due to the sale of Risk Solutions, the Medical Stop-Loss segment is in run-off. The Company has $2.3 million in reserves at December 31, 2017. Liabilities for policy benefits and claims on medical stop-loss coverage are computed using completion factors and expected Net Loss Ratios derived from actual historical premium and claim data. Policy benefits and claims for medical stop-loss insurance are more volatile in nature than those for specialty health medical insurance. This is primarily due to the excess nature of medical stop-loss, with very high deductibles applying to specific claims on any individual claimant and in the aggregate for a given group. The level of these deductibles makes it more difficult to predict the amount and payment pattern of such claims. Furthermore, these excess claims are highly sensitive to changes in factors such as medical trend, provider contracts and medical treatment protocols, adding to the difficulty in predicting claim values and estimating reserves. Also, because medical stop-loss is in excess of an underlying benefit plan, there is an additional layer of claim reporting and processing that can affect claim payment patterns. Finally, changes in the distribution of business by effective month can affect reserve estimates due to the timing of claim occurrences and the time required to accumulate claims against the stop-loss deductible.
Predicting ultimate claims and estimating reserves in Medical Stop-Loss is more complex than specialty health medical and disability business due to the “excess of loss” nature of these products with very high deductibles applying to specific claims on any individual claimant and in the aggregate for a given group. The level of these deductibles makes it more difficult to predict the amount and payment pattern of such claims. Fluctuations in results for specific coverage are primarily due to the severity and frequency of individual claims, whereas fluctuations in aggregate coverage are largely attributable to frequency of underlying claims rather than severity. Liabilities for first dollar medical reserves and disability coverages are computed using completion factors and expected Net Loss Ratios derived from actual historical premium and claim data.
Due to the short-term nature of Medical Stop-Loss, redundancies or deficiencies will typically emerge during the course of the following year rather than over a number of years. For Medical Stop-Loss, as noted above, the Company maintains its reserves based on underlying assumptions until it determines that an adjustment is appropriate based on emerging experience from all of its prior underwriting years.
Individual Accident and Health and Other
This segment is a combination of closed lines of business as well as certain small existing lines. While the assumptions used in setting reserves vary between these different lines of business, the assumptions would generally relate to the following: (i) the rate of disability; (ii) the morbidity rates on specific diseases; and (iii) accident rates. The reported reserves are based on management’s best estimate for each line within this segment. General uncertainties that surround all insurance reserving methodologies would apply. However, since the Company has so few policies of this type, volatility may occur due to the small number of claims.
Management believes that the Company's methods of estimating the liabilities for policy benefits and claims provided appropriate levels of reserves at December 31, 2017. Changes in the Company's policy benefits and claims estimates are recorded through a charge or credit to its earnings.
Future Policy Benefits
The liability for future policy benefits consists of the liabilities related to insured events for the Company’s long-duration contracts, primarily its life and annuity products. For traditional life insurance
products, the Company computes the liability for future policy benefits primarily using the net premium method based on anticipated investment yield, mortality, and withdrawals. These methods are widely used in the life insurance industry to estimate the liabilities for insurance reserves. Inherent in these calculations are management and actuarial judgments and estimates that could significantly impact the ending reserve liabilities and, consequently, operating results. Actual results may differ, and these estimates are subject to interpretation and change.
Management believes that the Company's methods of estimating the liabilities for future policy benefits provided appropriate levels of reserves at December 31, 2017 and 2016. Changes in the Company's future policy benefits estimates are recorded through a charge or credit to its earnings.
Other Policyholders’ Funds
Other policyholders’ funds represent interest-bearing liabilities arising from the sales of products, such as universal life, interest-sensitive life and annuities. Policyholder funds are primarily comprised of deposits received and interest credited to the benefit of the policyholder less surrenders and withdrawals, mortality charges and administrative expenses.
Interest credited to policyholder funds represents interest accrued or paid on interest-sensitive life policies and investment policies. These amounts are reported in insurance benefits, claims and reserves on the Consolidated Statements of Income. Credit rates for certain annuities and interest-sensitive life policies are adjusted periodically by the Company to reflect current market conditions, subject to contractually guaranteed minimum rates.
Investments
The Company has classified all of its investments as either available-for-sale or trading securities. These investments are carried at fair value with unrealized gains and losses reported through other comprehensive income (loss) for available-for-sale securities or as unrealized gains or losses in the Consolidated Statements of Income for trading securities. Available-for-sale securities totaled $447.5 million and $454.8 million at December 31, 2017 and 2016, respectively. Premiums and discounts on debt securities purchased at other than par value are amortized and accreted, respectively, to interest income in the Consolidated Statements of Income, using the constant yield method over the period to maturity. Net realized gains and losses on investments are computed using the specific identification method and are reported in the Consolidated Statements of Income on the trade date.
Fair value is determined using quoted market prices when available. In some cases, we use quoted market prices for similar instruments in active markets and/or model-derived valuations where inputs are observable in active markets. When there are limited or inactive trading markets, we use industry-standard pricing methodologies, including discounted cash flow models, whose inputs are based on management assumptions and available current market information. Further, we retain independent pricing vendors to assist in valuing certain instruments. Most of the securities in our portfolio are classified in either Level 1 or Level 2 of the Fair Value Hierarchy.
The Company periodically reviews and assesses the vendor’s qualifications and the design and appropriateness of its pricing methodologies. Management will on occasion challenge pricing information on certain individual securities and, through communications with the vendor, obtain information about the assumptions, inputs and methodologies used in pricing those securities, and corroborate it against documented pricing methodologies. Validation procedures are in place to determine completeness and accuracy of pricing information, including, but not limited to: (i) review of exception reports that (a) identify any zero or un-priced securities; (b) identify securities with no price change; and (c) identify securities with significant price changes; (ii) performance of trend analyses; (iii) periodic comparison of pricing to alternative pricing sources; and (iv) comparison of pricing changes to expectations based on rating changes, benchmarks or control groups. In certain circumstances, pricing is unavailable from the vendor and broker
pricing information is used to determine fair value. In these instances, management will assess the quality of the data sources, the underlying assumptions and the reasonableness of the broker quotes based on the current market information available. To determine if an exception represents an error, management will often have to exercise judgment. Procedures to resolve an exception vary depending on the significance of the security and its related class, the frequency of the exception, the risk of material misstatement, and the availability of information for the security. These procedures include, but are not limited to: (i) a price challenge process with the vendor; (ii) pricing from a different vendor; (iii) a reasonableness review; and (iv) a change in price based on better information, such as an actual market trade, among other things. Management considers all facts and relevant information obtained during the above procedures to determine the proper classification of each security in the Fair Value Hierarchy.
Declines in value of securities available-for-sale that are judged to be other-than-temporary are determined based on the specific identification method. The Company reviews its investment securities regularly and determines whether other-than-temporary impairments have occurred. The factors considered by management in its regular review to identify and recognize other-than-temporary impairment losses on fixed maturities include, but are not limited to: the length of time and extent to which the fair value has been less than cost; the Company's intent to sell, or be required to sell, the debt security before the anticipated recovery of its remaining amortized cost basis; the financial condition and near-term prospects of the issuer; adverse changes in ratings announced by one or more rating agencies; subordinated credit support; whether the issuer of a debt security has remained current on principal and interest payments; current expected cash flows; whether the decline in fair value appears to be issuer specific or, alternatively, a reflection of general market or industry conditions including the effect of changes in market interest rates. If the Company intends to sell a debt security, or it is more likely than not that it would be required to sell a debt security before the recovery of its amortized cost basis, the entire difference between the security's amortized cost basis and its fair value at the balance sheet date would be recognized by a charge to total other-than-temporary impairment losses in the Consolidated Statement of Income. If a decline in fair value of a debt security is judged by management to be other-than-temporary and; (i) the Company does not intend to sell the security; and (ii) it is not more likely than not that it will be required to sell the security prior to recovery of the security’s amortized cost, the Company assesses whether the present value of the cash flows to be collected from the security is less than its amortized cost basis. To the extent that the present value of the cash flows generated by a debt security is less than the amortized cost basis, a credit loss exists. For any such security, the impairment is bifurcated into (a) the amount of the total impairment related to the credit loss, and (b) the amount of the total impairment related to all other factors. The amount of the other-than-temporary impairment related to the credit loss is recognized by a charge to total other-than-temporary impairment losses in the Consolidated Statement of Income, establishing a new cost basis for the security. The amount of the other-than-temporary impairment related to all other factors is recognized in other comprehensive income (loss). It is reasonably possible that further declines in estimated fair values of such investments, or changes in assumptions or estimates of anticipated recoveries and/or cash flows, may cause further other-than-temporary impairments in the near term, which could be significant.
In assessing corporate debt securities for other-than-temporary impairment, the Company evaluates the ability of the issuer to meet its debt obligations and the value of the company or specific collateral securing the debt position. For mortgage-backed securities where loan level data is not available, the Company uses a cash flow model based on the collateral characteristics. Assumptions about loss severity and defaults used in the model are primarily based on actual losses experienced and defaults in the collateral pool. Prepayment speeds, both actual and estimated, are also considered. The cash flows generated by the collateral securing these securities are then determined with these default, loss severity and prepayment assumptions. These collateral cash flows are then utilized, along with consideration for the issue’s position in the overall structure, to determine the cash flows associated with the mortgage-backed security held by the Company. In addition, the Company evaluates other asset-backed securities for other-than-temporary impairment by examining similar characteristics referenced above for mortgage-backed securities. The Company evaluates U.S. Treasury securities and obligations of U.S. Government corporations, U.S.
Government agencies, and obligations of states and political subdivisions for other-than-temporary impairment by examining the terms and collateral of the security.
Equity securities may experience other-than-temporary impairment in the future based on the prospects for full recovery in value in a reasonable period of time and the Company’s ability and intent to hold the security to recovery. If a decline in fair value is judged by management to be other-than-temporary or management does not have the intent or ability to hold a security, a loss is recognized by a charge to total other-than-temporary impairment losses in the Consolidated Statement of Income. For the purpose of other-than-temporary impairment evaluations, redeemable preferred stocks are evaluated in a manner similar to debt securities. Declines in the creditworthiness of the issuer of debt securities with both debt and equity-like features are evaluated using the equity model in consideration of other-than-temporary impairment.
Goodwill and Other Intangible Assets
Goodwill carrying amounts are evaluated for impairment, at least annually, at the reporting unit level that is equivalent to an operating segment. If the fair value of a reporting unit is less than its carrying amount, further evaluation is required to determine if a write-down of goodwill is required. In determining the fair value of each reporting unit, we used an income approach, applying a discounted cash flow method that included a residual value. Based on historical experience, we make assumptions as to: (i) expected future performance and future economic conditions, (ii) projected operating earnings, (iii) projected new and renewal business as well as profit margins on such business, and (iv) a discount rate that incorporated an appropriate risk level for the reporting unit. Any impairment of goodwill would be charged to expense.
At December 31, 2017, the Company’s market capitalization was less than its book value indicating a potential impairment of goodwill. As a result, the Company assessed the factors contributing to the performance of IHC stock in 2017, and concluded that the market capitalization does not represent the fair value of the Company. The Company noted several factors that have led to a difference between the market capitalization and the fair value of the Company, including (i) the Company’s stock is thinly traded and a sale of even a small number of shares can have a large percentage impact on the price of the stock, (ii) Geneve Corporation and insiders own approximately 67% of the outstanding shares, which has had a significant adverse impact on the number of shares available for sale and therefore the trading potential of IHC stock, and (iii) lack of analyst coverage of the Company. If we experience a sustained decline in our results of operations and cash flows, or other indicators of impairment exist, we may incur a material non-cash charge to earnings relating to impairment of our goodwill, which could have a material adverse effect on our results. No impairment charge for goodwill was required in 2017, 2016 or 2015.
Other intangible assets are amortized to expense over their estimated useful lives and are subject to impairment testing. Any impairment of other intangible assets would be charged to expense. No impairment charges for intangible assets were required in 2017, 2016 or 2015.
Deferred Income Taxes
The provision for deferred income taxes is based on the asset and liability method of accounting for income taxes. Under this method, deferred income taxes are recognized by applying enacted statutory tax rates to temporary differences between amounts reported in the Consolidated Financial Statements and the tax bases of existing assets and liabilities in the years in which those temporary differences are expected to be recovered or settled. A valuation allowance is recognized for the portion of deferred tax assets that, in management's judgment, is not likely to be realized. A liability for uncertain tax positions is recorded when it is more likely than not that a tax position will not be sustained upon examination by taxing authorities. The effect on deferred income taxes of a change in tax rates or laws is recognized in income tax expense in the period that includes the enactment date.
RESULTS OF OPERATIONS
Results of Operations for the Year Ended December 31, 2017 Compared to the Year Ended December 31, 2016
Information by business segment for the periods indicated is as follows (in thousands):
|
|
|
| Insurance |
|
| ||||||
|
|
|
| Benefits, | Selling, |
| ||||||
|
| Net | Fee and | Claims | General |
| ||||||
December 31, 2017 | Premiums | Investment | Other | and | and |
| ||||||
| Earned | Income | Income | Reserves | Administrative | Total | ||||||
|
|
|
|
|
|
| ||||||
Specialty Health | $ | 181,851 | $ | 5,299 | $ | 16,660 | $ | 84,380 | $ | 106,223 | $ | 13,207 |
Group disability, |
|
|
|
|
|
|
|
|
|
|
|
|
life and DBL |
| 99,953 |
| 6,469 |
| 505 |
| 52,792 |
| 35,857 |
| 18,278 |
Individual life, |
|
|
|
|
|
|
|
|
|
|
|
|
annuities and other |
| 210 |
| 1,536 |
| 393 |
| 241 |
| 2,411 |
| (513) |
Medical Stop-Loss |
| 252 |
| 1,111 |
| 1,244 |
| (2,359) |
| 2,127 |
| 2,839 |
Corporate |
| - |
| 1,861 |
| 611 |
| - |
| 10,486 |
| (8,014) |
Sub total | $ | 282,266 | $ | 16,276 | $ | 19,413 | $ | 135,054 | $ | 157,104 |
| 25,797 |
|
|
| ||||||||||
Net realized investment gains |
| 2,539 | ||||||||||
Income from continuing operations before income taxes |
| 28,336 | ||||||||||
Income tax benefits |
| (13,794) | ||||||||||
Income from continuing operations, net of tax | $ | 42,130 | ||||||||||
|
|
|
| Insurance |
|
| ||||||
|
|
|
| Benefits, | Selling, |
| ||||||
|
| Net | Fee and | Claims | General |
| ||||||
December 31, 2016 | Premiums | Investment | Other | and | and |
| ||||||
| Earned | Income | Income | Reserves | Administrative | Total | ||||||
|
|
|
|
|
|
| ||||||
Specialty Health | $ | 154,397 | $ | 3,272 | $ | 15,478 | $ | 81,215 | $ | 84,730 | $ | 7,202 |
Group disability, |
|
|
|
|
|
|
|
|
|
|
|
|
life and DBL |
| 96,190 |
| 6,469 |
| 876 |
| 52,245 |
| 33,386 |
| 17,904 |
Individual life, |
|
|
|
|
|
|
|
|
|
|
|
|
annuities and other |
| 47 |
| 2,255 |
| 454 |
| 1,344 |
| 3,952 |
| (2,540) |
Medical Stop-Loss |
| 12,070 |
| 1,700 |
| 11,844 |
| 10,427 |
| (1,546) |
| 16,733 |
Corporate |
| - |
| 2,874 |
| 51 |
| - |
| 11,652 |
| (8,727) |
Sub total | $ | 262,704 | $ | 16,570 | $ | 28,703 | $ | 145,231 | $ | 132,174 |
| 30,572 |
|
|
| ||||||||||
Net realized investment gains |
| 4,502 | ||||||||||
Net impairment losses recognized in earnings |
| (1,475) | ||||||||||
Interest expense on debt |
| (1,534) | ||||||||||
Income from continuing operations before income taxes |
| 32,065 | ||||||||||
Income taxes |
| 9,555 | ||||||||||
Income from continuing operations, net of tax | $ | 22,510 | ||||||||||
Premiums Earned
In 2017, premiums earned increased $19.6 million over the comparable period of 2016. The increase is primarily due to: (i) an increase of $27.5 million in the Specialty Health segment principally as a result of a $36.7 million increase in the fixed indemnity limited benefit line, a $9.7 million increase in premiums from the short term medical line of business, and a $0.9 million increase in the pet line of business, partially offset by a decrease of $9.9 million in occupational accident business premiums due to the run-off of this line following the sale of our primary producer of this business, in the third quarter of 2016, a decrease of $4.1 million in the dental line of business and a $5.9 million decline in international premiums; (ii) a $3.7 million increase in earned premiums from the Group disability, life, annuities and DBL segment primarily due to increased volume in the LTD, DBL and group term life lines; and (iii) an increase of $0.2 million in the Individual life, annuities and other segment; partially offset by (iv) a decrease of $11.8 million in the Medical Stop-Loss segment as a result of the sale of Risk Solutions and exit from the medical stop-loss business, further described in Note 3.
Net Investment Income
Total net investment income decreased $0.3 million over the comparable period in 2016. The overall annualized investment yields for the years ended December 31, 2017 and 2016 were 3.2% and 2.7%, respectively. The overall decrease was primarily the result of lower average invested assets in 2017 largely due to the retirement of debt in the fourth quarter of 2016 partially offset by higher returns on partnership investment.
The annualized investment yields on bonds, equities and short-term investments for the years ended December 31, 2017 and 2016 were 3.0% and 2.9%, respectively. IHC has approximately $176.9 million in highly rated shorter duration securities earning on average 1.8%. A portfolio that is shorter in duration enables us, if we deem prudent, the flexibility to reinvest in much higher yielding longer-term securities, which would significantly increase investment income.
Net Realized Investment Gains and Net Impairment Losses Recognized in Earnings
The Company had net realized investment gains of $2.5 million in 2017 compared to $4.5 million in 2016. These amounts include gains and losses from sales of fixed maturities and equity securities available-for-sale and other investments. Decisions to sell securities are based on management's ongoing evaluation of investment opportunities and economic and market conditions, thus creating fluctuations in gains and losses from period to period.
In 2016, the Company recognized $1.5 million of other-than-temporary impairment losses on certain fixed maturities available-for-sale due to credit losses. The Company determined that it was more likely than not that the securities would be sold before the recovery of their amortized cost basis.
Fee Income and Other Income
Fee income increased $.3 million for the year ended December 31, 2017 compared to the comparable period in 2016 primarily due to fee income earned by PetPartners, our recently acquired subsidiary, with no comparable amounts in 2016, partially offset by a decrease in fee income related to occupational accident business as a result of the sale of our primary producer of that business in 2016.
Other income in 2017 decreased $9.6 million from the same period in 2016 primarily due to the run-off of fees received in conjunction with the diminished administration of the Medical Stop-Loss segment.
Insurance Benefits, Claims and Reserves
In 2017, insurance benefits, claims and reserves decreased $10.1 million over the comparable period in 2016. The decrease is primarily attributable to: (i) a decrease of $12.8 million in the Medical Stop-Loss segment primarily as a result of the sale of Risk Solutions and exit from the medical stop-loss business, further described in Note 3; (ii) a decrease of $1.1 million in the Individual life, annuity and other segment; partially offset by (iii) an increase of $3.2 million in the Specialty Health segment, primarily due to an increase of $3.8 million in the small group major medical line of business due to favorable development of this line in 2016 with no comparable amount in 2017, and increases of $8.6 million, $6.3 million and $1.3 million in the benefits and claims of fixed indemnity limited benefit, short term medical and pet lines of business, respectively, due to increases in volume, partially offset by a $9.4 million decrease in benefits, claims and reserves related to the run-off of the occupational accident line of business and decreases of $4.6 million and $2.6 million in the dental and international lines, respectively, due to lower premiums; and (iv) an increase of $0.6 million in benefits, claims and reserves in the Group disability, life, annuities and DBL segment, primarily due to growth in this line partially offset by improved experience in the DBL line.
Selling, General and Administrative Expenses
Total selling, general and administrative expenses increased $24.9 million over the comparable period in 2016. The increase is primarily attributable to: (i) a $21.5 million increase in the Specialty Health segment primarily due to administrative and commission expenses associated with the increased premium volume in the short term medical and fixed indemnity limited benefit lines, and agency expenses from PetPartners with no comparable expenses in the prior year, partially offset by a decrease in administrative expenses in 2017 from Accident Insurance Services, Inc., our primary producer of Occupational Accident line of business, which was sold in the third quarter of 2016; (ii) an increase of $3.6 million in the Medical Stop-Loss segment primarily due to a credit in premium taxes in 2016 with no comparable amount for 2017; (iii) an increase of $2.5 million in the Group disability, life, annuities and DBL segment due principally to higher general expenses on increased volume; partially offset by (iv) a decrease of $1.5 million in the Individual life, annuity and other segment largely due to lower amortization of deferred costs and general expenses from business in run-off; (v) a decrease of $1.2 million in Corporate due to a decrease in audit and consulting fees.
Income Taxes
The effective tax (benefit) rate was (48.7)% in 2017 compared to 29.8% for the same period in 2016. The Company has completed its accounting for the impact of the Tax Act as of December 31, 2017 and recorded a deferred income tax expense of $9.4 million due to the re-measurement of deferred tax assets, liabilities and related valuation allowance. Also in 2017, the Company wound down the operations and dissolved a subsidiary recognizing an estimated $11.6 million income tax benefit on a worthless stock deduction of $33.1 million, representing the Company’s tax basis on its unrecovered investment in that subsidiary. In addition, the Company recorded a $20.3 million credit to federal income taxes in 2017 as a result of the reduction in AMIC’s valuation allowance for increased income projections and associated utilization of Federal net operating loss carryforwards. AMIC’s valuation allowance was due to the probability that AMIC might not be able to fully utilize its prior tax year federal net operating loss carryforwards ("NOLs"). Income taxes for the year ended December 31, 2016, also include an income tax benefit of $3.9 million on a worthless stock deduction of $11.2 million representing the Company’s tax basis in its unrecovered investment in a subsidiary.
Excluding the impact of the Tax Act in 2017, the worthless stock deductions in both 2017 and 2016, and the reduction in the valuation allowance in 2017, the effective rate was significantly lower in 2017 due to: (i) a decrease in non-deductible expenses in 2017; (ii) tax benefits realized in 2017 upon the exercise and vesting of sharebased compensation awards with no comparable amounts in 2016; and (iii) a decrease in state taxes as a percentage of income.
Results of Operations for the Year Ended December 31, 2016 Compared to the Year Ended December 31, 2015
Information by business segment for the periods indicated is as follows (in thousands):
|
|
|
| Insurance |
|
| |||||||
|
|
|
| Benefits, | Selling, |
| |||||||
|
| Net | Fee and | Claims | General |
| |||||||
December 31, 2016 | Premiums | Investment | Other | and | and |
| |||||||
| Earned | Income | Income | Reserves | Administrative | Total | |||||||
|
|
|
|
|
|
| |||||||
Medical Stop-Loss | $ | 12,070 | $ | 1,700 | $ | 11,844 | $ | 10,427 | $ | (1,546) | $ | 16,733 | |
Specialty Health |
| 154,397 |
| 3,272 |
| 15,478 |
| 81,215 |
| 84,730 |
| 7,202 | |
Group disability, |
|
|
|
|
|
|
|
|
|
|
|
| |
| life and DBL |
| 96,190 |
| 6,469 |
| 876 |
| 52,245 |
| 33,386 |
| 17,904 |
Individual life, |
|
|
|
|
|
|
|
|
|
|
|
| |
| annuities and other |
| 47 |
| 2,255 |
| 454 |
| 1,344 |
| 3,952 |
| (2,540) |
Corporate |
| - |
| 2,874 |
| 51 |
| - |
| 11,652 |
| (8,727) | |
Sub total | $ | 262,704 | $ | 16,570 | $ | 28,703 | $ | 145,231 | $ | 132,174 |
| 30,572 | |
|
|
| |||||||||||
Net realized investment gains |
| 4,502 | |||||||||||
Net impairment losses recognized in earnings |
| (1,475) | |||||||||||
Interest expense on debt |
| (1,534) | |||||||||||
Income from continuing operations before income taxes |
| 32,065 | |||||||||||
Income taxes |
| 9,555 | |||||||||||
Income from continuing operations | $ | 22,510 | |||||||||||
|
|
|
| Insurance |
|
| |||||||
|
|
|
| Benefits, | Selling, |
| |||||||
|
| Net | Fee and | Claims | General |
| |||||||
December 31, 2015 | Premiums | Investment | Other | and | And |
| |||||||
| Earned | Income | Income | Reserves | Administrative | Total | |||||||
|
|
|
|
|
|
| |||||||
Medical Stop-Loss | $ | 209,765 | $ | 4,374 | $ | - | $ | 153,919 | $ | 41,392 | $ | 18,828 | |
Specialty Health |
| 171,912 |
| 1,813 |
| 12,187 |
| 93,916 |
| 85,506 |
| 6,490 | |
Group disability, |
|
|
|
|
|
|
|
|
|
|
|
| |
| life and DBL |
| 85,953 |
| 3,699 |
| 662 |
| 47,646 |
| 26,857 |
| 15,811 |
Individual life, |
|
|
|
|
|
|
|
|
|
|
|
| |
| annuities and other |
| 11,904 |
| 7,146 |
| 8,069 |
| 11,697 |
| 15,544 |
| (122) |
Corporate |
| - |
| 205 |
| - |
| - |
| 8,342 |
| (8,137) | |
Sub total | $ | 479,534 | $ | 17,237 | $ | 20,918 | $ | 307,178 | $ | 177,641 |
| 32,870 | |
|
|
| |||||||||||
Gain on sale of subsidiary to joint venture |
| 9,940 | |||||||||||
Net realized investment gains |
| 3,094 | |||||||||||
Net impairment losses recognized in earnings |
| (228) | |||||||||||
Interest expense on debt |
| (1,798) | |||||||||||
Income from continuing operations before income taxes |
| 43,878 | |||||||||||
Income taxes |
| 15,904 | |||||||||||
Income from continuing operations | $ | 27,974 | |||||||||||
Premiums Earned
In 2016, premiums earned decreased $216.8 million over the comparable period of 2015. The decrease is primarily due to: (i) a decrease of $197.7 million in the Stop Loss segment as a result of the sale of Risk Solutions and exit from the medical stop-loss business, further described in Note 3; (ii) a decrease of $17.5 million in the Specialty Health segment principally as a result of a $26.8 million decrease in premiums from exiting the Major Medical line, a $11.9 million decrease in the fixed indemnity limited benefit line due to the cancellation of a distribution source, and a $1.4 million decrease in international medical business premiums due to lower retention, partially offset by premium increases in the short-term medical, pet and occupational accident lines of business of $17.7 million, $4.7 million and $1.6 million, respectively, as a result of higher volume; and (iii) a decrease of $11.8 million in the Individual life, annuities and other segment as a result of this business being in run-off; partially offset by (iv) a $10.2 million increase in earned premiums from the Group disability, life, annuities and DBL segment primarily due to increased volume and retention in the LTD and group term life lines and increased volume in DBL business.
Net Investment Income
Total net investment income decreased $0.7 million. The overall annualized investment yields for the year ended December 31, 2016 and 2015 were 2.7% and 2.8%, respectively. The overall decrease was primarily the result of a decrease in investment income on bonds, equities and short-term investments due to cash transferred out in the third quarter of 2015 in connection with a coinsurance and sale transaction, partially offset by cash received in connection with the sale of Risk Solutions in the first quarter of 2016. Additionally, income from partnerships was lower in 2016.
The annualized investment yields on bonds, equities and short-term investments were 2.9% and 2.8% for 2016 and 2015, respectively. IHC has approximately $168.7 million in highly rated shorter duration securities earning on average 1.5%. A portfolio that is shorter in duration enables us, if we deem prudent, the flexibility to reinvest in much higher yielding longer-term securities, which would significantly increase investment income.
Gain on Sale of Subsidiary to Joint Venture
In the third quarter of 2015, the Company finalized a joint venture with Ebix, Inc. in which IHC sold its wholly owned administrative subsidiary, IHC Health Solutions (now known as Ebix Health Administration Exchange, Inc.), in exchange for a 60% ownership interest in Ebix Health Exchange and $6.0 million in cash proceeds. The transaction resulted in a loss of control over the subsidiary (due to a lack of the majority of the voting interest on the Board of Managers) and therefore the subsidiary was deconsolidated from the Company’s financial statements. The Company recognized a net gain of $9.9 million, pre-tax, on the transaction (see Note 7). There was no comparable transaction in 2016.
Net Realized Investment Gains and Net Impairment Losses Recognized in Earnings
The Company had net realized investment gains of $4.5 million in 2016 compared to $3.1 million in 2015. These amounts include gains and losses from sales of fixed maturities and equity securities available-for-sale and other investments. Decisions to sell securities are based on management's ongoing evaluation of investment opportunities and economic and market conditions, thus creating fluctuations in gains and losses from period to period.
The Company recognized $1.5 million of other-than-temporary impairment losses on certain fixed maturities available-for-sale during 2016. The Company determined that it is more likely than not that we will sell the securities before recovery of their amortized cost basis. In 2015, the Company recognized $0.2 million of other-than-temporary impairment losses on equity securities available-for-sale due to the length of time and extent an equity security was below cost.
Fee Income and Other Income
Fee income increased $5.8 million in 2016 compared to 2015 primarily due to increased fee income from the Specialty Health segment partially offset by decreased fees due to the partial sale and deconsolidation of a previously wholly owned third party administrator.
Other income increased $2.0 million. Other income in 2016 consists primarily of fees received in connection with the ceding of the Medical Stop Loss business; whereas, 2015 includes a gain recorded in connection with the ceding of individual life and annuity policies and sale of the related infrastructure.
Insurance Benefits, Claims and Reserves
In 2016, insurance benefits, claims and reserves decreased $161.9 million over the comparable period in 2015. The decrease is primarily attributable to: (i) a decrease of $143.5 million in the Medical Stop Loss segment primarily as a result of the sale of Risk Solutions and exit from the medical stop-loss business, further described in Note 3; (ii) a decrease of $12.7 million in the Specialty Health segment, primarily due to a decrease of $23.8 million in benefits, claims and reserves related to the run-off of the Major Medical business, a $3.5 million decrease due to lower volume in the fixed indemnity business, and a $2.1 million decrease due to lower retention in the international line; partially offset by increases of $5.4 million in claims in the occupational accident lines due to higher claim activity and increases of $9.3 million and $2.3 million in the short term medical and pet, respectively, due to the increase in volume of both lines of business; and (iii) a decrease of $10.3 million in the Individual life, annuity and other segment, primarily as a result of business in run-off; partially offset by (iv) an increase of $4.6 million in benefits, claims and reserves in the group disability, life, annuities and DBL segment, primarily due to increased retention and higher loss ratios on LTD lines.
Selling, General and Administrative Expenses
Total selling, general and administrative expenses decreased $45.5 million over the comparable period in 2015. The decrease is primarily attributable to: (i) a decrease of $42.9 million in the Medical Stop Loss segment primarily as a result of the sale of Risk Solutions and exit from the medical stop-loss business, further described in Note 3, (ii) a decrease of $0.8 million in the Specialty Health segment primarily due to decreased expenses from the run-off of Major Medical and lower volume of fixed indemnity business, partially offset by an increase in expenses due to increased volume in the short term medical line; and (iii) a decrease of $11.6 million in the Individual life, annuity and other segment largely due to a decrease in amortization of deferred acquisition costs as a result of ceding life and annuity policies in 2015 and lower general expenses from business in run-off; partially offset by (iv) an increase of $6.5 million in the group disability, life, annuities and DBL segment primarily due to increased commission and other expenses in the LTD line as a result of volume; and (v) an increase of $3.3 million in Corporate principally from increased compensation costs in addition to higher audit and consulting fees in 2016.
