Back to Form 10-K Exhibit 10.40
Medicaid Managed Care Contract
WellCare of Kentucky, Inc.
Table of Contents
| |
| 3. | Abbreviations and Acronyms |
| |
| 4.1 | Contractor Representations and Warranties |
| |
| 4.2 | Organization and Valid Authorization |
| |
| 4.3 | Licensure of the Contractor – To Be Supplemented |
| |
| 4.5 | Licensure of Providers |
| |
| 4.6 | Ownership or Controlling Interest/Fraud and Abuse |
| |
| 4.7 | Pending or Threatened Litigation |
| |
| 5.2 | Administration and Management |
| |
| 5.3 | Delegations of Authority |
| |
| 5.4 | Contractor Conformance with Applicable Law, Policies and Procedures |
6. Department Policies and Procedures
6.1 Commonwealth and Federal Law
6.2 Nondiscrimination and Affirmative Action
6.3 Employment Practices
6.4 Governance
6.5 Access to Premises
| |
| 7.1 | Subcontractor Indemnity |
7.3 Disclosure of Subcontractor
7.4 Remedies
8. Contract Term
8.1 Term
8.2 Effective Date for Payment
8.3 Social Security
8.4 Contractor Attestation
9. Readiness Review
10. Organization
| |
| 10.1 | Administration/Staffing |
11. Capitation Payment Information
11.1 Monthly Payment
11.2 Payment in Full
11.3 Payment Adjustments
11.4 Contractor Recoupment from Member for Fraud, Waste and Abuse
12. Rate Component
12.1 Calculation of Rates
12.2 Rate Adjustments
12.3 Risk Adjustments
12.4 Rate Proposals
| |
| 12.5 | Physician Compensation Plans |
| |
| 12.6 | Contractor Provider Payments |
13. Service Area
14. Contractor’s Financial Security Obligations
14.1 Solvency Requirements and Protections
14.2 Contractor Indemnity
14.3 Insurance
14.4 Advances, Distributions and Loans
14.5 Accumulated Fund Deficit
14.6 Provider Risks
15. Third Party Resources
| |
| 15.1 | Coordination of Benefits (COB) |
| |
| 15.2 | Third Party Liability |
16. Management Information System
| |
| 16.1 | Contractor MIS Requirements |
| |
| 16.3 | Third Party Liability (TPL) Subsystem |
| |
| 16.6 | Claims Processing Subsystem |
| |
| 16.8 | Utilization/Quality Improvement Subsystem |
| |
| 16.9 | Surveillance Utilization Review Subsystem (SURS) |
| |
| 16.10 | Analysis and Reporting Function |
| |
| 16.11 | Interface Capability |
| |
| 16.12 | Access to Contractor’s MIS |
17. Encounter Data
17.1 Encounter Data Submission
17.2 Technical Workgroup
18. Kentucky Health Information Exchange (KHIE)
19. Quality Assessment/Performance Improvement (QAPI)
19.1 QAPI Program
19.2 Annual QAPI Review
19.3 QAPI Plan
19.4 QAPI Monitoring and Evaluation
20. Kentucky Healthcare Outcomes
| |
| 20.1 | Kentucky Outcomes Measures and Health Care Effectiveness Data and Information Set (HEDIS) Measures |
| |
| 20.2 | HEDIS Performance Measures |
| |
| 20.3 | Accreditation of Contractor by National Accrediting Body |
| |
| 20.4 | Performance Improvement Projects (PIPs) |
| |
| 20.5 | Quality and Member Access Committee |
| |
| 20.6 | Utilization Management |
| |
| 20.7 | Adverse Actions Related to Medical Necessity or Coverage Denials |
| |
| 20.8 | Assessment of Member and Provider Satisfaction and Access |
| |
| 21. | Monitoring and Evaluation |
| |
| 21.1 | Financial Performance Measures |
| |
| 21.2 | Monitoring Requirements |
| |
| 22.3 | External Quality Review |
| |
| 22.4 | EQR Administrative Reviews |
| |
| 22.3 | Member Education and Outreach |
| |
| 22.4 | Outreach to Homeless Persons |
| |
| 22.5 | Member Information Materials |
| |
| 22.6 | Member Rights and Responsibilities |
| |
| 22.8 | Membership Identification Cards |
23. Member Selection of Primary Care Provider
23.1 Members without SSI
23.2 Members who have SSI and Non Dual Eligibles
23.3 Enrollment Procedures for Foster Children, Adoption and Guardianship
23.4 Primary Care Provider Changes
24. General Requirements for Grievances and Appeals
24.1 Grievance Process
24.2 Appeal Process
24.3 Expedited Resolution of Appeals
24.4 State Hearings for Members
25. Marketing
25.1 Marketing Activities
25.2 Marketing Rules
25.3 Marketing and Enrollment Agent
26. Member Eligibility, Enrollment and Disenrollment
26.1 Eligibility Determination
26.2 Managed Care Mass Enrollment Initial Assignment
26.3 General Enrollment Provisions
26.4 Enrollment Procedures
26.5 Enrollment Levels
26.6 Enrollment Period
26.7 Member Eligibility File (HIPAA 834)
26.8 Persons Eligible for Enrollment
26.9 Newborn Infants
26.10 Dual Eligibles
26.11 Persons Ineligible for Enrollment
26.12 Reinstatement of Medicaid Eligibility
26.13 Moving Out of the Contractor’s Region
26.14 Member Request for Disenrollment
26.15 Contractor Request for Disenrollment
26.16 Effective Date of Disenrollment
26.17 Continuity of Care upon Disenrollment
26.18 Death Notification
27. Provider Services
27.1 Required Functions
27.2 Provider Credentialing and Recredentialing
27.3 Primary Care Provider Responsibilities
27.4 Provider Manual
27.5 Provider Orientation and Education
27.6 Medical Records
27.7 Advance Medical Directives
27.8 Provider Grievances and Appeals
27.9 Other Related Processes
27.10 Release for Ethical Reasons
28. Provider Network
28.1 Network Providers to Be Enrolled
28.2 Out-of-Network Providers
28.3 Contractor’s Provider Network
28.4 Enrolling Current Medicaid Providers
28.5 Enrolling New Providers and Providers not
Participating in Medicaid
28.6 Termination of Network Providers or Subcontractors
28.7 Provider Program Capacity Demonstration
28.8 Program Mapping
28.9 Expansion and/or Changes in the Network
28.10 Provider Electronic Transmission of Data
28.11 Provider System Specifications and Data Definitions
28.12 Cultural Consideration and Competency
29. Provider Payment Provisions
29.1 Claims Payments
29.2 Payment to Out-of-Network Providers
29.3 Payment to Providers for Serving Dual Eligible Members
29.4 Payment of Federally Qualified Health Centers (“FQHC”) and Rural Health Clinics (“RHC”)
29.5 Commission for Children with Special Needs
29.6 Payment of Teaching Hospitals
29.7 Intensity Operating Allowance
29.8 Urban Trauma
29.9 Critical Access Hospitals
29.10 Supplemental Payments –
30.1 Medicaid Covered Services
30.2 Direct Access Service
30.3 Second Opinions
30.4 Billing Members for Covered Services
30.5 Referrals for Services Not Covered by Contractor
30.6 Interface with State Mental Health Agency
31.1 Pharmacy Requirements
31.2 Formulary and Non-Formulary Services
31.3 Pharmacy Claims Administration
31.4 Pharmacy Rebate Administration
31.5 Pharmacy Program Management
31.6 Pharmacy Provider Relations and Prior Authorizations
32. Special Program Requirements
32.1 EPSDT Early and Periodic Screening, Diagnosis and Treatment
32.2 Dental Services
32.3 Emergency Care, Urgent Care and Post Stabilization Care
32.4 Out-of-Network Emergency Care
32.5 Maternity Care
32.6 Voluntary Family Planning
32.7 Nonemergency Medical Transportation
32.8 Pediatric Interface
32.9 Pediatric Sexual Abuse Examination
32.10 Lock-In Program
33. Behavioral Health Services
33.1 Department for Behavioral Health, Developmental and Intellectual Disabilities (DBHDID) Responsibilities
33.2 DBHDID Goals for Behavioral Health Services
33.3 General Behavioral Health Requirements
33.4 Covered Behavioral Health Services
33.5 Behavioral Health Provider Network
33.6 Behavioral Health Services Hotline
33.7 Coordination between the Behavioral Health Provider and the PCP
33.8 Follow-up after Hospitalization for Behavioral Health Services
33.9 Court-Ordered Services
33.10 Community Mental Health Center (CMHC)
33.11 Program and Standards
34. Case Management
34.1 Health Risk Assessment (HRA)
34.2 Care Management System
34.3 Care Coordination
34.4 Coordination with Women, Infants and Children (WIC)
35. Enrollees with Special Health Care Needs
35.1 Individuals with Special Health Care Needs (ISHCN)
35.2 DCBS and Department for Aging and Independent Living DAIL Protection and Permanency Clients
35.3 Adult Guardianship Clients
35.4 Children in Foster Care
35.5 Children Receiving Adoption Assistance
35.6 Legal Guardians
36. Program Integrity
37. Contractor Reporting Requirements
37.1 General Reporting and Data Requirements
37.2 Record System Requirements
37.3 Reporting Requirements and Standards
37.4 COB Reporting Requirements
37.5 QAPI Reporting Requirements
37.6 Enrollment Reconciliation
37.7 Member Services Report
37.8 Grievance and Appeal Reporting Requirements
37.9 EPSDT Reports
37.10 Contractor’s Provider Network Reporting
37.11 DCBS and DAIL Service Plans Reporting
37.12 Prospective Drug Utilization Review Report
37.13 Management Reports
37.14 Financial Reports
37.15 Ownership and Financial Disclosure
37.16 Utilization and Quality Improvement Reporting
38. Records Maintenance and Audit Rights
38.1 Medical Records
38.2 Confidentiality of Records
39. Remedies for Violation, Breach, or Non-Performance of Contract
39.1 Performance Bond
39.2 Requirement of Corrective Action
39.3 Notice of Contractor Breach
39.4 Health Care Data Sanctions
39.5 Reporting
39.6 Annual Contract Monitoring
39.7 Intermediate Sanction and Civil Money Penalties
39.8 Termination for Convenience
39.9 Termination for Default
39.10 Obligations upon Termination
39.11 Liquidated Damages
39.12 Right of Set Off
39.13 Termination by Contractor
39.14 Documents Constituting Contract
39.15 Definitions and Construction
39.16 Amendments
40. Miscellaneous
40.1 Notice of Legal Action
40.2 Conflict of Interest
40.3 Offer of Gratuities/Purchasing and Specifications
40.4 Independent Capacity of the Contractor and Subcontractors
40.5 Assignment
40.6 No Waiver
40.7 Severability
40.8 Force Majeure
40.9 Disputes
40.10 Modifications or Rescission of Section 1915 Waiver / State Plan Amendment
40.11 Choice of Law
40.12 Health Insurance Portability and Accountability Act
40.13 Notices
40.14 Survival
40.15 Prohibition on Use of Funds for Lobbying Activities
40.16 Adoption of Auditor of Public Account (APA) Standards for Public and Nonprofit Boards
40.17 Review of Distributions
40.18 Audits
40.19 Cost Effective Analyses
40.20 Open Meetings and Open Records
40.21 Disclosure of Certain Financial Information
Contract Appendix
A.Service Area
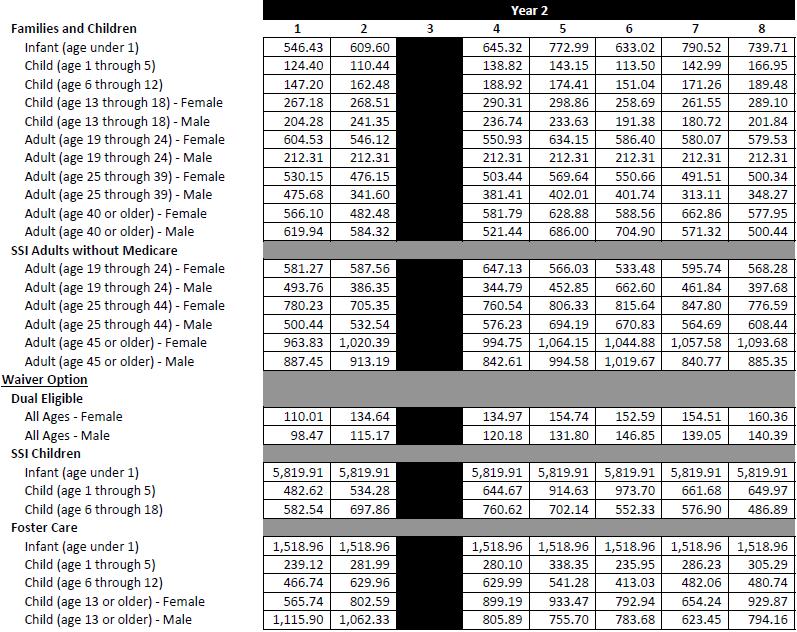
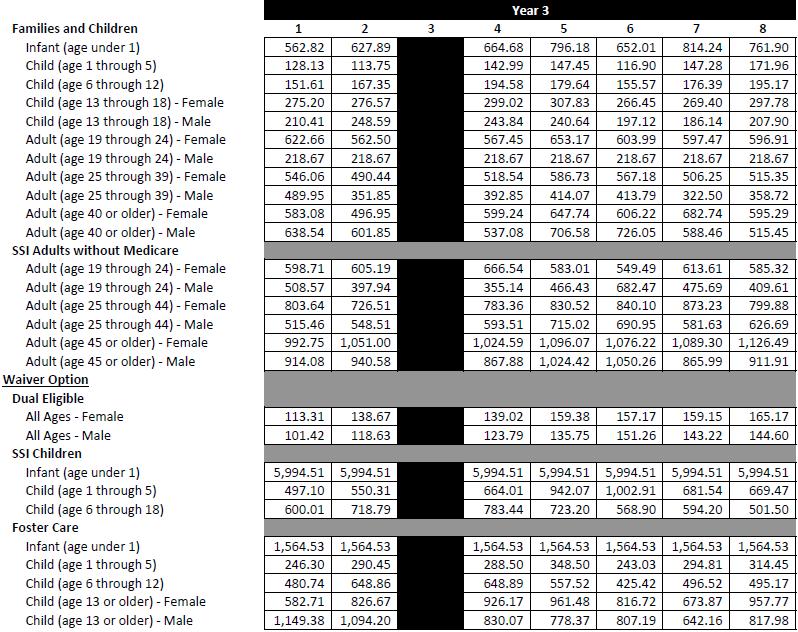
B.Approved Capitation Payment Rates
C.Management Information System Requirements
D.Encounter Data Submission Requirements
E.Encounter Data Submission Quality Standards
F.Third Party Liability/Coordination of Benefits Requirements
G.Network Provider File Layout Requirements
H.Credentialing Process Coversheet
I.Covered Services
J.Early and Periodic Screening, Diagnosis and Treatment Program Periodicity Schedule
K.Reporting Requirements Reporting Deliverables –
L.Program Integrity Requirements
M.Performance Improvement Projects
N.Health Outcomes, Indicators, Goals and Performance Measures
O.Business Associates Agreement
P.Annual Contract Monitoring Tools
This Contract is entered into among the Commonwealth of Kentucky, Finance and Administration Cabinet (“Finance”), and WellCare Health Insurance of Illinois, Inc., an Illinois corporation, doing business as WellCare of Kentucky, Inc. (“Contractor”).
WHEREAS, the Kentucky Department of Medicaid Services within the Cabinet for Health and Family Services is charged with the administration of the Kentucky Plan for Medical Assistance in accordance with the requirements of Title XIX of the Social Security Act of 1935, as amended (the “Act”), and the statutes, laws, and regulations of Kentucky; and the Kentucky Children’s Health Insurance Program (KCHIP) in accordance with the requirements of the Title XXI of the Social Security Act, as amended, and
WHEREAS, the Contractor is eligible to enter into a risk contract in accordance with Section 1903(m) of the Act and 42 CFR 438.6, is engaged in the business of providing prepaid comprehensive health care services as defined in 42 C.F.R. 438.2, and Contractor is licensed as a HMO, as defined in KRS 304.38 et seq. or as an insurer under Subtitle 3 of the Kentucky Insurance Code with a health line of authority; and
WHEREAS, the parties are entering into this agreement regarding services for the benefit of Members residing or otherwise located in the Medicaid Managed Care Region(s), and the Contractor has represented that the Contractor will exercise appropriate financial responsibility during the term of this Contract, including adequate protection against the risk of insolvency, and that the Contractor can and shall provide quality services efficiently, effectively and economically during the term of this Contract, and further the Contractor shall monitor the quality and provision of those services during the term of this Contract, representations upon which - Finance and Administration Cabinet and the Department of Medicaid Services rely in entering into this Contract;
NOW THEREFORE, in consideration of the monthly payment of predetermined Capitated Rates by the Department, the assumption of risk by the Contractor, and the mutual promises and benefits contained herein, the parties hereby agree as follows:
Abuse means Provider Abuse and Member Abuse, as defined in KRS 205.8451.
Action means, as defined in 42 CFR 438.400(b), the
| |
| A. | denial or limited authorization of a requested service, including the type or level of service; |
| |
| B. | reduction, suspension, or termination of a service previously authorized by the Department, its agent or Contractor; |
| |
| C. | denial, in whole or in part, of payment for a service; |
| |
| D. | failure to provide services in a timely manner, as defined by Department; |
| |
| E. | failure of an MCO or Prepaid Health Insurance Plan (PHIP) to act within the timeframes required by 42 CFR 438.408(b); or |
| |
| F. | for a resident of a rural area with only one MCO, the denial of a Medicaid enrollee’s request to exercise his or her right, under 42 CFR 438.52(b)(2)(ii), to obtain services outside a Contractor’s Region. |
Affiliate means an entity that directly, or indirectly through one or more intermediaries, controls or is controlled by, or is under common control with, the entity specified.
Affordable Care Act means the Patient Protection and Affordable Act (PPACA), P.L. 111-148, enacted on March 23, 2010 and the Health Care and Education Reconciliation Act of 2010 (HCERA), P.L. 111-152, enacted on March 30, 2010.
Appeal means a request for review of an Action, or a decision by the Contractor related to Covered Services or services provided.
Behavioral Health Services means clinical, rehabilitative, and support services in inpatient and outpatient settings to treat a mental illness, emotional disability, or substance abuse disorder.
Business Associate means parties authorized to exchange electronic data interchange (EDI) transactions on the Trading Partner’s behalf, as defined by HIPAA.
Cabinet means the Cabinet for Health and Family Services.
Capitation Payment means the total per Member per month amount paid by the Commonwealth to the Contractor, for providing Covered Services to Members enrolled.
Capitation Rate(s) means the amount(s) to be paid monthly to the Contractor by the Commonwealth for Members enrolled based on such factors as the Member’s aid category, age, gender and service.
Care Coordination means the integration of all processes in response to a Member’s needs and strengths to ensure the achievement of desired outcomes and the effectiveness of services.
Care Management System includes a comprehensive assessment and care plan care coordination and case management services. This includes a set of processes that arrange, deliver, monitor and evaluate care, treatment and medical and social services to a member.
Care Plan means written documentation of decisions made in advance of care provided, based on a Comprehensive Assessment of a Member’s needs, preference and abilities, regarding how services will be provided. This includes establishing objectives with the Member and determining the most appropriate types, timing and supplier(s) of services. This is an ongoing activity as long as care is provided.
Case Management is a collaborative process that assesses, plans, implements, coordinates, monitors, and evaluates the options and services required to meet the client’s health and human service needs. It is characterized by advocacy, communication, and resource management and promotes quality and cost-effective interventions and outcomes.
C.F.R. means the Code of Federal Regulations.
Children with Special Health Care Needs means Members who have or are at increased risk for chronic physical, developmental, behavioral, or emotional conditions and who also require health and related services of a type or amount beyond that required by children generally and who may be enrolled in a Children with Special Health Care Needs program operated by a local Title V funded Maternal and Child Health Program.
CHIPRA means the Children's Health Insurance Program Reauthorization Act of 2009 which reauthorized the Children's Health Insurance Program (CHIP) under Title XXI of the Social Security Act. It assures that a State is able to continue its existing program and expands insurance coverage to additional low-income, uninsured children.
Claim means any 1) bill for services, 2) line item of service, or 3) all services for a Member within a bill.
CLIA means the federal legislation commonly known as the Clinical Laboratories Improvement Amendments of 1988 as found at Section 353 of the federal Public Health Services Act (42 U.S.C. §§ 201, 263a) and regulations promulgated hereunder.
CMS means the U.S. Department of Health and Human Services, Centers for Medicare and Medicaid, formerly the Health Care Financing Administration.
Commonwealth means the Commonwealth of Kentucky.
Commission for Children with Special Health Care Needs is a Title V agency which provides specialty medical services for children with specific diagnoses and health care services needs that make them eligible to participate in Commission sponsored programs, including provision of Medical care. The Commission is an essential part of the Commonwealth’s health safety net.
Comprehensive Assessment means the detailed assessment of the nature and cause of a person’s specific conditions and needs as well as personal resources and abilities. This is generally performed by an individual or a team of specialists and may involve family, or other significant people. The assessment may be done in conjunction with care planning.
Contract means this Contract between Finance and the Contractor and any amendments, including, corrections or modifications thereto incorporating and
making a part hereof the documents described in Section 39.14 “Documents Constituting Contract” of this Contract.
Contractor’s Network means collectively, all of the Providers that have contracts with the Contractor to provide Covered Services to Members.
Contract Term means the term of this Contract as set forth in Section 8.1.
Control (including the terms controlling, controlled by and under common control with) means the possession, direct or indirect, of the power to direct or cause the direction of the management and policies of a person, whether through the ownership of voting securities, by contract, or otherwise.
Covered Services means services that the Contractor is required to provide under this Contract, as identified in Addendum I of this Contract.
Critical Access Hospitals means a health care facility designation of the federal Centers for Medicare and Medicaid Services (CMS) that provides for cost-based reimbursement.
Days mean calendar days except as otherwise noted. “Working day” or “business day” means a day on which the Contractor is officially open to conduct its affairs.
Delegated Subcontract means any agreement entered into, directly or indirectly, by a Contractor to provide or arrange for the provision of core functions required under this Agreement, or in the case of a Provider, the provision of both Covered Services and such core functions. Examples of core functions include but are not limited to customer service and call center functions, the provision of printed materials to Members, utilization management, claims processing, appeals and grievances, and credentialing.
The term “Delegated Subcontract” does not include a policy of insurance for the purpose of fulfilling a Contractor’s obligations under this Agreement or reinsurance purchased by a Contractor or a Delegated Subcontractor to limit its specific or aggregate loss with respect to Covered Services provided to Members hereunder provided the Contractor or its risk-assuming Subcontractor assumes some portion of the underwriting risk for providing health care services to Members.
Delegated Subcontractor means any person or entity that enters into a Delegated Subcontract directly or indirectly with Contractor. The term Delegated Subcontractor does not include a Provider unless that provider has been delegated core functions other than credentialing.
Denial means the termination, suspension or reduction in the amount, scope or duration of a Covered Service or the refusal or failure to provide a Covered Service.
Department means the Department for Medicaid Services (DMS) within the Cabinet, or its designee.
Department for Aging and Independent Living (DAIL) is the Department within the Cabinet which oversees the administration of statewide programs and services on behalf of Kentucky's elders and individuals with disabilities.
Department for Community Based Services (DCBS) is the Department within the Cabinet that oversees the eligibility determinations for the DMS and the management of the foster care program. DCBS has offices in every county of the Commonwealth.
Disenrollment means an action taken by the Department to remove a Member’s name from the HIPAA 834 following the Department’s receipt and approval of a request for Disenrollment or a determination that the Member is no longer eligible for Enrollment.
Dual Eligible Member means a Member who is simultaneously eligible for Medicaid and Medicare benefits.
Emergency Medical Condition is defined in 42 USC 1395dd(e) and 42 CFR 438.114 and means:
| |
| A. | a medical condition manifesting itself by acute symptoms of sufficient severity (including severe pain) that a prudent layperson, who possesses an average knowledge of health and medicine, could reasonably expect that the absence of immediate medical attention to result in |
| |
| (1) | placing the health of the individual (or with respect to a pregnant woman, the health of the woman or her unborn child) in serious jeopardy, |
| |
| (2) | serious impairment of bodily functions, or |
| |
| (3) | serious dysfunction of any bodily organ or part; or |
| |
| B. | with respect to a pregnant woman having contractions |
| |
| (1) | that there is an inadequate time to effect a safe transfer to another hospital before delivery, or |
| |
| (2) | that transfer may pose a threat to the health or safety of the woman or the unborn child. |
Emergency Medical Services or Emergency Care means care for a condition as defined in 42 USC 1395dd and 42 CFR 438.114.
Encounter means a service or item provided to a patient through the healthcare system that include but are not limited to:
| |
| C. | Radiology, including professional and/or technical components; |
| |
| D. | Prescribed drugs including mental/behavioral drugs; |
| |
| I. | A service or item not directly provided by the Plan, but for which the Plan is financially responsible. An example would include an emergency service provided by an out-of-network provider or facility. |
Encounter Record means the electronically formatted list of Encounter data elements per Encounter as established by the Department and specified in Appendix D.
Encounter Technical Workgroup means a workgroup composed of representatives from Contractor, the Department, the Fiscal Agent, and EQRO.
Encounter Void means an accepted or Erred Encounter Record that has been removed from all Encounter Records.
Enrollment means an action taken by the Department to add a Member’s name to the HIPAA834 following approval by the Department of an eligible Member to be enrolled.
EPSDT means Early and Periodic Screening, Diagnosis and Treatment Program.
EPSDT Special Services means any necessary health care, diagnostic services, treatment, and other measure described in section 1905(a) of the Social Security Act to correct or ameliorate defects and physical and mental illnesses, and conditions identified by EPSDT screening services, whether or not such services are covered under the State Medicaid Plan.
EQRO means the external quality review organization, and its affiliates, with which the Commonwealth may contract as established under 42 CFR 438, Subpart E.
Erred Encounter Record means an encounter record that has failed an edit when a correction is expected by the Department.
Execution Date means the date upon which this Contract is executed by –Finance, the Department, and the Contractor.
Family Planning Services means counseling services, medical services, and pharmaceutical supplies and devices to aid those who decide to prevent or delay pregnancy.
Fiscal Agent means the agent contracted by the Department to audit Provider Claims: process and audit Encounter data; and, to provide the Contractor with eligibility, provider, and processing files.
Finance means the Commonwealth of Kentucky Finance and Administration Cabinet.
Fraud means any act that constitutes fraud under applicable federal law or KRS 205.8451-KRS 205.8483.
Federally Qualified Health Center (FQHC) means a facility that meets the requirements of Social Security Act at 1905(l)(2).
Foster Care means the DCBS program which provides temporary care for children placed in the custody of the Commonwealth who are waiting for permanent homes.
FTE means full-time equivalent, based on forty (40) hours worked per week.
Grievance means the definition established in 42 CFR 438.400.
Grievance System means a comprehensive system that includes a grievance process, an appeal process, and access to the Commonwealth’s fair hearing system.
Health Care Effectiveness Data and Information Set (HEDIS) means a tool used to measure performance on important dimensions of care of services.
HHS means the United States Department for Health and Human Services.
HHS Transaction Standard Regulation means 45 CFR, at Title 45, Parts 160 and 162, as may be amended.
HIPAA means the Health Insurance Portability and Accountability Act of 1996, and its implementing regulations (45 C.F. R. sections 142, 160, 162, and 164), all as may be amended.
HMO means a Health Maintenance Organization licensed in the Commonwealth pursuant to KRS 304.38, et.seq.
Homeless Person means one who lacks a fixed, regular or nighttime residence; is at risk of becoming homeless in a rural or urban area because the residence is not safe, decent, sanitary or secure; has a primary nighttime residence at a publicly or privately operated shelter designed to provide temporary living accommodations; has a primary nighttime residence at a public or private place not designed as regular sleeping accommodations; or is a person who does not have access to normal accommodations due to violence or the threat of violence from a cohabitant.
Health Risk Assessment (HRA) means a screening tool used to collect information on a member’s health status that includes, but is not limited to member demographics, personal and family medical history, and lifestyle. The assessment will be used to determine member’s needs for care management, disease management, behavioral health services and/or other health or community services.
HIPAA 820 means a monthly transaction file prepared by the Department that indicates Member’s cap payment.
HIPAA 834 means a monthly transaction file prepared by the Department that indicates all Members enrolled.
Individuals with Disabilities Education Act (IDEA) is a law ensuring services to children with disabilities. IDEA governs how states and public agencies provide early intervention, special education and related services to eligible infants, toddlers, children and youth with disabilities.
Individual Education Plan (IEP) means medically necessary services for an eligible child coordinated between the schools and the Contractor that complement
school services and promote the highest level of function for the child and is coordinated between the schools and the Contractor.
Information means any “health information” provided and/or made available by the Department to a Trading Partner, and has the same meaning as the term “health information” as defined by 45 CFR Part 160.103.
Insolvency means the inability of the Contractor to pay its obligations when they are due, or when its admitted assets do not exceed its liabilities. “Liabilities,” for purposes of the definition of Insolvency, shall include, but not be limited to, Claims payable required by the Kentucky Department of Insurance pursuant to Kentucky statutes, laws or regulations.
Individuals with Special Healthcare Needs (ISHCN) are Members who have or are at high risk for chronic physical, developmental, behavioral, neurological, or emotional condition and who may require a broad range of primary, specialized medical, behavioral health, and/or related services. ISHCN may have an increased need for healthcare or related services due to their respective conditions. The primary purpose of the definition is to identify these Members so the MCO can facilitate access to appropriate services.
Insurer is an insurer under Subtitle 3 of the Kentucky Insurance Code with a health line of authority
Kentucky Department of Insurance (DOI) regulates the Commonwealth's insurance market, licenses insurance agents and other insurance professionals and monitors the financial condition of insurance companies, educates consumers to make wise choices and ensures that Kentuckians are treated fairly in the marketplace.
Kentucky Health Information Exchange (KHIE) means the secure electronic information infrastructure created by the Commonwealth for sharing health information among health care providers and organizations and offers health care providers the functionality to support meaningful use and a high level of patient-centered care.
Legal Entity means any form of corporation, insurance company, Limited Liability Company, – partnership, or other business entity recognized as being able to enter into contracts and bear risk under the laws of both the Commonwealth and the United States.
Managed Care Organization (MCO) means a health maintenance organization (HMO) or insurer which has a contract with the DMS services to provide services to its Medicaid enrollees as accessible (in terms of timeliness, amount, duration, and scope) as those services are to other Medicaid Members within the area served by the entity.
Marketing means any activity conducted by or on behalf of the Contractor, in which information regarding the services offered by the Contractor is disseminated in order to educate eligible Members about Enrollment in and services of the Contractor.
Medical Detoxification means management of symptoms during the acute withdrawal phase from a substance to which the individual has been addicted.
Medical Record means a single complete record that documents all of the treatment plans developed for, and medical services received by, the Member including inpatient, outpatient, referral services and Emergency Care whether provided by Contractor’s Network or Out of Network Providers.
Medically Necessary or Medical Necessity means Covered Services which are medically necessary as defined under 907 KAR 3:130, and provided in accordance with 42 CFR § 440.230, including children’s services pursuant to 42 U.S.C. 1396d(r).
Member means a Member who is an enrollee as defined in 42 CFR 438.10(a).
MIS means Management Information System.
National Correct Coding Initiative (NCCI) means CMS developed coding policies based on coding conventions defined in the American Medical Association’s CPT manual, national and local policies and edits.
Non-covered Services means health care services that the Contractor is not required to provide under the terms of this Contract.
NPI means the national provider identifier, required under the HIPAA.
Office of Inspector General (OIG) is Kentucky's regulatory agency for licensing all health care, day care and long-term care facilities and child adoption/child-placing agencies in the Commonwealth. The OIG is responsible for the prevention, detection and investigation of fraud, abuse, waste, mismanagement and misconduct by the Cabinet's clients, employees, medical providers, vendors, contractors and subcontractors and it conducts special investigations into matters related to the Cabinet or its programs as requested by the cabinet secretary, commissioners or office heads.
Office of Attorney General (OAG) The Attorney General is the chief law officer of the Commonwealth of Kentucky and all of its departments, commissions, agencies, and political subdivisions, and the legal adviser of all state officers, departments, commissions, and agencies.
Out-of-Network Provider means any person or entity that has not entered into a participating provider agreement with Contractor or any of the Contractor’s Delegated Subcontractors for the provision of Covered Services.
Point-of-Sale (POS) means state-of-the-art, online and real-time rules-based Claims processing services with prospective drug utilization review including an accounts receivable process;
Post Stabilization Services means Covered Services, related to an Emergency Medical Condition, that are provided after a Member is stabilized in order to maintain
the stabilized condition, or under the circumstances described in 42 CFR 438.114(e) to improve or resolve the Member’s condition.
Presumptive eligibility means eligibility granted for Medicaid-covered services as specified in administrative regulation 907 KAR 1:810, Section 6 to a qualified pregnant woman based on an income screening performed by a qualified provider.
Primary Care Provider or “PCP” means a licensed or certified health care practitioner, including a doctor of medicine, doctor of osteopathy, advanced practice registered nurse, physician assistant, or health clinic, including an FQHC, primary care center, or RHC that functions within the scope of licensure or certification, has admitting privileges at a hospital or a formal referral agreement with a provider possessing admitting privileges, and agrees to provide twenty-four (24) hours a day, seven (7) days a week primary health care services to individuals, and for a Member who has a gynecological or obstetrical health care needs, disability or chronic illness, is a specialist who agrees to provide and arrange for all appropriate primary and preventive care.
Prior Authorization means Contractor’s act of authorizing specific services before they are rendered.
Program Integrity means the process of identifying and referring any suspected Fraud or Abuse activities or program vulnerabilities concerning the health care services to the Cabinet’s Office of the Inspector General.
Protected Health Information (PHI) means individual patient demographic information, Claims data, insurance information, diagnosis information, and any other care or payment for health care that identifies the individual (or there is reasonable reason to believe could identify the individual), as defined by HIPAA.
Provider means any person or entity under contract with the Contractor or its contractual agent that provides Covered Services to Members.
Psychiatric Residential Treatment Facilities (PRTF) means a non-hospital facility that has a provider agreement with the Department to provide inpatient services to Medicaid-eligible individuals under the age of 21 who require treatment on a continuous basis as a result of a severe mental or psychiatric illness. The facility must be accredited by JCAHO or other accrediting organization with comparable standards recognized by the Commonwealth. PRTFs must also meet the requirements in §441.151 through 441.182 of the CFR.
QAPI means quality assessment and performance improvement.
Quality Improvement or QI means the process of assuring that Covered Services provided to Members are appropriate, timely, accessible, available and Medically Necessary and the level of performance of key processes and outcomes of the healthcare delivery system are improved through the Contractor’s policies and procedures.
Quality Management means the integrative process that links knowledge, structure and processes together throughout the Contractor’s organization to assess and improve quality.
Rural Health Clinic or RHC means an entity that meets all of the requirements for designation as a rural health clinic under 1861(aa)(1) of the Social Security Act and approved for participation in the Kentucky Medicaid Program.
Service Location means any location at which a Member may obtain any Covered Services from the Contractor’s Network Provider.
Specialty Care means any service provided that is not provided by a PCP.
State means the Commonwealth of Kentucky.
State Fair Hearing means the administrative hearing provided by the Cabinet pursuant to KRS Chapter 13B and contained in 907 KAR 1:560.
Supplemental Security Income (SSI) is a program administered by the Social Security Administration (SSA) that pays benefits to disabled adults and children who have limited income and resources. SSI benefits are also payable to people 65 and older without disability who meet the financial limits.
Teaching hospital means a hospital providing the services of interns or residents-in-training under a teaching program approved by the appropriate approving body of the American Medical Association or, in the case of an osteopathic hospital, approved by the Committee on Hospitals of the Bureau of Professional Education of the American Osteopathic Association. In the case of interns or residents-in-training in the field of dentistry in a general or osteopathic hospital, the teaching program shall have the approval of the Council on Dental Education of the American Dental Association. In the case of interns or resident-in-training in the field of podiatry in a general or osteopathic hospital, the teaching program shall have the approval of the Council on Podiatry Education of the American Podiatry Association.
Third-Party Liability/Resource means any resource available to a Member for the payment of expenses associated with the provision of Covered Services, including but not limited to, Medicare, other health insurance coverage or amounts recovered as a result of settlement, dispute resolution, award or litigation. Third Party Resources do not include amounts that are exempt under Title XIX of the Social Security Act.
Trading Partner means a provider or a health plan that transmits health information in electronic form in connection with a transaction covered by 45 CFR Parts 160 and 162, or a business associate authorized to submit health information on the Trading Partner’s behalf, as defined by HIPAA.
Transaction means the exchange of information between two (2) parties to carry out financial or administrative activities related to health care as defined by 45 CFR Part 160.103, as defined by HIPAA.
Urgent Care means care for a condition not likely to cause death or lasting harm but for which treatment should not wait for a normally scheduled appointment.
Women, Infants and Children (WIC) means a federally-funded health and nutrition program for women, infants, and children.
| |
| 3. | Abbreviations and Acronyms |
ADA - American Dental Association
AFDC - Aid to Families with Dependent Children
AHRQ - Agency for Health Care Research and Quality
AIDS - Acquired Immune Deficiency Syndrome
AM - Ante Meridian
APRN - Advanced Practice Registered Nurse
A/R - Accounts Receivable
BBA - Balanced Budget Act
BCCTP - Breast and Cervical Cancer Treatment Program
BH - Behavioral Health
CAHPS - Consumer Assessment of Health Care Providers and Systems
CAP - Corrective Action Plan
CCD - Continuity of Care Document
CD - Compact Disc
CFR - Code of Federal Regulations
CHFS - Cabinet for Health and Family Services
CIT - Crisis Intervention Team
CLIA - Clinical Laboratory Improvement Amendments
CMHC - Community Mental Health Center
CMS - Centers for Medicare and Medicaid Services
CMS-416 - Centers for Medicare and Medicaid Services-416 (form)
CMS-1500 - Centers for Medicare and Medicaid Services-1500 (form)
COB - Coordination of Benefits
COPD - Chronic Obstructive Pulmonary Disease
CPT - Current Procedural Terminology
CVA - Cerebrovascular Accident
D (Rh) - Disease (Rheus)
DAIL - Department for Aging and Independent Living
DBHDID - Department for Behavioral Health, Developmental and Intellectual Disabilities
DCBS - Department for Community Based Services
DIVERTS - Direct Intervention: Vital Early Responsive Treatment Systems
Department - Department for Medicaid Services
DOI - Department of Insurance
DSH - Disproportionate Share Hospital
DSM-IV - Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition
DSS - Department for Social Services
EBP - Evidence-based Practice
ED - Emergency Department
EEO - Equal Employment Opportunity
EPSDT - Early and Periodic Screening, Diagnosis and Treatment
EQR - External Quality Review
EQRO - External Quality Review Organization
EST - Eastern Standard Time
FDA - Food and Drug Administration
FQHC - Federally Qualified Health Center
FTE - Full-time Equivalent
HCC - Health Call Center
HCPCS - Health Care Common Procedure Coding System
HEDIS - Health Care Effectiveness Data and Information Set
HIPAA - Health Insurance Portability and Accountability Act
HIV - Human Immunodeficiency Virus
HRA - Health Risk Assessment
HTTP - Hyper Text Transport Protocol or Hyper Text Transfer Protocol
ICD-9-CM - International Classification of Diseases, Ninth Revision, Clinical Modification
ICD-10-CM - International Classification of Diseases, Tenth Revision, Clinical Modification
ICF-MR - Intermediate Care Facility for Mentally Retarded
IDEA - Individuals with Disabilities Education Act
IEP - Individualized Education Program
ISHCN - Individuals with Special Health Care Needs
ISS - Interactive Survey System
IT - Information Technology
KAR - Kentucky Administrative Regulation
KRS - Kentucky Revised Statute
KHIE - Kentucky Health Information Exchange
LPN - Licensed Practical Nurse
MCO - Managed Care Organization
MIS - Management Information System
MMIS - Medicaid Management Information System
NAIC - National Association of Insurance Commissioners
NCCI – National Correct Coding Initiative
NCPDP - National Council for Prescription Drug Programs
NCQA - National Committee for Quality Assurance
NDC - National Drug Code
NEMT – Nonemergency Medical Transportation
NPI – National Provider Identification
OSCAR – Online Survey Certification and Reporting
PCP - Primary Care Provider
P&T – Pharmacy and Therapeutic (Committee)
PDL – Preferred Drug List
PIP - Performance Improvement Project
PM - Post Meridian
POS – Point of Sale
PRTF - Psychiatric Residential Treatment Facility
PSN - Provider-Sponsored Integrated Health Delivery Network
QAPI - Quality Assessment and Performance Improvement
QDWI - Qualified Disabled Working Individual
QI - Quality Improvement
QIC – Quality Improvement Committee
QID - Quality Improvement Directive
QMB - Qualified Medicare Beneficiary
RAC – Recovery Audit Contractor
RFP - Request for Proposal
RHC - Rural Health Clinic
RN - Registered Nurse
SED - Serious Emotional Disturbance
SLMB - Specified Low Income Medicare Beneficiary
SMI - Serious Mental Illness
SOBRA - Sixth Omnibus Budget Reconciliation Act
SSI - Supplemental Security Income
TANF - Temporary Assistance for Needy Families
TPL - Third Party Liability
UB-92 - Universal Billing 1992 (form)
UB-04 - Universal Billing 2004 (form)
UM - Utilization Management
URAC - Utilization Review Accreditation Commission
USC - United States Code
VFC - Vaccines for Children
VPN - Virtual Private Network
WIC - Women, Infants and Children
WS-Security - Web Services-Security
XDS - Cross-enterprise Document Sharing
4. Contractor Terms
4.1 Contractor Representations and Warranties
The Contractor represents and warrants that the following are true, accurate and complete statements of fact as of the Execution Date and that the Contractor shall take all actions and fulfill all obligations required so that the representations and warranties made in this section shall remain true, accurate and complete statements of fact throughout the term of the Contract.
| |
| 4.2 | Organization and Valid Authorization |
Contractor is a Legal Entity duly organized, validly existing and in good standing under the laws of the Commonwealth, and each is in full compliance with all material Commonwealth requirements and all material municipal, Commonwealth and federal tax obligations related to its organization as a Legal Entity. The obligations and responsibilities set forth in this Contract have been duly authorized under the terms of the laws of the Commonwealth and the actions taken are consistent with the Articles of Incorporation and By-laws of Contractor.
This Contract has been duly authorized and validly executed by individuals who have the legal capacity and authorization to bind the Contractor as set forth in this Contract. Likewise, execution and delivery of all other documents relied upon by Finance and the Department in entering into this Contract have been duly authorized and validly executed by individuals who have the legal capacity and corporate authorization to represent the Contractor.
| |
| 4.3 | Licensure of the Contractor |
Contractor has a valid license to operate as an HMO or insurer, issued by the DOI. There are no outstanding unresolved material Appeals or Grievances filed against Contractor with DOI. Contractor has timely filed all reports required by DOI and DOI has taken no adverse action against Contractor’s Name of which the Finance has not been notified.
As of the Execution Date, Contractor’s statutory surplus is at or above the Regulatory Action Level as defined in the risk-based capital regulations applicable to designated HMO or insurer’s licenses in the Commonwealth. The Contractor is not aware of any impending changes to its financial structure that could adversely impact its compliance with these requirements or its ability to pay its debts as they come due generally. The Contractor has not filed for protection under any Commonwealth or federal bankruptcy laws. None of the Contractor’s property, plant or equipment has been subject to foreclosure or repossession within the preceding ten-year period, and the Contractor has not had any debt called prior to expiration within the preceding ten-year period.
| |
| 4.5 | Licensure of Providers |
Each of the Providers, including individuals and facilities, which will provide health care services in Contractor’s Network is validly licensed or, where required, certified to provide those services in the Commonwealth, including
certification under CLIA, if applicable. Each Provider in the Contractor’s Network has a valid Drug Enforcement Agency (“DEA”) registration number, if applicable. Each provider in the Contractor’s Network shall have a valid NPI and taxonomy, if applicable.
| |
| 4.6 | Ownership or Controlling Interest/Fraud and Abuse |
Neither the Contractor nor any individual who has a controlling interest or who has a direct or indirect ownership interest of five (5) percent or more of the Contractor, nor any officer, director, agent or managing employee (i.e., general manager, business manager, administrator, director or like individual who exercises operational or managerial control over the Contractor or who directly or indirectly conducts the day-to-day operation of the Contractor) of the Contractor is an entity or individual (1) who has been convicted of any offense under Section 1128(a) of the Social Security Act (42 U.S.C. §1320a-7(a)) or of any offense related to fraud or obstruction of an investigation or a controlled substance described in Section 1128(b)(1)-(3) of the Social Security Act (42 U.S.C. §1320a-7(b)(1)-(3)); or (2) against whom a civil monetary penalty has been assessed under Section 1128A or 1129 of the Social Security Act (42 U.S.C. §1320a-7a; 42 U.S.C. §1320a-8); or (3) who has been excluded from participation in a program under Title XVIII, 1902(a)(39) and (41) of the Social Security Act, Section 4724 of the BBA or under a Commonwealth health care program.
Contractor shall require by contract that neither any Provider of health care services in the Contractor’s Network, nor any individual who has a direct or indirect ownership or controlling interest of 5% or more of the Provider, nor any officer, director, agent or managing employee (i.e., general manager, business manager, administrator, director or like individual who exercises operational or managerial control over the Provider or who directly or indirectly conducts the day-to-day operation of the Provider) is an entity or individual (1) who has been convicted of any offense under Section 1128(a) of the Social Security Act (42 U.S.C. §1320a-7(a)) or of any offense related to fraud or obstruction of an investigation or a controlled substance described in Section 1128(b)(1)-(3) of the Social Security Act (42 U.S.C. §1320a-7(b)(1)-(3)); or (2) against whom a civil monetary penalty has been assessed under Section 1128A or 1129 of the Social Security Act (42 U.S.C. §1320a-7a; 42 U.S.C. §1320a-8); or (3) who has been excluded from participation in a program under Title XVIII, 1902(a)(39) and (41) of the Social Security Act, Section 4724 of the BBA or under a Commonwealth health care program.
The Contractor shall certify its compliance with 42 CFR 438.610(a)(b) and have processes and/or procedures in place to ensure ongoing compliance throughout the life of the contract.
| |
| 4.7 | Pending or Threatened Litigation |
All material pending litigation against the Contractor or its Affiliates has been disclosed in writing to Finance prior to the Execution Date. For purposes of this section, litigation is material if a final finding of liability
against the Contractor or its Affiliate(s), would create a substantial likelihood that the Contractor’s ability to perform its obligations under this Agreement would be significantly impaired. Any new material litigation filed against the Contractor or its Affiliates after the Execution Date will be disclosed in writing to Finance within ten (10) business days of receipt by the Contractor of notice new pending litigation. For purposes of this Section the term “litigation” shall mean any formal judicial or administrative proceeding.
5. Contractor Functions
The Contractor shall perform or cause to be performed all of the Covered Services and shall develop, produce and deliver to the Department all of the statements, reports, data, accounting, Claims and documentation described and required by the provisions of this Contract, and the Department shall make payments to the Contractor on a capitated basis as described in this Contract. The Contractor acknowledges that failure to comply with the provisions of this Contract may result in Finance taking action pursuant to Remedies for Violation, Breach, or Non-Performance of Contract herein. The Contractor shall meet the applicable terms and conditions imposed upon Medicaid managed care organizations as set forth in 42 United States Code Section 1396b(m), 42 CFR 438, other related managed care regulations and the 1915 Waiver, as applicable.
| |
| 5.2 | Administration and Management |
The Contractor shall be responsible for the administration and management of all aspects of the performance of all of the covenants, conditions and obligations imposed upon the Contractor pursuant to this Contract. No delegation of responsibility, whether by Subcontract or otherwise, shall terminate or limit in any way the liability of the Contractor to the Department for the full performance of this Contract.
The Contractor shall, directly or indirectly, maintain the staff and staff functions as specified in Section 10.1, Administration/Staffing. The Contractor shall submit to the Department any material changes to the Contractor’s organization, and whenever requested by the Department, a current organizational chart depicting all staff functions, including but not limited to mandatory staff functions, the number of employees serving each function, and a description of the qualifications of each individual with key management responsibility for any mandatory function specified in Section 10.1.
The Contractor agrees that its administrative costs shall not exceed ten percent (10%) of the total Medicaid managed care contract cost.
| |
| 5.3 | Delegations of Authority |
The Contractor shall oversee and remain accountable for any functions and responsibilities that it delegates to any Delegated Subcontractor. In addition to the provision set forth in Subcontracts, Contractor agrees to the following provisions.
| |
| A. | There shall be a written agreement that specifies the delegated activities and reporting responsibilities of the Delegated Subcontractor and provides for revocation of the delegation or imposition of other sanctions if the Delegated Subcontractor’s performance is inadequate. |
| |
| B. | Before any delegation, the Contractor shall evaluate the prospective Delegated Subcontractor’s ability to perform the activities to be delegated. |
| |
| C. | The Contractor shall monitor the Delegated Subcontractor’s performance on an ongoing basis and subject the Delegated Subcontractor to a formal review at least once a year. |
| |
| D. | If the Contractor identifies deficiencies or areas for improvement, the Contractor and the Delegated Subcontractor shall take corrective action. |
| |
| E. | If the Contractor delegates selection of providers to another entity, the Contractor retains the right to approve, suspend, or terminate any provider selected by that Delegated Subcontractor. |
| |
| F. | The Contractor shall assure that the Delegated Subcontractor is in compliance with the requirement in 42 CFR 438. |
| |
| 6. | Contractor Conformance with Applicable Law, Policies and Procedures |
| |
| 6.1 | Department Policies and Procedures |
The Contractor shall comply with the applicable policies and procedures of the Department, specifically including without limitation the policies and procedures for MCO services, and all policies and procedures applicable to each category of Covered Services as required by the terms of this Contract. In no instance may the limitations or exclusions imposed by the Contractor with respect to Covered Services be more stringent than those specified in the applicable Department’s policies and procedures. The Department shall provide reasonable prior written notice to Contractor of any material changes to its policies and procedures, or any changes to its policies and procedures that would materially change Contractor’s performance under this Contract.
| |
| 6.2 | Commonwealth and Federal Law |
At all times during the term of this Contract and in the performance of every aspect of this Contract, the Contractor shall strictly adhere to all applicable federal and Commonwealth law (statutory and case law), regulations and standards, in effect when this Contract is signed or which may come into effect during the term of this Contract, except where waivers of said laws, regulations or standards are granted by applicable federal or Commonwealth authority. In addition to the other laws specifically identified herein, Contractor agrees to comply with the Davis-Bacon Act and the Clean Air Act and Federal Water
Pollution Control Act. The Contractor agrees to comply with the terms of 45 CFR 93 Appendix A, as applicable.
Any change mandated by the Affordable Care Act which pertain to Managed Care Organizations (MCO) and/or Medicaid Services shall be implemented by the Contractor. One such requirement listed in Section 2501 of PPACA pertains to the States collecting drug rebates for drugs covered under a MCO. The Contractor shall create and transmit a file according to the Department specifications which will allow for the Department or its contractors to bill drug rebates to manufacturers. The Contractor shall fully cooperate with Department and Department’s contractors to ensure file transmissions are complete, accurate and delivered by the Department’s specified deadlines. In addition, the Contractor shall assist and provide detailed Claim information requested by the Department or Department contractors to support rebate dispute and resolution activities.
6.3 Nondiscrimination and Affirmative Action
During the performance of this Contract, the Contractor agrees as follows:
| |
| A. | The Contractor shall not discriminate against any employee or applicant for employment because of race, religion, color, national origin, sex or age. The Contractor further agrees to comply with the provision of the Americans with Disabilities Act of 1990 (Public Law 101- 336) (ADA), 42 USC 12101, and applicable federal regulations relating thereto prohibiting discrimination against otherwise qualified disabled individuals under any program or activity. The Contractor agrees to provide, upon request, needed reasonable accommodations. The Contractor will take affirmative action to ensure that applicants are employed and that employees are treated during employment without regard to their race, religion, color, national origin, sex, age or disability. Such action shall include, but not be limited to the following: employment, upgrading, demotion or transfer; recruitment or recruitment advertising; layoff or termination; rates of pay or other forms of compensation; and selection for training, including apprenticeship. The Contractor agrees to post in conspicuous places, available to employees and applicants for employment, notices setting forth the provisions of this nondiscrimination clause or its nondiscriminatory practices. |
| |
| B. | The Contractor shall, in all solicitations or advertisements for employees placed by or on behalf of the Contractor; state that all qualified applicants will receive consideration for employment without regard to race, religion, color, national origin, sex, age or disability. |
| |
| C. | The Contractor shall send to each labor union or representative of workers with which they have a collective bargaining agreement or other contract understanding, a notice advising the said labor union or workers’ representative of the Contractor’s commitments under this |
section, and shall post copies of the notice in conspicuous places available to employees and applicants for employment. The Contractor will take such action with respect to any Subcontract or purchase order as Finance may direct as a means of enforcing such provisions, including sanctions for noncompliance.
| |
| D. | The Contractor shall comply with all applicable provisions and furnish all information and reports required by Executive Order No. 11246 of September 24, 1965, as amended, and by the rules, regulations and orders of the Secretary of Labor, or pursuant thereto, and will permit access to their books, records and accounts by the administering agency and the Secretary of Labor for purposes of investigation to ascertain compliance with such rules, regulations and orders. |
| |
| E. | In the event of the Contractor’s noncompliance with the nondiscrimination clauses of this Contract or with any of the said rules, regulations or orders, this Contract may be canceled, terminated or suspended in whole or in part and the Contractor may be declared ineligible for further government contracts or federally-assisted construction contracts in accordance with procedures authorized in Executive Order No. 11246 of September 24, 1965, as amended, and such other sanctions may be imposed and remedies invoked as provided in or as otherwise provided by law. |
| |
| F. | As this Contract involves the expenditure of federal assistance or contract grant funds, the awarded contractor shall comply with federal law and authorized regulations that are mandatorily applicable and that are not set forth in this Contract. |
| |
| G. | The Equal Employment Opportunity Act of 1978, KRS 45.560 – 45.640 applies to All State government projects with an estimated value exceeding $500,000. The Contractor shall comply with all terms and conditions of the Act. |
The Contractor agrees to comply with each of the following requirements, and to include in any Subcontracts that any Delegated Subcontractor, supplier, or any other person or entity who receives compensation pursuant to performance of this Contract, a requirement to also comply with the following laws:
| |
| A. | Title VI of the Civil Rights Act of 1964 (Public Law 88-352); |
| |
| B. | Rules and regulations prescribed by the United States Department of Labor in accordance with 41 C.F.R. Parts 60-741; and |
| |
| C. | Regulations of the United States Department of Labor recited in 20 C.F.R. Part 741, and Section 504 of the Federal Rehabilitation Act of 1973 (Public Law 93-112). |
As a Managed Care Organization responsible for providing Medicaid Covered Services to eligible residents of Kentucky, the Contractor’s governing body which has direct responsibility for fulfilling this Contract shall have a mechanism for Kentucky recipients, advocates, public sector representatives and providers to contribute meaningful guidance to ensure that the quality and adequacy of such Covered Services are provided.
Upon reasonable notice, the Contractor shall allow duly authorized agents or representatives of the Commonwealth or federal government or the independent external quality review organization required by Section 1902 (a)(30)(c) of the Social Security Act, 42 U.S. Code Section 1396a(a)(30), access to the Contractor’s premises during normal business hours, and shall cause similar access or availability to the Contractor’s Subcontractors’ premises to inspect, audit, investigate, monitor or otherwise evaluate the performance of the Contractor and/or its Subcontractors. The Contractor and/or Subcontractors shall forthwith produce all records, documents, or other data requested as part of such review, investigation, or audit.
In the event right of access is requested under this Section, the Contractor or Subcontractor shall provide and make available staff to assist in the audit or inspection effort, and provide adequate space on the premises to reasonably accommodate the Commonwealth, federal, or external quality review personnel conducting the audit, investigation, or inspection effort. All inspections or audits shall be conducted in a manner as will not unduly interfere with the performance of the Contractor’s or Subcontractors’ activities. The Contractor will be given twenty (20) business days to respond to any findings of an audit made by Finance, the Department or their agent before the findings are finalized. The Contractor shall cooperate with Finance, the Department or their agent as necessary to resolve audit findings. All information obtained will be accorded confidential treatment as provided under applicable laws, rules and regulations.
7. Provider Contracts and Delegated Subcontracts
The Contractor shall provide its proposed form of Provider contracts to the Department for review and approval prior to their use.
Except as otherwise provided in this Contract, all subcontracts between the Contractor and its Providers and Delegated Subcontractors, shall contain an agreement by the Providers and Delegated Subcontractors to indemnify, defend and hold harmless the Commonwealth, its officers, agents, and employees, and each and every Member from any liability whatsoever arising
in connection with this Contract for the payment of any debt of or the fulfillment of any obligation of the Provider and Delegated Subcontractor.
Each such Provider and Delegated Subcontractor shall further covenant and agree that in the event of a breach of the Provider and Delegated Subcontract by the Contractor, termination of the Provider and Delegated Subcontract, or insolvency of the Contractor, each Provider and Delegated Subcontractor shall provide all services and fulfill all of its obligations pursuant to the Provider and Delegated Subcontract for the remainder of any month for which the Department has made payments to the Contractor, and shall fulfill all of its obligations respecting the transfer of Members to other Providers or Delegated Subcontractors, including record maintenance, access and reporting requirements all such covenants, agreements, and obligations of which shall survive the termination of this Contract and any Provider and Delegated Subcontract.
The Contractor may, with the approval of the Department, enter into Delegated Subcontracts for the performance of its core administrative functions or core administrative functions in addition to the provision of various Covered Services to Members. All Delegated Subcontractors that provide Covered Services must be eligible for participation in the Medicaid program. The Contractor must disclose all Delegated Subcontracts to the Department. The Contractor shall submit for review to the Department each proposed Delegated Subcontract prior to signing. The Department may approve, approve with modification, or deny Delegated Subcontracts under this contract with cause if the Delegated Subcontract does not satisfy the requirements of this Contract. In determining whether the Department will impose conditions or limitations on its approval of a Delegated Subcontract, the Department may consider such factors as it deems appropriate to protect the Commonwealth and Members, including but not limited to, the proposed Delegated Subcontractor’s past performance. Each Delegated Subcontract, and any material amendment to an approved Delegated Subcontract, shall be in writing, and in form and content approved by the Department. In the event the Department has not approved the Delegated Subcontract prior to the scheduled effective date, Contractor agrees to execute said subcontract contingent upon receiving the Department’s approval. No Delegated Subcontract shall in any way relieve the Contractor of any responsibility for the performance of its duties pursuant to this Contract. The Contractor shall notify the Department in writing of the status of all Delegated Subcontractors on a quarterly basis and of the termination of any approved Delegated Subcontract within ten (10) days following termination.
The Department’s Delegated Subcontract review shall assure that all Delegated Subcontracts:
| |
| A. | Identify the population covered by the Delegated Subcontract; |
| |
| B. | Specify the amount, duration and scope of services to be provided by the Delegated Subcontractor; |
| |
| C. | Specify the term and the procedures and criteria for termination; |
| |
| D. | Specify that Delegated Subcontractors use only Commonwealth participating Medicaid providers in accordance with this Contract; |
| |
| E. | Make full disclosure of the method and amount of compensation or other consideration to be received from the Contractor; |
| |
| F. | Provide for monitoring by the Contractor of the quality of services rendered to Members, in accordance with the terms of this Contract; |
| |
| G. | Where the Delegated Subcontractor agrees to provide Covered Services, contain no provision that provides incentives, monetary or otherwise, for the withholding from Members of Medically Necessary Covered Services; |
| |
| H. | Contain a prohibition on assignment, or on any further subcontracting, without the prior written consent of the Subcontractor (note consider for example a delegated dental subcontract, this provision would preclude the subcontracting to individual dentists without Department approval) |
| |
| I. | Contain an explicit provision that the Commonwealth is the intended third-party beneficiary of the Delegated Subcontract and, as such, the Commonwealth is entitled to all remedies entitled to third-party beneficiaries under law; |
| |
| J. | Specify that Delegated Subcontractor agrees to submit Encounter Records in the format specified by the Department so that the Contractor can meet the Department’s specifications required by this Contract; |
| |
| K. | Incorporate all provisions of this Contract to the fullest extent applicable to the service or activity delegated pursuant to the Delegated Subcontract, including without limitation, the obligation to comply with all applicable federal and Commonwealth law and regulations, including but not limited to, KRS 205.8451-8483, all rules, policies and procedures of Finance and the Department, and all standards governing the provision of Covered Services and information to Members, all QAPI requirements, all record keeping and reporting requirements, all obligations to maintain the confidentiality of information, all rights of Finance, the Department, the Office of the Inspector General, the Attorney General, Auditor of Public Accounts and other authorized federal and Commonwealth agents to inspect, investigate, monitor and audit operations, all indemnification and insurance requirements, and all obligations upon termination; |
| |
| L. | Provide for Contractor to monitor the Delegated Subcontractor’s performance on an ongoing basis, including those with accreditation: the frequency and method of reporting to the Contractor; the process by which the Contractor evaluates the Delegated Subcontractor’s performance; and subjecting it to formal review according to a periodic schedule consistent with industry standards, but no less than annually. |
| |
| M. | A Delegated Subcontractor with NCQA/URAC or other national accreditation shall provide the Contractor with a copy of its’ current certificate of accreditation together with a copy of the survey report. |
| |
| N. | Provide a process for the Delegated Subcontractor to identify deficiencies or areas of improvement, and any necessary corrective action. |
| |
| O. | The remedies up to, and including, revocation of the Delegated Subcontract available to the Contractor if the Delegated Subcontractor does not fulfill its obligations. |
| |
| P. | Contain provisions that suspected fraud and abuse be reported to the contractor. |
| |
| 7.3 | Disclosure of Certain Delegated Subcontractor’s subcontracts |
The Contractor shall inform the Department of any Delegated Subcontractor which engages a subcontractor in any transaction or series of transactions, in performance of any term of this Contract, which in one fiscal year exceeds the lesser of $250,000 or five percent (5%) of the Subcontractor’s operating expense. For purposes of such disclosure, Delegated Subcontractors that provide Covered Services to Members may exclude amounts paid to their contracted Providers for the provision of Covered Services to Members.
Finance shall have the right to invoke against any Subcontractor any remedy set forth in this Contract, including the right to require the termination of any Subcontract, for each and every reason for which it may invoke such a remedy against the Contractor or require the termination of this Contract.
The initial term of the Contract shall be for a period of three (3) years from the Execution Date of the Contract.
This Contract may be renewed at the completion of the initial Contract period for four (4) additional one (1) year periods upon the mutual agreement of the Parties. Such mutual agreement shall take the form of an addendum to the Contract under RFP Section 40.050 – Changes and Modifications to the Contract. The Department shall use its best efforts to commence negotiations with the Contractor for the next term of the Agreement, within one hundred and eighty (180) days prior to the expiration of the current term, and propose rates at least ninety (90) days prior to the expiration of the current term, unless the Department elects to terminate the Agreement hereunder.
The Commonwealth reserves the right not to exercise any or all renewal options. The Commonwealth reserves the right to extend the Contract for a period less than the length of the above-referenced renewal period if such an extension is determined by Finance and the Department to be in the best interest of the Commonwealth and agreed to by the Contractor.
The Commonwealth reserves the right to renegotiate any terms and/or conditions as may be necessary to meet requirements for the extended period.
If the parties cannot agree on terms for renewal prior to June 30, 2014, then Contractor agrees to continue to provide services to Department for up to six (6) months after the end of the term, or until such time as any applicable 1915(b) waiver(s) expires, whichever is less. During such period the Department will pay Contractor under the same Provider and Capitation Rate structure as during the preceding twelve (12) months set forth herein increased by three (3%) percent per annum.
This Contract is not effective and binding until approved by the Secretary of the Finance and Administration Cabinet. Payment under this Contract is contingent upon approval by CMS of the Waiver or State Plan Amendment and this Contract.
The Department shall direct the Contractor to commence Managed Care Services under this Contract on October 1, 2011 unless doing so would violate this Contract or the requirement under 42 CFR Part 438 to provide Members with a choice between at least two Managed Care Organizations. In that event, the Department reserves the right to start Managed Care Services under the Contract November 1, 2011.
8.3 Social Security
The parties are cognizant that the Commonwealth is not liable for Social Security contributions pursuant to 42 U.S. Code Section 418, relative to the compensation of the Contractor for this Contract.
| |
| 8.4 | Contractor Attestation |
The Chief Executive Officer (CEO), the Chief Financial Officer (CFO) or Designee must attest to the best of their knowledge to the truthfulness, accuracy, and completeness of all data submitted to the Department at the time of submission. This includes encounter data or any other data in which the contractor paid Claims.
The Department or its duly authorized representative shall conduct a readiness review which will be phased over six (6) weeks and will include a minimum of one site visit for the Department. This review will be completed prior to providing Covered Services to Members by the Contractor and shall commence within thirty (30) calendar days of the Execution Date of the Contract. The purpose of the review is to provide the Department with assurances the Contractor is able and prepared to perform all administrative functions and to provide high-quality services to enrolled Members. Specifically, the review will assess the Contractor’s ability to meet the requirements set forth in the Contract and federal requirements outlined in 42 CFR 438.
The readiness review activities will be conducted by a team appointed by the Department and may include contract staff. The scope of the readiness review will include, but not be limited to, review and/or verification of: administration and organization structure, quality assurance, provider relations, member services; enrollment, third party liability and program integrity, grievances system, marketing, record keeping, adequate network provider composition and access, financial solvency and financial performance monitoring and information systems performance and interfacing capabilities.
The readiness review will require a mix of document review and interviews with Contractor’s staff to assess the various areas of operation. Written documents will be examined to ensure that they are compliant with the policies set forth by the Medicaid program and federal and state law. Reviewers will supplement the policy and procedure review with interviews (in person or by phone) with Contractor’s staff. These interviews will assure that qualified staff is aware of and able to implement the written policies and procedures and confirm the Contractor’s required systems are in place.
The Contractor shall not provide Members Covered Services until the Department has determined that the Contractor is capable of meeting these standards. A Contractor’s failure to pass the readiness review within ninety (90) days of the execution of a Contract may be in default and may result in Contract termination pursuant to Section 29.
The Department will provide the Contractor with a summary of the findings as well as the areas requiring remedial attention.
During the first one hundred and eighty (180) days after the Execution Date the Department may give tentative approval of Contractor’s required policies and procedures, temporary relief from most reporting requirements, and shall not impose penalties for failure to report or reporting late except for the following reports which shall be provided as scheduled upon commencement of providing Covered Services: Primary Care Provider reports, Provider Network Report, Benefit Prior Authorization Reports, Grievance and Appeals reports, Claims Data reports, and Call Center data reports.
A Provider currently credentialed by the Department shall be deemed credentialed for purposes of satisfying the Contractor’s requirement under this Contract to credential Providers until March 1, 2012 or when the Provider’s credential expires, whichever comes first.
The Department and Contractor shall meet weekly upon execution of the Contract or as frequently as necessary to ensure the successful transition of Members into the Managed Care Organization with no break in Covered Services. Contractor shall have one-hundred and eighty days from Execution Date to complete Health Risk Assessments under Section 34.1 for Members assigned during the initial enrollment period.
The Contractor shall have an office located within eighty (80) miles of Frankfort, Kentucky within thirty (30) days of contract execution. Prior to October 1, 2011 such office shall, at a minimum, provide for the following staff functions:
A. Executive Director for the Kentucky account
B. Member Services for Grievances and Appeals
C. Provider Services for Provider Relations and Enrollment
Other functions required to be available may be located outside of an eighty (80) mile radius of Frankfort, Kentucky.
The Contractor may subcontract for any functions; however, the above functions, if subcontracted, shall be approved by the Department and shall be carried out within an eighty (80) mile radius of Frankfort, Kentucky. All Subcontractors shall meet appropriate licensing and contract requirements specified in applicable State and Federal laws and regulations.
| |
| 10.1 | Administration/Staffing |
The Contractor shall provide the following functions that shall be staffed by a sufficient number of qualified persons to adequately provide for the member enrollment and services provided. Responsibility for these functions or staff positions may be provided by, combined with or split among Contractor’s departments, people or Subcontractors and carry such titles as Contractor designates and provides to the Department. The Executive Management shall be capable and responsible for the oversight of the entire operation.
| |
| A. | An Executive Director who is to act as liaison to the Department for all issues that relate to the Contract between the Department and the Contractor. The Executive Director shall act as the primary contact and will be authorized to represent the Contractor regarding inquiries pertaining to the contract, will be available during normal business hours, and will have decision-making authority in regard to urgent situations that arise. The Executive Director will be responsible for follow-up on contract inquiries initiated by the Department. |
| |
| B. | A Compliance Director whose responsibilities shall be to ensure financial and programmatic accountability, transparency and integrity. The Compliance Director shall maintain current knowledge of Federal and State legislation, legislative initiatives, and regulations relating to Contractor and oversee the Contractor’s compliance with the laws and Contract requirements of the Department. The Compliance Director shall also serve as the primary contact for and facilitate communications between Contractor leadership and the Department relating to Contract compliance issues. The Compliance Director shall also oversee Contractor implementation of and evaluate any actions required to correct a deficiency or address noncompliance with Contract requirements as identified by the Department. |
| |
| C. | A Medical Director who shall be a Kentucky-licensed physician. The Medical Director shall be actively involved in all major clinical programs and Quality Improvement components. The Medical Director shall devote sufficient time to ensure timely medical decisions, including after-hours consultation as needed. |
| |
| D. | A Dental Director who shall be a dentist licensed by a Dental Board of Licensure in any state. The Dental Director shall be actively involved in all major dental programs. The Dental Director shall devote sufficient time to ensure timely dental decisions, including after-hours consultation as needed. |
| |
| E. | A Finance Officer and function or designee, to oversee the budget and accounting systems implemented by the Contractor. An internal auditor shall ensure compliance with adopted standards and review expenditures for reasonableness and necessity. |
| |
| F. | A Member Services Director and function to coordinate all communications with Members and act as Member advocates. This function shall include sufficient Member Services staff to respond in a timely manner to Member seeking prompt resolution to their problems or inquiries. |
| |
| G. | A Provider Services Director and function to coordinate all communications with Contractor’s providers and Subcontractors. This function shall include sufficient Provider Services staff to respond in a timely manner to Providers seeking prompt resolution to their problems or inquires. |
| |
| H. | A Quality Improvement Director who shall be responsible for the operation of the Contractor’s QAPI Program and any QAPI Program of its subcontractors. |
| |
| I. | A Guardianship Liaison who shall serve as the Contractor’s primary liaison for meeting the needs of Members who are adult guardianship clients. |
| |
| J. | A Case Management Coordinator who shall be responsible for coordination and oversight of case management services and continuity of care for the Contractor’s Members. |
| |
| K. | An Early and Periodic Screening, Diagnosis and Treatment (EPSDT) Coordinator who shall coordinate and arrange for the provision of EPSDT services and EPSDT special services for Members. |
| |
| L. | A Foster Care/Subsidized Adoption Liaison who shall serve as the Contractor’s primary liaison for meeting the needs of Members who are children in foster care and subsidized adoptive children. |
| |
| M. | A Management Information System Director and function who shall oversee, manage and maintain the Contractor’s management information system (MIS). |
| |
| N. | A Behavioral Health Director who shall be a behavioral health practitioner and actively involved in all programs or initiatives relating to behavioral health. The Behavioral Health Director shall also coordinate efforts to provide behavioral health services by the Contractor or any behavioral health subcontractors. |
| |
| O. | A Pharmacy Director who shall coordinate, manage and oversee the provision of pharmacy services to Members. |
| |
| P. | A Claims Processing Director and function who shall ensure the timely and accurate processing of original Claims, corrected Claims, re-submissions and overall adjudication of Claims. |
| |
| Q. | A Program Integrity Coordinator who shall coordinate, manage and oversee the Contractor’s Program Integrity unit to reduce fraud and abuse of Medicaid Services. |
The Contractor shall submit to the Department on annual basis and upon request by the Department, a current organizational chart depicting all functions including mandatory functions, number of employees in each functional department and key managers responsible for the functions. The Contractor shall notify the Department in writing of any staffing change in the Executive Director, Finance Director, Medical Director, Pharmacy Director, Dental Director, Behavioral Health Director, Compliance Director or Quality Improvement Director positions within ten (10) business days. The Commonwealth reserves the right to approve or disapprove all key personnel (initial or replacement) prior to their assignment with the Contractor. The Contractor shall ensure that all staff, Providers and Subcontractors have appropriate training, education, experience, liability coverage and orientation to fulfill the requirements of their positions.
