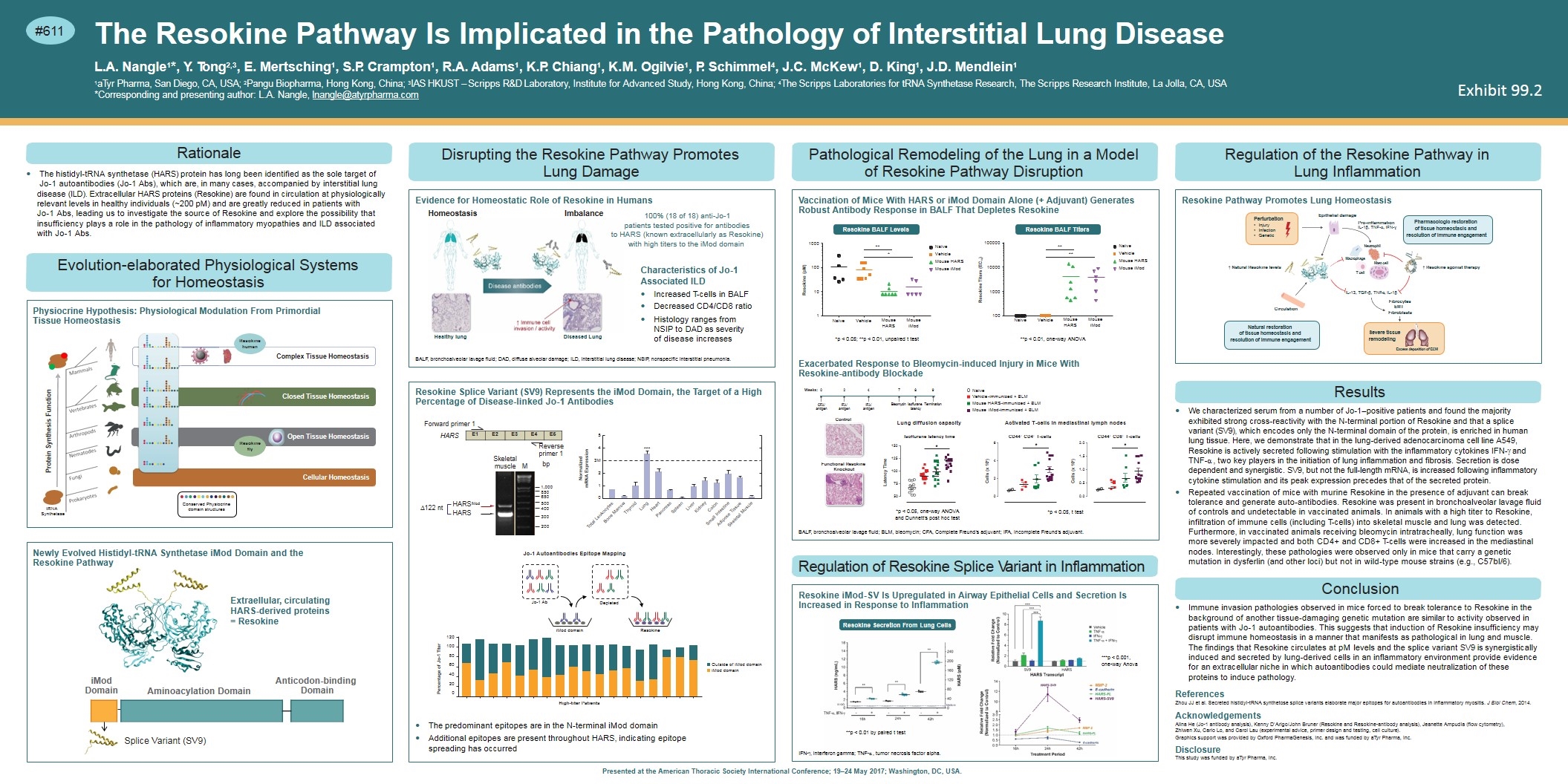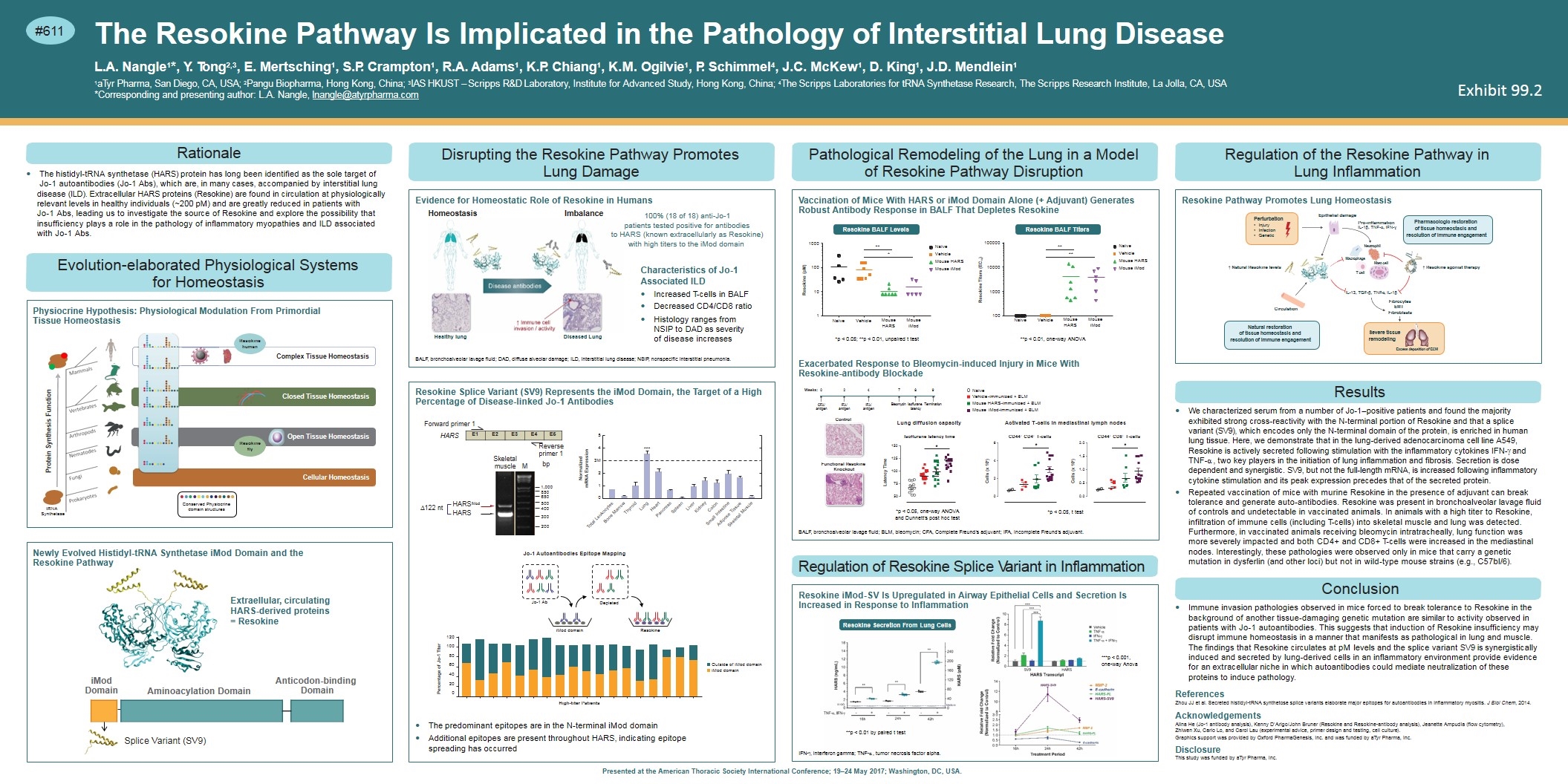
#611 Presented at the American Thoracic Society International Conference; 19–24 May 2017; Washington, DC, USA. The Resokine Pathway Is Implicated in the Pathology of Interstitial Lung Disease L.A. Nangle1*, Y. Tong2,3, E. Mertsching1, S.P. Crampton1, R.A. Adams1, K.P. Chiang1, K.M. Ogilvie1, P. Schimmel4, J.C. McKew1, D. King1, J.D. Mendlein1 1aTyr Pharma, San Diego, CA, USA; 2Pangu Biopharma, Hong Kong, China; 3IAS HKUST – Scripps R&D Laboratory, Institute for Advanced Study, Hong Kong, China; 4The Scripps Laboratories for tRNA Synthetase Research, The Scripps Research Institute, La Jolla, CA, USA *Corresponding and presenting author: L.A. Nangle, lnangle@atyrpharma.com Rationale The histidyl-tRNA synthetase (HARS) protein has long been identified as the sole target of Jo-1 autoantibodies (Jo-1 Abs), which are, in many cases, accompanied by interstitial lung disease (ILD). Extracellular HARS proteins (Resokine) are found in circulation at physiologically relevant levels in healthy individuals (~200 pM) and are greatly reduced in patients with Jo-1 Abs, leading us to investigate the source of Resokine and explore the possibility that insufficiency plays a role in the pathology of inflammatory myopathies and ILD associated with Jo-1 Abs. Evolution-elaborated Physiological Systems for Homeostasis Closed Tissue Homeostasis Complex Tissue Homeostasis Open Tissue Homeostasis Conserved Physiocrine domain structures Cellular Homeostasis tRNA Synthetase Protein Synthesis Function Resokine fly Resokine human Physiocrine Hypothesis: Physiological Modulation From Primordial Tissue Homeostasis Extraellular, circulating HARS-derived proteins = Resokine Anticodon-binding Domain DomainAminoacylation D Splice Variant (SV9) Newly Evolved Histidyl-tRNA Synthetase iMod Domain and the Resokine Pathway Pathological Remodeling of the Lung in a Model of Resokine Pathway Disruption Naïve Vehicle Mouse HARS Mouse iMod Naïve Vehicle Mouse HARS Mouse