Income Taxes
The effective tax rate was 29.8% in 2016 compared to 36.2% for the same period in 2015. The lower effective tax rate is primarily due to the liquidation of a subsidiary in 2016 that resulted in tax benefits of approximately $3.9 million recognized for IHC’s unrecovered investment in that subsidiary.
LIQUIDITY |
Insurance Group
The Insurance Group normally provides cash flow from: (i) operations; (ii) the receipt of scheduled principal payments on its portfolio of fixed maturities; and (iii) earnings on investments. Such cash flow is partially used to fund liabilities for insurance policy benefits. These liabilities represent long-term and short-term obligations.
Corporate
Corporate derives its funds principally from: (i) dividends from the Insurance Group; (ii) management fees from its subsidiaries; and (iii) investment income from Corporate liquidity. Regulatory constraints historically have not affected the Company's consolidated liquidity, although state insurance laws have provisions relating to the ability of the parent company to use cash generated by the Insurance Group. The Insurance Group declared and paid $18.0 million, $18.4 million and $10.6 million of cash dividends to Corporate in 2017, 2016 and 2015, respectively.
Corporate utilizes cash primarily for the payment of general overhead expenses, common stock dividends, and common stock repurchases.
Cash Flows
The Company had $26.5 million and $22.0 million of cash and cash equivalents as of December 31, 2017 and 2016, respectively.
Operating activities provided $28.6 million of cash. Investment activities provided $27.6 million of cash, primarily the result of sales of investment securities, partially offset by $12.3 million net cash outflow to acquire PetPartners. Financing activities utilized $51.7 million of cash, of which $46.4 million was utilized for treasury share purchases.
The Company repurchased 2,289,502 shares of its common stock. Of that amount, 703,000 shares were repurchased in private transactions for an aggregate cost of $14.0 million; 1,385,118 shares were repurchased for an aggregate cost of $27.7 million pursuant to the terms of a tender offer; and the remaining shares were repurchased in the open market.. The tender offer was fully funded through corporate liquidity.
At December 31, 2017, the Company had $544.1 million of insurance liabilities that it expects to ultimately pay out of current assets and cash flows from future business. If necessary, the Company could utilize the cash received from maturities and repayments of its fixed maturity investments if the timing of claim payments associated with the Company's insurance resources does not coincide with future cash flows. For the year ended December 31, 2017, cash received from the maturities and other repayments of fixed maturities was $28.4 million.
The Company believes it has sufficient cash to meet its currently anticipated business requirements over the next twelve months including working capital requirements and capital investments.
BALANCE SHEET |
The Company had receivables from reinsurers of $380.6 million at December 31, 2017 compared to $440.3 million at December 31, 2016. All of such reinsurance receivables are from highly rated companies or are adequately secured. No allowance for doubtful accounts was necessary at December 31, 2017.
The $5.0 million decrease in IHC’s stockholders' equity in 2017 is primarily due to $46.5 million of treasury stock purchases, $2.4 million in common stock dividends declared and $1.3 million related to share-based compensation, partially offset by $42.0 million of net income attributable to IHC and $3.2 million of other comprehensive income attributable to IHC.
Asset Quality and Investment Impairments |
The nature and quality of insurance company investments must comply with all applicable statutes and regulations, which have been promulgated primarily for the protection of policyholders. Although the Company's gross unrealized losses on available-for-sale securities totaled $7.4 million at December 31, 2017, 100% of the Company’s fixed maturities were investment grade and continue to be rated on average AA. The Company marks all of its available-for-sale securities to fair value through accumulated other comprehensive income or loss. These investments tend to carry less default risk and, therefore, lower interest rates than other types of fixed maturity investments. The Company does not have any non-performing fixed maturity investments at December 31, 2017.
Certain fixed maturities, primarily municipal obligations, in our investment portfolio are insured by financial guaranty insurance companies. The insurance, however, does not enhance the credit ratings on these securities. The following table summarizes the credit quality of our fixed maturity portfolio, as rated, at December 31, 2017:
|
|
Bond Ratings | As Rated |
|
|
AAA | 12.9% |
AA | 59.1% |
A | 25.3% |
BBB | 2.7% |
|
|
Total Investment Grade | 100.0% |
|
|
Changes in interest rates, credit spreads, and investment quality ratings may cause the market value of the Company’s investments to fluctuate. The Company does not have the intent to sell nor is it more likely than not that the Company will have to sell debt securities in unrealized loss positions that are not other-than-temporarily impaired before recovery. In the event that the Company’s liquidity needs require the sale of fixed maturity securities in unfavorable interest rate, liquidity or credit spread environments, the Company may realize investment losses.
The Company reviews its investments regularly and monitors its investments continually for impairments, as discussed in Note 1(F) (iv) of the Notes to Consolidated Financial Statements in Item 8 of this report. The Company did not record any other-than-temporary impairment losses in 2017. The Company recognized $1.5 million of other-than-temporary impairment losses on certain fixed maturities available-for-sale during 2016. The Company determined that it was more likely than not that we will sell the securities before recovery of their amortized cost basis. At December 31, 2017, there were no securities with fair values less than 80% of their amortized cost.
The unrealized losses on all available-for-sale securities have been evaluated in accordance with the Company's impairment policy and were determined to be temporary in nature at December 31, 2017. From time to time, as warranted, the Company may employ investment strategies to mitigate interest rate and other market exposures. Further deterioration in credit quality of the companies backing the securities, further deterioration in the condition of the financial services industry, imbalances in liquidity that exist in the marketplace, worsening of the current economic recession, or declines in real estate values may further affect the fair value of these securities and increase the potential that certain unrealized losses be designated as other-than-temporary in future periods and the Company may incur additional write-downs.
Goodwill
Goodwill represents the excess of the amount we paid to acquire subsidiaries and other businesses over the fair value of their net assets at the date of acquisition. The Company tests goodwill for impairment at least annually and between annual tests if an event or circumstances change that would more likely than not reduce the fair value of a reporting unit below its carrying amount. Goodwill is considered impaired when the carrying amount of goodwill exceeds its implied fair value.
All goodwill carrying amounts are evaluated for impairment at the reporting unit level which is equivalent to an operating segment. Goodwill was allocated to each reporting unit or operating segment at the time of acquisition. At December 31, 2017, total goodwill was $50.7 million, all of which was attributable to the Specialty Health segment.
Based upon the goodwill impairment testing performed at December 31, 2017, the fair value of each reporting unit exceeded its carrying value and no impairment charge was required. Fair value exceeded carrying value by more than 10% in the Specialty Health segment.
In determining the fair value of each reporting unit, we used an income approach, applying a discounted cash flow method that included a residual value. Based on historical experience, we made assumptions as to: (i) expected future performance and future economic conditions, (ii) projected operating earnings, (iii) projected new and renewal business as well as profit margins on such business, and (iv) a discount rate that incorporated an appropriate risk level for the reporting unit.
Management uses a significant amount of judgment in estimating the fair value of the Company’s reporting units. The key assumptions underlying the fair value process are subject to uncertainty and change. The following represent some of the potential risks that could impact these assumptions and the related expected future cash flows: (i) increased competition; (ii) an adverse change in the insurance industry and overall business climate; (iii) changes in state and federal regulations; (iv) rating agency downgrades of our insurance companies; and (v) a sustained and significant decrease in our share price and market capitalization. Our market capitalization as of December 31, 2017 was below the sum of our reporting units’ fair values. As a result, the Company assessed the factors contributing to the performance of IHC stock in 2017, and concluded that the market capitalization does not represent the fair value of the Company. The Company noted several factors that have led to a difference between the market capitalization and the fair value of the Company, including (i) the Company’s stock is thinly traded and a sale of even a small number of shares can have a large percentage impact on the price of the stock, (ii) Geneve Corporation and insiders own approximately 67% of the outstanding shares, which has had a significant adverse impact on the number of shares available for sale and therefore the trading potential of IHC stock, and (iii) lack of analyst coverage of the Company. If we experience a sustained decline in our results of operations and cash flows, or other indicators of impairment exist, we may incur a material non-cash charge to earnings relating to impairment of our goodwill, which could have a material adverse effect on our results.
Liability for Policy Benefits and Claims
The following table summarizes the prior year net favorable amount of policy benefits and claims incurred in 2017 according to the year in which it relates, together with the opening balances of the corresponding liability for policy benefits and claims (net of reinsurance recoverable) (in thousands):
| Policy Benefits and Claims |
| Prior Year Amount | ||
|
| at January 1, 2017 |
|
| Incurred in 2017 |
|
|
|
|
|
|
2016 | $ | 71,136 |
| $ | (2,691) |
2015 |
| 20,475 |
|
| (5,930) |
2014 |
| 6,951 |
|
| (311) |
2013 and Prior |
| 31,698 |
|
| 924 |
|
|
|
|
|
|
Total | $ | 130,260 |
| $ | (8,008) |
The following sections describe, for each segment, the unfavorable (favorable) development in the liability for policy benefits and claims experienced in 2017, together with the key assumptions and changes therein affecting the reserve estimates.
Specialty Health
The Specialty Health segment had a net unfavorable development of $1.4 million related to prior years. The Company experienced net unfavorable developments of $2.2 million in the STM line and $1.5 million in our occupational accident business. Due to a system conversion there was a claim processing and inventory backlog at the end of 2016 and as that backlog and those processing issues were resolved it revealed a much more favorable dental and vision block of experience than what was expected. The short-term medical line of business also had a processing and backlog issue, however, as the inventory was paid down the block experienced a worse development than what was expected revealing higher trend levels than expected. Some pricing changes and reserve strengthening has occurred on the STM block prior to this year-end. The occupational accident line of business has some low frequency and high severity components to it and we had a few rather large claims develop during the year. Since this is a small product for us that was not performing well, the Company has since sold the principal agency that produced this occupational accident business and discontinued risk exposure to the rather high severity features of the product. These developments were partially offset by a favorable development of $1.1 million in dental business.
Group Disability
The Group Disability segment had a net favorable development of $3.7 million primarily related to $2.1 million of DBL benefits and claims and $1.1 million of LTD benefits and claims experience primarily related to the 2015 business.
Due to the long-term nature of LTD, in establishing the liability for policy benefits and claims, the Company must make estimates for case reserves, IBNR, and reserves for Loss Adjustment Expenses (“LAE”). Case reserves generally equal the actuarial present value of the liability for future benefits to be paid on claims incurred as of the balance sheet date. The IBNR reserve is established based upon historical trends of existing incurred claims that were reported after the balance sheet date. The LAE reserve is calculated based on an actuarial expense study. Since the LTD block of policies is relatively small, with the potential for very large claims on individual policies, results can vary from year to year. If a small number of claimants with large claim reserves were to recover or several very large claims were incurred, the results could distort the Company’s policy benefits and claims estimates from year to year. With respect to DBL, the liability for policy benefits and claims for the most recent quarter of earned premium is established using a Net Loss Ratio methodology. The Net Loss Ratio is determined by applying the completed prior four quarters of historical Net Loss Ratios to the last quarter of earned premium. Policy
benefits and claims associated with the premium earned prior to the last quarter are established using a completion factor methodology. The completion factors are developed using the historical payment patterns for DBL. The favorable DBL development is due to lower than anticipated claims, in addition, the Company establishes a reserve for a potential premium refund for better than mandated experience which was not required to be paid in 2017.
Medical Stop-Loss
The Company experienced a net favorable development of $2.6 million related to the Medical Stop-Loss segment. Our Medical Stop-Loss business is currently in run-off.
Individual Life, Annuities and Other
All other lines, primarily life and other individual health products, experienced favorable development of $3.1 million. The favorable development in life reserves is partially due to a decrease in Paid Up Life (“PUL”) and additional reserves within the group term life line of business. The PUL change was due to a decrease in the number of eligible members and a decrease in the number of groups with the PUL benefit. Additionally, the Ordinary line of business had a pre-reinsurance true-up and released the remaining pre-reinsurance IBNR reserves.
.
CAPITAL RESOURCES |
Due to its strong capital ratios, broad licensing and excellent asset quality and credit-worthiness, the Insurance Group remains well positioned to increase or diversify its current activities. It is anticipated that future acquisitions or other expansion of operations will be funded internally from existing capital and surplus and parent company liquidity. In the event additional funds are required, it is expected that they would be borrowed or raised in the public or private capital markets to the extent determined to be necessary or desirable. The Company has no long-term debt outstanding at December 31, 2017 or 2016. See Note 11 of the Notes to Consolidated Financial Statements in Item 8 of this report.
IHC enters into a variety of contractual obligations with third parties in the ordinary course of its operations, including liabilities for insurance reserves, funds on deposit, debt and operating lease obligations. However, IHC does not believe that its cash flow requirements can be fully assessed based solely upon an analysis of these obligations. Future cash outflows, whether they are contractual obligations or not, also will vary based upon IHC’s future needs. Although some outflows are fixed, others depend on future events.
The chart below reflects the maturity distribution of IHC’s contractual obligations at December 31, 2017 (in thousands):
|
|
|
| Insurance |
| Funds |
|
|
|
|
|
| Policy |
| on |
|
|
|
| Leases |
| Benefits |
| Deposit |
| Total |
|
|
|
|
|
|
|
|
|
2018 | $ | 2,251 | $ | 105,767 | $ | 14,543 | $ | 122,561 |
2019 |
| 1,953 |
| 35,031 |
| 13,981 |
| 50,965 |
2020 |
| 1,929 |
| 28,705 |
| 13,477 |
| 44,111 |
2021 |
| 1,460 |
| 26,055 |
| 12,993 |
| 40,508 |
2022 |
| 1,125 |
| 24,224 |
| 12,630 |
| 37,979 |
2023 and thereafter |
| 195 |
| 138,326 |
| 75,913 |
| 214,434 |
|
|
|
|
|
|
|
|
|
Totals | $ | 8,913 | $ | 358,108 | $ | 143,537 | $ | 510,558 |
OUTLOOK |
For 2018, the Company anticipates that it will:
Continue to show significant increases in specialty health premiums (including STM, hospital indemnity, group limited medical and group gap and other supplemental health products, such as accident medical, gap and critical illness (“CI”) products). Given the extremely high cost and high deductible nature of ACA-compliant plans, IHC has found an increasing demand for its STM and hospital indemnity, accident and critical illness plans as either an alternative to ACA-compliant plans or in order to provide affordable ways for insureds to finance high deductibles and co-pays. We have found that consumers who do not receive significant subsidies for ACA-compliant plans are worried about how they will pay for deductible and co-pays in the event they are hospitalized are attracted to hospital indemnity, accident and CI products. Consumers who are looking for coverage that also covers out-patient services are typically more interested in purchasing STM plans and often combine it with one or more of our HIP and/or gap plans. IHC continued to sell record numbers of STM policies in 2017 despite the federal government imposing a restriction on duration of these policies to 90 days. In February 2018, three federal agencies issued a proposed rule that would reverse such executive order and return to the states the ability to determine the duration of STM in each state. Assuming the proposed rule is enacted, the Company believes the demand for STM will increase. The Company further believes that these packages (which combine STM with other benefits such as hospital indemnity, accident and critical illness, telemedicine and dental plans) will also become much more attractive once the duration of our STM products is increased to 364 days, subject to state law. In anticipation of this growth we have begun to make material enhancements to our systems and infrastructure. For all the preceding reasons, we believe that we will continue in 2018 the solid sales growth we experienced in 2017.
Continue to increase IHC’s emphasis on lead generation for its direct-to-consumer and career advisor distribution initiatives, as well as expanding our controlled sales through our call center, career model and transactional websites: HealtheDeals.com, PetPlace.com, akcpetinsurance, AspiraAmas and HealthInsurance.org.
Expand sales of our specialty health products as a result of private-label and white-label distribution arrangements with large national partners and our equity investments in two call center agencies and a worksite marketing company. We expect to continue our relationship with eHealth to sell packages of specialty health products.
Continue to diversify the distribution and administration of our pet insurance as a result of the acquisition of Pet Partners Inc. and several new distribution relationships that we expect to begin selling through in 2018.
Effective January 1, 2018, Standard Security Life began selling a new rider (“Paid Family Leave” or “PFL”) as part of our New York DBL policies in 2018. This is a result of New York State requiring employers to provide PFL, which would cover job-protected paid leave to care for a new child or sick family member or to assist when someone is called to active military service. Standard Security Life anticipates that the implementation of this coverage will more than double our current $30 million DBL block. The rates for PFL are set by New York State and as this is a new product, with no historical experience, there is no certainty as to the adequacy of the rate and therefore underwriting profitability.
Experience increases in both long-term and short-term disability premiums in 2018 generated from new distribution relationships.
Continue to evaluate strategic transactions. We plan to continue to deploy some of our cash to make additional investments and acquisitions that will continue to bolster existing or new lines of business.
Continue to focus on administrative efficiencies.
On March 31, 2016, IHC and a subsidiary of AMIC sold the stock of Risk Solutions. In addition, under the purchase and sale agreement, all of the in-force stop-loss business of Standard Security Life and Independence American produced by Risk Solutions was co-insured by Westport as of January 1, 2016. The aggregate purchase price was $152.5 million in cash, subject to adjustments and settlements. This transaction resulted in a gain of $100.8 million for the year ended December 31, 2016, net of taxes and amounts attributable to noncontrolling interests.
As a result of the sale of Risk Solutions, IHC remains highly liquid with excess capital; however, we have used some of this capital to make equity investments, retire debt and purchase IHC stock. If the Specialty Health business were to grow exponentially as a result of the turmoil in the major medical markets, IHC may need to contribute additional capital to one or more of its carriers. While the run-off of the Medical Stop-Loss line of business had a negative impact on future earnings in 2017, the growth in our other lines of business has offset this reduction in earnings.
Subject to making additional repurchases, acquisitions, investments and capital contributions to support growth, the Company will remain highly liquid in 2018 as a result of the continuing shorter duration of the portfolio. IHC has approximately $176.9 million in highly rated shorter duration securities earning on average 1.8%; our portfolio as a whole is rated, on average, AA. The low duration of our portfolio enables us, if we deem prudent, the flexibility to reinvest in much higher yielding longer-term securities, which would significantly increase investment income in the future. A low duration portfolio such as ours also mitigates the adverse impact of potential inflation. IHC will continue to monitor the financial markets and invest accordingly.
Our results depend on the adequacy of our product pricing, our underwriting, the accuracy of our reserving methodology, returns on our invested assets, and our ability to manage expenses. We will also need to be diligent with increased rate review scrutiny to effect timely rate changes and will need to stay focused on the management of medical cost drivers as medical trend levels cause margin pressures. Factors affecting these items, as well as unemployment and global financial markets, may have a material adverse effect on our results of operations and financial condition.
ITEM 7A.QUANTITATIVE AND QUALITATIVE DISCLOSURES ABOUT
MARKET RISK
The Company manages interest rate risk by seeking to maintain an investment portfolio with a duration and average life that falls within the band of the duration and average life of the applicable liabilities. Options may be utilized to modify the duration and average life of such assets.
The following summarizes the estimated pre-tax change in fair value (based upon hypothetical parallel shifts in the U.S. Treasury yield curve) of the fixed income portfolio (excluding redeemable preferred stocks) assuming immediate changes in interest rates at specified levels at December 31, 2017:
|
| Change in Interest Rates | ||||||||
|
|
|
|
|
|
|
|
|
|
|
|
| 200 basis point rise |
| 100 basis point rise |
| Base scenario |
| 100 basis point decline |
| 200 basis point decline |
|
|
|
|
|
|
|
|
|
|
|
Corporate securities | $ | 135,053 | $ | 140,589 | $ | 146,447 | $ | 152,612 | $ | 159,173 |
CMO’s |
| 6,080 |
| 6,367 |
| 6,677 |
| 7,018 |
| 7,391 |
U.S. Government obligations |
| 82,100 |
| 83,590 |
| 85,114 |
| 86,680 |
| 88,280 |
Agency MBSs |
| 13 |
| 13 |
| 14 |
| 13 |
| 13 |
GSEs |
| 8,996 |
| 9,326 |
| 9,682 |
| 10,071 |
| 10,492 |
State & Political Subdivisions |
| 159,308 |
| 169,386 |
| 179,643 |
| 189,919 |
| 200,410 |
Foreign governments |
| 3,846 |
| 3,995 |
| 4,150 |
| 4,317 |
| 4,493 |
|
|
|
|
|
|
|
|
|
|
|
Total estimated fair value | $ | 395,396 | $ | 413,266 | $ | 431,727 | $ | 450,630 | $ | 470,252 |
|
|
|
|
|
|
|
|
|
|
|
Estimated change in value | $ | (36,331) | $ | (18,461) |
|
| $ | 18,903 | $ | 38,525 |
|
|
|
|
|
|
|
|
|
|
|
The Company monitors its investment portfolio on a continuous basis and believes that the liquidity of the Insurance Group will not be adversely affected by its current investments. This monitoring includes the maintenance of an asset-liability model that matches current insurance liability cash flows with current investment cash flows. This is accomplished by first creating an insurance model of the Company's in-force policies using current assumptions on mortality, lapses and expenses. Then, current investments are assigned to specific insurance blocks in the model using appropriate prepayment schedules and future reinvestment patterns.
The results of the model specify whether the investments and their related cash flows can support the related current insurance cash flows. Additionally, various scenarios are developed changing interest rates and other related assumptions. These scenarios help evaluate the market risk due to changing interest rates in relation to the business of the Insurance Group.
In the Company's analysis of the asset-liability model, a 100 to 200 basis point change in interest rates on the Insurance Group's liabilities would not be expected to have a material adverse effect on the Company. With respect to its liabilities, if interest rates were to increase, the risk to the Company is that policies would be surrendered and assets would need to be sold. This is not a material exposure to the Company since a large portion of the Insurance Group's interest sensitive policies are burial policies that are not subject to the typical surrender patterns of other interest sensitive policies, and many of the Insurance Group's universal life and annuity policies were acquired from liquidated companies which tend to exhibit lower surrender rates than such policies of continuing companies. Additionally, there are charges to help offset the benefits being surrendered. If interest rates were to decrease substantially, the risk to the Company is that some of its investment assets would be subject to early redemption. This is not a material exposure because the Company would have additional unrealized gains in its investment portfolio to help offset the future reduction of investment income. With respect to its investments, the Company employs (from time to time as warranted) investment strategies to mitigate interest rate and other market exposures.
ITEM 8. FINANCIAL STATEMENTS AND SUPPLEMENTARY DATA
See Index to Consolidated Financial Statements and Schedules on page 61.
ITEM 9.CHANGES IN AND DISAGREEMENTS WITH ACCOUNTANTS ON
ACCOUNTING AND FINANCIAL DISCLOSURE
On October 6, 2016, the registrant filed a Form 8-K stating that the registrant has engaged RSM US LLP as its principal accountant to replace its former principal accountant KPMG LLP, effective September 13, 2016. The decision to change accountant was approved by the Audit Committee of the registrant. Neither of the reports of the former principal accountants on the financial statements for the periods ending December 31, 2015 and December 31, 2014, respectively, and through the subsequent interim periods ending September 13, 2016, contained an adverse opinion nor disclaimer of opinion, nor was either qualified or modified as to uncertainty, audit scope, or accounting principles.
During the audited period, there were no disagreements with the former principal accountant on any matter of accounting principles or practices, financial statement disclosure, or auditing scope or procedure, which disagreements, if not resolved to the satisfaction of the former accountant, would have caused the registrant to make reference to the subject matter in connection with this report.
ITEM 9A.CONTROLS AND PROCEDURES
Management’s Report on Internal Control Over Financial Reporting
Management of the Company is responsible for establishing and maintaining adequate internal control over financial reporting as such term is defined in the Securities Exchange Act of 1934 (“the Exchange Act”) Rule 13a-15(f). The Company’s internal controls are designed to provide reasonable assurance as to the reliability of its financial reporting and the preparation of financial statements for external purposes in accordance with U.S. generally accepted accounting principles.
Due to inherent limitations, internal control over financial reporting may not prevent or detect misstatement. Also, projections of any evaluation of effectiveness to future periods are subject to the risk that controls may become inadequate because of changes in conditions, or that the degree of compliance with the policies or procedures may deteriorate.
On March 24, 2017, the Company acquired 85% of the stock of PetPartners, Inc. (“PetPartners”). Management excluded from its assessment of internal control over financial reporting PetPartners’ internal control over financial reporting. PetPartners constituted approximately 1.9% of total assets as of December 31, 2017, and approximately 1.4% of total revenues for the year ended December 31, 2017, which are included in the Company’s consolidated financial statements as of and for the year ended December 31, 2017. The Company will incorporate PetPartners into its assessment of internal control over financial reporting in 2018.
With the participation of the Chief Executive Officer (“CEO”) and the Chief Financial Officer (“CFO”), our management conducted an evaluation of the effectiveness of our internal control over financial reporting based on the criteria established in Internal Control - Integrated Framework (2013) issued by the Committee of Sponsoring Organizations of the Treadway Commission. Based on this evaluation, our management has concluded that our internal control over financial reporting was effective as of December 31, 2017.
Remediation of Prior Year Material Weakness
We previously identified and disclosed in our Form 10-K for the years ended December 31, 2015 and 2016, a material weakness in our internal control over financial reporting as we did not maintain
adequate controls over the completeness and accuracy of our financial reporting for income taxes. Throughout fiscal years 2016 and 2017, we implemented changes to our processes to improve our internal control over financial reporting related to the controls over the accounting for income taxes. The following steps have been taken to remediate the conditions leading to the above stated material weakness: (i) strengthened existing tax resources by engaging independent tax consultants, and financial reporting staff attended training related to the design and operation of tax related financial reporting and corresponding internal controls; (ii) implemented enhanced risk assessment processes over accounting for income taxes, with a focus on tax accounting and disclosure for unusual and complex transactions; and (iii) improved existing and established new processes and controls to measure and record transactions related to tax accounting to enhance the effectiveness of the design and operation of those controls.
We will continue to focus on maintaining the system of internal controls that was developed and implemented over the last two years and make enhancements when and where necessary.
Evaluation of Disclosure Controls and Procedures
At the end of the period covered by this Annual Report on Form 10-K, we carried out an evaluation, under the supervision and with the participation of management, including the CEO and the CFO, of the effectiveness of our disclosure controls and procedures (as defined in Rules 13a-15(e) and 15d-15(e) under the Exchange Act). Based upon that evaluation, our CEO and CFO have concluded that our disclosure controls and procedures (as defined in Rule 13a-15(e) under the Exchange Act, as amended) were effective.
Changes in Internal Control Over Financial Reporting
Our management identified no change in our internal control over financial reporting that occurred during the fourth quarter ended December 31, 2017, that has materially affected, or is reasonably likely to materially affect, our internal control over financial reporting other than the remediation of the material weakness in our internal controls over financial reporting for income taxes as noted above.
ITEM 9B. OTHER INFORMATION
None.
PART III |
ITEM 10.DIRECTORS, EXECUTIVE OFFICERS AND CORPORATE
GOVERNANCE
The information required by this Item is hereby incorporated by reference from our definitive proxy statement relating to IHC’s 2018 annual meeting of stockholders, which definitive proxy statement will be filed with the Securities and Exchange Commission (“SEC”).
Our written Code of Business Ethics and Corporate Code of Conduct may be found on our website, www.ihcgroup.com, under the Corporate Information / Corporate Governance tabs. Both Codes apply to all of our directors, officers and employees, including our principal executive officer and our senior financial officers. Any amendment to or waiver from either of the Codes will be posted to the same location on our website, to the extent such disclosure is legally required.
ITEM 11.EXECUTIVE COMPENSATION
The information required by this Item is hereby incorporated by reference from our definitive proxy statement relating to IHC’s 2018 annual meeting of stockholders, which definitive proxy statement will be filed with the SEC.
ITEM 12.SECURITY OWNERSHIP OF CERTAIN BENEFICIAL OWNERS AND
MANAGEMENT AND RELATED STOCKHOLDER MATTERS
The information required by this Item is hereby incorporated by reference from our definitive proxy statement relating to IHC’s 2018 annual meeting of stockholders, which definitive proxy statement will be filed with the SEC.
ITEM 13.CERTAIN RELATIONSHIPS, RELATED TRANSACTIONS AND DIRECTOR INDEPENDENCE
The information required by this Item is hereby incorporated by reference from our definitive proxy statement relating to IHC’s 2018 annual meeting of stockholders, which definitive proxy statement will be filed with the SEC.
ITEM 14.PRINCIPAL ACCOUNTING FEES AND SERVICES
The information required by this Item is hereby incorporated by reference from our definitive proxy statement relating to IHC’s 2018 annual meeting of stockholders, which definitive proxy statement will be filed with the SEC.
PART IV
ITEM 15.EXHIBITS AND FINANCIAL STATEMENT SCHEDULES
(a) (1) and (2)
See Index to Consolidated Financial Statements and Schedules on page 61.
(a) (3) EXHIBITS
See Exhibit Index on page 124.
SIGNATURES
Pursuant to the requirements of Section 13 or Section 15(d) of the Securities Exchange Act of 1934, the Registrant has duly caused this report to be signed on its behalf by the undersigned, thereunto duly authorized, on March 26, 2017.
INDEPENDENCE HOLDING COMPANY
REGISTRANT
By:/s/ Roy T. K. Thung
Roy T.K. Thung
Chief Executive Officer
(Principal Executive Officer)
By:/s/ Teresa A. Herbert
Teresa A. Herbert
Senior Vice President and Chief Financial Officer
(Principal Financial and Accounting Officer)
Pursuant to the requirements of the Securities Exchange Act of 1934, this report has been signed below by the following persons on behalf of the Registrant and in the capacities indicated as of the 26th day of March, 2018.
/s/ Larry R. Graber | /s/ Steven B. Lapin |
Larry R. Graber | Steven B. Lapin |
Director and Senior Vice President | Vice Chairman of the Board of Directors |
/s/ Allan C. Kirkman | /s/ Ronald I. Simon |
Allan C. Kirkman | Ronald I. Simon |
Director | Director |
/s/ John L. Lahey | /s/ James G. Tatum |
John L. Lahey | James G. Tatum |
Director | Director |
/s/ Roy T.K. Thung | /s/ David T. Kettig |
Roy T.K. Thung | David T. Kettig |
Chairman of the Board of Directors and | Director, President and Chief Operating Officer |
Chief Executive Officer |
|
(Principal Executive Officer) |
|
/s/ Teresa A. Herbert |
|
Teresa A. Herbert |
|
Director, Senior Vice President and |
|
Chief Financial Officer |
|
(Principal Financial and Accounting Officer) |
|
INDEPENDENCE HOLDING COMPANY AND SUBSIDIARIES | ||||
| ||||
INDEX TO CONSOLIDATED FINANCIAL STATEMENTS AND SCHEDULES | ||||
| ||||
|
|
| PAGE | |
|
|
|
| |
|
| 62 | ||
|
|
|
| |
CONSOLIDATED FINANCIAL STATEMENTS: |
|
|
| |
|
|
|
| |
|
| 66 | ||
|
|
|
| |
|
| 67 | ||
|
|
|
| |
|
| 68 | ||
|
|
|
| |
|
| 69 | ||
|
|
|
| |
|
| 70 | ||
|
|
|
| |
|
| 71 | ||
|
|
|
| |
SCHEDULES:* |
|
|
| |
|
|
|
| |
Summary of Investments - Other Than Investments in Related Parties (Schedule I) |
|
| 118 | |
|
|
|
| |
Condensed Financial Information of Parent Company (Schedule II) |
|
| 119 | |
|
|
|
|
|
|
| 122 | ||
|
|
|
| |
|
| 123 | ||
|
|
|
| |
*All other schedules have been omitted as they are not applicable or not required, or the information is included in the Consolidated Financial Statements or Notes thereto.