Contractor shall provide notice to the Department of any changes relating to the personnel of its management staff, including a change in duties or time commitments. Contractor shall assure the adequacy of its administrator’s staffing to properly service the needs of Contractor if changes are proposed in the personnel, duties or time commitments of administrator’s staff from those in place on the Effective Date of each Contract. Contractor shall provide those assurances to the Department before permitting its administrator to implement such changes.
| |
| 11. | Capitation Payment Information |
On or before the eighth (8th) day of each month during the term of this Contract, the Department shall remit to the Contractor the Capitation Payment specified in Appendix B for each Member determined to be enrolled for the upcoming month. The Contractor shall reconcile the capitation payment against the HIPAA 820. The Contractor shall receive a full month’s capitation payment for the month in which enrollment occurs except for a Member enrolled based on a determination of eligibility due to being unemployed in accordance with 45 CFR 233.100. The monthly capitation payment for such a member shall be pro-rated from the date of eligibility based on unemployment.
The Contractor shall accept the Capitation Payment and any adjustments made pursuant to Rate Adjustments of this Contract from the Department as payment in full for all services to be provided pursuant to this Contract and all administrative costs associated with performance of this Contract. Members
shall be entitled to receive all Covered Services for the entire period for which the Department has made payment. Any and all costs incurred by the Contractor in excess of the Capitation Payment will be borne in full by the Contractor. Interest generated through investment of funds paid to the Contractor pursuant to this Contract shall be the property of the Contractor to use for eligible expenditures under this Contract. The Contractor and Department acknowledge that contracts for Medicaid capitated rates and services are subject to approval by CMS.
In accordance with KRS 45.454, interest in the amount of one (1%) percent of any amount approved and unpaid shall be added to the amount approved for each month or fraction thereof thirty (30) working days after when due under this Contract. Contractor may pursue any unpaid amounts form the Commonwealth in accordance with KRS 45A.245.
Monthly Capitation Payments will be adjusted to reflect corrections to the Member eligibility information. In the event that a Member is eligible and enrolled, but does not appear on the HIPAA 820, the Contractor may submit a payment adjustment request. Each request must contain the following Member information:
| |
| A. | Name (last, first, middle initial) and Medicaid identification number; |
| |
| C. | Age and aid category; and |
| |
| D. | Month for which payment is being requested. |
In the event that a Member does not appear on the HIPAA 834, but the Department has paid the Contractor for a Member, the Department may request and obtain a refund of, or it may recoup from subsequent payments, any payment previously made to the Contractor for which the Contractor has not provided Covered Services to the Member or otherwise made payments on behalf of the Member.
In the event a Member appears on the HIPAA 834 but is determined to be ineligible, the Department may request and obtain a refund of, or it may recoup from subsequent payments, any payment previously made to the Contractor. Such refund or recoupment is limited to the previous payment amounts in excess of the amount of the costs for Covered Services provided to the Member or payments otherwise made on behalf of the Member. In the event that the payments for covered services exceed the capitation amount the Department will reimburse the difference to the Contractor. This reconciliation is based on accepted encounter records into the Department’s MMIS. For cases involving member ineligibility due to fraud, waste and abuse, the Department will only recoup the capitation amount and the Contractor shall establish procedures pursuant to Ineligibility Due to Fraud, Waste and Abuse Cases to recover paid Claims. Any adjustment by the Department hereunder for retroactive
disenrollments of Enrollees shall not exceed twelve (12) months from the effective date of disenrollment
| |
| 11.4 | Contractor Recoupment from Member for Fraud, Waste and Abuse |
If permitted by state and federal law, the Contractor shall request a refund from the Member for all paid Claims in the event the Department has established that the Member was not eligible to be a Member through an administrative determination or adjudication of fraud for cases handled by the OIG. The Contractor shall, upon receipt of a completed OIG investigation of a Contractor’s Member that calls for administrative recoupment, send a request letter to member seeking voluntary repayment of all Fee-For-Service Claims paid by contractor on behalf of member during time period member was found to be ineligible to receive services. The request letter should include the following as provided by the Department: the reason for the member’s ineligibility, time period of ineligibility, and amount paid during the period of ineligibility. The Contractor shall report, on a monthly basis, to the Commonwealth any monies collected from administrative request letters during the previous month and provide a listing of all administrative request letters sent to Members(s) during the previous month. The Contractor is only required to mail the initial letter to the Member requesting repayment of funds and accept repayment on behalf of the Department. The contractor is not required to address any due process issues should those arise. The Contractor shall work with Department’s agent to obtain monies collected through court ordered payments. Any outstanding payments not collected within six (6) months shall be subject to be collected by the Commonwealth and shall be maintained by the Commonwealth. The foregoing provisions shall be construed to require Contractor’s reasonable cooperation with the Commonwealth in its efforts to recover payments made on behalf of ineligible persons, and shall not create any liability on the part of the Contractor to reimburse amounts paid due to fraud that the Contractor has been unable to recover.
The Capitation Rate shall be established in accordance with 42 CFR 438. The Capitation Rates are attached as Appendix B and shall be deemed incorporated into this Agreement and shall be binding to the Contractor and the Department.
Prospective adjustments to the rates may be required. Funds previously paid may be adjusted when the Capitation Rate revision is the result of legislative, executive or judicial mandated changes in Medicaid services, or when Capitation Rate calculations are determined to have been in error (including but not limited to errors in calculation due to mislabeling of Claims as not
properly payable.) Changes mandated by state or federal legislation, or executive or judicial mandates, will take effect on the dates specified in the legislation or mandate. Any rate adjustments shall be made through the Contract amendment process.
The Affordable Care Act increases Medicaid payment rates for primary care services delivered by Primary Care Physicians to Medicare’s payment levels for the same services for calendar years 2013 and 2014. Existing rates do not include this increase as specific rules have not been promulgated by CMS. Three months prior to any increase or at the time of promulgation of rules, whichever is later, the Department’s actuary in consultation with the Department and participating MCOs, shall quantify the effect of the rate increase by applying the new required fee schedule to the claims records with the applicable codes. Capitation rates will be adjusted accordingly.
Risk adjustment shall be applied Contractor’s rates. The methods used to determine the risk assessment and risk adjustment amount will be designed to be budget neutral to the Commonwealth. The latest version of the Chronic Illness Disability Payment System (CPDS) available at the time of execution of this Contract shall be used; future updated versions of CPDS will be used as deemed appropriate. An initial meeting between the Contractor, the Department, and the Department’s actuary to discuss the technical characteristics of the model shall occur no later than sixty (60) days after contract execution. Upon agreement by all participating MCOs regarding a specified component(s) of a budget neutral risk adjust methodology; the Department shall adopt those recommended components as part of the risk adjustment process. For components of the risk adjustment methodology upon which all participating MCO’s cannot agree, the Department in consultation with its Actuary shall determine the method used for that component (s) of the risk adjustment process. Final recommendations of the group shall be provided to the Department no later than 90 days subsequent to contract execution.
| |
| 12.4 | Physician Compensation Plans |
A template for any compensation arrangement between the Contractor and a physician, or physician group as that term is defined in 42 C.F.R. § 417.479(c), or between the Contractor and any other Primary Care Providers within the meaning of this Contract, or between the Contractor and any other Subcontractor or entity to Members must be submitted to the Department for approval prior to its implementation. Approval is preconditioned on compliance with all applicable federal and Commonwealth laws and regulations. The Contractor must provide information to any Member upon request about any Physician Incentive Plan and/or any payments to Provider made pursuant to an incentive arrangement under this Section to a provider as required by applicable state or federal law.
| |
| 12.5 | Contractor Provider Payments |
If a Contractor includes a Physician Incentive Plan, the activities included shall comply with requirements set forth in 42 CFR 422.208 and 42 CFR 422.210. The Disclosures to the Department for Contractors with Physician Incentive Plans include the following:
| |
| A. | The Contractor shall report whether services not furnished by a physician/group are covered by the incentive plan. No further disclosure is required if the Physician Incentive Payment does not cover services not furnished by a physician/group. |
| |
| B. | The Contractor shall report type of incentive arrangement, e.g. withhold, bonus, capitation. |
| |
| C. | The Contractor shall report percent of withhold or bonus (if applicable). |
| |
| D. | The Contractor shall report panel size, and if patients are pooled, the approved method used. |
| |
| E. | If the physician/group is at substantial financial risk, the Contractor shall report proof the physician/group has adequate stop loss coverage, including amount and type of stop-loss. |
The Contractor’s service area shall be State-wide excluding Medicaid Managed Care Region Three as depicted in Appendix A of this Contract. Such service area is the specific geographic area within which Members shall reside to enroll with the Contractor.
| |
| 14. | Contractor’s Financial Security Obligations |
| |
| 14.1 | Solvency Requirements and Protections |
The Contractor will be subject to requirements contained in KRS Chapter 304 and related administrative regulations regarding protection against insolvency and risk-based capital requirements. In addition, pursuant to KRS 304.3-125, the Commissioner has authority to require additional capital and surplus if it appears that an insurer is in a financially hazardous condition.
The Contractor shall cover continuation of services to Members during insolvency, for the duration of the period for which payment has been made, as well as for inpatient admissions up until discharge.
In the event of the Contractor’s insolvency, the Contractor shall not hold its Members liable, except in instances of Member fraud:
| |
| A. | For the Contractor’s debts; |
| |
| B. | For the covered services provided to the Member, for which the Department does not pay the Contractor; |
| |
| C. | For the covered services provided to the Member for which the Department or the Contractor does not pay the individual or health care |
provider that furnishes the services under a contractual, referral, or other arrangement; and
| |
| D. | For covered services furnished under a contract, referral, or other arrangement, to the extent that those payments are in excess of the amount that the Member would owe if the Contractor provided the services directly. |
In no event shall the Commonwealth, Finance, the Department or Member be liable for the payment of any debt or fulfillment of any obligation of the Contractor or any Subcontractor to any Subcontractor, supplier, Out-of-Network Provider or any other party, for any reason whatsoever, including the insolvency of the Contractor or any Subcontractor. The Contractor agrees that any Subcontract will contain a hold harmless provision.
The Contractor agrees to indemnify, defend, save and hold harmless the Commonwealth, Finance, the Department, its officers, agents, and employees (collectively, the “Indemnified Parties”) from all claims, demands, liabilities, suits, judgments, or damages, including court costs and attorney fees made or asserted against or assessed to the Indemnified Parties (collectively the “Losses”), arising out of or connected in any way with this Contract or the performance or nonperformance by the Contractor, its officers, agents, employees; and suppliers, Subcontractors, or Providers, including without limitation any claim attributable to:
| |
| A. | The improper performance of any service, or improper provision of any materials or supplies, irrespective of whether the Department knew or should have known such service, supplies or materials were improper or defective; |
| |
| B. | The erroneous or negligent acts or omissions, including without limitation, disregard of federal or Commonwealth law or regulations, irrespective of whether the Department knew or should have known of such erroneous or negligent acts; |
| |
| C. | The publication, translation, reproduction, delivery, collection, data processing, use, or disposition of any information to which access is obtained pursuant to this Contract in a manner not authorized by this Contract or by federal or Commonwealth law or regulations, irrespective of whether the Department knew or should have known of such publication, translation, reproduction, delivery, collection, data processing, use, or disposition; or |
| |
| D. | Any failure to observe federal or Commonwealth law or regulations, including but not limited to, insurance and labor laws, irrespective of whether the Department knew or should have known of such failure. |
Upon receiving notice, the Department shall give the Contractor written notice of any claim made against the Contractor for which the Indemnified Parties are entitled to indemnification, so that the Contractor shall have the opportunity to appear and defend such claim. The Indemnified Parties shall have the right
to intervene in any proceeding or negotiation respecting a claim and to procure independent representation, all at the sole cost and expense of the Indemnified Parties. Under no circumstances shall the Contractor be deemed to have the right to represent the Commonwealth in any legal matter. Notwithstanding the above, Contractor shall have no obligation to indemnify the Indemnified Parties for any losses due to the negligent acts or omissions or intentional misconduct of the Indemnified Parties.
The Contractor shall secure and maintain during the entire term of the Contract, and for any additional periods following termination of the Contract during which it is obligated to perform any obligations pursuant to this Contract, original, prepaid policies of insurance, in amounts, form and substance satisfactory to Finance, and non cancelable except upon thirty (30) days prior written notice to Finance, providing coverage for property damage (all risks), business interruption, comprehensive general liability, motor vehicles, workers’ compensation and such additional coverage as is reasonable or customary for the conduct of the Contractor’s business in the Commonwealth.
| |
| 14.4 | Advances, Distributions and Loans |
The Contractor shall not, without thirty (30) day prior written notice make any distribution, loan or loan guarantee to an Affiliate. Written notice is to be submitted to the Department’s Commissioner and if applicable to DOI. The foregoing shall not be construed as a prohibition on advances to subcontractors and shall not apply to Capitation Payments or other payments made by the Contractor contemplated by service or Provider contracts previously disclosed and approved by the Department.
14. 5 Provider Risks
If a Provider assumes substantial financial risk for contracted services, the Contractor must ensure that the Provider has adequate stop-loss protection. The Contractor must provide the Department proof the Provider has adequate stop-loss coverage, including an amount and type of stop-loss.
| |
| 15.1 | Coordination of Benefits (COB) |
The Contractor shall actively pursue, collect and retain all monies available from all available resources for services to Members under this Contract except where the amount of reimbursement the Contractor can reasonably expect to receive is less than estimated cost of recovery.
Cost effectiveness of recovery is determined by, but not limited to, time, effort, and capital outlay required in performing the activity. The Contractor shall specify the threshold amount or other guidelines used in determining whether
to seek reimbursement from a liable third party, or describe the process by which the Contractor determines seeking reimbursement would not be cost effective. The Contractor shall provide the guidelines to the Department for review and approval.
COB collections are the responsibility of the Contractor or its Subcontractors. Subcontractors must report COB information to the Contractor. Contractor and Subcontractors shall not pursue collection from the Member but directly from the third party payer or the provider. Access to Covered Services shall not be restricted due to COB collection.
The Contractor shall maintain records of all COB collections. The Contractor must be able to demonstrate that appropriate collection efforts and appropriate recovery actions were pursued. The Department has the right to review all billing histories and other data related to COB activities for Members. The Contractor shall seek information on other available resources from all Members.
In order to comply with CMS reporting requirements, the Contractor shall submit a monthly COB Report for all member activity which the Department or its agent shall audit no less than every six (6) months. Additionally, Contractor shall submit a report that includes subrogation collections from auto, homeowners, or malpractice insurance, etc.
| |
| 15.2 | Third Party Liability |
By law, Medicaid is the payer of last resort and as a result shall be used as a source of payment for covered services only after all other sources of payment have been exhausted. If a Member has Third Party Resources available for payment of expenses associated with the provision of Covered Services, other than those which are exempt under Title XIX of the Social Security Act, such resources are primary to the coverage provided by the Contractor, pursuant to this Agreement, and must be exhausted prior to payment by the Contractor. The Capitation Rate set forth in this Contract has been adjusted to account for the primary liability of third parties to pay such expenses. The Contractor shall be responsible for determining the legal liability of third parties to pay for services rendered to Members pursuant to this Contract. All funds recovered by the Contractor from Third Party Resources shall be treated as income to the Contractor to be used for eligible expenses under this Contract. The Contractor and all Providers in the Contractor’s Network are prohibited from directly receiving payment or any type of compensation from the Member, except for Member co-pays or deductibles from Members for providing Covered Services. Member co-pay, co-insurance or deductible amounts cannot exceed amounts specified in 907 KAR 1:604. Co-pays, co-insurance or deductible amounts may be increased only with the approval of the Department.
42 CFR 433.138 requires that as a condition of Medicaid eligibility each Member will be required to:
| |
| A. | Assign, in writing, his/her rights to the Contractor for any medical support or other Third Party Payments for medical services provided by the Contractor; and |
| |
| B. | Cooperate in identifying and providing information to assist the Contractor in pursuing third parties that may be liable to pay for care and services provided by the Contractor. |
42 CFR 433.138 requires the Contractor be responsible for actively seeking and identifying third party resources, i.e. health or casualty insurance, liability insurance and attorneys retained for tort action, through contact with the Members, participating providers, and the Medicaid Agency.
42 CFR 433.139 requires the Contractor be responsible to assure that the Medicaid Program is the payer of last resort when other Third Party Resources are available to cover the costs of medical services provided to Medicaid Members. When the Contractor is aware of other Third Party Resources, the Contractor shall avoid payment by “cost avoiding” (denying) the Claim and redirecting the provider to bill the other Third Party Resource as a primary payer. If the Contractor does not become aware of another Third Party Resource until after the payment for service, the Contractor is responsible to seek recovery from the Third Party Resource or the provider on a post-payment basis. See Appendix F. The Department or its agent will audit the Contractor’s Third Party practices and collections at least every six (6) months.
| |
| 16. | Management Information System |
The Contractor shall maintain a Management Information System (MIS) that will provide support for all aspects of a managed care operation to include the following subsystems: Member, third party liability, provider, reference, encounter/Claims processing, financial, utilization data/quality improvement and Surveillance Utilization Review Subsystem. The Contractor will also be required to demonstrate sufficient analysis and interface capacities. The Contractor’s MIS shall assure medical information will be kept confidential through security protocol, especially as that information relates to personal identifiers and sensitive services.
The Contractor shall provide such information in accordance with the format and file specifications for all data elements as specified in Appendix C hereto, and as may be amended from time to time.
The Contractor shall transmit all data directly to the Department in accordance with 42 CFR 438. If the Contractor utilizes subcontractors for services, all data from the subcontractors shall be provided to the Contractor and the Contractor shall be responsible for transmitting the subcontractors’ data to the Department in a format specified by the Department in accordance with 42 CFR 438.
The Contractor will execute a Business Associate Agreement (BAA) in Appendix P with the Department, pursuant to Sections 261 through 264 of the federal Health Insurance Portability and Accountability Act of 1996, Public Law 104-191, known as “the Administrative Simplification provisions,” direct
the Department of Health and Human Services to develop standards to protect the security, confidentiality and integrity of health information. The execution of the BAA is required prior to data exchanges being implemented.
The Contractor shall be responsible for meeting all system requirements as required by the Department. The Contractor shall be responsible for meeting all 5010 transaction changes, ICD-10-CM diagnosis code changes and required testing.
The Contractor shall notify the Department of all significant changes to the system that may impact the integrity of the data, including such changes as new Claims processing software, new Claims processing vendors and significant changes in personnel.
| |
| 16.1 | Contractor MIS Requirements |
The Department’s MIS system utilizes eight (8) subsystems to carry out the functions of the Medicaid program. The Contractor is not required to have actual subsystems as listed below, provided the requirements are met in other ways which may be mapped to the subsystem concept. The Contractor shall have the capacity to capture necessary data and provide it in formats and files that are consistent with the Commonwealth's functional subsystems as described below. The Contractor shall maintain flexibility to accommodate the Department’s needs if a new system is implemented by the Commonwealth. These subsystems focus on the individual systems functions or capabilities which provide support for the following areas:
| |
| B. | Third Party Liability (TPL); |
| |
| E. | Claims Processing Subsystem (to include Encounter Data); |
| |
| G. | Utilization/Quality Improvement Subsystem; and |
| |
| H. | Surveillance Utilization Review Subsystem (SURS). |
The Contractor shall ensure that data received from Providers and Subcontractors is accurate and complete by:
| |
| A. | Verifying, through edits and audits, the accuracy and timeliness of reported data; |
| |
| B. | Screening the data for completeness, logic and consistency; |
| |
| C. | Collecting service information in standardized formats to the extent feasible and appropriate; |
| |
| D. | Compiling and storing all Claims and encounter data from the Subcontractors in a data warehouse in a central location in the Contractor’s MIS; and |
| |
| E. | At a minimum, edits and audits must comply with NCCI. |
The primary purpose of the member subsystem is to accept and maintain an accurate, current, and historical source of demographic information on Members to be enrolled by the Contractor.
The maintenance of enrollment/member data is required to support Claims and encounter processing, third party liability (TPL) processing and reporting functions. The major source of enrollment/member data will be electronically transmitted by the Department to the Contractor on a daily basis in a HIPAA 834 file format. The daily transaction file will include new, changed and terminated member information. The Contractor shall be required to process and utilize the daily transaction files immediately upon receipt. A monthly HIPAA 834 file of members will be electronically transmitted to the Contractor. The Contractor must reconcile Member and Capitation Payment information with the Department for Medicaid Services.
Specific data item requirements for the Contractor’s Member subsystem shall contain such items as maintenance of demographic data, matching Primary Care Providers with Members, maintenance information on Enrollments/Disenrollments, identification of TPL information, tracking EPSDT preventive services and referrals.
| |
| 16.3 | Third Party Liability (TPL) Subsystem |
In order to ensure that federal third party liability requirements are met and to maximize savings from available Third Party Resources, identification and recovery of Third Party Resources must be a joint effort between the Department and the Contractor. The Department will provide Contractor with the Medicare effective dates.
The Third Party Liability (TPL) processing function permits the Contractor to utilize the private health, Medicare, and other Third-Party Resources of its Members and ensures that the Contractor is the payer of last resort. This function works through a combination of cost avoidance (non-payment of billed amounts for which a third party may be liable) and post-payment recovery (post-payment collection of Contractor paid amounts for which a third party is liable).
Cost avoidance is the preferred method for processing Claims with TPL. This method is implemented automatically by the MIS through application of edits and audits which check Claim information against various data fields on Member, TPL, reference, or other MIS files. Post-payment recovery is primarily a back-up process to cost avoidance, and is also used in certain situations where cost avoidance is impractical or unallowable.
The provider subsystem accepts and maintains comprehensive, current and historical information about Providers eligible to participate in the Contractor’s
Network. The maintenance of provider data is required to support Claims and encounter processing, utilization/quality processing, financial processing and report functions. The Contractor shall electronically transmit provider enrollment information to the Department on a monthly basis, by the first Friday of the month following the month reported.
The Contractor’s provider subsystem shall contain such items as demographic data, identification of provider type, specialty codes, maintenance of payment information, identification of licensing, credentialing/re-credentialing information and monitoring of Primary Care Provider capacity for enrollment purposes.
The Contractor shall demonstrate compliance with standards of provider network capacity and member access to services by producing reports illustrating that services, service locations, and service sites are available and accessible in terms of timeliness, amount, duration and personnel sufficient to provide all Covered Services on an emergency or urgent care basis, 24 hours a day, seven days a week.
The Department shall monitor the Contractor’s Network capacity and member access by use of a Decision Support System. The Encounter Record submitted will be used to display Primary Care Provider location, Service Location, Member distribution, patterns of referral, quality measures, and other analytical data.
The reference subsystem maintains pricing files for procedures and drugs, and maintains other general reference information such as diagnoses, edit/audit criteria, edit dispositions and reimbursement parameters/modifiers. The reference subsystem provides a consolidated source of reference information which is accessed by the MIS during the performance of other functions, including Claims and encounter processing, TPL processing and utilization/quality reporting functions.
The Contractor’s reference subsystem shall contain such items as maintenance of procedure codes/NDC codes and diagnosis codes, identification of pricing files, maintenance of edit and audit criteria.
| |
| 16.6 | Claims Processing Subsystem |
The Claims processing subsystem collects, processes, and stores data on all health services delivered. The functions of this subsystem are Claims payment processing and capturing medical service utilization data. Claims are screened against the provider and Member subsystems. The Claims processing subsystem captures all medically related services, including medical supplies, using standard codes (e.g. HCPCS, ICD9-CM/ICD-10 CM/PCS diagnosis and procedure code, Revenue Codes, ADA Dental Codes and NDCs) rendered by medical providers to a Member regardless of remuneration arrangement (e.g. capitation/fee-for-service). The Contractor shall be required to electronically
transmit Encounter Record to the Department on a weekly basis, or on a department approved schedule that is determined by the Contractor’s financial schedule.
The Contractor’s Claims processing/encounter subsystem shall contain such items as: apply edit and audit criteria to verify timely, accurate and complete Encounter Record; edit for prior-authorized Claims; identify error codes for Claims.
The Financial subsystem function encompasses Claim payment processing, adjustment processing, accounts receivable processing, and all other financial transaction processing. This subsystem ensures that all funds are appropriately disbursed for Claim payments and all post-payment transactions are applied accurately. The financial processing function is the last step in Claims processing and produces remittance advice statements/explanation of benefits and financial reports.
The Contractor’s financial subsystem shall contain such items as: update of provider payment data, tracking of financial transactions, including TPL recoveries and maintenance of adjustment and recoupment processes.
| |
| 16.8 | Utilization/Quality Improvement Subsystem |
The Contractor shall capture and maintain a patient-level record of each service provided to Members using CMS 1500, UBO4, NCPDP, HIPAA code sets or other Claim or Claim formats that shall meet the reporting requirements in this Contract. The computerized database must contain and hold a complete and accurate representation of all services covered by the Contractor, and by all providers and Subcontractors rendering services for the contract period. The Contractor shall be responsible for monitoring the integrity of the database and facilitating its appropriate use for such required reports as encounter data, and targeted performance improvement studies.
Contractor shall comply with the requirements of 42 CFR 455.20 (a) by employing a selected sample method approved by CMS and the Department of verifying with Members whether the services billed by provider were received.
The utilization/quality improvement subsystem combines data from other subsystems, and/or external systems, to produce reports for analysis which focus on the review and assessment of access, availability and continuity of services, quality of care given, detection of over and under utilization of services, and the development of user-defined reporting criteria and standards. This system profiles utilization of Providers and Members and compares them against experience and norms for comparable individuals.
The subsystem shall support tracking utilization control function(s) and monitoring activities, including Geo Network for all Encounters in all settings
particularly in-patient and outpatient care, emergency room use, outpatient drug therapy, EPSDT and out-of-area services. It shall complete provider profiles; occurrence reporting, including adverse incidents and complications, monitoring and evaluation studies; Members and Providers aggregate Grievances and Appeals; effects of educational programs; and Member/Provider satisfaction survey compilations. The subsystem may integrate the Contractor’s manual and automated processes or incorporate other software reporting and/or analysis programs.
The Contractor’s utilization/quality improvement subsystem shall contain such items as: monitoring of primary care and specialty provider referral patterns processes to monitor and identify deviations in patterns of treatment from established standards or norms, performance and health outcome measures using standardized indicators. The quality improvement subsystem will be based upon nationally recognized standards and guidelines, including but not limited to, a measurement system based upon the most current version of HEDIS published by the National Committee for Quality Assurance.
| |
| 16.9 | Surveillance Utilization Review Subsystem (SURS) |
In accordance with 42 CFR 455, the Contractor shall establish a SURS function which provides the capability to identify potential fraud and/or abuse of providers or Members. The SURS component supports profiling, random sampling, groupers (for example Episode Treatment Grouper), ad hoc and targeted queries.
| |
| 16.10 | Analysis and Reporting Function |
The analysis capacity function supports reporting requirements for the Contractor and the Department with regard to the QAPI program and managed care operations. The Contractor shall show sufficient capacity to support special requests and studies that may be part of the financial and quality systems. The reporting subsystem allows the Contractor to develop various reports to enable Contractor management and the Department to make informed decisions regarding managed care activity, costs and quality.
The Contractor’s reporting subsystem shall contain such items as: specifications for a decision support system; capacity to collect, analyze and report performance data sets such as may be required under this Contract; HEDIS performance measures; report on Provider rates, federally required services, reports such as family planning services, abortions, sterilizations and EPSDT services.
| |
| 16.11 | Interface Capability |
The interface subsystems support incoming and outgoing data from other organizations and allow the Contractor to maintain Member Enrollment information and Member-related information. It might include information from secondary sources to allow the tracking of population outcome data or other population information. At a minimum, there will be a Provider, Member,
Encounter Record and capitation interface. Specific requirements for the interface subsystem shall include such items as: defined data elements, formats, file layouts.
| |
| 16.12 | Access to Contractor’s MIS |
The Contractor shall provide appropriate Department staff individual access to their eligibility files, Claims and prior authorization attached to a Claim, provider enrollment and other information as necessary via an online real time connection. The Department shall work with the Contractor on the most expedient way to provide this access.
| |
| 17.1 | Encounter Data Submission |
The Contractor shall ensure that Encounter Records are consistent with the terms of this Contract and all applicable state and federal laws. (See Appendix D and Appendix E.) The Contractor shall have a computer and data processing system sufficient to accurately produce the data, reports and Encounter Record set in formats and timelines prescribed by the Department as defined in the Contract. The system shall be capable of following or tracing an Encounter within its system using a unique Encounter Record identification number for each Encounter. At a minimum, the Contractor shall be required to electronically provide Encounter Record to the Department, on a weekly schedule. Encounter Record must follow the format, data elements and method of transmission specified by the Department. All changes to edits and processing requirements due to Federal or State law changes shall be provided to the Contractor in writing no less than sixty (60) working days prior to implementation, whenever possible. The Contractor shall submit electronic test data files as required by the Department in the format referenced in this Contract and as specified by the Department. The electronic test files are subject to Department review and approval before production of data. The Department will process the Encounter Record through defined edit and audit requirements and reject Encounter Record that does not meet its requirements. Threshold and informational editing shall apply. The Department reserves the right to change the number of, and the types of edits used for threshold processing based on its review of the Contractor’s monthly transmissions. The Department and Contractor will work together to implement threshold edits or deletions and will consider the alignment of edits and threshold edits for encounters with Department fee-for-service claim submissions and provider notification and required change timelines. Provided, however, this process shall not delay the implementation of the changes by the Department by more than sixty (60) business days. The Encounter Record will be utilized by the Department for the following:
| |
| A. | To evaluate access to health care, availability of services, quality of care and cost effectiveness of services; |
| |
| B. | To evaluate contractual performance; |
| |
| C. | To validate required reporting of utilization of services; |
| |
| D. | To develop and evaluate proposed or existing Capitation Rates; |
| |
| E. | To meet CMS Medicaid reporting requirements; and |
| |
| F. | For any purpose the Department deems necessary. |
Data quality efforts of the Department shall incorporate the following standards for monitoring and validation:
| |
| A. | Edit each data element on the Encounter Record for required presence, format, consistency, reasonableness and/or allowable values; |
| |
| B. | Edit for Member eligibility; |
| |
| C. | Perform automated audit processing (e.g. duplicate, conflict, etc.) using history Encounter Record and same-cycle Encounter Record; |
| |
| D. | Identify exact duplicate Encounter Record; |
| |
| E. | Maintain an audit trail of all error code occurrences linked to a specific Encounter; and |
| |
| F. | Update Encounter history files with both processed and incomplete Encounter Record. |
The Contractor shall have the capacity to track and report on all Erred Encounter Records.
The Contractor shall be required to use procedure codes, diagnosis codes and other codes used for reporting Encounter Record in accordance with guidelines defined by the Department in writing. The Contractor must also use appropriate NPI/Provider numbers for Encounter Records as directed by the Department. The Encounter Record shall be received and processed by the Department’s Fiscal Agent and shall be stored in the existing MMIS.
All Subcontracts with Providers or other vendors of service must have provisions requiring that Encounter Record is reported/submitted in an accurate and timely fashion.
The Contractor shall specify to the Department the name of the primary contact person assigned responsibility for submitting and correcting Encounter Record, and a secondary contact person in the event the primary contact person is not available.
The Contractor shall assign staff to participate in the Encounter Technical Workgroup periodically scheduled by the Department. The workgroup’s purpose is to enhance the data submission requirements and improve the accuracy, quality and completeness of the Encounter Record. In the event of a change in the Fiscal Agent, the Encounter Technical Workgroup shall cooperate to minimize any burden on the Department and the Contractor resulting from the change.
| |
| 18. | Kentucky Health Information Exchange (KHIE) |
The contractor shall provide all adjudicated Claims data within twenty-four (24) hours of final claim adjudication in support of KHIE. The Contractor shall provide the KHIE with all clinical data as soon as it is available. The Contractor will also share with the KHIE any Member patient clinical data. This requirement can be met in one of following ways:
| |
| A. | Provide a secure Web Service that serves up Continuity of Care Documents (CCD’s) in real time to the KHIE. |
| |
| (1) | This service shall be secured using WS-Security and an unsecure HTTP transport. (A VPN tunnel may be used in addition to WS-Security, but not in place of it. If VPN is chosen, the entire cost of the VPN tunnel shall be borne by the contractor including cost of equipment and any rack charges or other regular or irregular charges.) |
| |
| (2) | This service shall utilize web service description language (WSDL) approved by KHIE. Approval decisions rest solely with KHIE and will be based upon interoperability with no respect given to other concerns of the contractor. |
| |
| (3) | This service shall provide a response time of no more than fifteen (15) seconds as measured from the first Internet relay point outside of the contractor’s data center. The contractor is responsible for its own environment plus its connection to the Internet. |
| |
| B. | Provide a Cross Enterprise Document Sharing (XDS) repository and publish Continuity of Care Documents (CCD’s) to it for the purpose of real time as needed retrieval by KHIE. |
| |
| (1) | If this option is chosen, the contractor shall send messages to the KHIE registry informing it of the presence of these documents at the same time that these documents are published to the repository. |
| |
| (2) | This service shall provide a response time of no more than fifteen (15) seconds as measured from the first Internet relay point outside of the contractor’s data center. The contractor is responsible for its own environment plus its connection to the Internet. |
| |
| (3) | This service shall be secured using techniques specified by KHIE, which are still to be determined |
| |
| (4) | This service shall utilize transports, schemas and techniques approved or specified by the KHIE, which are still to be determined. |
The Contractor shall make a good faith effort to have PCPs in the Contractor’s network connect to KHIE within one (1) year of the effective date of the contract with the Contractor or other schedule as determined by the Department. Furthermore, the Contractor shall encourage all Providers in their Network to establish connectivity with the KHIE.
The Department for Medicaid Services will continue to administer the EHR Incentive Payment Program. DMS will make the vendors aware of which providers have received incentive payments and will continue to update the contractor when additional payments are made.
| |
| 19. | Quality Assessment/Performance Improvement (QAPI) |
The Contractor QAPI Program shall conform to requirements of 42 CFR 438, Subpart D. The Contractor shall implement and operate a comprehensive QAPI program that assesses, monitors, evaluates and improves the quality of care provided to Members. The program shall also have processes that provide for the evaluation of access to care, continuity of care, health care outcomes, and services provided or arranged for by the Contractor. The Contractor’s QI structures and processes shall be planned, systematic and clearly defined. The Contractor’s QI activities shall demonstrate the linkage of QI projects to findings from multiple quality evaluations, such as the EQR annual evaluation, opportunities for improvement identified from the annual HEDIS indicators and the consumer and provider surveys, internal surveillance and monitoring, as well as any findings identified by an accreditation body. The QAPI program shall be developed in collaboration with input from Members. The Contractor shall maintain documentation of all member input; response; conduct of performance improvement activities; and feedback to Members. The Contractor shall have or obtain within two (2) to four (4) years and maintain National Committee for Quality Assurance (NCQA) accreditation for its Medicaid product line. The Contractor shall provide the Department a copy of its current certificate of accreditation together with a copy of the complete survey report every three years including the scoring at the category, Standard, and element levels, as well as NCQA recommendations, as presented via the NCQA Interactive Survey System (ISS): Status, Summarized & Detailed Results, Performance, Performance Measures, Must Pass Results Recommendations and History. Annually, the Contractor shall submit the QAPI program description document to the Department for review by July 31 of each contract year.
As the Contractor will provide Behavioral Health services, the Contractor shall integrate Behavioral Health indicators into its QAPI program and include a systematic, on-going process for monitoring, evaluating, and improving the quality and appropriateness of Behavioral Health Services provided to Members. The Contractor shall collect data, and monitor and evaluate for improvements to physical health outcomes resulting from behavioral health integration into the Member’s overall care.
The Contractor shall annually review and evaluate the overall effectiveness of the QAPI program to determine whether the program has demonstrated improvement in the quality of care and service provided to Members. The Contractor shall modify as necessary, the QAPI program, including Quality Improvement policies and procedures; clinical care standards; practice guidelines and patient protocols; utilization and access to Covered Services; and treatment outcomes. The Contractor shall prepare a written report to the Department, detailing the annual review and shall include a review of
completed and continuing QI activities that address the quality of clinical care and service; trending of measures to assess performance in quality of clinical care and quality of service; any corrective actions implemented; corrective actions which are recommended or in progress; and any modifications to the program. There shall be evidence that QI activities have contributed to meaningful improvement in the quality of clinical care and quality of service, including preventive and behavioral health care, provided to Members. The Contractor shall submit this report by July 31 of each contract year.
The Contractor shall have a written QAPI work plan that outlines the scope of activities and the goals, objectives and timelines for the QAPI program. New goals and objectives must be set at least annually based on findings from quality improvement activities and studies, survey results, Grievances and Appeals, performance measures and EQRO findings. The Contractor is accountable to the Department for the quality of care provided to Members. The Contractor’s responsibilities of this include, at a minimum: approval of the overall QAPI program and annual QAPI work plan; designation of an accountable entity within the organization to provide direct oversight of QAPI; review of written reports from the designated entity on a periodic basis, which shall include a description of QAPI activities, progress on objectives, and improvements made; review on an annual basis of the QAPI program; and modifications to the QAPI program on an ongoing basis to accommodate review findings and issues of concern within the organization.
The Contractor shall have in place an organizational Quality Improvement Committee that shall be responsible for all aspects of the QAPI program. The committee structure shall be interdisciplinary and be made up of both providers and administrative staff. It should include a variety of medical disciplines, health professions and individual(s) with specialized knowledge and experience with Individuals with Special Health Care needs. The committee shall meet on a regular basis and activities of the committee must be documented; all committee minutes and reports shall be available to the Department upon request.
QAPI activities of Providers and Subcontractors, if separate from the Contractor’s QAPI activities, shall be integrated into the overall QAPI program. Requirements to participate in QAPI activities, including submission of complete Encounter Record, are incorporated into all Provider and Subcontractor contracts and employment agreements. The Contractor’s QAPI program shall provide feedback to the Providers and Subcontractors regarding integration of, operation of, and corrective actions necessary in Provider and Subcontractor QAPI activities.
The Contractor shall integrate other Management activities such as Utilization Management, Risk Management, Member Services, Grievances and Appeals, Provider Credentialing, and Provider Services in its QAPI program. Qualifications, staffing levels and available resources must be sufficient to meet the goals and objectives of the QAPI program and related QAPI activities,
including but not limited to monitoring and evaluation of Member’s care and services, including the care and services of Members with special health care needs: use of preventive services; coordination of behavioral and physical health care needs, monitoring and providing feedback on provider performance, involving Members in QAPI initiatives; and conducting performance improvement projects. Written documentation listing staffing resources, including total FTE’s percentage of time, experience and roles, shall be submitted to the Department, upon request.
| |
| 19.4 | QAPI Monitoring and Evaluation |
| |
| A. | The Contractor, through the QAPI program, shall monitor and evaluate the quality of health care on an ongoing basis. Health care needs such as acute or chronic physical or behavioral conditions, high volume, and high risk, special needs populations, preventive care, and behavioral health shall be studied and prioritized for performance measurement, performance improvement and/or development of practice guidelines. Standardized quality indicators shall be used to assess improvement, assure achievement of at least minimum performance levels, monitor adherence to guidelines and identify patterns of over- and under-utilization. The measurement of quality indicators selected by the Contractor must be supported by valid data collection and analysis methods and shall be used to improve clinical care and services. |
| |
| B. | Providers shall be measured against practice guidelines and standards adopted by the Quality Improvement Committee. Areas identified for improvement shall be tracked and corrective actions taken as indicated. The effectiveness of corrective actions must be monitored until problem resolution occurs. The Contractor shall perform reevaluations to assure that improvement is sustained. |
| |
| C. | The Contractor shall use appropriate multidisciplinary teams to analyze and address data or systems issues. |
| |
| D. | The Contractor shall submit to the Department upon request documentation regarding quality and performance improvement (QAPI) projects/performance improvement projects (PIPs) and assessment that relates to enrolled members. Refer to Section 5.6 Performance Improvement Projects for further detail. |
| |
| E. | The Contractor shall develop or adopt practice guidelines that are disseminated to Providers and to Members upon request. The guidelines shall be based on valid and reliable medical evidence or consensus of health professionals; consider the needs of Members; developed or adopted in consultation with contracting health professionals, and reviewed and updated periodically. Decisions with respect to UM, member education, covered services, and other areas to which the practice guidelines apply shall be consistent with the guidelines. |
Contractor shall implement its innovative program as presented in the response to the RFP and report quarterly on its program to improve and reform
the management of the pharmacy program as contained in the Contractor’s response to the Request for Proposal. (See Appendix K.)
| |
| 20. | Kentucky Healthcare Outcomes |
| |
| 20.1 | Kentucky Outcomes Measures and Health Care Effectiveness Data and Information Set (HEDIS) Measures |
A goal of the Commonwealth’s Medicaid Program is to improve the health status of Medicaid Members. Therefore, the Department has established statewide goals, health care outcomes, and health indicators targeted and designated to accomplish this goal and comply with federal requirements established under 42 CFR.438.24 (C)(1) and (C)(2) relating to Contractor performance and reporting. The Department shall work with the Contractor to establish a set of unique Kentucky Medicaid Managed Care Performance Measures, which are aligned with national and state preventive initiatives (such as CHIPRA) which focus on improving health, including but not limited to Healthy People 2010 and Healthy Kentuckians 2010. Based upon these goals and requirements in Appendix O, a Contractor shall implement steps targeted at health improvement for these selected performance measures in either the actual outcomes or processes used to affect those outcomes. Once performance goals are met, select measures may be retired, and new measures, based on CMS guidelines and/or developed collaboratively with the Contractor, may be implemented if either federal or state priorities change; findings and/or recommendations from the EQRO; or identification of quality concerns; or findings related to calculation and implementation of the measures require amended or different performance measures, the parties agree to amend the previously identified measures. Additionally, the Department, the Contractor, and the EQRO will review and evaluate the feasibility and strategy for rotation of measures requiring hybrid or medical record data collection to reduce the burden of measure production. The group may consider the annual HEDIS measure rotation schedule as part of this process. The Contractor in collaboration with the Department and the EQRO shall develop and initiate a performance measure specific to Individual Members with Special Health Care Needs (ISHCN).
The Department shall assess the Contractor’s achievement of performance improvement related to the health outcome measures. The Contractor shall be expected to achieve demonstrable and sustained improvement for each measure. Specific quantitative performance targets and goals are to be set by the workgroup. The Contractor shall report activities on the performance measures in the QAPI work plan quarterly and shall submit an annual report after collection of performance data. The Contractor shall stratify the data to each measure by the Medicaid eligibility category, race ethnicity, gender and age to the extent such information has been provide by the Department to Contractor. This information will be used to determine disparities in health care.
| |
| 20.2 | HEDIS Performance Measures |
The Contractor shall be required to collect and report HEDIS data annually. After completion of the Contractor’s annual HEDIS data collection, reporting and performance measure audit, the Contractor shall submit to the Department the Final Auditor’s Report issued by the NCQA certified audit organization and an electronic (preferred) or printed copy of the interactive data submission system tool (formerly the Data Submission tool) by no later than August 31st.
In addition, for each measure being reported, the Contractor shall provide trending of the results from all previous years in chart and table format. Where applicable, benchmark data and performance goals established for the reporting year shall be indicated. The Contractor shall include the values for the denominator and numerator used to calculate the measures.
For all reportable Effectiveness of Care and Access/Availability of Care measures, the Contractor shall stratify each measure by Medicaid eligibility category, race, ethnicity, gender and age.
Annually, the Contractor and the department will select a subset of targeted performance from the HEDIS reported measures on which the Department will evaluate the Contractor’s performance. The Department shall inform the Contractor of its performance on each measure, whether the Contractor satisfied the goal established by the Department, and whether the Contractor shall be required to implement a performance improvement initiative. The Contractor shall have sixty (60) days to review and respond to the Departments performance report.
The Department reserves the right to evaluate the Contractor’s performance on targeted measures based on the Contractors submitted encounter data. The Contractor shall have 60 days to review and respond to findings reported as a result of these activities.
| |
| 20.3 | Accreditation of Contractor by National Accrediting Body |
A Contractor which holds current NCQA accreditation status shall submit a copy of its current certificate of accreditation with a copy of the complete accreditation survey report, including scoring of each category, standard, and element levels, and recommendations, as presented via the NCQA Interactive Survey System (ISS): Status. Summarized & Detailed Results, Performance, Performance Measures, Must Pass Results Recommendations and History to the Department in accordance with timelines established by the Department.
If a Contractor has not earned accreditation of its Medicaid product through the National Committee for Quality Assurance (NCQA) Health Plan, the MCO shall be required to obtain such accreditation within two (2) to four (4) years from the effective date of this contract.
| |
| 20.4 | Performance Improvement Projects (PIPs) |
Performance Improvement Projects (PIPs) are required to address and achieve significant (demonstrable) and sustained improvement in focus areas over time. The projects are designed to measure diverse aspects of care, and care provided to diverse populations of Members. The Contractor must ensure that the chosen topic areas for PIP’s are not limited to only recurring, easily measured subsets of the health care needs of its Members. The selected PIPs topics must consider: the prevalence of a condition in the enrolled population; the need(s) for a specific service(s); member demographic characteristics and health risks; and the interest of Members in the aspect of care/services to be addressed.
The Contractor shall continuously monitor its own performance on a variety of dimensions of care and services for Members, identify areas for potential improvement, carry out individual PIPs, undertake system interventions to improve care and services, and monitor the effectiveness of those interventions. The Contractor shall develop and implement PIPs to address aspects of clinical care and non-clinical services and are expected to have a positive effect on health outcomes and Member satisfaction. While undertaking a PIP, no specific payments shall be made directly or indirectly to a provider or provider group as an inducement to reduce or limit medically necessary services furnished to a Member. Clinical PIPs should address preventive and chronic healthcare needs of Members, including the Member population as a whole and subpopulations, including, but not limited to Medicaid eligibility category, type of disability or special healthcare need, race, ethnicity, gender and age. PIPs shall also address the specific clinical needs of Members with conditions and illnesses that have a higher prevalence in the enrolled population. Non-clinical PIPs should address improving the quality, availability, and accessibility of services provided by the Contractor to Members and Providers. Such aspects of service should include, but not be limited to availability, accessibility, cultural competency of services, and complaints, grievances, and appeals.
The Contractor shall develop collaborative relationships with local health departments, behavioral health agencies and other community based health/social agencies to achieve improvements in priority areas. Linkage between the Contractor and public health agencies is an essential element for the achievement of public health objectives. The Contractor shall be committed to on-going collaboration in the area of service and clinical care improvements by the development of best practices and use of encounter data–driven performance measures.
The Contractor shall monitor and evaluate the quality of care and services by initiating a minimum of two (2) PIPs each year, including one (1) relating to physical health and one (1) relating to behavioral health. However, the Contractor may propose an alternative topic(s) for its annual PIPs to meet the unique needs of its Members if the proposal and justification for the alternative(s) are submitted to and approved by the Department.
Additionally, the Department may require the Contractor to (1) implement an additional PIP specific to the Contractor, if findings from an EQR review or audit indicate the need for a PIP, or if directed by CMS; and (2) assist the Department in one (1) annual statewide PIP, if requested. In assisting the Department with implementation of an annual statewide PIP, the Contractor’s participation shall be limited to providing the Department with readily available data from the Contractor’s region. The Contractor shall submit reports on PIPs as specified by the Department.
The Department has identified four clinical areas and non-clinical topics for PIPs as a baseline assessment of Medicaid members in Appendix N.
The Contractor shall report on each PIP utilizing the template provided by the Department and must address all of the following in order for the Department to evaluate the reliability and validity of the data and the conclusions drawn:
| |
| A. | Topic and its importance to enrolled members; |
| |
| B. | Methodology for topic selection; |
| |
| D. | Data sources/collection; |
| |
| E. | Intervention(s) – not required for projects to establish baseline; and |
| |
| F. | Results and interpretations – clearly state whether performance goals were met, and if not met, analysis of the intervention and a plan for future action. |
The final report shall also answer the following questions and provide information on:
| |
| A. | Was Member confidentiality protected; |
| |
| B. | Did Members participate in the performance improvement project? |
| |
| C. | Did the performance improvement project include cost/benefit analysis or other consideration of financial impact; |
| |
| D. | Were the results and conclusions made available to members, providers and any other interested bodies |
| |
| E. | Is there an executive summary |
| |
| F. | Do illustrations – graphs, figures, tables – convey information clearly |
Performance reporting shall utilize standardized indicators appropriate to the performance improvement area. Minimum performance levels shall be specified for each performance improvement area, using standards derived from regional or national norms or from norms established by an appropriate practice organization. The norms and/or goals shall be pre-determined at the commencement of each performance improvement goal and the Contractor shall be monitored for achievement of demonstrable and/or sustained improvement.
The Contractor shall validate if improvements were sustained through periodic audits of the relevant data and maintenance of the interventions that resulted in improvement. The timeframes for reporting:
| |
| A. | Project Proposal – due September 1 of each contract year. If PIP identified as a result of Department/EQRO review, the project proposal shall be due sixty (60) days after notification of requirement. |
| |
| B. | Baseline Measurement – due at a maximum, one calendar year after the project proposal and no later than September 1 of the contract year. |
| |
| C. | 1st Remeasurement – no more than two calendar years after baseline measurement and no later than September 1 of the contract year |
| |
| D. | 2nd Remeasurement – no more than one calendar year after the first remeasurement and no later than September 1 of the contract year. |
| |
| 20.5 | Quality and Member Access Committee |
The Contractor shall establish and maintain an ongoing Quality and Member Access Committee (QMAC) composed of Members, individuals from consumer advocacy groups or the community who represent the interests of the Member population.
Members of the committee shall be consistent with the composition of the Member population, including such factors as aid category, gender, geographic distribution, parents, as well as adult members and representation of racial and ethnic minority groups. Member participation may be excused by the Department upon a showing by Contractor of good faith efforts to obtain Member participation. Good faith efforts will be subject to audit by the Department. Responsibilities of the committee shall include:
| |
| A. | Providing review and comment on quality and access standards; |
| |
| B. | Providing review and comment on the Grievance and Appeals process as well as policy modifications needed based on review of aggregate Grievance and Appeals data; |
| |
| C. | Proving review and comment on Member Handbooks; |
| |
| D. | Reviewing Member education materials prepared by the Contractor; |
| |
| E. | Recommending community outreach activities; and |
| |
| F. | Providing reviews of and comments on Contractor and Department policies that affect Members. |
The list of the Members participating with the QMAC shall be submitted to the Department annually.
| |
| 20.6 | Utilization Management |
The Utilization Management (UM) program, processes and timeframes shall be in accordance with 42 CFR 456, 42 CFR431, 42 CFR 438 and the private review agent requirements of KRS 304.17A as applicable. The Contractor shall have a comprehensive UM program that reviews services for Medical Necessity and that monitors and evaluates on an ongoing basis the appropriateness of care and services. A written description of the UM program shall outline the program structure and include a clear definition of authority and accountability for all activities between the Contractor and entities to which the Contractor delegates UM activities. The description shall include the scope of the program; the processes and information sources used to determine service coverage; clinical necessity, appropriateness and effectiveness; policies and procedures to evaluate care coordination, discharge criteria, site of services, levels of care, triage decisions and cultural competence of care delivery; processes to review, approve and deny services, as needed. The UM program shall be evaluated annually, including an evaluation of clinical and service outcomes. The UM program evaluation along with any changes to the UM program as a result of the evaluation findings, will be reviewed and approved annually by the Medical Director or the QI Committee.
The Contractor shall adopt national recognized standards and criteria which shall be approved by the Department. The Contractor shall include appropriate physicians and other providers in Contractor’s Network in the review and adoption of Medical Necessity criteria. The Contractor shall have in place mechanisms to check the consistency of application of review criteria. The written clinical criteria and protocols shall provide for mechanisms to obtain all necessary information, including pertinent clinical information, and consultation with the attending physician or other health care provider as appropriate. The Medical Director shall supervise the UM program and shall be accessible and available for consultation as needed. Decisions to deny a service authorization request or to authorize a service in an amount, duration, or scope that is less than requested, must be made by a physician who has appropriate clinical expertise in treating the Member’s condition or disease. The reason for the denial shall be cited. Physician consultants from appropriate medical and surgical specialties shall be accessible and available for consultation as needed. The Medical Necessity review process shall be timely and shall include a provision for expedited reviews in urgent decisions.
| |
| A. | The Contractor shall submit its request to change any prior authorization requirement to the Department for review. |
| |
| B. | For the processing of requests for initial and continuing authorization of services, the Contractor shall require that its subcontractors have in place written policies and procedures and have in effect a mechanism to ensure consistent application of review criteria for authorization decisions. |
| |
| C. | In the event that a Member or Provider requests written confirmation of an approval, the Contractor shall provide written confirmation of its |
decision within two working days of providing notification of a decision if the initial decision was not in writing. The written confirmation shall be written in accordance with Member Rights and Responsibilities.
| |
| D. | The Contractor shall have written policies and procedures that show how the Contractor will monitor to ensure clinical appropriate overall continuity of care. |
| |
| E. | The Contractor shall have written policies and procedures that explain how prior authorization data will be incorporated into the Contractor’s overall Quality Improvement Plan. |
Each subcontract must provide that consistent with 42 CFR Sections 438.6(h) and 422.208, compensation to individuals or entities that conduct UM activities is not structured so as to provide incentives for the individual or entity to deny, limit, or discontinue medically necessary services to a Member.
The program shall identify and describe the mechanisms to detect under-utilization as well as over-utilization of services. The written program description shall address the procedures used to evaluate Medical Necessity, the criteria used, information sources, timeframes and the process used to review and approve the provision of medical services. The Contractor shall evaluate Member satisfaction (using the CAHPS survey) and provider satisfaction with the UM program as part of its satisfaction surveys. The UM program will be evaluated by the Department on an annual basis.
| |
| 20.7 | Adverse Actions Related to Medical Necessity or Coverage Denials |
The Contractor shall provide the Member written notice that meets the language and formatting requirements for Member materials, of any action (not just service authorization actions) within the timeframes for each type of action pursuant to 42 CFR 438.210(c). The notice must explain:
| |
| A. | The action the Contractor has taken or intends to take; |
| |
| B. | The reasons for the action; |
| |
| C. | The Member’s right to appeal; |
| |
| D. | The Member’s right to request a State hearing; |
| |
| E. | Procedures for exercising Member’s rights to Appeal or file a Grievance; |
| |
| F. | Circumstances under which expedited resolution is available and how to request it; and |
| |
| G. | The Member’s rights to have benefits continue pending the resolution of the Appeal, how to request that benefits be continued, and the circumstances under which the Member may be required to pay the costs of these services. |
The Contractor must give notice at least:
| |
| A. | Ten (10) Days before the date of Action when the Action is a termination, suspension or reduction of a covered service authorized by the Department, its agent or Contractor, except the period of advanced |
notice is shortened to five (5) Days if Member Fraud or Abuse has been determined.
| |
| B. | The Contractor must give notice by the date of the Action for the following: |
| |
| (1) | In the death of a Member; |
| |
| (2) | A signed written Member statement requesting service termination or giving information requiring termination or reduction of services (where he understands that this must be the result of supplying that information); |
| |
| (3) | The Member’s admission to an institution where he is ineligible for further services; |
| |
| (4) | The Member’s address is unknown and mail directed to him has no forwarding address; |
| |
| (5) | The Member has been accepted for Medicaid services by another local jurisdiction; |
| |
| (6) | The Member’s physician prescribes the change in the level of medical care; |
| |
| (7) | An adverse determination made with regard to the preadmission screening requirements for nursing facility admissions on or after January 1, 1989; |
| |
| (8) | The safety or health of individuals in the facility would be endangered, the Member’s health improves sufficiently to allow a more immediate transfer or discharge, an immediate transfer or discharge is required by the Member’s urgent medical needs, or a Member has not resided in the nursing facility for thirty (30) days. |
| |
| C. | The Contractor must give notice on the date of Action when the Action is a denial of payment. |
| |
| D. | The Contractor must give notice as expeditiously as the Member’s health condition requires and within State-established timeframes that may not exceed two (2) business days following receipt of the request for service, with a possible extension of up to fourteen (14) additional days, if the Member, or the Provider, requests an extension, or the Contractor justifies a need for additional information and how the extension is in the Member’s interest. If the Contractor extends the time frame, the Contractor must give the Member written notice of the reason for the decision to extend the timeframe and inform the Member of the right to file a Grievance if he or she disagrees with that decision; and issue and carry out the determination as expeditiously as the Member’s health condition requires and no later than the date the extension expires. |
| |
| E. | For cases in which a Provider indicates, or the Contractor determines, that following the standard timeframe could seriously jeopardize the Member’s life or health or ability to attain, maintain or regain maximum function, the Contractor shall make an expedited authorization decision and provide notice as expeditiously as the Member’s health condition requires and no later than two (2) business days after receipt of the request for service. |
| |
| F. | The Contractor shall give notice on the date that the timeframes expire when service authorization decisions not reached within the timeframes |
for either standard or expedited service authorizations. An untimely service authorization constitutes a denial and is thus an adverse action.
| |
| 20.8 | Assessment of Member and Provider Satisfaction and Access |
The Contractor shall conduct an annual survey of Members’ and Providers’ satisfaction with the quality of services provided and their degree of access to services. The member satisfaction survey requirement shall be satisfied by the Contractor participating in the Agency for Health Research and Quality’s (AHRQ) current Consumer Assessment of Healthcare Providers and Systems survey (“CAHPS”) for Medicaid Adults and Children, administered by an NCQA certified survey vendor. The Contractor shall provide a copy of the current CAHPS survey tool to the Department. Annually, the Contractor shall assess the need for conducting special surveys to support quality/performance improvement initiatives that target subpopulations perspective and experience with access, treatment and services. To meet the provider satisfaction survey requirement the Contractor shall submit to the Department for review and approval the Contractor’s provider satisfaction survey tool. The Department shall review and approve any Member and Provider survey instruments and shall provide a written response to the Contractor within fifteen (15) days of receipt. The Contractor shall provide the Department a copy of all survey results. A description of the methodology to be used conducting the Provider or other special surveys, the number and percentage of the Providers or Members to be surveyed, response rates, and a sample survey instrument, shall be submitted to the Department along with the findings and interventions conducted or planned. All survey results must be reported to the Department, and upon request, disclosed to Members.
| |
| 21. | Monitoring and Evaluation |
| |
| 21.1 | Financial Performance Measures |
Contractor shall provide reports quarterly on trends in utilization for each category of eligibility in a format as directed by the Department. These categories of eligibility trends should include but not necessarily be limited to:
| |
| • | inpatient hospital admissions and days per thousand Member months; |
| |
| • | outpatient hospital visits per thousand Member month; |
| |
| • | emergency room visits per thousand Member months; |
| |
| • | percent of emergency room visits resulting in admission; |
| |
| • | ambulatory surgery / procedures per thousand Member months; hospital readmissions within 30 days per thousand Member months; |
| |
| • | average visits per provider by major provider type; |
| |
| • | PRTF admits and days per thousand; |
| |
| • | mental hospital admits and days per thousand; |
| |
| • | prescriptions dispensed by major drug class per thousand Member months; |
| |
| • | pharmacy cost per Member per month. |
In addition a report shall be provided that displays expenditures by category of service by both month of service and month of payment; this report should distinguish between the five major categories of eligibility (i.e. Families and Children, SSI Adults, SSI Children, Foster Care, and Dual Eligibles).
| |
| 21.2 | Monitoring Requirements |
The Contractor is responsible for the faithful performance of the contract and shall have internal monitoring procedures and processes in place to ensure compliance. The Contractor shall cooperate with the Department, its agent and/or Contractor in the annual contract monitoring, tracking and/or auditing activity, which may require the Contractor to report progress and problems, provide documents, allow random inspections of its facilities, participate in scheduled meetings and monitoring, respond to requests for corrective action plans and provide reports as requested by the Department. Cooperation in the annual contract monitoring and provision of documents during contract monitoring will be at no additional cost to the Department.
| |
| 21.3 | External Quality Review |
Section 1902(a)(30)(c) of Title XIX of the Social Security Act, requires the Commonwealth to acquire an independent external review body for the purpose of performing an annual review of the quality of services provided by an MCO under contract with the Commonwealth, including the evaluation of quality outcomes and timeliness of access to services. Requirements relating to the External Quality Review (EQR) are further defined and described under 42 CFR 433 and 438. The results of EQR are made available, upon request, to specified groups and to interested stakeholders. The Contractor shall provide information to the External Quality Review Organization EQRO as requested to fulfill the requirements of the mandatory and optional activities required in 42 CFR Parts 433 and 438.
The Contractor shall cooperate and participate in EQR activities in accordance with protocols identified under 42 CFR 438, Subpart E. These protocols guide the independent external review of quality outcomes and timeliness of and access to services provided by a Contractor providing Medicaid services.
In an effort to avoid duplication, the Department may also use, in place of such audit, information obtained about the Contractor from a Medicare or private accreditation review in accordance with 42 CFR 438.360.
| |
| 21.4 | EQR Administrative Reviews |
In the event that the Department selects an EQRO, it will obtain an agreement from EQRO to hold and keep all information and materials it reviews from the Contractor as part of such audit with the utmost confidence, and for the EQRO to agree that it will not use such information in any matter whatsoever, including
for its own benefit, and that it will not provide comparable services of Contractor in the Service Area for twelve months after this Contractor no longer provides services to the Department in the Service Area, and to further hold the Contractor and the Department harmless for any and all damages for its violation of the agreement, including but not limited to attorneys fees and court costs.
The Contractor shall assist the EQRO in completing all Contractor reviews and evaluations in accordance with established protocols previously described. The Contractor shall assist the Department and the EQRO in identification of Provider and Member information required to carry out annual, external independent reviews of the quality outcomes, and timeliness of on-site or off-site medical chart reviews. Timely notification of Providers and subcontractors of any necessary medical chart review shall be the responsibility of the Contractor.
If during the conduct of an EQR by an EQRO acting on behalf of the Department, an adverse quality finding or deficiency is identified, the Contractor shall respond to and correct the finding or deficiency in a timely manner in accordance with guidelines established by the Department and EQRO. The Contractor shall:
| |
| A. | Assign a staff person(s) to conduct follow-up concerning review findings; |
| |
| B. | Inform the Contractor’s Quality Improvement Committee of the final findings and involve the committee in the development, implementation and monitoring of the corrective action plan; |
| |
| C. | Submit a corrective action plan in writing to the EQRO and Department within 60 days that addresses the measures the Contractor intends to take to resolve the finding. The Contractor’s final resolution of all potential quality concerns shall be completed within six (6) months of the Contractor’s notification; |
| |
| D. | The Contractor shall demonstrate how the results of the External Quality Review (EQR) are incorporated into the Contractor’s overall Quality Improvement Plan and demonstrate progressive and measurable improvement during the term of this Contract; and |
| |
| E. | If Contractor disagrees with the EQRO’s findings, it shall submit its position to the Commissioner of the Department whose decision is final. |
The Contractor shall have a Member Services function that includes a call center which is staffed and available by telephone Monday through Friday 7
am to 7 pm Eastern Standard Time (EST). The call center shall meet the current American Accreditation Health Care Commission/URAC-designed Health Call Center Standard (HCC) for call center abandonment rate, blockage rate and average speed of answer. If a Contractor has separate telephone lines for different Medicaid populations, the Contractor shall report performance for each individual line separately. The Department will inform the Contractor of any changes/updates to these URAC call center standards.
The Contractor shall also provide access to medical advice and direction through a centralized toll-free call-in system, available twenty-four (24) hours a day, seven (7) days a week nationwide. The twenty-four/seven (24/7) call-in system shall be staffed by appropriately trained medical personnel. For the purposes of meeting this requirement, trained medical professionals are defined as physicians, physician assistants, licensed practical nurses (LPN), and registered nurses (RNs).
The Contractor shall self-report their prior month performance in the three areas listed above, call center abandonment rate, blockage rate and average speed of answer, for their member services and twenty-four/seven (24/7) hour toll-free medical call-in system to the Department.
Appropriate foreign language interpreters shall be provided by the Contractor and available free of charge and as necessary to ensure availability of effective communication regarding treatment, medical history, or health education. Member materials shall be provided and printed in each language spoken by five (5) percent or more of the Members in each county. The Contractor staff shall be able to respond to the special communication need of the disabled, blind, deaf and aged and effectively interpersonally relate with economically and ethnically diverse populations. The Contractor shall provide ongoing training to its staff and Providers on matters related to meeting the needs of economically disadvantaged and culturally diverse individuals.
The Contractor shall require that all Service Locations meet the requirements of the Americans with Disabilities Act, Commonwealth and local requirements pertaining to adequate space, supplies, sanitation, and fire and safety procedures applicable to health care facilities. The Contractor shall cooperate with the Cabinet for Health and Family Services’ independent ombudsman program, including providing immediate access to a Member’s records when written Member consent is provided.
The Contractor’s Member Services function shall also be responsible for:
| |
| A. | Ensuring that Members are informed of their rights and responsibilities; |
| |
| B. | Monitoring the selection and assignment process of PCPs; |
| |
| C. | Identifying, investigating, and resolving Member Grievances about health care services; |
| |
| D. | Assisting Members with filing formal Appeals regarding plan determinations; |
| |
| E. | Providing each Member with an identification card that identifies the Member as a participant with the Contractor, unless otherwise approved by the Department; |
| |
| F. | Explaining rights and responsibilities to members or to those who are unclear about their rights or responsibilities including reporting of suspected fraud and abuse; |
| |
| G. | Explaining Contractor’s rights and responsibilities, including the responsibility to assure minimal waiting periods for scheduled member office visits and telephone requests, and avoiding undue pressure to select specific Providers or services; |
| |
| H. | Providing within five (5) business days of the Contractor being notified of the enrollment of a new Member, by a method that will not take more than three (3) days to reach the Member, and whenever requested by member, guardian or authorized representative, a Member Handbook and information on how to access services; (alternate notification methods shall be available for persons who have reading difficulties or visual impairments); |
| |
| I. | Explaining or answering any questions regarding the Member Handbook; |
| |
| J. | Facilitating the selection of or explaining the process to select or change Primary Care Providers through telephone or face-to-face contact where appropriate. The Contractor shall assist members to make the most appropriate Primary Care Provider selection based on previous or current Primary Care Provider relationship, providers of other family members, medical history, language needs, provider location and other factors that are important to the Member. The Contractor shall notify members within thirty (30) days prior to the effective date of voluntary termination (or if Provider notifies Contractor less than thirty (30) days prior to the effective date, as soon as Contractor receives notice), and within fifteen (15) days prior to the effective date of involuntary termination if their Primary Care Provider leaves the Program and assist members in selecting a new Primary Care Provider; |
| |
| K. | Facilitating direct access to specialty physicians in the circumstances of: |
| |
| (1) | Members with long-term, complex health conditions; |
| |
| (2) | Aged, blind, deaf, or disabled persons; and |
| |
| (3) | Members who have been identified as having special healthcare needs and who require a course of treatment or regular healthcare monitoring. This access can be achieved through referrals from the Primary Care Provider or by the specialty physician being permitted to serve as the Primary Care Provider. |
| |
| L. | Arranging for and assisting with scheduling EPSDT Services in conformance with federal law governing EPSDT for persons under the age of twenty-one (21) years; |
| |
| M. | Providing Members with information or referring to support services offered outside the Contractor’s Network such as WIC, child nutrition, elderly and child abuse, parenting skills, stress control, exercise, smoking cessation, weight loss, behavioral health and substance abuse; |
| |
| N. | Facilitating direct access to primary care vision services; primary dental and oral surgery services, and evaluations by orthodontists and prosthodontists; women’s health specialists; voluntary family planning; maternity care for Members under age 18; childhood immunizations; sexually transmitted disease screening, evaluation and treatment; tuberculosis screening, evaluation and treatment; and testing for HIV, HIV-related conditions and other communicable diseases; all as further described in Appendix I of this Contract; |
| |
| O. | Facilitating access to behavioral health services and pharmaceutical services; |
| |
| P. | Facilitating access to the services of public health departments, Community Mental Health Centers, rural health clinics, Federally Qualified Health Centers, the Commission for Children with Special Health Care Needs and charitable care providers, such as Shriner’s Hospital for Children; |
| |
| Q. | Assisting members in making appointments with Providers and obtaining services. When the Contractor is unable to meet the accessibility standards for access to Primary Care Providers or referrals to specialty providers, the Member Services staff function shall document and refer such problems to the designated Member Services Director for resolution; |
| |
| R. | Assisting members in obtaining transportation for both emergency and appropriate non-emergency situations; |
| |
| S. | Handling, recording and tracking Member Grievances properly and timely and acting as an advocate to assure Members receive adequate representation when seeking an expedited Appeal; |
| |
| T. | Facilitating access to Member Health Education Programs; |
| |
| U. | Assisting members in completing the Health Risk Assessment (HRA) as outlined in Covered Services upon any telephone contact; and referring Members to the appropriate areas to learn how to access the health education and prevention opportunities available to them including referral to case management or disease management; and |
| |
| V. | The Member Services staff shall be responsible for making an annual report to management about any changes needed in member services functions to improve either the quality of care provided or the method of delivery. A copy of the report shall be provided to the Department |
The Contractor shall publish a Member Handbook in and make the handbook available to Members upon enrollment, to be delivered to the Member within five (5) business days of Contractor’s notification of Member’s enrollment. Contractor is in compliance with this requirement if the Member’s handbook is mailed within five (5) business days by a method that will not take more than three (3) days to reach the Member. The Member Handbook shall be available in English, Spanish and any other language spoken by five (5) percent of the potential enrollee or enrollee population. The Member Handbook shall be available in a hardcopy format as well as an electronic format online. The Contractor shall review the handbook at least annually and shall communicate
any changes to Members in written form. Revision dates shall be added to the Member Handbook so that it is evident which version is the most current. Changes shall be approved by the Department prior to printing. The Department has the authority to review the Contractor’s Member Handbook at any time.