iMod 1 10 100 1000100000 Resokine (pM) Naïve Vehicle Mouse HARS Mouse iMod ** * ** ** Naïve Vehicle Mouse HARS Mouse iMod 100 1000 10000 Resokine Titers (EC50) Vaccination of Mice With HARS or iMod Domain Alone (+ Adjuvant) Generates Robust Antibody Response in BALF That Depletes Resokine Resokine BALF LevelsResokine BALF Titers Control Functional Resokine Knockout Weeks: 024 CFA/ antigen IFA/ antigen IFA/ antigen 789 Bleomycin Isoflurane Termination latency Naïve Vehicle-immunized + BLM Mouse HARS-immunized + BLM Mouse iMod-immunized + BLM Lung diffusion capacity Isoflurane latency time * CD44+ CD4+ T-cells * CD44+ CD8+ T-cells * Cells (x 106) Cells (x 106) Latency Time 50 75 100 125 150 Activated T-cells in mediastinal lymph nodes 0 2 4 6 0.0 0.5 1.0 1.5 2.0 Exacerbated Response to Bleomycin-induced Injury in Mice With Resokine-antibody Blockade BALF, bronchoalveolar lavage fluid; BLM, bleomycin; CFA, Complete Freund’s adjuvant; IFA, Incomplete Freund’s adjuvant. Regulation of Resokine Splice Variant in Inflammation Resokine Secretion From Lung Cells Resokine iMod-SV Is Upregulated in Airway Epithelial Cells and Secretion Is Increased in Response to Inflammation IFN-g, interferon gamma; TNF-α, tumor necrosis factor alpha. Regulation of the Resokine Pathway in Lung Inflammation IL-13, TGF-β, TNF-α, IL-1β Fibrocytes EMT Fibroblasts ↑ Resokine agonist therapy Pharmacologic restoration of tissue homeostasis and resolution of immune engagement Natural restoration of tissue homeostasis and resolution of immune engagement Perturbation Injury Infection Genetic Severe tissue remodeling Excess deposition of ECM Pro-inflammation IL-1β, TNF-α, IFN-ɣ Circulation ↑ Natural Resokine levels T cell Macrophage Neutrophil Mast cell Resokine Pathway Promotes Lung Homeostasis Epithelial damage Results We characterized serum from a number of Jo-1–positive patients and found the majority exhibited strong cross-reactivity with the N-terminal portion of Resokine and that a splice variant (SV9), which encodes only the