The Board of Directors and Stockholders |
Independence Holding Company: |
Opinion on the Internal Control Over Financial Reporting
We have audited Independence Holding Company's (the Company) internal control over financial reporting as of December 31, 2017, based on criteria established in Internal Control — Integrated Framework issued by the Committee of Sponsoring Organizations of the Treadway Commission in 2013. In our opinion, the Company maintained, in all material respects, effective internal control over financial reporting as of December 31, 2017, based on criteria established in Internal Control — Integrated Framework issued by the Committee of Sponsoring Organizations of the Treadway Commission in 2013.
We have also audited, in accordance with the standards of the Public Company Accounting Oversight Board (United States) (PCAOB), the consolidated balance sheets as of December 31, 2017 and 2016, the related consolidated statements of income, comprehensive income, changes in stockholders' equity and cash flows for the years then ended, and the related notes to the consolidated financial statements (collectively, the financial statements) of the Company and our report dated March 26, 2018 expressed an unqualified opinion.
As described in Management’s Report on Internal Control Over Financial Reporting, management has excluded PetPartners, Inc. from its assessment of internal control over financial reporting as of December 31, 2017, because it was acquired by the Company in a purchase business combination in the first quarter of 2017. We have also excluded PetPartners, Inc. from our audit of internal control over financial reporting. PetPartners, Inc. is a majority owned subsidiary whose total assets and total revenue represent approximately 1.9% percent and 1.4% percent, respectively, of the related consolidated financial statement amounts as of and for the year ended December 31, 2017.
Basis for Opinion
The Company’s management is responsible for maintaining effective internal control over financial reporting and for its assessment of the effectiveness of internal control over financial reporting in the accompanying Management’s Report of Internal Control over Financial Reporting. Our responsibility is to express an opinion on the Company’s internal control over financial reporting based on our audit. We are a public accounting firm registered with the PCAOB and are required to be independent with respect to the Company in accordance with U.S. federal securities laws and the applicable rules and regulations of the Securities and Exchange Commission and the PCAOB.
We conducted our audit in accordance with the standards of the PCAOB. Those standards require that we plan and perform the audit to obtain reasonable assurance about whether effective internal control over financial reporting was maintained in all material respects. Our audit included obtaining an understanding of internal control over financial reporting, assessing the risk that a material weakness exists, and testing and evaluating the design and operating effectiveness of internal control based on the assessed risk. Our audit also included performing such other procedures as we considered necessary in the circumstances. We believe that our audit provides a reasonable basis for our opinion.
Definition and Limitations of Internal Control Over Financial Reporting
A company's internal control over financial reporting is a process designed to provide reasonable assurance regarding the reliability of financial reporting and the preparation of financial statements for external purposes in accordance with generally accepted accounting principles. A company's internal control over financial reporting includes those policies and procedures that (1) pertain to the maintenance of records that, in reasonable detail, accurately and fairly reflect the transactions and dispositions of the assets of the company; (2) provide reasonable assurance that transactions are recorded as necessary to permit preparation of financial statements in accordance with generally accepted accounting principles, and that receipts and expenditures of the company are being made only in accordance with authorizations of management and directors of the company; and (3) provide reasonable assurance regarding prevention or timely detection of unauthorized acquisition, use or disposition of the company's assets that could have a material effect on the financial statements.
Because of its inherent limitations, internal control over financial reporting may not prevent or detect misstatements. Also, projections of any evaluation of effectiveness to future periods are subject to the risk that controls may become inadequate because of changes in conditions, or that the degree of compliance with the policies or procedures may deteriorate.
/s/ RSM US LLP
Jacksonville, Florida
March 26, 2018
Report of Independent Registered Public Accounting Firm |
To the Stockholders and the Board of Directors of Independence Holding Company |
Opinion on the Financial Statements
We have audited the accompanying consolidated balance sheets of Independence Holding Company and its subsidiaries (the Company) as of December 31, 2017 and 2016, the related consolidated statements of income, comprehensive income, changes in stockholders' equity and cash flows for the years then ended, and the related notes to the consolidated financial statements and schedules (collectively, the financial statements). In our opinion, the financial statements present fairly, in all material respects, the financial position of the Company as of December 31, 2017 and 2016, and the results of its operations and its cash flows for the years then ended, in conformity with accounting principles generally accepted in the United States of America.
We have also audited, in accordance with the standards of the Public Company Accounting Oversight Board (United States) (PCAOB), the Company's internal control over financial reporting as of December 31, 2017, based on criteria established in Internal Control — Integrated Framework issued by the Committee of Sponsoring Organizations of the Treadway Commission in 2013, and our report dated March 26, 2018 expressed an unqualified opinion on the effectiveness of the Company's internal control over financial reporting.
As discussed in Note 3 to the financial statements, the Company sold Risk Solutions, LLC and accounted for the sale as discontinued operations. We audited the adjustments described in Note 3 that were applied to restate the 2015 financial statements. In our opinion, such adjustments are appropriate and have been properly applied.
Basis for Opinion
These financial statements are the responsibility of the Company’s management. Our responsibility is to express an opinion on the Company’s financial statements based on our audits. We are a public accounting firm registered with the PCAOB and are required to be independent with respect to the Company in accordance with U.S. federal securities laws and the applicable rules and regulations of the Securities and Exchange Commission and the PCAOB.
We conducted our audits in accordance with the standards of the PCAOB. Those standards require that we plan and perform the audits to obtain reasonable assurance about whether the financial statements are free of material misstatement, whether due to error or fraud. Our audits included performing procedures to assess the risks of material misstatement of the financial statements, whether due to error or fraud, and performing procedures that respond to those risks. Such procedures included examining, on a test basis, evidence regarding the amounts and disclosures in the financial statements. Our audits also included evaluating the accounting principles used and significant estimates made by management, as well as evaluating the overall presentation of the financial statements. We believe that our audits provide a reasonable basis for our opinion.
/s/ RSM US LLP
We have served as the Company's auditor since 2016.
Jacksonville, Florida
March 26, 2018
Report of Independent Registered Public Accounting Firm |
The Board of Directors and Stockholders |
Independence Holding Company: |
We have audited, before the effects of the adjustments to retrospectively reflect discontinued operations discussed in Note 3 to the consolidated financial statements, the consolidated statements of income, comprehensive income (loss), changes in stockholders’ equity, and cash flows of Independence Holding Company and subsidiaries (the Company) for the year ended December 31, 2015. In connection with our audit of the consolidated financial statements, we also have audited, before the effects of the adjustments to retrospectively reflect the discontinued operations discussed in Note 3 to the consolidated financial statements, the consolidated financial statement schedules II to IV, as of December 31, 2015 and for the year ended December 31, 2015. The 2015 financial statements and schedules before the effects of these adjustments discussed in Note 3 are not presented herein. The 2015 consolidated financial statements and financial statement schedules are the responsibility of the Company’s management. Our responsibility is to express an opinion on these consolidated financial statements and financial statement schedules based on our audit.
We conducted our audit in accordance with the standards of the Public Company Accounting Oversight Board (United States). Those standards require that we plan and perform the audit to obtain reasonable assurance about whether the financial statements are free of material misstatement. An audit includes examining, on a test basis, evidence supporting the amounts and disclosures in the financial statements. An audit also includes assessing the accounting principles used and significant estimates made by management, as well as evaluating the overall financial statement presentation. We believe that our audit provides a reasonable basis for our opinion.
In our opinion, the consolidated financial statements referred to above, before the effects of the adjustments to retrospectively reflect discontinued operations discussed in Note 3 to the consolidated financial statements, present fairly, in all material respects, the results of operations and cash flows of Independence Holding Company and subsidiaries for the year ended December 31, 2015, in conformity with U.S. generally accepted accounting principles. Also in our opinion, the related financial statement schedules for 2015, when considered in relation to the basic consolidated financial statements taken as a whole, present fairly, in all material respects, the information set forth therein.
We were not engaged to audit, review, or apply any procedures to the adjustments to retrospectively reflect discontinued operations discussed in Note 3 to the consolidated financial statements, we do not express an opinion or any other form of assurance about whether such adjustments are appropriate and have been properly applied. Those adjustments were audited by a successor auditor.
/s/ KPMG LLP
New York, New York
June 3, 2016
INDEPENDENCE HOLDING COMPANY AND SUBSIDIARIES | ||||||
CONSOLIDATED BALANCE SHEETS (In thousands, except share data) | ||||||
DECEMBER 31, | ||||||
| ||||||
|
|
| 2017 |
|
| 2016 |
|
|
|
|
|
|
|
ASSETS: |
|
|
|
|
|
|
Investments: |
|
|
|
|
|
|
Short-term investments |
| $ | 50 |
| $ | 6,912 |
Securities purchased under agreements to resell |
|
| 10,269 |
|
| 28,962 |
Trading securities |
|
| 490 |
|
| 592 |
Fixed maturities, available-for-sale |
|
| 441,912 |
|
| 449,487 |
Equity securities, available-for-sale |
|
| 5,630 |
|
| 5,333 |
Other investments |
|
| 18,547 |
|
| 23,534 |
Total investments |
|
| 476,898 |
|
| 514,820 |
|
|
|
|
|
|
|
Cash and cash equivalents |
|
| 26,465 |
|
| 22,010 |
Due and unpaid premiums |
|
| 21,950 |
|
| 42,896 |
Due from reinsurers |
|
| 380,593 |
|
| 440,285 |
Premium and claim funds |
|
| 11,108 |
|
| 17,952 |
Goodwill |
|
| 50,697 |
|
| 41,573 |
Other assets |
|
| 72,912 |
|
| 54,928 |
|
|
|
|
|
|
|
TOTAL ASSETS |
| $ | 1,040,623 |
| $ | 1,134,464 |
|
|
|
|
|
|
|
LIABILITIES AND EQUITY: |
|
|
|
|
|
|
LIABILITIES: |
|
|
|
|
|
|
Policy benefits and claims |
| $ | 168,683 |
| $ | 219,113 |
Future policy benefits |
|
| 214,766 |
|
| 219,450 |
Funds on deposit |
|
| 143,537 |
|
| 145,749 |
Unearned premiums |
|
| 6,666 |
|
| 9,786 |
Other policyholders' funds |
|
| 10,402 |
|
| 9,769 |
Due to reinsurers |
|
| 3,808 |
|
| 35,796 |
Accounts payable, accruals and other liabilities |
|
| 56,453 |
|
| 55,477 |
Liabilities attributable to discontinued operations |
|
| - |
|
| 68 |
|
|
|
|
|
|
|
TOTAL LIABILITIES |
|
| 604,315 |
|
| 695,208 |
|
|
|
|
|
|
|
Commitments and contingencies (Note 15) |
|
|
|
|
|
|
Redeemable noncontrolling interest |
|
| 2,065 |
|
| - |
|
|
|
|
|
|
|
STOCKHOLDERS’ EQUITY: |
|
|
|
|
|
|
Preferred stock $1.00 par value, 100,000 shares authorized; |
|
|
|
|
|
|
none issued or outstanding |
|
| - |
|
| - |
Common stock $1.00 par value, 23,000,000 shares authorized; |
|
|
|
|
|
|
18,625,458 and 18,620,508 shares issued; and 14,890,285 and |
|
|
|
|
|
|
17,102,525 shares outstanding |
|
| 18,625 |
|
| 18,620 |
Paid-in capital |
|
| 124,538 |
|
| 126,468 |
Accumulated other comprehensive loss |
|
| (4,598) |
|
| (6,964) |
Treasury stock, at cost; 3,735,173 and 1,517,983 shares |
|
| (63,404) |
|
| (17,483) |
Retained earnings |
|
| 356,383 |
|
| 315,918 |
|
|
|
|
|
|
|
TOTAL IHC STOCKHOLDERS’ EQUITY |
|
| 431,544 |
|
| 436,559 |
NONREDEEMABLE NONCONTROLLING INTERESTS |
|
| 2,699 |
|
| 2,697 |
|
|
|
|
|
|
|
TOTAL EQUITY |
|
| 434,243 |
|
| 439,256 |
|
|
|
|
|
|
|
TOTAL LIABILITIES AND EQUITY |
| $ | 1,040,623 |
| $ | 1,134,464 |
See accompanying notes to consolidated financial statements. |
INDEPENDENCE HOLDING COMPANY AND SUBSIDIARIES | ||||||||
CONSOLIDATED STATEMENTS OF INCOME (In thousands, except per share data) | ||||||||
YEARS ENDED DECEMBER 31, |
|
|
|
|
|
|
|
|
|
| 2017 |
|
| 2016 |
|
| 2015 |
REVENUES: |
|
|
|
|
|
|
|
|
Premiums earned | $ | 282,266 |
| $ | 262,704 |
| $ | 479,534 |
Net investment income |
| 16,276 |
|
| 16,570 |
|
| 17,237 |
Fee income |
| 16,765 |
|
| 16,446 |
|
| 10,651 |
Other income |
| 2,648 |
|
| 12,257 |
|
| 10,267 |
Gain on sale of subsidiary to joint venture |
| - |
|
| - |
|
| 9,940 |
Net realized investment gains |
| 2,539 |
|
| 4,502 |
|
| 3,094 |
Other-than-temporary impairment losses: |
|
|
|
|
|
|
|
|
Total other-than-temporary impairment losses |
| - |
|
| (1,475) |
|
| (228) |
Portion of losses recognized in other comprehensive income (loss) |
| - |
|
| - |
|
| - |
Net impairment losses recognized in earnings |
| - |
|
| (1,475) |
|
| (228) |
|
|
|
|
|
|
|
|
|
|
| 320,494 |
|
| 311,004 |
|
| 530,495 |
|
|
|
|
|
|
|
|
|
EXPENSES: |
|
|
|
|
|
|
|
|
Insurance benefits, claims and reserves |
| 135,054 |
|
| 145,231 |
|
| 307,178 |
Selling, general and administrative expenses |
| 157,104 |
|
| 132,174 |
|
| 177,641 |
Interest expense on debt |
| - |
|
| 1,534 |
|
| 1,798 |
|
|
|
|
|
|
|
|
|
|
| 292,158 |
|
| 278,939 |
|
| 486,617 |
|
|
|
|
|
|
|
|
|
Income from continuing operations before income taxes |
| 28,336 |
|
| 32,065 |
|
| 43,878 |
Income taxes (benefits) |
| (13,794) |
|
| 9,555 |
|
| 15,904 |
|
|
|
|
|
|
|
|
|
Income from continuing operations, net of tax |
| 42,130 |
|
| 22,510 |
|
| 27,974 |
|
|
|
|
|
|
|
|
|
Discontinued operations: |
|
|
|
|
|
|
|
|
Income from discontinued operations, before income taxes |
| - |
|
| 117,617 |
|
| 4,310 |
Income taxes on discontinued operations |
| - |
|
| 6,813 |
|
| 1,762 |
Income from discontinued operations, net of tax |
| - |
|
| 110,804 |
|
| 2,548 |
|
|
|
|
|
|
|
|
|
Net income |
| 42,130 |
|
| 133,314 |
|
| 30,522 |
(Income) from nonredeemable noncontrolling interests |
| (27) |
|
| (10,016) |
|
| (578) |
(Income) from redeemable noncontrolling interests |
| (61) |
|
| - |
|
| - |
|
|
|
|
|
|
|
|
|
NET INCOME ATTRIBUTABLE TO IHC | $ | 42,042 |
| $ | 123,298 |
| $ | 29,944 |
|
|
|
|
|
|
|
|
|
Basic income per common share (Note 2) |
|
|
|
|
|
|
|
|
Income from continuing operations | $ | 2.67 |
| $ | 1.28 |
| $ | 1.59 |
Income from discontinued operations |
| - |
|
| 5.90 |
|
| 0.14 |
Basic income per common share | $ | 2.67 |
| $ | 7.18 |
| $ | 1.73 |
|
|
|
|
|
|
|
|
|
WEIGHTED AVERAGE SHARES OUTSTANDING |
| 15,718 |
|
| 17,162 |
|
| 17,314 |
|
|
|
|
|
|
|
|
|
Diluted income per common share (Note 2) |
|
|
|
|
|
|
|
|
Income from continuing operations | $ | 2.63 |
| $ | 1.27 |
| $ | 1.58 |
Income from discontinued operations |
| - |
|
| 5.82 |
|
| 0.13 |
Diluted income per common share | $ | 2.63 |
| $ | 7.09 |
| $ | 1.71 |
|
|
|
|
|
|
|
|
|
WEIGHTED AVERAGE DILUTED SHARES OUTSTANDING |
| 16,008 |
|
| 17,379 |
|
| 17,484 |
|
|
|
|
|
|
|
|
|
See accompanying notes to consolidated financial statements. |
INDEPENDENCE HOLDING COMPANY AND SUBSIDIARIES | ||||||
CONSOLIDATED STATEMENTS OF COMPREHENSIVE INCOME (In thousands) | ||||||
YEARS ENDED DECEMBER 31, | ||||||
|
| 2017 |
| 2016 |
| 2015 |
|
|
|
|
|
|
|
Net income | $ | 42,130 | $ | 133,314 | $ | 30,522 |
Other comprehensive income (loss): |
|
|
|
|
|
|
Available-for-sale securities: |
|
|
|
|
|
|
Unrealized gains (losses) on available-for-sale securities, pre-tax |
| 4,996 |
| (5,424) |
| (5,475) |
Tax expense (benefit) on unrealized gains (losses) on available-for-sale securities |
| 1,815 |
| (1,916) |
| (2,013) |
Unrealized gains (losses) on available-for-sale securities, net of taxes |
| 3,181 |
| (3,508) |
| (3,462) |
|
|
|
|
|
|
|
Other comprehensive income (loss), net of tax |
| 3,181 |
| (3,508) |
| (3,462) |
|
|
|
|
|
|
|
COMPREHENSIVE INCOME, NET OF TAX |
| 45,311 |
| 129,806 |
| 27,060 |
|
|
|
|
|
|
|
Comprehensive (income) loss, net of tax, attributable to noncontrolling interests: |
|
|
|
|
|
|
(Income) loss from noncontrolling interests in subsidiaries |
| (88) |
| (10,016) |
| (578) |
Other comprehensive (income) loss, net of tax, attributable to noncontrolling interests: |
|
|
|
|
|
|
Unrealized (gains) losses on available-for-sale securities, net of tax |
| - |
| (118) |
| (5) |
|
|
|
|
|
|
|
Other comprehensive (income) loss, net of tax, attributable to noncontrolling interests |
| - |
| (118) |
| (5) |
|
|
|
|
|
|
|
COMPREHENSIVE (INCOME) LOSS, NET OF TAX, |
|
|
|
|
|
|
ATTRIBUTABLE TO NONCONTROLLING INTERESTS |
| (88) |
| (10,134) |
| (583) |
|
|
|
|
|
|
|
COMPREHENSIVE INCOME, NET OF TAX, |
|
|
|
|
|
|
ATTRIBUTABLE TO IHC | $ | 45,223 | $ | 119,672 | $ | 26,477 |
See accompanying notes to consolidated financial statements.
INDEPENDENCE HOLDING COMPANY AND SUBSIDIARIES | ||||||||||||||||||||
CONSOLIDATED STATEMENTS OF CHANGES IN STOCKHOLDERS' EQUITY (In thousands, except share data) | ||||||||||||||||||||
| ||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| |||||
|
|
|
|
| ACCUMULATED |
|
|
|
|
|
|
| NONREDEEMABLE |
|
| |||||
|
|
|
|
| OTHER |
|
|
|
|
| TOTAL IHC |
| NONCONTROLLING |
|
| |||||
| COMMON STOCK |
| PAID-IN |
| COMPREHENSIVE |
| TREASURY STOCK, AT COST |
| RETAINED |
| STOCKHOLDERS' |
| INTERESTS IN |
| TOTAL | |||||
| SHARES |
| AMOUNT |
| CAPITAL |
| INCOME (LOSS) |
| SHARES |
| AMOUNT |
| EARNINGS |
| EQUITY |
| SUBSIDIARIES |
| EQUITY | |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| |
BALANCE AT DECEMBER 31, 2014 | 18,531,158 | $ | 18,531 | $ | 127,098 | $ | 22 |
| (1,160,118) | $ | (12,141) | $ | 166,177 | $ | 299,687 | $ | 9,925 | $ | 309,612 | |
Net income |
|
|
|
|
|
|
|
|
|
|
|
| 29,944 |
| 29,944 |
| 578 |
| 30,522 | |
Other comprehensive loss, net of tax |
|
|
|
|
|
| (3,467) |
|
|
|
|
|
|
| (3,467) |
| 5 |
| (3,462) | |
Repurchases of common stock |
|
|
|
|
|
|
|
| (143,307) |
| (1,820) |
|
|
| (1,820) |
| - |
| (1,820) | |
Acquisition of subsidiary |
|
|
|
|
|
|
|
|
|
|
|
|
|
| - |
| 608 |
| 608 | |
Purchases of noncontrolling interests |
|
|
|
| 112 |
| 5 |
|
|
|
|
|
|
| 117 |
| (1,851) |
| (1,734) | |
Common stock dividends ($0.09 per share) |
|
|
|
|
|
|
|
|
|
|
|
| (1,562) |
| (1,562) |
| - |
| (1,562) | |
Share-based compensation | 38,025 |
| 38 |
| 408 |
|
|
|
|
|
|
|
|
| 446 |
| - |
| 446 | |
Other capital transactions |
|
|
|
| 115 |
|
|
|
|
|
|
| (109) |
| 6 |
| 88 |
| 94 | |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| |
BALANCE AT DECEMBER 31, 2015 | 18,569,183 | $ | 18,569 | $ | 127,733 | $ | (3,440) |
| (1,303,425) | $ | (13,961) | $ | 194,450 | $ | 323,351 | $ | 9,353 | $ | 332,704 | |
Net income |
|
|
|
|
|
|
|
|
|
|
|
| 123,298 |
| 123,298 |
| 10,016 |
| 133,314 | |
Other comprehensive income, net of tax |
|
|
|
|
|
| (3,626) |
|
|
|
|
|
|
| (3,626) |
| 118 |
| (3,508) | |
Repurchases of common stock |
|
|
|
|
|
|
|
| (214,558) |
| (3,522) |
|
|
| (3,522) |
| - |
| (3,522) | |
Purchases of noncontrolling interests |
|
|
|
| (2,302) |
| 102 |
|
|
|
|
|
|
| (2,200) |
| (15,911) |
| (18,111) | |
Common stock dividends ($0.105 per share) |
|
|
|
|
|
|
|
|
|
|
|
| (1,800) |
| (1,800) |
| - |
| (1,800) | |
Share-based compensation | 51,325 |
| 51 |
| 727 |
|
|
|
|
|
|
|
|
| 778 |
| - |
| 778 | |
Distributions to noncontrolling interests |
|
|
|
|
|
|
|
|
|
|
|
|
|
| - |
| (947) |
| (947) | |
Other capital transactions |
|
|
|
| 310 |
|
|
|
|
|
|
| (30) |
| 280 |
| 68 |
| 348 | |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| |
BALANCE AT DECEMBER 31, 2016 | 18,620,508 | $ | 18,620 | $ | 126,468 | $ | (6,964) |
| (1,517,983) | $ | (17,483) | $ | 315,918 | $ | 436,559 | $ | 2,697 | $ | 439,256 | |
Net income |
|
|
|
|
|
|
|
|
|
|
|
| 42,042 |
| 42,042 |
| 27 |
| 42,069 | |
Other comprehensive income, net of tax |
|
|
|
|
|
| 3,181 |
|
|
|
|
|
|
| 3,181 |
| - |
| 3,181 | |
Repurchases of common stock |
|
|
|
|
|
|
|
| (2,289,502) |
| (46,527) |
|
|
| (46,527) |
| - |
| (46,527) | |
Common stock dividends ($0.16 per share) |
|
|
|
|
|
|
|
|
|
|
|
| (2,392) |
| (2,392) |
| - |
| (2,392) | |
Share-based compensation | 4,950 |
| 5 |
| (1,930) |
|
|
| 72,312 |
| 606 |
|
|
| (1,319) |
| - |
| (1,319) | |
Distributions to noncontrolling interests |
|
|
|
|
|
|
|
|
|
|
|
|
|
| - |
| (25) |
| (25) | |
Reclassification of the stranded tax effects |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| |
in accumulated other comprehensive income |
|
|
|
|
|
| (815) |
|
|
|
|
| 815 |
| - |
|
|
| - | |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| |
BALANCE AT DECEMBER 31, 2017 | 18,625,458 | $ | 18,625 | $ | 124,538 | $ | (4,598) |
| (3,735,173) | $ | (63,404) | $ | 356,383 | $ | 431,544 | $ | 2,699 | $ | 434,243 | |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| |
See accompanying notes to consolidated financial statements. |
INDEPENDENCE HOLDING COMPANY AND SUBSIDIARIES | ||||||||
CONSOLIDATED STATEMENTS OF CASH FLOWS (In thousands) | ||||||||
YEARS ENDED DECEMBER 31, | ||||||||
|
| 2017 |
|
| 2016 |
|
| 2015 |
CASH FLOWS PROVIDED BY (USED BY) OPERATING ACTIVITIES: |
|
|
|
|
|
|
|
|
Net income | $ | 42,130 |
| $ | 133,314 |
| $ | 30,522 |
Adjustments to reconcile net income to net change in cash from |
|
|
|
|
|
|
|
|
operating activities: |
|
|
|
|
|
|
|
|
Gain on disposal of discontinued operations, net of tax |
| - |
|
| (110,337) |
|
| - |
Gain on sale of subsidiary to joint venture |
| - |
|
| - |
|
| (9,940) |
Gain on disposition of assets |
| - |
|
| - |
|
| (5,053) |
Amortization of deferred acquisition costs |
| 340 |
|
| 319 |
|
| 3,524 |
Net realized investment gains |
| (2,539) |
|
| (4,502) |
|
| (3,094) |
Other-than-temporary impairment losses |
| - |
|
| 1,475 |
|
| 228 |
Equity income from equity method investments |
| (1,846) |
|
| (62) |
|
| (405) |
Depreciation and amortization |
| 1,920 |
|
| 1,831 |
|
| 2,313 |
Deferred tax expense |
| (9,746) |
|
| 4,445 |
|
| 614 |
Other |
| 6,535 |
|
| 7,809 |
|
| 6,724 |
Changes in assets and liabilities: |
|
|
|
|
|
|
|
|
Net purchases (sales) of trading securities |
| - |
|
| 3,727 |
|
| 5,356 |
Change in insurance liabilities |
| (90,065) |
|
| (120,064) |
|
| (18,907) |
Change in deferred acquisition costs |
| (353) |
|
| (296) |
|
| 26,774 |
Change in amounts due from reinsurers |
| 59,692 |
|
| 42,787 |
|
| (202,617) |
Change in premium and claim funds |
| 6,844 |
|
| 3,094 |
|
| (1,891) |
Change in current income tax liability |
| (5,979) |
|
| (9,146) |
|
| 3,386 |
Change in due and unpaid premiums |
| 20,946 |
|
| 26,179 |
|
| (6,447) |
Other operating activities |
| 725 |
|
| (11,571) |
|
| 4,189 |
Net change in cash from operating activities |
| 28,604 |
|
| (30,998) |
|
| (164,724) |
|
|
|
|
|
|
|
|
|
CASH FLOWS PROVIDED BY (USED BY) INVESTING ACTIVITIES: |
|
|
|
|
|
|
|
|
Net (purchases) sales and maturities of short-term investments |
| 6,849 |
|
| (6,870) |
|
| - |
Net (purchases) sales of securities under resale agreements |
| 18,693 |
|
| (677) |
|
| (11,495) |
Sales of equity securities |
| - |
|
| 3,577 |
|
| 11,986 |
Purchases of equity securities |
| - |
|
| - |
|
| (6,601) |
Sales of fixed maturities |
| 193,930 |
|
| 410,983 |
|
| 629,376 |
Maturities and other repayments of fixed maturities |
| 28,355 |
|
| 47,285 |
|
| 42,630 |
Purchases of fixed maturities |
| (210,694) |
|
| (486,398) |
|
| (521,417) |
Payments to acquire business, net of cash acquired |
| (12,323) |
|
| - |
|
| 511 |
Proceeds on sales of subsidiaries, net of cash divested |
| - |
|
| 135,736 |
|
| 4,518 |
Proceeds on sales of assets |
| - |
|
| - |
|
| 8,000 |
Change in policy loans |
| - |
|
| 1 |
|
| 10,629 |
Sales of and distributions from other investments |
| 5,246 |
|
| 4,210 |
|
| 1,000 |
Purchases of other investments |
| (602) |
|
| (4,371) |
|
| - |
Other investing activities |
| (1,854) |
|
| (4,601) |
|
| (809) |
Net change in cash from investing activities |
| 27,600 |
|
| 98,875 |
|
| 168,328 |
|
|
|
|
|
|
|
|
|
CASH FLOWS PROVIDED BY (USED BY) FINANCING ACTIVITIES: |
|
|
|
|
|
|
|
|
Repurchases of common stock |
| (46,401) |
|
| (3,522) |
|
| (1,820) |
Cash paid in acquisitions of noncontrolling interests |
| - |
|
| (18,111) |
|
| (1,734) |
(Withdrawals of) proceeds from investment-type insurance contracts |
| (1,736) |
|
| 1,898 |
|
| (2,306) |
Repayments of debt |
| - |
|
| (42,935) |
|
| (2,617) |
Dividends paid |
| (1,928) |
|
| (1,553) |
|
| (1,392) |
Payments related to tax withholding for sharebased compensation |
| (1,659) |
|
| - |
|
| - |
Other financing activities |
| (25) |
|
| (815) |
|
| 353 |
Net change in cash from financing activities |
| (51,749) |
|
| (65,038) |
|
| (9,516) |
|
|
|
|
|
|
|
|
|
Net change in cash and cash equivalents, including discontinued operations |
| 4,455 |
|
| 2,839 |
|
| (5,912) |
Cash and cash equivalents, beginning of year, including discontinued operations |
| 22,010 |
|
| 19,171 |
|
| 25,083 |
|
|
|
|
|
|
|
|
|
Cash and cash equivalents, end of year, including discontinued operations | $ | 26,465 |
| $ | 22,010 |
| $ | 19,171 |
|
|
|
|
|
|
|
|
|
See accompanying notes to consolidated financial statements.
Note 1. Organization, Consolidation, Basis of Presentation and Accounting Policies
(A)Business and Organization
Independence Holding Company, a Delaware corporation (“IHC”), is a holding company principally engaged in the life and health insurance business through: (i) its insurance companies, Standard Security Life Insurance Company of New York ("Standard Security Life"), Madison National Life Insurance Company, Inc. ("Madison National Life"), and Independence American Insurance Company (“Independence American”); and (ii) its marketing and administrative companies, including IHC Specialty Benefits Inc., IHC Carrier Solutions, Inc. and a majority interest in PetPartners, Inc. (“PetPartners”). IHC also owns a significant equity interest in: (i) Ebix Health Exchange Holdings, LLC (“Ebix Health Exchange”), an administration exchange for health insurance. Standard Security Life, Madison National Life and Independence American are sometimes collectively referred to as the “Insurance Group”. IHC and its subsidiaries (including the Insurance Group) are sometimes collectively referred to as the "Company", or “IHC”, or are implicit in the terms “we”, “us” and “our”.