The handbook shall be written at the sixth grade reading comprehension level and shall include at a minimum the following information:
| |
| A. | The Contractor’s Network of Primary Care Providers, including a list of the names, telephone numbers, and service site addresses of PCPs available for Primary Care Providers in the network listing. The network listing may be combined with the Member Handbook or distributed as a stand-alone document; |
| |
| B. | The procedures for selecting a PCP and scheduling an initial health appointment; |
| |
| C. | The name of the Contractor and address and telephone number from which it conducts its business; the hours of business; and the Member Services telephone number and twenty-four/seven (24/7) toll-free medical call-in system; |
| |
| D. | A list of all available Covered Services, an explanation of any service limitations or exclusions from coverage and a notice stating that the Contractor will be liable only for those services authorized by the Contractor; |
| |
| E. | Member rights and responsibilities including reporting suspected fraud and abuse; |
| |
| F. | Procedures for obtaining Emergency Care and non-emergency care after hours. For a life-threatening situation, instruct Members to use the emergency medical services available or to activate emergency medical services by dialing 911; |
| |
| G. | Procedures for obtaining transportation for both emergency and non-emergency situations; |
| |
| H. | Information on the availability of maternity, family planning and sexually transmitted disease services and methods of accessing those services; |
| |
| I. | Procedures for arranging EPSDT for persons under the age of twenty-one (21) years; |
| |
| J. | Procedures for obtaining access to Long Term Care Services; |
| |
| K. | Procedures for notifying the Department for Community Based Services (DCBS) of family size changes, births, address changes, death notifications; |
| |
| L. | A list of direct access services that may be accessed without the authorization of a PCP; |
| |
| M. | Information about procedures for selecting a PCP or requesting a change of PCP and specialists; reasons for which a request may be denied; and reasons a Provider may request a change; |
| |
| N. | Information about how to access care before a PCP is assigned or chosen; |
| |
| O. | A Member’s right to obtain second opinion and information on obtaining second opinions related to surgical procedures, complex and/or chronic conditions; |
| |
| P. | Procedures for obtaining Covered Services from non-network providers; |
| |
| Q. | Procedures for filing a Grievance or Appeal. This shall include the title, address and telephone number of the person responsible for processing and resolving Grievances and Appeals; |
| |
| R. | Information about the Cabinet for Health and Family Services’ independent ombudsman program for Members; |
| |
| S. | Information on the availability of, and procedures for obtaining behavioral health/substance abuse health services; |
| |
| T. | Information on the availability of health education services; |
| |
| U. | Information deemed mandatory by the Department; and |
| |
| V. | The availability of care coordination case management and disease management provided by the Contractor. |
| |
| 22.3 | Member Education and Outreach |
The Contractor shall develop, administer, implement, monitor and evaluate a Member and community education and outreach program that incorporates information on the benefits and services of the Contractor’s Program to all Members. The Outreach Program shall encourage Members and community partners to use the information provided to best utilize services and benefits.
Educational and outreach efforts shall be carried on throughout the Contractor’s Region. Creative methods will be used to reach Members and community partners. These will include but not be limited to collaborations with schools, homeless centers, youth service centers, family resource centers, public health departments, school-based health clinics, chamber of commerce, faith-based organizations, and other appropriate sites.
The Contractor shall submit an annual outreach plan to the Department for review and approval. The plan shall include the frequency of activities, the staff person responsible for the activities and how the activities will be documented and evaluated for effectiveness and need for change.
| |
| 22.4 | Outreach to Homeless Persons |
The Contractor shall assess the homeless population within the Contractor’s Region by implementing and maintaining a customized outreach plan for Homeless Persons population, including victims of domestic violence. The plan shall include:
| |
| A. | Utilizing existing community resources such as shelters and clinics; and |
| |
| B. | Face-to-face encounters. |
The Contractor will not provide a differentiation of services for Members who are homeless. Victims of domestic violence should be a target for outreach
as they are frequently homeless. Assistance with transportation to access health care may be provided via bus tokens, taxi vouchers or other arrangements when applicable.
| |
| 22.5 | Member Information Materials |
All written materials provided to Members, including marketing materials, new member information, and grievance and appeal information shall be geared toward persons who read at a sixth-grade level, be published in at least a fourteen (14) point font size, and shall comply with the Americans with Disabilities Act of 1990 (Public Law USC 101-336). Font size requirements shall not apply to Member identification Cards. Braille and audio tapes shall be available for the partially blind and blind. Provisions to review written materials for the illiterate shall be available. Telecommunication devices for the deaf shall be available. Language translation shall be available if five (5) percent of the population in any county has a native language other than English. Materials shall be updated as necessary to maintain accuracy, particularly with regard to the list of participating providers.
All written materials provided to Members, including forms used to notify Members of Contractor actions and decisions, with the exception of written materials unique to individual Members, unless otherwise required by the Department shall be submitted to the Department for review and, approval prior to publication and distribution to Members.
| |
| 22.6 | Member Rights and Responsibilities |
The Contractor shall have written policies and procedures that are designed to protect the rights of Members and enumerate the responsibilities of each Member. A written description of the rights and responsibilities of Members shall be included in the Member information materials provided to new Members. A copy of these policies and procedures shall be provided to all of the Contractor’s Network Providers to whom Members may be referred. In addition, these policies and procedures shall be provided to any Out-of-Network Provider upon request from the Provider.
The Contractor’s written policies and procedures that are designed to protect the rights of Members shall include, without limitation, the right to:
| |
| A. | Respect, dignity, privacy, confidentiality and nondiscrimination; |
| |
| B. | A reasonable opportunity to choose a PCP and to change to another Provider in a reasonable manner; |
| |
| C. | Consent for or refusal of treatment and active participation in decision choices; |
| |
| D. | Ask questions and receive complete information relating to the Member’s medical condition and treatment options, including specialty care; |
| |
| E. | Voice Grievances and receive access to the Grievance process, receive assistance in filing an Appeal, and request a state fair hearing from the Contractor and/or the Department; |
| |
| F. | Timely access to care that does not have any communication or physical access barriers; |
| |
| G. | Prepare Advance Medical Directives pursuant to KRS 311.621 to KRS 311.643; |
| |
| H. | Assistance with Medical Records in accordance with applicable federal and state laws; |
| |
| I. | Timely referral and access to medically indicated specialty care; and |
| |
| J. | Be free from any form of restraint or seclusion used as a means of coercion, discipline, convenience, or retaliation. |
The Contractor shall also have policies addressing the responsibility of each Member to:
| |
| A. | Become informed about Member rights; |
| |
| B. | Abide by the Contractor’s and Department’s policies and procedures; |
| |
| C. | Become informed about service and treatment options; |
| |
| D. | Actively participate in personal health and care decisions, practice healthy lifestyles; |
| |
| E. | Report suspected Fraud and Abuse; and |
| |
| F. | Keep appointments or call to cancel. |
The Department will enroll and disenroll eligible Members in the MCO. To enroll in an MCO, the Members permanent residence shall be located within the Contractor’s region. The Contractor is not allowed to induce or accept disenrollment from a Member. The Contractor shall direct the Member to contact the Department for enrollment or disenrollment questions.
The Department makes no guarantees or representations to the Contractor regarding the number of eligible members who will ultimately be enrolled with the Contractor or the length of time any Member will remain enrolled with the Contractor.
The Department will electronically transmit to the Contractor new Member information monthly and will electronically transmit demographic changes regarding Members daily.
| |
| 22.8 | Membership Identification Cards |
Each Member will receive two (2) identification cards. One will be issued by the Department or its agent for Medicaid eligibility, and the other will be issued by the Contractor (for membership). The Membership card will also include the PCP, if applicable.
Dual Eligible Members, Members who are presumptively eligible, disabled children, and foster care children are not required to have a PCP. All other
Members in the MCO shall choose or have the Contractor select a PCP for their medical home.
The Contractor shall have two processes in place for Members to choose a PCP:
| |
| A. | A process for Members who have SSI coverage but are not Dual Eligible Members; and |
| |
| B. | A process for other Members. |
23. Member Selection of Primary Care Provider
A Member without SSI shall be offered an opportunity to: (1) choose a new PCP who is affiliated with the Contractor’s network or (2) stay with their current PCP as long as such PCP is affiliated with the Contractor’s network. Each Member shall be allowed to choose his or her Primary Care Provider from among all available Contractor Network Primary Care Providers and specialists as is reasonable and appropriate for Member.
The Contractor shall have procedures for serving Members from the date of notification of enrollment, whether or not the Member has selected a Primary Care Provider. The Contractor shall send Members a written explanation of the Primary Care Provider selection process within ten (10) business days of receiving enrollment notification from the Department, either as a part of the Member Handbook or by separate mailing. Members will be asked to select a Primary Care Provider by contacting the Contractor’s Member Services department with their selection. The written communication shall include the timeframe for selection of a Primary Care Provider, an explanation of the process for assignment of a Primary Care Provider if the Member does not select a Primary Care Provider and information on where to call for assistance with the selection process.
A Member shall be allowed to select, from all available, but not less than two (2) Primary Care Providers in the Contractor’s Network.
Contractor shall assign the Member to a Primary Care Provider:
| |
| A. | Who has historically provided services to the Member, meets the Primary Care Provider criteria and participates in the Contractor’s Network; |
| |
| B. | If there is no such Primary Care Provider who has historically provided services, the Contractor shall assign the Member to a Primary Care Provider, who participates in the Contractor’s Network and is within thirty (30) miles or thirty (30) minutes from the Member’s residence or place of employment in an urban area or within forty-five (45) miles or forty-five (45) minutes from the Member’s residence or place of |
employment in a rural area. The assignment shall be based on the following:
| |
| (1) | The need of children and adolescents to be followed by pediatric or adolescent specialists; |
| |
| (2) | Any special medical needs, including pregnancy; |
| |
| (3) | Any language needs made known to the Contractor; and |
| |
| (4) | Area of residence and access to transportation. |
| |
| C. | If there is no Primary Care Provider in the Contractor’s Network that meets the criteria listed in paragraphs A and B directly above, the Contractor shall assign the Member to any Network Primary Care Provider in an adjoining county to the Member’s county of residence or within the Contractor’s Region. |
The Contractor shall monitor and document in a quarterly report to the Department the number of eligible individuals that are assigned a PCP. The Contractor shall notify the Member, in writing, of the PCP assignment, including the Provider’s name, and office telephone number. The Contractor shall make available to the PCP a roster on the first day of each month of Members who have selected or been assigned to his/her care.
| |
| 23.2 | Members who have SSI and Non Dual Eligibles |
A Member who has SSI but is not a dual eligible shall be offered an opportunity to: (1) choose a new PCP who is affiliated with the Contractor’s network or (2) stay with their current PCP as long as such PCP is affiliated with the Contractor’s network. Each Member shall be allowed to choose his or her Primary Care Provider from among all available Contractor Network Primary Care Providers and specialists as is reasonable and appropriate for Member.
The Contractor will send Members information regarding the requirement to select a PCP, or one will be assigned to them accordingly to the following:
| |
| A. | Upon Enrollment, Member will receive a letter requesting them to select a PCP. This letter may be included in the Member Welcome Kit. After one month, if the Member has not selected a PCP, the Contractor must send a second letter requesting the Member to select a PCP within thirty (30) days or one will be chosen for the Member. |
| |
| B. | At the end of the third thirty (30) day period, if the Member has not selected a PCP, the Contractor may select a PCP for the Member and send a card identifying the PCP selected for the Member and informing the Member specifically that the Member can contact the Contractor and make a PCP change. |
| |
| C. | Except for Members who were previously enrolled, the Contractor cannot auto-assign a PCP to a member with SSI within the first ninety (90) days from the date of the Member’s initial enrollment. |
| |
| 23.3 | Enrollment Procedures for Foster Children, Adoption and Guardianship |
DCBS and DAIL staff will apply for Medicaid on behalf of foster children (DCBS) and guardianship clients (DAIL) through an expedited application process agreed on by the Department and the DCBS and DAIL.
Members who are children in foster care and adult guardianship clients may move frequently from one placement to another. The parties agree that the following procedures will be used to determine the residence of these Members for the purpose of maintaining Enrollment.
Foster Children. For members who are in foster care, assignment will be based on where the foster child’s DCBS case is located (which is usually the region where the child’s family of origin resides). When a foster child is placed outside the Contractor’s Region but DCBS continues to maintain the child’s case within the Contractor’s Region, the Contractor’s Region shall remain as the child’s official residence and Contractor shall be responsible for arranging medical care for the Member. It is the responsibility of the DCBS to notify the Contractor of a foster child’s change in placement. Within ten (10) Days of notification, the Contractor must assign a PCP based on the DCBS selection.
Adopted Children. For members who have been adopted, the Member’s region of residence shall be determined by the adoptive parent’s official residence.
Adult Guardianship. For members who are in adult guardianship status, the county of residence shall be where the Member is living. Brief absences, such as for respite care or hospitalization, not to exceed one month, do not change the county of residence. When a Member is transferred outside of the region, the Contractor will continue to be responsible for arranging care for the Member until removed from the HIPAA 834.
The DCBS shall notify the Department when a Member’s case is transferred outside the Contractor’s Region. The Department will include notice of the transfer in the HIPAA 834.
| |
| 23.4 | Primary Care Provider Changes |
The Contractor shall have written policies and procedures for allowing Members to select or be assigned to a new PCP when such a change is mutually agreed to by the Contractor and Member, when a PCP is terminated from coverage, or when a PCP change is as part of the resolution to an Appeal. The Contractor shall allow Members to select another PCP within ten (10) days of the approved change or the Contractor shall assign a PCP to the Member if a selection is not made within the time frame.
A Member shall have the right to change the PCP ninety (90) days after the initial assignment and once a year regardless of reason, and at any time for any reason as approved by the Member’s Contractor. The Member may also change the PCP if there has been a temporary loss of eligibility and this loss caused the Member to miss the annual opportunity, if Medicaid or Medicare imposes sanctions on the PCP, or if the Member and/or the PCP are no longer located in the Contractor’s Region.
The Member shall also have the right to change the PCP at any time for cause. Good cause includes the Member was denied access to needed medical services; the Member received poor quality of care; and the Member does not have access to providers qualified to treat his or her health care needs. If the Contractor approves the Member’s request, the assignment will occur no later than the first day of the second month following the month of the request.
PCPs shall have the right to request a Member’s Disenrollment from his/her practice and be reassigned to a new PCP in the following circumstances: incompatibility of the PCP/patient relationship or inability to meet the medical needs of the Member. PCPs shall not have the right to request a Member’s Disenrollment from their practice for the following: a change in the Member’s health status or need for treatment; a Member’s utilization of medical services; a Member’s diminished mental capacity; or, disruptive behavior that results from the Member’s special health care needs unless the behavior impairs the ability of the PCP to furnish services to the Member or others. Transfer requests shall not be based on race, color, national origin, handicap, age or gender. The Contractor shall authority to approve all transfers.
The initial Provider must serve until the new Provider begins serving the Member, barring ethical or legal issues. The Member has the right to Appeal such a transfer in the formal Appeals process.
The provider shall make the change for request in writing. Member may request a PCP change in writing, face to face or via telephone.
The Contractor shall provide written notice within fifteen (15) Days to a member whose PCP has been voluntarily or involuntarily disenrolled or been terminated from participation in the Contractor’s network.
| |
| 24. | General Requirements for Grievances and Appeals |
The Contractor shall have a grievance system in place for Members that includes a grievance process related to “dissatisfaction” and an appeals process related to a Contractor “action,” including the opportunity to request a State fair hearing pursuant to KRS Chapter 13B.
The Contractor shall implement written policies and procedures describing how the Member may submit a request for a grievance or an appeal with the Contractor or submit a request for a state fair hearing with the State. The policy shall include a description of how the Contractor resolves the grievance or appeal.
The Contractor shall provide to all Providers in the Contractor’s network a written description of its grievance and appeal process and how providers can submit a grievance or appeal for a Member or on their own behalf.
The Contractor shall make available reasonable assistance in completing forms and taking other procedural steps. This includes, but is not limited to,
providing interpreter services and toll-free numbers that have adequate TTY/TTD and interpreter capability.
The Contractor shall name a specific individual(s) designated as the Contractor’s Medicaid Member grievances or appeals coordinator with the authority to administer the policies and procedures for resolution of a grievance or appeal, to review patterns/trends in grievances or appeals, and to initiate corrective action.
The Contractor shall ensure that the individuals who make decisions on grievances or appeals are not involved in any previous level of review or decision-making. The Contractor shall also ensure that health care professionals with appropriate clinical expertise shall make decisions for the following:
| |
| A. | An appeal of a Contractor denial that is based on lack of medical necessity; |
| |
| B. | A Contractor denial that is upheld in an expedited resolution; and |
| |
| C. | A grievance or appeal that involves clinical issues. |
The Contractor shall provide Members, separately or as a part of the Member handbook, information on how they or their representative(s) can file a grievance or an appeal, and the resolution process. The Member information shall also advise Members of their right to file a request for a state fair hearing with the Cabinet, upon notification of a Contractor action, or concurrent with, subsequent to or in lieu of an appeal of the Contractor action.
The Contractor shall ensure that punitive or retaliatory action is not taken against a Member or service provider that files a grievance or an appeal, or a provider that supports a Member’s grievance or appeal.
A grievance is an expression of dissatisfaction about any matter or aspect of the Contractor or its operation, other than a Contractor action as defined in this contract.
A Member may file a grievance either orally or in writing with the Contractor within thirty (30) calendar days of the date of the event causing the dissatisfaction. The legal guardian of the Member for a minor or an incapacitated adult, a representative of the Member as designated in writing to the Contractor, or a service provider acting on behalf of the Member and with the Member’s written consent, have the right to file a grievance on behalf of the Member.
Within five (5) working days of receipt of the grievance, the Contractor shall provide the grievant with written notice that the grievance has been received and the expected date of its resolution.
The investigation and final Contractor resolution process for grievances shall be completed within thirty (30) calendar days of the date the grievance is received by the Contractor and shall include a resolution letter to the grievant.
The Contractor may extend by of up to fourteen (14) calendar days if the Member requests the extension, or the Contractor determines that there is need for additional information and the extension is in the Member’s interest. For any extension not requested by the Member, the Contractor shall give the Member written notice of the reason for the extension within two working days of the decision to extend the timeframe.
Upon resolution of the grievance, the Contractor shall mail a resolution letter to the Member. This resolution letter may not take the place of the acknowledgment letter referred to in Section B above, unless the resolution of the grievance has been completed and can be communicated to the Member in the same correspondence acknowledging receipt of the grievance. The resolution letter shall include, but not be limited to, the following:
| |
| A. | All information considered in investigating the grievance; |
| |
| B. | Findings and conclusions based on the investigation; and |
| |
| C. | The disposition of the grievance. |
An appeal is a request for review by the Contractor of a Contractor action.
| |
| A. | An action for purpose of an appeal is: |
| |
| (1) | the denial or limited authorization of a requested service, including the type or level of service; |
| |
| (2) | the reduction, suspension, or termination of a previously authorized service; |
| |
| (3) | the denial, in whole or in part, of payment for a service; |
| |
| (4) | the failure of the Contractor to provide services in a timely manner, as defined by the Department or its designee; or |
| |
| (5) | the failure of the Contractor to complete the authorization request in a timely manner as defined in 42 CFR 438.408. |
| |
| (6) | for a resident of a rural area with only one Contractor, the denial of a Member’s request to exercise his or her right under 42 CFR 438.52(b)(2)(ii) to obtain services outside the network. |
| |
| B. | The Contractor shall mail a notice of action to the Member or service provider. The notice shall comply with 42 CFR 438.10(c) regarding language and (d) regarding format and shall contain, but not be limited to, the following: |
| |
| (1) | the action the Contractor has taken or intends to take; |
| |
| (2) | the reasons for the action; |
| |
| (3) | the Member’s or the service provider’s right, as applicable, to file an appeal of the Contractor action through the Contractor; |
| |
| (4) | the Member’s right to request a state fair hearing and what the process would be; |
| |
| (5) | the procedures for exercising the rights specified; |
| |
| (6) | the circumstances under which expedited resolution of an appeal is available and how to request it; and |
| |
| (7) | the Member’s right to have benefits continue pending resolution of an appeal or state fair hearing, how to request the continuation of benefits, and the circumstances under which the Member may be required to pay the costs of continuing these benefits. |
The notice shall be mailed within ten (10) days of the date of the action for previously authorized services as permitted under 42 CFR 431.213 and 431.214, and within fourteen (14) days of the date of the action for newly requested services. Denials of Claims that may result in Member financial liability require immediate notification.
| |
| C. | A Member may file an appeal either orally or in writing of a Contractor action within thirty (30) calendar days of receiving the Contractor’s notice of action. The legal guardian of the Member for a minor or an incapacitated adult, a representative of the Member as designated in writing to the Contractor, or a provider acting on behalf of the Member with the Member’s written consent, have the right to file an appeal of an action on behalf of the Member. The Contractor shall consider the Member, representative, or estate representative of a deceased Member as parties to the appeal. |
| |
| D. | The Contractor has thirty (30) calendar days from the date the initial oral or written appeal is received by the Contractor to resolve the appeal. The Contractor shall appoint at least one person to review the appeal who was not involved in the initial decision and who is not the subordinate of any person involved in the initial decision. |
| |
| E. | The Contractor shall have a process in place that ensures that an oral or written inquiry from a Member seeking to appeal an action is treated as an appeal (to establish the earliest possible filing date for the appeal). An oral appeal shall be followed by a written appeal that is signed by the Member within ten (10) calendar days. The Contractor shall use its best efforts to assist Members as needed with the written appeal and may continue to process the appeal. |
| |
| F. | Within five working days of receipt of the appeal, the Contractor shall provide the grievant with written notice that the appeal has been received and the expected date of its resolution. The Contractor shall confirm in writing receipt of oral appeals, unless the Member or the service provider requests an expedited resolution. |
| |
| G. | The Contractor may extend the thirty (30) day timeframe by fourteen (14) calendar days if the Member requests the extension, or the Contractor determines that there is need for additional information, and the extension is in the Member’s interest. For any extension not requested by the Member, the Contractor shall give the Member written notice of the extension and the reason for the extension within two working days of the decision to extend the timeframe. |
| |
| H. | The Contractor shall provide the Member or the Member’s representative a reasonable opportunity to present evidence of the facts or law, in person as well as in writing. |
| |
| I. | The Contractor shall provide the Member or the representative the opportunity, before and during the appeals process, to examine the Member’s case file, including medical or clinical records (subject to HIPAA requirements), and any other documents and records considered during the appeals process. The Contractor shall include as parties to the appeal the Member and his or her representative, or the legal representative of a deceased Member’s estate. |
| |
| J. | For all appeals, the Contractor shall provide written notice within the thirty (30) calendar-day timeframe for resolutions to the Member or the provider, if the provider filed the appeal. The written notice of the appeal resolution shall include, but not be limited to, the following information: |
| |
| (1) | the results and reasoning behind the appeal resolution; and |
| |
| (2) | the date it was completed. |
| |
| K. | The written notice of the appeal resolution for appeals not resolved wholly in favor of the Member shall include, but not be limited to, the following information: |
| |
| (1) | the right to request a state fair hearing and how to do so; |
| |
| (2) | the right to request receipt of benefits while the state fair hearing is pending, and how to make the request; and |
| |
| (3) | that the Member may be held liable for the cost of continuing benefits if the state fair hearing decision upholds the Contractor’s action. |
| |
| L. | The Contractor shall continue the Member’s benefits if all of the following are met: |
| |
| (1) | the Member or the service provider files a timely appeal of the Contractor action or the Member asks for a state fair hearing within 30 days from the date on the Contractor notice of action; |
| |
| (2) | the appeal involves the termination, suspension, or reduction of a previously authorized course of treatment; |
| |
| (3) | the services were ordered by an authorized service provider; |
| |
| (4) | the time period covered by the original authorization has not expired; and |
| |
| (5) | the Member requests extension of the benefits. |
| |
| M. | The Contractor shall provide benefits until one of the following occurs: |
| |
| (1) | The Member withdraws the appeal; |
| |
| (2) | Fourteen (14) days have passed since the date of the resolution letter, provided the resolution of the appeal was against the Member and the Member has not requested a state fair hearing or taken any further action; |
| |
| (3) | The Cabinet issues a state fair hearing decision adverse to the Member; |
| |
| (4) | The time period or service limits of a previously authorized service has expired. |
| |
| N. | If the final resolution of the appeal is adverse to the Member, that is, the Contractor’s action is upheld, the Contractor may recover the cost of the services furnished to the Member while the appeal was pending, |
to the extent that services were furnished solely because of the requirements of this section and in accordance with the policy in 42 CFR 431.230(b).
| |
| O. | If the Contractor or the Cabinet reverses a decision to deny, limit, or delay services, and these services were not furnished while the appeal was pending, the Contractor shall authorize or provide the disputed services promptly and as expeditiously as the Member’s health condition requires. If the Contractor or the Cabinet reverses a decision to deny, limit or delay services and the Member received the disputed services while the appeal was pending, the Contractor shall pay for these services. |
| |
| 24.3 | Expedited Resolution of Appeals |
An expedited resolution of an appeal is an expedited review by the Contractor of a Contractor action.
| |
| A. | The Contractor shall establish and maintain an expedited review process for appeals when the Contractor determines that allowing the time for a standard resolution could seriously jeopardize the Member’s life or health or ability to attain, maintain, or regain maximum function. Such a determination is based on: |
| |
| (1) | a request from the Member; |
| |
| (2) | a provider’s support of the Member’s request; |
| |
| (3) | a provider’s request on behalf of the Member; or |
| |
| (4) | the Contractor’s independent determination. |
The Contractor shall ensure that the expedited review process is convenient and efficient for the Member.
| |
| B. | The Contractor shall resolve the appeal within three working days of receipt of the request for an expedited appeal. In addition to written resolution notice, the Contractor shall also make reasonable efforts to provide and document oral notice. |
| |
| C. | The Contractor may extend the timeframe by up to fourteen (14) calendar days if the Member requests the extension, or the Contractor demonstrates to the Department that there is need for additional information and the extension is in the Member’s interest. For any extension not requested by the Member, the Contractor shall give the Member written notice of the reason for the delay. |
| |
| E. | The Contractor shall ensure that punitive action is not taken against a Member or a service provider who requests an expedited resolution or supports a Member’s expedited appeal. |
| |
| F. | The Contractor shall provide an expedited resolution, if the request meets the definition of an expedited appeal, in response to an oral or written request from the Member or service provider on behalf of the Member. |
| |
| G. | The Contractor shall inform the Member of the limited time available to present evidence and allegations in fact or law. |
| |
| H. | If the Contractor denies a request for an expedited resolution of an appeal, it shall: |
| |
| (1) | transfer the appeal to the thirty (30) day timeframe for standard resolution, in which the thirty (30) day period begins on the date the Contractor received the original request for appeal; and |
| |
| (2) | make reasonable efforts to give the Member prompt oral notice of the denial, and follow up with a written notice within two-calendar days. |
| |
| I. | The Contractor shall document in writing all oral requests for expedited resolution and shall maintain the documentation in the case file. |
| |
| 24.4 | State Hearings for Members |
A Member may request a State Fair Hearing if he or she is dissatisfied with an Action that has been taken by the Contractor, within thirty (30) days of receiving notice of the Action or within thirty (30) days of the final decision by the Contractor
All documents supporting the Contractor’s Action must be received by the Department no later than five (5) days from the date the Contractor receives notice from the Department that a State Fair Hearing has been filed. These records shall be made available to the Member upon request by either the Member or the Member’s legal counsel. The Department will provide the Member with a hearing process that shall adhere to 907 KAR 1:563, 42 CFR 438 Subpart F and 42 CFR 431 Subpart E.
Failure of the Contractor to comply with the State Fair Hearing requirements of the state and federal Medicaid law in regard to an Action taken by the Contractor or to appear and present evidence will result in an automatic ruling in favor of the Member.
The Contractor shall abide by the requirements in 42 CFR 438.104 regarding Marketing activities. The Contractor shall establish and at all times maintain a system of control over the content, form, and method of dissemination of its marketing and information materials. The Contractor shall submit any marketing plans and all marketing materials to the Department and shall obtain the written approval of the Department prior to implementing any marketing plan or arranging for the distribution of any marketing materials to potential enrollees. The Contractor shall provide marketing materials in English, Spanish and any other language spoken by five (5) percent of the potential enrollee or enrollee population. The marketing plan shall include methods and procedures to log and resolve marketing Grievances. The Contractor shall conduct mass media advertising directed to enrollees in the entire service area pursuant to the marketing plan.
Marketing by mail, mass media advertising and community oriented marketing directed at potential Members shall be allowed, subject to the Department’s prior approval. The Contractor shall be responsible for all costs of mailing, including labor costs.
Any marketing materials referring to the Contactor must be approved in writing by the Department prior to dissemination, including mailings sent only to Members. The Contractor agrees to engage only in marketing activities that are pre-approved in writing by the Department. The Contractor must correct problems and errors subsequently identified by the Department after notification by the Department.
The Contractor shall abide by the requirements in 42 CFR Section 438.104 regarding Marketing activities. Face to face marketing by the Contractor directed at Members or potential Members is strictly prohibited. In developing marketing materials such as written brochures, fact sheets, and posters, the Contractor shall abide by the following rules:
| |
| A. | No fraudulent, misleading, or misrepresentative information shall be used in the marketing materials; |
| |
| B. | No offers of material or financial gain shall be made to potential enrollees as an inducement to select a particular provider or use a product; |
| |
| C. | No offers of material or financial gain shall be made to any person for the purpose of soliciting, referring or otherwise facilitating the enrollment of any enrollee; |
| |
| D. | No direct telephone marketing to enrollees and potential enrollees who are not enrolled in the Contractor’s Region; |
| |
| E. | No direct or indirect door-to-door, telephone or other cold-call marketing activities; |
| |
| F. | All marketing materials comply with information requirements of 42 CFR 438.10; and |
| |
| G. | No materials shall contain any assertion or statement (whether written or oral) that CMS, the federal government, the Commonwealth, or any other similar entity endorses the Contractor. |
The following are inappropriate marketing activities, and the Contractor shall not:
| |
| A. | Provide cash to Members or potential Members, except for stipends, in an amount approved by the Department and reimbursement of expenses provided to Members for participation on committees or advisory groups; |
| |
| B. | Provide gifts or incentives to Members or potential Members unless such gifts or incentives: (1) are also provided to the general public; (2) do not exceed ten dollars per individual gift or incentive; and (3) have been pre-approved by the Department; |
| |
| C. | Provide gifts or incentives to Members unless such gifts or incentives: (1) are provided conditionally based on the Member receiving preventive care or other Covered Services; (2) are not in the form of cash or an instrument that may be converted easily to cash; and (3) have been pre-approved by the Department; |
| |
| D. | Seek to influence a potential Member’s enrollment with the Contractor in conjunction with the sale of any private insurance; |
| |
| E. | Induce providers or employees of the Department to reveal confidential information regarding Members or otherwise use such confidential information in a fraudulent manner; or |
| |
| F. | Threaten, coerce or make untruthful or misleading statements to potential Members or Members regarding the merits of enrollment with the Contractor or any other plan. |
| |
| 25.3 | Marketing and Enrollment Agent |
The Department reserves the right to delegate to an independent agent or agents, the responsibility for determining the eligibility of Members for enrollment pursuant to Eligibility of this Contract; and disenrolling Members in accordance with Disenrollment of this Contract.
In the event an agent is designated according to the terms of this Contract, the Department shall have the right to prescribe the application and Disenrollment forms to be used by the Contractor and the agent. The Department shall provide written notice to the Contractor identifying the agent or agents, if any, selected by the Department pursuant to this subsection, and setting forth the functions of the agent or agents, and procedures to be followed by the Contractor and its agents.
| |
| 26. | Member Eligibility, Enrollment and Disenrollment |
| |
| 26.1 | Eligibility Determination |
The Department shall have the exclusive right to determine an individual’s eligibility for the Medicaid Program and eligibility to become a Member of the Contractor. Such determination shall be final and is not subject to review or appeal by the Contractor. Nothing in this section prevents the Contractor from providing the Department with information the Contractor believes indicates that the Member’s eligibility has changed.
| |
| 26.2 | Managed Care Mass Enrollment Initial Assignment |
For a successful transition of a Medicaid program from a Fee for Service model to a sustainable Managed Care Organization (MCO) model it is imperative that due consideration be given to:
| |
| A. | Provider Network – Only MCOs which have adequate provider network and have successfully completed the readiness assessment |
as defined by the Department will be considered for the mass enrollment process.
| |
| B. | Keeping the family together - Assign members of a family to the same MCO. |
| |
| C. | Continuity of Care - Preserve the family’s pre-established relationship with providers to the extent possible |
| |
| D. | Robust MCO Competition - equitable distribution of the participants among the MCOs |
The mass initial auto-assignment process is based upon algorithms that take into consideration continuity of care, preference of MCO or of MCO providers, or cost, in that order, with a particular focus on needs of children and individuals with specialized health care needs. These factors are considered within a system with enrollment limits imposed to assure that MCOs do not have excessive or inadequate numbers of enrollees. In order to ensure equitable distribution of members there will be a MCO maximum threshold and a minimum threshold assigned per region. DMS will set the maximum and minimum thresholds by region based on the number of MCOs per region. The maximum threshold per region shall be 55% and the minimum threshold per region shall be 20%.
| |
| A. | All managed care members of a Medicaid family will be assigned to the same MCO. |
| |
| B. | Continuity of Care – The Department will use Claims history to determine the most recent, regularly visited primary care physicians (PCP). The top three PCP providers for each member will be considered. This determination will be based on the last 12 months of history with relative weights based on the time period of the visits.. The weight will be 1 thru 3 with 3 being assigned to visits in the most recent four months; 1 being assigned to visits in the earliest four month period, and 2 being assigned to the visits in the middle four month period. Next, each member’s top three PCP Providers will be matched against the provider network of the region’s MCOs and a “MCO network suitability score” will be assigned to each family member. |
| |
| C. | In order to give due consideration to children and individuals with specialized health care needs it is important that all family members are not treated equally in developing the family unit’s overall MCO score. The ratio between the number of children eligible for managed care versus the number of adults eligible for managed care is almost 1.9 to 1. Therefore the “MCO network suitability score” for a child will be further multiplied by a factor of 1.9. Similarly individuals with special health care needs (identified as SSI Adults, SSI Children, and Foster Care) will have their score adjusted bya factor of 1.6 which represents the relative cost of these individuals relative |
to the cost of adults over 18. In the case of SSI Children and Foster Care both the child factor (1.9) and the special needs factor (1.6) will be applied. After these adjustments, , each family member’s individual “MCO net work suitability score” will be added together to determine the family unit’s “MCO network suitability score”
| |
| D. | The family will be assigned to the MCO with the highest “MCO network suitability score” unless that MCO has exceeded their region’s maximum threshold. Two maximum thresholds are defined for each region: Families and Children, and Others. If the family unit has both categories of individuals, then both thresholds will apply. In a scenario where the applicable threshold(s) are exceeded, the family will be assigned to the MCO with next highest score. If a tie exists between two eligible MCOs, see the following step used. |
| |
| E. | In scenarios where multiple eligible MCOs have the same score for the family “MCO network suitability score”, the MCOs which are under the minimum threshold will be given preference, until the MCO reaches the minimum threshold. |
| |
| F. | In scenarios where multiple MCOs have the same score for the family “MCO network suitability score” and all MCOs are above the minimum threshold, the MCO with the lowest capitation rate for the family will be assigned. |
| |
| 26.3 | General Enrollment Provisions |
The Department shall notify the Contractor of the Members to be enrolled with the Contractor. The Contractor shall provide for a continuous open enrollment period throughout the term of the Contract. The Contractor shall not discriminate against potential Members on the basis of an individual’s health status, need for health services, race, color, religion, or national origin, and shall not use any policy or practice that has the effect of discriminating on the basis of a Member’s health status, need for health services, race, color, religion, or national origin.
The Department shall be responsible for the enrollment. The Department shall develop an enrollment packet to be sent to potential Members. The Contractor shall have an opportunity to review and comment on the information to be included in the enrollment packet, and may be asked to provide material for the enrollment packet.
Generally, during the first ninety (90) calendar days after the effective date of initial enrollment, whether the Member selected the Contractor or was assigned through an automatic process, the Member shall have the opportunity to change their Contractor and once a year thereafter in accordance with 42 CFR 438.
| |
| 26.4 | Enrollment Procedures |
Each Member shall be provided with a Kentucky Medical Assistance Identification Card.
Within five (5) business days after receipt of notification of new Member enrollment, the Contractor shall send a confirmation letter to the Member by a method that will not take more than three (3) days to reach the Member. The confirmation letter shall include at least the following information: the effective date of enrollment; Site and PCP contact information; how to obtain referrals; the role of the Care Coordinator and Contractor; the benefits of preventive health care; Member identification card; copy of the Member Handbook; and list of covered services. The identification card may be sent separately from the confirmation letter as long as it is sent within five (5) business days after receipt of notification of new Member enrollment.
The Contractor shall accept all Members, regardless of overall plan enrollment. Enrollment shall be without restriction and shall be in the order in which potential Members apply or are assigned. The Contractor shall maintain staffing and service delivery network necessary to adhere to minimum standards for Covered Services set forth in Appendix I.
Members may voluntarily choose a Contractor. Members who do not select a Contractor will be auto-assigned to a Contractor by the Department. The Department shall design an algorithm for the auto-assignment process. The Department reserves the right to re-evaluate and modify the auto-assignment algorithm anytime for any reason, provided however, after April 1, 2012, the Department shall provide written notice to Contractor of any modification of the auto-assignment algorithm at least sixty (60) days before the implementation of such modification.
The Department may develop specific limitations regarding Member enrollment with the Contractor to take into consideration quality, cost, competition and adverse selection.
Enrollment begins at 12:01 a.m. on the first day of the first calendar month for which eligibility is indicated on the eligibility file (HIPAA 834) transmitted to the Contractor, and shall remain until the Member is disenrolled in accordance with Disenrollment of this Contract. Applicable state and federal law determines membership for newborns. Membership begins on day of application for members who are presumptive eligible.
The Contractor shall be responsible for the provision and costs of all Covered Services beginning on or after the beginning date of Enrollment. In the event a Member entering is receiving Medically Necessary Covered Services the
day before Enrollment, the Contractor shall be responsible for the costs of continuation of such Medically Necessary Covered Services, without any form of prior approval and without regard to whether such services are being provided within or outside the Contractor’s Network until such time as the Contractor can reasonably transfer the Member to a service and/or Network Provider without impeding service delivery that might be harmful to the Member’s health.
| |
| 26.7 | Member Eligibility File (HIPAA 834) |
The Department will electronically transmit to the Contractor a HIPAA 834 transaction file daily to indicate new, terminated and changed members and a monthly listing of all Contractor’s Members. The Department will submit with the monthly HIPAA 834 transaction file, a reconciliation of enrollment information pursuant to policies and procedures determined by the Department. The Department shall send the first enrollment data to Contractor in HIPAA 834 format.
All Enrollments and Disenrollments shall become effective on the dates specified on the HIPAA 834 transaction files and shall serve as the basis for Capitated Payments to the Contractor.
The Contractor will be responsible for promptly notifying the Department of Members of whom it has knowledge were not included on the HIPAA 834 transaction file and should have been enrolled with the Contractor. Should the Contractor become aware of any changes in demographic information the Contractor shall advise the Member of the need to report information to the appropriate source, i.e. the DCBS office or the Social Security Administration. The Contractor should not attempt to report these types of changes on behalf of the member, but should monitor the HIPAA 834 for appropriate changes. In the event that the change does not appear on the HIPAA 834 within sixty (60) days, Contractor shall report the conflicting information to the Department. The Department will evaluate and address the inconsistencies as appropriate.
| |
| 26.8 | Persons Eligible for Enrollment |
To be enrolled with a Contractor, the individual shall be a resident of the Contractor Region, and shall be eligible to receive Medicaid assistance under one of the aid categories defined below:
Eligible Member Categories*
| |
| A. | Temporary Assistance to Needy Families (TANF); |
| |
| B. | Children and family related; |
| |
| C. | Aged, blind, and disabled Medicaid only; |
| |
| E. | Poverty level pregnant women and children, including presumptive eligibility; |
| |
| F. | Aged, blind, and disabled receiving State Supplementation; |
| |
| G. | Aged, blind, and disabled receiving Supplemental Security Income (SSI); or |
| |
| H. | Under the age of twenty-one (21) years and in an inpatient psychiatric facility. |
*The populations identified in 42 CFR 438.50(d) will be included in the eligible member categories. These eligibles may be voluntarily enrolled prior to the Department receiving approval of the waiver.
Members eligible to enroll with the Contractor will be enrolled beginning with the first day of the application month with the exception of (1) newborns who are enrolled beginning with their date of birth and (2) unemployed parent program Members who are enrolled beginning with the date the definition of unemployment in accordance with 45 CFR 233.100 is met.
The Contractor shall also be responsible for providing coverage to individuals who are retro-actively determined eligible for Medicaid. Retro-active Medicaid coverage is defined as a period of time up to three (3) months prior to the application month. For SSI Members, Medicaid coverage may also include previous months or years in situations where an individual appealed a SSI denial, and were subsequently approved as of the original application date.
Newborn infants of non-presumptive eligible Members shall be deemed eligible for Medicaid and automatically enrolled with the Contractor as individual Members for sixty (60) days. Deemed eligible newborns are auto enrolled in Medicaid and enrollment is coordinated within the Cabinet. The delivery hospital is required to enter the birth record in the birth record system called KY CHILD (Kentucky’s Certificate of Live Birth, Hearing, Immunization, and Lab Data). That information is used to auto enroll the deemed eligible newborn within twenty-four (24) hours of birth. The Contractor is required to use the newborn’s Medicaid ID for any costs associated with child.
The Contractor shall utilize the HIPAA 834 to identify Members who are Dual Eligible shall be identified within the MMIS. The Contractor and Medicare providers shall work together to coordinate the care for such Members in order to reduce over utilization and duplication of services and cost.
| |
| 26.11 | Persons Ineligible for Enrollment |
Members who are not eligible to enroll in the MCO Program are defined below:
INELIGIBLE MEMBER CATEGORIES
| |
| A. | Individuals who shall spend down to meet eligibility income criteria; |
| |
| B. | Individuals currently Medicaid eligible and have been in a nursing facility for more than thirty (30) days*; |
| |
| C. | Individuals determined eligible for Medicaid due to a nursing facility admission including those individuals eligible for institutionalized hospice; |
| |
| D. | Individuals served under the Supports for Community Living, Michele P, home and community-based, or other 1915(c) Medicaid waivers; |
| |
| E. | Qualified Medicare Beneficiaries (QMBs), specified low income Medicare beneficiaries (SLMBs) or qualified Disabled Working Individuals (QDWIs); |
| |
| F. | Timed limited coverage for illegal aliens for emergency medical conditions; |
| |
| G. | Working Disabled Program; |
| |
| H. | Individuals in an intermediate care facility for mentally retarded (ICF-MR); and |
| |
| I. | Individuals who are eligible for the Breast or Cervical Cancer Treatment Program. |
* The Contractor shall not be responsible for a Member’s nursing facility costs during the first thirty (30) days; however, if a Member is admitted to a nursing facility, the Contractor will be responsible for covering the costs of health services, exclusive of nursing facility costs, provided to the Member while in the nursing facility until the Member is either discharged from the nursing facility or disenrolled from the Contractor (after the thirty-first day in the nursing facility). Contractor costs may include those of physicians, physician assistants, APRNs, or any other medical services that are not included in the nursing home facility per diem rate.
The Contractor shall not be responsible for Waiver Services furnished to MCO Members.
| |
| 26.12 | Reinstatement of Medicaid Eligibility |
A Member whose membership is terminated because the Member no longer qualifies for medical assistance under one of the aid categories listed in Persons Eligible for Enrollment of this Contract shall be automatically reenrolled with the Contractor if eligibility for medical assistance is re-established within two (2) months. The Contractor shall be given a new enrollment date once a Member has been reinstated.
A Member whose Medicaid coverage has been reinstated in the last two calendar months shall be re-enrolled with the same Contractor in which they were previously enrolled provided the Member’s eligibility status and county of residence is still valid for participation in the Contractor.
| |
| 26.13 | Moving Out of the Contractor’s Region |
The Contractor shall continue to be responsible for the provision and cost of medical care of any Member moving out of the Contractor’s Region until such
time as the Member is removed from the HIPAA 834. The Department shall continue Capitation Payments to the Contractor on behalf of the Member until such time as the Member’s change of residence is updated in the eligibility system and the Member’s name is removed from the HIPAA 834. The Department shall notify the Contractor promptly upon the removal of the Member.
| |
| 26.14 | Member Request for Disenrollment |
A Member may request Disenrollment only with cause. The Member shall submit a written request for a hearing to request Disenrollment to either the Contractor or the Department giving the reason(s) for the request. If submitted to the Contractor, the Contractor shall transmit the Member’s request to the Contract Compliance Officer of the Department. If submitted to the Department, the Department shall transmit a copy to Contractor.
| |
| 26.15 | Contractor Request for Disenrollment |
The Contractor shall recommend to the Department Disenrollment of a Member when the Member pursuant to 42 CFR 438.56:
| |
| A. | Is found guilty of Fraud in a court of law or administratively determined to have committed Fraud related to the Medicaid Program; |
| |
| B. | Is abusive or threatening as defined by and reported in Guidelines for Preventing Workplace Violence for Health Care and Social Service Workers to either Contractor, Contractor’s agents, or providers; |
| |
| C. | No longer resides in the Contractor’s Region; |
| |
| D. | Is admitted to a nursing facility for more than 31 days; or |
| |
| E. | Is incarcerated in a correctional facility; |
| |
| F. | No longer qualifies for Medical Assistance under one of the aid categories listed in Eligibility of this Contract. |
All requests by the Contractor for the Department to disenroll a Member shall be in writing and shall specify the basis for the request. If applicable, the Contractor’s request must document that reasonable steps were taken to educate the Member regarding proper behavior, and that the Member refused to comply. The Contractor may not request Disenrollment of a Member based on an adverse change in the Member’s health.
| |
| 26.16 | Effective Date of Disenrollment |
Disenrollment shall be effective on the first day of the calendar month for which the Disenrollment appears on the HIPAA 834 transaction file. Requested Disenrollment shall be effective no later than the first day of the second month following the month the Member or the Contractor files the request. If the Department fails to make a determination within the timeframes the Disenrollment shall be considered approved.
| |
| 26.17 | Continuity of Care upon Disenrollment |
The Contractor shall take all reasonable and appropriate actions necessary to ensure the continuity of a Member’s care upon Disenrollment. Such actions shall include: assisting in the selection of a new Primary Care Provider, cooperating with the new Primary Care Provider in transitioning the Member’s care, and making the Member’s Medical Record available to the new the Primary Care Provider, in accordance with applicable state and federal law.
The Contractor shall notify the Department or Social Security Administration in the appropriate county, within five (5) working days of receiving notice of the death of any Member.
The Contractor shall demonstrate compliance with standards of provider network capacity and member access to services by producing reports illustrating that services, service locations, and service sites are available and accessible in terms of timeliness, amount, duration and personnel sufficient to provide all Covered Services on an emergency or urgent care basis, twenty-four (24) hours a day, seven days a week.
The Department shall use multiple tools to monitor the Contractor’s Network adequacy and Member access. The Encounter Record submitted will be used to display Primary Care Provider location, Service Location, Member distribution, patterns of referral, quality measures, and other analytical data.
The Contractor shall maintain a Provider Services function that is responsible for the following services and tasks:
| |
| A. | Enrolling, credentialing and recredentialing and performance review of providers; |
| |
| B. | Assisting Providers with Member Enrollment status questions; |
| |
| C. | Assisting Providers with Prior Authorization and referral procedures; |
| |
| D. | Assisting Providers with Claims submissions and payments; |
| |
| E. | Explaining to Providers their rights and responsibilities as a member of Contractor’s Network; |
| |
| F. | Handling, recording and tracking Provider Grievances and Appeals properly and timely; |
| |
| G. | Developing, distributing and maintaining a Provider manual; |
| |
| H. | Developing, conducting, and assuring Provider orientation/training; |
| |
| I. | Explaining to Providers the extent of Medicaid benefit coverage including EPSDT preventive health screening services and EPSDT Special Services; |
| |
| J. | Communicating Medicaid policies and procedures, including state and federal mandates and any new policies and procedures; |
| |
| K. | Assisting Providers in coordination of care for child and adult members with complex and/or chronic conditions; |
| |
| L. | Encouraging and coordinating the enrollment of Primary Care Providers in the Department for Public Health and the Department for Medicaid Services Vaccines for Children Program. This program offers certain vaccines free of charge to Medicaid members under the age of 21 years; |
| |
| M. | Coordinating workshops relating to the Contractor’s policies and procedures; |
| |
| N. | Providing necessary technical support to Providers who experience unique problems with certain Members in their provision of services; and |
| |
| O. | Annually addressing fraud, waste and abuse with providers |
Provider Services shall be staffed, at a minimum, Monday through Friday 8am – 6pm Eastern Standard Time. Staff members shall be available to speak with providers any time during open hours. The Contractor shall operate a provider call center that meets standards as determined by the Department.
Provider Services staff shall be instructed to follow all contractually-required provider relation functions including, policies, procedures and scope of services.
| |
| 27.2 | Provider Credentialing and Recredentialing |
In compliance with 907 KAR 1:672 and federal law the Contractor shall document the procedure, which shall comply with the Department’s current policies and procedures, for credentialing and recredentialing of providers with whom it contracts or employs to treat Members. This documentation shall include, but not be limited to, defining the scope of providers covered, the criteria and the primary source verification of information used to meet the criteria, the process used to make decisions and the extent of delegated credentialing and recredentialing arrangements. The Contractor shall have a process for receiving input from participating providers regarding credentialing and recredentialing of providers. Those providers accountable to a formal governing body for review of credentials shall include physicians, dentists, advanced registered nurse practitioners, audiologist, CRNA, optometrist, podiatrist, chiropractor, physician assistant and other licensed or certified practitioners. Providers required to be recredentialed by the Contractor per Department policy are physicians, audiologists, certified registered nurse anesthetists, advanced registered nurse practitioners, podiatrists, chiropractors and physician assistants. However, if any of these providers are hospital-based, credentialing will be performed by the Department. The Contractor shall be responsible for the ongoing review of provider performance and credentialing as specified below:
| |
| A. | The Contractor shall verify that its enrolled network Providers to whom Members may be referred are properly licensed in accordance with all applicable Commonwealth law and regulations and have in effect such current policies of malpractice insurance as may be required by the Contractor. |
| |
| B. | The process for verification of Provider credentials and insurance, and any additional facts for further verification and periodic review of Provider |
performance, shall be embodied in written policies and procedures, approved in writing by the Department.
| |
| C. | The Contractor shall maintain a file for each Provider containing a copy of the Provider’s current license issued by the Commonwealth and such additional information as may be specified by the Department. |
| |
| D. | The process for verification of Provider credentials and insurance shall be in conformance with the Department’s policies and procedures. The Contractor shall meet requirements under KRS 205.560(12) related to credentialing. The Contractor’s enrolled providers shall complete a credentialing application in accordance with the Department’s policies and procedures. |
The process for verification of Provider credentials and insurance shall include the following:
| |
| A. | Written policies and procedures that include the Contractor’s initial process for credentialing as well as its re-credentialing process that must occur, at a minimum, every three (3) years; |
| |
| B. | A governing body, or the groups or individuals to whom the governing body has formally delegated the credentialing function; |
| |
| C. | A review of the credentialing policies and procedures by the formal body; |
| |
| D. | A credentialing committee which makes recommendations regarding credentialing; |
| |
| E. | Written procedures, if the Contractor delegates the credentialing function, as well as evidence that the effectiveness is monitored; |
| |
| F. | Written procedures for the termination or suspension of Providers; and |
| |
| G. | Written procedures for, and implementation of, reporting to the appropriate authorities serious quality deficiencies resulting in suspension or termination of a provider. |
The contractor shall meet requirements under KRS 205.560(12) related to credentialing. Verification of Provider’s credentials shall include the following:
| |
| A. | A current valid license or certificate to practice in the Commonwealth of Kentucky; |
| |
| B. | A Drug Enforcement Administration (DEA) certificate and number, if applicable; |
| |
| C. | Primary source of graduation from medical school and completion of an appropriate residency, or accredited nursing, dental, physician assistant or vision program as applicable; if provider is not board certified. |
| |
| D. | Board certification if the practitioner states on the application that the practitioner is board certified in a specialty; |
| |
| E. | Professional board certification, eligibility for certification, or graduation from a training program to serve children with special health care needs under twenty-one (21) years of age; |
| |
| F. | Previous five (5) years work history; |
| |
| G. | Professional liability claims history; |
| |
| H. | Clinical privileges and performance in good standing at the hospital designated by the Provider as the primary admitting facility, for all providers whose practice requires access to a hospital, as verified through attestation; |
| |
| I. | Current, adequate malpractice insurance, as verified through attestation; |
| |
| J. | Documentation of revocation, suspension or probation of a state license or DEA/BNDD number; |
| |
| K. | Documentation of curtailment or suspension of medical staff privileges; |
| |
| L. | Documentation of sanctions or penalties imposed by Medicare or Medicaid; |
| |
| M. | Documentation of censure by the State or County professional association; and |
| |
| N. | Most recent information available from the National Practitioner Data Bank. |
The provider shall complete a credentialing application that includes a statement by the applicant regarding:
| |
| A. | The ability to perform the essential functions of the positions, with or without accommodation; |
| |
| B. | Lack of present illegal drug use; |
| |
| C. | History of loss of license and felony convictions; |
| |
| D. | History of loss or limitation of privileges or disciplinary activity; |
| |
| E. | Sanctions, suspensions or terminations imposed by Medicare or Medicaid; and |
| |
| F. | Applicants attest to the correctness and completeness of the application. |
Before a practitioner is credentialed, the Contractor shall verify information from the following organizations and shall include the information in the credentialing files:
| |
| A. | National practitioner data bank, if applicable; |
| |
| B. | Information about sanctions or limitations on licensure from the appropriate state boards applicable to the practitioner type; and |
| |
| C. | Other recognized monitoring organizations appropriate to the practitioner’s discipline. |
At the time of credentialing, the Contractor shall perform an initial visit to potential providers as it deems necessary and/or as required by law. The Contractor shall document a structured review to evaluate the site against the Contractors organizational standards and those specified by this contract. The Contractor shall document an evaluation of the medical record documentation and keeping practices at each site for conformity with the Contractors organizational standards and this contract.
The Contractor shall have formalized recredentialing procedures. The Contractor shall formally recredential its providers at least every three (3) years. The Contractor shall comply with the Department’s recredentialing policies and procedures. There shall be evidence that before making a recredentialing decision, the Contractor has verified information about sanctions or limitations on practitioner from:
| |
| A. | A current license to practice; |
| |
| B. | The status of clinical privileges at the hospital designated by the practitioner as the primary admitting facility; |
| |
| C. | A valid DEA number, if applicable; |
| |
| D. | Board certification, if the practitioner was due to be recertified or become board certified since last credentialed or recredentialed; |
| |
| E. | Five (5) year history of professional liability claims that resulted in settlement or judgment paid by or on behalf of the practitioner; and |
| |
| F. | A current signed attestation statement by the applicant regarding: |
| |
| (1) | The ability to perform the essential functions of the position, with or without accommodation; |
| |
| (2) | The lack of current illegal drug use; |
| |
| (3) | A history of loss, limitation of privileges or any disciplinary action; and |
| |
| (4) | Current malpractice insurance. |
There shall be evidence that before making a recredentialing decision, the Contractor has verified information about sanctions or limitations on practitioner from:
| |
| A. | The national practitioner data bank; |
| |
| C. | State boards of practice, as applicable; and |
| |
| D. | Other recognized monitoring organizations appropriate to the practitioner’s specialty. |
The Contractor will use the format provided in Appendix H to transmit the listed provider credentialing elements to the Department. A Credentialing Process Coversheet will be generated per provider. The Credentialing Process Coversheet will be submitted electronically to the Department’s fiscal agent.
The Contractor shall establish ongoing monitoring of provider sanctions, complaints and quality issues between recredentialing cycles, and take appropriate action.
The Contractor shall have written policies and procedures for the initial and on-going assessment of organizational providers with whom it intends to contract or which it is contracted. Providers include, but are not limited to, hospitals, home health agencies, free-standing surgical centers, residential treatment centers, and clinics. At least every three (3) years, the Contractor shall confirm that the provider is in good standing with state and federal regulatory bodies, including the Department, and, has been accredited or certified by the appropriate accrediting body and state certification agency or has met standards of participation required by the Contractor.
The Contractor shall have policies and procedures for altering conditions of the practitioners participation with the Contractor based on issues of quality of care and services. The Contractor shall have procedures for reporting to the appropriate authorities, including the Department, serious quality deficiencies that could result in a practitioner’s suspension or termination.
If a provider requires review by the Contractor’s credentialing Committee, based on the Contractor’s quality criteria, the Contractor will notify the Department regarding the facts and outcomes of the review in support of the State Medicaid credentialing process.
The contractor shall use the provider type summaries listed at http://chfs.ky.gov/dms/provEnr/Prvoider+Types.htm.
| |
| 27.3 | Primary Care Provider Responsibilities |
A primary care provider (PCP) is a licensed or certified health care practitioner, including a doctor of medicine, doctor of osteopathy, advanced practice registered nurse (including a nurse practitioner, nurse midwife and clinical specialist), physician assistant, or clinic (including a FQHC, primary care center and rural health clinic), that functions within the scope of licensure or certification, has admitting privileges at a hospital or a formal referral agreement with a provider possessing admitting privileges, and agrees to provide twenty-four (24) hours per day, seven (7) days a week primary health care services to individuals. Primary care physician residents may function as PCPs. The PCP shall serve as the member's initial and most important point of contact with the Contractor. This role requires a responsibility to both the Contractor and the Member. Although PCPs are given this responsibility, the Contractors shall retain the ultimate responsibility for monitoring PCP actions to ensure they comply with the Contractor and Department policies.
Specialty providers may serve as PCPs under certain circumstances, depending on the Member’s needs. The decision to utilize a specialist as the PCP shall be based on agreement among the Member or family, the specialist,
and the Contractor’s medical director. The Member has the right to Appeal such a decision in the formal Appeals process.
The Contractor shall monitor PCP’s actions to ensure he/she complies with the Contractor’s and Department’s policies including but not limited to the following:
| |
| A. | Maintaining continuity of the Member’s health care; |
| |
| B. | Making referrals for specialty care and other Medically Necessary services, both in and out of network, if such services are not available within the Contractor’s network; |
| |
| C. | Maintaining a current medical record for the Member, including documentation of all PCP and specialty care services; |
| |
| D. | Discussing Advance Medical Directives with all Members as appropriate; |
| |
| E. | Providing primary and preventative care, recommending or arranging for all necessary preventive health care, including EPSDT for persons under the age of 21 years; |
| |
| F. | Documenting all care rendered in a complete and accurate medical record that meets or exceeds the Department’s specifications; and |
| |
| G. | Arranging and referring members when clinically appropriate, to behavioral health providers. |
Maintaining formalized relationships with other PCPs to refer their Members for after hours care, during certain days, for certain services, or other reasons to extend their practice. The PCP remains solely responsible for the PCP functions (A) through (G) above.
The Contractor shall ensure that the following acceptable after-hours phone arrangements are implemented by PCPs in Contractor’s Network and that the unacceptable arrangements are not implemented:
| |
| (1) | Office phone is answered after hours by an answering service that can contact the PCP or another designated medical practitioner and the PCP or designee is available to return the call within a maximum of thirty (30) minutes; |
| |
| (2) | Office phone is answered after hours by a recording directing the Member to call another number to reach the PCP or another medical practitioner whom the Provider has designated to return the call within a maximum of thirty (30) minutes; and |
| |
| (3) | Office phone is transferred after office hours to another location where someone will answer the phone and be able to contact the PCP or another designated medical practitioner within a maximum of thirty (30) minutes. |
| |
| (1) | Office phone is only answered during office hours; |
| |
| (2) | Office phone is answered after hours by a recording that tells Members to leave a message; |
| |
| (3) | Office phone is answered after hours by a recording that directs Members to go to the emergency room for any services needed; and |
| |
| (4) | Returning after-hours calls outside of thirty (30) minutes. |
The Contractor shall prepare and issue a Provider Manual(s), including any necessary specialty manuals (e.g. Behavioral Health) to all network Providers. For newly contracted providers, the Contractor shall issue copies of the Provider Manual(s) within five (5) working days from inclusion of the provider in the network.
Department shall approve the Provider Manual, and any updates to the Provider Manual, prior to publication and distribution to Providers.
All Provider Manuals shall be available in hard copy format and online.
The Provider Manual and updates shall serve as a source of information to Providers regarding Covered Services, Contractor’s Policies and Procedures, provider credentialing and recredentialing, including Member Grievances and Appeals, claims submission requirements, reporting fraud and abuse, prior authorization procedures, Medicaid laws and regulations, telephone access, the QAPI program, standards for preventive health services and other requirements when identified by the Contractor.
| |
| 27.5 | Provider Orientation and Education |
The Contractor shall conduct initial orientation for all Providers within thirty (30) days after the Contractor places a newly contracted Provider on an active status. The Contractor shall ensure that all Providers receive initial and ongoing orientation in order to operate in full compliance with the Contract and all applicable Federal and Commonwealth requirements. The Contractor shall maintain and make available upon request enrollment or attendance rosters dated and signed by each attendee or other written evidence of training of each Provider and their staff. The Contractor shall ensure that Provider education includes: Contractor coverage requirements for Medicaid services; policies or procedures and any modifications to existing services, reporting fraud and abuse; Medicaid populations/eligibility; standards for preventive health services; special needs of Members in general that affect access to and delivery of services; Advance Medical Directives; EPSDT services; Claims submission and payment requirements; special health/care management programs that Members may enroll in; cultural sensitivity; responding to needs of Members with mental, developmental and physical disabilities; reporting of communicable disease; the Contractors QAPI program; medical records review; EQRO and; the rights and responsibilities of both Members and
Providers. The Contractor shall ensure that ongoing education is conducted relating to findings from the QAPI program when deemed necessary by either the Contractor or Department.
The Contractor shall require their Providers to maintain Member medical records on paper or in an electronic format. Member Medical Records shall be maintained timely, legible, current, detailed and organized to permit effective and confidential patient care and quality review. Complete Medical Records include, but are not limited to, medical charts, prescription files, hospital records, provider specialist reports, consultant and other health care professionals’ findings, appointment records, and other documentation sufficient to disclose the quantity, quality, appropriateness, and timeliness of services provided under the Contract. The medical record shall be signed by the provider of service.
The Member’s Medical Record is the property of the Provider who generates the record. However, each Member or their representative is entitled to one free copy of his/her medical record. Additional copies shall be made available to Members at cost. Medical records shall generally be preserved and maintained for a minimum of five (5) years unless federal requirements mandate a longer retention period (i.e. immunization and tuberculosis records are required to be kept for a person’s lifetime).
The Contractor shall ensure that the PCP maintains a primary medical record for each member, which contains sufficient medical information from all providers involved in the Member’s care, to ensure continuity of care. The medical chart organization and documentation shall, at a minimum, require the following:
A. Member/patient identification information, on each page;
| |
| B. | Personal/biographical data, including date of birth, age, gender, marital status, race or ethnicity, mailing address, home and work addresses and telephone numbers, employer, school, name and telephone numbers (if no phone contact name and number) of emergency contacts, consent forms, identify language spoken and guardianship information; |
C. Date of data entry and date of encounter;
D. Provider identification by name;
| |
| E. | Allergies, adverse reactions and any known allergies shall be noted in a prominent location; |
| |
| F. | Past medical history, including serious accidents, operations, illnesses. For children, past medical history includes prenatal care and birth |
information, operations, and childhood illnesses (i.e. documentation of chickenpox);
| |
| G. | Identification of current problems; |
| |
| H. | The consultation, laboratory, and radiology reports filed in the medical record shall contain the ordering provider’s initials or other documentation indicating review; |
| |
| I. | Documentation of immunizations pursuant to 902 KAR 2:060; |
| |
| J. | Identification and history of nicotine, alcohol use or substance abuse; |
| |
| K. | Documentation of reportable diseases and conditions to the local health department serving the jurisdiction in which the patient resides or Department for Public Health pursuant to 902 KAR 2:020; |
| |
| L. | Follow-up visits provided secondary to reports of emergency room care; |
M. Hospital discharge summaries;
N. Advanced Medical Directives, for adults;
O. All written denials of service and the reason for the denial; and
| |
| P. | Record legibility to at least a peer of the writer. Any record judged illegible by one reviewer shall be evaluated by another reviewer. |
A Member’s medical record shall include the following minimal detail for individual clinical encounters:
| |
| A. | History and physical examination for presenting complaints containing relevant psychological and social conditions affecting the patient’s medical/behavioral health, including mental health, and substance abuse status; |
| |
| B. | Unresolved problems, referrals and results from diagnostic tests including results and/or status of preventive screening services (EPSDT) are addressed from previous visits |
| |
| C. | Plan of treatment including: |
| |
| 1. | Medication history, medications prescribed, including the strength, amount, directions for use and refills; and |
| |
| 2. | Therapies and other prescribed regimen; and |
| |
| 3. | Follow-up plans including consultation and referrals and directions, including time to return. |
| |
| 27.7 | Advance Medical Directives |
The Contractor shall comply with laws relating to Advance Medical Directives pursuant to KRS 311.621 - 311.643 and 42 CFR Part 489, Subpart I and 42 CFR 422.128, 438.6 and 438.10 Advance Medical Directives, including living wills or durable powers of attorney for health care, allow adult Members to initiate directions about their future medical care in those circumstances where Members are unable to make their own health care decisions. The Contractor shall, at a minimum, provide written information on Advance Medical Directives to all Members and shall notify all Members of any changes in the rules and regulations governing Advance Medical Directives within ninety (90) Days of the change and provide information to its PCPs via the Provider Manual and Member Services staff on informing Members about Advance Medical Directives. PCPs have the responsibility to discuss Advance Medical Directives with adult Members at the first medical appointment and chart that discussion in the medical record of the Member.
| |
| 27.8 | Provider Grievances and Appeals |
The Contractor shall establish and maintain written policies and procedures for the filing of Provider grievances and appeals. A provider shall have the right to file a grievance or an appeal with the Contractor. Provider grievances or appeals shall be resolved within thirty (30) calendar days. If the grievance or appeal is not resolved within thirty (30) days, the Contractor shall request a fourteen (14) day extension from the provider. If the Provider requests the extension, the extension shall be approved by the Contractor. A Provider may not file a grievance or an appeal on behalf of a Member without written designation by the Member as the Member’s representative. A Provider shall have the right to file an appeal with the Contractor regarding provider payment or contractual issues.
| |
| 27.9 | Other Related Processes |
The Contractor shall provide information specified in 42 CFR 438.10(g)(1) about the grievance system to all service providers and subcontractors at the time they enter into a contract.
All grievance or appeal files shall be maintained in a secure and designated area and be accessible to the Department or its designee, upon request, for review. Grievance or appeal files shall be retained for ten (10) years following the final decision by the Contractor, HSD, an administrative law judge, judicial appeal, or closure of a file, whichever occurs later.
The Contractor shall have procedures for assuring that files contain sufficient information to identify the grievance or appeal, the date it was received, the nature of the grievance or appeal, notice to the Member of receipt of the grievance or appeal, all correspondence between the Contractor and the Member, the date the grievance or appeal is resolved, the resolution, the notices of final decision to the Member, and all other pertinent information.
Documentation regarding the grievance shall be made available to the Member, if requested.
| |
| 27.10 | Release for Ethical Reasons |
The Contractor shall not require Providers to perform any treatment or procedure that is contrary to the Provider’s conscience, religious beliefs, or ethical principles in accordance with 42 CFR 438.102.
The Contractor shall have a referral process in place for situations where a Provider declines to perform a service because of ethical reasons. The Member shall be referred to another Provider licensed, certified or accredited to provide care for the individual service, or assigned to another PCP licensed, certified or accredited to provide care appropriate to the Member’s medical condition.
A release for ethical reasons only applies to Contractor’s Network Providers; it does not apply to the Contractor.
The Contractor shall not prohibit or restrict a Provider from advising a Member about his or her health status, medical care or treatment, regardless of whether benefits for such care are provided under the Contract, if the Provider is acting within the lawful scope of practice.
| |
| 28.1 | Network Providers to Be Enrolled |
The Contractor’s Network shall include Providers from throughout the provider community. The Contractor shall comply with the any willing provider statute as described in 907 KAR 1:672 or as amended and KRS 304.17A-270. Neither the Contractor nor any of its Subcontractors shall require a Provider to enroll exclusively with its network to provide Covered Services under this Contract as such would violate the requirement of 42 CFR Part 438 to provide Members with continuity of care and choice. The Contractor shall enroll at least one (1) Federally Qualified Health Centers (FQHCs) into its network if there is a FQHC appropriately licensed to provide services in the region or service area and at least one teaching hospital In addition the Contractor shall enroll the following types of providers who are willing to meet the terms and conditions for participation established by the Contractor: physicians, advanced practice registered nurses, physician assistants, birthing centers, dentists, primary care centers including, home health agencies, rural health clinics, opticians, optometrists, audiologists, hearing aid vendors, pharmacies, durable medical equipment suppliers, podiatrists, renal dialysis clinics, ambulatory surgical centers, family planning providers, emergency medical transportation provider, non-emergency medical transportation providers as specified by the Department, other laboratory and x-ray providers, individuals and clinics providing Early and Periodic Screening, Diagnosis, and Treatment services, chiropractors, community mental health centers, psychiatric residential treatment facilities, hospitals (including acute care, critical access,
rehabilitation, and psychiatric hospitals), local health departments, and providers of EPSDT Special Services. The Contractor may also enroll other providers, which meet the credentialing requirements, to the extent necessary to provide covered services to the Members. Enrollment forms shall include those used by the Kentucky Medicaid Program as pertains to the provider type. The Contractor shall use such enrollment forms as required by the Department.
The Department will continue to enroll and certify hospitals, nursing facilities, home health agencies, independent laboratories, preventive health care providers, and hospices. The Medicaid provider file will be available for review by the Contractor so that the Contractor can ascertain the status of a Provider with the Medicaid Program and the provider number assigned by the Kentucky Medicaid Program.
Providers performing laboratory tests are required to be certified under the CLIA. The Department will continue to update the provider file with CLIA information from the OSCAR file provided by the Centers for Medicare & Medicaid Services for all appropriate providers. This will make laboratory certification information available to the Contractor on the Medicaid provider file.
The Contractor shall have written policies and procedures regarding the selection and retention of Contractor’s Network. The policies and procedures regarding selection and retention must not discriminate against providers who service high-risk populations or who specialize in conditions that require costly treatment or based upon that Provider’s licensure or certification.
If the Contractor declines to include individuals or groups of providers in its network, it shall give affected providers written notice of the reason for its decision.
The Contractor must offer participation agreements with currently enrolled Medicaid providers who have received electronic health record incentive funds who are willing to meet the terms and conditions for participation established by the Contractor.