N-terminal domain of the protein, is enriched in human lung tissue. Here, we demonstrate that in the lung-derived adenocarcinoma cell line A549, Resokine is actively secreted following stimulation with the inflammatory cytokines IFN-g and TNF-α, two key players in the initiation of lung inflammation and fibrosis. Secretion is dose dependent and synergistic. SV9, but not the full-length mRNA, is increased following inflammatory cytokine stimulation and its peak expression precedes that of the secreted protein. Repeated vaccination of mice with murine Resokine in the presence of adjuvant can break tolerance and generate auto-antibodies. Resokine was present in bronchoalveolar lavage fluid of controls and undetectable in vaccinated animals. In animals with a high titer to Resokine, infiltration of immune cells (including T-cells) into skeletal muscle and lung was detected. Furthermore, in vaccinated animals receiving bleomycin intratracheally, lung function was more severely impacted and both CD4+ and CD8+ T-cells were increased in the mediastinal nodes. Interestingly, these pathologies were observed only in mice that carry a genetic mutation in dysferlin (and other loci) but not in wild-type mouse strains (e.g., C57bl/6). Conclusion Immune invasion pathologies observed in mice forced to break tolerance to Resokine in the background of another tissue-damaging genetic mutation are similar to activity observed in patients with Jo-1 autoantibodies. This suggests that induction of Resokine insufficiency may disrupt immune homeostasis in a manner that manifests as pathological in lung and muscle. The findings that Resokine circulates at pM levels and the splice variant SV9 is synergistically induced and secreted by lung-derived cells in an inflammatory environment provide evidence for an extracellular niche in which autoantibodies could mediate neutralization of these proteins to induce pathology. References Zhou JJ et al. Secreted histidyl-tRNA synthetose splice variants elaborate major epitopes for autoantibodies