Geneve Corporation, a diversified financial holding company, and its affiliated entities, held approximately 61% of IHC's outstanding common stock at December 31, 2017.
(B)Consolidation
AMIC Holdings, Inc.
AMIC Holdings, Inc., formerly known as American Independence Corp., (“AMIC”) is an insurance holding company engaged in the insurance and reinsurance business. At December 31, 2015, the Company owned approximately 92% of its outstanding common stock. On August 31, 2016, IHC took AMIC private by way of a statutory “short-form" merger. The Company paid $18,111,000 for the remaining shares of AMIC common stock owned by noncontrolling interests and as a result, the Company now owns all of the outstanding common stock of AMIC. In connection with the transaction, $2,200,000 was charged to paid-in capital representing: (i) the difference between the fair value of the consideration paid for the shares and the carrying amount of noncontrolling interests; plus (ii) specific, direct costs of the transaction.
In 2015, IHC purchased shares of AMIC common stock increasing its ownership interest in AMIC from 90% to approximately 92%.
Effects of Ownership Changes in Subsidiaries
The following table summarizes the effects of any changes in the Company’s ownership interests in its less than wholly owned subsidiaries on IHC’s equity for the years indicated (in thousands).
|
|
| 2017 |
| 2016 |
| 2015 |
|
|
|
|
|
|
|
|
Changes in IHC’s paid-in capital: |
|
|
|
|
|
|
|
Purchases of AMIC shares |
| $ | - | $ | (2,200) | $ | (199) |
Purchase remaining IPA Family, LLC interests |
|
| - |
| - |
| 311 |
|
|
|
|
|
|
|
|
Net transfers from (to) noncontrolling interests |
| $ | - | $ | (2,200) | $ | 112 |
(C)Basis of Presentation
The Consolidated Financial Statements have been prepared in conformity with U.S. generally accepted accounting principles (“GAAP”) and include the accounts of IHC and its consolidated subsidiaries. All significant intercompany transactions have been eliminated in consolidation. The preparation of financial statements in conformity with U.S. GAAP requires management to make estimates and assumptions that affect: (i) the reported amounts of assets and liabilities and the disclosure of contingent assets and liabilities at the date of the financial statements; and (ii) the reported amounts of revenues and expenses during the reporting period. Actual results could differ from those estimates.
On March 31, 2016, the Company sold Risk Solutions, its managing general underwriter of excess or stop-loss insurance for self-insured employer groups that desire to manage the risk of large medical claims (“Medical Stop-Loss”). In addition, under the purchase and sale agreement, all of the in-force stop-loss business of Standard Security Life and Independence American produced by Risk Solutions was 100% co-insured as of January 1, 2016. IHC’s block of medical stop-loss business is in run-off. The sale of Risk Solutions and exit from the medical stop-loss business represents a strategic shift that will have a major effect on the Company’s operations and financial results. The disposal transaction qualified for reporting as discontinued operations in the first quarter of 2016 as a result of the Board of Directors commitment to a plan for its disposal in January 2016. The assets, liabilities, and related income and expenses associated with the disposal group are presented as discontinued operations in the accompanying consolidated financial statements and Notes thereto for all periods presented. The results of discontinued operations reflect the operations of the disposed managing general underwriters (see Note 3). The run-off of IHC’s remaining block of medical stop-loss business is in continuing operations.
Effective September 1, 2015 (“Deconsolidation Date”), pursuant to the terms of a contribution agreement, IHC contributed all of its shares in its subsidiary, IHC Health Solutions, Inc. (“IHC Health Solutions”) to Ebix Health Exchange, a newly formed joint venture with Ebix, Inc. (“Ebix”), and, as a result, IHC deconsolidated IHC Health Solutions (see Note 7). In accordance with U.S. GAAP, the accompanying Consolidated Financial Statements include the operating results of IHC Health Solutions prior to the Deconsolidation Date. Subsequent to the Deconsolidation Date, the Company’s equity interest in the joint venture is accounted for under the equity method of accounting.
(D) Cash, Cash Equivalents and Short-Term Investments
Cash equivalents are carried at cost which approximates fair value, and include principally interest-bearing deposits at brokers, money market instruments and U.S. Treasury securities with original maturities of less than 91 days. Investments with original maturities of 91 days to one year are considered short-term investments and are carried at cost, which approximates fair value.
The following is a reconciliation of cash and cash equivalents as reported in the Consolidated Balance Sheets to the ending cash and cash equivalents, including discontinued operations, as reported in the Consolidated Statements of Cash Flows as of December 31 of each year indicated (in thousands):
|
| December 31, | ||||
|
| 2017 |
| 2016 |
| 2015 |
|
|
|
|
|
|
|
Cash and cash equivalents | $ | 26,465 | $ | 22,010 | $ | 17,500 |
Cash and cash equivalents attributable to discontinued operations |
| - |
| - |
| 1,671 |
|
|
|
|
|
|
|
Cash and cash equivalents, including discontinued operations | $ | 26,465 | $ | 22,010 | $ | 19,171 |
|
|
|
|
|
|
|
(E) Securities Purchased Under Agreements to Resell
Securities purchased under agreements to resell ("resale agreements") are carried at the amounts at which the securities will be subsequently resold as specified in the agreements. Resale agreements are utilized to invest excess funds on a short-term basis. At December 31, 2017, the Company had $10,269,000 invested in resale agreements, all of which settled on January 2, 2018 and were subsequently reinvested. The Company maintains control of securities purchased under resale agreements, values the collateral on a daily basis (102% is required) and obtains additional collateral, if necessary, to protect the Company in the event of default by the counterparties.
(F)Investment Securities
(i) Investments in fixed maturities, redeemable preferred securities and equity securities are accounted for as follows:
(a) Securities that are held for trading purposes are carried at estimated fair value ("fair value"). Changes in fair value are credited or charged, as appropriate, to net realized investment gains (losses) in the Consolidated Statements of Income.
(b) Securities not held for trading purposes that may or may not be held to maturity ("available-for-sale securities") are carried at fair value. Unrealized gains and losses deemed temporary, net of deferred income taxes, are credited or charged, as appropriate, to other comprehensive income or loss. Premiums and discounts on debt securities purchased at other than par value are amortized and accreted, respectively, to interest income in the Consolidated Statements of Income, using the constant yield method over the period to maturity.
(ii) Gains or losses on sales of securities are determined on the basis of specific identification and are recorded in net realized investment gains (losses) in the Consolidated Statements of Income on the trade date.
(iii) Fair value is determined using quoted market prices when available. In some cases, we use quoted market prices for similar instruments in active markets and/or model-derived valuations where inputs are observable in active markets. When there are limited or inactive trading markets, we use industry-standard pricing methodologies, including discounted cash flow models, whose inputs are based on management assumptions and available current market information. Further, we retain independent pricing vendors to assist in valuing certain instruments. Most of the securities in our portfolio are classified in either Level 1 or Level 2 of the Fair Value Hierarchy.
The Company periodically reviews and assesses the vendor’s qualifications and the design and appropriateness of its pricing methodologies. Management will on occasion challenge pricing information on certain individual securities and, through communications with the vendor, obtain information about the assumptions, inputs and methodologies used in pricing those securities, and corroborate it against documented pricing methodologies. Validation procedures are in place to determine completeness and accuracy of pricing information, including, but not limited to: (i) review of exception reports that (a) identify any zero or un-priced securities; (b) identify securities with no price change; and (c) identify securities with significant price changes; (ii) performance of trend analyses; (iii) periodic comparison of pricing to alternative pricing sources; and (iv) comparison of pricing changes to expectations based on rating changes, benchmarks or control groups. In certain circumstances, pricing is unavailable from the vendor and broker-pricing information is used to determine fair value. In these instances, management will assess the quality of the data sources, the underlying assumptions and the reasonableness of the broker quotes based on the current market information available. To determine if an exception represents an error, management will often have to exercise judgment. Procedures to resolve an exception vary depending on the significance of the security and its related class, the frequency of the exception, the risk of material misstatement, and the availability of information for the security. These procedures include, but are not limited to; (i) a price challenge process with the vendor; (ii) pricing from a different vendor; (iii) a reasonableness review; and (iv) a change in price based on better information, such as an actual market trade, among other things. Management considers all facts and relevant information obtained during the above procedures to determine the proper classification of each security in the Fair Value Hierarchy.
(iv) The Company reviews its investment securities regularly and determines whether other-than-temporary impairments have occurred. The factors considered by management in its regular review to identify and recognize other-than-temporary impairment losses on fixed maturities include, but are not limited to: the length of time and extent to which the fair value has been less than cost; the Company's intent to sell, or be required to sell, the debt security before the anticipated recovery of its remaining amortized cost basis; the financial condition and near-term prospects of the issuer; adverse changes in ratings announced by one or more rating agencies; subordinated credit support; whether the issuer of a debt security has remained current on principal and interest payments; current expected cash flows; whether the decline in fair value appears to be issuer specific or, alternatively, a reflection of general market or industry conditions including the effect of changes in market interest rates. If the Company intends to sell a debt security, or it is more likely than not that it would be required to sell a debt security before the recovery of its amortized cost basis, the entire difference between the security's amortized cost basis and its fair value at the balance sheet date would be recognized by a charge to total other-than-temporary impairment losses in the Consolidated Statement of Income. If a decline in fair value of a debt security is judged by management to be other-than-temporary and; (i) the Company does not intend to sell the security; and (ii) it is not more likely than not that it will be required to sell the security prior to recovery of the security’s amortized cost, the Company assesses whether the present value of the cash flows to be collected from the security is less than its amortized cost basis. To the extent that the present value of the cash flows generated by a debt security is less than the amortized cost basis, a credit loss exists. For any such security, the impairment is bifurcated into (a) the amount of the total impairment related to the credit loss, and (b) the amount of the total impairment related to all other factors. The amount of the other-than-temporary impairment related to the credit loss is recognized by a charge to total other-than-temporary impairment losses in the Consolidated Statement of Income, establishing a new cost basis for the security. The amount of the other-than-temporary impairment related to all other factors is recognized in other comprehensive income (loss). It is reasonably possible that further declines in estimated fair values of such investments, or changes in assumptions or estimates of anticipated recoveries and/or cash flows, may cause further other-than-temporary impairments in the near term, which could be significant.
In assessing corporate debt securities for other-than-temporary impairment, the Company evaluates the ability of the issuer to meet its debt obligations and the value of the company or specific collateral securing the debt position. For mortgage-backed securities where loan level data is not available, the Company uses a cash flow model based on the collateral characteristics. Assumptions about loss severity and defaults used in the model are primarily based on actual losses experienced and defaults in the collateral pool. Prepayment speeds, both actual and estimated, are also considered. The cash flows generated by the collateral securing these securities are then determined with these default, loss severity and prepayment assumptions. These collateral cash flows are then utilized, along with consideration for the issue’s position in the overall structure, to determine the cash flows associated with the mortgage-backed security held by the Company. In addition, the Company evaluates other asset-backed securities for other-than-temporary impairment by examining similar characteristics referenced above for mortgage-backed securities. The Company evaluates U.S. Treasury securities and obligations of U.S. Government corporations, U.S. Government agencies, and obligations of states and political subdivisions for other-than-temporary impairment by examining the terms and collateral of the security.
Equity securities may experience other-than-temporary impairment in the future based on the prospects for full recovery in value in a reasonable period of time and the Company’s ability and intent to hold the security to recovery. If a decline in fair value is judged by management to be other-than-temporary or management does not have the intent or ability to hold a security, a loss is recognized by a charge to total other-than-temporary impairment losses in the Consolidated Statement of Income. For the purpose of other-than-temporary impairment evaluations, redeemable preferred stocks are evaluated in a manner similar to debt securities. Declines in the creditworthiness of the issuer of debt securities with both debt and equity-like features are evaluated using the equity model in consideration of other-than-temporary impairment.
Subsequent increases and decreases, if not an other-than-temporary impairment, in the fair value of available-for-sale securities that were previously impaired, are recorded in other comprehensive income (loss).
(G)Other Investments
Other investments primarily consist of limited partnership interests carried on the equity method, which approximates the Company's equity in the underlying net assets of the partnership. Equity income or loss on partnership interests is credited or charged, as appropriate, to the Consolidated Statements of Income. For cost method investments, dividends received are recognized in earnings to the extent that they were distributed from the net accumulated earnings of the investee. Dividends received in excess of the investee’s net accumulated earnings are considered a return of investment and are recorded as reductions of cost of the investment.
(H)Property and Equipment
Property and equipment of $2,786,000 and $2,029,000 are included in other assets at December 31, 2017 and 2016, respectively, net of accumulated depreciation and amortization of $4,188,000 and $3,348,000, respectively.
Improvements are capitalized while repair and maintenance costs are charged to operations as incurred. Depreciation of property and equipment has been provided on the straight-line method over the estimated useful lives of the respective assets. Amortization of leasehold improvements has been provided on the straight-line method over the shorter of the lease term or the estimated useful life of the asset.
(I) Goodwill and Other Intangible Assets
Goodwill carrying amounts are evaluated for impairment, at least annually, at the reporting unit level that is equivalent to an operating segment. If the fair value of a reporting unit is less than its carrying amount, further evaluation is required to determine if a write-down of goodwill is required. In determining the fair value of each reporting unit, we used an income approach, applying a discounted cash flow method that included a residual value. Based on historical experience, we make assumptions as to: (i) expected future performance and future economic conditions, (ii) projected operating earnings, (iii) projected new and renewal business as well as profit margins on such business, and (iv) a discount rate that incorporated an appropriate risk level for the reporting unit. Any impairment of goodwill would be charged to expense.
Other intangible assets are amortized to expense over their estimated useful lives and are subject to impairment testing. Any impairment of other intangible assets would be charged to expense.
(J)Insurance Liabilities
Policy Benefits and Claims
The Company maintains loss reserves to cover its estimated liability for unpaid losses and loss adjustment expenses, where material, including legal, other fees, and costs not associated with specific claims but related to the claims payment function), for reported and unreported claims incurred as of the end of each accounting period. These loss reserves are based on actuarial assumptions and are maintained at levels that are in accordance with U.S. GAAP. Many factors could affect these reserves, including economic and social conditions, frequency and severity of claims, medical trend resulting from the influences of underlying cost inflation, changes in utilization and demand for medical services, and changes in doctrines of legal liability and damage awards in litigation. Therefore, the Company’s reserves are necessarily based on estimates, assumptions and analysis of historical experience. The Company’s results depend upon the variation between actual claims experience and the assumptions used in determining reserves and pricing products. Reserve assumptions and estimates require significant judgment and, therefore, are inherently uncertain. The Company cannot determine with precision the ultimate amounts that will be paid for actual claims or the timing of those payments. The Company's estimate of loss represents management's best estimate of the Company's liability at the balance sheet date.
Loss reserves differ for short-duration and long-duration insurance policies, including annuities. Reserves are based on approved actuarial methods, but necessarily include assumptions about expenses, mortality, morbidity, lapse rates and future yield on related investments.
All of the Company’s short-duration contracts are generated from its accident, health, disability and pet insurance business, and are accounted for based on actuarial estimates of the amount of loss inherent in that period’s claims, including losses incurred for which claims have not been reported. Short-duration contract loss estimates rely on actuarial observations of ultimate loss experience for similar historical events.
Specialty Health
For the Specialty Health business, incurred but not reported (“IBNR”) claims liabilities plus expected development on reported claims are calculated using standard actuarial methods and practices. The “primary” assumption in the determination of Specialty Health reserves is that historical Claim Development Patterns are representative of future Claim Development Patterns. Factors that may affect this assumption include changes in claim payment processing times and procedures, changes in time delay in submission of claims, and the incidence of unusually large claims. Liabilities for policy benefits and claims for specialty health medical and disability coverage are computed using completion factors and expected Net Loss Ratios derived from actual historical premium and claim data. The reserving analysis includes a review of claim processing statistical measures and large claim early notifications; the potential impacts of any changes in these factors are not material. The Company has business that is serviced by third-party administrators. From time to time, there are changes in the timing of claims processing due to any number of factors including, but not limited to, system conversions and staffing changes during the year. These changes are monitored by the Company and the effects of these changes are taken into consideration during the claim reserving process. Other than these considerations, there have been no significant changes to methodologies and assumptions from the prior year.
While these calculations are based on standard methodologies, they are estimates based on historical patterns. To the extent that actual claim payment patterns differ from historical patterns, such estimated reserves may be redundant or inadequate. The effects of such deviations are evaluated by considering claim backlog statistics and reviewing the reasonableness of projected claim ratios. Other factors which may affect the accuracy of policy benefits and claim estimates include the proportion of large claims which may take longer to adjudicate, changes in billing patterns by providers and changes in claim management practices such as hospital bill audits.
Disability
The Company’s disability business is primarily comprised of New York short-term disability (“DBL”) and group disability.
With respect to DBL, the liability for policy benefits and claims for the most recent quarter of earned premium is established using a Net Loss Ratio methodology. The Net Loss Ratio is determined by applying the completed prior four quarters of historical Net Loss Ratios to the last quarter of earned premium. Policy benefits and claims associated with the premium earned prior to the last quarter are established using a completion factor methodology. The completion factors are developed using the historical payment patterns for DBL. There have been no significant changes to methodologies and assumptions from the prior year.
Policy benefits and claims for the Company’s group disability products are developed using actuarial principles and assumptions that consider, among other things, future offsets and recoveries, elimination periods, interest rates, probability of rehabilitation or mortality, incidence and termination rates based on the Company’s experience. The liability for policy benefits and claims is made up of case reserves,
IBNR and reopen reserves and Loss Adjustment Expenses (“LAE”). IBNR and reopen reserves are calculated by a hind-sight study, which takes historical experience and develops the reserve as a percentage of premiums from prior years.
The two “primary” assumptions on which group disability reserves are based are: (i) morbidity levels; and (ii) recovery rates. If morbidity levels increase, for example due to an epidemic or a recessionary environment, the Company would increase reserves because there would be more new claims than expected. In regard to the assumed recovery rate, if disabled lives recover more quickly than anticipated then the existing claims reserves would be reduced; if less quickly, the existing claims reserves would be increased.
Due to the long-term nature of LTD, in establishing the liability for policy benefits and claims, the Company must make estimates for case reserves, IBNR, and reserves for LAE. Case reserves generally equal the actuarial present value of the liability for future benefits to be paid on claims incurred as of the balance sheet date. The IBNR reserve is established based upon historical trends of existing incurred claims that were reported after the balance sheet date. The LAE reserve is calculated based on an actuarial expense study. There have been no significant changes to methodologies and assumptions from the prior year.
Medical Stop-Loss
Due to the sale of Risk Solutions, the Medical Stop-Loss segment is in run-off. The Company has $2.3 million in reserves at December 31, 2017. Liabilities for policy benefits and claims on medical stop-loss coverage are computed using completion factors and expected Net Loss Ratios derived from actual historical premium and claim data. Policy benefits and claims for medical stop-loss insurance are more volatile in nature than those for specialty health medical insurance. This is primarily due to the excess nature of medical stop-loss, with very high deductibles applying to specific claims on any individual claimant and in the aggregate for a given group. The level of these deductibles makes it more difficult to predict the amount and payment pattern of such claims. Furthermore, these excess claims are highly sensitive to changes in factors such as medical trend, provider contracts and medical treatment protocols, adding to the difficulty in predicting claim values and estimating reserves. Also, because medical stop-loss is in excess of an underlying benefit plan, there is an additional layer of claim reporting and processing that can affect claim payment patterns. Finally, changes in the distribution of business by effective month can affect reserve estimates due to the timing of claim occurrences and the time required to accumulate claims against the stop-loss deductible.
Predicting ultimate claims and estimating reserves in Medical Stop-Loss is more complex than specialty health medical and disability business due to the “excess of loss” nature of these products with very high deductibles applying to specific claims on any individual claimant and in the aggregate for a given group. The level of these deductibles makes it more difficult to predict the amount and payment pattern of such claims. Fluctuations in results for specific coverage are primarily due to the severity and frequency of individual claims, whereas fluctuations in aggregate coverage are largely attributable to frequency of underlying claims rather than severity. Liabilities for first dollar medical reserves and disability coverages are computed using completion factors and expected Net Loss Ratios derived from actual historical premium and claim data.
Due to the short-term nature of Medical Stop-Loss, redundancies or deficiencies will typically emerge during the course of the following year rather than over a number of years. For Medical Stop-Loss, as noted above, the Company maintains its reserves based on underlying assumptions until it determines that an adjustment is appropriate based on emerging experience from all of its prior underwriting years.
Management believes that the Company's methods of estimating the liabilities for policy benefits and claims provided appropriate levels of reserves at December 31, 2017. Changes in the Company's policy benefits and claims estimates are generally recorded through a charge or credit to its earnings. There have been no significant changes to methodologies and assumptions from the prior year.
Future Policy Benefits
The liability for future policy benefits consists of the liabilities related to insured events for the Company’s long-duration contracts, primarily its life and annuity products. For traditional life insurance products, the Company computes the liability for future policy benefits primarily using the net premium method based on anticipated investment yield, mortality, and withdrawals. These methods are widely used in the life insurance industry to estimate the liabilities for future policy benefits. Inherent in these calculations are management and actuarial judgments and estimates that could significantly impact the ending reserve liabilities and, consequently, operating results. Actual results may differ, and these estimates are subject to interpretation and change.
Management believes that the Company's methods of estimating the liabilities for future policy benefits provided appropriate levels of reserves at December 31, 2017. Changes in the Company's future policy benefits estimates are recorded through a charge or credit to its earnings.
Funds on Deposit
Funds received (net of mortality and expense charges) for certain long-duration contracts (principally deferred annuities and universal life policies) are credited directly to a policyholder liability account, funds on deposit. Withdrawals are recorded directly as a reduction of respective policyholders' funds on deposit.
Amounts on deposit were credited at annual rates ranging from 3.0% to 6.0% in 2017, 3.0% to 6.0% in 2016, and 3.0% to 7.0% in 2015.
Other Policyholders’ Funds
Other policyholders’ funds represent interest-bearing liabilities arising from the sale of products, such as universal life, interest-sensitive life and annuities. Policyholder funds are primarily comprised of deposits received and interest credited to the benefit of the policyholder less surrenders and withdrawals, mortality charges and administrative expenses.
Interest credited to policyholder funds represents interest accrued or paid on interest-sensitive life policies and investment policies. These amounts are reported in insurance benefits, claims and reserves on the Consolidated Statements of Income. Credit rates for certain annuities and interest-sensitive life policies are adjusted periodically by the Company to reflect current market conditions, subject to contractually guaranteed minimum rates.
(K)Deferred Income Taxes
The provision for deferred income taxes is based on the asset and liability method of accounting for income taxes. Under this method, deferred income taxes are recognized by applying enacted statutory tax rates to temporary differences between amounts reported in the Consolidated Financial Statements and the tax bases of existing assets and liabilities in the years in which those temporary differences are expected to be recovered or settled. A valuation allowance is recognized for the portion of deferred tax assets that, in management's judgment, is not likely to be realized. A liability for uncertain tax positions is recorded when it is more likely than not that a tax position will not be sustained upon examination by taxing authorities. The effect on deferred income taxes of a change in tax rates or laws is recognized in income tax expense in the period that includes the enactment date.
The Company uses a portfolio approach to release income tax effects from accumulated other comprehensive income. The portfolio approach involves a strict period-by-period cumulative incremental allocation of income taxes to the change in unrealized gains and losses reflected in other comprehensive income. Under this approach, the net cumulative tax effect is ignored. The net change in unrealized gains or losses recorded in accumulated other comprehensive income under this approach would be eliminated only on the date the entire inventory of available-for-sale securities is sold or otherwise disposed of.
Interest and penalties, if any, are classified as other interest expense and are included in selling, general and administrative expenses in the Consolidated Statements of Income.
(L)Reinsurance
Amounts paid for or recoverable under reinsurance contracts are included in total assets or total liabilities as due from reinsurers or due to reinsurers. The cost of reinsurance related to long-duration contracts is accounted for over the life of the underlying reinsured policies using assumptions consistent with those used to account for the underlying policies.
(M)Insurance Premium Revenue Recognition and Policy Charges
Premiums from short-duration medical insurance contracts are intended to cover expected claim costs resulting from insured events that occur during a fixed period of short duration. The Company has the ability to not renew the contract or to revise the premium rates at the end of each annual contract period to cover future insured events. Insurance premiums from annual health contracts are collected monthly and are recognized as revenue evenly as insurance protection is provided.
Premiums related to long-term and short-term disability contracts are recognized on a pro rata basis over the applicable contract term.
Traditional life insurance products consist principally of products with fixed and guaranteed premiums and benefits, primarily term and whole life insurance products. Revenue from these products are recognized as premium when due.
Annuities and interest-sensitive life contracts, such as universal life and interest sensitive whole life, are contracts whose terms are not fixed and guaranteed. Premiums from these policies are reported as funds on deposit. Policy charges consist of fees assessed against the policyholder for cost of insurance (mortality risk), policy administration and early surrender. These revenues are recognized when assessed against the policyholder account balance.
Policies that do not subject the Company to significant risk arising from mortality or morbidity are considered investment contracts. Deposits received for such contracts are reported as other policyholder funds. Policy charges for investment contracts consist of fees assessed against the policyholder account for maintenance, administration and surrender of the policy prior to contractually specified dates, and are recognized when assessed against the policyholder account balance.
(N)Income Per Common Share
Income per common share is computed using the treasury stock method.
(O)Share-Based Compensation
Compensation costs for equity awards, such as stock options and non-vested restricted stock, are measured based on grant-date fair value and are recognized in the Consolidated Statements of Income over the requisite service period (which is usually the vesting period). For such awards with only service conditions, the Company recognizes the compensation cost on a straight-line basis over the requisite service period for the entire award.
Compensation costs for liability-classified awards, such as share appreciation rights (“SARs”), are measured and accrued each reporting period in the Consolidated Statements of Income as the requisite service or performance conditions are met.
(P)Recent Accounting Pronouncements
Recently Adopted Accounting Standards
In February 2018, the Financial Accounting Standards Board (“FASB”) issued guidance allowing entities to reclassify, from accumulated other comprehensive income to retained earnings, the stranded tax effects resulting from the Tax Cuts and Jobs Act (“Tax Reform”). The amendments in this Update are effective for all entities for fiscal years beginning after December 15, 2018 and interim periods within those fiscal years. Early adoption is permitted. The amendments should be applied in the period of adoption or retrospectively to each period in which the effect of the change in the U. S. Federal corporate income tax rate in Tax Reform is recognized. The Company has elected to adopt the amendments in this Update on December 31, 2017. Accordingly, the Company has reclassified the effect of the change in the U. S. Federal corporate income tax rate on its gross deferred tax amounts, and related valuation allowances, remaining in accumulated other comprehensive income at December 31, 2017 to retained earnings. The adoption of this guidance did not have a material effect on the Company’s consolidated financial statements.
In October 2016, the FASB issued guidance that amends the consolidation analysis for a reporting entity that is the single decision maker of a variable interest entity. The amendments in this guidance require the decision maker’s evaluation of its interests held through related parties that are under common control on a proportionate basis rather than in their entirety when determining whether it is the primary beneficiary of that variable interest entity. The adoption of this guidance did not have a material effect on the Company’s consolidated financial statements.
In March 2016, the FASB issued guidance that simplify several aspects of accounting for share-based payment transactions, including the income tax consequences, classification of awards as either equity or liabilities, and classification in the statement of cash flows. New guidance related to the classifications in the statement of cash flows were applied on a prospective transition basis. The adoption of this guidance did not have a material effect on the Company’s consolidated financial statements.
In March 2016, the FASB issued guidance that eliminates the requirement for retroactive adjustments on the date that a previously held investment qualifies for the equity method of accounting as a result of an increase in ownership interest or degree of influence. The adoption of this guidance did not have a material effect on the Company’s consolidated financial statements.
Recently Issued Accounting Standards Not Yet Adopted
In May 2017, the FASB issued guidance to provide clarity and reduce both (i) diversity in practice; and (ii) cost and complexity when accounting for a change in the terms or conditions of a share-based payment award. The amendments in this guidance will be applied prospectively in annual periods beginning after December 15, 2017, including interim periods within those periods. The adoption of this guidance is not expected to have a material effect on the Company’s consolidated financial statements.
In March 2017, the FASB issued guidance requiring premium amortization on callable debt securities to be amortized to the earliest call date to more closely align the amortization period with expectations incorporated in market pricing of the underlying securities. The amendments in this guidance should be applied using a modified retrospective approach for annual periods beginning after December 15, 2018, including interim periods within those periods. Additional disclosures are required in the period of adoption. Early adoption is permitted. The adoption of this guidance is not expected to have a material effect on the Company’s consolidated financial statements.
In January 2017, the FASB issued guidance to simplify the test for goodwill impairment by eliminating Step 2 in the goodwill impairment test. Instead, under the amendments in this Update, an entity should perform its annual or interim, goodwill impairment test by comparing the fair value of a reporting unit with its carrying amount. An entity should recognize an impairment charge for the amount by which the carrying amount exceeds the reporting unit’s fair value. Additionally, an entity should consider income tax effects from any tax-deductible goodwill on the carrying amount of the reporting unit when measuring the goodwill impairment loss, if applicable. The amendments in this guidance are effective for public business entities for annual, or any interim, goodwill impairment tests in fiscal years beginning after December 15, 2019. The adoption of this guidance is not expected to have a material effect on the Company’s consolidated financial statements.
In January 2017, the FASB issued guidance that clarifies the definition of a business to assist entities with evaluating when a set of transferred assets and activities is a business. The amendments in this guidance will be applied prospectively in annual periods beginning after December 15, 2017, including interim periods within those periods, with early adoption permitted. The adoption of this guidance is not expected to have a material effect on the Company’s consolidated financial statements.
In November 2016, the FASB issued guidance requiring entities to show the changes in the total cash, cash equivalents, restricted cash and restricted cash equivalent in the statement of cash flows. The amendments in this guidance will be applied retrospectively and is effective for public business entities for fiscal years beginning after December 15, 2017, and interim periods within those fiscal years. The adoption of this guidance will not have a material effect on the Company’s consolidated financial statements.
In October 2016, the FASB issued guidance requiring an entity to recognize the income tax consequences of an intra-entity transfer of an asset other than inventory when the transfer occurs. The amendments in this guidance should be applied on a modified retrospective basis through a cumulative-effect adjustment directly to retained earnings as of the beginning of the period of adoption and are effective for annual reporting periods beginning after December 15, 2017, including interim reporting periods within those annual reporting periods. The adoption of this guidance is not expected to have a material effect on the Company’s consolidated financial statements.
In August 2016, the FASB issued guidance that changes how certain cash receipts and cash payments are presented and classified in the cash flows statement. The amendments in this Update are effective for annual periods beginning after December 15, 2017, and interim periods within those annual periods. The adoption of this guidance will not have a material effect on the Company’s consolidated financial statements.
In June 2016, the FASB issued guidance requiring financial assets measured at amortized cost basis
to be presented at the net amount expected to be collected. An allowance for credit losses will be deducted from the amortized cost basis to present the net carrying value at the amount expected to be collected with changes in the allowance recorded in earnings. Credit losses relating to available-for-sale debt securities will also be recorded through an allowance for credit losses rather than the currently applied U.S. GAAP method of taking a permanent impairment of the security, which would be limited to the amount by which fair value is below the amortized cost. Certain existing requirements used to evaluate credit losses have been removed. For public entities that are SEC filers, the amendments in this Update are effective for fiscal years beginning after December 15, 2019, including interim periods within those years. Early adoption is permitted for fiscal years beginning after December 15, 2018. The amendments in this guidance should be applied through a cumulative effect adjustment to retained earnings upon adoption as of the beginning of the first reporting period in which the guidance is effective. Management is evaluating the requirements and potential impact that the adoption of this guidance will have on the Company’s consolidated financial statements.