28.2 Out-of-Network Providers
The Department will provide the Contractor with a streamlined enrollment process to assign provider numbers for Out-of-network providers. Only out-of-network hospitals and physicians are allowed to complete the Registration short form in emergency situations. The Contractor shall, in a format specified by the Department report all out-of-network utilization by Members.
| |
| 28.3 | Contractor’s Provider Network |
The Contractor may enroll providers in their network who are not participating in the Kentucky Medicaid Program. Providers shall meet the credentialing standards described in Provider Credentialing and Re-Credentialing of this
Contract and be eligible to enroll with the Kentucky Medicaid Program. A provider joining the Contractor’s Network shall meet the Medicaid provider enrollment requirements set forth in the Kentucky Administrative Regulations and in the Medicaid policy and procedures manual for fee-for-service providers of the appropriate provider type. The Contractor shall provide written notice to Providers not accepted into the network along with the reasons for the non-acceptance. A provider cannot enroll in the Contractor’s Network if the provider has active sanctions imposed by Medicare or Medicaid or SCHIP, if required licenses and certifications are not current, if money is owed to the Medicaid Program, or if the Office of the Attorney General has an active fraud investigation involving the Provider or the Provider otherwise fails to satisfactorily complete the credentialing process. The Contractor shall obtain access to the National Practitioner Database as part of their credentialing process in order to verify the Provider’s eligibility for network participation. Federal Financial Participation is not available for amounts expended for providers excluded by Medicare, Medicaid, or SCHIP, except for Emergency Medical Services.
| |
| 28.4 | Enrolling Current Medicaid Providers |
The Contractor will have access to the Department Medicaid provider file either by direct on-line inquiry access, by electronic file transfer, or by means of an extract provided by the Department. The Medicaid provider master file is to be used by the Contractor to obtain the ten-digit provider number assigned to a medical provider by the Department, the Provider’s status with the Medicaid program, CLIA certification, and other information. The Contractor shall use the Medicaid Provider number as the provider identifier when transmitting information or communicating about any provider to the Department or its Fiscal Agent The Contractor shall transmit a file of Provider data specified in this Contract for all credentialed Providers in the Contractor’s network on a monthly basis and when any information changes.
| |
| 28.5 | Enrolling New Providers and Providers not Participating in Medicaid |
A medical provider is not required to participate in the Kentucky Medicaid Program as a condition of participation with the Contractor’s Network. If a potential Provider has not had a Medicaid number assigned, the Contractor will obtain all data and forms necessary to enroll within the Contractor’s Network, and include the required data in any transmission of the provider file information with the exception of the Medicaid provider number. Provider file records transmitted without a provider number will be suspended until verification of the provider’s Medicaid enrollment status and for the assignment of the provider number. When eligibility is confirmed, the Department will enter the provider number on the master provider file and the transmitted data will be loaded to the provider file. The Contractor will receive a report within two weeks of transactions being accepted, suspended or denied.
All documentation regarding a provider’s qualifications and services provided shall be available for review by the Department or its agents at the Contractor’s offices during business hours upon reasonable advance notice.
| |
| 28.6 | Termination of Network Providers or Subcontractors |
Any Provider or Subcontractor who engages in activities that result in suspension, termination, or exclusion from the Medicare or Medicaid program shall be terminated from participation.
The Department shall notify the Contractor of suspension, termination, and exclusion actions taken against Medicaid providers by the Kentucky Medicaid program within three business days via e-mail. The Department will notify the Contractor of voluntary terminations within five business days via email.
The Contractor shall notify the Department of suspension, termination, and exclusion from Contractor’s network taken against a Provider within three business days via email. The Contractor shall notify the Department of voluntary terminations within five business days via email. The Contractor will provide all terminations monthly, via the Provider Termination Report as referenced in Appendix K. The Contractor shall terminate the Provider effective the same date as the Medicaid program termination.
| |
| 28.7 | Provider Program Capacity Demonstration |
The Contractor shall assure that all covered services are as accessible to Members (in terms of timeliness, amount, duration, and scope) as the same services are available to commercial insurance members in the Contractor’s Region; and that no incentive is provided, monetary or otherwise, to providers for the withholding from Members of medically-necessary services. The Contractor shall make available and accessible facilities, service locations, and personnel sufficient to provide covered services consistent with the requirements specified in this section. Emergency medical services shall be made available to Members twenty-four (24) hours a day, seven (7) days a week. Urgent care services by any provider in the Contractor's Program shall be made available within 48 hours of request. The Contractor shall provide the following:
| |
| A. | Primary Care Provider (PCP) delivery sites that are: no more than thirty (30) miles or thirty (30) minutes from Members in urban areas, and for Members in non-urban areas, no more than forty-five (45) minutes or forty-five (45) miles from Member residence; with a member to PCP (FTE) ratio not to exceed 1500:1; and with appointment and waiting times, not to exceed thirty (30) days from date of a Member’s request for routine and preventive services and forty-eight (48) hours for Urgent Care. |
| |
| B. | Specialty care in which referral appointments to specialists shall not exceed thirty (30) days for routine care or forty-eight (48) hours for Urgent Care; except for Behavioral Health Services for which emergency care with crisis stabilization must be provided within twenty-four (24) hours, urgent care which must be provided within forty-eight (48) hours, services may not exceed fourteen (14) days post discharge |
from an acute Psychiatric Hospital and sixty (60) days for other referrals. Specialists shall be commensurate with the subpopulations designated by the Department, and include sufficient pediatric specialists to meet the needs of Members younger than twenty-one (21) years of age.
| |
| C. | Immediate treatment for Emergency Care at a health facility that is most suitable for the type of injury, illness or condition, regardless of whether the facility is in Contractor’s Network. |
| |
| D. | Hospital care for which transport time shall not exceed thirty (30) minutes, except in non-urban areas where access time may not exceed sixty (60) minutes, with the exception of Behavioral Health Services and physical rehabilitative services where access shall not exceed sixty (60) minutes. |
| |
| E. | General dental services for which transport time shall not exceed one (1) hour. Any exceptions shall be justified and documented by the Contractor. Appointment and waiting times shall not exceed three (3) weeks for regular appointments and forty eight (48) hours for urgent care. |
| |
| F. | General vision, laboratory and radiology services for which transport time shall not exceed one (1) hour. Any exceptions shall be justified and documented by the Contractor. Appointment and waiting times shall not exceed thirty (30) days for regular appointments and forty eight (48) hours for Urgent Care. |
| |
| G. | For Pharmacy services, travel time shall not exceed one (1) hour or the delivery site shall not be further than fifty (50) miles from the Member’s residence. The Contractor is not required to provide transportation services to Pharmacy services. |
The Contractor shall attempt to enroll the following Providers in its network as follows:
| |
| B. | FQHCs and rural health clinics; |
| |
| C. | The Kentucky Commission for Children with Special Health Care Needs; and |
| |
| D. | Community Mental Health Centers |
If the Contractor is not able to reach agreement on terms and conditions with these specified providers, it shall submit to the Department, for approval, documentation which supports that adequate services and service sites as required in this Contract shall be provided to meet the needs of its Members without contracting with these specified providers.
In consideration of the role that Department for Public Health, which contracts with the local health departments play in promoting population health of the provision of safety net services, the Contractor shall offer a participation agreement to public health departments. Such participation agreements shall include the following provisions:
| |
| A. | Coverage of the Preventive Health Package pursuant to 907 KAR 1:360. |
| |
| B. | Provide reimbursement at rates commensurate with those provided under Medicare. |
The Contractor may also include any charitable providers which serve Members in the Contractor Region, provided that such providers meet credentialing standards.
The Contractor shall demonstrate the extent to which it has included providers who have traditionally provided a significant level of care to Medicaid Members. The Contractor shall have participating providers of sufficient types, numbers, and specialties in the service area to assure quality and access to health care services as required for the Quality Improvement program as outlined in Management Information Systems. If the Contractor is unable to contract with these providers, it shall submit to the Department, for approval, documentation which supports that adequate services and service sites as required in the Contract shall be available to meet the needs of its Members.
The Contractor shall initially submit a series of maps and charts in a format prescribed by the Department that describes the Contractor’s Provider Network, as set forth below. The use of computer-generated maps is preferred. Maps shall include geographic detail including highways, major streets and the boundaries of the Contractor’s network. In addition to the maps and charts, the Contractor shall provide an analysis of the capacity to serve all categories of Members. The analysis shall address the standards for access to care.
Maps shall include the location of all categories of Providers or provider sites as follows:
| |
| A. | Primary Care Providers (designated by a “P”); |
| |
| B. | Primary Care Centers, non FQHC and RHC (designated by a “C”); |
| |
| C. | Dentists (designated by a “D”); |
| |
| D. | Other Specialty Providers (designated by a “S”); |
| |
| E. | Non-Physician Providers - including nurse practitioners, (designated by a “N”) nurse mid-wives (designated by a “M”) and physician assistants (designated by a “A”); |
| |
| F. | Hospitals (designated by a “H”); |
| |
| G. | After hours Urgent Care Centers (designated by a “U”); |
| |
| H. | Local health departments (designated by a “L”); |
| |
| I. | Federally Qualified Health Centers/Rural Health Clinics (designated by a “F” or “R” respectively); |
| |
| J. | Pharmacies (designated by a “X”); |
| |
| K. | Family Planning Clinics (designated by an “Z”); |
| |
| L. | Significant traditional Providers (designated by an “*”); |
| |
| M. | Maternity Care Physicians (designated by a “o”); |
| |
| N. | Vision Providers (designated by a “V”); and |
| |
| O. | Community Mental Health Centers (designated by a “M” |
The Contractor shall update these maps to reflect changes in the Contractor’s Network on an annual basis, or upon request by the Department.
| |
| 28.9 | Expansion and/or Changes in the Network |
If at any time, the Contractor determines that its Contractor Network is not adequate to comply with the access standards specified above, the Contractor shall notify the Department of this situation and submit a corrective action plan to remedy the deficiency. The corrective action plan shall describe the deficiency in detail, including the geographic location and specific regions where the problem exists, and identify specific action steps to be taken by the Contractor and time-frames to correct the deficiency.
In addition to expanding the service delivery network to remedy access problems, the Contractor shall also make reasonable efforts to recruit additional providers based on Member requests. When Members ask to receive services from a provider not currently enrolled in the network, the Contractor shall contact that provider to determine an interest in enrolling and willingness to meet the Contractor’s terms and conditions.
| |
| 28.10 | Provider Electronic Transmission of Data |
The Contractor shall transmit any additions or changes to the Contractor’s Network as specified in Appendix G. Encounter Record containing provider numbers that are not on the Medicaid master provider file will not be accepted.
| |
| 28.11 | Provider System Specifications and Data Definitions |
Appendix G contains the file layouts, data element definitions, and other information relevant to maintenance of the provider file by Contractor.
| |
| 28.12 | Cultural Consideration and Competency |
The Contractor shall participate in the Department’s effort to promote the delivery of services in a culturally competent manner to all Members, including those with limited English proficiency and diverse cultural and ethnic backgrounds. The Contractor shall address the special health care needs of its members needing culturally sensitive services. The Contractor shall incorporate in policies, administration and service practice the values of: recognizing the Member’s beliefs; addressing cultural differences in a competent manner; fostering in staff and Providers attitudes and interpersonal communication styles which respect Member’s cultural background. The Contractor shall communicate such policies to Subcontractors.
| |
| 29. | Provider Payment Provisions |
In accordance with the Balanced Budget Act (BBA) Section 4708, the Contractor shall implement Claims payment procedures that ensure 90% of all Provider Claims for which no further written information or substantiation is required in order to make payment are paid or denied within thirty (30) days of the date of receipt of such Claims and that 99% of all Claims are processed within ninety (90) days of the date of receipt of such Claims. In addition, the Contractor shall comply with the Prompt-Pay statute, codified within KRS 304.17A-700-730, as may be amended, and KRS 205.593, and KRS 304.14-135 and 99-123, as may be amended.
The Contractor shall, notify the requesting provider of any decision to deny a Claim, or to authorize a service in an amount, duration, or scope that is less than requested. The notice to the provider need not be in writing.
Any conflict between the BBA and Commonwealth law will default to the BBA unless the Commonwealth requirements are stricter.
| |
| 29.2 | Payment to Out-of-Network Providers |
The Contractor shall reimburse Out-of-Network Providers in accordance with Section 29.1 Provider Claims payments for the following Covered Services:
| |
| A. | Specialty care for which the Contractor has approved a authorization for the Member to receive services from an Out-of-Network Provider; |
| |
| B. | Emergency Care that could not be provided by the Contractor’s Network Provider because the time to reach the Contractor’s Network Provider would have resulted in risk of serious damage to the Member’s health; |
| |
| C. | Services provided for family planning; and |
| |
| D. | Services for children in Foster Care. |
Covered Services shall be reimbursed at no less than 100 percent of the Medicaid fee schedule/rate until January 1, 2012 and after January 1, 2012, no less than 90% of the Medicaid fee schedule/rate. Covered services except for emergency services provided to a Member from an Out-of-Network Provider that has not sought Prior Authorization within thirty (30) days need not be reimbursed.
For services not covered above, the Contractor shall submit to the Department for review and approval a process for Out-of-Network reimbursement.
| |
| 29.3 | Payment to Providers for Serving Dual Eligible Members |
The Contractor shall coordinate benefits for Dual Eligible Members by paying the lesser amount of:
| |
| A. | The Contractor’s allowed amount minus the Medicare payment, or |
| |
| B. | The Medicare co-insurance and deductible up to Contractor’s allowed amount. |
The Contractor shall further assist Dual Eligible Members in coordination of benefits required under Delegations of Authority.
| |
| 29.4 | Payment of Federally Qualified Health Centers (“FQHC”) and Rural Health Clinics (“RHC”) |
The Contractor shall assure that payment for services provided to FQHCs and RHCs is not less than the level and amount of payment the Contractor would make for the services if the services were furnished by other clinic or primary care Providers. The Department shall reimburse, by making payments directly to FQHCs and RHCs, the difference if the rate is less than the amount paid under Kentucky’s established prospective payment system (PPS) rate for the federally certified facilities.
The Contractor shall report to the Department within forty-five (45) calendar days of the end of each quarter the total amount paid to each FQHC per month.
| |
| 29.5 | Commission for Children with Special Needs |
The case management and care coordination needs of the medically fragile children serviced by the Commission for Children with Special Needs must be recognized by the Contractor in that a special payment rate shall be developed for the Commission by a process of negotiation between the Contractor and the Commission. The rate to be established shall be not less than seventy-eight (78) percent of the Medicaid allowable cost based on the most recent available cost report of the Commission and shall be subject to negotiation at annual intervals.
| |
| 29.6 | Payment of Teaching Hospitals |
In establishing payments for teaching hospitals in its Contractor’s Network, the Contractor shall recognize costs for graduate medical education, including adjustments required by KRS 205.565 and 907 KAR 1:825.
| |
| 29.7 | Intensity Operating Allowance |
The Department acknowledges and agrees that Contractor is subject to the legislatively mandated intensity operating allowance and hospital rate increase. Contractor shall receive capitation payments that reflect these mandated items. (See 907 KAR 10:825)
The contractor shall agree that payment for Urban Trauma Center amount is contingent upon the Commonwealth's receipt of the necessary state matching funds from the Contractor to support such payment and shall so do in a manner necessary to meet all federal requirements governing such transactions. (See 907 KAR 10:825)
| |
| 29.9 | Critical Access Hospitals |
The Contractor shall reimburse Critical Access Hospitals at rates that are at least equal to those established by CMS for Medicare reimbursement to a critical access hospital in accordance with 907 KAR 10:815.
| |
| 29.10 | Supplemental Payments |
The Department and Contractor recognize the Department’s desire to provide enhanced reimbursement to provider entities through supplemental payments in order to preserve the ability of the provider entities to provide essential services to Commonwealth residents.
The Department currently makes supplemental payments in addition to adjudicated claims payments to a number of provider entities. Those categories of providers receiving supplemental payments are as follows:
| |
| • | Intensity Operating Allowance for Pediatric Teaching hospitals |
| |
| • | A State Designated Urban Trauma Center |
| |
| • | State Owned or Operated University Teaching Hospital Faculty |
| |
| • | Psychiatric Access Supplement to a Designated Psychiatric Hospital |
Descriptions of these payments are found in other sections of the contract. State owned or operated university teaching hospitals include a hospital operated by a related party organization as defined in 42 CFR 413.17, which is operated as part of an approved School of Medicine or Dentistry.
Amounts were included in the data book, as used by the Contractor in establishing base period rates reflecting these payment amounts, which have been trended by the Contractor using their trends and trend assumptions for capitation payments covered under the contract.
Contractor is required to make monthly supplemental payments to the specified providers on or before the last business day of the month of service for which capitation is paid. The payment shall be an amount equal to the amount included in the data book for each respective provider entity increased by the increase in the contractor’s weighted average rate for each year of the contract based on capitation rates displayed in Appendix B, multiplied by the Contractor’s share of monthly enrollment as calculated by the Department. The Department shall provide the detailed amounts by provider entity included in the data book upon contractor request
The Contractor agrees, upon the request of the Department, to submit to the Department claims-level cost data for payment verification purposes.
Contractor will work with the Department to assure that information is provided to allow for provider entities to remit the state matching portion of the payments to the Department, as applicable.
| |
| 30.1 | Medicaid Covered Services |
The Contractor shall provide, or arrange for the provision of, the Covered Services listed in Appendix I to Members in accordance with the Contract standards, and according to the Department’s regulations, state plan, policies and procedures applicable to each category of Covered Services. The Contractor shall be required to provide Covered Services to the extent services are covered for Members at the time of Enrollment. The Contractor shall ensure that the care of new enrollees is not disrupted or interrupted. The Contractor shall ensure continuity of care for new Members receiving health care under fee for service prior to enrollment in the Plan. Appendix I shall serve as a summary of currently Covered Services that the Contractor shall be responsible for providing to Members. However, it is not intended, nor shall it serve as a substitute for the more detailed information relating to Covered Services which is contained in applicable administrative regulations governing Kentucky Medicaid services provision (907 KAR Chapter 1 and 907 KAR 3:005) and individual Medicaid program services manuals incorporated by reference in the administrative regulations.
After the Execution Date, to the extent a new or expanded Covered Service is added by the Department to Contractor’s responsibilities under this Contract, (“New Covered Service”) the financial impact of such New Covered Service will be evaluated from an actuarial perspective by the Department, and Capitation Rates to be paid to Contractor hereunder will be adjusted accordingly to 12.2 and 39.17 herein. The determination that a Covered Service is a New Covered Service is at the discretion of the Department. At least ninety (90) days before the effective date of the addition of a New Covered Service, the Department will provide written notice to Contractor of any such New Covered Service and any adjustment to the Capitation Rates herein as a result of such New Covered Service. This notice shall include: (i) an explanation of the New Covered Service; (ii) the amount of any adjustment to Capitation Rates herein as a result of such New Covered Service; and (iii) the methodology for any such adjustment.
The Contractor may provide, or arrange to provide, services in addition to the services described in Appendix I, provided quality and access are not diminished, the services are Medically Necessary health services and cost-effective. The cost for these additional services shall not be included in the Capitation Rate. The Contractor shall notify and obtain approval from Department for any new services prior to implementation. The Contractor shall notify the Department by submitting a proposed plan for additional services and specify the level of services in the proposal.
If coverage of any Medicaid service provided by the Contractor requires the completion of a specific form (e.g., hospice, sterilization, hysterectomy, or abortion), the form shall be properly completed according to the appropriate Kentucky Administrative Regulation (KAR). The Contractor shall require its
Subcontractor or Provider to retain the form in the event of audit and a copy shall be submitted to the Department upon request.
The Contractor shall not prohibit or restrict a Provider from advising a Member about his or her health status, medical care, or treatment, regardless of whether benefits for such care are provided under the Contract, if the Provider is acting within the lawful scope of practice.
If the Contractor is unable to provide within its network necessary medical services covered under Appendix I, it shall timely and adequately cover these services out of network for the Member for as long as Contractor is unable to provide the services in accordance with 42 CFR 438.206. The Contractor shall coordinate with out-of-network providers with respect to payment. The Contractor will ensure that cost to the Member is no greater than it would be if the services were provided within the Contractor’s Network.
A Member who has received Prior Authorization from the Contractor for referral to a specialist physician or for inpatient care shall be allowed to choose from among all the available specialists and hospitals within the Contractor’s Network, to the extent reasonable and appropriate.
| |
| 30.2 | Direct Access Services |
The Contractor shall make Covered Services available and accessible to Members as specified in Appendix I -. The Contractor shall routinely evaluate Out-of-Network utilization and shall contact high volume providers to determine if they are qualified and interested in enrolling in the Contractor’s network. If so, the Contractor shall enroll the provider as soon as the necessary procedures have been completed. When a Member wishes to receive a direct access service or receives a direct access service from an Out-of-Network Provider, the Contractor shall contact the provider to determine if it is qualified and interested in enrolling in the network. If so, the Contractor shall enroll the provider as soon as the necessary enrollment procedures have been completed.
The Contractor shall ensure direct access and may not restrict the choice of a qualified provider by a Member for the following services within the Contractor’s Network:
| |
| A. | Primary care vision services, including the fitting of eye-glasses, provided by ophthalmologists, optometrists and opticians; |
| |
| B. | Primary care dental and oral surgery services and evaluations by orthodontists and prosthodontists; |
| |
| C. | Voluntary family planning in accordance with federal and state laws and judicial opinion; |
D. Maternity care for Members under eighteen (18) years of age;
E. Immunizations to Members under twenty-one (21) years of age;
F. Sexually transmitted disease screening, evaluation and treatment;
G. Tuberculosis screening, evaluation and treatment;
| |
| H. | Testing for Human Immunodeficiency Virus (HIV), HIV-related conditions, and other communicable diseases as defined by 902 KAR 2:020; |
I. Chiropractic services; and
J. Women’s health specialists.
The Contractor shall ensure direct access and may not restrict the Member’s access to services in accordance with 42 CFR 438 and applicable state statutes and regulations.
The Contractor shall provide for a second opinion related to surgical procedures and diagnosis and treatment of complex and/or chronic conditions within the Contractor’s network, at the Member’s request. The Contractor shall inform the Member, in writing, at the time of Enrollment of the Member’s right to request a second opinion.
| |
| 30.4 | Billing Members for Covered Services |
The Contractor and its Providers and Subcontractors shall not bill a Member for Medically Necessary Covered Services with the exception of applicable co-pays or other cost sharing requirements provided under this contract. Any Provider who knowingly and willfully bills a Member for a Medicaid Covered Service shall be guilty of a felony and upon conviction shall be fined, imprisoned, or both, as defined in Section 1128B(d)(1) 42 U.S.C. 1320a-7b of the Social Security Act. This provision shall remain in effect even if the Contractor becomes insolvent.
However, if a Member agrees in advance in writing to pay for a Non-Medicaid covered service, then the Contractor, the Contractor’s Provider, or Contractor’s Subcontractor may bill the Member. The standard release form signed by the Member at the time of services does not relieve the Contractor, Providers and Subcontractors from the prohibition against billing a Medicaid Member in the absence of a knowing assumption of liability for a Non-Medicaid covered Service. The form or other type of acknowledgement relevant to Medicaid Member liability must specifically state the services or procedures that are not covered by Medicaid.
| |
| 30.5 | Referrals for Services not Covered by Contractor |
When it is necessary for a Member to receive a Medicaid service that is outside the scope of the Contract, the Contractor shall refer the Member to a provider
enrolled in the Medicaid fee-for-service program. The Contractor shall have written policies and procedures for the referral of Members for Non-Covered Services that shall provide for the transition to a qualified health care provider and, where necessary, assistance to Members in obtaining a new Primary Care Provider. The Contractor shall submit any desired changes to the established written referral policies and procedures to the Department for review and approval.
| |
| 30.6 | Interface with State Mental Health Agency |
| |
| A. | Contractor’s Behavioral Health Director or designee will meet with the Department monthly to discuss State Mental Health Authority and Single State (substance abuse) Agency (SSA) protocols, rules and regulations including but not limited to: |
| |
| • | SMI and SED operating definitions |
| |
| • | Other priority populations |
| |
| • | Targeted Case Management and Peer Support provider certification training and process |
| |
| • | IMPACT Plus program operations |
| |
| • | Satisfaction survey requirements |
| |
| • | Priority training topics (e.g. trauma-informed care, suicide prevention, co-occurring disorders, evidence-based practices) |
| |
| • | Behavioral health services hotline |
| |
| • | Behavioral health crisis services (referrals; emergency, urgent and routine care) |
| |
| B. | Contractor will coordinate IMPACT Plus Covered Services to ensure existing services are provided, rates are set, and encounter and cost data are provided. |
| |
| C. | Contractor will coordinate: |
| |
| 1. | Member education process for individuals with serious mental illnesses (SMI) and children and youth with serious emotional disturbances (SED) with the department. Contractor will provide the Department with proposed materials and protocols. |
| |
| 2. | With the Department and CMHCs a process for integrating Behavioral Health Services’ hotlines with processes planned by the Contractor to meet system requirements. |
| |
| 3. | With the Department on establishing collaborative agreements with state operated or stated contracted psychiatric hospitals, as well as with other the Department facilities that individuals with co-occurring behavioral health and developmental and intellectual disabilities (DID). |
| |
| 31.1 | Pharmacy Requirements |
The Contractor shall provide pharmacy benefits in accordance with this section in addition to other requirements specified in this contract. Pharmacy benefit requirements shall include, but not be limited to:
| |
| A. | State-of-the-art, online and real-time rules-based point-of-sale (POS) Claims processing services with prospective drug utilization review including an accounts receivable process; |
| |
| B. | Retrospective utilization review services; |
| |
| C. | Formulary and non-formulary services, including prior authorization services; |
| |
| D. | Pharmacy provider relations and call center services, in addition to Provider Services specified elsewhere; and |
| |
| E. | Seamless interfaces with the information systems of the Commonwealth and as needed, any related vendors. |
| |
| 31.2 | Formulary and Non-Formulary Services |
The Contractor shall maintain a preferred drug list and make information available to pharmacy providers and Members the co-pay tiers or other information as necessary. The Contractor shall utilize a Pharmacy and Therapeutics Committee (P&T Committee). The committee shall meet periodically throughout the calendar year as necessary and make recommendations to the Contractor for changes to the drug formulary. The Contractor shall provide information to its pharmacy providers regarding the Preferred Drug List (PDL) for Medicaid Members. This list updated by the Contract throughout the year shall reflect changes in the status of a drug or to the addition of new drugs, as required.
| |
| 31.3 | Pharmacy Claims Administration |
The Contractor shall process, adjudicate, and pay pharmacy Claims for Members via an online real-time POS system, including voids and full or partial adjustments. The Contractor shall maintain prospective drug utilization review edits and apply these edits at the POS. The Contractor shall be responsible for processing components required for paper Claims.
The Contractor maintains, through an online system, appropriate accounts receivable (A/R) records for the Commonwealth to systematically track adjustments, recoupments, manual payments and other required identifying A/R and Claim information.
The Contractor shall interface with the Commonwealth’s information systems to provide data and other information, as needed, to properly administer the pharmacy benefit program.
| |
| 31.4 | Pharmacy Rebate Administration |
The Patient and Affordable Care Act (PPACA) signed into law in March 2010 require states to collect CMS level rebates on all Medicaid MCO utilization. In order for the Department to comply with this requirement the Contractor shall be required to submit NDC level information including J-code conversions consistent with CMS requirements. The Department will provide this Claims level detail to manufacturers to assist in dispute resolutions. However, since the Department is not the POS Claims processor, resolutions of unit disputes are dependent upon cooperation of the Contractor. The Contractor shall assist the Department in resolving drug rebate disputes with the manufacture. The Contractor also shall be responsible for rebate administration for pharmacy services provided through other settings such as physician services.
| |
| 31.5 | Pharmacy Program Management |
The Contractor shall assure that pharmacy benefits are administered in accordance with the state and Federal laws and regulations. In the event the prescription is for a non-preferred drug and the pharmacist cannot reach the physician or the Contractor or its agent for approval and the pharmacist deems it necessary, a seventy-two (72) hour emergency supply shall be provided. If the physician prescribed an amount of the medicine that is less than a seventy-two (72) hour supply, the pharmacist shall only dispense the amount prescribed.
Kentucky Medicaid members may be limited to three (3) brand prescriptions and four (4) total prescriptions, based upon their diagnoses and/or medical condition.
For example co-payments are typically one dollar ($1.00), two dollars ($2.00), three dollars ($3.00), or five percent (5%) up to a maximum of twenty dollars ($20.00) per prescription, based upon member’s age, status, or category of eligibility. The Contractor shall track and reports on the Members’ usage and co-payments, including accumulation of maximum out-of-pocket co-payments. The co-payments requirements for the Kentucky Medicaid Program can be found in 907 KAR 1:604.
| |
| 31.6 | Pharmacy Provider Relations and Prior Authorizations |
The Contractor shall operate a toll-free call center twenty-four (24) hours a day, seven (7) days a week for access by pharmacies and physicians/prescribers. The call center shall respond to pharmacy related questions that require clinical intervention and requests for prior authorizations. The call center shall process prior authorization requests received from prescribers by facsimile, telephone or postal service.
| |
| 32. | Special Program Requirements |
| |
| 32.1 | EPSDT Early and Periodic Screening, Diagnosis and Treatment |
The Contractor shall provide all Members under the age of twenty-one (21) years EPSDT services in compliance with the terms of this Contract and policy statements issued during the term of this Contract by the Department or CMS. The Contractor shall file EPSDT reports in the format and within the time-frames required by the terms of this Contract as indicated in Appendix J. The Contractor shall comply with 907 KAR 1:034 that delineates the requirements of all EPSDT providers participating in the Medicaid program. Health care professionals who meet the standards established in the above-referenced regulation shall provide EPSDT services. Additionally, the Contractor shall:
| |
| A. | Provide, through direct employment with the Contractor or by Subcontract, accessible and fully trained EPSDT Providers who meet the requirements set forth under 907 KAR 1:034, and who are supported by adequately equipped offices to perform EPSDT services. |
| |
| B. | Effectively communicate information (e.g. written notices, verbal explanations, face to face counseling or home visits when appropriate or necessary) with members and their families who are eligible for EPSDT services [(i.e. Medicaid eligible persons who are under the age of twenty-one (21)] regarding the value of preventive health care, benefits provided as part of EPSDT services, how to access these services, and the member’s right to access these services. Members and their families shall be informed about EPSDT and the right to Appeal any decision relating to Medicaid services, including EPSDT services, upon initial enrollment and annually thereafter where Members have not accessed services during the year. |
| |
| C. | Provide EPSDT services to all eligible Members in accordance with EPSDT guidelines issued by the Commonwealth and federal government and in conformance with the Department’s approved periodicity schedule, a sample of which is included in Appendix J. |
| |
| D. | Provide all needed initial, periodic and inter-periodic health assessments in accordance with 907 KAR 1:034. The Primary Care Provider assigned to each eligible member shall be responsible for providing or arranging for complete assessments at the intervals specified by the Department’s approved periodicity schedule and at other times when Medically Necessary. |
| |
| E. | Provide all needed diagnosis and treatment for eligible Members in accordance with 907 KAR 1:034. The Primary Care Provider and other Providers in the Contractor’s Network shall provide diagnosis and treatment and or Out-of-network Providers shall provide treatment if the service is not available within the Contractor’s network. |
| |
| F. | Provide EPSDT Special Services for eligible members, including identifying providers who can deliver the Medically Necessary services described in federal Medicaid law and developing procedures for authorization and payment for these services. Current requirements for EPSDT Special Services are included in Appendix J. |
| |
| G. | Establish and maintain a tracking system to monitor acceptance and refusal of EPSDT services, whether eligible Members are receiving the recommended health assessments and all necessary diagnosis and treatment, including EPSDT Special Services when needed. |
| |
| H. | Establish and maintain an effective and on-going Member Services case management function for eligible members and their families to provide education and counseling with regard to Member compliance with prescribed treatment programs and compliance with EPSDT appointments. This function shall assist eligible members or their families in obtaining sufficient information so they can make medically informed decisions about their health care, provide support services including transportation and scheduling assistance to EPSDT services, and follow up with eligible members and their families when recommended assessments and treatment are not received. |
| |
| I. | Maintain a consolidated record for each eligible member, including reports of informing about EPSDT, information received from other providers and dates of contact regarding appointments and rescheduling when necessary for EPSDT screening, recommended diagnostic or treatment services and follow-up with referral compliance and reports from referral physicians or providers. |
| |
| J. | Establish and maintain a protocol for coordination of physical health services and Behavioral Health Services for eligible members with behavioral health or developmentally disabling conditions. Coordination procedures shall be established for other services needed by eligible members that are outside the usual scope of Contractor services. Examples include early intervention services for infants and toddlers with disabilities, services for students with disabilities included in the child’s individual education plan at school, WIC, Head Start, DCBS, etc. |
| |
| K. | Participate in any state or federally required chart audit or quality assurance study; |
| |
| L. | Maintain an effective education/information program for health professionals on EPSDT compliance (including changes in state or federal requirements or guidelines). At a minimum, training shall be provided concerning the components of an EPSDT assessment, EPSDT Special Services, and emerging health status issues among members which should be addressed as part of EPSDT services to all appropriate staff and Providers, including medical residents and specialists delivering EPSDT services. In addition, training shall be provided concerning physical assessment procedures for nurse practitioners, registered nurses and physician assistants who provide EPSDT screening services. |
| |
| M. | Submit Encounter Record for each EPSDT service provided according to requirements provided by the Department, including use of specified EPSDT procedure codes and referral codes. Submit quarterly and annual reports on EPSDT services including the current Form CMS-416. |
| |
| N. | Provide an EPSDT Coordinator staff function with adequate staff or subcontract personnel to serve the Contractor’s enrollment or projected enrollment. |
The Contractor shall provide preventive and primary care dental services for oral health conditions and illness in a timely manner on an emergent, urgent care or non-urgent care basis in accordance with 42 CFR 438. Covered dental services shall be provided in accordance with 907 KAR 1:026.
The Contractor shall enroll providers of dental services in accordance with KRS 304.17A-270, and establish written policies and procedures to ensure the timely provision of services in an amount, duration, and scope that is no less than the amount, duration, and scope for the same services provided to fee-for-service Medicaid Members. The Contractor shall assess the oral health of Members and develop a plan for improving oral health in Members, particularly in children and persons with special health care needs.
The Contractor shall have ultimate responsibility for the provision of dental services and shall oversee and coordinate the delivery of or access to all member health information and other date relating to dental services, as requested by the Department.
| |
| 32.3 | Emergency Care, Urgent Care and Post Stabilization Care |
Emergency Care shall be available to Members twenty-four (24) hours a day, seven (7) days a week. Urgent Care services shall be made available within forty-eight (48) hours of request. Post Stabilization Care services are covered and reimbursed in accordance with 42 CFR 422.113(c) and 438.114(c).
| |
| 32.4 | Out-of-Network Emergency Care |
The Contractor shall provide, or arrange for the provision of Emergency Care, even though the services may be received outside the Contractor’s network, in accordance with 42 CFR 431.52 and 907 KAR 1:084. These regulations require that the Commonwealth, including Department and its Contractor, cover not only Medically Necessary services due to a medical emergency, but also out-of-state emergency medical services if medical services are needed and the Member’s health would be endangered if he/she were required to travel to his/her state of residence;
Payment for Emergency Services covered by a non-contracting provider shall not exceed the Medicaid fee-for service rate as required by Section 6085 of the Deficit Reduction Act of 2005. For services provided by non-contracting hospitals, this amount must be less any payments for indirect costs of medical education and direct costs of graduate medical education that would have been included in fee-for-service payments.
When a woman has entered prenatal care before enrolling with the Contractor shall take every effort to allow her to continue with the same prenatal care provider throughout the entire pregnancy. Contractor shall also establish procedures to assure either prompt initiation of prenatal care or continuation of care without interruption for women who are pregnant when they enroll. The Contractor shall provide maternity care that includes prenatal, delivery, and postpartum care as well as care for conditions that complicate pregnancies. All newborn Members shall be screened for those disorders specified in the Commonwealth of Kentucky metabolic screen.
| |
| 32.6 | Voluntary Family Planning |
The Contractor shall ensure direct access for any Member to a Provider, qualified by experience and training, to provide Family Planning Services, as such services are described in Appendix I to this Contract. The Contractor may not restrict a Member’s choice of his or her provider for Family Planning Services. Contractor must assure access to any qualified provider of Family Planning Services without requiring a referral from the PCP.
The Contractor shall maintain confidentiality for Family Planning Services in accordance with applicable federal and state laws and judicial opinions for Members less than eighteen (18) years of age pursuant to Title X. 42 CFR 59.11, and KRS 214.185. Situations under which confidentiality may not be guaranteed are described in KRS 620.030, KRS 209.010 et seq., KRS 202A, and KRS 214.185.
| |
| 32.7 | Nonemergency Medical Transportation |
The Department contracts with the Office of Transportation and Delivery to provide non-emergency medical transportation (NEMT) services to select Medicaid Members. Through the NEMT program, members receive safe and reliable transportation to Medicaid covered services. The Department shall continue to provide NEMT services for Medicaid Members. The Contractor shall provide educational materials regarding the availability of transportation services and refers Members for NEMT. NEMT means medical transportation not of an emergency nature, excluding ambulance stretcher services, provided to a Medicaid Member by the Transportation Cabinet pursuant to an agreement between the Transportation Cabinet and the Department.
The Contractor shall establish procedures to coordinate care for children receiving school-based health services and early intervention services, in a manner that prevents duplication of Contractor provided services. The Contractor shall monitor the continuity and coordination of care for these children as part of its QAPI program.
Services provided under these programs are authorized under the Federal Individuals with Disabilities Education Act, but typically excluded from Contractor coverage except in situations where a child’s course of treatment is interrupted due to school breaks, after school hours or during summer months, the Contractor is responsible for providing all Medically Necessary Covered Services. IEP services should not be duplicated.
School-Based Services provided by schools are excluded from Contractor coverage and are paid by the Department through fee-for-service Medicaid when provided by a Medicaid enrolled provider. School-Based Services provided by public health departments are included in Contractor coverage. However, in situations where a child’s course of treatment is interrupted due to school breaks, after school hours or during summer months, the Contractor is responsible for providing all Medically Necessary Covered Services. Coordination between the schools and the Contractor shall ensure that Members receive medically necessary services that complement the individual education plan (IEP) services and promote the highest level of function for the child.
The Contractor shall coordinate services between the First Steps program and Contractor coverage. The First Steps program is an entitlement program established by the Federal Individuals with Disabilities Education Act (IDEA) and is funded by federal, state and local funds. The goal of the program is to provide early intervention services to children from birth up to age three who have developmental disabilities or delays. The intended outcome of the program is to ensure maximum amelioration of the impact of developmental disabilities or delays on infants and toddlers by early and ongoing provision of rehabilitation services.
In order for the Contractor and its Providers to effectively manage care for Members who qualify for these services, it will be necessary to coordinate the care provided through both programs as children who are receiving these services are identified, to share information with early intervention/school-based service providers with appropriate permission from parents.
Services provided under HANDS shall be excluded from Contractor coverage. HANDS is a home visitation program for first-time parents. It services children under three (3) years of age and it promotes good parenting skills.
| |
| 32.9 | Pediatric Sexual Abuse Examination |
Contractor shall have Providers in its network that have the capacity to perform a forensic pediatric sexual abuse examination. This examination must be conducted for Members at the request of the DCBS.
The Contractor shall develop a program to address and contain Member over utilization of services, for pharmacy and non-emergent care provided in an
emergency setting. The program shall be in accordance with 907 KAR 1:677. The criteria for this program shall be submitted to the Department for approval.
| |
| 33. | Behavioral Health Services |
| |
| 33.1 | Department for Behavioral Health, Developmental and Intellectual Disabilities (DBHDID) Responsibilities |
The Department for Behavioral Health, Developmental and Intellectual Disabilities (DBHDID) is part of the Cabinet for Health and Family Services. It is responsible for planning and overseeing mental health, intellectual disability, and developmental disability services using state and federal funds. DBHDID contracts with outpatient mental health services through fourteen (14) regional mental health centers and four psychiatric hospitals (three of which are state operated and one private) to assure that community and inpatient mental health services are available to Kentucky citizens. DBHDID works collaboratively with Department, to assure that Medicaid Members receive quality services.
Kentucky’s mental health system strengths include the following:
| |
| A. | In the area, of criminal justice, police Crisis Intervention Teams (CIT) are expanding throughout the Commonwealth. A statewide telephonic triage system continues to screen jail inmates and provide linkages to treatment. In addition, DBHDID also received a grant to develop a strategic plan for pre-and post-booking programs. DBHDID also provides a peer support specialist training program and a Peer Leadership Academy. |
| |
| B. | Additionally, community mental health centers receive department funds for a new statewide program call Direct Intervention, Vital Early Response Treatment systems (DIVERTS) to specifically help reduce the number of persons becoming homeless or going to jail. Each of the fourteen (14) regions work with DBHDID to tailor the DIVERTS program to its particular needs. |
| |
| C. | A new psychiatric facility to replace Eastern State Hospital in Lexington has begun construction in Lexington. The new hospital will replace the second oldest state hospital in the nation (opened in 1824). Kentucky’s state hospitals have reduced the use of seclusion and restraints. |
Additional work needs to be done in assuring that evidence-based practices (EBPs) are routinely used in all behavior health services and that they meet the standards of national models. Primary focus shall be on further development and expansion of supported housing, supported employment, development of peer support and recovery models of care. Additionally, there are shortages of mental health professionals, especially psychiatrists, in rural areas.
| |
| 33.2 | DBHDID Goals for Behavioral Health Services |
The Department, working with the behavioral health state agency, DBHDID, desires that Kentucky become a national leader in the wellness and recovery approach to behavioral health services, including psychosocial rehabilitation. Through health promotion efforts, psychotropic medication management, suicide prevention and overall person centered treatment approaches, the Commonwealth seeks to lower morbidity among Members with serious mental illnesses, including Members with co-occurring developmental disabilities. Through the Contractor, Members will have the ability to access other valuable health programs such as smoking cessation programs.
The Contractor in its design and operation shall incorporate Department and DBHDID’s core values for Medicaid Members receiving behavioral health services which are:
| |
| A. | Maintaining basic personal rights. Individuals with mental illness have the same rights and obligations as other citizens of the Commonwealth. Consumers have the right to choice, to retain the fullest possible control over their own lives and to have opportunities to be involved in their communities. |
| |
| B. | Being responsive to the consumer and community. The Contractor’s provision of mental health services shall be responsive to the people it serves, coherently organized, and accessible to those who require mental health care. |
| |
| C. | Empowering the consumer and community. The Contractor’s provision of mental health services shall involve consumers and families in decision-making processes, both individually at the treatment level as well as collectively. Services and programs are responsive to consumer needs and choices and are culturally relevant. |
| |
| D. | Providing family support and education. The Contractor shall provide families with the assistance they need in order to maintain or enhance the support they give to their family members and to keep families united whenever possible. |
| |
| E. | Providing care in the most appropriate setting. The Contractor shall provide the most normative care in the least restrictive setting and permit Members to be served in the community when appropriate. |
| |
| F. | Working collaboratively with all stakeholders. The Contractor shall foster collaboration and integration with relevant stakeholders to assist Members in all activities of life. |
| |
| G. | Having well-managed services. The Contractor shall promote cost effective services and hold all components accountable by requiring monitoring and self-evaluation, responding rapidly to identify weaknesses, adapting to changing needs, and improving technology. The Contractor shall place a high priority on measuring Members’ satisfaction with the services they receive. Outcome measures are a key component for evaluating program effectiveness. The Contractor shall require local planning to improve continuity of care, coordination and quality of services and resources. The Contractor shall require |
local planning and coordination of services to improve continuity of care and concurrence of services and resources.
| |
| H. | Having resources to provide adequate and qualified staff. The Contractor shall promote provider competence and opportunities for skill-enhancement training or retraining as changes in the service system take place. |
| |
| I. | Educating the community. The Contractor shall promote early identification and prevention for at-risk groups of all ages through public education and early intervention programs, and it promotes efforts that support families and communities. |
| |
| 33.3 | General Behavioral Health Requirements |
The Department requires the Contractor’s provision of mental health services to be recovery and resiliency focused. This means that services will be provided to allow individuals, or in the case of, a minor, family or guardian, to have the greatest opportunities for decision making and participation in the individual’s treatment and rehabilitation plans.
| |
| 33.4 | Covered Behavioral Health Services |
The Contractor shall assure the provision of all Medically Necessary Behavioral Health Services for Members. These services are described in Appendix I. All Behavioral Health services shall be provided in conformance with the access standards established by the Department. When assessing Members for BH Services, the Contractor and its providers shall use the DSM-IV multi-axial classification. The Contractor may require use of other diagnostic and assessment instrument/outcome measures in addition to the DSM-IV. Providers shall document DSM-IV diagnosis and assessment/outcome information in the Member’s medical record.
| |
| 33.5 | Behavioral Health Provider Network |
The Contractor must emphasize utilization management, assuring the services authorized are provided, are medically necessary and produce positive health outcomes. The Department and DBHDID will coordinate on the requirement of data collection and reporting to assure that state and federal funds utilized in financing behavioral health services are efficiently utilized and meet the overall goals of health outcomes.
The Contractor shall utilize DSM-IV classification for Behavioral Health billings.
The Contractor shall provide access to psychiatrists, psychologists, and other behavioral health service providers. In order to meet the provider network requirement for BH services, Community Mental Health Centers (CMHCs) located within the Contractor service region shall be offered participation in the Contractor provider network. Network providers shall have experience serving children and adolescents, persons with disabilities, the elderly, and
cultural or linguistic minorities. The Contractor shall ensure accessibility and availability of qualified providers to all Members in the service area pursuant to Provider Program Capacity Demonstration as contained in the RFP.0 When necessary to meet the access standards for Behavioral Health Services for its Members, the Contractor may include in its provider network other specialty care clinic providers with comparable core services of the CMHC’s. To the extent that non-psychiatrists and other providers of Behavioral health services may also be provided as a component of FQHC and RHC services, these facilities shall be offered the opportunity to participate in the Behavioral Health network. FQHC and RHC providers can continue to provide the same services they currently provide under their licenses.
Since the Contractors shall offer participation agreements to the Community Mental Health Centers to participate in their Behavioral Health network, should a Community Mental Health Center decline participation in the Contractor in that service area, or if the Contractor fails to meet access or any other terms and conditions of the contract the Contractor may meet its BH network requirements by offering participation to other qualified specialty care clinic providers with comparable core CMHC services.
The Contractor shall maintain a Member education process to help Members know where and how to obtain Behavioral Health Services.
The Contractor shall permit Members to participate in the selection of the appropriate behavioral health individual practitioner(s) who will serve them and shall provide the Member with information on accessible in-network Providers with relevant experience.
| |
| 33.6 | Behavioral Health Services Hotline |
The Contractor shall have an emergency and crisis Behavioral Health Services Hotline staffed by trained personnel twenty-four (24) hours a day, seven (7) days a week, three hundred sixty-five (365) days a year, toll-free throughout the Contractor’s region. Crisis hotline staff must include or have access to qualified Behavioral Health Services professionals to assess, triage and address specific behavioral health emergencies. Emergency and crisis Behavioral Health Services may be arranged through mobile crisis teams. Face to face emergency services shall be available twenty-four (24) hours a day, seven (7) days a week. It is not acceptable for an intake line to be answered by an answering machine.
The Contractor shall ensure that the toll-free Behavioral Health Services Hotline meets the following minimum performance requirements for all Contractor Programs and Service Areas:
| |
| A. | Ninety-nine percent (99%) of call are answered by the fourth ring or an automated call pick-up system; |
| |
| B. | No incoming calls receive a busy signal; |
| |
| C. | At least eighty percent (80%) of calls must be answered by toll-free line staff within thirty (30) seconds measured from the time the call is placed in queue after selecting an option; |
| |
| D. | The call abandonment rate is seven percent (7%) or less; |
| |
| E. | The average hold time is two (2) minutes or less; and |
| |
| F. | The system can immediately connect to the local Suicide Hotline’s telephone number and other Crisis Response Systems and have patch capabilities to 911 emergency services. |
The Contractor may operate one hotline to handle emergency and crisis calls and routine Member calls. The Contractor cannot impose maximum call duration limits and shall allow calls to be of sufficient length to ensure adequate information is provided to the Member. Hotline services shall meet Cultural Competency requirements and provide linguistic access to all Members, including the interpretive services required for effective communication.
The Behavioral Health Services Hotline may serve multiple Contractor Programs if the Hotline staff is knowledgeable about all of the Contractor Programs. The Behavioral Health Services Hotline may serve multiple Service Areas if the Hotline staff is knowledgeable about all such Service Areas, including the Behavioral Health Provider Network in each Service Area.
The Contractor shall conduct on-going quality assurance to ensure these standards are met.
The Contractor shall monitor its performance against the Behavioral Health Services Hotline standards and submit performance reports summarizing call center performance as indicated.
If Department determines that it is necessary to conduct onsite monitoring of the Contractor's Behavioral Health Services Hotline functions, the Contractors responsible for all reasonable costs incurred by Department or its authorized agent(s) relating to such monitoring.
| |
| 33.7 | Coordination between the Behavioral Health Provider and the PCP |
The Contractor shall require, through contract provisions, that PCPs have screening and evaluation procedures for the detection and treatment of, or referral for, any known or suspected behavioral health problems and disorders. PCPs may provide any clinically appropriate Behavioral Health Services within the scope of their practice.
The Contractor shall provide training to network PCPs on how to screen for and identify behavioral health disorders, the Contractor's referral process for Behavioral Health Services and clinical coordination requirements for such services. The Contractor shall include training on coordination and quality of care such as behavioral health screening techniques for PCPs and new models of behavioral health interventions.
The Contractor shall develop policies and procedures and provide to the Department for approval regarding clinical coordination between Behavioral Health Service Providers and PCPs. The Contractor shall require that Behavioral Health Service Providers refer Members with known or suspected and untreated physical health problems or disorders to their PCP for examination and treatment, with the Member's or the Member's legal guardian's consent. Behavioral Health Providers may only provide physical health care services if they are licensed to do so. This requirement shall be specified in all Provider Manuals.
The Contractor shall require that behavioral health Providers send initial and quarterly (or more frequently if clinically indicated) summary reports of a Members' behavioral health status to the PCP, with the Member's or the Member's legal guardian's consent. This requirement shall be specified in all Provider Manuals.
| |
| 33.8 | Follow-up after Hospitalization for Behavioral Health Services |
The Contractor shall require, through Provider contract provision, that all Members receiving inpatient psychiatric services are scheduled for outpatient follow-up and/or continuing treatment prior to discharge. The outpatient treatment must occur within fourteen (14) days from the date of discharge. The Contractor shall ensure that Behavioral Health Service Providers contact Members who have missed appointment within twenty-four (24) hours to reschedule appointments.
| |
| 33.9 | Court-Ordered Services |
“Court-Ordered Commitment” means an involuntary commitment of a Member to a psychiatric facility for treatment that is ordered by a court of law pursuant to Kentucky statutes.
The Contractor must provide inpatient psychiatric services to Members under the age of twenty-one (21) and over the age of sixty-five (65), up to the annual limit, who have been ordered to receive the services by a court of competent jurisdiction under the provisions of KRS 645, Kentucky Mental Health Act of The Unified Juvenile Code and KRS 202A, Kentucky Mental Health Hospitalization Act.
The Contractor cannot deny, reduce or controvert the Medical Necessity of inpatient psychiatric services provided pursuant to a Court ordered commitment for Members under the age of twenty-one (21) or over the age of sixty-five (65). Any modification or termination of services must be presented to the court with jurisdiction over the matter for determination.
| |
| 33.10 | Community Mental Health Center (CMHC) |
The Contractor shall coordinate with the Community Mental Health Center (CMHC) or other qualified special health care providers, other providers of
behavioral health services, and state operated or state contracted psychiatric hospitals and nursing facilities regarding admission and discharge planning, treatment objectives and projected length of stay for Members committed by a court of law to the state psychiatric hospital. The Contractor shall enter into a collaborative agreement with the state operated or state contracted psychiatric hospital assigned to their region in accordance with 908 KAR 3:040 and in accordance with federal Olmstead law. At a minimum the agreement shall include responsibilities of the Behavioral Health Service Provider to assure continuity of care for successful transition back into community-based supports. In addition, the Contractor Behavioral Health Service Providers shall participate in quarterly Continuity of Care meetings hosted by the state operated or state contracted psychiatric hospital.
The Contractor shall ensure the Behavioral Health Service Providers assign a case manager prior to or on the date of discharge and provide case management services to Members with severe mental illness and co-occurring developmental disabilities who are discharged from a state operated or state contracted psychiatric facility or state operated nursing facility for Members with severe mental illness. The Case Manager and other identified behavioral health service providers shall participate in discharge planning meetings to ensure compliance with federal Olmstead and other applicable laws. Appropriate discharge planning shall be focused on ensuring needed supports and services are available in the least restrictive environment to meet the Member’s behavioral and physical health needs, including psychosocial rehabilitation and health promotion. Appropriate follow up by the Behavioral Health Service provider shall occur to ensure the community supports are meeting the needs of the Member discharged from a state operated or state contracted psychiatric hospital.
The Contractor shall ensure the Behavioral Health Service Providers assist Members in accessing free or discounted medication through the Kentucky Prescription Assistance Program (KPAP) or other similar assistance programs.
| |
| 33.11 | Program and Standards |
Appropriate information sharing and careful monitoring of diagnosis, treatment, and follow-up and medication usage are especially important when Members use physical and behavioral health systems simultaneously. The Contractor shall:
| |
| A. | Establish guidelines and procedures to ensure accessibility, availability, referral and triage to effective physical and behavioral health care, including emergency behavioral health services, (i.e. Suicide Prevention and community crisis stabilization); |
| |
| B. | Facilitate the exchange of information among providers to reduce inappropriate or excessive use of psychopharmacological medications and adverse drug reactions; |
| |
| C. | Identify a method to evaluate the continuity and coordination of care, including member-approved communications between behavioral health care providers and primary care providers; |
| |
| D. | Protect the confidentiality of Member information and records; and |
| |
| E. | Monitor and evaluate the above, which shall be a part of the Quality Improvement Plan. |
The Department and DBHDID shall monitor referral patterns between physical and behavioral providers to evaluate coordination and continuity of care. Drug utilization patterns of psychopharmacological medications shall be closely monitored. The findings of these evaluations will be provided to the Contractor.
| |
| 34.1 | Health Risk Assessment (HRA) |
The Contractor shall have programs and processes in place to address the preventive and chronic healthcare needs of its population. The Contractor shall implement processes to assess, monitor, and evaluate services to all subpopulations, including but not limited to, the on-going special conditions that require a course of treatment or regular care monitoring, Medicaid eligibility category, type of disability or chronic conditions, race, ethnicity, gender and age.
The Contractor shall conduct initial health screening assessments of new Members who have not been enrolled in the prior twelve (12) month period for the purpose, of accessing the Members need for any special health care needs within ninety (90) days of Enrollment. Members whose Contractor has a reasonable belief to be pregnant shall be screened within thirty (30) days of Enrollment, and if pregnant, referred for appropriate prenatal care. The Contractor agrees to make all reasonable efforts to contact new Members in person, by telephone, or by mail to have Members complete the initial health screening questionnaire.
Information to be collected shall include demographic information, current health and behavioral health status to determine the Member’s need for care management, disease management, behavioral health services and/or any other health or community services.
The Contractor shall use appropriate health care professionals in the assessment process. Members shall be offered assistance in arranging an initial visit to their PCP for a baseline medical assessment and other preventive services, including an assessment or screening of the Members potential risk, if any, for specific diseases or conditions.
The Contractor shall submit a quarterly report on the number of new Member assessment; number of assessment completed; number of assessment not completed after reasonable effort; number of refusals.
The Contractor shall be responsible for the management and continuity of health care for all Members.
| |
| 34.2 | Care Management System |
As part of the Care Management System, the Contractor shall employ care coordinators and case managers to arrange, assure delivery of, monitor and evaluate basic and comprehensive care, treatment and services to a Member. Members needing Care Management Services shall be identified through the health risk assessment, evaluation of Claims data, Physician referral or other mechanisms that may be utilized by the Contractor. The Contractor shall develop guidelines for Care Coordination that will be submitted to the Department for review and approval. The Contractor shall have approval from the Department for any subsequent changes prior to implementation of such changes. Care coordination shall be linked to other Contractor systems, such as QI, Member Services and Grievances.
The care coordinators and case managers will work with the primary care providers as teams to provide appropriate services for Members. Care coordination is a process to assure that the physical and behavioral health needs of Members are identified and services are facilitated and coordinated with all service providers, individual Members and family, if appropriate, and authorized by the Member. The Contractor shall identify the primary elements for care coordination and submit the plan to the Department for approval.
The Contractor shall identify a Member with special health care needs, including but not limited to Members identified in Member Services. A Member with special health care needs shall have a Comprehensive Assessment completed upon admission to a Care Management program. The Member will be referred to Care Management. Guidelines for referral to the appropriate care management programs shall be pre-approved by the Department. The guidelines will also include the criteria for development of Care Plans. The Care Plan shall include both appropriate medical, behavioral and social services and be consistent with the Primary Care Provider’s clinical treatment plan and medical diagnosis.
The Contractor shall first complete a Care Coordination Assessment for these Members the elements of which shall comply with policies and procedures approved by the Department.
The Care Plan shall be developed in accordance with 42 CFR 438.208.
The Contractor shall develop and implement policies and procedures to ensure access to care coordination for all DCBS clients. The Contractor shall track, analyze, report, and when indicated, develop corrective action plans on indicators that measure utilization, access, complaints and grievances, and satisfaction with care and services specific to the DCBS population.
Members, Member representatives and providers shall be provided information relating to care management services, including case management, and information on how to request and obtain these services.
| |
| 34.4 | Coordination with Women, Infants and Children (WIC) |
The Contractor shall comply with Section 1902(a)(11)(C) of the Social Security Act which requires coordination between Medicaid MCOs and WIC. This coordination includes the referral of potentially eligible women, infants and children to the WIC program and the provision of medical information by providers working within Medicaid managed care plans to the WIC program if requested by WIC agencies and if permitted by applicable law. Typical types of medical information requested by WIC agencies include information on nutrition-related metabolic disease, diabetes, low birth weight, failure to thrive, prematurity, infants of alcoholics, mentally retarded or drug-addicted mothers, AIDS, allergy or intolerance that affects nutritional status and anemia.
| |
| 35. | Enrollees with Special Health Care Needs |
| |
| 35.1 | Individuals with Special Health Care Needs (ISHCN) |
Individuals with Special Health Care Needs (ISHCN) are persons who have or are at high risk for chronic physical, developmental, behavioral, neurological, or emotional condition and who may require a broad range of primary, specialized medical, behavioral health, and/or related services. ISCHN may have an increased need for healthcare or related services due to their respective conditions. The primary purpose of the definition is to identify these individuals so the Contractor can facilitate access to appropriate services.
As per the requirement of 42 CFR 438.208, the Department has defined the following categories of individuals who shall be identified as ISHCN. The Contractor shall have written policies and procedures in place which govern how Members with these multiple and complex physical and behavioral health care needs are further identified. The Contractor shall have an internal operational process, in accordance with policy and procedure, to target Members for the purpose of screening and identifying ISHCN's. The Contractor shall assess each member identified as ISHCN in order to identify any ongoing special conditions that require a course of treatment or regular care monitoring. The assessment process shall use appropriate health professionals. The Contractor shall employ reasonable efforts to identify ISHCN's based on the following populations:
| |
| A. | Children in/or receiving Foster Care or adoption assistance ; |
| |
| B. | Blind/Disabled Children under age 19 and Related Populations eligible for SSI; |
| |
| C. | Adults over the age of 65; |
| |
| D. | Homeless (upon identification); |
| |
| E. | Individuals with chronic physical health illnesses; and |
| |
| F. | Individuals with chronic behavioral health illnesses. |
The Contractor shall develop and distribute to ISHCN Members caregivers, parents and/or legal guardians, information and materials specific to the needs of the member, as appropriate. This information shall include health educational material as appropriate to assist ISHCN and /or caregivers in understanding their chronic illness.
The contractor shall have in place policies governing the mechanisms utilized to identify, screen and assess individuals with special health care needs. The Contractor will produce a treatment plan for enrollees with special health care needs who are determined through assessment to need a course of treatment or regular care monitoring.
The Contractor shall develop practice guidelines and other criteria that consider that needs of ISHCN and provide guidance in the provision of acute and chronic physical and behavioral health care services to this population.
| |
| 35.2 | DCBS and Department for Aging and Independent Living DAIL Protection and Permanency Clients |
Members who are adult guardianship clients or foster care children shall be identified as ISHCN and shall be enrolled in the Contractor through a service plan that will be completed on each such Member by DCBS and Department for Aging and Independent Living (DAIL) prior to being enrolled with the Contractor. The service plan will be completed by DCBS or DAIL and forwarded to the Contractor prior to Enrollment and will be used by DCBS and or DAIL and the Contractor to determine the individual’s medical needs and identify the need for placement in case management. The Contractor shall be responsible for the ongoing care coordination of these members whether or not enrolled in case management to ensure access to needed social, community, medical and behavioral health services. A monthly report of Foster Care Cases shall be sent to Department thirty (30) days after the end of each month.
| |
| 35.3 | Adult Guardianship Clients |
Upon Enrollment with the Contractor, each adult in Guardianship shall have a service plan prepared by DAIL. The service plan shall indicate DAIL level of responsibility for making medical decisions for each Member. If the service plan identifies the need for case management, the Contractor shall work with Guardianship staff and/or the Member, as appropriate, to develop a case management care plan.
| |
| 35.4 | Children in Foster Care |
Upon Enrollment with the Contractor, each child in Foster Care shall have a service plan prepared by DCBS. DCBS shall forward a copy of the service plan to the Contractor on each newly enrolled Foster Care child. No less than monthly, DCBS staff shall meet with Contractor’s staff to identify, discuss and resolve any health care issues and needs of the child as identified in the service plan. Examples of these issues include needed specialized Medicaid Covered
Services, community services and whether the child’s current primary and specialty care providers are enrolled in the Contractor’s Network.
If DCBS service plan identifies the need for case management or DCBS staff requests case management for a Member, the foster parent and/or DCBS staff will work with Contractor’s staff to develop a case management care plan.
The Contractor will consult with DCBS staff before the development of a new case management care plan (on a newly identified health care issue) or modification of an existing case management care plan.
The DCBS and designated Contractor staff will sign each service plan to indicate their agreement with the plan. If the DCBS and Contractor staff cannot reach agreement on the service plan for a Member, information about that Member’s physical health care needs, unresolved issues in developing the case management plan, and a summary of resolutions discussed by the DCBS and Contractor staff will be forwarded to the designated county DCBS worker. That DCBS staff member shall work with the designated Contractor representative and a designated Department representative, if needed, to agree on a service plan. If agreement is not reached through mediation, the service plan shall be referred to the Department for resolution through the appeals process.
| |
| 35.5 | Children Receiving Adoption Assistance |
Upon Enrollment with the Contractor, each Member receiving adoption assistance shall have a service plan prepared by DCBS. The process for enrollment of children receiving adoption assistance shall follow that outlined for Children in Foster Care above.
The Contractor shall permit a parent, custodial parent, person exercising custodial control or supervision, or an agency with legal responsibility for a child by virtue of voluntary commitment or emergency or temporary custody orders to act on behalf of a Member under the age of eighteen (18), potential member or former Member for purposes of selecting a PCP, filing Grievances or Appeals, and otherwise acting on behalf of the child in interactions with the Contractor.
A legal guardian of an adult Member appointed pursuant to KRS 387.500 to 387.800 shall be allowed to act on behalf of a ward as defined in that statute, and a person authorized to make health care decisions pursuant to KRS 311.621, et seq. shall be allowed to act on behalf of a Member, prospective Member or former Member. A Member may represent her/himself, or use legal counsel, a relative, a friend, or other spokesperson.
The Contractor shall have arrangements and policies and procedures that comply with all state and federal statutes and regulations including 42 CFR 438.608 and Section 6032 of the Federal Deficit Reduction Act of 2005, governing fraud, waste and abuse requirements.
The Contractor shall develop in accordance with Appendix M, a Program Integrity plan of internal controls and policies and procedures for preventing, identifying and investigating enrollee and provider fraud, waste and abuse. This plan shall include, at a minimum:
| |
| A. | Written policies, procedures, and standards of conduct that articulate the organization’s commitment to comply with all applicable federal and state standards; |
| |
| B. | The designation of a compliance officer and a compliance committee that are accountable to senior management; |
| |
| C. | Effective training and education for the compliance officer, the organization’s employees, subcontractors, providers and members regarding fraud, waste and abuse; |
| |
| D. | Effective lines of communication between the compliance officer and the organization’s employees; |
| |
| E. | Enforcement of standards through disciplinary guidelines; |
| |
| F. | Provision for internal monitoring and auditing of the member and provider; |
| |
| G. | Provision for prompt response to detected offenses, and for development of corrective action initiatives relating to the Contractor’s contract; |
| |
| H. | Provision for internal monitoring and auditing of Contractor and its subcontractors; if issues are found Contractor shall provide corrective action taken to the department |
| |
| I. | Contractor shall be subject to on-site review; and comply with requests from the department to supply documentation and records; |
| |
| J. | Contractor shall create an account receivables process to collect outstanding debt from members or providers; and provide monthly reports of activity and collections to the department; |
| |
| K. | Contractor shall provide procedures for appeal process; |
| |
| L. | Contractor shall comply with the expectations of 42 CFR 455.20 by employing a method of verifying with member whether the services billed by provider were received by randomly selecting a minimum sample of 500 Claims on a monthly basis; |
| |
| M. | Contractor shall create a process for card sharing cases; |
| |
| N. | Contractor shall run algorithms on Claims data and develop a process and report quarterly to the department all algorithms run, issues identified, actions taken to address those issues and the overpayments collected; |
| |
| O. | Contractor shall follow cases from the time they are opened until they are closed; and |
| |
| P. | Contractor shall attend any training given by the Commonwealth/Fiscal Agent or other Contractor’s organizations provided reasonable advance notice is given to Contractor of the scheduled training. |
The plan shall be made available to the Department for review and approval.
| |
| 37. | Contractor Reporting Requirements |
| |
| 37.1 | General Reporting and Data Requirements |
The Contractor shall provide to the Department managerial, financial, delegation, utilization, quality, Program Integrity and enrollment reports. The parties acknowledge that CMS has requested Department to provide certain reports concerning Contractor. Contractor agrees to provide Department with the reports CMS has requested or does request. Additionally, the parties agree for Contractor to provide any additional reports requested by Department upon mutual agreement of the parties. The parties agree that Appendix K and Appendix L may be amended outside the scope of this agreement The Department may require the Contractor to prepare and submit adhoc reports.
The Contractor shall respond to any Department request for information or documents within the timeframe specified by the Department in its request. If the Contractor is unable to respond within the specified timeframe, the Contractor shall immediately notify the Department in writing and shall include an explanation for the inability to meet the timeframe and a request for approval of an extension of time. The Department may approve, within it sole discretion, any such extension of time upon a showing of good cause by the Contractor. To avoid delayed responses by Contractor caused by a high volume of information or document requests by the Department, the Parties shall devise and agree upon a functional method of prioritizing requests so that urgent requests are given appropriate priority.
| |
| 37.2 | Record System Requirements |
The Contractor shall maintain or cause to be maintained detailed records relating to the operation including but not limited to the following:
| |
| A. | Administrative costs and expenses incurred pursuant to this Contract; |
| |
| B. | Member enrollment status; |
| |
| C. | Provision of Covered Services; |
| |
| D. | All relevant medical information relating to individual Members for the purpose of audit, evaluation or investigation by the Department, the Office of Inspector General, the Attorney General and other authorized federal or state personnel; |
| |
| E. | Quality Improvement and utilization; |
| |
| F. | All financial records, including all financial reports required under Financial Reports of this Contract and A/R activity, rebate data, DSH requests and etc; |
| |
| G. | Performance reports to indicate Contractor’s compliance with contract requirements; |
| |
| I. | Member/Provider satisfaction and |
All records shall be maintained and available for review by authorized federal and state personnel during the entire term of this Contract and for a period of five (5) years after termination of this Contract, except that when an audit has been conducted, or audit findings are unresolved. In such case records shall be kept for a period of five (5) years in accordance with 907 KAR 1:672, or as amended or until all issues are finally resolved, whichever is later.
| |
| 37.3 | Reporting Requirements and Standards |
The Contractor shall verify the accuracy for data and other information on reports submitted. Reports or other required data shall be received on or before scheduled due dates. Reports or other required data shall conform to the Department’s defined standards. All required information shall be fully disclosed in a manner that is responsive and without material omission.
The Contractor shall analyze all required reports internally before submitting to the Department. The Contractor shall analyze the reports for any early patterns of change, identified trends, or outliers and shall submit this analysis with the required report. The Contractor shall submit a written narrative with the report documenting the Contractor’s interpretation of the early patterns of change, identified trend or outlier.
The Contractor shall be responsible for complying with the reporting requirements set forth in this Contract. The Contractor shall be responsible for assuring the accuracy, completeness and timely submission of each report. Reports shall be submitted in electronic format, paper or disk. The Contractor shall provide such additional data and reports as may be reasonably requested by the Department. The Department shall furnish the Contractor with the appropriate reporting formats, instructions, timetables for submission and such technical assistance in filing reports and data as may be permitted by the Department’s available resources. The Department reserves the right to modify from time to time the form, nature, content, instructions and timetables for the collection and reporting of data. Any requested modification will take cost into consideration.
If the Contractor and the Department are in agreement, the reporting requirements outlined in Appendix K and Appendix L may be amended with a written agreement.
| |
| 37.4 | COB Reporting Requirements |
In order to comply with CMS reporting requirements, the Contractor shall submit a monthly COB Report for all member activity. Additionally, Contractor shall submit a report that includes subrogation collections from auto, homeowners, or malpractice insurance, etc.
| |
| 37.5 | QAPI Reporting Requirements |
The Contractor shall provide status reports of the QAPI program and work plan to the Department on a quarterly basis thirty (30) working days after the end of the quarter and as required under this section and upon request. All reports shall be submitted in electronic and paper format.
| |
| 24.6 | Enrollment Reconciliation |
The Contractor shall reconcile each Member payment identified in a HIPAA 820 transaction with information contained in the HIPAA 834 transaction. The Contractor shall submit all requested corrections to the Department within forty-five (45) days of receipt of HIPAA 820 transaction. Adjustments shall be made to the next HIPAA 820 transaction and/or next available HIPAA 834 transactions to reflect corrections.
| |
| 37.7 | Member Services Report |
By the tenth (10th) of each month, Contractor s shall self-report their prior month performance in these three areas for their member services and twenty-four/seven (24/7) hour toll-free medical call-in system to the Department.
| |
| 37.8 | Grievance and Appeal Reporting Requirements |
The Contractor shall submit to the Department on a quarterly basis the total number of Member Grievances and Appeals and their disposition. The report shall be in a format approved by the Department and shall include at least the following information:
| |
| A. | Number of Grievances and Appeals, including expedited appeal requests; |
| |
| B. | Nature of Grievances and Appeals; |
| |
| D. | Timeframe for resolution; and |
| |
| E. | QAPI initiatives or administrative changes as a result of analysis of Grievances and Appeals. |
The Department or its contracted agent may conduct reviews or onsite visits to follow up on patterns of repeated Grievances or Appeals. Any patterns of suspected Fraud or Abuse identified through the data shall be immediately referred to the Contractor’s Program Integrity Unit.
The Contractor shall submit Encounter Records to the Department’s Fiscal Agent for each Member who receives EPSDT Services. This Encounter Record shall be completed according to the requirements provided by the Department, including use of specified EPSDT procedure codes and referral codes. Annually the Contractor shall submit a report on EPSDT activities, utilization and services and the current Form CMS-416 to the Department.
| |
| 37.10 | Contractor’s Provider Network Reporting |
The Contractor shall submit to the Department on a quarterly basis, in a format specified by the Department, a report summarizing changes in the Contractor’s Network. The Contractor shall report to the Department all provider groups, clinics, facilities and individual physician practices and sites in its network that are not accepting new Medicaid Members. The Contractor shall have procedures to address changes in its network that reduce Member access to services. Significant changes in Contractor’s network composition that reduce Member access to services may be grounds for contract termination.