in inflammatory myositis. J Biol Chem, 2014. Acknowledgements Alina He (Jo-1 antibody analysis), Kenny D’Arigo/John Bruner (Resokine and Resokine-antibody analysis), Jeanette Ampudia (flow cytometry), Zhiwen Xu, Cario Lo, and Carol Lau (experimental advice, primer design and testing, cell culture). Graphics support was provided by Oxford PharmaGenesis, Inc. and was funded by aTyr Pharma, Inc. Disclosure This study was funded by aTyr Pharma, Inc. Disrupting the Resokine Pathway Promotes Lung Damage Evidence for Homeostatic Role of Resokine in Humans BALF, bronchoalveolar lavage fluid; DAD, diffuse alveolar damage; ILD, interstitial lung disease; NSIP, nonspecific interstitial pneumonia. Reverse primer 1 bp Forward primer 1 *** Normalized mRNA Expression 5 4 3M 2 1 0 Total Leukocytes Bone Marrow Thyroid Lung Heart Pancreas Spleen Liver Kidney Colon Small Intestine Adipose Tissue Skeletal Muscle HARS 1,000 850 650 500 400 300 200 Skeletal muscle M High-titer Patients Jo-1 Autoantibodies Epitope Mapping Percentage of Jo-1 Titer 120 100 80 60 40 20 0 Outside of iMod domain iMod domain iMod domain Depleted Resokine Jo-1 Ab Resokine Splice Variant (SV9) Represents the iMod Domain, the Target of a High Percentage of Disease-linked Jo-1 Antibodies The predominant epitopes are in the N-terminal iMod domain Additional epitopes are present throughout HARS, indicating epitope spreading has occurred Characteristics of Jo-1 Associated ILD Increased T-cells in BALF Decreased CD4/CD8 ratio Histology ranges from NSIP to DAD as severity of disease increases *p < 0.05; **p < 0.01, unpaired t test **p < 0.01 by paired t test ***p < 0.001, one-way Anova **p < 0.01, one-way ANOVA *p < 0.05, one-way ANOVA and Dunnett’s post hoc test *p < 0.05, t test E1 E2 E3 E4 E5 Aminoacylation Domain iMod Domain HomeostasisImbalance Diseased Lung Healthy lung 100% (18 of 18) anti-Jo-1 patients tested positive for antibodies to HARS (known extracellularly as Resokine) with high titers to the iMod domain ∆122 nt HARSiMod HARS Exhibit 99.2