In February 2016, the FASB issued guidance that requires lessees to recognize the assets and liabilities that arise from leases, including operating leases, on the statement of financial position. The amendments in this guidance are effective for fiscal years beginning after December 31, 2018, including interim periods within those fiscal years, using a modified retrospective approach. The adoption of this guidance is not expected to have a material effect on the Company’s consolidated financial statements.
In January 2016, the FASB issued guidance that eliminates the requirement to classify equity securities with readily determinable fair values as trading or available-for-sale. The guidance requires equity securities, other than those that result in consolidation or are accounted for under the equity method, (including other ownership interests, such as partnerships, unincorporated joint ventures, and limited liability companies) to be measured at fair value with changes in the fair value recognized through net income, simplifies the impairment assessment of equity securities without readily determinable fair values and requires changes in disclosure requirements. For public entities, the amendments in this Update are effective for fiscal years beginning after December 15, 2017, including interim periods within those fiscal years. The amendments in this Update will be applied by means of a cumulative-effect adjustment to the balance sheet as of the beginning of the fiscal year of adoption. The amendments related to equity securities without readily determinable fair values (including disclosure requirements) will be applied prospectively to equity investments that exist as of the date of adoption of the guidance. The adoption of this guidance will not have a material effect on the Company’s Consolidated Balance Sheet or IHC’s stockholders’ equity.
In May 2014, the FASB issued revenue recognition guidance for entities that either enter into contracts with customers to transfer goods or services or enter into contracts for the transfer of nonfinancial assets unless those contracts are within the scope of other standards such as insurance contracts or lease contracts. The amendment provides specific steps that an entity should apply in order to achieve its main objective which is recognizing revenue to depict the transfer of promised goods or services to customers in an amount that reflects the consideration to which the entity expects to be entitled in exchange for those goods or services. In 2016, additional guidance and technical corrections were issued to clarify certain aspects of the implementation guidance and to clarify the identification of performance obligations. In August 2015, the effective date of this guidance was deferred. For public entities, this guidance is effective for annual reporting periods beginning after December 15, 2017, including interim periods within that reporting period, and requires one of two specified retrospective methods of application. The Company has substantially completed its process to implement this guidance and as a result, has determined that substantially all of our revenue sources are excluded from the scope of the standard. For those revenue sources within the scope of the standard (included in the Fee income line of the Consolidated Statement of Income), there were no material changes in the timing or measurement of revenues. The adoption of this guidance will not have a material effect on the Company’s consolidated financial condition, results of operations, cash flows or required disclosures. The guidance will be applied retrospectively with a cumulative effect adjustment on the date of initial application.
Note 2.Income Per Common Share
Included in the diluted earnings per share calculation for 2017, 2016 and 2015 are 290,000, 217,000 and 170,000 of incremental common shares, respectively, primarily from the dilutive effect of share-based payment awards.
The following is a reconciliation of income available to common shareholders used to calculate income per share for the periods indicated (in thousands):
|
| 2017 |
| 2016 |
| 2015 |
|
|
|
|
|
|
|
Income from continuing operations, net of tax | $ | 42,130 | $ | 22,510 | $ | 27,974 |
Less: Income from continuing operations attributable to |
|
|
|
|
|
|
noncontrolling interests |
| (88) |
| (458) |
| (405) |
|
|
|
|
|
|
|
Income from continuing operations attributable to IHC |
|
|
|
|
|
|
common shareholders | $ | 42,042 | $ | 22,052 | $ | 27,569 |
|
|
|
|
|
|
|
Income from discontinued operations, net of tax | $ | - | $ | 110,804 | $ | 2,548 |
Less: Income from discontinued operations attributable to |
|
|
|
|
|
|
noncontrolling interests |
| - |
| (9,558) |
| (173) |
|
|
|
|
|
|
|
Income from discontinued operations attributable to |
|
|
|
|
|
|
IHC common shareholders | $ | - | $ | 101,246 | $ | 2,375 |
|
|
|
|
|
|
|
Net income attributable to IHC | $ | 42,042 | $ | 123,298 | $ | 29,944 |
|
|
|
|
|
|
|
Note 3.Discontinued Operations
On March 31, 2016, IHC and a subsidiary of AMIC sold the stock of Risk Solutions to Swiss Re Corporate Solutions, a division of Swiss Re (“Swiss Re”). In addition, under the purchase and sale agreement, all of the in-force stop-loss business of Standard Security Life and Independence American produced by Risk Solutions is co-insured by Westport Insurance Corporation (“Westport”), Swiss Re’s largest US carrier, as of January 1, 2016. The aggregate purchase price was $152,500,000 in cash, subject to adjustments and settlements. Approximately 89% of the purchase price was allocated to AMIC and its subsidiaries, with the balance being paid to Standard Security Life and other IHC subsidiaries. The Company recorded a gain of $100,819,000, net of taxes and amounts attributable to noncontrolling interests, as a result of the transaction. The aforementioned transaction, which includes the sale of Risk Solutions and the corresponding coinsurance agreement, is collectively referred to as the “Risk Solutions Sale and Coinsurance Transaction”. IHC’s block of Medical Stop-Loss business is in run-off. The sale of Risk Solutions and exit from the medical stop-loss business represents a strategic shift that will have a major effect on the Company’s operations and financial results. The disposal transaction qualified for reporting as discontinued operations in the first quarter of 2016 as a result of the Board of Directors commitment to a plan for its disposal in January 2016. Aside from reinsurance and marketing of Westport small group stop-loss, there will be no further involvement with the discontinued operation.
The following is a reconciliation of the major line items constituting the pretax profit of discontinued operations, including adjustments for amounts previously eliminated in consolidation, for the periods indicated (in thousands):
|
| 2017 |
| 2016 |
| 2015 |
|
|
|
|
|
|
|
Revenue | $ | - | $ | 6,406 | $ | 2,373 |
Selling, general and administrative expenses |
| - |
| 5,689 |
| (1,937) |
|
|
|
|
|
|
|
Pretax profit of discontinued operations |
| - |
| 717 |
| 4,310 |
Gain on disposal of discontinued operations, pretax |
| - |
| 116,900 |
| - |
|
|
|
|
|
|
|
Income from discontinued operations before income taxes |
| - |
| 117,617 |
| 4,310 |
Income taxes on discontinued operations |
| - |
| 6,813 |
| 1,762 |
|
|
|
|
|
|
|
Income from discontinued operations, net of tax | $ | - | $ | 110,804 | $ | 2,548 |
|
|
|
|
|
|
|
Liabilities attributable to discontinued operations at December 31, 2017 and 2016 consist of $0 and $68,000, respectively, of accounts payable and accrued liabilities.
Total operating and investing cash flows from discontinued operations were $128,000 and $(132,000), respectively, in 2015. In 2016, the Company elected to classify the proceeds received from the sale of discontinued operations in the investing activities section of the Consolidated Statement of Cash Flows. There were no other operating or investing cash flows from discontinued operations in 2017 or 2016.
In connection with the Risk Solutions Sale and Coinsurance Transaction in March 2016, AMIC utilized a significant amount of its Federal NOL carryforwards and made a corresponding adjustment to its valuation allowance (see Note 12). On a consolidated basis, the Company recorded income taxes on discontinued operations of $6,813,000 for the year ended December 31, 2016, consisting of $3,819,000 of state income taxes and $2,994,000 of Federal taxes. Federal income taxes differ from applying the Federal statutory income tax rate of 35% to pretax income from discontinued operations principally as the result of tax benefits from state income taxes and AMIC’s $38,169,000 decrease in its valuation allowance, net of a tax provision from limits on compensation deductions.
Note 4.Investment Securities
The cost (amortized cost with respect to certain fixed maturities), gross unrealized gains, gross unrealized losses and fair value of investment securities are as follows for the periods indicated (in thousands):
|
| December 31, 2017 | ||||||
|
|
|
| GROSS |
| GROSS |
|
|
|
| AMORTIZED |
| UNREALIZED |
| UNREALIZED |
| FAIR |
|
| COST |
| GAINS |
| LOSSES |
| VALUE |
|
|
|
|
|
|
|
|
|
FIXED MATURITIES |
|
|
|
|
|
|
|
|
AVAILABLE-FOR-SALE: |
|
|
|
|
|
|
|
|
Corporate securities | $ | 148,996 | $ | 298 | $ | (2,847) | $ | 146,447 |
CMOs - residential (1) |
| 6,857 |
| - |
| (180) |
| 6,677 |
U.S. Government obligations |
| 85,510 |
| - |
| (396) |
| 85,114 |
Agency MBS - residential (2) |
| 14 |
| - |
| - |
| 14 |
GSEs (3) |
| 9,887 |
| - |
| (205) |
| 9,682 |
States and political subdivisions |
| 182,664 |
| 598 |
| (3,619) |
| 179,643 |
Foreign government obligations |
| 4,227 |
| 13 |
| (90) |
| 4,150 |
Redeemable preferred stocks |
| 10,006 |
| 179 |
| - |
| 10,185 |
|
|
|
|
|
|
|
|
|
Total fixed maturities | $ | 448,161 | $ | 1,088 | $ | (7,337) | $ | 441,912 |
EQUITY SECURITIES |
|
|
|
|
|
|
|
|
AVAILABLE-FOR-SALE: |
|
|
|
|
|
|
|
|
Common stocks | $ | 1,612 | $ | 388 | $ | - | $ | 2,000 |
Nonredeemable preferred stocks |
| 3,588 |
| 60 |
| (18) |
| 3,630 |
|
|
|
|
|
|
|
|
|
Total equity securities | $ | 5,200 | $ | 448 | $ | (18) | $ | 5,630 |
|
| December 31, 2016 | ||||||
|
|
|
| GROSS |
| GROSS |
|
|
|
| AMORTIZED |
| UNREALIZED |
| UNREALIZED |
| FAIR |
|
| COST |
| GAINS |
| LOSSES |
| VALUE |
|
|
|
|
|
|
|
|
|
FIXED MATURITIES |
|
|
|
|
|
|
|
|
AVAILABLE-FOR-SALE: |
|
|
|
|
|
|
|
|
Corporate securities | $ | 192,976 | $ | 209 | $ | (5,490) | $ | 187,695 |
CMOs - residential (1) |
| 6,021 |
| 8 |
| (116) |
| 5,913 |
U.S. Government obligations |
| 43,417 |
| 133 |
| (441) |
| 43,109 |
Agency MBS - residential (2) |
| 22 |
| 1 |
| - |
| 23 |
GSEs (3) |
| 10,301 |
| 1 |
| (422) |
| 9,880 |
States and political subdivisions |
| 191,146 |
| 780 |
| (5,115) |
| 186,811 |
Foreign government obligations |
| 5,098 |
| 13 |
| (157) |
| 4,954 |
Redeemable preferred stocks |
| 11,454 |
| 96 |
| (448) |
| 11,102 |
|
|
|
|
|
|
|
|
|
Total fixed maturities | $ | 460,435 | $ | 1,241 | $ | (12,189) | $ | 449,487 |
EQUITY SECURITIES |
|
|
|
|
|
|
|
|
AVAILABLE-FOR-SALE: |
|
|
|
|
|
|
|
|
Common stocks | $ | 1,612 | $ | 178 | $ | - | $ | 1,790 |
Nonredeemable preferred stocks |
| 3,588 |
| 30 |
| (75) |
| 3,543 |
|
|
|
|
|
|
|
|
|
Total equity securities | $ | 5,200 | $ | 208 | $ | (75) | $ | 5,333 |
(1)Collateralized mortgage obligations (“CMOs”).
(2) Mortgage-backed securities (“MBS”).
(3)Government-sponsored enterprises (“GSEs”) are private enterprises established and chartered by the Federal Government or its various insurance and lease programs which carry the full faith and credit obligation of the U.S. Government.
The amortized cost and fair value of fixed maturities available-for-sale at December 31, 2017, by contractual maturity, are shown below (in thousands). Expected maturities will differ from contractual maturities because borrowers may have the right to call or prepay obligations with or without call or prepayment penalties.
|
|
| AMORTIZED |
|
| FAIR |
|
|
| COST |
|
| VALUE |
|
|
|
|
|
|
|
Due in one year or less |
| $ | 17,554 |
| $ | 17,492 |
Due after one year through five years |
|
| 165,260 |
|
| 163,826 |
Due after five years through ten years |
|
| 140,361 |
|
| 138,909 |
Due after ten years |
|
| 108,228 |
|
| 105,312 |
Fixed maturities with no single maturity date |
|
| 16,758 |
|
| 16,373 |
|
|
|
|
|
|
|
|
| $ | 448,161 |
| $ | 441,912 |
The following tables summarize, for all available-for-sale securities in an unrealized loss position, the aggregate fair value and gross unrealized loss by length of time those securities that have continuously been in an unrealized loss position for the periods indicated (in thousands):
|
| December 31, 2017 | ||||||||||||||
|
|
|
|
|
|
|
|
| ||||||||
|
| Less than 12 Months |
|
| 12 Months or Longer |
|
| Total | ||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Fair |
|
| Unrealized |
|
| Fair |
|
| Unrealized |
|
| Fair |
| Unrealized |
|
| Value |
|
| Losses |
|
| Value |
|
| Losses |
|
| Value |
| Losses |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Corporate securities | $ | 85,642 |
| $ | 1,250 |
| $ | 44,640 |
| $ | 1,597 |
| $ | 130,282 | $ | 2,847 |
CMOs - residential |
| 1,381 |
|
| 45 |
|
| 5,237 |
|
| 135 |
|
| 6,618 |
| 180 |
U.S. Government obligations |
| 75,811 |
|
| 198 |
|
| 9,302 |
|
| 198 |
|
| 85,113 |
| 396 |
GSEs |
| - |
|
| - |
|
| 9,669 |
|
| 205 |
|
| 9,669 |
| 205 |
States and political subdivisions |
| 83,682 |
|
| 1,348 |
|
| 66,617 |
|
| 2,271 |
|
| 150,299 |
| 3,619 |
Foreign government obligations |
| 2,959 |
|
| 90 |
|
| - |
|
| - |
|
| 2,959 |
| 90 |
Total fixed maturities |
| 249,475 |
|
| 2,931 |
|
| 135,465 |
|
| 4,406 |
|
| 384,940 |
| 7,337 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Nonredeemable preferred stocks |
| 2,160 |
|
| 18 |
|
| - |
|
| - |
|
| 2,160 |
| 18 |
Total equity securities |
| 2,160 |
|
| 18 |
|
| - |
|
| - |
|
| 2,160 |
| 18 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Total temporarily impaired |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
securities | $ | 251,635 |
| $ | 2,949 |
| $ | 135,465 |
| $ | 4,406 |
| $ | 387,100 | $ | 7,355 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Number of securities in an |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
unrealized loss position |
| 61 |
|
|
|
|
| 76 |
|
|
|
|
| 137 |
|
|
|
| December 31, 2016 | ||||||||||||||
|
|
|
|
|
|
|
|
| ||||||||
|
| Less than 12 Months |
|
| 12 Months or Longer |
|
| Total | ||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Fair |
|
| Unrealized |
|
| Fair |
|
| Unrealized |
|
| Fair |
| Unrealized |
|
| Value |
|
| Losses |
|
| Value |
|
| Losses |
|
| Value |
| Losses |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Corporate securities | $ | 145,205 |
| $ | 3,818 |
| $ | 19,841 |
| $ | 1,672 |
| $ | 165,046 | $ | 5,490 |
CMO’s - residential |
| 5,038 |
|
| 116 |
|
| - |
|
| - |
|
| 5,038 |
| 116 |
U.S. Government obligations |
| 28,406 |
|
| 441 |
|
| - |
|
| - |
|
| 28,406 |
| 441 |
GSEs |
| 3,640 |
|
| 166 |
|
| 6,220 |
|
| 256 |
|
| 9,860 |
| 422 |
States and political subdivisions |
| 144,357 |
|
| 4,561 |
|
| 18,132 |
|
| 554 |
|
| 162,489 |
| 5,115 |
Foreign government obligations |
| 3,738 |
|
| 157 |
|
| - |
|
| - |
|
| 3,738 |
| 157 |
Redeemable preferred stocks |
| - |
|
| - |
|
| 3,315 |
|
| 448 |
|
| 3,315 |
| 448 |
Total fixed maturities |
| 330,384 |
|
| 9,259 |
|
| 47,508 |
|
| 2,930 |
|
| 377,892 |
| 12,189 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Nonredeemable preferred stocks |
| 826 |
|
| 25 |
|
| 1,277 |
|
| 50 |
|
| 2,103 |
| 75 |
Total equity securities |
| 826 |
|
| 25 |
|
| 1,277 |
|
| 50 |
|
| 2,103 |
| 75 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Total temporarily impaired |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
securities | $ | 331,210 |
| $ | 9,284 |
| $ | 48,785 |
| $ | 2,980 |
| $ | 379,995 | $ | 12,264 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Number of securities in an |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
unrealized loss position |
| 156 |
|
|
|
|
| 23 |
|
|
|
|
| 179 |
|
|
Substantially all of the unrealized losses on fixed maturities available-for-sale at December 31, 2017 and December 31, 2016 relate to investment grade securities and are attributable to changes in market interest rates. Because the Company does not intend to sell, nor is it more likely than not that the Company will have to sell such investments before recovery of their amortized cost bases, which may be maturity, the Company does not consider these investments to be other-than-temporarily impaired at December 31, 2017.
The following table summarizes the Company’s net investment income for the years indicated (in thousands):
|
| 2017 |
|
| 2016 |
|
| 2015 |
|
|
|
|
|
|
|
|
|
Fixed maturities | $ | 13,397 |
| $ | 14,960 |
| $ | 15,364 |
Equity securities |
| 613 |
|
| 676 |
|
| 845 |
Cash, cash equivalents and other short-term investments |
| 264 |
|
| 1,088 |
|
| 66 |
Equity method investments |
| 1,846 |
|
| 62 |
|
| 405 |
Other |
| 221 |
|
| (135) |
|
| 661 |
|
|
|
|
|
|
|
|
|
Investment income, gross |
| 16,341 |
|
| 16,651 |
|
| 17,341 |
Investment expenses |
| (65) |
|
| (81) |
|
| (104) |
|
|
|
|
|
|
|
|
|
Net investment income | $ | 16,276 |
| $ | 16,570 |
| $ | 17,237 |
The following table summarizes the Company’s net realized investment gains (losses) for the years indicated (in thousands):
|
| 2017 |
|
| 2016 |
|
| 2015 |
|
|
|
|
|
|
|
|
|
Available-for-sale securities: |
|
|
|
|
|
|
|
|
Fixed maturities | $ | 2,640 |
| $ | 4,275 |
| $ | 3,533 |
Common stocks |
| - |
|
| 263 |
|
| 1,519 |
Nonredeemable preferred stocks |
| - |
|
| - |
|
| 151 |
Total available-for-sale securities |
| 2,640 |
|
| 4,538 |
|
| 5,203 |
|
|
|
|
|
|
|
|
|
Trading securities |
| - |
|
| (409) |
|
| (1,653) |
Total realized gains |
| 2,640 |
|
| 4,129 |
|
| 3,550 |
|
|
|
|
|
|
|
|
|
Unrealized gains (losses) on trading securities: |
|
|
|
|
|
|
|
|
Change in unrealized gains (losses) on trading securities |
| (102) |
|
| 289 |
|
| (452) |
Total unrealized gains (losses) on trading securities |
| (102) |
|
| 289 |
|
| (452) |
|
|
|
|
|
|
|
|
|
Gains (losses) on other investments |
| 1 |
|
| 84 |
|
| (4) |
|
|
|
|
|
|
|
|
|
Net realized investment gains | $ | 2,539 |
| $ | 4,502 |
| $ | 3,094 |
For the years ended December 31, 2017, 2016 and 2015, proceeds from sales of available-for-sale securities, excluding paydowns and maturities, were $193,638,000, $414,997,000 and $640,902,000, respectively, and the company realized gross gains of $3,746,000, $5,356,000 and $6,412,000, respectively, and gross losses of $895,000, $480,000 and $805,000, respectively, on those sales.
We recognize other-than-temporary impairment losses in earnings in the period that we determine: 1) we intend to sell the security; 2) it is more likely than not that we will be required to sell the security before recovery of its amortized cost basis; or 3) the security has a credit loss. Any non-credit portion of the other-than-temporary impairment loss is recognized in other comprehensive income (loss). The Company did not recognize any other-than-temporary impairments on available-for-sale securities in 2017. In 2016, the Company recognized an other-than-temporary impairment loss of $1,475,000 on certain fixed maturities available-for-sale. The Company determined that it was more likely than not that we would sell the securities before the recovery of their amortized cost basis. In 2015, the Company recognized $228,000 of other-than-temporary impairment losses in earnings on equity securities available-for-sale due to the length of time and extent an equity security was below cost.
Credit losses were recognized on certain fixed maturities for which each security also had an impairment loss recognized in other comprehensive income (loss). The rollforward of these credit losses were as follows for the years indicated (in thousands):
|
| 2017 |
| 2016 |
| 2015 |
|
|
|
|
|
|
|
Balance at beginning of year | $ | - | $ | 473 | $ | 473 |
Securities sold |
| - |
| (473) |
| - |
|
|
|
|
|
|
|
Balance at end of period | $ | - | $ | - | $ | 473 |
Note 5.Fair Value Disclosures
For all financial and non-financial assets and liabilities accounted for at fair value on a recurring basis, the Company utilizes valuation techniques based upon observable and unobservable inputs. Observable inputs reflect market data obtained from independent sources, while unobservable inputs reflect our market expectations. These two types of inputs create the following fair value hierarchy:
Level 1 - Quoted prices for identical instruments in active markets.
Level 2 - Quoted prices for similar instruments in active markets; quoted prices for identical or similar instruments in markets that are not active; and model-derived valuations whose inputs are observable or whose significant value drivers are observable.
Level 3 - Instruments where significant value drivers are unobservable.
The following section describes the valuation methodologies we use to measure different assets and liabilities at fair value.
Investments in fixed maturities and equity securities:
Available-for-sale securities included in Level 1 are equities with quoted market prices. Level 2 is primarily comprised of our portfolio of government securities, agency mortgage-backed securities, corporate fixed income securities, foreign government obligations, collateralized mortgage obligations, municipals and GSEs that were priced with observable market inputs. Level 3 securities consist primarily of municipal tax credit strips. The valuation method used to determine the fair value of municipal tax credit strips is the present value of the remaining future tax credits (at the original issue discount rate) as presented in the redemption tables in the Municipal Prospectuses. This original issue discount is accreted into income on a constant yield basis over the term of the debt instrument. Further we retain independent pricing vendors to assist in valuing certain instruments.
Trading securities:
Trading securities included in Level 1 are equity securities with quoted market prices.
The following tables present our financial assets measured at fair value on a recurring basis for the periods indicated (in thousands):
|
| December 31, 2017 | |||||||
|
| Level 1 |
|
| Level 2 |
| Level 3 |
| Total |
|
|
|
|
|
|
|
|
|
|
FINANCIAL ASSETS: |
|
|
|
|
|
|
|
|
|
Fixed maturities available-for-sale: |
|
|
|
|
|
|
|
|
|
Corporate securities | $ | - |
| $ | 146,447 | $ | - | $ | 146,447 |
CMOs - residential |
| - |
|
| 6,677 |
| - |
| 6,677 |
US Government obligations |
| - |
|
| 85,114 |
| - |
| 85,114 |
Agency MBS - residential |
| - |
|
| 14 |
| - |
| 14 |
GSEs |
| - |
|
| 9,682 |
| - |
| 9,682 |
States and political subdivisions |
| - |
|
| 177,767 |
| 1,876 |
| 179,643 |
Foreign government obligations |
| - |
|
| 4,150 |
| - |
| 4,150 |
Redeemable preferred stocks |
| 10,185 |
|
| - |
| - |
| 10,185 |
Total fixed maturities |
| 10,185 |
|
| 429,851 |
| 1,876 |
| 441,912 |
|
|
|
|
|
|
|
|
|
|
Equity securities available-for-sale: |
|
|
|
|
|
|
|
|
|
Common stocks |
| 2,000 |
|
| - |
| - |
| 2,000 |
Nonredeemable preferred stocks |
| 3,630 |
|
| - |
| - |
| 3,630 |
Total equity securities |
| 5,630 |
|
| - |
| - |
| 5,630 |
|
|
|
|
|
|
|
|
|
|
Trading securities - equities |
| 490 |
|
| - |
| - |
| 490 |
Total trading securities |
| 490 |
|
| - |
| - |
| 490 |
|
|
|
|
|
|
|
|
|
|
Total Financial Assets | $ | 16,305 |
| $ | 429,851 | $ | 1,876 | $ | 448,032 |
|
| December 31, 2016 | |||||||
|
| Level 1 |
|
| Level 2 |
| Level 3 |
| Total |
|
|
|
|
|
|
|
|
|
|
FINANCIAL ASSETS: |
|
|
|
|
|
|
|
|
|
Fixed maturities available-for-sale: |
|
|
|
|
|
|
|
|
|
Corporate securities | $ | - |
| $ | 187,695 | $ | - | $ | 187,695 |
CMOs - residential |
| - |
|
| 5,913 |
| - |
| 5,913 |
US Government obligations |
| - |
|
| 43,109 |
| - |
| 43,109 |
Agency MBS - residential |
| - |
|
| 23 |
| - |
| 23 |
GSEs |
| - |
|
| 9,880 |
| - |
| 9,880 |
States and political subdivisions |
| - |
|
| 184,778 |
| 2,033 |
| 186,811 |
Foreign government obligations |
| - |
|
| 4,954 |
| - |
| 4,954 |
Redeemable preferred stocks |
| 11,102 |
|
| - |
| - |
| 11,102 |
Total fixed maturities |
| 11,102 |
|
| 436,352 |
| 2,033 |
| 449,487 |
|
|
|
|
|
|
|
|
|
|
Equity securities available-for-sale: |
|
|
|
|
|
|
|
|
|
Common stocks |
| 1,790 |
|
| - |
| - |
| 1,790 |
Nonredeemable preferred stocks |
| 3,543 |
|
| - |
| - |
| 3,543 |
Total equity securities |
| 5,333 |
|
| - |
| - |
| 5,333 |
|
|
|
|
|
|
|
|
|
|
Trading securities - equities |
| 592 |
|
| - |
| - |
| 592 |
Total trading securities |
| 592 |
|
| - |
| - |
| 592 |
|
|
|
|
|
|
|
|
|
|
Total Financial Assets | $ | 17,027 |
| $ | 436,352 | $ | 2,033 | $ | 455,412 |
It is the Company’s policy to recognize transfers of assets and liabilities between levels of the fair value hierarchy at the end of a reporting period. The Company does not transfer out of Level 3 and into Level 2 until such time as observable inputs become available and reliable or the range of available independent prices narrow. The Company did not transfer any securities between Level 1, Level 2 or Level 3 in 2017 or 2016.
The following table presents the changes in fair value of our Level 3 financial assets for the years indicated (in thousands):
|
| 2017 |
| 2016 | |||||||||
|
| States and |
| Total |
|
|
| States and |
| Total | |||
|
| Political |
| Level 3 |
| CMOs |
| Political |
| Level 3 | |||
|
| Subdivisions |
| Assets |
| Commercial |
| Subdivisions |
| Assets | |||
|
|
|
|
|
|
|
|
|
|
| |||
Beginning balance | $ | 2,033 | $ | 2,033 | $ | 1,195 | $ | 2,179 | $ | 3,374 | |||
|
|
|
|
|
|
|
|
|
|
| |||
Gains (losses) included in earnings: |
|
|
|
|
|
|
|
|
|
| |||
Net realized investment gains |
| - |
| - |
| 141 |
| - |
| 141 | |||
|
|
|
|
|
|
|
|
|
|
| |||
Gains (losses) included in other |
|
|
|
|
|
|
|
|
|
| |||
comprehensive income (loss): |
|
|
|
|
|
|
|
|
|
| |||
Net unrealized gains (losses) |
| (35) |
| (35) |
| (296) |
| (40) |
| (336) | |||
|
|
|
|
|
|
|
|
|
|
| |||
Repayments and amortization of |
|
|
|
|
|
|
|
|
|
| |||
fixed maturities |
| (122) |
| (122) |
| (74) |
| (106) |
| (180) | |||
Sales |
| - |
| - |
| (966) |
| - |
| (966) | |||
|
|
|
|
|
|
|
|
|
|
| |||
Balance at end of period | $ | 1,876 | $ | 1,876 | $ | - | $ | 2,033 | $ | 2,033 | |||
During 2016, the Company had contingent liabilities classified in Level 3 of the fair value hierarchy. These liabilities were paid out prior to December 31, 2016; there were no comparable amounts for 2017. The following table presents the changes in fair value of our Level 3 financial liabilities for the year indicated (in thousands):
|
| Year Ended December 31, 2016 | ||
|
|
|
| Total |
|
| Contingent |
| Level 3 |
|
| Liabilities |
| Liabilities |
|
|
|
|
|
|
|
|
|
|
Beginning balance | $ | 1,650 | $ | 1,650 |
|
|
|
|
|
Gains (losses) included in earnings: |
|
|
|
|
Net investment income |
| (1,038) |
| (1,038) |
Other income |
| 88 |
| 88 |
|
|
|
|
|
Payment of contingent liability |
| (700) |
| (700) |
|
|
|
|
|
Balance at end of period | $ | - | $ | - |
The following table provides carrying values, fair values and classification in the fair value hierarchy of the Company’s financial instruments, for the periods indicated, that are not carried at fair value but are subject to fair value disclosure requirements, for the periods indicated (in thousands):
|
| December 31, 2017 |
| December 31, 2016 | ||||||||
|
| Level 1 |
| Level 2 |
|
|
| Level 1 |
| Level 2 |
|
|
|
| Fair |
| Fair |
| Carrying |
| Fair |
| Fair |
| Carrying |
|
| Value |
| Value |
| Value |
| Value |
| Value |
| Value |
|
|
|
|
|
|
|
|
|
|
|
|
|
FINANCIAL ASSETS: |
|
|
|
|
|
|
|
|
|
|
|
|
Short-term investments | $ | 50 | $ | - | $ | 50 | $ | 6,912 | $ | - | $ | 6,912 |
|
|
|
|
|
|
|
|
|
|
|
|
|
FINANCIAL LIABILITIES: |
|
|
|
|
|
|
|
|
|
|
|
|
Funds on deposit | $ | - | $ | 143,702 | $ | 143,537 | $ | - | $ | 146,098 | $ | 145,749 |
The following methods and assumptions were used to estimate the fair value of the financial instruments that are not carried at fair value in the Consolidated Financial Statements:
Short-term Investments
Investments with original maturities of 91 days to one year are considered short-term investments and are carried at cost, which approximates fair value.
Funds on Deposit
The Company has two types of funds on deposit. The first type is credited with a current market interest rate, resulting in a fair value which approximates the carrying amount. The second type carries fixed interest rates which are higher than current market interest rates. The fair value of these deposits was estimated by discounting the payments using current market interest rates. The Company's universal life policies are also credited with current market interest rates, resulting in a fair value which approximates the carrying amount. Both types of funds on deposit are included in Level 2 of the fair value hierarchy.