In the event a PCP ceases participation voluntarily in the network, the Contractor shall notify the Department, in writing, at least thirty (30) calendar days prior to the PCP termination date, or of the Contractor’s notification to the PCP to terminate the Provider’s participation. In the event a PCP ceases participation involuntarily in the network, the Contractor shall notify the Department, in writing, at least fifteen (15) days after the PCP termination date. The Contractor shall indicate in its notice to the Department the reason or reasons for which the PCP ceases participation.
| |
| 37.11 | DCBS and DAIL Service Plans Reporting |
Thirty (30) days after the end of each quarter, the Contractor shall submit a quarterly report detailing the number of service plan reviews conducted for Guardianship, Foster and Adoption assistance Members outcome decisions, such as referral to case management, and rationale for decisions.
| |
| 37.12 | Prospective Drug Utilization Review Report |
The Contractor shall perform Prospective Drug Utilization Review (Pro-DUR) at the POS. They also provide Retrospective Drug Utilization Review (Retro-DUR) services by producing multiple reports for use by the Department.
The Contractor shall submit to the Department on a quarterly basis, in a format specified by the Department, a report summarizing changes in the Contractor’s Network. The Contractor shall report to the Department all provider groups, clinics, facilities and individual physician practices and sites in its network that are not accepting new Medicaid Members. The Contractor shall have procedures to address changes in its network that reduce Member access to services. Significant changes in Contractor’s network composition that reduce Member access to services may be grounds for contract termination.
Managerial reports demonstrate compliance with operational requirements of the contract. These reports shall include, but not be limited to, information on such topics as:
| |
| A. | Composition of current provider networks and capacity to take on new Medicaid members; |
| |
| B. | Changes in the composition and capacity of the provider network; |
| |
| E. | Grievance and appeals resolution activities; |
| |
| F. | Fraud and abuse activities; |
| |
| G. | Delegation oversight activities; and |
Financial reports demonstrate the Contractor’s ability to meet its’ commitments under the terms of this contract. The Contractor and its subcontractors shall maintain their accounting systems in accordance with statutory accounting principles, generally accepted accounting principles, or other generally accepted system of accounting. The accounting system shall clearly document all financial transactions between the Contractor and its subcontractors and the Contractor and the Department. These transactions shall include, but not be limited to, Claims payment, refunds and adjustment of payments.
The Contractor shall file, in the form and content prescribed by the National Association of Insurance Commissioners (NAIC), within one hundred and twenty days (120) days following the end of each fiscal year an annual audited financial statements at the end of the fiscal year that has been prepared by an independent Certified Public Accountant on an accrual basis, in accordance with generally accepted accounting principles as established by the American Institute of Certified Public Accountants.
The Contractor shall also file, within seventy-five (75) days following the end of each fiscal year, certified copies of the annual statement and reports as prescribed and adopted by the DOI. The Department may request information in the form of a consolidated financial statement.
The Contractor shall file within sixty (60) days following the end of each calendar quarter, quarterly financial reports in form and content as prescribed by the NAIC.
The Contractor shall file with Finance and the Department, within seven (7) days after issuance, a true, correct and complete copy of any report or notice issued in connection with a financial examination conducted by or on behalf of the DOI.
| |
| 37.15 | Ownership and Financial Disclosure |
The Contractor agrees to comply with the provisions of 42 CFR 455.104. The Contractor shall provide true and complete disclosures of the following information to Finance, the Department, CMS, and/or their agents or designees, in a form designated by the Department (1) at the time of each annual audit, (2) at the time of each Medicaid survey, (3) prior to entry into a new contract with the Department, (4) upon any change in operations which
affects the most recent disclosure report, or (5) within thirty-five (35) days following the date of each written request for such information:
| |
| A. | The name and address of each person with an ownership or control interest in (i) the Contractor or (ii) any Subcontractor or supplier in which the Contractor has a direct or indirect ownership of five percent (5%) or more, specifying the relationship of any listed persons who are related as spouse, parent, child, or sibling; |
| |
| B. | The name of any other entity receiving reimbursement through the Medicare or Medicaid programs in which a person listed in response to subsection (a) has an ownership or control interest; |
| |
| C. | The same information requested in subsections (a) and (b) for any Subcontractors or suppliers with whom the Contractor has had business transactions totaling more than $250,000 during the immediately preceding twelve-month period; |
| |
| D. | A description of any significant business transactions between the Contractor and any wholly-owned supplier, or between the Contractor and any Subcontractor, during the immediately preceding five‑year period; |
| |
| E. | The identity of any person who has an ownership or control interest in the Contractor, any Subcontractor or supplier, or is an agent or managing employee of the Contractor, any Subcontractor or supplier, who has been convicted of a criminal offense related to that person’s involvement in any program under Medicare, Medicaid, or the services program under Title XX of the Act, since the inception of those programs; |
| |
| F. | The name of any officer, director, employee or agent of, or any person with an ownership or controlling interest in, the Contractor, any Subcontractor or supplier, who is also employed by the Commonwealth or any of its agencies and |
| |
| G. | The Contractor shall be required to notify the Department immediately when any change in ownership is anticipated. The Contractor shall submit a detailed work plan to the Department and to the DOI during the transition period no later than the date of the sale that identifies areas of the contract that may be impacted by the change in ownership including management and staff. |
| |
| 37.16 | Utilization and Quality Improvement Reporting |
Utilization and Quality Improvement reports demonstrate compliance with the Departments service delivery and quality standards. These reports shall include, but not be limited to:
| |
| A. | Trending and analysis reports on areas such as quality of care, access to care, or service delivery access; |
| |
| B. | Encounter data as specified by the Department; |
| |
| C. | Utilization review and management activities data; and |
| |
| D. | Other required reports as determined by the Department, including, but not limited to, performance and tracking measures. |
| |
| 38. | Records Maintenance and Audit Rights |
Member Medical Records if maintained by the Contractor shall be maintained timely, legible, current, detailed and organized to permit effective and confidential patient care and quality review. Complete Medical Records include, but are not limited to, medical charts, prescription files, hospital records, provider specialist reports, consultant and other health care professionals’ findings, appointment records, and other documentation sufficient to disclose the quantity, quality, appropriateness, and timeliness of services provided under the Contract. The medical record shall be signed by the provider of service.
The Contractor shall have medical record confidentiality policies and procedures in compliance with state and federal guidelines and HIPAA. The Contractor shall protect Member information from unauthorized disclosure as set forth in Confidentiality of Records of this Agreement.
The Contractor shall conduct HIPAA privacy and security audits of providers as prescribed by the Department.
The Contractor shall include provisions in its Subcontracts for access to the Medical Records of its Members by the Contractor, the Department, the Office of the Inspector General and other authorized Commonwealth and federal agents thereof, for purposes of auditing. Additionally, Provider contracts shall provide that when a Member changes PCP, the Medical Records or copies of Medical Records shall be forwarded to the new PCP or Partnership within ten (10) Days from receipt of request. The Contractor’s PCPs shall have Members sign a release of Medical Records before a Medical Record transfer occurs.
The Contractor shall have a process to systematically review provider medical records to ensure compliance with the medical records standards. The Contractor shall institute improvement and actions when standards are not met. The Contractor shall have a mechanism to assess the effectiveness of practice-site follow-up plans to increase compliance with the Contractor’s established medical records standards and goals.
The Contractor shall develop methodologies for assessing performance/compliance to medical record standards of PCP’s/PCP sites, high risk/high volume specialist, dental providers, providers of ancillaries services not less than every three (3) years. Audit activity shall, at a minimum;
| |
| A. | Demonstrate the degree to which providers are complying with clinical and preventative care guidelines adopted by the Contractor; |
| |
| B. | Allow for the tracking and trending of individual and plan wide provider performance over time; |
| |
| C. | Include mechanism and processes that allow for the identification, investigation and resolution of quality of care concerns; and |
| |
| D. | Include mechanism for detecting instances of over-utilization, under-utilization, and miss utilization. |
| |
| 38.2 | Confidentiality of Records |
The parties agree that all information, records, and data collected in connection with this Contract, including Medical Records, shall be protected from unauthorized disclosure as provided in 42 C.F.R. Section 431, subpart F, KRS 194.060A, KRS 214.185, KRS 434.840 to 434.860, and any applicable state and federal laws, including the laws specified in Section 40.12.
The Contractor shall have written policies and procedures for maintaining the confidentiality of Member information consistent with applicable laws. Policies and procedures shall include but not be limited to, adequate provisions for assuring confidentiality of services for minors who consent to diagnosis and treatment for sexually transmitted disease, alcohol and other drug abuse or addiction, contraception, or pregnancy or childbirth without parental notification or consent as specified in KRS 214.185. The policies and procedures shall also address such issues as how to contact the minor Member for any needed follow-up and limitations on telephone or mail contact to the home.
The Contractor on behalf of its employees, agents and assigns, shall sign a confidentiality agreement.
Except as otherwise required by law, regulations, or this Contract, access to such information shall be limited by the Contractor and the Department, to persons who or agencies which require the information in order to perform their duties related to the administration of the Department, including but not limited to the U.S. Department of Health and Human Services, U.S. Attorney’s Office, the Office of the Inspector General, the Office of Attorney General, and such others as may be required by the Department.
Any data, information, records or reports which may be disclosed to the Department by the Contractor pursuant to the express terms of this Contract shall not be disclosed or divulged by the Department in whole or in part to any other third person, other than expressly provided for in this Contract, or the Kentucky Open Records Act, KRS 61.870-61.882. The Department and the Contractor agree that this confidentiality provision will survive the termination of this Contract.
Proprietary information, which consists of data, information or records relating to the Contractor, its affiliates’ or subsidiaries’ business operations and structure, sales methods, practices and techniques, advertising, methods and practices, provider relationships unless otherwise expressly provided for in this Contract, non-Medicaid member or enrollee lists, trade secrets, and the Contractor’s, its affiliates’ or subsidiaries’ relationships with its suppliers, providers, potential members or enrollees and potential providers, is supplied under the terms of this Contract based on the Department’s representation that the information is not subject to disclosure, except as otherwise provided
by the Kentucky Open Records Act, KRS 61.870-61.882 or 200 KAR 5:314. The Contractor understands that it must designate information it has which it considers proprietary so that the Department or Finance may Claim the proprietary information exemption to KRS 61.878(1)(c) if a request for such information is made. The Contractor also understands that it shall be responsible for defending its Claim that such designated information is proprietary before any applicable adjudicator.
Any requests for disclosure of information received by the Contractor pursuant to this section of the Contract shall be submitted to and received by the Department’s Contract Compliance Officer within twenty-four (24) hours as specified in Section 40.13of this Contract, and no information for which an exemption from disclosure exists shall be disclosed pursuant to such a request without prior written authorization from the Department. The Department shall notify Contractor if its records are being requested under the Open Records Law.
| |
| 39. | Remedies for Violation, Breach, or Non-Performance of Contract |
Finance or the Department shall have the right to enforce the Contractor’s Performance Bond pursuant to the terms thereof for any material breach of this Contract after prior written notice to Contractor and an opportunity to cure such material breach within thirty (30) days of the date of the notice, and subject to Contractor's appeal rights pursuant to Section 40.9.
| |
| 39.2 | Requirement of Corrective Action |
Finance or the Department may require corrective action in the event that any report, filing, examination, audit, survey, inspection, or investigation should indicate that the Contractor, or any Subcontractor or supplier is not in substantial compliance with any material provision of this Contract, or in the event that the Department receives a substantiated Grievance or Appeal respecting the standard of care rendered by the Contractor, or any Subcontractor or supplier. The Department may also require the modification of any policies or procedures of the Contractor relating to the fulfillment of its obligations pursuant to this Contract. Should Finance or the Department desire to take any such corrective action it must issue a written deficiency notice and require a corrective action plan to be filed by the Contractor within fifteen (15) days following the date of the notice. A corrective action plan shall delineate the time and manner in which each deficiency is to be corrected. The plan shall be subject to approval by Finance or the Department, which may accept the plan as submitted, accept the plan with specified modifications, or reject the plan. Finance or the Department may extend or reduce the time allowed for corrective action depending upon the nature of the deficiency.
| |
| 39.3 | Notice of Contractor Breach |
If the Contractor fails to cure a default in accordance with a plan of correction under Section 14.1, or comply with Sections 1932, 1903(m) and 1905(t) of the Social Security Act, Finance shall issue a written notice to the Contractor indicating the violation(s) and advising the Contractor that failure to cure the violation(s) within a defined time period not less than thirty (30) days to the satisfaction of the Department, may lead to the imposition of any sanction or combination of sanctions provided by the terms of this Contract, or otherwise provided by law, including but not limited to the following:
| |
| A. | Suspension of further Enrollment for a defined time period; When the Department determines the Contractor is out of compliance with the Contract, Finance may suspend the Contractor’s right to new Enrollment under this contract. The suspension will take effect if the non-compliance remains uncorrected at the end of the notice period. Finance may suspend Enrollment sooner than the time period specified in this paragraph if the Department finds that Member’s health or welfare is jeopardized. The suspension period may be for any length of time specified by the Department, or may be indefinite. The suspension period may extend to the expiration of this Contract. |
| |
| B. | Suspension of Capitation Payments; |
| |
| C. | Suspension or recoupment of the Capitation Rate paid for any month for any Member who was denied the full extent of Covered Services meeting the standards set by this Contract, or who received or is receiving substandard services; |
| |
| D. | A claim against Contractor’s Performance Bond; or |
| |
| E. | Termination of this Contract. |
| |
| A. | Encounter data is due on a weekly basis and shall be considered late if not received after four (4) calendar days from the weekly due date. Beginning on the fifth calendar day late, the Department shall withhold Five Hundred ($500.00) Dollars a day for each day late from the Contractor’s Capitation Payment for the month following non-submission. |
| |
| B. | If the Contractor fails to submit health care data derived from processed Claims or Encounter data in the required form or format required by the terms of this Contract for one calendar month the Department shall withhold an amount equaling five(5%) percent of the Contractor’s Capitation Payment for the month following non-submission. The Department shall retain the amount withheld until the data is received and accepted by the Department less Five Hundred ($500.00) Dollars per day for each day late. |
| |
| C. | An Erred Encounter Record File shall be transmitted to the Contractor electronically on 997 acknowledgement file and 277U response file for |
correction and submission. The Contractor shall have ten (10) days to resubmit the corrected Encounter Record File. The Department may assess and withhold for the month following non-submission, an amount equaling one-tenth (0.1%) of a percent of the Contractor’s Capitation Payment a day until the Encounter Record File is received and accepted by the Department EPSDT Encounter Record shall be completed in accordance with EPSDT Reports and these penalties may apply.
| |
| D. | Any other health care information/data requested by the Department or required pursuant to this Contract, including social and demographic data, shall be submitted to the Department in accordance with the time-frames developed by the Department which shall take into consideration the purpose for the data requested, the availability of information, the capabilities of the Contractor to collect and assemble the data in readable form and the cost. |
If the Department elects not to exercise any of the retention clauses herein in a particular instance, this decision shall not be construed as a waiver of the Department’s right to pursue the future assessment of that performance standard requirement and associated reduction in compensation.
The Department will work with the Contractor to resolve problems in obtaining data at all times. The Contractor acknowledges its responsibility to provide data on Members upon request. It is further understood that no withholding will be applied if the reason for delay is beyond control of the Contractor as reasonably determined by the Department.
The submission of late, inaccurate or otherwise incomplete reports shall be considered failure to report. Sanctions may be imposed by Finance for failure to submit accurate and timely reports following failure on the part of the Contractor to cure a default in accordance with a plan of correction under Section 39.2.
| |
| 39.6 | Annual Contract Monitoring |
Finance retains the right to withhold payment if the Contractor does not comply with programmatic and fiscal reporting and monitoring requirements following failure on the part of the Contractor to cure a default in accordance with a plan of correction under Section 39.2.
| |
| 39.7 | Intermediate Sanction and Civil Money Penalties |
In the event the Contractor fails to comply with the terms and conditions of 42 United States Code Section 1396b(m), Finance may do any of the following:
| |
| A. | Appoint temporary management to oversee the entity if a plan engages in continued egregious behavior or there is a substantial risk to the health of enrollees; |
| |
| B. | Permit individuals to disenroll without cause; |
| |
| C. | Suspend default Enrollment; or |
| |
| D. | Suspend payment for new enrollees. |
Prior to imposing the intermediate sanctions, Finance must give the Contractor timely written notice that explains the basis and nature of the sanction and any other due process protections that Finance elects to provide.
Before terminating the Contract under 42 CFR 438.708, Finance must provide the Contractor with a pre-termination hearing. The State shall give the Contractor written notice of its intent to terminate, the reason for termination, and the time and place of hearing. Finance shall give the Contractor, after the hearing, written notice of the decision affirming or reversing the proposed termination of the Contract, and for an affirming decision, the effective date of termination. For an affirming decision, the Department shall give Members notice of the termination and information, consistent with 42 CFR 438.10 on their options for receiving Medicaid services following the effective date of termination.
Following failure on the part of the Contractor to cure a default in accordance with a plan of correction under Section 39.2, Finance may impose civil money penalties in the circumstances and the amounts set forth below if the Contractor does any of the following:
| |
| A. | Fails substantially to provide Medically Necessary items and services that are required under law and under this Contract ($25,000); |
| |
| B. | Imposes excess premiums and charges; (doubles the excess amount charged); |
| |
| C. | Acts to discriminate among Members; (an amount not to exceed $100,000; |
| |
| D. | Misrepresents or falsifies information; (an amount not to exceed $100,000); or |
| |
| E. | Violates marketing guidelines ($10,000). |
| |
| 39.8 | Termination for Convenience |
Finance upon thirty (30) days prior written notice to the Contractor may terminate this Contract without cause. Termination shall be effective only at midnight of the last day of a calendar month, except for termination notices received in June, which termination shall be effective on June 30. In the event of such a termination, Contractor shall have a transition period of not less than three (3) nor more than six (6) months to transition services, during which time the terms and conditions of this Contract shall continue to apply, and Contractor shall provide Covered Services to, and shall be paid pursuant to the Capitation
Rate set forth herein for, each Member up to and including the date of transition of such Member.
| |
| 39.9 | Termination for Default |
In addition to nonperformance of the particular terms and conditions of this Contract by the Contractor, each of the following shall constitute breach of the Contract by Contractor for which any of the remedies set forth in the Contract are available to Finance, as well as a remedy of immediate termination of this Contract if the problem is not cured in the time frame specified by the Department:
| |
| A. | The conduct of the Contractor, any Subcontractor or supplier, or the standard of services provided by or on behalf of the Contractor, fails to meet the Department’s minimum standards of care or threatens to place the health or safety of any group of Members in jeopardy; |
| |
| B. | The Contractor is either expelled or suspended from the federal health insurance programs under Title XVIII or Title XIX of the Social Security Act; |
| |
| C. | Contractor’s Name’s license to operate as an HMO is suspended or terminated by the DOI, or any adverse action is taken by the DOI which is deemed by the Department to affect the ability of the Contractor to provide health care services as set forth in this Contract to Members; |
| |
| D. | The Contractor fails to maintain protection against fiscal insolvency as required under state or federal law, or as required by the terms of this Contract, or the Contractor fails to meet its financial obligations as they become due other than with respect to contested or challenged Claims filed by Members or Providers; |
| |
| E. | The Contractor fails to or knowingly permits any Subcontractor, supplier, or any other person or entity who receives compensation pursuant to performance of this Contract, to fail to comply with the nondiscrimination and affirmative action requirements of Nondiscrimination and Affirmative Action of this Contract; |
| |
| F. | The Contractor provides or knowingly permits any Subcontractor to provide fraudulent, or intentionally misleading or misrepresentative information to any Member, or to any agent of the Commonwealth or the United States in connection with; or |
| |
| G. | Gratuities other than de-minimus or otherwise legal gratuities are offered to, or received by, any public official, employee or agent of the Commonwealth from the Contractor, its agent’s employees, Subcontractors or suppliers, in violation of Offer of Gratuities and Affirmative Action of this Contract; or |
| |
| H. | The Contractor violates any of the confidentiality provisions of this Contract. |
As part of Finance’s option to terminate, if the Contractor is in uncured material breach of the Contract or is insolvent, the Department has the option to assume
the rights and obligations of the Contractor and directly operate the Contractor’s network, using the existing Contractor’s administrative organization, to ensure delivery of care to Members through the Contractor’s Network until cure by the Contractor of the breach or by demonstrated financial solvency, or until the successful transition of those Members to Fee for Service Medicaid providers at the expense of the Contractor.
The certification by the Commissioner of the Department of the occurrence of any of the events stated above shall be conclusive. The Contractor, however, shall retain all rights to dispute resolution specified in Disputes of this Contract.
| |
| 39.10 | Obligations upon Termination |
Upon termination of this Contract by Finance for convenience, lack of funds or for default, the Contractor shall be solely responsible for the provision and payment for all Covered Services for all Members for the remainder of any month for which the Department has paid the monthly Capitation Rate. Contractor may be requested to continue in place for two additional months. Upon final notice of termination, on the date, and to the extent specified in the notice of termination, the Contractor shall:
| |
| A. | Continue providing Covered Services to all Members until midnight on the last day of the calendar month for which a Capitation Payment has been made by the Department; |
| |
| B. | Continue providing all Covered Services to all infants of female Members who have not been discharged from the hospital following birth, until each infant is discharged, or for the period specified in (a) above, whichever period is shorter; |
| |
| C. | Continue providing inpatient hospital services to any Members who are hospitalized on the termination date, until each Member is discharged, or for the period specified in (a) above, whichever period is shorter; |
| |
| D. | Arrange for the transfer of Members and Medical Records to other appropriate Providers; |
| |
| E. | Promptly supply to the Department such information as it may request respecting any unpaid Claims submitted by Out-of- Network Providers and arrange for the payment of such Claims within the time periods provided herein; |
| |
| F. | Take such action as may be necessary, or as the Department may direct, for the protection of property related to this Contract, which is in the possession of the Contractor and in which the Department has or may acquire an interest; and |
| |
| G. | Provide for the maintenance of all records for audit and inspection by the Department, CMS and other authorized government officials, in accordance with terms and conditions specified in this Contract including the transfer of all such data and records, or copies thereof, to the Department or its agents as may be requested by the |
Department; and the preparation and delivery of any reports, forms or other documents to the Department as may be required pursuant to this Contract or any applicable policies and procedures of the Department.
The covenants set forth in this Section shall survive the termination of this Contract and shall remain fully enforceable by Finance against the Contractor. In the event that the Contractor fails to fulfill each covenant set forth in this Section, the Department shall have the right, but not the obligation, to arrange for the provision of such services and the fulfillment of such covenants, all at the sole cost and expense of the Contractor and the Contractor shall refund to the Department all sums expended by the Department in so doing.
After Finance notifies the Contractor that it intends to terminate the Contract, the Department may provide the Members written notice of Finance’s intent to terminate the Contract and allow the Members to disenroll immediately without cause.
If the Commonwealth terminates this Contract under Section 39.9, Contractor acknowledges and agrees that the Department will incur substantial inconvenience and additional expenses and costs which are difficult or impossible to accurately estimate. The Contractor shall pay to the Department liquidated damages up to ten percent (10%) of the Contractor’s monthly Capitation Payment. Such payment is to be made no later than thirty (30) days following the date of the notice of termination. Finance and the Contractor agree that the sum set forth herein as liquidated damages is a reasonable pre-estimate of the probable loss which will be incurred by the Department in the event this Contract is terminated prior to the end of the Contract term.
If this Contract is terminated by Finance for convenience as specified in Section 39.8 of this Contract, the Contractor may seek a remedy pursuant to 200 KAR 5:312.
The Contractor hereby grants to Finance a lien and right of set off for any refund and liquidated damages due the Department pursuant to this Contract, upon and against any deposits, credits, payments due or other property of the Contractor at any time in the possession or control of the Department or in transit to the Department.
| |
| 39.13 | Termination by Contractor |
The Contractor may terminate this Contract with notice given in accordance with the requirements of Section 40.13 at least six (6) months but no more than seven (7) months prior to the end of the initial term of this Contract or any renewal terms.
| |
| 39.14 | Documents Constituting Contract |
This Contract shall include
1. This Medicaid Managed Care agreement;
2. The Appendices to this agreement;
3. The Request for Proposal and all attachments and addendums thereto, including Section 40--Terms and Conditions of a Contract with the Commonwealth of Kentucky, where applicable;
4. General Conditions contained in 200 KAR 5:021 and Office of Procurement Services’ FAP110-10-00;
5. Any clarifications concerning the Contractor’s proposal in response to the RFP;
6. The Contractor’s proposal in response to the RFP. Provided however, by submitting materials in response to the RFP, the Contractor has not fulfilled any obligation under this Contract to submit plans, programs, policies, procedures, forms or documents, etc. to the Department for approval as required by this Contract.
In the event of any conflict between or among the provisions contained in the Contract, the order of precedence shall be as enumerated above.
The documents listed above constitute the entire agreement between the parties.
| |
| 39.15 | Definitions and Construction |
The terms used in this Contract shall have the definitions set forth in Section 2, unless this Contract expressly provides otherwise. References to numbered sections refer to the designated sections contained in this Contract. Titles of sections used in this Contract are for reference only and shall not be deemed to be a part of this Contract.
This Contract may be amended at any time by written mutual consent of the Contractor and Finance and the Department, and upon approval of CMS. In the event that changes in state or federal law require the Department to amend its Contract with the Contractor, notice shall be made to the Contractor in writing and any such amendment shall be subject to the applicable payment rate revision provisions as described in Section 12. The Department may, from time to time provide clarification of the Providers’ and the Contractor’s responsibilities, provided, however, such clarification shall not expand or amend the duties and obligations under this Contract without an amendment. The reporting requirements in the Appendices to this Contract may be modified by mutual agreement between the Contractor and the Department by a signed letter of agreement.
| |
| 40.1 | Notice of Legal Action |
The Contractor shall provide written notice to Finance of any legal action or notice listed below, within ten (10) days following the date the Contractor receives written notice of:
| |
| A. | Any action, proposed action, lawsuit or counterclaim filed against the Contractor, or against any Subcontractor or supplier, related in any way to this Contract; |
| |
| B. | Any administrative or regulatory action, or proposed action, respecting the business or operations of the Contractor, any Subcontractor or supplier, related in any way to this Contract; |
| |
| C. | Any notice received from the DOI or the Cabinet for Health and Family Services; |
| |
| D. | Any claim made against the Contractor by a Member, Subcontractor or supplier having the potential to result in litigation related in any way to this Contract; |
| |
| E. | The filing of a petition in bankruptcy by or against a Subcontractor or supplier, or the insolvency of a Subcontractor or supplier; and |
| |
| F. | The payment of a civil fine or conviction of any person who has an ownership or controlling interest in the Contractor, any Subcontractor or supplier, or who is an agent or managing employee of the Contractor, any Subcontractor or supplier, of a criminal offense related to that person’s involvement in an program under Medicare, Medicaid, or Title XX of the Act, or of Fraud, or unlawful manufacture, distribution, prescription or dispensing of a controlled substance, as specified in 42 USC 1320a-7. |
A complete copy of all documents, filings or notices received by the Contractor shall accompany the notice to Finance. A complete copy of all further filings and other documents generated in connection with any such legal action shall be provided to Finance within ten (10) days following the date the Contractor receives such documents.
By the signature of its authorized representative, the Contractor certifies that it is legally entitled to enter into this Contract with the Commonwealth, and in holding and performing this Contract, the Contractor does not and will not violate either applicable conflict of interest statutes (KRS 45A.330‑45A.340, 45A.990, 164.390), or KRS 11A.040 of the Executive Branch Code of Ethics, relating to the employment of former public servants.
| |
| 40.3 | Offer of Gratuities/Purchasing and Specifications |
The Contractor certifies that no member or delegate of Congress, nor any elected or appointed official, employee or agent of the Commonwealth, the
Kentucky Cabinet for Health and Family Services, CMS, or any other federal agency, has or will benefit financially or materially from this procurement. This Contract may be terminated by Finance pursuant to Section 39.9 herein if it is determined that gratuities were offered to or received by any of the aforementioned officials or employees from the Contractor, its agents, employees, Subcontractors or suppliers.
The Contractor certifies by its signatories hereinafter that it will not attempt in any manner to influence any specifications to be restrictive in any way or respect nor will it attempt in any way to influence any purchasing of services, commodities or equipment by the Commonwealth. For the purpose of this paragraph, “it” is construed to mean any person with an interest therein, as required by applicable law.
| |
| 40.4 | Independent Capacity of the Contractor and Subcontractors |
It is expressly agreed that the Contractor and any Subcontractors and agents, officers, and employees of the Contractor or any Subcontractors shall act in an independent capacity in the performance of this Contract and not as officers or employees of the Department or the Commonwealth. It is further expressly agreed that this Contract shall not be construed as a partnership or joint venture between the Contractor or any Subcontractor and the Department or the Commonwealth.
Except as allowed through Subcontracting, this Contract and any payments that may become due hereunder, shall not be assignable by the Contractor, either in whole or in part, without prior written approval of Finance. The transfer of five percent (5%) or more of the beneficial ownership in the Contractor at any time during the term of this Contract shall be deemed an assignment of this Contract. Finance shall be entitled to assign this Contract to any other agency of the Commonwealth which may assume the duties or responsibilities of the Department relating to this Contract. Finance shall provide written notice of any such assignment to the Contractor, whereupon the Department shall be discharged from any further obligation or liability under this Contract arising on or after the date of such assignment.
No covenant, condition, duty, obligation, or undertaking contained in or made a part of this Contract may be waived except by written agreement of the parties. The forbearance or indulgence in any form or manner by either party shall not constitute a waiver of any covenant, condition, duty, obligation, or undertaking to be kept, performed, or discharged by the party to which the same may apply. Until complete performance or satisfaction of all such covenants, conditions, duties, obligations, or undertakings, the other party shall have the right to invoke any remedy available under law or equity, notwithstanding any such forbearance or indulgence.
In the event that any provision of this Contract (including items incorporated by reference) is found to be unlawful, invalid or unenforceable, such provision shall be deemed severed from this Contract and Finance the Department and the Contractor shall be relieved of all obligations arising under such provision. If the remaining parts of this Contract are capable of performance, this Contract shall continue in full force and effect, and all remaining provisions shall be binding upon each party to this Contract as if no such unlawful, invalid or unenforceable provision had been part of this Contract. If the laws or regulations governing this Contract should be amended or judicially interpreted so as to render the fulfillment of this Contract impossible or economically not feasible, as determined jointly by Finance, the Department and the Contractor, Finance, the Department and the Contractor shall be discharged from any further obligations created under the terms of this Contract.
The parties shall be excused from performance thereunder for any period that it is prevented from providing, arranging for, or paying for services as a result of a catastrophic occurrence or natural disaster including but not limited to an act of war, and excluding labor disputes.
Any disputes arising under this Contract which cannot be disposed of by agreement between the parties, shall be decided by the Secretary of the Cabinet for Health and Family Services or his/her duly authorized representative. Such decision shall be produced in writing and sent via first-class mail to the Contract Compliance Officer for the Contractor at the address specified in Notices of this Contract. The decision of the Secretary or his representative shall be final and conclusive unless, within ten (10) working days following the date of notice to the Contractor of such decision, the Contractor mails or otherwise furnishes a written appeal to the Secretary of the Finance and Administration Cabinet.
The Contractor shall be afforded an opportunity to be heard and to offer evidence in support of its appeal to the Secretary of the Cabinet for Health and Family Services. Any appeal to the Secretary of the Finance and Administration Cabinet shall be in accordance with KRS Chapter 45A.225 et seq. and regulations promulgated thereunder. The Contractor shall proceed diligently with the performance of this Contract in accordance with the decision rendered by the Secretary of the Cabinet for Health and Family Services until the Secretary of the Finance and Administration Cabinet renders a final decision.
The Contractor acknowledges that, pursuant to KRS Chapter 45A.225 et seq., the Secretary of the Finance and Administration Cabinet is the final arbiter of any and all disputes concerning the Contract or the Department, subject to
the right of the Contractor to appeal any such determination to the Circuit Court of Franklin County, Kentucky.
| |
| 40.10 | Modifications or Rescission of Section 1915 Waiver / State Plan Amendment |
It is understood Contractor operates either pursuant to authority granted to the Department under a 1932(a) State Plan Amendment or 1915(b) waiver granted by CMS. Notwithstanding any other provision contained herein, if at any time the waiver is rescinded or materially changed in scope, format, funding or SPA is withdrawn or modified the Department reserves the right to immediately and without notice suspend or terminate this Contract pursuant to Remedies for Violation, Breach or Non-Performance of Contract herein.
The Contract shall be governed by and construed in accordance with the laws of the Commonwealth and applicable federal law and regulations. The Contractor shall be required to bring all legal proceedings against the Commonwealth in the Franklin County Circuit Court of the Commonwealth and the Contractor shall accept jurisdiction of the Kentucky courts over all matters arising out of this Contract.
| |
| 40.12 | Health Insurance Portability and Accountability Act |
The Contractor agrees to abide by the rules and regulations regarding the confidentiality of protected health information as defined and mandated by the Health Insurance Portability and Accountability Act (42 USC 1320d) and set forth in federal regulations at 45 CFR Parts 160 and 164. Any Subcontract entered by the Contractor as a result of this agreement shall mandate that the Subcontractor be required to abide by the same statutes and regulations regarding confidentiality of protected health information as is the Contractor.
All notices required by, or pursuant to, this Contract shall be deemed duly given upon delivery, if delivered by hand (against receipt), or three (3) business days after posting, if sent by registered or certified mail, return receipt requested, to a party’s representative or representatives, as designated in this Contract at the address or addresses designated in this Contract. Notices to Finance and the Department, except those specified to be given to the Department’s Fiscal Agent, shall be given to both of the following:
Finance and Administration Cabinet
Office of Procurement Services
Attn: Executive Director
Room 96 Capitol Annex
Frankfort, Kentucky 40601
and
Department for Medicaid Services
Commissioner
275 East Main Street
Frankfort, Kentucky 40621
Notices to the Contractor shall be given to the following:
WellCare of Kentucky, Inc.
211 Perimeter Center Parkway
Suite 800
Atlanta, GA 30346
The provisions of this Contract which relate to the obligations of the Contractor to maintain records and reports shall survive the expiration of earlier termination of this Contract for a period of five (5) years or such other period as may be required by record retention policies of the Commonwealth or CMS, or otherwise required by law. Each party’s right to recoupment pursuant to Ineligibility Due to Fraud, Waste and Abuse Cases of this Contract shall survive the expiration or earlier termination of this Contract until such time as all payments and/or recoupment have been finally settled. Finance’s, the Department’s and the Contractor’s rights pursuant to Section 14.0 of this Contract shall survive expiration, or earlier termination of this Contract, until such time as the Contractor has satisfactorily complied with the terms thereof.
| |
| 40.15 | Prohibition on Use of Funds for Lobbying Activities |
The contractor agrees that no funding derived directly or indirectly from funds pursuant to this contract shall be used to support lobbying activities or expenses of state or federal government agencies or state or federal lawmakers.
| |
| 40.16 | Adoption of Auditor of Public Account (APA) Standards for Public and Nonprofit Boards |
The contractor agrees to adopt the APA Standards for Public and Nonprofit Boards, if applicable. The contractor agrees to provide documentation of this adoption within thirty (30) days of execution of the contract.
| |
| 40.17 | Review of Distributions |
The Contractor agrees to provide notice to the Department at the same time of submission of a request for approval of the Contractor’s domiciliary Insurance Commissioner of any distributions of capital and surplus that are subject to the provisions of its State Insurance Code. The parties agree that capital and surplus amounts in excess of the required minimum amount required to be maintained under its Insurance Code represents net worth
assets for the purposes of benefitting the Commonwealth of Kentucky’s Medicaid Program and its beneficiaries. The parties agree to make a good faith effort to cooperatively decide how much excess capital and surplus is needed by the Contractor and possible uses of excess capital and surplus that should not be retained by the Contractor.
The Contractor agrees that the Department, the Finance and Administration Cabinet, the Auditor of Public Accounts, and the Legislative Research Commission, or their duly authorized representatives, shall have access to any books, documents, papers, records, or other evidence, which are directly pertinent to this contract for the purpose of financial audit or program review. Records and other prequalification information confidentially disclosed as part of the bid process shall not be deemed as directly pertinent to the contract and shall be exempt from disclosure as provided in KRS 61.878(1)(c). The contractor also recognizes that any books, documents, papers, records, or other evidence, received during a financial audit or program review shall be subject to the Kentucky Open Records Act, KRS 61.870 to 61.884 subject to applicable exceptions
| |
| 40.19 | Cost Effective Analyses |
The Contractor will cooperate with any analyses conducted by the Department or its agent(s) of the cost effectiveness of the contract for any period. Such analyses may review cost effectiveness from any number of comparisons. Such analyses will be used to assist the Department to meet federal requirements, program management and provide accountability and transparency to the public.
| |
| 40.20 | Open Meetings and Open Records |
The Contractor agrees that only those portions of its Board of Directors meetings or parts of its meetings that are with the Department shall be open to the public.
The Contractor for the purpose of this Contract and any documents or records pertaining to this Contract shall be considered a “public agency” under the Open Records Act, KRS 61.870 through KRS 61.884.
| |
| 40.21 | Disclosure of Certain Financial Information |
The Contractor agrees to provide the Department within thirty (30) days of contract execution a business plan that outlines proposed annual expenditures under the contract for items including but not limited to proposed budgets for salaries, bonus, other compensation, travel, other expenditures (i.e. sponsorships, grants, donations, insurance cost and medical expenses) and other items in APA’s report.
The Contractor agrees to provide the Department upon request information regarding salaries, travel, other compensation, and other expenses listed in Appendix K. The contractor agrees to provide any information requested by the Department regarding expenditures related to this contract. Including but not limited to any findings of the Medicaid Managed Care Operations Examination.
Approvals:
This Contract is subject to the terms and conditions as stated. The parties certify that they are authorized to bind this agreement between parties and that they accept the terms of this agreement.
CONTRACTOR: WELLCARE OF KENTUCKY, INC.
/s/ Jesse Thomas President, South Division
SIGNATURE TITLE
Jesse Thomas July 4, 2011
PRINTED NAME DATE
COMMONWEALTH OF KENTUCKY
CABINET FOR FINANCE AND ADMINISTRATION
/s/ Donald R. Speer Executive Director
SIGNATURE TITLE
Donald R. Speer July 6, 2011
PRINTED NAME DATE
Approved As To Form And Legality:
/s/ E. Jeffrey Mosley
GENERAL COUNSEL
CABINET FOR FINANCE AND ADMINISTRATION
WellCare of Kentucky, Inc.
APPENDICES
Table of Contents
| |
| B. | Approved Capitation Payment Rates |
| |
| C. | Management Information System Requirements |
| |
| D. | Encounter Data Submission Requirements |
| |
| E. | Encounter Data Submission Quality Standards |
| |
| F. | Third Party Liability/Coordination of Benefits Requirements |
| |
| G. | Network Provider File Layout Requirements |
| |
| H. | Credentialing Process Coversheet |
| |
| J. | Early and Periodic Screening, Diagnosis and Treatment Program Periodicity Schedule |
| |
| M. | Program Integrity Requirements |
| |
| N. | Performance Improvement Projects |
| |
| O. | Health Outcomes, Indicators, Goals and Performance Measures |
| |
| P. | Business Associates Agreement |
| |
| Q. | Annual Contract Monitoring Tools |
Appendix A
Commonwealth of Kentucky
Medicaid Managed Care Organization (MCO) Regions
Service Area - Statewide Excluding Region 3
MCO Region 1 (includes the following 12 counties)
Ballard
Caldwell
Calloway
Carlisle
Crittenden
Fulton
Graves
Hickman
Livingston
Lyon
Marshall
McCracken
MCO Region 2 (includes the following 12 counties)
Christian
Daviess
Hancock
Henderson
Hopkins
McLean
Muhlenberg
Ohio
Todd
Trigg
Union
Webster
MCO Region 4 (includes the following 20 counties)
Adair
Allen
Barren
Butler
Casey
Clinton
Cumberland
Appendix A
Commonwealth of Kentucky
Medicaid Managed Care Organization (MCO) Regions
Service Area - Statewide Excluding Region 3
MCO Region 4 (includes the following 20 counties) - Continued
Edmonson
Green
Hart
Logan
McCreary
Metcalfe
Monroe
Pulaski
Russell
Simpson
Taylor
Warren
Wayne
MCO Region 5 (includes the following 21 counties)
Anderson
Bourbon
Boyle
Clark
Estill
Fayette
Franklin
Garrard
Harrison
Jackson
Jessamine
Lincoln
Madison
Mercer
Montgomery
Nicholas
Owen
Powell
Rockcastle
Scott
Woodford
Appendix A
Commonwealth of Kentucky
Medicaid Managed Care Organization (MCO) Regions
Service Area - Statewide Excluding Region 3
MCO Region 6 (includes the following 6 counties)
Boone
Campbell
Gallatin
Grant
Kenton
Pendleton
MCO Region 7 (includes the following 14 counties)
Bath
Boyd
Bracken
Carter
Elliott
Fleming
Greenup
Lawrence
Lewis
Mason
Menifee
Morgan
Robertson
Rowan
MCO Region 8 (includes the following 19 counties)
Bell
Breathitt
Clay
Floyd
Harlan
Johnson
Knott
Knox
Laurel
Lee
Leslie
Appendix A
Commonwealth of Kentucky
Medicaid Managed Care Organization (MCO) Regions
Service Area - Statewide Excluding Region 3
MCO Region 8 (includes the following 19 counties) -Continued
Letcher
Magoffin
Martin
Owsley
Perry
Pike
Whitley
Wolfe
Appendix B
Approved Capitation Payment Rates
WellCare of Kentucky, Inc.
YEAR 1 – OCTOBER 1, 2011 THROUGH SEPTEMBER 30, 2012
Appendix B (cont.)
Approved Capitation Payment Rates
WellCare of Kentucky, Inc.
YEAR 2 – OCTOBER 1, 2012 THROUGH SEPTEMBER 30, 2013
Appendix B (cont.)
Approved Capitation Payment Rates
WellCare of Kentucky, Inc.
YEAR 3 – OCTOBER 1, 2013 THROUGH JUNE 30, 2014
Appendix C
Management Information System Requirements
As specified in Management Information Systems Section in the Contract, The Contractor’s MIS must enable the Contractor to provide format and file specifications for all data elements as specified below for all of the required seven subsystems.
The Recipient Data Maintenance function will accept input from various sources to add, change, or close records on the file(s). Inputs to the Recipient Data Maintenance function include:
| |
| 1. | Daily and monthly electronic member eligibility updates (HIPAA ASC X12 834) |
| |
| 2. | Claim/encounter history – sequential file; file description to be determined |
| |
| 3. | Social demographic information |
| |
| 4. | Initial Implementation of the Contract, the following inputs shall be provide to the contractor: |
| |
| • | Initial Member assignment file (sequential file; format to be supplemented at contract execution); a file will be sent approximately sixty (60) calendar days prior to the Contractor effective date of operations |
| |
| • | Member claim history file – twelve (12) months of member claim history (sequential file; format to be supplemented at Contract execution) |
| |
| • | Member Prior Authorizations in force file (medical and pharmacy; sequential file; format will be supplemented at Contract execution) |
| |
| B. | Processing Requirements |
The Recipient Data Maintenance function must include the following capabilities:
| |
| 1. | Accept a daily/monthly member eligibility file from the Department in a specified format. |
| |
| 2. | Transmit a file of health status information to the Department in a specified format. |
| |
| 3. | Transmit a file of social demographic data to the Department in a specified format. |
| |
| 4. | Transmit a primary care provider (PCP) enrollment file to the Department in a specified format. |
| |
| 5. | Edit data transmitted from the Department for completeness and consistency, editing all data in the transaction. |
| |
| 6. | Identify potential duplicate Member records during update processing. |
| |
| 7. | Maintain on-line access to all current and historical Member information, with inquiry capability by case number, Medicaid Recipient ID number, social security number (SSN), HIC number, full name or |
partial name, and the ability to use other factors such as date of birth and/or county code to limit the search by name.
| |
| 8. | Maintain identification of Member eligibility in special eligibility programs, such as hospice, etc., with effective date ranges/spans and other data required by the Department. |
| |
| 9. | Maintain current and historical date-specific managed care eligibility data for basic program eligibility, special program eligibility, and all other Member data required to support Claims processing, Prior Authorization processing, managed care processing, etc. |
| |
| 10. | Maintain and display the same values as the Department for eligibility codes and other related data. |
| |
| 11. | Produce, issue and mail a managed care ID card pursuant to the Department’s approval within Department determined time requirements. |
| |
| 12. | Identify Member changes in the primary care provider (PCP) and the reason(s) for those changes to include effective dates. |
| |
| 13. | Monitor PCP capacity and limitations prior to Enrollment of a Member to the PCP. |
| |
| 14. | Generate and track PCP referrals if applicable. |
| |
| 15. | Assign applicable Member to PCP if one is not selected within thirty (30) Days, except Members with SSI without Medicare, who are allowed ninety (90) Days. |
Reports for Member function are described in Appendix XI.
| |
| D. | On-line Inquiry Screens |
On-line inquiry screens that meet the user interface requirements of this section and provide access to the following data:
| |
| 1. | Member basic demographic data |
| |
| 3. | Member characteristics and service utilization data |
| |
| 4. | Member current and historical managed care eligibility data |
| |
| 5. | Member special program data |
| |
| 6. | Member social/demographic data |
The Member Data Maintenance function must accommodate an external electronic interface (HIPAA ASC X12 834, both 4010A1 and 5010 after January 1, 2012) with the Department.
| |
| II. | Third Party Liability (TPL) Subsystem |
The Third Party Liability (TPL) processing function permits the Contractor to utilize the private health, Medicare, and other third-party resources of its Members and ensures that the Contractor is the payer of last resort. This function works through a combination of cost avoidance (non-payment of billed amounts for which a third party
may be liable) and post-payment recovery (post-payment collection of Contractor paid amounts for which a third party is liable).
Cost avoidance is the preferred method for processing claims with TPL. This method is implemented automatically by the MIS through application of edits and audits which check claim information against various data fields on recipient, TPL, reference, or other MIS files. Post-payment recovery is primarily a back-up process to cost avoidance, and is also used in certain situations where cost avoidance is impractical or unallowable.
The TPL information maintained by the MIS must include Member TPL resource data, insurance carrier data, health plan coverage data, threshold information, and post payment recovery tracking data. The TPL processing function will assure the presence of this information for use by the Edit/Audit Processing, Financial Processing, and Claim Pricing functions, and will also use it to perform the functions described in this subsection for TPL Processing.
The following are required inputs to the TPL function of the MIS:
| |
| 1. | Member eligibility, Medicare, and TPL, information from the Department via proprietary file formats. |
| |
| 2. | Enrollment and coverage information from private insurers/health plans, state plans, and government plans. |
| |
| 3. | TPL-related data from claims, claim attachments, or claims history files, including but not limited to: |
| |
| • | diagnosis codes, procedure codes, or other indicators suggesting trauma or accident; |
| |
| • | indication that a TPL payment has been made for the claim (including Medicare); |
| |
| • | indication that the Member has reported the existence of TPL to the Provider submitting the claim; |
| |
| • | indication that TPL is not available for the service claimed. |
| |
| 4. | Correspondence and phone calls from Members, carriers, and Providers and DMS. |
| |
| B. | Processing Requirements |
The TPL processing function must include the following capabilities:
| |
| 1. | Maintain accurate third-party resource information by Member including but not limited to: |
| |
| • | Name, ID number, date of birth, SSN of eligible Member; |
| |
| • | Policy number or Medicare HIC number and group number; |
| |
| • | Name and address of policyholder, relationship to Member, |
| |
| • | Court-ordered support indicator; |
| |
| • | Employer name and tax identification number and address of policyholder; |
| |
| • | Type of policy, type of coverage, and inclusive dates of coverage; |
| |
| • | Date and source of TPL resource verification; and |
| |
| • | Insurance carrier name and tax identification and ID. |
| |
| 1. | Provide for multiple, date-specific TPL resources (including Medicare) for each Member. |
| |
| 2. | Maintain current and historical information on third-party resources for each Member. |
| |
| 3. | Maintain third-party carrier information that includes but is not limited to: |
| |
| • | Corporate correspondence address and phone number |
| |
| • | Claims submission address(s) and phone number |
| |
| 1. | Identify all payment costs avoided due to established TPL, as defined by the Department. |
| |
| 2. | Maintain a process to identify previously paid claims for recovery when TPL resources are identified or verified retroactively, and to initiate recovery within sixty (60) Days of the date the TPL resource is known to the Contractor. |
| |
| 3. | Maintain an automated tracking and follow-up capability for all TPL questionnaires. |
| |
| 4. | Maintain an automated tracking and follow-up capability for post payment recovery actions which applies to health insurance, casualty insurance, and all other types of recoveries, and which can track individual or group claims from the initiation of recovery efforts to closure. |
| |
| 5. | Provide for the initiation of recovery action at any point in the claim processing cycle. |
| |
| 6. | Maintain a process to adjust paid claims history for a claim when a recovery is received. |
| |
| 7. | Provide for unique identification of recovery records. |
| |
| 8. | Provide for on-line display, inquiry, and updating of recovery case records with access by claim, Member, carrier, Provider or a combination of these data elements. |
| |
| 9. | Accept, edit and update with all TPL and Medicare information received from the Department through the Member eligibility update or other TPL updates specified by the Department. |
| |
| 10. | Implement processing procedures that correctly identify and cost avoid claims having potential TPL, and flag claims for future recovery to the appropriate level of detail. |
| |
| 11. | Provide verified Member TPL resource information generated from data matches and claims, to the Department for Medicaid Services, in an agreed upon format and media, on a monthly basis. |
The following types of reports must be available from the TPL Processing function by the last day of the month for the previous month:
| |
| 1. | Cost-avoidance summary savings reports, including Medicare but identifying it separately; |
| |
| 2. | Listings and totals of cost-avoided claims; |
| |
| 3. | Listings and totals of third-party resources utilized; |
| |
| 4. | Reports of amounts billed and collected, current and historical, from the TPL recovery tracking system, by carrier and Member; |
| |
| 5. | Detailed aging report for attempted recoveries by carrier and Member; |
| |
| 6. | Report on the number and amount of recoveries by type; for example, fraud collections, private insurance, and the like; |
| |
| 7. | Report on the unrecoverable amounts by type and reason, carrier, and other relevant data, on an aged basis and in potential dollar ranges; |
| |
| 8. | Report on the potential trauma and/or accident claims for claims that meet specified dollar threshold amounts; |
| |
| 9. | Report on services subject to potential recovery when date of death is reported; |
| |
| 10. | Unduplicated cost-avoidance reporting by program category and by type of service, with accurate totals and subtotals; |
| |
| 11. | Listings of TPL carrier coverage data; |
| |
| 12. | Audit trails of changes to TPL data. |
| |
| D. | On-line Inquiry Screens |
On-line inquiry screens that meet the user interface requirements of this section and provide the following data:
| |
| 1. | Member current and historical TPL data |
Automatically generate letters/questionnaires to carriers, employers, Members, and Providers when recoveries are initiated, when TPL resource data is needed, or when accident information is required and was not supplied with the incoming claim.
Automatically generate claim facsimiles, which can be sent to carriers, attorneys, or other parties.
Provide absent parent canceled court order information generated from data matches with the Division of Child Support Enforcement, to the Department, in an agreed upon format and media, on an annual basis.
The provider function accepts and maintains comprehensive, current and historical information about Providers eligible to participate in the Contractor’s Network. The maintenance of provider data is required to support Claims and Encounter processing, utilization/quality processing, financial processing and report functions. The Contractor will be required to electronically transmit provider enrollment information to the Department as requested.
The inputs to the provider Data Maintenance function include:
| |
| 1. | Provider update transactions |
| |
| 2. | Licensure information, including electronic input from other governmental agencies |
| |
| 3. | Financial payment, adjustment, and accounts receivable data from the Financial Processing function. |
| |
| B. | Processing Requirements |
The Provider Data Maintenance function must have the capabilities to:
| |
| 1. | Transmit a provider enrollment file to the Department in a specified format; |
| |
| 2. | Maintain current and historical provider enrollment applications from receipt to final disposition (approval only); |
| |
| 3. | Maintain on-line access to all current and historical provider information, including Provider rates and effective dates, Provider program and status codes, and summary payment data; |
| |
| 4. | Maintain on-line access to Provider information with inquiry by Provider name, partial name characters, provider number, NPI, SSN, FEIN, CLIA number, Provider type and specialty, County, Zip Code, and electronic billing status; |
| |
| 5. | Edit all update data for presence, format, and consistency with other data in the update transaction; |
| |
| 6. | Edits to prevent duplicate Provider enrollment during an update transaction; |
| |
| 7. | Accept and maintain the National Provider Identification (NPI); |
| |
| 8. | Provide a Geographic Information System (GIS) to identify Member populations, service utilization, and corresponding Provider coverage to support the Provider recruitment, enrollment, and participation; |
| |
| 9. | Maintain on-line audit trail of Provider names, Provider numbers (including old and new numbers, NPI), locations, and status changes by program; |
| |
| 10. | Identify by Provider any applicable type code, NPI/TAXONOMY code, location code, practice type code, category of service code, and medical specialty and sub-specialty code which is used in the Kentucky Medicaid program, and which affects Provider billing, claim pricing, or other processing activities; |
| |
| 11. | Maintain effective dates for Provider membership, Enrollment status, restriction and on-review data, certification(s), specialty, sub-specialty, claim types, and other user-specified Provider status codes and indicators; |
| |
| 12. | Accept group provider numbers, and relate individual Providers to their groups, as well as a group to its individual member Providers, with effective date ranges/spans. A single group provider record must be able to identify an unlimited number of individuals who are associated with the group; |
| |
| 13. | Maintain multiple, provider-specific reimbursement rates, including, but not necessarily limited to, per diems, case mix, rates based on licensed levels of care, specific provider agreements, volume purchase contracts, and capitation, with beginning and ending effective dates for a minimum of sixty (60) months. |
| |
| 14. | Maintain provider-specific rates by program, type of capitation, Member program category, specific demographic classes, Covered Services, |
and service area for any prepaid health plan or managed care providers;
| |
| 15. | Provide the capability to identify a Provider as a PCP and maintain an inventory of available enrollment slots; |
| |
| 16. | Identify multiple practice locations for a single provider and associate all relevant data items with the location, such as address and CLIA certification; |
| |
| 17. | Maintain multiple addresses for a Provider, including but not limited to: |
| |
| 18. | Create, maintain and define provider enrollment status codes with associated date spans. For example, the enrollment codes must include but not be limited to: |
| |
| • | Limited time-span enrollment |
| |
| • | Terminated-voluntary/involuntary |
| |
| 19. | Maintain a National Provider Identifier (NPI) and taxonomies; |
| |
| 20. | Maintain specific codes for restricting the services for which Providers may bill to those for which they have the proper certifications (for example, CLIA certification codes); |
| |
| 21. | Maintain summary-level accounts receivable and payable data in the provider file that is automatically updated after each payment cycle; |
| |
| 22. | Provide the capability to calculate and maintain separate 1099 and associated payment data by FEIN number for Providers with changes of ownership, based upon effective dates entered by the Contractor; |
| |
| 23. | Generate a file of specified providers, selected based on the Department identified parameters, in an agreed upon Department approved format and media, to be provided to the Department on an agreed upon periodic basis; and |
| |
| 24. | Generate a file of provider 1099 information. |
| |
| 25. | Reports – Reports for Provider functions are as described in Appendices s K and L. |
| |
| C. | On-line Inquiry Screens |
On-line inquiry screens that meet the user interface requirements of this contract and provide access to the following data:
| |
| 1. | Provider eligibility history |
| |
| 2. | Basic information about a Provider (for example, name, location, number, program, provider type, specialty, sub-specialty, certification dates, effective dates) |
| |
| 3. | Provider group inquiry, by individual provider number displaying groups and by group number displaying individuals in group (with effective and end dates for those individuals within the group) |
| |
| 5. | Provider accounts receivable and payable data, including claims adjusted but not yet paid |
| |
| 6. | Provider Medicare number(s) by Medicare number, Medicaid number, and SSN/FEIN |
| |
| 7. | Demographic reports and maps from the GIS, for performing, billing, and/or enrolled provider, listing provider name, address, and telephone number to assist in the provider recruitment process and provider relations |
The Provider Data Maintenance function must accommodate an external interface with:
| |
| 2. | Other governmental agencies to receive licensure information. |
The reference function maintains pricing files for procedures and drugs including Mental/Behavioral Health Drugs and maintains other general reference information such as diagnoses and reimbursement parameters/modifiers. The reference function provides a consolidated source of reference information which is accessed by the MIS during performance of other functions, including claims and encounter processing, TPL processing and utilization/quality reporting functions.
The contractor must maintain sufficient reference data (NDC codes, HCPCS, CPT4, Revenue codes, etc.) to accurately process fee for service claims and develop encounter data for transmission to the Department as well as support Department required reporting.
The inputs to the Reference Data Maintenance function are:
| |
| 3. | ICD-9-CM or 10 and DSM III diagnosis and procedure updates |
B. Processing Requirements
The Reference Processing function must include the following capabilities:
| |
| 1. | Maintain current and historical reference data, assuring that updates do not overlay or otherwise make historical information inaccessible. |
| |
| 2. | Maintain a Procedure data set which is keyed to the five-character HCPCS code for medical-surgical and other professional services, ADA dental codes; a two-character field for HCPCS pricing modifiers; and the Department’s specific codes for other medical services; in addition, the procedure data set will contain, at a minimum, the following elements for each procedure: |
| |
| • | Thirty-six (36) months of date-specific pricing segments, including a pricing action code, effective beginning and end dates, and allowed amounts for each segment. |
| |
| • | Thirty-six (36) months of status code segments with effective beginning and end dates for each segment. |
| |
| • | Multiple modifiers and the percentage of the allowed price applicable to each modifier. |
| |
| • | Indication of TPL actions, such as Cost Avoidance, Benefit Recovery or Pay, by procedure code. |
| |
| • | Other information such as accident-related indicators for possible TPL, federal cost-sharing indicators, Medicare coverage and allowed amounts. |
| |
| 3. | Maintain a diagnosis data set utilizing the three (3), four (4), and five (5) character for ICD-9-CM and 7 digits for ICD-10 and DSM III coding system, which supports relationship editing between diagnosis code and claim information including but not limited to: |
| |
| • | Family planning indicator |
| |
| • | Prior authorization requirements |
| |
| • | Trauma diagnosis and accident cause codes |
| |
| • | Description of the diagnosis |
| |
| • | Permitted primary and secondary diagnosis code usage |
| |
| 4. | Maintain descriptions of diagnoses. |
| |
| 5. | Maintain flexibility in the diagnosis file to accommodate expanded diagnosis codes with the implementation of ICD-10 by October 1, 2013. |
| |
| 6. | Maintain a drug data set of the eleven (11) digit National Drug Code (NDC), including package size, which can accommodate updates from a drug pricing service and the CMS Drug Rebate file updates; the Drug data set must contain, at a minimum: |
| |
| • | Unlimited date-specific pricing segments that include all prices and pricing action codes needed to adjudicate drug claims. |
| |
| • | Indicator for multiple dispensing fees |
| |
| • | Indicator for drug rebate including name of manufacturer and labeler codes. |
| |
| • | Description and purpose of the drug code. |
| |
| • | Identification of the therapeutic class. |
| |
| • | Identification of discontinued NDCs and the termination date. |
| |
| • | Identification of CMS Rebate program status. |
| |
| • | Identification of strength, units, and quantity on which price is based. |
| |
| • | Indication of DESI status (designated as less than effective), and IRS status (identical, related or similar to DESI drugs). |
| |
| 7. | Maintain a Revenue Center Code data set for use in processing claims for hospital inpatient/outpatient services, home health, hospice, and such. |
| |
| 8. | Maintain flexibility to accommodate multiple reimbursement methodologies, including but not limited to fee-for-service, capitation and carve-outs from Capitated or other “all inclusive” rate systems, and DRG reimbursement for inpatient hospital care, etc. |
| |
| 9. | Maintain pricing files based on: |
| |
| • | Federal maximum allowable cost (FMAC), estimated acquisition (EAC) for drugs |
| |
| • | Percentage of charge allowance |
| |
| • | Contracted amounts for certain services |
| |
| • | Fee schedule that would pay at variable percentages. |
| |
| • | (MAC) Maximum allowable cost pricing structure |
C. On-line Inquiry Screens
Maintain on-line access to all Reference files with inquiry by the appropriate service code, depending on the file or table being accessed.
Maintain on-line inquiry to procedure and diagnosis files by name or description including support for phonetic and partial name search.
Provide inquiry screens that display:
| |
| • | All relevant pricing data and restrictive limitations for claims processing including historical information, and |
| |
| • | All pertinent data for claims processing and report generation. |
D. Interfaces
The Reference Data Maintenance function must interface with:
| |
| 3. | ICD-9, ICD-10, DSM, or other diagnosis/surgery code updating service; and |
The financial function encompasses claim payment processing, adjustment processing, accounts receivable processing, and all other financial transaction processing. This function ensures that all funds are appropriately disbursed for claim payments and all post-payment transactions are applied accurately. The financial processing function is the last step in claims processing and produces remittance advice statements/explanation of benefits and financial reports.
The Financial Processing function must accept the following inputs:
| |
| 1. | On-line entered, non-claim-specific financial transactions, such as recoupments, mass adjustments, cash transactions, etc; |
| |
| 2. | Retroactive changes to Member financial liability and TPL retroactive changes from the Member data maintenance function; |
| |
| 3. | Provider, Member, and reference data from the MIS. |
| |
| B. | Processing Requirements |
The MIS must perform three types of financial processing: 1) payment processing; 2) adjustment processing; 3) other financial processing. Required
system capabilities are classified under one of these headings in this subsection.
C. Payment Processing
Claims that have passed all edit, audit, and pricing processing, or which have been denied, must be processed for payment by the Contractor if the contractor has fee for service arrangements. Payment processing must include the capability to:
| |
| 1. | Maintain a consolidated accounts receivable function and deduct/add appropriate amounts and/or percentages from processed payments. |
| |
| 2. | Update individual provider payment data and 1099 data on the Provider database. |
D. Adjustment Processing
The MIS adjustment processing function must have the capabilities to:
| |
| 1. | Maintain complete audit trails of adjustment processing activities on the claims history files. |
| |
| 2. | Update provider payment history and recipient claims history with all appropriate financial information and reflect adjustments in subsequent reporting, including claim-specific and non claim-specific recoveries. |
| |
| 3. | Maintain the original claim and the results of all adjustment transactions in claims history; link all claims and subsequent adjustments by control number, providing for identification of previous adjustment and original claim number. |
| |
| 4. | Reverse the amount previously paid/recovered and then processes the adjustment so that the adjustment can be easily identified. |
| |
| 5. | Re-edit, re-price, and re-audit each adjustment including checking for duplication against other regular and adjustment claims, in history and in process. |
| |
| 6. | Maintain adjustment information which indicates who initiated the adjustment, the reason for the adjustment, and the disposition of the claim (additional payment, recovery, history only, etc.) for use in reporting the adjustment. |
| |
| 7. | Maintain an adjustment function to re-price claims, within the same adjudication cycle, for retroactive pricing changes, Member liability changes, Member or provider eligibility changes, and other changes necessitating reprocessing of multiple claims. |
| |
| 8. | Maintain a retroactive rate adjustment capability which will automatically identify all Claims affected by the adjustment, create adjustment records for them, reprocess them, and maintain a link between the original and adjusted Claim. |
E. Other Financial Processing
Financial transactions such as stop payments, voids, reissues, manual checks, cash receipts, repayments, cost settlements, overpayment adjustments, recoupments, and financial transactions processed outside the MIS are to be processed as part of the Financial Processing function. To process these transactions, the MIS must have the capability to:
1. Maintain the following information:
| |
| • | Program identification (for example, TPL recovery, rate adjustment); |
| |
| • | Transaction source (for example, system generated, refund, Department generated); |
| |
| • | Provider number/entity name and identification number; |
| |
| • | Payment/recoupment detail (for example, dates, amounts, cash or recoupment); |
| |
| • | Reason indicator for the transaction (for example, returned dollars from provider for TPL, unidentified returned dollars, patient financial liability adjustment); |
| |
| • | Type of collection (for example, recoupment, cash receipt); |
| |
| • | Adjustment indicator; and |
| |
| • | Internal control number (ICN) (if applicable). |
| |
| 2. | Accept manual or automated updates including payments, changes, deletions, suspensions, and write-offs, of financial transactions and incorporate them as MIS financial transactions for purposes of updating claims history, Provider/Member history, current month financial reporting, accounts receivable, and other appropriate files and reports. |
| |
| 3. | Maintain sufficient controls to track each financial transaction, balance each batch, and maintain appropriate audit trails on the claims history and consolidated accounts receivable system, including a mechanism for adding user narrative. |
| |
| 4. | Maintain on-line inquiry to current and historical financial information with access by Provider ID or entity identification, at a minimum to include: |
| |
| • | Current amount payable/due |
| |
| • | Total amount of claims adjudication for the period |
| |
| • | Aging of receivable information, according to user defined aging parameters |
| |
| • | Receivable account balance and established date |
| |
| • | Percentages and/or dollar amounts to be deducted from future payments |
| |
| • | Type and amounts of collections made and dates |
| |
| • | Both non-claim-specific, and |
| |
| • | Data to meet the Department’s reporting. |
| |
| 5. | Maintain a recoupment process that sets up Provider accounts receivable that can be either automatically recouped from claims payments or satisfied by repayments from the provider or both. |
| |
| 6. | Maintain a methodology to apply monies received toward the established recoupment to the accounts receivable file, including the remittance advice date, number, and amount, program, and transfer that data to an on-line provider paid claims summary. |
| |
| 7. | Identify a type, reason, and disposition on recoupments, payouts, and other financial transactions. |
| |
| 8. | Provide a method to link full or partial refunds to the specific Claim affected, according to guidelines established by the Department. |
| |
| 9. | Generate provider 1099 information annually, which indicate the total paid claims plus or minus any appropriate adjustments and financial transactions. |
| |
| 10. | Maintain a process to adjust providers’ 1099 earnings with payout or recoupment or transaction amounts through the accounts receivable transactions. |
| |
| 11. | Maintain a process to accommodate the issuance and tracking of non-provider-related payments through the MIS (for example, a refund or an insurance company overpayment) and adjust expenditure reporting appropriately. |
| |
| 12. | Track all financial transactions, by program and source, to include TPL recoveries, Fraud, Waste and Abuse recoveries, provider payments, drug rebates, and so forth. |
| |
| 13. | Determine the correct federal fiscal year within claim adjustments and other financial transactions are to be reported. |
| |
| 14. | Provide a method to direct payments resulting from an escrow or lien request to facilitate any court order or legal directive received. |
Reports from the financial processing function are described in Appendix L and Contractor Reporting Requirements Section of Contract.
| |
| II. | Utilization/Quality Improvement |
The utilization/quality improvement function combines data from other external systems, such as Geo Network to produce reports for analysis which focus on the review and assessment of access and availability of services and quality of care given, detection of over and under utilization, and the development of user-defined reporting criteria and standards. This system profiles utilization of Providers and Members and compares them against experience and norms for comparable individuals.
This system supports tracking utilization control function(s) and monitoring activities for inpatient admissions, emergency room use, and out-of-area services. It completes Provider profiles, occurrence reporting, monitoring and evaluation studies, and Member/Provider satisfaction survey compilations. The subsystem may integrate the Contractor’s manual and automated processes or incorporate other software reporting and/or analysis programs.
This system also supports and maintains information from Member surveys, Provider and Member Grievances, Appeal processes.
The Utilization/Quality Improvement system must accept the following inputs:
| |
| 1. | Adjudicated Claims/encounters from the claims processing subsystem; |
| |
| 2. | Provider data from the provider subsystem; |
| |
| 3. | Member data from the Member subsystem. |
| |
| B. | Processing Requirements |
The Utilization/Quality Improvement function must include the following capabilities:
| |
| 1. | Maintain Provider credentialing and recredentialing activities. |
| |
| 2. | Maintain Contractor’s processes to monitor and identify deviations in patterns of treatment from established standards or norms. Provide feedback information for monitoring progress toward goals, identifying optimal practices, and promoting continuous improvement. |
| |
| 3. | Maintain development of cost and utilization data by Provider and services. |
| |
| 4. | Provide aggregate performance and outcome measures using standardized quality indicators similar to Medicaid HEDIS as specified by the Department. |
| |
| 5. | Support focused quality of care studies. |
| |
| 6. | Support the management of referral/utilization control processes and procedures. |
| |
| 7. | Monitor PCP referral patterns. |
| |
| 8. | Support functions of reviewing access, use and coordination of services (i.e. actions of peer review and alert/flag for review and/or follow-up; laboratory, x-ray and other ancillary service utilization per visit). |
| |
| 9. | Store and report Member satisfaction data through use of Member surveys, Grievance/Appeals processes, etc. |
| |
| 10. | Provide Fraud, Waste and Abuse detection, monitoring and reporting. |
Utilization/quality improvement reports are listed in Appendices K and L.
| |
| III. | Claims Control and Entry |
The Claims Control function ensures that all claims are captured at the earliest possible time and in an accurate manner. Claims must be adjudicated within the parameters of Prompt Pay standards set by CMS and the American Recovery and Reinvestment Act (ARRA).
The Edit/Audit Processing function ensures that Claims are processed in accordance with Department and Contractor policy and the development of accurate encounters to be transmitted to the department. This processing includes application of non-history-related edits and history-related audits to the Claim. Claims are screened against Member and Provider eligibility information; pended and paid/denied claims history; and procedure, drug, diagnosis, and edit/audit information. Those Claims that exceed Program limitations or do not satisfy Program or processing requirements, suspend or deny with system assigned error messages related to the Claim.
Claims also need to be edited utilizing all components of the CMS mandated National Correct Coding Initiative (NCCI)
The inputs to the Edit/Audit Processing function are:
| |
| 1. | The Claims that have been entered into the claims processing system from the claims entry function; |
| |
| 2. | Member, Provider, reference data required to perform the edits and audits. |
| |
| B. | Processing Requirements |
Basic editing necessary to pass the Claims onto subsequent processing requires that the MIS have the capabilities to:
| |
| 1. | Edit each data element on the Claim record for required presence, format, consistency, reasonableness, and/or allowable values. |
| |
| 2. | Edit to assure that the services for which payment is requested are covered. |
| |
| 3. | Edit to assure that all required attachments are present. |
| |
| 4. | Maintain a function to process all Claims against an edit/audit criteria table and an error disposition file (maintained in the Reference Data Maintenance function) to provide flexibility in edit and audit processing. |
| |
| 5. | Edit for prior authorization requirements and to assure that a prior authorization number is present on the Claim and matches to an active Prior Authorization on the MIS. |
| |
| 6. | Edit Prior-Authorized claims and cut back billed units or dollars, as appropriate, to remaining authorized units or dollars, including Claims and adjustments processed within the same cycle. |
| |
| 7. | Maintain edit disposition to deny Claims for services that require Prior Authorization if no Prior Authorization is identified or active. |
| |
| 8. | Update the Prior Authorization record to reflect the services paid on the Claim and the number of services still remaining to be used. |
| |
| 9. | Perform relationship and consistency edits on data within a single Claim for all Claims. |
| |
| 10. | Perform automated audit processing (e.g., duplicate, conflict, etc.) using history Claims, suspended Claims, and same cycle Claims. |
| |
| 11. | Edit for potential duplicate claims by taking into account group and rendering Provider, multiple Provider locations, and across Provider and Claim types. |
| |
| 12. | Identify exact duplicate claims. |
| |
| 13. | Perform automated audits using duplicate and suspect-duplicate criteria to validate against history and same cycle claims. |
| |
| 14. | Perform all components of National Correct Coding Initiative (NCCI) edits |
| |
| 15. | Maintain audit trail of all error code occurrences linked to a specific Claim line or service, if appropriate. |
| |
| 16. | Edit and suspend each line on a multi-line Claim independently. |
| |
| 17. | Edit each Claim record completely during an edit or audit cycle, when appropriate, rather than ceasing the edit process when an edit failure is encountered. |
| |
| 18. | Identify and track all edits and audits posted to the claim from suspense through adjudication. |
| |
| 19. | Update Claim history files with both paid and denied Claims from the previous audit run. |
| |
| 20. | Maintain a record of services needed for audit processing where the audit criteria covers a period longer than thirty-six (36) months (such as once-in-a-lifetime procedures). |
| |
| 21. | Edit fields in Appendices D and E for validity (numerical field, appropriate dates, values, etc.). |
The Claims Pricing function calculates the payment amount for each service according to the rules and limitations applicable to each Claim type, category of service, type of provider, and provider reimbursement code. This process takes into consideration the Contractor allowed amount, TPL payments, Medicare payments, Member age, prior authorized amounts, and any co-payment requirements. Prices are maintained on the Reference files (e.g., by service, procedure, supply, drug, etc.) or provider-specific rate files and are date-specific.
The Contractor MIS must process and pay Medicare Crossover Claims and adjustments.
The inputs into the Claims Pricing function are the Claims that have been passed from the edit/audit process.
The Reference and Provider files containing pricing information are also inputs to this function.
| |
| B. | Processing Requirements |
The Claims Pricing function for those Fee For Service contracts the vendor has with providers of the MIS must have the capabilities to:
| |
| 1. | Calculate payment amounts according to the fee schedules, per diems, rates, formulas, and rules established by the Contractor. |
| |
| 2. | Maintain access to pricing and reimbursement methodologies to appropriately price claims at the Contractor’s allowable amount. |
| |
| 3. | Maintain flexibility to accommodate future changes and expanded implementation of co pays. |
| |
| 4. | Deduct Member liability amounts from payment amounts as defined by the Department. |
| |
| 5. | Deduct TPL amounts from payments amounts. |
| |
| 6. | Provide adjustment processing capabilities. |
| |
| VI. | Claims Operations Management |
The Claims Operations Management function provides the overall support and reporting for all of the Claims processing functions.
The inputs to the Claims Operations Management function must include all the claim records from each processing cycle and other inputs described for the Claims Control and Entry function.
| |
| B. | Processing Requirements |
The primary processes of Claims Operations Management are to maintain sufficient on-line claims information, provide on-line access to this information, and produce claims processing reports. The claims operations management function of the MIS must:
| |
| 1. | Maintain Claim history at the level of service line detail. |
| |
| 2. | Maintain all adjudicated (paid and denied) claims history. Claims history must include at a minimum: |
| |
| • | All submitted diagnosis codes (including service line detail, if applicable); |
| |
| • | Line item procedure codes, including modifiers; |
| |
| • | Member ID and medical coverage group identifier; |
| |
| • | Billing, performing, referring, and attending provider Ids and corresponding provider types; |
| |
| • | All error codes associated with service line detail, if applicable; |
| |
| • | Billed, allowed, and paid amounts; |
| |
| • | TPL and Member liability amounts, if any; |
| |
| • | Prior Authorization number; |
| |
| • | Procedure, drug, or other service codes; |
| |
| • | Date of service, date of entry, date of adjudication, date of payment, date of adjustment, if applicable. |
| |
| 3. | Maintain non-claim-specific financial transactions as a logical component of Claims history. |
| |
| 4. | Provide access to the adjudicated and Claims in process, showing service line detail and the edit/audits applied to the Claim. |
| |
| 5. | Maintain accurate inventory control status on all Claims. |
The following reports must be available from the Claims processing function ten days after the end of each month:
| |
| 1. | Number of Claims received, paid, denied, and suspended for the previous month by provider type with a reason for the denied or suspended claim. |
| |
| 2. | Number and type of services that are prior-authorized (PA) for the previous month (approved and denied). |
| |
| 3. | Amount paid to providers for the previous month by provider type. |
| |
| 4. | Number of Claims by provider type for the previous month, which exceed processing timelines standards defined by the Department. |
Claim Prompt Pay reports as defined by ARRA
Additional detail found in Appendix L.
Appendix D
Encounter Data Submission Requirements
| |
| I. | Contractor’s Encounter Record |
At a minimum, the Contractor will be required to electronically provide encounter Record to the Department on a weekly basis. Encounter Records must follow the format, data elements and method of transmission specified by the Department.
Encounter data will be utilized by the Department for the following purposes: 1) to evaluate access to health care, availability of services, quality of care and cost effectiveness of services, 2) to evaluate contractual performance, 3) to validate required reporting of utilization of services, 4) to develop and evaluate proposed or existing capitation rates, and 5) to meet CMS Medicaid reporting requirements.
The Contractor is required to electronically submit Encounter Record to the Department on a weekly scheduled basis. The submission is to include all adjudicated (paid and denied) Claims, corrected claims and adjusted claims processed by the Contractor for the previous month. Monthly Encounter Record transmissions that exceed a 5% threshold error rate (total claims/documents in error equal to or exceed 5% of claims/documents records submitted) will be returned to the Contractor in their entirety for correction and resubmission by the Contractor. Encounter data transmissions with a threshold error rate not exceeding 5% will be accepted and processed by the Department. Only those encounters that hit threshold edits will be returned to the contractor for correction and resubmission. Denied claims submitted for encounter processing will not be held to normal edit requirements and rejections of denied claims will not count towards the minimum 5% rejection.
Encounter Record must be submitted in the format defined by the Department as follows:
| |
| 1. | Health Insurance Portability and Accountability Act (HIPAA) Accredited Standards Committee (ASC) X12 version 4010A1 to ASC X12 version 5010 transaction 837 and National Council for Prescription Drug Programs (NCPDP) version 5.1 to NCPDP version 2.2 by January 1, 2012. Example transactions include the following: |
| |
| • | 837I – Instructional Transactions |
| |
| • | 837P – Professional Transactions |
| |
| • | 837D – Dental Transactions |
| |
| • | 278 – Prior Authorization Transactions |
| |
| • | 834 – Enrollment/Disenrollment |
| |
| • | 276/277 Claims Status Transactions |
| |
| • | 270/271 Eligibility Transactions |
| |
| • | 999 – Functional Acknowledgement |
| |
| 2. | Conversion from ICD-9 to ICD-10 for medical diagnosis and inpatient procedure coding by October 1, 2013. |
The Contractor is required to use procedure codes, diagnosis codes and other codes used for reporting Encounter data in accordance with guidelines defined by the Department. The Contractor must also use appropriate provider numbers as directed by the Department for Encounter data. The Encounter Record will be received and processed by Fiscal Agent and will be stored in the existing MIS.
Encounter corrections (encounter returned to the Contractor for correction, i.e., incorrect procedure code, blank value for diagnosis codes) will be transmitted to the Contractor electronically for correction and resubmission. Penalties will be assessed against the Contractor for each Encounter record, which is not resubmitted within thirty (30) days of the date the record is returned. The Contractor shall have the opportunity to dispute appropriateness of assessment of penalties prior to them occurring to attest to ongoing efforts regarding data acceptance.
The Department will conduct an annual validity study to determine the completeness, accuracy and timeliness of the Encounter Record provided by the Contractor.
Completeness will be determined by assessing whether the Encounter record transmitted includes each service that was provided. Accuracy will be determined by evaluating whether or not the values in each field of the Encounter record accurately represent the service that was provided. Timeliness will be determined by assuring that the Encounter record was transmitted to the Department the month after adjudication. The
Department will randomly select an adequate sample which will include hospital claims, provider claims, drug claims and other claims (any claims except in-patient hospital, provider and drug), to be designated as the Encounter Processing Assessment Sample (EPAS). The Contractor will be responsible to provide to the Department the following information as it relates to each Claim in order to substantiate that the Contractor and the Department processed the claim correctly:
| |
| • | A copy of the claim, either paper or a generated hard copy for electronic claims; |
| |
| • | Data from the paid claim’s file; |
| |
| • | Member eligibility/enrollment data; |
| |
| • | Provider eligibility data; |
| |
| • | Reference data (i.e., diagnosis code, procedure rates, etc.) pertaining to the Claim; |
| |
| • | Edit and audit procedures for the Claim; |
| |
| • | A copy of the remittance advice statement/explanation of benefits; |
| |
| • | A copy of the Encounter Record transmitted to the Department; and |
| |
| • | A listing of Covered Services. |
The Department will review each Claim from the EPAS to determine if complete, accurate and timely Encounter Record was provided to the Department. Results of the review will be provided to the Contractor. The Contractor will be required to provide a corrective action plan to the Department within sixty (60) Days if deficiencies are found.
| |
| II. | Encounter Data Requirements |
A. HIPAA 4010 Companion Guides
DMS Encounter Data Requirements are defined by HIPAA 4010 Companion Guides and are available at: https://ddipwb.kymmis.com-/KYXIXDDI/Subsystem/EDI and Claim Capture/Companion Guides/KY New MMIS Companion Guides
B. HIPAA 5010 Companion Guides
Effective January 1, 2012 the Department will be implementing HIPAA 5010 Companion Guides and will be provide upon completion.
III. Department’s Utilization of Submitted Encounter Records
The Contractor’s Encounter Records will be utilized by the Department for the following:
| |
| A. | To evaluate access to health care, availability of services, quality of care and cost effectiveness of services; |
| |
| B. | To evaluate contractual performance; |
| |
| C. | To validate required reporting of utilization of services; |
| |
| D. | To develop and evaluate proposed or existing Capitation Rates; |
| |
| E. | To meet CMS Medicaid reporting requirements; and |
| |
| F. | For any purpose the Department deems necessary. |
Appendix E
Encounter Data Submission Quality Standards
| |
| I. | Data quality efforts of the Department shall incorporate the following standards for monitoring and validation: |
| |
| A. | Edit each data element on the Encounter Record for required presence, format, consistency, reasonableness and/or allowable values; |
| |
| B. | Edit for Member eligibility; |
| |
| C. | Perform automated audit processing (e.g. duplicate, conflict, etc.) using history Encounter Record and same-cycle Encounter Record; |
| |
| D. | Identify exact duplicate Encounter Record; |
| |
| E. | Maintain an audit trail of all error code occurrences linked to a specific Encounter; and |
| |
| F. | Update Encounter history files with both processed and incomplete Encounter Record. |
II. Data Quality Standards for Evaluation of Submitted Encounter Data Fields
|
| | |
DATA QUALITY STANDARDS FOR EVALUATION OF SUBMITTED ENCOUNTER DATA FIELDS Based on CMS Encounter Validation Protocol |
| Data Element | Expectation | Validity Criteria |
| Enrollee ID | Should be valid ID as found in the State’s eligibility file. Can use State’s ID unless State also accepts SSN. | 100% valid |
| Enrollee Name | Should be captured in such a way that makes separating pieces of name easy. There may be some confidentiality issues that make this difficult to obtain. If collectable, expect data to be present and of good quality | 85% present. Lengths should vary and there should be at least some last names >8 digits and some first names < 8 digits. This will validate that fields have not been truncated. Also verify that a high percentage have at least a middle initial. |
| Enrollee Date of Birth | Should not be missing and should be a valid date. | 2% missing or invalid |
| MCO/PIHP ID | Critical Data Element | 100% valid |
| Provider ID | Should be an enrolled provider listed in provider enrollment file. | 95% valid |
| Attending Provider NPI | Should be an enrolled provider listed in provider enrollment file (also accept the MD license number if listed in provider enrollment file). | > 85% match with provider file using either provider ID or MD license number |
| Provider Location | Minimal requirement is county code, with zip code being strongly advised. | • 95% with valid county code • > 95% with valid zip code (if available) |
Appendix F
Third Party Liability/Coordination of Benefits Requirements
| |
| I. | To meet the requirements of 42 CFR 433.138 through 433.139, the Contractor shall be responsible for: |
| |
| A. | Maintaining an MIS that includes: |
| |
| 1. | Third Party Liability Resource File |
| |
| • | Insurance Company Address |
| |
| a) | Cost Avoidance - Use automated daily and monthly TPL files to update the Contractor’s MIS TPL files as appropriate. This information is to cost avoid claims for members who have other insurance. |
| |
| b) | DMS shall require the Contractor to do data matches with insurers. DMS shall require the Contractor to obtain subscriber data and perform data matches with a specified list of insurance companies, as defined by DMS. |
| |
| c) | Department for Community Based Services (DCBS) - Apply Third Party Liability (TPL) information provided electronically on a daily basis by DMS through its contract with DCBS to have eligibility caseworkers collect third party liability information during the Recipient application process and reinvestigation process. |
| |
| d) | Workers’ Compensation -. The data is provided electronically on a quarterly basis by DMS to the Contractor. This data should be applied to TPL files referenced in I.A.1.a (Commercial Data Matching) in this Appendix. |
| |
| 2. | Third Party Liability Billing File |
| |
| • | TCN Status Code (Code identifies if claim was denied and the reason for the denial) |
| |
| • | Billing Type (Code identifies claim was billed to insurance policy) |
| |
| a) | Commercial Insurance/Medicare Part B Billing - The Contractor’s MIS should automatically search paid claim history and recover from providers, insurance companies or Medicare Part B in a nationally accepted billing format for all claim types whenever other commercial insurance or Medicare Part B coverage is discovered and added to the Contractor’s MIS that was unknown to the Contractor at the time of payment of a claim or when a claim could not be cost avoided due to federal regulations (pay and chase) which should have been paid by the health plan. Within sixty (60) Days from the date of identification of the other third party resource billings must be generated and sent to liable parties. |
| |
| b) | Medicare Part A - The Contractor’s MIS should automatically search paid claim history and generate reports by Provider of the billings applicable to Medicare Part A coverage whenever Medicare Part A coverage is discovered and added to the Contractor’s MIS that was unknown to the Contractor at the time of payment of a claim. Providers who do not dispute the Medicare coverage should be instructed to bill Medicare immediately. The Contractor’s MIS should recoup the previous payment from the Provider within sixty (60) days from the date the reports are sent to the Providers, if they do not dispute that Medicare coverage exists. |
| |
| c) | Manual Research/System Billing - System should include capability for the manual setup for billings applicable to workers’ compensation, casualty, absent parents and other liability coverage that require manual research to determine payable claims. |
| |
| • | Type of Questionnaire Sent |
All questionnaires should be tracked in a Questionnaire history file on the MIS.
| |
| B. | Coordination of Third Party Information (COB) |
| |
| 1. | Division of Child Support Enforcement (DCSE) |
Provide county attorneys and the Division of Child Support Enforcement (DCSE) upon request with amounts paid by the Contractor in order to seek restitution for the payment of past medical bills and to obtain insurance coverage to cost avoid payment of future medical bills.
Actively pursue recovery from carriers or members with settlements. Contractor shall provide the necessary information regarding paid claims to necessary parties in order to seek recovery from liable parties in legal actions involving Members.
Notify DMS with information regarding casualty or liability insurance (i.e. auto, homeowner's, malpractice insurance, etc.) when lawsuits are filed and attorneys are retained as a result of tort action. This information should be referred in writing within five (5) working Days of identifying such information.
In cases where an attorney has been retained, a lawsuit filed or a lump sum settlement offer is made, the Contractor shall notify Medicaid within five days of identifying such information so that recovery efforts can be coordinated and monthly through a comprehensive report.
| |
| • | Edit and cost avoid Claims when Member has Medicare coverage; |
| |
| • | Edit and cost avoid Claims when Provider indicates other insurance on claim but does not identify payment or denial from third party; |
| |
| • | Edit and cost avoid Claims when Provider indicates services provided were work related and does not indicate denial from workers’ compensation carrier; |
| |
| • | Edit and cost avoid or pay and chase as required by federal regulations when Member has other insurance coverage. When cost avoiding, the Contractor’s MIS should supply the Provider with information on the remittance advice that would be needed to bill the other insurance, such as carrier name, address, policy #, etc.; |
| |
| • | Edit Claims as required by federal regulations for accident/trauma diagnosis codes. Claims with the accident/trauma diagnosis codes should be flagged and accumulated for ninety (90) Days and if the amount accumulated exceeds $250, a questionnaire should be sent to the Member in an effort to identify whether other third party resources may be liable to pay for these medical bills; |
| |
| • | The Contractor is prohibited from cost avoiding Claims when the source of the insurance coverage was due to a court order. All Claims with the exception of hospital Claims must be paid and chased. Hospital claims may be cost avoided; and |
| |
| • | A questionnaire should be generated and mailed to Members and/or Providers for claims processed with other insurance coverage indicated on the claim and where no insurance coverage is indicated on the Contractor’s MIS Third Party Files. |
| |
| II. | DMS shall be responsible for the following: |
| |
| A. | Provide the Contractor with an initial third party information proprietary file; |
| |
| B. | Provide, through a proprietary data file, copies of insurance company’s subscriber eligibility files that are received by DMS; |
| |
| C. | Provide proprietary data files of third party information transmitted from DCBS; |
| |
| D. | Ensuring the Contractors obtain a data match file from the Labor Cabinet on a quarterly basis; |
| |
| E. | Provide the Contractor with a list of the Division of Child Support Contracting Officials. |
| |
| F. | Ensure coordination of calls from attorneys to the Contractor in order for their Claims to be included in casualty settlements; and |
| |
| G. | Monitoring Encounter Claims and reports submitted by the Contractor to ensure that the Contractor performs all required activities. |
Appendix G
Network Provider File Layout Requirements
I. MCO Provider Network
Submit one delimited text file per network. Submit one record for each provider type to include the values in the layout. Template to be supplemented with additional requirements.
|
| | |
| Field Name | Field Size | Valid Values |
| Provider Type | 2 | Utilize valid values from sheet titled Medicaid Provider Types |
| Provider Contracted | 1 | Valid values are C or L. C=provider has a signed contract to be a participating provider in the network or L=provider has signed a letter of intent stating they will be a participating provider in the network. |
| Provider License | 10 | Must be submitted for physicians and leave blank if physician is licensed in a state other than Kentucky. |
| National Provider Identifier (NPI) | 10 | Must be submitted for providers required to have an NPI. |
| Medicaid Provider ID | 10 | Provider ID assigned by Kentucky Medicaid. Must be submitted - if known. |
| Primary Specialty Code | 3 | Utilize valid values from sheet titled Medicaid Provider Specialties (Required Field even for PCPs) |
| Secondary Specialty Code | 3 | Utilize valid values from sheet titled Medicaid Provider Specialties |
| Name | 50 | If a physician name, enter as last name, first name, MI. |
| Address Line 1 | 50 | DO NOT SUBMIT PO BOX OR MAILING ADDRESS. THIS MUST BE LOCATION ADDRESS! |
| Address Line 2 | 50 | DO NOT SUBMIT PO BOX OR MAILING ADDRESS. THIS MUST BE LOCATION ADDRESS! |
| City | 50 | |
|
| | |
| State | 2 | |
| Zip Code | 5 | |
| County Code | 3 | County Code of the Provider's location address. See sheet titled for Kentucky County Codes |
| Phone Number | 15 | Do not include dashes, etc. |
| Latitude | 11 | Latitude of the Provider's location address. Precision to the 6th digit. Must be in format 99.999999 |
| Longitude | 11 | Longitude of the Provider's location address. Precision to the 6th digit. Must be in format -99.999999 |
| PCP Specialist or Both | 1 | Valid entries are P, S or B. P=PCP, S=Speciatity, B=Both. Leave blank for all other providers. |
| PCP Open or Closed Panel | 1 | Mandatory for PCP. Valid entries are O or C. O=Open, C=Closed. Leave blank for all other providers. |
| PCP Panel Size | 9 | PCP Provider's maximum panel size |
| PCP Panel Enrollment | 9 | PCP Provider's current panel enrollment count |
Appendix H
Credentialing Process Coversheet
| |
| 2. | Address-Physical & telephone number |
| |
| 6. | Address-1099 & telephone number |
| |
| 12. | Begin and End date of Eligibility |
| |
| 17. | Previous Provider Number (if applicable) this also includes Change in Ownership |
| |
| 18. | Existing provider number if EPSDT |
| |
| 22. | Supervising Physician (for Physician Assist) |
| |
| 23. | Map 347 (need group# and effective date) |
| |
| 24. | EFT (Account # and ABA #) |
| |
| 26. | DEA (Effective and Expiration dates) |
| |
| 28. | Document Control Number |
| |
| 29. | Contractor Credentialing Date |
| |
| 30. | Credentialing Required |
Appendix I
Covered Services
| |
| I. | Contractor Covered Services |
| |
| A. | Alternative Birthing Center Services |
| |
| B. | Ambulatory Surgical Center Services |
| |
| D. | Community Mental Health Center Services |
| |
| E. | Dental Services, including Oral Surgery, Orthodontics and Prosthodontics |
| |
| F. | Durable Medical Equipment, including Prosthetic and Orthotic Devices, and Disposable Medical Supplies |
| |
| G. | Early and Periodic Screening, Diagnosis & Treatment (EPSDT) screening and special services |
| |
| H. | End Stage Renal Dialysis Services |
| |
| I. | Family Planning Clinic Services in accordance with federal and state law and judicial opinion |
| |
| J. | Hearing Services, including Hearing Aids for Members Under age 21 |
| |
| L. | Hospice Services (non-institutional only) |
| |
| N. | Independent Laboratory Services |
| |
| O. | Inpatient Hospital Services |
| |
| P. | Inpatient Mental Health Services |
| |
| Q. | Meals and Lodging for Appropriate Escort of Members |
| |
| R. | Medical Detoxification as defined in 907 KAR 1:705 |
| |
| S. | Medical Services, including but not limited to, those provided by Physicians, Advanced Practice Registered Nurses, Physicians Assistants and FQHCs, Primary Care Centers and Rural Health Clinics |
| |
| T. | Organ Transplant Services not Considered Investigational by FDA |
| |
| U. | Other Laboratory and X-ray Services |
| |
| V. | Outpatient Hospital Services |
| |
| W. | Outpatient Mental Health Services |
| |
| X. | Pharmacy and Limited Over-the-Counter Drugs including Mental/Behavioral Health Drugs |
| |
| Z. | Preventive Health Services, including those currently provided in Public Health Departments, FQHCs/Primary Care Centers, and Rural Health Clinics |
| |
| AA. | Psychiatric Residential Treatment Facilities (Level I and Level II) |
| |
| BB. | Specialized Case Management Services for Members with Complex Chronic Illnesses (Includes adult and child targeted case management) |
| |
| CC. | Therapeutic Evaluation and Treatment, including Physical Therapy, Speech Therapy, Occupational Therapy |
| |
| DD. | Transportation to Covered Services, including Emergency and Ambulance Stretcher Services |
| |
| EE. | Urgent and Emergency Care Services |
| |
| FF. | Vision Care, including Vision Examinations, Services of Opticians, Optometrists and Ophthalmologists, including eyeglasses for Members Under age 21 |
| |
| GG. | Specialized Children’s Services Clinics |
| |
| II. | Member Covered Services and Summary of Benefits Plan |
| |
| A. | General Requirements and Limitations |
The Contractor shall provide, or arrange for the provision of, health services, including Emergency Medical Services, to the extent services are covered for Members under the then current Kentucky State Medicaid Plan, as designated by the department in administrative regulations adopted in accordance with KRS Chapter 13A and as required by federal and state regulations, guidelines, transmittals, and procedures.
This Appendix was developed to provide, for illustration purposes only, the Contractor with a summary of currently covered Kentucky Medicaid services and to communicate guidelines for the submission of specified Medicaid reports. The summary is not meant to act, nor serve as a substitute for the then current administrative regulations and the more detailed information relating to services which is contained in administrative regulations governing provision of Medicaid services (907 KAR Chapters 1, 3 4, 10 and 11) and in individual Medicaid program services benefits summaries incorporated by reference in the administrative regulations. If the Contractor questions whether a service is a Covered Service or Non-Covered Service, the Department reserves the right to make the final determination, based on the then current administrative regulations in effect at the time of the contract.
Administrative regulations and incorporated by reference Medicaid program services benefits summaries may be accessed by contacting:
Kentucky Cabinet for Health and Family Services
Department for Medicaid Services
275 East Main Street, 6th Floor
Frankfort, Kentucky 40621
Kentucky’s administrative regulations are also accessible via the Internet at http//www.ky.gov
Kentucky Medicaid covers only Medically Necessary services. These services are considered by the Department to be those which are reasonable and necessary to establish a diagnosis and provide preventive, palliative, curative or restorative treatment for physical or mental conditions in accordance with the standards of health care generally accepted at the time services are provided, including but not limited to services for children in accordance with 42 USC 1396d(r). Each service must be sufficient in amount, duration, and scope to reasonably achieve its purpose. The amount, duration, or scope of coverage must not be arbitrarily denied or reduced solely because of the diagnosis, scope of illness, or condition.
The Contractor shall provide any Covered Services ordered to be provided to a Member by a Court, to the extent not in conflict with federal laws. The Department shall provide written notification to the Contractor of any court-ordered service. The Contractor shall additionally cover forensic pediatric and adult sexual abuse examinations performed by health care professional(s) credentialed to perform such examinations and any physical and sexual abuse examination(s) for any Member when the Department for Community Based Services is conducting an investigation and determines that the examination(s) is necessary.
| |
| III. | EMERGENCY CARE SERVICES (42 CFR 431.52) |
The Contractor must provide, or arrange for the provision of, all covered emergency care immediately using health care providers most suitable for the type of injury or illness in accordance with Medicaid policies and procedures, even when services are provided outside the Contractor’s region or are not available using Contractor enrolled providers. Conditions related to provision of emergency care are shown in 42 CFR 438.144.
| |
| IV. | MEDICAID SERVICES COVERED AND NOT COVERED BY THE CONTRACTOR |
The Contractor must provide Covered Services under current administrative regulations. The scope of services may be expanded with approval of the Department and as necessary to comply with federal mandates and state laws. Certain Medicaid services are currently excluded from the Contractor benefits package, but continue to be covered through the traditional fee-for-service Medicaid Program. The Contractor will be expected to be familiar with these Contractor excluded services, designated Medicaid “wrap-around” services and to coordinate with the Department’s providers in the delivery of these services to Members.
Information relating to these excluded services’ programs may be accessed by the Contractor from the Department to aid in the coordination of the services.
| |
| A. | Health Services Not Covered Under Kentucky Medicaid |
Under federal law, Medicaid does not receive federal matching funds for certain services. Some of these excluded services are optional services that the Department may or may not elect to cover. The Contractor is not required to cover services that Kentucky Medicaid has elected not to cover for Members.
Following are services currently not covered by the Kentucky Medicaid Program:
| |
| • | Any laboratory service performed by a provider without current certification in accordance with the Clinical Laboratory Improvement Amendment (CLIA). This requirement applies to all facilities and individual providers of any laboratory service; |
| |
| • | Cosmetic procedures or services performed solely to improve appearance; |
| |
| • | Hysterectomy procedures, if performed for hygienic reasons or for sterilization only; |
| |
| • | Medical or surgical treatment of infertility (e.g., the reversal of sterilization, invitro fertilization, etc.); |
| |
| • | Induced abortion and miscarriage performed out-of-compliance with federal and Kentucky laws and judicial opinions; |
| |
| • | Personal service or comfort items; |
| |
| • | Services, including but not limited to drugs, that are investigational, mainly for research purposes or experimental in nature; |
| |
| • | Sex transformation services; |
| |
| • | Sterilization of a mentally incompetent or institutionalized member; |
| |
| • | Services provided in countries other than the United States, unless approved by the Secretary of the Kentucky Cabinet for Health and Family Services; |
| |
| • | Services or supplies in excess of limitations or maximums set forth in federal or state laws, judicial opinions and Kentucky Medicaid program regulations referenced herein; |
| |
| • | Services for which the Member has no obligation to pay and for which no other person has a legal obligation to pay are excluded from coverage; and |
| |
| • | Services for substance abuse diagnoses in adults except for pregnant women, or in cases where acute care physical health services related to substance abuse or detoxification are necessarily required. |
| |
| V. | Health Services Limited by Prior Authorization |
The following services are currently limited by Prior Authorization of the Department for Members. Other than the Prior Authorization of organ transplants, the Contractor may establish its own policies and procedures relating to Prior Authorization.
| |
| • | Early and Periodic Screening, Diagnosis and Treatment (EPSDT) Special Services |
The Contractor is responsible for providing and coordinating Early and Periodic Screening, Diagnosis and Treatment Services (EPSDT), and EPSDT Special Services, through the primary care provider (PCP), for any Member under the age of twenty-one (21) years.
EPSDT Special Services must be covered by the Contractor and include any Medically Necessary health care, diagnostic, preventive, rehabilitative or therapeutic service that is Medically Necessary for a Member under the age of twenty-one (21) years to correct or ameliorate defects, physical and mental illness, or other conditions whether the needed service is covered by the Kentucky Medicaid State Plan in accordance with Section 1905 (a) of the Social Security Act.
| |
| • | Transplantation of Organs and Tissue (907 KAR 1:350) |
| |
| • | Other Prior Authorized Medicaid Services |
Other Medicaid services limited by Prior Authorization are identified in the individual program coverage areas in Section VI.
| |
| VI. | Current Medicaid Programs’ Services and Extent of Coverage |
The Contractor shall cover all services for its Members at the appropriate level, in the appropriate setting and as necessary to meet Members’ needs to the extent services are currently covered. The Contractor may expand coverage to include other services not routinely covered by Kentucky Medicaid, if the expansion is approved by the Department, if the services are deemed cost effective and Medically Necessary, and as long as the costs of the additional services do not affect the Capitation Rate.
The Contractor shall provide covered services as required by the following statutes or administrative regulations:
| |
| • | Medical Necessity and Clinical Appropriate Determination Basis |
(907 KAR 3:130)
| |
| • | Alternative Birthing Center Services (907 KAR 1:180) |
| |
| • | Ambulatory Surgical Center and Anesthesia Services (907 KAR 1:008) |
| |
| • | Chiropractic Services (907 KAR 3:125) |
| |
| • | Commission for Children with Special Health Care Needs |
(907 KAR 1:440)
Certain Medically Necessary services provided by the Commission for Children with Special Health Care Needs for Members identified with special needs. Coverage includes physician, EPSDT, dental, occupational therapy, physical therapy, speech therapy, durable medical equipment, genetic screening and counseling, audiological, vision, case management, laboratory and x-ray, psychological and hemophilia treatment and related services.
| |
| • | Community Mental Health Center Services (907 KAR 1:044 and 907 KAR 3:110) |
| |
| • | Dental Health Services (907 KAR 1:026) |
| |
| • | Dialysis Center Services (907 KAR 1:400) |
| |
| • | Durable Medical Equipment, Medical Supplies, Orthotic and Prosthetic Devices (907 KAR 1:479) |
| |
| • | Early and Periodic Screening, Diagnosis and Treatment (EPSDT) Services (907 KAR 11:034) |
| |
| • | Family Planning Clinic Services (907 KAR 1:048 & 1:434) |
| |
| • | Hearing Program Services (907 KAR 1:038) |
| |
| • | Home Health Services (907 KAR 1:030) |
| |
| • | Hospice Services – non-institutional (907 KAR 1:330 & 1: 436) |
| |
| • | Hospital Inpatient Services (907 KAR 10:012 & 10:376) |
| |
| • | Hospital Outpatient Services (907 KAR 10:014 & 10:376) |
| |
| • | Laboratory Services (907 KAR 1:028) |
| |
| • | Medicare Non-Covered Services (907 KAR 1:006) |
| |
| • | Mental Health Inpatient Services (907 KAR 10:016) |
| |
| • | Mental Health Outpatient Services (see physician, community mental health |
center, FQHC and RHC)
| |
| • | Nursing Facility Services (907 KAR 1:022 & 1:374) |
| |
| • | Other Laboratory and X-ray Provider Services (907 KAR 1:028) |
| |
| • | Outpatient Pharmacy Prescriptions and Over-the-Counter Drugs including |
| |
| • | Mental/Behavioral Health Drugs (907 KAR 1:019, KRS 205.5631, 205,5632, |
| |
| • | KS 205.560) Psychiatric Residential Treatment Facility Services – (907 KAR 1:505) |
| |
| • | Physicians and Nurses in Advanced Practice Medical Services (907 KAR 3:005 and 907 KAR 1:102) |
| |
| • | Podiatry Services (907 KAR 1:270) |
| |
| • | Preventive Health Services (907 KAR 1:360) |
| |
| • | Primary Care and Rural Health Center Services (907 KAR 1:054, 1:082, 1:418 and 1:427) |
| |
| • | Sterilization, Hysterectomy and Induced Termination of Pregnancy Procedures (Sterilizations of both male and female Members are covered only when performed in compliance with federal regulations 42 CFR 441.250.) |
These services are covered in accordance with Kentucky Law (KRS 205.560) and a United States District Court judge ruling in the case of Glenda Hope, et al. v. Masten Childers, et al.
| |
| • | Targeted Case Management Services (907 KAR 1:515, 907 KAR 1:525, 907 KAR 1:550 and 907 KAR 1:555) |
| |
| • | Transportation, including Emergency and Non-emergency Ambulance (907 KAR 1:060) |
| |
| • | Vaccines for Children (VFC) Program (907 KAR 1:680) Vision Services (907 KAR 1:038) |
| |
| • | Specialized Children’s Services Clinics (907 KAR 3:160) |
Appendix J
Early and Periodic Screening, Diagnosis and Treatment Program Periodicity Schedule *
Infancy
-- 3 to 5 days
-- < 1 month
-- 2 months
-- 4 months
-- 6 months
-- 9 months
-- 12 months
Early Childhood
-- 15 months
-- 18 months
-- 24 months
-- 30 months
-- 3 years
-- 4 years
Middle Childhood
-- 5 years
-- 6 years
-- 7 years
-- 8 years
-- 9 years
-- 10 years
Adolescence
-- 11 years
-- 12 years
-- 13 years
-- 14 years
-- 15 years
-- 16 years
-- 17 years
-- 18 years
-- 19 years
-- 20 years
| |
| • | EPSDT Periodicity Schedule is based on American Academy Pediatric Guidelines and is subject to change with these guidelines. |
Early and Periodic Screening, Diagnosis and Treatment
Required Components - Initial and Periodic Health Assessments
|
| |
Health History:
| |
Complete History Interval History | Initial Visit Each Visit |
By History /Physical Exam: | |
| Developmental Assessment | Each Visit |
| (Age appropriate physical and mental health milestones) | |
| Nutritional Assessment | Each Visit |
| Lead Exposure Assessment | 6 mo. through 6 yr. age visits |
| | |
Physical Exam:
| |
| Complete/ Unclothed | Each Visit |
| Growth Chart | Each Visit |
| Vision Screen | Assessed each visit *According to recommended medical standards (AAP1) |
| Hearing Screen | Assessed Each Visit *According to recommended medical standards (AAP1) |
| Laboratory: | |
| Hemoglobin/ Hematocrit | *According to recommended medical standards (AAP1) |
| Urinalysis | *According to recommended medical stans (AAP1) |
| Lead Blood Level (Low Risk History) | 12 mo. and 2 year age visit |
| Lead Blood Level (High Risk History) | Immediately |
| Cholesterol Screening | *According to recommended medical standards (AAP1) |
| Sickle Cell Screening | Documentation X 1 |
| Hereditary/ Metabolic Screening | * According to Kentucky statute |
| (Newborn Screening) | |
| Sexually Transmitted Disease Screening | *According to recommended medical standards (AAP1) |
| Pelvic Exam (pap smear) | *According to recommended medical standards (AAP1) |
| Immunizations: | |
| DPT | Assessed Each Visit |
| DTaP | *According to recommended OPVmedical standards (AAP1, ACIP2, Hepatitis BAAFP3) |
| HiB | |
|
| |
| Immunizations: Cont. | |
| MMR | |
| Varicella | |
| Td | |
| PPD | |
| | |
| Health Education/ Anticipatory Guidance | |
| (Age Appropriate) | Each Visit |
| | |
| Dental Referral | Age 1 |
1. AAP American Academy of Pediatrics
(Committee on Practice and Ambulatory Medicine)
2. ACIP Advisory Committee on Immunization Practices
3. AAFP American Academy of Family Physicians
EPSDT provides any Medically Necessary diagnosis and treatment for Members under the age of 21 indicated as the result of an EPSDT health assessment or any other encounter with a licensed or certified health care professional, even if the service is not otherwise covered by the Kentucky Medicaid Program. These services which are not otherwise covered by the Kentucky Medicaid Program are called EPSDT Special Services.
The Contractor shall provide EPSDT Special Services as required by 42 USC Section 1396 and by 907 KAR 1:034, Section 7 and Section 8.
The Contractor shall provide the following medically necessary health care, diagnostic services, preventive services, rehabilitative services, treatment and other measures, described in 42 USC Section 1396d(a), to all members under the age of 21:
| |
| (a) | Inpatient Hospital Services; |
| |
| (b) | Outpatient Services; Rural Health Clinics; Federally Qualified Health Center Services; |
| |
| (c) | Other Laboratory and X-Ray Services; |
| |
| (d) | Early and Periodic Screening, Diagnosis, and Treatment Services; Family Planning Services and Supplies; |
| |
| (e) | Physicians Services; Medical and Surgical Services furnished by a Dentist; |
| |
| (f) | Medical Care by Other Licensed Practitioners; |
| |
| (g) | Home Health Care Services; |
| |
| (h) | Private Duty Nursing Services; |
| |
| (k) | Physical Therapy and Related Services; |
| |
| (l) | Prescribed Drugs including Mental/Behavioral Health Drugs, Dentures, and Prosthetic Devices; and Eyeglasses; |
| |
| (m) | Other Diagnostic, Screening, Preventive and Rehabilitative Services; |
| |
| (n) | Nurse-Midwife Services; |
| |
| (p) | Case Management Services; |
| |
| (q) | Respiratory Care Services; |
| |
| (r) | Services provided by a certified pediatric nurse practitioner or certified family; |
Nurse practitioner (to the extent permitted under state law);
| |
| (s) | Other Medical and Remedial Care Specified by the Secretary; and |
| |
| (t) | Other Medical or Remedial Care Recognized by the Secretary but which are not covered in the Plan Including Services of Christian Science Nurses, Care and Services Provided in Christian Science Sanitariums, and Personal Care Services in a Recipient’s Home. |
Those EPSDT diagnosis and treatment services and EPSDT Special Services which are not otherwise covered by the Kentucky Medicaid Program shall be covered subject to Prior Authorization by the Contractor, as specified in 907 KAR 1:034, Section 9. Approval of requests for EPSDT Special Services shall be based on the standard of Medical Necessity specified in 907 KAR 1:034, Section 9.
The Contractor shall be responsible for identifying Providers who can deliver the EPSDT special services needed by Members under the age of 21, and for enrolling these Providers into the Contractor’s Network, consistent with requirements specified in this Contract.
Appendix K
Reporting Requirements
These report formats and accompanying report templates are used by the Kentucky Department for Medicaid Services (DMS) to monitor and evaluate the Contractor’s performance and to inform CMS and other interested parties of activities and progress on a quarterly basis. The reports should be a detailed rather than a general treatment of issues and events of the reporting period. All information in these reports should be for the most recent three-month period unless otherwise noted and submitted within ten (10) days of the end of each reporting period.
The Contractor shall review all reports for accuracy and completeness prior to submitting to the Department. Any noticeable variances identified in report comparisons shall include a detailed explanation which explains the reason for the discrepancy and the actions taken to resolve the problem, if applicable.
Utilization data for reports in Appendices K and L should be reported annually for the twelve (12) month period beginning with January 1 through December 31 and should allow a 90-day run out period past the end of the twelve-month period.
Provide an overview of the content of the report summarizing each topic. The Contractor should include summarize significant activities during the reporting period, problems or issues during the reporting period, and any program modifications that occurred during the reporting period. The overview should also contain success stories or positive results that were achieved during the reporting period, any specific problem area that the Contractor plans to address in the future, and a summary of all press releases and issues covered by the press.
| |
| II. | ELIGIBILITY/ENROLLMENT |
| |
| A. | Enrollment Changes During the Quarter |
Summarize all changes in the number of persons enrolled during the report period. Include a summary discussion of enrollees by aid category and by age according to Utilization Report #1, Enrollment Summary (see example table below). Discuss the trends in enrollment and any issues or concerns related to enrollment. Discuss any plans or outreach efforts to expand enrollment to qualified potential members.
| |
| B. | PCP Changes During the Report Period |
(These reports are required on a quarterly basis, and once annually. The Annual Report is produced by analyzing the top 10% providers for each quarter, combining them into one report. Any physician/group can be listed up to four times in the table for the annual report.)
Identify PCPs with voluntary member enrollment change activity and the percent change in members per PCP. A member enrollment change is defined as any change in a members PCP assignment for reasons other than member disenrollment. This report should be based on the PCP’s total panel size, not his/her office location panel size. The following tables provide example layouts:
PCP Changes During the Report Period
|
| | | | | | | |
Physician/Group ID |
Physician/Group Name |
Beginning Panel Enrollment Size |
Number of Members that requested voluntary change
|
Overall Net Change (+-) in Panel Enrollment Size |
Ending Panel Enrollment Size |
Percent Change |
PCP Assignment initiated by who: Member, Provider or Contractor
|
| |
| C. | PCP’s with Panel Changes Greater than 50 or 10% |
Briefly narrate reasons for those voluntary member transfers that exceed the lessor of 50 or 10% of total panel. The purpose for the change is to place emphasis on looking at reasons for voluntary changes and less on routine member transfers due to new enrollment activity. (See note under B. above for annual report
PCP’s with Panel Changes Greater than 50 or 10%
|
| | | | | | |
| Provide an electronic copy of PCPs w/n panel changes greater than 50% or 10% format below | Physician/Group ID |
Physician/Group Name |
Beginning Panel Enrollment Size |
Number of Members that requested voluntary change
|
Percent Change |
Ending Panel Enrollment Size |
| |
| III. | ACCESS/DELIVERY NETWORK |
| |
| A. | GeoNetworks Reports and Maps |
Distribution and Analysis of Current Provider Network and Beneficiaries
Annually, due on July 31 of each year include the following GeoNetworks reports: Title page, table of contents, accessibility standard comparison, accessibility standard detail, accessibility detail, accessibility summary, member map, provider listing, provider map, service area detail. Discuss monitoring and analysis of the GeoNetwork reports and maps to determine utilization patterns especially those of Members with special healthcare needs. Do not include member listing. Include a 3 computer diskette containing the GeoNetworks .dbf files used for the members and providers as well as the GeoNetworks .rpt file(s).
| |
| B. | Access Issues/Problems Identified During the Report Period and/or Remedial Action Taken |
Provide specific information on the nature of any access problems identified and any plans or remedial action taken. Include a summary of all provider and member complaints about access issues, responses to member and provider survey questions dealing with access, analysis of GeoAccess reports, and notification of the Contractor by DMS of network access problems.
| |
| C. | Listing of Providers Denied Participation |
Provide a listing of providers that requested participation in the MCO network during the report period but were denied. Include reasons for denials.
Provide a summary (count) of providers that terminated their contract(s) with the Contractor during the report period and the reasons for the terminations. (Sample listing of termination reasons below. Add other reasons as needed.)
|
| |
| Reason for Provider Termination | Number |
| Retired | |
| Deceased | |
| Moving Out of Service Area | |
| Cap/Fees Too Low | |
| No Longer Accepting Medicaid | |
| Does Not Meet Credentialing Criteria | |
| Terminated Due to Quality Assurance | |
| Administrative | |
| Site Closed - Bankrupt | |
| Group Practice Dissolved Doctors Billing | |
| Moved New Location Unknown | |
| Rates Too Low | |
| Request By Provider | |
| Closed Office | |
| Precluded From Medicaid | |
| Due to IPA Contracting | |
| Refused MAID Application | |
| No Medicaid ID# | |
| Total Terminated Providers | |
| |
| D. | Subcontracting Issues/Monitoring Efforts |
Provide an overview of all monitoring efforts of all subcontractors and vendors, including those responsible for the delivery of ancillary services, i.e., pharmacy, dental, vision, and transportation (if applicable), as well as information systems, utilization review, and credentialing vendors. Provide brief summaries of all delegation oversight committee reports/minutes for the report period and attach quarterly reports.
| |
| IV. | QUALITY ASSURANCE AND IMPROVEMENT |
| |
| A. | Internal Quality Assurance Activities During the Report Period |
| |
| 1. | Summary of QI Activities |
Describe the quality assurance activities during the report period directed at improving the availability, continuity, and quality of services. Examples include problems identified from utilization review to be investigated, medical management committee recommendations based on findings, special research into suspected problems and research into practice guidelines or disease management.
| |
| 2. | Monitoring of Indicators, Benchmarks and Outcomes |
Include a narrative on the Contractor’s progress in developing or obtaining baseline data and the required health outcomes, including proposed sampling methods and methods to validate data, to be used as a progress comparison for the Contractor’s quality improvement plan. The report should include how the baseline
data for comparison will be obtained or developed and what indicators of quality will be used to determine if the desired outcomes are achieved.
| |
| 3. | Performance Improvement Projects |
Report on the progress and status of performance improvement projects.
| |
| 4. | Utilization of Sub-Populations and Individuals with Special Healthcare Needs |
Discuss any issues that arose during the report period that related to persons associated with sub-populations and individuals with special healthcare needs. Examples of sup-populations and individuals with special health care needs include members with chronic and disabling conditions, minorities, children enrolled with the Commission for Children with Special Health Care Needs, persons receiving SSI, persons with mental illness, the disabled, homeless, and any groups identified by the Contractor for targeted study. Discuss progress in the development of new or ongoing outreach and education to these special populations.
Describe results of any satisfaction survey that was conducted by the Contractor during the report period, if applicable. (Note: surveys are conducted each year, so this section will be completed during one quarter for the providers and one for the members.)
| |
| 6. | Evidence-based guidelines for practitioners |
Report on assessment activities during the report period resulting in development and distribution of practice guidelines for providers. Provide an analysis of the effectiveness in improving patterns of care.
| |
| B. | Activities Related to EPSDT, Pregnant Women, Maternal and Infant Health |
Provide a summary of the activities of these programs, and trends noted in prenatal visit appropriateness, birth outcomes including death, and program interventions, during the last reporting period. If any of the programs have changed during the reporting period, please describe the change in the programs.
Describe activities of the EPSDT staff, including outreach, education, and case management. Provide data on levels of compliance during the report period (including screening rates) with EPSDT regulations.
The CMS-416 report is an additional report required annually. The Department specifications for the CMS 416 (EPSDT) shall be in
compliance with the CMS-416: Annual EPSDT Participation Report and shall be based on Federal Fiscal Year (FFY).
| |
| C. | Credentialing and Re-credentialing Activities During the Report Period |
Summarize the Contractor’s credentialing and re-credentialing activities.
| |
| D. | Fraud, Waste and Abuse Activities During the Report Period |
Discuss Contractor efforts to monitor Fraud, Waste and Abuse.
| |
| A. | Grievance Activities During the Report Period |
Summarize the grievances received by the Contractor during the reporting period. Provide the number, type and resolution of grievances during the report period. (Note: these logs are the “number, type and resolution.” Also under the BBA – complaint and grievances are the same.)
| |
| B. | Appeal Activities during the Report Period |
Summarize the appeals received by the Contractor during the reporting period. Provide the number, type and resolution of appeals during the report period.
| |
| C. | Trends or Problem Areas |
Discuss any trends or problem areas identified in the appeals and grievances, and the Contractor’s efforts to address any trends.
| |
| VI. | BUDGET NEUTRALITY/FISCAL ISSUES |
| |
A. | Budgetary Issues for the Report Period |
Provide a narrative of budgetary issues including changes in appropriations, adjustments in the upper payment limits, etc.
| |
B. | Potential/Anticipated Fiscal Problems |
Provide a narrative of anticipated fiscal problems or issues at the Contractor level. Include such topics as payment of claims, financial solvency, etc.
| |
| A. | Utilization Summary Data Reports |
| |
| 1. | Enrollment Summary Report |
| |
| 2. | Ambulatory Care by Age Breakdown |
| |
| 3. | Emergency Care and Ambulatory Surgery Resulting in Hospital Admission |
| |
| 4. | Emergency Care by ICD-9 Diagnosis (Emergency Care by ICD-10 Diagnosis upon implementation) |
| |
| 6. | Ambulatory Care by Provider Category and Category of Aid |
| |
| a) | Top 50 Drugs – Cost, Number of Prescriptions |
| |
| b) | Top Therapeutic Classes based on top 50 Drugs – Cost and Number of Prescriptions |
| |
| c) | Pharmacy Utilization Statistics |
| |
| B. | Templates for Utilization Reports |
The Department for Medicaid Services and the Contractor will review the utilization reporting formats regarding any necessary updates to the formatting of the reports. This review will be completed for the purposes of ensuring accuracy of the reports and meaningful information sharing.
|
| | | | | | | | |
| UTILIZATION REPORT 1 - ENROLLMENT SUMMARY |
| Region XX |
| Reporting Period Covers: _/_/_ - _/_/_ |
| First Month of The Report Period |
| Unduplicated Number of Members During the Month By Age And Category of Medicaid Eligibility |
| AGE | AFDC | SOBRA | FOSTER | KCHIP | SSI W/ MEDICARE | SSI WO/ MEDICARE | TOTAL |
| < 1 | | | | | | | |
| 1 < 2 | | | | | | | |
| 2 < 3 | | | | | | | |
| 3 < 6 | | | | | | | |
| 6 < 10 | | | | | | | |
| 1 - 9 | | | | | | | |
| 10 - 19 | | | | | | | |
| 20 - 44 | | | | | | | |
| 45 -64 | | | | | | | |
| 65 - 74 | | | | | | | |
| 75 - 84 | | | | | | | |
| 85+ | | | | | | | |
| Total | | | | | | | |
|
| | | | | | | | |
| | | | | | | | |
| Second Month of The Report Period |
| Unduplicated Number of Members During the Month By Age And Category of Medicaid Eligibility |
| | | | | | | | |
| AGE | AFDC | SOBRA | FOSTER | KCHIP | SSI W/ MEDICARE | SSI WO/ MEDICARE | TOTAL |
| < 1 | | | | | | | |
| 1 < 2 | | | | | | | |
| 2 < 3 | | | | | | | |
| 3 < 6 | | | | | | | |
| 6 < 10 | | | | | | | |
| 1 - 9 | | | | | | | |
| 10 - 19 | | | | | | | |
| 20 - 44 | | | | | | | |
| 45 -64 | | | | | | | |
| 65 - 74 | | | | | | | |
| 75 - 84 | | | | | | | |
| 85+ | | | | | | | |
| Total | | | | | | | |
| Third Month of the Report Period |
| Unduplicated Number of Members During the Month By Age And Category of Medicaid Eligibility |
| AGE | AFDC | SOBRA | FOSTER | KCHIP | SSI W/ MEDICARE | SSI WO/ MEDICARE | TOTAL |
| < 1 | | | | | | | |
| 1 < 2 | | | | | | | |
| 2 < 3 | | | | | | | |
| 3 < 6 | | | | | | | |
| 6 < 10 | | | | | | | |
| 1 - 9 | | | | | | | |
| 10 - 19 | | | | | | | |
| 20 - 44 | | | | | | | |
| 45 -64 | | | | | | | |
| 65 - 74 | | | | | | | |
| 75 - 84 | | | | | | | |
| 85+ | | | | | | | |
| Total | | | | | | | |
| | | | | | | | |
| Total Member Months During the Report Period By Age And Category of Medicaid Eligibility (Note: Sum the months above for each cell) |
| AGE | AFDC | SOBRA | FOSTER | KCHIP | SSI W/ MEDICARE | SSI WO/ MEDICARE | TOTAL |
|
| | | | | | | | |
| < 1 | | | | | | | |
| 1 < 2 | | | | | | | |
| 2 < 3 | | | | | | | |
| 3 < 6 | | | | | | | |
| 6 < 10 | | | | | | | |
| 1 - 9 | | | | | | | |
| 10 - 19 | | | | | | | |
| 20 - 44 | | | | | | | |
| 45 -64 | | | | | | | |
| 65 - 74 | | | | | | | |
| 75 - 84 | | | | | | | |
| 85+ | | | | | | | |
| Total | | | | | | | |
| Version: DMS Approved 06/2011 |
| Notes: All reports are based on date of service |
| Unduplicated members include all members eligible at any time during the month regardless of date. |
Retroactive eligibility shall be included in the "total" table. Footnote accordingly. |
| For report periods greater than 3 months, simply include a table for each month. |
|
| | | | | | | | |
| Utilization Report 2 |
| Region XX |
| Reporting Period Covers: _/_/_ - _/_/_ |
| Ambulatory Care by Age Breakdown |
| | Outpatient Visits (Excludes MH/CD) | All Emergency Room Visits (Include outpatient ER and ER resulting in inpatient admissions) | Ambulatory Surgery / Procedures | Observation Room Stays Resulting in Discharge |
| Age | Visits | Visits / 1,000 Member Months | Visits | Visits / 1,000 Member Months | Procedures | Procedures / 1,000 Member Months | Stays | Stays / 1,000 Member Months |
| <1 | | | | | | | | |
| 1-9 | | | | | | | | |
| 10-19 | | | | | | | | |
| 20-44 | | | | | | | | |
| 45-64 | | | | | | | | |
| 65-74 | | | | | | | | |
| 75-84 | | | | | | | | |
| 85+ | | | | | | | | |
| Total | | | | | | | | |
| | | | | | | | | |
| Version: DMS Approved 06/2011 |
| Notes: All reports are based on date of service |
| ER Utilization shall be according to HEDIS specifications to include HCFA-1500 Claims with Place of Service code 23. |
|
| | | | |
| UTILIZATION REPORT 3 |
| Region XX |
| Reporting Period Covers: _/_/_ - _/_/_ |
| Emergency Care and Ambulatory Surgery Resulting in Hospital Admission |
| | Emergency Room Visits Resulting in Inpatient Admission Same Day | Ambulatory Surgery / Procedures* Resulting in Inpatient Admission within 30 days |
| Age | Visits | Visits / 1,000 Member Months | Procedures | Procedures / 1,000 Member Months |
| <1 | | | | |
| 1-9 | | | | |
| 10-19 | | | | |
| 20-44 | | | | |
| 45-64 | | | | |
| 65-74 | | | | |
| 75-84 | | | | |
| 85+ | | | | |
| Total | | | | |
| | | | | |
| Version: DMS Approved 06/2011 |
| * Use the Medicare base rate file for ambulatory surgery procedures |
|
| | | | | | |
| UTILIZATION REPORT 4 |
| Region XX |
| Reporting Period Covers: _/_/_ - _/_/_ |
| Emergency Care by ICD-9 code |
| ICD-9 Diagnosis 3 digit prefix | Diagnosis Description | In-Plan ER Visits | Out-of-Plan ER Visits | In-Plan Urgent Care Visits | Total ER and Urgent Care Visits | ER-UC Visits / 1,000 Member Months |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| | | | | | | |
| Report includes the top 50 Primary ICD-9 CM Diagnosis Codes appearing on the UB-92 using the first three (3) digit prefix. |
| "In-Plan" is defined as an ER provider under contract or letter of agreement with the Contractor. |
| Per 1000 calculations are monthly average |
| Version: DMS Approved 06/2011 |
|
| | | | | | | | | | | | | | |
| UTILIZATION REPORT 5 |
| Region XX |
| Reporting Period Covers: _/_/_ - _/_/_ |
| Home Health Utilization |
| Age | Unduplicated Patients Served | Visits for Infusion Therapy | Visits for Oxygen and/or Respiratory Therapy | Visits for Physical Therapy | Visits for Occupational Therapy | Visits for Speech Therapy | Other Visits | Total Visits | Total Visits / 1,000 Member Months |
| <1 | | | | | | | | | |
| 1-9 | | | | | | | | | |
| 10-19 | | | | | | | | | |
| 20-44 | | | | | | | | | |
| 45-64 | | | | | | | | | |
| 65-74 | | | | | | | | | |
| 75-84 | | | | | | | | | |
| 85+ | | | | | | | | | |
| Total | | | | | | | | | |
| | | | | | | | | | |
| Use revenue codes and HCPC codes appropriate for RN, LPN, RT, OT, PT, ST, CNA, Oxygen and Respiratory Therapy, Infusion Therapy. | |
| Do not include DME in this report. | | | | | | |
| Version: DMS Approved 06/2011 |
| Note: All reports based on date of service. |
|
| | | | |
| Utilization 6 |
| Region XX |
| Reporting Period Covers: _/_/_ - _/_/_ |
| Ambulatory Care by Provider Type and Category of Aid |
| Category | Visits w/ Participating Providers | Visits w/ Non-participating Providers | Total Visits | Visits / 1,000 Member Months |
| 1. Primary Care Providers | | | | |
| AFDC | | | | |
| SOBRA | | | | |
| Foster Care | | | | |
| KCHIP | | | | |
| SSI w/o Medicare | | | | |
| SSI w/ Medicare | | | | |
| 2. FQHC & RHC | | | | |
| AFDC | | | | |
| SOBRA | | | | |
| Foster Care | | | | |
| KCHIP | | | | |
| SSI w/o Medicare | | | | |
| SSI w/ Medicare | | | | |
| 3. Eye Care Providers | | | | |
| AFDC | | | | |
| SOBRA | | | | |
| Foster Care | | | | |
| KCHIP | | | | |
| SSI w/o Medicare | | | | |
| SSI w/ Medicare | | | | |
| 4. Dentists | | | | |
|
| | | | |
| AFDC | | | | |
| SOBRA | | | | |
| Foster Care | | | | |
| KCHIP | | | | |
| SSI w/o Medicare | | | | |
| SSI w/ Medicare | | | | |
| 5. Physician Specialists | | | | |
| AFDC | | | | |
| SOBRA | | | | |
| Foster Care | | | | |
| KCHIP | | | | |
| SSI w/o Medicare | | | | |
| SSI w/ Medicare | | | | |
| 6. Home Health | | | | |
| AFDC | | | | |
| SOBRA | | | | |
| Foster Care | | | | |
| KCHIP | | | | |
| SSI w/o Medicare | | | | |
| SSI w/ Medicare | | | | |
| Version: DMS Approved 06/2011 |
| Notes: All reports are by date of service. |
|
| | | |
| UTILIZATION REPORT 7A - Top 50 Drugs |
| Region XX |
| Reporting Period Covers: _/_/_ - _/_/_ |
| Drug | Cost | Number of RX per Quarter |
| 1 | |
| |
| 2 | | | |
| 3 | | | |
| 4 | | | |
| 5 | | | |
| 6 | | | |
| 7 | | | |
| 8 | | | |
| 9 | | | |
| 10 | | | |
| 11 | | | |
| 12 | | | |
| 13 | | | |
| 14 | | | |
| 15 | | | |
| 16 | | | |
| 17 | | | |
| 18 | | | |
| 19 | | | |
| 20 | | | |
| 21 | | | |
| 22 | | | |
| 23 | | | |
| 24 | | | |
| 25 | | | |
| 26 | | | |
| 27 | | | |
| 28 | | | |
| 29 | | | |
| 30 | | | |
| 31 | | | |
| 32 | | | |
| 33 | | | |
| 34 | | | |
| 35 | | | |
| 36 | | | |
| 37 | | | |
|
| | | |
| 38 | | | |
| 39 | | | |
| 40 | | | |
| 41 | | | |
| 42 | | | |
| 43 | | | |
| 44 | | | |
| 45 | | | |
| 46 | | | |
| 47 | | | |
| 48 | | | |
| 49 | | | |
| 50 | | | |
|
| | | | | |
| UTILIZATION REPORT 7B - Top Therapeutic Classes (Based on Top 50 Drugs) |
| Region XX |
| Reporting Period Covers: _/_/_ - _/_/_ |
| Top Therapeutic Class | Cost | Total Number of RX | | |
| 1 | | | | | |
| 2 | | | | | |
| 3 | | | | | |
| 4 | | | | | |
| 5 | | | | | |
| 6 | | | | | |
| 7 | | | | | |
| 8 | | | | | |
| 9 | | | | | |
| 10 | | | | | |
| | | | | | |
| (Add more rows as needed per the top 50 drugs.) | | | |
|
| | | | |
| UTILIZATION REPORT 7C - Pharmacy Utilization by Month |
| Region XX |
| Reporting Period Covers: _/_/_ - _/_/_ |
| Month | # Members utilizing RX benefit | Total RX per month | Cost PMPM (All drug Costs) |
| January | | | | |
| February | | | | |
| March | | | | |
| April | | | | |
| May | | | | |
| June | | | | |
| July | | | | |
| August | | | | |
| September | | | | |
| October | | | | |
| November | | | | |
| December | | | | |
| Yearly Total: | | | | |
| |
| | Total RX Utilization Brand Vs. Generic |
| Month | Generic Rx Total | Percent of Total | Brand Rx Total | Percent of Total |
| January | | | | |
| February | | | | |
| March | | | | |
| April | | | | |
| May | | | | |
| June | | | | |
| July | | | | |
| August | | | | |
| September | | | | |
| October | | | | |
| November | | | | |
| December | | | | |
| Yearly Total: | | | | |
| |
| C. | Monitoring Activities Related to Utilization and Access to Care |
Discuss the Contractor’s use of encounter data and utilization reports to monitor utilization of services and access to care.
| |
| D. | Utilization Trends/Patterns Identified During the Report Period |
Analyze and discuss trends in utilization and any unusual patterns about which the Contractor will take subsequent action. Also, discuss areas where over- or under-utilization has been influenced appropriately, i.e., pharmacy and ER utilization management.
| |
| E. | Summary of Denials Rendered during the Report Period |
Analyze and discuss any unusual patters in the denials rendered during the reporting period.
| |
| VIII. | Quarterly Benefit Payment Report |
The Quarterly Benefit Payments Report summarizes Medicaid payments by category of service for each month during the reporting quarter. In addition, KCHIP, reinsurance and pharmacy rebate totals are included to calculate a grand total for the program. KCHIP monthly totals are derived from the Quarterly Benefit Payments – KCHIP Members Only Report. Reports shall:
| |
| • | Include column headings on each page; |
| |
| • | Be submitted in Excel format; |
| |
| • | Be completed for each MCO region, in addition to a summary of all MCO regions; and |
|
| | | | | |
| | CONTRACTOR REGION X DEPARTMENT FOR MEDICAID SERVICES QUARTERLY BENEFIT PAYMENTS STATE FISCAL YEAR XXXX |
| | | | | | |
| COS # | Category of Service | October- | November- | December- | Quarterly Total |
| |
Medicaid Mandatory Services | | | | |
| 2 | Inpatient Hospital | | | | |
| 12 | Outpatient Hospital | | | | |
| 32 | EPSDT Related | | | | |
| 34 | Clinical Social Worker | | | | |
| 37 | Physical Therapist Crossover | | | | |
| 38 | Occupational Therapist | | | | |
| 39 | Psychologist Crossover | | | | |
| 40 | DME | | | | |
| 41 | Primary Care | | | | |
| 43 | Rural Health Clinic | | | | |
| 44 | Nurse Midwife | | | | |
| 45 | Family Planning | | | | |
| 46 | Home Health | | | | |
| 47 | Independent Laboratory | | | | |
| 48 | EPSDT Preventive | | | | |
| 62 | Emergency Transportation | | | | |
| 63 | Non-Emergency Transportation | | | | |
| 67 | Vision | | | | |
| 72 | Dental | | | | |
| 74 | Physician | | | | |
| 75 | Certified Nurse Practitioner | | | | |
| 81 | Hearing | | | | |
| 90 | Comprehensive Outpatient Rehab Facility (CORF) | | | | |
| 92 | Psychiatric Distinct Part Unit | | | | |
| 93 | Rehab Distinct Part Unit | | | | |
| 94 | Physician Assistant | | | | |
| | Subtotal | $ | $ | $ | $ |
| | | | | | |
| | Medicaid Optional Services | | | | |
| 3 | Mental Hospital | | | | |
|
| | | | | |
| 4 | Renal Dialysis Clinic | | | | |
| 8 | Psychiatric Residential Treatment Facility (PRTF) | | | | |
| 13 | Ambulatory Surgery | | | | |
| 16 | Impact Plus | | | | |
| 17 | Specialized Children’s Services Clinic | | | | |
| 20 | Targeted Case Management – Adults | | | | |
| 21 | Targeted Case Management – Children | | | | |
| 24 | Commission for Children with Special Health Care Needs | | | | |
| 29 | Preventive Health | | | | |
| 35 | Chiropractor | | | | |
| 36 | Other Lab & X-Ray | | | | |
| 42 | Community Mental Health Center (CMHC) | | | | |
| 54 | Nurse Anesthetist | | | | |
| 55 | Hospice – Non Institutional | | | | |
| 64 | Pharmacy | | | | |
| 88 | Podiatry | | | | |
| 99 | Unknown Type | | | | |
| | Subtotal | $ | $ | $ | $ |
| | | | | | |
| | KCHIP | $ | $ | $ | $ |
| | | | | | |
| | TOTAL | $ | $ | $ | $ |
| | | | | | |
| | Reinsurance | $ | $ | $ | $ |
| | | | | | |
| | Pharmacy Rebates | $ | $ | $ | $ |
| | | | | | |
| | GRAND TOTAL | $ | $ | $ | $ |
|
| | | | | |
| | CONTRACTOR REGION X DEPARTMENT FOR MEDICAID SERVICES QUARTERLY BENEFIT PAYMENTS – KCHIP MEMBERS ONLY STATE FISCAL YEAR XXXX |
| | | | | | |
| COS # | Category of Service | October- | November- | December- | Quarterly Total |
| |
Medicaid Mandatory Services | | | | |
| 2 | Inpatient Hospital | | | | |
| 12 | Outpatient Hospital | | | | |
| 32 | EPSDT Related | | | | |
| 34 | Clinical Social Worker | | | | |
| 37 | Physical Therapist Crossover | | | | |
| 38 | Occupational Therapist | | | | |
| 39 | Psychologist Crossover | | | | |
| 40 | DME | | | | |
| 41 | Primary Care | | | | |
| 43 | Rural Health Clinic | | | | |
| 44 | Nurse Midwife | | | | |
| 45 | Family Planning | | | | |
| 46 | Home Health | | | | |
| 47 | Independent Laboratory | | | | |
| 48 | EPSDT Preventive | | | | |
| 62 | Emergency Transportation | | | | |
| 63 | Non-Emergency Transportation | | | | |
| 67 | Vision | | | | |
| 72 | Dental | | | | |
| 74 | Physician | | | | |
| 75 | Certified Nurse Practitioner | | | | |
| 81 | Hearing | | | | |
| 90 | Comprehensive Outpatient Rehab Facility (CORF) | | | | |
| 92 | Psychiatric Distinct Part Unit | | | | |
| 93 | Rehab Distinct Part Unit | | | | |
| 94 | Physician Assistant | | | | |
| | Subtotal | $ | $ | $ | $ |
| | | | | | |
| | Medicaid Optional Services | | | | |
| 3 | Mental Hospital | | | | |
|
| | | | | |
| 4 | Renal Dialysis Clinic | | | | |
| 8 | Psychiatric Residential Treatment Facility (PRTF) | | | | |
| 13 | Ambulatory Surgery | | | | |
| 16 | Impact Plus | | | | |
| 17 | Specialized Children’s Services Clinic | | | | |
| 20 | Targeted Case Management – Adults | | | | |
| 21 | Targeted Case Management – Children | | | | |
| 24 | Commission for Children with Special Health Care Needs | | | | |
| 29 | Preventive Health | | | | |
| 35 | Chiropractor | | | | |
| 36 | Other Lab & X-Ray | | | | |
| 42 | Community Mental Health Center (CMHC) | | | | |
| 54 | Nurse Anesthetist | | | | |
| 55 | Hospice – Non Institutional | | | | |
| 64 | Pharmacy | | | | |
| 88 | Podiatry | | | | |
| 99 | Unknown Type | | | | |
| | Subtotal | $ | $ | $ | $ |
| | | | | | |
| | TOTAL | $ | $ | $ | $ |
| | | | | | |
| | Reinsurance | $ | $ | $ | $ |
| | | | | | |
| | Pharmacy Rebates | $ | $ | $ | $ |
| | | | | | |
| | GRAND TOTAL | $ | $ | $ | $ |
IX. Abortion Procedure Report
An Abortion Procedure Report shall be submitted each quarter to the Department. The report shall list all claims paid with an abortions procedure code and be submitted with supporting documentation (i.e. doctor’s notes, etc.) that justify the service was performed in accordance with federal and state laws and judicial opinions. Currently, abortion claims can only be paid by Medicaid for three reasons (rape, incest and when the mother’s life is at risk). The Abortion Procedure Report shall contain the following fields:
| |
| • | FDOS (First Date of Service) |
| |
| • | LDOS (Last Date of Service) |
X. Systems
A. Systems and Data Development Issues
Discuss the status of systems and data development and issues. Include information on plan modification and expected outcomes.
| |
| B. | Claims Processing Timeliness/Encounter Data Reporting |
Provide a discussion of the status on the timeliness of encounter data reporting and the processing of claims, including steps taken by the Contractor to correct problems.
| |
| XI. | OTHER CONTRACTOR ACTIVITIES |
Identify organizational changes relating to the Contractor.
Identify administrative changes relating to the Contractor.
Provide information on additional or innovative program solutions implemented by the Contractor as referenced in the RFP.