Note 6.Other Investments, Including Variable Interest Entities
Other investments consist of the following for the periods indicated (in thousands):
|
|
| December 31, | |||
|
|
| 2017 |
|
| 2016 |
|
|
|
|
|
|
|
Equity method investments |
| $ | 15,385 |
| $ | 19,747 |
Cost method investments |
|
| 3,125 |
|
| 3,750 |
Other investments and securities, at cost |
|
| 37 |
|
| 37 |
|
|
|
|
|
|
|
|
| $ | 18,547 |
| $ | 23,534 |
In 2017 the Company received a $5,246,000 cash distribution from an equity investment representing a return of capital.
Included in equity method investments above is our investment in Ebix Health Exchange. Ebix Health Exchange administers various lines of health insurance for IHC’s insurance subsidiaries. The carrying value of the Company’s equity investment in Ebix Health Exchange amounted to $8,188,000 and $8,770,000 at December 31, 2017 and 2016, respectively, and the Company recorded $629,000, $(743,000) and $(271,000), respectively, of equity income (loss) from its investment for the years ended December 31, 2017, 2016 and 2015.
Effective July 1, 2016, Ebix exercised its right to increase its ownership in Ebix Health Exchange by purchasing an additional 11% of Ebix Health Exchange for $2,000,000. As a result of the transaction, the Company’s ownership interest in Ebix Health Exchange decreased to 49%. In accordance with the terms of the original sale and joint venture agreement, IHC was obligated to fund any negative cash flow through December 31, 2016 in the form of a loan to the joint venture. A portion of the loan at December 31, 2016 was converted to capital. In 2016, the Company reduced the contingent liability, previously recognized on the acquisition date (see Note 7), by $1,038,000, for cash operating losses reported during the period.
At December 31, 2017 and 2016, the Company’s Consolidated Balance Sheets includes $1,859,000 and $570,000, respectively, of notes and other amounts receivable from Ebix Health Exchange, and include $1,139,000 and $938,000, respectively, of administrative fees and other expenses payable to Ebix Health Exchange, which are included in other assets and accounts payable, accruals and other liabilities, respectively. For the years ended December 31, 2017, 2016 and 2015, the Company’s Consolidated Statements of Income include $0, $366,000 and $80,000, respectively, in fee income from Ebix Health Exchange, and include $10,306,000, $5,937,000 and $1,477,000, respectively, of administrative fee expenses to Ebix Health Exchange, which are included in fee income and selling, general and administrative expenses, respectively.
During 2016, the Company acquired several other investments, including an equity method investment and certain cost method investments, for an aggregate $5,250,000.
Investments in certain unconsolidated trust subsidiaries were liquidated in connection with the Company’s redemption of its junior subordinated debt in 2016 (see Note 11).
Variable Interest Entities
Other investments at December 31, 2017 and 2016 include $3,993,000 and $8,961,000, respectively, of noncontrolling interests in certain limited partnerships that we have determined to be Variable Interest Entities (“VIEs”). The aforementioned VIEs are not required to be consolidated in the Company’s consolidated financial statements as we are not the primary beneficiary since we do not have the power to direct the activities that most significantly impact the VIEs’ economic performance.
The Company will periodically reassess whether it is the primary beneficiary in any of these investments. The reassessment process will consider whether it has acquired the power to direct the most significant activities of the VIEs through changes in governing documents or other circumstances. The Company’s maximum loss exposure is limited to the combined $3,993,000 carrying value in these equity investments and the Company has no future funding obligations to them.
Note 7.Acquisitions, Sales and Deconsolidations of Subsidiaries
Acquisitions
A)PetPartners, Inc.
On March 24, 2017 (the "Acquisition Date"), the Company acquired 85% of the stock of PetPartners, a pet insurance marketing and administration company, for a purchase price of $12,713,000, subject to certain post-closing adjustments. The Company acquired PetPartners for the purpose of owning additional distribution and administration sources for its pet insurance. Any time after March 24, 2019, shares owned by the noncontrolling interest are putable to the Company at fair value and are therefore presented on the balance sheet as a redeemable noncontrolling interest.
Upon the acquisition, the Company consolidated the assets and liabilities of PetPartners. The following table presents the identifiable assets acquired and liabilities assumed in the acquisition of PetPartners on the Acquisition Date based on their respective fair values (in thousands):
Cash |
| $ | 390 |
Intangible assets |
|
| 5,880 |
Other assets |
|
| 567 |
|
|
|
|
Total identifiable assets |
|
| 6,837 |
|
|
|
|
Other liabilities |
|
| 174 |
Deferred tax liability |
|
| 1,069 |
|
|
|
|
Total liabilities |
|
| 1,243 |
|
|
|
|
Net identifiable assets acquired |
| $ | 5,594 |
|
|
|
|
Redeemable noncontrolling interest |
| $ | 2,005 |
In connection with the acquisition, the Company recorded $9,124,000 of goodwill and $5,880,000 of intangible assets (see Note 8). Goodwill reflects the synergies between PetPartners and Independence American as PetPartners will provide Independence American with increased distribution sources for its pet insurance business through its marketing relationship with the American Kennel Club. Goodwill was calculated as the excess of the sum of: (i) the acquisition date fair value of total cash consideration transferred of $12,713,000; and (ii) the fair value of the redeemable noncontrolling interest in PetPartners of $2,005,000 on the acquisition date; over (iii) the net identifiable assets of $5,594,000 that were acquired. The enterprise value of PetPartners was determined by an independent appraisal using a discounted cash flow model based upon the projected future earnings of PetPartners including a control premium. The fair value of the redeemable noncontrolling interest was determined based upon their percentage of the PetPartners enterprise value discounted for a lack of control. Acquisition-related costs, primarily legal and consulting fees, were expensed and are included in selling, general and administrative expenses in the Consolidated Statement of Income.
For the period from the Acquisition Date to December 31, 2017, the Company’s Consolidated Statement of Income includes revenues and net income of $4,468,000 and $691,000, respectively, from PetPartners.
Pro forma adjustments to present the Company’s consolidated revenues and net income as if the acquisition date was January 1, 2016 are not material and accordingly are omitted.
B)Global Accident Facilities, LLC
On April 30, 2015 (the "Acquisition Date"), through a settlement with a former owner, AMIC increased its ownership in Global Accident Facilities, LLC (“GAF) from 40% to 80%, in order to obtain control of the business it produced for Independence American. GAF and its subsidiaries are principally engaged in the marketing, underwriting and administration of specialty risk insurance, referred to as Occupational Accident and Injury on Duty for Independence American, which are offered exclusively in Texas and Massachusetts, respectively. The consideration transferred in exchange for the additional 40% voting interest consisted of: (i) $325,000 in cash; and (ii) non-monetary consideration, primarily consisting of the settlement of a pre-existing relationship with a former owner, with a fair value of $1,195,000 at the Acquisition Date. The fair value of the settlement of the pre-exiting relationship was based on projected future underwriting results discounted for collectability. The acquisition resulted in AMIC obtaining control of GAF. Immediately preceding the transaction, AMIC’s carrying value of its investment in GAF was $1,908,000.
As a result of AMIC obtaining control, the Company has included GAF’s consolidated assets and liabilities and results of operations, subsequent to the Acquisition Date, in its consolidated financial results as of and for the periods ended December 31, 2015. Accordingly, the individual line items on the Consolidated Statements of Income for 2015 reflect approximately eight months of the operations of GAF.
On the Acquisition Date, the Company recognized a net pre-tax gain of $503,000 as follows: (i) a loss of $692,000 was recognized by AMIC as a result of re-measuring its equity interest in GAF to its fair value of $1,216,000 immediately before the acquisition; and (ii) a gain of $1,195,000 was recognized by AMIC as a result of settling the pre-existing relationship with the former owner. The net pre-tax gain of $503,000 is included in the “Other income” line in the Consolidated Statements of Income.
Upon the acquisition of a controlling interest, the Company consolidated the assets and liabilities of GAF. Accordingly, the Company determined the fair value of the identifiable assets acquired and liabilities assumed from GAF on the Acquisition Date. The following table presents the identifiable assets acquired and liabilities assumed in the acquisition of GAF on the Acquisition Date based on their respective fair values (in thousands):
Cash |
| $ | 836 |
Intangible assets |
|
| 5,500 |
Other assets |
|
| 1,405 |
|
|
|
|
Total identifiable assets |
|
| 7,741 |
|
|
|
|
Other liabilities |
|
| 4,369 |
Deferred tax liability |
|
| 1,925 |
Debt |
|
| 3,806 |
|
|
|
|
Total liabilities |
|
| 10,100 |
|
|
|
|
Net identifiable liabilities assumed |
| $ | 2,359 |
Other liabilities assumed included a $1,000,000 contingent liability recorded in connection with an earn-out agreement with a former owner of a subsidiary of GAF. The fair value of the contingent liability was estimated based on projected income.
In connection with the acquisition, the Company recorded $5,703,000 of goodwill and $5,500,000 of intangible assets (see Note 8). None of the goodwill is deductible for income tax purposes. Goodwill reflects the synergies between GAF and Independence American as GAF was the primary writer of Occupational Accident and Injury on Duty business for Independence American. Goodwill was calculated as the excess of the sum of: (i) the acquisition date fair value of total consideration transferred of $1,520,000; (ii) the acquisition date fair value of the equity interest in GAF immediately preceding the acquisition of $1,216,000; and (iii) the fair value of the noncontrolling interest in GAF of $608,000 on the acquisition date; over (iv) the net liabilities of $2,359,000 that were assumed. The enterprise value of GAF was determined by an independent appraisal using a discounted cash flow model based upon the projected future earnings of GAF including a control premium. The fair value of the non-controlling interest was determined based upon their percentage of the GAF enterprise value discounted for a lack of control.
For the period from the Acquisition Date to December 31, 2015, the Company’s Consolidated Statement of Income includes revenues and net income of $6,954,000 and $607,000, respectively, from GAF.
In 2016, the Company paid off the remaining outstanding balance of the aforementioned contingent liability, amounting to $700,000, in connection with the sale of Accident Insurance Services, Inc. (“AIS”) discussed below.
Deconsolidations
A)Accident Insurance Services
On September 30, 2016, the Company sold the assets and the stock of its wholly owned subsidiary, AIS, to unrelated parties for an aggregate $9,000,000 of cash. Upon the sale, AIS was deconsolidated from the Company’s financial statements. The Company recognized a loss of $558,000 on the transaction, pre-tax, which is included in Other Income on the Consolidated Statement of Income in 2016. The loss was measured as the difference between the fair value of the consideration received and: (i) the carrying amount of the former subsidiary’s assets and liabilities, including certain intangible assets (see Note 8); (ii) the
divestiture of associated goodwill (see Note 8), and (iii) other expenses directly attributable to the transaction. There will be no further involvement with AIS other than with respect to the run-out of the business it produced for our insurance companies.
B)Ebix Health Administration Exchange, Inc.
Effective September 1, 2015, IHC and Ebix, a non-related party and international supplier of On-Demand software and E-commerce services to the insurance, financial and healthcare industries, entered into a joint venture in which IHC sold its wholly owned administrative subsidiary, IHC Health Solutions (now known as Ebix Health Administration Exchange, Inc.), in exchange for a 60% ownership interest in Ebix Health Exchange and $6,000,000 in cash proceeds. Ebix contributed $6,000,000 of cash and a pet insurance software license, valued by Ebix Health Exchange at $2,000,000, for its 40%. IHC and Ebix have equal voting interest on the Board of Managers of Ebix Health Exchange. The transaction resulted in a loss of control over the subsidiary (due to a lack of the majority of the voting interest on the Board of Managers) and therefore the subsidiary was deconsolidated from the Company’s financial statements.
In 2015, the Company recognized a gain of $9,940,000, pre-tax, on the transaction consisting of: (i) a pre-tax gain on the deconsolidation of $11,441,000, measured as the fair value of the consideration received and the fair value of the retained investment in Ebix Health Exchange less the carrying amount of the former subsidiary’s net assets; partially offset by (ii) a contingent liability of $1,501,000 representing the Company’s estimated obligation to fund future cash operating losses through December 31, 2016 per the terms of the joint venture agreement. The fair value of the contingent liability was estimated based on expected future operating cash shortfalls. Approximately $5,441,000 of the pre-tax gain is attributable to the re-measurement of the retained investment in the former subsidiary to its current value. The fair value of the retained investment was determined by an independent appraisal using a discounted cash flow model based upon the projected future earnings.
See Note 6 for more information about our investment in Ebix Health Exchange subsequent to its deconsolidation in 2015.
C)Innovative Medical Risk Management, Inc.
On December 31, 2015, the Company sold all of the stock of its wholly owned subsidiary, Innovative Medical Risk Management, Inc. (“IMRM”), to an unrelated party for $1,084,000 cash consideration. Upon the sale, IMRM was deconsolidated from the Company’s financial statements. The Company recognized a gain of $679,000 on the transaction, pre-tax, which is included in Other Income on the Consolidated Statement of Income in 2015. The gain was measured as the difference between the fair value of the consideration received and the carrying amount of the former subsidiary’s assets and liabilities. The sale transaction also included an earn-out agreement with the new owners of IMRM. Other than the aforementioned earn-out agreement, there will be no further involvement with IMRM.
Note 8.Goodwill and Other Intangible Assets
Changes in goodwill and goodwill balances by reportable segment are as follows for the periods indicated (in thousands):
|
|
| Specialty |
|
|
|
|
| Health |
| Total |
|
|
|
|
|
|
Balance at December 31, 2015 |
| $ | 47,276 | $ | 47,276 |
Sale of subsidiary/business (see Note 7) |
|
| (5,703) |
| (5,703) |
|
|
|
|
|
|
Balance at December 31, 2016 |
|
| 41,573 |
| 41,573 |
Acquisition (see Note 7) |
|
| 9,124 |
| 9,124 |
|
|
|
|
|
|
Balance at December 31, 2017 |
| $ | 50,697 | $ | 50,697 |
The Company has net other intangible assets of $14,669,000 and $10,122,000 at December 31, 2017 and 2016, respectively, which are included in other assets in the Consolidated Balance Sheets. These intangible assets consist of: (i) finite-lived intangible assets, principally the fair value of acquired agent and broker relationships, which are subject to amortization; and (ii) indefinite-lived intangible assets which consist of the estimated fair value of insurance licenses that are not subject to amortization.
The gross carrying amounts of these other intangible assets are as follows for the periods indicated (in thousands):
|
| December 31, 2017 |
| December 31, 2016 | ||||
|
| Gross |
|
|
| Gross |
|
|
|
| Carrying |
| Accumulated |
| Carrying |
| Accumulated |
|
| Amount |
| Amortization |
| Amount |
| Amortization |
|
|
|
|
|
|
|
|
|
Finite-lived Intangible Assets: |
|
|
|
|
|
|
|
|
Agent and broker relationships | $ | 17,253 | $ | 12,140 | $ | 13,052 | $ | 11,882 |
Domain |
| 1,000 |
| 125 |
| 1,000 |
| 25 |
Software systems |
| 780 |
| 76 |
| - |
| - |
Total finite-lived | $ | 19,033 | $ | 12,341 | $ | 14,052 | $ | 11,907 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| December 31, | ||
|
|
|
|
|
| 2017 |
| 2016 |
Indefinite-lived Intangible Assets: |
|
|
|
|
|
|
|
|
Insurance licenses |
|
|
|
| $ | 7,977 | $ | 7,977 |
Total indefinite-lived |
|
|
|
| $ | 7,977 | $ | 7,977 |
Changes in net other intangible assets are as follows for the periods indicated (in thousands):
|
| 2017 |
| 2016 |
| 2015 |
|
|
|
|
|
|
|
Balance at beginning of year | $ | 10,122 | $ | 14,598 | $ | 10,620 |
Intangible assets acquired (see Note 7) |
| 5,880 |
| 1,000 |
| 5,500 |
Sale of subsidiaries/businesses (see Note 7) |
| - |
| (4,233) |
| (122) |
Amortization expense |
| (1,333) |
| (1,243) |
| (1,400) |
|
|
|
|
|
|
|
Balance at end of year | $ | 14,669 | $ | 10,122 | $ | 14,598 |
As discussed in Note 7, in connection with the acquisition of PetPartners in 2017, the Company recorded $9,124,000 of goodwill and $5,880,000 of intangible assets associated with the Specialty Health segment. None of the goodwill is deductible for income tax purposes. The intangible assets primarily represent the fair value of customer relationships and are being amortized over a weighted average period of 9.6 years.
Estimated amortization expense for each of the next five years is as follows (in thousands):
|
|
| Amortization |
Year |
|
| Expense |
|
|
|
|
2018 |
| $ | 1,506 |
2019 |
|
| 1,138 |
2020 |
|
| 862 |
2021 |
|
| 667 |
2022 |
|
| 579 |
Note 9.Reinsurance
The Insurance Group reinsures portions of certain business in order to limit the assumption of disproportionate risks. Amounts not retained are ceded to other companies on an automatic or facultative basis. In addition, the Insurance Group participates in various coinsurance treaties on a quota share or excess basis. The Company is contingently liable with respect to reinsurance in the unlikely event that the assuming reinsurers are unable to meet their obligations. The ceding of reinsurance does not discharge the primary liability of the original insurer to the insured.
The effects of reinsurance on premiums earned and insurance benefits, claims and reserves are shown below for the periods indicated (in thousands).
|
|
|
| ASSUMED |
| CEDED |
|
|
|
| GROSS |
| FROM OTHER |
| TO OTHER |
| NET |
|
| AMOUNT |
| COMPANIES |
| COMPANIES |
| AMOUNT |
|
|
|
|
|
|
|
|
|
Premiums Earned: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
December 31, 2017 |
|
|
|
|
|
|
|
|
Accident and health | $ | 249,134 | $ | 7,574 | $ | 32,290 | $ | 224,418 |
Life and annuity |
| 56,194 |
| 795 |
| 38,899 |
| 18,090 |
Property and liability |
| 40,139 |
| - |
| 381 |
| 39,758 |
| $ | 345,467 | $ | 8,369 | $ | 71,570 | $ | 282,266 |
|
|
|
|
|
|
|
|
|
December 31, 2016 |
|
|
|
|
|
|
|
|
Accident and health | $ | 461,467 | $ | 19,744 | $ | 276,392 | $ | 204,819 |
Life and annuity |
| 57,938 |
| 1,595 |
| 42,078 |
| 17,455 |
Property and liability |
| 40,697 |
| - |
| 267 |
| 40,430 |
| $ | 560,102 | $ | 21,339 | $ | 318,737 | $ | 262,704 |
|
|
|
|
|
|
|
|
|
December 31, 2015 |
|
|
|
|
|
|
|
|
Accident and health | $ | 513,814 | $ | 28,822 | $ | 126,613 | $ | 416,023 |
Life and annuity |
| 46,699 |
| 4,330 |
| 23,078 |
| 27,951 |
Property and liability |
| 35,812 |
| - |
| 252 |
| 35,560 |
| $ | 596,325 | $ | 33,152 | $ | 149,943 | $ | 479,534 |
|
|
|
|
|
|
|
|
|
Insurance benefits, claims and reserves: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
December 31, 2017 | $ | 199,063 | $ | 5,965 | $ | 69,974 | $ | 135,054 |
December 31, 2016 | $ | 335,968 | $ | (5,512) | $ | 185,225 | $ | 145,231 |
December 31, 2015 | $ | 365,634 | $ | 24,956 | $ | 83,412 | $ | 307,178 |
Effective January 1, 2016, all of the in-force stop-loss business of Standard Security Life and Independence American produced by Risk Solutions was co-insured in connection with the Risk Solutions Sale and Coinsurance Transaction (see Note 3).
On July 31, 2015, Madison National Life and Standard Security Life together entered into a coinsurance and sale agreement with an unaffiliated reinsurer, National Guardian Life Insurance Company, to: (i) cede substantially all of their individual life and annuity policy blocks currently in run-off; and (ii) sell the related infrastructure associated with the administration of such policies. In 2016, a large block of assumed policies were novated, thereby relieving the Company of its liability with regards to those policies.
Note 10.Policy Benefits and Claims
Policy benefits and claims is the liability for unpaid loss and loss adjustment expenses. It is comprised of unpaid claims and estimated IBNR reserves. Summarized below are the changes in the total liability for policy benefits and claims for the periods indicated (in thousands).
|
| 2017 |
|
| 2016 |
|
| 2015 |
|
|
|
|
|
|
|
|
|
Balance at beginning of year | $ | 219,113 |
| $ | 245,443 |
| $ | 236,803 |
Less: reinsurance recoverable |
| 88,853 |
|
| 65,362 |
|
| 78,531 |
Net balance at beginning of year |
| 130,260 |
|
| 180,081 |
|
| 158,272 |
|
|
|
|
|
|
|
|
|
Amount assumed |
| - |
|
| - |
|
| 10,343 |
|
|
|
|
|
|
|
|
|
Amount incurred, related to: |
|
|
|
|
|
|
|
|
Current year |
| 147,603 |
|
| 155,044 |
|
| 294,390 |
Prior years |
| (8,008) |
|
| (5,496) |
|
| (8,488) |
|
|
|
|
|
|
|
|
|
Total incurred |
| 139,595 |
|
| 149,548 |
|
| 285,902 |
|
|
|
|
|
|
|
|
|
Amount paid, related to: |
|
|
|
|
|
|
|
|
Current year |
| 80,839 |
|
| 78,159 |
|
| 169,488 |
Prior years |
| 62,469 |
|
| 121,210 |
|
| 104,948 |
|
|
|
|
|
|
|
|
|
Total paid |
| 143,308 |
|
| 199,369 |
|
| 274,436 |
|
|
|
|
|
|
|
|
|
Net balance at end of year |
| 126,547 |
|
| 130,260 |
|
| 180,081 |
Plus: reinsurance recoverable |
| 42,136 |
|
| 88,853 |
|
| 65,362 |
Balance at end of year | $ | 168,683 |
| $ | 219,113 |
| $ | 245,443 |
Since unpaid loss and loss adjustment expenses are estimates, actual losses incurred may be more or less than the Company’s previously developed estimates and is referred to as either unfavorable or favorable development, respectively. The overall net favorable development of $8,008,000 in 2017 related to prior years consists of favorable developments of $3,742,000 in the group disability reserves, $3,084,000 in the other individual life, annuities and other reserves, and $2,607,000 in Medical Stop-Loss reserves, partially offset by an unfavorable development of $1,425,000 in the Specialty Health reserves. The overall net favorable development of $5,496,000 in 2016 related to prior years consists of favorable developments of $1,392,000 in the Specialty Health reserves, $2,728,000 in the group disability reserves and $1,728,000 in the other individual life, annuities and other reserves, partially offset by an unfavorable development of $352,000 in Medical Stop-Loss reserves. The overall net favorable development of $8,488,000 in 2015 related to prior years consists of favorable developments of $7,977,000 in the Specialty Health reserves and $4,464,000 in the group disability reserves, partially offset by an unfavorable development of $3,628,000 in Medical Stop-Loss reserves and $325,000 in other individual accident and health reserves.
Specialty Health Segment
The following tables provide undiscounted information about net incurred and paid claims development by accident year for significant short-duration contract liabilities for policy benefits and claims in our Specialty Health segment. All amounts are shown net of reinsurance. In addition, the tables present the total IBNR plus expected development on reported claims by accident year and the cumulative number of reported claims (in thousands, except number of reported claims). Refer to Note 1 for information on the methods we use to estimate IBNR plus expected development, as well as changes to those methodologies and assumptions. Five years of claims development data is presented for lines that are included in our Specialty Health segment since a majority of the claims are fully developed in that time. Certain information about incurred and paid claims is presented as supplementary information and unaudited where indicated.
Specialty Health Segment –Claims Development | ||||||||||
|
|
|
| December 31, 2017 | ||||||
|
| Incurred Claims and Claim Adjustment Expenses, Net of Reinsurance |
| Incurred But | Cumulative | |||||
|
| For the years ended December 31, |
| Not Reported | Number of | |||||
Accident |
| 2013 | 2014 | 2015 | 2016 |
|
|
| Plus Expected | Reported |
Year |
| (unaudited) | (unaudited) | (unaudited) | (unaudited) |
| 2017 |
| Development | Claims |
|
|
|
|
|
|
|
|
|
| (Actual) |
2013 | $ | 180,649 | 181,454 | 180,595 | 181,114 | $ | 181,113 | $ | 660 | 447,248 |
2014 |
|
| 146,060 | 140,139 | 141,869 |
| 142,110 |
| 1,739 | 405,798 |
2015 |
|
|
| 104,497 | 100,988 |
| 101,241 |
| 3,638 | 392,846 |
2016 |
|
|
|
| 85,426 |
| 86,446 |
| 7,835 | 441,619 |
2017 |
|
|
|
|
|
| 87,070 |
| 37,781 | 436,623 |
Total | $ | 597,980 |
|
|
| |||||
|
|
|
|
|
| |||||
Specialty Health Segment –Claims Development | |||||||||
|
|
| |||||||
|
| Cumulative Paid Claims and Claim Adjustment Expenses, Net of Reinsurance | |||||||
|
| For the years ended December 31, | |||||||
Accident |
|
|
| 2013 | 2014 | 2015 | 2016 |
|
|
Year |
|
|
| (unaudited) | (unaudited) | (unaudited) | (unaudited) |
| 2017 |
|
|
|
|
|
|
|
|
|
|
2013 |
|
| $ | 131,801 | 179,023 | 179,750 | 180,520 | $ | 180,453 |
2014 |
|
|
|
| 103,064 | 134,557 | 139,162 |
| 140,371 |
2015 |
|
|
|
|
| 70,090 | 94,757 |
| 97,603 |
2016 |
|
|
|
|
|
| 45,454 |
| 78,611 |
2017 |
|
|
|
|
|
|
|
| 49,289 |
|
|
| |||||||
Total | $ | 546,327 | |||||||
|
|
| |||||||
Outstanding policy benefits and claims payable before 2013, net of reinsurance |
| 57 | |||||||
|
|
| |||||||
Total policy benefits and claims, net of reinsurance | $ | 51,710 | |||||||
|
|
| |||||||
The claim frequency information consists of the count of claims submitted. Each claim was counted as one claim whether or not multiple claim lines were submitted with that claim, and each claim was counted whether or not it resulted in a liability. For those portions of business that did not have claim records readily available, a reasonable count assumption was made based on a comparison to the known records of a similar business type. Cumulative claim count information is not a precise tool for calculating claim severity. Factors, such as changes in provider billing practices, the mix of services, benefit designs or processing systems could impact this type of analysis. The Company does not necessarily use the cumulative number of reported claims disclosed above in its claims analysis but has provided this information to comply with accounting standards.
The following is supplementary information about the average historical policy claims duration for the Specialty Health segment as of December 31, 2017:
Average Annual Percentage Payout of Incurred Claims by Age, Net of Reinsurance (unaudited) | |||||
|
|
|
|
|
|
| Year 1 | Year 2 | Year 3 | Year 4 | Year 5 |
Specialty Health Segment | 64.7% | 27.7% | 2.2% | 0.6% | 0.0% |
|
|
|
|
|
|
The liability for policy benefits and claims associated with the Company’s health insurance lines are embedded within the Specialty Health segment. The table below summarizes the components of the change in the liability for policy benefits and claims that are specific to the health insurance claims that are included in our Specialty Health segment for the periods indicated (in thousands).
|
| Specialty Health Segment | ||||||
|
| Health Insurance Claims | ||||||
|
| 2017 |
|
| 2016 |
|
| 2015 |
|
|
|
|
|
|
|
| (unaudited) |
|
|
|
|
|
|
|
|
|
Balance at beginning of year | $ | 27,183 |
| $ | 23,425 |
| $ | 35,620 |
Less: reinsurance recoverable |
| 1,179 |
|
| 1,362 |
|
| 3,584 |
Net balance at beginning of year |
| 26,004 |
|
| 22,063 |
|
| 32,036 |
|
|
|
|
|
|
|
|
|
Amount incurred, related to: |
|
|
|
|
|
|
|
|
Current year |
| 54,333 |
|
| 44,243 |
|
| 63,122 |
Prior years |
| 158 |
|
| (4,702) |
|
| (8,410) |
|
|
|
|
|
|
|
|
|
Total incurred |
| 54,491 |
|
| 39,541 |
|
| 54,712 |
|
|
|
|
|
|
|
|
|
Amount paid, related to: |
|
|
|
|
|
|
|
|
Current year |
| 24,370 |
|
| 19,371 |
|
| 42,419 |
Prior years |
| 23,983 |
|
| 16,229 |
|
| 22,266 |
|
|
|
|
|
|
|
|
|
Total paid |
| 48,353 |
|
| 35,600 |
|
| 64,685 |
|
|
|
|
|
|
|
|
|
Net balance at end of year |
| 32,142 |
|
| 26,004 |
|
| 22,063 |
Plus: reinsurance recoverable |
| 762 |
|
| 1,179 |
|
| 1,362 |
Balance at end of year | $ | 32,904 |
| $ | 27,183 |
| $ | 23,425 |
The liability for the IBNR plus expected development on reported claims associated with the Company’s health insurance claims was $32,142,000 at December 31, 2017.
Group Disability; Life and DBL Segment
The following tables provide undiscounted information about net incurred and paid claims development by accident year for significant short-duration contract liabilities for policy benefits and claims related to our DBL and group disability policy claims (in thousands). All amounts are shown net of reinsurance. Refer to Note 1 for information on the methods we use to estimate IBNR plus expected development, as well as changes to those methodologies.
One year of claims development data is presented for our DBL claim liabilities since claims are developed in less than six months. The liability for IBNR plus expected development related to our DBL business was $6,579,000 at December 31, 2017. The cumulative number of reported claims was approximately 11,000 at December 31, 2017 and consists of the number of claims either paid or accrued.
Group disability; life and DBL Segment – DBL Claims Development | ||||
Incurred Claims and Claim Adjustment Expenses, Net of Reinsurance | ||||
For the year ended December 31, | ||||
|
|
|
|
|
Accident |
|
|
|
|
Year |
|
|
| 2017 |
|
|
|
|
|
2017 |
| Total | $ | 20,428 |
|
|
|
|
|
Group disability; life and DBL Segment – DBL Claims Development | ||||
Cumulative Paid Claims and Claim Adjustment Expenses, Net of Reinsurance | ||||
For the year ended December 31, | ||||
|
|
|
|
|
Accident |
|
|
|
|
Year |
|
|
| 2017 |
|
|
|
|
|
2017 |
| Total | $ | 13,849 |
|
|
|
|
|
|
| Total policy benefits and claims, net of reinsurance | $ | 6,579 |
|
|
|
|
|
Eight years of undiscounted claims development data is presented for our group disability contract liabilities (in thousands) and we will add one year going forward for each subsequent year until we reach ten years of disclosure. In addition, total IBNR plus expected development on reported claims by accident year is presented with the cumulative number of reported claims (in thousands, except number of reported claims). Certain information about incurred and paid claims is presented as supplementary information and unaudited where indicated.