MCO shall recommend innovative programs to assist in controlling pharmacy and other medical costs through such mechanisms
Provide any information relevant to the operation of the Contractor not otherwise covered herein.
| |
| XII. | Behavioral Health, Developmental and Intellectual Disabilities (BHDID) |
| |
| A. | BHDID General Reporting Requirements |
BHDID reports shall be provided with display of the following fields and should have detailed report definitions. Report should include “totals” and be delineated by the following:
| |
| 1. | Age (0 - <18, 18 - <21 receiving service under child benefit), 18 and above for those receiving services under adult benefit |
| |
| 3. | Diagnostic category or diagnoses |
B. BHDID Additional Reporting Requirements
1. Network Capacity
MCO will provide quarterly reports on staffing within the behavioral health network to include:
a) FTEs per 1000 Chronic Cases
| |
| • | Ph.D. psychologists/1000 |
| |
| • | Total licensed (for independent practice) therapists FTE/1000 (by discipline LMFT, LPCC, LCSW, etc.) |
| |
| • | Total master’s level therapists under supervision FTE/1000 (by discipline) |
| |
| • | Targeted case managers /1000 |
| |
| • | Other support staff / 1000 |
| |
| • | Peer support specialists / 1000 |
b) Utilization by Chronic Cases
| |
| • | Number of crisis calls/1000 |
| |
| • | Number of counseling sessions/1000 |
c) Number of days wait for initial appointment
d) Utilization by Medicaid Enrollees
| |
| • | Number of crisis calls/1000 |
| |
| • | Number of counseling sessions/1000 |
| |
| • | Number of days wait for initial appointment (Should include: Total; Emergency; Urgent; and Routine) |
| |
| • | Number of Minutes to Reach a Clinician by Telephone in an Emergency |
| |
| • | Number of Days to Reach a Clinician by Telephone (non-emergency) |
| |
| • | Prevention Visits per 1000 Medicaid Enrollees |
e) Outcomes for Chronic Cases (SMI,SED)
| |
| • | Number of psychiatric hospitalizations/1000 |
| |
| • | Pharmaceutical expenditures/1000 |
| |
| • | Percent adhering to recommended course of mental health treatment |
| |
| • | Percent of clients satisfied with access and quality of mental health services |
| |
| • | Percent maintaining employment or staying in school while in mental health treatment |
| |
| • | Percent with permanent housing after mental health treatment |
| |
| • | Percent arrested or incarcerated after mental health treatment |
f) Outcomes for Medicaid Enrollees
| |
| • | Number of psychiatric hospitalizations/1000 |
| |
| • | Percent hospitalized for psychiatric problems |
| |
| • | Pharmaceutical expenditures/1000 |
| |
| • | Percent adhering to recommended course of behavioral health treatment |
| |
| • | Percent of clients satisfied with access and quality of behavioral health services |
| |
| • | Percent maintaining employment or staying in school while in mental health treatment |
| |
| • | Percent with permanent housing after mental health treatment |
| |
| • | Percent arrested or incarcerated after mental health treatment |
2. Financial / Payment
| |
| a) | MCO shall be required to make payments to providers upon receipt of filed claims (not to exceed thirty days or with respective penalty after sixty days, ninety days, etc.) |
| |
| b) | MCO shall report monthly on per member, per month expenses for behavioral health services for children / youth and for adults |
| |
| c) | MCO shall report monthly on per member, per month expenses for behavioral health services for adults with SMI and children/youth with SED |
XIII. Other Quarterly Report
Personal Information Form Template
|
| | | | | | | |
| | | | | | | | |
| | | Total # of New Member Packets Mailed by Month | | Total # of PIFs Received by Month | |
| | | | | | | | |
| October | | 0 | | 0 | |
| November | | 0 | | 0 | |
| December | | 0 | | 0 | |
| Total for Quarter | | 0 | | 0 | |
| | | | | | | | |
| New Member Enrollment Report: Phone Call Results by Date Span |
| 00/00/00 to 00/00/00 |
| | | | | | | | |
| | | | | | | | |
| Call Result | | 1st Attempt: Call Results | | 2nd Attempt: Call Results | | Grand Total: Call Results | |
| | | | |
| No Answer | | 0 | | 0 | | 0 | |
| | | | | | | | |
| Phone number incorrect | | 0 | | 0 | | 0 | |
| Left message | | 0 | | 0 | | 0 | |
| Phone number not listed | | 0 | | 0 | | 0 | |
|
| | | | | | | |
| Member disenrolled from Contractor | | 0 | | 0 | | 0 | |
| Not convenient time | | 0 | | 0 | | 0 | |
| Member not home | | 0 | | 0 | | 0 | |
| Did Not Want Assistance | | 0 | | 0 | | 0 | |
| Phone Busy | | 0 | | 0 | | 0 | |
| Assisted Member to Fill Out PIF | 0 | | 0 | | 0 | |
| Doesn't speak English | | 0 | | 0 | | 0 | |
| Filled Out PIF and Mailed | | 0 | | 0 | | 0 | |
| Total # of call results: | | 0 | | 0 | | 0 | |
| | | | | | | | |
| Health/Disease Management and Case Management follow-up Report: |
| 00/00/00 to 00/00/00 |
| | | | | | | | |
| Call Result | | Total Number: | | | | | |
| Filled Out PIF and Mailed | | 0 | | | | | |
| Completed Call | | 0 | | | | | |
| Member no longer at this phone number | 0 | | | | | |
| No Phone Number Listed | | 0 | | | | | |
| Phone number incorrect | | 0 | | | | | |
| Assisted Member to Fill Out PIF | 0 | | | | | |
| Left Message | | 0 | | | | | |
| Member not home | | 0 | | | | | |
| No Answer | | 0 | | | | | |
| Total # of call results | | 0 | | | | | |
| | | | | | | | |
| | | | | | | | |
| | | | | | | | |
|
| | | | | | | | | | | |
Provider Termination Report
Monthly Report - Month/Year
Ran as of Date - MM/DD/YY |
| NPI | Last | First | Title | Group | Add 1 | Add 2 | City | St | Zip | County | Reason |
| | | | | | | | | | | | |
| | | | | | | | | | | | |
| | | | | | | | | | | | |
|
| | | | | | | | | | | |
Provider Denial Report
Monthly Report - Month/Year
Ran as of Date - MM/DD/YY |
| NPI | Last | First | Title | Group | Add 1 | Add 2 | City | St | Zip | County | Reason |
| | | | | | | | | | | | |
| | | | | | | | | | | | |
| | | | | | | | | | | | |
|
| | | | | | | | | | | |
| | | Outstanding Accounts Receivable Report
Monthly Report - Month/Year
Ran as of Date - MM/DD/YY | |
| |
| |
| | Provider FEIN/SSN | Medicaid ID | Provider NPI | Provider Name | Date of AR Setup | Age of AR | Reason for Setup | Original Amount of AR | Balance of AR | TPL Indicator | |
| | | | | | | | | | | | |
| | | | | | | | | | | | |
| | | | | | | | | | | | |
|
| | | | | | | | | | | | | | | | |
| Provider Case Report |
| Quarterly Report - Quarter/Year |
| Ran as of Date - MM/DD/YY |
| Case Number | Investigator | Subject Type | Date Opened | Date Closed | Original Report Summary | Findings | Potential Recovery |
| | | | | | | | |
| | | | | | | | |
| | | | | | | | |
| | | | | | | | |
| | Member Case Report
Quarterly Report - Quarter/Year
Ran as of Date - MM/DD/YY | |
| | Case Number | Investigator | Subject Type | Date Opened | Date Closed | Original Report Summary | Findings | Potential Recovery | |
| | | | | | | | | | |
| | | | | | | | | | |
| | | | | | | | | | |
| | | | | | | | | | |
| | | | | | | | | | |
|
| | | | | | | | |
| Monthly Provider Enrollment Report | |
| NPI | Provider Name | Tax ID | Owner | Address | City | State | Zip | County |
| | | | | | | | | |
| | | | | | | | | |
| | | | | | | | | |
| | | | | | | | | |
| | | | | | | | | |
Expenditures Related to Contractor’s Operations
|
| | | | | | | | |
| | | | | Other | | Other | Reporting Period |
| Category | Positions | Salary 1 | Bonus 2 | Compensation 3 | Travel | Expenses | Begin Date | End Date |
| Executive Management | Executive Officer/CEO | | | | | | | |
| Executive Management | Medical Director | | | | | | | |
| Executive Management | Pharmacy Director | | | | | | | |
| Executive Management | Dental Director | | | | | | | |
| Executive Management | CFO | | | | | | | |
| Executive Management | Compliance Director | | | | | | | |
| Executive Management | Quality Improvement Director | | | | | | | |
| | Sub-Total | | | | | | | |
| Executive Management | All other Executive Management Staff | | | | | | | |
| Executive Management | All Other Non-Executive Management Staff | | | | | | | |
| All Categories | Total | | | | | | | |
1Where an individual serves Contractor lines of business other than Kentucky Medicaid Managed Care, the Contractor may disclose an estimated allocation based on the time allocated to its Kentucky Medicaid Managed Care line of business. Information related to the Contractor's ultimate parent company's executive management need not be disclosed.
2Unless guaranteed, or actually paid during the period, bonuses disclosed may be target amounts for the period disclosed expressed as a percentage of base salary.
3 “Other Compensation” is limited to other cash compensation actually paid during the period, and may exclude amounts realized or realizable during the period through the grant, vesting, or exercise of stock options, restricted stock, stock appreciation rights, phantom stock plans, or other long term non-cash incentives.
Appendix L
Reporting Deliverables
To Be Supplemented
|
| | | | | | | | | | | | | | | | | | | | | | | | |
| Report Name | Report
Description | Report Frequency | Submitted to |
| WKL | MTH | QTR | ANN | As Revised / Other | Due Date |
| Financial |
Annual
Financial Statements | Contractor must provide a copy to the DMS of the most recent annual financial statements, as submitted to and required by DOI for each covered contract year | | | | X | 120 days following each fiscal year | | DOI |
Annual Audited
Financial Statements | Contractor must provide a copy to the DMS of the most recent annual audited financial statements, as submitted to and required by DOI for each covered contract year | | | | X |
Concurrant with filing same with the domiciliary Insurance regulator | | DOI and DMS |
| Quarterly Financial Reports | Provide financial reports in format and content as prescribed by NAIC and cover letter | | | X | | Concurrant with filing same with the domiciliary Insurance regulator d | | DMS |
| Executive Summary |
| Executive Summary | Include a summary of any significant activities, problems or issues and any program modifications | | | X | | 30 days after quarter end | | DMS |
|
| | | | | | | | | | | | | | | | | | | | | | | | |
| Eligibility/Enrollment |
| Enrollment Changes During the Quarter | Summarize all changes in the number of persons enrolled during the report period | | | X | | 30 days after quarter end | | DMS |
| PCP Changes During the Report Period | Identify PCPs with voluntary member enrollment change activity and percent change in members per PCP | | | X | X | 30 days after quarter end | April
30th | DMS |
| PCP Assignments Initiated by the Contractor | Provide number of PCP assignments initiated by the Contractor | | | X | | 30 days after quarter end | | DMS |
| PCP Changes by Member | Provider number of all member PCP changes | | | X | | 30 days after quarter end | | DMS |
| PCP's with Panel Changes Greater than 50 or 10% - Table | Provide an electronic file of all PCPs with panel changes greater than 50 or 10% | | | X | | 30 days after quarter end | | DMS |
| PCP's with Panel Changes Greater than 50 or 10% - Narrative Summarization | Briefly narrate reasons for those voluntary member transfers that exceed the lesser of 50 or 10% of total panel | | | X | | 30 days after quarter end | | DMS |
| Member Services Report | Provide self-report on prior month's performance in the areas of call center abandonment, blockage rate and average speed of answer | | X | | | By the 10th of Every Month | | DMS |
| Access/Delivery Network |
Geo Access Networks Reports & Maps | Distribution and analysis of current provider network and beneficiaries | | X | | | By the 15th of Every Month | | DMS |
| Access Issues/Problems Identified During the Quarter and/or Remedial Action Taken | Provide specific information on the nature of any access problems identified and any plans or remedial action taken | | | X | | 30 days after quarter end | | DMS |
| Listing of Providers Denied Participation | Provide a complete listing of providers that requested participation during the report period and were denied | | | X | | 30 days after quarter end | | DMS |
| Subcontracting Issues/Monitoring Efforts | Provide overview of all monitoring efforts of all subcontractors | | | X | | 30 days after quarter end | | DMS |
|
| | | | | | | | | | | | | | | | | | | | | | | | |
| Quality Assurance and Improvement |
| Summary of QI Activities | Describe the quality assurance activities during the report period | | | X | | 30 days after quarter end | | DMS |
| QI Work plan | Outlines scope of activities, goals, objectives and timelines for QAPI program | | | X | | 30 days after quarter end | | DMS |
| Monitoring of Indicators, Benchmarks and Outcomes | Report should include progress in baseline data, sampling methods to validate used a comparison for QI plan and health outcomes | | | | X | | July 31st | DMS |
| Performance Improvement Projects | Progress and status updates of PIPs | | | | X | | July 31st | DMS |
| Utilization of Subpopulations and individuals with special healthcare needs | Discuss any issues during the report period related to members associated with populations and individuals with special health care needs | | | X | | 30 days after quarter end | | DMS |
| Committee activities, including any decisions regarding quality and appropriateness of care | Provide a summary of the activities within Contractor and committees that met during the report period | | | X | | 30 days after quarter end | | DMS |
| Satisfaction Survey(s) | Describe results of any satisfaction survey that was conducted during the report period | | | | X | | July 31st | DMS |
| Evidence-Based guidelines for practitioners | Report on assessment activities during the report period in development and distribution of practice guidelines for providers | | | X | | 30 days after quarter end | | DMS |
| Activities Related to EPSDT, Pregnant Women, Maternal and Infant Death | Provide summary of activities of these programs changes or trends including outreach and informative activities | | | X | | 30 days after quarter end | | DMS |
| Overview of Activities | Provide summary of activities of these programs changes or trends and provide a summary of approved and denied EPSDT Special Services | | | X | | 30 days after quarter end | | DMS |
| Credentialing and Recredentialing Activities During the Quarter | Summarize credentialing and re-credentialing activities | | | X | | 30 days after quarter end | | DMS |
| Grievances/Appeals |
|
| | | | | | | | | | | | | | | | | | | | | | | | |
| Grievance Activities During the Quarter | Provide of all member and provider grievances and appeals | | | X | | 30 days after quarter end | | DMS |
| Appeal Activities During the Quarter | Provide of all member and provider grievances and appeals | | | X | | 30 days after quarter end | | DMS |
| Trends or Problem Areas | Discuss any trends or problem areas identified in grievances or appeals and the effort to address any trends | | | X | | 30 days after quarter end | | DMS |
| Budget Neutrality/Fiscal Impact |
| Budgetary Issues for the Quarter | Provide discussion of budgetary issues including changes in appropriations, adjustments in the upper limit or etc | | | X | | 30 days after quarter end | | DMS |
| Potential/Anticipated Fiscal Problems | Include a discussion of anticipated fiscal | | | X | | 30 days after quarter end | | DMS |
| Utilization |
| Enrollment Summary Report | (1/1-3/31 enrollment submitted 7/30, 1/1-6/30 submitted 10/30, 1/1-9/30 submitted 1/30 and 1/1-12/31 submitted 4/30.) | | | X | | 30 days after quarter end | | DMS |
| Ambulatory Care by Age Breakdown | Provide utilization data during the report period | | | | X | | April
30th | DMS |
| Emergency and Ambulatory Care Resulting in Hospital Admission | Provide utilization data during the report period | | | | X | | April
30th | DMS |
| Emergency Care by ICD-9 Diagnosis | Provide utilization data during the report period | | | | X | | April
30th | DMS |
| Home Health Utilization | Provide utilization data during the report period | | | | X | | April
30th | DMS |
| Ambulatory Care by Provider Type and Category of Aid | Provide utilization data during the report period | | | | X | | April
30th | DMS |
| EPSDT Special Services | Provide utilization during the report period | | | | X | | April
30th | DMS |
| Pharmacy |
|
| | | | | | | | | | | | | | | | | | | | | | | | |
| Top 50 Drugs - cost, number of prescriptions | Provide utilization data during the report period | | | | X | | April
30th | DMS |
| Top therapeutic classes based on Top 50 drugs - cost, number of prescriptions | Provide utilization data during the report period | | | | X | | April
30th | DMS |
| Pharmacy Utilization (# of Members, # of Rx, PMPM cost, Brand vs. Generic) | Provide utilization data during the report period | | | | X | | April
30th | DMS |
| Monitoring Activities Related to Utilization and Access to Care | Provide utilization data during the report period | | | X | | 30 days after quarter end | | DMS |
| Utilization Trends/Patterns Identified During the Quarter | Provide utilization data during the report period | | | X | | 30 days after quarter end | | DMS |
| Summary of Denials Rendered During the Quarter | Provide utilization data during the report period | | | X | | 30 days after quarter end | | DMS |
| UM Call Statistics | Provide utilization data during the report period | | | X | | 30 days after quarter end | | DMS |
| Systems |
| Systems and Data Development Issues | Discuss the status of systems, data development and issues | | | X | | 30 days after quarter end | | DMS |
| Claims Processing Timeliness/Encounter Data Processing | Provide status on the timeliness of encounter data reporting, processing of claims including steps taken to correct problems | | | X | | 30 days after quarter end | | DMS |
| Other Activities |
| Organizational Changes | Identify any organizational changes during the report period | | | X | | 30 days after quarter end | | DMS |
| Administration Changes | Identify any administrative changes during the report period | | | X | | 30 days after quarter end | | DMS |
| Innovations / Solutions | Provide information on additional or innovative program solutions during the report period | | | X | | 30 days after quarter end | | DMS |
| Other | Provide any information relevant to the operation during the report period | | | X | | 30 days after quarter end | | DMS |
| Expenditures Related to MCO’s Operations | Provide business plan that outlines proposed annual expenditures | | | X | | 30 days after quarter end | | DMS |
|
| | | | | | | | | | | | | | | | | | | | | | | | |
| DOI Claims | The current (as of 11-02) reporting requirement from DOI became effective for the reporting period beginning 7/1/02 and includes claims received within the quarter | | | X | | 180 days after quarter end | | DOI and
DMS |
| COB Savings | Provide report on insurance contractor has on file and pays claims accordingly | | X | | | By the 15th of Every Month | | DMS |
| Cost Avoidance Summary Savings (Medicare only) | Provide report for claims that have been denied due to Medicare | | X | | | By the 15th of Every Month | | DMS |
| Cost Avoidance Summary Savings (no Medicare) | Provide report for claims that have been denied due to other insurance | | X | | | By the 15th of Every Month | | DMS |
| Potential Subrogation | Provide reports for cases where the contractor's member has had an accident and there is a possible liable third party | | X | | | By the 15th of Every Month | | DMS |
| Claims Processing | Report from claims processing function in the format agreed upon | | X | | | By the 15th of Every Month | | DMS |
| Prior Authorization | Provide number and type of services both approved and denied in the format agreed upon | | X | | | By the 15th of Every Month | | DMS |
| Claims Processing Summary by Provider Type-Paid | Provide number of claims paid by provider in the format agreed upon | | X | | | By the 15th of Every Month | | DMS |
| Claims Processing Summary by Provider Type-Denied | Provide number of claims denied by provider with a reason for the denied claim in the format agreed upon | | X | | | By the 15th of Every Month | | DMS |
| Claims Processing Summary by Provider Type-Suspended | Provide number of claims suspended by provider with a reason for the suspended claim in the format agreed upon | | X | | | By the 15th of Every Month | | DMS |
| Claims Inventory | Provide number of claims by provider type which exceed processing timeliness standards defined by the department in the format agreed upon | | X | | | By the 15th of Every Month | | DMS |
|
| | | | | | | | | | | | | | | | | | | | | | | | |
| Encounter Data | Required to provide encounter records/transactions | X | | | | | | DMS |
| Foster Care Report | Provide foster care case reports in the format agreed upon | | X | | | By the 15th of Every Month | | DMS |
| Guardianship Report | Provide guardianship case reports in format agreed upon | | X | | | By the 15th of Every Month | | DMS |
| Credentialed Providers Report | Provide number of provider applications received, credentialed, processed, enrolled and not enrolled/reason for termination | | X | | | By the 15th of Every Month | | DMS |
| Provider Enrollment Report | Electronically transmit provider enrollment information | | X | | | By the 15th of Every Month | | DMS |
| Provider Termination Report | Report should include any provider or subcontractor who engages in activities that result in suspension, termination or exclusion | | X | | | By the 15th of Every Month | | DMS |
| Provider Denial Report | Report should include any provider or subcontractor who is denied participation | | X | | | By the 15th of Every Month | | DMS |
| Provider Outstanding Accounts Receivables Report | Report should contain all outstanding accounts with an age of 180 days or older | | X | | | By the 15th of Every Month | | DMS |
| Member Program Violation Collections and Letters | Report should provide how much collected on all member cases whether begun internally or in court. Provide number of mailed letters, responses/results and collections | | X | | | By the 15th of Every Month | | DMS |
| Summary of Member EOB Report | Report should contain number of letters Contractor sent out, how many responses were received, actions taken and collections | | X | | | By the 15th of Every Month | | DMS |
| Lock-In Report | Report should contain number of members locked into PCP, pharmacy and hospital and provide year before lock in and year after paid amounts | | | X | | 30 days after quarter end | | DMS |
|
| | | | | | | | | | | | | | | | | | | | | | | | |
| Algorithms Report | Report should contain number ran and results. | | X | | | By the 15th of Every Month | | DMS |
| Provider Fraud, Waste and Abuse Report | Report should contain all open cases and closed previous quarter cases and their status as of the date of the report | | | X | | 30 days after quarter end | �� | DMS |
| Member Fraud, Waste and Abuse Report | Report should contain all open cases and closed previous quarter cases and their status as of the date of the report | | | X | | 30 days after quarter end | | DMS |
| Quarterly Benefits Payment | Provider report summarizing Medicaid payments by category of service for each month during quarter | | | X | | 30 days after quarter end | | DMS |
| Health Risk Assessments | Provide HRA's on new members, number completed, number not completed and number of refusals | | | X | | 30 days after quarter end | | DMS |
| Provider Changes in Network Report | Report should contain providers in network accepting new member, not accepting members and panel size | | | X | | 30 days after quarter end | | DMS |
| Out of Network Utilization by Members | Provide report for within MCO region providers not participating with Contractor's provider network and those providers providing services outside of the MCO region | | | X | | 30 days after quarter end | | DMS |
| Status of all Subcontractors | Provide an overview of all monitoring efforts of all subcontractors/vendors | | | X | | 30 days after quarter end | | DMS |
| Member TPL Resource Information (format) | Provide report of other insurance information on contractor's members | | X | | | By the 15th of Every Month | | DMS |
| QAPI Program Description | Provide QAPI program description documents | | | | X | | July
31st | DMS |
| Quality Improvement Plan and Evaluation | Provide details the annual review and include review of completed and continuing QI activities | | | | X | | July
31st | DMS |
|
| | | | | | | | | | | | | | | | | | | | | | | | |
| Outreach Plan | Provide both EPSDT and non-EPSDT outreach activities, frequency, responsible staff, activities and evaluated | | | | X | | July
31st | DMS |
| DMS copied on Report to Management of any changes in Member Services function to improve quality of care provided or method of delivery | Provide report to improve Member Services functions in providing quality of care provided and delivered | | | | X | | July
31st | DMS |
| Absent parent cancelled court order information | Provide report from court order information generated from data matches the Division of Child Support Enforcement/Department in the format agreed upon | | | | X | | July
31st | DMS |
| List of the Members participating with the Quality Member Access Advisory Committee | Provide list of members participating on committee | | | | X | | July
31st | DMS |
| Performance Improvement Projects (PIP) Proposal | Provide project proposal for clinical and non-clinical focus areas | | | | X | | September 1st | DMS |
| Abortion Procedure Report | Provide report by quarter on claims paid with abortion procedure code and be submitted with appropriate documentation | | | X | | 30 days after end of quarter | | DMS |
| Performance Improvement Project Measurement | Provide project measurements for clinical and non-clinical focus areas | | | | X | | September 1st | DMS |
| CMS-416 (EPSDT) | Provide reports on EPSDT services including the current CMS-416 format | | | | X | | March 15th | DMS |
| Member Survey(s) | Provide survey instruments for review and a copy of all results | | | | X | | August 31st | DMS |
| Provider Survey(s) | Provide survey instruments for review and a copy of all results | | | | X | | August 31 | DMS |
| Submit the final audited HEDIS report to DMS and NCQA | Provide final auditor's report issued by NCQA certified audit and data submission tool | | | | X | | August 31st | DMS |
| Behavioral Health |
| Member Receiving Behavioral Health Services |
| Number of Unduplicated Adults and Children/Youth | Provide monthly and year-to-date reports of the unduplicated number of adults and the unduplicated number of children/youth who have received a mental health and/or a substance abuse service** (to be reported separately unless delivered as an integrated service) | | X | | | By the 15th of Every Month | | DBHDID |
|
| | | | | | | | | | | | | | | | | | | | | | | | |
| Number of Unduplicated Pregnant and Postpartum Members | Provide monthly and year-to-date reports of the unduplicated number of pregnant and postpartum (60 days) patients who have received substance abuse services | | X | | | By the 15th of Every Month | | DBHDID |
| Number of Unduplicated of Intravenous Drug using Members | MCO to provide monthly and year-to-date reports of the unduplicated number of intravenous drug using patients who have received substance abuse services | | X | | | By the 15th of Every Month | | DBHDID |
| EPSDT and Behavioral Health Services | Provide EPSDT monthly and year-to-date reports for behavioral health services provided (by procedure code) | | X | | | By the 15th of Every Month | | DBHDID |
| Unduplicated Number and Percentage of Adults with SMI | Provide monthly and year-to-date reports of the unduplicated number and percentage of adults with SMI who are receiving peer support services | | X | | | By the 15th of Every Month | | DBHDID |
| Unduplicated Number and Percentage of Adults and Children/Youth with Mental Health and Substance Abuse Services | MCO to provide monthly and year-to-date reports of the unduplicated number and percentage of adults and the unduplicated number and percentage of children/youth of who have received both mental health and substance abuse services. | | X | | | By the 15th of Every Month | | DBHDID |
| Unduplicated Number of Children/Youth Receiving Impact Plus | Provide monthly and year-to-date reports of the unduplicated number of children/youth (up to age 21) who are assessed for IMPACT Plus covered service eligibility. | | X | | | By the 15th of Every Month | | DBHDID |
| Unduplicated Number of Children/Youth Receiving Impact Plus Prior Authorizations | Provide monthly and year-to-date reports of the unduplicated number of children/youth who receive services under IMPACT Plus eligibility, and the resulting services, by type and unit, that were prior authorized including the type and units of those prior authorized services that were rendered | | X | | | By the 15th of Every Month | | DBHDID |
| Unduplicated Number of Adults and Children/Youth Received Services under 907 KAR 3:110 | MCO to provide monthly and year-to-date reports of the unduplicated number of adults and unduplicated number of children/youth who have received each of the following level of substance abuse services, as defined in 907 KAR 3:110: Prevention, Assessment, Outpatient, Intensive Outpatient, Residential and Case Management | | X | | | By the 15th of Every Month | | DBHDID |
| Pharmacy use and Cost for Adults and Children/Youth with Behavioral Health Diagnoses | MCO will provide monthly and year-to-date reports of all pharmacy use and cost for adults (18 +) and children/youth (up to age 21) with behavioral health diagnoses | | X | | | By the 15th of Every Month | | DBHDID |
| Pharmacy use and Cost for Children/Youth Received Impact Plus Services | MCO will provide monthly and year-to-date reports of all pharmacy use and cost for children/youth (up to age 21) who receive IMPACT Plus covered services | | X | | | By the 15th of Every Month | | DBHDID |
| Inpatient Psychiatric Hospitalization / Level I and II PRTFs - Admissions / Readmissions |
|
| | | | | | | | | | | | | | | | | | | | | | | | |
| Unduplicated Number of Adults and Children/Youth Received PRTF - Level I and Level II | Provide monthly and year-to-date reports of the unduplicated number of adults and the unduplicated number children/youth who have received inpatient psychiatric hospitalization, psychiatric residential treatment (PRTF- Level I and Level II) and residential substance abuse treatment. This report shall include length of stay and “discharged to” information and must delineate those placed out-of-state. This report also shall include placements covered by the insurer (including KCHIP and EPSDT) and those covered by other payor sources | | X | | | By the 15th of Every Month | | DBHDID |
| Unduplicated Number and Percentage of Adults and Children/Youth Readmitted to PRTF | Track and report quarterly and year-to-date the number and percentage of children/youth and adults who have been readmitted within 30 days and within 180 days to an inpatient psychiatric setting and/or PRTF | | X | | | | | DBHDID |
| Services Provided |
| Behavioral Health Services Provided by Procedure Code | Provide monthly and year-to-date reports of behavioral health (mental health and substance abuse) by procedure code. The report should delineate number of unduplicated members receiving the service, units of service and paid amount of claim (by procedure code) | | X | | | By the 15th of Every Month | | DBHDID |
| Member Best Practices Outcomes |
| Unduplicated Number and Percentage of Adults with SMI | Provide monthly and year-to-date reports of the unduplicated number and percentage of adults with SMI who live in independent, permanent housing | | X | | | By the 15th of Every Month | | DBHDID |
| | | | | | | | | |
|
| | | | | | | | | | | | | | | | | | | | | | | | |
| | | | | | | | | |
| Unduplicated Number and Percentage of Adults with SMI and Children/Youth with SED Received with Co-occurring Mental Health and Substance Abuse Disorders | Provide monthly and year-to-date reports of the unduplicated number and percentage of adults with SMI and children/youth with SED who received Assertive Community Treatment, Supported Employment, Supportive Housing, Family Psycho education, Integrated treatment for co-occurring mental health and substance abuse disorders, Illness Management/Recovery, or Medication Management | | X | | | By the 15th of Every Month | | DBHDID |
| Unduplicated Number and Percentage of Children/Youth with SED Therapy or Family Functional Therapy | Provide monthly and year-to-date reports of the unduplicated number and percentage of children/youth with SED who received Therapeutic Foster Care, Multisystem Therapy or Family Functional Therapy | | X | | | By the 15th of Every Month | | |
| Unduplicated Number and Percentage of Children/Youth with SED who were assessed for Trauma History | Provide monthly and year-to-date reports of the unduplicated number and percentage of children/youth with SED who were assessed for trauma history | | X | | | By the 15th of Every Month | | |
| Unduplicated Number of Adults and Children/Youth of their Caregivers Received Peer Support Service | Provide monthly and year-to-date reports of the unduplicated number of adults and children/youth or their caregivers who received a Peer Support Service from an individual credentialed by the DBHDID | | X | | | By the 15th of Every Month | | DBHDID |
| Member Access |
| Unduplicated Number and Percentage of Pregnant and Post-partum women with Substance use Disorders Received First Treatment within 48 hours | Report monthly and year-to-date on the number and percentage of pregnant and post-partum women with substance use disorders who receive their first treatment visit within 48 hours of initial request for services | | X | | | By the 15th of Every Month | | DBHDID |
| Continuity of Care |
| Unduplicated Number and Percentage of Children/Youth Discharged from PRTF | Report quarterly and year-to-date on number and percentage of children/youth (under 21) and adults (18 +) discharged from an inpatient psychiatric facility or PRTF who participate in an outpatient visit within seven (7) and 14 days of discharge | | X | | | By the 15th of Every Month | | DBHDID |
| Unduplicated Number and Percentage of Children/Youth Discharged from a Residential Substance Abuse Treatment Program | Report quarterly and year-to-date on number and percentage of youth (under 21) and adults (18 +) discharged from a residential substance abuse treatment program who participate in an outpatient visit within seven (7) and 14 days of discharge | | X | | | By the 15th of Every Month | | DBHDID |
| Member Satisfaction |
| Mental Health Statistics Improvement Project (MHSIP) Adult Survey | Provide annual report on the results of the administration of the Mental Health Statistics Improvement Project (MHSIP) adult survey. Results should be displayed as the number of individuals surveyed and the percentage reporting positively in the following seven domains: General satisfaction, Access, Quality / Appropriateness, Participation in Treatment Planning, Outcomes, Social Connectedness and Functioning | | | | X | | August 31st | DBHDID |
| Administration of the Youth Services Satisfaction Caregiver (YSS-F) | Provide annual report on the results of the administration of the Youth Services Satisfaction Caregiver (YSS-F) survey for children/youth. Results should be displayed as the number of individuals surveyed and the percentage rating positively in the following seven domains: General satisfaction, Access, Quality / Appropriateness, Participation in Treatment Planning, Outcomes, Social Connectedness and Functioning | | | | X | | August 31st | DBHDID |
| Interface with Criminal Justice / Education |
| Interface with Primary Care / Physical Health |
| Unduplicated Number of Adults and Children/Youth with Behavioral Health Diagnosis's with PCP | Provide quarterly and year-to-date reports of the number of children/youth and adults, with behavioral health diagnoses, who have a known Primary Care Provider (PCP) | | | X | | 30 days after quarter end | | DBHDID |
| Unduplicated Number of Children/Youth with Behavioral Health Diagnoses Received Annual Wellness Check/Health Exam | Provide quarterly and year-to-date reports of the number of children/youth (up to age 21) and adults (18 +) with behavioral health diagnoses who receive annual wellness check/annual physical health exams | | | X | | 30 days after quarter end | | DBHDID |
|
| | | | | | | | | | | | | | | | | | | | | | | | |
| Unduplicated Number of Adults and Children/Youth General Behavioral Health Diagnosis and Chronic Physical Health Diagnosis | Provide quarterly and year-to-date reports of the number of children/youth (up to age 21) and adults (general behavioral health and with SMI designation) with both an Axis I behavioral health diagnosis(as) and a chronic (physical) health diagnosis(as). Exclusions are permitted in instances where the behavioral health diagnosis is well documented as directly attributable to the physical health condition | | | X | | 30 days after quarter end | | DBHDID |
| Unduplicated Number of Adults and Children/Youth with Regular use of Tobacco Products | Provide annual report of the number of children/youth (up to age 18) and adults (18+) who report regular use (once a week or greater) of tobacco products (all types). | | | | X | | April
30th | DBHDID |
| Unduplicated Number of Adults and Children/Youth Screened for Substance Use Disorder in Physical Care Setting | Provide quarterly and year-to-date report on the number of children/youth (up to age 18) and adults (18+) who are screened for a substance use disorder in a physical care setting (including ER, primary care, specialized care, other) | | | X | | 30 days after quarter end | | DBHDID |
| | | | | | | | | | |
Appendix M
Program Integrity Requirements
I. Organization
A. The Contractor’s Program Integrity Unit (PIU) shall be organized so that:
| |
| 1. | Required Fraud, Waste and Abuse activities shall be conducted by staff that shall have sufficient authority to direct PIU activities; and shall include written policies, procedures, and standards of conduct that articulate the organization’s commitment to comply with all applicable federal and state regulations and standards; |
| |
| 2. | The unit shall be able to establish, control, evaluate and revise Fraud, Waste and Abuse detection, deterrent and prevention procedures to ensure their compliance with Federal and State requirements; |
| |
| 3. | Adequate staff shall be assigned to the PIU to enable them to conduct the functions specified in this Appendix on a continuous and on-going basis and staffing shall consist of a compliance officer, auditing and clinical staff; |
| |
| 4. | The unit shall be able to prioritize work coming into the unit to ensure that cases with the greatest potential program impact are given the highest priority. Allegations or cases having the greatest program impact include cases involving: |
| |
| • | Multi-State fraud or problems of national scope, or Fraud or Abuse crossing service area boundaries; |
| |
| • | High dollar amount of potential overpayment; or |
| |
| • | Likelihood for an increase in the amount of Fraud or Abuse or enlargement of a pattern. |
| |
| 5. | Contract shall provide ongoing education to Contractor staff on Fraud, Waste and abuse trends including CMS initiatives; |
| |
| 6. | Contractor shall attend any training given by the Commonwealth/Fiscal Agent or other Contractor’s organizations provided reasonable advance notice is given to Contractor of the scheduled training. |
II. Function
The Contractor shall establish a PIU to identify and refer to the Department any suspected Fraud or Abuse of Members and Providers.
A. The Contractor’s PIU shall be responsible for:
| |
| 1. | Preventing Fraud, Waste and Abuse by identifying vulnerabilities in the Contractor’s program including identification of member and provide Fraud, Waste and Abuse by and taking appropriate action including but not limited to the following: |
| |
| • | Recoupment of overpayments; |
| |
| • | Dispute resolution meetings; and |
| |
| 2. | Proactively detecting incidents of Fraud, Waste and Abuse that exist within the Contractor’s program through the use of algorithm, investigations and record reviews; |
| |
| 3. | Determining the factual basis of allegations through investigation concerning fraud or abuse made by Members, Providers and other sources; |
| |
| 4. | Initiating appropriate administrative actions to collect overpayments, deny or suspend payments that should not be made; |
| |
| 5. | Referring potential Fraud, Waste and Abuse cases to the OIG (and copying DMS) for preliminary investigation and possible referral for civil and criminal prosecution and administrative sanctions; |
| |
| 6. | Initiating and maintaining network and outreach activities to ensure effective interaction and exchange of information with all internal components of the Contractor as well as outside groups; |
| |
| 7. | Making and receiving recommendations to enhance the Contractor ability to prevent, detect and deter Fraud, Waste or Abuse; |
| |
| 8. | Providing prompt response to detected offenses and developing corrective action initiatives relating to the Contractor’s contract; |
| |
| (i) | Providing for internal monitoring and auditing of Contractor and its subcontractors; and supply the department with quarterly reports on the activity and ad hocs as necessary; |
| |
| 9. | Being subject to on-site review and fully complying with requests from the department to supply documentation and records; and |
| |
| 10. | Creating an account receivables process to collect outstanding debt from members or providers and providing monthly reports of activity and collections to the department. |
B. The Contractor’s PIU shall:
| |
| 1. | Conduct continuous and on-going reviews of all MIS data including, Member and Provider Grievances and appeals, for the purpose of identifying potentially fraudulent acts; |
| |
| 2. | Conduct regularly scheduled post-payment audits of provider billings, investigate payment errors, produce printouts and queries |
of data and report the results of their work to the Contractor, the Department and OIG;
| |
| 3. | Conduct onsite and desk audits of providers and report the results to the Department, including any overpayments identified; |
| |
| 4. | Maintain locally cases under investigation for possible Fraud, Waste or Abuse activities and provide these lists and entire case files to the Department and OIG upon demand; |
| |
| 5. | Designate a contact person to work with investigators and attorneys from the Department and OIG; |
| |
| 6. | Ensure the integrity of PIU referrals to the Department. Referrals if appropriate by the unit shall not be subject to the approval of the Contractor’s management or officials; |
| |
| 7. | Comply with the expectations of 42 CFR 455.20 by employing a method of verifying with member whether the services billed by providers were received by randomly selecting a minimum sample of 500 claims on a monthly basis; |
| |
| 8. | Run algorithms on claims data and develop a process and report quarterly to the department all algorithms run, issues identified, actions taken to address those issues and the overpayments collected; |
| |
| 9. | Have a method for collecting administratively on member overpayments that were declined prosecution, known as Medicaid Program Violations (MPV) letters, and recover payments from the member; |
| |
| 10. | Comply with the program integrity requirements set forth in 42 CFR 438.608 and provide policies and procedures to the Department for review; |
| |
| 11. | Report any provider denied enrollment by Contractor for any reason, including those contained in 42 CFR 455.106, to the Department within 5 days of the enrollment denial; |
| |
| 12. | Have a method for recovering overpayments from providers; |
| |
| 13. | Comply with the program integrity requirements of the Patient Protection and Affordable Care Act as directed by the Department; |
| |
| 14. | Correct any weaknesses, deficiencies, or noncompliance items that are identified as a result of a review or audit conducted by DMS, CMS, or by any other State or Federal Agency that has oversight of the Medicaid program. Corrective action shall be completed the earlier of 30 calendar days or the timeframes established by Federal and state laws and regulations; and |
| |
| 15. | Work cooperatively and collaboratively with the Department to enhance the contractors PIU and to address any deficiencies identified. |
Incidents or allegations concerning physical or mental abuse of Members shall be immediately reported to the Department for Community Based Services in accordance with state law and carbon copy the Department for Medicaid Services and OIG.
The Contractor’s PIU shall operate a process to receive, investigate and track the status of Fraud, Waste and Abuse complaints received from members, providers and all other sources which may be made against the Contractor, providers or members.
A. The process shall contain the following:
| |
| 1. | Upon receipt of a complaint or other indication of potential fraud or abuse, the Contractor’s PIU shall conduct a preliminary inquiry to determine the validity of the complaint; |
| |
| 2. | The PIU should review background information and MIS data; however, the preliminary inquiry should not include interviews with the subject concerning the alleged instance of Fraud or Abuse; |
| |
| 3. | Should the preliminary inquiry result in a reasonable belief that the complaint does not constitute Fraud or Abuse, the PIU should not refer the case to OIG; however, the PI should take whatever actions may be necessary, up to and including, administrative recovery of identified overpayments; |
| |
| 4. | Should the preliminary inquiry result in a reasonable belief that Fraud or Abuse has occurred, the PI should refer the case and all supporting documentation to the Department, with a copy to OIG; |
| |
| 5. | OIG will review the referral and attached documentation and make a determination as to whether OIG will investigate the case or return it to the PIU for them to conduct a preliminary investigation; |
| |
| 6. | OIG will notify the PIU in a timely manner as to whether the OIG will investigate or whether the PIU should conduct a preliminary investigation; |
| |
| 7. | If in the process of conducting a preliminary investigation the PIU suspects a violation of either criminal Medicaid fraud statutes or the Federal False Claims Act, the PIU shall immediately notify the Department with a copy to the OIG of their findings and proceed only in accordance with instructions received from the OIG; |
| |
| 8. | If OIG determines that it will keep a case referred by the PIU, the OIG will conduct an investigation, gather evidence, write a report and forward information to Department and the PIU for appropriate actions; |
| |
| 9. | If OIG opens an investigation based on a complaint received from a source other than the Contractor, OIG will, upon completion of the |
investigation, provide a copy of the investigative report to DMS and the PIU for appropriate actions;
| |
| 10. | If OIG investigation results in a referral to the Attorney General’s Medicaid Fraud Control Unit and/or the U.S. Attorney, the OIG will notify DMS and the PIU of the referral. DMS and the PIU should only take actions concerning these cases in coordination with the law enforcement agencies that received the OIG referral; |
| |
| 11. | Upon approval of the Department, Contractor shall suspend provider payments in accordance with Section 6402 (h)(2) of the Affordable Care Act pending investigation of credible allegation of fraud; these efforts shall be coordinated through the Department; |
| |
| 12. | Upon completion of the PIU’s preliminary investigation, the PIU should provide the Department and OIG a copy of their investigative report, which should contain the following elements: |
| |
| • | Name and address of subject; |
| |
| • | Medicaid identification number; |
| |
| • | The complaint/allegation; |
| |
| • | Date assigned to the investigator; |
| |
| • | Methodology used during investigation; |
| |
| • | Facts discovered by the investigation as well as the full case report and supporting documentation; |
| |
| • | All exhibits or supporting documentation; |
| |
| • | Recommendations as considered necessary, for administrative action or policy revision; |
| |
| • | Overpayment identified, if any, and recommendation concerning collection; |
| |
| 13. | The Contractor’s PIU shall provide OIG and DMS a quarterly member and provider status report of all cases including actions taken to implement recommendations and collection of overpayments; |
| |
| 14. | The Contractor’s PIU shall maintain access to a follow-up system, which can report the status of a particular complaint or grievance process or the status of a specific recoupment; and |
| |
| 15. | The Contractor’s PIU shall assure a Grievance and appeal process for Members and Providers in accordance with 907 KAR 1:671 and 907 KAR 1:563. |
The Contractor’s PIU shall provide a quarterly in narrative report format all activities and processes for each investigative case (from opening to closure) to the Department within 30 calendar days of investigation closure.
If any internal component of the Contractor discovers or is made aware of an incident of possible Member or Provider Fraud, Waste or Abuse, the incident shall be immediately reported to the PIU Coordinator.
The Contractor’s PIU shall report all cases of suspected Fraud, Waste, Abuse or inappropriate practices by Subcontractors, Members or employees to the Department and OIG.
| |
| A. | The Contractor is required to report the following data elements to the Department and the OIG on a quarterly basis, in an excel format: |
| |
| 4. | Provider/Member number; |
| |
| 5. | Date complaint received by Contractor; |
| |
| 6. | Source of complaint,-unless the complainant prefers to remain anonymous |
| |
| 9. | Is complaint substantiated or not substantiated (Y or N answer only under this column), |
| |
| 10. | PIU Action Taken (only provide the most current update); |
| |
| 11. | Amount of overpayment (if any); |
| |
| 12. | Administrative actions taken to resolve findings of completed cases including the following information: |
| |
| • | The overpayment required to be repaid and overpayment collected to date; |
| |
| • | Describe sanctions/withholds applied to Providers/Members, if any; |
| |
| • | Provider/Members appeal regarding overpayment or requested sanctions. If so, list the date an appeal was requested, date the hearing was held, the date of the final decision, and to the extent they have occurred; |
| |
| • | Revision of the Contractor’s policies to reduce potential risk from similar situations with a description of the policy recommendation, implemented of aforementioned revision and date of implementation; and |
| |
| • | Make MIS system edit and audit recommendations as applicable. |
| |
| VI. | Availability and Access to Data |
A. The Contractor shall:
| |
| 1. | Gather, produce, keep and maintain records including, but not limited to, ownership disclosure, for all providers and subcontractors, submissions, applications, evaluations, qualifications, member information, enrollment lists, grievances, Encounter data, desk reviews, investigations, investigative supporting documentation, finding letters and subcontracts for a period of 5 years after contract end date; |
| |
| 2. | Regularly report enrollment, Provider and Encounter data in a format that is useable by the Department, and the OIG; |
| |
| 3. | Backup, store and be able to recreate reported data upon demand for the Department and the OIG; |
| |
| 4. | Permit reviews, investigations or audits of all books, records or other data, at the discretion of the Department or OIG, or other authorized federal or state agency; and shall provide access to Contractor records and other data on the same basis and at least to the same extent that the Department would have access to those same records; |
| |
| 5. | Produce records in electronic format for review and manipulation by the Department and the OIG; |
| |
| 6. | Allow designated Department staff read access to ALL data in the Contractor’s MIS systems; and |
| |
| 7. | Provide all contracted rates for providers upon request. |
The Contractor’s PIU shall have access to any and all records and other data of the Contractor for purposes of carrying out the functions and responsibilities specified in this Contract.
The Contractor shall fully cooperate with the OIG, the United States Attorney’s Office and other law enforcement agencies in the investigation of fraud or abuse cases.
In the event no action toward collection of overpayments is taken by the Contractor after one hundred and eight (180) days the Commonwealth may begin collection activity and shall retain any overpayments collected. If the Contractor shall takes appropriate action to collect overpayments, the Commonwealth will not intervene.
The Contractor shall provide identity and cover documents and information for law enforcement investigators under cover.
Appendix N
Performance Improvement Projects
The Performance Improvement Projects (PIPs) shall include one project (1) relating to physical health, one (1) project relating to behavioral health, and one (1) project relating to a statewide care or services issue. Following is a table which identifies the four (4) clinical care and non-clinical services topics which will be implemented Year One of the Contract as well as justification (reasons) for selecting these topics.
| |
| A. | The topic relates to clinical care and non clinical services and represents a national and/or statewide health issue; |
| |
| B. | There are current guidelines/standards available to guide the development/implementation of a PIP; |
| |
| C. | There are identifiable measures for performance improvement (HEDIS or claims data); and |
| |
| D. | The topic is associated with historical over- or underutilization of Medicaid Services. |
|
| | | | | | |
| TOPIC | JUSTIFICATION (REASON) |
| | Clinical Care or Non-clinical Service | National &/or State Care or Services Burden | Performance Guidelines/ Standards of Care are Available | HEDIS or Other Measures for Performance are Available | Assoc with Under – &/or Over utilization (High Costs)
| Other Reasons |
|
| | | | | | |
Access to & Availability of Services
| Non-clinical Svc. | YES | YES | YES | YES | The Ensuring Access to Care in Medicaid under Health Reform report **** cited concerns regarding the expansion of Medicaid eligibility under the 2010 ACA & movement of states toward using Contractors for management of health & healthcare costs of Medicaid Members. Concerns were also expressed regarding Medicaid’s comprehensive benefits & ensuring access to provider/delivery systems equipped to serve low-income populations with complex health needs. Additionally, 1)Access to/availability of Medicaid participating primary care providers & specialists is a major concern, as reimbursement levels are reduced due to state Medicaid budget deficits & demands on state resources increase. 2)Contractors express concerns regarding the “churning,” which results from short Medicaid eligibility/enrollment periods, as this is viewed as key obstacle in managing care & incompatible with efforts to manage chronic conditions & prevent disruptions in care.
|
Depression
| Clinical Care | YES | YES | YES | YES | The State of Health Care Quality report** indicated that depression affects 15 million Americans, & if untreated, can lead to other physical/mental health conditions. The American Psychiatric Association recommends use of antidepressant & behavioral therapies (at the primary care level) to treat depression. Additionally, in 2009, 49.6% of Medicaid Members, 18 years of age/older diagnosed with a new episode of major depression, were treated with antidepressant medication for a specified period of time, as compared to 62.9 % of individuals 18 years of age/older who were covered under commercial HMO health plans. |
|
| | | | | | |
Emergency Department (ED) Use Management
| Clinical Care | YES | NO | YES | YES | The data on emergency room utilization of FFS KY Medicaid claims for ED visits in CY 2008 indicated that the major difference between “high fliers” (having 12 or more ER visits/yr) & “single timers” (having one visit/yr), is that high fliers are most over-represented in 3-digit primary diagnosis codes for abdominal symptoms, migraines & back conditions, which may be effectively treated (on a primary care level). Additionally, of FFS Medical claims for ED services provided in SFY 2010, indicated that a total of $151,897,739 was spent on illnesses/conditions such as upper respiratory infection, otitis media, acute pharyngitis, viral infection and lumbago.
|
|
| | | | | | |
Screenings for Breast Cancer, Cervical Cancer, & Chlamydia
| Clinical Care | YES | YES | YES | YES | The Aggregate Medicaid Plan Report* for CY 2009, indicated that the KY Medicaid Average rate of mammograms performed (45%) & Medicaid Average rate of PAP tests performed (57%) were lower, as compared to the KY Average rate of mammograms performed (68%) and KY Average rate of PAP tests performed (72%). Additionally, The State of Health Care Quality report** indicated that: 1)Breast cancer is one of the most common forms of cancer in American women, accounting for the deaths of 40, 170 women in 2009. In that same year, 52.4% of Medicaid women 50-69 years of age were screened by mammography, as compared to 71.3 % of women 50-69 years of age covered under Commercial HMO health plans. 2)As one of the most treatable cancers, cervical cancer is the second most common cancer worldwide & 10th leading cause of cancer in females. In 2009, 65.8% of Medicaid women 21 to 64 years of age received PAP tests, as compared to 77.3% of women 21–64 years of age covered under Commercial HMO plans. 3)Chlamydia is a sexually transmitted disease that may have serious consequences (e.g., HIV, syphilis, reproductive health conditions). Although screening rates for Chlamydia in 2009 are higher in Medicaid populations (61.6%), as compared to Commercial HMO rates (45.4%) according to this report, the screening is not complicated & can save $45 annually for every woman screened. |
References
*Aggregate Medicaid Plan Report, Select Preventive Care Measures, January 09 – December 09 distributed by The Kentuckiana Health Collaborative in 2010.
**The State of Health Care Quality 2010, published by the National Committee for Quality Assurance in 2011.
****Ensuring Access to Care in Medicaid under Health Reform, Report #8187, published by Kaiser Family Foundation in May 2011.
Appendix O
Health Outcomes, Indicators, Goals and Performance Measures
A goal of the Medicaid Program is to improve the health status of Medicaid recipients. Statewide health care outcomes, health indicators, and goals have been targeted and designated by the Department in collaboration with the Departments for Public Health (DPH) and Behavioral Health, Developmental and Intellectual Disabilities. Federal Medicaid Managed Care regulations, 438.24 (C ) (1) and (C) 2 Performance Measurement, require that the Contractor measure and report to the State its performance, using standard measures required by the State and/or submit to the State data, specified by the State that enables the State to measure the Contractor’s performance.
In accordance with this, the Department has established a set of Medicaid Managed Care Performance Measures. The measure set was originally designed to align with the Healthy Kentuckians 2010 Goals. Healthy Kentuckians is the state’s commitment to national preventive initiative, Healthy People 2010, with the overarching goals to increase years of healthy life and eliminate health disparities and includes objectives and targets set to meet the needs of Kentuckians. The document includes ten leading health indicators with related goals and objectives. Select indicators, goals and objectives that are the basis of the Performance Measures are displayed in the table below.
Other Performance Measures are derived from the managed care Healthcare Effectiveness Data and Information Set (HEDIS®)4 set, which are reported by managed care organizations nationally and have national benchmarks for comparison of performance. Performance Measures have also been developed collaboratively by the Department and the EQRO based on key areas of interest of the Department. Together, the measures address the access to, timeliness of, and quality of care provided to children, adolescents enrolled in Managed Care; and focus on preventive care, health screenings, prenatal care, as well as special populations (adults with hypertension, children with special health care needs (CSHCN).
4HEDIS is a registered trademark of the National Committee for Quality Assurance (NCQA).
|
| | | |
Healthy Kentuckians Leading Health Indicator(s)5 | Healthy Kentuckians Goals | Health Kentuckians Objectives6 | Related Medicaid Managed Care Performance Measure(s) |
Physical Activity and Fitness
Nutrition | ▪ Improve the health, fitness, and quality of life of all Kentuckians through the adoption and maintenance of regular, daily physical activity. ▪ To promote health and reduce chronic disease risk, disease progression, debilitation, and premature death associated with dietary factors and nutritional status among all people in Kentucky. | ▪ Reduce overweight to a prevalence of no more than 25 percent among Kentuckians ages 18 and older. ▪ Reduce the percentage of Kentuckians age 18 and older who are either overweight or obese. ▪ Decrease the percentage of Kentuckians reporting no leisure time physical activity (by BMI category, i.e., normal weight, overweight, obese class I, obese class II, obese class III). ▪ To increase to at least 24 percent the proportion of young people in grades 9-12 who engage in, | ▪ Height/Weight/BMI Assessment and Assessment/counseling for Nutrition and Physical Activity for Adults7
▪ Height/Weight/BMI Assessment and Assessment/ Counseling for Nutrition and Physical Activity for Children and Adolescents8
|
5 See the Healthy Kentuckians 2010 Mid-Decade Review for full details on all indicators, goals, and objectives. Available at: http://chfs.ky.gov/dph/hk2010MidDecade.htm.
6 Stated State and National Performance Target goals are for reference only and reflect the Healthy Kentuckians goals, and do not apply to health plan contract requirements.
7 The performance measure for this goal will follow a combination of the HEDIS measure specifications for Adult BMI assessment and State-specific numerator(s).
8 The performance measure for this goal will follow a combination of the HEDIS measure specifications for Weight Assessment and Counseling for Nutrition and Physical Activity for Children and Adolescent s and State-specific numerator(s).
|
| | | |
Healthy Kentuckians Leading Health Indicator(s)5 | Healthy Kentuckians Goals | Health Kentuckians Objectives6 | Related Medicaid Managed Care Performance Measure(s) |
| | | moderate physical activity for at least 30 minutes on five or more of the previous seven days. ▪ Increase to at least 50 percent the prevalence of healthy weight (defined as a body mass index (BMI) greater than 19.0 and less than 25.0) among all people aged 20 and older. ▪ Reduce to less than 15 percent the prevalence of BMI at or above 30.0 among people aged 20 and older. ▪ Reduce to 5 percent or less the prevalence of overweight and obesity (at or above the sex and age-specific 95th percentile of BMI from the revised NCHS/CDC growth charts) in children (aged 1 - 5 and 6 - 11) and adolescents (aged 12 - 19). ▪ Increase to at least 40 percent the proportion of people age 2 and older who meet the Dietary
| |
|
| | | |
Healthy Kentuckians Leading Health Indicator(s)5 | Healthy Kentuckians Goals | Health Kentuckians Objectives6 | Related Medicaid Managed Care Performance Measure(s) |
| | | guidelines' minimum average daily goal of at least five servings of vegetables and fruits | |
Heart Disease and Stroke
| Enhance the cardiovascular health and quality of life of all Kentuckians through improvement of medical management, prevention and control of risk factors, and promotion of healthy lifestyle behaviors. | ▪ To increase to at least 85 percent the proportion of adults who have had their blood cholesterol checked within the preceding five years. ▪ Reduce heart disease deaths to no more than 250 deaths per 100,000 people (age adjusted to the year 2000 standard). ▪ To decrease to at least 20 percent the proportion of adult Kentuckians with high blood pressure. ▪ Reduce heart disease deaths to no more than 250 deaths per 100,000 people (age adjusted to the year 2000 standard).
| ▪ Cholesterol Screening for Adults ▪ HEDIS Controlling High Blood Pressure The performance measure for this goal will follow the HEDIS measure specifications for Controlling High Blood Pressure. 9
|
9The performance measure for this goal will follow the HEDIS measure specifications for Controlling High Blood Pressure.
|
| | | |
Healthy Kentuckians Leading Health Indicator(s)5 | Healthy Kentuckians Goals | Health Kentuckians Objectives6 | Related Medicaid Managed Care Performance Measure(s) |
| Tobacco Use | ▪ Reduce the burden of tobacco-related addiction, disease, and mortality, thereby improving the health and well being of adults and youth in Kentucky. This includes decreasing tobacco use among adults, pregnant women, youth, and disparate populations, eliminating exposure to secondhand smoke, and building capacity in communities for tobacco prevention and cessation. | ▪ Increase to 95 percent the proportion of patients who receive advice to quit smoking from a health care provider. ▪ Increase to 32 percent the proportion of young people in grades 9 to 12 who have never smoked. ▪ Reduce the proportion of high school and middle school students who think smoking cigarettes makes young people look cool or fit in. ▪ Increase to 100 percent the proportion of high school students who think secondhand smoke is harmful. ▪ Reduce cigarette smoking among pregnant women to a prevalence of no more than 17 percent. ▪ Of new mothers who smoked in the first three months before becoming pregnant, increase the percentage who abstained from using tobacco
| |
|
| | | |
Healthy Kentuckians Leading Health Indicator(s)5 | Healthy Kentuckians Goals | Health Kentuckians Objectives6 | Related Medicaid Managed Care Performance Measure(s) |
| | | during their pregnancy. | |
Oral health 7 | To improve the health and quality of life for individuals and communities by preventing and controlling oral disease and injuries, and to improve access to oral health care for all Kentuckians. | ▪ Increase to at least 70 percent the proportion of children ages 6, 7, 12, and 15 who have participated in an oral health screening, including those who have been referred, and those who have received the appropriate follow-up. | ▪ HEDIS Annual Dental Visit.10 |
| Access to quality health services | Improve access to a continuum of comprehensive, high quality health care using both the public and private sectors in Kentucky. | ▪ Increase to at least 90 percent the proportion of people who have a specific source of ongoing primary care. ▪ Reduce by 25 percent the number of individuals lacking access to a primary care provider in underserved areas. | ▪ HEDIS Well Child Visits in the First 15 Months: 6+ visits.11 ▪ HEDIS Well Child Visits in the 3rd, 4th, 5th and 6th Years of Life ▪ HEDIS Adolescent Well Care ▪ HEDIS Children's Access to PCP's
|
10The performance measure for this goal will follow the HEDIS measure specifications for Annual Dental Visit.
11The performance measures for this goal will follow the HEDIS measure specifications for Well Child Visits 15 months (6+ visits), Well Child Visits 3rd, 4th, 5th & 6th Years of Life, and Adolescent Well-Care Visits, and Children's and Adolescents' Access to PCPs.
|
| | | |
Healthy Kentuckians Leading Health Indicator(s)5 | Healthy Kentuckians Goals | Health Kentuckians Objectives6 | Related Medicaid Managed Care Performance Measure(s) |
Adolescent Screening/ Counseling: Tobacco Use12, See Healthy Kentuckians Indicator for Tobacco Use for additional details on this numerator., Alcohol/Substance Use, Sexual Activity, and/or Mental Health Assessment
|
Tobacco Use Substance Abuse Alcohol Abuse | To increase abstinence from substances while reducing experimentation, use and abuse, especially among Kentucky's youth, thereby reducing the consequences -- violence, crime, illness, death and disability -- that result from abuse of substances at d harm to individuals and society. | ▪ Increase the proportion of 8th grade students who report strong disapproval for use of tobacco, alcohol, and other drugs to: tobacco, 60 percent; alcohol, 65 percent; marijuana, 85 percent, and other drugs 98 percent. ▪ Increase the proportion of 8th grade students who report that none of their friends use substances to: tobacco: 70 percent; alcohol: 70 percent; marijuana: 90 percent, and other drugs: 95 percent. ▪ Increase the proportion of 8th grade students who perceive great risk of personal harm and/or trouble associated with regular use of substances: tobacco: 50 percent, alcohol: 35 percent, and marijuana: 80 percent. ▪
| Adolescent Screening/ Counseling: Tobacco, Alcohol, and Substance Use |
12See Healthy Kentuckians Indicator for Tobacco Use for additional details on this numerator.
|
| | | |
Healthy Kentuckians Leading Health Indicator(s)5 | Healthy Kentuckians Goals | Health Kentuckians Objectives6 | Related Medicaid Managed Care Performance Measure(s) |
| | | ▪ Increase the percentages of 8th grade students who report having never used tobacco, alcohol, and other drugs: tobacco: 65 percent; alcohol: 65 percent; marijuana: 90 percent; cocaine: 98 percent. | |
Family Planning Sexually Transmitted Diseases | A society where healthy sexual relationships free of infection is the standard. | ▪ Reduce pregnancies among females ages 15-17 to no more than 20 per 1,000 adolescents. ▪ Increase by at least 10 percent the proportion of sexually active individuals, ages 15-19, who use barrier method contraception with or without hormonal contraception to prevent sexually transmitted disease and prevent pregnancy. ▪ To increase to at least 68 percent the number of sexually active, unmarried high school-aged youth who used a latex condom at last sexual intercourse. ▪
| Adolescent Screening/ Counseling: Sexual Activity |
|
| | | |
Healthy Kentuckians Leading Health Indicator(s)5 | Healthy Kentuckians Goals | Health Kentuckians Objectives6 | Related Medicaid Managed Care Performance Measure(s) |
| Mental Health Screening | Improve the mental health of all Kentuckians by ensuring appropriate, high-quality services informed by scientific research to those with mental health needs. | ▪ Reduce by half the proportion of Kentucky adolescents who report considering or attempting suicide during the past year. | Adolescent Screening/ Counseling: Mental Health |
| Environmental Health | Health for all through a healthy environment. | ▪ Increase the number of abatement permits for lead housing projects to 115 per grant fiscal year. | HEDIS Lead Screening in Children13 |
Access to Quality Health Services
Disability and Secondary Conditions
| Improve access to a continuum of comprehensive, high quality health care using both the public and private sectors in Kentucky.
Promote health and prevent secondary conditions among persons with disabilities, including eliminating disparities between persons with disabilities and the U.S. population.
| ▪ Increase to at least 90 percent the proportion of people who have a specific source of ongoing primary care.
▪ Ensure that 100 percent of persons with a developmental disability who receive services from the state receive a yearly physical examination. ▪ Ensure that 100 percent of persons with a ▪
| Children with Special Health Care Needs (CSCHN) |
13The performance measure for this goal will follow the HEDIS measure specifications for Lead Screening in Children.
|
| | | |
Healthy Kentuckians Leading Health Indicator(s)5 | Healthy Kentuckians Goals | Health Kentuckians Objectives6 | Related Medicaid Managed Care Performance Measure(s) |
| | | developmental disability who receive services from the state receive a dental examination every six months. | |
Medicaid Managed Care Performance Measures
The Department, in collaboration with the EQRO, have developed a set of measures that are clinically sound, consistent with Healthy Kentuckians goals, and that complement the Managed Care Organizations’ quality improvement goals. Annually, the Department, with input from the Contractor and the EQRO, will determine measures that should be retired, revised, rotated or determine if new measures should be developed. The Contractor is expected to demonstrate, through repeat measurement of the quality indicators, meaningful improvement in performance relative to the baseline measurement. Meaningful improvement shall be defined by: 1) reaching a prospectively set benchmark, or 2) improving performance and sustaining that improvement. The specific performance targets and timeframes are to be determined by the Department with input from the Contractor and EQRO. Annually, the non-HEDIS® measures shall be validated by the EQRO and the Contractor shall submit all data, documentation, etc., used to calculate the measures. Below is the current list of performance measures. Full specifications for calculating and reporting the non-HEDIS measures will be provided to the Contractor.
|
| | | |
Kentucky Medicaid Managed Care Performance Measures
|
| Measure Name | HEDIS/State-specific/Both | Admin/Hybrid | Baseline Measurement Period |
| Adult BMI, Nutritional Screening/Counseling, Physical Activity Counseling, Height and Weight | Both | Hybrid/Medical Record Review | TBD |
| Adult Cholesterol Screening | HK | Administrative | TBD |
| Controlling High Blood Pressure | HEDIS | Hybrid | TBD |
| Prenatal Risk Assessment Counseling and Education | State-specific | Hybrid/Medical Record Review | TBD
|
| BMI, Nutritional Screening/Counseling, Physical Activity Counseling, Height and Weight for Children and Adolescents | Both | Hybrid/Medical Record Review | TBD |
| Annual Dental Visit | HEDIS | Administrative | TBD |
| Lead Screening | HEDIS | Hybrid | TBD |
| Adolescent Screening/Counseling | State-specific
| Hybrid | TBD |
| EPSDT Hearing Assessments | State-specific | Administrative | TBD |
| EPSDT Vision Assessment | State-specific | Administrative | TBD |
| Well Child 15 months | HEDIS | Administrative | TBD |
| Well Child Ages 3-6 | HEDIS | Administrative | TBD |
| Adolescent Well Care Visits | HEDIS | Administrative | TBD |
| Children’s and Adolescent’s to PCPs | HEDIS
| Administrative | TBD |
| Children with Special Health Care Needs (CSHCN) | State-specific | | TBD |
Appendix P
Business Associates Agreement
This Business Associate Agreement (“Agreement”), effective on this the ____ day of ______________,20___, (“Effective Date”), is entered into by and between ________________ (the “Business Associate”) and ___________________________________________, with an address at ____________________________________________________________ (the “Covered Entity”) (each a “Party” and collectively the “Parties”).
The Business Associate is a _____________________. The Covered Entity is the executive agency of the Commonwealth of Kentucky vested with the authority to administer the ([Kentucky Medical Assistance Program (hereinafter the “Medicaid Program”), in accordance with the requirements of Title XIX of the Social Security Act (42 U.S.C. §1396 et. seq.) and KRS Chapter 205] or [Cabinet for Health and Family Services, Department for Behavioral Health, Developmental and Intellectual Disabilities, Kentucky Correctional Psychiatric Center (“KCPC”) vested as a licensed hospital with the authority to administer care to patients as stated in KRS Chapter 216B], etc.). The Parties entered into a Master Contract _________ (the “Contract”) on the ___ day of ____________, 20___, under which the Business Associate may use and/or disclose Protected Health Information in its performance of the Services described in the Contract. This Agreement sets forth the terms and conditions pursuant to which Protected Health Information that is provided by Covered Entity to Business Associate, or created or received by the Business Associate from or on behalf of the Covered Entity, will be handled between the Business Associate and the Covered Entity and with third parties during the term of their Contract and after its termination. The Parties agree as follows:
WITNESSETH:
WHEREAS, Sections 261 through 264 of the federal Health Insurance Portability and Accountability Act of 1996, Public Law 104-191, known as “the Administrative Simplification provisions,” direct the Department of Health and Human Services to develop standards to protect the security, confidentiality and integrity of health information; and
WHEREAS, pursuant to the Administrative Simplification provisions, the Secretary of Health and Human Services has issued regulations modifying 45 CFR Parts 160 and 164 (the “HIPAA Privacy Rule”); and
WHEREAS, the Parties wish to enter into or have entered into an arrangement whereby the Business Associate will provide certain services to the Covered Entity, and, pursuant to such arrangement, Business Associate may be considered a “business associate” of the Covered Entity as defined in the HIPAA Privacy Rule; and
WHEREAS, Business Associate may have access to Protected Health Information (as defined below) in fulfilling its responsibilities under the Contract.
THEREFORE, in consideration of the Parties’ continuing obligations under the Contract, the Parties agree to the provisions of this Agreement in order to address the requirements of the HIPAA Privacy Rule and to protect the interests of both Parties.