Group disability; life and DBL Segment – Group Disability Claims Development | |||||||||||||
|
|
|
| December 31, 2017 | |||||||||
|
| Incurred Claims and Claim Adjustment Expenses, Net of Reinsurance |
| Incurred But | Cumulative | ||||||||
|
| For the years ended December 31, |
| Not Reported | Number of | ||||||||
Accident |
| 2010 | 2011 | 2012 | 2013 | 2014 | 2015 |
|
|
|
| Plus Expected | Reported |
Year |
| (unaudited) | (unaudited) | (unaudited) | (unaudited) | (unaudited) | (unaudited) | 2016 |
| 2017 |
| Development | Claims |
|
|
|
|
|
|
|
|
|
|
|
|
| (Actual) |
2010 | $ | 12,329 | 11,218 | 7,142 | 5,222 | 5,049 | 4,220 | 7,925 | $ | 8,658 | $ | - | 2,311 |
2011 |
|
| 18,669 | 17,301 | 16,569 | 15,699 | 16,179 | 17,157 |
| 17,224 |
| 60 | 2,337 |
2012 |
|
|
| 15,510 | 13,999 | 12,522 | 12,535 | 12,965 |
| 12,876 |
| 172 | 2,263 |
2013 |
|
|
|
| 33,143 | 31,323 | 30,546 | 32,888 |
| 32,575 |
| 241 | 2,629 |
2014 |
|
|
|
|
| 16,469 | 13,678 | 15,228 |
| 14,881 |
| 314 | 2,781 |
2015 |
|
|
|
|
|
| 25,621 | 19,929 |
| 17,427 |
| 579 | 3,246 |
2016 |
|
|
|
|
|
|
| 28,907 |
| 29,382 |
| 1,407 | 3,475 |
2017 |
|
|
|
|
|
|
|
|
| 30,273 |
| 11,151 | 2,944 |
Total | $ | 163,296 |
|
|
| ||||||||
|
|
|
|
|
| ||||||||
| Group disability; life and DBL Segment – Group Disability Claims Development | |||||||||||
|
|
|
| |||||||||
|
|
| Cumulative Paid Claims and Claim Adjustment Expenses, Net of Reinsurance | |||||||||
|
|
| For the years ended December 31, | |||||||||
Accident |
| 2010 | 2011 | 2012 | 2013 | 2014 | 2015 |
|
|
| ||
Year |
| (unaudited) | (unaudited) | (unaudited) | (unaudited) | (unaudited) | (unaudited) | 2016 |
| 2017 | ||
|
|
|
|
|
|
|
|
|
|
| ||
2010 | $ | 3,288 | 8,456 | 10,135 | 10,700 | 11,135 | 11,678 | 12,219 | $ | 12,641 | ||
2011 |
|
| 3,463 | 8,544 | 10,025 | 10,613 | 11,186 | 11,847 |
| 12,505 | ||
2012 |
|
|
| 3,222 | 7,294 | 8,367 | 8,949 | 9,377 |
| 9,912 | ||
2013 |
|
|
|
| 5,645 | 13,032 | 17,077 | 20,246 |
| 22,448 | ||
2014 |
|
|
|
|
| 3,818 | 8,823 | 10,355 |
| 11,090 | ||
2015 |
|
|
|
|
|
| 7,111 | 14,715 |
| 17,430 | ||
2016 |
|
|
|
|
|
|
| 8,790 |
| 17,193 | ||
2017 |
|
|
|
|
|
|
|
|
| 8,834 | ||
|
|
| ||||||||||
Total | $ | 112,053 | ||||||||||
|
|
| ||||||||||
Outstanding policy benefits and claims payable before 2010, net of reinsurance |
| 21,189 | ||||||||||
|
|
| ||||||||||
Total policy benefits and claims, net of reinsurance | $ | 72,432 | ||||||||||
|
|
| ||||||||||
The incurred claims and claim adjustment expenses, net, for the 2013 accident year include the acquisition of $15,384,000 of disability policy benefits and claims liabilities from a Receivership.
Claim frequency information consists of the count of unique claims where a benefit has been paid, whether that benefit was paid for one month or multiple months. Any claims where a benefit has not been paid are not in the count. Cumulative claim count information is not a precise tool for calculating claim severity. Changes in reinsurance and other factors, such as those described in Note 1, could impact this type of analysis with regards to our group disability business. The Company does not necessarily use the cumulative number of reported claims disclosed above in its claims analysis but has provided this information to comply with accounting standards.
Unpaid claim liabilities related to our group disability policies is presented at present value. The following is additional information on unpaid claims liabilities presented at present value (in thousands):
|
| Carrying Value of |
|
| Aggregate Amount | ||||
|
| Unpaid Claim Liabilities |
|
| of Discount | ||||
|
| December 31, |
|
| December 31 | ||||
|
| 2017 |
| 2016 |
|
| 2017 |
| 2016 |
|
|
|
|
|
|
|
|
|
|
Group disability | $ | 60,724 | $ | 60,194 |
| $ | 11,707 | $ | 11,475 |
|
|
|
|
|
|
|
|
|
|
Discount rates for each of the years ended December 31, 2017 and 2016 ranged from 3% to 6%. Insurance benefits, claims and reserves on the Consolidated Statements of Income for the years ended December 31, 2017, 2016 and 2015, include the accretion of interest amounting to $1,706,000, $1,571,000 and $1,451,000, respectively.
The following is supplementary information about the average historical claims duration for our group disability business as of December 31, 2017:
Average Annual Percentage Payout of Incurred Claims by Age, Net of Reinsurance (unaudited) |
| |||||||
|
|
|
|
|
|
|
|
|
| Year 1 | Year 2 | Year 3 | Year 4 | Year 5 | Year 6 | Year 7 | Year 8 |
Group disability | 18.3% | 22.5% | 7.4% | 3.5% | 2.4% | 1.4% | 1.0% | 0.4% |
The following table reconciles the above disclosures of undiscounted net incurred and paid claims development for significant short-duration contract liabilities to the liability for policy benefits and claims on the consolidated balance sheet (in thousands).
|
| December 31, 2017 |
|
|
|
Net outstanding balances: |
|
|
Specialty Health Segment | $ | 51,710 |
DBL |
| 6,579 |
Group disability |
| 72,432 |
Other short-duration insurance lines |
| 7,410 |
|
|
|
Policy benefits and claims, net of reinsurance |
| 138,131 |
|
|
|
Reinsurance recoverable on unpaid claims: |
|
|
Specialty Health Segment |
| 1,821 |
DBL |
| 1,124 |
Group disability |
| 26,849 |
Other short-duration insurance lines |
| 6,168 |
|
|
|
Reinsurance recoverable on unpaid claims |
| 35,962 |
|
|
|
Insurance lines other than short-duration |
| 6,297 |
Aggregate discount |
| (11,707) |
|
|
|
Total policy benefit and claims | $ | 168,683 |
|
|
|
Note 11.Debt and Junior Subordinated Debt Securities
The Company has no long term debt outstanding at December 31, 2017 or 2016. In 2016, the Company made aggregate cash payments of $38,146,000 to redeem all of its outstanding junior subordinated debt securities at the redemption price of 100%. During the years ended December 31, 2016 and 2015, the Company also made aggregate cash payments of $4,789,000 and $2,617,000, respectively, for the repayment of other debt.
Aggregate cash payments for interest on debt and junior subordinated debt securities totaled $0, $1,865,000 and $1,738,000 for the years ended December 31, 2017, 2016 and 2015, respectively.
Note 12.Income Taxes
IHC and its subsidiaries file a consolidated Federal income tax return on a June 30 fiscal year.
The provision for income tax expense (benefit) attributable to income from continuing operations, as shown in the Consolidated Statements of Income, is as follows for the years indicated (in thousands):
|
| 2017 |
|
| 2016 |
|
| 2015 |
|
|
|
|
|
|
|
|
|
CURRENT: |
|
|
|
|
|
|
|
|
U.S. Federal | $ | (4,077) |
| $ | 4,637 |
| $ | 14,278 |
State and Local |
| 29 |
|
| 473 |
|
| 1,012 |
|
| (4,048) |
|
| 5,110 |
|
| 15,290 |
|
|
|
|
|
|
|
|
|
DEFERRED: |
|
|
|
|
|
|
|
|
U.S. Federal |
| (9,780) |
|
| 4,390 |
|
| 673 |
State and Local |
| 34 |
|
| 55 |
|
| (59) |
|
| (9,746) |
|
| 4,445 |
|
| 614 |
|
|
|
|
|
|
|
|
|
| $ | (13,794) |
| $ | 9,555 |
| $ | 15,904 |
Taxes computed at the Federal statutory rate of 35%, attributable to pretax income, are reconciled to the Company's actual income tax expense as follows for the years indicated (in thousands):
|
| 2017 |
|
| 2016 |
|
| 2015 |
|
|
|
|
|
|
|
|
|
Tax computed at the statutory rate | $ | 9,918 |
| $ | 11,223 |
| $ | 15,357 |
Dividends received deduction and tax |
|
|
|
|
|
|
|
|
exempt interest |
| (423) |
|
| (641) |
|
| (796) |
State and local income taxes, net of Federal effect |
| 42 |
|
| 331 |
|
| 619 |
Subsidiary stock basis write-off |
| (11,589) |
|
| (3,903) |
|
| - |
Health insurance excise tax |
| - |
|
| 146 |
|
| 526 |
Health insurer compensation limit |
| 192 |
|
| 594 |
|
| 379 |
Impact of enacted tax reform |
| 9,402 |
|
| - |
|
| - |
AMIC valuation allowance adjustment |
| (20,261) |
|
| - |
|
| - |
Sharebased compensation |
| (867) |
|
| - |
|
| - |
Other, net |
| (208) |
|
| 1,805 |
|
| (181) |
|
|
|
|
|
|
|
|
|
Income tax expense | $ | (13,794) |
| $ | 9,555 |
| $ | 15,904 |
As a result of the winding down of operations and dissolution of IHC Administrative Services, Inc. (“IHC AS”), a subsidiary of IHC, in 2017, the Company recognized an estimated $11,589,000 income tax benefit on a worthless stock deduction of $33,110,000 representing the Company’s tax basis in its unrecovered investment in IHC AS. In 2016, as a result of the dissolution of Health Plan Administrators, Inc. (“HPA”), a subsidiary of IHC, income tax benefits of approximately $3,903,000 were also recognized on a worthless stock deduction of $11,150,000 representing the Company’s tax basis in its unrecovered investment in HPA.
On December 22, 2017, President Trump enacted tax legislation commonly referred to as the Tax Cuts and Jobs Act (the “Tax Act”). The Tax Act makes broad and complex changes to the U.S. tax code, including, but not limited to reducing the Federal corporate income tax rate from 35% to 21%. We are required to recognize the income tax effect of a change in tax rates in the period the tax rate change was enacted. As the result of IHC’s June 30 fiscal tax year, the Tax Act subjects IHC to a blended tax rate of 28% for its fiscal tax year ended June 30, 2018. Due to IHC’s NOL carryforward position at December 31, 2017, there was no impact of the Tax Act’s blended tax rate on current income tax expense for the year ended December 31, 2017. The Company recorded a one-time, non-cash charge to deferred income tax expense of $9,402,000 for the year ended December 31, 2017.
Temporary differences between the Consolidated Financial Statement carrying amounts and tax bases of assets and liabilities that give rise to the deferred tax assets and liabilities at December 31, 2017 and 2016 are summarized below (in thousands). The net deferred tax asset or liability is included in Other Assets or Other Liabilities, as appropriate, in the Consolidated Balance Sheets. IHC and its subsidiaries, excluding AMIC and its subsidiaries, considered the reversal of deferred tax liabilities and projected future taxable income in determining that a valuation allowance was not necessary on their deferred tax assets at December 31, 2017 or 2016. The net deferred tax asset relative to AMIC and its subsidiaries included in other assets on IHC’s Consolidated Balance Sheets at December 31, 2017 and 2016 was $18,602,000 and $15,427,000, respectively.
|
|
| 2017 |
|
| 2016 |
DEFERRED TAX ASSETS: |
|
|
|
|
|
|
Unrealized losses on investment securities |
| $ | 1,222 |
| $ | 3,851 |
Investment write-downs |
|
| 48 |
|
| 596 |
Loss carryforwards |
|
| 30,928 |
|
| 50,735 |
Other |
|
| 1,938 |
|
| 4,322 |
Total gross deferred tax assets |
|
| 34,136 |
|
| 59,504 |
Less AMIC valuation allowance |
|
| (9,394) |
|
| (35,918) |
|
|
|
|
|
|
|
Net deferred tax assets |
|
| 24,742 |
|
| 23,586 |
|
|
|
|
|
|
|
DEFERRED TAX LIABILITIES: |
|
|
|
|
|
|
Deferred insurance policy acquisition costs |
|
| (105) |
|
| (114) |
Insurance reserves |
|
| (3,252) |
|
| (4,947) |
Goodwill and intangible assets |
|
| (4,115) |
|
| (5,274) |
Other |
|
| (1,625) |
|
| (4,097) |
|
|
|
|
|
|
|
Total gross deferred tax liabilities |
|
| (9,097) |
|
| (14,432) |
|
|
|
|
|
|
|
Net deferred tax asset |
| $ | 15,645 |
| $ | 9,154 |
As of December 31, 2017, IHC, excluding AMIC and its subsidiaries, had a Federal NOL carryforward of approximately $338,000 at December 31, 2017, which expires in 2037.
At December 31, 2017, AMIC and its subsidiaries had Federal SRLY NOL carryforwards of approximately $144,830,000, which expire in varying amounts through the year 2034, with a significant portion expiring in 2020. As a result of the Risk Solutions Sale and Coinsurance Transaction (see Note 3), AMIC utilized approximately $109,055,000 of its operating loss carryforwards in 2016.
In 2017, the Company decreased AMIC’s valuation allowance by $20,261,000 for an increase in projected income and associated utilization of Federal net operating losses allocated to operations and by $6,263,000 as a result of the change in enacted tax rates. AMIC’s valuation allowance at December 31, 2017 and 2016 was primarily related to net operating loss carryforwards that, in the judgment of management, were not considered realizable.
In assessing the realizability of deferred tax assets, management considers whether it is more likely than not that some portion or all of the deferred tax assets will not be realized. The ultimate realization of deferred tax assets is dependent upon the generation of future taxable income during the period in which those temporary differences become deductible. Management considers the scheduled reversal of deferred tax liabilities, projected future taxable income, and tax planning strategies in making this assessment. Management believes that it is more likely than not that IHC and its subsidiaries, including AMIC and its subsidiaries, will realize the benefits of these net deferred tax assets recorded at December 31, 2017. As of December 31, 2017, IHC and its subsidiaries, and AMIC and its subsidiaries, believe there were no material uncertain tax positions that would require disclosure under U.S. GAAP.
Interest expense and penalties for the years ended December 31, 2017, 2016 and 2015 are insignificant. Tax years ending June 30, 2014 and forward are subject to examination by the Internal Revenue Service. The Company’s 2015 consolidated income tax return was selected for examination by the Internal Revenue Service.
Net cash payments (receipts) for income taxes were $397,000, $12,585,000 and $10,974,000 in 2017, 2016 and 2015, respectively.
Note 13.Stockholders’ Equity
Treasury Stock
In 1991, IHC initiated a program of repurchasing shares of its common stock. In August 2016, the Board of Directors increased the number of shares that can be repurchased to 3,000,000 shares of IHC common stock. At December 31, 2017, there were 1,991,058 shares still authorized to be repurchased under the plan authorized by the Board of Directors.
In 2017, the Company repurchased 2,289,502 shares of its common stock for an aggregate cost of $46,527,000. Of that amount, 703,000 shares were repurchased in private transactions for an aggregate cost of $13,975,000; 1,385,118 shares were repurchased for an aggregate cost of $27,702,000 pursuant to the terms of a tender offer; and the remaining shares were repurchased in the open market.
In 2017, the Company reissued 72,312 shares previously held in treasury. Of that amount, 69,012 shares were reissued to satisfy net-share settlements of option exercises during the period.
Accumulated Other Comprehensive Income (Loss)
The components of other comprehensive income (loss) include the after-tax net unrealized gains and losses on investment securities available-for-sale, including the subsequent increases and decreases in fair value of available-for-sale securities previously impaired and the non-credit related component of other-than-temporary impairments of fixed maturities.
Changes in the balances for each component of accumulated other comprehensive income (loss), shown net of taxes, for the years indicated were as follows (in thousands):
|
| 2017 |
| 2016 |
| 2015 |
|
|
|
|
|
|
|
Beginning balance | $ | (6,964) | $ | (3,440) | $ | 22 |
|
|
|
|
|
|
|
Other comprehensive income (loss) before reclassifications |
| 4,892 |
| (1,582) |
| (256) |
Amounts reclassified from accumulated OCI |
| (1,711) |
| (1,926) |
| (3,206) |
Net other comprehensive income (loss) |
| 3,181 |
| (3,508) |
| (3,462) |
|
|
|
|
|
|
|
Less: Other comprehensive loss attributable |
|
|
|
|
|
|
to noncontrolling interests |
| - |
| (118) |
| (5) |
Acquired from noncontrolling interests |
| - |
| 102 |
| 5 |
Reclassification of the stranded tax effects in accumulated |
|
|
|
|
|
|
other comprehensive income |
| (815) |
| - |
| - |
|
|
|
|
|
|
|
Ending balance | $ | (4,598) | $ | (6,964) | $ | (3,440) |
Presented below are the amounts reclassified out of accumulated other comprehensive income (loss) and recognized in earnings for each of the years indicated (in thousands):
|
| 2017 |
| 2016 |
| 2015 |
|
|
|
|
|
|
|
Unrealized gains (losses) on available-for-sale securities |
|
|
|
|
|
|
reclassified during the period to the following income |
|
|
|
|
|
|
statement line items: |
|
|
|
|
|
|
Net realized investment gains | $ | 2,640 | $ | 4,538 | $ | 5,202 |
Net impairment losses recognized in earnings |
| - |
| (1,475) |
| (228) |
|
|
|
|
|
|
|
Income before income tax |
| 2,640 |
| 3,063 |
| 4,974 |
Tax effect |
| 929 |
| 1,137 |
| 1,768 |
|
|
|
|
|
|
|
Net income | $ | 1,711 | $ | 1,926 | $ | 3,206 |
Note 14.Share-Based Compensation
IHC and AMIC each have a share-based compensation plan. The following is a summary of the activity pertaining to each of these plans.
(A)IHC Share-Based Compensation Plan
In November 2016, the stockholders approved the Independence Holding Company 2016 Stock Incentive Plan (the “2016 Plan"). The 2016 Plan permits grants of options, SARs, restricted shares, restricted share units, unrestricted shares, deferred share units and performance awards. Under the terms of the 2016 Plan: (i) the exercise price of an option may not be less than the fair market value of an IHC share on the grant date and the terms of an option may not exceed 10 years from the grant date; and (ii) the exercise price of a SAR may not be less than the fair market value of an IHC share on the grant date and SAR terms may not exceed 10 years from the date of grant.
The fair value of an option award is estimated on the date of grant using the Black-Scholes option valuation model. In general, the vesting period for an option grant is 3
years. Restricted share units are valued at the quoted market price of the shares at the date of grant and generally vest over 3 years. Compensation costs for options and restricted share units are recognized over the stated vesting periods on a straight-line basis. The fair value of a SAR is calculated using the Black-Scholes valuation model at the grant date and each subsequent reporting period until settlement. Compensation cost is based on the proportionate amount of the requisite service that has been rendered to date. Once fully vested, changes in the fair value of a SAR continue to be recognized as compensation expense in the period of the change until settlement. The Company accounts for forfeitures of share-based compensation awards in the period that they occur.
At December 31, 2017, there were 859,300 shares available for future stock-based compensation grants under the 2016 Plan. The following table summarizes share-based compensation expense, which is included in selling, general and administrative expenses on the Consolidated Statements of Income, applicable to the IHC plans (by award type) for each of the years indicated (in thousands):
|
|
| 2017 |
| 2016 |
| 2015 |
IHC’s Share-based Compensation Plan: |
|
|
|
|
|
|
|
Stock options |
| $ | 224 | $ | 181 | $ | 55 |
Restricted stock units |
|
| 116 |
| 83 |
| 89 |
SARs |
|
| 454 |
| 435 |
| 13 |
|
|
|
|
|
|
|
|
Share-based compensation expense, pre-tax |
|
| 794 |
| 699 |
| 157 |
Tax benefits |
|
| 316 |
| 279 |
| 63 |
|
|
|
|
|
|
|
|
Share-based compensation expense, net |
| $ | 478 | $ | 420 | $ | 94 |
Stock Options
The Company’s stock option activity during 2017 was as follows:
|
| Shares |
| Weighted- Average | |
|
| Under Option |
| Exercise Price | |
|
|
|
|
|
|
December 31, 2016 |
| 697,180 |
| $ | 11.75 |
Granted |
| 199,000 |
|
| 26.72 |
Exercised |
| (203,800) |
|
| 9.82 |
December 31, 2017 |
| 692,380 |
| $ | 16.62 |
The weighted average grant-date fair-values of options granted during the years ended December 31, 2017 and 2016 were $8.66 and $2.65, respectively. No options were granted in 2015. The assumptions set forth in the table below were used to value the stock options granted during the periods indicated:
| 2017 |
| 2016 |
|
|
|
|
Weighted-average risk-free interest rate | 2.02% |
| 1.87% |
Expected annual dividend rate per share | 0.58% |
| 0.60% |
Expected volatility factor of the Company's common stock | 37.44% |
| 12.95% |
Weighted-average expected term of options | 4.5 years |
| 4.5 years |
In 2017, IHC received no cash from the exercise of stock options, as option exercises were net settled in IHC shares. As part of the net-share settlements in 2017, cash outflows to satisfy employees’ income tax withholding obligations amounted to $1,659,000. Stock options exercised in 2017 had an aggregate intrinsic value of $3,535,000 and IHC realized $834,000 of tax benefits. In 2016, option agreements affecting 13 employees were modified to extend the expirations of their terms from 2017 to 2019 and as a result, the Company recorded incremental compensation costs of $170,000. In 2016, IHC received $399,000 in cash from the exercise of stock options with an aggregate intrinsic value of $416,000 and realized $104,000 of tax benefits. In 2015, IHC received $278,000 in cash from the exercise of stock options with an aggregate intrinsic value of $132,000 and realized $22,000 of tax benefits.
The following table summarizes information regarding options outstanding and exercisable:
|
| December 31, 2017 | ||
|
| Outstanding |
| Exercisable |
|
|
|
|
|
Number of options |
| 692,380 |
| 388,713 |
Weighted average exercise price per share | $ | 16.62 | $ | 10.55 |
Aggregate intrinsic value for all options (in thousands) | $ | 7,499 | $ | 6,568 |
Weighted average contractual term remaining |
| 2.8 years |
| 1.4 years |
At December 31, 2017, the total unrecognized compensation cost related to IHC’s non-vested stock options was $1,904,000 and it is expected to be recognized as compensation expense over a weighted average period of 2.4 years.
Restricted Stock
The following table summarizes IHC’s restricted stock activity for the year ended December 31, 2016:
|
| No. of |
| Weighted-Average | ||
|
| Non-vested |
| Grant-Date | ||
|
| Shares |
| Fair Value | ||
|
|
|
|
|
|
|
December 31, 2016 |
| 17,325 |
| $ | 16.20 |
|
Granted |
| 9,900 |
|
| 28.20 |
|
Vested |
| (8,250) |
|
| 15.18 |
|
|
|
|
|
|
|
|
December 31, 2017 |
| 18,975 |
| $ | 22.91 |
|
IHC granted 9,900, 9,900 and 7,425 of restricted stock units during each of the years ended December 31, 2017, 2016 and 2015, respectively, with weighted-average grant-date fair values of $28.20, $19.15 and $11.78 per share, respectively. The total fair value of restricted stock units that vested in 2017, 2016 and 2015 was $187,000, $120,000 and $89,000, respectively.
At December 31, 2017, the total unrecognized compensation cost related to non-vested restricted stock unit awards was $398,000 which is expected to be recognized as compensation expense over a weighted average period of 2.2 years.
SARs and Share-Based Performance Awards
IHC had 64,900 and 71,500 SAR awards outstanding at December 31, 2017 and 2016, respectively. In 2017, 64,900 shares were granted; and 71,500 shares were exercised with an aggregate intrinsic value of $1,309,000. In 2016, 54,350 SARs were exercised with an aggregate intrinsic value of $449,000. In 2015, 11,000 SARs were exercised with an aggregate intrinsic value of $61,000. Included in Other Liabilities in the Company’s Consolidated Balance Sheets at December 31, 2017 and December 31, 2016 are liabilities of $22,000 and $876,000, respectively, pertaining to SARs.
(B)AMIC Share-Based Compensation Plans
As a result of a short-form merger discussed in Note 1 (B), AMIC’s 2009 Stock Incentive Plan (“AMIC 2009 Plan”) was terminated in 2016. Under the terms of the AMIC 2009 Plan, prior to its termination, option exercise prices were equal to the quoted market price of the shares at the date of grant; option terms were a maximum of ten years; and vesting periods generally ranged from three to four years. The fair value of an option award was estimated on the date of grant using the Black-Scholes option valuation model.
For the years ended December 31, 2016 and 2015, AMIC recorded $14,000 and $28,000 of share-based compensation expense, respectively, net of tax benefits of $7,000, and $15,000, respectively.
In 2016, AMIC received $262,000 in cash from the exercise of stock options with an aggregate intrinsic value of $212,000. In connection with the short-form merger transaction discussed in Note 1 (B), option agreements affecting 7 employees and directors were cancelled and as a result, the Company recorded incremental compensation costs of $646,000. These costs were accounted for as part of the equity transaction to take AMIC private. In 2015, AMIC received $52,000 in cash from the exercise of stock options with an aggregate intrinsic value of $37,000.
Note 15.Commitments and Contingencies
Certain subsidiaries of the Company are obligated under non-cancelable operating lease agreements for office space. Total rental expense for the years 2017, 2016 and 2015 for operating leases was $2,117,000, $2,316,000 and $3,088,000, respectively.
The approximate minimum annual rental payments under operating leases that have remaining non-cancelable lease terms in excess of one year at December 31, 2017 are as follows (in thousands):
|
|
|
|
2018 |
| $ | 2,251 |
2019 |
|
| 1,953 |
2020 |
|
| 1,929 |
2021 |
|
| 1,460 |
2022 |
|
| 1,125 |
2023 and thereafter |
|
| 195 |
|
|
|
|
Total |
| $ | 8,913 |
|
|
|
|
We are involved in legal proceedings and claims that arise in the ordinary course of our businesses. We have established reserves that we believe are sufficient given information presently available relating to our outstanding legal proceedings and claims. We do not anticipate that the result of any pending legal proceeding or claim will have a material adverse effect on our financial condition or cash flows, although there could be such an effect on our results of operations for any particular period.
A third party administrator with whom we formerly did business (“Plaintiff”) filed a Complaint dated May 17, 2017 in the United States District Court, Northern District of Texas, Dallas Division, naming IHC, Madison National Life, Standard Security Life, and IHC Carrier Solutions, Inc. (collectively referred to as “Defendants”). The Complaint concerns agreements entered into by Standard Security Life and Madison National Life with Plaintiff, as well as other allegations made by Plaintiff against the Defendants. The Complaint seeks injunctive relief and damages in an amount exceeding $50,000,000, profit share payments allegedly owed to Plaintiff under the agreements totaling at least $3,082,000 through 2014, plus additional amounts for 2015 and 2016, and exemplary and punitive damages as allowed by law and fees and costs. The Defendants believe these claims to be without merit. The Defendants moved to Compel Arbitration and Dismiss or Stay the original Complaint. The Plaintiff filed an Amended Complaint on August 18, 2017. The Defendants filed a Motion to Compel Arbitration or Stay the Amended Complaint, which is still pending. Madison National Life and Standard Security Life have demanded arbitration against this third party administrator. In the fourth quarter of 2017, Madison National Life paid fines in the state of Texas primarily related to the claims payment practices of the Plaintiff.
Note 16.Concentration of Credit Risk
At December 31, 2017, the Company had no investment securities of any one issuer or in any one industry which exceeded 10% of stockholders' equity, except for investments in obligations of the U.S. Government and its agencies and mortgage-backed securities issued by GSEs, as summarized in Note 4.
Fixed maturities with carrying values of $12,819,000 and $12,577,000 were on deposit with various state insurance departments at December 31, 2017 and 2016, respectively.
At December 31, 2017, the Company had reinsurance recoverable from the following reinsurers that individually exceed 10% of stockholders’ equity (in thousands):
|
| AM Best |
| Due from |
Reinsurer |
| Rating |
| Reinsurer |
|
|
|
|
|
National Guardian Life Insurance Company |
| A- | $ | 223,402 |
Guggenheim Life and Annuity Company |
| B++ |
| 96,664 |
|
|
|
|
|
The Company believes that these receivables are fully collectible.
Note 17.Dividend Payment Restrictions and Statutory Information
Our insurance subsidiaries are restricted by state laws and regulations as to the amount of dividends they may pay to their parent without regulatory approval in any year. Any dividends in excess of limits are deemed “extraordinary” and require approval. Based on statutory results as of December 31, 2017, in accordance with applicable dividend restrictions, our insurance subsidiaries could pay dividends of approximately $23,606,000 in 2018 without obtaining regulatory approval. There are no regulatory restrictions on the ability of our holding company, IHC, to pay dividends. Under Delaware law, IHC is permitted to pay dividends from surplus or net profits for the fiscal year in which the dividend is declared and/or the preceding fiscal year. Dividends to shareholders are paid from funds available at the corporate holding company level.
Non-“extraordinary” dividend payments were as follows: (i) Madison National Life declared and paid cash dividends of $11,000,000, $5,290,000 and $4,600,000 to its parent in 2017, 2016 and 2015, respectively; (ii) Standard Security Life declared and paid dividends of $7,000,000, $12,500,000 and $6,000,000 to its parent in 2017, 2016 and 2015, respectively; and (iii) Independence American declared and paid $0 dividends to its parent in 2017, 2016 or 2015. IHC declared cash dividends of $2,392,000 in 2017, $1,800,000 in 2016 and $1,562,000 in 2015.
In December 2016, regulatory approvals were received for the following “extraordinary” dividend payments: (i) Madison National Life declared and paid an “extraordinary” dividend in the amount of $10,546,000 to its parent; and (ii) Standard Security Life declared and paid an “extraordinary” dividend in the amount of $60,000,000 to its parent.
The Company’s insurance subsidiaries are required to prepare statutory financial statements in accordance with statutory accounting practices prescribed or permitted by the insurance department of their state of domicile. Statutory accounting practices differ from U.S. GAAP in several respects causing differences in reported net income and stockholder’s equity. The Company’s insurance subsidiaries have no permitted accounting practices, which encompass all accounting practices not so prescribed that have been specifically allowed by the state insurance authorities.
The statutory net income and statutory capital and surplus for each of the Company’s insurance subsidiaries are as follows for the periods indicated (in thousands):
|
| Years Ended December 31, | ||||
|
| 2017 |
| 2016 |
| 2015 |
|
|
|
|
|
|
|
Statutory net income: |
|
|
|
|
|
|
Madison National Life | $ | 12,794 | $ | (1,615) | $ | 20,326 |
Standard Security Life |
| 3,555 |
| (10,480) |
| 13,198 |
Independence American |
| 8,728 |
| 4,048 |
| 2,960 |
|
| December 31, | ||
|
| 2017 |
| 2016 |
|
|
|
|
|
Statutory capital and surplus: |
|
|
|
|
Madison National Life | $ | 179,648 | $ | 178,978 |
Standard Security Life |
| 65,600 |
| 70,620 |
Independence American |
| 72,083 |
| 66,812 |
The insurance subsidiaries are also required to maintain certain minimum amounts of statutory surplus to satisfy their various state insurance departments of domicile. Risk-based capital (“RBC”) requirements are designed to assess capital adequacy and to raise the level of protection that statutory surplus provides for policyholders. At December 31, 2017 and 2016, the statutory capital of our insurance subsidiaries is significantly in excess of their regulatory RBC requirements.
Note 18.Segment Reporting
The Insurance Group principally engages in the life and health insurance business. Interest expense, taxes, and general expenses associated with parent company activities are included in Corporate. Identifiable assets by segment are those assets that are utilized in each segment and are allocated based upon the mean reserves and liabilities of each such segment. Corporate assets are composed principally of cash equivalents, resale agreements, fixed maturities, equity securities, partnership interests and certain other investments.