Unless otherwise specified in this Agreement, all capitalized terms used in this Agreement not otherwise defined in this Agreement shall have the meanings established for purposes of the Health Insurance Portability and Accountability Act of 1996 and its implementing regulations (collectively, “HIPAA”) and ARRA (as defined below), as each is amended from time to time.
| |
| 2. | PERMITTED USES AND DISCLOSURES OF PROTECTED HEALTH INFORMATION |
| |
| 2.1 | Services. Pursuant to the Contract, Business Associate provides services (“Services”) for the Covered Entity that involve the use and/or disclosure of Protected Health Information. Except as otherwise specified herein, the Business Associate may make any and all uses and/or disclosures of Protected Health Information necessary to perform its obligations under the Contract, provided that such use would not violate the Privacy and Security Regulations if done by Covered Entity or the minimum necessary policies and procedures of HIPAA. All other uses not authorized by this Agreement are prohibited. Moreover, Business Associate may disclose Protected Health Information for the purposes authorized by this Agreement only, (i) to its employees, subcontractors and agents, in accordance with Section 2.1(e), (ii) as directed by the Covered Entity, or (iii) as otherwise permitted by the terms of this Agreement including, but not limited to, Section 1.2(b) below, provided that such disclosure would not violate the Privacy or Security Regulations if done by Covered Entity or the minimum necessary policies and procedures of HIPAA. |
| |
| 2.2 | Business Activities of the Business Associate. Unless otherwise limited herein, the Business Associate may: |
| |
| a. | Use the Protected Health Information in its possession for its proper management and administration and to fulfill any present or future legal responsibilities of the Business Associate provided that such uses are permitted under state and federal confidentiality laws. |
| |
| b. | Disclose the Protected Health Information in its possession to third parties for the purpose of its proper management and administration or to fulfill any present or future legal responsibilities of the Business Associate, provided that the Business |
Associate represents to the Covered Entity, in writing, that (i) the disclosures are Required by Law, as that phrase is defined in 45 CFR §164.501 or (ii) the Business Associate has received from the third party written assurances regarding its confidential handling of such Protected Health Information as required under 45 CFR §164.504(e)(4), and the third party agrees in writing to notify Business Associate of any instances of which it becomes aware that the confidentiality of the information has been breached.
| |
| c. | Notwithstanding anything to the contrary contained herein, the parties understand and agree that inasmuch as may be necessary to perform its services under the Contract, Business Associate shall be permitted to use, access, disclose and transfer PHI. |
| |
| 3. | RESPONSIBILITIES OF THE PARTIES WITH RESPECT TO PROTECTED HEALTH INFORMATION |
| |
| 3.1 | Responsibilities of the Business Associate. With regard to its use and/or disclosure of Protected Health Information, the Business Associate hereby agrees to do the following: |
| |
| a. | Shall use and disclose the Protected Health Information only in the amount minimally necessary to perform the services of the Contract, provided that such use or disclosure would not violate the Privacy and Security Regulations if done by the Covered Entity. |
| |
| b. | Shall, within five (5) business days, report to the designated Privacy Officer of the Covered Entity, in writing, any use and/or disclosure of the Protected Health Information of which Business Associate becomes aware that is not permitted or authorized by the Contract or this Agreement. |
| |
| c. | Establish procedures for mitigating, to the greatest extent possible, any deleterious effects from any improper use and/or disclosure of Protected Health Information that the Business Associate reports to the Covered Entity. |
| |
| d. | Use appropriate administrative, technical and physical safeguards to maintain the privacy and security of the Protected Health Information and to prevent uses and/or disclosures of such Protected Health Information other than as provided for in this Agreement and in the Contract. |
| |
| e. | Require all of its subcontractors and agents that receive or use, or have access to, Protected Health Information under this Agreement to agree, in writing, to adhere to the same restrictions and conditions on the use and/or disclosure of Protected Health Information that apply to the Business Associate pursuant to this Agreement and the Contract. |
| |
| f. | Make available all records, books, agreements, policies and procedures relating to the use and/or disclosure of Protected Health Information to the Secretary of the Department for Health and Human Services for purposes of determining the Covered Entity’s compliance with the Privacy Regulation. |
| |
| g. | Upon prior written request in accordance with the Contact, make available during normal business hours at Business Associate’s offices all records, books, agreements, policies and procedures relating to the use and/or disclosure of Protected Health Information under this Agreement to the Covered Entity to determine the Business Associate’s compliance with the terms of this Agreement. |
| |
| h. | Upon Covered Entity’s written request but in no event less than ten (10) business days prior written notice, Business Associate shall provide to Covered Entity an accounting of each Disclosure of PHI made by Business Associate or its employees, agents, representatives, or subcontractors in accordance with 45 CFR §164.528. Business Associate shall implement a process that allows for an accounting to be collected and maintained for any Disclosure of PHI for which Covered Entity is required to maintain in accordance with 45 CFR §164.528. Business Associate shall include in the accounting: (a) the date of the Disclosure; (b) the name, and address if known, of the entity or person who received the PHI; (c) a brief description of the PHI disclosed; and (d) a brief statement of the purpose of the Disclosure. For each Disclosure that requires an accounting under this section, Business Associate shall document the information specified in (a) through (d), above, and shall securely retain this documentation for six (6) years from the date of the Disclosure. To the extent that Business Associate maintains PHI in an Electronic Health Record, Business Associate shall maintain an accounting of Disclosure for treatment, payment, and health care operations purposes for three (3) years from the date of Disclosure. Notwithstanding anything to the contrary, this requirement shall become effective upon either of the following: (a) on or after January 1, 2014, if Business Associate acquired Electronic Health Record before January 1, 2009; or (b) on or after January 1, 2011 if Business Associate acquired an Electronic Health Record after January 1, 2009, or such later date as determined by the Secretary of the Department for Health and Human Services. |
| |
| i. | Subject to Section 4.5 below, return to the Covered Entity or destroy, at the termination of this Agreement, the Protected Health Information in its possession and retain no copies (which for purposes of this Agreement shall mean without limitation the destruction of all backup tapes). However, in the event Business Associate is continuing to need access to or use of the Protected Health Information pursuant to other agreements, contracts, purchase orders or services rendered to the Covered Entity, this paragraph shall not apply. |
| |
| j. | Disclose to its subcontractors, agents, or other third parties, and request from the Covered Entity, only the minimum Protected Health Information necessary to perform or fulfill a specific function required or permitted hereunder. |
| |
| k. | Business Associate agrees to report to the Covered Entity any security incident of which it becomes aware involving the attempted or successful unauthorized access, use, disclosure, modification, or destruction of Covered Entity’s electronic Protected Health Information or interference with systems operations in an information system that involves Covered Entity’s electronic Protected Health Information within five (5) business days of Business Associate’s knowledge. An attempted unauthorized access, for purposes of reporting to the Covered Entity, means any attempted unauthorized access that prompts Business Associate to investigate the attempt, or review or change its current security measures. The parties acknowledge that the foregoing does not require Business Associate to report attempted unauthorized access that results in Business Associate: (i) investigating but merely reviewing and/or noting the attempt, but rather requires notification only when such attempted unauthorized access results in Business Associate conducting a material and full-scale investigation (a “Material Attempt”); and (ii) continuously reviewing, updating and modifying its security measures to guard against unauthorized access to its systems, but rather requires notification only when a Material Attempt results in significant modifications to Business Associate’s security measures in order to prevent such Material Attempt in the future. |
| |
| l. | Business Associate agrees to use appropriate administrative, physical and technical safeguards that reasonably and appropriately protect the confidentiality, integrity and availability of the electronic protected health information (EPHI) that it creates, receives, maintains, or transmits on behalf of the Covered Entity as required by 45 CFR part 164.308/310/312 & 164.314. |
| |
| m. | Business Associate agrees that any EPHI it acquires, maintains or transmits will be maintained or transmitted in a manner that fits the definition of secure PHI as that term is defined by the American Recovery and Reinvestment Act of 2009 (ARRA) and any subsequent regulations or guidance from the Secretary of the Department of Health and Human Services (DHHS) promulgated under ARRA. |
| |
| n. | Business Associate agrees to ensure that any agent, including a subcontractor, to whom it provides EPHI agrees to implement reasonable and appropriate safeguards to protect it as required by 45 CFR part 164.308/310/312 & 164.314. |
| |
| o. | Within five (5) business days of Business Associate’s knowledge, the Business Associate agrees to notify the Covered Entity of any breach of unsecure PHI, as that term is defined in the ARRA and any subsequent regulations and/or guidance from the Secretary of DHHS, caused by Business Associate or any Business Associate agent or subcontractor performing under the Contract. Notice of such a breach shall include the identification of each individual whose unsecured |
protected health information has been, or is reasonably believed by the business associate to have been, accessed, acquired, or disclosed during such breach. Business Associate further agrees to make available in a reasonable time and manner any information needed by Covered Entity to respond to individuals’ inquiries regarding said breach.
| |
| p. | In the event of a breach of unsecured PHI caused by Business Associate or any Business Associate agent or subcontractor performing under this Agreement, Business Associate shall pay for the reasonable and actual costs associated with notifications required pursuant to 42 U.S.C. §17932 and 45 C.F.R. Parts 160 & 164 subparts A, D & E as of their respective Compliance Dates. Business Associate further shall indemnify the Covered Entity and shall pay for the reasonable and actual costs associated and for any cost or damages, including attorney fees or fines, incurred by Covered Entity as a result of the breach by Business Associate, including but not limited to any identity theft related prevention or monitoring costs if the Covered Entity determines these services are appropriate as a result of the breach. |
| |
| q. | Business Associate agrees to comply with any and all privacy and security provisions not otherwise specifically addressed in the Contract made applicable to Business Associate by the ARRA on the applicable effective date as designated by ARRA and any subsequent regulations promulgated under ARRA and/or guidance thereto. |
| |
| 3.2 | Responsibilities of the Covered Entity. With regard to the use and/or disclosure of Protected Health Information by the Business Associate, the Covered Entity hereby agrees: |
| |
| a. | To inform the Business Associate of any changes in the form of notice of privacy practices (the “Notice”) that the Covered Entity provides to individuals pursuant to 45 CFR §164.520, and provide, upon request, the Business Associate a copy of the Notice currently in use. |
| |
| b. | To inform the Business Associate of any changes in, or revocation of, the authorization provided to the Covered Entity by individuals pursuant to 45 CFR §164.508. |
| |
| c. | To inform the Business Associate of any opt-outs exercised by any individual from fundraising activities of the Covered Entity pursuant to 45 CFR §164.514(f). |
| |
| d. | To notify the Business Associate, in writing and in a timely manner, of any arrangements permitted or required of the Covered Entity under 45 CFR § part 160 and 164 that may impact in any manner the use and/or disclosure of Protected Health Information by the Business Associate under this Agreement, including, but |
not limited to, restrictions on use and/or disclosure of Protected Health Information as provided for in 45 CFR §164.522 agreed to by the Covered Entity.
| |
| e. | Within ten (10) business days of Covered Entity’s knowledge, the Covered Entity agrees to notify the Covered Entity of any breach of unsecure PHI, as that term is defined in the ARRA and any subsequent regulations and/or guidance from the Secretary of DHHS, caused by Business Associate or any Business Associate agent or subcontractor performing under the Contract. |
ADDITIONAL RESPONSIBILITIES OF THE PARTIES WITH RESPECT TO PROTECTED HEALTH INFORMATION
| |
| 3.3 | Responsibilities of the Business Associate with Respect to Handling of Designated Record Set. In the event that Business Associate maintains Protected Health Information received from, or created or received by Business Associate on behalf of, Covered Entity, in a Designated Record Set, the Business Associate hereby agrees to do the following: |
| |
| a. | At the request of, and in the reasonable time and manner designated by the Covered Entity, provide access to the Protected Health Information to the Covered Entity or the individual to whom such Protected Health Information relates or his or her authorized representative in order for the Covered Entity to meet a request by such individual under 45 CFR §164.524. |
| |
| b. | At the request of, and in the reasonable time and manner designated by the Covered Entity, make any amendment(s) to the Protected Health Information that the Covered Entity directs pursuant to 45 CFR §164.526. |
| |
| 3.4 | Additional Responsibilities of the Covered Entity. The Covered Entity hereby agrees to do the following: |
| |
| a. | Notify the Business Associate, in writing, of any Protected Health Information that Covered Entity seeks to make available to an individual pursuant to 45 CFR §164.524 and the time, manner, and form in which the Business Associate shall provide such access, if Business Associate maintains Protected Health Information received from, or created or received by Business Associate on behalf of, Covered Entity, in a Designated Record Set. |
| |
| b. | Notify the Business Associate, in writing, of any amendment(s) to the Protected Health Information in the possession of the Business Associate that the Business Associate shall make and inform the Business Associate of the time, form, and manner in which such amendment(s) shall be made. |
| |
| 4. | REPRESENTATIONS AND WARRANTIES |
| |
| 4.1 | Mutual Representations and Warranties of the Parties. Each Party represents and warrants to the other party that it is duly organized, validly existing, and in good standing under the laws of the jurisdiction in which it is organized or licensed, it has the full power to enter into this Agreement and to perform its obligations hereunder, and that the performance by it of its obligations under this Agreement have been duly authorized by all necessary corporate or other actions and will not violate any provision of any license, corporate charter or bylaws. |
| |
| 5.1 | Term. This Agreement shall become effective on the Effective Date and shall continue in effect until all obligations of the Parties have been met, unless terminated as provided in this Section 4. In addition, certain provisions and requirements of this Agreement shall survive its expiration or other termination in accordance with Section 6.3 herein. |
| |
| 5.2 | Termination by the Covered Entity. As provided for under 45 C.F.R. §164.504(e)(2)(iii), the Covered Entity may immediately terminate this Agreement and any related agreements if the Covered Entity makes the determination that the Business Associate has breached a material term of this Agreement. Alternatively, the Covered Entity may choose to: (i) provide the Business Associate with thirty (30) days written notice of the existence of an alleged material breach; and (ii) afford the Business Associate an opportunity to cure said alleged material breach upon mutually agreeable terms. Nonetheless, in the event that mutually agreeable terms cannot be achieved within thirty (30) days, Business Associate must cure said breach to the satisfaction of the Covered Entity within thirty (30) days. Failure to cure in the manner set forth in this paragraph is grounds for the immediate termination of this Agreement. |
| |
| 5.3 | Termination by Business Associate. If the Business Associate makes the determination that a material condition of performance has changed under the Contract or this Agreement, or that the Covered Entity has breached a material term of this Agreement, Business Associate may provide thirty (30) days notice of its intention to terminate this Agreement. Business Associate agrees, however, to cooperate with Covered Entity to find a mutually satisfactory resolution to the matter prior to terminating and further agrees that, notwithstanding this provision, it shall only terminate this Agreement in accordance with the Contract. |
| |
| 5.4 | Automatic Termination. This Agreement will automatically terminate without any further action of the Parties upon the termination or expiration of the Contract. |
| |
| 5.5 | Effect of Termination. Upon the event of termination pursuant to this Section 4, Business Associate agrees to return or destroy all Protected Health Information of the Covered Entity, as defined herein, pursuant to 45 C.F.R. §164.504(e)(2)(I), if it is feasible to do so. Prior to doing so, the Business Associate further agrees to recover any Protected Health Information in the possession of its subcontractors or agents. If the Business Associate determines that it is not feasible to return or destroy said |
Protected Health Information, the Business Associate will notify the Covered Entity in writing. Upon mutual agreement of the Parties that the return or destruction is not feasible, Business Associate further agrees to extend any and all protections, limitations and restrictions contained in this Agreement to the Business Associate’s use and/or disclosure of any Protected Health Information retained after the termination of this Agreement, and to limit any further uses and/or disclosures to the purposes that make the return or destruction of the Protected Health Information infeasible. If it is infeasible for the Business Associate to obtain, from a subcontractor or agent any Protected Health Information in the possession of the subcontractor or agent, the Business Associate must provide a written explanation to the Covered Entity and require the subcontractors and agents to agree to extend any and all protections, limitations and restrictions contained in this Agreement to the subcontractors’ and/or agents’ use and/or disclosure of any Protected Health Information retained after the termination of this Agreement, and to limit any further uses and/or disclosures to the purposes that make the return or destruction of the Protected Health Information infeasible.
| |
| 6.1 | Covered Entity. For purposes of this Agreement, Covered Entity shall include all entities covered by the notice of privacy practices (or privacy notice) and who are parties to this Agreement. |
| |
| 6.2 | Business Associate. For purposes of this Agreement, Business Associate shall include the named Business Associate herein. However, in the event that the Business Associate is otherwise a hybrid entity under the Privacy Regulation, that entity may appropriately designate a health care component of the entity, pursuant to 45 C.F.R. §164.504(a), as the Business Associate for purposes of this Agreement. |
| |
| 6.3 | Survival. The respective rights and obligations of Business Associate and Covered Entity under the provisions of Sections 4.5, and Section 2.1 solely with respect to Protected Health Information Business Associate retains in accordance with Sections 2.1 and 4.5 because it is not feasible to return or destroy such Protected Health Information, shall survive termination of this Agreement. |
| |
| 6.4 | Amendments; Waiver. This Agreement may not be modified, nor shall any provision hereof be waived or amended, except in a writing duly signed by authorized representatives of the Parties. A waiver with respect to one event shall not be construed as continuing, or as a bar to or waiver of any right or remedy as to subsequent events. |
| |
| 6.5 | No Third Party Beneficiaries. Nothing express or implied in this Agreement is intended to confer, nor shall anything herein confer, upon any person other than the Parties and the respective successors or assigns of the Parties, any rights, remedies, obligations, or liabilities whatsoever. |
| |
| 6.6 | Notices. Any notices to be given hereunder to a Party shall be made via U.S. Mail or express courier to such Party’s address given below, and/or (other than for the delivery of fees) via facsimile to the facsimile telephone numbers listed below. |
If to Business Associate, to:
Attention:
Phone:
Fax:
With a copy (which shall not constitute notice) to:
Attention:
Phone:
Fax:
If to Covered Entity, to:
Department for Medicaid Services
275 East Main Street, 6W-A
Frankfort, KY 40621
Attention: Commissioner
Phone: 502-564-4321
Fax: 502-564-0509
With a copy (which shall not constitute notice) to:
Office of Legal Services
Cabinet for Health and Family Services
275 East Main Street, 5W-B
Frankfort, Kentucky 40621
Attention: Privacy Officer
Phone: (502) 564-7905
Fax: (502) 564-7573
With a copy (which shall not constitute notice) to:
Office of Administrative & Technology Services
Cabinet for Health and Family Services
275 East Main Street, 4W-E
Frankfort, Kentucky 40621
Attention: Security Officer
Phone: (502) 564-6478
Fax: (502) 564-0203
Each Party named above may change its address and that of its representative for notice by the giving of notice thereof in the manner hereinabove provided.
| |
| 6.7 | Counterparts; Facsimiles. This Agreement may be executed in any number of counterparts, each of which shall be deemed an original. Facsimile copies hereof shall be deemed to be originals. |
| |
| 6.8 | Disputes. If any controversy, dispute or claim arises between the Parties with respect to this Agreement, the Parties shall make good faith efforts to resolve such matters informally. |
| |
| 7.1 | Designated Record Set. Designated Record Set shall have the meaning set out in its definition at 45 CFR §164.501, as such provision is currently drafted and as it is subsequently updated, amended, or revised. |
| |
| 7.2 | Health Care Operations. Health Care Operations shall have the meaning set out in its definition at 45 CFR §164.501, as such provision is currently drafted and as it is subsequently updated, amended, or revised. |
| |
| 7.3 | Privacy Officer. Privacy Officer shall mean the privacy official referred to in 45 CFR §164.530(a)(1) as such provision is currently drafted and as it is subsequently updated, amended, or revised. |
| |
| 7.4 | Protected Health Information. Protected Health Information (“PHI”) shall have the meaning as set out in its definition at 45 CFR §164.501, as such provision is currently drafted and as it is subsequently updated, amended, or revised. |
IN WITNESS WHEREOF, each of the undersigned has caused this Agreement to be duly executed in its name and on its behalf effective as of this day of 20 .
COVERED ENTITY
By: _____________________________
Neville Wise______________________
Printed Name
Department for Medicaid Services, Acting Commissioner
Printed Title
________________________________
Date
BUSINESS ASSOCIATE
By: _____________________________
________________________________
Printed Name
________________________________
Printed Title
________________________________
Date
Appendix Q
Annual Contract Monitoring Tools
Department for Medicaid Services
Site Visit ___
Desk Review ___
Administrative Monitoring Tool—FY 20XX
Contract Name: Contract Number:
Monitoring Date(s): Monitor:
Person(s) Interviewed:
|
| | | | |
| Monitoring Items | Yes | No | N/A | Documentation |
1. Corrective Action Plans resultant from the most recent Department for Medicaid Services (DMS) contract monitoring have been implemented by the Contractor. |
|
|
| |
| 2. Notices, employment, advertisements, information pamphlets, research reports, and similar public notices prepared and released by the Contractor, pursuant to this contract, include a statement identifying the appropriate source of funds for the project or service, including but not limited to, identifying whether the funding is in whole or in part from federal, Cabinet for Health and Family Services (CHFS), or other state funds. |
|
|
| |
| 3. Travel expenses are being paid by DMS. | | | | |
| 4. If Contractor is a non-Federal entity and expends $500,000 or more in a year in Federal awards, a single or program-specific audit has been conducted. |
|
|
| |
|
| | | | |
| 5. For any and all subcontractors, the Contractor: | | | | |
| A. Maintains a contract with the subcontractor; | | | | |
| B. Specifies in the contract that all requirements of the contract between the Contractor and DMS are applicable and binding on the subcontractor; and, |
|
|
| |
| C. Monitors the subcontractor for programmatic and fiscal compliance. | | | | |
| 6. The Contractor maintains a property control ledger/log that lists all property and/or furniture provided (whether leased or purchased) by CHFS with funds from this contract. |
|
|
|
|
7. The Contractor maintains liability insurance for directors and officers, workers’ compensation insurance, and employer liability insurance. |
|
|
| |
| 8. The Contractor maintains a file of confidentiality agreements for all employees who have access to confidential information provided by CHFS. |
|
|
| |
Comments/Observations
Department for Medicaid Services
Site Visit ____
Desk Review ____
FY 20XX Monitoring Tool
Managed Care
Contract Name: ______ Contract Number: _____
Contract Monitor: _______ Monitoring Date(s):
|
| | | | |
| Monitoring Items | Yes | No | N/A | Documentation |
| 1. Contractor provides medical services under a pre-paid capitated risk method for Medicaid eligible recipients. | | | | |
| Organization |
| 2. Contractor has an office located within eighty (80) miles of Frankfort, KY that provides, at a minimum, the following staff functions: | | | | |
| A. Executive Director for the KY account; | | | | |
| B. Member Services for Grievances and Appeals; and, | | | | |
| C. Provider Services for Provider Relations and Enrollment. | | | | |
| 3. Contractor ensures at least the following: | | | | |
| A. At least one teaching hospital; | | | | |
| B. Regional representation of all provider types on the Council’s Board; | | | | |
| C. A network of providers that includes: | | | | |
| (1) Hospitals; | | | | |
| (2) Home health; | | | | |
| (3) Dentists; | | | | |
| (4) Vision; | | | | |
| (5) Hospice; | | | | |
| (6) Pharmacy; | | | | |
| (7) Prevention; | | | | |
| (8) Primary care; and, | | | | |
| (9) Maternity care providers. | | | | |
| D. A provider network representing the complete array of provider types including: | | | | |
| (1) Primary care providers; | | | | |
| (2) Primary care centers; | | | | |
|
| | | | |
| (3) Federally qualified health centers and rural health clinics; | | | | |
| (4) Local health departments; and, | | | | |
| (5) Ky Commission for Children with Special Health Care Needs. | | | | |
| E. Licensed or contain an entity that is licensed as a health maintenance organization or provider-sponsored integrated health delivery program in the Commonwealth. | | | | |
| Administration/Staffing |
| 4. Contractor provides staff for the following (functions may be combined or split among departments, people or subcontractors): | | | | |
| A. Executive Management that provides oversight of the entire operation; | | | | |
| B. Corporate Compliance Officer who ensures financial and programmatic accountability, transparency and integrity; | | | | |
| C. Medical Director who is: | | | | |
| (1) A KY-licensed physician; | | | | |
| (2) Involved in all major clinical programs; and, | | | | |
| (3) Involved in Quality Improvement components. | | | | |
| D. Dental Director who is: | | | | |
| (1) A dentist licensed by a Dental Board of Licensure in any state; and, | | | | |
| (2) Actively involved in all major dental programs. | | | | |
| E. Finance Officer and function, or designee to: | | | | |
| (1) Oversee the budget and accounting systems implemented by the Contractor; and, | | | | |
| (2) An internal auditor who ensures compliance with adopted standards and reviews expenditures for reasonableness and necessity. | | | | |
|
| | | | |
| F. Member Services Director and function to coordinate communication with members and act as member advocates; | | | | |
| G. Provider Services Director and function to coordinate all communications with Contractor’s providers and subcontractors; | | | | |
| H. Quality Improvement Director who is responsible for the operation of the QAPI Program or any subcontractors; | | | | |
| I. Guardianship Liaison who serves as the Contractor’s primary liaison for meeting the needs of members who are adult guardianship clients; | | | | |
| J. Case Management Coordinator who is responsible for coordination and oversight of case management services and continuity of care for the Contractor’s members; | | | | |
| K. Early and Periodic Screening, Diagnosis and Treatment (EPSDT) Coordinator who coordinates and arranges for the provision of EPSDT services and EPSDT special services for members; | | | | |
| L. Foster Care/Subsidized Adoption Liaison who serves as the Contractor’s primary liaison for meeting the needs of members who are children in foster care and subsidized adoptive children; | | | | |
| M. Management Information System Director and function who oversees, manages and maintains the Contractor’s management information system (MIS); | | | | |
|
| | | | |
| N. Behavioral Health Director who is a behavioral health practitioner and actively involved in all program or initiatives relating to behavioral health, and coordinates efforts to provide behavioral health services by the Contractor or any behavioral health subcontractors; | | | | |
| O. Compliance Director who: | | | | |
| (1) Oversees the Contractor’s compliance with laws and contract requirements of the Department for Medicaid Services (DMS); | | | | |
| (2) Serves as the primary contact for and facilitate communications between Contractor leadership and DMS relating to contract compliance issues; and, | | | | |
|
| | | | | | | | | | | | |
| Monitoring Items | Yes | No | N/A | Documentation |
| (3) Oversees Contractor implementation of and evaluate any actions required to correct deficiency or address noncompliance with contract requirements as identified by DMS. | | | | |
| P. Pharmacy Coordinator who coordinates, manages and oversees the provision of pharmacy services to members; | | | | |
| Q. Claims processing function to ensure the timely and accurate processing of original claims, corrected claims, re-submissions and overall adjudication of claims; | | | | |
| R. Program Integrity Coordinator to coordinate, manage and oversee the Contractor’s Program Integrity unit to reduce fraud and abuse of Medicaid Services; and, | | | | |
| S. Liaison to the Department for Medicaid Services (DMS) for all issues that relate to the contract between DMS and the Contractor. | | | | |
| 5. Contractor submits to DMS, annually, a current organizational chart depicting all functions including mandatory ones, number of employees in each functional department, and key managers responsible for the functions. | | | | |
| Management Information System (MIS) Requirements |
| 6. Contractor maintains a MIS that provides support for all aspects of a managed care operation to include the following subsystems: | | | | |
| A. Recipient; | | | | |
| B. Third Party Liability (TPL); | | | | |
| C. Provider; | | | | |
| D. Reference; | | | | |
| E. Encounter/Claims Processing; | | | | |
| F. Financial; | | | | |
| G. Utilization Data/Quality Improvement; and, | | | | |
| H. Surveillance Utilization Review. | | | | |
|
| | | | | | | | | | | | |
| 7. Contractor ensures that data received from providers and subcontractors is accurate and complete by: | | | | |
| A. Verifying, through edits and audits, the accuracy and timeliness of reported data; | | | | |
| B. Screening the data for completeness, logic and consistency; | | | | |
| C. Collecting service information in standardized formats to the extent feasible and appropriate; and, | | | | |
| D. Compiling and storing all claims and encounter data from the subcontractors in a data warehouse in a central location in the Contractor’s MIS. | | | | |
| Quality Assessment/Performance Improvement (QAPI) |
| 8. Contractor provides to DMS by July 31 the QAPI program description document. | | | | |
| 9. Contractor provides DMS a copy every three (3) years of its current National Committee for Quality Assurance (NCQA) certificate of accreditation and the complete survey report. | | | | |
| 10. Contractor prepares and submits to DMS by July 31 a written report detailing the annual QAPI review and evaluation. | | | | |
| 11. The QAPI work plan sets new goals and objectives annually based of findings from: | | | | |
| A. Quality improvement activities and studies; | | | | |
| B. Survey results; | | | | |
| C. Grievances and appeals; | | | | |
| D. Performance measures; and, | | | | |
| E. External quality review findings. | | | | |
| 12. Contractor monitors and evaluates the quality of clinical care on an ongoing basis. | | | | |
|
| | | | | | | | | | | | |
| 13. The following health care needs are studied and prioritized for performance improvement and/or development of practice guidelines: | | | | |
| A. Acute or chronic conditions; | | | | |
| B. High volume; | | | | |
| C. High risk; | | | | |
| D. Special needs populations; and, | | | | |
| E. Preventive care. | | | | |
14. In relation to Health Care Effectiveness Data and Information Set (HEDIS), Contractor collects and reports to DMS, by August 31st, the Final Auditor’s Report issued by the NCQA. | | | | |
| 15. Contractor conducts a minimum of two (2) performance improvement projects (PIPs) each year, including one relating to physical health and one relating to behavioral health. | | | | |
| 16. Contractor establishes and maintains an ongoing Quality and Member Access Advisory Committee (QMAC) composed of : | | | | |
| A. Members; | | | | |
| B. Individuals from consumer advocacy groups or the community who represent the interests of the member population; and, | | | | |
| C. Public health representatives. | | | | |
| 17. Contractor has a Utilization Management (UM) program that reviews services for medical necessity, and monitors and evaluates on an ongoing basis the appropriateness of care and services. | | | | |
| 18. The UM program is evaluated annually, the evaluation reviewed and approved annually by the Medical Director or the QI Committee. | | | | |
| Adverse Actions Related to Medical Necessity or Coverage Denials |
|
| | | | | | | | | | | | |
| 19. Contractor gives members written notice of any action within the timeframes for each type of action that explains: | | | | |
| A. The action the Contractor has taken or intends to take; | | | | |
| B. The reasons for the action; | | | | |
| C. The member’s right to appeal; | | | | |
| D. The member’s right to request a State hearing; | | | | |
| E. Procedures for exercising member’s rights to appeal or file a grievance; | | | | |
| F. Circumstances under which expedited resolution is available and how to request it; and, | | | | |
| G. The member’s rights to have benefits continue pending the resolution of the appeal, how to request that benefits be continued, and the circumstances under which the member may be required to pay the costs of these services. | | | | |
| 20. Contractor gives notice at least: | | | | |
| A. Ten (10) days before the date of action when the action is a termination, suspension, or reduction of a previously authorized covered service; or, five (5) days if member fraud or abuse has been determined | | | | |
| B. By the date of the action for the following: | | | | |
| (1) In the death of a member; | | | | |
| (2) A signed written member statement requesting service termination or giving information requiring termination or reduction of services; | | | | |
| (3) The member’s admission to an institution where he is ineligible for further services; | | | | |
| (4) The member’s address is unknown and mail directed to him has no forwarding address; | | | | |
|
| | | | | | | | | | | | |
| (5) The member has been accepted for Medicaid services by another local jurisdiction; | | | | |
| (6) The member’s physician prescribes the change in the level of medical care; | | | | |
| (7) An adverse determination made with regard to the preadmission screening requirements for nursing facility admissions on or after January 1, 1989; | | | | |
| 8) The safety or health of individuals in the facility would be endangered, the member’s health improves sufficiently to allow a more immediate transfer or discharge, an immediate transfer or discharge is required by the member’s urgent medical needs, or a member has not resided in the nursing facility for thirty (30) days. | | | | |
| C. On the date of action when the action is a denial of payment. | | | | |
| 21. Contractor gives notice as expeditiously as the member’s health condition requires and within State-established timeframes that do not exceed two (2) working days following receipt of the request for service (with an extension of up to fourteen [14] additional days if the member or provider requests an extension or the Contractor justifies a need for additional information and how the extension is in the member’s interest). | | | | |
| 22. If the Contractor extends the timeframe, the member is given written notice of the reason for the decision to extend and is informed of the right to file a grievance if he/she disagrees with that decision. | | | | |
|
| | | | | | | | | | | | |
| 23. For cases in which a provider indicates or the Contractor determines that following the standard timeframe could seriously jeopardize the member’s life or health or ability to attain, maintain or regain maximum function, the Contractor makes an expedited authorization decision and provides notice as expeditiously as the member’s health condition requires and no later than two (2) working days after receipt of the request for service. | | | | |
| 24. Contractor gives notice on the date the timeframes expire when service authorization decisions are not reached within the timeframes for either standard or expedited service authorizations. | | | | |
| Assessment of Member and Provider Satisfaction and Access |
| 25. Contractor conducts an annual survey of members’ and providers’ satisfaction with the quality of services provided and their degree of access to services. | | | | |
| 26. Contractor provides DMS a copy of the current Consumer Assessment of Healthcare Providers and Systems (CAHPS) survey tool as approved. | | | | |
| 27. Contractor submits to DMS a copy of all survey tools and results including: | | | | |
| A. A description of the methodology to be used conducting the provider or other special surveys; | | | | |
| B. The number and percentage of the providers or members to be surveyed; | | | | |
| C. Response rates; | | | | |
| D. A sample survey instrument; and, | | | | |
| E. Findings and interventions conducted or planned. | | | | |
| Member Services Functions |
| 28. Contractor’s member services function includes: | | | | |
|
| | | | | | | | | | | | |
| A. A call center which is staffed and available by telephone Monday through Friday 7 a.m. to 7 p.m. Eastern Standard Time; | | | | |
| B. A centralized toll-free call-in system, available 24/7, seven days a week nationwide, staffed by physicians, physician assistants, licensed practical nurses, or registered nurses; | | | | |
C. Providing a report to DMS, by the 10th of each month, prior month performance related to the call-in systems; | | | | |
| D. Make available foreign language interpreters free of charge; | | | | |
| E. Ensuring that member materials are provided and printed in each language spoken by five percent (5%) or more of the members in each county; | | | | |
| F. Ability to respond to special communication needs of the disabled, blind, deaf and aged; | | | | |
| G. Providing ongoing training to staff and providers on matters related to meeting the needs of economically disadvantaged and culturally diverse individuals; | | | | |
| H. Requiring all service locations to meet the requirements of the Americans with Disabilities Act, Commonwealth and local requirements pertaining to adequate space, supplies, sanitation, and fire and safety procedures applicable to health care facilities; | | | | |
| I. Ensuring that members are informed of their rights and responsibilities; | | | | |
| J. Monitoring the selection and assignment process of Primary Care Providers (PCPs); | | | | |
| K. Identifying, investigating, and resolving member grievances about health care services; | | | | |
|
| | | | | | | | | | | | |
| L. Assisting members with filing formal appeals regarding plan determinations; | | | | |
|
| | | | | | | | |
| Monitoring Items | Yes | No | N/A | Documentation |
| M. Providing each member with an identification card that identifies the member as a participant within the Contractor’s Network, unless otherwise approved by the Department; | | | | |
| N. Explaining rights and responsibilities to members or to those who are unclear about their rights or responsibilities including reporting of suspected fraud or abuse; | | | | |
| O. Explaining Contractor’s rights and responsibilities, including the responsibility to assure minimal waiting periods for scheduled member office visits and telephone requests, and avoiding undue pressure to select specific providers or services; | | | | |
| P. Within three (3) business days of enrollment notification of a new member, by a method that will not take more than five (5) days to reach the member, and whenever requested by member, guardian or authorized representative, provide a Member Handbook and information on how to access services (alternate notification methods are available for persons who have reading difficulties or visual impairments); | | | | |
| Q. Explaining or answering any questions regarding the Member Handbook; | | | | |
| R. Facilitating the selection of or explaining the process to select or change PCPs through telephone or face-to-face contact where appropriate. | | | | |
|
| | | | | | | | |
| (1) Contractor notifies members within thirty (30) days prior to the effective date of voluntary termination or as soon as Contractor receives notice, if notified less than thirty (30) days prior to the effective date. | | | | |
| (2) Contractor notifies members within fifteen (15) days prior to the effective date of involuntary termination if their PCP leaves the programs. | | | | |
| S. Facilitating direct access to specialty physicians in the circumstances of: | | | | |
| (1) Members with long-term, complex conditions; | | | | |
| (2) Aged, blind, deaf, or disabled persons; and, | | | | |
| (3) Individuals who have been identified as having special healthcare needs and who require a course of treatment or regular healthcare monitoring. | | | | |
| T. Arranging for and assisting with scheduling EPSDT Services in conformance with federal law governing EPSDT for persons under the age of twenty-one (21) years; | | | | |
| U. Making referrals for relevant non-program provider services such as the Women, Infants and Children (WIC) supplemental nutrition program and Protection and Permanency; | | | | |
| V. Facilitating direct access to: | | | | |
| (1) Primary care vision services; | | | | |
| (2) Primary dental and oral surgery services and evaluations by orthodontists and prosthodontists; | | | | |
| (3) Women’s health specialists; | | | | |
| (4) Voluntary family planning; | | | | |
| (5) Maternity care for members under age 18; | | | | |
|
| | | | | | | | |
| (6) Childhood immunizations; | | | | |
| (7) Sexually transmitted disease screening, evaluation and treatment; | | | | |
| (8) Tuberculosis screening, evaluation and treatment; and, | | | | |
| (9) Testing for HIV, HIV-related conditions and other communicable diseases. | | | | |
| W. Facilitating access to behavioral health services and pharmaceutical services; | | | | |
| X. Facilitating access to the services of public health departments, rural health clinics, Federally Qualified Health Centers, the Commission for Children with Special Health Care Needs and charitable care providers; | | | | |
| Y. Assisting members in making appointments with providers and obtaining services; | | | | |
| Z. Assisting members in obtaining transportation for both emergency and appropriate non-emergency situations; | | | | |
| AA. Handling, recording and tracking member grievances properly and timely and acting as an advocate to assure members receive adequate representation when seeking an expedited appeal; | | | | |
| BB. Facilitating access to member health education programs; and, | | | | |
| CC. Assisting members in completing the Health Risk Assessment (HRA) form upon any telephone contact, and referring members to the appropriate areas to learn how to access the health education and prevention opportunities available to them including referral to case management or disease management. | | | | |
| Member Handbook |
|
| | | | | | | | |
| 29. Contractor publishes a Member Handbook and makes the handbook available to members upon enrollment, to be delivered within five (5) business days to the member. | | | | |
| 30. Contractor reviews the handbook at least annually and communicates any changes to all members in written form. | | | | |
| 31. Revision dates are added to the handbook. | | | | |
| 32. Contractor ensures the handbook is written at the sixth grade reading comprehension level. | | | | |
| 33. The handbook includes: | | | | |
| A. Contractor’s network of primary care providers, including a list of the name, telephone numbers, and service site addresses of the PCPs available for primary care providers in the network listing; | | | | |
| B. The procedures for selecting an individual physician and scheduling an initial health appointment; | | | | |
| C. The name of the Contractor and address and telephone number from which it conducts its business; the hours of business; and, the member services telephone numbers and toll-free 24-hour medical call-in system; | | | | |
| D. A list of all available covered services, an explanation of any service limitations or exclusions from coverage and a notice stating that the Contractor will be liable only for those services authorized by the Contractor; | | | | |
| E. Member rights and responsibilities including reporting suspected fraud and abuse; | | | | |
| F. Procedures for obtaining emergency care and non-emergency after hours care; | | | | |
|
| | | | | | | | |
| G. Procedures for obtaining transportation for both emergency and non-emergency situations; | | | | |
| H. Information on the availability of maternity, family planning and sexually transmitted disease services and methods of accessing those services; | | | | |
| I. Procedures for arranging EPSDT for persons under the age of 21 years; | | | | |
| J. Procedures for obtaining access to Long Term Care Services; | | | | |
| K. Procedures for notifying DCBS of family size changes, births, address changes, death notifications; | | | | |
| L. A list of direct access services that may be accessed without the authorization of a PCP; | | | | |
| M. Information about procedures for selecting a PCP or requesting a change of PCP and specialists; reasons for which a request may be denied; and, reasons a provider may request a change; | | | | |
| N. Information about how to access care before a PCP is assigned or chosen; | | | | |
| O. Information about how to obtain second opinions related to surgical procedures, complex and/or chronic conditions; | | | | |
| P. Procedures for obtaining covered services from non-network providers; | | | | |
| Q. Procedures for filing a grievance or appeal, including the title, address and telephone number of the person responsible for processing and resolving grievances and appeals; | | | | |
| R. Information about CHFS independent ombudsman program for members; | | | | |
|
| | | | | | | | |
| S. Information on the availability of, and procedures for obtaining behavioral health/substance abuse health services; | | | | |
| T. Information on the availability of health education services; | | | | |
| U. Information deemed mandatory by DMS; and, | | | | |
| V. The availability of care coordination case management and disease management provided by the Contractor. | | | | |
| Member Services--Member Education and Outreach |
| 34. Contractor makes educational and outreach efforts with: | | | | |
| A. Schools; | | | | |
| B. Homeless centers; | | | | |
| C. Youth service centers; | | | | |
| D. Family resource centers; | | | | |
| E. Public Health departments; | | | | |
| F. School-based health clinics; | | | | |
| G. Chamber of commerce; and, | | | | |
| H. Faith-based community. | | | | |
| 35. Contractor submits an annual outreach plan to DMS for review and approval. | | | | |
| 36. The annual outreach plan includes; | | | | |
| A. Frequency of activities; | | | | |
| B. The staff person responsible for the activities; and, | | | | |
| C. How the activities will be documented and evaluated for effectiveness and need for change. | | | | |
| Member Services—Outreach to Homeless Persons |
| 37. Contractor assesses the homeless population within the region by implementing and maintaining a customized outreach plan for homeless population. | | | | |
| 38. The plan includes: | | | | |
| A. Utilizing existing community resources such as shelters and clinics; and, | | | | |
|
| | | | | | | | |
| B. Face-to-face encounters. | | | | |
| Member Services—Member Information Materials |
| 39. Contractor ensures that all written materials provided to members are: | | | | |
A. Geared toward persons who read at a 6th grade level; | | | | |
| B. Published in at least a fourteen (14) point font size; and, | | | | |
| C. Comply with the Americans with Disabilities Act of 1990. | | | | |
| 40. Contractor ensures that Braille and audio tapes are available for the partially blind and blind. | | | | |
| 41. Contractor ensures provisions to review written materials for the illiterate are available. | | | | |
| 42. Contractor ensures that telecommunication devices for the deaf are available. | | | | |
| 43. Contractor ensures that language translation is available if five percent (5%) of the population in any county has a native language other than English. | | | | |
| Member Rights and Responsibilities |
| 44. Contractor has written policies and procedures designed to protect the rights of members that include: | | | | |
| A. Respect, dignity, privacy, confidentiality and nondiscrimination; | | | | |
| B. A reasonable opportunity to choose a PCP and to change to another provider in a reasonable manner; | | | | |
| C. Consent for or refusal of treatment and active participation in decision choices; | | | | |
| D. To ask questions and receive complete information relating to the member’s medical condition and treatment options, including specialty care; | | | | |
|
| | | | | | | | |
| E. Voice grievances and receive access to the grievance process, receive assistance in filing an appeal, and receive a hearing from the Contractor and/or the Department; | | | | |
| F. Timely access to care that does not have any communication or physical access barriers; | | | | |
| G. To prepare advance medical directives; | | | | |
| H. To have access to medical records; | | | | |
| I. Timely referral and access to medically indicated specialty care; and, | | | | |
| J. To be free from any form of restraint or seclusion used as a means of coercion, discipline, convenience, or retaliation. | | | | |
| Member Selection of Primary Care Provider Members Without SSI |
| 45. Contractor ensures a member without SSI is offered an opportunity to: | | | | |
| A. Choose a new PCP who is affiliated with the Contractor’s network; or, | | | | |
| B. Stay with their current PCP as long as such PCP is affiliated with the Contractor’s network. | | | | |
| Monitoring Items | Yes | No | N/A | Documentation |
| 46. Contractor sends members written explanations of the PCP selection process within ten (10) business days of receiving enrollment notification from DMS. | | | | |
| 47. The written communication includes: | | | | |
| A. Timeframe for selection of a PCP; | | | | |
| B. Explanation of the process for assignment of a PCP if the member does not select a PCP; and, | | | | |
| C. Information on where to call for assistance with the selection process. | | | | |
|
| | | | | | | | |
| 48. Contractor ensures that members are allowed to select, from all available, but not less than two (2) PCPs in the Contractor’s network. | | | | |
| 49. Contractor assigns the member to a PCP: | | | | |
| A. Who has historically provided services to the member, meets the PCP criteria and participates in the Contractor’s network; | | | | |
| B. If there is no such PCP who has historically provided services, the Contractor assigns the member to a PCP, who participates in the Contractor’s network and is within thirty (30) miles or thirty (30) minutes from the member’s residence or place of employment in an urban area or within forty-five (45) miles or forty-five (45) minutes from the member’s residence or place of employment in a rural area. | | | | |
| 50. Assigning of PCPs is based on: | | | | |
| A. The need of children and adolescents to be followed by pediatric or adolescent specialists; | | | | |
| B. Any special medical needs, including pregnancy; | | | | |
| C. Any language needs made known to the Contractor; and, | | | | |
| D. Area of residence and access to transportation. | | | | |
| Members Who Have SSI and Non-Dual Eligibles |
| 51. Contractor sends members information regarding the requirement to select a PCP or one will be assigned to them according to the following: | | | | |
|
| | | | | | | | |
A. Upon enrollment, member will receive a letter requesting them to select a PCP. After one month, if the member has not selected a PCP, the Contractor sends a 2nd letter requesting the member to select a PCP within thirty (30) days or one will be chosen for the member. | | | | |
| B. At the end of the third thirty (30) day period, if the member has not selected a PCP, the Contractor may select a PCP for the member and sends a card identifying the PCP selected for the member and informing the member specifically that the member can contact the Contractor and make a PCP change. | | | | |
| C. Except for members who were previously enrolled, the Contractor cannot auto-assign a PCP to a member with SSI within the first ninety (90) days from the date of the member’s initial enrollment. | | | | |
| Primary Care Provider Changes |
| 52. Contractor has written policies and procedures for allowing members to select or be assigned to a new PCP when: | | | | |
| A. Such a change is mutually agreed to by the Contractor and Member; | | | | |
| Monitoring Items | Yes | No | N/A | Documentation |
| B. A PCP is terminated from coverage; or, | | | | |
| C. A PCP change is as part of the resolution to an appeal. | | | | |
| 53. Contractor allows members to select another PCP within ten (10) days of the approved change. | | | | |
| 54. Contractor allows the member to change the PCP ninety (90) days after the initial assignment and once a year regardless of reason. | | | | |
| Grievances and Appeals |
|
| | | | | | | | |
| 55. Contractor has a grievance system that includes a grievance process, an appeal process, and access for members to the State’s hearing system. | | | | |
| 56. Contractor ensures a grievance documentation process that includes: | | | | |
| A. Member name and identification number; | | | | |
| B. Member’s telephone number, when available; | | | | |
| C. Nature of grievance; | | | | |
| D. Date of grievance; | | | | |
| E. Member’s PCP or provider; | | | | |
| F. Member’s county of residence; | | | | |
| G. Resolution; | | | | |
| H. Date of resolution; | | | | |
| I. Corrective action taken or required; and, | | | | |
| J. Person recording grievance. | | | | |
| 57. Contractor has policies and procedures for the receipt, handling and disposition of grievances that: | | | | |
| A. Are approved by the Contractor’s governing bodies or board of directors; | | | | |
| B. Are approved in writing by DMS prior to implementation; | | | | |
| C. Include a process for evaluating patterns of grievances for impact on formulation of policy and procedures, access and utilization; | | | | |
| D. Establish procedures for maintenance of records of grievances separate from medical case records and in a manner which protects the confidentiality of members who file a grievance or appeal; | | | | |
|
| | | | | | | | |
| E. Inform members orally and/or in writing, about the Contractor’s and State’s grievance and appeal process, and by making information available at the Contractor’s offices and service locations, and by distributing information to members upon enrollment and to subcontractors at time of contract; | | | | |
| F. Provide assistance to member in filing grievances or appeals if requested or needed; | | | | |
| G. Include assurance that there will be no discrimination against a member solely on the basis of the member filing a grievance or appeal; and, | | | | |
| H. Include notification to members regarding how to access the Cabinet’s ombudsman’s office regarding grievance, appeals and state hearings. | | | | |
| 58. Contractor provides oral or written notice of the grievance resolution that includes: | | | | |
| A. The results of the resolution process; | | | | |
| B. The date it was completed; and, | | | | |
| C. Any written response is provided within ninety (90) days following the initial filing of the grievance. | | | | |
| Monitoring Items | Yes | No | N/A | Documentation |
| 59. Contractor ensures written policies and procedures for responding to and resolving appeals by members. | | | | |
| 60. Contractor establishes written policies and procedures for the receipt, handling and disposition of appeals that includes: | | | | |
| A. All appeals are submitted in writing within thirty (30) days of the aggrieved occurrence, either by the member or member’s authorized representative, or a provider acting on behalf of a member with the member’s written consent; | | | | |
|
| | | | | | | | |
| B. The Contractor responds in writing within three (3) business days to the member filing the appeal, and includes the name and phone number of the staff to contact regarding the appeal; | | | | |
| C. The Contractor provided an explanation regarding the continuation of services pending resolution of an appeal, if applicable; | | | | |
| D. The Contractor continues to provide benefits for the member’s services if: | | | | |
| (1) The appeal is filed on or before the later of the following: | | | | |
| a. Within ten (10) days of the Contractor mailing the notice; and, | | | | |
| b. The intended effective date of the Contractor’s proposed action. | | | | |
| (2) The appeal involves the termination, suspension, or reduction of a previously authorized course of treatment; | | | | |
| (3) The services were ordered by an authorized provider; | | | | |
| (4) The authorized period has not expired; | | | | |
| (5) The member requests extension of benefits; | | | | |
| (6) If the Contractor continues or reinstates the member’s services while an appeal is pending, the services continue until one of the following occurs: | | | | |
| a. The member withdraws the appeal; | | | | |
| b. The member does not request a state hearing within ten (10) days from the date when the Contractor mails notices of an adverse decision; | | | | |
| c. A state hearing decision adverse to the member is made; or, | | | | |
| d. The authorization expires or authorization service limits are met. | | | | |
|
| | | | | | | | |
| E. Contractor includes provisions for notifying members of the right to appeal the Contractor’s disposition of an appeal to the state hearing process, including expedited time frames; | | | | |
| F. Expedited appeals relating to matters which could place the member at risk or which could seriously jeopardize the member’s health or well being are resolved with three (3) business days; | | | | |
| G. Contractor allows the member and/or the member’s authorized representative opportunity before and during the appeals process, to examine the member’s appeals case file, including medical records and any other documents; | | | | |
| Monitoring Items | Yes | No | N/A | Documentation |
| H. Contractor includes, as parties to the appeals: | | | | |
| (1) The member and his or her authorized representative; or, | | | | |
| (2) The legal representative of a deceased member’s estate. | | | | |
| 61. Contractor provides written notice of the appeal resolution that includes: | | | | |
| A. The results of the resolution process; | | | | |
| B. The date it was completed; | | | | |
| C. For appeals not resolved in favor of the member: | | | | |
| (1) The right to request a state hearing and how to do so; | | | | |
| (2) The right to request continuation of benefits, if applicable, while the state hearing is pending and how to make the request; and, | | | | |
| (3) If the Contractor action is upheld in a state hearing, the member may be liable for the cost of any continued benefits. | | | | |
|
| | | | | | | | |
| D. The written response is provided within thirty (30) days of the initial filing of the appeal. | | | | |
| Enrollment |
| 62. Contractor sends a confirmation letter to the member, within three (3) business days after receipt of notification of new member enrollment, that includes: | | | | |
| A. The effective date of enrollment; | | | | |
| B. Site and PCP contact information; | | | | |
| C. How to obtain referrals; | | | | |
| D. The role of the Care Coordinator and Contractor; | | | | |
| E. The benefits of preventive health care; | | | | |
| F. Member identification card; | | | | |
| G. Copy of the Member Handbook; and, | | | | |
| H. List of covered services. | | | | |
| Provider Services |
| 63. Contractor maintains a provider services function that includes: | | | | |
| A. Enrolling, credentialing and recredentialing and performance review of providers; | | | | |
| B. Assisting providers with member enrollment status questions; | | | | |
| C. Assisting providers with prior authorization and referral procedures; | | | | |
| D. Assisting providers with claims submissions and payments; | | | | |
| E. Explaining to providers their rights and responsibilities as a member of Contractor’s network; | | | | |
| F. Handling, recording and tracking provider grievances and appeals; | | | | |
| G. Developing, distributing and maintaining a provider manual; | | | | |
| H. Developing, conducting, and assuring provider orientation/training; | | | | |
|
| | | | | | | | |
| I. Explaining the extent of Medicaid benefit coverage to providers including EPSDT preventive health screening services and EPSDT Special Services; | | | | |
|
| | | | |
| Monitoring Items | Yes | No | N/A | Documentation |
| J. Communicating Medicaid policies and procedures, including state and federal mandates and new policies and procedures; | | | | |
| K. Assisting providers in coordination of care for child and adult members with complex and/or chronic conditions; | | | | |
| L. Encouraging and coordinating the enrollment of primary care providers in the Department for Public Health and DMS Services for Vaccines for Children Program; | | | | |
| M. Coordinating workshops relating to the Contractor’s policies and procedures; and, | | | | |
| N. Providing technical support to providers who experience unique problems with certain members in their provision of services. | | | | |
| 64. Contractor ensures that providers services is staffed, at a minimum, Monday through Friday 8 A.M through 6 P.M. Eastern Standard Time. | | | | |
| 65. Contractor operates a provider call center. | | | | |
| Provider Credentialing and Recredentialing |
| 66. Contractor documents the procedure for credentialing and recredentialing of providers that includes: | | | | |
| A. Defining the scope of providers covered; | | | | |
| B. The criteria and the primary source verification of information used to meet the criteria; | | | | |
| C. The process used to make decisions; and, | | | | |
| D. The extent of delegated credentialing and recredentialing arrangements. | | | | |
|
| | | | |
| 67. Contractor has a process for receiving input from participating providers regarding credentialing and recredentialing. | | | | |
| 68. Contractor has written policies and procedures of the process for verifying that specific providers are licensed and have current policies of malpractice insurance. | | | | |
| 69. Contractor maintains a file for each provider containing a copy of the provider’s current license issued by the Commonwealth. | | | | |
| 70. Contractor ensures the process for verification of provider credentials and insurance includes: | | | | |
| A. Written policies and procedures that include the Contractor’s initial process for credentialing, as well as its recredentialing process that occurs, at a minimum, every three (3) years; | | | | |
| B. A governing body, or the groups or individuals to whom the governing body has formally delegated the credentialing function; | | | | |
| C. A review of the credentialing policies and procedures by the formal body; | | | | |
| D. A credentialing committee which makes recommendations regarding credentialing; | | | | |
| E. Written procedures, if the Contractor delegates the credentialing function, as well as evidence that the effectiveness is monitored; | | | | |
| F. Written procedures for the termination or suspension of providers; and, | | | | |
|
| | | | | | | | | | | | | | | | |
| G. Written procedures for, and implementation of, reporting to the appropriate authorities serious quality deficiencies resulting in suspension or termination of a provider. | | | | |
| 71. Verification of provider’s credentials includes: | | | | |
| A. A current valid license or certificate to practice in the Commonwealth of Kentucky; | | | | |
| B. A Drug Enforcement Administration (DEA) certificate and number, if applicable; | | | | |
| C. Primary source of graduation from medical school and completion of an appropriate residency, or accredited nursing, dental, physician assistant or vision program as applicable, if provider is not board certified; | | | | |
| D. Board certification if the practitioner states on the application that the practitioner is board certified in a specialty; | | | | |
| E. Professional board certification, eligibility for certification, or graduation from a training program to serve children with special health care needs under twenty-one (21) years of age; | | | | |
| F. Previous five (5) years work history; | | | | |
| G. Professional liability claims history; | | | | |
| H. Clinical privileges and performance in good standing at the hospital designated by the provider as the primary admitting facility, for all providers whose practice requires access to a hospital, as verified through attestation; | | | | |
| I. Current, adequate malpractice insurance, as verified through attestation; | | | | |
| J. Documentation of revocation, suspension or probation of a state license or DEA/Bureau of Narcotics and Dangerous Drugs (BNDD) number; | | | | |
|
| | | | | | | | | | | | | | | | |
| K. Documentation of curtailment or suspension of medical staff privileges; | | | | |
| L. Documentation of sanctions or penalties imposed by Medicare or Medicaid; | | | | |
| M. Documentation of censure of the State or County professional association; and, | | | | |
| N. Most recent information available from the National Practitioner Data Bank. | | | | |
| 72. Before a practitioner is credentialed, the Contractor receives information from the following organizations and includes the information in the credentialing files: | | | | |
| A. National practitioner data bank, if applicable; | | | | |
| B. Information about sanctions or limitations on licensure from the appropriate state boards applicable to the practitioner type; and, | | | | |
| C. Other recognized monitoring organizations appropriate to the practitioner’s discipline. | | | | |
| 73. Contractor has evidence that before making a recredentialing decision, information about sanctions or limitations on practitioner has been verified from: | | | | |
| A. A current license to practice; | | | | |
| B. The status of clinical privileges at the hospital designated by the practitioner as the primary admitting facility; | | | | |
| C. A valid DEA number, if applicable; | | | | |
| D. Board certification, if the practitioner was due to be recertified or become board certified since last credentialed or recredentialed; | | | | |
| E. Five (5) year history of professional liability claims that resulted in settlement or judgment paid by or on behalf of the practitioner; and, | | | | |
|
| | | | | | | | | | | | | | | | |
| F. A current signed attestation statement by the applicant regarding: | | | | |
| (1) The ability to perform the essential functions of the position with or without accommodation; | | | | |
| (2) The lack of current illegal drug use; | | | | |
| (3) A history of loss, limitation or privileges or any disciplinary action; and, | | | | |
| (4) Current malpractice insurance. | | | | |
| 74. Contractor generates a Credentialing Process Coversheet per provider that is submitted electronically to DMS’ fiscal agent. | | | | |
| 75. Contractor establishes ongoing monitoring of provider sanctions, complaints and quality issues between recredentialing cycles. | | | | |
| Primary Care Providers |
| 76. Contractor monitors primary care provider actions to ensure compliance with the Contractor’s and DMS’ policies that include: | | | | |
| A. Maintaining continuity of the member’s health care; | | | | |
| B. Making referrals for specialty care and other medically necessary services, both in and out of plan, if such services are not available within the Contractor’s network; | | | | |
| C. Maintaining a current medical record for the member, including documentation of all PCP and specialty care services; | | | | |
| D. Discussing advance medical directives with all members as appropriate; | | | | |
| E. Providing primary and preventative care, recommending or arranging for all necessary preventive health care, including EPSDT for persons under the age of 21 years; | | | | |
| F. Documenting all care rendered in a complete and accurate medical record that meets or exceeds DMS’s specification; and, | | | | |
|
| | | | | | | | | | | | | | | | |
| G. Arranging and referring members when clinically appropriate to behavioral health providers. | | | | |
| 77. Contractor ensures the following after-hours phone arrangements are implemented by PCPs in Contractor’s network: | | | | |
| A. Office phone is answered after hours by an answering service that can contact the PCP or another designated medical practitioner and the PCP or designee is available to return the call within a maximum of thirty (30) minutes; | | | | |
| B. Office phone is answered after hours by a recording directing the member to call another number to reach the PCP or another medical practitioner whom the provider has designated to return the call within a maximum of thirty (30) minutes; and, | | | | |
| Monitoring Items | Yes | No | N/A | Documentation |
| C. Office phone is transferred after office hours to another location where someone will answer the phone and be able to contact the PCP or another designated medical practitioner within a maximum of thirty (30) minutes. | | | | |
| Provider Manual |
| 78. Contractor prepares and issues a provider manual to all existing network providers. | | | | |
| 79. Contractor issues to newly contracted providers copies of the provider manual within five (5) working days from inclusion of the provider into the network. | | | | |
| 80. Contractor ensures the provider manual is the source of information to providers regarding: | | | | |
| A. Covered services; | | | | |
| B. Provider credentialing and recredentialing; | | | | |
| C. Member grievances and appeals policies and procedures; | | | | |
| D. Reporting fraud and abuse; | | | | |
|
| | | | | | | | | | | | | | | | |
| E. Prior authorization procedures; | | | | |
| F. Medicaid laws and regulations; | | | | |
| G. Telephone access; | | | | |
| H. The QAPI program; and, | | | | |
| I. Standards for preventive health services. | | | | |
| Provider Orientation and Education |
| 81. Contractor conducts initial orientation for all providers within thirty (30) days after the Contractor places a newly contracted provider on an active status. | | | | |
| 82. Contractor ensures that provider education includes: | | | | |
| A. Contractor coverage requirements for Medicaid services; | | | | |
| B. Policies or procedures and any modifications to existing services; | | | | |
| C. Reporting fraud and abuse; | | | | |
| D. Medicaid populations/eligibility; | | | | |
| E. Standards for preventive health services; | | | | |
| F. Special needs of members in general that affect access to and delivery of services; | | | | |
| G. Advance medical directives; | | | | |
| H. EPSDT services; | | | | |
| I. Claims submission and payment requirements; | | | | |
| J. Special health/care management programs that members may enroll in; | | | | |
| K. Cultural sensitivity; | | | | |
| L. Responding to needs of members with mental, developmental and physical disabilities; | | | | |
| M. Reporting of communicable disease; | | | | |
| N. The Contractors QAPI program; | | | | |
| O. Medical records review; and, | | | | |
| P. Rights and responsibilities of both members and providers. | | | | |
| Medical Records |
|
| | | | | | | | | | | | | | | | |
| 83. Contractor ensures that member medical records are maintained either hard copy or electronically and include: | | | | |
| A. Medical charts; | | | | |
| B. Prescription files; | | | | |
| C. Hospital records; | | | | |
| D. Provider specialist reports; | | | | |
| E. Consultant and other health care professionals’ findings; | | | | |
| F. Appointment records; and, | | | | |
| G. Other documentation sufficient to disclose the quantity, quality, appropriateness, and timeliness of services. | | | | |
| 84. Contractor ensures medical records are signed by the provider of service. | | | | |
| 85. Contractor ensures the medical chart organization and documentation include: | | | | |
| A. Member/patient identification information on each page; | | | | |
| B. Personal/biographical data, including: | | | | |
| (1) Date of birth; | | | | |
| (2) Age; | | | | |
| (3) Gender; | | | | |
| (4) Marital status; | | | | |
| (5) Race or ethnicity; | | | | |
| (6) Mailing address; | | | | |
| (7) Home and work addresses and telephone numbers; | | | | |
| (8) Employer; | | | | |
| (9) School; | | | | |
| (10) Name and telephone numbers (if no phone, contact name and number) of emergency contacts; | | | | |
| (11) Consent forms; | | | | |
| (12) Identify language spoken; and, | | | | |
| (13) Guardianship information. | | | | |
| C. Date of data entry and date of encounter; | | | | |
|
| | | | | | | | | | | | | | | | |
| D. Provider identification by name; | | | | |
| E. Allergies, adverse reactions and no known allergies are noted in a prominent location; | | | | |
| F. Past medical history including serious accidents, operations, illnesses (for children, past medical history includes prenatal care and birth information, operations, and childhood illnesses); | | | | |
| G. Identification of current problems; | | | | |
| H. The consultation, laboratory, and radiology reports filed in the medical record contain the ordering provider’s initials or other documentation indicating review; | | | | |
| I. Documentation of immunizations; | | | | |
| J. Identification and history of nicotine, alcohol use or substance abuse; | | | | |
| K. Documentation of reportable diseases and conditions to the local health department serving the jurisdiction in which the patient resides or Dept. for Public Health; | | | | |
| L. Follow-up visits provided secondary to reports of emergency room care; | | | | |
| M. Hospital discharge summaries; | | | | |
| N. Advanced medical directives, for adults; | | | | |
| O. All written denials of service and the reason for the denial; and, | | | | |
| P. Record legibility to at least a peer of the writer. | | | | |
| 86. Contractor ensures members’ medical records include the following minimal detail for individual clinical encounters: | | | | |
| A. History and physical examination for presenting complaints containing relevant psychological and social conditions affecting the patient’s medical/behavioral health, including mental health, and substance abuse status; | | | | |
|
| | | | | | | | | | | | | | | | |
| B. Unresolved problems, referrals and results from diagnostic tests including results and/or status of preventive screening services (EPSDT) are addressed from previous visits; | | | | |
| C. Plan of treatment; | | | | |
| D. Medication history, medications prescriber, including the strength, amount, directions for use and refills; | | | | |
| E. Therapies and other prescribed regimen; and, | | | | |
| F. Follow-up plans including consultation and referrals and directions, including time to return. | | | | |
| Provider Grievances and Appeals |
| 87. Contractor implements a process to ensure that all appeals from providers are reviewed and the following details recorded in a written record and logged: | | | | |
| A. Date; | | | | |
| B. Nature of appeal; | | | | |
| C. Identification of the individual filing the appeal; | | | | |
| D. Identification of the individual recording the appeal; | | | | |
| E. Disposition of the appeal; | | | | |
| F. Corrective action required; and, | | | | |
| G. Date resolved. | | | | |
| 88. Contractor ensures that every grievance received is documented in the MIS and contains the following: | | | | |
| A. Provider name and identification number; | | | | |
| B. Provider telephone number, when available; | | | | |
| C. Nature of grievance; | | | | |
| D. Date of grievance; | | | | |
| E. Provider’s county; | | | | |
| F. Resolution; | | | | |
| G. Date of resolution; | | | | |
|
| | | | | | | | | | | | | | | | |
| H. Corrective action taken or required; and, | | | | |
| I. Person recording the grievance. | | | | |
| Release for Ethical Reasons |
| 89. Contractor ensures, in situations where a provider declines to perform a service because of ethical reasons, that members are referred to another provider licensed, certified or accredited to provide care for the individual service or assigned to another PCP licensed, certified or accredited to provide case appropriate to the member’s medical condition. | | | | |
| Network Providers to Be Enrolled |
| 90. Contractor enrolls the following into its network: | | | | |
| A. At least one (1) Federally Qualified Health Center (FQHC) if there is a FQHC appropriately licensed to provide services in the region or service area; | | | | |
| B. Physicians; | | | | |
| C. Advanced practice registered nurses; | | | | |
| D. Physician assistants; | | | | |
| E. Birthing centers; | | | | |
| F. Dentists; | | | | |
| G. Primary care centers: | | | | |
| H. Home health agencies; | | | | |
| I. Rural health clinics; | | | | |
| J. Opticians; | | | | |
| K. Optometrists; | | | | |
| L. Audiologists; | | | | |
| M. Hearing aid vendors; | | | | |
| N. Pharmacies; | | | | |
| O. Durable medical equipment suppliers; | | | | |
| P. Podiatrists; | | | | |
| Q. Renal dialysis clinics; | | | | |
| R. Ambulatory surgical centers; | | | | |
| S. Family planning providers; | | | | |
|
| | | | | | | | | | | | | | | | |
| T. Emergency medical transportation provider; | | | | |
| U. Non-emergency medical transportation providers; | | | | |
| V. Other laboratory and x-ray providers; | | | | |
| W. Individuals and clinics providing EPSDT services; | | | | |
| X. Chiropractors; | | | | |
| Y. Community mental health centers; | | | | |
| Z. Psychiatric residential treatment facilities; | | | | |
| AA. Hospitals (including acute care, critical access, rehabilitation, and psychiatric hospitals); | | | | |
| BB. Local health departments; and, | | | | |
| CC. Providers of EPSDT Special services. | | | | |
| 91. Contractor has written policies and procedures regarding the selection and retention of Contractor’s network. | | | | |
| 92. Contractor provides written notice to providers not accepted into the network along with the reasons for the non-acceptance. | | | | |
| Termination of Network Providers or Subcontractors |
| 93. Contractor notifies DMS of suspension, termination and exclusion taken against a provider within three (3) business days via email. | | | | |
| 94. Contractor notifies DMS of voluntary terminations within five (5) business days via email. | | | | |
| 95. Contractor provides written notice within fifteen (15) days to a member whose PCP has been involuntary disenrolled and within thirty (30) days of a PCP who has voluntarily terminated participation in the Contractor’s network. | | | | |
| Provider Program Capacity Demonstration |
|
| | | | | | | | | | | | | | | | |
| 96. Contractor ensures that emergency medical services are made available to members twenty-four (24) hours a day, seven (7) days a week. | | | | |
| 97. Contractor ensures that urgent care services by any provider in the Contractor’s program are made available within 48 hours of request. | | | | |
| 98. Contractor provides the following: | | | | |
| A. PCP delivery sites that: | | | | |
| (1) Are no more than forty-five (45) minutes or forty-five (45) miles from member residence; | | | | |
| (2) Have no more than member to PCP ratio of 1500:1; | | | | |
| (3) Have appointment and waiting times not to exceed thirty (30) days from date of a member’s request for routine and preventive services and forty-eight (48) hours for urgent care. | | | | |
| B. Have specialty care in which referral appointments to specialists do not exceed thirty (30) days for routine care or forty-eight (48) hours for urgent care; | | | | |
| C. Have immediate treatment for emergency care at a health facility that is most suitable for the type of injury, illness or condition, regardless of whether the facility is in Contractor’s network; | | | | |
| D. Have hospital care for which transport time does not exceed thirty (30) minutes, except in non-urban areas where access time does not exceed sixty (60) minutes; | | | | |
|
| | | | | | | | | | | | | | | | |
| E. Have general dental services for which transport time does not exceed one (1) hour (appointment and waiting times do not exceed three (3) weeks for regular appointments and forty-eight (48) hours for urgent care); | | | | |
| F. Have general vision, laboratory and radiology services for which transport time does not exceed one (1) hour (appointment and waiting times do not exceed thirty (30) days for regular appointments and forty-eight (48) hours for urgent care); | | | | |
| G. Have pharmacy services with travel time not exceeding one (1) hour or the delivery site is no further than fifty (50) miles from the member’s residence. | | | | |
| Program Mapping |
| 99. Contractor submits maps and charts that include geographic details including highways, major streets and boundaries. | | | | |
| 100. Maps include the location of all categories of providers or provider sites as follows: | | | | |
| A. Primary Care Providers (designated by “P”); | | | | |
| B. Primary Care Centers, non-FQHC and RHC (designated by “C”); | | | | |
| C. Dentists (designated by “D”); | | | | |
| D. Other Specialty Providers (designated by “S”); | | | | |
| E. Non-Physician Providers, including: | | | | |
| (1) Nurse practitioners (designated by “N”); | | | | |
| (2) Nurse mid-wives (designated by “M”); and, | | | | |
| (3) Physician assistants (designated by “A”); | | | | |
| F. Hospitals (designated by “H”); | | | | |
| G. After hours Urgent Care Centers (designated by “U”); | | | | |
|
| | | | | | | | | | | | | | | | |
| H. Local Health Departments (designated by “L”); | | | | |
| I. Federally Qualified Health Centers/Rural Health Clinics (designated by “F” or “R” respectively); | | | | |
| J. Pharmacies (designated by “X”); | | | | |
| K. Family Planning Clinics (designated by “Z”); | | | | |
| L. Significant traditional providers (designated by “*”); | | | | |
M. Maternity Care Physicians (designated by “o”; and, | | | | |
| N. Vision Providers (designated by “V”). | | | | |
| Reporting Requirements |
| 101. Contractor monitors and documents in a quarterly report to DMS the number of eligible individuals that are assigned a PCP. | | | | |
| 102. Contractor submits to DMS on a quarterly basis the total number of member grievances and appeals and their disposition. | | | | |
| 103. The member grievances and appeals report includes: | | | | |
| A. Number of grievances and appeals, including expedited appeal requests; | | | | |
| B. Nature of grievances and appeals; | | | | |
| C. Resolution; | | | | |
| D. Timeframe for resolution; and, | | | | |
| E. QAPI initiatives or administrative changes as a result of analysis of grievances and appeals | | | | |
| 104. Contractor monitors and evaluates in quarterly reports provider grievances and appeals regarding: | | | | |
| A. The number of grievances and appeals; | | | | |
| B. Type of grievances and appeals; and, | | | | |
| C. Outcomes of provider grievances and appeals. | | | | |
|
| | | | | | | | | | | | | | | | |
| 105. Contractor provides all provider terminations in the monthly Provider Termination Report. | | | | |
| 106. Contractor submits to DMS on a quarterly basis a report summarizing changes in the Contractor’s network. | | | | |
| 107. Contractor submits a quarterly report on EPSDT services. | | | | |
| 108. Contractor submits an annual report on EPSDT services. | | | | |
| 109. Contractor submits a quarterly report on the number of new member assessments; number of assessments completed, number of assessments not completed after reasonable efforts, and the number of refusals. | | | | |
| 110. Contractor submits a report of foster care cases thirty (30) days after the end of each month. | | | | |
| 111. Contractor submits thirty (30) days after the end of each quarter a report detailing the number of service plan reviews conducted for guardianship, foster and adoption assistance members outcome decisions, such as referral to case management, and rationale for decisions. | | | | |
| 112. Contractor provides to DMS a status report of the QAPI program and work plan on a quarterly basis thirty (30) days after the end of the quarter. | | | | |
| Record System Requirements |
| 113. Contractor ensures the maintenance of detailed records relating to the operation of the Contractor, including: | | | | |
| A. The administrative costs and expenses incurred pursuant to this contract; | | | | |
| B. Member enrollment status; | | | | |
| C. Provision of covered services; | | | | |
|
| | | | | | | | | | | | | | | | |
| D. All relevant medical information relating to individual members for the purpose of audit, evaluation or investigation by DMS, the Office of Inspector General, the Attorney General and other authorized federal or state personnel; | | | | |
| E. Quality improvement and utilization; | | | | |
| F. All financial records; | | | | |
| G. Performance reports indicating compliance with contract requirements; | | | | |
| H. Fraud and abuse; and, | | | | |
| I. Managerial reports. | | | | |
| Reporting Requirements and Standards |
| 114. Contractor ensures that submitted reports meet these standards: | | | | |
| A. Contractor verifies the accuracy for data and other information on reports submitted; | | | | |
| B. Reports or other required data is received on or before scheduled due dates; | | | | |
| C. Reports or other required data conforms to DMS’ defined standards; and, | | | | |
| D. All required information is fully disclosed in a manner that is responsive and without material omission. | | | | |
| Ownership and Financial Disclosure |
| 115. Contractor provides disclosures of the following: | | | | |
| A. Name and address of each person with an ownership or control interest in (i) the Contractor or (ii) any subcontractor or supplier in which the Contractor has a direct or indirect ownership of five percent (5%) or more, specifying the relationship of any listed persons who are related as spouse, parent, child, or sibling; | | | | |
|
| | | | | | | | | | | | | | | | |
| B. Name of any other entity receiving reimbursement through the Medicare or Medicaid programs in which a person listed in response to subsection A has an ownership or control interest; | | | | |
| C. The same information requested in subsection A and B for any subcontractors or suppliers with whom the Contractor has had business transactions totaling more than $25,000 during the immediately preceding twelve-month period; | | | | |
| D. A description of any significant business transactions between the Contractor and any wholly-owned supplier, or between the Contactor and any subcontractor, during the immediately preceding five-year period; | | | | |
| E. The identity of any person who has an ownership or control interest in the Contractor, any subcontractor or supplier, or is an agent or managing employee of the Contractor, any subcontractor or supplier, who has been convicted of a criminal offense related to that person’s involvement in any program under Medicare, Medicaid, or the services program under Title XX of the Act, since the inception of those programs; | | | | |
| F. The name of any officer, director, employee or agent of, or any person with an ownership or controlling interest in, the Contractor, any subcontractor or supplier, who is also employed by the Commonwealth or any of its agencies; and, | | | | |
|
| | | | |
| Monitoring Items | Yes | No | N/A | Documentation |
| G. The Contractor shall be required to notify DMS immediately when any change in ownership is anticipated. The Contractor shall submit a detailed work plan to DMS and to the Department of Insurance during the transition period no later than the date of the sale that identifies areas of the contract that may be impacted by the change in ownership, including management and staff. | | | | |
| 116. Contractor provides disclosures to DMS: | | | | |
| A. At the time of each annual audit; | | | | |
| B. At the time of each Medicaid survey; | | | | |
| C. Prior to entry into a new contract with DMS; | | | | |
| D. Upon any change in operations which affects the most recent disclosure report; or, | | | | |
| E. Within thirty-five (35) days following the date of each written request for such information. | | | | |
Comments/Observations