Information by business segment is presented below for the years indicated (in thousands).
|
|
| 2017 |
|
| 2016 |
|
| 2015 |
Revenues: |
|
|
|
|
|
|
|
|
|
Specialty Health |
| $ | 203,810 |
| $ | 173,147 |
| $ | 185,912 |
Group disability; life and DBL |
|
| 106,927 |
|
| 103,535 |
|
| 90,314 |
Individual life, annuities and other (A) |
|
| 2,139 |
|
| 2,756 |
|
| 27,119 |
Medical Stop-Loss (A) |
|
| 2,607 |
|
| 25,614 |
|
| 214,139 |
Corporate |
|
| 2,472 |
|
| 2,925 |
|
| 205 |
|
|
| 317,955 |
|
| 307,977 |
|
| 517,689 |
Gain on sale of subsidiary to joint venture |
|
| - |
|
| - |
|
| 9,940 |
Net realized investment gains |
|
| 2,539 |
|
| 4,502 |
|
| 3,094 |
Net impairment losses recognized in earnings |
|
| - |
|
| (1,475) |
|
| (228) |
|
|
|
|
|
|
|
|
|
|
Total revenues |
| $ | 320,494 |
| $ | 311,004 |
| $ | 530,495 |
|
|
|
|
|
|
|
|
|
|
Income from continuing operations before income taxes: |
|
|
|
|
|
|
|
|
|
Specialty Health (B) |
| $ | 13,207 |
| $ | 7,202 |
| $ | 6,490 |
Group disability; life and DBL |
|
| 18,278 |
|
| 17,904 |
|
| 15,811 |
Individual life, annuities and other (A) (C) |
|
| (513) |
|
| (2,540) |
|
| (122) |
Medical Stop-Loss (A) |
|
| 2,839 |
|
| 16,733 |
|
| 18,828 |
Corporate |
|
| (8,014) |
|
| (8,727) |
|
| (8,137) |
|
|
| 25,797 |
|
| 30,572 |
|
| 32,870 |
Gain on sale of subsidiary to joint venture |
|
| - |
|
| - |
|
| 9,940 |
Net realized investment gains |
|
| 2,539 |
|
| 4,502 |
|
| 3,094 |
Net impairment losses recognized in earnings |
|
| - |
|
| (1,475) |
|
| (228) |
Interest expense |
|
| - |
|
| (1,534) |
|
| (1,798) |
|
|
|
|
|
|
|
|
|
|
Income from continuing operations before income taxes |
| $ | 28,336 |
| $ | 32,065 |
| $ | 43,878 |
(A)Substantially all of the business in the segment is coinsured. Activity in this segment primarily reflects income or expenses related to the coinsurance and the run-off of any remaining blocks that were not coinsured.
(B)The Specialty Health segment includes amortization of intangible assets recorded as a result of purchase accounting for previous acquisitions. Total amortization expense was $1,333,000, $1,243,000 and $1,488,000 for the years ended December 31, 2017, 2016 and 2015, respectively. There is no amortization expense attributable to the other segments.
(C)The Individual life, annuities and other segment includes amortization of deferred charges in connection with the assumptions of certain ceded life and annuity policies amounting to $1,196,000, $2,340,000 and $1,323,000 for the years ended December 31, 2017, 2016 and 2015, respectively.
|
|
| December 31, | |||
|
|
| 2017 |
|
| 2016 |
IDENTIFIABLE ASSETS AT YEAR END |
|
|
|
|
|
|
Specialty Health |
| $ | 223,896 |
| $ | 172,275 |
Group disability; life and DBL |
|
| 246,877 |
|
| 243,421 |
Individual life, annuities and other |
|
| 363,693 |
|
| 363,119 |
Medical Stop-Loss |
|
| 78,234 |
|
| 200,026 |
Corporate |
|
| 127,923 |
|
| 155,623 |
|
|
|
|
|
|
|
|
| $ | 1,040,623 |
| $ | 1,134,464 |
Note 19.Quarterly Data (Unaudited)
The quarterly results of operations for the years indicated are summarized below (in thousands, except per share data):
|
| FIRST |
| SECOND |
| THIRD |
| FOURTH |
|
| QUARTER |
| QUARTER |
| QUARTER |
| QUARTER |
2017 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Total revenues | $ | 71,840 | $ | 82,237 | $ | 83,752 | $ | 82,665 |
|
|
|
|
|
|
|
|
|
Income from continuing operations, net of tax | $ | 5,009 | $ | 14,307 | $ | 5,213 | $ | 17,601 |
Income from discontinued operations, net of tax |
| - |
| - |
| - |
| - |
Net income |
| 5,009 |
| 14,307 |
| 5,213 |
| 17,601 |
(Income) loss from nonredeemable noncontrolling interests |
| (62) |
| 26 |
| 32 |
| (23) |
(Income) from redeemable noncontrolling interests |
| (11) |
| (2) |
| (16) |
| (32) |
|
|
|
|
|
|
|
|
|
Net income attributable to IHC | $ | 4,936 | $ | 14,331 | $ | 5,229 | $ | 17,546 |
|
|
|
|
|
|
|
|
|
Basic income per common share: |
|
|
|
|
|
|
|
|
Income from continuing operations | $ | 0.30 | $ | 0.88 | $ | 0.35 | $ | 1.18 |
Income from discontinued operations |
| - |
| - |
| - |
| - |
Basic income per common share | $ | 0.30 | $ | 0.88 | $ | 0.35 | $ | 1.18 |
|
|
|
|
|
|
|
|
|
Diluted income per share: |
|
|
|
|
|
|
|
|
Income from continuing operations | $ | 0.29 | $ | 0.86 | $ | 0.34 | $ | 1.16 |
Income from discontinued operations |
| - |
| - |
| - |
| - |
Diluted income per common share | $ | 0.29 | $ | 0.86 | $ | 0.34 | $ | 1.16 |
|
|
|
|
|
|
|
|
|
|
| FIRST |
|
| SECOND |
|
| THIRD |
|
| FOURTH |
|
| QUARTER |
|
| QUARTER |
|
| QUARTER |
|
| QUARTER |
|
|
|
|
|
|
|
|
|
|
|
|
2016 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Total revenues | $ | 75,895 |
| $ | 77,696 |
| $ | 78,542 |
| $ | 78,871 |
|
|
|
|
|
|
|
|
|
|
|
|
Income from continuing operations, net of tax | $ | 5,896 |
| $ | 4,495 |
| $ | 4,366 |
| $ | 7,753 |
Income from discontinued operations, net of tax |
| 109,770 |
|
| 142 |
|
| - |
|
| 892 |
Net income |
| 115,666 |
|
| 4,637 |
|
| 4,366 |
|
| 8,645 |
Less income from noncontrolling interests |
|
|
|
|
|
|
|
|
|
|
|
in subsidiaries |
| (9,656) |
|
| (201) |
|
| (43) |
|
| (116) |
|
|
|
|
|
|
|
|
|
|
|
|
Net income attributable to IHC | $ | 106,010 |
| $ | 4,436 |
| $ | 4,323 |
| $ | 8,529 |
|
|
|
|
|
|
|
|
|
|
|
|
Basic income per common share: |
|
|
|
|
|
|
|
|
|
|
|
Income from continuing operations | $ | 0.34 |
| $ | 0.25 |
| $ | 0.25 |
| $ | 0.45 |
Income from discontinued operations |
| 5.81 |
|
| 0.01 |
|
| 0.00 |
|
| 0.05 |
Basic income per common share | $ | 6.15 |
| $ | 0.26 |
| $ | 0.25 |
| $ | 0.50 |
|
|
|
|
|
|
|
|
|
|
|
|
Diluted income per share: |
|
|
|
|
|
|
|
|
|
|
|
Income from continuing operations | $ | 0.33 |
| $ | 0.25 |
| $ | 0.25 |
| $ | 0.44 |
Income from discontinued operations |
| 5.75 |
|
| 0.01 |
|
| 0.00 |
|
| 0.05 |
Diluted income per common share | $ | 6.08 |
| $ | 0.26 |
| $ | 0.25 |
| $ | 0.49 |
|
|
|
|
|
|
|
|
|
|
|
|
SCHEDULE I | ||||||
| ||||||
INDEPENDENCE HOLDING COMPANY AND SUBSIDIARIES | ||||||
SUMMARY OF INVESTMENTS – OTHER THAN INVESTMENTS IN RELATED PARTIES | ||||||
DECEMBER 31, 2017 | ||||||
(In thousands) | ||||||
|
|
|
|
|
| AMOUNT |
|
|
|
|
|
| SHOWN IN |
|
|
|
|
|
| BALANCE |
TYPE OF INVESTMENT |
| COST |
| VALUE |
| SHEET |
|
|
|
|
|
|
|
FIXED MATURITIES - AVAILABLE-FOR-SALE: |
|
|
|
|
|
|
Bonds: |
|
|
|
|
|
|
United States Government and Government |
|
|
|
|
|
|
agencies and authorities | $ | 95,411 | $ | 94,810 | $ | 94,810 |
States, municipalities and political subdivisions |
| 182,664 |
| 179,643 |
| 179,643 |
Foreign governments |
| 4,227 |
| 4,150 |
| 4,150 |
Public utilities |
| 15,865 |
| 15,717 |
| 15,717 |
All other corporate bonds |
| 139,988 |
| 137,407 |
| 137,407 |
Redeemable preferred stock |
| 10,006 |
| 10,185 |
| 10,185 |
|
|
|
|
|
|
|
TOTAL FIXED MATURITIES |
| 448,161 |
| 441,912 |
| 441,912 |
|
|
|
|
|
|
|
EQUITY SECURITIES - AVAILABLE-FOR-SALE |
|
|
|
|
|
|
AND TRADING: |
|
|
|
|
|
|
Common stocks: |
|
|
|
|
|
|
Industrial, miscellaneous and all other |
| 2,612 |
| 2,490 |
| 2,490 |
Non-redeemable preferred stocks |
| 3,588 |
| 3,630 |
| 3,630 |
|
|
|
|
|
|
|
TOTAL EQUITY SECURITIES |
| 6,200 |
| 6,120 |
| 6,120 |
|
|
|
|
|
|
|
Short-term investments and resale agreements |
| 10,319 |
| 10,319 |
| 10,319 |
Other long-term investments |
| 18,547 |
| 18,547 |
| 18,547 |
|
|
|
|
|
|
|
TOTAL INVESTMENTS | $ | 483,227 | $ | 476,898 | $ | 476,898 |
SCHEDULE II | ||||||
| ||||||
INDEPENDENCE HOLDING COMPANY | ||||||
CONDENSED BALANCE SHEETS (In thousands, except share data) | ||||||
(PARENT COMPANY ONLY) | ||||||
| ||||||
|
|
| DECEMBER 31, | |||
|
|
| 2017 |
|
| 2016 |
|
|
|
|
|
|
|
ASSETS: |
|
|
|
|
|
|
Cash and cash equivalents |
| $ | 2,304 |
| $ | 3,667 |
Short-term investments |
|
| - |
|
| 3,500 |
Fixed maturities, available-for-sale |
|
| 27,270 |
|
| 48,819 |
Investments in consolidated subsidiaries |
|
| 445,697 |
|
| 425,677 |
Other assets |
|
| 235 |
|
| 408 |
|
|
|
|
|
|
|
TOTAL ASSETS |
| $ | 475,506 |
| $ | 482,071 |
|
|
|
|
|
|
|
LIABILITIES AND STOCKHOLDERS' EQUITY |
|
|
|
|
|
|
LIABILITIES: |
|
|
|
|
|
|
Accounts payable and other liabilities |
| $ | 8,886 |
| $ | 8,732 |
Amounts due to consolidated subsidiaries, net |
|
| 25,318 |
|
| 28,697 |
Income taxes payable |
|
| 3,411 |
|
| 4,236 |
Dividends payable |
|
| 1,583 |
|
| 1,082 |
Liabilities attributable to discontinued operations |
|
| - |
|
| 68 |
|
|
|
|
|
|
|
TOTAL LIABILITIES |
|
| 39,198 |
|
| 42,815 |
|
|
|
|
|
|
|
Redeemable noncontrolling interest |
|
| 2,065 |
|
| - |
|
|
|
|
|
|
|
STOCKHOLDERS' EQUITY: |
|
|
|
|
|
|
Preferred stock (none issued)(A) |
|
| - |
|
| - |
Common stock (B) |
|
| 18,625 |
|
| 18,620 |
Paid-in capital |
|
| 124,538 |
|
| 126,468 |
Accumulated other comprehensive loss |
|
| (4,598) |
|
| (6,964) |
Treasury stock, at cost (C) |
|
| (63,404) |
|
| (17,483) |
Retained earnings |
|
| 356,383 |
|
| 315,918 |
|
|
|
|
|
|
|
TOTAL IHC’S STOCKHOLDERS' EQUITY |
|
| 431,544 |
|
| 436,559 |
NONREDEEMABLE NONCONTROLLING INTERESTS |
|
| 2,699 |
|
| 2,697 |
|
|
|
|
|
|
|
TOTAL EQUITY |
|
| 434,243 |
|
| 439,256 |
|
|
|
|
|
|
|
TOTAL LIABILITIES AND EQUITY |
| $ | 475,506 |
| $ | 482,071 |
(A)Preferred stock $1.00 par value, 100,000 shares authorized; none issued or outstanding.
(B)Common stock $1.00 par value, 23,000,000 shares authorized; 18,625,458 and 18,620,508 shares issued, respectively, 14,890,285 and 17,102,525 shares outstanding, respectively.
(C)Treasury stock, at cost; 3,735,173 and 1,517,983 shares, respectively, outstanding.
The financial information of Independence Holding Company (Parent Company Only) should be read in conjunction with the Consolidated Financial Statements and Notes thereto.
SCHEDULE II | ||||||||
(Continued) | ||||||||
| ||||||||
INDEPENDENCE HOLDING COMPANY | ||||||||
CONDENSED STATEMENTS OF INCOME AND COMPREHENSIVE INCOME (In thousands) | ||||||||
(PARENT COMPANY ONLY) | ||||||||
| ||||||||
|
| 2017 |
|
| 2016 |
|
| 2015 |
REVENUES: |
|
|
|
|
|
|
|
|
Net investment income | $ | 576 |
| $ | 146 |
| $ | 112 |
Net realized investment gains (losses) |
| 189 |
|
| (121) |
|
| (506) |
Other income |
| 1,533 |
|
| 1,619 |
|
| 1,800 |
|
|
|
|
|
|
|
|
|
|
| 2,298 |
|
| 1,644 |
|
| 1,406 |
EXPENSES: |
|
|
|
|
|
|
|
|
Interest expense on debt |
| - |
|
| 1,443 |
|
| 1,567 |
General and administrative expenses |
| 7,675 |
|
| 8,837 |
|
| 5,506 |
|
|
|
|
|
|
|
|
|
|
| 7,675 |
|
| 10,280 |
|
| 7,073 |
|
|
|
|
|
|
|
|
|
Loss from continuing operations before income tax benefits and |
|
|
|
|
|
|
|
|
equity in net income from continuing operations of subsidiaries |
| (5,377) |
|
| (8,636) |
|
| (5,667) |
|
|
|
|
|
|
|
|
|
Equity in net income from continuing operations of subsidiaries |
| 44,854 |
|
| 28,843 |
|
| 32,118 |
|
|
|
|
|
|
|
|
|
Income from continuing operations before income tax benefits |
| 39,477 |
|
| 20,207 |
|
| 26,451 |
|
|
|
|
|
|
|
|
|
Income tax (benefits) |
| (2,653) |
|
| (2,303) |
|
| (1,523) |
|
|
|
|
|
|
|
|
|
Income from continuing operations, net of tax |
| 42,130 |
|
| 22,510 |
|
| 27,974 |
|
|
|
|
|
|
|
|
|
Discontinued operations (Note 3): |
|
|
|
|
|
|
|
|
Income from discontinued operations, before income taxes |
| - |
|
| 117,617 |
|
| 4,310 |
Income taxes on discontinued operations |
| - |
|
| 6,813 |
|
| 1,762 |
Income from discontinued operations, net of tax |
| - |
|
| 110,804 |
|
| 2,548 |
|
|
|
|
|
|
|
|
|
Net income |
| 42,130 |
|
| 133,314 |
|
| 30,522 |
|
|
|
|
|
|
|
|
|
Less income from noncontrolling interests in subsidiaries |
| (88) |
|
| (10,016) |
|
| (578) |
|
|
|
|
|
|
|
|
|
Net income attributable to IHC |
| 42,042 |
|
| 123,298 |
|
| 29,944 |
|
|
|
|
|
|
|
|
|
Comprehensive Income: |
|
|
|
|
|
|
|
|
Net income |
| 42,130 |
|
| 133,314 |
|
| 30,522 |
Other comprehensive income (loss), net of tax: |
|
|
|
|
|
|
|
|
Unrealized gains (losses) on available-for-sale securities |
| 73 |
|
| 114 |
|
| (51) |
Equity in unrealized gains (losses) on available-for-sale |
|
|
|
|
|
|
|
|
securities of subsidiaries |
| 3,108 |
|
| (3,622) |
|
| (3,411) |
Other comprehensive income (loss), net of tax |
| 3,181 |
|
| (3,508) |
|
| (3,462) |
|
|
|
|
|
|
|
|
|
Comprehensive income, net of tax |
| 45,311 |
|
| 129,806 |
|
| 27,060 |
Less: comprehensive income attributable to noncontrolling interests |
| (88) |
|
| (10,134) |
|
| (583) |
|
|
|
|
|
|
|
|
|
Comprehensive income, net of tax, attributable to IHC | $ | 45,223 |
| $ | 119,672 |
| $ | 26,477 |
The financial information of Independence Holding Company (Parent Company Only) should be read in conjunction with the Consolidated Financial Statements and Notes thereto.
SCHEDULE II | ||||||||
(Continued) | ||||||||
| ||||||||
INDEPENDENCE HOLDING COMPANY | ||||||||
CONDENSED STATEMENTS OF CASH FLOWS (In thousands) | ||||||||
(PARENT COMPANY ONLY) | ||||||||
| ||||||||
|
| 2017 |
|
| 2016 |
|
| 2015 |
|
|
|
|
|
|
|
|
|
CASH FLOWS PROVIDED BY (USED BY) |
|
|
|
|
|
|
|
|
OPERATING ACTIVITIES: |
|
|
|
|
|
|
|
|
Net income | $ | 42,130 |
| $ | 133,314 |
| $ | 30,522 |
Adjustments to net income: |
|
|
|
|
|
|
|
|
Gain on disposal of discontinued operations, net of tax |
| - |
|
| (110,337) |
|
| - |
Equity in net income of subsidiaries, including discontinued operations |
| (44,854) |
|
| (28,843) |
|
| (34,698) |
Other |
| 2,521 |
|
| 3,396 |
|
| 9,204 |
Changes in other assets and liabilities |
| (3,121) |
|
| (1,939) |
|
| 550 |
|
|
|
|
|
|
|
|
|
Net change in cash from operating activities |
| (3,324) |
|
| (4,409) |
|
| 5,578 |
|
|
|
|
|
|
|
|
|
CASH FLOWS PROVIDED BY (USED BY) |
|
|
|
|
|
|
|
|
INVESTING ACTIVITIES: |
|
|
|
|
|
|
|
|
Change in investments in and advances to subsidiaries (A) |
| 26,847 |
|
| 81,762 |
|
| 12,398 |
Net (purchases) sales and maturities of short-term investments |
| 3,499 |
|
| (3,501) |
|
| - |
Purchases of fixed maturities |
| (46,605) |
|
| (94,850) |
|
| (20,857) |
Sales of fixed maturities |
| 63,568 |
|
| 70,745 |
|
| 5,915 |
Maturities and other repayments of fixed maturities |
| 4,640 |
|
| - |
|
| - |
Other investing activities |
| - |
|
| (2,995) |
|
| - |
|
|
|
|
|
|
|
|
|
Net change in cash from investing activities |
| 51,949 |
|
| 51,161 |
|
| (2,544) |
|
|
|
|
|
|
|
|
|
CASH FLOWS PROVIDED BY (USED BY) |
|
|
|
|
|
|
|
|
FINANCING ACTIVITIES: |
|
|
|
|
|
|
|
|
Repurchases of common stock |
| (46,401) |
|
| (3,925) |
|
| (1,820) |
Cash paid in acquisitions of noncontrolling interests |
| - |
|
| (486) |
|
| - |
Repayments of debt |
| - |
|
| (38,146) |
|
| - |
Dividends paid |
| (1,928) |
|
| (1,553) |
|
| (1,392) |
Payments related to tax withholding for sharebased compensation |
| (1,659) |
|
| - |
|
| - |
Other financing activities |
| - |
|
| 513 |
|
| 301 |
|
|
|
|
|
|
|
|
|
Net change in cash from financing activities |
| (49,988) |
|
| (43,597) |
|
| (2,911) |
|
|
|
|
|
|
|
|
|
Net change in cash and cash equivalents |
| (1,363) |
|
| 3,155 |
|
| 123 |
Cash and cash equivalents, beginning of year |
| 3,667 |
|
| 512 |
|
| 389 |
|
|
|
|
|
|
|
|
|
Cash and cash equivalents, end of year | $ | 2,304 |
| $ | 3,667 |
| $ | 512 |
|
|
|
|
|
|
|
|
|
(A)Includes $12,100,000, $29,800,000 and $0 of cash dividends paid to parent company by consolidated subsidiaries for the years ended December 31, 2017, 2016 and 2015, respectively.
The financial information of Independence Holding Company (Parent Company Only) should be read in conjunction with the Consolidated Financial Statements and Notes thereto.
| SCHEDULE III | ||||||||||
| INDEPENDENCE HOLDING COMPANY | ||||||||||
| SUPPLEMENTARY INSURANCE INFORMATION | ||||||||||
| (in thousands) | ||||||||||
|
| ||||||||||
|
|
| FUTURE |
|
|
|
|
|
|
|
|
|
|
| POLICY |
|
|
| INSURANCE | AMORTIZATION | SELLING |
|
|
|
| DEFERRED | BENEFITS, |
| NET | NET | BENEFITS, | OF DEFERRED | GENERAL & |
| NET |
|
| ACQUISITION | LOSSES & | UNEARNED | PREMIUMS | INVESTMENT | CLAIMS & | ACQUISTION | ADMINISTRATIVE |
| PREMIUMS |
|
| COSTS (1) | CLAIMS | PREMIUMS | EARNED | INCOME (2) | RESERVES | COSTS (1) | EXPENSES (3) |
| WRITTEN |
December 31, 2017 |
|
|
|
|
|
|
|
|
|
|
|
Specialty Health | $ | - | 53,859 | 3,292 | 181,851 | 5,299 | 84,380 | - | 106,223 | $ | 179,164 |
Group disability; life |
|
|
|
|
|
|
|
|
|
|
|
and DBL |
| - | 137,765 | 3,193 | 99,953 | 6,469 | 52,792 | - | 35,857 |
| 99,495 |
Individual life, annuities |
|
|
|
|
|
|
|
|
|
|
|
and other |
| - | 333,105 | 181 | 210 | 1,536 | 241 | - | 2,411 |
| 209 |
Medical Stop-Loss |
| - | 2,257 | - | 252 | 1,111 | (2,359) | - | 2,127 |
| 253 |
Corporate |
| - | - | - | - | 1,861 | - | - | 10,486 |
| - |
| $ | - | 526,986 | 6,666 | 282,266 | 16,276 | 135,054 | - | 157,104 | $ | 279,121 |
|
|
|
|
|
|
|
|
|
|
|
|
December 31, 2016 |
|
|
|
|
|
|
|
|
|
|
|
Specialty Health | $ | - | 50,943 | 6,320 | 154,397 | 3,272 | 81,215 | - | 84,730 | $ | 154,333 |
Group disability; life |
|
|
|
|
|
|
|
|
|
|
|
and DBL |
| - | 137,428 | 3,305 | 96,190 | 6,469 | 52,245 | - | 33,386 |
| 96,454 |
Individual life, annuities |
|
|
|
|
|
|
|
|
|
|
|
and other |
| - | 341,181 | 161 | 47 | 2,255 | 1,344 | - | 3,952 |
| 46 |
Medical Stop-Loss |
| - | 54,760 | - | 12,070 | 1,700 | 10,427 | - | (1,546) |
| 12,070 |
Corporate |
| - | - | - | - | 2,874 | - | - | 11,652 |
| - |
| $ | - | 584,312 | 9,786 | 262,704 | 16,570 | 145,231 | - | 132,174 | $ | 262,903 |
|
|
|
|
|
|
|
|
|
|
|
|
December 31, 2015 |
|
|
|
|
|
|
|
|
|
|
|
Specialty Health | $ | - | 42,165 | 7,005 | 171,912 | 1,813 | 93,916 | - | 85,506 | $ | 171,731 |
Group disability; life |
|
|
|
|
|
|
|
|
|
|
|
and DBL |
| - | 141,837 | 3,060 | 85,953 | 3,699 | 47,646 | - | 26,857 |
| 86,304 |
Individual life, annuities |
|
|
|
|
|
|
|
|
|
|
|
and other |
| - | 405,327 | 171 | 11,904 | 7,146 | 11,697 | - | 15,544 |
| 11,901 |
Medical Stop-Loss |
| - | 100,088 | - | 209,765 | 4,374 | 153,919 | - | 41,392 |
| 209,765 |
Corporate |
| - | - | - | - | 205 | - | - | 8,342 |
| - |
| $ | - | 689,417 | 10,236 | 479,534 | 17,237 | 307,178 | - | 177,641 | $ | 479,701 |
|
|
|
|
|
|
|
|
|
|
|
|
(1)In 2015, the Company ceded substantially all of its individual life and annuity policy blocks in run-off and as a result, the remaining balance of deferred acquisition costs is insignificant at December 31, 2017 and 2016 and is included in other assets on the accompanying Consolidated Balance Sheets. Amortization of deferred acquisition costs was $340,000, $319,000 and $3,524,000 for the years ended December 31, 2017, 2016 and 2015, respectively, and is included in selling, general and administrative expenses on the Consolidated Statements of Income for those periods.
(2)Net investment income is allocated between product lines based on the mean reserve method.
(3)Where possible, direct operating expenses are specifically identified and charged to product lines. Indirect expenses are allocated based on time studies; however, other acceptable methods of allocation might produce different results.
SCHEDULE IV | ||||||||||
INDEPENDENCE HOLDING COMPANY | ||||||||||
REINSURANCE | ||||||||||
(In thousands) | ||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| PERCENTAGE |
|
|
|
| ASSUMED |
| CEDED |
|
|
| OF AMOUNT |
|
| GROSS |
| FROM OTHER |
| TO OTHER |
| NET |
| ASSUMED |
|
| AMOUNT |
| COMPANIES |
| COMPANIES |
| AMOUNT |
| TO NET |
|
|
|
|
|
|
|
|
|
|
|
Life Insurance In-Force: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
December 31, 2017 | $ | 13,770,999 | $ | 7,054 | $ | 6,878,689 | $ | 6,899,364 |
| 0.1% |
December 31, 2016 | $ | 12,466,127 | $ | 7,848 | $ | 6,303,742 | $ | 6,170,233 |
| 0.1% |
December 31, 2015 | $ | 12,063,911 | $ | 129,231 | $ | 6,365,993 | $ | 5,827,149 |
| 2.2% |
|
|
|
|
|
|
|
|
|
|
|
Premiums Earned: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
December 31, 2017 |
|
|
|
|
|
|
|
|
|
|
Accident and health | $ | 249,134 | $ | 7,574 | $ | 32,290 | $ | 224,418 |
| 3.4% |
Life and annuity |
| 56,194 |
| 795 |
| 38,899 |
| 18,090 |
| 4.4% |
Property and liability (1) |
| 40,139 |
| - |
| 381 |
| 39,758 |
| 0.0% |
| $ | 345,467 | $ | 8,369 | $ | 71,570 | $ | 282,266 |
| 3.0% |
|
|
|
|
|
|
|
|
|
|
|
December 31, 2016 |
|
|
|
|
|
|
|
|
|
|
Accident and health | $ | 461,467 | $ | 19,744 | $ | 276,392 | $ | 204,819 |
| 9.6% |
Life and annuity |
| 57,938 |
| 1,595 |
| 42,078 |
| 17,455 |
| 9.1% |
Property and liability (1) |
| 40,697 |
| - |
| 267 |
| 40,430 |
| 0.0% |
| $ | 560,102 | $ | 21,339 | $ | 318,737 | $ | 262,704 |
| 8.1% |
|
|
|
|
|
|
|
|
|
|
|
December 31, 2015 |
|
|
|
|
|
|
|
|
|
|
Accident and health | $ | 513,814 | $ | 28,822 | $ | 126,613 | $ | 416,023 |
| 6.9% |
Life and annuity |
| 46,699 |
| 4,330 |
| 23,078 |
| 27,951 |
| 15.5% |
Property and liability (1) |
| 35,812 |
| - |
| 252 |
| 35,560 |
| 0.0% |
| $ | 596,325 | $ | 33,152 | $ | 149,943 | $ | 479,534 |
| 6.9% |
|
|
|
|
|
|
|
|
|
|
|
(1)Property and liability products consist primarily of our pet and liability portion of our occupational accident insurance lines.
Exhibit Number |
3.1 Restated Certificate of Incorporation of Independence Holding Company (Filed as Exhibit 3(i) to our Quarterly Report on Form 10-Q for the quarter ended June 30, 1996 and incorporated herein by reference).
3.3 By-Laws of Independence Holding Company (Filed as Exhibit 3.3 to our Annual Report on Form 10-K for the year ended December 31, 2006 and incorporated herein by reference), as amended by Amendment to By-Laws of Independence Holding Company (Filed as Exhibit 3.2 to our Quarterly Report on Form 10-Q for the quarter ended September 30, 2013 and incorporated herein by reference).
10.6 Retirement Benefit Agreement, dated as of September 30, 1991, between Independence Holding Company and Mr. Roy T.K. Thung, as amended. (Filed as an Exhibit to our Annual Report on Form 10-K for the year ended December 31, 1993 and incorporated herein by reference; Amendment No. 1 filed as Exhibit 10(iii)(A)(4a) to our Annual Report on Form 10-K for the year ended December 31, 2003 and incorporated herein by reference; Amendment No. 2 filed as Exhibit 10(iii)(4)(b) to our Current Report on Form 8-K filed with the SEC on June 22, 2005 and incorporated herein by reference; Amendment No. 3 filed as Exhibit 10.1 to our Current Report on Form 8-K filed with the SEC on January 7, 2009 and incorporated herein by reference.)
10.7Purchase Agreement, made and entered into on June 15, 2015, by and among Madison National Life Insurance Company, Inc., Standard Security Life Insurance Company of New York and
21Subsidiaries of Independence Holding Company, as of December 31, 2017.*
23.1Consent of RSM US LLP, independent registered public accounting firm.*
23.2Consent of KPMG LLP, independent registered public accounting firm.*
101.INSXBRL Instance Document. The instance document does not appear in the Interactive Data File because its XBRL tags are embedded within the Inline XBRL document.
101.SCHXBRL Taxonomy Extension Schema Document. *
101.CALXBRL Taxonomy Extension Calculation Linkbase Document. *
101.LABXBRL Taxonomy Extension Label Linkbase Document. *
101.PREXBRL Taxonomy Extension Presentation Linkbase Document. *
101.DEFXBRL Taxonomy Extension Definition Linkbase Document. *
* Filed herewith.